Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/177/14. The contractual start date was in March 2014. The final report began editorial review in April 2016 and was accepted for publication in October 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Edwin van Teijlingen declares membership of the HTA Clinical Trials Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Pitchforth et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
Community hospitals form an established component of health-care provision. 1 Historically, in the UK, community hospitals have been defined as local hospitals that are typically staffed mainly by general practitioners (GPs) and nurses to provide care in a hospital setting, often for predominantly rural populations. 2 However, the notion of a community hospital has evolved over time, with a wider range of service delivery arrangements and models developing across England and the UK more widely. These include services that support the rehabilitation and recovery of patients, allowing them to resume independent living more quickly,3 and community care homes or service models that do not include inpatient beds but that provide specialist care alongside primary care and outreach services. 4 Thus, community hospitals exist in a variety of forms, differing in the nature and scope of services provided, the models of ownership and management, and the level of integration with other services. This diversity of service delivery models reflects the needs of the local populations served, as well as broader changes in the nature of the delivery of health-care services. 5 For example, advances in medical technology have made it possible to provide many services closer to the patient, with interventions that would previously have required a hospital environment now carried out in ambulatory settings. 6 With concerns about the perceived high costs of hospital care, there is increasing interest in moving care into the community in order to increase accessibility, in particular in dispersed populations, and so enhance the responsiveness of the system, and, potentially, to reduce costs.
Available evidence suggests that community hospitals may offer advantages over larger hospitals for some patients. For example, studies examining the impact of rehabilitation care for older people found that the community hospital setting was associated with greater independence at 6 months than the district general hospital setting. 7–11 Other work has pointed to the potential role of community hospitals in providing palliative care. 12 It is reported that community hospitals are perceived as friendly and service-user centred; for example, evidence from the 2011 Scottish Inpatient Patient Experience Survey found that community hospitals scored above the national average on many questions concerning patient experience,13 and it has been suggested that community hospitals offer a better experience of care than acute hospitals by allowing more integration with patients’ families and home life.
Others have pointed to a strong tradition of community hospitals providing more integrated care. 14 This core feature of the ‘traditional’ community hospital assumes a renewed importance given the rising burden of chronic disease, creating a complex set of health and social care needs, in particular among those with multiple chronic conditions, alongside frailty at old age. Meeting those needs requires the development of delivery systems that bring together a range of professionals and skills from both the cure (health-care) and care (long-term and social care) sectors. 15 Failure to better integrate or co-ordinate services along the care continuum may result in suboptimal outcomes, such as potentially preventable hospitalisation, medication errors or adverse drug events. 16 A recent commitment by national partners to support service integration emphasised the use of existing structures to align the NHS, public health and adult social care outcomes,17 and it has been suggested that community hospitals may act as a hub for care integration and the provision of care closer to home. 14 More recently, the NHS England Five Year Forward View18 has called for the removal of barriers in how care is provided, including between primary and secondary care and between health and social care, and a small number of vanguard sites have included community hospitals as part of integrated primary and acute care systems and multispecialty community providers. 19
Against this background, there is thus potential for community hospitals and related service delivery models to assume a more strategic role in the local health economy to integrate service provision and thereby address some of the challenges arising from service fragmentation in particular. Furthermore, there is an opportunity to learn from the experiences of other countries in order to inform and help advance the future development of community hospitals in England. However, given the evolving nature of the notion of the community hospital in England and across the UK, there is a need to understand better the role of different models of community hospital provision within the wider health economy and their capacity and capability to integrate services locally. It will be particularly important to understand the nature and scope of services provided by what may be considered a ‘community hospital’, as well as its specific functions and delivery models.
The proposed research seeks to contribute to filling this gap by, first, reviewing the evidence base on community hospitals and equivalent service delivery models nationally and internationally, examining a range of organisational characteristics as well as outcomes. Second, we draw on experiences in other countries on the contribution of community hospitals to the health-care system by assessing equivalent service delivery models. Scotland has a long and rich tradition of community hospitals,13 and relevant approaches have also been described with reference to, for example, Finland,20 Norway,21,22 and, more recently, Italy, in the context of the 2012 reorganisation of hospital care. 23 Evidence from other countries offers opportunities for mutual learning and consideration of alternative policies, or policy transfer, where appropriate. 24
Aims and objectives
The proposed research seeks to answer five principal research questions:
-
What is the nature and scope of service provision models that can be considered under the umbrella term ‘community hospital’ in England and other high-income countries?
-
What is the evidence of effectiveness and efficiency of community hospitals and comparable service models in England and other high-income countries, including in terms of patient outcomes?
-
What is the wider role and impact of community engagement in community hospital service development and provision?
-
How do models that are comparable to community hospitals in England operate, and what is their role within the wider system of service provision in other countries?
-
What is the potential for models that are comparable to community hospitals in England to perform an integrative role in the delivery of health and social care in other countries?
To address these questions, we used a range of methods: a scoping review, a systematic review, a review of five countries (Australia, Finland, Italy, Norway and Scotland) and in-depth case studies (four cases in three countries – Finland, Italy, Scotland).
Structure of the report
The report is organised as two main parts: (1) reviews of current literature and an evidence synthesis; and (2) international country review and comparison. Chapters are broadly organised, within this structure, in line with the principal research questions. In Part 1, Chapters 2 and 3 relate to research questions 1 and 2, respectively, both of which report literature reviews that draw on the same search strategy but employ different methodological approaches. Specifically, Chapter 2 uses a scoping review to describe the nature and scope of service models that can be considered as ‘community hospital’, whereas Chapter 3 presents the findings of a systematic review of the evidence of the effectiveness and cost-effectiveness of such models. In Part 2, Chapters 4, 5 and 6 address research question 4, that is, how models that are comparable to community hospitals in England operate and their role within the wider system of service provision in other countries. Chapter 6 presents a comparative analysis of the nature, scope and distribution of relevant service delivery models in Australia, Finland, Italy, Norway and Scotland, using a review of the published and grey literature following a structured data collection template and key informant interviews. Chapter 5 reports on a detailed multiple case-study analysis of two innovative models of community hospitals in Scotland, and Chapter 6 describes a cross-case analysis of four case studies, including those in Scotland and one each in Finland and Italy. Research question 3 on the wider role and impact of community engagement in community hospital service development and provision and question 5 on the potential for relevant models to perform an integrative role in the delivery of health and social care were understood as aspects to be addressed across the different components of this study. However, as demonstrated, we were unable, as part of the evidence reviews, to identify robust published evidence that assessed the aspect of community engagement (question 3) in a systematic way. Important issues relating to community engagement were brought out in the case studies but this did not emerge as a key area of focus in the country review.
The report concludes with Chapter 7, which provides overarching observations emerging from the different study components, discusses options for community hospital provision that are relevant to NHS England and makes a set of recommendations for future research. The appendices provide supplementary materials relating to data collection and provide individual country and case-study reports. The country reviews reported here reflect the situation in the relevant setting as of March 2016.
Patient and public involvement
Patient and public involvement (PPI) was important throughout our study, particularly as patients were not among our study participants. We outline how we worked with PPI representatives throughout the project from the proposal stage to completion.
Proposal stage
In preparation for the research proposal, we shared our research plan with a PPI panel, INsPIRE. Panel members were asked to comment on the following:
-
Is the lay/plain English summary understandable (if not, please could you offer suggestions from a lay perspective)?
-
Is the extent and quality of service user and carer involvement in the research satisfactory and could people be involved in any other way?
-
Are the proposed research questions important and relevant to service users?
-
Is the proposed research likely to be beneficial to service users?
-
Do you have any other comments on the research plan, research questions or methods suggested?
-
Is our plan for PPI involvement throughout the study appropriate?
Patient and public involvement respondents commented that the proposed research was of value and made suggestions for improvement, noticing that some of the wording remained too technical. PPI members also suggested that it may be useful to present the models of community hospital that we identify in diagrammatic or schematic form. We have used schematic representation as appropriate in Chapter 2.
During the project
For the duration of the project, we sought to recruit two PPI representatives. Following conversation with the co-ordinator of the INsPIRE group, we drafted a job description to explain the project and what would be expected of the representatives (see Appendix 1).
We were able to recruit two patient representatives, Kate Massey and Hamish McBride. Kate Massey commented on the research plan at the proposal stage as a member of INsPIRE and was recruited to the study from there. Hamish McBride was recruited though professional networks. Kate Massey has been an active PPI member on several health service research projects. Hamish McBride is a retired GP with experience of working in a community hospital in rural Scotland. In addition to providing PPI support to this project, Kate Massey was a member of the cross-project steering group. She attended one meeting in person and when unable to attend in person, she provided input remotely.
A number of the points made by the patient representatives during the meetings related more generally to the relevance and accessibility of the work to patients and members of the public. The representatives also commented on each individual component of the study, highlighting issues that seemed particularly important and seeking clarification from the research team in some cases. We noted all of these points for development of the next draft.
Towards the end of the study, we shared drafts of the outputs and followed up individuals for comment and suggestions, which were useful in finalising our report. At this stage, comments from the representatives were particularly useful with regard to the abstract and plain English summary. Once the final report is submitted, we shall seek our PPI representatives’ advice in order to maximise the impact of our study and effectively implement our dissemination plan.
Steering group and co-ordination with related studies
This study was one of three studies that were funded by the Health Services and Delivery Research programme of the National Institute for Health Research (NIHR) to undertake research into community hospitals. The concurrent studies were ‘A comprehensive profile and comparative analysis of the characteristics, patient experience and community value of the classic community hospital’ (HSDR project number 12/177/13) led by Professor Jon Glasby at the University of Birmingham and ‘A study to understand and optimise community hospital ward care in the NHS’ (HSDR project number 12/177/04) led by Professor John Young at Bradford Teaching Hospitals NHS Foundation Trust. The three projects were supported by a cross-project steering group to provide guidance for the research in order to maximise synergies between the three studies. Chaired by Professor Sir Lewis Ritchie, University of Aberdeen, the steering group included representation from the Community Hospitals Association, research, and patient and public associations. The steering group met with members of the three research teams three times over the course of the research presented in this report. The steering group created an open environment in which to share findings and experiences between the projects, as well as to avoid duplication of efforts. For example, our international study was commissioned specifically not to include England or to focus on patients and the role of community in detail, as these issues are central to the study being led by Professor Jon Glasby (HSDR project number 12/177/13). The projects have different durations but the findings from the international experience, presented in this report, have been actively incorporated into the other two studies where appropriate. Joint publications, which synthesise the results of the different studies, will also be pursued, strengthening the relevance of the international evidence to England.
Ethics approval and research governance
Ethics approval was granted by the University of Bournemouth Research Ethics Committee (reference 4857) on 2 October 2014. Details of the ethics application and process are available upon request from the corresponding author. All appropriate local research governance checks were made and approvals given. For the case studies, each research site was responsible for obtaining the appropriate local research governance approvals as per local guidance.
Part 1 Literature reviews and evidence synthesis
Chapter 2 Community hospitals in selected high-income countries: a scoping review of approaches and models
Introduction
Community hospitals have been an established component of health-care provision in the UK for many decades, frequently evolving from local cottage hospitals, which predated the formation of the NHS in 1948. 1 Community hospitals have typically been staffed mainly by GPs and nurses to provide care in a hospital setting, often for predominantly rural populations. 2 They usually sit at the interface between primary and secondary care25 and may provide a diverse range of services including inpatient, outpatient, diagnostic, day care, primary care and outreach services. 1
In England there has been increasing policy focus and government investment into shifting the delivery of medical care to community settings,26,27 with calls for the development of a new generation of community hospitals and services that would be responsive to local needs and at the forefront of health-care innovation. 28–30 The 2014 NHS Five Year Forward View proposed new models of care to be developed in England, which would allow for integration across organisational boundaries, and highlighted the potential role for community hospitals in delivering more integrated care locally by bringing together community, primary and secondary care services. 18 Similar visions have been expressed in other system contexts. 13,23 Although there is potential for community hospitals to assume a more strategic role in service delivery, the precise role that these service structures should take is not clear. A 2006 review by Heaney et al. 1 found that the role of community hospitals has been viewed in different ways, as step-down facilities, as an extension of primary care or as an alternative to secondary care. A wider range of service delivery arrangements have also been described, such as community care resource centres, community care homes and intermediate care or rehabilitation units. 28,29,31,32 Heaney et al. 1 also found that community hospitals serve primarily an older population and are staffed by a range of professionals, including GPs, nurses, allied health professionals and visiting specialists. However, the authors highlighted a lack of robust evidence for the role of community hospitals, indicating a need to understand better the different roles that community hospitals can fulfil, and their capacity and capability to integrate or collaborate with other health and care services.
Commissioned by the National Institute for Health Research (England and Wales), this scoping review updates a review by Heaney et al. 1 published in 2006. It aims to describe different models of community hospitals in selected high-income countries. From this understanding of the nature and scope of services provided and their specific functions, we seek to inform the future development of community hospitals.
Methods
We carried out a scoping review33 following the approach proposed by Levac et al. 34 Given our interest in comprehensively mapping literature that provides insight into community hospital models, we chose a scoping review methodology, which does not exclude evidence based on study design or quality. The review extends the 1984–2005 time frame of the Heaney et al. 1 integrative thematic review and builds on it using comparable search terms and conceptual understanding of the ‘community hospital’. However, it differs fundamentally in its specific interest in models of care and thus in the scope and nature of its reported findings. In addition, unlike Heaney et al. ,1 our review includes non-English language papers.
Given the range of definitions of a community hospital available in the literature (Table 1), we developed a working definition to guide our review. After reviewing these definitions, and having sought expert opinion from members of our cross-project steering group, we stipulated that a community hospital (1) provides a range of services to a local community; (2) is led by community-based health professionals; and (3) provides inpatient beds.
| Definition | Reference |
|---|---|
| A GP community hospital can be defined as a hospital where the admission, care and discharge of patients is under the direct control of a GP who is paid for this service through a bed fund, or its equivalent | Royal College of General Practitioners2 |
| A community hospital is a local hospital, unit or centre providing an appropriate range and format of accessible health-care facilities and resources. Medical care is normally led by GPs, in liaison with consultant, nursing and allied health professional colleagues as necessary, and may also incorporate consultant long-stay beds, primary care nurse-led and midwife services | Ritchie and Robinson25 |
| Many countries have a lower tier of hospital, sometimes called a community hospital. These typically have ≤ 50 beds and provide basic diagnostic services, minor surgery and care for patients who need nursing care but not the facilities of a district general hospital | McKee and Healy35 |
| A service that offers integrated health and social care and is supported by community-based professionals | UK Department of Health26 |
| A local hospital, unit or centre that is community based, providing an appropriate range and format of accessible health-care facilities and resources. These will include inpatient beds and may include outpatients, diagnostics, surgery, day care, nurse-led care, maternity, primary care and outreach services for patients provided by multidisciplinary teams | Community Hospitals Association4 |
We searched PubMed, EMBASE, Scopus, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO, British Nursing Index, Health Management Information Consortium (HMIC), Social Care Online, and Health Business Elite in June 2014 for literature published since 2005, using the principal search terms ‘community hospital’, ‘cottage hospital’, ‘GP beds’ or ‘intermediate care’. The full PubMed search strategy, which was adapted for the other databases we used, is shown in Box 1.
“Hospitals, Community”[Mesh] OR “Hospitals, Group Practice”[Mesh] OR “Hospitals, Rural”[Mesh] OR (“Hospitals”[Mesh] AND “Family Practice”[Mesh]) OR (“Hospitals”[Mesh] AND “Rural Health Services”[Mesh]) OR (“Family Practice”[Mesh] AND “Hospital-Physician Relations”[Mesh]) OR “Hospital Bed Capacity, under 100”[Mesh] OR (“Family Practice”[Mesh] AND “Bed Occupancy”[Mesh]) OR “Intermediate care facilities”[Mesh]
OR
“cottage hospital”[All Fields] OR “cottage hospitals”[All Fields] OR “community hospital”[All Fields] OR “community hospitals”[All Fields] OR (“gp”[All Fields] AND (“beds”[MeSH Terms] OR “beds”[All Fields] OR “bed”[All Fields])) OR “gp beds”[All Fields] OR “general practitioner hospital”[All Fields] OR “general practitioner hospitals”[All Fields] OR ((“community”[All Fields] OR “rural”[All Fields]) AND “hospitals, maternity”[MeSH Terms]) OR “intermediate care” [All Fields]
NOT
(“Africa”[Mesh] OR “Africa, Western”[Mesh] OR “Africa, Central”[Mesh] OR “South Africa”[Mesh] OR “Africa, Southern”[Mesh] OR “Africa, Northern”[Mesh] OR “India”[Mesh] OR “China”[Mesh] OR “South America”[Mesh] OR “Developing Countries”[Mesh])
Limit results to years 2005–present.
Reproduced from Winpenny EM, Corbett J, Miani C, King S, Pitchforth E, Ling T, et al. Community hospitals in selected high income countries: a scoping review of approaches and models. Int J Integr Care 2016;16:13. 36 This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0.
Three researchers (CM, SK and JC) screened titles and abstracts of identified records against a set of inclusion and exclusion criteria (Table 2), which were informed by our working definition. The researchers independently screened the same 300 records and compared their results in order to ensure consistency in deciding on study eligibility. The remaining titles and abstracts were then screened by one of the three researchers. Full texts of potentially eligible studies were retrieved and reassessed against the inclusion and exclusion criteria by one reviewer, and checked by a second reviewer. Disagreements or uncertainties between reviewers were resolved by discussion within the wider research team.
| Study characteristics | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Setting | High-income country with comparable health-care systems that provide universal access (i.e. Canada, Australia, New Zealand and high-income countries in Europe) | Low- and middle-income country; non-European country (except Canada, Australia, New Zealand) |
| Facility type | Meets all of the following criteria:
|
Facility that offers specialist services only GP- or nurse-led beds within secondary or tertiary hospitals |
| Outcomes | A description of the nature and scope of delivery models or services provided | Provides synthesis and discussion of the delivery model only Does not describe the delivery model or services provided by individual community hospitals |
| Study type | Experimental study (RCT, cluster-RCT, quasi-RCT), qualitative study and observational study | Editorial, commentary, review |
| Publication type | Journal article, report, dissertation, book and professional journal | Conference abstract, study protocol |
| Publication year | Published in 2005 and after | Published before 2005 |
| Language | All languages | N/A |
Data were extracted from each study on the features of the hospital model (e.g. management, staffing, ownership) and the specific services offered. Data extraction was undertaken by the three researchers with some duplicate extraction to check for consistency of the approach. Data were analysed drawing on the principles of narrative synthesis, which has been recommended as the most appropriate approach for analysing diverse evidence. 37
Given this diversity, and the fact that this was designed as a scoping review aimed to provide an overview of the existing literature, a formal quality assessment of the included studies was not conducted. However, during data extraction researchers commented on the nature of the evidence presented and any particular concerns as to the quality of the study.
Findings
Our searches identified a total of 15,555 records following the removal of duplicates. After initial screening of titles and abstracts, we considered 604 references for full-text review, and, of these, 75 studies were identified as eligible for inclusion (Figure 1).
FIGURE 1.
Studies eligible for inclusion. Reproduced from Winpenny EM, Corbett J, Miani C, King S, Pitchforth E, Ling T, et al. Community hospitals in selected high income countries: a scoping review of approaches and models. Int J Integr Care 2016;16:13. 36 This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0.
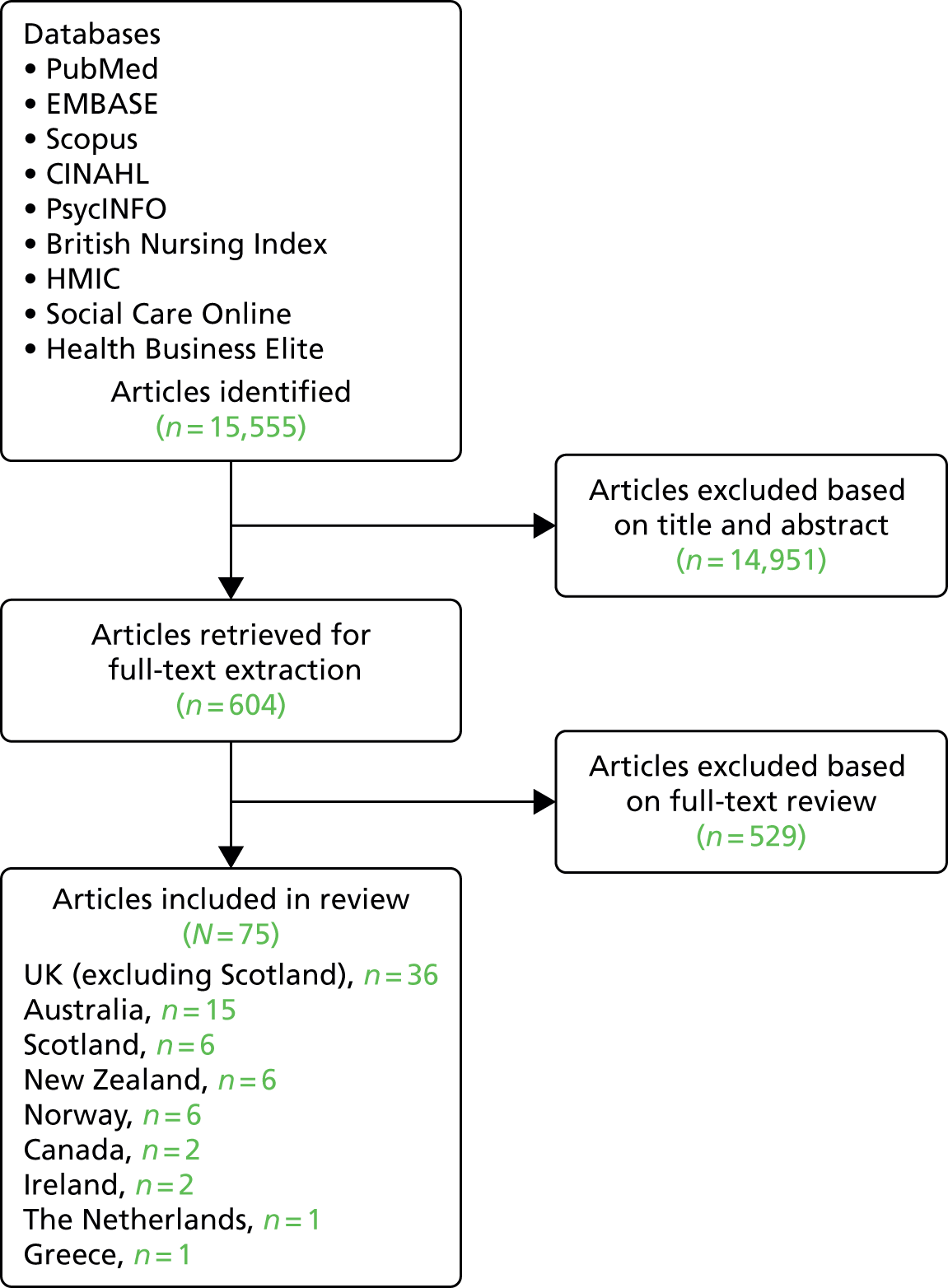
The majority of studies were descriptive or used a qualitative design, while 11 studies used a randomised controlled trial (RCT) design. Included studies fell broadly into the following categories: descriptions of one or more community hospitals (n = 14); descriptions of development of new facilities or procedures within a community hospital (n = 9); reports of particular services within community hospitals (n = 12); studies of patients’ or family members’ experiences of care within community hospitals (n = 4); studies presenting surveys of community hospitals or units within community hospitals (n = 5); or studies reporting on specific outcomes of care delivered by community hospitals (n = 9). The largest number of studies were set in England and Wales (n = 36), followed by Australia (15), New Zealand (6), Norway (6), Scotland (6), Canada (2), Ireland (2), the Netherlands (1) and Greece (1).
Table 3 provides an overview of selected data from eligible studies, including the range of services provided by the community hospitals, as well as the types of staff involved in delivering the services. It should be noted that for many of the studies found, reporting of details of the hospital model was not the primary aim, and information presented here was taken from background or introductory information provided.
| Country | Number of papers retrieved | Facility designation | Services discussed in the literature | Staffing |
|---|---|---|---|---|
| England and Wales | 36 | Community hospital | A large proportion of articles focused on non-acute inpatient services (e.g. post-acute care, rehabilitation or palliative care). Fewer articles looked at outpatient services, urgent care such as in minor injury units, and acute inpatient care. Other services that were discussed more rarely include health promotion, surgery, mental health care, primary care, social care and maternity care | Care led by GPs, nurses and/or community geriatricians, supported by specialist consultants and other practitioners |
| Scotland | 6 | Community hospital | Studies reported on non-acute inpatient services, outpatient services, urgent care services, acute inpatient care, surgery, mental health care and maternity care | Not reported |
| Norway | 6 | Intermediate care hospital Community hospital |
All articles discussed provision of non-acute inpatient services, particularly intermediate care. Other services included outpatient services, urgent care services, acute inpatient care, mental health care and maternity care | GPs, nurses and allied health professionals |
| New Zealand | 6 | Rural hospital | Articles reported on the provision of non-acute inpatient services, outpatient services, urgent care services, acute inpatient care, surgery and primary care | GPs, MOSSes, nurses and allied health professionals, visiting specialists |
| Australia | 15 | Rural hospital | Articles reported on the provision of non-acute inpatient services, outpatient services, urgent care services, acute inpatient care, surgery and primary care | GPs, nurses, midwives and allied health professionals |
| Regional hospital | ||||
| Base hospital | ||||
| Canada | 2 | Rural hospital | Articles report on provision of acute and non-acute inpatient care, urgent care services, surgery, mental health care and maternity care | Family physicians |
| Greece | 1 | Hospital-health centre | Reports on provision of inpatient, outpatient, primary care and preventative health services | Doctors and nurses |
| Ireland | 2 | Community hospital | The articles report on provision of non-acute inpatient services and outpatient services | Nurses and allied health professionals, with input from GPs and geriatricians |
| Netherlands | 1 | GP hospital | The article reports on provision of acute and non-acute inpatient care, outpatient services | GPs and nurses with support from paramedics and specialists |
Range of services provided by community hospitals
Community hospitals provide a wide range of services, across a broad spectrum of care provision, from preventative38,39 and primary care40,41 through to outpatient services,42–44 inpatient medical care,21,45 surgery,46,47 minor injury care48 and accident and emergency (A&E) care. 40,49 Within these broad areas, there was considerable diversity of the types of services provided, and a number of studies further reported on the implementation of new types and methods of service provision not previously available within the community hospital setting, such as point-of-care testing,41 fracture clinics50 or chemotherapy. 51 Community hospitals that provided a wide range of services were common in Australia, New Zealand and Canada, reflecting the geographical needs of these countries in ensuring provision of locally accessible primary, secondary and emergency care services in remote rural areas.
However, providing comprehensive services in these settings was reported to be challenging, because of limited capacity or access to specialist expertise to deliver services required to meet the needs of the local population. For example, one study set in New Zealand reported that of 35 selected medical conditions and procedures that may be needed for acutely ill patients, only about 70% could be performed in any one of a group of rural hospitals. 52 A cross-sectional survey of emergency departments in rural hospitals in Canada found that, with the exception of basic laboratory and radiography services, the majority had limited access to professional and support services. For example, only 5% of hospitals had access to a paediatrician, 26% had access to a surgeon and less than one-third had access to ultrasound equipment (28%), a computerised tomography scanner (20%) or an intensive care unit (17%). 53
Studies of community hospitals in England and Scotland typically reported on the provision of non-acute inpatient services, particularly post-acute geriatric care, rehabilitation services and palliative care. 7,54–58 Indeed, several UK community hospitals provide exclusively, or largely, non-acute inpatient care to chronically ill or older populations. 7,38,56 Similarly, community hospitals in Ireland tend to focus on services for older people such as respite care, rehabilitation, palliative care long-stay facilities and community-based assessment. 59,60
Studies of community hospitals in Norway also described a focus on intermediate care, targeted at people who would otherwise face unnecessarily prolonged hospital stays or inappropriate admission to acute inpatient care, including chronically ill and older patients. 9,61,62 A specific case of a community hospital is Hallingdal Sjukestugu in central Norway. 21,22 Described as a ‘decentralised specialist healthcare service’, it is led by GPs under telephone supervision by hospital specialists who are located in an acute hospital (Ringerike sykehus), which is 170 km away and administers and funds the community hospital. It includes an inpatient department, which functions as an intermediate care unit, along with outpatient psychiatric and somatic services, somatic day care, a somatic inpatient department, as well as a pre-hospital ambulance and air ambulance services.
There were only a small number of studies of community hospitals in countries other than England, Scotland, Australia, New Zealand and Norway, as noted earlier. One study set in the Netherlands described a community hospital that was established as an experiment after closure of a former district general hospital west of Amsterdam. 63 Its 20 beds were designated as ‘GP beds’ for GPs treating their own patients, ‘recovery beds’ for the rehabilitation of post-surgery patients or ‘nursing home beds’ for patients awaiting a place in a nursing home. Services reported were low-level care and observation and included diagnostic facilities (e.g. laboratory and radiography), allied health services (e.g. physiotherapy, occupational therapy and speech therapy) and outpatient clinics.
A number of studies described and evaluated the development of new outpatient services in community hospitals. Examples include a treatment and diagnostic centre for gynaecology,64 and a nurse-consultant-led clinic for patients with chronic musculoskeletal pain,42 both set in the UK. Several studies reported on outpatient services that were developed in collaboration with larger hospitals, such as services for people with eating disorders, which used videoconferencing to connect participants in community hospital sites and a specialist service within a large urban hospital for weekly therapy sessions. 65 Another example was the development of a teleopthalmology service by a regional hospital in Western Australia together with eye specialists in Perth, which allowed digital images to be transmitted to the specialists for diagnosis. 44 Two studies described outreach chemotherapy services, delivering chemotherapy cycles in community hospitals by staff based at a larger hospital or care centre. 51,66 Finally, two studies described the role of community hospitals in the provision of maternity services. This included one study set in Australia, which reported on a rural community hospital providing pregnant women with access to monthly ultrasound, specialist maternity advice by telephone, and an obstetrician outpatient clinic several times a year. 67 Another study, also set in Australia, described a midwifery-led model of care within a rural hospital, providing low-risk women the option to give birth at their local hospital. 68
Staffing of community hospitals
The community hospital workforce includes GPs, generalist and specialist nurses, allied health professionals (e.g. physiotherapists, occupational therapists, dietitians) and health-care assistants. This staff mix is described in studies of community hospitals in the UK,56 Norway,61 the Netherlands63 and Australia. 69 In many hospitals GPs are in charge of hospital management70 or have ultimate responsibility for patients and beds. 63,71 In New Zealand the community hospital workforce also includes the non-specialist Medical Officers of Special Scale (MOSSes),52,72 a non-training position for a doctor who has not yet specialised. 73
Staffing models were described in which MOSSes constitute the core of the medical workforce, supported by nursing staff and allied health professionals, together with back-up GPs or visiting specialists. 72,74 In many community hospitals, medical doctors were reported to represent a small proportion of community hospital staff, and were not available on site at all times. For example, a survey of New Zealand rural hospitals reported that 14% of hospitals had a GP on site at all times and 41% had a facility for the GP to spend the night in the hospital,52 whereas a study of the 10 community hospitals of the Powys region in Wales noted that none of these had resident medical doctors, including GPs. 71 Elsewhere, studies reported on-site availability of GPs only during weekdays, such as in a 12-bed intermediate care hospital in Norway;61 however, GPs are generally available to provide care at night and at weekends, with on-call GPs committed to provide out-of-hours cover. 41,71,74,75
In some countries, a shortage of medical staff is reportedly an issue. This was the case in New Zealand, where 9% of medical staff positions were unfilled and 24% were filled by locums,76 and in Greece. 39 One study in Australia68 described difficulties experienced by a rural hospital in recruiting sufficiently skilled hospital medical officers, eventually leading to the closure of the maternity service. However, in this particular case it was possible to substitute medical officers with midwives, permitting reopening of the service 6 weeks after its initial closure.
The role of specialists
Given that many community hospitals described in studies included in this review do not tend to have GPs on site full time, it is perhaps not surprising that on-site presence of specialists is even less common. In most cases, the specialist tends to perform an intermittent or remote supervisory role. 59,68 Models of such supervision include weekly oversight by a consultant from the nearest acute hospital,54 or regular educational visits. 59 One study from New Zealand reported on consultant surgeons who undertake visits to community hospitals over a distance of 150 km at least twice per week. 72 In more remote areas, specialist visits may be less frequent, as in the case of the delivery of obstetrician outpatient clinics several times per year,67 or of specialist eye care offered by visiting specialists for 1 week two times a year in Australia. 44
This limited or remote specialist involvement means that GPs and nurses are required to be flexible in their roles and to demonstrate a broad spectrum of skills. 21,41 For example, GPs may perform minor surgery or caesarean sections68 and have ‘multiple roles’, which include ward duty, GP clinics and emergency unit on-call, such as in a 20-bed rural hospital in Victoria, Australia. 77 Small regional hospitals in the Northern Territory in Australia are staffed with GPs trained to perform emergency and elective surgery. 47 As for nurses, they may have to demonstrate skills in areas such as clinical procedures, diagnosis, leadership, patient-centred care, interprofessional communication, spiritual guidance and bereavement support,78 or to master some relatively complex diagnostic tools (e.g. for stroke54 or chest pain48).
The role of nurses
The importance of the nurse’s role was particularly emphasised in community hospitals where, in addition to requirements for a broader skill set, they hold greater managerial 59 and patient-related responsibility than in larger hospitals. 79 Senior nurses or midwifes are often in charge of managing a unit or the whole hospital, as in the case of the 18 community hospitals reported on in Ireland. 59 They may be responsible for the patient from admission to discharge,80 without the patient seeing a doctor. 77 In other cases, nurses were in charge of the development and implementation of a specific specialist service, such as a chronic musculoskeletal pain service42 or a mental health liaison service. 81 Steers et al. ,82 based on a review of the evidence of providing palliative care in community hospitals in the UK, concluded that GPs generally acknowledged their dependence on nursing staff to support them to make timely management decisions following the admission of patients.
Collaboration and integration with other services
Community hospitals tend to be highly collaborative and integrated with primary care and secondary care as well as with third-sector or community organisations. 83 This is facilitated through the community hospitals’ role along the patient pathway, its function as a physical site for the co-location of services, and through a shared workforce with primary care and close collaborative working with acute specialists, described above.
For example, one of the functions community hospitals may take on is the provision of post-acute care. A study of the effect of an intermediate care hospital in central Norway on the discharge process from acute to community care found that the community hospital had a role in facilitating integration between care levels. 61 Staff at the acute hospital saw the community hospital providing ‘an extension of a hospital department’, while those in primary care viewed it ‘as a buffer that provided preparations for discharge of the patients’. Staff of the community hospital were reported to liaise effectively with both acute and primary care, sharing information through medical records as well as further direct communication where necessary.
Physical co-location of different services also offers opportunity for collaboration and integration. Included studies report co-location of primary care, community care and social care services within the community hospital. 38,84,85 A perhaps unusual case is that of a community hospital in Oxford, England, which was transferred to form a unit within a large tertiary teaching hospital. Special financial arrangements (a monthly fee) allows for staff from the acute hospital, such as the specialist gerontologist, senior registrar and senior house officer, to support community hospital staff. 56
Given the core involvement of GPs in the delivery of community hospital services as described above, typically working in their practice in addition to delivering shifts in the hospital, they provide opportunity to build strong links between the community hospital and primary care. 52,63 Indeed, in the UK, continuity of care delivered by local GPs known to the patient and their family was cited as one of the benefits of care in a community hospital. 45
Strong collaboration was also reported between community hospitals and specialists located in acute hospitals, and a number of studies described different models of collaboration. For example, specialists from a nearby acute hospital are frequently reported to be available to provide remote advice and support when needed, for example by telephone or videoconferencing. 80 We described earlier the example of the community hospital Hallingdal Sjukestugu in central Norway, which is funded and administered by an acute hospital with patients legally under the acute hospital’s professional responsibility. 21 As such, the specialist at the acute hospital must approve admissions to the community hospital and the community hospital GPs are under remote supervision from acute hospital specialists.
In many cases, collaboration between community hospitals and larger hospitals or specialists has been described as a means to maximise local provision of services. 47 One example is the reopening of the maternity unit in Mareeba District Hospital in Queensland, Australia, as a midwifery-led model of care, described above. 68 The unit is supported by an obstetrician at the base hospital who oversees all emergency care and pregnancy complications.
In many cases, collaboration between the community hospital and other health services is supported by the introduction of new technologies. Examples include a shared electronic health record to help facilitate links between the community hospital and primary care in Norway61 or a telemedicine link between the community hospital and a larger hospital. Use of telemedicine often involved direct interaction between the specialist and the patient, such as a teleophthalmology service in Australia. 44 Other examples include the provision of a medical oncology outreach clinic, whereby oncologists from a larger hospital review patients in the community hospital using video conferencing equipment,69 therapy sessions delivered by videoconference,65 videoconference fracture clinics,50 telepharmacy86 and remote commenting by radiographers. 87 In the Grampian region of Scotland, a minor injuries telemedicine network connects 15 minor injury units in community hospitals to the emergency department at the regional teaching hospital. 80 Patients are seen by trained community hospital nurses, who can seek advice as required from medical staff and consultants based at the teaching hospital emergency department.
Ownership of community hospitals
Most community hospitals described in studies included in this review are public hospitals, which are the responsibility of local or regional health authorities (RHAs) with regard to funding, management and commissioning of services. However, reflecting the specific system context in different countries, ownership and management may take different forms. For example, an intermediate care department in Trondheim in the north of Norway was established at a teaching nursing home to provide care for older patients initially admitted to the city acute hospital, but who no longer require acute medical supervision. 9 The goal was to create a new link between specialist care at a general acute hospital and community home care to aid recovery before final discharge of the patient to their own home. Under the Norwegian decentralised model of health-care provision, the nursing home falls under the responsibility of the municipality.
One other example is that of a community hospital in Norfolk in the east of England, which is operated as a social enterprise following the closure of inpatient beds previously operated by the NHS in 2005. 88 In addition, a 28-bed community hospital in Oxford, England, was described earlier. Considered ‘unfit for purpose’, it was integrated as a unit within a nearby acute tertiary hospital. 56
Discussion
This scoping review explored the range of community hospitals in high-income countries as described in the published literature. We note that there is not one definition of a community hospital, and we identified a number of service delivery ‘models’ than can be broadly subsumed under the heading of a community hospital, which we defined as (1) providing a range of services to a local community; (2) being led by community-based health professionals; and (3) providing inpatient beds. We found that community hospitals may provide a wide spectrum of health services, including preventative and primary care, inpatient and outpatient services, medical and surgical care, and acute and chronic care. Within these broad categories there is wide variation in the specific services and level of service provided, typically reflecting the needs of the local population and the availability of other health services, as well as the interests of local practitioners in service development.
Figure 2 presents a graphical depiction of our understanding of the nature and scope of services provided by community hospitals, based on our review of the evidence presented in this study. This diagram may provide a helpful way to conceptualise the remit of community hospitals, obviating the need to provide a precise definition for this inherently diverse concept.
FIGURE 2.
Nature and scope of services provided by community hospitals. Reproduced from Winpenny EM, Corbett J, Miani C, King S, Pitchforth E, Ling T, et al. Community hospitals in selected high income countries: a scoping review of approaches and models. Int J Integr Care 2016;16:13. 36 This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0.
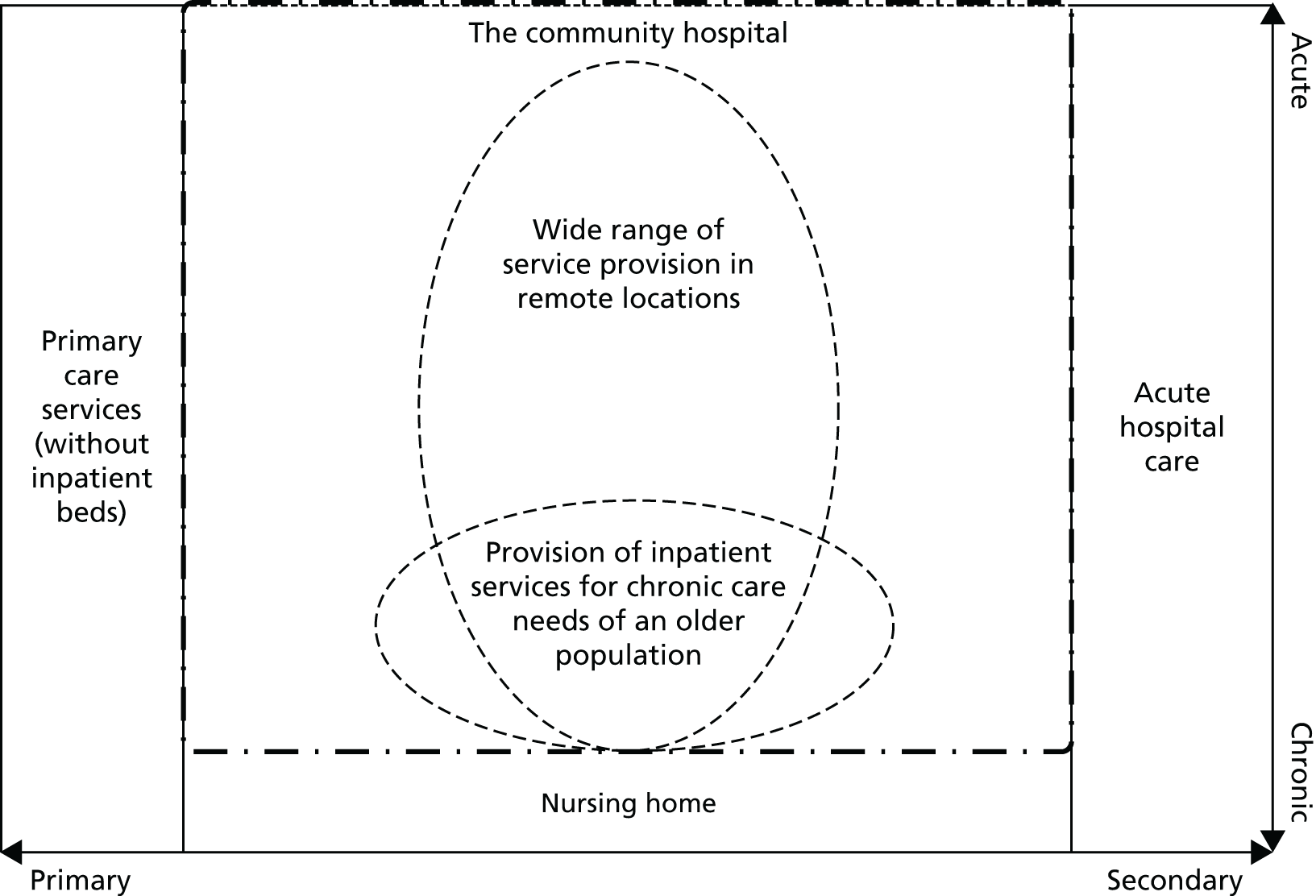
As shown, community hospitals occupy the space between, and to some extent encompass, primary care services and acute hospital care. The dashed box outline in Figure 2 indicates this flexibility in the boundaries between community hospital services and other levels of care. In addition, community hospitals may deliver care across a range of services from acute to chronic care. There are examples of community hospitals that focus on the delivery of non-acute inpatient care, such as post-acute care or rehabilitation care for an older population, and others that deliver a wide range of health care to a whole population, often in geographically remote locations where alternative services are not readily available. These potential areas of focus are indicated by the dashed circles in Figure 2; however, as we have seen, community hospitals are characterised by their wide diversity.
Our literature search considered studies that have been published since 2005, building on a previous review by Heaney et al. 1 We note that our findings show many similarities with the previous review regarding the role of community hospitals within health-care provision and the types of services offered. We did not identify studies on certain specific services described by Heaney et al. ,1 such as cardiac care; however, the literature reviewed in the present study reported on a more diverse range of service provision with such services often supported by acute specialists working remotely. We also found evidence of a wider use of telemedicine than described previously.
Limitations of the review
Our review has a number of limitations. We focused on community hospitals defined as those that provide inpatient beds, are led by community-based health professionals, and provide a range of services to a local community, and our findings are thus constrained within these a priori definitions. We also have captured literature pertaining to services that may form part of a community hospital, but for which the relevant study does not mention the community hospital itself, for example those studies examining midwifery units that may be located in community hospitals. 89
As a scoping review, which aimed to map the evidence on community hospitals, this review did not assess the quality of the evidence, nor did it assess the effectiveness of the different types of community hospitals. Although not within the remit of our scoping review methodology, the heterogeneity of the studies identified would have precluded any meta-analysis. We therefore cannot derive any conclusion about which service formations may be most appropriate. Furthermore, our review focused on published studies and we therefore do not capture information on factors that have not been studied or, indeed, on community hospitals that have not been reported on in the range of sources we considered for the review. Similarly, we have found little evidence on topics that are difficult to measure or analyse. These limitations suggest the need for more systematic interrogation of practice in community hospitals through primary research.
Despite these limitations, our review enhances understanding of the current role of community hospitals in a number of high-income countries, allowing it to help inform future policy and practice. One key feature that is apparent is the flexibility and adaptability of the community hospital model. This may be an important advantage allowing response to future changes in population health needs and other changes in health service delivery. In England, the 2014 NHS Five Year Forward View set out how the health service should better adapt to the changing system environment. 18 The rising number of people with multiple chronic conditions, an ageing population and increasing patient expectations, alongside technological advances and new approaches to practice and funding, are all altering the way health care is delivered by providers and accessed by service users. 18 Among the measures set out in this long-term view, a set of new care delivery options have been proposed as a means to better meet the changing needs and challenges the system is facing. Within these the community hospital may be seen to take a core role through provision of a community hub which already hosts a wide range of services, provides a setting for integration between different health and social care organisations, and has strong links with the local community.
Evidence reviewed provided many examples for the provision of particular specialist services in community hospital settings, including inpatient and outpatient services, which can be delivered in community hospital settings on a routine or intermittent basis, often with the aid of technology. These findings provide important insights to inform the wider policy debate on shifting care into the community. 20 Joint working arrangements such as visits by travelling surgeons, shared posts across community and acute hospitals, or the use of telemedicine have allowed an increase in the range of services available in community hospitals, as well as the level of specialisation of care delivered within community hospitals. Future technological developments allowing medical care to be delivered at a distance may be able to expand the role of community hospitals further.
One important issue to consider, which was outside the scope of this study, will be the cost-effectiveness of provision of services in a community hospital compared with in other settings. Despite ongoing government interest in provision of services closer to home, it may be that some services are most cost-effective when provided at scale in a specialist centre. This will vary by service and it will be important to examine in detail the different services provided and the costs and benefits of provision in different settings.
Conclusion
This scoping review, drawing on literature from 10 high-income countries over the past 10 years, found that community hospitals reported in the literature operate in a manner that situates them at the boundary of primary care, acute hospital care and nursing home care and may provide services which span each of these domains. Different community hospitals offer services that range from preventative and primary care to inpatient surgical or medical care, and service provision tends to be delivered by generalist doctors and nurses, with specialist physicians visiting occasionally to deliver particular services in some cases. Our analysis suggests that community hospitals can provide a diverse range of services, responding to different geographical and health system contexts. The literature highlighted the collaborative working at community hospitals between those from primary, community and secondary care, and this integrative role may be particularly important in the design of future models of care delivery, where emphasis is placed on continuity of care and collaboration between those traditionally situated in different care sectors.
Chapter 3 Community hospitals in high-income countries: a systematic review of the evidence on effectiveness and cost-effectiveness
Introduction
As countries are striving to find ways to create systems that are more responsive to the changing needs of an ageing population, different service delivery models are being considered that seek to better integrate services along the care continuum to meet the often complex care needs of people with multiple chronic and long-term conditions. 90 In England, a growing policy focus on care integration and on shifting services closer to people’s homes has led to renewed interest in community hospitals and the potential role they can have in delivering more integrated care at local levels. 18
Community hospitals have formed an established component of health-care provision in the UK for decades. 1 Defined as local hospitals that are typically staffed mainly by GPs and nurses and provide a diverse range of care to mostly rural populations, community hospitals have been associated with a wide range of benefits for patients, in particular around accessibility and a sense of a friendly atmosphere but also improved outcomes in terms of independence and rehabilitation. 29,58,91 Comparable models have also developed outside the UK, offering services that sit on the continuum between primary and secondary care, often with a particular focus on older patients. 22,92 However, as demonstrated elsewhere, the overall evidence for their effectiveness and cost-effectiveness has remained limited. 1
Given the renewed policy interest, highlighting the potential for a more strategic role of community hospitals in shaping service delivery locally, it seems timely to revisit the evidence base on their clinical effectiveness and cost-effectiveness. Linked to the scoping review exploring international approaches and models of community hospital care (see Chapter 2), this chapter examines the available evidence on the effectiveness and cost-effectiveness of community hospitals nationally and internationally. With an identical search strategy, time frame and definition of ‘community hospital’ to the scoping review, this review further updates and expands on the thematic review by Heaney et al. 1 However, by addressing the specific question of the effectiveness and cost-effectiveness of community hospitals, it differs fundamentally in its thematic interest and thus in the focus of its reporting.
Methods
This review is reported in line with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). 93 Chapter 2 presents the full search strategy (see Box 1) and the definition of ‘community hospital’ (see Table 1) used. The protocol for this review was not registered.
Unlike our scoping review methodology (see Chapter 2), to be included in this review studies had to assess patient health outcomes, patient and carer experience or satisfaction measures, organisational outcomes or cost-effectiveness compared with other hospital settings, including acute hospitals. Measures assessed could be qualitative or quantitative and studies had to be set in high-income countries with health-care systems comparable with that of England (Table 4).
| Study characteristics | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Countries | High-income countries with comparable health-care systems that provide universal access (i.e. Canada, Australia, New Zealand and high-income countries in Europe) | Low- and middle-income countries; non-European countries (except Canada, Australia, New Zealand) |
| Hospital type | Community hospitals that meet all of the following criteria:
|
|
| Comparators | Care provided in other settings, including general hospitals | Audits of care provided in a community hospital, with no comparison |
| Comparison made in the discussion (e.g. against best practice, guidelines or data from the literature) | ||
| Outcomes | Quantitative measures of efficiency | No outcomes measured |
| Quantitative measures of effectiveness | ||
| Qualitative measures of effectiveness | ||
| Patient outcomes to include health measures, patient satisfaction, patient experience | ||
| Study types | Experimental (RCTs, cluster RCTs, quasi-RCTs), qualitative and observational studies | Conference abstracts |
| Editorials, letters or commentaries | ||
| Vignette studies or hypothetical cases | ||
| RCT protocols | ||
| Publication year | Published in 2005 and after | Published before 2005 |
| Language | All languages | – |
Screening and data extraction proceeded as described in Chapter 2, Methods, and papers were assessed against the inclusion and exclusion criteria for this review (see Table 4) at the stage of full-text screening. Titles and abstracts were screened by three researchers (CM, SK and JC) against the inclusion and exclusion criteria, and the process was repeated for full texts. Data were extracted on features of the hospital model, population covered and outcomes evaluated. Extraction was undertaken by the same three researchers and data were checked for consistency between the three; disagreements or uncertainties were resolved by discussion within the wider research team.
Papers were assessed for quality of reporting of underlying studies by three researchers (EW, JC and SK), following checklists provided by the National Institute for Health and Care Excellence in their Guidelines Manual. 94–96 For cost-effectiveness studies, we drew on a checklist for assessing economic evaluations. 97 Assessments were verified by a second researcher for accuracy, and disagreements were resolved through discussion. Quality assessments were used to inform an understanding of the weight of the evidence base and not as a basis to exclude papers. Given the diverse nature of evidence, a narrative synthesis approach was used for analysis. 37 Meta-analysis of data was not conducted owing to the small number of studies included and the diversity of outcome measures applied therein.
Findings
We identified 15,555 independent records, of which 604 studies were retrieved for full-text extraction (Figure 3). A total of eight studies (represented by 17 papers) met our inclusion criteria.
FIGURE 3.
Literature included in the study.

An overview of the included studies is given in Table 5. There were seven papers reporting on four RCTs,7,9,10,62,66,98,100 and two papers reporting on qualitative research embedded in two of the RCTs. 8,55 There were a further four papers reporting on three qualitative studies, and one paper on an observational cohort study. 45,54,58,61,102 An additional three papers reported on cost (effectiveness) analyses embedded in three of the aforementioned RCTs. 11,62,99 Of the aforementioned papers, the cohort study and a RCT also reported on some cost-analyses. 66,102 Two of the studies (across four papers) reported on research conducted in Norway, and the remainder were set in England.
| Study description | Paper | Design | Primary outcomes measured | Study setting | Overall quality assessment |
|---|---|---|---|---|---|
| Single-centre post-acute care RCT, underpinning the PATCH study | Green et al. (2005)7 | RCT |
|
A community hospital and an acute hospital in England | Low risk of bias |
| Young et al. (2007)98 | Secondary analysis of RCT |
|
Unclear | ||
| O’Reilly et al. (2006)99 | Cost-effectiveness analysis embedded within RCT |
|
High quality | ||
| Green et al. (2008)55 | Qualitative interview study embedded within RCT |
|
Medium quality | ||
| PATCH study | Young et al. (2007)10 | RCT |
|
Five acute hospitals and seven community hospitals in England | High quality |
| Young and Green (2010)100 | Secondary analysis of RCT |
|
Unclear | ||
| O’Reilly et al. (2008)11 | Cost-effectiveness analysis embedded within RCT |
|
High quality | ||
| Small et al. (2009)8 | Qualitative interview study embedded within RCT |
|
Medium quality | ||
| Intermediate care at a community hospital as an alternative to long-term acute hospital care | Garåsen et al. (2007)9 | RCT |
|
A community hospital and an acute hospital in Norway | Low risk of bias |
| Garåsen et al. (2008)62 | 12 month follow up of RCT |
|
Low risk of bias | ||
| Garåsen et al. (2008)101 | Cost analysis embedded within RCT |
|
Medium quality | ||
| Chemotherapy provision in community hospitals | Pace et al. (2009)66 | Crossover RCT with some cost analysis |
|
Specialised cancer centre and chemotherapy outreach clinics in four community hospitals in England | Low risk of bias |
| Emergency admissions of older patients | Stapley et al. (2007)102 | Observational (cohort) study and cost analysis |
|
An acute hospital and five community hospitals in England | Unclear |
| End-of-life care in community hospitals | Hawker et al. (2006)45 | Qualitative interview study |
|
Six community hospitals in England (comparisons drawn with acute hospital care) | Medium quality |
| Payne et al. (2007)58 | Qualitative interview study |
|
Medium quality | ||
| Stroke rehabilitation | Dobrzanska et al. (2006)54 | Qualitative focus group study |
|
A community hospital in England (comparisons drawn with acute hospital care) | Low quality |
| Role of intermediate care community hospital in patient discharge to primary care | Dahl et al. (2014)61 | Qualitative interview and focus group study | Health professionals’ experiences of patient discharge to primary care | Acute hospital, community hospital and primary care service in Norway | Medium quality |
Five studies in 13 papers reported on the provision of post-acute care at community hospitals,7–11,54,55,61,62,98–101 one examined chemotherapy at community hospitals,66 one considered emergency admissions102 and one study presented data on end-of-life care across two papers. 45,58 The majority of papers focused on patient outcomes (health,7,9,10,61,62,66,98,100 experience and satisfaction7,8,10,54,55,58,66), whereas two measured staff experience. 8,61 Other outcomes measured included organisational and resource efficiencies61 and family and carer experience. 7,45,58 With the exception of one study on chemotherapy, all studies concerned an older population (aged ≥ 55 years). 66
All studies reported in the papers compared community hospital care with care delivered in an acute hospital setting. The quality of papers included varied from high (n = 7) (i.e. all aspects of study methodology were well reported and the authors used an acceptable methodology), medium/moderate (n = 6) (i.e. details were not fully reported for some criteria, but otherwise the authors used an acceptable methodology) and low (n = 1) (i.e. an unacceptable methodology was used) to unclear or unknown quality (n = 3) (i.e. there was insufficient evidence to make a firm judgement) (see Appendix 2).
Patient health outcomes
Post-acute care
Four studies in seven papers evaluated health outcomes in a post-acute setting. 7,9,10,61,62,98,100 In their high-quality RCT, Young et al. 10 used the Nottingham Extended Activities of Daily Living Scale to assess independence 6 months after treatment in patients randomised to receive either intermediate care at a community hospital or usual care at an acute hospital. The study showed a significant increase in independence at 6 months in the community hospital compared with usual care [mean difference = 3.27, 95% confidence interval (CI) = 0.26 to 6.28; p = 0.03], supporting findings from the previous single-centre study by the same group (mean difference = 5.30, CI = 0.64 to 9.96). 7 In the multicentre trial, similar proportions of both groups died before follow-up (p = 0.33), and, among those living at home before admission, similar proportions of both groups were discharged to a care home, died before discharge (p = 0.08) or continued to live at home (p = 0.426) at 6 months. 10 Conversely, anxiety levels 1 week post discharge showed a greater increase in the community hospital group (p = 0.03) as assessed using the Hospital Anxiety and Depression Scale (HADS).
Additional analyses of both RCTs found a trend towards worse independence outcomes for patients who were transferred to the community hospital late or not at all (p = 0.072 for the multicentre trial). 98,100 Pairwise comparisons in both studies showed significant differences in favour of patients who were transferred to the community hospitals early compared with those who remained at the acute hospital for longer.
A high-quality RCT set in Norway compared provision of intermediate care at a community hospital with continued care at an acute hospital. 9 Care at the community hospital was associated with a decrease in readmissions for the same complaint within 60 days [odds ratio (OR) 2.77, 95% CI = 1.18 to 6.49; p = 0.03] and an increase in independence from home care (OR 1.21, 95% CI = 0.59 to 2.52; p = 0.02) compared with the acute hospital. There was no significant difference in the proportion of deaths at 6 months (p = 0.23), but at 12 months a significantly smaller proportion of patients had died in the community hospital group (p = 0.03). 62 The number of patients living in nursing homes and total number of bed-days at 6 months did not differ significantly between settings, but the acute hospital group had fewer days of initial inpatient care (p = 0.00) and the community hospital group had fewer inpatient days for readmissions (p = 0.04). 9 No significant differences were found at 12 months in the number of admissions, acute hospital bed-days or for long-term primary-level care needs, which the authors link to a loss of power to reveal differences owing to the high proportion of deaths during follow-up. 62
Chemotherapy provision
A high-quality crossover RCT compared chemotherapy in outreach locations at four community hospitals with chemotherapy delivered in a dedicated cancer centre. 66 The community hospitals had not previously delivered chemotherapy and in all settings treatment was delivered by a hospital chemotherapy team. No safety issues or adverse reactions were reported in community hospitals and there were no significant differences between the treatment groups either in toxicity levels (using Chemotherapy Symptom Assessment Scale) or in anxiety and depression (using HADS).
Patient and carer experience and satisfaction
Palliative care
One qualitative study on end-of-life care (in two medium-quality papers) asked patients and their family carers about care in community hospitals compared with acute hospital care, and suggested that the community hospital was perceived as preferable. 45,58 Hawker et al. 45 reported that bereaved carers expressed more satisfaction with community hospitals than with their nearest acute hospital, valuing ease of access for visits, pleasant environment and facilities, familiarity between staff and families and sensitive and kind nursing staff. Participants also commented that staff seemed to care more for the patients and had more time to spend with them than at the acute hospital. These findings were supported in Payne et al. ,58 as patients reported the community hospital to be cleaner, more comfortable, better located and more flexible in responding to individual needs. Study participants also particularly valued the continuity of care offered by GP-led community hospitals. Both papers, however, reported concerns related to a lack of contact with qualified nursing staff and noise levels in community hospitals. Older patients also highlighted the lack of facilities and qualified staff for complex medical procedures, when compared with the acute setting. 58
Chemotherapy provision
In Pace et al. ’s66 crossover RCT, some 97% of patients chose to receive their remaining chemotherapy treatment at a community hospital rather than a cancer centre. Data from the Chemotherapy Patient Satisfaction Questionnaire showed that patients were significantly more satisfied with the community hospital than with the cancer centre for accessibility (mean difference = 1.05, p < 0.001), environment (mean difference = 2.79, p < 0.001), technical aspects of nursing care (mean difference = 0.58, p < 0.01) and interpersonal aspects of nursing care (mean difference = 0.4, p < 0.05) . There was no significant difference in global satisfaction between the settings.
Post-acute care
Three studies set in England reported high patient satisfaction and preference for community hospitals for post-acute care and rehabilitation across five papers. 7,8,10,54,55 One low-quality qualitative study reported that patients discharged to the community hospital for rehabilitation after stroke appreciated the convenient location, which made it easier for relatives to visit. 54 The community hospital was also perceived to be less confusing and safer than the acute hospital because of its small size, and patients appreciated having a choice of location.
Young et al. ’s10 multicentre and Green et al. ’s7 single-centre RCTs found only minor differences in patient and carer satisfaction between community and acute hospital groups. In the Young et al. 10 trial, patient satisfaction with their own recovery was similar for both groups but greater at 1 week after discharge for community hospital groups (OR 2.12, 95% CI = 1.3 to 3.46; p = 0.004). Green et al. 7 reported that patient and carer satisfaction with community services was also similar for both groups, but greater for the community hospital group at 3 months after recruitment (OR 3.43, 95% CI = 1.05 to 11.24). They found no difference between groups for emotional distress in carers, or in effect on the carer burden.
Two medium-quality qualitative papers nested within the two RCTs found patients’ and carers’ experiences of care in community hospitals generally compared favourably to equivalent care in acute hospitals. 8,55 Patients were reported to value the location, food, staff attitudes, the physical environment and the ambience of the community hospital, including single-bed accommodation, which was perceived to be more home-like. 55 These findings were supported by Small et al. ,8 who reported that patients and carers described the community hospital as more ‘homely’ and valued its accessibility. There was a perception, as expressed by one carer, that the community hospital’s home-like environment would promote recovery through encouraging the self-care activities needed after discharge. This was contrasted with views on the acute hospital, where the philosophy of care was seen to be focused on ‘medical efficiency’.
Staff experience and organisational effectiveness
Post-acute care
Staff experiences of delivering post-acute care to older patients in community hospitals were generally described to be positive in two studies reported in two qualitative papers set in England and Norway. 8,61 In England, Small et al. 8 carried out interviews with community hospital staff, who reported that the community hospital provided a distinctly homely, calm and pleasant setting, where social interaction was encouraged and patients’ relatives were involved in patient care. Community hospitals’ orientation towards older people was also considered important. Conversely, in describing their workplace, acute hospital staff emphasised care attributes such as ‘medical efficiency’ and high standards and described a lack of stimulation for patients. At the same time, staff in both settings highlighted shared understandings of the importance of providing holistic and patient-centred post-acute care.
The study in Norway reported that the introduction of a community hospital as a ‘bridge’ between acute and primary care had improved staff experience of discharge processes, including timeliness, patient preparation for transition and communication between the different levels of care. 61 Primary care staff were satisfied that patients with complex needs were ‘shielded’ from fast discharge from the acute hospital. Staff interviewed for the study felt that, overall, the community hospital liaised effectively with both acute and primary care, with staff at the acute hospital describing the community hospital ‘as an extension of a hospital department’, whereas those in primary care commented that the community hospital served ‘as a buffer that provided preparations for discharge of the patients’.
Cost and cost-effectiveness
Treatment costs in post-acute care
Garåsen et al. ’s62 medium-quality cost analysis of intermediate care in Norway was nested within a RCT and calculated average costs per day of treatment from randomisation up to 12 months after discharge from a community hospital or an acute hospital. It found treatment costs in the community hospital group to be lower than in the acute hospital group. Lower costs were mainly attributable to reductions in the number of readmissions and days readmitted, as well as lower average costs per day at the community hospital. Total average costs per patient per day in the community hospital group were £56.12 (p = 0.026) compared with the acute hospital group at £74.27 (p = 0.026) [converted from Norwegian kroner (NOK) by the authors using historical rates (GBP 0.0926 per NOK)]. Similarly, the total average cost per patient per treatment episode, including readmission within 60 days after discharge, were lower at the community hospital than at the acute hospital, at £3671.59 (p = 0.002) compared with £6798.41 (p = 0.002). There were no significant differences between groups in hospital costs during the follow-up year or for after treatment. The costs of long-term hospitalisation were highest in the community hospital group, but the difference was not statistically significant.
In two high-quality papers embedded in linked RCTs, O’Reilly et al. 11,99 reported on the cost-effectiveness of post-acute care for older people in community hospitals in England, which they found to be similar to that provided in acute hospitals. This was attributed to similar mean length of stay in hospital, similar resource use per patient and similar mean costs per patient of health and social care over 6 months of follow-up. There were non-significant differences for changes in quality-adjusted life-years (QALY) at 6 months after baseline in favour of the community hospital groups. The incremental cost-effectiveness ratio estimate was £16,324 per QALY for the multicentre study and suggested similar cost-effectiveness in the single-centre study. A cost-effectiveness acceptability curve for the multicentre study suggested that if decision-makers’ willingness to pay per QALY was £10,000, community hospital care would be cost-effective in 47% of cases. At a willingness-to-pay threshold of £30,000, this increased to 50%. 11 For the single-centre study, the acceptability curve suggested cost-effectiveness at the same thresholds in 51% and 53% of cases, respectively. 99
Treatment and drug costs in emergency care
Stapley et al. ,102 in a cohort study of uncertain quality, compared the use and cost of medicines and investigations for emergency admissions of older patients to five community hospitals and an acute hospital in England. They found the mean values for the total cost of investigations during the hospital stay per patient to be higher in the acute hospital, at £323.94 [standard deviation (SD) £245.73] than in the community hospitals, at £65.94 (SD £74.27). Similarly, the mean cost of drugs prescribed during hospital stay per patient was higher in the acute hospital (£102.74 vs. £41.86), as were the mean costs of prescriptions at admission and discharge. Overall, the median total number and cost of drugs prescribed per patient in the community hospitals was lower (p = 0.001). The authors noted that, overall, cost differences were relatively small compared with capital and staffing costs of the hospitals. The paper concludes that considerable extra resources were used in emergency treatment of older patients at an acute hospital, without yielding mortality or morbidity benefits (conclusions around clinical benefits refer to a linked paper not included in our review). 103
Patient and service costs for chemotherapy
Pace et al. 66 compared patient and service costs incurred providing chemotherapy in community hospitals and a cancer centre. Patient travel costs to attend chemotherapy in the community hospitals were found to be lower by almost half, as patients tended to live closer to the community hospitals (estimated additional patient cost of £6.29 per cancer centre visit over community hospital visit). However, when considering service costs, the need to relocate nurses to deliver chemotherapy at the community hospitals was associated with additional travel costs, both direct (£12.83 per clinic attended) and indirect (opportunity cost; £32.08 per clinic attended). Overall, the cost of delivering chemotherapy in the community hospitals was found to be marginally higher than in the cancer centre.
Discussion
This review has explored the available evidence on the effectiveness and efficiency of community hospitals compared with acute hospitals in selected high-income countries. Overall, the evidence that has been published since the 2006 review by Heaney et al. 1 has remained relatively scarce and comparative studies that met our inclusion criteria were available for England and Norway only. Reviewed studies described equivalent or improved outcomes and experiences in community hospitals compared with acute hospital settings for a range of services. This includes improved or equivalent outcomes for measures of patient health including mortality, measures of independence and community or nursing care needs, and toxicity levels following chemotherapy. 7,9,10,62,66,98,100 The evidence on measures of anxiety and depression varied, with outcomes for those receiving chemotherapy in community hospitals reported to be equivalent to those treated in acute care hospitals, but not for post-acute care, which tended to be worse for those receiving care in community hospitals. 7,10,66 Evidence on process measures such as readmissions and number of bed-days showed favourable reductions in community hospitals. 9,62 Staff, carer and patient experiences of community hospital care were comparatively favourable. Qualitative evidence identified key features of care at community hospitals that were perceived to be important for recovery as part of rehabilitative care, such as ease of access and the provision of a familiar and homely environment. 8,45,54,55,58 Patient accounts may also serve as representations of a more intangible sense of being valued and prioritised in the community hospital, rather than lost in the possibly more disorienting acute hospital setting. 55
Evidence on the cost and cost-effectiveness of care delivered in community hospitals was scarce. Two linked studies of post-acute care in England found cost-effectiveness to be similar. 11,99 Cost analyses tended to show lower costs for community hospitals, mainly because of fewer and shorter readmissions, as well as lower average costs per day, or fewer and less expensive drugs prescribed and interventions carried out. 62,102 However, staff travel costs meant that delivering chemotherapy in community hospitals was more costly than in a cancer centre. 66 Cost analyses generally did not take account of capital costs that would be incurred in the development of the community hospital estate, which would inevitably have implications for the cost-effectiveness of any future expansion.
A key strength of our review was that it considered evidence on current models of community hospitals not reported in previous reviews. 1 In addition, the extraction of a large number of records has contributed to the quality of the review. This study also has limitations. The range of studies to be included was constrained within our a priori definition of a community hospital, which followed previous definitions of community hospitals, and whether the community hospital setting was specified in the paper. 1,104 As a result, studies of comparable service models that are not labelled in the same way but that could offer additional insights could have been excluded (e.g. independent units within acute hospitals).
Based on the findings of our review it is perhaps fair to conclude that in some areas, particularly post-acute care, the quality of the evidence for the clinical effectiveness and cost-effectiveness of delivering services in community hospitals has strengthened since the 2006 review by Heaney et al. 1 Four high-quality RCTs using robust measures of clinical effectiveness and the Post-Acute care Trial of Community Hospitals (PATCH) study’s measurement of cost-effectiveness in terms of QALYs have significantly contributed to this improvement. 7,9,10,66 Findings indicate that care in community hospitals can offer a viable, and often preferable, alternative to care in acute hospitals for a number of services, in terms of clinical outcomes, patient, carer and staff experience, and cost. The reviewed evidence suggests that community hospitals can add value to service delivery systems by improving patient and carer experience and facilitating the establishment of improved ways of working.
In England, community hospitals are seen to have a role in breaking down traditional boundaries between primary care, community services and hospitals in order to better meet the changing needs of an ageing population against the background of a rising burden of chronic disease. 18 However, conclusions around the suitability of community hospitals as a service delivery model to fulfil this role crucially depends on our understanding of the primary challenges that they are expected to solve. Although evidence indicates that they can offer a safe and often cost-effective alternative to acute hospital care, their role within a given health economy remains less clear.
Other researchers have highlighted the need for further research on the clinical effectiveness and cost-effectiveness of delivering services in community hospitals. 1,9 Although the evidence has improved significantly in recent years with regard to post-acute care, the continuing lack of robust empirical evidence of the impacts of different forms of service delivery that can be offered by community hospitals highlights the need for continuous evaluation of new delivery models and their contribution to wider system effectiveness. The range of services offered in community hospitals span from acute to chronic, primary and specialist care, but the literature has largely focused on post-acute and inpatient services, offering little insight into the potential for community hospitals to deliver specialist and outpatient care. Existing evidence is also limited in geographical scope, and the lack of evidence from countries with developed community hospital provision, such as Scotland, is notable. As the policy vision for community hospitals continues to develop in the UK and internationally, further research is needed to underpin service design and to inform the optimum role of community hospital provision across the full range of services and system contexts.
Part 2 International review and comparison
Chapter 4 Understanding the role of community hospitals within the wider system of service provision: a comparative analysis of experiences in five countries
Introduction
Although the acute hospital will always have an important role in the provision of health care, both as a key locale for teaching, training and research and in the management of complex and rare disorders, there have been increasing concerns about health systems’ dependence on hospital-based delivery and the efficiency of such services given the changing disease burden and associated demand for services. 6 There are also concerns about the perceived high costs of hospital care and, consequently, health-care systems have been experimenting with new ways of shifting specialist services from hospital into the community as a means to increase the accessibility of services and responsiveness of the system, and, potentially, to reduce costs. 20,105,106
In England, a policy focus on moving health care closer to people’s homes has led to renewed interest in community hospitals and the potential role they can have in delivering more integrated care at the local level. 18 Countries such as Italy and Norway are implementing community hospital-type delivery models in an effort to reduce reliance on acute hospital care and to provide more integrated care within the community. 107,108 However, as shown in Chapter 2 and highlighted elsewhere,1 the concept of a community hospital is not uniform across high-income countries and, indeed, there are a number of service delivery models than can be broadly subsumed under this heading. This variation is likely to reflect the specific health system context within which community hospitals have been or are being implemented. It also highlights the range of options that countries might wish to consider in their efforts to more effectively respond to changing local population and service needs.
Against this background, it seems timely to explore the nature, scope and distribution of community hospitals in selected high-income countries to understand better (1) the policy drivers behind the implementation or advancement of such delivery models, (2) their function and role within the wider system of service provision and (3) the degree to which such models contribute to enhanced integration of service delivery and benefit the population more broadly. Better understanding of the nature and the possible role of the community hospital within the service delivery structure will be invaluable to those seeking to understand alternative forms of health service organisation and delivery in England and elsewhere.
Methods
Marmor et al. 109 distinguish three principal purposes of comparative analysis in health policy: (1) learning about national health systems and polices, (2) learning why they take the forms they do and (3) learning from other countries for potential application of policies elsewhere. The first seeks to explore systems and policies in different countries without necessarily aiming at a causal explanation of observed phenomena or seeking the transfer of policies. Such analysis typically remains at a descriptive level, while often forming the basis for more analytical enquiries. 110 The second type of analysis aims to explain why systems and policies exist the way they do and why they have developed in a certain way. They commonly seek to explain an observation from which to generalise by identifying factors that appear relevant to generating a particular outcome. The third type of studies seeks to understand processes and developments in one group of countries to inform policy learning in another. This approach would treat cross-national experience as ‘quasi-experimental’ in order to draw lessons for possible transfer elsewhere.
In the present study, the emphasis is on the first analytical approach. Given the scarcity of documented developments around community hospitals in different settings, it appears crucial to establish an evidence base that explores the evolution and general trends of related policies as a foundation for further analytical work. It is against this background that the methodological approach is at its core descriptive, principally drawing on documented evidence and key informant interviews to explore observed developments and policies. This approach principally allows for drawing lessons to inform policy learning elsewhere, although it should be emphasised that this can only be tentative and is to be seen as a first step for further analytical work.
Country selection
A key criterion for selecting countries for in-depth review was the existence of community hospitals, or of organisational structures that can be considered community hospital according to the definition guiding our work as set out in Chapter 2. Identification of countries meeting this condition was principally informed by three sources. First, our scoping review of the published evidence on community hospitals describes community hospitals in eight countries: Australia, Canada, Greece, Ireland, the Netherlands, New Zealand, Norway and the UK (England and Wales and Scotland) (see Chapter 2). Second, previous work in a related area provides evidence of organisational structures that are comparable to community hospitals as defined in the present study in Finland. 20,106 Third, consultation with members of the steering group for this project identified unpublished reports on organisational structures that are comparable to community hospitals as defined in the present study in Italy. Starting from this sample of countries, a further consideration for country selection was comparability to the English NHS on key characteristics while acknowledging differences in countries’ political, societal and cultural contexts within which health service delivery systems operate, alongside variation in demographic and geographical features. We stipulated that countries for inclusion should operate a largely tax-funded system that provides health care to every legal resident, with most services free at the point of use. Considering the embeddedness of community hospitals in primary care, a further criterion for inclusion was comparability in the organisation of, and access to, primary care services. Finally, there should be evidence that community hospitals, or comparable organisational structures, form an integral part of the service delivery structure. Based on these considerations, we included five countries for further review: Australia, Finland, Italy, Norway and Scotland. These countries all use tax-based funding mechanisms while drawing on different combinations of local and national taxes and, more importantly, they present diversity in terms of the governance of health and social care at local and national levels. We excluded the Netherlands, as available evidence identified one community hospital only, which was established as an experiment but not rolled out further. 10 We also excluded Greece and Ireland on the grounds that, although both countries ensure, in principle, universal access to primary care services, in practice parts of the population have faced challenges accessing these services, although efforts are ongoing to address these challenges. 111 Canada and New Zealand were excluded on pragmatic grounds, as for reasons of feasibility it was necessary to limit the number or countries for in-depth review to five.
Data collection
We carried out reviews of each of the five countries, using two principal instruments for data collection: (1) a structured data collection template; and (2) key informant interviews.
Data collection template and draft country reports
The data collection template sought to capture information on the basic features of the system context within which health care is governed, financed, organised and delivered more broadly. In particular, the template sought to capture the different types of models of community hospital, including the nature and scope of services provided, ownership, the interface with other forms of care, evidence of effectiveness and future development. Data were collected by means of a review of the published and grey literature, which was identified through an iterative search of the biomedical database PubMed, the world wide web using common search engines [Google Scholar (Google Inc., Mountain View, CA, USA)], and of governmental and non-governmental agencies and organisations with a remit in the area of health service and system organisation, financing and governance in the countries under review. We included documents written in English, Finnish, Italian and Norwegian. The detailed template for data collection is presented in Appendix 3.
The data compiled using the template formed the basis for draft country reports, which were shared with one expert in each of the five countries. Country experts were identified from the Health Systems and Policy Monitor hosted by the European Observatory on Health Systems and Policies112 and the authors’ own professional networks as established through earlier international comparative work. 113 Experts were asked to review the draft report for their country and to comment on and verify the information presented, and, where appropriate and relevant, to provide additional information, in particular on areas that are not well documented or that require in-depth understanding of the country context.
Key informant interviews
Interviews with key informants in the five countries sought to enhance understanding of the more salient issues pertaining to the context and processes within which community hospitals operate and function in the different systems. Key informants were identified through a combination of purposive and ‘snowball’ strategies using the published literature, official websites, the authors’ professional networks and recommendations from other study participants. We focused on a range of stakeholders involved in the organisation, governance or delivery of health services, considering representatives from national and local authorities, professional and hospital associations, and research organisations.
Potential study participants were invited to participate by e-mail and provided with background information. Interviews explored broad topics around community hospitals, including their role in the health system, types of community hospitals, funding, perceived benefits and challenges of community hospital provision and anticipated future developments, according to an interview topic guide. The interview topic guide, which was shared with participants before the interview, is presented in Appendix 4. Interviews followed ethics principles of conducting research involving human subjects. Key informants were approached in their professional role only, and no sensitive personal information was collected. As part of the consent process, study participants were assured that neither they nor their organisations would be identified in any reports of the study findings. In line with the approved study protocol, consent for participation in the interview and for the interview to be audio-recorded was sought at the beginning of each interview.
All but one interview were carried out by telephone between June and November 2015. All interviews were conducted in English. Two researchers were present during interviews, with one leading the discussion while the second person listened for key areas to explore further. One interview was undertaken in person and with only one researcher present. Interviews lasted 45–60 minutes, were audio-recorded following consent and were transcribed verbatim. Two study participants were unable to participate in interviews but provided written information according to the interview topic guide. Interview data were analysed by country according to the pre-defined topics that guided the collection of evidence for country reports (see Appendix 3). The main purpose of key informant interviews was to gather additional insight into the role of community hospitals in a given health system and their positioning in wider context of service delivery. As such, interview data were not subjected to a formal framework analysis although data were analysed following the principal steps of thematic analysis, including familiarisation of data through reading and rereading transcripts and organising data according to pre-defined topics. 114,115 Interview data were incorporated into country draft reports, which were then shared again with country experts for a final review. Country reports were updated as required to reflect changes in the policy context that concerned, directly or indirectly, community hospitals. Completed country reports formed the basis for the analysis presented here; the full country reports can be found in Appendix 5. We principally followed a thematic approach, synthesising and contrasting data according to the core themes leading the individual country reviews. We therefore begin by briefly setting out the key characteristics of the health systems in the five countries as they relate to governance, financing and principles of service organisation, in particular of hospital services. We then assess how community hospitals have evolved and we describe the types of services provided, including their role in the wider system of service delivery. We consider the evidence of benefits and the challenges faced by community hospitals in each country, and conclude with an assessment of anticipated future changes. Data derived from key informant interviews are indicated as key informant (KI) in combination with the initial of the country represented (Table 6) (e.g. KI-F03 signifies key informant number 3 from Finland). Data reported here represent reviewed countries’ policy context as of March 2016.
| Country (initial) | National government | Regional or local government | Provider or provider association | Academia | Other | Total |
|---|---|---|---|---|---|---|
| Australia (A) | 1 | 1 | 1 | 2 | 1 | 6 |
| Finland (F) | 1 | 2 | 1 | 1 | – | 5 |
| Italy (I) | 1 | 2 | – | 2 | – | 5 |
| Norway (N) | 2 | 1 | 1 | 1 | 1 | 6 |
| Scotland (S) | 2 | 2 | 1 | 1 | – | 6 |
| Total | 7 | 8 | 4 | 7 | 2 | 28 |
Findings
We conducted a total of 28 interviews with key informants who represented different stakeholders involved in, or close observers of, the organisation, governance or delivery of health services (see Table 6).
Principal features of health system governance, finance and organisation
Australia, Finland, Italy, Norway and Scotland all provide universal and reasonably equitable access to health care for their populations. 116–120 Financed primarily through taxation, the five countries have similar levels of health spending in terms of percentage of gross domestic product (GDP), at 8–9% in 2013 [Organisation for Economic Co-operation and Development (OECD) average: 8.9%], although not in terms of per capita spending, which was considerably higher in Norway than elsewhere (Table 7). 121 The reviewed countries vary in relation to health-care governance structures and organisation, although all have devolved certain functions fully or in part to local and regional authorities or states (Australia).
| Country | Population (density) | Sources of funding (% total health expenditure) | Spending (% GDP) | Per capita spending (US$ PPP) | Governance of the publicly funded system |
|---|---|---|---|---|---|
| Australia (2012) | 23.6 million (3 per km2) | General taxation: 67.6% | 8.8 | 3866 | Fiscal and functional responsibilities are divided between Australian government and six states/two territories; federal government funds and administers Medicare and PBS, regulates much of the health system; states administer public hospitals and regulate all hospitals and community-based health services; public hospital funding is shared between the states and federal government |
| VHI: 8.9% | |||||
| OOP: 19.9% | |||||
| Finland | 5.6 million (18 per km2) | National and regional taxation: 61.0% | 8.6 | 3442 | Shared by central government and 313 self-governing municipalities; central government has mainly a steering function; municipalities are responsible for provision of health and social care services and organise primary care; they also fund specialised care through 20 hospital districts, which are responsible for the provision of specialised health care |
| NHI: 14.3% | |||||
| OOP: 18.5% | |||||
| Italy | 61 million (200 per km2) | National and regional taxation: 77.1% | 8.8 | 3077 | Highly decentralised: central government provides legislative framework for health care and defines basic principles and objectives for the national health service; 20 regions are responsible for organising and funding health care, with considerable variation in how they exercise autonomy |
| OOP: 18.8% | |||||
| Norway | 5.3 million (13.5 per km2) | General taxation: 75% | 8.9 | 5862 | ‘Semi-decentralised’: many functions delegated to the regions and municipalities; four RHAs are responsible for the planning, organisation and provision of specialist care; 429 municipalities are responsible for the organisation of primary care, public health services, and provision of and access to emergency care |
| NHI: 10% | |||||
| OOP: 14.6% | |||||
| Scotland | 5.3 million (69 per km2) | General taxation: 83.3% | 8.5 | 3235 | Scottish government is responsible for health care, providing strategic leadership for public health, the NHS and social care; planning and delivery functions are delegated to 14 regional NHS Boards, seven Special NHS Boards and one public health body. From 2016 Integrated Joint Boards, formed by Health Boards and local authorities, will have overall responsibility for the planning, resourcing and delivery of all integrated health and social care services |
| VHI: 3.5% | |||||
| OOP 9.9% (UK figures) |
In all five countries, the GP (or family physician) typically serves as the first point of contact for non-urgent care. All offer (some) choice of GP or health centre, with Finland, Norway and Scotland requiring patient registration (see Appendix 6). All five countries also operate a gatekeeping system in which the GP controls access to specialist care in non-urgent cases, although patients in Italy can access some specialists directly118 and, in Australia, GPs act as gatekeepers to specialist care in so far as patients will receive only the Medicare subsidy for referred consultations. 122 With the exception of Finland, GPs are usually self-employed and work in their own practices, with group practices increasingly becoming the most common model. The level of involvement of other health professionals varies. For example, Italy has only recently begun to move to group practices that also include nurses,123 whereas multiprofessional teams in health centres have traditionally formed the core of primary care in Finland. 117
Organisation and funding of hospital services
Reflecting the principal governance structure in the five countries, the organisation and funding of hospital services varies. All reviewed countries have devolved hospital administration and funding to the regional or local levels (NHS Boards in Scotland), although the central government may still play a part in setting the regulatory framework, such as in Italy,118 or contributing funding, such as in Australia (see Table 7). 124
Payment of hospital services is typically based on activity, using diagnosis-related groups (DRGs), complemented by block grants based on past or predicted service use; in Australia, small rural and regional hospitals are funded from block grants only (Table 8). In Scotland, a national tariff using health resource groups (comparable to DRGs) is used to support NHS Boards in agreeing cross-boundary inpatient flows for acute inpatients and day cases. 120 Similarly, in Italy, the tariff for DRGs is generally set at the national level, although regions may adapt the tariff for local service delivery. 118 As a consequence, there is considerable variation in the way hospital payment and monitoring are implemented across Italy. In Finland, as hospital districts determine the payment methods used to reimburse hospitals, approaches vary between districts. The first national guidelines for specialised care DRGs were published at the end of 2012, and this was expected to reduce the degree of variation between districts regarding the principles and rules of DRG usage. 127
| Country | Categorisation of hospitals | Payment for hospital services | Number of hospitalsa | Number of hospital beds per 1000 populationa | Community hospital is considered to be a hospital |
|---|---|---|---|---|---|
| Australia | Principally distinguishes hospitals into acute care hospitals, psychiatric hospitals and day hospitals or centres | Activity-based funding using a ‘national efficient price’ (based on diagnosis related groups) from July 2012 | 1347 hospitals (55% public) (2012) | 3.8 all beds: 3.4 acute beds (2012); 65% public beds | Yes |
| Block funding for small rural and regional hospitals based on ‘national efficient cost’ | Small decline in number of public hospitals; 20% increase in private hospitals since 1990s | ||||
| Further categorisation according to peer groupings, which define hospitals based on shared characteristics into: principal referral hospitals, acute hospitals of different sizes, small hospitals, women’s and children’s hospitals, psychiatric hospitals, subacute and non-acute hospital, and outpatient clinics |
|
||||
| Finland | 20 hospital districts cover populations of 50,000–1.2 million; organise and provide all inpatient and outpatient specialised health care within region |
|
263 hospitals (2012) (down from 391 in 1995) | 4.9 all beds: 2.8 acute beds (2013); 96% public beds | Yes |
| Most hospital districts have a central hospital, sometimes supplemented by small regional hospitals | Steady decline since 1990s | ||||
| Each hospital district belongs to one of five university hospital catchment areas | |||||
| Italy | Basic hospital: catchment population 80,000–150,000; emergency services and some specialist services | Prospective payment system using DRGs, complemented by capitation and/or grants for specific services | 1152 hospitals (55% public) (2012) (down from 1760 in 1990) | 3.4 all beds: 2.8 acute beds (2012); 69% public beds | No |
| Level I hospital: 150,000–300,000; first-level A&E, large number of specialties available on call – 24/7 | Tariffs set at the national level but regions can modify the tariffs implemented locally | Steady decline since 1990s | |||
| Level II hospital: 600,000–1.2 million; hospital trusts, university hospitals and IRCCS; same as Level I with more specialised services added | Bed-day rate for hospitals directly operated by ASLs, rehabilitation and long-term care facilities | ||||
| Norway | Regional or university hospital (1 per region) | Block grants (60%), complemented by activity-based financing from the central government using DRGs | 21 hospital trusts with > 100 sites (2012) | 3.9 all beds: 2.3 acute beds (2013); 75% public beds | Some (cottage hospital) |
| Large acute care hospital: 60,000–80,000 population; emergency care, surgery, several specialties | |||||
| Acute care hospital: emergency care, elective surgery, some acute surgery | Block grants for certain types of specialist care (such as mental health) | Steady decline since 1990s | |||
| Hospitals without acute care functions (elective surgery only) | |||||
| Scotland |
|
NHS Boards are responsible for allocating resources locally to meet their strategic objectives | 287 hospitalsb (2015) | Staffed bedsb: 3.7 all beds; 2.6 acute beds (2014–15) | Yes |
The nature of the type of services that are formally considered hospital services varies across countries. All tend to distinguish acute care or general hospitals, which are typically further categorised by the size and range of services delivered, from specialist service providers such as psychiatric hospitals and women’s and children’s hospitals, although the latter form a distinct category in Australia and Scotland only. Community hospitals or their equivalent, such as very small hospitals in Australia,128 tend to form an integral part of the overall hospital infrastructure in all countries except Italy, where community hospitals are not considered part of the hospital network. In Finland, the national data on inpatient care beds also include long-term care beds that are provided in municipal health centres (‘health centre hospitals’; see Community hospitals in five countries: types and services provided). 125 This in part explains the larger number of total hospital beds of 4.9 per 1000 population in Finland in 2013 than in the other countries, while the number of acute care beds per 1000 population was fairly similar across countries, at between 2.3 in Norway and 2.8 in Finland and Italy, although this figure was somewhat higher in Australia (3.4 per 1000) (see Table 8).
Community hospitals in five countries: types and services provided
Defining the community hospital
Table 9 provides a summary overview of selected principal features of service delivery models in the five countries reviewed, which can be broadly subsumed under the term ‘community hospital’. Models can be seen to lie on a continuum. At one end of this continuum we observe the ‘traditional,’ small community or cottage hospital based in a typically rural or remote setting and which serves a ‘geographic purpose’ (KI-A01), that is, it provides a range of services to the local population including emergency care, minor surgery, low-acuity acute general medical care, obstetric care and basic diagnostics. These types of models are found mainly in Australia, Norway and Scotland. At the other end lie structures that are dedicated to specific population groups, primarily older people at different stages of dependency. These services may include sub- and post-acute care, intermediate care, rehabilitation, and, in some instances, palliative or end-of-life care and long-term or residential care. These structures are found predominantly in Finland, in the form of health centre inpatient wards (also referred to as health centre hospitals), and in Italy.
| Country | Definition of community hospital | Service focus | Size: number of beds | Average length of stay (days) |
|---|---|---|---|---|
| Australia | Varies across states but most commonly refer to a small (district) hospital in rural and remote areas | ‘Geographic purpose’, most typically providing obstetric care, emergency care, minor surgery and/or emergency stabilisation, management of simple conditions, hospitalisation for uncomplicated general medical patients, subacute care or step-down care | Varies by state, between fewer than 10 and up to 75 beds | Very small public hospitals: 13.2 (2011–12) |
| Finland | Inpatient wards in municipal hospitals (erveyskeskusten laitoshoito), commonly referred to as ‘health centre hospitals’: ‘A person in need of urgent institutional care shall always be assigned to a health centre hospital bed’129 | Sub- and post-acute care, intermediate care following discharge from acute care hospital, rehabilitation, palliative care | 20–40 beds | 11–53 (2014) |
| Italy | Ospedale di Comunità: ‘[A] structure with a limited number of beds (15-20) [that is] managed by nurses, and in which medical care is provided by general practitioners or paediatricians or other medical staff contracted by the [Italian NHS]’107 | Varies by region; most commonly sub- and post-acute care or intermediate care, rehabilitation, palliative care | 15–20 beds as per national regulation but varies across regions, typically between 20–30 beds in regions for which data are available | 15–20 days as per national regulation; some regions have set maximum length of stay of up to 6 weeks (Emilia Romagna, Veneto) |
| Community hospitals in Marche provide 24-hour emergency services and a wide range of medical specialist clinics, including dialysis | ||||
| Norway | Includes four principal structures:
|
Varies by structure: generally sub- and post-acute care, intermediate care, rehabilitation, palliative care | Cottage hospitals: up to 10 beds | Not reported |
| Cottage hospitals provide wider range of services including obstetrics, day surgery and some specialist services such as chemotherapy | Municipal acute care beds and local medical centres: typically up to or around 10 beds | |||
| Scotland | A community hospital is a health-care facility undertaking patient care with typically fewer than 60 beds130 | Most likely to include GP acute medical inpatient care, inpatient care for older people, rehabilitation, end-of-life care, outpatient clinics, minor injuries, diagnostics, community midwifery | Up to 60 beds, although there are a few with more beds | 17 days for GP acute inpatient medical care |
| Hospital may be a base for the provision of community services |
However, this distinction is not clear-cut. For example, community hospitals in Scotland may also provide intermediate care, rehabilitation services and end-of-life care,130 whereas community hospitals in some Italian regions, such as the Marche region, are more akin to the conceptualisation of a traditional cottage hospital which sees the provision of a wider range of services including selected medical specialist services (see Table 9). In other parts of Italy, such as Friuli Venezia Giulia, regional legislation has defined the community hospital as an intermediate care structure131 but it is mostly conceptualised in the context of residential care, as part of rehabilitation and long-term care (KI-I03).
Evolution of community hospitals
The diversity of community hospitals illustrated in Table 9 has to be interpreted in the context of the evolution of the overall hospital service delivery structure in place in different countries. Thus, some regions in Norway, such as the northernmost county of Finnmark, have a long history of operating cottage hospitals (in Finnmark this history dates back to the 1850s), which are seen to have formed a core component of health service delivery. 132 Formally defined in the 1969 Hospital Act,133 cottage hospitals in Norway are generally seen as organisational structures that deliver health care in rural areas, have overnight inpatient beds and typically also provide a selection of specialist outpatient services (KI-N04). This description also includes small general hospitals that have experienced changes in the service delivery structure over time in response to changing local population needs. Examples include the Hallingdal hospital in southern Norway (see Chapter 2), which, from the 1980s, has gradually developed specialist health-care services in an attempt to reduce acute hospital admissions. 21 More recently, such localised efforts have been placed on a more strategic footing with the 2012 Coordination Reform, which sought to enhance integrated care in the community and improve co-ordination between different levels of care as part of an overall movement to shift services from the hospital sector into primary care. The reform introduced new structures in the form of municipal acute care beds [kommunale akutte døgnplasser (KAD)] to complement or potentially substitute the traditional cottage hospital model. 108 KAD can be set up in a variety of settings [e.g. nursing homes, (newly established) local medical centres, wards in a hospital]. They aim to address the needs of patients with acute but manageable conditions, who need 24-hour supervision, but not necessarily in an acute hospital setting. All municipalities in Norway are required to provide municipal acute care beds from 2016. 134
Similar to Norway, many community hospitals in Scotland pre-date the formation of the NHS in 1948. 13 Often originally established by local benefactors in response to the needs of the local community, many have subsequently evolved into what has generally been described as GP hospitals. For example, by 1980, some 70 hospitals in Scotland could be classified as GP hospitals, estimated to account for some 3% of all hospital beds across the country. 135 Despite forming an integral component of the service delivery system in Scotland, in 2006 community hospitals received renewed attention as part of a wider government strategy that foresaw an expansion of community-based, primary care-led services. 31 The strategy envisaged new models of community hospital to operate as ‘local community resource centres’ for the provision of ‘more holistic and integrated services quicker and closer to home’. This was followed by the 2012 Community Hospitals Strategy Refresh, which sought to place the 2006 vision for community hospitals in the context of more recent strategic priorities, seeing them as having a key part to play in the health and social care integration reforms, acting as a base for community services, or as a community hub for health and social care services. 13 The role of community hospitals was also seen to have been strengthened in the context of the 2020 strategic vision for the delivery of health-care services in Scotland, with its aims to provide care close to people’s homes within an integrated health and social care system. 136 Compared with Norway and Scotland, the evolution of community hospitals in Finland has been a fairly recent phenomenon, following the 1972 primary care reform which established municipal health centres. These emerged in part from small local or district hospitals and as a result they offer a wide range of services, including GP-led inpatient units (also referred to as health centre hospitals). 117 Newly formed municipal health centres that were not linked to a former local hospital also established inpatient wards. However, in contrast to the traditional community hospital in Scotland or the cottage hospital in Norway, health centre inpatient wards aim primarily to address the needs of dependent older people, who do not require hospitalisation but who cannot be cared for in their own homes (KI-F04). This focus on older people has intensified over time, following a reform in 1993 which made municipalities responsible for all secondary and tertiary care costs. 117 It led to a change in the composition of patient population cared for in health centre inpatient wards, as ‘they lost much of their professional attraction and gradually became long-term care facilities for the elderly, especially those with memory disorders’ (KI-F05). 117
Somewhat similar to Finland, community hospitals in Italy also evolved more recently. They were set up from the mid-1990s onwards, partly in response to the changing needs of an ageing population. 137 They seek to provide medium-to-low-level clinical management of chronic degenerative diseases and of predominantly older people with a range of social care needs. 138 The development of community hospitals in Italy can also be seen as a response to national policies that from the 1990s onwards have sought to make acute care provision the primary focus of hospitals and to reduce the length of acute hospital stay. Community hospitals are expected to provide a ‘protected place’ for patients who are not yet sufficiently stable to be cared for in their own homes following discharge from acute care (KI-I01, KI-I02). They also provide a solution to the threat of hospital closures through the repurposing of existing local hospitals into multifunction facilities:
So we save the small local hospital, we keep it over there. We try to name it hospital . . . its written in big [letters] . . . so they [patients] feel comfortable to go there, but I mean no expert would ever name it a hospital.
KI-I01
Importantly, the development of community hospitals in Italy has largely relied on regional efforts. Indeed, it was only in 2006 that community hospitals were formally mentioned in a national-level document in the context of a proposed reorganisation of primary care, highlighting the need for the development of intermediate care services and of GP-led community hospitals. 139 The potential value of this form of service delivery was formally recognised following the 2012 legislation on the reorganisation of hospital care, with the 2014–16 health agreement mandating the establishment of community hospitals for the delivery of subacute care, seeking to reduce the number of inappropriate admissions to acute care hospitals and to facilitate the discharge of patients from acute care. 140
Although the notion of a community hospital is difficult to clearly delineate in all countries reviewed above, it remains a particular challenge in Australia. This is in part because of the way health services are governed in the Australian context, with states assuming responsibility for regulating hospitals. Hospitals tend to be small, particularly in regions that cover large geographical areas. The majority of beds tend to be in larger hospitals and in more densely populated areas, whereas some 70% of hospitals have 50 or fewer beds. 141 This poses considerable challenges, with an observed increase in closures of a number of small hospitals over the past decade:142
Rationally, they can’t operate [. . .] and the occupancy rates is so low, it’s very hard to argue that they’re operating efficiently and it’s increasingly evident that it’s hard to operate things safely, for anything with fairly low security levels.
KI-A05
At the same time, such facilities are seen to be indispensable in remote communities ‘where a patient can be stabilised and evacuated because the distances are significant’ (KI-A01), although this service might not necessarily be provided by a hospital as such. In response, most states have started transforming small rural hospitals into alternative settings, such as residential aged care facilities, community medical centres or multipurpose health centres. For example, states have invested in the redevelopment of small rural hospitals into so-called ‘multipurpose services’ as part of the Multipurpose Service (MPS) Program, which was established in 1993. 143 A joint initiative of the federal and state governments, these services are designed specifically to address the needs of small rural and remote communities that could not viably support stand-alone hospitals or aged care homes. MPSs may or may not include inpatient beds and are not generally considered ‘community hospitals’ in the Australian context.
Nature and scope of services delivered
Although countries, or regions within countries, offer a wide range of community hospital and similar service delivery structures, one area of commonality is that the local GP usually holds clinical responsibility and has oversight of the medical care provided, as well as admission rights. This reflects the general function of community hospitals, sitting ‘in the middle of the patient journey between home and the district general hospital’ (KI-S03). In some instances, having a GP lead can be seen to have evolved out of necessity, particularly in the cases of rural and remote regions, due to the fact that ‘the specialists aren’t there’ (KI-A01). Elsewhere, the central role of the GP has been a consequence of the historical development, such as in health centre hospitals in Finland, cottage hospitals in Norway and community hospitals in Scotland, as noted earlier.
Where community hospital-type delivery models are newly established, such as in Italy and Norway (municipal acute care beds), the formal assignment of clinical authority to a GP has been intentional because these structures are seen to form an integral part of the (reorganised) primary care system. 134,140 However, in some instances, and reflecting the specific function of the community hospital, the clinical lead may also be a geriatrician. This is the case for some structures in the Veneto region in Italy144 and for geriatric hospitals in Scotland, which have primarily long-stay beds, although there is some debate over whether or not this latter example should be included within the community hospital definition (KI-S03, KI-S05).
Service delivery typically involves multiprofessional teams, which, in addition to GPs, may comprise nurses, health-care assistants, and allied health professionals (most commonly physiotherapists and occupational therapists). Health centre hospitals in Finland (KI-F02) and community hospitals in some regions in Italy may also include social workers as part of their teams,145 and community hospitals in Scotland have seen an increase in the co-location of social care practitioners in recent years. 13 In terms of the actual management of the hospital, in all the settings reviewed, this is typically the responsibility of a head nurse or nurse manager.
The involvement of medical specialists generally varies according to the range of services provided, the size and location of the community hospital, and the population serviced. For example, in Finland, health centres in larger municipalities would typically have medical specialists in internal medicine and geriatrics, for example, available on site. Community hospitals in Italy have to ensure access to specialist advice on site, which is frequently done through co-location of community hospitals with a so-called ‘house of health’, which has been established in a number of regions. Houses of health oversee access to and provision of health and social care services in the district and their aim is to provide a single point of access and initial needs assessment through the co-ordination of primary care units with other service providers in the district, including specialist and inpatient care, public health, and mental health. 146 As a consequence, community hospitals in Italy might have access to a wide range of specialist clinics.
Elsewhere, community hospitals tend to rely on visiting specialists from the acute care hospital. For example, in Scotland, patient care at the community hospital is typically provided by multidisciplinary primary care teams, with support from secondary care specialists as required. 13 Similar models are in place in Australia, where visiting clinicians provide specialist expertise, although the precise mechanism by which this is facilitated varies across states. For example, in the Northern Territory, local GPs would typically have a network of specialists whom they can phone for advice or for evacuating patients if required. In these cases, ‘the specialists fly in and out, and, you know, run clinics or have surgical lists, that sort of thing’ (KI-A02). In Queensland, small public hospitals are managed by one of the 17 Hospital and Health Services and the community hospital would be embedded within wider service provision, which might be facilitated by telehealth links between the main hospital and the local small hospital (KI-A01). Such an approach can also be found in Norway; one example is the aforementioned Hallingdal hospital in Norway, a small hospital with 14 intermediate care beds, which is managed and funded by a general hospital (see Chapter 2). 22 The inpatient department is led by GPs who are supervised, via telephone, by specialists located at the general hospital; outpatient clinics are also hosted by specialists visiting from the general hospital.
Benefits of community hospitals
As earlier parts of this report have shown, the evidence of effectiveness of community hospitals is relatively scarce. Among the five countries examined in this paper, robust empirical evidence of some degree of impact is available for Norway (see Chapter 3) and Finland only. Research in Norway found, for example, evidence of reduced service utilisation such as readmissions or community services use among those treated in a community hospital compared with those treated in a general hospital. 9 An unpublished study by Swanson and Hagen147 examined early evidence of benefit that can be associated with municipal acute care beds in Norway, which were introduced from 2012 as described above. The authors demonstrated a correlation between the introduction of these beds and a small, but significant, reduction in acute care admissions, highlighting the potential of municipal acute care beds to alleviate the burden on acute care hospitals. 147 In Finland, an analysis of the management of people with chronic obstructive pulmonary disease (COPD) treated in primary care hospitals (health centre hospitals) compared with secondary care hospitals observed a reduced risk of death among those managed by a GP relative to those managed by a pulmonary specialist, at 0.83 (95% CI 0.75 to 0.91). 148 Conversely, a related study showed that COPD patients discharged from primary care hospitals had a greater risk of readmission within 7 days of discharge than those discharged from secondary care. However, the risk of readmission to a primary care hospital was reduced for those who had received home care on initial discharge. 149 The authors attributed these observations to likely differences in treatment procedures, disease severity and admission threshold between the two levels of care, which they were, however, unable to study further given the study design, which used national hospital admissions data.
Key informants interviewed for this study recognised the challenges involved in demonstrating evidence of impact of community-based programmes, given their small size. It was, however, noted that ‘there is a great deal of belief so you end up with this knowledge gap which is a challenge when we try and protect the funding of smaller services’ (KI-A03). Thus, much of what is known about the impact of community hospitals on patient and service outcomes in the countries reviewed tends to be informed by anecdotal evidence and presumed benefits [‘Based on just my past experience and talking to people’ (KI-A02)]. The main benefit attributed to community hospitals across the five countries by the majority of key informants interviewed for this study was seen to be their size and proximity to people’s homes. This was considered especially important for those places characterised by geographic dispersion of the population, as well as for older people who can stay near their families:
[The community hospital is] seen as part of a local support system for people, particularly but not uniquely perhaps older people or those who may require additional support. So I think that there’s a kind of intangible value there. It’s actually quite hard to demonstrate the . . . the value in, kind of, cash terms but in terms of emotional support as well as the physical support which is given, these local facilities have very significant value.
KI-S01
This view has some grounding in the international evidence reviewed in Chapter 2 of this report; for example, one study that examined the aforementioned Hallingdal hospital in Norway observed that patients admitted to the community hospital reported statistically significant greater satisfaction with several care aspects than those admitted to the general hospital. 150 Specific factors highlighted by patients included a ‘quiet and homelike atmosphere’, the hospital’s proximity to the local community and a perceived continuity in the patient–staff relationship.
Key informants in Scotland further highlighted the potential part that community hospitals can play in facilitating service integration locally, citing their function as an ‘integrator’ of services and as a locale for the development of a ‘single point of access to integrated services’ (KI-S02). 13 This perspective was perhaps less obvious in other countries reviewed here, where community hospitals were seen to form an integral part of local service delivery but where other structures are expected to provide the single point of access to integrated services, such as the municipal health centre in Finland,151 the house of health in some regions in Italy146 or the local (community) medical centre in Norway. 134
Challenges faced by community hospitals
While acknowledging the value of community hospitals and their potential as a key locale for, or complement to, local service delivery, key informants interviewed for this study cited a range of challenges faced by this delivery structure. Although the specific issues that were identified varied across countries, reflecting the policy context within which they exist, two overarching themes emerged, which focus on (1) workforce and skills and (2) the role of community hospitals within the local service delivery structure.
Attracting health-care workers and skills
Key informants from across the five reviewed countries all noted workforce challenges in relation to the delivery of care in community hospitals. One particular issue noted by commentators from Australia, Finland and Scotland was the difficulty to attract health-care workers, especially in rural or remote areas. However, this challenge has to be seen in the general context of workforce issues in the different settings; for example, key informants from Finland highlighted the problem of recruiting a sufficient number of doctors to work in municipal health centres more generally (KI-F05):
[T]o work on the [inpatient] ward it’s more demanding than in [outpatients], so that it is not so easy but because if you go to work to the health centre you are [a] worker there then the employer can decide that you are working in the open or in the ward. But of course, we always try to find people who really can and want to do those works because there are a lot of jobs to choose [from] so that if they say they have to go there then the workers say goodbye.
KI-F02
Key informants from Scotland also noted that an overall shortage of GPs and nurses in the country was further compounded by the fact that priority was typically given to staffing acute hospitals, which means that community hospitals can become short staffed (KI-S05, KI-S04).
There was agreement among key informants from Australia, Finland, Norway and Scotland that working in a community hospital required some additional skills, for example the ability to treat complex and acute cases (KI-N01). Commentators from Scotland highlighted that it would take some time for new staff who have received standard nursing or GP training to develop the additional skills required for working in a community hospital (KI-S05).
In Australia, GPs working in small rural hospitals or municipal health centres traditionally had a wider range of skills, meaning that they were able to perform, for example, basic surgery following some additional training. This model of ‘procedural GPs’ was reported to have been common (KI-A02, KI-A03) but to have ‘waned over a period of time, as there were closures of small country hospitals across the country because of cost pressures’ (KI-A02). However, it was noted that the general policy direction in Australia now was to (re-)encourage the development of rural generalists, that is, GPs who have additional skills, such as in anaesthesia or surgery or obstetrics (KI-A01, KI-A02). Training is provided through the Australian College of Rural and Remote Medicine, for example. 152 In Scotland, there is a recognised need to provide further support to GPs in particular, with investment in additional skills training such as the Rural Fellowships in General Practice. 153 In Norway, workforce issues were recently acknowledged by the government, which proposed to rethink hospital staffing and medical training in the context of the recent health services changes. 154
However, challenges remain, in particular where national workforce policies conflict with local requirements. For example, in Australia it was noted that while the number of medical graduates has increased, this increase was unlikely to address the challenge of attracting them to work in rural and remote settings. This was in part because GPs can set up practice anywhere in the country, and most settle in inner cities, and ‘there is nothing you can do to reallocate those GPs, you have to attract them to small rural communities’ (KI-A03). A similar challenge was reported in Finland, where one potential solution has been to provide opportunities for GPs and nurses to work with specialists in, for example, internal medicine or geriatrics (KI-F02). This was seen to be particularly attractive for more junior health-care workers given the characteristics of the patient population, that is, older patients with complex health and care problems. One key informant highlighted the need to offer flexible terms of employment and to allow workers to for example ‘continue their studies or do research, or work in private sector also [. . .] It has to be some kind of a combination that this kind of a people and specialists are willing to work in a public sector and city hospital’ (KI-F03).
A challenge of a different nature was reported for Italy, where policies introduced by the national government in the wake of the 2008 financial crisis involved a cut in workforce capacity among health-care workers, and a concurrent fall in national health-care expenditure of about 5% between 2011 and 2014. 155 Much of the cuts in the physician workforce have been achieved through a freeze on the restaffing of vacant posts following retirement. This has created challenges, as the restrictions on replacing staff coincides with an increasing need for services, and, regardless of cuts, medical staff have ‘to continue with the job, because if you have beds and you need to ensure 24 hour [care] you need to have at least six nurses, six nurses in a day, because you need to [cover services 24/7]’ (KI-I03).
The role of the community hospital within the local service delivery structure
There was a perception among key informants from several countries that as delivery systems are evolving, boundaries between services provided by community hospitals and those offered elsewhere locally might blur or indeed, overlap, impacting on the effectiveness and efficiency of service delivery, and potentially undermining the value of the community hospital and similar structures. For example, commentators from Norway expressed concerns about how the various service innovations that have been promoted following the 2012 Care Coordination reform sit alongside each other, in particular with reference to the newly introduced municipal acute care beds (KAD). There was some apprehension that the shift towards the development of intermediate care facilities at the municipality level might create tensions with local cottage hospitals and small general hospitals, which will have to compete not only with each other, but also with the newly introduced structures for funding (KI03).
Key informants in Scotland highlighted a further set of challenges arising from service restrictions elsewhere. For example, there were concerns about a perceived rise in the use of the community hospital as a step-down facility from the acute hospital (KI-S04), owing to the pressure to free bed use in acute hospitals. This was seen to have reduced the number of beds available for GP admissions (KI-S05). It was also noted that there had been delays in discharge from the community hospital to community care because of a lack of care home placements or the availability of home carers, which in turn would lead to a longer length of stay at the community hospital than was seen to be appropriate (KI-S05, KI-S04).
A related issue was reported by key informants in Italy, who described the challenges faced by regions seeking to balance the implementation of national level reforms, which place restrictions on the maximum number of hospital beds and length of stay in acute care, with an increasing need to deliver services that address the combined pressures arising from multiple chronic disease and population ageing (KI-I02). Against this background, the way that local or regional systems have evolved can be regarded as opportunistic rather than needs-based, driven by the need to reduce capacity in the acute care sector and which may impact on the delivery of appropriate care to those in need (KI-I-01):
So you may have in one local health authority twice as much subacute as the other one, the neighbour local health authority, who has half of these and twice of those. Or three times nursing beds or four times this here, so very random. So, what we have found is that, the sum of all this kind of beds are moving towards an increasing number because of the reduction of [acute] hospital beds and because the development of nursing homes, paid by families. But the combination is quite emergent, with no real rationale [. . .] But having such big differences in the mix, in the infrastructure mix, what happens is that, independent of your physical or psychological condition, you can end in one of those settings just depending on the offer you find over there.
KI-I01
A perhaps extreme example of an opportunistic approach seeking to reconcile national stipulations with local need is that taken by the Marche region in Italy, which, in response to the nationally mandated requirement to establish community hospitals, proposed, in 2015, to redefine its 13 houses of health as community hospitals. 156
Pursuing a needs-based approach may be particularly challenging in places where community hospital-type structures have developed historically, which can result in discrepancies between, or duplication of, services delivered in the same districts. We have already highlighted concerns expressed by key informants in Norway as they relate to the implementation of new services models vis-à-vis existing ones. It was also reported to pose challenges in Finland, where some larger municipalities operate city hospitals, in addition to health centre inpatient wards; these should be complementary to the specialist services provided for by the hospital district (central and university hospitals) but services frequently overlap (KI-F01, KI-F04). In Scotland, extended role community hospitals provide a larger range of services than the typical community hospital (such as more complex types of surgery), as these have commonly developed from previous district general hospitals, and they maintain larger sites. These hospitals have often assumed a community hospital function following the development of a new acute hospital nearby (KI-S03), which poses the risk of service duplication.
Future changes in community hospital provision
Key informants interviewed for this study agreed that the future of community hospitals should be seen in the context of the wider challenges faced by health systems. For example, in Scotland, the perceived role of community hospitals was to provide ‘a hub for community services’,13 with specific functions continuing to evolve in response to changing population needs but also as a result of advances in treatment and technology:
People who 20 years ago would be in a community hospital are now at home and people who 20 years ago might have been in an acute hospital are now probably in the community hospital.
KI-S03
The further development of community hospitals was seen to lie in these advances, with potential future functions including the provision of a greater proportion of outpatient and investigatory services, as well as ambulatory care (KI-S01, KI-S04).
These types of functions were not explicitly mentioned by key informants in the other four countries reviewed. This is partly because the role of community hospitals in these other countries is less seen to be a resource for community-based services as such; instead, it forms one among other important components of a more integrated health and care system locally, led by local health centres, for example in Italy (houses of health) and Norway (local medical centres). Here, the major determinant of the future community hospital was seen to lie in ongoing efforts to reform service delivery more broadly, as indicated above.
In Finland, municipal health centre inpatient wards have witnessed a steady decline in recent years, as seen in the closure of beds or in the transition to other services. 157 This reflects, in part, an ongoing policy focus across Finland on moving people out of institutional care and into alternative settings. This trend is anticipated to continue in light of a major reform that foresees the ‘complete horizontal and vertical integration of services’ and the creation of seamless service delivery,158 as well as related reforms of hospital organisation and financing to be implemented from 2017 onwards (KI-F05). There was consensus among key informants that the ongoing reforms could provide considerable opportunities to rethink the processes by which health care is delivered, and which is expected to eventually help to reduce the number of beds in municipal health centres:
And I’m sure that after 10 years we still have those wards in smaller, not in so many municipalities as we have now. But we are going to have them but I’m sure we are also having much [. . .] better processes [. . .] I hope there are no more so strict borders between primary health care and specialised health care and we are concentrating more on the process and during the process patient’s needs different kind of professionals.
KI-F02
In Australia, the role of the small rural hospital remains somewhat different from the way community hospitals are evolving elsewhere, reflecting the particular geographical challenges in ensuring access to health services. As noted above, states are investing in alternative settings. MPSs in particular are increasingly assuming the role of a local service integrator, bringing together a range of health and residential aged care services on one site, with co-location of GP and ambulance services. Available evidence has shown that the MPS model is able to tailor services to individual community needs:143
It is a good model actually [. . .] It is a way of transforming small acute care facilities to meet acute, age care residential care facilities. So that is quite common now and is a very successful model with the aging of the rural population.
KI-A02
These efforts form part of ongoing reforms across Australia to strengthen co-ordination between primary and hospital care, as well as aged care, to better meet the challenges posed by the rising burden of chronic disease and Australia’s ageing population. 159 They will be likely to impact on the future evolution of small rural hospitals in the country.
Discussion
This chapter explored the nature, scope and distribution of community hospitals in Australia, Finland, Italy, Norway and Scotland in an effort to understand better the policy drivers behind implementing or advancing such delivery models, their function and role within the wider system of service provision, and the degree to which such models contribute to enhanced integration of service delivery and benefit the population more broadly.
Overall, we find that the term community hospital, historically defined in the UK context as a local hospital that is typically staffed mainly by GPs and nurses to provide care in a hospital setting, often for predominantly rural populations,2 is not easily transferable to other system settings. Indeed, even within the UK, the notion of a community hospital encompasses a range of service delivery models that defy the formulation of a single, overarching definition, reflecting the evolution of the nature and scope of services delivered by community hospitals over time, in response to changing population needs as well as the broader change in the nature of the delivery of health-care services.
These observations mirror the findings of our scoping review of the range of community hospitals in high-income countries as described in the published literature, which noted that there is not one definition of a community hospital (see Chapter 2). In line with the scoping review, the present analysis shows that community hospitals and related structures in five countries provide a wide spectrum of health services, occupying the space between, and to some extent encompassing, primary care services and acute hospital care. Evidence from the scoping review suggests that community hospitals deliver care across a range of services from acute to chronic care. In the context of the country review this can be further conceptualised as a continuum between community hospitals serving a ‘geographic purpose’, typically rural populations, at one end, to a specific population focus, mainly older and frail people, at the other end. However, boundaries may be blurred where the local community constitutes a specific group, such as indigenous populations. In addition, as rural communities are ageing, service delivery will have to accommodate the changing needs. This is seen, for example, in Scotland, where community hospitals are increasingly focusing on services for older people. 13 Likewise, in Australia, the repurposing of small, rural hospitals into alternative care settings, such as residential aged care facilities, community medical centres or multipurpose health services reflects the changing focus on ageing populations. 143
Overall, we find that the diversity of community hospitals in different countries has to be interpreted in the context of the evolution of the overall hospital service delivery structure, and so has their future development, very much reflecting the characteristics of individual health systems as it relates to the relationships between, and responsibilities of, different stakeholders in the regulation, funding and delivery of health care. At the risk of simplifying what is inherently complex, it is perhaps fair to say that the community hospital as such presents a ‘fluid’ concept, with the greatest advantage perhaps being their flexibility to respond to local need,13 again an observation raised in our earlier scoping review (see Chapter 2). We have noted how this may be an important advantage as it allows a response to future changes in population health needs and other changes in health service delivery, and the evidence presented here underlines the potential for community hospitals to occupy this niche within the local service delivery structure. This ‘niche’ may stretch from viewing community hospitals as a locale for service integration locally, as in Scotland,13 to their function as a component of locally integrated health and care services, such as in Finland,151 Italy146 and the newly established local medical centres in Norway. 134
However, as service delivery systems continue to evolve there is a risk that boundaries between services provided by community hospitals and those offered elsewhere locally might blur or indeed overlap, impacting on the effectiveness and efficiency of service delivery and potentially undermining the value of the community hospital and similar structures. All countries reviewed are in the midst of ongoing reform efforts, striving to achieve greater integration of services and it will be important that system-level efforts take account of the existing delivery structure in order to optimise service delivery locally.
Chapter 5 Innovative models of community hospitals in Scotland: a multiple case study
Introduction
In the UK and elsewhere, community hospitals are currently high on policy agendas13,18,23 and have a key role in plans to improve service integration and health-care provision in community settings. 18 In Scotland, community hospitals have played a key part in the national health system for over a century and remain central to current government strategy to provide accessible health and social care services to rural and growing frail elderly populations in particular. 13 In the context of the country’s 2016 reforms to enhance the integration of health and social care,160,161 their role as facilitators of integrated services will be increasingly relevant.
Primarily staffed by nurses and GPs, community hospitals sit between primary and secondary care25 and provide diverse local services including inpatient, outpatient, diagnostic, primary care and community services. 1 However, it is unclear from existing research what role precisely community hospitals can and will have, especially in relation to the integration of health and social care. To inform the development of community hospital provision, there is a need for an in-depth understanding of current service models, how community hospitals sit within wider systems of care provision and the barriers to and enablers of the delivery of services.
This multiple case study aims to explore the role and functioning of two innovative community hospitals in Scotland and the factors influencing their implementation and development. Given the long-established role of community hospitals within the Scottish health system, particularly in serving the country’s expansive rural areas, Scotland offers a rich setting to explore service models and delivery in-depth. In addition, close parallels with the English NHS enhance applicability of findings from Scotland in other health system contexts. This paper compares and contrasts two models of service provision and draws out possible implications for the planning of community hospital provision, both in Scotland and more widely.
Methods
Study design
A case-study methodology162,163 using a multiple case-study design allowed us to explore whether or not the functioning of two community hospitals was affected by common or specific factors across the cases.
The study was designed to test three propositions, based on the literature, which suggest that community hospitals:
-
provide friendly, service-user focused care leading to better patient experience than in other hospital types;13
-
focus more on some patient groups (e.g. elderly7 or palliative care12) than others with better or equivalent patient outcomes than larger hospitals for certain services;10
-
act as a hub for care integration and provision of care closer to home. 83
These propositions informed the selection of the community hospital cases, the selection of interview participants, the development of the interview topic guide and the collection of additional data and documents.
Sampling
Informed by a desk-based review and advice from national experts, six potential community hospitals were short-listed according to four main criteria (Box 2).
To be included, a facility must:
-
provide a range of services to a local community
-
be led by community-based health professionals
-
provide inpatient beds
-
be perceived as being innovative in approach or service provision in Scotland.
Two cases were selected in accordance with sampling guidance162,163 and were perceived to vary with respect to accessibility of acute hospital; rural/urban catchment; demographic characteristics of population; notable or innovative features of service; degree of community involvement; and number and specialty of inpatient beds.
Data collection
The same methodological approach was used across the two case studies to examine the role and function of the selected community hospitals. This approach incorporated three main data collection components: stakeholder interviews (informed by stakeholder mapping); non-participant observation; and document review. These are described in turn below. Researchers followed a common protocol. Site field visits of approximately 1 week’s duration were completed for each case (Case A in November 2014; Case B in March 2015). Desk-based tasks were conducted between September 2014 and November 2015.
Stakeholder interviews
Semistructured interviews were conducted at each site (see Table 10). Potential participants were identified via a stakeholder mapping exercise and were sampled purposively. Most interviews were conducted during field visits, with a small number of telephone interviews conducted shortly before or after. Interviews lasted for between 30 and 60 minutes. Interviews for Case A were conducted by JC and EvT and for Case B by JC. A semistructured interview guide was used, although the approach remained flexible, both for the researchers and the participants, and participants were encouraged to talk from their own perspective. The common interview guide covered origins and likely future development of community hospitals; staffing and staff roles; local system of services; relationships with other providers and community; vision for the community hospital; and challenges to provision of services (see Appendix 7). Informed written consent was obtained from each interviewee and interviews were audio-recorded and transcribed verbatim, with permission. Permission to record was refused only once and notes were taken instead. Transcripts and notes were anonymised.
Non-participant observation
Non-participant observation was conducted in the selected community hospital settings as a means of gaining an understanding of organisational functioning. Observations were conducted in the public areas of each community hospital (reception, corridors, waiting rooms) and during multidisciplinary team meetings. No observations of patient care were conducted. Observations were conducted on a variety of days of the week and times of day in order to gain an understanding of the full range and levels of activity. Observations were recorded using a semistructured observation framework. 164 Management permission for non-participant observation was sought before commencing field visits but consent was not sought from everybody observed. Names or identifiable information was not recorded as part of observation notes.
Document review
Documents describing the organisations, their mission, status, activities and working relationships were reviewed to provide a historical perspective and contextualise the hospitals’ development and functioning. Documents were sourced through internet searching and signposting by stakeholders and included records related to the structure, infrastructure and governance; community hospitals’ setting within the wider health system; minutes of management meetings; and communication materials. In addition, we profiled the population served, using routinely collected anonymised data. 165,166
Analysis
Multiple case-study analysis was conducted in line with the approach outlined by Stake. 162 Analysis began with the first data collected. Two researchers (JC and SB) constructed detailed case descriptions in order to describe the history, context and organisation of the community hospitals (see Table 11) and the two cases were analysed independently in the first instance. A thematic analysis was conducted based on the principles outlined by Boyatzis. 167 For Case A, JC and SB developed a coding frame based on the interview topic guide and initial reading of interview transcripts and field notes. JC and SB each coded half the transcripts, meeting regularly to discuss meaningful themes and to make refinements to the coding frame in an iterative manner as required. As analysis progressed, codes were organised into overarching or organising themes, using QSR NVivo 10 software (QSR International, Warrington, UK). Emerging findings were discussed with the wider study team and with the external study steering group to guide analysis. Sourced documents, observations and field-notes were read (and reread) to identify contextual and historical data and to triangulate interview findings.
The coding frame developed for Case A was then used for the analysis of Case B, with further refinements based on emerging findings. Cross-case analysis was then undertaken, whereby the two case studies were systematically compared and contrasted according to the major themes identified previously. Emphasis was placed on context in the cross-case analysis in order to understand similarities and differences between the cases. JC and SB independently compared and contrasted across the two case studies before discussing and agreeing themes as part of an iterative process of writing and analysis.
Findings
Table 10 presents the 27 stakeholders interviewed.
| Stakeholder group | Community hospital Case A (n = 13) | Community hospital Case B (n = 14) |
|---|---|---|
| Implementers and managers of the community hospital (current and former) | S1_A: Clinical leadership (GP) S9_A: Nursing leadership/clinical management S11_A: Former clinical leadership (GP) |
S6_B: Community hospital management S10_B: Nursing leadership (former community hospital management) S4_B: Former CHP clinical leadership S9_B: Former facilities management; management of PFI relationship |
| Community hospital clinicians and frontline staff (current and former) | S3_A: Ward clerk S6_A: Referral assessment officer S2_A: Ambulance service S10_A: District nursing management S4_A: Physiotherapy management S5_A: Adult social care management |
S3_B: Nursing management S11_B: District nursing management S7_B: Physiotherapy management GP1_B: GP involved in teaching S8_B: Former visiting specialist |
| Broader health and social care system actors | S7_A: Clinical management, Operational Unit S8_A: Operations management, Operational Unit |
S12_B: Senior Health Board leadership; former Health Board primary care clinical leadership S1_B: Clinical leadership, CHP S5_B: Organisational development and training, Health Board |
| Representatives of the wider community | C1_A: Patient group representative C2_A: Local councillor |
C1_B: Community hospital volunteering representative C2_B: Public Partnership Forum chair |
Table 11 offers detailed descriptions of the two cases.
| Site characteristics | Case A | Case B |
|---|---|---|
| Overview of services and facilities |
|
|
| Management, funding and governance structure |
|
|
| Geographical setting and catchment population |
|
|
| Performance and setting within the wider health system |
|
|
| History and development of community hospitals |
|
|
Key roles and functions of community hospitals
Providing both step-up and step-down care
Staff at both hospitals shared a vision of the ideal community hospital role within the wider health system. It focused primarily on the provision of timely, effective preventative and step-up care locally. Especially with regard to elderly patients and those with chronic illnesses, they sought to keep patients out of hospital where possible.
However, both community hospitals regularly accommodated patient transfers from overstretched nearby acute hospitals, providing step-down beds to ease patient discharge through intermediate care and often taking on delayed discharges to relieve pressure from the wider system. With shortages in home care causing delayed discharges in both settings, it was often challenging to balance the demand for step-down beds with the imperative to provide step-up care to local populations.
Establishing a flexible service model to meet changing needs
Despite the range of primary and specialist care services offered at the community hospitals, staff and management in both settings felt that the potential for local provision had not yet been fully realised. As local elderly frail populations grew, building acute skills and being able to expand flexibly the range of services at the community level were seen as key to the community hospital role within regional health-care systems and their relationship with acute services. The delivery of ‘enhanced’ services, towards the specialist end of the care spectrum, and the ability of GP, nursing and allied health staff to support specialist services were seen as important ways for the hospitals to relieve the pressure on acute provision and to improve patient access. In Case A, some GPs were trained in specialist procedures such as minor surgery and joint injections, as well as dermatology. Satellite services by visiting consultants were another approach to service diversification. In challenging GPs and other staff to extend their skills in this way, both hospitals served to address a wider clinical skills gap in the community for dealing with complex patients.
The ability to provide a community resource that could adapt to accommodate future needs and complement regional acute provision was crucial and as such, had been a key design consideration during the facilities’ redevelopments. In Case B, one participant described this as ‘future-proofing’ (S1_B).
Providing integrated services from a central hub
Both hospitals were designed to serve as ‘hubs’ for a wide range of health and social care services that were previously separately located (see Table 11), and to therefore catalyse improved integration and collaboration across teams and disciplines. The primary reported benefits of co-location in both settings centred around the facilitation of informal interactions and relationship-building between teams. According to participants, this allowed staff to communicate more efficiently and to understand each other’s roles.
Weekly multidisciplinary team meetings were the foundation of interservice co-operation in both settings, where discharge plans were discussed with input from representatives of relevant services, including GPs, nursing, physiotherapy, district nursing, occupational therapy, adult social care and mental health. Participants described how co-location had directly benefited patients, enabling more joined-up care, quicker referrals and closer communication between disciplines. In both hospitals, GPs and other professionals appreciated having easier access to diagnostic facilities than they had had previously.
In both settings, the integration (formal or otherwise) of health and social care services was particularly helpful in responding to home care shortages, although this occurred in different ways. In Case A, formal integration had allowed the Health Board to fast-track the registration of a new home care operator, whereas in Case B, close co-operation between the integrated community health (including hospital at home, intermediate care and district nurses) and home care teams had led to the development of joint care for patients in the community.
Providing local, holistic and patient-centred care in a home-like environment
At both sites, a key defining function identified by participants was the provision of care close to home that was personalised, holistic and patient-centred, often defined in contrast to care in larger acute hospitals. The role of GPs in the leadership and delivery of hospital services was central, as their prior patient knowledge and relationships were considered beneficial to patient experience as well as to the community-oriented character of the hospitals more broadly. The importance of community feeling and a sense of duty to the local population were also clear in the operation of the hospitals. This was particularly visible in Case A, as staff sought to prioritise admissions from the local community.
Participants reported that by facilitating more joined-up working, the integration of services at the community hospitals led to a more holistic and personalised approach to care. The hospitals’ homely and friendly environment was also appreciated by patients and staff, and the decor and layout of the wards in both hospitals counteracted the medicalised setting. Walls were observed to carry community notices, pictures and local historical information. Wards were spacious and bright, with well-used common rooms for patients, with views looking out on to the grounds. For elderly inpatients in particular, the community hospitals were considered better for recovery than acute hospitals.
Factors affecting the functioning of community hospitals
The degree to which the community hospitals were able to fulfil the roles and functions described above was reported to be affected by a range of factors. These are considered in turn below and their effects are compared and contrasted between the two sites.
Balancing the optimum community hospital function with wider system needs
Interviews revealed a tension in both community hospitals between their optimum role and the needs of resource-constrained systems, in particular in relation to long-term care of delayed discharges and bed shortages in nearby acute hospitals. Participants in Case A in particular emphasised a tension between their own understanding of the hospital’s function as a provider of step-up care, and expectations of wider health system actors. However, although Case A regularly accommodated acute referrals, local admissions were prioritised and efforts made to retain a ‘community bed’ at the weekend, just in case a local patient needed it.
This sense of competing objectives was potentially reinforced by blurred boundaries between the levels of care and misperceptions of the function and limits of community hospital provision. In both cases, staff reported that acute hospital colleagues had limited understanding of the community hospitals’ capabilities: ‘I think our understanding of what goes on in hospitals is possibly better than the hospitals understanding of what we can do in the community’ (S1_B). In Case A, a staff member reported that acute hospital clinicians were at times reluctant to refer certain patients to the community hospital as they underestimated staff skills. Conversely, in Case B, it was reported that pressure to free up beds at times led to the premature transfer of acute patients with care needs that stretched staff’s skill sets.
In addition, in seeking to expand the delivery of specialist services, the hospitals also faced the challenge of managing the ‘tension between local and central around efficiencies and costs’ (S4_B) and the tendency for long-term gains around patient access and local skills to be stymied by expense and efficiency concerns. In Case B in particular, under-utilised facilities, including a fully equipped minor surgery suite, highlighted the complexity of planning for future community service needs.
Enabling general practitioner ownership and continuity of care
The integration of GP services into the community hospitals was deemed beneficial in two key ways: (1) they provided valuable local input and leadership to wards; and (2) the traditional GP role was enhanced by improved access to facilities and treatment options (e.g. hospital at home, diagnostic facilities, beds). The degree to which they were able to effectively and confidently fulfil their roles on the wards and in the multidisciplinary hospital environment more widely was affected by both the system used among GPs to share responsibility for ward cover, and how their role was funded and defined by the Health Board.
In Case A, GP leadership was considered key both to driving the redevelopment of the hospital and to maintaining services. The rota system used allocated one GP to ward cover for 1 full week at a time, and minimising GP rotation was considered important to the maintenance of skills and continuity.
In contrast, in Case B continuity of care on the wards and maintaining GP skills and confidence had been a challenge. Inefficiencies were created by the division of responsibility and inpatient load among three separate practices. One GP from each practice took primary responsibility for ward cover and thus maintained a regular presence but, in their absence, some of the other GPs struggled. This occasional lack of continuity, combined with a heavy workload and time pressures, reportedly made it difficult for some GPs to take confident ownership of patient care on the wards:
They know there’s no way they can get a complete handle on the patient, in one sitting, without sitting and reading the notes, and spending half an hour talking to the nurses about what’s going on.
S8_B
Contractual and funding arrangements defining the GP’s support for the hospitals, beyond their practice responsibilities, were also key to the GPs’ function. Whereas in Case A, GP input was contracted through a clearly defined service level agreement, which could be supplemented when enhanced services were added, in Case B, the complexity of GPs’ roles were reported to be insufficiently defined in contractual and funding arrangements with the Health Board. A GP reported that, although the move to the new facility had significantly increased the complexity and volume of workload, GPs still received the blanket funding for bed cover that they had previously. One participant described the mismatch:
You’ve got multidisciplinary team meetings, there is that complexity, you need to speak to the [occupational therapist] OT, the physio. So it’s completely changed, but it’s still funded as if you were just, you know, it was just like a home visit or something like that.
S1_B
Given their pivotal role as managers and leaders, participants in both hospitals highlighted the importance of respect for GP autonomy in order to sustain the model of service delivery and staffing.
Meeting community hospital staffing and training needs
Referring to GPs as well as other service staff, participants in both hospitals repeatedly emphasised that community hospitals attracted a ‘different’ kind of individual, who sought to stretch their skills and challenge themselves beyond their traditional role.
Management staff in both hospitals underlined the importance of encouraging innovation and exploiting the smaller setting to do things differently:
We have been encouraged and allowed to be innovative, to try different ways of working, to have that discussion and to get on with it to make a difference . . .
S10_A
However, understaffing was reported as a pressing issue in both hospitals, especially among nursing and home care services, which necessitated flexibility and close collaboration among the small teams to maintain services. Maintaining and building the skills required by the community hospital setting was an ongoing challenge for both hospitals. Staff often dealt with a wide range of techniques too infrequently to maintain expertise and confidence. Although nurses and GPs were commonly trained in more specialist procedures, in the context of increasingly complex and frail patient loads, staff expressed concern about having the necessary skills:
We sometimes feel a wee bit isolated when, you know, something . . . a patient’s really quite unwell and we can’t just run along the corridor or the consultant’s not just along the corridor to give that extra advice. They’re on the phone but, you know, they’re not just next door to come along and see a patient.
S10_B
In Case B, achieving the right balance between GP and consultant oversight of palliative care also demonstrated the challenge created by delivering more specialist care in the community hospital. Interviews indicated that some GPs lacked the confidence to take some palliative care decisions, preferring to defer them until the consultant’s weekly visit.
Overcoming challenges of co-location and integration
Although service integration and co-location were generally viewed positively, interview participants also identified challenges related to the sharing and division of workspace, differing work cultures and a lack of shared information technology (IT) systems. These concerns were reported to affect the degree to which the full potential of joined-up working was realised.
In Case A, where responsibility for adult social care was already under the Health Board, integration was seen as a long-running work in progress by the health and social care teams. According to interviews, different cultures of working and difficulties around defining team workspace and perceived differential power relationships were the main challenges. In Case B, the health and social care teams’ co-location within an open-plan office was reported to have improved collaboration, despite no formal integration having taken place. Shared break and dining areas in both facilities reinforced the co-operative environment.
A lack of upfront planning and investment in IT system interoperability limited service teams’ abilities to reap the full benefits of co-location. Although some IT systems in both hospitals did enable information sharing, separate systems were in use in both hospitals and they did not ‘speak’ to each other at all. Initiatives of limited scope demonstrated the value of interoperable systems. In Case A, GPs had shared access to their system with community staff, and found it extremely helpful to book physiotherapy appointments directly. In Case B, the integrated community health team’s shared system was also reported to have helped to build efficient and collaborative working practices.
Defining the ‘community’: equity, management and mission
Although Case B was managed by a community health partnership (CHP), which also oversaw two other community hospitals, Case A maintained and defended strong locality-level control. These differing management models had a strong impact on the approaches of the two hospitals and were reflected in their understanding of the ‘community’ they served.
With a perspective on district-wide needs, the CHP placed no formal boundaries on Case B’s community served and consciously extended services to patients beyond its immediate locality. The effect of this approach was most clearly manifest on the wards, where many beds were occupied by referrals from nearby acute hospitals and patients from the wider region. Health Board investment in the redevelopment of Case B was justified in part by this wide geographic coverage and the hospital’s ability to address district-wide needs:
. . . if you used a locality here to provide services you’re taking some of the pressure off another part of the system. So that was to our mind was the quid pro quo, you know.
S4_B
This function was also important to addressing equity concerns in service provision across the local region.
District-level planning was also seen as an effective approach to rationalising resources. Close relationships between the CHP’s three community hospitals strengthened local service delivery. For example, outpatient clinics were co-ordinated between the CHP hospitals in order to avoid overlap and if one was full, a patient could often find a bed in another.
However, the emphasis in Case A differed significantly, as staff emphasised a strong sense of community boundaries and the value of locality control for effective planning and resource management. Although structurally part of a district partnership, management was still taking place at the locality level in practice. This locality focus was also reflected in interactions between the ward and the acute hospital, where staff strongly prioritised local admissions over transfers of patients from beyond their locality and proactively reached out to other regional services to bring local patients into their care, where possible.
Community ownership and engagement
Despite the differences in approach to defining their ‘community’, in both settings a sense of community ownership, through engagement and use of facilities, was significant. Community engagement was seen as important, to the hospitals’ initial development, as well as their day-to-day operation and mission. It was also seen as a feature of the hospital models that distinguished them from acute hospitals:
The community hospital is at the centre of community so you should be reflecting on what the community is thinking.
S8_A
In both sites, volunteering was an important way for local people to engage in the life of the hospital. Local chapters of the League of Friends (Attend, London, UK) worked actively with staff to fundraise for equipment, for example. In Case B, volunteers maintained a continuous presence, directing patients and visitors in the reception areas, and visiting inpatients to bring newspapers, serve tea and keep them company. A staff member described the effect on the hospital’s function:
There is always a real community feel in that the community gets behind the community hospitals and they’ll fight for it.
S10_B
In both hospitals, staff participants were eager to leverage these aspects of the service models to develop the community hospital as a ‘community hub’, which could function as a space to deliver health messages even to those not receiving treatment as well as to bring people together and alleviate social isolation. In Case A, participants highlighted the importance of hospital facilities for social interaction, following complaints about the lack of a café and from elderly patients who had been attended to too quickly without having time to enjoy the outing. In Case B, the hospital’s café was observed to be continuously busy and according to interviews, was often used by members of the public without a hospital appointment.
Dialogue with the local community ensured buy-in at the planning stages. In Case A, although a community representative was included on the redevelopment panel, no formal public consultation took place. Despite the fact that the vocal and at times oppositional engagement of local media and community with hospital matters signalled the strong sense of ownership felt, the absence of a formal mechanism for direct engagement meant that some participants still sorely felt the lack of a community voice and channel for information-sharing. The picture differed considerably in Case B, where comprehensive public consultations at the planning stage facilitated community buy-in.
Discussion
This study addresses a gap in our understanding of the role and functioning of community hospitals, and the factors influencing their implementation and development. Our findings confirm the three propositions that the study was designed to test, namely that community hospitals provide friendly, service-user focused care,13 have a focus on elderly7 or palliative care,12 and act as a hub for care integration and provision of care closer to home,83 but also suggest a much broader role. The community hospitals studied occupied a space between primary, secondary and chronic care and provided step-up, step-down and community care to patients both within and beyond their localities. In doing so, they endeavoured to prevent hospital admissions and ease the transition from hospital to home, as well as to relieve pressure from overburdened acute services. Both funded under the private finance initiative (PFI) route after a series of failed attempts by GPs and other local stakeholders to secure capital funding, they established flexible service models which, thanks to adaptable facilities and the maintenance of a motivated staff with ‘enhanced’ skill sets, offered scope to respond to changing needs. By exemplifying the diversity of management models and approaches that exist, the case studies showed that community hospitals can serve a variety of system priorities, both in terms of addressing regional equity and demands for joined-up, accessible provision for local populations.
Our findings around the capacity of community hospitals to facilitate integrated working support those of a previous study of a community hospital providing intermediate care in Norway. 61 This study also reinforces the findings of other authors8,55,58 on the less tangible, experiential benefits of delivering care in a community hospital for patients and staff, as opposed to larger, acute facilities.
At a local level, a range of contextual factors affected both the ways in which the hospitals functioned and the degree to which they were perceived to be successful in fulfilling their intended role. Enabling GP ownership and continuity of care, maintaining clinical skills and confidence to support the range of services offered, ensuring adequate mechanisms and space for community engagement and overcoming the challenges of co-location and service integration were all identified as important considerations. This reflects a range of existing literature on the various internal barriers to and facilitators of the integration of care services, including the challenge of defining professional identities and power balances between newly integrated teams,171 and the value of personal interaction172 and shared IT systems. 173 The experiences of staff reflect the evidence on the challenge of maintaining clinical skills and confidence for low-frequency procedures faced by rural physicians in particular. 77,174 If the scope of care delivered in the community is to expand, our case studies indicate a need for strategic investment in maintaining the clinical skills and confidence of community practitioners. The association of social isolation in older people with increased mortality and numerous other health risks is well-established175 and, as such, the value of considering isolation as part of any preventative health strategy is acknowledged. 176,177 In this sense, community hospitals’ potential role as social hubs and community members’ apparent desire to engage with them are important. By offering a friendly, safe setting to socialise, and attracting community members through various mechanisms (i.e. volunteering, public cafés), hospitals can enhance their preventative role. Although less formally integrated into the development and operation of Case B, local community identification and engagement were viewed as important in both settings, and the desired prioritisation of local community needs was seen to distinguish the community hospitals from acute services. However, with constrained resource availability, our findings suggest that the extent to which community hospitals can fulfil their local mission may be inhibited by competing priorities in the wider system.
This study has some possible limitations. First, it was undertaken in only two settings, which may limit the applicability of the findings to other contexts. However, the case studies were located in different regions and were selected for the differences in setting, accessibility, population, size, and services that they were expected to offer. Significant variations between the settings facilitate wider applicability. Second, although it was attempted, it was not possible to speak to certain key categories of stakeholder. For example, in Case B, interviews could not be arranged with a social care representative. However, data from interviews with other stakeholders did not differ considerably from each other on key topics of interest. In addition, all interview findings were triangulated with data from observations and document review to enhance their richness.
Conclusion
From the findings presented, this study should reinforce the place of community hospitals in current policy plans to enhance service integration locally and to organise services more effectively for the elderly and chronically ill. 13,18,23 However, without sufficient delineation of their role within the wider system, community hospitals may risk being relied upon to plug shortfalls in acute provision, thus constraining their ability to fulfil their preventative and step-up function that could help to keep local populations healthy and maintain patients in the community.
Chapter 6 Comparing community hospitals in Europe: a cross-case analysis of models in Finland, Italy and Scotland
Introduction
Community hospitals are featuring more and more prominently in government policy agendas in the UK and in a range of European countries. 107,108 There are a number of drivers for this, including the requirement to meet the health and social care needs of increasingly elderly populations with multiple health conditions, and an increasing focus on integrated care. 18 This issue is particularly acute in rural areas, which often struggle with longstanding difficulties in recruiting and sustaining a skilled workforce. 178 Community hospitals sit between primary care and secondary care and are traditionally defined as local hospitals that are staffed mainly by GPs and nurses to provide care in a hospital setting, predominantly for rural populations. 2 Our scoping review (see Chapter 2) found that community hospitals provide a wide spectrum of services to care for acute and chronic needs and hence occupy a space between, and to some extent encompass, community-based primary care and acute hospitals. They have also been highlighted as being highly collaborative in nature and representing many forms of integration in their operation. 83 They have, however, evolved to exist in a variety of forms, differing in the nature and scope of services, models of ownership and management or level of service integration. Often defined in terms of locality and the population that they serve, there is limited understanding of specific organisational and governance features of different community hospital models, how they may sit within local systems of service delivery and the wider context in which they operate. There is also little known of the challenges and facilitators of service provision for community hospitals, particularly in light of sociodemographic changes and economic pressures.
This chapter presents a cross-case analysis of four case studies of community hospitals in three European countries, which sought to address these gaps in understanding. Making comparisons between countries at the subnational level can provide useful and important information for national policy and health-care service delivery. 179 The cross-case analysis in this chapter starts to fill some of the gap in our knowledge of community hospital models.
Methods
Case-study selection
The case-study approach is widely used in health-care research. Case studies can provide richness and detail of data that may be difficult to obtain through other methods. 180 Creswell181 defines a case study as ‘An exploration of a ‘bounded system’ or case (or multiple cases) over time through detailed, in-depth data collection involving multiple sources of information rich in context.’
A case-study approach is appropriate in order to generate a more in-depth and context-specific understanding to help inform the further development of community hospitals to best meet the health and social care needs of the local populations.
The case-study selection involved two stages: (1) selection of country and (2) selection of community hospitals as cases. The purpose of country selection was to understand the experience of community hospitals within a range of countries, all with predominantly tax-funded health-care systems, but with differing governance arrangements and means of organising health care to facilitate meaningful comparisons. Restricted to high-income countries, countries were also selected based on having recent and/or significant developments in terms of community hospital models, or policies and strategies supporting community hospitals. Case studies of different models in Scotland, Italy and Finland were selected. All three countries have relatively recently highlighted community hospitals or equivalent models within health and social care policies: in Scotland, this has been through the Community Hospitals Refresh Strategy published in 2012,13 which envisages a key role for community hospitals in Scotland, particularly in respect of delivering more integrated health and social care; in Finland, through the Health Care Act (2010);182 and in Italy through the National Health Plan 2006–8. 139
The selection of innovative models of community hospitals within each of the countries was informed by the scoping review reported in Chapter 2, as well as by discussion with expert in-country advisors and the cross-project steering group. Two case studies were carried out in Scotland to reflect its long-established community hospitals, the 2012 Community Hospitals Refresh Strategy and because Scotland is closest to England in terms of health system context and the historical development of community hospitals. 13
Case-study methodology
Description of methods used across the different countries
The same methodological approach was used across all four case studies to examine the role and function of the selected community hospitals in the three countries. Table 12 details the three main data collection components: stakeholder interviews (informed by a stakeholder mapping), non-participant observation and document review. Researchers followed a common protocol. For each case, site field visits were made, lasting between 4 and 10 days. Observations were carried out on different days and at a range of times in order to capture a variety of activity and any differences in workload and staffing within the community hospitals.
| Method | Purpose | Participants/sampling |
|---|---|---|
| Semistructured interviews with stakeholders | To understand the evolving nature of community hospitals, their role within the local health economy, staffing and staff roles, relationships with other providers, relationship with communities served, vision and opportunities and challenges to future provision | Range of stakeholders to include a number of representatives from the community hospital (senior management and frontline staff), funders, other local providers and patient group representatives |
| Non-participant observation | To gain an in-depth understanding of organisational functioning of the community hospital, for example, to understand the full range of activities and activity levels | Observations were restricted to public areas within community hospitals (reception, corridors, waiting rooms) and staff meetings. No observations of patient care were conducted |
| Document review | Review of relevant documentation to understand community hospital mission, status, governance and organisation, activities, working relationships, historical development and performance | Documents sourced through internet search and through stakeholders and interviewees |
When interviews could not be completed during field visits, these were completed by telephone. A semistructured interview guide (see Appendix 7) and observation framework was used,183 although the approach remained flexible, both for the researchers and the participants. Informed written consent was obtained from each interviewee and interviews were audio-recorded and transcribed verbatim, with permission. Permission to record was declined once, and in this case, notes were taken instead. Researchers in Italy and Finland were bilingual and translated interviews into English. Permission for non-participant observation was sought before commencing field visits but consent was not sought from everybody observed. No names or identifiable information were recorded as part of observation notes. Data collection took place between November 2014 and August 2015.
Analysis
Each case study was analysed individually in the first instance. Detailed case descriptions were developed in order to describe the history, context and organisation of the community hospitals. Thematic analysis was conducted based on principles outlined by Boyatzis. 167 For the analysis of Case A, a coding frame was developed by JC and SB based on the interview topic guide and initial reading of interview transcripts and field notes. Using the coding frame, JC and SB each coded half of the transcripts for Case A, meeting regularly to discuss themes and refining the coding frame in an iterative manner as required. As analysis progressed, codes were organised into overarching or organising themes, using NVivo 10. Sourced documents, observations and field notes were read (and reread) to identify contextual and historical data and to triangulate interview findings. The coding frame for Case A was used for subsequent cases, with further refinements based on emerging findings. Cross-case analysis was then undertaken where case-study reports were systematically compared and contrasted according to the major themes identified previously. Context was emphasised in the cross-case analysis in order to understand similarities and differences between the cases. Three researchers (EP, EvT and NE) independently compared and contrasted the four case studies and identified emerging themes before discussing and agreeing themes as part of an iterative process of writing and analysis.
Case-study country settings
Health system and policy context
Chapter 4 provides an overview of the sources of health expenditure, governance, hospital bed capacity and number of community hospitals in the three countries. Italy and Finland are highly decentralised, with municipalities, or regions, having responsibility for the funding and organisation of health care, whereas in Scotland the responsibility is retained by central government (although devolved from the UK government to Scotland) with planning and delivery functions lying with territorial Health Boards. The number of community hospitals varies by country but is lower in Italy, relative to population.
Chapter 4 further summarises key legislation and policies in each of the countries that are relevant to community hospital provision. The policy context provides useful background against which to understand the different hospital models considered. It can be seen that in Scotland since 2011 there has been a series of strategies and policies specific to community hospitals and a bill to integrate health and social care. In contrast, in Italy driving policies are largely around reductions in hospitals, hospital beds and length of acute hospital stay, and in Finland around merging municipalities. This may in some part be a reflection of the longevity of community hospital within the three countries. In Scotland, community hospitals predate the setting up of the NHS in 1948. In Finland, community health centres, which have several of the same features as community hospitals, have been established since 1972, and in Italy community hospitals were established only in the mid-1990s. Community hospitals are thus at a different stage of evolution in each country. In Finland and Italy they may be seen as part of a reaction and solution to wider reorganisation within the health system, whereas in Scotland they have become perhaps more embedded in the health system.
Community hospital provision
‘Community hospitals’ are not necessarily well defined, even in Scotland where they are long established. Chapter 4 provides an overview of the definition and service focus of community hospitals in each of the countries. As noted, Finland does not use the term ‘community hospital’ but its health centre hospitals (or, more precisely, health centre inpatient wards) can be seen to be similar in terms of structure and function. We use the term ‘community hospital’ to encompass these health centres and equivalent models for the remainder of the chapter. As noted in Chapter 4 community hospitals tend to serve a ‘geographic purpose’ with a broad range of services, including low-acuity acute general medical care, whereas community hospitals in Finland and Italy tend to be dedicated to specific population groups, primarily older people, and have a service focus on sub- and post-acute care, intermediate care and rehabilitation, with some variation. An important similarity across all of the countries studied here is that GPs, often with additional specialist training, have a key operational role, leading the management and medical care. Community hospitals in Finland and Scotland offer a comparable number of beds (between 20 and 60 typically), whereas those in Italy tend to offer up to 20 beds, although this varies within and across regions (see Chapter 4). In Italy, this may be representative of the move from providing the majority of primary and secondary care in district and regional hospitals to community hospitals; a transition, which has largely already taken place in Scotland and Finland.
Findings
The case studies were selected on the basis of being perceived as innovative models within the three countries. All were also relatively recently (post-2000) opened in their current form. Table 13 provides a summary description for each case. Table 14 lists details of stakeholder interviews conducted for each case study.
| Site characteristics | Case A (Scotland) | Case B (Scotland) | Case C (Italy) | Case D (Finland) |
|---|---|---|---|---|
| Geographical setting | Small town | Edge of small town | Small rural town | Centre of municipality |
| Population served | 15,000 (increased in summer) | 20,000–30,000 (+ 8000 students) | 6000 | 30,000 |
| Mixed urban/rural | Mixed urban/rural | Sparsely populated valley, two main villages | ||
| Demographic characteristics | Growing elderly population (22% aged 65+ years) | Growing elderly population (22% aged 65+ years) | Largely elderly (23.8% aged 65+ years) | Largely elderly (27.1% aged 65+ years) |
| Child poverty (11%) | Lower than country average income level | |||
| Date opened | 2009 (replacing hospital built in 20th century) | 2009 | 1996 | Late 2000s |
| Beds | 20 | 40 (two wards) | 16 | 84 (three wards) |
| Bed occupancy (%) | 90 | 89 | 78.5 | Ward 1: 93.1 |
| Ward 2: 91.7 | ||||
| Ward 3: 87.2 (closed for 2 months during summer 2015) | ||||
| Average length of stay (days) | 15 | 41.5 | 31.6 | 6–8 days (acute inpatient ward); 18–20 days (rehabilitation ward) |
| Indicative range of services and facilities |
|
|
|
|
| Staff numbers (approximately) | 250 | 200 | 32 | 80 |
| Management and finance characteristics |
|
|
|
|
| Stakeholder group | Case A (Scotland) | Case B (Scotland) | Case C (Italy) | Case D (Finland) |
|---|---|---|---|---|
| Implementers and managers of the community hospital (current and former) |
|
|
|
|
| Community hospital clinicians and frontline staff (current and former) |
|
|
|
|
| Broader health and social care system actors |
|
|
|
|
| Representatives of the wider community |
|
|
|
Five overarching prominent themes emerged in our analysis: (1) community hospitals evolving within health systems settings; (2) function and environment; (3) integration versus co-location; (4) staffing and management; and (5) the role of the community. The themes were found to be intrinsically linked; however, for analytical clarity, they will each be discussed separately below.
Community hospitals evolving within health systems settings
In each case, it was apparent that the community hospitals had some flexibility to develop according to population needs but that tensions could be created in implementation because of their place in the wider health system. There was a sense that the community hospitals were at times ‘stuck in the middle’ between the needs of the community they were serving, the needs of the acute hospital and their own needs and visions of what they wanted to achieve. The redevelopment of services in Cases A and B (Scotland) had allowed for purpose-built modern facilities but most notably greater co-location of a range of services including general practices, social care, district and school nursing, home care and specialist outpatient services as well as inpatient beds (see Table 13). Both Cases A and B had the explicit goals of focusing on the provision of timely and preventative step-up care and sought to keep patients out of hospital wherever possible; however, the place of the community hospitals within the health system meant that they were not able to function fully in this way. Most notably, the place of the community hospitals within the health system meant that they both felt considerable pressure to accommodate referrals from larger hospitals that in turn were facing pressure to free up beds. Interviewees in Case A reported that they had taken a stance to strongly resist filling community hospital beds with acute referrals but this was a point of tension within the system.
In Case C (Italy), community hospitals were reported by interviewees to be compensation for communities that were losing a hospital and a means to retain skilled health service staff within communities and provide patient care locally. Case C was innovative in being the first of its kind where GPs decided to work in synergy with other doctors and health professionals while keeping their own patients in outpatient service. One distinct Italian feature was that they had identified a need to provide palliative care closer to home for an increasingly elderly population and to operate in a nursing home function to allow families time to find accommodation that is more suitable. The model was initially designed and created at municipality and district levels and subsequently recognised and supervised by the regional level. In practice, the ability to do this was constrained through changes in payment mechanisms and regulation at a regional level, which would restrict maximum length of stay to 6 weeks. There was a further tension in this as the palliative care function was reported to have come about in part owing to the societal taboo around specifically designed rooms for palliative care, considered ‘the anterooms of death’ by patients. Therefore, if the region recognised that the hospital performed palliative care, it could lead to an increase of funding but also the application of a ‘label’ that would not be well received by the community. At the time of data collection, Case C was therefore considering how it would adapt to be more sustainable, which would involve either agreement at a regional level to extend length of stay in end-of-life situations (GP2_C) or further development of home-based end-of-life care (D1_C).
The Finnish community hospital had been created following major structural reform of the municipal system that sought to enhance co-operation between municipalities, to provide unified health and social care services across several areas. Community hospitals have thus evolved to serve larger populations and to act as gatekeepers to specialist care. Case D reported that the tensions arose from their physical closeness to the acute hospital (directly adjacent to the community hospital), which resulted in confusion among patients as regards the function and services provided by each and was thought to contribute to the unnecessary use of specialised medical services, which was somewhat in contrast with the ethos of the community hospital. Furthermore, although changes at the municipality level had driven the move to unified health and social care services, the perceived lack of flexibility in the organisation of the municipality resulted in reported constraints to the development of new operating models.
Function and environment
All four case studies conformed to the traditional definition of a community hospital and their function seemed to be a product of their environment, which, in some cases, showed in the buildings they occupied. Three of the cases (A, B and C) were particularly highlighted as having a ‘home-like’ physical environment in terms of layout, décor and atmosphere, counteracting the medicalised setting of larger acute hospitals, and cited as being of importance to patients and staff. In Cases A and B, there were community notices and information relating to the history of the local area, and rooms were spacious and bright with patient common rooms looking out onto the grounds. In Case C, the building was surrounded by gardens and a courtyard. In Cases A and B, this internal design of the hospitals did seem to be a reflection of a philosophy of working and there was strong emphasis on holistic and patient-centred care. However, in Cases C and D it was less clear whether or not this was the case.
All of the cases were set in a rural or semi-rural location (although there was generally reasonable access from public transport so locations were not particularly remote). The buildings themselves were a mixture of purpose built and redevelopments of existing hospital buildings. This sometimes resulted in structural limitations for use. For example, Case C reported that the exterior elevator did not have sufficient space to carry patients on a stretcher, and three steps preceded the internal lift.
With the exception of Case D, which was based next door to the district hospital but operated five satellite hospitals, all of the community hospitals studied were closer than the acute hospitals for the communities they served, reducing travel time for patients and improving accessibility. Having a sense of ‘localness’ appeared to be central to the operation of the hospitals, although the degree to which this was demonstrated varied. For example, Case C placed great emphasis and pride in the staff being local, whereas in Case D this emphasis was placed on patients being able to be supported at home.
Despite the differing country settings, each community hospital model performed similar functions. There was an emphasis on providing rehabilitative or long stay care for the community. Palliative or end-of-life care was a commonly cited function across each of the cases, although, as noted, it varied depending on whether or not this was formally recognised within the wider health system. There was also an emphasis on the existence of other enhanced services across the four cases, creating a step-up approach to care provision. Cases A and B had explicit aims of step-up care provision and operated a large number of services from within the hospital, including mental health services, endoscopy, renal dialysis, physiotherapy and podiatry. In contrast, Case C offered fewer services within the hospital itself, instead referring out to the nearest district hospital. Given the historical context of Case C, (opened in replacement of a district hospital), this may be reflective of the wider health-care context and aims to reduce health-care expenditure. Similarly, Case D does not explicitly focus on operating a step-up approach. The hospital is adjacent to the main district hospital and the lack of step-up care provision may be a product of this, as barriers around referrals to the main hospital may be reduced in comparison to the other cases.
Integration versus co-location
Integration was a significant theme that emerged from the analyses. Co-location was reported to promote integration but a number of other factors also influenced the degree to which integration could take place, some of which appeared out of the control of the hospitals and implied that a wider system overhaul would further aid collaborative working.
A common obstacle everywhere was IT and the ability to practically share patient information through existing systems. All hospitals reported that a lack of shared IT systems, particularly between health and social care, prevented or reduced integrated working. Case C also reported that the reliance of external services for technological equipment caused delays in patient care and treatment. Case B reported cross-location integration within disciplines (e.g. the paramedic service) but patient data could not be shared with other disciplines, such as primary care professionals.
Integration that was perceived to be more forced or procedural, for example, through local or regional restructuring such as practice mergers or closures, hospital closures, or as a result of location such as shared space, resulted in tension for the community hospital staff. For example, staff in Case B cited the large open-plan office as a facilitator to integrated working; however, in order for staff or disciplines to retain some sense of identity and privacy the use of physical barriers within the office increased, providing evidence that boundaries were still in place. Similarly, interviewees at Case D reported poor communication with the regional hospital despite co-location and having district policies in place, which were aimed to promote collaborative working.
In contrast, regular multidisciplinary team meetings, transfer of skills through staff rotation and specialised training, such as in Case D, appeared to demonstrate an embedding of multidisciplinary working, which in turn helped to enable the provision of integrated services. Cases A, B and D appeared well developed in terms of multidisciplinary working, although this was achieved through a variety of approaches and this may be linked to differences between the role or vision of the community hospital and contracting and staffing models. Case A and B reported regular (weekly) multidisciplinary meetings which aided care and discharge decisions. Case D used a system of staff rotation, district policy and allocation of GP–nursing partnerships to patients. In contrast, Case C seemed relatively underdeveloped in this area and instead ran ad hoc meetings between GPs and nurses on the request of the head nurse. Only specialist doctors met on a weekly basis, and wider multidisciplinary meetings did not yet take place. Some interviewees at this site agreed that multidisciplinary meetings were important to achieving holistic care, but felt that some GPs did not want to give up their autonomy.
Staffing and management
There were particular features of staffing and management across the different case studies. A common feature across Cases A, B and D was a perception that GPs in particular had to be particular kinds of individuals, willing to embrace challenges and responsible for personal and professional development. This could lead to some challenges in retention and recruitment. In Case D, which operates five satellite clinics from the community hospital, staff were difficult to recruit and retain, reportedly owing to the location of the clinics. Both Scottish cases (A and B) reported understaffing, particularly for nursing and home care services. The difficulties in recruitment and retention in turn had implications for patient care, notably in the ability to achieve continuity of care, which was felt across the cases to be a crucial strength of the care that community hospitals could provide. This was evident in Cases A and B. GPs in Case B provided ward care in 1-week blocks in a bid to maintain continuity. However, on occasions of absence or heavy workload, GPs who provided ward cover lacked the confidence to take ownership of patient care and instead waited for the regular GP to return, meaning that patient’s treatment or care could sometimes be delayed and that continuity was more challenging.
Further innovation in staffing was reported in Case D, where GP–nurse pairs were assigned to patients with chronic illness, in an aim to improve interdisciplinary collaboration. This was noted as being unusual within this setting. In a subsequent evaluation of this model, staff reported being very satisfied with this model of working, which reportedly resulted in more effective time management, reduced waiting times for patients and clarity over workload distribution for staff.
In contrast, working in a community hospital was not necessarily seen as being an enhancement of the traditional GP role in Case C. As noted above, GPs were reported to be unwilling to give up their autonomy, which meant that multidisciplinary working was challenging. However, Case C also reported excellent retention of staff, reportedly owing to the staff living very locally in relation to the hospital, in a relatively rural and sparsely populated area.
Overarching management for each of the cases was found to be an important factor affecting the operations of the community hospitals. Contrasting management approaches were evident and generally appeared to take a top-down or a bottom-up approach. All but one of the cases were run by GPs, which is traditional for community hospitals. In comparison, Case D was operated jointly by the Chief Medical Director and the Chief Nursing director in a more top-down managerial structure and appeared to demonstrate a commitment to collaborative working, through staff motivation and a sense of ‘togetherness’ throughout the management structure of the hospital. However, it was reported that at times this approach hindered development because of outdated thinking and prevailing hierarchy between secondary and primary care.
There was a strong sense of staff ownership particularly in Cases A, B and C, and, again, the contrast to this was Case D, where this sense of ownership was less strong. In some cases, this created some tensions for the community hospital. In Cases B and D, external contracts or shared services were used. In Case B, this created tensions whereby staff who were employed by the regional Health Board, rather than the community hospital itself, appeared disloyal or uncommitted to the overall vision and goals of the community hospital. Interviewees suggested, for example, that a particular type of individual and external contract employees who did not stay late were regarded as less committed to the community hospital.
The role of the community
The role of the community was emphasised heavily in each of the cases, although the level of involvement varied, ranging from an active to the more passive role of the community. In Case B, where the building was purpose built, the community was consulted at each stage of planning and development through comprehensive public consultations, which helped to facilitate community buy-in. Furthermore, Case B has also maintained regular volunteers in the hospital and emphasises the shared use of facilities such as the hospital cafeteria. The community was generally discussed positively. Active and structured volunteering was unique to Case B and appeared to be more grounded in the general approach to operational management.
In contrast, Case A had no formal public consultation of the redevelopment of the community hospital and management took the decision to disband the existing patient participation group after a breakdown of trust between the community hospital management and some vocal and critical members. It was highlighted that the community contribution was challenging, as it sometimes resulted in conflict after areas for concern have been raised through local media, affecting staff morale. There was a sense of disconnect between the community hospital and the community and some interviewees were dissatisfied with the lack of an engagement mechanism. This added to the pressure the hospital is under in trying to meet the needs and preferences of all stakeholders. Despite this, the staff talked positively about the importance of the community and their involvement in the hospital development.
Case C narratively maintained the importance of community involvement in hospital working, after fierce community opposition to the closure of the original district hospital, but the evidence to support this was sparse. Community involvement appeared to be more linked to the localness of the staff, and their base within the community setting, rather than to the patients themselves. There was little evidence of active involvement by the community, through either volunteering or consultation. There were also no shared spaces for patients and staff to use, as was the case in Case B with the hospital cafeteria. The identified lack of active community involvement may be a reflection of the novelty of community hospitals in this setting and a lack of clear strategy in which to maintain community involvement from patients rather than a conscious decision against community involvement.
Case D stood out, as it seems to place less emphasis on the role of the community in the hospital and focused more on integration and collaboration within the workforce. There are no established voluntary work activities and the only reported link to involvement of the community was the regular collection of patient feedback. This was described as being systematic but it was unclear how feedback was collected. There was some evidence of change resulting from the patient feedback but this appeared to be at a basic operational level rather than service design.
Discussion
Our cross-case analysis of innovative community hospital models in three countries show that, although models have evolved differently, they commonly provide a range of health and social care services in a less medicalised environment than in acute hospitals and function as a potential bridge between primary and secondary care. It was also evident that all placed priority on preventative services and home rather than hospital care. There was scope in all of the models for community hospitals to be flexible in how they developed services but also evidence that this could be constrained by a number of factors such as the constraints of physical space to organisational changes and pressures in the wider health-care system. It was clear from the different cases that community hospitals had great potential in integrating services that may have been traditionally separated. Creating a place for co-location of these services was seen to promote multidisciplinary working, but a number of challenges remained. The ability to effectively share patient information was hampered by the incompatibility of IT systems. The importance of maintaining professional identity and traditional boundaries also prevailed to a greater or lesser extent. Although a sense of ‘localness’ was important in all of the models, the extent to which communities were involved and engaged varied considerably from no involvement beyond care transactions to co-design and the creation of public spaces. Finally, staffing requirements often created opportunities and challenges for hospitals. Work within community hospitals was considered to provide a layer of challenge on top of typical roles in primary care, yet this in itself meant that recruitment and retention could be difficult. In the discussion below, we use these findings to consider three important aspects relating to our analysis: the place that community hospitals have in more traditional rural settings; indications for how community hospitals may operate in more urban areas; and lessons around the role of community and integration of services.
Three of the four case studies show that part of the function of community hospitals is to improve accessibility, providing inpatient and specialist outpatient services closer to home. However, it is clear that community hospitals are considered by staff not to be defined by their geographic setting or physical structures as hospital buildings but as a model of care, distinguishable by their ethos and the nature of care provided compared with other settings. Rural health-care structures have previously been characterised in terms of having broader co-operation, greater teamwork and an approach to illness that is inclusively medical and holistic. 60,150 They are also reportedly associated with a strong sense of ownership among staff. 150 This was confirmed in our case studies, particularly for Cases A and B, which had been longer established.
The discourse of insiders and outsiders has been noted with reference to community participation in health care in rural settings, most recently as a means to prioritise rural authenticity. 184,185 The sense of ownership and difference created in speaking about the community hospitals seemed important in three of our cases. This was demonstrated for example through staffing in Case B, whereby professionals not employed by the community hospital were seen to be lacking in commitment to the vision of the community hospital or in necessary skills to take over patient care. Community hospitals were also to some extent defined by what they did in comparison to others, often deliberately offering services that others could not and developing in direct response to changes in the wider health system, for example, in maintenance of palliative care in Case C. It is likely that the reported sense of being in the middle afforded community hospitals an ability to adapt as well as causing frustrations as a result of having to be reactive rather than proactive in response to the wider health system, particularly acute hospitals. If countries are seeking to develop more strategic roles for community hospitals in the health system, it may be important to consider whether such flexibility, which can be afforded through a lack of a rigid legislative framework,138 should and could be maintained, recognising that it may be two-sided. 186 In contrast, staff ownership and community involvement appeared less evident in Case D, which was based in a larger town, although still serving a rural population, and alongside a regional hospital. The management structure in the context of Case D, with nursing and medical leadership, through the innovative GP–nurse pairs, seemed to serve to foster a sense of togetherness among staff. The contrast, however, suggests that considerations in developing models of care in urban or rural settings will differ; in the case of the latter, the relationship between community hospitals, staff, community and place is possibly more integral and mutually dependent. 187,188
Interestingly, previous research has also suggested that geographic situation will affect the networks formed through integrated care, arguing that in rural areas, the limited labour market may reinforce longstanding and close professional networks, whereas urban settings may be more likely to lead to more open networks and a diversity of services stimulated. 189 Our case studies showed that, partly through the co-location of services, community hospitals had great potential in integrating services. The degree to which this translated into integrated care pathways and multidisciplinary working varied. In Case C for example, some saw multidisciplinary working as a threat to the autonomy of physicians, whereas in Cases A and B it seemed to be much longer established. Consideration of how integrated care is implemented through community hospitals is likely to be dependent on locality and national context. 151,189 The recent evolution of community hospital models in Scotland, for example, has coincided with the introduction of integrated Health Boards,165 whereas in Italy the national and regional drivers have been the need to reduce inappropriate utilisation of acute care hospitals 140 and a drive to maintain professional workforces in rural areas.
The way in which community hospitals adapted was reportedly based on the needs of local populations. However, there was little or no evidence of systematic needs assessments in any of the cases. The different levels of involvement of the community and volunteers most probably reflect differences in historical, social and cultural norms within the countries. 190,191 Interestingly, even in the context of Scotland, where there is a stated requirement for communities to be involved in all stages of development and delivery of services in community hospitals13 and where the role of volunteering is formalised,192 this is not without its challenges. Thus, although alignment with community needs were reported to be an integral part of the community hospital model, it is not clear how or if this is achieved. Particular challenges of community participation in rural health care have been noted elsewhere. 185,193
Our analysis starts to address some of the highlighted gaps in knowledge around the role of community hospitals and points to factors that will be important to consider, at a local and national level, in the future development of models. There are, however, a number of limitations. The cross-case analysis was based on only four models, two of which were based in the same country, which may limit the generalisability of findings. In addition, we have used the term ‘community hospital’ to encompass what we regarded to be similar models in each country but this may have led us to overlook important differences. The cross-case analyses were conducted from pre-existing case-study analyses, and, therefore, these data have already been subject to interpretation, which may have influenced the findings reported here. However, authors of the four individual case studies have contributed to the interpretation presented in this chapter. We sought to gain a range of perspectives in all case studies and bring together data from different sources and methods but key viewpoints may be missing. Future research would benefit from including the views and experiences of patients and carers.
Conclusion
Community hospitals have evolved differently within the same country and between countries. Common features include the breadth of services provided within an overarching ethos, often encompassing primary care, preventative services, social care and specialist care and care given to predominantly older populations. There are local and national contexts that will be important to consider in terms of how models of community hospitals develop across different countries. Important questions include how transferable models are from one setting to another given the perceived interrelationship with place and community, how barriers to integration beyond location may be overcome and how community should be best represented in ‘community hospitals’. Future research should consider how community hospital models might be implemented in more urban settings.
Chapter 7 Conclusions and recommendations
This study demonstrates that community hospitals form an integral component of local health-care delivery systems, providing care closer to people’s homes and addressing challenges arising from service fragmentation. They have the potential to assume a more strategic role as hubs for care integration locally, although this will depend on the specific context within which they are implemented. This multimethod study comprised, first, a synthesis of the literature on models of community hospitals in the UK and other high-income countries and an assessment of the evidence of their effectiveness, and, second, a detailed assessment of experiences in five high-income countries and case studies of individual community hospitals in three countries to understand better the roles, functions and contributions of community hospitals in different health system governance and service delivery contexts. We summarise the findings below and suggest options for their future role in the context of the changing policy environment of the NHS in England.
Evidence synthesis: roles and features, and evidence of effectiveness and cost-effectiveness of community hospitals
Our scoping review found that community hospitals in the UK and elsewhere operate in a manner that situates them at the boundary of primary care, acute hospital care and nursing home care, with services provided spanning each of these domains. There is a diversity of community hospital models, which offer the full spectrum of service provision, from preventative and primary care to inpatient surgical or medical care. Services tend to be provided by GPs and nurses, with visiting medical specialists supporting delivery through providing additional services such as outpatient clinics. Our analyses suggest that the types of services offered in community hospitals respond to the needs created by different geographical and health system contexts, for example, where acute hospital services are not easily accessible. The literature identified collaborative working to be a key characteristic of community hospitals, highlighting the potential for community hospitals to assume an integrative role locally by bringing together primary, secondary and community care. This observation may be particularly important in the design of future models of care delivery. At the time of writing, community hospitals have been included explicitly as part of NHS England’s plans to develop new models of working in relation to integrated primary and acute care systems and multispecialty community providers. 18,19 The evidence on the range of services provided in community hospitals and their integrative role suggests that there may be further potential to include community hospitals, and learning from these new models will be important. Our conceptualisation of community hospitals offers the basis from which to classify the purpose of community hospitals and informs thinking about further strategic development of their role.
Our systematic review of studies of the effectiveness and cost-effectiveness of community hospitals has highlighted the continued scarcity of robust evidence, an issue already highlighted in an earlier review by Heaney et al. 1 Eligible studies were available from England and Norway only, describing equivalent or improved outcomes for community hospitals compared with acute hospital settings on a range of measures for different service dimensions. Measures of effect included health outcomes such as mortality, process measures such as readmissions and number of bed-days and indicators of independence and community or nursing care needs. Staff, carer and patient experiences of community hospitals were also found to be favourable in comparison to acute hospitals and, from the available evidence, factors such as ease of access and the provision of a familiar and homely environment were perceived to be important to staff, carers and patients.
There was limited evidence on the cost and cost-effectiveness of community hospitals. Evidence that was available was narrow in its focus on post-acute care, suggesting that cost-effectiveness is comparable between community hospitals and acute hospitals. Evidence further suggested that the cost of some services provided by community hospitals was lower as a result of fewer readmissions, lower average costs per day and fewer interventions carried out, but this had to be balanced with higher costs incurred elsewhere, such as the need for visiting specialists. Studies tended to focus on recurrent expenditure, whereas investment costs were typically not considered; moreover, cost assessments tended to take a hospital perspective, which risks overlooking potential benefits to other parts of the system, such as community care or wider social care. It will be important for these aspects to be considered in future research, in particular where community hospitals are being viewed as a hub for integration locally.
Learning from international experience
We combined breadth and depth of analysis by undertaking a review of community hospital provision in five high-income countries along with four in-depth case studies of innovative community hospital models in three of these countries. In some cases, the country studies allowed us to access evidence that was not yet published or captured in our review of existing literature.
Experiences of community hospitals in five countries
Our review of the nature, scope and distribution of community hospitals in Australia, Finland, Italy, Norway and Scotland showed that the term ‘community hospital’ is not easily transferable to other system settings. Indeed, even within the UK, the notion of a community hospital encompasses a range of service delivery models that defy the formulation of a single, overarching definition. This reflects the evolution of the nature and scope of services delivered by community hospitals over time in response to changing population needs as well as the broader change in the nature of the delivery of health-care services themselves.
In line with our scoping review, the country review showed that community hospitals and related structures provide a wide spectrum of health services, which can be further conceptualised as a continuum between community hospitals serving a ‘geographic purpose’, typically for rural populations, at one end, to a specific population focus, mainly older and frail people, at the other. However, boundaries may be blurred where the local community constitutes a specific group, such as indigenous populations. In addition, as rural communities are ageing, service delivery will have to accommodate their changing needs.
Overall, and again in line with the scoping review, the country review suggests that the community hospital presents a ‘fluid’ concept, with the greatest advantage perhaps being its flexibility to respond to local needs. The evidence presented underlines the potential for community hospitals to occupy this niche within the local service delivery structure. This ‘niche’ may stretch from viewing community hospitals as a locale for service integration locally, as in Scotland, to their function as a component of locally integrated health and care services, such as in Finland, Italy and the newly established local (community) health centres in Norway.
Community hospitals in different systems face a number of common challenges, such as attracting suitable staff and maintaining a diverse skill set. There was also a perception that, as delivery systems are evolving, boundaries between services provided by community hospitals and those offered elsewhere locally might blur or indeed overlap, thus impacting on the effectiveness and efficiency of service delivery and potentially undermining the value of the community hospital and similar structures within the wider system.
Case studies of innovative models of community hospitals in three countries
The cross-case analysis of four community hospitals, or equivalent models, showed that they commonly provide a range of health and social care services in a less medicalised environment than acute hospitals and function as a bridge between primary and secondary care. The case studies, which offered a more nuanced understanding, particularly of the challenges faced by community hospitals, also mirrored our scoping review with respect to the range of services offered and in terms of evidence of an integrative role between community, primary and secondary care.
A number of findings presented may be important to consider in the development of community hospitals in the context of the NHS in England. Community hospitals have the ability to be flexible and innovative but can be constrained by pressure elsewhere in the health-care system (especially in overstretched acute hospitals) resulting in them operating more reactively than proactively in order to plug gaps in provision. Thus, there is an important distinction between ‘flexibility’ as (1) something created within the health system by having community hospitals, and (2) the flexibility within community hospitals to innovate and be adaptable to local need. This was demonstrated particularly in the Scottish cases, which called for greater delineation of the role of community hospitals to fulfil preventative and step-up functions. However, it will be interesting to examine whether and how a formalisation of the community hospital role within the health system affects service model flexibility.
Case studies found that community hospitals can have an important integrative function, but co-location of different services and professional disciplines is not sufficient to ensure this. Factors such as IT infrastructure were common barriers to information sharing and integrated care across all sites. Recruitment and the maintenance of skills was also a challenge in some cases; hence, it is important to consider the training role that community hospitals can have recognising, for example, that doctors need to be capable of providing general care in broad specialties across a range of different settings194 but also how sustainable staffing models can be developed in community hospitals. The reliance of community hospitals on GPs for both managerial and medical roles in countries with a shortage of GPs underlines the need for innovative reforms of the medical education and training systems that would attract more medical students to a general medicine career. 195
Finally, international experience highlighted the challenges of service decentralisation, fragmentation of local health authorities and the pivotal role of local commissioners. Difficulties in co-ordinating local care for an ever-growing patient population suggests that it would be beneficial if some level of central planning or strategic thinking supported the development of knowledge, competencies and responsibilities at the local level.
Limitations of this study
The limitations of the individual elements of the study are noted in each chapter. A common challenge across all elements of this study is the definition of community hospital. For the purposes of this study, we defined community hospital as a service model that (1) provides a range of services to a local community, (2) is led by community-based health professionals, and (3) provides inpatient beds. This definition was informed by a review of existing definitions of community hospitals and by consultation with members of the steering group for this project. By using this somewhat restricted definition, in particular the requirement of the model to have inpatient beds, our evidence reviews may have excluded some service models that might have usefully informed the work presented here. 4 However, the definition helped to identify service delivery models in other countries that could be considered comparable to the community hospital model in the UK. However, it is important to note that even within the UK there is not one definition that would capture that wide range of service delivery models that are presently considered under the umbrella term of a community hospital in England and the UK more broadly. Our findings emphasise that the notion of a single, overarching definition for community hospitals may be misleading, when the concept and range of services are so inherently diverse.
In this study, we were able to draw on only a small number of countries to explore the diversity of community hospitals in system settings other than England, and on even fewer studies for a detailed analysis of individual community hospital models. Clearly, it remains challenging to derive lessons from other systems contexts, given different policy contexts. At the same time, it is important to recognise that health systems are facing similar challenges and there is considerable potential to learn from approaches implemented elsewhere to inform domestic policy choices.
Our research also set out to investigate the wider role(s) and impact of community engagement in community hospital service development and provision. We were unable, as part of the evidence reviews, to identify robust published evidence that assessed this issue in a systematic way. Important issues relating to community engagement were brought out in the case studies but it did not emerge as a key area of focus in the country review. We note that a concurrent study, ‘A comprehensive profile and comparative analysis of the characteristics, patient experience and community value of the classic community hospital’ (HSDR project 12/777/13) examined more systematically community engagement and we shared relevant findings with that project team in order to prevent duplication of work.
Finally, we acknowledge that, although our research benefited from valuable advice from PPI representatives throughout, the public and patients were lacking as a participant group within the research, partly as a result of our focus on organisational, governance and service delivery features of community hospitals. As community hospital models are developed further and our research recommendations are taken forward, it will be particularly important to ensure a strong patient and public voice in this. The aforementioned project (HSDR project 12/777/13) will also bring important findings in this regard and we shall work in future publications to combine those findings with our international learning.
Research recommendations
Our study provided a range of insights that we believe will be important in informing the further development of a more integrated service delivery structure within the English NHS and where community hospitals might be afforded a key role. However, we also identified a range of challenges associated with the available evidence base that currently limits generalisation of our observations overall. We highlight these challenges below but do not seek to prioritise their ordering, as all will be important to address and should not be taken forward in isolation from each other.
First, there is a particular lack of research into the effectiveness, efficiency and cost-effectiveness of community hospitals that offer services other than post-acute care in different settings. In particular, there appears to be a mismatch between the available literature and findings from the review of international experiences, which highlights the role of community hospitals in relation to preventative services, step-up care and care integration. Evaluating the cost-effectiveness of these broader functions is challenging, but there is a need to better capture costs against value gained at the whole system level and beyond individual interventions.
Second, at a time when emphasis is being placed on integrated care and community-based service delivery, it seems particularly important for research to understand how community hospitals can and do contribute to developing related models of care.
Third, the role of the community in community hospitals varies across settings, and it remains unclear to what extent services are configured based on any assessment of community needs and which approaches to community engagement would best serve this purpose.
Fourth, there is a particular need for research into optimal staffing profiles and training needs of health professionals in community hospitals.
Finally, there is a need to assess the extent to which characteristics of community hospitals identified in this study reflect a unique combination of geographical location and specifics of the community hospital in a given setting, which was largely, although not exclusively, rural, and whether these can be transferred to larger urban settings.
Acknowledgements
We would like to thank a number of people who contributed to the successful completion of this study. Jody Larkin (Research Librarian, Knowledge Services, RAND Corporation) conducted the literature searches for the literature review. David Steel (University of Aberdeen, UK), Jane Farmer (La Trobe University, Australia), Marja Kaunonen (University of Tampere, Finland), Giovanni Fattore (Bocconi University) and Ingrid Sperre Saunes (The Norwegian Knowledge Centre for the Health Services) provided important suggestions and feedback on country reports on community hospitals in Scotland, Australia, Finland, Italy and Norway, respectively, which informed Chapter 4; the individual country reports are presented in full in Appendix 5. Irja Nieminen and Marja Kaunonen (University of Tampere, Finland) and Michela Meregaglia and Giovanni Fattore (Bocconi University) contributed to Chapter 6, conducting the case studies in Finland and Italy, respectively (shown in full in Appendix 8). Katherine Stewart and Calum MacLure (both RAND Europe) provided administrative assistance throughout the project. Professor Martin Roland (University of Cambridge) acted in a quality assurance role and provided valuable insight throughout the project. We thank all members of the cross-project steering group, chaired by Professor Sir Lewis Ritchie (University of Aberdeen). Helen Tucker (Community Hospital Association, England) provided very helpful comments and insights on the research protocol and draft chapters of the report. The Community Hospital Association has an organisational aim to promote the retention and development of Community Hospitals. Finally, we would like to thank our PPI representatives, Kate Massey and Hamish McBride, for their continuous support and comments, as well as all our study participants who contributed to this study through participation in interviews and site visits.
Contributions of authors
Emma Pitchforth (Associate Director, CCHSR, RAND Europe) co-designed the study, contributed to the scoping review, the systematic review and case studies, led and prepared for publication the cross-case analysis, and contributed to the overall synthesis and final report.
Ellen Nolte (Hub Coordinator, European Observatory on Health Systems and Policies, London School of Economics and Political Science and London School of Hygiene & Tropical Medicine) conceived the study, provided intellectual oversight for the whole study, contributed to all chapters and the final report, led on the country reports and conducted and prepared for publication the cross-country analysis. She was principal investigator on the project until September 2014.
Jennie Corbett (Analyst, CCHSR, RAND Europe) contributed to the scoping review, co-led and prepared for publication the systematic review and co-led and prepared for publication the Scotland case study.
Céline Miani (Senior Analyst, CCHSR, RAND Europe) co-led the scoping review, contributed to the systematic review, contributed to the Scotland country report and the Scotland case study, co-led the Norway country report, and co-ordinated the preparation of this report for publication.
Eleanor Winpenny (Career Development Fellow, University of Cambridge) co-led and prepared for publication the scoping review, co-led the systematic review and contributed to all the country reports.
Edwin van Teijlingen (University of Bournemouth) contributed to the cross-case analysis and supervised the Scotland case studies, conducting one of them.
Natasha Elmore (Research Assistant, CCHSR, University of Cambridge) contributed to the Scotland country report, the cross-case analysis and writing of the final report.
Sarah King (Visiting Fellow, University of Cambridge) contributed to the scoping review and the systematic review.
Sarah Ball (Analyst, CCHSR, RAND Europe) co-led and prepared for publication the Scotland case study.
Joanna Miler (Research Associate, University of Glasgow) contributed to the country reports.
Tom Ling (Senior Research Fellow, CCHSR, RAND Europe) was principal investigator on the project from September 2014. He was involved in the analysis of findings and provided oversight for the study.
Publication
Winpenny EM, Corbett J, Miani C, King S, Pitchforth E, Ling T, et al. Community hospitals in selected high income countries: a scoping review of approaches and models. Int J Integr Care 2016;16:13.
Data sharing statement
Requests for data obtained as part of this study should be directed to the corresponding author in the first instance. However, no names of study participants or sensitive information will be provided, in order to respect participant anonymity and confidentiality.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Heaney D, Black C, O’Donnell CA, Stark C, van Teijlingen E. Community hospitals - the place of local service provision in a modernising NHS: an integrative thematic literature review. BMC Public Health 2006;6. https://doi.org/10.1186/1471-2458-6-309.
- Royal College of General Practitioners . Community hospitals – preparing for the future. Occas Pap R Coll Gen Pract 1990;43:1-51.
- The NHS Plan. London: The Stationery Office; 2000.
- Profiling Community Hospitals in England: 1998–2008. London: Community Hospitals Association; 2008.
- Cacace M, Nolte E, Walshe K, Smith J. Healthcare Management. Maidenhead: Open University Press; 2011.
- Rechel B, Wright S, Edwards N, Dowdeswell B, McKee M. Investing in Hospitals of the Future. Copenhagen: World Health Organization, on behalf of the European Observatory on Health Systems and Policies; 2009.
- Green J, Forster A, Mallinder K, Bogle S, Lowson K, Small N. Effects of locality based community hospital care on independence in older people needing rehabilitation: randomised controlled trial. BMJ 2005;331:317-20.
- Small N, Green J, Spink J, Forster A, Young J. Post-acute rehabilitation care for older people in community hospitals and general hospitals – philosophies of care and patients’ and caregivers’ reported experiences: a qualitative study. Disabil Rehabil 2009;31:1862-72. http://dx.doi.org/10.1080/09638280902847002.
- Garåsen H, Windspoll R, Johnsen R. Intermediate care at a community hospital as an alternative to prolonged general hospital care for elderly patients: a randomised controlled trial. BMC Public Health 2007;7:1-9. http://dx.doi.org/10.1186/1471-2458-7-68.
- Young J, Green J, Forster A, Small N, Lowson K, Bogle S, et al. Postacute care for older people in community hospitals: a multicenter randomized, controlled trial. J Am Geriatr Soc 2007;55:1995-2002. https://doi.org/10.1111/j.1532-5415.2007.01456.x.
- O’Reilly J, Lowson K, Green J, Young JB, Forster A. Post-acute care for older people in community hospitals – a cost-effectiveness analysis within a multi-centre randomised controlled trial. Age Ageing 2008;37:513-20. http://dx.doi.org/10.1093/ageing/afn120.
- Thorne CP, Seamark DA, Lawrence C, Gray DJ. The influence of general practitioner community hospitals on the place of death of cancer patients. Palliat Med 1994;8:122-8. https://doi.org/10.1177/026921639400800205.
- Community Hospitals Strategy Refresh. Edinburgh: The Scottish Government; 2012.
- Tucker H. Integrating care in community hospitals. J Integr Care 2006;14:3-10.
- Nolte E, McKee M. Caring for People with Chronic Conditions: a Health System Perspective. Maidenhead: Open University Press; 2008.
- Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med 2007;22:391-5. http://dx.doi.org/10.1007/s11606-007-0322-1.
- Integrated Care and Support: Our Shared Commitment. London: National Collaboration for Integrated Care and Support; 2013.
- The NHS Five Year Forward View. London: NHS England; 2014.
- NHS England . New Care Models. Vanguards: Developing a Blueprint for the Future of NHS and Care Services 2016. www.england.nhs.uk/wp-content/uploads/2015/11/new_care_models.pdf (accessed March 2016).
- Ettelt S, Nolte E, Mays N, Thomson S, McKee M. Health Care Outside Hospital: Accessing Generalist and Specialist Care in Eight Countries. Copenhagen: World Health Organization on behalf of the European Observatory on Health Systems and Policies; 2006.
- Lappegard Ø, Hjortdahl P. Acute admissions to a community hospital: experiences from Hallingdal sjukestugu. Scand J Public Health 2012;40:309-15. http://dx.doi.org/10.1177/1403494812450372.
- Lappegard Ø, Hjortdahl P. The choice of alternatives to acute hospitalization: a descriptive study from Hallingdal, Norway. BMC Fam Pract 2013;14. http://dx.doi.org/10.1186/1471-2296-14-87.
- Ministero della Salute . Regolamento Recante: ‘Definizione Degli Standard Qualitativi, Strutturali, Tecnologici E Quantitativi Relativi all’assistenza Ospedaliera, in Attuazione dell’articolo 1, Comma 169, Della Legge 30 Dicembre 2004, N. 311’ E dell’articolo 15, Comma 13, Lettera c), Del Decreto-Legge 6 Luglio 2012, N. 95 Convertito, Con Modificazioni Dalla Legge 7 Agosto 2012, N. 135 2014. www.sinpia.eu/atom/allegato/1250.pdf (accessed March 2017).
- Nolte E, Ettelt S, Thomson S, Mays N. Learning from other countries: an on-call facility for health care policy. J Health Serv Res Policy 2008;13:58-64. http://dx.doi.org/10.1258/jhsrp.2007.007146.
- Ritchie LD, Robinson K. Community hospitals: new wine in old bottles?. Br J Gen Pract 1998;48:1039-40.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: The Stationery Office; 2006.
- Future Hospital: Caring for Medical Patients. London: Royal College of Physicians; 2013.
- Developing Community Hospitals: Models of Ownership: Options for Community Hospitals. London: Department of Health; 2006.
- Our Health, Our Care, Our Community: Investing in the Future of Community Hospitals and Services. London: The Stationery Office; 2006.
- Delivering Care Closer to Home: Meeting the Challenge. London: DH; 2008.
- Developing Community Hospitals: A Strategy for Scotland. Edinburgh: Scottish Executive; 2006.
- Reviews of Community Hospital/Intermediate Care Provision: Good Practice Guide. London: Department of Health; 2008.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-69.
- McKee M, Healy J. Hospitals in a Changing Europe. Buckingham: Open University Press; 2002.
- Winpenny EM, Corbett J, Miani C, King S, Pitchforth E, Ling T, et al. Community hospitals in selected high income countries: a scoping review of approaches and models. Int J Integr Care 2016;16. http://dx.doi.org/10.5334/ijic.2463.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. A Product from the ESRC Methods Programme. Lancaster: Lancaster University; 2006.
- Baillie J. Green ‘heart’ for new community hospital. Health Estate 2013;67:47-52.
- Kontodimopoulos N, Nanos P, Niakas D. Balancing efficiency of health services and equity of access in remote areas in Greece. Health Policy 2006;76:49-57. https://doi.org/10.1016/j.healthpol.2005.04.006.
- Tescher P, Chen TM. Emergency department performance at a small rural hospital: an independent in-depth review. Aust J Rural Health 2009;17:292-7. http://dx.doi.org/10.1111/j.1440-1584.2009.01101.x.
- Blattner K, Nixon G, Jaye C, Dovey S. Introducing point-of-care testing into a rural hospital setting: thematic analysis of interviews with providers. J Prim Health Care 2010;2:54-60.
- Ryan S, Hassell A, Thwaites C, Manley K, Home D. Developing a new model of care for patients with chronic musculoskeletal pain. J Nurs Manag 2007;15:825-9. https://doi.org/10.1111/j.1365-2934.2007.00761.x.
- Wong M, Rietzschel J, Mulherin D, David C. Evaluation of a multidisciplinary outpatient pain management programme based at a community hospital. Musculoskeletal Care 2009;7:106-20. http://dx.doi.org/10.1002/msc.147.
- Kumar S, Yogesan K, Hudson B, Tay-Kearney ML, Constable IJ. Emergency eye care in rural Australia: role of internet. Eye 2006;20:1342-4. https://doi.org/10.1038/sj.eye.6702104.
- Hawker S, Kerr C, Payne S, Seamark D, Davis C, Roberts H, et al. End-of-life care in community hospitals: the perceptions of bereaved family members. Palliat Med 2006;20:541-7. https://doi.org/10.1191/0269216306pm1170oa.
- Menakuru SR, Philip T, Ravindranath N, Fisher PW. Outcome of inguinal hernia repair at two rural hospitals in northern Scotland. Surgeon 2006;4:343-5. http://dx.doi.org/10.1016/S1479-666X(06)80109-5.
- Carson PJ. Providing specialist services in Australia across barriers of distance and culture. World J Surg 2009;33:1562-7. http://dx.doi.org/10.1007/s00268-009-0088-1.
- Paynter M. Evaluating use of telemedicine within a minor injury unit. Nurs Times 2008;104:30-1.
- Mensour M, Pineau R, Sahai V, Michaud J. Emergency department procedural sedation and analgesia: A Canadian Community Effectiveness and Safety Study (ACCESS). CJEM 2006;8:94-9. https://doi.org/10.1017/S1481803500013531.
- McGill A, North J. An analysis of an ongoing trial of rural videoconference fracture clinics. J Telemed Telecare 2012;18:470-2. http://dx.doi.org/10.1258/jtt.2012.GTH110.
- Neame B. Delivering chemotherapy with a nurse-led cancer outreach service. Nurs Times 2008;104:28-9.
- Williamson M, Gormley A, Dovey S, Farry P. Rural hospitals in New Zealand: results from a survey. N Z Med J 2010;123:20-9.
- Fleet R, Poitras J, Maltais-Giguère J, Villa J, Archambault P. A descriptive study of access to services in a random sample of Canadian rural emergency departments. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003876.
- Dobrzanska L, Young L, Patterson C. Piloting stroke rehabilitation in a community hospital. Nursing Times 2006;102.
- Green J, Forster A, Young J, Small N, Spink J. Older people’s care experience in community and general hospitals: a comparative study. Nurs Older People 2008;20:33-9. http://dx.doi.org/10.7748/nop2008.07.20.6.33.c6617.
- Owen V. Community care in a hospital setting. Nurs Stand 2010;24:20-1. https://doi.org/10.7748/ns.24.45.20.s25.
- Kerr C, Payne S, Hawker S. End-of-life care for older people in community hospitals. End Life Care 2008;2.
- Payne S, Hawker S, Kerr C, Seamark D, Roberts H, Jarrett N, et al. Experiences of end-of-life care in community hospitals. Health Soc Care Community 2007;15:494-501. https://doi.org/10.1111/j.1365-2524.2007.00714.x.
- O’Hanlon S, Liston R. Education in geriatric medicine for community hospital staff. Br J Community Nurs 2010;15:583-6. http://dx.doi.org/10.12968/bjcn.2010.15.12.583.
- Kelly M, McSweeney E. Re-visioning respite: a culture change initiative in a long-term care setting in Eire. Qual Ageing Older Adults 2009;10. https://doi.org/10.1108/14717794200900020.
- Dahl U, Steinsbekk A, Jenssen S, Johnsen R. Hospital discharge of elderly patients to primary health care, with and without an intermediate care hospital – a qualitative study of health professionals’ experiences. Int J Integr Care 2014;14:1-11.
- Garåsen H, Windspoll R, Johnsen R. Long-term patients’ outcomes after intermediate care at a community hospital for elderly patients: 12-month follow-up of a randomized controlled trial. Scand J Public Health 2008;36:197-204. http://dx.doi.org/10.1177/1403494808089685.
- Moll van Charante EP, Hartman EE, Ijzermans CJ, Voogt E, Klazinga NS, Bindels PJE. The general practice clinic in Ijmuiden: a special transmural experiment. Huisarts En Wetenschap 2005;48:102-8.
- Penfold J. Introducing convenience and calm to gynaecology. Primary Health Care 2013;23. https://doi.org/10.7748/phc2013.11.23.9.8.s9.
- Simpson S, Bell L, Knox J, Mitchell D. Therapy via videoconferencing: a route to client empowerment?. Clin Psychol Psychother 2005;12:156-65.
- Pace E, Dennison S, Morris J, Barton A, Pritchard C, Rule SA. Chemotherapy in the community: what do patients want?. Eur J Cancer Care 2009;18:209-15. http://dx.doi.org/10.1111/j.1365-2354.2008.01051.x.
- Schultz R, Lockey R, Oats JJ. Birthing in the Barkly: births to Barkly women in 2010. Rural Remote Health 2013;13.
- Scherman S, Smith J, Davidson M. The first year of a midwifery-led model of care in Far North Queensland. Med J Aust 2008;188:85-8.
- Sabesan S, Van Houts B, Parkinson C. Factors to consider when starting up a videoconference medical oncology outreach clinic. Aust J Rural Health 2010;18:89-90. http://dx.doi.org/10.1111/j.1440-1584.2010.01132.x.
- Green J, Young J, Forster A. Background to the post-acute care trial of community hospital rehabilitation for older people. Int J Ther Rehabil 2006;13:66-72.
- Wolfenden J, Dunn A, Holmes A, Davies C, Buchan J. Track and trigger system for use in community hospitals. Nurs Stand 2010;24:35-9. http://dx.doi.org/10.7748/ns2010.07.24.45.35.c7905.
- Ryan SM, Milsom P, Yang J, Snyman G. Travelling surgeons--a clinical audit of laparoscopic cholecystectomy procedures in Northland, New Zealand. N Z Med J 2009;122:34-40.
- Medical Council of New Zealand . Glossary 2015. www.mcnz.org.nz/glossary/#M (accessed April 2015).
- Williamson M, Gormley A, Farry P. Otago rural hospitals study: what do utilisation rates tell us about the performance of New Zealand rural hospitals?. N Z Med J 2006;119.
- Kerr C, Hawker S, Payne S, Lloyd-Williams M, Seamark D. Out-of-hours medical cover in community hospitals: implications for palliative care. Int J Palliat Nurs 2006;12:75-80. http://dx.doi.org/10.12968/ijpn.2006.12.2.20534.
- Lawrenson RA, Nixon G, Steed RH. The rural hospital doctors workforce in New Zealand. Rural Remote Health 2011;11.
- Chen TM, Tescher P. Emergency department demographics at a small Australian rural hospital. Rural Remote Health 2010;10.
- Payne S, Hawker S, Kerr C, Seamark D, Jarrett N, Roberts H, et al. Healthcare workers’ skills: perceived competence and experiences of end-of-life care in community hospitals. Prog Palliat Care 2007;15:118-25.
- Tucker J, Hundley V, Kiger A, Bryers H, Caldow J, Farmer J, et al. Sustainable maternity services in remote and rural Scotland? A qualitative survey of staff views on required skills, competencies and training. Qual Saf Health Care 2005;14:34-40. https://doi.org/10.1136/qshc.2004.010561.
- Miller DR, Alam K, Fraser S, Ferguson J. The delivery of a minor injuries telemedicine service by Emergency Nurse Practitioners. J Telemed Telecare 2008;14:143-4. http://dx.doi.org/10.1258/jtt.2008.003013.
- Hughes CP. The development of a nurse-led liaison mental health service for older people in Chesterfield, Derbyshire, UK. J Psychiatr Ment Health Nurs 2008;15:595-604. http://dx.doi.org/10.1111/j.1365-2850.2008.001279.x.
- Steers J, Brereton L, Ingleton C. Palliative care for all? A review of the evidence in community hospitals. Int J Palliat Nurs 2007;13:392-9. http://dx.doi.org/10.12968/ijpn.2007.13.8.24538.
- Tucker H. Discovering integrated care in community hospitals. J Integr Care 2013;21:336-46.
- Baillie J. Health Estate 2009;63:56-9.
- Moore A. Community services: why all’s ending well in Wells. Health Serv J 2011;121:19-21.
- Poulson LK, Nissen L, Coombes I. Pharmaceutical review using telemedicine – a before and after feasibility study. J Telemed Telecare 2010;16:95-9. http://dx.doi.org/10.1258/jtt.2009.090716.
- Howard ML. An exploratory study of radiographer’s perceptions of radiographer commenting on musculo-skeletal trauma images in rural community based hospitals. Radiography 2013;19:137-41.
- Wallis L. The business of community spirit. Nurs Stand 2008;22:62-3. http://dx.doi.org/10.7748/ns2008.05.22.35.62.p4166.
- Birthplace in England Collaborative Group . Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ 2011;343:1-13.
- Nolte E KC, Saltman R. Assessing Chronic Disease Management in European Health Systems. Concepts and Approaches. Copenhagen: World Health Organization, on behalf of the European Observatory on Health Systems and Policies; 2014.
- Royal College of General Practitioners . Distribution of general practitioner community hospitals in Great Britain and Northern Ireland. Occas Pap R Coll Gen Pract 1990;14.
- Pryor J. Building rehabilitation capacity in rural in New South Wales. Rural Remote Health 2009;9.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b2535.
- NICE . The Guidelines Manual. Appendix C: Methodology Checklist: Randomised Controlled Trials 2012. www.nice.org.uk/process/pmg6/resources/the-guidelines-manual-appendices-bi-1967364/chapter/2-appendix-c-methodology-checklist-randomised-controlled-trials#notes-on-use-of-methodology-checklist-randomised-controlled-trials (accessed 8 August 2016).
- NICE . The Guidelines Manual. Appendix D: Methodology Checklist: Cohort Studies 2012. www.nice.org.uk/process/pmg6/resources/the-guidelines-manual-appendices-bi-1967364/chapter/3-appendix-d-methodology-checklist-cohort-studies (accessed 8 August 2016).
- NICE . The Guidelines Manual. Appendix H: Methodology Checklist: Qualitative Studies 2012. www.nice.org.uk/process/pmg6/resources/the-guidelines-manual-appendices-bi-1967364/chapter/7-appendix-h-methodology-checklist-qualitative-studies#checklist-6 (accessed 8 August 2016).
- Drummond MO, Stoddart G, Torrance G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 1997.
- Young J, Forster A, Green J, Bogle S. Post-acute transfer of older people to intermediate care services: the sooner the better?. Age Ageing 2007;36:589-92. https://doi.org/10.1093/ageing/afm057.
- O’Reilly J, Lowson K, Young J, Forster A, Green J, Small N. A cost effectiveness analysis within a randomised controlled trial of post-acute care of older people in a community hospital. BMJ 2006;333. https://doi.org/10.1136/bmj.38887.558576.7C.
- Young J, Green J. Effects of delays in transfer on independence outcomes for older people requiring postacute care in community hospitals in England. J Clin Gerontol Geriatr 2010;1:48-52.
- Garåsen H, Magnussen J, Windspoll R, Johnsen R. Elderly patients in general hospitals or in intermediate care units in community hospitals – a cost analysis. Tidsskr Nor Laegeforen 2008;128:283-5.
- Stapley S, Crabb T, Round A, Hollinghurst S, Hamilton W. Use of medication and investigations in community hospitals and a district general hospital: A cohort study of emergency admissions in the elderly. Prim Health Care Res Dev 2007;8:105-11.
- Round A, Crabb T, Buckingham K, Mejzner R, Pearce V, Ayres R, et al. Six month outcomes after emergency admission of elderly patients to a community or a district general hospital. Fam Pract 2004;21:173-9. https://doi.org/10.1093/fampra/cmh212.
- Ritchie L. Community Hospitals in Scotland – Promoting Progress. Aberdeen: University of Aberdeen; 1996.
- Sibbald B, McDonald R, Roland M. Shifting care from hospitals to the community: a review of the evidence on quality and efficiency. J Health Serv Res Policy 2007;12:110-17. http://dx.doi.org/10.1258/135581907780279611.
- Winpenny E, Miani C, Pitchforth E, Ball S, Nolte E, King S, et al. Outpatient services and primary care: scoping reviews, case studies and international comparisons. Health Serv Deliv Res 2016;4.
- Ministero della Salute . DECRETO 2 Aprile 2015, N. 70. Regolamento Recante Definizione Degli Standard Qualitativi, Strutturali, Tecnologici E Quantitativi Relativi all’assistenza Ospedaliera. 2015 n.d. www.gazzettaufficiale.it/eli/id/2015/06/04/15G00084/sg (accessed February 2016).
- Medisinskfaglig veileder for kommunale akutte døgnplasser (KAD). Oslo: Den Norske Legeforening; 2014.
- Marmor T, Freeman R, Okma K. Comparative perspectives and policy learning in the world of health care. J Comparative Policy Analysis 2005;7:331-48. https://doi.org/10.1080/13876980500319253.
- Cacace M, Ettelt S, Mays N, Nolte E. Assessing quality in cross-country comparisons of health systems and policies: towards a set of generic quality criteria. Health Policy 2013;112:156-62. http://dx.doi.org/10.1016/j.healthpol.2013.03.020.
- Maresso A, Mladovsky P, Thomson S, Sagan A, Karanikolos M, Richardson E, et al. Economic crisis, health systems and health in Europe. Country experience. Copenhagen: World Health Organization, acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies; 2015.
- European Observatory on Health Systems and Policies . Health Systems and Policy Monitor 2015. www.hspm.org/mainpage.aspx (accessed February 2016).
- International Healthcare Comparisons . About Us n.d. www.international-comparisons.org.uk/about-us/ (accessed February 2016).
- Green J, Thorogood N. Qualitative Methods for Health Research. London: Sage; 2009.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114-16. https://doi.org/10.1136/bmj.320.7227.114.
- Healy J, Dugbale P, Thomson S, Osborne R, Squires D, Jun M. International Profiles of Health Care Systems. New York, NY: The Commonwealth Fund; 2013.
- Vuorenkoski L, Mladovsky P, Mossialos E. Health Syst Transit. Finland: Health system review; 2008.
- Ferré F, de Belvis AG, Valerio L, Longhi S, Lazzari A, Fattore G, et al. Health Syst Transit. Italy: health system review; 2014.
- Ringard Å, Sagan A, Sperre Saunes I, Lindahl AK. Health Syst Transit. Norway: health system review; 2013.
- Steel D, Cylus J. Health Syst Transit. United Kingdom (Scotland): Health system review; 2012.
- OECD . OECD Health Statistics 2015 (last Updated 12 November 2015) 2015. www.oecd.org/els/health-systems/health-data.htm (accessed December 2015).
- Glover L, Mossialos E, Wenzl M, Osborn R, Sarnak D. International Profiles of Health Care Systems. New York, NY: The Commonwealth Fund; 2016.
- Bosio A. L’evoluzione Delle Cure Primarie in Italia 2013. www.istud.it/up_media/cureprimarie13/vance.pdf (accessed March 2016).
- Department of the Prime Minister and Cabinet . Reform of the Federation White Paper. Roles and Responsibilities in Health 2014. https://federation.dpmc.gov.au/sites/default/files/issues-paper/Health_Issues_Paper.pdf (accessed February 2016).
- Health at a Glance. Paris: OECD; 2015.
- Information Services Division Scotland . Hospital Care 2015. www.isdscotland.org/Health-Topics/Hospital-Care/Hospitals/ (accessed June 2015).
- Ministry of Social Affairs and Health Finland . Act in Specialized Medical Care (1062 1989 2012. www.finlex.fi/en/laki/kaannokset/1989/en19891062.pdf (accessed February 2016).
- Australian Hospital Peer Groups. Canberra: AIHW; 2015.
- Ministry of Social Affairs and Health Finland . Primary Health Care Act (66 1972) 2007. www.finlex.fi/en/laki/kaannokset/1972/en19720066.pdf (accessed February 2016).
- Community Hospitals and Intermediate Care Networks . Data Collection Enhancement 2015. www.knowledge.scot.nhs.uk/chin/community-hospitals/resources-page/data-collection-enhancement.aspx (accessed June 2015).
- Regione Autonoma Friuli Venezia Giulia . Legge Regionale 16 Ottobre 2014, N. 17. Riordino dell’assetto Istituzionale E Organizzativo Del Servizio Sanitario Regionale E Norme in Materia Di Programmazione Sanitaria E Sociosanitaria 2014;43:9-48. http://lexview-int.regione.fvg.it/fontinormative/xml/IndiceLex.aspx?anno=2014&legge=17&fx=lex (accessed January 2016).
- Aaraas I. The Finnmark general practitioner hospital study. Patient characteristics, patient flow and alternative care level. Scand J Prim Health Care 1995;13:250-6. https://doi.org/10.3109/02813439508996771.
- Hospitals Act of 19 June 1969 n.d. http://app.uio.no/ub/ujur/oversatte-lover/data/lov-19690619-057-eng.pdf (accessed January 2016).
- National Health and Care Services Plan (2011–2015) -Meld. St.16 (2010-2011) Report to the Storting (White Paper) Summary. Oslo: Ministry of Health and Care Services; 2012.
- Grant JA. Contribution of general practitioner hospitals in Scotland. Br Med J 1984;288:1366-8. https://doi.org/10.1136/bmj.288.6427.1366.
- The Scottish Government . 2020 Vision 2011. www.gov.scot/Topics/Health/Policy/2020-Vision (accessed June 2015).
- Aulizio G, Mazzeo M, Milillo G, Cicchetti A, Meloncelli A. L’Assistenza primaria in Italia dale condotte mediche al lavoro di squadra. Rome: Edizioni Iniziative Sanitaire; 2009.
- Federazione Italiana Medici di Medicina Generale (FIMMG) . L’Ospedale Di Comunità: Linee Guida Fimmg 2003. www.fimmg.livorno.it/drupal/node/83 (accessed April 2015).
- Ministero della Salute . Piano Sanitario Nazionale 2006–2008 2006. www.cisl.it/sito-sociali.nsf/432be92ec43b2fbec1256e5f0053653b/75b69e5a7be0fc9bc12571640036c657/$FILE/Psn2006_2008.pdf (accessed May 2015).
- Conferenza delle Regioni e delle Province autonome . Patto Della Salute 2014-2016: Il Testo 2014. www.regioni.it/newsletter/n-2539/del-16-07-2014/patto-della-salute-2014-2016-il-testo-12784/ (accessed January 2016).
- Hospital Resources 2013–14. Australian Hospital Statistics. Canberra: AIHW; 2015.
- Nancarrow SA, Roots A, Grace S, Saberi V. Models of care involving district hospitals: a rapid review to inform the Australian rural and remote context. Aust Health Rev 2015;39:494-507. https://doi.org/10.1071/AH14137.
- Anderson J, Malone L. Suitability of the multi-purpose service model for rural and remote communities of Australia. Asia Pacific J Health Manage 2014;9:14-8.
- Regione del Veneto . Deliberazione Della Giunta Regionale N. 2718 Del 24 Dicembre 2012. Legge Regionale 29 Giugno 2012 N. 23, Art. 10. Definizione Delle Tipologie Di Strutture Di Ricovero Intermedie E Approvazione Dei Requisiti Di Autorizzazione all’esercizio dell’Ospedale Di Comunità E dell’Unità Riabilitativa Territoriale Ai Sensi Della Legge Regionale 16 Agosto 2002 N. 22 2013:215-39. http://bur.regione.veneto.it/BurvServices/Pubblica/DettaglioDgr.aspx?id=244978 (accessed January 2016).
- Regione Emilia-Romagna . Ospedali Di Communita (OsCo) Per Le Cure Intermedie Sanitarie Della Regione Emilia Romagna. Documento Programmatico 2013–2015 2013. www.fper.cisl.it/sanita/sanita-pubblica/item/download/263_eacab1f1de3423947d33898f3a547c81.html (accessed January 2016).
- Curcetti C, Parisini L, Brambilla A. Le ‘Case della Salute’ in Emilia-Romagna: il monitoraggio regionale in Emilia-Romagna: il monitoraggio regionale. Bologna: Regione Emilia-Romagna, Assessorato Politiche per la Salute, Direzione Generale Sanità e Politiche Sociali e per l’Integrazion; 2015.
- Swanson JO, Hagen TP. Reinventing the Community Hospital n.d.
- Lampela P, Säynäjäkangas O, Jokelainen J, Keistinen T. Does place of treatment affect prognosis for chronic obstructive pulmonary disease (COPD)?. Eur J Gen Pract 2008;14:123-8. http://dx.doi.org/10.1080/13814780802444410.
- Lampela P, Säynäjäkangas O, Jokelainen J, Keistinen T. Differences in COPD-related readmissions to primary and secondary care hospitals. Scand J Prim Health Care 2009;27:80-4. http://dx.doi.org/10.1080/02813430802673501.
- Lappegard Ø, Hjortdahl P. Perceived quality of an alternative to acute hospitalization: an analytical study at a community hospital in Hallingdal, Norway. Soc Sci Med 2014;119:27-35. http://dx.doi.org/10.1016/j.socscimed.2014.08.014.
- Kokko S. Integrated primary health care: Finnish solutions and experiences. Int J Integr Care 2009;9. https://doi.org/10.5334/ijic.310.
- Australian College of Rural and Remote Medicine . Rural Generalist Programs 2015. www.acrrm.org.au/preparing-for-your-career/rural-generalist-programs (accessed February 2016).
- NHS Education for Scotland . GP Fellowships. 2015. www.nes.scot.nhs.uk/education-and-training/by-discipline/medicine/general-practice/gp-fellowships.aspx (accessed June 2015).
- Ministry of Health and Care Services . Nasjonal Helse-Og Sykehusplan -I Korte Trekk 2015. www.regjeringen.no/contentassets/1bc33e0b23ef4e968d7fd90eb1f191d1/no/pdfs/nhsp-kortversjon.pdf (accessed January 2016).
- Longo F. Lessons from the Italian NHS retrenchment policy. Health Policy 2016;120:306-15. http://dx.doi.org/10.1016/j.healthpol.2016.02.001.
- Regione Marche . Richiesta Di Parere Alla Competente Commissione Consiliare Sullo Schema Di Deliberazione Delle Case Della Salute Tipo C, Ridefinite Ospedali Di Communita, in Coerenza Con Gli Standard Qualitativi, Strutturali, Tecnologici E Quantitativi Relativi all’assistenza Ospedaliera Di Cui Al DM 70 2015. Revisione Della DGR 735 2013 E DGR 920 2013 E DGR 1476 2013 2015. www.norme.marche.it/Delibere/2015/DGR1183_15.pdf (accessed February 2015).
- Rintanen H, Puromäki H, Heinämäki L. Terveyskeskusten avosairaanhoidon järjestelyt Suomessa Kysely terveyskeskuksille keväällä 2013. Tampere: Terveyden ja hyvinvoinnin laitos; 2013.
- Finland, a Land of Solutions. Strategic Programme of Prime Minister Juha Sipilä’s Government. Helsinki: Prime Minister’s Office Finland; 2015.
- Australian Government . Reform of the Federation, Discussion Paper 2015 2015. https://federation.dpmc.gov.au/sites/default/files/publications/reform_of_the_federation_discussion_paper.pdf (accessed February 2016).
- Public Bodies (Joint Working) (Scotland) Act 2014 no. 2014 asp 9. Norwich: The Stationery Office; 2014.
- SPICe Briefing: Public Bodies (Joint Working) (Scotland) Bill. Edinburgh: The Scottish Parliament; 2013.
- Stake R. Multiple Case Study Analysis. New York, NY: Guilford Press; 2006.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: Sage; 2009.
- Cohen L, Manion L, Morrision K. Research Methods in Education. London and New York, NY: Routledge; 2011.
- The Scottish Government . Rural Scotland Key Facts 2015 2015. www.gov.scot/Publications/2015/03/5411/2 (accessed June 2015).
- National Records of Scotland . Mid-Year Population Estimates. 2015. www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/population/population-estimates/mid-year-population-estimates/population-estimates-time-series-data (accessed March 2016).
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA, London and New Delhi: SAGE Publications; 1998.
- The Scottish Government . Scottish Government Urban Rural Classification 2013–2014 (Online) 2014. www.gov.scot/Publications/2014/11/2763/downloads (accessed February 2016).
- End Child Poverty . End Child Poverty Report, 2014 2014. www.endchildpoverty.org.uk/poverty-in-your-area/ (accessed February 2016).
- Information Services Division Scotland . Available Beds by Specialty &Amp; NHS Board of Treatment 2015. www.isdscotland.org/Health-Topics/Hospital-Care/Beds/ (accessed February 2016).
- Glendinning C. Breaking down barriers: integrating health and care services for older people in England. Health Policy 2003;65:139-51. https://doi.org/10.1016/S0168-8510(02)00205-1.
- Goodwin N, Dixon A, Anderson G, Wodchis W. Providing Integrated Care for Older People with Complex Needs: Lessons from Seven International Case Studies. London: The King’s Fund; 2014.
- Timmins N, Ham C. The Quest for Integrated Health and Social Care: A Case Study in Canterbury, New Zealand. London: The King’s Fund; 2013.
- Glazebrook RM, Harrison SL. Obstacles and solutions to maintenance of advanced procedural skills for rural and remote medical practitioners in Australia. Rural Remote Health 2006;6.
- Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA 2013;110:5797-801. http://dx.doi.org/10.1073/pnas.1219686110.
- Windle K, Francis J, Coomber C. Preventing Loneliness and Social Isolation: Interventions and Outcomes. London: Social Care Institute for Excellence; 2011.
- Nicholson NR. A review of social isolation: an important but underassessed condition in older adults. J Prim Prev 2012;33:137-52. http://dx.doi.org/10.1007/s10935-012-0271-2.
- Mack M, Maxwell H, Hogg D, Gillies J. Being Rural: Exploring Sustainable Solutions for Remote and Rural Healthcare RCGP Scotland Policy Paper Written by the Rural Strategy Group Scotland. Edinburgh: Royal College of General Practitioners Scotland; 2014.
- van Teijlingen E, Benoit C, Bourgeault I, DeVries R, Sandall J, Wrede S. Learning from health care in other countries: the prospect of comparative research. Health Prospect 2015;14:8-12.
- Abercrombie N, Hill S, Turner BS. The Penguin Dictionary of Sociology. Harmondsworth: Penguin; 1988.
- Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Traditions. London: SAGE; 1998.
- Health Care Act. Helsinki: Ministry of Social Affairs and Health; 2012.
- McNaughton Nicholls C, Mills L, Kotecha M, Ritchie J, Lewis J, McNaughton Nicholls C, et al. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE; 2014.
- Farmer J, Currie M, Kenny A, Munoz SA. An exploration of the longer-term impacts of community participation in rural health services design. Soc Sci Med 2015;141:64-71. http://dx.doi.org/10.1016/j.socscimed.2015.07.021.
- Nimegeer A, Farmer J. Prioritising rural authenticity: community members’ use of discourse in rural healthcare participation and why it matters. J Rural Stud 2016;43:94-103.
- Pitchforth E, Roland M. Future Hosp J 2015;2:173-9.
- Farmer J, Philip L, King G, Farrington J, Macleod M. Territorial tensions: misaligned management and community perspectives on health services for older people in remote rural areas. Health Place 2010;16:275-83. http://dx.doi.org/10.1016/j.healthplace.2009.10.010.
- Farmer J, Lauder W, Richards H, Sharkey S. Dr. John has gone: assessing health professionals’ contribution to remote rural community sustainability in the UK. Soc Sci Med 2003;57. http://dx.doi.org/10.1016/s0277-9536(02)00410-0.
- Kümpers S, Mur I, Hardy B, van Raak A, Maarse H. Integrating dementia care in England and The Netherlands: four comparative local case studies. Health Place 2006;12:404-20. https://doi.org/10.1016/j.healthplace.2005.04.001.
- Anheier HK, Salamon LM. Volunteering in cross-national perspective: initial comparisons. Law Contemp Prob 1999;62:43-65.
- Volunteering in the European Union. Brussels: GHK; 2010.
- Refreshed Strategy for Volunteering in the NHS in Scotland. Edinburgh: The Scottish Government, Healthcare Policy and Strategy Directorate; 2008.
- Nimegeer A, Farmer J, West C, Currie M. Addressing the problem of rural community engagement in healthcare service design. Health Place 2011;17:1004-6. http://dx.doi.org/10.1016/j.healthplace.2011.04.013.
- Shape of Training . Securing the Future of Excellent Patient Care. Final Report of the Independent Review Led by Professor David Greenaway 2014. www.shapeoftraining.co.uk/static/documents/content/Shape_of_training_FINAL_Report.pdf_53977887.pdf (accessed March 2016).
- Miani C, Hinrichs S, Pitchforth E, Bienkowska-Gibbs T, Disbeschl S, Roland M, et al. Best Practice: Medical Education from an International Perspective. Santa Monica, CA: RAND Corporation; 2015.
- Australia in Brief. Barton: Department of Foreign Affairs and Trade; 2014.
- Australian Bureau of Statistics . Australian Demographic Statistics, Dec 2014 2015. www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 (accessed August 2015).
- Australia’s Health 2014. The 14th Biennial Health Report of the Australian Institute of Health and Welfare. Canberra: AIHW; 2014.
- Australian Prudential Regulation Authority . Private Health Insurance Statistical Trends 2015. www.apra.gov.au/PHI/Publications/Pages/Statistical-Trends.aspx (accessed November 2015).
- Council of Australian Governments . National Health Reform Agreement 2011. www.federalfinancialrelations.gov.au/content/npa/health_reform/national-agreement.pdf (accessed December 2015).
- National Health Performance Authority . About Us 2015. www.nhpa.gov.au/internet/nhpa/publishing.nsf/Content/About-us (accessed November 2015).
- Independent Hospital Pricing Authority . The Independent Hospital Pricing Authority (IHPA) 2015. www.ihpa.gov.au/ (accessed December 2015).
- Hall J. Australian Health Care – The Challenge of Reform in a Fragmented System. N Engl J Med 2015;373:493-7. http://dx.doi.org/10.1056/NEJMp1410737.
- Healthier Medicare. London: DH; 2015.
- Medicare Benefits Schedule Review. London: DH; 2016.
- Primary Health Care Advisory Group . Better Outcomes for People With Chronic and Complex Health Conditions Through Primary Health Care. Discussion Paper 2015. www.health.gov.au/internet/main/publishing.nsf/content/2D8BCF439DE725CACA257E93001B462A/$File/discussion.pdf (accessed December 2015).
- Schweppenstedde D, Hinrichs S, Ogbu U, Schneider E, Kringos D, Klazinga N, et al. Regulating Quality and Safety of Health and Social Care: International Experiences. Santa Monica, CA: RAND Corporation; 2014.
- Department of Social Services . Ageing and Aged Care 2016. www.dss.gov.au/ageing-and-aged-care.
- Health Expenditure Australia 2013–14. Canberra: AIHW; 2015.
- Health Expenditure Australia 2013–14: Analysis by Sector. Canberra: AIHW; 2015.
- Australian Institute of Health and Welfare (AIHW) . Australia’s Medical Workforce 2016. www.aihw.gov.au/workforce/medical/ (accessed February 2016).
- Department of Health . General Practice Statistics 2015. www.health.gov.au/internet/main/publishing.nsf/content/general+practice+statistics-1 (accessed February 2016).
- Department of Health . Primary Care (GP, Nursing, Allied Health) 2014. www.health.gov.au/internet/main/publishing.nsf/Content/mbs-primary-care (accessed February 2016).
- Department of Human Services . General Practice 2016. www.humanservices.gov.au/health-professionals/professions/general-practitioners (accessed February 2016).
- Davies PK. Divisions of General Practice: will they transform, or die?. Med J Aust 2010;193:75-7.
- Robinson S, Varhol R, Ramamurthy V, Denehy M, Hendrie D, O’Leary P, et al. The Australian primary healthcare experiment: a national survey of Medicare Locals. BMJ Open 2015;5. http://dx.doi.org/10.1136/bmjopen-2014-007191.
- Horvath J. Review of Medicare Locals. Report to the Minister for Health and Minister for Sport 2014. www.health.gov.au/internet/main/publishing.nsf/Content/A69978FAABB1225ECA257CD3001810B7/$File/Review-of-Medicare-Locals-may2014.pdf (accessed February 2016).
- Department of Health . Primary Health Networks 2014. www.health.gov.au/internet/main/publishing.nsf/Content/00069147C384180DCA257F14008364CB/$File/guidelines.pdf (accessed February 2016).
- Australian Institute of Health and Welfare . Establishment – Establishment Type, Sector and Services Provided Code AN.N{.N} 2015. http://meteor.aihw.gov.au/content/publish/export.phtml?media=pdf&type=list&items[]=269971&form=long (accessed February 2016).
- National Strategic Framework for Rural and Remote Health. Canberra: Commonwealth of Australia; 2011.
- Administrator National Health Funding Pool . Local Hospital Network (LHN) Directory 2015. www.publichospitalfunding.gov.au/directory (accessed February 2016).
- Cairns and Hinterland Hospital and Health Service . 2013–14 Annual Report 2014. www.health.qld.gov.au/cairns_hinterland/docs/chhhs-annual-report13-14.pdf (accessed February 2016).
- Queensland Government . Cairns and Hinterland Hospital and Health Service 2016. www.health.qld.gov.au/services/cairns-hinterland/default.asp (accessed February 2016).
- Northern Territory Government . Katherine Hospital 2016. www.health.nt.gov.au/Hospitals/Katherine_Hospital/index.aspx (accessed February 2016).
- HealthStats NSW . Potentially Avoidable Deaths 2016. www.healthstats.nsw.gov.au/Indicator/bod_avodth/bod_avodth_aria (accessed February 2016).
- Greenhill JA, Walker J, Playford D. Outcomes of Australian rural clinical schools: a decade of success building the rural medical workforce through the education and training continuum. Rural Remote Health 2015;15.
- Shires L, Allen P, Cheek C, Deb W. Regional universities and rural clinical schools contribute to rural medical workforce, a cohort study of 2002 to 2013 graduates. Rural Remote Health 2015;15.
- The Rural Way: Implementation of a National Rural Generalist Pathway. Brisbane: ACRRM; 2014.
- NSW Government . Rural Hospital and Health Services: Multipurpose Services (MPS) 2015. www.health.nsw.gov.au/rural/rhhsp/pages/default.aspx (accessed February 2016).
- Department of Social Services . Multi-Purpose Services for Small Rural and Remote Communities 2015. www.myagedcare.gov.au/multi-purpose-services-programme (accessed February 2016).
- Statistics Finland . Population Structure 2015. http://tilastokeskus.fi/til/vaerak/2014/vaerak_2014_2015-03-27_tie_001_en.html (accessed May 2015).
- Association of Finnish Local and Regional Authorities . Local Authorities 2016. www.localfinland.fi/en/statistics/Pages/default.aspx (accessed February 2016).
- Ministry of Social Affairs and Health Finland . Social Welfare and Health Care System in Finland, Responsibilities 2016. http://stm.fi/en/social-and-health-services/responsible-agencies (accessed February 2016).
- Tynkkynen L. The New Health Care Act – Follow Up. Helsinki: National Institute for Health and Welfare; 2010.
- Better Regulation in Europe: Finland. Paris: OECD; 2010.
- Ministry of Social Affairs and Health Finland . Healthcare, Social Welfare and Regional Government Reform Package 2016. http://alueuudistus.fi/en/frontpage (accessed February 2016).
- Tynkkynen LK, Chydenius M, Saloranta A, Keskimäki I. Expanding choice of primary care in Finland: much debate but little change so far. Health Policy 2016;120:227-34. http://dx.doi.org/10.1016/j.healthpol.2016.01.015.
- Terveydenhuollon menot ja rahoitus 2013. Hälso- och sjukvårdsutgifter samt deras finansiering 2013. [Health Expenditure and Financing 2013.]. Helsinki: National Institute for Health and Welfare; 2015.
- Association of Finnish Local and Regional Authorities . Health Services 2015. www.localfinland.fi/en/authorities/social-and-health-services/health-services/Pages/default.aspx (accessed February 2016).
- Tynkkynen LK, Keskimäki I, Lehto J. Purchaser-provider splits in health care-the case of Finland. Health Policy 2013;111:221-5. http://dx.doi.org/10.1016/j.healthpol.2013.05.012.
- Lehto J, Vrangbæk K, Winblad U. The reactions to macro-economic crises in Nordic health system policies: Denmark, Finland and Sweden, 1980-2013. Health Econ Policy Law 2015;10:61-8. http://dx.doi.org/10.1017/S1744133114000243.
- Ministry of Social Affairs and Health Finland . Private Social and Health Services 2016. http://stm.fi/en/private-health-care (accessed February 2016).
- Winell K, Dedeu T, Kringos D, Boerma W, Hutchinson A, Saltman R. Building Primary Care in a Changing Europe. Case Studies. Copenhagen: World Health Organization, acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies; 2015.
- André C, García C. Local Public Finances and Municipal Reform in Finland. OECD Economics Department Working Papers, No. 1121. Paris: OECD; 2014.
- Hämäläinen K, Moisio A. One or Two Tiers of Local Government? – The Cost Effects of Regional Experiment. Helsinki: Government Institute for Economic Research; 2011.
- Ministry of Social Affairs and Health Finland . Health Care in Finland 2013.
- Saarivirta T, Consoli D, Dhondt P. The Position of Hospitals in the Finnish Health Care System: An Historical Approach. SENTE Working Papers 29/2010. Tampere: University of Tampere; 2010.
- Constitution of the Åland Islands: August 16, 1991 (as Amended to July 12, 1996) (Finland [fi]) n.d. http://oxcon.ouplaw.com/view/10.1093/law:ocw/cd1009-H1996.regGroup.1/law-ocw-cd1009-H1996 (accessed April 2016).
- Ettelt S, Nolte E, Noikolentzos A, Mays N. Decision-Making in Health Care: Roles and Responsibilities at Local, Regional and National Level. London: London School of Hygiene & Tropical Medicine; 2008.
- Kautiainen K, Häkkinen U, Lauharanta J, Busse R, Geissler A, Quentin W, et al. Diagnosis-Related Groups in Europe. Moving Towards Transparency, Efficiency and Quality in Hospitals. Maidenhead: Open University Press; 2011.
- Ettelt S, Nolte E, Thomson S, Mays N. Capacity Planning in Health Care: Reviewing the International Experience. Copenhagen: World Health Organization on behalf of the European Observatory on Health Systems and Policies; 2008.
- Johansson E. The Long-Term Care System for the Elderly in Finland. ENEPRI Research Report No. 76 2010. www.ancien-longtermcare.eu/sites/default/files/ANCIEN%20RR%2076%20Finland_0.pdf (accessed February 2016).
- Pulkki J, Jylhä M, Forma L, Aaltonen M, Raitanen J, Rissanen P. Long-term care use among old people in their last 2 years of life: variations across Finland. Health Soc Care Community 2016;24:439-49. https://doi.org/10.1111/hsc.12224.
- Pekurinen M, Erhola M, Häkkinen U, Jonsson P, Keskimäki I, Kokko S, et al. Sosiaali - ja terveydenhuollon monikanavaisen rahoituksen edut, haitat ja kehittämistarpeet. Helsinki: National Institute for Health and Welfare; 2010.
- The Crisis, Hospitals and Healthcare. Brussels: HOPE; 2011.
- Ministry of Social Affairs and Health Finland . National Development Programme for Social Welfare and Health Care (Kaste) 2016. http://stm.fi/en/kaste-progamme (accessed February 2016).
- Sosiaali- ja terveysalan tilastollinen vuosikirja 2015. Statistisk årsbok om social- och hälsovården 2015. Tampere: National Institute for Health and Welfare; 2015.
- Kilpeläinen T. Satakunta Centre for Economic Development, Transport and the Environment. Foreign Nurses’ Guide to Finnish Working Life 2010. https://seure.fi/Global/Polku/Foreign_Nurses_Guide_to_Finnish_Working_Life.pdf (accessed February 2016).
- Lampela P, Säynäjäkangas O, Keistinen T. Is the treatment of acute COPD exacerbations in Finland shifting to general practitioners?. Scand J Prim Health Care 2006;24:140-4. https://doi.org/10.1080/02813430600830832.
- Istat . Demografia in Cifre 2014 2015. http://demo.istat.it/ (accessed March 2016).
- Nuti S, Vola F, Bonini A, Vainieri M. Making governance work in the health care sector: evidence from a ‘natural experiment’ in Italy. Health Econ Policy Law 2016;11:17-38. http://dx.doi.org/10.1017/S1744133115000067.
- Cavalieri M. Geographical variation of unmet medical needs in Italy: a multivariate logistic regression analysis. Int J Health Geogr 2013;12. http://dx.doi.org/10.1186/1476-072X-12-27.
- Donatini A, Mossialos E, Wenzl M, Osborn R, Sarnak D. International Profiles of Health Care Systems, 2015. New York, NY: The Commonwealth Fund; 2016.
- Conferenza delle Regioni e delle Province autonome . CONFERENZA STATO-REGIONI DEL 02.07.2015: Intesa Tra Governo, Regioni E Province Autonome Di Trento E Di Bolzano Concernente l’individuazione Di Misure Di Razionalizzazione E Di Efficientamento Della Spesa Del Servizio Sanitario Nazionale 2015. www.regioni.it/sanita/2015/07/24/conferenza-stato-regioni-del-02-07-2015-intesa-tra-governo-regioni-e-province-autonome-di-trento-e-di-bolzano-concernente-lindividuazione-di-misure-di-razionalizzazione-e-di-efficientamento-415145/ (accessed January 2016).
- Ferré F. New Financial Measures to Contain Public Health Expenditures 2015. www.hspm.org/countries/italy25062012/countrypage.aspx (accessed January 2016).
- OECD Reviews of Health Care Quality: Italy. Raising Standards. Paris: OECD; 2014.
- Paterlini M. Italy’s health system reforms on hold. Lancet 2013;381:1085-6. https://doi.org/10.1016/S0140-6736(13)60745-X.
- Cislaghi C, Zocchetti C. Regional pro capite funding: how to unscramble it. Epidemiol Prev 2012;36:221-3.
- Ricciardi W, De Belvis A, Specchia M, Valerio L, Nolte E, Nolte E, et al. Assessing Chronic Disease Management in European Health Systems. Country Reports. Copenhagen: World Health Organization, acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies; 2015.
- Armeni P, Cantù E, Carbone C, Longo F, Petracca F, Sommariva S, et al. Osservatorio sulle aziende e sul sistema sanitario italiano. Milan: CERGAS; 2015.
- Tedeschi P, Kringos DS, Boerma WGW, Hutchinson A, Saltman RB. Building Primary Care in a Changing Europe. Case Studies. Copenhagen: World Health Organization, acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies; 2015.
- Salute E-R. Ospedali Di Comunità 2015. http://salute.regione.emilia-romagna.it/cure-primarie/ospedali-di-comunita (accessed February 2016).
- Regione Marche . Riduzione Della Frammentazione Della Rete Ospedaliera, Riconversione Delle Piccole Struture Ospedaliere E Riorganizzazione Delle Rete Territoriale Della Emergenza-Urgenza Delle Regione Marche in Attuazione Della DGR 1696 2012 2013. www.norme.marche.it/Delibere/2013/DGR0735_13.pdf (accessed January 2016).
- Melchiorre MG, Greco C, Lucchetti M, Chiatti C, Lamura G, Genet N, et al. Home Care across Europe. Case Studies. Copenhagen: World Health Organization, on behalf of the European Observatory on Health Systems and Policies; 2013.
- Ettelt S, Nolte E. Funding Intensive Care – Approaches in Systems Using Diagnosis-Related Groups. Santa Monica, CA and London: RAND Corporation/London School of Hygiene & Tropical Medicine; 2010.
- Sindacato Italiano Medici del Territorio . Linee Guida Per Un Modello Di Country Hospital 1998. www.simetsind.it/linee+guida.html (accessed April 2015).
- Polloli R. Il Riordino Delle Cure Primarie E Del Servizio Sanitario Regionale Della Regione Toscana 2013. www.quotidianosanita.it/allegati/allegato7510096.pdf (accessed January 2016).
- Regione Toscana . Aziende Sanitarie 2015. www.regione.toscana.it/sst/organizzazione/aziende-sanitarie (accessed January 2016).
- La Giunta della Regione Emilia-Romagna . Riorganizzazione Dalla Rete Ospedaliera Secondo Gli Standard Previsti Dalla Legge 135 2012, Dal Patto Per La Salute 2014 2016 E Dal DM Salute 70 2015 2015. http://salute.regione.emilia-romagna.it/assistenza-ospedaliera/ospedali (accessed January 2016).
- Rodelli PM. Casa Della Salute Di San Secondo Parmense. Modelli E Strumenti Per Il Governo Della Rete dell’assistenza Territoriale. Milano 3-4 Novembre 2014 2014. http://cureprimarie.altervista.org/lavori/cds/Cerismas.pdf (accessed February 2016).
- Regione del Veneto . Cure Intermedia 2015. http://cureintermedie.regione.veneto.it/area-odc-urt/atti (accessed February 2016).
- Regione del Veneto . LEGGE REGIONALE 29 Giugno 2012, N. 23. Norme in Materia Di Programmazione Socio Sanitaria E Approvazione Del Piano Socio-Sanitario Regionale 2012-2016 2012.
- Regione del Veneto . Deliberazione Della Giunta Regionale N. 2683 Del 29 Dicembre 2014. Approvazione Dei Requisiti Generali E Specifici Per l’accreditamento Istituzionale, Del Contenuto Assistenziale Delle Prestazioni Mediche, Del Tracciato Del Sistema Informativo Per Il Monitoraggio dell’assistenza Erogata E Degli Indicatori Di Attività E Risultato Per Ospedali Di Comunità E Unità Riabilitative Territoriali. L.R. 16 Agosto 2002, N. 22 2015.
- Regione del Veneto . Adeguamento Delle Schede Di Dotazione Ospedaliera Delle Strutture Pubbliche E Private Accreditate, Di Cui Alla l.R. 39 1993, E Definizione Delle Schede Di Dotazione Territoriale Delle Unità Organizzative Dei Servizi E Delle Strutture Di Ricovero Intermedie. PSSR 2012-2016 2013. http://web.consiglioveneto.it/commissioni/quintacommissione/allegati/68CR_18_06_2013_SchOspTer.pdf (accessed January 2016).
- Regione Autonoma Friuli Venezia Giulia . Residenze Sanitarie Assistenziali (RSA) 2011. www.regione.fvg.it/rafvg/cms/RAFVG/salute-sociale/sistema-sociale-sanitario/FOGLIA8/ (accessed January 2016).
- Statistics Norway . Population 2015. www.ssb.no/en/befolkning/statistikker/folkemengde (accessed December 2015).
- OECD . Data on Health Expenditure 2015. www.oecd.org/els/health-systems/health-expenditure.htm (accessed January 2016).
- Norway and Health. An Introduction. Oslo: Directorate of Health; 2012.
- Shifting Care Away from the Hospital Sector and Toward Primary Care Settings in Norway. Paris: OECD; 2014.
- Ministry of Health and Care Services . Meld. St. 26 (2014-2015). The Primary Health and Care Services of Tomorrow – Localised and Integrated 2016. www.regjeringen.no/en/dokumenter/meld.-st.-26-20142015/id2409890/?ch=1&q (accessed February 2016).
- Sperre Saunes I. Reforming the Local Government – Restructuring and Reforming the Role of Municipalities 2015. http://www.hspm.org/countries/norway08012014/countrypage.aspx (accessed February 2016).
- Statistics Norway . Health Expenditure 2015. www.regjeringen.no/no/aktuelt/Hva-er-et-sykehus/id753210/ (accessed December 2015).
- Long Term Care – Future Challenges. Care Plan 2015 Report No.25 (2005-2006) to the Storting Chapter 1, 2 and 3. Oslo: Ministry of Health and Care Services; 2007.
- Statistics Norway . Long-Term Care 2015. www.ssb.no/statistikkbanken/selectvarval/saveselections.asp (accessed December 2015).
- Miani C, Pitchforth E, Nolte E. Choice of Primary Care Provider: A Review of Experiences in Three Countries. London: Policy Innovation Research Unit; 2013.
- Magnussen J, Vrangbæk K, Saltman R. Nordic Health Care Systems: Recent Reforms and Current Policy Challenges. London: Open University Press; 2009.
- Lov Om Spesialisthelsetjenesten m.M. (spesialisthelsetjenesteloven) n.d. https://lovdata.no/dokument/NL/lov/1999-07-02-61 (accessed April 2016).
- Romøren TI, Torjesen DO, Landmark B. Promoting coordination in Norwegian health care. Int J Integr Care 2011;11. https://doi.org/10.5334/ijic.581.
- Statistics Norway . Specialist Health Service. Activity and Number of Beds, by Type of Service and Health Enterprise 2015. www.ssb.no/statistikkbanken/selectvarval/saveselections.asp (accessed January 2016).
- Statistics Norway . Specialist Health Service. Activity and Number of Beds, by Type of Service, Contents and Time 2015. www.ssb.no/statistikkbanken/selectvarval/Define.asp?subjectcode=&ProductId=&MainTable=AktivDogn&nvl=&PLanguage=1&nyTmpVar=true&CMSSubjectArea=helse&Kort (accessed December 2015).
- Eurostat . Healthcare Resource Statistics – Beds 2015. http://ec.europa.eu/eurostat/statistics-explained/index.php/Healthcare_resource_statistics_-_beds (accessed February 2016).
- Sperre Saunes I, Lindhal AK, Ringard Å. Online HiT, Norway: New National Agency for Hospital Construction 2014. www.hspm.org/_layouts/LivingHiT/Archive.aspx?type=Reformlog&siteid=0dd2ce6a-573f-4651-9cf3-674face81b36 (accessed January 2016).
- Nordlandssykehuset . Nordland Hospital 2013. www.nordlandssykehuset.no/?lang=en_US (accessed January 2016).
- Aaraas I. General Practitioner Hospitals: Use and Usefulness. A Study from Finnmark County in North Norway. ISM skriftserie 45. Tromsø: University of Tromsø; 1998.
- Iversen H. Pasienters erfaringer med sykestuene i Finnmark. Oslo: Kunnskapssenteret; 2014.
- Helse Nord RHF. Final Report: Examination of Specialist Health Care in Alta/Western Finnmark. Bodø: Helse Nord RHF; 2014.
- Centre for Development of Institutional and Home Care Services . About the Centre for Development of Institutional and Home Care Services 2015. www.utviklingssenter.no/english.180221.no.html (accessed February 2016).
- Barnett K. Exploring the Teaching Nursing Home Model: Literature Review to Inform the National Evaluation of the TRACS Program. Adelaide: Australian Workplace Innovation and Social Research Centre, University of Adelaide; 2014.
- Ministry of Health and Care Services . Øyeblikkelig Hjelp døgntilbud 2014. www.regjeringen.no/no/tema/helse-og-omsorg/helse--og-omsorgstjenester-i-kommunene/innsikt/oyeblikkelig-hjelp-dogntilbud/id2356317/ (accessed March 2016).
- Kartlegging av data om lokalmedisinske sentre. Oslo: Statistics Norway; 2012.
- Helse Nord-Trøndelag HF. Videreføring av prosjekt - Distriktsmedisinsk senter i Stjørdalsregionen [Follow-up project: The intermediate care hospital in Stjørdal municipality. Levanger; 2006.
- Distriktsmedisinsk senter i Stjørdal. Kommunestyresak 13/06. Stjørdal; 2006.
- Aaraas I, Søråsdekkan H, Kristiansen IS. Are general practitioner hospitals cost-saving? Evidence from a rural area of Norway. Fam Pract 1997;14:397-402. https://doi.org/10.1093/fampra/14.5.397.
- Aaraas II, Bing-Johnsson PC, Bjøru H, Folgerø T, Jensvold M, Olsen A, et al. Healthcare for the Sick Elderly. Report of Experts Appointed by Norwegian Ministry of Health and Care Services November 2010 2010. www.nsdm.no/filarkiv/File/Eksterne_rapporter/110124Rapport_HelsetjenesterSykeEldre24jan.pdf (accessed 23 January 2017).
- Minister of Health and Care Services . Trygge Sykehus Og Bedre Helsetjenester Der Folk Bor 2015. www.regjeringen.no/no/aktuelt/trygge-sykehus-og-bedre-helsetjenester-der-folk-bor/id2462563/ (accessed January 2016).
- Office for National Statistics . UK Statistics – Population and Migration 2015. www.ons.gov.uk/ons/guide-method/compendiums/compendium-of-uk-statistics/population-and-migration/index.html (accessed June 2015).
- OECD . OECD Statistics, Health Status 2015 2015. http://stats.oecd.org/index.aspx?DataSetCode=HEALTH_STAT# (accessed September 2015).
- Bevan G, Karanikolos M, Exley J, Nolte E, Connolly S, Mays N. The Four Health Systems of the United Kingdom: How Do they Compare?. London: Nuffield Trust; 2014.
- The Scottish Government . Health and Social Care 2014. www.scotland.gov.uk/Topics/Health (accessed October 2014).
- NHS Scotland . About NHS Scotland – Scotland’s Health On the Web 2014. www.show.scot.nhs.uk/about-nhs-scotland/ (accessed June 2015).
- Communications Toolkit – A Guide to Support the Local Implementation of Health and Social Care Integration. Edinburgh: The Scottish Government; 2015.
- The Scottish Government . Health and Social Care Integration Narrative 2014. www.gov.scot/Resource/0044/00447596.pdf (accessed June 2015).
- Scottish Health Service Costs: Year Ended 31 March 2013. Edinburgh: Information Services Division Scotland; 2013.
- Boyle S. United Kingdom (England): Health system review. Health Syst Transit 2011;13:1-483.
- National Services Division . National Managed Networks (NMCNs) n.d. www.nsd.scot.nhs.uk/%5C%5C/services/nmcn/index.html#a2 (accessed March 2016).
- Hospice Aid UK . Guide to Hospice Care 2016. www.hospiceaid.org.uk/guide-to-hospice-care (accessed March 2016).
- Information Services Division Scotland . Data Dictionary A–Z 2014. www.ndc.scot.nhs.uk/Dictionary-A-Z/Definitions/index.asp?Search=H&ID=288&Title=Hospital (accessed October 2014).
- Information Services Division Scotland . Finance | Costs | Reference Information 2013 2014. www.isdscotland.org/Health-Topics/Finance/Costs/Reference-Information.asp (accessed October 2014).
- NHS Greater Glasgow and Clyde . NHS Board 2015 2015. www.nhsggc.org.uk/about-us/nhs-board/ (accessed September 2015).
- NHS Scotland 2020: Local Delivery Plan Guidance. Edinburgh: The Scottish Government; 2013.
- ISD Scotland . Personal Communication 2015.
- Stark C, Oliver K, Hopkins P. Effect of general practitioner hospitals on district general hospital bed use in the Highlands of Scotland. Health Bull 2000;58:385-9.
- Greenaway D. Securing the Future of Excellent Patient Care. London: General Medical Council; 2013.
- Mattila K. Perusterveydenhuolto. Lääkärikirja Duodecim 2005. www.terveyskirjasto.fi (accessed March 2016).
- Finlex . Primary Health Care Act n.d. www.finlex.fi/en/laki/kaannokset/1972/19720066 (accessed April 2016).
- Finlex . Health Care Act n.d. www.finlex.fi/en/laki/kaannokset/2010/en20101326 (accessed April 2016).
- Lofland J, Lofland L. Analyzing Social Settings: A Guide to Qualitative Observation and Analysis. Belmont, CA: Wadsworth; 1995.
- Heinämäki L. Yhteistoiminta-alueiden sosiaali- ja terveyspalvelut 2010 Järjestämisen, tuottamisen ja hallinnon kysymyksiä uusissa palvelurakenteissa. Raportti 41/2011. Tampere: Juvenes Print; 2011.
- Statistics Finland . Sastamala 2013. www.stat.fi/tup/kunnat/kuntatiedot/790.html (accessed November 2015).
- Terveyden ja Hyvinvoinnin Laitos . N Sairastavuusindeksi, ikävakioitu – 2010-2012 2012. www.terveytemme.fi/sairastavuusindeksi/2012/kunnat_taulukot/report_Kunnat_i0_2010-2012.html (accessed March 2016).
- Hanhijärvi J, Pylsy K. Sastamalan Maaseutuohjelma 2014–2017 2014.
- Kaikkonen R, Murto J, Pentala O, Koskela T, Virtala E, Härkänen T, et al. Alueellisen Terveys- Ja Hyvinvointitutkimuksen Perustulokset 2010-2015 2015. www.thl.fi/ath (accessed April 2016).
- Statistics Finland . Total Statistics on Income Distribution 2014. www.stat.fi/til/tjkt/tau_en.html (accessed February 2016).
- Ministry of Social Affairs and Health Finland . Hallitus Linjasi Sote- Ja Aluehallintouudistusta 2015. http://stm.fi/sote-uudistus (accessed December 2015).
- Guzzanti E. L’assistenza Primaria in Italia. Dalle Condotte Mediche Al Lavoro Di Squadra 2009.
- Strippoli S. Sanità, La Rivoluzione Dolce Del Ricovero a Domicilio Cure Migliori E Costi Ridotti. Quando l’ Ospedale Trasloca a Casa Del Paziente. La Repubblica.It (20 Nov. 2010) 2010. http://ricerca.repubblica.it/repubblica/archivio/repubblica/2010/11/20/sanita-la-rivoluzione-dolce-del-ricovero-domicilio.html?refresh_ce (accessed April 2016).
- Ministero dell’Economia e delle Finanze . Libro Verde Sulla Spesa Pubblica 2007. www.rgs.mef.gov.it/_Documenti/VERSIONE-I/Attivit--i/Bilancio_di_previsione/Missioni_e_programmi_delle_ACdS/LaPrecedentestrutturadelbilancio468/Libro-verde-sulla-spesa-pubblica/Sanit-.pdf (accessed April 2016).
- Caruso Y. Il Ruolo dell’ospedale Di comunita’ Nella Rete Dei Servizi Sanitari Territoriali E Ospedalieri. Convegno: ‘Evoluzione Della Organizzazione Sanitaria territoriale’ 2008. www.socialwiki.it/it/kDownload.asp?n=1000000218 (accessed April 2016).
- Financial Law 1992 (n.412, 30th December 1991). 1992. www.rgs.mef.gov.it/_Documenti/VERSIONE-I/Attivit--i/Contabilit_e_finanza_pubblica/Archivio-d/Finanziari/1992/LF1992_coll.pdf (accessed March 2016).
- Fattore G, Frosini F, Salvatore D, Tozzi V. Social network analysis in primary care: the impact of interactions on prescribing behaviour. Health Policy 2009;92:141-8. http://dx.doi.org/10.1016/j.healthpol.2009.03.005.
- Mossialos E, Wenzl M, Osborn R, Anderson C. 2014 International Profiles on Healthcare Systems. Australia, Canada, Denmark, England, France, Germany, Italy, Japan, the Netherlands, New Zealand, Norway, Singapore, Sweden, Switzerland, and the United States. New York, NY: The Commonwealth Fund; 2015.
- Tuttitalia . Statistiche Demografiche Italia 2016. www.tuttitalia.it/statistiche/ (accessed March 2016).
- International Classification of Diseases. Atlanta, GA: Centers for Disease Control and Prevention; 2011.
- Aulizio G. Il Country Hospital Ha 10 Anni. Anello Di Congiunzione Tra Ospedale E Territorio E Basato Sui MMG 2006.
Appendix 1 Patient and public involvement: role description
Background to the study
This research aims to further our understanding of the nature and scope of services provided by community hospitals in England, and, by drawing on experiences in other countries, to inform the further development of community hospital models for the health and social care system. The research will involve a detailed review of existing evidence around community hospital services in the UK and comparable services in other high-income countries. It will then draw on experiences of innovation in other countries that have comparable models to help inform how community hospitals in England may best meet the health and social care needs of the populations that they serve. The research will inform national and local policy-makers and commissioners, setting out the current and future options for community hospital provision, with contextual information to allow local commissioners to assess those models of provision that might be applicable to their own context. More effective provision of community care will benefit patients, allowing a more streamlined service and care that is more suited to their needs.
The aims of the study are to understand (1) the nature and scope of service provision models that can be considered under the umbrella term ‘community hospital’ in the UK and in other high-income countries, (2) the evidence of effectiveness and efficiency of community hospitals and comparable service models in the UK and in other high-income countries, (3) the wider role and impact of community engagement in community hospital service development and provision, (4) how models that are comparable to community hospitals in England operate and their role within the wider system of service provision in other countries; and (5) the potential for such models to perform an integrative role on the delivery of health and social care in other countries.
The work will be undertaken in two work streams. We will first undertake a comprehensive scoping review to understand how community hospitals have been conceptualised and defined in the UK and other high-income countries. We will seek to identify the range of organisational models of service delivery that can be broadly covered by the heading of a ‘community hospital’ and what is already known about service provision and their role in the local and wider health-care economy. Second, we will conduct five country reviews to gain a detailed understanding of the nature, scope and distribution of service delivery models that can be considered comparable to community hospitals in England. We will also undertake detailed case studies of community hospital models in a small subset of countries to provide an in-depth understanding of particular models that appear innovative and to offer learning to service development in England. The case studies will follow a structured approach and will include a local stakeholder mapping, document review, population assessment, interviews and non-participant observation. We will not directly observe any patient care but instead shall focus on aspects of the organisation function, the range of services delivered from the community hospital and the wider role of community hospitals, including community engagement. We will seek approval from the appropriate research ethics committees in each country before the case studies begin.
Request for patient and public involvement members
-
We would like two regular PPI members to join our project.
-
PPI members will contribute throughout the research process, in an advisory capacity.
-
PPI members will also join the National Steering Group, which is being formed across this and two other parallel projects, which are all conducting research on community hospitals.
Roles and responsibilities of the patient and public involvement members
-
To ensure the relevance of the research to the public and service users at all stages.
-
To contribute to the design of the research and communication materials.
-
To contribute to the interpretation of results at key points.
-
To ensure the validity of conclusions from a public perspective.
-
To contribute to the project dissemination strategy.
-
To attend two National Steering Group meetings, planned to be held in London.
Our responsibilities
-
We look forward to introducing PPI members to the research team and wider advisory group.
-
Emma Pitchforth, the main point of contact for PPI members, will be responsible for communicating with and providing support for PPI members. In the event that Emma is not available, we will ensure that there is always a clear point of contact within the research team.
Duration of role
-
The study will run from April 2014 to February 2016.
Payment and expenses
-
We will pay PPI members at an hourly rate of £15 to cover time spent reviewing materials and at meetings. We have budgeted for 36 hours of time per member over the course of the project.
-
All reasonable travel expenses will also be paid. Receipts for public transport will be required or, if travelling by car, postcode of origin and destination will be needed.
Person specification
We are looking for PPI members with an interest in the research topic. We hope that members will have an active role in the project expert group and be able to commit for the duration of the project.
Contact details
Please contact Emma Pitchforth, Research Leader, RAND Europe.
E-mail: epitchfo@rand.org; Tel: 01223 353329
Appendix 2 Quality assessment tables for the systematic review of the evidence on effectiveness and cost-effectiveness
| Reference | Theoretical approach | Study design | Data collection | Validity | Analysis | Ethics | Overall quality assessment | First reviewer | Checker | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Is a qualitative approach appropriate? | Is the study clear in what it seeks to do? | How defensible/rigorous is the research design/methodology | How well was the data collection carried out? | Is the context clearly described? | Were the methods reliable? | Are the data ‘rich’? | Is the analysis reliable? | Are the findings convincing? | Are the conclusions adequate? | Was the study approved by an ethics committee? | Is the role of the researcher clearly described? | ||||
| Dahl et al. (2014)61 | Appropriate | Clear | Defensible | Adequately | Clear | Reliable | Uncertain/not reported | Reliable | Convincing | Adequate | Yes | Uncertain/not reported | Medium quality | EW | JC |
| Dobrzanska et al. (2006)54 | Appropriate | Unclear | Not defensible | Inadequately reported | Clear | Uncertain | Poor | Uncertain/not reported | Not convincing | Inadequate | Not reported | Not clear | Low quality | EW | JC |
| Green et al. (2008)55 | Appropriate | Clear | Defensible | Adequately | Clear | Reliable | Rich | Reliable | Convincing | Adequate | Yes | Uncertain/not reported | Medium quality | JC | EW |
| Hawker et al. (2006)45 | Appropriate | Clear | Defensible | Adequately | Clear | Reliable | Rich | Reliable | Convincing | Adequate | Yes | Not clear | Medium quality | EW | JC |
| Payne (2007)58 | Appropriate | Clear | Defensible | Adequately | Clear | Reliable | Rich | Reliable | Uncertain | Adequate | Yes | Uncertain/not reported | Medium quality | JC | EW |
| Small et al. (2009)8 | Appropriate | Clear | Defensible | Adequately | Clear | Reliable | Uncertain/not reported | Reliable | Convincing | Adequate | Yes | Not clear | Medium quality | EW | JC |
| Reference | Garåsen et al. (2007)9 | Garåsen et al. (2008)62 | Green et al. (2005)7 | Pace et al. (2009)66 | Young et al. (2007)98 | Young et al. (2007)10 | Young and Green (2010)100 | |
|---|---|---|---|---|---|---|---|---|
| Study type | RCT | RCT follow-up | RCT | Quasi-RCT | RCT | RCT | RCT | |
| Selection bias | An appropriate method of randomisation was used to allocate participants to treatment groups | Yes | Yes | Yes | Yes | Unclear | Unclear | Unclear |
| State method of randomisation | Blinded randomisation was performed using random number tables in blocks. | Blinded randomisation was performed using random number tables in blocks | Patients stratified on abbreviated mental test and by activity restriction, then randomised using random numbers tables | Randomisation was in the ratio of 1 : 1 in blocks of 10 | Patients were randomised (in a ratio of 2 : 1, CH to acute hospital) to receive rehabilitation in the CH or to remain in the acute hospital | Patients were stratified and then randomised in blocks | Patients were randomised in predetermined, fixed ratios (1 : 1, 2 : 1 or 1 : 2) for each centre to transfer to the CH or to remain in acute hospital | |
| There was adequate concealment of allocation | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | |
| State method of allocation concealment | Blinded randomisation was performed by the Clinical Research Department at the Faculty of Medicine | Blinded randomisation was performed by the Clinical Research Department, Norwegian University of Science and Technology | Numbered, sealed, opaque envelopes. The research nurse responsible was unaware of the stratification boundaries and block length | Telephone randomisation to local NHS R&D Support Unit | Randomisation was carried out away from the clinical setting and ward staff were blind to allocation. Transfer to the CH was arranged independently of the research team by a member of a case management team employed by the primary care trust | Randomisation was performed independently, away from the clinical setting, was concealed and used short length blocks. The researchers responsible for recruitment were unaware of block length | Patients were recruited by research nurses who were independent of the ward teams and transfer to the CH was arranged independently of the research team | |
| The groups were comparable at baseline including all major confounding and prognostic factors | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Based on your answers, in your opinion was selection bias present? | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Unclear/unknown risk | Low risk of bias | Unclear/unknown risk | |
| If so what was the likely direction of effect? | Hospital staff refused access to some eligible patients (n = 42) | Five patients chose not to take part because they preferred to be treated at the cancer centre | Before randomisation, some patients refused consent (n = 144); staff refused access to some eligible patients (n = 136) | |||||
| Performance bias | The comparison groups received the same care apart from the intervention(s) studied | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Participants receiving care were kept ‘blind’ to treatment allocation | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| Individuals administering care were kept ‘blind’ to treatment allocation | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| Based on your answers, in your opinion was performance bias present? | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | |
| If so, what was the likely direction of effect? | Patients sent to CH may have been more likely to believe that they were in better health. However, this would be common to all CH treatments, and blinding would not have been possible | |||||||
| Attrition bias | All groups were followed up for an equal length of time (or analysis was adjusted to allow for differences) | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| How many participants did not complete treatment in each group? | Eight patients randomised to CH were not transferred; three patients died during treatment in CH; one patient died during treatment at acute hospital | CH group: 22 dead; acute hospital group: 13 dead | 30 patients did not complete treatment: 17 died in CH group; 12 died and 1 withdrew in usual care group | Not reported by group, only 66% completed the six cycles of chemotherapy | Early transfer to CH group: 19 (17 died; 2 withdrew). Late transfer to CH group: 12 died CH group: 19 allocated to this group were not transferred at all (16 discharged; 3 died). Usual care group: 29 (10 transferred to CH; 18 died; 1 withdrew) | In CH group, 38 patients died and 6 patients withdrew before 1 week after discharge. In usual care group, 35 patients died and 7 patients withdrew before 1 week after discharge. Some patients were not treated as randomised (n = 69) | Early transfer to CH group: 30 (26 died; 4 withdrew). Late transfer to CH group: 39 (34 died; 5 withdrew). No transfer group: 89 (30 transferred to CH; 50 died; 9 withdrew) 46 patients allocated to CH group were not transferred (39 were discharged; 2 died) | |
| The groups were comparable for treatment completion | Unclear | Yes | Unclear | Unclear | Unclear | Unclear | Unclear | |
| For how many participants in each group were no outcome data available? | None | None | Only those who did not complete treatment (n = 30) | Not reported by group | Early transfer to CH group: 19 (17 died; 2 withdrew). Late transfer to CH group: 12 died CH group: 19 allocated to this group were not transferred at all (16 discharged; 3 died) Usual care group: 29 (10 transferred to CH; 18 died; 1 withdrew) | Only those who did not complete treatment: n = 44 in CH group, n = 42 in usual care group | Early transfer to CH group: 30 (26 died; 4 withdrew). Late transfer to CH group: 39 (34 died; 5 withdrew). No transfer group: 89 (30 transferred to CH; 50 died; 9 withdrew). 46 patients allocated to CH group were not transferred (39 were discharged; 2 died) | |
| The groups were comparable with respect to the availability of outcome data | Yes | Yes | Unclear | Unclear | Unclear | Unclear | Unclear | |
| Based on your answers, in your opinion was attrition bias present? | Low risk of bias | Low risk of bias | Low risk of bias | Unclear/unknown risk | Unclear/unknown risk | Unclear/unknown risk | Unclear/unknown risk | |
| If so, what is the probable direction of its effect? | It is possible that patients in the CH may have been healthier; eight patients referred to CH (intervention) were too sick and were treated at general hospital. However, data were presented both including and excluding these patients and little difference in effects was evident | Both intention to treat and treatment group analysis conducted | It is difficult to determine attrition bias as raw data are not reported | |||||
| Detection bias | The study had an appropriate length of follow-up | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| The study used a precise definition of outcome | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| A valid and reliable method was used to determine the outcome | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Investigators were kept ‘blind’ to participants’ exposure to the intervention | Yes | Unclear | No | Unclear | No | Yes | Unclear | |
| Investigators were kept ‘blind’ to other important confounding and prognostic factors | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | |
| In your opinion, was detection bias present? | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | |
| If so what is the likely direction of its effect | ||||||||
| Comments | Unblinding of patient allocation to the investigator was recorded. The investigator was unblinded by 18 patients and carers in the treatment group and 6 patients and carers in the control group. Deviations in treatment allocation may have introduced bias: some patients were not treated as randomised and some transfers were delayed. Results need to be confirmed by further studies | Very experienced personnel were used to deliver the chemotherapy, which possibly impacts on results for patient satisfaction | This paper reports on subgroup analyses of the single centre RCT described in Green et al.7 The authors note that analyses are exploratory and findings provisional. Ill health caused a delay in transfer for 14% of patients, which may have led to worse outcomes for members of that group. However, the majority of the late transfer group were delayed for other reasons. Also, study may be subject to bias as only those patients treated according to randomised allocation and assessed at 6 months (141/220 = 64% of the RCT study group) have been included | This paper reports on subgroup analyses of the multicentre RCT reported by Young et al.98 The authors note that analyses should be considered exploratory. Ill health may have caused a delay in transfer for some patients, which may have led to worse outcomes for members of that group. Also, study may be subject to bias as only those patients treated according to randomised allocation and assessed at 6 months have been included | ||||
| Overall assessment | Low risk of bias | Low risk of bias | Low risk of bias | Low risk of bias | Unclear | High quality | Unclear | |
| First reviewer | EW | JC | EW | EW | JC | EW | JC | |
| Checker | SK | EW | JC | JC | EW | JC | EW | |
| Reference | Study type | Is there a well- defined question? | Is there comprehensive description of alternatives? | Are all important and relevant costs and outcomes for each alternative identified? | Has clinical effectiveness been established? | Validity | Inclusivity & Generalisability | Comments | Overall assessment | First reviewer | Checker | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Are costs and outcomes measured accurately? | Are costs and outcomes valued credibly? | Are costs and outcomes adjusted for differential timing? | Is there an incremental analysis of costs and consequences? | Were sensitivity analyses conducted to investigate uncertainty in estimates of cost or consequences? | How far do study results include all issues of concern to users? | Are the results generalisable to the setting of interest in the review? | ||||||||||
| Garåsen et al. (2008)101 | Cost-analysis within a RCT | Yes | Yes | Unclear | No | Unclear | Yes | N/A | No | Unclear | Inadequate extent | Unclear | The study would benefit from justification of the lack of consideration of incremental costs | Medium quality | JC | EW |
| O’Reilly et al. (2006)99 | Cost-effectiveness study within a RCT | Yes | Yes | Yes | Yes | Yes | Yes | N/A | Yes | Yes | Adequate extent | Unclear | The reliability of participants’ recall for services used was a concern | High quality | JC | EW |
| O’Reilly (2008)11 | Cost-effectiveness study within a RCT | Yes | Yes | Yes | Yes | Yes | Yes | N/A | Yes | Yes | Adequate extent | Yes | – | High quality | JC | EW |
| Reference | Study type | Selection bias | Performance bias | Attrition bias | Detection bias | Overall assessment | Comments | First reviewer | Checker | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| The method of allocation to treatment groups was unrelated to potential confounding factors | Attempts were made within the design or analysis to balance the comparison groups for potential confounders | The groups were comparable at baseline, including all major confounding and prognostic factors | Based on your answers, in your opinion was selection bias present? | The comparison groups received the same care apart from the intervention(s) studied | Participants receiving care were kept ‘blind’ to treatment allocation | Individuals administering care were kept ‘blind’ to treatment allocation | Based on your answers, in your opinion was performance bias present? | All groups were followed up for an equal length of time (or analysis was adjusted to allow for differences) | How many participants did not complete treatment in each group? | The groups were comparable for treatment completion | For how many participants in each group were no outcome data available? | The groups were comparable with respect to the availability of outcome data | Based on your answers, in your opinion was attrition bias present? | The study had an appropriate length of follow-up | The study used a precise definition of outcome | A valid and reliable method was used to determine the outcome | Investigators were kept ‘blind’ to participants’ exposure to the intervention | Investigators were kept ‘blind’ to other important confounding and prognostic factors | In your opinion, was detection bias present? | ||||||
| Stapley et al. (2007)102 | Cohort study | N/A | Unclear | No | Unclear/unknown risk | Yes | N/A | N/A | Low risk of bias | Yes | Due to death or withdrawal: CH: 70 Acute: 52 | Unclear | Due to death or withdrawal: CH: 70 Acute: 52 | Unclear | Unclear/unknown risk | Yes | Yes | Yes | No | No | Unclear/unknown risk | Unclear | The paper states that multivariable regressions were used to control for age and sex, but the results reported seem to be unadjusted (comparison was by means and t-tests) | JC | EW |
Appendix 3 Country report data collection template
Health system context
Please provide a brief description of the health system context in [country], approx. 500 words.
-
Brief description of the country.
-
Financing of health-care provision – public/private.
-
Overall responsibility for health-care provision.
-
Breakdown of health expenditure by major category (primary care, hospital care, pharmaceuticals, etc.).
Organisation of the health-care system
-
Role of primary care/secondary care and if possible information on integration between primary and secondary care – if anything is going on.
-
Responsibility for planning and delivery of services at a local level.
-
Integration with social care.
Organisation, financing and delivery of hospital care
-
How is ‘hospital’ defined, what categories of hospital are there [e.g. according to function (teaching, general, specialist, other); legal status (e.g. operated under public law, as private enterprise); ownership (public, private non-profit, private for profit), etc.]?
-
Please provide an overview of the current number and size of hospitals (number of sites, number of beds, staff composition, etc.) (latest data), by hospital category (e.g. ownership, function).
-
Please provide an overview of trends in the number of hospitals and hospital beds over the past 10–15 years (by ownership, status, function where appropriate).
-
Please describe the principal mechanisms for the planning of hospital capacity and whether and how this has changed over the past 10–15 years (approx. 500 words).
-
Please describe the principal mechanisms for financing hospitals and hospital care (capital investment, operating costs) and whether and how this has changed over the past 10–15 years (approx. 500 words).
Community hospital models
-
What forms of hospital are there that fit within our definition of ‘community hospitals’? [Provides beds, is led by community-based health professional usually a doctor (e.g. GP or community-based specialist), number of beds is < 100; and delivers services locally to the patient.]
-
For each of these models:
-
What is the name of the hospital type?
-
What services do these hospitals deliver?
-
Typical size, staffing, management, ownership of community hospital.
-
Role of community hospital in health-care provision, and interface with other forms of care.
-
Any evidence of community hospital effectiveness/efficiency?
-
Environmental and cultural factors
-
What is the history of the development of community hospitals? Did it develop in response to a particular need or a particular policy direction?
-
What were the main reasons for community hospital development in this context?
-
What is the view of health-care professionals, doctors and the public on community hospitals?
-
How widespread are community hospitals? Are they increasing/decreasing in number/popularity?
-
Are there plans for future changes in community hospital provision?
Appendix 4 Country report interview protocol
Information for the interviewer
Before commencing the interview, please remind the interviewee of the research project, and the purpose of our study (see below). Please ask the interviewee if they are happy for the interview to be recorded, reassuring them that what they say will be confidential, and, although quotations may be used, they will not be attributed.
About the study and its objectives
This section will link in with the interviewer’s duties detailed above and will serve to ensure that the participant understands and accepts both the details of their participation and the broader aims of the study.
Thank you for speaking to me today.
We are from RAND Europe, which is an independent not-for-profit research institute. We are conducting a research study to understand the use of models of care similar to community hospitals in international contexts, and draw learning for the future development of community hospitals in England.
The aim of this interview is to aid our understanding of the [country] health system context, and the role of community hospitals within that context.
Key questions and prompts
Introduction to the interview participant
-
Could you briefly introduce yourself and your role, and describe your area of expertise?
The role of community hospitals in the health system
-
Which types of hospitals or facilities in your country would be described as community hospitals and why?
-
is there a ‘definition’ (perhaps there is document where this has been described)
-
estimated number of hospitals/facilities that would be considered as a community hospital (absolute number or proportion or both)
-
do they typically have beds, how many on average?
-
-
How would you describe the role/s or function of community hospitals in the service delivery structure in your country overall?
-
E.g. they serve communities in remote settings (definition of ‘remote’); they serve a predominantly older population; they fulfil a step-down/intermediate care function for patients who do not require full inpatient monitoring but are not yet ready to be discharged to their home, other.
-
To be adapted to the country in question:
-
(where community hospitals have a long tradition/have been part of the service infrastructure for some time), how has their role or function changed over time?
-
(where community hospitals are a new feature in the system), what was the motivation for introducing these?
-
To what extent is the current model of operation a consequence of their history of development?
-
Types of community hospitals
-
What do you see as the main role of community hospitals in health-care provision?
-
(prompt: in relation to acute hospitals and primary/community care)
-
-
Are there different types of community hospital in your country and how would you describe these?
-
GP-led, nurse-led, specialist-led
-
rural/remote hospital, facility for provision of ‘step-down’ or ‘step-up’ care
-
different ownership/funding arrangements.
-
-
What services are typically provided by community hospitals?
-
Would you say that [name of community hospital, or known community hospitals from the literature] represents a typical community hospital in your country?
-
if yes what would you see as ‘typical’ features (e.g. nurse-led, targets older populations, etc.)
-
if not, what makes this ‘model’ different from others (e.g. it is very innovative, provides services to a very selected population, is located in a geographically isolated area)
-
-
How does service provision differ from services provided by a ‘typical’ general district hospital or services that are provided in the community?
-
How much duplication of service provision is there between community hospital and district general hospitals?
-
-
Can you tell me about the relationship between services provided by community hospitals and those offered by other local health and social care services? (to include: district general hospital, nursing homes, home care)
-
Are there examples where the community hospital hosts services provided by others?
-
What forms of collaboration are there between community hospital and other services?
-
Are there staff working across the community hospital and other organisations?
-
For Scotland: We have heard that there are some services provided from the community hospital, and some are merely hosted by the community hospital. How does the split work between core provide services and hosted services? Does the funding come from different places?
-
Are all community hospitals owned and managed by the Scottish NHS?
-
-
Who owns and who manages community hospitals? Has this changed over time and how?
Community hospital funding
-
How are services provided by community hospitals financed?
-
is payment based on the population covered, on historical spending, activity (case-based), or a combination)
-
-
Are community hospitals contracted directly by local government/health authority and how are contracts arranged
-
who is involved in negotiations, are contracts put out for tender and do community hospital have to compete to get them, who decides that community hospital should be contracted
-
-
Are staff employed directly by the community hospital or contracted in from elsewhere?
-
e.g. GPs or consultants who have other roles may be contracted.
-
-
How are decisions made about investment in community hospitals, compared with investment in other forms of health-care provision?
-
Who funds capital costs for community hospitals?
-
Who makes community hospital funding decisions? (compared to other parts of the health system)
-
Is decision to fund capital costs for community hospitals part of a wider planning processes? If so at what level?
-
Perceived benefits and challenges of community hospitals provision
-
What do you see as the particular benefits or disadvantages for patients of care provision in community hospitals?
-
Are you aware of any evidence from studies of community hospitals in your country, for example looking at patient outcomes?
-
What do you see as the key current challenges for community hospitals in your country? (prompt on the following: staffing)
-
What do you think should be done to address these challenges? (refer back to those mentioned)
-
What are the particular skills required to work in a community hospital?
-
What training is provided to allow people to gain these skills?
-
Do people just learn on the job?
-
Are there specific ‘rural medical schools’ or training centres?
-
-
What is being done to attract staff to work in a community hospital?
-
Does working in a community hospital attract additional payments?
-
E.g. are staff offered additional training they would not get otherwise which provides them with a competitive advantage
-
Other?
-
The future role of community hospitals
-
To what extent do you think that community hospitals are efficient and effective in their provision of care?
-
Cost-effectiveness?
-
Meeting population needs?
-
-
What ongoing or anticipated health system changes will affect the future role of community hospitals in your country? (e.g. integration of care)
-
How do you see the future of community hospitals in terms of their number and role?
-
Do you think that there are opportunities for further adaptation of the community hospitals role?
-
Integration and communication
-
-
Should there be changes to the community hospital’s role to improve service delivery, and what would these be?
-
Is the notion of ‘community hospital’ a useful one?
-
Difficult to define the concept from other types of hospital – is it a useful concept?
-
Any other comments
This will give an opportunity for the interviewee to raise any additional points or other comments which have not been covered elsewhere in the interview.
Do you have suggestions for other people that we should talk to?
Wrap up
Thank you for your time and your input. If I need to follow up anything discussed today or clarify some points later, would you be happy if I gave you a call?
As we mentioned before, the information you’ve given us will be used as part of a country review within a larger published report. Once this report is ready, it will be made available on the RAND Europe website.
Appendix 5 International experiences: individual country reports
Australia
Australia, formally the Commonwealth of Australia, is the sixth largest country by area, comprising the mainland of the Australian continent, the island of Tasmania and several smaller islands. It is both a representative democracy and a constitutional monarchy, with Queen Elizabeth II as head of state. 196 At a total population of 23.6 million at the end of 2014, population density is low, at 3 persons per km2, with most parts of the country uninhabited or sparsely settled. 197 Australia’s population is mostly concentrated in the east and south-east of the country, with about 70% of Australians living in major cities, while the remainder of the population resides in areas characterised by increasing levels of ‘remoteness’, including so-called ‘inner regional areas’ (i.e. areas where geographic distance imposes some restriction upon accessibility to the widest range of goods, services and opportunities for social interaction, 18%), outer regional areas (9%), and remote and very remote areas (1%). 198
Health system context
The tax-funded public Medicare programme, established in 1984, provides health insurance for all citizens and permanent residents, with full or partial coverage of all medical services, including hospital stays, according to a fee schedule. In 2012, 67.6% of total health expenditure was funded from general taxation, 8.9% from private health insurance, 19.9% from out-of-pocket payments and the remainder (3.6%) from other sources. 121 By June 2015, some 47% of the population had private hospital insurance and 56% had general treatment coverage (for ancillary treatments not covered under the public system such as dental care or physiotherapy). 199 Uptake is promoted by the federal government and subsidised by its tax policy. 116 In 2012 (latest available year), national health expenditure was 8.8% of GDP, which was similar to the OECD average at 8.9% (for 2013) (UK: 8.5% in 2013). 121 However, when expressed as per capita expenditure, health spending was higher than the OECD average, at US$3866 purchasing power parity (PPP) (2012) compared with US$3453 PPP (2013) (UK: US$3235 PPP in 2013).
A federal form of government, fiscal and functional responsibilities are divided between the Australian government and the six states (New South Wales, Victoria, Queensland, Western Australia, South Australia and Tasmania) and two territories (Australian Capital Territory and Northern Territory) (hereafter referred to as ‘states’), which administer regional systems for health and social care. The federal government funds and administers the Medicare Benefits Scheme (MBS) and pharmaceutical benefits through the Pharmaceutical Benefits Scheme (PBS). It regulates much of the health system and has the main funding and regulatory responsibility for aged care programmes and government-subsidised residential care facilities. 116 Together with the states, the Australian government funds public hospitals and public health programmes, whereas the states administer public hospitals and regulate all hospitals. Local government also plays a small part in funding health care and it is involved in the delivery of community health and preventative programmes. 124
The past decade has seen a series of changes in the Australian health system, with more recent reforms shifting the focus of health policy to public hospital funding. The 2011 National Health Reform Agreement,200 negotiated by the Council of Australian Governments, forms one of the key reforms of the Australian health system in the more recent past. It set out a range of arrangements seeking to improve health outcomes for all Australians and to ensure the sustainability of the Australian health system. 200 Among other things, it established a new basis for the federal government’s contribution to public hospital funding and introduced activity-based funding of public hospitals (see Organisation, financing and delivery of hospital care). 124
It also established new statutory bodies to enhance quality and transparency in the system. These include the National Health Performance Authority, which is tasked with the monitoring and reporting on the performance of public and private hospitals, primary health-care organisations and other providers of community health-care services,201 and the Independent Hospital Pricing Authority (IHPA), which delivers the pricing framework for public hospital services in Australia. 202
In an effort to enhance the systems’ responsiveness to local need, the reform further established local hospital networks (LHNs) as a means by which to decentralise public hospital management and increase local accountability and so drive improvements in performance. It also introduced Medicare Locals, which were tasked with supporting and enabling better integrated and responsive local GP and primary health-care services. 200 However, following the 2013 change in the federal government, a number of aspects of the reform have since been revised, with, for example, Medicare Locals being replaced by Primary Health Networks (PHNs) from 2015. 203 In 2015, the government also established a programme of work that seeks to deliver a ‘Healthier Medicare’ to ensure high-quality, appropriate and efficient health care. 204 This involved the establishment of a Medicare Benefits Schedule Review Taskforce to review the MBS schedule205 and a Primary Health Care Advisory Group, which is tasked with examining options for reforming primary care to improve the management of people with complex and chronic disease. 206 Additional reform efforts include an ongoing programme to change the aged care system; commencing in 2012, the 10-year reform programme prioritises increasing support and care in the home, enhancing access to residential care, increasing support for those with dementia and strengthening the aged care workforce to better meet the social and economic challenges of Australia’s ageing population. 207 In 2015, responsibility for ageing and aged care was shifted from the Department of Social Services to the Department of Health. 208
Organisation of the health-care system
Figure 4 shows health-care expenditure in Australia by sector. In 2013–14, public and private hospital services accounted for around 40% of total recurrent health expenditure, of which 31% was spent on public hospital services, followed by medical services outside hospital, including other health practitioner services (22%) and pharmaceuticals, aids and devices (16%). 209
FIGURE 4.
Health-care expenditure by function as percentage of total recurrent health expenditure, Australia, 2013–14. Note: the category ‘other’ includes patient transport (2.1%), administration (2.2%) and research (3.5%). Based on Australian Institute of Health and Welfare. 209

Figure 5 further disaggregates the allocation of health-care spending to the different sectors by funding source, illustrating the involvement of different funders (federal government, states and territories, private health insurance, individuals and other sources). This shows that the federal government is the largest government funder of the health system, providing 64% of recurrent government funding in health in 2013–14. 210 It also illustrates that, although expenditure on public hospital services is shared between the federal government and the states, primary health-care funding is from a wide range of sources, with federal funding covering just over 40% of services, mainly GP services and pharmaceuticals falling under the PBS.
FIGURE 5.
Health-care expenditure (recurrent) by sector and funding source, in AU$M, Australia, 2013–14. Note: the category ‘medical services (unreferred)’ relates, mainly, to GP services. Source: Australian Institute of Health and Welfare. 209
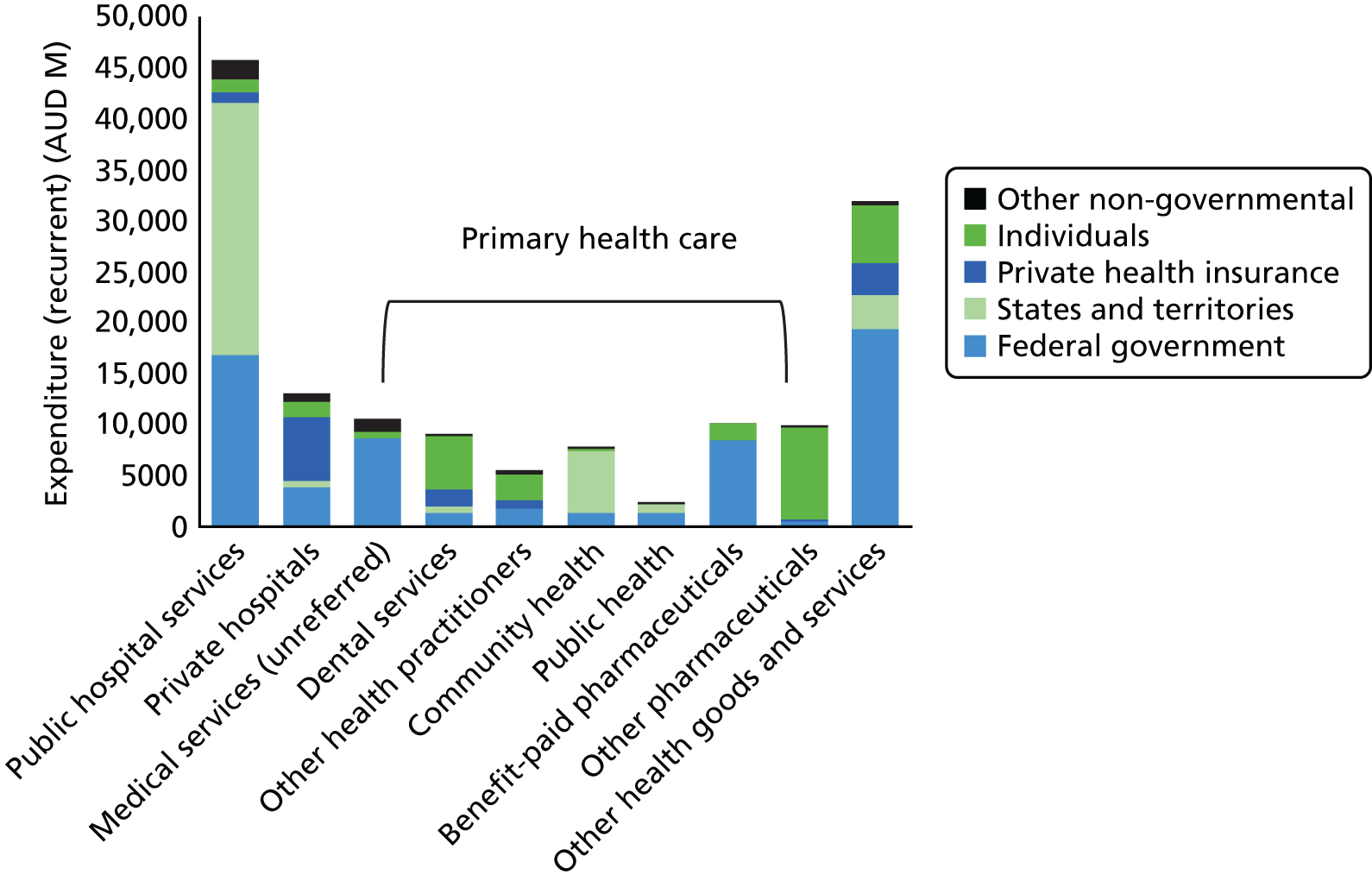
In Australia’s mixed system, health care is delivered by public and private providers. Medical services outside hospital (ambulatory care) are provided by GPs and specialists. General practice forms a core part of primary health-care services, along with community health centres and allied health practices, such as physiotherapy, dietetic and chiropractic practices. 209
In 2014, about one-third of medical practitioners working in medicine were GPs, which is slightly lower than the proportion of medical specialists (35%). 211 There has been a general increase in the number of GPs since the mid-2000s, both in terms of absolute numbers and per head of population. 212 In 2014, the supply of GPs as measured in full-time equivalents (FTEs) was 111 FTE per 100,000 population. 211
General practitioners work mostly in private practice and they may establish their practice where they wish. The number of solo practices has declined over time and practices with multiple GPs now constitute the majority. In 2014, 87% of GPs worked in group practices,211 with about four practitioners per practice on average. 122 Medical specialists work in public and/or private hospitals and private practices; those working outside hospital are more likely to work in solo practices (2014: 54.4%) than in group practices. 211
Office-based physicians in private practice are paid on a fee-for-service basis, with generalist and specialist services either fully or partly reimbursed based on the MBS. All Australians are eligible for a full rebate of the schedule fee for GP services, whereas specialist services are subsidised for 85% of the schedule fee. The Medicare fee schedule is set by the federal government. Doctors may charge more than the Medicare fee, which leaves the patient with a copayment plus any additional charges.
The fee schedule for GPs is based on payment for each consultation provided, with the fee increasing with the level of complexity and consultation length. Medicare has introduced additional rebates for a range of services provided by GPs and other primary care providers such as nurse practitioners, practice nurses and allied health providers, in order to incentivise selected activities. These include, for example, rebates for chronic disease management services that seek to enable GPs to plan and co-ordinate the health care of patients with chronic or terminal medical conditions. 213 In addition, there are separate incentive payment schemes, such as the Practice Incentive Program (PIP), which aims to encourage continuing improvements, enhance capacity and improve quality and access for patients in general practice, and the General Practice Rural Incentives Program, which seeks to encourage GPs to work in rural and remote areas of Australia. 214 PIP payments have been estimated to account for about 5% of federal spending on general practice. 122
Community health services involve non-residential health services that are provided by, or on behalf of, state and territory governments. 210 Community health centres usually employ multiprofessional teams122 and services include, for example, health services provided to particular population groups, such as Aboriginal and Torres Strait Islander people, women, youth and migrants, or for particular services such as family planning, or alcohol and drug treatment services. 210 They may also include specialised mental health programmes that are delivered in a community setting.
Patients have free choice of primary care doctor and there is no requirement for patients to register with a GP. GPs act as gatekeepers to specialist care insofar as patients will receive the Medicare subsidy only for referred consultations. 122
In 1992, divisions of general practice were established to encourage GPs to collaborate and form links with other health professionals to improve the quality of health service delivery to local communities. 215 Subsequently, as part of the 2011 National Health Reform Agreement described above, the divisions were replaced or substituted by ‘Medicare Locals’, meso-level organisations with the aim to support better service integration and co-ordination and improve the quality of patient care in local communities. 200 During 2012, a total of 61 Medicare Locals were established as not-for-profit companies, but following a change in the federal government in 2013, Medicare Locals were subsequently disbanded. 216 This was based on recommendations of a government-commissioned review suggesting that, in the form in which they were set up, Medical Locals were not suitable to achieve their strategic aims. 217 From July 2015, Medicare Locals were replaced by 31 PHNs, with the key objectives of increasing the efficiency and effectiveness of medical services for patients, and improving the co-ordination of care. 218 PHNs are expected to achieve this by providing support to GP practices to improve patient care and by working with other funders of services and providers of services to facilitate improved outcomes for patients.
Organisation, financing and delivery of hospital care
The Australian national data collection system principally distinguishes hospitals into acute care hospitals, psychiatric hospitals and day hospitals or centres. Acute care hospitals are defined as ‘[e]stablishments which provide at least minimal medical, surgical or obstetric services for inpatient treatment and/or care, and which provide round-the-clock comprehensive qualified nursing service as well as other necessary professional services’. 219 They must be licensed by the state health department. Psychiatric hospitals are defined as establishments for the treatment and care of inpatients with psychiatric, mental or behavioural disorders, and day centres or hospitals provide ‘a course of acute treatment on a full-day or part-day non-residential attendance basis at specified intervals over a period of time’. 219
Hospitals are further categorised according to peer groupings, which define hospitals based on shared characteristics (see below), distinguishing public and private entities. 128 Public hospitals are controlled by a state or territory health authority and they offer free diagnostic services, treatment, care and accommodation to all eligible patients. Private hospitals are owned and operated privately, and patients are charged for accommodation and other services provided.
In 2013–14, there were 1359 hospitals in Australia, of which 55% were public (747 hospitals) and the remainder private (612 hospitals). 141 Overall, there has been a small decline in the number of public hospitals since the mid-1990s, whereas the number of private hospitals has steadily increased, by around 20% between 1997 and 2012 (Figure 6). 121
FIGURE 6.
Total number of hospitals and hospitals per million population in Australia, 1997–2012. Based on OECD. 121
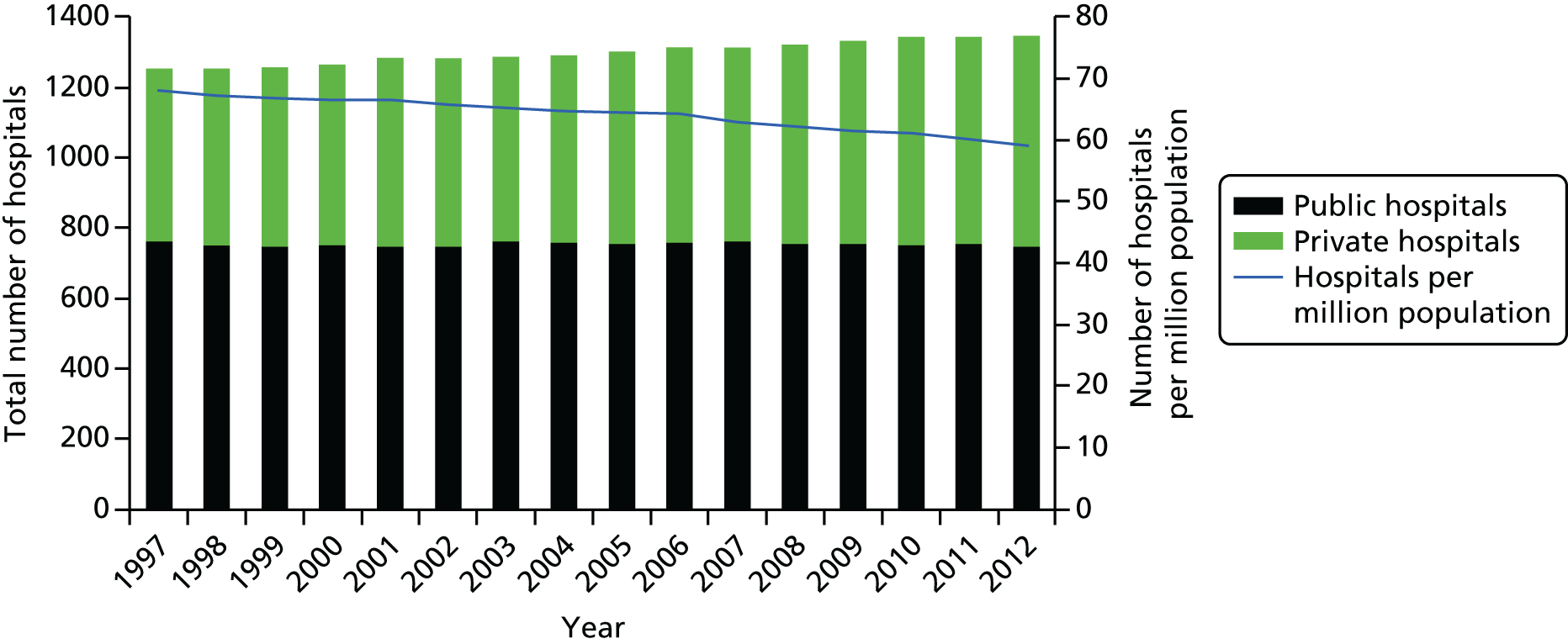
Also in 2013–14, public hospitals accounted for two-thirds of hospital beds, at 58,567 (65%), whereas private hospitals accounted for 35% (30,920). 141 This equated to 2.5 beds per 1000 population in the public sector and 1.3 beds per 1000 population in private facilities. Overall, there has been a small but steady decline in the number of hospital beds during the past decade, both in the public and private sectors (Figure 7).
Of hospital beds in the public sector, some 96% were acute beds, whereas same-day beds accounted for about 12% of available public hospital beds. Although the absolute number of public hospital beds was highest in major cities, their number in relation to the resident population was highest in remote areas, at 3.5 beds per 1000 population compared with 2.4 beds per 1000 in major cities. The availability of beds also varied across states, with the highest number in New South Wales, at 5.0 beds per 1000 population and the lowest number in Tasmania (1.5 beds per 1000).
Public and private hospitals in Australia are very diverse, and, to enable comparison between hospitals and across states, the Australian Institute of Health and Welfare has been developing, in collaboration with other stakeholders, hospital peer groupings, which define hospitals based on shared characteristics, as noted above. This distinguishes, for example, five categories of acute hospitals in the public sector according to the range of services provided, namely principal referral hospitals and four public acute groups hospitals (A–D), with the public acute groups hospitals descending in range and number of services provided and size in terms of number of beds. There are also private acute hospitals but they are not directly comparable to public acute hospitals, as most of the latter provide emergency services, whereas most private acute hospitals do not. Private hospitals also tend to be more specialised than public hospitals. 128 It furthermore includes very small hospitals, with an average of about 10 beds, which provide care for a small number of admitted patients; most do not perform surgery. Generally, the size and type of hospital service changes with increasing remoteness, with large, specialised hospitals mainly concentrated in major cities and more remote areas’ hospital facilities tending to be smaller and more likely to provide multipurpose and non-acute services (see Annex A below). 220
As noted earlier, the funding of public hospitals is principally shared by the states and the federal government, although the degree of federal government involvement has varied over time. Indeed, there has been an ongoing debate about the funding and administration of public hospitals in Australia for several years, including a threat by the federal government to take over public hospitals from the states. 207 This debate was only resolved in 2011, when the Council of Australian Governments agreed on a hospital reform strategy including changes to the funding formula, the National Health Reform Agreement described above. The reform introduced activity-based funding using a ‘national efficient price’ (based on diagnosis-related groups), which was to form the foundation for public hospital funding distribution from July 2012. Small rural and regional hospitals were to continue to be block funded, as were teaching and training functions. The federal government committed to funding 45% of growth in efficient prices or costs of public hospital services for the period 2014–17. 200 The efficient price (for activity-based funding) or cost (for block grant funding) is determined annually by the aforementioned IHPA, taking account of changes in use, the scope of services provided and the cost of those services. Initially, the federal contribution was to increase to 50% from 2017, but this agreement was recently reversed, and beginning in July 2017, the federal government’s additional contributions will be based only on population growth and inflation and no longer will be provided on the basis of activity. 124
The 2011 National Health Reform Agreement also established LHNs, formed by small groups of public hospitals governed by their local management board to increase local accountability for budget management, service delivery and treatment outcomes. 200 LHNs comprise small groups of local hospitals, or an individual hospital, linking services within a region or through specialist networks across a state or territory. 141 A LHN is usually defined as a business group, geographical area or community, and every public hospital in Australia is part of a LHN. 221 LHNs vary widely in location, size and type. For example, there were 138 LHNs in 2013–14, and their number ranged from one in the Australian Capital Territory to 88 in Victoria. 141 However, many LHNs consist of a single hospital, in particular in Victoria, with 56 out of 88 LHNs (63%) containing one hospital only. Other LHNs comprise a principal referral hospital or a public acute group. Although LHNs have their own local boards, state health departments continue to be the overall administrators of their public hospitals. 116
Physicians in public hospitals are either salaried (with options to undertake limited private practice) or combine private medical practice with a visiting medical officer engagement at one or more public hospitals. 207 Physicians working in private hospitals are in private practice and do not concurrently hold salaried positions in public hospitals.
Community hospitals in Australia
Defining the community hospital
It is difficult to define a community hospital in the Australian context. Key informants interviewed for this study suggested that the concept has to be understood in the context of the general way the hospital infrastructure is organised in the different states:
[Hospital models] are driven by not only by state government policy but also by the demography really [. . .] [For example, in the Northern Territory] the population is very scattered over very vast lots of very small communities. We really don’t have community hospitals per se [. . .] most of these very remote communities we have something that you would characterise more as a community health centre [. . .] We do have in a couple of regional centres larger hospitals that are largely GP run and they are in larger population centres of you know 3000 to 6000 that sort of size. They will have visiting specialist services and they would still have procedural GPs in one of those towns but not in the other.
KI-A02
In Australia, hospitals tend to be small, particularly in regions that cover large geographical areas. The majority of beds tend to be in larger hospitals and in more densely populated areas. In 2013–14, some 70% of hospitals had 50 or fewer beds. 141 Figure 8 illustrates the distribution of public hospitals by size across states. This shows that, in 2013–14, the Northern Territory did not have any public hospitals with > 500 beds or ≤ 10 beds. Queensland had the highest number of hospitals with < 10 beds, and New South Wales the highest number of hospitals with 11–50 beds.
FIGURE 8.
Public acute and psychiatric hospitals, by hospital size, Australian states and territories, 2013–14. Based on Australian Institute of Health and Welfare material. 141
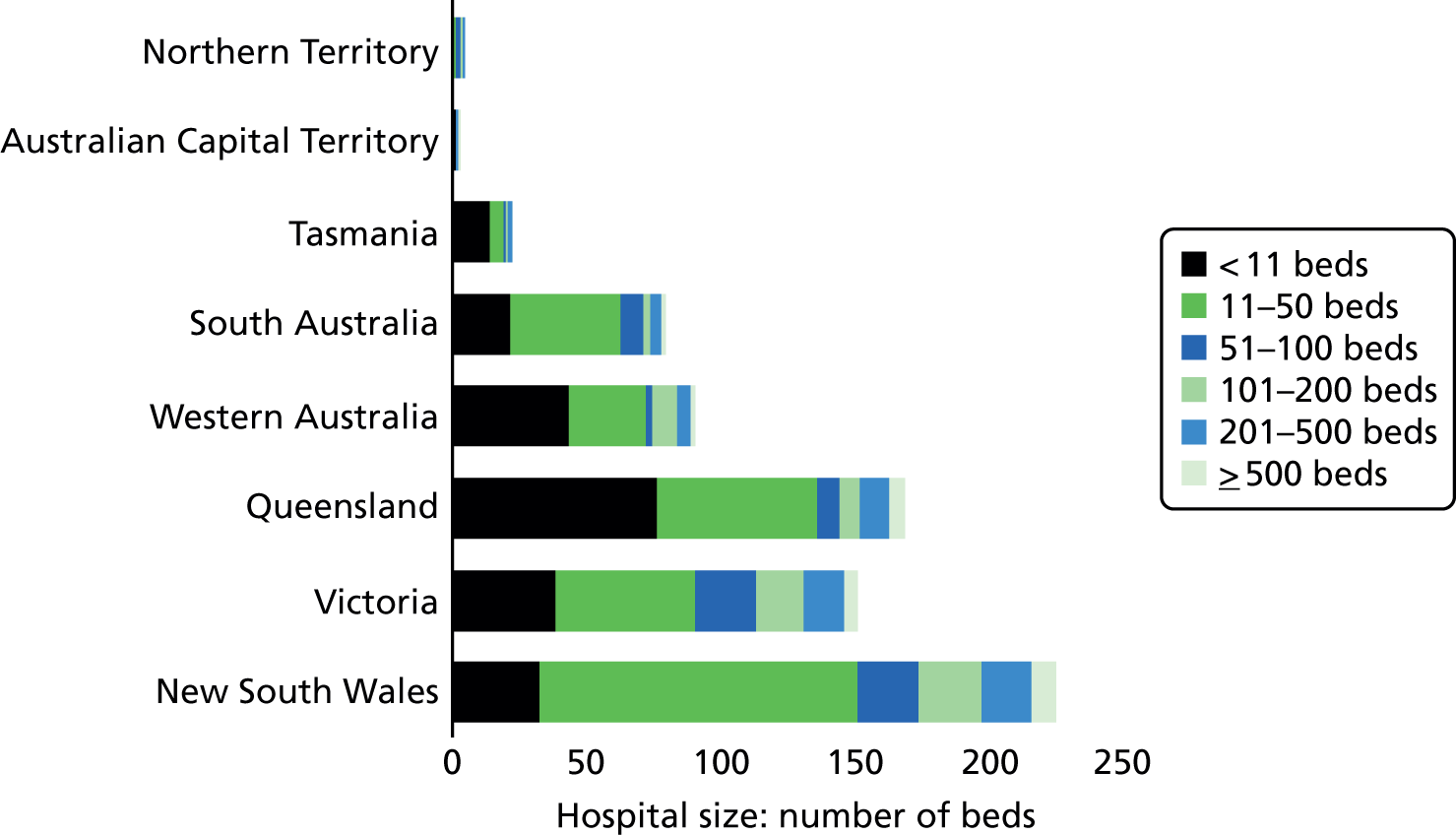
It is these small (district) hospitals in rural and remote areas that perhaps most closely resemble the traditional community hospital found in the UK:
[Community hospitals] are hospitals that perform less than 2000 separations [hospital discharges] a year and either have surgery or no surgery attached. So conceptually [this] includes most of our small rural towns, looking at populations between about 2000 and 10,000.
KI-A04
Community hospitals in this sense would typically be run by GPs, partly because ‘the specialists aren’t there’ (KI-A01); these types of hospitals are not common in metropolitan areas. Set-up and size will, however, vary by state. One key informant noted that the most common model in Queensland would be in the form of ‘GP-run hospitals where the GP you know provides anaesthetics and [does] basic surgery [. . .] There might be between 500 and a couple of a thousand people in a town or a district’ (KI-A02), while in New South Wales they would be somewhat bigger:
Probably around maybe 40 to 100 beds which are generally in smaller rural towns. And they provide surgery on low risk patients and do medicine, treat gastro[intestinal conditions], [intravenous] antibiotics, that sort of thing. A lot of them do chemotherapy as an example, a lot of them do renal dialysis; so they provide . . . they have what we call close observation units, so they don’t really provide intensive care.
KI-A06
One other key informant highlighted the specific situation in the state of Victoria, where public hospitals would have a comparatively high number of residential care beds, between 40 and 50, but only a small number (up to 10) of acute care beds, which are ‘mainly filled with people at the very low acuity categories and some of them might have as few as two (beds)’ (KI-A03).
One commonality observed by all key informants interviewed for this study is that the focus of community hospitals in the Australian context tends to be geographical rather than on specific population groups (KI-A01). However, boundaries may be blurred where the local community constitutes a specific group, such as indigenous populations. In addition, as rural communities are ageing, service delivery will have to accommodate the changing needs (KI-A06), as perhaps illustrated by the example of Victoria.
Types of community hospitals and services provided
Reflecting the purpose and settings of community hospitals in the Australian context, the range of services provided can vary across states and across regions within states. For example, in some settings, community hospitals would provide emergency stabilisation, management of simple conditions, hospitalisation for uncomplicated general medical patients, or subacute care or step-down care (KI-A04). Elsewhere, services would include obstetric care, emergency care and minor surgical procedures, which would be delivered by GPs (KI-A01):
GPs that are trained [. . .] in both anaesthetics and basic surgery so they might have a graduate diploma in anaesthetics so they are not trained anaesthetists but they do some general anaesthetic training. They also can do some surgical training, so they can do basic surgical procedures. So they can do you know severe infection, appendectomy, that sort of thing. So procedural GPs can do those, really it is around emergency surgical procedures.
KI-A02
Key informants commented that this model of ‘procedural GPs’ used to be quite common (KI-A02, KI-A03) but ‘waned over a period of time, as there were closures of small country hospitals across the country because of cost pressures, but now it has come back’ (KI-A02) as part of the rural generalist pathway (see also below).
Access to specialist expertise varies across settings and states, reflecting, in part, the governance models in place, as well as the level of collaboration and co-operation across the health system in individual states. For example, in Queensland, small public hospitals are managed by one of the 17 Hospital and Health Services (previously Health Service Districts) and the community hospital would be embedded within wider service provision (Box 3):
[T]here’d be a director of nursing at the local site or there may not even been a director of nursing, depending on what the industrial agreements say, but they’d be totally integrated in a management sense and clinically they would have built up referral relationships depending on where the hospitals are and very often there might also be telehealth links between the main hospital and the local hospital.
KI-A01
The Cairns and Hinterland Hospital and Health Service (CHHHS) is responsible for providing primary health, community and public health services to a population of just over 280,000 which is culturally diverse and dispersed over a wide geographical area in the north of Queensland. CHHHS is in charge of the direct management of the facilities within its geographical boundaries, which includes nine hospitals and multipurpose health centres, of which half have < 50 beds, and only one provides > 100 beds (Cairns Hospital with 347 overnight beds and 124 day beds).
Among the smaller hospitals is Tully Hospital with 20 beds, which offers primary health clinics (antenatal, diabetes mellitus, gynaecology, immunisation, obstetrics, women’s health and wound management), allied health services (occupational therapy, physiotherapy, social work, speech pathology and dietetics) and co-located services (community health, community mental health and dental health). It operates a 24-hours a day, 7-days a week emergency department. Telehealth services are available for linking with other facilities via video-conference for patients.
Facilities also include the Babinda Multi-Purpose Health Centre, which employs allied health staff and provides inpatient (22 beds) and outpatient services. It provides a home-based nursing service and visiting health services include gerontology, aged care assessment, speech pathology, dietetics, midwifery group practice, radiography, mental health, alcohol and drugs services, and women’s health. Home and community care services are managed by the director of nursing and include centre-based respite 2 days a week, transport and in-home respite for carers.
Source: Cairns and Hinterland Hospital and Health Service,222 Queensland Government. 223
This would be somewhat different in the state of Victoria where hospital governance has been devolved so that most hospitals, including the smaller ones, will be their own organisation (KI-A03). However, hospitals tend to collaborate closely, with the regional hospital providing support for services that are not available in the smaller hospital:
[In] a local hospital, you’re not going to have an obstetrician or you’re not going to have even a permanent medical director, but you might essentially borrow that staff member from the larger hospital so that you can still have those services provided in your hospital without actually having to employ the person and that works quite well in some cases. It means [. . .] that there’s maybe somebody coming in once a month or whatever it might be who is overseen by somebody from a larger service or who is based in a larger service, so that it takes some of the clinical governance burden away from that smaller service and they don’t need to have a clinical governance framework for cancer care for example.
KI-A03
Key informants described similar examples in other states, such as the Northern Territory, where the local GPs would have a network of specialists whom they could telephone for advice or for evacuating patients if required and where ‘the specialists fly in and out, and you know run clinics or have surgical lists, that sort of thing’ (KI-A02) (Box 4). Such a model was also described for diagnostic services in small hospitals in New South Wales, where basic radiology or pathology services may be available on site, with the local GP and nursing staff functioning as ‘remote operators’ while a visiting clinician would provide the specialist expertise (KI-A04).
Katherine District Hospital is an accredited 60-bed non-specialist medical, diagnostic and treatment facility, which services a population of approximately 19,000 in the Northern Territory, covering an area which is approximately 1.5 times that of the UK. It provides a 24-hour emergency service, a maternity ward with 14 beds, a general medical and surgical ward with 28 beds (including 1 palliative care bed), an 18-bed children’s ward, a renal dialysis unit, a radiology department, pathology and the Northern Territory Aerial Medical Services, which provides a 24-hour emergency retrieval service, co-ordinated with Gove District Hospital and the Royal Darwin Hospital, where the on-call doctor is based. The renal dialysis unit is staffed by a trained Aboriginal Health Worker and renal trained registered nurses, with clinical nursing support provided by Royal Darwin Hospital:
[T]here aren’t any specialist staff resident in the hospital and it is 300 kilometres from Darwin so it is not too far for a specialist to travel to do clinics and do lists and that sort of thing. There is no plan to expand it because the population is not expanding very quickly and it works reasonably well.
KI-A02
Source: Northern Territory Government. 224
Several key informants highlighted the key role of telehealth technology in supporting the provision of services in rural and remote settings (KI-A01, KI-A02, KI-A04, KI-A06), although one expert interviewed for this study highlighted that the development of telehealth had not been progressed as far as it could have [‘We also have very poor internet infrastructure in Australia so that does not help’ (KI-A03)].
Benefits and disadvantages of community hospitals
There is some empirical evidence about the impacts of community hospitals on patient and service outcomes in the Australian context, but this tends to draw on small case studies analysing the feasibility of providing a given service and typically involving a before–after assessment of impact only. For example, two linked studies described the provision of emergency services in a small rural hospital in Victoria, which provided a 17-bed ward for medical, surgical and palliative inpatient care, radiography, ultrasound and pathology services and an on-site GP clinic, as well as three emergency department beds. 40,77 This found that the small size and lack of dedicated emergency department staff restricted the ability of the hospital to match the performance of major metropolitan emergency departments. This was seen to be particularly challenging in view of an ageing population and large proportion of after-hours presentations.
A small number of studies examined the use and impact of telehealth services such as teleophthalmology,44 rural videoconference fracture clinics50 or telepharmacy. 86 These found evidence of varying quality and robustness on the potential for telehealth technology to enhance patient and service outcomes, such as earlier diagnosis and treatment, a shorter hospital stay (where required) and avoided travel for an eye care service using internet consultation provided by a small regional hospital in Western Australia. 44 A reduction in unnecessary patient transfers to the tertiary referral centre was also reported for videoconference fracture clinics provided by a small rural hospital in Queensland. 50 The latter study also showed that, although the cost of running the videoconferencing clinic was initially higher than the costs saved because of avoided patient transfers, there was an overall saving for the health service in the second year of operating the clinic. A third study assessed the feasibility of implementing pharmaceutical review using videoconferencing between remote pharmacists and patients in two rural hospitals in Queensland, finding the service to lead to improved documentation of medications and reduced medication risk. 86
Aside from these studies, much of what is known about the benefits of small rural hospitals in Australia tends to be anecdotal:
Based on just my past experience and talking to people [. . .] So you know we do have an aging population, in many of these towns they have lost populations. There is no point in maintaining larger hospital facilities that are no longer needed whilst the population is aging and you know needing care. So I think that they are successful because they have actually been responsive to changes in the population.
KI-A02
One key informant highlighted the challenges of evaluating community-based programmes and service delivery models, because of their small size, ‘but there is a great deal of belief so you end up with this knowledge gap which is a challenge when we try and protect the funding of smaller services’ (KI-A03). What is known is that populations in rural and remote settings tend to have a higher utilisation of services, with evidence of higher rates of potentially avoidable deaths,225 although the degree to which this is attributable to the quality of service delivery locally remains poorly understood (KI-A04).
Challenges faced by community hospitals
Key informants interviewed for this study pointed to a number of challenges faced by community hospitals, and these related mostly to workforce and funding issues. There were differing views about the nature of workforce challenges, although there was agreement that rural and remote communities faced particular difficulties:
So especially if there are only a couple of GPs they can get quite isolated and the life can be quite difficult [on] 24/7 call, 7 days a week, 365 days a year and very often in these rural remote communities they might be staffed by international medical graduates who are, you know, have to work in a rural and remote area to get [the] full licence [. . .] So workforce issues are pretty dramatic in remote Australia.
KI-A01
There have been efforts to try to address these challenges, through, for example, the establishment of rural clinical and regional medical schools,226 with emerging evidence pointing to a positive impact in terms of attracting and retaining graduates to work in rural areas. 227 One key informant commented that this gave cause for optimism to ‘get on top of the workforce issue’ (KI-A02), while another key informant noted that, although there had been a ‘massive expansion in the number of medical students’, this was unlikely to address the challenge of attracting graduates to work in rural and remote settings ‘because most of the medical students are living in the cities and they’re not going to go and work in the country’ (KI-A01). This is in part because GPs can set up practice anywhere in the country, and most settle in inner cities and in the more attractive rural communities, and ‘there is nothing you can do to reallocate those GPs, you have to attract them to small rural communities’ (KI-A03).
The overall role of the GP varies across states and regions within states. One key informant noted that it was financially attractive for GPs to provide services in rural hospitals because general practices generate income through Medicare plus additional charging where they operate private practices (which is, however, not typically the case in very remote communities) (KI-A02). The state government, which funds hospitals, would then pay an additional stipend to the GP to run the hospital, as for example in Queensland:
[It] is a substantial amount that makes it worth their while to run the hospital. For a lot of them where general practice might not be as viable as it could be, that makes the big difference between you know make or break in maintaining their practice in that country town. So what they get from the state government is actually quite important to sustain those services.
KI-A02
In other states, small rural hospitals would not have a GP as clinical lead but it would be attended by a visiting medical officer. A GP cannot be formal lead because they are a private provider and, as such, the GP cannot be employed by the hospital (KI-A06). Instead, there would be a facility manager or a health service manager who would then contract a GP as visiting medical officer or some other form of agreement that would involve the GP providing clinics at the hospital on a fee-for-service basis. This situation can, however, become challenging in places where services are organised in a different way, such as in Victoria where many smaller hospitals operate as single organisations. One key informant noted that these hospitals will find it increasingly difficult to pay for after-hours services delivered by GPs, because ‘[GPs are] starting to increase the amount that they’re asking for beyond what the small hospitals are funded’ (KI-A03).
Overall, the funding situation is complex because of multiple funding sources, which is particularly challenging for small health services because they have to report back (on different performance indicators) to multiple funders (KI-A02):
[B]ecause we have a federal level of government and a state level of government, it is a very confusing policy space from the perspective of those small hospitals [. . .] There are things that are caused by our federal state system, like the fact that a hospital cannot employ a GP or finds it very difficult to contact with a GP because of the fact that they are federal rather than state, which sort of blurs some of what they do.
KI-A03
Future changes in community hospital provision
Small hospitals in rural and remote areas in Australia are facing several challenges, such as maintaining services and attracting staff, along with economic viability within constrained resources. This has led to an increase in closures of a number of small hospitals over the past decade (KI-A04):142
Rationally, they can’t operate [. . .] and the occupancy rates is so low, it’s very hard to argue that they’re operating efficiently and it’s increasingly evident that it’s hard to operate things safely, for anything with fairly low security levels.
KI-A05
However, at the same time, such facilities are seen to be indispensable in remote communities ‘where a patient can be stabilised and evacuated because the distances are significant’ (KI-A01), although this service might not necessarily be provided by a hospital as such. One key informant interviewed for this study noted that the general policy direction was to (re-)encourage the development of rural generalists, that is, GPs who have additional skills, such as in anaesthesia or surgery or obstetrics (KI-A01). Rural generalists (or rural generalist medicine) have been defined as practitioners who have the skills to provide unsupervised community or primary care, inpatient and emergency care in a hospital or related setting, extended specialised services in at least one approved medical discipline required to sustain comprehensive health-care services in regional, rural and remote communities, services across the continuum of care in a range of settings and service delivery models including outreach where required, such as community paediatrics or palliative care, and who are able to apply a population-health approach with relevance to the community in which they practice. 228 Training is provided, for example, through the Australian College of Rural and Remote Medicine. 228
There has also been a move, in most states, to transform small rural hospitals into alternative settings, such as residential aged care facilities, community medical centres or multipurpose health centres (KI-A05, KI-A06). This is illustrated by the example of Victoria, where public hospitals have a relatively high number of residential care beds, in effect representing residential aged care facilities, with community health visiting specialists (KI-A05). New South Wales has invested in the redevelopment of small rural hospitals into MPSs in response to an ageing population and the need to ensure appropriate care (KI-A06). This was part of the MPS Program, which was established in 1993. 229 A joint initiative of the federal and state governments, the services are designed to specifically address the needs of small rural and remote communities that could not viably support stand-alone hospitals or aged care homes. 143 Usually administered by the state or territory health department, MPSs bring together a range of health and residential aged care services on one site, with co-location of GP and ambulance services through pooling the funding across programme boundaries, so overcoming some of the challenges posed by the otherwise fragmenting system of health services and aged care funding. 230 They are available in all states except for the Australian Capital Territory:
It is a good model actually [. . .] It is a way of transforming small acute care facilities to meet acute, aged care residential care facilities. So that is quite common now and is a very successful model with the aging of the rural population.
KI-A02
Some will have inpatient beds or are co-located with a residential care facility. MPSs typically provide up to 10 beds, but they can be flexible and, depending on demand, beds can be redefined as acute beds or as respite beds to meet the needs of the local community (KI-A04). Available evidence has shown that the MPS model is responsive to community needs and able to tailor services to individual community needs. 143 The model allows sharing of staff among services, which may lead to the achievement of economies of scale through the amalgamation of acute and aged care services, which will be particularly important to enable small communities to sustain services.
These efforts form part of ongoing reforms across Australia to strengthen co-ordination between primary and hospital care as well as aged care to better meet the challenges of the rising burden of chronic disease and Australia’s ageing population. There are ongoing discussions of options for reforming the roles and responsibilities of the federal and the state governments in regulating and funding health services in Australia. These developments will probably impact on the future evolution of community hospitals in the country.
Annex A: public hospital categories in Australia, 2013–14
| Hospital peer group | Description | Average number of beds (range)a | Average length of stay, days (range)a | Typical location | Number in 2013/14 |
|---|---|---|---|---|---|
| Principal referral hospitals | Acute hospitals that provide a broad range of services, have a range of highly specialised service units and very large patient volumes. Most include an intensive care unit, a cardiac surgery unit, a neurosurgery unit, an infectious diseases unit and a 24-hour emergency department | 651 (358–1023) | 3.5 (2.5–4.7) | Mostly major cities | 29 |
| Public acute group A hospitals | Provide a wide range of services, typically including a 24-hour emergency department, intensive care unit, coronary care unit and oncology unit | 254 (79–503) | 3.1 (1.4–5.6) | Major cities and regional areas | 62 |
| Public acute group B hospitals | Provide a 24-hour emergency department, elective surgery and specialised service units such as obstetric, paediatric and psychiatric units | 123 (66–373) | 2.7 (1.9–4.1) | Major cities and regional areas | 45 |
| Public acute group C hospitals | Usually provide an obstetric unit, surgical services and some form of emergency facility | 42 (10–181) | 3.1 (1.4–12) | Mostly regional areas | 143 |
| Public acute group D hospitals | Offer a smaller range of services relative to the other public acute hospital groups | 17 (0–75) | 4.7 (1.1–25.7) | Mostly regional and remote areas | 191 |
| Very small hospitals | Have few beds and provide care for few admitted patients; most do not perform surgery | 8 (0–34) (public) | 13.2 (0–193.2) (public) | Mostly regional and remote areas | 136 |
| Women’s and children’s hospitals | Specialise in the treatment and care of women and/or children | Children’s: 216 (141–290); women’s: 168 (122–252) | Children’s: 2.7 (2.4–4.1); women’s: 3.7 (2.8–4.6) | Major cities | 13 |
| Psychiatric hospitals | Specialising in providing psychiatric care and/or treatment for people with a mental disorder or psychiatric disability | Varies by type | Varies by type | Mostly major cities | 19 |
| Subacute and non-acute hospitals | Include hospitals that primarily provide rehabilitation care and geriatric evaluation and management, as well as mixed subacute and non-acute hospitals that provide palliative care, geriatric evaluation and management, psychogeriatric care and non-acute (maintenance) care | Varies by type | Varies by type | Major cities and regional areas | 39 |
| Outpatient hospitals | Provide a range of non-admitted patient services and do not usually admit patients | N/A | N/A | Mostly remote areas | 42 |
| Other | Diverse group of hospitals not grouped under any of the above | Varies by type | Varies by type | Mostly major cities | 28 |
| TOTAL | 747 | ||||
Finland
Finland is a parliamentary republic located in Northern Europe, bordered by Norway to the north, Sweden to the west, the Russian Federation to the east and Estonia to the south, across the Gulf of Finland. 117 Finland is among the largest countries in Europe in terms of area covered, but with a population of 5.47 million at the end of 2014,231 it is among the most sparsely populated, at an average of 18 inhabitants per km2. The majority of the population is located in the urban areas in the southern and western parts of the country; around one-third of the population lives in rural areas. The country is divided into 18 regions plus the Åland Islands and, in early 2016, 313 self-governing municipalities. 232
Health system context
Finland’s highly decentralised health system is mainly funded through local and national taxation. Delivery of health care is predominantly public, with municipal taxes accounting for almost half of all funding, which is supplemented by state subsidies, national health insurance (NHI) contributions and some copayments. In 2013, taxation accounted for 61.0% of total health expenditure, with another 14.3% financed from NHI and 18.5% from out-of-pocket payments. 121 Out-of-pocket payments are mainly patient copayments for pharmaceuticals, physician appointments in health centres, outpatient specialist visits, and day and inpatient care, among other services. 117 Preventative, maternal and child health services are free at the point of use. In 2013, national health expenditure was 8.6% of GDP, which was lower than the OECD average at 8.9% (UK: 8.5%). 121 However, per capita expenditure was fairly similar, at US$3,442 PPP in Finland (2013) compared with an OECD average of US$3,453 PPP (UK: US$3,235 PPP).
Health system governance in Finland is shared by central government and the municipalities. The role of central government in health and social care is largely that of a steering function; the Ministry of Social Affairs and Health directs social welfare and health-care policy and services at the national level. It prepares major reforms and proposals for legislation, monitors their implementation and supports the government in decision-making. 233 Municipalities are responsible for organising health and social services; they organise primary care and, following the 1993 state subsidy for public services reform, they are also responsible for all secondary and tertiary care costs. 207 Employed persons can also access occupational health services, which are free at the point of use, and which are part-funded through the NHI, with approximately 80% of employed persons covered by employer-purchased primary care-level services. 234
The past 10 years have seen a series of reforms seeking to restructure local administration to enhance the sustainability of service provision in view of an ageing population. Initiated in 2005, the Paras reform project sought to create a larger population base for service delivery (with a population of 20,000 set as the minimum for primary care services) through the voluntary merger of municipalities, and their number subsequently decreased by some 70 to around 350 in 2009, while municipality co-operation in organising primary care services increased. 235 The Paras reform project was followed by a new local government reform in 2011, which sought to further decrease the number of municipalities and to restructure the health-care system, with a particular view to strengthen the primary care infrastructure and address rising health inequalities. In 2013, municipalities in Finland had an average population of about 17,000, although half had < 6000 residents. 232 The government has committed to further reform the administrative system to enhance productivity and effectiveness in the delivery of public services (see below).
In parallel, the 2010 Health Care Act, which came into force in May 2011, sought to enhance access to services by introducing patient choice of primary care and secondary care provider outside their area of residence and a joint register of patient records between primary and secondary care. 234 It also introduced provisions for all local authority health centres to co-ordinate services.
More recently, the government has embarked, as part of a new government strategic programme 2015–2018, on a major social welfare and health-care reform, which seeks to ensure equitable health-care and social welfare services and to bridge a sustainability gap of EUR 3M. 236 It includes the creation of 18 larger, autonomous regions that will be responsible for a wider range of tasks, including the organisation of social welfare and health services, as of January 2019. 237 The reform foresees the ‘complete horizontal and vertical integration of services’ and aims to create their seamless delivery. 158 Importantly, local authorities will no longer be responsible for financing health-care and social welfare services, and the government is currently exploring alternative funding options. Central government supervision of social welfare and health care is expected to be strengthened overall. The regions will be governed by elected councils, which will be responsible for organising services in their area through providing services themselves or together with other autonomous regions, or through purchasing services from the private or third sector. The reform foresees, in preparation for the Social Welfare and Health Care Arrangements Act, an exploration of local or central government funding models as alternative funding options. The draft bill was expected to be presented to Parliament by the end of 2016.
Organisation of the health-care system
Figure 9 shows health-care expenditure in Finland by function, highlighting that in 2013 specialised health care accounted for over one-third of total health expenditure, of which about half (18%) was spent on (somatic) inpatient care, followed by primary health care (17%) and pharmaceuticals (13%). 238
FIGURE 9.
Health-care expenditure by function as percentage of total health expenditure, Finland, 2013. Note: the category ‘other’ includes therapeutically appliances such as spectacles (2.3%), administration (178%), capital investment (5.6%) and transport (1.8%). Based on National Institute for Health and Welfare material. 238
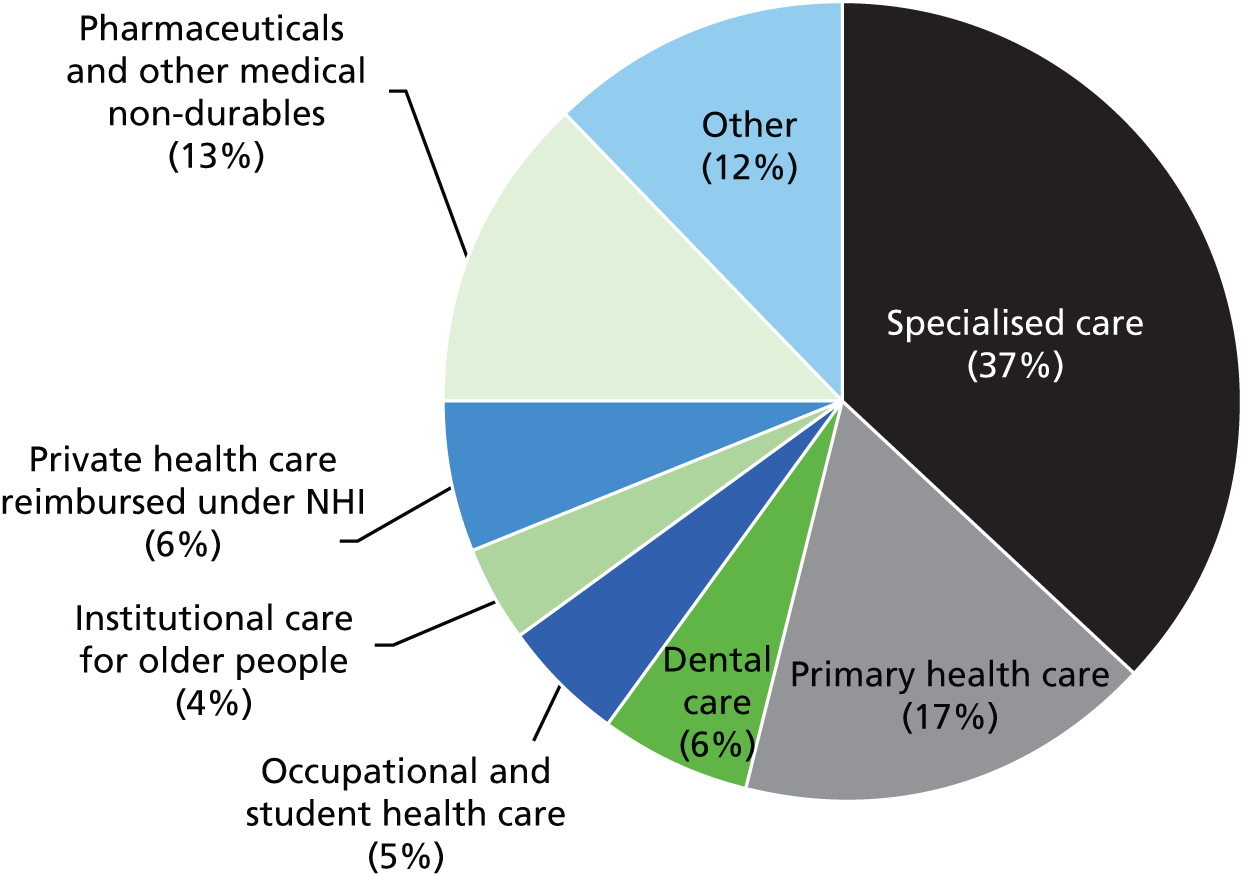
As noted above, in Finland, municipalities are currently responsible for the organisation of health and social services. They organise primary care and, through participation in hospital districts, secondary and tertiary care. As per the 1972 Primary Health Care Act they are obliged to maintain health centres for the provision of primary care services, and they do so either on their own or jointly through a local federation of municipalities. 117 They may also purchase services from other municipalities, third-sector organisations or for-profit providers.
In 2014, local authorities operated some 172 health centres; 106 of these were municipal health centres, and the remainder belonged to joint municipal authorities formed by several local authorities. 239 Employers also provide primary care services for their employees as part of occupational health services; these are jointly financed by NHI, employers and employees, and are offered by company-owned health-care units, municipal health centres or, in most cases, private providers. 117 Private health-care providers such as enterprises and third-sector organisations and foundations must be licensed; they can provide services directly to patients or contract with local authorities or joint municipal authorities. In 2009, Finland introduced a new law on social and health-care vouchers, which sought to create more flexible conditions for local authorities to contract with private providers; however, although this was seen to have resulted in several municipalities increasing their purchasing of health and social care services from the private sector, others sought to reduce the role of private provision in their local systems because of the higher costs associated with private provision. 240,241 According to the Ministry of Social Affairs and Health, private providers currently account for about one-quarter of all social welfare and health-care services. 242
Finland operates a gatekeeping system in which patients are assigned to a GP at their local health centre, with recent moves to broaden choice of primary care provider within geographical limits in line with the aforementioned 2010 Health Care Act. 237 However, in contrast to other countries that operate gatekeeping systems, services offered within primary care in Finland can include those that elsewhere would be considered specialist care. 151 This can be seen to have its origins in the development of the health-care sector before the 1972 primary care reform. That reform introduced municipal health centres, which partly evolved from small local hospitals and, as a result, health centres can offer a wide range of services, including GP-led inpatient units, and they are well equipped with medical technology, including facilities for minor surgery and diagnostic equipment. 117 This means that services such as minor surgery or the availability of equipment for near patient diagnostic testing in general practice form a core part of primary care in Finland.
Municipal health centres comprise a range of professionals including GPs, nurses, midwives, social workers, dentists, physiotherapists and psychologists. Physicians working in municipal health centres are typically employed by the municipality and they receive a combination of basic salary and variable added payments and bonuses. The exact remuneration method varies among municipalities. 243 Physicians working in occupational health centres are reimbursed by the NHI and by employers, each of which contributes 50%. The NHI also reimburses private physicians who provide primary care services, which, until recently, was for about 30% of the costs, but this has been reduced since. They also receive direct patient payments.
The 1993 state subsidy for public services reform mentioned above, which made local municipalities responsible for all secondary and tertiary care costs, prompted the introduction of alternatives to specialist care in hospital, such as the contracting of specialists to provide clinics in primary care. 234 In larger cities, the co-location of primary care teams and specialists in newly integrated organisations is common. 151 Some health centres directly employ geriatricians as internal consultants, while in other cases a visiting consulting doctor will perform this task in the health centre. In 2013, more than one-third of health centres provided specialist consultations, including psychiatry, typically by contracting relevant services from the respective hospital district. 157
During the past 10–15 years, there have been moves to merge primary and secondary care providers into single organisations. These reforms aim to improve the co-ordination of services, which are typically organised separately by municipalities and hospital districts, and to reduce inefficiencies of care provision, especially in smaller municipalities. One specific example is the Kainuu region in the eastern part of Finland, which, since 2005, has been experimenting with transferring about 60% of municipal activities, including health and social care, to the regional level to enhance the efficiency of public service delivery and to promote regional development. 244 There is some evidence that the experiment has led to improved availability and quality of services, although evidence on whether or not this experiment has led to tangible cost savings remains uncertain. 245 The experiment came to an end in 2012, following a decision by the municipalities involved. 244
Organisation, financing and delivery of hospital care
Municipalities form hospital districts that are responsible for the provision of specialised health care, and each municipality must belong to a hospital district. 246 There are 20 hospital districts in mainland Finland, which were established in the mid-20th century;247 the autonomous Åland Islands organise and provide health care according to the Act on the Autonomy of Åland. 248 The 1989 Act on Specialised Medical Care brought all municipal hospitals under the ownership and management of the hospital districts. 182
Hospital districts cover populations of between 50,000 and 1.2 million inhabitants, and they are responsible for organising and providing all inpatient and outpatient specialised health care within a region, as well as supplying them with the necessary funding. 249 Hospital districts provide specialist services that cannot be delivered at the primary care level, although this varies considerably between hospital districts. They are also responsible for the co-ordination and quality control of municipal laboratory and imaging services, medical rehabilitation and other specialised services, as well as research, development, education and training along with the harmonisation of municipal health-care information systems. 246
Most hospital districts have a central hospital and in some districts specialised care is supplemented by small regional hospitals. 250 However, it is difficult to distinguish categories, as there is no formal definition of what constitutes a ‘regional hospital’. Each hospital district belongs to one of the five university hospital catchment areas; districts are expected to co-ordinate the provision of specialised care, information systems, medical rehabilitation and procurement. 246 University hospitals provide tertiary care and also act as the central hospital for their respective hospital district. Hospitals provide inpatient and outpatient services. In 2013, about half of resources allocated to specialised care were spent on inpatient care, around 30% on outpatient services and 4% on day-care surgery; the remaining 15% were allocated to other specialised care, largely psychiatric inpatient and day care. 238 As indicated above, some acute somatic care is also provided by health centres that are owned by municipalities or joint municipality authorities, or private hospitals.
Each hospital district is governed by a council and an executive board, whose members are appointed by the participating municipal councils, in proportion to the size of each municipality. 251 District councils are thus directly accountable to the municipalities.
The number of hospitals in Finland has declined over the past decades, as has the number of hospital beds (Figures 10 and 11). In 2013, there were 259 hospitals in Finland, down from 391 in 1995, whereas the total number of beds was 26,429 (including general hospital, long-term care and other specialised hospital beds). 121 This equated to 4.9 beds per 1000 population, similar to the OECD average of 4.8 beds per 1000 population in 2012 but higher than the UK, at 2.8.
FIGURE 10.
Total number of hospitals and hospitals per million population Finland, 1995–2013 (all hospitals). Based on OECD. 121
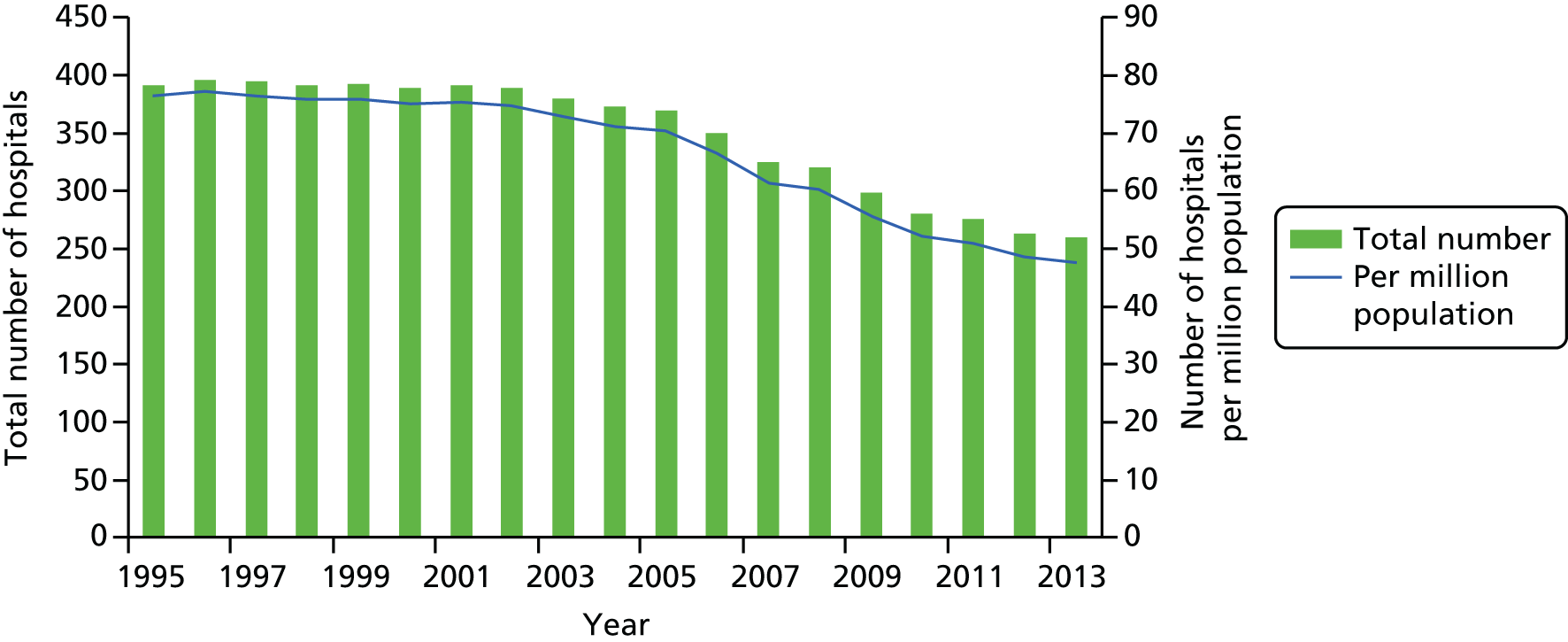
In addition, in 2013 about 58% of beds were acute care beds, up from 47% in 2000, while the proportion of long-term beds was 27%, down from 39% in 2000. When relating the number of long-term care beds to the population aged ≥ 65 years, the proportion of long-term beds has fallen by almost 75% over the past 15 years, reflecting Finland’s efforts during the 2000s to shift long-term beds from hospital to other settings and an overall trend to help older people remain independent in their own homes through the provision of home care and supporting informal carers or, where this is not possible, offering community-based solutions such as sheltered accommodation instead of residential care homes. 252,253 In 2013, of all hospital beds, around 96% were public beds and 4% were private for-profit; these proportions have changed only slightly compared with figures in 2000, when some 97% of hospital beds were public and just over 3% were private for-profit. 121
The steady reduction in the number of hospitals and hospital beds over the past 10–15 years mirrors trends seen in other European countries, partly reflecting a shift from inpatient to day care, and from specialised outpatient provided in hospital to the community. 254 However, Figures 10 and 11 also indicate that the fall in the number of hospitals and hospital beds appears to have accelerated from 2007/8. This trend has been attributed, at least in part, to the global financial crisis of the late 2000s, and the introduction of policies encouraging the centralisation of emergency and specialised care in particular. 255
Overall, and as a result of these various efforts, the number of all hospital discharges has fallen by almost 20% since 2000, from 213 per 1000 population in 2001 to 173 in 2013 (OECD average in 2013: 155/1000; UK: 129/1000). 121
Responsibility for planning health services, including hospital services, is currently largely devolved to the municipalities, which receive a lump sum subsidy for health care from the central government. The subsidy is calculated for each of five service categories (care for the elderly and long-term hospital care; consultations with primary care physicians and nurses; other primary care such as preventative services and occupational health care; specialised care; and psychiatric care), although municipalities may also use subsidies for purposes other than health care. 251
The role of the central government in planning has so far been limited mainly to establishing the general framework for the organisation and principles of health care, largely through national legislation. Until recently, the steering tool at national level was the National Development Plan for Social Welfare and Health Care (Kaste Programme), drawn up by each incoming government for the forthcoming four years in government, with the latest covering the period 2012–15. 256 The programme defined the key social and health policy targets, priority action areas, guidelines and recommendations with the aim for actors at national, regional and local level to work together to implement the reforms. 256
The main mechanism for planning involves annual negotiations and agreements between the hospital districts and individual municipalities, with different contractual or negotiation mechanisms between hospital districts and municipalities for agreeing target volumes and payments, reflecting differences in geographic size, number of facilities and other factors. 251
Hospital districts also plan capital investments, in consultation with their member municipalities. There are only a few general standards for capacity planning in the hospital sector and no national norms for bed capacity.
As noted, hospital districts negotiate targets for services that they have to provide with municipalities or groups of municipalities (the so-called ‘steering by agreement’ approach; however, agreements do not constitute a formal contract). Targets apply to outpatient and inpatient services and are usually based on historical service utilisation figures, although some areas also include projections of anticipated changes in demography and morbidity. Many of these targets are defined on the basis of case classifications, using DRGs.
Hospital districts are managed and funded by the member municipalities, with funding mainly based on municipalities’ payments to hospital districts,250 as per the aforementioned 1993 state subsidy reform. In 2013, the share of state and municipal payments of all costs for specialised somatic care was 92%; the remaining 8% was from private sources, half of which was direct household expenditure, while the other half was covered by voluntary health insurance. 238 The Government defines the maximum fees that hospitals may charge for inpatient day, outpatient visits and day surgery; in practice, hospitals tend to charge the maximum fees. 250 An annual ceiling applies to user charges, after which services are provided free of charge for the patient.
The budget of each hospital district is formally decided by its council; it also approves the financial statements (such as payment methods and prices). Hospital payments made by municipalities are based on the total budget and the predicted use of services. 250 Each hospital district determines the payment methods used to reimburse its hospitals and approaches vary between districts. Over the years, districts have gradually moved away from a price-per-bed-day approach towards case-based pricing, using DRGs. The first national guidelines for specialised care DRGs were published at the end of 2012, and this was expected to reduce the variation among districts regarding the principles and rules for DRG usage. A compensation scheme has been introduced to reduce municipalities’ financial risk from expensive patients; this scheme allows for the cost of treatment per patient that exceeds a certain threshold to be shared between all the member municipalities of a hospital district. 250
The approach to hospital organisation and financing will be subject to considerable change following the 2015–18 government programme mentioned earlier. Specifically, it foresees a reform of the division of responsibilities of hospitals in order to centralise part of specialised health care in catchment areas under the direction of the Ministry of Social Affairs and Health. 236 The hospital reform was drawn up in February 2016 and will be implemented during 2017–18, in advance of the comprehensive social and health-care reform (KI-F05). Among the key features of the hospital reform will be gradual centralisation of all hospital care to 18 central hospitals, involving the transfer of 24/7 services to 12 ‘full service’ acute hospitals in addition to six to eight 24/7 emergency hospitals with more limited service provision.
Community hospitals in Finland
Defining the community hospital
In Finland, the term community hospital as used in the context of the NHS in the UK does not exist. However, there are service delivery models in place that resemble some of the key features of the traditional community hospital as conceptualised in the UK. The previous sections have shown that municipal health centres, which were established following the 1972 primary care reform in Finland, partly evolved from small local hospitals and that they offer a wide range of services, including GP-led inpatient units. 117 These are frequently referred to as health centre hospitals [‘We do not talk about community hospitals we talk of health centre hospitals’ (KI-F04)] or health centre inpatient wards and they provide short- and long-term (≥ 90 days) inpatient care. 252,253
There is no clear definition of the ‘health centre hospital’. The 1972 Primary Health Care Act describes the purpose of hospital beds provided at health centres, specifying that these beds:
Shall primarily be assigned to the patients that it is most expedient to care for [. . .] in view of the nature of the illness and the need for examinations, care and medical rehabilitation, or the degree of convalescence. A person in need of urgent institutional care shall always be assigned to a health centre hospital bed or, if the necessary examinations or care cannot be provided there, must be instructed to use, or consigned to, an appropriate medical care institution. 129
As noted, health centre hospitals partly evolved from the conversion of small local or district hospitals into municipal health centres in the context of the 1972 primary care reform. Subsequent to the reform, newly formed municipal health centres that were not linked to a former local or district hospital also established inpatient wards, for the reason:
That not all patients needing inpatient care are in need of specialised care led by specialists. Typically, frail, elderly, terminal care patients and so on, could quite as well be placed in smaller units closer to their home community, so that’s the explicit reason for that.
KI-F04
Care provided in health centre hospitals is considered inpatient care, as set out in the 2010 Health Care Act, while explicitly falling under primary care services. 182 It is for this reason that national data formally distinguish inpatient primary health care from inpatient specialised care. 238 Furthermore, a health centre may also comprise a specialist-led hospital. 257 This tends to be the case in larger cities that have a city hospital (KI-F04, KI-F05), which is administratively overseen by the municipal health centre ‘but the actual care given in those units is typical specialised care’ (KI-F04). This complicates interpreting national data on the utilisation of health centre inpatient care services at present.
For example, in 2014, just under 143,000 patients received health centre inpatient care, accounting for some 4.4 million care days. 257 Although the annual number of patients has remained at around 145,000 since the early 2000s, the number of care days has almost halved since then, as reflected in the average length of stay, which fell from just over 30 days in 2003 to 22.3 days in 2014. About two-thirds of patients were aged 75 years and older, accounting for about 75% of all health centre inpatient care days; those aged 85 years and over accounted for about one-third of patients and for about 40% of inpatient care days. The number of patients and of inpatient days varied by region, as does average length of stay, ranging from 11.3 days to 54 days.
The most common primary diagnosis for inpatients in health centres were circulatory diseases, with an average length of stay of 29 days, followed by injury and poisoning and other selected external causes (23 days), respiratory diseases (14.5 days) and mental and behavioural disorders (45 days).
As noted above, health centre hospitals offer short- and long-term care beds, although the latter form only a small proportion of the total number of patients in health centre hospitals. For example, in 2014, the number of patients aged 75 years and older residing in health centre hospitals as long-term inpatients was 2920 (3% of all patients in health centre hospitals), or 0.6% of the population in this age group, with proportions ranging from 0.2% in the Satakunta region in the south-west of Finland to 1.9% in North Karelia. 257 The proportion of older people receiving institutional care in health centres has fallen substantially since the early 2000s (Figure 12), in particular from 2009 onwards, reflecting the increasing trend away from institutionalised care towards the home-based care and sheltered accommodation alternatives mentioned earlier. 253 It is worth noting, however, that the proportion of older people receiving regular home care has changed only slightly during the 2000s, fluctuating between 11% and 12%,257 because the regular use of home care has tended to focus on those in greatest need. 253
FIGURE 12.
Long-term inpatients in health centres (as a proportion of the population in the relevant age group), 2000–14. Based on National Institute for Health and Welfare. 257

The total expenditure on inpatient primary care has declined from 6.8% of total health expenditure in 2000 to 5.8% in 2013, with much of the decline attributable to a large reduction in expenditure on long-term care, by 55%, while expenditure on short-term inpatient care rose from 3.2% to 3.8%. 238
Types of community hospitals and services provided
Health centre hospitals provide subacute and post-acute or intermediate care following discharge from an acute care hospital (KI-F01, KI-F02, KI-F05). Their role is to look after people who are not sufficiently unwell to be in an acute care hospital but who are clinically too unstable to be in their own home or the nursing home. The subacute function includes an entire spectrum of cases, from ‘simple’ infections requiring the administering of intravenous antibiotics to terminally ill people requiring palliative care (KI-F02). Health centre hospitals previously also provided 24/7 emergency services but this function has been transferred to general acute care hospitals during recent years (KI-F05).
Health centre hospitals are seen to be principally very similar in terms of the type of patients they take care of; the main difference is that of local context in terms of size of the community and the availability of other services provided (KI-F01, KI-F02):
Like the line between elderly persons’ homes and these inpatient health centres, so in some municipality’s maybe a more chronically ill patient is taken care of in the elderly persons’ homes and in some municipalities the same person would be taken care of at the [health centre] patient ward – the line can vary between municipalities, but not I think very much.
KI-F01
One key informant interviewed for this study highlighted the impact of the 1993 state subsidy for public services reform. As described above, it made local municipalities responsible for all secondary and tertiary care costs and this led to a change in the composition of patients cared for in health centre hospitals, and ‘they lost much of their professional attraction and gradually became long-term care facilities for the elderly, especially those with memory disorders’ (KI-F05).
Health centre hospital staffing would typically include a GP, a head nurse, physiotherapists, nurses, health-care assistants and, depending on the size of the municipality, social workers (KI-F02). In larger municipalities or cities, health centres would also have medical specialists such as in internal medicine and geriatrics available, and in places such as Helsinki neurology as well. The work of the GP can be exclusively on the ward, depending on the organisation and size of the health centre. For example, centres might divide work differently, having for example three GPs looking after patients on the ward while also taking care of regular health centre patients (KI-F02).
The lead physician of the health centre determines whether or not a patient requires admission to the health centre hospital as stipulated in the 1972 Primary Health Care Act; the lead physician is also in charge of determining any transfers of patients to other medical care institutions. 129 Admission can be from acute care, nursing homes or people’s own homes.
Given the origins of health centres as described above, the range of services provided would typically include the inpatient ward, an outpatient clinic, physiotherapy and a small radiography unit and very basic laboratory services (KI-F01) (Box 5). Some municipal health centres would also employ specialists such as a surgeon or a specialist in internal medicine. One key informant interviewed for this study pointed to the example of a municipal health centre in the very northern part of Finland, where the inpatient ward would be doing ‘a bit more than normal’ (KI-F01), because of its remote location.
The Northern Satakunta basic-service–public-utility federation of municipalities was established in 2009. Located in south-western Finland, it brings together five municipalities and provides residents with a wide range of social and health care including parental and child health clinics, adult health clinics and adult social work, health clinics for senior citizens and home care, specialist services including physician and nursing care, oral health care, physical therapy and radiography, along with a range of support services.
There is one main health centre located in Kankaanpää municipality, plus five basic service centres in each of the five municipalities that form the federation. The main health centre offers urgent care services provided by physicians and nurses, as well as inpatient care, rehabilitation, radiography and medical examinations such as gastrointestinal endoscopies and urological examinations. These can be accessed on referral by a speciality and health centre physician. Speciality services also include dental care provided at the basic service centres and at Kankaanpää dental clinic.
The main health centre includes two inpatient wards, each with 40 beds. Patient referral to the inpatient ward can be through an emergency care physician, their treating physician or speciality care nurses. The main objective of the inpatient ward is to provide high-quality, GP-led services to residents in the region in collaboration with the patient and their carers. The two inpatient wards are similar in terms of their organisational structure. The operational principle is based on rehabilitative nursing, with patients encouraged and supported to manage their condition according to their own resources.
Source: Kilpeläinen. 258
At present, it is difficult to determine the number of beds in municipal health centres with certainty, and there appears to be no central guidance on the planning of beds to be hosted by health centre hospitals. Typically, there would be between 25 and 40 in one ward, but some health centres have two wards (KI-F02). The decision about size of the health centre and number of beds in inpatient wards is usually made by the municipal council (KI-F01, KI-F02).
Benefits and disadvantages of community hospitals
There is some empirical evidence on the impacts of community hospitals on processes and outcomes of care in Finland. A small number of studies examined the outcomes of people with COPD treated in primary care hospitals compared with secondary care hospitals. Lampela et al. 259 analysed hospitalisations for acute exacerbations of COPD among patients aged ≥ 45 years during the period 1995–2001 by specialty (general practice, pulmonary medicine, internal medicine). They found a general increase in the number of admissions during the observation period, of 11%, with the largest rise seen among those supervised by a GP (36.8%), suggesting a shift in the responsibility for COPD to primary care. This was attributed, in part, to a national programme for COPD and the related training provided for GPs, but also to financial motivations. Subsequently, the same authors specifically examined outcomes of COPD treatment by hospital site for the period 1995/6–2004. They found a reduced risk of death among those managed by a GP relative to those managed by a pulmonary specialist, at 0.83 (95% CI 0.75 to 0.91). 148 Conversely, a related study showed that COPD patients discharged from primary care hospitals had a greater risk of readmission within 7 days of discharge, compared with those discharged from secondary care. 149 The readmission risk was highest among those aged < 65 years, but not among those aged ≥ 85 years. The authors discussed a range of possible explanations for this observation, including differences in treatment procedures and arrangement of subsequent care, along with differences in disease severity (which they were unable to assess) and admission threshold, which may differ between the different levels of care.
Four key informants interviewed for this study generally believed that health centre hospitals could provide a useful ‘buffer between specialised healthcare and then nursing homes, residential homes or [sheltered] accommodation’ (KI-F01). The main benefit was seen to be the location of the health centre hospital close to people’s homes, which was considered to be an important feature given the geographic dispersion of the population in Finland, in particular for older people who can stay close to their relatives (KI-F02, KI-F05). One key informant commented that care provided in health centre hospitals can be seen to be more holistic or person-centred because the patients and their circumstances are known to health centre staff, as are the local services that are available to patients, such as home care services or sheltered accommodation. It can also be seen to be efficient in that they allow more specialised care provided by the hospital district ‘to concentrate on the real work, on the specialised care’ (KI-F02).
Challenges faced by community hospitals
Key informants also recognised the challenges posed by the current system:
We have also an amount of people with, I would say in the wrong place, because we don’t have always enough sheltered housing. So when the people need [. . .] during the whole day or 24 hours a day some kind of help and they have to wait for that kind of housing place, we have these also in there. That is the problem in the process.
KI-F02
It was noted that where health centre hospitals worked well, they were very successful in meeting their ambition of keeping people out of acute care hospitals, through for example investing in intensive rehabilitation for people following discharge from acute care (KI-F04, KI-F05):
Those advanced municipalities. So they have lots of rehabilitation type of activities for the elderly, in this unit. They know that if the specialised care hospital makes the elderly stay in bed for a week or two, that game is lost. So the more advanced municipalities try to invest in this type of rehabilitation wards, in the health centre hospitals.
KI-F04
However, key informants also highlighted that in several cases this was not achieved and, instead, that health centre hospitals had tended to develop into geriatric long-term care units, a ‘very long term geriatric patient repository type of thing which was not the idea’ (KI-F04).
There were some concerns among those interviewed for this study with regard to attracting health-care workers, especially in rural or remote areas in eastern and northern Finland with younger people moving away (KI-F01). However, the challenge to attract health-care workers has to be seen in the general context of workforce challenges in Finland (KI-F05):
[W]e have problems with finding enough doctors to work in the primary health-care centres. And to work on the ward it’s more demanding than in [outpatients], so that it is not so easy but because if you go to work to the health centre you are [a] worker there then the employer can decide that you are working in the open or in the ward. But of course, we always try to find people who really can and want to do those works because there are a lot of jobs to choose [from] so that if they say they have to go there then the workers say goodbye.
KI-F02
A recent increase in medical graduates is expected to overcome some of these challenges (KI-F05). Larger health centres may find it easier to recruit because they provide opportunity for GPs and nurses to work with specialists in internal medicine or geriatrics, for example (KI-F02). This may be particularly attractive for younger doctors given the characteristics of the patient population, that is, older patients with complex health and care problems. One key informant reported on experiences of ways to attract workers, highlighting the need to offer flexible terms of employment and allowing workers to, for example, ‘continue their studies or do research, or work in private sector also [. . .] It has to be some kind of a combination that this kind of a people and specialists are willing to work in a public sector and city hospital’ (KI-F03).
Future changes in community hospital provision
Key informants interviewed for this study agreed that the future of health centre hospitals should be seen in the context of the wider challenges faced by the health system in Finland:
One of the questions which is topical at the moment, and which should be discussed in all the Finnish municipalities, is how to develop the ambulatory specialised care, or, as I would say, how to abolish the division between primary and secondary care.
KI-F04
There was a perception among those interviewed for this study that health centre hospitals should be complementary to the specialist services provided for by the hospital district (central and university hospitals) to avoid duplication of services, because the municipality has to cover the associated cost either way (KI-F01). However, there may be a risk of duplication in regions where there is a city hospital, which is administratively overseen by the municipal health centre, and the central hospital provided by the hospital district (KI-F01, KI-F04). There was consensus about the probable impact of the ongoing government reforms, in particular for those municipal health centres that are operating specialised health-care services, and the need to cut these services, although perhaps not affecting those health centre hospitals that really provide GP-led care (KI-F04).
Earlier sections of this report noted that there has been a substantial fall in the proportion of older people receiving institutional care in health centres, in particular from the mid-2000s. One survey of municipal health centres carried out in 2013 noted that about 40% of the centres that had responded to the survey (141 of 151 approached) had reported changes in inpatient care, such as the closure or transition of services to other settings. 157 That study did not provide any further detail about the nature of these reported changes but this is likely to reflect, at least in part, the ongoing trend across Finland towards moving people out of institutional care into alternative settings. The main driver is seen to have been financial but the change was also seen to be motivated by the ‘ideology of promoting home care as long as possible’ (KI-F05). One key informant interviewed for this study questioned the success of these policies and noted:
So one thing municipalities actually do is they’ll change the name of the nursing home to [sheltered] housing, everything stays the same, but it’s a positive step for the municipality and social institutions will pay the bills [. . .] there won’t be any change for the people living there.
KI-F01
This statement is somewhat in contrast to the perception of one other key informant from one municipality that has begun moving patients from the health centre hospital to sheltered accommodation who reported anecdotal evidence that the quality of life had improved for those concerned:
Not in every case, but it might be with the majority of the patients [. . .] They have a lot of open possibilities for different kind of activities. They have their own rooms and so on, so I guess we are sure that we have a better quality in [sheltered accommodation] than how the hospital works’.
KI-F03
It is not possible, on the basis of these two contrasting views, to arrive at an overall conclusion about the best way forward, although there was consensus among all key informants interviewed for this study that the organisation of specialist services in the present system would need to change, in particular those provided in smaller hospitals, because of their perceived lower quality (KI-F01). There was also recognition, however, that this is going to take ‘a long time because it’s the small municipalities that have these regional hospitals and they don’t like the idea that it’s going to be taken away from them’ (KI-F01). Furthermore, where health centre hospitals are closed altogether this would require support for workers, especially nurses who would be expected to work in a different environment (home care services, city or regional hospital), and providing this type of support should form a key part of the ongoing reform efforts (KI-F-03).
There was consensus among key informants that the ongoing reforms could provide considerable opportunities to rethink the processes by which health care is being delivered. Key informants (KI-F02, KI-F04) saw the reform to provide an opportunity to enhance seamless care between primary care and specialist care that will then eventually also help to reduce the number of beds in health centre hospitals:
And I’m sure that after 10 years we still have those wards in smaller, not in so many municipalities as we have now. But we are going to have them but I’m sure we are also having much [. . .] better processes [. . .] I hope there are no more so strict borders between primary health care and specialised health care and we are concentrating more on the process and during the process patient’s needs different kind of professionals.
KI-F02
They also noted that these sorts of changes needed to be developed in a measured way, rather than forcing the reforms through too fast in order to achieve sustainable transformation.
Italy
Italy is a parliamentary republic located in southern Europe. 118 It borders France, Switzerland, Austria and Slovenia to the north and south, and comprises the Italian Peninsula and the two Mediterranean islands of Sicily and Sardinia, along with a cluster of smaller islands. With a population of just under 61 million in 2014 and an average population density of 200 inhabitants per km2,260 Italy is among the most densely populated countries in the European Union. Most of the population is centred around metropolitan areas and along the coast, whereas the mountainous parts of the country, which cover about half of the territory, account for < 20% of the total population.
Health system context
Health care in Italy is provided through the National Health Service [Servizio Sanitario Nazionale (SSN)]. Established in 1978, the SSN guarantees universal access to comprehensive care throughout the country. The system is funded through national and regional taxation, accounting for 77.1% of total health expenditure (2013), with another 18.8% financed from out-of-pocket payments; social security contributions and voluntary health insurance play a minor role. 121 Out-of-pocket payments are mainly patient copayments for diagnostic procedures, pharmaceuticals, specialist visits and non-urgent care in hospital emergency departments. 118 Primary and inpatient care are free at the point of use. In 2013, national health expenditure was 8.8% of GDP,121 which was only slightly lower than the OECD average at 8.9% (UK: 8.5%). Per capita expenditure was also slightly lower than the OECD average, at US$3077 PPP (2013) compared with US$3453 PPP (UK: US$3235 PPP).
Following a gradual process of decentralisation, regions have assumed considerable legislative, administrative and regulatory powers over the years, which was substantially strengthened following the 2001 constitutional reform. 118 Overall responsibility for health-care governance is shared between the central government and the 20 regions (with the region of Trentino-Alto-Adige being split into the Autonomous Province of Trento and the Autonomous Province of Bolzano). 261 The central government provides the legislative framework for health care and defines the basic principles and objectives within which the SSN operates. It defines, through the Ministry of Health, the core benefit basket and standard of health services provided by the regions [Livelli Essenziali di Assistenza (LEA); ‘essential levels of care’],251 with the State-Regions Conference having an important role in priority setting and determining criteria for resource allocation. The regions are responsible for organising and funding health care, by means of allocating resources set at the national level, and there is considerable variation in how regions exercise their autonomy.
During the past decade, reform efforts have focused on containing health-care expenditure without reducing access to health services. 155 The regionalised nature of the health system remains a challenge, with differences in performance regarding service delivery and large variations between the northern and southern parts of the country. 262 The most recent attempt at comprehensive reform was the 2012 Balduzzi decree, which, among other things, revised the basic benefit basket for the first time since 2001 and involved a restructuring of the governance of hospitals and local health units. 118 It further proposed a reorganisation of primary care into teams of professionals to provide 24-hour coverage and ensure continuity of care, continuing attempts at the regional level to strengthen primary care through promoting the collaboration between GPs and other providers. These provisions were to be further strengthened as per the 2014–16 health agreement (Patto per la Salute), a 3-year financial and planning agreement between the central government and the regions. It explicitly set out to strengthen system governance and to enhance the quality and efficiency of services, for example through the reorganisation of primary care and the establishment of community hospitals for the delivery of subacute care. 140,263 A subsequent review introduced further explicit measures to control costs, including a reduction of the national health-care budget by 1.8% for 2015, along with measures to reduce the inappropriate use of specialist services through requiring GPs to provide evidence of the need for a referral, with failure to do so incurring a financial penalty, while inappropriate hospital rehabilitation stays will be only partially reimbursed when not aligned with national guidelines. 264,265 However, although the 2014–16 health agreement has provided further support for the stipulations set out in the Balduzzi decree,266 it has yet to be fully implemented. 263,267
Organisation of the health-care system
The accounting system in place for the Italian SSN does currently not allow the disaggregation of health-care expenditure according to the different sectors of spending. However, drawing on the present accounting classification, which provides information about some but not all levels of care and SSN directives about financing rules, Cislaghi and Zucchetti268 estimated that, in 2011, some 44% of the budget allocation was on hospital care, just over half (51%) of which was for services delivered at the district level and the remainder of which was for prevention services (Figure 13).
FIGURE 13.
Allocation of resources to the basic benefit package (LEA) items (percentage of national health fund), Italy, 2011. Based on data from Cislaghi and Zucchetti. 268
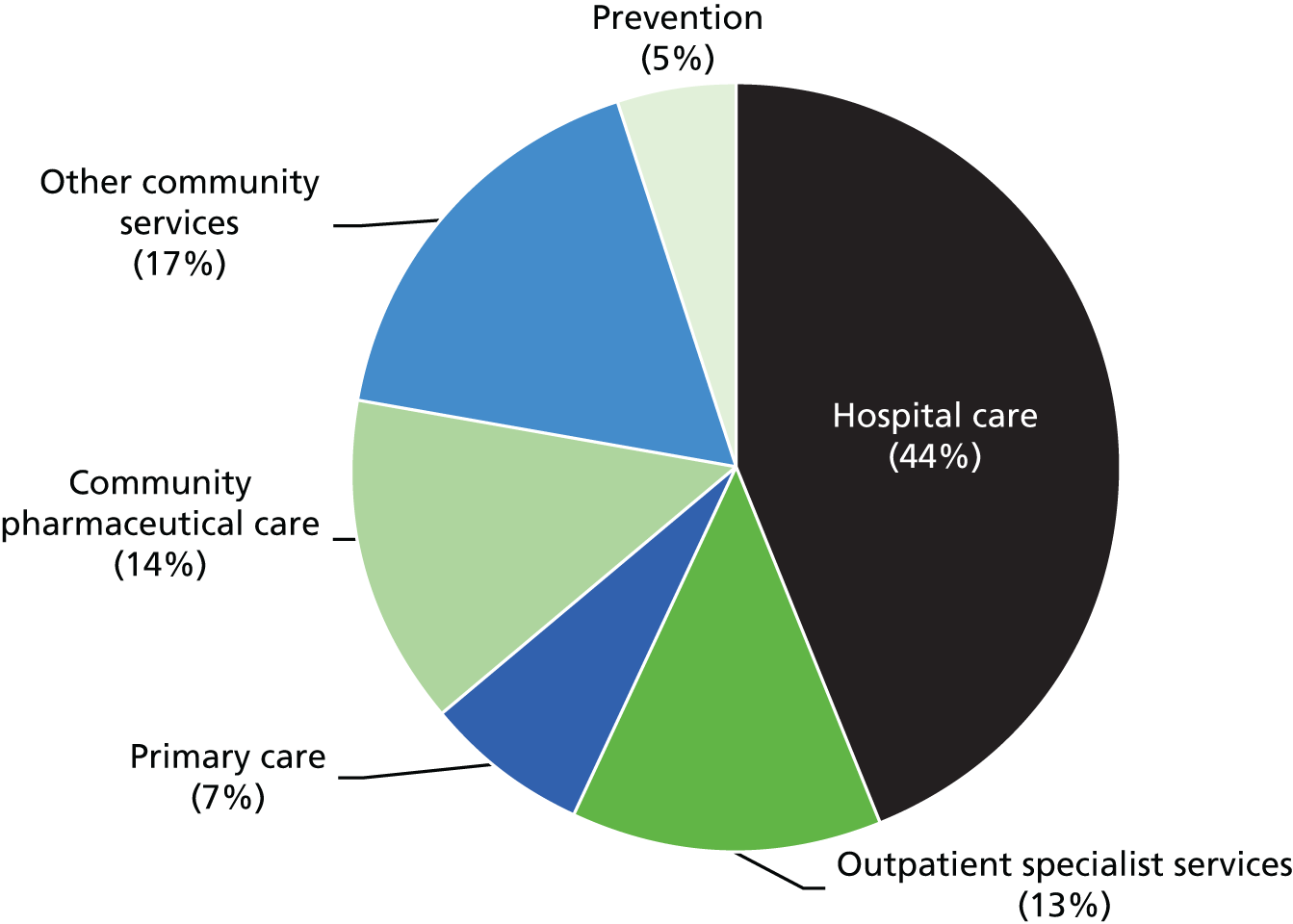
Health-care delivery rests with geographically defined, population-based local health authorities, the Aziende Sanitarie Locali (ASL). 118 Further divided into districts, ASLs organise primary, secondary and tertiary health care by contracting with public and private hospitals and overseeing office-based GPs. 269 In 2015, there were 139 ASLs, down from 228 in 1995. 270
Primary care is defined as the ‘hub’ for delivering first contact care in the Italian SSN. It is tasked with health promotion and education, the diagnosis and treatment of acute and chronic diseases in different settings from ambulatory care to home care, and ensuring continuity of care through appropriate co-ordination. 118 GPs and paediatricians are at the core of delivering ambulatory care outside hospital and they are, organisationally, included within health districts. GPs and paediatricians (acting as GPs for children) are self-employed and operate under a national contract, which is complemented by regional agreements. They are paid a capitation fee related to the number of patients registered with their practice (up to 1500 for GPs and 800 for paediatricians) plus a share based on participation in public health interventions (vaccination and screening) and other activities (e.g. home visits), as well as additional payments according to specific performance indicators (typically set at regional and local level). 118,269 Residents are free to choose a GP who will act as a gatekeeper to specialist care, and they may access certain specialists, such as gynaecologists, directly. Direct access is also guaranteed for private specialist services. Specialist care is provided by public and private providers in hospital outpatient departments, clinics and doctors’ offices, generally delivered by self-employed specialist physicians contracted by the SSN. 263
Over the past 15 years there have been attempts to reorganise the delivery of primary care away from the traditional model of GPs and other health professionals working in solo practice to a more integrated approach that brings together the different health-care providers in multiprofessional teams to better meet the health and social care needs of the local population. 118 This has included, as part of the 2000 national GP contract (ACN), the introduction of financial incentives to encourage the development of new forms of collaboration and working in group practices. This has led to the formation of different forms of teamworking, from the co-ordination of individual practices with regard to opening times (medicina in associazione) to advanced group practices (medicina di gruppo), which involves the sharing by GPs of a clinic or practice. 271 Subsequent efforts included the introduction, in 2005, of primary care centres (Unità Territoriali per l’Assistenza Primaria), and, in 2009, of the (multiprofessional) complex primary care unit [Unità Complesse di Cure Primarie (UCCP)], involving GPs, specialists, nurses and social workers, and of functional (monoprofessional) territorial collective practices (Aggregazioni Funzionali Territoriali). The 2009 ACN also made the participation of GPs in any existing form of group practice compulsory. 271
Following these changes, a wide range of models have been implemented in different regions, with GPs in advanced group practices and in network group practices tending to be the most common model, while more complex group practice formations involving multiprofessional teams are evolving more slowly. 123 For example, Emilia-Romagna has established primary care units (Nuclei delle cure primarie), which bring together GPs, paediatricians and other professionals in the district, who share care facilities, nursing resources and specialist resources in order to ensure continuity of care, extended access to out-of-hours care services and improved home care services. 272 More recently, following a resolution by the Regional Council in 2010, Emilia-Romagna has introduced the ‘house of health’ (Case della salute), which oversees access to and provision of health and social care services in the district. The aim is to ensure continuity of care 24 hours a day 7 days a week by providing a single point of access and initial needs assessment, through co-ordinating the primary care units with other service providers in the district, including specialist and inpatient care, public health and mental health by means of nurse-led case management. 146 Campania, Marche, Lazio and Tuscany regions are in the process of implementing, or have already implemented, similar models, frequently involving the conversion of the existing hospital infrastructure to house these new integrated models of care. 123,273
More recently, the 2014–16 Health Agreement has made it a requirement for all regions to establish multiprofessional complex primary care units (UCCPs) and linked territorial collective practices (Aggregazioni Funzionali Territoriali) to replace all GP group practices and networks described above. 263 However, challenges remain regarding the implementation of multiprofessional group practices and more integrated service delivery models. A core challenge is the separation of (financial) responsibility for health services, which rests with the ASLs, from that for social care, which is overseen by the municipality (Box 6). Only a few regions, including those mentioned above, along with Veneto and Marche regions, have so far been able to partly overcome these challenges through combining the management and financing of health and social care services. 118
In Italy, municipalities have responsibility for supporting non-self-sufficient individuals with assets that fall below a certain threshold. Financial support is on a means-tested basis and covers home help (housework and personal care) and nursing homes. Conversely, health services that are delivered in nursing homes and in the community setting more broadly, such as the home nursing service, home hospitalisation and programmed home care assistance by GPs, are funded by the SSN,274 and this creates challenges for the provision of seamless care across sectors. In some Italian regions municipalities have delegated part of their social care duties to ASLs, which is expected to improve the co-ordination between health-care and social care activities. However, the non-universal nature of social care makes co-ordination challenging and often dependent on the local context.
Organisation, financing and delivery of hospital care
Public hospitals are either directly managed by ASLs or are independent hospital enterprises or trusts (Aziende Ospedaliere), with a larger degree of financial and technical autonomy. 251 Private hospitals require accreditation according to regionally defined standards to qualify for SSN reimbursement. Hospitals typically provide both outpatient and inpatient care and, in addition to the aforementioned independent hospital trusts (Aziende Ospedaliere), which are accountable to the regions and provide tertiary care with a high level of specialisation, they are formally distinguished into teaching hospitals (Aziende Ospedaliere Universitarie and Policlinici Universitari); national hospitals for scientific research [Istituti di ricovero e cura a carattere scientifico (IRCCS)]; district general hospitals (Presidi Ospedalieri), which are directly managed by ASLs; single-specialty hospitals, such as those for maternity services or orthopaedics; and religious hospitals (Ospedali classificati). Virtually all psychiatric hospitals were closed following psychiatric reform legislation in 1978, which prohibited new admissions and were thus discontinued. 118 Mental health care is now provided in specialised units in general hospitals or managed in community facilities.
On a functional level, according to the national legislation, Italy’s hospital network is organised into three levels according to specialisation and capacity to provide emergency care. 118 Basic hospitals cover a catchment population of between 80,000 and 150,000 residents; they provide emergency services and a small set of specialist services. Level I hospitals serve a population of 150,000–300,000; they host a first-level A&E department and provide a large number of specialty medical services that are available on call. This includes the provision of radiology services, ultrasound, laboratory services and immune transfusion services that have to be available 24 hours a day, either on site or through other arrangements. Level II hospitals serve a catchment area of 600,000 to 1.2 million residents; they mainly comprise hospital trusts, university hospitals and IRCCS and provide the same set of services as level I hospitals, with the added provision of more specialised services to address more complex health conditions. Given the powers of regions on organisational matters, the free choice of hospital by patients and the presence of the private sector in many jurisdictions, the organisation of hospital networks varies across regions.
Community hospitals (see below) are not considered part of the hospital sector, as they do not meet the defined infrastructure, technological and staff requirements for the provision of hospital care; consequently, they are not reimbursed according to the DRG system. They are managed by the ASLs. Residential facilities with long-term care beds [Residenza Sanitaria Assistenziale (RSAs)] are either private or public and, if private, are not under the direct control of the SSN. 118 In some publications, RSAs are also referred to as nursing homes but the function fulfilled by these structures varies across regions.
Doctors working in public hospitals are salaried employees, as are those working in public health and occupational medicine. About 20% of a doctor’s salary is determined by grade and performance; they may also practise privately, as long as they are not in competition with the employing hospital’s interests. 269
The number of hospitals in Italy has declined over the past decades, as has the number of hospital beds (Figures 14 and 15). According to the latest data available, in 2012, there were 1152 hospitals in Italy, compared with just under 1760 in 1990, while the total number of beds was 203,723 (including acute care and specialised hospital beds), or 3.4 beds per 1000 population (OECD average 2013: 4.8 beds per 1000 population; UK: 2.8). 121
FIGURE 14.
Total number of hospitals and hospitals per million population in Italy, 1990–2012. Based on OECD. 121
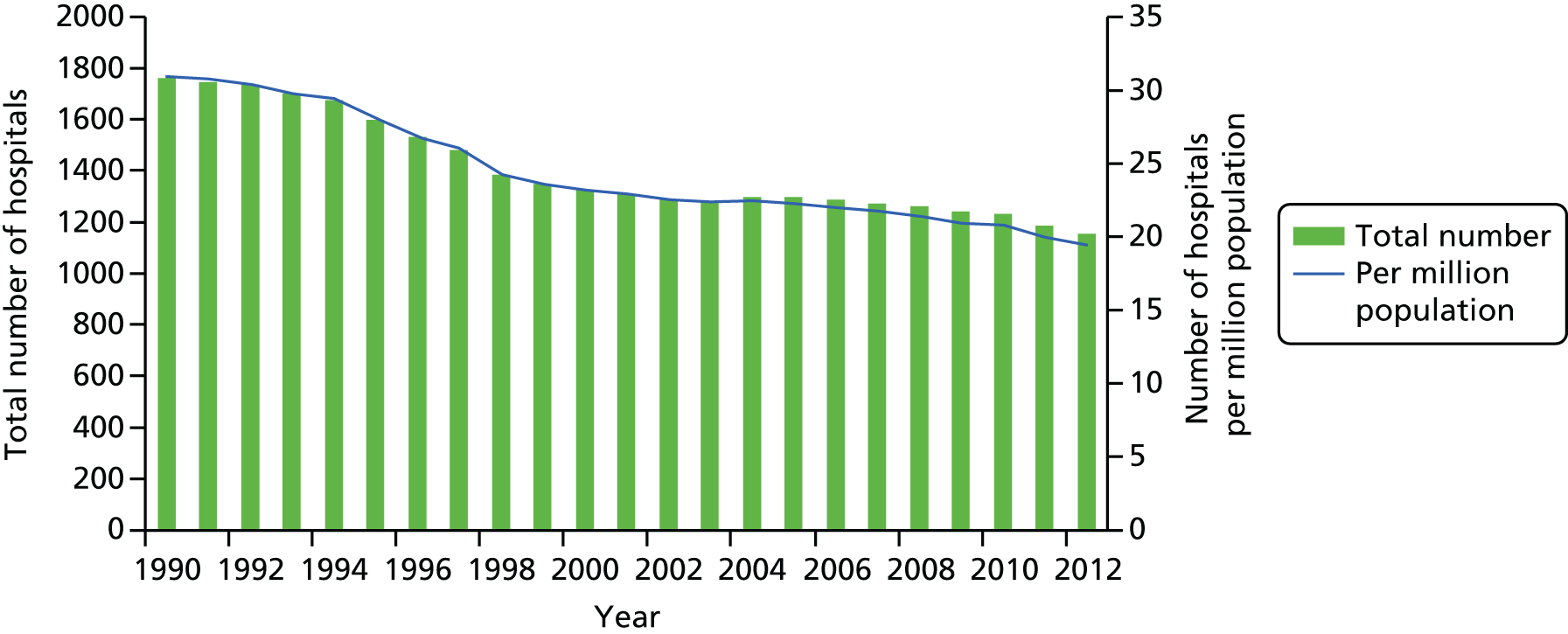
In addition, in 2012, around 80% of beds were acute care beds. Although over half (55%) of all hospitals were in the private for-profit sector, the share of private for-profit beds was 28%; the majority of beds were in the public sector, at 68.5% and the remainder were in the private not-for-profit sector. 121 These proportions have changed only slightly compared with the early 2000s, when some 70% of hospital beds were public and 27% were private for-profit. 121 The highest number of beds in private facilities accredited by the SSN were in the regions of Lazio, Campania and Lombardy. 118
The steady reduction in the number of hospitals and hospital beds reflects a policy context aimed at controlling health expenditure, increasing hospital efficiency and improving quality. 118 For example, the 2001 legislation defined a standardised number of beds per acute care facility (affecting public and private SSN accredited institutions), which was further revised in the 2010–12 health agreement, setting a regional standard for the average number of beds at four beds per 1000 population (including 0.7 beds per 1000 for rehabilitation and long-term care). This was to be achieved through shifting from inpatient to day care, and from day hospital to ambulatory care along with better provision of home care services for those requiring long-term care. More recent stipulations (Law 135/2012, commonly referred to as ‘spending review’ and subsequent decree no. 70/2015) introduced a new target for an overall national average of 3.7 beds per 1000 population, of which 0.7/1000 were to be dedicated to rehabilitation and long-term care. The 2012 legislation also set a target of 160 hospitalisations per 1000 population, of which 25% should be provided in a day-hospital setting.
The reduction in the number of hospital facilities (and beds) occurred mainly through the closure of small hospitals or the conversion of acute care facilities into other types of facilities and services in order to better meet the changing needs of an ageing population. 118 The way hospitals are organised and managed has also changed, and there has been development of new innovative approaches to capital assets and working practices.
Overall, and as a result of these various efforts, the number of all hospital discharges fell by almost 30% since 2000, from 173 per 1000 population in 2001 to 124 in 2013 (OECD average in 2013: 155/1000; UK: 129/1000),121 with reductions most pronounced in regions such as Calabria, Friuli Venezia Giulia, Apulia and Campania. 118
The planning of capital investments, expensive health technologies and bed capacity has been devolved to the regions. This is executed within the regional health plan, which every region has to adopt within 150 days of the introduction of the triennial national health plan, the main instrument for national-level health-care planning. 118 The regional health plan typically includes aspects such as the distribution of beds in secondary, emergency and long-term care, the size and location of hospitals, and the integration between health and social care. Regional planning usually involves all providers of health care, both public and private (for-profit and not-for-profit), although approaches vary widely across regions. 249 At present, eleven regions, mainly those in the north of the country, have established a regional agency for health that is responsible for supporting the regional health department in its executive functions as well as providing technical and scientific support to the ASLs and hospitals. According to Ferré et al. ,118 several regions are increasingly moving away from a hospital-centred form of regional planning towards one that integrates primary and community health services and encompasses the whole range of health-care services.
Since 1995, hospitals have been partly funded through a DRG-based prospective payment system, complemented by capitation and/or grants for a number of specific services. 275 DRG tariffs are set at the national level, although regions can modify the tariffs implemented in their own health systems within the limits set by the national framework. As a consequence, there is considerable variation across regions in the way payment and monitoring are implemented. 118 The DRG system does not apply to hospitals that are directly operated by ASLs, or to long-term care, which is paid for using a bed-day rate. However, as in the case for acute care, in order to prevent long stays, a progressive rate reduction scheme is applied to both rehabilitation and long-term care. Outpatient specialist care, diagnostic services and imaging are reimbursed using tariffs that are defined by unit of service. Regions are permitted to set their own tariff which is, however, guided by a national rate; as a result, there is considerable variation among regions.
Community hospitals in Italy
Defining the community hospital
In Italy, the development of community hospitals (Ospedale di Comunità) has been described as ‘a very fragmented experience’ (KI-I02). They were set up from the mid-1990s onwards, with the Emilia-Romagna region being the first to introduce such structures in the provinces of Premilcuore (1995) and Modigliana (1996). 138 Adapted from models in place in the UK, the concept of the community hospital in Italy spread steadily in a number of regions, including, as well as Emilia-Romagna, the regions of Tuscany and Marche, followed by Umbria, Puglia, Friuli Venezia Giulia, Piedmont and Lazio, with the majority having incorporated community hospitals into their regional health legislation. 137
A common feature of the early community hospitals in Italy was their ‘bottom up’ evolution in the absence of a national framework on how to address the rising need for integrated health and social care planning and provision. 138 Initially also referred to as ‘country hospital’, the Italian National Syndicate of Territorial Doctors described this new structure as ‘a territorial social health facility, developed in response to the health needs of those who do not require, in the view of the family doctor, the complexity of secondary care but at the same time whose health and social care needs cannot, for various reasons, be adequately addressed in his/her home environment’. 276 Subsequently, the Italian Federation of General Practitioners offered, in 2003, a refined definition, which describes the community hospital as a regional health structure within the network of district services, which:
-
provides for the direct management of beds by GPs of that catchment area, aimed at service users, mainly dependent older people, who do not require hospitalisation but who cannot be cared for in their own homes
-
is managed by GPs and allows for person-centred care and medium- to low-level clinical interventions appropriate for the management of chronic degenerative diseases and people with a range of social care needs
-
is placed at the interface (‘buffer’ or ‘bridge’) between the hospital and the community through a network of home care services and nursing homes.
A review of the early experiences of community hospitals in Italy presented in 2003 noted that their nature and scope varied considerably, reflecting to a great extent the local context in which they were implemented. 138 It further highlighted that the flexibility of the community hospital model was to be seen to be one of its major advantages and was the result of the absence of a rigid legislative framework. This permitted multiple experimentations but has posed challenges to the systematic comparison of different models. Despite this heterogeneity, the review identified three basic models:
-
The ‘rural model’ (modello rurale): defined by the hourly availability of a defined number of GPs who individually agree to be present for a set number of hours/time slots in the facility to provide care where required. GPs are remunerated by a set daily fee against specific goals of care that they are committed to achieve. Bed numbers vary between 5 and 8 beds up to a maximum of 12–15 beds. As is typical for small and medium-sized towns, the model was most commonly found in Emilia-Romagna and Marche.
-
In the ‘metropolitan model’ (modello metropolitano), the GPs sign up with the facility on the basis of a programme that is agreed in advance (with the district director, etc.) and with fixed dates (weekly, biweekly, monthly) to monitor inpatients. Usually found in urban centres, where the number of doctors who can provide care is high, the model varies widely, with the number of beds ranging from 8 to 12 up to a few tens. It appeared to be the most common approach in Tuscany, Umbria and Friuli Venezia Giulia.
-
In the joint (misto) model, the clinical responsibility of GPs is shared with specialists or other staff. The model provides for the simultaneous presence of the GP (access or time slot) and medical staff in various forms of integration. It was most common in Marche and Umbria.
A further model that did emerge in some parts of Italy was described as the ‘hospital model’, which, in contrast to the community hospital that is normally managed by a GP, is managed by hospital doctors.
The first formal mention of the community hospital in national-level strategies came only in the national health plan 2006–8, which, in the context of a proposed reorganisation of primary care, highlighted the need for the development of intermediate care services and of GP-led community hospitals. 139 This notion of a community hospital as a structure within the Italian health-care system was only recently strengthened further, following the aforementioned Law 135/2012 on the reorganisation of hospital care, which envisaged that community hospitals to would play an important part in the delivery of more integrated services at the local level. This was further detailed in subsequent regulations (Box 7), and the 2014–16 health agreement described above requires the establishment of community hospitals for the delivery of subacute care, with the overarching aim of reducing the number of inappropriate admissions to acute care hospitals and facilitating the discharge of patients from acute care. 140
National regulation defines the community hospital as ‘a structure with a limited number of beds (15-20) [that is] managed by nurses, and in which medical care is provided by GPs or paediatricians or other medical staff contracted by the SSN’. 23 The district holds the organisational and managerial responsibility and also ensures ‘the necessary specialist advice’. 107 In line with the regulations, the core function of the community hospital is to take charge of patients who require health care that cannot be provided in the home environment of the patient (because of structural and/or family reasons) or who need continuous nursing supervision. The average stay in the community hospital is expected to be around 15–20 days, and admission can be from the patient’s home or a residential care facility upon referral by the patient’s GP, the hospital ward or directly from the emergency room. Care is expected to be provided on a 24-hour basis by nursing and health-care assistant staff, GPs, paediatricians and out-of-hours or continuous care physicians. The community hospital can be physically located in converted hospitals or residential care facilities.
The number of community hospitals in Italy slowly increased over time, from 23 in 2003138 to 57 in 2009. 137 Distributed across eleven regions (Emilia-Romagna, Tuscany, Marche, Umbria, Puglia, Friuli Venezia Giulia, Piedmont, Lazio, Liguria, Veneto, Lombardy), some 200 municipalities were involved in the provision of community hospitals in 2009, covering a population of about 2 million. The total number of beds provided was about 700, which were overseen by an estimated 500 GPs and at least 1000 nurses and other health-care workers. It is difficult to arrive at more recent estimates for the number of community hospitals across Italy. This is in part because of the continued evolution of the role of the community hospital in the local context, and, perhaps more importantly and as we shall see below, because of the 2015 national legislation, which required regions to implement the stipulations set out in the national framework. 107
Types of community hospitals and services provided
Despite the recent formal definition of a community hospital in the national regulation, it remains difficult to map this conceptualisation to facilities ‘on the ground’ (KI-I01). One way of describing community hospitals in Italy is by identifying what they are not. Thus, the community hospital is generally not seen to be a long-term care institution for the chronically ill. This function is fulfilled by the RSAs, which have wards for seriously chronically ill patients. Community hospitals are not hospices either, as they are not designed to admit patients in the very terminal phase of their life. However, boundaries are not clear cut, with some community hospitals hosting or co-located with RSAs or providing a hospice function.
One key informant suggested differentiating two principal types or functions of community hospitals in the contemporary health system in Italy, namely subacute and post-acute functions (KI-I01):
-
Subacute: targeted at people aged ≥ 75 years with multiple conditions, who require (nursing) assistance that cannot be provided by their informal carers in their own homes; aimed at preventing admission to acute care hospital. They tend to be more common in rural areas.
-
Post-acute: intermediate care delivered in small hospitals or in separate units in larger hospitals; nurse-led, with support from health-care assistants; aimed at reducing length of stay in acute care hospitals. Post-acute care units or facilities tend to be located in urban areas.
A further form of community hospital are long-stay (lungodegenza)/rehabilitation beds, a combination of long-term care and geriatric rehabilitation with an average length of stay of about 60 days, which aims to stabilise the patient and support the family in the transition of the patient to a nursing home.
It is beyond the scope of this study to present an inventory of the wide range of community hospitals that have been established across Italy. Instead, we report on a small set of regions that have had experiences of community hospitals and for which publicly available documentation allowed for an assessment of the most recent developments. These are Emilia Romagna, Veneto, Marche and Friuli Venezia Giulia. Tuscany, which was also among the regions with experiences in developing community hospital-type structures, pursued, from 2013, a reorganisation of the regional health service, which foresaw, among other things, the integration of primary care with intermediate and hospital care of medium to low intensity, by means of establishing houses of health and the use of community hospitals, RSA and hospices as locations for intermediate care delivery. 277 However, from January 2016, the Tuscan health system has undergone a major reform, involving the merger of its 12 ASLs into three larger co-ordinating authorities (area vasta), which will further impact the organisation of regional health services. 278
Emilia-Romagna
The health authority of Emilia-Romagna described, in a 2013 programmatic document, community hospitals as structures that are designed ‘to achieve specific health goals through the provision of intermediate care models that sit between home care and hospitalisation, for particular types of patients who would unnecessarily be kept in (an acute care) hospital, could be treated appropriately outside hospital, but not in their own home’. 145 A model of care that ‘represents a healthcare setting, and not a substitute for social care’,279 the community hospital principally targets two types of eligible patients:145
-
patients, mainly older people, who have been discharged from acute care or rehabilitation because they are medically stable but not in a position to be appropriately cared for in their own homes (e.g. patients with chronic heart failure, or with neurological conditions), or who are otherwise unable to continue rehabilitation therapy because of the complexity of their condition. This reduces the length of hospital stay and ensures that the patient is cared for in a protected environment (post acute).
-
fragile patients or those with chronic conditions who are referred from their homes or from residential care homes because they are clinically unstable (e.g. exacerbation of pre-existing chronic disease, or new destabilising event, such as the after-effects of cancer treatment).
Referral to the community hospital can be through the treating GP or the treating physician of other facilities (residential care home, nursing home, etc.), as well as from acute care, following specific protocols developed at the regional level (KI-I04).
Medical care is provided by the treating community hospital GP or the GP of the house of health, which hosts the community hospital, where applicable. A nursing co-ordinator is in charge of the managerial and organisational operation of a unit of 20 beds, overseeing the management of hospital admissions and discharges and the planning of the activities of health-care assistants and other professionals required to carry out the individualised care plan. This includes physical therapists, psychologists, community nurses (case manager), social workers, caregivers, as well as the GPs or specialists who have referred the patient to the facility.
The average length of stay in the hospital should not exceed 6 weeks and should be around 15 days. The discharge process follows regional protocols (KI-I04) and involves a multidimensional assessment by the attending physician, the nurse case manager and home care and social care providers, as well as any appropriate specialists, to help develop the subsequent care plan addressing the health and social care needs of the patient. 145
The 2013 programmatic document further emphasises the active involvement of patients and their caregivers to be among the primary objectives of the recovery process. This is to be delivered through providing training for the management of the condition/s and the early detection of any signs of instability. 145
As described above, Emilia-Romagna was the first region to have developed the community hospital concept, with many such structures emerging as a consequence of converting acute care hospitals. This development was accelerated as part of the 2013–14 regional health plan, with nine local hospitals converted into community hospitals during 2013 and 2014, and this is expected to continue in order to comply with the national standards for hospital care issued in 2015. 279 As of July 2015, there were 10 community hospitals operating in Emilia-Romagna, with a total of 232 beds, including 17 in other residential facilities. 272 Of these, the majority operate as part of or are co-located or co-ordinated with houses of health, which have been established in Emilia-Romagna since 2010. 146 The number of beds per community hospital varies, from a low of six beds provided by the community hospital ‘L.Cappelli’ in the municipality of Mercato Saraceno to 40 beds offered by ‘San Secondo Parmense’ in the Parma municipality. 280 The majority of community hospitals in the region provide between 20 and 30 beds. 279
Veneto
Following a period of experimentation with intermediate care structures, regional legislation issued in 2012 stipulated the specific licensing requirements for the implementation of community hospitals and regional rehabilitation units. 281 The 2012 law, and subsequent regulatory documents that further define the specific features of community hospitals,144,282,283 describe the community hospital as ‘a structure providing intermediate care, that is, care for patients who are medically stable and do not require hospital care but are not stable enough to be treated in a classic outpatient or residential setting and that is required for a limited period of time (4-6 weeks)’. 144 It is seen to provide a functional link between health facilities, social care and residential care, principally targeting post-acute patients with some functional loss [e.g. activities of daily living (ADL)] who are clinically stable. These are usually adults and older people, with three different possible prognostic trajectories:
-
patients whose functions or abilities are possibly recoverable following a period of convalescence involving mobilisation, reactivation and the regaining of some ADL, with a path starting at the community hospital and possibly continuing in rehabilitation (referred functional recovery)
-
patients whose functions or abilities are permanently lost and not recoverable, and who (and their family) have to adapt to the use of prosthetic aids and their home environment. The stay at the community hospital allows observation of whether the new functional state is consistent with a return of the patient to their own home or whether institutionalisation is required (adaptation to a disability)
-
patients whose functions or abilities are definitely lost, and whose condition has a short-term fatal prognosis but does not make them eligible for hospice care.
Referral to the community hospital can be from the patient’s own home or residential care facility on proposals from the treating GP, or from acute care by the treating physician of other facilities (residential care home, nursing home, etc.). Admission involves the development, within 7 days, of a personalised care plan. 282
The clinical responsibility is held by a physician; depending on the organisation this can be a geriatrician, a GP or another medical practitioner. Patients in palliative care are preferably cared for by the palliative care team. A nursing organisation is responsible for nursing tasks and case management, with at least one nurse care manager who (1) co-ordinates the patient’s care from admission to the ultimate destination; and (2) is responsible for restoring, mobilising or preparing the patient for discharge with the support from allied health staff, which includes at least one part-time physiotherapist or occupational therapist for every 24 patients. 144
The hospital will have to ensure access to specialist advice on site, including in palliative care, a physiatrist, a geriatrician and a psychologist. It should also provide access to a social worker to facilitate the patient’s transition to the care setting most appropriate to the patient’s health and social care needs.
The expected length of stay is set at no more than 30 days, although this may be re-evaluated on a case-by-case basis in the light of the patient prognosis. The discharge process involves comprehensive functional, mobility and cognitive assessment. Family involvement in the patient’s functional recovery process is desirable and facilitated by the free access of family members to the structure and to its staff. The patient, their family or caregiver are to be involved in the development of the care plan upon admission, and its periodic evaluation.
The number of beds in community hospitals is determined in line with the overall norm for intermediate care, which is set at 1.2 beds per 1000 population. Earlier documentation noted that community hospitals should have no fewer than 24–25 beds to ensure the cost-efficient use of human resources,144 and more recent stipulations set the maximum number of beds in community hospitals at 30. 283
Available data suggest that, in 2011, there were a total of 1775 beds in intermediate care facilities, of which 236 were located in community hospitals. 284 It is difficult to arrive at more up-to-date figures about the number of community hospitals in the region. This may be interpreted against the background of a continued defining of the key features of these structures, with most recent stipulations providing for specific minimum standards to be met by facilities, and requirements for accreditation, the definition of the content of medical care provided, and specific indicators for the measurement of activities and outcomes. 283
Marche
Along with Emilia-Romagna and Tuscany, Marche was among the early adopters of the community hospital concept in Italy. This approach was recently reinforced in the light of the national requirements set out in 2015 as described above, and, in particular, in order to comply with the expected reduction of hospital fragmentation. 156 Specifically, the Marche region reviewed, in 2015, the houses of health structures that it had formally established in 2013273 and proposed, at the end of 2015, to redefine these as community hospitals. 156 In doing so, it sought to reduce the share of care paid for by the hospital component through converting day surgery, rehabilitation and long-term stay beds into intermediate care beds.
Houses of health in Marche as per 2013 regional regulation provide a wide range of services, and, as a consequence of the 2015 review and having emerged from the houses of health, the 13 community hospitals will also offer a wide range of services. Thus, all community hospitals will provide for the integration of primary care with GP or paediatrician surgeries, continuous medical care as well as 24-hour emergency medical care (mezzo di soccorso avanzato). They will also provide for access to clinics for a wide range of medical specialities (from seven to > 20), which may include cardiology, surgery, diabetology or endocrinology, endoscopy, geriatrics, gynaecology, urology, neurology, dermatology, ophthalmology, obstetrics and gynaecology, orthopaedics, diagnostic imaging, rehabilitation and physiotherapy, or psychiatry, with some also hosting a dialysis centre (with limited or decentralised assistance), along with internal medicine capacity for minor illnesses or multispecialist outpatient surgery on site. The proposed number of intermediate care beds ranges from 10 to 50, with the average number of beds being around 30. Several community hospitals also provide for residential care and hospice beds.
Friuli Venezia Giulia
Defining the community hospital in the context of Friuli Venezia Giulia has been described by one key informant interviewed for this study to be ‘tricky, because what we have are not really hospitals, in this sense’ (KI-I03). Instead, this function has been provided by long-term care facilities (RSA), which were established from the mid-1990s onwards and which are intended to provide continuous health and rehabilitative care to older, dependent people, those with temporary dependency and those with a physical or learning disability. 285 These facilities would provide intermediate care for people discharged from hospital who do not have a place to stay, require rehabilitation, or ‘maybe they come from their home, because their family needs a [temporary] relief from their assistance’ (KI-I03). Referral into the facility can be from acute care or the patient’s GP, with the needs assessed by nurses and social care assistants. The RSAs are usually staffed with nurses, physiotherapists, assistants and GPs, or by specialists in internal medicine providing services in the RSA (KI-I03).
More recently, regional legislation has described the community hospital more specifically as an intermediate care structure that addresses ‘in the most appropriate and effective way the problems of particular patients, especially those with complex health and care needs, who require assistance in a protected healthcare setting; clinical responsibility and the patient’s overall management is the responsibility of the GP’. 131 However, community hospitals remain defined in the context of residential care as part of rehabilitation and long-term care.
Benefits and disadvantages of community hospitals
There is very little empirical evidence on the impacts of community hospitals on processes and outcomes of care in Italy. Much of what is known appears to be anecdotal and based on presumed benefits, with one key informant interviewed for this study citing the rising number of people aged ≥ 75 years who are surviving with chronic disease as indirect evidence of the impact of improvements in intermediate care (KI-I04).
There appeared to be agreement among interviewees about the implicit benefit of community hospitals, as they relate to their size, their closeness to the community and the active involvement of patients and their families and carers in the recovery process:
The other thing is [they provide opportunity] to train the patient, or the relatives, to use some facilities, where they have a rehabilitation programme, so use wheelchairs, or other things [. . .] So I think that this is quite a good place, it’s not so crowded, not too many beds, and also where the organisation is different from the hospital. Where the people can be referred and the relatives can understand what they need to do after.
KI-I03
Alongside these perceived benefits, study participants also noted a number of challenges faced by regions in developing community hospitals as part of a more integrated system locally. One of the main challenges described by key informants is for regions to have to strike a balance between implementing the national level norms on the number of beds and length of stay in acute care in particular [‘You cannot stay in acute, a real acute hospital more than seven days and then you are out. . . We don’t want to see you any more’ (KI-I-01)], against an increasing need for services because of the combined pressures arising from multiple chronic diseases and population ageing:
First of all a very big push for reducing the beds in the hospitals, as you know we have a regional standard [. . .] suddenly now we are down to three, three beds for 1000 persons. We were [. . .] at [bed] occupancy of 75% and now they require 90% of occupancy. And we had the pressure on the emergency rooms, so all the territorial structures are created first of all by looking at the problems of the hospitals [. . .] but if you don’t resolve the problem of the territorial assistance, you will never be able to keep the people out of the hospitals.
KI-I02
This key informant further noted that there was no ‘clear definition of what the continuity of care should be at a territorial level’, combined with a perceived lack of a ‘clear capacity of stewardship if you want from the national level’ (KI-I02), leading the regions to take different approaches, which has implications for the accessibility and performance of health care across the country, a challenge that was also mentioned to be a wider challenge for the Italian health system.
Against this background, the way the systems at local or regional level have evolved can be seen to be opportunistic rather than needs-based, driven by the need to reduce capacity in the acute care sector, which may impact on the delivery of appropriate care to those in need:
So you may have in one local health authority twice as much subacute as the other one, the neighbour local health authority, who has half of these and twice of those. Or three times nursing beds or four times this here, so very random. So, what we have found is that, the sum of all this kind of beds are moving towards an increasing number because of the reduction of [acute] hospital beds and because the development of nursing homes, paid by families. But the combination is quite emergent, with no real rationale [. . .] But having such big differences in the mix, in the infrastructure mix, what happens is that, independent of your physical or psychological condition, you can end in one of those settings just depending on the offer you find over there.
KI-I-01
This challenge was seen to be further compounded by staffing policies introduced by government in the wake of the 2008 financial crisis. In brief, following the crisis there was a push to cut capacity among health-care workers, with national expenditure on the public health workforce falling by about 5% between 2011 and 2014. 155 Many of the ‘cuts’ in the physician workforce have been the result of a freeze on the restaffing of vacant posts following retirement, with a complete freeze in regions subject to central government-imposed regional recovery plans (i.e. regions with financial deficits in health-care budgets, mostly those in the south of Italy), whereas stronger regions that were in fiscal balance were permitted to restaff 50% of retired staff (typically in northern Italy).
This has created challenges, as the need for services is increasing; however, there are restrictions on replacing staff who have left alongside a need ‘to continue with the job, because if you have beds and you need to ensure 24 hour [care] you need to have at least six nurses, six nurses in a day, because you need to [cover services 24/7]’ (KI-I03).
As well as these broader pressures, one key informant also highlighted more local challenges around collaboration and integration, both within and between the health and social care sectors. For example, districts are generally responsible for ensuring that community hospitals have access to specialist expertise, which is typically based in the acute care hospital. And although community hospitals might have a list of specialists to call upon for a second opinion, this might not be the same the other way round and, as a consequence
It is possible we lose some patients now because doctors and nurses are in acute care level [do] not know there is [a] country hospital near the hospital or in the same district. But I think hospital doctors and hospital nurses need to have another thing after acute care because acute care is so, so fast now.
KI-I04
The same key informant also highlighted the challenges of working across sectors, including the introduction of social workers in the intermediate care team, while recognising that time had been among the most important factors that had helped to facilitate this collaboration:
So they are used not to working with the health-care system. They add a further professional in the unit, evaluation unit for elderly, for disabled, for access to the social factor and they go also in hospitals to evaluate people . . . Now it is more developed than the start because it was really difficult the first years, but now no they have used to work with us and we are used to working with them.
KI-I04
Future changes in community hospital provision
Community hospitals in Italy emerged as one of the possible responses to national policies that sought to focus hospital services on acute care and to reduce length of stay. They are seen to provide a means by which to prevent the hospitalisation of a patient or the provision of a ‘protected place’ following discharge because the patient is not fully stabilised or does not have appropriate support in their own home.
The development of community hospitals can also be seen as a policy response to the decision to close hospitals. Traditionally, municipalities have strongly opposed hospital closure in their territories, even if these performed poorly. Community hospitals provide one option to retain a health-care facility in small to medium-sized municipalities. Indeed, as we have seen, several regions have ‘closed’ old local hospitals by means of restructuring and reorganising these into multifunction facilities: ‘So we save the small local hospital, we keep it over there. We try to name it hospital . . . its written in big [letters] . . . so they [patients] feel comfortable to go there, but I mean no expert would ever name it a hospital’ (KI-I-01). These buildings may host a nursing home, a community hospital, specialist clinics and GP group practices.
The future evolution of community hospital provision in Italy can be seen to continue to be driven to a great degree by the national regulation of July 2015, as highlighted in a number of recent regional reorganisation activities targeting the hospital sector in particular.
Norway
Norway, located in northern Europe, is one of the Scandinavian countries. It has an extensive coastline facing the North Atlantic Ocean and the North Sea and shares physical borders with Sweden, Finland and Russia. Norway is a parliamentary democracy, divided into three administrative levels: the state, the 19 counties and the 429 municipalities. Norway is a member of the European Economic Area (but not of the European Union) and it retains close co-operation with the other Scandinavian countries. 119 With a population of around 5.2 million people286 spread over a territory of nearly 400,000 km2, Norway is one of the most sparsely populated countries in Europe (density of 13.5 inhabitant per km2).
Health system context
The Norwegian health system is largely tax funded, with taxation accounting for approximately 75% of total health expenditure. Social security in the form of the National Insurance Scheme accounts for just over 10% of health expenditure, while the remainder comprises private out-of-pocket spending, mostly involving copayments for pharmaceuticals and dental care. In 2013, total health expenditure accounted for 8.9% of GDP, which was in line with the OECD average (UK: 8.5%). However, per capita expenditure was almost twice the OECD average, at US$5862 PPP compared with US$3453 PPP (UK: US$3,235 PPP in 2013). 287
The Ministry of Health and Care Services retains overall responsibility for the health-care sector at the national level. It determines the national health policy, prepares and oversees legislation, decides on the allocation of funds within the health sector and implements national health policy, with many tasks delegated to subordinate institutions such as the Directorate of Health. 288 Since 2009, the Ministry of Health and Care Services and its Directorate of Health have been responsible for the health-care element of the National Insurance Scheme budget, which is administered by the Norwegian Health Economics Administration (HELFO), which sits within the Directorate of Health.
The health system in Norway has been characterised as ‘semi-decentralised’, with many functions delegated to the regions and municipalities. 119 Norway has four state-owned enterprises known as RHAs, which are responsible for the planning, organisation and provision of specialist care; they also oversee investment in the hospital infrastructure. At the local level, 429 municipalities are responsible for the organisation of primary care, public health services and the provision of and access to emergency care. The four RHAs are co-owners of centralised services such as the Health Agency Procurement Service, the National Air Ambulance Services of Norway and the Center for Patient Travels. Each RHA also owns a hospital pharmacy enterprise, and they are all part of a national drug procurement co-operation. RHAs and municipalities enjoy considerable autonomy in exercising their responsibilities, although RHAs have to consult the Ministry of Health for major investments in infrastructure (e.g. the building of new hospitals). The central government is also responsible for large infrastructure projects, such as the Norwegian Health Network, which enables the electronic exchange of patient information throughout the health and social services sectors. Since the early 2000s, there have been a number of significant health reforms in Norway, including a reform of primary care in 2001, a national plan for mental health (1999–2008), hospital sector and specialist health-care service reforms in 2002, and, most recently, the 2012 Coordination Reform. 289 These reforms focused on (1) structural changes in the delivery and organisation of care, placing the emphasis on increased co-ordination between the primary and secondary care sector to better address the needs of the ageing population; and (2) policies intended to empower patients and users with the development of schemes that improve continuity of care, management of patient data and overall patient experience with care services.
Other reforms are under way, with, for example, the 2015 National Health and Hospital Plan, which seeks to clarify the roles and responsibilities of hospitals at different tiers of the system, their interdependencies, task sharing and collaboration, among other things,154 the 2015 White Paper on the future of primary care proposing a range of organisational and structural changes, including the distribution of tasks, the strengthening of public health and preventative services and of interdisciplinary team working as the primary building blocks,290 and the preparation for the Local Government Reform passed in 2014, which foresees the merger of municipalities by 2018 and the allocation of new responsibilities, with impacts on the organisation and delivery of primary and secondary care services. 291
Organisation of the health-care system
Figure 16 shows health-care expenditure in Norway by function, highlighting that in 2014 specialist health care accounted for more than one-third of total health expenditure (hospital care, 27% and outpatient specialised care, 9%), closely followed by long-term care (29%; including care in institutions and home-based care). 292
FIGURE 16.
Health-care expenditure by function as percentage of total health expenditure, Norway, 2014. Based on Statistics Norway. 292
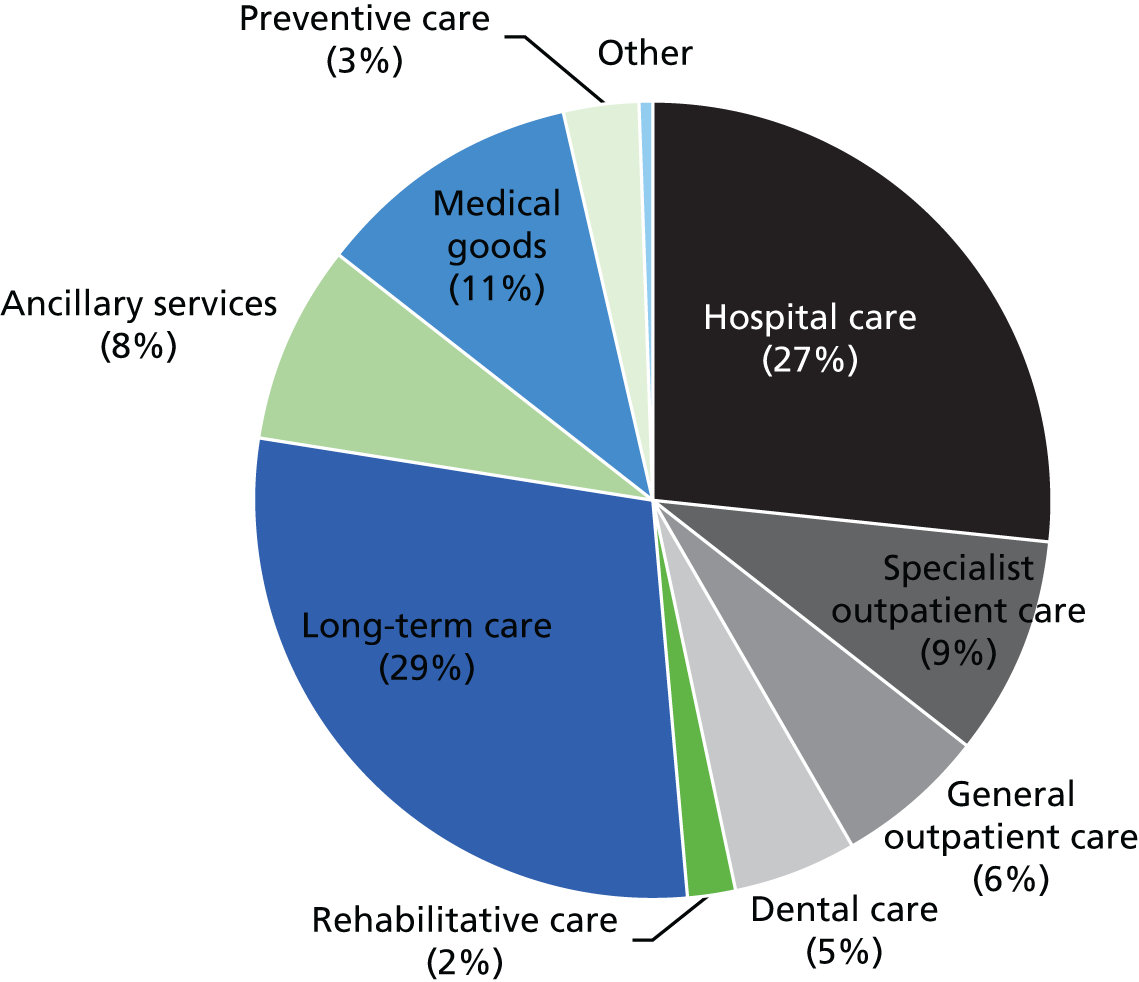
Primary care is provided at the municipal level, mostly by office-based, self-employed GPs (within office hours) and on-call GPs (outside office hours), supported by telephone services, and as part of municipal public services (e.g. nursing homes and home-based services). GPs act as gatekeepers to specialist care. Primary care services are financed through a combination of capitation (allocated at municipal level and accounting for approximately 30% of GPs’ income), fee-for-service (financed through HELFO at the Directorate of Health) and patient copayments. 119 GPs are obliged, through their contracts with municipalities, to serve as on-call physicians in local emergency centres. 119 Inpatient care is provided by public and private hospitals contracted by the RHAs, whereas outpatient specialist services are provided by hospitals’ outpatient departments or by self-employed, private specialists (mostly obstetricians, specialists in internal medicine, etc.), who work in their own practices under a contractual agreement with one of the RHAs. 119 Rehabilitation is provided at both the primary (physiotherapy, occupational therapy) and secondary (specialised rehabilitation) levels, whereas palliative care services are provided at all levels of care. Children and adolescents receive statutory dental care services, whereas adults see private dentists and pay the full fee. 119
Long-term care is provided as home care in people’s homes, nursing homes or municipality-run sheltered homes. The municipalities offer nursing homes with long-stay places, short-stay places and day places. They also provide sheltered housing for people with varying needs for care services. The state encourages the development of sheltered housing and nursing homes facilities through the provision of earmarked funding. 293 The aim is to enable independent living and individualised care for as long as possible and to ensure long-term facility capacity at the municipal level. The number of people receiving care at home rose from 162,000 in 2002 to > 180,000 in 2014,294 and spending on social care services is now greater for care at home than for care provided in institutions.
As noted above, during the 2000s, the Norwegian government introduced a range of reforms to enhance the co-ordination and quality of care. For example, the aforementioned 2001 primary care reform introduced a requirement for residents to register with a ‘regular’ GP, and those choosing not to participate in this scheme have to pay higher user fees when consulting a GP. This move aimed to improve the quality of GP services and to enable GPs to more effectively manage their patient list and patient load while planning and delivering care in a more equitable manner. 295 The reform led to the entry of new primary care providers into the system, which may have contributed to an enhanced geographical distribution of GPs across the country. 296
The 2012 Coordination Reform described earlier sought to enhance integrated care in the community, strengthen health care at the municipal level and improve co-ordination between different levels of care as part of an overall movement to shift services from the hospital sector into primary care. Specifically, the reform requires, in an extension of responsibilities at municipal level, the provision of municipal acute care beds by 2016 (KAD; see Community hospitals in Norway). This is part of a broader objective of the reform, which seeks to encourage the experimentation with and diffusion of new models of care provision to expand the role of primary health-care services through the establishment of local medical centres (Distriktsmedisinsk senter). 289 These are jointly financed by hospitals and municipalities, catering for patients with intermediate needs for institutionalised care. It also foresees economic incentives to strengthen post-acute care provision by municipalities. 134 As municipalities enjoy considerable autonomy in how they organise services, various approaches are being used to meet the requirements of the reform. 289
Organisation, financing and delivery of hospital care
According to the 1969 Hospital Act, a hospital is ‘a medical institution which examines or treats patients and admits patients to stay for such short or long periods as the examination or treatment may require’. 133 The 1999 Specialist Health Services Act §§ 3–8297 further states that the primary objective of hospitals is the treatment of patients, training of health personnel, research and education of patients and their next of kin.
The 1969 Hospital Act made counties responsible for planning, building and managing hospitals in their geographical areas. 298 The 2002 hospital reform transferred responsibility for hospital care from the counties to initially five (now four) newly established health regions (RHAs), which converted the traditional three-tier structure into a two-tier system, distinguishing university hospitals (teaching hospitals with a national responsibility) and hospital trusts. 119 A hospital trust consists of one large and several smaller hospitals, which are administered as one trust. In addition to the publicly owned hospital trusts, there are not-for-profit hospitals or institutions that are set up as foundations. They are financed from public sources and are seen as an integral part of public health services. Examples include the Diaconal hospital foundation in Oslo, which is owned by the Norwegian Church. 119 All hospitals, whether public or private, must be approved by the Ministry of Health and Care Services if they wish to provide health services within the publicly funded system.
Hospitals in Norway are generally classified into three categories: local hospitals, medium specialised hospitals and highly specialised hospitals. In addition, in rural areas there are cottage hospitals (sykestue). These are local care organisations, which assess patients’ need for hospitalisation or provide subacute care for those who cannot be cared for in their own homes but who do not require admission to hospital. 133
More recently, the 2015 National Health and Hospital Plan further specified the hospital landscape in Norway, in order to clarify the role of the different stakeholders and administrative levels and to redistribute resources and skills across specialist services in a more efficient manner. It distinguishes hospitals into four tiers: regional hospital or university hospital (one in each region: Universitetssykehuset i Nord-Norge, St. Olavs Hospital, Haukeland universitetssykehus and Oslo universitetssykehus); large acute care hospitals (serving populations of 60,000–80,000, emergency care, surgery and several medical specialities); acute care hospitals, which provide emergency care for internal medicine as well as elective surgery, and which may offer acute surgery (depending on a number of factors such as distance and access to larger hospitals); and hospitals without acute care functions (elective care). 154
In 2012, there were 21 public hospital trusts in Norway, with > 100 hospital sites. 119 Hospitals are mainly situated in urban areas, with some smaller local hospitals located in remote areas. A very large geographical area can be covered by just one hospital trust (e.g. Nordland county with distances of > 500 kilometres between hospitals serving a population of approximately 131,000). Population density and the number of hospitals are generally positively correlated, and the largest number of hospitals is in the South-Eastern RHA, although the average density of beds is lower here (at 347 per 100,000 population) compared with other RHAs. 119 The size of the hospital trusts varies, ranging from Sunnaas trust with 159 beds and the Oslo University Hospital with almost 2000 beds (both located in the south-eastern RHA). Six trusts have > 1000 hospital beds, eight have between 500 and 1000 beds, and eight have < 500 beds. 299
In 2014 there were a total of 19,751 beds (four per 1000 population) in the hospital sector, down from 22,662 in 2002 (5/1000) (Figure 17). 300 Beds in public health-care institutions account for approximately three-quarters of all beds.
The fall in the number of beds continues a steady decline in the number of beds from 1990 onwards. Thus, between 1990 and 2010, the number of acute hospital beds declined by 37%, that of general hospital beds declined by 29% and that of psychiatric hospital beds declined by 7%. This decline has been attributed to the government’s efforts to enhance resource allocation, through, for example, shifting inpatient care to outpatient settings and to day-care surgery. 119 Average length of stay in hospital also fell, from 8.9 days in 2000 to 6.1 days in 2013,125 while bed occupancy rate has remained comparatively high, at 91% in 2013. 301 High bed occupancy rates in Norway have been linked to long waiting times for elective surgery. 119
Most specialist care is financed through block grants (60%), complemented by activity-based financing from the central government using DRGs. 119 The other types of specialist care are financed mainly through block grants (e.g. for mental health). The size of the block grant is contingent on the type of service provided by the RHA (in 2010: somatic care, 73%; psychiatric care, 18%, ambulance/patient transport, 6%; and substance abuse treatment, 3%). The size of the block grant also depends on other factors such as the number of residents in the catchment area and the demographic profile of the population covered. As noted above, RHAs enjoy considerable autonomy in exercising their responsibilities, although for investments with a budget of > NOK 500M (approx. £41.5M) they have to consult with the ministry. Investments are financed through the basic funding budget allocated to RHAs, with loans from the Ministry of Health and Social Care and the health trusts’ own capital. In 2014, the four RHAs established a new Agency for Hospital Construction, which serves as a national centre of competence for hospital planning and construction, with expertise available for all hospital trusts. 302 The estimated annual investment budget for the four RHAs is expected to be NOK 10B (around £0.83B).
Community hospitals in Norway
Defining the community hospital
In Norway, the concept of a community hospital is not well defined and, among those interviewed for this study, some struggled with the idea itself and the difficulty to translate it into Norwegian (KI-N01, KI-N05). Some interview participants compared community hospitals with the traditional cottage hospitals in rural areas, especially in the northern parts of Norway (KI-N05), while others equated them to what is referred to as teaching nursing homes (KI-N06).
One approach to defining a community hospital in the Norwegian context is through its function within the health system, as there are several types of organisational structures that serve a similar purpose. More specifically, community hospital-type structures are generally understood as those that provide subacute and post-acute care (also referred to as step-up and step-down care) with the overall aim of increasing hospital efficiency, through preventing unnecessary admission to an acute care hospital, while providing care as close as possible to the patient home. Following this line of reasoning, there are essentially four basic structures that can be distinguished within the Norwegian system that fulfil this function and that we will describe in turn:
-
cottage hospitals
-
small general hospitals
-
municipal acute care beds (KAD)
-
local medical centres.
Types of community hospitals and services provided
Cottage hospitals (sykestue)
The 1969 Hospital Act defined a cottage hospital as ‘a medical institution which admits patients in order to investigate whether they should be admitted to hospital, or for simple treatment which cannot appropriately take place at the patient’s home, but does not warrant admission to a hospital’. 133 It was suggested that the size and organisational structure of these institutions vary, as well as the services they provide but:
The main thing is that they are delivering health care in rural areas, there are overnight beds, and then there’s also usually outpatient [services] that can give maybe radiology, specialty services and a variable degree of collaboration with the many people doing these activities.
KI-N04
Accordingly, there are a number of facilities that can be described as community hospitals following this definition, including, for example, the Nordland Hospital Trust (the second largest hospital trust in northern Norway), which serves a population of approximately 131,000 and operates community hospitals in three locations [Salten (Bodø), Lofoten and Vesterålen]. 303 It is important to note that some regions have a long history of operating cottage hospitals, with, for example, the northernmost county of Finnmark operating such hospitals for > 150 years (KI03) (Box 8).
Finnmark county has a long tradition of cottage hospitals, which has been attributed, mainly, to its geography as the northern-most and eastern-most county in Norway and its size, being larger than Denmark but with a population of about 75,000 (the least populated of all Norwegian counties). 304 In 2014 there were 16 cottage hospitals in Finnmark. 305 They co-operate with the Helse Finnmark hospital trust and the Northern RHA and in 2013 a total of 3000 day and overnight stays were registered at the cottage hospitals. From 2009, activity-based funding was piloted in the cottage hospitals. The largest cottage hospital, with nine beds, is Alta helsesenter. Seen as a hybrid, it provides traditional cottage hospital services, as well as specialist care in agreement with Finnmarkssykehuset Kirkenes (a clinic department of the Helse Finnmark HF),306 such as chemotherapy (KI-N03). In 2012, Alta helsesenter registered 470 admissions, 3357 ambulance transports, 97 deliveries in the maternity ward, 132 cases of day-surgery and 4803 radiology examinations. 306 There are plans for Alta helsesenter to increase the number of beds to 20, of which six beds will be owned by the municipalities and 14 by the hospital trust. 306
Hallingdal hospital
Hallingdal hospital is a decentralised, specialist health-care provider, which is managed and funded by the Ringerike general hospital (which is 170 km away). 22 This hospital serves six municipalities with a total population of 20,000. The inpatient department is run by GPs, who work daytime hours but who can be consulted by telephone during evenings and at weekends. The GPs are supervised, by telephone, by specialists located at Ringerike general hospital and can also consult with intermunicipal medical emergency services located in the same building. 21 In 2009–10 the inpatient department, an intermediate care unit with 14 beds, had an average of 605 admissions annually, with a mean length of stay of 6.3 days. 21 Generally, patients are admitted for acute conditions or to receive follow-up care, rehabilitation or palliative treatment. Outpatient clinics hosted by specialists visiting from Ringerike general hospital include internal medicine, surgery, orthopaedics, oncology, paediatrics, ophthalmology, neurology, rheumatology and psychiatric (KI-N05). It was suggested by one interview participant that Hallingdal hospital is not dissimilar to the Finnmark cottage hospitals, in particular Alta elsesenter (Box 9) and some local medical centres (KI-N05).
The concept of teaching nursing homes was developed from 1996 onwards and, following continued success of the pilot facilities, extended to the entire country. 307 Aiming primarily to improve the quality of care provided in nursing homes and to ensure the recruitment of qualified staff, teaching nursing homes soon contributed to the development of strong links between the universities, hospitals and the tertiary education sector. Teaching nursing homes in Norway also often deliver intermediate care for the older population,308 and Trondheim teaching nursing home provides an example of this type of facility. In 2001, it established an intermediate care department for older patients who were initially admitted to the city general hospital but who no longer required more specialised hospital care. 9 The goal was to establish a link between advanced care provided at the general hospital and community home care and so optimise patient recovery before their return home. More specifically, the transformation involved the reassigning, in 2002, of 20 beds at Søbstad nursing home as intermediate care beds. This was accompanied by an increase in staffing in terms of staff-time equivalents for both trained nurses and doctors, alongside training provided by the general hospital. The department was also equipped with laboratory facilities including intravenous pumps, equipment for continuously monitoring of oxygen-saturation in blood, laboratory equipment to measure infectious variables, haemoglobin and blood glucose levels. 9 Although the establishment of the intermediate care department at Trondheim teaching nursing home precedes the introduction of municipal acute care beds from 2012 onwards, the experience can be seen to provide useful lessons for similar arrangements elsewhere in the country.
Municipal acute care beds
As noted above, in 2012, the Coordination Reform introduced municipal acute care beds (KAD) for patients with acute, but manageable conditions such as worsening COPD and infections, who need 24-hour supervision but not necessarily in an acute hospital setting. 108 Guidance from the College of General Practice stipulates that the beds are the responsibility of the municipality and under the authority of family physicians, although there is a need to co-ordinate and communicate with specialised services. A range of diagnostic tools should be available, as well as treatments. KAD beds can be set up in a variety of settings (e.g. nursing homes, see Box 9; local medical centres; ward in a hospital) and are staffed mostly by nurses. Gradually introduced from 2012 with support from the state, all municipalities are required to provide KAD beds from 2016. The KADs are expected to form an integral part of the municipality’s health service and not a new local hospital service in addition to other services. Because KAD beds were not clearly defined in the regulation, a variety of models has emerged so far. The government highlighted that at the end of 2014, > 60% of the municipalities had introduced acute care beds (275 of 429). 309
Local medical centres
As noted earlier, local medical centres (Distriktsmedisinsk senter) were introduced against a broader aim to expand the role of primary health-care services. Local (community) medical centres are defined as structures that provide municipal health care in co-operation with specialist health care (hospitals). 134 They specifically cater for patients with intermediate needs for institutionalised care, that is, patients upon discharge from hospital, or those at risk of admission when the condition could be appropriately managed at a lower-intensity care setting. 289
There is a wide range of local medical centres and data on staffing and the range of services provided are not easily accessible. 310 However, it is possible to distinguish two principal models of organisation and financing of local medical centres. The first model is one financed and operated by the local hospital trust/RHA, whereas the second model is generally operated by the municipality or several municipalities and funded through a block grant from the hospital trust/RHA, with each partner (hospital trust, RHA, municipality) most commonly contributing one-third of the funding.
Local medical centres that cater for more than one municipality principally operate according to one of three models:
-
host-municipality, where municipalities delegate authority to the host-municipality in which the centre is located
-
co-municipality, where two or more municipalities enter a contractual agreement of task sharing and are mutually responsible; they are operated by a co-municipality board; this is a new legal entity from 2012
-
intermunicipal company, which is owned by several municipalities and regulated by the Municipal Act.
The local medical centre in Stjørdal is an example of a local medical centre model 2 and is described further in Box 10. Annex B provides an overview of all organisations and facilities that qualified as a local medical centre in Norway in 2015.
In 2007, Stjørdal municipality, which covers a population of 22,000 residents and is located in central Norway, established an intermediate care service in collaboration with the general hospital and the RHA. 311,312 Considering itself an intermediate care hospital, it provides an inpatient ward with 12 beds that are co-located with primary health-care services; it is located in a municipality other than the one that hosts the hospital (a distance of 50 km away). 61 Services are targeted at patients who were discharged from the general hospital and who require additional support that cannot be provided within regular primary care services. The goals are to develop an integrated care pathway for older people and those with chronic conditions, and it is also anticipated that this will enable professional collaboration, with the exchange of information and knowledge between the general hospital and primary care. 311 The intermediate care hospital’s criteria for admission have gradually been adjusted to prevent prolonged stay at the general hospital and the mean length of stay at the intermediate care hospital is approximately 10 days. 61 The intermediate care hospital is staffed mainly with nurses of whom many are specialised and have previous experience in hospital settings. In addition, there are occupational therapists and physiotherapists, and a GP is present on weekdays. There is an emphasis on follow-up treatment, ADL, motivation and promotion of safety to enable as many patients as possible to return to their own homes.
Benefits and disadvantages of community hospitals
There is some evidence from Norway examining the impact of community hospitals on service and patient outcomes. For example, Aaraas et al.,313 in an early study of admissions to what they referred to as GP hospitals in Finnmark county, found that admissions to community hospitals can lead to lower readmission rates and cost savings compared with general hospital admissions. More recently, evidence from Hallingdal hospital, described above, suggests that of patients initially admitted to the community hospital, only 17% were subsequently transferred to the general hospital for further treatment. 21 Although the study did not use a comparative design, the authors argued that the community hospital was able to resolve the vast majority of acute care admissions (> 80% during the observation period) and therefore demonstrated its role as a ‘buffer’, protecting the general hospital from unnecessary admissions while filtering out those patients in need of further diagnostic work or treatment. A subsequent study found that patients admitted to the community hospital reported statistically significant greater satisfaction with several care aspects than those admitted to the general hospital. 150 Specific factors that were highlighted by patients included the ‘quiet and homelike atmosphere’ of the hospital, its close ties to the local community and a perceived continuity in the patient–staff relationship.
Garåsen et al. 9 examined more specifically the benefits of intermediate care in the Norwegian setting, exploring the experience of the Trondheim teaching nursing home. Using a RCT design, they showed that among patients allocated to intermediate care provided by Trondheim teaching nursing home, a significantly smaller proportion (19.4%) was readmitted for the same condition than for admissions to the general hospital (35.7%). Furthermore, after 26 weeks, among those initially admitted to intermediate care, 25% did not require community care compared with 10% in the general hospital group. On average, treatment costs in the intermediate care group were, at almost half the cost, significantly lower than for the general hospital group, at NOK 39,650 and NOK 73,417, respectively. 62 However, there were no significant differences in the number of patients who had died at 12 months’ follow-up. 62
More recently, Swanson and Hagen147 examined early evidence of benefit that can be associated with municipal acute care beds. Using a retrospective before–after cohort study, they found a correlation between the introduction of these beds and a small but significant reduction in overall hospital admissions (–1.3%, p = 0.041 for the general population and –1.7%, p = 0.041 for those aged ≥ 80 years). In particular, acute admissions and acute internal medicine admissions fell significantly for all age categories (–3.6%, p < 0.01 and –3.5%, p < 0.01 for the general population; –3%, p < 0.01 and –3.1%, p < 0.01 for patients aged 70–79 years; and –2.9%, p < 0.01 and –2.8%, p < 0.05 for patients aged ≥ 80 years). Based on these findings, the authors concluded that municipal acute care beds are likely to have alleviated the burden on hospitals by reducing acute care admissions. 147
In addition to the empirical evidence, those interviewed for this study pointed to a number of additional benefits for patients, citing anecdotal evidence in particular in relation to older people, who make up a large proportion of community hospitals’ patients:
Patients report greater satisfaction [. . .] And other factors enhanced are this interdisciplinary approach, the holistic approach, proximity to local GPs and the local health and care system but also a close co-operation with specialist health services at the hospital.
KI-N05
Another interview participant also noted the benefits associated with reduced distances to travel for treatment and its importance for older people in particular (KI-N01).
Challenges faced by community hospitals
Despite the observed and perceived benefits of community hospitals, there were reports of increasing professional objections to acute admissions of older patients to community hospitals, with concerns over the medical challenge that those with multiple health problems and complex needs, in particular, represent. 314 Key informants commented on the difficulty over deciding whether or not a patient qualifies for a community hospital admission (KI-N02), a responsibility that sits with the GPs: ‘It’s a difficult decision for the referring GP to decide whether the patient should go one place or another place.’ (KI-N05).
Several study participants also highlighted issues around skills, training and staff recruitment (KI-N01, KI-N02, KI-N04), with one key informant emphasising the need for GPs to attend ‘extra specialist training’ (KI-N01) to be able to treat complex and acute cases, and another participant pointing to the need to provide additional training to ambulance staff, who will have to deal with an ever-growing number of emergencies locally (KI-N04). Workforce issues were recently acknowledged by the government, which proposed to rethink hospital staffing and medical training in the context of the recent health service changes. 315
Interview participants also expressed concerns about how the various service innovations that have been promoted following the 2012 Care Coordination reform sit alongside each other, in particular with reference to the newly introduced municipal acute care beds (KAD). One study participant noted that municipalities would require more guidance from the state to support them in implementing these new models of care (KI-N01). This concern was also highlighted in a recent review of the quality of care in Norway. 289 It noted that, in order for the new vision introduced by the reform to be implemented fully, it was necessary to ensure that basic structures to support changes are in place, including appropriate payment systems and meaningful engagement between key stakeholders.
Future changes in community hospital provision
Increasing financial pressure and growing health-care needs are contributing to shaping the future of community hospital provision in Norway. The role of community hospital is reported to be changing, from small cottage hospitals providing care to remote population to a (hopefully) cost-effective alternative to specialist health care that can manage the needs of complex older patients through integrating all parts of the health system (e.g. local health centres, nursing homes) (KI-N05). Therefore, community hospitals are bound to become an even more diverse and flexible concept, with structures that are co-financed and co-managed by a range of stakeholders who will have the autonomy to design local agreements and collaborations. 154 Community hospitals will have to find their place in an evolving system in which the centralisation of more specialised services (especially acute surgery) and the investment in intermediate care services in local hospitals will be concomitant. This shift towards the development of intermediate care facilities under the authority of the municipalities is likely to create some tensions: local providers of specialist care such as the cottage hospitals and small general hospitals will have to compete not only with each other but also with newer facilities such as the local medical centres for funding (KI-N03).
Annex B: local medical centres
| RHA | County | Municipalities | Co-operating hospital trust | Local medical centre |
|---|---|---|---|---|
| Western | Hordaland | Fjell, Sund og Øygarden | Helse Bergen HF | Straume LMS |
| Rogaland | Helse Fonna HF | Sauda DMS | ||
| Sogn og Fjordane | Årdal, Lærdal, Aurland and Leikanger | Helse Førde HF | Sogn LMS (in Lærdal) | |
| Florø | Helse Førde HF | Sunnfjord medisinske senter | ||
| Central | Nord-Trøndelag | Verran, Snåsa, Inderøy og Steinkjer | Helse Nord-Trøndelag HF | DMS Inn-Trøndelag, Steinkjer |
| Stjørdal og Meråker | Helse Nord-Trøndelag HF | Værnesregionen DMS, Stjørdal | ||
| St. Olavs Hospital HF | ||||
| Sør-Trøndelag | Selbu og Tydal | |||
| Røros og Holtålen [and Os from Hedmark county (South-Eastern RHA)] | St. Olavs Hospital HF | Røros sykehus | ||
| Agdenes, Frøya, Hemne, Hitra, Meldal, Orkdal, Rennebu, Skaun and Snillfjord | St. Olavs Hospital HF | SiO – Samhandling i Orkdalsregionen | ||
| Møre og Romsdal | Rindal, Halsa og Surnadal | |||
| Sør-Trøndelag | Oppdal kommune | St. Olavs Hospital | Oppdal DMS | |
| Ørland, Bjugn, Åfjord, Roan og Rissa | St. Olavs Hospital og Helse Nord-Trøndelag | Fosen Helse IKS | ||
| Nord-Trøndelag | Leksvik | |||
| Sør-Trøndelag | Malvik, Midtre Gaudal. Melhus, Klæbu og Trondheim | St. Olavs Hospital | Øya Helsehus | |
| Møre og Romsdal | Kristiansund, Averøy, Gjemnes og Tingvoll | Kristiansund – korttidsavdeling og øyeblikkelig hjelp | ||
| Molde | Molde – kirkebakken helsehus | |||
| Sunndal | Helse Møre og Romsdal HF | Sunndal DMS | ||
| South-eastern | Østfold | Sarpsborg | Helsehuset Sarpsborg | |
| Askim, Eidsberg, Hobøl, Marker, Skiptvet, Spydeberg og Trøgstad | Helsehuset – Indre Østfold Medisinske Kompetansesenter IKS | |||
| Moss | Peer Gynt helsehus | |||
| Fredrikstad og Hvaler | Helsehuset Fredrikstad | |||
| Oppland | Sel, Skjåk, Lom, Vågå, Dovre and Lesja | Sykehuset Innlandet HF | NGLMS | |
| Oppland | Bagn, Etnedal, Fagernes, Nes, Nord-Aurdal, Slidre, Vang and Øystre Slidre | Sykehuset Innlandet HF | Valdres lokalmedisinske senter | |
| Lillehammer, Gausdal, Øyer | Sykehuset Innlandet HF | Lillehammer Helsehus | ||
| Ringebu, Ringsaker (Nord Fron & Sør Fron) | ||||
| Buskerud | Flå, Gol, Hemsedal, Hol, Nes and Ås | Vestre Viken HF | Hallingdal lokalmedisinske senter | |
| Akershus | Skedsmo, Lørenskog, Rælingen, Nittedal, Fet, Sørum and Enebakk | AHUS HF | Nedre Romerike Kommunal akutt døgnenhet | |
| Oslo | Oslo | AHUS HF | Aker samhandlingsarena | |
| Vest-Agder | Birkenes, Lillesand og Kristiansand | Sørlandet Sykehus Kristiansand | Valhalla helsesenter | |
| Northern | Svalbard | UNN HF | UNN HF – Longyearbyen sykehus | |
| Nordland | Rana, Hemnes, Nesna, Lurøy og | Helgelandssykehuset HF | Helseparken Rana | |
| Rødøy | ||||
| Troms | Skjervøy, Nordreisa, Kåfjord og Kvænangen | UNN HF | Helsesenteret Sonjatun (DMS Nord-Troms) | |
| Troms | Berg, Torsken, Tranøy, Lenvik, Sørreisa, Målselv, Dyrøy, Salangen, Lavangen og Bardu | UNN HF | DMS Finnsnes | |
| Finnmark | Alta og Vest-Finnmark (Loppa, Hasvik, Kvalsund, Måsøy, Nordkapp, Porsanger, Kautokeino og Karasjok) | UNN HF | Alta helsesenter | |
| Helse Finnmark HF |
Scotland
Scotland is the northern-most country of the UK, with an estimated population of 5.3 million in 2013. The population density is low, at 69 persons per square kilometre in 2014 (compared with 413 persons per square kilometre in England in 2013),316 and there is wide variation between local authorities from 3433 persons per square kilometre in Glasgow City to nine persons per square kilometre in Eilean Siar, Highland, and the Western Isles. 166 In 2009, > 82% of the population of Scotland lived in urban areas, mainly concentrated in the central belt around the cities of Glasgow and Edinburgh, which covers only 2% of Scotland’s land area. The remainder of the land area is defined as accessible rural areas (27%) or remote rural areas (70%) and contained 18% of the population in 2013. 165
Health system context
Health services in Scotland are delivered through a NHS. Health services provided through the NHS are financed primarily through general taxation, including a small national insurance contribution. The NHS covers all residents, and health services are free at the point of use. There are only very few exceptions, such as dental care for which there are copayments. In the UK as a whole, government expenditure on health accounted for 83.3% of total health expenditure in 2013. 317 Voluntary insurance accounted for 3.5% of total health expenditure across all of the UK (covering 8.5% of the population in Scotland), with out-of-pocket payments accounting for another 9.9%. 317 It is difficult to interpret the data, as requirements for user charges vary across the UK, with Scotland abolishing prescription charges in 2011. 120
Prior to 1997, health-care organisation and delivery in Scotland was similar to that in the rest of the UK. However, following the political devolution of powers to the four constituent countries of the UK in 1999, the responsibility for health in Scotland has been held by the Scottish government and the Scottish health system has evolved into one that is different from the other countries within the UK, following an approach focused on integration and partnership across the Scottish NHS120 and moving away from the purchaser–provider split introduced in the UK in 1991. 318
In 2012, health spending accounted for 10% of GDP in Scotland and, because the devolved governments control only some parts of public expenditure, with the remaining being under the control of the UK government, for 34% of the Scottish Government budget. 120
Responsibility for health and health services in Scotland rests with the Scottish Cabinet Secretary for Health and Wellbeing. The Cabinet Secretary is supported by the Scottish Government Health and Social Care Directorate, which provides strategic leadership for public health, the NHS and social care in Scotland and is responsible for ensuring high standards of health and social care provision. 319 Planning and delivery functions are delegated to 14 regional NHS Boards. Seven Special NHS Boards and one public health body support the regional NHS Boards by providing a range of specialist and national services. The regional NHS Boards are responsible for the protection and improvement of their population’s health and for the delivery of frontline health-care services. The seven Special NHS Boards and the public health body support the regional NHS Boards through the provision of specialist and national services. 320
The 14 regional NHS Boards were, until recently, responsible for planning and delivering all health services – acute, primary and community services – to the population in their areas, and were responsible for the strategic leadership and performance management of the entire local NHS system. However, more recently, plans have been put in place to enhance the integration between Health Boards and local authorities. The Public Bodies (Joint Working) (Scotland) Bill was passed by the Scottish Parliament on 25 February 2014 and received Royal Assent on 1 April 2014. It puts in place the framework for integrating health and social care in Scotland. 160,161 Health Boards and local authorities are required to establish integrated partnership arrangements. In most areas of Scotland, Integrated Joint Boards are being established, which will hold an integrated budget for both health and social care and take over strategic planning functions from the NHS Boards as well as Local Authority. 321 From April 2016, Integrated Joint Boards have had overall responsibility for the planning, resourcing and delivery of all integrated health and social care services (to include adult community health services and some acute health-care services). 322
Organisation of the health-care system
Figure 18 sets out the division of Scottish health service costs by different sectors, presenting primary care services broken down into ‘community services’ and ‘family health services’. Community services include community hospitals, as well as community services delivered outside hospitals, such as home visits by district nurses or prevention services such as breast screening and health promotion. Family health services include local GP practices, local pharmacy services (including the costs of drugs dispensed), dental and ophthalmic services. 323
FIGURE 18.
Operating costs (in £B) in NHS Scotland, by sector in NHS Scotland, 2012–13. Hospital services includes costs for larger hospitals; community services includes community hospital costs, as well as costs of community services delivered outside hospital; family health services includes local GP practices, local pharmacy (including the costs of drugs dispensed), dental and ophthalmic services. Resource transfer refers to NHS funds transferred to local authorities for the continued care of patients. 323 Based on Information Services Division Scotland. 323
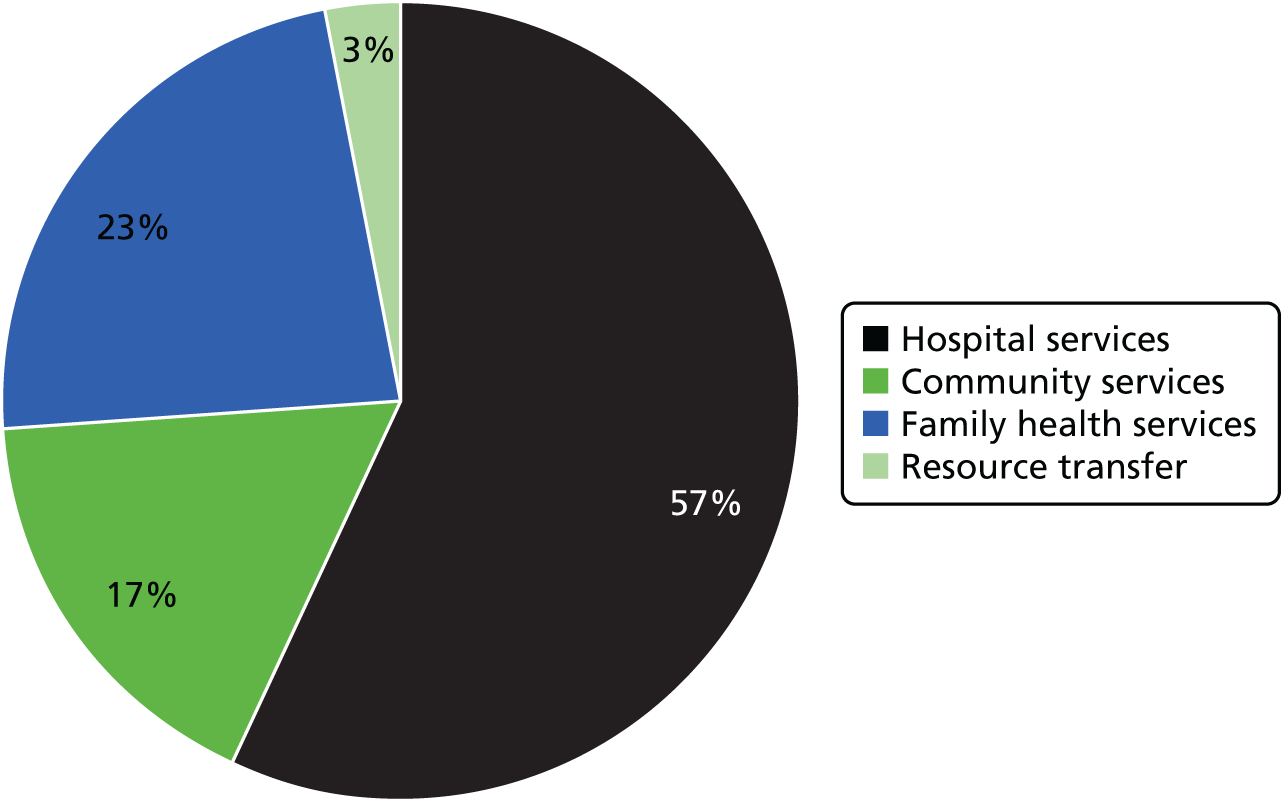
The majority of patient contacts with publicly financed NHS care take place in non-hospital settings, through the provision of primary care services. Primary care is provided by a range of health-care professionals, including GPs, dentists, pharmacists and opticians. GPs often work as part of a multidisciplinary team along with practice nurses, midwives, health visitors, allied health professionals and managers. GPs are usually self-employed and work as partners within their practices, although they can be employed directly by the NHS Boards to work in the community. They are often the first point of contact for general medical care. Primary care has a ‘gatekeeping role’, such that access to secondary and tertiary services is usually available only upon referral. Patients are able to choose their GP provider and where they are treated, provided the practitioner is willing to refer them. 120 However, since the 1990s there has been a move to allow more self-referral to physiotherapy services within the UK.
Secondary care within the NHS is provided by specialist consultants, nurses and allied health professionals, who are employed directly by the NHS, mostly in a hospital setting, although there is a small private sector. 120
Tertiary care includes further specialised services for rare or complex conditions and is provided by seven NHS-funded teaching hospitals and additional secondary care services. 120 Access to these services often requires referral from a secondary care specialist, although referral can also be from primary care. 324 There are also a number of National Managed Clinical Networks, which link groups of health professionals and organisations from primary, secondary and tertiary care to provide co-ordinated clinical services across NHS Board boundaries. 325
Long-term care is provided either through care at home or sheltered housing, residential care homes or nursing homes and does not require referral from primary or secondary care. Nursing homes are distinct from care homes, as they provide 24-hour qualified nursing care, whereas care homes receive visits from community and district nurses. Both receive regular and ad hoc visits from a GP. Residential care homes and nursing homes are usually privately owned organisations, which may or may not be for profit. Care at home is funded by the local authority in cases in which the care is deemed to be required, although non-personal care is funded by the individual. Residential care is divided into three constituent parts: accommodation care, nursing care and personal care. Only accommodation is financially means-tested and the amount that the individual would be expected to contribute towards their accommodation costs would depend on their financial assessment.
Palliative or end-of-life care can take place in any of the above settings, or, alternatively, patients may be transferred to a hospice by their hospital doctor or GP. However, historically, this is mostly the case for patients with terminal cancer or other life-limiting conditions, for whom further treatment is no longer beneficial or desired by the patient. 326 Palliative care has been predominantly funded by the voluntary sector but, more recently, the government has taken a more strategic approach and NHS provision is increasing. 120
Organisation, financing and delivery of hospital care
The Information Services Division (ISD) of NHS National Services Scotland defines a hospital as ‘An institution which is managed, staffed and equipped for the provision of health care services. Hospitals comprise facilities for the diagnosis and treatment of disease.’327
The ISD of NHS National Services Scotland listed 287 hospitals in Scotland as of September 2015. 126 Of the 196 hospitals for which further detail was provided, the majority were classified as community hospitals (31%), followed by long-stay hospitals (21%), general hospitals (19%) and mental health hospitals (14%), with psychiatry or learning disabilities hospitals, maternity hospitals, dental hospitals, community hospitals and other constituting the remainder (Figure 19). Further information on the different types of hospital is provided in Annex C. 328
FIGURE 19.
Hospitals in Scotland, by major category (absolute number), 2015. ‘Other’ includes the hospital categories ‘Maternity Hospitals’, ‘Dental Hospitals’, ‘Clinics’ and ‘Other’. Based on ISD Scotland. 126
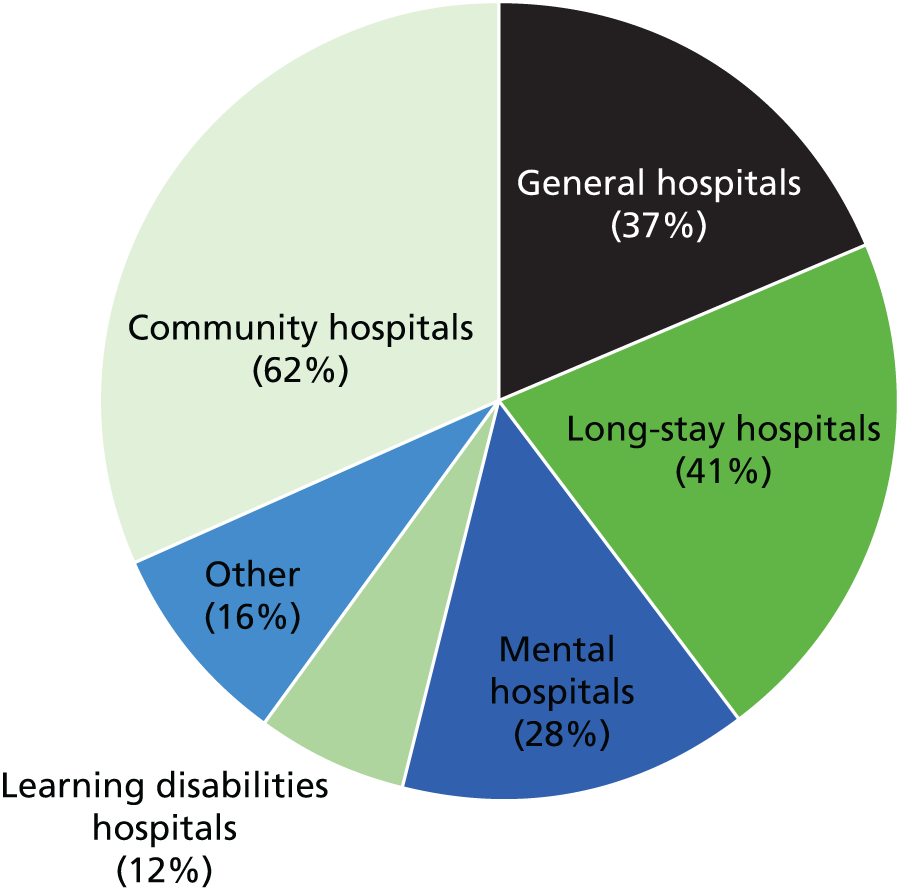
Figure 20 shows each of these categories of hospital disaggregated by size in terms of the average number of staffed beds, that is, bed-days available to a specialty or significant facility over a given period of time. The majority of general hospitals (75%) hold > 100 beds, with one-third having > 500 beds. In contrast, the majority of community hospitals as defined by ISD Scotland (95%) have < 50 beds, and only three community hospitals hold between 50 and 100 beds.
FIGURE 20.
Hospitals in Scotland by category and size (average staffed beds), 2015. Based on ISD Scotland. 170
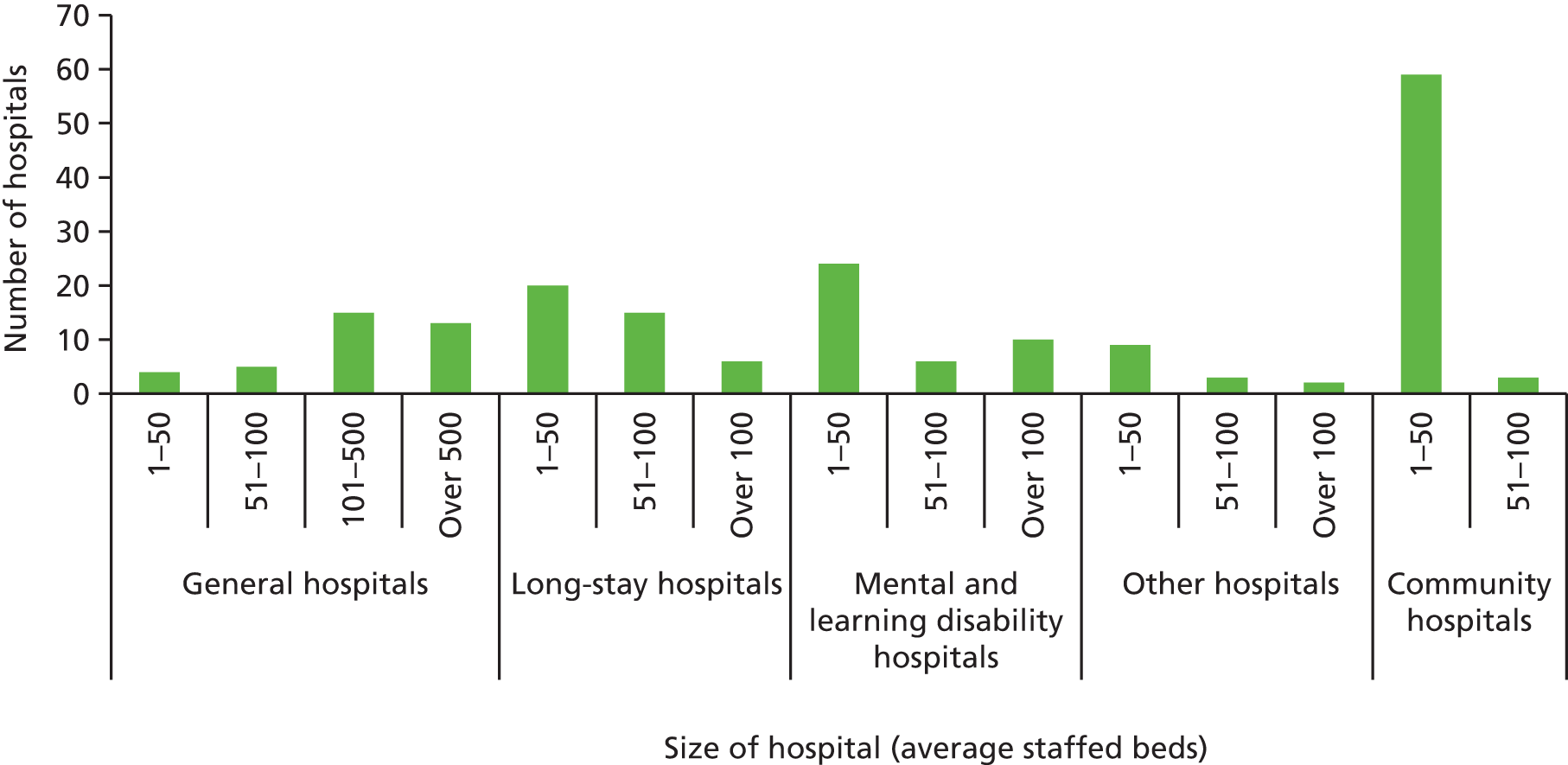
In recent years, hospital bed numbers have remained steady for general hospitals and have fallen for other hospital types (Figure 21).
Planning of hospital capacity is the responsibility of each NHS Board and includes the following:329
-
strategy development: to develop a single Local Health Plan for each NHS Board area, which addresses the health priorities and health-care needs of the resident population, and within which all aspects of NHS activity, in relation to health improvement, acute services and primary care will be specified
-
resource allocation to address local priorities: funds will flow to the NHS Board, which will be responsible for deciding how these resources are deployed locally to meet its strategic objectives
-
implementation of the Local Health Plan and Local Delivery Plan
-
performance management of the local NHS system, including risk management.
NHS Boards develop a local delivery plan that is agreed with the Scottish Government Health Directorate, which also includes financial plans. Each NHS Board is allocated funding from the Scottish budget. NHS Scotland provides guidance on development of the local delivery plan. 330
In 2011, the Scottish Government set out a vision for delivery of health-care services by 2020, noting that ‘by 2020 everyone is able to live longer healthier lives at home, or in a homely setting’136 by means of a health-care system that has integrated health and social care, with a focus on prevention and on anticipatory and supported self-management, and in which hospital treatment, where required and where not able to be provided in a community setting, was to be delivered as day-case treatment where possible. The vision further set out that care was to be provided to the highest standards of quality and safety and to be centred on the person, while ensuring that people are transferred back into their home or community environment as soon as appropriate.
Community hospitals in Scotland
Defining the community hospital
Many community hospitals in Scotland pre-date the formation of the NHS. 13 As such, these hospitals developed independently, often established by local benefactors in response to the needs of the local community. Thus, some developed from early fever hospitals or war memorial hospitals,13 whereas others evolved from local authority facilities that provided care for older people or people with mental health problems (KI-S01). By 1980, a study estimated that approximately 70 hospitals could be classified as GP hospitals, estimated to contain 3% of all hospital beds in Scotland. 135 According to the Royal College of General Practitioners, by 1990, there were 73 community hospitals in Scotland. 91
Against this background, it is perhaps not surprising that defining a community hospital in the Scottish (and the wider UK) context has remained challenging. A commonly used definition describes the community hospital as:
A local hospital, unit or centre providing an appropriate range and format of accessible health-care facilities and resources. Medical care is normally led by GPs, in liaison with consultant, nursing and allied health professional colleagues as necessary and may also incorporate consultant long stay beds, primary care nurse-led and midwife services. 104
However, there is no official definition adopted by the Scottish Government, and while ISD Scotland lists 60 community hospitals,331 the Community Hospitals Improvement Network lists around 80 community hospitals (KI-S03) as well as a proposed definition (Box 11). Since early 2015, the Community Hospital Improvement Network has been working together with ISD Scotland and four NHS Boards to agree a revised definition of a Community Hospital (KI-S03, KI-S04).
A community hospital is a health-care facility undertaking patient care with typically < 60 beds (there are a few with more). The services provided are likely to include a number of the following:
-
GP acute medical inpatient care
-
inpatient care for older people
-
rehabilitation
-
end-of-life care
-
outpatient clinics
-
minor injuries
-
diagnostics
-
community midwifery.
The hospital may be a base for the provision of community services.
Community hospitals:
-
do not have consultant-led A&E departments
-
do not carry out complex surgery
-
do not have primarily long-stay patients.
Non-bypass community hospitals, typically more than 1 hour’s journey time from a 24-hour A&E department, provide 24-hour a day, 365-day a year response to accidents and emergencies including stabilising patients prior to transfer to an acute hospital.
Reproduced from Community Hospitals and Intermediate Care Networks130 under a Creative Commons Attribution – Noncommercial 2.5 UK : Scotland License, which permits others to distribute, remix, adapt and build upon this work for non-commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc/2.5/scotland/
Types of community hospitals and services provided
Services provided at community hospitals vary widely and can include not only inpatient facilities, but also outpatient, diagnostic, day care, primary care and outreach services for patients, provided by multidisciplinary teams. 1 In response to technological advances and demographic pressures, community hospitals are reported to be expanding the range of outpatient and inpatient services, diagnostics and procedures that they can undertake. 13
The 2012 Community Hospitals Strategy Refresh by the Scottish Government sets out three main functions of community hospitals in Scotland:13
-
supporting the rehabilitation and recovery of patients after a stay in an acute hospital
-
providing the specialist end of community services, whether this be co-ordinating care around high-risk patients, providing/co-locating services that patients have traditionally had to travel to bigger sites for and beds for clinical specialties (such as palliative care and mental health)
-
providing some diagnostic and outpatient services.
However, many community hospitals provide further services, for example, dementia care, diagnostic tests and procedures, minor injury services or general clinical services. In addition, the co-location of other services on community hospital sites has increased in recent years, including social care practitioners, minor injury units and the Scottish Ambulance Service. 13
The 2015 Community Hospital Improvement Network working definition of community hospitals (Box 12) suggests a number of services that are likely to be provided within a community hospital, and key informants interviewed for this study were largely in agreement about the types of services that might be offered. 130 There was some divergence of opinion, however, with some key informants suggesting that all community hospitals should have inpatient beds (KI-S03), but others suggesting that a less restrictive definition might be more appropriate as community hospitals continue to evolve (KI-S02).
-
Social care and health-care administration.
-
Family and social services.
-
Home care services for elderly people.
-
Residential services for elderly people.
-
Primary health care (in the health centre).
-
Environment health care.
-
Special health care and emergency room.
Within the overall community hospital definition, a number of different models of community hospital were noted by key informants:
-
non-bypass community hospitals
-
extended role community hospitals
-
long-stay geriatric hospitals.
Non-bypass community hospitals are those that are typically more than 1 hour’s journey time from an acute hospital, and they provide a wider range of services. These include 24-hour a day, 7-day a week A&E services to stabilise patients in need of emergency care prior to transfer to the acute hospital (KI-S03). 130
Extended role community hospitals provide a larger range of services than the typical community hospital (e.g. more complex surgery), as they have typically developed from a previous district general hospital and maintain a larger site. The hospital often changed to a community hospital function following the development of a new acute hospital nearby (KI-S03).
Long-stay geriatric hospitals, which have primarily long-stay beds and may be led by a consultant rather than a GP, may also be considered under the community hospital definition, although there was no consensus among those interviewed for this study on this point (KI-S03, KI-S05).
Community hospitals in Scotland were seen to sit ‘in the middle of the patient journey between home and the district general hospital’ (KI-S03) and have been described as an ‘integrator’ as well as a location for the development of a ‘single point of access to integrated services’ (KI-S02). It has been suggested that discharge of patients for rehabilitation to a community hospital can provide better integration with community and social care services. 13 In addition to their direct provision of inpatient services, community hospitals often host a wide range of different service providers on the hospital site, which may include GP practices, dentistry, community nursing, allied health professionals, social work, social care services and local council staff (KI-S03).
So you’ve got your district nursing base, usually at the community hospital, occupational therapy, physiotherapy base at the community hospital. Some have got dentistry. Some do minor surgery. You’ve got social work based there, children’s services, and in terms of somewhere to put staff within their local area, it’s a very good facility. And they also form out-of-hours hubs as well in a lot of cases.
KI-S05
Of the key informants interviewed for this study, several commented on the ongoing development of the integrative role of community hospitals, articulating an opportunity for community hospitals to develop into ‘local resource centres’ working within the broader health and social care environment as a hub for further non-inpatient activities (KI-S01).
Community hospitals are presently managed and owned by the local NHS Board. The NHS Board is responsible for funding recurrent and capital costs of the community hospital, balancing priorities with funding for acute care and other community care. Key informants suggested that changes in the organisation of health service delivery as a result of the 2014 Public Bodies (Joint Working) (Scotland) Act160 will mean that, from 2016, strategic plans will be developed by Integrated Joint Boards and wider decisions about funding commitments may be taken at this level (KI-S02, KI-S01).
Key informants further noted that local communities would feel a strong sense of ownership for their local community hospital. This sense of ownership was seen to be very powerful and particularly manifested in situations in which there are proposals to remove services or close a community hospital: ‘If you say to an area, “We’re going to get rid of your community hospital,” well, it’s all hell breaks loose’ (KI-S03).
Community hospitals are staffed predominantly by nurses and allied health professionals who are employed directly by the Health Board and who deliver the majority of patient care. 13 Medical leadership is generally provided by one or several GPs, and GP contracts for community hospital work are being negotiated locally between the GPs and the relevant Health Board (KI-S03). Patient care at the community hospital is typically provided by primary care multidisciplinary teams, with support from secondary care consultants as necessary. 13 Outpatient clinics may also be provided by visiting specialists from the acute hospital (KI-S04).
Benefits and disadvantages of community hospitals
There is little empirical evidence for the effectiveness and efficiency of community hospitals in Scotland. One study conducted in the Highlands found that general practices with access to GP beds used substantially fewer district general hospital bed-days per 1000 population than general practices without access to GP beds. 332 One key informant interviewed for this study reported on an unpublished evaluation of two GP practices, one with and one without a community hospital, which suggested that the community hospital practice was able to decrease overall costs of care through a reduction in outpatient referrals, A&E admissions and emergency admissions, with cost per bed at the community hospital reported to be lower than that at the acute hospital (KI-S05). Despite the scarcity of published empirical evidence, key informants cited a wide range of perceived benefits for patients cared for in community hospitals as opposed to acute hospitals, referring to a ‘calmer’, ‘more homely’ and ‘enabling’ environment, which may allow for better recovery of confidence and skills after an episode of acute illness (KI-S03, KI-S02, KI-S04). They also cited a shorter travelling distance for urgent care or outpatient appointments as a benefit (KI-S02), particularly for those frail older people who may find such travel exhausting (KI-S03), alongside increased ability for friends and relatives to visit (who may also be older) (KI-S03, KI4), facilitated discharge planning owing to ease of liaison with community services (KI-S02, KI-S05, KI-S04), reduced risk of hospital-acquired infection and of delirium and falls (KI-S02), reduced overinvestigation or overtreatment of patients (KI-S05) and better-quality food (KI-S05). One key informant further observed:
[The community hospital is] seen as part of a local support system for people, particularly but not uniquely perhaps older people or those who may require additional support. So I think that there’s a kind of intangible value there. It’s actually quite hard to demonstrate the . . . the value in, kind of, cash terms but in terms of emotional support as well as the physical support which is given, these local facilities have very significant value.
KI-S01
Key informants were also asked about perceived disadvantages of community hospitals, and the only observation cited was that some severely ill patients would require transfer to the acute hospital, although this was seen as less of a disadvantage of the community hospital as such compared with spending the whole hospital stay in the acute hospital.
Challenges faced by community hospitals
One main challenge noted for the delivery of care in community hospitals was seen in the difficulty of staffing community hospitals (KI-S03), along with workforce capability and skills. Despite a perceived high retention of the community hospital workforce, shortages in GPs and nurses, and the priority given to staffing of acute hospitals, have meant that community hospitals can become short-staffed (KI-S05, KI-S04). In addition, it was reported that it takes some time for new staff, who have received standard nursing or GP training, to develop the additional skills required for working in a community hospital. As one key informant stated:
It takes a couple of years, to be honest, to get people from having gone through a standard GP training programme to being comfortable about working here.
KI-S05
There have been some developments recently in the provision of further training for GPs. As an example, an additional year of community hospital training as an optional addition following the completion of the standard GP training is soon to be piloted (KI-S01, KI-S03, KI-S04). Other schemes also exist, for example Rural Fellowships in General Practice. 153 Other than these special schemes, it was reported that most of those going to work in community hospitals will learn on the job, through intensive mentoring by senior staff (KI-S05).
This need for additional workforce development may be part of a pattern that is changing at a national level. A 2013 UK-wide report identified a need for change in the medical workforce in response to changing patient needs in order to better respond to the rising burden of chronic disease, in particular multiple comorbidities. 333 It suggested that more generalist doctors will be needed who will be able to work in community-based multiprofessional health and social care teams and proposed changes in training pathways to facilitate this.
A further challenge that was reported to have emerged over the past few years was a perceived rise in the use of the community hospital as a step-down facility from the acute hospital (KI-S04) owing to pressures to free bed use in acute hospitals. This was seen to have reduced the number of beds available for GP admission (KI-S05). Furthermore, key informants noted that there had been delays in discharge from the community hospital to community care because of a lack of care home placements or the availability of home carers, which in turn would lead to longer length of stay at the community hospital than was seen to be appropriate (KI-S05, KI-S04).
Other challenges reported for community hospitals included the age of the infrastructure of some community hospitals (KI-S03), swift access to diagnostics (KI-S02), as well as constraints on health-care spending (KI-S02), which were seen to pose a challenge for the entire health-care system.
Future changes in community hospital provision
In 2006, a report from the Scottish Executive set out a strategy to refocus community hospitals, to contribute towards a shift in the balance of care from an acute setting to a primary and community setting and to an increasing emphasis on patient-centred care. 31 The report recommended that ‘NHS Boards should consider using new community hospitals as local resource centres in which to provide people with more holistic and integrated services quicker and closer to home’. 31 More recently, the 2012 Community Hospitals Strategy Refresh set out a number of suggestions for how community hospitals could improve patient outcomes. It suggested that community hospitals needed to be better integrated into the wider care provision, including acute hospitals, care homes and social care services. 13 Community hospitals were proposed to play a key part in the health and social care integration reforms, acting as a base for community services, or as a community hub for health and social care services. As we have seen, community hospitals are already providing an integrative role, and key informants interviewed for this study suggested that this role would develop in the future, with the potential of the community hospital to function as an integrated health and care facility for the community, hosting a range of statutory and non-statutory agencies (KI-S01). However, it was highlighted that the community hospital model needed to remain flexible to be able to respond to the diversity of local communities and their needs (KI-S01).
Key informants suggested that the ongoing aim of provision of care as close to home as possible, as set out in the 2020 vision for Scotland136 (KI-S02, KI-S03), had strengthened the role of the community hospital in recent years, given their ability to provide hospital care closer to people’s homes.
Key informants reported changes in the function of community hospitals in recent decades, particularly a move towards the use of community hospital beds for shorter-term acute stays, moving away from housing long-stay patients (KI-S03, KI-S01). One exception to this is dementia care and palliative care, where community hospitals may continue to provide care for a longer period (KI-S01). It was also reported that community hospitals now receive patients who are more acutely ill than would have been the case in the past:
People who 20 years ago would be in a community hospital are now at home and people who 20 years ago might have been in an acute hospital are now probably in the community hospital.
KI-S03
It was suggested that if more people can be looked after in their own homes in the future there would be a reduced need for community hospital inpatient facilities, which may result in a reduction in the number of inpatient beds provided (KI-S04). There has been a small decrease in the number of community hospital beds in recent years, from 1473 in 2010 to 1328 in 2013,170 although it is unclear whether or not this was driven by a shift to home care. Key informants suggested that community hospitals might change their focus to provide increased support through outpatient services, investigatory services and ambulatory care (KI-S01, K-S0I4). Advances in technologies have increased the scope of procedures and investigations that can be performed and conducted in local facilities,13 with additional support from specialists through telemedicine (KI-S01).
Annex C: hospital classification
| Main category | Subcategory | Title |
|---|---|---|
| General hospitals (mainly acute) | ||
| A | 1 | Teaching hospitals – major teaching hospitals covering a full range of services and with special units |
| 2 | Large general hospitals – general hospitals with some teaching units, usually > 250 average staffed beds | |
| 3 | General hospitals – mixed specialist hospitals (may have maternity units). Consultant type surgery undertaken, usually ≤ 250 average staffed beds | |
| 4 | Sick children’s hospitals – large teaching hospitals for children covering a range of medicine and surgery | |
| Long-stay hospitals | ||
| B | 6 | Long-stay hospitals (> 100 average staffed beds) – long-stay geriatric units controlled by geriatrician. May be with young chronic sick unit |
| 7 | Small long-stay hospitals (≤ 100 average staffed beds) – long-stay geriatric units controlled by geriatrician. May be with young chronic sick unit | |
| 8 | Long-stay/acute hospitals – long-stay geriatric units with some medical and surgical services | |
| 9 | Long-stay/psychiatric hospitals – long-stay geriatric units with geriatric psychiatry | |
| 11 | Geriatric day hospitals | |
| Mental health hospitals | ||
| C | 12 | Teaching mental illness hospitals with major teaching or research units |
| 13 | Large mental illness hospitals with > 250 average staffed beds, may have some teaching elements | |
| 14 | Mental illness hospitals with ≤ 250 average staffed beds | |
| 15 | Mental illness day hospitals | |
| Psychiatry of learning disabilities hospitals | ||
| D | 16 | Large learning disabilities hospitals (> 150 average staffed beds) |
| 17 | Learning disabilities hospitals (≤ 150 average staffed beds) | |
| 18 | Learning disabilities day hospitals | |
| Maternity hospitals | ||
| E | 19 | Maternity hospitals |
| Dental hospitals | ||
| F | 20 | Dental hospitals |
| Other | ||
| G | 21 | Other – miscellaneous hospitals in which function and/or costs are not comparable with other hospitals |
| 22 | Other – new/closed locations – hospitals subject to cost but in the process of retraction or closure (may include new hospitals with costs for part year) | |
| Clinics | ||
| H | 24 | Hospital clinics |
| 25 | Non-hospital clinics | |
| Community hospitals | ||
| J | 26 | Community hospitals |
Appendix 6 Key features of service provision and payment in primary and ambulatory care in five countries
| Country | Provision of primary/ambulatory care | Choice of provider in primary care | GP gatekeeping | Payment of GPs |
|---|---|---|---|---|
| Australia | Office-based GPs (typically four per practice) | Yes | Yes; access to specialist care upon referral only | Combination of fee-for-service according to national MBS fee schedule plus small pay-for-performance component |
| Finland | (Joint) municipal health centres | From 2012 registration with health centre of choice in municipality of residence; from 2014 choice of any centre in the countrya | Yes; access to specialist care upon referral only | Those working in municipal health centres typically are employed by municipality and receive combination of basic salary and variable added payments and bonuses; exact remuneration method varies among municipalities |
| Italy | Office-based GPs; traditionally solo practices with group practices emerging | Yes | Yes; access to specialist care upon referral only, some specialists can be accessed directly | Operate under a national contract, complemented by regional agreements; capitation fee related to the number of patients registered with practice plus a share based on participation in public health interventions and other activities |
| Norway | Office-based GPs with typically two to six GPs | Yes; registration with ‘regular GP’ required | Yes; access to specialist care upon referral only | Combination of capitation (allocated at municipal level, approximately 30% of GPs’ income), fee-for-service (financed through HELFO at the Directorate of Health) and patient copayments |
| Scotland | Primary care team in GP practices or health centres | Within specified small area only; registration with GP required | Yes; access to specialist care upon referral only | Combination of capitation and fee-for service based on centrally negotiated contract; voluntary pay-for-performance element (until 2015) |
Appendix 7 Case studies in Scotland: interview topic guide
Information for the interviewer
Before commencing the interview, please remind the interviewee of the project information sheet he/she has received and ensure that they have read, understood, and signed the interview consent form. Ensure that there are no further questions or doubts.
About the study and its objectives
This section will link in with the interviewer’s duties detailed above and will serve to ensure that the participant understands and accepts both the details of their participation and the broader aims of the study.
Thank you for meeting with me today. The aim of this interview is to find out your views and experiences regarding how [insert name of community hospital] functions and the factors that are important in delivering the model of care. It is hoped that through this research lessons can be learned that will inform the future development of community hospitals.
Key questions and prompts:
About the participant and their role in the community hospital
This section will briefly explore the role of the participant in the community hospital or in relation to it. Specifically, we want to understand how the participant is involved in the hospital and in what role, whether and how this involvement has changed over time.
-
Can you tell me about your role in/in relation to the hospital?
-
How long have you been in that role?
[Probe on the following: how their role has changed over time and why; which services they are involved with; which service teams they work with and how closely; time commitment of role; nature of work with patients]
The role of the hospital and its services in the community
This section will seek to understand what the participant understands to be the role of the community hospital, the services provided, population served and how these have evolved over time.
-
Can you tell me about the hospital (model) and the services it provides?
[Probe on the following: physical location/buildings; specialties provided by the hospital and by related services on site – and how these are grouped and how they interact with each other; how services are accessed; how the patient journey is managed; workforce – type and number of staff; history of the hospital and how it developed into the present model; how the hospital is financed]
-
Can you tell me about how you understand the community served by the hospital?
-
How do you know about the needs of the community?
-
How is this knowledge used to inform service development?
-
[If appropriate, probe on data available and where from]
-
Can you describe the characteristics of patients that typically attend the hospital?
-
How are they likely to have come to be there/here?
-
Can you describe a typical ‘patient journey’?
-
How the community hospital contributes to the wider health economy
This section will seek to understand how the hospital affects the wider health economy in the local area, what it contributes and how it fits in. It will try to explore the aims and outcomes of this service delivery model, as well as changes that may have been implemented.
-
Can you tell me about how the services provided fit with other local health and social care services?
[Probe on the following: relationships between providers; inter-agency working and formal processes of engagement]
-
Can you tell me about how the hospital works with the closest general hospital(s)?
[Probe on the following: referrals, discharge & admissions; mechanisms to ensure services provided complement each other; communication; strategic co-ordination and co-operation]
-
What would you describe as the main aims and expectations of delivering services in this community hospital setting (as opposed to a general hospital setting, for example)?
[Probe on the following: mission statement/vision; patient outcomes, costs, efficiencies; effects on wider health economy]
-
What do you feel are the benefits of the approach taken here over other approaches? And what are the disadvantages?
Ensure some discussion of benefits/disadvantages related to the community hospital model, rather than focusing on external issues alone.
[Probe on the following: patient outcomes; costs; effects on wider health economy; how setting compares to general hospital; hospital philosophy; staff attitudes; importance and value of ‘local feeling’ for staff and patients; better alternative approaches]
-
Have you been aware of changes in how services are provided? If so, please describe them.
[Probe on the following: Why were changes made? Who initiated them? What was the result of these changes?]
Challenges and enablers found in the local context
This section will explore in more detail the barriers and enablers that are found in the local context. It goes on to probe participant’s perceptions of the hospital’s future and the broader acceptability of the model for other contexts.
-
What do you consider have been the main enablers in developing and delivering services?
-
What do you consider have been the main challenges?
-
What were the consequences of this?
-
What measures have been put in place to overcome them?
-
Ensure some discussion of challenges/enablers related to the community hospital model, rather than focusing on external issues related to local structural/funding context alone, for example.
[Probe on the following: staffing and recruitment difficulties (different skill-set requirements, use of incentives); finances; infrastructure; leadership; variation in challenges associated with different types of service]
-
How do you see the hospital and the services it provides developing in the future?
[Probe on the following: long term sustainability; possible expansion of role; future challenges; impact of technological advances on types of service provided – e.g. more specialist services, telemedicine]
-
How well-perceived is the hospital by:
-
Staff and people providing services in the hospital?
-
Patients and other members of the community?
-
[Prompt on the following: perceptions of the model as a whole and perceived added-value of such a model; Partner organisations? How do you think that your view might compare to the views of others?]
Other considerations
This will give an opportunity for the interviewee to raise any additional points or other comments which have not been covered elsewhere in the interview.
Wrap up
Thank you for your time and your input. If I need to follow up anything discussed today or clarify some points later, would you be happy if I gave you a call? What’s your number?
As we mentioned before, the information you have given us may be used as part of a case study within a larger published report. Once this report is ready, it will be made available on the RAND Europe website. We’ll also send a few hard copies to the local library.
Appendix 8 International experiences: individual case studies
An innovative health centre in Finland: a case-study review
Introduction
The structure of local health services in Finland can be traced to the early 1900s. At that time Finland was a sparsely populated country, where small local hospitals formed the backbone of health-care provision. 151 In 1972 primary health care was reformed through the Primary Health Care Act and health centres were established, evolving partly from the small local hospitals. Primary health care is the foundation of the Finnish health-care system, and its services are provided by health centres and an occupational health service as well as by the private sector. 334
Health centres can offer a wide range of services, including GP-led inpatient units (sometimes also referred to as health centre hospitals), and they are well equipped with medical technology, including facilities for minor surgery and diagnostic equipment. This means that services such as minor surgery or the availability of equipment for patient diagnostic testing in general practice form a core part of primary care in Finland. 117 In 2014, there were 172 health centres in Finland,239 and there is only one per municipality.
Primary health care is organised by municipalities or joint municipal authorities. Municipalities also form 20 hospital districts, which are responsible for organising specialised care. 246 The operations of health centres are based primarily on the legislation on municipal health care: the Primary Health Care Act of 1972 (L66/1972)335 and the Health Care Act of 2011 (L1326/2010). 336 Health centre services are either provided by the municipality or purchased by the municipality from a third-party provider. If the municipality cannot afford to maintain a health centre, it is required to provide services in another way, most often by forming a federation of municipalities.
This case study was conducted in a health centre in Finland. The purpose of the study was to explore the role and functioning of the selected health centre hospital and the factors influencing its implementation and development. It aims to describe the model of service provision, its role within the wider health economy, the challenges and facilitators to the provision of services and staff and community experiences. As an example of an innovative hospital model within its local system of service delivery, comparable to what is understood as a ‘community hospital’, the in-depth understanding gleaned will inform the future development of community hospitals and comparable models in Finland and elsewhere.
Methods
We used a case-study methodology to examine the role and function of a health centre hospital in Finland. The case-study hospital was selected from a short-list of six potential health centres compiled based on the assessment of national experts, with in-depth knowledge of the primary health-care system. Findings from a country review, part of a wider research project on community hospitals, as well as internet searches, also informed the hospital selection. The site selected had to meet the following inclusion criteria:
-
perceived as a community hospital (i.e. services are provided to a local community, are led by GP and include inpatient beds)
-
perceived as innovative by national experts, in terms of services provided and developed
-
located in Finland.
Multiple data collection procedures were used in order to gain rich, detailed information about the case. Desk-based tasks were conducted between June and September 2015, and fieldwork was conducted during a field visit of approximately 10 days in August 2015.
Semistructured interviews were conducted with stakeholders within specific stakeholder groups described in Table 23. Potential participants were identified via a stakeholder mapping exercise, involving an internet search, and consultations with a key local collaborator in the health centre hospital. The majority of interviews were conducted during field visits to the site by one researcher (IN), with a small number of interviews conducted by telephone shortly before or after this visit. Informed consent was sought for participation and interviews lasted for between 30 and 60 minutes. A common semistructured topic guide was used for each interview and they were audio-recorded with permission. Interviews were then transcribed verbatim and anonymised. Non-participant observation was conducted in the public areas of the health centre for a total of 5 hours over the course of 1 week. Observations were conducted on a variety of days of the week and times of day in order to gain an understanding of the full range of activities and activity levels. Observations were recorded using a semistructured observation framework template. The observation data were used to complement and reinforce the information gathered through other methods.
| Stakeholder interviewees | Roles |
|---|---|
| Health centre | S2 – Registered nurse S4 – Senior medical management/primary care S5 – Senior nursing management/primary care S6 – Senior nursing staff S8 – Senior GP staff S9 – Senior nursing staff |
| Social services | S1 – Senior management / family and social services S3 – Social worker |
| Social and health services (co-operation area) | S7 – Director of social and health services S10 – Representative of Board of social and Health Care |
In addition, we conducted a review of available documents and online resources describing the hospital and its mission, status, activities and working relationships, in order to provide a historical and contextual perspective on its implementation, development and functioning. These documents were sourced through internet searches and through signposting by the stakeholders contacted. In addition, we sought to profile the population served, using statistics available online to develop a detailed assessment and to understand the health centre hospital in relation to other health and social care services.
Data were analysed using a thematic content analysis approach according to the principles outlined by Lofland and Lofland. 337 Interview transcripts were read several times to gain an overall sense of the text. An initial coding frame was used based on the interview topic guide with further codes derived inductively from the data, following the initial readings of interview transcripts. As analysis progressed, codes were organised into overarching or organising themes. Emerging findings were shared and discussed with the wider study team. Sourced documents, observations and field-notes were read (and reread) to identify contextual/historical data, and to triangulate findings from interview data.
Findings
Context and background of a health centre
The health centre was established in its current form in the late 2000s in the context of a merger of three municipalities into a single one (Municipality A). In 2012, the organisation and management of social care and health-care services in the municipality was consolidated through the creation of a ‘co-operation area’, which also included a neighbouring municipality (Municipality B). As a consequence, the health centre provides social and health-care services across two municipalities, with a catchment population of just under 30,000 residents. These mergers followed a major structural reform of the municipal system in Finland that sought to enhance co-operation between municipalities in order to ensure the availability of services (L169/2007). One of the key objectives of the reform was to integrate health and social services. 338 The organisation of the social and health services is agreed on in a co-operation agreement between the municipalities concerned.
According to interviews, the health centre served mainly an elderly population, with working age people being a minority among its service users. Table 24 presents the municipalities’ demographic information.
| Age (years) | % of population of Municipality A | % of population of Municipality B |
|---|---|---|
| 0–14 | 15.9 | 13.3 |
| 15–64 | 59.7 | 56.9 |
| Over 64 | 24.4 | 29.8 |
In 2010–12, the morbidity of the population in Municipality A was 107.3, and in Municipality B was 103.1. This compares with the Finnish average of 100. 340
The health centre serves a mixed rural and urban population; however, two-thirds of the population served live in a rural area. 341 Public transport services to the health centre are available, but were perceived to be poorer than the general standard in Finland (Kaikkonen et al. 342). The income level of the population served by the health centre is a bit lower than average level in Finland. 343
The Board of Social and Health Care (sosiaali-ja terveyslautakunta) is responsible for managing and organising the social and health services in the municipality co-operation area. The Director of Social and Health Services has financial responsibility for social and health-care services in the area. The range of social care and health-care services provided under the auspices of the board is presented in Box 12.
Overview of the health centre model
Location and facilities
The health centre is located in the centre of Municipality A. The building comprises three inpatient wards, an emergency room, facilities for general practice, rehabilitation, laboratory and radiography services, as well as for endoscopy and occupational health services. The inpatient rooms on wards have one to three beds, but most of them have two. A cafeteria serves service users, staff and members of the public in the reception area of the general practice surgery.
In addition to the central facility, the health centre manages five satellite clinics in different locations across the municipalities. These clinics originate from services in the historically separate municipalities. Distances between the main health centre and the satellites vary from 17 to 35 kilometres, and the clinics’ sizes and service offerings also differ (Table 25).
| Main health centre | ||||
|---|---|---|---|---|
| General practice | Emergency room | Health centre hospital | Dental clinic | School and student health care |
|
|
|
|
|
|
||||
Services
The health centre aims to provide all residents of the municipality with equal access to basic health-care services. The purpose of the health centre is to promote, support and maintain the health and well-being of the population by providing health services. The principal services availed of by municipality residents are appointments with physicians, nurses, public health nurses, dentists, oral hygienists, dental nurses and physiotherapists, as well as round-the-clock nursing care, and rehabilitation in the health centre hospital. Services are also delivered close to service users’ homes by means of networked co-operation with other providers in the region, such as a hospice for people with memory problems.
The health centre hospital has three wards, with 28 beds each. Each ward fulfils certain specialised functions, such as acute care and monitoring, including out-of-hours wound care or intravenous therapy; end-of-life care; and rehabilitation for, for example, stroke patients or those recovering from endoprosthetic procedures. Services also include respite care, involving nursing support in the centre for periods ranging from 2 days to 3 weeks to provide relief for family carers and those they care for. The average length of stay in acute inpatient wards is 6–8 days, whereas in the rehabilitation ward it is 18–20 days.
Admission to the health centre hospital occurs through a number of different routes, and decision-making responsibility lies with the treating GP. Admission can occur via the emergency room; referral from a GP appointment; home care (when the need for inpatient care has been assessed and agreed upon in advance); or specialised care in the acute hospital. Admission may also occur from a patient’s home to receive scheduled respite nursing. In terms of home care, treatment plans are prepared by GPs, with criteria for possible hospital admission defined in advance. Thus, admission decisions in these cases can be made by home care nurses if the service user’s condition satisfies the pre-defined criteria. Service users being monitored at home may also arrive directly at the ward, if needed; the goal is always to have one bed available for them. According to the interviewees the most common route for admission is via the emergency room.
The health centre also offers a range of specialised services in the following areas: pulmonary diseases, paediatrics, gynaecology, psychiatry, physiotherapy and geriatrics. General practice specialists, who in the Finnish health-care system are usually GPs, operate in the health centre primarily in general practice, apart from geriatricians who also work in the wards.
An overview of health centre services is presented in Table 25 and of services offered in the satellite health clinics in Table 26.
| Satellite health clinics | ||||
|---|---|---|---|---|
| A: distance from health centre = 26 km | B: distance from health centre = 28 km | C: distance from health centre = 30 km | D: distance from health centre = 35 km | E: distance from health centre = 17 km |
| Services available | ||||
|
|
|
|
|
Multidisciplinary teamwork is another essential part of service delivery. A multidisciplinary care consultation is organised for those who have three treatment periods in an inpatient ward within 6 months, as well as for palliative care service users within 1 week of admission. If needed, the care consultation can also be organised for other service users. Participants in the consultation include the service user, a relative, a GP in charge of ward operation, a nurse or staff members from local sheltered accommodation. When necessary, a social worker, physiotherapist, occupational therapist and speech therapist also attend. The aim of the care consultation is to create jointly the best possible care pathway for the service user and to ensure continuity of care. A user-centred approach is also emphasised, ensuring that the service user and relatives are listened to.
Management and finance
The medical director, who manages the health centre’s operations jointly with the chief nursing director, holds overall responsibility for the health centre. This leadership structure represents a contrast to the more common approach in Finland, under which nursing would fall under medical leadership. According to interviews, it illustrates the willingness of the organisation to facilitate both medical and nursing leadership:
I think it also indicates the prevailing mind set that having two leaders in primary health care is needed: a medical director and a nursing director.
S5
The health centre’s inpatient wards are managed by the chief GP, who also has medical responsibility for emergency services and the endoscopy services.
A management group consisting of directors of a range of services, including primary health care (medical and nursing), home care and the housing service, manages and allocates the budget for all social and health-care services. For primary care, the medical director administers the budget jointly with the nursing director. It was indicated in interviews that managers at all levels were expected to be aware of financial issues, in order to increase the sense of joint responsibility.
Changing nature of inpatient care
The health centre hospital has undergone extensive changes over the past 25 years. In the past, health centre hospitals were mainly for people who needed long-term care. An interviewee described her experience of change:
When I started working here, there was a so-called chronic patient ward, in other words a ward for patients with long-term illnesses. Some patients were there for short periods, for example, when their family member was ill and could not care for them. But the majority were long-term patients. Now we do not have long-term beds anymore, so things have changed a lot since 1989.
S2
The scope of services provided on the wards today tends to be acute in nature and focuses on rehabilitation, along with home care services designed to support people in their own home. If home care is not deemed sufficient, sheltered accommodation is also available for municipality residents. According to one interviewee, the average length of stay in the centre hospital has fallen considerably as a result of these changes.
Staff
The total number of health-care staff working in the co-operation area is 223, of whom 80.5 work in the health centre hospital (Table 27). All staff members are employed by the municipality.
Paying for services
Social and health services in Finland are financed through municipal taxes and state subsidies. The municipality council decides on the annual allocation of funds to the health and social care sector based on a draft budget prepared by the social services and health-care board. Within the overall allocation, the health centre receives its own budget.
The municipality also purchases services from municipal enterprises, which are part of the municipality/joint municipal authority organisation. Services purchased in this manner in the health centre include catering and hygiene, radiography, occupational health and laboratory services.
Balancing primary and specialised health care
The health centre is located on the same campus as a regional acute hospital, which is the nearest acute hospital and also part of one of the five university hospitals in Finland. The regional hospital provides specialised somatic and psychiatric services (Table 28).
| Type of services | Distance from health centre | Number of beds | Management structure |
|---|---|---|---|
| Somatic and psychiatric services Outpatient and inpatient clinics |
N/A, on same campus | 64 | Part of hospital district Council and board of hospital district oversee the operation of the hospital Hospital board manages the operation of the hospital |
The close proximity of the regional hospital was seen to facilitate co-operation with the health centre and access to specialised care services. According to interviews, this close co-operation made it easier for GPs and specialists to provide joint consultations and seek each other’s advice. Health centre GPs may also consult specialists at the nearby university hospital in writing and by telephone. Nurses in the health centre and the regional hospital were also reported to co-operate and consult with each other on service user care. In addition, the health centres’ rehabilitation function has also been strengthened by increased physiotherapy services on wards, especially since the rehabilitation ward was established and physiotherapy service was merged with the regional hospital.
However, according to interviewees, the physical proximity of the regional hospital also created confusion for service users, which has at times affected service provision. Municipality residents have been confused concerning the lines of division between the two organisational structures and the range of the services they offer, at times meaning that they are not aware of whether they are using health centre or regional hospital services. The physical proximity has also caused confusion around which hospital service users belong to, leading to the unnecessary use of specialised services.
One interviewee also highlighted that the proximity of the regional hospital had increased the use of specialist care services overall:
Traditionally, we have been using specialised medical care more than other municipalities have, simply because they are so readily available in the regional hospital. This closeness definitely has an impact.
S10
The interviewee perceived this situation as a conflicting one, within the context of municipalities’ purchase of health services:
[The] regional hospital is politically, concerning livelihood, a very important institution for us, but it has been threatened for years. Municipalities, which use services, have heavily reduced the purchase of these services, so the use of the regional hospital has been upheld, it has been very expensive for the municipalities.
S10
Indeed, in a difficult economic context, the health centre was seen to be somewhat deprioritised in terms of resource allocation in favour of the regional hospital, as specialised care has traditionally been most emphasised in the municipality under study. This was highlighted in interviews: ‘The regional hospital has always been powerful, so primary health care has been cast aside a little’ (S1).
Study participants reported pressure and demands for developing and improving service provision in the health centre using existing or even fewer resources. However, financial scarcity also acted as a driver for development:
If we have a limited amount of money and that is what we have to work with to provide the best possible care for people, the financial situation may be a motivator for finding new ways of doing things.
S4
Even if interview participants found that providing primary health-care services was expensive for the municipality, they emphasised the role of the health centre as a gatekeeper to specialised care, as well as the long-term savings that early intervention and prevention can offer. Participants noted that increasing attention had been paid to the health centre’s role in health promotion and disease prevention and that there was an expectation that this would eventually reduce the need for specialised care. The health centre was also seen as an essential local service for the residents of the municipality, and the proximity of the services was perceived to reduce costs. In addition, the provision of some specialised care in the health centre offered cost savings for acute services as well:
The most important thing is probably the fact that we can treat service users who were previously always referred to specialised medical care. In this way, service users receive care in their own locality. On the other hand, it has to do with financial matters as well I think . . . we also have our own special expertise, which may sometimes be quite advanced.
S6
The care provided by the health centre was considered to be more holistic than specialised care offered in the acute hospitals, as one interviewee expressed: ‘Specialised medical care only treats the hand, for example, whereas in primary health care, the person seeking care is seen more holistically’ (S5). Furthermore, the small size of the organisation and the familiarity of staff involved were perceived to enable more organisational flexibility and collaboration between teams, as one of the interviewees described: ‘Smaller-scale operations mean smaller personnel, which enables everyone to know each other and work flexibly together and not stick to your own duties only’ (S8).
Focus on service user independence
In the interviews, the objective of the health centre was defined as providing service users with comprehensive care and supporting them in their daily life, helping them to regain mobility as quickly as possible and supporting them in their ability to function:
Coping in the daily activities should be the starting point of development, whether we are talking about inpatient care or care in general practice. In any case, we should keep in mind what the needs of the person in question are.
S5
There was also an emphasis on person-centred service provision: ‘We should implement the idea that instead of the patient running from one desk to another, the physicians would go to the patient’ (S9).
When the co-operation area was established, the integration of social and health-care services was an interest shared by both parties. The integration resulted in the development of a shared culture for social and health-care services, and the operations adhere to shared objectives. With integration, care can be more easily brought to where the service users are:
Concrete manifestations of the co-operation between the social and health-care services include the ‘one-bed principle’ we have been applying for approximately 2 years. The principle means that if a patient already has a bed somewhere, then why not bring care there. In an acute situation where the patient requires medical care 24 hours per day, that bed is in the health centre hospital. Otherwise, care can be provided at home.
S7
Interviews indicated that the idea of the one-bed principle was based on user-centeredness, giving users the option to stay at home instead of in a hospital ward and for services to be brought to them. It required multiprofessional co-operation and the staff’s wide-ranging competence. At the time of data collection, services that could be brought to the users’ homes under this principle included intravenous treatments such as infusions.
There was a perception among interviewees that the integration of social and health-care services in this way had also helped to distribute health-care expenses more evenly. One reason for this was that service users could be transferred from a ward to their sheltered accommodation, where less expensive treatment could be continued. In addition, with this approach beds in the wards were freed up for service users to be transferred from specialised care for post-acute treatment.
Clinical skills and staff experience in the health centre setting
The health centre staff felt a sense of togetherness with their colleagues and in interviews were conscious of the importance of their work, as one interviewee indicated:
Now that we’ve been under the co-operation area for a while, we’re starting to feel like we belong. Achieving this team spirit just takes some time; to feel that this is our thing, our hospital, and we are really good at what we do here.
S2
Staff described the homeliness and innovation-friendly environment of the health centre, in which they felt comfortable. Interviews also indicated that there was high long-term employment and low numbers of sick leave days among the staff. In 2015, short-term sick leave days decreased significantly according to one interviewee. They also said that job rotation among staff members worked well and that colleagues were generally ready to cover shifts in the case of sudden sickness absence. All this may reflect a kind of loyalty to the health centre on the part of staff and strong job satisfaction.
The health centre as a whole was credited in interviews as being a pleasant place to work. Senior staff attributed this to the development opportunities offered to staff as well as openness to innovation:
We have not had a shortage of physicians since the joint municipal authority was dissolved and the co-operation area was launched. We have a good reputation as an employer, which is probably because we offer development opportunities and require that the personnel develop themselves. Employee input is also welcome, and personnel are given fairly free hands to innovate. This culture has attracted to our hospital acclaimed senior physicians, and younger doctors like to come learn from them.
S7
There was a perception among senior managers that staff in the health centre understood their role in contributing to successful recruitment:
We realise that unless we want to be understaffed in the future, every one of us must do our part to ensure successful recruitment. After all, people value the way they are treated far more than the money they earn.
S6
However, it remains unclear, from the data collected, whether or not this assumption was shared among all staff.
On the other hand, recruiting staff to the satellite clinics was difficult as it required lone working without the support of a larger working community. This was especially challenging in situations in which more junior GPs need support from senior GPs. Recruitment difficulties made the system vulnerable, for example in the case of sickness absence. For this reason, interviews indicated concern that the quality and availability of services could not be guaranteed in the satellite clinics.
In order to maintain and develop staff skills, an annual staff training plan was implemented for each operating area across the entire organisation. Training is provided within the hospital as well as in co-operation with the university hospitals. It was reported that requirements for staff competence have increased because of the expanding service provision of the health centre. It is providing increasingly comprehensive and advanced care, since the treatment periods at the health centre are becoming shorter and some specialised care is being provided. Training needs have also increased owing to the launch of new operations, such as mental health services. This was caused by functional changes in the hospital district when a psychiatric hospital was closed in 2015.
Staff pharmaceutical competence was maintained by regional pharmaceutical treatment training, which is mandatory for the entire nursing staff. The training enabled nurses to administer IV hydration in home environments, for example, supporting the ‘one bed’ principle.
The comprehensive and more specialised care offered in the health centre has also created a need to more clearly delineate staff roles. Practice nurses worked increasingly in home care and assisted living services, with registered nurses remaining at the health centre. This enabled registered nurses to co-ordinate service users’ care during the whole treatment period.
Furthermore, all staff (except for dentists) were required to participate in job rotation across different units of the health centre in order to maintain a wide range of skills. Job rotation was carried out in accordance with the individual’s needs and wishes, enabling them to align their choices with professional interests. In this way, skills-building work in the health centre aimed to equip staff to work in areas to which they were best suited; one interviewee described the principle as ‘[the] right people to [the] right place’ (S5).
The health centre also functions as a training site for GPs specialise in palliative care. This kind of specialism among GPs is rare in Finnish primary health care:
It’s one of the ‘crown jewels’. After all, we are one of the few health centres that are authorised to provide physicians with training leading to a special qualification in palliative care. Of course, there are such units at university hospitals and central hospitals, but these kinds of health centres and wards with that kind of training authorisation are few and far between in Finland.
S4
This function has increased co-operation with the relevant unit in the university hospital and the local hospice. It has also motivated health centre GPs to participate in training and increase palliative care competence in the health centre.
The importance of leadership training for supervisors was also emphasised in the interviews, in order to facilitate innovation and change management:
I believe that supervisors also need training in modern leadership. A solution-oriented way of thinking will help them implement changes in the organisation and provides them with leadership skills.
S5
Co-location and integration of services: benefits and challenges
Benefits and enablers
The interview data showed that active steps had been taken to intensify co-operation between primary care and specialised care, and this had been enhanced by the co-location of services. Since the beginning of 2015, the hospital district promoted a ‘one hospital’ concept, which encouraged close co-operation between primary care and acute care. Driven by the idea that the university hospital and other hospitals in the district should form a coherent whole, joint discussions took place between services on service development, their respective roles and ensuring the provision of appropriate services:
Our co-operation is based on the campus management team model. The campus management team is not a judicial organisation and it does not have actual decision-making power, but it is used to co-ordinate the overall operations. We talk about a well-being campus, formed by the health centre and the regional hospital together. Since we are physically located so close to one another, it makes sense to co-ordinate the operations as one entity, apply new operating methods together and to not operate as two separate organisations.
S4
In practice, this has meant the consolidation of overlapping services between the health centre and the regional hospital and the associated integration of relevant staff. Services shared in this manner include physiotherapy and endoscopic procedures. As mentioned, previously separate physiotherapy services in the health centre and the regional hospital were merged in the health centre. Anecdotally, interviewees reported that this consolidation of services reduced costs, although actual data supporting this were not yet available.
In addition, the Centre of Primary Care was an institution that enhanced integration between primary and specialised care in the region by co-ordinating and developing co-operation links and training. Physically located at the university hospital, the Centre establishes and co-ordinates regional care chains, enhances quality in further and specialised training and education in health centres and at the same time develops and promotes research in health centres. It was perceived to be a workable communication channel for both parties: ‘In a way, the Centre is the link that communicates this message to both’ (S7).
Furthermore, developing links and closer co-operation with the sheltered accommodation service reportedly increased the health centre’s scope to offer service users unable to cope at home an opportunity to live in a supported setting. According to the interviews it was perceived to have reduced costs and freed up resources for those who needed hospital care. At the time of data collection, plans were under way to further enhance this co-operation, including a pilot to expand the range of procedures delivered in sheltered accommodation (e.g. intravenous antibiotics) and the establishment of a nursing position dedicated to visits to sheltered accommodation and home care.
The reorganisation of operations also encompassed general practice services in the health centre. The new model, in which the GP and a nurse work in pairs, was perceived as satisfactory by staff, according to interviews and a questionnaire administered by the health centre. The reorganisation resulted in a clarified distribution of staff roles and more effective time management, minimising service user waiting times.
A permanent nurse–GP pair is assigned to service users with chronic illnesses. According to interviews, the quality of the care relationship improves since the relationship between service user and staff can build over time:
The fact that patient wishes and the effect of care do not meet will always be a challenge. Our solution to this misalignment is to try and find a balance by focusing on patients with long-term illnesses and offer well-prepared appointment visits, longer appointments and GP-nurse pairs who specialise in certain aspects. We focus on these kinds of arrangements since they offer genuine health benefits and effects. We also reserve appointments for patients who come in because of, for example, a cold and need a quick response even though their condition is not that serious. However, they are the ones who give us feedback on the quality of the services.
S7
The value of care plans, prepared by GP–nurse pairs for chronic service users, for service integration was highlighted in the interviews. They form the basis of smooth collaboration between health care, home care and sheltered accommodation services, enabling a comprehensive picture of the service user’s condition for all parties. Furthermore, the care plan contributes to the continuity of care and improves the efficiency of possible hospital stays, because treatment would have been planned in advance.
In order to further enhance service user flow and integrated care pathways, the health centre also established a post for a co-ordinating nurse to oversee the discharge of inpatients. Specifically, the nurse is responsible for actively monitoring the pathway as the service user passes through the health centre hospital and to co-ordinate appropriate arrangements for care post-discharge through liaising with relevant staff in a timely manner. There was a perception among participants that the introduction of this post has contributed to reducing length of hospital stay and, potentially, costs.
Transferring tasks from GPs to registered nurses also allowed GPs to prioritise their tasks more effectively and reduced service user waiting times. Under these arrangements, and with proper training and permits, a registered nurse was allowed to determine a dosage for anticoagulant treatment for example, when a physician had already initiated the treatment and a public health nurse could conduct a follow-up check 3 months after a normal childbirth.
Leadership was seen to be one of the key factors in promoting these service developments:
The way I see it is that proper management and organisation of the operations at social and health-care services help to overcome potential obstacles. Therefore, in principle, there are no obstacles.
S5
It seemed that health centre leadership succeeded in creating an atmosphere that motivates staff to work together in order to meet shared objectives. The attitude of top management had a significant impact:
Currently, the social and health services management is enthusiastic about getting things done. It works hard to ensure a motivating atmosphere for personnel, and this drives things forward.
S2
Open communication throughout the organisation, enhanced by co-location and the ease of interaction it brings, was also seen as important for improving co-operation:
Co-operation happens only by working together and being together. Simply having a cup of coffee together might be enough to spark it. But if you are not in contact with others, making co-operation happen between people in different localities is very difficult by phone or via the internet or e-mail.
S7
Challenges
However, although service co-location and enhanced integration in the health centre had brought a range of benefits, staff also reported a number of challenges that they had faced. Interviewees found that differences in the viewpoints of decision-makers occasionally hindered the implementation and development of services. Attitudes played a part in this:
Could the attitude be at all adjusted so that they would see how something repays itself easily in the future? This is not always necessarily understood.
S8
In addition, difficulties related to communication and information-sharing on service user care between the health centre hospital and the regional hospital weakened co-operation links:
A patient may visit the psychiatric ward, but we don’t receive any information on it; they have kept their doors closed and the attitude has been ‘stay away, I know what I am doing here’. There is no transparency.
S9
In terms of information-sharing, lack of shared electronic service user records between social services, primary care and the regional hospital further hindered co-operation, and privacy requirements caused problems for communication:
We can’t talk about any service user without his/her permission, so there is a problem in data transfer . . . it sometimes may appear that same service user has used our (social) services and has been in the regional hospital or in the health centre and all of us have not known about it.
S3
According to interviews, this risked weakening continuity of care and often resulted in duplicated efforts:
Unfortunately, this is seen in situations where examinations are prescribed although primary health care already had them done; only we don’t see any information on it.
S9
However, investments were made on the national level to improve information sharing and from 2015 service user data would be stored in a shared database. This database is intended to eventually cover the whole country, but pre-2015 data would not be stored.
Historical barriers between the health centre hospital and the regional hospital and the traditional emphasis on specialised rather than primary care created challenges, too. Fundamentally, interviewees saw it as a question of values, as one noted:
What may be a hindrance is the old-fashioned thinking, which is probably now decreasing but which was very visible at least a couple of years ago: that specialised care in the regional hospital is something great, something that should be preserved no matter what. In practice, this kind of clinging to old structures means fewer resources for primary health care.
S7
Furthermore, some interviewees reported a perceived inflexibility at the municipality level, which had also posed a challenge to service integration and reorganisation owing to the delays around decision-making on staff recruitment, for example. It was speculated that this may relate to traditionally conservative, reform-shy operating models in primary care and made service development more difficult:
Previously we have been quite conservative in primary health care, clinging to our old ways. Switching to the new model, in which the focus is on strong customer orientation and the coping of the patient, it is not necessarily an obstacle but naturally, it slows things down a bit, culture is changing and it takes time.
S4
Owing to the consolidation of the municipalities that formed the current health centre catchment area, the proximity of health and social care services for residents varied, as some were inevitably located farther from the main campus of the health centre than others. In interviews, it was reported that, for the more remote areas, services were perceived as too heavily centralised in the health centre. This was especially the case for acute and more technologically demanding services, such as laboratory and imaging. However, study participants also indicated that this consolidated arrangement reduced the need to disruptively transfer service users from one site to another.
Community engagement and demand
In Finland, a health centre is seen as a facility to which people go only to avail themselves of its services. There are no established voluntary work activities in Finnish health services. According to interviews, for municipality residents primary care was similar throughout Finland and the idea of a local identity for local services was not familiar:
Somehow I think that primary health care in Finland is quite a bit similar everywhere, if you go any municipality I think it has not very much local identity or at least I have not experienced it.
S1
However, it remained unclear whether the health centre studied did have a specific local identity for the surrounding community, as no service users were interviewed for this study.
The residents’ need for health services is assessed based on demand. This was demonstrated by the length of waiting lists, the quantity of referrals, as well as the service need observed by staff. Service user feedback was collected systematically and assessed, and used to inform service development. One example of a change implemented as a result of service user feedback was the introduction of a noticeboard in the waiting area of the emergency room, entitled ‘What am I waiting for?’. The noticeboard explained the operational model of the emergency room, as service users had complained about long and varying waiting times.
According to interviews, feedback received indicated that service users were relatively satisfied with the services at the health centre. Although the volume of feedback was not high, according to one participant this may indicate a positive, rather than a negative attitude:
But in practice, we receive very little verbal feedback. When the emergency service started here at the beginning of the year, it was a big change and resulted in a high volume of verbal feedback during the first month. We reviewed the feedback to determine what should be changed and implemented the changes. I can’t recall if I have received any feedback since March, and in practice, the feedback that comes to my level is usually major outbursts. The feedback volume is so low that I take it as a sign that people are happy with the services. If they weren’t, they would let me know.
S7
Negative media messages around primary health care, with little attention paid to the role of health centres, reportedly impacted on the residents’ perception of care provided in the health centre. However, systematic collection of feedback, information sharing and a service user-centred approach to care had had a positive effect on attitudes:
One patient in the specialised care hospital informed that she doesn’t want to go to the health centre, she demanded to be admitted to the regional hospital, but then the care provided by the health centre was described to her and finally she agreed to be admitted to the health centre. A couple of days was difficult for her but in the end of the treatment period she was very satisfied with the care and explained that she could have never imagined that the health centre can offer this good care.
S6
Future and the sustainability of the health centre
Interviewees supposed that the role of health centres would be reinforced in the future, and that this was in line with the apparent aims of the planned social and health service reforms in Finland:
I think there will be a lot of development for the better in the strengthening of primary health care. Also, although the social and health service areas [created under the reforms] will be large, the basic idea there, too, will be to strengthen primary health care.
S1
Maximising the care that can be delivered in health centres will also be made possible by increased specialised expertise in health centres in the future. Participants were optimistic about the potential for reforms to facilitate improved holistic, integrated and service user-centred care:
Let’s talk about the term ‘well-being campus’ that we’re trying to introduce. I think it would be great if our special fields would result in bringing down the silos and blocks between wards. After all, in practice, the majority of the patients are elderly, who would benefit more from an evaluation carried out at the general practice than a narrow assessment by an internist or a surgeon. Perhaps in the future we could use these special fields increasingly as consultants: our ward would be more of a general ward and specialists would come see patients here and we would discuss the situation together.
S4
In addition, the importance of the health centre’s future role as a preventative and health-promoting facility was highlighted:
We should find elements that help individuals take responsibility for the management of their own life and health. This would reduce the need for health-care services. Thus, prevention is important but new operating models should also be supported. The task of the health centre is also to treat illnesses at as early a stage as possible to prevent complications or the worsening of the condition, which would result in high costs.
S7
Advances in technology were also expected to help to allocate scarce resources to the most crucial areas of service user care and bring the services closer to the service user:
Laboratory tests even carried out by service users themselves and the results of the tests will be sent to their mobile phone.
S7
Summary and conclusions
The purpose of the health centre is to promote, support and maintain the health, well-being and ability to function of the population it serves by providing health-care and social care services close to the service users’ homes. It aims to do this by means of networked co-operation with other providers in the region and offers certain specialised services and residential services to support service user independence. Working closely with other social and health-care services in the district in question, including two acute hospitals and sheltered accommodation services for example, the health centre under review must be viewed as being embedded within a wider system of provision.
The health centre’s role in health promotion and preventative services was viewed as increasingly important within the wider system, and its delivery of a range of specialised services was seen to complement and produce cost savings for other acute services, such as the adjoining regional hospital.
The findings of this case study also revealed that a holistic, user-centred approach to service provision was another primary objective of the health centre. Interviews indicated that service reorganisation and other efforts undertaken to enhance the integration of social and health care facilitated the delivery of user-centred care.
Maintaining and developing the clinical skills of staff in the health centre was a continuous priority for the organisation, and this was supported by systems such as job rotation and undertaken partly in co-operation with the adjoining regional hospital and supported by the Centre of Primary Care. It offered staff continual opportunities to widen and deepen their professional skills, as well as an unofficial forum for dialogue between primary and specialised health-care staff. Job rotation in particular helped to broaden staff expertise, which may be advantageous in the context of the widening range of specialised services being offered in the health centre.
Strong leadership that emphasised development and innovation was seen as important by staff interviewed. Management were seen to have worked hard to create a motivating atmosphere and a supportive working environment between colleagues at all levels. This environment was seen to contribute to the strong commitment staff had to their work. The health centre’s unusual leadership structure, whereby the medical director managed operations jointly with the chief nursing director, may have facilitated the observed emphasis on interdisciplinary co-operation and teamwork with a set of shared objectives for the whole organisation. In the context of continuous change and service development observed in the case study, strong leadership and clear, shared aims become all the more important.
The benefits of integrating services were seen across the organisation. Co-operation between GPs and nurses was viewed to have contributed to the quality and continuity of care. In addition, the nurse–GP work pairings model may have promoted multidisciplinary co-operation and efficient task distribution, reducing waiting times and improving effectiveness and efficiency of care.
Despite these achievements, the health centre also faced a number of challenges in its drive to improve service delivery. These included the lack of IT interoperability and shared service user records between acute and primary care, limited information sharing on service user care and the persistence of traditional attitudes, which devalued the work and role of the health centre and primary care more generally.
The Finnish system of health and social care is currently facing a time of profound change and reform. In 2015 the national government decided to form 18 larger, autonomous regions in Finland, which as of 2019 will be responsible for a range of areas including the organisation of social care and health-care services. 237 Under this reform, municipalities no longer hold responsibility for financing health and social care services, and the regions would be responsible for organising social services, primary health-care services and specialised care services. The aim of the reform is to further enhance the integration of services and to streamline care chains for more timely, responsive care. The government is currently exploring options for how services will be funded and legislation on the reforms was expected during 2016. 344
In the context of these ongoing reforms, this study shows that the health centre’s ongoing emphasis on service and skills development, as well as its networked co-operation with acute and community care, will probably facilitate its ability to adapt to the coming changes. With an emphasis on staff flexibility, continual skills development and increasing specialised expertise, the health centre indicates its willingness to reinforce and expand its role in service provision.
An innovative community hospital model in Italy: a case study
Introduction
In the past two decades, acute hospital bed numbers and lengths of stay have reduced in all Italian regions. These measures, driven by economic pressures, have impacted on the provision of rehabilitation services and accentuated the need for a viable alternative to acute hospital care. Care in community hospitals is one of these alternatives and in recent years it has become an increasingly important component of the post-acute care pathway for elderly people in Italy and elsewhere. 345
The community hospitals models developed in Italy were inspired by those first instituted in the UK in the 1920s, where small hospitals were entrusted to GPs and were characterised by close integration with social services and local community engagement. 345 In general terms, community hospitals in Italy are characterised by a number of distinctive elements: (1) admissions only for local residents; (2) clinical responsibility of the patient entrusted to GPs; (3) high average age of the patients (i.e. around 78 years); and (4) low cost (i.e. EUR 146 per bed per day vs. EUR 550–600 per bed per day in acute hospital wards345–347). In 2009, 57 community hospitals were operating across 11 Italian regions, covering > 200 municipalities and 2 million inhabitants. These community hospitals comprised about 700 beds, and employed > 500 GPs and at least 1000 nurses and health and social care workers. 345,348 However, this model of care in Italy is still relatively unexplored in the literature; national legislative references are scarce and the available data are usually based on occasional surveys at the local level.
In Italy, the first community hospitals were established in the 1990s and were especially favoured in the northern and central areas of the country. The rationale for their institution dates back to the 1980s, when Emilia-Romagna was considered to have a surplus of acute hospital beds and the region sought to design and implement policies to reduce the number of hospitals and expand community services. However, attempts to close or downsize hospitals faced strong opposition and on a number of occasions such plans had to be negotiated by the regional government with local communities that feared and resisted reduced access to health services.
The introduction of community hospitals (at that time termed ‘country hospitals’) should be understood in this context. Communities that were losing their local acute hospitals had to be ‘compensated’ with new community health services that would allow the retention of some of the health service staff and provide patient care locally. These new services included community hospitals, nursing homes and multispecialty centres, intended to shift patients from the acute setting to the community and often created by repurposing acute hospital facilities. In this case study, we seek to explore the role and functioning of a community hospital that was established in this context and the factors influencing its implementation and development. It aims to describe the model of service provision, its role within the wider health economy, the challenges and facilitators to the provision of services and staff and community experiences. As an example of an innovative hospital model within its local system of service delivery, an in-depth understanding of its role and functioning will inform the future development of community hospitals in Italy and elsewhere.
Methods
We used a case-study methodology to examine the role and function of a community hospital based in a small town of approximately 4500 inhabitants, located in Italy. With a history running for more than 20 years, the case-study selection was justified by the established nature of the hospital service model and the opportunity this provided to study the development of the facility over time.
Multiple data collection procedures were used in order to gain rich, detailed information about the case. Desk-based tasks were conducted between June and July 2015, and fieldwork was conducted during a site visit by one researcher (MM) over the course of 4 days in July 2015.
Semistructured interviews were conducted with eight relevant stakeholders to learn about the type of services provided by the community hospital and the main financial and organisational factors that affected its functioning (Table 29). Participants were first identified through a mapping exercise consisting of three main steps: (1) desk-based research, (2) identification of main stakeholders and (3) a ‘snowballing’ approach to identify further stakeholders. Interviews and non-participant observation took place during the field visit. In synthesis, six stakeholders were interviewed face-to-face during this period, and two were interviewed subsequently by telephone. Only one member of community hospital staff (a physiotherapist) refused to take part in the study. Informed consent was sought for participation. The interviews lasted for between 30 and 60 minutes and were conducted in a semistructured format in accordance with a topic guide provided by RAND Europe (see Appendix 7). The interview schedule comprised four general question areas (participant role; hospital services; contribution to the wider health economy; challenges and enablers) and was sufficiently flexible to allow respondents to introduce new themes. The interviews were audio-recorded with permission, transcribed verbatim and anonymised.
| Participant code | Participant’s role | Mode of contact |
|---|---|---|
| GP1 | GP management (community hospital) | Face-to-face |
| GP2 | GP (community hospital) | Face-to-face |
| S1 | Nurse management (community hospital) | Face-to-face |
| D1 | Nursing management (district level) | Face-to-face |
| CR1 | Senior municipal representative | Face-to-face |
| CR2 | Municipal Councillor | Face-to-face |
| S2 | Social Assistant (community hospital) | By telephone |
| D2 | Health and social care management (district level) | By telephone |
Non-participant observation was conducted in the public areas of the hospital for a total of 6 hours over the course of the 4 days. Observations were conducted on a variety of days of the week and times of day in order to gain an understanding of the full range of activities and activity levels. Observations were recorded using a semistructured observation framework template. A camera was also used to take pictures of the community hospital’s public spaces and of the village where it is located.
We also conducted a review of available documents and online resources describing the hospital and its mission, status, activities and working relationships, in order to provide a historical and contextual perspective on its implementation, development and functioning. These documents were sourced through internet search and through signposting by the stakeholders contacted. In addition, we developed a profile of the population served, and used local statistics to understand the hospital in relation to other health and social care services.
Data were analysed using a thematic content analysis approach according to the principles outlined by Lofland and Lofland. 337 Analysis was carried out by one researcher (MM) and supervised by a senior researcher (GF). An initial coding frame was used based on the interview topic guide with further codes derived inductively from the data, following the initial readings of interview transcripts. As analysis progressed, codes were organised into overarching or organising themes. Emerging findings were shared and discussed with the wider study team. Shared views and dissenting opinions were identified in relation to different job roles. 8,150 Sourced documents, observations and field-notes were read to identify contextual/historical data, and to triangulate findings from interviews. The two qualitative researchers (GF and MM) involved in the study were independent of the hospital(s).
Findings
Context and background of the community hospital
The community hospital in question opened in a small village in a remote, hilly area of Italy in January 1996. Initially an eight-bed facility, it was established following the formal closure of the local acute hospital, by two municipalities belonging to the same valley. With funding from the local district, the former acute hospital premises were converted to house the new GP-run facility, which was considered an alternative response to the health-care needs of people living in the area.
After its establishment in the 18th century thanks to a bequest, the acute hospital had gradually increased in size and with regional funding became the main health centre of the valley in the 1970s. Since 1980, however, the number of wards was progressively reduced by the region from four to one, leaving only a general medicine ward with 20 beds. The hospital finally stopped functioning in 1993, after national registration349 required the closure (or conversion) of hospitals with < 120 beds. After 3 years of popular protests, the community hospital replaced the former acute hospital. In 2007, it was incorporated into a larger Casa della Salute (‘house of health’), with outpatient clinics on the first floor and inpatient beds on the third. Initially opened with eight beds in 1996, the number of beds in the community hospital had increased to 12 by 2001, and increased again to 18 in 2007 (Figure 22).
FIGURE 22.
Historical timeline.
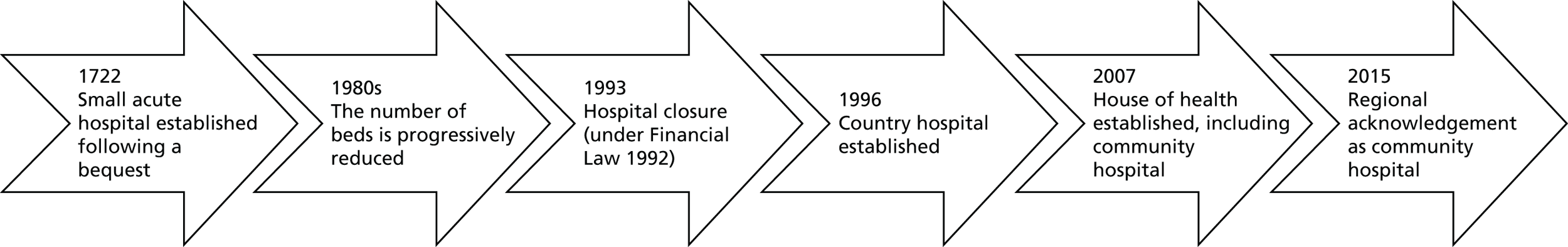
Primary care in Italy has been traditionally provided by self-employed and independent physicians, GPs and paediatricians, under contract and paid according to their patient list, adjusted for age. In recent years, this independent practice model has been progressively modified and GPs are being encouraged to participate in collaborative arrangements to share practice space and resources with paediatricians and other professionals. 350,351 In this context, when faced with acute hospital closure, GPs in the two municipalities felt that working in a collaborative, interdisciplinary manner in the community hospital was the only option to avoid the complete removal of hospital beds in their area. The facility was established shortly after a similar but smaller hospital was introduced in a nearby village.
In 1996 our case study represented the first national experience of its type, in terms of the degree of local interdisciplinary team working, complex medical association and multiprofessional integration. 345 As never before, GPs jointly decided to work in synergy with other doctors and health professionals while maintaining their own patients through an outpatient service. This interdisciplinary collaboration allowed the community hospital to deliver a range of services in outpatient care, limiting the use of outside resources. The community hospital model established in 1996 also represented an innovation in the sense that clinical management, previously under the charge of hospital doctors, was awarded to GPs and out-of-hours care, to dedicated care continuity service physicians. Moreover, legislative references at the time of establishment were very limited (community hospitals were first cited in the National Health Plan 2006–8) and provided little formal guidance to the municipalities in their endeavour. Indeed, as one participant stated, ‘GPs had to use a huge amount of imagination’ (GP2), and to refer to international experience in order to develop the service model.
Following its establishment, the five GPs operating in the two municipalities agreed to conduct a 3-year experimental phase. In 1998, the local district’s evaluation of the testing phase produced positive results: types of admissions to the community hospital were comparable, at 92%, to those of the former hospital’s general medicine ward during its last year of operation. Thus, ‘the ex-general medicine ward and the community hospital were treating the same types of medical conditions, but with relevant cost savings in the latter case as it was entirely run by GPs’ (GP2).
In official terms, the facility was recognised as a ‘community hospital’ by its region only in May 2015, and before that operated for 20 years as a ‘country hospital’. Like the smaller hospital nearby (still categorised as a ‘country hospital’), from 1996 to 2015 the case-study hospital was entirely managed and financed at the municipality and district levels (from here onwards, when referring to the case study, we use the term ‘community hospital’, despite the fact that prior to May 2015 the facility was officially termed a ‘country hospital’). Although the services provided and the staff involved in the community hospital remained the same, accreditation as a ‘community hospital’ meant that the facility would now be financed by the region on the basis of a number of variables reported into a tailored database, the Regional Community Hospitals Information System (SIRCO). In addition to basic clinical, diagnostic and intervention data, the system focuses on measurements of patients’ conditions and independence, nursing care and social issues (D1, S1). These data do not serve as performance indicators, but rather as elements that characterise the admissions and determine the level of reimbursement by the region.
At the time of data collection, the community hospital was going through a phase of change triggered by the region’s recognition. The important changes to the financing and service model that this recategorisation entailed are detailed in Table 30.
| Country hospital (1996–2015) | Community hospital (after May 2015) |
|---|---|
| Local financing (district budget) | Regional financing (on the basis of SIRCO data) |
| Copayment by the patient after the 20th hospitalisation day (EUR 41.16/day) | Free hospital admissions |
| Flexibility in extending the length of stay | Length of stay should not exceed 6 weeks |
| GPs are fully responsible for patients’ admissions and discharges | Other health professionals (e.g. social assistants) are involved in admission/discharge processes |
| Lack of computerisation (e.g. paper medical records) | Management software [Log 80 (Log 80 S.r.l., Forlì, Italy)] and electronic case report forms used |
| Community hospital patients are considered as ‘external users’ by the district acute hospitals | Community hospital admissions are part of regional hospitalisations with priority access to external services (e.g. laboratory testing) |
| Knowledge services and network limited to the local context | Training opportunities and regular visits by the district co-ordinator |
A brief profile of the population served by the community hospital is presented in Table 31. The valley, encompassing an area of around 126 km2, includes two villages (Village 1 and Village 2) that are about 10 kilometres apart. Its inhabitants include many elderly people who frequently live in an isolated manner, as suggested by the low population density. This is particularly evident in the smaller (and more peripheral) Village 2 compared with the Village 1, where the case study is located. The hospital mostly served the elderly population, and also accepts medically stable patients for short-term rehabilitation, social care assessment and palliative care. Over the years, ‘the community hospital became a landmark for the whole valley, providing locality-based care for patients without age limits, but predominantly older people’ (GP2).
| Key indicators | Village 1 (community hospital location) | Village 2 | Italy |
|---|---|---|---|
| Population | 4654 | 1243 | 60,795,612 |
| Population density (inhabitants/km2) | 46 | 20 | 201 |
| Male to female ratio | 98.5 | 94.5 | 94.3 |
| Ageing index (> 65 years/0–14) | 191.3 | 286.2 | 154.1 |
| Household size (mean) | 2.25 | 2.06 | 2.34 |
| Birth rate (per 1000/year) | 7.5 | 4.8 | 8.3 |
| Death rate (per 1000/year) | 12.6 | 18.4 | 9.8 |
Overview of the community hospital model
Currently located in a four-floor house of health, the community hospital is surrounded by gardens and a courtyard, with space for ambulance parking. An external lift facilitates access to the building for disabled people. The ground floor is dedicated to GP clinics and rehabilitation services, including a physiatrist and physiotherapist. The first floor hosts the outpatient clinics of specialist doctors (e.g. cardiologist) who also act as consultants for the community hospital on the GPs’ request. On the second floor, there are meeting rooms, offices and communal spaces. At the time of data collection, the community hospital ward consisted of 16 beds in total and occupied the entire third floor. It was composed of a single corridor with eight double rooms, a doctors’ hall and a space for intravenous therapy.
However, the building hosting the community hospital was reported to present some structural deficiencies that posed problems for patient accessibility. In particular, the exterior elevator was not spacious enough to carry patients on a stretcher, whereas the inner one was rendered difficult to access by the three steps that led to it (S1).
Staffing and services available in the house of health (encompassing the community hospital) are listed in Box 13.
-
Five GPs (from the two municipalities) who are entirely responsible for admissions and clinical pathways.
-
Six nurses and eight health and social care workers.
-
One physician belonging to continuity care service (operating during weekends, public holidays and at night-time).
-
Specialists [e.g. ophthalmologist, otolaryngologist (ear, nose and throat), cardiologist, neurologist, gynaecologist, paediatrician, physiatrist, dermatologist, psychiatrist].
-
Non-medical health professionals (e.g. psychologist, speech therapist, physiotherapist, social assistant).
Source: authors’ elaboration from interview data and site observation.
Five GPs work collaboratively in the hospital and primarily manage patients belonging to their own list in the outpatient service. They dedicate 5 hours per week to covering the community hospital ward, divided into two weekly sessions of 2 hours each, as well as a weekly 1-hour GP meeting. The rest of their working time is spent at the outpatient service or in the community (e.g. home and nursing home visits). Meetings with nurses occur when requested by the nurse co-ordinator, and some participants considered additional meetings with other house of health professionals to be something that would be necessary in the future (S1, S2).
Medical and paramedical assistance is assured 24 hours a day by nurses, the care continuity service and GP shifts. Specialists who are not present in the house of health but whose expertise are often relevant to patient needs (i.e. urologists, orthopaedics, pulmonologists, diabetologists) can be found in the district acute hospitals or in the private system. In the event of complex medical issues, patients are transferred by GPs to the nearest acute hospitals or, in rare instances, a private specialist is invited to the community hospital by the patient (or the families) themselves (GP1). One ambulance with a nurse and a driver is ready to transport emergency cases to the nearest emergency service 24 hours a day.
The average bed occupancy is 12.6 (i.e. around 75%) and peaks during the winter period (for flu epidemics or COPD). Despite the number of beds increasing over time from eight to 16, bed occupancy is still below the target of almost 100% recently imposed by the region for community hospitals. Thus, some concerns were expressed by the staff about a possible cut in the number of beds in the near future (S1). As stated above, the community hospital admitted mainly elderly patients, most of whom were female. This is perhaps explained by demographic factors in the local area, as in 2014 there were almost five times more widows than widowers among the population aged over 70 years in the community hospital village (Village 1). 352 The key data on community hospital activity are reported in Table 32.
| Number of beds | 16 |
| Average length of stay (days) | 31.6 |
| Number of hospital admissions/year | 145 (male: 56; female: 89) |
| Waiting times | N/A |
| Bed occupancy rate (%) | 78.5 |
| Average occupancy (beds) | 12.6 |
| Male to female ratio | 0.63 |
| Age, years (mean) | 81 (male: 79; female: 83) |
| Cost/hospitalisation day (2008) | EUR 143.5 |
Capital costs to transform the previous small acute hospital into the country hospital were covered by the local district. Up until the time of data collection, the hospital’s operating budget was also covered by the district, with occasional assistance from the region for capital expenditure. However, with the recent change in status, the region was expected to take control of the hospital’s operational budget in the near future.
Community hospital’s role in the local health economy
According to interviews, the community hospital represented the ‘bridge’ between traditional acute hospitals and local services: ‘the community hospital was the ‘missing link’ between acute care hospital and community health services’ (GP2). It was seen as ‘the community service with the higher healthcare intensity’ (GP2). The GPs interviewed defined the community hospital as ‘the strongest response to the healthcare needs of citizens in the area’, underlining the local value of this model together with its relevance within the wider health economy. The community hospital responds to the needs of patients suffering from an exacerbation of chronic diseases, consequences of surgical interventions and terminal conditions that do not require intensive therapies or technology-intensive diagnostics. As mentioned above, patients are mainly elderly, with many in situations of isolation or living with inappropriate housing conditions for their health status (GP1). The conditions commonly treated in the hospital are listed in more detail in Table 33.
| Main diagnoses | ICD-9-CM353 | Frequency (%) |
|---|---|---|
| Neoplasms (even in terminal phase) | 140–239 | 21 (14.5) |
| Traumatism and poisoning | 800–999 | 21 (14.5) |
| Myocardial diseases | 425–429 | 16 (11.0) |
| Vascular diseases (e.g. stroke, TIA, venous thrombosis) | 390–459 | 14 (9.6) |
| Blood diseases (e.g. anaemia) | 280–289 | 11 (7.6) |
| Digestive tract diseases (e.g. dyspeptic syndrome, gastroenteritis, colitis) | 520–579 | 7 (4.8) |
| Musculoskeletal system diseases | 710–739 | 6 (4.1) |
| Diabetes mellitus | 250 | 5 (3.4) |
| Urinary tract infections (with or without retention of urine) | 580–629 | 4 (2.8) |
| Lung diseases (e.g. COPD) | 490–493 | 4 (2.8) |
| Mental disorders | 290–319 | 4 (2.8) |
| Other respiratory tract diseases | 460–519 | 2 (1.4) |
| Other endocrine diseases | 240–279 | 2 (1.4) |
| CNS degenerative diseases (e.g. Parkinson’s disease) | 320–389 | 1 (0.7) |
| Not defined diseases | 780–799 | 20 (13.8) |
| Other | 6 (4.1) | |
| Not specified | 1 (0.7) | |
| Total | 145 (100.0) |
Although its primary aims are rehabilitation and safe discharge home, the community hospital has regularly served as a ‘hospice’ for terminally ill patients, especially those affected by cancer. Hospital admissions for oncological diseases were estimated at about 15% (GP2). Despite not being formally qualified as a hospice, in practice the decision to admit end-of-life patients to the community hospital has been justified by the distance to the closest hospice (16 km). Moreover, patients and their families prefer to be cared for close to home and ‘refuse to be treated in facilities expressly dedicated to palliative care, which are perceived as “anterooms of death”’. Finally, according to one interviewee, terminally ill patients not suffering from cancer had difficulty finding adequate care in traditional hospices, as they have only recently begun reorganising their services to manage non-cancer-related end-of-life conditions (D2).
Following the formal transition to community hospital status in May 2015 and the subsequent reduction of hospital stays to a maximum of 6 weeks imposed by the region (see Table 30), the issue of terminally ill patients is likely to become more pressing. Moreover, the new regulations will affect also non-terminal patients who have completed their treatment (or rehabilitation) at the community hospital but who are not yet ready for discharge. Indeed, community hospital beds were often used for extended periods while families were finding a suitable accommodation for the elderly. As one GP stated: ‘the community hospital was used as a temporary nursing home’ (GP1). A possible solution advocated by some of the interviewed stakeholders is ‘the enhancement of nursing home care service in order to allow most of cancer patients (or frail elderly) to end their lives in a family setting’ (D1).
Among community hospital admissions, staff interviewed distinguished two primary patient origins: (1) patients coming from acute hospitals for clinical stabilisation after an acute admission (mainly orthopaedic or cardiac surgery); and (2) patients coming from home (even under nursing care) who require hospitalisation owing to a worsening of their clinical condition (D2). Of 145 admissions in 2014, five patients came from the own district’s main acute hospital, 60 from another nearby acute hospital (belonging to another district), 77 from their own home and three from other facilities (e.g. nursing homes). As regards hospital discharges, 63.4% of patients returned home, 17.9% were readmitted to an acute hospital, 9.7% were admitted to a nursing home and 13 patients (9%) died in the community hospital.
The geographical location of the community hospital within the regional territory is peculiar. The two municipalities in its catchment belong to the same district, but the closest acute hospital (around 320 beds) is located in a neighbouring district. GPs therefore generally choose to refer to their own acute hospital (around 480 beds) for medical expertise not present locally (e.g. advanced diabetes mellitus care), even though it is further away. However, emergency cases are sent to the hospital of the neighbouring district owing to geographical proximity. For this reason, one interviewee stated that ‘the relationship with the district level is double and complex’ (GP1). In some cases, participants reported a lack of information exchange and co-ordination in patient management between the two acute hospitals (GP1, S2). In other cases, complaints related to long waiting time for patients admitted to the community hospital but referred to the district acute hospital for diagnostic tests emerged from the interviews (GP2).
As reported in Table 34, the distances between the two villages and the nearest hospitals are significant. The isolation is exacerbated by the lack of a rail connection (there is only a bus service). Travel distance represents a challenge in terms of time and fuel costs for families who care for patients admitted to one of the acute hospitals.
| Distances to local acute and emergency care services | Village 1 | Village 2 |
|---|---|---|
| Distance from the closest emergency room/acute hospital | 20 km | 32 km |
| Distance from the district acute hospital | 38 km | 50 km |
In this context, the community hospital has an important role in the wider health economy of its region. According to interviews, admissions to the community hospital can often prevent rehospitalisation to the acute hospitals or shorten the length of stay after acute admissions or surgery (GP2). Indeed, in October 2001 it was reported that the hospitalisation rate in the district had been reduced by 10% owing to the opening of the community hospital and the small country hospital operating nearby. According to interviews with GPs, emergency room visits were reduced, as patients could approach another doctor within the same health facility when their GPs were not on duty.
From an economic perspective, interviewees reported that the community hospital enables the containment of both health-care costs (as admissions are cheaper, in particular as a result of lower pay of GPs compared with medical specialists) and family expenses (owing to lower travel costs) (GP2, CR1).
Philosophy and aims of care in the community hospital setting
Interviewees reported a number of key clinical aims of the community hospital, which can be summarised as follows: (1) stabilising the overall clinical state and maintaining treatment outcomes achieved by the acute hospital; (2) preventing complications and recovering patient independence to allow a safe return home; (3) facilitating early discharge from the acute hospital and preventing rehospitalisation; (4) promoting access and engagement of family members and reducing their costs (i.e. travel expenses and productivity losses); and (5) enhancing the role of GPs and nurses by increasing their clinical and managerial responsibilities. 354
According to interviews, the philosophy of care in the community hospital relies on a ‘holistic approach’ to the patient, whereby the whole person, and not a single disease, is given full consideration (S1). In contrast to acute hospitals, the primary objectives of which are the diagnosis and treatment of severe acute conditions, the community hospital aims for the patient’s complete post-acute rehabilitation and social integration once discharged. A particular focus is put on psychological and social needs thanks to the co-operation of GPs with different professionals present in the house of health. As patients and doctors belong to the same community and they have already established a relationship in outpatient care ‘the local doctors’ deep knowledge of their patients is at the heart of this approach’ (GP1, GP2).
According to one of the GPs interviewed, the geographical location of the community hospital allows easier access to patients’ family, friends and the local community. Caregivers have a relevant role in treatment and rehabilitation and, for GPs, act as important source of health data, especially for patients with poor cognitive skills: ‘The involvement of patient’s relatives is particularly relevant in end-of-life situations and allows [us] to minimise the risk of legal issues and public complaints’ (GP1). The atmosphere was reported to be relaxed and friendly compared with the acute hospital and, at the time of data collection, there was greater tolerance for extending the length of stay and visiting hours. In referring to the community hospital, one of the doctors interviewed (GP1) spoke about ‘a facility rich in humanity and poor in technology’, pointing out that structural deficiencies (i.e. limited traditional equipment) are offset by a patient-friendly environment.
Clinical skills and staffing in a community hospital setting
Medical and nursing staff at the community hospital have been stable for several years and are mainly composed of professionals from the local area. Given that both patients and staff belong to the same community, they share knowledge and values shaped by similar local contexts and are also likely to know each other well. The staff interviewed confirmed that ‘the community hospital has a good working environment with friendly and established relations between different professionals’ (GP2, S1). With such stable staffing, the community hospital has not experienced any recruitment difficulties. In addition, the introduction of the community hospital has had positive effects on local employment, enhancing local skills and avoiding the depopulation of young people (CR1, CR2).
The community hospital also allowed for a welcome expansion of the traditional role for the GPs working there. GPs interviewed were grateful to have the opportunity to act as hospital doctors and to improve their clinical (and managerial) skills, a role that is not normally given to GPs in Italy (GP1).
Co-location and integration of services: challenges and benefits
The co-location of hospital and other health and social services within the larger house of health facilitated the integration of a number of care services. As mentioned, the availability of key medical specialties prevented the displacement of patients to acute hospitals. Moreover, the regular presence of a physiotherapist and other professionals allowed patients to spend the full period of post-acute rehabilitation at the community hospital. Co-operation among different professionals was enhanced by the introduction of the electronic case report forms, which enabled quicker information exchange (S1).
The GPs’ leadership style was reported to be participative (S2) and the importance of teamwork was emphasised in interviews. Indeed, in interview a member of GP management described himself as a ‘one among peers’ (GP1). Although in charge of liaising with district management, he did not consider himself to have enhanced power over other GPs either at the outpatient service or in the hospital (GP1). However, although the hospital GPs held weekly meetings, according to staff interviews, multidisciplinary team meetings were not regularly conducted. This was reported to be due to reluctance on the part of the GPs to share their leadership role with other staff. At the time of data collection, such meetings were expected to be periodically scheduled in the future. Moreover, according to some staff interviewed, future admissions and discharges to and from the community hospital would be agreed within a multidisciplinary team composed of GPs, nurses and other health professionals, in order to allow a more holistic perspective on patient care (S2, S1). Meetings with the district management occurred monthly to review economic data or to update clinical guidelines (GP1, S1).
In carrying out its core business of post-acute treatment and rehabilitation, the community hospital also depended on co-operation with acute hospitals which, while essential, also posed some challenges for patient care (GP1, GP2). With relatively modest medical equipment (comprising one electrocardiograph and two defibrillators along with common medical instruments), the community hospital relied upon the acute hospitals for access to a range of technologies. In terms of diagnostics, blood samples were sent daily to the acute hospital laboratory and the community hospital relied on the acute hospital for a range of other diagnostic tests (e.g. computed tomography). Although the community hospital lacked sufficient economies of scale to maintain these services, interviewees reported that reliance on the acute hospitals for such services at times led to unacceptable delays in patient care:
Their outsourcing inevitably creates some delays to the detriment of patients; the issue of waiting time will require a further evaluation in the near future.
GP2
According to interviews, the provision of appropriate care for the elderly demanded improved integration between health, psychosocial and social care services. Interviewees stated that with an ageing population, hospitals, and especially community hospitals, were increasingly required to meet social and psychological needs, which went beyond their traditional function (GP1, GP2, CR2). Social assistants, who may already propose hospital admissions for individuals living in poor conditions or without adequate family support, were expected to play a key role in this domain. Until May 2015, the social assistant’s collaboration with the community hospital was voluntary and informal. However, following regional recognition, their role was intended to become more formalised, with enhanced involvement in decision-making around patient admission and discharge. Historically, the social assistant has been in charge of assessing the needs of the elderly (through home visits or meetings with families), referral to services (e.g. meals at home, placement in nursing homes) and monitoring vulnerable people (through home visits or telephone calls) (S2).
The community hospital also works together with three nursing homes: one 28-bed public home adjacent to the community hospital; one 85-bed private home in Village 1 and a 39-bed private nursing home in Village 2 (CR2). Around 10% of patients discharged by the community hospital enter a nursing home. The facilities services (i.e. catering, cleaning) on which the community hospital relied were provided by a co-operative shared with the public nursing home.
Community ownership and engagement
Interviews indicated that the community hospital had a good reputation among the local inhabitants, which had been consolidated over time. Community representatives interviewed expressed a sense of ‘local ownership’ of the community hospital.
The strength of community feeling around local health provision and hospital beds was also indicated by the 3-year period of strong opposition among local inhabitants to the closure of the former acute hospital, which preceded the establishment of the community hospital. Indeed, in the early 1990s, delegations of citizens went to the regional authority’s offices to protest against the closure. The acute hospital, which had operated in the valley since the 18th century, had also been deeply rooted in the community.
The local community expressed a strong appreciation for community hospital provision. In the collective imagination ‘the [acute] hospital has never closed’ (GP2) and the community hospital was perceived as a direct continuation of the closed facility. Moreover, the community hospital staff is almost exclusively composed of local residents, which also contributed to the sense of local ownership and positive feeling. Indeed, the establishment of the community hospital allowed nurses and other staff members to return to live in their village after periods spent working elsewhere (S1, CR1).
Some participants outlined other key reasons for community satisfaction with the hospital, including (1) the proximity of family and friends during patient care and rehabilitation; (2) patient trust in the GPs thanks to their relationship established over time; (3) the sense of protection provided by the community hospital’s presence, which represents a beacon for chronic and post-acute care in the remote valley; and (4) the community hospital’s function in providing care for the elderly, which relieves the caring burden of the working population (CR1, CR2, GP2).
Volunteering activities in the valley are not particularly focused on health and social care, despite some initiatives that help to transport isolated elderly people to and from the hospital(s). No volunteers regularly work at the community hospital (S2, S1).
Future and sustainability of the community hospital
As described above, the community hospital is currently undergoing an important transitional phase. As with any change, the shift to different organisational and financing structures has posed some challenges for the community hospital. The passage from ‘country hospital’ to ‘community hospital’ will require GPs to give up some of their autonomy in favour of other professionals, as part of the multidisciplinary discharge meetings described above, for example. Moreover, the timely discharge of patients may be affected by the removal of the disincentive of a patient copayment after the 20th hospitalisation day.
As mentioned above, the community hospital’s role as an unofficial ‘hospice’, which it has had for the last 20 years, might also be subject to change. However, according to interviews, it is likely that the 6-week limit on length of stay will be extended for terminally ill patients. In addition, some interviewees indicated that the 6-week limit might be interpreted as average length of stay across admitted patients, rather than a strict deadline for each admission. Discussions with the region were ongoing at the time of data collection (GP2, D2).
With formal recognition as a ‘community hospital’ in May 2015, the region acknowledged the important part that the hospital has played in the regional health system in the recent past and is expected to play in the future.
Towards a common language: a push for regional standardisation and co-operation
Another challenge faced by community hospital staff as part of the transition to regional management has been the implementation of new management software, which is already widely used by acute hospitals. The system offered the possibility of connecting the community hospital with all the other district health facilities allowing them, for example to book laboratory tests directly. Despite attending training organised by the district, nurses and GPs reported that the programme does not fit the needs of the community hospital, as a facility that mainly deals with chronic and post-acute conditions. In particular, difficulties have been experienced in reporting complex therapeutic plans for chronic patients, with doses modulated according to patient characteristics. Moreover, one interviewee complained that the software was unsuitable for certain demands of clinical work and lacked sufficient technical support (GP1).
The ongoing transition from ‘country hospital’ to ‘community hospital’ was also reported to require the standardisation of clinical guidelines and practices among the case-study hospital and the other 28-bed community hospital in the district, located 40 kilometres away. These changes and moves for standardisation were intended to enhance community hospital integration with regional hospital provision, while still preserving the community hospital’s strong local identity and role (S1).
Co-operation between the community hospital and other regional health-care actors was also intended to be enhanced in other ways. Interviews also mentioned the potential for the development of a telemedicine service for the community hospital in the coming years. Telemedicine will allow doctors in the community hospital to receive the results of diagnostic tests (e.g. spirometry) in real time from the acute hospital and to share clinical information with isolated inhabitants in the valley while they are at home (GP1, S2).
Summary and conclusions
The community hospital reviewed in this case study provides a strong example of the response of the Italian health system to the need for enhanced health-care options between acute hospital care and home care. The establishment of the community hospital was justified by the need to provide accessible health services to those living in isolated areas, especially the elderly. As such, the case study’s rural, remote setting was the ideal location to implement this new model of care in Italy. The positive perceptions expressed by the community hospital staff and community representatives confirm the achievements of this model of care, which inspired about 70 similar developments across a number of Italian regions in the years since its establishment in 1996 (GP1). Moreover, as the first hospital model of its type in Italy, it raised great interest and has hosted > 400 delegations of doctors, nurses, journalists and managers who sought to study it.
The community hospital also faced a number of difficulties, related to disjointed co-operation and co-ordination with acute services and managing changes to systems and processes. Prior to regional recognition as a community hospital, the qualification of its patients as ‘external users’ by district acute hospitals caused delays in performing diagnostic tests and, according to interviews, potentially negatively affected patient care. Similarly, the community hospital’s interaction with two different acute hospitals (rather than only one) generated challenges in terms of co-ordination and communication in the management of emergency and other patients who required acute care. Moreover, the fulfilment of regional requirements with regard to clinical management software and limits of lengths of stay were an ongoing concern and point of discussion. In addition, enhanced multidisciplinary working in the form of shared decision-making between GPs and other health-care professionals (e.g. nurses, social assistants) was perceived by some to undermine the strong leadership that doctors have traditionally played at the community hospital (and in other hospitals in Italy).
Despite these challenges, the case study suggests that the community hospital may represent a promising alternative to acute hospital care, which is highly appreciated by patients and community members. The community hospital was greatly appreciated by the GPs as well, who valued the unique opportunity in Italy to spend part of their working time on hospital care. The community hospital was considered particularly important for the elderly population who often lived in relative isolation. In a time of limited health-care resources and continual cuts in public health financing, the community hospital may represent an affordable way of managing post-acute and chronic conditions in the increasingly elderly population. This is particularly relevant in areas that are located far away from larger health service providers (GP2).
In the future, the enhancement of multidisciplinary integration at the community hospital may allow it to meet patient needs in a more holistic way. Moreover, as part of a regional network of community hospitals, benchmarking with other facilities may help to improve clinical and economic performance.
Many of the positive findings reported here can be seen as a function of local knowledge and relationships developed over time. However, the community hospital’s role in facilitating early discharge from acute hospital and avoiding unnecessary acute hospital admissions indicates a potential for health gains and cost containment and a valuable example for community hospitals in Italy and elsewhere.
List of abbreviations
- A&E
- accident and emergency
- ADL
- activities of daily living
- ASL
- Aziende Sanitarie Locali
- CHP
- community health partnership
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- COPD
- chronic obstructive pulmonary disease
- DRG
- diagnosis-related group
- FTE
- full-time equivalent
- GDP
- gross domestic product
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HELFO
- Norwegian Health Economics Administration
- HMIC
- Health Management Information Consortium
- IHPA
- Independent Hospital Pricing Authority
- IRCCS
- Istituti di ricovero e cura a carattere scientifico
- ISD
- Information Services Division
- IT
- information technology
- KAD
- kommunale akutte døgnplasser
- LEA
- Livelli Essenziali di Assistenza
- LHN
- local hospital network
- MBS
- Medicare Benefits Scheme
- MOSS
- Medical Officer of Special Scale
- MPS
- Multipurpose Service
- NETSCC
- NIHR Evaluation, Trials and Studies Coordinating Centre
- NHI
- National Health Insurance
- NIHR
- National Institute for Health Research
- NOK
- Norwegian kroner
- OECD
- Organisation for Economic Co-operation and Development
- OR
- odds ratio
- PBS
- Pharmaceutical Benefits Scheme
- PFI
- private finance initiative
- PHN
- Primary Health Network
- PIP
- Practice Incentive Program
- PPI
- patient and public involvement
- PPP
- purchasing power parity
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RHA
- regional health authority
- RSA
- Residenza Sanitaria Assistenziale
- SD
- standard deviation
- SIRCO
- Regional Community Hospitals Information System
- SSN
- Servizio Sanitario Nazionale
- UCCP
- Unità Complesse di Cure Primarie