Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5001/25. The contractual start date was in May 2013. The final report began editorial review in September 2016 and was accepted for publication in March 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Iestyn Williams is a member of the Health Services and Delivery Research (HSDR) Prioritisation Commissioning Panel. Glenn Robert is a member of the HSDR Prioritisation Researcher-led Panel.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Williams et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Context
All publicly funded health-care systems grapple with the challenge of meeting expanding health need with constrained resources, and this is exacerbated by long-term demographic and cultural trends. Allied to this, the NHS in England is currently facing one of the most challenging financial periods in its history, and the 2016 referendum on membership of the European Union has once again seen funding of health care return to the centre of political and media debate. 1 Part of the strategy for meeting this challenge involves the replacement or discontinuation of outmoded, obsolete, unaffordable or cost-ineffective services. This has led to the development of low-value treatment lists such as those recently advocated in the UK Academy of Medical Royal Colleges’ version of the international ‘Choosing Wisely’ initiative,2 the establishment of the Royal College of General Practitioners standing group on overdiagnosis3 and the British Medical Journal’s ‘Too Much Medicine’ campaign (see www.bmj.com/too-much-medicine). The importance of this is not just in reducing inappropriate spending but also in creating space for more innovative and effective ways of providing and delivering services.
The concern with the oversupply of medicine is one of the reasons why decommissioning – defined as the replacement, removal or reduction of health-care services and interventions – has been advocated. 4 However, in the absence of clear, evidence-informed guidance on effective decommissioning practice, the danger is that blunt and unsophisticated instruments are employed, leading to unnecessary turmoil, with no guarantee of positive outcomes,5 or to the simple avoidance of decommissioning. There is currently a lack of theoretically informed, evidence-based guidance to inform the design and implementation of decommissioning programmes. Therefore, developing a better understanding of how decommissioning programmes unfold in the NHS and elsewhere is a crucial first step towards improving policy and practice. The study reported here explores the experience of the NHS as it seeks to grapple with the challenge of decommissioning, and puts forward evidence-based suggestions for future practice.
As well as the need to address ‘too much’ medicine, the case for more substantial reconfiguration of NHS services has become a familiar theme in health policy and practice in recent years. An ageing population, increasing numbers of people living with long-term and complex conditions, and advances in medical technology and innovation mean that traditional models of care have come under political and clinical scrutiny. In addition, concerns about the quality of services following high-profile scandals such as Winterbourne View and Mid Staffordshire6 are reflected in the establishment of new regulatory structures and regimes. Reconfiguration of NHS services to meet these various challenges was a feature of the NHS Five Year Forward View published in 2014,7 which proposed new models of care such as multispeciality community providers, primary and acute care systems and a shift in investment towards primary care, prevention and self-management. This approach is intended to help reduce the £30B funding gap identified in the review7 with Clinical Commissioning Groups (CCGs), as the local health-care budget holders, taking responsibility for delivering such programmes of service reconfiguration. CCGs were formed in 2012 as part of a significant restructure of the NHS in England following the Health and Social Care Act (2012),8 which saw the abolishment of primary care trusts (PCTs) and strategic health authorities at regional level. In the current system, CCGs fund, plan and procure health-care services for their local communities, while NHS England, with the support of regionally based area teams, has responsibility for commissioning specialised services and selected other primary care services. Thus, decommissioning, particularly as part of wider processes of service reconfiguration, is one in a continuum of skills and activities that CCGs are expected to learn.
Most recently, the NHS has been asked to develop place-based sustainability and transformation plans (STPs) to cover all areas of NHS spending in England. 9 Local NHS leaders are required to work with local government partners to identify local priorities and reorganise services in order to improve efficiency and financial balance. Given the challenging financial climate, these plans are likely to involve some decommissioning of services and therefore to generate controversy, and the early signs are that the relative lack of public engagement in STPs will lead to opposition. 10
Changes at these levels of decision-making also fall within our definition of decommissioning, which includes interventions ranging from medicines and equipment to clinical services and patient pathways. The mechanisms and drivers for decommissioning also vary. For example, services might be reduced or removed through the application of eligibility criteria, practice guidelines and other forms of service restriction and scale-back. They may be withdrawn as a result of in-house service closure, external contract termination, service reconfiguration and formulary delisting. Quality, affordability and cost-effectiveness are typically cited as drivers of decommissioning, but other concerns such as safety, changes in demand and political imperatives may also be influential. Decommissioning implies an explicit approach in which the rationale and aims of decisions are made clear to all those involved. This definition excludes passive decommissioning, whereby interventions and services ‘wither on the vine’ through lack of use, or through processes such as organisational mergers and takeovers, which may result in de facto decommissioning of services but which are not presented as such. Our definition of active decommissioning implies a deliberate, intentional decision followed by explicit actions, irrespective of the success or otherwise of these actions in bringing about their intended aims.
In these ways we distinguish decommissioning from associated activities such as priority-setting, pathway redesign and technology coverage decision-making. Although each of these may be employed as mechanisms within a decommissioning programme, they do not necessarily involve the withdrawal and reduction of health-care interventions. Therefore, it is the explicit aim of removing, replacing or reducing existing interventions that distinguishes decommissioning from other forms of resource allocation and service-improvement initiatives that may or may not be adopted as part of a decommissioning programme.
Our definition of decommissioning is therefore broad and designed to encompass related activities such as divestment, deinsurance, discontinuance and service termination,11,12 as well as concepts such as exnovation and reverse innovation, which have also been used to describe health-care decommissioning. 13,14 The most commonly used concept in the recent health services literature is disinvestment. Typically this refers to decision-making in relation to the removal and reduction of clinical and therapeutic interventions (as opposed to broader services and organisations) and stems from health technology assessment (HTA) and the application of economic principles of cost-effectiveness analysis. While subsuming these activities, our definition of decommissioning also includes programme and service closure and/or relocation and is not confined to narrow notions of value maximisation. For example, decommissioning programmes driven by policy, patient acceptability and affordability fall within our sphere of interest.
Decommissioning as used here shares some characteristics of commissioning and the commissioning ‘cycle’. 15 Whereas the latter refers to a series of specific functions, including needs assessment, procurement and contract management, decommissioning refers to programmes of activity concerned with withdrawal or reduction in the scale and volume of services delivered. As such, decommissioning may be seen as part of a continuum of activities – alongside commissioning and recommissioning – that are often interconnected in the NHS. 16 For example, when an existing service or care pathway is being decommissioned, an alternative may need to be commissioned in order for this retreat to take place. However, decommissioning is not reducible to the commissioning function and may, for example, be instigated by provider organisations. Similarly, decommissioning takes place in health-care systems that do not have a commissioning function, whether led by government or other planners and resource allocators. 4,17
Examples of decommissioning activities include:
-
reducing investment in or access to a specific treatment (e.g. through altering formulary listing or changing treatment protocols)
-
replacing existing services with ones deemed to provide greater cost-effectiveness or a lower overall cost (including the transfer of the delivery of services into more cost-effective settings)
-
closure or discontinuation of health-care programmes and organisations, for example through non-renewal of contracts and agency downgrading.
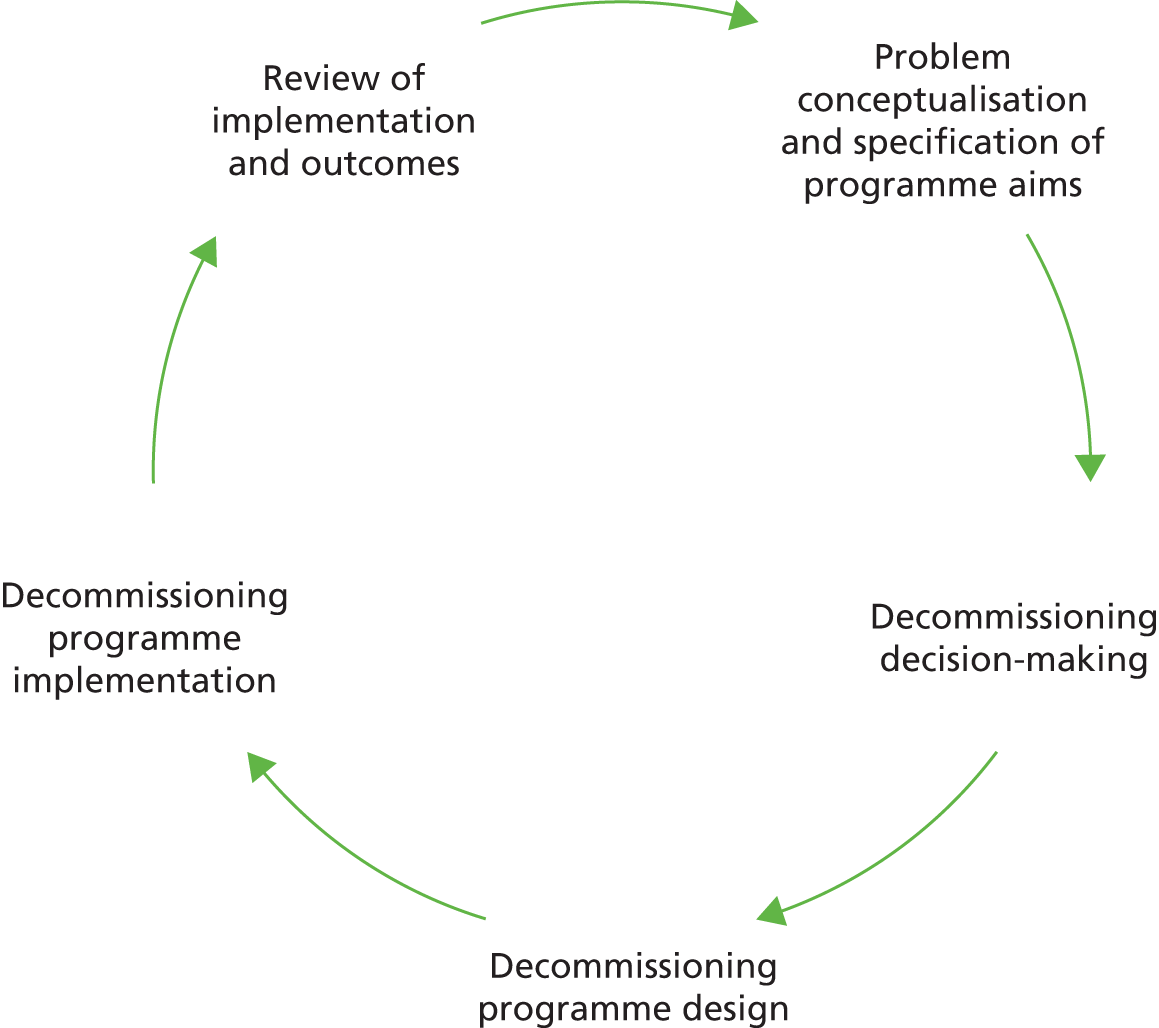
Key to each of these is the need to identify the candidates for decommissioning, as well as a requirement to design effective policies for the practical implementation of decommissioning programmes. Accordingly, at the outset of the research we developed a heuristic model of the ‘stages’ required for a typical decommissioning cycle, including the identification of need, processes for arriving at decommissioning decisions, and processes of implementation and review (Figure 1). In practice, however, progress through these stages is unlikely to be entirely predictable in terms of the exact distinction between, and the duration and sequencing of, stages.
FIGURE 1.
Stages of the decommissioning process.
Chapter 2 Research aims and objectives
The primary aim of this research is to formulate theoretically informed best-practice guidance for health-care managers by identifying and studying the factors and processes that influence the implementation and outcomes of decommissioning in the English NHS and other health systems. The study addresses the following research questions:
-
What is the international evidence and expert opinion regarding best practice for decommissioning in health care?
-
How and to what extent are NHS organisations currently implementing decommissioning?
-
What factors and processes influence the implementation and outcomes of decommissioning?
-
What are the perspectives and experiences of citizens, patient/service user representatives, carers, third-sector organisations and local community groups in relation to decommissioning?
The objectives of the research are to:
-
synthesise the existing international evidence and expert opinion on implementing decommissioning in health care
-
establish the extent and nature of decommissioning across the NHS by means of a national survey of NHS commissioners
-
carry out in-depth case studies of decommissioning in the English NHS
-
gauge the views and experiences of citizens, patient/service users, carers, third-sector organisations and local community groups in relation to decommissioning
-
develop evidence-based guidance on decommissioning for policy-makers and senior managers.
Chapter 3 Methodology
This chapter describes all aspects of study design, data collection and data analysis.
Conceptual framework for analysis
Much of the current literature on decommissioning in health care derives from evidence-based medicine and population health disciplines, and this study sought to complement this by drawing on insights from politics, systems and organisational/institutional analysis. Decommissioning programmes combine multiple interlocking processes and decision points, which mean that outcomes may be hard to predict. As well as this, theory and evidence suggests that perceived and real ‘losses’ can inhibit rates of decommissioning, thereby contributing to financial and administrative pressures on publicly funded health systems. 5 For example, Kahneman and Tversky’s prospect theory18 holds that, when faced with a risky decision, people’s attitudes concerning potential loss will be significantly different from their attitudes concerning possible gains. In other words, we value goods (or services) in our possession more highly than an equivalent service not yet experienced. The overarching theoretical framework for this project was made up of the following considerations:
-
the influence of ideas, interests and institutions on decommissioning decision-making and implementation
-
the stages of decommissioning programme design and implementation and how these influence outcomes
-
the complex processes of organisational change required to carry out decommissioning
-
process of translation associated with actor–network theory (ANT)
-
the concept of loss aversion.
Beyond this general orientation, we sought to be led in our analysis by findings from early work packages so that our most substantive work package, namely the case studies in work package 3, would be informed by a thorough appreciation of relevant aspects of context. This chapter explains how the project was sequenced so as to build our analytical tools and insights for the final synthesis and discussion of main messages and details all aspects of data collection.
Study design
The study comprises a multilevel investigation of decommissioning policies and programmes structured into four distinct but interconnecting work packages. Work package 1 was designed to address the first research question and also to inform the foci of the national survey and four case studies (work packages 2 and 3). Work packages 1 and 2 also provided a context for the analysis of findings from work package 3, enabling reflections on the transferability of findings. The case studies enabled us to explore gaps and unanswered questions identified in work packages 1 and 2. Finally, work package 4 (citizen, patient/service user representative, carer, third-sector and local community group perspectives) was added to the study following application for additional funds from the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme. We devised and implemented this final work package in order to build upon the engagement with patients and service user representatives in work packages 1–3.
Work package 1: synthesis of evidence and expert opinion
Work package 1 addressed the research question ‘What is the international evidence and expert opinion regarding best practice for decommissioning in health care?’. This involved four activities: a summary of the extant literature, a Delphi panel of decommissioning experts, a mapping exercise and collection of qualitative decommissioning narrative vignettes.
Summary of the extant literature
At the time of commencement of the research, a number of structured evidence reviews had been completed or commissioned in which the authors identify practical constraints caused by poor indexing of decommissioning and its synonyms. 17 In order to build on work under way and to avoid these well-documented indexing problems, we opted to collate and synthesise learning from existing literature reviews.
Our approach to synthesising the existing literature therefore took the form of a ‘review of reviews’. The aim was to distil relevant messages from the evidence base on decommissioning and how this relates and applies to the specific context of the English NHS, as well as to identify knowledge gaps and unanswered questions to be pursued in subsequent phases of our research. To these ends we analysed existing reviews from the period 1990–2016 to address the following questions:
-
How are terms such as ‘decommissioning’ and ‘disinvestment’ employed in the literature?
-
What are considered to be the main determinants of successful decommissioning programmes?
-
What models and frameworks are available to guide decommissioning and how have these been evaluated?
-
What are the remaining knowledge gaps in terms of evidence and practice?
Search terms were identified from a scoping search of the literature drawing on the expertise of the authors and project advisors (Table 1 and Figure 2). Searches were carried out at the beginning and end of the project to ensure that results were up to date at the time of writing and that early results were available to inform subsequent phases of research design and analysis. Existing reviews were identified in the first instance through searches of health databases. From the initial list of search terms, ‘termination’, ‘replacement’ and ‘closure’ were removed from the searches of MEDLINE as they generated unmanageable volumes of results. The term ‘health’ was added to searches of the non-health-specific database (Social Sciences Citation Index). Snowballing searches were also conducted, including citation analysis and bibliography scanning.
| Review components | Details |
|---|---|
| Dates | No restrictions |
| Reporting | English language |
| Search terms | ‘Decommissioning’ ‘Disinvestment’ ‘Divestment’ ‘Deinsurance’ ‘Exnovation’ ‘Discontinuation’ ‘Exit’ ‘Cutback’ ‘Replacement’ ‘Delisting’ ‘Deimplementation’ ‘Undiffusion’ ‘De-adoption’ and ’review’ or ‘synthesis’ or ‘evidence’ |
| Other inclusion criteria | Included documents were reviews of empirical literature related to the replacement, removal or reduction of services (broadly defined) in health-care settings internationally |
| Database hits | HMIC (128 hits), MEDLINE (409) CINAHL (126) SSCI (44) |
FIGURE 2.
Filtering flow chart.
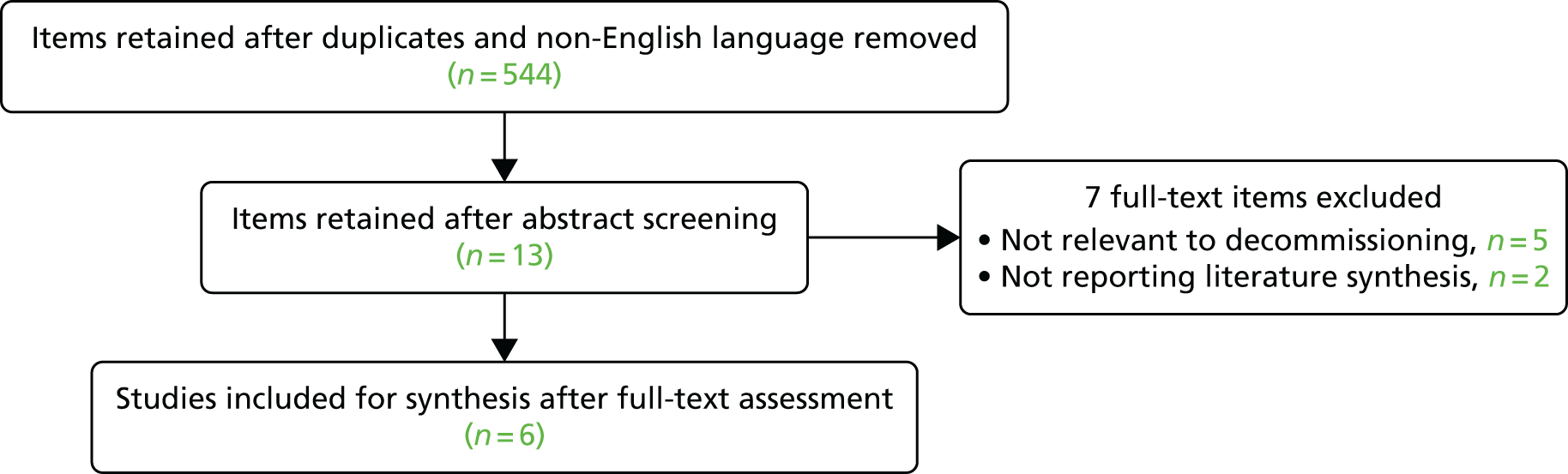
Synthesis of the six included literature reviews took the form of structured data extraction and tabulation against the five research questions (see Appendix 1). As the included reviews contained studies with a range of methodologies, our approach to synthesis was primarily descriptive, involving presentation rather than translation of main findings. 19 Results are presented in narrative form in Chapter 4.
Included reviews were confined to health settings and this is reflected in our synthesis. Although the scope for inclusion was wide in other respects, included reviews were somewhat skewed towards a narrow range of decommissioning types and were drawn largely from cognate disciplinary fields. In recognition of this, additional literature items uncovered during the search and retrieval process were summarised and incorporated in an unsystematic fashion. These were selected for inclusion if they were judged by the research team to complement the included reviews, for example by focusing on a wider range of decommissioning types or on relatively neglected stages of the decommissioning process (e.g. implementation). However, this process was opportunistic and non-replicable and a more in-depth evidence review was beyond the scope of our research. We put forward recommendations for future evidence synthesis in the conclusions chapter of this report (see Chapter 8).
Mapping the decommissioning landscape
In order to develop our understanding of the current decommissioning ‘landscape’ we conducted a mapping exercise of the roles and remit of agencies that might be expected to play a part in decommissioning in the NHS. No further sampling logic was employed. A list of potential organisations was drawn up by the research team and the project advisory group. Telephone interviews and/or searches of websites and official documents were carried out by two of the authors (JH and IW) in relation to each organisation, with the aim of establishing:
-
current roles and responsibilities with regard to decommissioning
-
current and planned decommissioning-related activities
-
perceptions regarding the challenges facing those leading decommissioning
-
any available good-practice guidance and other resources.
One interview was conducted at short notice and therefore was not audio-recorded, with note-taking carried out instead by the interviewer.
A key intended outcome of the mapping exercise was to inform the design of subsequent work packages and to provide a context to results emanating from the survey and case studies. Table 2 presents a list of organisations included and the method of data collection employed in each.
| Organisation | Data collection |
|---|---|
| Specialised commissioning area teams | Audio-recorded telephone interview |
| NHS Improving Quality | Audio-recorded telephone interview |
| IRP | Audio-recorded telephone interview |
| Care Quality Commission | Audio-recorded telephone interview |
| HealthWatch England | Audio-recorded telephone interview |
| Local government association | Audio-recorded telephone interview |
| NHS Clinical Commissioners | Written response and desktop research |
| NHS Confederation | Telephone interview, not recorded |
| NHS England Commissioning Development Directorate | Audio-recorded telephone interview |
| NHS Quality Board | Audio-recorded telephone interview |
| NICE | Audio-recorded telephone interview |
| NHS Alliance | Audio-recorded telephone interview |
| Monitor | Audio-recorded telephone interview |
| NCAT | Desktop research |
| OSCs | Desktop research |
Collecting qualitative decommissioning vignettes
To augment these assessments of the published research and the decommissioning landscape, we compiled a sample of retrospective accounts from individuals who had led decommissioning programmes within health and social care contexts in England. These narrative vignettes were collected through seven semistructured interviews carried out by two of the authors (JH and IW) with an opportunistic sample of local leaders of decommissioning processes identified through early mapping work and other suggestions of the advisory group. 20 The aims were to:
-
explore the stages and activities involved in a sample of recent decommissioning journeys
-
identify the actors and agencies involved in local processes of decommissioning to inform sampling for case studies conducted in work package 3
-
gain additional insight into the challenges, contexts and determinants of contemporary decommissioning processes in the NHS and related service areas.
Interviews were semistructured so as to enable core issues to be covered while allowing new themes to emerge. Three interviews were not audio-recorded at the request of interviewees, although note-taking was carried out. Table 3 provides further details of data collection.
| Interviewee | Decommissioning example | Method | Length of interview |
|---|---|---|---|
| Health-care review project lead (PCT) | Closure and relocation of walk-in centres to emergency department | Audio-recorded face-to-face interview | 1 hour |
| Public health specialist | Attempt to remove and replace a drug from a formulary | Audio-recorded telephone interview | 45 minutes |
| Commissioning manager (CCG) | Attempt to relocate anticoagulation services from acute to community settings | Audio-recorded telephone interview | 45 minutes |
| Programme manager | Planned care home closures by a County Council Adult Social Services department | Audio-recorded face-to-face interview | 1 hour |
| Clinical lead for one strand of the reconfiguration | Nationally instigated reconfiguration of children’s health-care services (paediatrics, neonatal services and obstetrics) | Audio-recorded telephone interview | 1 hour |
| CCG accountable officer | Recommissioning of a non-emergency patient transport service to an alternative provider | Telephone interview, not recorded | 45 minutes |
| CCG accountable officer | Transfer of chronic pain management service from acute to community setting | Telephone interview, not recorded | 45 minutes |
| Programme lead (CCG) | Reconfiguration of local maternity services by a CCG | Telephone interview, not recorded | 30 minutes |
Data from the mapping interviews and from the narrative vignettes were gathered, stored and analysed in accordance with best practice. Coding was carried out by two members of the research team (IW and JH) and differences resolved in discussion with a third member (GR). The primary aim of the mapping exercise was to help understand the wider context within which decommissioning activities were enacted. The primary function of the vignettes was to sensitise the research team to themes and issues to be explored in subsequent work packages. Findings from these two activities are presented in short descriptive form in the following chapter of the report (see Chapter 4).
Delphi study of research, policy and practice opinion
To help fill some of the gaps in the published evidence as regards ‘what works’ in decommissioning, we carried out an international Delphi study of expert opinion. Delphi surveys build a consensus through iterative questionnaires sent to a panel of experts and are effective in establishing a consensus in complex topic areas. 21 Developed by the RAND Corporation in the 1950s, the Delphi method was used to forecast the emergence of new technologies22 and has subsequently been used to establish research priorities in health care,23–28 as well as to generate a consensus on policy issues. 29–31 Delphi studies on policy themes share key features of the original approach including multiple rounds in which data are analysed and fed back as the basis for subsequent rounds with at least one opportunity for participants to revisit and revise their judgements on the basis of wider group responses, and anonymity for the participants who never meet or interact directly.
The first round of the Delphi study usually involves participants suggesting factors or cues that form the basis of subsequent closed questions. Participants are then sent a second questionnaire asking for their individual views on the items that they and their co-participants suggested previously. Responses are collated and returned to the participants in summary form, indicating both the group judgement and the individual’s initial judgement. Participants are then given the opportunity to revise their responses in the light of group feedback. This process may be repeated a number of times before the judgements of the participants are aggregated. 27
In this study, individuals were purposively selected from three groups (total n = 30) with expertise on the topic of decommissioning. These were researchers, policy-makers and regulators, and commissioners and providers of health-care services (Table 4). In this context ‘experts’ were understood to be individuals with experience in decommissioning in one or more of these capacities.
| Participant characteristics | Participants (n) |
|---|---|
| Country | |
| Australia | 6 |
| Canada | 3 |
| UK | 20 |
| Republic of Ireland | 1 |
| Perspective | |
| Researcher | 8 |
| Policy-maker | 10 |
| Practitioner | 12 |
| Expertise in forms of decommissioning | |
| Removal or replacement of a treatment from a formulary or patient pathway | 2 |
| Relocation/replacement of a service as part of reconfiguration | 5 |
| Relocation/replacement of a service from an acute to a community setting | 1 |
| Closure or partial closure of a service | 2 |
| Closure or partial closure of an acute health-care organisation | 1 |
| More than one of the above (and including ‘research/policy development’) | 19 |
Candidates for the ‘research’ group were identified through the previously described searches of the published literature. Candidates for the ‘policy’ and ‘practice’ groups were identified through desktop searches and nominations from an international advisory group for the research project. An initial list of approximately 100 target respondents from the UK, Europe, North America, Australia and New Zealand were invited via e-mail to participate (see Appendix 2). Of these, 30 agreed to participate. As Table 4 shows, participants were drawn from the UK, Australia, Canada and the Republic of Ireland, although the final sample contained an over-representation of UK respondents, especially in the ‘practice’ category.
Participants were requested to consider, define and rate criteria and factors that shape the process and outcomes of decommissioning programmes. They were invited to complete three online rounds (with 1 week for completion of each one) and to suggest examples of ‘best practice’ in decommissioning. Open comment responses were analysed by the research team using open coding and constant comparison. Similar codes were grouped to identify concepts emerging from the data. A consensus was statistically operationalised by measuring whether or not group ratings were strongly polarised (e.g. 50% of respondents strongly agreeing and 50% strongly disagreeing with any statement is a strongly polarised distribution).
In round 1, participants were asked for up to five nominations for each of the following:
-
considerations that should inform decisions to implement decommissioning
-
considerations that do inform decisions to implement decommissioning
-
factors that positively shape the process of decommissioning
-
factors that negatively shape the process of decommissioning
-
factors that positively shape the outcome of decommissioning
-
factors that negatively shape the outcome of decommissioning.
They were also invited to suggest best-practice recommendations for the implementation of decommissioning decisions. Open comment fields enabled respondents to explain and/or justify their suggestions, and to raise any other issues. The anonymised, cumulative responses were then fed back to the whole panel to inform the design of round 2.
For the second round, participants were requested to rank their level of agreement with statements derived from round 1, using a four-point Likert rating scale (strongly disagree, disagree, agree and strongly agree). They were also asked to rank relative importance of the factors proposed in round 1 in shaping the process and outcomes of decommissioning, again using a Likert rating scale (very low importance, little importance, high importance and very high importance). Open comment fields enabled respondents to explain responses. The research team calculated the level of consensus in relation to the total of 88 rating scale questions in round 2 using the following thresholds:32
-
high = 70% of ratings in one category or 80% in two contiguous categories (e.g. agree and strongly agree)
-
medium = 60% of ratings in one category or 70% in two contiguous categories
-
low = 50% of ratings in one category or 60% in two contiguous categories
-
none ≤ 60% in two contiguous categories.
Anonymised, aggregated responses relating to factors with no consensus or a low level of consensus were then fed back to the Delphi panel to inform the design of round 3.
For the third round, participants were invited to reflect and comment on the round 2 results for the 17 statements that achieved no consensus or a low level of consensus, and to rank their level of agreement with the 17 statements, having had an opportunity to review the results from the panel as a whole. The final outcomes from rounds 1 to 3 were fed back to all participants and an opportunity to make further open comments provided.
Work package 2: national survey of Clinical Commissioning Groups
Work package 2 addressed the research question ‘How and to what extent are NHS organisations currently implementing decommissioning?’. This was addressed via an online national survey of NHS CCGs. The aim of the survey was to identify the volume and types of decommissioning activities planned and under way across England by CCGs and to derive self-reported data, where possible, on the implementation and outcomes of decommissioning programmes. The survey tool was developed with guidance from the project advisory group and survey questions were designed to follow up findings from work package 1 concerning the drivers of decommissioning and factors that shape and influence the process and outcome of decommissioning activities. The survey addressed the following themes:
-
extent of current engagement with decommissioning
-
current/recent decommissioning programmes
-
aims and intended outcomes of decommissioning
-
challenges and key determinants of decommissioning
-
attitudes, experiences and competencies in relation to decommissioning.
The survey was designed in SurveyMonkey® (Palo Alto, CA, USA). Before being implemented nationally, the survey was piloted with local CCG representatives identified through project team networks. The finalised data collection instrument (see Appendix 3) combined tick boxes and attitudinal questions rated according to Likert scales with additional opportunities to provide free-text responses. An additional question at the end of the survey asked respondents if they would be willing to be contacted for further information and to discuss the potential to feature as a case study in the research.
In order to administer the survey, contact details for all 211 CCGs in England (at the time of the research) were compiled from NHS England and Department of Health websites and an e-mail invitation and accompanying information sheet was sent to each CCG (see Appendix 3). Within each CCG we sought a single survey response from a member of the senior team (e.g. chair, clinical lead, accountable officer, chief finance officer or other member of senior management and/or board), and our e-mail invitation offered the option for CCGs to nominate a suitable respondent. The seniority of the respondent was an important prerequisite in order for respondents to be able to offer an authoritative account, as well as to provide strategic oversight of decommissioning activities planned or already completed by the CCG. A link to the survey was included in the e-mail invitation and respondents were provided with a time frame of 1 month in which to complete the survey. The e-mail invitation also offered CCGs the option of accessing a hard copy of the survey from the research team.
E-mail reminders and telephone follow-up were employed during the 1-month response period. The survey was also promoted via professional bodies and networks such as the NHS Confederation and NHS Clinical Commissioners. A final response rate of 27% (56 CCGs) was achieved, with the majority of CCGs opting to complete the survey via the online method and eight opting to complete it via hard copy. This response rate is comparable to other CCG surveys undertaken at the time (such as the NHS Confederation survey33). Feedback from CCGs that declined to take part suggested that time pressures and lack of capacity were key reasons.
The final sample of respondent organisations is broadly representative of the wider CCG population in terms of size, rural-to-urban ratio and performance against financial targets (see www.england.nhs.uk/2013/12/ccg-allocations and www.nhs.uk/service-search/performance/search). The sample includes an over-representation of CCGs in the Midlands, perhaps reflecting the location and profile of the lead research institution (University of Birmingham). This notwithstanding, the broadly representative sample would suggest that extrapolation of findings is warranted. However, the research team were conscious of possible selection bias with CCGs more engaged in the decommissioning agenda perhaps more likely to respond. This has led us to be cautious with regard to the claims made.
Quantitative data derived from the CCG survey were uploaded into Statistical Product and Service Solutions (SPSS) version 22 (SPSS Inc., Chicago, IL, USA) and subjected to descriptive statistical analysis (primarily involving counting and calculation of percentages) in order to generate results about the frequency and types of decommissioning, aims and intended outcomes, methods used in decommissioning and key factors affecting decommissioning programmes. Qualitative free-text responses were coded into themes and reported alongside the quantitative data to provide further insight. As well as providing a sample of contemporary CCG decommissioning activity, the survey sensitised us to the range of types of decommissioning activities planned or under way within CCGs and their experiences of implementation thus far. These insights were important for refining our case study selection. A list of potential candidates was also compiled from CCGs that indicated that they would be willing to feature as a case study in the research.
Work package 3: decommissioning case studies
In combination with work packages 1 and 2, work package 3 addressed the research question ‘What factors and processes influence the implementation and outcomes of decommissioning?’. We used a comparative case study design across multiple study sites to generalise theoretically from within and between cases,34,35 to map the multiple interacting actors and influences and to uncover the intended/unintended consequences of decommissioning initiatives. Although each case had its own integrity in terms of theory building and potential to generate practice recommendations, we also developed common themes across case study sites using comparative case study methods and pattern matching. 35–37
Case selection
We selected four case studies in which a planned and explicit approach to decommissioning had been adopted. These were at varying stages of progression (as mapped against the stages model) in order to enable us to follow decommissioning journeys from initiation and development to implementation and, where possible, direct and indirect outcomes.
To identify potential case studies, we adopted a snowballing approach using existing contacts from the project principal investigator, advisory group, decommissioning narratives, survey responses and mapping exercise. Using these approaches, we developed a matrix of potential case study options structured around four sampling criteria (Table 5), intended to capture a diversity of decommissioning activities:
-
geography – including programmes implemented in both rural and urban settings in England
-
scale and complexity – including decommissioning programmes that vary from the relatively simple (e.g. implementation of National Institute for Health and Care Excellence (NICE) disinvestment guidance) to the highly complex (e.g. reorganisation of services across organisational and sector boundaries)
-
conflict – including programmes with a high degree of stakeholder buy-in and support and others for which there are currently (or it is anticipated that there will be) high levels of resistance and stakeholder challenge
-
programme instigation – including decommissioning programmes where national bodies play an important role and others that have been instigated and led entirely by local organisations such as CCGs.
| Criterion | Case study | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Geography | Urban | Urban | Rural | Rural/urban |
| Scale and complexity | High | Low | Low | High |
| Conflict | High | Low | Low | High |
| Programme instigation | National/regional | Local (CCG) | National (NICE) | Local (CCG) |
| Stage of decommissioning at data collection | Programme design | Programme implementation | Decision-making/programme implementation | Decision-making |
Based on these provisional sampling criteria we selected the following case studies.
-
Reorganisation of specialist services for paediatric burn care in England.
This case study was selected to fulfil the criteria of being a nationally led, complex reorganisation process involving planned service removal or reduction. The case was identified through the national mapping exercise, and access was negotiated between the project principal investigator and NHS England. In these conversations it was established that the burn care reorganisation would incorporate the decommissioning (by downgrading) of some services and that it would be closest to the ‘programme design’ phase at the commencement of fieldwork. As a national reorganisation it was anticipated that it would generate relatively high levels of conflict and that the specialised services sites would be in predominantly urban areas.
-
CCG-led decommissioning of an end-of-life (EOL) home support service.
This case study was selected to fulfil the criteria of having relatively low complexity and low conflict (although we could not be sure of this at the outset) and of being in an urban area and closest to the implementation phase of the decommissioning process. The CCG was initially identified as a potential case study through networks of the research team and access was negotiated with the CCG programme manager for the decommissioning programme.
-
Decommissioning activity by an Area Prescribing Committee (APC).
This case study was selected to fulfil the criteria of being rural, and having low complexity and relatively low conflict (although again this could not be fully established prior to commencing the case study). The intention was to observe implementation of NICE guidance by the committee and any additional decommissioning undertaken. The APC was identified following the mapping exercise through an e-mail invitation to a number of APC representatives in suitable areas, asking if they wished to showcase work in the area of decommissioning. Access was negotiated through the APC chair and research lead for the host CCG.
-
CCG-led review and planned reorganisation of local primary and acute care services.
This case study was selected to fulfil the criteria of covering an area with rural parts, which had high levels of scale, complexity and likely conflict. This case study was closest to the decision-making phase of our stages model. Access was negotiated with the programme manager for the service transformation programme following an initial approach to the research team.
Data collection
For each case study, the primary unit of analysis was the decommissioning process itself and we compiled narrative accounts of the programme of work intended and/or under way. We employed non-participant observation techniques as used successfully by the applicants in previous research. 38 Detailed field notes were taken to record the processes through which decommissioning plans were identified and drawn up, and the role of decision-making tools and frameworks in this.
For each case study, semistructured interviews were conducted with a sample of those involved (see Table 6 and Appendix 4). In all case studies, the interview sample comprised individuals involved in the design and implementation of the decommissioning programme. For case studies in the early stages of progression, a second round of interviews was conducted approximately 12 months after the initial round. These were intended to update the research team on programme progress. For case studies in the implementation phase (e.g. case study 2) the primary focus of a first round of interviews was on design and enactment of the implementation plan with a follow-up round planned to explore outcomes.
Interviews focused on:
-
the origins, aims and intended outcomes of the decommissioning programmes
-
decision-making tools and other information used to inform decommissioning programmes
-
the web of relationships between internal and external actors and influences in decommissioning design and implementation processes
-
the role of key interest groups in decommissioning, including politicians, clinicians and the public
-
outcomes, experiences and attitudes towards future decommissioning.
In summary, a total of 59 interviews were carried out in work package 3. This is somewhat less than the 90 interviews anticipated in our project plan. The main reasons for this discrepancy are as follows:
-
We placed a greater emphasis than was initially intended on observation over interviews in the case studies, as these provided a rich source of data (Table 6).
-
Data saturation was reached early in interviews for case study 3.
-
We were unable to gain access to respondents for follow-up interviews in case study 2 as some individuals had moved on from their posts.
| Case study | Number of | |
|---|---|---|
| Interviews | Observations | |
| 1. Paediatric burn care reorganisation | 17 | 3 |
| 2. Decommissioning EOL service | 13 | 0 |
| 3. Decommissioning in an APC | 10 | 4 |
| 4. CCG reorganisation of primary and secondary care | 19 | 11 |
| Total | 59 | 18 |
Data analysis
Informed by our theoretical framework, we inductively analysed interview data to explore participants’ perspectives and experiences. Analysis involved comparative case study methods and pattern matching. 36,37,39 In order to facilitate internal validity,40 all interviews were fully transcribed and we used qualitative coding software [NVivo version 11 (QSR International, Warrington, UK)] to support data storage and retrieval during the analysis phases. Two members of the research team (IW and JH) were involved in building coding frames for themes from qualitative data and compared independent coding of a subset of data to identify and address coding differences and ensure consistency. All identified themes were discussed at ‘analysis days’ attended by the core project team. External validity and transferability of analysis was addressed through detailed description and data triangulation between work packages. 40 Respondent validation was facilitated through sharing of draft case study reports with respondents (with four individuals taking up the offer to review and comment), and additional clinical expertise was drawn on in case study 1 to ensure the accurate presentation of clinical information.
In our approach to case study analysis we drew on our theoretical framework, including concepts derived from the ANT research tradition. ANT was developed by Bruno Latour, Michel Callon and John Law41 as part of the academic field of ‘Science and Technology Studies’ during the 1980s. Although it has ‘theory’ in its name, ANT is better understood as a range of methods for conducting research that aims to describe the connections that link together humans and non-humans (e.g. objects, technologies, policies and ideas). 42,43 In particular, ANT seeks to describe how these connections come to be formed, what holds them together and what they produce.
In the context of health-care service and delivery, ANT has typically been forwarded as a framework for investigating technology implementations in health-care settings (e.g. 44–46). Aside from technology implementation, ANT has also informed studies of implementing ‘Lean thinking’ in health-care organisations,47 exploring the effectiveness of quality-improvement interventions48 and the evolution of indoor smoke-free regulations (a policy innovation). 49
A key concept in ANT – particularly pertinent to the study of decommissioning processes – is what Latour called ‘the sociology of translation’. 50 By this, he meant that players interact to build heterogeneous networks of human and non-human actors, forming alliances and mobilising resources as they strive to convert an idea into reality. The central focus of ANT in the context of our study is, therefore, the process by which a decommissioning project is ‘brought into being’ through the process of translation and how it changes over time. The picture is always a dynamic one, as actors interrelate, define one another and realise their goals (or not) by mobilising intermediaries, such as technical artefacts, texts, human skills and other resources. 51,52 Translation is achieved by displacements that require discourse and the exercise of power, and it may or may not achieve the desired outcome. This continuous, organic realignment of people and non-human actors is what Latour50 calls the ‘chain of transformation’. What emerges may not be a unified, shared goal; indeed, the concept of the ‘network’ is that different actors often have conflicting goals, and outcomes are the result of struggles between different interest groups and the flow of power through the network. Callon51,52 summarised the process of translation as four ‘moments’ or phases:
-
problematisation – the definition of the nature of the problem in a specific situation by an actor (a group or an individual) and the consequential establishment of dependency
-
interessement – ‘locking’ other actors into the roles that were proposed for them in the actor’s programme for resolving that problem
-
enrolment – the definition and interrelation of the roles that were allocated to other actors in the previous step
-
mobilisation – ensuring that supposed spokespersons for relevant collective entities are properly representative of those entities.
Prior to beginning our study we felt that ANT and the concepts briefly outlined above would enable us to explore decommissioning processes in novel ways by helping to describe the multiple interacting actors and influences in our four case studies; to consider why such actors and processes appear to ‘behave’ differently in different settings or at different times; and to draw attention to the unintended consequences of decommissioning processes (as well as the anticipated ones). We also proposed that applying an ANT perspective would help us to explore several common themes that, from the literature, appear to impede successful outcomes of decommissioning processes, namely:
-
one or more interest groups may feel threatened by substantive change
-
external actors may feel insufficiently consulted and involved in decision-making processes
-
stalemates between coalitions of interests
-
the role of power and politics.
In drawing on ANT, we needed to ‘follow the actors’ in our case studies and to analyse how these actors themselves define what is going on. However, it should be noted that the empirical scope of the case studies was not as expansive as is usually found in the ANT tradition and precluded us from, for example, extending our analysis into all levels of health-care decision-making and activity. It would therefore be inappropriate to cast our case studies as full actor–network analyses or to make inferences about the full actor networks at play. Instead, we have drawn on Callon’s51 summary of the translation process to make sense of smaller-scale case studies that were primarily interview led and supported with observational and documentary analysis. We have recast the Callon framework in the following language to be more accessible to practitioner audiences. These form a structure for presenting and analysing findings:
-
the role of evidence and other resources in identifying and framing a need for decommissioning
-
alliance building (e.g. analysing context, attending to interests and power relations) as part of a decommissioning process
-
social acceptance (analysing engagement strategies, attempts to gain wider acceptance) for the solution of decommissioning
-
implementation and institutionalisation of a decommissioning decision.
It is important to note that several criticisms have been made of ANT that are relevant to our study of decommissioning processes. Building on Robert et al. ,53 these include the following:
-
ANT fails to attend to the various ways in which macro-level structures (e.g. external regulatory bodies or the Department of Health in the context of our study) shape and modify the process of social interaction and practices; by ignoring such institutional sources of power, ANT is criticised for having little to say about the systematic exclusion that prevents some social groups from having a voice in, for example, decommissioning processes.
-
How to delineate an actor network (with a view to studying it) presents a methodological problem. The network is open, and hence must be artificially defined by the researcher. There is an argument for not defining the actor networks in advance but rather seeing what emerges as key in any particular study.
-
May54 suggests that ANT may also be limited in terms of accounting for everyday micro-level practice and assisting with practical problem-solving.
Summary of patient and public involvement activities in work packages 1–3
A key aim in each of these work packages was that public, service user and patient (PSUP) expertise and input voices would be included. PSUP expertise was recruited to the research team and advisory group and a subgroup was convened to discuss PSUP activities at strategic intervals during the research. We also sought to build PSUP activities into the research design in a number of ways. In work package 1, patients and service user representatives were invited to form part of the Delphi panel. However, all of those invited declined to participate, citing concerns that they did not consider themselves sufficiently ‘expert’ to take part. In work package 3 we anticipated that patient input would feature in each of the decommissioning case studies and that public engagement or consultation would feature in a subset of these. We therefore utilised site-specific mechanisms for involvement, for example by observing and participating in public engagement events held as part of the case study 4. However, in case studies 1, 2 and 3, opportunities for engagement beyond interviews with individual patient/public representatives were limited by the modest PSUP activities of the decommissioning processes themselves. As a result, and acting within the constraints of our research ethics approval, we were limited in the extent of additional engagement that we were able to undertake. This raised concerns with regard to (1) the breadth of perspectives on the research topic that we were able to collect and (2) opportunities to feed back research findings to these audiences.
As a result of these concerns, the research team applied for and secured NIHR HSDR funds to build an additional work package into the project, designed to strengthen our understanding of decommissioning from citizen, patient/service user representative, carer, third-sector organisation and local community group perspectives.
Work package 4: citizen, patient/service user representative, carer, third-sector organisation and local community group perspectives
To mitigate for gaps in the data, a further work package was put in place that was targeted towards a series of further stakeholder groups for whom decommissioning might be important. It was intended to recruit participants representing citizens, patient/service user groups, carers and community/third-sector organisations. The aim of the work package was to investigate the perspectives and experiences of citizens, patient/service user representatives, carers, third-sector organisations and local community groups in relation to decommissioning, and to address the following research questions:
-
What are the views and experiences of citizens, patient/service user representatives, carers, third-sector organisations and local community groups in relation to health and social care decommissioning?
-
How do these compare with those of policy-makers, practitioners, health-care leaders and researchers?
-
How might these perspectives be brought together in order to improve equity and acceptability in decommissioning?
To address these questions we undertook the data collection activities described below.
Focus group discussions
We carried out three deliberative focus groups, each with approximately 10 participants sampled with the intention of achieving a diversity of age, gender and ethnicity. 55 Focus groups involved combinations of citizens/members of the public, representatives of national citizen organisations (e.g. HealthWatch) and patient organisations (general and specific), community organisations and independent third-sector organisations. In the focus groups, some participants also self-identified as NHS patients/service users. The logic of this sampling was simply to recruit individuals more likely to be affected by (as opposed to being responsible for) decommissioning.
Potential participants for the focus groups were contacted through HealthWatch England, National Voices, the Department of Health Voluntary Sector Strategic Partner Programme, Carers UK, patient representative and advocacy organisations such as the National Association for Patient Participation and Shaping Our Lives, researchers with particular expertise and interest in patient and public experience and engagement and individuals involved in patient and public engagement identified in work package 3. No NHS organisations were contacted, in accordance with the terms of our research ethics approval. Participants were not required to have direct previous experience of decommissioning, although it transpired that a substantial proportion of those who consented to take part did have, having been directly affected by decommissioning.
The focus groups were intended to sensitise us to the issues and perspectives and so questions were open ended, encouraging wide-ranging discussion. At least two facilitators were involved in each of the focus groups (IW, SB and JH) and examples of decommissioning scenarios were used to prompt discussion (see Appendix 5). Each discussion lasted for approximately 1.5 hours and the final 30 minutes was taken up with the co-design of questions for a follow-up Delphi study of expert opinion, drawing specifically on the experiences and perspectives of citizens, patient/service users, carers, third-sector organisations and local community groups.
Delphi study of citizen, patient/service user representatives, carer and community groups, and third-sector organisations
Drawing on these insights we implemented a second three-round, online Delphi survey in order to compare views on drivers of decommissioning with those expressed by the first Delphi panel (work package 1) on drivers of decommissioning and to elucidate a consensus on best practice for the engagement of patients and the public in decommissioning processes, from the perspective of citizens, patients/service user representatives, carers and community groups and third-sector organisations. 28,30 The letter of introduction (see Appendix 6) incorporated the suggestions of participants in the focus groups about accessibility, as did the decision to replace the term ‘decommissioning’ with the phrase ‘move or take away services’.
The approach to analysis and consensus-building was as described in Chapter 3, Delphi study of research, policy and practice opinion. The final sample for the second Delphi study comprised third-sector organisations that provide support to, and advocacy/representation of, service users and carers (including, among others, Shaping our Lives, National Voices, Carers UK, National Development Team for Inclusion, the Mental Health Providers Forum, the Voluntary Organisations Disability Group, the National Care Forum and National Association for Voluntary and Community Action); other patient and public representative organisations (including HealthWatch England, National Association for Patient Participation, the Race Equality Foundation and patient expert groups); and selected academics specialising in public involvement and/or patient experience. Following advice from our advisory group, we restricted the scope to the English NHS rather than seeking respondents from other countries. More detail on respondents is provided in Table 7.
| Role (self-identified) | Participants, n (%) |
|---|---|
| Patient | 14 (56) |
| Service user | 8 (32) |
| Carer | 8 (32) |
| Community/third sector | 14 (56) |
| Member of the public | 11 (44) |
| Academic specialist in PPI | 2 (8) |
| NHS patient representative | 2 (8) |
| No response | 1 (4) |
| Total responsesa | 25 |
Of the 50 individuals and organisations invited, 26 agreed to participate. Female participants made up the majority of respondents (15, 60%). Eighteen described themselves as ‘white British’ or ‘white English’, with five describing themselves as ‘non-white’, ‘European’ or ‘other’. Ten respondents indicated that they had a disability and a further two provided no response to this question. Older age groups were over-represented within the sample, with two respondents aged between 25 and 34 years, four between 35 and 44 years, four between 45 and 54 years, seven between 54 and 65 years and seven > 65 years.
In round 1, participants were asked about their experiences of decommissioning, including good and bad aspects of these experiences. They were then asked ‘What if any do you think are good reasons to move or take away services?’ The same question was then asked in relation to ‘bad’ reasons and the reasons behind such a decision in reality. They were also asked how they would wish to be involved ‘if the NHS was thinking about moving or taking away services in your local area or nationally’. Open-text comment boxes were provided in relation to each of the questions. The anonymised, cumulative responses were then fed back to the whole panel to inform round 2.
In round 2, participants were asked to rank their level of agreement with statements derived from round 1, using the four-point Likert rating scale and consensus thresholds employed in Delphi study 1. The statements related to:
-
good reasons to move or take away services
-
bad reasons to remove or take away services
-
the reasons why these decisions were made in practice.
Respondents were also asked to choose the three reasons that they considered were most justifiable/least justifiable/most influential in practice.
Two more questions asked respondents to review lists of statements deriving from their first-round comments about how they would like to be involved and which methods they thought most important to employ. They were then invited to select the three that they considered most important.
The anonymised, cumulative responses relating to those factors that achieved a low level of consensus or no consensus were fed back to the whole Delphi panel to inform round 3. In round 3, participants were asked to reflect and comment on the round 2 results for the 19 statements that achieved a low level of/no consensus and to rank their agreement with these statements, having had an opportunity to review the results from the panel as a whole. They were also given an opportunity to comment on the combined three highest and lowest ranking statements from each of the questions.
The final outcomes from rounds 1 to 3 were fed back to all participants and further open comments were invited.
Integrating across the empirical strands of the study
Work package 1 informed the foci of the national survey and four case studies (work packages 2 and 3). The case studies enabled us to explore gaps and unanswered questions identified in work packages 1 and 2. Work packages 1 and 2 gave a context to the analysis of findings from work package 3, enabling reflections on transferability of findings. Finally, work package 4 enabled us to compare and contrast these perspectives with those of patients, community groups and carers and to mitigate shortcomings in the involvement of these groups in earlier work packages. In these ways, the various stages of the project were integrated.
As well as using data from work packages to inform the development of subsequent work packages, each was designed to answer specific research questions. Work package 1 addressed the question ‘What is the international evidence and expert opinion regarding best practice in decommissioning health care?’. Work package 2 addressed the question ‘How and to what extent are NHS organisations currently implementing decommissioning?’. Work package 3 addressed the question ‘What factors and processes facilitate the successful implementation and outcomes of decommissioning?’. Finally, work package 4 addressed the question ‘What are the perspectives and experiences of citizens, patient/service user representatives, carers, third-sector organisations and local community groups in relation to decommissioning?’. In our final synthesis and discussion, we brought together insights from each of these data sources to address the main aim of the research, which was to formulate theoretically grounded, best-practice guidance for health-care managers by identifying the factors and processes that influence the successful implementation and outcomes of decommissioning health services.
Research ethics approval
Research ethics approval was secured from the University of Birmingham. As well as having all research plans and materials approved, the research team discussed ethical dimensions throughout the research project, including, for example, issues of informed consent, anonymity and researcher–respondent relations.
Chapter 4 Findings from the review of reviews, mapping and narrative vignettes and Delphi study of experts
This chapter presents results from the various strands of work package 1, including the evidence summary, the mapping exercise, the narrative vignettes and the Delphi panel.
Evidence summary
In this section we present findings from a narrative synthesis of the existing literature against our research questions. 19 Table 8 provides details of the included reviews.
| Author/year | Relevant research aims/question | Review type | Scope | Data sources | Findings |
|---|---|---|---|---|---|
| Gallego et al. 201056 | To identify current approaches to reducing ineffective or cost-ineffective interventions and programmes | Systematic |
|
Seven papers identified | Approaches to disinvestment found to employ CER and/or PBMA. Authors note barriers relating to evidence, politics and ethics |
| Leggett et al. 201257 | To review the literature on health technology reassessment in practice | Systematic |
|
40 literature items identified | Authors conclude that the field of health technology reassessment is in its infancy and there is a lack of practical knowledge to guide implementation. There is a need to build expertise and knowledge in this regard |
| Polisena et al. 201358 | To identify case studies of disinvestment in health care | Systematic search for case studies |
|
14 case studies identified | Approaches to decommissioning include tools such as PBMA, CER and procedural justice models such as A4R |
| Mayer and Nachtnebel 201559 | To elucidate factors that facilitate implementation | Systematic database search and unsystematic hand search |
|
Seven programmes identified | Authors identify the following as important to implementation: political will, transparent processes and physician engagement |
| Niven et al. 201560 | To describe the literature on de-adoption, document current terminology and frameworks | Systematic |
|
109 literature items identified (65% original research) | Identifies a ‘large body of literature’ describing current approaches, although additional research is required to determine an ‘ideal strategy’ |
| Parkinson et al. 201517 | To review how reimbursement policy decision makers have sought to . . . disinvest from drugs | Expert |
|
Unclear | Full decommissioning (referred to as ‘delisting’) is rare. Other methods include restricting treatment, price/reimbursement reductions and encouraging generic prescribing |
How are terms such as ‘decommissioning’ and ‘disinvestment’ employed in the literature?
In their review, Niven et al. 60 document the terminology employed in the literature, identifying 43 separate terms currently in usage, which they go on to map on to a conceptual framework made up of de-adoption ‘phases’ (identification of low-value practices, facilitation of the de-adoption process, evaluation of de-adoption outcomes, and sustaining de-adoption). This mirrors to some extent the stages model that we outlined in Chapter 1, albeit without the ‘programme design’ stage, reflecting the authors’ focus on clinical rather than organisational interventions. ‘Disinvestment’ is reported to be the most prevalent term in the literature, although the authors advocate ‘de-adoption’ as more suited to a process rather than a decision point.
Four of five other reviews employ the more established term ‘disinvestment’,17,56,58,59 whereas Leggett et al. 57 employ the term ‘reassessment’ in keeping with their specific interest in this area. The earliest of the six reviews56 locates the term ‘disinvestment’ within the HTA movement and notes the tendency for prescriptions for practice following a HTA model. As noted, each of the reviews confines its scope to clinical/therapeutic interventions and, notwithstanding Niven et al. ’s60 preference for ‘de-adoption’, this area of decommissioning has become synonymous with the term ‘disinvestment’. In most definitions of the term, ‘disinvestment’ contains a normative component in its emphasis on improved health outcomes:
The complete or partial withdrawal of resources from health care services and technologies that are regarded as unsafe, ineffective or inefficient, with those resources shifted to health services and technologies with greater clinical- or cost-effectiveness.
Polisena et al. 58
Parkinson et al. 17 employ the term ‘disinvestment’ in a more expansive way to include restrictions on prescribing, price negotiations and the encouragement of generic prescribing, with ‘delisting’ used to refer to complete disinvestment. This very broad definition appears to signal a break with the narrower scope of previous usages of the term.
What are the current and previous levels and types of health-care decommissioning as reported in previous studies?
The scope of each of the six reviews is primarily confined to (1) activity that is commonly known as disinvestment (incorporating the principle of cost-effectiveness maximisation) and (2) health technologies (i.e. treatments and interventions). The reviews’ reporting of decommissioning activity rates is similarly circumscribed. Furthermore, the approach taken to reporting prevalence of decommissioning varies across the reviews. Leggett et al. 57 and Parkinson et al. 17 focus on formal programmes instigated at the national level. Polisena et al. 58 and Mayer and Nachtnebel59 identify and analyse case study decommissioning programmes (n = 14 and n = 7, respectively). Niven et al. 60 offer the most extensive synthesis of decommissioning (or disinvestment) levels, from candidate identification through to ‘sustaining de-adoption’. In summary, the following messages can be identified in relation to levels of decommissioning (with particular focus on the NHS in England):
-
Some decommissioning has been instigated at national and local levels across Organisation for Economic Cooperation and Development (OECD) countries.
-
Overall rates are reported as being somewhat low, although recent reviews appear to show an increase.
-
At the national level, the focus has been on comparative effectiveness research and HTA, whereas for lower tiers of decision-making, economic frameworks such as programme budgeting and marginal analysis (PBMA) have been advocated.
-
NICE is often the main focus of reported decommissioning activities in England.
-
Safety (or harm reduction) is the most common driver of decommissioning programmes that are successfully implemented, with cost-effectiveness, for example, being far less likely to be cited as the primary driver.
-
‘Passive’ or ‘implicit’ forms of decommissioning are more common than ‘active’ or ‘explicit’ forms.
-
Restriction (e.g. to patient subgroups) is more common than full withdrawal (or ‘delisting’).
-
Considerable attention has been paid to the identification of decommissioning candidate interventions and the assembling of lists of those deemed suitable for either removal or reduction in provision.
What are considered to be the main determinants of successful decommissioning programmes?
The reviews report some common impediments (or ‘barriers’) to the implementation of planned decommissioning. These include a lack of resource for research into candidate technologies for replacement or removal. 56 Later reviews, for example by Mayer and Nachtnebel,59 note that attempts have since been made to address this evidence deficit.
The reviews also identify consistent and widespread ‘resistance to change’ from stakeholders, including patients and clinicians. 58 This can be because of ‘sunk costs’57 or ‘losses’ experienced by clinicians, patients and manufacturers of interventions considered for decommissioning. Parkinson et al. 17 elaborate on the logic of these impediments, referring to restrictions to ‘patient and prescriber choice’ and ‘perverse incentives’ created by payment regimes for clinicians. They observe that ‘there may be resistance to changing prescribing behaviours in the face of established clinical training and practice paradigms’. 17 The resulting lack of ‘will’ among political, clinical and administrative actors is the most consistently cited barrier. 56,59 Perhaps not surprisingly, early and effective stakeholder management is foregrounded in good-practice recommendations in the reviews.
What models and frameworks are available to guide decommissioning and how have these been evaluated?
Gallego et al. 56 report HTA and other methods for establishing lists of candidates for disinvestment as being one of the main sources of support for health systems and techniques, such as PBMA, as a means of putting these into practice. Beyond this, the authors identify a lack of ‘formal structures, processes or mechanisms’ to support practice. 56 Polisena et al. 58 also identify PBMA and HTA as two of the most prominent tools for supporting decommissioning, even though these are not deployed simultaneously in their case study examples. They also identify the application of the accountability for reasonableness (A4R) model – based on four process conditions for decision-making – in three case study disinvestment processes. Leggett et al. 57 focus on health technology reassessment (HTR) programmes and find one ‘model’ for reassessment.
In relation to implementation, Mayer and Nachtnebel59 compare top-down approaches based on mandated decisions and forced compliance, with bottom-up approaches where disinvestment is encouraged and facilitated and led by those working at the ‘coal-face’. They conclude that while top-down approaches can engender resistance, bottom-up approaches require voluntary engagement that may not be forthcoming in all cases. They therefore advocate a combination of both approaches.
As well as low-value lists, Niven et al. 60 identify the following ‘common mechanisms’ for supporting de-adoption processes:
Restructuring of funding associated with the given practice, changes to local and/or regional policies, and more consistent integration of health technology reassessment within existing health technology assessment programs.
Niven et al. 60
Parkinson et al. 17 identify a variety of means by which candidates for disinvestment might be identified, including assessment processes for new and existing drugs and consultation with stakeholders. In relation to implementation, they considered restricting the use of drugs and reducing the process to be more ‘acceptable politically’ than full withdrawal.
Mayer and Nachtnebel59 devote some attention to the need to sustain change and the need for financial/human resource capacity and organisational levers:
For government-initiated programs, tying a program to existing controlling tools (e.g., maintenance of a catalogue of benefits, conditional coverage, coverage under evidence development) and establishing new tools (e.g., coverage of new technologies provided only that ineffective technologies are removed concurrently) could facilitate the implementation of reassessment processes.
Niven et al. 60
Although none of the reviews set out to document existing guidance on decommissioning, we identified two such guides in the process of synthesis,16,61 although each of these reviews is somewhat narrow in focus. Overall, the evaluations presented in the reviews chart a realisation of the limits of tools such as low-value lists and HTA in addressing the full range of decommissioning stages. 60 To this we would add their limits as tools for the decommissioning of wider services and programmes. Of more obvious practical value is PBMA, which enables varied forms of investment areas to be compared from within fixed budgets. However, PBMA remains primarily an economic (normative) model and is not always aligned with the constraints of local decision-making contexts. 4,62,63
What are the remaining knowledge gaps in terms of evidence and practice?
Of the reviews that present recommendations for future research, Gallego et al. ,56 writing in 2010, note the prevalence of case studies in the grey literature and the absence of published research; Polisena et al. 58 focus on the need to support the process of identifying candidate technologies; Leggett et al. 57 note the ‘negligible’ focus on the monitoring and implementation of HTR and Mayer and Nachtnebel59 argue for further research on the impact of decommissioning programmes. Niven et al. 60 identify a lack of clarity over the threshold for agreeing to decommission:
There are multiple factors that likely determine when a practice should be de-adopted (e.g., nature of the intervention, lack of effectiveness or degree of harm, nature of the evidence) but the role of each factor and the interplay among them that ultimately determines when to de-adopt is not clear.
Niven et al. 60
They also argue the need for a ‘taxonomy of de-adoption terminology’ and to:
Summarise barriers and facilitators to de-adoption, and quantify the impact of past examples of de-adoption. We also need empirical research to examine optimal strategies for identifying candidate low-value practices, and to determine which de-adoption strategies are likely to have the most impact.
Niven et al. 60
All of the reviews contain examples of planned and successfully implemented decommissioning, although these tend to have been driven by safety concerns. The scope of the identified reviews means that it is difficult to draw conclusions about rates and outcomes of decommissioning programmes involving wider services and organisations. We would therefore add to the knowledge gaps identified in the reviews the need to take empirical research beyond discrete technologies (interventions) to wider management and service changes. There remains a need for process-based research into the organisational and political dimensions of decommissioning in general and specific investigation of programmes involving wider service withdrawal, closures or reorganisation. There is currently a lack of robust evidence and guidance to inform design and implementation of decommissioning programmes. Therefore, developing a better understanding of how decommissioning programmes unfold in the NHS and elsewhere is a crucial first step towards providing evidence-based guidance for the successful implementation of decommissioning in the NHS.
Additional literature items
As explained in Chapter 3, we collated and analysed additional literature items identified during the search and retrieval phase. These were retained for further analysis if they (1) were not reviewed by the authors of the six literature reviews and (2) provided additional insight in one or more of the following ways:
-
They reported more recent research of relevance to our study.
-
They focused specifically on decommissioning in England.
-
They focused on different decommissioning types to the those covered in the reviews.
-
They focused on stages of the decommissioning process not routinely included in the reviews (e.g. programme design and implementation stages).
The items are presented in Table 9.
| Author/year | Research aims/question | Literature type | Relevance to the study |
|---|---|---|---|
| Massatti et al. 200864 | To understand the factors involved in decisions to de-adopt ‘innovative mental health practices’ | Empirical research – survey and interviews with de-adopting organisations | Takes an organisational perspective and focuses on decommissioning beyond clinical interventions. Looks at all stages of decision-making and implementation and draws on a ‘diffusion of innovation’ lens |
| Rooshenas et al. 201565 | To investigate how disinvestment is understood and enacted at the local level of decision-making in two areas of the UK and to explore facilitators of and barriers to this | Empirical research – prospective case studies | Reports recent study of decommissioning practice among local medicines committees in the English NHS |
| Johns et al. 201666 | Examine the origins, development and decline of the CDC’s ‘counselling and testing’ paradigm for HIV infection prevention | Empirical research – interviews and archival research | Looks at a public health programme and focuses retrospectively on the factor shaping implementation of the policy. Uses the term ‘de-implementation’ |
| Fulop et al. 201267 | To analyse factors important in the process and results of reconfiguration of hospital services at a local level | Empirical research – three cases of reconfiguration in the English NHS | ‘Reconfiguration’ is often seen as reflecting a cost-cutting agenda and also often actively involves removal or relocation of services. As such, the study of these processes is of relevance to the decommissioning field, especially when situated in the context of the English NHS |
| Greenwood et al. 201668 | To examine differences in the rates of abandonment of medical technologies (stents) in hospitals | Empirical research – analysis of census data on patients admitted to Florida hospitals (1995–2007) | Considers the influence of institutional form on decisions to abandon technologies when triggered by new alternative treatments or new evidence of limited effectiveness |
Johns et al. 66 analyse how the Centers for Disease Control and Prevention, the leading national public health institute of the USA, announced withdrawal of its long-standing support for an approach to human immunodeficiency virus (HIV) prevention that combined risk reduction counselling and HIV testing. This followed a review of evidence of effectiveness and cost-effectiveness, and expert opinion foregrounding the benefits of screening. The authors pose the question: ‘What could explain the persistence of HIV test counselling despite numerous questions about its effectiveness in altering the sexual behaviour of persons testing negative?’. 66 They note the difficulties of establishing an evidence base for public health interventions and emphasise how institutions and interests impede change:
. . . public health policies are frequently developed and disseminated through a broad organisational infrastructure into which they become deeply embedded. Implementation presses policy into networks of stakeholders who may guard their positions and develop a sense of ownership over the unfolding project. This infrastructural inertia makes reversal particularly difficult . . .
Johns et al. 66
Rooshenas et al. ’s65 study of local commissioning found that there was no formalised process in place for decommissioning and that it was ‘largely absent from observed commissioning group meetings’. The authors identify a reticence among those making decisions to use terms associated with scarcity (such as ‘rationing’), as well as:
. . . practical and ideological barriers to disinvestment, including an absence of guidance and capacity to engage in disinvestment, difficulties in collaboration, reluctance to engage in explicit rationing, and a perceived lack of central/political support.
Rooshenas et al. 65
Massatti et al. 64 examined the factors influencing decisions to de-adopt new practices in mental health providers in Ohio, USA. The focus was on the discontinuation of the implementation of new practices rather than the discontinuation of existing (entrenched) practices and is therefore similar, but not equivalent, to decommissioning. The study found that the availability of fiscal resources was a major determinant of decisions to cease implementation and to de-adopt. Other influential factors related to staff attitudes towards the interventions and a general organisational predisposition to the new way of working. This study is important in drawing attention to these wider factors, with the authors finding in several cases that ‘the innovation was not compatible with the organisation’s philosophy and/or the community was neutral in its support’. 64 The authors recommend that ‘future research should collect more detailed information about and examine characteristics of de-adopter organisations’. 64
Fulop et al. 67 sought to understand the factors influencing the implementation of hospital reconfiguration at the local level. These were found to include the financial context and the role of senior management and stakeholders, including community ‘opposition’. The authors conclude that the experiences of three cases show that the nature of the proposed changes and local politics is more influential than the evidence for change in shaping outcomes. They also make specific observations in relation to decommissioning:
Where reconfiguration was perceived as a ‘downgrading’ of service provision, there was more active internal (professional) and external stakeholder involvement . . . whereas in cases where changes were not perceived as ‘downgrading’ because services were not being moved from one site to another or closing . . . there was less conflict.
Fulop et al. 67
Finally, Greenwood et al. 68 compare ‘abandonment’ of medical practices in US hospitals across public and private sectors, focusing on organisational determinants. They examine data on patients in Florida hospitals from the period 1995–2007, and, in particular, the use of stents. The authors conclude that organisational factors are more influential than physician differences in explaining abandonment. They note the need for:
deeper theorising about how organisations respond to differences in the underlying triggers for abandonment, and the interplay of these responses with different organisational types.
Greenwood et al. 68
Summary of additional literature
These additional studies give some insight into the determinants of decommissioning in forms that go beyond those addressed in the six literature reviews. They suggest that such processes are influenced by organisational and institutional factors, and by staff and user attitudes, local politics and language and how this is deployed. This in turn suggests the need to develop explanations of the phenomena of decommissioning that draw not just on an evidence-based decision-making paradigm, but also take into consideration:
-
how wider financial drivers and the availability of financial resources influence decommissioning programmes
-
how organisational types and characteristics might influence levels of predisposition to decommissioning
-
how staff attitudes might shape and be shaped by organisational factors
-
how wider organisational networks and infrastructure can engender inertia among stakeholders
-
how wider political factors and the absence of a shared language to discuss decommissioning might inhibit programmes at the local level
-
how community groups might come together to oppose decommissioning plans.
Mapping the external landscape of decommissioning
This section presents results of the mapping exercise. The aim was to develop a thorough appreciation of the current decommissioning landscape and specifically to understand:
-
current roles and responsibilities of national bodies with regard to decommissioning
-
decommissioning activities and projects current and planned by those bodies
-
perceptions regarding the challenges facing those leading decommissioning programmes
-
any currently existing good-practice guidance and resources for local leaders.
A secondary aim was to inform the design of subsequent research activities as well as an analysis of the case studies conducted in work package 3. This section provides a summary of findings for each organisation against aims (Table 10). The information included relates to the time of data collection (2012–13).
| Organisation | Summary |
|---|---|
| Specialised commissioning area teams | Area teams are regional teams that support the commissioning of high-quality services and directly commission primary care and specialised services. Areas include the South of England, London, North of England, the Midlands and East of England. Area teams operate as part of the national Operations Directorate, NHS England. No specific resources on decommissioning were identified, but these teams do consider decommissioning and service reconfiguration as part of the commissioning function |
| NHSIQ | Hosted by NHS England, NHSIQ seeks to provide expert support to the NHS in areas of service improvement and management of change. No specific resources on decommissioning were identified, but this is considered to be part of service reorganisation and the commissioning function |
| IRP | The IRP provides expert advice on proposed NHS reconfigurations or significant service changes. Proposals are referred to the panel by government ministers. The panel comprises independent experts on a rotating basis and considers whether or not referred proposals will provide safe, sustainable and accessible services for the local population, taking account of clinical and service quality; the current or likely impact of patients’ choices and the rigour of public involvement and consultation processes; the views and future referral needs of local GPs who commission services; the wider configuration of the NHS and other services locally; and any other relevant matters |
| CQC | This was the regulatory body for quality and safety standards in health and care services at the time of data collection. Where it is found that a service is not meeting standards, CQC can require providers to deliver a plan of action or can use enforcement powers, which can pertain to decommissioning. These powers include issuing a warning notice requiring improvements within a short period of time; restricting the services that the provider can offer; stopping admissions into the care service; issuing fixed penalty notices; suspending or cancelling the service’s registration; and prosecution. The CQC works with various bodies to enforce the standards. Depending on the service and the circumstances, the CQC can work with local authorities, regulatory bodies and agencies and even the police to ensure that action is taken |
| HealthWatch England | This is the national consumer champion for health and care in England that supports local HealthWatch organisations, of which there are 152. It reports on the issues that affect people who use services and works with other national bodies to ensure patient and public interests are represented in policy and decision-making. Local HealthWatch organisations, which are represented on local Health and Wellbeing Boards, give patients and communities a voice in decisions that affect them. Local HealthWatch organisations report their views and concerns to HealthWatch England so that issues can also be raised at a national level. No specific resources on decommissioning identified |
| LGA | The LGA is a membership organisation that represents the interests of local councils in England and Wales, lobbying and influencing policy development at the national level and providing support, advice, information and improvement for local government. The LGA gets involved in service redesign plans and programmes (without actively using terms such as ‘decommissioning’ and ‘disinvestment’). Through personalisation, services have closed as a result of lack of demand from individual budget holders |
| NHSCC | This is the representative body for CCGs in the English NHS. In 2016, NHSCC began work on a support document for CCGs entitled Making Difficult Decisions: Commissioning Healthcare in Changing Times.69 This put forward recommendations for decommissioning (and priority setting) including advanced planning, managing public perceptions, stakeholder engagement and political backing. This was the first formal support for decommissioning provided by NHSCC |
| NHS Confederation | This is the membership body for NHS providers and commissioners. The NHS Confederation has joined up with the Academy of Royal Colleges and National Voices (a third-sector representative body for patients and the public) to explore service change/reconfiguration and best practice. It has produced a series of case studies on reconfiguration and a survey of CCGs’ confidence in achieving change |
| NHS England Commissioning Development Directorate | This directorate of NHS England supports the development of the commissioning system in England, providing guidance on how clinical commissioning and commissioning support can deliver improvements in quality, outcomes and value for money. Specific support to CCGs to build skills and capacity for commissioning is provided. No specific resources on decommissioning have been produced |
| NHS Quality Board | This is a policy advisory group that aims to improve the quality and outcomes of NHS services. Provides leadership and works with clinicians, regulators, commissioners and patient groups to embed quality principles in the NHS. Key areas of quality policy include ensuring the overall alignment of the NHS systems for managing and improving quality, improving quality indicators, contributing to NICE quality standards, quality accounts, patient experience, accreditation and clinical audit policy areas and ensuring quality in service transformation. No specific resources on decommissioning identified |
| NICE | NICE identifies candidates for disinvestment through its technology appraisals and clinical guidelines programmes. The NICE website includes a ‘do not do’ database, although plans to more proactively identify options for removal and replacement have yet to be implemented |
| NHS Alliance | This is a national organisation representing and providing a voice for primary care, front-line staff, providers and patients (rather than commissioners). No specific resources on decommissioning identified |
| Monitor | Monitor is the sector (and competition) regulator for health services with powers granted by Parliament, including setting and enforcing a framework of rules for providers and commissioners, implemented in part through licences issued to NHS-funded providers (e.g. foundation hospitals, ambulance trusts and mental health and community care organisations). It also helps commissioners to ensure that essential local services continue if providers get into serious difficulty. No specific resources produced in relation to decommissioning |
| NCAT | NCAT responded to requests to review plans for reconfiguration from those leading the processes or other interested parties. Reviewed key documentation such as the Case for Change70 and the supporting business case and strategies before producing a report of its assessment. No specific support for decommissioning provided |
| OSCs | These are based in local government, are made up of councillors and are responsible for scrutinising local NHS policy, planning and impact against local needs and inequalities |
Summary of findings from the mapping interviews
The mapping interviews show that at the time of research there was a range of bodies with responsibilities in relation to decommissioning. However, these national roles and responsibilities were neither joined up nor mutually informed, and not all respondents indicated a detailed awareness of the remit of the other bodies in relation to decommissioning. Many of the national bodies included within the mapping review, with the exception of NICE, were not providing active support for locally led decommissioning. Others had a responsibility to intervene, for example in a review role, as in the case of the Independent Reconfiguration Panel (IRP), National Clinical Advisory Team (NCAT) and Overview and Scrutiny Committees (OSCs), on a case-by-case basis. This national context was highly fluid during the lifetime of the project, with some of the bodies either merged or discontinued.
Narrative vignettes
This section presents vignettes of the seven decommissioning stories recounted in the interviews (Boxes 1–7). Our main aim in collecting these was to sensitise ourselves to some of the features and determinants of decommissioning processes so that we could build these in to the design of research instruments in subsequent work packages.
Following a review of patient attendance at a local A&E department and two walk-in centres, it emerged that there was duplication in the treatments being carried out for the same patient group with some treatments also being carried out at local primary care practices. Early consultation with clinicians and staff produced a majority decision to relocate one walk-in centre to the A&E department and close the remaining centre. Backlash from patients, the public, local elected politicians and also a small number of secondary care clinicians located at the A&E department resulted in a review of the decision by the local OSC, and subsequently the Secretary of State for Health and national IRP. The decision was upheld. Continuous clinical backing and leadership were considered to be important for successful implementation of the decision.
A&E, accident and emergency.
Clinical sensory specialists sought to replace a drug for treatment of a sensory condition with an effective but less expensive alternative. Both drugs are manufactured by the same parent pharmaceutical company. The substitute drug was currently not licensed for treatment for the sensory condition and not recommended by NICE for that use in England. However, early trials revealed effective results and the (unlicensed) drug was widely used internationally for the condition in private health-care systems. Legal and licensing challenges and the longevity of research trials meant that attempts to replace the drug were, thus far, unsuccessful. This resulted in tensions for health-care commissioners who perceived that the current treatment option consumed a disproportionate amount of resources.
Changing patterns in health demand and the effects of these on skill levels led to a planned service transformation initiated in the mid-2000s. A well-resourced reconfiguration programme was put in place over a long period of time, with widespread buy-in and a thorough media and communications strategy. A clinical discussion of options was followed by public consultation, including with the paediatric population. The IRP reviewed the process and agreed that it was appropriate to decommission paediatric, obstetric and neonatal services in some hospitals and strengthen larger units, with support for staff in the transition. However, lengthy consultation and approval processes – including a second intervention following a change of government – meant that, overall, the process took many years to implement. Eventual success in implementation was considered to be because of an inclusive, generously funded approach with genuine (rather than belated and constrained) public consultation instead of organisations ‘sharing out the spoils’. Some of the intended reinvestment in community services was not as successful as planned and attendance at A&E did not reduce as anticipated.
A&E, accident and emergency.
In 2009, a CCG sought to decommission the local acute hospital homeopathy service. The commissioner gave 6 months’ formal notice that it would no longer fund this service. Three years had passed at the time of interview and the trust continued to invoice the CCG for the service, claiming that it had not been appropriately ‘repatriated’ out of general practice and that it was still receiving GP referrals (this was contested by the interviewee). One of the difficulties was identified as being unable to present a ‘united front’ between commissioners and the reluctance of commissioners to take the matter to arbitration.
GP, general practitioner.
A county council decided to reduce its reliance on care homes and thus embarked on a process of closing local care homes and relocating residents to neighbouring boroughs. A 3-month consultation process with residents, relatives and local community organisations took place before deciding to proceed with the programme of closures. Homes were closed one by one over a period of 4 years to allow the market to respond to the demand for alternative beds. Each home took approximately 9 months to close. An experienced officer was designated to project manage each closure and liaise with residents and relatives, as well as care staff and medical professionals supporting residents to ensure a smooth transition. Planned time scales, communication with residents and their families, and engaging the whole support circle of care staff and medical professionals were key factors to success. Having ‘supportive politicians’ was also cited as crucial.
In 2013, a CCG considered options for the future of maternity care within the area. Data on patterns of usage were reviewed, and existing maternity care service users and women of child-bearing age were consulted on their preferences. After consultation with midwives and clinicians, it was agreed that the only option was to close and transfer a maternity care unit to a hospital approximately 3 miles away. The changes were planned for summer 2015. A formal patient and public engagement consultation was led by a ‘highly skilled’ communications professional and the team were able to deal with enquiries and questions effectively. The consultation also involved local radio coverage and public meetings. However, the consultation revealed that the existing inpatient post-natal service was highly valued by patients and at the time of interview, alternative ways to improve services were being considered.
A CCG reviewed its services for the management of chronic pain, as it was found that there was heavy reliance on injections for pain relief. The CCG preferred a supported self-management model including coping strategies, psychology, occupational therapy and physiotherapy. It gathered data on the volume/types of injections and frequency of administration, and found that high levels of spinal epidural injections were carried out in acute/secondary care settings under tariffs. Clinicians, patient groups and commissioners were consulted on what they thought would be the best approach for care and on a new specification for the service. A rigorous selection process took place for the new contract and it was awarded to the community trust. Notice of the intention to decommission the injection service was sent to the acute trust and it was ultimately removed from the contract. Funding for the previous service and staff was redistributed among 10 local providers, with the intention that the service would be provided closer to home for patients. The experience of new patients was reported to be positive. Training for GPs on chronic pain management was included as part of the new service model and the referrals process was reviewed. However, existing patient views are reported to be largely negative and patients have struggled to adjust to the new model.
GP, general practitioner.
Taken together, these vignettes draw attention to a number of issues pertinent to the implementation of decommissioning policies. First, they show that mechanisms and levers for decommissioning vary. For example, CCGs within the sample employed contracts, formularies and consultation processes. Relationships of power shape the selection of levers and the success or otherwise of their implementation.
Second, the vignettes suggest that macro-political involvement was rarely experienced as predictable or indeed helpful. By contrast, local political (and clinical) buy-in was seen as important in making progress. Regional decommissioning plans were often subject to national involvement and processes that involved independent review became extremely lengthy in some cases.
Each of the stages of our model was observed in the narratives, albeit not in the linear manner implied by the model. Although the case studies hint at aspects of good practice, there is no apparent blueprint that guarantees delivery against aims, and much clearly depends on context (including changes in the political environment).
The vignettes appear to demonstrate the importance of engagement with patient groups and the wider public if ambitious decommissioning plans are to be implemented. The sample also contains an example (Box 6) of plans being abandoned following engagement activities.
Delphi study of researchers, policy-makers and practitioners
This section presents findings from the Delphi survey of expert opinion. Numerical results are included with illustrative quotations of the main findings from the analysis of the open comments provided by respondents in each round. For each quotation, a country and categorisation is provided using our tripartite sampling frame of ‘research’, ‘policy’ and ‘practice’.
Round 1 results
Thirty respondents provided a total of 142 criteria that they considered should inform decisions to carry out decommissioning and 126 criteria that they considered did inform such decisions in practice. After grouping of similar suggestions by the research team (Box 8), 16 criteria were identified as informing decisions to carry out decommissioning, both as it should be done and as it is done in practice. An additional eight considerations were identified for the latter. Open comments in support of these suggestions included scepticism as regards the evidence base of decommissioning decisions and a belief that cost considerations are most influential:
[We] need to acknowledge that health services are delivered within a dynamic policy and political context that on occasions drive decommissioning contrary to evidence.
Australia, policy/practice
Whilst the ideal is decommissioning of services that don’t represent high quality care or value for money, the reality is that decommissioning decisions are generally made as a money-saving mechanism.
UK, practice
Cutting costs is a legitimate reason for change but it is often hidden from public view or presented within the case for change as a subsidiary factor.
UK, policy
Common considerations that both (a) should and (b) do inform decisions:
-
addressing inequalities
-
alignment with strategic priorities
-
availability of alternative services/interventions
-
capital costs/condition (buildings, maintenance)
-
clinical effectiveness
-
cost/budgetary pressures
-
cost-effectiveness/efficient use of resources
-
cost of implementation of decommissioning
-
duplication of services
-
equitable resource allocation
-
evidence base
-
maximising population health
-
new service developments/innovations
-
patient and public views
-
quality and patient safety
-
responding to changing demographics/population needs.
Additional considerations in practice:
-
complexity of implementation of decommissioning
-
government intervention, for example, legislation
-
impact on workforce
-
marginal groups not heard (e.g. homeless people)
-
prejudice against public-sector provision
-
support from clinicians
-
support from elected politicians
-
support from industry and other interest groups.
Respondents also put forward 463 factors that shape the process or outcomes of decommissioning (either positively or negatively). These were grouped by the research team into the 30 factors, listed in Box 9. The sheer volume of identified factors meant that categorisation was challenging. In order to present findings back to respondents in an accessible format, we grouped the factors into three broad themes (below). However, we recognise that they are not entirely mutually exclusive:
-
change management and implementation strategy – this includes factors such as strategic planning, project management, communication and leadership
-
evidence and information – this includes formal evidence of effectiveness and cost-effectiveness of candidates for decommissioning as well as, for example, information from implementers elsewhere
-
relationships and political dimensions – this includes factors such as relationship with communities, national political influence and the media.
Change management and implementation strategy:
-
attention throughout to human aspects of process of change
-
availability of resources to support decision-making and implementation processes
-
clarity of incentives and levers to support change
-
clarity of specific aims and objectives at the start
-
extent of cultural and behavioural change
-
pace of change
-
quality of strategic planning
-
quality of project management
-
complexity of decommissioning programme
-
quality of communication
-
strength of clinical leadership
-
strength of executive leadership
-
training and preparedness of staff.
Evidence and information:
-
availability of alternative services
-
clarity around new patient pathways
-
clarity of evidence/data to support business case, ongoing monitoring and impact assessment
-
demonstrable benefits
-
extent of adoption elsewhere of new intervention/service
-
review/evaluation of process.
Relationships and political dimensions:
-
clarity of rationale/case for change
-
extent to which change challenges vested interests
-
level of political support
-
meets community expectations
-
nature and extent of clinician engagement/involvement
-
nature and extent of media coverage
-
nature and extent of patient/public involvement
-
quality of partnership working with relevant agencies
-
reputation of existing providers
-
stability within the local health economy during transition
-
transparency of decision-making process.
Participant comments included reflections on politics and evidence:
Decommissioning health care services is difficult unless you have clinicians onside. This also needs to be complemented by political support at the local and national level. Without these and a clear narrative of what these changes are and why these are necessary then decommissioning is difficult to bring about.
Australia, research
Lots of decommissioning I see seems to focus on a technical, rational decision to change services but doesn’t pay sufficient attention to the politics of such change (at its peril).
UK, policy
A very rigid ‘science of health care’ and therefore what is worth commissioning is causing the decommissioning of ‘non evidence-based’ services in a way that appears fair but is hugely damaging. The evidence-base used is flawed.
UK, practice
Finally, in round 1, participants generated a total of 125 ‘best-practice’ recommendations to guide effective decommissioning, which were grouped by the research team into 19 ‘best-practice’ recommendations (Box 10). Again, participant comments provided further explanation of these recommendations:
Once a decision has been taken it should be stuck to as long as the appropriate process has been followed. Many decommissioning projects fail to achieve what they set out to achieve because commissioners and organisations go back on their decisions. Among the main reasons why commissioners may change their minds are the influences of staff groups who may not have been fully engaged in the decision making process and politicians who may have been influenced by public opinion to oppose change.
UK, research
Decommissioning services is a taboo subject. In order to manage it effectively you need a good strong clinical leader so that the service is decommissioned from a clinical perspective on quality issues and ineffectual clinical outcomes.
UK, practice
-
Adopt a whole-systems perspective from the beginning.
-
Base decisions on evidence of what works.
-
Be proactive in engaging with the media.
-
Clear and thorough project planning and governance.
-
Collect and analyse relevant data before, during and after.
-
Do not decommission until there are alternative services in place.
-
Engage and involve clinical leaders from an early stage.
-
Engage and involve service users from an early stage.
-
Ensure a transparent decision-making process.
-
Establish a clear rationale and narrative for change.
-
Establish clear criteria by which to measure outcomes.
-
Focus on improved patient experience and quality.
-
Identify and establish a strong top leadership team.
-
Pay attention to the human elements of change and the impact that decommissioning can have on those involved.
-
Pay equal attention to implementation and decision-making phases.
-
Place emphasis on public engagement and communication.
-
Provide regular feedback on progress.
-
Resource the process and retain a budget for contingencies.
-
Secure high-level political support (national and local) at an early stage.
Round 2 results
Of the 30 participants in round 1, 27 completed the round 2 questionnaire, which assessed the extent to which there was a consensus regarding which of the considerations identified in round 1 should inform decisions to carry out decommissioning, and which do inform decisions in practice. Appendix 7 presents these results. Respondents were also asked to rank the relative importance of the factors proposed in round 1 as shaping – either positively or negatively – the process or outcomes of decommissioning. The results are shown in Appendix 7. The politically contested nature of decommissioning and the importance of clinical buy-in featured in open-text comments:
Politicians may not instigate decommissioning decisions themselves but they can bully senior decision makers into changing their plans if they feel that they will adversely effect their election chances. Other decommissioning decisions are taken at short notice and they need to deliver savings quickly and effectively. If a decommissioning decision costs money in the short term or is hard to implement and will take too long then it won’t happen.
UK, research
Decommissioning projects fail when the clinical case is not clear or supported by clinicians and the public.
UK, policy
Calculation of the degree of consensus in responses to the 88 rating scale questions from round 2 found that 59 questions achieved a high degree of consensus among participants, 11 achieved a medium degree of consensus, 10 achieved a low degree of consensus and 8 achieved ‘no consensus’. The nine statements and three ‘best-practice recommendations’ with the highest degree of consensus are shown in Box 11.
‘Cost-effectiveness/efficient use of resources’ considerations should ideally inform decisions to carry out decommissioning (strongly agree).
‘Quality and patient safety’ considerations should ideally inform decisions to carry out decommissioning (strongly agree).
‘Clinical effectiveness’ considerations should ideally inform decisions to carry out decommissioning (strongly agree).
‘Cost/budgetary pressures’ considerations do actually – in practice – inform decisions to carry out decommissioning (strongly agree).
‘Addressing inequalities’ considerations do actually – in practice – inform decisions to carry out decommissioning (disagree).
‘Strength of executive leadership’ has very high importance for shaping the extent to which decommissioning is implemented as planned.
‘Strength of clinical leadership’ has very high importance for shaping the extent to which decommissioning is implemented as planned.
‘Clarity of rationale/case for change’ has very high importance for shaping the extent to which decommissioning is implemented as planned.
‘Quality of partnership working with relevant agencies’ has high importance for shaping the extent to which decommissioning is implemented as planned.
Best-practice recommendation: identify and establish a strong top leadership team (very high importance).
Best-practice recommendation: establish a clear rationale and narrative for change (very high importance).
Best-practice recommendation: engage and involve clinical leaders from an early stage.
Of the 18 questions with a relatively low level of (or no) consensus, 14 related to the factors that participants put forward as informing decisions to carry out decommissioning in practice. By contrast, the other five sections in round 2 generated much higher overall consensus levels. All of the questions in the section exploring the extent to which the nominated factors should inform decisions to carry out decommissioning achieved a medium or high degree of consensus.
In descending order of importance, the following good-practice recommendations were identified as being the most important:
-
identify and establish a strong leadership team
-
engage and involve clinical leaders from an early stage
-
establish a clear rationale and narrative for change
-
ensure clear and thorough project planning and governance
-
secure high-level political support (national and local) at an early stage
-
base decisions on evidence of what works
-
adopt a whole-systems perspective from the beginning.
Round 3 results
Of the 27 respondents in round 2, 25 participated in the third round of the survey, and Appendix 7 presents the full results. Because of the marked contrast between the judgement of what should happen and what happens in practice in relation to decommissioning decisions, we explored this theme further in the third and final round. Participants were invited to reconsider the 18 questions in round 2 that registered a low level of/no group consensus, 13 of which related to the ‘what happens in practice’ section. Participants also reflected on the possible reasons for the low consensus levels. For example, in relation to whether or not the costs of decommissioning do in practice inform decisions, participants reflected that:
I can remember 4 years of meetings with officers from a handful of other bodies all relating to a decommissioning which was mainly intended to secure a service improvement, rather than a cash saving. The time we spent on the exercise was never counted as a cost.
UK, practice
There is a major misconception of cost. The costs incurred are far more complex than I believe is considered.
UK, practice
I don’t really think the costs per se are relevant – it is more about skills, having the right framework in place, leadership and political will . . . the failure to see priority setting as a programme . . . which needs resources attached to it is one of the reasons we have poor priority setting . . . it is a lack of understanding and will to establish priority setting as a major programme needing a team and resources to support it.
UK, policy/practice
Results from the third round show a low level of/no consensus in relation to five of the original 88 statements generated in round 1:
-
‘The evidence base’ does inform decisions to carry out decommissioning.
-
‘Responding to changing demographics/population needs’ does inform decisions to carry out decommissioning.
-
‘Support from industry and other interest groups’ does inform decisions to carry out decommissioning.
-
‘Impact on workforce’ does inform decisions to carry out decommissioning.
-
What is the relative importance of the ‘pace of change’ for shaping the extent to which decommissioning is implemented as planned?
The first of these generated the widest range of reactions to the round 2 rankings, and the role played by evidence was a source of notable differences of opinion:
Very disconcerting ‘disagree’ response rate. Evidence certainly ought to inform decisions and in my applied experience it is central. Please unpack and report the reasons for the ‘disagree’ responses.
Australia, research
I think we have all experienced decisions that were taken in the absence of a robust evidence base. I don’t think I have personally experienced decisions that were taken in flat contradiction of a robust evidence base. For that reason I choose ‘agree’ but recognise others may choose ‘disagree’.
UK, practice
I’m afraid I just don’t buy the standard textbook answer here – it feels more an issue of responding to national/local politics and a pragmatic sense of what we can get away with in practice.
UK, policy
In my experience, I still feel that a lot of decommissioning decisions are taken on ‘gut feeling’ rather than necessarily on the basis of hard evidence or facts.
UK, research
My experience is that a highly reductionist approach to evidence base and efficacy tends to negate what actually works/the effectiveness in real life . . . services that work on paper often don’t work in practice. The biggest block to truly evidence-based decommissioning is a lack of effectiveness data and a lack of review of the beliefs around efficacy.
UK, practice
Changes between rounds 2 and 3
Following round 3, 9 of the 13 statements moved from a low level of/no consensus to a medium or high degree of consensus with three statements added to the list of statements with a high level of consensus (Box 12).
‘Maximising population health’ does actually in practice inform decisions to carry out decommissioning (disagree).
‘Patient and public views’ do actually in practice inform decisions to carry out decommissioning (disagree).
‘Complexity of implementing decommissioning’ does actually in practice inform decisions to carry out decommissioning (agree).
After the third round there was a high level of consensus that ‘reputation of existing providers for shaping the extent to which decommissioning is implemented as planned’ had high or very high importance.
Overall results from the Delphi survey suggested areas of agreement and disagreement and a notable gap between what the panel believed should and does inform decommissioning. The panel agreed on six good-practice recommendations related to leadership: clinical engagement, creating a change narrative, project planning and governance, political support, evidence and whole-systems thinking.
Summary of findings across work package 1
The summary of previous reviews shows that in the years since 2004 there has been increased investigation of health-care decommissioning, and that this has been dominated by the study of ‘disinvestment’ decision-making at macro and meso levels within health systems. This literature has been somewhat normative in its identification with promoting evidence-based decision-making, drawing on principles of cost-effectiveness and opportunity cost, and applying tools and methods such as HTA (and reassessment), low-value lists and PBMA. This literature seems to confirm a general picture of patchy or low levels of decommissioning at the local level despite some national and international initiatives. The focus on the decommissioning of medicines or therapeutic interventions (rather than services or organisations) prevents us from drawing conclusions from the literature about planned decommissioning of these types. However, it does highlight some potential determinants of successful implementation, including the availability of relevant evidence, overcoming resistance to change and generating ‘will’ among political, clinical and management actors.
The Delphi study of expert opinion enables us to further develop these insights and is designed to combine perspectives on a broader range of decommissioning types. Our findings indicate that the considerations that experts believe ought to drive decommissioning (cost-effectiveness, quality and patient safety, clinical effectiveness) are different from those that often do in practice (cost/budgetary pressures). The four factors that drew the highest degree of consensus as being important in shaping whether or not decommissioning is implemented as planned were (1) strength of executive leadership, (2) strength of clinical leadership, (3) clarity of rationale/case for change and (4) quality of partnership working with relevant agencies.
Finally, the mapping exercise and narrative vignettes suggest that although there are national bodies that play a role in decommissioning, there is an absence of leading organisations at the national or regional level. This preparatory work suggests the importance of examining the complex relationships between macro and meso levels with the NHS (and local government) and the reticence at both levels towards explicitly pursuing a decommissioning agenda. The narrative vignettes in particular suggest that decommissioning is not always ordered and linear and is therefore likely to deviate from our stages model. The importance of implementation levers and mechanisms, and the play of power more generally, are also lessons from these data sources.
Chapter 5 Findings from a national survey of Clinical Commissioning Groups
The aims of the national survey of CCGs were to identify the volume and types of decommissioning activities planned and under way across England, and to gain insight into the implementation and outcomes of decommissioning programmes. A total of 56 CCGs responded to the survey (27% of all CCGs) and we asked respondents to report their experiences in relation to the following:
-
extent of current engagement with decommissioning
-
types of current/recent decommissioning programmes
-
aims and intended outcomes of decommissioning programmes
-
challenges and key determinants of decommissioning
-
attitudes and competencies regarding decommissioning.
Extent and nature of decommissioning
Of the 56 responding CCGs, 77% had decommissioning activities planned and 67% had decommissioning activities currently being implemented, with a total of 91 projects reported and 50 being implemented. The responses are summarised in Table 11.
| Decommissioning activity | Percentage | n |
|---|---|---|
| Planned | 77 | 91 |
| Being implemented | 67 | 50 |
| Completeda | 55 | 35 |
The number of CCGs that reported carrying out decommissioning was higher than might have been expected given the low levels reported in our evidence synthesis. This may reflect selection bias, with those CCGs that were engaged in decommissioning being more likely to respond. However, open comments provided by participants suggested that decommissioning was viewed as increasingly necessary in the current financial climate and that wider policy and strategy regarding the NHS required significant service transformation, to be led by CCGs. For example, one respondent commented:
The nature of NHS finance assumptions means the CCG needs to agree bold and ambitious change programmes into the future.
Survey respondent 18
The most common type of decommissioning activity reported as being undertaken by CCGs in our survey was the relocation or replacement of a service from an acute to a community setting (28%). The second most common was removal or replacement of a service as part of a reconfiguration of services (25%) and the third most common was closure of a service (14%). The results are reported in Table 12 and Figure 3.
| Decommissioning type | Frequency | Percentage of total |
|---|---|---|
| Relocation/replacement of a service from an acute to a community setting | 49 | 28 |
| Relocation or replacement of a service as part of reconfiguration | 44 | 25 |
| Closure of a service | 25 | 14 |
| Removal or replacement of a treatment from a formulary or pathway | 20 | 12 |
| Partial closure of a service | 15 | 9 |
| Closure of an acute health-care organisation | 6 | 3 |
| Partial closure of a primary health-care organisation | 4 | 2 |
| Closure of a primary health-care organisation | 2 | 1 |
| Partial closure of an acute health-care organisation | 2 | 1 |
| Other | 7 | 4 |
FIGURE 3.
Number and types of decommissioning projects.
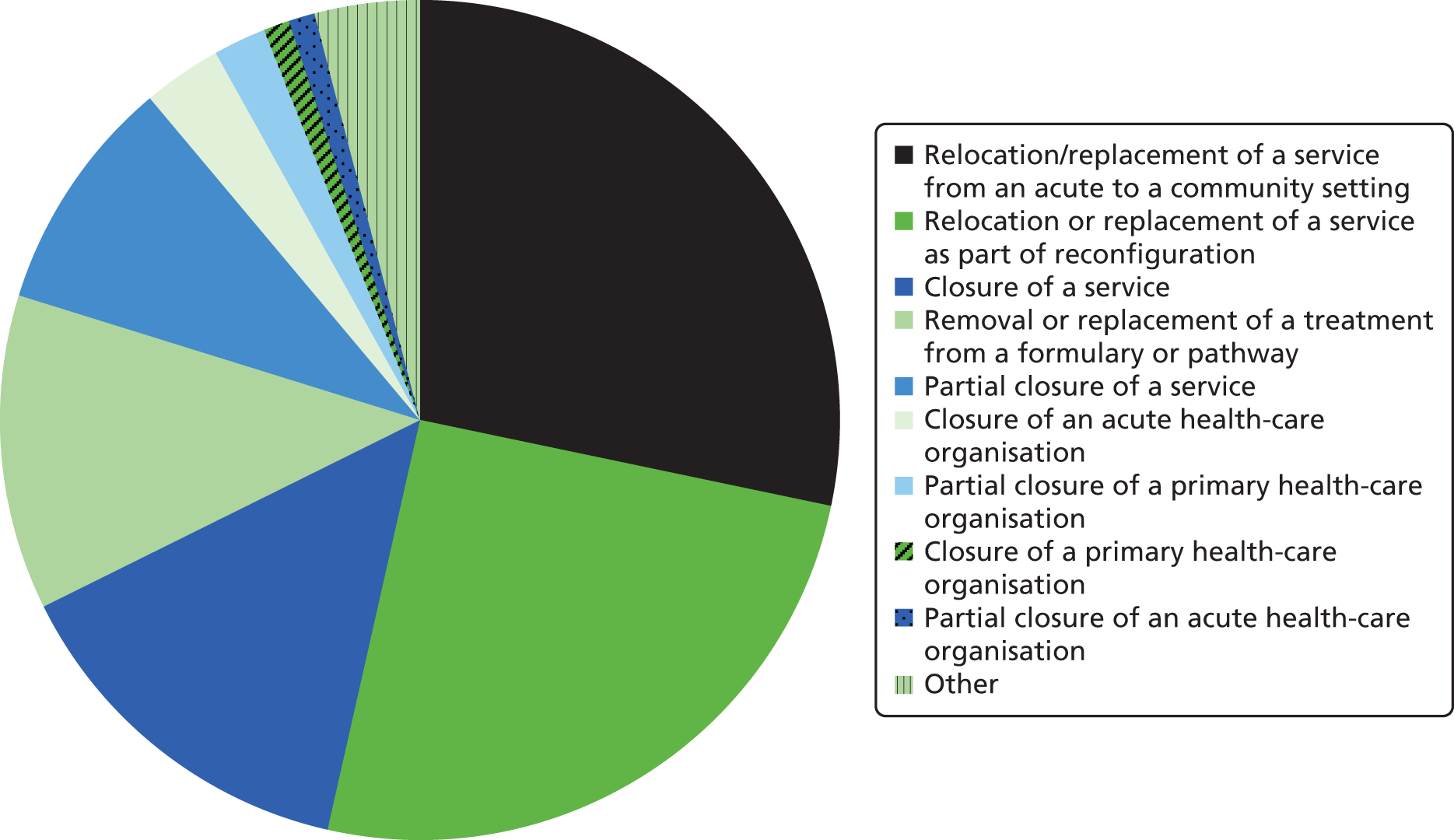
Open comments provided by participants shed further light on these responses and suggest that CCGs were aiming to invest more in primary and community care and to provide services closer to home for patients and the public:
Part of our 5-year plan is to shrink back the acute sector and to redesign and reprovide within primary and community care where appropriate.
Survey respondent 38
The integration agenda means a shift in resource from hospital to community and primary care.
Survey respondent 10
. . . mostly changing care pathways and setting up intermediary services in the community, e.g. cardiology, dermatology, MSK [musculoskeletal].
Survey respondent 43
Other types of decommissioning reported by CCGs included decommissioning services and recommissioning them to alternative providers, and rationing access to specific services and treatments:
Decommission of a service and recommission.
Survey respondent 45
Recommissioning of non-emergency patient transport, from acute provider commissioning to CCG-commissioned service.
Survey respondent 27
Review of commissioning policy may restrict access to certain treatments.
Survey respondent 46
Aims and intended outcomes of decommissioning
In order to gain insight into the aims, outcomes and experiences of contemporary decommissioning activities, we asked CCGs to respond to questions in relation to the decommissioning project that they had most recently completed. Our survey results indicated that the most common intended outcome of decommissioning activities was to improve cost-effectiveness (reported by 38% of CCGs). The second most common driver was improved patient experience (36%), followed by improved clinical effectiveness and greater alignment with strategic priorities (both 30%). The results are summarised in Table 13.
| Decommissioning outcome | Frequency | Percentage |
|---|---|---|
| Improved cost-effectiveness | 21 | 38 |
| Improved patient experience | 20 | 36 |
| Improved clinical effectiveness | 17 | 31 |
| Greater alignment with strategic priorities | 17 | 31 |
| Improved access to services | 14 | 26 |
| Cost/budgetary savings | 13 | 23 |
| Improved patient safety | 10 | 18 |
| Reduced inequalities | 9 | 16 |
| Improved population health/well-being | 6 | 11 |
| Other | 2 | 4 |
Overall, 38% agreed and 19% strongly agreed that decommissioning had achieved its intended outcomes, with 38% reporting that it was too early to tell and 5% strongly disagreeing that decommissioning activities had achieved their intended outcomes overall. We asked CCGs to tell us the extent to which specific outcomes were observed for decommissioning programmes (Table 14).
| Decommissioning outcome | Increased | Decreased | Too early to tell | No change | No evidence | Not sure |
|---|---|---|---|---|---|---|
| Cost/budgetary savings | 25 | 6 | 56 | 6 | 0 | 6 |
| Cost-effectiveness | 38 | 0 | 56 | 0 | 0 | 6 |
| Duplication of services | 0 | 50 | 25 | 13 | 6 | 6 |
| Patient safety | 40 | 13 | 33 | 13 | 0 | 0 |
| Clinical effectiveness | 40 | 0 | 53 | 7 | 0 | 0 |
| Patient experience | 19 | 13 | 44 | 13 | 0 | 13 |
| Population health/well-being | 19 | 0 | 44 | 13 | 19 | 6 |
| Inequalities/lack of access to services | 13 | 19 | 50 | 6 | 0 | 13 |
| Alignment with strategic priorities | 63 | 0 | 25 | 13 | 0 | 0 |
Responses were mixed, and again it was often too early to tell if specific outcomes had been achieved. This may be because of the timing of the survey, as many decommissioning activities may only recently have been completed so that outcomes were not yet known; this is particularly likely given the recent formation of CCGs and given that only 55% reported that they had fully implemented decommissioning activities overall. Other reasons for the lack of clarity about outcomes may be related to the capacity of CCGs to collect and analyse data, and the time frames required to realise outcomes. Elaborating further on their responses, respondents also indicated that outcomes and impacts were often subjective and varied according to position in the health-care system:
There have been positives and negatives. From a clinical safety perspective and in evaluating clinical and performance outcomes these have either improved or not been adversely affected. From a public perspective, some people have to travel further so this could be classed as a negative.
Survey respondent 26
Early feedback indicates that new patients are very happy with the service (community pain service); existing patients who had a different pathway before feedback is varied.
Survey respondent 27
Methods and stakeholder involvement
Our review of the literature in work package 1 indicated that a number of methods have been developed for use in decommissioning and disinvestment processes. We asked CCGs in our survey to indicate the extent to which such methods featured in the decommissioning activities they reported (Table 15).
| Method | Frequency | Percentage |
|---|---|---|
| Public engagement and involvement | 24 | 44 |
| Needs assessment | 22 | 40 |
| Stakeholder workshops | 21 | 38 |
| Stakeholder mapping | 16 | 29 |
| PBMA | 13 | 24 |
| Scenario planning | 10 | 18 |
| HTA | 4 | 7 |
| No formal methods | 3 | 6 |
| Other | 4 | 7 |
‘Public engagement and involvement’ was the most common method undertaken by CCGs in their decommissioning programmes, and this was followed closely by ‘needs assessment and stakeholder workshops’. ‘PBMA’ was also used by a significant minority. ‘Scenario planning’ and ‘HTA’ were not widely used.
Further questions in our survey aimed to gauge the extent to which different stakeholders were involved in the various stages of decommissioning and the nature of that involvement. The results in Table 16 report the degree to which stakeholders were actively involved in the decommissioning process.
| Stakeholder | Decision-making | Planning | Implementation | Review |
|---|---|---|---|---|
| CCG | 97 | 90 | 90 | 87 |
| Clinical professionals (primary care) | 68 | 61 | 59 | 68 |
| Clinical professionals (secondary care) | 33 | 50 | 39 | 36 |
| Local provider organisation(s) | 24 | 47 | 59 | 45 |
| Patient and community groups | 29 | 18 | 11 | 18 |
| Public/citizens | 14 | 14 | 11 | 19 |
| Other | 14 | 17 | 14 | 29 |
From the results it appears that patient and community groups and the public/citizens have the least active involvement throughout the decommissioning process. Provider organisations also have lower involvement in decision-making regarding decommissioning, but are more involved in the planning, implementation and review of decommissioning activities. This would appear to correspond to our work package 1 and subsequent case study findings, suggesting that providers often have a key role in the implementation of decommissioning plans and activities, with key responsibilities in managing and implementing changes to services and the transition of patients and users from those services.
The finding of active involvement of clinical professionals (particularly in primary care) across the decommissioning stages also corresponds to our results from work package 1, which suggested that obtaining the support of clinicians early on for decommissioning activities was key to their success.
Determinants of decommissioning processes
A key aim of the survey was to understand the factors – positive and negative – that influenced the decommissioning processes reported by CCGs. Using the Delphi study results reported in work package 1, we compiled a list of challenges and issues experienced in decommissioning and asked respondents to tell us whether or not and how these influenced their reported decommissioning processes. The results are summarised in Table 17.
| Factor | Positive | Negative | No influence | Not sure |
|---|---|---|---|---|
| Executive leadership/management | 36 | 0 | 0 | 0 |
| Quality of evidence base | 32 | 0 | 2 | 2 |
| Clinical engagement and support | 29 | 7 | 2 | 2 |
| Quality of implementation plans/planning | 27 | 6 | 4 | 0 |
| Staff training and skills | 24 | 6 | 7 | 2 |
| Patient and public views | 20 | 7 | 4 | 9 |
| Scale of project (e.g. geography, number of organisations involved) | 16 | 6 | 15 | 0 |
| Implementation costs | 13 | 2 | 28 | 2 |
| Views of local elected politicians | 9 | 3 | 18 | 7 |
| National government | 4 | 0 | 29 | 4 |
| Media coverage | 4 | 13 | 15 | 6 |
| Other | 2 | 0 | 2 | 0 |
The three most common factors that were seen to hinder decommissioning and affect the process negatively were ‘media coverage’, ‘clinical engagement and support’ and ‘patient and public views’. Notably, ‘clinical engagement and support’ also featured among the most common factors that enabled decommissioning, suggesting that clinicians are a powerful stakeholder group that can both hinder and facilitate the decommissioning process. The next most common factors reported to have a positive influence on decommissioning were ‘executive leadership/management’, ‘quality of evidence base’ and ‘quality of implementation plans/planning’. These findings broadly reflect the best-practice recommendations reported by the Delphi panel in work package 1.
Only three CCGs reported that planned decommissioning projects had been discontinued. These included one partial closure of a primary health-care organisation, two relocation/replacements of a service as part of a reconfiguration, and one removal/replacement of a treatment from a formulary or patient pathway. Reported reasons for discontinuation included:
Clinical and patient views in engagement process.
Survey respondent 48 – regarding removal/replacement of a treatment from a formulary or patient pathway
On basis of evidence base.
Survey respondent 47 – regarding relocation/replacement of a service as part of a reconfiguration
Lack of organisational appetite to disinvest in a service delivered by member practices as this may lead to disengagement.
Survey respondent 35 – regarding partial closure of primary health-care organisation
Awaiting impact of new primary care contract – was decommissioning a local enhanced service.
Survey respondent 29 – regarding relocation/replacement of a service as part of a reconfiguration
The reported reasons for discontinuation correspond with the most common reported factors that were said to hinder or support decommissioning in the survey: clinician engagement and support, patient and public views and quality of evidence base.
Attitudes and competencies
The survey sought to identify which organisational bodies were initiating decommissioning. Perhaps not surprisingly, given the target population of the survey, 81% of decommissioning projects were reported as being led by CCGs, with 7% led by local provider organisations, 3% jointly led by the CCG and another partner/organisation, and 10% led by another organisation [including Commissioning Support Units (CSUs), other CCGs and local government].
Clinical Commissioning Groups were also asked to assess their capacity, capability and resources for decommissioning (Table 18). A narrow majority either agreed or strongly agreed that they had the necessary capacity and resources, while a larger percentage (78%) felt that they had the necessary capabilities. This suggests that shortages of human and fiscal resources were considered to be a bigger hindrance than shortages of the necessary skills for decommissioning.
| Statement | Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree |
|---|---|---|---|---|---|
| My organisation has the necessary capacity (dedicated time and personnel) to undertake decommissioning | 5 | 16 | 27 | 43 | 8 |
| My organisation has the necessary capability (skills, expertise and authority) to undertake decommissioning | 8 | 5 | 11 | 57 | 19 |
| My organisation has the necessary financial resources to undertake decommissioning | 8 | 19 | 19 | 49 | 5 |
Some responding CCGs (40%) reported having accessed support from CSUs to undertake decommissioning. This was the most common type of support accessed overall. By contrast, 6% had accessed support from private providers to undertake decommissioning, 7% had accessed support from a university department and 6% had accessed support from voluntary sector providers to undertake decommissioning. Other types of accessed support reported by CCGs in the survey included ‘legal advice’ (survey respondent 28), support from local authorities and public health teams and the NCAT.
Open comments provided by CCGs suggested that a number of factors had detracted from the capacity, resources and capabilities that they required to perform this role. These included a perceived lack of guidance designed to support their decision-making, the turbulence caused by NHS reforms and restructuring (and associated turnover of staff and expertise), and limits to the local support offered by bodies such as CSUs:
The PCT undertook a decommissioning process during the year prior to CCG coming into place therefore a large element of this work already completed. However, what is missing is a clear framework CCGs can use to help them make decisions.
Survey respondent 31
Disinvestment is going to be necessary to stay in financial balance. The CCG has a robust process. The PCT never grasped this nettle. Other commissioners such as Public Health, NHSE [NHS England] and spec[ialised] services will have to face this difficult decision, but for now the CCGs will be criticised, especially by the media for having the courage and integrity to take difficult decisions.
Survey respondent 32
The lack of capacity/resources relates largely to CSUs. They have spent so much time reacting to changes relating to their own future rather than developing their own expertise.
Survey respondent 53
Summary of findings from work package 2
Overall, the survey would appear to indicate increased levels of activity in the area of planned decommissioning, but at the time of data collection there had been insufficient time (including since the setting up of most CCGs) to record implementation rates, outputs and outcomes. In keeping with the more ambitious plans reported, there was less of a focus on tools such as low-value lists and HTA/HTR than reported in the reviews included in Chapter 4. More commonly, respondents had employed stakeholder engagement techniques and needs assessment, with PBMA used in a smaller number of cases. Findings support those from work package 1, including concerns over the level of information and other support available from national and local bodies; low levels of patient and especially public input into decommissioning stages; and the influential role of senior leadership to decommissioning processes and evidence to support decision-making.
Chapter 6 Findings from longitudinal case studies of four decommissioning processes
Introduction
This section presents results from the four in-depth case studies carried out in order to develop our response to the question: what factors and processes influence the implementation and outcomes of decommissioning? Each narrative account explores the origins, aims and intended outcomes of the decommissioning programmes. They examine the use of evidence and analysis in the decision-making process before exploring the web of relationships between internal and external actors and influences in decommissioning design and implementation processes. The role of interest groups such as politicians and clinicians, and the public, are analysed and, finally, attention is given to any outcomes of the processes and the attitudes of those involved towards future decommissioning.
Case study 1: decommissioning as part of the national reorganisation of paediatric burn care services in England
The incidence of severe burns in both children and adults has decreased over time71 and there have been repeated calls for a rebalancing of specialised service provision to reflect changing demand. This case study focused on the reorganisation of burn care services for children across England and Wales during the period of September 2014 to May 2016. This was led by NHS England’s Trauma National Programme of Care and, specifically, the national Burn Care Clinical Reference Group (CRG), which was one of many set up to advise NHS England on new drugs and innovations, and the development of policy and reorganisation. At the time of the case study, the CRG was advising the commissioner on the reorganisation of paediatric services. As described in Chapter 3, this case study was selected to fulfil the criteria of being a nationally led, complex reorganisation process involving planned service removal or reduction.
This report presents case study findings against research aims and questions. In accordance with our overall analytical framework, it provides a narrative account to describe how interactions between actors were recounted by participants and documented in written evidence, and how these unfolded during observation. It focuses on the following broad processes:
-
the role of evidence and actors in identifying and framing a need for decommissioning
-
alliance-building as part of a decommissioning process
-
gaining acceptance for the solution of decommissioning
-
implementation and institutionalisation of a decommissioning decision.
The report finishes with reflections on case study findings and implications for our understanding of decommissioning.
Reorganisation of burn care services in England: a brief history
Burn severity is measured according to size, depth and location of the injury, and patient characteristics. Specialist paediatric burn care in England is low in volume and high in cost. Traditionally, burns services have developed incrementally across the country, and the national Burn Care Review of 200172 was the first time that a co-ordinated assessment was carried out of the effectiveness of these arrangements. This led to a series of national and regional initiatives intended, at least in part, to reconfigure services in line with changing patterns in demand (Box 13). A key outcome was the tripartite categorisation of burn services according to severity, with levels of care designated as ‘unit’, ‘facility’ or ‘centre’, with the most specialised (centre level) requiring multiprofessional specialist care support.
2001: Burn Care Review72 posits three levels of care (‘facility’, ‘unit’ and ‘centre’).
2003: National Burn Care Group set up and secures statutory funding.
2004–5: services measured against Burn Care Standards (‘designation’).
2005: Burn Injury Database set up.
2007: four regional networks set up under umbrella of a National Network for Burn Care.
2008–11: standards revised and reorganisation processes attempted but not implemented in all regions.
2012–13: creation of NHS England and the Burn Care CRG replacing previous National Network for Burn Care. National contract replaces regional designation process.
2013: standards revised and new service specifications used to carry out an NHS England review of compliance.
2014: non-compliant services considered for derogation.
2015: Options put forward by the CRG for the reorganisation of paediatric services.
2016: NHS England merges the Burn Care CRG with larger specialities.
In 2003, the National Burn Care Group was set up with Department of Health funding and allocated responsibility for the assessment of services against the national burn care standards, and the designation of these according to the three orders of specialty. However, differential rates of progress led to the formation of four regional networks covering England and Wales (Northern Burn Care Network, Midlands Burn Care Network, South West UK Burn Care Network and London and the South East of England Burns Network) and charged with continuing the process of change under the oversight of a national network that is itself a subgroup of the predecessor to NHS England (the NHS Commissioning Board). In 2005 a Burn Injury Database was set up to enable monitoring of provider activity and outputs, and, in each of the regions, recommendations were subsequently made to reduce the number of centre-level providers. However, in two of these regions (the North West in 2007 and London/the South East in 2012) proposals were opposed by provider organisations threatened with decommissioning and no significant service changes resulted. In these regions, the landscape of paediatric burn care provision has therefore remained largely unchanged since 2001.
The Health and Social Care Act 20128 and subsequent establishment of NHS England saw responsibility for the commissioning of specialist burn services move from local and regional arrangements to a national commissioning contract, with clinical advice provided by the Burn Care CRG comprised of nurses, doctors, patient and lay representatives, NHS England and Public Health England, and intended to be geographically representative of the country. In 2012 the CRG led a review and revision of the Burn Care Standards, and confirmed the following minimum specifications for provider designation at (paediatric) centre level:
-
on-site access to designated paediatric intensive care (PIC) and paediatric high-dependency care
-
burn-competent paediatric anaesthetists
-
sustainable 24/7 consultant burn surgeon rota
-
24/7 access to paediatric-related specialties (including paediatric surgery and paediatric renal medicine).
At the time of the research, assessing compliance against these specifications was the responsibility of NHS England Local Area Teams reporting to NHS England and the CRG. Regional operational delivery networks (ODNs), coterminous with the former regional networks, had responsibility for the implementation of national policies and plans. These arrangements afford two main mechanisms for delivering service changes, each of which involves the CRG. These are:
-
identification of ‘derogation’, that is, a failure to comply with one or more of the minimum standards (in accordance with the legal origins of the term, derogation implies a temporary relaxing of the rules while arrangements are put in place to enable compliance)
-
wider reorganisation initiatives intended to concentrate high-level paediatric burn care in fewer provider sites.
Both mechanisms had been activated at the time of the commencement of the case study. One centre – hospital A – had self-assessed as non-compliant with the requirement for a co-located PIC unit, and assessment of other centre-level providers was under way. Furthermore, the CRG was in the process of preparing an options statement for the reconfiguration of paediatric centre-level burn care in England. The target date for resolving the issue of hospital A’s derogation and gaining approval for implementation of the wider changes was 31 March 2015.
Case study activity
During the period of fieldwork the CRG met five times and observations were conducted by the research team in September 2014, September 2015 and April 2016. Key documents were retrieved and added to the analysis and a total of 17 telephone interviews were conducted (including four follow-up interviews). Access to interviewees was negotiated through the chair of the CRG and the NHS England programme lead. Consent was secured collectively from participants at the September 2014 CRG meeting and individually prior to each interview. The sample of interviewees included representatives from each of the four regions, eight CRG members and six non-members, including NHS England employees at national and local level, and clinical staff. Interviewees were identified on an iterative basis following initial advice from the CRG chair. All participants approached agreed to be interviewed in either first or second rounds. The chair was a regular point of contact for the case study and as such is not quoted verbatim in this report. Further details of data sources are provided in Appendix 8.
Defining the problem and mobilisation
Rationale for change
The history of reform of burn care services – including the development of national standards, the national database, and successive national and regional service reviews over a 15-year period – had led to some degree of consensus over the case for change among those directly involved. This case rested on a combination of theoretical assumptions – for example, linking levels of clinical activity to the maintenance of expertise – and evidence collected from the scientific literature and service data (e.g. Palmieri et al. 73). These were combined and codified in the burn care specifications against which services were assessed. However, there were differences in emphasis in interviewee descriptions of the drivers of the programme. Some saw the main driver as being clinical (‘the major case for all this is clinical . . . that’s what everybody’s arguing over’), whereas others emphasised performance management (‘it’s about meeting national standards isn’t it?’). A small number considered cost-effectiveness to be the main driver. Most commonly, the proposed changes were justified on the dual grounds of promoting quality and maintaining service sustainability:
If we’re going to really try to meet the standards and to improve the level of the quality of burns care and to secure the outcomes for people, the current distribution of service and the current use of manpower is just not sustainable. We need to group them into bigger and fewer services and that’s particularly true at the top end.
Interviewee 4
We’ve got too many providers as it is. The expertise is far too wide spread, particularly for children. Expertise is used very, very infrequently in some places.
Interviewee 1
The case for change was always clinical. It was clinical and it was about sustainability. It was to give uniformity that was sustainable.
Interviewee 10
The emphasis on clinical quality, national standards and concentration of activity and expertise tallied with documents including the 2001 Burn Care Review. 72 However, this consensus was challenged by a subset of interviewees who were more equivocal in their support for the need for change, or else expressed some concerns about the risks of reducing capacity:
There’s a volume and outcome argument which I think a lot of people do not accept and I think most people are happy with the status quo.
Interviewee 5
I now don’t really see the value of designation because I fear the harmful effects more than I see that there’ll be benefit from it, on a clinical level.
Interviewee 2
There was also less of a consensus as regards what a rationalised service would look like. For example, the ‘ideal’ number of centres posited by interviewees ranged from one to four. All agreed, at least in theory, that the solution should be based on a national plan, and a number of interviewees raised the issue of parity in tariffs for burn services across the country. These areas of agreement seemed to have been built up through relatively long-standing networks stretching back to the 2001 review. 72 Almost all interviewees were able to lay claim to prolonged involvement in the service area and each cited the pivotal role played by the standards in raising the profile and status of burn services:
You know there was a lot of very poor burn care offered around the country in various places, particularly for paediatrics, and the burn care review did a great deal of good in highlighting that problem and getting money into burns and, from that point of view, I support it.
Interviewee 2
As a result of the relatively small scale of the sector, the protagonists were well known to one another and it was clear that strong interpersonal and professional relationships had built up over the period since 2001.
Translating (contested) evidence into practice
The mobilisation of evidence had been and continued to be critical to the case for reducing the number of centre-level paediatric services. However, there was an acknowledged paucity of independent research, a function in part of small patient numbers and the low service profile. This was compounded by an absence of national clinical guidance or structured synthesis of the international evidence base. A lack of granularity in outcome indicators made meaningful assessment and comparison of service results difficult. The UK burn care community – including many of those included in the case study – was engaged in responding to these gaps through retrieval, analysis and peer review of service data, and preparation of funded research grant applications. Despite this work, the strength of evidence for change remained contested:
We’re in the development of the reporting stage and gathering the evidence as a case for change. That has been an incredibly painful process in terms of seeking a consensus on the evidence base, which is very limited, and we had to use international evidence around volume and outputs and outcomes. And what we recognise is that in the UK the outcome data is very limited on burns and therefore it’s very difficult to make assessments or assumptions on whether one unit is better than the other . . . And because the numbers are so small, clinicians will always question it.
Interviewee 11
The evidence and data embodied in the standards, and the development of these into a performance measurement and management tool, gave rise to some contestation:
Strictly speaking I shouldn’t even be allowed to manage a burn that’s two per cent on the hand. But if you look at my healing times, if you look at my complication rates, if you look at my patient satisfaction, if you look at the functional outcome of the patients that I treat, curiously enough they’re as good as if not better than most of my colleagues who work in the services which tick all the boxes.
Interviewee 3
Derogation
Some of the dissent voiced in relation to the designation and derogation process was crystallised in the case of hospital A, which, having previously been allocated responsibility for major paediatrics in the region, had now self-assessed as non-compliant with the requirement for a co-located PIC unit. Those opposed to the withdrawal of hospital A’s centre-level status cited its continued geographical importance, and contrasted this to regions with an apparent over-supply of centre-level care. This was considered a flaw of the case-by-case strategy that designated services irrespective of wider population health and access factors:
From the paediatric perspective I would be saying yes it’s correct to have standards that you should have a PICU [paediatric intensive care unit] there so that you’ve got somewhere that the kids that are sick can go to with the knowledge and expertise. However, it’s getting that balance. At the moment there is not a PICU anywhere near a burns unit in the [de-identified region] so therefore you’ve got the choice of sending them right outside of the region and losing that expertise, and then you’ve lost it from the whole of that region.
Interviewee 6
I still think the burn care review was generated for the right motives and did a lot of good but I think the designation process was done the wrong way round and I think it was very divisive and very damaging for relations and communication . . . It would have been far better to have established at the beginning who is going to treat the minor burns and where the small ones should go, and trying to work it out from that.
Interviewee 9
Allied to this objection, interviewees believed that many centres not apparently under derogation were also non-compliant with aspects of the specifications. A third objection stemmed from data suggesting positive mortality outcomes at hospital A, with respondents supporting this with reports from the popular media and peer-reviewed sources (e.g. Roberts et al. 74)
Building alliances and networks
Overall, and notwithstanding these points of contestation, the case study was notable for the recognition among most interviewees of the need for some service change. However, there was significant resistance to the twin-track direction of travel and disputes over the evidence base were central to this. The espoused values of interviewees were apparently shared, but these were filtered through perceptions of unfairness with regard to implementation of the derogation process, and these perceptions appeared in turn to shape how resources such as evidence and theory were mobilised. Despite some agreement over the drivers for change, discussion of the specific decommissioning plans uncovered differences of emphasis, between, for example, a focus on safety (i.e. co-location with PIC), sustainability and organisational performance. There was also concern expressed at the apparent influence of institutional power and prestige in the derogation process. For example, representatives from hospital A felt that their status vis-à-vis more prestigious trusts was a factor in the decision-making, with one remarking: ‘they are all big institutions, teaching hospitals, strongly supported by their local health economy. We are a little pimple in [de-identified] aren’t we?’.
The formal role of the Clinical Reference Group
The group of stakeholders advocating changes to paediatric burn care services had long antecedents and yet exhibited signs of flux and change. The current focal point was the CRG and its appointed NHS England programme leads. This group was made up of individuals who had been ‘translated’ away in part from their professional roles, as typified by one interviewee who stated ‘my whole consultant career has been centred around some of the reconfiguration of burns services in various roles’. By contrast, NHS England was a relatively new presence and turnover of NHS England personnel was a feature of the case study. There was also some uncertainty over the precise responsibilities and authority granted to the CRG. As well as providing advice to the wider programme of care and to the NHS England board, the CRG had de facto authority to make decision recommendations and plans in relation to both derogation and wider reorganisation. However, in CRG meetings, frustrations were frequently voiced at the slow response to these outputs from higher chains of NHS command and, in particular, the delays in taking reorganisation plans forward. In interview, some of those not currently on the CRG questioned its independence, while some CRG members felt that they were being charged with leading review processes that went beyond their remit and expertise:
At the moment we’re being asked to undertake an option appraisal on the children’s specialised central levels of care. But is a clinical group the right group to run an option appraisal on its own? . . . What I’m saying is: is it actually only a clinical question? We could come up with an answer that was complete pie in the sky. I don’t think we would, but we could.
Interviewee 4
Some of this lack of role clarity was observed during the case study. For example, at a CRG meeting a non-member consultant enquired as to the designation process for his specific unit and was informed that he should consult the local area team rather than the CRG, but this was then disputed by others present. Although the CRG appeared to be the main architect of the proposed changes, its intended relationship with NHS England and with ODNs and other pre-existing regional networks was not clear to all respondents. Those interviewees not directly involved in the CRG highlighted limits to the flow of information on proposed service changes, with one senior burn clinician noting:
When you read all the documents for how it should work the information coming down and information going back up, that in my opinion doesn’t work as well as it should do. And often we find out about things after the decisions have been made.
Interviewee 6
The balance in the CRG and wider networks between those seeking to take a national perspective and those perceived as representing a regional or local perspective was raised frequently in both meetings and interviews (e.g. with references to the ‘old conflict between local decision making and national direction’).
Acceptance of the problem and the solution
Patients and workforce
As a result of these difficulties, although a nucleus of established professional opinion had formed, there were still significant differences in terms of desired outcomes, especially where organisational interests were implicated. In turn, this immediate group was connected through fairly weak ties to wider actors, such as the burn care workforce, organised patient and public opinion and national decision-making bodies. In relation to the workforce, some interviewees advocated a reframing of the decommissioning components of the changes:
[The burns workforce] don’t understand what’s going on so all that they will see is ‘we’re being told to do this, we don’t think it’s a good idea, it’s a change and we don’t know or understand the rationale behind it’. Whereas I think if you’ve got more confidence with what you’re being told to do, you understand the rationale behind it, etc. then I think things are implemented a lot better.
Interviewee 6
It’s perceived as downgrading but in my view it’s about being more realistic about the things that we can and can’t do. And I think if we could use a slightly different terminology . . . the language is extraordinarily important.
Interviewee 4
The CRG included long-standing individual patient representatives who were supportive of the changes, but this involvement did not extend routinely to wider patient and public voices, and these individuals were keen to emphasise that they did not claim to represent a wider patient view in any direct sense. Interviewees noted that the nature of burn injuries contributed to reticence and low levels of patient mobilisation. In general, burn care was considered to be lower in profile than many other specialties. While some pointed to the risk of patient backlash against explicit decommissioning, others felt that patients would acquiesce if the position was explained. For example, one commissioner asked ‘do you want to travel a bit further and get top quality? I think most people probably do. I do not think it’s that difficult to sell really’. In general, interviewees felt that while the workforce and patients could be better engaged, these stakeholders were unlikely by themselves to prevent the translation of the reorganisation plans into reality. From the research team’s perspective, it would have been invaluable to have had the opportunity to compare these perspectives with those of a more extensive patient group. However, it became clear that this would require us to make contact with current service providers through channels not permitted by our research ethics agreement.
Political context
Participants in the case study demonstrated far greater concern over the impediments presented by organisational resistance and wider political imperatives. For example, one interviewee asserted that ‘timing is critical: don’t try and do anything that could be controversial in a period leading up to a general election’, and another stated:
What I think will happen is there’ll be a project plan drawn up to do this and then it’ll not get done. Because either short-term political interests will overtake the procedure or short-term professional, clinical interests will overtake the procedure and people won’t be allowed to get the message out.
Interviewee 1
Organisational interests were seen as an important impediment to the plans, with one interviewee noting that ‘people will accept the theory until it gets applied to them’. This linked to concerns over profile and influence of the CRG as a vehicle for pushing plans forward:
My sense is less clear now on how that change can happen. So is it within NHS England, is it within the local area team? Is it the specific commissioners of individual trusts? And so this is, you know, I don’t have clarity in my own mind about how that change can happen.
Interviewee 12
Many interviewees lamented the absence of a recognised and mandated authority that could shift the balance of opinion towards implementation. Those in the most senior positions felt that they were neither mandated nor supported to adopt a directive brand of leadership while, at the same time, resource gaps were seen as weakening local leadership of service transformation:
There needs to be someone who has the authority to make executive decisions which may be unpopular and which the government doesn’t want to do when it comes up to an election. But actually, ensure that you’re delivering quality of care at a cost that the NHS can afford.
Interviewee 9
Institutionalisation and implementation
Levers and resources for change
Supporters of the new commissioning landscape noted the opportunity it presented to put ‘teeth’ into the process of change, describing it as a ‘clean slate’ and a process with ‘penalties’ attached to non-compliance. However, others saw the new commissioning arrangements as having weakened implementation levers, partly because of the level of confusion created:
There have been various commissioning models utilised for burns care. There were burns consortia, there was regional commissioning . . . and then there’s obviously now the potential for national commissioning and the impending potential change going back to co-commissioning . . . To some extent I think it’s all very confusing.
Interviewee 13
Interviewees were keenly aware that to be brought to fruition their plans required financial and management resources, and this was seen by many as a potentially decisive impediment to success, as encapsulated in the statement ‘you can’t make changes, you know, real changes without dosh and there ain’t none at the moment’. Another interviewee feared the effects of a compromised approach:
My concern is that there will be [a response] but it will be along the lines of: we can’t afford this therefore we’re going to do that. We can’t afford to do it properly therefore we’re going to come up with some sort of half-baked fudgoplasty that is going to allow us to say we’ve done a good job and in fact is going to ruin paediatric burns care in the South East for the next 20 years.
Interviewee 10
Towards the end of the case study, NHS England’s plans to overhaul its CRG structure fuelled concerns that the paediatric service review would be marginalised. Members of the CRG felt that their influence did not extend sufficiently into the arenas of senior decision-making and that the proposed NHS England changes – including a merger with a larger CRG – would further weaken their influence. These matters were discussed at an unofficial CRG meeting in April 2016 where concerns were raised regarding the review and its implementation. One participant characterised NHS England’s plans as ‘isolating CRGs by dilution’. Concerns were also expressed at the general reliance on regional ‘goodwill’ in place of properly resourced and mandated implementation:
We feel that the political weight is around major trauma and not around burns and therefore the burns within a merged CRG would be – marginalised is possibly too strong a word but it’s diluted, quite a lot.
Interviewee 4
Although a small number of interviewees saw the challenging economic climate as increasing the likelihood of implementation, others voiced concerns that the relatively modest projected savings would mean that political will and resources would be directed elsewhere:
We’re too small. They’re keen to centralise other services because they cost a shed load. They’re a significant slice of the financial NHS pie whereas we aren’t. We are never going to make a financial hole in anybody in which case we’re below the event horizon as far as they’re concerned . . . I must admit I think it is one of the best examples of reorganisation or attempted reorganisation because it wasn’t on the back of a disaster, it was actually one that was done reasonably objectively and in reasonable time, but it doesn’t seem to have helped it move forward. And perhaps not having a crisis and a disaster has actually held us up.
Interviewee 10
In this context, concerns were expressed that by identifying lack of compliance without a credible and supported change plan (‘I think everybody individually knows it’s broken, but the answer, the solution, is too big, is too difficult’) they risked demoralising providers of services without delivering intended changes.
Interim solution
Despite having laid the ground for reorganisation and having established derogation procedures, during the lifetime of the case study attempts to move these processes forward remained frustrated. Throughout the fieldwork period, conversations with CRG members indicated that they were awaiting confirmation from NHS England of the commitment of resources to the process. Meanwhile, an interim arrangement was put in place in hospital A whereby children exceeding an identified clinical threshold were transferred to a service with a co-located PIC unit outside the area. Interviewees pointed out that while this temporarily resolved the issue of derogation, it only exacerbated the imbalance in allocation of services:
If the whole process of clinical derogation means anything, then it must mean that that change has to be brought, and if they have to – you know, the answer to this is not to say, ‘Pitch off a lot of your children to other centres’. This is about [de-identified region] not having a compliant paediatric burns centre.
Interviewee 1
At the final CRG meeting observed during the case study (April 2016), two proposal documents were tabled and discussed. The first was a national strategy options paper for reorganising paediatric centre-level burn care with options including concentration in fewer centres (see Appendix 8). The second was an outline case for development of paediatric burn services in the relevant region to make them compliant with service specifications. The latter changes required investment from NHS England with approval required by 31 March 2016 in order to be active by 1 April 2017 (a deadline that had already elapsed). Although both of these interventions were well received in the meeting, it was felt that resources would not be found for the new centre despite the current derogation being ‘unsupportable’, leaving the CRG ‘between a rock and a hard place’. These factors, and the experience of prior, failed attempts at service reorganisation, contributed to pessimism about the likelihood of success:
What I’m really trying to say is you can produce the most wonderful case for change in the world but don’t think that solves your problems. I think you’ve got to do it, but it doesn’t mean that people won’t you know at the eleventh and half hour actually challenge the basis on which you even started.
Interviewee 4
I’ve been involved in burn care and burn care planning in and around London, particularly with regards to paediatric care, for 15 years. Nothing has changed. I’ve got reports in my office somewhere from the 90s about reorganisation of burn care in London, South East, what should happen and we’re still – in fact guess what we’re having next year? Another review of paediatric burn care.
Interviewee 5
Reflections
The purpose of the case study was not to ascertain if or in what way the changes to paediatric burn care should proceed, and it is important to note limitations in our methodology. For example, we were unable to engage further with service user representatives on issues such as travel times and geography and our approach did not extend to modelling the effects of proposed changes in other parts of the system [e.g. ambulance services, accident and emergency (A&E), and so on] or assessing their resilience to major events. Instead, our focus was on the social processes involved and how plans were formulated and received. When considered over a longer time horizon, the network of actors advocating the reorganisation of burn care services had made progress in building a clinical case and mobilising such resources as were available. However, the period of case study fieldwork coincided with something of an impasse. One interviewee’s summation was that ‘there’s been review after review after review, and all of them come up with the same answer, but nobody can come up with a solution’. At the time of the case study, those advocating change had formulated a solution but appeared to lack access to the range of resources required to implement their plans. The work put in by a small but dedicated group towards profile and alliance-building, and mobilisation of evidence and other resources did not look as though it would henceforth be sufficient to overcome organisational and political counter-forces, and interviewees voiced fears that the network advocating change itself was at risk of atrophy in the light of slow progress. The political arena in which the CRG operated was felt to be either disengaged or non-committal in respect of its plans, reflecting a perception that the service itself was somewhat lacking in profile and voice. Ultimately, this apparent intransigence appeared to prevent the CRG from being able to overcome or circumvent the resistance of those in the immediate and extended network that opposed the changes. The problem of inertia was compounded by the absence of a mandated lead body with sufficient authority and resources to implement the changes. As a result, the CRG was hampered in its attempts to influence upwards through the confusing and ever-changing chains of NHS authority, and downwards through formal and informal implementation channels.
As an example of decommissioning, the reorganisation of paediatric burn services is perhaps unusual in not being driven to any great extent by the imperative to control spending. Indeed, the lack of a strong financial case may have led to the plan’s low profile in wider decision-making circles (although engagement with these bodies was beyond the scope of the research). In cases such as this, in which decommissioning is likely to require some prior investment, both in the change process and in the development of new service arrangements, the payoff is perhaps more difficult to promote.
The dual nature of the burn care plans, including system-wide transformation and redesignation of non-compliant services, may have increased disaffection as they appeared to rest on separate logics. The identification of specific units in derogation implied a case-by-case approach that seemed at odds with the parallel national plan and was interpreted as unfair by some. This is redolent of Charles Levine’s75 distinction between ‘organisational atrophy’ and ‘problem depletion’ as reasons for service ‘cutbacks’. The two following quotations exemplify the two approaches:
I’m happy for a visitor to come to me and say, ‘You don’t provide good enough care. Your outcomes don’t meet the standards of your neighbours’. Then that’s my real concern, because that is my primary focus. And if they can’t say that to me, but what they can say is, ‘Your wards are too far away from theatres’. That’s not good enough to me.
Interviewee 3
We’ve got a lot of really good burn units that have been burn units for as long as I’ve known them, that actually do not meet the criteria and actually if you were sitting down with a blank piece of paper you would never have put the burn unit there in the first place.
Interviewee 6
The aim of achieving a sustainable distribution of burn services is arguably in tension with the iterative designation of individual service providers. In the strategic review options document an explicit attempt had been made to reconcile the two approaches as sequential ‘phases’ of reorganisation. However, in the absence of an arbitrating body with authority and resources to ‘redraw’ the service map on strategic (rather than performance) grounds, progress on ‘phase 2’ had faltered.
Case study 2: local decommissioning of an end-of-life home support service
Introduction
This case study report presents findings from a CCG-led decommissioning of an EOL home support service provided by an independent organisation in 2014. Decommissioning of this service took place over a period of 3 months, following a 6-month review by the CCG. This case study was selected to fulfil the criteria of being locally led and having relatively low complexity and low conflict. Drawing on Callon’s51 four processes as a framework, this report explains how the CCG was able to propose and subsequently manage the closing down of the service. Key to the success of implementing the decision to decommission was the management of the relationship with the provider. Wider lessons highlighted by this particular case study concern the availability of alternative patient pathways during service changes and the challenge of post-discharge patient monitoring.
Background: the end-of-life home support service
The EOL home support service was originally commissioned by the predecessor PCT in 2009 under preferred provider status for a 1-year pilot. The EOL home support service was a non-clinical service designed to provide support to patients, their families and carers at home during the last 12 months of life. The decision to commission the service by the PCT originally had three intended outcomes: to increase the percentage of patients dying in their preferred place of death, to improve the amount of support given to carers and to decrease the number of unnecessary admissions to hospital in the last year of life.
Under the EOL home support service, patients were provided with a named nurse co-ordinator, who provided regular contact and home visits as assessed as necessary by the co-ordinator, as well as telephone access to a ‘care bureau’ providing triaging and nursing advice and support, 24 hours a day, 365 days a year. The 12-month pilot was extended for 3 years in 2010 by the then PCT, and inherited by the newly formed CCG in 2013. The contract was extended for a further 6 months for existing patients in October 2013 to allow for a review of the service to be undertaken, followed by a further 3-month managed close-down process beginning in April 2014 (Table 19).
| Date | Activity |
|---|---|
| Summer 2013 | Plans for the review of the EOL home support service |
| October 2013 | 6-month extension to the service contract agreed in order to carry out the review |
| October 2013–March 2014 | Review undertaken |
| March 2014 | Review document published and presented to decision-makers, 3-month extension to the service contract agreed to manage the close down of the service |
| April 2014 | Close down and discharge of patients from the service begins |
| July–August 2014 | Final patients discharged from service |
Case study activity
Our fieldwork took place between May and October 2014 in the final stages of implementation and review of the decommissioning process. Interviews with 13 individuals involved in leading and managing the decommissioning process were carried out from the CCG, CSU and provider organisations involved, and two meetings were observed between the CCG and provider. Some interviews occurred retrospectively. Further details of data sources are provided in Appendix 8. In order to protect the anonymity of individuals, identifiers are removed from verbatim quotations.
The following sections use Callon’s51 four processes to consider how the CCG was able to propose and then successfully implement decommissioning of the EOL home support service. Consistent with this approach, the activity of decommissioning in this case study has been divided into four overlapping processes: (1) defining the problem and mobilisation; (2) building alliances/networks; (3) gaining acceptance of (a) the problem and (b) the solution; and (4) implementation and institutionalisation. It is important to note that these processes are not necessarily linear or sequential; rather, they (re)occurred at various points throughout the decommissioning process.
Defining the problem and mobilisation
As explained in previous chapters, establishing current service arrangements as a ‘problem’ requiring a ‘solution’ represents the first stage in the process of institutionalising and implementing decommissioning. In this case study, this process began when a Local Commissioning Network requested that a review of the EOL home support service contract be undertaken by the CCG owing to concerns over value for money and clinical effectiveness of the service, with a potential £1.98M saving projected.
It transpired to be quite an expensive service in relation to what it provided . . . it was a service liked by patients, but not medically of paramount importance.
They were very, very keen to disinvest because they were needing to find huge savings. But they were quite right in what they’d identified as being a service which wasn’t providing value for money.
The fact that the contract was due to end in October 2013 after its 3-year extension was also a key factor for the CCG in mobilising the process.
In October 2013, the CCG extended the contract for the service (for existing patients only) for approximately 6 months (until 31 March 2014) so that a review of the service could be carried out, in order to decide its future. General practitioners (GPs) were notified of changes to the arrangements and no new referrals were made during the 6-month review period. A review team was established to oversee the process and included representatives from the finance, contracting, procurement, quality, patient engagement, communications and data intelligence teams within the CCG and CSU. A clinical lead was also appointed.
The review document and mobilising evidence
The review team compiled a document that set out the nature of the problem. This mobilising of evidence was critical to establish the case for change. However, interviewees from the review team reported that this proved to be very challenging because of the lack of existing patient-level activity data from the provider, partly as a result of unclear monitoring and reporting specifications and the ‘block’ nature of the contract, which meant that no precise costs per patient were available. There was also a lack of available clinical data on users of the service. Some of these were held by the provider and by referring GPs; however, interviewees explained that the CCG had no direct access to the clinical data held by the provider, and commissioners stated that they were wary of ‘asking too much’ of GPs. In addition, significant changes to the service’s role, scope and patient population had taken place since its inception, with a ‘relaxed’ definition of EOL being employed by PCT commissioners and also, therefore, by referring GPs. As a result, a number of patients were using the service who were defined in the final review document as not being at the EOL (i.e. within 12 months of death), including particularly frail elderly people and/or patients with dementia. One interviewee expressed the challenges regarding the data collection process as a ‘steep learning curve’ for the CCG:
. . . really looking at what needs to be reported and making sure we’ve got the appropriate information being reported by the providers I think, because that’s something that, you know, a lot of these contracts have not got and that’s historic.
Unfortunately it was a bit of a botched job contract with no key performance indicators within it. There was no requirement for lots of information although the company was a very proactive company and they were supplying some information, it was not needed within the contract.
An estimate of the cost per patient was therefore calculated for existing patients with the provider, and the preparedness of the provider and GP practices to provide information was said by the review team to be important in this process. Based on the available data and the modelling undertaken by the review team, the review document reported that there was significant variation in the number of EOL home support service patients per GP practice, ranging from 1 to 49 referrals, with a total of 804 people using the service at the time, and the cost per patient was calculated to be approximately £153.26 per month.
Patient and carer evidence
The review team obtained feedback about the EOL service from patients and their families/carers using the service. A patient/user survey was developed by the CSU and CCG communications and engagement teams, with input from the CCG quality team and provider, and sent to all patients using the service via the provider over a 3-month period. The objective of the survey was ‘to understand if the service is delivering what it set out to do, and if patients value the service’ (review document). Again, the preparedness of the provider to mobilise the survey with patients was said by interviewees to be important in this process.
There were 215 responses from users of the service received, which indicated that the majority of contact with the service was on a monthly basis, via home visits. Overall, patients were found to value the service highly. The review document summarised the participant responses as follows:
Most of the respondents who completed the survey highly value the service and are strongly against [de-identified] changing. They particularly value the home visits; the unrushed nature of visits – time to talk and discuss worries; the reassurance that comes of having someone they know that they can call; the practical help with advice and contacts; the liaison/coordination of services including GP liaison; equipment provided that makes living at home practical.
Retrospective interviews with the CCG and CSU communications and engagement teams revealed some different views about the nature of the engagement process with patients and users of the service for the review. These related to whether or not a wider public engagement process was required; the depth of the consultation process with patients/users and the particular use of the survey method; and how the survey results were then used to inform subsequent decision-making. Interviewees commented:
I think we did make best efforts to involve patients in the process but I think it would have been more helpful to have actually been able to bring members of the family or people that are actually receiving that particular service . . . I mean as in a really qualitative approach either bringing those people in for a conversation or meeting with them personally . . . I would have preferred to have been able to have more time to work with the people in the service in order to shape that up. Sort of say to them ‘does this make sense to you, does this work for you?’ and have that sort of collaboration on that.
I felt that there should have been proper consultations because it was a closure and because it was going to have impact . . . approach was to do more of a patient experience exercise, patient survey.
In explaining further the differences in views, interviewees referred in general terms to paucity of (national) guidance about procedures for service closure; organisational capacity and resources for patient/public consultation; tight time frames for decision-making; and the loss of some expertise and experience caused by reorganisation and the newness of CCG and CSU organisations. Some interviewees also questioned using the provider to administer the survey and possible response bias, and this was commented on in the final review document.
General practices’ evidence
Evidence from patients/users of the service was presented in the final review document alongside evidence from referring GPs. A survey with referring GPs was undertaken during the review process to understand both the evolution and nature of referrals to the EOL service and to gauge views and opinions on the service. The survey responses, reported in the main review document, were mixed, with a number of referrers highly valuing the service and others being less positive. Responses indicated different understandings among referring GPs about the criteria for referral to the service, the objectives of the service and how it fitted into the wider landscape of services for EOL patients. Responses also indicated that GPs found the service particularly useful for dementia patients and those with fluctuating EOL or other long-term conditions, and GPs commented on ‘confusing messages’ (review document) from commissioners about referral criteria. The review document summarised the responses of GPs as follows:
The service is generally liked by GPs as it does provide a further source of support for certain patients. Results from practices in [de-identified], the largest users of the service, were equivocal about its value; however multiple practices highlighted the benefit of additional support for dementia patients and their carers.
These results supported the message of the review document that while the service was valued by (most) patients and referring practices, there was greater ambivalence about its clinical value and effectiveness for EOL patients and how it related to other available EOL services.
Availability of alternative services
The availability of alternative services for patients was addressed as a key issue in the review document. This also emerged in interviews about the implementation stage of the process. Interviewees explained retrospectively that it had been challenging to ascertain what alternative support patients might currently, or in the future, access, beyond contact with their GP:
If they were end of life then probably they had alternative services already, you know, in attendance etc., but obviously again instantly it became impossible – you can’t look at that number patients records in any detail and you can’t access that number – those records anyway. So that was a bit of a stopper instantly.
Forecasting the impact on other services, especially secondary care, was experienced as especially problematic:
We had to make some broad assumptions around that as well . . . we couldn’t actually say what impact would it have, other than wait and see what happens after 6 months and see if those providers sort of say ‘well actually activities increased by this amount and we can’t sustain it on the value that you’ve given at the moment.
However, a comparison of secondary care activity for patients receiving the service against a control group of other, non-similar EOL patients not receiving the service was undertaken by the CSU. The final review document suggested that patients were likely already to be in receipt of other sources of support (such as social care), anticipating no significant impact on these services’ capacity if the EOL home support service were decommissioned. A mapping of existing commissioned alternative services was also undertaken and appended to the review document.
Conclusions of the review
Based on the data gathered during the review process from the provider, referring GP practices, patients/users and the modelling undertaken by NHS organisations involved, the review document concluded that:
-
a significant number of patients did not fit the original service specification definition of EOL patients
-
there appeared to be significant overlap with other services commissioned by the CCG; and
-
the service achieved a number of key performance indicators (KPIs) but did not achieve the KPI to reduce the average number of unplanned hospital admissions for people in their last year of life from three admissions to two.
The review process and the evidence presented in the review document therefore had a significant role in defining the problem and mobilising the decommissioning process. Combined with the fact that the contract was coming to the end of its natural life, the willingness of the provider to mobilise data for the review and the fact that stakeholders, including the provider, did not actively contest the review process itself meant that the service was rendered early on as an option for decommissioning.
Building alliances and networks
Building alliances and managing relationships with key stakeholders was the second important process in ensuring the successful mobilisation and completion of decommissioning the EOL service in this case.
The review process and preparation of the review document helped to build a foundation for the successful completion of the decommissioning process by bringing together individuals internally to co-ordinate the process and building relationships with key decision-making bodies. During the review process the review team, driven by the CCG and led by the appointed clinical lead, presented review findings to the relevant commissioning board and approached Health Overview and Scrutiny officials early on to begin discussions about the proposed decommissioning of the service. This relationship-building was felt by interviewees to help facilitate the review process. In addition, two sets of relationships were reported retrospectively by the review team to have been important in managing and implementing the decommissioning process successfully: the relationships with the provider and with GP practices.
Managing relations with the provider
Review team interviewees reported that the provider was engaged early on and notified of the CCG’s decision to review the service. Early communication and discussion with the provider over plans was said to be important to facilitate a good working relationship through the process, particularly as the team was relying on the provider to provide information and data to inform the review:
I think that was one of the keys was, you know, being open and honest with the provider as early as we could be once the decision had been made and that we knew that that was going to happen.
Meetings were held by the CCG and review team with the provider to update on progress, and the preparedness and willingness of the provider to supply required data to inform the review was recognised by interviewees as being very important to the success of the process:
The [provider] were helpful in the process even if they recognised they were sort of arranging their own funeral, if you like. They did continue to be helpful throughout.
The review team also stressed the importance of developing the patient survey in collaboration with the provider. Language and patient impression management were key factors in the development of the survey, as well as communication with front-line provider staff about plans for the survey:
We agreed semantics and all that kind of thing with them. So there was negotiation around both the leaflet and the survey so that it was deemed to be fair and because for them they were concerned about their workforce so we had to be sensitive in that regard as well. So as a sort of piece of work it was done in a consultative style with the provider as part of that process.
Managing relations with general practitioner practices
General practices were similarly engaged early on by the CCG. General practices were identified by interviewees as a particularly significant stakeholder in this case because of their responsibility for referring patients to the EOL service. Decommissioning the EOL service also required patients to be discharged back to their GP as a primary care service. Establishing and maintaining their involvement throughout the process was important to manage the transition and avoid risk to patients. One interviewee explained:
We really needed to sort of work through the GPs ensuring that the GPs knew exactly what was happening because the GPs would be there as pivotal as part of the support and that every patient would need to have an individual monitor of plan.
Interviewees also stressed the importance of gathering data about patient referrals to the EOL service and GPs’ views on the performance of the service to inform the review. Key considerations that shaped the review team’s approach to engaging GP practices were to minimise the impact on their time and resources, and ensure that they were informed and consulted as the process progressed. One interviewee commented:
We had to be careful not to impose too much on the GPs whose job, if you like, it wasn’t to provide us with a lot of detailed information about all these patients. They’ve got other things to do as well as answer questions. We had to be very careful not to impose too much onto their time, and merely just get them to deal with those who had a clinical need at the end of the discharge process.
Maintaining GP involvement and GP relationships with the provider became important later in the process as patients were discharged from the EOL service, and this is discussed in more detail in the implementation phase below.
Acceptance of the problem and solution
As explained above, the final review document produced at the end of the review process was significant in defining and framing the issue as one of clinical effectiveness and value for money. After establishing this as the ‘problem’, three options for decommissioning the service were proposed in the review document, thus embedding decommissioning as the ‘solution’:
-
option 1 – do nothing (i.e. contract ends on 31 March 2014)
-
option 2 – allow the contract to continue for existing patients only until the wider EOL strategy had been developed
-
option 3 – a managed close-down process over a short period of time. Patients would be discharged to GPs for re-referral to alternative services as appropriate. The contract would be extended to allow that process to take place.
An analysis of pros and cons for each option was presented in the review document. The analysis suggested options 1 and 2 to be unfeasible in terms of patient risk and cost, and option 3 was recommended. This was presented by the CCG and debated with the commissioning board and Health Overview and Scrutiny officials. A consensus was reached with these governing bodies to extend the contract for 3 months at a cost of £370,000 to manage the close-down process and transition patients.
Interviewees reflected that involving and engaging key stakeholders and decision-makers early on was important to the consensus-building process, as well as having strong supporting evidence. This was felt to be particularly the case for building a consensus with GP practices. Here, the clinical lead took an active engagement role and no contestation was reportedly experienced, despite mixed views about the service expressed during the review process. Interviewees reflected:
Locally when we made the views early on it was done basically on the basis of the GPs first of all who said ‘yes we can save some money if we were not to continue to use this service, so let’s look at that’. So I think the GPs were inherently on-board to begin with which is better.
Keep GPs on-board – we’ll keep GPs involved in the decision making process so that they are happy with the decisions that they’ve got to make and be involved, and be happy with the position. They can’t have decisions made to them they need to be involved in it.
The provider perspective
Although the decision to decommission the service was not contested by the provider at the time and no obvious contestation was displayed in observed meetings between the provider and CCG during the implementation phase, retrospective interviews with provider staff revealed mixed feelings about the conclusions of the review. Clarity over drivers and timelines for the process, the influence of the patient survey views on decision-making, and the availability of alternative services for patients were all areas where provider staff expressed some ambivalence. One member of the provider staff commented:
For me that was the main disappointment, it was the kind of the justification for the decision I thought wasn’t necessarily being made in the patients’ interests. My sense was that it was much more of a cost-saving discussion.
The provider also expressed disappointment that opportunities to renegotiate the contract and nature of the service were not explored or debated further as part of the review:
We were quite willing and flexible to want to try and do whatever really it took but they never gave us an opportunity to ever, you know, to kind of negotiate . . . you know, you could have used the contract to spend the money in a way that could have tested different things, expanded the service, you could have done lots of things but they just didn’t quite want to do it.
Interviews revealed that managing ongoing relationships with the CCG and concern for commercial reputation were key considerations that shaped the provider’s approach to the review and subsequent closure process. Interviewees stressed the importance of maintaining objectivity, pragmatism and a positive working relationship throughout the process, and the provider was particularly keen to ensure that future commissioning opportunities were not jeopardised. The provider summarised their view as follows:
In the end I think we just took a reasonably pragmatic view which is that we know that the quality of the services we provided has been of very high standards . . . the decision had been made, and I think it would have been churlish to challenge the decision of the CCG. You know, we didn’t want to be confrontational about this.
First and foremost try and help the commissioner to come to a sensible decision; that’s number one, and that’s what I felt we tried to do. The second thing is that if a decision has been made, is remain professional and keep the patients central to everything you do. It maintains relationships for the future, you know, just because things have happened now, you never know what will happen in the future and really what you don’t want to do is bite your nose to spite your face.
Relations between the CCG and provider also continued to be important for managing the implementation of the closure and transferring patients from the service (see Institutionalisation and implementation). The absence of active challenges to the decision to decommission by the provider was therefore critical in shaping the process in this case.
Institutionalisation and implementation
A project group, comprising two leads from the CCG, a senior project manager and the service manager from the provider, was set up to manage the closure and transfer of patients from the service. Discharging patients from the EOL service involved a series of negotiations between key stakeholders, which are described below.
Managing the transition with patients
The discharge of patients from the service was managed in a joint process between the provider and CCG, with the CCG taking overall responsibility for the transition and referrals back to GPs and pathway planning. Each patient was sent a letter of communication by the CCG to notify them of the service closure and followed up by the provider if necessary. Provider and CCG staff indicated in an observed meeting that the level of contact required with patients was determined on an individual basis, usually by the provider who was in direct contact with patients.
Patient and carer reactions to the service closure were discussed in an observed meeting between the provider and CCG. Front-line provider staff reported experiencing mistrust from patients since the decision to decommission the service and handling difficult conversations with aggrieved patients about the closure:
Ultimately us as the provider were, you know, were the kind of coal face of that. Patients became very unhappy because they felt that they’d be able to say, you know, they felt they were being listened to by taking the time, filling in all the questionnaires and they got a relatively good response rate and then the decision was that the service was, you know, decommissioned.
Carers were concerned about the loss of support and difficulties were experienced by the provider in informing dementia patients about the process. Patient deaths during the transition also had to be managed as part of the process because of the nature of the service in this case study, and the provider noted the sensitivity required to deal with families and carers in these circumstances, while the service was removed.
The vulnerability of patients was a key issue throughout the transition and influenced the pace of the discharge process. The most vulnerable or those deemed at high risk were prioritised in the discharge process and individual cases were discussed with GP practices by the provider where there were concerns. Another factor that influenced the pace of the discharge process was the size of the patient population. In an observed meeting the CCG and provider commented that ‘the bigger numbers carry bigger risks’ and discussed strategies to minimise the ‘danger of patients falling through the net’. These factors meant that the discharge process was extended beyond original time scales.
Managing the transition with general practices
The CCG and provider reported mixed responses among general practices to the process of discharging patients back to GPs and primary care services. Patients were discharged in cohorts to GP services, with ‘gold standard’ GP practices approached first; this was followed by the vulnerability of the patient as the determining criterion. General practices were notified of the discharge by letter, telephone call and e-mail, and the provider attended some meetings with general practices where referral levels to the EOL service had been highest.
During an observed meeting with the CCG, the provider expressed some concerns about patient follow-up at some general practices. When there were particularly strong concerns, the provider and CCG agreed to delay discharge to these practices and the provider provided information on the cases in question to the CCG for follow-up. Staff reflected on the challenges with implementing the decommissioning process with some GP practices:
They’ve got so many patients . . . the CCG’s following them up and the GPs are saying ‘oh I didn’t even know that these patients had been discharged’ and even though discharge letters had been sent. So the additional thing we’ve had to do is send an e-mail to each of the GP practices with a list of all the patients to say these are the patients and this is the date that they were discharged.
With the GP practices obviously you’re dealing with dozens of different organisations. So getting that complete set of data is going to be quite difficult. As you say, we’ll be asking for returns from practices, we’re not paying them to do the return so uptake may be an issue. They will quite rightly point out that there are a lot of demands on their time and they can’t allocate the resource.
Comment made during observed meeting
A performance management tool was developed part-way through the discharge process to assess the discharge and follow-up process with general practices. However, interviewees commented on the limited capacity and time of GPs to complete the tool and to provide information on individual patients, and both the CCG and provider expressed frustration with the difficulties in following up patient cases with some general practices. CCG staff also described a lack of leverage over general practices and reflected on capacity issues to undertake post-discharge monitoring about what alternative services had been accessed. This was viewed partly as an effect of the recent reorganisation: interviewees indicated that they felt more at ‘arms’ length from the process’ and lacked infrastructure to carry out such activities.
An important issue throughout the discharge process was the availability of alternative services, and this was discussed at length in observed meetings between the provider and CCG. Variation in the availability of alternative services geographically, variations in GP knowledge about alternative services for patient referral and the particular lack of alternative services for dementia patients were discussed as key issues. Both the provider and CCG commented that planning exit routes for patients had been the most challenging, despite previous mapping work undertaken in the review:
There’s not necessarily a clear pathway for these patients. They have a lower medical need but increasing social need.
Comment made during observed meeting
GPs are unclear about access to other services e.g. voluntary organisations, social services. Patient access is a big issue. Can patients get there physically?
Comment made during observed meeting
An absence noted by both the provider and CCG in planning for the discharge and re-referral process was the input of social services. Both provider and CCG staff reflected on the difficulties in engaging social services in the process because of the ‘siloed’ nature of both health and social care and the differences in accessing care, including procedural, process and eligibility issues. In addition, provider, CCG and CSU staff all reflected in interviews on the difficulties in sharing information about patients and patient outcomes across the system, which created additional challenges in pathway planning for patients and undertaking post-discharge monitoring.
The provider: Clinical Commissioning Group relationship
Key to the overall management of the transition was the relationship between the provider and the CCG. The provider reflected that:
I think we got through this decommissioning because actually we had some very good people on both sides . . . taking this seriously.
The importance of individual attitudes, as well as a general attitude of mutual co-operation and communication through the process, were said to be crucial to the management of the transition. Active awareness and avoidance of potential tensions on both sides were highlighted retrospectively in interviews as factors that helped to facilitate the process, as well as the need to focus on patients who were affected:
I think we all did a very good job but I could see had people been placing less focus on the tensions of it, and on the patients, it potentially had the risk of going wrong.
Particular areas of tension that needed to be managed were the impact on provider staff who not only were directly affected by the closure of the service themselves, but also had to manage patient and carer concerns during the transition. Managing the communication of the decision to patients and GPs also required careful negotiation. Although the CCG had formal responsibility for this, the provider reflected retrospectively that as they were in direct contact with patients and GPs and because of CCG capacity issues they were, in practice, more heavily involved in this aspect of the process. Patient follow-up and post-discharge monitoring were also areas in which both the provider and CCG reflected that further support and information-sharing would have been beneficial.
In addition, both the provider and the CCG stressed the evolving nature of the process, and the lack of formal guidance or a template for managing the process. Working together to therefore plan the process and utilising strong project management skills were highlighted by both the provider and CCG as key strengths of their approach, particularly given the vulnerability of patients using the service. Interviewees commented:
We did a pretty good job. There wasn’t much to go on. We had to kind of feel our way through it. We only had a skeleton structure . . . We kind of used common sense and just general project management skills to kind of get through it.
Reflections
Overall, the management of the relationship between provider and commissioner was key to the success of the decommissioning process in this case study, and as an example of decommissioning this case is perhaps unusual in the preparedness of the provider to co-operate with the process. The process of preparing the review document was important in drawing together and maintaining the network of stakeholders involved and in informing decision-makers, and the strong financial case presented in the review document appears to have been instrumental to the decision to decommission. Meanwhile, the lack of strong patient and provider resistance and the lack of wider public or political voices and profile in this case meant that potential counter forces were not mobilised. The availability of financial resources to manage the 3-month close-down and transition of patients from the service also appears to have negated potential disaffection. This case illustrates the challenges of monitoring the impact of decommissioning on users of services and on alternative services in the health economy. Second-round interviews suggested that activity had moved on and capacity and resources were directed elsewhere in the commissioning chain; individual patient pathway monitoring happened elsewhere in the health system.
Case study 3: decommissioning in the work of an Area Prescribing Committee
The APC was set up in its current form in 2013 and served a coastal CCG area containing single acute, mental health and community health trusts. At the time of research, membership of the APC was made up of approximately 20 individuals representing each of these organisations, as well as GPs and patient/lay representatives. As described in Chapter 3, this case study was selected to fulfil the criteria of being rural and having low complexity, and of focusing on the implementation of decommissioning decisions instigated at the national level. This report presents case study findings against research aims and questions. In accordance with our overall analytical framework, it provides a narrative account to describe how interactions between actors were recounted by participants and documented in written evidence, and how these unfolded during observation. It focuses on the following broad processes:
-
the role of evidence and actors in identifying and framing a need for decommissioning
-
alliance-building around the decommissioning process
-
gaining acceptance for the solution of decommissioning
-
implementation and institutionalisation of decommissioning.
It finishes with reflections on case study findings and implications for our understanding of decommissioning.
The Area Prescribing Committee
The focus of the APC’s work was on the implementation of coverage and medicines management guidance from national bodies such as NICE, as well as the development of care pathways and the governance of local prescribing behaviour and responsibilities across primary and secondary care sectors. To this end, the APC was engaged in the production of policies and guidance and oversight of a joint formulary for the area. The formulary itself was formally described as ‘output of processes to support the managed introduction, utilisation or withdrawal of healthcare treatments’ (see the APC website),76 and the APC was accountable to the governing body of the CCG. The formulary application form employed by the APC included an option for removal, and the committee operated a traffic light system that placed restrictions on usage (e.g. confinement to secondary care initiation). At the time of writing, the APC did not employ a formal multicriteria decision tool in their decision-making.
In order to encourage joint ownership from the main provider, the APC had a rotating chair between heads of pharmacy at the CCG and acute trust. In relation to decommissioning, the APC operated as both a vehicle for implementation of NICE disinvestment guidance and a source of further local decisions on replacement and withdrawal:
The Area Prescribing Committee is our principal sort of governing meeting which therefore makes the investment/disinvestment decisions in terms of medicines management across the patch and it’s very much instrumental in terms of setting up and devising our sort of medicines/drug formulary that we have in operation within our health economy.
Interviewee 8
The work of the APC was supported by three members of the CCG pharmacy team who attended meetings and were responsible for drafting policies, supporting governance of medicines management and transference of prescribing responsibilities, working on care pathways and formulary development.
Case study activity
The APC was recruited to the study following conversations with the clinical lead for medicines management and the head of medicines management for the CCG (and cochair of the APC). The APC convened every 2 months and, during the fieldwork period, three such meetings were attended and observed by the research team, along with two meetings of the acute trust ‘medicines optimisation committee’ (MOC). Relevant documents were retrieved and added to the analysis and a total of 10 telephone interviews were conducted, including one follow-up interview with the current APC chair. Consent was secured collectively from participants at the November 2014 meeting of the APC and individually prior to each interview. The sample of interviewees included clinical and non-clinical representatives, members of each of the participating organisations and patient representatives on the APC. All participants approached agreed to be interviewed. During the fieldwork period no instance of implementation of NICE decommissioning guidance was observed and no locally identified programmes were instigated. As a result, the data presented here are drawn from general observations and comments in regard to the committee’s decommissioning work. Further details of data sources are provided in Appendix 8.
Defining the problem and mobilisation
Decommissioning activities and plans
At the meeting at which the proposed research was explained, APC members expressed an interest in the topic. One noted a ‘lack of fit’ between guidance produced at national level and pressures of local decision-makers, and expressed a hope that the project could help with this. Interviewees discussed examples of where decommissioning had previously been attempted, including reducing the number of testing strips for diabetics and changes to gluten-free prescribing. Gluten-free products (including dressings, appliances and stoma products) were seen as having a high growth rate and as being outside the usual prescribing expertise of GPs. The APC had previously worked with stakeholder groups such as the Coeliac Society and the British Gastroenterology Society to identify legitimate restrictions as to what people could access:
I would see that as being one of our really true disinvestment decisions albeit the amount of money we’re talking about is not huge. Actually it’s a bit of a low hanging fruit and personally I’m thinking many of these products are available in many supermarkets anyway so why are we giving loaves of bread out to patients when clearly they can just buy it and pay an extra 50p for a loaf of bread?
Interviewee 8
However, these and other previous attempts to disinvest were experienced as ‘arduous’ and the gluten-free initiative had experienced setbacks and challenges, with the APC consequently keen to ensure that any future decommissioning recommendations were robust to challenge.
These examples apart, the primary emphasis in meetings was on ‘managed entry’ and ‘cost-effective investment’ rather than ‘exit’ or ‘disinvestment’. During the meetings observed in both hospital and APC settings, no specific plans for removal or replacement were discussed. Most of the data relating specifically to decommissioning were therefore generated in interviews, where the topic was raised by the researcher. Here it was noted by most interviewees that the act of setting up the formulary had led to de facto decommissioning as, prior to this, prescribers ‘had the entire BNF [British National Formulary] to choose from’. Apart from this, it was considered to be rare:
I can’t say it’s a strong theme . . . I suppose the big thing is we’ve recently had to do the new formulary and probably in that process they did disinvest in things that maybe they had before . . . But you know, if something new is put on I’ve not heard anyone say ‘Well we have definitely got to take something off’. Which maybe some APCs do, I don’t know.
Interviewee 4
Interviewees recalled only a few situations in which the APC had made decisions on whether or not to remove something already available unless this was instigated by a NICE appraisal. However, some cited programmes or instances of decommissioning in their organisations (e.g. through the CCG’s ‘low priority procedures’ policy). The acute trust medicines team indicated that they were reviewing internal prescribing for decommissioning options and also seeking to draw up a list of ‘about five or six’ drugs for assessment in conjunction with the CCG.
Drivers for decommissioning
The ‘problem’ that decommissioning was intended to solve was interpreted in different ways by interviewees. Although all saw it as a legitimate activity, the grounds cited for removing interventions varied. There was a consensus over the need to reduce unnecessary duplication and to decommission in response to safety concerns:
There are too many drugs out there. The NHS needs to streamline what it offers because it can’t continue doing what it’s doing at the minute. At GP level, how do the GPs possibly start making a decision as to what patient to treat with what when you’ve got so much to choose from?
Interviewee 1
Well I think a lot of it is about me-too drugs. Me-too drugs can be designed in order to produce a patent that will last longer and therefore keep the price up for longer . . . And then they’ve really milked their marketing authorisations. So that’s one way in which me-too drugs can work. And so in that sense it’s disinvestment if we’re countering that strategy by the drug companies.
Interviewee 6
By contrast, many respondents felt cost drivers to be insufficient grounds for decommissioning:
The disinvestment should not happen purely for financial reasons. Clearly there’s a cost-effectiveness decision to be made and some treatments will be very expensive but that doesn’t necessarily mean they shouldn’t be used. For me, basing things purely on a budgetary basis would not be helpful.
Interviewee 3
I mean obviously in an ideal world you would say that money is no object and that our decision making processes aren’t based on money. Unfortunately it does have a heavily influencing factor. But we wouldn’t ever stop a treatment purely on cost grounds . . . We would never ever say ‘right that’s too expensive, we can’t have it’. If it’s supported and there is a place for its use in the care pathway somewhere then you wouldn’t stop its use just on cost.
Interviewee 2
Observations of meetings of the APC and the MOC confirmed the general focus on prudent formulary management rather than decommissioning. However, a subset of interviewees believed that this pattern would have to be revisited in a challenging economic climate:
For the first time probably during my career we cannot afford evidenced-based care. For some things difficult decisions have to be made. So before, you could say ‘If there’s no evidence base behind this, then we’re not going to do it’. But just because something now has the evidence base, it doesn’t necessarily mean it’s affordable . . . One of the greatest problems we have now is we just don’t have the money for reinvestments. It’s all about making savings, and I think that’s a much more difficult thing to sell.
Interviewee 9
Another respondent referred to the CCG as one of the ‘most expensive in the land’ in support of his claim that greater emphasis on replacement and removal would be required.
Using evidence to create the case for decommissioning
One of the reasons cited for decommissioning remaining marginal to the APC’s work was the perceived lack of robust and credible evidence to support this work, as well as deficits in analytical capacity:
I think the biggest challenge from my perspective is gaining sufficiently robust evidence to show that one or another treatment might be more or less effective or cost-effective. I think that is very difficult. There is competing evidence, there are competing interests, there are conflicts of interest, I mean it is just really, really difficult to get the absolutely concrete evidence.
Interviewee 3
The problem is we don’t always have evidence for things, and if you work in a specialist area, sometimes you have to work outside of best evidence, because it doesn’t exist.
Interviewee 5
The expertise that feeds into the Area Prescribing Committee to support the evidence base, the health economics, anything else: that is better done I think at scale. It’s actually very difficult as a CCG finding somewhere that you can either buy or share that expertise from.
Interviewee 10
The National Institute for Health and Care Excellence was cited as the main external trigger of decommissioning processes, confirming that implementation was more common than initiation of decommissioning decisions within the APC. Since its merger with the National Prescribing Committee, interviewees indicated that NICE had become the primary source of evidence-based disinvestment guidance, although this was considered to have limitations. Comparative data indicating better performance elsewhere was seen as important in creating momentum for greater decommissioning activity:
When we’ve got good data that’s robust, when we can compare our practice to the practice of our peers . . . That, for me, is the powerful bit with our clinicians that if we’re able to say ‘we’re using lots of this drug here, other people aren’t using it and yet their patients are still recovering from surgery or still have a length of stay of three days and therefore . . .’
Interviewee 7
Building alliances and networks
An important strand of the committee’s work in the time since its inception was securing buy-in from the range of prescribing organisations and individuals in the area. In general this was considered an area of relative strength, with high levels of ‘trust’ cited and increasing levels of adherence to formulary guidance. The medicines team published both APC decisions and the formulary so that these were accessible, and engaged in a range of activities designed to encourage compliance with these. However, interviewees regularly referred to some lack of adherence among both primary and secondary care prescribers, and also identified gaming strategies sometimes employed in order to gain access to non-approved treatments. In general, this was considered to be of greater immediate concern than relatively low rates of explicit and planned decommissioning:
I’m not really seeing huge amounts of disinvestment as such. Clearly, the emphasis for my commissioning colleagues is about getting the pathway streamlined for the activity out of secondary care where it doesn’t need to be. That seems to be the sort of tactic to date so I’ve not really seen any complete disinvestment.
Interviewee 8
There hasn’t been a particularly strong focus on disinvestment as yet. Although there are workstreams in process and de-prescribing, they’re some of the things that have come much later down the line. With trying to get the formulary in place and staffing in place to manage it, and the engagement of the secondary care colleagues as well.
Interviewee 2
Local opposition to decommissioning
The concern for some was that decommissioning would incur a negative reaction, for example from patients and clinicians:
Well I mean, I suppose the other thing is people. It’s much easier to add something than take something off. I mean, that’s just life. It’s politically easier to do. Let’s be honest, you know, we keep adding clothes to our wardrobe, don’t we? And we don’t say ‘Right, I’ve bought a shirt. I’m definitely throwing one away’.
Interviewee 4
The reaction of patients and patient representative groups was seen as a strong determinant of whether or not a treatment could be successfully withdrawn – both as a positive potential facilitator and a potential impediment:
The main problem with implementation is I suppose the doctor/patient relationship, that some people feel that this is the best thing for their patient irrespective of how you present any data: ‘I have made this decision. I think it’s the best for them’. And sometimes that’s without actually any clinical justification of why that’s the case.
Interviewee 9
It’s much harder to withdraw a treatment from a patient than it is to give a new one. I think the voice of the public would be much louder, much stronger. If you’ve got say somebody with Parkinson’s who is on a certain level of medication and the commissioning group through the APC decide that no they’re not going to fund this particular drug any more those Parkinson’s patients would be up in arms. I think it’s too difficult.
Interviewee 1
Lay representatives on the committee felt that they played a full and respected part in the deliberations. However, as a function in general, engagement was seen as limited:
I’ll hold my hands up: we’re not good at it, patient engagement. Because I think the patient and public engagement in these tough decisions is really key and given a set of understandable, patient-friendly language facts an awful lot of patients would come to the same decision as the clinicians in the room. But if perhaps patients think decisions are being made about their care without them that then puts the difficulties in implementing disinvestment and taking disinvestment or investment decisions . . . Because I think patients can often see that ‘well, it doesn’t make sense to be using branded X if you can use generic Y at a much lower cost, I would like to have more money for cataracts thank you very much’. So I think that’s something the NHS doesn’t do well, we need to do better and all Area Prescribing Committees need to do better.
Interviewee 10
Regional partners
A common theme among interviewees was the importance of bolstering and galvanising support for medicines management in general, and for decommissioning in particular. Some felt that, despite a strong overall relationship with the wider CCG, there was room for a greater profiling of medicines management and for more direct support for limit-setting:
But [disinvestment] would need to be formal policy. You would want to have your CCG at your back covering you because you might get an awful lot of flak.
Interviewee 10
When mentioned, drug companies were generally portrayed as being antithetical to disinvestment:
The influence of industry which sometimes is there and sometimes is not. So I think, again I think the reps aren’t necessarily as pushy here as they possibly are in some places but you certainly see a certain amount of influence.
Interviewee 7
Gaining acceptance of the problem and the solution
As noted, the APC had been unsuccessful in previous attempts to implement decommissioning, including as a result of media interventions. This had induced some risk aversion and reluctance to take a lead. Interviewees referred to ‘protests’ creating ‘disincentives for others to do the same thing’:
We had a big problem with trying to change the commissioning of [musculoskeletal services], which caused a lot of public outcry locally. Although there was nothing for them to be worried about – we were trying to improve the service, not actually take it away. But the hospital trust ran a very good media campaign to try and stop that. And it was thought at that time that approaching something like coeliac disease and decommissioning was not a . . . it was too sensitive to do that at that particular time.
Interviewee 9
The media are always going to give the sad story about, you know, poor Flopsy who can’t get this drug. And they’re always going to focus on the individual case, often with inaccurate clinical data and what have you. So you’re always going to have that problem and the only defence against that is really authoritative well-based guidance.
Interviewee 6
National leaders
In meetings, members of the APC and MOC identified national policy, such as Innovation Health and Wealth,14 as driving inflated levels of drug expenditure and creating cost pressures on local budgets. Towards the end of the case study, NHS England began consultation on plans for ‘regional optimisation committees’ and this was received with cautious optimism by leaders of the APC. 77 In particular, it was felt that responsibility for tough coverage decisions might be better set at a regional or national level, leaving local APCs to focus on implementation strategies:
I think that perhaps what needs to happen is that rather than each commissioning group reinventing the wheel, that these decisions are made at a very high level within the National Health Service and applied blanketly across the country and you make this decision once for everybody.
Interviewee 1
We might be much more successful in withstanding flak from very loud patient groups and also withstanding media interest or anything else if we worked in collaboration with other CCGs . . . Sometimes disinvestment decisions are better done at scale.
Interviewee 10
Ideally I would like to think that, you know, there’s no point in reinventing the research and the assessment process – that NICE does – at district level.
Interviewee 6
This linked to a widely expressed concern that there was a national vacuum in leadership in relation to the difficult task of decommissioning:
I think it’s politically very difficult for NICE to be able to say ‘we don’t think the NHS should be investing in X, Y, Z’ or that there are better alternatives . . . They appear afraid to put their head above the parapet when it comes to a disinvestment decision . . . They appear to be afraid to be really clear ‘the NHS should not be using this’. Even if it’s something that they’ve turned down as a technology appraisal very often it’s turned down because the manufacturer hasn’t produced sufficient economic evidence or something. It’s not turned down because ‘you know what? The NHS shouldn’t be using this’. So they’re kind of a bit mealy-mouthed about it sometimes and that doesn’t give confidence to those of us who would be on the front line of the flak if we need to make a hard decision. You don’t have that confidence that NICE is there at your back being forthright with you.
Interviewee 10
I think there needs to be some national responsibility, I think, so it backs up the disinvestment of things, so it actually is OK to say, ‘We don’t have enough money’. And I think the politicians are very happy to say that, you know, ‘this is all available from your CCGs’.
Interviewee 9
In response to this perceived lack of national leadership, the APC employed less controversial strategies to control expenditure:
I don’t recall making a formal decision on a disinvestment situation due to health economics in the APC. It’s very often a bit more subtle than that and we would advise and encourage prescribers to use drug X instead of drug Y and back that up with appropriate cost-effectiveness messages through decision support software and that would be normal medicines optimisation advice and good practice, but not necessarily an APC policy decision.
Interviewee 10
Increasing decommissioning
As well as citing the importance of national support, interviewees offered reflections on strategies for increasing or improving decommissioning. These included the partial reinvestment of any funds generated:
So ‘let’s recycle the cash’ I think is a means by which I’m trying to invigorate others to thinking actually it might require a bit more extra work but what we’re doing here is we’re providing treatment options for other people. I don’t know whether people think along my lines but I thought that’s quite a nice way of thinking about it.
Interviewee 8
Other suggestions included small-scale ‘pilot schemes’ to demonstrate the benefits of replacement and removal, as well as the need for clinical champions:
People won’t change their habits if they think they’re being done to, but if they’ve got another health care professional from their profession with that credibility there advising them then it makes a big difference.
Interviewee 10
Those in favour of increased rates of decommissioning emphasised the importance of consistent and defensible processes:
Maybe there ought to be a discipline that if we’re adding something we take something off. I’m not saying we’ve ever done that, but it would be a good discipline to say ‘unless there was a damn good reason not to . . . there should be a product we could take off this formulary, if we’re adding’.
Interviewee 4
I actually think it’s important for the same approach and principles to be used for disinvestment as investment decisions. So you need to make sure you are absolutely squeaky clean on your due diligence so that if you get challenged you can show that you’ve done everything in the right way.
Interviewee 10
Overall, however, interviewees felt that other strategies for managing financial difficulties were often preferable to the politically contentious option of service reduction or removal.
Institutionalisation and implementation
A key mechanism for decommissioning was the formulary. The process of establishing it had provided an opportunity to place limits on prescribing and to both support this with evidence, and persuade clinical stakeholders of the importance of this. Not surprisingly, however, it was rare for decommissioning options to be put forward by prescribers. A more common approach was the ranking of treatments:
So there’s always going to be that small group that fall into that problematic basket of ‘OK we take this away, what do we then do with them?’ So more often than not, rather than going for a drug that is a formulary choice whether it be secondary or primary care prescribed to then making it non-formulary, it would more often than not be recoded or knocked down the preference list so there was still the option to prescribe for that small group of patients.
Interviewee 2
Adherence to the formulary was not mandatory at the time of writing, although this was under review by the APC. Interviewees identified a tension between allowing for reasonable exceptionality while standardising care where this was warranted. They were also conscious of the relative lack of contractual levers to enforce GP adherence.
A small number of respondents questioned the approach of focusing on single medicines:
I’ve been talking lots of in terms of disinvestment as in probably stop using one drug or change drug A for drug B. For me, there is a whole bigger agenda that we sometimes forget about with disinvestment and it’s a more holistic approach to the patient and it’s the whole thing of are we just using too much of everything in the first place?
Interviewee 7
Implementation of decommissioning, and of APC guidance more generally, was seen as dependent again on the co-operation of patients and their clinicians. Transfer of patients was invariably a gradual process at best and rarely imposed as a blanket restriction:
When we’ve tried to change people as prescriptions come up, some of them are very reluctant to actually change it, and some do return back. And they’re willing to take on an element of safety risk because the drug is actually effective for them.
Interviewee 9
It doesn’t often happen that you will actually go out and actually switch everybody over to a new drug. I think it has happened once or twice but most times it’s when you start new drugs, or if the patient comes in for another reason, you might open them up to that suggestion.
Interviewee 5
As well as foregrounding patient preferences, a small number of interviewees cited institutional inhibitors to implementation:
They have very different procurement mechanisms in the secondary care environment in that they have things they’d procure centrally via the central hub which they have no control over. They also have more local bulk purchase contracts, so the more that they use the greater the discount. But unfortunately those savings aren’t then passed onto primary care. So that then poses a problem if they don’t want to adopt a specific drug because it’s not what they’re getting their bulk discount on.
Interviewee 2
Reflections
Overall, the formulary appeared to be the main mechanism for enacting replacement or removal within the APC. In particular, during the initial setting up of the shared formulary, the team had worked to reduce the number of similar agents in use for the same condition. Implementation of such changes was typically tackled through a gradual process of incremental patient initiation and some historical prescribing was permitted. Although the APC was proactively engaged in managing medicine and prescribing across the patch, planned decommissioning had not emerged as a mechanism in the committee’s work, and this can perhaps be understood as a response to the competing priorities they faced and the unique challenges that decommissioning poses. This was encapsulated in the following quotation:
Occasionally there is a fairly clear cut disinvestment decision where it might be as a result of a NICE recommendation or appraisal or it might be as a result of a change in the market availability where it becomes fairly clear cut that one sort of medicine should not be used in favour of a newer or a different medicine that would give the same or better benefits for the patients. Those aren’t all that common because most often a formal disinvestment decision doesn’t need to be made, it’s a matter of custom and practice and it almost happens by default. But occasionally it might be necessary to put the added weight of a formal policy decision behind something.
Interviewee 10
Previous experiences of decommissioning had reinforced the reticence of the APC, and some pessimism was expressed over the likelihood of future success. Although decommissioning, especially when informed by safety concerns, was seen as legitimate, the consequences of taking a more proactive approach were considered to be prohibitive, especially in light of the other challenges faced by the APC. Where decommissioning had been implemented, this often coincided with NICE guidance recommending replacement of a treatment, albeit this scenario did not arise during the case study. Interviewees felt that leadership or greater support would be required from bodies such as NICE if decommissioning was to be tackled more substantially.
Case study 4: local service reorganisation
Introduction
This case study report presents findings from a CCG-led review and planned reorganisation of local primary and acute care services, involving decommissioning of a local hospital and centralisation of acute services at alternative sites. This case study was selected to fulfil criteria of covering both an urban and a rural area and being high in levels of scale, complexity and probable conflict. The review and strategic planning for the reorganisation took place over a period of 18 months between 2014 and 2016. Drawing on the four processes described by Callon,51 this chapter explains how the CCG was able to propose and plan the reorganisation of local services, and why the implementation and mobilisation of plans subsequently stalled. Key issues highlighted by this particular case study are relationships between providers, system complexity, and the scale and scope of the proposed reorganisation.
Background: the proposed reorganisation of local primary and acute care
The geographical area overseen by the CCG in this case study was made up of four localities, with a population of approximately 592,600. In 2012, the CCG employed mainly new staff, as the majority of staff from the predecessor PCT went to CCGs in other parts of the local area. A strategic review to inform a reorganisation of local primary and acute care was proposed by the newly established CCG in summer 2014, following the publication of its own clinical strategy in 2013 and driven significantly by long-standing financial and estates difficulties in the local hospital trust.
The initial plans in summer 2014 were for a 12-week review/consultation period employing an external consultant company to draft plans for a reorganisation of health services locally (to include social care), and a programme manager, who was seconded from another part of the NHS, to co-ordinate and deliver the review. However, a longer consultation and review period (18 months) was eventually decided on, with one external consultancy providing expert advice to the process, and another employed to deliver the communications and engagement work for the review. This change was due in part to concerns around the feasibility of a 12-week period, and also to the legacy of several previous controversial attempts at review and reorganisation of acute services in the area, including the loss of A&E services from one locality. The programme management team was also extended to include two supporting officers to the programme manager in January 2015 (Table 20).
| Date | Activity |
|---|---|
| Summer 2014 | Plans for the review set out |
| September 2014 | Appointment of external consultants to advise on the review and appointment of the programme manager |
| October–November 2014 | Plans and decision-making regarding governance of the review |
| November 2014 | Official launch of the review |
| Winter 2014 | Building the case for change, data gathering, stakeholder meetings and engagement |
| March 2015 | Launch of the interim Need for Change78 document |
| May 2015 | Reflection and analysis (purdah period to coincide with elections) |
| July 2015 | Launch of the final case for change and potential options for change |
| Autumn 2015 | Engagement on options for change and launch of strategic outline case |
| Winter 2015–Spring 2016 | Decision-making around options for change and plans for implementation |
Case study activity
Fieldwork took place between September 2014 and March 2016 during the review of local services. Interviews with 13 individuals involved in leading and managing the reorganisation process were carried out from the CCG, local acute and other provider organisations involved, the county council, and local HealthWatch. A second round of interviews was carried out with six of the individuals towards the final stages of the fieldwork. A total of 11 key meetings and public engagement events were observed during the review period. Further details of data sources are provided in Appendix 8. In order to protect the anonymity of individuals, identifiers are removed from verbatim quotations.
The following sections draw on Callon’s51 four processes to explain how the CCG proposed and planned the reorganisation of local health services, involving the proposed decommissioning of a local hospital. Consistent with this approach, the process of reorganisation in this case study has been separated into four overlapping processes: defining the problem and mobilisation; building alliances/networks; gaining acceptance of (1) the problem and (2) the solution; and implementation and institutionalisation. It is important to restate that these processes are not necessarily linear or sequential, but that they (re)occurred at various points throughout the review period to significantly shape the journey.
Defining the problem and mobilisation
Establishing the issue and drivers for the review
The process of establishing current service arrangements as a ‘problem’ requiring a ‘solution’ was formally initiated by the CCG in this case study, who proposed plans for a strategic review of local health services in the summer of 2014. Informal discussions between the CCG and providers about a potential reorganisation had been taking place for some time, however, in the context of pressing financial challenges.
A driver behind the decision to formally review services was the significant financial and estates challenges facing the local hospital trust. Approximately one-third of the sites owned by the hospital trust had historically been designated unsuitable and/or were unoccupied, with a significant debt and maintenance backlog, and other organisations within the local health economy were also projecting significant challenges in response to demographic and financial pressures. The Community Trust and the partnership foundation trust (PFT) in particular were experiencing workforce and estates difficulties, and the PFT was already implementing a strategy of rationalisation. Another driver was frustration within the CCG over lack of progress with implementing their own clinical strategy and plans to develop community provision, as a result of current commissioning arrangements. Interviewees comments included the following:
The chief exec[utive] system has been meeting on a regular basis for a couple of years and one day we agreed that we would all share our financial position . . . The hospitals are the ones with the obvious financial deficit but all of us were saying . . . over the next 3 to 5 years, they were going to find themselves going into deficit. So suddenly we realised actually, that in the medium to longer term, we had got a financial problem so that was the first driver. The second driver was that we had not made sufficient progress in terms of development of community-based provision for our local population . . . care closer to the home, looking after people in their own home and actually, we were really struggling to make progress with that because all of our money kept getting soaked into the hospital.
If the patch continued to operate as it currently did, it wouldn’t be delivering the best outcomes to the local population and along that journey, on a kind of 2 to 5 year basis, some of those organisations were going, at different rates, to struggle to be sustainable.
Building the case for change
The strategic review itself was structured around four questions that were designed to inform decision-making around the final model(s) of care for the area:
how well (how effectively and efficiently) are patients’ needs met by the current health and social care system across [de-identified]?
what are the opportunities to meet future health and social care needs of the [de-identified] population more effectively and efficiently?
how should health and social care services across [de-identified] be configured to realise these opportunities?
what organisational form(s) and commissioning/contracting model(s) best support the delivery of the preferred future configuration of services?
Board to Boards document
Two key documents were produced – the Need for Change78 and the Case for Change70 (see Appendix 8) – summarising the purpose of the review for public and wider stakeholders, and these were launched at two engagement events to which patient representatives and other stakeholders were invited. The documents set out a case for why change was needed in the health and social care system and presented a selection of evidence from patients, clinicians and other stakeholders gathered through feedback events. The documents emphasised the demographic challenge, aspirations for a healthier population and the system-wide nature of the problem, including social care:
we want everyone to benefit from excellent care in the right place when they need it
we want to prevent more people from becoming ill in the first place
we’d like health and social care staff to work together – not in isolation – to meet your needs and to involve you in your care.
Need for Change document,78 p. 2
It was clear from interviews and observations that less emphasis was deliberately put on the financial challenges informing the proposed changes, as this might engender opposition. In reflecting on the narrative in the case for change, interviewees commented:
I think what’s been good from my perspective, it does feel like it isn’t just a hospital trust because what often happens in these initiatives, it can just look like it’s about hospitals, so it’s the tangible building and therefore people can dissociate with this whereas actually it does feel like the CCG and others are active in this and therefore it feels like it is a proper partnership and not just about the hospital building and what’s going to shut.
When we had the case for change launch, it’s great to see, you know, social services up there alongside the mental health trust, not just about the hospital . . . explain it to people in that way and actually because there’s six of us who are working in this way, the solutions could be better.
Here the external consultants provided support and capacity to undertake analysis, garnering international evidence about models of care, and communicating the review to wider stakeholders. Although establishing the case for change was seen as an important precursor to reorganisation, some interviewees expressed ambivalence about the direction of the overall process and were anxious to direct resources to implementation planning.
Building alliances and networks
Programme governance and the role of the programme manager
As explained in previous chapters, alliance-building is the process by which the ‘innovator’ of the decommissioning process garners allies who can tie it into extended networks (and their resources) and who, crucially, can contribute to and support the process – often against others who may wish to derail or detract from it. In this case study the role of the programme manager was key in managing stakeholder relationships and engagement with the process, and co-ordinating the strategic review. The programme manager explained:
The stakeholder management bit is something I’ve spent probably 60% of my time on, making sure that people feel as if they’re connected into it and understand where it’s getting to, what it’s doing. So that we don’t get to a point in the summer or the autumn where people say ‘You’ve been doing this in the bubble, I don’t recognise it and I’m going to snooker it’.
Alliance building also took place informally through conversations and interactions between stakeholders outside the formal review process, and different tactics were used to move the process forward:
Often it’s just sufficient to say to people ‘You know, you agreed that you’re going to be part of this, here we go, we’re here to help you’ and try to make it easy for people. There’s a bit of competition, so you know, we play on the fact that planned and primary are making great progress, so people think, ‘Oh God, maybe I ought to make great progress’. I have offline conversations with people that help them understand where we need to be, and how we can get there.
A governance system was also established for the strategic review by the programme manager and the CCG. The system comprised a programme executive made up of the CCG and provider chief executives, a communications and engagement group, a care advisory group and a series of operational groups including information technology (IT), estates, workforce and finance. A series of themed working groups meanwhile focused on specific service user groups and the design of care pathways for these users. Each group within the system had mechanisms to draw in or connect with their wider stakeholders, for example by using patient forums or engaging existing working groups on these issues, and by having a lead to champion the issue. In this way, the governance structure of the programme was designed to include stakeholders and thereby militate against potential challenges to the process.
Provider relationships
Interviewees stressed the importance of adopting an attitude of ‘partnership working’ among the providers and of fostering a shared sense of ownership of the review in order for it to achieve its objectives. Considerable time was spent at the beginning of the review developing the governance structure and ‘vision’ to ensure this sense of ownership, and this was revisited regularly throughout the review process at observed meetings. One interviewee commented:
It’s important that it’s owned by the patch. What we didn’t want is a thing over here devising the answer, coming back to the patch and saying, ‘Here’s the answer’ and people going, ‘Where on earth did that come . . .?’ So we’re trying to do it from within.
Interviewees also commented that key personalities were disposed favourably to working together and that this had a positive influence on the process:
All of the leaders are committed to common cause. And they’re saying that to their teams, so whilst there will be difficult stuff to agree, their level of commitment and the commitment from their boards is very high. So they’re pulling in the same direction and I think that isn’t always as evident in other places.
Clinical engagement
Interviewees stressed the importance of having clinicians involved and committed to the objectives of the review process. Clinicians were felt to command trust and authority among patients and the wider public, and held the clinical expertise and knowledge necessary to shape and design patient pathways in a reorganised system. However, their involvement in the review process was hampered by lack of capacity to engage and also what was described as a sense of reorganisation ‘fatigue’, caused by the longevity of challenges and past attempts at reorganisation. One interviewee commented:
Initially from clinicians it would be ‘not another strategic review. Why is it so different this time?’ The other bit of it was the capacity; the frustration that even if it’s something that they really want to do, it’s just not physically having the time to do it.
Clinicians were engaged in the process via a clinical advisory group with a clinical lead, and were also invited to take part in a survey to inform the review. In general, while the review team felt that clinicians could be better engaged and that there was a risk of some disaffection, they were not in themselves viewed as a risk to the reorganisation process.
Patient and public engagement
Patient and public engagement in this case study involved a range of methods to collect and synthesise views. Because of past attempts at reorganisation and the loss of some acute services in recent years, the review team were keen to reassure patients and the public and to negate potential disaffection. This was evident in the Need for Change,78 the Case for Change70 and the Strategic Outline Case documents, as well as at public engagement events, which stressed the need to improve services and recognised the legacy of challenges in the case study area.
In order to engage patients and the public in the process, existing patient groups and platforms were used, as well as mechanisms to engage the wider public. A website was devised to coordinate the collation of evidence from all stakeholders and provide a public point of contact and visibility for the review, including updates on progress. A survey was produced and made available online and in hard copy form, and face-to-face engagement was carried out at shopping centres and at local train stations to raise wider public awareness, distribute the survey and collate views. A series of evening events were held with patients via GP practices and with existing patient forums/representative groups in each locality and two conversation cafes were held at public spaces to discuss the review and collate community views. Patient representation groups were also invited to stakeholder events as part of the review programme, including the launch of the case for change in March 2015.
Gaining acceptance of the problem and the solution
Gaining acceptance of the problem
Throughout the review and during observed meetings, the necessity of change was emphasised by the programme management team and the Need for Change,78 Case for Change70 and Strategic Outline Case documents were important to reinforce this narrative and message. Fear that the severity of the financial and estates challenges facing the hospital trust would prompt external intervention in the future was also a strong factor in generating a consensus among the provider organisations of the necessity for change and gaining acceptance of the problem. Participants commented:
We’re better off doing something ourselves that we can all agree on before it’s done to us.
Comment made during observed meeting
It’s not like they’ve got a do-nothing scenario. The trust is bankrupt basically so it’s not like people can just look at it and go ‘Oh let’s not do anything then’.
We all recognise that the services we’ve got are no longer fit for purpose and the estate that we’ve got is no longer fit for purpose. So we’ve got to do, you know we don’t want to get to the point where we are tripping over and we can’t manage the finances, we’ve got to do something different.
. . . an overheated hospital with major pressures, whether it’s financial or clinical, and we know that that’s not sustainable. We are so overheating and I think people here know that something has to change, you know, we’re in buildings that are unfit, and they’re definitely not fit for purpose. Everything is a challenge as a result of that and as a result of the capacity issues; you know . . . I think people get that. So I think they’re going to buy into it.
Interviews with local HealthWatch and observation during patient engagement events suggested that patients were broadly supportive of the need for change, citing in particular dissatisfaction with the quality of local hospital services, perceived siloes in provision, and difficulties in accessing and navigating current services. Interviewees from the review team remarked that there was less cynicism and disengagement from patients and the public than anticipated:
I think that we all thought before there would be, that people were feeling less positive about it actually, in the sense that either they would be thinking, as I said, you know, ‘we told you what we think years ago, and with this programme and that programme, and just calling it something else’ and actually we’ve had much less of that cynicism than I was expecting.
Concerns about current provision and recognition of the need for change appeared to be echoed by clinicians and the workforce in observed engagement events, and interviewees reflected that adopting an honest approach regarding affordability and the national profile of the financial pressures facing the NHS contributed to a more benign environment for engagement. However, some hostility from patients and the public was encountered in later engagement events when proposals for the future configuration of services were presented, and this honest approach was tempered somewhat in the written justification for the changes, as already noted.
Gaining acceptance of the solution
Although there was broad agreement over the need for change among stakeholders, including patients and the public, agreeing the solution proved more contentious. Broad agreement within the programme executive was achieved for proposals for health-care community ‘hubs’ that would provide a single point of contact for most primary care and some social care services. However, it was less clear how these services would be organised in practice. Debate meanwhile focused particularly on the hospital provision. The configuration and location of acute services presented a challenge for the hospital trust because of strong patient and public views about travelling distances to access care (observed during engagement events), the complexity of the clinical design of the system and resources required at each acute site including workforce, affordability and the quality and suitability of existing buildings. Reconciling these points of tension proved challenging for the review team and programme executive. However, three options for the configuration of acute services were provisionally agreed and shared with wider stakeholders. Proposals consisted of a new hospital build for the area in a central location, the centralisation of all acute services at one existing site and the centralisation of acute services (planned and emergency) between two existing sites. At the time of writing, feedback and debate on proposals was ongoing. During the fieldwork period a number of other factors were observed that shaped and influenced the debate about the future design of the system in this case study and these are discussed below.
Provider relationships
As the review progressed, tension between provider organisations increased as discussions took place over the future organisation of services. A particular point of tension was the intended future role of community services. The Community Trust, PFT and County Council Social Services all voiced aspirations to play a more significant role in the provision of community services and questioned the current configuration and viability of the provider landscape. Interviewees commented:
I think that the relationships remain decent so we’re not shouting at each other or anything like that but actually it’s probably a bit too cosy at the moment and we need a bit of grit in there.
We can’t really have open dialogue. There’s this elephant in the room about having an organisation who are all very nice, it’s not about personalities, it’s just broad economics, we can’t afford to keep it and we should do something about that. We can’t just limp along for another 3 or 4 years, we need to do something about the community trust and how we divvy that work up. So that will be a difficult conversation.
This issue was remarked upon in interviews with a local HealthWatch representative, who feared that dynamics between providers may unduly influence local solutions:
The organisations themselves are all providers. Some are either foundation trusts or applying for foundation trust status, so you’ve got a bit financial best interest in making sure they maintain that income. So that’s my conflict of interest concern that they may not quite put across the best plan for our population because it might not serve their own interests and I guess it’s difficult with all the organisations, as I say we hope that they’ll, sort of, help each other out but it’s difficult to actually say, you know, truly whether or not that has been solved.
Review fatigue and cynicism
A second issue raised by interviewees was the need to maintain the momentum of the review, as discussions around the precise configuration of services and their practical implementation continued. Interviewees expressed a sense of ‘review fatigue’ in second-round interviews and progress had appeared to slow as stakeholders continued to debate the potential solutions. Some interviewees were beginning to question more urgently the time and resources required to sustain the review and were struggling to maintain the level of input that had so far been provided both personally and from their workforces. Some interviewees also expressed their frustration at what they saw as the protracted nature of the review process and a lack of critical decision-making:
I think it’s taken longer, been slower than people maybe hoped for but I think, I’m not sure that there was really full recognition or even is now, of the real scale of what we’re talking about and hence I guess my comments are around the need to focus. I’d rather that we agreed the things that really would make a difference that we could actually implement and then really focus on how we deliver those, than you try and solve everything and come up with the best model in the world but actually, you get no traction around any of it and I think we’re still wrestling with that. I think there was a lot of time put into establishing the base line, understanding where we are now but probably didn’t tell us a huge amount more than what we already knew but was important in terms of the buy-in process.
So we’re turning up to meetings, we’re looking at what the other groups have discussed, but for me it doesn’t yet feel like we’ve fundamentally talked about what the new model of care will be. It feels like we’re turning up looking at a load of slides and then all agreeing that they’re very fancy and going away again.
Differences of opinion between stakeholders and interviewees about the pace at which the review needed to take place emerged during second-round interviews and in observed meetings later in the process. Frustration was expressed particularly by social services representatives who referred to differences in the decision-making culture of health and social services and the financial pressures they were facing, which were impacting on their capacity to commit time and resources to the review. Interviewees were particularly fearful of disengagement from clinicians, whose involvement had so far already been more limited than intended:
I think they just need to see something a bit more tangible before they start walking up the hill again.
They’ve had so many of these that don’t deliver that makes it hard, makes it really hard to get people involved as well as doing their day job, which is, you know, as I said, we’re an overheated hospital, so that does make it difficult.
The programme manager described his attempts to manage these various tensions between stakeholders and the challenge of maintaining the momentum of the review and keeping it aligned:
The longer it runs out the less people think it’s really going to deliver. You’ve got to have a degree of momentum to it. But equally you can’t short-circuit something that’s not ready. It’s like baking a cake, isn’t it? You don’t want to have it in the oven for too long, because it will just be inedible. But at the same time, you’ve got to cook it for the right amount of time. But if you do it too slow, then stuff comes along, alongside, so you know for instance in this patch, we’ve got one organisation in turnaround. Do people want to wait for the outcome of the strategic review to take some pretty critical decisions, or would the system just fast track those? And that’s always been the worry of one of the chief exec[utive]s, is that you know stuff just gets decided as you go anyway. And at what point does that reduce the credibility of the review process itself?
Implementation and institutionalisation
Clinical Commissioning Group leadership and commissioning levers
An issue raised by case study participants in interviews was the role and leadership of the CCG in progressing agreement for and implementation of the proposals. The relatively recent formation of the CCG, with new staff, was considered by some interviewees to have weakened their ability to push particular solutions and manage dynamics between providers. One interviewee commented that:
It just feels like we haven’t been tight enough in specifying what we want and I think that’s about possibly the CCG not being as clear as they need to be. Whilst we’re all partners in this they are most actively engaged with the programme director and [de-identified consultant] so you know there’s a bit of a discussion to be had about where we’re going with all of this at the moment.
Other interviewees expressed a view that responsibility for leadership of the reorganisation needed to shift from the CCG to the providers, as the latter had important responsibilities for implementing services changes and organising themselves differently in the new system. Reflecting on the evolvement of their role, the CCG discussed the necessity to commission services differently in the future, but remained cautious about both the availability and impact of using contractual levers to commission differently from providers:
Ultimately, in my view, there’s going to have to be some strong commissioning around it to set a direction, set some centres that align to it and bake that into contracts, going forward because I think that’s the only way that it will be, you know, that ultimately it will be pushed through, but there are dangers in that.
So this is about the chickens coming home to roost I think and people thinking, everybody thinking, this will be alright for them, it’s everybody else that’s going to have to give and there’s going to have to be some give and that’s the only way around it. But our commissioners, we will have, obviously, alternative options. If the providers don’t work collaboratively to deliver the solutions and that might mean mergers, it might mean a very different model, very different stance of organisation, if they don’t come together and collaboratively do that, then we’ll commission for an alternative model and that will take longer but, but that’s what we’ll do so there are solutions that can be put into place.
Maintaining system stability was a concern for interviewees, but this was at odds with the logic of change, and tensions between providers continued to shape discussions about future models of care.
System complexity
As an example of reorganisation, this case study was ambitious in the scale and scope of its proposals. The complexity of the proposed service configuration appeared to hamper both agreement for, and the implementation of, proposals. The review featured both primary and acute care services and included mental health, community services and social care. While this meant that a holistic, whole-systems approach was adopted with a view to providing more joined-up care, aligning these services and their patient/care pathways proved challenging for the review team. The competitive dynamics between providers further complicated organisational design, and the disparate cultures and operational processes of health and social services were viewed as a barrier to greater integration and system alignment, particularly in areas such as services for children and older people. One interviewee commented that:
I think the biggest challenge to this programme is its broad scope. So in other areas these types of things would be about an acute services review or it would be about health review or it would be about bits of services, you know what I mean? They were very ambitious in saying ‘Let’s put everything on the table’ so this is about prevention, it’s about self-care, it’s about voluntary sector, it’s about community support, it’s about acute, it’s about specialist services. And whilst that is helpful, because it makes it holistic and you can come at it with a strategic overview and it probably has a better resonance with communities, it makes it much more complex to mobilise.
A further issue that the review team was struggling to reconcile concerned operating boundaries between providers and the CCG, as most of the providers were delivering services beyond the CCG catchment area. The effects of changing service configuration – on operations outside the CCG area and on the users of those services – were therefore a key consideration for providers. An interviewee commented:
Three of the partners are county wide, not [CCG area] wide. You might want that in [CCG area] but I can’t help you organise that type of service design because I run it on a county-wide basis not a [CCG area] basis. I think the other thing that we pay attention to through the strategic advisory group, which is part of the governance jigsaw, is what’s happening around our borders. So when we get to issues around travel times analysis, specialist services, the population looks beyond the boundaries of [de-identified area] for a number of services. It creates another set of problems around the borders.
In addition, the review team was undertaking an in-depth analysis of the clinical design of the acute provision to ensure the viability of clinical procedures and pathways in a changed system and to minimise clinical risks to patients. Because of these various factors, interviewees reflected on the probable longevity and delay of achieving reorganisation in their second-round interviews and were preparing for a protracted implementation process.
Reflections
As an example of reorganisation, this case study was ambitious in its scale and scope, involving a range of providers and stakeholders in the strategic review and reorganisation process. Recognition of the severity of the financial and estates situation initially appears to have underpinned commitment to the strategic review process among providers and other stakeholders. However, at the time of fieldwork completion, input levels were becoming more difficult to sustain as the review progressed past original time scales and friction increased as providers ‘jostled for position’ in the new system.
System complexity appears meanwhile to have been the most significant barrier to gaining agreement for proposed solutions and moving towards implementation. This case study has revealed a number of tension points and variables that must be reconciled in any reorganisation process, including travelling distances for services users and equity of access to care; provider and commissioner boundaries of provision; care pathways and clinical design of the system; and system stability through the transition. Affordability was meanwhile an underlying driver throughout the review and strategic planning and is likely to shape the process and outcome of any attempted reorganisation.
An intensive engagement process was carried out by the review team in anticipation of strong public and political opposition, and an external consultant was recruited to assist with the development and communication of key messages and to add capacity to the engagement process. Unexpectedly, however, patient and public controversy over proposals was not experienced to levels anticipated by the review team. Observed events and interviews with patient representatives suggested moderate support for the review process in order to improve the quality of services, especially hospital provision, and to help integrate care. However, the timing of fieldwork means that limited data collection took place as more concrete proposals for future models of care were being shared and it was not possible to garner public opinion. Efforts to secure local political support were meanwhile initiated at the beginning of the process and a pause in the review was scheduled to coincide with the elections in May 2015 to avoid undue political attention or ‘hijacking’.
Overall, learning from this case study suggests that even planned and well-resourced change programmes may be subject to delay and lengthy time scales and that reconciling provider, commissioner and patient perspectives is likely to prove challenging. As an example of reorganisation, this case study has most relevance and learning for STPs, suggesting that pre-identified implementation mechanisms and honesty about the financial drivers are important prerequisites of change.
Summary of findings across the case studies
With regard to the research question ‘what factors and processes influence the implementation and outcomes of decommissioning’, the case studies offer some important insights. As these were selected according to criteria of diversity, it is difficult to draw inferences from our small sample with regard to geography and location. However, when combined with our narrative vignettes, our analysis appears to confirm that scale and complexity are related to the amount of ‘work’ required to secure progression through the decommissioning stages, and to the chances of (and time scales for) completion. We anticipated that the EOL closure would generate less controversy than in other case studies and this was confirmed in practice. This also appeared to enable a short-circuiting through the stages and processes observed elsewhere. Our aim to compare nationally and locally instigated decommissioning was hampered somewhat by the absence of implementation of NICE guidance in case study 3. However, overall, the case studies underline the influence of national context and system actors on the progress of local decommissioning, as well as confirming the unique challenges of nationally led programmes of reorganisation.
Using our four processes framework, we can make the following additional observations:
-
The role of evidence and networks in identifying and framing a need for decommissioning.
In case study 3, the process of translation towards decommissioning had been halted in an early phase and effectively put on hold. None of the relevant actors on the APC sought actively to define the nature of the problems it faced as requiring systematic decisions to remove or replace services. In each of the other three case studies, decommissioning advocates sought to mobilise evidence in support of decommissioning, sometimes in the face of conflicting goals and competing interests. For the closure of the EOL service, a key influencer was the review of the contract with a view to achieving savings, led by the CCG, which identified inappropriate service usage as well as availability of other services. This evidence proved more persuasive in the mobilisation phase than patient support for continuation. In case study 4, namely the CCG-led reorganisation, support for decommissioning rested on widely recognised finance, workforce and estates dysfunctions and/or shortages. These were crystallised in two documents arguing the case for change. Similarly, the burn care review was predicated on a broadly accepted problem of sustainability in the face of plunging demand for intensive care.
-
Alliance-building as part of a decommissioning process.
In the case of the EOL service, a narrow constituency of pro-decommissioning actors was formed and this extended to the provider threatened with decommissioning (which was therefore characterised as ‘arranging their own funeral’). This co-option into the advocacy group of the provider, who chose not to be ‘confrontational’, sealed the acceptance of decommissioning as a solution. By contrast, alliances in favour of the burn care programme of change proved to be somewhat brittle and subject to mutual doubt and suspicion. Ultimately, some of the actors required for the changes to be accepted proved not to have been successfully co-opted into the roles required of them. The local reorganisation saw perhaps the most concerted attempt at co-option of all relevant actors, including provider organisations, clinicians and patient and public groups.
-
Social acceptance for the solution of decommissioning.
Closure of the EOL service required negotiation between four actors: the CCG, the provider, referrers (predominantly GPs) and the patient population. The process was notable for its achievement of acceptance in all but the last of these groups. By contrast, social acceptance had not been sought or achieved by advocates of the burn care reorganisation, and interviews with those outside the nucleus of actors indicated a lack of support for the proposed direction of travel. In the local reorganisation, leaders had employed a deliberate strategy of engagement and co-option – in accordance with accepted principles of good practice – but had not succeeded in gaining wider acceptance of the legitimacy of their preferred course of action. As with the burn care proposals, the proposed solution proved harder to sell, despite acceptance of the need for change. Patient and public views were more powerfully expressed than in the EOL closure and, as tension between provider bodies increased, progress stalled.
-
Institutionalisation of a decommissioning decision.
Only one of our case studies, the EOL service, reached a point of implementation and institutionalisation in which the changes could not be ceased or reversed. The availability of an implementation mechanism (in the form of a simple two-party contract) and a compliant provider meant that enactment of the policy was simple, despite some concerns expressed retrospectively about efficacy and equity of the transition and outcomes. Implementation was clearly more challenging for the two wider reviews and even for the APC, which was unable to mandate compliance with its guidance.
Chapter 7 Findings from the focus groups and Delphi study involving citizens, patient/service user representatives, carers and representatives from third-sector organisations and community groups
Introduction
The aim of work package 4 was to investigate the perspectives and experiences of citizens, patient/service user representatives, carers, third-sector organisations and local community groups in relation to decommissioning, by addressing the following research questions:
-
What are the views and experiences of citizens, patient/service users, carers, third-sector organisations and local community groups in relation to health and social care decommissioning?
-
How do these compare with those of policy-makers, practitioners, health-care leaders and researchers?
-
How might these perspectives be brought together in order to improve equity and acceptability in decommissioning?
The first of these questions is addressed through focus groups and a Delphi survey. The Delphi survey also enables us to provide a direct comparison with the views of policy-makers, practitioners, health-care leaders and researchers. The third question requires us to synthesise findings from across the work packages, and this is carried out in Chapter 8 (see Bringing together perspectives of the stakeholders in decommissioning).
Focus groups
As explained in Chapter 3 of this report, the focus groups were conducted in three regions of the country – Liverpool, Birmingham and London – although some participants travelled from further afield to attend. In total there were 30 participants spread over the three events and these included patient representatives, carers, members of the public and members of organisations working with these groups, including third-sector health-care providers. The first aim of the focus groups was to understand participants’ experiences of and perspectives on decommissioning. Participants were therefore encouraged to share and discuss their views about decommissioning, and to reflect on their involvement in decommissioning processes. We employed short descriptions of decommissioning examples (see Appendix 5) to stimulate discussion among participants. A second aim of the focus groups was to sensitise us to the language used by patients/service user representatives, carers, third-sector organisations and community groups when discussing decommissioning, in order to inform a subsequent Delphi study. The discussions involved working with participants to design questions for the Delphi study, as well as discussing recruitment strategies, potential participants and methods for disseminating findings. Below we present findings against these aims.
Participant views and experiences of decommissioning
Some key themes of the focus group discussions included mistrust of decision-makers, the importance of patient and public involvement in decommissioning processes, experiences of loss and uncertainty associated with decommissioning and views on the impacts and outcomes of decommissioning. These are discussed in turn below. Where excerpts are included verbatim from focus group discussions, ‘F’ denotes a female participant, ‘M’ denotes a male participant and ‘I’ denotes the interviewer (or facilitator).
Examples of decommissioning
Participants were asked to describe examples of decommissioning that (1) they were aware of, (2) they had been directly or indirectly involved with or (3) they had been affected by. In response they cited a range of examples that varied in terms of scale and scope, service area (including social care) and type. Examples included:
-
removal of a community-based nurse-led service for patients with heart failure (Birmingham focus group)
-
closure of residential mental health services (Liverpool focus group)
-
closure of small rural hospitals (Birmingham focus group)
-
reductions in funding for, and restriction of access to, hearing aids (Birmingham and London focus groups)
-
closure of local day-centre services (Liverpool focus group)
-
reduction of transport provision for people with learning disabilities (Liverpool focus group)
-
reductions in funding of support for black and minority ethnic (BME) advocacy services (Liverpool focus group)
-
removal of hydrotherapy services (London focus group)
-
removal of tertiary referral pathways (London focus group).
These examples correspond in scope and range to those discussed in previous work packages, enabling comparison with these earlier findings.
When discussing the term ‘decommissioning’, participants noted that this can have both active and passive forms:
I suppose for me it sounds like it is an active thing, doing decommissioning. Like you said the comparisons of decommissioning oil rigs was interesting.
Well I saw it as an engineering term.
Yeah I think that’s really interesting, but it does sound like it’s something active you do and sometimes it is, in the NHS, it is something active people try to do.
But sometimes it’s a sort of passive thing, like they commission services and they’re just not commissioning what you have, you know, every year we have our commissioning intentions and you might have just left out something or bits of what people had before. So it’s a sort of passive ‘oh, we’re not doing that any more’ rather than . . .
Discussion in focus group 2
Participants generally agreed that adopting a planned, active approach was preferable to passive decommissioning, as it was more likely to avoid disproportionate adverse impacts on patient populations. However, it was also notable throughout the focus groups that many participants associated decommissioning with the wider context of financial restraint and austerity in the public sector, and for many participants it had become synonymous with reductions in public spending, financial pressures and ‘cuts’.
The issue of ‘privatisation’ was also raised in discussions, with some participants raising objections to the use of private-sector providers in the delivery of NHS services. In these discussions, these respondents clearly linked decommissioning with an agenda of increased private involvement in NHS service delivery.
Mistrust of decision-makers and motives
Discussions suggested a wariness of the motives behind both the specific examples of decommissioning cited by participants (including closure of community services, reduction in transport opportunities and so on) and of decommissioning and health-care reorganisation more generally. As already noted, there was a strongly articulated view across the three focus groups that decommissioning was driven frequently by financial pressures and the requirement to make cost savings, rather than primarily to improve services. Furthermore, some participants perceived that particular services were decommissioned because they were seen as ‘easy targets’ by funders/commissioners, and as being less likely to cause political or public controversy. Examples included third-sector and community services and non-life-saving interventions such as audiology and fertility services:
I think I’m with [de-identified] on the thin end of the wedge and I think when these sorts of things come up the commissioners are picking off things they can get away with.
OK.
And then they’ll look at the next one they think they can get away with and they think they can get away with it. You know, it’s the reason for having a service there because any of these reasons it’s expensive and it’s not life threatening and it’s not urgent and it’s very mild. But because they have to sort of have some reason, but really they think ‘well, we might be able to get this through’ because there are people, the public, who think ‘oh yes fertility treatment, there’s enough kids in the world we don’t need any more kids. Hearing aids, oh well yes, it’s only mild . . .’
Discussion in focus group 2
In addition, there was strong agreement among participants across the focus groups that preventative and rehabilitative services tended to be more greatly affected by decommissioning or disinvestment, and that resources tended to be targeted into curative services when planning and commissioning services:
It seems that if it’s for a surgical procedure and hospitals are going to make some money, that that could be provided or they can do the surgical procedure. But they don’t want to put anything into services that get people well quickly afterwards or ways of preventing all of this in the first place.
OK, so you think it’s easier to underinvest let’s say in a rehab out in the community or some kind of prevention rather than some surgical intervention or some curative?
Yes.
And why would it be easier?
I think it’s to do with commissioning because it’s easier to commission something specific than it is something that is, well OK, it might be a few sessions of physiotherapy, it might involve a little bit of psychology, it might involve a bit of this and I think they just think ‘we can’t deal with this, it’s too complex for us, we want it simple, we want it straightforward, that’s cut and dried’.
It’s because everybody deals with their own little budget.
Yeah.
And they don’t think about the overall cost of an operation is pre the actual operation, the recovery, social help to go with it, the looking after the families, the benefits paid because you’ve got somebody not working in the family, all those things they’re all separate and they’re not looked at as a whole.
Discussion in focus group 2
There was some disagreement among participants over what were perceived to be justifiable circumstances for decommissioning, with some participants expressing the view that because of financial and staffing pressures some decommissioning was acceptable and others believing that decommissioning was legitimate only where services were of demonstrable poor quality or where there was evidence of reduced need.
In discussion, participants identified a perceived lack of transparency and accountability in decision-making:
I just wanted to ask a question really because as we’re talking about these Clinical Commissioning Groups I’m realising I’m quite ignorant on their construction and, you know, are people appointed or are people nominated? I know GPs sit on the Clinical Commissioning Groups, but what other sorts of people? I mean are they public appointments? How do these people understand the needs, the complex needs of the areas that they serve? Do they make their own choices based on what they see sort of coming through the door?
Participant in focus group 1
Low levels of patient and public involvement
In addition to the concern expressed in relation to decision-making, some participants also reported a sense of frustration at being ‘removed’ from decision-making processes about services and of decisions happening in what were perceived as ‘closed’ environments with little meaningful patient or public involvement. The degree to which participants had been directly involved in decommissioning processes varied, but a strong view expressed across the focus groups was that involvement tended to take the form of consultation or information-giving (e.g. about plans for service changes) rather than sustained engagement and genuine opportunity to influence decision-making.
Where participants had been directly involved in a decommissioning process, they described a range of methods for facilitating their engagement, including filling in surveys, attending public meetings and acting as patient representatives through existing platforms such as patient advisory or reference groups, or via local HealthWatch organisations. Experiences of engagement were mixed, with many participants expressing dissatisfaction about short time scales for involvement and poor communication with those leading the process.
Participants appeared to agree that the language used by commissioners/funders was often inaccessible and made engagement difficult and that, as a result, involvement was often limited to patients and members of the public with greater understanding and prior knowledge of the health-care system:
They were using words like ‘what do you think about the consultation process?’ and of course they were getting blanked as if ‘have you ever experienced a consultation process?’ Well some of them might have but they’re not using the right terminology.
Participant in focus group 3
Other participants meanwhile described feeling overwhelmed by the level of time and commitment required by commissioners for engagement processes, and that the same people were often called upon to be consulted:
The CCG is just sending surveys and surveys and surveys and they say, you know, we want you . . .
Your opinions, tick boxes.
. . . yes, now it should be my beneficiaries’ or my service users’ opinions, you know.
You don’t always know what happens to that information either perhaps or . . .
Exactly and then we’re getting four emails on the one subject. I’ve just started deleting them now because we haven’t got the time.
. . . very, very, very complex questionnaires which ask the same questions, not in a logical order.
Discussion in focus group 3
Many participants voiced doubt about the influence their input had on decision-making and in general did not feel that patient and public views alone would sway decision-making. Some expressed the view that, for example in relation to hospital closure proposals, decommissioning decisions were reversed or renegotiated only in response to negative media coverage or political intervention, and that therefore this is where patient and public energy should be directed. Participants also identified differences in the relative influence of different patient subpopulations in terms of their profile, how easy it was for them to mobilise and the strength of their networks and political representation. For example, patients with very rare conditions or dementia were cited as being especially vulnerable in this regard. In general, participants expressed dissatisfaction with engagement methods that depended on single lay or patient representative membership of decision-making bodies, as this was seen as placing unfair demands on the individuals concerned, while failing to capture the full range of views held.
During the focus group discussions, representatives of third-sector and community organisations emphasised the difficulties they experienced in communicating decisions about the future of services to their users. One respondent, for example, had heard on the morning of the focus group that their application for continued funding of an audiology service for older people had been unsuccessful. This made the requirement to inform patients, hitherto postponed, unavoidable, especially as staff departures in light of the uncertainty over funding had made continued delivery of the service increasingly difficult.
Loss and uncertainty
Loss was articulated and experienced by participants in a range of ways. For example, in relation to the closure of services, discussion included terms such as ‘grief-stricken’, ‘upset’, ‘anxious’ and ‘sad’. A concern among participants was that commissioners and decision-makers did not understand or value the attachment of users to long-standing services and the subsequent emotional experience of loss when these were taken away, even in cases where an alternative service was being commissioned. As one participant explained in relation to decisions to remove services from community settings:
Some of the decommissioning that’s been going on have been a loss and I think the commissioners have underestimated and undervalued that sense of loss. I would say, I’ve worked with community groups who are most grief stricken with the loss of the service and they don’t see anything to replace it and so there’s no trade-off, there’s no like ‘you know, well this is about improving the NHS, we’ve got new clinical developments. The reason why we’re making a change is for your benefit’, you’re not having those dialogues. You’re having like ‘well we’re just taking this service away and you – members of the public – will have to travel four times as far to go somewhere else but you can do that’.
Participant in focus group 1
Another experience of loss discussed by participants was the erosion of relationships with coservice users and staff as a result of decommissioning and/or reorganisation. As well as the personal loss of these relationships, participants lamented the wasted energies expended in the establishment of the relationship and the associated programmes of work. This was cited for example in relation to the closure of local day-centre services and reduction of transport opportunities for people with learning disabilities.
Participants also talked about the uncertainty associated with decommissioning. This was notably felt by third-sector organisations and community groups involved in delivering and providing services. These participants expressed a sense of anxiety over the continuation of their funding streams and, where they had already experienced reductions in funding, concern about the implications for the future sustainability and continuation of their organisation. Communication from commissioners and time scales for notification of contract renegotiations were also felt to be poor by these participants and compounded their experiences of uncertainty and insecurity:
You know, so organisations can be waiting until 30th March to find out whether they’re going to be commissioned the next month. Now that’s not just impacting on their service users . . .
The staff.
. . . it’s the staff.
Discussion in focus group 2
Carer impact was cited particularly in relation to day-centre services, hospital closures and the cessation of audiology services. Carers described being unsure of how to access and navigate new services following reorganisation or replacement. Some also related experiences whereby new or replacement services did not retain complete patient or case histories, and expressed their anxiety over the loss of personal relationships as carers with staff who knew and understood patients’ particular conditions and experiences.
Impacts and outcomes of decommissioning
Some of the focus group participants had been personally affected by the loss of services, treatments or changes to local decommissioning of day services and transport for people with learning disabilities. Participants described a sense of increased isolation, loss of relationships established via the day-centre services, disruption to weekly routines and increased reliance on carers. One focus group discussed at length the impact of reduced funding for hearing loss services. Implications included increased difficulties in communication for people with hearing loss, reduced confidence, increased isolation for service users and increased travel and related expenses to access alternative hearing-loss services.
Participants shared experiences and concerns about having to travel further for services where reorganisations or local service closures had taken place. Availability and ease of access to personal or public transport were significant issues and shaped the extent to which participants felt that they were able to access alternative services; however, they reported that they did not feel that these issues were often considered sufficiently by decision-makers and health-care commissioners. Participants also discussed their experiences and perceptions of reductions in the quality of care received by patients and service users as a result of reduced funding/resources or withdrawal of certain services. One example was given as follows:
But without [a replacement hearing aid], that lady sat in the hospital bed for the few days that I was there and she was in for a lot longer than myself, every morning they came along and they said ‘morning ladies, for breakfast we’ve got blah, blah, blah’ and this poor lady sat in total oblivion. The doctor came and he talked to her and she sat in total oblivion because nobody had taken on board that while she looked happy and she was smiling, she couldn’t hear a word anybody said unless they walked up to her, spoke face-to-face to give her a bit of help with lip-reading and to actually make her understand why she was in hospital. She didn’t even know why.
Participant in focus group 1
Participants also referred to what they saw as a lack of ‘joined-up thinking’ about health care and a failure to view the system as a whole. They recounted experiences of disruption to familiar patient pathways such as referral processes and to after-care and post-surgery support, which created difficulties for patients, service users and carers in navigating and accessing appropriate treatment. Participants also expressed the view that where a service or part of a health-care system was affected by decommissioning, another part of the health-care system would have to compensate. An example discussed was the additional pressures on GP services as a result of the decommissioning of some district nursing, home care and social care services.
Designing the Delphi survey
The final part of the focus group discussions focused on the design of the subsequent Delphi survey. This involved crafting questions and sense-checking language with participants, identifying potential participants and recruitment strategies and generating suggestions for the dissemination of findings among participant groups.
Recruitment and sampling
Participants suggested a range of both national and local organisations to contact for the Delphi study, including patient and service user organisations, lobby and advocacy groups, condition-specific organisations and charities, carer organisations and third-sector umbrella groups. Some focus group participants stressed the importance of targeting seldom-heard groups, particularly young people’s organisations and organisations representing BME groups. We also asked for suggestions from the project team and project advisory group and compiled these together with the focus group suggestions to generate a list of potential participant organisations. Where possible, we identified named individuals within the suggested organisations to invite to take part.
We also asked focus group participants to advise on recruitment to the study and how to encourage participation, particularly given the under-representation in our first Delphi panel. Responses suggested the need for initial communication to make clear the purpose of the study, what was intended to happen to the results and, in particular, the plans for feeding back the findings to participants. Feedback was felt to be particularly important by focus group participants, as some recounted experiences of being involved in research and then excluded from dissemination.
Participants also emphasised the importance of making clear the probable impact of the research:
More people are more likely to want to take part in research in the future if you can actually show tangible change. So if you can communicate a tangible change even if it takes you a year or whatever to do that.
Participant in focus group 3
I think it would be helpful to tell people what you’re going to do with the information. You know back to the old deal ‘what difference is it going to make?’ And if you’re doing it to produce a research paper well good luck to you, but if in fact you are going to use that in a fairly productive way to try to shift or influence decisions in the NHS and you see some possibility that that might help, I think people would be a lot more willing to participate.
Participant in focus group 1
Other recommendations included the provision of clear and accurate information about what participation is likely to involve; covering expenses (although payment was seen as unnecessary); inviting participants to a final event to share findings; sending timely and frequent reminders to participants; and providing contact details for the research team to answer participants’ questions or concerns. Each of these suggestions was implemented.
Accessibility and design
A further suggestion that was incorporated in the Delphi study design was making the survey available in different formats, and with the option of facilitated completion. A key issue regarding the design of the Delphi study concerned terminology, language and the phrasing of questions to ensure that they were accessible and easy for respondents to understand. In particular, focus group participants recommended the avoidance of the use of technical, clinical or managerial language, and avoidance of the term ‘expert’ when inviting people to take part. Providing a clear explanation of decommissioning was also considered to be important by focus group participants, as they anticipated different understandings and connotations associated with the term:
Don’t use any jargon whatsoever. Decommissioning meant nothing at all to me. It’s got to be in plain English.
Participant in focus group 1
Participants discussed suggestions for how the research team could explain decommissioning in the invitation to take part in the Delphi survey. Recommendations that we included in our final Delphi survey were the terms ‘stopping’, ‘taking away’ and ‘moving’ services:
Eliminate, you want to eliminate a service.
Take away the service.
That sounds like . . .
Take away.
Stopping a service.
I would put restructure.
Restructure.
Restructure it, yeah.
[All talking together.]
Service transformation.
[All talking together.]
I think they use decommissioning because they think . . .
It’s the right word.
No, because they think maybe the public think one day we’ll start it again, that it’s not totally out of action, but as I said, I didn’t understand what it meant, you know.
Yeah, OK, not many people do, they think of the military or . . .
Yeah, yeah. But you’re taking away a service.
Taking away, OK.
We’re moving a service.
Stopping.
Or stopping funding or stopping paying for a service.
Discussion in focus group 1
Another suggestion made by participants was to include an example to illustrate the meaning of decommissioning to participants.
I was just thinking depending on the experience of the people that you target it might be an idea that you include a case study, like you did with us.
OK a scenario.
And then actually say ‘this is a decommissioning, this is actually decommissioning, making these choices of decommissioning’ then say ‘have you ever been involved in that kind of choice affecting you personally?’
What do other people think about that?
I think that’s a brilliant idea because that was really –
It is a good idea, yeah.
I mean it was really, it was very clear.
Because it’s not abstract any more then is it?
Right.
It becomes a reality.
So you would say ‘this is an example of decommissioning in health care’ and then they know and then ‘have you ever had to face this experience?’
Yeah, OK.
That’s really terrific.
Discussion in focus group 1
The research team also asked focus group participants to suggest questions for the first round of the Delphi survey, on the theme of decommissioning. Suggestions for questions that were adapted and included in the final design of the first round of the Delphi study were:
-
Have you had experience of a service changing in your area (i.e. something being taken away and something in its place)?
-
Have you been involved in decisions about stopping services in your area?
-
How could it have been done differently?
-
How would you want to be more active?
-
What’s the best way for you to be involved?
Participants were also supportive of asking for respondent views on methods for involvement and whether or not these methods were likely to make a meaningful difference to the process. Thus, this was also included as a question in our Delphi survey:
Put one more. Ask, what about people feeling that they’ve made a difference. So in this commission there’s no question there of how involved were you made to feel in the decision?
OK, yeah.
And did you feel that your involvement made a difference or just –
Yeah and how, how do you feel this involvement made a difference?
How is a great way to phrase things because it almost demands an answer other than yes or no.
It gives you a text then doesn’t it?
Yeah, OK.
Yeah, that’s a good way that you can be involved very well, but actually if your involvement doesn’t end up making any difference to the final decision that’s taken, that’s –
That’s right and that affects people as well if they think they’ve made, like I said, made a difference then.
Discussion in focus group 1
Dissemination
Finally, focus group participants were asked for suggestions about appropriate ways to share findings with Delphi study participants. In general, face-to-face events were felt to be preferable to written feedback. However, some participants recognised the practical challenges in arranging and co-ordinating events that were accessible for all respondents/delegates, and felt that a short plain-language summary of written feedback was appropriate.
Delphi study of patient and service user representatives, carers, the third sector and the public
Each of these suggestions was incorporated into the design of the second Delphi survey (see Appendix 6). The aim of the second Delphi study was to obtain a consensus on (1) best practice for the engagement of patients and the public in decommissioning processes and (2) the drivers of decommissioning, to facilitate comparison with the Delphi study in work package 1. In this section, numerical results are presented with illustrative quotations of the main findings from the analysis of the open comments provided by respondents in each round. For each open-text quotation, a participant categorisation is provided.
Round 1 results: the views and experiences of participants in relation to health and social care decommissioning
In round 1, respondents were asked to briefly describe their experiences of services being ‘moved or taken away’. Five respondents indicated having no direct experience. The remaining 18 referred to a range of decommissioning types (Box 14).
-
Closure of A&E departments (three respondents).
-
Closure/transfer of paediatric services (two respondents).
-
Closure of maternity services (two respondents).
-
Community hospital bed closures.
-
Community hospital closures.
-
CCG non-renewal of community nurse specialist service for patients with heart failure.
-
Reconfiguration of mental health day services.
-
Reduction in number of psychiatric beds.
-
(Attempted) closure of children’s heart unit.
-
Shifting social care out of the statutory sector.
-
Removal of IVF service.
-
Centralisation as part of large-scale reorganisation.
-
Moving radiographic services.
-
Moving hearing centre services.
-
Learning difficulties day care and respite service reductions.
-
Medication dose reductions for patients with rare diseases.
-
Moving a rheumatology service from hospital to community.
-
Reducing GP referrals.
-
Closure of specialist homeless services (social care).
IVF, in vitro fertilisation.
Some participants indicated having been affected by, or involved with, these decommissioning projects – for example petitioning decision-makers or submitting views in the consultation process. Some indicated that they had not sought involvement, whereas others expressed frustration and/or resentment at the limited opportunities to do so:
No account was taken of views of those affected by closure. Insufficient information given to those concerned. Decision taken to close in spite of overwhelming views to the contrary from patients and staff. Not enough time or skill to explain the alternative and reassure.
Member of the public/carer/service user/patient
Denied services. Went private but not everyone has the option to do that.
Patient/service user/member of the public
Exhausting and hard work trying to find the truth.
Carer
Each of these experiences and perspectives is likely to have informed the responses that participants provided to the subsequent questions. In total, the 26 individual respondents put forward 42 criteria that they believed were good reasons to carry out decommissioning, 33 criteria that they believed were bad reasons to carry out decommissioning and 44 criteria that they believed inform such decisions in practice. Unlike in the previous Delphi study (work package 1), the research team did not combine these lists as we wished to ensure that respondents were able to recognise the language employed in rounds 2 and 3 as deriving from their round 1 responses. However, as Box 15 shows, within each question we were able to combine and aggregate similar suggestions to arrive at lists of 14, 6 and 14 criteria. Two of the statements relating to ‘good’ reasons reflect the view of some participants that there are no such reasons (in italics in Box 16).
-
It is important that people like you (e.g. patient, service provider, researcher or member of the public) have a chance to be involved in these discussions.
-
It is important that outcomes of involving people like you actually influence decisions.
-
It is important that there are consultations held with the public over such decisions.
-
Involving people like you will take time and this should be built into the decision-making process.
-
People like you should be involved in all stages of decisions (e.g. including whether or not to move/replace services; which ones to include; how to implement changes).
-
Involving the public and organisations such as charities can lead to bias and therefore should not be done.
-
It is important for people like you to have the opportunity to challenge and if necessary oppose any changes to services.
-
Any changes should be ‘co-produced’ – in other words made in true partnership between staff and patients.
-
Good involvement depends on having a relationship of trust with decision-makers.
In addition, in round 1 individual responses were combined into a total of nine recommendations relating to how participants would like to be involved in decisions to move or take away services (Box 15).
Good reasons:
-
If the service is performing poorly.
-
If a service is not being used very much.
-
If other similar services are available.
-
If there are changes in patient/service user need.
-
If a service is not an efficient use of money.
-
If a service is not in line with patient values.
-
In order to develop centres of excellence.
-
If a service is high in cost.
-
If a service lacks accountability and/or transparency.
-
If new developments have been made in clinical research.
-
If a service does not meet national policy.
-
If a service is not being used by patients/service users in the way intended.
-
There are no good reasons to move services.
-
There are no good reasons to replace services.
Bad reasons:
-
To make financial savings.
-
There is a shortage of staff with the right expertise.
-
There is a shortage of other resources (e.g. buildings).
-
To meet the interests of organisations (e.g. hospitals) or individuals (e.g. professionals).
-
Political pressures at the local level.
-
Meeting national policies and targets.
In practice:
-
To make financial savings.
-
Political pressures at the local level.
-
Meeting national policies and targets.
-
Evidence suggests it is the right thing to do.
-
The public are in favour.
-
Professionals (e.g. doctors) are in favour.
-
Decision-makers (e.g. commissioners) are in favour.
-
Concerns over quality and safety.
-
The service is not considered to be good value for money.
-
There is a shortage of staff with the right expertise.
-
The service is not being used much.
-
New models of care are available.
-
Other services are available that deliver the same thing.
-
There are changes in patient or service user need.
Finally, individual responses were combined into a total of seven methods for involving people in decisions to move or take away services (Box 17).
-
Online engagement (e.g. through social media).
-
Patient panels (e.g. being part of a group that is formally consulted on plans for service changes).
-
Using surveys to reach a wide range of people.
-
Inviting postal feedback on proposals to change services.
-
Holding engagement events and meetings.
-
Focus groups in which 4–6 patients meet together and discuss in detail any plans for service change.
-
Petitions against proposals to replace or move services.
Round 2 results: developing a consensus and comparing with the views of policy-makers, practitioners, health-care leaders and researchers
Of the 26 respondents in round 1, 23 participated in the round 2 survey that assessed the extent to which there was a consensus among the respondents regarding drivers of decommissioning decisions. Appendix 9 shows levels of consensus in relation to good reasons, bad reasons and reasons for moving or taking away services in practice. In each case, respondents were asked to identify the three drivers that they considered to be (1) most justifiable (2) least justifiable and (3) most influential in practice, in order of preference. Results are shown in Table 21.
| Placing in top three by respondents | Most justifiable reasons for moving or taking away services (n) | Least justifiable reasons for moving or taking away services (n) | Reasons why services are actually moved or taken away in practice (n) |
|---|---|---|---|
| Most votes | If there are changes in patient/service user need (12) | To make financial savings (12) | To make financial savings (17) |
| If a service is not being used very much (7) | Political pressures at the local level (12) | Decision-makers (e.g. commissioners) are in favour (14) | |
| If other similar services are available (7) | To meet the interests of organisations (e.g. hospitals) or individuals (e.g. professionals) (9) | Political pressures at the local level (7) | |
| Least votes | If a service is not an efficient use of money (0) | There is a shortage of staff with the right expertise (7) | There are changes in patient/service user need (1) |
| If a service is high in cost (1) | Meeting national policies and targets (7) | Concerns over quality and safety (1) | |
| If a service does not meet national policy (3) | There is a shortage of other resources (e.g. buildings) (7) | Professionals (e.g. doctors) are in favour (1) |
Open-text comments provide some elaboration on these preferences. The majority of comments focused on the reasons for moving or replacing services in practice and the dominance in this of political and financial factors. Other comments emphasised the cost-effectiveness of patient empowerment, and some expressed cynicism about the motives of decision-makers and clinicians:
Before taking away a service it’s important there is a session with the people who regularly use the service to have input. As this could effect there health and well-being! Then how much would it cost you, when other services have to be put in place? If a good service was done then maybe you wouldn’t need to keep going back. That saves money. Or making people be in more control with the service they use is more cost-effective.
Patient
Care needs to be patient led and not organisation led.
Member of the public
Political and resource consideration outweigh patient need in practice.
Patient
Do not think that evidence or patient/carer/community opinion is taken into account as fully as needs to be. More commissioner led and finance driven.
Carer
One comment ran counter to the others with regard to the role played by politics in decommissioning:
Political pressures are usually a reason not to move or take away services (i.e. local opposition to reconfiguration, etc.).
Member of the public
An analysis of the degree of consensus in the panel’s responses to the 34 rating scale questions included in round 2 found that eight questions achieved a high degree of consensus among participants, seven achieved a medium degree of consensus, eight achieved a low degree of consensus and 11 achieved no consensus. The statements with a high degree of consensus among respondents are shown in Box 18.
‘If other similar services are available’ is a good reason to move or replace services (agree).
‘If there are changes in patient/service user need’ is a good reason to move or replace services (agree).
‘If a service is high in cost’ is a good reason to move or replace services (disagree).
‘Political pressures at the local level’ is a bad reason to move or replace services (agree).
‘To make financial savings’ is a reason why services are actually moved or taken away in practice (agree).
‘Meeting national policies and targets’ is a reason why services are actually moved or taken away in practice (agree).
‘Decision-makers (e.g. commissioners) are in favour’ is a reason why services are actually moved or taken away in practice (agree).
‘The service is not considered to be good value for money’ is a reason why services are actually moved or taken away in practice (agree).
Overall, compared with the Delphi study in work package 1, there was less of a consensus expressed over the factors put forward in each category for round 2. No consensus or a low degree of consensus was found in 8 out of 14 factors that participants put forward as good reasons to move or take away services; 3 out of the 6 factors put forward as bad considerations; and 8 out of 11 of the factors put forward as influential in practice.
Statements derived from round 1 relating to approach/methods of involvement showed a preference for in-depth and substantive involvement, for example through co-production, patient panels and focus group discussions (Table 22).
| Placing in top three by respondents | Statements about engaging (n) | Statements about methods of engaging (n) |
|---|---|---|
| Most votes | Any changes should be ‘co-produced’ – in other words made in true partnership between staff and patients (14) | Patient panels (e.g. being part of a group that is formally consulted on plans for service changes) (17) |
| It is important that outcomes of involving people like you actually influence decisions (10) | Focus groups in which 4–6 patients meet together and discuss in detail any plans for service change (17) | |
| It is important for people like you to have the opportunity to challenge and if necessary oppose any changes to services (9) | Holding engagement events and meetings (12) | |
| Least votes | Involving the public and organisations such as charities can lead to bias and therefore should not be done (0) | Petitions against proposals to replace or move services (0) |
| It is important that there are consultations held with the public over such decisions (6) | Inviting postal feedback on proposals to change services (2) | |
| Involving people like you will take time and this should be built into the decision-making process (6) | Online engagement (e.g. through social media) (3) |
In open-text comments, participants confirmed the general lack of agreement with the statement ‘Involving the public and organisations such as charities can lead to bias and therefore should not be done’ (e.g. ‘I agree with all the above statements except for . . .’, ‘All statements other than . . . make sense’). Other comments elaborated on respondent preferences in relation to the other statements:
The method is less important that the commitment to genuine engagement, and building trust. All the above methods are fine, but there are countless examples of where they have been done well, and where they have been done badly. So I’m reluctant to rank ‘top three′ methods, because this suggests that particular methods are better than others and this isn’t the case.
Researcher working in the field of user and public involvement
Where a decision will affect someone’s health, there should be a patient who has recently received treatment present in regards to involvement.
Patient
One respondent expressed views not fully captured in the statements submitted and categorised during round 1:
These aren’t ways of involving patients in these decisions, these are ways of engaging patients with decisions that have already been made. What about patients actually having a seat at the table, being members of the bodies that actually make the decisions on an equal basis with commissioners and clinicians?
Patient/representing a community/third-sector organisation
Round 3 results
In the final round we asked participants to reconsider the 19 questions in round 2 that registered little or no group consensus. All of the 23 respondents in round 2 participated in the round 3 survey. Appendix 9 presents the full results.
Extent of changes between rounds 2 and 3
Following the third round, 8 of the 19 statements moved from having a low degree of consensus/no consensus to having a medium or high degree of consensus. These included two additional statements with a high level of consensus (Box 19).
‘There is a shortage of staff with the right expertise’ is a bad reason to move or replace services (agree).
‘The public are in favour’ is a reason why services are actually moved or taken away in practice (disagree).
Of the seven factors carried forward as good reasons to move or take away services from round 2 (because of a low level of or no consensus), four recorded higher levels of disagreement and two recorded no change, with only one recording greater agreement (‘in order to develop centres of excellence’). For the remaining driver (‘if new developments have been made in clinical research’) the change was in the direction of a reduced consensus (from ‘low agreement’ to ‘none’). Of the three reasons carried forward as bad reasons to move or take away services (i.e. those with a low level of or no consensus in round 2), one showed no change and two showed higher levels of agreement that the reasons were bad. Of the eight reasons carried forward for taking these decisions in practice, four showed greater levels of agreement. Of the remaining four, two reasons showed higher levels of disagreement and two remained the same.
Comments on statements with a low level of or no consensus from round 2
Fourteen of the 23 respondents left additional comments in relation to each of the factors brought forward from round 2. Across the three areas of questioning related to drivers of decommissioning some common themes were identified from these comments.
Improving instead of removing
Many of the explanatory open-text comments reflected a preference for finding ways to address any service deficiencies other than through decommissioning. Overall, there was a marked reticence, compared with the first Delphi study in work package 1, to opt for decommissioning, while other options for addressing the reasons identified had not yet been exhausted. In relation to poor performance the following comments were made:
The service should be brought up to standard.
Representing a community/third-sector organisation
If the service is important the over-riding objective should be to improve it.
Service user/representing a community/third-sector organisation/member of the public
Surely it would make sense to look at improving the services, how they are delivered where they are delivered and how reliant people are on the services, before just removing.
Carer
A poorly performing service may be one that is badly managed. It does not indicate whether it is a service is needed such as for clinical needs. With good management it may improve. So it does not provide a basis for closing a service as poor performance can be rectified and does not give any indication of need.
Patient/carer/representing a community/third-sector organisation
This is often used as an excuse to save money. Often there is no evidence to support that the service is performing poorly.
Representing a community/third-sector organisation
In relation to staffing shortages or lack of accountability the following comments were made:
It is far better to address the question of appropriate staffing before cutting services.
Carer
The reasons for lack of accountability and/or transparency should be investigated. This has been used by management as an excuse to move [unclear] from one area to another.
Representing a community/third-sector organisation
Decommissioning is not always cost-effective
Another theme of the additional comments added in round 3 was the claim that decommissioning (or taking away and moving services) was likely in some instances to be a less cost-effective option than improving or modifying the services:
Improve the service as start-up costs for the same service elsewhere are more expensive. I strongly disagree with this – not logical thinking.
Member of the public/carer/service user/patient
I also disagree. If a service is performing poorly it should not be moved or taken away because it gives an opportunity to improve the service. It is more cost-effective to build on what you have. Moving or taking away a service can create other more dramatic problems.
Member of the public/representing a community/third-sector organisation/patient
There is always room to look at delivery of service and making efficient changes (not necessarily making cuts). Often a small change to administration, how things are done can make the services more cost-effective.
Carer
Expressed doubt over decision-maker motives
The principle of building ‘centres of excellence’ was questioned and doubt expressed over the imperative of meeting national policy. Overall, a strong strain of doubt ran through comments from a substantial subset of respondents. These mainly related to distrust of the motives behind decommissioning and the belief that cited motives for this are a ‘smokescreen’ for a cost-cutting agenda or ‘closure by stealth’. In one or two instances this cynicism extended to the research process itself. Responses also expressed their appreciation of the apparent cynicism (or distrust) manifested in responses of the wider participant group:
It shows that the NHS is not explaining their reasons or proving there is justification for removing a service. We are cynical of their reasons. Patients and the public need to be told facts and reasons.
Carer
This fits with public perception that decommissioning is always carried out for the ‘wrong’ reasons.
Patient/representing a community/third-sector organisation
It shows a lot of people were ‘conned’ by the question and have answered simplistically without considering why the service is poor and whether alternatives such as reasonable resourcing might be preferable. It’s the type of question that a government looking to cut costs might employ to find a way of demonstrating public approval when the public clearly do not.
Patient
Polarisation and consensus
As noted, the overall extent of consensus was relatively low when compared with the Delphi study from work package 1. Some respondents expressed surprise or puzzlement at the spread of responses from round 2, and only a small number referred to an inclination to shift their position.
Surprised that so many people would support continuation of a service that isn’t achieving its objectives. If it doesn’t work why support it when you could support something that does work.
Member of the public
Am surprised at the level of disagreement.
Patient/service user/representing a community/third-sector organisation
[National policy] should be an acceptable feature but for some reason it has divided opinion remarkably.
Patient/service user/representing a community/third-sector organisation
I’m somewhat surprised by the rate of strongly disagrees, considering the responses to previous questions.
Patient/representing a community/third-sector organisation
I can see the logic of this argument better now than before.
Patient/service user/representing a community/third-sector organisation
Unable to respond
A small number of respondents referred repeatedly to the difficulty or undesirability of responding to the questions. Reasons for this included the perceived interdependence of factors and/or the lack of contextual information afforded by the Delphi study format.
It’s hard to know without knowing more information. What factors are causing poor performance?
Representing a community/third-sector organisation
Difficult to isolate one factor as often they are interdependent. So finance alone would not be a strong basis for removing a service but if it was also linked to poor outcomes and low patient satisfaction then it would be appropriate. So the triple aim to include quality cost and need would be best considered together rather than as separate factors. Isolating each factor oversimplifies a detailed and nuanced debate. Patient need, preference, outcome etc. ideally take priority but within a financial envelope and according to quality standards and whether the service is feasible (staffing etc.).
Patient/carer
Don’t know enough about local politics to answer this – examples would have helped.
Patient
Analysis of overall responses on good and bad reasons for decommissioning and reasons in practice
When fed back to participants, the results of the ‘top three’ ranking questions in relation to reasons for moving or taking away services were generally confirmed in open-text comments (e.g. ‘No surprises there’, ‘makes sense to me’, ‘some I agree with, others not’, ‘would fit with my assessment’). Overall, the Delphi study found two factors that might constitute good reasons for moving or replacing services. These were ‘if other similar services are available’ and ‘if there are changes in patient or service user need’. This was supported by the ranking of the three most justifiable reasons, which comprised these two reasons and a third: ‘if a service is not being used very much’. The third instance of a high level of consensus was in disagreement with the statement that ‘“if a service is high in cost” is a good reason to move or take away services’.
There was a high degree of consensus around two bad reasons: ‘there is a shortage of staff with the right expertise’ and ‘political pressures at the local level’. This was again supported by the ‘top three’ rankings of bad reasons, which were ‘to make financial savings’, ‘political pressures at the local level’ and ‘to meet the interests of organisations (e.g. hospitals) or individuals (e.g. professionals)’.
After three rounds there was a high degree of consensus that four considerations do actually drive decisions in practice:
-
to make financial savings
-
meeting national policies and targets
-
decision-makers (e.g. commissioners) are in favour
-
the service is not considered to be good value for money.
There was also a high degree of consensus that ‘the public are in favour’ is not a reason for services actually to be moved or taken away in practice. These findings were supported by the ‘top three’ rankings, which were ‘to make financial savings’, ‘decision-makers (e.g. commissioners) are in favour’ and ‘political pressures at the local level’.
Overall, the ratings and rankings indicate a match between bad reasons identified by participants and those that participants felt were most likely to be drivers of decommissioning in practice. In other words, the consensus was that, in practice, decisions to move or take away services were made for bad reasons.
Analysis of overall responses on approaches to engagement
The rankings of statements related to engagement were largely supported by the open-text responses (e.g. ‘I would agree with the rankings’, ‘seems reasonable’, ‘fair distribution’, ‘cannot argue with any of that’). The same was broadly true for the ranking of involvement methods albeit with some exceptions:
There seems to be broad agreement that bringing patients together and encouraging participation and discussion in decision-making is most effective in influencing decision-making.
Patient/service user/carer/member of the public
Idealism with the top three then no effective robust processes to complain about changes in services in the bottom three. Very worrying stats.
Member of the public/carer/service user/patient
It’s interesting that online engagement received so few votes – might this reflect the demographic involved in the Delphi study? Do you have any representation from younger people (who I suspect are more interested in social media as a vehicle for involvement)?
Researcher working in the field of user and public involvement
These seem sensible arrangements with attention to patient panels & focus groups.
Patient/carer/representing a community/third-sector organisation
This supports the above: people want to be active decision-makers, not passively consulted after a decision has already been made.
Patient/representing a community/third-sector organisation
However, in other sections of the survey there were some specific concerns expressed about the public as an influence over decommissioning decisions. The following quotations were included in response to the suggestion that public opinion shapes decisions in practice:
Public are frequently misinformed by newspapers but not sure they have that much influence as they can’t stop it in practice, in my experience.
Patient
Public will normally be emotionally motivated, for example, would prefer a veterans service over a young people/homeless service.
Carer
‘The public’ generally speaking have no idea what services encompass and are unlikely to make such a contribution to the process.
Patient/representing a community/third-sector organisation
Reflections on the methodology
The decontextualising of some questions in the third round (e.g. ‘there are no good reasons to move services’) led to some confusion, with two respondents indicating lack of clarity over the aim of the question. Some questions involved a potential double negative (e.g. ‘I disagree that this is a bad reason’), which one respondent reflected may have affected responses. We recognise this limitation, although sense-checking against open-text comments would appear to show good levels of understanding of the task as set. One respondent referred multiple times to the small sample group for the Delphi survey and others expressed a general desire for more information.
All of my responses would be subject to more information and reliant on specific circumstances, so this is very generalistic.
Member of the public
It’s difficult to answer some of the above without knowing what the alternative to move/take away is – the alternative might be nothing (i.e. the service stays as it is), it might be work to improve the service and bring it back to standard. In some of the above cases, giving services time to improve or to change what they do is more desirable as a first line response than the more radical option than moving it or taking it away.
Patient
Summary and reflections
The focus group discussions served a number of functions in the context of the wider study. They enabled us to recast the questions posed in the first Delphi survey (work package 1) so that these better reflected the language and concerns of the respondent group while still enabling us to address our overarching aims and generate findings that could be compared with the previous Delphi survey. The first question for this work package was ‘what are the views and experiences of citizens, patient/service users, carers, third-sector organisations and local community groups in relation to health and social care decommissioning?’. The focus groups and Delphi survey raised issues not covered in the prior work packages and that we therefore report here as valuable findings in their own right. For example, the exchanges between participants in the focus groups covered experiences of loss and adversity that we would not have otherwise captured, as well as uncovering a cynicism and mistrust in the decision-making process that has far-reaching implications for our wider analysis of the topic of decommissioning in health care. In the Delphi study we were able to overcome the previous impediments to recruitment of service user and patient representative groups, as well as obtaining the other perspectives sought.
Our second question related to how these views compare with those of policy-makers, practitioners, health-care leaders and researchers. The findings show areas of agreement with the first Delphi panel. However, there are also key differences of opinion relating to (1) the validity of cost as a driver of decision-making and (2) the role that should be played by citizens, patient/service users, carers, third-sector organisations and local community groups in decommissioning processes. For example, the Delphi survey from this work package suggests a clear preference for deliberative co-production of decommissioning programmes with those groups affected by them. The implications of this divergence of opinion as well as analysis in relation to our third question, ‘how might these perspectives be brought together in order to improve equity and acceptability in decommissioning?’, are addressed in the following chapter.
Chapter 8 Conclusions and research implications
Introduction
Health systems around the globe have begun to grasp the challenge of removing, replacing and reducing health-care service provision, in relation to medicines, discrete services and wider configurations of care. However, these challenges are not well theorised or researched. Against this background, this study sought to add to the theoretical and empirical evidence base underpinning decommissioning in health, and to apply the findings to the NHS in England. In this section we draw together and integrate the findings from each of the work packages and consider them in the light of current knowledge about decommissioning research both in England and internationally. We begin by identifying the main findings in relation to each of the research questions set out at the beginning of the report. We then consider the implications of these for the development of theory, health-care policy and practice, before looking ahead at the future research agenda in this area. As has been shown in Chapter 4, there is a growing body of literature on decommissioning in health care. However, there is a requirement to go beyond a focus on clinical or therapeutic interventions and to incorporate other forms of service change. There is also a need for process-based research into the organisational and political dimensions of decommissioning, as well as specific investigation of programmes involving wider service withdrawal, closures or reorganisation. This study sought to address these gaps by:
-
considering a broad range of decommissioning forms
-
applying analytical lenses to the topic derived from disciplines outside evidence-based medicine, HTA and health economics
-
extending a critical focus to all stages of decommissioning processes, from conception through to full implementation and review
-
employing a combination of data collection methods, including longitudinal case studies, national and expert surveys
-
mapping the multiple levels and actors that shape or are affected by decommissioning.
In these ways the study provides an original contribution to the literature in terms of scope, theoretical framing and methodological approach. External validity and transferability of the research is addressed through detailed description and data triangulation between the four interlinked work packages.
Revisiting the research questions
The overall approach to data collection and analysis is informed by a conceptual framework drawing on elements of political science (interests, institutions and ideas), complex service change, aspects of ANT, loss aversion and a stages heuristic. Drawing on each work package as appropriate, this section revisits the main research questions of the study and draws conclusions deriving from and commensurate with the nature of the evidence presented so far.
What is the international evidence and expert opinion regarding best practice in decommissioning health-care services?
From the summary of previous reviews presented in Chapter 4, it is clear that the international evidence on health-care decommissioning is skewed towards clinical interventions and, in particular, the replacement or withdrawal of medicines, and this applies to England and the wider UK. The most commonly used term in the recent health-care literature – ‘disinvestment’ – is synonymous with this form of decommissioning, and with a suite of tools (e.g. low-value lists, HTA) designed with such activity in mind. Most definitions of disinvestment incorporate principles of cost-effectiveness and opportunity cost and are therefore embedded in a health economics paradigm. 58,79 Furthermore, the literature in this area is primarily (although by no means exclusively) concerned with the use of evaluative evidence to promote population health and to improve clinical decision-making. However, this is a relatively fast-moving field and recent contributions have begun to reflect critically on the limitations of the disinvestment ‘movement’, and in particular to argue the need to develop strategies for overcoming obstacles to disinvestment practices. 60 Our study adds to this developing appreciation of the determinants of decommissioning of clinical interventions, and how these interact in practice with tools and formal resource allocation frameworks (including PBMA, HTA, low-value treatment lists and so on).
Across the world, the study of disinvestment is thus in a nascent phase and in its current form does not extend far beyond the removal and replacement of clinical interventions. However, this somewhat narrow focus is in contrast to the range and scope of decommissioning observed in the research carried out for this report. For example, five of our seven narrative vignettes, three of our four case studies and 89% of the decommissioning reported by our 56 CCG survey respondents (as well as the majority of examples put forward by participants in work package 4) all fall outside the purview of the extant disinvestment literature and of the tools and frameworks advanced within it. Our study therefore redresses the relative inattention paid to other forms of decommissioning such as service/organisational relocation and closure.
The review of reviews, and in particular the evidence synthesis provided by Niven et al. ,60 suggests a shift in the literature from an initial focus predominantly on problem identification and decision-making towards a greater awareness of decommissioning programme design and implementation mechanisms and strategies. Our study is one of the first to take a longitudinal approach incorporating the stages of decommissioning, and to reflect on how each of these is subject to influencing factors. In this we have drawn on additional literature such as Fulop et al. ,67 who examine the implementation of reconfiguration programmes and find that the nature of the programme of change and ‘local politics’ are more significant in shaping outcomes than the strength of the evidence, and that public resistance is greater when reconfiguration is perceived to include hospital downgrading. Similarly, Greenwood et al. 68 identify organisational determinants of abandonment (albeit in non-health settings) and Johns et al. 66 identify an ‘infrastructural inertia’ that inhibits abandonment of established services. To this, Younkin80 adds the notion of ‘de-commitment’ as a prerequisite of abandonment of practices and supports the conceptualisation of decommissioning as a dynamic, multistage process rather than a discrete decision point. Although drawn from research in a range of countries, each of these insights into more diverse forms of decommissioning (and/or related activity) has shaped our appreciation of the factors shaping the phenomena observed in our study.
Despite these insights, there remains an absence of published evidence with regard to ‘good practice’ in the implementation of the full range of decommissioning types. We therefore conducted a Delphi panel of expert opinion designed to combine perspectives on a broad range of decommissioning types, and to go beyond the normative case for decommissioning (i.e. what should the drivers be?) to reflect on what drives decommissioning in practice. This was international in scope, albeit with strong UK representation.
Our findings indicate that the considerations that experts from a number of health-care systems believe ought to drive decommissioning (cost-effectiveness, quality and patient safety, clinical effectiveness) are different from those that they believe do so in practice (e.g. cost/budgetary pressures, political imperatives). This disjuncture suggests the importance of taking a critical approach to research inquiry and avoiding decommissioning strategies that rely purely on gathering evidence to support decision-making and/or exhorting individuals to change their practice.
The four factors that drew the highest level of consensus as being important in shaping whether or not decommissioning is implemented as planned were found to be strength of executive leadership, strength of clinical leadership, clarity of rationale/case for change and quality of partnership working with relevant agencies. When asked to identify good-practice principles, the six statements for which there was most support were:
-
Engage and involve clinical leaders from an early stage.
-
Establish a clear rationale and narrative for change.
-
Ensure clear and thorough project planning and governance.
-
Secure high-level political support (national and local) at an early stage.
-
Base decisions on evidence of what works.
-
Adopt a whole-systems perspective from the beginning.
How and to what extent are organisations currently decommissioning services?
Subsequent work packages enabled us to explore the phenomenon of decommissioning in the specific context of the English NHS. This is the most recent study to gauge rates of local decommissioning activity in the English NHS, and the first dedicated solely to exploring this area of activity. Hitherto, the literature has focused on the work of NICE or else has been confined to a relatively small number of case studies. 65,81 Evidence related to wider activity rates at the meso level in England is thus somewhat limited. However, reviews appear to show a shift in activity levels, with later reviews (e.g. Niven et al. 60) apparently uncovering a greater volume of examples than earlier reviews (e.g. Gallego et al. 56) (notwithstanding differences in approach to inclusion). Despite this, the published evidence in England, as elsewhere, suggests that decommissioning at the local level remains relatively rare, especially for reasons other than safety. 60 Furthermore, our mapping interviews indicate that while there are sources of assistance for CCGs in carrying out commissioning and service reconfiguration, very little of this is tailored specifically to meet the challenges of decommissioning. The most active national body in this area, NICE, produces ‘do not do’ recommendations through their appraisal and guidance processes. However, this covers a relatively small proportion of the existing interventions in the NHS, and NICE has yet to launch a programme specifically designed to identify disinvestment opportunities. 81
Our sample of 27% CCG survey responses contained notably higher levels of reported decommissioning than both these previous reviews and a similar survey published in 2011. 82 What is more, much of this activity goes beyond the ‘low-hanging fruit’ described in the study of Daniels et al. 83 to include programmes of significant scale and scope. In support of this work, our survey suggests that CCGs were employing ‘public engagement’, ‘stakeholder workshops’ and ‘needs assessment’ most commonly, and ‘stakeholder mapping’, ‘PBMA’ and ‘scenario planning’ to a lesser extent. The most cited drivers of decommissioning were ‘cost-effectiveness’ and ‘patient experience’, with ‘alignment with strategic priorities’, ‘clinical effectiveness’ and ‘cost/budgetary savings’ also cited by a minority of respondents. These data would appear to suggest that decommissioning activities are both more prevalent and more ambitious than they have previously been, and that cost-related criteria are among those currently driving this change.
What factors and processes facilitate the successful implementation of decisions to decommission services?
The CCG survey findings suggest that the key determinants of successful implementation include:
-
executive leadership/management
-
quality of evidence base
-
clinical engagement and support (both as enabler and inhibitor); and
-
quality of implementation plans/planning.
Open-text comments from the survey suggest a perceived lack of guidance to support decision-making, limited local sources of support for decommissioning, and difficulties deriving from NHS restructuring and associated staff turnover and loss of expertise. We have noted that the first Delphi panel identified areas of consensus with regard to good practice. As helpful as these are, they remain somewhat abstract, and the aim of our case studies was to delve deeper into the decommissioning experience in a range of settings.
In case study 1, the review and reorganisation of intensive paediatric burn care, implementation was not achieved in the lifetime of the project and doubt was expressed over future prospects. It became clear that the national political context inhibited progress in a number of respects. First, the specialty area was not felt to be sufficiently high profile in media or government spheres and was therefore considered unlikely to command very high resources in support of change. These factors marked it as different from, for example, the reconfiguration of paediatric services recounted in one of the narrative vignettes, despite both being nationally led specialty reconfigurations. Somewhat paradoxically, the drive for NHS efficiencies was felt to impede implementation of the burn care review, as no large-scale savings were projected to flow from what was likely to be an expensive implementation process. To compound this, the mechanisms for implementation of the decommissioning components of the changes were both limited and subject to challenge, which in turn had led to something of a standstill. Taken in isolation, this experience would suggest the following implications for future national decommissioning:
-
Reviews and reorganisations are more likely to succeed to implementation phase when the potential gains in efficiencies promise to make worthwhile the short-term political and financial costs of change.
-
Executive authority and power of implementation granted to an identifiable and credible body, which in turn is granted autonomy and political support from relevant national system actors, are prerequisites of successful implementation.
-
There are merits to adopting an approach with a simple and coherent case for change supported with evidence that opinion-formers accept as legitimate.
Of course, these propositions are highly aspirational and in practice may generate other sources of difficulty. For example, executive authority and discretion can often be challenged or undermined and higher-profile service areas are more likely to be subject to opposition from interest groups, the media and organised patient and public opinion. Indeed, our narrative vignettes confirm that even very well-resourced decommissioning processes that satisfy the above requirements can suffer from delay and, in some cases, discontinuation.
In our case study of the closure of an EOL service, implementation was achieved and, as such, this was unusual within our sample. The CCG was able to propose and manage the closure of the EOL home support service over a relatively short implementation period, following a 6-month review of the contract with the provider. The most important factors in achieving this outcome appear to have been a relatively powerless patient group and a provider organisation that was resigned to the fate assigned to it following the CCG review. Outcomes of the decommissioning were subsequently questioned by some of those involved and doubts were raised over the availability of alternative patient pathways during service changes and the challenge of post-discharge patient monitoring. Unfortunately, we were unable to explore these stages within our case study.
Case study 3 focused on the decommissioning activity of an APC. Leaders of the APC adopted an approach that largely precluded substantive, planned decommissioning. Instead, they had chosen to focus on building mechanisms and processes of decision-making and governance that might later be employed in pursuit of decommissioning, but that were for the time being directed towards promoting evidence-based prescribing (rather than de-prescribing) throughout the patch. These mechanisms and processes included a shared formulary, auditing of compliance with APC guidelines, initiatives to align prescribing across care sectors and development of economies of scale in decision support. Decommissioning had been undertaken but had remained somewhat peripheral and there was recognition, albeit tacit in some cases, that the risks generated outweighed the promised benefits. This position seems rational when considered in the light of the decommissioning failure reported elsewhere, while also perhaps at odds with a wider financial context of acute fiscal constraint.
Case study 4 was a major CCG-led review and planned reorganisation of local primary and acute care services. Successful implementation was not facilitated during the period of research, despite a lengthy and generously resourced process of preparation and stakeholder engagement. The CCG was able to propose and plan the reorganisation but implementation faltered as tensions grew between the provider organisations involved. This example offers a cautionary tale against the assumption that following procedural good practice can ensure delivery of decommissioning outcomes, especially where complexity makes prediction of effects extremely difficult.
In combination, these case studies suggest that the good-practice principles generated in our Delphi study have some limitations. Within the case study sample we found examples of good practice apparently being followed but success nevertheless remaining elusive (e.g. case study 4). Conversely, many of the good-practice recommendations were not observed in case study 2 but implementation was nevertheless achieved. This would suggest either that these recommendations are erroneous or, more likely, that their application is highly dependent on local contingencies. Their merit may reside primarily in their function as general principles of approach and we should perhaps avoid the temptation to codify and apply them mechanistically across contexts.
The case studies also highlight how the role played by evidence and actors in identifying and framing a need for decommissioning depends in turn on factors such as the scope of the project and the number of actors implicated in or affected by the decommissioning, as well as the resources that these can mobilise to oppose plans. The proposed closure of the EOL service generated a muted response in which the patient voice was not loudly heard, and the provider organisation elected not to challenge the decision. This apparently unusual set of circumstances may have negated the requirement for Delphi panel recommendations such as securing high-level political support, engaging service users and stakeholders, and adopting a whole-systems perspective. By contrast, case study 4, drawing on frameworks employed in reconfiguration programmes elsewhere in the NHS, employed expensive and somewhat elaborate processes of option appraisal, consultation and engagement. Despite this, at the time of writing, acceptance of the ‘solution’ of decommissioning remained elusive. Furthermore, the reconfiguration involved considerable complexity in the implementation phase, in contrast to expedient removal of the EOL service, which was ultimately implemented via the cessation of a contract between two parties. The case studies also provide insight into how evidence thresholds required to build the case for decommissioning vary, in terms of both volume and rigour, and this has important implications, how high-quality evidence to inform decommissioning changes is often hard to generate or access, and how professional consensus is therefore frequently employed as a proxy. However, this consensus can be hard won, as illustrated by the three case studies that had been unsuccessful in implementing their plans. The case studies also show how the mobilisation of evidence is often inextricably interwoven with the politics of decommissioning.
What are the perspectives and experiences of citizens, patient/service user representatives, carers, third-sector organisations and local community groups in relation to decommissioning?
The conclusions we have drawn so far reflect something of a management bias, drawing disproportionately as they do on the views and experiences of health-system actors, as well as academics and national bodies with an interest in this field. The fourth work package enabled us to directly address the perspectives of citizens, patient/service user representatives, carers, third-sector organisations and local community groups through focus group discussions and a second Delphi survey, both of which recruited from within these groups.
Findings from work package 4 suggest some commonalities with the views of participants in work package 1. First of all, there was support for the principle that decommissioning in some circumstances is legitimate (although the same consensus was not found in relation to moving services). Both Delphi panels also considered decommissioning, in practice, to be at least partly a function of financial pressures and the need to make cost-savings. The majority of participants in work package 4, however, felt this to be an unjustified basis upon which to make decommissioning decisions. Their rejection of cost pressures as a basis for decommissioning was therefore emphatic.
Results from across each of the work packages suggest a perception that patients and the public are rarely influential in decommissioning decision-making. For example, Delphi study 1 participants strongly disagreed with the statement ‘patient and public views do actually in practice inform decisions to carry out decommissioning’ and Delphi study 2 participants strongly disagreed with the statement ‘the public are in favour’ as a reason why services are actually moved or taken away in practice. This apparent consensus with regard to the relative lack of influence of patients and the public was supported by the CCG survey finding that ‘patient and community groups’ and ‘public/citizens’ are among the least-involved stakeholders in each stage of the decommissioning process. Opinions diverged, however, on the normative question of engagement: while the first Delphi panel did not rank patient and public engagement high on the list of good-practice principles, the second Delphi panel expressed an appetite for substantive engagement and co-production of decisions.
These findings are of crucial importance to understanding attitudes to decommissioning. They appear to suggest that patients and the public are rarely influential in decommissioning and that decommissioning is informed, in part, by considerations that these groups are unlikely to consider to be justified. Given this confluence of factors, it was not surprising to hear frustration and mistrust in decision-making voiced by participants in work package 4. Few had faith that calculations of patient benefit or cost-effectiveness (for example) trumped financial pressures and political considerations in the selection of targets for removal.
Allied to this was resentment expressed at the lack of apparent awareness in decision-making of the lived experience of service users. It was felt that little or no value is placed on the relationships that make up service provision and the damage done to these in the process of service removal or replacement, or of the benefits of service continuity as a counterweight to the projected benefits of service replacement. Third-sector providers involved in the focus groups voiced their distress at having to communicate service removal decisions to vulnerable user groups, and their own feelings of uncertainty when under threat of decommissioning. Others participants emphasised the harms to carers and service users of extending travel times resulting from service changes.
Bringing together the perspectives of stakeholders in decommissioning
One of our research aims was to consider how this range of perspectives might be brought together in order to improve equity and acceptability in decommissioning. The study suggests a number of ways in which this ambitious aim might be tackled. The first relates to language and the need to avoid terminology that is confusing or misleading. The language used in work package 4 was notably different from that employed in work packages 1–3. In place of ‘transformation’, ‘disinvestment’ and ‘decommissioning’, respondents recommended terms such as ‘stopping’, ‘taking away’ and ‘moving’ services. These terms had the twin benefits of greater clarity and apparently greater honesty in their description of what was planned.
The study also has important implications for engagement of wider stakeholders, an enterprise that is likely to require greater prioritisation than suggested by our first Delphi panel. Our findings suggest that established approaches to engagement and involvement require rethinking. On the one hand, for example, our study supports Dalton et al. ’s84 suggestions for engagement in reconfiguration such as early and wide engagement, local partnership working and shared ownership of change and use of multiple, deliberative approaches that target different groups. On the other hand, our findings cast some doubt over the injunction to ‘demonstrate the clinical-led case for change, with focus on service improvement rather than cost savings’. 84 In the case of decommissioning, which often has financial pressure as one of its major drivers, to attempt to downplay cost-savings runs the risk of increasing cynicism and challenge from stakeholders who are often fully aware of the financial ‘big picture’.
We would argue that the presence of decommissioning alters the dynamic between health-care leaders and the patient and public groups affected, such that challenge and veto become more likely. Any ambitious plans stand a greater chance of implementation success if they are genuinely co-produced with a public/patient constituency that has been given the time and resources to contribute constructively. 85 The example of local STPs is instructive here, as negative media reactions have prompted NHS guidance on how STPs can use lay representatives and patient reference groups and carry out public consultations. 86 Whether this will be sufficient to enable plans to be completed and implemented remains to be seen. We finish this section with a plea for greater candidness from one of our second Delphi panellists:
Usually [decommissioning is for] a combination of clinical and financial reasons – clinical in terms of the delivery of effective and safe care, financial in terms of what can be paid for within the NHS ‘envelope’. So often the NHS doesn’t want to talk about the financial element of these decisions, but the public knows full well (especially in the current context) that finances are a major driver in reconfiguration. The service has got to be able to have a more sensible conversation with the public about finances, acknowledging that they are a driver for change, but also pledging to the public that any changes made will always either maintain or improve standards of care. The trouble, of course, is that the public often doesn’t trust decision-makers and so any conversation of this kind gets derailed quickly because the public suspects hidden agendas and personal motives.
Making sense of decommissioning
Previous research65,87 has indicated a low success rate for decommissioning, and this was reflected in our sample of case studies and narrative vignettes (with survey results too early to assess). Although this sample is not large it would appear to support the proposition that implementing decommissioning in health-care contexts is harder to achieve than other forms of decision-making and service change. Our study suggests that in seeking to understand why this might be, it is important to separate factors that are specific to decommissioning from those factors present in other health actions and processes. There are obvious parallels to be drawn between decommissioning and the following cognate fields.
Priority setting. It is clear that much learning can be transferred to the pursuit of decommissioning, for example from PBMA, HTR and so on. 57,63,88,89 Our study underscores the role that these tools can have in decommissioning without suggesting that in themselves they offer a panacea for solving the range of challenges to decommissioning.
Innovation adoption and diffusion. Decommissioning can also learn from the organisational insights contained within the innovation and diffusion literature. In 2004, Greenhalgh et al. 90 posed the question ‘why and how do people (and organisations) reject an innovation after adopting it?’. Organisational perspectives on decommissioning (or undiffusion, deimplementation and exnovation91,92) offer additional frames of analysis to those contained in the priority-setting literature. These include, for example, the notion of a ‘negative tipping point’ at which support for decommissioning reaches a critical mass and implementation is quickened. 93 While our study focused predominantly on inter- (or supra-) organisational processes, there are clear overlaps with these questions and much that is shared with the study of organisational processes more generally.
Service reconfiguration. Finally, as already described, the more ambitious of our decommissioning types have much in common with the literature on service transformation in health settings. Indeed, the good-practice recommendations of our first Delphi panel are redolent of prescriptions for practice put forward in the service transformation literature. 94
However, despite these areas of overlap and commonality, our study also suggests the need to consider decommissioning as something of a special case. This is partly the result of the likelihood of heightened resistance when decommissioning is part of the proposed activity. There are a number of components to this.
Stakeholder resistance. Our study shows that decommissioning plans are often opposed by coalitions of stakeholders, including health-service managers, independent service providers, user and patient groups, advocacy and campaign groups, clinical professionals, and industry. However, the groups that might be expected to routinely support decommissioning plans are few and far between. Therefore, although the range and number of groups involved in opposing decommissioning varies according to the scope and scale of the plans, the high proportion of opposers appears largely constant. In this context, decommissioning can be seen as a complicated and often expensive process that is likely to encounter resistance from stakeholders at multiple stages of design and implementation.
Institutional inertia. As well as this stakeholder resistance, ‘dynamic conservatism’ has been shown to attenuate the implementation of decommissioning decisions. 95 Organisations and wider institutions are often somewhat impervious to change and this can be especially pronounced in relation to decommissioning. For example, in relation to innovation there is a marked imbalance between ebb and flow, with newly introduced practices far outweighing the number of replaced practices. 96 This would support our finding that determinants at organisational and suborganisational levels that impede change are more successfully mobilised against attempts to dislodge and/or undo established ways of working, as evidenced in our case study of the APC. 97
Patient and public mistrust. Allied to these raised levels of system and interest group resistance is the additional ingredient of heightened patient and public mistrust. Our two Delphi panels indicate something of a fissure between perspectives from research, policy and practice on the one hand and those of patient/service user representatives, citizens and third-sector organisations, especially with regard to the acceptability of financial constraint as a factor in decision-making, on the other. Our research, including the case studies and the CCG survey, indicates that decommissioning is likely to be driven, at least in part, by the imperative to save money, but that the emphasis in making the case for decommissioning is often placed on more palatable drivers such as service improvement and/or reduction in service duplication. The research suggests that establishing these more positive narratives is hard to achieve with a sceptical patient and public constituency.
Lack of political will and support. Finally, the study confirms the frequent lack of a macro-political environment conducive to the difficult business of decommissioning. The language of ‘rationing’ and ‘cuts’ is as damaging to health-care decision-making as it is attractive to the popular media, and this can increase the appeal of decommissioning strategies based on avoidance and/or subterfuge. Our study suggests that while local politics can sometimes (albeit not always) be mobilised in support of decommissioning, the national political context is more likely to hinder than help progress. Longer-term decommissioning plans in particular can be prey to electoral cycles and political upheaval in the system more generally.
The combination of these factors means that leaders of decommissioning programmes are seldom fully in control of the processes, as these are frequently more politically charged and more vulnerable to challenge and veto than other decision-making and implementation processes. Needless to say, this has implications for the strategies that might be deployed and what might be expected to result from these.
Theoretical reflections
We noted in the introduction to this study that, while the disinvestment literature offers theories of how removal and replacement should proceed, there is currently less theoretical consensus in relation to how it proceeds in practice. The importance of this distinction was further underlined in the first Delphi study, which found that the most desirable drivers of decommissioning (cost-effectiveness, quality and patient safety, clinical effectiveness) are different from the actual drivers (cost/budgetary pressures, political imperatives). In recognition of this, we operated with a descriptive theoretical framework made up in part of concepts drawn from the literature on policy processes. This oriented us to the ways in which internal and external interest groups seek to influence policy, and how institutional contexts (e.g. funding arrangements, governance and regulatory regimes, legal mandates) constrain the range of policy options available to those designing and leading decommissioning programmes. 98 Our case studies illustrate some of the ways in which decommissioning reflects a contest of ideas or narratives, as protagonists seek to establish their preferred policy frames and outcomes.
Our study design also reflected a conceptualisation of decommissioning as a journey, in the same way as Van de Ven et al. 99 depict innovation processes as having a number of components that, while not necessarily happening in a predictable and orderly sequence, take them from initiation, through development, to implementation or termination, in which case the new practice either becomes part of the mainstream or is closed. This enabled us to disaggregate the stages and processes of decommissioning in our case studies and to examine how actors and contexts shifted and changed at points along the way.
A further element of our theoretical framework was provided by Callon’s51 four processes of translation, which we have modified and applied in order to help us to understand rates of progress observed in the case studies. This points to the critical importance of successfully establishing a ‘problem’ for which decommissioning can be proposed as a solution. In the case of the burn care review, this case for change had been painstakingly compiled over many years and contained multiple component parts. Similarly, the locally led hospital reconfiguration employed numerous review and evidence-generating techniques to arrive at a case for change involving service decommissioning. By contrast, the EOL service, as a more modest change plan, established the problem quickly via a service review, whereas the APC, after tentative first steps, postponed grasping of the nettle. External factors such as the availability of evidence were crucial in this problem-conceptualisation phase.
Alliance-building around the legitimacy of decommissioning as a solution to these problems was a necessary next step to enable progression, and in the case of the burn care review, the local reorganisation was followed by the seeking of wider acceptance for the decommissioning plans. In both cases the majority of internal stakeholders accepted the need for change; however, wider social acceptance was not fully established. By contrast, in the case of the EOL service, although wider acceptance had not been sought, alliances between the main organisational and clinical actors were sufficient to see the plans move to the implementation phase. This would suggest that the importance of gaining wider acceptance increases according to the scale of the proposed changes and the strength of feeling outside the immediate context of service delivery.
Finally, with regard to implementation, it was clear from the case studies that, while the CCG in case study 2 had a relatively straightforward implementation mechanism available to it, the burn care review and local reorganisation foundered at the implementation phase.
As we noted in Chapter 3, there are some limitations to the actor–network approach as applied in this study. Many of the phenomena reported across the work packages were apparently influenced by a macro context of service upheaval, huge financial pressures and a highly charged political atmosphere. These forces are relatively absent from the conceptualisation offered by Callon’s51 four processes, as is the structural alignment of power and interests more generally, and this hinders its efficacy in explaining phenomena observed in the study.
Allied to descriptive frameworks for understanding the processes at play in our study, we also drew on the notion of ‘loss aversion’18 to understand impediments to decommissioning. Our study supports the claim that in cases in which options have been identified for withdrawal or replacement, implementation can be confounded by individual loss aversion – whereby people fear losses more than appreciate gains – but also by the forces of inertia that often characterise health-care environments. 100
Overall, we would argue that the hitherto predominantly psychological theory of loss aversion requires development or augmentation to incorporate other arenas in which loss is felt and maintenance preferred to change. For example, Greenwood et al. 68 find that ‘organisational factors dominate physician differences as explanatory factors for abandonment’. Our study supports the development of organisational, professional and system-level components to the concept of loss aversion. We advocate broadening the theoretical lens to include dynamics operating at organisational and institutional (as well as psychological) levels. We further advocate the development of theoretical constructs that include the unique dynamics of the different ‘stages’ of decommissioning as well as how these vary according to decommissioning type. Finally, we recommend continued interrogation of the intersection between active processes of problematisation, alliance-building, gaining acceptance and implementing, on the one hand, and wider determinants related to institutions, ideas, economics, etc., on the other.
Implications for health care
Allied to the good-practice principles put forward for leadership and engagement in decommissioning, we offer the following thoughts on the implications of our study for decommissioning in practice.
Decommissioning is highly context dependent
Despite generating consensus around areas of good practice, we conclude that a formula for decommissioning is not only unavailable but also impossible given its dependence on local context and the apparent unpredictability of outcomes. Furthermore, it is likely that managerial approaches adopted elsewhere in health will not always be sufficient in the face of the additional dynamics associated with decommissioning. We emphasise the need for greater levels of honesty with regard to the rationale for removal and for co-production with affected parties at each stage of the process with the possible exception of decommissioning where low levels of controversy are projected.
Approaches to decommissioning should be modified according to type
Our definition of decommissioning encompasses reduction and replacement in, as well as removal of, services. It also includes medicines, discrete services and whole-provider organisations. Our study points to the differences between these forms of decommissioning, as well as factors held in common. In relation to medicines we believe that the relatively embryonic field of replacement and withdrawal would be well served by learning lessons from the longer-standing field of evidence-based medicine. This includes the need to mobilise and incorporate the experiential evidence of practitioners and patients, on the grounds that end-user intelligence is required if replacement and withdrawal is to be implemented without unintended consequences. 101,102 In this, professional stewardship of limited resources will be key. 103 Other, more substantive forms of decommissioning at the organisational or interorganisational level require greater attention to factors such as context, scale and scope (along with interests and systems). Inclusion of decommissioning in health-care improvement stands an increased chance of success if it is based on a more sophisticated appreciation of each of these aspects and how they cohere and conflict in local service settings.
Terminology is important
The literature on removal and replacement employs multiple terms and there is a danger of this becoming something of an obsession for the research community. The proliferation of terms has aided theoretical development but has not increased clarity or accessibility. Debates over the merits of candidate terms such as ‘de-adoption’, ‘de-implementation’ and ‘undiffusion’ will no doubt continue. Our aim in employing the term decommissioning is merely to denote the phenomenon of study and we revert to the terms suggested by our participants (including ‘stopping’, ‘moving’ and ‘replacing’) when disseminating our work outside research settings.
Successful decommissioning is a long-term pursuit
Our study suggests that successful decommissioning is likely to be the end point of a process in which the case for change has been shared and argued widely. This ‘de-commitment’ is important to the building of acceptance of both problem and solution in relation to decommissioning. 80 Where this was not achieved, for example in the case of our APC, the preference of those involved was for more passive approaches to decommissioning. Our case studies also reaffirm the importance of developing long-term engagement strategies and addressing issues of trust and public legitimacy before embarking on substantive decommissioning activities. 104 This in turn suggests that reliance on a combination of evidence and exhortation is likely to be insufficient in making the case for decommissioning, and that a more root-and-branch analysis of the politics and processes involved is required.
Delineating decommissioning decision-making
In our case studies and vignettes there is evidence of some confusion over roles and responsibilities for decision-making and it is clear that the challenges of decommissioning are exacerbated by lack of clarity and authority in this regard. There is a further requirement for clarity over the specific terms of decision-making. For example, do decision options include reduction in investment or full withdrawal? Is substitution or partial reinvestment built into the decision-making parameters? Once these questions are answered, more informed choices over the use of decision-support tools and frameworks can be made.
Substantive decommissioning requires attention to programme design
The design of effective decommissioning requires evidence to support the causal efficacy ascribed to the programme in meeting its aims, as well as a grasp of the technical and political feasibility of putting the programme in place. 105 This study suggests that local commissioning processes and frameworks may not be sufficient in themselves to deliver effective decommissioning. While decommissioning and commissioning may be seen in normative terms as elements of the same processes (i.e. needs assessment, service review, contracting and procurement and so on), in practice our study suggests that received NHS models of commissioning good practice may be insufficient to meet the challenges of decommissioning. Key to this are the additional implementation challenges involved in dislodging entrenched services and practices. Our study suggests that the more ambitious a programme of change is, the more likely it is that this will require active participation from the organisations implicated in the changes, because, as we have seen, resistant provider organisations can call upon an array of strategies to delay or derail changes. The requirement for some degree of service self-sacrifice (or ‘arranging their own funeral’, as our interviewee described it) sets decommissioning apart from other commissioning activities.
Decommissioning programme implementation
Key considerations at the implementation phase include how the extent of ambiguity and conflict surrounding a policy can mediate and constrain approaches to implementation. 106 For example, the implementation of decommissioning in the NHS is often characterised by high levels of conflict as well as ambiguity over the different priorities and criteria that should inform and guide decisions, leading to implementation slow-down and/or failure. 89 We have seen that services can be reduced or removed through the application of eligibility criteria, practice guidelines and other forms of service restriction and scale-back. Alternatively, they may be withdrawn as a result of in-house service closure, external contract termination, service reconfiguration and formulary delisting. As above, our study suggests that full implementation of decommissioning requires the active support (e.g. through temporary double-running of services) of the affected provider, which suggests the need for their co-option into the process.
Management and community engagement in decommissioning
This study expands and refines understanding of the processes related to decommissioning across a range of health-care settings and contexts. Overall, we conclude that no decommissioning blueprint exists and that outcomes, especially of more ambitious programmes, are hard to predict. Approaches to planning and management should reflect the factors found to shape the outcomes of decommissioning, including change management and implementation, evidence and information, and relationships and politics. Those planning decommissioning will need to account for history, culture and quality of interprofessional relationships. In a highly politicised and contested landscape, skills in negotiation, sense-making and leadership are paramount. Furthermore, the contentiousness of decommissioning suggests that an explicit and proactive media strategy is more likely to be required, as is the political acumen to negotiate the inevitable influence of power and interests. 107
Without community support, it is often difficult to achieve planned changes. Evidence-based models for working with communities are required to support difficult decisions of this kind. Our findings suggest that established approaches to engagement and involvement require rethinking. In particular, in cases in which decommissioning is driven in part or in full by financial pressure, we find that attempts to downplay cost-savings run the risk of increasing cynicism and challenge from stakeholders who are often fully aware of the financial ‘big picture’.
Limitations of the study
Sampling
In most aspects of the study we have sought to recruit participants who have experienced or are currently involved with some form of decommissioning. For work package 1 this included national bodies with a possible role in decommissioning (mapping exercise), previous leaders of decommissioning processes (decommissioning stories), and ‘experts’ in decommissioning from research, policy and practice backgrounds (Delphi study). In work package 3 this included individuals involved in current and/or recent decommissioning processes (case studies). In work package 4 this included citizens, patient/service user representatives, carers, third-sector organisations and local community groups, many of whom will have had direct experience, in these capacities, of decommissioning. This is a deliberate sampling strategy intended to draw on the perspectives and experiences of those with a ‘take on’, as well as possibly a ‘stake in’, decommissioning. Results will therefore be different from what might have been expected if we had either deliberately sought to target those with no involvement in decommissioning or pursued a sampling strategy in which we were blinded to this information. Our results are therefore not intended to be automatically generalisable to, or typical of, wider managerial or stakeholder populations.
Clinical Commissioning Group survey response rate
By contrast, work package 3 targeted all CCGs in England. Although the response rate reached over one-quarter (27%), the potential for self-selection bias has led us to be cautious in our approach to extrapolation. In Chapter 3, we acknowledged the possibility of response bias in our survey of CCGs, with responding CCGs perhaps more likely to be actively engaged in decommissioning than non-responders. We also noted that, with the exception of an over-representation of Midlands CCGs (perhaps reflecting the location of the lead research institution), the sample of responding organisations shows no obvious atypical characteristics. Although we consider that a response rate of 27% enables us to infer some general patterns across the wider population of CCGs, we acknowledge that a larger sample size would have reduced the chances of sampling error and that we could have mitigated for gaps in the national data with, for example, a detailed mapping of decommissioning in one region or locality.
Public and service user involvement
As noted in Chapter 3 of this report, our aim was for the perspectives of patient and service user representatives and members of the public to form an integral element of the study. Although this was partially achieved in work packages 1 and 3, this was not to the intended degree of depth and breadth. This is a product of the limited engagement and participation activities enacted in the case study processes, but which nevertheless means that incorporation of these perspectives into our case study analysis has been hindered. In more general terms, we have sought to mitigate these deficiencies. The research team applied for and secured NIHR HSDR funds to build an additional work package into the project designed to strengthen our understanding of decommissioning from a service user, patient and public perspective.
Case study progress
Our study is inevitably constrained by the phenomena we observed within it. Although instructive, the modest progress against aims of the case studies means that some stages of our hypothetical decommissioning model – notably implementation and review – are given less attention than others. We were unable, for example, to analyse how organisational close-down periods were managed (i.e. the time from an announcement until the final day)108 and still less to measure the outcomes and impacts of decommissioning processes. In the single case study in which close-down was enacted (the EOL service), we were unable to re-establish contact with case study sites after key respondents moved on to new posts.
Case study interviews
Although we had intended to conduct a total of 90 interviews across the four case studies, the eventual number was 59. There are a number of reasons for this shortfall. First, we had intended to interview higher numbers of patient and public representatives in case studies. A greater part of the gap is accounted for by a deliberate decision to shift fieldwork in the direction of non-participant observation, as this began to yield important insights (e.g. in case studies 1 and 4), periods of stasis in case studies 1, 3 and 4, which meant less follow-up interviewing was warranted, and key staff moving on from their posts and becoming unavailable for interview during case study 4. We consider the level of overall data to be commensurate with that required for the case studies, notwithstanding the lack of follow-up in case study 4. The addition of unexpectedly fertile opportunities for observation mitigates gaps in the interview data set.
Recommendations for future research
To build on the work presented here we recommend the below areas of future study.
Realist synthesis of the evidence contexts, mechanisms and outcomes in decommissioning
To further enhance understanding of the theory and practice of decommissioning, we recommend that future evidence synthesis takes a realist approach, incorporating insights generated in studies such as this one. 109 In particular, as the volume of empirical case studies increases, future research should identify context–mechanism–outcome configurations and pathways to successful implementation and outcomes. This would provide development of the empirical findings presented here and a complement to the methods employed in evidence reviews to date.
Conceptual and empirical development of loss aversion
We believe that there is a need for theoretical and empirical development of a broader concept of loss than that advanced in prospect theory. 18 It is unclear whether the multiple layers of impact and resistance, including at levels of organisation, institution, politics and community, can be incorporated into an expanded concept of loss and loss aversion or these require separate theoretical constructs reflecting the distinct dynamics at play.
Exploration of the role of financial pressures in limit-setting decisions
The importance of financial constraint runs through all aspects of the study and the experiences of those leading and affected by decommissioning processes. Although it is far from clear what the proper place of affordability considerations should be, our study clearly shows a fissure between the two Delphi panels with regard to the acceptability of financial constraint as a factor in decommissioning. We advocate further investigation, for example using large-scale and deliberative data collection techniques, of the place of financial considerations in health-care limit-setting. There is often talk of the need for a national conversation on limit-setting in the NHS, and we believe that this would be a fruitful way to initiate such a conversation. Our study suggests the further need in future work to disaggregate the perspectives of patients/service users, carers, citizens and third-sector providers so that the subtle differences of emphasis identified in work package 4 can be explored.
Research into community engagement in decision-making
Research is required into the specifics of engaging communities in decommissioning. This would address questions such as:
-
How have communities participated in plans for decommissioning of local service provision?
-
What dynamics are at play in these processes?
-
How might future engagement processes build greater credibility into such processes?
Given the frequency of organisational change in health care, the scale of current reorganisations, the costs involved and the level of community mobilisation against changes, this research is strategically important and urgently needed.
Exploration of decommissioning outcomes
A key limitation of our study is the lack of data on outcomes of decommissioning, either in the CCG survey or the case studies. This would be a valuable focus for future studies, including, for example, through follow-up of case studies included in this study. In case study 3 the decommissioning objectives were largely achieved, but only through follow-up would we be able to determine whether the decommissioning ultimately increased or reduced equality of outcomes. Areas to explore in future research therefore include the impact on patients of the changes as well as budget impact and benefits accrued from released resources. Prior phases of organisational decommissioning processes also require further research, especially linking to organisational closure and how such processes can be managed in ways that minimise harm to employees and service users.
Acknowledgements
The financial support of the NIHR HSDR programme is acknowledged, along with the very helpful and constructive comments of NIHR peer reviewers and editors.
We would like to thank our advisory group for their expert advice and support: Bernd Sass, Jeffrey Braithwaite, Stirling Bryan, Paul Chrisp, Chris Clough, Andrew Coward, Roz Dixon, Adam Elshaug, Tracy Madge, Diane Ketley, John Kimberly, Craig Mitton, Suzanne Robinson and Julia Simon.
We would also like to thank Krissie Styles for providing clinical advice on case study 1.
Finally, we would like to thank each of our research participants for their invaluable contribution to the project.
Contributions of authors
Dr Iestyn Williams (University of Birmingham) led the project, was the first author of the final report and participated in all aspects of the research and analysis.
Dr Jenny Harlock (University of Birmingham) was the second author of the final report, participated in all aspects of the research and analysis and was co-lead of work package 4.
Dr Glenn Robert (King’s College London) was the third author of the final report, participated in all aspects of the research, helped design the national survey questionnaires and led on analysis of the first Delphi survey.
Professor Russell Mannion (University of Birmingham) was the fourth author of the final report, was involved in study design and analysis and acted as a mentor to the principal investigator.
Ms Sally Brearley (King’s College London) was the fifth author of the final report, was involved in data collection for the patient and public involvement focus groups and provided expert input on patient and public involvement activities throughout the study.
Dr Kelly Hall (University of Birmingham) was the sixth author of the final report, helped to design and analyse the national survey and advised on all aspects of the research.
Publication
Robert G, Harlock J, Williams I. Disentangling rhetoric and reality: an international Delphi study of factors and processes that facilitate the successful implementation of decisions to decommission healthcare services. Implement Sci 2014;9:123.
Data sharing statement
Data can be obtained from the corresponding author in such a way that safeguards the confidentiality and anonymity of participants and organisations.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- McKee M. Brexit: the NHS is far safer inside the European Union. BMJ 2016;353. https://doi.org/10.1136/bmj.i2489.
- Malhotra A, Maughan D, Ansell J, Lehman R, Henderson A, Gray M, et al. Choosing Wisely in the UK: the Academy of Medical Royal Colleges’ initiative to reduce the harms of too much medicine. BMJ 2015;350. https://doi.org/10.1136/bmj.h2308.
- McCartney M, Treadwell J. The RCGP’s new standing group on overdiagnosis. BMJ 2014;349. https://doi.org/10.1136/bmj.g4454.
- Robert G, Harlock J, Williams I. Disentangling rhetoric and reality: an international Delphi study of factors and processes that facilitate the successful implementation of decisions to decommission healthcare services. Implement Sci 2014;9. https://doi.org/10.1186/s13012-014-0123-y.
- Donaldson C, Bate A, Mitton C, Dionne F, Ruta D. Rational disinvestment. QJM 2010;103:801-7. https://doi.org/10.1093/qjmed/hcq086.
- Francis, R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Five Year Forward View. London: NHS; 2014.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Sustainability and Transformation Plans (STPs) Explained. London: The King’s Fund; 2016.
- Edwards N. So Much to Do, So Little Time: Turning STPs into Action. London: Nuffield Trust; 2016.
- Giacomini M, Hurley J, Stoddart G. The many meanings of deinsuring a health service: the case of in vitro fertilization in Ontario. Soc Sci Med 2000;50:1485-500. https://doi.org/10.1016/S0277-9536(99)00394-9.
- Geva-May I. Riding the wave of opportunity: termination in public policy. J Public Admin Res Theory 2004;14:309-33. https://doi.org/10.1093/jopart/muh020.
- Kimberly JR, Nystrom PC, Starbuck WH. Handbook of Organizational Design. New York, NY: Oxford University Press; 1981.
- Innovation Health and Wealth: Accelerating Adoption and Diffusion in the NHS. London: DH; 2011.
- Ovretveit J. Purchasing for Health: A Multi-Disciplinary Introduction to the Theory and Practice of Purchasing. Buckingham: Open University Press; 1995.
- How to Decommission Public Services Delivered by Civil Society Organisations and Maintain Value for Money. London: NAO; 2011.
- Parkinson B, Sermet C, Clement F, Crausaz S, Godman B, Garner S, et al. Disinvestment and value-based purchasing strategies for pharmaceuticals: an international review. PharmacoEconomics 2015;33:905-24. https://doi.org/10.1007/s40273-015-0293-8.
- Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica 1979;47:263-91. https://doi.org/10.2307/1914185.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10:6-20. https://doi.org/10.1258/1355819054308576.
- Sandelowski M. Telling stories: narrative approaches in qualitative research. Image J Nurs Sch 1991;23:161-6. https://doi.org/10.1111/j.1547-5069.1991.tb00662.x.
- de Meyrick J. The Delphi method and health research. Health Educ 2003;103:7-16. https://doi.org/10.1108/09654280310459112.
- Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Manag Sci 1963;9:458-67. https://doi.org/10.1287/mnsc.9.3.458.
- Bond S, Bond J. A Delphi survey of clinical nursing research priorities. J Adv Nurs 1982;7:565-75. https://doi.org/10.1111/j.1365-2648.1982.tb00277.x.
- Burns TJ, Batavia AI, Smith QW, DeJong G. Primary health care needs of persons with physical disabilities: what are the research and service priorities?. Arch Phys Med Rehabil 1990;71:138-43.
- Bayley EW, Richmond T, Noroian EL, Allen LR. A Delphi study on research priorities for trauma nursing. Am J Crit Care 1994;3:208-16.
- Harrington JM. Research priorities in occupational medicine: a survey of United Kingdom medical opinion by the Delphi technique. Occup Environ Med 1994;51:289-94. https://doi.org/10.1136/oem.51.5.289.
- Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al. Consensus development methods and their use in clinical guideline development. Health Technol Assess 1998;2.
- Robert G, Milne R. A Delphi study to establish national cost-effectiveness research priorities for positron emission tomography. Eur J Radiol 1999;30:54-60. https://doi.org/10.1016/S0720-048X(98)00139-9.
- Turoff M. The design of a policy Delphi. Technol Forecast Soc Change 1970;2. https://doi.org/10.1016/0040-1625(70)90161-7.
- Linstone HA, Turoff M. The Delphi Method: Techniques and Applications. Reading, MA: Addison-Wesley Publishing Company; 1975.
- O’Loughlin R, Kelly A. Equity in resource allocation in the Irish health service: a policy Delphi study. Health Policy 2004;67:271-80. https://doi.org/10.1016/j.healthpol.2003.07.001.
- De Loe RC. Exploring complex policy questions using the policy Delphi. A multi-round, interactive survey method. Appl Geogr 1995;15:53-68. https://doi.org/10.1016/0143-6228(95)91062-3.
- NHS Confederation . The Views of Healthcare Leaders on the Future of the NHS 2014. www.nhsconfed.org/resources/2014/03/the-views-of-healthcare-leaders-on-the-future-of-the-nhs (accessed 20 February 2016).
- Yin R. Case-Study Research Design and Methods. Beverley Hills, CA: Sage; 1984.
- Yin R. Enhancing the quality of case-studies in health services research. Health Serv Res 1999;34:1209-24.
- Ovretveit J. Comparative and Cross-Cultural Health Research: A Practical Guide. Abingdon: Radcliffe Medical Press; 1998.
- Eisenhardt K. Building theories from case-study research. Acad Manag Rev 1989;14:532-50.
- Williams I, McIver S, Moore D, Bryan S. The use of economic evaluations in NHS decision-making: a review and empirical investigation. Health Technol Assess 2008;12. https://doi.org/10.3310/hta12070.
- Thomas G. How to Do your Case-Study. London: Sage; 2011.
- Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage; 1985.
- Law J, Hassard J. Actor Network Theory and After. Oxford: Blackwell Publishing/The Sociological Review; 1999.
- Latour B. Science in Action: How to Follow Scientists and Engineers Through Society. Milton Keynes: Open University Press; 1987.
- Latour B. Reassembling the Social: An Introduction to Actor-Network-Theory. Oxford: Oxford University Press; 2005.
- Cresswell KM, Worth A, Sheikh A. Actor-Network Theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med Inform Decis Mak 2010;10. https://doi.org/10.1186/1472-6947-10-67.
- Cresswell K, Worth A, Sheikh A. Implementing and adopting electronic health record systems: how actor network theory can support evaluation. Clin Gov 2011;16:320-36. https://doi.org/10.1108/14777271111175369.
- Nguyen L, Bakewell L, Wickramasinghe N, Haddad P, Muhammad I, Moghimi H, et al. Transition from paper to electronic nursing documentation in residential aged care: an actor network theory analysis. Electron J Health Inform 2015;9.
- Papadopoulos T, Radnor Z, Yasmin M. The role of actor associations in understanding the implementation of Lean thinking in healthcare. Int J Operations Prod Manag 2011;31:167-91. https://doi.org/10.1108/01443571111104755.
- Broer T, Nieboer AP, Bal RA. Opening the black box of quality improvement collaboratives: an Actor-Network theory approach. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-265.
- Young D, Borland R, Coghill K. An actor-network theory analysis of policy innovation for smoke-free places: understanding change in complex systems. Am J Public Health 2010;100:1208-17. https://doi.org/10.2105/AJPH.2009.184705.
- Latour B, Bijker WE, Law J. Shaping Technology/Building Society: Studies in Sociotechnical Change. Cambridge, MA: MIT Press; 1992.
- Callon M, Callon M, Law J, Rip A. Mapping the Dynamics of Science and Technology. London: Macmillan; 1986.
- Callon M, Law J. A Sociology of Monsters? Essays on Power, Technology and Domination. Sociological Review Monograph. London: Routledge; 1991.
- Robert G, Greenhalgh T, MacFarlane F, Peacock R. Adopting and assimilating non-pharmaceutical technological innovations into health care practice: a systematic review. J Health Serv Res Policy 2010;15:243-50. https://doi.org/10.1258/jhsrp.2010.009137.
- May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-86.
- Halcomb EJ, Gholizadeh L, DiGiacomo M, Phillips J, Davidson PM. Literature review: considerations in undertaking focus group research with culturally and linguistically diverse groups. J Clin Nurs 2007;16:1000-11. https://doi.org/10.1111/j.1365-2702.2006.01760.x.
- Gallego G, Haas M, Hall J, Viney R. Reducing the Use of Ineffective Health Care Interventions: A Rapid Review. An Evidence Check review brokered by the Sax Institute, for the NSW Treasury. Sydney, NSW: Sax Institute; 2010.
- Leggett L, Noseworthy TW, Zarrabi M, Lorenzetti D, Sutherland LR, Clement FM. Health technology reassessment of non-drug technologies: current practices. Int J Technol Assess Healthc 2012;28:220-7. https://doi.org/10.1017/S0266462312000438.
- Polisena J, Clifford T, Elshaug AG, Mitton C, Russell E, Skidmore B. Case studies that illustrate disinvestment and resource allocation decision-making processes in health care: a systematic review. Int J Technol Assess Healthc 2013;29:174-84. https://doi.org/10.1017/S0266462313000068.
- Mayer J, Nachtnebel A. Disinvesting from ineffective technologies: lessons learned from current programs. Int J Technol Assess Healthc 2015;31:355-62. https://doi.org/10.1017/S0266462315000641.
- Niven DJ, Mrklas KJ, Holodinsky JK, Straus SE, Hemmelgarn BR, Jeffs LP, et al. Towards understanding the de-adoption of low-value clinical practices: a scoping review. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0488-z.
- Ibargoyen-Roteta N, Gutiérrez-Ibarluzea I, Asua J. Guiding the process of health technology disinvestment. Health Policy 2010;98:218-26. https://doi.org/10.1016/j.healthpol.2010.06.018.
- Mortimer D. Reorienting programme budgeting and marginal analysis (PBMA) towards disinvestment. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-288.
- Mitton C, Dionne F, Damji R, Campbell D, Bryan S. Difficult decisions in times of constraint: criteria based resource allocation in the Vancouver Coastal Health Authority. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-169.
- Massatti RR, Sweeney HA, Panzano PC, Roth D. The de-adoption of innovative mental health practices (IMHP): why organizations choose not to sustain an IMHP. Adm Policy Ment Health 2008;35:50-65. https://doi.org/10.1007/s10488-007-0141-z.
- Rooshenas L, Owen-Smith A, Hollingworth W, Badrinath P, Beynon C, Donovan JL. ‘I won’t call it rationing . . .’: an ethnographic study of healthcare disinvestment in theory and practice. Soc Sci Med 2015;128:273-81. https://doi.org/10.1016/j.socscimed.2015.01.020.
- Johns DM, Bayer R, Fairchild AL. Evidence and the politics of deimplementation: the rise and decline of the ‘counseling and testing’ paradigm for HIV prevention at the US Centers for Disease Control and Prevention. Milbank Q 2016;94:126-62. https://doi.org/10.1111/1468-0009.12183.
- Fulop N, Walters R, Spurgeon P. Implementing changes to hospital services: factors influencing the process and ‘results’ of reconfiguration. Health Policy 2012;104:128-35. https://doi.org/10.1016/j.healthpol.2011.05.015.
- Greenwood BN, Agarwal R, Agarwal R, Gopal A. The when and why of abandonment: the role of organizational differences in medical technology lifecycles. Soc Sci Res Netw 2016.
- NHS Clinical Commissioners . Making Difficult Decisions: Commissioning Healthcare In Changing Times 2016. www.nhscc.org/policy-briefing/making-difficult-decisions/ (accessed March 2017).
- NHS Organisations in West Hertfordshire . Working Together for a Healthier West Hertfordshire: The Case for Change n.d. www.yourcareyourfuture.org.uk/case-for-change (accessed December 2016).
- Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care 2010;14. https://doi.org/10.1186/cc9300.
- National Burn Care Review . Standards and Strategy for Burn Care: A Review of Burn Care in the British Isles 2001. www.britishburnassociation.org/nbcr (accessed May 2014).
- Palmieri TL, Taylor S, Lawless M, Curri T, Sen S, Greenhalgh DG. Burn center volume makes a difference for burned children. Pediatr Crit Care Med 2015;16:319-24. https://doi.org/10.1097/PCC.0000000000000366.
- Roberts G, Lloyd M, Parker M, Martin R, Philp B, Shelley O, et al. The Baux score is dead. Long live the Baux score: a 27-year retrospective cohort study of mortality at a regional burns service. J Trauma Acute Care Surg 2012;72:251-6. https://doi.org/10.1097/TA.0b013e31824052bb.
- Levine CH. Organizational decline and cutback management. Public Admin Rev 1978;38:316-25. https://doi.org/10.2307/975813.
- Coastal West Sussex . Local Health Economy Formulary Application (version 2) 2015. www.coastalwestsussexformulary.nhs.uk (accessed 5 July 2016).
- NHS England . Regional Medicines Optimisation Committees – Workshop Outputs from 20 April 2016 2016. www.england.nhs.uk/wp-content/uploads/2014/06/rmoc-note.pdf (accessed September 2016).
- NHS Organisations in West Hertfordshire . Working Together for a Healthier West Hertfordshire: The Need for Change n.d. www.yourcareyourfuture.org.uk/site_assets/files/nhs%20Herts%20Report%20single%20page.pdf (accessed December 2016).
- Elshaug AG, Hiller JE, Tunis SR, Moss JR. Challenges in Australian policy processes for disinvestment from existing, ineffective health care practices. Aust N Z Health Policy 2007;4. https://doi.org/10.1186/1743-8462-4-23.
- Younkin P. Complicating abandonment: how a multi-stage theory of abandonment clarifies the evolution of an adopted practice. Organ Stud 2016;37:1017-53. https://doi.org/10.1177/0170840615613376.
- Garner S, Littlejohns P. Disinvestment from low value clinical interventions: NICEly done?. BMJ 2011;343. https://doi.org/10.1136/bmj.d4519.
- Robinson S, Dickinson H, Williams I, Freeman T, Rumbold B, Spence K. Setting priorities in health: a study of English primary care trusts. London: Nuffield Trust; 2011.
- Daniels T, Williams I, Robinson S, Spence K. Tackling disinvestment in health care services. The views of resource allocators in the English NHS. J Health Organ Manag 2013;27:762-80. https://doi.org/10.1108/JHOM-11-2012-0225.
- Dalton J, Chambers D, Harden M, Street A, Parker G, Eastwood A. Service user engagement in health service reconfiguration: a rapid evidence synthesis. Health Serv Deliv Res 2015;17.
- Durose C, Richardson L, Dickinson H, Williams I. Dos and don’ts for involving citizens in the design and delivery of health and social care. J Integr Care 2013;21:326-35. https://doi.org/10.1108/JICA-10-2013-0039.
- NHS England . Engaging Local People: A Guide for Local Areas Developing Sustainability and Transformation Plans 2016. www.england.nhs.uk/wp-content/uploads/2016/09/engag-local-people-stps.pdf (accessed September 2016).
- Harris C, Allen K, Waller C, Hille V, Dyer T, Voutier C, et al. SHARE – Sustainability in Health care by Allocating Resources Effectively – an evidence-based approach to investment and disinvestment in health technologies in a regional health service. Int J Evid Based Healthc 2011;9:296-7. https://doi.org/10.1097/01258363-201109000-00035.
- Peacock S, Mitton C, Bate A, McCoy B, Donaldson C. Overcoming barriers to priority setting using interdisciplinary methods. Health Policy 2009;92:124-32. https://doi.org/10.1016/j.healthpol.2009.02.006.
- Williams I, Walshe K, Smith J. Allocating Resources for Health Care: Setting and Managing Priorities. Basingstoke: Open University Press; 2016.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Davidoff F. On the undiffusion of established practices. JAMA Intern Med 2015;175:809-11. https://doi.org/10.1001/jamainternmed.2015.0167.
- Rye CB, Kimberly JR. The adoption of innovations by provider organisations in health care. Med Care Res Rev 2007;64:235-78. https://doi.org/10.1177/1077558707299865.
- Rogers EM. Diffusion of Innovations. New York, NY: Free Press; 2003.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. https://doi.org/10.1111/j.1468-0009.2012.00670.x.
- Frantz JE. The high cost of policy termination. Int J Public Admin 1997;20:2097-119.
- Clancy TR, Delaney CW. Complex nursing systems. J Nurs Manag 2005;13:192-201.
- Wiltsey Stirman S, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-17.
- Smith N, Mitton C, Davidson A, Williams I. A politics of priority setting: ideas, interests and institutions in healthcare resource allocation. Public Policy Admin 2014;29:331-47.
- Van de Ven A, Polley D, Garud R. The Innovation Journey. Oxford: Oxford University Press; 1999.
- Williams I. Who wants to live forever? Organizational decline in health care. J Health Serv Res Policy 2015;20:189-91. https://doi.org/10.1177/1355819614564813.
- Gray JM, Nagel E, Lauerer M. Prioritization in Medicine. Springer International Publishing; 2016.
- Saini V, Brownlee S, Elshaug AG, Glasziou P, Heath I. Addressing overuse and underuse around the world [published online ahead of print January 6 2017]. Lancet 2017. https://doi.org/10.1016/S0140-6736(16)32573-9.
- Reuben DB, Cassel CK. Physician stewardship of health care in an era of finite resources. JAMA 2011;306:430-1. https://doi.org/10.1001/jama.2011.999.
- O’Cathain A, Musson G, Munro J. Shifting services from secondary to primary care: stakeholders’ views of the barriers. J Health Serv Res Policy 1999;4:154-60. https://doi.org/10.1177/135581969900400306.
- Wolman H. The determinants of programme success and failure. J Public Policy 1981;1:433-64. https://doi.org/10.1017/S0143814X00002336.
- Matland RE. Synthesising the implementation literature: the ambiguity–conflict model of policy implementation. J Public Admin Res Theory 1995;5:145-57.
- Hartley J, Alford J, Hughes O, Yates S. Public value and political astuteness in the work of public managers: the art of the possible. Public Admin 2015;93:195-211. https://doi.org/10.1111/padm.12125.
- Wigblad R, Lewer J. Organisational Closure: A Critique of the Literature and Some Research Propositions 2007.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-33.
- National Network for Burn Care . National Burn Care Standards 2013. www.britishburnassociation.org/downloads/National_Burn_Care_Standards_2013.pdf (accessed May 2015).
Appendix 1 Review of reviews data extraction form
Appendix 2 Delphi study 1 letter of introduction and round 1 questionnaire
Appendix 3 Clinical Commissioning Group survey information sheet and questionnaire
Appendix 4 Sample interview schedules for mapping exercise, narrative vignettes and case studies
Work package 1: interview schedule (a)
Representatives of agencies with a role in decommissioning (telephone interviews)
Introductions, preamble and consent
Q1 Please describe your current role and responsibilities.
Q2 How is your role/organisation involved with decommissioning?
Q3 Please describe any current and/or planned activities linked to decommissioning.
Q4 What, in your view, are the main challenges facing those leading decommissioning programmes?
Q5 Are you aware of any good-practice guidance or other resources relating to decommissioning?
Q6 Is there anything else you would like to add?
Work package 1: topic guide (b)
Decommissioning narratives (telephone interviews)
Introductions, preamble and consent
In relation to the decommissioning programmes you have led/been involved with, please tell me about your experience of the following aspects:
-
The aims and drivers behind the decommissioning exercise.
-
The experience of attempting to implement the programme.
-
Any outcomes of the decommissioning programme.
-
The key actors and agencies involved.
-
Your views on the challenges of decommissioning.
-
Important points of learning for others attempting to lead decommissioning projects.
-
Is there anything else you would like to add?
Work package 3: interview schedule (c)
Case study interviews round 1 (telephone and face to face)
Introductions, preamble and consent
Q1 Please describe your current roles and responsibilities.
Q2 Please describe current or planned decommissioning projects that you are involved with, including:
origins and aims
intended outcomes.
Q3 What, if any, methods are to be used to support decommissioning?
(prompt – e.g. decision tools, service improvement frameworks)
Q4 Who are the key interest groups involved in the decommissioning project and what is their role?
(prompt – e.g. public, professional, political)
Q5 What do you consider to be the key relationships required for effective decommissioning?
Q6 What, in your view, is the role of evidence and information in decommissioning?
Q7 How would you characterise your experiences so far of carrying out/being involved with decommissioning?
Q8 Is there anything else you would like to add?
Work package 3: interview schedule (d)
Case study interviews round 2 (telephone and face to face)
Introductions, preamble and consent
Q1 Please provide an update on the progress of the decommissioning programme since the last interview. In particular, I would like to hear about:
-
the experience of attempting to implement the programme
-
any outcomes of the decommissioning programme
-
the key actors and agencies involved
-
your views on the challenges involved
-
important points of learning for others attempting to lead decommissioning projects.
Q2 Do you have plans to:
-
continue the programme of decommissioning?
-
– (prompt – please explain why)
-
-
develop new programmes?
-
– (prompt – please explain why)
-
Q3 Is there anything else you would like to add?
Appendix 5 Materials used in focus groups
[Slide 1]
Have a conversation about these types of decisions and processes in health care.
Discuss your experiences.
Look at a couple of examples in more detail.
Ask for your views on what we do next . . .
[Slide 2]
We want you to do the talking! Our job is to make sure everyone has a chance to contribute.
There are no right or wrong answers and everyone’s opinions are important. Feel free to disagree!
Everything you say will stay in the room – nothing will be attributed to you so you can speak freely.
[Slide 3]
Harlock-Brearley CCG is considering options to help it meet its spending targets. The CCG is responsible for funding 65% of NHS services in the area but budgets are tight. As a result they are considering current treatments that they might withdraw from those offered to their patient populations. Examples under consideration include:
-
fertility treatment – it is expensive and infertility is not life-threatening
-
hearing aids – for those with mild hearing loss
-
vasectomies – it is a non-urgent service and there are alternatives.
[Slide 4]
Williams CCG is considering options for reducing the number of hospital sites in its local area. The hospitals have all been graded poorly by inspectors, and parts of one of the hospitals are currently unused. The hospital trust is accumulating a lot of debt (£66M) to maintain all three hospitals. Currently the hospitals are located in three of the four districts overseen by the CCG. Options are:
-
Build a brand new, modern hospital in one of the districts.
-
Centralise all services at one of the existing hospitals.
-
Centralise services at two of the three existing hospitals: hospital 1 – emergency/acute care; hospital 2 – planned surgery and complex diagnostics.
[Slide 5]
The organisation NHS England is responsible for overseeing specialised services across the NHS in England. It is currently developing proposals to reduce the number of hospitals providing intensive burn care for children. Its main concerns are how to maintain high standards of care while making best use of limited resources.
[Slide 6]
The Delphi survey is aimed at generating consensus on difficult topics. It involves asking for opinions from groups of people through three rounds of questions. After each round of questions, the responses are summarised and shared for discussion in the next round. By the third round, conclusions are drawn on areas of agreement and disagreement.
Appendix 6 Delphi study 2 letter of introduction and round 1 questionnaire
Appendix 7 Detailed findings from Delphi study 1 (rounds 2 and 3)
Round 2 results: to what extent do you agree that the following considerations should ideally inform decisions to carry out decommissioning? (% responses, in descending order of average strength of agreement.)
| Consideration | Strongly disagree | Disagree | Agree | Strongly agree | Do not know |
|---|---|---|---|---|---|
| Quality and patient safety | 0 | 0 | 7.4 | 92.6 | 0 |
| Clinical effectiveness | 0 | 0 | 11.1 | 88.9 | 0 |
| Cost-effectiveness/efficient use of resources | 0 | 0 | 18.5 | 81.5 | 0 |
| Duplication of services | 0 | 0 | 33.3 | 66.7 | 0 |
| Evidence base | 0 | 3.7 | 29.6 | 63.0 | 3.7 |
| Responding to changing demographics/population needs | 0 | 0 | 48.1 | 48.1 | 3.7 |
| Addressing inequalities | 0 | 7.7 | 30.8 | 61.5 | 0 |
| Maximising population health | 0 | 7.4 | 37.0 | 55.6 | 0 |
| Alignment with strategic priorities | 0 | 11.1 | 40.7 | 48.1 | 0 |
| New service developments/innovations | 0 | 0 | 66.7 | 29.6 | 3.7 |
| Equitable resource allocation | 3.7 | 7.4 | 48.1 | 40.7 | 0 |
| Patient and public views | 0 | 18.5 | 40.7 | 40.7 | 0 |
| Cost/budgetary pressures | 0 | 18.5 | 48.1 | 33.3 | 0 |
| Availability of alternative services/interventions | 0 | 14.8 | 63.0 | 22.2 | 0 |
| Cost of implementation of decommissioning | 14.8 | 11.1 | 44.4 | 25.9 | 3.7 |
Round 2 results: to what extent do you agree that the following considerations do actually – in practice – inform decisions to carry out decommissioning? (% responses, in descending order of average strength of agreement.)
| Consideration | Strongly disagree | Disagree | Agree | Strongly agree | Do not know |
|---|---|---|---|---|---|
| Cost/budgetary pressures | 3.7 | 0 | 22.2 | 74.1 | 0 |
| Government intervention (e.g. legislation) | 7.4 | 3.7 | 37.0 | 51.9 | 0 |
| Capital costs/condition (buildings, maintenance) | 3.8 | 15.4 | 42.3 | 30.8 | 7.7 |
| Quality and patient safety | 0 | 7.4 | 66.7 | 25.9 | 0 |
| Complexity of implementation of decommissioning | 0 | 29.6 | 40.7 | 18.5 | 11.1 |
| Support from clinicians | 7.4 | 18.5 | 37.0 | 33.3 | 3.7 |
| Cost-effectiveness/efficient use of resources | 3.7 | 22.2 | 48.1 | 25.9 | 0 |
| Support from industry and other interest groups | 7.4 | 29.6 | 37.0 | 14.8 | 11.1 |
| Clinical effectiveness | 3.7 | 11.1 | 74.1 | 11.1 | 0 |
| Availability of alternative services/interventions | 3.7 | 29.6 | 44.4 | 18.5 | 3.7 |
| Cost of implementation of decommissioning | 0 | 33.3 | 48.1 | 14.8 | 3.7 |
| Alignment with strategic priorities | 7.4 | 29.6 | 37.0 | 22.2 | 3.7 |
| Support from elected politicians | 11.1 | 14.8 | 51.9 | 22.2 | 0 |
| New service developments/innovations | 8.0 | 28.0 | 44.0 | 16.0 | 4.0 |
| Prejudice against public-sector provision | 3.7 | 51.9 | 22.2 | 7.4 | 14.8 |
| Duplication of services | 7.4 | 33.3 | 40.7 | 14.8 | 3.7 |
| Responding to changing demographics/population needs | 7.4 | 37.0 | 40.7 | 11.1 | 3.7 |
| Evidence base | 3.7 | 37.0 | 51.9 | 7.4 | 0 |
| Impact on workforce | 3.7 | 59.3 | 18.5 | 14.8 | 3.7 |
| Patient and public views | 11.1 | 40.7 | 37.0 | 7.4 | 3.7 |
| Maximising population health | 11.1 | 48.1 | 37.0 | 0 | 3.7 |
| Addressing inequalities | 11.1 | 70.4 | 14.8 | 3.7 | 0 |
| Equitable resource allocation | 11.1 | 74.1 | 11.1 | 3.7 | 0 |
| Marginal groups not heard (e.g. homeless) | 22.2 | 66.7 | 7.4 | 0 | 3.7 |
Round 2 results: please rate each of the factors in terms of their relative importance within each category in shaping the extent to which decommissioning is implemented as planned, using the four-point scale below (% responses, in descending order of importance within each category.)
| Factor | Very low importance | Little importance | High importance | Very high importance | Do not know |
|---|---|---|---|---|---|
| Change management and implementation strategy | |||||
| Strength of executive leadership | 0 | 0 | 7.4 | 92.6 | 0 |
| Strength of clinical leadership | 0 | 3.7 | 14.8 | 74.1 | 7.4 |
| Quality of communication | 0 | 3.7 | 33.3 | 63.0 | 0 |
| Clarity of specific aims and objectives at the start | 0 | 3.7 | 48.1 | 48.1 | 0 |
| Extent of cultural and behavioural change | 0 | 7.4 | 51.9 | 40.7 | 0 |
| Attention throughout to human aspects of process of change | 0 | 11.5 | 46.2 | 42.3 | 0 |
| Quality of project management | 0 | 11.1 | 48.1 | 40.7 | 0 |
| Availability of resources to support decision-making and implementation processes | 0 | 14.8 | 48.1 | 33.3 | 3.7 |
| Quality of strategic planning | 0 | 11.1 | 63.0 | 25.9 | 0 |
| Training and preparation of staff | 0 | 18.5 | 63.0 | 18.5 | 0 |
| Clarity of incentives and levers to support change | 0 | 22.2 | 59.3 | 18.5 | 0 |
| Complexity of decommissioning programme | 0 | 29.6 | 59.3 | 11.1 | 0 |
| Pace of change | 3.7 | 40.7 | 51.9 | 0 | 3.7 |
| Evidence and information | |||||
| Demonstrable benefits | 0 | 0 | 37.0 | 63.0 | 0 |
| Clarity of evidence/data to support business case, ongoing monitoring and impact assessment | 0 | 0 | 63.0 | 37.0 | 0 |
| Clarity around new patient pathways | 0 | 14.8 | 63.0 | 18.5 | 3.7 |
| Review/evaluation of process | 3.7 | 11.1 | 59.3 | 25.9 | 0 |
| Availability of alternative services | 0 | 25.9 | 51.9 | 22.2 | 0 |
| Extent of adoption elsewhere of new intervention/service | 0 | 33.3 | 48.1 | 18.5 | 0 |
| Relationships and political dimensions | |||||
| Clarity of rationale/case for change | 0 | 0 | 29.6 | 70.4 | 0 |
| Nature and extent of clinician engagement/involvement | 0 | 7.4 | 33.3 | 59.3 | 0 |
| Level of political support | 0 | 14.8 | 29.6 | 55.6 | 0 |
| Transparency of decision-making process | 0 | 7.4 | 63.0 | 29.6 | 0 |
| Nature and extent of patient/public engagement/involvement | 0 | 14.8 | 51.9 | 29.6 | 3.7 |
| Quality of partnership working with relevant agencies | 0 | 7.7 | 76.9 | 11.5 | 3.8 |
| Extent to which it challenges vested interests | 0 | 23.1 | 46.2 | 30.8 | 0 |
| Nature and extent of media coverage | 0 | 25.9 | 51.9 | 18.5 | 3.7 |
| Stability within the local health economy during transition | 3.7 | 18.5 | 66.7 | 11.1 | 0 |
| Reputation of existing providers | 0 | 33.3 | 55.6 | 3.7 | 7.4 |
| Meets community expectations | 0 | 37.0 | 51.9 | 7.4 | 3.7 |
Comparisons of round 2 and round 3 responses for statements attracting no or low consensus in round 2.
| Statement | Strongly disagree | Disagree | Agree | Strongly agree | Do not know | Change in level of consensus | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | ||
| ‘Costs of implementation of decommissioning’ do actually in practice inform decision to carry out decommissioning | 0 | 0 | 33.3 | 32.0 | 48.7 | 60.0 | 14.8 | 8.0 | 3.7 | 0 | Low → medium (agree) |
| ‘Duplication of services’ does actually in practice inform decision to carry out decommissioning | 7.4 | 0 | 33.3 | 24.0 | 40.7 | 68.0 | 14.8 | 8.0 | 3.7 | 0 | None → medium (agree) |
| The ‘evidence base’ does actually in practice inform decision to carry out decommissioning | 3.7 | 0 | 37.0 | 32.0 | 51.9 | 52.0 | 7.4 | 16.0 | 0 | 0 | No change (low) |
| ‘Maximising population health’ does actually in practice inform decisions to carry out decommissioning | 11.1 | 4.0 | 48.1 | 76.0 | 37.0 | 20.0 | 0 | 0 | 3.7 | 0 | None → high (disagree) |
| ‘Availability of alternative services/interventions’ does actually in practice inform decisions to carry out decommissioning | 3.7 | 0 | 29.6 | 16.0 | 44.4 | 68.0 | 18.5 | 12.0 | 3.7 | 4.0 | Low → medium (agree) |
| ‘Responding to changing demographics/population needs’ does actually in practice inform decisions to carry out decommissioning | 7.4 | 0 | 37.0 | 44.0 | 40.7 | 48.0 | 11.1 | 4.0 | 3.7 | 4.0 | No change (none) |
| ‘New service developments/innovations’ do actually in practice inform decisions to carry out decommissioning | 8.0 | 0.0 | 28.0 | 24.0 | 44.0 | 72.0 | 16.0 | 4.0 | 4.0 | 0 | Low → medium (agree) |
| ‘Alignment with strategic priorities’ does actually in practice inform decisions to carry out decommissioning | 7.4 | 0 | 29.6 | 28.0 | 37.0 | 64.0 | 22.2 | 8.0 | 3.7 | 0 | None → medium (agree) |
| ‘Patient and public views’ do actually in practice inform decisions to carry out decommissioning | 11.1 | 8.0 | 40.7 | 72.0 | 37.0 | 16.0 | 7.4 | 4.0 | 3.7 | 0 | None → high (disagree) |
| ‘Support from industry and other interest groups’ does actually in practice inform decisions to carry out decommissioning | 7.4 | 0 | 29.6 | 32.0 | 37.0 | 48.0 | 14.8 | 4.0 | 3.7 | 16.0 | No change (none) |
| ‘Prejudice against public sector provision’ does actually in practice inform decisions to carry out decommissioning | 3.7 | 8.0 | 51.9 | 60.0 | 22.2 | 8.0 | 7.4 | 8.0 | 14.8 | 16.0 | Low → medium (disagree) |
| ‘Complexity of implementing decommissioning’ does actually in practice inform decisions to carry out decommissioning | 0 | 0 | 29.6 | 8.0 | 40.7 | 72.0 | 18.5 | 16.0 | 11.1 | 4.0 | None → high (agree) |
| ‘Impact on workforce’ does actually in practice inform decisions to carry out decommissioning | 3.7 | 8.0 | 59.3 | 48.0 | 18.5 | 28.0 | 14.8 | 12.0 | 3.7 | 4.0 | Low → none |
| Statement | Very little importance | Little importance | High importance | Very high importance | Do not know | Change in level of consensus | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | ||
| What is the relative importance of the ‘pace of change’ for shaping the extent to which decommissioning is implemented as planned? | 3.7 | 0 | 40.7 | 33.3 | 51.9 | 50.0 | 0.0 | 4.2 | 3.7 | 12.5 | No change (none) |
| What is the relative importance of the ‘extent of adoption elsewhere of new intervention/service’ for shaping the extent to which decommissioning is implemented as planned? | 0 | 0 | 33.3 | 24.0 | 48.1 | 60.0 | 18.5 | 8.0 | 0 | 8.0 | Low → medium (high/very high) |
| What is the relative importance of ‘meets community expectations’ for shaping the extent to which decommissioning is implemented as planned? | 0 | 0 | 37.0 | 28.0 | 51.9 | 64.0 | 7.4 | 4.0 | 3.7 | 4.0 | None → low (high/very high) |
| What is the relative importance of the ‘reputation of existing providers’ for shaping the extent to which decommissioning is implemented as planned? | 0 | 0 | 33.3 | 12.0 | 55.6 | 76.0 | 3.7 | 4.0 | 7.4 | 8.0 | None → high (high/very high) |
Appendix 8 Details of case study data collection
Case study 1: reorganisation of paediatric burn care services
| Interviewee | Professional role | Other affiliations |
|---|---|---|
| 1 | Local commissioner/area team | Longstanding involvement in specialised commissioning and the regional network containing hospital A |
| 2 | Burn consultant | Not on the CRG. Member of regional network where previous reorganisation plans were not implemented |
| 3 | Burn consultant | CRG member and member of the network containing hospital A |
| 4 | Patient representative | Retired NHS manager and former commissioner of burn care. Previously part of the national burn care group and the national network |
| 5 | Burn consultant | Not on the CRG, member of the regional network containing hospital A |
| 6 | Senior burn nurse | Not on the CRG, member of a regional network |
| 7 | Senior service specialist | Responsible for services in a region |
| 8 | Senior service specialist | Responsible for services in a region |
| 9 | Burn consultant | CRG member and member of the network containing Hospital A |
| 10 | Burn consultant | CRG and regional network member |
| 11 | NHS England programme lead | NHS England Trauma Programme of Care |
| 12 | Patient representative | Works for a national charity involved with burn care |
| 13 | Burn consultant | Chair of CRG and regional network member |
| Observations | Date | Summary of relevant discussions |
| 1 | 19 September 2014 | Hospital A representatives not present at this meeting. The review of compliance in other centres led by area teams reported to be ongoing and therefore derogation will be completed, with a final decision regarding hospital A, by 31 March 2015. The national strategic review for paediatric care is under development |
| 2 | 2 September 2015 | The strategic service review is under consideration by the senior NHS England management team. The next step would be a project plan with resources for implementation of the reorganisation. Discussion of delay in time scales. A provider representative (non-member) expresses frustration at the process of being designated a ‘facility’ and wishes to clarify who makes designation decisions |
| 3 | 6 April 2016 | Meeting not officially chaired since the current chair stepped down and with uncertainty over the CRG’s future. Lots of discussion about these changes. Discussion of the lack of resources/levers to implement service review plans through the ODNs. A proposed new centre-level unit in the relevant region discussed and considered a sensible response to the derogation at hospital A. However, doubt expressed over likelihood of resourcing the plans |
| Document | Title | Content and influence |
| 1 | Burn Care Review (2001)72 | Brought together stakeholders from across the burn care sector (including professional and patient associations, royal colleges and academic partners). Advocated ‘substantial reorganisation of the current burn care network’ (p. 1) over a 5- to 7-year period |
| 2 | National Burn Care Standards (revised 2013)110 | Undertaken by a subgroup of the National Network for Burn Care, with input from the four regional networks and other stakeholders such as the British Burns Association. Recommends that providers self-assess against the standards |
| 3 | Developing a National Strategy for Paediatric Centre Level Burn Care in England: Options Paper (2015, Burns Clinical Reference Group, NHS England, unpublished) | Prepared by the NHS England programme leads and the CRG. Reiterates that a ‘co-located PIC unit is an essential requirement for a paediatric specialised burn centre’. The case for change articulated in terms of integration of services and provision of interdependencies, as well as the need for critical mass in order to maintain safe levels, and finally workforce specialty training levels. Options put forward, including status quo, two centres, three centres and four centres |
Case study 2: closure of an end-of-life home support service
| Interviewee | Professional role | Organisational affiliation |
|---|---|---|
| 1 | Senior Operations Officer | CCG |
| 2 | Delivery Officer | CCG |
| 3 | Contracting Manager | CCG |
| 4 | Clinical Lead (GP) | CCG |
| 5 | Finance Manager | CCG |
| 6 | Nurse, Quality Team | CCG |
| 7 | Patient and Public Engagement Officer | CCG |
| 8 | Contracting Officer, Third Sector Contracts Team | CSU |
| 9 | Manager, Communications Team | CSU |
| 10 | Communications and Engagement Officer | CSU |
| 11 | Analytics and Intelligence Senior Manager | CSU |
| 12 | Project Manager, NHS Projects | Provider |
| 13 | Commercial Director, NHS Projects | Provider |
| Document | Title | Content and Influence |
| 1 | Review of EOL Home Support Service (de-identified) | Presented evidence from the Review of the EOL Home Support Service regarding clinical effectiveness and cost-effectiveness. Highlighted potential cost savings of £1.98M. Three options for the close-down of the EOL home support service and strengths and weaknesses for each option presented |
| Date | Observations | Summary of relevant discussions |
| July 2014 | Meeting between provider and CCG | Update on managed close-down of service discussed. Approximately 100 patients remaining to be transferred from the service. Some issues with referring patients back to GPs reported by the provider and challenges of post-discharge monitoring discussed |
Case study 3: Area Prescribing Committee
| Interviews | Role/affiliation |
|---|---|
| 1 | Lay member |
| 2 | Senior Pharmaceutical Commissioning Technician |
| 3 | GP and Local Medical Committee representative |
| 4 | Chief Pharmacist at the partnership (mental health) trust |
| 5 | Lead nurse at the acute trust |
| 6 | GP, previously an area representative on the APC |
| 7 | Head of Pharmacy at the acute trust |
| 8 | CCG Deputy Head of Medicines Management |
| 9 | CCG Clinical Lead for Medicines Management |
| 10 | CCG Head of Medicines Management |
| Observations | Summary of relevant discussions |
| 1. APC 19 November 2014 | NICE tags tabled as agenda item but no action or discussion required. Discussion focused on pathways and guidelines, unlicensed drug use, adherence to formulary, access to non-formulary drugs |
| 2. APC 13 May 2015 | Application for new diabetes treatment considered with attendant discussion of cost implications. Disinvestment not considered. NICE tags considered and discussion of bio-similars although no action required. Discussion of industry legal verdicts, guidelines and shared care agreements |
| 3. MOC 20 November 2015 | Discussion of bio-similars, metrics, electronic prescribing. Consideration of drug application, unlicensed prescribing. Strategy document for medicines management circulated for discussion next time. Updates on shared formulary, cancer drugs fund. Efficiency programme discussed |
| 4. MOC 7 December 2015 | Audit results and NICE guidelines discussed. Nutrition policies discussed. Unlicensed medicines policy discussed. Discussion of top 35 drug expenditures – indicating growth in the high-cost drugs ‘driven by CDF and NICE tag’. Only one tariff drug in the list |
Case study 4: Clinical Commissioning Group-led reorganisation of services
| Interviewee | Professional role | Organisational affiliation |
|---|---|---|
| 1 | Programme Manager | Seconded from NHS |
| 2 | Accountable Officer | CCG |
| 3 | Chair | CCG |
| 4 | Communications and Engagement Lead | CCG |
| 5 | Chair, Clinical Advisory Group | Secondary Care Board Representative, CCG |
| 6 | Director of Transformation | Hospital Trust |
| 7 | Director of Strategy and Improvement | Partnerships Foundation Trust |
| 8 | Chief Executive | Community Trust |
| 9 | Director | Local HealthWatch |
| 10 | Medical Director | Community Trust |
| 11 | Director of Communications | Hospital Trust |
| 12 | Director of Strategy and Transformation | CCG |
| 13 | Director, Adult Social Services | County Council |
| Document | Title | Content and influence |
|---|---|---|
| 1 | Need for Change78 (March 2015) | Summarised the purpose of the Strategic Review for the public and wider stakeholders. Advocated the need for change in the health and social care system in response to demographic and funding challenges. Presented evidence and feedback from initial engagement with patients, public, clinicians and wider stakeholders |
| 2 | Case for Change70 (July 2015) | Built on the Need for Change document and updated on the review for public and wider stakeholders. Set out a vision for health care based on ‘prevention’, integration’ and ‘more services closer to people’s homes’ (p. 2) |
| 4 | Board to Boards workshop report (October 2015) | Summarised discussions between CCG, providers and social services held at executive boards meeting and set out next steps for the Review. Highlighted system configuration and implementation issues as key areas for focus |
| 5 | Strategic Outline Case (autumn, 2015) | Updated on review progress for public and wider stakeholders and set out options for models of care, with a strengths and weaknesses analysis for each option. Provided detailed information about the financial and estate challenges faced, current patient pathways and potential system design for different service user groups |
| Date | Observations | Summary of relevant discussions |
| October 11 2015 | Board to Boards workshop | Update on progress with strategic review. Implementation issues discussed by break-out groups. Target areas identified and discussed included estates/buildings, IT systems, workforce and clinical system/pathways |
| June 2015 | Stakeholder Advisory Group meeting | Update on progress with strategic review presented and shared vision for future system reaffirmed by programme executive. Options for future service configuration shared with wider stakeholders and feedback invited. Some disaffection with proposals expressed by patient representatives concerned about travelling distances for acute care |
| June 2015 | Clinical Advisory Group meeting | Clinicians and workforce invited to reflect on clinical design of the new system and propose systems/pathways for particular patient groups through break-out sessions. Tension points and bottle-necks in existing system were highlighted |
| March 2015 | Programme Executive meeting | Presentation of financial analysis and projections by finance team and estates challenges discussed across providers, but with particular focus on the hospital trust. Challenge of closing the financial gap discussed at length |
| March 2015 | Launch of the Need for Change document | Half-day event to launch the Need for Change document. Local NHS staff and some patient representatives in attendance. Key members of the programme executive and other stakeholders presented views on the case for change and invited questions from the audience |
| January 2015 | Health OSC meeting | Strategic review process presented by the Programme Manager and discussed by the OCS. Key issues raised included impact on patients and local citizens travelling distances to access care. Committee asked to be kept updated regularly on progress |
| January 2015 | Programme Executive meeting | Update on production of the Need for Change document shared by Programme Manager and team agreed sign-off date and launch. Discussed mobilisation of care working groups to assist in designing models of care. Barriers to greater integration were discussed and clinical engagement was identified as lower than anticipated in the review |
| January 2015 | Meeting with local patient forum and patient representation group | Strategic review plans were presented to patient representatives by the Programme Manager and feedback was sought on proposals. Greater integration between services, improved quality of care and travelling distances for service users were identified as priorities for the review by patient representatives |
| January 2015 | Communications and engagement group meeting | Engagement strategy shared and discussed by the communications team. Reported 800 responses to the survey received and stakeholder forums, patient and GP forums were in progress. Ensuring the accessibility of engagement documentation identified as a key issue |
| September 2014 | Appointment of consultant | Series of presentations by external consultants addressing plans and proposals for the strategic review. Strengths and weaknesses of the observed presentations discussed by the review team and decision-making process agreed around appointment of consultant |
Appendix 9 Detailed findings from Delphi study 2 (rounds 2 and 3)
Round 2 results: to what extent do you agree that the following considerations are good reasons to move or replace services? (% responses in descending order of average strength of agreement.)
| Consideration | Strongly disagree | Disagree | Agree | Strongly agree | Do not know |
|---|---|---|---|---|---|
| If there are changes in patient/service user need | 0 | 4 | 52 | 35 | 9 |
| If other similar services are available | 4 | 9 | 65 | 17 | 4 |
| If a service is not in line with patient values | 9 | 13 | 50 | 22 | 9 |
| If a service is not being used very much | 4 | 17 | 61 | 9 | 9 |
| If new developments have been made in clinical research | 9 | 13 | 43 | 22 | 13 |
| In order to develop centres of excellence | 13 | 26 | 50 | 9 | 4 |
| If a service lacks accountability and/or transparency | 9 | 30 | 30 | 22 | 9 |
| If a service is being not being used in the way intended by patients/service users | 4 | 30 | 43 | 9 | 13 |
| If the service is performing poorly | 13 | 43 | 30 | 13 | 0 |
| If a service does not meet national policy | 9 | 35 | 30 | 13 | 13 |
| If a service is not an efficient use of money | 5 | 45 | 32 | 9 | 9 |
| There are no good reasons to move services | 22 | 39 | 17 | 9 | 13 |
| There are no good reasons to take away services | 26 | 48 | 22 | 0 | 4 |
| If a service is high in cost | 30 | 61 | 4 | 0 | 4 |
Round 2 results: to what extent do you agree that the following considerations are bad reasons to move or replace services? (% responses in descending order of average strength of agreement.)
| Consideration | Strongly disagree | Disagree | Agree | Strongly agree | Do not know |
|---|---|---|---|---|---|
| Political pressures at the local level | 0 | 13 | 30 | 57 | 0 |
| To make financial savings | 9 | 13 | 26 | 50 | 4 |
| To meet the interests of organisations (e.g. hospitals) or individuals (e.g. professionals) | 4 | 9 | 35 | 35 | 17 |
| There is a shortage of staff with the right expertise | 4 | 26 | 39 | 26 | 4 |
| Meeting national policies and targets | 4 | 26 | 17 | 39 | 13 |
| There is a shortage of other resources (e.g. buildings) | 4 | 43 | 17 | 26 | 9 |
Round 2 results: to what extent do you agree that the following considerations are reasons why services are actually moved or taken away in practice? (% responses in descending order of average strength of agreement.)
| Consideration | Strongly disagree | Disagree | Agree | Strongly agree | Do not know |
|---|---|---|---|---|---|
| To make financial savings | 0 | 9 | 17 | 74 | 0 |
| The service is not considered to be good value for money | 0 | 9 | 39 | 52 | 0 |
| Meeting national policies and targets | 4 | 4 | 48 | 44 | 0 |
| Decision makers (e.g. commissioners) are in favour | 4 | 9 | 13 | 70 | 4 |
| Other services are available that deliver the same thing | 4 | 17 | 61 | 17 | 0 |
| Political pressures at the local level | 9 | 17 | 30 | 34 | 9 |
| The service is not being used much | 4 | 26 | 43 | 22 | 4 |
| Concerns over quality and safety | 9 | 22 | 61 | 4 | 4 |
| New models of care are available | 4 | 26 | 43 | 17 | 9 |
| Professionals (e.g. doctors) are in favour | 13 | 17 | 35 | 22 | 13 |
| There are changes in patient/service user need | 9 | 35 | 43 | 9 | 4 |
| There is a shortage of staff with the right expertise | 4 | 30 | 39 | 9 | 17 |
| Evidence suggests that it is the right thing to do | 26 | 30 | 13 | 22 | 9 |
| The public are in favour | 30 | 35 | 17 | 13 | 4 |
Comparisons of round 2 and round 3 responses for statements attracting a low level of or no consensus in round 2 (% calculated based on total number of responses, which varies from 21 to 23 across the questions)
| Statement | Strongly disagree, n (%) | Disagree, n (%) | Agree, n (%) | Strongly agree, n (%) | Do not know, n (%) | Change in level of consensus | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | Round 2 | Round 3 | ||
| ‘If the service is performing poorly’ is a good reason to move or replace services | 3 (13) | 6 (27) | 10 (43) | 9 (41) | 7 (30) | 6 (27) | 3 (13) | 1 (4) | 0 | 0 | None → low disagree |
| ‘If a service is not an efficient use of money’ is a good reason to move or replace services | 1 (5) | 3 (14) | 10 (45) | 13 (59) | 7 (32) | 5 (23) | 2 (9) | 1 (4) | 2 (9) | 0 | None → medium disagree |
| ‘In order to develop centres of excellence’ is a good reason to move or replace services | 3 (13) | 1 (4) | 6 (26) | 7 (32) | 11 (48) | 13 (59) | 2 (9) | 1 (4) | 1 (4) | 0 | None → low agree |
| ‘If a service lacks accountability and/or transparency’ is a good reason to move or replace services | 2 (9) | 0 | 7 (30) | 10 (45) | 7 (30) | 7 (32) | 5 (22) | 5 (23) | 2 (9) | 0 | No change (none) |
| ‘If new developments have been made in clinical research’ is a good reason to move or replace services | 2 (9) | 1 (4) | 3 (13) | 6 (27) | 10 (43) | 11 (50) | 5 (22) | 2 (9) | 3 (13) | 2 (9) | Low agree → none |
| ‘If a service doesn’t meet national policy’ is a good reason to move or replace services | 2 (9) | 5 (23) | 8 (35) | 11 (50) | 7 (30) | 5 (23) | 3 (13) | 0 | 3 (13) | 1 (4) | None → medium disagree |
| ‘If a service is not being used in the way intended by patients/service users’ is a good reason to move or replace services | 1 (4) | 3 (14) | 7 (30) | 10 (45) | 10 (43) | 5 (23) | 2 (9) | 3 (14) | 3 (13) | 1 (4) | No change (none) |
| ‘There are no good reasons to move services’ | 5 (22) | 6 (29) | 9 (39) | 10 (48) | 4 (17) | 2 (9) | 2 (9) | 1 (5) | 3 (13) | 2 (9) | Low disagree → medium disagree |
| ‘There is a shortage of staff with the right expertise’ is a bad reason to move or replace services | 1 (4) | 1 (4) | 6 (26) | 3 (13) | 9 (39) | 11 (48) | 6 (26) | 8 (35) | 1 (4) | 0 | Low agree → High agree |
| ‘There is a shortage of other resources (e.g. buildings)’ is a bad reason to move or replace services | 1 (4) | 3 (13) | 10 (43) | 8 (35) | 4 (17) | 6 (26) | 6 (26) | 6 (26) | 2 (9) | 0 | No change (none) |
| ‘Meeting national policies and targets’ is a bad reason to move or replace services | 1 (4) | 1 (4) | 6 (26) | 4 (17) | 4 (17) | 6 (26) | 9 (39) | 11 (48) | 3 (13) | 1 (4) | None → low agree |
| ‘Political pressures at the local level’ is a reason why services are actually moved or taken away in practice | 2 (9) | 2 (9) | 4 (17) | 3 (14) | 7 (30) | 6 (27) | 8 (34) | 9 (41) | 2 (9) | 2 (9) | No change (low agree) |
| ‘Evidence suggests that it is the right thing to do’ is a reason why services are actually moved or taken away in practice | 6 (26) | 4 (18) | 7 (30) | 12 (54) | 3 (13) | 5 (23) | 5 (22) | 1 (4) | 2 (9) | 0 | None → medium disagree |
| ‘The public are in favour’ is a reason why services are actually moved or taken away in practice | 7 (30) | 6 (27) | 8 (35) | 14 (64) | 4 (17) | 1 (4) | 3 (13) | 1(4) | 1 (4) | 0 | Low disagree → high disagree |
| ‘Professionals (e.g. doctors) are in favour’ is a reason why services are actually moved or taken away in practice | 3 (13) | 1 (5) | 4 (17) | 4 (19) | 8 (35) | 12 (57) | 5 (22) | 1 (4) | 3 (13) | 3 (14) | None → low agree |
| ‘There is a shortage of staff with the right expertise’ is a reason why services are actually moved or taken away in practice | 1 (4) | 2 (9) | 7 (30) | 7 (32) | 9 (39) | 11 (50) | 2 (9) | 2 (9) | 4 (17) | 0 | No change (none) |
| ‘The service is not being used much’ is a reason why services are actually moved or taken away in practice | 1 (4) | 1 (9) | 6 (26) | 3 (14) | 10 (43) | 10 (45) | 5 (22) | 6 (27) | 1 (9) | 2 (9) | Low agree → medium agree |
| ‘New models of care are available’ is a reason why services are actually moved or taken away in practice | 1 (4) | 1 (4) | 6 (26) | 4 (18) | 10 (43) | 14 (64) | 4 (17) | 3 (14) | 2 (9) | 0 | Low agree → medium agree |
| ‘There are changes in patient/service user need’ is a reason why services are actually moved or taken away in practice | 2 (9) | 1 (5) | 8 (35) | 5 (24) | 10 (43) | 11 (52) | 2 (9) | 3 (14) | 1 (4) | 1 (5) | None → low agree |
Glossary
- Coproduction
- An equal and reciprocal relationship between people providing and using services.
- De-adoption
- The processes of removing a practice or technology previously introduced.
- Decommissioning
- The removal, reduction and/or replacement of health-care services and interventions.
- Decommitment
- The process of reducing support for an intervention prior to a decision to decommission.
- Deimplementation
- The process of removing a practice or technology previously introduced.
- Deinsurance
- Removal of a service/intervention from a health insurance plan.
- Delisting
- Removal of an intervention from a formulary, insurance plan or other (e.g. a register of approved interventions).
- Derogation
- Failure to be in compliance with one or more pre-set standards.
- Disinvestment
- Withdrawal of funding from treatments and technologies that deliver insufficient health gain for their cost.
- Divestment
- Disposal of part of a health organisation, for example through closure.
- Downgrading
- Reduction in the range or level of specialism of an organisation’s function.
- Exnovation
- The process of removing a practice or technology previously introduced.
- Termination
- The closure or discontinuation of initiatives and/or services.
- Undiffusion
- The process of removing a practice or technology previously introduced.
List of abbreviations
- A&E
- accident and emergency
- A4R
- accountability for reasonableness
- ANT
- actor–network theory
- APC
- Area Prescribing Committee
- BME
- black and minority ethnic
- CCG
- Clinical Commissioning Group
- CER
- comparative effectiveness research
- CRG
- Clinical Reference Group
- CSU
- Commissioning Support Unit
- EOL
- end of life
- GP
- general practitioner
- HIV
- human immunodeficiency virus
- HSDR
- Health Services and Delivery Research
- HTA
- health technology assessment
- HTR
- health technology reassessment
- IRP
- Independent Reconfiguration Panel
- IT
- information technology
- MOC
- medicines optimisation committee
- NCAT
- National Clinical Advisory Team
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- ODN
- operational delivery network
- OECD
- Organisation for Economic Cooperation and Development
- OSC
- Overview and Scrutiny Committee
- PBMA
- programme budgeting and marginal analysis
- PCT
- primary care trust
- PFT
- partnership foundation trust
- PIC
- paediatric intensive care
- PSUP
- public, service user and patient
- STP
- sustainability and transformation plan