Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1025/05. The contractual start date was in April 2013. The final report began editorial review in May 2016 and was accepted for publication in November 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Jacobs et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Context and literature review
The organisation of community pharmacy in the UK
As private businesses contracted to provide NHS dispensing and medicines-related services, community pharmacies play a key role in UK health-care systems. Community pharmacies constitute a range of organisational forms under different types of ownership, such as national multiple (chain) pharmacies and supermarkets, small and medium-sized chains, and local independent pharmacies operating between one and five premises.
The community pharmacy contractual framework for England was introduced in 2005 (with revisions in 2011 and 2015) to meet the objectives set out in the 2003 White Paper, A Vision for Pharmacy in the New NHS. 1 These included helping to tackle health inequalities, supporting self-care and responding to the diverse needs of patients and communities. The contract specifies three levels of service provision. Essential services, which all community pharmacies are required to provide, include dispensing, repeat dispensing and clinical governance requirements. Advanced services, including medicines use reviews (MURs), the new medicines service (NMS) introduced in 2011, and the influenza vaccination service introduced in 2015, are not mandatory and require training and a declaration of competence by the pharmacist. Enhanced and locally commissioned services, which until 2013 were commissioned by primary care trusts (PCTs), are now commissioned by NHS England, clinical commissioning groups (CCGs) and local authorities. These services are commissioned to meet locally assessed needs and include minor ailment schemes, smoking cessation clinics and medicines management services for long-term conditions. Similar contractual frameworks exist for Wales, Scotland and Northern Ireland, although there are some regional differences.
The extension of the community pharmacist’s role from traditional dispensing duties into a range of clinical areas that were once the remit of only family doctors is part of a general move to embrace the philosophy of ‘pharmaceutical care’ within the profession. 2 It is widely supported by pharmacists3 – who see it as an opportunity to utilise their extensive clinical knowledge of medicines to greater effect – and service commissioners – who recognise the opportunities to improve service access and quality for patients, reduce some of the burden on general practitioners (GPs)’ workload and potentially to save money through role substitution, the reduction of waste medicines (through improved medicines understanding and adherence) and the prevention of medicines-related unplanned hospital admissions.
One important aspect of recent health-care policy in the UK has been to increase patient choice and access to services. Together with a raft of pro-market policies, this has sought to increase the range and diversity of professionals and provider organisations able to offer advice and services. The election of the Conservative–Liberal Democrat coalition government in 2010 saw the introduction of further health-care reforms, with the drive towards independent sector provision of health care being stepped up (‘any qualified provider’). 4 However, concerns have been raised over the quality and safety of patient care delivered by private sector organisations,5 which need to balance the pressures of delivering quality services within the context of a for-profit business. Community pharmacies are private businesses and established providers of NHS-funded services. As such, they provide an ideal exemplar in which to begin to unpack concerns over conflicting commercial pressures versus improving quality and safety.
Definitions of clinical productivity
Productivity can be simply defined as the ratio of outputs to inputs in the production process. In industry, ‘outputs’ can be measured as the number of units of production per day, for example. However, in health care, where a positive patient experience and high-quality services are necessary to ensure maximum patient benefit, the amount of time spent per patient may be more important than the volume of services delivered. In this way, ‘clinical’ productivity, it could be argued, differs from more traditional definitions of productivity in that it encompasses not only the quantity of services provided, but also the quality of those services. Indeed, in 2005, the University of York’s Centre for Health Economics and the National Institute for Economic and Social Research suggested improved methods for measuring productivity that captured measures of quality as well as service activity. 6 ‘Inputs’ often refer to expenditure on labour, capital and materials.
The majority of studies examining clinical productivity in health care have been conducted in hospital settings in the USA and have measured clinical productivity in purely quantitative terms, for example numbers of procedures performed or patients seen, hours per case or, often, ‘relative value units’, which are a measure of value used in the USA to reimburse health-care services that take into account the time, training, skills and intensity needed to deliver a particular service. Studies of clinical productivity generally do not take into account the quality or outcomes of the services delivered.
For the purposes of this study, we sought to examine clinical productivity in terms of both the quantity and quality of services delivered by community pharmacies. The quality of pharmacy services is associated with individual patient benefit and is important to consider alongside the quantity (range and volume) of services delivered because the more patients that receive a high-quality service, the greater the effect the service will have on patient benefit and the health of the public. Conversely, high volumes of low-quality services have a potential cost both to the NHS and to patients/customers. The study did not seek to derive a single metric of ‘clinical productivity’ (obtaining ‘input’ data for individual pharmacies would not have been possible due to commercial sensitivities); rather, it explored the different components of clinical productivity simultaneously to gain a better understanding of how they might vary, their inter-relationships and the influence of organisational characteristics.
No commonly accepted definition of quality in community pharmacy has yet been developed7 and robust measures of quality in community pharmacy of proven validity and reliability are rare. 8 Moreover, it can be difficult to attribute patient outcomes to the quality of the service delivered by the community pharmacy when that is only one element of the care pathway experienced by the patient. For the purposes of this study, the quality of community pharmacy services has been operationalised in terms of overall patient satisfaction, satisfaction with the information received by the patient about their medication, their adherence to their medication and the safety climate within which the pharmacy operates. These measures of quality were selected on the basis of the availability of validated instruments and because they are likely to be influenced directly by the pharmacy itself. However, the construct of quality in community pharmacy and the influence of organisational characteristics were also explored more widely in the qualitative study (see Chapter 6, Definitions of quality).
The relationship between organisational characteristics and clinical productivity in health care
Research into variation in clinical productivity within health care and the organisational factors that influence this is inconclusive. In their extensive review of the relationship between organisational factors and performance, Sheaff et al. 9 concluded that, ‘There is no consistent or strong relationship between organisational size, ownership, leadership style, contractual arrangements for staff or economic environment (competition, performance management) and performance’. In primary care the evidence is even more limited. However, more recent studies have been able to utilise data now available from the UK Quality and Outcomes Framework (QOF) to investigate variation in the performance of general practices. Studies have found that some practice characteristics, notably practice size, ratio of practitioners to patients, levels of nurse staffing and team climate, may be associated with variation in performance, in addition to local levels of population deprivation and need. 10–14 A study of the role of incentives in a range of primary care settings concluded that incentives led to higher levels of attainment of quality targets and a reduction in variation in quality relating to deprivation in general practice; a shift towards treatments that pay more in general dental practice; and the provision of increased volumes of incentivised services in community pharmacy. However, it also found that incentives had some unintended consequences in relation to whether or not the additional investment actually represented value for money with a number of opportunity costs arising out of an increasing focus on incentivised activities. 15,16
The relationship between organisational characteristics and clinical productivity in community pharmacy
Evidence is emerging to suggest that organisational factors may influence the levels of clinical productivity in community pharmacies. MURs aim to help patients manage their medicines more effectively, by increasing their understanding, identifying problems and providing feedback to prescribers. Research published not long after the introduction of the 2005 contractual framework suggested that the volume of MUR provision by pharmacy chains was almost twice that of independent pharmacies17,18 and that this difference may be primarily profit driven, prioritising service quantity over quality. 18 There is also some evidence that locally commissioned enhanced services were more likely to be provided by chain pharmacies than independent pharmacies and that provision was greater in deprived and urban areas. 19 Other research into the implementation of pharmaceutical care services by community pharmacies worldwide has identified a number of organisational barriers to and facilitators of their provision, including the physical environment (particularly adequate space and privacy), organisational culture and leadership, having the necessary staffing and skill mix, relationships with GPs, equipment and technology, and work overload/conflicting workloads. 20 Studies of the implementation of MURs in English pharmacies suggest that although delegation of dispensing duties to pharmacy technicians or other support staff (to free up pharmacists’ time) is supported by pharmacists, constant workload demands and interruptions still prevent pharmacists from conducting MURs. 15 Yet pharmacists, particularly those working for large chain pharmacy organisations (‘multiples’), are under intense pressure to meet financial targets, including conducting specified numbers of MURs. 18 This may detract from not only the effectiveness of the MURs conducted,21 but also the extent to which they may represent true role substitution and cost efficiency.
Previous research also suggests that the quality of community pharmacy services may be influenced by organisational factors. A realist review of studies describing aspects of organisational culture in community pharmacy, its antecedents and outcomes, highlighted longstanding evidence of the dichotomy in organisational values in this sector (professional vs. business) as a result of community pharmacy services being provided by private sector organisations. 22 A subsequent survey of community pharmacists provided evidence of a significant relationship between organisational culture, particularly the balance between business and professional values, and pharmacists’ work stress and the potentially detrimental effect on patient safety of working within an intensely targets-driven culture. 23,24 Moreover, there is evidence that the organisational culture extant within pharmacies under different types of ownership may differ (Dr Sally Jacobs, University of Manchester, 2012, personal communication) and that ownership type may be associated with variation in work stress. 23 Evidence from a number of studies has described a relationship between workload and working patterns on pharmacists’ work-related stress,23,25,26 and the role of the pharmacist’s manager (particularly whether or not they are a pharmacist themselves) in determining job satisfaction. 27 Other research has suggested that organisational factors may be associated with the occurrence of dispensing errors24,28 and qualitative research on locum pharmacists has raised concerns that patients are put at risk because of the increasing reliance on temporary staff. 29 This is of particular importance in a sector of health care in which around one-quarter of all pharmacists work as self-employed locums. 30
Clinical productivity in community pharmacy and the wider health-care economy
Research suggests that up to 50% of patients with a chronic condition do not take medicines as prescribed. 31 Non-adherence to medicines is known to cause poorer health outcomes and unscheduled hospital admissions. In the UK, as many as 6.5% of adult hospital admissions are estimated to be medicines related and 30% of these cases are caused by non-adherence to medicines for chronic illness. 32 In 2014/15, £15.6B was spent on non-elective inpatient costs and £2.5B on accident and emergency admissions. 33 Therefore, it could be estimated that approximately £352M was spent on such unplanned hospital admissions in relation to medicines non-adherence.
Another key concern in health care is medicines waste in the primary and community sectors, which has been estimated to cost the NHS approximately £300M per year, equivalent to approximately £1 in every £25 spent on primary care and community pharmaceutical and allied products use, and 0.3% of total NHS expenditure. 34 This figure includes an estimated £110M worth of unused prescription medicines that are returned to community pharmacies over the course of the year and an additional £90M retained in individuals’ homes at any one time.
Community pharmacies are well placed to deliver services to improve patients’ understanding of medicines and their use. Interventions such as pharmacist-led medication reviews have been shown to improve adherence,35 and there is some evidence that increased adherence has a direct impact on treatment success and patient outcomes,36 thus improving health-care efficiency. It is for this reason that MURs were originally introduced to ensure that patients have a better understanding of their medicines, thus achieving better adherence and avoiding unnecessary waste and unplanned hospital readmissions.
NHS investment in community pharmacy services is substantial and, until 2015, was growing year on year. The total budget agreed for the provision of pharmaceutical services in England was £2.8B in 2014/15,37 making up a considerable part of overall NHS expenditure. Over 978 million prescriptions were dispensed by community pharmacists in England in 2014/15, an increase of almost 48.5% over the previous 10 years. 38 The number of enhanced services delivered had risen to 30,962 in 2010/11 and almost 3.2 million MURs and 0.8 million NMS interventions were conducted in England in 2014/15. 38
Service payments for advanced and enhanced pharmaceutical services are based on a fee-for-service structure, although there is a cap of 400 on the number of MURs for which a pharmacy will be paid annually. This raises questions over whether or not the NHS is getting value for money, particularly in light of the concerns raised above that commercial pressures may drive some community pharmacy organisations to prioritise quantity over quality in delivering MURs. To try to address these concerns, targeted MURs and the NMS were introduced in 2011. However, there is still a pressing need for the NHS as service commissioners to gain an understanding of the relationship between the quantity and quality of service provision as key elements of clinical productivity in the context of private businesses such as community pharmacy organisations. This need has been heightened by the reorganisation of the NHS and the dissolution of PCTs in 2013. With the commissioning of community pharmacy services passing to the newly formed NHS England area teams, CCGs and, for the first time, local authorities, the commissioning landscape has become fractured; there has been a loss of organisational memory and a depletion of pharmacy commissioning manpower, knowledge and skills.
This study was designed to address this need for service commissioners. An understanding of the organisational requirements for maximising clinical productivity in terms of both quantity and quality of service provision could help in the development of a set of organisational standards against which to assess applying pharmacies as part of the pharmacy contract approval process or for commissioning advanced and enhanced services. A better understanding of the inter-relationships between the quality and quantity of service provision in private sector organisations could also help to inform improvements in service payment structures and contract monitoring processes to help ensure that the NHS is getting value for money from the services it commissions. With studies of the impact of community pharmacy services on patient outcomes – in particular medicines understanding and adherence – still scarce, this study sought to provide such insights. Finally, for community pharmacy organisations themselves, knowledge of the organisational characteristics associated with higher levels of productivity (both quality and quantity) are likely to be of benefit to them as businesses and employers without compromising benefits to patients and customers.
Chapter 2 Aim and objectives
The overarching aim of this study was to inform the commissioning of NHS general pharmaceutical services in England by exploring variation in clinical productivity (levels of service delivery and service quality) in community pharmacy organisations and identifying the organisational factors associated with this variation.
The objectives were to:
-
explore variation in levels of service delivery across a representative sample of community pharmacies in England
-
investigate the relationships between organisational characteristics and levels of service delivery
-
investigate the inter-relationships between organisational characteristics, levels of service delivery and service quality
-
examine the mechanisms by which organisational factors influence both levels of service delivery and service quality
-
develop a toolkit to inform commissioning processes to improve clinical productivity in community pharmacy.
Chapter 3 Design and methodology
Theoretical framework
The design of this study was informed by organisational theory, in particular the framework proposed by Michie and West39 describing the relationships between organisational context (environment, structure and culture) and performance in health care. Moreover, it utilised the theoretical framework developed by Halsall et al. 7,40 for assessing the quality of community pharmacy services in terms of ‘accessibility’ (influenced by available structures and processes), ‘effectiveness’ (measured through patient, pharmacy, societal and health outcomes) and ‘positive perception of the experience’ (both from the patients’ and the pharmacists’/staff’s perspective). In addition, the study design was influenced by the comprehensive review of the body of work previously conducted by Jacobs et al. 22 describing the culture of community pharmacy organisations, its antecedents and outcomes. Each of these theoretical perspectives underpinned the design of both quantitative and qualitative data collection tools and informed the analysis, integration and interpretation of the data collected in this mixed-methods study.
As described previously (see Chapter 1, Definitions of clinical productivity), ‘clinical productivity’ has been defined and operationalised in a number of different ways in the research literature, but it is not commonly used in the context of community pharmacy. For the purposes of this study, clinical productivity was defined in terms of both quantity of service delivery (e.g. volume and range of essential and advanced services delivered) and service quality (e.g. satisfaction with information about and adherence to medicines).
Stakeholder engagement
From the outset, the study engaged a multidisciplinary project advisory group. Membership of this group consisted of lead pharmacists from NHS commissioning organisations in each of the five original study sites, senior representatives from two community pharmacy provider organisations, an independent pharmacist and representative of the Pharmaceutical Services Negotiating Committee (PSNC), two patient representatives (see Chapter 3, Patient and public involvement) and members of the research team. Each of these individuals was given the opportunity to contribute to the study design of the original proposal, for example, on methods of data collection, the disclosure of commercially sensitive information and other ethical issues, and patient and public involvement (PPI). The advisory group met together four times over the duration of the project, keeping the study grounded in the needs of the different stakeholder groups, providing guidance throughout the study and facilitating access to research sites.
In addition, concerted efforts were made to engage with the community pharmacy sector. Early on, a number of concerns had been voiced by community pharmacy organisations about the study including the workload demands on participating pharmacists, study access to commercially sensitive data and how the findings would be interpreted and used. The study was also due to commence at the time of the 2013 reorganisation of the NHS, which had led to fears of decommissioning of community pharmacy services within the sector and further sensitivities around the research. Advice was sought from the PSNC in relation to obtaining consent from participating organisations. The PSNC also disseminated the study plans to local pharmaceutical committees (LPCs) covering the areas in which the study was to be conducted. Subsequently, the study team contacted each of these LPCs and attended a number of LPC meetings (although others declined the offer). Explicit support for the study was obtained from four LPCs.
Also approached were the Company Chemists’ Association (CCA), which represents the nine biggest pharmacy multiples [Boots (Boots UK Ltd, Nottingham, UK), LloydsPharmacy (LloydsPharmacy Ltd, Coventry, UK), The Co-operative Pharmacy (Co-operative Pharmacy, Manchester, UK), Rowlands Pharmacy (Rowlands Pharmacy, Runcorn, UK), Tesco Pharmacy (Tesco plc, Welwyn Garden City, UK), Morrisons (Morrisons Supermarkets plc, Bradford, UK), Sainsbury’s (J Sainsbury plc, London, UK), Superdrug (Superdrug Stores plc, Croydon, UK) and Asda (Asda Stores Ltd, Leeds, UK)], which together make up approximately 50% of the community pharmacy market). The CCA would not offer its endorsement of the study, but instead requested that its member companies were approached individually to ascertain their level of support. This process led to four of the nine multiples declining to participate, which had important consequences for the stage 1 sample size and representativeness and, thus, led to a significant study amendment (see Chapter 3, Study Design, Stage 1, Sample).
Patient and public involvement
This study sought to integrate PPI into all stages in the research process from the design of the study through to interpretation of the data, toolkit development and dissemination of the findings.
Advice was received on early drafts of the original project proposal from an involvement and partnership manager of a local NHS trust, which not only helped with the design of the PPI element but also informed the research design. Their involvement at this stage also helped with the recruitment of PPI representatives to the project advisory group.
Two PPI representatives were recruited to the project advisory group, both of whom had previous experience advising on health services research studies. One was an older patient with a number of long-term conditions and who was involved in running a hospital-based cardiac patient group. The other was the main carer for a sibling with mental health (MH) problems and who was involved in running a carers’ support group. Both were regular users of community pharmacy services to support medicines usage. Both were given the opportunity to feed into the research proposal, which helped inform the methodology and strategies for dissemination from a patient/public viewpoint. Involvement in the project advisory group aimed to provide grounding for the study throughout in the experiences and needs of pharmacy patients.
In addition, presentations were made to local patient groups at key stages of the study to explain what we were doing and why, describe aspects of the methodology (e.g. patient survey) and to present early findings. Feedback was invited after each presentation to inform the development of data collection tools and survey methodology, and to help with interpretation of the findings.
Last, the two PPI advisory group representatives and two other members of the public recruited through an external PPI group were invited to contribute to the workshop for service commissioners and other pharmacy stakeholders held towards the end of the study to inform the development of the commissioning toolkit (see Chapter 3, Commissioners’ workshop and toolkit development).
Setting
The study was originally designed to be conducted in five geographical locations across England described by now obsolete PCT administrative boundaries. This design was appropriate given the original plan of obtaining pharmacy service activity data from the PCTs as service commissioners (although this was later changed – see Chapter 3, Study Design, Stage 1, Data sources). The original five sites were purposively selected to cover a geographically diverse range of affluent/deprived areas of dense/sparse populations and included one healthy living pharmacy (HLP) pathfinder site.
However, non-participation in the study by a number of national community pharmacy chains (see Chapter 3, Stakeholder engagement) necessitated an expansion of the number of sites from five to nine to maintain sample size. A pragmatic decision was made to expand the original five areas to adjoining sites to build on the now-existing relationships made with local National Institute for Health Research (NIHR) clinical research networks (CRNs) that were helping with aspects of data collection while maintaining the geographical and sociodemographic diversity of the sites. A brief description of each area and its community pharmacy provision is provided in Table 1.
| Commissioning locality (based on original PCT boundaries) | Description | Number of community pharmacies | Number of independents (five or fewer branches) (%) | Average number of prescription items dispensed per month per pharmacy 2010–11 | Average number of MURs per pharmacy 2010–11 |
|---|---|---|---|---|---|
| Merseyside (pop. 1,160,000) | An extensive area of NW England with a mixture of urban and rural areas, with areas of affluence and high deprivation | 314 | 123 (39.2) | 6899 | 207 |
| Trafford (pop. 212,800) | Predominantly affluent urban area of NW England with some areas of deprivation | 59 | 22 (37.3) | 6413 | 244 |
| Central and Eastern Cheshire (pop. 453,000) | Predominantly affluent suburban/rural area of NW England with pockets of deprivation | 98 | 20 (20.4) | 6672 | 241 |
| Cambridgeshire (pop. 607,000) | Predominantly rural county in SE England with few urban settlements. Predominantly affluent with pockets of deprivation | 101 | 35 (34.7) | 6311 | 200 |
| Peterborough (pop. 178,000) | Urban area in SE England, ethnically diverse with areas of high deprivation | 41 | 19 (46.3) | 6013 | 168 |
| Hertfordshire (pop. 1,095,000) | A large rural and suburban area of SE England. Predominantly affluent with pockets of deprivation | 238 | 137 (57.6) | 5712 | 218 |
| Sheffield (pop. 547,000) | Large urban area, ethnically diverse with areas of high deprivation. HLP pathfinder site | 118 | 29 (24.6) | 7663 | 217 |
| Doncaster (pop. 291,600) | Predominantly urban area of NE England with some rural areas. Areas of high deprivation | 73 | 13 (17.8) | 7235 | 218 |
| Rotherham (pop. 255,000) | Predominantly urban area of NE England with some rural areas. Areas of high deprivation | 58 | 13 (22.0) | 7535 | 219 |
Study design
This was a mixed-methods study with a number of strands of both quantitative and qualitative data collection over two stages, followed by a workshop for service commissioners and other community pharmacy stakeholders designed to inform the development of a commissioning toolkit through discussion of the study findings.
Stage 1
The first stage of the study was purely quantitative, combining analysis of existing data sets with primary data collection to examine variation in levels of service delivery across community pharmacies (objective i) and to investigate associations between organisational characteristics and levels of service delivery (objective ii).
Sample
The original plan was to approach all community pharmacies in the original five study areas to participate (n ≈ 632). Based on a 5% level of statistical significance and assuming a non-response rate of 33% (i.e. 420 pharmacies would respond), this would have provided the study with > 90% power to detect a correlation as small as 0.16 between organisational factors and clinical productivity. Even if the non-response rate reached 50%, the study would still have > 80% power to detect such a correlation.
However, non-participation in the study by four national community pharmacy chains (see Chapter 3, Stakeholder engagement) required the exclusion of all associated pharmacies from the original sample. Extending the study into nine geographical areas (as described above), with the exclusion of the non-participating chains, provided an overall sample size of n = 817. Based on a 5% level of statistical significance and assuming a non-response rate of 50% (i.e. 410 pharmacies would respond), this gave the study 90% power to detect a correlation as small as 0.16 between organisational factors and clinical productivity. Even if the non-response rate reached 66%, the study would still have 77% power to detect such a correlation. A lower response rate was anticipated following the negative response to the study received from some parties during the stakeholder engagement process (see Chapter 3, Stakeholder engagement).
Lists of names and full addresses for all pharmacies commissioned to provide NHS services in their area were obtained from each PCT (subsequently NHS England area teams) represented in the study, together with their organisational ‘F’ code (a unique NHS organisational identifier), obtained with the permission of LPCs. Pharmacies belonging to non-participating chains were removed manually.
Data sources
Community pharmacy activity data
The original plan had been to obtain monthly service activity data for pharmacies in the sample from service commissioners (PCTs at the time the study was designed). PCTs were then responsible for the routine collection of data from pharmacies in respect of delivery of the general pharmaceutical services contract including monthly dispensing volume and numbers of advanced (MURs and NMS interventions) and enhanced services. Provisional agreement from PCT lead pharmacists that these data would be provided for each pharmacy, identified by postcode and organisational ‘F’ code, had been obtained from the original five study sites.
However, the 2013 reorganisation of the NHS and subsequent fragmentation of the commissioning of general pharmaceutical services between NHS England (essential and advanced services), CCGs (locally commissioned services – previously enhanced services) and local authorities (locally commissioned services – public health) coincided with the start of this study. In order to ensure consistency in the data obtained and to lessen the burden placed on the new, pared down, commissioning bodies, it was decided to request these data instead from the NHS Business Services Authority (BSA), which are responsible for collating the data on the community pharmacy contract for payment purposes.
With approval from the NHS England Senior Information Risk Owner, monthly data for all pharmacies in England for the period April 2011 to October 2013, inclusive, were requested from the NHS BSA. Variables included numbers of dispensed items, numbers of MURs declared, numbers of NMS interventions declared and numbers of a range of (unspecified) enhanced services. The data set requested also included the organisational ‘F’ code (premises), ‘Y’ code (head office) and postcode identifiers for each pharmacy for data linkage purposes only. Once all data sets (including stage 2 survey data) were linked, however, all data were anonymised through removal of these identifiers.
Survey of community pharmacies
An 8-sided self-completion questionnaire (see Appendix 1) was distributed to all pharmacies (bar those belonging to non-participating chains) in the nine study areas in February 2014 to collect data on their organisational characteristics. Distribution of the questionnaire, together with a participant information sheet, covering letter and reply-paid envelope, was by post, addressed to the lead pharmacist, with an option to complete a web-based version developed using the Qualtrics (Qualtrics, Provo, UT, USA) online survey platform. Two postal reminders (including additional copies of the questionnaire) were sent at 3-week intervals.
Information was collected on key organisational characteristics, which have been shown in previous research to influence care provision. 18,19,22–24,26,27,29 These included items on:
-
ownership type [supermarket, multiple (> 200 branches), medium-sized chain (26–200 branches), small chain (6–25 branches), independent (< 6 branches)]
-
location (geographical and physical)
-
contract and opening hours
-
staffing and skill mix (numbers and types of pharmacists and other pharmacy staff)
-
use of locums (number, frequency and regularity of locum use)
-
working hours/patterns of main pharmacist (hours worked per week, shift patterns)
-
management structure (pharmacy manager is pharmacist or not, pharmacist managed by pharmacist or non-pharmacist)
-
pharmacy/general practice integration
-
organisational culture
-
safety climate.
Most of these items were developed from items validated through previous community pharmacy surveys conducted by the research team.
Organisational culture was measured using the Pharmacy Service Orientation (PSO) tool validated for use in community pharmacies,42 which has been used successfully in a recent postal survey of English community pharmacies to discriminate between different types of pharmacy organisation (Dr Sally Jacobs, personal communication). This short tool is scored on the basis of three 1–10 semantic differential scales whereby respondents are asked to rate their pharmacy’s ‘orientation’ (patient vs. product), ‘focus’ (quality vs. quantity) and ‘pharmacists’ work’ (professional vs. technical). A tick placed on a vertical line is scored as a whole number between 1 and 10; a tick placed between two vertical lines is scored as the halfway point (e.g. 1.5, 2.5, etc.). The PSO variable for each pharmacy is calculated as the mean of the three semantic differential scales. Higher scores indicate a pharmacy more closely aligned to the patient, quality and professional work (the pharmaceutical care paradigm)2 than to the product, quantity and technical work (the traditional pharmacy role).
The questionnaire also collected data on safety climate using the validated Pharmacy Safety Climate Questionnaire (PSCQ), which captures the pharmacy’s collective attitudes and behaviours regarding patient safety. 43,44 This 24-item questionnaire, scored on a five-point Likert scale (from 1 = strongly disagree to 5 = strongly agree) elicits four domains of safety climate: organisational learning (willingness to develop and maintain safety), blame culture (propensity to blame individuals when an incident occurs), working conditions (the extent to which the working environment supports safe working) and safety focus (the priority given to safety in day-to-day work). Higher scores correlate with safer working conditions apart from for ‘blame culture’, which is reverse scored.
The questionnaire was piloted with a sample of community pharmacy managers, recruited through existing contacts, using cognitive interviewing techniques. 45 Nine interviews were carried out with pharmacists and non-pharmacist pharmacy managers based at separate pharmacies, covering six different companies (two independents, three large multiples and one medium-sized multiple). The questions were redrafted, through an iterative process, during the cognitive interviewing period, to allow suggested changes to be piloted in later interviews. Further piloting was undertaken on the final version and pharmacist and non-pharmacist colleagues within Manchester Pharmacy School piloted the online questionnaire.
Secondary demographic and socioeconomic data sets
Determinants of the demographic, socioeconomic and health-needs status of the population within the immediate individual pharmacy locality were obtained from national secondary data sets. These included (1) the income deprivation domain of the 2010 English Indices of Multiple Deprivation (IMDs),46 allowing the comparison of relative levels of material deprivation local to community pharmacies; (2) Office for National Statistics 2011 Census data47 reporting the proportion of the local population who, for example, have a self-reported limiting long-term illness or are aged ≥ 65 years. Local determinants were attributed to pharmacies by linking pharmacy postcodes to super output areas, which are geographical units of approximately 1500 people. Super output areas are commonly used to measure and compare the local concentration, extent or weighted averages of population characteristics; and (3) local area health need and pharmaceutical services information were sourced from the 2011/12 QOF disease prevalence data48 for conditions for which community pharmacies (can) provide clinical services [e.g. coronary heart disease (CHD), asthma].
There are some limitations to attaching super output area data to individual community pharmacies, particularly in the case of supermarket pharmacies and city centre/shopping centre pharmacies, which are more likely to serve a wider and less easily defined population. However, almost 90% of people either visit the same pharmacy all of the time or one pharmacy most often and for a similar proportion, the main pharmacy they visit is located near where they live or their GP. These proportions are even greater for those with long-term conditions (i.e. those more likely to take in prescriptions to dispense or to be offered a MUR). In the absence of pharmacy lists or data collected directly in relation to pharmacy customers, these are therefore the best available data.
Data preparation and analysis
Data from paper questionnaires returned (n = 260) were entered onto a SPSS database (version 20; IBM Corporation, Armonk, NY, USA) and merged with data extracted from online questionnaire returns (n = 25). Frequencies and cross-tabulation were used to check for outliers, missing data, double-digit entry and variable inconsistencies, and all errors corrected with reference to original questionnaire returns. A double data entry check was performed on a 15% sample of responses (41/285) to assess the accuracy of data entry (0.4% errors detected).
Data from the community pharmacy questionnaire were ‘merged’ with both the national activity data and the demographic and socioeconomic data using the organisational ‘F’ code and postcode. Data for only one pharmacy could not be matched to the national data sources due to the removal of the study identification (ID) by the respondent.
Two series of regressions were conducted: one on the stage 1 survey data set (n = 277, following removal of returns from distance selling pharmacies; linked to activity and demographic/socioeconomic data); the other on the national data set [n = 10,973 following exclusion of pharmacies with extremely high or low annual dispensing volumes relative to other pharmacies (outliers, n = 60) and those for which a full set of data for 2012/13 was unavailable] of community pharmacy activity (linked to demographic and socioeconomic data sets but not to organisational variables).
The unit of analysis was the individual pharmacy. When analysing the subset of pharmacies that participated in the survey, the geographical study site was treated as a fixed effect given that we were not planning to generalise to pharmacies outside the nine study sites. For the national data, we had the entire population of pharmacies at the time and, in such circumstances, hypothesis testing is not recommended as there is no wider population to which the results are generalisable. However, we treat this exploratory analysis as though it were on a sample of pharmacies that could ever have existed (in the past, currently or in the future).
The outcomes of primary interest were yearly dispensing volume and yearly volume of advanced services (separately, MURs conducted and NMS interventions claimed for). These were calculated by summing individual monthly data for the latest financial year available in the national data set (April 2012 to March 2013 inclusive). The secondary outcomes of interest were numbers and volume of enhanced services and safety climate (domains of the PSCQ). However, the data on enhanced services obtained from the NHS BSA proved to be incomplete because of local payment mechanisms for these services often bypassing the BSA management information system; therefore, the planned analysis of enhanced service activity was not possible.
Initially, the variation in our primary and secondary outcome measures was investigated using appropriate summary statistics [mean/standard deviation (SD) or median/interquartile range (IQR)]: these are also reported by key organisational factors (e.g. ownership type). Using Stata statistical software (version 13; StataCorp LP, College Station, TX, USA), a series of univariable linear (for dispensing volume), ordered logistic (for advanced services, following categorisation of the original scale variables) or multivariate linear (for safety climate) regression models were fitted to determine which pharmacy-level organisational variables (for the survey sample only) and/or areal-specific demographic, socioeconomic and health-needs variables were associated with each outcome. To ensure the multivariable examination of all variables likely to have an association with the outcome, a conservative p-value of 0.2 was employed to indicate a significant association. Independent variables meeting this criterion were then included in an appropriate multivariable regression model to determine if their association persisted on controlling for other factors. Study site and pharmacy ownership type were added to the model at this point. Variables were retained in the ‘final’ model, along with ownership type and study site and after removal of collinear ones, if significance at p = 0.05 was achieved.
When analysing data from the survey of pharmacies from each of the nine study sites, probability weights were applied, in order to make the sample of respondent pharmacies more representative of the population of pharmacies in their area. The weight equates to the number of pharmacies of each ownership type, within their commissioning locality (as described by the original PCT or PCT cluster), that each respondent pharmacy ‘represents’ and is calculated as the ratio of the number of each pharmacy type within the locality to the number of each pharmacy type within the locality that responded to the survey (i.e. the inverse of the probability of response). Weights varied from 4/3 to 6.5, which is a narrow range.
Stage 2
The second stage of data collection incorporated both quantitative and qualitative elements. Quantitative methods examined the inter-relationships between organisational characteristics, levels of service delivery and service quality (objective iii). Qualitative methods explored issues around levels of service delivery and service quality in community pharmacies, their relationship and the mechanisms by which they are influenced by organisational characteristics (objective iv).
Sample
Study sites
Forty-one community pharmacies were randomly selected from the stage 1 community pharmacy survey respondents to be invited to participate in stage 2 using the stratified sampling strategy outlined in Table 2. The plan in the original proposal had been to select 40 pharmacies from across the original five study sites – two of each ownership type (supermarket, multiple, small/medium-sized chain, independent) from each NHS area – but this was modified slightly following the expansion in the number of study sites and once the distribution of respondents to the stage 1 survey was known. To recruit pharmacies, letters of invitation, study information sheets and letters of endorsement from the corresponding LPC (when available) were sent out by post, addressed to a named pharmacist. This was followed up 1 week later with a telephone call to discuss the study with the lead pharmacist and further e-mail and telephone communication as required to recruit pharmacies. Agreement from the head office was also sought for pharmacies belonging to chains. When a selected pharmacy declined to participate in stage 2, or when the selected pharmacy did not offer MURs or was unlikely to conduct enough MURs to provide the required sample of patients for the patient survey, they were substituted by another pharmacy of the same type, from the same NHS area, chosen at random. This process of substitution continued until all potential pharmacies in each cell were used up. Thereafter a ‘next best’ approach was taken to maintain the overall distribution of the sample as far as possible.
| Site | Independents | Small and medium-sized multiples | Large multiples and supermarkets | N/K | Total |
|---|---|---|---|---|---|
| Cambridgeshire and Peterborough | 2 (17) | 2 (5) | 2 (15) | (0) | 6 (37) |
| C&E Cheshire | 2 (5) | 2 (5) | 2 (13) | (0) | 6 (23) |
| Doncaster and Rotherham | 2 (6) | 2 (6) | 2 (15) | (0) | 6 (27) |
| Hertfordshire | 2 (37) | 2 (9) | 2 (19) | (1) | 6 (66) |
| Merseyside | 3 (29) | 3 (28) | 3 (32) | (3) | 9 (92) |
| Sheffield | 2 (8) | 2 (5) | 2 (10) | (0) | 6 (23) |
| Trafford | 1 (5)a | 0 (0)b | 1 (5) | (0) | 2 (10) |
| Total | 14 (107) | 13 (58) | 14 (109) | (4) | 41 (278) |
Once pharmacies had agreed to participate, a training session lasting up to 1 hour was organised for the lead pharmacist and any other staff who may be involved. Pharmacies were provided with the study materials (patient questionnaire packs, distribution instructions booklets, study poster, prompt stickers, eligibility flow charts, log sheets) and taken through the process of questionnaire distribution and eligibility/ineligibility criteria.
Pharmacies were offered a flat fee of £200 for participating in the study, which recognised their involvement in the training session, logging and monitoring of questionnaire distribution, and optional participation in the stage 2 stakeholder interviews. In addition, service support costs were offered by the NIHR CRNs at a rate of £11 for each patient questionnaire returned to the research team.
Subjects (patient survey)
Each pharmacy recruited for stage 2 of the study was asked to distribute a self-completion questionnaire to two samples of 30 consecutive walk-in patients following receipt of (a) dispensing and (b) MUR services. Calculation of the size of the sample required was based on detecting a 2-point difference in patient-average Satisfaction with Information about Medicines Scale (SIMS) scores (see Data sources) between any pair of ownership types. Assuming that the population SD of SIMS scores is 5 points,49–51 in a sample of 40 pharmacies, 30 patients per pharmacy would be required to detect such a difference with 80% power, at the 5% level of statistical significance. Furthermore, assuming a non-response rate of 50% and an intrapharmacy correlation coefficient of 0.05, 1200 patients in receipt of dispensing services and 1200 patients undergoing a MUR would need to be surveyed (n = 2400 in total).
Patients who had received the NMS were not surveyed as this was a newly introduced service still requiring time to ‘bed in’. Furthermore, the NMS was, at the time, undergoing a national evaluation having only been commissioned until March 2013 and it was not known if the service would continue to be commissioned. Patients in receipt of enhanced or locally commissioned services were not surveyed as the provision of these services in different pharmacies and geographical locations is highly variable.
A number of inclusion and exclusion criteria were applied to the sample.
The inclusion criteria were as follows:
-
walk-in patients only
-
received either a MUR or a NHS dispensing service from the pharmacy
-
aged ≥ 18 years
-
sufficiently fluent in English to be able to understand and complete the questionnaire.
The exclusion criteria were as follows:
-
those presenting private prescriptions (including veterinary prescriptions)
-
those presenting NHS prescriptions for appliances (elasticated garments, wound management products) or borderline substances
-
emergency supplies requested by a member of the public or a prescriber
-
patients receiving supervised consumption (including, but not limited to, methadone and buprenorphine).
Selecting only walk-in patients excluded those unable to visit the pharmacy themselves (often those more disabled or ill and older people) who account for, on average, around 1 in 4 prescriptions dispensed. 52 However, this was done for a number of methodological reasons. First, MURs are conducted opportunistically and in store in the vast majority of patients, already excluding those not visiting the pharmacy in person. Second, for those using dispensing services by proxy, variation in satisfaction with information received about medicines is far less likely to relate to the quality of the service provided by the pharmacist or pharmacy staff (e.g. it may relate to the way in which their proxy relayed the information given; the patient may be more likely to rely on a different health professional for information about their medicine). Furthermore, including both walk-in patients and those collecting medicines by proxy using consecutive sampling would risk wide variation in the proportions of each type of patient in the samples achieved for different pharmacies (contingent on population demographics), thus making direct comparisons of outcomes less robust.
To avoid the potential problem of cherry-picking, the importance of distributing questionnaires to consecutive patients to avoid research bias was stressed during the training session described above and pharmacies were informed that spot checks would be made on progress. To facilitate this, pharmacists/pharmacy staff were required to keep a log of all questionnaires distributed and researchers remained in regular telephone contact with each of the pharmacies throughout the period of recruitment.
Subjects (qualitative interviews)
Semistructured interviews were conducted during stage 2 of the study with front-line and superintendent pharmacists and service commissioners. Up to 50 interviews were sought with stakeholders, selected purposively to include at least one service commissioner (representatives from NHS England area teams and CCGs) from each of the nine geographical areas and a cross-section of front-line/superintendent pharmacists and pharmacy ownership categories across the study sites. As rules of thumb, between six and eight in-depth interviewees are required to reach data saturation in homogenous samples (i.e. no new themes will emerge by recruiting further participants), or between 30 and 50 per study, taking into account the nature and diversity of the population. 53
Data sources
Patient survey
A self-completion questionnaire (see Appendix 2) was distributed by the pharmacist/pharmacy staff in each of the participating pharmacies to two consecutive samples of eligible patients as described above. After their MUR or on receipt of their prescribed medication, patients were handed an envelope containing the questionnaire, participant information sheet and cover letter, and a reply-paid envelope for return of the completed questionnaire directly to the research team.
The eight-sided questionnaire contained the following sections:
-
reasons for visiting the pharmacy (service received, usual pharmacy or not, choice of pharmacy)
-
a 15-item community pharmacy patient satisfaction scale54 and a single item measuring overall satisfaction with visit
-
medication and information/advice received (number of medicines taken, new or repeat medication received, nature of information/advice received, category and continuity of advice-giver)
-
the 17-item SIMS55
-
the 5-item Medication Adherence Report Scale (MARS)56
-
the 8-item Beliefs about Medicines Questionnaire (BMQ)57
-
background data (sociodemographic, existing conditions).
There is a lack of validated instruments for measuring overall satisfaction with community pharmacy services based on sound theoretical underpinning. 58 Tinelli et al. ’s54 patient satisfaction scale was selected as it was developed in the UK, was relatively brief, was non-disease or medication specific, and it had been validated in a study of cognitive services in community pharmacy. The SIMS, MARS and BMQ are of proven reliability and validity, and have been widely used in research studies in a number of settings (including pharmacy) across a range of conditions and in several countries. 49–51,55,59–62
The patient satisfaction scale lists 15 statements that respondents are asked to rate on a five-point Likert scale, from 1 (strongly disagree) to 5 (strongly agree) according to how they felt about their visit to a pharmacy. In addition, following cognitive interview piloting, a ‘not applicable’ option was provided, which was scored 3 (equivalent to ‘neither agree nor disagree’). Following recoding of items 14 and 15, which are reverse scored, the mean item response was calculated (to take account of any missing items, up to a maximum of two) to give an overall satisfaction score ranging from 1 to 5, whereby higher scores indicate higher levels of self-reported satisfaction with the pharmacy visit.
The SIMS lists 17 statements that respondents are asked to rate according to the amount of information that they have received as follows: ‘too much’, ‘about right’, ‘too little’, ‘none received’ or ‘none needed’. Responses indicating that the patient is satisfied with the amount of information received (‘about right’ or ‘none needed’) are scored 1. Responses indicating that the patient is dissatisfied with the amount of information received (‘too much’, ‘too little’ or ‘none received’) are scored 0. In this study, missing data imputation was undertaken on a per-item, per-person basis, up to a maximum of two items. For each missing item, a unit response was imputed if a uniformly distributed random number (between 0 and 1) exceeded the observed probability of a unit response on that item in participants who had completed all SIMS items and had the same SIMS score prior to the imputation of that item. A zero response was imputed otherwise. Responses for all items were summed to give a total satisfaction score ranging from 0 to 17, where higher scores indicate higher levels of self-reported satisfaction with information received. For the purposes of this study, because of a highly skewed distribution (see Chapter 5, Service quality: stage 2 patient survey data set analysis), this score was recategorised as follows: 0–5, 6–10, 11–16 and 17.
The MARS lists five statements that respondents are asked to rate according to the frequency with which they engage in non-adherent behaviour as follows: ‘always’, ‘often’, ‘sometimes’, ‘rarely’ or ‘never’. Responses are scored from 1 (always) to 5 (never) and summed giving a scale ranging from 5 to 25, whereby higher scores indicate higher levels of self-reported adherence. No imputation of missing data was carried out for MARS items as it was fully completed by > 90% of respondents. For the purposes of this study, due to a highly skewed distribution (see Chapter 5, Service quality: stage 2 patient survey data set analysis), this score was dichotomised as follows: ≤ 20 = ‘low adherers’; > 20 = ‘high adherers’.
The BMQ lists eight statements that respondents are asked to rate according to the strength of their views about medicines in general as follows: ‘strongly agree’, ‘agree’, ‘uncertain’, ‘disagree’ or ‘strongly disagree’. Responses are scored from 5 (strongly agree) to 1 (strongly disagree). Two scales (‘general harm’ and ‘general overuse’), ranging from 4 to 20, are derived through summation of four of these items each, in which higher scores indicate stronger beliefs that medicines are harmful or that medicines are overused by doctors, respectively.
The questionnaire was piloted with a sample of community pharmacy users, recruited through existing contacts, using cognitive interviewing techniques. 45 Nine interviews were carried out. The questions were redrafted, through an iterative process, during the cognitive interviewing period, to allow suggested changes to be piloted in later interviews. Further piloting was undertaken on the final version through presentation and feedback at project advisory group and PPI group meetings.
Qualitative interviews
The qualitative study took a broadly phenomenological approach63 to explore the views and experiences of pharmacists, pharmacy managers and commissioners directly involved in the provision of community pharmacy services. This approach uses one-to-one interviews to develop first-hand accounts of the subjective experiences of individuals. From these accounts, common themes can be derived to understand the meanings individuals attach to the lived experience. 64
Semistructured, face-to-face and telephone interviews were conducted with pharmacy and commissioning representatives from across all study sites, as described above. Topic guides specific to each stakeholder group (see Appendix 3 for the pharmacist interview topic guide) were developed from the aims of the research and the research literature and covered the following areas:
-
background information about the respondent and their organisation
-
defining clinical productivity
-
the quality and quantity of community pharmacy services (definitions, levels achieved, organisational and other influences)
-
recent changes in clinical productivity (organisational and other influences)
-
maximising clinical productivity and how this could be achieved
-
measuring and monitoring clinical productivity.
Lines of questioning explored the relationship between the quantity and quality of service provision in community pharmacies, opportunities and barriers to maximising clinical productivity in this setting and the mechanisms by which different organisational characteristics may help or hinder this objective. A prompt sheet listing the organisational factors of interest to the study (see Appendix 3) was sent to interviewees in advance for reference during the interview.
Data preparation and analysis
Quantitative data
Data from patient questionnaires returned were entered onto a SPSS database. Frequencies and cross-tabulation were used to check for outliers, missing data, double digit entry and variable inconsistencies, and all errors corrected with reference to original questionnaire returns. A double-data entry check was performed on a 10 per cent sample of responses (100/1008) to assess the accuracy of data entry (0.06% errors detected).
Data from the patient questionnaire were merged with data from the pharmacy questionnaire using the pharmacy organisational F code. Of course, data from the latter source did not vary between patients attending the same pharmacy and, with this in mind, the responses of such patients to the patient questionnaire could be correlated; this was accounted for in all analyses in order to ensure that incorrect inferences were not made.
The unit of analysis was the patient. As alluded to above, patients are ‘clustered’ within pharmacy and this ‘multilevel’ structure was taken into account in all analyses at this stage. In addition, all regression models ‘control’ for the type of questionnaire distributed (dispensing or MUR).
The outcomes of primary interest were overall patient satisfaction, satisfaction with information about medication (measured on the SIMS) and self-reported medication adherence (measured on the MARS). Initially, each of these outcomes was tabulated and/or summarised using appropriate summary statistics; they are also reported by pharmacy ownership type.
Using Stata statistical software, a series of univariable linear (for overall satisfaction), ordered logistic (for SIMS) or binary logistic (for MARS) regression models were fitted to determine which patient- and pharmacy-level organisational variables and/or areal-specific demographic, socioeconomic and health-needs variables were associated with each outcome. To ensure the multivariable examination of all variables likely to have an association with the outcome, a conservative p-value of 0.2 was employed to indicate a significant association. Independent variables meeting this criterion were then included in an appropriate multivariable regression model to determine if their association persisted on controlling for other factors. Variables were retained in the ‘final’ model, after removal of collinear ones, if significance at p = 0.05 was achieved.
In order to simplify the calculation of the weights at this stage, we decided not to include any of the information from the stage 1 sampling process, but to create weights that represented only the stage 2 responses of the patients from the individual participating pharmacies. Pharmacies do not have a ‘fixed patient list’ (such as is the case for general practice) and we therefore made the assumption that pharmacy ‘population size’ was proportional to its dispensing volume (as calculated in stage 1). The stage 2 weight (which was equivalent for each patient attending the same pharmacy) was then derived as the inverse of the ratio of the percentage of the overall response at each pharmacy (n/1008) to the percentage of the dispensing volume reported at each pharmacy (when the denominator here is the total number of items dispensed across the participating pharmacies).
Qualitative data
All interviews were audio-recorded with consent and transcribed verbatim for analysis by a University of Manchester-approved supplier following strict data protection policies and procedures for data storage and transfer.
Interview data were thematically analysed using the framework approach65 using NVivo 10 (QSR International, Warrington, UK) qualitative analysis software to manage the process. Framework analysis involves five steps: (1) familiarisation, (2) developing a thematic framework, (3) indexing, (4) charting and (5) mapping and interpretation. In the current study, two researchers (TF and FB) undertook the first four steps collaboratively, developing the thematic framework through independent familiarisation with different sets of interview transcripts initially, followed by close discussion and agreement of the themes identified. Themes were derived from the interview topic guide in the first instance and latterly from the data themselves. When consensus could not be reached, a third researcher (SJ) was brought in. The agreed thematic framework was applied to the data and charted by TF and FB, but the final stage of mapping and interpretation was undertaken by the chief investigator (SJ).
Integration of stage 1 and stage 2 findings
Integration of the findings from the different stages and methodologies employed by the study was an important final step to building a rounded picture of the factors associated with variation in clinical productivity in community pharmacies. Methods of synthesis incorporated elements of triangulation of the data and also illustration and explanation of one set of findings by another. 66 For example, when findings from the survey indicated a significant association between particular organisational characteristics and productivity in terms of quantity of service provided, the qualitative data from interviews with stakeholders were interrogated to obtain information on the mechanisms of that association. We also looked for alternative explanations when findings from different stages of data collection diverged. This process of integration formed the basis of the discussion (see Chapter 8) and will provide the basis for any recommendations we make to service commissioners regarding commissioning processes, to community pharmacy organisations regarding their provision of NHS pharmaceutical services and to patient/public audiences regarding medicines usage.
Commissioners’ workshop and toolkit development
The final objective (v) of the study was to develop a toolkit informed by the study findings to help service commissioners improve their contracting processes with community pharmacies to promote clinical productivity (both quality and quantity) and, hence, value for money. To do this, a half-day workshop was organised in July 2015, in partnership with NHS Primary Care Commissioning (PCC), to which commissioners from the new NHS commissioning structures (NHS England and CCGs) from across the North West of England and further afield were invited. In addition, a number of community pharmacy representatives were invited, including from the PSNC, Pharmacy Voice (umbrella organisation incorporating the CCA, Association of Independent Multiple Pharmacies and National Pharmacy Association) and community pharmacy multiples, together with four members of the public.
The workshop was used to present the findings from the study and invite discussion and feedback in small mixed-group sessions, facilitated by the PCC (see Appendix 4 for the programme). The groups each recorded key discussion points on flipcharts and these were brought back to the larger group for final discussion. The PCC collated the findings of the discussions and these directly informed the first draft of the toolkit to which the research team added supporting summaries of the research evidence from the study. The toolkit (see Appendix 5), which will be made available electronically to service commissioners nationally through PCC channels, links to the six stages in the NHS commissioning cycle67 and provides guidance and supporting evidence for commissioners at each stage.
Research ethics
Research ethics approval was obtained for this study from the National Research Ethics Service Committee West Midlands – Edgbaston (13/WM/0137), which was subsequently endorsed by the University of Manchester Research Ethics Committee (reference number 13025). Site-specific NHS research governance approval was obtained from all of the relevant local NHS research and development offices.
Chapter 4 Findings: associations between organisational characteristics and levels of service delivery
Community pharmacy survey response rate and sample characteristics
Of the 817 questionnaires distributed, 285 were returned completed to the research team, 260 by post and 25 online. A further nine were returned undelivered. Eight questionnaires that had been completed by distance-selling pharmacies (those dispensing by post and not face to face) were removed from the sample. The total valid response rate was therefore 34.6% (277/800).
Descriptive statistics for each of the key independent variables used in the analysis of community pharmacy activity in the survey data set (and, later, in the analysis of quality outcomes in Chapter 5) are presented in Table 3.
| Variable | Sample data, n (%) | N |
|---|---|---|
| Job title (respondent) | ||
| Owner | 55 (20.1) | 273 |
| Manager | 168 (61.5) | |
| Other pharmacist | 50 (18.3) | |
| Type of pharmacy | ||
| Independent (< 6 stores) | 111 (40.1) | 277 |
| Small multiple (6–25 stores) | 41 (14.8) | |
| Medium-sized multiple (26–200 stores) | 9 (3.2) | |
| Large multiple (> 200 stores) | 91 (32.9) | |
| Supermarket | 25 (9.0) | |
| Geographical location | ||
| City centre | 18 (6.6) | 274 |
| Large town | 43 (15.7) | |
| Small town | 81 (29.6) | |
| Suburb | 96 (35.0) | |
| Village/rural | 36 (13.1) | |
| Pharmacy open for ≥ 3 years | ||
| No | 22 (8.0) | 274 |
| Yes | 252 (92.0) | |
| HLP | ||
| No | 192 (72.2) | 266 |
| Yes | 74 (27.8) | |
| Pharmacy contract held | ||
| Standard 40 hours | 230 (84.2) | 273 |
| 100 hours | 30 (11.0) | |
| Other | 13 (4.8) | |
| Opening hours per week | ||
| Mean (SD) | 55.8 (17.4) | 274 |
| Median (IQR) | 50 (45–56) | |
| Range | 36–104 | |
| Number of staff working on a typical day | ||
| Mean (SD) | 5.4 (2.2) | 268 |
| Median (IQR) | 5 (4–6.5) | |
| Range | 1–18 | |
| Pharmacists working on a typical day | ||
| 1 | 219 (80.5) | 272 |
| ≥ 2 | 53 (19.5) | |
| Registered pharmacy technician (typical day) | ||
| No | 159 (58.2) | 273 |
| Yes | 114 (41.8) | |
| ACT (typical day) | ||
| No | 209 (75.7) | 276 |
| Yes | 67 (24.3) | |
| Use of locums | ||
| Not regularly | 118 (42.6) | 277 |
| Regularly | 159 (57.4) | |
| Is the pharmacy manager a pharmacist? | ||
| No | 30 (10.9) | 274 |
| Yes | 244 (89.1) | |
| Work pattern of main pharmacist | ||
| Standard hours (8 a.m.–6 p.m.) | 165 (59.6) | 277 |
| Non-standard | 112 (40.4) | |
| Average daily working hours of main pharmacist | ||
| Mean (SD) | 9.2 (1.1) | 270 |
| Median (IQR) | 9.0 (8.5–9.75) | |
| Range | 5–15 | |
| Organisational culture (PSO) | ||
| Mean (SD) | 7.3 (1.4) | 269 |
| Median (IQR) | 7.5 (6.5–8.2) | |
| Range | 3.5–10 | |
| Relationship with nearest GP surgery | ||
| Very good | 136 (49.1) | 277 |
| Good | 83 (30.0) | |
| Satisfactory/poor/none | 43 (15.5) | |
| No GP surgery identified | 15 (5.4) | |
The proportion of independently owned pharmacies in this sample of respondents was comparable to the national figure of 38.9% in March 2014. 38 Nearly two-thirds were located in small towns or suburbs with only a small proportion in city centres or rural settings. Most were established pharmacies operating on a standard contract; over one-quarter were either accredited as having, or working towards, HLP status.
There was a wide range of staffing levels with three-fifths of the pharmacies in this sample operating on a one-pharmacist model. Approximately two-fifths of pharmacies employed a pharmacy technician on a typical day, one-quarter employed an accuracy checker or accuracy-checking technician (ACT), and around 10% had a non-pharmacist pharmacy manager. Over half regularly used locum pharmacists on a daily or weekly basis. Weekly opening hours varied between 36 and 104 hours, and the average daily working hours of the main pharmacist, two-fifths of whom worked non-standard hours (shifts or extended working days), ranged from 5 to 15 hours.
As a measure of organisational culture, the mean (SD) PSO score in this sample was 7.3 (1.4), which was higher (i.e. more closely aligned to the patient, quality and professional work than to the medicine, quantity and technical work) than the mean value of 6.3 (1.8) found in a previous survey of 903 English community pharmacists (Dr Sally Jacobs, personal communication). The majority of pharmacies reported good or very good working relationships with their main GP surgery, where one could be identified: only 14% of pharmacies had not had any face-to-face contact with their main GP surgery over the previous 12 months and that contact had most commonly been made with the practice receptionist (82% of pharmacies) and least often with a practice pharmacist (17%). Sixty-four per cent of pharmacies in contact with their main GP surgery reported having had face-to-face contact with a GP in the previous 12 months.
Community pharmacy activity: stage 1 community pharmacy survey data set analysis
The first series of regression analyses conducted in stage 1 of the study were on quantity: annual dispensing volume, MURs and NMS interventions for 2012/13 for those pharmacies responding to the stage 1 survey (n = 277). This was to explore the associations between the organisational characteristics of the pharmacy, the socioeconomic and demographic characteristics of the local population and pharmacy activity.
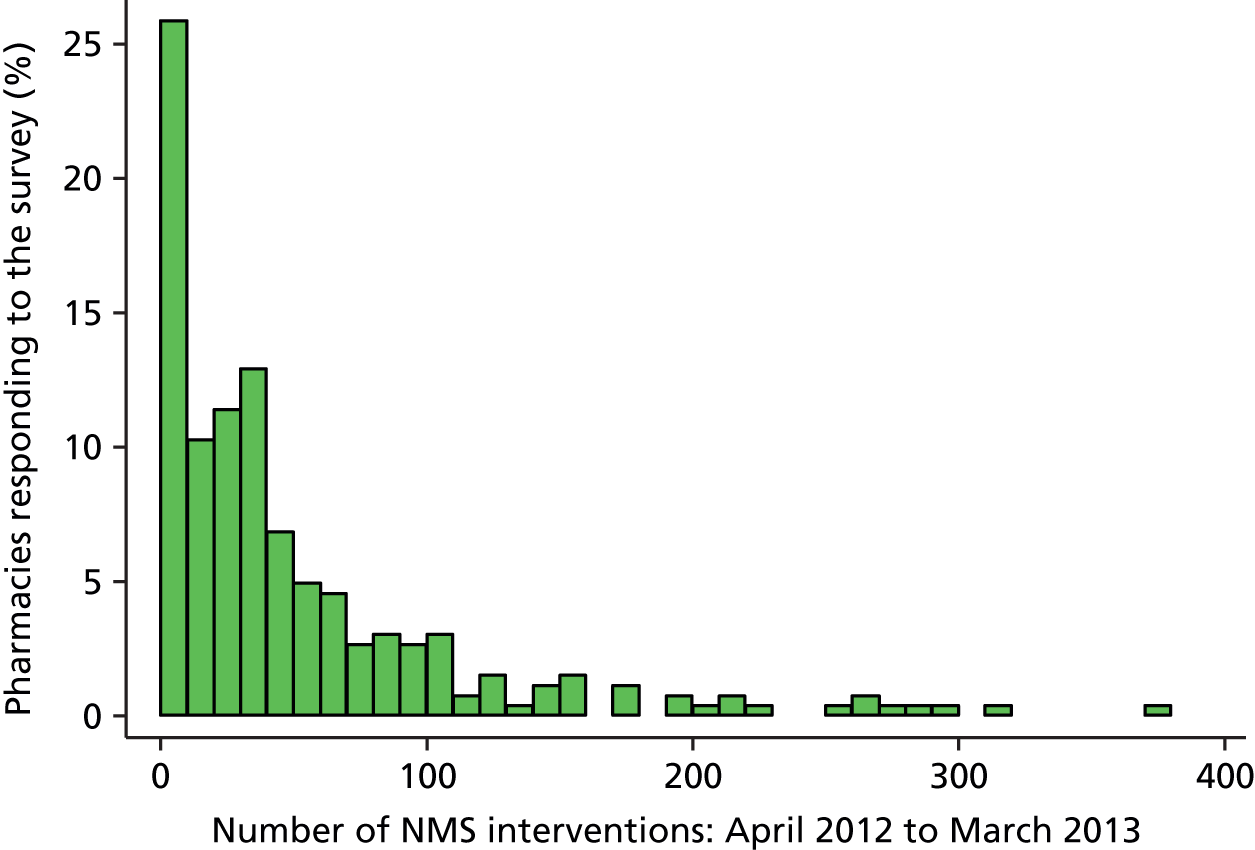
Summary statistics for annual dispensing volume, MURs conducted and NMS interventions, broken down by pharmacy ownership type, are presented in Table 4. Although this table presents summary statistics for each pharmacy ownership category, for the purposes of the subsequent regression analyses, ‘ownership type’ was collapsed into three categories – (1) independent, (2) small/medium-sized multiple and (3) large multiple/supermarket – to account for the small numbers of medium-sized multiples and supermarkets. The distributions of each of these primary outcome variables are given in Figures 1–3.
| Pharmacy ownership type | Number of items dispensed | Number of MURs | Number of NMS interventions |
|---|---|---|---|
| Independent (< 6 stores), n = 103 | |||
| Mean (SD) | 87,523 (55,181) | 165.2 (150.8) | 48.5 (76.2) |
| Median | 70,846 | 127 | 19 |
| IQR | 51,410–106,247 | 14–298 | 0–49 |
| Range | 5529–326,961 | 0–509 | 0–376 |
| Small multiple (6–25 stores), n = 35 | |||
| Mean (SD) | 76,271 (27,963) | 273.9 (139.6) | 53.3 (57.1) |
| Median | 72,338 | 312 | 38 |
| IQR | 59,796–93,441 | 154–402 | 14–68 |
| Range | 19,313–143,981 | 0–415 | 0–258 |
| Medium-sized multiple (26–200 stores), n = 9 | |||
| Mean (SD) | 72,688 (36,223) | 226.3 (128.6) | 48.1 (51.2) |
| Median | 59,135 | 219 | 29 |
| IQR | 51,025–101,212 | 131–320 | 2–68 |
| Range | 33,499–141,046 | 52–412 | 0–148 |
| Large multiple (> 200 stores), n = 91 | |||
| Mean (SD) | 90,131 (37,567) | 283.7 (114.8) | 49.6 (53.4) |
| Median | 82,814 | 303 | 32 |
| IQR | 62,607–120,209 | 196–397 | 15–67 |
| Range | 22,536–225,460 | 0–473 | 0–297 |
| Supermarket, n = 25 | |||
| Mean (SD) | 53,868 (30,142) | 333.5 (95.8) | 67.2 (50.4) |
| Median | 56,547 | 386 | 46 |
| IQR | 25,595–75,730 | 281–400 | 33–101 |
| Range | 13,654–126,993 | 113–408 | 17–201 |
| Total, n = 277 | |||
| Mean (SD) | 83,221 (44,848) | 238.7 (145.3) | 51.3 (63.3) |
| Median | 74,187 | 261 | 31 |
| IQR | 53,869–104,810 | 114–386 | 8–67 |
| Range | 5529–326,961 | 0–509 | 0–376 |
FIGURE 1.
Distribution of the annual dispensing volume for pharmacies responding to the stage 1 survey (n = 277).

FIGURE 2.
Distribution of the annual number of MURs conducted by pharmacies responding to the stage 1 survey (n = 277).
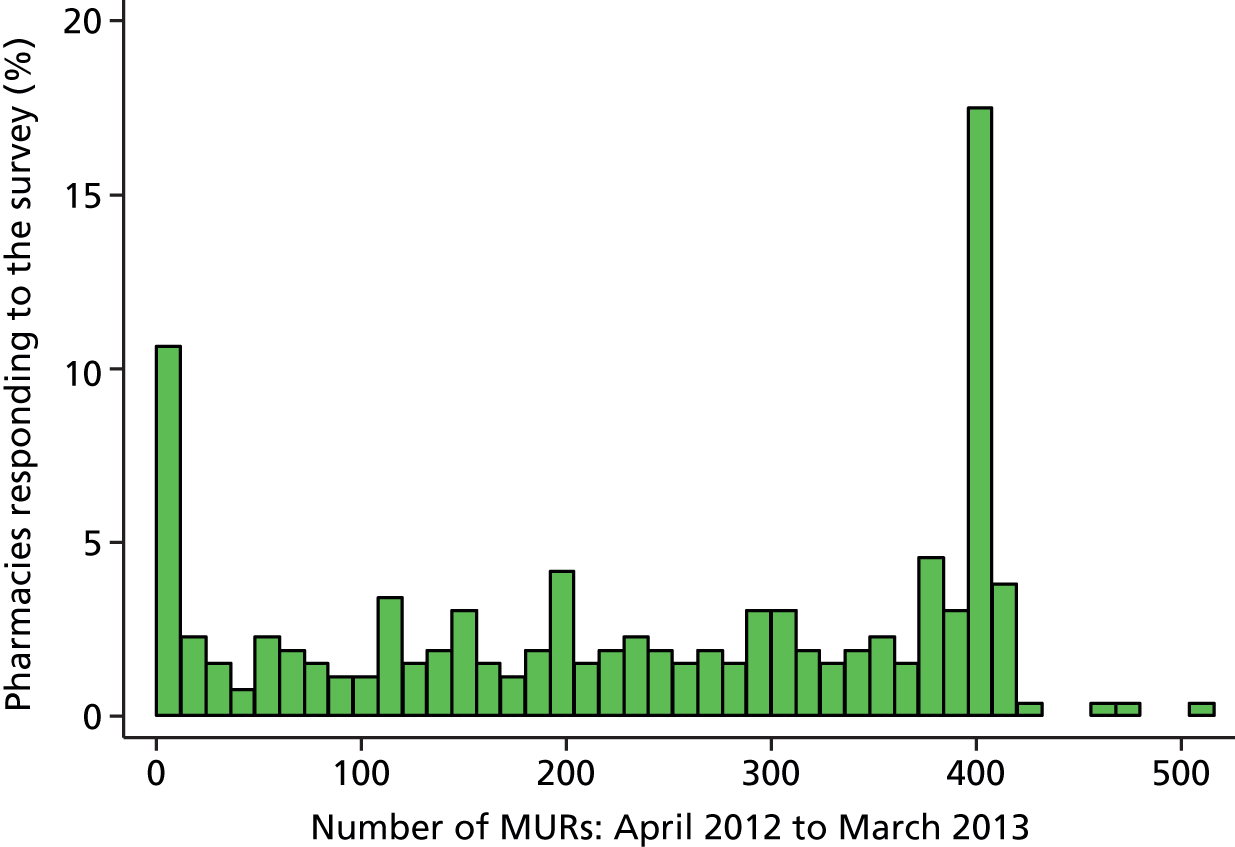
FIGURE 3.
Distribution of the annual number of NMS interventions conducted by pharmacies responding to the stage 1 survey (n = 277).
The median dispensing volume for the sample was 74,187 items per year with an IQR of 53,869–104,810. Supermarkets had the lowest annual dispensing volumes and large multiples had the highest (see Table 4). The distribution of annual dispensing volumes was positively skewed (see Figure 1); linear regression of the logarithmic value of dispensing volume was therefore used in its analysis to eliminate the long right-hand tail.
The distribution of the number of MURs conducted per year was fairly uniform (see Figure 2) except for a pronounced spike at 400 (the maximum number paid for) and another, smaller, spike at zero. The median value was 261 with an IQR of 114–386. Independent pharmacies conducted the fewest MURs annually (see Table 4). To account for the unusual distribution, this outcome variable was categorised as follows: 0–12, 13–200, 201–365, > 365 and ordinal logistic regression was used in its analysis.
The distribution of the number of NMS interventions conducted per year was highly positively skewed but with a pronounced spike at zero (see Figure 3). The median value for the sample was 31 with an IQR of 8–67. Independent pharmacies conducted the fewest NMS interventions overall (see Table 4), although a small number conducted the highest volume in this sample. As a logarithmic transformation would not have eliminated the spike at zero, this outcome variable was categorised as follows: 0, 1–12, 13–31, 32–52, 53–104, ≥ 105, and ordinal logistic regression was used in its analysis.
Dispensing volume
The full findings of the univariable and subsequent multivariable linear regressions of annual dispensing volume for stage 1 pharmacy survey respondents can be found in Appendix 6: a summarised version is presented in Table 5.
| Variable | Dispensing volume (2012/13), multivariable model | ||
|---|---|---|---|
| Coefficient | 95% CI | p-value | |
| Pharmacy open ≥ 3 years | |||
| No | Reference | 0.001 | |
| Yes | 0.3147 | 0.1233 to 0.5062 | |
| Pharmacists working (typical day) | |||
| 1 | Reference | 0.015 | |
| ≥ 2 | 0.0949 | 0.0188 to 0.1710 | |
| Registered pharmacy technician (typical day) | |||
| No | Reference | < 0.001 | |
| Yes | 0.1120 | 0.0599 to 0.1641 | |
| ACT (typical day) | |||
| No | Reference | < 0.001 | |
| Yes | 0.1655 | 0.1112 to 0.2197 | |
| Average daily working hours of main pharmacist | |||
| 1-hour change | 0.0314 | 0.0086 to 0.0541 | 0.007 |
| Organisational culture (PSO) | |||
| 1-unit change | –0.0194 | –0.0373 to –0.0014 | 0.035 |
| IMD score | |||
| 10-unit change | 0.0164 | 0.0024 to 0.0304 | 0.022 |
Staffing levels and skill mix had important associations with dispensing volume: pharmacies with higher dispensing volumes were significantly more likely to employ two or more pharmacists, have a registered pharmacy technician or an accuracy checker; a univariate analysis also demonstrated a positive association with the overall staff number (however, this was correlated with skill mix and, as we were more interested in skill mix, this variable was dropped from the multivariable analyses). The organisational culture of the pharmacy (measured using the PSO tool) also proved to be significantly associated with dispensing volume: pharmacies with higher dispensing volumes were assessed as having a greater focus on quantity, technical work and medicine than on quality, professional work and the patient. Pharmacies that had been open for ≥ 3 years also had significantly higher dispensing volumes. Dispensing volume was not associated with pharmacy ownership type.
As expected, the level of deprivation in the local population (IMD score) was significantly associated with dispensing volume. Although the local prevalence of a number of health-related variables was also significantly associated with dispensing volume (univariable analyses), some of these variables were dropped from the final multivariable model as a result of collinearity with IMD score and intercorrelation; those that were tested were not significantly associated with dispensing volume.
Volume of medicines use reviews conducted
The full findings of the univariable and subsequent multivariable ordered logistic regressions of annual volume of MURs conducted by the stage 1 pharmacy survey respondents can be found in Appendix 6: a summarised version is presented in Table 6.
| Variable | MURs (2012/13), multivariable model | ||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Weekly opening hours | |||
| 10-hour change | 1.25 | 1.06 to 1.49 | 0.010 |
| Patients with asthma (%) | |||
| 1% change | 0.42 | 0.21 to 0.86 | 0.018 |
| Log(dispensing volume) | |||
| 1-unit change | 5.88 | 1.76 to 19.6 | 0.004 |
| Type of pharmacy | |||
| Independent | Reference | < 0.001 | |
| Small/medium-sized multiple | 2.67 | 1.39 to 5.15 | |
| Large multiple/supermarket | 4.86 | 2.63 to 8.96 | |
The volume of MURs conducted by these pharmacies was strongly associated with annual dispensing volume. Controlling for this in the multivariable regression, pharmacy ownership type had the strongest association of the organisational variables with volume of MUR provision, with multiples, particularly large multiples and supermarkets, conducting significantly more MURs annually than independent pharmacies. Although a number of organisational factors were univariably associated with volume of MURs (HLPs, 100-hour pharmacies, those with more staff or employing a pharmacy technician or accuracy checker all conducted higher volumes of MURs), the only other organisational factor remaining in the final multivariable model was opening hours; pharmacies with longer opening hours conducted more MURs.
Unlike dispensing volume, the volume of MURs conducted was not related to the level of deprivation in the local population (IMD score). A significant association was seen, however, with the prevalence of asthma – although this was a negative association – with higher numbers of MURs being conducted in pharmacies with lower proportions of asthma in the local population. This significant association was seen in both univariable and multivariable models. There were no other significant associations with any demographic or socioeconomic variables.
Volume of new medicines service interventions
The full findings of the univariable and subsequent multivariable ordered logistic regressions of annual volume of NMS interventions conducted by the stage 1 pharmacy survey respondents can be found in Appendix 6: a summarised version is presented in Table 7.
| Variable | NMS interventions (2012/13), multivariable model | ||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Geographical location | |||
| City centre | 0.29 | 0.12 to 0.67 | |
| Large town | 1.84 | 0.69 to 4.96 | |
| Small town | Reference | < 0.001 | |
| Suburb | 1.61 | 0.85 to 3.03 | |
| Village/rural | 1.67 | 0.78 to 3.60 | |
| Pharmacists working on a typical day | |||
| 1 | Reference | 0.001 | |
| ≥ 2 | 3.25 | 1.67 to 6.32 | |
| Relationship with the nearest GP surgery | |||
| Very good | Reference | 0.017 | |
| Good | 1.15 | 0.60 to 2.17 | |
| Poor/none | 0.66 | 0.35 to 1.23 | |
| No GP surgery identified | 0.19 | 0.06 to 0.59 | |
| Type of pharmacy | |||
| Independent | Reference | < 0.001 | |
| Small/medium-sized multiple | 2.60 | 1.37 to 4.94 | |
| Large multiple/supermarket | 3.18 | 1.81 to 5.61 | |
Similar to MURs, pharmacy ownership type had one of the strongest associations with annual volume of NMS interventions with multiples, particularly large multiples and supermarkets, again conducting significantly more NMS interventions annually than independent pharmacies. Although dispensing volume was significantly positively associated with NMS volume in the univariable models, this relationship was found to be non-significant in the multivariable analysis. Another organisational characteristic strongly associated with annual volume of NMS interventions conducted was the number of pharmacists employed on a typical day, with those employing two or more conducting significantly more NMS interventions annually. Although overall staffing levels, weekly opening hours, the working pattern of the main pharmacist and HLP status were also significantly associated with NMS provision in the univariable analysis, none of these associations remained in the final multivariable model.
Unlike dispensing volume and MUR provision, both the geographical location of the pharmacy and the strength of its relationship with the local GP surgery were significantly associated with the volume of NMS interventions conducted annually. In particular, pharmacies located in city centres conducted significantly fewer NMS interventions than pharmacies in other locations and those unable to identify a local GP surgery with which they had a working relationship conducted significantly fewer than those indicating very good working relationships with their nearest GP surgery.
There were no significant associations found between annual volume of NMS interventions conducted and any demographic or socioeconomic variables.
Community pharmacy activity: national data set analysis
The second series of regressions conducted in stage 1 of the study, again focused on quantity of services provided, were on annual dispensing volume, MURs and NMS interventions for all pharmacies for which a full set of activity data was obtained from the NHS BSA for 2012/13, excluding outliers (n = 10,973). This was to explore the associations between pharmacy ownership type, the socioeconomic and demographic characteristics of the local population and pharmacy activity nationally.
Summary statistics for annual dispensing volume, MURs conducted and NMS interventions, broken down by pharmacy ownership type, are presented in Table 8. The distribution of each of these primary outcome variables are given in Figures 4–6.
| Pharmacy ownership type | Dispensing volume | Volume of MURs | Volume of NMS interventions |
|---|---|---|---|
| Independent (< 6 stores), n = 4081 | |||
| Mean (SD) | 77,640 (45,997) | 154.9 (148.5) | 48.8 (85.9) |
| Median | 67,549 | 109 | 13 |
| IQR | 46,623–98,010 | 12–280 | 0–61 |
| Range | 5277–466,277 | 0–902 | 0–1315 |
| Small multiple (6–25 stores), n = 984 | |||
| Mean (SD) | 80,278 (42,396) | 260.4 (143.2) | 59.2 (97.5) |
| Median | 72,724 | 297.5 | 27 |
| IQR | 49,741–101,391 | 138–400 | 5–73 |
| Range | 6012–350,514 | 0–810 | 0–1435 |
| Medium-sized multiple (26–200 stores), n = 809 | |||
| Mean (SD) | 78,440 (46,926) | 258.9 (129.7) | 53.6 (72.8) |
| Median | 69,756 | 257 | 27 |
| IQR | 43,192–106,614 | 143–400 | 8–70 |
| Range | 5352–381,181 | 0–526 | 0–644 |
| Large multiple (> 200 stores), n = 4208 | |||
| Mean (SD) | 91,700 (46,219) | 334.9 (104.6) | 72.1 (70.5) |
| Median | 83,306 | 391 | 52 |
| IQR | 59,465–114,860 | 295–400 | 25–98 |
| Range | 6861–411,618 | 0–797 | 0–697 |
| Supermarket, n = 891 | |||
| Mean (SD) | 55,760 (26,748) | 308.1 (103.9) | 39.9 (44.5) |
| Median | 52,308 | 354 | 27 |
| IQR | 36,210–71,374 | 229–399 | 7–57 |
| Range | 6526–172,644 | 0–474 | 0–280 |
| Total, n = 10,973 | |||
| Mean (SD) | 81,550 (45,685) | 253.5 (150.8) | 58.3 (78.7) |
| Median | 72,325 | 297 | 33 |
| IQR | 49,569–103,213 | 116–399 | 6–80 |
| Range | 5277–466,277 | 0–902 | 0–1435 |
FIGURE 4.
Distribution of annual dispensing volume for pharmacies in national data set (n = 10,973).

FIGURE 5.
Distribution of annual number of MURs conducted by pharmacies in national data set (n = 10,973).

FIGURE 6.
Distribution of annual number of NMS interventions conducted by pharmacies in national data set (n = 10,973).
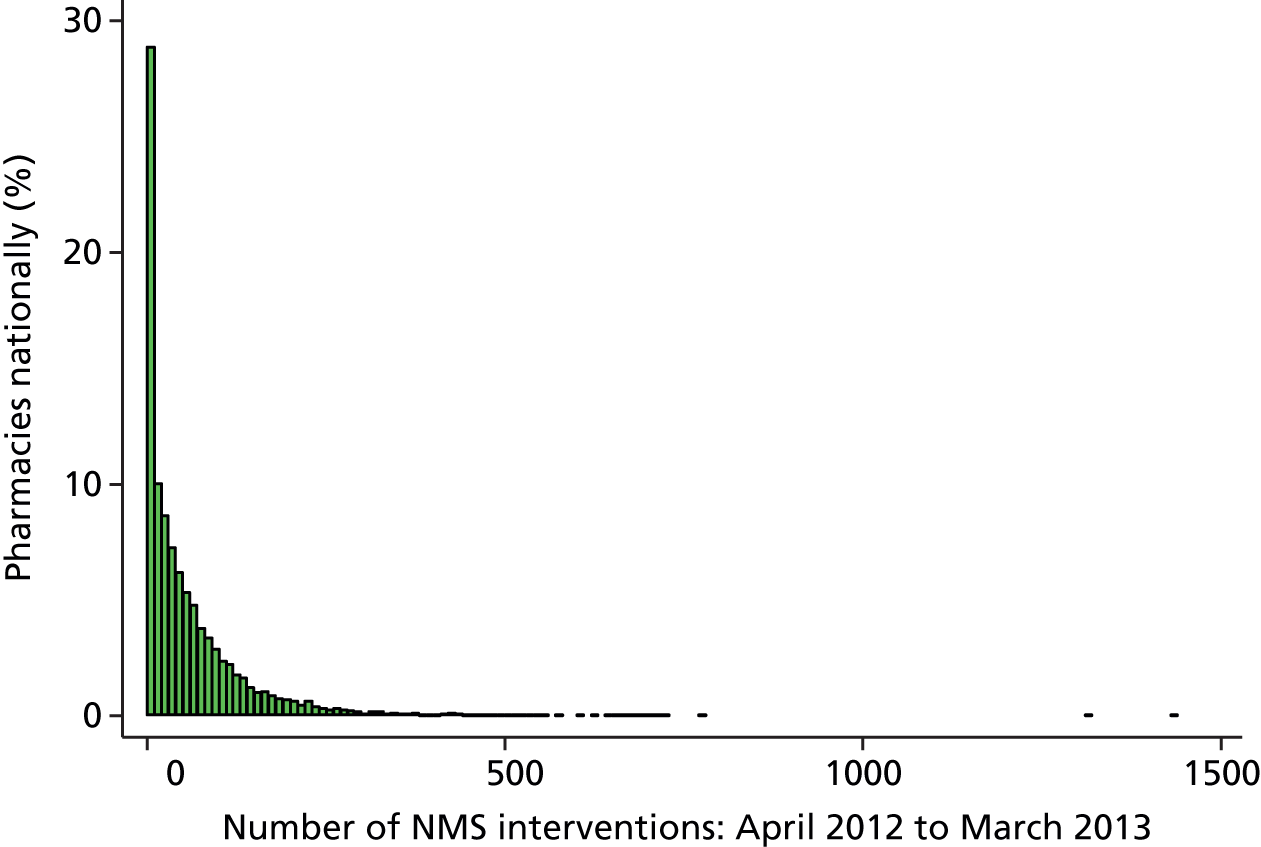
The median dispensing volume for the national data set was 72,325 items per year with an IQR of 49,569–103,213. Supermarkets again had the lowest annual dispensing volumes and large multiples had the highest. The distribution of annual dispensing volume was positively skewed (see Figure 4); linear regression of the logarithmic value of dispensing volume was therefore used in its analysis to eliminate the long right-hand tail.
The distribution of the number of MURs conducted per year was again fairly uniform, but with an even more pronounced spike at 400 than the survey sample and another, smaller, spike at zero (see Figure 5). The median value was 297 with an IQR of 116–399. Independent pharmacies conducted the fewest MURs annually and large multiples/supermarkets conducted the most. This outcome variable was again categorised as follows: 0–12, 13–200, 201–365, > 365, and ordered logistic regression was used in its analysis.
The distribution of the number of NMS interventions conducted per year was highly positively skewed (similar to an exponential distribution), again with a pronounced spike at zero (see Figure 6). The median value was 33 with an IQR of 6–80. Independent pharmacies conducted the fewest NMS interventions and large multiples conducted the most. This outcome variable was again categorised as follows: 0, 1–12, 13–31, 32–52, 53–104, ≥ 105, and ordered logistic regression was used in its analysis.
Dispensing volume
The findings of the univariable and subsequent multivariable linear regressions of annual dispensing volume of pharmacies in the national data set are presented in Table 9.
| Dispensing volume | Univariable models | Multivariable model | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| IMD scorea | ||||||
| 10-unit change | 0.0065 | 0.0038 to 0.0093 | < 0.001 | 0.0115 | 0.0080 to 0.0149 | < 0.001 |
| Aged 0–4 years (%)a | ||||||
| 1% change | –0.0036 | –0.0058 to –0.0013 | 0.002 | 0.0044 | 0.0015 to 0.0073 | 0.003 |
| Aged ≥ 75 years (%)a | ||||||
| 1% change | 0.0077 | 0.0067 to 0.0087 | < 0.001 | 0.0050 | 0.0038 to 0.0062 | < 0.001 |
| Percentage with CHD (%)a | ||||||
| 1% change | 0.0629 | 0.0574 to 0.0684 | < 0.001 | 0.0385 | 0.0323 to 0.0447 | < 0.001 |
| Percentage with a MH condition (%)a | ||||||
| 1% change | –0.2181 | –0.2461 to –0.1901 | < 0.001 | –0.1599 | –0.1919 to –0.1279 | < 0.001 |
| Percentage with depression (%)a | ||||||
| 1% change | 0.0277 | 0.0236 to 0.0319 | < 0.001 | 0.0079 | 0.0032 to 0.0126 | 0.001 |
| Percentage with asthma (%)a | ||||||
| 1% change | 0.0656 | 0.0590 to 0.0723 | < 0.001 | NSb | ||
| Pharmacy type | ||||||
| Independent | Reference | < 0.001 | ||||
| Small multiple | 0.0166 | 0.0000 to 0.0331 | ||||
| Medium multiple | –0.0221 | –0.0429 to –0.0013 | ||||
| Large multiple | 0.0644 | 0.0539 to 0.0748 | ||||
| Supermarket | –0.1428 | –0.1601 to –0.1255 | ||||
There was a significant association between pharmacy ownership type and dispensing volume with large multiples dispensing significantly more and supermarkets significantly fewer items than independents.
Dispensing volume was significantly and positively associated with local population deprivation scores, the proportion of older people and the local prevalence of some long-term conditions (CHD, depression). Although univariably associated with dispensing volume, the local prevalence of asthma did not remain so in the multivariable analysis. The prevalence of MH problems in the local population was significantly but negatively associated with pharmacy dispensing volume.
Volume of medicines use reviews conducted
The findings of the univariable and subsequent multivariable ordered logistic regressions of the volume of MURs conducted by pharmacies in the national data set are presented in Table 10.
| MURs | Univariable models | Multivariable model | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| IMD scorea | ||||||
| 10-unit change | 0.98 | 0.96 to 1.00 | 0.028 | 0.95 | 0.93 to 0.97 | < 0.001 |
| Percentage aged 0–4 yearsa | ||||||
| 1% change | 0.98 | 0.97 to 1.00 | 0.047 | 0.99 | 0.99 to 1.00 | 0.014 |
| Percentage aged ≥ 75 yearsa | ||||||
| 1% change | 1.03 | 1.02 to 1.04 | < 0.001 | NSb | ||
| Percentage with CHDa | ||||||
| 1% change | 1.00 | 0.96 to 1.04 | > 0.200c | NS | ||
| Percentage with MH conditiona | ||||||
| 1% change | 0.40 | 0.33 to 0.49 | < 0.001 | NS | ||
| Percentage with depressiona | ||||||
| 1% change | 0.99 | 0.96 to 1.01 | > 0.200 | NS | ||
| Percentage with asthmaa | ||||||
| 1% change | 1.05 | 0.99 to 1.10 | < 0.081 | 0.68 | 0.64 to 0.71 | < 0.001 |
| Pharmacy type | ||||||
| Independent | Reference | < 0.001 | ||||
| Small multiple | 4.50 | 3.91 to 5.17 | ||||
| Medium multiple | 4.74 | 4.13 to 5.43 | ||||
| Large multiple | 11.6 | 10.5 to 12.8 | ||||
| Supermarket | 11.3 | 9.91 to 12.9 | ||||
| log(dispensing volume) | 8.56 | 7.47 to 9.80 | < 0.001 | 10.5 | 8.97 to 12.2 | < 0.001 |
There was a strong association between pharmacy ownership type and the volume of MURs conducted, with pharmacy multiples, particularly large multiples and supermarkets, conducting significantly more MURs than independent pharmacies. There was also a strong positive association between the volume of MURs conducted and a pharmacy’s dispensing volume.
As in the pharmacy survey data analysis, the volume of MURs conducted was negatively associated with the prevalence of asthma in the local population. Local prevalence of MH problems was also univariably associated with the volume of MURs conducted but did not remain so in the multivariable analysis. The volume of MURs conducted was negatively associated with local population deprivation score and the proportion of young children in the local population. Although more MURs were conducted in pharmacies situated in areas with a higher proportion of older people, this association did not persist in the multivariable analysis controlling for the stronger effects of dispensing volume and pharmacy ownership type.
Volume of new medicines service interventions
The findings of the univariable and subsequent multivariable ordered logistic regressions of the volume of NMS interventions conducted by pharmacies in the national data set are presented in Table 11.
| NMS interventions | Univariable models | Multivariable model | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| IMD scorea | ||||||
| 10-unit change | 0.96 | 0.94 to 0.98 | < 0.001 | 0.95 | 0.93 to 0.97 | < 0.001 |
| Percentage aged 0–4 yearsa | ||||||
| 1% change | 0.97 | 0.96 to 0.99 | 0.001 | NSb | ||
| Percentage aged ≥ 75 yearsa | ||||||
| 1% change | 1.03 | 1.02 to 1.04 | < 0.001 | NS | ||
| Percentage with CHDa | ||||||
| 1% change | 1.02 | 0.98 to 1.06 | > 0.200c | |||
| Percentage with MH conditiona | ||||||
| 1% change | 0.44 | 0.36 to 0.54 | < 0.001 | 0.74 | 0.59 to 0.93 | 0.010 |
| Percentage with depressiona | ||||||
| 1% change | 0.99 | 0.96 to 1.02 | > 0.200 | |||
| Percentage with asthmaa | ||||||
| 1% change | 1.03 | 0.98 to 1.08 | 0.188 | 0.77 | 0.73 to 0.81 | < 0.001 |
| Pharmacy type | ||||||
| Independent | Reference | < 0.001 | ||||
| Small multiple | 1.83 | 1.60 to 2.10 | ||||
| Medium multiple | 2.26 | 1.99 to 2.57 | ||||
| Large multiple | 3.59 | 3.29 to 3.92 | ||||
| Supermarket | 2.31 | 2.03 to 2.62 | ||||
| log(dispensing volume) | 8.79 | 7.69 to 10.1 | < 0.001 | 8.06 | 7.00 to 9.29 | < 0.001 |
As with MURs, there was a significant association between the numbers of NMS interventions conducted, dispensing volume and pharmacy ownership type with all multiples, particularly large multiples, conducting significantly more NMS interventions than independent pharmacies.
Again, similar to MUR provision, the volume of NMS interventions conducted was inversely related to a number of markers of ‘need’ (deprivation score, local prevalence of MH conditions and asthma prevalence). Although the age of the local population showed significant associations with the volume of NMS interventions conducted in the univariable analysis, these relationships did not persist in the multivariable model controlling for the stronger effects of dispensing volume and pharmacy ownership type.
Chapter 5 Findings: associations between organisational characteristics, levels of service delivery and service quality
In the quantitative study, service quality was measured in terms of overall patient satisfaction with their pharmacy visit, patient satisfaction with the information they received about their medication and self-reported medication adherence using validated tools in the stage 2 patient survey. It was also measured using a validated safety climate instrument included in the stage 1 pharmacy survey. This chapter therefore reports the findings of two series of regressions: the first using data from the stage 2 patient survey data set; the second going back to the stage 1 pharmacy survey data set.
Patient survey response rate and sample characteristics
In total, 78 pharmacies were approached to participate in stage 2. Of these, 39 pharmacies were recruited to the study, two fewer than the target number. Independent pharmacies proved the most difficult to recruit. The distribution of the participating pharmacies is given in Table 12.
| Site | Independents | Small and medium-sized multiples | Large multiples and supermarkets | Total |
|---|---|---|---|---|
| Cambridgeshire and Peterborough | 1 | 1 | 2 | 4 |
| C&E Cheshire | 1 | 2 | 2 | 5 |
| Doncaster and Rotherham | 0 | 4 | 2 | 6 |
| Hertfordshire | 3 | 2 | 2 | 7 |
| Merseyside | 3 | 3 | 3 | 9 |
| Sheffield | 2 | 2 | 2 | 6 |
| Trafford | 0 | 1 | 1 | 2 |
| Total | 10 | 15 | 14 | 39 |
A total of 2124 questionnaires were distributed by these pharmacies, 1160 to patients who had prescriptions dispensed and 964 to patients who had received a MUR. One pharmacy only distributed questionnaires to dispensing patients. Of these, 1008 questionnaires were returned to the research team, 546 from the dispensing sample and 462 from the MUR sample, giving an overall response rate of 47.5% (47.1% for the dispensing sample and 47.9% for the MUR sample). Of these, 37 questionnaires were excluded from the analysis as the respondent indicated that they had visited the pharmacy on behalf of somebody else, giving a valid response rate of 46.5% (971/2087).
Descriptive statistics for each of the key independent variables from the patient survey used in the analysis of quality outcomes are presented in Table 13.
| Variable | Sample data, n (%) | N |
|---|---|---|
| Why did you choose this pharmacy on this occasion? (Number of selected categories) | ||
| 1 | 287 (30.6) | 939 |
| 2 | 518 (55.2) | |
| 3 | 134 (14.3) | |
| How many medicines are you currently being prescribed? | ||
| 1 | 86 (8.9) | 962 |
| 2–3 | 281 (29.2) | |
| 4–10 | 527 (54.8) | |
| > 10 | 68 (7.1) | |
| Received medicine(s) for the first time? | ||
| No | 750 (78.5) | 956 |
| Yes | 206 (21.5) | |
| Who did you receive information/advice from? | ||
| Do not know/NA | 459 (50.4) | 911 |
| Pharmacist only | 380 (41.7) | |
| Other staff combination | 72 (7.9) | |
| Do you usually receive information/advice from the same person? | ||
| Do not know/NA | 167 (17.5) | 952 |
| No | 281 (29.5) | |
| Yes | 504 (52.9) | |
| Overuse of medication (BMQ) | ||
| Mean (SD) | 10.9 (3.1) | 890 |
| Median (IQR) | 11 (9–13) | |
| Range | 4–20 | |
| Harm from medication (BMQ) | ||
| Mean (SD) | 8.8 (2.9) | 896 |
| Median (IQR) | 9 (7–10.5) | |
| Range | 4–20 | |
| Gender | ||
| Female | 502 (52.2) | 961 |
| Male | 459 (47.8) | |
| Number of long-term conditions | ||
| 0 | 68 (7.0) | 968 |
| 1 | 217 (22.4) | |
| 2 | 249 (25.7) | |
| 3 | 200 (20.7) | |
| 4 | 131 (13.5) | |
| ≥ 5 | 103 (10.6) | |
Respondents ranged in age from 18 to 93 years but the average age was in the mid-sixties. Slightly more women than men completed questionnaires. Most respondents indicated that they had at least one long-term condition, with 70% indicating that they had two or more.
Respondents were asked to select the reason(s) why they chose to visit that particular pharmacy. Nine options were available: three related to ease of access, four related to quality of service and two related to value/range of products. Responses were scored 1–3 depending on the number of categories (access, service or products) from which reasons were selected. Most respondents (93.7%) selected a reason relating to access, three-quarters of respondents (74.8%) selected a reason relating to service and 15.2% selected a product-related response. Just over half indicated that the reasons for their visit spanned two of these categories, with only around one in seven selecting reasons from all three categories.
More than half of these pharmacy patients were currently prescribed four or more medicines, with just over one-fifth receiving a medicine for the first time at that pharmacy visit. Approximately half either received no information about their medication (n = 457; 48.5%) or were unable to identify which member of pharmacy staff they received information from. A further two-fifths received information or advice from the pharmacist.
The mean score on the overuse of medication scale of the BMQ was around 11, slightly lower (i.e. weaker beliefs that medicines are overused by doctors) than values reported elsewhere. 57 The mean score on the harm from medication scale of the BMQ was around 9, again slightly lower (i.e. weaker beliefs that medicines cause harm) than reported previously. Both scales are strongly correlated (r = 0.68); therefore, we fit the ‘overuse’ subscale only in subsequent regressions to avoid problems with collinearity.
Service quality: stage 2 patient survey data set analysis
The first series of regressions conducted to explore the associations between the organisational characteristics of the pharmacy, pharmacy activity and service quality were on satisfaction with pharmacy visit, satisfaction with information received about medicines (SIMS) and self-reported medication adherence (MARS) for those eligible patients responding to the stage 2 survey (n = 971).
Summary statistics for satisfaction with pharmacy visit, SIMS score and MARS score, broken down by pharmacy ownership type, are presented in Table 14. As in previous analysis (see Chapter 4, Community pharmacy activity: stage 1 community pharmacy survey data set analysis) ownership type was collapsed into three categories for subsequent regressions. The distribution of each of these primary outcome variables is given in Figures 7–9.
| Pharmacy ownership type | Satisfaction | SIMS | MARS |
|---|---|---|---|
| Independents | |||
| n | 227 | 233 | 237 |
| Mean (SD) | 3.81 (0.56) | 13.25 (5.20) | 22.38 (3.65) |
| Median | 3.73 | 17 | 24 |
| IQR | 3.40–4.13 | 10–17 | 21–25 |
| Range | 1.93–5.00 | 0–17 | 5–25 |
| Small multiples | |||
| n | 201 | 212 | 206 |
| Mean (SD) | 3.76 (0.59) | 14.00 (5.01) | 23.21 (2.17) |
| Median | 3.67 | 17 | 24 |
| IQR | 3.36–4.20 | 13–17 | 23–25 |
| Range | 2.00–5.00 | 0–17 | 15–25 |
| Medium-sized multiples | |||
| n | 104 | 114 | 105 |
| Mean (SD) | 3.90 (0.61) | 14.70 (4.36) | 22.58 (2.72) |
| Median | 3.93 | 17 | 24 |
| IQR | 3.59–4.27 | 14–17 | 21–25 |
| Range | 1.53–5.00 | 0–17 | 15–25 |
| Large multiples | |||
| n | 272 | 290 | 309 |
| Mean (SD) | 3.84 (0.61) | 13.46 (5.06) | 23.45 (2.12) |
| Median | 3.80 | 17 | 24 |
| IQR | 3.45–4.27 | 11–17 | 23–25 |
| Range | 2.00–5.00 | 0–17 | 11–25 |
| Supermarkets | |||
| n | 17 | 18 | 19 |
| Mean (SD) | 3.68 (0.74) | 13.11 (5.80) | 22.95 (2.17) |
| Median | 3.53 | 16.5 | 24 |
| IQR | 3.40–4.07 | 11–17 | 23–24 |
| Range | 2.33–5.00 | 0–17 | 18–25 |
| Total | |||
| n | 821 | 867 | 876 |
| Mean (SD) | 3.81 (0.59) | 13.69 (5.03) | 22.99 (2.73) |
| Median | 3.80 | 17 | 24 |
| IQR | 3.40–4.20 | 12–17 | 22–25 |
| Range | 1.53–5.00 | 0–17 | 5–25 |
FIGURE 7.
Distribution of overall satisfaction with pharmacy visit (mean item score) for patients responding to the stage 2 survey.

FIGURE 8.
Distribution of satisfaction with information received about medicines (SIMS score) for patients responding to the stage 2 survey.
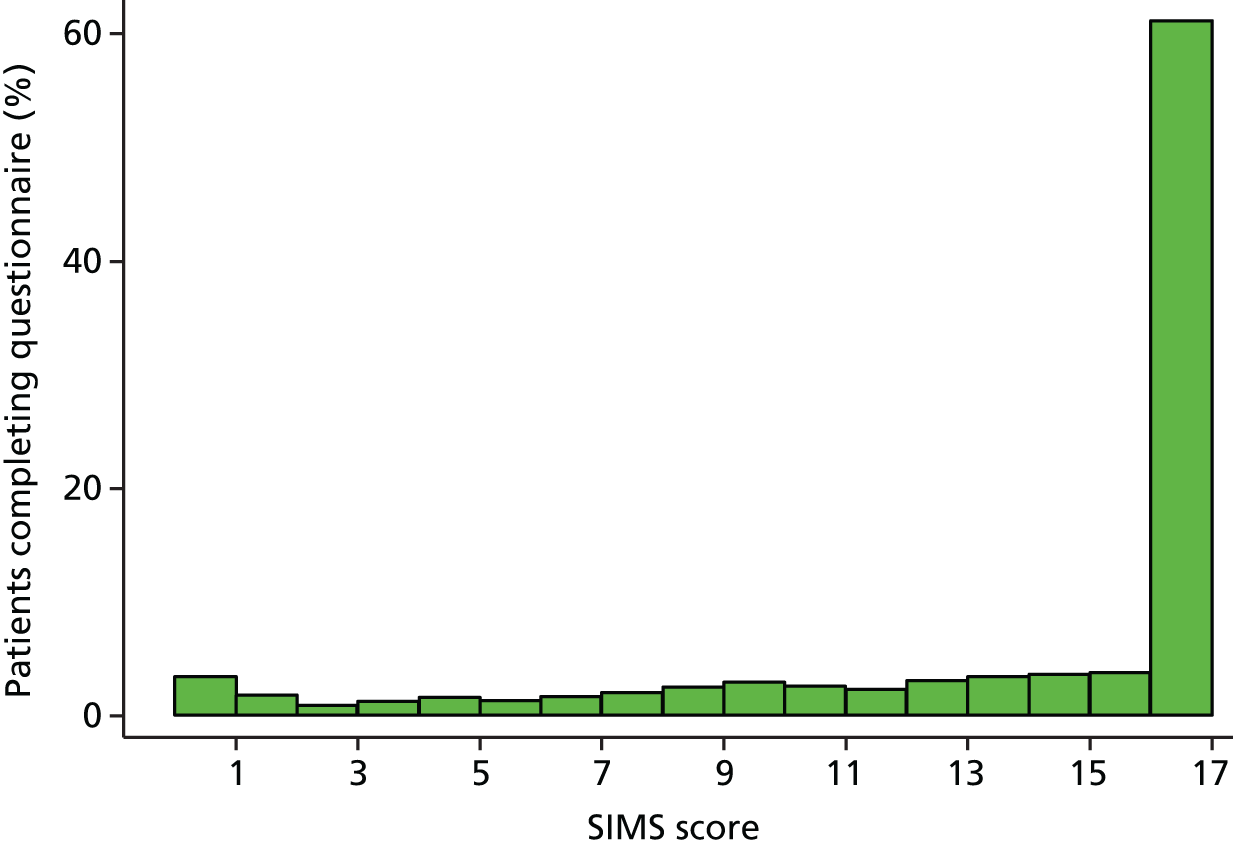
FIGURE 9.
Distribution of self-reported adherence (MARS score) for patients responding to the stage 2 survey.
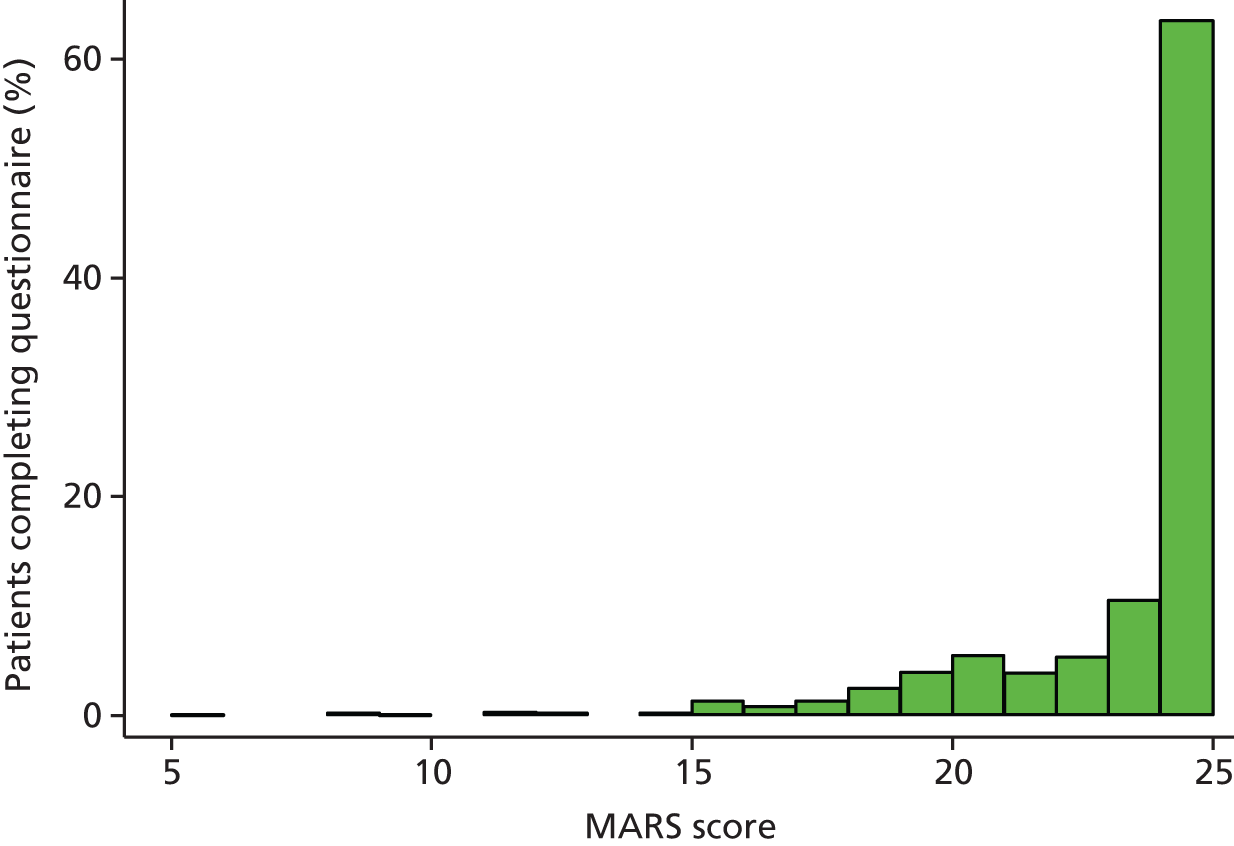
The mean item score for overall satisfaction ranged from 1.53 to 5, where higher scores indicate higher levels of self-reported satisfaction with the pharmacy visit. The sample mean was 3.81 (0.59) for survey respondents, higher (i.e. more satisfaction) than that reported elsewhere. 54 There was little difference in overall satisfaction between pharmacies of different ownership type. The distribution of overall satisfaction had a negative skew; however, given the large respondent sample, the distribution of its mean is very likely to be normal and so linear regression was used in its analysis.
Summed SIMS scores ranged from 0 to 17, where higher scores indicate higher levels of self-reported satisfaction with information received. The median SIMS score for this sample of pharmacy patients was 17, with an IQR of 12–17. There was little difference in SIMS score between pharmacies of different ownership type. The distribution of SIMS scores was highly negatively skewed with a pronounced peak at 17 (> 60% of respondents ‘scored’ 17). Therefore, this score was categorised (0–5, 6–10, 11–16 and 17) and analysed using ordered logistic regression.
Medication Adherence Report Scale scores ranged from 5 to 25, where higher scores indicate higher levels of self-reported adherence. The median MARS score for this sample of pharmacy patients was 24, with an IQR of 22–25. There was again little difference in MARS scores between pharmacies of different ownership type. The distribution of MARS scores was also highly negatively skewed with a pronounced peak at 25. Consistent with previous research,59 this score was dichotomised into ≤ 20 (‘low adherers’) and > 20 (‘high adherers’), and analysed using binary logistic regression.
Satisfaction with pharmacy visit
The full findings of the univariable and subsequent multivariable linear regressions of overall satisfaction with pharmacy visit for stage 2 patient survey respondents can be found in Appendix 6: a summarised version is presented in Table 15.
| Patient Satisfaction Scale | Multivariable model | ||
|---|---|---|---|
| Coefficient | 95% CI | p-value | |
| Pharmacy contract held | |||
| Standard 40 hours | Reference | 0.001 | |
| 100 hours | –0.0052 | –0.1925 to 0.1821 | |
| Other | 0.1771 | 0.0867 to 0.2675 | |
| Registered pharmacy technician | |||
| No | Reference | 0.036 | |
| Yes | 0.0998 | 0.0070 to 0.1926 | |
| Why did you choose this pharmacy on this occasion? (Number of selected categories) | |||
| 1 | Reference | < 0.001 | |
| 2 | 0.2235 | 0.1049 to 0.3421 | |
| 3 | 0.3943 | 0.2644 to 0.5242 | |
| Who did you receive information/advice from? | |||
| Do not know/NA | Reference | < 0.001 | |
| Pharmacist only | 0.2141 | 0.1143 to 0.3139 | |
| Other staff combination | 0.3376 | 0.1890 to 0.4862 | |
| Do you usually receive information/advice from the same person? | |||
| Do not know/NA | –0.0492 | –0.1463 to 0.0479 | |
| No | Reference | < 0.001 | |
| Yes | 0.2593 | 0.1251 to 0.3935 | |
| Overuse of medication (BMQ) | |||
| 1-unit change | –0.0293 | –0.0494 to –0.0092 | 0.005 |
| Volume of MURs | |||
| ≤ 12 | –0.2545 | –0.3631 to –0.1448 | |
| 13–200 | –0.0007 | –0.1191 to 0.1177 | |
| 201–365 | –0.0270 | –0.1087 to 0.0548 | |
| > 365 | Reference | < 0.001 | |
Patients who had chosen to visit a pharmacy for reasons that spanned a greater number of categories than just one (access, service, products) were significantly more satisfied with their visit. Patients who had received information from either the pharmacist or another member of staff were more satisfied with their visit than those who had not received any information. Furthermore, those who usually received advice from the same person were more satisfied than those who did not. Patients with higher scores on the ‘overuse of medication’ scale of the BMQ – indicating that they believed more strongly that medicines were overused – were significantly less satisfied with their pharmacy visit. Number of long-term conditions was positively associated with patient satisfaction in the univariable but not the multivariable analysis.
Significantly higher levels of patient satisfaction with their pharmacy visit were measured in patients who had visited pharmacies holding an ‘other’ type of contract (e.g. essential small pharmacy or local pharmaceutical services compared with a standard 40-hour contract) and those employing a registered pharmacy technician. Patients were also more satisfied following a visit to a pharmacy with an organisational culture more closely aligned to the patient, quality and professional work than to the medicine, quantity and technical work (univariable regression). However, this significant association did not persist in the multivariable model. Patient satisfaction was not significantly associated with pharmacy ownership type.
Overall patient satisfaction was not significantly associated with the annual dispensing volume of the pharmacy. However, patients were significantly more satisfied if they had visited a pharmacy that conducted over 365 MURs per year compared with those who had visited a pharmacy conducting fewer than 12. It should be noted, however, that only one pharmacy in the stage 2 sample conducted fewer than 12 MURs per year. Above 12 MURs per year, there was no indication that volume of MURs was significantly associated with overall patient satisfaction.
Although the geographical location of the pharmacy and a small number of socioeconomic and demographic indicators were associated with patient satisfaction in the univariable analyses, they did not remain so in the final multivariable model.
Satisfaction with information received about medicines
The full findings of the univariable and subsequent multivariable ordered logistic regressions of SIMS score for stage 2 patient survey respondents can be found in Appendix 6: a summarised version is presented in Table 16.
| SIMS | Multivariable model | ||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Mean age (population, years) | |||
| 1-year change | 1.07 | 1.02 to 1.12 | 0.002 |
| Do you usually receive information/advice from the same person? | |||
| Do not know/NA | 1.72 | 0.98 to 3.01 | |
| No | Reference | 0.001 | |
| Yes | 1.96 | 1.36 to 2.82 | |
| Overuse of medication (BMQ) | |||
| 1-unit change | 0.92 | 0.88 to 0.96 | < 0.001 |
| Patient age (years) | |||
| Linear component | 1.02 | 1.01 to 1.03 | 0.002 |
| Quadratic component | 1.00 | 1.00 to 1.00 | |
| Volume of MURs | |||
| ≤ 12 | 0.15 | 0.08 to 0.29 | |
| 13–200 | 0.79 | 0.49 to 1.27 | |
| 201–365 | 0.72 | 0.49 to 1.07 | |
| > 365 | Reference | < 0.001 | |
| Type of pharmacy | |||
| Independent | Reference | 0.008 | |
| Small/medium-sized multiple | 1.88 | 1.13 to 3.11 | |
| Large multiple/supermarket | 1.15 | 0.68 to 1.94 | |
Patients who usually received advice from the same person at their pharmacy were more satisfied with the information that they had received about medicines. Younger patients, and those with higher scores on the ‘overuse of medication’ scale of the BMQ, had significantly lower SIMS scores. Patients who had chosen to visit their pharmacy for reasons that spanned a greater number of domains (access, service, products) had significantly higher SIMS scores in the univariable analysis, but not in the final multivariable model. Although patients receiving their medication for the first time were significantly less satisfied with the information received (univariable analysis), this association also did not persist in the multivariable analysis.
Satisfaction with Information about Medicines Scale scores were significantly associated with pharmacy type, being significantly higher in small and medium multiples than in independent pharmacies. Although two other organisational characteristics (100-hour pharmacies and those with longer opening hours) were associated with higher SIMS scores in the univariable analysis, neither remained in the final multivariable model.
Other than the mean age of the local population, which was positively associated with SIMS score, no other socioeconomic or demographic variables were significantly associated with patient satisfaction with information received about medicines.
There was again no indication that the magnitude of this outcome was associated with the dispensing volume of the pharmacy. However, as for overall satisfaction, SIMS scores were significantly higher for patients visiting pharmacies that conducted more than 365 MURs per year than for those visiting pharmacies conducting fewer than 12 MURs per year. However, it should again be noted that only one pharmacy in the stage 2 sample conducted fewer than 12 MURs per year. Above 12 MURs per year, there was no indication that volume of MURs was significantly associated with patient satisfaction with information received about their medication.
Self-reported medication adherence
The full findings of the univariable and subsequent multivariable binary logistic regressions of MARS score for stage 2 patient survey respondents can be found in Appendix 6: a summarised version is presented in Table 17.
| MARS | Multivariable model | ||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Use of locums | |||
| Not regularly | Reference | 0.008 | |
| Regularly | 0.50 | 0.30 to 0.84 | |
| Do you usually receive information/advice from the same person? | |||
| Do not know/NA | 2.50 | 1.20 to 5.23 | |
| No | Reference | 0.044 | |
| Yes | 1.45 | 0.73 to 2.89 | |
| Overuse of medication (BMQ) | |||
| 1-unit change | 0.88 | 0.81 to 0.95 | 0.002 |
| Patient age (years) | |||
| Linear component | 1.04 | 1.01 to 1.07 | < 0.001 |
| Quadratic component | 1.00 | 1.00 to 1.00 | |
Patients who did not usually receive information or advice from the same person were significantly (weak association) more likely to be classified as ‘low adherers’ than either those who did or those who could not identify who they received their information from or for whom this question was not applicable (had not received any information or advice). As with SIMS scores, younger patients, and those with higher scores on the ‘overuse of medication’ scale of the BMQ, were significantly more likely to be classified as ‘low adherers’. Other patient characteristics shown to be associated with self-reported adherence in the unvariable analyses (receiving medicine for the first time, member of staff information was received from, number of long-term conditions, SIMS score) did not remain so in the multivariable analysis.
The only organisational characteristic significantly associated with self-reported adherence was use of locums; patients who had visited pharmacies who regularly (on a daily/weekly basis) used locums were significantly more likely to be classified as ‘low adherers’ according to their MARS score. There was no association with pharmacy ownership type.
Other than the mean age of the local population, which was weakly associated with MARS classification in the unvariable analysis, no socioeconomic or demographic variables were significantly associated with self-reported adherence in the multivariable model. There was no indication that self-reported adherence was significantly associated with the volume of services (dispensing or MURs) provided by the pharmacy.
Service quality: stage 1 community pharmacy survey data set analysis – safety climate
The second series of regressions conducted to explore the associations between the organisational characteristics of the pharmacy, pharmacy activity and service quality were on safety climate (the four domains of the PSCQ for those pharmacies responding to the stage 1 survey (n = 277).
Summary statistics for each of the domains of the PSCQ – organisational learning, blame culture, working conditions, safety focus – broken down by pharmacy ownership type are presented in Table 18. The distribution of each of these secondary outcome variables is given in Figures 10–13.
| Pharmacy ownership type | Organisational learning | Blame culture | Working conditions | Safety focus |
|---|---|---|---|---|
| Independents (< 6 stores) | ||||
| n | 107 | 106 | 106 | 106 |
| Mean (SD) | 40.29 (7.54) | 4.60 (2.50) | 12.70 (2.55) | 9.99 (1.92) |
| Median | 40 | 5 | 13 | 10 |
| IQR | 37–44 | 3–6 | 11–14 | 9–11 |
| Range | 13–53 | 1–13 | 7–17 | 5–13 |
| Small multiples (6–25 stores) | ||||
| n | 36 | 38 | 39 | 37 |
| Mean (SD) | 40.61 (6.51) | 5.00 (3.03) | 12.21 (3.04) | 9.65 (1.70) |
| Median | 41 | 5 | 12 | 10 |
| IQR | 38–44 | 2–7 | 10–14 | 9–11 |
| Range | 19–53 | 1–12 | 7–17 | 6–13 |
| Medium-sized multiples (26–200 stores) | ||||
| n | 8 | 9 | 9 | 9 |
| Mean (SD) | 41.75 (5.34) | 4.33 (2.74) | 12.89 (2.26) | 10.22 (1.20) |
| Median | 41 | 5 | 13 | 10 |
| IQR | 37.5–45 | 2–5 | 12–15 | 10–11 |
| Range | 36–51 | 1–10 | 8–15 | 8–12 |
| Large multiples (> 200 stores) | ||||
| n | 87 | 89 | 91 | 88 |
| Mean (SD) | 39.84 (7.14) | 5.49 (2.95) | 10.53 (3.16) | 9.53 (2.09) |
| Median | 40 | 5 | 11 | 10 |
| IQR | 36–44 | 3–8 | 8–13 | 9–11 |
| Range | 12–53 | 1–14 | 2–16 | 2–13 |
| Supermarkets | ||||
| n | 24 | 24 | 24 | 24 |
| Mean (SD) | 41.25 (7.64) | 5.79 (3.13) | 10.75 (3.34) | 10.04 (2.01) |
| Median | 41.5 | 6 | 12 | 10 |
| IQR | 38–45.5 | 3.5–7.5 | 8.5–13.5 | 9–11 |
| Range | 16–53 | 1–13 | 4–16 | 5–13 |
| Total | ||||
| n | 262 | 266 | 269 | 264 |
| Mean (SD) | 40.32 (7.19) | 5.06 (2.82) | 11.72 (3.06) | 9.80 (1.94) |
| Median | 40 | 5 | 12 | 10 |
| IQR | 37–44 | 3–7 | 10–14 | 9–11 |
| Range | 12–53 | 1–14 | 2–17 | 2–13 |
FIGURE 10.
Distribution of the PSCQ: organisational learning scores for pharmacies responding to the stage 1 survey.
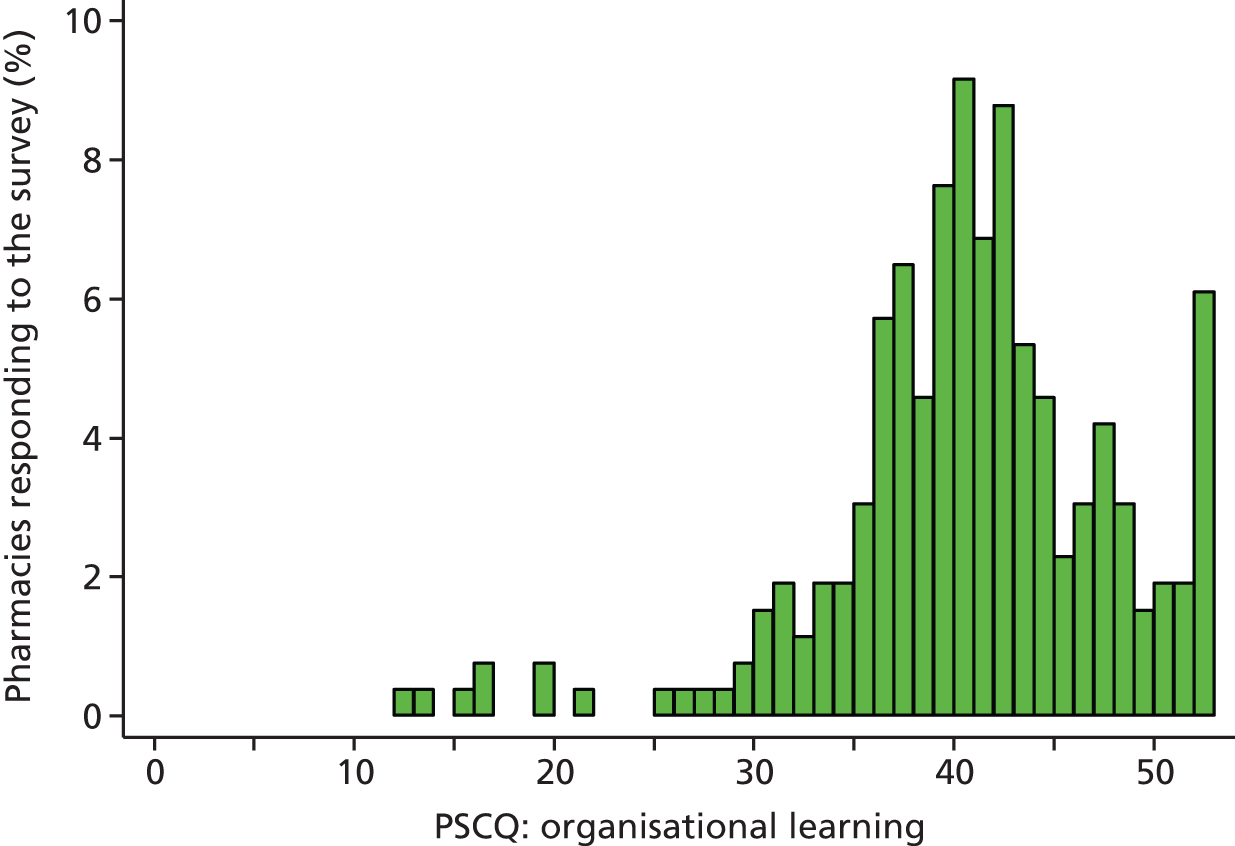
FIGURE 11.
Distribution of the PSCQ: blame culture scores for pharmacies responding to the stage 1 survey.

FIGURE 12.
Distribution of PSCQ: working condition scores for pharmacies responding to the stage 1 survey.
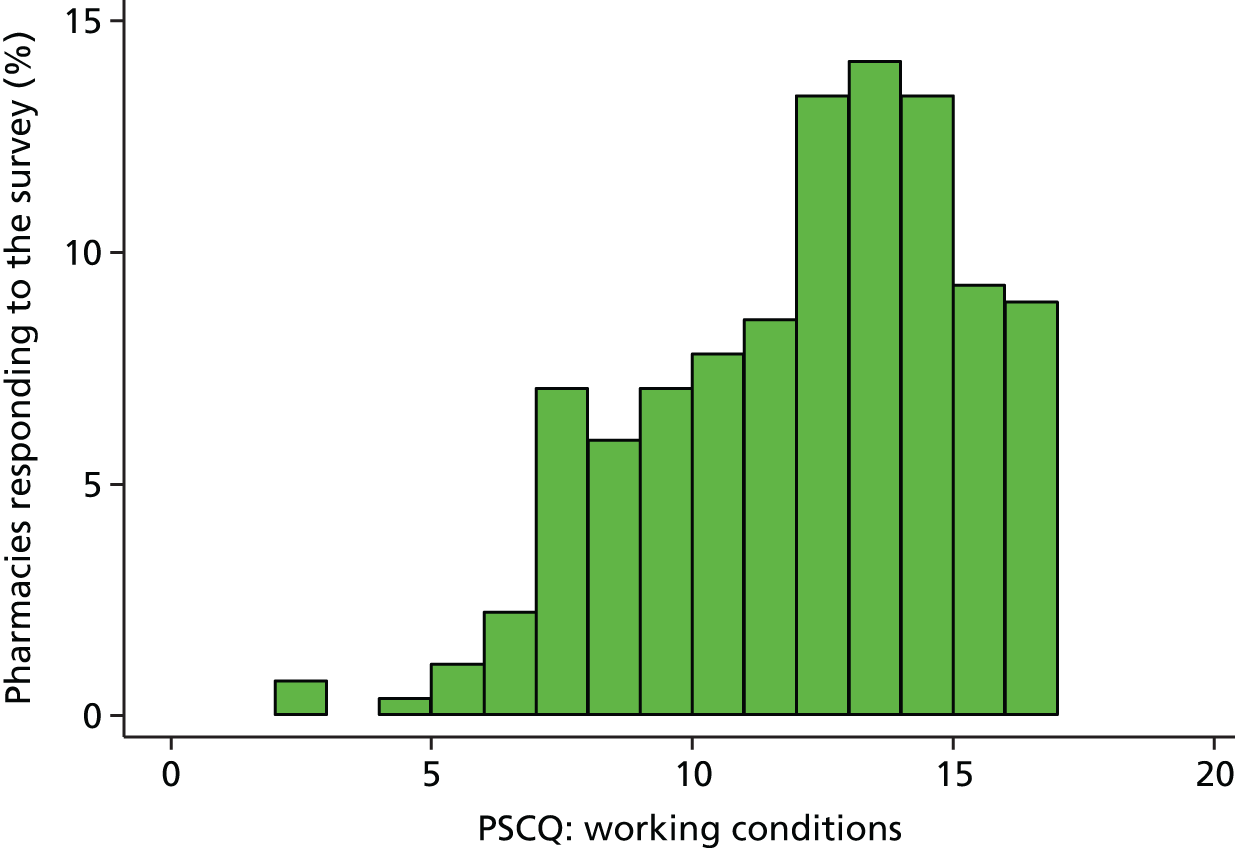
FIGURE 13.
Distribution of PSCQ: safety focus scores for pharmacies responding to the stage 1 survey.
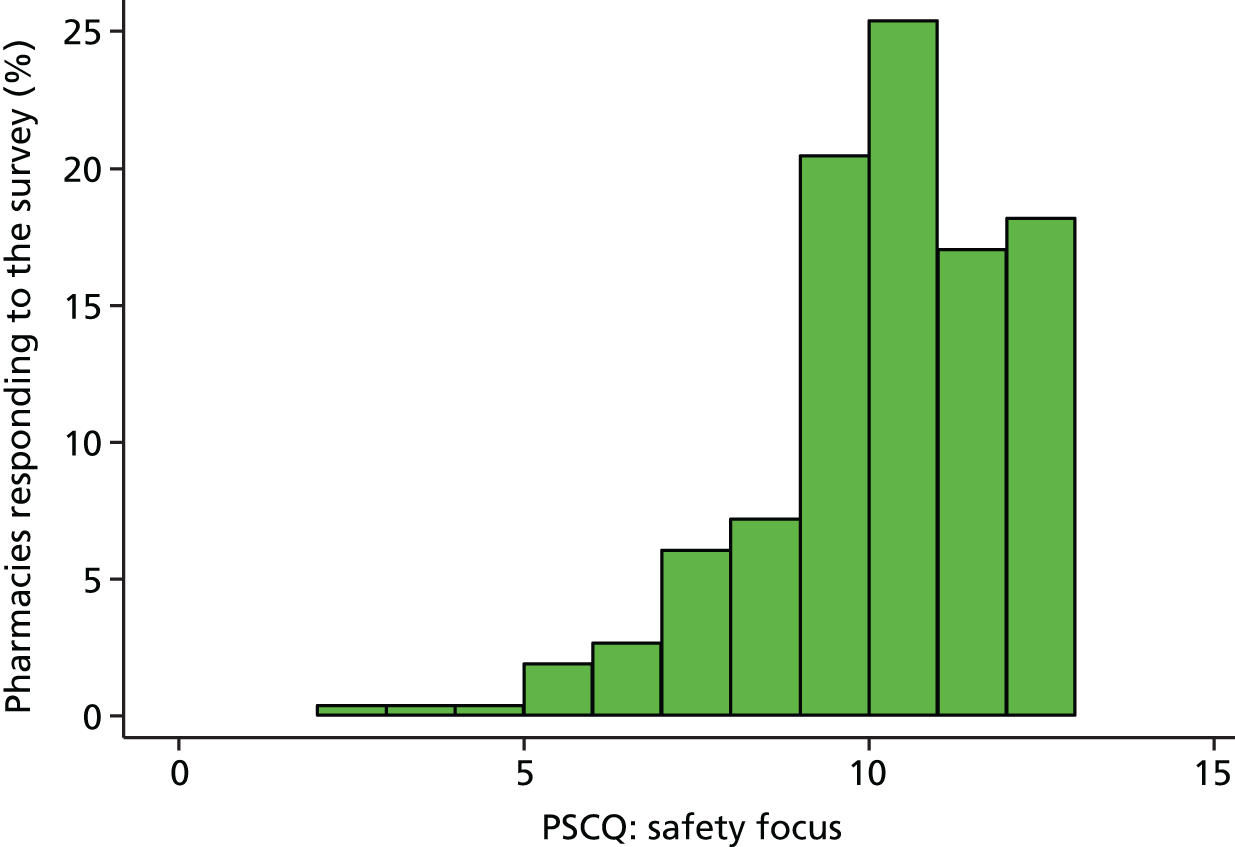
Mean and median values for each of the four PSCQ domain scores (see Table 18) varied as a result of the different number of items in each subscale (from 13 in organisational learning to only three in safety focus). For three of the domains (organisational learning, working conditions, safety focus), higher scores indicate a more favourable safety climate; for the fourth domain (blame culture), which is reverse scored, higher scores indicate a less favourable safety climate. Some differences were apparent between organisational types, particularly in relation to blame culture and working conditions, both of which were least favourable in larger organisational types, particularly supermarkets. This reflects previous research findings. 68
The distribution of scores on each of the domains of the PSCQ was somewhat skewed: negatively in all cases, given that blame culture was reverse scored (see Figures 10–13). However, the sample size is again sufficient to be able to utilise ‘normality-based’ methods. Given that each scale measured a different aspect of the same construct (safety climate) and that interdomain correlation was expected (and observed), a multivariate linear regression analysis was used to fit multivariable models to each domain simultaneously. Independent variables only remained in the model if a composite hypothesis test, conducted across all four domains, was ‘significant’ (as previously, p < 0.2 in univariable models; p < 0.05 in multivariable models). This meant that the same subset of independent variables was retained in the model for each domain, although not necessarily significantly associated with each.
The full findings of the univariable and subsequent multivariable multivariate linear regression of the PSCQ domains for stage 1 pharmacy survey respondents can be found in Appendix 6: a summarised version is presented in Table 19.
| PSCQ | Multivariable model, coefficients (95% CI) | ||||
|---|---|---|---|---|---|
| Organisational learning | Blame culture | Working conditions | Safety focus | Composite hypothesis test | |
| Job title | |||||
| Pharmacist | Reference | F4,225 = 3.65; p = 0.007 | |||
| Owner/manager | 1.74 (–0.51 to 3.98) | –0.90 (–1.81 to 0.00) | 1.73 (0.80 to 2.65) | 0.64 (0.01 to 1.28) | |
| ACT | |||||
| No | Reference | F4,225 = 4.55; p = 0.002 | |||
| Yes | –0.87 (–2.72 to 0.98) | 0.38 (–0.36 to 1.13) | –0.97 (–1.73 to –0.20) | –1.01 (–1.53 to –0.49) | |
| Work pattern of main pharmacist | |||||
| Standard hours (8 a.m.–6 p.m.) | Reference | F4,225 = 2.61; p = 0.037 | |||
| Non-standard | 1.03 (–0.77 to 2.83) | –0.70 (–1.43 to 0.03) | –0.13 (–0.87 to 0.61) | 0.69 (0.18 to 1.20) | |
| Average daily working hours of main pharmacist | |||||
| 1-hour change | –0.37 (–1.19 to 0.46) | 0.03 (–0.30 to 0.37) | –0.51 (–0.85 to –0.17) | –0.17 (–0.41 to 0.06) | F4,225 = 2.68; p = 0.032 |
| Organisational culture (PSO) | |||||
| 1-unit change | 2.11 (1.49 to 2.73) | –0.40 (–0.65 to –0.15) | 0.46 (0.21 to 0.72) | 0.39 (0.21 to 0.56) | F4,225 = 12.44; p < 0.001 |
| Relationship with nearest GP surgery | |||||
| Very good | Reference | F12,225 = 2.44; p = 0.005 | |||
| Good | –1.43 (–3.44 to 0.60) | 1.02 (0.20 to 1.84) | –0.23 (–1.06 to 0.61) | –0.32 (–0.89 to 0.26) | |
| Satisfactory/poor/none | –3.09 (–5.38 to –0.80) | 1.18 (0.25 to 2.11) | –0.60 (–1.54 to 0.35) | –1.08 (–1.73 to –0.43) | |
| No GP surgery identified | –6.31 (–10.6 to –2.07) | 3.03 (1.32 to 4.75) | –1.11 (–2.85 to 0.63) | –0.60 (–1.80 to 0.61) | |
| Type of pharmacy | |||||
| Independent | Reference | F8,225 = 4.36; p < 0.001 | |||
| Small/medium-sized multiple | 1.99 (–0.56 to 4.54) | –0.56 (–1.59 to 0.47) | 0.39 (–0.66 to 1.44) | 0.17 (–0.55 to 0.89) | |
| Large multiple/supermarket | 2.07 (0.18 to 3.95) | 0.27 (–0.50 to 1.03) | –1.64 (–2.42 to –0.87) | 0.01 (–0.53 to 0.54) | |
Survey respondents who were pharmacy owners or managers were more likely to report a more favourable safety climate across all four domains than those who were another type of employee pharmacist (taking into account the inverse scoring of the ‘blame culture’ domain, where higher scores indicate a less favourable safety culture).
The extant organisational culture (PSO score) in the pharmacy was strongly associated with safety climate. Pharmacies with cultures more closely aligned to the patient, professional work and quality also had more favourable scores across all four domains of the PSCQ. Safety climate was also significantly related to organisational type, with larger chains (large multiples/supermarkets) having less favourable scores in the ‘working conditions’ domain but more favourable scores around ‘organisational learning’ than independent pharmacies.
Higher daily working hours for the main pharmacist were associated with a less favourable safety climate particularly in relation to the ‘working conditions’ domain of the PSCQ. However, in pharmacies where the main pharmacist worked non-standard hours (which included extended working hours and shift work patterns), a more favourable safety climate prevailed in relation to ‘safety focus’. Unexpectedly perhaps, pharmacies employing an accuracy checker reported a less favourable safety climate in relation to both ‘working conditions’ and ‘safety focus’.
Finally, there was a significant association demonstrated in the multivariable analysis between a pharmacy’s relationship with its nearest GP surgery and its safety climate. Compared with pharmacies reporting a ‘very good’ relationship with their nearest GP surgery, those reporting ‘good’, ‘satisfactory, poor or no’ relationships and those unable to identify a single GP surgery with which they had the closest working relationship had increasingly less favourable safety climates in relation to both ‘organisational learning’ and ‘blame culture’.
Chapter 6 Findings: mechanisms of associations between organisational characteristics and clinical productivity
Stakeholder interviews: overview
Forty semistructured interviews were conducted in total in stage 2 of the study, 30 with pharmacists and 10 with service commissioners. Of the 30 pharmacists, five were superintendent pharmacists, one from a small chain and four from large multiples. A further six had a dual superintendent/patient-facing pharmacist role in independent pharmacies. The remaining 19 pharmacist interviewees each had a patient-facing role: nine in large multiples/supermarkets, six in small/medium-sized multiples and four in independent pharmacies. Of the 10 service commissioners, five were from NHS England area teams and five from CCGs. Interviews were conducted either face to face (n = 21) or by telephone (n = 19) and lasted between 33 minutes and 1 hour 37 minutes.
The findings from both pharmacist and commissioner interviews are presented together under the main themes of the derived framework: definitions of quality; organisational characteristics associated with variation in clinical productivity; extraorganisational factors associated with clinical productivity; and monitoring clinical productivity.
Definitions of quality
Given the definition of clinical productivity used in this study as being a factor of both the quantity (range and volume) and quality of services provided by community pharmacies, it was important to explore with interviewees their own understandings and definitions of service quality. To facilitate discussions of service quality, and to link to the focus of the quantitative analysis, interviewees were asked specifically about how they defined the quality of dispensing services and MURs.
Quality of dispensing services
In relation to dispensing, speed and accuracy were the most commonly described elements of service quality. Most pharmacists and superintendent pharmacists believed that speed of dispensing was valued by patients above anything else:
. . . often it’s public expectation, I mean people expect you to just basically . . . have a prescription within 2 minutes or whatever. The fact that whatever is on that prescription, they’d say, ‘oh, you can just pick it off a shelf and put its label on’; their expectation is for speed, but not always for quality or for anything else.
Pharmacist 35
Although speed was also felt to be important by pharmacists themselves, more often accuracy was described as being paramount to service quality and many expressed the need to balance speed with accuracy. A number of commissioners also highlighted the importance of accuracy in the dispensing process:
So, the waiting times are important to the patient, I suppose, it’s important to us as well in the pharmacy, but I suppose it’s more important to us to make sure that it’s right.
Pharmacist 29
A number of pharmacists and commissioners believed that, alongside speed and accuracy, the clinical input of the pharmacist was an important element of the quality of dispensing. This could either be about the provision of counselling or advice-giving alongside dispensing or else interventions made as a result of the clinical check:
So there is the accuracy, and then there is our role as pharmacists, to check the prescribing and the clinical side of the thing, just to make sure that it is right for the patient, and challenge a little bit, GPs, if necessary.
Pharmacist 1
I would want a really strong cognitive element at the beginning in terms of the clinical check so people really thinking about what they’re doing rather than necessarily looking at prescriptions thinking ‘have we got this in stock?’. Thinking critically about that prescription and at the end of the process making sure that patients know what they’re taking and why they’re taking it and recognising that there is somebody that they can call upon should they have any problems. So there’s the whole of the patient counselling piece at the end which I think is often forgotten about in the spirit of getting prescriptions done as quickly as possible to meet customer demand.
Superintendent pharmacist 3
Although sometimes not perceived as being as important as speed and accuracy, most interviewees also felt that a full supply of medication to enable every prescription to be filled when first presented was another aspect of a high-quality dispensing service. This prevented prolonged waits for medication or patients having to return to the pharmacy for ‘owings’:
And having a good level of stock as well . . . if people keep coming in and every month you’re having to owe them the same tablet then they’re sort of thinking, ‘Well, they never have my tablets in stock’. So having the right stock levels is important as well.
Pharmacist 32
Having a patient-centred approach and offering good customer service were also mentioned by several pharmacists as important elements of a high-quality dispensing service:
I think [patients] think it’s high quality when we’re genuinely interested in them, their medication, and helping them with their medication.
Pharmacist 21
Quality of medicines use reviews
For the majority of interviewees, a high-quality MUR was one that had made an impact on the patient. The types of impact described included increasing the patient’s knowledge or understanding of their medication and why it had been prescribed; improving patients’ adherence to their medication, ensuring that they take it, at the right times and in the right way; identifying and addressing side effects; improving clinical outcomes and quality of life; and providing reassurance to the patient:
I guess it’s still reassuring for the patient to know that they’re taking everything properly and everything’s fine and it’s just like a quick check. But I only find them worthwhile when you have an outcome at the end of it. So if, say for example, they’ve been experiencing a side effect and they haven’t linked it to a particular drug, or you’ve actually offered something more to them to either improve their regime, or to resolve a problem that they’ve been having, or there’s been some kind of positive outcome where they either feel more reassured about taking the medication or there’s been some kind of change, or something else that you have to offer which has helped in any kind of way – then I find them worthwhile.
Pharmacist 38
However, a number of interviewees were keen to highlight that a high-quality MUR stopped short of being a full clinical medication review and that MURs should be about the patient’s use of existing prescribed medications and not a review of what they should or should not be prescribed:
. . . I think there still is a misconception around what actually we should do in a medicines use review and then what would then tip into being a clinical medication review. I’ve seen MURs where it’s come back and said, ‘This patient’s got heart disease, so you should really put them on a statin’. Whereas I’ve seen some really good quality ones . . . [saying] ‘I’m a bit concerned because this lady takes a diuretic and only . . . in the morning, because she worries about going to the . . . ’, so . . . she wasn’t taking her diuretic properly . . . for fear of she had to run to the toilet.
Commissioner 8
Several respondents suggested that a high-quality MUR service was one that was targeted at the people most likely to benefit: those taking a larger number of medicines or those in particular patient groups, for example those with long-term respiratory conditions or those with cardiovascular disease:
I bet you get a lot of MURs that are just . . . two or three item ones where they’re not really making much difference to the patient. Someone who’s in their forties who’s on two blood pressure medications, they know what they’re doing with it, probably. But then still an MUR because you check to see that they’re happy and they know what they’re doing. And I don’t think that’s the point of MURs. I think it’s to make an impact on people.
Pharmacist 23
At the moment the ones where I feel that we do something is respiratory MURs, because we can use them to test their inhaler technique, that’s something quite quick and quite simple and you can tell that providing they then comply and carry on with the technique you’ve shown them, you feel, yes, well, that’s benefited the patient.
Pharmacist 35
There was a perception among many interviewees that a MUR should be patient centred to be of high quality. This involved effective listening and communication skills, and tailoring the consultation to the individual patient rather than sticking rigidly to a set of questions that risked restricting the consultation to a tick-box exercise. It was suggested that a patient-centred MUR would be more likely to affect positive outcomes for the patient:
I always find that having a relaxed less formal approach to the MUR, people are more likely to open up to you and it’s like a conversation rather than a step-by-step going through each of their medicines . . . I often find that I’ll ask them about something and they say, ‘Oh well, no one’s ever said that to me’. So it’s more having a relaxed conversation about all their medicines and how the medicines are fitting into lifestyles . . . I would say, for them, [that] is a high-quality MUR.
Pharmacist 19
The length of the consultation was another important element of a high-quality MUR for some interviewees. Devoting adequate time to a MUR prevented the consultation being rushed, provided sufficient time for patients to air their concerns about their medication and facilitated a patient-centred approach:
It’s a balance between getting patients when there’s plenty of time for you to actually sit with them and make sure it’s going to be a good MUR, rather just coming in and rushing through . . . we’ve got 5 minutes to rush through this while someone waits outside and they get the script done, and then you’re dashing in and out all the time. So that’s the main thing, to make sure the quality is there and make sure that patients . . . the other customers aren’t waiting because you are sat for 20 minutes doing an MUR.
Pharmacist 26
Less frequently, interviewees mentioned the opportunities for added value that contributed to the quality of a MUR consultation. These included the provision of healthy living advice, signposting to or integration with other pharmacy services and integration with GP services:
. . . as part of MUR you don’t always cover that sort of thing [healthy living advice]. There’s normally a tick box, ‘yes, I have covered it’, but with the time space you get it’s . . . we do really push it here and make sure the patients understand lifestyle advice, things like diet, exercise, smoking, obesity, that sort of thing . . . and we have a stand outside . . . lots of leaflets and things. So we’ll always show people, ‘have a read about your condition’, so they’ve obviously got something to take home with them as well.
Pharmacist 40
I think we’ve got a pretty good one [relationship with local GPs], which is unusual, because we’re not located in the surgery, or we haven’t got a surgery nearby. But we do work with surgeries across the city, and generally, we have a very good relationship with GPs. And we’ve had some really positive feedback about our MURs, especially where we’ve been able to solve a problem as part of the MUR, rather than just write to them with a list of problems. We’ve been able to actually do something. Then I think we’ve been very well received.
Pharmacist 2
Finally, although less within the control of the pharmacist, a number of interviewees suggested that a high-quality MUR was one in which the patient was engaged with the process:
Some patients don’t want to spend 2 minutes with you, and I don’t call that an MUR. You’ll get those patients who, ‘I know what I’m doing, don’t worry about it’. Even trying to get something out of them it’s just like talking to a brick wall. Everything you fire just comes back to you. So those aren’t high-quality MURs.
Pharmacist 15
Organisational characteristics associated with variation in clinical productivity
Staffing and skill mix
All of the pharmacist and superintendent pharmacists and most of the service commissioners we interviewed mentioned aspects of staffing and skill mix as important, if not the most important, organisational factors determining the level of clinical productivity achieved by community pharmacies (both the quantity and quality of services provided). This was in relation to overall staffing levels, skill mix (including second pharmacists, dispensers, accuracy checkers, pharmacy technicians, counter staff, pre-registration pharmacists, locum pharmacists, drivers), training, teamwork, delegation and continuity of staff.
Overall staffing levels
Many pharmacist interviewees spoke about the necessity of having a sufficient number of staff or staff hours to enable them to deliver the current volume and/or range of pharmacy services:
Staffing’s very important. Obviously we need the right amount of staff so we can provide the services. If we haven’t got the right amount of staff in . . . the waiting time increases, which means people go elsewhere.
Pharmacist 32
Often, however, staffing levels were reported to be insufficient, either having reduced in recent years, or not increased in line with growing dispensing volumes and expanding service provision. Interviewees cited changes in NHS remuneration and the need for organisations to make savings as possible reasons for this:
. . . because of the squeezes on funding . . . one of the first things to get squeezed is staffing levels, unfortunately. So, as the contracts have . . . changed over the last few years, and it’s become more service orientated . . . the funding has not gone up, but been moved around a bit . . . the first thing companies have done is to streamline the staff.
Pharmacist 29
Perceived shortfalls in staffing levels meant that cover for absent staff was not always available and some pharmacies struggled to provide MURs or the full range of services available, with dispensing services prioritised (particularly at busier periods). In addition, both the quality (particularly in relation to the time that could be spent counselling patients) and safety (particularly in relation to dispensing errors) of services was also sometimes seen to be put at risk. Some interviewees talked about community pharmacy being at a ‘tipping point’ in which any further demands could not be met safely without additional resources:
I’ve worked in three different companies, and it’s always been one of the main issues I think, where they try and scrape the most they can from the minimum. I suppose it’s a business, but my regional manager came to see this branch . . . she was happy with our performance as such, and I said to her ‘I’ve asked for some more hours, more staff’ . . . what they tell you always is, ‘Everybody would like more staff!’. It’s fine, but you can’t operate or get any more performance . . . you want to be performing but you want to be safe at the same time. When you said about the quantity and the quality there is a balance there. So I told them, ‘I might not be able to increase their figures more because I’m reaching that point where we’ll not be able to do that’.
Pharmacist 1
Low staffing levels were also a concern for commissioners, who were critical of pharmacy organisations that operated with only the bare minimum of staff. One commissioner suggested that basing staffing levels on the minimum outlined in Part VIA of the Drug Tariff69 left pharmacies with no capacity to provide advanced, enhanced or locally commissioned services:
Obviously, they’ve got to have the correct staffing levels but there’s a difference between what legally you should staff that pharmacy at and what ideally you would staff that pharmacy at, do you know what I mean?
Commissioner 3
For many commissioners, turnover and continuity of pharmacy staff was also a problem. Commissioners spoke about how frequent pharmacist turnover or the high use of locum pharmacists affected both the commissioners’ knowledge of, and communication with, local pharmacies, and also the confidence they had that the services they had commissioned could be reliably and consistently offered to patients. In some cases, training and accreditation was identified as a problem with locums or relief pharmacists not being appropriately trained to offer a particular service, or training not being applicable to other areas, which therefore led to gaps in service provision. In other cases, commissioners felt that the individual drive and interest of a pharmacist was crucially important to the success of a service. If a particular pharmacist left the pharmacy or went on a period of leave the service would grind to a halt:
Turnover, I think, is a massive thing because . . . if you give a contract to a big organisation, and they have staff members that move around, at least the organisation retains the memory. But with the pharmacy services, it’s often the individual pharmacist that’s either keen or not keen. And so we very often, have the experience of phoning or going into a pharmacy and saying, ‘Oh hello, can I ask you if you’re providing the minor ailments service today?’, for example. And they’ll say, ‘Oh no, we’ve only got a locum on today’, or, ‘Oh, well, we used to but our regular manager’s gone off on maternity leave and we’re covered by temporary staff now’ . . . our experience is . . . they’re delivering fine, and then suddenly, it goes from several consultations a month, down to zero, and it’s just because that keen person has moved on.
Commissioner 1
. . . I think what we’ve commissioned, would be a good service. It’s just that we can’t rely on it. So, all the commissioning toolkits in the world aren’t going to help if the provider isn’t ready to provide. Well, they will help . . . but they won’t solve, what I see, as the biggest issue, which is the workforce and their consistency of provision.
Commissioner 10
Skill mix
More commonly discussed by pharmacist and superintendent interviewees than overall staffing levels, however, was the skill mix of the pharmacy team and how that could influence the clinical productivity of the pharmacy.
A key enabling factor, described by a number of pharmacists, was the support of a trusted and competent team, each trained to an appropriate level. Having appropriate skill mix could free up the pharmacist to take on a more patient-facing role, provide more clinical services and deliver a higher-quality service by spending more time with patients. It was suggested that this would be more likely to achieve better patient outcomes (e.g. improving adherence) and reduce waste:
Staff. Qualified staff. Good dispensing staff [can maximise clinical productivity], so that if there’s an MUR, an NMS opportunity, EHC [emergency hormonal contraception], I’m quite happy to leave the dispensary for the 10 minutes or whatever that you’re going to be in the consulting room. Head lice, the staff are all trained, so it doesn’t require me to do it. Smoking cessation, the same, in fact I’m not trained, the staff do it. So I think the staff, having good, qualified staff.
Pharmacist 41
The importance of different components of that team were highlighted by interviewees, including the dispensing staff, accuracy checkers, pharmacy technicians, the pharmacists themselves (and having a second pharmacist, pre-registration pharmacists and locums), counter staff and the delivery driver.
A number of interviewees believed that it was important that all (or most) staff were trained to a certain level in dispensing so that each member of the team could stand in for others who may be absent or to release the pharmacist from the dispensary:
I think it’s just that we’ve got a range of staff that they can all do everyone else’s job, so everyone can dispense, everyone can go on the till. Everyone just chips in, there’s no delineation between roles.
Pharmacist 7
When the skill set of the pharmacy team was more limited, this could be perceived as a barrier to clinical productivity:
You get some other shops, where I worked before, where you have people that are only counter assistants, so they are quite limited. So they are there, and they’re serving all the time. But if they’re on holiday, or if somebody else is on holiday in the dispensary, you don’t have anybody to replace that person.
Pharmacist 1
Training dispensary and medicines counter assistants to deliver aspects of services such as smoking cessation or minor ailments was also seen as a way of maximising clinical productivity (see Pharmacist 41, above). A small number had help from a non-pharmacist pharmacy manager who could take responsibility for much of the administrative side of running the pharmacy. One interviewee mentioned that employing a second delivery driver had increased their dispensing volume.
The knowledge and ability of the pharmacist themselves was also recognised by some as an enabler of clinical productivity (or barrier to, in situations where skills were lacking). For example, training in the delivery of particular services was seen to be a necessary, although not sufficient, investment for the delivery of high-quality services, with experience in the delivery of those services an additional requirement to instil confidence in the pharmacist. A small number of pharmacists who had undertaken postgraduate diplomas believed that these had been instrumental in building their confidence as a health-care provider. Interviewees highlighted the need to enhance not only clinical skills but also management and leadership skills to be able to maximise clinical productivity. In particular, skills around time management, delegation and team leadership were identified as important facilitators of being able to get the most out the pharmacy team. It was also suggested, however, that the lack of available time was a barrier to pharmacists accessing training opportunities.
Many interviewees (both pharmacist and commissioner) emphasised the role of accuracy checkers in the dispensing process as a successful way of freeing up pharmacists’ time to focus on more clinical services, extending the range offered, volume delivered and also the quality of those services (e.g. time spent with a patient for a MUR):
I think a big thing is if you can get an ACT . . . it frees up your time incredibly. You have a dispenser and an ACT you’ve got nothing to worry on the dispensing side, then you’ll become fully patient focused . . . you can offer other services, diabetes screening and blood pressure monitoring.
Pharmacist 15
Well if you then have a number of things that have already been clinically checked, and so the item is there, just needing to be accuracy checked before it goes out, it then means you can still have items going out, whilst the pharmacist is actually involved in an MUR. It just keeps the flow going, and you don’t have people hanging around for ages.
Commissioner 4
Barriers to employing and using an accuracy checker effectively included financial barriers (although this could be offset by the additional income generated through the ability to provide more services), overall staffing levels (in which accuracy checkers were required to take on additional roles in the dispensary that prevented them from focusing on accuracy checking) and the reluctance of some pharmacists to delegate tasks that they retain responsibility for:
. . . I haven’t worked with an ACT. Personally I’m still a bit dubious to do with, not the legal side but if something goes wrong, who takes the rap? . . . I’m not sure how I’d feel about that, I think I’ve been qualified for many years, long in the tooth and it would be a bit of a change in role I think . . . I just worry that if we did go wrong, you’re still overall responsible.
Pharmacist 41
Some pharmacist interviewees suggested that the one-pharmacist model, common in community pharmacies, was a particular barrier to increasing clinical productivity and that having a second pharmacist would be the preferred solution. With pharmacists still required for the clinical check in the dispensing process, a second pharmacist was viewed by some as the best way to increase clinical productivity in relation to both the quantity and quality of clinical services such as MURs and locally commissioned services. In addition, a second pharmacist would provide opportunities for domiciliary visits to allow those with potentially greater health-care needs to have access to pharmacy services. Similar to pharmacists, commissioners felt that the main benefit to adopting the second pharmacist model would be an ability to share the workload, enabling pharmacists to spend more time on clinical activities with patients conducting MUR consultations, for example, and also enabling one pharmacist to leave the premises to conduct other services such as MURs for housebound patients:
[Having a second pharmacist] that provides the ability to actually go out and do MURs in a patient’s home, where the patient is housebound, and often they’re the ones that need it the most . . . I don’t think it would be a waste of money if the NHS just overnight said, right, we’re going to provide the cost of a full-time equivalent for every community pharmacy . . . community pharmacy especially would then have the opportunity to really prove their worth, and I think it might not save the NHS money this year or the year after, but it should be really showing a big difference 3/4/5/10 years down the line, if we’re doing what we’re supposed to be doing.
Commissioner 2
In some pharmacies, for example the busier stores and 100-hour pharmacies where pharmacist shifts can overlap, a two-pharmacist model was already practised and this was valued by those involved. A more recent development in some chains was also described in which newly qualified pharmacists were employed to focus on dispensing alongside more experienced pharmacists who would take responsibility for the clinical services:
We actually offered our pre-reg [pre-registration trainee pharmacists]’s a pharmacist position when they’ve finished, so we now have a number of second pharmacists in the business, so that’s like an extra investment for us . . . part of what we want them to be doing is actually enabling that pharmacy to do more service delivery . . . that’s the main principle, but . . . having the second pharmacist, there’s a bit of a mentoring role between the two of them, so . . . we want to be developing the second pharmacist into our pharmacy managers of the future . . . but principally yes, it would be they need to learn the basic pharmacy business and have the confidence of another pharmacist there if they need it, and the experienced one is the one that does more of the patient facing service. I think it works really well . . . we’ve seen the number of MURs increasing in the stores where we’ve invested in a second pharmacist.
Superintendent pharmacist 5
There was some scepticism among commissioners, however, that pharmacy organisations would adopt the second pharmacist model due to the financial costs involved. One commissioner stated that it would need to be made a contractual obligation in order for the model to be successfully implemented:
I would really like to see two pharmacists in every premises, so that they could cover for each other and provide the clinical services that I would want to see from community pharmacy. I don’t think that’s going to happen until it’s part of the national contract. And perhaps the national contract has to move away from an item-based fee basis, onto more of a population, well-being basis.
Commissioner 10
Other commissioners felt that the second pharmacist model may not be required full time, but more periodically, such as 1 or 2 days per week. One commissioner gave an example of the use of ‘parachute pharmacists’, employed by companies to move around pharmacy stores as and when needed to relieve workload pressure; another stated:
With the increasing number of pharmacists and the stabilisation of the number of pharmacies, it’s suggested now that we’re getting more pharmacies that are then doubling up on their pharmacist numbers, if not every day, but certainly for 1 or 2 days of the week . . . that then . . . is going to greatly increase the capacity to be delivering other services than dispensing, within each pharmacy.
Commissioner 4
Finally, the use of locum pharmacists in community pharmacies had the potential both to help and to hinder clinical productivity according to these interviewees. When locums were seen as beneficial, this tended to be in circumstances where they acted as a second pharmacist, allowing the main pharmacist to provide more services. Moreover, when regular locums were used, this was seen as allowing familiarity and continuity of care for pharmacy staff, patients and local GP surgeries, and a certain guarantee of the quality of service they would provide:
I think the customers are used to having the regular locum on a Monday who’s been here for a few years. She obviously has her holidays and when she’s not in they’ll notice. And she has a different way of working to me and they’ll perhaps come on a Monday just to see her . . . And Saturday I have a locum . . . he used to co-own a pharmacy and he’s a good pharmacist and he likes doing MURs. I’ve every confidence that, [when I’m not here] things are getting done to the same standard, if not better, than my standard.
Pharmacist 25
In one small chain, the superintendent pharmacist described how they would encourage such continuity and quality of service provision by treating regular locums almost like employees, giving them access to training and involving them in team meetings and communications:
So our locums, I always to say to them, ‘Don’t think about yourself as a locum, as far as I’m concerned you’re a full member of the team who works part time’. The idea being that if . . . you come in and today’s the pharmacist’s day off and we’ve got a locum, as a consumer you wouldn’t know the difference, you get the same service. So we embrace our locums within our training, within our management meetings, within our e-mail round. And if we want to take out a new service then all the regular locums are encouraged, we can’t make them, but all the regular locums are encouraged to engage with the service as well.
Superintendent pharmacist 4
Conversely, other interviewees spoke of locums as being at best ‘hit and miss’ in terms of the impact they could have on both the quality and quantity of services provided by the pharmacy, or else a distinct barrier to clinical productivity. In particular, a locum pharmacist’s unfamiliarity with the pharmacy premises and staff could be a barrier to the quality of service they could achieve as could the lack of continuity from the patient/customer’s perspective:
If you’re a locum pharmacist it must be really difficult, because you’re going to be going into a branch where you’re expected to keep the dispensing going, but you’re also expected to deliver two, three, four MURs, and your two, three, four, NMS’s in the day. But, you don’t know what’s happening when you’re doing those, and you may not know any of the staff, and that’s got to put a lot of pressure on.
Pharmacist 29
Furthermore, there was a perception among some interviewees that locum pharmacists were either unwilling to provide services (MURs or enhanced services) or unlikely to be accredited to do so, which was a barrier to the range and volume of services provided:
I think locums, generally speaking, when it comes to services, I think most people like [the] flu [influenza] [vaccination service] but . . . nobody wants to do medicine reviews, I don’t think, or NMS. I think they’d all rather not bother. So I don’t think the locums are effective at all.
Pharmacist 34
Management of workload
Relationships between workload and clinical productivity
Most interviewees believed that time constraints were and would continue to be a ubiquitous barrier to clinical productivity in community pharmacy:
I think time is often a factor in any pharmacy, you know. I think because you don’t have a lot of time with any one person, or if you do spend that time, something else gives basically, so having time is always a factor.
Pharmacist 28
It’s going to get to tipping point, I think, where there’s so much pressure on the teams. And, not just the pharmacist time, the dispensers I’ve worked with, I can’t say enough good things about them . . . sometimes they’re in the back and they’re in tears because they’re that stretched. They know they’re working at absolute capacity and it’s still not enough, and they still can’t get through the work.
Pharmacist 29
I think the volume of scripts has increased to such a level, that that’s probably affected the quantity of provision of clinical services, but when those interactions happen, they’re probably at the same quality as they were before, if you see what I mean? So I think the capacity has diminished, to offer clinical services, but the capability’s probably the same. If they were given the time they could do it, but they’ve got less time.
Commissioner 10
Several factors were identified by interviewees to increase demands placed on pharmacists’ time: reduced staffing (see Overall staffing levels); rising dispensing volumes; the greater and growing range of pharmacist-led services; the greater administrative and regulatory burden associated with service delivery; procurement difficulties (stock shortages); the number of different ways that prescriptions are presented [e.g. electronic transfer of prescriptions (ETP), prescription collection, walk-ins]; pharmacy staff training; and inadequate pharmacy premises and technology:
So everything that’s in the promotions, on the telly, on the adverts, pharmacy, first line of defence, go to the pharmacist, speak to the pharmacist, but then the NHS come through the back door and put a shed-load of work for me to work through and they still expect me to fit in the time to go out and speak to the patient and to go out and deliver the service when I’ve got 400 or 500 items to check a day, in addition to managing the shop, in addition to all of the paperwork, in addition to the e-mails that are coming through, in addition to actioning an MHRA [Medicines and Healthcare Regulatory Authority] alert.
Pharmacist 31
Time constraints were seen to challenge clinical productivity, both in terms of service quality and also in terms of the level or volume of services delivered. There were reports that high (and fluctuating) dispensing volumes were problematic, reducing patient contact time for counselling and/or follow-up, thereby lowering the quality of dispensing services:
. . . if there’s a high volume of prescriptions then . . . we’re basically likely to spend less time with a patient then we would otherwise. So the basics do get done in terms of the pharmacist being available for patient advice, but in terms of how much time you spend with people following things up . . . it’s more the follow-up and things that we would be able to spend more time with if we were less busy.
Pharmacist 19
Pressures on the dispensary to deliver a speedy dispensing service could also adversely affect the quality of the dispensing service. This could be exacerbated by patient expectations and was sometimes fuelled by organisational targets around waiting times that could be displayed in the pharmacy:
However, you do get times when you just are inundated and people do have to wait longer, so then they’re not happy about that, but you’re faced with, well either we quicken up and reduce our accuracy, or we slow it down and get it right, which obviously I’d rather do.
Pharmacist 28
As well as pressures on the quality of dispensing services, many interviewees also stated that existing workloads limited both the quality and quantity of the advanced and enhanced/locally commissioned services provided. Because of the reactive nature of the dispensing service, this was often prioritised over other services, particularly at busy times. Therefore, managing high dispensing volumes could reduce opportunities to offer other clinical services to patients, encourage pharmacists to select less complex cases to offer MURs to, or limit the time they could spend with patients receiving these services.
I think the problem with MURs at the moment is it’s a very numbers-led service which I think generally impacts on the quality. So I mean I’m guilty of it myself, you look at the two-item MURs where you hope that there’s not really any issues and you can be in and out relatively quickly. I mean you never can tell, someone on two items might not know what they’re doing, there might be a lot of other issues going on, you can’t tell. But generally you’d expect them to be less complicated and less time-consuming.
Pharmacist 23
The likelihood that pharmacies would take up any additional services from service commissioners was also mentioned as a limiting factor to pharmacies’ clinical productivity. Commissioners also recognised that high volumes of work, particularly dispensing volumes, were a major barrier to the uptake of the services that they were commissioning and also to increasing clinical productivity in the future.
I think, one of the main things is, that there’s just so much dispensing, that the pharmacists really haven’t got the capacity to take on more and the services that I’ve commissioned, all have to be delivered by the pharmacist.
Commissioner 10
There was a perception among many interviewees that rising workloads would continue to challenge the capacity of pharmacies to remain clinically productive, and would place greater importance on optimal workload management strategies to overcome these challenges.
Strategies for workload management
A number of workload (re)organisation strategies, perceived to help facilitate clinical productivity in community pharmacy, were described by pharmacist interviewees. These included appointment systems for MURs and other services, mechanisms for handling repeat dispensing, pharmacy-level procedures and the use of technology. This was endorsed by service commissioners who felt that there was a need for pharmacies to adopt better workload management systems.
Some pharmacists reported deferring MURs during busy periods and offering appointments or inviting patients to re-visit the pharmacy at a quieter period, in order to secure delivery of the service, maintain the length of MUR consultations and therefore maximise the quality of the MUR service:
I think being open Saturday helps a lot. Saturdays are very quiet here . . . So I do tell a lot of people if they want to come back and we can do their MUR on Saturday that’s fine. A lot of my stuff’s been clinics, when I have appointments, they’re normally on Saturdays as well because it’s just so quiet.
Pharmacist 15
Several commissioners agreed that identifying quiet times in order to book in appointments with patients for services was one solution to improving workflow and maximising service delivery. One commissioner stated that he was aware that some of the larger pharmacy companies were attempting to do this by analysing their patterns of business throughout the day:
Everybody gets lulls in the day . . . so it might be that if you’re quiet from 2 ‘til 3 before the sort of late afternoon surge kicks in, then it might be that if, you were offering . . . a pre-bookable service, like health checks . . . you would say to your staff ‘well, look, that’s a really good slot for . . .’ . That’s what the companies are good at doing . . . they literally look at the till receipts, so they can see the surges in business . . . and the dispensing flow and everything, and they target the services around those dips in walk-in.
Commissioner 3
However, although some pharmacists were able to use an appointments system for managing competing workloads, others felt that this was not workable because of the unpredictable nature of their walk-in business:
We have an appointment system but you may as well not, because you book someone in but you can’t control what time someone comes to buy their paracetamol, and you can’t control what time someone, a stranger walks in with their prescription. So you book someone in at seven o’clock to see them, the world and his wife could turn up at seven o’clock.
Pharmacist 34
One view expressed by commissioners was that pharmacists needed to move away from the mentality that dispensing should always be prioritised over other work and embrace the idea of spreading out prescription work over the working week:
I think there’s a little bit around the pharmacists managing workflow . . . so okay, Monday to Friday you’re really busy . . . and you’re not doing very many MURs. On a Sunday, you don’t have the people in, so you can’t deliver MURs . . .’why aren’t you managing some of your prescription load on the Sunday, so on a Monday when you’ve now got more patients, you can do some MURs?’ . . . I think there’s a little bit of a mentality of pharmacists as well that the prescription’s waiting, ‘we need to do them’, rather than thinking . . . ’we’ve got plenty of time, we’ve got a 7-day lag before that patient comes in . . .’ . That isn’t necessarily a priority, your priority is serving that patient with the needs of that patient, which might be an MUR. But pharmacists . . . their tick at the end of the day, the bench is clear and ‘I’ve done my work’.
Commissioner 5
A number of methods of organising the more predictable workload associated with repeat prescription dispensing was described by the pharmacist interviewees, including the use of collection services, off-site dispensing services and pharmacy-level procedures for managing dispensing workflow, all of which helped some pharmacies free up time to maximise both the quantity and quality of service provision.
Many interviewees believed that a prescription collection service increased the quality and quantity of pharmacy service provision, by changing the balance of workflow from reactive to proactive and enabling pharmacies to manage high volumes of repeat dispensing work during quieter periods. This created time for unpredictable ‘walk-ins’ and also released pharmacists to perform clinical activities. By enabling the pharmacy to decide when to dispense these repeat prescriptions, this service was perceived to reduce waiting times for both patients on repeat prescriptions and walk-in patients to whom they were able to react more quickly. Some also felt that the prescription collection service tied patients to the pharmacy, which additionally helped to maximise productivity:
Also we offer the repeat dispensing system where we collect prescriptions directly from the GP for the patient . . . [if an item has] not been issued or there’s been some form of delay . . . because we’ve got a good relationship with the surgery, we can actually go and get a prescription done immediately. So doing this keeps this kind of the patient tied to us because they’re kind of happy with our service and they want to continue to be with us.
Pharmacist 11
. . . it’s all interwoven, your items are increasing, people are now more willing to want to come and have a chat because they’ve not had to wait that long. They’re happy to have you call them if it’s a new medication for them . . . even the shop floor, OTC [over the counter] sales, they’re now happy to use that extra time they’ve got to just go around, see what they can buy. So it’s increased your sales over the counter . . . to them that’s quality of service when they come to your pharmacy [and] their prescription is ready and they don’t have to waste time here.
Pharmacist 20
However, some perceived that the prescription collection service created challenges to workflow, creating more work for pharmacies without increased capacity, as a result of this ‘extra’ work not being remunerated. Moreover, this service [like dispensing and monitored dosage system (MDS) services] also relies on partnerships with GP practices, with interviewees describing difficulties resolving prescription issues in a timely manner as having the greatest detrimental impact on quality during periods of high volumes of work. A small number of commissioners also felt that the prescription collection service could lead to medicines waste:
A lot of the big companies are running these repeat dispensing services, where the company will order the prescription, get it ready. That’s fantastic for the patient, absolutely brilliant, but companies have taken on all that extra admin[istration], and obviously with that it’s your responsibility, you can’t just do it slapdash. You’ve got to have audit trails, it’s got to be properly done, that’s got a massive administrative burden to do that properly, you know, without doing it in a slapdash way [. . .] The income that we get from a repeat dispensing service is still just the prescription fee, at the end of the day, and whatever the cost of the medication is, we don’t get paid by the patient for managing their prescription. So, the money that comes into the business is still the same, but the work that we do to get that money has increased.
Pharmacist 29
There was a perception that off-site (or ‘hub and spoke’) dispensing, which assembles repeat prescriptions outside the branch, removed the branch-level burden of repeat dispensing and therefore provided in-branch pharmacists with time to deliver additional services and spend time with patients to improve clinical productivity:
And I do think that that [hub and spoke dispensing]’s the way forward, and I do think, at some point down the line, probably with the pick-up in the electronic prescription service, that we’ll move to more centralised dispensing factories, and patient packs being delivered to pharmacies rather than the individual products being sent out there to then be assembled in pharmacies.
Commissioner 4
I think as more pharmacies take on off-site dispensing . . . all the repeat business will go offsite which will free up more time for support staff and pharmacists to spend more time with patients and to actually get involved in more services.
Pharmacist 23
In addition to the prescription collection service and dispensing ‘hubs’, a number of interviewees also described how pharmacy-level procedures (e.g. prioritising walk-in patients, MDSs and stock management) helped to manage workflow to maintain clinical productivity:
We try and set it up so that if we’ve got patients actually walking in and waiting for prescriptions, they get priority rather than the people that might be coming in later to collect or people that are being delivered to at a certain time, then we’ve got a system for managing that so that the people that are actually the ones in the actual pharmacy are the ones that get dealt with first.
Superintendent pharmacist 5
However, a few reported delegating labelling to dispensary staff during periods of high workload in order to minimise waiting times, thereby improving the speed of the service but potentially reducing other aspects of quality (e.g. clinical check, ID of new medicines) and failing to link the dispensing service to other services (e.g. NMS and MUR services):
. . . when we get very busy, [I] try to work it in such a way that all I’m doing is checking prescriptions and it’s whether the member of staff is thinking about it, understands it etc. when they’re labelling to identify that it’s actually a new medicine, so, I would say, the kind of shop we are, we do probably miss a lot of new medicines.
Pharmacist 28
During periods of high workload, some pharmacists also described ways of managing patients’ expectations and waiting times to help manage demand:
You try and manage people’s wait in so much as, if, for example, someone comes in with a 10-, 15-item prescription . . . [and then] someone comes in after with one item you would maybe bump them up a little bit. Because I think if you bring in a large prescription you know there’s going to be a wait and I think you have to be prepared for that if you’re insisting on waiting . . . so . . . you would try and jiggle things about to try and make sure as few people are waiting a long time as possible.
Pharmacist 23
Finally, respondents’ views were mixed concerning the effectiveness of technology to help pharmacies manage workload and maximise their clinical productivity. Pharmacy computers and the associated software could facilitate data recording in relation to services provided, the ID of eligible patients and stock management, particularly when systems were up to date and when more than one computer terminal was available:
Well, we use the computers because they identify a potential patient for us . . . otherwise you’d be trying to find records, is this patient suitable? And the fact it’s on the computer, the MUR forms, so you just sit them down in front of the computer screen and it’s there for you . . . you can print the consent form off. So the main thing is the computers. I wouldn’t like to try to do paper-based ones.
Pharmacist 41
Conversely, only having one computer in the pharmacy and cumbersome data recording systems could add to the pharmacists’ workload and thus hinder clinical productivity:
In the pharmacy, because of the amount of paperwork, sometimes that can be time consuming . . . we tend to . . . have either one or two computers, and everything has got to go on the computer, so you’re always fighting for that one space.
Pharmacist 35
Some commissioners were similarly critical of pharmacies’ current information technology (IT) systems, which they felt were not always fit for purpose and were time-consuming for staff. Commissioners felt that investment in IT systems by pharmacy companies and owners could help to improve clinical productivity, but was not always viewed as a high priority. Again, having only one patient medication record terminal in a very busy pharmacy was identified as an obvious hindrance, along with IT systems that were not capable of easily recording interventions and allowing basic reports of these interventions to be made:
I think one of the major stumbling blocks that we’re finding, when we’re going out and doing our contract monitoring visits, is the poor level of support that most, if not all of, our pharmacies have, from their IT system . . . difficulties around recording things in a quick and easy manner . . . and having gone through and seen how they need to record it . . . I can’t help but agree with them . . . [it] could be easily sorted with a bit of thought and possibly a bit of investment . . . but at the moment we seem to be banging our heads against a brick wall, trying to get that message across . . . with the multiples, they’re then saying that it’s not high enough on their priority to then invest in that area, and for the independents, they’re telling us that they’ve tried to push back to their suppliers, but their suppliers are just saying, ‘well that’s our kit, take it or leave it’.
Commissioner 4
Electronic transfer of prescriptions or the Electronic Prescriptions Service (EPS) similarly evoked mixed views from respondents on whether they were a help or a hindrance to workload management and maximising clinical productivity. Some pharmacist interviewees perceived that ETP increased the speed at which interventions could be made and addressed by GPs or prescriptions issued, increasing the quality of the dispensing service. This, in turn, created more time for pharmacists, increasing their clinical productivity:
We’re doing a lot of ETPs – that’s grown massively . . . I think it improves the quality because it means that the prescription is here quicker . . . we can now put a prescription repeat in in the morning and we can get the prescription back by the afternoon on the computer, which is great . . . Sometimes [the patient’s] gone to see [the GP] and by the time they’ve walked here they’ve sent the prescription down . . . it will increase the number of people that are coming to pharmacy, because obviously they’re going to be registered here, and they’ve nominated us, [and] we’re not going to lose the odd script.
Pharmacist 21
Conversely, others had experienced difficulties with the introduction of ETP, which, rather than freeing up time to enhance productivity, was adding to pharmacists’ workload. For example, some had experienced delays in the arrival of prescriptions; others complained about irregular or constant streams of prescriptions. Some highlighted the inability of the EPS to issue controlled drug prescriptions (now addressed through legislation);70 others, the time and costs associated with printing:
. . . about 75% of our prescriptions are coming through ETP now . . . which is causing a problem with our workloads . . . The ETP is hard to get our heads around, because it’s coming all the time and we’ve never finished dispensing . . . even at half past six at night there’ll always be a full page . . . because they’ve just come down online . . . You come in on a morning you know there’s going to be a pile there . . . The ETP aren’t coming through in a logical sequence. So you have to look down the whole list to see if there’s more than one prescription for that person, which takes time. Also having printed it off, because you print it off and then dispense it, that takes longer than if somebody walked in with a prescription . . . We’re finding it’s taking considerably longer to claim for them than it used to be for just counting and filing at the end of the day. So that’s added to the workload.
Pharmacist 25
Similarly, ETP was viewed by commissioners as having the potential to help pharmacies to manage workload more efficiently in the future. However, the initial set up and accompanying teething problems of the service were believed to have increased the workload for pharmacies:
[I think EPS has] increased the workload within the pharmacy, in terms of printing off tokens and managing the sort of administrative side of it. I think the burden of EPS has fallen much more on community pharmacy than general practice. So I think that’s been a big factor.
Commissioner 10
Another technological advance perceived by some pharmacists and commissioners to improve or have the potential to improve clinical productivity in community pharmacy, by freeing up pharmacist and staff time for other services, was automated or robotic dispensing:
[Robotic dispensing] frees up that time, you don’t have to be there having to check boxes and all that. It’s been done automatically and maybe a pharmacist in the hub somewhere is making sure everything has been entered well and checked . . . it just frees up that time for you to do other things, have time to sit with patients.
Pharmacist 20
One commissioner gave an example of a pharmacy using robotic dispensing in his area; he felt that the robot along with a high level of staff had enabled the pharmacy to cope with a very high dispensing volume, while maintaining a quality clinical service and good compliance in terms of the making and recording of interventions. However, as with ETP, robotic dispensing was not without its perceived disadvantages. The cost of purchasing and installing systems could be prohibitively high. Moreover, the following respondent did not believe that they were effective in releasing pharmacists’ time:
I just don’t think we’re there yet in terms of automation of pharmacies. I think it will work in selected pharmacies potentially but those pharmacies are so few and far between . . . the cost of the robot and the complications that result from putting a robot in . . . just create other headaches that end up consuming pharmacists’ time. This is my view. It’s a pet project for quite a lot of people. I’ve not seen a dramatic change in practice anywhere because of them.
Superintendent pharmacist 2
Organisational culture
Many of these interviews highlighted the role of organisational culture in determining a pharmacy’s clinical productivity. Organisational culture, or ‘the way things get done around here’, was described in terms of the value the organisation (head office, the superintendent pharmacist or pharmacy owner) placed on investing in staffing and skill mix, the extent to which business targets or quantity was prioritised over quality of service, and management style and structure:
How things get done around here . . . I think that’s really key, actually. The organisational culture, because you get some people who are really positive and really want to make things work and really want to succeed and they normally have more staff than other people, to be fair, and others who are just kind of . . . they can only just about get through the day job and they just haven’t got the energy. They don’t have the vision, they don’t have the understanding of their importance or the fact that they’re part of a much bigger NHS family and they’re just part of one of the jigsaw pieces in that family of providing services to patients.
Commissioner 6
Organisational culture, staffing and skill mix
In pharmacies where the culture imbued by head office supported investment in staffing levels, skill mix and training for staff, the perception held was that this improved clinical productivity:
And [the owner] is quite encouraging in the sense that if he feels we need more staff, more support, then he’s more than happy to provide us with that, which is good . . . He also encouraged us to have a delivery driver . . . so it’s definitely improved the number of deliveries we do, or increased, let’s put it that way.
So has that increased the dispensing volumes?
It has, definitely.
So we have a very rich staffing body, so it’s probably double what you’d find in your average multiple. So our plan is that every branch would have a tech[nician] and an ACT to free the pharmacist and we would have one or two counter staff on at any time as well, so that’s the basic staffing model. And in a bigger branch we’d have a second pharmacist some of the time or all of the time . . . So in our business branch we’ve got two full time pharmacists, we’ve got two or three ACTs, two or three technicians and three counter staff on most of the time.
Superintendent pharmacist 4
Conversely, others believed that when head office applied minimal staffing levels, this limited the level of clinical productivity that could be achieved:
And they’re not giving us the staff and they’re doing cutbacks. On one hand they’re wanting us to do these extra services and be out there for the face of the public, but we’re not getting anything extra. In fact, they’re reducing all our resources really staff wise.
Pharmacist 25
In addition to overall staffing levels, an organisational culture perceived to prioritise investment in team development and deploying the necessary skill mix was recognised by some as a way of maximising clinical productivity by freeing up the pharmacist’s time to deliver clinical services:
Skill mix we very much believe in, that’s why we have ACTs, and we train staff up as much as we can, as long as we feel that they’re going to be able to practise their new role and use those skills. We pretty much believe that the majority of our staff . . . should be at least pharmacy-assistant trained. And, we’re quite happy to use our ACTs, such to enable pharmacists to carry out the services, and that’s the philosophy of the company.
Superintendent pharmacist 3
A small number of interviewees identified barriers to this approach, including the low levels of pay offered to dispensing assistants demotivating individuals from taking on additional roles and the levels of remuneration offered by some service commissioners being insufficient to be able to invest in more highly trained staff:
I think it’s about investment, where you’ve got, as we have in [another commissioning region], a consistent credible reliable additional income strain you can make an investment in more ACTs, second pharmacists, a lot more IT, because you get a return. Where you’ve just got like we have here a few sporadic services none of which are really economic to provide, it’s impossible to make the investment.
Superintendent pharmacist 4
Organisational culture and targets
Most pharmacists interviewed for this study reported the existence of service targets to help maximise the volume of service provision. Some recognised that targets could be helpful as a way of ensuring that a range of services was provided. However, when the culture of the organisation was one where the pressure to meet targets was perceived as excessive or as prioritising profit over meeting the needs of patients, this could be viewed as detrimental to service quality:
I think most of . . . the pharmacists I speak to . . . I think everybody I know thinks it’s quantity, not quality, and it’s because . . . if you don’t set targets, maybe nothing will ever get done. But then setting targets just creates rubbish, you just end up with rubbish being done to just earn some money. So I don’t know what the way is.
Pharmacist 34
Quality was seen to be compromised for both MUR services, for which these targets were commonly set, and for dispensing services. The quality of MURs could thus be affected by pharmacists identifying ‘easy’ patients to offer MURs to (i.e. those on less complex medications who would therefore be less likely to benefit from a MUR), by pharmacists treating MURs as a tick-box exercise or by pharmacists not having the time to conduct a thorough MUR. The quality of dispensing services could be affected by pharmacists not spending enough time with walk-in patients in order to find the time to conduct MURs:
I’ve heard dreadful instances of pharmacists being bullied and saying ‘you’ve got to do your quota’ and being given targets each week . . . That is not clinical, is it? . . . So it’s not been a good environment at all and I think for some pharmacists I think they just put their head down and they’ll just do them because it’s easier than not really because of the pressure . . .
And that’s affecting the quality?
Absolutely. Because pharmacists have said to me . . . some pharmacists have stuck out and said ‘I will not do them’ and have been very strong but have had flak from higher management and that depends on the individual pharmacist as to how strong they can hold that. You’re thinking professionally you shouldn’t have to do that. You should have the backing of your company and so on, but that has been down to individuals, yes.
The monitoring of these targets varied from pharmacists submitting daily reports of targets to the delivery of targets being managed by the pharmacist:
It’s company policy. Only because when we have our daily reports the total number of MURs and NMSs that are performed each day, they’re the only two figures that are reported on a daily basis without fail across the whole estate, so from a business point of view they’re the two priority things regardless of all the peripheral stuff that other pharmacies may do, even though they might be beneficial.
Pharmacist 7
There weren’t any targets for MURs initially, they have introduced them recently, and they’ve said that we want you to complete 400 by the end of the year. But there’s no pressure so if there’s a week where you’ve done none you will never get a call from your line manager to say, ‘why weren’t any MURs done?’. That kind of pressure doesn’t exist in the company, they tell you what your target is, but then they leave you to do it in your own time.
Pharmacist 38
Medicines use reviews and NMS interventions were widely perceived to be the services for which pharmacy management were most likely to set and enforce targets. Targets were not perceived to be set for other services to the same extent:
I mean MURs, NMS, obviously we’ve got a lot of pressure on, but other things like chlamydia screening, smoking cessation, there’s not the same level of pressure.
Pharmacist 23
Organisational culture and management
The role of management structures in helping or hindering clinical productivity was also highlighted in relation to the extant culture of the organisation. For example, having a non-pharmacist area manager could be seen to be detrimental to productivity when they were unreceptive to the problems faced by pharmacists; having a non-pharmacist store manager, on the other hand, could be seen to be beneficial by taking on pharmacy management and administrative tasks, and freeing up the pharmacist’s time to deliver services:
. . . for our area, we have an area manager that is a pharmacist, yeah. I don’t think it’s a rule, but . . . we’re lucky enough to have a pharmacist. I think it helps because they can understand certain issues or the role better than if they were non-pharmacists . . . I’ve had experience before, in other companies, where area managers were not pharmacists, and one of them told me that even trained monkeys can do our job! And so that wasn’t very nice! But if they’re pharmacists, they have an insight in our role and our job better.
Pharmacist 1
[The non-pharmacist manager’s] role in the store was much more focused on the retail side of things. She was responsible for the pharmacy side of things as well, but she always said, ‘Clinically, I’ll leave you to make any decision you want to make. I’ll never question you on anything clinically, or how you want to run the dispensary, I’ll leave that to you, unless I think it’s illegal or unsafe I’ll leave that to you’. That worked brilliantly for me, because I got to still manage the dispensary team, and everything that went on in the dispensary. Not so much I didn’t have to worry about the retail side of things, as I’m still legally responsible as the RP [responsible pharmacist] for everything that’s going on with the selling of medicines. But just, you know, silly things, like planograms, and have you got enough deodorants and toothpaste on the shelf, that wasn’t a worry for me anymore, which was great.
Pharmacist 29
Managerial style was also thought to influence clinical productivity in terms of the way service targets were enforced. Reported managerial strategies to enforce targets varied from collaborative, supportive and encouraging to autocratic, discouraging and humiliating:
But we’ve had area managers that liked to name and shame those that don’t meet targets and say you could do better. I personally prefer to be encouraged rather than discouraged. And ones that can listen and understand what the problems are, but they’ve also got things to do. So I’ve not really found an area manager that’s been supportive of our needs. They’ll implement the extra services, but they’re not really supportive of helping us at the branch level.
Pharmacist 25
Ownership type
A number of opportunities and barriers to clinical productivity were identified by interviewees in relation to the type of organisation a pharmacy belonged to (e.g. large multiple, supermarket, smaller chains and independents). These often related to the organisational cultures associated with these different ownership types. However, they also related to organisational size and infrastructure, pharmacy staffing and skill mix, pharmacists’ autonomy and the relationship with the customer.
Ownership type and organisational size, structure and culture
In the view of some pharmacists, multiples were better able to provide a greater quantity of services, but sometimes this could be at the expense of quality through pressure to meet targets. Large multiples were perceived to be target-driven, a view expressed most commonly by pharmacists working for small chain or independent pharmacy organisations. Although a target-driven culture was sometimes believed to increase the volume of MURs conducted, this could be perceived to be at the risk of compromising service quality for both MUR and dispensing services, the latter due to longer waiting times while pharmacists were tied up delivering other services. In contrast, it was suggested that smaller chains were associated with a ‘clinically led’ culture, which improved the quality of service provision:
I suppose for some people they need to be monitored or need to have targets and things to . . . improve their services. I think if you’re quite driven to giving those services already it wouldn’t necessarily make much difference, but I guess yes, it’s good to have targets because you’ve got something to aim towards . . . The only thing is . . . for example with [large multiple], they had very high targets so people would do MURs that probably weren’t very good MURs just to make sure that they hit the target . . . I think if you haven’t got such high targets then the quality is higher because you’re not under that kind of pressure to perform. You’re actually doing it because you want to do it and do it properly rather than anything else.
Pharmacist 21
Although it was recognised that all pharmacy organisations placed some pressure on pharmacists to maximise productivity, some perceived that in the large multiples this pressure was excessive. The point was made that the funding changes introduced in the 2005 contractual framework had produced financial incentives to maximise the number of MURs to recover funding that had been redirected from dispensing. However, one superintendent pharmacist from a large multiple stressed the importance of delivering high-quality MURs in order to secure the service’s long-term future:
There is a bigger picture here in terms of . . . if we don’t prove the quality of MURs as a profession we will face losing the service. Unfortunately because there is a ceiling of 400, and because it was money that was previously earned through dispensing, . . . there was an inevitability there that, ‘well, actually if we need to do 400 in order to earn the same amount of money that previously we used to get’, then there was going to be a notional, ‘well, let’s make sure that we are maximising the number of MURs that we’re able to do’.
Superintendent pharmacist 3
The size and structure of different organisational types were also thought to influence clinical productivity. Some superintendent pharmacists felt that their organisational structure and centralised operations around performance management, policy development, standard operating procedures and off-site dispensing enabled large multiples to maximise the volume of MUR provision and increase efficiency. Other pharmacist interviewees, however, perceived that these same attributes placed constraints on pharmacies. For example, one believed that pharmacists working in large multiples were unable to influence their pharmacy at branch level because of centralised decision-making. Another felt that decisions made centrally could create difficulties in the branch and went on to describe the greater administrative burden for pharmacy staff created by the repeat prescription dispensing service.
There was a perception that smaller pharmacy organisations faced procurement difficulties compared with the buying power of larger organisations (although one pharmacist reported that many patients complained that large multiples ‘never have anything in stock’, which lowered the quality of the dispensing service).
I think there must come a time where independent pharmacies who don’t have the buying power of the big groups will become non-profitable, forcing them to sell. And that the numbers of independent pharmacies will go down even more than they have done already.
Pharmacist 4
Conversely, smaller organisations could also be seen to benefit from increased pharmacist autonomy, closer working relationships and reduced professional isolation compared with multiples.
Because it’s an independent, we have a lot of flexibility. So, yes, within reason it’s pretty much it’s up to me to if we think that we should keep certain things then basically I’ll make that decision and say ‘yes we’ll get that’. And also . . . I guess because we are a small chain I can compare what other stores are doing, what other pharmacists are doing with what I’m doing.
Pharmacist 19
Ownership type and staffing
Some pharmacist interviewees perceived that staffing levels in the larger multiples in particular were not increasing with the increasing workload and in some cases being pared back such that the capacity of the pharmacy team to provide additional services was limited and patient safety might be put at risk. Some commissioners agreed that, in their experience, independent pharmacies could be more willing to increase staffing levels to meet demand than multiples, which helped engender a better patient experience:
[Patients] said, we’re treated with courtesy, we’re treated with respect, we’re dealt with promptly and it’s all the sort of things that the patients value. They’ve always got time for you. There’s always a pharmacist there, so I can quickly talk to them and stuff like that . . . Despite the sheer volume of prescriptions that they deal with . . . Definitely the independents have that ability because they always have more staff, whereas the multiples are very much it’s down to that nth degree of the staffing.
Commissioner 1
However, one interviewee felt that all pharmacy organisations were ‘as bad for running things to the bone and people feeling massive pressure’ (pharmacist 34).
Conversely, some interviewees felt that a better quality of service could be delivered by the pharmacy team in the large multiples because of investment in training for the pharmacist and pharmacy staff. A small number also perceived that this was augmented by the level of support for the pharmacy team from head office:
One of the downsides of working for a big company – like I work for a multiple – is that you’ll always be squeezed for staff, because ultimately that’s what all companies do. But, it’s got its benefits as well, because there is plenty of support, so things like SOPs [standard operating procedures], and everything like that, are all provided for you, you’ve got a head office team to phone up. Training is all provided, and it’s normally provided during your working day so you don’t have to go out in your own time in an evening, or anything, so we get a chance to do that if we want to. So, I think it’s easy to have a go at the big companies, but at the same time there are the benefits as well, because they do give you a fair bit of support.
Pharmacist 29
A number of commissioners stated that although ownership type may play a role in clinical productivity variation, the impact of the individual pharmacist and/or pharmacy team should not be underestimated:
. . . there is a supermarket pharmacy very close to here who . . . had a regular pharmacy manager for as long as I’ve been in the PCT . . . for me, a good-quality service [is] someone you can talk to. She . . . speaks very regularly to her local GP practice . . . has built that relationship up. So sometimes I think it’s about the personnel, isn’t it? As well as . . . the organisation . . . [She] has been very influential and has made the pharmacy very different to how the rest of the shop operate.
Commissioner 8
Ownership type and the relationship with the customer
Smaller chains and independents were sometimes seen to have the edge over larger multiples and supermarkets in terms of service quality, offering a more patient-centred service and continuity of care through stability of the workforce:
But I think that’s where independents have that advantage over big chains and supermarkets because there’s always the same pharmacist, and I have the same locum every Tuesday, so they only see two faces every time. So it’s not like there’s too many different faces. Our staff have been the same for years as well.
Pharmacist 15
Others achieved this through not using locums at all. One pharmacist felt that inconsistency of accreditation to provide services within the locum workforce meant that using only employed pharmacists not only ensured continuity of care but also helped to deliver a wider range of services. The pharmacy type (i.e. employee-owned) and staff benefits were believed to be reasons that attracted pharmacists to employee positions within that organisation.
It was suggested that the patient experience could also be enhanced by supermarket pharmacies, which took some pressure off dispensing times by allowing customers to do their shopping while waiting. However, supermarkets were also viewed as offering a poorer quality service as a result of a clash in culture/priorities between the wider store and the pharmacy:
. . . there’s still a lot of structural things wrong within supermarkets. Well, I imagine it’s like that across all the different chains, the way things are done. I think pharmacy’s an afterthought within the company and because of that . . . you may as well be the bakery.
Pharmacist 34
Ownership type and ease of commissioning services
Some commissioners felt that, in their experience, there was greater willingness by independent pharmacies to participate in the provision of enhanced or locally commissioned services because of the additional income this generated. By recognising this as an important source of income, independents were said to be more willing to invest in additional staff to deal with the resultant increased workload. In contrast, there was less incentive for employee pharmacists at multiple chain pharmacies to participate in such services as they did not directly reap the financial benefit:
Independents are always very, very keen to commission services. They recognise it as an income stream . . . as do the chains . . . but obviously as a general rule, the independents will say, ‘Right, OK, well, if we’ve got these services’ and they might buy in some extra hours off their staff . . . whereas . . . unfortunately, the chains tend to just want more out of you.
Commissioner 3
One commissioner felt, however, that although independents may be keen to try new services, from a commissioner’s point of view, multiple chain pharmacies were often the most straightforward to commission from, and once ‘on board’ could offer widespread provision of a service:
I think independents probably struggle slightly more in the whole. There are some very good ones, but they have to have a very solid business and some very committed people to really sort of branch out into other services. Multiples, well, they’ll do some services and not be interested in others, so the only thing is that sometimes it’s a bit easier to manage because you can talk to one person about a whole group of pharmacies, whereas an independent you’ve got to take in all those people . . . working with a chain you might be able to get something organised on a bit more of a national basis . . . some of the [smoking cessation] quit packs that were issued a couple of years back . . . that was all mainly done through two chains . . . That was done at a very high level.
Commissioner 6
Healthy living pharmacies
The HLP concept was not one that was discussed widely by interviewees in relation to clinical productivity, even though 13 pharmacies selected for stage 2 of the study were either accredited HLPs or else working towards HLP accreditation. For those that did, there were mixed views about the impact HLP status had on a pharmacy’s clinical productivity, ranging from commitment and buy-in to scepticism. Service commissioners were similarly ambivalent:
In terms of healthy living pharmacy, well it is quality; it’s a quality framework around healthy living services. So it’s a quality framework which we’re very much committed to, so that’s a good thing.
Superintendent pharmacist 4
I think we do HLP, we’re just doing it a different way . . . and that’s the way we’ve done our business for the last 10 years or so. So we’ve trialled HLP but we’ve seen no benefit in terms of the stores I’ve operated, but we’ve kind of been doing it for 10 years anyway.
Superintendent pharmacist 2
What we were finding was healthy living pharmacy in [locality] was different to healthy living pharmacy in [other localities]. There’s not a standardised approach and that’s a shame. We need a standard national kite mark so that people know that when you’re in a healthy living pharmacy you’re going to have a certain standard and certain information of messages being given out.
Commissioner 1
Some believed that the quality of service delivery was improved by the knowledge and skills gained by staff from the HLP accreditation process:
We are a healthy living pharmacy and I think that has been useful, in terms of staff member engagement and perhaps the increase in the added value. So before, when we might have just sold a bottle of Gaviscon [Gaviscon®, Reckitt Benckiser, Slough, UK] with some advice on how to take it that might now include, for example, alcohol use, other lifestyle things, in terms of diet and perhaps change mind sets in the team, around other advice we give.
Pharmacist 2
Others, however, considered that providing healthy living advice was already part of their role and that HLP status conferred no additional advantage:
To be honest, I think all pharmacies whether they’re branded ‘healthy living’ or not should be offering the healthy living advice. I don’t think you can be a pharmacy without offering healthy living advice.
Pharmacist 40
In terms of the advantage HLP status may or may not give pharmacies in the commissioning process, one superintendent pharmacist believed it gave them additional negotiating power with service commissioners, whereas others felt that this was limited:
I think what it’s done very well is branded a type of service delivery, especially to commissioners, and it’s given people a concept that they can wrap their heads round, which is quite important in negotiation.
Superintendent pharmacist 2
I don’t think the benefits have quite kicked in yet. What the CCG thought, and what we thought we were going to get from health living pharmacy hasn’t quite been the case . . . we thought we’d get . . . them pushing more stuff towards us and then we would have a campaign around that.
Pharmacist 3
Although HLPs could be seen as a way of increasing the skills of the pharmacy team and alleviating some of the pressure on the pharmacist for delivering services through effective use of skill mix, this was not always successful and some felt that further investment in training was required to deliver the model successfully:
. . . We were at some point nominated by our manager, to work towards the healthy living pharmacies, but then it just sort of flopped . . . we were too busy doing the basic things and trying to get that right . . . You need to have people that are properly trained to do things, so it’s investing in training, not only pharmacists, but the staff, for us to get more involved in healthy living advice . . . at the moment we’re struggling with just being able to dispense normally . . . and do MURs and those few services that we do.
Pharmacist 1
Extraorganisational factors associated with variation in clinical productivity
Patient and population factors
Local population characteristics
A number of features of the local population served by the pharmacy was perceived by the pharmacists we interviewed to contribute to the level of clinical productivity attainable by the pharmacy, particularly in relation to the volume and range of services delivered.
A number of pharmacists highlighted that being situated in an area with a large proportion of older residents limited both the number of MURs that they were able to conduct and also the range of other (locally commissioned/enhanced/private) services they could offer. In particular, the number of housebound older people who either had medication delivered or else collected by a spouse or other carer prevented direct contact with the pharmacist and the ability to offer MURs or other potentially useful services in store. Although it was recognised that domiciliary MURs could be conducted, regulatory and organisational barriers often meant that they were not:
. . . unfortunately, those people that . . . most need our services, are quite often housebound patients that you never see in the pharmacy . . . things like MURs, NMS, are completely useless, because you’re not seeing the patient . . . the only person that possibly sees the patient is the delivery driver, or their relative, and so you’re reliant upon a lot of information from these people that aren’t medically trained at all . . . where you can make the most impact, I think it’s that group of patients but, in order for that to occur, with current economics, then you need to move to more of a remote supervision basis.
Pharmacist 3
There was also the perception that older people were more likely than those aged > 65 years to visit their GP for services that could otherwise be provided by the pharmacy (e.g. influenza vaccinations or glucose monitoring) either through preference or service age restriction. For pharmacies serving a large population of those aged > 65 years, this could result in limited uptake of certain pharmacy services. Some services, particularly sexual health services (e.g. chlamydia testing), were felt by a small number of interviewees to be less appropriate to be offered in areas with high proportions of older people, thus limiting the range of services that could be offered by some pharmacies.
Conversely, a small minority of the pharmacists we spoke to suggested that older people might be more willing to speak to pharmacists about their medication, offering up opportunities for providing medicines optimisation advice. Furthermore, an older population offered opportunities to increase the number of compliance aids provided:
I especially like the elderly. They do like to sit, and sometimes they do like to have a good chat . . . most of them are lonely, and it’s just getting the time to be able to sit down with the patient and talk, which if it is busy that can be difficult.
Pharmacist 40
The level of deprivation in the local area was also perceived by some pharmacists and a small number of commissioners as either an opportunity for or a barrier to clinical productivity. For example, one pharmacist suggested that being situated in an affluent area where the local population was more educated meant that people were less likely to seek advice about their medication:
. . . it’s quite an affluent area . . . they’re all ex-teachers and retired cops . . . so they tend to be quite knowledgeable about what they’re using and how they’re using and they tend to have quite a good product knowledge really.
Pharmacist 26
Levels of high deprivation, on the other hand, could either be seen as an opportunity to provide some services, for example needle exchange or minor ailments services, or else as a barrier to providing private services that the local population would be less willing to pay for:
Well, there’s demand for [the minor ailments scheme], there’s GP support. We’ve seen the highest levels of use of it in the most deprived parts of the city . . . evaluations we’ve done indicate that if those patients weren’t treated in minor ailments, they would certainly be at their GPs.
Commissioner 7
The only thing is, living on this estate, private services are really pointless, just because that’s the infrastructure of this area. We’re on a council estate . . . So private PGDs [patient group directions], child clinics, they’re probably a no go in this area, and I don’t think they’d be worth even opening up.
Pharmacist 15
One superintendent pharmacist with city centre pharmacies noted that for them, the customer base was quite different from patients visiting a local pharmacy or one close to their GP surgery. This provided opportunities to offer a range of private services aimed at busy working adults:
. . . we have probably a higher proportion than other pharmacies of patients and customers that are used to paying for their prescriptions and other services . . . we see a lot of people that are workers in our locations because we’re in town centre locations, so they don’t want to have to take time off work because they’re ill so actually having access to a flu jab is really important for them because that’s about keeping well.
Superintendent pharmacist 4
Finally, some interviewees perceived that there might be a difference in the culture of the local population in relation to the extent to which customers/patients were willing to talk to pharmacists about their medication or how receptive they were to new services:
. . . sometime in other places, where you do get the odd patient who wants you to go and discuss their medication with them, whatever you’re dispensing . . . I’ve found it in other chemists, but we don’t tend to have that here.
Pharmacist 28
Public perceptions of community pharmacy and patient expectations
A number of the pharmacists and commissioners we spoke to also perceived that public perceptions of community pharmacy – of the services available and of pharmacists’ roles – could influence the level of clinical productivity achieved. In addition, patient expectations of their pharmacy visit and how receptive they might be to other services on offer was identified as a challenge to both the volume and quality of services delivered.
It has been 10 years since the introduction of the 2005 contractual framework heralded the availability of MURs and an extended range of other medicines optimisation and public health services from community pharmacies. Yet interviewees identified that the public’s perception that pharmacies are only there to dispense prescriptions remains an important barrier to maximising their clinical productivity:
No one ever actually requests an MUR.
Pharmacist 3
. . . if you’re going to collect your medicines and then the pharmacist said, ‘oh, can I have a chat with you about your medicines?’, you’re like, ‘Well, no, I’ve got things to do and I’ve got shopping or the kids to pick up and things’. I know pharmacists have said, ‘it’s really, really hard sometimes to recruit patients’.
Commissioner 1
Although some interviewees recognised that there had been a gradual shift in perceptions, many felt that more still needed to be done by the NHS (both GPs and commissioners) and pharmacies themselves to promote the range of services available:
. . . pharmacy is sort of like the forgotten bit in the NHS sometimes, especially community pharmacy, and I think if they just keep plugging away at raising awareness that we are skilled professionals and we can do minor ailments . . . they need to keep at it and I think it’s just a bit of a culture change because people aren’t used to going to the pharmacy even now for minor ailments.
Pharmacist 7
A lack of awareness of a pharmacist’s role in the dispensing process was thought to contribute to a commonly held perception that patients were sometimes not willing to wait long for prescriptions to be dispensed. This increased time pressures for some pharmacists and could not only affect the quality of the dispensing service, reducing counselling opportunities, but also limited opportunities to offer other services, such as MURs, when speed of dispensing is a priority:
So there’s the whole of the patient counselling piece at the end which I think is often forgotten about in the spirit of getting prescriptions done as quickly as possible to meet customer demand.
Superintendent pharmacist 3
I pretty much feel under pressure because I’ve got waiters and the fact that I’ve got waiters, then conducting the MUR, I wouldn’t really get to the point I would want to get to because I’m constrained with time. So I don’t have enough time to conduct that service.
Pharmacist 11
The perception that patients were unwilling to spend much time in the pharmacy also contributed to difficulties in providing a high-quality MUR to patients who appeared unreceptive. Patient uptake of MURs and achieving a high-quality MUR (one with a positive outcome for the patient) were seen to be very much dependent on how receptive an individual was to having their medication reviewed by a pharmacist:
So basically time is the biggest factor . . . if they’re in a rush and you’re trying to rush an MUR then they’re less likely to talk to you about any of that, they’re more likely to just agree with whatever you’re saying.
Pharmacist 19
Some people tend to look at you and say, ‘Why are you asking me these questions? I go to my GP for this’, so they don’t have any value whatsoever … If they have a problem or a side effect or a query, or something that’s bothered them for a while, but they’ve never spoke about it, if they’re given a forum to then speak about it, I think they consider it a good service.
Pharmacist 28
A small number of interviewees suggested that past experience of a high-quality service from a pharmacist would encourage patients to come back again, gradually increasing demand:
. . . delivery [of the MUR] has to be good . . . because when they know you can deliver and what they get from the service, then the next time you ask them, even if they’ve not got time they’ll tell you ‘yes, yes, yes’ . . . where I was before, you have some locums who the presentation or the delivery of the MUR is so poor that you have patients saying they will never ever do an MUR again. So I think that does help, to deliver very, very good-quality MURs.
Pharmacist 20
Community pharmacy/general practice relationships
The nature of the pharmacy’s relationship with local GP surgeries was cited by a large number of pharmacist and superintendent pharmacist interviewees as a factor influencing clinical productivity. The overarching finding was that positive relationships with GPs and practice staff helped to nurture interdisciplinary practice, fostering greater co-operation and working together for patients, increasing effective signposting and opening channels of communication. Respondents were fairly evenly split between those who described relationships with local practices in positive terms and those who described those relationships as being more problematic or strained.
All of the commissioners interviewed also spoke about the importance of good pharmacist–GP relationships for improved clinical productivity. Several aspects of the relationship were mentioned, including the need for clear and direct communication channels between the pharmacist and the GP to enable prescription queries to be resolved efficiently and swiftly, thus ensuring that the patient receives the appropriate medication promptly without impacting on both the pharmacist and GPs’ workload and affecting clinical productivity.
I also think that good communications and relationships . . . makes a huge, huge difference to the working lives of pharmacists and GPs . . . if you have those relationships in your working day in itself, it will be so much smoother, and so reduced in terms of hassle, then you can only use that to your benefit to get the work through and get the work done at a quality that you wish to produce. So the wider working relationships are as important as the staff to underpin that service, I think.
Commissioner 5
Many pharmacists believed that good relationships with local practices enabled prompt resolution of issues, for example problems with prescriptions and repeat prescriptions, clinical interventions and stock shortages. This had a positive effect on the quality of the pharmacy service as experienced by the patient.
If there was something that I was concerned about or needed changing . . . if I have a good rapport with the surgery then I’m more likely to pick up the phone and say ‘can I sort this out this afternoon?’ . . . Whereas if the surgery you don’t have a good rapport with . . . you’re less likely to be able to . . . do that or it might take longer to do . . . So the better rapport you have with them the easier it is to sort things out for patients, it will always impact on the quality of the service.
Pharmacist 19
Conversely, when poorer relationships existed, this could be perceived as a barrier to the timely resolution of problems, adversely affecting the quality of the dispensing service.
Sometime we have problems, you know, with the GP . . . the receptionist, but I suppose that everybody’s got the same problem. The way you’re to trying to help a situation, they will hinder it basically. That causes a massive problem with the flow of things, but there’s no way round that. It just seems to have always been the way.
Pharmacist 28
One commissioner mentioned that in her area there had been a number of reports of pharmacists being blocked from directly speaking to GPs; however, some progress had been made with encouragement from the area team:
We encourage pharmacies to foster that good relationship . . . There is still this reluctance although the barriers are being broken down a little bit . . . pharmacists talk about being blocked; not being able to speak to the GP when they’ve got a query on a prescription and that happens a lot. I’ve been in meetings certainly with GPs and I’ve thrown that back to them and they’ve said, ‘Oh, right, well, we hadn’t realised that . . . we have our own special numbers’ and I said, ‘But you’re not releasing them to pharmacists’ . . . one particular very forward GP . . . he said, ‘This is ridiculous!’ . . . when I saw him again recently he said, ‘I’ve made sure that local pharmacies round me have got that number now that they ring up if they need to speak to me or send me an e-mail or whatever.
Commissioner 1
A number of pharmacists felt that positive relationships encouraged GPs to initiate contact with pharmacists, for example, to request advice and follow up recommendations from MURs. Indeed, some perceived that effective working relationships were optimised when local GPs had developed a certain level of trust in the pharmacist. Good working relationships with local practices could therefore help to increase the volume and range of services pharmacies were able to deliver through referral or signposting of patients to pharmacy services:
And to be honest ever since that my relationship with the surgery has skyrocketed. I think they actually appreciate you looking out for things . . . now I get . . . one [doctor] especially keeps phoning me up asking what he should prescribe.
Pharmacist 23
We sometimes get a letter from the GP saying, ‘Dear pharmacist, we would be grateful if you could provide an MUR to this patient, she’s having the following difficulties with taking her medicines’. Or it might be just via the patient, ‘Go and see the pharmacist and they’ll provide you with some help with medicines taking’. So it varies from formal to informal. It’s mainly informal, but it would be much better if there was a proper commissioning pathway for this. So if it was formalised it would be better.
Superintendent pharmacist 4
Commissioners also spoke about the importance of GP endorsement of pharmacy services, to increase patient participation and, thus, clinical productivity. Commissioners felt that if the GP and pharmacist had a good relationship, the GP or practice staff were more likely to signpost patients to a pharmacy for consultation:
If a GP said to a patient, ‘Oh, by the way the pharmacy down the road offers this really good service called an MUR and I think it’s really important that you go and talk to them about your inhaler technique’, the patient is far more likely to do that . . . if you get that endorsement from GPs around pharmacy services I think that carries a lot of weight with patients.
Commissioner 6
However, for some pharmacists, referral or signposting to pharmacy was believed to be, at best, selective for some services, with competition between pharmacies and general practices to provide some services encouraging silo behaviours and acting as a barrier to service uptake by patients from community pharmacies. The seasonal influenza vaccination service, which at the time of these interviews was yet to be introduced as an ‘advanced’ service, was provided as an example of when competition between GPs and pharmacists was straining relationships as a result of traditional income streams for GPs being challenged:
. . . pharmacy/GP integration is something that needs to be focused upon . . . The problem is . . . they’re two competing businesses . . . there is certain cross-over areas, such as flu vaccinations and things like that . . . If we work together . . . pharmacists can help the GPs to achieve their targets . . . [and] at the same time . . . also enable the pharmacist to provide another service.
Pharmacist 3
Finally, some believed that patient perceptions were another barrier to pharmacist–GP integration and any subsequent benefits for clinical productivity in community pharmacies. Some pharmacists perceived that patients objected to pharmacists encroaching on GPs’ territory or, given the general lack of patient awareness of the pharmacist’s extended role described above and an absence of signposting or referral by GPs to pharmacy services, that patients chose GP service provision over pharmacy service provision:
I think a lot of it is a culture shock to them . . . in terms of . . . ’My doctor does that, I go to the doctor for this’ . . . If pharmacy is going to take on all these new roles, and new services, that’s something that needs to be broken down, I suppose. Or, the patients informed that actually we’re better placed than the doctors’ service, and . . . you don’t have to wait to see us.
Pharmacist 29
A number of possible solutions to improving pharmacist–GP integration was suggested by interviewees including pharmacists themselves being proactive in establishing and maintaining good working relationships with GPs through regular communication and face-to-face meetings; the interprofessional education of trainee doctors; GP endorsement of pharmacy services with increased signposting and referral to pharmacies; and closer alignment of the general medical and general pharmaceutical services contracts:
Once in a while I go and sit with the doctors and have coffee and just discuss, ‘OK, these are the difficulties, I think you guys should do this, this way . . . If you are prescribing batch prescriptions these are the kind of people that should be on batch’. They hear from me and I hear also their struggles. The surgery next door is also educational because they get student doctors there . . . [who] come here once in a while to see how things are and we can also explain to them how prescribing should be done, pack sizes. So it’s a good combination for us and them . . . it’s a good relationship and one that I want to keep and maintain.
Pharmacist 20
I do think that if there was closer alignment of the two contracts, so there was a shared and common interest in how both clinicians are then delivering their services to the patient, that we might get more effective targeting of MURs to those patients that are not taking their medicines appropriately, and that we might then be able to improve their use of medicines and . . . help inform some of the prescribing decisions that GPs might make in the future as a result of both their own clinical reviews of medicines, and also the medicine use review . . . [they are] different, but they’re highly complementary and both really inform each other.
Commissioner 4
At a more strategic level, some commissioners felt that clinical productivity generally could be improved by having more community pharmacy representation in CCGs, which would foster greater GP–pharmacist integration:
A lot of CCGs are still coming across as representing the GPs rather than actually representing the patients, and we said right at the beginning that they missed a trick, the government, by not insisting on having a community pharmacy representative on the board of every CCG who could . . . encourage working together, because community pharmacy and GPs are so interlinked.
Commissioner 2
One commissioner from a CCG that did have community pharmacy representation stated that having this input had been useful in terms of reducing wastage and providing valuable information to the CCG about drug switches and supplier problems, to ensure that both GP practices and pharmacies could plan and accommodate these.
Commissioning structures and processes
This study was conducted at a time of significant reorganisation within the NHS, which had a marked impact on the commissioning landscape for community pharmacy services. PCTs were dissolved in 2012 and replaced by CCGs. However, the commissioning of community pharmacy services became fragmented between the new area teams of NHS England (primarily for essential and advanced services but including some enhanced services), CCGs (for locally commissioned medicines-related health-care services – previously enhanced services) and, for the first time, local authorities (for locally commissioned public health services – previously enhanced services). It is therefore unsurprising that many interviewees discussed commissioning as a factor influencing clinical productivity – particularly in terms of the reorganisation, the geographical variation and a new GP dominance of local NHS commissioning processes.
The reorganisation of commissioning caused confusion among many pharmacy interviewees about the sources of remuneration and the commissioning process for different services. The resulting increase in the variety of commissioners (NHS England, CCGs, local authorities) caused further confusion and increased the bureaucratic process to bid for services. In addition, some perceived that as services transferred from PCTs to the new CCGs and local authorities, there had been a degree of decommissioning of services. As a consequence, the quantity of service provision was reduced following the reorganisation, reducing pharmacies’ sources of income, threatening the viability of some businesses and investment in staffing in others. This reduction in service provision, by reducing service accessibility to patients, was also seen as lowering the quality of NHS services.
There was almost a false sense of security, I think, initially, because services were just rolled over because it was probably too much as part of the changes that were going on to do anything about them . . . over the last probably 12 months, there’s been quite a lot of recommissioning . . . Most of the public health initiative-type services, have gone onto the local authority tendering format which has put a much increased burden bureaucratically on community pharmacies . . . there are a number of pharmacies that have said, . . . ’That’s too much like hard work to complete all of that paperwork and maybe I will and maybe I won’t be successful at the end of it. Actually I’m busy enough as it is; I’m not going to bother.’ . . . That leads to poorer quality of service because there’ll probably be fewer pharmacies delivering certain services and therefore you haven’t got the accessibility for the service that was previously available.
Superintendent pharmacist 5
There were conflicting views about the way in which individual pharmacies or pharmacy chains were commissioned to provide different services in different localities. Some believed that selective commissioning within a geographical area meant that their pharmacy’s income and viability was challenged, especially when training had been undertaken to deliver a service. It also influenced the pharmacy’s ability to compete with other pharmacies.
I worked in an area . . . the teen pregnancy rate was just off the scale like the highest in the country. And we commissioned and commissioned and I did months of training to get the emergency contraceptive and they just said, ‘it’s in five pharmacies already . . . we’re not giving it to any more’ . . . We said ‘look we’ve sent people up to [large multiple] in [location], and there’s no pharmacist on board who’s trained so they’ve had to come back and buy it or we’ve had to refer it to the GPs’. We’ve got a pharmacist here 6 days a week and who’s willing to provide the service, he’s totally trained, I’ve done all the child protection stuff . . . and they just said ‘No funding . . . we’re not commissioning it in your pharmacy’. That’s the thing that we worked on with the LPC was commissioning on all services for any pharmacy that wants to do it. So if you want emergency contraceptive, if you can provide the training to us now, you can provide the certificates, if you can say look this is what we’ve got, this is our opening hours then every pharmacy should be able to provide every service.
Pharmacist 26
Conversely, one pharmacist believed that uniform commissioning of all pharmacies across a geographical area could be inappropriate as local population need could vary drastically. This could lead to an underutilisation of the skills of the pharmacy workforce and could reduce the quality of the service delivered.
Variation in commissioning activity between commissioners caused disruption to the remuneration process in one pharmacy located on the border of different commissioning areas, which led to reduced quantity of services provided. Variation in commissioning arrangements across commissioning borders was also seen as a barrier to clinical productivity when service delivery required local accreditation for the pharmacist, the requirements of which differed between commissioners. Pharmacy chains with branches in different commissioning areas were also affected by variation in service commissioning between different CCGs and local authorities, some of which were seen to be more proactive in commissioning from community pharmacies than others. This could be seen as a threat to that pharmacy chain’s income and the investment that they were able to make in staffing and infrastructure.
So unfortunately in [county] because there’s very little commissioning we’re really constrained by the lack of any commissioning that we can engage with . . . in [adjacent county], where there’s a lot more imaginative commissioning we’re also doing MDS . . . weight management and we do a much broader sexual health service . . . and we’ve got a huge warfarin service including home visiting . . . it’s a massive service . . . where you’ve got . . . a consistent credible reliable additional income stream you can make an investment in more ACTs, second pharmacists a lot more IT, because you get a return. Where you’ve just got like we have here a few sporadic services none of which are really economic to provide it’s impossible to make the investment.
Superintendent pharmacist 4
The commissioners we spoke to were themselves still learning about the new commissioning structures and processes. Some NHS England commissioners had commissioned a pharmacy-enhanced service on behalf of their local CCG, meaning that the CCG held responsibility for managing the service but NHS England held overall accountability. This arrangement had arisen as a result of the service previously having been commissioned as an enhanced service by the PCT and, to minimise administrative work, had remained as an enhanced service rather than transferring to a CCG locally commissioned service. Many commissioners engaged with LPCs to design services and to gain endorsement to attract providers. Input from LPCs was seen as a way of helping to improve the quality of commissioning.
Last year’s flu campaign . . . it was probably commissioned a bit rushed . . . it probably wasn’t the highest quality commissioning cycle. As a result, the uptake through pharmacies was really poor . . . this year it was different, we set about it earlier, we engaged with the LPC. We used the LPC to advertise and roll out the service, and somebody within the LPC who was well known was the point of contact and everything. And as a result, we got loads of pharmacies signed up and they really got behind it . . . within about 4 weeks of the service start, we’d done 1000 flu jabs in pharmacies.
Commissioner 3
Contractual framework and remuneration
The nature of the community pharmacy contractual framework and the levels of remuneration available for essential, advanced and enhanced/locally commissioned services were seen by many to have both a direct and indirect impact on clinical productivity.
As private businesses, community pharmacies are required to make a profit. Many pharmacists and superintendent pharmacists interviewed perceived that the level of remuneration for services was insufficient for the pharmacy to invest in the levels of staffing (number of pharmacists and/or other pharmacy staff) and infrastructure (consultation rooms/IT) necessary to be able to deliver these services at high enough quality and to still make a profit. This perceived insufficiency of remuneration could have the effect of minimising investment in the number and skill mix of staff employed by pharmacies, limiting the range of services taken up by pharmacies, and/or reducing the volume of those services delivered. One superintendent used the MUR service as an example of this.
To enable you to do MURs you have to invest in a consultation room . . . Then you need . . . a second PMR [patient medication record] system to use in that room. In order to free the pharmacist up you need a team of better-trained counter staff and dispensary assistants. When you add up all those costs you would be much better off to forget the MURs . . . it just doesn’t work, the economics don’t work.
Superintendent pharmacist 4
Overall, remuneration by the NHS was seen by many pharmacists not to have increased in line with increasing workloads and expectations. Although the contract was still weighted towards dispensing (essential services), remuneration for these services was seen to have been cut, with the overall global sum redistributed towards payments for advanced services (MURs and NMS interventions). Although one respondent believed that the redistribution of funding away from dispensing and towards services had a positive effect on the clinical impact of community pharmacy, the majority felt that, together with Category M (of the Drug Tariff, which relates to reimbursement prices set for over 500 generic medicines, subject to regular review and negotiation between the PSNC and Department of Health) ‘clawbacks’, this had led to a perceived squeeze overall on profit margins leading to cuts in staffing and the consequent threat to clinical productivity (described in more detail in Staffing and skill mix):
I think number one [barrier to maximising clinical productivity] is definitely the income we get . . . it’s just being eroded year after year. So it is hard sometimes to keep upping your game when they keep reducing your dispensing fees . . . you can’t employ more staff and it just filters down from there.
Pharmacist 7
Other contract-related issues having a detrimental effect on clinical productivity included the short commissioning cycle operated by NHS commissioners, seen as a barrier to investment in staffing and training of staff, remuneration on the basis of service volume rather than service quality and the cap on the provision of MURs at 400 per year:
. . . the financial outlook is, in the NHS and in pharmacy with the various contracts, can be quite . . . [Pharmacies] don’t know whether it’s worthwhile doing [services] because 2 years down the line they mightn’t get paid for it, or they might be expected to do it without the same reimbursement.
Pharmacist 35
Obviously when we get to the limit for the year then we don’t do any more after that really. Once we’ve done the 400 we don’t provide any more.
Pharmacist 32
Suggestions made by interviewees for counteracting these financial constraints included increasing the overall global sum; increasing the levels of remuneration for advanced and enhanced/locally commissioned services to more accurately reflect the cost of delivery; an increase in the level of local commissioning of pharmacy services; and changing the basis of remuneration from fee-for-service to one reflecting aspects of service quality or outcome, for example having a pharmacy QOF in line with general practice. The perceived benefits of such changes included not only increased investment in staffing, which could lead to an increase in the quantity and quality of services a community pharmacy was able to deliver, but also an alleviation of pressure on general practice workloads:
. . . if they were to commission more services here then obviously we can work our way around that . . . [if] they are viable in this area and I can make them successful then obviously I would get in the staff, I would go out of my way to get an ACT, so I wouldn’t have to worry about other things.
Pharmacist 15
They need to be thinking about the contract in a very different way. So a QOF for pharmacy would be good . . . [The pharmacy contract] doesn’t appear to be aligned particularly well to the GP contract so we’ve not necessarily got two professions working in the best interests of patients. I think a route and branch review of the pharmacy contract would be a good start and start to recognise the clinical value that pharmacists add through their interaction with patients.
Superintendent pharmacist 3
Legal and regulatory constraints
Some legal and regulatory constraints to maximising clinical productivity in community pharmacy were identified by interviewees, most notably around the existing consideration of dispensing errors as ‘strict liability’ or criminal offences and the Medicines (Pharmacies) (Responsible Pharmacist) Regulations 200871 and associated provisions for supervision under the Medicines Act 196872 and the National Health Service (Pharmaceutical and Local Pharmaceutical Services) Regulations 201373 (under review at the time of writing and likely to change in the near future).
A number of interviewees identified the existing consideration of dispensing errors as criminal offences as a barrier to clinical productivity because it deterred the effective deployment of skill mix within the pharmacy:
They need to deregulate the criminal aspect of dispensing errors; that needs to not be an offence . . . and the dispensers . . . you should have a team of them, one dispensing it, one checking it . . . and one labelling it and it all gets done by three different people . . . and I could join in as well, but I’m not solely responsible for any cock-ups. So that then frees me up and them up as well to do things.
Pharmacist 34
Others felt that the existing responsible pharmacist regulations and associated supervision arrangements were unclear, not only leading to suboptimal utilisation of skill mix, thereby lowering the quantity and quality of service provision (as described in Skill mix), but also making it difficult to nurture effective relationships with local GPs and preventing pharmacists from providing services such as MURs to those who may benefit most, for example the housebound elderly:
. . . in order to free up pharmacists’ time, there’s probably going to have to be a change as far as the supervision regulations . . . there might be the possibility of remote supervision, which already . . . occurs in a number of other countries.
Pharmacist 3
. . . as a responsible pharmacist we can disappear off. I’m not sure how many of us do that, because we’re all worried about lack of business from a commercial point of view, and pressure, but we need to talk more and practice meetings at surgeries should probably involve the local pharmacies more.
Pharmacist 35
A small number of pharmacists believed that increases in staffing and improved skill mix could overcome these regulatory constraints, but that this would require increased levels of remuneration or else result in a drop in profit for the pharmacy. Two pharmacists believed that only a two-pharmacist model would provide a solution and allow pharmacies to increase their clinical productivity:
I think over 50 per cent of potential MURs we can’t do because they’re either deliveries or they’re collection by a relative, not the patient . . . I know you can apply to go off site and do them but maybe it’s something that . . . NHS England . . . look at making that sort of service easier to provide. But that would require a second pharmacist . . . which again would have to be extra payment. I suppose you could argue the extra MURs would pay for a second pharmacist. Maybe it’s an area that they need to look at, because there probably is those patients that are housebound or don’t get out very often.
Pharmacist 41
Supply chain problems
The importance of having well-managed stock to the delivery of a high-quality dispensing service has been described above (see Quality of dispensing services). It is therefore unsurprising that many pharmacists interviewed reported that supply chain problems were a barrier to clinical productivity in community pharmacy. Stock shortages, fluctuating prices, perceived quotas imposed by wholesalers, ‘direct-to-pharmacy’ schemes and perceived wholesaler preference or ties to larger pharmacy multiples all contributed to the difficulties reported by pharmacists in obtaining stock.
Supply chain problems were believed to be detrimental to service quality – sometimes forcing patients to revisit the pharmacy when the full prescribed order was not readily available – and on the pharmacy’s relationship with the patient. It was also seen to have an adverse effect on the workload of the pharmacy, increasing the time spent by pharmacists sourcing products, finding alternatives with prescribers, dispensing ‘owings’ and tying up dispensing staff restocking the dispensary. The volume or quantity of service provision was therefore also affected:
This is where I think as a pharmacist I waste a lot of my time, chasing stock and chasing prices.
Pharmacist 15
We’re spending hours just sourcing products now. Nobody takes into account the sheer workload involved in making sure you’ve got the drug for the patient which used to just be a given. Direct-to-pharmacy schemes [in which manufacturers supply pharmacies directly] have made it harder and harder to obtain products. It places huge constraints because if you’re spending an hour on the phone trying to get Mrs Smith’s products you haven’t got an hour to spend with her doing an MUR.
Superintendent pharmacist 4
Approaches to the management of supply chain problems described by interviewees included having good working relationships with local GPs, prescription collection services, having good working relationships with other local pharmacies and building relationships with trusted suppliers:
But [the local practice] are nice enough to, if we tell them that it’s not something that we can get hold of, with all these shortage issues with stock, then they try and change it to something else sometimes the doctors will call me and ask me if there is anything else I can think of.
Pharmacist 1
We have excellent relationships with both competitors . . . if I ever don’t have an item they’ll loan it to me . . . In other places where I’ve worked, if you requested that off another pharmacy they would tell you to simply send the prescription to them . . . that means that I’m never owing an item or I’m never owing an item for any longer than I should do for a patient, so we manage to process the prescription fairly quickly and the end result is that the patient is happy.
Pharmacist 31
Monitoring clinical productivity
Respondents were asked how clinical productivity (both the quantity and quality of service provision) was being monitored at the time, the benefits and drawbacks to monitoring clinical productivity, any opportunities or barriers to monitoring and whether or not more monitoring should take place, in what format and who should be responsible.
Current monitoring arrangements for clinical productivity
Community pharmacies’ monitoring arrangements
Most pharmacists and superintendent pharmacists interviewed reported that their pharmacies had internal mechanisms for monitoring the quantity of services provided, generally linked to payment systems:
We ask our stores to report on a monthly basis the number of items of service that they deliver, so we monitor and that’s so we can track when we get paid by the NHS that we’re being paid for everything that we’re delivering. As far as quality goes, hand on heart I can’t say that we measure that . . . if something hasn’t gone well then we know about it because either the customer or the patient tells us that they’re not happy, so it’s almost like if we don’t hear that something’s not good, we assume it’s good at the moment.
Superintendent pharmacist 5
A large number of pharmacy respondents similarly described that service quality was not monitored formally by their organisation. Instead a number of informal mechanisms were used to provide an indication of the level of quality of services being delivered. Most commonly, this was through patient feedback, although other sources of information were identified including the pharmacist’s own subjective assessment, GP feedback, customer loyalty and observed changes in a patient’s health or behaviour:
The only way we [know that we’re providing a high-quality service] . . . is by getting feedback from the GP, and also the patient . . . If the GP encourages patients to come to us for services, then we know that they’re happy with what we’re providing, and that helps us say, ‘OK, they’re happy with that’, and so we keep doing that and keep improving it.
Pharmacist 16
Well, I think we reach a high standard the majority of the time . . . personally, I think we give a very good service and we wouldn’t be as busy, because we haven’t got a surgery on our doorstep, so they don’t have to come to us.
Pharmacist 25
However, some aspects of service quality were monitored more formally by others. All pharmacies are contractually obliged to conduct a patient survey annually and some pharmacists recognised this as a way of monitoring service quality. Others supplemented this with their own customer surveys:
You’re given so many questionnaires; it’s pro rata depending on how busy you are. So they’re given out to patients and they basically fill out a questionnaire about their experience in the pharmacy. Then we get feedback from that in terms of any ways we can improve.
Pharmacist 29
Another common method for assessing quality (in terms of patient safety) was through monitoring errors and near misses in the dispensary (also a contractual obligation). A number of organisations had systems of formal weekly or monthly reviews of errors and near misses in order to encourage organisational learning and improve patient safety:
If there are any slight minor errors that are caught then they are noted down. We have monthly meetings to discuss anything serious or . . . we feel, as far as a member of the dispensary staff or counter staff, that they are making regular errors on a certain thing, to discuss it.
Pharmacist 3
Complaints from customers were also monitored by a number of respondents and used as an indication of the quality of services delivered alongside other mechanisms. Some organisations also employed mystery shoppers to assess the quality of over-the-counter sales. Less frequently mentioned were audits, area manager or superintendent pharmacist visits, monitoring the time taken to dispense prescriptions, recording and monitoring interventions, use of customer focus groups and escorted customer shops.
Commissioners’ monitoring arrangements
NHS England area teams are responsible for monitoring the community pharmacy contractual framework. Although highlighted by some respondents as a way in which concerns with the overall quality of community pharmacy provision might be identified, this was not the primary aim of contract monitoring. Furthermore, area teams were very much reliant on pharmacies’ self-assessments, with contract monitoring visits only taking place when there were concerns about adherence to the terms of the contractual framework. Contract monitoring was not, therefore, considered to be an adequate mechanism for monitoring the clinical productivity of community pharmacies:
With regard to quality, it’s only [monitored] against the community pharmacy framework, and often . . . we have to do a lot of that on trust, self-assessment, or by exception where there is evidence of one sort or another that they may not be providing the quality that is provided in the regulations for core contract.
Commissioner 2
The consensus among the commissioners interviewed for this study was that they did not monitor service quality, with several stating that they did not have any awareness of whether or not the services they commissioned from community pharmacies were of high quality. They only had access to pharmacy activity data (to measure quantity of service provision) and could only base quality assumptions on the complaints that they might receive from patients or any feedback they got from GPs:
You don’t [know that you’re getting a high-quality service]. I suppose the bottom line is you don’t. You would look at a number of things like patient complaints; although to be honest patients tend to be quite reluctant to complain.
Commissioner 1
We monitor activity and we monitor incidents as well, I suppose. So we would hear if things went wrong. We don’t hear so much if things go right . . . So all I can monitor at the moment is numbers and activity. And we can see the consultation forms if we need to, and that kind of thing, to see if there’s an issue. And we hear back from GPs, if people are being referred back to them and they think it’s inappropriate.
Commissioner 10
Benefits and drawbacks to monitoring clinical productivity
A number of benefits to monitoring both the quantity and quality of community pharmacy services was identified by respondents. For example, it was suggested that monitoring service activity levels by community pharmacies allowed benchmarking against other pharmacies, helped pharmacies to reach targets to maximise income, and generally increased the volume of service delivery and the number of patients reached:
[The pharmacy owner] wanted to firstly make sure that we’re on target . . . with MURs . . . he wants to make sure that we’re going to be getting the 400 a year, and if we’re starting to do like 10, 15 a month regularly he’ll say, ‘Well, you need to increase that’ . . . and items as well, I think he will quite often look at items and say, ‘You’ve had a busy month’, or he can quickly spot if we have 1 month which is far lower than normal and, again, he’ll say, ‘Well, what’s happened there?’.
Pharmacist 32
For commissioners, a reduction in service activity levels could be an indicator of wider problems within a pharmacy and a prompt for further investigation. It was also suggested that contract monitoring procedures, by improving record-keeping, ultimately led to improvements in service quality:
All I can say is that the monitoring, I believe, then leads to better record-keeping . . . I’m hoping that by improving the record-keeping and making pharmacies more aware of what it is that they should be doing in the service, will then lead, in turn, to improve the quality.
Commissioner 4
Monitoring and reviewing patient safety incidents (dispensing errors and near misses) was perceived as an opportunity for organisational learning – sometimes shared learning across pharmacies within a chain – and a way of improving patient safety within community pharmacies:
. . . if I feel that it’s linked to any particular person at any particular time then I like to get to the bottom of why that’s happening . . . I think sometimes people don’t necessarily assess themselves about how many errors they’re making unless it’s kind of pointed out to them, but it seems to have worked and it’s reduced the number of errors that are going to the patients.
Pharmacist 38
Monitoring quality, for example through the annual patient survey, was seen by some as a way of increasing service quality by identifying weaknesses and developing action plans for improvement. However, often the benefits of the patient survey were seen to be limited. It was recognised that pharmacies could ‘cherry pick’ those patients who received a questionnaire, that responses were generally very positive with little opportunity for making improvements and that commissioners did not review the findings, limiting opportunities for benchmarking or monitoring change in quality over time:
I suppose if there was negative feedback you would perhaps look into it and see how can we do things better. But it’s usually quite positive . . . I think we just use it as a tool and it’s something we have to put on the wall anyway to show people.
Pharmacist 17
Respondents also identified a number of drawbacks to monitoring clinical productivity in community pharmacies. These included pharmacies being overburdened with monitoring and inspection requirements, and the excessive bureaucracy involved in some of these processes; the fact that sometimes neither pharmacies nor commissioners reviewed or acted on the information obtained through monitoring processes; and the focus on quantity and business targets rather than the quality or clinical outcomes of services:
Inevitably the danger here is we then try and measure and monitor everything and you spend so much time recording things that you don’t actually have time to care.
Superintendent pharmacist 3
Opportunities and barriers to monitoring clinical productivity
Many interviewees recognised the difficulties inherent in measuring the quality of community pharmacy services that created a significant barrier to monitoring clinical productivity. A number indicated that there were no existing markers for quality or that they would not know what to measure. It was also suggested that the dissonance between a patient’s view of a quality dispensing service (speed) and one that was clinically of high quality was an additional hurdle to developing appropriate measures. Moreover, with few pharmacy services offering a follow-up of patients, it was difficult to measure their impact on the patient or wider health service:
[Quality] is enormously difficult to measure . . . because you’re not aware of anything bad, you’re hoping that the quality is going to be good. I suppose for us if you were looking at it more widely we would be looking from a commissioner’s point of view, the sort of stuff is, what about hospital admissions? . . . Is the level of disease going down in an area? . . . How on earth are we going to measure that? I don’t know.
Commissioner 1
When measures of quality did exist (e.g. patient surveys, records of errors and near misses, or records of pharmacist interventions) a number of barriers was identified to their effectiveness as tools with which to monitor clinical productivity. Community pharmacies did not always record interventions, sometimes because of a lack of time or because this was not supported by existing IT systems:
I think one of the major stumbling blocks that we’re finding, when we’re going out and doing our contract monitoring visits, is the poor level of support that most, if not all of, our pharmacies have, from their IT system . . . one of the prerequisites of the contractual framework is that pharmacies should be recording any interventions that they make around dispensing, around signposting, around support for self-care, and for support around public health initiatives, and yet, what we’re seeing is very, very low levels of interventions being recorded.
Commissioner 4
So if we’ve had to speak to a doctor or if there’s been an issue we are supposed to record interventions. But it’s finding the time to record them, it’s difficult, especially when you’ve got a high volume, you’re doing quite a lot of interventions. It’s difficult to find the time to do that.
Pharmacist 23
The barriers to monitoring clinical productivity faced by service commissioners also included the fragmentation of community pharmacy commissioning following the dissolution of PCTs. This not only meant that no one commissioning body had oversight of all elements of pharmacy service provision, but it also resulted in a significant reduction in the resources available to commissioners to monitor services. This fragmentation of commissioning responsibilities was compounded by barriers to data sharing and poor communication between pharmacies and commissioners, and between different commissioning bodies, sometimes in relation to data protection restrictions and terms of service:
. . . we don’t have the resource any more in the CCG to monitor pharmacies, because we lost all that resource when it went to NHS England . . . In PCT days, we had a programme of pharmacy visits . . . we had a pharmacy quality scheme . . . So we had a very good knowledge on the ground of what was happening . . . and we have a lot less confidence about the quality of what’s happening than we did . . . When we had our commitment to quality pharmacy scheme, with three levels of quality . . . we had a grid and we could have told you pretty much any pharmacy in [area], we could have given you chapter and verse about the quality of work, the number of indicators . . . We can’t do that anymore.
Commissioner 7
Nonetheless, there were some reports of opportunities taken by service commissioners to monitor clinical productivity. These included joint visits and data sharing with the local General Pharmaceutical Council inspectorate, use of the number of targeted MURs as a quality indicator, and the triangulation of existing data and intelligence to give an indication of clinical productivity in community pharmacies:
I think what we need to build on is working together with the GPhC [General Pharmaceutical Council] inspectors . . . when there was an issue that was both performance related and contractual related we did a joint visit to a pharmacist.
Commissioner 2
Future monitoring of clinical productivity
When asked if there should be more monitoring of clinical productivity in community pharmacies, the majority of respondents believed that there should be, with only a small number expressing ambivalence or disagreeing. In particular, it was suggested that there was a need to measure service quality or to be able to demonstrate the outcomes or benefits of pharmacy services. A number of aims of such monitoring was proposed, including ensuring accountability for spending taxpayers’ money, being able to demonstrate the benefits or value of community pharmacy services, improving quality and identifying areas of concern:
But if the regulations say that we’re going to pay them for 400 MURs every year, it’s public money, we should be getting value for money out of those MURs. And we don’t know that at the moment. It’s public money so we have a right to ensure, like anything, we are answerable to all of us.
Commissioner 3
The purported need for additional monitoring varied according to the type of service. For some services, for example influenza vaccinations, numbers and activity levels were thought to be sufficient. However, there was a consensus that services such as MURs and NMS interventions should have more quality markers:
But, yeah, I do think it’s important to get the patient’s reflection on things like MURs and NMS, and look at the information that they’re giving and see whether it’s actually worthwhile doing, whether they found them beneficial or not. I suppose that’s the only way you’re going to be able to measure [it].
Pharmacist 40
However, even among those who perceived monitoring as a good thing, there was some recognition that both commissioners and community pharmacies were already overstretched and had little capacity to undertake further monitoring activities. Other respondents questioned what further monitoring of clinical productivity would achieve, some seeing it as a tick-box exercise having no impact on quality improvement:
If you look at the wider NHS, what does monitoring achieve? . . . not in just the NHS, look at teaching, looking at Ofsted. Does it genuinely achieve long-term gain in quality or does it achieve a short-term gain in quality for the purpose of passing the inspection? . . . whereas if you get the structure and the management and the ethos within an organisation right, that will always lead to better quality.
Commissioner 3
Chapter 7 Commissioners’ workshop and toolkit development
A workshop for service commissioners and other community pharmacy stakeholders was held to meet objective (v) of the study. This section describes the outcomes of that workshop and how it informed the development of a toolkit to support the commissioning of medicines optimisation services from community pharmacies.
Workshop attendees and structure of the day
Of the 128 invitations sent out, 23 people attended: four patients/members of the public, nine with commissioning (or ex-commissioning) roles, nine community pharmacy provider representatives and one from the PSNC. Two attendees had additional roles on LPCs and two in Pharmacy Voice or its constituent organisations.
The programme for this half-day event, held in July 2015, was as follows:
-
welcome and introductions
-
presentation of preliminary study findings
-
small group discussions of study findings around two topics (with feedback to room):
-
face validity of findings
-
implications for patients (what does a ‘good’ medicines optimisation service look like?)
-
-
small-group discussions around three topics (with feedback to room):
-
implications for community pharmacies (how can pharmacies deliver a service to meet these expectations?)
-
implications for service commissioners (what actions do commissioners need to take?)
-
content of commissioning toolkit
-
-
round-up and next steps.
Table places for small-group discussions were allocated to ensure a mix of stakeholder representation. Notes were recorded by the groups on flipcharts.
Summary of group discussions
Face validity of study findings
There was general agreement in the room that the study findings had high face validity. However, some surprise was voiced regarding the inverse relationship between annual volume of MURs and indicators of local population need. The reasons for this inverse relationship were discussed with suggestions raised that it might relate to less complex cases being targeted for MURs in some instances because of either time constraints or pressure to reach targets, or that it may be related to public perceptions of the role of the pharmacist and that people do not ask for MURs. There was further discussion around the public perceptions of pharmacy presented in the qualitative findings and the need for the sector to obtain a better understanding of what patients want and need from medicines optimisation services. Finally, the role of HLP status on clinical productivity was discussed with the suggestion that it was probably more important for enhancing service quality than service quantity.
Implications for patients
There was some discussion about the role of the pharmacist in relation to other health-care providers, and patients’ perceptions and preferences around this. It was suggested that services should be designed around patient needs and expectations, and that patient experience should be monitored. This would, in turn, provide added value to any medicines optimisation service and patients would return, by choice, to the pharmacy. There was also a suggestion that pharmacists should become the primary contact for patients in relation to medicines and the need to manage patient expectations around this, and to obtain buy-in from other health-care professionals. It was also recognised that medicines optimisation should occur during the dispensing process (through the provision of counselling and advice) as well as through dedicated services such as MURs. The positive outcomes identified by groups from a well-designed medicines optimisation service included greater choice, flexibility and access to services for patients, informed patient decision-making, better health outcomes, improved trust, and partnerships between patients and pharmacists and between pharmacists and other health-care providers.
Implications for community pharmacies
Much of the discussion on the implications for pharmacies was around skill mix and the role of the whole pharmacy team in helping to free up the pharmacist to be able to deliver medicines optimisation services. To support this, there was a perceived need for services to be commissioned on a longer-term basis than annually to allow pharmacies to make the necessary investment in staffing and skill mix. Finally, it was recognised that all new services commissioned should have robust evaluations built into them to be able to demonstrate benefit and secure ongoing commissioning.
Implications for service commissioners
A number of themes arose from the small group discussions around what actions commissioners needed to take in relation to the study findings. First, there was a necessity for commissioners to identify the need for a particular medicines optimisation service and to define the cohort of patients for whom the service should be designed. Second, commissioners needed to consider the role of community pharmacy in relation to the other elements of the health-care system to help ensure integrated care pathways and remove competition between pharmacy and general practice. Suggestions were made here around incentivising GPs to refer patients to pharmacies, and aligning the GP and community pharmacy contracts. In designing the service, the views and needs of all stakeholders should be considered, particularly the patient’s, but including pharmacy providers (enlisting the help of LPCs) and other health-care providers. Delegates also identified the need for commissioners to take into account the organisation of community pharmacies, particularly making best use of the available skill mix (not just the pharmacist) and the capacity of pharmacies to deliver additional services within existing resources. In relation to this, the issues of funding and sustainability were discussed to facilitate pharmacies with making any necessary investment to deliver new services. It was also suggested that commissioners include the newly introduced Declaration of Competence system within service specifications. The need to build evaluation into the design of any new services was raised as was the marketing or advertising of services to patients to generate demand.
Content of commissioning toolkit
The final topic discussed during the workshop was the required content of a commissioning toolkit for medicines optimisation services. A number of suggestions was made in relation to content, starting with background information about pharmacies and how they operate, definitions of medicine optimisation, and local and national statistics around hospital admissions and GP data to support the commissioning of a new service. Contextual information about where medicines optimisation services fit into the wider commissioning landscape and contractual framework for community pharmacy, and with health-care services more widely, was similarly considered important. Guidance on developing a business case, possibly a template, was suggested as useful content, considering any potential cost savings and/or value for money. Advice around early stakeholder involvement, particularly PPI, in service design was suggested. Content around designing the service specification was discussed, taking into account any necessary training and the Declaration of Competence. Consideration should also be given in the toolkit to measuring and monitoring outcomes, data sharing and data protection, and the evaluation of services. Finally, it was suggested that the toolkit should cover funding and the sustainability of services.
Toolkit development and dissemination
Primary Care Commissioning was tasked with developing a commissioning toolkit for medicines optimisation services, organised around the commissioning cycle and drawing on the study findings and workshop discussions.
The toolkit (see Appendix 5) is structured under the following headings, each section being supported by summaries of supporting evidence from the study:
-
A. Introduction
-
A1. Foreword
-
A2. Aim of toolkit
-
A3. Supporting evidence
-
-
B. Background
-
B1. The case for commissioning medicines optimisation services
-
B2. Examples of medicines optimisation services
-
B3. Commissioners of services from community pharmacies
-
-
C. The commissioning process
-
C1. Strategic planning
-
C2. Procurement
-
C3. Monitoring and evaluation.
-
Once finalised, the toolkit will be disseminated through existing PCC channels, reaching NHS England area teams, CCGs, local authorities, commissioning support units, LPCs and pharmacy professional bodies [including the Royal Pharmaceutical Society (RPS), PSNC, and Pharmacy Voice and its constituent organisations].
Chapter 8 Discussion
This extensive, multimethod study aimed to explore variation in clinical productivity in English community pharmacies and examine the organisational characteristics associated with that variation. Clinical productivity was broadly defined as a combination of the quantity (range and volume) and quality of pharmacy services provided. In terms of quantity, it looked specifically at medicines optimisation services (dispensing, MURs and the NMS) as a result of the availability (or lack of availability) of activity data for all NHS services delivered. In terms of quality, the quantitative study used measures of patient satisfaction, self-reported medicines adherence and safety climate as these are domains for which validated measurement tools exist. However, the qualitative study allowed for a broader exploration of the quality of community pharmacy services, which for dispensing included elements of speed, accuracy, clinical input, supply and communication, and for MURs included the impact on patient knowledge, medicines adherence, clinical outcomes and reassurance, and that they were appropriately targeted, patient centred and unhurried. Furthermore, stakeholder interviews allowed exploration of the perceived mechanisms by which organisational factors (and extraorganisational factors) influence clinical productivity. Finally, study findings were used to stimulate discussion at a workshop for service commissioners and other pharmacy stakeholders, which, in turn, informed the development of a toolkit for commissioning medicines optimisation services from community pharmacies.
This chapter opens with an integrated summary of the study findings, drawn from both quantitative and qualitative elements of the study. After a consideration of the methodological strengths and limitations, it proceeds to discuss the key findings in the context of the existing literature and current community pharmacy policy, before concluding with a reflection of PPI in the study.
Integrated summary of findings
Organisational factors associated with clinical productivity in community pharmacies
Pharmacy ownership type was strongly associated with the volume of services provided by pharmacies, particularly the volume of MURs and NMS interventions, with large multiples and supermarkets providing a significantly greater volume of these services than independent pharmacies (although dispensing volumes in supermarkets were significantly lower than in other types of pharmacy).
Although the perception existed among some stakeholders that the greater volume of services provided by large multiples was associated with a poorer quality of service provision, there was little evidence from the quantitative study that ownership type was associated with service quality.
Pharmacies with higher dispensing volumes provided more MURs and NMS interventions; however, there was no association between dispensing volume and service quality. Pharmacies conducting the fewest MURs per year had significantly lower patient satisfaction and SIMS scores than those conducting close to the annual maximum of 400 per year. There was no other significant association between service volume and service quality.
Stakeholder interviews also suggested that ownership type influenced clinical productivity through variation in organisational culture, staffing and skill mix, the quality of the customer relationship and ease of commissioning.
Organisational culture was perceived by many stakeholders to be important in relation to the drive to reach business targets and the degree to which that was prioritised above service quality, as well as the importance placed on investment in staffing and staff and team development. The measure of organisational culture used in the pharmacy survey was strongly associated with higher dispensing volumes and with safety climate. Specifically, pharmacies with a culture more closely aligned to ‘quantity’, the ‘medicine’ and ‘technical’ work than to ‘quality’, the ‘patient’ and ‘professional’ work had higher dispensing volumes but a significantly less favourable safety climate. However, no association was demonstrated with any other measure of service quality or quantity.
Overall staffing levels and also the skill mix deployed in the pharmacy were identified by most stakeholders as crucial to the level of clinical productivity achieved. Although staffing levels were perceived to have been reduced, limiting both the quantity and the quality of services delivered, the availability of a trusted and competent team with appropriately trained pharmacy technicians, dispensers and medicines counter assistants was viewed as necessary to support the pharmacist to take on an effective clinical role. The value of accuracy checkers and a two-pharmacist staffing model was also discussed, as were the pros and cons of locum pharmacists.
In the quantitative study also, associations were demonstrated between staffing and skill mix, and service quantity and quality. Pharmacies with a higher dispensing volume were more likely to have longer pharmacist daily working hours or to employ a second pharmacist, pharmacy technicians or accuracy checkers. Pharmacies employing more than one pharmacist also conducted a greater volume of NMS interventions. Pharmacies in which the main pharmacist worked longer hours were associated with a less favourable safety climate. Unexpectedly, however, pharmacies with an accuracy checker were also associated with a less favourable safety climate. The employment of a pharmacy technician was associated with higher levels of patient satisfaction. Regular use of locums was associated with poorer patient self-reported medicines adherence.
Some ambivalence was shown by stakeholders over the value of HLP status to the clinical productivity of the pharmacy. Some believed that it might improve service quality in terms of the added value offered and that it was beneficial for staff development and skill mix. However, it was not perceived to increase the quantity of services delivered or to attract the commissioning of new or additional services. HLP status was not seen to be associated with any measures of service quantity or quality in the quantitative study.
Pharmacy–GP relationships were perceived by some stakeholders to have a bearing on the clinical productivity of the pharmacy. Good working relationships were seen to improve the quality of services provision, for example by allowing prompt resolution of prescribing or dispensing issues, or by ensuring GP follow-up of the pharmacist’s recommendations following a MUR. Good working relationships were also thought to help boost the quantity of service provision through increased signposting and referral to pharmacy services by the GP. The quantitative study demonstrated a significant positive association between the strength of the pharmacist–GP relationship and the volume of NMS interventions conducted.
Extraorganisational factors associated with clinical productivity in community pharmacies
Increasing levels of local area deprivation were associated with higher dispensing volumes but a lower volume of MURs and NMS interventions. In the qualitative interviews, however, stakeholders identified the level of local deprivation as either an opportunity or a barrier to clinical productivity. For example, in more affluent areas where the population was better educated, customers or patients were sometimes perceived to be less receptive to pharmacy services or advice. More deprived areas, on the other hand, offered opportunities to deliver some services (e.g. needle exchange or minor ailments) but the level of deprivation was a barrier to others (e.g. private services).
The age profile of the local population was also associated with dispensing volumes, with higher proportions of both older people (aged ≥ 75 years) and young children (aged 0–4 years) in the local population associated with higher dispensing volumes in the national data. A number of pharmacists interviewed also suggested that an older customer base limited the number of MURs and other services they could offer as a result of them either being housebound or receiving services for long-term conditions from their GP. Of those responding to the patient survey, older patients were significantly more satisfied with the information they received about medicines and were more likely to be self-reported adherers.
Local disease prevalence relating to a number of long-term conditions was positively associated with dispensing volumes but for asthma was negatively associated with the volume of MURs and NMS interventions conducted.
The location of the pharmacy was seen from both the qualitative and quantitative study to provide either opportunities or barriers to the volume of pharmacy service provision. NMS provision was significantly lower in city centre pharmacies than in pharmacies in other locations; city centre pharmacies being seen by stakeholders to cater for a different customer base than local or suburban pharmacies.
Public perceptions and expectations of the pharmacist’s role and the services available from pharmacies were described in the stakeholder interviews as influencing the clinical productivity of the pharmacy. A lack of understanding by patients of the complexity of the dispensing process and the clinical input of the pharmacist was thought to contribute to pharmacists’ prioritisation of speed over other aspects of quality and of dispensing over other services provided. Moreover, a lack of awareness of the range of services available from the pharmacy limited public demand and receptiveness to being offered information or advice. However, from the patient survey, when patients had more reasons for choosing to visit a particular pharmacy, this was significantly associated with greater patient satisfaction, as was continuity of advice-giving from the same member of pharmacy staff.
Supply chain problems were reported by many of the stakeholders interviewed to be a barrier to both the quantity and quality of pharmacy services provided. These could be caused by stock shortages, fluctuating prices, wholesaler quotas, direct-to-pharmacy schemes and a perceived wholesaler preference for some large multiples. Difficulties in obtaining stock could be detrimental to the patient experience and could also increase the pharmacist’s workload, reducing the time available to provide other services.
Since the 2013 NHS reorganisation, the commissioning structures and processes for pharmacy had become fragmented between NHS England, CCGs and local authorities. This caused confusion for some pharmacies, a perceived increase in commissioning-related bureaucracy and some decommissioning of services. Many interviewees viewed this as a threat to clinical productivity. Variation in commissioning, both between geographical areas and within the same locality was seen as a barrier to clinical productivity by others. The short commissioning cycle operated by many CCGs was also seen to hamper longer-term planning and the investment required for pharmacies to be able to deliver new services.
The existing contractual framework and associated levels of remuneration were seen by many pharmacists and superintendent pharmacists to have both a direct and an indirect negative impact on clinical productivity. Investment in staffing and infrastructure was reported to be limited by current levels of remuneration, which were perceived to be decreasing.
Finally, legal and regulatory constraints to maximising clinical productivity were reported by many stakeholders, including the continued consideration of dispensing errors as a criminal offence and the responsible pharmacist regulations and related supervision arrangements, all of which are under review at the time of writing.
Monitoring clinical productivity in community pharmacies
Arrangements for monitoring clinical productivity that already existed in community pharmacy organisations primarily focused on the quantity of service provision but also looked at quality in terms of obtaining informal customer feedback, patient survey returns, monitoring and analysing errors, and near misses and monitoring complaints.
Arrangements for monitoring clinical productivity by NHS commissioners were almost exclusively focused on the quantity of service provision. When quality was monitored, this was usually through self-assessment by the pharmacy or following reported incidents or complaints from patients.
A number of benefits and drawbacks to monitoring clinical productivity in community pharmacy were suggested by stakeholders including the ability to benchmark activity, helping to improve quality and safety, providing an indicator of underlying problems and the bureaucracy involved.
The barriers to monitoring clinical productivity identified by stakeholders included the inherent difficulty in measuring quality, poor recording by pharmacies, findings not being monitored by pharmacies or commissioners, a lack of resources and manpower, the fragmentation of commissioning and responsibilities for monitoring. However, some opportunities were highlighted through pockets of good practice.
Most stakeholders agreed that there should be more monitoring of clinical productivity in the future but highlighted the need for more quality markers to be developed and the additional regulatory burden that would entail.
Study strengths and limitations
This is the first study to describe variation in clinical productivity in community pharmacies in terms of both the quantity and quality of service delivery, and to investigate the organisational factors associated with this variation. Although previous studies have described an association between pharmacy ownership type and the volume of services delivered (MURs)18 or pharmacists’ perceptions of the relationship between ownership type, volume of services and service quality,15,74 none have taken a systematic approach on such a large scale to investigate all these inter-relationships. Furthermore, this study has, for the first time, looked further than ‘ownership type’ as an explanatory organisational variable and investigated a range of different organisational characteristics and configurations simultaneously to obtain a better understanding of the way in which pharmacies operate and how that might affect clinical productivity. In addition, by taking a mixed-methods approach, this study has been able to explore both the associations between these organisational characteristics and clinical productivity, and the mechanisms underpinning these relationships, many of which are complex and inter-related. Finally, the findings of this study have been incorporated into a commissioning toolkit, providing an output that will support service commissioners to design and commission medicines optimisation services from community pharmacies based on improved knowledge of what will help or hinder clinical productivity in that sector.
A number of study limitations should be taken into account when interpreting these findings. First, the strategy employed for selecting study sites was based on the original proposal to obtain pharmacy activity data from PCTs, which were then the commissioners of community pharmacy services. PCTs were originally selected to cover a diversity of geographical and socioeconomic locations but also pragmatically using existing contacts to ensure that the necessary data could be obtained. This, however, has implications for the generalisability of the quantitative findings. Ideally, had the study been designed around obtaining the data from the NHS BSA, a stratified random sampling approach could have been taken to ensure greater generalisability. However, this would also have had important practical implications for conducting the study in relation to obtaining buy-in from community pharmacy organisations and LPCs, and to obtaining assistance from the NIHR CRNs in setting up stage 2 of the study, which, in nine geographical areas spanning five different CRNs, was already particularly complex. Although it is not possible to state that the quantitative findings are statistically generalisable to all community pharmacies in England, the survey findings are generalisable to all pharmacies in those nine areas, and the distribution of pharmacy types (see Table 3) and pharmacy activity levels (see Table 4) are comparable to national figures (see Table 8).
The other threat to the generalisability of these findings was the non-participation in the study of a number of large community pharmacy multiples. Despite concerted efforts to engage with a range of community pharmacy organisations, commercial sensitivities, implications for pharmacists’ workload and the existing flux in the community pharmacy commissioning landscape prevented the researchers from obtaining support for the study from four out of the nine largest multiples (see Chapter 3, Stakeholder engagement). Despite this, the overall proportion of large multiples participating in the stage 1 survey mirrors the figure nationally. Variation in the organisational characteristics of pharmacies within this group will, however, be limited.
A third limitation of this study was its failure to obtain and analyse activity data for the range of enhanced or locally commissioned services provided by community pharmacies. This was as a result of the transfer of commissioning of these services from PCTs to NHS England, CCGs and local authorities, and the resulting fragmentation of responsibilities for collecting and collating these data. The data relating to these services held by the NHS BSA lacked the specific detail of the services provided and proved to be incomplete as payment mechanisms often bypassed that organisation. It is recognised that the resulting analysis does not, therefore, cover the full extent of NHS (and local authority) services provided by community pharmacies.
There are also limitations associated with the other measures of clinical productivity used in the pharmacy and patient surveys (safety climate, patient satisfaction, SIMS and MARS scales). Validated tools for measuring the quality of community pharmacy services are not widely available8 and those that are available are limited in the dimensions of quality that they can measure. In this study, quality was operationalised as patient safety (for which safety climate was used as a proxy measure), patient satisfaction (both overall satisfaction with the pharmacy visit and satisfaction with information received about medicines) and self-reported adherence to medicines. However, it is clear both from previous studies7 and from the stakeholder interviews in the current study that definitions of quality in community pharmacy extend more widely than that, incorporating additional elements of accessibility, effectiveness and experience. 7 Patient safety in terms of the occurrence of errors or near misses was not measured as these are not consistently recorded by pharmacies and self-reported errors may not be a true reflection of errors made. Patients’ self-reported medicines adherence is highly subjective and is similarly reliant on a survey respondent’s honesty. However, in the absence of any other validated measures of effectiveness that are non-disease specific, this was deemed to be the best approach. Moreover, a strong qualitative component to the study also allowed for a more holistic exploration of clinical productivity, encompassing a far wider definition of service quality as perceived by stakeholders and the mechanisms by which quality is influenced by different organisational (and extraorganisational) characteristics.
Finally, although this study was an investigation of different elements of clinical productivity in community pharmacy, it did not aim to produce a metric combining measures of ‘outputs’, both quality and quantity, over a common denominator or ‘inputs’ that would allow ranking of community pharmacy organisations or tracking over time. However, the findings of this study should help health economists seeking to take a reductive econometric approach to the measurement of clinical productivity in community pharmacy by describing variation in some of the outputs likely to be included in such an approach and how they relate both to each other and to the characteristics of the provider organisations.
Discussion of key findings
This study has highlighted the importance of pharmacy ownership type in determining the clinical productivity of community pharmacies, particularly the volume of services provided with large multiples consistently associated with higher annual dispensing volumes, annual volumes of MURs and NMS interventions. This is consistent with a previous study of MUR uptake undertaken soon after their introduction in 200518 and annual figures produced by the Health and Social Care information Centre,38 indicating that there has been little change in this position over time. Although the findings suggest that there are still perceived risks to quality when there is an emphasis on maximising the volume of services delivered, there is no evidence of reduced patient satisfaction or self-reported adherence associated with these larger organisations. Furthermore, although the safety climate in larger multiples is less favourable in relation to working conditions, their safety climate in relation to organisational learning is significantly better. Although these findings are reassuring, some caution is still needed in their interpretation. As a result of non-participation by a number of large multiples, this study did not capture the full extent of organisational variation within this group of pharmacies. This is reflected both in the lower service activity levels for large multiples in the stage 1 survey data set than in the corresponding national data and in the difference in the mean PSO (organisational culture) scores measured here compared with previous studies that have demonstrated that larger corporate chains are associated with cultures more aligned to quantity, the medicine and technical work than to quality, the patient and professional work (Dr Sally Jacobs, personal communication). 42
The relationship between the quantity and quality of service delivery is further illustrated by the finding that, although higher annual dispensing volumes are associated with higher volumes of MURs and NMS interventions conducted, there was no adverse effect of higher volumes of any of these services on quality in terms of patient satisfaction, self-reported adherence or safety climate. Again, this finding contradicts reported concerns both in the qualitative element of this study and in others18,21 that quality may be compromised in pharmacies enforcing maximum annual targets for MURs. Indeed, in the stage 2 pharmacy that conducted fewer than 12 MURs per year, patient satisfaction was seen to be lower than those conducting close to the maximum of 400. In pharmacies conducting very few MURs, it is possible that the greater focus on dispensing than on advanced services is indicative of a lack of skill, experience or engagement by the pharmacist. However, extreme caution is needed in extrapolating these results: having only one pharmacy in this category means that there is a likelihood that there may be other factors about this particular pharmacy (and indeed others) that have not been measured that explain these low ratings for patient satisfaction. Moreover, this study was limited in its quantitative exploration of service quality by the availability of validated measures of service quality in community pharmacy. It is therefore possible that compromises to service quality in high-volume pharmacies, particularly around MURs, were not captured.
The central role of staffing and skill mix to the levels of clinical productivity attainable by community pharmacies was clearly demonstrated in both the qualitative and quantitative findings from this study. Overall staffing levels and the employment by the pharmacy of a wider range of staff categories (e.g. second pharmacist, pharmacy technician, accuracy checker) were likely to be driven by dispensing volumes and, hence, the income of the pharmacy and the need for a larger and more diverse workforce. However, there were also indications from the quantitative findings that this could, in turn, provide the capacity for the pharmacy to provide additional services (pharmacies with more than one pharmacist conducted a greater volume of NMS interventions) and a higher-quality service (pharmacies employing a registered pharmacy technician were associated with higher levels of patient satisfaction). From the qualitative interviews, it was evident that the presence of a trusted, appropriately trained team with a range of skills was necessary for pharmacists to be able to delegate responsibilities for much of the dispensing process in order to free up their time to focus on their extended clinical role. Furthermore, pharmacies seen to value and invest in their staff and staff development were perceived as supporting higher levels of clinical productivity, in terms of both the quality and quantity of services delivered. However, it was also reported that pharmacies had been cutting back on staffing in recent years as a result of pressures on profit margins and that this was threatening levels of clinical productivity. With significant cuts to pharmacy remuneration on the horizon,75 this situation may get worse. However, it may force pharmacies to rethink and reorganise the way they work, making better use of pharmacy support staff (particularly pharmacy technicians) in the more technical aspects of the dispensing process and, indeed, other services. Pharmacy technicians and other support staff have been shown in recent studies to be able and, indeed, willing to take on such roles76–78 and this may free pharmacists’ own capacity to deliver a wider range of advanced and locally commissioned services and open up new income streams.
Good working relationships between community pharmacies and their local GP surgeries were described as beneficial for the clinical productivity of the pharmacy. This could be in terms of the ability to resolve prescribing issues swiftly for patients, to address supply chain problems, ensure GP follow-up of MUR recommendations and to promote signposting and referral to pharmacy services by the GP. There is supportive evidence from the quantitative findings that good working relationships with local GP surgeries are associated with increased clinical productivity in community pharmacies, with a significantly higher volume of NMS interventions being conducted in pharmacies where that relationship was described as very good than in those where the relationship was poor or non-existent. Pharmacies with very good relationships with their local GPs were also more likely to have a favourable safety climate, although the reasons for this are unclear and the relationship is unlikely to be causal but as a result of other latent factors. The pharmacist–GP relationship has previously been described as competitive and conflicting,79,80 with conflicts around the commercial aspects of pharmacy and medical dominance in the health-care professional hierarchy. 81 Such conflict and competition between the professions is still in evidence, for example in current tensions around the provision of a national pharmacy influenza vaccination service. 82 The findings from the stakeholder interviews suggest ways in which pharmacist–GP integration might be improved, including pharmacists being more proactive in establishing and maintaining regular communication, increased interprofessional education, incentives for GPs to signpost and refer patients to pharmacy services and closer alignment of the general medical and pharmaceutical services contracts. These findings reflect recommendations from previous investigations of pharmacist–GP collaboration81,83,84 suggesting that, to overcome existing barriers to collaboration, systems to enable more face-to-face contact were required to facilitate direct communication together with alignment of contracts and incentives for closer working. The need to find solutions to promote closer working between the sectors has been recognised by a recent joint RPS and National Association for Primary Care consultation on the integration of general practice and community pharmacy85 (building on the 2011 joint statement from the RPS and Royal College of General Practitioners),86 and the implementation of a pilot initiative to employ more clinical pharmacists in GP surgeries. 87
The findings of this study indicate that although annual dispensing volume is driven by local population need (deprivation, prevalence of long-term conditions, age profile), this is not the case for MURs or NMS interventions. Here, an inverse relationship between local population need and service delivery is apparent. This suggests that there has been little change since an earlier study of MUR uptake reported similar findings 1 year after their introduction in 2005,18 despite the introduction of target groups for MURs in 2011. Given stakeholders’ definition of a high-quality MUR in the current study as being one targeted to those most likely to benefit, this implies that the quality of the MUR service as currently implemented still falls short. The most significant drivers of MUR provision, therefore, still appear to be organisation related and not related to patient need. The association between dispensing volumes and MUR provision is likely to be caused by increased opportunities for pharmacists to offer MURs to patients given the perception that demand for such services is minimal. However, the limit of 400 MURs per year for which pharmacies will be reimbursed, together with the limited capacity for pharmacists to conduct any more within existing staffing models, may be a barrier to pharmacies increasing their service volume in areas with the greatest population need. Furthermore, the findings of this study suggest that structural barriers exist that relate to the responsible pharmacist regulations and associated supervision arrangements, and that these prevent pharmacists providing services outside of the pharmacy premises to some patients who stand to benefit most (e.g. housebound older people or those with multimorbidities).
The perception of patients’ limited awareness of the pharmacist’s role, the dispensing process and the range of services available from the pharmacy helps to explain the prioritisation of speed over other aspects of dispensing quality and of dispensing over other services being operated by some pharmacies and described by interviewees in the current study. Patient expectations of minimal waiting times for dispensing services were sometimes reinforced by pharmacies that displayed organisational targets around waiting times. A number of strategies to manage workloads and workflow were described by interviewees, including appointment systems for MURs and other services and systems for managing repeat dispensings, and these could be adopted by other pharmacies to help improve their productivity. Furthermore, previous studies have suggested that extended pharmacy services lack publicity89 and that the general public remains sceptical about pharmacists’ skills and abilities to provide such services,90 and do not take pharmacists as seriously as other health-care professionals. 91 This study therefore contributes to existing evidence that there may still be a need for information and marketing campaigns to moderate patient expectations, increase public awareness of the pharmacist’s role, knowledge and skills, and to create wider demand for services.
Stakeholder interviews also suggested that elements of the community pharmacy contractual framework, levels of remuneration and the commissioning process all had a negative impact on clinical productivity. Despite continued government policy supporting the expansion of community pharmacy services, in December 2015 the UK Department of Health announced for the first time a cut in the total funding available for pharmacies under the community pharmacy contractual framework (essential and advanced services) from £2.80B in 2015/16 to £2.63B in 2016/17. 75 The findings of this study suggest that current levels of contractual remuneration are already perceived by many to limit the level of clinical productivity possible in community pharmacies. Further cuts may therefore constitute not only a threat to the continued expansion of pharmacy services, but also a risk to both the quantity and quality of services already provided, with some pharmacies having to make cuts to staffing and others risking closure. 92 The UK Government has put out to consultation a number of proposals to increase community pharmacy efficiency including hub-and-spoke dispensing models. There is some evidence from this study that this and the other strategies mentioned above may be helpful for managing workload in community pharmacies. In particular, more effective use of the existing skill mix within the pharmacy team, as described above, may be one solution. However, further research and evaluation is required to understand what works best and for which types of pharmacy. Moreover, changes to existing supervision arrangements and the decriminalisation of dispensing errors may be required to encourage pharmacists to delegate responsibilities to pharmacy technicians and other support staff, something that they are sometimes reluctant to do. 76 An additional source of income for pharmacies could be an expansion of enhanced or locally commissioned services that would be facilitated by increased delegation of technical tasks to support staff to free pharmacists’ time to extend their clinical role. However, the study findings suggest that variation in the commissioning of these services, levels of remuneration and, commonly, a short commissioning cycle are further barriers to the investment necessary for the uptake of these services by community pharmacies.
Finally, this study has suggested that the fragmentation of community pharmacy commissioning responsibilities has resulted in no single entity retaining an overview of community pharmacy services in any locality. Clinical productivity is only generally monitored in terms of the quantity of service provision, primarily for the purposes of payment and, hampered by the lack of reliable and validated methods for measuring service quality, the quality of the services provided is effectively assumed until something goes wrong. There is little opportunity, therefore, for commissioners to monitor, ensure and potentially drive improvements in the quality of community pharmacy services. These findings have therefore highlighted the need for the development of validated tools for measuring service quality in community pharmacy and mechanisms that can be used by service commissioners to monitor and support quality improvement. One development suggested by the stakeholders interviewed, which could both aid the monitoring and improvement of service quality, and better integrate pharmacy services with the wider primary health-care system, would be the introduction to the community pharmacy contractual framework of a QOF aligned with the QOF for general practice. A pharmacy QOF, as proposed in the 2010 RPS of Great Britain manifesto,93 would reward pharmacies for the provision of ‘quality care’ across a number of standards; integration would be encouraged when these were aligned with existing QOF standards for GPs.
Reflection on patient and public involvement
This study benefited from the membership of two PPI contributors on the project advisory group. Both PPI members actively contributed to that group throughout the study, helping to advise on additional study plans for PPI, study progress (particularly around the development of the patient survey), recruiting PPI participants in the piloting of the stage 2 patient questionnaire and helping to interpret the study findings from a patient perspective. For example, PPI contributors highlighted the lack of awareness among the public of the range of services offered by pharmacists, and also a lack of understanding of the roles and responsibilities of pharmacists and how that may influence the perceived quality of services delivered (e.g. speed of dispensing). In this way, both members made valuable and substantial contributions to the ongoing study.
In addition, we invited patients and members of the public to pilot and comment on the design of the stage 2 patient questionnaire and accompanying letter and information sheet. As described, a series of cognitive interviews were conducted with nine patients. The study advisory group PPI contributors helped to identify patients for interview through their own networks and patient groups. Through an iterative process, questions in the questionnaire were redrafted during the interviewing period to allow suggested changes to be piloted in later interviews.
Patient and public involvement contributors also attended the commissioners’ workshop held to inform the development of the commissioning toolkit. Each discussion table at that workshop included one member of the public and all contributed freely to discussion. This helped to ensure that the discussion remained grounded in the needs of patients and the public, and was successful in that regard.
Finally, the original application stated that the research team would ‘piggyback’ onto existing patient group meetings to present material from the research. In May 2014, the study team presented the project to two CCG patient group meetings: HealthVoice in Eastern Cheshire and Manchester city-wide Patient and Public Advisory Group. The purpose of these meetings was to gain feedback from members about the design and process of the study, specifically focusing on the patient questionnaire and recruitment process for patients in stage 2. The study was well received by these CCG patient groups, with members expressing an interest in learning more about the study findings. As a result, the research team revisited one of these groups and a third general practice-based patient and public advisory group (at Cornishway Group Practice in Wythenshawe, Manchester) to consult with members again and to provide an overview of the study findings. Although this presentation of the study findings was, again, well received by both groups, the lack of time available for feedback and discussion with members limited the benefit for the study in relation to the interpretation of findings.
Chapter 9 Conclusions
This study of clinical productivity in community pharmacy and the organisational characteristics associated with its variation has built on existing knowledge of individual factors thought to influence the delivery of high-quality community pharmacy services and has, for the first time, provided systematic evidence for the organisational and extraorganisational factors associated with both the quantity and quality of service delivery.
The extent of variation in the levels of essential (dispensing) and advanced (MUR, NMS) service activity has been demonstrated (objective i). However, because of the lack of available data, variation in the levels of enhanced or locally commissioned service activity remains to be explored. Although staffing and skill mix were strongly associated with dispensing volume, organisational type was the strongest predictor of MUR and NMS activity (objective ii). Patient and interpersonal factors were stronger predictors of service quality (satisfaction with visit, satisfaction with information received about medicines, self-reported medicines adherence) than organisational characteristics, but no association was demonstrated between service quality and service quantity using these measures (objective iii). Qualitative findings suggested that clinical productivity (both quality and quantity) was influenced by staffing levels and skill mix; the presence of a trusted team; volume of work and competing demands; organisational culture; pharmacist–GP relationships; and a number of extraorganisational factors, including patient and population characteristics, supply chain problems, commissioning and contractual factors, and legal and regulatory constraints (objective iv). Finally, these findings have informed the development of a toolkit for commissioning medicines optimisation services from community pharmacies (objective v).
The findings of this study have important implications, both for pharmacies and for service commissioners, and are suggestive of a number of areas of future research.
Implications for health care
Findings from this study support existing evidence that, even when controlling for other organisational characteristics, there is a difference in the way in which large, corporate pharmacy organisations operate compared with smaller pharmacy chains and independents. Although this enables the larger multiples to deliver a greater quantity of services, questions have arisen from stakeholder interviews around the mechanisms by which these organisations are able to achieve this, placing undue pressure on pharmacists and pharmacy staff, and potentially compromising quality. Although there was no indication from the quantitative findings that service quality (in terms of patient satisfaction, satisfaction with information received about medicines or self-reported medicines adherence) was lower in large multiples, safety climate in relation to working conditions was significantly less favourable. This has important implications for pharmacies’ internal approaches to performance management to ensure that business targets are met without compromising pharmacists’ well-being or patient safety, and that the quest for profit is not prioritised over service quality and maximising patient benefit. However, the findings also suggest that current arrangements and levels of remuneration for the different levels of service under the global sum (essential and advanced services) incentivise this type of organisational behaviour. Therefore, the Department of Health, NHS and other service commissioners are also responsible for ensuring that contracts with community pharmacy create incentives to maximise the quality of services commissioned and patient benefit, not only the quantity of services provided.
The study also highlighted the central role of staffing and skill mix within the pharmacy for maximising clinical productivity. Findings demonstrated the importance of having a trusted and competent team to free pharmacists from the more technical and transactional work associated with dispensing to allow them to focus on more clinical and patient-centred work, and to enable pharmacies to deliver the growing range of services now expected. Particularly in light of the recently announced cuts to pharmacy funding, this suggests an urgent need for pharmacies to implement different models of skill mix and dispensing, possibly taking the lead from hospital pharmacy, to support community pharmacists with delegation and adopting an extended clinical role. Although much of this can be achieved within existing responsible pharmacist and supervision legislation, study findings suggest that these and the legal status of dispensing errors (both under review at the time of writing) still constitute a perceived barrier to change.
The fact that individual and interpersonal factors were more predictive of service quality (satisfaction with pharmacy visit and information received about medicines) than organisational characteristics in the quantitative study suggests that the ability of pharmacists and pharmacy staff to build relationships with their customers and foster customer loyalty may help to improve the quality of the services they provide as perceived by patients. Moreover, the association demonstrated between regular locum use and reduced self-reported medicines adherence is suggestive of the importance of continuity of care to improved patient outcomes. This also relates to the qualitative findings around patients being more receptive to pharmacy services having already had a positive experience, generating further demand and increasing their impact. These findings suggest that pharmacies encouraging continuity of staffing and providing or supporting training in interpersonal and communication skills may see increases in their clinical productivity. Indeed, the qualitative findings also suggest that pharmacy organisations with a culture of supporting and investing in staff supported higher levels of clinical productivity.
Existing commissioning structures and processes have been identified as barriers to clinical productivity in community pharmacy. The fragmentation of pharmacy commissioning and the resulting loss of manpower and local knowledge have impeded the planning, oversight and integration of pharmacy services in the wider health-care system with evidence of decommissioning or poor uptake of some services. Furthermore, findings suggest that the short-term nature of the commissioning cycle hinders longer-term planning for community pharmacies in terms of investment in staff, training and equipment. This can create challenges for pharmacies, particularly small chains and independents, seeking to expand the range and volume of services they deliver. This evidence suggests that there is a need for a collaborative endeavour in the planning and commissioning of local medicines-related health care and public health services, and that commissioning, when possible, should be conducted on a longer-term basis. New models of integrated care delivery in the NHS, such as vanguard sites, may provide important learning for how such problems may be overcome, particularly in areas where community pharmacy has been given a central role.
It was also apparent from these findings that the fragmentation of commissioning structures, coupled with the lack of available measures of service quality, has led to woefully inadequate monitoring by service commissioners of clinical productivity in community pharmacy. This is particularly around service quality but also includes a lack of centrally collated data on the range and volume of locally commissioned services delivered by pharmacies nationally. An inability to monitor service quality limits service commissioners’ capability to ensure the accountability of these publicly funded services and also hinders the potential for quality improvement in this sector. The lack of centrally collated locally commissioned service activity data is a barrier to the planning and commissioning of new services. The study findings suggest that there is general support from pharmacies and commissioners for additional monitoring of clinical productivity in community pharmacy, moreover that transparent and consistent monitoring processes would support both quality improvement and service planning in this sector.
Finally, the importance of good working relationships between pharmacists and GPs was highlighted by this study. The findings suggest that measures to enhance and encourage closer collaborative working, such as alignment of the general medical and general pharmaceutical services contracts or the introduction of a joint QOF, might overcome existing barriers and introduce incentives for GPs to refer or signpost patients to community pharmacy services, ensuring a more joined-up approach to commissioning primary care services around the needs of the patient. The little evidence we do have from existing research is that when care is integrated with or supported by the GP, patients are much more willing to access services through their community pharmacy. In relation to this, the evidence of a perceived lack of awareness among members of the public regarding the role of the pharmacist and range of services available indicates that increased marketing and public information campaigns may increase demand for extended community pharmacy services, taking some of the pressure off general practice. Furthermore, increased involvement of patients to identify their service needs and where community pharmacy can best contribute may also result in patients being more willing to engage with community pharmacy.
Recommendations for research
The experience of undertaking this study has highlighted the difficulties of obtaining existing pharmacy performance data and of engaging pharmacies and pharmacy organisations in the research process. Unlike NHS organisations, community pharmacies are private sector commercial enterprises. There is therefore a lack of clarity around ownership of any data relating to the delivery of NHS services that, although the services are publicly funded, are deemed to be ‘commercially sensitive’. This lack of transparency is at odds with current moves to increase transparency within the NHS to help improve the quality and safety of services. Although there have been some recent developments in this area in community pharmacy (e.g. the RPS ‘research-ready pharmacies’ initiative), progress is slow and the sector lags well behind other NHS providers.
How can service quality best be measured in community pharmacy?
The qualitative evidence from this study provides valuable insights into definitions of quality in relation to dispensing and MUR services in community pharmacy. Further research is needed to help develop reliable and validated quantitative tools to measure community pharmacy service quality over and above patient satisfaction. As interview respondents described, there are inherent difficulties in measuring patient outcomes that can link directly to community pharmacy services. However, there is a growing body of knowledge in this area that, if expanded, could provide both researchers and commissioners with the tools necessary to monitor and improve service quality. The development of such tools should draw on qualitative investigations of patient views and experiences of pharmacy services as well as those of pharmacists and GPs.
How cost-effective are different models of skill mix in community pharmacy?
To support the development of cost-effective models of skill mix in community pharmacy, research is needed to describe and evaluate existing developments in this area (including in hospital pharmacy where such developments have already been successfully implemented) to examine how they affect clinical productivity. This should include, but not be limited to, investigating the costs and effects of implementing a two-pharmacist model, different configurations and levels of support staff, and the implementation of different dispensing cascade models (i.e. conducting the clinical check at the beginning vs. at the end of the dispensing process), all of which aim to free up pharmacists to deliver more clinical, patient-centred services.
How are community pharmacy services commissioned and how does this relate to local need?
Research is also needed into the way in which services are commissioned locally from community pharmacies by CCGs, local authorities and NHS England, and the extent to which local needs are met. The evidence from this study suggests that, for MURs at least, services are not targeted at areas with greatest need. This may not be the case for locally commissioned services but, without the evidence, improvements cannot be made to the commissioning process to ensure that community pharmacy services are targeted at those in greatest need and integrated with other services around patient pathways.
Acknowledgements
We would like to thank all of the patients, pharmacies, pharmacists, pharmacy staff and other pharmacy stakeholders who took part in, or helped to facilitate, the different elements of this study – your contribution is gratefully acknowledged. In particular we are grateful to those pharmacy organisations who supported and encouraged participation by their constituent pharmacies and pharmacists, and without whom we would not have obtained sufficient representative data for our analysis.
Thank you to the project management team at the NIHR Health Services and Delivery Research programme for supporting the study through the necessary changes and project extension. In addition, thank you to the peer reviewers for the original application for funding and for their insightful and useful suggestions for improving the protocol.
Many thanks for the guidance provided by the members of our project advisory group: Philip Hough (public contributor), James Shillito (public contributor), Mark Burdon (independent pharmacist), Liz Stafford (Rowlands Pharmacy), Clare Kerr (Lloyds Pharmacy), Amy Lepiorz (NHS England), Kate Kinsey (NHS England), Jo Tsoneva (NHS Sheffield) and Kelvin Rowland-Jones (NHS England).
We would also like to acknowledge the support of Melanie Parmenter (NHS BSA), Graham Mitchell (NHS BSA), Narissa Leyland (NHS England), Natasha Davies (NHS England) and Alison Hemsworth (NHS England) in relation to study use of the community pharmacy activity data.
Thanks also to the members of the NIHR CRN who helped to implement the stage 2 patient survey: Michelle Horspool, Narinder Dhillon, Daniel Lawrence, Lisa Cheng and Clare Daly.
Finally, thanks to Helen Northall, Poppy Tipton and Charlotte Goodson of PCC for facilitating the commissioners workshop and subsequent work on the commissioning toolkit.
Contributions of authors
Sally Jacobs (Lecturer, Social Pharmacy), chief investigator, led on all aspects of the study and prepared the final report.
Fay Bradley (Research Fellow, Social Pharmacy) contributed to the design of research instruments, and conducted fieldwork and analysis for stage 2 of the study.
Rebecca Elvey (Research Fellow, Primary Care) contributed to the design of research instruments and conducted fieldwork for stage 1 of the study.
Tom Fegan (Research Assistant, Pharmacy Practice) contributed to the design of research instruments, and conducted fieldwork and analysis for stage 2 of the study.
Devina Halsall (Research Fellow, Pharmacy Practice) contributed to overall study design, stakeholder engagement activities, development of the commissioning toolkit, and a working knowledge of community pharmacy practice and commissioning.
Mark Hann (Research Fellow, Statistics) contributed to study design (quantitative sampling and analysis), undertook sampling, conducted all quantitative analysis and prepared the results for publication, and contributed to the final report.
Karen Hassell (Professor, Social Pharmacy) contributed to overall study design and stakeholder engagement activities.
Andrew Wagner (Information Manager) contributed to study design (use of secondary data sets), and obtained access to and prepared socioeconomic and demographic data sets.
Ellen Schafheutle (Senior Lecturer, Law and Professionalism in Pharmacy) contributed to overall study design, provided ongoing advice and support, and contributed to preparation of the final report.
Publications
Fegan T, Jacobs S, Bradley F, Halsall D, Schafheutle E, Elvey R, et al. Pharmacist views on organisational characteristics that affect clinical productivity in English community pharmacies. Int J Pharm Pract 2015;23(Suppl. 2):44.
Halsall D, Jacobs S, Elvey R, Bradley F, Fegan T, Hann M, et al. Engaging the community pharmacy sector in research: lessons learned from a national study of clinical productivity. Int J Pharm Pract 2015;23(Suppl. 1):19–20.
Jacobs S, Hann M, Elvey R, Bradley F, Fegan T, Halsall D, et al. Organisational factors associated with variation in dispensing and medicine use review (MUR) activity in a sample of English community pharmacies. Int J Pharm Pract 2015;23(Suppl. 1):47–8.
Jacobs S, Hann M, Wagner A, Schafheutle E. Medicines use review (MUR) activity in English community pharmacies: associations with pharmacy type and population need. Int J Pharm Pract 2015;23(Suppl. 2):48–9.
Jacobs S, Fegan T, Bradley F, Halsall D, Hann M, Hassell K, Schafheutle E. Pharmacists’ views of the extra-organisational factors affecting clinical productivity in English community pharmacies. Int J Pharm Pract 2016;24(Suppl. 1):17–18.
Hann M, Schafheutle EI, Bradley F, Elvey R, Wagner A, Halsall D, et al. Organisational and extraorganisational determinants of volume of service delivery by English community pharmacies: a cross-sectional survey and secondary data analysis. BMJ Open 2017;7:e017843.
A series of full peer-reviewed papers reporting the different elements of the study is planned.
Data sharing statement
We shall make quantitative study data available to the scientific community with as few restrictions as feasible, subject to anonymisation, while retaining exclusive use until the publication of major outputs. Qualitative study data are not suitable for sharing beyond that contained within the report. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- A Vision for Pharmacy in the New NHS. London: Department of Health; 2003.
- Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 1990;47:533-43.
- Edmunds J, Calnan MW. The reprofessionalisation of community pharmacy? An exploration of attitudes to extended roles for community pharmacists amongst pharmacists and general practioners in the United Kingdom. Soc Sci Med 2001;53:943-55. https://doi.org/10.1016/S0277-9536(00)00393-2.
- Operational Guidance to the NHS: Extending Patient Choice of Provider. London: Department of Health; 2011.
- Timmins N. Challenges of private provision in the NHS. BMJ 2005;331:1193-5. https://doi.org/10.1136/bmj.331.7526.1193.
- Dawson D, Gravelle H, O’Mahony M, Street A, Weale M, Castelli A, et al. Developing New Approaches to Measuring NHS Outputs and Productivity. York: University of York Centre for Health Economics, National Institute of Social and Economic Research; 2005.
- Halsall D, Noyce PR, Ashcroft DM. Characterizing healthcare quality in the community pharmacy setting: insights from a focus group study. Res Social Adm Pharm 2012;8:360-70. http://dx.doi.org/10.1016/j.sapharm.2011.09.001.
- Halsall D, Ashcroft D, Noyce P. Assessing quality in community pharmacy. Int J Pharm Pract 2008;16:137-48. http://dx.doi.org/10.1211/ijpp.16.3.0003.
- Sheaff R, Schofield J, Mannion R, Dowling B, Marshall M, McNally R. Organisational Factors and Performance: A Review of the Literature. Southampton: National Coordinating Centre for Service Delivery and Organisation; 2003.
- Ashworth M, Armstrong D. The relationship between general practice characteristics and quality of care: a national survey of quality indicators used in the UK Quality and Outcomes Framework, 2004–5. BMC Fam Pract 2006;7. https://doi.org/10.1186/1471-2296-7-68.
- Ashworth M, Seed P, Armstrong D, Durbaba S, Jones R. The relationship between social deprivation and the quality of primary care: a national survey using indicators from the UK Quality and Outcomes Framework. Br J Gen Pract 2007;57:441-8.
- Campbell SM, Hann M, Hacker J, Burns C, Oliver D, Thapar A, et al. Identifying predictors of high quality care in English general practice: observational study. BMJ 2001;323:784-7. https://doi.org/10.1136/bmj.323.7316.784.
- Doran T, Fullwood C, Gravelle H, Reeves D, Kontopantelis E, Hiroeh U, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med 2006;355:375-84. https://doi.org/10.1056/NEJMsa055505.
- Griffiths P, Murrells T, Maben J, Jones S, Ashworth M. Nurse staffing and quality of care in UK general practice: cross-sectional study using routinely collected data. Br J Gen Pract 2010;60:36-48. http://dx.doi.org/10.3399/bjgp10X482086.
- McDonald R, Cheraghi-Sohi S, Sanders C, Ashcroft D. Professional status in a changing world: the case of medicines use reviews in English community pharmacy. Soc Sci Med 2010;71:451-8. http://dx.doi.org/10.1016/j.socscimed.2010.04.021.
- McDonald R, Cheranghi-Sohi S, Tickle M, Roland M, Doran T, Campbell S, et al. The Impact of Incentives on the Behaviour and Performance of Primary Care Professionals. Southampton: NIHR Evaluations, Trials and Studies Coordinating Centre; 2010.
- Blenkinsopp A, Bond C, Celino G, Inch J, Gray N. Medicines use review: adoption and spread of a service innovation. Int J Pharm Pract 2008;16:271-6. http://dx.doi.org/10.1211/ijpp.16.4.0010.
- Bradley F, Wagner AC, Elvey R, Noyce PR, Ashcroft DM. Determinants of the uptake of medicines use reviews (MURs) by community pharmacies in England: a multi-method study. Health Policy 2008;88:258-68. http://dx.doi.org/10.1016/j.healthpol.2008.03.013.
- Wagner A, Noyce PR, Ashcroft DM. Changing patient consultation patterns in primary care: an investigation of uptake of the Minor Ailments Service in Scotland. Health Policy 2011;99:44-51. http://dx.doi.org/10.1016/j.healthpol.2010.07.002.
- Roberts AS, Benrimoj SI, Chen TF, Williams KA, Aslani P. Implementing cognitive services in community pharmacy: a review of facilitators used in practice change. Int J Pharm Pract 2006;14:163-70. http://dx.doi.org/10.1211/ijpp.14.3.0002.
- Harding G, Wilcock M. Community pharmacists’ perceptions of medicines use reviews and quality assurance by peer review. Pharm World Sci 2010;32:381-5. http://dx.doi.org/10.1007/s11096-010-9381-1.
- Jacobs S, Ashcroft D, Hassell K. Culture in community pharmacy organisations: what can we glean from the literature?. J Health Organ Manag 2011;25:420-54. http://dx.doi.org/10.1108/14777261111155047.
- Jacobs S, Hassell K, Ashcroft D, Johnson S, O’Connor E. Workplace stress in community pharmacies in England: associations with individual, organizational and job characteristics. J Health Serv Res Policy 2014;19:27-33. http://dx.doi.org/10.1177/1355819613500043.
- Johnson SJ, O’Connor EM, Jacobs S, Hassell K, Ashcroft DM. The relationships among work stress, strain and self-reported errors in UK community pharmacy. Res Social Adm Pharm 2014;10:885-95. http://dx.doi.org/10.1016/j.sapharm.2013.12.003.
- Lea VM, Corlett SA, Rodgers RM. Workload and its impact on community pharmacists’ job satisfaction and stress: a review of the literature. Int J Pharm Pract 2012;20:259-71. http://dx.doi.org/10.1111/j.2042-7174.2012.00192.x.
- Schafheutle EI, Seston EM, Hassell K. Factors influencing pharmacist performance: a review of the peer-reviewed literature. Health Policy 2011;102:178-92. http://dx.doi.org/10.1016/j.healthpol.2011.06.004.
- Ferguson J, Ashcroft D, Hassell K. Qualitative insights into job satisfaction and dissatisfaction with management among community and hospital pharmacists. Res Social Adm Pharm 2011;7:306-16. http://dx.doi.org/10.1016/j.sapharm.2010.06.001.
- Ashcroft DM, Quinlan P, Blenkinsopp A. Prospective study of the incidence, nature and causes of dispensing errors in community pharmacies. Pharmacoepidemiol Drug Saf 2005;14:327-32. http://dx.doi.org/10.1002/pds.1012.
- Shann P, Hassell K. Flexible working: understanding the locum pharmacist in Great Britain. Res Social Adm Pharm 2006;2:388-407. https://doi.org/10.1016/j.sapharm.2006.03.002.
- Phelps A, Agur M, Nass L, Blake M. GPhC Registrant Survey 2013. Findings. London: National Centre for Social Research and General Pharmaceutical Council; 2014.
- Horne R, Myers LB, Midence K. Adherence to Treatment in Medical Conditions. Amsterdam: Harwood Academic Press; 1998.
- Howard RL, Avery AJ, Howard PD, Partridge M. Investigation into the reasons for preventable drug related admissions to a medical admissions unit: observational study. Qual Saf Health Care 2003;12:280-5. https://doi.org/10.1136/qhc.12.4.280.
- NHS Reference Costs 2014–2015. London: Department of Health; 2015.
- Trueman P, Taylor DG, Lowson K, Bligh A, Meszaros A, Wright D, et al. Evaluation of the Scale, Causes and Costs of Waste Medicines. York: York Health Economics Consortium/School of Pharmacy, University of London; 2010.
- Van Wijk BL, Klungel OH, Heerdink ER, de Boer A. Effectiveness of interventions by community pharmacists to improve patient adherence to chronic medication: a systematic review. Ann Pharmacother 2005;39:319-28. https://doi.org/10.1345/aph.1E027.
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2008;2. http://dx.doi.org/10.1002/14651858.CD000011.pub3.
- PSNC . National Contract Funding 2016. www.psnc.org.uk/funding-and-statistics/historical-funding-arrangements/201415-funding-settlement/ (accessed 17 January 2017).
- General Pharmaceutical Services England 2005–06 to 2014–15. Leeds: Health and Social Care Information Centre; 2015.
- Michie S, West MA. Managing people and performance: an evidence based framework applied to health service organizations. Int J Manag Rev 2004;5:91-111. http://dx.doi.org/10.1111/j.1460-8545.2004.00098.x.
- Halsall D. Defining and Assessing Quality in Community Pharmacy 2010.
- Health and Social Care Information Centre . General Pharmaceutical Services in England, 2001–02 to 2010–11 2011. www.hscic.gov.uk/primary-care (accessed 10 March 2016).
- Clark BE, Mount JK. Pharmacy Service Orientation: a measure of organizational culture in pharmacy practice sites. Res Social Adm Pharm 2006;2:110-28. https://doi.org/10.1016/j.sapharm.2005.12.003.
- Ashcroft DM, Parker D. Development of the pharmacy safety climate questionnaire: a principal components analysis. Qual Saf Health Care 2009;18:28-31. http://dx.doi.org/10.1136/qshc.2006.022129.
- Phipps DL, De Bie J, Herborg H, Guerreiro M, Eickhoff C, Fernandez-Llimos F, et al. Evaluation of the Pharmacy Safety Climate Questionnaire in European community pharmacies. Int J Qual Health Care 2012;24:16-22. http://dx.doi.org/10.1093/intqhc/mzr070.
- Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res 2003;12:229-38. https://doi.org/10.1023/A:1023254226592.
- English Indices of Deprivation 2010. 2011.
- 2011 Census. 2012.
- Quality and Outcomes Framework – 2011–12. Leeds: NHS Digital; 2012.
- Glattacker M, Heyduck K, Meffert C. Illness beliefs, treatment beliefs and information needs as starting points for patient information – evaluation of an intervention for patients with chronic back pain. Patient Educ Couns 2012;86:378-89. http://dx.doi.org/10.1016/j.pec.2011.05.028.
- Mahler C, Hermann K, Horne R, Ludt S, Haefeli WE, Szecsenyi J, et al. Assessing reported adherence to pharmacological treatment recommendations. Translation and evaluation of the Medication Adherence Report Scale (MARS) in Germany. J Eval Clin Pract 2010;16:574-9. http://dx.doi.org/10.1111/j.1365-2753.2009.01169.x.
- Sahm L, Quinn L, Madden M, Richards HL. Does satisfaction with information equate to better anticoagulant control?. Int J Clin Pharm 2011;33:543-8. http://dx.doi.org/10.1007/s11096-011-9505-2.
- Hassell K, Noyce PR, Rogers A, Harris J, Wilkinson J. A pathway to the GP: the pharmaceutical ‘consultation’ as a first port of call in primary health care. Fam Pract 1997;14:498-502. https://doi.org/10.1093/fampra/14.6.498.
- Sobal J. Sample extensiveness in qualitative nutrition education research. J Nutr Educ 2001;33:184-92. https://doi.org/10.1016/S1499-4046(06)60030-4.
- Tinelli M, Blenkinsopp A, Bond C. Development, validation and application of a patient satisfaction scale for a community pharmacy medicines-management service. Int J Pharm Pract 2011;19:144-55. http://dx.doi.org/10.1111/j.2042-7174.2011.00110.x.
- Horne R, Hankins M, Jenkins R. The Satisfaction with Information about Medicines Scale (SIMS): a new measurement tool for audit and research. Qual Health Care 2001;10:135-40. https://doi.org/10.1136/qhc.0100135.
- Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 1999;47:555-67. https://doi.org/10.1016/S0022-3999(99)00057-4.
- Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health 1999;14:1-24. http://dx.doi.org/10.1080/08870449908407311.
- Naik Panvelkar P, Saini B, Armour C. Measurement of patient satisfaction with community pharmacy services: a review. Pharm World Sci 2009;31:525-37. http://dx.doi.org/10.1007/s11096-009-9311-2.
- Clatworthy J, Price D, Ryan D, Haughney J, Horne R. The value of self-report assessment of adherence, rhinitis and smoking in relation to asthma control. Prim Care Respir J 2009;18:300-5. http://dx.doi.org/10.4104/pcrj.2009.00037.
- Cohen JL, Mann DM, Wisnivesky JP, Home R, Leventhal H, Musumeci-Szabó TJ, et al. Assessing the validity of self-reported medication adherence among inner-city asthmatic adults: the Medication Adherence Report Scale for asthma. Ann Allergy Asthma Immunol 2009;103:325-31. https://doi.org/10.1016/S1081-1206(10)60532-7.
- Mårdby AC, Akerlind I, Jörgensen T. Beliefs about medicines and self-reported adherence among pharmacy clients. Patient Educ Couns 2007;69:158-64. https://doi.org/10.1016/j.pec.2007.08.011.
- Mora PA, Berkowitz A, Contrada RJ, Wisnivesky J, Horne R, Leventhal H, et al. Factor structure and longitudinal invariance of the Medical Adherence Report Scale-Asthma. Psychol Health 2011;26:713-27. http://dx.doi.org/10.1080/08870446.2010.490585.
- Schutz A. The Phenomenology of the Social World. Evanston, IL: Northwestern University Press; 1967.
- Reeves S, Albert M, Kuper A, Hodges BD. Why use theories in qualitative research?. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a949.
- Ritchie J, Spencer L, Bryman A. Analyzing Qualitative Data. London: Routledge; 1994.
- Bryman A. Integrating quantitative and qualitative research: how is it done?. Qual Res 2006;6:97-113. https://doi.org/10.1177/1468794106058877.
- NHS Library and Knowledge Services . The Commissioning Handbook for Librarians 2017. http://commissioning.libraryservices.nhs.uk/ (accessed 17 January 2017).
- Phipps DL, Ashcroft DM. Psychosocial influences on safety climate: evidence from community pharmacies. BMJ Qual Saf 2011;20:1062-8. http://dx.doi.org/10.1136/bmjqs.2011.051912.
- Drug Tariff. Newcastle upon Tyne: NHS BSA; 2017.
- The Misuse of Drugs (Amendment) (No. 2) (England, Wales and Scotland) Regulations 2015. London: The Stationery Office; 2015.
- The Medicines (Pharmacies) (Responsible Pharmacist) Regulations 2008. London: The Stationery Office; 2008.
- Medicines Act 1968. London: Her Majesty’s Stationery Office; 1968.
- The National Health Service (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013. London: The Stationery Office; 2013.
- Latif A, Boardman H. Community pharmacists’ attitudes towards medicines use reviews and factors affecting the numbers performed. Pharm World Sci 2008;30:536-43. http://dx.doi.org/10.1007/s11096-008-9203-x.
- Community Pharmacy in 2016/17 and Beyond – Proposals. London: Department of Health; 2015.
- Bradley F, Schafheutle EI, Willis SC, Noyce PR. Changes to supervision in community pharmacy: pharmacist and pharmacy support staff views. Health Soc Care Community 2013;21:644-54. http://dx.doi.org/10.1111/hsc.12053.
- Bradley F, Willis SC, Noyce PR, Schafheutle EI. Restructuring supervision and reconfiguration of skill mix in community pharmacy: classification of perceived safety and risk. Res Soc Admin Pharm 2015;12:733-46. https://doi.org/10.1016/j.sapharm.2015.10.009.
- Napier P, Norris P, Green J, Braund R. Can they do it? Comparing the views of pharmacists and technicians to the introduction of an advanced technician role. Int J Pharm Pract 2016;24:97-103. http://dx.doi.org/10.1111/ijpp.12225.
- Adamcik BA, Ransford HE, Oppenheimer PR, Brown JF, Eagan PA, Weissman FG. New clinical roles for pharmacists: a study of role expansion. Soc Sci Med 1986;23:1187-200. https://doi.org/10.1016/0277-9536(86)90338-2.
- Hughes CM, McCann S. Perceived interprofessional barriers between community pharmacists and general practitioners: a qualitative assessment. Br J Gen Pract 2003;53:600-6.
- Bradley F, Ashcroft DM, Noyce PR. Integration and differentiation: a conceptual model of general practitioner and community pharmacist collaboration. Res Social Adm Pharm 2012;8:36-4. http://dx.doi.org/10.1016/j.sapharm.2010.12.005.
- Millett D. GPC Warning over ‘Questionable’ Deal for Pharmacies to Deliver All NHS Flu Jabs 2015. www.gponline.com/gpc-warning-questionable-deal-pharmacies-deliver-nhs-flu-jabs/article/1356692 (accessed 1 April 2016).
- Bradley F. Exploring Collaboration Between General Practitioners and Community Pharmacists: A Novel Application of Social Network Analysis 2012.
- Bradley F, Elvey R, Ashcroft DM, Hassell K, Kendall J, Sibbald B, et al. The challenge of integrating community pharmacists into the primary health care team: a case study of local pharmaceutical services (LPS) pilots and interprofessional collaboration. J Interprof Care 2008;22:387-98. http://dx.doi.org/10.1080/13561820802137005.
- RPS . 12/08/2015/–/RPS/and/NAPC/Consult/on/Integration/of/General/Practice/and/Community/Pharmacy 2015. www.rpharms.com/pressreleases/pr_show.asp?id=2724 (accessed 15 April 2016).
- Joint Statement. Breaking Down the Barriers – How Community Pharmacists and GPs can Work Together to Improve Patient Care. London: RPS/RCGP; 2011.
- Clinical Pharmacists in General Practice Pilot. London: NHS England; 2015.
- Hann M, Schafheutle EI, Bradley F, Elvey R, Wagner A, Halsall D, et al. Organisational and extraorganisational determinants of volume of service delivery by English community pharmacies: a cross-sectional survey and secondary data analysis. BMJ Open 2017;7. http://doi.org/10.1136/bmjopen-2017-017843.
- Saramunee K, Krska J, Mackridge A, Richards J, Suttajit S, Phillips-Howard P. How to enhance public health service utilization in community pharmacy?: general public and health providers’ perspectives. Res Social Adm Pharm 2014;10:272-84. http://dx.doi.org/10.1016/j.sapharm.2012.05.006.
- Eades CE, Ferguson JS, O’Carroll RE. Public health in community pharmacy: a systematic review of pharmacist and consumer views. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-582.
- Rapport F, Doel MA, Hutchings HA, Wright S, Wainwright P, John DN, et al. Eleven themes of patient-centred professionalism in community pharmacy: innovative approaches to consulting. Int J Pharm Pract 2010;18:260-8. http://dx.doi.org/10.1111/j.2042-7174.2010.00056.x.
- Lam B. Government Cuts to Community Pharmacy: The Perspective of Leaders. London: The Pharmaceutical Journal; 2016.
- Promoting Patient Safety: The Pharmacy Manifesto. London: RPSGB; 2010.
Appendix 1 Stage 1 pharmacy questionnaire
Appendix 2 Stage 2 patient questionnaire
Appendix 3 Stage 2 pharmacist interview topic guide and prompt sheet
This was amended slightly for superintendent pharmacist and service commissioner interviews.
Background
First of all I would like to get a bit of background information about you.
-
What position do you currently hold?
-
How long have you been in your current post?
-
Have you had any pharmacy jobs before this one? (Probe: previous jobs/experience/qualifications)
-
Could you briefly describe your current roles and responsibilities?
We also need a bit of information about your pharmacy (cross-check with survey data where possible and KEEP BRIEF).
-
How would you describe the type of pharmacy you work for? (Probe: multiple, supermarket, small/medium-sized chain, independent? How many stores?)
-
In terms of how the pharmacy is managed, is the pharmacy manager a pharmacist (or are managers pharmacy technicians or non-pharmacy professional?)? And who manages the main pharmacist? Are they themselves a pharmacist?
-
What staff do you have working here? [Probe: levels, skill-mix (who does what?) and differences throughout the day/week] – KEEP BRIEF.
-
Roughly how many items do you usually dispense in a day? How many MURs would you normally conduct in a week/month? What other NHS services do you offer and what is the take-up of these? What about private services? How does the workload of the pharmacy vary throughout the day/week? – KEEP BRIEF.
Defining clinical productivity
This is a study of clinical productivity in community pharmacy and what pharmacies and service commissioners can do to maximise this.
-
Is ‘clinical productivity’ a term that is used much in community pharmacy? What does the term mean to you (if anything)?
We are looking at clinical productivity in terms of both the quality and quantity of service provision. The quality of the pharmacy service is associated with individual patient benefit. The quantity is also important because the more patients that receive a high-quality service, the greater the effect the service will have on public health. Conversely, high volumes of low-quality services have a potential cost both to the NHS and to patients/customers.
Quality and quantity of pharmacy service provision
1. Quantity
Thinking about the quantity of services provided by your pharmacy – and by quantity I mean both the number or range, and volume of different services provided by your pharmacy (essential, advanced and locally commissioned) – would you say that this level of activity is high (above average), about average, or low?
-
What aspects of the way your pharmacy operates do you think helps you to maximise this level of service delivery? (Probe: which organisational factors and how they help – PROMPT SHEET)
-
What aspects of the way your pharmacy operates do you think gets in the way of you maximising the quantity of the different services you deliver? (Probe: which organisational factors and how they get in the way – PROMPT SHEET)
2. Quality
I would now like to ask you about the quality of the services your pharmacy provides.
Thinking first of all about dispensing, what for you characterises a ‘high-quality’ dispensing service provided by a pharmacy?
-
What does a high quality dispensing service look like? (Probe: pharmacy team perspective, patient perspective)
How often do you feel the dispensing service provided by your pharmacy achieves this level of quality? (Probe: level of quality actually achieved, how this deviates from ‘high quality’)
-
Thinking about how this pharmacy operates, what aspects do you think help you to provide a high-quality dispensing service? (Probe: which organisational factors and how they help – PROMPT SHEET)
-
What aspects do you think get in the way of you providing a high-quality dispensing service? (Probe: which organisational factors and how they get in the way – PROMPT SHEET)
Thinking now about MURs, what for you characterises a ‘high-quality’ service provided by a pharmacy?
-
What does a high-quality MUR look like? (Probe: pharmacy team perspective, patient perspective)
How often do you feel that the MURs provided by your pharmacy achieve this level of quality? (Probe: level of quality actually achieved, how this deviates from ‘high quality’)
-
Thinking about how this pharmacy operates, what aspects do you think help you to provide high-quality MURs? (Probe: which organisational factors and how they help – PROMPT SHEET)
-
What aspects do you think get in the way of you providing high-quality MURs? (Probe: which organisational factors and how they get in the way – PROMPT SHEET)
Changes in clinical productivity
Have you been aware of any changes in the quantity (range and/or volume) of services delivered by this pharmacy over the past 5 years/since you have worked here?
-
(If yes) Could you describe these changes?
-
What do you think have been the main causes of these increases/decreases?
-
Has your organisation made any changes to the way it operates to adapt to these changes in levels of service delivery? (Probe: organisational factors – PROMPT SHEET)
-
(If yes) How successful do you feel these changes have been?
Have you been aware of any changes in the quality of service delivery in this pharmacy over the past 5 years/since you have worked here?
-
(If yes) Could you describe these changes?
-
What do you think have been the main causes of this increase/decrease in quality?
-
Are there any aspects of the way your pharmacy operates which you think have contributed to these changes in quality? (Probe: organisational factors – PROMPT SHEET)
Maximising clinical productivity
The NHS is continually seeking to maximise clinical productivity to get ‘more bang for its bucks’. We also know that, in general, dispensing volumes are rising and pharmacies are increasingly being commissioned to provide a wider range of services.
To what extent do you think it is possible for pharmacies to continue to provide a greater quantity of services while maintaining (or improving) the quality of the service provided?
-
What aspects of clinical productivity do you think could be improved?
-
What do you think community pharmacies need to be doing to help achieve this? (Probe: organisational factors – PROMPT SHEET)
-
What do you think are the main barriers to improving clinical productivity in community pharmacy? (Probe: organisational factors – PROMPT SHEET; external factors)
-
What do you think the NHS as service commissioners need to be doing to help achieve this in community pharmacy?
Measuring/monitoring clinical productivity
We are also interested in how clinical productivity might be measured and monitored.
How do you know if you are providing high-quality services at the appropriate level?
Does your pharmacy formally monitor/measure clinical productivity (i.e. both the quality and quantity of services provided)?
-
(If so) How? (Prompt: audits, patient survey)
-
How are the findings then used?
-
Do you think this helps to improve clinical productivity in your pharmacy?
-
(If not) Do you think it should?
-
How?
-
Do you think this would help to improve clinical productivity in your pharmacy?
Do service commissioners monitor/measure clinical productivity in your pharmacy? (Prompt: mystery shoppers, audits, quality-improvement instruments etc.)
-
(If so) How? For instance, what is done to measure the number of MURs performed and assess the quality of this service?
-
Do you know how these findings are used?
-
Do you think this helps to improve clinical productivity?
-
(If not) Do you think they should?
-
How?
-
Do you think this would help to improve clinical productivity in your pharmacy?
Do you think more should be done to monitor/measure clinical productivity in community pharmacy?
-
(If so) Who do you think should be responsible for monitoring/measuring clinical productivity in community pharmacy?
-
How do you think clinical productivity should be monitored/measured in community pharmacy?
-
What do you think the benefits might be? (Probe: to commissioners, to pharmacies, to patients)
-
What do you think the drawbacks might be?
-
(If not) Why not?
Is there anything else you would like to add about clinical productivity in community pharmacy that we have not already covered?
Interview prompt sheet
Organisational factors under investigation:
Location – geographical and physical.
Ownership (e.g. independent, chain, supermarket).
Type of contract (e.g. standard, 100-hour, essential small pharmacy).
Healthy Living Pharmacy status.
Volume of work – number, range and volume of different services offered by the pharmacy; how that fluctuates throughout the day, week, year.
Staffing – number and type of staff in pharmacy, turnover, experience.
Skill-mix – who does what?
Use of locums – frequency and turnover.
Continuity of care for patient – whether or not patients/customers see the same members of the pharmacy team on each visit.
Management – structure and style.
Working hours – opening hours, working hours, shift work.
Organisational culture (‘how things get done around here’) – the set of implicit or explicit values, beliefs, rules and behaviours that govern how the pharmacy operates.
Safety climate – the organisational culture in relation to patient safety.
Technology/automation – use of computers, automated dispensing, etc.
Pharmacist/GP integration – working relationship between pharmacy and nearby general practice(s).
Anything else?
Appendix 4 Commissioners’ workshop programme
Commissioning medicines optimisation services
| Time | Description |
|---|---|
| 09.00 | Registration and refreshments |
| 09.30 | Welcome and aims of the day |
| 09.45 | Presentation Findings of a NIHR study of clinical productivity in community pharmacy |
| 10.15 | Discussion on study findings Questions:
|
| 11.00 | Refreshments |
| 11.15 | Feedback from discussions Validity of findings What does good look like from a patient’s perspective for a medicines optimisation service? |
| 11.45 | Facilitated session How can we deliver a service that meets these expectations? What actions do commissioners need to take to commission this service? What would a toolkit include to help commissioners make this service improvement? |
| 12.40 | Feedback from discussions Actions commissioners need to take What needs to be in toolkit |
| 13.00 | Next steps |
| 13.15 | Close and lunch |
Appendix 5 Commissioning toolkit
Appendix 6 Full regression tables
| Dispensing volume (2012/13) | Univariable models | Multivariable model | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Job title | ||||||
| Pharmacist | Referencea | > 0.200b | ||||
| Owner/manager | –0.0147 | –0.1329 to 0.1036 | ||||
| Geographical location | ||||||
| City centre | 0.0454 | –0.1382 to 0.2289 | ||||
| Large town | –0.0018 | –0.1148 to 0.1111 | ||||
| Small town | Reference | > 0.200 | ||||
| Suburb | 0.0067 | –0.0622 to 0.0757 | ||||
| Village/rural | –0.0290 | –0.1483 to 0.0902 | ||||
| Pharmacy open for ≥ 3 years | ||||||
| No | Reference | 0.004 | Reference | 0.001 | ||
| Yes | 0.3277 | 0.1083 to 0.5470 | 0.3147 | 0.1233 to 0.5062 | ||
| HLP | ||||||
| No | Reference | > 0.200 | ||||
| Yes | –0.0367 | –0.1266 to 0.0531 | ||||
| Pharmacy contract held | ||||||
| Standard 40 hours | Reference | > 0.200 | ||||
| 100 hours | –0.0955 | –0.2369 to 0.0458 | ||||
| Other | –0.0848 | –0.3301 to 0.1605 | ||||
| Weekly opening hours | ||||||
| 10-hour change | –0.0007 | –0.0256 to 0.0243 | > 0.200 | |||
| Staff working on typical dayc | ||||||
| 1-person change | 0.0683 | 0.0570 to 0.0795 | < 0.001 | |||
| Pharmacists working on typical day | ||||||
| 1 | Reference | 0.109 | Reference | 0.015 | ||
| ≥ 2 | 0.0813 | –0.0182 to 0.1808 | 0.0949 | 0.0188 to 0.1710 | ||
| Registered pharmacy technician (typical day) | ||||||
| No | Reference | < 0.001 | Reference | < 0.001 | ||
| Yes | 0.1713 | 0.1103 to 0.2322 | 0.1120 | 0.0599 to 0.1641 | ||
| ACT (typical day) | ||||||
| No | Reference | < 0.001 | Reference | < 0.001 | ||
| Yes | 0.2497 | 0.1901 to 0.3092 | 0.1655 | 0.1112 to 0.2197 | ||
| Use of locums | ||||||
| Not regularly | Reference | > 0.200 | ||||
| Regularly | –0.0169 | –0.0828 to 0.0490 | ||||
| Pharmacy manager a pharmacist? | ||||||
| No | Reference | > 0.200 | ||||
| Yes | –0.0416 | –0.1158 to 0.0325 | ||||
| Work pattern of main pharmacist | ||||||
| Standard hours (8 a.m.–6 p.m.) | Reference | > 0.200 | ||||
| Non-standard | 0.0379 | –0.0276 to 0.1034 | ||||
| Average daily working hours of main pharmacist | ||||||
| 1-hour change | 0.0426 | 0.0126 to 0.0726 | 0.006 | 0.0314 | 0.0086 to 0.0541 | 0.007 |
| Organisational culture (PSO) | ||||||
| 1-unit change | –0.0263 | –0.0504 to –0.0022 | 0.033 | –0.0194 | –0.0373 to –0.0014 | 0.035 |
| Patient safety (PSCQ) | ||||||
| Organisational learning | –0.0033 | –0.0073 to 0.0007 | 0.107 | NSd | ||
| Blame culture | 0.0011 | –0.0098 to 0.0120 | > 0.200 | |||
| Working conditions | –0.0040 | –0.0137 to 0.0057 | > 0.200 | |||
| Safety focus | –0.0024 | –0.0191 to 0.0143 | > 0.200 | |||
| Relationship with nearest GP surgery | ||||||
| Very good | Reference | > 0.200 | ||||
| Good | –0.0069 | –0.0794 to 0.0656 | ||||
| Satisfactory/poor/none | –0.1036 | –0.2113 to 0.0041 | ||||
| No GP surgery identified | –0.0501 | –0.1720 to 0.0717 | ||||
| IMD score | ||||||
| 10-unit change | 0.0244 | 0.0092 to 0.0397 | 0.002 | 0.0164 | 0.0024 to 0.0304 | 0.022 |
| Mean age (years) | ||||||
| 1-year change | –0.0047 | –0.0142 to 0.0047 | > 0.200 | |||
| Percentage aged 0–4 | ||||||
| 1% change | 0.0071 | –0.0128 to 0.0270 | > 0.200 | |||
| Percentage aged ≥ 75 | ||||||
| 1% change | –0.0046 | –0.0134 to 0.0042 | > 0.200 | |||
| Percentage with very bad healthe | ||||||
| 1% change | 0.0356 | 0.0048 to 0.0664 | 0.024 | |||
| Percentage with CHDf | ||||||
| 1% change | 0.0662 | 0.0247 to 0.1076 | 0.002 | NS | ||
| Percentage with MH conditionf | ||||||
| 1% change | 0.2137 | 0.0384 to 0.3890 | 0.017 | NS | ||
| Percentage with depressionf | ||||||
| 1% change | 0.0252 | –0.0069 to 0.0573 | 0.123 | NS | ||
| Percentage with asthmaf | ||||||
| 1% change | 0.0318 | –0.0289 to 0.0926 | > 0.200 | |||
| Type of pharmacy | ||||||
| Independent | Reference | 0.368 | ||||
| Small/medium-sized multiple | –0.0091 | –0.0775 to 0.0593 | ||||
| Large multiple/supermarket | –0.0416 | –0.1021 to 0.0190 | ||||
| MURs (2012/13) | Univariable models | Multivariable model | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Job title | ||||||
| Pharmacist | Referencea | > 0.200b | ||||
| Owner/manager | 0.71 | 0.38 to 1.30 | ||||
| Geographical location | ||||||
| City centre | 0.78 | 0.30 to 1.99 | ||||
| Large town | 1.69 | 0.84 to 3.42 | ||||
| Small town | Reference | 0.112 | NSc | |||
| Suburb | 0.91 | 0.47 to 1.75 | ||||
| Village/rural | 0.62 | 0.27 to 1.39 | ||||
| Pharmacy open for ≥ 3 years | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.23 | 0.62 to 2.46 | ||||
| HLP | ||||||
| No | Reference | 0.003 | NS | |||
| Yes | 2.25 | 1.31 to 3.87 | ||||
| Pharmacy contract heldd | ||||||
| Standard 40 hours | Reference | 0.048 | ||||
| 100 hours | 2.29 | 1.11 to 4.73 | ||||
| Other | 0.83 | 0.47 to 1.47 | ||||
| Weekly opening hours | ||||||
| 10-hour change | 1.34 | 1.14 to 1.57 | < 0.001 | 1.25 | 1.06 to 1.49 | 0.010 |
| Staff working on typical daye | ||||||
| 1-person change | 1.24 | 1.06 to 1.45 | 0.006 | |||
| Pharmacists working on typical day | ||||||
| 1 | Reference | 0.105 | NS | |||
| ≥ 2 | 1.60 | 0.91 to 2.84 | ||||
| Registered pharmacy technician (typical day) | ||||||
| No | Reference | 0.002 | NS | |||
| Yes | 2.24 | 1.35 to 3.72 | ||||
| ACT (typical day) | ||||||
| No | Reference | 0.013 | NS | |||
| Yes | 2.05 | 1.17 to 3.59 | ||||
| Use of locums | ||||||
| Not regularly | Reference | > 0.200 | ||||
| Regularly | 1.06 | 0.66 to 1.69 | ||||
| Pharmacy manager a pharmacist? | ||||||
| No | Reference | 0.107 | NS | |||
| Yes | 0.44 | 0.16 to 1.20 | ||||
| Work pattern of main pharmacist | ||||||
| Standard hours (8 a.m.–6 p.m.) | Reference | > 0.200 | ||||
| Non-standard | 1.26 | 0.78 to 2.05 | ||||
| Average daily working hours of main pharmacist | ||||||
| 1-hour change | 1.27 | 0.97 to 1.65 | 0.078 | NS | ||
| Organisational culture (PSO) | ||||||
| 1-unit change | 0.84 | 0.68 to 1.04 | 0.102 | NS | ||
| Patient safety (PSCQ) | ||||||
| Organisational learning | 0.99 | 0.95 to 1.04 | > 0.200 | |||
| Blame culture | 1.07 | 0.99 to 1.16 | 0.083 | NS | ||
| Working conditions | 0.90 | 0.83 to 0.97 | 0.009 | NS | ||
| Safety focus | 0.93 | 0.82 to 1.06 | > 0.200 | |||
| Relationship with nearest GP surgery | ||||||
| Very good | Reference | 0.109 | NS | |||
| Good | 1.07 | 0.63 to 1.83 | ||||
| Poor/none | 0.67 | 0.37 to 1.20 | ||||
| No GP surgery identified | 0.16 | 0.03 to 0.98 | ||||
| IMD score | ||||||
| 10-unit change | 1.09 | 0.97 to 1.23 | 0.152 | NS | ||
| Mean age (years) | ||||||
| 1-year change | 0.97 | 0.91 to 1.04 | > 0.200 | |||
| Percentage aged 0–4 | ||||||
| 1% change | 1.13 | 1.00 to 1.29 | 0.053 | NS | ||
| Percentage aged ≥ 75 | ||||||
| 1% change | 0.97 | 0.91 to 1.04 | > 0.200 | |||
| Percentage with very bad healthf | ||||||
| 1% change | 1.22 | 0.93 to 1.59 | 0.154 | |||
| Percentage with CHD | ||||||
| 1% change | 1.18 | 0.84 to 1.66 | > 0.200 | |||
| Percentage with MH condition | ||||||
| 1% change | 2.35 | 0.70 to 7.94 | 0.169 | NS | ||
| Percentage with depression | ||||||
| 1% change | 0.96 | 0.73 to 1.24 | > 0.200 | |||
| Percentage with asthma | ||||||
| 1% change | 0.54 | 0.34 to 0.87 | 0.012 | 0.42 | 0.21 to 0.86 | 0.018 |
| log(dispensing volume) | ||||||
| 1-unit change | 3.90 | 1.54 to 9.83 | 0.004 | 5.88 | 1.76 to 19.6 | 0.004 |
| Type of pharmacy | ||||||
| Independent | Reference | < 0.001 | ||||
| Small/medium-sized multiple | 2.67 | 1.39 to 5.15 | ||||
| Large multiple/supermarket | 4.86 | 2.63 to 8.96 | ||||
| NMS interventions (2012/13) | Univariable models | Multivariable model | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Job title | ||||||
| Pharmacist | Referencea | > 0.200b | ||||
| Owner/manager | 0.98 | 0.55 to 1.75 | ||||
| Geographical location | ||||||
| City centre | 0.39 | 0.18 to 0.86 | 0.29 | 0.12 to 0.67 | ||
| Large town | 2.27 | 1.08 to 4.74 | 1.84 | 0.69 to 4.96 | ||
| Small town | Reference | 0.003 | Reference | < 0.001 | ||
| Suburb | 1.23 | 0.66 to 2.28 | 1.61 | 0.85 to 3.03 | ||
| Village/rural | 1.30 | 0.64 to 2.65 | 1.67 | 0.78 to 3.60 | ||
| Pharmacy open for ≥ 3 years | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.09 | 0.48 to 2.46 | ||||
| HLP | ||||||
| No | Reference | 0.014 | NSc | |||
| Yes | 1.94 | 1.15 to 3.28 | ||||
| Pharmacy contract held | ||||||
| Standard 40 hours | Reference | > 0.200 | ||||
| 100 hours | 1.29 | 0.71 to 2.34 | ||||
| Other | 1.54 | 0.68 to 3.52 | ||||
| Weekly opening hours | ||||||
| 10-hour change | 1.14 | 1.01 to 1.29 | 0.031 | NS | ||
| Staff working on typical dayd | ||||||
| 1-person change | 1.17 | 1.04 to 1.31 | 0.010 | |||
| Pharmacists working on typical day | ||||||
| 1 | Reference | < 0.001 | Reference | 0.001 | ||
| ≥ 2 | 2.79 | 1.59 to 4.89 | 3.25 | 1.67 to 6.32 | ||
| Registered pharmacy technician (typical day) | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.09 | 0.67 to 1.77 | ||||
| ACT (typical day) | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.04 | 0.58 to 1.87 | ||||
| Use of locums | ||||||
| Not regularly | Reference | > 0.200 | ||||
| Regularly | 0.88 | 0.54 to 1.42 | ||||
| Pharmacy manager a pharmacist? | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.08 | 0.60 to 1.93 | ||||
| Work pattern of main pharmacist | ||||||
| Standard hours (8 a.m.–6 p.m.) | Reference | 0.011 | NS | |||
| Non-standard | 1.86 | 1.15 to 3.00 | ||||
| Average daily working hours of main pharmacist | ||||||
| 1-hour change | 1.25 | 0.96 to 1.63 | 0.102 | NS | ||
| Organisational culture (PSO) | ||||||
| 1-unit change | 0.97 | 0.78 to 1.20 | > 0.200 | |||
| Patient safety (PSCQ) | ||||||
| Organisational learning | 1.00 | 0.96 to 1.03 | > 0.200 | |||
| Blame culture | 1.00 | 0.93 to 1.07 | > 0.200 | |||
| Working conditions | 0.94 | 0.87 to 1.02 | 0.154 | NS | ||
| Safety focus | 1.01 | 0.89 to 1.15 | > 0.200 | |||
| Relationship with nearest GP surgery | ||||||
| Very good | Reference | 0.007 | Reference | 0.017 | ||
| Good | 1.32 | 0.75 to 2.32 | 1.15 | 0.60 to 2.17 | ||
| Poor/none | 0.67 | 0.37 to 1.21 | 0.66 | 0.35 to 1.23 | ||
| No GP surgery identified | 0.20 | 0.06 to 0.60 | 0.19 | 0.06 to 0.59 | ||
| IMD score | ||||||
| 10-unit change | 1.01 | 0.91 to 1.12 | > 0.200 | |||
| Mean age (years) | ||||||
| 1-year change | 1.01 | 0.94 to 1.09 | > 0.200 | |||
| Percentage aged 0–4 | ||||||
| 1% change | 1.04 | 0.91 to 1.20 | > 0.200 | |||
| Percentage aged ≥ 75 | ||||||
| 1% change | 1.01 | 0.93 to 1.10 | > 0.200 | |||
| Percentage with very bad health | ||||||
| 1% change | 1.07 | 0.83 to 1.38 | > 0.200 | |||
| Percentage with CHD | ||||||
| 1% change | 0.76 | 0.53 to 1.08 | 0.125 | NS | ||
| Percentage with MH condition | ||||||
| 1% change | 0.64 | 0.16 to 2.63 | > 0.200 | |||
| Percentage with depression | ||||||
| 1% change | 0.87 | 0.67 to 1.13 | > 0.200 | |||
| Percentage with asthma | ||||||
| 1% change | 0.62 | 0.38 to 1.00 | 0.051 | NS | ||
| log(dispensing volume) | ||||||
| 1-unit change | 2.94 | 1.24 to 6.95 | 0.014 | NS | ||
| Type of pharmacy | ||||||
| Independent | Reference | < 0.001 | ||||
| Small/medium-sized multiple | 2.60 | 1.37 to 4.94 | ||||
| Large multiple/supermarket | 3.18 | 1.81 to 5.61 | ||||
| Patient satisfaction scale | Univariable models | Multivariable models | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Geographical location | ||||||
| City centre/large town | 0.1469 | –0.0954 to 0.3892 | ||||
| Small town | Referencea | 0.031 | NSb | |||
| Suburb | 0.0414 | –0.1218 to 0.2046 | ||||
| Village/rural | –0.1265 | –0.2826 to 0.0295 | ||||
| HLP | ||||||
| No | Reference | > 0.200c | ||||
| Yes | 0.0798 | –0.0823 to 0.2449 | ||||
| Pharmacy contract held | ||||||
| Standard 40 hours | Reference | < 0.001 | 0.001 | |||
| 100 hours | –0.1376 | –0.2360 to –0.0392 | –0.0052 | –0.1925 to 0.1821 | ||
| Other | 0.2637 | 0.1734 to 0.3539 | 0.1771 | 0.0867 to 0.2675 | ||
| Weekly opening hours | ||||||
| 10-hour change | 0.0128 | –0.0398 to 0.0655 | > 0.200 | |||
| Staff working on typical dayc | ||||||
| 1-person change | 0.0139 | –0.0028 to 0.0305 | 0.100 | NS | ||
| Pharmacists working on typical day | ||||||
| 1 | Reference | > 0.200 | ||||
| ≥ 2 | 0.1344 | –0.0856 to 0.3543 | ||||
| Registered pharmacy technician | ||||||
| No | Reference | 0.007 | Reference | 0.036 | ||
| Yes | 0.1777 | 0.0510 to 0.3043 | 0.0998 | 0.0070 to 0.1926 | ||
| ACT | ||||||
| No | Reference | > 0.200 | ||||
| Yes | –0.0063 | –0.1806 to 0.1680 | ||||
| Use of locums | ||||||
| Not regularly | Reference | > 0.200 | ||||
| Regularly | 0.0290 | –0.1167 to 0.1747 | ||||
| Pharmacy manager a pharmacist? | ||||||
| No | Reference | > 0.200 | ||||
| Yes | –0.0801 | –0.2225 to 0.0623 | ||||
| Work pattern of main pharmacist | ||||||
| Standard hours (8 a.m.–6 p.m.) | Reference | > 0.200 | ||||
| Non-standard | 0.0424 | –0.1108 to 0.1955 | ||||
| Average daily working hours of main pharmacist | ||||||
| 1-hour change | –0.0509 | –0.1315 to 0.0296 | > 0.200 | |||
| Organisational culture (PSO) | ||||||
| 1-unit change | 0.0834 | 0.0283 to 0.1385 | 0.004 | NS | ||
| Patient safety (PSCQ) | ||||||
| Organisational learning | 0.0146 | 0.0022 to 0.0271 | 0.022 | NS | ||
| Blame culture | –0.0049 | –0.0251 to 0.0154 | > 0.200 | |||
| Working conditions | 0.0032 | –0.0223 to 0.0286 | > 0.200 | |||
| Safety focus | 0.0071 | –0.0431 to 0.0574 | > 0.200 | |||
| Relationship with nearest GP surgery | ||||||
| Very good | Reference | > 0.200 | ||||
| Good | 0.1084 | –0.0400 to 0.2568 | ||||
| Poor/none/no GP identified | 0.0936 | –0.1786 to 0.3659 | ||||
| IMD score | ||||||
| 10-unit change | 0.0308 | –0.0020 to 0.0636 | 0.065 | NS | ||
| Mean age (years) | ||||||
| 1-year change | –0.0058 | –0.0205 to 0.0088 | > 0.200 | |||
| Percentage with very bad health | ||||||
| 1% change | 0.0345 | –0.0742 to 0.1431 | > 0.200 | |||
| Percentage with CHDd | ||||||
| 1% change | 0.1181 | 0.0154 to 0.2208 | 0.025 | NS | ||
| Percentage with MH conditiond | ||||||
| 1% change | 0.4335 | 0.0847 to 0.7823 | 0.016 | NS | ||
| Percentage with depressiond | ||||||
| 1% change | 0.0396 | –0.0057 to 0.0849 | 0.085 | NS | ||
| Percentage with asthmad | ||||||
| 1% change | 0.0606 | –0.0983 to 0.2195 | > 0.200 | |||
| Why did you choose this pharmacy on this occasion? (Number of selected categories) | ||||||
| 1 | Reference | < 0.001 | Reference | < 0.001 | ||
| 2 | 0.2990 | 0.1833 to 0.4147 | 0.2235 | 0.1049 to 0.3421 | ||
| 3 | 0.6412 | 0.5033 to 0.7791 | 0.3943 | 0.2644 to 0.5242 | ||
| How many medicines are you currently being prescribed? | ||||||
| 1 | Reference | > 0.200 | ||||
| 2–3 | –0.0098 | –0.2854 to 0.2659 | ||||
| 4–10 | 0.0467 | –0.2174 to 0.3107 | ||||
| > 10 | 0.1930 | –0.0508 to 0.4367 | ||||
| Received medicine(s) for first time? | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 0.0222 | –0.1225 to 0.1670 | ||||
| Who did you receive information/advice from? | ||||||
| Do not know/NA | Reference | < 0.001 | Reference | < 0.001 | ||
| Pharmacist only | 0.4039 | 0.3053 to 0.5025 | 0.2141 | 0.1143 to 0.3139 | ||
| Other staff combination | 0.4648 | 0.2962 to 0.6334 | 0.3376 | 0.1890 to 0.4862 | ||
| Do you usually receive information/advice from the same person? | ||||||
| Do not know/NA | –0.0179 | –0.1463 to 0.1105 | –0.0492 | –0.1463 to 0.0479 | ||
| No | Reference | < 0.001 | Reference | < 0.001 | ||
| Yes | 0.4063 | 0.3105 to 0.5022 | 0.2593 | 0.1251 to 0.3935 | ||
| Overuse of medication (BMQ) | ||||||
| 1-unit change | –0.0352 | –0.0538 to –0.0166 | < 0.001 | –0.0293 | –0.0494 to –0.0092 | 0.005 |
| Patient age (years) | ||||||
| Linear component | 0.0013 | –0.0036 to 0.0062 | > 0.200 | |||
| Quadratic component | 0.0001 | –0.0001 to 0.0002 | ||||
| Gender | ||||||
| Female | 0.0791 | –0.0533 to 0.2116 | ||||
| Male | Reference | > 0.200 | ||||
| Number of long-term conditions | ||||||
| 0 | Reference | 0.002 | NS | |||
| 1 | –0.0304 | –0.3103 to 0.2495 | ||||
| 2 | 0.0247 | –0.3065 to 0.3559 | ||||
| 3 | 0.0635 | –0.2110 to 0.3381 | ||||
| 4 | 0.1831 | –0.0158 to 0.3820 | ||||
| ≥ 5 | 0.2148 | –0.0006 to 0.4302 | ||||
| log(dispensing volume) | ||||||
| 1-unit change | 0.1540 | –0.2275 to 0.5355 | > 0.200 | |||
| Volume of MURs | ||||||
| ≤ 12 | –0.2970 | –0.4061 to –0.1878 | –0.2545 | –0.3631 to –0.1448 | ||
| 13–200 | 0.1604 | –0.0235 to 0.3443 | –0.0007 | –0.1191 to 0.1177 | ||
| 201–365 | 0.0669 | –0.0697 to 0.2036 | –0.0270 | –0.1087 to 0.0548 | ||
| > 365 | Reference | < 0.001 | Reference | < 0.001 | ||
| Type of pharmacy | ||||||
| Independent | Reference | 0.314 | ||||
| Small/medium-sized multiple | 0.0368 | –0.0230 to 0.0966 | ||||
| Large multiple/supermarket | 0.0769 | –0.0292 to 0.1831 | ||||
| SIMS | Univariable models | Multivariable models | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Geographical location | ||||||
| City centre/large town | 0.95 | 0.55 to 1.66 | ||||
| Small town | Referencea | > 0.200b | ||||
| Suburb | 0.81 | 0.47 to 1.37 | ||||
| Village/rural | 0.91 | 0.57 to 1.46 | ||||
| HLP | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 0.99 | 0.67 to 1.47 | ||||
| Pharmacy contract held | ||||||
| Standard 40 hours | Reference | 0.004 | NSc | |||
| 100 hours | 1.53 | 1.16 to 2.00 | ||||
| Other | 1.14 | 0.86 to 1.51 | ||||
| Weekly opening hours | ||||||
| 10-hour change | 1.06 | 1.00 to 1.12 | 0.044 | NS | ||
| Staff working on typical dayc | ||||||
| 1-person change | 1.01 | 0.99 to 1.03 | 0.178 | NS | ||
| Pharmacists working on typical day | ||||||
| 1 | Reference | 0.186 | NS | |||
| ≥ 2 | 1.19 | 0.92 to 1.55 | ||||
| Registered pharmacy technician | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.28 | 0.87 to 1.86 | ||||
| ACT | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 0.95 | 0.63 to 1.41 | ||||
| Use of locums | ||||||
| Not regularly | Reference | > 0.200 | ||||
| Regularly | 1.09 | 0.75 to 1.59 | ||||
| Pharmacy manager a pharmacist? | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.51 | 0.77 to 2.96 | ||||
| Work pattern of main pharmacist | ||||||
| Standard hours (8 a.m.–6 p.m.) | Reference | > 0.200 | ||||
| Non-standard | 0.79 | 0.54 to 1.17 | ||||
| Average daily working hours of main pharmacist | ||||||
| 1-hour change | 1.07 | 0.84 to 1.37 | > 0.200 | |||
| Organisational culture (PSO) | ||||||
| 1-unit change | 1.07 | 0.84 to 1.38 | > 0.200 | |||
| Patient safety (PSCQ) | ||||||
| Organisational learning | 0.99 | 0.95 to 1.04 | > 0.200 | |||
| Blame culture | 0.96 | 0.90 to 1.03 | > 0.200 | |||
| Working conditions | 1.07 | 1.00 to 1.14 | 0.055 | NS | ||
| Safety focus | 1.07 | 0.95 to 1.21 | > 0.200 | |||
| Relationship with nearest GP surgery | ||||||
| Very good | Reference | > 0.200 | ||||
| Good | 1.02 | 0.68 to 1.54 | ||||
| Poor/none/no GP identified | 0.77 | 0.49 to 1.21 | ||||
| IMD score | ||||||
| 10-unit change | 0.99 | 0.91 to 1.09 | > 0.200 | |||
| Mean age (years) | ||||||
| 1-year change | 1.05 | 1.00 to 1.10 | 0.054 | 1.07 | 1.02 to 1.12 | 0.002 |
| Percentage with very bad health | ||||||
| 1% change | 1.07 | 0.89 to 1.29 | > 0.200 | |||
| Percentage with CHD | ||||||
| 1% change | 1.22 | 0.86 to 1.72 | > 0.200 | |||
| Percentage with MH condition | ||||||
| 1% change | 2.20 | 0.84 to 5.80 | 0.110 | NS | ||
| Percentage with depression | ||||||
| 1% change | 1.00 | 0.82 to 1.22 | > 0.200 | |||
| Percentage with asthma | ||||||
| 1% change | 0.78 | 0.53 to 1.14 | > 0.200 | |||
| Why did you choose this pharmacy on this occasion? (Number of selected categories) | ||||||
| 1 | Reference | < 0.001 | NS | |||
| 2 | 1.77 | 1.23 to 2.55 | ||||
| 3 | 2.42 | 1.44 to 4.05 | ||||
| How many medicines are you currently being prescribed? | ||||||
| 1 | Reference | > 0.200 | ||||
| 2–3 | 1.10 | 0.68 to 1.77 | ||||
| 4–10 | 0.88 | 0.46 to 1.68 | ||||
| > 10 | 1.00 | 0.49 to 2.04 | ||||
| Received medicine(s) for first time? | ||||||
| No | Reference | 0.002 | NS | |||
| Yes | 0.53 | 0.35 to 0.80 | ||||
| Who did you receive information/advice from? | ||||||
| Do not know/NA | Reference | > 0.200 | ||||
| Pharmacist only | 1.17 | 0.75 to 1.82 | ||||
| Other staff combination | 1.33 | 0.83 to 2.13 | ||||
| Do you usually receive information/advice from the same person? | ||||||
| Do not know/NA | 1.90 | 1.23 to 2.94 | 1.72 | 0.98 to 3.01 | ||
| No | Reference | < 0.001 | Reference | 0.001 | ||
| Yes | 1.82 | 1.37 to 2.41 | 1.96 | 1.36 to 2.82 | ||
| Overuse of medication (BMQ) | ||||||
| 1-unit change | 0.91 | 0.87 to 0.95 | < 0.001 | 0.92 | 0.88 to 0.96 | < 0.001 |
| Patient age (years) | ||||||
| Linear component | 1.02 | 1.01 to 1.03 | 0.011 | 1.02 | 1.01 to 1.03 | 0.002 |
| Quadratic component | 1.00 | 1.00 to 1.00 | 1.00 | 1.00 to 1.00 | ||
| Gender | ||||||
| Female | 1.08 | 0.80 to 1.45 | ||||
| Male | Reference | > 0.200 | ||||
| Number of long-term conditions | ||||||
| 0 | Reference | > 0.200 | ||||
| 1 | 0.92 | 0.41 to 2.10 | ||||
| 2 | 0.92 | 0.37 to 2.31 | ||||
| 3 | 1.60 | 0.85 to 3.00 | ||||
| 4 | 1.14 | 0.53 to 2.43 | ||||
| ≥ 5 | 1.08 | 0.44 to 2.68 | ||||
| log(dispensing volume) | ||||||
| 1-unit change | 0.97 | 0.52 to 1.81 | > 0.200 | |||
| Volume of MURs | ||||||
| ≤ 12 | 0.47 | 0.32 to 0.70 | 0.15 | 0.08 to 0.29 | ||
| 13–200 | 1.14 | 0.71 to 1.85 | 0.79 | 0.49 to 1.27 | ||
| 201–365 | 0.92 | 0.58 to 1.44 | 0.72 | 0.49 to 1.07 | ||
| > 365 | Reference | < 0.001 | Reference | < 0.001 | ||
| Type of pharmacy | ||||||
| Independent | Reference | 0.008 | ||||
| Small/medium-sized multiple | 1.88 | 1.13 to 3.11 | ||||
| Large multiple/supermarket | 1.15 | 0.68 to 1.94 | ||||
| MARS | Univariable models | Multivariable models | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Geographical location | ||||||
| City centre/large town | 0.94 | 0.51 to 1.71 | ||||
| Small town | Referencea | > 0.200b | ||||
| Suburb | 0.59 | 0.32 to 1.06 | ||||
| Village/rural | 1.06 | 0.64 to 1.74 | ||||
| HLP | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 0.99 | 0.67 to 1.47 | ||||
| Pharmacy contract held | ||||||
| Standard 40 hours | Reference | > 0.200 | ||||
| 100 hours | 1.36 | 0.41 to 4.51 | ||||
| Other | 0.89 | 0.68 to 1.16 | ||||
| Weekly opening hours | ||||||
| 10-hour change | 1.01 | 0.88 to 1.15 | > 0.200 | |||
| Staff working on typical day | ||||||
| 1-person change | 1.00 | 0.97 to 1.04 | > 0.200 | |||
| Pharmacists working on typical day | ||||||
| 1 | Reference | 0.097 | NSc | |||
| ≥ 2 | 0.76 | 0.55 to 1.05 | ||||
| Registered pharmacy technician | ||||||
| No | Reference | 0.163 | NS | |||
| Yes | 0.71 | 0.44 to 1.15 | ||||
| ACT | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 1.26 | 0.79 to 2.01 | ||||
| Use of locums | ||||||
| Not regularly | Reference | 0.016 | Reference | 0.008 | ||
| Regularly | 0.51 | 0.30 to 0.88 | 0.50 | 0.30 to 0.84 | ||
| Pharmacy manager a pharmacist? | ||||||
| No | Reference | > 0.200 | ||||
| Yes | 0.85 | 0.40 to 1.79 | ||||
| Work pattern of main pharmacist | ||||||
| Standard hours (8 a.m.–6 p.m.) | Reference | > 0.200 | ||||
| Non-standard | 1.34 | 0.82 to 2.18 | ||||
| Average daily working hours of main pharmacist | ||||||
| 1-hour change | 1.13 | 0.88 to 1.45 | > 0.200 | |||
| Organisational culture (PSO) | ||||||
| 1-unit change | 1.06 | 0.89 to 1.27 | > 0.200 | |||
| Patient safety (PSCQ) | ||||||
| Organisational learning | 1.04 | 1.00 to 1.09 | 0.053 | NS | ||
| Blame culture | 1.04 | 0.99 to 1.10 | 0.119 | NS | ||
| Working conditions | 0.95 | 0.86 to 1.06 | > 0.200 | |||
| Safety focus | 1.09 | 0.98 to 1.21 | 0.111 | NS | ||
| Relationship with nearest GP surgery | ||||||
| Very good | Reference | > 0.200 | ||||
| Good | 0.88 | 0.47 to 1.65 | ||||
| Poor/none/no GP identified | 0.74 | 0.34 to 1.58 | ||||
| IMD score | ||||||
| 10-unit change | 1.05 | 0.94 to 1.17 | > 0.200 | |||
| Mean age (years) | ||||||
| 1-year change | 0.96 | 0.93 to 1.00 | 0.045 | NS | ||
| Percentage with very bad health | ||||||
| 1% change | 1.21 | 0.81 to 1.79 | > 0.200 | |||
| Percentage with CHD | ||||||
| 1% change | 1.07 | 0.62 to 1.84 | > 0.200 | |||
| Percentage with MH condition | ||||||
| 1% change | 0.38 | 0.14 to 1.08 | 0.068 | NS | ||
| Percentage with depression | ||||||
| 1% change | 0.83 | 0.61 to 1.14 | > 0.200 | |||
| Percentage with asthma | ||||||
| 1% change | 0.89 | 0.46 to 1.75 | > 0.200 | |||
| Why did you choose this pharmacy on this occasion? (Number of selected categories) | ||||||
| 1 | Reference | 0.108 | NS | |||
| 2 | 1.11 | 0.69 to 1.80 | ||||
| 3 | 2.62 | 0.99 to 6.94 | ||||
| How many medicines are you currently being prescribed? | ||||||
| 1 | Reference | > 0.200 | ||||
| 2–3 | 1.74 | 0.87 to 3.46 | ||||
| 4–10 | 1.33 | 0.68 to 2.58 | ||||
| > 10 | 1.22 | 0.40 to 3.69 | ||||
| Received medicine(s) for first time? | ||||||
| No | Reference | 0.014 | NS | |||
| Yes | 0.45 | 0.23 to 0.85 | ||||
| Who did you receive information/advice from? | ||||||
| Do not know/NA | Reference | 0.005 | NS | |||
| Pharmacist only | 0.67 | 0.36 to 1.26 | ||||
| Other staff combination | 0.26 | 0.12 to 0.59 | ||||
| Do you usually receive information/advice from the same person? | ||||||
| Do not know/NA | 2.29 | 1.10 to 4.77 | 2.50 | 1.20 to 5.23 | ||
| No | Reference | 0.080 | Reference | 0.044 | ||
| Yes | 1.65 | 0.89 to 3.04 | 1.45 | 0.73 to 2.89 | ||
| Overuse of medication (BMQ) | ||||||
| 1-unit change | 0.87 | 0.81 to 0.94 | < 0.001 | 0.88 | 0.81 to 0.95 | 0.002 |
| Patient age (years) | ||||||
| Linear component | 1.04 | 1.02 to 1.07 | < 0.001 | 1.04 | 1.01 to 1.07 | < 0.001 |
| Quadratic component | 1.00 | 1.00 to 1.00 | 1.00 | 1.00 to 1.00 | ||
| Gender | ||||||
| Female | 1.09 | 0.72 to 1.63 | ||||
| Male | Reference | > 0.200 | ||||
| Number of long-term conditions | ||||||
| 0 | Reference | 0.002 | NS | |||
| 1 | 0.51 | 0.18 to 1.51 | ||||
| 2 | 0.54 | 0.18 to 1.55 | ||||
| 3 | 0.90 | 0.41 to 1.96 | ||||
| 4 | 0.45 | 0.13 to 1.59 | ||||
| ≥ 5 | 0.81 | 0.28 to 2.34 | ||||
| log(dispensing volume) | ||||||
| 1-unit change | 1.34 | 0.56 to 3.23 | > 0.200 | |||
| Volume of MURs | ||||||
| ≤ 12 | 1.46 | 0.88 to 2.41 | ||||
| 13–200 | 1.21 | 0.66 to 2.25 | ||||
| 201–365 | 1.06 | 0.55 to 2.06 | ||||
| > 365 | Reference | 0.046 | NS | |||
| SIMS | ||||||
| Least satisfied | 0.43 | 0.23 to 0.78 | ||||
| 0.81 | 0.37 to 1.78 | |||||
| 0.39 | 0.17 to 0.88 | |||||
| Most satisfied | Reference | 0.005 | NS | |||
| Type of pharmacy | ||||||
| Independent | Reference | 0.113 | ||||
| Small/medium-sized multiple | 0.87 | 0.48 to 1.59 | ||||
| Large multiple/supermarket | 1.58 | 0.97 to 2.57 | ||||
| Patient safety climate (PSCQ) | Univariable model | Multivariable model, coefficient (95% CI) | ||||
|---|---|---|---|---|---|---|
| Composite hypothesis test | Organisational learning | Blame culture | Working conditions | Safety focus | Composite hypothesis test | |
| Job title | ||||||
| Pharmacist | F4,246 = 3.25; p = 0.013 | Referencea | F4,225 = 3.65; p = 0.007 | |||
| Owner/manager | 1.74 (–0.51 to 3.98) | –0.90 (–1.81 to 0.00) | 1.73 (0.80 to 2.65) | 0.64 (0.01 to 1.28) | ||
| Geographical location | ||||||
| City centre | F16,246 = 1.32; p = 0.186 | NSb | ||||
| Large town | ||||||
| Small town | ||||||
| Suburb | ||||||
| Village/rural | ||||||
| Pharmacy open for ≥ 3 years | ||||||
| No | F4,247 = 0.85; p > 0.200c | |||||
| Yes | ||||||
| HLP | ||||||
| No | F4,242 = 3.58; p = 0.007 | NS | ||||
| Yes | ||||||
| Pharmacy contract held | ||||||
| Standard 40 hours | F8,245 = 1.33; p > 0.200 | |||||
| 100 hours | ||||||
| Other | ||||||
| Weekly opening hours | ||||||
| 10-hour change | F4,247 = 0.95; p > 0.200 | |||||
| Staff working on typical day | ||||||
| 1-person change | F4,242 = 0.18; p > 0.200 | |||||
| Pharmacists working on typical day | ||||||
| 1 | F4,245 = 1.10; p > 0.200 | |||||
| ≥ 2 | ||||||
| Registered pharmacy technician | ||||||
| No | F4,245 = 0.25; p > 0.200 | |||||
| Yes | ||||||
| ACT | ||||||
| No | F4,248 = 3.66; p = 0.006 | Reference | F4,225 = 4.55; p = 0.002 | |||
| Yes | –0.87 (–2.72 to 0.98) | 0.38 (–0.36 to 1.13) | –0.97 (–1.73 to –0.20) | –1.01 (–1.53 to –0.49) | ||
| Use of locums | ||||||
| Not regularly | F4,249 = 0.58; p > 0.200 | |||||
| Regularly | ||||||
| Pharmacy manager a pharmacist? | ||||||
| No | F4,246 = 1.55; p = 0.188 | NS | ||||
| Yes | ||||||
| Work pattern of main pharmacist | ||||||
| Standard hours (8 a.m. – 6 p.m.) | F4,249 = 3.74; p = 0.006 | Reference | F4,225 = 2.61; p = 0.037 | |||
| Non-standard | 1.03 (–0.77 to 2.83) | –0.70 (–1.43 to 0.03) | –0.13 (–0.87 to 0.61) | 0.69 (0.18 to 1.20) | ||
| Average daily working hours of main pharmacist | ||||||
| 1-hour change | F4,247 = 4.39; p = 0.002 | –0.37 (–1.19 to 0.46) | 0.03 (–0.30 to 0.37) | –0.51 (–0.85 to –0.17) | –0.17 (–0.41 to 0.06) | F4,225 = 2.68; p = 0.032 |
| Organisational culture (PSO) | ||||||
| 1-unit change | F4,246 = 18.74; p < 0.001 | 2.11 (1.49 to 2.73) | –0.40 (–0.65 to –0.15) | 0.46 (0.21 to 0.72) | 0.39 (0.21 to 0.56) | F4,225 = 12.44; p < 0.001 |
| Relationship with nearest GP surgery | ||||||
| Very good | F12,247 = 2.46; p = 0.005 | Reference | F12,225 = 2.44; p = 0.005 | |||
| Good | –1.43 (–3.44 to 0.60) | 1.02 (0.20 to 1.84) | –0.23 (–1.06 to 0.61) | –0.32 (–0.89 to 0.26) | ||
| Satisfactory/poor/none | –3.09 (–5.38 to –0.80) | 1.18 (0.25 to 2.11) | –0.60 (–1.54 to 0.35) | –1.08 (–1.73 to –0.43) | ||
| No GP surgery identified | –6.31 (–10.6 to –2.07) | 3.03 (1.32 to 4.75) | –1.11 (–2.85 to 0.63) | –0.60 (–1.80 to 0.61) | ||
| IMD score | ||||||
| 10-unit change | F4,249 = 2.50; p = 0.043 | NS | ||||
| Mean age (years) | ||||||
| 1-year change | F4,239 = 1.26; p > 0.200 | |||||
| Percentage aged 0–4 | ||||||
| 1% change | F4,239 = 0.49; p > 0.200 | |||||
| Percentage aged ≥ 75 | ||||||
| 1% change | F4,239 = 0.47; p > 0.200 | |||||
| Percentage with very bad healthd | ||||||
| 1% change | F4,239 = 1.20; p > 0.200 | |||||
| Percentage with CHDe | ||||||
| 1% change | F4,249 = 2.00; p = 0.096 | NS | ||||
| Percentage with MH conditione | ||||||
| 1% change | F4,249 = 1.90; p = 0.110 | NS | ||||
| Percentage with depressione | ||||||
| 1% change | F4,249 = 0.72; p > 0.200 | |||||
| Percentage with asthmae | ||||||
| 1% change | F4,249 = 2.00; p = 0.095 | NS | ||||
| log(dispensing volume) | ||||||
| 1-unit change | F4,239 = 0.77; p > 0.200 | |||||
| MUR provision | ||||||
| F12,237 = 1.50; p = 0.126 | NS | |||||
| NMS interventions | ||||||
| F8,235 = 1.15; p > 0.200 | ||||||
| Type of pharmacy | ||||||
| Independent | Reference | F8,225 = 4.36; p < 0.001 | ||||
| Small/medium-sized multiple | 1.99 (–0.56 to 4.54) | –0.56 (–1.59 to 0.47) | 0.39 (–0.66 to 1.44) | 0.17 (–0.55 to 0.89) | ||
| Large multiple/supermarket | 2.07 (0.18 to 3.95) | 0.27 (–0.50 to 1.03) | –1.64 (–2.42 to –0.87) | 0.01 (–0.53 to 0.54) | ||
List of abbreviations
- ACT
- accuracy-checking technician
- BMQ
- Beliefs about Medicines Questionnaire
- BSA
- Business Services Authority
- CCA
- Company Chemists’ Association
- CCG
- clinical commissioning group
- CHD
- coronary heart disease
- CRN
- clinical research network
- EPS
- Electronic Prescriptions Service
- ETP
- electronic transfer of prescriptions
- GP
- general practitioner
- HLP
- healthy living pharmacy
- ID
- identification
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- IT
- information technology
- LPC
- local pharmaceutical committee
- MARS
- Medication Adherence Report Scale
- MDS
- monitored dosage system
- MH
- mental health
- MUR
- medicines use review
- NIHR
- National Institute for Health Research
- NMS
- new medicines service
- PCC
- Primary Care Commissioning
- PCT
- primary care trust
- PPI
- patient and public involvement
- PSCQ
- Pharmacy Safety Climate Questionnaire
- PSNC
- Pharmaceutical Services Negotiating Committee
- PSO
- Pharmacy Service Orientation
- QOF
- Quality and Outcomes Framework
- RPS
- Royal Pharmaceutical Society
- SD
- standard deviation
- SIMS
- Satisfaction with Information about Medicines Scale