Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1024/02. The contractual start date was in March 2013. The final report began editorial review in January 2016 and was accepted for publication in December 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Alex D Tulloch and Faisil Sethi work as consultant psychiatrists for South London and Maudsley NHS Foundation Trust. Faisil Sethi is vice chairperson of the National Association of Psychiatric Intensive Care Units.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Bowers et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Acute inpatient care
In psychiatric services, acute inpatient care may be defined as the short-term care and treatment of people with greater psychiatric symptom severity within accommodation that is secure and supervised 24 hours per day. Its primary purpose is to maintain the safety of patients and others, as well as to allow more substantial assessment and provide treatment that is not easily or safely deployed in community settings. Reflecting these objectives, acute inpatient care is often provided on a compulsory basis, via mental health legislation and its associated procedures. In the UK, acute inpatient care is provided primarily via the NHS, with small psychiatric hospitals or units consisting of several wards serving their local areas. These wards are staffed by a mix of qualified and unqualified nurses, supported by occupational therapists, psychologists and a range of medical staff, including consultant psychiatrists. Lengths of stay are generally between 2 and 3 weeks, and more than half of patients either are admitted compulsorily or become subject to compulsory care during the course of their stay.
Given that the justification for compulsory care is the risk that patients pose to themselves or others, and as all patients are admitted (compulsorily or not) because they are severely and acutely mentally ill, an acute psychiatric ward is typically populated by a mix of patients who may behave in a very disturbed, disorganised and risky way. Specifically, acute psychiatric inpatients may be verbally abusive, damage property, assault others, seek to escape, harm themselves, attempt suicide, refuse or resist treatment that will help them, refuse to eat, drink or wash, or behave in other ways that those around them find difficult to tolerate. In order to manage such behaviours safely and respectfully, in crisis situations the staff may use a number of different containment methods, ranging from oral sedating medication to special supervision and observation, manual restraint of the patient, rapid tranquillisation via injection, seclusion or transfer to a psychiatric intensive care unit (PICU). Although generally unheard of in current British psychiatric practice, related methods such as the use of net beds (a bed enclosed in a net cage) and mechanical restraints remain in use in other parts of the world.
Seclusion
Seclusion is the isolation of a disturbed psychiatric patient in a robust locked room. A recent literature review1 found that 12–48% of patients were secluded at least once during their admission to acute wards. Secluded patients were younger, more likely to be formally detained and less likely to suffer from depression than non-secluded patients. Sex, ethnicity and socioeconomic status had no influence on seclusion rates. Seclusion made patients feel angry, lonely, sad, hopeless, punished and vulnerable. The efficacy of seclusion in reducing aggression and injuries to staff and patients has not been evaluated. The City-128 study2 found that seclusion use on wards was associated with increased rather than reduced aggression, and that seclusion usage and provision were associated in complex ways with the proximity of a PICU and the use of locked doors on acute wards. However, these analyses were based on data aggregated at ward level at each time point and so it was not possible to estimate the effect of seclusion at the individual level. A study published in 20123 found that the outcome of seclusion (judged as the repetition of physical violence to others) was no better than that of time out (a request for the patient to stay in their own room for a period, without the door being locked); however, the sample size was modest and the analysis did not control for differences in patient characteristics.
Some hospitals in the UK have begun to end the use of seclusion. At the time of writing, around 25–50% of hospitals do not seclude patients at all and do not have seclusion rooms for acute psychiatric patients. However, in some hospitals, up to one-quarter of admitted patients are secluded once or more during the first 2 weeks of their admission. 2,3 Although many countries (e.g. the USA, Australia, the Netherlands) are running large-scale programmes to reduce seclusion use, with varying success, it is not known how some of our UK hospitals are achieving seclusion-free care or if the outcomes in terms of aggression rates and injuries are better or worse. We do know that access to seclusion rooms in UK hospitals is linked to when the unit concerned was built, with more modern units less likely to have such a room. 2 Presumably as new units have been built to replace older ones, seclusion has been eradicated with this move. However, it is not known whether or not this been accomplished by substitution (greater use of alternative forms of containment), early intervention (faster progression to manual restraint during crises leading to easier resolution), therapeutic intensity (behavioural or psychotherapeutic interventions to avert crises before they occur) or non-standard transfers (to other hospitals or services). The use of manual restraint is clearly critical, as this is a gateway measure to other coercive interventions (seclusion, a PICU, rapid tranquillisation) or a replacement for them if utilised continuously for longer durations.
The use of coercive containment methods is an area of primary concern to service users. Previous research has shown that patients rate seclusion as less acceptable than nearly every other form of containment. 4 In line with this finding, a recent report by MIND on acute inpatient care5 calls for the elimination of seclusion and manual restraint as soon as possible, and their replacement with a system based on co-operation, negotiation and mutual respect.
Most psychiatric services in the UK do use seclusion, yet there is a widespread aspiration to minimise the use of such interventions, which are unpalatable to nurses6 and patients. 5 A key practical question for managers is ‘what are the services that are not using seclusion actually doing to manage disturbed behaviour in a safe and successful manner?’. This is not a straightforward question and simply asking professionals does not generate an adequate answer. If you ask nurses at a hospital that does not use seclusion to explain how they manage without it, they will struggle to find an answer. They simply do not use it and do not feel the need for it. Yet nurses at hospitals that do use seclusion struggle to understand how others do without it and speculate that sedating drugs are given more often, and in higher doses, or that patients are held in manual restraint for long periods. These questions are critical for psychiatric service managers faced with demands to reduce reliance on coercive methods and make inpatient care more efficient. The absence of answers to these questions holds back many who might otherwise abolish seclusion use by simply decommissioning seclusion rooms or reducing the numbers of PICU beds.
Psychiatric intensive care units
When risks are higher than the norm for an acute psychiatric ward, patients can be transferred to a PICU. PICUs are small wards with higher levels of nursing and other staff, built on an open-plan design to ease observation, often (but not always) locked and sometimes (but not always) with facilities for seclusion. A recent literature review7 identified that typical PICU patients are male, younger, single, unemployed, suffering from schizophrenia or mania, from a black Caribbean or African background and legally detained, and have a forensic history. The most common reason for admission is aggression management and most patients stay for < 1 week. Only two studies provide any data on cost and, of these, only one is from the UK; this study gives a cost per patient per annum of £103,501, based mainly on staffing costs in the mid-1990s. 8 The other study, from Canada, gives a cost of CA$365 per patient per day, compared with CA$235 for an acute unit9 (i.e. a difference of 55%). Information on costs is lacking, and the cost-effectiveness of PICU care relative to acute care has never been identified or described. The same literature review7 concludes that PICUs have been very poorly evaluated for their efficacy, with only two small-scale studies carried out on single units reporting decreases in aggression. Given the expenditure on PICU care, it is anomalous that no systematic evaluation has ever taken place.
An analysis of data from the Service Delivery and Organisation-funded City-128 cross-sectional multivariate study of acute psychiatric wards of differences in access to PICU care has raised questions about outcomes. 10 Controlling for other factors, wards with greater ease of PICU access did not have lower rates of adverse incidents. PICU transfers were associated with seclusion, manual restraint and other severe containment measures, and were triggered by aggression, drug use and absconding. The findings suggest that transferring patients to a PICU may not be an effective means of reducing the frequency of adverse incidents on acute wards. Longitudinal research using individual patient-level data is required to assess whether or not this conclusion is valid.
The past few years have seen several innovations and changes to PICU provision. In some cases, a significant number of PICU beds have been allocated to the treatment of transfers of acutely mentally ill people from the prison system, leading to the reduced availability of a PICU for transfers of difficult and high-risk patients from acute psychiatric wards. At the same time, the increasing practice of keeping acute psychiatric wards locked is likely to have led to reduced transfers of patients to PICUs in order to prevent risk resulting from the patient absconding. 11,12 Finally, some new psychiatric units have opened that have no PICU provision at all, or, in other instances, PICU provision has been limited to a single site within a much larger multihospital NHS trust. The consequences and efficacy of these differing systems for managing high-risk patients has been neither compared nor evaluated on a wide scale.
Psychiatric intensive care unit care is a potentially very expensive intervention. The provision of a special ward with high staffing levels could not be anything other. However, this cost may be acceptable if outcomes are improved or savings occur as a result of reduced length of stay or reduced use of other services. Even the provision of a PICU may itself be cost neutral to some degree if it enables lower nurse staffing levels on the acute wards to which it provides a service. The question of cost and outcome, therefore, has a clear bearing on the choices service managers must make in this area. However, currently there is no research evidence on which they can draw, underscoring the need for the projects proposed here.
The Seclusion and Psychiatric Intensive Care Evaluation Study
Our research was devised to obtain answers to some of these questions and consisted of two linked studies. The first of these studies used the electronic patient record system of one NHS trust to compare patients transferred to a PICU with those who were not and, in addition, compare patients subject to seclusion with those who were not. We hoped to understand both the factors associated with the use of each intervention and if each intervention altered the associated outcomes and costs. The results of this study are presented in Chapters 2 and 3.
In the second study, the sets of all interventions used by nurses to manage disturbed behaviours were collected via structured interview and questionnaires. These data were collected across hospitals that did and did not have direct access of seclusion rooms or PICUs, thus making it possible to compare the differences in the management strategies used by nurses in the absence of seclusion or PICU facilities. The results of this study are presented in Chapters 4 and 5.
A final discussion (see Chapter 6) brings together the range of results obtained across the entire Seclusion and Psychiatric Intensive Care Evaluation Study (SPICES) and considers what these results might mean for future clinical care and research.
Chapter 2 Predictors of use of a psychiatric intensive care unit and seclusion
This chapter is based on data from Cullen et al. 13 under the terms of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0), which permits unrestricted reuse, distribution and reproduction in any medium, provided the original work is properly cited.
Introduction
Comprehensive reviews of PICU14 and seclusion1 practices indicate that PICU patients are typically male, young (aged ≈30 years), diagnosed with schizophrenia or bipolar disorder, and legally detained, with some evidence that PICU patients are more likely than non-PICU patients to be of black African or Caribbean heritage. Although secluded patients are also likely to be young and legally detained, seclusion has not been consistently associated with either patient sex or patient ethnicity. 1 Similar to PICU patients, however, secluded patients are commonly diagnosed with schizophrenia and bipolar disorder, with personality disorder also reported as more prevalent in this population. With regard to behavioural precursors, aggressive, disruptive and chaotic behaviour, acute psychosis, absconsion and self-harm are all strongly associated with the use of both a PICU and seclusion. 1,14 Although there is some evidence that these behavioural precursors differ between men and women, the extent to which patient sex is associated with PICU and seclusion duration (which one might expect to be influenced by preceding behaviours) has yet to be examined.
There are several notable limitations of the studies described in these reviews. First, many of the previous studies are descriptive in nature, for example reporting the average age or the proportion of men without reference to a control population. Furthermore, of those that have statistically compared patients receiving these treatments with general psychiatric patients, few have included an appropriate control group. Rather, studies often compare PICU and secluded patients with the entire hospital/ward population as opposed to identifying a subgroup of patients who are at risk but who do not receive these treatments. Finally, studies reporting differences in patient characteristics across treated and untreated groups have typically failed to adjust for patient behaviours that might account for these differences. In the light of these limitations, the aims of the current study were to:
-
use multiple logistic regression analyses, applied to two samples of treated (cases) and untreated subjects (controls), to determine the demographic, clinical and behavioural characteristics associated with both PICU care and seclusion
-
explore interactions between patient sex and other predictors of PICU and seclusion receipt.
Methods
The Biomedical Research Centre Clinical Records Interactive Search database
Source data
South London and Maudsley (SLaM) provides secondary mental health care to a population of approximately 1.1 million residents from four south-east London boroughs (Lambeth, Southwark, Lewisham and Croydon). The Biomedical Research Centre (BRC) Clinical Records Interactive Search (CRIS), described in detail in other studies,15–17 comprises the anonymised electronic medical records of over 200,000 patients who have been in contact with SLaM services since 2006, when electronic records were implemented across the trust. The available data are either structured data or free-text data. Structured data contain a variety of data types (numbers, dates or short standardised text) including personal details, demographic information and details of clinical activity such as appointments, dates of periods of service by clinical teams and details associated with free-text records (e.g. the date on which a particular item of correspondence was created and added to the case notes). Free-text data comprise mainly correspondence (e.g. documentation and communication concerning the patient) and progress notes that are recorded regularly by staff. CRIS is capable of extracting data in both formats, that is, information held in both structured fields and free-text entries.
Anonymisation process
The anonymisation procedure within CRIS consists of two stages. 18 In the first, patient-identifiable information is stripped from the structured data in CRIS; dates of birth are truncated to month and year of birth, ethnicity is grouped into broad categories, addresses are converted to the corresponding Office for National Statistics output area, and the names of the service user and contacts are removed. A pseudonymous identifier is created, replacing local and national identifying numbers. In a second stage, free-text data are cleaned of names: wherever names or recorded aliases for the user or their relatives are encountered in the free text, they are replaced with ‘ZZZZZ’ or similar. Once cleaned, data are organised into around 100 tables ranging from the small (tables containing infrequently used test scores) to the extremely large (e.g. the table containing free-text progress notes, which has over 10 million rows).
Ethics approval
The BRC CRIS security procedures have been reviewed by the Oxfordshire Research Ethics Committee (08/H0606/71) and the tool is treated for ethics purposes as an anonymised database: that is, access is granted after review of applications by an oversight committee. Approval for the current study was obtained from the oversight committee in March 2014.
Clinical Records Interactive Search data extraction techniques
Structured Query Language (SQL) can be used to extract data held in CRIS (both in structured fields and free text) to create data tables that can then be manipulated, merged (joined) and exported to other software such as Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) or Stata® (StataCorp LP, College Station, TX, USA). SQL allows the retrieval of records meeting specified criteria, such as those containing particular words or those that meet criteria in other linked fields (e.g. records made during a time interval defined separately for each sample of individuals). The use of SQL to interrogate the CRIS database has huge advantages, in terms of both time and accuracy, over manually searching data to identify records of relevance.
Psychiatric intensive care unit cohort
Identification of psychiatric intensive care unit cohort cases
Psychiatric intensive care unit cohort services in SLaM are provided by five wards: four in general adult services (three male only and one female only) and one within the forensic inpatient service. PICU cases (n = 986) were defined as all transfers of patients from general adult acute wards to a (non-forensic) PICU ward occurring during the study period of April 2008 to April 2013. Figure 1 summarises how these PICU cases relate to all admissions during the same period. Direct admissions to a PICU from the community were excluded primarily because our method depended on being able to code behaviours in the 3 days prior to entry into the PICU and the available notes for patients just admitted to hospital were considered unlikely to suffice. In addition, as we hypothesised that factors predicting PICU transfer would differ substantially among general adult and forensic wards (and our primary interest was in the former) we also excluded transfers from forensic wards to any PICU and all transfers into the forensic PICU.
FIGURE 1.
Identification of PICU cases (treated) and controls (untreated).
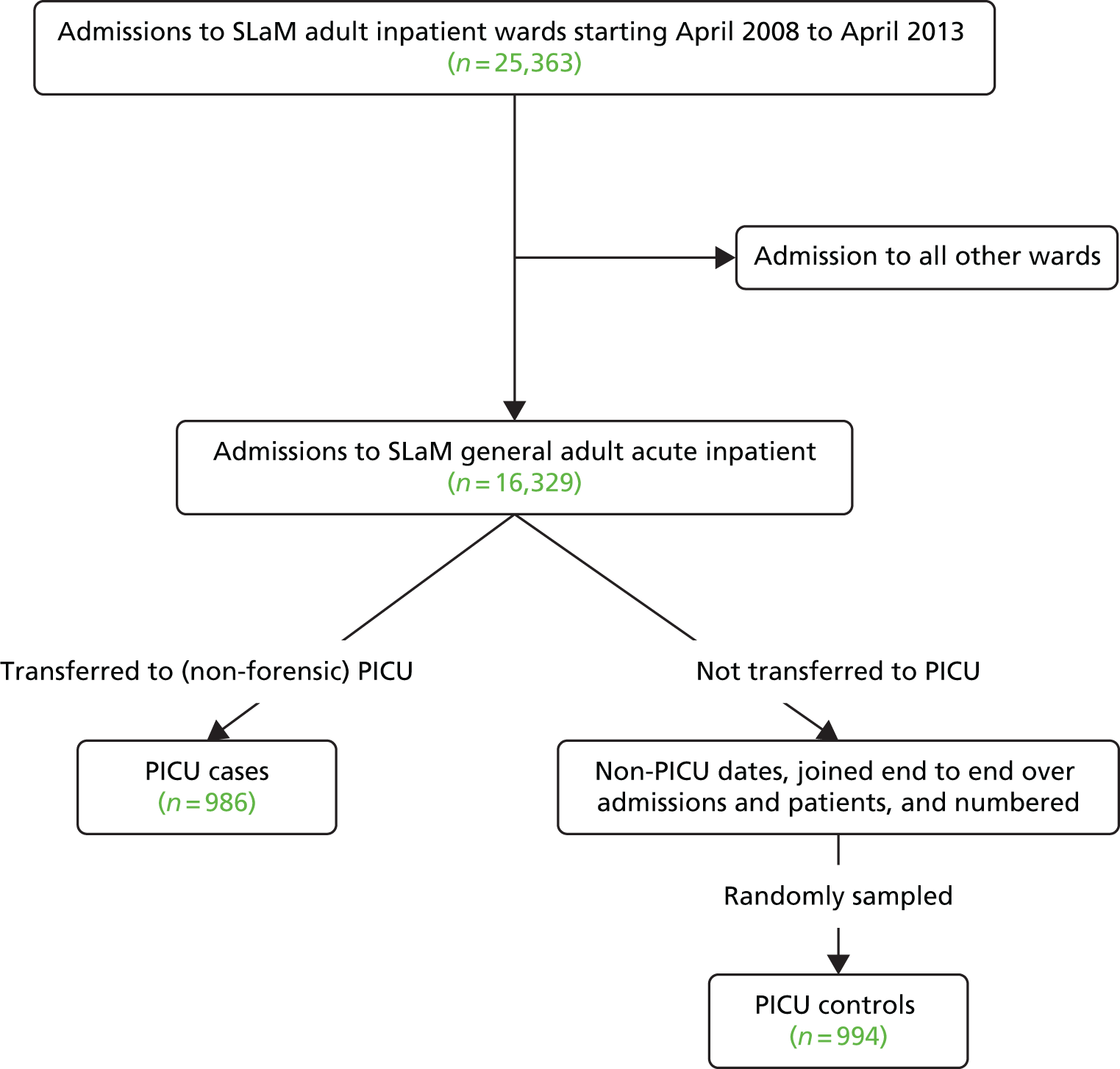
Identification of psychiatric intensive care unit controls
We used SQL to obtain a control group of patients treated in general adult wards to serve as a comparison for the PICU case group (see Figure 1). These controls were randomly selected from a population of patient-day combinations – the sum of all days on which a particular patient could have been transferred to a PICU but was not. The procedure followed was this: we first created a data set that comprised all admissions to general adult wards between April 2008 and April 2013; from these admissions, we then excluded dates corresponding to periods of treatment in PICU wards, including the date of transfer to and out of the PICU ward. These non-PICU periods of time were then combined to create a data set representing all general adult (non-PICU) inpatient-days for all patients admitted during the study period. These inpatient-days were then assigned a sequential number such that each number corresponded uniquely to a particular date, within a particular admission, for an individual patient. Random numbers, corresponding to a specific inpatient date, were then generated with a sampling probability rate of 0.0017 and used to identify a PICU control group of approximately equal size to the PICU case group (n = 994). This method is truly population based, avoiding the greatest threat to the validity of case–control studies. The way that it combines the selection of a subject and a non-transfer date also increases validity. Because the method for defining behavioural predictors depends on their measurement in the period directly before transfer or non-transfer to a PICU (see Preparation of intermediate data sets), definition of a non-transfer date subsequent to selection of controls would have introduced bias: whether or not because of differential length of the at-risk period between subjects (long vs. short admission) or systematic selection of a particular point in admission.
Seclusion cohort
Seclusion cases
The use of seclusion is recorded in free-text progress notes within the electronic patient record rather than in any structured field. Relevant free-text data were therefore extracted and used to identify seclusion spells. Using SQL, we initially extracted progress notes containing the words ‘seclusion’, ‘supervised confinement’ or ‘solitary confinement’. We manually cleaned these to create a database comprising details of all seclusion spells occurring during the study period (n = 1478). Based on the assumption that seclusion practices across general and forensic wards might also differ substantially, seclusions occurring on forensic wards (n = 240) were subsequently excluded from the data set. We also excluded seclusions on other non-PICU wards, which formed only a small proportion of the non-forensic seclusions (n = 248), in order to reduce heterogeneity. Seclusion episodes examined in the current study were therefore those that occurred on the four non-forensic PICU wards (n = 990). Figure 2 summarises the procedure used to construct the seclusion databases.
FIGURE 2.
Identification of seclusion cases (treated) and controls (untreated).
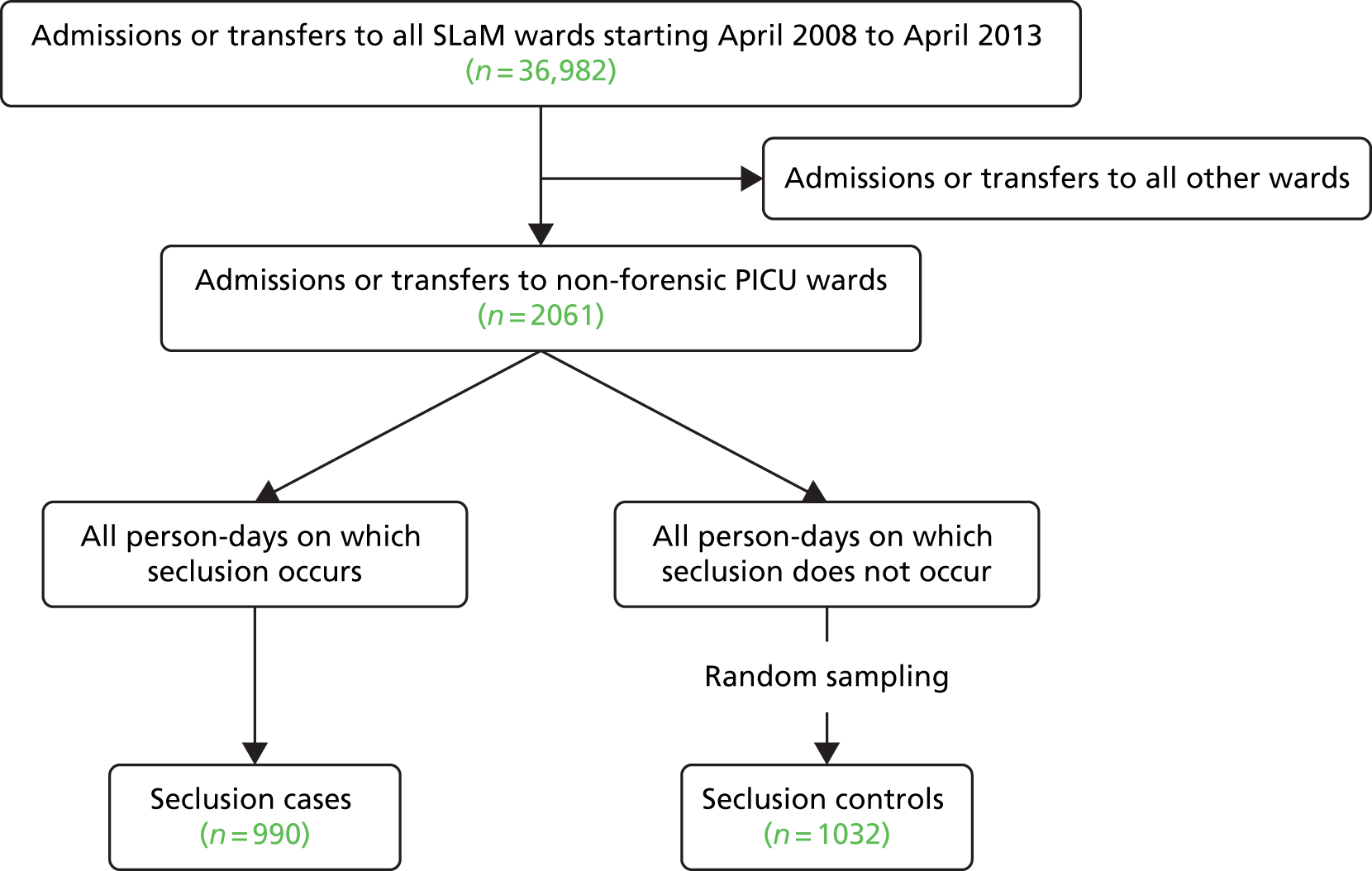
Seclusion controls
Seclusion controls were identified using a similar procedure to that used to identify PICU controls (summarised in Figure 2). As our seclusion cases were restricted to seclusion episodes occurring on PICU wards, seclusion controls were selected by randomly sampling dates from the set of patient-days on non-forensic PICU wards where the patient was neither in seclusion, sent to seclusion or returned from seclusion. To obtain these control dates, we first extracted a data set that included dates of all non-forensic PICU ward stays occurring between April 2008 and April 2013 (note that, as we did not exclude PICU patients admitted directly from the community, the base population from which potential controls were sampled exceeds the number of cases examined in the PICU analysis). Using the manually created seclusion database described above, dates corresponding to days when a patient was in seclusion at any time were excluded. These non-seclusion PICU periods were combined and numbered sequentially. Random numbers were then generated to identify dates that corresponded to time periods when a patient was not in seclusion using a sampling probability rate of 0.016. This yielded a seclusion control group of approximately equal size to the seclusion case group (n = 1032).
Consequences of how cases and controls were defined
It is important to note that at the analysis level, ‘cases’ refer to transfers into PICU treatment and into seclusion, and not to unique patients. Similarly, as set out above, controls are non-transfers of patients into a PICU or seclusion, rather than patients who are not transferred to a PICU or into seclusion. The same patient could, in principle, feature within a data set multiple times as a case (each time they are secluded or sent to a PICU) and also as a control (on any day during which they are not transferred). This respects the fundamental principle of case–control design, which is that any patient who is at risk of the outcome of interest should be eligible for selection as a control. The fact that an individual person may contribute more than one observation to the data set may create clustering within the data, a feature that must be taken account of by the selected method of analysis.
Treatment length
The number of days in PICU treatment was calculated as the difference between the date of transfer to the PICU ward and the data of transfer away from the PICU ward (or discharge, if the same). Length of time in seclusion was calculated as the number of days between the start and end data of seclusion; durations of 0 days indicated seclusion spells that were < 24 hours’ duration.
Extraction of predictor variables
Behavioural exposures
For each intervention (PICU and seclusion), we used a two-stage process to generate a set of potential behavioural predictors for later consideration alongside other potential predictors.
First, we generated a list of potentially relevant behavioural search terms directly from a sample of free-text progress notes. Specifically, a random sample of 500 such notes recorded on the day of PICU transfer or 2 days prior to these dates was extracted along with an analogous sample of notes made on the day of a seclusion commencement or the 2 days prior. The notes were manually reviewed to identify relevant incidents preceding PICU transfer and seclusion (e.g. aggressive/chaotic behaviour and absconsion), and words commonly used by clinical staff to describe these behaviours were recorded. Any behaviour that actually occurred after PICU transfer or after seclusion had started was excluded.
The second stage of this process involved limiting this list of words to those most strongly related to incidents that occurred prior to PICU transfer/seclusion. To achieve this, we extracted another random data set of 350 progress notes recorded within any psychiatric admission but that did not occur on the day of PICU transfer/seclusion or in the 2 days prior to these dates. These records were then manually coded to identify those containing the words generated in the previous step. Before analysis, related words were grouped together; for example, absconded was grouped with abscond, absconded and absconding. Because the resulting groups would be used in a later stage of the research as a means of tagging extracted records, they were represented as regular expressions, in which literal character strings were sometimes combined with the use of a wildcard operator (*) and could be combined with Boolean operators. Table 1 lists these ‘keywords’ along with potential matches and examples of relevant, related behaviours.
| Search term | Behaviours of interest | Examples of behaviours as recorded in notes | Use in seclusion analysis | Use in PICU analysis |
|---|---|---|---|---|
| Abscon* | Actual absconsion or serious attempts at absconsion |
|
Not screened | Retained |
| Abus* | Verbally abusive behaviour |
|
Retained | Retained |
| Aggress* | Verbal or physical aggression directed at others or objects |
|
Retained | Retained |
| Agitat* | Observed agitated behaviour |
|
Retained | Retained |
| Angry OR anger | Reported as behaving in an angry way |
|
Discarded | Not screened |
| Arous* | Observed aroused behaviour |
|
Discarded | Not screened |
| Assault* | Actual or attempted physical assault |
|
Retained | Discarded |
| Attack* | Actual or attempted attacks |
|
Not screened | Retained |
| AWOL | Patient recorded as AWOL |
|
Not screened | Retained |
| Demand* | Demanding of resources or change in treatment |
|
Retained | Retained |
| Hit* | Actual or attempted physical assault |
|
Retained | Not screened |
| Hostile | Reported as behaving in a hostile way |
|
Discarded | Not screened |
| Incident | Some kind of disorderly or violent incident occurred |
|
Not screened | Discarded |
| Irritable* | Observed irritable behaviour |
|
Not screened | Retained |
| Manic | Observed manic behaviour |
|
Not screened | Retained |
| Push | Pushing someone else |
|
Discarded | Not screened |
| Refus* | Refusal of staff requests/treatment |
|
Not screened | Retained |
| Restrain* | Restraint of patient by staff |
|
Retained | Not screened |
| Shout* | Shouting directed at others |
|
Retained | Retained |
| Threat* | Verbal threats of harm to others |
|
Retained | Retained |
| Threw OR throw* | Objects thrown at others or destruction of property |
|
Retained | Retained |
| Violen* | Actual physical violence |
|
Retained | Retained |
Having created two ‘transfer’ data sets and one ‘non-transfer’ data set, two multivariable logistic regression analyses were run. All keywords for PICU transfer and for seclusion transfer were entered into separate multivariable logistic regression analyses in order to identify the keywords that best discriminated between events that occurred prior to PICU transfer or, in the other analysis, seclusion and those that did not. Keywords that were significant at the 0.1 level in each of the multivariable analyses were used as search terms in the final data extraction. As will be described below, the numbers of data used in these initial steps were two orders of magnitude smaller than the row sets used for the final analyses.
Preparation of intermediate data sets
Having performed these preparatory steps, we proceeded to extract an intermediate, ‘working’ data set for each of the analyses using SQL. To the anonymous person identifier (ID) and sample date, we joined (1) sex, (2) ethnicity, (3) date of birth, (4) admission date for the current SLaM inpatient episode, (5) primary International Classification of Diseases, Tenth Edition19 diagnosis nearest to date of discharge and (6) legal status under the Mental Health Act (MHA)20 at midnight on the sampling date. Time between admission and the sample date was recoded as a four-level categorical variable (< 7 days, 8–21 days, 22–60 days, > 60 days) based on the distribution of the data. For a small number of observations (< 1%) we were able to code missing primary diagnosis manually based on correspondence. Primary diagnoses were extracted from structured fields or retrieved manually from admission, discharge or tribunal reports if unavailable (< 1%). When multiple records were available, which may arise, for example, when a patient receives different diagnoses at different admissions, we extracted the record closest to the sampling date (i.e. the date of PICU transfer or date of seclusion for cases and random sampling date for controls). MHA section was determined at midnight on the sampling date.
The ‘left-hand’ part of each data set described above was structured as a single row of data for each combination of person and sample date. We then joined this to any free-text progress note that (1) occurred on the sampling date – that is, the date of PICU transfer or seclusion for cases and the random sampling date for controls – or either of the 2 days prior to these dates, and (2) that contained at least one of the relevant search terms identified in the two-stage process described above. This join was performed such that each progress note required its own row in the data set; thus, for example, if three separate progress notes were joined to a single person–sample date combination, the pre-existing single row would be expanded to form three rows. Accordingly, the PICU intermediate data set comprised 22,504 data rows and the seclusion intermediate data set comprised 22,239 data rows.
The SQL script also generated additional columns containing an indicator variable for the presence or absence of each search term in the corresponding progress note. Once exported to a Microsoft Excel spreadsheet, each progress note was manually reviewed to determine whether or not the search term referred to a behaviour that actually occurred on the day of the event. The indicator variable was edited accordingly, such that in the final coded data set it represented the presence or absence of the behaviour in question. For example, a given record may have been identified using the SQL script that included the terms ‘Irritable’, ‘Aggress*’ and ‘Violen*’, with the columns associated with each of these three terms coded as 1. However, after reviewing the record, the text might actually state that the patient in question had been ‘irritable but had not shown any aggression or violence during the shift’; thus, the columns for ‘Aggress*’ and ‘Violen*’ would be changed from 1 (as coded by the SQL script) to 0.
After the data cleaning procedure was completed, both data sets were imported into Stata version 12 and the ‘max’ and ‘drop duplicates’ commands were used to collapse data across rows so that each combination of person and sample date was represented again by a single row within which each behavioural variable recorded the presence or absence of that behaviour over the entire 3-day period of sample date and two preceding days.
Statistical analyses
All analyses were conducted using Stata. The same procedure was used for the analysis of PICU and seclusion use; in all analyses, the BRC ID was included as a random effect in order to account for clustering at the patient level (i.e. within each data set a single patient could represent multiple cases or controls, by including the BRC ID as a random effect, correlations between data observations obtained by the same patient were accounted for). Univariable logistic regression analyses were first performed to examine associations between all predictor variables (demographic/clinical factors and behavioural precursors) and PICU/seclusion status. We then performed a multivariable analyses for each outcome (PICU and seclusion) that included all predictor variables, irrespective of whether or not they were significantly associated with the outcome in univariable analyses. We subsequently conducted exploratory multivariable analyses that included interaction effects between sex and all other predictor variables; that is, all predictor variables and all interaction effects (sex with all other predictors) were entered simultaneously, with subsequent removal of all effects with p ≥ 0.05. In the analyses presented in this chapter, we did not apply probability weight – as is typical in case–control studies – and therefore the intercept values are uninterpretable (weights were used in the derivation of propensity scores in Chapter 3).
Results
Predictors of psychiatric intensive care unit transfer
Sample
The PICU sample comprised 986 cases (PICU transfers) and 944 controls (PICU non-transfers). All of these observations originated from 1360 patients, of whom 693 contributed only non-PICU observations, 515 contributed only PICU observations and 152 contributed a mixture. The contribution that each group of people made to the total number of observations was as follows: those who were never transferred contributed a mean of 1.2 observations [standard deviation (SD) 0.4 observations], those who were only ever transferred to a PICU in our data set contributed a mean of 1.4 observations (SD 0.9 observations) and those who were both transferred and not transferred contributed a mean of 3.0 observations (SD 1.5 observations).
Univariable analyses
Table 2 presents the demographic and clinical characteristics for cases and controls, and the results of the univariable logistic regression analyses. PICU cases were significantly younger than controls (mean age 32.9 vs. 40.7 years, respectively; p < 0.001) and were less likely to be female [odds ratio (OR) 0.29; p < 0.001]. There was also a significant association between ethnicity and case status, whereby the likelihood of PICU transfer was approximately threefold higher among individuals of black African/Caribbean ethnicity than among those of white ethnicity (OR 2.97; p < 0.001); being of ‘other’ ethnicity was also associated with slightly elevated likelihood of PICU transfer, but this was not statistically significant. With regard to diagnosis, relative to patients with schizophrenia, those diagnosed with other psychotic disorders (including schizoaffective disorder) and bipolar disorder were significantly more likely to be transferred to a PICU ward (OR 2.04 and 3.69, respectively; p < 0.001), whereas the odds of transfer were significantly lower among those with ‘other’ diagnoses (OR 0.46; p < 0.001). Strong and highly significant associations were also observed between MHA section and PICU status, whereby patients on a civil section (section 2) and those on section 3 or a forensic section were significantly more likely to be transferred to a PICU than patients who were informal (OR 136.10 and 39.24, respectively; p < 0.001). Finally, the likelihood of PICU transfer decreased as the admission progressed in a dose–response fashion, whereby the odds of transfer were significantly lower at each subsequent time band relative to the first 7 days of the admission (p < 0.001 for all). Both ward and financial year were also significantly associated with the odds of transfer.
| Risk factor | Cases (N = 986), n (%) | Controls (N = 994), n (%) | Analyses | |||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | |||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | |||
| Age (years) | ||||||||
| ≥ 45 | 151 (15) | 365 (37) | 1 | – | – | 1 | – | – |
| 35–44 | 220 (22) | 273 (27) | 2.62 | 1.72 to 4.01 | < 0.001 | 2.53 | 1.43 to 4.47 | 0.001 |
| 25–34 | 342 (35) | 216 (22) | 7.24 | 4.59 to 11.41 | < 0.001 | 4.35 | 2.36 to 8.01 | < 0.001 |
| < 25 | 273 (28) | 140 (14) | 9.08 | 5.52 to 14.95 | < 0.001 | 5.66 | 2.86 to 11.19 | < 0.001 |
| Sex | ||||||||
| Female | 260 (26) | 429 (43) | 0.29 | 0.20 to 0.42 | < 0.001 | 0.11 | 0.04 to 0.28 | < 0.001 |
| Ethnicity | ||||||||
| White | 273 (28) | 423 (43) | 1 | – | – | 1 | – | – |
| Black African/Caribbean | 625 (63) | 465 (47) | 2.97 | 2.08 to 4.23 | < 0.001 | 1.44 | 0.93 to 2.25 | 0.104 |
| Other | 88 (9) | 106 (11) | 1.50 | 0.87 to 2.59 | 0.148 | 1.06 | 0.54 to 2.09 | 0.865 |
| Diagnosis | ||||||||
| Schizophrenia | 353 (36) | 434 (44) | 1 | – | – | 1 | – | – |
| Other psychotic | 258 (26) | 191 (19) | 2.04 | 1.38 to 3.01 | < 0.001 | 1.53 | 0.93 to 2.49 | 0.091 |
| Bipolar disorder | 264 (27) | 131 (13) | 3.69 | 2.37 to 5.76 | < 0.001 | 1.88 | 1.08 to 3.27 | 0.026 |
| Personality disorder | 27 (3) | 49 (5) | 0.60 | 0.27 to 1.34 | 0.215 | 0.89 | 0.24 to 3.30 | 0.862 |
| Other diagnosis | 84 (9) | 189 (19) | 0.46 | 0.29 to 0.73 | 0.001 | 0.81 | 0.41 to 1.57 | 0.526 |
| MHA section | ||||||||
| Informal | 37 (4) | 445 (45) | Reference | – | – | Reference | – | – |
| Section 2 | 379 (38) | 130 (13) | 136.10 | 67.18 to 275.74 | < 0.001 | 10.58 | 5.17 to 21.66 | < 0.001 |
| Section 3/forensic | 570 (58) | 419 (42) | 39.24 | 22.16 to 69.52 | < 0.001 | 10.14 | 5.29 to 19.44 | < 0.001 |
| Time since admission (days) | ||||||||
| Male and female | ||||||||
| ≤ 7 (all) | 409 (41) | 191 (19) | Reference | – | – | |||
| 8–21 | 199 (20) | 186 (18) | 0.33 | 0.21 to 0.52 | < 0.001 | |||
| 22–60 | 188 (19) | 291 (29) | 0.13 | 0.08 to 0.20 | < 0.001 | |||
| > 60 | 190 (19) | 326 (33) | 0.09 | 0.05 to 0.15 | < 0.001 | |||
| Male | ||||||||
| ≤ 7 (all) | 1 | – | – | |||||
| 8–21 | 0.34 | 0.17 to 0.70 | 0.004 | |||||
| 22–60 | 0.40 | 0.19 to 0.83 | 0.015 | |||||
| > 60 | 0.48 | 0.23 to 1.00 | 0.050 | |||||
| Female | ||||||||
| ≤ 7 (all) | 1 | – | – | |||||
| 8–21 | 2.45 | 0.92 to 6.53 | 0.074 | |||||
| 22–60 | 1.16 | 0.42 to 3.23 | 0.775 | |||||
| > 60 | 0.92 | 0.31 to 2.72 | 0.884 | |||||
| Financial year | ||||||||
| 2008–9 | 176 (18) | 270 (27) | Reference | – | – | Reference | – | – |
| 2009–10 | 181 (18) | 208 (21) | 1.24 | 0.81 to 1.90 | 0.322 | 0.79 | 0.45 to 1.40 | 0.423 |
| 2010–11 | 225 (23) | 194 (20) | 1.86 | 1.22 to 2.84 | 0.004 | 0.87 | 0.48 to 1.58 | 0.643 |
| 2011–12 | 225 (23) | 174 (18) | 2.29 | 1.48 to 3.53 | < 0.001 | 0.63 | 0.33 to 1.21 | 0.166 |
| 2012–13 | 179 (18) | 148 (15) | 2.00 | 1.27 to 3.16 | 0.003 | 0.60 | 0.31 to 1.16 | 0.129 |
| Warda | ||||||||
| Behavioural precursors | ||||||||
| Abscon* | 143 (15) | 14 (1) | 27.28 | 12.40 to 60.04 | < 0.001 | 4.24 | 1.63 to 11.01 | 0.003 |
| Abus* | 482 (49) | 70 (7) | 31.71 | 19.29 to 52.14 | < 0.001 | 1.93 | 1.14 to 3.28 | 0.015 |
| Aggress* | 602 (61) | 58 (6) | 61.68 | 36.04 to 105.57 | < 0.001 | 3.47 | 2.02 to 5.99 | < 0.001 |
| Agitat* | 670 (68) | 140 (14) | 35.24 | 21.77 to 57.03 | < 0.001 | 3.46 | 2.12 to 5.65 | < 0.001 |
| Attack* | 275 (28) | 6 (1) | 278.01 | 12.33 to 860.36 | < 0.001 | 29.07 | 9.23 to 91.57 | < 0.001 |
| AWOL* | 96 (10) | 24 (2) | 6.90 | 89.84 to 13.68 | < 0.001 | 4.37 | 1.97 to 9.68 | < 0.001 |
| Demand* | 456 (46) | 114 (12) | 11.10 | 3.48 to 16.03 | < 0.001 | 1.19 | 0.74 to 1.90 | 0.472 |
| Irritable* | 529 (54) | 144 (14) | 13.65 | 7.68 to 20.18 | < 0.001 | 1.40 | 0.89 to 2.22 | 0.145 |
| Manic | 144 (15) | 13 (1) | 29.40 | 9.23 to 66.05 | < 0.001 | 2.97 | 1.07 to 8.23 | 0.036 |
| Refus* | 773 (78) | 418 (42) | 11.33 | 7.75 to 16.58 | < 0.001 | 0.90 | 0.60 to 1.36 | 0.619 |
| Shout* | 536 (54) | 111 (11) | 20.60 | 13.48 to 31.47 | < 0.001 | 1.28 | 0.78 to 2.09 | 0.334 |
| Threat* | 633 (64) | 66 (7) | 59.81 | 35.44 to 100.93 | < 0.001 | 3.39 | 1.94 to 5.91 | < 0.001 |
| Threw* or throw* | ||||||||
| Male or female | 316 (32) | 21 (2) | 94.29 | 42.67 to 208.38 | < 0.001 | |||
| Male | 2.63 | 1.12 to 6.20 | 0.027 | |||||
| Female | 11.18 | 3.34 to 37.40 | < 0.001 | |||||
| Violen* | 199 (20) | 5 (1) | 163.15 | 53.28 to 505.77 | < 0.001 | 4.57 | 1.35 to 15.45 | 0.015 |
All potential behavioural precursors were strongly and significantly associated with PICU status in univariable analyses (p < 0.001). Estimates of effect were notably high for ‘Threat*’ (OR 59.81), ‘Aggress’ (OR 61.68), ‘Threw/Throw*’ (OR 94.29), ‘Violen*’ (OR 163.15) and ‘Attack*’ (OR 278.01), indicating that these behaviours showed excellent ability to discriminate between events that preceded PICU transfer and randomly selected control dates.
Multivariable analyses
Multivariable logistic regression results are presented in Table 2. Although the pattern of results was similar to the unadjusted analyses, estimates of effect for all demographic/clinical factors were slightly attenuated in the adjusted model with some effects no longer reaching statistical significance. When interactions with sex were tested, those with time since admission and with throwing (threw*/throw*) were modestly significant, so the model was refitted to include these.
In the fully adjusted model, PICU status was significantly associated with age, sex, legal status and having a diagnosis of bipolar disorder. Time since admission was associated with PICU transfer only among men. Ward remained significant. Estimates of effect for all behavioural precursors were also greatly attenuated in the fully adjusted model. PICU status remained significantly associated with ‘Abscon*’, ‘Abus*’, ‘Aggress*’, ‘Agitat*’, ‘AWOL’, ‘Threat*’, ‘Threw/Throw*’ and ‘Violen*’ (p < 0.05), with the strongest association observed for ‘Attack*’ (OR 29.07). Ethnicity and financial year were entirely non-significant.
Predictors of seclusion use
Sample
The seclusion sample comprised 990 cases (seclusion transfers) and 1032 controls (seclusion non-transfers). All of these observations originated from 771 patients, of whom 285 contributed only non-seclusion observations, 203 contributed only seclusion observations and 233 contributed a mixture. The contribution that each group of people made to the total number of observations was as follows: those who were never secluded contributed a mean of 1.8 observations (SD 1.5 observations), those who were only secluded contributed a mean of 1.8 observations (SD 1.4 observations) and those who were both secluded and not secluded contributed a mean of 5.0 observations (SD 3.7 observations).
Univariable analyses
The demographic and clinical characteristics for the seclusion cases and controls are presented in Table 3. In unadjusted analyses, the likelihood of seclusion was significantly higher among younger patients and female patients (OR 2.59; p < 0.001); there was a borderline significant increase for those with black African or Caribbean ethnicity (OR 1.42; p = 0.073). Relative to a diagnosis of schizophrenia, the odds of seclusion were significantly elevated for all other diagnoses (p < 0.05) and highest for those with personality disorder (OR 3.05; p < 0.001). Patients on a civil section (section 2), but not those on section 3 or a forensic section, were significantly more likely than informal patients to be secluded (OR 7.64; p < 0.001). In comparison with the first 7 days of the admission, the odds of seclusion for each subsequent time point were decreased (p < 0.001). The effects of financial year were non-significant, but there were significant differences between wards.
| Risk factor | Cases (N = 990), n (%) | Controls (N = 1032), n (%) | Analyses | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | |||||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | |||||
| Age (years) | ||||||||||
| ≥ 45 | 135 (14) | 231 (22) | 1 | – | – | 1 | – | – | ||
| 35–44 | 185 (19) | 216 (21) | 1.49 | 0.91 to 2.45 | 0.115 | 1.92 | 1.07 to 3.48 | 0.030 | ||
| 25–34 | 347 (35) | 366 (35) | 2.00 | 1.26 to 3.15 | 0.003 | 1.76 | 1.02 to 3.03 | 0.041 | ||
| < 25 | 323 (33) | 219 (21) | 2.98 | 1.83 to 4.86 | < 0.001 | 2.77 | 1.54 to 4.96 | 0.001 | ||
| Sex | ||||||||||
| Female | 354 (36) | 203 (20) | 2.59 | 1.80 to 3.73 | < 0.001 | 0.75 | 0.41 to 1.41 | 0.376 | ||
| Ethnicity | ||||||||||
| White | 199 (20) | 253 (24) | 1 | – | – | 1 | – | – | ||
| Black African/Caribbean | 690 (70) | 657 (64) | 1.42 | 0.97 to 2.08 | 0.073 | 1.17 | 0.73 to 1.87 | 0.518 | ||
| Other | 101 (10) | 122 (12) | 0.94 | 0.51 to 1.75 | 0.848 | 0.71 | 0.34 to 1.48 | 0.361 | ||
| Diagnosis | ||||||||||
| Schizophrenia | 323 (33) | 435 (42) | 1 | – | – | 1 | – | – | ||
| Other psychotic | 273 (28) | 262 (25) | 1.70 | 1.16 to 2.48 | 0.007 | 0.75 | 0.48 to 1.19 | 0.224 | ||
| Bipolar disorder | 283 (28) | 217 (21) | 2.60 | 1.72 to 3.93 | < 0.001 | 1.12 | 0.69 to 1.84 | 0.640 | ||
| Personality disorder | 24 (2) | 18 (2) | 3.05 | 1.15 to 8.13 | 0.025 | 1.56 | 0.44 to 5.50 | 0.486 | ||
| Other diagnosis | 87 (9) | 100 (10) | 1.76 | 1.03 to 3.02 | 0.039 | 1.13 | 0.58 to 2.22 | 0.715 | ||
| MHA section | ||||||||||
| Informal | 44 (4) | 119 (12) | 1 | – | – | 1 | – | – | ||
| Section 2 | 417 (42) | 170 (16) | 7.64 | 4.37 to 13.35 | < 0.001 | 1.89 | 0.90 to 3.99 | 0.094 | ||
| Section 3/forensic | 529 (53) | 743 (72) | 1.47 | 0.87 to 2.48 | 0.149 | 1.26 | 0.62 to 2.53 | 0.522 | ||
| Time since admission (days) | ||||||||||
| ≤ 7 | 395 (40) | 98 (10) | 1 | – | – | 1 | – | – | ||
| 8–21 | 235 (24) | 215 (21) | 0.16 | 0.11 to 0.24 | < 0.001 | 0.24 | 0.15 to 0.39 | < 0.001 | ||
| 22–60 | 204 (21) | 380 (37) | 0.06 | 0.04 to 0.09 | < 0.001 | 0.19 | 0.11 to 0.31 | < 0.001 | ||
| > 60 | 156 (16) | 339 (33) | 0.05 | 0.03 to 0.08 | < 0.001 | 0.24 | 0.15 to 0.43 | < 0.001 | ||
| Financial year | ||||||||||
| 2008–9 | 122 (12) | 177 (17) | 1 | – | – | 1 | – | – | ||
| 2009–10 | 171 (17) | 193 (19) | 1.15 | 0.74 to 1.81 | 0.548 | 1.23 | 0.68 to 2.21 | 0.488 | ||
| 2010–11 | 240 (24) | 215 (21) | 1.31 | 0.84 to 2.04 | 0.231 | 1.63 | 0.91 to 2.92 | 0.103 | ||
| 2011–12 | 256 (26) | 255 (25) | 1.34 | 0.87 to 2.07 | 0.188 | 1.69 | 0.96 to 2.97 | 0.070 | ||
| 2012–13 | 201 (20) | 192 (19) | 1.04 | 0.65 to 1.66 | 0.873 | 0.89 | 0.49 to 1.61 | 0.701 | ||
| Ward | ||||||||||
| A | 388 (39) | 258 (25) | 1 | – | – | 1 | – | – | ||
| B | 119 (12) | 323 (31) | 0.20 | 0.14 to 0.30 | < 0.001 | 0.19 | 0.10 to 0.35 | < 0.001 | ||
| C | 149 (15) | 237 (23) | 0.33 | 0.22 to 0.49 | < 0.001 | 0.42 | 0.23 to 0.77 | 0.005 | ||
| D | 334 (34) | 214 (21) | 1.02 | 1.10 to 1.83 | 0.922 | 1.17 | 0.72 to 1.90 | 0.533 | ||
| Behavioural precursors | ||||||||||
| Abus* | 570 (58) | 231 (22) | 7.62 | 5.70 to 10.17 | < 0.001 | 1.57 | 1.07 to 2.30 | 0.022 | ||
| Aggress* | 654 (66) | 192 (19) | 11.59 | 8.86 to 15.17 | < 0.001 | 1.96 | 1.36 to 2.83 | < 0.001 | ||
| Agitat* | 714 (72) | 286 (28) | 10.21 | 7.77 to 13.42 | < 0.001 | 1.77 | 1.25 to 2.49 | 0.001 | ||
| Arous* | 472 (48) | 124 (12) | 9.47 | 7.02 to 12.77 | < 0.001 | 1.75 | 1.19 to 2.57 | 0.004 | ||
| Assault* | 229 (23) | 25 (2) | 21.29 | 12.33 to 36.76 | < 0.001 | 3.37 | 1.81 to 6.28 | < 0.001 | ||
| Demand* | 531 (54) | 276 (27) | 3.82 | 2.97 to 4.93 | < 0.001 | 1.29 | 0.92 to 1.81 | 0.145 | ||
| Hit* | 266 (27) | 41 (4) | 11.58 | 7.55 to 17.78 | < 0.001 | 2.10 | 1.22 to 3.61 | 0.007 | ||
| Restrain* | ||||||||||
| Male and female | 554 (56) | 67 (6) | 34.47 | 23.26 to 51.09 | < 0.001 | |||||
| Male | 12.17 | 7.21 to 20.55 | < 0.001 | |||||||
| Female | 2.90 | 1.50 to 5.61 | < 0.001 | |||||||
| Shout* | ||||||||||
| Male and female | 573 (58) | 217 (21) | 6.40 | 4.93 to 8.31 | < 0.001 | |||||
| Male | 0.68 | 0.44 to 1.05 | 0.084 | |||||||
| Female | 2.97 | 1.63 to 5.42 | < 0.001 | |||||||
| Threat* | 689 (70) | 190 (18) | 18.94 | 13.75 to 26.09 | < 0.001 | 3.70 | 2.52 to 5.43 | < 0.001 | ||
| Threw/throw* | 328 (33) | 77 (7) | 8.31 | 5.86 to 11.80 | < 0.001 | 1.64 | 1.04 to 2.57 | 0.032 | ||
| Violen* | 247 (25) | 28 (3) | 16.36 | 10.06 to 26.62 | < 0.001 | 1.96 | 1.09 to 3.53 | 0.025 | ||
All behavioural precursors were significantly associated with seclusion status in univariable analyses (p < 0.001); estimates of effect were highest for ‘Violen*’ (OR 16.36), ‘Threat*’ (OR 18.94), ‘Assault*’ (OR 21.29) and ‘Restrain*’ (OR 34.47).
Multivariable analyses
The patterns of association between all demographic/clinical factors and seclusion were largely unchanged in the fully adjusted model. Seclusion status remained significantly associated with age, time since admission (p < 0.05) and ward. However, sex, ethnicity and diagnosis were not significantly associated with seclusion after adjustment for all demographic/clinical factors and behavioural precursors. Although ORs were substantially attenuated in the fully adjusted model, all precursors other than demanding behaviour remained significantly associated with seclusion (p < 0.05). There were significant interactions in the case of restraint and shouting, such that the effect of restraint was greater in men and there was no effect of shouting in men. An examination of variance inflation factors and standard errors (SEs) indicated minimal risk of multicollinearity (all variance inflation factors were < 4).
Discussion
In this large, methodologically robust study, we identified several demographic and clinical factors that distinguished between PICU/seclusion cases and randomly selected controls, including age, sex, ethnicity, diagnosis, MHA section and time since admission. With the exception of ethnicity and diagnosis, these factors remained significant predictors of both PICU and seclusion status after adjusting for behavioural precursors strongly associated with treatment receipt. In exploratory analyses, several statistically significant interactions were observed between patient sex and other predictors of transfer to a PICU and seclusion, indicating that the behaviours and circumstances contributing to these treatments differ between male and female patients.
Strengths and limitations
Our analyses examining the predictors of transfer to a PICU and seclusion have a number of strengths. First, the sample sizes that we achieved were distinctly in excess of those in other previous studies, increasing the precision of the estimates that we obtained. Second, we combined novel and robust measurement and sampling techniques so that we could estimate the effect of the time-varying behavioural factors that we assumed to be critically involved in selection for treatment, as well as the usually available demographic and basic clinical factors. There were, however, a number of notable limitations.
The current study was conducted within a single NHS trust, which potentially limits the extent to which the current findings can be generalised to other psychiatric hospitals (particularly those outside the UK). However, within this single NHS trust, we were able to examine practices across four PICU wards, including a female-only ward; thus, our findings may have greater generalisability than those of previous studies.
Although we examined a wide range of behavioural precursors that were identified directly from clinical events preceding treatment, we may have failed to account for some low-frequency behaviours that were not present in the initial screening subset but that may, nonetheless, be important precursors of treatment. Of note, we did not examine suicide or self-harm behaviours, both of which have been reported as antecedents of transfer to a PICU and of seclusion in previous studies. A further limitation relates to the fact that we focused only on patient characteristics. It is likely that a range of environmental factors influence the decision to initiate PICU transfer and seclusion (e.g. number of staff, staff sex, bed numbers); however, it was beyond the scope of the current study to examine these variables. Thus, we were unable to determine the impact of patient factors after accounting for external factors beyond the patient’s control. Environmental factors are particularly important as they are often dynamic (i.e. amenable to change) and, therefore, offer the opportunity to identify ways by which PICU and seclusion practices might be modified. A more difficult issue may be the potential for treatment selection to determine the recording of apparently relevant behaviours; these records may be as much accounts of a decision already taken as disinterested reports of behaviour. Naturally, there are normal concerns about the accuracy of data taken from electronic patient records, although in most cases these would be expected not to result in bias.
Finally, based on previous studies, we explored whether or not there might be important interactions between patient sex and other predictors of PICU/seclusion status. However, we did not examine other interaction effects identified in the extant literature (e.g. interactions with ethnicity and diagnosis).
Demographic and clinical predictors of treatment
Characteristics of psychiatric intensive care unit patients
In line with previous studies examining the characteristics of PICU patients, we observed that PICU patients were significantly younger and much more likely to be male than randomly selected controls. These findings are not surprising, given that both younger age and male sex are well-established risk factors for violence in acute psychiatric impatient settings. 21–23 That both factors remained highly significant predictors of PICU status after adjustment for all other demographic/clinical variables and a range of behavioural precursors (that were themselves strongly associated with PICU transfer) is, therefore, interesting, as this suggests that younger patients and men may be at greater risk of transfer to a PICU because of factors other than their aggressive behaviour. It is conceivable that this does represent a direct effect of patient sex, perhaps because of stereotyping of men as more violent and women as less violent. Thus, clinical staff may be more likely to perceive men as more risky and therefore requiring PICU admission. There may also be an important indirect effect of sex: SLaM, during the period of this study, operated three male PICU wards and one female ward, and, therefore, the supply of female PICU beds was distinctly limited. Alternatively, it may be that male and female psychiatric patients differ on other factors (e.g. frequency or severity of violence) that are relevant to PICU transfer but were not captured in the current study.
In unadjusted analyses, we additionally observed that patients of black African or Caribbean ethnicity were significantly more likely than white patients to be transferred to a PICU, a finding that is consistent with recent studies conducted in London and the South East. 24–26 This association between ethnicity and PICU status was greatly attenuated and rendered non-significant in the fully adjusted model. This finding is reassuring, as it suggests a lack of referral bias within the psychiatric inpatient system. That is, although black African or Caribbean patients were more likely than white patients to be transferred to a PICU, this was fully explained by other risk factors and behavioural precursors, indicating that PICU transfer was not associated with ethnicity per se. Similar conclusions were drawn in a previous study, conducted within the same NHS trust as that in the current investigation, which found that, although black African or Caribbean patients were more prevalent than expected (based on the ethnic composition of the entire hospital and the general population of the catchment area), black African or Caribbean PICU patients were characterised by higher levels of functional impairment than white PICU patients. 25 The current study extends these findings by statistically adjusting for a wide range of potential confounders, thereby demonstrating that these factors do indeed account for the higher likelihood of PICU transfer among black African or Caribbean patients.
In contrast to studies reporting that the majority of PICU patients have a diagnosis of schizophrenia,14 we observed that only 36% of patients transferred to a PICU had this disorder. Only patients with bipolar disorder were more likely to be transferred to a PICU after adjusting for a wide range of potential confounders. The fact that the elevated risk of PICU transfer among bipolar disorder patients remained even after adjusting for behaviours and traits commonly associated with this disorder (i.e. manic, agitated, demanding and irritable behaviour) suggests that patients with bipolar disorder may present with other behaviours that cause them to be viewed by clinical staff as needing PICU treatment.
In univariable analyses and multivariable analyses, legal status was very strongly associated with PICU status. Only 4% of PICU patients were informal (compared with 45% of non-PICU patients) and, indeed, we discovered from discussions with clinical staff that formal detention under the MHA was generally required on SLaM PICUs, suggesting that this very small number of apparently informal patients may in part even be attributable to data-coding errors (non-clinical staff were responsible for transforming MHA paperwork into the electronic patient record).
Among male patients we found a strong association between PICU transfer and time since admission, with a distinctly higher risk in the first 7 days. We are not aware of any previous studies to have investigated time since admission as a risk factor for PICU transfer, but the association is not surprising. Patients are often admitted to hospital during a period of acute illness that then improves following successful treatment; thus, we would expect chaotic/aggressive behaviour to be more prevalent early in the admission. Indeed, a large study of psychiatric inpatients reported that the majority of aggressive incidents occurred within the first 2 days of admission. 27 The fact that time since admission remained a very strong predictor of PICU transfer after adjusting for behavioural factors indicates, however, that high levels of aggression during the start of the admission may not fully account for this finding. Perhaps staff are more inclined to transfer newly admitted patients, whose behaviours and risks are not yet known, to PICU wards, whereas patients who remain in general inpatient care for longer periods may be viewed as less risky, even if both groups exhibit the same levels of aggression. Why the same pattern was not observed among women is unclear. We can formulate three potential explanations.
-
Given that the presence-specific behaviours were controlled for, there may be an underlying difference between men and women in how the intensity of disordered behaviour changes over time, with men exhibiting a greater intensity early on. This could be endogenous (determined by male illness alone) or exogenous (e.g. caused by differential patterns of substance use prior to admission).
-
Particular triggers, rather than just mental illness, are responsible in whole or in part for the kinds of incidents that lead to PICU transfer. If such triggers – for example conflicts over leave, possessions or access to mobile phones – occur in different ways for women or on female wards, then this might lead to a differential distribution of transfers over time.
-
There may a genuine issue of sex bias. Male patients may provoke greater fear early on in admission, with staff being more likely to think that they are capable of greater unpredictable violence and, therefore, being predisposed to initiate a PICU transfer.
Characteristics of secluded patients
Consistent with previous research,1 we observed that patients who were secluded during a period in a PICU were younger in age than randomly selected PICU patients who were not secluded. This association remained significant after adjusting for behavioural precursors; this again suggests that other (unmeasured) factors may contribute to the greater risk of seclusion among younger patients. We found no effect of sex on seclusion, consistent with previous case–control studies,1 but this is difficult to disentangle from the effect of ward and time period.
Previous case–control studies investigating the association between ethnicity and seclusion have yielded inconsistent findings. Studies conducted in the USA and New Zealand have reported that black/Asian patients and Maori/non-European patients, respectively, are more likely to be secluded than their white and European counterparts, yet more comprehensive studies conducted in these countries have observed no differences in seclusion rates across these ethnic groups. 1 Ethnic differences have, however, been observed in England and Wales; robust investigations conducted by the Healthcare Commission indicate that seclusion rates are higher among ethnic minority groups (black African, black Caribbean and white other) than among the white British group. 28 Our finding that seclusion status was not significantly associated with ethnicity in either unadjusted or adjusted analyses is, therefore, inconsistent with previous studies conducted in the UK. Again, it is likely that this difference in findings relates to our use of non-secluded PICU-based controls. In the underlying PICU population, individuals of black African or Caribbean ethnicity form the majority, constituting two-thirds of the total cohort (i.e. seclusion cases and seclusion controls). Thus, in the PICU population, being of black African or Caribbean ethnicity appears to confer no additional risk of seclusion.
Previous case–control studies have observed that patients with schizophrenia, other psychotic disorders, bipolar disorder and personality disorder are more likely to be secluded than other diagnostic groups, whereas patients diagnosed with depression are at lower risk. 14 We found no such effect in adjusted analyses. Thus, patient behaviours and other potential confounders appear to account for the observed differences in seclusion use across diagnostic groups.
Very few secluded patients were recorded as informally admitted to hospital (4%) on the date when transfer into seclusion occurred. Indeed, even this small number may be incorrectly coded as most PICUs require detention under the MHA as a condition of entry (see Characteristics of Psychiatric intensive care unit patients). As such, our finding that patients formally detained were not more likely to be secluded, although inconsistent with the extant literature,14 may be because we studied an entirely PICU-based sample.
Similar to the findings obtained in the PICU analyses, strong associations were observed between time since admission and seclusion status, whereby the likelihood of seclusion was greatly decreased at all subsequent time periods (although not in a dose–response fashion) relative to the first 7 days of the admission. This finding is consistent with several descriptive studies that report that the majority of seclusion incidents occur within the first 24 hours or within the first week of admission. 1 Effect sizes were attenuated in the fully adjusted model, suggesting that this finding is partially explained by higher levels of aggressive behaviour during the early stages of the admission; however, highly significant effects remained for all time periods, suggesting that we have not fully captured the range of factors that may contribute to the elevated risk of seclusion at the start of the admission. Anecdotally, it appeared from the clinical notes that many patients were transferred to a PICU in a state of distress/agitation and that seclusion was often initiated as soon as the patient arrived at the PICU ward as a precaution. Additionally, as the seclusion cohort (cases and controls) comprised all patients admitted to the PICU, including those admitted directly from the community, it is possible that we may not have been able to adequately capture (and subsequently adjust for) behavioural precursors occurring in the 3 days prior to seclusion. However, given that we observed a similar association between time since admission and PICU transfer, despite the fact that we excluded patients admitted directly from the community (for whom behavioural data would be unavailable) this suggests that this cannot be the only explanation for this finding and we again propose that this may be a strategy employed by clinical teams to safely manage patients who are newly admitted and whose level of risk is, therefore, unclear.
Behaviours associated with use of a psychiatric intensive care unit and seclusion
Behavioural precursors of psychiatric intensive care unit transfer
We identified a range of patient behaviours that preceded PICU transfer. In terms of prevalence, keywords related to difficult-to-manage and verbally aggressive behaviour (e.g. ‘Abus*’, ‘Aggress*’, ‘Agitat*, ‘Shout’ and ‘Threat*’) were common in the 3 days prior to PICU transfer and were observed in 49–68% of PICU cases. Those relating to physically aggressive behaviour (‘Threw/Throw*, ‘Attack*’ and ‘Violen*) were less frequently observed during this time period (20–32% of PICU cases) and absconsion (‘Abscon*’ and ‘AWOL’) was relatively rare (10–15% of PICU cases). These findings are broadly consistent with previous studies that have reported that aggression is the most common reason for PICU transfer (occurring in 30–50% of admissions), followed by disruptive/acutely psychotic behaviour and absconsion (each prevalent in 10–20% of cases). 7 Our findings demonstrate that, in addition to aggression and violence, a range of behaviours displayed by the patient, including rule-breaking behaviour, boundary pushing, reluctance, non-compliance and argumentativeness, underlie PICU transfer. Although these behaviours are not in themselves necessarily dangerous, by challenging the authority of staff members these behaviours often invoke an emotional reaction in staff (e.g. feelings of irritation and frustration), which may lead to staff needing to exert power and control, and, hence, initiate PICU transfer. The size of the associated effects varied, but ORs were typically in the range of 1.5 to 5; in the case of attacking behaviour, the adjusted OR was 29. The effect of throwing differed between men and women.
Contrasting with previous studies, self-harm appeared to be a very infrequent precursor to PICU transfer in the population that we studied. We did not identify any behavioural keywords relating to self-harm or suicidal behaviour when we reviewed a randomly selected subset of events occurring prior to PICU transfer (n = 500) from which the list of behavioural precursors was derived.
Behavioural precursors of seclusion
A comprehensive review of studies providing reasons for initiating seclusion (n = 47) indicated that the most common reason was aggression (typically aggression to objects but also verbal aggression, self-directed aggression and physical aggression), followed by psychiatric symptoms (e.g. delusion, disorientated, confused or disturbed behaviour), disruptive behaviour, absconsion and medication refusal. These findings are to a large extent consistent with those obtained in the current study. As was the case with PICU transfer, we identified several keywords related to verbally aggressive and agitated behaviour (‘Abus*’, ‘Aggress*’, ‘Agitat*’, ‘Arous*’, ‘Shout*’ and ‘Threat*’) that were highly prevalent in the period directly preceding seclusion (occurring in 48–72% of seclusion cases), whereas keywords indicating physical aggression (‘Assault*’, ‘Threw/Throw*’ and ‘Violen’) were less common (present in 23–33% of cases). Although we observed a considerable degree of overlap between PICU and seclusion keywords, there were some differences. First, absconsion keywords were notably absent in the pre-seclusion events. As noted above, this is somewhat surprising given that absconsion has been noted as an antecedent of seclusion. However, this may relate to the fact that we examined seclusions occurring on a PICU ward (as opposed to a general adult ward), where there may be fewer opportunities to abscond. Second, the clinical notes for over half of the seclusion cases were found to contain the word ‘Restrain*’. Although this keyword clearly relates to staff and not patient behaviour, and is therefore not a behavioural precursor per se, it was so strongly related to seclusion in the initial selection process that we felt that it was important to include this term in the final model.
Nearly all of the included behavioural precursors were significantly associated with seclusion status in the adjusted analysis; however, ORs were generally smaller than those observed for PICU transfer. This probably reflects the fact that although these behaviours are highly prevalent among patients who are secluded, they are also far more common in the underlying PICU population (from which seclusion controls were drawn) than among patients treated in general adult wards (from which PICU controls were drawn). The highest OR (12) was observed for ‘Restrain*’ among men, with all other remaining keywords being associated with ORs between 1.5 and 4. The effects of restraining and of shouting differed between men and women; the second finding has no obvious explanation, but it is notable that the occurrence of a restraint was much less commonly followed by seclusion among women, even though the association was still significant and of substantial size.
Implications
Previous studies have indicated that specific patient subgroups are at increased risk of PICU transfer and seclusion. However, these studies have typically lacked appropriate control groups and have also failed to account for patient behaviours that might explain this elevation in risk. In the current study, we found little evidence of referral bias in relation to ethnicity or diagnosis; after adjusting for a range of behavioural precursors and demographic/clinical factors, these factors were not associated with transfer to a PICU or seclusion. One exception to this is that patients with bipolar disorder were twice as likely to be transferred to a PICU than patients with schizophrenia, even after adjusting for behaviours typically associated with this diagnosis (i.e. mania, agitation and irritability). Presumably this simply reflects a degree of disturbance that our measures were not able to detect. However, further work to determine the reasons why clinical teams consider patients with bipolar disorder to be particularly difficult to manage in general adult wards might potentially bear fruit if it leads to strategies that can help to avoid PICU transfer.
One interesting finding was that even after accounting for a range of confounders, sex differences in the risk of transfer to a PICU and seclusion were still apparent, with men being more likely to be transferred to a PICU, whereas women demonstrated no difference in the use of seclusion that could be not be accounted for by the inclusion of other variables such as ward and time period. Overall, the influence of ward was substantial in the case of both transfer to a PICU and seclusion, supporting a key assumption of this project, which is that major differences in the use of coercive practices can coexist in apparently similar services and units.
Our findings emphasise the importance of adjusting for a wide range of demographic/clinical factors and behavioural precursors when conducting any non-randomised analyses examining the effects of transfer to a PICU and seclusion on outcomes. The work presented in this chapter, therefore, has important implications for the analyses performed in Chapter 3. Thus, having identified a range of factors that clearly distinguish treated patients (i.e. those receiving PICU care or seclusion) from untreated patients, it is essential to adjust for these variables when examining the effect of PICU care and seclusion on adverse incidents, length of stay and costs.
Conclusions
The findings presented in this chapter indicate that there are a number of demographic and clinical factors that distinguish between patients who are subject to PICU transfer/seclusion and those who are not. Moreover, some of these factors (notably, patient sex, age and time since admission) remain consistently associated with treatment receipt after adjusting for a range of behavioural precursors. Patient sex was found to modify the effect of other demographic/clinical factors and behavioural precursors on treatment receipt, and was also significantly associated with both PICU and seclusion duration. These findings highlight the importance of patient sex when examining predictors and outcomes of these treatments.
Chapter 3 Effects of treatment on adverse incidents, length of stay and costs
Introduction
Although numerous studies have investigated predictors of PICU transfer and seclusion, the effects of these interventions on the outcomes that they aim to reduce (e.g. aggressive and agitated behaviour, length of stay and costs) have scarcely been examined.
The few studies examining the effect of PICU transfer on symptoms and behaviour have indicated largely positive effects of PICU treatment. A study conducted in the USA compared patients admitted to a PICU ward with those admitted to an open voluntary ward, and observed that PICU patients showed greater reductions in psychotic and manic symptoms over time. 29 A further naturalistic study examining the impact of a new PICU ward in a psychiatric hospital reported a 38% reduction in staff time lost to injuries at work (when examined across the whole hospital) following PICU implementation. 30 With regard to seclusion, a number of studies, published between 1978 and 1996, have provided descriptions of patient behaviour both during and after seclusion. 1 Behaviours observed during seclusion were extremely varied and ranged from settled, sleeping and remorseful to destructive, aggressive, assaultive, abusive and agitated. Of the six studies examining post-seclusion behaviour, all reported a settling effect, although demanding, agitated, violent, absconding, self-injurious and abusive behaviour were also reported.
Although we are not aware of any previous studies investigating the effect of PICU transfer on future length of stay, a recent literature review identified 13 studies examining the impact of seclusion on this outcome. 1 Of these studies, 11 reported that length of stay was significantly longer among secluded patients than among non-secluded patients.
With regard to economic outcomes, a previous literature review identified only two studies examining costs associated with PICU transfer, of which one was conducted in the 1980s9 and the other was conducted in 1993. 8 However, one of these studies, published in Canada, reported that the cost per day for PICU care was approximately 1.5 times higher than the daily cost for acute care. 9 Thus, there is some evidence that PICU costs are higher than those of standard care. In contrast, we were unable to identify any previous studies examining the costs and cost-effectiveness of seclusion.
All of the studies described above are limited in the extent to which they can provide evidence of the effectiveness of PICU and seclusion practices. To our knowledge, no study to date has fully taken account of differences between patients receiving PICU treatment/seclusion and those who do not receive these interventions and their relationship to treatment selection; that there are such differences is demonstrated by the analyses in Chapter 2. Although there is evidence that length of stay is extended among those who are secluded compared with those who are not, similar comparisons have not been performed for PICU treatment. Furthermore, there appear to have been no robust investigations into the costs associated with PICU and seclusion; consequently, the cost-effectiveness of these treatments is unknown.
The aims of the current chapter are:
-
to derive propensity scores31 for treatment with PICU and for treatment with seclusion, and to use these scores to assess the feasibility of outcomes analyses satisfying the common support condition32–34
-
to report unadjusted (raw) differences in (a) adverse incidents (general aggression, general violence and serious incidents), (b) length of stay and (c) costs between those transferred to a PICU and those not transferred, and between those placed in seclusion and those not placed in seclusion
-
if feasible, to use Poisson regression weighted by the inverse probability of treatment selection35 to derive estimates of the causal effect of transfer to a PICU and seclusion, and to perform a cost-effectiveness analysis.
Methods
Identification of treated and untreated groups
Full details of the methods used to identify treated (cases) and untreated (controls) groups are provided in Chapter 2. The PICU case group comprised all transfers from general adult wards to non-forensic PICU wards during the study period (n = 986); PICU controls were randomly selected person–date combinations taken from the set of person–day combinations on general adult wards where PICU transfer did not occur and where the person had not just been transferred back from a PICU (n = 994). Similarly, the seclusion case group comprised all episodes of seclusion occurring on non-forensic PICU wards (n = 990); seclusion controls were randomly selected dates corresponding to periods of treatment in non-forensic PICU wards where seclusion was not in progress, started or ended (n = 1032).
Extraction of covariates
Demographic and clinical data for all cases and controls (PICU and seclusion) were extracted from CRIS using the procedure described in Chapter 2. These data were used to derive the following variables: age, sex, ethnicity, diagnosis, MHA section (at midnight on the day of sampling) and time since admission for the current SLaM inpatient episode. Chapter 2 additionally provides details of the two-stage process used to identify behavioural precursors of PICU transfer and seclusion from clinical ‘Events’ recorded prior to treatment (0, –1 and –2 days before the date of PICU transfer or date of seclusion) and the procedure used to extract, code and clean the final pre-PICU and pre-seclusion data sets, comprising behavioural precursor data for all cases and controls.
Extraction of violence and aggression outcomes subsequent to transfer/non-transfer
General aggression and violence
Incidents of general aggression and violence occurring in the 7 days following the sample date (i.e. date of PICU transfer/seclusion initiation for cases and random sampling date for controls) were identified from ‘Event’ records (i.e. free-text entries made by the clinical team at multiple times throughout the day). We first compiled a list of keywords relating to aggressive, disruptive and violent behaviour that included all PICU and seclusion behavioural precursors with the exception of those related to absconsion and with three additional keywords included to capture a broader range of incidents. The following keywords were included in the final list: ‘Abus*’, ‘Aggress*’, ‘Agitat*’, ‘Arous’, ‘Assault*’, ‘Attack*’, ‘Demand*’, ‘Hit*’, ‘Irritable’, ‘Manic’, ‘Punch*’, ‘Push*’, ‘Slap*’, ‘Refus*’, ‘Restrain*’, ‘Shout*’, ‘Threat*’, ‘Threw/Throw*’ and ‘Violen*’. For all cases and controls (PICU and seclusion) we then extracted all events occurring in the 7 days subsequent to the sample date that contained at least one of these keywords. This resulted in two data sets: one including all relevant events for PICU cases and controls (n = 21,628), and the other including all relevant events for seclusion cases and controls (n = 26,563). All relevant events were then manually reviewed to identify incidents of aggressive and violent behaviour. For each incident, the date, location and types of behaviours displayed during the incident (verbal aggression, aggression to objects, attempted violence and actual violence) were recorded. A single incident could include multiple behaviours, although each behaviour was coded as present/absent for that incident (i.e. we did not count the number of violent behaviours within a single incident, only the presence/absence of that behaviour within the incident). Behaviours separated temporally were treated as separate incidents. Within each data set, two outcome variables were subsequently derived:
-
the total number of aggressive incidents (sum of all incidents involving either verbal aggression, aggression to objects, attempted violence and actual violence)
-
the total number of violent incidents (sum of all incidents involving either attempted or actual violence).
Serious incidents
Serious incidents occurring within SLaM are recorded in a separate database (DATIX version 14.0.6; Datix Ltd, Wimbledon, UK), which is not linked to ePJS (Electronic Patient Journey System, version 5.6.5, Advanced, Datchet, UK) and therefore not accessible via CRIS. It is recommended, however, that DATIX incidents relating to individual patients (some incidents refer to issues of health and safety that are not relevant to any particular patient) are also recorded in ePJS. In such instances, the DATIX incident number and details of the incident are typically recorded within the ‘Events’ and ‘Risk Events’ tables. Using SQL, we searched these two tables to identify all entries occurring within 30 days from the sample date that contained the keywords ‘DATIX’, ‘Incident report’ or ‘Incident form’. This yielded a PICU–DATIX data set comprising relevant records for all PICU cases and controls (n = 999) and a seclusion–DATIX data set that included relevant records for seclusion cases and controls (n = 1392). All records were manually cleaned and coded to identify relevant incidents (i.e. those involving verbal aggression, aggression to objects, attempted violence, actual violence, self-harm and absconsion) in which a single incident could include more than one type of behaviour. A single variable, indicating the total number of serious incidents of any type, was subsequently derived.
Extraction of length of stay subsequent to transfer/non-transfer
In order to examine the effect of PICU transfer and seclusion on length of stay, we excluded that part of the admission occurring prior to PICU transfer/seclusion, defining length of stay for our purposes as the difference between the sample date (the date of transfer to PICU/seclusion for treated patients and the randomly selected date for controls) and the end of the admission.
Extraction of economic outcome data subsequent to transfer/non-transfer
Separately, we obtained SLaM internal financial data for the financial years covered by the study, comprising costs of each separate SLaM team or ward for each financial year. These data were examined carefully, locating budgets shared between services and services funded by more than one budget. Having grouped services and budgets when necessary, we extracted and totalled all service use data for the team(s) or ward(s) corresponding to each budget: at the ward level, we extracted inpatient nights and for teams, which were community based, we extracted face-to-face contacts. These data were used to create a unit cost for each service, along with a currency (inpatient night or face-to-face contact). The data were fully cleaned for inpatient services, general adult community mental health teams (CMHTs) and home treatment teams, and therefore encompassed the overwhelming majority of spending for adult mental health services. In the data extraction, we extracted total costs under each of these headings for 7, 30 and 365 days subsequent to the sampling date. We separated out PICU days and also separated PICU days into secluded and non-secluded, allowing for the possibility of sensitivity analyses modelling different relative costs of secluded and non-secluded time.
The primary measures for the economic analysis were therefore:
-
total health-care costs, including non-PICU inpatient care, seclusion and non-seclusion inpatient care within a PICU, community care provided by CMHTs, Mood, Anxiety & Personality outpatient and day services, psychotherapy care and home treatment care
-
health outcomes, including total 7-day general aggression and violent incidents, and 30-day total serious incidents
-
cost-effectiveness analysis of PICU transfer and of seclusion.
The total health-care costs were analysed for different time periods of 7, 30 and 365 days. The cost-effectiveness analysis considered only the weekly and monthly total costs, as these could be linked to the corresponding health outcomes.
Statistical analyses
Derivation and testing of propensity scores
The logistic regression analyses in Chapter 2 were rerun applying inverse probability weights based on the known sampling probability and using the estimation results to predict the probability of treatment conditional on the observed covariates (the propensity score). A preliminary Poisson regression of general violent incidents, omitting the treatment of interest (PICU or seclusion), was used to define a subset of variables specifically associated with the outcome of interest, and this was then used to create an alternative propensity score that would, in principle, be associated with reduced error. 36 Box plots grouped by treatment were used to visually assess the distribution of propensity score values and when these fell in relation to the interval 0.1 ≤ p ≤ 0.9, which has been shown to provide a basis for trimming observations in which inclusion would vitiate estimation by violating the common support condition. 34
Adverse incidents and length of stay
Unadjusted Poisson regression models with a person-level random effect were used to compare (1) the count of aggressive incidents (violent, destructive or disruptive), (2) the count of violent incidents and (3) the count of serious incidents between those transferred to a PICU and not transferred, and between those placed in seclusion and those not placed in seclusion. Similar unadjusted linear regression analyses with a person-level random effect were used to compare length of stay subsequent to transfer/non-transfer. Because of marked right skew, SEs were calculated with the non-parametric bootstrap and 1000 repetitions.
Dependent on the review of the box plot of propensity scores suggesting that (1) the common support condition could potentially be met and (2) there would be sufficient suitable observations, we planned to run Poisson regression analyses, weighting by the inverse of the probability of treatment selection (the inverse of the propensity score for treated observations; the inverse of one minus the propensity score for untreated observations35).
Economic analyses
For both the PICU and seclusion analyses, unadjusted random-effects linear regressions were used to compare costs and mean number of adverse incidents between those who were treated and those who were untreated. Because of the positively skewed distribution of the cost data and the likelihood of heteroscedasticity and non-normally distributed error terms, the non-parametric bootstrap method with 1000 samples was used to compute SEs. 37
Again dependent on the assessment of propensity scores suggesting the feasibility of deriving an estimate of causal effect (see Derivation and testing of propensity scores), we planned to perform analyses weighted by the inverse of the probability of treatment selection. These analyses were planned to comprise propensity-score-based models (1) estimating the differences in cost estimates between groups, (2) calculating the predicted difference in the mean number of adverse incidents between those receiving and not receiving each intervention and (3) extending these analyses by plotting cost-effectiveness planes and calculate incremental cost-effectiveness ratios based on simultaneous estimation of the effects on costs and outcomes within multiple bootstrap samples.
Results
Effect of psychiatric intensive care unit transfer on adverse incidents
Analysis of propensity scores
The distribution of propensity scores was markedly unequal between treated and untreated observations (Figure 3). Not one untreated observation fell in the interval 0.1–0.9. Even though the sampling frequency for untreated observations was 0.0017, equivalent to approximately 1/588, it seemed not only that there was no possibility of deriving a causal effect from the data set, but also that further samples would not necessarily find a usable number of comparison observations.
FIGURE 3.
Box plots of propensity scores for PICU: treated vs. untreated. Added lines at 0.1 and 0.9 represent the limits established in Crump et al. 34 as equivalent to the common support condition in standard matching and regression designs.
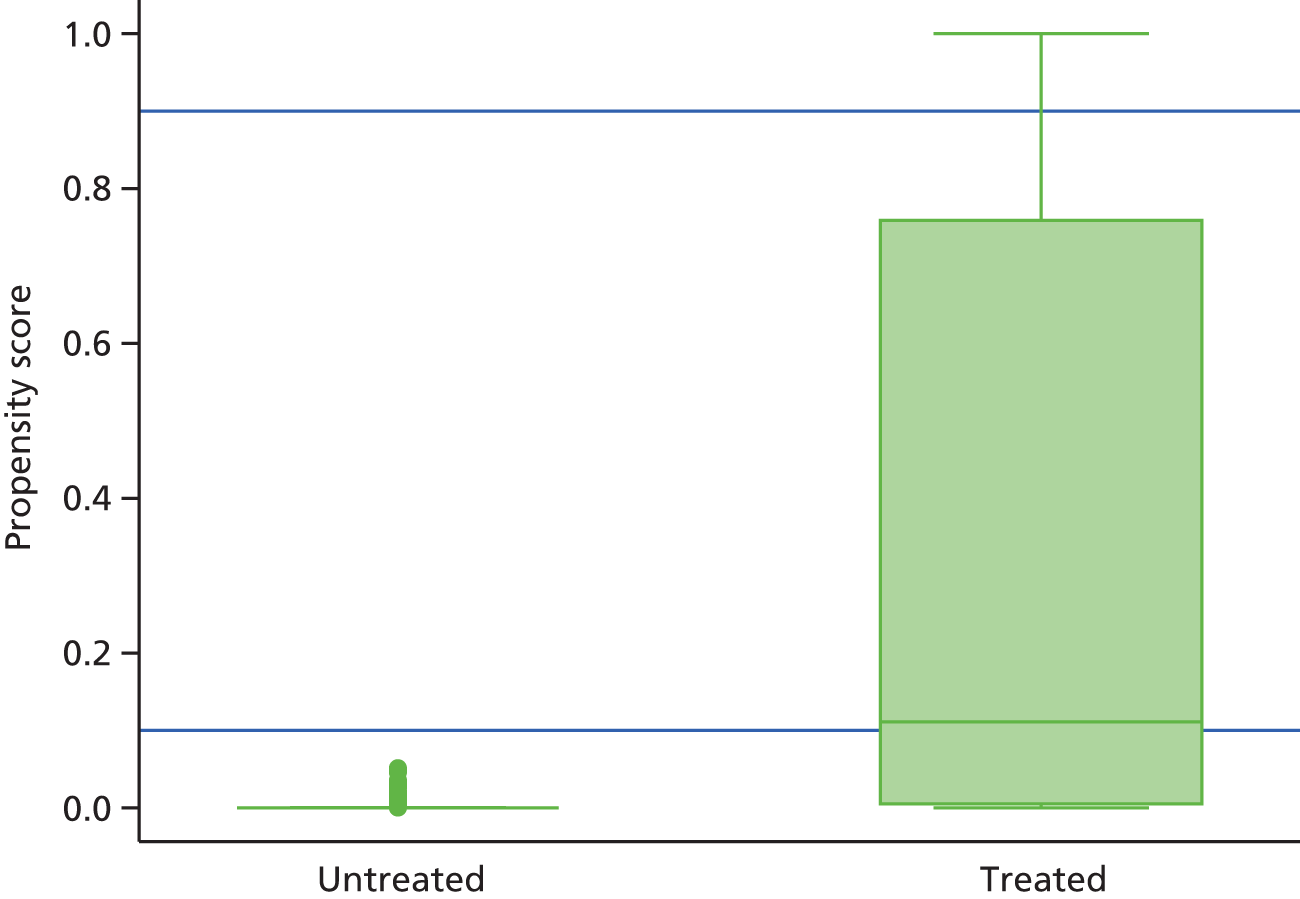
Unadjusted differences
In total, 3344 incidents of general aggression occurred during the 7 days following the sampling date; 2994 of these incidents were perpetrated by PICU cases whereas only 350 were instigated by PICU controls. The mean number of general aggressive incidents per PICU case was 3.04 (range 0–27) and 0.35 per PICU control (range 0–10). When restricted to incidents that included violent behaviour (i.e. examining a subset of the general aggression incidents), the total number occurring within the 7-day period was 878. Of these, 793 were committed by PICU cases (mean 0.80 per PICU case; range 0–14) and 85 by PICU controls (mean 0.09 per PICU control; range 0–5). During the 30-day follow-up period, 482 serious incidents were recorded; the majority of these incidents (n = 406) were perpetrated by PICU cases, whereas only 76 were perpetrated by PICU controls. The mean number of serious incidents per PICU case and PICU controls was 0.41 (range 0–7) and 0.08 (range 0–6), respectively.
Psychiatric intensive care unit transfer was associated with significantly higher rates of general aggression [incident risk ratio (IRR) 6.70; p < 0.001], general violence (IRR 8.76; p < 0.001) and recorded serious incidents (IRR 4.76; p < 0.001) in unadjusted Poisson regression analyses. As noted above, an analysis of propensity scores suggested that it would not be possible to derive an estimate of the causal effects of PICU transfer, and these unadjusted estimates should therefore be assumed to be biased, because of both confounding and lack of common support.
Effect of seclusion on adverse incidents
Analysis of propensity scores
The distribution of propensity scores was unequal between treated and untreated observations (Figure 4). However, 26 untreated observations fell in the interval 0.1 to 0.9. The sampling frequency for untreated observations was 0.016, equivalent to approximately 1/63, suggesting (by multiplication) the existence of 1638 candidate untreated observations within the entire sampling frame. However, the number of usable untreated observations was too low to perform adequately powered analyses.
FIGURE 4.
Box plot of propensity scores for seclusion: treated vs. untreated. Added lines at 0.1 and 0.9 represent the limits established in Crump et al. 34 as equivalent to the common support condition in standard matching and regression designs.

Adverse incidents
In total, during the 7 days following the sample date, 5057 incidents of aggression occurred. Of these, 3958 were perpetrated by seclusion cases (mean number per seclusion case 4.00; range 0–30) and 1099 were attributed to seclusion controls (mean number per seclusion control 1.06; range 0–17). In total, 1378 incidents were noted to involve violent behaviour, of which 1085 were committed by seclusion cases and 293 by seclusion controls. The mean number of violent incidents per seclusion case and seclusion control was 1.10 (range 0–13) and 0.28 (range 0–6), respectively. In total, 793 serious incidents were recorded during the 30 days following the sample date; 554 of these were perpetrated by seclusion cases and 239 by seclusion controls; the mean number of incidents during this period was 0.56 (range 0–7) and 0.23 (range 0–5), respectively.
In unadjusted Poisson regression analyses, incidents of general aggression and general violence were higher among seclusion cases than among seclusion controls (IRR 2.76 and 2.83, respectively; p < 0.001). Recorded serious incidents were significantly higher among seclusion cases than among seclusion controls (IRR 1.74; p < 0.001). Again, these estimates should be assumed to be biased because of both confounding and lack of common support.
Effect of psychiatric intensive care unit on length of stay
The extent to which those treated with PICU transfer and those untreated differed in length of stay between the sample date and the end of admission was estimated using unadjusted and adjusted random-effects linear regression, with SEs estimated using 1000 bootstrap samples. In the unadjusted analysis, PICU status was significantly associated with higher length of stay [b = 22.05, 95% confidence interval (CI) 6.35 to 37.75; p < 0.001].
Effect of seclusion on length of stay
The extent to which those who were placed in seclusion and those who were not differed in length of stay was estimated as for PICU transfer above. There was no significant unadjusted association between seclusion status and subsequent length of stay (b = 0.19, 95% CI –13.43 to 13.82; p = 0.98).
Psychiatric intensive care unit economic analyses
Inpatient and community contacts
Table 4 shows the number of patients who utilised inpatient and community services, and the number of contacts over 7, 30 and 365 days.
| Health-care services | Cases (N = 986) | Controls (N = 994) | ||
|---|---|---|---|---|
| n (%) | Mean (SD) | n (%) | Mean (SD) | |
| 7 days | ||||
| Non-PICU inpatient care | 79 (8) | 4.4 (2.5) | 927 (93) | 6.5 (1.4) |
| PICU non-seclusion inpatient care | 930 (94) | 6.5 (1.2) | 10 (1) | 4.1 (1.9) |
| PICU seclusion inpatient care | 167 (17) | 2.1 (1.5) | 1 (0) | 1.0 |
| CMHT care | 241 (24) | 1.8 (1.2) | 287 (29) | 1.8 (1.2) |
| Home treatment | 10 (1) | 2.2 (1.6) | 61 (6) | 5.3 (3.7) |
| 30 days | ||||
| Non-PICU inpatient care | 532 (54) | 12.1 (7.9) | 934 (94) | 22.4 (10.3) |
| PICU non-seclusion inpatient care | 942 (95) | 22.3 (8.5) | 29 (3) | 15.6 (7.4) |
| PICU seclusion inpatient care | 133 (13) | 2.3 (1.9) | 2 (0) | 6.0 (7.1) |
| CMHT care | 468 (47) | 4.1 (3.5) | 550 (55) | 4.7 (3.8) |
| Home treatment | 83 (8) | 8.0 (6.1) | 160 (16) | 12.8 (10.4) |
| 365 days | ||||
| Non-PICU inpatient care | 983 (99) | 80.8 (78.8) | 986 (99) | 97.2 (98.2) |
| PICU non-seclusion inpatient care | 986 (100) | 52.2 (52.9) | 97 (10) | 53.6 (51.3) |
| PICU seclusion inpatient care | 412 (42) | 4.2 (5.4) | 33 (3) | 4.5 (5.7) |
| CMHT care | 706 (72) | 43 (37) | 764 (77) | 42 (37) |
| Home treatment | 319 (32) | 21.8 (18.4) | 314 (31) | 25.5 (27.2) |
Among general adult wards, patients who were transferred to a PICU utilised similar inpatient care and community care services to patients in acute inpatient care units (non-PICU) during a week. The vast majority of PICU patients (94%) utilised inpatient care associated with non-seclusion. The mean number of inpatient-days associated with PICU and non-seclusion was 6.5 days for the PICU group compared with 4.1 days for the non-PICU group, and the majority of non-PICU patients (90%) had a mean number of 6.5 days of non-PICU inpatient care.
During the first 30 days, non-PICU patients utilised non-PICU inpatient care more intensively than PICU patients. Approximately half of PICU patients used non-PICU inpatient care, with a mean number of 12.1 days, compared with 22.4 days for the non-PICU group, 91% of whom utilised these services. The majority (95%) of the PICU patients and only a few (3%) non-PICU patients used non-seclusion PICU services; the mean number of non-seclusion inpatient-days were 22.3 and 15.6, respectively. Similarly, non-PICU patients had approximately 4 more days of seclusion inpatient care than PICU patients. Similar proportions of patients used community services, but, of these, the PICU group had fewer contacts on average.
During the year after the index date, the majority of PICU and non-PICU patients had non-PICU inpatient care days, with the PICU group having approximately 16 days fewer (80.8 vs. 97.2) than the non-PICU group. It should be noted that everyone in the PICU group used non-seclusion inpatient care services, whereas less than half of the PICU group (42%) used seclusion inpatient care. For PICU patients, the mean numbers of days for seclusion and non-seclusion inpatient care were 52.2 and 4.2, respectively. The mean number of days used by non-PICU patients for the same services was similar (53.6 and 4.5 days); however, utilisation of these services was < 10%. Throughout the year, the most frequently utilised community care services were CMHTs and home treatment. PICU patients had slightly more contacts with CMHTs and slightly fewer home treatment care contacts than the non-PICU patients (43 vs. 41.9 and 21.8 vs. 25.5 contacts).
Inpatient, community and total costs
Table 5 shows the number of patients who utilised inpatient and community services, and the incurred costs of these services during the 7, 30 and 365 days following the sample date. The total costs were significantly higher for the PICU patients than for the non-PICU patients in all periods, mostly because of the costs of inpatient care.
| Health-care services | Cases (N = 986) | Controls (N = 994) | Unadjusted differences | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Mean cost (£) | SD (£) | n (%) | Mean cost (£) | SD (£) | Mean cost (£) | SE (£) | p-value | 95% CI (£) | |
| 7 days | ||||||||||
| Non-PICU inpatient care | 79 (8) | 1647 | 1257 | 927 (93) | 1980 | 585 | –1714 | 32 | < 0.001 | –1777 to –1651 |
| PICU non-seclusion inpatient care | 930 (94) | 5311 | 1420 | 10 (1) | 3126 | 1637 | 4977 | 59 | < 0.001 | 4862 to 5092 |
| PICU seclusion inpatient care | 167 (17) | 1736 | 1232 | 1 (0) | 718 | 293 | 28 | < 0.001 | 238 to 348 | |
| CMHT | 241 (24) | 225 | 166 | 287 (29) | 224 | 162 | –10 | 6 | 0.137 | –22 to 3 |
| Home treatment | 10 (1) | 440 | 383 | 61 (6) | 951 | 713 | –54 | 10 | < 0.001 | –73 to –35 |
| Total | 973 (99) | 5568 | 1398 | 940 (95) | 2122 | 673 | 3488 | 60 | < 0.001 | 3371 to 3605 |
| 30 days | ||||||||||
| Non-PICU inpatient care | 532 (54) | 3838 | 3062 | 934 (95) | 6767 | 3391 | –4287 | 150 | < 0.001 | –4581 to –3994 |
| PICU non-seclusion inpatient care | 942 (96) | 17,867 | 7304 | 29 (3) | 11,934 | 5845 | 16,721 | 271 | < 0.001 | 16,189 to 17,253 |
| PICU seclusion inpatient care | 133 (13) | 1915 | 1746 | 2 (0) | 5964 | 7029 | 246 | 29 | < 0.001 | 190 to 302 |
| CMHT | 468 (47) | 501 | 468 | 550 (56) | 597 | 510 | –93 | 22 | < 0.001 | –136 to –49 |
| Home treatment | 83 (8) | 1428 | 1104 | 160 (16) | 2343 | 1948 | –257 | 42 | < 0.001 | –340 to –174 |
| Total | 980 (99) | 19,882 | 6328 | 951 (96) | 7781 | 3753 | 12,317 | 248 | < 0.001 | 11,830 to 12,803 |
| 365 days | ||||||||||
| Non-PICU inpatient care | 910 (92) | 27,997 | 33,078 | 974 (98) | 30,655 | 34,431 | –4199 | 1522 | 0.006 | –7182 to –1216 |
| PICU non-seclusion inpatient care | 956 (97) | 40,534 | 40,308 | 96 (10) | 41,407 | 39,928 | 35,302 | 1590 | < 0.001 | 32,186 to 38,418 |
| PICU seclusion inpatient care | 269 (27) | 2917 | 4096 | 18 (2) | 3647 | 4775 | 730 | 135 | < 0.001 | 464 to 995 |
| CMHT | 706 (72) | 5344 | 4921 | 764 (77) | 5277 | 5189 | –230 | 251 | 0.360 | –722 to 263 |
| Home treatment | 319 (32) | 3909 | 3233 | 314 (32) | 4516 | 4655 | –162 | 142 | 0.253 | –440 to 116 |
| Total | 985 (100) | 71,176 | 53,056 | 987 (99) | 40,358 | 39,689 | 31,030 | 2358 | < 0.001 | 26,409 to 35,651 |
Seclusion economic analyses
Inpatient and community contacts
Table 6 shows the number of PICU patients in seclusion and non-seclusion that utilised inpatient and community services and the number of contacts during 7, 30 and 365 days, respectively.
| Health-care services | Cases (N = 990) | Controls (N = 1032) | ||
|---|---|---|---|---|
| n (%) | Mean (SD) | n (%) | Mean (SD) | |
| 7 days | ||||
| Non-PICU inpatient care | 57 (6) | 4.2 (2.1) | 155 (15) | 4.2 (1.9) |
| PICU non-seclusion inpatient care | 956 (97) | 6.0 (1.5) | 1007 (98) | 6.4 (1.5) |
| PICU seclusion inpatient care | 425 (43) | 2.1 (1.5) | 11 (1) | 2.3 (1.5) |
| CMHT care | 222 (22) | 1.8 (1.3) | 227 (22) | 1.8 (1.7) |
| Home treatment care | 4 (0) | 1.3 (0.5) | 6 (1) | 3.7 (2.7) |
| 30 days | ||||
| Non-PICU inpatient care | 457 (46) | 11.3 (7.3) | 551 (53) | 15.1 (8.0) |
| PICU non-seclusion inpatient care | 965 (97) | 22.1 (8.6) | 1009 (98) | 20.2 (10.3) |
| PICU seclusion inpatient care | 463 (47) | 2.6 (2.7) | 38 (4) | 1.8 (1.2) |
| CMHT care | 447 (45) | 3.8 (2.9) | 442 (43) | 4.1 (4.6) |
| Home treatment care | 74 (7) | 9.1 (6.6) | 79 (8) | 12.2 (7.8) |
| 365 days | ||||
| Non-PICU inpatient care | 854 (86) | 76.9 (71.7) | 859 (83) | 96.7 (90.8) |
| PICU non-seclusion inpatient care | 971 (98) | 56.2 (54.6) | 1015 (98) | 59.5 (72.4) |
| PICU seclusion inpatient care | 520 (53) | 3.5 (4.3) | 101 (10) | 3.6 (4.4) |
| CMHT care | 677 (68) | 42.7 (31.7) | 653 (63) | 42.3 (43.7) |
| Home treatment | 362 (37) | 24.8 (22.2) | 225 (22) | 23.1 (20.4) |
Service use was fairly similar between the PICU patients in seclusion and not in seclusion during the 7-day period. The majority of PICU patients used non-seclusion-related inpatient care, with an average number of approximately 6 days per patient per week. Of the PICU patients in seclusion, 43% used inpatient care related to seclusion, with a mean of 2.1 days per patient per week. Community care offered by CMHTs was identical for secluded and non-secluded PICU patients, whereas home care treatment was used more intensively by the non-secluded PICU patients (3.7 vs. 1.3 contacts).
During the 30-day period, approximately half of patients from both groups utilised non-PICU inpatient care, with an average of 11.3 vs. 15.1 days per patient per month, whereas almost everyone used PICU non-seclusion inpatient care, with an average of 22.1 vs. 20.2 days per patient per month, for secluded and non-secluded patients, respectively. Community care service use was fairly similar between the two groups.
In 1 year, secluded patients used 56.2 days of non-seclusion inpatient care and non-secluded patients used 59.5 days. Approximately 85% of PICU patients used non-PICU inpatient care, with secluded patients having 19.8 fewer days than non-secluded patients. The mean number of inpatient-days related to seclusion was approximately 3.5 days per patient per year for both groups; however, these services were mostly used by the secluded patients (53% vs. 10%). Community care was dominated by CMHT and home treatment care, with more secluded than non-secluded patients receiving care through these services. However, the mean number of contacts remained similar between the two groups, with approximately 42 and 24 CMHT contacts and home treatment, respectively.
Table 7 shows the number of PICU patients in seclusion and non-seclusion that utilised inpatient and community services and the associated cost for these patients over 7, 30 and 365 days, respectively. The total costs were much higher in the treated group over the 7-day and 30-day periods, with the difference attributable to greater use of inpatient services.
| Health-care services | Cases (N = 990) | Controls (N = 1032) | Unadjusted differences | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Mean cost (£) | SD (£) | n (%) | Mean cost (£) | SD (£) | Mean cost (£) | SE (£) | p-value | 95% CI (£) | |
| 7 days | ||||||||||
| Non-PICU inpatient care | 57 (6) | 1715 | 1286 | 155 (15) | 1348 | 740 | –104 | 29 | < 0.001 | –162 to –46 |
| PICU non-seclusion inpatient care | 956 (97) | 4944 | 1550 | 1007 (98) | 4951 | 1441 | –57 | 93 | 0.545 | –240 to 127 |
| PICU seclusion inpatient care | 425 (43) | 1789 | 1330 | 11 (1) | 2031 | 1388 | 746 | 64 | < 0.001 | 621 to 872 |
| CMHT | 222 (22) | 212 | 151 | 227 (22) | 210 | 189 | 2 | 9 | 0.860 | –16 to 19 |
| Home treatment | 4 (0) | 240 | 128 | 6 (1) | 657 | 472 | –3 | 2 | 0.141 | –7 to 1 |
| Total | 990 (100) | 5690 | 1275 | 1029 (100) | 5120 | 1217 | 585 | 69 | < 0.001 | 450 to 720 |
| 30 days | ||||||||||
| Non-PICU inpatient care | 457 (46) | 3747 | 3377 | 551 (53) | 4768 | 3067 | –816 | 167 | < 0.001 | –1144 to –488 |
| PICU non-seclusion inpatient care | 965 (97) | 18,064 | 7534 | 1009 (98) | 15,521 | 8205 | 2433 | 480 | < 0.001 | 1492 to 3373 |
| PICU seclusion inpatient care | 463 (47) | 2256 | 2507 | 38 (4) | 1529 | 1135 | 999 | 128 | < 0.001 | 748 to 1250 |
| CMHT | 447 (45) | 455 | 359 | 442 (44) | 488 | 540 | –4 | 31 | 0.910 | –65 to 58 |
| Home treatment | 74 (7) | 1685 | 1285 | 79 (8) | 2160 | 1452 | –39 | 27 | 0.147 | –93 to 14 |
| Total | 990 (100) | 20,725 | 6688 | 1029 (100) | 18,204 | 6348 | 2574 | 381 | < 0.001 | 1826 to 3321 |
| 365 days | ||||||||||
| Non-PICU inpatient care | 854 (86) | 27,819 | 36,630 | 859 (83) | 36,412 | 45,339 | –6311 | 2315 | 0.006 | –10,848 to –1774 |
| PICU non-seclusion inpatient care | 971 (98) | 45,070 | 43,025 | 1015 (98) | 45,528 | 53,802 | –573 | 4567 | 0.900 | –9524 to 8377 |
| PICU seclusion inpatient care | 520 (53) | 2955 | 3824 | 101 (10) | 2933 | 3803 | 1265 | 242 | < 0.001 | 790 to 1740 |
| CMHT | 677 (68) | 5076 | 3867 | 653 (63) | 5027 | 5205 | 291 | 334 | 0.385 | –365 to 946 |
| Home treatment | 362 (37) | 4459 | 3907 | 225 (23) | 4136 | 3752 | 729 | 166 | < 0.001 | 402 to 1055 |
| Total | 990 (100) | 74,912 | 55,656 | 1030 (100) | 79,628 | 68,640 | –4562 | 5006 | 0.362 | –14,373 to 5249 |
Discussion
The current study was the first attempt to examine the effect of PICU and seclusion on (1) adverse incidents, (2) length of stay and (3) costs and cost-effectiveness using statistical approaches that afford proper protection against selection bias when using non-randomised data. In unadjusted analyses, PICU and seclusion were associated with increased aggression, violence and serious incidents. However, preliminary calculation and testing of propensity scores (probabilities of treatment conditional on observed covariates) indicated that there was limited overlap between treated and untreated observations, indicating that naive regression estimation would not remove selection bias and that, at least in the available samples, it would not be possible to use propensity scores to derive unbiased estimates. In the case of seclusion, the distribution of scores, when taken together with the sampling frequency, indicated that a different, higher-risk sample of controls could, in principle, be used to derive some estimate of the treatment effect. For similar reasons, it was not possible to generate unbiased estimates of effects on costs or cost-effectiveness.
Strengths and limitations
Notwithstanding the very obvious limitations of our findings, our methods were scrupulous. Without our sampling design and our associated strategy for measuring time-varying covariates, it would not have been possible to calculate propensity scores and, without those, we would not have been aware of the extent to which regression-based estimates would have been biased.
Implications and conclusions
The main implications are for further research. Our findings in relation to seclusion indicate that a modified design applied to our existing sampling frame – one that is not, for pragmatic reasons, limited to using the sample for investigation of predictors and investigation of effects – could yield a usable estimate of effect, bearing in mind the usual caveat regarding unmeasured confounding. It would be necessary to select a group of controls whose probability of treatment was similar to the small group identified in our analysis as having a conditional probability of treatment greater than 0.1, perhaps using more or less sophisticated text-mining approaches. In the case of PICU transfer, the most appropriate approach would be to study a number of provider organisations, including wards that have easy and frequent access to a PICU and wards that do not. Assuming a lack of systematic differences in behaviour between PICU- and non-PICU-using wards, this approach might be expected to yield a higher number of non-PICU untreated controls than was the case in the present study. Once plausible effect estimates have been calculated based on non-randomised data, it will be possible to judge whether further non-randomised or randomised studies are needed.
Chapter 4 Availability, attitudes and time to restraint
Background
Mental health problems in patients requiring admission to acute psychiatric wards are often associated with disturbed behaviour that can put at risk the health and safety of the patient concerned and that of the staff supporting them. One study investigating containment methods for aggressive behaviour in acute psychiatric wards reported almost one aggressive incident per day for every 20 patients. 38 Acute psychiatric wards manage patients whose actions may threaten their own safety and that of hospital staff. 39 To aid in management, wards may be fitted with a seclusion room and/or have direct or indirect access to a PICU.
The Code of Practice for the MHA 1983 (revised 2007) defines seclusion as the supervised confinement and isolation of a patient in a room that has been specifically designed for the purpose of seclusion and that serves no other function on the ward. 40 In this study, when we describe seclusion as ‘available’ this implies the existence of a defined seclusion room directly available to acute wards on the same ward site. When risks are higher than the norm for an acute psychiatric ward, patients can be transferred to a PICU. PICUs are services that provide psychiatric intensive care for patients who are in an acutely disturbed phase of a serious mental disorder and may have a loss of capacity for self-control, with corresponding increase in risk that prevents safe treatment in a general acute ward. 41 The units have higher ratios of nursing and other staff, and are often built on an open-plan design to ease observation and containment. 7 Acute wards may have direct access to an on-site PICU; alternatively, they may have restricted access to a PICU that is located on a different site and/or provided by a different organisation. The process of transferring a patient to a PICU may involve an initial referral, assessment of the patient by PICU staff and transfer to the unit. When PICUs are on site, transfer will often involve calling the rapid response team, which will aid in physical transfer of the patient. When PICUs are not on site, transfer will involve a team accompanying the patient to the unit via transportation, such as a mini-bus or van. The length of time taken for the process of patient transfer to a PICU can range from hours to several days and may be further complicated when the unit is not on site.
The management of acutely disturbed patients during periods of crisis presents the challenge of maintaining the safety of the patient and others while providing a safe environment. 42 Staff act in order to prevent or minimise harm through the use of a variety of containment methods designed to keep patients and staff safe. 43 These include the use of tranquillising medications, increased levels of observation, manual restraint and time out. A number of studies have reported that staff experience adverse and conflicting feelings when using containment methods44 and it has been suggested that this may lead to a preference of not having to use them. 45 Surveys have shown variation in the acceptability of different containment methods, with patients and staff having rated seclusion as one of the least acceptable interventions and PICU care is rated as more acceptable than seclusion, but is still not the most acceptable of interventions. 4 Despite the negative connotations of seclusion, one study suggested that staff with access to seclusion rated this method of containment as more effective in resolving an emergency than alternative methods of containment used in resolving the same emergency rated by staff from the same hospital (but without access to seclusion). 46 The study suggests that seclusion is regarded as more effective in aiding with emergency situations than other methods of containment; however, these other methods were not described and it is not yet clear what seclusion may be substituted with, when a seclusion unit is not directly available to the ward. Even less is known about the attitudes towards PICUs and how these may determine their use.
A literature review conducted by Stewart et al. 47 suggests that, on average, manual restraint is used up to five times per month on psychiatric wards, with each episode lasting approximately 10 minutes. Some forms of manual restraint involve face-down (prone) restraint, which has been associated with sudden death. 48 The struggle of the patient to gain control from restraint can itself lead to staff and patient injury. Information about the use of manual restraint as a management method in psychiatric hospitals is sparse and little is known about instances in which manual restraint might be used and the point at which it will be instigated when risk behaviour is displayed. Understanding at what point this method of management might be instigated is important to improve patient and staff safety. This may be associated with a range of factors, including staff perceptions of, or exposure to, differing levels of risk49 and the availability of facilities at each ward, such as access to seclusion and the use and acceptability to staff of other containment methods. 50
Aims and method
Aim
The purpose of this study was to examine the use and acceptability to staff of a range of containment methods currently utilised in acute psychiatric wards, as well as exploration of speed of initiation of manual restraint across service configuration, dependent on access to PICUs and seclusion.
Participants
Eight hospitals providing inpatient acute psychiatric care participated in the study. The hospitals were identified in a purposeful sample to include two of each of the following: (1) no seclusion and restricted PICU access, (2) no seclusion and full PICU access, (3) seclusion available and restricted PICU access and (4) seclusion available and full PICU access. In order to ensure greater national representativeness, half of the sample was drawn from hospitals in the north west of England and half from hospitals in Greater London. The study participants were acute ward staff members (qualified nurses, n = 130; health-care assistants, n = 69; others, n = 7) who were drawn from the eight hospitals included in the study. All eligible members of staff on duty during frequent researcher visits to the study wards were invited to participate, of whom 206 from 18 wards took part.
Measures
Demographic questionnaire
The demographic questionnaire was a self-administered instrument designed to ascertain information on the participant’s age, sex, ethnicity, relationship status, presence of cohabiting dependents and details of work experience. The participants were asked to provide details including years in current post, years working in psychiatry, occupation, exposure to mild physical violence during the past year, exposure to severe physical violence during the past year, grade of pay (as an indication of experience) and any prevention and management of aggression training (of at least 3 days). For each question, participants selected a response from a choice of pre-determined items.
Attitude to Containment Measures Questionnaire
The Attitude to Containment Measures Questionnaire, version two (ACMQv2), is a self-administered instrument assessing views on the acceptability of 11 different methods of containment for disturbed behaviour to include pro re nata (PRN) medication, seclusion, manual restraint, time out, intermittent observation, compulsory intramuscular sedation, psychiatric intensive care, mechanical restraint, constant observation, net bed and open-area seclusion. 51 Each listed coercive measure is accompanied by a short description and a visual illustration. The participant is asked to rate the acceptability of each method by selecting one response from a five-point Likert scale (strongly agree to strongly disagree) and is then asked to indicate (yes or no) whether or not he or she has ever used the method of containment.
The Moylan Progression of Aggression Tool
The Moylan Progression of Aggression Tool (MAPAT) was designed to identify differences in nurses’ decision-making in relation to the need for manual restraint of an aggressive patient. 52 The MAPAT consists of a 300-second video showing interactions between a nurse and a patient who is becoming increasingly agitated and aggressive, culminating in a serious physical attack on the nurse (strangulation at 280 seconds). The participant watching the video is told that he or she is a nurse standing by with a team of other nurses available to assist, should the situation escalate. The participant is asked to push a button when he or she considers that, was this a real situation occurring in the service context in which they work, restraint should be initiated. The MAPAT exhibits high test–retest validity (r = 0.89)52 and has shown associations with past experience of violent assault by a patient causing injury. 49
Procedure
Ethics approval was granted by the King’s College Ethics Committee, with NHS research and development approval obtained at each participating trust. After a complete description of the study, written informed consent was obtained. Staff members completed the study at their hospital site, on the ward on which they worked. After completion, participants were asked not to discuss the tasks with other staff members in order to prevent contamination. Testing took part in a quiet room; participants were asked to complete paper versions of both the demographic questionnaire and the ACMQv2, and the MAPAT was administered on a laptop computer. The participants were debriefed and thanked for their time.
Analysis
Spearman’s rank-order correlations were calculated to determine the relationship between service configuration and the items from the demographic questionnaire. Significant associations between service configuration and demographic variables were further examined using logistic regression modelling with seclusion provision and PICU provision.
Spearman’s rank-order correlations were calculated to determine the relationship between service configuration and individual items of the ACMQv2 with significant associations further tested using logistic regression.
Reactions during use of the MAPAT had a bimodal distribution and scores were categorised to match their distribution as follows: (1) ≤ 224 seconds, (2) 225–250 seconds and (3) ≥ 251 seconds. In time frame 1, a patient displays signs of agitation by pacing, fidgeting and becoming agitated when a nurse attempts to verbally de-escalate. In time frame 2, the patient displays similar agitation and is verbally abusive and threatening to the nurse. In time frame 3, the patient hits a piece of furniture and shoves a chair out of the way while approaching the nurse, finally attempting strangulation. Spearman’s rank-order correlations were run to determine the relationship between MAPAT time-to-restraint and other questionnaires. Chi-squared tests were performed to explore the relationships between MAPAT score and use of containment method. Using ordinal regression, MAPAT score was modelled using seclusion provision and PICU provision as predictors.
Results
Demographic information
Table 8 summarises the demographic features of the sample (counts and percentages).
| Demographic features | n (%) |
|---|---|
| Service configuration | |
| Seclusion used and PICU available | 49 (23.2) |
| Seclusion used but no PICU | 48 (22.7) |
| Seclusion not used but PICU available | 51 (24.2) |
| Seclusion not used and no PICU | 63 (29.9) |
| Demographics | |
| Age (years) | |
| 20–29 | 44 (21.6) |
| 30–39 | 44 (21.6) |
| 40–49 | 53 (25.9) |
| 50–59 | 54 (26.5) |
| > 60 | 9 (4.4) |
| Male sex | 86 (42.2) |
| Ethnicity | |
| White | 118 (58.1) |
| Caribbean | 9 (4.4) |
| African | 57 (28.1) |
| South Asian | 4 (19.7) |
| Other | 15 (7.4) |
| Relationship status | |
| Single | 64 (31.4) |
| Separated | 15 (7.4) |
| Widowed | 4 (1.9) |
| Married/cohabiting | 121 (59.3) |
| Dependants | |
| Aged < 12 years | 39 (19.3) |
| Aged 12–21 years | 46 (22.8) |
| Other | 3 (1.5) |
| None | 114 (56.4) |
| Details of current post | |
| Time in current post (years) | |
| < 1 | 43 (21.2) |
| 1–3 | 60 (29.6) |
| 3–5 | 29 (14.3) |
| > 5 | 71 (34.9) |
| Experience in psychiatry (years) | |
| < 1 | 15 (7.4) |
| 1–3 | 31 (15.2) |
| 3–5 | 30 (14.7) |
| > 5 | 128 (62.7) |
| Occupation | |
| Nurse | 130 (63.1) |
| HCA | 69 (33.5) |
| Therapist | 2 (0.9) |
| Other | 5 (2.5) |
| Pay grade | |
| 2 | 5 (2.7) |
| 3 | 65 (34.6) |
| 4 | 7 (3.7) |
| 5 | 74 (39.4) |
| 6 | 27 (14.4) |
| 7 | 8 (4.3) |
| 8 | 2 (1.1) |
| Received violence related training (past year) | 148 (90.2) |
| Exposure to mild violence (past year) | |
| Occasionally | 87 (42.3) |
| Sometimes | 48 (23.3) |
| Often | 30 (14.6) |
| Frequently | 31 (15) |
| Never | 10 (4.9) |
| Exposure to severe violence (past year) | |
| Occasionally | 43 (20.9) |
| Sometimes | 16 (7.8) |
| Often | 6 (2.9) |
| Frequently | 5 (2.4) |
| Never | 136 (66) |
The absence of a seclusion room was associated with younger staff (rS = –0.16, n = 204; p = 0.021) and fewer years’ experience of working in psychiatry (rS = –0.14, n = 204; p = 0.040). When further tested in a logistic regression equation with seclusion as the dependent variable and controlling for PICU access, neither of these two variables remained significant.
The absence of an on-site PICU was associated with higher numbers of female staff (rS = 0.15, n = 204; p = 0.028) and greater exposure to mild physical violence (rS = –0.14, n = 206; p = 0.047). When tested in a logistic regression controlling for seclusion availability, only sex (p = 0.034) remained significant.
Attitude to Containment Methods Questionnaire
The means and SDs of each item from the ACMQv2 are illustrated in Table 9. The containment methods have been ranked in order of acceptability, from most acceptable to least acceptable.
| Containment method | Mean (SD) | Used (n) | Used (%) |
|---|---|---|---|
| PICU | 4.46 (0.59) | 167 | 84.8 |
| Intermittent observation | 4.45 (0.77) | 195 | 97 |
| PRN medication | 4.37 (0.7) | 139 | 73.9 |
| Constant observations | 4.28 (0.77) | 194 | 97 |
| Time out | 4.24 (0.8) | 173 | 86.9 |
| Manual restraint | 4.06 (0.8) | 179 | 89.9 |
| Seclusion | 3.95 (0.96) | 132 | 67.3 |
| Intramuscular medication | 3.94 (0.92) | 135 | 68.9 |
| Open-area seclusion | 3.34 (1.02) | 53 | 26.4 |
| Mechanical restraint | 1.91 (0.99) | 5 | 2.5 |
| Net bed | 1.77 (0.89) | 1 | 0.5 |
Psychiatric intensive care unit, intermittent observations and PRN medication received the highest approval ratings, whereas mechanical restraint and net beds received the lowest. Approval scores with the greatest variability were open-area seclusion, mechanical restraint and seclusion.
Access to a seclusion room was associated with greater acceptability of seclusion as a method of containment (rS = 0.25, n = 198; p < 0.001) and lower acceptability of open-area seclusion (rS = –0.23, n = 199; p = 0.001). When tested in a logistic regression controlling for PICU access, seclusion acceptability remained significantly associated with seclusion availability (p < 0.001); however, open-area seclusion acceptability was no longer significant.
Participants were asked to identify whether or not they had ever used any of the 11 methods of containment indicated by a response of ‘yes’ or ‘no’. Frequency (and percentage) of total responses can be seen in Table 9. Intermittent observation, constant observation and manual restraint were the methods that had been used by most members of staff, whereas mechanical restraint and net beds had been used the least.
The availability of a seclusion room was associated with a greater reported use of seclusion (rS = 0.548, n = 196; p < 0.001) and time out (rS = 0.152, n = 200; p = 0.032), and a lesser use of open-area seclusion (rS = –0.181, n = 201; p = 0.010). When entered into a logistic regression controlling for PICU access, greater reported use of seclusion (p < 0.001) and less open-area seclusion use (p = 0.001) remained significant, whereas reported time-out use did not (p = 0.715).
The availability of an on-site PICU was not statistically associated with any containment method acceptability score. The availability of an on-site PICU was associated with less reported use of open-area seclusion (rS = –0.154, n = 201; p = 0.029). This usage association remained significant (p = 0.048) when tested in a logistic regression equation controlling for seclusion availability.
Moylan Progression of Aggression Tool
Using Spearman’s rank-order correlation, MAPAT time to restraint was not associated with demographic information or details of current post. Table 10 shows the frequency (and percentage) of responses for each of the three time frames during use of the MAPAT across seclusion and PICU provision.
| Technique and availability | MAPAT times (seconds) | ||
|---|---|---|---|
| < 224, n (%) | 225–50, n (%) | > 250, n (%) | |
| Seclusion access on site | |||
| Yes | 16 (19.5) | 38 (46.3) | 28 (34.1) |
| No | 6 (5.8) | 39 (37.5) | 59 (56.7) |
| PICU access on site | |||
| Yes | 12 (12.9) | 33 (35.5) | 48 (51.6) |
| No | 10 (10.8) | 44 (47.3) | 39 (41.9) |
Moylan Progression of Aggression Tool timings were inversely associated with seclusion availability (rS = –0.258, n = 186; p < 0.001) but were not associated with PICU availability. Using logistic regression with seclusion availability as the dependent variable, controlling for PICU availability, MAPAT times remained highly significant (p < 0.001). When there was no seclusion room available, staff took longer and allowed a greater degree of escalation before initiating restraint, as judged by their MAPAT scores.
Moylan Progression of Aggression Tool scores were also explored in relation to ACMQv2 scores. The MAPAT timings were positively associated with participants’ judgements of mechanical restraint acceptability (rS = 0.190, n = 179; p = 0.011) and net bed acceptability (rS = 0.168, n = 177; p = 0.025). A longer time before restraint was initiated was associated with greater acceptability of these containment methods. MAPAT scores were not associated with the reported use of any of the containment methods on the ACMQv2.
Discussion
Acute psychiatric wards, such as those taking part in the current study, manage patients whose actions may threaten their own safety and that of hospital staff. 53 Previous studies evaluating the acceptability and/or use of different containment methods in mental health services4,45,54 have not considered the association between access to seclusion and/or PICUs and acceptability/use of different containment methods. Those that have considered ratings of acceptability have shown that staff rate seclusion as less acceptable than nearly every other form of containment and PICU care as one of the most acceptable forms of containment. 4 In our results, transfer to a PICU was rated as the most acceptable form of containment. However, seclusion was rated as less acceptable than transfer to a PICU, intermittent observations, constraint observation, PRN, time out and manual restraint.
Service configuration is associated with acceptability of some containment methods
The acceptability and use of seclusion is related to its access. No such associations were found between PICU access and its acceptability and use. Seclusion use has been shown to increase when a seclusion room is directly available to the ward,2 suggesting that with first-hand experience of seclusion room use, staff members are more likely to approve of it as a method of containment. Seclusion is regarded as more effective in aiding with emergency situations than other methods of containment,46 and those with access to a seclusion room reported that without the use of this room, the unit could not operate effectively. 55 It is also possible that some form of cognitive dissonance56 process might underlie this association, with nurses exposed to, and therefore involved in, seclusion use, shifting their beliefs to fall in line with their behaviour. One study suggested that the availability of a seclusion room made staff believe that they were providing more effective care, with the use allowing staff to become more accustomed to it, leading them to rate seclusion as less intrusive to patients, compared with staff who had never secluded a patient on the same site. 57 Alternatively, it is possible that members of staff with strong feelings against seclusion room use perhaps avoid working at wards with direct access to one. All things considered, it is possible that seclusion rooms are being overused at sites with direct access to one, with evidence that some staff members conform to the use of seclusion rooms when seclusion rooms are available, feeling discriminated against if alternative methods are suggested. 58 The concern that seclusion could be abused, for example by being overused when available or used as a substitute when staffing levels are decreased, has been expressed by some authors. 51,59 This has important implications, as patients rate seclusion as unacceptable when compared with many other methods of containment. 4
For those without direct access to seclusion, staff members are more likely to approve of open-area seclusion and this method of containment was more commonly used by staff on wards without on-site seclusion and a PICU. Open-area seclusion is more often referred to as ‘nursing in a side room’ or as the use of an ‘extra care area’. The ACMQv2 defines seclusion as ‘a patient being isolated in a locked room’ and open-area seclusion as ‘a member of staff stays in the locked room with the patient’. Both seclusion and open-area seclusion fit under the umbrella term of seclusion in 2002 English guidance40 and it is possible that wards without defined seclusion rooms are simply substituting this for a different type of seclusion.
Seclusion provision, and not psychiatric intensive care unit provision, is associated with time to restraint in response to aggressive behaviour while using the MAPAT
Time to restraint in response to aggressive behaviour while using the MAPAT was strongly and significantly associated with seclusion provision but not PICU provision and, in places without seclusion, there was a longer time lapse before staff initiated restraint. In units without seclusion, staff members tolerated higher levels of aggression before choosing to restrain while using the MAPAT. Previous studies have suggested that staff without access to seclusion rate their methods of containment as less effective in resolving emergency situations. 46 This lack of confidence could explain delayed time to restraint during the MAPAT. There was no association between PICU access and MAPAT score, despite the fact that on-site PICU availability leads to increased use. 10 This may be because, unlike seclusion, which can be utilised immediately, a transfer to a PICU takes some time to organise and commonly occurs after the immediate crisis is over.
Other findings
There was no association between MAPAT time to restraint and manual restraint acceptability or between MAPAT time to restraint and use of manual restraint. Therefore, it was not the acceptability of restraint that was driving the difference in MAPAT scores, but perhaps more likely a rational calculation about managing outcomes, on which seclusion availability seems to be an influence.
Although mechanical restraint and net beds remain the two containment methods with lowest acceptability ratings, greater acceptability was associated with longer time to restraint during the MAPAT. Although the reasons for this are unclear, it is possible that staff members who are less judgemental of these methods of containment tolerate more extreme patient behaviours and, thus, react more slowly.
The current study found that initiation of restraint was not associated with exposure to either mild or severe physical violence. This conflicts with previous research by Moylan and Cullinan49 using the MAPAT, in which staff members who had suffered from injury at work took longer to initiate restraint than those with no history of injury. The authors suggested that it was fear itself that delayed the restraint process. Moylan and Cullinan’s study considered associations between injury and serious injury, in which type of injury was clearly defined (e.g. evidence of fracture). 49 Our study did not ask participants to be so detailed with their exposure to physical violence and was more subjective in comparison. Therefore, the different methods of investigation in these studies may account for the differences in findings.
Clinical implications
This study raises important questions about clinical practice, particularly the links between the availability, approval of and use of seclusion, coupled with the faster use of manual restraint as judged by the MAPAT. However, none of these findings constitute evidence that seclusion can be safely abandoned. Faster restraint may, in fact, be safer for staff and patients. Secluding a patient might be safer than not doing so (although findings elsewhere in this report suggest that this is not the case).
Limitations
The sample was representative of two urban regions in England (London and the North West). Not all staff participated in the study, with 9.71% of staff not completing the MAPAT. Some degree of response bias may be a possibility. Participants may have previously worked at hospitals with or without seclusion/PICU availability and this may have impacted on the results. ACMQv2 scores are valid and have previously been confirmed to be related to usage; however, generic acceptability ratings ignore potential variation by specific types of behaviour such as aggression, self-harm or mania. Different scenarios may influence judgments of acceptability. Although the MAPAT has been rigorously developed, the extent to which MAPAT scores correlate with actual restraint use in practice is not known, and nor are there any criteria for judging what score represents the optimum or best for a safe outcome. As such, the validity of the MAPAT is unclear.
Conclusions
Transfer to a PICU is a more acceptable form of containment to acute ward staff than seclusion and many other methods, yet staff members in some hospitals do not have easy and speedy access to it when they are managing disturbed high-risk patients. The availability of seclusion appears to drive both approval of it and its use, raising concerns that it may be overused when it is available. In the absence of a seclusion room, staff members are more likely to use open-area seclusion.
Absence of seclusion was associated with delayed time to restraint during the MAPAT task, yet the nature of this link is somewhat obscure as judgements of the acceptability of seclusion were not related to restraint thresholds, nor was the acceptability of manual restraint itself linked to that threshold. More research into the underlying staff psychology of containment evaluations, cognitions, emotions, morality and usage is clearly needed.
Chapter 5 Availability and escalation pathways
This chapter has been based on data from Pettit et al. 60 under the terms of the Creative Commons Attribution license (http://creativecommons.org/licenses/by-nc/4.0).
Background
One major rationale for psychiatric inpatient care is to keep acutely ill patients and those around them safe from harm. In the hospital a number of different methods are used either to directly prevent a patient from engaging in behaviour that is likely to result in injury or to curtail such behaviour should it occur. Two commonly used containment methods are seclusion and psychiatric intensive care. By seclusion we mean the isolation of a patient in a locked room. By psychiatric intensive care we mean a specialist ward with more robust security and higher nurse staffing levels.
Seclusion rooms are robustly designed with heavy security doors and locks, and solid fixtures and fittings that cannot be easily damaged. For the same reason, they commonly have bare walls, recessed light fittings with controls outside the room, limited ventilation, limited sanitary access, little external light and contain nothing more than a solid foam mattress, possibly with sheets or blankets. Such rooms always permit some form of observation from outside so that staff can monitor the patient. About one-quarter of UK acute psychiatric hospitals do not have a seclusion room. 10 It is not known for certain whether or not the provision of seclusion makes wards safer places; however, a large multivariate study has not shown the presence of a seclusion room to be associated with reduced levels of any high-risk behaviour such as aggression61 or self-harm. 62 How staff manage those same behaviours in the absence of a seclusion room is also not known.
Psychiatric intensive care units tend to be smaller wards with higher nurse staffing levels, heavier locks and security doors, stronger furnishings and greater levels of staff supervision and observation. Disturbed patients are transferred to the PICU and this transfer is easier to achieve if it is on the same site. About one-third of acute psychiatric hospitals do not have access to an on-site PICU10 and, just as with seclusion, on-site provision is not associated with fewer high-risk behaviours. Again, how staff manage high-risk behaviours in the absence of an on-site PICU is not known.
The aim of this study was, therefore, to describe how the same patient high-risk behaviours are managed in hospitals with differing access to a PICU and seclusion. By seclusion being available we mean that there is a defined seclusion room available to acute wards, which is on the same hospital site as the acute ward. By restricted PICU access we mean that a PICU might be available to the acute wards, but was on another site and/or in a different organisation and/or privately provided.
Aims and methods
Aim
Comparing units with differing access to a PICU and seclusion we (1) describe how the same patient high-risk behaviours are managed; and (2) explore and identify differing thresholds for the commencement of severe containment methods (manual restraint, rapid tranquillisation, seclusion and PICU transfer).
Objectives
To compare the management of disturbed behaviours in four different service configurations: (1) no seclusion and restricted PICU access; (2) no seclusion and full PICU access; (3) seclusion available and restricted PICU access; and (4) seclusion available and full PICU access.
By seclusion available we mean that there is a defined seclusion room available to acute wards, which is on the same hospital site as the acute ward. By restricted PICU access we mean that a PICU may be available to the acute wards, but is on another site and/or in a different organisation and/or privately provided.
Specific hypotheses explored
The absence of seclusion and/or restricted access to PICU care are managed through one or more of the following four mechanisms.
-
Substitution: seclusion for PICU (or vice versa) or other alternatives such as medication (regular in higher dose, more intensely sedating medications and/or routes of faster or more effective absorption, intramuscular/intravenous) and/or long duration of manual restraint, time out and open-area seclusion (confinement of a disturbed patient in a separate area together with nursing staff) of some form.
-
Early intervention: faster response to escalation, earlier physical intervention, leading to safer management and more benign outcomes, possibly accompanied by temporarily increased nurse staffing levels or the use of intensive forms of constant special observation (such as two staff to one patient).
-
Therapeutic intensity: deployment of a range of psychotherapeutic and behavioural interventions to manage, ameliorate and reduce the frequency of risky patient behaviours.
-
Non-standard transfer: move of the patient to another ward providing more secure or intensive care in some fashion, perhaps in a private hospital or in a neighbouring trust, or via a secure rehabilitation ward or a forensic ward of some type.
Design
Qualitative data collection was undertaken through interviews of nurses on the management of disturbed behaviour. The interviews used standardised vignettes to elicit what typically happened on the interviewee’s ward in response to particular types of disturbed behaviour. Interviews were conducted within the four different service configurations, systematically coded and subjected to quantitative analysis. The design therefore includes elements of both qualitative and quantitative design, straddling the border between the two.
Sample and sample size
Eight hospitals providing inpatient acute psychiatric care were identified in a purposeful sample, two in each of the following categories: no seclusion and restricted PICU access; no seclusion and full PICU access; seclusion available and restricted PICU access; and seclusion available and full PICU access. In order to ensure a less London-centric sample and greater national representativeness, half of the sample was drawn from hospitals in the north west of England, and half from hospitals in and around London. All NHS mental health hospitals in these areas were identified and one hospital in each category was randomly selected for inclusion (with replacement for any refusals). Thus, in the North West, four randomly selected hospitals (one in each category) were included in the study, and this was the same in London.
Our intention was to draw a random sample of 30 qualified nurses from acute wards in each category of hospital to participate in the threshold interview. This figure was a compromise between achieving a degree of representativeness of the nursing workforce at each hospital and, thus, being able to accurately describe their patient management systems and techniques, and being able to comprehensively manage the data analysis of a large number of interviews centrally.
These plans changed during execution in two respects. Development of the interview indicated that patient sex might influence the pathway and some randomly selected hospitals had separate male and female PICUs available on different sites. We therefore limited the sample to PICUs taking male patients and the sample of interviewees to all acute wards at the study site with male patients. The sample therefore included mixed-sex wards but not female-only wards. Second, and partly as a consequence, the eligible number of qualified nurses was smaller than anticipated at some sites and, instead of randomly selecting participants, we invited all eligible staff to participate.
Description of the Threshold and Escalation Pathway Interview and how it was utilised
The Threshold and Escalation Pathway Interview (TEPI) is a fully structured interview schedule that seeks to elicit from the interviewee the typical escalation pathways of interventions used to control and manage disturbed behaviour on the ward where they work. As such, it presented the interviewee with a number of behavioural scenarios and asked them to respond by describing in detail what typically happens and in what order, when this behaviour occurred on their ward. Three cases, each exhibiting a number of challenging behaviours, were presented one by one to the interviewee.
-
Mike (mania): medication refusal, public nakedness, giving away expensive property, shouting, attempting to abscond, sexual assault.
-
Steve (self-harm): suicidal ideation, scratching self, cutting self, attempt to hang self.
-
Alan (aggression): verbal abuse, property damage, wielding a club, assaulting a fellow patient, assaulting a fellow patient very seriously.
Each behaviour was presented independently to the interviewee for their description of responses, that is, free standing and independent of previously presented disturbed behaviours. The TEPI also contained additional questions to explore the possible impact of staffing levels, sex of the patient, vulnerability of the victim, intoxication, what explanation the patient might give, patient history of violence, etc. The interview was digitally recorded on the wards that were studied. Handwritten notes and check boxes were also completed by the interviewer as part of the process.
The TEPI is designed to be administered to qualified psychiatric nurses only and requires several hours of detailed study by potential interviewers, coupled with discussion and training. An online training module was designed as part of the research. Conducting a TEPI takes approximately 90 minutes.
The full TEPI and the instructions for its use are provided in Appendices 1 and 2, respectively.
Development of the Threshold and Escalation Pathway Interview
The development of the TEPI was a lengthy, sequential and iterative process. The initial ideas for the cases and their potential stages of increasingly difficult behaviour were developed via small group work by the mental health nursing research team under the direction of the principal investigator. These were subsequently synthesised and changed into a viable schedule, with some cases being dropped and others proposed, by the core SPICES collaborators. These then went back to the wider research team who split into five groups of three people (one note-taker, one subject, one interviewer) and the interviews were tried. A significant number of lessons were gained from this and the interview was revised. At this stage it was sent out to all the SPICES collaborators for comments and feedback and was taken to consultation with SUGAR (Service User and Carer Group Advising on Research), a service user and carer group,63 both leading to further amendments. Four trial interviews were then conducted with experienced clinical nurses by the principal investigator. These were recorded and carefully reviewed and, after each interview, changes were made to the TEPI schedule. Following these pilot interviews, the schedule was again presented to the main mental health nursing research team, to a group of prevention and management of aggression trainers and was reviewed by the SPICES qualitative research expert (AQ). These led to the final revision and the form of the TEPI used during the study: the interview schedule and its accompanying instructions that formed the basis for training interviewers. This TEPI development process took 8 months in total.
The issue that was the key focus throughout the development process was that of standardisation. It became apparent that many things might influence the direction of the escalation pathway in actual practice: the age, sex and ethnicity of the patient; nurses’ previous knowledge of the patient; their legal status; their history of violence; what the patient says about their behaviour; what other patients in the vicinity do; the patient’s degree of resistance to the interventions the staff deploy; the numbers of staff on duty; the general frequency of difficult behaviours on the wards, etc. All of these had to be standardised during the interview so that the influence of seclusion and PICU availability could be made visible. Additional care needed to be taken with the presentation of the problem behaviours and instructions produced on how to respond to a number of different but common ways that interviewees took the interview in directions not required by the research. Terminological differences had to be clarified, and at one point it became clear that many containment names in common use did not have any common meaning, necessitating extra questions in the TEPI to elicit the precise actual meaning of the words used by interviewees to describe interventions.
Data quality
The TEPI is a long and complex interview. It was conducted by a number of different interviewers (eight). Although all were trained in the same way to conduct the TEPI, each brought their individual experience of inpatient psychiatry, clinical work and their academic background to the way in which they conducted the interview. These factors in combination led to a number of identifiable problematic issues when the recorded interviews were being processed for analysis.
The most prominent difficulties were associated with changes to the way in which the interview was administered, either by adding questions or leaving them out. On the one hand, prompts were given as to possible interventions, such as ‘would you increase his level of observations?’, ‘would you restrain him?’ and ‘would you call the police at this point?’, even though interviewers had been asked not to do this. Such prompting seemed to be particularly prevalent in interviews conducted by clinically experienced nurses. When entering codes for analysis, the default position was to ignore any step that was prompted by the interviewer; however, these were sometimes included when they had already been given as steps in a previously covered similar pathway. On the other hand, interviewers were required to ask what would happen if an already discussed behaviour was to be repeated during the same shift, in the following shift and throughout the day, but we found that these three levels of repeats were often collapsed or asked idiosyncratically or not at all. These omissions seemed to be dependent on the perceived level of co-operation of the interview respondent.
More minor difficulties included large variation in the detail included when exploring different steps included in the pathway, such as who carries out the management method, what disciplines, how many staff are included, what exactly do they do and a full and detailed description. This was largely dependent on what the interview respondent was asked. The missing information was often relatively unimportant and not central to the analysis, but was problematic in the area of manual restraint practice. Planned explorations of resistance to the use of a low stimulus environment and how Mike’s treatment might have been different if he had a known history of violent behaviour were also not always discussed.
In rare cases, and contrary to their instructions, the interviewer would challenge the response of the respondent. Some examples included ‘do you really have time to do this?’ and ‘is that what would really happen, though?’. These responses were coded according to the initial response before the challenge.
It was typical for interviewees to reply in the first person singular, for example ‘I would – ‘. This often produced a response based on what they would do or what they believed should happen. The interviewers were asked to prompt the participant in the direction of what would typically happen on this ward. Although this did happen in most of the described cases, the use of this prompt was not absolutely consistent.
On occasion, interviewers introduced variations in delivery of the behaviours and some would extend the scenario or indulge in additional questioning, as would be more typical in a semistructured interview. For example, in the case of Mike, when he tries to abscond, one interviewer asked ‘what would happen if he actually escaped?’ and, in other cases, additional questions such as ‘and what if PICU [transfer] didn’t happen?’ and ‘but what if they didn’t come and you were alone?’. In such cases it felt as if the interviewer was probably curious, rather than intending to change the outcome of the scenario. The produced material was not included in the coding or analysis.
On occasion the interviewee would introduce more extreme behaviours such as ‘if he got violent we would – ‘. Usually (but not always) the interviewer would prompt the respondent back to the correct behaviour. Examples that were not controlled included ‘if Mike escapes we would . . .’ and ‘if he started assaulting people we would . . .’. In these examples and others like them the suggested pathways were simply ignored in the coding process.
These problems with data collection had several consequences. The use of the information on repeated behaviours by patients (in other words, what would typically happen on the ward if the patient performed the behaviour again and again) was avoided as much as possible. These data were considered to be less reliable than the first-line responses. A detailed evaluation of different manual restraint technique usage, particularly the issue of long duration restraint, could not be properly compared across categories of hospital, as in many cases details were sparse.
Some areas for which it was hoped to have further information from the interviews in addition to the main research questions about the impact of seclusion and PICU availability were not covered consistently enough to be usable.
Data analysis
The initial plan was that the interviews would be professionally transcribed and imported into qualitative data analysis software. However, the interviews were structured in such a way that this proved to be unnecessary and coding could be conducted directly from the digital audio recordings.
The interviews were thematically analysed for intervention themes (the treatment and management methods described by respondents). This generally resulted in a two-level hierarchy of codes, with the highest level being the most general and the lower having greater specificity. For example, the higher-level code ‘observation’ included a multiplicity of lower-level codes covering intermittent to continuous observation utilising various numbers of staff and differing time intervals. De-escalation, manual restraint and several other common intervention methods were hierarchically broken down in the same way. The codes and definitions utilised were initially derived from those used during the Sequences of Conflict and Containment Events Study (CONSEQ). 3 Additional codes were proposed by researchers coding the data based on the content of the interviews. These were reviewed with the principal investigator and the wider mental health nursing research team, who agreed a final definition for each code that was then deployed. The creation of additional codes ceased owing to saturation around half-way through the data entry process.
The coder would listen to the digital recording of the interview while examining the written notes of the interview taken by the interviewer. From this they would draw up on paper the escalation pathway as depicted by the interviewee. Codes were then entered directly into SPSS version 22 (IBM, Armonk, NY, USA) with their relative order in response to a specific challenging behaviour scenario and whether or not they were specified by the interviewee as a response to the first time the patient exhibited that behaviour or in response to repeats of the same behaviour.
It was initially planned that the escalation pathway of intervention responses to a particular challenging behaviour at any one hospital site could be summarised onto some form of network diagram or flow chart, so that these could be directly compared. Although this was attempted with the data from the first full hospital to be entered, it proved to be impossible to be confident that this was truly representative, given the huge variation in pathways between interviewees. A variety of other means of representing the data were tried in order to extract a visible pattern that could potentially be compared across hospitals, including heat maps, line graphs of mean order by intervention, sequence index plots and simple intervention frequency bar charts. This last simple method was more useful, but the variability highlighted that statistical testing would be required to identify which differences between hospital types were meaningful.
The frequency of interventions was statistically tested across the hospital categories using chi-squared tests. The frequencies were tabulated so that the differences could be seen in conjunction with the results of the statistical tests. When appropriate, multivariate models were applied using logistic regression. More complex multivariate modelling was not conducted in the light of both the small numbers of interviewees at each category of hospital and the difficulties already described in the standardisation of the data collection. Microsoft Excel, SPSS and Stata were all used during the analysis.
Results
Nurses completing the Threshold and Escalation Pathway Interview
Eighty-one TEPI interviews were completed at the eight selected hospitals. The numbers of eligible wards at each hospital site for sampling of staff ranged from 1 to 4 (mean 2.25, SD 1.16). The numbers of nurses recruited at each hospital ranged from 1 to 16 (mean 10.12, SD 6.77). Not all of the nurses who participated in the TEPI also completed the quantitative measures; however, these details were available for 75 of the 81 interviewees. Of those 75, the modal age group was aged 40–9 years, 43% were male, 45% were white British, 65% were married or cohabiting, and around half had been in their current post for > 3 years. Table 11 indicates the numbers from each of the four categories of hospital.
| Seclusion | On-site PICU | |
|---|---|---|
| No | Yes | |
| No | 29 | 16 |
| Yes | 19 | 17 |
There were a number of reasons why the sample size was smaller than initially planned. At some sites there were simply insufficient numbers of staff meeting the inclusion criteria. In addition, on some wards, support from the ward manager was less enthusiastic and recruitment was poor. It is worth bearing in mind that the participation of staff was a significant burden on wards, as key staff members were taken away from work for a period of up to 90 minutes. We extended our data collection period several times and made repeated visits to the study hospitals in order to increase recruitment. Although this incrementally increased the numbers, eventually it was clear that no further recruits could be obtained.
Nurse staffing and bed numbers compared
All interview participants were asked the following: ‘On your ward, how many staff are typically on duty mid-morning on a usual mid-week shift? Numbers of qualified nurses? Numbers of health-care assistants? Numbers of anyone else? What is the number of beds on your ward?’.
The purpose of collecting these data was to ascertain whether or not there was any indication that hospitals without seclusion or easy access to a PICU managed this situation by having higher numbers of staff available.
Figures were converted into staff numbers per 20 beds, to standardise for the different numbers of beds (and therefore patients) on the study wards. Replies to these questions were provided by 56 interviewees. The mean number of staff on duty per 20 beds on a mid-week morning was 5.00 (SD 0.89). Preliminary t-tests were applied to assess whether or not there was any indication of a difference by seclusion or PICU availability. These tests were not significant for all staff on duty or for qualified nurses or health-care assistants (unqualified nurses/nursing assistants) alone. Further statistical exploration controlling for clustering by ward was, therefore, deemed unnecessary.
There was no indication that wards differed in their staffing numbers by seclusion or PICU availability; therefore, staffing number differences are unlikely to account for any differences found in the escalation pathways reported.
Frequency or recency of adverse incidents on the study wards compared
At the end of the interview, participants were asked to report on how recently their ward had experienced any of the incidents covered in the preceding interview. For each incident type, participants were asked how often this typically occurred, if ever, and specifically if it had occurred in the past week, month, 6 months or year. Participants were asked both about one-off occurrences and about repeated incidents involving the same patient.
Table 12 shows part of the TEPI used to score such behaviours.
| Has this happened on your ward during the. . .? | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Once | Same patient, repeatedly during 24 hours | |||||||||
| Past week | Past month | Past 6 months | Year | Never | Past week | Past month | Past 6 months | Year | Never | |
| Aggression | ||||||||||
| Agitated, verbally abusive, shouting | ||||||||||
| Aggressive towards objects, breaking things | ||||||||||
| Brandishing a broken chair leg or similar as a weapon | ||||||||||
| Physically attacks a fellow patient, punches/kicks or equivalent | ||||||||||
| Self-harm and suicidality | ||||||||||
| Stated suicidal intent or threats of suicide | ||||||||||
| Scratches to skin with some form of sharp object | ||||||||||
| Deep cuts with a sharp item to limbs, or equivalent behaviour | ||||||||||
| Attempted suicide by tying a ligature round neck, attempted hanging, self-suffocation or other serious equivalent | ||||||||||
| Mania | ||||||||||
| Coming into the public areas of the ward naked | ||||||||||
| Giving away their own property to others | ||||||||||
| Loud, shouting, screaming | ||||||||||
| Attempting to abscond | ||||||||||
| Sexual assault, touching others inappropriately | ||||||||||
| Refusing to take his prescribed antipsychotic medication or equivalent on admission | ||||||||||
Spearman correlations were conducted between the above data items and the presence of a seclusion room or on-site PICU, thus allowing for the ordinal nature of the data. Positive correlations indicate less frequent incidents with either seclusion or PICU provision.
Seclusion was associated with less one-off self-harm by scratching with a sharp object (r = 0.341; p < 0.001; n = 66). There were no other significant findings.
An on-site PICU was associated with less repeated, recent verbal abuse (r = 0.376; p = 0.002; n = 63), less repeated damage to objects (r = 0.354; p = 0.005; n = 61), less one-off brandishing of a blunt weapon (r = 0.300; p = 0.015; n = 65), less one-off physical assault of a fellow patient (r = 0.324; p = 0.006; n = 69), less one-off threats of suicide (r = 0.303; p = 0.011; n = 69) and less one-off serious attempted suicide (r = 0.522; p < 0.001; n = 66), as well as less repeated attempted suicide (r = 0.286; p = 0.023; n = 63) and less repeated loud shouting (r = 0.269; p = 0.027; n = 67).
These findings do not support the hypothesis that hospitals without seclusion or a PICU are more quiescent places and experience fewer risky behaviours on the part of patients. On the contrary, there is support for the interpretation that having an on-site PICU (but not access to a seclusion room) results in significantly calmer and safer acute wards.
Relative frequency of the higher-level codes
Table 13 shows the frequency of the higher-level codes in the data set, separated into first-line responses and responses to repeated behaviour. These frequencies cannot represent the frequency of use of these interventions in clinical practice, as they were cited in response to the fixed vignettes and protocols of the TEPI. However, they are also likely to be related to frequency of use in practice, and gross differences in frequency may carry some implications. In particular, the low citation of calm-down methods, use of activity rooms and garden areas and, particularly, psychological therapy might indicate interventions that could be beneficially increased in clinical nursing practice.
| Definition | First line | Repeats | ||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| De-escalation, talking and engaging with the patient in order to manage, avert or resolve the situation | 1887 | 26.24 | 663 | 19.11 |
| Observation, any level of observation greater than the normal routine | 830 | 11.54 | 440 | 12.68 |
| Manual restraint, holding to prevent movement, resistance, aggression, self-harm or to move location of patient, compel treatment, retrieve an object | 765 | 10.64 | 262 | 7.55 |
| Request the assistance of other staff | 621 | 8.63 | 187 | 5.39 |
| Request to stay in a LSE or use a LSE such as their bedroom or a quiet room, TV room away from other patients. Includes a ‘time out’ period | 439 | 6.10 | 154 | 4.44 |
| PRN sedating/tranquillising medication, given orally, offered | 306 | 4.25 | 168 | 4.84 |
| Talk to others about the situation | 303 | 4.21 | 248 | 7.15 |
| A review of a patient | 285 | 3.96 | 331 | 9.54 |
| Coerced intramuscular medication, sedating/tranquillising medication given by injection without the patients consent | 279 | 3.88 | 166 | 4.78 |
| Any discussion about offering medication without specifying what | 233 | 3.24 | 171 | 4.93 |
| Involvement of the police | 208 | 2.89 | 56 | 1.61 |
| Referral to a PICU | 188 | 2.61 | 232 | 6.69 |
| Process of searching for and removing items in the ward, a room or persons that could be dangerous | 185 | 2.57 | 106 | 3.05 |
| Show of force, assembling staff in proximity to patient while requesting compliance with medication, movement or asking to stop | 175 | 2.43 | 68 | 1.96 |
| Deal with other patients on the ward or involved in an incident | 132 | 1.84 | 27 | 0.78 |
| Seclusion, isolated in a locked room | 88 | 1.22 | 39 | 1.12 |
| Sex-specific staff allocations to a patient | 76 | 1.06 | 32 | 0.92 |
| Calm-down methods: distract, offer tea, coffee, music, newspaper, cigarettes | 70 | 0.97 | 28 | 0.81 |
| Restrictions to where patients go and/or what they can use | 62 | 0.86 | 25 | 0.72 |
| Use of activity rooms, gardens, outside ward | 28 | 0.39 | 17 | 0.49 |
| Non-standard transfer, moving patient to a different hospital | 24 | 0.33 | 33 | 0.95 |
| Psychological therapy offered | 8 | 0.11 | 17 | 0.49 |
In first line and repeats, de-escalation and observation are the most common interventions mentioned by nurses. The repeat interventions lay a greater emphasis on talking to others, discussing medication and reviewing the case. They also place a greater emphasis on increasing medication, either oral offers or enforced injections, and are more likely to include interventions to transfer the difficult patient away from the ward, either to a PICU or to some other type of ward at a different hospital.
There is no escalation pathway
There was little evidence of any uniform escalation pathway at any one hospital. Instead, there was an extraordinary range of variation. This is illustrated in Table 14, which shows the responses of 15 qualified nurses at a single hospital in response to the following scenario as presented during the TEPI:
-
BA2 behaviour 2: Alan turns over furniture, throwing objects around the ward (not deliberately at others), picking up a chair and hitting the wall with it, on top of shouting and being verbally abusive.
| Intervention | Number of nurses endorsing (% of total) |
|---|---|
| Manual restraint | 13 (87) |
| Coerced intramuscular medication | 12 (80) |
| Request assistance from others | 10 (67) |
| Offer PRN medication | 8 (53) |
| De-escalation | 6 (40) |
| LSE | 6 (40) |
| Place on special observation | 5 (33) |
| Show of force | 4 (27) |
| Transfer to a PICU | 3 (20) |
| Call the police | 2 (13) |
| Discuss medication | 2 (13) |
| Talk to others | 1 (7) |
| Move other patients | 1 (7) |
Notably, there is not a single intervention on which everyone agrees. Considering that staff members were being asked not what their own responses would be, but what would typically happen on their ward, this level of variation is very high.
This level of variation was the same for every scenario in the TEPI. The researcher conducting the coding was clear that the vast majority of this variation was because of actual differences in the way interviewees considered the escalation pathway to operate on their ward, rather than because of differences between interviewers or the same interviewer on different occasions, in the way the interview was conducted. This confidence was based on the consistency and high degree of structure that was a feature of the application of the TEPI.
Pathway length
The length of the escalation pathways in general was explored and is depicted in Table 15. The mean length of an escalation pathway was 5.99 (SD 3.47) interventions and the modal number of interventions was 4.
| Length (interventions) | Frequency | % |
|---|---|---|
| 1 | 44 | 3.72 |
| 2 | 101 | 8.54 |
| 3 | 141 | 11.93 |
| 4 | 169 | 14.3 |
| 5 | 151 | 12.77 |
| 6 | 153 | 12.94 |
| 7 | 117 | 9.9 |
| 8 | 87 | 7.36 |
| 9 | 62 | 5.25 |
| 10 | 40 | 3.38 |
| 11 | 34 | 2.88 |
| 12 | 27 | 2.28 |
| 13 | 13 | 1.1 |
| 14 | 9 | 0.76 |
| 15 | 10 | 0.85 |
| 16 | 4 | 0.34 |
| 17 | 9 | 0.76 |
| 18 | 2 | 0.17 |
| 19 | 1 | 0.08 |
| 20 | 4 | 0.34 |
| 21 | 1 | 0.08 |
| 22 | 1 | 0.08 |
| 24 | 1 | 0.08 |
| 25 | 1 | 0.08 |
| Total | 1182 | 100 |
Tests were conducted for differences by seclusion and PICU availability. Pathways were significantly shorter in hospitals without access to seclusion (mean 5.61 vs. 6.47, t = 4.26; p < 0.001) and longer in hospitals without on-site access to a PICU (mean 6.35 vs. 5.47, t = 4.31; p < 0.001). Multiple regression of pathway length with both of these variables and an interaction term showed that having access to seclusion was significantly associated with a 1.57 (SE 0.26) longer pathway and access to both seclusion and an on-site PICU was associated with a 1.39 (SE 0.41) shorter pathway. PICU access by itself was not significant in the multiple regression equation.
These differences in pathway length complicate comparisons between the hospital types, as differences in frequencies of interventions might be partly a product of greater or lesser pathway length. Stronger comparisons are therefore likely to be those that compare the proportions of particular types of interventions within the differing types of hospitals (i.e. by chi-squared tests) rather than examination of the relative frequency of interventions by interviewee (i.e. by t-test).
Comparisons by proportion of use of interventions
This analysis compares, for example, the percentage of de-escalation as a proportion of all interventions cited by those in no-seclusion hospitals, with the same percentage in seclusion hospitals, using a chi-squared test. This method removes the influence of pathway length that complicates other types of analysis. Two levels of analysis were conducted, one at the level of the whole interview for interventions used when the described behaviours first occurred (i.e. without the interventions used on repetition of the problem behaviour) and the second level of analysis was by behaviour type (i.e. aggression separately, self-harm separately, mania separately). All degrees of freedom equal one in these chi-squared tests. At each level of analysis, significant variables were entered into a final logistic regression model controlling for the alternate condition (seclusion or PICU availability). Table 16 provides the frequencies of use by seclusion availability and Table 17 provides the same information by PICU availability. Statistically significant differences are detailed in the text.
| Intervention | All behaviours | Aggression | Self-harm | Mania | ||||
|---|---|---|---|---|---|---|---|---|
| No seclusion, n (%) | Seclusion, n (%) | No seclusion, n (%) | Seclusion, n (%) | No seclusion, n (%) | Seclusion, n (%) | No seclusion, n (%) | Seclusion, n (%) | |
| As-required medication | 177 (4.7) | 128 (3.7) | 89 (6.0) | 58 (5.0) | 32 (3.1) | 26 (2.6) | 56 (4.5) | 44 (3.5) |
| Calm-down methods | 27 (0.7) | 44 (1.3) | 0 (0.0) | 11 (0.9) | 8 (0.8) | 17 (1.7) | 19 (1.5) | 16 (1.3) |
| Coerced intramuscular medication | 168 (4.5) | 109 (3.2) | 125 (8.5) | 64 (5.5) | 11 (1.1) | 15 (1.5) | 32 (2.6) | 30 (2.4) |
| Deal with other patients | 69 (1.8) | 63 (1.8) | 50 (3.4) | 48 (4.1) | 10 (1.0) | 13 (1.3) | 9 (0.7) | 2 (0.2) |
| De-escalation | 980 (26.1) | 909 (26.6) | 268 (18.1) | 209 (17.8) | 295 (28.9) | 283 (28.4) | 417 (33.4) | 417 (33.3) |
| Sex-specific care | 42 (1.1) | 34 (1.0) | 5 (0.3) | 1 (0.1) | 0 (0.0) | 0 (0.0) | 37 (3.0) | 33 (2.6) |
| Impose restrictions | 35 (0.9) | 27 (0.8) | 16 (1.1) | 11 (0.9) | 9 (0.9) | 7 (0.7) | 10 (0.8) | 9 (0.7) |
| LSE | 201 (5.4) | 240 (7.0) | 85 (5.7) | 81 (6.9) | 31 (3.0) | 56 (5.6) | 85 (6.8) | 103 (8.2) |
| Manual restraint | 425 (11.3) | 338 (9.9) | 223 (15.1) | 149 (12.7) | 124 (12.1) | 100 (10.1) | 78 (6.3) | 89 (7.1) |
| Medication discussion | 107 (2.9) | 124 (3.6) | 57 (3.9) | 50 (4.3) | 12 (1.2) | 21 (2.1) | 38 (3.0) | 53 (4.2) |
| Non-standard transfer | 12 (0.3) | 11 (0.3) | 9 (0.6) | 9 (0.8) | 1 (0.1) | 1 (0.1) | 2 (0.2) | 1 (0.1) |
| Observation | 452 (12.1) | 374 (10.9) | 130 (8.8) | 69 (5.9) | 166 (16.3) | 150 (15.1) | 156 (12.5) | 155 (12.4) |
| PICU | 104 (2.8) | 79 (2.3) | 86 (5.8) | 55 (4.7) | 6 (0.6) | 11 (1.1) | 12 (1.0) | 13 (1.0) |
| Police call | 117 (3.1) | 91 (2.7) | 69 (4.7) | 60 (5.1) | 44 (4.3) | 24 (2.4) | 4 (0.3) | 7 (0.6) |
| Psychological therapy | 4 (0.1) | 4 (0.1) | 0 (0.0) | 0 (0.0) | 2 (0.2) | 3 (0.3) | 2 (0.2) | 1 (0.1) |
| Request assistance | 328 (8.8) | 290 (8.5) | 166 (11.2) | 127 (10.8) | 117 (11.5) | 116 (11.7) | 45 (3.6) | 47 (3.8) |
| Review of patient care | 174 (4.6) | 106 (3.1) | 22 (1.5) | 11 (0.9) | 61 (6.0) | 34 (3.4) | 91 (7.3) | 61 (4.9) |
| Search/remove items | 89 (2.4) | 95 (2.8) | 2 (0.1) | 11 (0.9) | 58 (5.7) | 50 (5.0) | 29 (2.3) | 34 (2.7) |
| Seclusion | 21 (0.6) | 67 (2.0) | 18 (1.2) | 64 (5.5) | 1 (0.1) | 1 (0.1) | 2 (0.2) | 2 (0.2) |
| Show of force | 59 (1.6) | 115 (3.4) | 34 (2.3) | 47 (4.0) | 7 (0.7) | 36 (3.6) | 18 (1.4) | 32 (2.6) |
| Talk to others | 140 (3.7) | 160 (4.7) | 21 (1.4) | 35 (3.0) | 20 (2.0) | 27 (2.7) | 99 (7.9) | 98 (7.8) |
| Use of gardens, room, etc. | 17 (0.5) | 11 (0.3) | 4 (0.3) | 1 (0.1) | 6 (0.6) | 4 (0.4) | 7 (0.6) | 6 (0.5) |
| Intervention | All behaviours | Aggression | Self-harm | Mania | ||||
|---|---|---|---|---|---|---|---|---|
| No PICU, n (%) | PICU, n (%) | No PICU, n (%) | PICU, n (%) | No PICU, n (%) | PICU, n (%) | No PICU, n (%) | PICU, n (%) | |
| As-required medication | 184 (4.1) | 121 (4.5) | 88 (5.1) | 59 (6.4) | 43 (3.5) | 15 (1.9) | 53 (3.5) | 47 (4.7) |
| Calm-down methods | 51 (1.1) | 20 (0.7) | 9 (0.5) | 2 (0.2) | 15 (1.2) | 10 (1.3) | 27 (1.8) | 8 (0.8) |
| Coerced intramuscular medication | 171 (3.8) | 106 (3.9) | 120 (7.0) | 69 (7.5) | 16 (1.3) | 10 (1.3) | 35 (2.3) | 27 (2.7) |
| Deal with other patients | 71 (1.6) | 61 (2.2) | 53 (3.1) | 45 (4.9) | 12 (1.0) | 11 (1.4) | 6 (0.4) | 5 (0.5) |
| De-escalation | 1184 (26.6) | 705 (25.9) | 330 (19.1) | 147 (15.9) | 353 (28.7) | 225 (28.6) | 501 (33.5) | 333 (33.1) |
| Sex-specific care | 49 (1.1) | 27 (1.0) | 5 (0.3) | 1 (0.1) | 0 (0) | 0 (0) | 44 (2.9) | 26 (2.6) |
| Impose restrictions | 43 (1.0) | 19 (0.7) | 20 (1.2) | 7 (0.8) | 9 (0.7) | 7 (0.9) | 14 (0.9) | 5 (0.5) |
| LSE | 280 (6.3) | 161 (5.9) | 108 (6.3) | 58 (6.3) | 48 (3.9) | 39 (5.0) | 124 (8.3) | 64 (6.4) |
| Manual restraint | 461 (10.4) | 302 (11.1) | 233 (13.5) | 139 (15.0) | 134 (10.9) | 90 (11.4) | 94 (6.3) | 73 (7.3) |
| Medication discussion | 126 (2.8) | 105 (3.9) | 65 (3.8) | 42 (4.5) | 18 (1.5) | 15 (1.9) | 43 (2.9) | 48 (4.8) |
| Non-standard transfer | 16 (0.4) | 7 (0.3) | 12 (0.7) | 6 (0.6) | 1 (0.1) | 1 (0.1) | 3 (0.2) | 0 (0.0) |
| Observation | 565 (12.7) | 261 (9.6) | 164 (9.5) | 35 (3.8) | 195 (15.9) | 121 (15.4) | 206 (13.8) | 105 (10.4) |
| PICU | 91 (2.0) | 92 (3.4) | 77 (4.5) | 64 (6.9) | 5 (0.4) | 12 (1.5) | 9 (0.6) | 16 (1.6) |
| Police call | 122 (2.7) | 86 (3.2) | 73 (4.2) | 56 (6.1) | 44 (3.6) | 24 (3.0) | 5 (0.3) | 6 (0.6) |
| Psychological therapy | 3 (0.1) | 5 (0.2) | 0 (0) | 0 (0) | 2 (0.2) | 3 (0.4) | 1 (0.1) | 2 (0.2) |
| Request assistance | 354 (8.0) | 264 (9.7) | 170 (9.8) | 123 (13.3) | 137 (11.1) | 96 (12.2) | 47 (3.1) | 45 (4.5) |
| Review of patient care | 172 (3.9) | 108 (4.0) | 27 (1.6) | 6 (0.6) | 57 (4.6) | 38 (4.8) | 88 (5.9) | 64 (6.4) |
| Search/remove items | 118 (2.7) | 66 (2.4) | 12 (0.7) | 1 (0.1) | 64 (5.2) | 44 (5.6) | 42 (2.8) | 21 (2.1) |
| Seclusion | 67 (1.5) | 21 (0.8) | 62 (3.6) | 20 (2.2) | 1 (0.1) | 1 (0.1) | 4 (0.3) | 0 (0.0) |
| Show of force | 134 (3.0) | 40 (1.5) | 61 (3.5) | 20 (2.2) | 40 (3.3) | 3 (0.4) | 33 (2.2) | 17 (1.7) |
| Talk to others | 169 (3.8) | 131 (4.8) | 34 (2.0) | 22 (2.4) | 28 (2.3) | 19 (2.4) | 107 (7.2) | 90 (8.9) |
| Use of gardens, rooms, etc. | 19 (0.4) | 9 (0.3) | 3 (0.2) | 2 (0.2) | 7 (0.6) | 3 (0.4) | 9 (0.6) | 4 (0.4) |
All problem behaviours
Seclusion
Responses from wards without seclusion were more likely to include PRN medication (4.7% vs. 3.7%, χ2 = 4.40; p = 0.036), manual restraint (11.3% vs. 9.9%, χ2 = 4.23; p = 0.040), coerced intramuscular medication (4.5% vs. 3.2%, χ2 = 7.95; p = 0.005) and review (4.6% vs. 3.1%, χ2 = 13.11; p < 0.001), and were less likely to include show of force (1.6% vs. 3.4%, χ2 = 23.35; p < 0.001), low-stimulus environment (5.4% vs. 7.0%, χ2 = 9.12; p = 0.003), calm-down methods (0.7% vs. 1.3%, χ2 = 6.51; p = 0.011) and seclusion (0.6% vs. 2.0%, χ2 = 28.89; p < 0.001). In multivariable logistic regression, controlling for PICU availability, all of these associations remained significant except for manual restraint.
Psychiatric intensive care unit
Responses from wards without an on-site PICU were more likely to include observation (12.7% vs. 9.6%, χ2 = 16.23; p < 0.001), show of force (3.0% vs. 1.5%, χ2 = 17.08; p < 0.001) and seclusion (1.5% vs. 0.8%, χ2 = 7.38; p = 0.007) and were less likely to include talking to others (3.8% vs. 4.8%, χ2 = 4.43; p = 0.035), moving other patients away (1.6% vs. 2.2%, χ2 = 4.02; p = 0.045), medication discussion (2.8% vs. 3.9%, χ2 = 5.37; p = 0.020), transfer to a PICU (2.0% vs. 3.4%, χ2 = 12.17; p < 0.001) and calling for help/assistance (8.0% vs. 9.7%, χ2 = 6.35; p = 0.012). In multivariate logistic regression controlling for seclusion availability, all of these associations remained significant except for talking to others.
Aggression only
Seclusion
Responses to aggression from wards without seclusion were more likely to include observation (8.8% vs. 5.9%, χ2 = 8.05; p = 0.005) and coerced intramuscular medication (8.5% vs. 5.5%, χ2 = 8.97; p = 0.003), and were less likely to include talking to others (1.4% vs. 3.0%, χ2 = 7.87; p = 0.005), show of force (2.3% vs. 4.0%, χ2 = 6.01; p = 0.014), calm-down methods (0% vs. 11.0%, χ2 = 14.01; p < 0.001), seclusion (1.2% vs. 5.5%, χ2 = 39.6; p < 0.001) and removal of items (0.1% vs. 0.9%, χ2 = 8.71; p = 0.003). In multivariate logistic regression controlling for PICU availability, all of these associations remained significant except for observation. Calm-down methods could not be included in this test because it predicted seclusion availability perfectly.
Psychiatric intensive care unit
Responses to aggression from wards without an on-site PICU were more likely to include de-escalation (19.1% vs. 15.9%, χ2 = 3.85; p = 0.050), observation (9.5% vs. 3.8%, χ2 = 28.41; p < 0.001), show of force (3.5% vs. 2.2%, χ2 = 4.01; p = 0.045), seclusion (3.6% vs. 2.2%, χ2 = 4.0; p = 0.045), removal of items (0.7% vs. 0.1%, χ2 = 4.22; p = 0.040) and review (1.6% vs. 0.6%, χ2 = 5.27; p = 0.022), and were less likely to include calling the police (4.2% vs. 6.1%, χ2 = 4.47; p = 0.034), moving other patients (3.1% vs. 4.9%, χ2 = 5.58; p = 0.018), transfer to a PICU (4.5% vs. 6.9%, χ2 = 7.62; p = 0.006) and calling for help/assistance (9.8% vs. 13.3%, χ2 = 7.30; p = 0.007). In multivariate logistic regression controlling for seclusion availability, all of these associations remained significant except for calling the police and moving other patients.
Self-harm only
Seclusion
Responses to self-harm from wards without seclusion were more likely to include call the police (4.3% vs. 2.4%, χ2 = 5.47; p = 0.019) and review (6.0% vs. 3.4%, χ2 = 7.21; p = 0.007), and were less likely to include show of force (0.7% vs. 3.6%, χ2 = 20.90; p < 0.001) and low-stimulus environment (3.0% vs. 5.6%, χ2 = 8.33; p = 0.004). In multivariate logistic regression, controlling for PICU availability, all of these associations remained significant.
Psychiatric intensive care unit
Responses to self-harm from wards without an on-site PICU were more likely to include PRN medication (3.5% vs.1.9%, χ2 = 4.28; p = 0.039) and show of force (3.3% vs. 0.4%, χ2 = 18.85; p < 0.001), and were less likely to include transfer to a PICU (0.4% vs. 1.5%, χ2 = 7.24; p = 0.007). In multivariate logistic regression controlling for seclusion availability, all of these associations remained significant.
Mania only
Seclusion
Responses to mania from wards without seclusion were more likely to include moving other patients (0.7% vs. 0.2%, χ2 = 4.55; p = 0.033) and review (7.3% vs. 4.9%, χ2 = 7.47; p = 0.006), and were less likely to include show of force (1.4% vs. 2.6%, χ2 = 3.84; p = 0.050). In multivariate logistic regression, controlling for PICU availability, moving other patients and review remained significant.
Psychiatric intensive care unit
Responses to mania from wards without an on-site PICU were more likely to include observation (13.8% vs. 10.4%, χ2 = 6.10; p = 0.013) and calm-down methods (1.8% vs. 0.8%, χ2 = 3.98; p = 0.046), and were less likely to include medication discussion (2.9% vs. 4.8%, χ2 = 5.70; p = 0.017) and PICU transfer (0.6% vs. 1.6%, χ2 = 4.96; p = 0.026). In multivariate logistic regression, controlling for seclusion availability, all of these associations remained significant.
Summary
Wards without seclusion managed difficult behaviour through a greater use of coerced intramuscular medication and review, particularly for aggressive behaviour. Show of force and calm-down methods appear to be positively associated with the provision of seclusion. Seclusion is still used when there is no room, but the provision of a room is strongly associated with its use.
Wards without on-site PICU availability managed difficult behaviour through observation and seclusion. In addition, more reviews were undertaken in the case of aggression; in the case of self-harm, there was more use of medication and show of force. The effect of PICU provision on the management of different disturbed behaviour types was more varied than that of seclusion. There is also evidence that seclusion can substitute for PICU transfer, but not vice versa.
Exploration of thresholds for the use of certain interventions
Seclusion
Figures 5 and 6 show the proportion of nurses who mention seclusion as one of the interventions in relation to the scenarios of aggression. It can be seen that as the scenarios get more serious, the proportion of nurses reporting that seclusion is used goes up. Nevertheless, it still remains a small proportion of the total numbers interviewed. There does not appear to be any specific behavioural threshold, that is, seclusion suddenly being used at a particular level of severity. Instead there seems to be a gradual rise in the propensity to cite the use of seclusion with increasing severity, with the differences caused by seclusion room availability becoming greater at higher levels of severity. The absence of a PICU also seems to slightly raise the frequency of reports of seclusion use. Similar charts for the self-harm questions (Figures 7 and 8) show that seclusion was hardly specified as an intervention for these questions, regardless of level of severity. S3 (deep cuts) was the only self-harm behaviour that a few nurses reported as likely to lead to seclusion on their ward and, even then, possibly only because the instrument of self-harm could be used as a weapon against staff attempting to manage the situation.
FIGURE 5.
Proportion of nurses citing seclusion as an intervention, by level of aggression and seclusion availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.
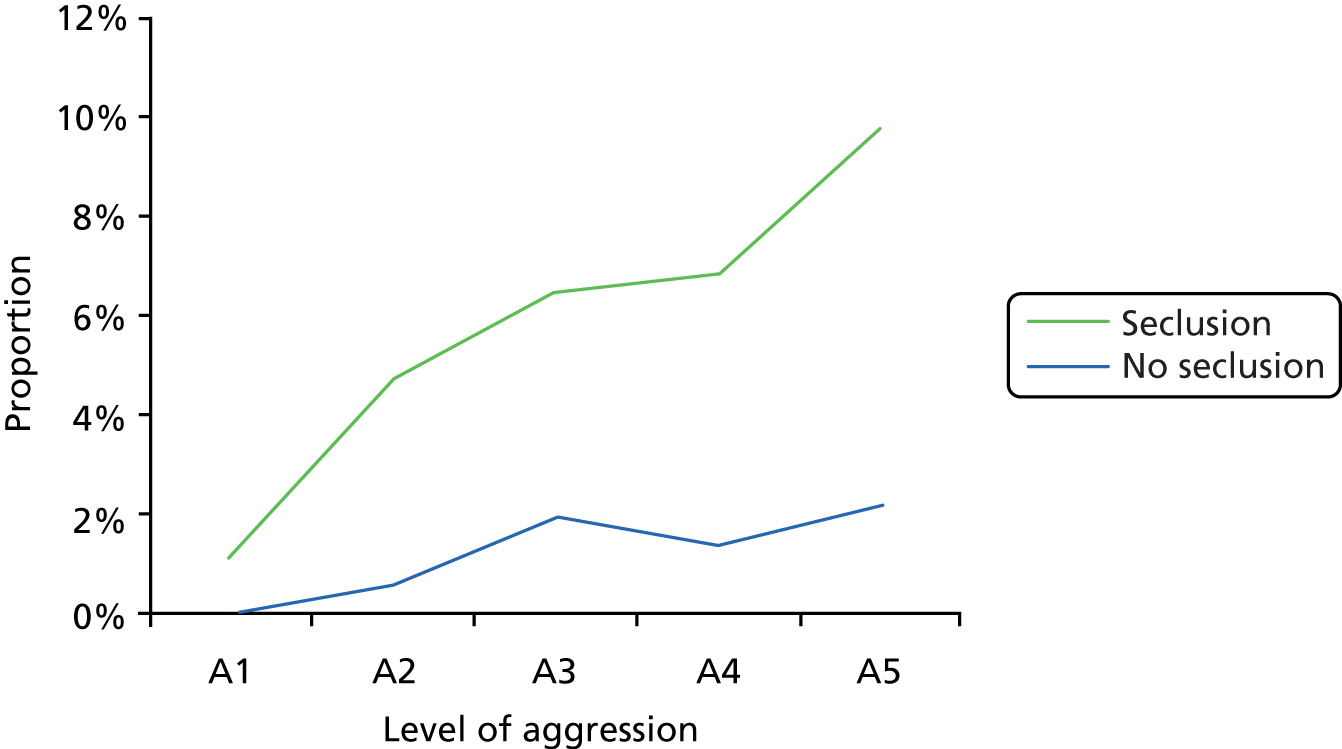
FIGURE 6.
Proportion of nurses citing seclusion as an intervention, by level of aggression and PICU availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.
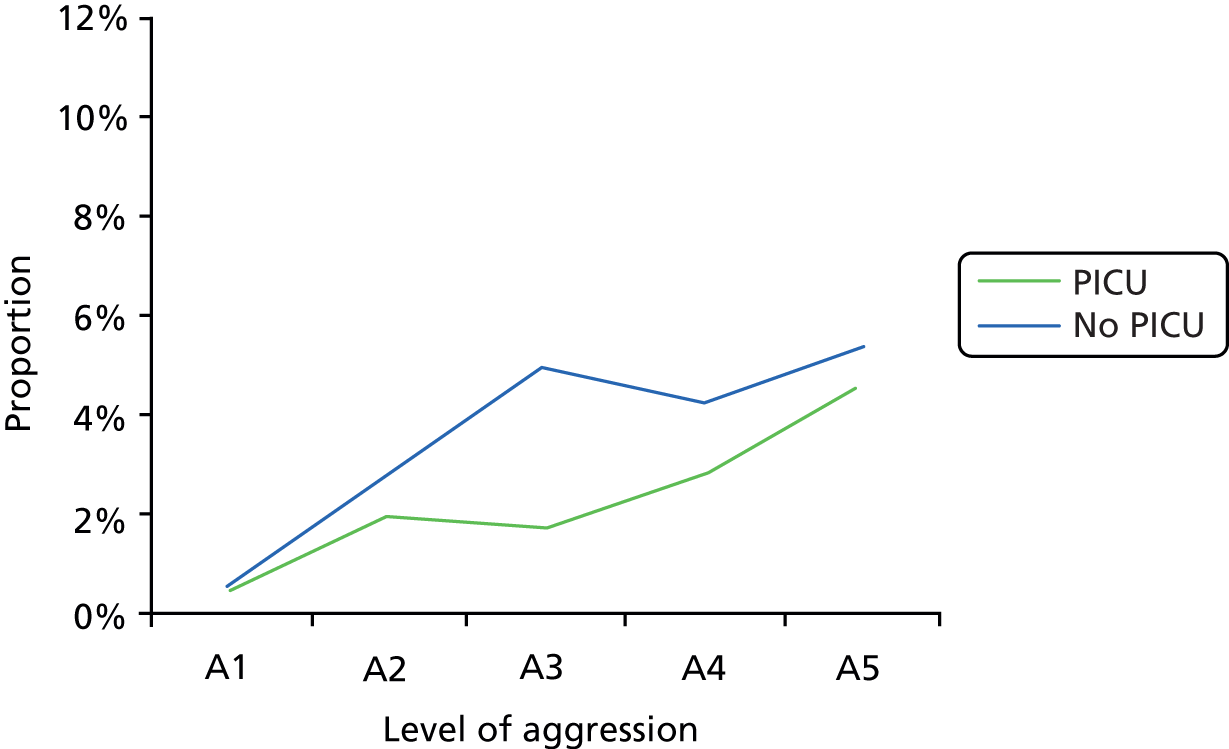
FIGURE 7.
Proportion of nurses citing seclusion as an intervention, by level of self-harm and seclusion availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
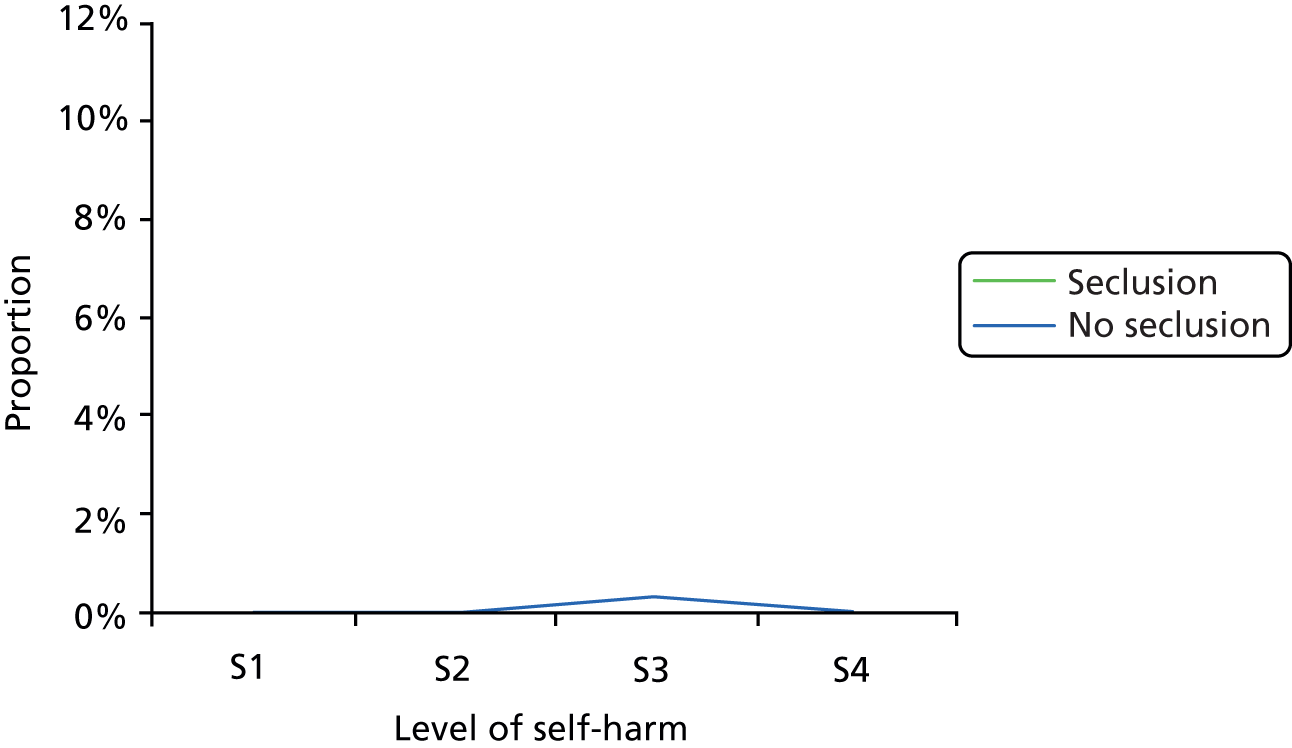
FIGURE 8.
Proportion of nurses citing seclusion as an intervention, by level of self-harm and PICU availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
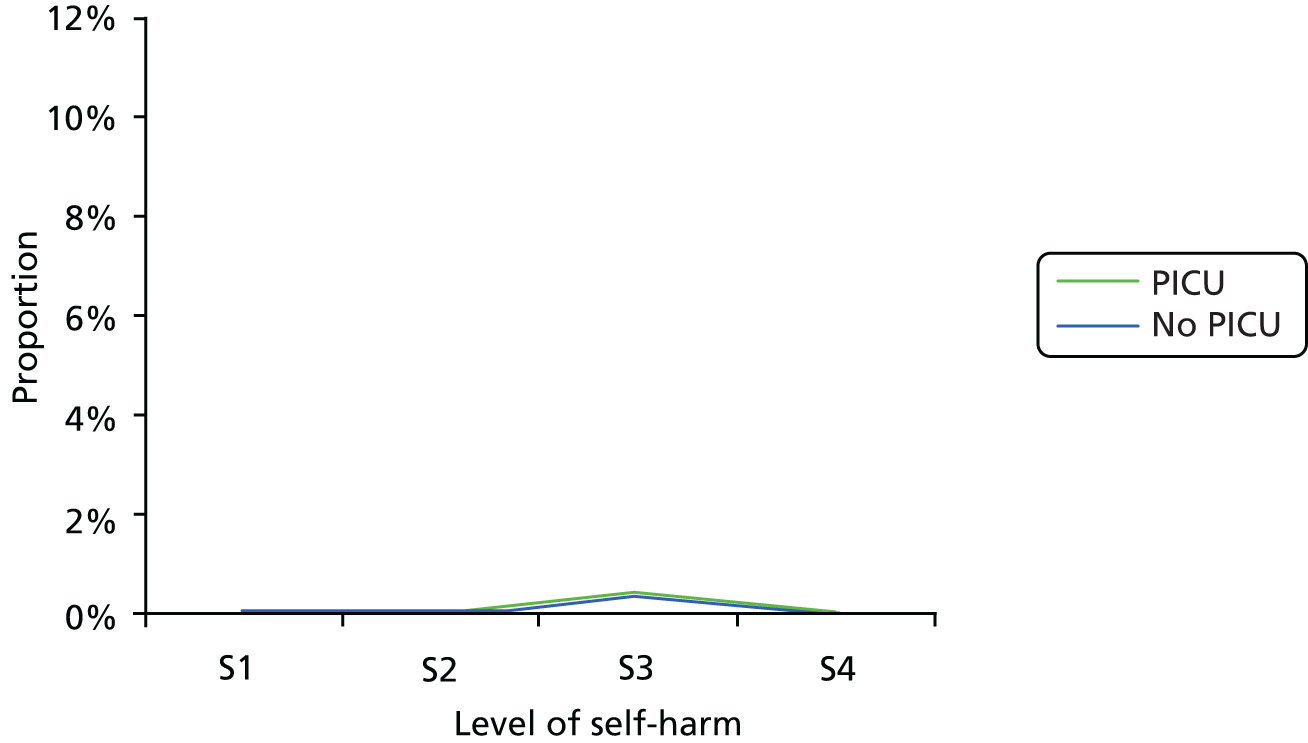
Psychiatric intensive care unit transfer
Figures 9 and 10 show the proportion of nurses who reported a PICU transfer in the escalation pathway for aggressive behaviour, broken down by the specific severity of aggressive behaviour (TEPI questions A1–A5) and by seclusion or PICU availability. It can be seen from Figure 10 that PICU transfer is more likely to be reported at hospitals with a PICU on site and that the difference increases with severity. However, the general level of difference is not as large as for the reporting of seclusion described in the preceding section. There is a notable dip in rates for question A4 (assault with punches and kicks) relative to A3 (wielding an object as weapon) suggesting that in terms of the interventions seen as necessary, A3 is perceived to be a more serious incident than A4.
FIGURE 9.
Proportion of nurses citing PICU transfer as an intervention, by level of aggression and seclusion availability. A1, verbal abuse; A2, property damage; A3, wielding a club; and A4, assaulting a fellow patient; A5, assaulting a fellow patient very seriously.
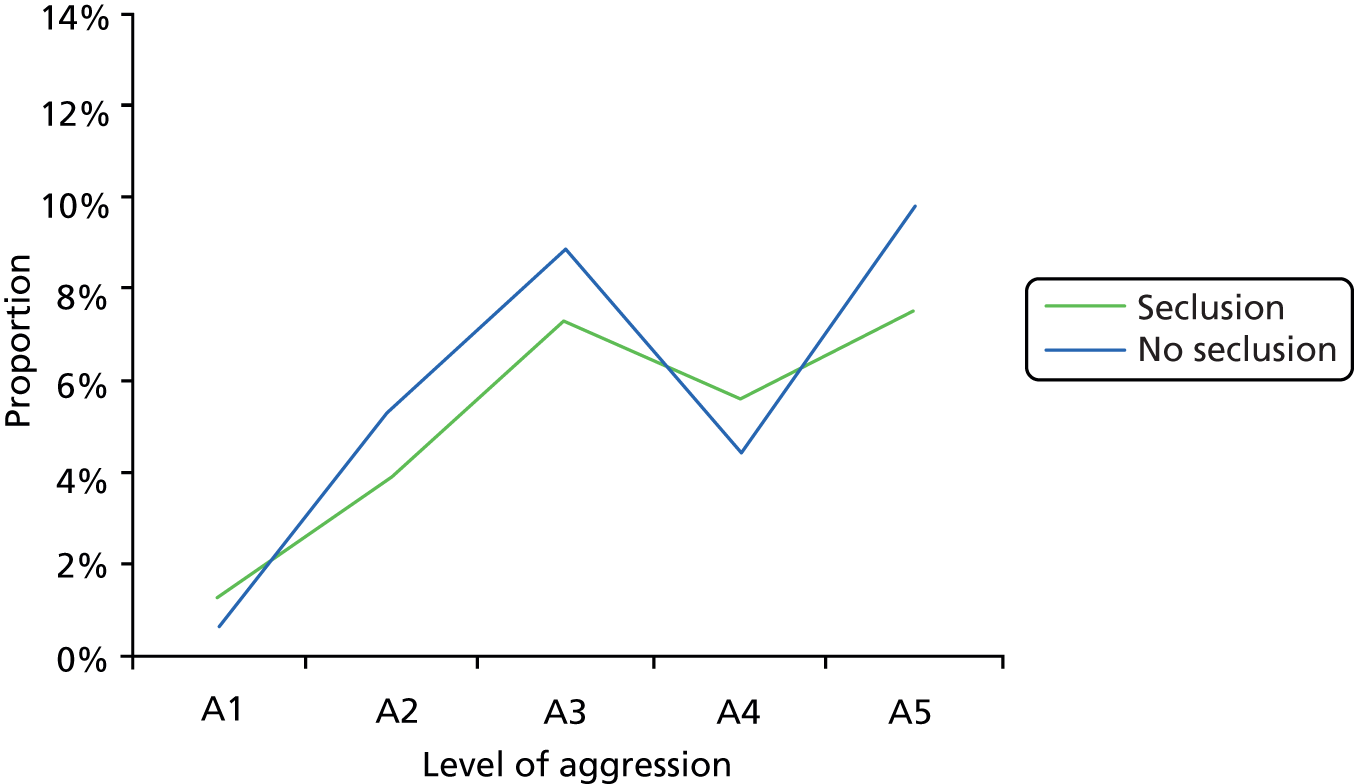
FIGURE 10.
Proportion of nurses citing PICU transfer as an intervention, by level of aggression and PICU availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.
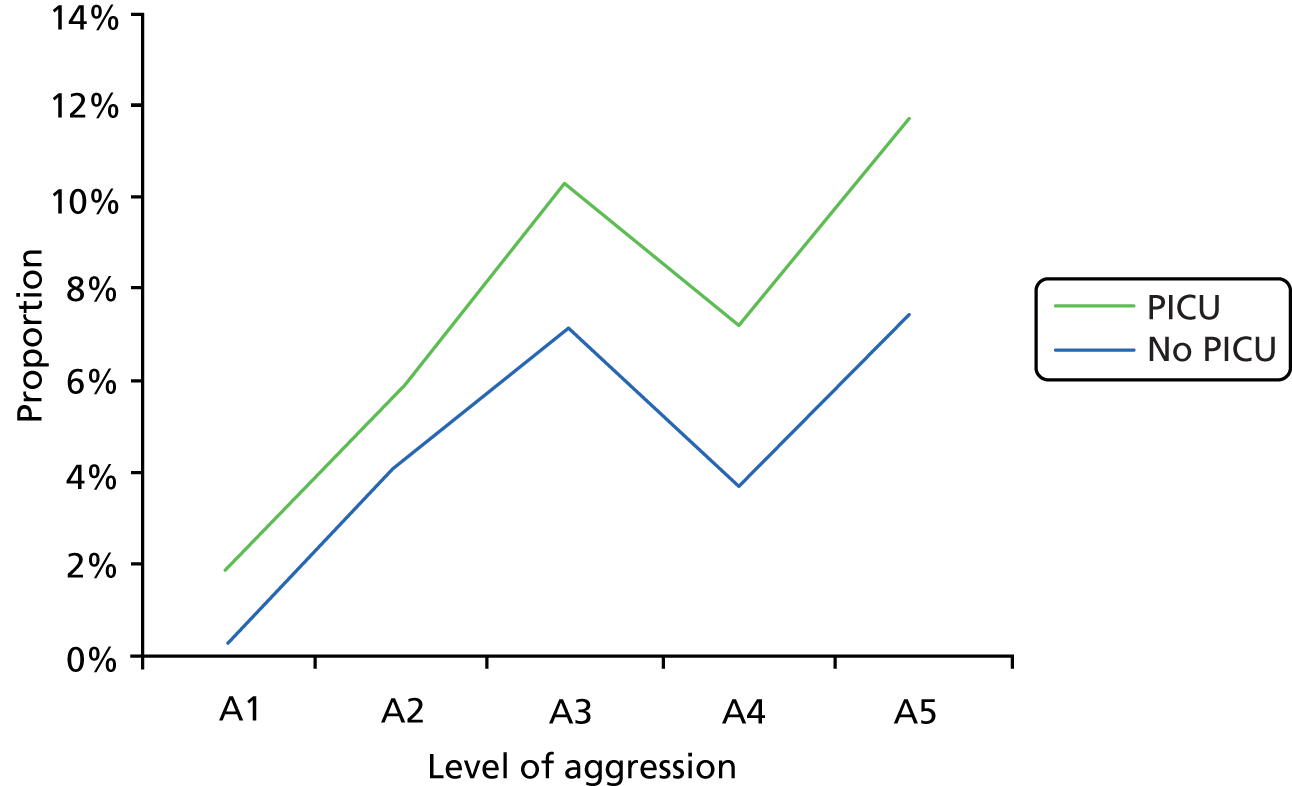
By comparison, Figures 11 and 12 make clear that PICU transfer is seldom seen as a relevant intervention for suicidal behaviour, even when that behaviour is severe. However, even at these low levels of reporting, a difference can be seen by whether or not a PICU is available on site. It is possible that the restriction of the TEPI to a consideration of male patients only may have influenced these particular findings.
FIGURE 11.
Proportion of nurses citing PICU transfer as an intervention, by level of self-harm and seclusion availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
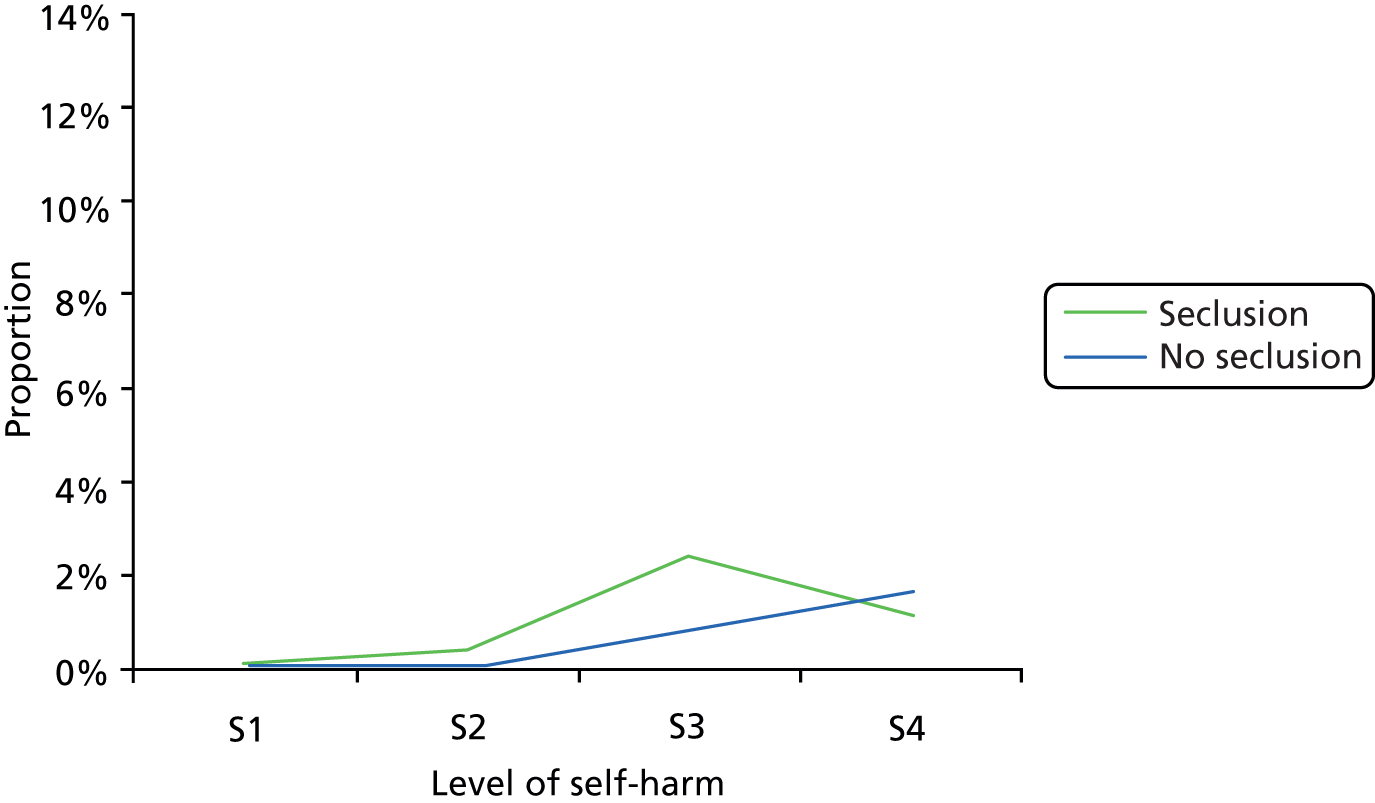
FIGURE 12.
Proportion of nurses citing PICU transfer as an intervention, by level of self-harm and PICU availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
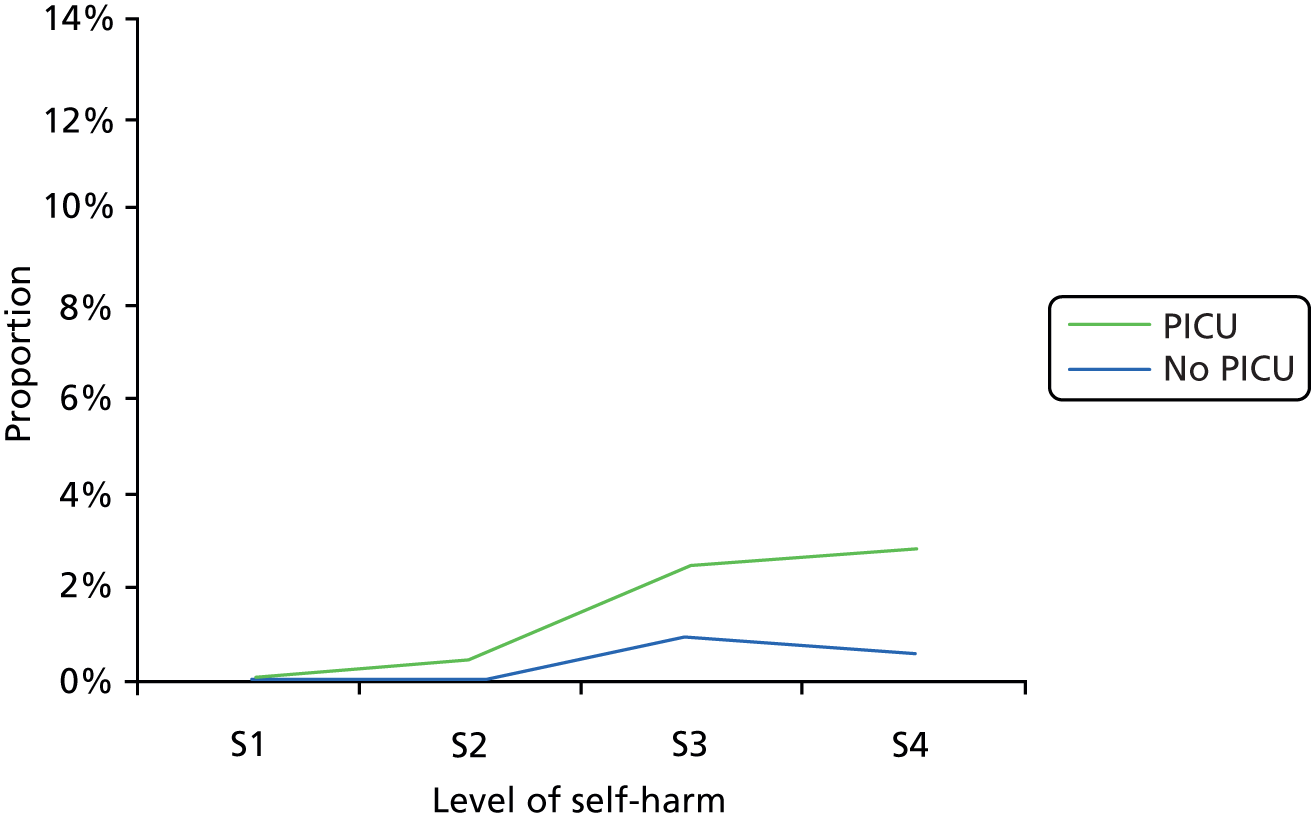
Manual restraint
Figures 13 and 14 show the proportions of nurses who reported manual restraint in the escalation pathway for aggressive behaviour, broken down by the specific severity of aggressive behaviour (TEPI questions A1–A5) and by seclusion or PICU availability. Figures 15 and 16 present the parallel information for self-harm. Use of manual restraint for aggression does not appear to differ by seclusion or PICU availability, although there is a notable dip in rates for question A3 (wielding a weapon) overall. The picture for self-harm is, again, identical regardless of seclusion and PICU availability, except for one question. For S4, which describes a very serious but prevented suicide attempt by hanging, manual restraint is reported more frequently when seclusion is not available.
FIGURE 13.
Proportion of nurses citing manual restraint as an intervention, by level of aggression and seclusion availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.

FIGURE 14.
Proportion of nurses citing manual restraint as an intervention, by level of aggression and PICU availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.
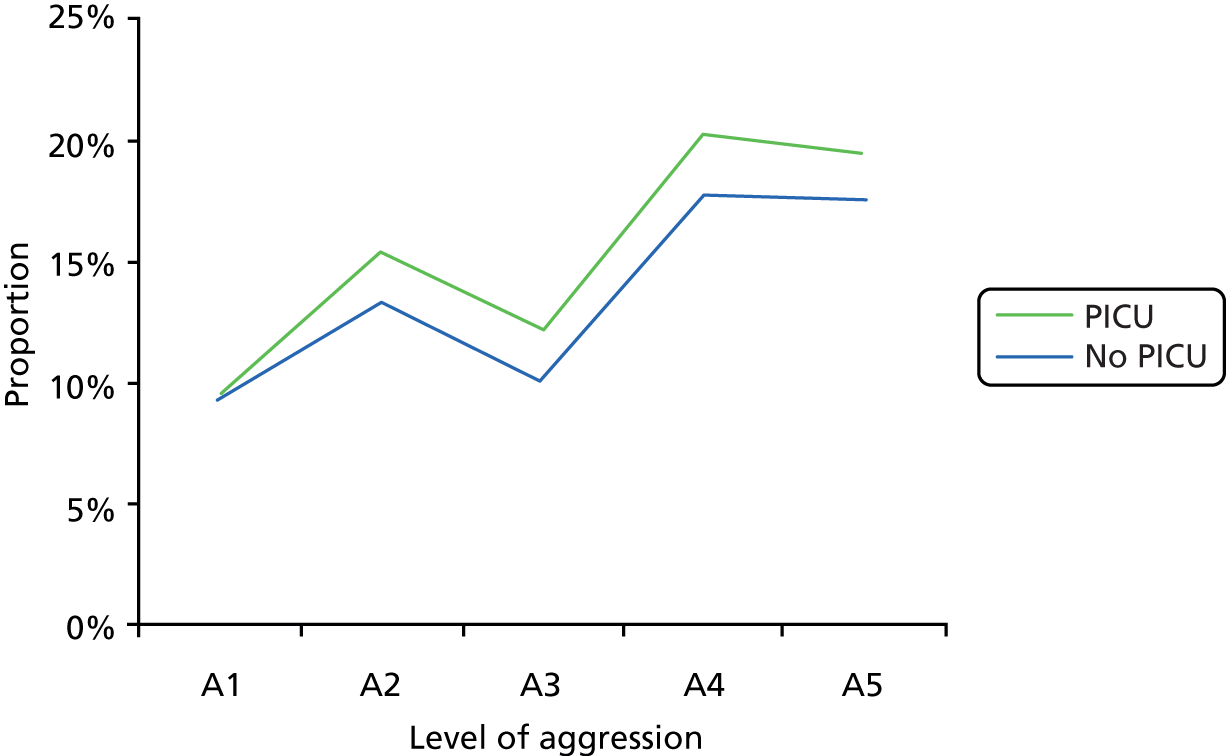
FIGURE 15.
Proportion of nurses citing manual restraint as an intervention, by level of self-harm and seclusion availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
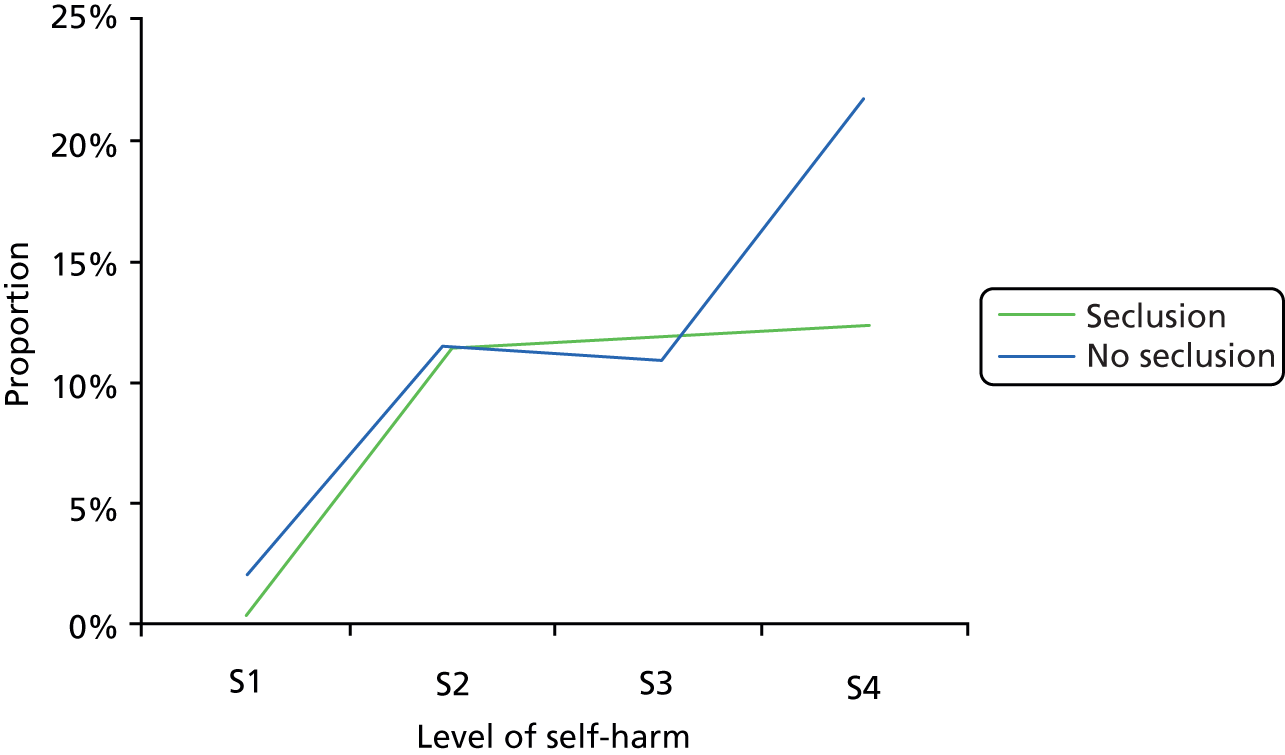
FIGURE 16.
Proportion of nurses citing manual restraint as an intervention, by level of self-harm and PICU availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
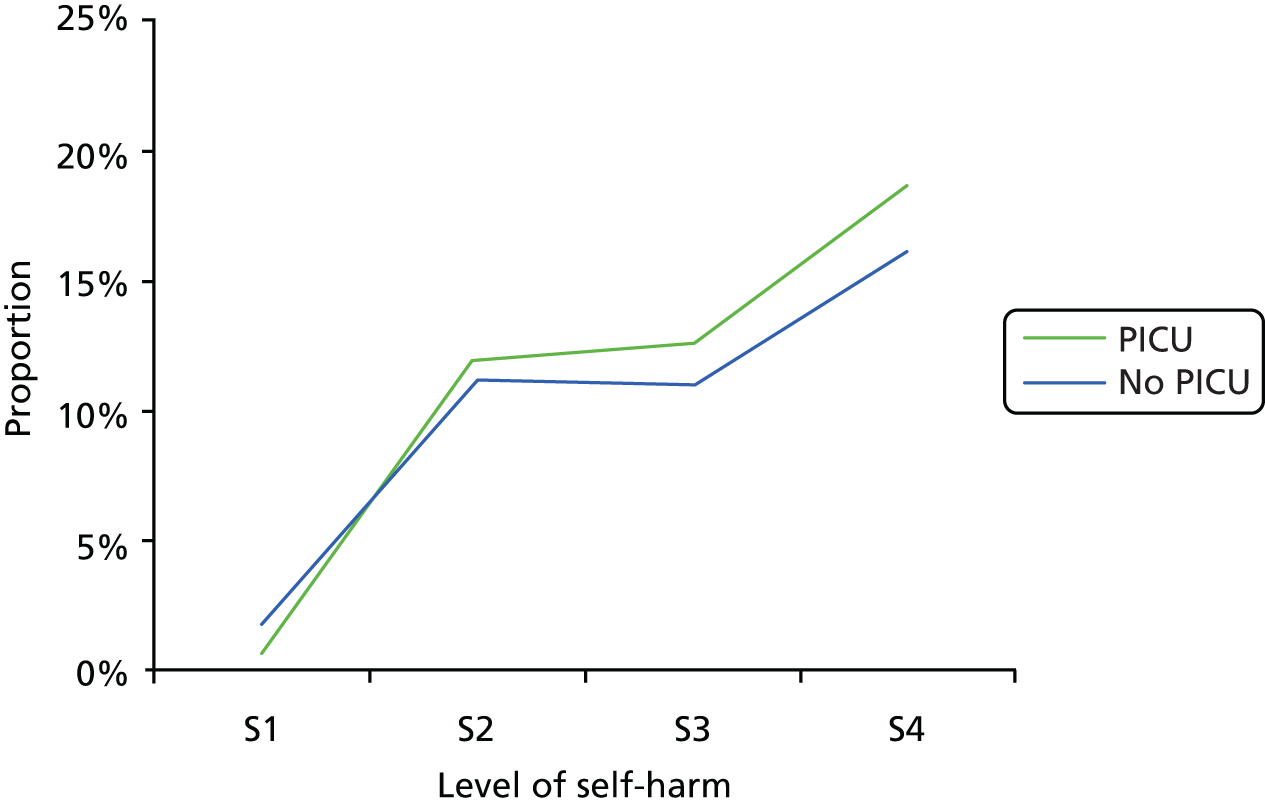
Observation
Figures 17 and 18 show the proportion of nurses who reported observation in the escalation pathway for aggressive behaviour, broken down by the specific severity of aggressive behaviour (TEPI questions A1–A5) and by seclusion or PICU availability. Figures 19 and 20 present the parallel information for self-harm. In general, the relevance of observation dwindles as aggression severity increases. However, this decrease is sharper in hospitals with seclusion availability and sharper still when an on-site PICU is available. For self-harm, observation is reported at similar frequencies for all severities of behaviour; the only difference emerging is for S3 (deep cuts), when observation dips in frequency when seclusion is available.
FIGURE 17.
Proportion of nurses citing observation as an intervention, by level of aggression and seclusion availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.
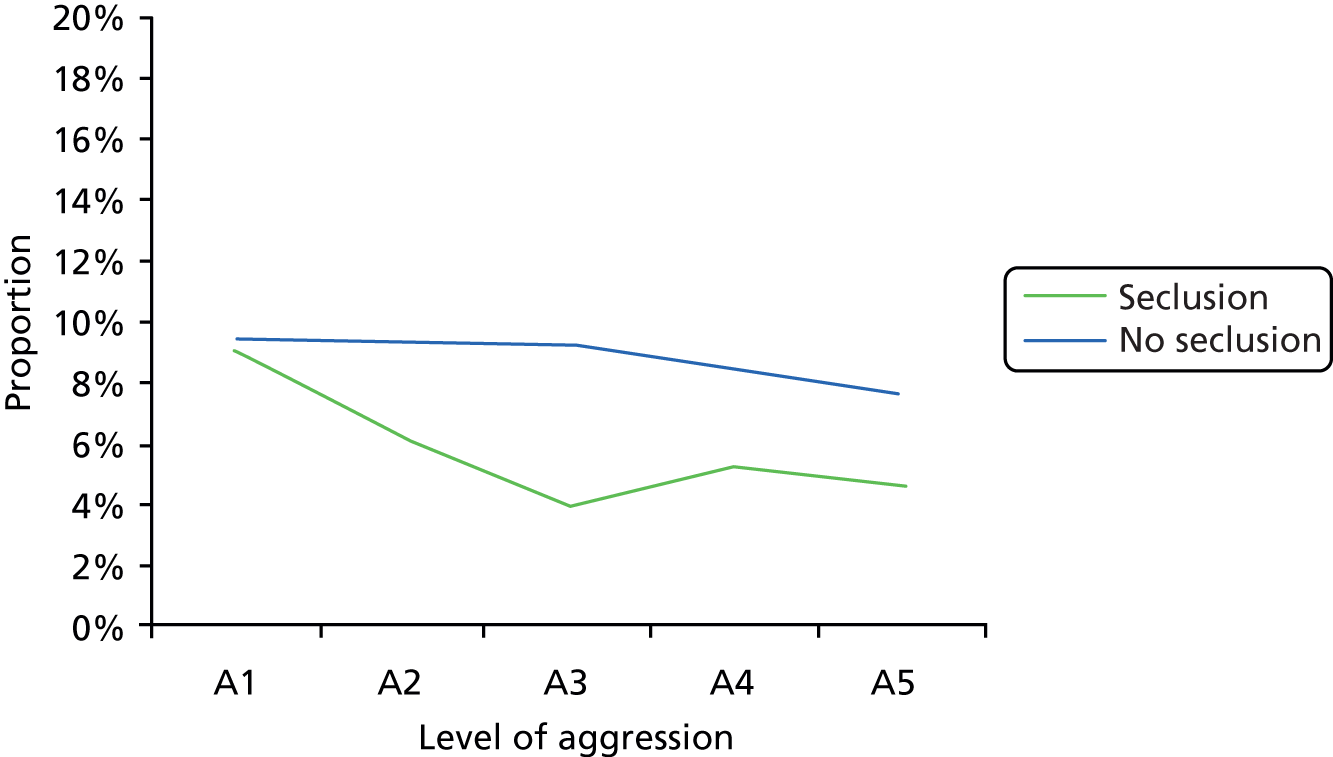
FIGURE 18.
Proportion of nurses citing observation as an intervention, by level of aggression and PICU availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.

FIGURE 19.
Proportion of nurses citing observation as an intervention, by level of self-harm and seclusion availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
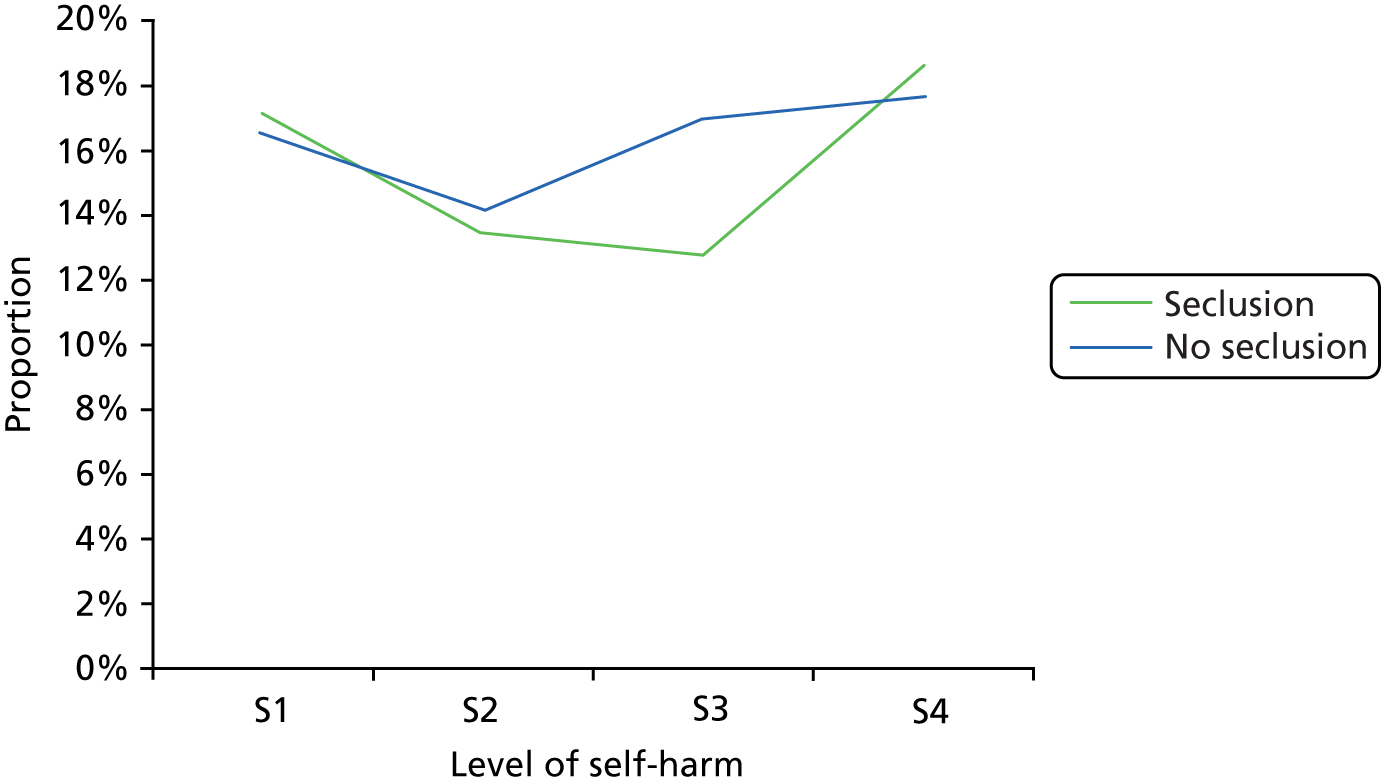
FIGURE 20.
Proportion of nurses citing observation as an intervention, by level of self-harm and PICU availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
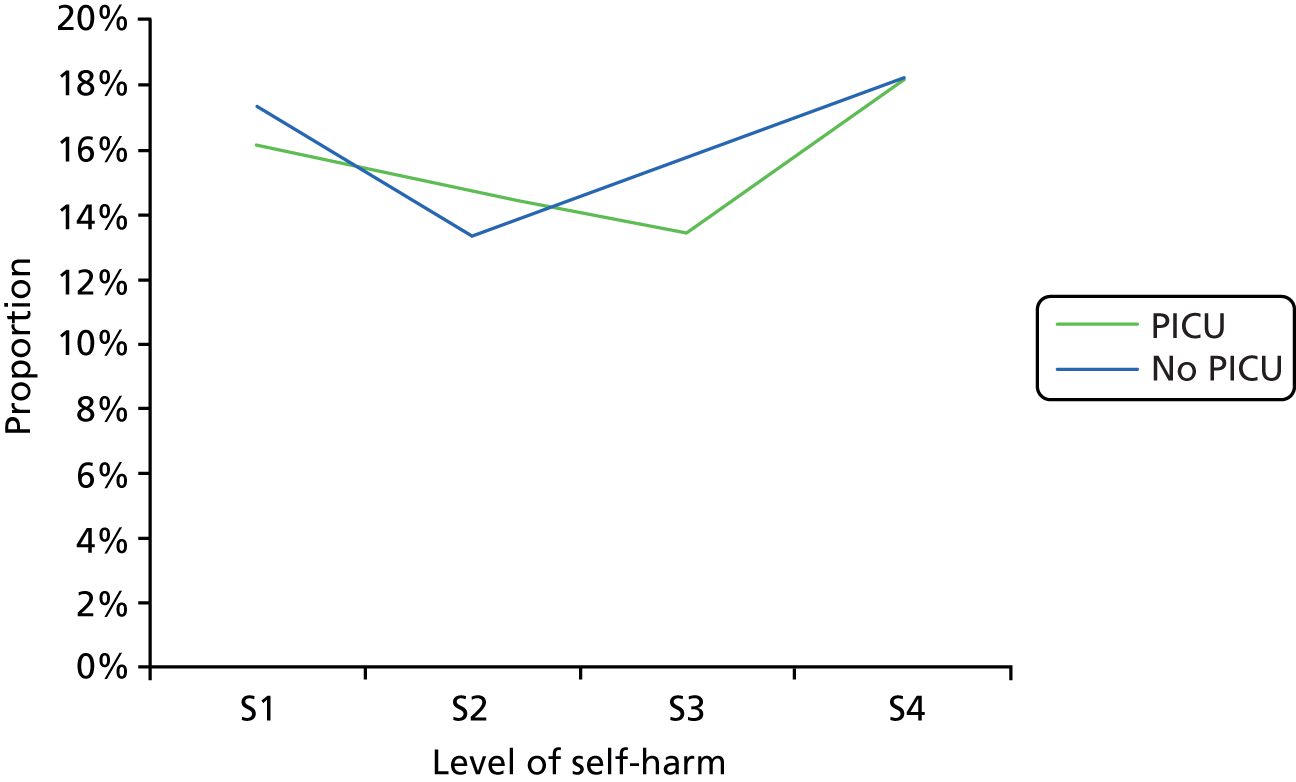
Coerced intramuscular medication
Figures 21 and 22 show the proportion of nurses who reported coerced intramuscular medication in the escalation pathway for aggressive behaviour, broken down by the specific severity of aggressive behaviour (TEPI questions A1–A5) and by seclusion or PICU availability. Figures 23 and 24 present the parallel information for self-harm. Overall, there is a slight decline in the perceived relevance of coerced intramuscular medication as aggression severity increases. Its use is reported more frequently for aggression across the spectrum of severity when there is no seclusion available. Coerced intramuscular medication is hardly seen as appropriate in the management of self-harm and was seldom reported for any level of severity of the behaviour.
FIGURE 21.
Proportion of nurses citing coerced intramuscular medication as an intervention, by level of aggression and seclusion availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.
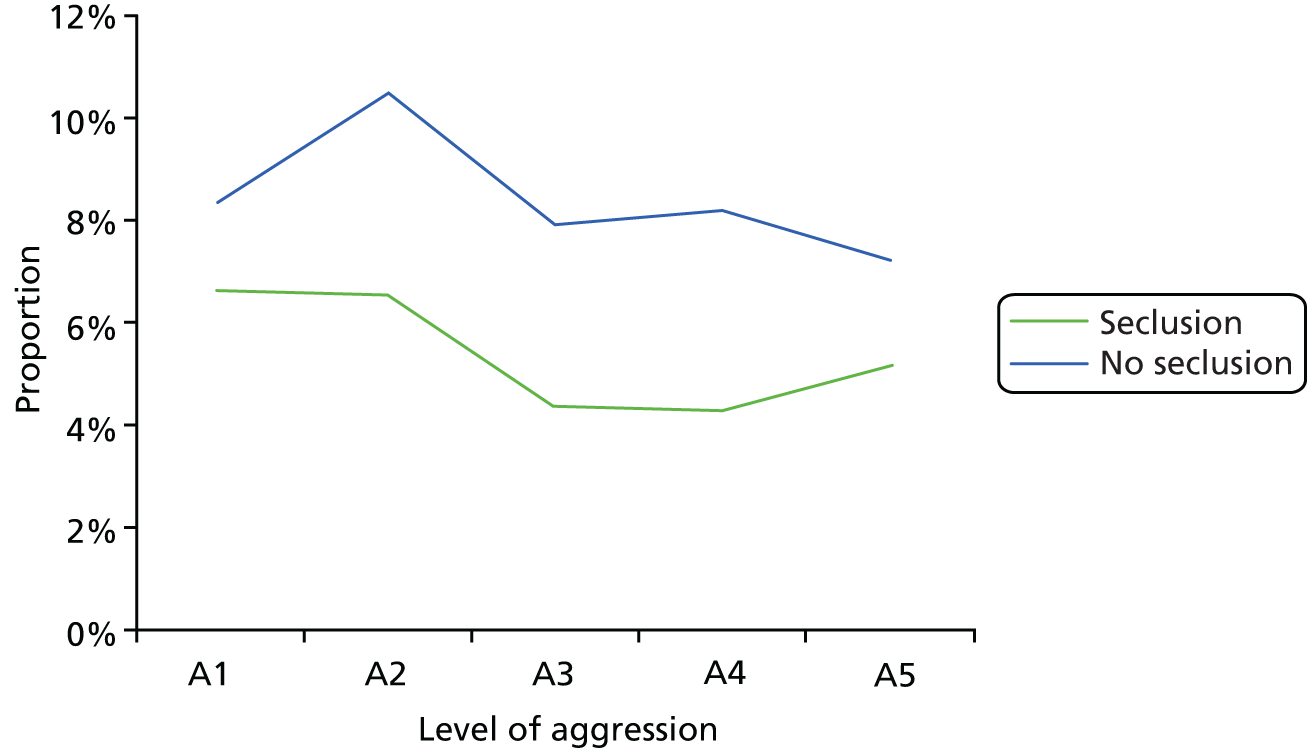
FIGURE 22.
Proportion of nurses citing coerced intramuscular medication as an intervention, by level of aggression and PICU availability. A1, verbal abuse; A2, property damage; A3, wielding a club; A4, assaulting a fellow patient; and A5, assaulting a fellow patient very seriously.
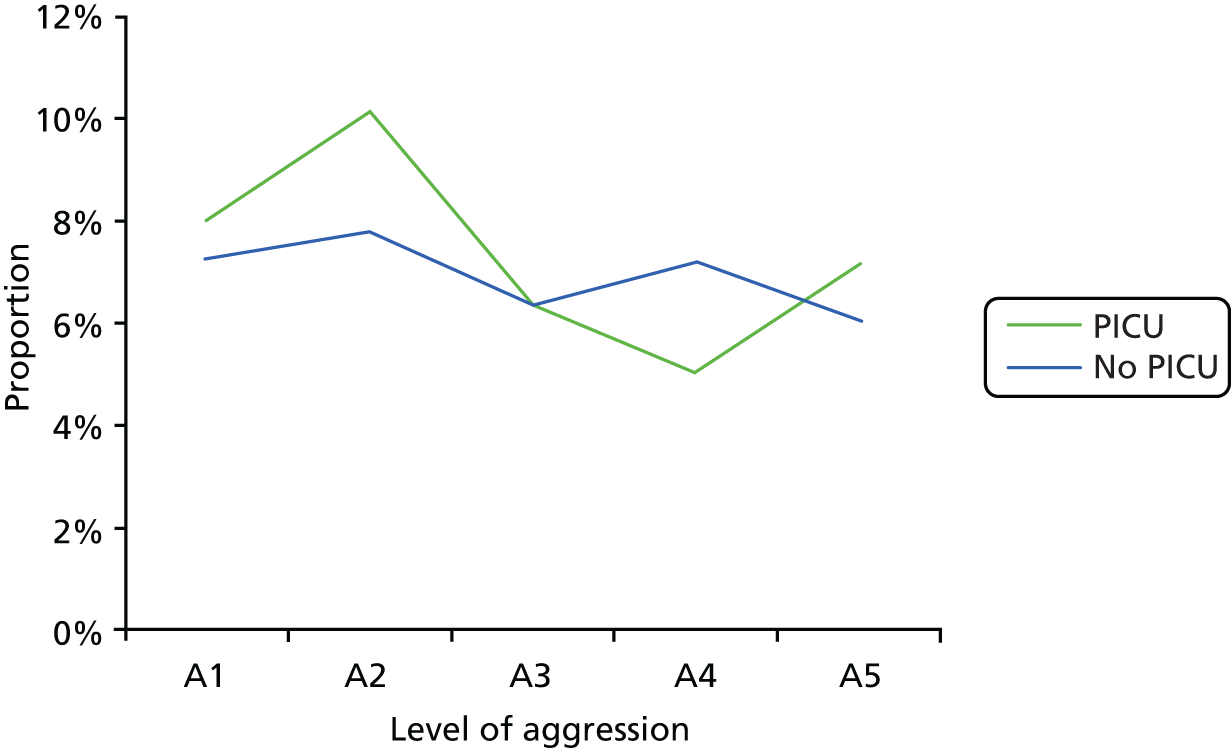
FIGURE 23.
Proportion of nurses citing coerced intramuscular medication as an intervention, by level of self-harm and seclusion availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.
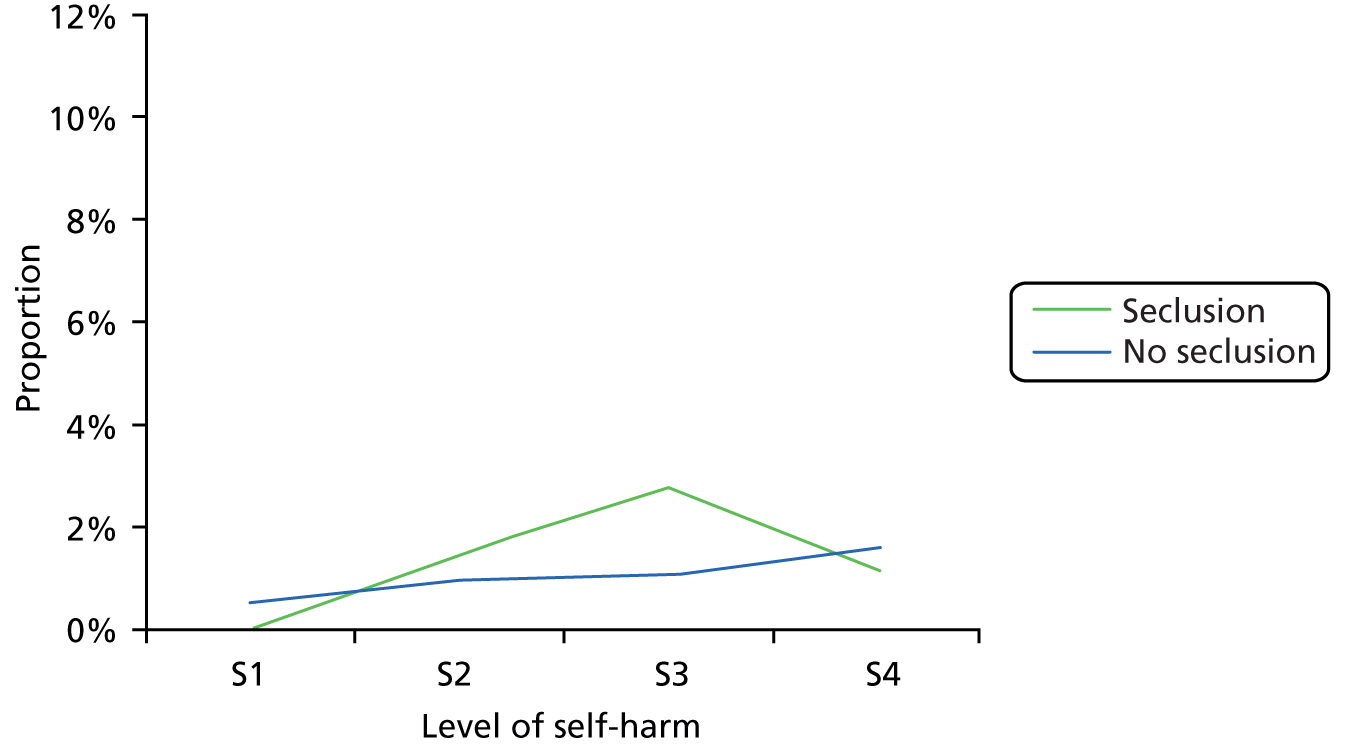
FIGURE 24.
Proportion of nurses citing coerced intramuscular medication as an intervention, by level of self-harm and PICU availability. S1, expressing suicidal ideation; S2, scratching self; S3, cutting self; and S4, attempt to hang self.

Exploration of lower-level intervention codes
Examination and exploration of the more fine-grained codes was undertaken to further illuminate those differences already discovered. Not all higher-level codes had such subcodes, but those with many were observation, de-escalation and manual restraint.
Breakdown of different types of observation
Figure 25 provides a bar chart of the frequencies of the different types of observation identified within the interviewee responses and Table 18 provides the codes and their definitions.
FIGURE 25.
Relative frequencies of observation.
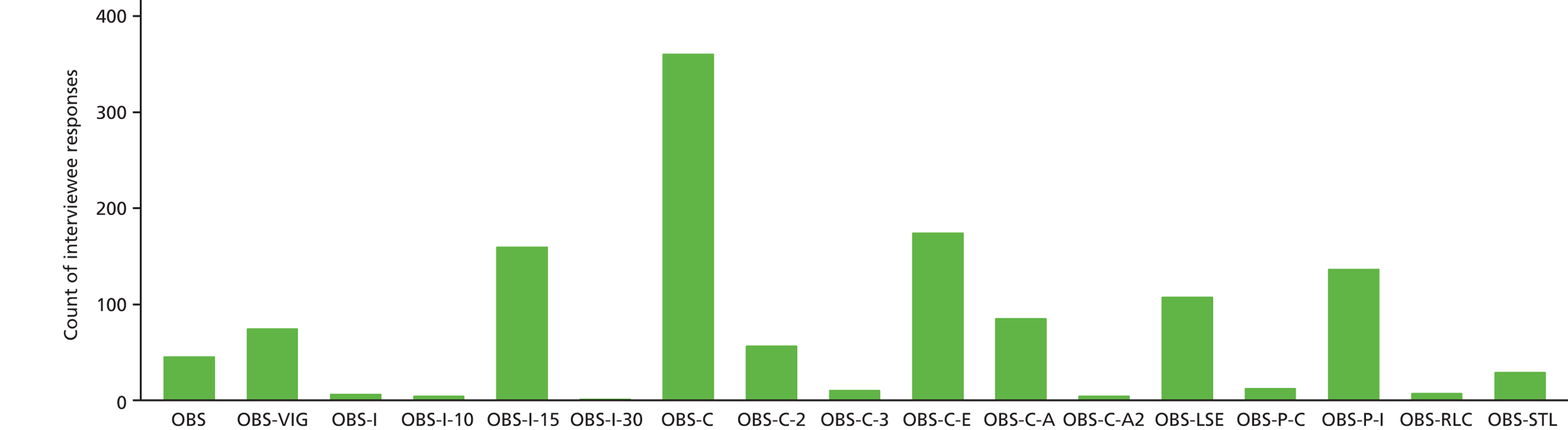
| Code | Definition |
|---|---|
| OBS | Unclassified |
| OBS-VIG | Vigilance, all staff on duty asked to be aware and keep their eyes open for the patient concerned, without them being placed on formal observation, including monitoring the outcome of treatment changes, give space, do nothing |
| OBS-I | Intermittent observation at unspecified intervals |
| OBS-I-10 | Intermittent observation at 10-minute intervals |
| OBS-I-15 | Intermittent observation at 15-minute intervals |
| OBS-I-30 | Intermittent observation at 30-minute intervals |
| OBS-C-E | Constant observation within eyesight |
| OBS-C-A | Constant observation within arm’s length |
| OBS-C-A2 | Constant observation within arm’s length, two staff, 2 : 1 |
| OBS-C | Constant observation, unspecified distance |
| OBS-C-2 | Constant observation by two staff, no distance specified |
| OBS-C-3 | Three staff on constant observation, no distance specified |
| OBS-LSE | Room observation – patients voluntarily stay in unlocked room |
| OBS-P-C | Policy of hospital to put on constant observation |
| OBS-P-I | Policy of hospital to be on intermittent observation (e.g. 15-minute intervals) |
| OBS-RLC | Relocate patient to a different bedroom to allow better observation of patient |
| OBS-STL | Staff assigned to a location to prevent conflict such as absconsion (e.g. ward door or patient door after coerced intramuscular injection) |
Intermittent observation clearly has a normative practice of around 15 minutes, this constituting the first data on observation intervals used during this practice. There is no clear uniformity or agreement around constant observation practice, with many different varieties being reported. Observation via team vigilance has not been previously described and does not form a part of hospitals’ observation policies. Its efficacy and impact are, therefore, unknown.
In the analyses that follow, using the same proportion-of-reports approach as previously used, it should be noted that some types of observation were mentioned in very low numbers. Such small differences in rates can be statistically significant without necessarily being of great clinical relevance. When the numbers are small, this has been indicated with the results.
Seclusion
When there is no access to seclusion, there is more generic constant observation (χ2 = 5.06; p = 0.024), constant observation by two staff (χ2 = 6.51; p = 0.011), constant observation by three staff (χ2 = 4.55; p = 0.033), constant observation in a low-stimulus environment (χ2 = 26.69; p < 0.001) and staff located to facilitate observation (χ2 = 13.13; p < 0.001). There is less use of 10-minute intermittent observation (small numbers, χ2 = 5.25; p = 0.022), constant observation within eyesight (χ2 = 5.81; p = 0.016), constant observation within arm’s length, two staff (small numbers, χ2 = 5.25; p = 0.022), intermittent observation by policy (χ2 = 65.24; p < 0.001) and relocating bedroom to facilitate observation (small numbers, χ2 = 9.21; p = 0.002). Using multivariate logistic regression, controlling for PICU availability, the only items still significant were constant observation in a low-stimulus environment, staff located to facilitate observation, constant observation within eyesight and intermittent observation by policy. A number of smaller items were dropped from the analysis because they predicted seclusion availability perfectly and could not, therefore, be included using this statistical method. The absence of seclusion therefore means that there is a greater emphasis on constant observation in a low-stimulus environment and staff being located to facilitate observation, and a lesser emphasis on constant observation within eyesight and intermittent observation by policy.
Psychiatric intensive care unit
When there is no access to a PICU on site, there is more constant observation by two staff (χ2 = 4.28; p = 0.039), constant observation by three staff (χ2 = 5.25; p = 0.022), constant observation within eyesight (χ2 = 46.37; p < 0.001), observation in a low-stimulus environment (χ2 = 6.15; p = 0.013) and constant observation by policy (χ2 = 6.31; p = 0.012). There is less use of generic observation (χ2 = 11.47; p = 0.001), 15-minute intermittent observation (χ2 = 4.25; p = 0.039) and generic constant observation (χ2 = 42.51; p < 0.001). Use of multivariate logistic regression controlling for seclusion availability only leaves constant observation within eyesight, generic observation and constant observation as significant. The absence of an on-site PICU therefore means that there is a greater emphasis on constant observation within eyesight and less use of generic forms of observation.
Summation
The absence of seclusion leads to a change of emphasis in observation use towards the constant observation of a patient in a separate room by themselves, accompanied by one or more staff members or with a staff member stationed at the door of the room. The absence of an on-site PICU leads to greater use of constant observation within eyesight.
Breakdown of different types of de-escalation
Figure 26 provides a bar chart of the frequencies of the different types of de-escalatory actions identified within the interviewee responses and Table 19 provides the codes and their definitions.
FIGURE 26.
Relative frequencies of de-escalation actions.
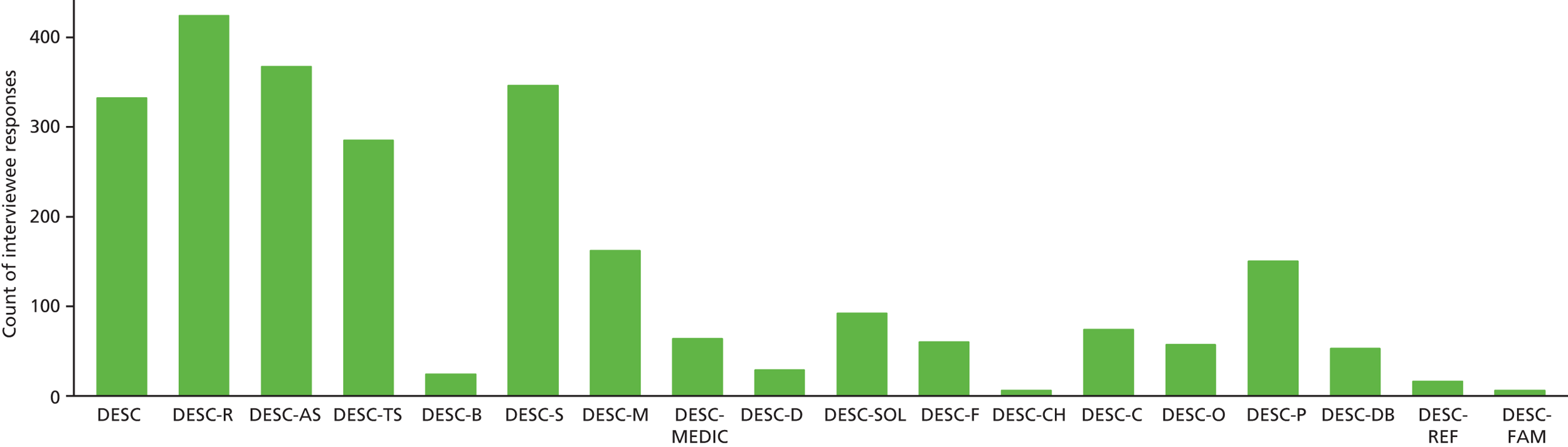
| Code | Definition |
|---|---|
| DESC | Unclassifiable de-escalation |
| DESC-R | Ask the reason for the behaviour, explore why the patient is doing what they are doing, what they are experiencing |
| DESC-CH | Consequences to patient’s health, problems with non-compliance |
| DESC-O | Orientate, give information about the ward, what is going on, who people are and why they are here |
| DESC-F | Give feedback about the impact of the behaviour on others, patients and staff to reflect on behaviour |
| DESC-D | Distract, talk about completely separate and different issues, make conversation |
| DESC-AS | Ask to stop and give/drop object (if appropriate) or similar |
| DESC-TS | Tell to stop, instruct, command, say behaviour is not acceptable |
| DESC-C | Inform of consequences to themselves (e.g. vulnerability to others’ actions) |
| DESC-SOL | Solutions, find out what has helped before, what can be done, what options are available, how can staff help |
| DESC-MEDIC | Get the doctor to talk to them |
| DESC-B | Set boundaries, explain boundaries, expectations |
| DESC-M | Encourage to take medication, providing information about it and the patient’s care plan |
| DESC-DB | Debrief patient about what has just happened |
| DESC-P | Talk about a plan that has been made and what is going to happen |
| DESC-FAM | Family speak to patient |
| DESC-REF | Ask other people to speak to patient (e.g. another health professional or expert in a non-health field) |
| DESC-S | Give reassurance, support, offer to help the patient and there to talk if they want |
Discounting those responses that were unclassifiable, the top six most frequently cited forms of de-escalation were (1) asking the reason for the behaviour (17%); (2) asking to stop (14%); (3) giving support and reassurance (14%); (4) telling to stop (11%); (5) encouraging to take medication (6%); and (6) talking about what is going to happen (6%). All other de-escalatory actions were mentioned at much lower frequencies (≤ 4%).
Differences in de-escalation by seclusion and PICU availability were tested using the difference-in-proportion-of-reports approach, followed by multivariate logistic regression including those items found to be significant, as before.
Seclusion
When there is no access to seclusion, de-escalation focuses more frequently on giving reassurance and support (χ2 = 12.44; p < 0.001), finding solutions (χ2 = 7.63; p = 0.006), telling to stop (χ2 = 25.7; p < 0.001) and asking to stop (χ2 = 13.48; p < 0.001), and focuses less frequently on giving feedback on the impact of the patient’s behaviour on others (χ2 = 12.11; p = 0.001), informing of the consequences for themselves (χ2 = 5.15; p = 0.023), orientating and giving information (χ2 = 5.15; p = 0.023), talking about or making plans (χ2 = 7.51; p = 0.006), discussing medication (χ2 = 5.58; p = 0.018) or unclassifiable ‘de-escalation’ (χ2 = 19.24; p < 0.001). Using multivariate logistic regression, controlling for PICU access, all of these variables remain significant except for discussing medication, making plans and informing of consequences. Orientation was excluded in this analysis due to collinearity (i.e. it was a perfect predictor and could not therefore be included). The absence of seclusion therefore means that there is a greater emphasis on reassurance, solutions, asking and telling to stop, and less emphasis on generic de-escalation or elaboration of the patient’s impact on others.
Psychiatric intensive care unit
When there is no on-site PICU, de-escalation focuses more frequently on unclassifiable ‘de-escalation’ (χ2 = 6.53; p = 0.011), debriefing patients about what has just happened (χ2 = 7.27; p = 0.007), distraction (χ2 = 9.88; p = 0.002), informing about medication or encouraging to take it (χ2 = 10.60; p = 0.001) and giving feedback on the impact of the patient’s behaviour on others (χ2 = 16.54, p < 0.001). De-escalation focuses less frequently on telling patients to stop (χ2 = 9.61; p = 0.002), asking patients to stop (χ2 = 6.13; p = 0.013) and asking for/exploring the reason for the patient’s behaviour (χ2 = 16.66; p < 0.001). Using multivariate logistic regression, controlling for seclusion access, all of these items remain significant. The absence of an on-site PICU, therefore, means that there is a greater emphasis on generic de-escalation, debriefing, distraction and encouraging medication, and less emphasis on asking or telling the patient to stop or exploring the reasons for their behaviour.
Summation
These findings resist a neat summary. It could be argued that the absence of seclusion leads to greater use of softer forms of de-escalation. Associations with PICU care availability are more opaque.
Breakdown of different types of manual restraint
A large number of codes were created to deal with information on manual restraint. These codes detailed the numbers of staff involved, the position of the patient and the location of the patient. However, the vast majority of the data collected during the interview were generic, providing no specific information about these aspects of the manual restraint process. It was particularly disappointing that a question about long-duration restraint was missed out so frequently that no useful information was collected. The questions in the TEPI were perhaps too detailed for the scenario being discussed, requiring a great deal of supposition and guesswork on the part of the interviewee, or possibly requests for clarifications from the interviewer that could not be provided. Alternatively, the issue of prone versus supine restraint was a matter of controversy at the time the data were collected, thus being an even more sensitive issue than usual. These may offer reasons as to why both parties seemed to avoid detailed discussion.
Some interviewers probed the participant for details, whereas others just left it at a generic description: ‘we would restrain him’. In some cases, the participant was asked about positions only (on the floor, sitting down, etc.) and not numbers. In others, they were just asked about the number of people involved in the restraint and not the position. So, in short, often ‘restraint’ was not investigated enough to include the correct level of detail. In many cases, as soon as the first restraint was described (usually in the case of Mike refusing his medication – behaviour 1, at some level of repeat or within the ‘if history’ prompt) this exact description was referred to from then on. For example, the participant would describe restraint for the first time. If restraint was then mentioned a second time at any point after, the interviewer would say ‘the same process as described first?’ and the participant would confirm ‘yes’. This would continue throughout the interview. This might have eliminated any variation in restraint between types of behaviour (e.g. mania vs. aggression). It also meant that if the first described form of restraint lacked in detail, this would follow through for every other behaviour thereafter. Owing to the difficulty in collecting these data comprehensively and consistently, the findings below should be taken with great caution.
It was necessary to collapse the many detailed lower-level codes to gain any useful information, and the results of this exercise can be found in Figure 27. This makes the high number of unspecified reports relative to others clearly visible. Setting these to one side, the most frequent patient position for restraint was lying, presumably on the floor as manual restraint on the bed was counted separately. There was insufficient information to say whether this was prone or supine. The next most frequently reported type of restraint was on the bed. Standing, sitting or kneeling positions were very infrequently reported.
FIGURE 27.
Frequencies of different types of manual restraint.
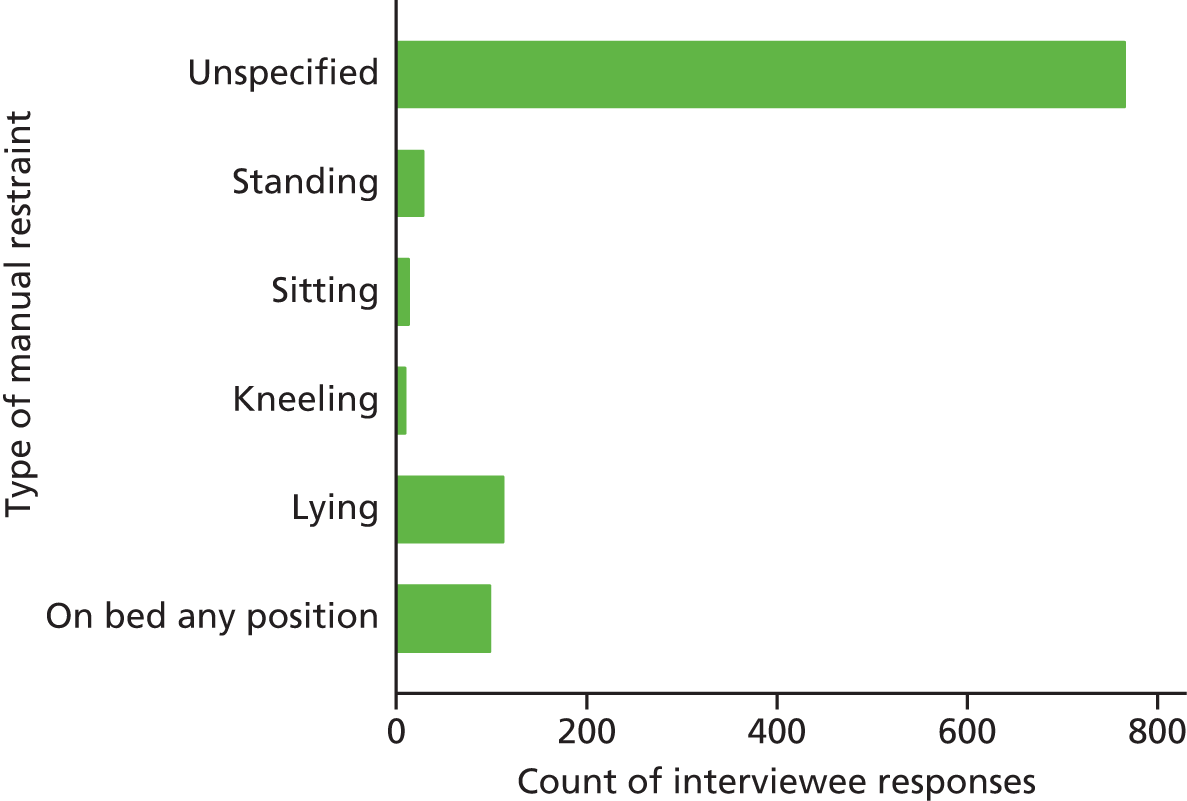
Seclusion
When there was no seclusion, manual restraint was less likely to be sitting (χ2 = 12.92; p < 0.001). This result remained significant when PICU availability was taken into account using multivariate logistic regression, although the numbers were very small.
Psychiatric intensive care unit
When there was no on-site PICU, restraint was more likely to be standing (χ2 = 11.99; p = 0.001) or on the bed (χ2 = 10.86; p = 0.001), and less likely to be sitting (χ2 = 20.98; p < 0.001) or lying (χ2 = 4.95; p = 0.026). Using multivariate logistic regression controlling for seclusion availability, standing and on the bed remained significant, whereas sitting was dropped from the analysis as it predicted PICU availability perfectly. The absence of an on-site PICU meant that restraint was more likely to be standing or on the bed.
Summation
Detailed data on manual restraint were sparse and to some degree unreliable. The most frequent position was lying, probably on the floor. However, restraint on a bed was nearly as frequent. Differences by seclusion or PICU availability were not susceptible to easy interpretation.
Repeated behaviours
The TEPI was constructed so that, for each behavioural scenario, the interviewer was to collect information about what would happen if the behaviour was repeated during the shift, in the next shift or for the whole day. Interviewers found it difficult to collect this information consistently and in a logical way. It was not always easy to say the behaviour was repeated if the previous account had ended in seclusion, PICU transfer or a period of close observation. The different time intervals were also impossible to separate. Furthermore, in the flow of this lengthy and difficult interview, interviewers sometimes omitted questions about repeats completely for some or many questions. Nevertheless, there was a substantial quantity of repeat information in the data set and this was therefore, with some caution, submitted to an analysis, using the proportion-of-reports approach. These frequency data are presented in Tables 20 and 21, with the statistically significant results in the text that follows.
| Intervention type | All behaviours, n (%) | Aggression, n (%) | Self-harm, n (%) | Mania, n (%) | ||||
|---|---|---|---|---|---|---|---|---|
| No seclusion | Seclusion | No seclusion | Seclusion | No seclusion | Seclusion | No seclusion | Seclusion | |
| As-required medication | 112 (5.8) | 56 (3.6) | 41 (7.1) | 9 (3.0) | 20 (5.7) | 12 (3.2) | 51 (5.1) | 35 (4.1) |
| Calm-down methods | 11 (0.6) | 17 (1.1) | 0 (0.0) | 1 (0.3) | 4 (1.1) | 5 (1.3) | 7 (0.7) | 11 (1.3) |
| Coerced intramuscular medication | 106 (5.5) | 60 (3.9) | 45 (7.8) | 17 (5.6) | 6 (1.7) | 3 (0.8) | 55 (5.5) | 40 (4.6) |
| Deal with other patients | 18 (0.9) | 9 (0.6) | 12 (2.1) | 3 (1.0) | 2 (0.6) | 4 (1.1) | 4 (0.4) | 2 (0.2) |
| De-escalation | 351 (18.2) | 312 (20.2) | 75 (13.0) | 35 (11.6) | 90 (25.6) | 90 (23.7) | 186 (18.7) | 187 (21.6) |
| Sex-specific care | 23 (1.2) | 9 (0.6) | 1 (0.2) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 22 (2.2) | 8 (0.9) |
| Impose restrictions | 8 (0.4) | 17 (1.1) | 3 (0.5) | 2 (0.7) | 2 (0.6) | 3 (0.8) | 3 (0.3) | 12 (1.4) |
| LSE | 95 (4.9) | 59 (3.8) | 35 (6.1) | 12 (4.0) | 7 (2.0) | 16 (4.2) | 53 (5.3) | 31 (3.6) |
| Manual restraint | 156 (8.1) | 106 (6.9) | 72 (12.5) | 29 (9.6) | 19 (5.4) | 19 (5.0) | 65 (6.5) | 58 (6.7) |
| Medication discussion | 80 (4.2) | 91 (5.9) | 19 (3.3) | 23 (7.6) | 8 (2.3) | 16 (4.2) | 53 (5.3) | 52 (6.0) |
| Non-standard transfer | 26 (1.4) | 7 (0.5) | 8 (1.4) | 3 (1.0) | 0 (0.0) | 0 (0.0) | 18 (1.8) | 4 (0.5) |
| Observation | 267 (13.9) | 173 (11.2) | 60 (10.4) | 16 (5.3) | 69 (19.7) | 63 (16.6) | 138 (13.8) | 94 (10.9) |
| PICU | 114 (5.9) | 118 (7.6) | 69 (12.0) | 59 (19.5) | 11 (3.1) | 10 (2.6) | 34 (3.4) | 49 (5.7) |
| Police call | 40 (2.1) | 16 (1.0) | 19 (3.3) | 5 (1.7) | 15 (4.3) | 6 (1.6) | 6 (0.6) | 5 (0.6) |
| Psychological therapy | 10 (0.5) | 7 (0.5) | 0 (0.0) | 0 (0.0) | 7 (2.0) | 6 (1.6) | 3 (0.3) | 1 (0.1) |
| Request assistance | 107 (5.6) | 80 (5.2) | 45 (7.8) | 16 (5.3) | 17 (4.8) | 24 (6.3) | 45 (4.5) | 40 (4.6) |
| Review of patient care | 162 (8.4) | 169 (10.9) | 23 (4.0) | 30 (9.9) | 34 (9.7) | 45 (11.8) | 105 (10.5) | 94 (10.9) |
| Search/remove items | 48 (2.5) | 58 (3.8) | 0 (0.0) | 1 (0.3) | 24 (6.8) | 38 (10.0) | 24 (2.4) | 19 (2.2) |
| Seclusion | 7 (0.4) | 32 (2.1) | 6 (1.0) | 20 (6.6) | 0 (0.0) | 0 (0.0) | 1 (0.1) | 12 (1.4) |
| Show of force | 40 (2.1) | 28 (1.8) | 16 (2.8) | 6 (2.0) | 2 (0.6) | 1 (0.3) | 22 (2.2) | 21 (2.4) |
| Talk to others | 131 (6.8) | 117 (7.6) | 25 (4.3) | 14 (4.6) | 9 (2.6) | 17 (4.5) | 97 (9.7) | 86 (10.0) |
| Use of gardens, rooms, etc. | 12 (0.6) | 5 (0.3) | 2 (0.3) | 0 (0.0) | 5 (1.4) | 2 (0.5) | 5 (0.5) | 3 (0.3) |
| Intervention type | All behaviours, n (%) | Aggression, n (%) | Self-harm, n (%) | Mania, n (%) | ||||
|---|---|---|---|---|---|---|---|---|
| No PICU | PICU | No PICU | PICU | No PICU | PICU | No PICU | PICU | |
| As-required medication | 95 (4.7) | 73 (5.1) | 31 (5.3) | 19 (6.4) | 20 (5.7) | 12 (3.2) | 44 (4.0) | 42 (5.6) |
| Calm-down methods | 19 (0.9) | 9 (0.6) | 0 (0.0) | 1 (0.3) | 5 (1.4) | 4 (1.1) | 14 (1.3) | 4 (0.5) |
| Coerced intramuscular medication | 107 (5.2) | 59 (4.1) | 38 (6.5) | 24 (8.1) | 4 (1.1) | 5 (1.3) | 65 (5.9) | 30 (4.0) |
| Deal with other patients | 13 (0.6) | 14 (1.0) | 8 (1.4) | 7 (2.4) | 1 (0.3) | 5 (1.3) | 4 (0.4) | 2 (0.3) |
| De-escalation | 383 (18.8) | 280 (19.6) | 82 (14.1) | 28 (9.4) | 89 (25.2) | 91 (24.1) | 212 (19.2) | 161 (21.3) |
| Sex-specific care | 22 (1.1) | 10 (0.7) | 1 (0.2) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 21 (1.9) | 9 (1.2) |
| Impose restrictions | 14 (0.7) | 11 (0.8) | 2 (0.3) | 3 (1.0) | 5 (1.4) | 0 (0.0) | 7 (0.6) | 8 (1.1) |
| LSE | 84 (4.1) | 70 (4.9) | 28 (4.8) | 19 (6.4) | 4 (1.1) | 19 (5.0) | 52 (4.7) | 32 (4.2) |
| Manual restraint | 168 (8.2) | 94 (6.6) | 67 (11.5) | 34 (11.4) | 13 (3.7) | 25 (6.6) | 88 (8.0) | 35 (4.6) |
| Medication discussion | 112 (5.5) | 59 (4.1) | 28 (4.8) | 14 (4.7) | 15 (4.2) | 9 (2.4) | 69 (6.2) | 36 (4.8) |
| Non-standard transfer | 22 (1.1) | 11 (0.8) | 9 (1.5) | 2 (0.7) | 0 (0.0) | 0 (0.0) | 13 (1.2) | 9 (1.2) |
| Observation | 266 (13.0) | 174 (12.2) | 62 (10.7) | 14 (4.7) | 58 (16.4) | 74 (19.6) | 146 (13.2) | 86 (11.4) |
| PICU | 128 (6.3) | 104 (7.3) | 82 (14.1) | 46 (15.5) | 12 (3.4) | 9 (2.4) | 34 (3.1) | 49 (6.5) |
| Police call | 33 (1.6) | 23 (1.6) | 12 (2.1) | 12 (4.0) | 15 (4.2) | 6 (1.6) | 6 (0.5) | 5 (0.7) |
| Psychological therapy | 6 (0.3) | 11 (0.8) | 0 (0.0) | 0 (0.0) | 3 (0.8) | 10 (2.6) | 3 (0.3) | 1 (0.1) |
| Request assistance | 115 (5.6) | 72 (5.0) | 39 (6.7) | 22 (7.4) | 17 (4.8) | 24 (6.3) | 59 (5.3) | 26 (3.4) |
| Review of patient care | 171 (8.4) | 160 (11.2) | 30 (5.2) | 23 (7.7) | 36 (10.2) | 43 (11.4) | 105 (9.5) | 94 (12.5) |
| Search/remove items | 59 (2.9) | 47 (3.3) | 1 (0.2) | 0 (0.0) | 34 (9.6) | 28 (7.4) | 24 (2.2) | 19 (2.5) |
| Seclusion | 36 (1.8) | 3 (0.2) | 23 (4.0) | 3 (1.0) | 0 (0.0) | 0 (0.0) | 13 (1.2) | 0 (0.0) |
| Show of force | 43 (2.1) | 25 (1.7) | 15 (2.6) | 7 (2.4) | 2 (0.6) | 1 (0.3) | 26 (2.4) | 17 (2.3) |
| Talk to others | 133 (6.5) | 115 (8.0) | 22 (3.8) | 17 (5.7) | 15 (4.2) | 11 (2.9) | 96 (8.7) | 87 (11.5) |
| Use of gardens, rooms, etc. | 11 (0.5) | 6 (0.4) | 1 (0.2) | 1 (0.3) | 5 (1.4) | 2 (0.5) | 5 (0.5) | 3 (0.4) |
All problem behaviours
Seclusion
The absence of a seclusion room was associated with a higher number of reports of calls to the police (χ2 = 5.88; p = 0.015), PRN medication (χ2 = 8.99; p = 0.003) and observation (χ2 = 5.59; p = 0.018), and a lower number of reports of medication discussion (χ2 = 5.46; p = 0.019), transfer to a PICU (χ2 = 4.01; p = 0.045), seclusion (χ2 = 22.45; p < 0.001), removal of objects (χ2 = 4.57; p = 0.032), reviews (χ2 = 6.27; p = 0.012) and restrictions (χ2 = 5.60; p = 0.018). In multivariate logistic regression, controlling for PICU availability, all these interventions remained significant except for observation.
Psychiatric intensive care unit
The absence of an on-site PICU was associated with a higher number of reports of seclusion (χ2 = 18.29; p < 0.001) and a lower number of reviews (χ2 = 7.67; p = 0.006) and psychological interventions (χ2 = 3.89; p = 0.048). In multivariate logistic regression controlling for seclusion availability, all of these interventions remained significant.
Aggression only
Seclusion
The absence of a seclusion room was associated with a higher number of reports of PRN medication (χ2 = 6.32; p = 0.012), observation (χ2 = 6.56; p = 0.010) and transfer to a PICU (χ2 = 9.09; p = 0.003), and a lower number of reports of medication discussion (χ2 = 8.11; p = 0.004), seclusion (χ2 = 21.47; p < 0.001) and review (χ2 = 12.33, p < 0.001). Using multivariate logistic regression, controlling for PICU availability, PRN medication and observation were no longer significant.
Psychiatric intensive care unit
The absence of an on-site PICU was associated with a higher number of reports of de-escalation (χ2 = 3.94; p = 0.047), observation (χ2 = 8.82; p = 0.003) and seclusion (χ2 = 5.94; p = 0.015). All three interventions remained significant when multivariate logistic regression was used, controlling for seclusion availability.
Self-harm only
Seclusion
The absence of a seclusion room was associated with a higher number of reports of calls to the police (χ2 = 4.75; p = 0.029). This was no longer significant when PICU availability was controlled for.
Psychiatric intensive care unit
The absence of an on-site PICU was associated with a higher number of reports of calls to the police (χ2 = 4.64; p = 0.031) and restrictions (χ2 = 5.39; p = 0.020), and a lesser use of a low-stimulus environment (χ2 = 9.08; p = 0.003). In multivariate logistic regression, controlling for seclusion availability, only the use of a low-stimulus environment remained significant. Restrictions were dropped from the analysis as they predicted PICU availability perfectly.
Mania only
Seclusion
The absence of a seclusion room was associated with a higher number of reports of sex-specific care (χ2 = 4.79; p = 0.029) and a lower number of reports of PICU transfer (χ2 = 5.55; p = 0.018), seclusion (χ2 = 11.08; p = 0.001) and restrictions (χ2 = 6.85; p = 0.009). In a multivariate logistic regression, controlling for PICU availability, only seclusion and restrictions remained significant.
Psychiatric intensive care unit
The absence of an on-site PICU was associated with a higher number of reports of seclusion (χ2 = 8.94; p = 0.003) and a lower number of reports of talking to others (χ2 = 4.09; p = 0.043), PICU transfer (χ2 = 12.29; p < 0.001) and review (χ2 = 4.11; p = 0.043). In a multivariate logistic regression controlling for seclusion availability, all items remained significant, although seclusion could not be included as it predicted PICU availability perfectly.
Summation
The message from the repeated data is not totally clear, but there are indications that the absence of seclusion leads to a higher use of PRN medication and number of reports of calls to the police, and a lower frequency of reviewing care. The absence of an on-site PICU was also associated with a lower frequency of reviewing care. The provision of seclusion was clearly associated with its use, as was the availability of an on-site PICU; however, the absence of an on-site PICU was also associated with the use of seclusion.
Discussion
Summary of findings
Hospitals and their staff do not have any common practice threshold and escalation pathways. Hospitals without a seclusion room available managed disturbed behaviour through:
-
less use of seclusion, although small numbers of seclusions still occur outside policy and utilising rooms not built for the purpose
-
greater use of coerced intramuscular medication
-
less use of calm-down methods and show of force
-
observation use by the constant observation of the patient in a separate room by themselves, accompanied by one or more staff members, or with a staff member stationed at the door of the room
-
indicative evidence of more use of PRN medication and calls to the police and fewer reviews of care.
Hospitals without an on-site PICU managed disturbed behaviour through:
-
less use of PICU transfer; transfers to PICUs at other sites did occur, but they were less frequent
-
greater use of seclusion
-
greater use of de-escalation
-
greater use of observation, specifically observation within eyesight
-
greater use of show of force
-
greater use of calm-down methods
-
indicative evidence of less use of psychological interventions and reviews of care.
These differences by seclusion and PICU availability are greatest for aggression, less prominent for self-harm and unclear for mania. The differences are also greater for the more severe expressions of these behaviours, although seclusion was not used for self-harm and PICU transfer was seldom reported. Coerced intramuscular medication was also not seen as relevant in the management of self-harm.
The normative interval for intermittent observation is every 15 minutes and a practice of team vigilance outside policy was described. The second most frequent manual restraint position was on a bed.
No escalation pathway
Although the absence of a common escalation pathway has been previously reported by a single hospital qualitative study in the USA,64 not to find one was surprising and also unwelcome, as this element of the overall research was predicated on finding and describing such pathways. It is possible that the interview process was flawed in some way and failed to detect pathways that actually existed, perhaps because interviewees failed to recollect or accurately describe common practice. Certainly, orthodox social researchers have succeeded in generating similar ‘ethnographic decision trees’ through quasi-naturalistic methods. 65 Alternatively, it could be that, as the TEPI development process revealed, managing crisis situations was dependent on so many moment-to-moment changes of behaviour and response by the individual patient, balanced with their known history and existing relationship with the nurse, that in fact a common pathway practised by a group of staff in one location is not possible. A third possibility is that such responses are first and foremost pragmatic moment-to-moment social judgements through which staff members actually create a meaningful structure to their actions and the way that they are sequenced. In this case, if escalation pathways do exist in any documentary or attestable form, they may not in any simple sense determine what staff members do; rather, they are oriented to by staff members as they either ‘do’ following an escalation pathway or attempt to perceive such structure in actions that they observe. Ethnomethodology66 and post-Wittgensteinian social theory67 may be relevant approaches to understanding this.
Nevertheless, despite methodological difficulties, there were differences in our sample dependent on the availability of seclusion and PICU care at hospitals, and we were able to describe these based on statistical testing. Lessons about practice can be drawn even without a common escalation pathway, for there were many intervention strategies, particularly types of de-escalation, that were mentioned only rarely by few staff. It could be that these methods were less mentioned because they were less useful, or it could be that nursing staff could gain through the expansion of their range of strategies for intervention, giving them a greater number of interventions to choose from to match the patient and situation.
Seclusion still used in the absence of a dedicated room and policy
Clearly this is not desirable. The absence of a specially constructed robust room means that a disturbed patient could easily break fixtures and fittings, harming themselves or staff members who go in to manage the situation. The use of seclusion without a policy means a deficit of recording, reporting and an absence of clinical oversight, mandated clinical reviews at intervals and managerial supervision of practice and rates of use. Although this practice was seldom mentioned in our data, it is not really possible to extrapolate from that how frequently it is occurring. Interviewees may have had some embarrassment or sensitivity about it and been disinclined to mention it for these reasons. This should, therefore, be an issue of concern at any acute psychiatric hospital without a dedicated seclusion room.
The existence of this practice, not previously documented, does explain data previously collected during the City-128 study, showing a rate of reported seclusion at hospitals without a seclusion room. 2 This was previously attributed to reporting error; however, now it is clear that the data were, in fact, likely to be close to accurate and this suggests that the rate of seclusion in English acute psychiatric wards that do not have access to a seclusion room is once every 20 days on a 20-bedded ward. This figure may seem high, but it is based on 6 months’ worth of end-of-shift reports (> 21,000 reports) submitted by 67 randomly selected acute wards where the ward managers reported no access to a seclusion room and using the same definition of seclusion used in this study.
Nursing in a side room as an alternative to seclusion
Hospitals without seclusion rooms also managed disturbed patients by two practices commonly referred to as ‘nursing the patient in a side room’: one in which the nurses sat outside the door of the room (often, but not always, the patient’s bedroom) and the other in which nurses (sometimes two or three) accompanied the patient into the room.
The first of these practices, stationing a nurse near the door either to disincline or to prevent the patient from leaving, or to observe them through the open door, is seen by some as being, in effect, seclusion. It would come under the definition of seclusion used in some policy documents, such as the UK MHA code of practice (2015, paragraph 26.103). 40 Whether or not it is useful to do so remains open to question as, in current practice, it can mean that the patient is restricted to their own bedroom, with access to all their own clothing and other items, and their own en-suite bathroom (if provided), compared with isolation from staff and patients in a separate robust seclusion room with a heavy locked door, observation panel, robust unbreakable furnishings, etc. There is a great deal of difference between these two practices and counting them together for the purpose of official statistics would equate both and fail to recognise the less severe and more acceptable end of practice. Exactly how seclusion is defined will also influence international comparison statistics and assessing where we are in the UK vis-à-vis other countries’ reductions in restrictive practices. At present there are no national statistics in the UK on seclusion rates, unlike many other countries where seclusion requires a formal report to the central government. 68 Clarity of definition and terminology in this and related areas is highly desirable. Good terminology and definitions have the capacity to exert beneficial influence. Poorly constructed or vague resolutions of the difficulties of describing different interventions may warp practice or the reporting of practice in unpredictable ways, at worst leading to a less desirable range of options for patients.
The second of these interventions, in which staff accompany the patient into the room, has been less well described in UK psychiatric nursing practice. The room could be the patient’s bedroom, but could also be a specialist de-escalation room of some sort, or those hospitals that do have a seclusion room can use it in this way. Some UK hospitals do have special extra care or intensive care areas where staff can accompany patients, locking the door behind them so that all are isolated together. This practice is referred to in Norway as ‘open-area seclusion’,69 and is the only form of seclusion used there. In Norway, the time with the patient is well used in a therapeutic way, to debrief the patient, work with their understanding of what has happened and what has to change in order for them to rejoin the rest of the patients. This may be an opportunity for nurses to forge and develop therapeutic interventions with patients. However, what happens during this time in the UK is unknown and the association of observation with untrained staff70,71 suggests that the practice here is likely to be more restrictive than therapeutic. This practice is also clearly more risky for the staff. Instead of the angry, agitated, deluded and hallucinating patient being on the other side of a hefty seclusion room door, nurses accompany the patient, potentially in sufficient numbers to instantly manually restrain them if their violence recommences. Any misjudgement about the timing of interventions could, in these circumstances, lead to injured nurses. In addition, the presence of the nurses implies a greater use of manual restraint, which carries risks both for the patient and the staff. 72 Finally, the use of staff members, if more than one, is bound to be costly relative to seclusion.
In previous research by our group, stationing a nurse at the doorway and a third option that did not differ by seclusion availability in this study (asking the patient to stay voluntarily in a side room for a period of time) were collectively referred to as ‘time out’. Our previous research had no special category for staff accompanying the patient in the side room, so this may have been categorised as constant observation or time out or both in that research and related reports. Bearing this in mind, our previous work has sought to examine the acceptability of different containment practices and their efficacy. Time out is seen as one of the most acceptable forms of containment by patients and staff,4 student nurses51 and the general public,54 all of these studies also demonstrating that it was rated very differently to seclusion, which was seen as one of the least acceptable containment methods currently in use in the UK. Several studies found, however, that time out was associated with less severe disturbed behaviour,2,3 although the use of time out following a violent assault appeared to be equally effective in preventing a repetition. 3
More evaluation studies are clearly required in this area and it has been demonstrated that it is possible to conduct randomised trials comparing different forms of containment. 73 More evaluation information has the potential to quickly shape practice into a safer and more effective form.
Coerced intramuscular medication as an alternative to seclusion
Nurses from hospitals without access to seclusion were more likely to report the use of coerced intramuscular medication (rapid tranquillisation) in their escalation pathways. The two are not mutually incompatible interventions and it is known that a small number of patients are given intramuscular medication as well as being secluded (5%), and more accept oral PRN medication during the seclusion process (24%). 74 The use of seclusion is also statistically associated with the use of coerced intramuscular medication. 2 The relative efficacy of coerced intramuscular medication and seclusion is not known, by any outcome indicator. In UK acute psychiatry, the vast majority of seclusions are terminated within a few hours. 3 However, it is a negative experience for patients, who feel a combination of anger, upset, abandonment, fear, humiliation and worthlessness, with the experience often being interpreted as punishment. 1 A similar range of negative emotions are reported by those subject to coerced intramuscular medication: angry, helpless, frightened,75 sadness, violation, panic and fear of becoming ill or dying as a result of the injection. 76 Any parenteral medication of sedating drugs carries some risk and the contribution of rapid tranquillisation to the (thankfully) rare deaths during manual restraint is not known. 72
Large-scale surveys of UK acute patients have shown slightly higher ratings of acceptability for seclusion than coerced intramuscular medication; however, the difference is not large and masks a wide variety of different opinions between patients. 4 Those patients who had experienced coerced intramuscular medication were less likely to consider it acceptable, whereas the experience of seclusion made no difference to acceptability ratings. A study with a smaller sample conducted in the Netherlands showed equal numbers with preference for seclusion or medication, with one-quarter of patients having no preference either way. 77 Acute care nurses in the UK, on the other hand, give significantly higher acceptability ratings to coerced intramuscular medication than seclusion,4 whereas nursing and non-nursing students rated their acceptability as equal. 54 Using some of the same data from the City-128 study, Dack et al. 45 examined the relationship between acceptability ratings and actual rates of usage on the wards. Greater use of seclusion was associated with higher acceptability ratings of seclusion by all patients (i.e. including, but not exclusively, those who had experienced it); however, greater use of coerced intramuscular medication was associated with lower acceptability ratings for coerced intramuscular medication itself and nearly every other form of containment, including seclusion. The authors suggested that this might be interpreted as the use of coerced medication having a ‘toxic’ effect on patient attitudes.
These different survey results on relative acceptability come out slightly in favour of seclusion rather than coerced intramuscular medication, albeit with significant variation in individual patient preferences. It is relatively easy to recommend that patient preferences be requested and acted on; however, in busy acute wards, with constantly changing staff and patients and unpredictable events in unpredictable circumstances, where, as we have seen, there are not even any consistent escalation pathways, getting such a system into practice would represent a significant challenge. When there is no seclusion room available, the choice cannot be offered.
Seclusion as an alternative to psychiatric intensive care unit care
The data from this study support the idea that when seclusion is available and an on-site PICU is not, seclusion is utilised as an alternative for the management of disturbed behaviour. This clarifies a relationship that is difficult to investigate because of the way seclusion is provided and care managed in some places. For example, in a significant number of places the available seclusion room is located in the PICU. In some of those hospitals, the patient must be transferred to the PICU in order to use the seclusion room, whereas in others, staff from the acute ward bring the patient into seclusion and stay outside the room to monitor and provide care, without any such transfer taking place. Cross-sectional studies looking at statistical associations are thus confounded by service provision and its associated policies.
With seclusion, once the person has calmed, they return to mix with the other patients on the acute ward where the disturbance took place. Such episodic seclusion seems likely to be a cheaper option than PICU care; however, it means that the risk of further conflict events remains on the acute ward, where staffing levels are lower and the environment is less robust. Moreover, the remaining patients on the acute ward must then accommodate their behaviour towards that potentially risky individual and may be more fearful as a consequence. 78
De-escalation as an alternative to psychiatric intensive care unit care
Greater use of de-escalation was a notable component of care pathways when no on-site PICU was available. Any judgement of the value of this depends on the efficacy of de-escalation, about which little is currently known. The components of de-escalation have only recently been brought together and described,79 and have been coded into a model80 that forms part of the Safewards interventions known to be effective in reducing rates of conflict and containment. 39 This account of de-escalation is further expanded by the de-escalatory interventions identified in this study. Around half of all incidents to which a rapid response team were called in one hospital were resolved without the use of restraint, although this may have been as much a product of show of force as de-escalation. 81 An analysis of the CONSEQ data,3 obtained during the first 2 weeks of a hospital admission for 522 randomly sampled patients, showed that 60% of uses of de-escalation were successful, although de-escalation was less likely to be successful with patients who had a history of violence. 82 Research into de-escalation is at an early stage; current evidence suggests that it can be effective and therefore could to some degree act as a substitute for PICU care.
Observation within eyesight as an alternative to psychiatric intensive care unit care
There is a great paucity of information or evidence on the efficacy of this type of observation. The analysis of thresholds shows that this use of within-eyesight observation as a substitute for PICU care is specific to aggressive behaviour. Placing a member of staff within eyesight does mean that the patient concerned can be promptly distracted from activities likely to trigger their irritation or aggression, that other patients can be warned away or diverted from putting themselves at risk, and that de-escalation and other interventions such as PRN medication are offered early and at times when they are most likely to be effective. When aggression does occur, it means that someone is present to call for assistance immediately and then intervene so as to prevent harm. However, within-eyesight observation might also place the observer at some risk, as it can be highly irritating to the patient to be followed around by another person and therefore actually evoke the behaviour that the team wishes to prevent. In some hospitals (known to the authors but not in the TEPI sample) this risk means that all such observation is done on a two-to-one basis (two nurses to one patient being observed) and therefore is an expensive option, as well as potentially being even more irritating to the patient who is subject to it. The only evidence that has a bearing on the efficacy of observation for aggression is a natural experiment in which observation was successfully substituted for seclusion in one PICU. 83 This does not really take us much further, and more research is urgently required on this topic.
Calm-down methods, show of force and seclusion/psychiatric intensive care unit availability
It was unclear why show of force and calm-down methods showed contrasting associations with PICU and seclusion availability. Their positive association with the provision of seclusion might indicate that they form part of a regular process of getting into seclusion, in other wards that show of force is used to persuade the patient to voluntarily enter the seclusion room and calm-down methods are offered to the patient once they are in seclusion. However, in relation to PICU availability, calm-down methods and show of force are associated with its absence, whereas it can be imagined that show of force might be needed to compel transfer. It is possible that as PICU transfers take time, the crisis is over before the transfer takes place and such interventions are not required. Nevertheless, the association of show of force with the absence of an on-site PICU remains without an explanation. Findings from the City-128 study offer no help here, as no relationship was found between seclusion/PICU availability and rates of show of force in that study. 84
Reviews of care and seclusion/psychiatric intensive care unit availability
Fewer reviews of care were reported when seclusion or a PICU were not available. This is probably because hospital policies for seclusion and PICU transfer generally specify that formal reviews should take place; in the case of seclusion, these may be repeated at fixed intervals once seclusion has started. Those places without access to one or the other might benefit from instituting formal reviews of care as part of the management of disturbed behaviour, unless those reviews have poor utility and fulfil only a bureaucratic function. Such reviews do have the potential for the joint exploration of psychological and social causes of the patient’s difficult behaviour and thus have the potential to form part of a therapeutic process. This is yet another topic in the area of disturbed behaviour management that requires further evaluative research.
Normative 15-minute intervals for intermittent observation
This study provides the first empirical data on the typically implemented intervals for intermittent observation in the UK. A previously unpublished review of the policies of 31 mental health trusts by D Stewart and L Bowers (King’s College London, 2012) reported that:
The minimum time period for checking patients was either 5, 10 or 15 minutes. Eight Trusts did not specify a minimum time, while a further two advised that checks should be entirely random. The maximum time interval included 10, 15, 30 and 60 minutes, although 30 minutes was the most frequent recommendation (n = 16). Seven policies did not specify a maximum interval for checking patients. The highest number of intervals specified in a single policy document was six, while two policies specified only one permissible interval (15 minutes in both cases). However, most Trusts (n = 21) did not provide guidance for the total number of possible time intervals for intermittent observation. Seven policies advised that checks on patients should vary within the specified interval. For example, where checks were prescribed to take place every 15 minutes, this should be conducted at different times within this period.
The issue of intervals is important because intermittent observation is one of several important mechanisms on acute psychiatric wards for the prevention of suicide, in that it has a demonstrable degree of efficacy, as it has been shown to be critical in stopping serious suicide attempts in progress. 85 Intermittent observation has been criticised, as some patients still successfully take their own lives in the intervals between checks;86 however, to deduce that it should therefore not be used is a logical fallacy. Some patients who are prescribed antidepressants still take their own lives, but this is not an argument to cease such prescriptions. Intermittent observation is one of a wide range of suicide prevention precautions taken by wards and their staff, and has a useful place when matched to the assessed risks for patients. However, clearly the interval length is going to have implications for its potential efficacy and it might be considered a relatively easy improvement to decrease the normative time interval to 10 minutes when intermittent observation is used.
Team vigilance as an observation method
Team vigilance may be an interesting addition to practice, involving the whole team on an informal basis and not carrying any bureaucratic burden of monitoring and reporting. To be more widely used it might be of benefit to consider in what circumstances it could be used and to manage what level and what types of risk. These questions being answered, it still needs to be made clear how the team of nurses are to put ‘vigilance’ into effect; in other words, what does it actually mean? Without such specification, alerting all of the staff members to be aware and vigilant regarding a specific patient may turn out to mean very little or even nothing, or might mean very different things to different members of staff. On the other side of such an equation, formalisation and regulation may actually make staff less likely to opt for using this as one tool to keep their ward safer for patients.
Manual restraint on the bed
The high number of manual restraints on the bed may be an issue of concern. Such restraints may arise when the patient is taken to a side room, for the sake of privacy, for the administration of medication by injection when some degree of force is being used. Alternatively, it may arise when the patient and the restrainers are seated on the edge of the bed and the patient’s arms are held. Perhaps most worrying would be the prone full-force restraint of a patient on the bed, as bedding, pillows and the soft nature of the mattress might all make it more difficult for the patient to breathe. Currently, manual restraint training in the UK is provided by a number of different organisations, none of which makes publicly available the range of techniques it teaches. It is, therefore, impossible to say whether or not restraint on a bed is covered during the training of staff. This is an issue of some concern. Further research on the actual practice of manual restraint (not just the teaching of it) is clearly required to guide staff.
The four initial hypotheses
These were that the absence of seclusion and/or restricted access to PICU care are managed through one or more of the following four mechanisms.
-
Substitution: seclusion for a PICU (or vice versa) or other alternatives such as medication (regular in higher-dose, more intensely sedating medications and/or routes of faster or more effective absorption, intramuscular/intravenous) and/or long-duration manual restraint, time out or open-area seclusion (confinement of a disturbed patient in a separate area together with nursing staff) of some form.
-
The process of substitution was supported by the data. In the absence of seclusion there was greater use of coerced intramuscular medication, PRN medication and nursing in a side room (open-area seclusion). In the absence of an on-site PICU there was greater use of seclusion, de-escalation and observation. No evidence was found for changes in the use of a low-stimulus environment (time out) other than nursing in a side room. Insufficient data were collected to provide an answer on the issue of long-duration manual restraint.
-
-
Early intervention: faster response to escalation, earlier physical intervention, leading to safer management and more benign outcomes, possibly accompanied by temporarily increased nurse staffing levels or the use of intensive forms of constant special observation (such as two staff to one patient).
-
This hypothesis was not supported. There were no differences found in rates of manual restraint use between the hospitals studied, although the failure to find such differences may be due to the precise content of the TEPI in relation to patient responses to staff actions.
-
-
Therapeutic intensity: deployment of a range of psychotherapeutic and behavioural interventions to manage, ameliorate and reduce the frequency of risky patient behaviours.
-
This was not supported. In fact, there was one indication that psychological interventions were more likely to be considered if a PICU was available on site. There were few reports at all of endeavours to psychologically understand disturbed behaviour or to respond to it in a creative or therapeutic way. As such, this study supports others demonstrating ‘therapeutic poverty’ in UK psychiatric nursing practice. 87
-
-
Non-standard transfer: move of the patient to another ward providing more secure or intensive care in some fashion, perhaps in a private hospital or in a neighbouring trust, or via a secure rehabilitation ward or a forensic ward of some type.
-
This was not supported. There were no differences in the rates of non-standard transfers reported as part of the escalation pathway, by whether seclusion or an on-site PICU were available.
-
Strengths and limitations
One of the strengths of this study is that data were collected directly from those people who were actively and directly in charge of taking decisions about the management of patient behaviour. Through the use of an interview format to obtain data, staff could be asked about the management of relatively rare events that would be difficult or impossible to collect information about in any other way, such as by observation. Standardised scenarios presented to the interviewees during a structured interview meant that differences in their responses were more likely to reflect differences in practices between the hospitals studied. For a qualitative study, this sample size was large, adding to the external validity of the results. Moreover, the sample was not limited to hospitals in London and was, therefore, more likely to be generalisable to acute psychiatric care in the UK as a whole. Differences between the different hospitals were not explicable by different rates of adverse incidents. In other words, hospitals that managed without seclusion of PICU care did not do so because they were caring for less disruptive, less ill and calmer patients. In fact, the indications were for the reverse in relation to PICU care, and it was the presence of an on-site PICU that was associated with calmer and more peaceful wards.
Nevertheless, there are several limitations to our findings. Only eight hospitals were part of the sample, moderating the generalisability of the findings, and the two research areas, London and the North West, may not be wholly comparable. Local policies for the use of seclusion and/or transfer to a PICU may have varied in important ways between the different hospitals, irrespective of the basic availability of each technique, giving rise to the results that have been obtained. The TEPI was a long and complex interview, and interviewers had difficulty in completing it precisely as asked on every occasion. The design of the TEPI itself was constrained by the many additional factors that could influence the escalation pathway, particularly the response of patients to each intervention attempted by the staff. Thus, many aspects of the scenarios had to be constrained to produce standardised situations that would allow us to identify differences between hospital practices. Not the least of these standardisations was the restriction of the scenarios and data collection to focus on male patients only. Although this was a practical necessity, it will have shaped the findings to some unknown degree. In addition, our data may be influenced by the desire of staff to show their wards in a good light; thus, they may have preferentially described ideal rather than actual practice on their wards. Differences in pathway length between the different types of hospitals remain unexplained, and it remains possible that the statistical differences we have described are caused by other local characteristics, rather than the availability or otherwise of seclusion or PICU care. Power and precision would have been reduced by our achieved sample size (n = 81), compared with that planned (n = 120).
Conclusions
Our analysis in itself does not provide clear evidence of the benefits or harms associated with seclusion or PICU. If a seclusion room is provided, it may perhaps be used more than strictly necessary. If it is not provided, other measures may be substituted that might be considered equally unpalatable or potentially more risky. On the other hand, the absence of seclusion does present a potential therapeutic opportunity via nursing the patient in a side room. PICU care might be considered superior to either of these alternatives, but without easy access to PICU care far more use is made of seclusion. There were fewer differences around PICU provision, as those hospitals without an on-site PICU could, albeit with more difficulty, access PICU care on other sites. This relationship between PICU availability and seclusion means that judgements about the appropriateness and utility of on-site PICU are inseperable from judgements about seclusion. There is clear scope for more therapeutic interventions and practice in the management of disturbed behaviour, and this should be a priority for practice development and education if necessary. Many issues came to light from the data of this study, indicating the urgent need for further research to guide practice in the management of disturbed behaviour. Rather than focus on the provision of specific interventions, services could address overall conflict and containment prevention via such evidence-based methods as Safewards. 39
Chapter 6 Conclusions and recommendations
Comparison of results
Together, our findings highlight the striking variation in how staff at different hospitals respond to challenging behaviour as well as the difficulty in ascertaining the effectiveness of the techniques that are used. When seclusion is available and used, members of staff view this practice more positively and are quicker to manually restrain patients whose behaviour is escalating, both factors being likely to lead to some degree of excessive and unnecessary use. Moreover, when seclusion rooms are present, less use is made of nursing patients in a side room under close observation and/or rapid tranquillisation, alternatives that may have better outcomes. When a PICU is more available locally, staff make less use of special observation and supervision of patients, a method known to be more acceptable to patients. Overall, accidental or historical factors are, therefore, presumed to dominate over the choice of interventions and only improved quantitative studies, perhaps of the types outlined in the discussion in Chapter 3, are likely to provide any impetus from research to change this.
Overall limitations
It is important to note that, although we have attempted to employ a wide range of robust methodological approaches to investigate seclusion and PICU care, there are a number of noteworthy limitations. The statistical modelling in Chapters 2 and 3 was based on electronic records obtained from a single NHS trust; these routinely collected records are, of course, characterised to some extent by biases and deficits. These limitations extend to the economic analyses that utilised the same electronic records. The escalation pathway interviews, although conducted with a wider sample (spanning several NHS trusts), were limited in number, and we experienced difficulties in standardised execution and analysis. In addition, all findings relate to acute inpatient care for adult patients only and therefore cannot be readily taken to apply to care of elderly, child/adolescent or forensic psychiatric patients. Serious questions about the efficacy and value of seclusion and PICU care remain, highlighting the urgent need for further rigorously designed outcome studies.
Research recommendations
The pressing need is for non-randomised studies that may yield unbiased estimates of the effects of PICU transfer, seclusion and, indeed, other coercive interventions on relevant outcomes and costs. Although we did not succeed in doing this, our results demonstrate the feasibility of doing so based on altered design. In the case of seclusion, even an enriched sample of controls from our own trust ought to enable the necessary comparisons; the problem we had was an insufficient number of control observations (n = 26) rather than their total lack. In the case of a PICU, the difficulty was more fundamental. Propensity scores barely overlapped between treated and control observations; here, as we have already suggested, it may be possible to take advantage of different service configurations to include subjects treated in settings where transfer to a PICU is unusual or does not occur.
Leaving aside the approach of evaluating existing interventions, there is also the possibility of actively intervening to reduce coercion in all its forms. What is required is research into therapeutic interventions for disturbed behaviour: managers, clinicians and service users would benefit from knowing whether or not there are particular approaches not based on coercion that are able to avert conflict and subsequent violence. This would not only be valuable in its own right, but also opens up the possibility of active control treatments for future randomised trials, should these ever be necessary.
Acknowledgements
Contributions of authors
Len Bowers (Professor of Psychiatric Nursing) was lead investigator for the research on nurse attitudes and escalation pathways, and conducted the analysis of the escalation pathway interviews. He was the primary investigator initially and throughout the study.
Alexis E Cullen (Postdoctoral Research Fellow and Honorary Lecturer) extracted and cleaned all data derived from electronic medical records, conducted analyses to determine predictors of treatment receipt, and performed analyses to examine the impact of PICU transfer/seclusion on adverse incidents and length of stay.
Evanthia Achilla [Doctor of Philosophy (PhD) Student] performed all analyses examining costs of a PICU and seclusion, including exploratory cost-effectiveness analyses not included in this report.
John Baker (Professor of Mental Health Nursing) co-ordinated data collection in the North of England and contributed to the design, analysis and interpretation of study 2.
Mizanur Khondoker (Senior Lecturer) provided guidance on the statistical analyses performed in Chapters 2 and 3.
Leonardo Koeser (PhD Student) cowrote the script to extract economic data and manually cleaned these data.
Lois Moylan (Professor of Nursing) provided the MAPAT and advised on the interpretation of all findings for study 2.
Sophie Pettit (Research Fellow) completed data entry and coding for the escalation pathway interviews, and also conducted the analysis of nurse attitudes.
Alan Quirk (Senior Research Fellow) aided and advised on interview construction and all parts of study 2.
Faisil Sethi (Consultant Psychiatrist) advised on the interpretation of the findings of study 2.
Duncan Stewart (Senior Research Fellow) contributed to study 2 design and interpretation.
Paul McCrone (Professor of Health Economics) was comodule lead for study 1 and provided overall direction of the economic analyses.
Alex D Tulloch (Lecturer and Consultant Psychiatrist) was comodule lead for study 1, provided overall direction of analyses in Chapters 2 and 3, produced scripts to derive study cohorts, cowrote the economic data script, extracted economic data and edited the final version of the report, acting as deputy to the primary investigator.
Publications
Patel R, Chesney E, Cullen AE, Tulloch AD, Broadbent M, Stewart R, McGuire P. Clinical outcomes and mortality associated with weekend admission to psychiatric hospital. Br J Psychiatry 2016;209:29–34.
Cullen AE, Bowers E, Khondoker M, Pettit S, Achilla A, Koeser L, et al. Factors associated with use of psychiatric intensive care and seclusion in adult inpatient mental health services [published online ahead of print 20 October 2016]. Epidemiol Psychiatr Sci 2016.
Pettit S, Bowers L, Tulloch AD, Cullen AE, Moylan L, Sethi F, et al. Acceptability and use of coercive methods across differing service configurations with and without seclusion and/or psychiatric intensive care units. J Adv Nursing 2017;73:966–76.
Forthcoming
A further paper will be prepared and submitted based on Chapter 4.
Data sharing statement
Data for study 1 may be available to interested parties via the Maudsley BRC, but cannot be distributed. Data for study 2 will be kept for 5 years and may be available for collaborative research that falls within the purposes outlined in the original ethics submission.
Because of information governance arrangements, data for study 1 cannot be shared; however, interested parties may contact the corresponding author (alex.tulloch@runbox.com or alex.tulloch@kcl.ac.uk) to discuss possibilities for reanalysis.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Van Der Merwe M, Muir-Cochrane E, Jones J, Tziggili M, Bowers L. Improving seclusion practice: implications of a review of staff and patient views. J Psychiatr Ment Health Nurs 2013;20:203-15. http://dx.doi.org/10.1111/j.1365-2850.2012.01903.x.
- Bowers L, Van Der Merwe M, Nijman H, Hamilton B, Noorthorn E, Stewart D, et al. The practice of seclusion and time-out on English acute psychiatric wards: the City-128 Study. Arch Psychiatr Nurs 2010;24:275-86. http://dx.doi.org/10.1016/j.apnu.2009.09.003.
- Bowers L, Ross J, Nijman H, Muir-Cochrane E, Noorthoorn E, Stewart D. The scope for replacing seclusion with time out in acute inpatient psychiatry in England. J Adv Nurs 2012;68:826-35. http://dx.doi.org/10.1111/j.1365-2648.2011.05784.x.
- Whittington R, Bowers L, Nolan P, Simpson A, Neil L. Approval ratings of inpatient coercive interventions in a national sample of mental health service users and staff in England. Psychiatr Serv 2009;60:792-8.
- Mind . Listening to Experience: An Independent Inquiry into Acute and Crisis Care 2011.
- Olofsson B, Jacobsson L, Gilje F, Norberg A. Being in conflict: physicians’ experience with using coercion in psychiatric care. Nord J Psychiatry 1999;53:203-10.
- Bowers L. TAWS Internet Paper 3: The Validity of the Patient-Staff Conflict Checklist-Shift Report (PCC-SR) Evaluated 2008. www.kcl.ac.uk/ioppn/depts/hspr/research/ciemh/mhn/projects/taws/TAWS-IP03.pdf (accessed 20 June 2017).
- Hyde CE, Harrower-Wilson C. Psychiatric intensive care in acute psychosis. Int Clin Psychopharmacol 1996;11:61-5. https://doi.org/10.1097/00004850-199605002-00010.
- Birnie WA, Matsuno K. The psychiatric acute observation unit in a general hospital. Can J Psychiatry 1988;33:707-10.
- Bowers L, Hammond N, James K, Quirk A, Robson D, Stewart D. Characteristics of acute wards associated with the presence of a psychiatric intensive care unit, and transfers of patients to it. J Psychiatr Intens Care 2012;8:66-77.
- Bowers L, Crowhurst N, Alexander J, Eales S, Guy S, McCann E. Psychiatric nurses’ views on criteria for psychiatric intensive care: acute and intensive care staff compared. Int J Nurs Stud 2003;40:145-52. https://doi.org/10.1016/S0020-7489(02)00043-3.
- Bowers L, Allan T, Haglund K, Muir-Cochrane E, Nijman H, Simpson A, et al. The City-128 extension. Locked Doors in Acute Psychiatry, Outcome and Acceptability. Report for the National Coordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO). London: Her Majesty’s Stationery Office; 2008.
- Cullen AE, Bowers E, Khondoker M, Pettit S, Achilla A, Koeser L, et al. Factors associated with use of psychiatric intensive care and seclusion in adult inpatient mental health services [published online ahead of print 20 October 2016]. Epidemiol Psychiatr Sci 2016.
- Bowers L. Psychiatric Intensive Care Units: A Literature Review. London: City University; 2006.
- Chang CK, Hayes RD, Perera G, Broadbent MT, Fernandes AC, Lee WE, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLOS ONE 2011;6. http://dx.doi.org/10.1371/journal.pone.0019590.
- Hayes RD, Chang CK, Fernandes A, Broadbent M, Lee W, Hotopf M, et al. Associations between substance use disorder sub-groups, life expectancy and all-cause mortality in a large British specialist mental healthcare service. Drug Alcohol Depend 2011;118:56-61. http://dx.doi.org/10.1016/j.drugalcdep.2011.02.021.
- Stewart R, Soremekun M, Perera G, Broadbent M, Callard F, Denis M, et al. The South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLAM BRC) case register: development and descriptive data. BMC Psychiatry 2009;9. http://dx.doi.org/10.1186/1471-244X-9-51.
- Fernandes AC, Cloete D, Broadbent MT, Hayes RD, Chang CK, Jackson RG, et al. Development and evaluation of a de-identification procedure for a case register sourced from mental health electronic records. BMC Med Inform Decis Mak 2013;13. http://dx.doi.org/10.1186/1472-6947-13-71.
- International Classification of Diseases. Geneva: World Health Organization; 2016.
- Mental Health Act. London: The Stationery Office; 1983.
- Dack C, Ross J, Papadopoulos C, Stewart D, Bowers L. A review and meta-analysis of the patient factors associated with psychiatric in-patient aggression. Acta Psychiatr Scand 2013;127:255-68. http://dx.doi.org/10.1111/acps.12053.
- Cornaggia CM, Beghi M, Pavone F, Barale F. Aggression in psychiatry wards: a systematic review. Psychiatry Res 2011;189:10-2. http://dx.doi.org/10.1016/j.psychres.2010.12.024.
- Iozzino L, Ferrari C, Large M, Nielssen O, de Girolamo G. Prevalence and risk factors of violence by psychiatric acute inpatients: a systematic review and meta-analysis. PLOS ONE 2015;10. http://dx.doi.org/10.1371/journal.pone.0128536.
- Brown S, Bass N. The psychiatric intensive care unit: patient characteristics, treatment and outcome. J Ment Health 2004;13:601-9. https://doi.org/10.1080/09638230400017095.
- Feinstein A, Holloway F. Evaluating the use of a psychiatric intensive care unit: is ethnicity a risk factor for admission?. Int J Soc Psychiatry 2002;48:38-46. https://doi.org/10.1177/002076402128783073.
- Pereira S, Sarsam S, Bhui K, Paton C. The London Survey of Psychiatric Intensive Care Units: psychiatric intensive care; patient characteristics and pathways for admission and discharge. J Psychiatr Intens Care 2006;1:17-24. https://doi.org/10.1017/S174264640500004X.
- Barlow K, Grenyer B, Ilkiw-Lavalle O. Prevalence and precipitants of aggression in psychiatric inpatient units. Aust N Z J Psychiatry 2000;34:967-74. https://doi.org/10.1080/000486700271.
- Mental Health Act Commission . Count Me in 2008: Results of the 2008 National Census of Inpatients in Mental Health Hospitals and Facilities in England and Wales 2008.
- Khan A, Cohen S, Chiles J, Stowell M, Hyde T, Robbins M. Therapeutic role of a psychiatric intensive care unit in acute psychosis. Compr Psychiatry 1987;28:264-9. https://doi.org/10.1016/0010-440X(87)90033-2.
- Musisi SM, Wasylenki DA, Rapp MS. A psychiatric intensive care unit in a psychiatric hospital. Can J Psychiatry 1989;34:200-4.
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983;70:41-55. https://doi.org/10.1093/biomet/70.1.41.
- Angrist JD, Pischke J-S. Mostly Harmless Econometrics: An Empiricist’s Companion. Princeton, NJ: Princeton University Press; 2009.
- Heckman J, Ichimura H, Smith J, Todd P. Characterizing selection bias using experimental data. Econometrica 1998;66:1017-98. https://doi.org/10.2307/2999630.
- Crump RK, Hotz VJ, Imbens GW, Mitnik OA. Dealing with limited overlap in estimation of average treatment effect. Biometrika 2009;96:187-99. https://doi.org/10.1093/biomet/asn055.
- Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 2015;34:3661-79. http://dx.doi.org/10.1002/sim.6607.
- Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol 2006;163:1149-56. https://doi.org/10.1093/aje/kwj149.
- Barber JA, Thompson SG. Analysis of cost data in randomized trials: an application of the non-parametric bootstrap. Stat Med 2000;19:3219-36. https://doi.org/10.1002/1097-0258(20001215)19:23<3219::AID-SIM623>3.0.CO;2-P.
- Nijman H, Allertz W, Merckelbach H, Ravelli D. Aggressive behaviour on an acute psychiatric admissions ward. Eur J Psychiat 1997;11:106-14.
- Bowers L, James K, Quirk A, Simpson A, Stewart D, Hodsoll J. SUGAR . Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. Int J Nurs Stud 2015;52:1412-22. http://dx.doi.org/10.1016/j.ijnurstu.2015.05.001.
- Code of Practice Mental Health Act 1983. London: The Stationery Office; 2015.
- National Minimum Standards for General Adult Services in Psychiatric Intensive Care Units (PICU) and Low Secure Environments. London: Department of Health; 2002.
- Muralidharan S, Fenton M. Containment strategies for people with serious mental illness. Cochrane Database Syst Rev 2006;3. http://dx.doi.org/10.1002/14651858.CD002084.pub2.
- Bowers L. On conflict, containment and the relationship between them. Nurs Inq 2006;13:172-80. https://doi.org/10.1111/j.1440-1800.2006.00319.x.
- Olofsson B, Norgberg A, Jacobsson L. Nurses’ experience with using force in institutional care of psychiatric patients. Nord J Psychiatry 1995;49:325-30. https://doi.org/10.3109/08039489509011924.
- Dack C, Ross J, Bowers L. The relationship between attitudes towards different containment measures and their usage in a national sample of psychiatric inpatients. J Psychiatr Ment Health Nurs 2011:577-86. http://dx.doi.org/10.1111/j.1365-2850.2011.01832.x.
- Cashin A. Seclusion: the quest to determine effectiveness. J Psychosoc Nurs Ment Health Serv 1996;34:17-21.
- Stewart D, Bowers L, Simpson A, Ryan C, Tziggili M. Manual restraint of adult psychiatric inpatients: a literature review. J Psychiatr Ment Health Nurs 2009;16:749-57. http://dx.doi.org/10.1111/j.1365-2850.2009.01475.x.
- Paterson B, Bradley P, Stark C, Saddler D, Leadbetter D, Allen D. Deaths associated with restraint use in health and social care in the UK. The results of a preliminary survey. J Psychiatr Ment Health Nurs 2003;10:3-15. https://doi.org/10.1046/j.1365-2850.2003.00523.x.
- Moylan LB, Cullinan M. Frequency of assault and severity of injury of psychiatric nurses in relation to the nurses’ decision to restrain. J Psychiatr Ment Health Nurs 2011;18:526-34. http://dx.doi.org/10.1111/j.1365-2850.2011.01699.x.
- Lemonidou C, Priami M, Merkouris A, Kalafati M, Tafas C, Plati C. Nurses’ perceptions toward seclusion and use of restraints for psychiatric patients in Greece. Eur J Psychiat 2002;16:81-90.
- Bowers L, Alexander J, Simpson A, Ryan C, Carr-Walker P. Cultures of psychiatry and the professional socialization process: the case of containment methods for disturbed patients. Nurse Educ Today 2004;24:435-42. http://dx.doi.org/10.1016/j.nedt.2004.04.008.
- Moylan LB. Physical restraint in acute care psychiatry: a humanistic and realistic nursing approach. J Psychosoc Nurs Ment Health Serv 2009;47:41-7. https://doi.org/10.3928/02793695-20090301-10.
- Bowers L, Simpson A, Alexander J, Hackney D, Nijman H, Grange A, et al. The nature and purpose of acute psychiatric wards: the Tompkins Acute Ward Study. J Ment Health 2005;14:625-35. https://doi.org/10.1080/09638230500389105.
- Muir-Cochrane E, Bowers L, Jeffery D. Comparison in attitudes between nursing and other students in relation to containment measures for disturbed psychiatric patients. Nurse Educ Today 2009;29:83-90. http://dx.doi.org/10.1016/j.nedt.2008.07.002.
- Alty A. Nurses’ learning experience and expressed opinions regarding seclusion practice within one NHS trust. J Adv Nurs 1997;25:786-93. https://doi.org/10.1046/j.1365-2648.1997.1997025786.x.
- Festinger L. A Theory of Cognitive Dissonance. Evanston, IL: Row Peterson; 1957.
- Harris G, Rice M, Preston D. Staff and patient perceptions of the least restrictive alternatives for the short-term control of disturbed behaviour. J Psychiatr Law 1989;17:239-63.
- Fisher A. The ethical problems encountered in psychiatric nursing practice with dangerous mentally ill persons. Sch Inq Nurs Pract 1995;9:193-208.
- Wynaden D, Orb A, McGowan S, Castle D, Zeeman Z, Headford C, et al. The use of seclusion in the year 2000: what has changed?. Collegian 2001;8:19-25. https://doi.org/10.1016/S1322-7696(08)60018-9.
- Pettit S, Bowers L, Tulloch AD, Cullen AE, Moylan L, Sethi F, et al. Acceptablility and use of coercive methods across differing service configurations with and without seclusion and/or psychiatric intensive care units. J Adv Nurs 2017;73:966-76. http://dx.doi.org/10.1111/jan.13197.
- Bowers L, Allan T, Simpson A, Jones J, Van Der Merwe M, Jeffery D. Identifying key factors associated with aggression on acute inpatient psychiatric wards. Issues Ment Health Nurs 2009;30:260-71. http://dx.doi.org/10.1080/01612840802710829.
- Bowers L, Whittington R, Nolan P, Parkin D, Curtis S, Bhui K, et al. Relationship between service ecology, special observation and self-harm during acute in-patient care: City-128 study. Br J Psychiatry 2008;193:395-401. http://dx.doi.org/10.1192/bjp.bp.107.037721.
- Anonymous, Service User and Carer Group Advising on Research (SUGAR) . About Us n.d. https://blogs.city.ac.uk/sugar/about-us/ (accessed 9 May 2017).
- Delaney KR, Johnson ME. Keeping the unit safe: mapping psychiatric nursing skills. J Am Psychiatr Nurses Assoc 2006;12:198-207.
- Gladwin CH. Ethnographic Decision Tree Modeling. Thousand Oaks, CA: Sage; 1989.
- Garfinkel H. Studies in Ethnomethodology. Oxford: Polity Press; 1967.
- Wittgenstein L. Philosophical Investigations. Oxford: Blackwell Publishers; 1968.
- Keski-Valkama A, Sailas E, Eronen M, Koivisto AM, Lönnqvist J, Kaltiala-Heino R. A 15-year national follow-up: legislation is not enough to reduce the use of seclusion and restraint. Soc Psychiatry Psychiatr Epidemiol 2007;42:747-52. http://dx.doi.org/10.1007/s00127-007-0219-7.
- Bjørkly S. Open-area seclusion in the long-term treatment of aggressive and disruptive psychotic patients, an introduction to a ward procedure. Psychol Rep 1995;76:147-57. http://dx.doi.org/10.2466/pr0.1995.76.1.147.
- Stewart D, Bowers L. Under the gaze of staff: special observation as surveillance. Perspect Psychiatr Care 2012;48:2-9. http://dx.doi.org/10.1111/j.1744-6163.2010.00299.x.
- Stewart D, Bowers L, Ross J. Managing risk and conflict behaviours in acute psychiatry: the dual role of constant special observation. J Adv Nurs 2012;68:1340-8. http://dx.doi.org/10.1111/j.1365-2648.2011.05844.x.
- Paterson B, Leadbetter D, McComish A. Restraint and sudden death from asphyxia. Nurs Times 1998;94:62-4.
- Bergk J, Einsiedler B, Flammer E, Steinert T. A randomized controlled comparison of seclusion and mechanical restraint in inpatient settings. Psychiatr Serv 2011;62:1310-17. http://dx.doi.org/10.1176/appi.ps.62.11.1310.
- Bowers L, Ross J, Owiti J, Baker J, Adams C, Stewart D. Event sequencing of forced intramuscular medication in England. J Psychiatr Ment Health Nurs 2012;19:799-806. http://dx.doi.org/10.1111/j.1365-2850.2011.01856.x.
- Greenberg WM, Moore-Duncan L, Herron R. Patients’ attitudes toward having been forcibly medicated. Bull Am Acad Psychiatry Law 1996;24:513-24.
- Haglund K, Von Knorring L, Von Essen L. Forced medication in psychiatric care: patient experiences and nurse perceptions. J Psychiatr Ment Health Nurs 2003;10:65-72. https://doi.org/10.1046/j.1365-2850.2003.00555.x.
- Veltkamp E, Nijman H, Stolker JJ, Frigge K, Dries P, Bowers L. Patients’ preferences for seclusion or forced medication in acute psychiatric emergency in the Netherlands. Psychiatr Serv 2008;59:209-11. http://dx.doi.org/10.1176/appi.ps.59.2.209.
- Quirk A, Lelliott P, Seale C. Service users’ strategies for managing risk in the volatile environment of an acute psychiatric ward. Soc Sci Med 2004;59:2573-83. https://doi.org/10.1016/j.socscimed.2004.04.005.
- Price O, Baker J. Key components of de-escalation techniques: a thematic synthesis. Int J Ment Health Nurs 2012;21:310-19. http://dx.doi.org/10.1111/j.1447-0349.2011.00793.x.
- Bowers L. A model of de-escalation. Ment Health Pract 2014;17:36-7. https://doi.org/10.7748/mhp.17.9.36.e924.
- Ryan CJ, Bowers L. An analysis of nurses’ post-incident manual restraint reports. J Psychiatr Ment Health Nurs 2006;13:527-32. https://doi.org/10.1111/j.1365-2850.2006.00975.x.
- Lavelle M, Stewart D, James K, Richardson M, Renwick L, Brennan G, et al. Predictors of effective de-escalation in acute inpatient psychiatric settings. J Clin Nurs 2016;25:2180-8. http://dx.doi.org/10.1111/jocn.13239.
- Lehane M, Rees C. Alternatives to seclusion in psychiatric care. Br J Nurs 1996;5. http://dx.doi.org/10.12968/bjon.1996.5.16.974.
- Bowers L, Van Der Merwe M, Paterson B, Stewart D. Manual restraint and shows of force: the City-128 study. Int J Ment Health Nurs 2012;21:30-4. http://dx.doi.org/10.1111/j.1447-0349.2011.00756.x.
- Bowers L, Dack C, Gul N, Thomas B, James K. Learning from prevented suicide in psychiatric inpatient care: an analysis of data from the National Patient Safety Agency. Int J Nurs Stud 2011;48:1459-65. http://dx.doi.org/10.1016/j.ijnurstu.2011.05.008.
- Appleby L, Shaw J, Kapur N, Windfuhr K, Ashton A, Swinson N, et al. Avoidable Deaths: Five Year Report of the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness. Manchester: University of Manchester; 2006.
- Bowers L, Wright S, Stewart D. Patients subject to high levels of coercion: staff’s understanding. Issues Ment Health Nurs 2014;35:364-71. http://dx.doi.org/10.3109/01612840.2013.871088.
Appendix 1 Threshold and Escalation Pathway Interview
Set-up
Consent.
Quiet room.
Agree not to be interrupted.
Switch on digital recording and make sure it is working (test).
Check battery life on equipment.
Participants
This interview is for qualified nurses only.
They must first have completed the demographic data sheet, the ACMQv2 and the MAPAT.
Name of interviewee . . .
Ward of interviewee . . .
Hospital of interviewee . . .
Introduction to the interview
Thank you for agreeing to be interviewed. During the interview, I am going to present you with three case studies of patients whose behaviour gradually becomes more difficult and challenging to manage. We’d like you to tell us how these would be managed if the patient was on your ward. We are interested to know what typically happens here on this ward in these circumstances. There are no right or wrong answers to the questions we are going to ask and we are not here to express any judgement or praise about what you tell us. We just need to find out what usually happens here so that we can compare it to other wards and hospitals.
The time it takes to complete this interview does vary, but we have learnt it usually takes between an hour and an hour and a half.
[State for the tape the name of the hospital, the name of the ward, and the research number of the participant.]
[Setting] Typical mid-week morning shift on your ward, the usual numbers of staff on duty (ask how many that would be, and proportion qualified/unqualified), no ward round being held during the shift.
[Content] We are going to present you with three cases of patients whose behaviour is disturbed. We will tell you a little bit of background about each patient, then give you an example of their behaviour, asking you to describe how such behaviour is usually managed on your ward. We will then give you an example of the patient behaving in an even more disturbed way, again asking you to tell us how they would be managed on your ward. We will continue to give you examples of ever more extreme behaviour, one by one, until we reach the worst case scenario.
So we are interested in how the staff manage difficult behaviours immediately, and how they manage them in the longer term. We’ll therefore be asking questions like ‘what happens if the patient doesn’t stop, or does certain things repeatedly’.
This can be a little uncomfortable, but be reassured this is not about how well you do your job. Instead it is to make sure we find out accurately how disturbed behaviour is managed on your ward.
We are specifically interested in the handling of male patients. All our example patients are male, and when we ask you questions about how patient behaviours are managed, we are talking about male patients only. Thanks for bearing this in mind.
Case 1: Mike
[Remind of setting] Typical mid-week morning shift on your ward, the usual numbers of staff on duty, no ward round being held during the shift.
[Cameo] Mike is an older white British man, 53 years, many previous admissions but new to the ward and area, having moved recently from elsewhere, long-term unemployed, he has a schizoaffective disorder and is in a manic state, has not been taking his medication and was admitted on a section 2 yesterday after causing a disruption in a shopping centre.
BM1Behaviour 1: Mike is refusing to take his prescribed oral mood stabiliser and antipsychotic medication.
How would the staff on this ward manage Mike and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
Special probe on confrontation
BM1 A: What if anything would be different if Mike was refusing his regular medication just after admission, but he had a long history of previous assaults on staff while manic, and he was clearly overactive and irritable?
BM2 Behaviour 2: Mike comes out of his bedroom completely naked, and walks through the day room then comes to the office door and asks for a cup of tea.
How would the staff on this ward manage Mike and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BM3 Behaviour 3: What if instead Mike is giving property away; you find out today he gave an expensive jacket to someone else (person unknown) last night, and gave all cigarettes to a fellow patient this morning and is now asking the staff for cigarettes.
How would the staff on this ward manage Mike and his behaviour (giving valuable personal property away)?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BM4 Behaviour 4: What if instead Mike is loud, shouting at voices, occasionally screaming at the top of his voice, annoying and irritating other patients who are starting to threaten him or lose their temper and shout at him to shut up.
How would the staff on this ward manage Mike and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BM5 Behaviour 5: What if instead Mike has just attempted to abscond, almost managing to get out by slipping through the door when something was being delivered by the porters.
Just to check, is the door on your ward always locked to patients trying to leave? Is it locked most of the time, or is it generally open?
Whichever is the case, Mike has been prevented from leaving without permission. How would the staff on this ward manage Mike and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BM6 Behaviour 6: What if instead Mike approaches one of the female members of staff, touches her breasts, stroking them, and suggests loudly that they have sex together in his bedroom.
How would the staff on this ward manage Mike and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
OK, we have come to the end of talking about Mike.
BME1: Do you want to say anything further about Mike and the management of his behaviour? Anything you can add about his management, or want to clarify about what you have already told us?
[Next question for staff from mixed-sex wards only.]
BME2: If the case we have been talking about was a woman, would your answers have been any different? If so, how?
[Refusing regular medication, stripping off clothing, giving away property, shouting, attempting to absconding, sexually touching a female member of staff.]
Case 2: Steve
[Remind of setting] Typical mid-week morning shift on your ward, the usual numbers of staff on duty, no ward round being held during the shift.
[Cameo] Steve is a middle-aged white British man, age 40, first admission yesterday following overdose of paracetomol, treated in hospital with antidote, lucky not to sustain liver damage. The attempt was prompted by his wife leaving the family home with children to live with another man and initiating divorce proceedings several months ago. Steve works as a secondary school English teacher but is currently off sick. On a section 2. Difficulty sleeping, not eating much or interacting with staff. Not engaging in ward activities.
BS1 Behaviour 1: You find him sitting on the floor in the TV room, he is crying. He tells you he does not want to live any more.
How would the staff on this ward manage Steve and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BS2 Behaviour 2: He pulls out a small piece of broken piece of glass from behind him and holds it tightly. It is half the size of a pen and is cutting into his hand. He is sobbing uncontrollably and says ‘I want to die’, and begins scratching his upper arms with the glass.
How would the staff on this ward manage Steve and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
Repetition questions can only be meaningfully asked here if the patient is not on constant observation – so be sure to ask how long the constant observation would last, and if it drops to intermittent within a shift or two, then ask about the repetition of the behaviour.
BS3 Behaviour 3: What if instead of a small piece of glass, Steve has a broken bottle which he is holding by the neck, and he is making deep cuts in his upper arm with jagged end. He says he wants to die.
How would the staff on this ward manage Steve and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
Repetition questions can only be meaningfully asked here if the patient is not on constant observation – so be sure to ask how long the constant observation would last, and if it drops to intermittent within a shift or two, then ask about the repetition of the behaviour.
BS4 Behaviour 4: What if instead of the cutting, Steve runs away to another part of the ward, and you catch up in time to see him grab a belt and lock himself in the toilet. You try to talk to him, but get no response, so you open the door and find him just starting to tie the belt around his neck.
How would the staff on this ward manage Steve and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
Repetition questions can only be meaningfully asked here if the patient is not on constant observation – so be sure to ask how long the constant observation would last, and if it drops to intermittent within a shift or two, then ask about the repetition of the behaviour.
BSE1: Do you want to say anything further about Steve and the management of his behaviour? Anything you can add about his management, or want to clarify about what you have already told us?
[Next question for staff from mixed-sex wards only.]
BSE2: If the case we have been talking about was a woman, would your answers have been any different? If so, how?
[Expressing suicidal ideation, scratching with glass, cutting with bottle, attempted suicide.]
Case 3: Alan
[Remind of setting] Typical mid-week morning shift on your ward, the usual numbers of staff on duty, no ward round being held during the shift.
[Cameo] First admission, admitted yesterday, Alan is a 20-year-old young white British man, average build and height, has worked as a building labourer, deluded, hallucinated, perplexed and without insight. It is difficult to have a conversation with him, he is thought disordered, angry and has been admitted under Section 2 of the Mental Health Act.
BA1 Behaviour 1: Alan is pacing up and down the ward restlessly, frowning, then becomes verbally abusive and shouting at other patients.
How would the staff on this ward manage Alan and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BA2 Behaviour 2: Alan turns over furniture, throwing objects around the ward (not deliberately at others), picking up a chair and hitting the wall with it, on top of shouting and being verbally abusive.
How would the staff on this ward manage Alan and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BA3 Behaviour 3: Same again, Alan has broken furniture and is being verbally abusive, but he has broken a chair against the wall and has picked up a chair leg which he is waving threateningly like a club.
How would the staff on this ward manage Alan and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
Special probe on weapons
[Ask the following questions only if the previous example did not elicit a call for the police. If the interviewee has already said this, we can assume he or she will report the same call for the following two weapon examples.]
BA3A: What if anything would be different if he had a broken bottle in his hand that he was waving threateningly?
or
BA3B: What if anything would be different if he had a kitchen carving knife in his hand that he was waving threateningly?
[No diagram necessary unless participant describes an entirely different chain of events.]
BA4 Behaviour 4: Alan is attacking a fellow patient with punches and kicks, and the assault is still under way when the nurse arrives on the scene.
How would the rest of the staff on this ward manage Alan and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
BA5 Behaviour 5: Alan is attacking a fellow patient very seriously by throwing him to the ground is kicking him with maximum available force.
How would the staff on this ward manage Alan and his behaviour?
| Who did | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
|
| What | ||
| Where | ||
| With what | ||
| While | ||
| Name | ||
| Duration | ||
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
[If at the end of this example, the interviewee has not yet talked of taking the patient to the floor, explore what happens when they are.]
Alan struggled so vigorously and has been so difficult to contain that the restraint team have taken him to the floor. What happens next? [Use over the page to make a record.]
Special probe on verbal thresholds and other issues
So, Alan has been verbally abusive, smashed furniture, and assaulted another patient. Previously we have said he is unable or unwilling to engage in discussion or negotiation about his behaviour.
BA5A: What if anything would be different in his management if he pleads self-defence on the grounds that he has paranoid beliefs about the person he attacked or hallucinatory experiences (e.g. he says ‘I heard him thinking bad things about me’, or ‘he was going to kill me when I turned my back’)?
[In questions BA4A to BA4F, allow the respondent to answer, then ask the following questions, circling their answer (i.e. whether staff would be ‘more likely’ or ‘less likely’ to respond in a certain way or be ‘just the same’). No diagram necessary unless participant describes an entirely different chain of events. Circle the interviewees’ choices so that we do not have to extract the data from each audio record!]
Would it be more likely or less likely that staff on this ward would invest time in talking to Alan before acting, or be just the same as when he could not communicate?
Would it be more likely or less likely, that staff on this ward would end up restraining Alan on the floor, or be just the same as when he could not communicate?
If restraint did occur, would it be more likely or less likely, that it would last for more than 10 minutes, or be just the same as when he could not communicate?
BA5B: What if anything would be different in his management if he apologises, saying he should not have done it, although the other patient gave him a funny look?
Would it be more likely or less likely, that staff on this ward would invest time in talking to Alan before acting, or be just the same as when he could not communicate?
Would it be more likely or less likely, that staff on this ward would end up restraining Alan on the floor, or be just the same as when he could not communicate?
If restraint did occur, would it be more likely or less likely, that it would last for more than 10 minutes, or be just the same as when he could not communicate?
BA5C: What if anything would be different in his management if he apologises, saying he should not have done it, although the other patient had been calling him names, threatening him, trying to get money and cigarettes from him, and being abusive (and there have been previous similar complaints from others about the patient who has been assaulted)?
Would it be more likely or less likely, that staff on this ward would invest time in talking to Alan before acting, or be just the same as when he could not communicate?
Would it be more likely or less likely, that staff on this ward would end up restraining Alan on the floor, or be just the same as when he could not communicate?
If restraint did occur, would it be more likely or less likely, that it would last for more than 10 minutes, or be just the same as when he could not communicate?
BA5D: What if anything would be different in his management if the person he has assaulted is a small and rather frail older person in their 60s who may have early dementia?
Would it be more likely or less likely, that staff on this ward would invest time in talking to Alan before acting, or be just the same as when the victim was a patient more similar in size and strength to himself?
Would it be more likely or less likely, that staff on this ward would end up restraining Alan on the floor, or be just the same as when the victim was a patient more similar in size and strength to himself?
If restraint did occur, would it be more likely or less likely, that it would last for more than 10 minutes, or be just the same as when the victim was a patient more similar in size and strength to himself?
BA5E: What if anything would be different in his management if the person Alan has assaulted is one of the ward nurses?
Would it be more likely or less likely, that staff on this ward would invest time in talking to Alan before acting, or be just the same as when the victim was a fellow patient?
Would it be more likely or less likely, that staff on this ward would end up restraining Alan on the floor, or be just the same as when the victim was a fellow patient?
If restraint did occur, would it be more likely or less likely, that it would last for more than 10 minutes, or be just the same as when the victim was a fellow patient?
BA5F: What if anything would be different in his management if it was noticed that Alan’s face was flushed, he was a bit unsteady on his feet and he smelt strongly of alcohol?
Would it be more likely or less likely, that staff on this ward would invest time in talking to Alan before acting, or be just the same as when he was sober?
Would it be more likely or less likely, that staff on this ward would end up restraining Alan on the floor, or be just the same as when he was sober?
If restraint did occur, would it be more likely or less likely, that it would last for more than 10 minutes, or be just the same as when he was sober?
Special probe on influence of known history
Can we just go back for a minute to the very first scenario with Alan? You’ll remember he was pacing up and down the ward restlessly, frowning, then becoming verbally abusive and shouting at other patients.
We have been talking about Alan as if he was a new patient that this was his first admission. What if this was actually his second admission, and the last time he was admitted he assaulted a member of staff quite badly, so that she was off work for a week with cuts and bruises?
Now think about Alan pacing up and down the ward restlessly, frowning, then becoming verbally abusive and shouting at other patients.
BA5G: How would the staff on this ward manage Alan and his behaviour?
[Be careful not to lead the interviewee; instead get them to expand on any differences in how they would respond and what they mean. Unpack the phrases they use so you get a good understanding of this.]
Would it be more likely or less likely, that staff on this ward would invest time in talking to Alan before acting, or be just the same as when he had no such history?
Would it be more likely or less likely, that staff on this ward would end up restraining Alan on the floor, or be just the same as when he had no such history?
If restraint did occur, would it be more likely or less likely, that it would last for more than 10 minutes, or be just the same as when he had no such history?
Thank you. We have come to the end of the questions about Alan.
BAE1: Do you want to say anything further about Alan and the management of his behaviour? Anything you can add about his management, or want to clarify about what you have already told us?
[Next question for staff from mixed-sex wards only.]
BAE2: If the case we have been talking about was a woman, would your answers have been any different? If so, how?
[Shouting/abusive, turning over furniture, breaking furniture and wielding chair leg as weapon, assaulting a fellow patient with punches and kicks, throwing patient to floor and kicking with maximum force.]
Is there anything else you would like to add to what you have said, or any additional comments you would like us to take note of?
Conclusion questions
On your ward, how many staff are typically on duty mid morning on a usual mid-week shift? Numbers of qualified nurses? Numbers of health-care assistants? Numbers of anyone else? What is the number of beds on your ward?
Is your ward an ordinary acute ward, or does it have a specialist function? Triage? Assessment? Treatment? Anything else, and if so, what does it mean?
For each of the behaviours in the case studies:
-
How often does a patient behave this way on your ward, typically? Has it (or something very similar) happened in the past week? Month? 6 months? Year? Ever in your experience? Never?
[Fill out the form below with the interviewee.]
| Has this happened on your ward during the. . .? | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Once | Same patient, repeatedly during 24 hours | |||||||||
| Past week | Past month | Past 6 months | Year | Never | Past week | Past month | Past 6 months | Year | Never | |
| Aggression | ||||||||||
| Agitated, verbally abusive, shouting | ||||||||||
| Aggressive towards objects, breaking things | ||||||||||
| Brandishing a broken chair leg or similar as a weapon | ||||||||||
| Physically attacks a fellow patient, punches/kicks or equivalent | ||||||||||
| Self harm and suicidality | ||||||||||
| Stated suicidal intent or threats of suicide | ||||||||||
| Scratches to skin with some form of sharp object | ||||||||||
| Deep cuts with a sharp item to limbs, or equivalent behaviour | ||||||||||
| Attempted suicide by tying a ligature round neck, attempted hanging, self-suffocation or other serious equivalent | ||||||||||
| Mania | ||||||||||
| Coming into the public areas of the ward naked | ||||||||||
| Giving away their own property to others | ||||||||||
| Loud, shouting, screaming | ||||||||||
| Attempting to abscond | ||||||||||
| Sexual assault, touching others inappropriately | ||||||||||
| Refusing to take his prescribed antipsychotic medication or equivalent on admission | ||||||||||
Concluding thanks
Thank you very much for participating in the interview. We really appreciate it, and this will help the development of nursing care of disturbed patients in the future. We’d be most grateful if you did not discuss your responses to the questions in the interview with other nurses at this hospital until we have finished doing all our interviews. That is because we would like to pose the questions fresh to each person, without them having any previous presuppositions.
Thank you again, and we will be letting the wards here at the hospital know what our results are when we have them – keep an eye out for a leaflet or small poster summarising the results, and giving a link to our final report.
Appendix 2 Threshold and Escalation Pathway Interview: instructions for interviewers
All case studies are male in order to rule out sex effects.
Anything in square brackets [ ] represents an instruction to you, the interviewer, and should not be read out.
All interviewees should have completed the demographic data sheet, the ACMQ and the MAPAT prior to undertaking this interview.
The purpose of the interview
We are interviewing nursing staff in order to ascertain the thresholds at which different patient management methods are deployed, and how increasingly difficult behaviours are managed. We want to know whether there are any methods not previously formally described in the literature, and we want to know the circumstances within which they are used. We know that the same behaviours must be managed differently between units that have and do not have seclusion. In this study we want to find out what those differences are, how the escalation pathways differs at hospitals without seclusion, or in those places that have more restricted access to psychiatric intensive care.
Method of the interview
We have devised three true to life case examples involving white British men: Mike (mania), Steve (self-harm and suicide) and Alan (aggression). For each case example we have descriptions of increasingly difficult behaviour to manage. It is your task to discover how those difficult behaviours are typically managed in the hospitals where you are conducting interviews. Not how the interviewees think they should be managed, but how they are generally managed.
As a result of the interview data you collect, we want to draw up an escalation pathway diagram for each hospital in the study, so we can show how things differ in different places, or what the differing solutions are.
The structure of the interview
The following diagram depicts the flow of the interview:
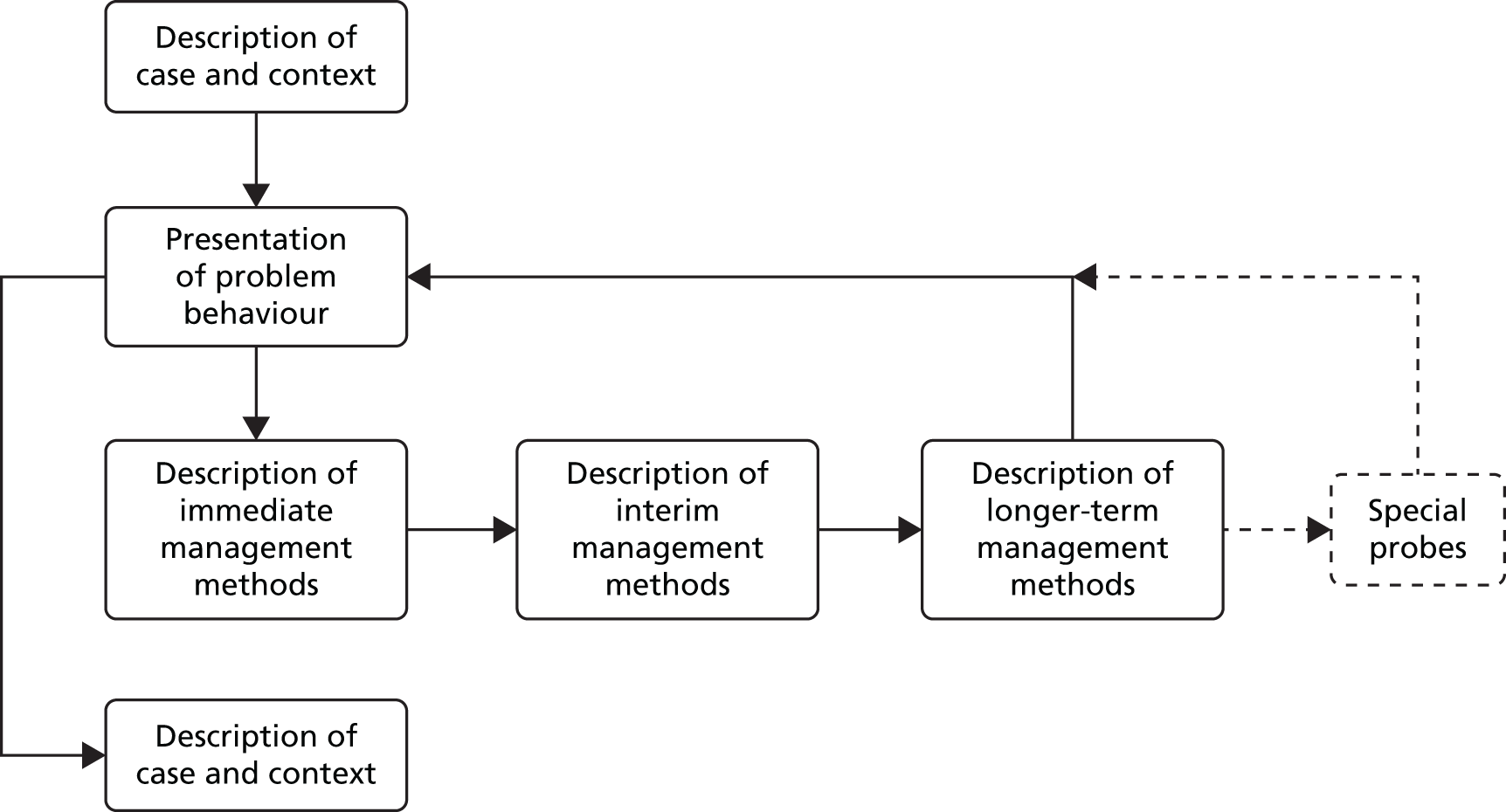
First you present a little cameo description of the case, then go on to present the first problem behaviour to the interviewee, and ask how that would be managed on the ward, including who carries out that procedure, how and where it is done and other details. If the management method is something that goes on continuously for more than a few minutes, further questions are asked about what happens if the patient continues or repeats the same behaviour. For selected containment methods responses to physical resistance are explored. Then finally questions are asked about what happens if the behaviour continues repeatedly over ever longer time periods. In some cases special probe questions follow. Once this is exhausted, then next problem behaviour is presented and the questions repeated. This goes on until all the problem behaviours for that particular case are dealt with, after which the next case is presented.
Each case is not linear in terms of escalation. Each behaviour for each individual patient should be taken largely on its own. To put this another way, you are not presenting a staged cumulative picture of the patient’s behaviour: Alan is first verbally abusive, then afterwards he is aggressive to objects, then he assaults another patient, etc. When you are presenting the interviewee with the assault on a fellow patient, there is no implication that the verbal abuse or aggression to objects has already taken place. Each behaviour is to be considered de novo, as if it arises by itself on the mid-week morning shift under discussion.
Using the grid of reminders
Below each problem behaviour example is a grid of reminder questions. This grid is to remind you to remember to ask all the relevant questions. When a management method is mentioned, label a column with a shorthand name (e.g. ‘Time out’), then tick the boxes when you have asked the relevant questions. Put a cross in boxes where the question is clearly not relevant to the management method being discussed.
| Time out | ||
|---|---|---|
| Who did | ✓ | Time out (in room by self with door unlocked): the first time this is mentioned, explore what happens if the patient comes out of the room once, then repeatedly Manual restraint on the floor: the first time this is mentioned explore what happens if the patient continues to physically struggle |
| What | ✓ | |
| Where | ✓ | |
| With what | ✗ | |
| While | ✓ | |
| Name | ✗ | |
| Duration | ✓ | |
| Then repetition within shift, through to following shift, then through to next day, then several days | ||
-
Who did: who does the management method, what disciplines, how many of them and who decides to use it
-
Who’s involved, how many staff, what sort of staff (discipline, size, sex, extra staff such as bank or agency, staff from this ward or other wards, any particular requirements)? If they give a wide range of staff numbers (e.g. 3 to 10), ask what determines the number who are used?
-
Who takes the decision and how? Is there some sort of consultation process, does someone have to be called, how long does that take, what happens while it is going on etc.?
-
-
What: what exactly do they do, a full and detailed description
-
Alarms: if raising the alarm, or pressing the alarm, or making a call for help is mentioned, find out the details of the alarm system. How does it work? Where is the button, where does it sound, what does it sound like? How long it takes to get a response from others in the ward and other staff on other wards? How many people come, and what happens while the staff are waiting for them to arrive?
-
Movement of the patient to another place: where does this take place? If not on the ward, how far away is it (stairs, corridors, journey in the open air to get there)? How is the patient moved to the location?
-
Intensive care: how it is done organisationally from referral, what type of assessment through to how the patient is transferred in what sort of vehicle if necessary accompanied by what staff numbers, and how long everything takes.
-
Observation: intermittent (what intervals) or constant? Within eyesight? Within arms length? Whereabouts on the ward? Maintaining physical contact? What would you see if you were there? Is time in the toilet supervised? Is the observation carried out by one, two or more staff?
-
Restraint: how many people, holding what? Is the patient seated, on the bed, on the floor, prone or face up? Standing, being walked, or led by the hand?
-
Time out: does someone stay with the patient? How many? Physical contact? Inside the room, or outside the room, or in the doorway?
-
Seclusion: does someone stay with the patient, so with constant observation? If not, how frequent are checks?
-
Medication: what drugs are used? What form are used if oral – tablets, liquid, fastmelt, or what?
-
De-escalation: talk to him or de-escalate the situation. Ask what this means – seeking cause to resolve, or telling impacts on others and not appropriate, or what?
-
Police: if the police are called, then who calls, how long does it take them to arrive, what do you do with the patient until they arrive, how many police arrive and with what equipment, what happens then, and what happens to the patient after they leave?
-
Medical emergency: medical response team, 222 or other numbers dialled to activate teams of people. Make sure you know who comes with what equipment and what skills, and how long they take to arrive
-
-
Where: where does this happen, what location on the ward?
-
With what: what equipment or special room is used, size, shape, features? Is any special equipment, kit or room(s) required? What is it? Where is it: on the ward, somewhere else? What does it look like, how is it constructed?
-
If taken to the de-escalation suite, extra care area, quiet room, sensory room, time out room, etc., what does this room or suite look like, where is it on the ward, what is in the room?
-
Seclusion: CCTV, observation window, toilet facilities, temperature control, music, etc.
-
-
While: what else is happening while this is going on, in other words if the staff are with the patient in time out, or holding them in restraint, are they doing anything else at the same time (do not prompt for de-escalation but see if it is mentioned and what they mean by it)?
-
What do the staff say to the patient, how do they interact with them during this procedure?
-
-
Name: is there a local name for the method, what do you call it here?
-
Duration: how long will this go on for, when does it stop and by what criteria?
Please differentiate between management methods. For manual restraint, any change of position or location of the patient, or the numbers of staff involved equals a new management method for which all the relevant grid questions are asked. Similarly, for time out, a person in the room with the patient constitutes a different intervention from that person being outside, the door wide open is different from, the door being closed, etc.
Obtain detailed information about the management method, in words that would be understood by a person without professional or specialist nursing knowledge. Phrases like ‘counselled about his behaviour’, ‘setting limits’, ‘specialled’ or ‘time out’ need to be unpacked, because they can mean different things on different wards. To find out what they mean, ask ‘Can you tell me what you mean by [that]?’ or words to that effect.
Other terms used by the interviewee may also need behavioural definition, for example ‘escalating behaviour’, ‘kicking off’, ‘given access to fresh air’, ‘cigarette break’.
There is no need to duplicate these descriptions if the person mentions the same terminology a second time, just check with the interviewee that they mean exactly the same thing. If exactly the same, move on, if not get them to describe the variation and then move on.
Bear in mind that we are just as interested in therapy interventions if they are mentioned, such as referral to a psychologist, dialectical behaviour therapy (DBT) sessions, specific groups, occupational therapy (OT) referrals, activity programmes, etc., and we would need just as much detail about what these actually mean, how long they take to organise, who does them, etc.
Dealing with two interventions mentioned together – ask the grid questions in reference to both, especially the description of exactly what these mean. An example might be ‘then we’d talk to him to calm him down while we moved him in the direction of his bedroom’. Here, the grid questions need to be asked with reference to (1) the talking and (2) the moving.
If the interviewee offers a conditional management strategy (e.g. ‘we’d restrain him sitting down, but if that failed to work we’d take him to the floor’), then reply ‘let’s talk about the first thing (sitting down) first, and we will come to the follow up afterwards’.
If respondents offer a choice of what might happen, find out which of them is more likely on their ward, and then proceed with questions on that. If they really refuse to choose, then you choose whatever you consider to be the more severe strategy, and continue the interview on that basis.
Do not prompt the interviewee with suggestions as to what might happen. Do not ask questions like ‘and would you give any medication?’ or ‘wouldn’t the police be called?’. The interviewees must be allowed to determine their own responses even if they miss obvious things out. Over the 15 interviews at the same site, a general pattern will emerge.
We are not really primarily asking for staff’s rationales for using different containment methods at different thresholds, what we are trying to find out is what the ward’s typical escalation pathway is. So do not follow up with ‘why’ questions unless they are germane to answering this primary question.
Repetition/duration
The questions about duration may be particularly important and should be asked and followed up carefully. What is tolerable and manageable for one shift becomes very difficult after a period (we do not know how long, or if this varies from place to place).
Present the interviewee with the behaviour you are asking about being repeated once the management method proposed is over, i.e. the patient is no longer restrained, is out of seclusion, has had intramuscular (IM) or PRN oral medication, or if the proposed management method is intermittent or constant observation or some type.
-
OK, that is how you manage the patient in the short term: what about for the rest of the shift if they behave in the same way repeatedly or continually?
-
What about if the problem continues through to the next day, even after you have tried that?
-
What about over several days, even after you have tried those things?
Pursue these questions until the interviewees says they have no further ideas on what to do. If a new management question is introduced by the interviewee, repeat the grid questions.
Transfer to PICU at any point terminates exploration of the behaviour, once the process of transfer has been described (i.e. how it is organised, how long it takes, how the patient is transported, etc). Placing the patient in seclusion means you can continue to ask about the behaviour being repeated after seclusion terminated. The same applies to restraint and most other management methods.
Patient scenarios: patient resistance
Theoretically there are three increasingly more severe types of resistance that a patient might offer to attempts by staff to contain their behaviour: (1) verbal refusal to comply with a management method, ‘No!’ when asked to do something or move somewhere; (2) passive resistance, physical non co-operation, not moving of own volition, but not struggling either; (3) physically struggling against some form of manual restraint holds, or other physical noncompliance (e.g. moving away).
Except where indicated otherwise, portray the patient as passively resistant. In other words the patient will not move unless physically forced, but does not struggle against the use of such physical force. So, more than just verbal resistance (1), but less than active physical resistance (3). With respect to oral PRN medication, this means that whenever it is offered, the patient refuses to accept it, and you proceed with exploring the staff response on this basis.
In only two cases do we want you to explore responses to actual physical resistance.
Firstly, when time out with the patient in the room by him or herself is first encountered, we want you to explore what happens when the patient refuses to stay in the room, coming out counter to the commands of staff.
Secondly when manual restraint on the floor is first encountered, we want you to explore what happens when the patient continues to struggle against the holding done by staff.
This means that in these two cases there will be a fork in the chain of events you explore – first you will finish what happens if the patient only passively resists. Then you will return to the time out or to the manual restraint on the floor, and explore what happens if they are physically resisted by the patient, drawing out a description of a new branch of the escalation pathway.
It is particularly important here to elicit how long the staff will stop and tolerate the given active physical resistance before moving on to a more severe form of containment, if at all. So always elicit this timing, unless it is obvious from the reply that the staff step up to another containment method immediately, then just check this is so – ‘So, straight away then?’.
These explorations of physical resistance only need to be done once during the interview, if these management methods (time out by self in room, or manual restraint on the floor) are mentioned thereafter, passive resistance only should be described, and the following events to that should have already been elicited by you.
Keeping the interviewee on track
Do not let the interviewee control the interview. For example, you might start asking how they would manage a verbally abusive Alan, the interviewee might themselves introduce more extreme behaviours, saying for example ‘We’d try verbal de-escalation, but if the patient started to be physically violent we would restrain them’. In cases like this you need to prompt the interviewee back to task: at the moment we are only thinking about verbal abuse and how that is generally managed on this ward.
Similarly, if they say their response would depend on why the patient acted in that way, you should respond that the patient is unable or unwilling to say why. If the interviewee says the response depends on whether staff member X or Y is on duty, you should ask what the response is the way things are done most of the time.
If they lapse into talking about a specific patient: ‘we had someone who did this last week, and we did so and so’, please respond by saying that we do not want to know about an individual patient, what we want to know is what happens usually or typically.
Keeping participants on topic
Remind the interviewee frequently of the behaviour you are talking about.
Use constant prompts (e.g. what typically happens on this ward, what generally happens here, what usually goes on, how patients like this are managed most of the time). We do not want to know about ideal, or best possible practice, we want to find out what generally really does happen.
Experience of conducting this interview shows that interviewees often slip into talking about what they would do, or what they believe should happen in the cases you are presenting. A slip from the first person plural (‘we usually do. . ..’) to the first person singular (‘I would. . .’) often indicates such a change in thinking. If they do start to describe ‘what I prefer to do’ or ‘what I think should happen’, please reply that ‘For the purpose of this interview we want to know what actually happens here on the ward, rather than your preferences. What does usually happen in this situation?’.
If they ask for more details about the case, you should answer: ‘I am unable to tell you any more about this patient’ or ‘I don’t know any more about this patient. Please answer based on the details you have’. You can repeat the cameo at the participants request as often as they wish.
Very important: Be careful not to add to or expand the case study or behaviours yourself. Stick with the interview guide, and do not be tempted to elaborate. If you make your own variations, your results will not be comparable to those of other interviewers. In other words you will be making the interview unreliable.
Dealing with potential impasse
Might reach a point when they say that they have never encountered a patient that bad on their ward, or that they would not know what to do. If so, ask them what they would recommend, or what they think was likely to occur if it did happen? Thankfully some of the scenarios we are putting to the interviewees are very rare, so no interviewee is likely to have experienced them all. Thus, you need to push for their recommendation, perhaps coupled with a statement that although such situations are rare, they do sometimes happen.
If they say: ‘we don’t admit patients like this’, reply that in this case they have come on duty and found them to have been admitted contrary to the ward’s normal practice. If they say they would discharge them, you can respond that the events described happen while they are trying to organise and authorise such a discharge.
If the interviewee asks how many staff are on duty, replay as many as are on a typical mid-week morning shift. How many are there usually? Please answer as if that is the case.
Alternatively the interview may get stuck for reasons we have not anticipated (it is a complex interview). If this happens, be creative in how you resolve it, bearing in mind the intent of the research.
List of abbreviations
- ACMQv2
- Attitude to Containment Measures Questionnaire, version two
- BRC
- Biomedical Research Centre
- CI
- confidence interval
- CMHT
- community mental health team
- CONSEQ
- Sequences of Conflict and Containment Events study
- CRIS
- Clinical Records Interactive Search
- ID
- identifier
- IRR
- incident risk ratio
- MAPAT
- Moylan Progression of Aggression Tool
- MHA
- Mental Health Act
- OR
- odds ratio
- PICU
- psychiatric intensive care unit
- PRN
- pro re nata
- SD
- standard deviation
- SE
- standard error
- SLaM
- South London and Maudsley NHS Foundation Trust
- SPICES
- Seclusion and Psychiatric Intensive Care Evaluation Study
- SQL
- Structured Query Language
- TEPI
- Threshold and Escalation Pathway Interview