Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1021/02. The contractual start date was in January 2013. The final report began editorial review in July 2016 and was accepted for publication in March 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Claire Goodman is a Senior Investigator at the National Institute for Health Research.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Goodman et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2017 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Introduction
Older people living in care homes are some of the oldest and frailest in society. They have entered a care home because they can no longer live in their own homes. 1 Care homes provide 24-hour personal care, and some care homes provide nursing care; however, residents still rely on primary health-care services for access to medical care and referral to specialist services.
The relationship between the NHS and care homes is a symbiotic one. 2–5 Care homes, as independent providers, are the main providers of long-term care for older people and, increasingly, respite and end-of-life care. The majority of care home residents have cognitive impairment, multiple morbidities and complex care needs defined by high functional dependency and unpredictable clinical trajectories. 6–8 In this context, good health outcomes depend on effective day-to-day social care and vice versa.
Despite this, how the NHS works with care homes is variable and often inequitable. 9,10 A number of different models of care provision have developed to address the identified inequity. This study considers what elements or characteristics of these different services support residents’ health and maintain efficient and effective working between NHS services and care homes.
Care homes
Approximately 433,000 older or physically disabled people live in care homes in the UK, with 90% of residential and nursing care services now delivered by independent providers. A care home can offer personal care and 24-hour support (previously called ‘residential homes’), on-site nursing in addition to this (previously called ‘nursing homes’) or both types of care (sometimes referred to as ‘dual registered homes’). Care home residents account for 4% of the population aged 65 years or older. 11,12 There are over three times as many care home beds as there are acute hospital beds in the UK, and approximately 10% of care home residents receive funding from the NHS. For the majority of residents their care is either self-funded, paid for from the state social care budget or via a mix of state social care funding with top-up from residents or their families. 12,13 Care homes are heterogeneous in terms of how these different funding sources make up their income and in how they structure themselves as businesses. A report described the sector as a ‘highly polarised marketplace’. 12 Providers that focus on private payers are relatively financially secure, while those reliant on public funding are vulnerable to the government’s austerity measures, financial losses and threat of closure. 12
The Burstow Commission on Residential Care14 found that only one in four people would consider moving into a care home if they became frailer in later life, while 43% said that they would definitely not move. Care homes were represented by many as an accommodation of last resort. The Commission argued that negative media coverage of care homes, despite many examples of innovative high-quality care for people with complex needs and dementia, has an impact on how staff and managers feel about their jobs and how their work is valued by wider society.
Most care home residents are female, over 85 years old and in the last years of life. The majority of care home residents have dementia, are in receipt of seven or more medications and a significant proportion live with depression, mobility problems, incontinence and pain. 6,9,15–18 They are a population that needs access to health care and ongoing review. The common perception that care homes are a ‘problem’ to the NHS is open to challenge. In addition to being the main providers of long-term care for older people, care homes provide multiple services to the NHS, including respite care, intermediate care and re-enablement services. Admission to emergency departments and acute hospitals from care homes may, contrary to the public narrative, be as much a consequence of how primary and emergency health-care services respond to calls for help from the care home sector as they are a reflection of care decisions by care home staff. 19 Residents’ close proximity to the end of life, however, provides an opportunity to establish advanced care plans enabling care homes to play an active role in responding to health concerns in situ, avoiding emergency hospital admissions as a consequence. 20
Health-care provision to care homes
There is a lack of shared understanding about what represents an ideal package of care that should be provided by the NHS to care homes. 21–24 Aspects of care related to the management of health problems are often undertaken by care home staff, whether or not they are qualified nurses. 25 These include non-pharmacological management of behavioural and psychological symptoms of dementia, monitoring the impact of pharmacological and non-pharmacological therapies, doing routine dressings and administering complex drug regimens. These arrangements are usually informally negotiated and vary between different homes and parts of the country. As a consequence, the extent to which the opportunity and financial costs of such health-care interventions are borne by the care home sector vary between regions.
Effective working between the health and residential care sectors is fundamental to residents’ quality of life and may influence how often residents are admitted to hospital and how long they stay there once admitted. But models of service delivery to care homes are many and ill defined. 26,27 Services at the interface between care homes and the NHS often have differing goals and funding sources, and operate in diverse ways. Although most regard integrated working as a vital objective, definitions of integrated care differ and few interventions to improve health-care delivery have been developed in collaboration with care home staff, residents and their families. Primary care services are frequently delivered from a distance and are reliant on how care home staff interpret residents’ health status. Inherent tensions can develop when NHS services favour models of care that focus on diagnosis, treatment and episodic involvement, while care home providers prioritise ongoing support and relationships that foster continuous review of care. 19 How to establish effective integrated working, and the models of service delivery that could facilitate this, remain unclear.
Rationale for the research
We have described a heterogeneous care home market and a range of context-sensitive variables that shape how services are provided. Cumulatively, these make it unlikely that a single model of health service delivery can promote effective working for all care homes and at all times. If there are generalisable patterns that underpin effective models of care, it is more likely that these will be at the level of recurrent features or explanatory mechanisms already manifested within multiple service models and potentially applicable across multiple models in the future. As Pawson et al. 28 have noted, much that is effective in health-care delivery is submerged, routine and taken for granted. Identifying these features and making them explicit is key to delivering effective care.
Aims and objectives
This study set out to identify, map and test the features or explanatory mechanisms of existing approaches to health-care provision to care homes in relation to five key outcomes: (1) medication use and review; (2) use of out-of-hours services; (3) hospital admissions, including emergency department attendances and length of hospital stay; (4) resource use; and (5) user satisfaction.
The overall aim of this study was to use a theory-driven realist evaluation approach29 to identify ways in which the delivery of existing NHS services to care homes may be optimised for the ongoing benefit of residents, relatives and staff, and the best use of NHS resources. It addressed the following research questions.
-
What is the range of health service delivery models designed to maintain care home residents outside hospital?
-
What features (in realist evaluation terms: mechanisms) of these delivery models are the ‘active ingredients’ associated with positive outcomes for care home residents?
-
How are these features/mechanisms associated with key outcomes, including medication use; use of out-of-hours services; resident, carer and staff satisfaction; unplanned hospital admissions (including A&E); and length of hospital stay?
-
How are these features/mechanisms associated with costs to the NHS and from a societal perspective?
-
What configuration of these features/mechanisms would be recommended to promote continuity of care at a reasonable cost for older people resident in care homes?
Structure of the report
Chapter 1 describes the background and the rationale for the study. Chapter 2 describes the research approach and methods, providing detail about the study design, data collection and analysis. Chapter 3 presents the findings of the review of surveys of health-care provision to care homes and the review of reviews. This is followed by the realist synthesis of health-care provision to care homes in Chapter 4. Chapter 5 introduces phase 2, with detail about the case study sites’ recruitment, participant characteristics and the organisation of health care in each site. Chapter 6 summarises the case study findings on care home residents’ service use and related costs, medication use and staff satisfaction. Chapter 7 revisits the findings of phase 1 and, based on phase 2 findings, presents context–mechanism–outcomes (CMOs), which capture how health-care services work (or not) with care homes. Chapter 8 discusses the findings and their implications for commissioning and the organisation and provision of NHS services to care homes.
Chapter 2 Research approach and methods
This study built on earlier descriptive work that had mapped how the NHS works with care homes without on-site nursing provision. 2 This chapter provides a brief overview of how the study was organised and managed. It also gives the rationale for using realist-driven approaches to evidence synthesis and evaluation in order to answer the research questions and to move beyond descriptive accounts of the NHS working with care homes. It describes the two phases of the study, data collection and analysis and, finally, notes the changes that were made to the originally funded protocol. This chapter is complemented by two published protocols on phases 1 and 2. 1,30
Study organisation and management
The study was overseen by a management group made up of the researchers and the study research team, which met four times a year, and a Study Steering Committee (SSC) that met twice a year. The overall role of the SSC was to ensure that the study was conducted in line with the protocol, and that the design, execution and findings were valid and appropriate for care home residents, relatives and the organisations involved in their care. A list of members and their relevant expertise is provided in the appendices (see Appendix 1).
Specifically, the study steering group were asked to do the following:
-
provide expert advice and guidance on all aspects of the study; individual members provided expertise for the different study phases
-
ensure that the project was running according to the time schedule
-
address any identified risks within the study and ensure that the appropriate procedures were in place to militate against these
-
contribute to a discussion of any issues arising from either the conduct or analysis of the study
-
debate the emergent theoretical propositions from phase 1 of what supported health-care working with care homes and the emergent findings from phase 2
-
read and comment on any reports and other relevant study outcomes
-
act as a link between the project and other related research studies, NHS and charitable organisations interested in the way that care homes work together with the NHS.
Public involvement in research
Public involvement in research (PIR) was integrated into the study from project design and management to dissemination. This was achieved through PIR review of the study design and research process, PIR support with resident recruitment and feedback on emergent findings presented at the SSC meetings and the analysis workshop.
Public involvement in research members with direct experience of visiting close relatives and friends over long periods of time (years) in care homes were recruited through two established university patient and public involvement groups. One member had supported recruitment of care home residents in a previous study. Her role had been to spend time talking with those residents who wanted more time to talk about their involvement in the study.
User involvement in the study design and research process
Members of the PIR group at the University of Hertfordshire (John Wilmott and Marion Cowe) and the University of Nottingham (Kate Sartain and Michael Osborn) were involved in the development of the study proposal and were also asked to review resident information booklets, summary and consent forms. PIR members also attended the SSC meetings.
Users as participants in recruitment with care home residents
Public involvement in research members who had an honorary contract with the university were involved in the support of resident recruitment in the care homes. PIR members were also involved in the development of a study information video for care home residents.
Analysis workshop
A member of the PIR group (Kate Sartain) actively participated in a 2-day analysis workshop together with the study management group where the emergent findings from the study sites were discussed.
Realist methods
Realist methods are based on a theory-driven approach to evidence review and evaluation that argues that reality is ‘objective’ and knowable but interpreted through cognition and senses. To explain why interventions work, these methods seek to identify the underlying mechanisms that can elucidate how different outcomes are obtained and how contexts influenced this process. 28,29,31
We defined health-care provision to care homes as a series of complex social processes involving multiple contributors over extended periods of time, where uptake and use of resources can vary widely depending on residents’ needs, organisational structures and local resources. Thinking of service delivery to care homes in this way enabled us to consider the heterogeneity of approaches used and consider the multiplicity of conditions in which they are enacted to provide an explanatory account of how one approach may work, when, for whom and why. It allowed us to go beyond descriptive accounts of the organisation of care, and the perceived barriers to and enablers of this, to provide plausible, evidenced explanations of observed outcomes and the mechanisms associated with these, while acknowledging and explaining the influence of context. We conceptualised different approaches to health-care provision to care homes as programmes that can be deconstructed to understand how key elements or factors in their working (mechanisms) may trigger a change or effect (outcome), and which contextual conditions or resources (context) are necessary to sustain changes. Box 1 describes how context (C), mechanism (M), outcomes (O) and programme theory as the analytical tools of realist approaches were operationalised for the purposes of this study.
Context can be broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism, that is, the ‘backdrop’ conditions (which may change over time). For example, education and qualifications of care home staff, history of working relationships between visiting HCPs and care home staff and residents’ functional abilities.
Mechanism (M)A mechanism is the generative force that leads to outcomes. Often denotes the reasoning (cognitive or emotional) of the various ‘actors’, that is, care home staff, residents, relatives and visiting HCPs. Identifying the mechanisms goes beyond describing ‘what happened’ to theorising ‘why it happened, for whom, and under what circumstances.’
Outcomes (O)Intervention outcomes, for example a reduction in episodes of unplanned hospital admissions, medication management, staff confidence and costs.
Programme theorySpecifies what mechanisms are associated with which outcomes and what features of the context will affect whether or not those mechanisms operate. The programme theory encapsulates ideas about what needs to be changed or improved in how NHS services work with care home staff, and what needs to be in place to achieve an improvement in residents’ health and organisations’ use of resources.
HCP, health-care professional.
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review — a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21–34. 32
Wong G, Greenhalgh T, Westhorp G, Pawson R. Realist methods in medical education research: what are they and what can they contribute? Med Educ 2012;46:89–96. 33
This realist evaluation included a realist synthesis as part of the process of developing and refining programme theory. Integrating different forms of knowledge (using both primary and secondary sources) to explain complex phenomena in this way is consistent with a realist understanding of research. It enables us to identify those contextual factors that are necessary across a range of interventions to trigger the desired mechanisms.
Method
Phase 1
This was designed to address questions 1 and 2 as outlined in Chapter 1, which were:
-
What is the range of health service delivery models designed to maintain care home residents outside hospital?
-
What features (in realist evaluation terms: mechanisms) of these delivery models are the ‘active ingredients’ associated with positive outcomes for care home residents?
Phase 1 completed a realist review of existing evidence to develop a theoretical understanding and working propositions of how different contexts and mechanisms influence how the NHS works with care homes, paying specific attention to five outcomes of interest that could then be refined and tested in the case studies that comprised phase 2.
The five outcomes of interest were identified by the research team as consistent with service priorities across the NHS, care home and local authority organisations. These were agreed through consultation with the SSC and the stakeholder organisations that they represented. These were as follows.
Admission to hospital, including emergency department attendances and length of hospital stay
The extent to which residents are enabled to receive care in situ in the care home can reflect both care home staff confidence and how they are able to access services, support and guidance from health-care services. Repeated admissions, particularly in the context of ambulatory care-sensitive conditions or towards the end of life where they might be regarded as inappropriate, can be avoided where proactive collaborative advanced clinical planning is embedded within systems of care. 19,20,34–36
Often the decision to admit an older person to hospital is appropriate and cannot be avoided. However, the length of hospital stay is influenced by how easy it is to discharge the older person to the care home, which in turn is influenced by the relationship between care homes and primary care services, and the relationship of both with secondary care. 37
Use of out-of-hours services
Use of out-of-hours services can be an indication of the level of anticipatory care, joint planning, day-to-day NHS support received and care home staff capacity, confidence and ability to deal with residents’ unexpected health-care needs. For care homes, the quality of advice and support they receive out of hours, often over the telephone, can influence decisions to support a person in the care home or call an ambulance. 38
Medication use and review
The majority of care home residents take seven or more medications. 1,17 Evidence suggests that residents are vulnerable to prescribing and administration errors and that review of medication, using agreed criteria,17 can improve the quality of prescribing and medication use. Regular review can also highlight other issues and act as a focus for making proactive decisions about care.
User satisfaction
Older people, including those with cognitive problems, can express what is important to them in their health care, their preferences for who else is involved in discussing health-care decisions and who should take responsibility for the day-to-day management of their health care. 39 Satisfaction with care in this setting needs to include the multiple perspectives of residents, family members and care home staff as recipients of health-care services. 40
The realist review took an iterative three-stage approach and was structured in line with Realist And MEta-narrative Evidence Syntheses: Evolving Standards (RAMESES) guidance on the organisation and reporting of realist syntheses. 31 First, scoping searches and stakeholder interviews were used to identify sources of policy, legislative and professional thinking that could help to explain how health-care services and care homes work with each other. Second, the findings were used to develop theoretical propositions that could be tested using the literature on health-care provision to care homes, in order to explain why an intervention may be effective in some situations and not others. Third, the findings were reviewed with our study steering group. We have published the phase 1 protocol. 30
Concept mining, scoping of the evidence and development of programme theories
To gain a preliminary understanding of what supported good health-care provision to care homes, we conducted a series of stakeholder interviews with key informants involved in the commissioning, provision and regulation of health care to care homes, as well as recipients of care (residents and relatives). This was followed by a review of surveys of health-care services provided to care homes, a review of reviews on care home interventions and a supplementary scoping literature review to begin to identify further the underlying assumptions and theories of what supported effective working in care homes.
Stakeholder interviews
The purpose of the interviews was to help inform and refine the focus of the evidence review, clarify terms, identify key headings or ‘theory areas’ and linked questions that should be asked in the development of data extraction forms in the evidence review. 41,42 A more detailed account of the method and findings is published elsewhere. 43
The interviews explored a number of areas of uncertainty. The priority that the NHS places on cost management, appropriate use of resources and service efficiency is well known. There is, however, less clarity about the level of evidence commissioners require in order to make judgements about services to care homes and how to measure effectiveness when working in and with care homes. It is also unclear how contexts of care (e.g. history of provision, size of care homes, leadership, care homes with on-site nursing and those without) influence demand on NHS services. Finally, it is unclear what care homes and their representatives, residents and relatives recognise as constituting effective health care.
For the purposes of this study, a stakeholder was defined as someone who had the relevant experience or knowledge to be able to express the view of the group or organisation that they represented. 44 Consequently, we selected individuals who either had responsibility for the commissioning, organisation or monitoring of NHS provision to care homes, or direct experience as care home residents. The interviews addressed current patterns of commissioning and provision, examples of success and failure, how continuity of care was achieved, processes that supported integrated working and the anticipated impact of policy change in rapidly changing health and social care economies.
Recruitment
To capture regional, historical and organisational differences, we identified a purposive sample of NHS and local authority commissioners, senior managers from care home organisations and the Care Quality Commission (CQC). Relevant organisations were approached and invited to nominate people we could approach to interview. We also interviewed a small sample of care home managers and residents who were invited to take part through My Home Life, an organisation that works with care homes to promote best practice. The extended time required to secure resident stakeholder interviews limited the number who participated and, following discussion with the SSC, we supplemented these interviews with a secondary data analysis on 34 resident interviews from an earlier study, looking specifically at how they described what constituted ‘good health care’. 2
Interviews
Interviews were conducted face to face unless a participant requested a telephone interview. Participants were asked to provide a stakeholder view, in other words to use their experience and expertise, for example, as a care home manager, to inform what a good service should look like, rather than to provide a solely personal account. To facilitate this, the interview prompts addressed current patterns of commissioning and provision. Prompts for residents focused on what they believed good health care to care homes should comprise to inform and test our understanding of the processes that characterise how health care is provided to care homes and how these work. Interviews asked about examples of success and failure, how continuity of care was achieved, what ‘good’ working between NHS services and care homes looked like, and the mechanisms of particular service models necessary to achieve the desired outcomes. All interviews were recorded and fully transcribed. To organise and structure the analysis, data were entered into NVivo version 11 (QSR International, Warrington, UK).
The secondary analysis of the resident interviews enabled us to consider what their descriptions revealed about being health-care recipients and what they identified as important.
The interview element of the study was reviewed and supported by the University of Hertfordshire Ethics Committee (reference number NMSCC/12/12/2/A).
Analysis
Data were initially mapped against the interview prompts. There were three stages to the analysis. First, there was a process of familiarisation, decontextualisation and segmenting of data into separate and defined categories that were close to how participants had described the issues. Second, there was a comparison within and between categories and identification of preoccupations, differences and themes. Third, there was identification of relationships and emergent hypotheses about how the favoured approaches worked, and what was necessary to support their implementation.
Scoping of the published evidence
To provide an overview of current provision of health care to care homes we reviewed published sources using a review of surveys of the range and type of services provided to care homes, a review of existing systematic reviews and a supplementary scoping review to ensure that the literature had been adequately summarised.
We had initially proposed to survey the care home field in the UK to understand the current range of provision to the sector. The review of surveys was suggested as an alternative approach by the SSC based on the assertion that the care home field had been subject to a number of large national surveys in the period immediately prior to our period of research but that there had been a systematic failure to collate these surveys or to consider how they informed each other to establish an overview of care provision in care homes. To be eligible for inclusion in the review of surveys, publications had to focus on health-care delivery to care homes in the UK and had to have been completed since 2008.
The review of existing systematic reviews was added to further enable us to capture a range of approaches to service provision for care homes that may not have been identified in the review of surveys. A review of reviews was chosen as a way of approaching the published literature based on the assumption that detailed summaries of the included studies would be an efficient way of identifying the bulk of potentially relevant studies. It allowed us to examine relevant studies in a consistent way. Literature published since 2006 was included. This was a pragmatic decision to capture literature that was likely to be relevant to current systems of health-care provision to care homes.
As a final step, a further scoping review was undertaken to ensure that no key literature considering models of health-care delivery to care homes had been overlooked in the review of surveys or review of reviews. Box 2 summarises the search terms, databases and e-networks used in phase 1 (i.e. the review of surveys, review of reviews and scoping of the literature). Realist review approaches are iterative, so these searches were refined, expanded and repeated as we tested emergent ideas about what supported health-care services to achieve the outcomes of interest. Database searches were supplemented by online searches conducted on the websites of prominent care home research groups, voluntary sector providers of care homes, other care home organisations and their representative and professional organisations. The websites of NHS strategic health authorities were searched to identify care home initiatives referred to in their annual reports (up to March 2013).
‘Care homes health care survey’, ‘residential care health care survey’, ‘nursing homes health care survey’, ‘older people health care homes survey’, ‘older people health residential care survey’, ‘older people health nursing homes survey’, ‘health service provision care homes survey’, ‘health service provision nursing homes survey’, ‘health service provision residential care homes survey’, ‘long term care health care survey’ and ‘long term care health service provision survey’.
Electronic databasesMEDLINE (PubMed), CINAHL, BNI, EMBASE, PsycINFO, DH Data and The King’s Fund were searched. In addition, we contacted care home-related interest groups and used lateral search techniques, such as checking reference lists of relevant papers and using the ‘cited by’ option on WoS, Google Scholar (Google Inc., Mountain View, CA, USA) and Scopus, and the ‘related articles’ option on PubMed and WoS.
E-networksE-networks requests for information were made to ECCA (now known as Care England), Care Home Providers Alliance, My Home Life Network, National Care Home Research and Development Forum, the PCRN, clinical study groups of the NIHR DeNDRoN and NIHR Age and Ageing network.
Inclusion criteriaPublications post 2006 of any research design, unpublished and grey literature, policy documents and information reported in specialist conferences. Studies relevant to UK systems of health care that addressed one or more of the outcomes of interest. Studies that were not UK-based but where there was transferable learning relevant to the UK models of service provision were included.
Exclusion criteriaStudies where the health-care provision to care homes was very different from UK models of care were treated with caution or excluded, for example where medical support is in house (as in the Netherlands) or the level of care would be closer to hospital-level provision (as can be the case in the USA). Studies were excluded if the focus of the intervention or project only involved care home staff and/or a research team, that is, there was no input from visiting HCPs.
BNI, British Nursing Index; CINAHL, Cumulative Index to Nursing and Allied Health Literature; DeNDRoN, Dementias and Neurodegenerative Diseases Research Network; DH, Department of Health; ECCA, England Community Care Association; HCP, health-care professional; NIHR, National Institute for Health Research; PCRN, Primary Care Research Network; WoS, Web of Science.
Citations yielded from the above searches were downloaded into and organised using EndNote [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] bibliographic software. All papers were independently screened by two members of the research team.
For the review of surveys, data extraction was structured to capture forms of NHS service provision for care homes in England in terms of frequency, location, focus and purpose and, where possible, funding.
The review of reviews and scoping review also extracted data about the structure and function of the different types of service provision to care homes as well as considering in greater detail how services were developed, who was involved and how they had affected, or considered, the outcomes of interest for our study (admissions to hospital, length of stay, out-of-hours service use, medication use and user satisfaction). Because of substantial heterogeneity in the studies reviewed we did not pool studies in a meta-analysis. Instead a narrative summary of findings was completed.
The combined findings of the above were used to develop propositions about possible CMO configurations and linked ‘if then’ statements that were debated and refined within the team about what might support health-care provision to care home residents.
Theory refinement and testing
This step involved taking the theoretical propositions and possible CMO configurations derived from the interviews, review of surveys and review of reviews that captured the emergent programme theories of how health-care services worked with care homes.
Detailed reading of the literature from the earlier stages of the review was accompanied by lateral searches of references retrieved from article bibliographies, driven by emerging theoretical constructs where it was clear that additional data were required from underpinning research studies. This more in-depth consultation of the literature was used to look for data that supported, refuted or augmented the possible CMO configurations identified in the earlier reviews. Analysis focused on interventions that drew on theories about the assessment of frail older people in the last years of life, system-driven quality improvement schemes in primary care and theories of integrated working that emphasised relational, participatory and context-sensitive approaches in care home settings (see Appendices 2 and 3).
In keeping with realist enquiry methods, equal consideration was given to negative and positive outcomes and inconsistencies in accounts of what works, when and with what outcomes. We retained the inclusion and exclusion criteria used for the initial scoping. Quality assessment was based on the opportunities for learning and testing emergent theory. Thus practitioner accounts of innovation were considered as evidence alongside empirical research.
Four reviewers (CG, SLD, MZ and MH) independently screened titles and abstracts to identify relevant documents, which were retrieved and assessed according to the inclusion criteria. All included papers were read by Claire Goodman and one of the three reviewers.
Data extraction focused on how health care was organised, funded, provided and delivered, how the underlying assumptions and theoretical framework (if identified within a particular study or group of studies) were articulated, and whether or not this fitted with the focus of our review in terms of the underlying theory and the impact of the intervention on the outcomes of interest. Our approach drew on Rycroft-Malone et al. ’s42 approach to data extraction in realist synthesis that questions the integrity of each theory, considers the competing theories as explanations to why certain outcomes are achieved in similar and different settings and compares the stated theory with observed practice.
Analysis and synthesis
A realist analysis of data adheres to a generative explanation for causation and looks for recurrent patterns of outcomes and their associated mechanisms and contexts (CMO configurations). 31 As the review progressed, the discussion focused on particular papers and sources that offered competing accounts of why or how an intervention was chosen and why it had, or had not, worked. We concentrated on what appeared to be recurrent patterns of contexts and outcomes in the data (demi-regularities) and then sought to explain these through the means (mechanisms) by which they occurred.
The review’s preliminary findings were presented to the study advisory group for further discussion and challenge. This iterative discussion process compared the stated theory with the evidence reviewed. We discussed how and why different mechanisms were triggered by the different approaches to providing health care to care homes. The findings were then used to structure the recruitment and sampling approach for testing in phase 2.
Phase 2
The case study phase of the project addressed research questions 3 to 5:
-
How are these features/mechanisms associated with key outcomes, including medication use; use of out-of-hours services; resident, carer and staff satisfaction; unplanned hospital admissions (including to an A&E department); and length of hospital stay?
-
How are these features/mechanisms associated with costs to the NHS and from a societal perspective?
-
What configuration of these features/mechanisms would be recommended to promote continuity of care at reasonable cost for older people resident in care homes?
Phase 1 findings indicated that we should target service delivery models that acknowledge and support the interactional nature of decision-making between care home staff and visiting health-care professionals (HCPs), for example by supporting increased contact from NHS practitioners, structured meetings and joint review of residents’ needs. The explanatory theory of interest and supporting CMO configurations, with the potential to explain why some or all of the outcomes were achieved (or not), was one that specified what needed to be in place to trigger, support and sustain mechanisms that generated trust, mutual obligation, recognition of how care homes worked and a common purpose. The review suggested that particular activities within different service models were important contextual factors (or possibly mechanisms). These included education, training and ongoing support of care home staff; employment of HCPs to work with care homes; opportunities for regular review and discussions between care home staff and professionals; and the allocation of resources to increase the frequency of visits by and involvement of primary care service staff.
A case study approach was chosen to facilitate a detailed description of processes of care and a comparison of the delivery of health care over a sustained period of time to care homes and their residents, across three geographically discrete sites. Specifically, we aimed to identify three sites where health-care provision had been designed to reflect some or all of the contexts identified in the review and particularly those that might support relational working.
Ethics approval
The phase 2 case study was reviewed and given a favourable opinion by the Social Care Research Ethics Committee on 29 January 2014 (Ethics Committee reference number 13/IEC08/0048).
Sampling and recruitment
Initially we proposed to select one Clinical Commissioning Group (CCG) area as an example of usual care, that is, one with an approach to commissioning and care delivery for care homes in its area where there was little or no differentiation between commissioning of services provided to people living at home and those in care homes. It became clear, however, that national preoccupations with unplanned hospital admissions meant that it was unlikely that a site would not have any intervention or initiative operating that involved care homes. We therefore approached and recruited a site where the main route for access to medical and specialist care was through the general practitioner (GP) and the General Medical Services (GMS) contract, but the county had also invested in care home manager leadership training (site E below).
We identified six CCGs/geographical areas within England that were each operating a distinctive approach to delivering health care in care homes and within 2 hours’ travelling distance of our two research centres.
-
Site A: CCG investment in care home specialist provision, which included care home specialist teams, linked specialist dementia care, falls prevention teams and involvement of community geriatricians.
-
Site B: CCG provision of financial payments to specific GP practices to work with care homes and deliver on specific areas of care complemented by the commissioning of training and education in care homes for residents with complex care needs. The initiative required care homes to register with one practice, CCG investment in a multidisciplinary out-of-hospital team, a 24/7 resource covering health and social care to avoid admission to hospital, supported early discharge and home-based rehabilitation. The team included care homes in its remit and had access to beds with care within a care home environment where a patient needed added intensity of care.
-
Site C: CCG investment in community matron support for care homes and a series of topic-specific initiatives to improve medication management and access to end-of-life care, and to prevent and reduce pressure ulcers in care homes.
-
Site D: CCG investment in support to care homes that focused on the creation of a single team for care homes led by a community matron, set up to work closely with GP practices.
-
Site E: geographical area that had a long history of innovation in care home working, for example pioneered intermediate care beds in care homes and where multiple care homes were actively involved in the Enabling Research in Care Homes (ENRICH45) network.
-
Site F: geographical area where there had been training and investment across the county in care home manager leadership training and development. CCG investment in care homes was based on GMS contracts with linked services designed to reduce unplanned admissions from across the community.
In four sites (A, B, C and D) the service proposition to care homes was delimited by the geographical boundaries of the local CCG, as the models of care had been specifically commissioned by CCGs in response to the challenge of providing health care to care homes. To fully understand the service proposition in these areas, it was necessary to ensure both the permission and the engagement of the local CCG to ensure that the necessary access to sites and staff stakeholders would be supported. These sites were therefore approached for recruitment by the research team contacting the CCG and the commissioners with responsibility for care homes and one via the organisation that had organised the training and development programme for care home staff in the county.
Two CCGs (C and D) expressed an initial interest in participating and received information about the study, and the researchers had preliminary telephone conversations with commissioner/site representatives. In one area the chairperson of the CCG decided against participation and in the other site the research team decided not to pursue the collaboration, as the CCG was still in the early stages of introducing changes as to how it worked with care homes.
In site E interest was expressed from specific care home managers; despite this interest, geographical proximity and participation in the ENRICH45 network, the team decided that site F offered more opportunities for learning.
At the last site (F), the relevant contextual factor – investment in a leadership and management framework – was not geographically bounded within a single CCG’s footprint because the service was delivered as a county-wide initiative by a national charity. The approach to the local care home leadership and management network was therefore made through the national charity, rather than the multiple CCGs that commissioned services with which the care homes might be required to interface. The managers comprising the network agreed, unanimously, to participate in the study.
When the sites were confirmed, 72 care homes that met our inclusion criteria were invited to participate in the study.
Selecting and recruiting homes for involvement in the study
Area A (investment in specialist care home provision) was recruited to the study and identified as study site 1, area B (provision of financial incentives to GPs) was identified as study site 2 and area F (care home leadership and management framework) as study site 3; four care homes were recruited in each site. All sites were in England and were located in the Midlands and the east of England (including the east coast).
Although the identification of service delivery models was theory driven, based on the findings of phase 1 we focused, as far as possible, on ‘typical’ homes, that is, those with 25 beds or more (the median size of care homes with and without nursing provision is 25 beds and 48 beds, respectively) and those identified as having contact with a range of NHS services comparable to the common patterns of service delivery identified in phase 1. We aimed to recruit care homes from a range of ownership categories, including large corporate providers, more localised single-home providers or small chains and third-sector charitably funded homes. We did not specifically seek to recruit either NHS- or local authority-funded homes as these now represent exceptional models of funding care. 12
Our exclusion criteria were care homes with specialist registration for alcohol and drug abuse or learning difficulties; those with bed numbers outside the interquartile range; those whose manager had been in post for < 6 months; and those providing specialist care services commissioned by the NHS. From the remaining homes, in sites 1 and 2, all homes that had contact with the services of interest were sent a letter inviting them to participate in the study. This was followed up by a telephone call from the study researcher to give them further information and to set up a meeting with managers who were interested in participating. In site 3, initial contact with care homes was made by the charitable organisation that provided leadership training. Here the details of interested managers, following their consent to be contacted, were passed on to the researcher to communicate directly. In all sites, meetings were arranged with managers to give them further information and to answer any queries about the study and what it involved.
From those willing to participate in the study in principle, care homes were selected to include those with and without on-site nursing and registration for dementia care. To enhance opportunities for comparison we aimed, as far as possible, to match the first four care homes recruited in site 1 with the remaining eight care homes in the other two sites, based on resident population, staffing ratios and geographical proximity to a NHS acute hospital providing secondary care.
Support for recruitment and participation was achieved in one of the sites through collaboration with the local Clinical Research Network, which recruited participating homes to be part of the ENRICH45 network alongside the research undertaken as part of this study.
Recruiting residents from participant homes
The challenges of recruiting older people to research in care homes are well documented. 46,47 Based on previous studies, and with the support of the ENRICH45 network and experienced PIR members, we aimed to achieve the maximum possible recruitment of residents. Where residents lacked mental capacity to give consent and had no contactable personal consultee, we employed a robust protocol using nominated consultees to boost recruitment. Those residents attending for respite care only, or those who were identified by care home staff as terminally ill (i.e. in the last weeks of life) or too ill to participate were excluded.
Sample size
Based on three areas and the purposive sampling framework outlined, we expected to recruit a resident sample of 263–438 based on 60–100% recruitment. Our target number of care home staff was 60 (five per home) to reflect a range of seniority and skill and – depending on GP attachment and models of service delivery – between two and three GPs, two and three NHS nurses (district nurses/specialist nurses) and two and three therapists per home, representing a maximum of 168 participants. Where possible we aimed to interview the chairperson or members of the participating CCG (between three and five) and the Health and Wellbeing Boards (n = 3) about current and projected patterns of service delivery to care homes.
Conducting the case studies
The longitudinal mixed-methods design enabled us to do two things: (1) to track the resource use of residents, particularly their use of emergency and out-of-hours services and (2) to understand how over time the different expressions of relational working between NHS and care staff were achieved and with what outcomes. It also enabled us to study if particular residents (e.g. those who frequently used resources) benefited more or less from the different mechanisms of care provision and whether or not there were differences in responsiveness and flexibility as residents’ needs changed over time.
Data collection with each of the study care homes was conducted over a period of 12 months following the baseline data collection.
Baseline data collection
Baseline descriptors for residents were collected from their care home records to provide the basis for a comparison of the population studied within the four care homes across the three study sites.
Following piloting with care home staff, we used a modified version of the international Resident Assessment Instrument (interRAI) items for use in assisted living facilities, to record information on residents’ clinical and functional status48 for modified interRAI-assisted living. 49 This tool was amended to allow for differences in terminology between Australia – where the tool was developed – and the UK and to remove sections that were not relevant to care home residents in UK care homes. It combined assessment items relating to clinical characteristics with activities of daily living (ADL) and cognitive function that relate to staff care time. 50 interRAI is a standardised assessment instrument for older adults with frailty,49 widely used outside the UK and internationally validated, that provided the study with data of cross-national comparability. The tool comes with a number of validated protocols that automatically generate subscores for a number of clinical syndromes, common diagnoses and patterns of dependency. Based on the experience of the SHELTER study,51 which collected data from 4156 care home residents across eight countries using a version of the interRAI for long-term care facilities (LTCFs) and included 507 residents across nine facilities in the UK, it was believed to be feasible for the interRAI to be completed by care home staff (including care assistants) following training from the research team.
Data on medication use at baseline were collected from Medication Administration Record (MAR) sheets. Thereafter, monthly changes to medications (additions, subtractions, substitutions) were collected from the MAR sheets and annotated longhand into the study database.
Descriptive case studies of continuing care as delivered to care home residents
The case studies provided descriptive data on resident characteristics and resource use, and qualitative data about how health-care provision to care homes was seen as supporting (or not supporting) relational working between the NHS and care homes. Case descriptions were built iteratively, taking account of audio-recorded interviews with residents and family members, care home staff, health and social care commissioners, GPs, NHS nurses and allied health professionals. Observation of NHS care delivery occurred when researchers were in the care homes; this included, for example, observation of meetings between NHS and care home staff and their contact with residents. These were documented as fieldwork notes and included in the qualitative analysis as memos. Care home policies and procedures that focused on residents’ health care were also reviewed. Participants were interviewed at least once over the 12 months. Interviews were semistructured. Interview schedules were initially focused to further inform and enable iteration of the CMO relationships and mid-range theory emerging from phase 1 of the study and were modified over time as these conceptual frameworks evolved. Schedules drew on work on continuity of care and work52–54 on integrative processes, which previously highlighted that service provision can only be meaningfully understood from the level of the patient or, in this case, the resident. All interviews were recorded and fully transcribed.
Care home staff were recruited as volunteers from among the broader workforce of the care homes. Posters were placed in staff areas of the care homes. In addition, staff were made aware of the study and the opportunity to participate in focus groups/interviews when researchers were visiting homes to support routine collection of resident-level outcome measures. Managers played a supporting role in helping to recruit staff but were advised not to coerce them to participate.
Health-care professionals were identified for interview on the basis that they were frequent visitors to the care homes, as established through the monthly service use reviews of participating residents and liaison with the care home link staff. Where required, permission was sought from service managers for the researchers to contact individual HCPs inviting them to participate in the study. To maximise recruitment from this group, telephone interviews were conducted with those staff unable to meet face to face, rather than risk losing their relevant perspectives from the study altogether.
General practitioners who had a role in providing residents with the care homes were identified through discussions with care home staff and were then contacted individually to request participation in a one-to-one interview. Where this failed to recruit participants, GPs were approached collectively via the CCG to take part in a focus group discussion on working with care homes.
Informed by the findings of the realist synthesis, interviews focused on the experience of providing and receiving health care in care homes. For residents and carers, we focused on what was important in relation to satisfaction with the services and how they saw relationships with care home staff and health-care practitioners contributing to this. For care home staff we focused on their satisfaction with the health-care services provided to the care homes and what they viewed as the priorities for NHS services when supporting residents’ health care. Researchers provided feedback about how residents had been found to use services and used these to elicit care home staff views and experiences of working together with health-care practitioners. Face-to-face interviews with care home managers at this stage aimed to capture any changes in the way that health services were provided over the data collection period and to compare and contrast their satisfaction with, and perceptions of, health service provision with those of their staff. Health-care staff were asked to consider the research team’s understanding of how they worked with care home staff, and other HCPs, NHS priorities for residents’ care and how satisfied they were in working with the care home. For GPs, we focused on how they worked together with care homes to provide care for residents, their level and type of contact with other NHS HCPs and their priorities for care, with a greater focus on their role in medication management. A final set of interviews and focus groups shared details from the process analysis and the emergent conceptual frameworks regarding the outcomes of interest and asked care home managers to consider the extent to which these resonated with their experiences.
Care home staff satisfaction surveys (staff outcomes)
To supplement qualitative data on staff satisfaction, we conducted a survey to take account of staff members’ overall satisfaction with continuing health-care services. We used the Quality-Work-Competence (QWC) questionnaire as the basis of this, developed and validated by Hasson and Arnetz55 as a mechanism for collecting data on care home staff competence, work stress, strain and satisfaction. The key area of interest, in keeping with the outcomes of interests stated at the start of the study and reflecting the focus of our programme of work specifically around health care and the contextual and mechanistic factors required to support good health outcomes, was the extent to which staff were satisfied with the health services provided within and between regions. We therefore only used the subset of QWC questions focused around quality of care.
Resource use outcome measures
A bespoke pro forma for collecting service use data was developed with the participating care homes to collect data on the community services that visited participating residents. These discussions were informed by the review of surveys undertaken in phase 1 that reported the range and variability in services accessed by care home residents. Following initial discussions, the specific services to be recorded for residents on a monthly basis were collated in a pro forma, which included the main service use outcomes of interest – namely out-of-hours services, unplanned hospital admissions (including A&E) and length of hospital stay. Each care home was visited by a researcher on a monthly basis at least, but usually more frequently. This helped to maintain working relationships with the care homes to verify and support up-to-date contemporaneous completion of forms.
Two designated members of the care home staff (study link staff) were identified who had responsibility for supporting resident and relative recruitment, day-to-day data collection on resource use, informing us of key events in the care home (e.g. CQC inspections, staff changes, etc.) and liaising with NHS services (see Appendix 5). These data were checked and the details were clarified by researchers from care home records and in discussion with the care home staff.
We had planned to cross-check the service use data obtained from the reviews of residents’ care home notes with data extracted from their medical notes, including information on hospital admission and length of stay, out-of-hours and emergency ambulance service use and referrals to other health-care services in the preceding 12 months. If this was not acceptable we aimed to do a 10% reliability check with residents’ GP records. At the end of data collection and despite multiple attempts, including support from the Clinical Research Network, we were unable to access resident data from GP notes. This reflected real difficulties in recruiting GP colleagues to all parts of the research study.
Analysis and synthesis
Qualitative data were analysed in stages (see also Figure 1).
FIGURE 1.
Data synthesis. CH, care home; MHL, My Home Life.
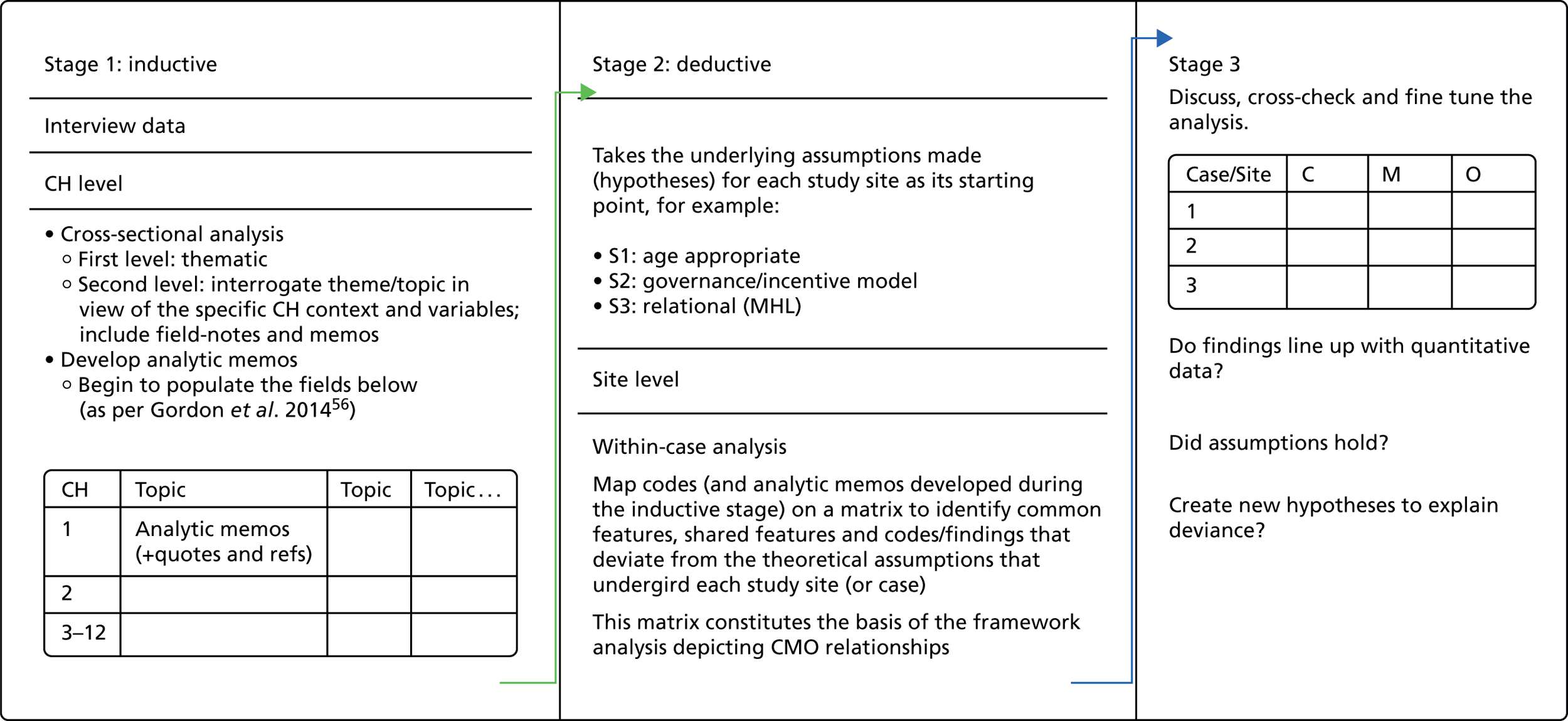
Stage 1
The initial data analysis commenced with the participant interviews, on the basis that an understanding of the provision and structure of health-care services to care homes would facilitate interpretation of the data from the other participant groups. The first level of analysis focused on the participants’ transcripts. The data were analysed both inductively and deductively, initially at the care home level, followed by a within-case analysis of the three study sites. All interview and focus group transcripts were entered into NVivo. Each transcript was coded thematically according to the responses given to the interview questions together with other variables including role, remit and the use of shared documentation. At the second level of analysis, each theme or topic was interrogated to identify the features and structure of health-care delivery to the care homes and the way that the services were organised. This included field notes and memos that were compiled during the data collection process. Analysis at the care home level was followed by a within-case analysis in which each study site, and the four care homes within it, constituted a case.
Stage 2
In stage 2, deductive data analysis was driven by the theoretical assumptions on which each study site had been selected for the study from the phase 1 findings and possible within- and cross-case CMO configurations, that is, sites were loosely characterised as study site 1, an ‘age-appropriate model of care’, study site 2, a ‘governance model’ and study site 3, a ‘relational model’ of working. 57 Drawing on the analysis from stage 1, the characteristics of each model were identified as well as the common features and differences across the sites, together with any data that did not rest on the assumptions underpinning the models. Coding of the transcripts was also conducted for the study outcomes, medication use and management, satisfaction, unplanned hospitalisation including length of stay, out-of-hours service use and A&E use. In line with the findings from the realist review, examples of relational working between HCPs and care home staff were identified and analysed to highlight their associated features.
The resulting data were used to provide a detailed description of the intervention, the outcomes at different levels, context conditions and mechanisms in order to facilitate the identification of the emerging CMOs. 58
Quantitative data analysis
In order to assess the economic outcomes for each of the sites, it was necessary to apply costs to the service use frequency data, collected by month from the patient records. Unit costs were identified from national and published sources. These unit costs were multiplied by the frequency of events for each of the resource use items and a new variable was generated containing the costs, at an individual resident level for that resource item. The frequency variables and costs were then aggregated over time and resource type. The resulting data set contained a set of eight frequency variables of resource use and the corresponding eight variables containing the summative total costs for that resource type, at an individual resident level. Two total cost variables were also generated: the summative total costs at an individual resident level, including all eight health resource types, and all costs, except hospital admissions, which were separated out because inpatient episodes were infrequent events, but costly when they occurred.
Missing data were assessed across all resource use items by way of frequency tables. When a positive response had been recorded for one or more health resource variables for a particular time point, nested by individual resident, any missing values for other resource items were assumed to be zero values. When this rule led to missing data for one or more time points for an individual, the observations for the resident were counted as missing and the resident was dropped from the complete-case analysis. Using this approach, the percentage of complete cases at each month was calculated. Beyond 6 months, when 85% of resident records were complete, the frequency of missing data increased to > 20% (and was 45% at 12 months). Hence 6 months was selected as the primary end point for the analysis.
To verify that inadvertent bias was not introduced by conducting the economic analyses based on those residents with complete data at 6 months, we compared the distribution of baseline variables for all residents recruited to the cohort as a whole and those included in the economic analysis, and no statistically significant difference in baseline variables was detected.
Considering associations between baseline variables, costs and outcome variables
The mean and standard deviation (SD) for each of the summary categories of service use and costs and total costs, broken down by site, were computed. Pairwise comparison between sites for health resource use was conducted using Pearson chi-squared tests; sample t-tests were used for site comparisons of costs.
We used Poisson regression to explore whether or not the site was a significant predictor of service use and total costs after the interRAI scores and the derived variables that we had developed for this study (cognitive impairment, number of comorbidities and medication count), as well as the interaction between the site and these variables, were entered in the regression equation. Poisson regression is a technique that can be used with infrequent count data, such as the service use data. We first entered each of the interRAI clinical syndrome variables [ADL hierarchy scale (sADLH), short ADL hierarchy scale (sADLSF), cognitive performance scale (sCPS), communication scale (sCOMM), clinical syndrome for pain (sPAIN_1) and pressure ulcer risk scale (sPURS)], as well as each of the derived variables (cognitive impairment, number of comorbidities and medication count) in a Poisson regression equation with each of the service use variables separately.
As an example, a regression equation would use sADLH to predict primary care contacts, GP contacts, out-of-hours contacts, community contacts, A&E visits, ambulance use, secondary care number of admissions, secondary care duration and secondary care non-admissions separately. Then, another regression equation would use sADLSF to predict each of the service use variables separately. As this was an exploratory analysis, we selected predictors based on whether or not they were significant in the univariate analysis at a p-value of < 0.10.
Medication analysis
Medication analysis focused on total medication, antibiotic and opioid counts and anticholinergic burden (ACB) scoring using the ACB scale produced by Aging Brain Care [www.agingbraincare.org/uploads/products/ACB_scale_-_legal_size.pdf (accessed October 2017)]. This was based on the guidance of the study steering group that identified an expansive list of prescribing decisions that could indicate optimal or suboptimal prescribing in the care home setting – ranging from number of antibiotics, painkillers and antihypertensives to more comprehensive indices including the STOPP/START criteria59 and Medication Appropriateness Indices. 60 The eventual recommendation of this group was to use the ACB scale as a proxy measure that incorporated antipsychotic and antihypertensive prescribing rates, and to count opioids and antibiotics separately. ACB scoring and the allocation of medications to antibiotic and opioid categories were conducted by a consultant geriatrician (ALG).
For baseline medication data, counts and distributions were summarised using means (SDs) and medians (range) for parametric and non-parametric data, respectively. Differences between sites were considered using the analysis of variance (ANOVA) statistical method and Kruskal–Wallis one-way ANOVA for parametric and non-parametric data, respectively. Opioid and antibiotic prescription were treated as dichotomous variables (present/absent) – because the majority of residents were taking only one of each of these medications – and were thus compared between sites using Pearson’s chi-squared test.
Follow-up data comprised total drug, antibiotic and opioid counts, and ACB scores for each month of follow-up. These were used to calculate total drugs/resident, antibiotics/resident, opioid/resident and ACB/resident, which were plotted as line graphs with 95% confidence intervals (CIs) to enable comparison in prescribing trends over time.
Staff satisfaction
Staff satisfaction questionnaires were analysed similarly to medication data, with counts and distributions summarised using means (SDs) and medians (range) for parametric and non-parametric data, respectively. Differences between sites were considered using ANOVA and Kruskal–Wallis one-way ANOVA for parametric and non-parametric data, respectively. Categorical variables were compared between sites using Pearson’s chi-squared test.
Analysis workshop
A 2-day analysis workshop was used to feed back emergent findings from the three sites to the research management team together with a member of the PIR group (Kate Sartain), in order to discuss the results from the quantitative data and the qualitative data and evidence supporting different CMO configurations both within and across the case study sites.
To enable comparison, home-, resident- and staff-level data were analysed and reported on a site-by-site basis. A matrix61 was generated, with the rows representing sites and columns organised to reflect both the key propositions developed from phase 1 and the data generated from resource use. This was used to facilitate qualitative cross-case analysis, taking account of similarities and differences between and across the three sites. Attention was paid to what the data revealed about the inter-relationships between the mechanism and context of care and how these linked to the outcomes of interest. 52,54
Analysis was iterative and reflected the analytic stages followed in phase 1; it focused on what was revealed about the actual intervention or mechanism, the observed outcomes, the context conditions and underlying mechanisms. This was compared with the theoretical propositions from phase 1 to establish the conditions under which the mechanisms work (or not) and their transferability across different settings.
Chapter 3 Results from the review of surveys and the review of reviews
Introduction
This chapter presents the findings that address the first question of the OPTIMAL study:
-
What is the range of health service delivery models designed to maintain care home residents outside hospital?
The first half of the chapter concerns the analysis from the review of published surveys of health-care provision to care homes. The second half provides a summary of the review of published reviews’ findings about the focus and priorities of health-care research in and with care homes. The chapter provides an overview of the organisation of health care for care homes with a particular, but not exclusive, focus on UK services. A paper on the review of surveys has been published elsewhere. 4
Review of surveys
To complement the searches of the databases (summarised in Chapter 2), forward citations and online searches of NHS websites and e-mail requests, we reviewed the websites of eight academic centres known for their work in care home research, four charities, seven care home provider representative bodies and 12 NHS, social care and professional organisation sites with responsibilities for care homes. Data extraction and analysis were completed in 2013.
Sixteen surveys completed since 2008 were identified and fifteen were included. Five focused on GP service provision to care homes, while also collecting data on specialist services. Ten focused on specialist services to care homes or were topic specific, for example, focusing on dementia services or end-of-life care. One survey62 considered the care home nurses’ work environment, staffing levels, quality of care, meeting residents’ needs and financial pressures on the home, but this was not included as there were no data on externally provided health-care provision/nursing support to care homes. Only two surveys included residents, one of which also included relatives of residents who were unable to participate because of cognitive impairment. The main methods of data collection were postal or online surveys, although some used face-to-face interviews with care home residents and telephone interviews with GPs.
The surveys are summarised in Tables 1 and 2. Table 1 shows, in order of publication date, those surveys that focused on GP services, and Table 2 lists those focusing on specialist services or topics.
| Author, title; year (home type) | Aims | Survey details | Sample size/response | GP services | Other services |
|---|---|---|---|---|---|
| 1. Morris J, Patients Association/University College London/BGS Clinical Quality Steering Group, 2008, personal communication, internal report (nursing homes in England) | Do care home staff and GPs get enough information about new residents? | Face-to-face or telephone interviews on one occasion with 11 care home managers and six GPs who worked with them using standardised questionnaires for care home managers and GPs, including some overlapping questions. Service-related questions included the following services: GPs, tissue viability, mental health, end-of-life and palliative care, geriatrician, old age psychiatry, audiology, ophthalmology, podiatry, physiotherapy, occupational therapy and community pharmacist | Eleven care homes selected to reflect a range of care homes in terms of size, location and residents | From nursing home interviews (n = 9), seven out of nine care homes had a single designated GP – five did weekly clinics, one visited daily and the other 2-weekly | All care homes had access to an ophthalmologist or optician, tissue viability support and support with mental health/behavioural problems |
| Do GPs and care home staff feel supported by primary and secondary care? | The care homes ranged in size from 39–118 beds | From GP interviews (n = 6), three out of six did either yearly or 6-monthly medication reviews | According to GPs, five care homes had access to palliative care support | ||
| Four homes had access to audiology and podiatry, two of which were provided by the care home organisation | |||||
| Three care homes had access to the geriatrician and old age psychiatrist; the others had no or ad hoc access | |||||
| Three had access to a physiotherapist whom they employed directly | |||||
| No care homes had access to occupational therapy services or a community pharmacist | |||||
| 2. Gladman and Chikura, Medical Crises in Older People;63 2011 (care homes with and without on-site nursing) | To conduct a review of current service provision to elderly residents in 252 care homes across the county | Postal survey. Data were collected on 20 services, including falls, GP, pharmacist, physiotherapy, occupational therapy, end of life, mental health, DN, podiatry, community geriatrician, nurse practitioner, dietitian, community matron, long-term conditions, tissue viability, continence, dementia, optometrist, SALT, stroke rehabilitation | One hundred and eighteen responses (47% response rate) | All homes allowed their residents to register with the practice of their choice – (one care home was served by up to 16 practices) | Ninety-seven per cent of care homes had access to pharmacy, 92% to a DN and 89% to a dietitian |
| Most visits were on request, GPs offered regular surgeries, others found it hard to get visits | Most services available on request rather than routinely with the exception of pharmacists | ||||
| Forty-two per cent of care homes did not have regular GP visits | The services available to the least number of care homes included nurse practitioner (34%), community geriatrician (42%; 9% of care homes had regular visits from the community geriatrician) and long-term conditions team (43%) | ||||
| Twenty-three per cent of care homes could not access SALT, physiotherapy or occupational therapy services | |||||
| An example of specific care home services: a nurse-led team that worked closely with care homes to liaise with NHS services and offer training and support to care homes, medication reviews | |||||
| 3. Gage et al., Integrated working between residential care homes and primary care: a survey of care homes in England;64 2012 (care homes without on-site nursing) | The APPROACH study survey 1: to establish the extent of integrated working between care homes and primary and community health and social services | A self-completion, online questionnaire of open and closed questions designed by the research team to establish the primary health-care service provision to care homes and their experience of integrated working with those services | Sent to a random sample of residential care homes in England in 2009 (n = 621) with more than 25 beds | All care homes received GP services – 81% worked with more than one practice |
More than 90% of homes reported using DNs and opticians Other frequently accessed services (> 80%) included CPNs, podiatrists Between half and three-quarters of homes reported visits from continence nurses, pharmacists, dentists, hearing services and old-age psychiatrists Difficulty accessing specialist services was a consistent theme |
| Ninety-three out of 587 care homes responded (a 15.8% response rate) | Consultation arrangements varied from weekly GP clinics to as required. Seven (8%) paid a retainer to the GP but these were seen as unfair | ||||
| 4. Quince, Low Expectations: Attitudes on Choice, Care and Community for People with Dementia in Care Homes;65 2013 (care homes with and without on-site nursing in England, Wales and Northern Ireland) | To explore attitudes on choice, care and community for people with dementia in care homes | Interviewed staff and observed care provided to 386 residentsa | Twenty-seven care homes with nursing: 144 adults aged > 65 years were observed or interviewed | Variability in GP services received: 44% had scheduled surgeries or visits; unclear who pays for GP services. Fifty-three per cent said the NHS paid for GP services | Only addressed GP provision |
| Twenty-seven care homes without nursing: 153 residents aged > 65 years were observed or interviewed and 90 staff were interviewed | Thirty-three per cent of GPs did not do the assessment post resident admission | ||||
| 5. Carter, Failing the Frail: A Chaotic Approach to Commissioning Healthcare Services for Care Homes;66 2011 (report to the British Geriatrics Societyb) | To establish what health-care services are commissioned by PCTs for older people living in care homes | Online survey by CQC to seek information about health services provided to care homes and older people living in the community in all PCTs in England (152 PCTs in England) | The survey noted that some responses provided minimal information.c ‘Do not know’ and missing answers were treated as negative answers | Fifty-one per cent (n = 77) of PCTs had enhanced service agreements with GPs for their work in care homes | There were significant variations in specialist provision to older people with 52 different possible combinations identified |
| Forty-three per cent (n = 65) of PCTs provided all the services that the CQC considers appropriate for all older people | |||||
| Sixty per cent (n = 91) of PCTs provided a geriatrician service to all older people | |||||
| The survey focused on nine key services: geriatricians, psychiatry, dietetics, occupational therapy, physiotherapy, podiatry, continence, falls prevention and tissue viability | It was not always possible in the analysis to separate the findings for care homes from those that applied to all older people living in the community. The focus of the analysis was on commissioning intentions | Sixty-seven per cent of PCTs did not think that care homes needed additional medication reviews | Most specialist services made visits on request | ||
| PCTs were also asked about additional services provided by GPs to care homes and payment for enhanced services to care homes. The CQC focused on seven activities that GPs could perform in care homes: health assessments on admission, specialist assessments, regular visits, support with end-of-life care planning, general support, liaison with other services and additional medication reviews | Seventy-seven per cent of PCTs provided at least one activity considered to be an enhanced activity for care homes | Scheduled visits were most likely to be offered by continence services, podiatry, dietetics and psychiatry |
| Author, title; year (home type) | Aims | Survey details | Sample size/response rate | GP services | Other services |
|---|---|---|---|---|---|
| 1. Steves et al., Geriatricians and care homes: perspectives from geriatric medicine departments and primary care trusts;21 2009 (all types of care homes in England) | To test concordance with the Royal College of Physicians, Royal College of Nursing and the British Geriatrics Society’s 2000 guidelines on clinical practice for care homes | Complementary surveys for PCTs and GMDs 2006 – to the lead clinician in each GMD in England and the lead nurse in each PCT in England | Responses from 109 of the 167 (65%) GMDs in England and 141 of the 303 (47%) PCTs | N/A | Seventeen (15.7%) GMDs specifically allocated sessions to care home work, mostly with nursing homes |
| Some PCTs funding geriatrician involvement in care homes (18.4%), but 52% of PCTs (n = 74) required either geriatrician’s involvement in the admissions process (20%) and/or the support of ongoing care of care home residents (40%) | |||||
| Twenty-four per cent (26/109) of GMDs gave ongoing input to care homes | |||||
| Most PCTs had a standardised assessment for admission to care homes with assessment of need for nursing mainly completed by a social worker and/or nurse | |||||
| 2. Monaghan and Morgan, Oral health policy and access to dentistry in care homes;67 2010 (all types of care homes, Wales) | To explore the factors that may facilitate or impede access to dental care and arrangements within care homes in Wales | All care homes in Wales. Postal survey with 10% random sample interviewed. Questions focused on new residents, dental assessment and access to routine and emergency care, dental care facilities, oral awareness, hygiene practice, diet and nutrition | Six hundred and seventy-three care homes without on-site nursing, 88 with nursing and 186 dual. Eighty-one per cent response rate, 957 out of 1185 | N/A | Managers reported more difficulty in accessing routine dental care than emergency dental care of the reported findings. Twenty-four per cent of care homes reported ‘always’ having problems accessing routine dental care. Eighteen per cent of care homes reported ‘always’ having problems accessing emergency dental care |
| 3. Darton, Study of Care Home Residents’ and Relatives’ Expectations and Experiences;68 2011 (all care homes, England) | To examine older people’s expectations and experiences of living in a care home and to collect information from relatives about choosing a care home | Focus was on residents’ decision to move into a care home and the difference between their expectations and experiences. Some data were collected on health service use before and after the move. An initial interview was conducted with a follow-up 3 months later | Random sample of 150 care homes approached in six regions of England, located via the CQC website. Sixty-seven per cent response rate: 605 out of 900 homes recruited. Sixty-nine residents participated and 33 relatives from 46 care homes | Since admission, 80% of residents had had a consultation with a GP or a practice nurse and 30% had been to hospital | Prior to admission over one-third of residents received chiropody services but few received other services. After moving in, twice as many receive chiropody. Few residents received occupational therapy and none received speech therapy. Relatives reported that residents were no more likely to receive other therapy services than before admission. Relatives reported that 79% of residents had hospital treatment prior to moving in and that the medical or nursing care provided in the home was of a higher standard |
| Relatives reported that 92% had had a consultation with a GP or a practice nurse and 46% had been to hospital | |||||
| 4. Seymour et al., Do nursing homes for older people have the support they need to provide end-of-life care? A Mixed-Methods Enquiry in England;69 2011 (nursing homes, Northern England) | To identify key factors in the wider health and social care system influencing the quality of end-of-life care provided in nursing homes | A postal survey to 180 nursing home managers. It included questions about the profile of deaths in the homes, access to external support and barriers to and perceived priorities for improving end-of-life care. A mixed-methods study – including two qualitative case studies comprising interviews with seven care home staff and ten stakeholders nominated by them | There was a 46% response rate (82/180) | Most external support for end-of-life care was provided by GPs – of the 72% (n = 59) of care home managers who responded to this question, 97% (n = 58) of them reported that they received ‘some’ or ‘ a lot’ of support from GPs | Eighty per cent of care homes received support from specialist nurses, 51% from DNs (n = 30) and 54% from specialist palliative care nurses |
| One-quarter of homes did not request help from specialist palliative care teams (24%) | |||||
| The majority of responders – 93% (n = 76) reported liaising with between 1 and 11 practices (mean, n = 5) and a range of 1–34 individual GPs (mean, n = 12) | Sixty-six per cent of responding care home managers reported that they accessed palliative care support via a direct advice line to the local hospice or Macmillan nurses | ||||
| Variability of support from GPs with end-of-life care highlighted | Support for residents with cancer was viewed as better than support given to those with dementia | ||||
| 5. Briggs et al., Standards of medical care for nursing home residents in Europe;70 2012 (nursing homes, in 25 European countries) | To investigate whether or not 25 countries in Europe have guidelines to formalise the medical care delivered to older people living in nursing homes | Survey e-mailed to representatives of 25 European geriatric medicine societies asking if their health service or professional group:
|
One hundred per cent response rate from 25 geriatric medicine societies in 25 European countries | The Netherlands was the only country where the national GP society had written medical care standards for nursing homes | Five out of 25 (20%) health services required specific training in geriatric medicine for doctors working in nursing homes |
| Four out of 25 (16%) geriatric medicine societies had written medical care standards for nursing homes – four out of 25 countries had a nursing home doctor society and one had published medical care standards for residents | |||||
| 6. British Dental Association, Dentistry in Care Homes Research;71 2012 (England, Wales, Northern Ireland and Scotland) | To investigate care home residents’ dental care, including access to dentists, care home staff input and knowledge | Semistructured in-depth qualitative telephone interviews with a core framework of topics were conducted with managers from 13 care homes and an online survey was sent to 39 clinical directors who reported to deliver services to care homes | Homes chosen that covered a range of sizes, ownership, location and resident needs | N/A | Half of the care home managers reported that their residents received regular check-ups. Homes were evenly split between those that used high-street dentists and those that used salaried primary care dentists |
| No information on how homes were recruited and how many declined to take part | Managers reported a lack of information about NHS providers and those willing to provide domiciliary care | ||||
| A purposive sample of 39 respondents who completed the annual survey of clinical directors and indicated that they provided dentistry to care homes, were approached to take part in an online survey. Twenty-six responded, a 67% response rate | Homes with salaried dentists were more likely to have regular check-ups and to receive domiciliary care | ||||
| 7. CQC, Health Care in Care Homes. A Special Review of the Provision of Health Care to Those in Care Homes;72 2012 (all homes, England) | Provides new evidence on the key issues affecting older people with dementia living in care homes | Three questionnaire surveys distributed to the Alzheimer’s Society members (and care homes’ contact details obtained from regulators, and through some Alzheimer’s Society staff and online. No details of how they were recruited) | Relatives of older people – 1139 responses | Relatives: 56% (n = 637) of respondents said access to and support from GPs was good | Large numbers of respondents did not know about access to dental services. Care home staff views on support from dentists was mixed, with only 23% (n = 259) saying access was good; 44% (n = 286) said that residents got enough support from the dentist |
| Care home staff) – 647 responses from a direct mailing to 300 care homes in England, Wales and Northern Ireland | Care home staff: 55% (n = 354) reported that the resident got enough support from the GP | Thirty-six per cent (n = 408) of relatives were positive about access to, and support from, other health-care services | |||
| YouGov/Alzheimer’s Society 2012 survey of UK adults regarding dementia and care homes65 (n = 2060 adults) | YouGov: 34 out of 2060 responses | Forty-three per cent (n = 281) of care home staff were positive about residents getting enough support from other health services | |||
| 8. Morgan et al., Wales Care Home Dental Survey 2010–2011;73 2012 (no details of homes, Wales) | To investigate any unmet dental care needs in a sample of care home residents | Supplemented the Adult Dental Health Survey 2009: common oral health conditions and their impact on the population74 to compare with older people living at home | Twenty-eight care homes randomly selected and five residents in each randomly selected to take part. No details on response rate and sample size; approximately 708 residents were examined and/or questioned about dental care, unknown how many participated | N/A | The majority of residents would only attend the dentist when having trouble. Residents with their own teeth were much less likely to report regular dental check-ups (19%) than older people living at home |
| Clinical data collected by dentists and questionnaire data on service use by dental nurses. Excluded residents who could not consent | |||||
| 9. Morris J, Patients Association/University College London/BGS Clinical Steering Group, 2013, personal communication; nursing homes, care home organisation specific | To identify good practice and barriers to the delivery of an integrated approach to end-of-life care in 10 Barchester homes | Face-to-face or telephone interviews with 10 care home managers and eight GPs | Ten care home managers, eight GPs (10 approached) | Nine out of 10 care homes had attached GPs; one care home worked with multiple GPs | Seven care homes had access to palliative care services |
| Focus was on how GPs work with care homes in relation to end-of-life care | Four out of eight care homes worked closely with the GP; the other four had problems getting them to visit | Three care homes had access to the DN | |||
| Two care homes had access to the old age psychiatrist | |||||
| One care home had access to the geriatrician | |||||
| 10. Leemrijse et al., The availability and use of allied health care in care homes in the Midlands, UK;75 2009 (all care home types) | To establish the access to, and use of, services provided by allied health professionals to care homes in Oxfordshire and Warwickshire | Cross-sectional postal survey on use of service, frequency of use, referral mechanisms, funding and most common problems service sought for | Ninety-five per cent (115/121) response rate from care homes | N/A | The majority of care homes had access to chiropody (91%), optician (86%), audiology (63%) and physiotherapist (65%). Less than half had access to an OT (41%), dietitian (44%), SALT (39%). One-third used an alternative therapist and social activities organiser. Sources of funding for services were variable with up to 15 variations and a high proportion of allied health care was privately funded. Referral mechanisms were complex, with care homes uncertain how to refer residents to the NHS and social services |
| Included in the survey were physiotherapy, occupational therapy, chiropody, dietetics, optometry, speech and language therapy, complementary (alternative) therapy, hearing services and social activity organisation services |
General practitioners were seen in most studies as key to the provision of good-quality health care for care home residents, including end-of-life care. There was no consensus, however, about how GP and other primary care services should be organised in relation to the care homes or what they should do. For example, some GPs carried out regular medication reviews (6-monthly or yearly), while some did post-admission assessments. Invariably, the care homes surveyed worked with multiple practices and multiple GPs – the largest number of practices visiting one care home was 30 – although some had a single designated GP. Consultation arrangements were also variable, with weekly clinics or visits being made only on request.
This unevenness of provision was mirrored in family and residents’ views: one survey found that only 56% reported good access to, and support from, GPs, with 55% of staff also reporting that residents got enough support from GPs. 72
There was limited information in the surveys about how wider NHS provision was organised for care homes, although some information on geriatrician services was reported in the survey by Steves et al. ,21 and on dental care by the British Dental Association’s survey. 71 Reports that focused on specialist or topic-specific service provision for care homes are summarised in Table 2. 76
Nurses with different areas of specialism visited the homes; eight types were identified. Community psychiatric nurses (CPNs), however, were not mentioned and overall mental health services were under-represented.
District nurses were the most frequently mentioned group, but nursing care could be organised as nurse-led teams or nurse specialists dedicated to working with care homes, falls prevention services, continence care, tissue viability, Parkinson’s disease nurse and palliative care nurse specialists.
Access to specialist services and general dentistry services was reported as problematic for some care homes but not all. Although most surveys reported frequency of contact and range of services, there was minimal information about how services were organised, who was seen and how often or whether or not the quality or range of provision of the care was assessed. In the surveys reviewed, it was not possible to differentiate between services that care homes could theoretically have access to and what was actually being delivered to care homes. This was the case even in surveys that included care home-specific services. Moving into a care home did not improve access to health-care services,68 although some nursing home residents were more likely to see a geriatrician.
The variation in the organisation, provision and funding of health services, both generalist and specialist, to care homes could not be explained by resident need or care home type. Two consistent findings emerged: first, wide variability in the provision of services to care homes and, second, widespread lack of dental services. Both signal inadequate care for residents.
The surveys reviewed were heterogeneous and their quality, although not formally assessed, was variable. Consequently, caution should be exercised in generalising these results. There have been several surveys published between 2007 and 2015 and, although their findings are variable, they all point to a picture in which there is little agreement between commissioners and providers as to how services to care homes should be organised. Little has changed in this regard since the first national survey in 2001. 77
The findings indicate that there is limited value in further descriptive work on NHS health-care service provision to care homes that is not linked to an understanding of how the services work with care home staff to improve care home residents’ health-related outcomes.
Review of reviews
The review of reviews complemented the review of surveys in addressing the first research question about the range and type of provision with the aim of establishing an evidence base for existing approaches to service delivery.
We identified 13 systematic and narrative reviews that focused on care homes and health-care provision. Seven were excluded: four because they focused on care home working and health-care provision without reference to working with external health-care provision,78–81 and three because they provided overviews of health-care provision to care homes,82–84 but referenced rather than discussed relevant research studies. Six reviews were included, which comprised two Cochrane reviews;85,86 one scoping review on the provision of oral health care to care homes;87 one annotated bibliography of research in care homes that developed a thematic review of models for improving care in residential care homes;26 one on predictors of hospitalisation from US nursing homes;88 and a systematic review of qualitative research89 on resident accounts of living well in care homes that included studies relevant to the experience of care. Table 3 provides a summary of the included studies.
| Title and type of review | Primary aim/objective | Included studies | Interventions/models of service provision | Relevant outcomes considered | Findings relevant to service delivery to care homes |
|---|---|---|---|---|---|
| 1. Interventions for improving palliative care for older people living in nursing care homes;86 systematic review | To determine effectiveness of multicomponent palliative care service delivery interventions for residents of care homes for older people | Two RCTs and one controlled before-and-after trial | Interventions differed in the three studies:
|
Use of hospice care, hospital admissions | Improved quality of care as assessed by family. Improved residents’ comfort, but did not address behaviours associated with dementia or physical complications |
| Length of hospital stay | |||||
| Place of death | All interventions relied on effective communication between clinicians and care home staff and training being provided | ||||
| Family ratings of quality of care | |||||
| Seven hundred and thirty-five participants | Residents’ symptoms: pain, discomfort, distress, complications | Authors’ comments suggested effective communication was likely to be essential but not sufficient to achieve change | |||
| All based in the USA (studies graded as poor quality and at risk of bias) | Documentation, for example ACP | ||||
| 2. Interventions to optimise prescribing for older people in care homes;85 systematic review | To determine the effect of interventions to optimise prescribing for older people living in care homes | Eight studies: six cluster RCTs and two patient RCTs | Diverse, multicomponent interventions | Adverse drug outcomes | Interventions led to the identification of medication-related problems and some evidence that medication appropriateness was improved. No effect on adverse drug events, hospital admission and mortality. Equivocal findings on costs. Need for a consensus on what are important resident-related outcomes |
| Hospital admissions | |||||
| Medication review part of seven studies | Mortality | ||||
| Multidisciplinary case conferencing three studies | Quality of life | ||||
| Two studies, education for care home staff | Medication-related problems | ||||
| Residents (n = 7653) in 262 care homes in six countries | Decision support technology, one study | Medication appropriateness | |||
| Overall quality rated as low or very low | Majority involved multidisciplinary working with pharmacists completing the review | Medicine costs | |||
| 3. Predictors of nursing home hospitalization: a review of the literature;88 literature review | To review the evidence for the association between the decision to hospitalise and factors related to the residents’ welfare and preferences, the providers’ attitudes and the financial implications of hospitalisation | Fifty-nine studies (including two RCTS) examining predictors of nursing home hospitalisationsa | Resident-level data collected prospectively and retrospectively: studies using nursing home data (n = 27), hospital data (n = 10), multiple data sources (n = 19), interviews and survey (n = 3) | Hospitalisations | Variability in how hospitalisations are defined in the literature: preventable/avoidable/discretionary |
| Reviewed papers from 1980 to 2006 | Use of the emergency department | Age and specific health conditions are associated with admissions, for example congestive heart failure, respiratory infections; however, severe cognitive impairment is not associated with admissions and the authors ask if this reflects a reluctance to treat people with dementia | |||
| Past hospitalisations associated with future hospitalisations | |||||
| Patient preferences were an influence on referral to hospital | |||||
| Presence of nurse practitioners/physician assistant may reduce hospitalisations (less clear about access to a physician) | |||||
| Equivocal findings about nursing staffing levels | |||||
| Access to hospice care reduced hospitalisations in some studies | |||||
| How residents were funded = negative incentive to reduce hospitalisation for some state-funded residents | |||||
| 4. In-reach specialist nursing teams for residential care homes;27 literature review | To bring together available evidence relevant to various approaches to improving care in residential care homes | Thematic review | Annotated bibliography under seven themes | Narrative account | Evidence mainly related to nursing homes |
| Residents’ and relatives’ views on care (73 papers) | |||||
| Clinical areas (107 papers) | |||||
| Medication in care homes (34 papers) | Debate about the relationship between quality of care and quality of life in nursing and residential homes. Measures of social care, as well as clinical care, needed | ||||
| Medical input into care homes (21 papers) | Notes absence of resource use outcomes | Need for better management of medication in nursing homes | |||
| Nursing care in care homes (66 papers) | Medical cover is suboptimal. GP workload should be more proactive | ||||
| Hospital Admissions (43 papers) | Medicine appropriateness outcomes | The quality of interinstitutional transfers and patient safety across settings is important | |||
| Models of care improvement in care homes (113 papers) | Partnership working between DNs and care home staff intermittent, with less evidence on therapist input to care homes | ||||
| 5. Living well in care homes: a systematic review of qualitative studies;89 systematic review | To conduct a systematic qualitative review of care home life | Systematic review | Thematic accounts of residents’ and relatives’ viewsb | Maintaining independence | Main focus was on the care received in the care home and not from visiting HCPs |
| Thirty-one studies | Safety | Continuity of care and less rigid time schedules and routines were important to residents. This has implications for how they experienced care | |||
| Carers’ technical knowledge and competency in nursing | Attitudes of staff and caring practices were also important | ||||
| 6. A scoping review and research synthesis on financing and regulating oral care in long-term care facilities;87 scoping review | How is oral health care for frail elders financed and regulated in LTCFs? | Scoping/realist review with stakeholder involvement | Different systems: financing systems for oral health care – public funding, insurance systems, managed care and contractual agreements | Access to oral health care in LTCFs | Inadequate regulation of oral health care in long-term care a reason for lack of provision |
| Uncertainty of treatment needs | |||||
| Despite government-sponsored incentives for dentists, very few dentists work with special populations | |||||
| Regulations | How dental services are financed and organised affects access to care | ||||
| Fee-for-service or salaried appointments | Portable dental equipment possible, but not liked by dentists | ||||
| Sixty-eight papers | Professional segregation between dentistry and medicine | MDS systems are not used to complete assessments of oral health and not prioritised by staff in long-term care |
All the included reviews highlighted the absence of agreement in the studies about outcomes and how these were defined (e.g. what is the difference between a discretionary hospitalisation and an avoidable hospitalisation?). How interventions in the different studies could be translated into improvements in resident-related outcomes, and particularly quality of life, were also either not considered in detail or discussed.
Findings on the prescribing of medication had similar findings. The reviews that focused on care home-specific service provision26 and topic-specific services such as palliative care,86,90 oral health care87 and prescribing of medication85 also confirmed what the review of surveys found, namely that health-care support and provision were erratic and access to care was often limited and constrained by funding and how limited resources were allocated.
Interventions were characterised by their heterogeneity of approach. For example, the multicomponent nature of palliative care and medication-related interventions often involved education of care home staff and structured and informal approaches to communication between clinicians and care home staff. This meant that it was unclear which elements of the intervention were essential to either supporting or triggering change in the observed outcomes. One review in its discussion of the evidence observed that ‘. . . none of the studies attempted to disentangle the “black box” effect, that is to understand the effects of the contributing components’. 85
Two reviews considered relatives’ and residents’ accounts/views of care. 26,89 Bradshaw et al. ’s89 review of residents’ and relatives’ accounts of what was important to them focused mainly on life within the care home and relationships with care home staff rather than the care provided by HCPs.
Although it is possible that residents do not differentiate between different professionals, their insights remain relevant. For example, residents identified continuity of care, and that nursing staff were technically competent and knowledgeable, as important. Interestingly, and relevant for the organisation of health care from outside the care home, the routines of the care home were also identified as important and the ability to be flexible in how and when care was scheduled. The review by Szczepura et al. 27 identified US work that established that high catheter use, poor skin care and residents’ low participation in organised activities are associated with negative outcomes for residents and that this was improved when staffing levels were higher and nurse turnover was lower. Bradshaw et al. 89 concluded that a key theme was how care was provided (summarised as caring practices) and that this was possibly predicated on the resource constraints such as lack of staff, availability of training and supervision, which was also suggested by Szczepura et al. ’s27 review. These are issues that link to how visiting health-care services work with care homes and whether or not they emphasise support and education of care home staff as some or part of their role and responsibilities. The review that focused on hospitalisations from nursing homes limited its scope to North American studies. 88 As already noted, this has implications for transferability to the UK setting. However, it did provide a useful overview of resident characteristics that are more or less likely to influence hospitalisations.
The majority of included studies could draw on large minimum data sets about residents’ characteristics and resource use. Resident numbers in the included studies ranged from 67 to 36,702, and, when included, from 1 to 527 nursing homes. The reviewers were able to identify with confidence the associations between age, particular conditions (e.g. pneumonia) and hospitalisations and raised some interesting questions about why residents with cognitive impairment had lower service use than those who were cognitively intact.
Summary
In summary, the review of surveys and the review of reviews provided a complementary and comprehensive commentary on the erratic provision of services to care homes. The lack of consensus on what needs to be in place to support care homes was compounded by limited evidence about how to measure effectiveness and whether certain approaches to providing health care were more or less effective or acceptable to care home residents and staff. The multicomponent nature of interventions and the impact of contextual factors such as local history, funding and staffing on outcomes were consistently highlighted. More recent work emphasised the lack of residents’ access to oral health and dentistry services.
The findings reinforced the value of taking a theory-driven approach to try and understand the multicomponent nature of provision, and the people, structures and organisations that (possibly) need to be in place for health-care provision to be effective. It provided a platform for a theory-driven review of the evidence and development of programme theories for testing in the case study phase.
Chapter 4 Realist synthesis
Introduction
The realist synthesis was undertaken to investigate what happens when different models of health-care delivery attempt to achieve improved outcomes for care home residents, and to develop a programme theory for further testing in the study. Specifically, the realist review addressed the second question of the project:
-
What features (mechanisms) of health service delivery models are the ‘active ingredients’ – defined as being associated with positive outcomes for care home residents?
Our previous findings from the review of surveys and review of reviews established the range and type of approaches to health-care provision and how outcomes were defined in the literature (see Figure 1). For the realist review we focused on research that yielded information on one or more of five outcomes for residents: medication use; use of out-of-hours services; hospital admissions, including emergency department attendances; length of hospital stay; and user satisfaction.
This chapter provides an account of the findings from the three stages of the synthesis. The review protocol30 and a detailed account of the stakeholder interviews from phase 191 are published elsewhere.
Stage 1 stakeholder involvement
Stakeholders were interviewed to explore their perspectives on health-care provision (Table 4). Twenty-one people were interviewed as representative of the views and experiences of care home organisations, residents, the regulator, and commissioners of health and social care for care homes. We were only able to interview three residents face to face. The resident data were therefore supplemented with a secondary data analysis (led by CV) of 34 residents’ interviews from an earlier care home study in which residents had been asked to discuss what they thought about the health care they received. 2
| Role | Number of stakeholders |
|---|---|
| Care home organisation owner/representatives | 7 |
| Residents’ representatives | 4 |
| CQC (regulator) | 4 |
| Commissioners of health and social care for care homes: CCGs (health) and local authority (social care) | 6 |
| Care home residents (34, secondary data analysis) | 37 |
| Total | 58 |
All the stakeholders were asked to consider what ‘good health-care provision’ might look like. The insights provided by participants drew on observations of good practice, hearsay and personal experience. There was a consensus that ‘the rule of thumb’ should be that residents have equivalent access to health care to those who live at home, specifically, access to a GP when needed. Stakeholders’ aspirations for health care were analysed and interpreted to identify their implicit theories of change, concerning how to implement evidence-based practice, manage risk in primary health care and achieve integrated working between health and social care. The following summarises what the different stakeholder groups highlighted as important.
Care home organisation owner and care home representatives
The narratives found in the care home managers’ and their representatives’ accounts stressed the importance of responsive access to care and services that reflected the residents’ needs. These views were supplemented by the frequently stated belief that services to care homes were rationed. This was attributed to ageism and a misunderstanding of the knowledge and skills of care home staff. ‘Good care’ was therefore characterised by both the frequency and the quality of contact with the GP and linked community services that the care home received:
‘Good’ means for me, for example, GPs who proactively go into care homes, who have good relationships with the staff, who have the proactive work but who are also prepared to be reactive, who might have good links to their general hospital as well so that they know when to admit and that they’re comprehensive in their approach to wider admitting. They communicate well with the staff at the care home as well.
Care home representative organisation stakeholder
Activities that supported continuity of the contact with health-care providers, mutual respect and shared opportunities for learning appeared to be key. This was seen as important in developing a common understanding of when and how to involve services if care home personnel were concerned about a resident’s health. Examples of such activities included joint training events and care home staff being consulted by NHS providers. Mutual confidence was built on previous experience of having resolved problems together. One care home manager described how residents’ needs were met and hospital admissions avoided because she knew that GPs would respond when asked, would listen to the home’s assessment of a resident’s needs and would support care home staff to provide care. Although the GP was identified as the linchpin, it was the quality of the association with the care home that was emphasised as crucial.
Residents’ and residents’ representatives’ accounts
Residents’ accounts presented them as being in the centre of a flow of HCPs (doctors, nurses, opticians, podiatrists, dentists), who all visited them at various times, perceived as ad hoc and unco-ordinated. Residents compared this experience with the service they had received while living at home. They felt that some provision was not available in the home, or that they now had to purchase it (e.g. podiatry and dentistry). They were unclear about the organisation of health care and did not understand the roles and responsibilities of visiting HCPs. The lack of a personal relationship with visiting health-care staff was also highlighted, for instance district nurses and GPs being too busy to talk or being task focused and not engaging with the resident.
Residents did identify the key role of care home staff in liaising on their behalf with care home staff, knowing their health-care needs and deciding when to refer to a GP. One resident with a leg wound saw that her needs were secondary to the needs of other, possibly more unwell, residents. She described a protracted process of decision-making as increasingly senior staff decided if a HCP should be called:
Well that I don’t know. I just feel I’m on a sort of, waiting, I’m not as ill as a lot of people so I think I’m just left to tick over . . . this morning, I was seeing the senior nurse who comes with the others [care staff] and tell her and she’s had a look and she’s going to be in touch, get in touch with somebody else who is higher up still, who is going to look at it this afternoon.
Resident 14
Residents were also aware that care home staff may not be trained adequately to undertake the assessment and monitoring role expected of them by residents; this created some uncertainty. This point was emphasised by a stakeholder from a resident representative organisation who linked it to the need for specialist input into care homes:
People are very worried about post-stroke patients not having the kind of rehab [rehabilitation] they’d get if they were at home or staying longer in hospital . . . It’s not just GPs, think about dental care . . . You know, you really need people like geriatricians who are specialist in the care of older people . . . the people who specialise in old age psychiatry also need to have a key role . . . there needs to be an all-round service plan.
Stakeholder SH11
Commissioners’ accounts
Commissioners recognised that many of the challenges surrounding health care for care homes came down to efficient integration of health and social care. Negotiations about what provision should be publicly funded as health care and what should come under the jurisdiction of the care home were a significant preoccupation. It could be a ‘juggling act’, having to reconcile the different priorities of care homes and health-care providers. Commissioners saw their priority as purchasing activities likely to reduce demands on hospital services; specifically, opportunities for health care and care home staff to work together. They saw the objective as pre-empting crises and reducing misuse of secondary services such as A&E, which could arise because of a lack of confidence or clinical knowledge in care home staff. Typical activities to achieve this end included financial incentives for GPs, which could be applied to more frequent visits to work more closely with care home staff, the creation of Care Home Specialist roles or the servicing of existing working relationships. One GP commissioner, drawing on personal experience, said that it was possible to maintain continuity and the desired outcomes of care if there was a specific key worker in the care home for NHS staff to liaise with. Similarly, a local authority commissioner identified the importance of nominated care home staff (‘champions’) being allocated to work with visiting NHS staff. This was considered to structure their working together, which was often needed in situations of pressure and limited resources:
It’s getting the right people from these particular homes to have that spare time to come along and get involved . . . It’s having champions; it’s making sure that each home has their particular champion on particular (health) topics and they’ve got ownership of that particular subject.
Local Authority Commissioner – Stakeholder SH5
Commissioners also emphasised the importance of audit and review of health-care service delivery to care homes. Although internal quality assurance is undertaken by commissioners, independent audit is the role of the CQC, as the regulator.
The accounts of the regulator
Regulator representatives, with responsibilities for regulation of services, highlighted the use of incentives or performance management as a means to support residents’ access to health care. They characterised good health care as evidence based and age appropriate, as well as being continuous in terms of the relationships between residents and visiting professionals. In keeping with the role of the CQC inspectorate, interviewees highlighted the consideration of untoward incidents and suboptimal care. Examples of elder abuse, avoidable deaths, high rates of pressure sores and unnecessary antipsychotic prescribing were given as the reasons why monitoring needed to be in place. One stakeholder acknowledged the importance of good GP–care home relationships, but saw that these need to be underwritten by explicit agreements and what was characterised as a ‘proper’ system of care:
It’s where they’ve got a proper agreed arrangement with that GP surgery around, you know, they visit at certain times of the week and they can be contacted if there are any problems. Ensuring then that people have a properly planned package of care that is really focused on their needs.
Stakeholder SH13
Inferences from interviews
Stakeholders placed different emphases on what was contextual and what was seen as essential to the achievement of effective health care for care home residents. They had different implicit theories about why they thought that practitioners responded to various approaches used. These conceptual frameworks informed how effective models of service delivery were described. They therefore shaped our first reading of the literature and how we elaborated ideas about CMO configurations for further review.
Scoping of the literature
In parallel to the interviews reported above, we completed an initial scoping of the literature. This added to the findings from the review of surveys and the review of reviews.
The database searches initially considered care home-wide interventions and then topic-led interventions that were linked to one or more of the five outcomes. This generated 556 records. Following screening and de-duplication, 64 full-text articles were assessed (see Appendix 9 for a table of included studies by design and focus). These papers were read by Sue L Davies, Melanie Handley, Maria Zubair and Claire Goodman and grouped by their study design, topic, approach and outcomes. A realist approach to inclusion of evidence and data extraction recognises that within one document different types of data can illuminate or build one theory, refute another or offer an alternative interpretation. This guided the selection (for inclusion or exclusion) and appraisal of the contribution of pieces of data within a document. Quality was assessed based on the level of detail the paper provided; specifically, the amount of information provided about the intervention and participants’ responses, acknowledgement of the underlying theories or assumptions guiding the study and discussion of what the findings revealed about health care and care home staff working together. Quality of the research design and method were assessed on the basis of rigour and clarity. Although we did not apply a hierarchy of evidence, descriptive accounts that focused on achievement or innovation, but provided minimal information about the process, were excluded. Evidence that came from professional opinion (e.g. blogs or commentaries or detailed accounts of an innovation) was treated as ‘special cases’ to be discussed at team meetings.
Within-team discussion and preliminary mapping of the scoping results focused on what the studies revealed about different possible CMO configurations. For example, discussions focused on the significance of how the organisation and make-up of multidisciplinary teams (MDTs) or single disciplinary groups working with care home teams and their patterns of contact were associated with learning opportunity uptake by care home staff. We also explored how shared protocols were introduced into care homes and who was involved in their implementation; what kind of feedback on HCPs’ performance was thought to lead to change in visiting professionals’ responses; the use of sanctions and financial incentives; and which groups of practitioners were expected to implement change. (Note that these searches were rerun and a more detailed data extraction completed for the detailed review of the evidence.)
In light of the stakeholder interviews, the scoping of the literature, review of surveys and review of reviews, we developed six statements. These were drafted to seek to capture the possible explanations for what needs to be in place for the provision of health care to care home residents and rewritten as ‘if then’ statements as the basis for refinement into potential programme theories for consideration by the SSC. Our purpose was to test each statement’s plausibility and ultimately to guide the in-depth evidence review of how health-care services to care homes improved the health of residents and use of services.
The following statements posited that health outcomes for care home residents could be improved under certain conditions.
-
If tailored education and support for care home staff are provided by clinical experts and supported by the use of structured documentation and protocols then resident outcomes will be improved. This will come about through prioritising specific assessment/care activities that trigger changes in how residents’ care is planned, and in how care home staff recognise and frame their need for training and support from visiting clinicians.
-
If contracts and financial incentives are provided to GPs to provide dedicated services to care homes and monitored against prespecified process and outcome measures, then the pattern and frequency of GP contact with residents and staff will change. This will come about through increasing the time and opportunities for screening and review of care, and enhancing staff confidence that they can access a GP. This will reduce demand on emergency and secondary care services.
-
If formalised recognition and ongoing facilitated support are provided to care home staff to equip them to build relationships and work with health service providers, this will increase their confidence when working with visiting HCPs and enable them to identify priorities for residents’ health care with visiting HCPs. This will come about through enhancing and validating the expertise of care home staff. It will reduce demand on emergency and secondary care services.
-
If care home champions are appointed, who have expertise in quality of care for older people and designated responsibility to work with care homes then they will facilitate continuity of support to the care home staff workforce. This will come about through their promotion of knowledge exchange and encouragement of skills acquisition by care home staff. The result will be that staff are more proactive in providing age-appropriate health care to residents.
-
If the commissioning and provision of services focuses on specific problems of old age and reflects the health-care needs frequently experienced by care home residents (e.g. falls prevention, end-of-life care, continence management) then the focus of services will shift to a more individualised pattern of care. As a result the health care provided will be perceived by residents as equivalent to that which they received living in their own homes.
-
If there is investment in the creation of interorganisational and intersectoral networks at the organisational level; between health and social care providers in the public and private sectors, then this will change how different services work together. It will come about through highlighting gaps and overlaps in service provision. It will trigger conversations and planning between services about resource use and who is responsible for providing health care. As a result, provision will become more efficient.
Further presentation and discussion within the team and the study steering group focused on areas of overlap and fit with their experience of health-care provision to care homes. This generated three broad programme areas from which the team then developed possible CMO configurations for rigorous testing in the detailed review of the evidence:
-
system change and cross-organisational working between care home and visiting health-care staff
-
age-appropriate care accessed by older people resident in long-term care
-
relational approaches to promote integrated working between visiting health-care and care home staff that emphasise interpersonal skills and shared decision-making.
The search strategy and derived theories are shown in Figure 2. The three programme areas are now discussed in turn.
FIGURE 2.
Search strategy for stages 1 and 2 of the realist review. ASSIA, Applied Social Sciences Index and Abstracts; CINAHL, Cumulative Index to Nursing and Allied Health Literature; CRN, Clinical Research Network; DARE, Database of Abstracts of Reviews of Effects; DeNDRoN, Dementia and Neurodegenerative Diseases Research Network; HTA, Health Technology Assessment; NHS EED, NHS Economic Evaluation Database; NIHR, National Institute for Health Research; Soc Abs, Sociological Abstracts.
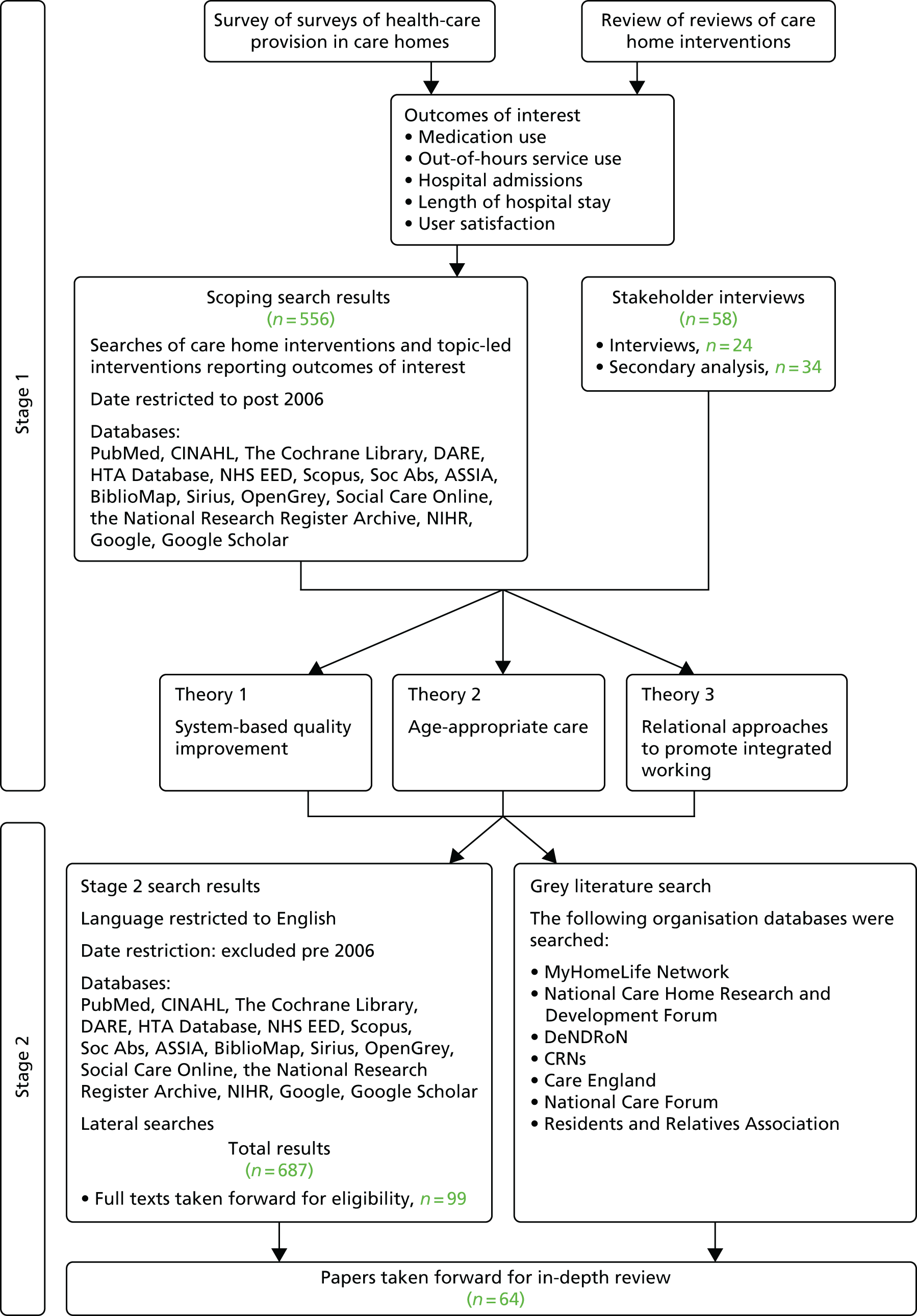
System-based quality improvement mechanisms to improve health-care outcomes: the use of incentives, sanctions and targets
The assumptions underlying system-based incentives, targets and sanctions are that they prompt behavioural change through targeting particular professional groups or organisations, focusing on the improvement of specific processes or outcomes, and thereby improve quality of care and reduce inequity of provision. 92 The Quality and Outcomes Framework (QOF), introduced for GPs in England in 2003, linked financial incentives to the quality of care that is provided by practices93 and has been described as a lever to reduce health inequalities and reinforce evidence-based practice. 94
Based on the different theoretical perspectives about how system-based approaches might work to improve one or more of the five outcomes we posited a possible CMO configuration to test and refine the evidence reviewed on the use of incentives, sanctions and targets (Box 3); it made explicit how we understood the intervention.
There is intermittent and unpredictable contact by GPs visiting residents in care homes; encounters with primary care are usually unplanned and in response to an urgent need and this affects the proactive identification of residents’ health-care needs, access to, and quality of, care and frequency of acute episodes of ill health.
ContextGPs are provided with a range of incentives and admonitions (intervention) to visit regularly (context) and undertake structured resident assessments (context) in key areas of care (context) (e.g. medication review) and to provide the care home with support and advice in addition to individual patient visits.
MechanismsGPs are motivated to engage with the care home staff. The incentives and sanctions prompt them to be more present in the care homes, complete reviews of care home residents and work with care home staff to plan care and identify residents in need of additional support and care.
OutcomesBoth care home staff and primary care professionals are more confident and satisfied working with each other. Residents have access to services required. There are improvements in care, specifically medication management and reduced use of out-of-hours emergency services and avoidable secondary care.
For GPs working with care homes, rewards linked to particular clinical activities are used as incentives to define and increase the length and frequency of their visits in order to achieve the desired outcomes of continuity of contact and proactive approaches to patient care95 together with improved medication management. 85 The literature suggests that additional payments to GPs and pharmacists to do specific activities can improve monitoring of medication use. 96 However, the use of payments or sanctions alone to trigger GP involvement in resident assessment and review did not appear to be sufficient. 94,95,97
Three additional contextual factors were identified from the evidence reviewed: the need for an accountability structure; the need to identify the named professional responsible for delivering a specified intervention; and care home-sensitive protocols that addressed the high number of residents living with dementia. 98–100 The need to consider those residents at particular risk and also care home staff needs for ongoing support and training were also flagged as important.
Generally, the literature would appear to support the view that, although incentives can improve the process of care and productivity (e.g. better adherence to protocols and care pathways), the evidence is limited about their impact on patient outcomes. 96,101 Charlesworth et al. 96 argued that:
Incentive schemes can only work if the organisations and clinicians whose behaviour they are trying to change understand what is required [our emphasis]. Too often, the incentives are blurred or inconsistent. In part, this is a result of the complexity of the current system.
Charlesworth et al. ,96 p. 14
The main pay-for-performance approach in UK primary care (QOF) allows practices to exclude patients for reasons such as extreme frailty or evidence of decline. Moreover, individuals with dementia in care homes achieve lower quality indicators in the QOF pay-for-performance system than their community-dwelling counterparts. 100 This arguably creates an implicit expectation that QOF incentives are less relevant to care homes. 100 Indeed, as QOF indicators focus on very specific aspects of disease management, care home residents as a discrete population may not be recognised by GPs as a priority group in need of identification and active management. Therefore payments alone may not be sufficient to motivate GPs to make care home residents a priority, nor to address issues of accessibility, appropriateness or system co-ordination. 102 Incentives work when they are aligned with what GPs believe they should be doing. The mechanism is encouragement to practice what they already recognise as doctors’ work:
They [incentives] work best when all the ducks are lined up in a row: financial, organisational, and professional incentives, then the incentives are providing encouragement [our emphasis] to do the things that doctors believe they should be doing anyway.
Roland103
One small study focused on early identification and support of frail older people and the implementation of anticipatory care. It audited cases of residents’ admissions to hospital as a trigger to identify and discuss with GPs the factors influencing hospital admissions from care homes. As a result of the discussion, the authors reported a change in GP behaviour, with an increase in care home visit rates and a reduction in overall hospital admissions. 97 However, audit and review of residents admitted to hospital had no impact on the numbers of hospital admissions sought by care home staff. The authors suggested that care home staff needed greater support from visiting HCPs and involvement in anticipatory planning for residents at risk of hospital admission – particularly where there was no on-site nursing provision. This was the only study we found that explored, and reported how, the mechanism of providing feedback on GP performance could influence how GPs worked with care homes.
Other studies suggested that formal notification to GPs of the need to improve care or guidance on good practice (prescribing) did not provoke change. 104,105 A possible explanation is that feedback on medication management does not have the same impact as alerts about unplanned hospital admissions that are recognised as avoidable and costly. The urgency of the issue to the health service, as opposed to its impact on individual residents or care homes, may be the contextual factor that influences when audit and feedback mechanisms trigger increased engagement with care homes by NHS services.
We found no evidence that targeted payments alone were a trigger to change practitioner behaviour or proactive assessment of care home residents’ health-care and medication needs. One US study found that financial payments, when paid directly to care homes rather than to HCPs, improved resident outcomes, but this was for specific projects identified by care home staff. The incentive was to introduce new approaches to care, not to ensure that health care was provided. 106
Age-appropriate care accessed by older people resident in long-term care
There is evidence that systematic approaches to the assessment and management of older people can reduce mortality and improve function. 107–109 These interventions rely on the involvement of clinicians with expertise in the care of frail older people and their ability to work with others to implement care plans (Box 4).
Care homes have unpredictable access to health-care services, the majority of staff are not clinically qualified and residents are frail and in the last years of life with complex health and social care needs.
ContextExperts in care of older people (intervention) visit care homes regularly (context) to compensate for known deficits in knowledge and skills (context) and facilitate (context) in-house learning and review.
MechanismsCare home staff feel supported and trained in how to recognise and manage symptoms and provide care to frail older people. They are motivated to consult with visiting HCPs and learn new skills because of the facilitation and ongoing expert support they receive.
OutcomesCare home staff are more confident and skilled in looking after care home residents and specific areas of care. Residents’ function is improved or maintained. Staff have higher levels of job satisfaction. Care homes are less likely to use emergency and out-of-hours services for residents’ symptoms that are non-urgent.
An increasing body of work has developed interventions for care home residents that have focused on specific processes such as assessment, targeted interventions and protocol-based care. Objectives include comprehensive assessment,110 depression,111–113 dementia,114 falls prevention,115 nutrition,39,116–118 recovery from stroke,119 medication management,120 end-of-life care,121–123 tissue viability,124 oral hygiene125 and occupational therapy. 126,127 Most of these interventions were multicomponent, but had in common the detailed assessment of residents’ functional abilities and the teaching of new skills to care home staff to improve residents’ health and well-being.
Most, but not all, interventions were appreciated by care home staff, often with reports of increased staff confidence that could have acted as a feedback loop and a potential additional mechanism to influence the improvement of residents’ health. However, the positive response of staff was as likely to have been a reflection of care home staff’s previously limited experience of professional support and encouragement. This arguably suggests that the mechanism that triggered a change in staff (or not) was the process of working together and receiving clinical support. The underlying assumption of many of the studies was that the allocation of professional (biomedical) expertise, education and training of staff, together with proactive identification of people at risk, would lead to improved health outcomes. Overall, this assumption was not supported. Our inference is that these were important contextual factors necessary for change, but not the key mechanisms that provided the generative force to alter resident outcomes.
Several contextual factors have been suggested that may inhibit care homes and/or residents’ ability to engage with interventions, but these remain largely untested. Putative factors include care home size and ownership, staff turnover, percentage of residents who have been resident in the care home for less than 12 months, and the absence of additional triggers or mechanisms such as the involvement of care home leadership, staff qualifications and the duration of programmes. 113 Two studies on end-of-life training programmes found that the manager’s length of employment was positively associated with use of advanced care planning documentation, improved staff satisfaction and reduced hospital deaths. Low staff turnover was also implicated as an important contextual factor. 121,128
One study with a positive outcome appears to have been successful because of particular contextual factors. The key differences between the intervention process described in this study and that of the others reviewed was that it was a single, time-specific intervention that could be co-ordinated by one member of staff per care home. It was a simple intervention with a quantifiable outcome in which the proposed health benefits to both staff and residents were clear for staff and residents. 129 Researchers129 tested the effectiveness of an influenza vaccine programme for care home staff (not residents) to prevent death, morbidity and health service use. The mechanisms of interest within the programme were the identification of a key link worker within the care home and the development of tailored processes to encourage vaccination uptake by care home staff. These were supported by a care home policy for immunisation. It achieved significantly lower mortality of residents in intervention homes than that of residents in control homes. An expert practitioner appeared to be important as a resource that enabled the link worker in the care home to implement the immunisation process that generated the positive outcomes.
Relational approaches to promote integrated working between visiting health-care professionals and care home staff that emphasise interpersonal skills and shared decision-making
The competing priorities of health and social care staff, inherent power imbalances between qualified and unqualified staff, staff turnover and the difficulties HCPs have in understanding the predominantly private care home environment are well-documented barriers to effective collaboration between visiting HCPs and care home staff. 15,84,118,130,131 Relational working draws on theories that emphasise strategies that co-ordinate and support shared problem-solving (and not blaming). Working relationships are grounded in common goals, shared knowledge and mutual respect. 132–134 In the extraction of data in this stage of the review, relational working was characterised as those activities and processes that emphasise shared decision-making, planning and learning, and continuity of contact between staff from different sectors (Box 5).
The expertise of care home staff in providing care for older people with frailty and/or dementia is seldom recognised by visiting HCPs. Health-care interventions, emphasising physical health, do not fit well with care home priorities of providing a homely setting and working practices that seek to balance positive risk-taking with patient safety. Working patterns to facilitate in-reach from numerous health professionals are difficult to accommodate by care home staff with limited resources who want to achieve a more personalised environment for residents.
ContextModels of care (interventions) that introduce opportunities for joint priority setting between care home and NHS personnel (context) and processes that support ongoing discussion and review of residents’ health-care needs between care homes and visiting HCPs (context).
MechanismsIdentification of key personnel in the care home to work with visiting HCPs triggers a response whereby staff are motivated to develop shared priorities for care and a sense of common purpose because their views are valued. They develop approaches that fit with the care home working patterns and incorporate care home staff knowledge. Priorities are jointly agreed, enacted and reviewed.
OutcomesCare home staff and visiting HCPs are motivated to work together and improve care for residents in agreed areas of practice. Residents’ function is improved or maintained, staff experience job satisfaction and the care homes are less likely to use emergency and out-of-hours services.
The organisation of care between the resident, their relatives, care home staff and visiting HCPs requires more than the one-on-one encounter between clinician and patient. It is a negotiated process over time, within a changing environment. Over time, there may be individual and organisational changes in who has responsibility for providing and/or paying for care, and changes in the arrangements for commissioning health and social elements of care. Roles and responsibilities for a resident’s care can shift as a consequence of an acute health event and/or a gradual shift in need from ‘social’ to ‘health’ care as complex long-term conditions progress, and/or as part of a transition to end-of-life care. 5,135 Three contextual factors reflecting aspects of relational working were identified as important for triggering activities and processes that were likely to lead to improved outcomes. These were important whether or not the intervention being reported had an explicit focus on working with care homes collaboratively. They were (1) the active involvement of care staff in implementing an initiative; (2) a nominated link person; and (3) some flexibility in how an initiative could be implemented.
Most of the health-care interventions reviewed were multicomponent (e.g. completion of education and training programmes, improved documentation of residents’ care). These were more likely to have positive uptake and promising outcomes when they focused on a concern of mutual interest to care home and health-care staff and/or residents and family, for example end-of-life care that avoided unplanned hospital admissions and enabled the person to die in the care home fitted with care home staff views that they were the person’s proxy family. The care home was the person’s home, and being with strangers (hospital staff) at the end of life was distressing for residents. 26,122
Where the initiative was identified as a priority, based on a review of resident need, but not recognised by staff as such (particularly where it added to their workload) it was unlikely to be implemented or sustained. 113,136 As one informant concerning a study that introduced a therapy-led intervention to reduce depression observed:
At times it was difficult to explain our remit to staff. We had little time to change attitudes of some staff to issues of mobility; making it hard to facilitate a change in practice.
Ellard et al. ,113 p. 4
This relates to who the HCPs worked with and their role in care delivery. Having a nominated link person in the care home, particularly when this person could play a collaborative role in reviewing, planning and supporting care, was helpful. 129
There was evidence of improved outcomes where care home staff had flexibility in how an intervention was implemented. 104,129,137 This was particularly the case when there was access to expert facilitation and support. Emphasis on preparatory work, structured assessment of a care home’s readiness to participate, collaborative and bottom-up approaches, shared learning and the development of a common understanding between care home staff and health-care providers were key mechanisms for improvement and involvement of care home staff in the intervention. 124,131,138 In one study this involved developing an intervention with care home managers that built on previous staff learning in end-of-life care, it was an iterative and reflective process that involved day and night staff and sought to address care home-specific issues such as supporting people with dementia:
We think this success (reduction in hospital deaths, improvement in quality of life for residents with dementia) is related to the training addressing staff fears and problems [our emphasis] as well as increasing knowledge.
Livingston et al. ,121 p. 1587
The involvement of care home staff, particularly senior staff, and other psychological and contextual factors that could be characterised collectively as a care home’s readiness for change had a positive impact on the uptake of innovation. 118,139 Bamford et al. 118 found that, while some changes could be achieved in staff understanding of nutrition, the implementation of nutrition guidelines in care homes foundered because:
It proved difficult to build collective understanding of and commitment to the study resulting in inconsistent implementation . . . Managers’ commitment to the nutrition guidelines did not extend to using scarce resources to facilitate implementation.
Bamford et al. ,118 p. 10
This finding was resonant with multiple references in the reviewed texts to the probable influence of the leadership and culture of particular care homes on health-care outcomes and staff satisfaction.
The literature on the attachment of a given GP practice to a care home did not support the goal of improved working relationships and resident outcomes. In fact there was evidence that such a system did not in practice lead to continuity of support. It could have the unintended consequence of rationing care because GPs set regular, but fixed, times for their availability. 2 There was also evidence that one-practice-per-home arrangements could effectively trap providers in dysfunctional relationships, providing an adverse context for appropriate health-care delivery. 5 Ongoing support from a clinician or team with relevant expertise was nevertheless important, depending on how this was delivered. Where the facilitator or lead clinician was able to be present and responsive to the needs of particular residents as they arose, and to engage staff in action learning that focused on issues of interest to them, there were higher levels of staff engagement and fidelity with training26,104,137,140,141 than in interventions where the clinician input was episodic or task focused. 116,120,137,142 The mechanism identified here was one in which the HCP worked with staff as the ‘bridge’ to connect between interventions to improve health care of residents over time in a way that could be incorporated into existing patterns of working.
Discussion
The realist synthesis in phase 1 has identified recurring themes and emergent patterns or demi-regularities that underline the importance of how HCPs introduce and provide health-care support to care homes. The way in which they work with care home staff, residents and their families, and the duration of this relational working, appear to be important, regardless of the specific health issue targeted.
Broad mechanisms within a programme that can help deliver appropriate health care to care home residents are those activities that ensure that an intervention is specific to the care home, aligning with the goals and priorities of care home staff. They should not be adapted from other care settings and patient groups, but from the outset they should focus on activities that aim to build relationships between care home staff and visiting HCPs. Contextual elements that shape the achievement of these outcomes and help to sustain participation have been identified as:
-
care home readiness to work with health-care staff (e.g. care home leadership and previous history of collaboration)
-
availability of structured assessment and care plans
-
involvement of a HCP to support change and reinforce learning
-
organisational endorsement
-
financial remuneration
-
staff incentives.
This is consistent with what is known generally about integrated working. 143
From the evidence reviewed the relevance and usefulness of the health-care interventions – and, ultimately, their impact – were diminished in situations in which there was either little evidence of prior collaborations or failure to engage in a period of exploration and preparation that could shape how HCPs and care home staff could work together. It highlights the levels (structural, service and personal) at which care homes and the NHS have to work together to achieve the desired outcomes.
Interventions alter context, that is, they attempt to change the care home environment so that the correct mechanisms are ‘triggered’ to generate the desired outcome. Interventions do not in themselves have causal powers. When care home and visiting NHS staff believed that they were working together and that there was ‘common ground’, change was more likely to occur. An example of this was interventions that introduced new knowledge by linking it with existing ways of working, using care planning and ongoing conversations to find a way to reconcile the innovation with competing priorities in the care home. This was achieved by connecting new knowledge with existing practice and knowledge, using processes such as care planning and ongoing conversations to reconcile competing priorities in the care home.
These findings resonate with international studies on the implementation of evidence-based care in residential care facilities and on working with care home staff to improve residents’ well-being. 144,145 A review on the use of advanced care planning that included care homes146 argued that no amount of facilitation or structured tools is sufficient to reduce the effects of those things that undermine them. Interventions that were feasible to be delivered within time-pressured environments, the mechanisms of which support dialogue, experimentation and collaboration, and allow the system to evolve and self-organise over time, were most likely to be effective. Financial incentives or sanctions, agreed protocols, continuity of contact and evidence-based approaches to assessment and care planning provided the necessary equipment or resources to enable those mechanisms to achieve improved resident and staff outcomes.
Conclusion
We drew together a disparate literature on care home residents’ access to health care. The interpretation of the possible CMO configurations was constrained by the lack of detail of the processes at work in the various interventions and by studies’ focus on staff satisfaction and confidence, rather than resident priorities, observed changes in practice or measurable changes in resident outcomes.
Previous review and survey work has demonstrated the complexity of the setting, the paucity of evidence and the shortcomings and inadequacies of either care home providers or health-care providers. 4,5 In realist terms, even when the desired outcomes are not achieved there is an opportunity to learn from the evidence and develop a theoretical understanding of what needs to be in place.
This conceptual model for further development in phase 2 proposes that interventions (regardless of their use of sanctions and incentives, specialist practitioners or care home-specific resources) are more likely to achieve the outcomes of interest when they trigger the engagement of care home staff from the outset and create opportunities for health-care and care home staff to work together and structure the intervention to fit with the priorities and working practices of the care home. This principle became the basis for the identification and selection of the case study sites in phase 2 and further refinement of the proposed programme theory of how and why NHS services work with care homes to achieve the five outcomes of interest.
Chapter 5 Phase 2 case studies: comparative description of the study sites
Introduction
Together, Chapters 5, 6 and 7 provide the basis for the development of an explanatory account of how NHS support to care homes works, for whom, in what circumstances and with what outcomes. This addresses research questions 3–5:
-
How are the features/mechanisms (as identified in phase 1 of the research) associated with key outcomes, including medication use; use of out-of-hours services; resident, carer and staff satisfaction; unplanned hospital admissions (including A&E); and length of hospital stay?
-
How are these features/mechanisms associated with costs of care from a NHS perspective?
-
What configuration of these features/mechanisms would be recommended to promote continuity of care at a reasonable cost for older people resident in care homes?
Chapter 5 summarises recruitment of care homes to the study and provides a detailed description of the phase 2 case studies on a site-by-site basis. It provides a within- and cross-case narrative of NHS provision to care homes that focuses on the different activities and responses that related to the areas of interest identified in phase 1, namely how the services were provided and received, and how they were thought to work. This provides the necessary detail to be able to understand how service models influenced the outcomes of interest, which is discussed in greater detail in Chapter 6.
Details of the protocol are published elsewhere. 56 The chapter is divided into two sections. The first section describes the case study sites, recruitment and participant details. The second section describes the services provided at each study site in greater detail.
Case study sites, recruitment and participant details
Study sites 1, 2 and 3 covered three geographically discrete areas in England comprising an inner area of a major city, a suburban area and a coastal area, respectively (Table 5). Sites 1 and 2 were each located within a single CCG area, but in site 3 recruitment was based on a county and around care homes’ engagement with the MyHomeLife leadership and management programme (see Chapter 2).
| Site | Characteristic | ||||||
|---|---|---|---|---|---|---|---|
| Population | Life expectancy (years): female (England, 82.8) | Aged > 85 years, % (England, 2.3) | Dementia prevalence (England, 4.27) | Nursing home patients, % (0.5) | Number of care homes | Number of GP practices | |
| 1 | 342,000 | 81.2 | 1.6 | 5.35 | 0.2 | 83 | 59 |
| 2 | 580,000 | 83.2 | 2.3 | 5.62 | 0.5 | 92 | 60 |
| 3a | 885,255 | 83.2 | 2.8 | 3.83 | 0.5 | 49 | 117 |
Seventy-two care homes were contacted across the three sites. Care home recruitment is summarised in Table 5. Care homes in site 1 were recruited first, in accordance with the purposive sampling framework outlined in Chapter 2. Following the confirmation of care homes in site 1, care homes with similar characteristics in terms of size, ownership and registration were identified in the other two sites. Care homes in site 2 were eligible if they were included in the site’s GP care home scheme that reimbursed specific practices to work with designated care homes. Care homes in site 3 were eligible if they participated in the local MyHomeLife network. For each site, the e-mail or letter invitation was followed by a telephone call and then a face-to-face meeting. After this, managers could express an interest in participating in the study. This process is outlined in Table 6 while the factors that facilitated and inhibited care home recruitment are given in Table 7.
| Site | Number of care homes contacted | Number of face-to-face meetings with managers | Number of care homes interested | Total number of care homes recruited | Time to recruit care homes (months) |
|---|---|---|---|---|---|
| 1 | 8 | 6 | 5 | 4 | 4 |
| 2 | 15 | 6 | 5 | 4 | 4 |
| 3 | 49 | 6 | 5 | 4 | 4 |
| Factors | |
|---|---|
| Facilitating care home recruitment | Inhibiting care home recruitment |
|
|
At all three sites the managers who had confirmed their intention to participate signed an agreement outlining their commitment to the study and their understanding of what taking part involved, and nominated two staff members to take on the role of care home link staff members with the OPTIMAL study.
The characteristics of the individual care homes and a summary of the services accessed by all the residents in the care homes at baseline are summarised in Tables 8 and 9.
| Care home ID | Short ID | Care home characteristic | |||
|---|---|---|---|---|---|
| Description | Number of rooms, n | Type of beds | Special registration | ||
| Site 1, care home 1 | S1CH1 | City; privately owned; converted house; single care home provider | Single rooms, 19 | Residential | Old age and dementia |
| Site 1, care home 2 | S1CH2 | City; not for profit; purpose-built two units across two floors | Single rooms, 62 | Residential | Dementia, old age and physical disability |
| Site 1, care home 3 | S1CH3 | City; privately owned; purpose built | Single rooms, 77 | Dual registered; 47 residential; 30 nursing | Old age and dementia |
| Site 1, care home 4 | S1CH4 | City; privately owned; purpose built | Single rooms, 40 | Residential | Old age and dementia |
| Site 2, care home 1 | S2CH1 | Town; privately owned; converted house | Single rooms, 19 | Residential | Old age and dementia |
| Site 2, care home 2 | S2CH2 | Town; not for profit; purpose built on two floors, split into separate units | Single rooms, 51 | Residential | Old age and dementia |
| Site 2, care home 3 | S2CH3 | Town; not for profit; purpose built on two floors and split into five different units | Single rooms, 60 | Residential | Old age, dementia and physical disability |
| Site 2, care home 4 | S2CH4 | Town; not for profit; modern, purpose built on two floors split into five separate units, three of which took part in the study | Single rooms, 93 | Nursing | Old age, dementia and physical disability |
| Site 3, care home 1 | S3CH1 | Town; for profit; large corporate provider; modern, purpose built on two floors split into two units | Single beds, 50 | Residential | Old age and dementia |
| Site 3, care home 2 | S3CH2 | Town; for profit; small chain provider; converted house | Rooms, 20 (18 single and two shared) | Residential | Old age and dementia |
| Site 3, care home 3 | S3CH3 | Town; for profit; small chain provider; converted house | Rooms, 34 | Residential | Old age and dementia |
| Site 3, care home 4 | S3CH4 | Town; for profit; privately owned; converted house | Rooms, 51 (50 single and one shared) | Dual registered, nursing and residential | Old age, dementia, physical disability, mental health and sensory impairment |
| Care home | Service | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DN | CHNP | SW | OOH | DOT | PT | OT | Falls team | TVN | CPN | CNS | DNS | PCN | PDNS | ACNS | Geriatrician | Dietitian | Chiropody | Optician | Dentist | Psychiatrist | Psychologist | Audiology | SALT | Phleb | |
| S1CH1 | +++ | +++ | +++ | ++ | ++ | – | – | +++ | ++ | ++ | ++ | ++ | ++ | – | – | ++ | ++ | ++ | ++a | ++a | – | – | – | – | ++ |
| S1CH2 | +++ | +++ | +++ | ++ | +++ | – | – | +++ | ++ | ++ | +++ | ++ | ++ | ++ | + | + | ++ | +++ | +++ | +a | ++ | + | + | ++ | + |
| S1CH3 | +++ | ++ | +++ | ++ | +++ | – | – | ++ | ++ | ++ | +++ | ++ | +++ | – | ++ | ++ | +++ | +++a | ++ | ++ | ++ | ++ | – | +++ | ++ |
| S1CH4 | +++ | ++ | +++ | +++ | +++ | – | – | +++ | ++ | ++ | +++ | ++ | – | – | ++ | – | +++ | +++a | +++a | +++ | ++ | – | – | +++ | +++ |
| S2CH1 | +++ | – | – | ++ | ++ | ++ | ++ | – | – | ++ | – | – | ++ | – | – | – | – | ++a | ++ | ++ | – | – | – | – | ++ |
| S2CH2 | +++ | – | – | ++ | ++ | ++ | ++ | ++ | – | ++ | ++ | – | ++ | – | – | – | ++ | ++ | ++ | ++ | – | – | – | ++ | – |
| S2CH3 | +++ | – | – | ++ | ++ | ++ | ++ | ++ | – | ++ | ++ | – | – | – | – | – | ++ | ++ | ++ | ++ | – | – | – | ++ | ++ |
| S2CH4 | – | – | – | ++ | ++ | ++ | ++ | – | ++ | ++ | – | – | ++ | – | – | – | – | ++ | ++ | ++ | – | – | – | – | – |
| S3CH1 | ++ | +++ | – | ++ | ++ | ++ | ++ | ++ | – | ++ | ++ | ++ | ++ | – | – | – | ++ | ++ | ++ | – | – | – | – | ++ | ++ |
| S3CH2 | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | – | ++ | ++ | – | – | – | – | – | ++ | ++ | ++ | ++ | – | – | – | ++ | – |
| S3CH3 | ++ | – | – | ++ | ++ | ++ | ++ | ++ | – | ++ | ++ | ++ | – | – | – | – | – | ++ | ++ | ++ | – | – | – | ++ | ++ |
| S3CH4 | +/– | – | – | ++ | ++ | – | ++ | – | ++ | ++ | ++ | – | ++ | ++ | – | – | ++ | ++a | – | ++ | – | – | – | ++ | – |
Changes in service provision and care home-specific changes across the study
The study took place against a recent backdrop of the reorganisation of primary care trusts into CCGs. In sites 1 and 2, the majority of NHS services were provided by a single trust, apart from mental health services. In site 3, most services were provided by a single trust, apart from mental health services and dietetics, even though the services were commissioned through three separate CCGs. In site 2, complex care payments were beginning to be introduced for particular residents with multiple comorbidities linked to staff having completed a specific training programme. This had not been implemented in the study care homes by the close of the study.
There were some changes in how services were structured over the course of the case studies. In site 2, personalised care plans were introduced by GPs for residents in three of the care homes. In site 3, there was a 6-month pilot study for a small number of GP practices to hold monthly clinics in care homes to review residents’ health and medication that involved care homes 2 and 3. The other care home in site 3 witnessed an increased tendency for specialist nurses to substitute for GP visits over the course of the study as locums replaced regular GPs who had retired from the practice, or who were on sick or maternity leave. Domiciliary dental services were withdrawn from two care homes in both sites 2 and 3 and, subsequently, replaced with another (domiciliary) service in site 2, but not in care homes 2 and 3 in site 3. District nursing teams were reorganised for care homes in sites 2 and 3. One care home that was dual registered at the start of the study became a nursing home. This change of registration was used as the basis of a decision that district nurses would no longer visit the remaining residential care residents.
These changes are summarised in Table 10 alongside a summary of care home staffing changes over the period of the study. These findings are compatible with previous studies describing high levels of staff turnover in the care home sector. One consequence was difficulty in maintaining the study link role. We had reimbursed this at market rates, emphasising the importance of continuity; however, staff were frequently required to prioritise care delivery over research.
| Changes in the organisation of care to and within care homes | Site | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Changes in NHS provision to care homes | An electronic prescription process was introduced by the GP practices linked with two of the care homes. One of these homes had three different GP practices. This resulted in variable usage of paper and electronic prescriptions, depending on which practice the resident was registered with | GPs introduced personalised care plans for care home residents in care homes 3 and 4 | In care home 1, GP locums were reported as not wanting to visit care homes. The locums had replaced a retired GP and one on sick leave |
| Monthly GP clinic pilot was introduced for 6 months in care homes 2 and 3 | |||
| Domiciliary dentist ceased visiting care homes 2 and 3 with no replacement | |||
| The community dentist who visited residents in care home 4 retired and was replaced by a temporary locum | Reorganisation of district nursing teams for care homes 1 and 3 integrated with therapists | New DN teams linked with care home 2 | |
| Change in the district nursing provision to care homes 3 and 4 resulting from the geographical extension of the Care Homes Team to the local area of these homes. Existing DNs visiting homes 3 and 4 were replaced by the Care Homes Nursing Team | New domiciliary dental service visiting care homes 1 and 3 | To reduce needs for SALT team visits, care home staff trained for swallowing assessments | |
| Care home changes | Three consecutive managers from one of the study care homes and four study link staff from two of the study care homes left their employment with these care homes. Two further study link staff from a third care home, while remaining in their existing posts within the same care home, withdrew from their study link staff role as a result of the continuing demands of their care home workloads | Five link staff members left in two different care homes, including two managers in one care home. One care home closed a unit to refurbish it for older people with dementia | Four care home link staff, in three different care homes, left before the end of data collection and one became deputy manager but remained as the dedicated staff member for the study |
| One care home was sold out to a different independent large chain corporate care home provider. The care home manager remained in post in this care home but was assigned additional responsibility for another care home owned by the same company | |||
Resident recruitment and retention
Identifying care homes and recruiting eligible residents to participate was a protracted process. Recruitment commenced in site 1, followed by site 3 and then site 2. Site 1 took 7 months to recruit 93 residents, site 2 took 8 months to recruit 92 residents and site 3 took 5 months to recruit 57 residents. Site 2 was the last to be included to allow sufficient time for a newly established GP care home scheme to be embedded. After exclusions, 472 residents were eligible for recruitment across the sites; the overall recruitment rate was 55% for site 1, 52% for site 2 and 46% for site 3 (see Tables 11–13). In sites 1 and 3, where the care homes with nursing beds were based in homes dual registered for personal care, the percentages of residents recruited who were in nursing beds were comparable at 13% and 14%, respectively. In site 2, where the fourth care home was nursing only, the proportion of residents in nursing beds was higher at 39%.
In total, 242 residents were recruited across the three sites; 93 in site 1, 92 in site 2 and 57 in site 3. Thirty per cent of the sample (n = 73) was made up of those residents with capacity to consent and these residents were recruited using standard consent procedures without the need to refer to consultees. The majority (n = 169) of residents were recruited via a consultee process, as outlined in Chapter 2. Nominated consultees, who were independent to the study, were appointed to act on behalf of eight residents. In site 3, it was not possible to identify a nominated consultee. Table 11 gives the breakdown of recruitment numbers including number of beds, those excluded and those with and without capacity to consent.
| Care home | Number of beds | Number of residents | Excluded | Number after exclusions | With capacity: agreed to participate | Letters sent out | Consultee (yes) | Consultee (no) | Total (yes) | Recruited after exclusions (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Site 1 | ||||||||||
| S1CH1 | 19 | 15 | 0 | 15 | 6 | 5 | 5 | 0 | 11 | 73 |
| S1CH2 | 62 | 60 | 11 | 49 | 10 | 31 | 18 | 10 | 28 | 57 |
| S1CH3 | 47 (R) | 45 (R) | 7 | 68 | 11 | 38 | 19 | 15 | 18 (R) | 44 |
| 30 (N) | 28 (N) | 12 (N) | ||||||||
| 77 (total) | 73 (total) | 30 (total) | ||||||||
| S1CH4 | 40 | 40 | 3 | 37 | 10 | 18 | 14 | 4 | 24 | 65 |
| Totals | 198 | 188 | 19 | 169 | 37 | 92 | 56 | 29 | 93 | 55 |
| Site 2 | ||||||||||
| S2CH1 | 19 | 11 | 0 | 11 | 1 | 9 | 2 | 0 | 3 | 27 |
| S2CH2 | 51 | 51 | 9 | 42 | - | 50 | 27 | 7 | 27 | 64 |
| S2CH3 | 60 | 54 | 5 | 49 | 2 | 54 | 24 | 4 | 26 | 53 |
| S2CH4 | 93 (N) | 76 | 2 | 74 | 5 | 53 | 31 | 7 | 36 (N) | 49 |
| Totals | 206 | 192 | 16 | 176 | 8 | 166 | 84 | 18 | 92 | 52 |
| Site 3 | ||||||||||
| S3CH1 | 50 | 49 | 2 | 47 | 10 | 28 | 9 | 6 | 19 | 42 |
| S3CH2 | 24 | 19 | 1 | 18 | 4 | 16 | 6 | 1 | 10 | 56 |
| S3CH3 | 34 | 31 | 6 | 25 | 8 | 15 | 7 | 0 | 15 | 60 |
| S3CH4 | 14 (R) | 14 (R) | 7 | 37 | 6 | 32 | 7 | 1 | 5 (R) | 35 |
| 37 (N) | 30 (N) | 8 (N) | ||||||||
| 53 (total) | 44 (total) | 13 (total) | ||||||||
| Totals | 161 | 143 | 16 | 127 | 28 | 105 | 29 | 8 | 57 | 45 |
| All sites | ||||||||||
| Totals | 565 | 523 | 51 | 472 | 73 | 363 | 169 | 55 | 242 | 51 |
Although the financial incentives paid to the care homes to compensate for the staff time involved in the study appeared to facilitate the recruitment of care homes at an institutional level, it did not appear to have an impact on resident recruitment and data collection. Apart from at one care home, funding was not used to employ extra staff to cover study involvement. Monies received by care homes were instead put aside for a variety of planned projects including the purchase of special adjustable beds for use by one or two of the older residents in the care home, a minibus for taking residents on outings, a sensory garden, the refurbishment of a sitting room for residents with dementia and staff training on wound management.
Baseline interRAI data were collected for 234 residents, with medication data for 228 residents and baseline service use for 235 residents (see Table 13). Monthly health service use, medication changes and reviews were collected for 12 months post baseline for 11 out of the 12 care homes. A delay between the 12th care home agreeing to take part and their availability to commence recruitment meant that monthly resident data were collected only for 9 months post baseline. Across the three sites, 85 residents (35%) were lost to the study, predominantly through death, although three residents were transferred to other care settings (Table 12). A complete set of service use data was collected for all residents in site 3, but in sites 1 and 2 this was incomplete. Fourteen residents, two in site 1 and 12 in site 2, had missing service use data equivalent to 36 months of service use (Table 13). This was because the information could not be located in archived notes as a result of the variable archiving policies across the 12 homes, which had not been accounted for in the study design.
| Retention and loss to follow-up | Site | All, n (%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||||||||||||
| Care home | Total, n (%) | Care home | Total, n (%) | Care home | Total, n (%) | |||||||||||
| 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | |||||
| Retention | ||||||||||||||||
| Baseline total number of residents recruited | 11 | 28 | 30 | 24 | 93 | 3 | 27 | 26 | 36 | 92 | 19 | 10 | 15 | 13 | 57 | 242 |
| Number of residents retained at 3 months | 9 | 27 | 26 | 22 | 84 (90) | 3 | 27 | 23 | 28 | 81 (88) | 19 | 10 | 15 | 10 | 54 (95) | 219 (90) |
| Number of residents retained at 6 months | 8 | 26 | 25 | 18 | 77 (83) | 3 | 26 | 21 | 27 | 77 (84) | 18 | 10 | 15 | 6 | 49 (86) | 203 (84) |
| Number of residents retained at 9 months | 6 | 24 | 23 | 14 | 67 (72) | 3 | 20 | 17 | 24 | 64 (70) | 15 | 7 | 13 | 6 | 41 (72) | 172 (71) |
| Number of residents retained at 12 months | 5 | 22 | 19 | 12 | 58 (62) | 3 | 18 | 16 | 0a | 37 (40) | 11 | 7 | 12 | 6 | 36 (63) | 131 (54) |
| Reasons for loss to follow-up | ||||||||||||||||
| Total number of residents lost to follow-up at 12 months | 6 | 7 | 9 | 12 | 34 (37) | 0 | 9 | 10 | 24 | 43 (47) | 8 | 3 | 3 | 7 | 21 (37) | 98 (40) |
| Number of residents who moved care facility | 1 | 1 | 0 | 0 | 2 (2) | 0 | 1 | 0 | 0 | 1 (1) | 0 | 0 | 0 | 0 | 0 | 3 (1) |
| Number of residents who are deceased | 5 | 6 | 9 | 12 | 32 (34) | 0 | 8 | 10 | 13 | 31 (34) | 8 | 3 | 3 | 7 | 21 (37) | 84 (35) |
| Site | Number of residents recruited | Number of residents deceased or left the care home | interRAI data collected | Number of MAR sheets collected | Number of baseline service use | Number of residents: month of service use | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||||||
| 1 | 93 | 32 | 90 | 90 | 90 | 88 | 87 | 84 | 84 | 82 | 77 | 73 | 69 | 67 | 66 | 63 | 58 |
| 2 | 92 | 32 | 92 | 81 | 88 | 79 | 83 | 79 | 78 | 74 | 73 | 67 | 64 | 64 | 38 | 37 | 37 |
| 3 | 57 | 21 | 57 | 57 | 57 | 56 | 55 | 54 | 53 | 49 | 49 | 44 | 43 | 41 | 40 | 38 | 36 |
| Total | 242 | 85 | 239 | 228 | 235 | 223 | 225 | 217 | 215 | 205 | 199 | 184 | 176 | 172 | 144 | 138 | 131 |
Recruitment of interview subjects
In total, 181 individuals, including residents, relatives, HCPs (such as community nurses, allied health professionals and GPs), care home staff and managers took part in individual interviews or focus groups (Table 14). Across the sites, 116 interviews took place. Eleven focus groups were conducted with care home staff in 11 care homes, one with GPs in sites 2 and 3 and with commissioners (including GP commissioners) in sites 2 and 3.
| Participants | Site | Total | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| HCPs | 18 | 9 | 16 | 43 |
| Residents | 17 | 3 | 15 | 35 |
| Relatives | 10 | 4 | 4 | 18 |
| Care home staff | 18 | 13 | 15 | 46 |
| Care home managers | 5 | 4 | 4 | 13 |
| GPs | 5 | 9 | 5 | 19 |
| Stakeholders | 3 | 2 | 2 | 7 |
| Total | 76 | 44 | 61 | 181 |
Residents with capacity to consent to interview were more difficult to recruit in site 2, where a significantly greater proportion of care home residents had cognitive impairment and lacked capacity. Thirty-five resident interviews were completed in total, but one interview was not used as the resident was unable to focus on questions about health and service use and no meaningful data relevant to the study were obtained (see Table 14).
In addition to the 18 interviews conducted with family members, four family members were present during resident interviews and in each case presented data additional to those provided by the resident, adding to the interview transcript. Relatives were harder to recruit in site 2, where a significant number of residents had no identified next of kin, and site 3, where the care home staff reported that it was difficult to engage relatives in care home-related activities. To counteract this the researcher attended residents’ and relatives’ meetings where possible in site 2 and set up evening meetings for relatives in site 3 care homes to inform them about the study and invite them to take part in an interview. Despite this, no relatives from the meetings in site 2 expressed an interest in taking part and no family members attended the evening meetings in site 3.
The care home staff represented a range of experience and roles including care provision, catering and training for care home staff. Staff were interviewed in the care home. Fewer HCPs were interviewed in site 2, which reflected the fact that care home provision at this site came from a relatively small pool of staff from the primary care organisation – thus there was significant overlap between the team members supporting individual homes. The breakdown of HCPs interviewed is summarised in Table 15.
| Site | Community nurses | Allied HCPs | Total |
|---|---|---|---|
| 1 | 9 (including care home, dementia, Parkinson’s disease, continence, falls and DNs) | 9 (including dentist, optician, chiropodist, falls, rehabilitation and dementia OTs, falls team, dementia and rehabilitation physiotherapists) | 18 |
| 2 | 6 (including district, palliative care, tissue viability, mental health and continuing health-care nurses) | 3 (including chiropodist, optician and a therapist assistant) | 9 |
| 3 | 9 (including care home, district, dementia, heart failure and tissue viability nurses) | 7 (including dietitian, OT, rehabilitation and stroke physiotherapists, dentist, optician and chiropodist | 16 |
| 24 | 19 | 43 |
General practitioner interviews were the most challenging to arrange and were not completed until after care home data collection had stopped. Interviews and focus group discussions were time constrained and arranged either to coincide with other meetings at the CCG or as individual interviews completed at the end of the study. On two occasions, in two sites, agreement to participate was withdrawn. One GP declined an interview but did complete a written questionnaire comprising the interview prompts about how they worked with care homes. Consequently, the focus of these interviews was not exclusively on the study care homes. They did, however, all consider care taking place within GP practices aligned to the CCGs included in the case studies. The breakdown of GP research contact is provided in Table 16.
| Sites | Number of transcripts | Number of GP participants |
|---|---|---|
| 1 | 1 completed questionnaire | 5 |
| 4 interviews | ||
| 2 | 1 focus group | 11 |
| 1 interview | ||
| 3 | 1 focus group | 5 (plus one practice manager) |
Resident characteristics at baseline
Resident characteristics by care home and site are summarised in Appendix 10. Gender and the age of the cohort were similar between sites and were broadly representative of the UK care home population. 148 Comorbidities were limited to those that could be retrieved from the care home notes and are significantly lower than the numbers seen in other large care home studies where medical records were used to count comorbidities. They serve here to act as a comparator looking for baseline confounding between sites where no significant difference was seen, rather than to represent a definitive picture of comorbidities across the cohort. A significantly greater number of self-funders were seen in site 2 than in site 1 (p < 0.05). Despite efforts to closely match the care home populations, a significantly higher number of nursing home residents were recruited in site 2 than in sites 1 or 3 (p < 0.01). Site 3 reported significantly lower levels of functional dependency, communication difficulties and cognitive impairment, as well as significantly lower scores for the interRAI summary scores for ADL, cognitive performance, communication (p < 0.01 for all) and pressure ulcer risk (p = 0.05). Site 3 reported significantly lower levels of functional dependency, communication difficulties and cognitive impairment, as well as significantly lower interRAI summary scores for ADL, cognitive performance, communication (p < 0.01 for all) and pressure ulcer risk (p = 0.05) – we were not aware of any particular recruitment bias that led to this.
Services provided at each study site in detail
Health-care professionals’ accounts of working with care homes and other HCPs were used to provide a description of service provision in each site and how it was structured. Specific attention was paid to how the different characteristics of the service models in each site were recognised and understood by participants.
Across all three sites, six aspects of the services were identified as being key to understanding how care was organised and operationalised:
-
the system for referrals
-
availability of dedicated health services for care homes
-
team working
-
the use of case management
-
care home-based training
-
length of time HCPs had worked with care homes and each other.
Engagement with care homes for each of the three sites is considered under the headings below.
Site 1: age-appropriate care
In site 1, HCPs’ pattern of engagement and working with care homes was characterised by:
-
multiple MDTs that either worked exclusively with care homes or had explicit responsibility for care homes as part of their work (dementia care, fractures and falls prevention)
-
a nurse-led care home service that had been in place in different iterations for more than 15 years. This included proactive approaches to working with care homes including case management of new and continuing health-care-funded residents.
-
formal and informal systems for team-to-team referrals about specific residents, including access to specialist dementia knowledge
-
a history of innovations around working with care homes with evidence of consultations with care home managers about health-care priorities and the need for support and training
-
ongoing structured training and forums to support both care home staff and managers.
Figure 3 gives a detailed outline of the way that services were structured in site 1 and interactions between them. Services that were care home specific and those that had significant contact with care homes or provided peer support or training for care homes are highlighted in green text. The figure is drawn from 18 interviews with HCPs. It may not capture the full picture of working relationships and practices, but it does reflect practitioner understanding of what was available and how the system worked.
FIGURE 3.
Overview of health services provision in site 1. Green font indicates care home-specific services, direct referral, high care home input or organised training. Circular boxes indicate teams, square boxes indicate individual HCPs. AHP, allied health professional; CHC, continuing health care; DN, district nurse; MRSA, meticillin-resistant Staphylococcus aureus; OT, occupational therapist; SALT, speech and language therapist.
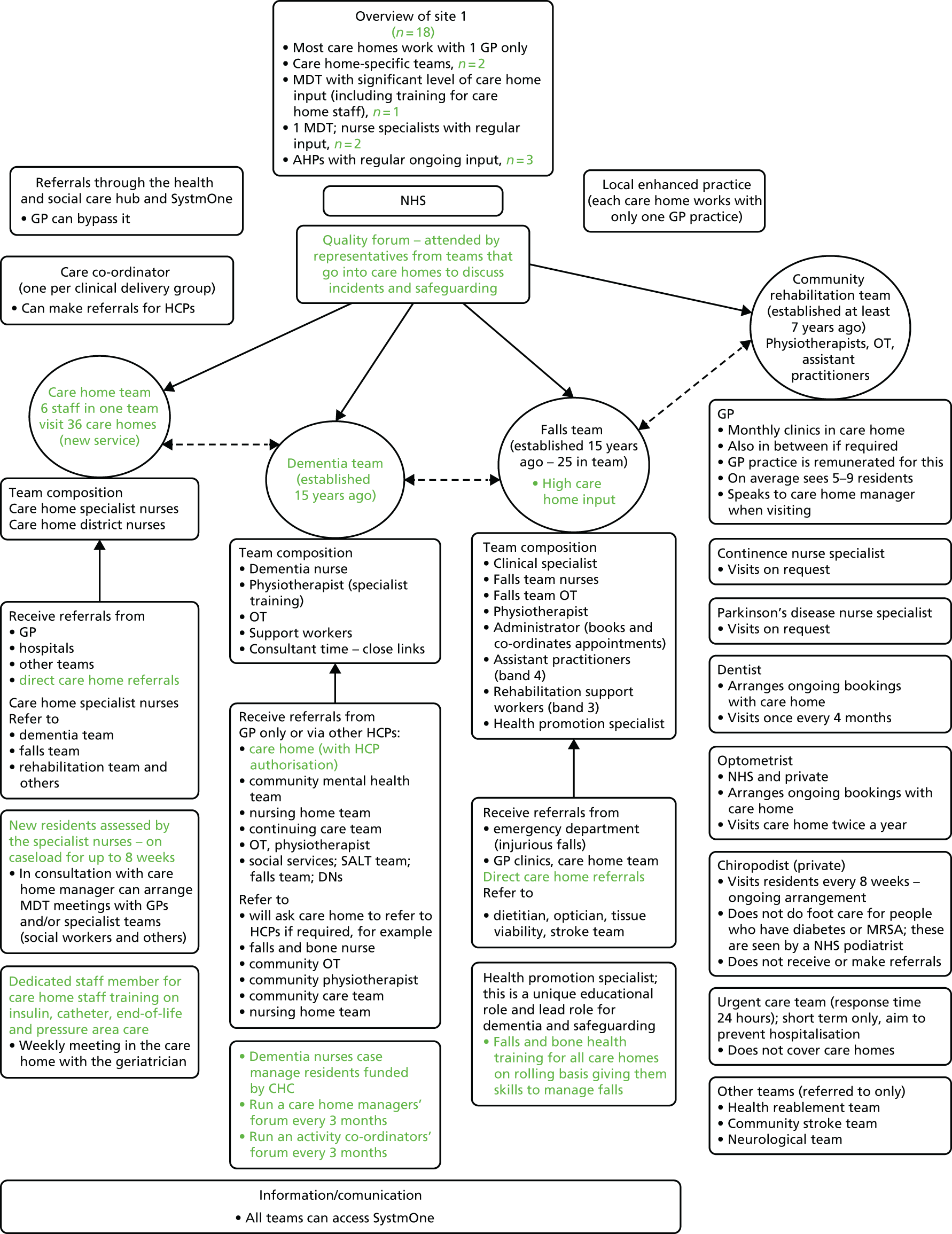
Referral systems
Most referrals on behalf of residents by care home staff and HCPs to other services were made through a single hub for both health and social care by telephone or electronically through a shared system between the services working in care homes. GP practices could choose to use or bypass the hub. Referrals to the optician, chiropodist and dentist were usually arranged separately by care home staff. According to the HCPs, this system worked well.
The hub referral system was intended to simplify the decision for care home staff as to whom they should make a referral. However, in practice, this was not always the case and there was limited evidence of triaging by resident need. In some instances care home staff had referred a resident to more than one team, generating duplicate visits and assessments, because they found knowing who to refer to unclear. HCPs from the same discipline were frequently part of multiple different specialist teams that either provided input, or potentially could provide input, to the same care home. For example, if a resident had a fall, they could be referred to a physiotherapist from either the falls team or the rehabilitation team and it was not always clear to professionals from outside these teams which was most appropriate. This confusion was not confined to care homes but was also found with other HCPs who were not part of the teams with care home responsibilities, including the GPs. Referrals made by GPs that bypassed the hub could also cause duplication. To offset this, some teams introduced an informal system of checking with each other when picking up a referral, to ensure that the care was not being duplicated. An informal network of communication developed over time helped to mitigate these problems.
Team working
Health-care provision in site 1 was characterised by numerous MDTs each with a specific focus of care and specialist knowledge (e.g. falls prevention) who liaised and worked closely with each other. These teams carried out joint visits to care homes and frequently made referrals both within their own team and across teams. Initial assessments of residents’ health needs were reported to be ‘holistic’ in order to highlight which aspects of care might require GP involvement and which might mandate specialist referral. One example described a situation in which a resident with dementia was seen at a fracture clinic but then followed up in situ by two physiotherapists, one each from the dementia and rehabilitation teams, who worked together to ensure the resident was assessed in the care home. This took the place of routine outpatient fracture clinic physiotherapy follow-up and allowed access to specific expertise in both musculoskeletal rehabilitation and modification of rehabilitation regimes to take account of cognitive impairment. Figure 3 illustrates a complex network in which there could be multiple teams working with a resident, each with rapid access to specialist services. This could lead to duplication of work and confusion for care home staff, especially if they are given contradictory advice regarding an individual resident’s care. A HCP described addressing this problem as follows:
. . . I think one of the other difficulties they [care home staff] have is often people [residents] end up having multiple teams involved, often giving slightly contradictory advice, and they’re like ‘Well what are we supposed to do? You’re telling me one thing, someone is telling me another thing’ and you can see they’re just in the middle going ‘Well what am I, whatever I do, someone’s going to be annoyed with me’. What we always do in the Falls Team is we always make sure we write in the professional’s bit of the records and then we send a recommendations letter saying ‘This is what we’ve recommended’, so if another professional from another team looks in the care plan they can see what we’ve done . . .
S1CH2HP01
Dedicated health services for care homes
Site 1 was the only site with HCP teams funded to work exclusively with care homes providing direct care for residents. Two teams worked specifically with care homes, including a nurse-led care home team and a dementia care home-specific team. In addition, a third team had substantial input into care homes mainly for staff training and support around falls prevention in addition to working with older people living at home.
The nurse-led care home team included district nurses and community nurses who provided on-demand nursing support to residents without on-site nursing provision and specialist nurses whose role was to assess all new admissions to all care homes and support the transition into the care home. They would then oversee care of residents (case management) during the first 8 weeks in the care home. This team met weekly with a consultant community geriatrician to review residents and discuss care planning. The dementia outreach team included physiotherapists, occupational therapists and mental health nurses. They provided assessments of the care needs of individual residents living with dementia and support to care home staff. Their work was not defined exclusively as health and social care. For example, support workers within the team had the remit to focus on residents’ engagement with dementia-related activities in the care home, such as reminiscence techniques.
Case management
Site 1 was the only site that had case management for new admissions to care homes. This was led by specialist nurses in the care home team, who worked exclusively with the care homes and thus had more time for talking to and supporting care home staff than their district nurse counterparts. Their presence meant that they were also able to respond to staff queries about other patients without needing a scheduled appointment. The specialist nurses from the dementia team had a case co-ordinator role for those residents in receipt of NHS continuing health-care funding. These residents stayed on their caseload, which also facilitated regular contact and relationship building with the care home staff.
Care home training and monitoring
A programme of planned training was available to care home staff in site 1. This was delivered by staff members of the dementia, falls and NHS care home nursing teams and targeted a range of staff from care home managers to activities organisers. This was supplemented by training that was available on request and in response to care home priorities from the tissue viability, diabetes mellitus and nutrition teams. The dementia team ran a programme of care home forums with meetings every 3 months that aimed to provide a programme of training while also providing an opportunity for more informal interaction, peer support and relationship-building.
Safeguarding and reviews of the quality of care provided in care homes were monitored and discussed at specific quality meetings attended by the NHS service leads. The approach taken was to identify homes with particular problems and to offer support to address any identified problems. Quality meetings augmented the teaching and were seen as a vehicle to highlight and share good practice in care homes for future learning and practice. They were not, however, attended by representatives from the care home sector and so communicating constructive outputs from this forum were contingent upon members liaising with the care homes afterwards:
What we tend to do is, apart from the incidents that are already recorded, that have already been safeguarded or dated, we also have . . . areas of good practice that we want to share. So, homes . . . that we have identified as improving or have shown, you know, really good ideas around that improved practice . . . that are good. So you know, praise where it’s due, I always say, because I think they get bashed so much, it’s about saying, ‘Actually this is really good, can we share that good practice? How have you done that? You know, can we sort of use that as a model and you know, pass that on, and pass that knowledge on to other homes?’
S1CH1HP06
Prior history of working with care homes
From the interview transcripts it was evident that some of the individual HCPs had long-standing working relationships with care homes, which had a positive impact on their ability to engage with each other. The care home teams in this site were built on a history of projects conducted with care homes. An earlier pilot had provided a small group of care homes with training from specialist nurses, which focused on six core areas: tissue viability, nutrition, hydration, medicine management, end-of-life care and continence. There was evidence that as pilot projects had drawn to a close, the NHS staff involved had tended to move into employment upon the next wave of care home initiatives being developed within the area, thus allowing and facilitating relationship-building over time. Continuity of relationships were maintained over a number of years, even as National Government Services projects stopped, started and were reconfigured.
Site 2: incentives, sanctions and targets
In site 2, HCP working with care homes was characterised by:
-
a focus on the GP as the organiser and partner in the co-ordination of services provided to the care homes
-
specific GP practices receiving extra payments to work with care homes; care homes were asked to register with one of these practices
-
a nurse specialist in palliative care who had a designated role to work with care homes
-
structured training for care homes commissioned by the CCG and provided by a training organisation; a focus on knowledge and skills needed to support people with complex needs to stay in the care home and avoid hospitalisation; completion of training meant that the care home was eligible to receive additional payments for residents recognised as needing extra care and support.
In addition, the following services were available to, and accessed by, care homes, but were not specifically targeted at the care home sector, nor did they have care homes as a priority within their service specification.
-
A newly established, integrated team of nurses and therapists that provided ‘wrap-around ‘care to older people living at home, which included care homes.
-
Dementia-specific advice and support provided via mental health services to older people living at home, which included care homes.
This led to the following.
-
Services were focused around individual residents, with few opportunities to meet with managers and care home staff about more generic issues affecting care across the resident cohort as a whole.
-
Care home staff and HCPs were uncertain about who to approach about specific problems and HCPs were similarly uncertain about how to signpost them.
The service model at site 2 is summarised in Figure 4.
FIGURE 4.
Overview of health service provision in site 2. Green font indicates care home-specific services, direct referral, high care home input or organised training. Circular boxes indicate teams, square boxes indicate individual HCPs. AHP, allied health professional; CNS, clinical nurse specialist; DN, district nurse; HCA, health-care assistant; OT, occupational therapist; SALT, speech and language therapist.
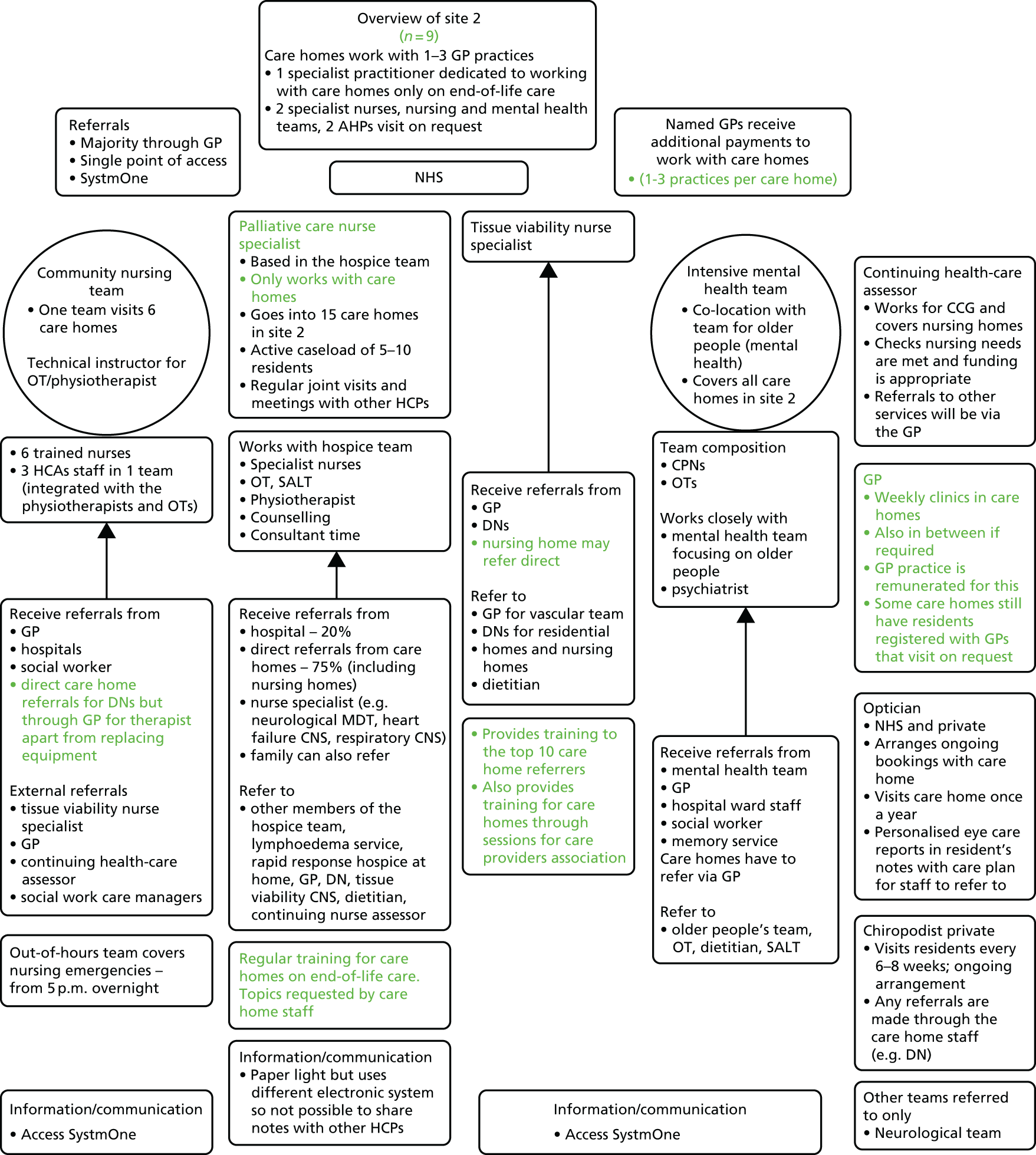
Referral systems
Health-care professionals in site 2 had access to a variety of referral routes, including a single point of access and electronic referrals through a shared system, but there was an emphasis on GPs acting as co-ordinators and conduits for such referrals. There were some differences across the teams; for example, for one district nurse team the care home could make referrals directly through the single point of contact, whereas for the other, which covered two of the study care homes, all referrals had to go through the GP. It was not clear, even to those involved, whether this was because of formal differences in service specification or simply a consequence of different working practices across GP surgeries. There was evidence that once a resident was being looked after by one member of the integrated care team, members of that team would make direct referrals from one to another, for example between district nurse and physiotherapist, without having to go back through the GP. There were examples of care home residents receiving joint assessment visits when, for example, some GPs would visit care homes together with members of the mental health team or when the palliative care nurse would attend together with other members of the hospice team whose input she had identified as likely to be important or helpful. In contrast to site 1, there were no formal or informal referral systems organised around the care homes and their residents. As in site 1, referrals from the optician and chiropodist were separately organised. Duplication occurred when, because there were no shared records, care home staff were unaware that the district nurse had already visited. In this site there were frequent references to ‘inappropriate’ referrals by care homes. As the following quotation demonstrates, inappropriate referrals were underpinned by care home staff not knowing that they could initiate conversations and few opportunities for meaningful dialogue between care homes and visiting HCPs; what might be regarded as an appropriate referral or how staff might differentiate between urgent and non-urgent reasons for referral were not discussed:
Anything else you’d like to say about working with care homes, or setting up a new service to provide health services to them?
. . . a lot of the times we do see patients at maybe inappropriate referrals, and maybe because of the lack of teaching and a lack of referral knowledge [of the care home staff] they refer when they shouldn’t, and maybe they should just ask us a question before they refer to us. So like if someone said, ‘Oh, can I just ask you a question, just for a bit of advice?’ And then we’ll say, ‘Yeah, that’s fine, refer that person,’ and then we can see them, rather than referring them to us when actually there was nothing there [no reason to visit] in the first place. So sometimes it can be a bit of time wasting on both sides, that’s it [laughs].
Team working
Specialist teams played a part in the organisation and provision of health services in site 2. Although they visited care homes, they also had responsibilities for community-dwelling older people. Their responsibility for care home residents and how much time they should allow for work in these settings were not specified. A notable exception, and one that was closer to the patterns of visiting reported in site 1, was the input of the palliative care nurse specialist. She worked exclusively with care homes and had regular meetings with a hospice team and a neurological specialist team as well as other HCPs who visited the care homes as part of their broader responsibilities. Her key roles were to advise on the care of residents who were dying, liaise with specialist nurses so that the homes could access their services more easily and provide ongoing support and training to care home staff. Her remit was care home wide and not limited to individual resident episodes of care:
So, asking about the level of contact you have with the care home staff when you go in, how the visit works, you know . . . ?
Yeah, so I would say I always have contact with the care home staff. Many patients do not have full mental capacity so care home staff help with assessing of situation, feedback and education is given to the care home staff on drug management, symptom control, psychological and spiritual support. If a new member of staff is there, I try to encourage them to work alongside me so I’m teaching them how to manage without me when having End of Life discussions, advanced care planning discussions and difficult conversations. Yeah, so I hope that this facilitates education of staff and helps continuity and coordination, the ability of the staff to communicate well with families of patients and MDT is vital.
Access to dementia specialist support for care home residents was identified by several respondents as a particular issue and there were accounts of where the lack of access to specialist support had led to residents receiving poor care from NHS services and, in one example, police involvement – the staff who discussed this case felt that proactive engagement by a specialist team with co-ordination of the services involved could have avoided this outcome. Dementia training (3 hours, internet based) had recently been made mandatory for one district nurse team but not the other. Several HCPs identified that they felt particularly uncertain in situations where they had to respond to residents whose behaviours they found challenging. There were examples of HCPs who showed in their language a tendency to depersonalise people living with dementia, referring to care homes as ‘all dementia’ and assuming that aggressive behaviour was an inevitable consequence of the illness:
Not so much the residents because in care home X, all the residents are dementia so but the thing is on the nursing side we can go in and because we know how they’re [residents] specialist going to react, i.e. there’s a couple that will call you everything under the sun, kick and bite you and everything, but I know how to work around them so I think that’s why it’s a really good thing to have the same people going in, especially on the dementia side because you know how that patient is going to react. Some of them will just sit there and put their arm out, another one will call you everything under the sun but you don’t take offence to it because you know that they don’t mean what they’re saying, you’re just going in to do your job and look after those patients. So, but again, I do ask for somebody to be with me [care home staff member], especially if I know that they’re going to lash out anyway.
S2CH3HCP01, community nursing team member
Dedicated health services for care homes
All health services in site 2 worked with care homes as part of a broader remit to care for older people in the community. When care home strategies had been developed, the focus was on GP provision and the use of enhanced payments to increase access and frequency of visiting.
Care home training and monitoring
Some of the district nurses thought that care home staff training should be a priority, especially in relation to catheter care and pressure area care; however, none of them was involved in delivering any such training. The majority of the HCPs, including the community and mental health nurses, focused on what they saw as the inadequacy of training and their monitoring role in highlighting safeguarding and quality issues. There was a perception that it was not their responsibility to provide training:
There should be better training I think for carers [care home staff], I mean because at the end of the day some of our referrals, we aren’t actually required in a home . . . I feel they need more updating on pressure care for sure, definitely, and their competence when it comes to pressure area and care is poor, very poor. And also their moving and handling skills are atrocious, I mean I’ve had to report quite a few times the way I’ve seen people handled in a home and then the girls that I’ve worked with, they’ve been like near to tears telling me that they go on courses and this is how they’ve been shown and then when I’ve gone to . . . the manager of the home, she said ‘No, this isn’t how we have shown them, they should know different’.
S2CH3HCP01 p. 7, community nurse – district nursing team
The structured training that was being provided (paid for by the CCG) during the time of data collection included some of the HCPs working with a social care training provider and was linked to care homes receiving extra funding. Partitioning training off in this way could possibly have had an unintended consequence of reinforcing other HCPs’ beliefs that supporting staff learning was not their responsibility.
Prior history of working with care homes
The palliative care home nurse specialist had a long history of working with the care homes. She had been a district nurse before becoming a specialist nurse and had built relationships with care home staff when working in that capacity. In the last 3 years in which she had been explicitly responsible for supporting care homes, she had worked with care home staff to roll out an online training package in end-of-life care. She interpreted her role as providing expertise, support and advocacy for both residents and staff:
What does your role involve?
So to go into the care home after a referral’s been sent and to support the care home staff to support their patient, to support the family or carers of that patient, to provide holistic support for that patient and their family, to liaise and co-ordinate the other MDT services, provide specialist drug advice.
The palliative care nurse was, however, the exception at this site. For the other HCPs interviewed they did not have this history of association or care home focus. The reason for visiting was to see particular residents, which meant that their involvement with the care homes and contact with care home staff fluctuated according to the needs of individual residents and was not structured to promote engagement at the care home level. In addition, care often focused around specific care episodes with intensive periods of involvement followed by withdrawal as things stabilised. Sustained and continuous engagement, even with individual residents, was not a feature of this way of working.
Site 3: General Medical Services plus investment in care home leadership and relational working within the care home
Health-care professionals working with care homes in site 3 was characterised by:
-
a range of services that were largely reactive, unco-ordinated and did not differentiate between services provided to older people living in their own homes and those in care homes
-
individual expert practitioners with competencies relevant to management of care home residents (e.g. tissue viability nurse specialist, cardiac nurse specialist) who received referrals about care home residents through separate routes and usually operated independently of each other
-
evidence that some individual HCPs worked with care homes at an institutional, rather than individual resident, level
-
limited formal or informal opportunities to meet with managers and care home staff beyond seeing residents.
Specialist nurse roles for care homes were integrated into district nursing teams with a remit to prevent unplanned hospitalisations and compensate for what was perceived as limited access to GP services.The service model is summarised in Figure 5.
FIGURE 5.
Overview of health service provision in site 3. Green font indicates care home-specific services, direct referral, high care home input or organised training. Circular boxes indicate teams, square boxes indicate individual HCPs. AHP, allied health professional; COPD, chronic obstructive pulmonary disease; DN, district nurse; OT, occupational therapist; PDNS, Parkinson’s disease nurse specialist; SALT, speech and language therapist.

Referral process
In site 3 there were a variety of referral routes, including a single point of access, electronic referrals through a shared system, GP referrals and informal referrals through HCPs visiting the care home. Care homes also had access to direct lines for a number of individual practitioners including the care home nurse and dementia nurse specialists, dietitian and community nurses. As with site 1, care home staff faced a challenge as to how to decide where to refer a resident and in what circumstances. The care home nurse specialist was designated as the ‘first port of call’. However, this only applied during office hours and their remit only covered specific conditions. There were guidelines for care home staff, but ultimately, their referral decision depended on a number of factors, including their level of experience and the quality of the working relationships with the HCP concerned:
So how do they [care home staff] decide whether to contact you directly or the contact point or the GP?
Well, [laughs] . . . it’s regards preference on who’s on duty to be fair, I mean we, they have got information regarding the Community Matrons and almost like a spider diagram which would say that Community Matrons support a residential care homes and give us an idea of the sort of things that we would see for all the patients. Some carers [care home staff] would always call a doctor, where some more senior carer would call us direct, I think if I’ve got a relationship with the home, I’ve been going for a long time, they know me very well, then they’re more likely to call me direct and we’d go from there.
In some areas, the referral system was further complicated by care home providers giving referral guidance to their care home staff that did not fit with the NHS protocols:
So sometimes . . . we find that, especially the big chains with care homes, they have set guidelines as to when to refer and who to refer and that might not actually tie in with our referral guidance where we’ve had referrals and we get . . . Some care homes are told to refer to us if somebody loses a kilogram which actually wouldn’t be significant or it might be two kilograms but if you’ve somebody who’s actually overweight and they lose two kilograms, you know, it wouldn’t be a factor, it wouldn’t be a referral criteria so that’s something that, you know, it depends on (the ownership).
S3CH2HCP01, dietitian
Team working
As in site 2, there was limited evidence of HCPs from different disciplines or teams working together on behalf of care home residents, or of referrals within and across teams. One exception to this was the dementia nurse specialist, who worked closely with the community mental health team via the psychiatrist and an intensive dementia service that provided day-to-day support for care homes, as well as working to a specific care pathway for medication reviews in collaboration with the memory service (Figure 6).
FIGURE 6.
Dementia nurse specialist role and integration with other services. a, Same clinical manager. CMHT, community mental health team; OOH, out of hours.
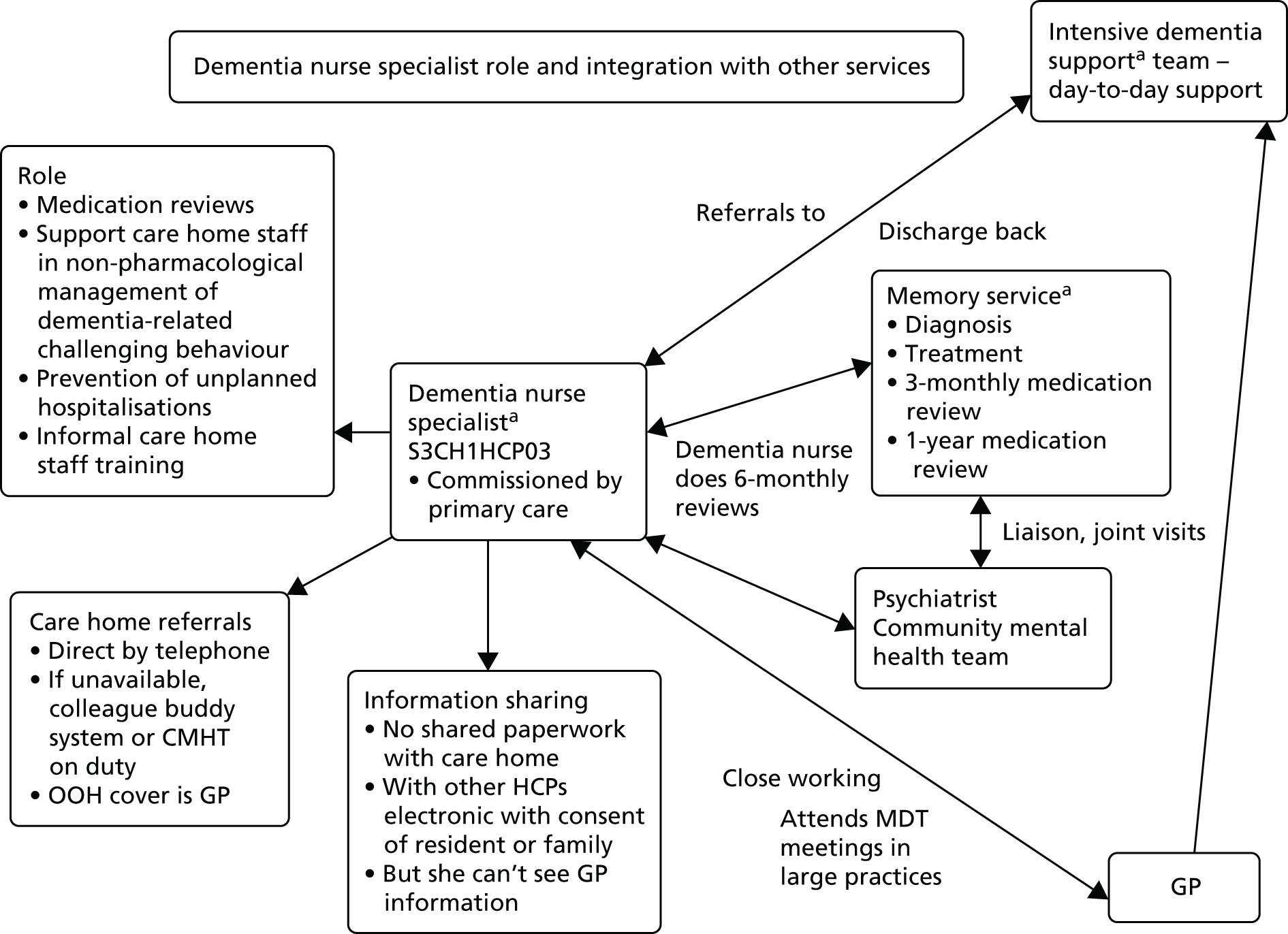
Dedicated health services for care homes
The care homes in site 3 had been recruited on the basis of their involvement in the MyHomeLife leadership training programme. Although geographically close, they were not all within the same CCG area because multiple CCGs had contracts with the same NHS provider organisation; the same NHS practitioner often visited more than one of the care homes in the case study. Individual nurse practitioners dedicated to work with care homes were a feature of service provision in site 3. These practitioners were co-located with the community nurse teams. Their service specification was oriented around compensating for care homes’ lack of access to GPs with an aim to preventing unnecessary hospitalisation. There was, however, evidence of a lack of clarity in how these terms had been established with some practitioners conflating protecting vulnerable older patients from the harms of hospitalisation with rationing care on the basis of age:
. . . Um, I think the main aim that we . . . We try to prevent hospital admission, so if we can do something in the home, especially with our dementia patients that are in homes, you know, we don’t want any disorientation, sending someone in, say for instance for, I don’t know, because they’re constipated for instance, if we can manage that in the home so they’re comfortable in their own room, IV antibiotics to prevent them going into hospital. It has to be an utter emergency for us to send them into hospital because they are, you know, elderly.
S3CH23HCP03, district nurse team leader
The care home nurse practitioners had prescribing rights but they often deferred to the GP regarding medication reviews, especially if the GP had initiated the medication. Not all residents were seen by the care home nurse specialists because some GPs employed a nurse practitioner to visit in their place, and preferred for them to co-ordinate care for care home residents on their list.
The nursing home at site 3 did not receive any care home-specific services.
The dementia nurse specialist was employed by a secondary care provider organisation. She appeared to be one of the only practitioners with specific dementia expertise. She had a significant level of input into care homes but also worked with older people living with dementia at home. Her role was to support the care home staff to use non-pharmacological approaches to manage dementia-related behaviours that staff found challenging. She reviewed antipsychotic medication for care home residents as part of a structured care pathway. However, this approach was restricted by the limited time that care home staff had available to work with her or to provide one-to-one input with residents:
So the strategy is really sometimes it’s already in the care plan but what we find within the care home sometimes it’s written in the care plan but it’s not actually being implemented . . . so it’s really about occupying the patient, providing that facility, using distraction techniques, using other methods of music and getting to know the patient. So it’s really, it’s quite a challenge for the care homes because sometimes the staffing level is quite low so trying to provide some form of like complete care for, one-to-one type of care for a patient with dementia who’s quite distressed I think that’s where the challenging bits come and that’s where a lot of the time you find they will either use medication to just sort of help the situation at that moment rather than just looking at the whole, somebody just spending a bit of time, you know. Sometimes it takes more than just 10 minutes; really you’re talking about an hour or so with the patient just to sort of calm situations.
S3CH1HCP03, dementia nurse specialist
Care home training and monitoring
Health-care professionals offered opportunistic training on request from care home staff. The enthusiasm shown for such a role was variable, with some staff reporting that they would have liked to have had the time and resources to offer more, whereas others did not see it as part of their role. In common with the community nurses in this site, the physiotherapists and occupational therapists only provided training to care home staff that focused on the needs of individual residents, for example to demonstrate postural management or exercises. However, three services provided dedicated training to the care home staff in the care home at no cost: the dietitian, the community dental team (which offered oral health promotion training) and the community optician (who provided visual awareness training).
One example of an integrated approach was the dietetic service training for both care home and catering staff. This 6-monthly training programme focused on working together with the care home staff using a specific protocol and a standardised tool. Care home staff were trained to use MUST (Malnutrition Universal Screening Tool; modified to include pressure sore-related nutritional requirements) as a tool for picking up any nutrition-related problems in conjunction with a related care plan and protocol to follow. This linked to information on how to refer residents to the dietetic service and what to do if a resident had swallowing problems or nausea. This was reinforced by the establishment of a specific area on the trust website for care homes to refer to, including information on MUST, food and body mass index record charts and a regular care home newsletter with features such as areas of best practice. Dementia-related training was included when talking about the impact it had on residents’ eating behaviours with catering and care home staff:
. . . When we’ve done training we’ve also . . . had people from the dementia care service who came along to do part of the talk and the last time, when we were talking to the catering staff we also talked about things like the colours of tablecloths because we had . . . And we told them about we had a lady who had a glass that had a flower pattern on it and she’d sit and try and pick the flower out, so she never drank anything out of it because she was too busy trying to get the flower and the same with if there’s a pattern on the tablecloth . . . and we talked about, you know, coloured plates and how the food looks on plates . . . so if you have white food on a white plate somebody with dementia’s not going to be able to eat it because they’re not going to be able to compute what it is. So things like that we will talk about.
S3CH2HCP01
Prior history of working with care homes
There was reference to a history of pilot projects in the education of dementia-related hospitalisations in secondary care prior to introducing the dementia nurse specialist role in 2013. The care home nurse specialist roles had been implemented 10 years ago. The dietitian had previously received funding by the medicines management group to undertake a nutrition project that informed the way in which they currently worked with and provided training to care homes. There was evidence that these initiatives had been more ‘stop–start’ than those described in site 1, with less opportunity for staff from one NHS initiative to move onto the next, with consequent loss of continuity.
General practitioner involvement with care homes across the sites
The GP accounts are set apart from the site-by-site presentation because, out of necessity, not all GP participants recruited were directly involved with the study care homes. The GPs eventually recruited were, however, all working directly with care homes within the case study sites.
Key to the use of incentives across the three sites was how their purpose was interpreted by the GP, as the means to do work they valued or as payment for activities that were compensating for care home staff shortcomings or firefighting to reduce the number of hospitalisations. Table 17 provides a summary of these accounts by site.
| Characteristic | Site | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| GP involvement | Minimum bimonthly regular visit/clinic (most do every week or every 2 weeks) plus responsive visits to urgent calls plus examples of monitoring ‘at-risk’ residents, popping in, messaging, texting and telephone conversations | Practice allocated to specific care homes. Emphasis on responsive working but visiting two or three times a week to facilitate this. One GP described fixed Friday visits as ‘popping in’ before the weekend |
|
| Winter pressures money = GPs proactive visiting every day, 7 days a week, emphasis maintained on responding to crisis and avoiding admissions at an individual resident level | |||
| How services are provided | Clinic seeing 6–18 people at a time. Operationalised differently in different practices. One GP described setting aside 4 hours one week and shorter clinic the next, whereas another consistently did a 1-hour clinic each week | Regular visiting, where GPs were frequently asked to see more than one resident. A care home visit combined urgent and planned care (something that GPs struggled to accommodate within fixed duration visits) | In response to request to see residents |
| Specialist nurses with remit to reduce hospitalisation worked in three care homes | |||
| Working relationships | Different demands from care home with and without nursing but established relationships. GPs encouraged to work with care home at an institutional level to establish explicit arrangements for joint working | Acknowledgement of variability within the sector. Certain care homes identified as ‘not a problem’, whereas others struggled to hold problems pending the next GP visit | Expectation that care homes will have some ability to triage call-outs and establish which residents require more urgent medical attention |
| History of working with care homes | Owing to duration of current and preceding locally enhanced service agreements, GPs have > 2 years’ experience of working with care homes | Worries that closer working with care homes could ‘raise expectations’ and establish ‘unsustainable patterns of working’, creating dependency on GPs | Past history of GPs having private retainer fee arrangements with care homes – paid for at an institutional level – in exchange for more frequent visiting |
Across all sites, GP participants consistently stated that, if their time was allocated and resourced to work with care homes, they would do more than respond to urgent care requests. Site 2 had an example of a time when they had used winter pressures funding to visit care homes 7 days a week, and GPs were sure that this had averted hospitalisations. However, such proactive working was not seen universally as a good thing. Several GPs at site 2 stated concerns that increased input would create dependency on GPs by care home staff. They were worried that this might reinforce reluctance among care home staff to take responsibility for decision-making about what was urgent and what was not. This worry, that additional funding could seed unmanageable levels of demand that would persist beyond the time-limited nature of the additional payments, was used by several GP respondents as the rationale for focusing on individual resident contacts, rather than engaging with the care home more structurally.
In site 3, GPs described how they had provided a care home-based clinic when there was funding, but that when that funding was no longer available, it ceased. In site 1, additional payments to GPs had been perceived as legitimising more structured engagement with care homes. This was, however, in the context of the other comprehensive care home services (see Figure 4). The GP interviews, however, did not suggest that they recognised this provision as sharing the burden; it was not clear how much the GPs collaborated with the care home teams. It was more that the site 1 GP accounts suggested that they had more time and opportunities to think more constructively about engagement with the sector.
There was cross-site recognition of the importance of having confident, well-established care home staff who had been there for years, which in turn influenced how staff managed their anxieties about patient care and communicated these to GPs. None of the GPs interviewed believed that they should be involved in education or training of care home staff.
In site 1, the GPs had worked in individual 1 : 1 relations with care homes, underpinned by formal contractual arrangements, for at least 2 years, and had established ways of working. There was an emphasis on the personal relationship they had built up with care homes. Site 1 had multiple accounts of a history of working together and multiple methods of communicating by, for example, using text messages and telephone calls to facilitate and support direct face-to-face contacts. The GPs interviewed were interested in care homes and gave accounts of being involved in fund-raising for homes and setting up protocols for shared working. Interestingly, this relationship was represented as separate to the work done by the specialist care home team and other services; indeed, there were some doubts around whether or not the care home specialist team hindered GP work because of a perceived reluctance to share information about residents:
You mentioned difficulties in communication with the care home nursing team?
That’s the only thing . . . I mean it works perfectly fine, I mean I can see what they’ve written in the notes and they can see what I’ve written, but there is no one person like.
Not a main person you can contact?
Yeah, I mean recently there seems to be one nurse who’s coming, I met her, and we’ll see if it progresses to anything.
Inappropriate calls were seen as the biggest threat to working relationships in sites 2 and 3. The conflation of planned care and urgent (and thus unpredictable) requests was highlighted as problematic. One GP observed that it was not the residents who were challenging, it was more that care home staff could not (or would not) differentiate between what was urgent and what could wait:
If it was just the residents and not the repeat call-outs for nothing very much then I think that would be fine that would be workable.
Site 2 GPI01
This was acknowledged but not represented so negatively by site 1 GPs. This may be because the other care home services in site 1 absorbed some of the demands experienced by GPs in other sites. The organisation of NHS care in and around care homes was unclear to GPs in all the sites. They were aware of some but not all services (e.g. dementia outreach team or a particular nurse specialist), but did not work closely with them and in some cases these were regarded as being unhelpful (e.g. also prescribing for their patients).
A cross-cutting issue when providing health care that GPs raised was the support of people with dementia whose behaviours care home staff did not know how to handle.
Continuum of association
The organisation and funding of NHS services to care homes in the three sites reflected a continuum of association that in part reflects how relational patterns of working have developed over time. Figure 7 provides a graphic illustration of how the different services described were organised around the care homes and the level of horizontal integration achieved. The pale green circles denote an explicit (funded) commitment to spend time working with care homes. Site 1 HCPs working with care homes also liaised with each other in how they worked with care homes. Sites 2 and 3 individual HCPs involved other services, but this was on a resident-by-resident basis and there was limited evidence of shared working. The green circles denote those services that visited care homes, but the frequency and intensity of their involvement were at the discretion of the HCPs involved. This was in turn influenced by the demands of their wider caseload.
FIGURE 7.
Continuum of horizontal integration of health services with care homes across the sites. AHP, allied health professional; DN, district nurse.

Conclusion
Chapter 5 has summarised in detail a within- and cross-case narrative of NHS provision to care homes from the three case study sites, with specific reference to those activities related to the areas of interest identified in phase 1. Resident baseline characteristics were very similar across the three sites, indicating broad comparability in terms of the resident cohorts and providing justification for cross-site analysis.There were differences in length of association, intensity of contact and opportunities for consultation, how particular services were organised and used, how participants worked with each other and how they interpreted their responsibilities. Chapter 6 will now go on to report a detailed site-by-site analysis of the outcomes of interest.
Chapter 6 Phase 2 case studies: case study outcomes of interest
Introduction
This chapter focuses on describing the outcomes of interest, identified through the earlier realist synthesis described in Chapter 4. These were medication use; use of out-of-hours service; resident, carer and staff satisfaction; unplanned hospital admissions (including A&E); and length of hospital stay. These are described across the three case study sites before a cross-case analysis of differences and commonalities across the three sites.
Service use data by site
Service use data were analysed based on complete cases at 6 months (85% of the baseline sample) because this provided the best balance of duration of follow-up and completeness of the data set, in order to avoid confounding introduced by missing data after the 6-month cut-off point.
Service use contacts are summarised by site in Table 18. Most residents had infrequent health service use of many health services over the 6-month period, resulting in high levels of no utilisation for many of the resource items when considered on their own. For this reason, services were combined into eight categories. GPs were the most heavily utilised group; over 90% of residents in each site had some level of general practice contact during the 6 months. Community care contact, which was made up of community nurses, allied health professionals and other specialist community care contacts, was the next most utilised group with approximately 88% of residents in sites 1 and 3, and 86% in site 2, having some level of community care. All other services were used by relatively small proportions of residents. There was significantly more use of primary care (other than GPs, i.e. dentists, opticians, chiropodists) in site 3, than in sites 1 and 2. Secondary care (ambulatory/no admission) was significantly higher in site 3, than in site 2. Although more residents in site 3 had hospital admissions than in the other two sites, the differences were not statistically significant.
| Care/service type | Site, contacts per resident | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 (n = 77) | 2 (n = 69) | 3 (n = 49) | |||||||
| Mean (SD) | Median (range) | Mean (SD) | Median (range) | Mean (SD) | Median (range) | Site 1 vs. 2 | Site 1 vs. 3 | Site 2 vs. 3 | |
| GP care contacts | 4.06 (2.97) | 4 (0–17) | 6.04 (4.49) | 5 (3–8) | 4.45 (3.98) | 4 (0–20) | 0.36 | 0.19 | 0.20 |
| Community care contacts | 9.74 (22.02) | 5 (0–189) | 14.39 (51.39) | 3 (1–7) | 24.10 (76.05) | 3 (0–376) | 0.49 | 0.33 | 0.18 |
| Primary care (optician, dentist, pharmacist) | 0.30 (0.51) | 0 (0–2) | 0.39 (0.79) | 0 (0–1) | 0.76 (0.78) | 1 (0–3) | 0.40 | < 0.01* | 0.01* |
| Out-of-hours care (GP or nurse) contacts | 0.25 (0.91) | 0 (0–7) | 0.35 (0.61) | 0 (0–1) | 0.31 (0.74) | 0 (0–4) | 0.08 | 0.46 | 0.45 |
| A&E visits | 0.23 (0.79) | 0 (0–6) | 0.14 (0.49) | 0 (0–0) | 0.06 (0.24) | 0 (0–1) | 0.61 | 0.43 | 0.68 |
| Secondary care non-admitted contacts | 0.43 (0.97) | 0 (0–5) | 0.19 (0.69) | 0 (0–0) | 0.65 (1.07) | 0 (0–5) | 0.37 | 0.42 | 0.01* |
| Secondary care admissions | 0.25 (0.61) | 0 (0–3) | 0.17 (0.42) | 0 (0–0) | 0.33 (0.55) | 0 (0–2) | 0.61 | 0.22 | 0.24 |
| Ambulance use | 0.35 (0.82) | 0 (0–5) | 0.28 (0.70) | 0 (0–4) | 0.35 (0.56) | 0 (0–1) | 0.19 | 0.08 | 0.31 |
Costs by site
Costs are summarised by site inferences and other covariates (Table 19). Average cost of hospital stay per resident was the single greatest contributor to costs at all three sites and did not show statistically significant differences between sites. The average total cost of 6 months of health resources per participant, excluding in-hospital stays, was £634 for site 1, £730 for site 2 and £880 for site 3; when the cost of hospital admissions was included, the means increased to £1160, £1190 and £2096, respectively. Excluding hospital stays, GP and community costs accounted for most costs. GP costs were significantly higher in site 2, where financial incentives provided to GPs to increase frequency of contact were a mainstay of the service model, than those in sites 1 and 3. Costs for dentistry, opticians and chiropody were higher in site 3 than in site 2. Although not statistically significant, it is notable that costs were higher in site 3, where care models were less specified and structured, than in sites 1 and 2. This was largely because of the increased expense associated with hospitalisation. Site 3, however, was associated with greater access for residents to dentists, opticians and chiropody services.
| NHS service used | Site, cost (£) per resident | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | Site 1 vs. 2 | Site 1 vs. 3 | Site 2 vs. 3 | ||||
| Mean (SD) | Median (range) | Mean (SD) | Median (range) | Mean (SD) | Median (range) | ||||
| GP (GP and practice staff) | 175 (132) | 146.31 (90–225) | 270 (194) | 225 (135–360) | 189 (174) | 135 (56–270) | < 0.01* | 0.64 | 0.02* |
| Communitya | 224 (384) | 143 (44–281) | 292 (876) | 70 (17–184) | 450 (1275) | 79 (50–215) | 0.56 | 0.23 | 0.46 |
| Primary care (other)b | 18 (34) | 0 (0–39) | 20 (41) | 0 (0–39) | 40 (60) | 39 (0–39) | 0.70 | 0.02* | 0.05* |
| Out of hours | 17 (62) | 0 (0) | 23 (40) | 0 (0–0) | 21 (51) | 0 (0–0) | 0.50 | 0.69 | 0.84 |
| A&E not admitted | 32 (107) | 0 (0) | 20 (67) | 0 (0–0) | 8 (33) | 0 (0–0) | 0.41 | 0.08 | 0.23 |
| Secondary care not admitted | 88 (231) | 0 (0) | 42 (225) | 0 (0–0) | 99 (205) | 0 (0–134) | 0.23 | 0.77 | 0.15 |
| Admissions (cost) | 525 (1888) | 0 (0) | 519 (1913) | 0 (0–0) | 1202 (3326) | 0 (0–512) | 0.99 | 0.20 | 0.20 |
| Ambulance use | 81 (190) | 0 (0) | 64 (163) | 0 (0–0) | 80 (130) | 0 (0–231) | 0.55 | 0.98 | 0.54 |
| Total cost | 1160 (2184) | 492 (239–740) | 1190 (2250) | 439 (257–893) | 2069 (3745) | 682 (264–1918) | 0.94 | 0.13 | 0.15 |
| Total cost excluding hospital admissions | 634 (687) | 458 (239–708) | 730 (991) | 413 (230–742) | 880 (1320) | 493 (264–865) | 0.51 | 0.23 | 0.50 |
There are some caveats to this analysis. In particular, no account is taken of the on-site nursing resource in nursing homes. Residents in residential homes without on-site nursing receive care from community or district nurses, and this was reflected in the service use frequencies collected from residential homes, and in the cost calculations. No data were available, however, on use of on-site nurses by residents in the sample who were living in nursing homes. The Care of Older People UK Market Report 2014/1512 suggests a difference of £226 per week in the average fees of private nursing and residential homes (£821 vs. £595, respectively), and this might be taken as an indicative cost to be added to the cost of other services used by nursing home residents. This is a particular problem because the proportion of residents from nursing (vs. residential homes) included in the study was not the same between sites. There were three and four times as many nursing home residents in site 2 as in sites 1 and 3, respectively, thus it is possible that the costs for community care on site 2 would have been greater had it been possible to account for this nursing resource use in the costing model. A further hidden cost is that of the financial incentives paid to GPs in site 2 for enhanced services to care homes, implying that the full economic cost of GP services in that site is higher than shown. The service frequency and cost comparisons are based on the differences in unconditional means. The subsequent analysis controls for baseline differences and other covariates.
Regression analysis of outcomes taking account of baseline variables by site
As described in Chapter 2, we used Poisson regression to consider whether or not a site was a significant predictor of service use. Total costs after the baseline interRAI scores and the derived interRAI scales, as well as the interaction between the site and these variables, were taken into account. We first entered each of the baseline interRAI scores and the derived variables into a Poisson regression equation in univariate analyses using each of the categories of service use and total costs as dependent variables. The results from this analysis are shown in Appendix 11.
Using a significance level of 0.10, we then tested interaction terms for each site and each baseline variable or derived variable found to be statistically significant in the univariate analysis. In a third and final step, significant interaction terms were entered along with the site and the variables found to be significant in the univariate analysis to determine whether or not the site was a significant determinant of differences between outcomes. Gender, age, bed type (residential or nursing) and payment source (self-funder vs. received state contributions) were included in the analysis based upon pre hoc assumptions derived from the existing literature about the likely role that they might play in confounding outcomes. The continuous predictors were mean centred; the mean was subtracted from the score to facilitate interpretation of the main effect of the site. The outputs of this process are summarised in Tables 20–22. For GP contacts we found that site 2 had 1.40 times as many GP contacts as site 1 (p < 0.01). This remained significant after the effect of other associated variables, namely comorbidities, pain and medication count, and the interaction term between site 3 and pressure ulcer risk were taken into account. For primary care (optician, dentist and pharmacist) contacts, we found that site 3 had almost twice as many of these as site 1 (p < 0.05). This remained significant after the effect of other associated variables, namely payment source and cognitive impairment, were taken into account. For out-of-hours contacts, we found that sites 2 and 3 had more than four times as many contacts as site 1 (p < 0.05 for both).
| Variable | IRR | SE | z | p-value | 95% CI | Pearson’s R2 |
|---|---|---|---|---|---|---|
| Site 2 | 1.39 | 0.17 | 2.74 | < 0.01 | 1.10 to 1.76 | 0.13 |
| Site 3 | 1.13 | 0.15 | 0.98 | 0.33 | 0.88 to 1.46 | |
| Gender | 0.94 | 0.10 | –0.60 | 0.55 | 0.75 to 1.16 | |
| Age | 1.01 | 0.01 | 1.05 | 0.29 | 0.99 to 1.02 | |
| Bed type | 0.89 | 0.12 | –0.81 | 0.41 | 0.68 to 1.17 | |
| Payment source | 1.00 | 0.00 | 1.36 | 0.17 | 1.00 to 1.01 | |
| sPURS: site 1 | 1.01 | 0.05 | 0.25 | 0.80 | 0.92 to 1.11 | |
| Comorbidities | 1.10 | 0.05 | 2.06 | < 0.05 | 1.00 to 1.20 | |
| sPAIN_1 | 1.30 | 0.14 | 2.41 | < 0.05 | 1.05 to 1.61 | |
| Medication count | 1.06 | 0.01 | 4.50 | < 0.01 | 1.03 to 1.09 | |
| sPURS: site 2 | 0.89 | 0.05 | –2.13 | < 0.05 | 0.80 to 0.99 | |
| sPURS: site 3 | 1.16 | 0.07 | 2.42 | < 0.05 | 1.03 to 1.31 |
| Variable | IRR | SE | z | p-value | 95% CI | Pearson’s R2 |
|---|---|---|---|---|---|---|
| Site 2 | 1.32 | 0.39 | 0.97 | 0.33 | 0.75 to 2.34 | 0.07 |
| Site 3 | 1.97 | 0.56 | 2.38 | < 0.05 | 1.13 to 3.44 | |
| Gender | 0.81 | 0.21 | –0.81 | 0.42 | 0.49 to 1.34 | |
| Age | 1.01 | 0.02 | 0.67 | 0.50 | 0.98 to 1.04 | |
| Bed type | 1.31 | 0.44 | 0.80 | 0.42 | 0.68 to 2.52 | |
| Payment source | 1.01 | 0.00 | 1.54 | 0.12 | 1.00 to 1.02 | |
| sCPS | 1.03 | 0.10 | 0.36 | 0.72 | 0.86 to 1.24 | |
| Cognitive impairment | 0.49 | 0.15 | –2.27 | < 0.05 | 0.27 to 0.91 |
| Variable | IRR | SE | z | p-value | 95% CI | Pearson’s R2 |
|---|---|---|---|---|---|---|
| Site 2 | 4.23 | 2.80 | 2.18 | < 0.05 | 1.16 to 15.48 | 0.13 |
| Site 3 | 4.50 | 3.44 | 1.97 | < 0.05 | 1.01 to 20.13 | |
| Gender | 0.54 | 0.29 | –1.13 | 0.26 | 0.18 to 1.57 | |
| Age | 1.01 | 0.02 | 0.53 | 0.59 | 0.97 to 1.06 | |
| Bed type | 0.49 | 0.31 | –1.12 | 0.26 | 0.14 to 1.70 | |
| Payment source | 0.99 | 0.01 | –1.12 | 0.26 | 0.97 to 1.01 | |
| sPURS | 0.92 | 0.15 | –0.51 | 0.61 | 0.67 to 1.26 | |
| sADLSF | 1.10 | 0.06 | 1.86 | 0.06 | 0.99 to 1.21 | |
| Comorbidities | 1.34 | 0.20 | 1.93 | 0.05 | 1.00 to 1.80 | |
| sPAIN_1 | 2.32 | 1.66 | 1.17 | 0.24 | 0.57 to 9.45 |
Interpreting service use data from the case studies
Before moving on to consider the specific substudies around unplanned hospitalisations and medication use data, and the qualitative data about the outcomes of interest, the quantitative outcome data will be discussed. Within the broader analysis, these contain important, albeit unsurprising, insights about service use; namely that pain, pressure ulcer prevalence, medication use and comorbidities are predicted for increased health service utilisation among care home residents (see Appendix 12).
For the most part there were no compelling differences in service use or costs between sites. Site 3 might have been expected to have been substantially cheaper, given that the cohort recruited here was substantially less dependent; however, this was not in fact the case. Site 1 might have been expected to have been substantially more expensive because of markedly different models of service provision that were more formalised and not primarily focused around the GP, but this was not the case.
Site 3 used more chiropody, pharmacy and optician resource than sites 1 or 2 and spent significantly more money on doing so, although, in real terms, the excess expense was small. This may have indicated better access to these services on this site, rather than excessive use of these resources. Site 3 also had a greater number of secondary care non-admitted contacts, as well as a trend towards higher costs associated with hospital admissions. This may indicate a tendency at this site to refer residents into hospital, rather than provide care in situ.
General practitioner attendances at site 2 cost more than in either sites 1 or 3. This is consistent with the model of care at this site where additional payments were designed to increase the frequency of GP attendances in care homes. Once baseline variables (including the functional dependency and comorbidities of the cohorts) were controlled for, there was evidence that GPs attended more frequently in site 2 than in site 1 and that there were more frequent out-of-hours attendances in sites 2 and 3.
Site 1 was no more expensive in any domain than the other two sites. It did not see a greater number of contacts for any one service than the other two sites.
Substudy of unplanned hospitalisations
To gain a better understanding of the nature and type of unplanned hospital admissions, we conducted a descriptive analysis of the data, summarised in Table 23 (see also Appendices 11 and 12). In total, 39 residents were hospitalised at some point during the 12-month data collection period, just 16% of the total number of residents recruited to the study. The length of stay ranged between one night (n = 17) and 47 nights for one case involving a dementia-related mental health assessment, with 22 residents being hospitalised for more than five nights in one episode. These support the findings from the quantitative analysis above of a greater reliance upon secondary care in site 3, but also highlight the tendency for patients to stay much longer in hospital in this site.
| Site | Number of residents hospitalised | Hospitalisations as a percentage of the total number of residents recruited | Number of residents hospitalised for . . . | |||
|---|---|---|---|---|---|---|
| 1 occasion | > 1 occasion | 1 night | ≥ 5 nights | |||
| 1 | 14 | 15% (n = 93) | 9 | 5 | 9 | 6 |
| 2 | 11 | 12% (n = 92) | 9 | 2 | 7 | 5 |
| 3 | 14 | 25% (n = 57) | 9 | 5 | 1 | 11 |
| Total | 39 | 16% of all residents | 27 | 12 | 17 | 22 |
The reasons for residents being hospitalised did not differ much across the three sites (Table 24). The most common reason was falls (n = 13), eight of which resulted in a fracture, followed by respiratory-related conditions (n = 6), including pneumonia, chest infection and breathing difficulties. No information was available in the care home record about the reason for admission or discharge diagnosis for six admissions.
| Site | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| Reason for admission | Number of admissions | Reason for admission | Number of admissions | Reason for admission | Number of admissions |
| Fall | 1 | Fall | 2 | Fall | 2 |
| Fall and fracture | 3 | Fall and fracture | 3 | Fall and fracture | 2 |
| Respiratory conditions | 2 | Respiratory conditions | 2 | Respiratory conditions | 2 |
| UTI | 3 | Urinary retention | 2 | Urinary retention | 1 |
| Syncope | 1 | Osteomyelitis | 1 | Hypotension | 2 |
| Pyrexia | 2 | Pyrexia | 1 | Abdominal pain | 1 |
| Transient ischaemic attack | 1 | Chest pain | 1 | Clostridium difficile infection | 2 |
| Chest pain | 1 | No information | 1 | Rectal bleed | 1 |
| Vomiting | 1 | Mental health assessment | 1 | ||
| No information | 3 | Not eating or drinking | 1 | ||
| No information | 2 | ||||
Substudy of medication data
Medication data were available from 214 out of 239 residents. All residents from site 1 had full medication data. Twenty-four residents from site 2 had missing data, related to difficulties in obtaining baseline medication data from one care home. One resident from site 3 was not taking any medication. Where baseline data were successfully retrieved, our mechanism for collecting follow-up data from the care home yielded a full follow-up data set. Thus, there were 90, 68 and 56 residents from each of sites 1, 2 and 3, respectively, with fully analysable medication data.
The mean number of medications at baseline for all sites was 8.28 (SD 3.4), and –8.00 (SD 3.5), 8.24 (SD 3.6), 8.77 (SD 3.1) for sites 1, 2 and 3, respectively, with no statistically significant difference between sites. The range of medications was 1–21. Forty-nine residents were taking opioids at baseline, with 47 of those taking a single opioid medication. Two were taking two opioid medications. Participants were significantly less likely to be taking opioids at site 1 (p < 0.01). Thirty-four residents were taking antibiotics at baseline. Participants were significantly less likely to be taking antibiotics at site 3 (p < 0.01). The median (range) ACB score was 1 (0–14), with no statistically significant difference in distribution of ACB scores between sites.
Over the study period, there were 366 medication changes (starting, stopping or substituting a medicine) in site 1, 261 changes in site 2 and 266 in site 3. This represents 0.40 (SD 0.66), 0.44 (SD 0.84) and 0.49 (SD 0.79) changes per resident per month in sites 1, 2 and 3, respectively.
Follow-up data did not demonstrate consistent trends in antibiotic or opioid prescribing. Site 3 reported the lowest ACB score throughout the study, with evidence of a rising ACB score in sites 1 and 2 (Figure 8).
FIGURE 8.
Mean ACB score across the three study sites over 12 months. Error bars: 95% CI.
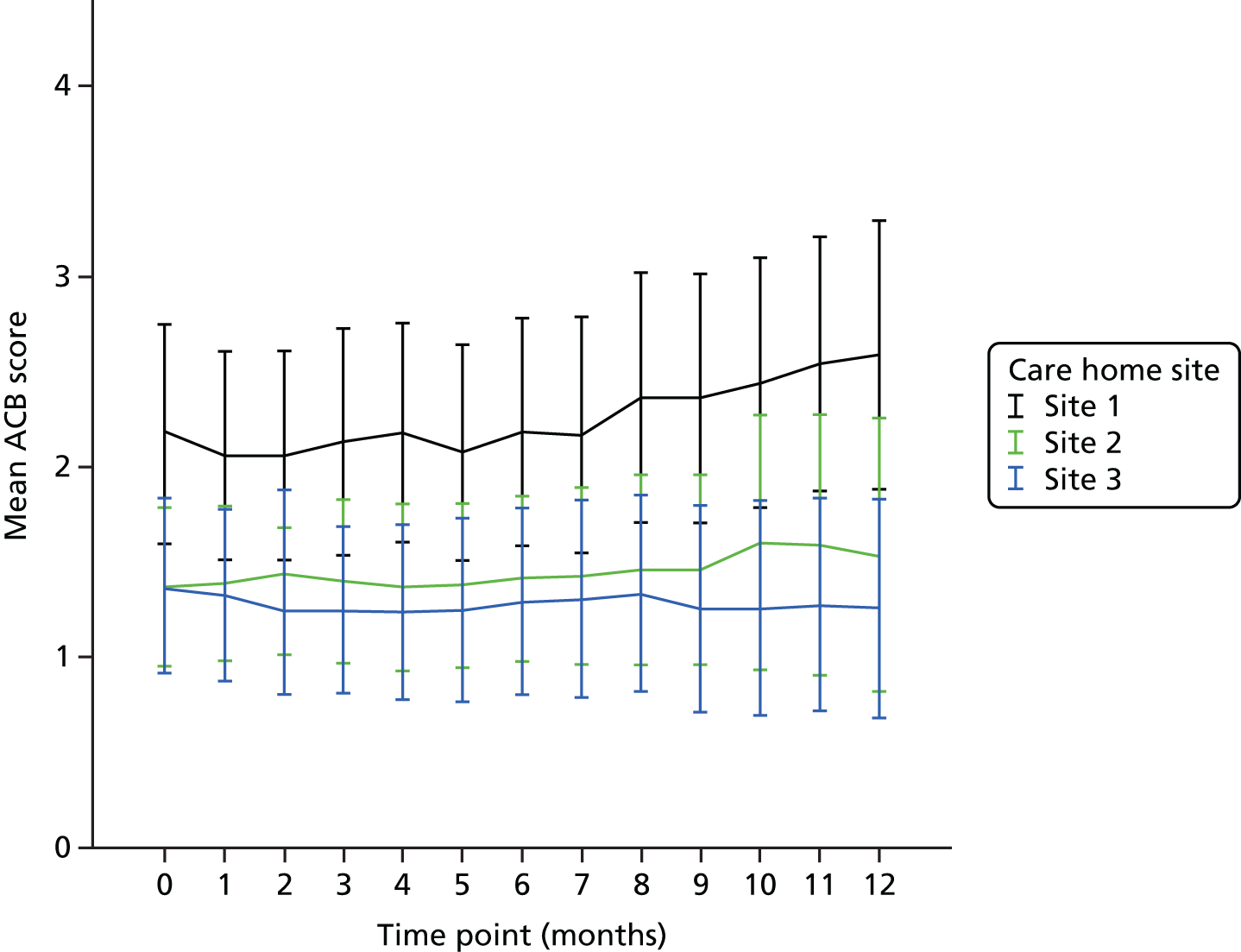
In summary, the cohort was representative of UK care homes generally in terms of the prescribing rates seen. For most variables measured, the sites were not substantively different at baseline and differences seen at baseline in antibiotic and opioid prescribing disappeared with follow-up. The implications of the tendency towards lower ACB scores in site 3 are unclear; it could either be attributable to the dementia specialist nurse’s involvement in the reduction of antipsychotic prescribing in the study care homes or be indicative of a different culture of care within the care homes in site 3, consistent with their participation in the My Home Life leadership training programme. There is, however, no evidence to suggest that increased GP contact in site 2, or case management as part of ‘wrap-around’ care, worked to optimise prescribing in any way over the more traditional models of working seen at site 3.
Staff satisfaction substudy
Data collection for this substudy took place towards the end of the case studies, by which time the research team were aware that the care homes were suffering from ‘research fatigue’ following the case study process, and it was anticipated that engagement might be suboptimal. A total of 562 questionnaires were sent out by post, with two rounds of follow-up telephone reminders on a weekly basis to maximise response rates. The forms were mislaid at two sites and further copies were sent. One care home subsequently refused to return their staff questionnaires because of a change in management and a decision that supporting this final stage of the study was no longer a priority.
Consequently, out of a potential total of 562 questionnaires, only 94 were returned, a response rate of 16.7%. Sites 1, 2 and 3 returned 55, 14 and 25 questionnaires, respectively. The bulk of responses from sites 1 and 3 came from care assistants, while in site 2, the number of responses was low overall (Table 25).
| Profession | Site, number of responses | Total | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Care assistant | 32 | 5 | 17 | 54 |
| Registered nurse | 0 | 5 | 1 | 6 |
| Care home manager | 2 | 2 | 2 | 6 |
| Activity co-ordinator | 0 | 1 | 1 | 2 |
| Other | 21 | 1 | 4 | 26 |
| No reply | 0 | 0 | 0 | 0 |
There were no differences between the sites in respondents’ age, duration in current profession or current post. Patterns of working differed, with participants significantly more likely to undertake split shift working on site 1 (Table 26).
| How are working hours organised? | Site, number of participants | Total | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Scheduled working hours with split shifts | 21 | 2 | 13 | 36 |
| Scheduled working hours without split shifts | 33 | 10 | 10 | 53 |
| Part-time sick leave | 0 | 0 | 0 | 0 |
| Full-time sick leave | 0 | 0 | 0 | 0 |
| Leave of absence | 0 | 0 | 0 | 0 |
| Other | 0 | 2 | 2 | 4 |
| No reply | 1 | 0 | 0 | 1 |
A total of 83 out of 94 (88%) respondents thought that their workplace was staffed sufficiently, either sometimes or usually, with only 10 out of 94 (11%) respondents raising concern about staffing levels; 91 out of 94 (97%) respondents were somewhat or absolutely satisfied with their current working hours; and 79 out of 94 (84%) respondents felt able to influence their current patterns of working. There were no significant differences between sites for any of these variables. In all sites, the bulk of the working week was spent caring directly for residents (Table 27).
| Activity | How working hours are distributed on an average week: all sites | No reply | ||||
|---|---|---|---|---|---|---|
| 0% | < 25% | 25–50% | 51–75% | > 75% | ||
| Working directly with residents | 7 | 11 | 16 | 10 | 40 | 10 |
| Administration | 25 | 19 | 8 | 6 | 9 | 27 |
| Cleaning/service | 31 | 15 | 4 | 1 | 3 | 40 |
| Travel | 29 | 19 | 5 | 1 | 3 | 37 |
| Other | 24 | 6 | 4 | 0 | 3 | 57 |
Satisfaction with the care provided within the care homes was high across all sites (Table 28), but was significantly higher for ‘information provided to residents about work routines and nurse in charge’ and ‘activities provided to residents’ in site 1 (p < 0.05).
| Satisfaction | No reply | |||||
|---|---|---|---|---|---|---|
| Very good | Quite good | Quite poor | Very poor | Cannot judge | ||
| Site 1 | ||||||
| Information, work routines, nurse in charge | 40 | 5 | 0 | 1 | 4 | 5 |
| Staff | 31 | 13 | 3 | 1 | 5 | 2 |
| Activity | 36 | 8 | 1 | 1 | 6 | 3 |
| Care | 34 | 9 | 0 | 2 | 4 | 6 |
| Site 2 | ||||||
| Information, work routines, nurse in charge | 2 | 12 | 0 | 0 | 0 | 0 |
| Staff | 2 | 12 | 0 | 0 | 0 | 0 |
| Activity | 0 | 14 | 0 | 0 | 0 | 0 |
| Care | 3 | 11 | 0 | 0 | 0 | 0 |
| Site 3 | ||||||
| Information, work routines, nurse in charge | 15 | 6 | 1 | 0 | 0 | 3 |
| Staff | 12 | 11 | 0 | 2 | 0 | 0 |
| Activity | 10 | 10 | 0 | 2 | 1 | 2 |
| Care | 15 | 10 | 0 | 0 | 0 | 0 |
Almost all (96%) of the sample responded to the question about quality of care provided to residents by the NHS on an analogue scale from 0 to 10, whereby 10 represented extremely satisfied and 0 represented not at all satisfied. The mean score was 7.5 (range 3–10), with no significant difference between sites.
The low response rate means that the data may well be biased in favour of positive responses from those staff members who had remained enthusiastic about the project throughout. Despite this, the staff responses suggest a staff group that, on the whole, reported high levels of job control, job satisfaction and satisfaction with the services provided by their employing care homes and the NHS services with which they interfaced. This is somewhat contrary to the narrative of a sector commonly portrayed as beleaguered and on the edge of collapse. Few significant differences were observed between sites, but where they did occur they tended to favour site 1.
Qualitative data on the outcomes of interest
This section focuses on findings that related to the five outcomes of interest: medication use; use of out-of-hours services; resident, carer and staff satisfaction; unplanned hospital admissions (including A&E); and length of hospital stay. The findings were drawn from all participants’ accounts (residents, family, care home staff, HCPs, GPs and commissioners). This section considers what these accounts revealed about the elements within the service delivery models offered in the three sites that phase 1 findings had theorised were important to achieve the outcomes of interest. Specifically, how different contexts generated (or did not generate) staff responses that supported relational working, which in turn supported residents’ care and integration of services, was considered. These data should be seen as complementary to the quantitative data about the outcomes of interest already presented.
Use of medications
Across all three sites, HCP accounts identified a range of issues that were medication specific and could not be identified as site specific. These included concerns about administration and recording errors, care home staff knowledge of pharmacology, difficulties of prescribing for wound management, the challenges of multiple prescribers visiting care homes and the importance of access to emergency end-of-life medication out of hours. A lack of pharmacist involvement in medication reviews was highlighted as a gap in service provision across the sites.
Site 1 appeared to have the highest number of nurse prescribers. Specialist nurses were involved in reviewing specific medications in sites 1 and 3, including medications for dementia and osteoporosis. However, in all the sites nurse prescribing was not a substitute for GP involvement. There were situations when nurse prescribers deferred to the GP, for example when it was quicker to access the medication through the GP prescribing route, where the GP had initiated the medication or where there was a protocol in place for GPs to review medications once the resident’s condition was stable.
In site 2, the tissue viability nurse specialist highlighted that nurses working as part of the care home staff did not identify products from the same formulary for wound care products as the tissue viability service and so requested different products from the GP. There were multiple routes to obtaining a prescription for a resident and it was difficult to identify how care home staff decided whom to approach and involve.
In site 3, there were no referral guidelines for care home staff in relation to dietary supplements. This was seen as leading to duplication of consultations with the dietitian, nurse practitioner and GP, inconsistent prescribing practices and a lack of clarity for the care home. The introduction of antipsychotic reviews by the dementia nurse specialist was reported to have resulted in significant reductions in prescribing of these medications and there was evidence of lower ACB scores in residents at this site. These reviews were sustained over the length of the study (Table 29).
| Site | Cross-cutting theme | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Mixed approach to medication review, but evidence of systematic approaches (taking patient records to care home) and working to reduce total medication burden |
|
|
|
The care home staff interviews and focus groups provided an alternative perspective on medication management, with three main themes emerging: medication reviews, ‘over-the-phone’ prescribing and chasing prescriptions and medications. Differences between accounts from the three sites were apparent. When GPs held regular clinics in the care homes, there were few or no references to medication-related problems, and reviews were conducted more frequently. In site 3, apart from a time-limited pilot when GPs had offered care home-based clinics, GPs visited only on request. Care home staff were either unaware that the GPs had completed reviews or reported having to remind GPs to complete them. ‘Over-the-phone’ prescribing was a particular issue for the care homes in site 3. In site 1 this only occurred occasionally and care home staff were generally of the opinion that the practice was unacceptable unless there were exceptional circumstances, for example for the benefit of a resident with specific needs such as end-of-life care:
No, majority, they [GPs] will come out. If I’ve got someone on end of life, and say like they’ve got thrush in the mouth, then they will prescribe over the phone because this person’s end of life, especially if it’s a Friday, we’re not going to wait until the Monday because it’s going to be uncomfortable, they’re not going to drink, they’re not going to want mouth care. So I think certain aspects they will, but nine out of ten I think the doctor will come out.
S1CH3, care home staff 01 interview
For care home staff, the logistics of obtaining prescriptions for residents were often described as being difficult. In sites 2 and 3, care staff described being continuously on the telephone ‘chasing prescriptions’ and acting as the ‘go-betweens’ for GPs or district nurses and pharmacists to sort out medication issues. Some staff in site 2 residential care homes found this particularly difficult to negotiate as a result of their lack of medication-related knowledge. Care home staff across the sites also talked about district nurses prescribing dressings or other items for residents and expecting them to arrange their delivery, which they did not see as part of their role. This was work for care home staff that arose from HCP visits and that was unknown and unacknowledged:
So when things don’t work so well with pharmacy, what’s that about?
What it is, isn’t it, it’s when the doctor’s signed a prescription and it’s our responsibility to do medication, blah blah. When it’s the district nurses right, it’s happened a lot, hasn’t it, where they expect us to get it across or whatever, dressings, but they order the, don’t they, at the side of the . . . and they’ll turn up and the item’s not here. That’s not our responsibility to order that item, that’s in their department, whereas ours is with the pharmacy medication.
Care home staff who participated in the interviews did not appear to have received specific education or training in medication management from the visiting NHS services, including those in site 3 where there had been a focus on reducing antipsychotic prescribing. This may be a reflection of the level of staff turnover in care homes or that those interviewed had not been involved in this programme of work.
In all three sites residents identified access to medications as a concern. In Site 1, residents knew that the GP visited regularly and at predictable times and wanted to have the opportunity to ask questions concerning their medication and treatment. To be seen, however, residents had to ensure that they or staff had written their name into a book. If this was not done, or the GP was fully booked, this arrangement was perceived as delaying rather than facilitating access to care and, specifically, prescriptions. An awareness of GP involvement raised expectations about access that were not so apparent in the other sites as the following quotation shows:
I have been waiting over a week for my prescriptions now. But I have marvellous treatment here. The girls are marvellous.
S1CH3R01, resident
Family members across the sites discussed medication. Several acknowledged the complexity of the medication regimes and the importance of getting it right. For some, how medication was managed was a proxy measure for the quality and personalised care provided by the care home:
Yeah, because he’s got a very complicated medication routine, and that’s . . . so he’s got, you know, he’s given tablets every 2 hours, 2 and a half hours, so somebody, somebody does that for him, and he always, you know, if he’s not feeling well, that’s monitored fairly closely.
S1CH2F03
In all sites, the medication management was perceived as being mostly good, but there were some bad experiences. Examples came from sites 2 and 3 and included not being informed about medication changes, ‘over-the-phone’ prescribing, delayed prescriptions and errors in dispensing. Family members also emphasised the importance of access to the GP to review, revise and access their relative’s medication. The drawbacks of not involving family members in decisions about starting and stopping medication were highlighted by one relative, where a medication’s positive effects were seen as having been lost:
Now unbeknownst to us, the doctor put mum on a very mild antidepressant, without any consultation with us at all. But both us and the home noticed a significant change in mum’s attitude, outlook, she became much brighter . . . about a year they said that the doctor had just done a routine visit and decided that he was going to take her off of them . . . [this was seen as having resulted in a severe depression].
S3CH4F01
Out-of-hours services
All HCPs recognised that part of their involvement with care homes was to reduce unnecessary hospitalisations. In sites 2 and 3, some HCP posts had been introduced with a specific remit to reduce out-of-hours and emergency service use. This included the dementia nurse specialist and care home nurse specialists in site 3. In site 1, avoiding crisis admissions and GP call-outs was the underlying rationale for the case management work with new care home admissions. Despite this provision, additional training for care home staff on sites and access to specialist nurses were not always seen as being able to compensate for other service and system limitations.
Apart from the GPs, all of the care home services worked office hours, and out-of-hours service provision did not always fit around the needs of older people living with dementia in care homes. An example was that residents had to be admitted to the emergency department at the weekend if they needed to be seen by the psychiatrist, running the risk that they might be admitted to a receiving medical unit even when a primary psychiatric diagnosis had been identified as the main issue by the care home staff or visiting HCPs.
Staff at three care homes in site 1 had positive experiences of out-of-hours services responding quickly once they had been contacted. However, in sites 2 and 3, care home staff experiences of these services were poor. In particular, no account was taken of care home staff knowledge of residents or experience, together with out-of-hours practitioners not differentiating between nursing homes and residential care homes in terms of staff knowledge and skills. They found the out-of-hours process protracted, with long delays between speaking to an advisor and residents receiving a visit. Care home staff could wait for anything up to 12 hours for an out-of-hours GP to visit from the first contact with the service:
But with the doctor ooh you can wait up to all night long. Sometimes if you phone them at lunchtime it can be five o’clock in the morning sometimes.
So what’s the shortest length of time before somebody will visit?
4 hours.
And what’s the longest?
About 4–12 hours. They say 4–6 if someone is on end of life.
Some out-of-hours services were perceived as having negative attitudes towards care homes and staff. Examples were given of do-not-attempt cardiopulmonary resuscitation paperwork being ignored on occasion, and there was a perception that care home residents were a low priority for out-of-hours and emergency services. It could therefore mean that an out-of-hours service that was perceived as responsive was more likely to be used by care home staff.
Hospitalisation and length of stay
Prevention of hospitalisation was a priority for HCPs but the process of hospitalisation, length of stay and facilitation of discharge did not feature in the HCP staff interviews and discussions, despite prompts in their interviews. The absence was striking. Care home staff, in contrast, were more preoccupied with how admissions and discharge were managed and the failure of hospitals to look after their residents or plan ahead. Hospital staff were perceived as having little dementia expertise and no insight into how care homes might work or the difference between care homes with and without on-site nursing. The consequences of this lack of communication and common understanding were unplanned or unannounced discharges back to the care home, with no communication about the resident when they were in hospital or prior to discharge, and discharges at times when senior staff were not available. This posed particular problems, as staff recognised that admission and discharge from hospital were often associated with deterioration in a resident’s condition:
OK, and what about when somebody has been in hospital and gets discharged back to you, what’s that like, how does that work?
Well we check them for bed sores (laughs).
Resident, carer and staff satisfaction
General practitioner services
Where GPs held regular clinics in care homes, as in sites 1 and 2, the level of satisfaction with the services provided was generally high. The highest levels of satisfaction were in site 1 where care homes 1 and 2 described their GP services as ‘excellent’ and care home 4 reported that GP services were ‘hugely improved’ as a consequence of the introduction of single GP practices working with care homes. Regular contact appeared to facilitate both working and interpersonal relationships as well as GPs’ knowledge of residents’ health-care needs. Care home staff highlighted continuity of care and the opportunity to build rapport as being key to satisfaction when working with GPs. The importance of a good relationship with the GP in the provision of residents’ care was highlighted by one care home manager:
We’ve always had a close rapport with the GP surgery so we couldn’t do what we do without them to be honest.
S2CH2, manager
In site 3, where GPs visited on request and specialist nurses often substituted for them, there was a marked contrast, as opportunities to establish relationships were limited and, correspondingly, levels of satisfaction were much lower. Care home staff focused on the difficulty of getting GPs to visit and the knock-on effects such as the high levels of ‘over-the-phone’ prescribing. As the following quotation demonstrates, if the care home manager was not satisfied with the nurse practitioner employed by the GP practice, then she would request a GP visit; substitution did not necessarily lead to reduction in demands on GP time:
Well if I was phoning doctor this morning for somebody, there’s a good chance I’ll get a nurse practitioner rather than a doctor but, at the end of the day, if that nurse practitioner doesn’t feel happy with who she’s seeing, then I’ll get a doctor later on.
S3CH3, care home manager
In S3CH1, access to GPs was further reduced over the course of the study as a result of their regular GPs being replaced by locums who were reluctant to visit the care home. This increased the care home’s reliance on specialist nurses. Satisfaction with GPs was lowest in S3CH4, where some GPs showed a lack of awareness of care home staff or their working patterns:
Doctors just come strolling in like they’re god’s gift sometimes still and you know, they want to see the nurse and they want to know this and it doesn’t matter if it’s lunchtime, tablet time, you have to accommodate them and it is just sometimes you want to say hang on a minute . . .
S3CH4, care home manager
The benefits of regular clinics on relationships and the quality of care were evident to staff when comparing the different experiences of two care homes. In S1CH4, care home staff were dissatisfied with the quality of service they received from GPs who visited only on request, as such visits tended to be rushed:
. . . because sometimes they [GPs visiting on a resident-by-resident basis] want to assess them [residents] so quickly . . .
S1CH4FG
Staff in S3CH2 had the contrasting experience of being able to compare the impact of the introduction of a monthly GP clinic for residents as part of a pilot scheme with their usual on-request GP service. Regular clinics were perceived to be a good service because of their focus on residents’ well-being and the proactive approach to residents’ health care:
Monthly GP clinic is good because they [GPs] are taking an interest in their [residents’] well-being and their patients, and they have check-ups every month. You might get somebody go for ages and be fine on the inside but when they come round and do checks [they find a health-care need].
S3CH4FG
However, it did not resolve the problem of not obtaining residents’ prescriptions promptly.
Other services
There appeared to be a similar pattern in terms of overall satisfaction with other health-care services, in that sites 1 and 2 were focused on what worked and site 3 showed the lowest level of satisfaction. Comparing types of care homes, the nursing home staff in sites 2 and 3 appeared to be the least satisfied with health services. In S2CH4, nursing home staff perceptions were that they had little access to health-care services in general and in site 3 the nursing home staff struggled to identify a service with which they were satisfied, with the exception of the chiropodist, optician and pharmacist. However, when care home staff deliberated their satisfaction with specific services there were wide variations, in some cases for the same services, within a site.
In site 1, two contrasting accounts were given by two different care homes about the care home team; one was extremely positive, especially in relation to the case management of new residents, and the other depicted staff as not knowing the residents and having little knowledge about dementia. In most cases it was individual HCPs that they found difficult to work with rather than the service. For example, staff in S1CH4 were of the opinion that some district nurses could ‘learn from the dementia team or the GPs’.
In sites 2 and 3, two care homes reported that district nursing services were outstanding, but two care homes with on-site nursing did not receive district nursing services. It was recognised that it took time to develop relationships; the manager in S3CH1 recounted that, as their relationship with the district nurses developed, so the performance of the care home team had also improved:
District nurses, when I first came here in 2012 there was a fractured relationship . . . and the relationship then with the district nurses improved, because they could see the performance improving and the environment had improved and then they were coming on board with things to the point where we’ve got an excellent relationship with them.
S1CH3, care home manager
In S1CH2 overall satisfaction with services was focused on how they worked together as a team to meet residents’ health-care needs, a narrative of NHS staff ‘helping out’:
What is it exactly about them you feel that works well?
I think they all work really well and I think depending on what services they are, I think they all do their job and help us out and everything else and they visit when required so I can’t complain that way and obviously every one of them services all link together and provide the overall care for the residents here and not one of them don’t do their job properly or help you out.
When evaluating satisfaction with services in all sites, the speed of access to the service was important, but in sites 2 and 3 relocation of NHS staff and their heavy workload were factors that affected satisfaction. In two of the care homes, the district nurses’ high caseloads limited the time they could spend in care homes and compromised the development of relationships with care home staff. However, the palliative nurse specialist in site 2 and the dietitian in site 3, who both had an explicit and specified care home component to their role, were able to establish a good rapport with the staff and give them regular support with residents’ health care.
Residents’ and relatives’ perspectives on their health and the services received
The overarching theme for residents and their relatives across all three sites was the need to be ‘looked after,’ or ‘checked over’, irrespective of whether this involved care home staff or HCPs, although one resident attributed her satisfaction with her health care as reflecting the care received in the care home rather than that received from the visiting professionals:
The health service is marvellous, it’s not the health service itself, it’s the people that work there that cure the patients.
S1CH1R04
When asked what was most important about their health on a day-to-day basis, the majority mentioned having their physical conditions managed and the ability to engage with ADL. These accounts echoed the phase 1 findings. Most residents did not distinguish between personal care and health care when talking about good health care and, with a few exceptions, resident satisfaction with care was high. The only visiting service that was consistently referred to by both residents and relatives was the GP, and satisfaction was linked to access, continuity of care and whether or not the GP was pleasant:
. . . the GP is alright . . . he has a sense of humour . . . no – I think they are all reasonable . . .
S3CH2R06
There were areas identified for improvement: access to dentists, therapists and podiatry; advice and support; and monitoring for specific conditions such as pain secondary to arthritis and diabetes mellitus. One relative wondered if a diagnosis of dementia had reduced her mother’s access to specialist care and commented that it would be different if she had cancer. One need identified by two residents living with diabetes mellitus in different sites was that medication and advice around the management of their condition should be linked to how meals were prepared and offered. Apart from this there was a lack of specificity about services received. Some relatives were uncertain about service eligibility and wondered in hindsight if they should have asked for services or challenged or been included in care-related decisions. For example, this relative wondered if physiotherapy services could have maintained or improved the resident’s function and mobility post admission and regretted not asking:
. . . Family [wife] felt that the resident [husband] needed physiotherapy to increase mobility, small movements such as eating, and bigger movements . . . but they have not spoken to anyone about it . . . and I feel guilty about that now really.
S1F02
Health-care professionals’ satisfaction with the service delivered to care homes
Health-care professionals across the sites generally showed high levels of satisfaction when working with care homes but there were differences in how HCPs and GPs talked about care homes. Satisfaction was based on the quality of the interpersonal relationships and was experienced when care home staff did as they were instructed by HCPs. Frustration was expressed where handovers between care home staff did not ensure HCPs’ instructions were communicated and implemented:
I think getting the information to start with for my assessment works quite well because there’s always someone there ready to give me the information. Sometimes it doesn’t work as well when I’ve put a particular recommendation in place that needs to be done regularly and it’s not handed over well in the care home so the morning shift don’t handover to the afternoon shift. So when I go in they haven’t got a clue what I’m on about so that’s quite frustrating really when that patient needs. For example, if I’ve advised that the patient needs regular standing and mobility and it’s not been handed over how far the patient can walk and they’re only doing two steps when in fact they can do 22 steps, they’re not carrying out the correct recommendations. That’s sometimes quite frustrating because there’s such a big staff ratio in the home, if it’s not handed over to every single carer it doesn’t get done for one particular reason.
S1CH4HCP04, physiotherapist dementia team
The importance of the role of the manager and the management structure were contributing factors to the overall experience of working with care homes identified in both sites 1 and 2. The palliative care nurse specialist talked about a high level of satisfaction when working with care homes, based on mutual trust and relationships that had taken 5 years to establish. Some HCPs, including the tissue viability nurse specialist in site 2 and the dietitian in site 3, noted that satisfaction was predicated on the extent to which care home staff were engaged in working with them. As one physiotherapist in site 3 stated:
If care homes are not ‘on board’ you are almost wasting your time.
S3CH3HCP02
Resident behaviour secondary to dementia and its impact on service provision and working relationships
Implicit in the phase 1 findings was that the majority of residents had a dementia diagnosis. However, we had not considered or recognised how this affected patterns of working and response between the care homes and the visiting health-care services. An assumption that primary health care and generalist community services had the relevant skills and, more importantly, referral networks was not supported in two of the three sites.
Across the sites, but particularly in sites 2 and 3, dementia-related behaviour was identified as the most challenging condition because of its unpredictability and staff not knowing how to respond. In particular, aggression and repetitive behaviours had an impact at all levels of care and could adversely influence the daily life of the care home: for the resident, it was the level of distress experienced; for staff, it caused challenges related to knowing how to respond to the individual’s needs, but also to those of other residents affected by the behaviours; and for visiting HCPs and GPs, it affected their confidence in knowing what to do and who to involve by way of additional expert support. Even when support was available, referrals were either slow in achieving a response or perceived as ineffective; in these situations, it was an unsatisfactory outcome for all involved. Box 6 provides one account of a situation in which multiple services were ultimately involved, but where there was little evidence of the care being co-ordinated or the key issues resolved.
Care home staff review with her relative possible reasons and if she is in pain, in discomfort or distressed by something or someone in the care home. She calls out slightly less when there is a member of staff available to hold her hand. Other interventions to distract, provide activities and reduce sources of possible distress have not worked. Other residents, staff and visitors are increasingly upset by the woman’s calling out. GP visits and suggests that the dementia specialist team visit; a member of the team visits and suggests the community mental health team, which visits and suggests a visit from the psychogeriatrician. The sequence of referrals takes several months and the woman’s symptoms at the time of data collection were still unresolved.
In sites 2 and 3, without access to a specialist team with care home responsibilities, there were case examples of police being involved and residents being sectioned from the care home to specialist psychiatric inpatient units. Even with access to a dedicated dementia team, the outcomes were mixed and, as the following quotation suggests, it needed more liaison with the care home staff about timing and frequency of visits, so that the HCPs could be present to witness when and how a resident was aggressive:
You try a lot of things but they just don’t always work do they? And then Dementia Outreach come back and they try a different strategy but it doesn’t always work.
You know like your [specialist nurse] can’t just come in and like we say she’s got aggression when we’re changing her, all personal care, if she’s [specialist nurse] coming in on a morning and that, well really it’s absolutely fine, you know, that’s a good day. But then they need to do a few days in seeing this aggression that these people are giving . . .
S1CHFG
Similarly, in site 2, the care home staff gave an example of how often the assessment of the issues was inappropriate and did not consider the context of care as well as the presenting behaviours. One bad experience made them reluctant to re-engage with the service or trust the HCPs’ expertise:
And was it helpful when they came out?
Not really because they’re all about, oh, looking on paperwork, what’s this resident been like . . . rather than go and look at the resident’s health, yeah, it’s only happened once, this has only happened once, yeah, but once is enough, yeah.
Site 2 provided another example of a situation not resolved. This led to a safeguarding referral, which was subsequently handled unsatisfactorily and resulted in a formal complaint from the care home manager. Only then was there a satisfactory response. This was the only example of care home staff formally complaining about the quality of the service provided by the NHS:
Yeah. We’ve had to put a formal complaint in before because they wouldn’t safeguard this resident and we tried desperately to safeguard him. His behaviour was getting a lot worse and in the end we had to put a formal complaint in to the mental health team. And it’s funny how quick they came out, the psychiatrist, doctor and sectioned the guy because he was just getting even worse.
S2CH2FG
Not only were behaviours problematic, but a lack of dementia knowledge and skill was shown by some HCPs, for example dentists expecting residents to visit the surgery when care could have been delivered in the home.
The care home staff believed that they had received adequate training in dementia, so they did not see that as the solution. In complex cases or situations when it was not clear why the person was distressed, staff wanted practical and expert support. Across the sites, care home staff talked about their frustration at being asked to complete behavioural charts for weeks, the purpose of which they did not understand, rather than working together with the specialist teams and the resident. GPs were perceived as doing little to manage a behavioural crisis other than referring to mental health services:
I’ve had residents who have been, got themselves on the floor and have decided they’re going to start kicking cupboard doors and everything like that and the GP doesn’t even look at them.
S2CHFG
This observation was substantiated by GPs in site 2 who highlighted dealing with aggression and violence in people living with dementia as the most difficult aspect of their work in care homes.
Cross-case comparison
To develop and refine the programme theory from phase 1, we wanted to know how HCPs interpreted their responsibilities to work with care homes. Specifically, what do the care homes require from them, who is the focus of their care and what influences how they provide their services? In our interviews, we asked HCPs about activities that might support (or not support) relational working. We looked for evidence of the ways in which health-care services were responsive to how care homes worked and what were their priorities and patterns of working. We considered the extent to which service development reflected co-design or a shared view of practice.
Several common narratives emerged from the HCP interview transcripts that suggested different mechanisms were at play (Table 30). In site 1, there appeared to be an ethos of HCPs working together with care home staff and a view that they were all ‘there for the same reason’. This was explained as having developed because of infrastructure and resources that were designated for care homes and patterns of working that had evolved over several years. These had evolved as HCPs had learnt to work with care homes within the context of a specifically commissioned care homes service. Individual practitioners appeared to share an understanding that to work with care homes they had to adjust how and when they visited, and that there was care home staff expertise that could inform their discussions and practice when working with residents:
What sort of things does the contact with the care home staff involve?
So it would be speaking to them to find out, you know, what, how they perceive, what, you know, the problem, or what the issue is, you know, find out from their point of view what’s working and what isn’t working, and then I would, you know, I obviously do my assessment and do kind of, normally do like a demonstration with carers. Provide education and advice on, you know, why I’m recommending something. I would spend time looking at the care plan and advising on, you know, maybe what else needs to be included in the care plan, or updated following my visit. You know, education on different risk assessments that can be used to make sure that they’ve got the right equipment in place. So you know, for example, like the use of like the Braden Pressure Care Tool, making sure that they’ve got that, that they understand how to use that. Yeah, I think that’s it.
| Site | ||
|---|---|---|
| 1 | 2 | 3 |
| Language of working together for residents, ‘all being there for the same reason’ | Frequent references from HCPs to ‘care homes they have issues with’ | Working with care homes presented as a challenge (apart from one AHP) |
| HCPs recognise the importance of focusing on care home staff’s perceptions of the issues | Narrative of having to fit visiting residents in with other work demands; few examples of meeting with care home staff apart from resident specific visits | Represented residents and older people living at home as eligible for the same services. Did not differentiate between care home residents and other patients on the caseload |
| HCPs plan their time to talk with the staff; they recognise the ‘oral culture’ for sharing information and care planning | HCPs’ threshold for support and care home staff’s need are not agreed, frequent references to inappropriate requests and call-outs | Examples of community nurses taking a prescriptive approach to residents’ care rather than engaging with care home staff in the care planning process |
| HCPs talk about achievable goals for care home staff and working with residents | Expectations differ between care homes and HCPs as to what care home staff should know and do | Some HCPs recognised care home staff expertise and knowledge of residents’ needs and their role as mediators for residents |
| Numerous examples of working with care homes – recognising care home staff experience, highlighting good practice and interventions to de-escalate situations when residents were distressed | HCPs think that care homes need to improve their quality of care – HCPs not seen as integral to this process | Perception that working relationships with care home staff were facilitated if care home staff had previous NHS experience or knowledge |
In site 1 there were numerous examples of HCPs engaging with care home staff in an appreciative way. During interviews, HCPs frequently highlighted good practice from care homes without prompting. This contrasted markedly with more negative portrayals of care homes depicted within the transcripts from sites 2 and 3. ‘Care homes we have issues with’ was a common phrase used by HCPs when discussing their working relationships with care homes in these sites. More HCPs in site 3 and, to a lesser extent, in site 2, made derogatory comments about the standards and quality of care provided in care homes. They described approaches to working with care homes that were prescriptive about the range of services and support that they would and would not provide, and this was presented as a strategy to manage what was seen as uncontrollable demand.
There were two notable exceptions in sites 2 and 3 where practitioners described a pattern of working that was not resident dependent, involved care home staff in discussing care and offered training and support to staff, and where a HCP assumed responsibility for liaising with the GP and referring residents to specialist services on the care home’s behalf. One was a palliative care nurse specialist (site 2) and the other a dietitian (site 3). Both practitioners described their personal interest in the support of care home residents, had worked for several years with care homes and knew (and were known within) the local ‘care economy’ and working with care homes was a designated element of their work. Their choice of language and descriptions of how they worked with care homes, examples of where care home staff had achieved good care and who they liaised with within the care home and within the local care economy on behalf of the care home, were similar to the HCP accounts in site 1.
Regardless of service delivery model or the infrastructure of care, there were common experiences that HCPs highlighted around access to services, electronic systems and sharing of information (Table 31). In site 1, the MDTs were meeting away from the care homes, but it was unclear how this affected residents’ care. Across all sites the opportunities for the different services to work together for the care homes were limited.
| Consultations and services | Paperwork and electronic systems |
|---|---|
| Nurses and therapists’ consultations with residents were arranged by referrals on request | There was no shared paperwork with care homes, but most services would record information in the HCP section of residents’ care home notes or annotate care plans |
| Clinics were not run by specialists (regular consultation sessions) in the home apart from one care home nurse specialist in site 3 and the GPs in sites 1 and 2. Multidisciplinary working limited to individual residents or meetings away from the care home that did not involve care home staff | Electronic systems, mainly SystmOne (The Phoenix Partnership, Leeds, UK), were used in all three sites by most HCPs for referrals, recording consultations and assessments; however, not everyone was on the same system. Where nurses and therapists were using SystmOne, only skeleton notes were left in the care home so care home staff did not have a record of the HCP consultation |
| Optician and podiatrist worked directly with the care homes; visits 6-monthly or yearly to see all residents | Most HCPs could access each other’s information on residents if they or their relatives had given their permission |
| Domiciliary dentist in site 1 worked in the same way, but in site 3 the community dentist visited only on request by care home staff, relatives or residents (it was not possible to access a dentist for interview in site 2) | Some GPs accessed information from other HCPs, but did not share their information |
| Dedicated care home services in sites 1 and 3 worked ‘office hours’ |
Conclusion
In summary, between sites, resident and relatives’ satisfaction with care and service use was not strikingly different. There were differences in the ability of services to engage with the issues and care needs of people living and dying with dementia and questions about the different reasons and type of residents’ hospitalisations across the sites.
Chapter 7 will use these findings, and the detailed service descriptions outlined in Chapter 5, to revisit the findings and emergent programme theory and possible CMO configurations of phase 1 and refine these in light of the phase 2 findings.
Chapter 7 Using the phase 2 case study findings to refine context–mechanism–outcome configurations and the explanatory framework
Introduction
Phase 1 (described in Chapters 3 and 4) mapped the range of NHS provision to care homes. Based on stakeholder views and linked evidence synthesis, we suggested different contexts and possible mechanisms that supported care home residents’ access to health care. This chapter revisits these arguments in light of the findings from the case studies in phase 2, as described in Chapters 5 and 6. Based on a cross-case analysis of recurring patterns within the phase 2 findings, it sets out a series of CMO configurations that challenge and refine the explanatory framework of phase 1.
Phase 1 posited that within the different types of service provision it is how and if a sense of ‘common ground’ is achieved between HCPs and care home staff that is important. The activities within an intervention that we identified as key were those that aligned health-care provision with the goals and priorities of care home staff, and aimed to build relationships between care home staff and visiting HCPs. Activities, such as discussions, before setting up a service to identify shared challenges and priorities, use of shared protocols and guidance and regular meetings were the contexts necessary to generate mechanisms of co-working. Box 7 summarises the emergent programme theory that informed the case study recruitment and structure for data collection and analysis.
Interventions (whether or not they use sanctions and incentives, specialist practitioners or care home-specific resources) are more likely to achieve the outcomes of interest when the activities:
-
trigger the engagement of care home staff from the outset
-
create opportunities for health-care and care home staff to work together
-
structure the intervention to fit with the priorities and working practices of the care home as an institution.
NHS interventions that use processes and approaches to working that reconcile competing priorities between care home staff and visiting health-care staff will engage the interest of the care home staff and generate opportunities for shared planning and working.
NHS interventions that provide and fund visiting HCPs, and that recognise that engagement with care homes at an institutional level is important, increase the potential for engagement across organisations and the association and engagement with care home residents and staff when there is clarity and an agreed understanding of each service’s roles and responsibilities.
Mechanisms of successful programmes are characterised by activities that provide visiting HCPs and care home staff allocated time together for discussion and reflection and which allow reconfiguration of the intervention to match care home workflow and priorities in different care home settings. Contextual influences, such as financial incentives or sanctions, continuity of contact and evidence-based approaches to assessment and care planning, are needed to enable these mechanisms/staff responses to occur and to achieve improved resident and staff outcomes.
Achieving common ground
The cross-case analysis broadly supported achieving common ground as a mechanism that supported effective working between health-care services and care homes. In site 1, with funding of care home teams and GPs to work with care homes, the narrative was one of co-operation, highlighting best practice in care homes and finding shared health-care solutions. This was replicated in specific instances in sites 2 and 3, where individual practitioners were employed to improve end-of-life care and nutrition in care homes. As the following quotation demonstrates, there was an appreciation of each other’s skills and evidence of collaboration:
. . . So you know, kind of educating staff on how to, you know, apply the sling on the stand aid [referring to hoist] more effectively and more efficiently. One of the, one of the carers in particular was excellent, because the person that I went, the resident had quite advanced dementia, and the carer was particularly good at communicating and putting the resident at ease. In that, in that case I did, I wrote an e-mail to the manager of care home 2 and complimented the particular carer, because she was very good.
S1CH2HP03, occupational therapy rehabilitation team
. . . It worked and it worked really well, the feedback was positive and then we rolled it out . . . But because we, because we go into the homes, then it’s not just a trainer delivering a training session, they could come back and say, ‘You know what you said on the course or could you explain more. I didn’t understand about this and can we go through it again?’ So, there’s open communication with them. And they, at that one (care home), they all, I’m always greeted with a smile, I’m always greeted with, ‘Oh really nice to see you again, where’ve you been? But it is a case of they feel confident that we have got a two-way communication and they feel that they can open up to me and I can open up to them as well and just to see that it is an open communication and that’s what works well there and . . . And the staff are consistent, which also works, where if you have got a place where they have not got consistent staff, then you’re sort of going over the same things all the time . . .
S1CH4HP02, specialist nurse care home team
What was evident as a shared narrative across the care home teams and some of the practitioners in site 1, was echoed in individual practitioner accounts in sites 2 and 3 from the palliative nurse specialist and the dietitian, respectively:
Yeah, so I would say I always have contact with the care home staff. Many patients do not have full mental capacity so care home staff help with assessing of situation, feedback and education is given to the care home staff on drug management, symptom control, psychological and spiritual support. If a new member of staff is there, I try to encourage them to work alongside me so I’m teaching them how to manage without me . . . the ability of the staff to communicate well with families of patients and MDT.
Yes, so they can sort of learn from each other’s experience.
Yeah . . . if there’s a care home that we know that the chef is really involved, we get them to come in and talk to the catering staff in other care homes . . . So some of our training is aimed at the care staff but some of it is aimed at the catering staff so that we can try to get things going that way.
OK, so it’s sort of brought some . . . It’s encouraging them to think about how to do that with their residents as well?
Yeah, and with the newsletter that we send out . . . we would put up areas of best practice as well so if we see something in a care home that we think is really good, like the midnight snack menu, we will highlight that on the thing so that other care homes can think about it as well.
When these activities did not happen (because of lack of funding, clarity of role, staff availability or time to meet), both NHS professionals and care home staff struggled to find an agreed way of working together. In particular, under such circumstances, NHS professionals did not adapt how they worked with care homes to accommodate the different residents’ needs or care home and NHS staff patterns of working. This was most evident in site 3 where, in comparison with the other sites, response to residents’ needs and NHS services was observed to be reactive and unco-ordinated with changing levels of service involvement.
Findings from phase 2 identified further contexts that informed the way in which NHS and care home staff worked together that generated mechanisms of mutual trust and willingness to work together. These were:
-
learning and working
-
wrap-around care for frail older people
-
living and dying with dementia.
Learning and working
Commissioners and HCPs needed to develop a language for an understanding of the complexities of supporting frail older people in non-medical, non-NHS settings. It took time for those NHS services funded to work with care homes to adapt and become embedded as a recognised part of the wider health-care provision to older people. The three case study sites and the services within them represented a continuum of experience and intensity of association between the NHS and care homes. The case studies suggested that, in addition to activities that fostered opportunities for collaboration, if commissioners and services had piloted and trialled different ways of working together, this increased confidence and trust between the services.
Site 1 had a long history of learning how to work with care homes and had either retrained NHS staff to work with care homes or staff had moved between services, taking their care home expertise with them. Site 2 had begun to invest in staff, changing how often staff visited care homes and expanding their range of activities. Site 3 had recognised the need for transformation but had invested in single practitioners and some GP pilot clinics to achieve specific outcomes rather than system change. Staff from the site had, for example, met with care homes to discuss how to reduce the number of call-outs to the ambulance service for residents who had fallen. As the following commissioner quotation demonstrates, site 3 was focused on reducing unplanned admissions from care homes but was still learning about the care homes in the surrounding area, who the staff were and how the care homes were run:
. . . So our focus is predominantly on admission avoidance themes predominantly, and obviously care homes is one that always comes up as a significant issue for us in terms of the level of demand that they create, we’ve got a huge number of care homes in our locality, so we’ve done some various things to try and improve our working relationship with care homes. We ran a pilot with GPs last year . . . we are just at the really early stages of trying to do that [work with care homes], so at the moment we do not have one definitive list for all care homes in the area, but I’m not sure that we have got sort of one list with all of our contacts for our homes that we can send something out to because we have got so many. We have got over 200 care homes in the area and obviously there’s some small independent companies that run homes as well as the bigger common ones, so it’s difficult to make contact with them all. So what we are starting to do is we are trying to build a list of those that we sort of engage with. But also we’re working very closely with our County Council in terms of they’re setting up some forums where they have invited all the care home managers to, and it’s a way of sharing information and getting them engaged, so we’re working with them to attend those and having a bit of joint approach really . . . it’s the fact that I do not think we have ever had care homes round the table before when we have come up with schemes you know. Every winter we talk about what schemes we need to put in place to support demand but we’ve never really had care homes as part of those discussions.
DS500042, commissioners interview site 3
Where patterns of working had evolved over several years, practitioners who were interested in working with care homes were supported by the commissioning organisation to develop their work. They were able to absorb or address what other practitioners had described as ‘challenges’. Continuity of HCP and team input, being accessible, responsive and willing to provide education and training could mitigate the effects of staff turnover in the care homes and support collaborative working. Such patterns of shared understanding and mutual professional development provided a platform through which more structured innovations could be introduced (such as facilitating end-of-life care training and nutritional assessment, risk assessment or guidelines on when to call out a GP). Care home staff tended to be more confident and could expect to receive ongoing support (as opposed to time-limited or single issue input) as part of such initiatives. Consequently, they were less threatened by interventions designed to improve resident outcomes. Equally, NHS staff were able to take the ‘long view’, linking work that supported individual residents with wider initiatives to improve care for all residents.
When NHS professionals did not modify how they worked to acknowledge differences between care home residents and older people living at home or in hospital, this triggered a sense of frustration among both the NHS service provider and care home staff that residents did not ‘fit’ with the service as offered. Such frustration was compounded when:
-
NHS staff defined their work solely by individual resident encounters and were reluctant or had limited incentives to engage with care homes as an organisation
-
visiting NHS staff felt that they lacked particular expertise in the care of those living and dying with dementia
-
the purpose or desired outcomes from working with care homes had not been identified or agreed by the commissioners in discussion with NHS practitioners involved or care home staff.
An observed consequence of some or all of the above was that a lack of constructive contact between the visiting NHS staff and care home organisations/staff could become self-perpetuating. NHS staff connecting primarily with individual residents, rather than with care homes as organisations, described a reluctance to engage with care home staff because of fears of being overwhelmed by requests to visit. Where NHS staff either felt coerced to visit or perceived that the number of care homes they were working in was unmanageable, there was an observed resistance to work with care homes to provide training and education to staff.
Funding of posts and time to increase the contact NHS staff had with care homes was necessary, but generated greater impact when they created the opportunities to work together. When (because of experience, an interest in working with care homes or an interest in peer-to-peer learning) NHS staff had an explicit commitment to working with care homes, this triggered responses that emphasised the value of the work.
Table 32 provides a revised CMO that explains how investment in additional resources and services for care homes can be theorised in certain circumstances to achieve outcomes of care home staff satisfaction and residents’ access to health care.
| Context | + | Mechanism | = | Outcome | |
|---|---|---|---|---|---|
| Resource | Response | ||||
| NHS services funded to visit care homes on a regular basis | NHS services staff working for care homes see this as a legitimate use of their time and skills | Practitioners willing to work with care homes, value their work and find ways to provide a package of care that supports residents and care home staff | Services engage with care homes and residents have access to specialist services | ||
| Length of time the service staff have been working with care homes/have known particular staff and care home routines | Staff develop ways of working and communicating with care home staff (both formal and informal) and are willing to be accessible and flexible | Services visit at times that fit with care home routines | |||
| Number of care homes staff work with that are seen as manageable | Care home staff concerns about individual residents are described as being addressed before they become a crisis | ||||
| NHS services’ care home responsibilities understood and accepted. The role has been through several iterations | Focus on residents’ access to health care (not just prevention of admissions or monitoring) | Willing to engage in proactive care and discuss residents with vague or uncertain symptoms | Resident crises and GP call-outs because of staff concerns are seen as either being reduced and dealt with by care home staff or accepted by visiting NHS professionals as reasonable use of the NHS services | ||
| Allocation of time and resource and to work in care homes | Value the work | ||||
In phase 1, the review of patterns of working with care homes and the realist synthesis focused on particular services, for example GP provision, care home teams and specific care home practitioners, including pharmacists and therapists. The realist synthesis addressed the cross-cutting learning from different CMO configurations within particular approaches to health-care delivery. Phase 2 findings identified how the presence or absence of other services around the care homes also affected residents’ access to health care and specifically specialist services. To understand what worked when and in what circumstances it was important to know to what extent NHS provision to care homes linked to other primary care-based services and the local hospitals.
Phase 2 found no measurable difference in costs per resident across the three sites, but identified that the way in which resources were allocated and organised (support of single practitioners or teams, care home focus or not) triggered different responses from the NHS and patterns of referral. The structure of support either brought care homes ‘into’ the economy of health care with formal methods for referrals and linking services and practitioners, or provided episodic outreach from health care to care homes. This influenced the ability of the service to respond to residents with complex ongoing needs or who needed support from more than one professional group.
Prevention of hospitalisations and quality monitoring were major preoccupations of all the health and social care commissioners and these were seen as important in all the sites. However, where this was the only focus, it could have an isolating effect on services and visiting HCPs. It also risked ‘short-termism’ in how NHS services were organised. They were under pressure to ‘fix’ something or avert a crisis, both of which were difficult to sustain, especially when single practitioners were expected to achieve outcomes that were, often, consequences of patterns of practice across the wider health and social care economy. In two of the three sites, there were examples of intensive interventions through which GPs were funded to improve medication reviews and reduce hospitalisations that had ended when the practitioner left or the funding ceased. This approach militated against forming working relationships both with care home staff and, just as importantly, other NHS services that had links to care homes. Where differences between health-care resource use and costs at sites were demonstrable, it was for the number of GP consultations, which tended to suggest that these were both more frequent and more expensive in site 2, and use of acute hospital beds, where there was a trend towards increased use and increased length of stay in site 3. Focusing service provision primarily around GPs did not reduce costs and did not reduce acute care utilisation.
Site 1 had an infrastructure around the care homes that was characterised by a network of NHS teams and a relatively loose connection with GPs. Site 2 used shared data sets and developed services that could link together around the care homes. Being able to refer residents to colleagues in a care home team or to other specialist teams with a care home-specific responsibility meant that residents had the potential to be ‘held’ within a framework of referrals and expertise. In these circumstances, care home staff appeared less likely to seek help on an ad hoc basis from outside the supporting infrastructure. This was important, for example, when care home staff were unable to manage or resolve residents’ behaviours that they found challenging. In such situations, the ability to co-ordinate the care of the resident within the caseload of interconnected specialist practitioners who visited the home militated against the tendency to call for help from outside services when things went wrong:
OK. How do your visits work when you are at this care home, so this particular care home?
Right, at this care home I’ll arrange an appointment as usual and I’ll either speak to the manager or a senior carer and we will discuss whatever plan we’ve put in place, if it’s being effective, I’ll go and talk to the patient. And then of course if the plan’s been effective and it’s useful and helping them we’ll continue with that and if not we’ll discuss how we can change and modify it. Then we’ll come back, talk to other members of the team for advice for us or we can refer to, because we’re a multidisciplinary team we’ve got physiotherapists, occupational therapists, support workers and so we can refer on if there’s any physiotherapy needs, occupational therapy needs, whatever, get support from support workers and we can do that so, and we’ve got consultant time as well, so that’s broadly how the visits work.
The ‘wrap-around’ effect of a range of older people-specific services being available to care homes, either through a formal infrastructure or informally through the connections of particular practitioners working on the residents’ behalf, helped to co-ordinate residents’ care. This could also have other beneficial effects. Residents whose health was deteriorating would be referred earlier for assessment, even if this was initiated by the NHS services. Care home staff could enjoy better access to education and training from specialist services. Investment in care home-specific services and GP time was an important underlying contextual factor in securing care home residents’ access to health care for problems besides urgent care needs.
The quality and consistency of access to the service that this investment prompted, however, was also linked to how well the referral systems and the different practitioners’ contributions were known and understood by the care home staff. If this was not understood, diverse providers could trigger multiple referrals or, when uncertain, a default response by care home staff of referring to the GP. In these situations, the outcomes and benefits of having the availability of a range of older people-specific services for care homes were reported more negatively or cautiously by care home staff. Care home staff found it difficult to control the number of NHS services visiting them. At times, they could perceive this as a form of surveillance or covert quality monitoring:
Different bodies. Different, you know, sometimes we can have three different professionals come in to see one person, you know and it’s a bit too much. I think care home life is like traffic, road traffic, everybody just coming and going, and demanding, and if you do not do this then the next thing you know you’re in Safeguarding.
S1CH1, care home manager
The role of the GP was important in all sites, even when services had been developed to supplement or substitute for care homes’ access to GP services. In site 1, it appeared that GPs were not overwhelmed by the demands from the care homes. This was possibly for two reasons. First, other NHS-funded services predicated to support care homes absorbed those referrals that GPs at other sites regarded as ‘inappropriate’ or trivial and as resulting from staff inexperience or anxiety. Care home staff had permission and the opportunity to seek advice and help from the services that visited about multiple residents or problems that were not patient specific. Second, the GPs had responsibility for fewer than three care homes. There was no evidence that GPs withdrew from care in site 1. The number of GP contacts was not lower than in site 3, even after controlling for the greater comorbidity and dependency at site 1. Sites 2 and 3 had GPs who received extra funding to visit care homes and, as part of these arrangements, in site 2, practices took over primary responsibility for care homes whose residents had previously been registered with other practices. They offered clinics in the care home, but the activities they described were very similar to how they would see patients in their own health centre and at home. Only in site 3 was greater attention (for the short time the service was funded) paid by GPs to medication reviews. This may have had an impact on prescribing as a consistently lower ACB score was recorded for residents at this site. The issue for many of the GPs, particularly in site 2, was that working in care homes conflated urgent and planned care. This required a shift in approach that they either could not or were not prepared to make, ostensibly because of the commitments associated with their wider caseload. As the following quotation also shows, this moved decision-making about what is urgent care from the GP to the care home staff:
Is it that you are saying there is dissonance between what you think you should be doing as a GP and what you are doing when you are in a care home?
I am not sure that I would call it dissonance, I think that it is not good use of my time, care homes are probably one of the only places where the GP is having to do urgent and planned work in the same place and at the same time. When you see other patients it is a booked appointment or an urgent call, there is some planning and anticipation it is harder to repeat that in care homes. I think that is an important difference. When I go in to see a patient then I can find myself dealing with what the care home staff think are urgent cases.
We were unable to explore how NHS practitioner caseload affected patterns of working, although there were references in sites 2 and 3 to the difficulties of prioritising care home work over other responsibilities. The negative accounts about GPs carefully managing their contact with care homes suggest that there may be a tipping point beyond which adding additional responsibilities or roles to already overburdened practitioners may become self-defeating. Care home ownership and the level of investment in training and education of care home staff may also have shaped demand on NHS resources. In the interviews, NHS practitioners recognised that particular staff were easier to work with than others, particularly if they were qualified nurses, but they did not attribute this to who managed or owned the care home. Table 33 provides a revised CMO that explains how commissioning multiple NHS services to work with care homes on a regular basis, including those with dementia expertise, where the referral networks are explicit may lead to outcomes including service engagement with care home staff, access to specialist services for residents and the reduced need for hospitalisation.
| Context | + | Mechanism | = | Outcome | |
|---|---|---|---|---|---|
| Resource | Response | ||||
| Multiple NHS services staff commissioned to work with care homes on a regular basis | Referral systems for residents’ needs (e.g. dementia, falls prevention) | Practitioners confident that they can provide or access services for residents and know the care home staff they work with | Services engage with care home staff and residents have access to specialist services for the support of people with complex needs | ||
| Known referral network, including services with staff who have dementia-specific expertise | Infrastructure supports review, feedback and opportunities to change patterns of service delivery | ||||
| NHS services staff know other services because of the length of association and stability of teams or structure of provision, or through staff moving between services | Staff with other responsibilities to other patient groups have capacity to work with care homes | Referral systems are clear to care home staff | Reduce the need for hospitalisation | ||
Living and dying with dementia
A cross-cutting theme in the case study sites was how the local NHS responded to the health needs of residents with dementia. Access to a linked dementia outreach team or specialist expertise allowed both rapid responses to crises and the provision of staff training and support:
You have described the challenges of working with care homes. Are there any issues in terms of resident health-care needs that you would say, is complex, and stretches you as a GP?
I think physical violence is the biggest issue that I have to deal with and how to best manage that.
With people living with dementia?
Yes, it can be very difficult to manage and to know what is best for the person and still think about the needs of the other residents. Symptoms of dementia that are not resolved. That has been an increasing area of my work.
I agree, that and safeguarding issues and deprivation of liberties, you can get drawn into that and that is quite difficult, who to work with and how to resolve it.
The responsiveness of the local NHS to residents with dementia was a key mechanism in securing residents’ timely access to services and the identification of dementia-sensitive solutions to minimise distress that could be supported in the care homes. This was, however, a resource that was separate from other care home-focused services, and the reviews of medication did not suggest that any of the study care home staff were more skilled than others in avoiding or reducing the use of antipsychotics. The problems that could arise when there was separation of dementia expertise from other sources of NHS support were most evident in the accounts of residents whose behaviours and distress could not be managed by care home staff, visiting primary care services or crisis-response mental health teams. The narratives in these situations were those of visible need, unco-ordinated responses, escalation of service involvement and demand on emergency services. The case study findings led us to hypothesise that resident and organisational outcomes would improve where there is ongoing access to dementia expertise within the care home support services (Table 34).
| Context | + | Mechanism | = | Outcome | |
|---|---|---|---|---|---|
| Resource | Response | ||||
| Care homes and visiting NHS practitioners have ongoing access to dementia expertise | Ability to provide training and support for the care of people living and dying with dementia | Visiting practitioners and care home staff have a shared skill set to draw on to support people living with dementia | Reduced use of antipsychotic prescribing | ||
| Expertise in dementia care a prerequisite for working with care homes | Range of resources and skills to anticipate and moderate the signs, and symptoms, of dementia that cause the resident distress, and address care home concerns around risk management and deprivation of liberty | Visiting health-care staff are confident when providing care to people living and dying with dementia | Care of people living with dementia whose behaviours staff and residents find challenging is managed within the care home | ||
Summary
The phase 2 findings broadly supported the explanatory framework proposed in phase 1 around mechanisms that promoted relational working between visiting NHS professionals and care home staff.
When NHS professionals, including GPs, did not receive dedicated funding for working with care homes, but were still required to visit care home residents across the sites, this triggered responses of stress, resentment and frustration, and resulted in unco-ordinated care for residents. For GPs, in particular, care home work was difficult to manage within existing caseloads. Established patterns of working with older people that were perceived to be successful in other settings were difficult to replicate or sustain in care homes. As a consequence, HCPs and GPs were more likely to emphasise care home staff shortcomings, the unacceptability of being asked to see urgent cases when making planned care home visits and the belief that care home staff should be better trained (though not by HCPs and GPs).
The additional resources needed to sustain NHS input to care homes should aim to build over time a shared recognition and common narrative that care homes are integral to the health-care economy. A skill set that is relevant to residents with dementia is especially important here. Clarity about how services were organised around and for care homes and their roles in managing different problems were important mechanisms for ensuring that care homes and NHS staff saw each other as valued partners. It was important that they could recognise how homes ‘sit’ within wider care provision for older people care. Services that comprised isolated single practitioners or services that offered episodic contact focused on a single objective, such as medication review or avoidance of unplanned admissions, were less likely to be sustained or understood by care home staff and residents or other services working with care homes.
Service staff were motivated when they recognised care homes at an organisational level and when engagement with care home managers, staff and structures was legitimised as part of the role for NHS staff. This was more readily fostered where service implementation and delivery was undertaken in the context of agreed or known goals. Shared priorities fostered by collaborative working over periods of several years were also important in this regard. It appeared difficult to build, sustain or embed proactive models of health-care delivery when NHS services and NHS practitioners did not acknowledge care home staff as integral to how they worked, and when they treated residents as individuals who were similar to those encountered in their own home. Continuity of care for care home residents was more likely to be achieved when planned meetings with care home staff and ad hoc conversations were possible and expected.
Chapter 8 Discussion and conclusions
Introduction
This chapter brings together the findings to discuss what needs to be in place to commission and provide health care for older people living in care homes. The starting point of this study was that it was unlikely that there was one model of service delivery that would be effective in all situations. Older people resident in care homes are similar in age and characteristics. However, long-term care provision and NHS services provided to care home residents are quite heterogeneous. Consequently, we required a theory-driven explanation of what works when, for whom and in what circumstances. To do this we took a long view. We considered competing accounts of how to support care home residents and the experiences of past and current initiatives to explore the underlying assumptions and supporting evidence. We then set out to test our candidate programme theories of what needs to be in place to work with care homes by conducting detailed case studies prospectively across three diverse health and social care economies.
The work built on what is already known about what supports integrated working,143,149,150 and specifically the findings of the APPROACH (Analysis and Perspectives of integrated working in PRimary care Organisations And Care Homes) study. 2 This study had described differing and competing priorities and interests of care home and NHS staff that needed to be negotiated to support integrated working between the services. It also drew on theories of co-production and co-design151 and social identity theory to develop a common understanding of what needs to be in place to reduce divisions in health and social care. 2,4,152
The goal of this study has been to develop a mid-range theory153 that, to quote Hedström and Ylikoski:154
. . . seeks to highlight the heart of the story by isolating a few explanatory factors that explain important but delimited aspects of the outcomes to be explained. A theory of the middle range can be used for partially explaining a range of different phenomena, but it makes no pretence of being able to explain all social phenomena, and it is not formed upon any form of extreme reductionism.
Hedström and Ylikoski (2010),154 p. 61
Specifically, we focused on how the provision of extra resources, or the reconfiguration of existing resources, shaped care home residents’ access to health care. We consider now the intended and unintended consequences of emphasising particular approaches and outcomes and how these influence the organisation and networks of co-operation with and around care homes.
Patterns of service provision
Our interviews with stakeholders, review of surveys and review of reviews4,30,91 have provided a comprehensive account of how health-care services can and do work with care homes, both in England and internationally. Phase 1 found that there was limited agreement in the intervention literature on how to measure the effectiveness of health-care provision to care homes or what quality health care might look like. This lack of consensus was evident in the review of surveys of health-care provision. Although there was evidence of the development of care home-specific services, these were the minority and it was impossible to establish how many residents they supported. The absence of a national minimum data set on the health-related characteristics of residents in care homes (as is available in the USA) makes it difficult to judge the relationship between service provided and needs observed. The wide variability in the provision of services to care homes and widespread lack of dental services signalled that erratic and inadequate care was a persistent feature of health-care provision to residents in care homes. The number of surveys identified and the consistent nature of their findings, despite their methodological diversity, provides a strong argument for the need to move beyond surveying or auditing the status quo.
Stakeholder interviews provided overlapping accounts of what was necessary to achieve ‘good’ health care. These included education and training of care home staff, access to clinical expertise, the use of incentives and sanctions to achieve minimum standards of care, the value of champions and designated workers working in and with care homes and the importance of activities that built robust working relationships between the two sectors. Combining this with the review evidence, and an initial scoping of the literature, the realist review theorised that it is activities that support and sustain relational working between care home staff and visiting HCPs that explain the observed differences in how health-care interventions are accepted and embedded into care home practice. Contextual factors such as financial incentives or sanctions, agreed protocols, clinical expertise and structured approaches to assessment and care planning could support relational working to occur. However, of themselves, these measures were likely to be insufficient to achieve change if they did not lead to visiting HCPs and care home staff working together to identify, plan and implement care home-appropriate protocols for care. This was the explanatory theory that was tested and refined in phase 2.
The case studies built on this to provide a detailed account of how different primary care, community services and secondary care outreach services could be resourced and structured and with what effect.
We selected the three sites on the basis of contrasting approaches and incentives for providing NHS services to care homes. Our selection was not based on how they referred residents between services or how they linked to other NHS services, but our findings indicated that these patterns were an important context for clinical practice. For example, patterns of service provision and referral influenced strongly what happened if more than one practitioner might need to be involved with a resident’s needs. We also found that these patterns affected the relationships between secondary care, care home staff and visiting NHS services.
Our findings corroborated a number of previously reported observations. For instance, care home residents have variable and inequitable access to health care and multiple services (GPs, nurses, therapists, specialists) are involved in delivering care. Care is often poorly co-ordinated and the paucity of strategic planning for care home residents is compounded by limited data about the costs and benefits of the services that are received by care homes. The new evidence presented here is less about the number and type of services available and more about how they work together, particularly if they are linked as services around the care home and for how long these patterns of association have existed.
The realist synthesis proposed that services for care homes had potential to improve access to care where there were opportunities for meetings between visiting practitioners and care home staff beyond direct clinician–patient contact.
Relational working
Activities that fostered patterns of working, which in turn supported the development of relationships based on trust and common interests, were more likely to increase care home staff confidence and create a sense of collegiality between the two groups. Possible mechanisms to bring this about could include activities that involved joint priority-setting and the shared use of assessments, protocols and documentation. The case studies broadly confirmed this.
We found little evidence, however, apart from adjusting times of visiting and improving access, of NHS services organising provision to fit with the wishes and suggestions of care home staff or residents. Where there were different patterns of NHS provision these were defined and controlled by the NHS. The care home staff and managers did not or could not exercise much influence over how the NHS worked with them, apart from restricting access or registering a complaint when a service was not provided. Care home residents and their representatives could not influence when they would be seen and by whom, especially when there were questions and issues around medication. Access was one of the few issues that residents raised in their interviews. Where the patterns of working and visiting created opportunities to meet and discuss care, however, there was a greater mutual appreciation of the challenges both NHS and care home staff faced each day.
The case studies suggested that mechanisms that facilitated relational working between NHS services around the care home as well as with the care home were important. Activities that fostered a sense of services working together for the care home and not just around individual residents were important. Using care homes as the hub of service provision was not more expensive than the alternative models (incentives to GPs and no specific arrangements outside the basic GMS contract) and no less efficient in the use of primary and secondary health-care services. Indeed, there was some evidence that this approach fostered access to a wider array of services, freed up GPs to focus on GMS tasks and enabled an approximation of care/case management, even when such roles were not made explicit.
At the macro or cross-organisational level of care, there were two approaches to relational working, which we have described as ‘outreach’ and ‘encircled’. In the ‘outreach’ approach, individual practitioners or single teams were funded to work systematically with care homes alongside the episodic involvement of existing primary care and specialist services. They were intended to be the link with other services, but this aspect of their role was not embedded into systems of care. In the ‘encircled’ approach, care home teams had formal links and referral mechanisms with other community-based and hospital outreach services, some team members also had care home working as an explicit part of their job specification.
We also found that reliance on individual practitioners or a single team risked isolation and service discontinuity. This approach was vulnerable to staff turnover, services being discontinued and residents being ‘handed over’ from one service to another without consultation or review. The published literature consistently highlights the problems of high turnover in care homes. The National Care Forum’s 2015 Personnel Statistics Survey155 found that more than half of social care staff (58.8%) leave within the first 3 years in post and almost one-third (30.7%) leave in their first year. This clearly was an issue for HCPs visiting care homes, as it prevents them from building working relationships with care staff who know the residents well. Conversely, NHS turbulence and NHS staff turnover were problematic for care homes, particularly in circumstances when the departure of an individual clinician led to the loss of the service.
An encircled approach to supporting care homes potentially provided a network of support that was not specific to a single person or team. It was therefore more likely to be robust against changes in the system. It also reinforced a view of care homes as one part of a system of care for frail older people. However, one unintended consequence of this network of support was evidence of duplication of effort, when multiple MDTs were involved, such as mental health outreach, a community falls team and a rehabilitation team, each with overlapping skill sets. It is possible that reducing this duplication may bring costs down, which would make this a more effective model of care overall. However, our data provide no evidence of this at present.
Importance of general practitioners
In all three sites, the involvement of the GP was important, even if other services had absorbed some of their activities, such as medication review, responsive care and case management. Taking specific tasks (e.g. regular medication review or initial comprehensive assessment on resident entry to the home) from GPs allowed their contact with care homes to be narrower and more focused. This appeared to facilitate relational working with care home staff, such that GPs were in effect allowed to practice in ways that they recognised (‘to concentrate on being a doctor’). Services that provided intensive care home support, through a model of relational working, still needed links to GPs for diagnosis, urgent care and discussions about unresolved issues of care with care home staff, residents and family.
The importance of the GP role is reflected in the larger number of hospitalisations in site 3. It is possible that this arose because the local systems were more chaotic. Specifically, site 3 was lacking in two contexts: (1) there was a lack of GPs and staff who were available and known to care home staff; and (2) referral systems or wrap-around care did not function between the NHS and care homes, nor between the different NHS services. We did not select the three sites on the basis of how they referred residents between services or how they linked to other NHS services but it appeared to be an important context in how practitioners responded, particularly when faced with residents who needed other specialist input. This was also related to the relationships between secondary care, care home staff and visiting NHS services.
Investment in care home-specific work
In all sites there was additional investment in providing NHS services to care homes. The realist synthesis had argued that financial incentives and targets were important resources (contexts) that could trigger activities that supported relational working. The case studies suggested that formal acknowledgement of working with care homes was important and valued work and not something that could be squeezed into a caseload of already overloaded primary care practitioners. Recognition of the importance of this area of work had a legitimising function that enabled NHS staff to engage more fully with care homes and their residents. It potentially freed them from anxiety that they were abrogating other competing responsibilities. This was most apparent when practitioners saw their role as focusing on providing continuity of support and access to expertise. Where this was the case, the funding acknowledged that working with care homes takes time. Perhaps more importantly it also recognised the need for the NHS to engage with care homes at an institutional level as well as with individual residents.
A different response and pattern of involvement was triggered when the need for investment was expressed predominantly as concern about care homes being a drain on NHS resources. This negative mindset did not appear to allow for shared discussions about what kind of health care or services residents needed. Instead, it led to a focus on specific issues, such as falls prevention and reduction of emergency call-outs, a commissioning approach we might call ‘hostile care’ (Dr Kenneth Rockwood, Dalhousie University, 2016, personal communication). When activities were focused on reducing expenditure, this triggered short-term, negative responses. In these circumstances, commissioners assumed the worst, and measured outcomes in terms of what had not happened and how resources had not been used, rather than focusing on the benefits to residents and potential job satisfaction for NHS and care home staff. This underlying rationale could affect outcomes, for example by an undue emphasis on safeguarding and addressing poor quality care. Where practitioners or services had an ongoing commitment to the care homes, concerns about quality of care were more likely to be presented as problems to be worked through rather than declaimed and reported. Without opportunities to work with care home staff, NHS practitioners experienced frustration, and focused on care home staff shortcomings or what care home staff should (following extra education and training) be able to do to support residents.
The realist synthesis argued that, for incentives to work, they needed to align with the interests and priorities of the practitioners involved. The cross-case study analysis suggested that the provision of intensive support or additional training to reduce demand on NHS resources and then a withdrawal of services satisfied no one. In such circumstances, NHS staff would not be likely to prioritise or value the development of close working relationships with care home staff.
Direct financial incentives appeared to generate more GP activity. The GPs were incentivised to work as GPs, gatekeeping access to secondary care. We showed that if you invest in GPs they spend more time in care homes, but this did not (as commissioners often hope) automatically lead to more proactive care, as it did not trigger a change in GP behaviour; as noted, behaviour change required the involvement of other services.
Without an explicit, ongoing commitment to working with care homes and other services on behalf of residents, GPs sought to control and limit the type and duration of interactions with care home staff, leaving care home staff struggling to find effective ways of working with NHS professionals. The commissioners shared common goals but they pursued different models of care. There was evidence that the site 1 models of commissioning had formalised aspects of care that were taking place organically elsewhere. There was also evidence that this responsive commissioning was informed by changes in patterns of working by front-line staff over time. Other sites were earlier in the evolution of service delivery models. What the case study findings demonstrated was, to quote Manzano-Santaella:156
. . . that programmes transform inexorably but mostly quietly from their original design.
Manzano-Santaella (2011),156 p. 21
In all three sites, there were examples of services and individual practitioners who, over time, had changed how they worked with care homes. This was because previous interventions had not been successful or, as they acknowledged, because the NHS had failed to understand how care homes worked. In the case of NHS professionals working with, and in, care homes, and drawing on the cross-case study analysis, several key mechanisms were identified; these included a shared focus on the older person as the recipient of care (and not solely as a potential drain on limited resources), flexibility in the service to accommodate the fluctuations in care home workforce and expertise and a shared clarity of purpose. The sense of shared purpose recognised that the care of frail older people living with dementia requires expertise and time, working in a care home is difficult and complex, and work is often provided by the least qualified members of the social care workforce. 84 These modifications and shifts in thinking were contextually necessary to trigger a different response to the demands of working with care homes. When funding of NHS services to care homes was not sustained or intermittent, and/or when practitioners left, there were fewer opportunities to adjust the focus and emphasis around what was important about working with care homes.
Access to age-appropriate expertise: the case of dementia care
In phase 1 we argued that an important resource (context) to improve health-related care is access to appropriate clinical assessment and care. We have suggested that this would lead to improvements in assessment and in health-related outcomes. Phase 2 supported the logic of this argument inasmuch as it found that pain, pressure ulcer prevalence, medication use and comorbidities were predictors of increased health service utilisation among care home residents.
Our findings suggest that access to NHS expertise in dementia care is particularly important. We found that the greater the severity of cognitive impairment, the less likely it was that a resident would see a primary care professional. The presence of dementia complicated care provision, and not all services could easily deal with this complexity. In addition, qualitative accounts from NHS staff described how difficult they found visiting residents with dementia, notably where there was no ready access to specialist dementia services. The detailed and sometimes extreme accounts of distress, police involvement and practitioners’ anxieties about helping care home staff to deal with violent episodes underlined the importance of access to, and integration of, dementia care expertise. Where a dedicated service of dementia specialist expertise was provided, it needed to have a remit to work with care home staff concerning referrals and working links with other NHS visiting services. Care home staff could then be more confident in caring for residents with behavioural and psychological symptoms of dementia. As others have found, this kind of specialist support can have other benefits, such as reduced prescribing of antipsychotic drugs and giving staff new skills in dementia care. 157,158
In some instances, however, services worked in parallel when they visited care homes or could only be mobilised at a time of crisis, so that residents were passed from one service to another without a clinician co-ordinating that process. This could then result in the resident being admitted to hospital.
Based on the care home staff accounts of how hospital staff provided care and the lack of communication with care homes, the lengths of stay observed for some residents were possibly more a reflection of secondary care’s inability to cope with older patients with dementia than deficiencies in the care home per se. A person living with dementia, on average, will stay twice as long as equivalent residents aged > 65 years and is three times more likely to have a fall while in hospital. 159 This may have been compounded when, as in site 3 (which also had the highest rate of hospitalisation overall), a lack of structure in working with care homes and HCPs with few links to hospitals meant that there were fewer opportunities to expedite residents’ discharge back to the care homes. Care home staff often felt that they knew more in this area than the HCPs with whom they interacted. Finding ways to harness and build dementia-specific expertise within the care home sector itself is a legitimate focus of ongoing enquiry.
Programme theory
In summary, our findings propose an explanatory theory that argues that specific commissioning arrangements are more likely to work well where:
-
there is a requirement and payment for dedicated care time as part of a job plan or service specification; this had a legitimising function and enabled staff to focus on ‘working with’ rather than ‘doing to’ care homes
-
the arrangements acknowledged the need to engage with care homes at an institutional level as well as with individual residents
-
the arrangements avoided a narrow description for health service input to achieve specific outcomes in a very short time; excessive focus on certain activities could trigger care home staff dependency upon the support received from the short-lived intervention; this could deter NHS staff from working to establish relational links with the care home team
-
the arrangements avoided reliance on individual practitioners or single staff groups with busy caseloads, such as GPs, without making space available for additional commitments and responsibilities.
Commissioning arrangements are likely to be beneficial if they lead to services being organised around the care home and can adapt over time. Then individual teams can co-ordinate their activities and act in a multidisciplinary fashion, without necessarily having explicit pathway navigation or case/care management. Building services around care homes as the hub of service provision does not necessarily require additional resources, or the use of secondary or primary care less productively than in settings where care was ad hoc, or where care was focused primarily around the GP.
This worked well when:
-
the different services saw care homes as a legitimate and shared part of their workload and respected the role of care homes as organisations in care delivery, rather than simply focusing on care delivery to individual residents
-
the GP was part of the care delivery team
-
it fostered access to a wider array of services, allowed GPs to focus on delivery of GMS and enabled an approximation of care/case management, even when such roles were not made explicit
-
ongoing, proactive topic-specific expertise in dementia care was included in the range of services provided.
Figure 9 sets out what needs to be in place to achieve a service that is sustainable and affordable. This figure summarises what we found to be the constituent CMOs that informed what is required to achieve improved access to health care. Figure 9 uses proxy outcomes, which are likely to transfer into improvements in the outcomes we have followed in this study, that is, those that are likely to lead to specific improvements in medication management and reduction of urgent and secondary care and continuity of care. In practice, these features have often arisen through a combination of trial and error, evolving systems of care and the voices of individual champions. The challenge for commissioners is how to build these mechanisms for good outcomes into their local health economy.
FIGURE 9.
Explanatory theory for NHS work with care homes.
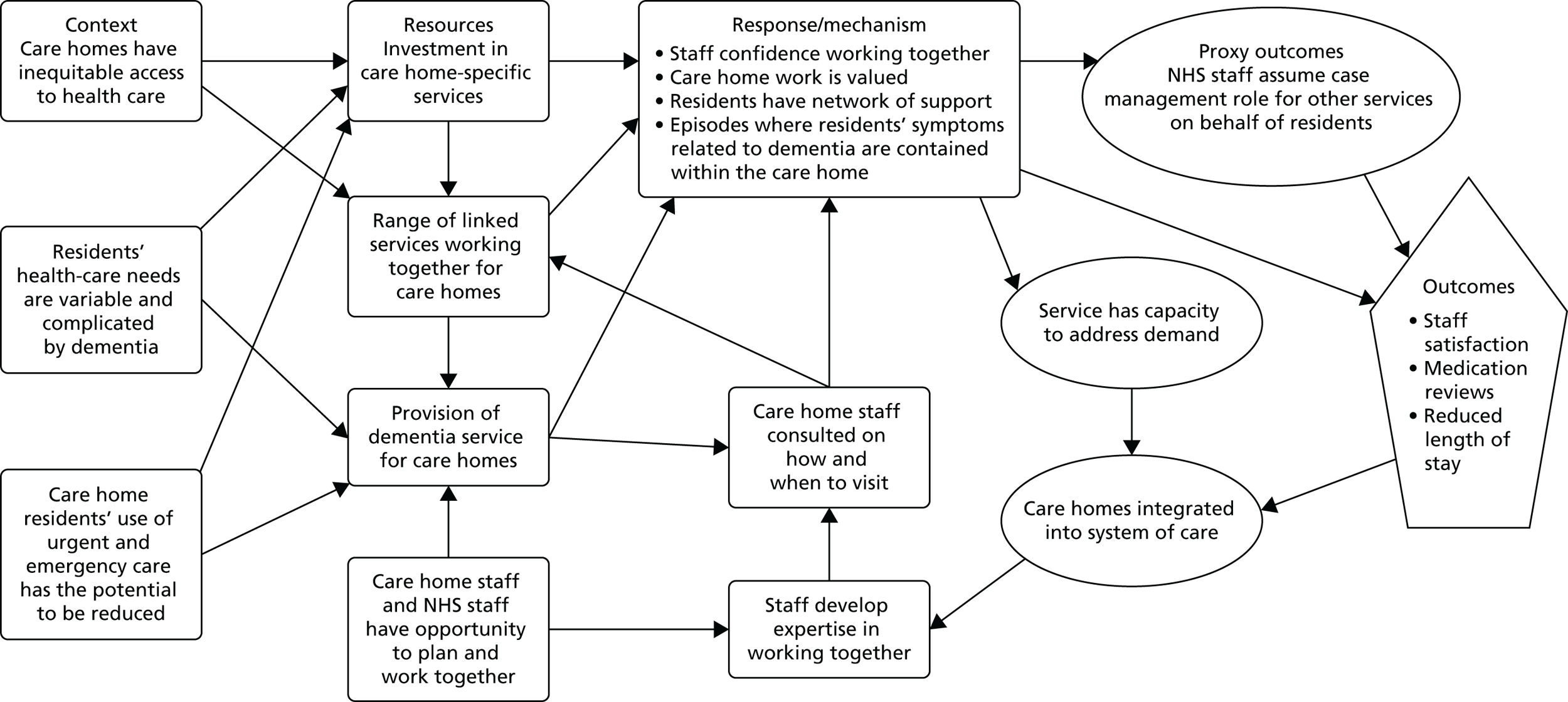
Strengths and limitations
A strength of this study is that it has been able to capture the range of NHS support to care homes and provide an explanatory account of how particular configurations of contexts and mechanisms are more or less likely to achieve certain outcomes. Integral to the design and analysis is the recognition that programmes are always affected by their contexts. In the rapidly changing care environment of the NHS, it provides a plausible account of what should be considered in different models of service delivery for care homes. This detailed examination of micro-level actions, and the relationships between NHS practitioners, care home staff and residents over time, enabled us to provide an explanatory account, one that identifies the causal processes that underlie what was observed. Our account describes the participants’ activities and their responses that characterise the delivery of health care to care homes and the environment in which this was achieved (or not).
The use of a modified version of interRAI is both a strength and a limitation; it is a strength in that it demonstrated the potential of minimum data sets for within- and cross-case comparisons of care home populations, and examination of particular residents’ service use; it is a limitation in that the findings are constrained by the number of residents we were able to recruit (50%) and the quality of the data over the 12-month period. This limited our ability to test our programme theory against observed use of secondary care. It raises a methodological question about the feasibility of prospective data collection for periods longer than 6 months. Despite financial incentives to participate and good working relationships with the research team, the care home staff’s capacity to support resident-based data collection was difficult to maintain for a year. The absence of a national minimum data set meant that a disproportionate amount of researcher time was given to obtaining consent from individual residents, capturing details of residents’ characteristics and service use, and chasing archived data (that were often not retrievable). In other countries this kind of resident-level information is readily available as anonymised data.
Our study design focused on care homes and the NHS services received from community providers and GPs. We recorded hospitalisations but were unable to review how NHS professionals became involved in co-ordinating residents’ discharge or confirm care home staff’s suspicion that hospitals were ill equipped to support people living with dementia. However, there is an increasing body of evidence that would support this. 159 Although we were able to provide an account of residents’ resource use, we were unable to establish the costs of running the different services provided to the study care homes.
An important limitation, with regard to the quantitative analysis, is that numbers were small and, therefore, the study was possibly underpowered to detect meaningful intersite differences in the outcomes measured. This was a recognised consequence of the trade-off between detailed data collection that enabled in-depth description of the cohort and the ability to recruit care home residents in large numbers. We have, however, taken account of the numbers of zero-count outcomes and have cross-referenced numerical data with qualitative observations to allow us to more fully understand any trends or statistically significant differences identified.
Our chosen method of realist synthesis and evaluation has certain strengths in terms of dealing with complicated situations where, for example, randomised controlled trials will never be possible. Our approach, unlike many realist studies, was not to look at a single intervention (e.g. care home specialist teams) implemented in different settings. Instead, we considered the contextual factors that are necessary to trigger the desired mechanisms. Distinguishing between contexts and mechanisms as part of the analytic process is challenging. 160 Over the course of the project we refined our understanding of how processes within the approach to health-care delivery could be recognised in, and across, the sites. It is a strength of the realist method and how it was applied that it enabled us to integrate and interrogate different forms of knowledge, using both primary and secondary sources. This allowed us to theorise and test how particular contextual factors, such as how long NHS staff had worked with care homes, triggered similar responses. Thus, in one site methods of working together that supported integrated working grew from a series of commissioning decisions over time. Similar relational approaches to working were observed elsewhere, developing organically over time as individual practitioners learnt how to work with care homes.
How language is used within realist evaluation is a recurring issue in the methodological literature. The study questions began by suggesting that we would focus on the ‘features’ of the different service delivery models, that is, what is done and how care is organised in order to understand the ‘mechanisms’ (the interaction of these features with people’s reasoning). This is arguably misleading and conflates elements or features of different service models with the observed mechanisms that emphasise the interaction of participants’ reasoning and resources.
This study report offers a theory-based explanatory account that can, and should, be tested further for its plausibility and relevance. The study was conducted in the UK, where the NHS creates a particular context, ways of working and professional (sub)cultures.
Conclusion
The study has focused on the experience of (and responses to) providing and being the recipients of NHS services to care homes. From this, we have provided a theory-driven account of the underlying causal processes that lead to some outcomes being achieved or not. The different contexts observed were not static. In all three sites studied, there were similar services, but in different concentrations, with different referral systems and frequencies of contact with each other and with care homes. We found that an interest in, and endorsement of, what care homes achieve for older people, combined with provision of time to consolidate together, were mechanisms associated with our outcomes of interest. Financial incentives and investment in care home specialist roles and teams made this achievable. When both practitioners and the provider organisations were able to meet frequently and take a wider interest in care home residents’ health, this provided an important context. From this position, care home staff became confident enough to accept, for example, critically ill patients because they knew they would be supported.
From the outset, a service delivery model therefore needs to recognise, record and accommodate the diversity of service groups involved in providing health care to residents, and find ways of building mutual familiarity among practitioners and the different systems of care represented. It is those activities that serve to break down the very real (and documented in this study) sense of ‘us’ and ‘them’ between NHS and care home services staff. We found that it took years, as well as targeted funding, to develop a recognition that working in care homes is difficult and complex work, which reflects that time is required to achieve shifts in attitude and approach. Our study represents a microcosm of the ongoing battles to break down what Lewis161 characterised as the hidden policy conflict that separates health and social care.
There is plenty of evidence that policy-makers see this as an important area, with the Five Year Forward View from the NHS,162 the introduction of vanguards163 and the continuing policy drive to achieve integrated care. However, our findings suggest that the social care sector (in this case, care homes) has an important contribution that so far has been underutilised to inform the commissioning of optimal health care for older citizens.
Implications for practice
There are multiple ways in which the NHS works with care homes and it is unlikely that there is one right way of working or model of service delivery. This study has argued, however, that there are common features or aspects of how care home and NHS staff work together that are more (or less) likely to support residents’ access to health care. This section sets out practice implications for commissioners of services for care homes, practitioners and care home staff and their organisations (a film of the findings is in preparation; see also Appendix 14 for the outline of the approach).
-
When commissioning and planning NHS service provision to care homes it is important that residents in care homes have access to health care that is equitable and equivalent to those received by older people living at home. We found that service provision to care homes is often ad hoc and reactive, and that some services (e.g. dental health care, speech and language therapy) were either not offered to all care homes or were limited in scope.
-
Health-care professionals’ work with care homes should be formally recognised by NHS managers as key to the support of integrated working for older people. Recognised referral links with other community and hospital services are more likely to support continuity of care and management of acute episodes in the care home. Where care home services are a stand-alone service or an adjunct to an existing role without protected time, practitioners can struggle to co-ordinate residents’ care and involve NHS services when needed.
-
Investment and incentives to NHS services and practitioners working with care homes should be structured to support joint working and planning before services are changed or modified. Where funding and sanctions are designed to reduce inappropriate demand on secondary care and other NHS services this can have the unintended consequences of focusing on failure. The study found that when funding supported care home teams and GPs to have more time to learn how to work with care homes and identify shared priorities and training needs, this was more likely to facilitate co-operation, affirm best practice and motivate staff to find shared health-care solutions.
-
Care home providers’ referral guidance needs to fit with NHS referral protocols together with opportunities for dialogue where they are uncertain about how to identify different NHS services. The study found that care home staff were often unsure who to involve when they were concerned about a resident. Established relationships that had developed over time between care home staff and HCPs were also observed to facilitate appropriate referrals that in turn helped to reinforce best practice.
-
Care home-based training needs to include all care home staff working with residents, not just the nurses or senior carers, to support them to work with the NHS and communicate with family carers. New care home staff in particular need to engage with NHS staff when working with residents and understanding their health-care needs. The study findings suggested that when training included all members of the workforce (e.g. catering staff and junior staff), there was more likely to be engagement at an organisational level and sustained implementation of service improvements.
-
General practitioners need to play a central role in residents’ health care. How their work complements other care home-focused services should be specified and agreed between all those involved in assessing, treating residents and making referrals. Regular GP clinics or patterns of visiting that were predictable were associated with higher levels of care home staff satisfaction with health care and fewer medication-related problems and more frequent medication reviews. This was particularly true when there were opportunities to discuss care provision across the care home and not just individual residents’ health care.
-
Dementia expertise needs to be integral to regular service provision, not part of a separate service. The study found that both care home and NHS staff could benefit from ongoing access to training and resources to equip them to support residents living with dementia.
-
Care home staff play a vital role in managing and monitoring residents’ medication, but may need further training and support in this area. The study found that this was an aspect of care that was of particular concern to both residents and their relatives.
Recommendations for future research
Our recommendations for future research relate both to aspects of research methods and to a number of research questions to further evaluate and explicate our programme theory. We conclude that there is limited value in further descriptive work on NHS health-care service provision to care homes that is not linked to an understanding of how the services work with care home staff to improve care home residents’ health-related outcomes.
-
There is an urgent need for research that can develop and refine a minimum data set for residents that can link with health and social care patient/client data systems.
-
The study findings suggest that when care home staff are confident in their decision-making and right to participate in planning care of their residents, this supported more equal patterns of working. Interventions that develop care home staff ability and confidence when working with visiting NHS staff need to test this further.
-
This study found limited evidence of care home residents, staff or families influencing or shaping how or what kind of health-care support was provided. Further research is needed that can build on the principles of relational working and co-design to test different ways of supporting the meaningful participation of residents, staff and families.
-
We found very little evidence of how family members contribute to, or monitor, the health care that their relatives receive. There is a need for further research to understand how their knowledge of the resident and insights might inform care.
-
Research is needed on how training and development in dementia care across the NHS and social care workforce (and not just for care home staff) can improve the quality of care of people living and dying with dementia.
Acknowledgements
We are extremely grateful to all the study participants including the residents, relatives, care home staff, HCPs and stakeholders who took part in the study. In particular, we are extremely grateful to everyone involved in the year-long duration of phase 2 for their time, input and ongoing interest in the study.
We would also like to thank the members of the SSC for their invaluable contributions and the PIR group members.
SSC members: Iain Carpenter, Sharon Blackburn, Eileen Burns, Kate Grisaffi, Jan Lockyer, Russell Pitchford, Caroline McGraw, Gill Duncan, Jackie Morris, Judy Downey, Alan Rosenbach and Angie Silva.
PIR group members: Michael Osborne, Karen Cooper, Kathleen Sartain and John Willmott.
We would also like to acknowledge and thank Elaine Argyle at Nottingham University for her work on the care home staff satisfaction survey and Lindsey Parker at the University of Hertfordshire for all her administrative support.
Contributions of authors
Claire Goodman (Professor of Health Care Research, University of Hertfordshire) was the principal investigator, led the study design, oversaw the whole study, was involved in all aspects of phases 1 and 2, and is lead author of the report.
Sue L Davies (Research Fellow, University of Hertfordshire) was a co-applicant, took day-to-day responsibility for project management, was involved in all aspects of phases 1 and 2, including recruitment and data collection for the case studies in sites 2 and 3, and was a co-author of the report.
Adam L Gordon (Clinical Associate Professor in Medicine of Older People, University of Nottingham) was a co-investigator, co-led the study design, was involved in all aspects of phases 1 and 2, oversaw the case studies in site 1, conducted the medication analysis and care home satisfaction survey, and was a co-author of the report.
Tom Dening (Professor of Dementia Research, University of Nottingham) was a member of the management group, involved in all aspects of both phases of the study, oversaw the case studies in site 1 together with Adam L Gordon and was a co-author of the report.
Heather Gage (Professor of Health Economics, University of Surrey) was a co-applicant, was a member of the management group, led the economic evaluation of phase 2 of the study and was a co-author of the report.
Julienne Meyer (Professor of Nursing Care for Older Adult, City, University of London) was a co-applicant and a member of the management group, contributed to phases 1 and 2, in particular facilitating recruitment of care homes in site 3 through the MyHomeLife programme, and design and development of the DVD, and was a co-author of the report.
Justine Schneider (Professor of Mental Health and Social Care, University of Nottingham) was a co-applicant, a member of the management group, contributed to phases 1 and 2 and was a co-author of the report.
Brian Bell (Research Fellow, University of Nottingham) was a member of the management team, provided the statistical support for phase 2 of the study and was a co-author of the report.
Jake Jordan (Research Fellow in Health Economics, University of Surrey) was a member of the management team for phase 2, provided the economic evaluation for the phase 2 case studies together with Heather Gage and was a co-author of the report.
Finbarr Martin (Professor of Medical Gerontology, Guy’s and St. Thomas’ NHS Foundation Trust) was a co-applicant and a member of the management team, contributed to all aspects of phases 1 and 2 of the study and was a co-author of the report.
Steve Iliffe (Professor of Primary Care for Older People, University College London) was a co-applicant and member of the management group, contributed to all aspects of phases 1 and 2, specifically the review of surveys in phase 1, and was a co-author of the report.
Clive Bowman (Honorary Visiting Professor, City, University of London) was a co-applicant and member of the management group, contributed to phases 1 and 2 of the study and was a co-author of the report.
John RF Gladman (Professor of the Medicine of Older People, University of Nottingham) was a co-applicant and member of the management group, contributed to all aspects of phases 1 and 2 and was a co-author of the report.
Christina Victor (Professor of Gerontology and Public Health, Brunel University) was a co-applicant and a member of the management team, and led on the secondary data analysis and write-up of residents’ interviews in phase 1 of the study.
Andrea Mayrhofer (Research Fellow, University of Hertfordshire) was involved in data collection and qualitative analysis for the phase 2 case studies in sites 2 and 3, was a member of the management team for that duration and was a co-author of the report.
Melanie Handley (Research Fellow, University of Hertfordshire) was involved in the phase 1 realist review, recruitment and data collection in sites 2 and 3 for the phase 2 case studies, was a member of the management team for that duration and was a co-author of the report.
Maria Zubair (Research Fellow, University of Nottingham), took day-to-day responsibility for one of the study sites, was involved in all aspects of phases 1 and 2, including recruitment and data analysis, and was a co-author of the report.
Publications
Goodman C, Gordon AL, Martin F, Davies SL, Iliffe S, Bowman C, et al. Effective health care for older people resident in care homes: the optimal study protocol for realist review. Syst Rev 2014;3:49.
Gordon AL, Goodman C, Dening T, Davies S, Gladman JR, Bell BG, et al. The optimal study: describing the key components of optimal healthcare delivery to UK care home residents: a research protocol. J Am Med Dir Assoc 2014;15:681–6.
Goodman C, Davies SL, Gordon AL, Meyer J, Dening T, Gladman JR. Relationships, expertise, incentives, and governance: supporting care home residents’ access to health care. An interview study from England. JAMA 2015;16:427–32.
Goodman C, Dening T, Gordon AL, Davies SL, Meyer J, Martin FC, et al. Effective health care for older people living and dying in care homes: a realist review. BMC Health Serv Res 2016;16:269.
Iliffe S, Davies SL, Gordon AL, Schneider J, Dening T, Bowman C, et al. Provision of NHS generalist and specialist services to care homes in England: review of surveys. Primary Health Care Res Dev 2016;17:122–37.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JR. Health status of UK care home residents: a cohort study. Age Ageing 2013;43:97-103. https://doi.org/10.1093/ageing/aft077.
- Goodman C, Davies SL, Dickinson A, Gage H, Froggatt K, Morbey H, et al. A Study to Develop Integrated Working between Primary Health Care Services and Care Homes. London: NIHR Service Delivery and Organisation programme; 2013.
- Goodman C, Robb N, Drennan V, Woolley R. Partnership working by default: district nurses and care home staff providing care for older people. Health Soc Care Community 2005;13:553-62. https://doi.org/10.1111/j.1365-2524.2005.00587.x.
- Iliffe S, Davies SL, Gordon AL, Schneider J, Dening T, Bowman C, et al. Provision of NHS generalist and specialist services to care homes in England: review of surveys. Prim Health Care Res Dev 2016;17:122-37. https://doi.org/10.1017/S1463423615000250.
- Robbins I, Gordon A, Dyas J, Logan P, Gladman J. Explaining the barriers to and tensions in delivering effective healthcare in UK care homes: a qualitative study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003178.
- Whittingham KA, Oldroyd LE. Using an SBAR - keeping it real! Demonstrating how improving safe care delivery has been incorporated into a top-up degree programme. Nurse Educ Today 2014;34:e47-52. https://doi.org/10.1016/j.nedt.2013.11.001.
- Prince M, Knapp M, Guerchet M, McCrone P, Prina P, Comas-Herrera A, et al. Dementia UK – Update. London: Alzheimer’s Society; 2014.
- Morley JE, Caplan G, Cesari M, Dong B, Flaherty JH, Grossberg GT, et al. International survey of nursing home research priorities. J Am Med Dir Assoc 2014;15:309-12. https://doi.org/10.1016/j.jamda.2014.03.003.
- Mayrhofer A, Goodman C, Smeeton N, Handley M, Amador S, Davies S. The feasibility of a train-the-trainer approach to end of life care training in care homes: an evaluation. BMC Palliat Care 2016;15. https://doi.org/10.1186/s12904-016-0081-z.
- Glendinning C, Powell MA, Rummery K. Partnerships, New Labour and the Governance of Welfare. Bristol: Policy Press, University of Bristol; 2002.
- Comas-Herrera A, Northey S, Wittenberg R, Knapp M, Bhattacharyya S, Burns A. Future costs of dementia-related long-term care: exploring future scenarios. Int Psychogeriatr 2011;23:20-3. https://doi.org/10.1017/S1041610210000025.
- Care of Older People UK Market Report 2014/15. London: Laing Buisson; 2015.
- Hancock R, Malley J, Wittenberg R, Morciano M, Pickard L, King D, et al. The role of care home fees in the public costs and distributional effects of potential reforms to care home funding for older people in England. Health Econ Policy Law 2013;8:47-73. https://doi.org/10.1017/S1744133112000035.
- The Commission on Residential Care chaired by Paul Burstow. London: Demos Magdalen House; 2014.
- Handley M, Goodman C, Froggatt K, Mathie E, Gage H, Manthorpe J, et al. Living and dying: responsibility for end-of-life care in care homes without on-site nursing provision – a prospective study. Health Soc Care Community 2014;22:22-9. https://doi.org/10.1111/hsc.12055.
- McCauley K, Cross W, Moss C, Walsh K, Schofield C, Handley C, et al. What does practice development (PD) offer mental health-care contexts? A comparative case study of PD methods and outcomes. J Psychiatr Ment Health Nurs 2014;21:724-37. https://doi.org/10.1111/jpm.12134.
- Parsons C, Johnston S, Mathie E, Baron N, Machen I, Amador S, et al. Potentially inappropriate prescribing in older people with dementia in care homes: a retrospective analysis. Drugs Aging 2012;29:143-55. https://doi.org/10.2165/11598560-000000000-00000.
- Forder JE, Caiels J. Measuring the outcomes of long-term care. Soc Sci Med 2011;73:1766-74. https://doi.org/10.1016/j.socscimed.2011.09.023.
- Witt E, Goodman C, Banerjee A, Scott T, Amador S. Patterns of attendance of care home residents to an Emergency Department. Eur J Emerg Med 2013;20:136-7. https://doi.org/10.1097/MEJ.0b013e32835608e1.
- Amador S, Goodman C, King D, Machen I, Elmore N, Mathie E, et al. Emergency ambulance service involvement with residential care homes in the support of older people with dementia: an observational study. BMC Geriatr 2014;14. https://doi.org/10.1186/1471-2318-14-95.
- Steves CJ, Schiff R, Martin FC. Geriatricians and care homes: perspectives from geriatric medicine departments and primary care trusts. Clin Med 2009;9:528-33. https://doi.org/10.7861/clinmedicine.9-6-528.
- Woods B, Aguirre E, Spector AE, Orrell M. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev 2012;2. https://doi.org/10.1002/14651858.CD005562.pub2.
- Quest for Quality: An Enquiry into the Quality of Healthcare Support for Older People in Care Homes: A Call for Leadership, Partnership and Improvement. London: British Geriatrics Society; 2011.
- Poltawski L, Goodman C, Iliffe S, Manthorpe J, Gage H, Shah D, et al. Frailty scales – their potential in interprofessional working with older people: a discussion paper. J Interprof Care 2011;25:280-6. https://doi.org/10.3109/13561820.2011.562332.
- Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. Int J Nurs Stud 2011;48:732-50. https://doi.org/10.1016/j.ijnurstu.2011.02.014.
- Amador S, Goodman C, King D, Ng YT, Elmore N, Mathie E, et al. Exploring resource use and associated costs in end-of-life care for older people with dementia in residential care homes. Int J Geriatr Psychiatry 2014;29:758-66. https://doi.org/10.1002/gps.4061.
- Szczepura A, Nelson S, Wild D. In-reach specialist nursing teams for residential care homes: uptake of services, impact on care provision and cost-effectiveness. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-269.
- Pawson R, Wong G, Owen L. Known knowns, known unknowns, unknown unknowns: the predicament of evidence-based policy. Am J Eval 2011;32:518-46. https://doi.org/10.1177/1098214011403831.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications Ltd; 1997.
- Goodman C, Gordon AL, Martin F, Davies SL, Iliffe S, Bowman C, et al. Effective health care for older people resident in care homes: the optimal study protocol for realist review. Syst Rev 2014;3. https://doi.org/10.1186/2046-4053-3-49.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review — a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Realist methods in medical education research: what are they and what can they contribute?. Med Educ 2012;46:89-96. https://doi.org/10.1111/j.1365-2923.2011.04045.x.
- Sherlaw-Johnson C, Smith P, Bardsley M. Continuous monitoring of emergency admissions of older care home residents to hospital. Age Ageing 2016;45:71-7. https://doi.org/10.1093/ageing/afv158.
- Connolly M, Broad J, Boyd M, Kerse N, Foster S, Lumley T, et al. Randomised controlled trial of packaged ‘evidenced’ interventions for reducing hospitalisations from residential aged care (RAC): first results from the ARCHUS study. Eur Geriatr Med 2013;4. https://doi.org/10.1016/j.eurger.2013.07.572.
- Molloy DW, Guyatt GH, Russo R, Goeree R, O’Brien BJ, Bédard M, et al. Systematic implementation of an advance directive program in nursing homes: a randomized controlled trial. JAMA 2000;283:1437-44. https://doi.org/10.1001/jama.283.11.1437.
- Lewis R, Edwards N. Improving Length of Stay: What Can Hospitals Do?. London: Nuffield Trust; 2015.
- Cowling TE, Harris MJ, Majeed A. Evidence and rhetoric about access to UK primary care. BMJ 2015;350. https://doi.org/10.1136/bmj.h1513.
- Bunn F, Burn AM, Goodman C, Rait G, Norton S, Robinson L, et al. Comorbidity and dementia: a scoping review of the literature. BMC Med 2014;12. https://doi.org/10.1186/s12916-014-0192-4.
- Bowers BJ, Fibich B, Jacobson N. Care-as-service, care-as-relating, care-as-comfort: understanding nursing home residents’ definitions of quality. Gerontologist 2001;41:539-45. https://doi.org/10.1093/geront/41.4.539.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. A realistic evaluation: the case of protocol-based care. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-38.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-33.
- Goodman C, Dening T, Gordon AL, Davies SL, Meyer J, Martin FC, et al. Effective health care for older people living and dying in care homes: a realist review. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1493-4.
- Brugha R, Varvasovszky Z. Stakeholder analysis: a review. Health Policy Plan 2000;15:239-46. https://doi.org/10.1093/heapol/15.3.239.
- Davies SL, Goodman C, Manthorpe J, Smith A, Carrick N, Iliffe S. Enabling research in care homes: an evaluation of a national network of research ready care homes. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-47.
- Goodman C, Baron NL, Machen I, Stevenson E, Evans C, Davies SL, et al. Culture, consent, costs and care homes: enabling older people with dementia to participate in research. Aging Ment Health 2011;15:475-81. https://doi.org/10.1080/13607863.2010.543659.
- McMurdo ME, Roberts H, Parker S, Wyatt N, May H, Goodman C, et al. Improving recruitment of older people to research through good practice. Age Ageing 2011;40:659-65. https://doi.org/10.1093/ageing/afr115.
- Mor V. A comprehensive clinical assessment tool to inform policy and practice: applications of the minimum data set. Med Care 2004;42:III50-9. https://doi.org/10.1097/01.mlr.0000120104.01232.5e.
- Carpenter I, Hirdes JP. A Good Life in Old Age. Paris: OECD/European Commission; 2013.
- Carpenter I, Perry M, Challis D, Hope K. Identification of registered nursing care of residents in English nursing homes using the Minimum Data Set Resident Assessment Instrument (MDS/RAI) and Resource Utilisation Groups version III (RUG-III). Age Ageing 2003;32:279-85. https://doi.org/10.1093/ageing/32.3.279.
- Onder G, Carpenter I, Finne-Soveri H, Gindin J, Frijters D, Henrard JC, et al. Assessment of nursing home residents in Europe: the Services and Health for Elderly in Long TERm care (SHELTER) study. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-5.
- Rosen R, Mountford J, Lewis G, Lewis R, Shand J, Shaw S. Integration in Action: Four International Case Studies. London: Nuffield Trust; 2011.
- Shaw S, Rosen R, Rumbold B. An Overview of Integrated Care in the NHS. What is Integrated Care?. London: Nuffield Trust; 2011.
- Parker G, Corden A, Heaton J. Experiences of and influences on continuity of care for service users and carers: synthesis of evidence from a research programme. Health Soc Care Community 2011;19:576-601. https://doi.org/10.1111/j.1365-2524.2011.01001.x.
- Hasson H, Arnetz JE. Nursing staff competence, work strain, stress and satisfaction in elderly care: a comparison of home-based care and nursing homes. J Clin Nurs 2008;17:468-81.
- Gordon AL, Goodman C, Dening T, Davies S, Gladman JR, Bell BG, et al. The optimal study: describing the key components of optimal health care delivery to UK care home residents: a research protocol. J Am Med Dir Assoc 2014;15:681-6. https://doi.org/10.1016/j.jamda.2014.06.011.
- Bunn F, Goodman C, Brayne C, Norton S, Rait G, Robinson L. Comorbidity and Dementia: Improving Healthcare for People with Dementia (CoDem). Southampton: NIHR HSDR programme; 2012.
- Marchal B, Dedzo M, Kegels G. A realist evaluation of the management of a well-performing regional hospital in Ghana. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-24.
- O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 2015;44:213-8. https://doi.org/10.1093/ageing/afu145.
- Spinewine A, Schmader KE, Barber N, Hughes C, Lapane KL, Swine C, et al. Appropriate prescribing in elderly people: how well can it be measured and optimised?. Lancet 2007;370:173-84. https://doi.org/10.1016/S0140-6736(07)61091-5.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- The Health and Care of Older People in Care Homes – A Comprehensive Interdisciplinary Approach. London: Royal College of Physicians; 2001.
- Gladman JRF, Chikura G. Medical Crises in Older People. University of Nottingham Discussion Paper 8. Nottingham: University of Nottingham; 2011.
- Gage H, Dickinson A, Victor C, Williams P, Cheynel J, Davies SL, et al. Integrated working between residential care homes and primary care: a survey of care homes in England. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-71.
- Quince C. Low Expectations: Attitudes on Choice, Care and Community for People with Dementia in Care Homes. London: Alzheimer’s Society; 2013.
- Carter C. Failing the Frail: A Chaotic Approach to Commissioning Healthcare Services for Care Homes. London: British Geriatrics Society; 2011.
- Monaghan N, Morgan M. Oral health policy and access to dentistry in care homes. J Disabil Oral Health 2010;11:61-8.
- Darton R. Study of Care Home Residents’ and Relatives’ Expectations and Experiences. Canterbury: Personal Social Services Research Unit, University of Kent; 2011.
- Seymour JE, Kumar A, Froggatt K. Do nursing homes for older people have the support they need to provide end-of-life care? A mixed methods enquiry in England. Palliat Med 2011;25:125-38. https://doi.org/10.1177/0269216310387964.
- Briggs R, Robinson S, Martin F, O’Neill D. Standards of medical care for nursing home residents in Europe. Eur Geriatr Med 2012;3:365-7. https://doi.org/10.1016/j.eurger.2012.07.455.
- British Dental Association . Dentistry in Care Homes Research - UK 2012. www.bda.org/dentists/policy-campaigns/research/patient-care/Documents/dentistry_in_care_homes.pdf (accessed 3 June 2017).
- Health Care in Care Homes – A Special Review of the Provision of Health Care to Those in Care Homes. London: The Stationery Office; 2012.
- Morgan MZ, Monaghan NP, Karki AJ. Wales Care Home Dental Survey 2010–2011 2012. www.cardiff.ac.uk/__data/assets/pdf_file/0010/47755/WALES-CARE-HOME.pdf (accessed 3 June 2017).
- White DA, Tsakos G, Pitts NB, Fuller E, Douglas GVA, Murray JJ, et al. Adult Dental Health Survey 2009: common oral health conditions and their impact on the population. Br Dent J 2012;213. https://doi.org/10.1038/sj.bdj.2012.1088.
- Leemrijse C, Veenhof C, Boer ME. The availability and use of allied health care in care homes in the Midlands, UK. Int J Ther Rehabil 2009;16:223-4.
- Gulliford M, Morgan M. Access to Health Care. London: Routledge; 2013.
- Jacobs S. A National Survey of Access to NHS Services of Older People in Residential and Nursing Care Homes. Manchester: National Centre for Primary Care and Research Development; 2001.
- Guaraldo L, Cano FG, Damasceno GS, Rozenfeld S. Inappropriate medication use among the elderly: a systematic review of administrative databases. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-79.
- Abbott RA, Whear R, Thompson-Coon J, Ukoumunne OC, Rogers M, Bethel A, et al. Effectiveness of mealtime interventions on nutritional outcomes for the elderly living in residential care: a systematic review and meta-analysis. Ageing Res Rev 2013;12:967-81. https://doi.org/10.1016/j.arr.2013.06.002.
- Rahman AN, Schnelle JF, Applebaum R, Lindabury K, Simmons S. Distance coursework and coaching to improve nursing home incontinence care: lessons learned. J Am Geriatr Soc 2012;60:1157-64. https://doi.org/10.1111/j.1532-5415.2012.03939.x.
- Shier V, Khodyakov D, Cohen LW, Zimmerman S, Saliba D. What does the evidence really say about culture change in nursing homes?. Gerontologist 2014;54:6-16. https://doi.org/10.1093/geront/gnt147.
- Donald IP, Gladman J, Conroy S, Vernon M, Kendrick E, Burns E. Care home medicine in the UK – in from the cold. Age Ageing 2008;37:618-20. https://doi.org/10.1093/ageing/afn207.
- A Quest for Quality in Care Homes – An Inquiry into the Quality of Healthcare Support for Older People in Care Homes. London: British Geriatrics Society; 2011.
- Dudman J, Meyer J. Understanding residential home issues to meet health-care needs. Br J Community Nurs 2012;17:434-8. https://doi.org/10.12968/bjcn.2012.17.9.434.
- Alldred DP, Raynor DK, Hughes C, Barber N, Chen TF, Spoor P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev 2013;2. https://doi.org/10.1002/14651858.CD009095.pub2.
- Hall S, Kolliakou A, Petkova H, Froggatt K, Higginson IJ. Interventions for improving palliative care for older people living in nursing care homes. Cochrane Database Syst Rev 2011;3. https://doi.org/10.1002/14651858.CD007132.pub2.
- MacEntee MI, Kazanjian A, Kozak JF, Hornby K, Thorne S, Kettratad-Pruksapong M. A scoping review and research synthesis on financing and regulating oral care in long-term care facilities. Gerodontology 2012;29:e41-52. https://doi.org/10.1111/j.1741-2358.2011.00575.x.
- Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev 2008;65:3-39. https://doi.org/10.1177/1077558707308754.
- Bradshaw SA, Playford ED, Riazi A. Living well in care homes: a systematic review of qualitative studies. Age Ageing 2012;41:429-40. https://doi.org/10.1093/ageing/afs069.
- Hall S, Goddard C, Stewart F, Higginson IJ. Implementing a quality improvement programme in palliative care in care homes: a qualitative study. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-31.
- Goodman C, Davies SL, Gordon AL, Meyer J, Dening T, Gladman JR, et al. Relationships, expertise, incentives, and governance: supporting care home residents’ access to health care. An interview study from England. J Am Med Dir Assoc 2015;16:427-32. https://doi.org/10.1016/j.jamda.2015.01.072.
- Mannion R, Davies HT. Payment for performance in health care. BMJ 2008;336:306-8. https://doi.org/10.1136/bmj.39463.454815.94.
- McDonald R, Harrison S, Checkland K, Campbell SM, Roland M. Impact of financial incentives on clinical autonomy and internal motivation in primary care: ethnographic study. BMJ 2007;334. https://doi.org/10.1136/bmj.39238.890810.BE.
- Doran T, Fullwood C, Kontopantelis E, Reeves D. Effect of financial incentives on inequalities in the delivery of primary clinical care in England: analysis of clinical activity indicators for the quality and outcomes framework. Lancet 2008;372:728-36. https://doi.org/10.1016/S0140-6736(08)61123-X.
- Roland M, Paddison C. Better management of patients with multimorbidity. BMJ 2013;346. https://doi.org/10.1136/bmj.f2510.
- Charlesworth A, Hawkins L, Marshall L. NHS Payment Reform: Lessons from the Past and Directions for the Future. London: Nuffield Trust; 2014.
- Evans G. Factors influencing emergency hospital admissions from nursing and residential homes: positive results from a practice-based audit. J Eval Clin Pract 2011;17:1045-9. https://doi.org/10.1111/j.1365-2753.2010.01471.x.
- Barber ND, Alldred DP, Raynor DK, Dickinson R, Garfield S, Jesson B, et al. Care homes’ use of medicines study: prevalence, causes and potential harm of medication errors in care homes for older people. Qual Saf Health Care 2009;18:341-6. https://doi.org/10.1136/qshc.2009.034231.
- Shah SM, Carey IM, Harris T, DeWilde S, Cook DG. Quality of prescribing in care homes and the community in England and Wales. Br J Gen Pract 2012;62:e329-36. https://doi.org/10.3399/bjgp12X641447.
- Shah SM, Carey IM, Harris T, Dewilde S, Cook DG. Quality of chronic disease care for older people in care homes and the community in a primary care pay for performance system: retrospective study. BMJ 2011;342. https://doi.org/10.1136/bmj.d912.
- Witter S, Fretheim A, Kessy FL, Lindahl AK. Paying for performance to improve the delivery of health interventions in low- and middle-income countries. Cochrane Database Syst Rev 2012;2. https://doi.org/10.1002/14651858.CD007899.pub2.
- Russell G. Does paying for performance in primary care save lives?. BMJ 2015;350. https://doi.org/10.1136/bmj.h1051.
- Roland M. When Incentives Go Wrong – £55 for Dementia Diagnosis Is a Dead Cert 2014. www.cchsr.iph.cam.ac.uk/2107 (accessed 2 June 2017).
- Fossey J, Ballard C, Juszczak E, James I, Alder N, Jacoby R, et al. Effect of enhanced psychosocial care on antipsychotic use in nursing home residents with severe dementia: cluster randomised trial. BMJ 2006;332:756-61. https://doi.org/10.1136/bmj.38782.575868.7C.
- Loganathan M, Singh S, Franklin BD, Bottle A, Majeed A. Interventions to optimise prescribing in care homes: systematic review. Age Ageing 2011;40:150-62. https://doi.org/10.1093/ageing/afq161.
- Cooke V, Arling G, Lewis T, Abrahamson KA, Mueller C, Edstrom L. Minnesota’s nursing facility performance-based incentive payment program: an innovative model for promoting care quality. Gerontologist 2010;50:556-63. https://doi.org/10.1093/geront/gnp140.
- Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet 1993;342:1032-6. https://doi.org/10.1016/0140-6736(93)92884-V.
- Ellis G, Whitehead MA, O’Neill D, Langhorne P, Robinson D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev 2011;7. https://doi.org/10.1002/14651858.CD006211.pub2.
- Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, Horwood J. Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet 2008;371:725-35. https://doi.org/10.1016/S0140-6736(08)60342-6.
- Gladman J, Harwood R, Conroy S, Logan P, Elliott R, Jones R, et al. Medical crises in older people. Programme Grants Appl Res 2015;3.
- Lyne KJ, Moxon S, Sinclair I, Young P, Kirk C, Ellison S. Analysis of a care planning intervention for reducing depression in older people in residential care. Aging Ment Health 2006;10:394-403. https://doi.org/10.1080/13607860600638347.
- Morrell CJ, Curran S, Topping A, Shaik K, Muthukrishnan V, Stephenson J. Identification of depressive disorder among older people in care homes – a feasibility study. Prim Health Care Res Dev 2011;12:255-65. https://doi.org/10.1017/S1463423611000144.
- Ellard DR, Thorogood M, Underwood M, Seale C, Taylor SJC. Whole home exercise intervention for depression in older care home residents (the OPERA study): a process evaluation. BMC Med 2014;12. https://doi.org/10.1186/1741-7015-12-1.
- Hancock GA, Woods B, Challis D, Orrell M. The needs of older people with dementia in residential care. Int J Geriatr Psychiatry 2006;21:43-9. https://doi.org/10.1002/gps.1421.
- Cox H, Puffer S, Morton V, Cooper C, Hodson J, Masud T, et al. Educating nursing home staff on fracture prevention: a cluster randomised trial. Age Ageing 2008;37:167-72. https://doi.org/10.1093/ageing/afm168.
- Kenkmann A, Price GM, Bolton J, Hooper L. Health, wellbeing and nutritional status of older people living in UK care homes: an exploratory evaluation of changes in food and drink provision. BMC Geriatr 2010;10. https://doi.org/10.1186/1471-2318-10-28.
- Merrell J, Philpin S, Warring J, Hobby D, Gregory V. Addressing the nutritional needs of older people in residential care homes. Health Soc Care Community 2012;20:208-15. https://doi.org/10.1111/j.1365-2524.2011.01033.x.
- Bamford C, Heaven B, May C, Moynihan P. Implementing nutrition guidelines for older people in residential care homes: a qualitative study using normalization process theory. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-106.
- Sackley C, Wade DT, Mant D, Atkinson JC, Yudkin P, Cardoso K, et al. Cluster randomized pilot controlled trial of an occupational therapy intervention for residents with stroke in UK care homes. Stroke 2006;37:2336-41. https://doi.org/10.1161/01.STR.0000237124.20596.92.
- Forsetlund L, Eike MC, Gjerberg E, Vist GE. Effect of interventions to reduce potentially inappropriate use of drugs in nursing homes: a systematic review of randomised controlled trials. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-16.
- Livingston G, Lewis-Holmes E, Pitfield C, Manela M, Chan D, Constant E, et al. Improving the end-of-life for people with dementia living in a care home: an intervention study. Int Psychogeriatr 2013;25:1849-58. https://doi.org/10.1017/S1041610213001221.
- Badger F, Plumridge G, Hewison A, Shaw KL, Thomas K, Clifford C. An evaluation of the impact of the Gold Standards Framework on collaboration in end-of-life care in nursing homes. A qualitative and quantitative evaluation. Int J Nurs Stud 2012;49:586-95. https://doi.org/10.1016/j.ijnurstu.2011.10.021.
- Hasson F, Kernohan WG, Waldron M, Whittaker E, McLaughlin D. The palliative care link nurse role in nursing homes: barriers and facilitators. J Adv Nurs 2008;64:233-42. https://doi.org/10.1111/j.1365-2648.2008.04803.x.
- Sprakes K, Tyrer J. Improving wound and pressure area care in a nursing home. Nurs Stand 2010;25:43-9. https://doi.org/10.7748/ns2010.11.25.10.43.c8092.
- De Visschere LM, van der Putten GJ, Vanobbergen JN, Schols JM, de Baat C. Dutch Association of Nursing Home Physicians . An oral health care guideline for institutionalised older people. Gerodontology 2011;28:307-10. https://doi.org/10.1111/j.1741-2358.2010.00406.x.
- Mozley CG, Schneider J, Cordingley L, Molineux M, Duggan S, Hart C, et al. The care home activity project: does introducing an occupational therapy programme reduce depression in care homes?. Aging Ment Health 2007;11:99-107. https://doi.org/10.1080/13607860600637810.
- Schneider J, Duggan S, Cordingley L, Mozley CG, Hart C. Costs of occupational therapy in residential homes and its impact on service use. Aging Ment Health 2007;11:108-14. https://doi.org/10.1080/13607860600963349.
- Goodman C. Evaluation of the End of Life Care Train the Trainer (TTT) Education Model. Hatfield: University of Hertfordshire; 2014.
- Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ 2006;333. https://doi.org/10.1136/bmj.39010.581354.55.
- Froggatt K, Hockley J, Parker D, Brazil K. A system lifeworld perspective on dying in long term care settings for older people: contested states in contested places. Health Place 2011;17:263-8. https://doi.org/10.1016/j.healthplace.2010.11.001.
- Masterson-Algar P, Burton CR, Rycroft-Malone J, Sackley CM, Walker MF. Towards a programme theory for fidelity in the evaluation of complex interventions. J Eval Clin Pract 2014;20:445-52. https://doi.org/10.1111/jep.12174.
- Cooperrider DL, Whitney DK. Appreciative Inquiry: A Positive Revolution in Change. San Francisco, CA: Berrett-Koehler Publishers; 2005.
- Gittell JH, Weinberg D, Pfefferle S, Bishop C. Impact of relational coordination on job satisfaction and quality outcomes: a study of nursing homes. Hum Resour Manag J 2008;18:154-70. https://doi.org/10.1111/j.1748-8583.2007.00063.x.
- Toles M, Anderson RA. State of the science: relationship-oriented management practices in nursing homes. Nurs Outlook 2011;59:221-7. https://doi.org/10.1016/j.outlook.2011.05.001.
- Goodman C, Amador S, Elmore N, Machen I, Mathie E. Preferences and priorities for ongoing and end-of-life care: a qualitative study of older people with dementia resident in care homes. Int J Nurs Stud 2013;50:1639-47. https://doi.org/10.1016/j.ijnurstu.2013.06.008.
- Sackley CM, van den Berg ME, Lett K, Patel S, Hollands K, Wright CC, et al. Effects of a physiotherapy and occupational therapy intervention on mobility and activity in care home residents: a cluster randomised controlled trial. BMJ 2009;339. https://doi.org/10.1136/bmj.b3123.
- Brooker DJ, Woolley RJ, Lee D. Enriching opportunities for people living with dementia in nursing homes: an evaluation of a multi-level activity-based model of care. Aging Ment Health 2007;11:361-70. https://doi.org/10.1080/13607860600963679.
- Mayrhofer A, Goodman C, Holman C. Establishing a community of practice for dementia champions (innovative practice). Dementia 2015;14:259-66. https://doi.org/10.1177/1471301214542534.
- Goodman C, L Davies S, Norton C, Fader M, Morris J, Wells M, et al. Can district nurses and care home staff improve bowel care for older people using a clinical benchmarking tool?. Br J Community Nurs 2013;18:580-7. https://doi.org/10.12968/bjcn.2013.18.12.580.
- Kinley J, Stone L, Dewey M, Levy J, Stewart R, McCrone P, et al. The effect of using high facilitation when implementing the Gold Standards Framework in Care Homes programme: a cluster randomised controlled trial. Palliat Med 2014;28:1099-109. https://doi.org/10.1177/0269216314539785.
- Chenoweth L, King MT, Jeon YH, Brodaty H, Stein-Parbury J, Norman R, et al. Caring for Aged Dementia Care Resident Study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: a cluster-randomised trial. Lancet Neurol 2009;8:317-25. https://doi.org/10.1016/S1474-4422(09)70045-6.
- Bakerjian D, Zisberg A. Applying the Advancing Excellence in America’s Nursing Homes Circle of Success to improving and sustaining quality. Geriatr Nurs 2013;34:402-11. https://doi.org/10.1016/j.gerinurse.2013.06.011.
- Kodner DL, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications – a discussion paper. Int J Integr Care 2002;2. https://doi.org/10.5334/ijic.67.
- Masso M, McCarthy G, Kitson A. Mechanisms which help explain implementation of evidence-based practice in residential aged care facilities: a grounded theory study. Int J Nurs Stud 2014;51:1014-26. https://doi.org/10.1016/j.ijnurstu.2013.11.010.
- Bolmsjö BB, Strandberg EL, Midlöv P, Brorsson A. ‘It is meaningful; I feel that I can make a difference’ – a qualitative study about GPs’ experiences of work at nursing homes in Sweden. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0326-6.
- Lund S, Richardson A, May C. Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0116629.
- Health Profiles. London: Public Health England; 2016.
- Changes in the Older Resident Care Home Population between 2001 and 2011. London: Office for National Statistics; 2014.
- Gilbert H. Supporting Integration Through New Roles and Working Across Boundaries. London: The King’s Fund; 2016.
- Larkin M, Boden ZV, Newton E. On the brink of genuinely collaborative care: experience-based co-design in mental health. Qual Health Res 2015;25:1463-76. https://doi.org/10.1177/1049732315576494.
- Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care 2006;15:307-10. https://doi.org/10.1136/qshc.2005.016527.
- Kreindler SA, Dowd DA, Dana Star N, Gottschalk T. Silos and social identity: the social identity approach as a framework for understanding and overcoming divisions in health care. Milbank Q 2012;90:347-74. https://doi.org/10.1111/j.1468-0009.2012.00666.x.
- Merton RK. Social Theory and Social Structure. New York, NY: Simon and Schuster; 1968.
- Hedström P, Ylikoski P. Causal mechanisms in the social sciences. Annu Rev Sociol 2010;36:49-67. https://doi.org/10.1146/annurev.soc.012809.102632.
- Personnel Statistics Survey. Coventry: National Care Forum; 2015.
- Manzano-Santaella A. A realistic evaluation of fines for hospital discharges: incorporating the history of programme evaluations in the analysis. Evaluation 2011;17:21-36. https://doi.org/10.1177/1356389010389913.
- Ballard C, O’Brien J, James I, Mynt P, Lana M, Potkins D, et al. Quality of life for people with dementia living in residential and nursing home care: the impact of performance on activities of daily living, behavioral and psychological symptoms, language skills and psychotropic drugs. Int Psychogeriatr 2001;13:93-106. https://doi.org/10.1017/S1041610201007499.
- Brooker DJ, Latham I, Evans SC, Jacobson N, Perry W, Bray J, et al. FITS into practice: translating research into practice in reducing the use of anti-psychotic medication for people with dementia living in care homes. Aging Ment Health 2016;20:709-18. https://doi.org/10.1080/13607863.2015.1063102.
- Fix Dementia Care. London: Alzheimer’s Society; 2016.
- Marchal B, van Belle S, van Olmen J, Hoerée T, Kegels G. Is realist evaluation keeping its promise? A review of published empirical studies in the field of health systems research. Eval 2012;18:192-21. https://doi.org/10.1177/1356389012442444.
- Lewis J. Older people and the health–social care boundary in the UK: half a century of hidden policy conflict. Soc Policy Adm 2001;35:343-59. https://doi.org/10.1111/1467-9515.00238.
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 22 February 2017).
- NHS England . New Care Models – Vanguard Sites 2015. www.england.nhs.uk/ourwork/futurenhs/new-care-models/ (accessed 22 February 2017).
- Curtis L, Burns A. Unit Costs of Health and Social Care. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- NHS England . National Careers Service NHS Agenda for Change Pay Scales 2015. www.nhsemployers.org/case-studies-and-resources/2015/04/agenda-for-change-pay-bands-and-points-april-2015 (accessed December 2015).
- Curtis L. Unit Costs of Health and Social Care. Canterbury: Personal Social Services Research Unit, University of Kent; 2014.
- Out of Hours GP Services in England. London: Department of Health and NHS England; 2014.
- Optical Business Regulation. Final report for the General Optical Council. London: Europe Economics; 2013.
- NHS Reference Costs 2014–2015. London: Department of Health; 2015.
- NHS Reference Costs 2013–2014. London: Department of Health; 2014.
- Ahearn DJ, Jackson TB, McIlmoyle J, Weatherburn AJ. Improving end of life care for nursing home residents: an analysis of hospital mortality and readmission rates. Postgrad Med J 2010;86:131-5. https://doi.org/10.1136/pgmj.2008.076430.
- Alldred DP, Standage C, Fletcher O, Savage I, Carpenter J, Barber N, et al. The influence of formulation and medicine delivery system on medication administration errors in care homes for older people. Qual Saf Health Care 2011;20:397-401. https://doi.org/10.1136/bmjqs.2010.046318.
- Badger F, Clifford C, Hewison A, Thomas K. An evaluation of the implementation of a programme to improve end-of-life care in nursing homes. Palliat Med 2009;23:502-11. https://doi.org/10.1177/0269216309105893.
- Barnes L, Cheek J, Nation RL, Gilbert A, Paradiso L, Ballantyne A. Making sure the residents get their tablets: medication administration in care homes for older people. J Adv Nurs 2006;56:190-9. https://doi.org/10.1111/j.1365-2648.2006.03997.x.
- Barnett K, McCowan C, Evans JMM, Gillespie ND, Davey PG, Fahey T. Prevalence and outcomes of use of potentially inappropriate medicines in older people: cohort study stratified by residence in nursing home or in the community. Qual Saf Health Care 2011;20:275-81. https://doi.org/10.1136/bmjqs.2009.039818.
- Boumans NP, Berkhout AJ, Vijgen SM, Nijhuis FJ, Vasse RM. The effects of integrated care on quality of work in nursing homes: a quasi-experiment. Int J Nurs Stud 2008;45:1122-36. https://doi.org/10.1016/j.ijnurstu.2007.09.001.
- Clegg A, Clingo D, Hinchcliffe S. Developing the community matron role in care homes. Br J Community Nurs 2006;11:469-70. https://doi.org/10.12968/bjcn.2006.11.11.22274.
- Cooney A, Murphy K, O’Shea E. Resident perspectives of the determinants of quality of life in residential care in Ireland. J Adv Nurs 2009;65:1029-38. https://doi.org/10.1111/j.1365-2648.2008.04960.x.
- Davidson S, Koritsas S, O’Connnor DW, Clarke D. The feasibility of a GP led screening intervention for depression among nursing home residents. Int J Geriatr Psychiatry 2006;21:1026-30. https://doi.org/10.1002/gps.1601.
- Dening T, Milne A. Mental Health in Care Homes. Oxford: Oxford University Press; 2011.
- Doran T, Kontopantelis E, Valderas JM, Campbell S, Roland M, Salisbury C, et al. Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK Quality and Outcomes Framework. BMJ 2011;342. https://doi.org/10.1136/bmj.d3590.
- Froggatt K, Davies S, Meyer J. Understanding Care Homes: A Research and Development Perspective. London: Jessica Kingsley Publishers; 2008.
- Gadsby R, Galloway M, Barker P, Sinclair A. Prescribed medicines for elderly frail people with diabetes resident in nursing homes — issues of polypharmacy and medication costs. Diabet Med 2012;29:136-9. https://doi.org/10.1111/j.1464-5491.2011.03494.x.
- Gittell JH, Fairfield KM, Bierbaum B, Head W, Jackson R, Kelly M, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care 2000;38:807-19. https://doi.org/10.1097/00005650-200008000-00005.
- Orrell M, Hancock G, Hoe J, Woods B, Livingston G, Challis D. A cluster randomised controlled trial to reduce the unmet needs of people with dementia living in residential care. Int J Geriatr Psychiatry 2007;22:1127-34. https://doi.org/10.1002/gps.1801.
- Hockley J, Watson J, Oxenham D, Murray SA. The integrated implementation of two end-of-life care tools in nursing care homes in the UK: an in-depth evaluation. Palliat Med 2010;24:828-38. https://doi.org/10.1177/0269216310373162.
- Livingston G, Pitfield C, Morris J, Manela M, Lewis-Holmes E, Jacobs H. Care at the end of life for people with dementia living in a care home: a qualitative study of staff experience and attitudes. Int J Geriatr Psychiatry 2012;27:643-50. https://doi.org/10.1002/gps.2772.
- McCormack B, Dewing J, Breslin L, Coyne-Nevin A, Kennedy K, Manning M, et al. Developing person-centred practice: nursing outcomes arising from changes to the care environment in residential settings for older people. Int J Older People Nurs 2010;5:93-107. https://doi.org/10.1111/j.1748-3743.2010.00216.x.
- McDermott C, Coppin R, Little P, Leydon G. Hospital admissions from nursing homes: a qualitative study of GP decision making. Br J Gen Pract 2012;62:e538-45. https://doi.org/10.3399/bjgp12X653589.
- Moylan T, Roberts M, Murray S. Medical needs and survival of NHS continuing care residents. Scottish Med J 2008;53:21-3. https://doi.org/10.1258/RSMSMJ.53.3.21.
- Nyman SR, Victor CR. Older people’s recruitment, sustained participation, and adherence to falls prevention interventions in institutional settings: a supplement to the Cochrane systematic review. Age Ageing 2011;40:430-6. https://doi.org/10.1093/ageing/afr016.
- Ong AC, Sabanathan K, Potter JF, Myint PK. High mortality of older patients admitted to hospital from care homes and insight into potential interventions to reduce hospital admissions from care homes: the Norfolk experience. Arch Gerontol Geriatr 2011;53:316-19. https://doi.org/10.1016/j.archger.2010.12.004.
- Parsons C, Alldred D, Daiello L, Hughes C. Prescribing for older people in nursing homes: strategies to improve prescribing and medicines use in nursing homes. Int J Older People Nurs 2011;6:55-62. https://doi.org/10.1111/j.1748-3743.2010.00263.x.
- Quinn T. Emergency hospital admissions from care-homes: who, why and what happens? A cross-sectional study. Gerontology 2011;57:115-20. https://doi.org/10.1159/000314962.
- South A, Tandy C, Watt R, Corrado OJ. Comment on ‘Care home medicine in the UK—in from the cold’. Age Ageing 2009;38. https://doi.org/10.1093/ageing/afp031.
- Szczepura A, Wild D, Nelson S. Medication administration errors for older people in long-term residential care. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-82.
- Zermansky AG, Alldred DP, Petty DR, Raynor DK, Freemantle N, Eastaugh J, et al. Clinical medication review by a pharmacist of elderly people living in care homes — randomised controlled trial. Age Ageing 2006;35:586-91. https://doi.org/10.1093/ageing/afl075.
Appendix 1 OPTIMAL Study Steering Committee members: 30 August 2013
| Member | Expertise |
|---|---|
| 1. Professor Iain Carpenter (chairperson) | Emeritus Professor (Human Ageing), Centre for Health Services Study, University of Kent |
| 2. Jan Lockyer | Innovations lead, quality improvement, Essex County Council |
| 3. Russell Pitchford | Commissioning Manager for Older People at Nottingham City CCG |
| 4/5. Des Kelly/Sharon Blackburn | National Care Forum |
| 6. Caroline McGraw | District nurse and lecturer in public health, City, University of London |
| 7. Dr Eileen Burns | Community geriatrician |
| 8. Angie Silva | Care home manager |
| 9. Karen Cooper | Care home manager |
| 10. John Willmott | University of Hertfordshire PIR Group member |
| 11. Dr Kate Grisaffi | GP |
| 12. Dr Jackie Morris | Dignity champion/researcher in care homes |
| 13. Alan Rosenbach | Policy lead, CQC |
| 14. Gill Duncan | Director of Adult Services at Hampshire County Council, the Association of Directors of Adult Social Services representative for nursing and care forum |
| 15. Judy Downey | Chairperson of the Relatives and Residents Association |
| 16. Kathleen Sartain | PIR group member, Nottingham |
| 17. Michael Osborne | PIR group member, Nottingham |
Appendix 2 Screening form for OPTIMAL
Appendix 3 Data extraction form used for theory area 1
Appendix 4 Manager summary
Appendix 5 Care home link staff role
Role of the OPTIMAL care home link staff
The OPTIMAL study aims to understand how the NHS works with care homes and to see whether or not specific ways of working improve the health care that residents receive. Each care home that takes part will be asked to identify two members of staff to act as OPTIMAL link staff to work with and support the research team. As part of this role they will be asked to do the following:
-
act as a first point of contact and liaison in the care home for the study researchers visiting the care home
-
provide support to the researchers with recruitment of study participants and collection of some of the study information.
The care home staff working with OPTIMAL will help with the following activities:
-
introducing researchers to care home residents for recruitment purposes
-
introducing researchers to interested relatives/family members of residents for recruitment purposes
-
introducing researchers to other care home staff working with them
-
identify and introduce researchers to the various NHS HCPs who visit the care home
-
assist researchers with access to residents’ care home notes (where consent is in place)
-
assist researchers with the recording of information relating to the participating residents’ (1) health and day-to-day function and (2) use of NHS health-care services (e.g. GP visits, hospital admissions, outpatient appointments) – this service information will be collected every month.
The data collection for the study will take place over 12 months. During this time, the OPTIMAL care home link staff will have contact with the researchers on a regular basis, for example weekly or fortnightly. This will be agreed between them on the days and times that are most convenient for everyone. We think that the amount of time put into the study for each OPTIMAL link staff member would be somewhere around 4–8 hours every month. We would need more help at the beginning when residents are being recruited and to collect information from their notes, but following on from this, collecting information on residents’ monthly NHS service use would take much less time.
There will be no change in care delivery as a result of the staff’s involvement in the study. The researchers will work closely with the staff and residents’ care will always take priority; no residents or staff will be pressured or coerced into taking part in the study.
Appendix 6 Staff satisfaction questionnaire
Appendix 7 Resident service log
Appendix 8 Unit cost table and references
| Resource item | Setting | Cost (£) | Unit | Source | Comment | Applied unit cost (£) per recorded item | Additional |
|---|---|---|---|---|---|---|---|
| Continence nurse/diabetes mellitus nurse/continuing health-care nurse assessor/CHANT nurse/Parkinson’s disease nurse/COPD nurse specialist/cardiac nurse specialist/nutrition specialist nurse/anticoagulant nurse/palliative care team | Community | 75.00 | Hour | PSSRU (2015).164 10.4 | PSSRU (2015).164 10.4 nurse specialist. Community. £75 per hour. Patient-facing work. With qualification. Assume 25-minute community care appointment. As per 10.7. Nurse advance. 25 home visit. 15 minutes in surgery | 31.25 | – |
| Registered mental health nurse, CPN | Community | 75.00 | Hour | PSSRU (2015).164 10.4 | PSSRU (2015).164 10.2 mental health nurse. Community. £75 per hour. Patient-facing work. With qualification. Assume 1-hour session | 75.00 | – |
| Mental health team | Community | 42.00 | Hour | PSSRU (2015).164 12.1 (community mental health team) | PSSRU (2015).164 12.1 Mental health team. 1 hour of one employee. 1 hour of contact | 42.00 | Assumed the same level of contact as a psychiatric assessment of 1 hour |
| Best interests assessment | Community | 79.00 | Hour | PSSRU (2015).164 11.2 (social worker) | PSSRU (2015).164 11.2 Social worker. Community. £79 per hour. Patient-facing work. With qualification. Assume 1-hour session | 79.00 | Assumed the same level of contact as a psychiatric assessment of 1 hour |
| Community matron | Community | 91.00 | Hour | PSSRU (2015).164 10.7 (advanced nurse) | PSSRU (2015).164 p. 175: £81 (£91) per hour of client contact cost. Length of consultation: home – 25 minutes. Assume 25-minute consultation | 37.92 | – |
| Physiotherapist/SALT/dietitian | Community | 38.00 | Hour | PSSRU (2015).164 13.1/13.2/13.3/13.4, page 217/218 | £34 (£38) per hour | 38.00 | – |
| OT | Community | 44.00 | Hour | PSSRU (2015).164 11.5 p. 191 | £41 (£44) per hour* (community OT – local authority) | 44.00 | – |
| Audiology | Community | 38.76 | Session | National Careers Service NHS Agenda for Change Pay Scales,165 UK | £21,692–28,180 per annum. Mid-point of the band used in calculation of the unit cost using the PSSRU approach | 38.76 | – |
| Psychological therapy/psychologist | Community | 138.00 | Hour | PSSRU (2014).166 9.5, p. 183 | £61 per hour; £138 per hour of client contact (including A&E) | 138.00 | – |
| Social worker | Community | 79.00 | Hour | PSSRU (2015).164 p. 188 | £40 (£57) per hour; £55 (£79) per hour of client-related work | 79.00 | Assume 1-hour appointment |
| Chiropodist | Community | 32.00 | Hour | PSSRU (2014).166 p. 182 | £32 per hour | 32.00 | – |
| Other dementia | Community | 42.00 | Hour | PSSRU (2015).164 12.1 (community mental health team) | PSSRU (2015).164 12.1 mental health team. 1 hour of one employee. 1 hour of contact | 42.00 | Assumed the same level of contact as a psychiatric assessment of 1 hour |
| Other phlebotomist | Community | 20.00 | Hour | PSSRU (2015).164 p. 173 | £20.00 per hour | 5.00 | Assume 15 minutes |
| Other falls prevention | Community | 75.00 | Hour | PSSRU (2015).164 10.4 | This is a programme involving various interventions and specialists, for example risk assessments, physical activities physiotherapy, etc., and can be done by nurses, administrators, care home managers, falls physiotherapists | 75.00 | Assume community nurse performs this function; assume 1 hour of activity |
| Other long-term needs | Community | 75.00 | Hour | PSSRU (2015).164 10.4 | PSSRU (2015).164 10.4 nurse specialist. Community. £75 per hour. Patient-facing work. With qualification. Assume 25-minute community care appointment | 31.25 | – |
| Geriatrician | Community | 137.00 | Hour | PSSRU (2015).164 p. 235 | Consultant – medical: £105 (£137) per contract hour | 57.08 | Assume 25-minute consultation |
| Other specialist | Community | 75.00 | Hour | PSSRU (2015).164 10.4 | PSSRU (2015).164 10.4 Nurse specialist. Community. £75 per hour. Patient-facing work. With qualification. Assume 25-minute community care appointment | 31.25 | – |
| GP | GP | 45.00 | Consult | PSSRU (2015).164 p. 117 | Per-patient contact lasting 11.7 minutes [including carbon emissions (6 kgCO2e)]. £45.00 with qualification and £38.00 without qualification | 45.00 | – |
| Practice matron | GP | 65.83 | Hour | National Careers Service NHS Agenda for Change Pay Scales,165 UK | £41,281–49,208 per annum. Mid-point of the band used in calculation of the unit cost using the PSSRU approach | 12.84 | Assume 14-minute consultation |
| £36 (£43) per hour; £47 (£58) per hour of face-to-face contact | |||||||
| Practice nurse/nurse practitioner | GP | 58.00 | Hour | PSSRU (2015).164 p. 174 | – | 11.31 | Per consultation |
| Out-of-hours nurse | Out of hours | 75.00 | Hour | PSSRU (2015).164 10.4 | PSSRU (2015).164 10.4 nurse specialist. Community. £75 per hour. Patient-facing work. With qualification. Assume 25-minute community care appointment. As per 10.7. Nurse advance. 25 home visit. 15 minutes in surgery | 31.25 | Assume equivalent to a home visit of 25 minutes. No explicit costs for nurses’ out-of-hours work in the community |
| Out-of-hours GP | Out of hours | 68.30 | Consult | Report on out-of-hours GP services in England by National Audit Office 2013–14,167 pp. 15–16 | Average £68.30 per case – 2013–14. Owing to capitation could also assume OOH work would fall under on-call home appointments. As per PSSRU. Home visits last 11.4 minutes at a cost of £231 per hour. £43 for a home visit | 68.3 | – |
| Pharmacist | Primary care | 71.00 | Hour | PSSRU (2014).166 9.6 community pharmacist | £51 (£57) per hour; £128 (£142) per hour of direct clinical services; £64 (£71) per hour of patient-related activities | 17.75 | Assume 15 minutes |
| Optician | Primary care | 91.00 | Hour | PSSRU (2015)164 and General Optical Council168 | PSSRU p. 193: £81 (£91) per hour of client contact cost. Length of consultation: home, 25 minutes. Optician specific: industry standard is 20 minutes but usually more than that. A study identified mean duration as 25.8 minutes (ranging from 15 to 40 minutes) – p. 9 of the final report for the General Optical Council (2013)168 | 39.13 | Use 25.8 minutes. Assumed pay is similar to a specialist community worker (PSSRU 10.7) |
| Dentist | Primary care | 208.00 | Hour | PSSRU (2015).164 10.11. Dentist providing-performer | Performer only: £71 per hour; £88 per hour of patient contact. Providing performer: £147 per hour; £208 per hour of patient contact. This is a community-based setting | 104 | Assume 30-minute appointment |
| Hospital admissions/total nights in hospital | Secondary care admitted | 512.00 | Per night | NHS Reference Costs 2014–2015.169 NES- and NEL-weighted average bed-days. £512/night | Non-elective figure used. Long and short stay | 512 | Per night, not using trim points for longer stays |
| Ambulance use | Ambulance use | 231.00 | Per use | NHS Reference Costs 2013–2014 170 | See and treat and convey. ASS02 | 231 | – |
| A&E visits | A&E | 135.00 | Per attendance | NHS Reference Costs 2013–2014 170 | Weighted average. Service code 180 | 135 | – |
| Hospital day case | Secondary care non-admitted | 721.00 | Per day case | NHS Reference Costs 2014–2015.169 DCs. Weighted average of all day cases | – | 721 | – |
| Outpatient | Secondary care non-admitted | 134.00 | Per attendance | NHS Reference Costs 2014–2015.169 DCs. Weighted average of all outpatient procedures | – | 134 | – |
Appendix 9 Included studies (for phases 1 and 2)
| Study | Design | Topic | Approach | Theory area | Outcomes/issues relevant to review |
|---|---|---|---|---|---|
| Abbot et al.,79 2013 | Review | Nutrition | Systematic review and meta-analysis | Age-appropriate health care | Nutrition-related outcomes |
| Resident satisfaction | |||||
| Ahearn et al.,171 2010 | Secondary analysis | Survival and readmission rates of nursing home patients admitted acutely to general medicine | A comparison of all hospital admission rates between nursing home residents and older people living at home | System-based quality improvement | Hospitalisations |
| Alldred et al.,172 2011 | Observational | Study of administration errors in care homes (pharmacists) | Observed two drug rounds of random selection of residents from a purposive sample of nursing home and residential care errors were classified and analysed by formulation and MDS | System-based quality improvement | Medication administration errors |
| Amador et al.,26 2014 | Prospective | Intervention to promote co-design approaches to end-of-life care | Review of service receipt data | Relational approaches | Costs and resource use |
| Co-design | Hospitalisations | ||||
| Badger et al.,122 2012 | Survey and case studies | End-of-life care using the Gold Standard Framework in care homes | Postal and telephone surveys with care home staff | Access to age-appropriate care | Staff satisfaction |
| Relational working | |||||
| Badger et al.,173 2009 | Survey | End-of-life care using Gold Standard Framework in care homes | Pre–post survey with care home staff | Access to age-appropriate care | Hospitalisations |
| Staff satisfaction | |||||
| Bakerjian and Zisberg,142 2013 | Case study | Quality improvement and role of nurses in nursing homes improving prevalence of pressure sores | Description of process of structured intervention | System-based quality improvement | Nurse satisfaction |
| Relational working | |||||
| Co-design | |||||
| Access to age-appropriate care | |||||
| Bamford et al.,118 2012 | A process evaluation of the introduction of the Food Standards Authority guidance for care homes in five residential care homes | Use of nutritional guidance in care homes | Observation and interviews | System-based quality improvement |
Staff satisfaction Health/nutritional benefits to residents |
| Barber et al.,98 2009 | Prospective study of a random sample of residents in three areas | Prevalence and potential harm of prescribing, monitoring, dispensing and administration errors in UK care homes | Patient interviews, notes’ reviews, observation of practice and dispensed items | System-based quality improvement | Medication error |
| Patients, care home staff, doctors, pharmacists and expert judges | |||||
| Barnes et al.,174 2006 | Exploratory study | Medication | Semistructured interviews | System-based quality improvement | Medication administration |
| Barnett et al.,175 2011 | Cohort study stratified by residence in nursing home or in the community | Prescribing for older people in care homes and the community | Using Beers criteria to assess prescribing | System-based quality improvement | Potentially inappropriate medications |
| Boumans et al.,176 2008 | Pre-test/post-test control group design | Care home-led intervention to enable the elaboration and implementation of an integrated care model (note that implemented in care homes) | Characteristics of participants | Co-design | Staff and resident satisfaction |
| Integrated care measure | |||||
| British Geriatrics Society,83 2011 | Consultation document and evidence synthesis | Professional account of what needs to be in place to support care homes | Synthesis of expert opinion and summaries of recent research | Relational approaches | Hospitalisations |
| Staff satisfaction | |||||
| Resident satisfaction | |||||
| Age-appropriate care | Cost | ||||
| Brooker et al.,137 2007 | Evaluation | The Enriched Opportunities programme using dementia care mapping (facilitated) | Structured observation | System-based quality improvement | Resident and staff satisfaction |
| Education and training | |||||
| Charlesworth et al.,96 2014 | Discussion and synthesis | The role of incentive payments in health care | Commentary | System-based quality improvement | Resource use/costs |
| Age-appropriate health care | Health outcomes | ||||
| Chenoweth et al.,141 2009 | Cluster RCT | The effectiveness of person-centred care and dementia care mapping | Fifteen sites focused on residents with persistent need-driven behaviours that staff found difficult to manage | Age-appropriate health care | Resident benefit (satisfaction) |
| Relational approaches | |||||
| Education and training | |||||
| Clegg et al.,177 2006 | Service innovation | Role of community matrons using case finding | Survey of care home managers and community matrons | Age-appropriate care | Resident satisfaction |
| Staff satisfaction | |||||
| Hospitalisations | |||||
| Cooke et al.,106 2010 | Evaluation | Use of incentives combined with specialist support to improve quality of care | Description of schemes and uptake by nursing homes | System-based quality improvement | Staff and resident satisfaction |
| Co-design/relational approaches | Access to health care | ||||
| Hospitalisations | |||||
| Cooney et al.,178 2009 | Grounded theory | Quality of life | Interview study with 101 participants | Age-appropriate care | Resident satisfaction |
| Cox et al.,115 2008 | Cluster RCT | Specialist nurse training support to reduce fractures and improve treatment choices | A total of 230 care homes | Education and training | Hospitalisations (fractures) |
| Age-appropriate care | Medication management | ||||
| Davidson et al.,179 2006 | Feasibility study | GPs attended an education session on depression and trained in the use of the Cornell Scale for Depression in Dementia | Review of residents’ notes | Access to age-appropriate health care | Resident and staff satisfaction |
| Clinical benefits/medication used | |||||
| Staff knowledge | |||||
| De Visschere et al.,125 2011 | Review | Oral health care | Narrative account of principles and linked evidence | Age-appropriate care | Resident health (satisfaction) |
| Governance and audit | |||||
| Dening and Milne,180 2011 | Edited book | Chapters on care homes’ access to health care | Mix of researchers’ and practitioners’ accounts of providing health care to care homes | Age-appropriate care | Resident satisfaction |
| Education and training | Medication | ||||
| Hospitalisation | |||||
| Staff satisfaction | |||||
| Doran et al.,181 2011 | Longitudinal analysis | Use of financial incentives | Reviewed the uptake of incentive payment on clinical work across 148 GP practices | System-based quality improvement | Recorded clinical activities following payment of GP incentives |
| Access to age-appropriate care | |||||
| Evans,97 2011 | Audit | Admission during out of hours and use of data to give feedback to practitioners | Review of case notes | System-based quality improvement | Unplanned hospitalisations |
| Access to health care | Length of hospital stay | ||||
| Frequency of contact (resource use) | |||||
| Out of hours | |||||
| Forsetlund et al.,120 2011 | Systematic review of RCTs | Education to reduce potentially inappropriate prescribing in nursing homes | Narrative review of educational interventions/on-site education | Governance | Medication administration (potentially inappropriate medications) |
| Access to age-appropriate health care | |||||
| Co-design | |||||
| Froggatt et al.,182 2008 | Edited book of research and commentary on care homes | Chapters on the support of care home staff and residents | Written by members of the National Care Home Research and Development Forum | Education and training | Resident satisfaction |
| Relational approaches | Staff satisfaction | ||||
| Hospitalisations | |||||
| Medication | |||||
| Gadsby et al.,183 2012 | Documentary review | Care of people with diabetes mellitus living in care homes | Eleven care homes’ reviews of notes from residents with diabetes mellitus (n = 75) | System-based quality improvement | Cost |
| Medication management | |||||
| Gittell et al.,184 2000 | Interview study | Relational approaches to co-ordination on outcomes | Questionnaires on satisfaction and relational co-ordination | Relational approaches | Staff satisfaction |
| Goodman et al.,139 2013 | Quasi-experimental design | Quality improvement tool used by DN and care home staff for continence care based on group workshops to review and agree goals of care | Care notes review | Relational approaches | Staff satisfaction |
| Interviews | Co-design | Cost and resource use | |||
| Access to age-appropriate care | Resident health | ||||
| Hall et al.,86 2011 | Systematic review | Palliative care for nursing home residents | Included RCTs/CCTs/CBA/ITS | Education and training | Hospitalisations |
| Three US studies included | Age-appropriate health care | Resident satisfaction | |||
| Staff satisfaction | |||||
| Hancock et al.,114 2006; and Orrell et al.,185 2007 | Survey of residents | Health-care needs of residents | Resident assessment using structured tool | Age-appropriate health care | Level of observed health need |
| Cluster RCT | In care homes without on-site nursing | Medication | |||
| Liaison service to intervention care homes | |||||
| Hayward et al.,129 2006 | Cluster RCT | Prevention of death secondary to influenza: vaccination offered to staff in intervention homes | Documented uptake, residents’ morbidity and mortality | Access to age-appropriate care | Resident mortality |
| Co-design | Hospitalisations | ||||
| Relational working | Service use (cost) | ||||
| Hockley et al.,186 2010 | Evaluation | End-of-life care and implementation of two tools facilitated by specialist nurse and in-house training | Care notes review | Relational working | Hospitalisations |
| Staff audit | Education and training | Staff satisfaction | |||
| Seven care homes | |||||
| Kenkmann et al.,116 2010 | Evaluation | Intervention to improve dining atmosphere and food choice, with snacks and drinks | Measured the health and well-being and national status of residents in six care homes using routine care data | Access to age-appropriate care | Resource use (e.g. UTIs, number of falls) |
| Resident questionnaire | Co-design | Resident satisfaction | |||
| Livingston et al.,121 2013 | Quasi-experimental design | End-of-life care with training and support | Interviews with staff and family | Education and training | Staff satisfaction |
| Care notes review | Relational approaches | Hospitalisations | |||
| Livingston et al.,187 2012 | Qualitative study completed within a pre and post intervention | End-of-life care education intervention manual with facilitated support | Interviews | Relational approaches | Staff satisfaction |
| Loganathan et al.,105 2011 | Systematic review | Mixed approaches | Systematic review of 16 studies | Co-design/relational approaches | Medication administration (potentially inappropriate medication) |
| Randomised or non-randomised controlled studies | Staff education | System-based quality improvement | |||
| Pharmacist review | Education and training | ||||
| Team review | |||||
| Assistive technology | |||||
| Lyne et al.,111 2006 | Intervention study | Impact of specialist input and training on care home staff | Brief mental health training. Care home staff had four 3-hourly sessions in recognising depression, its impact, and how to respond | Co-design/relational working | Identification of depression |
| Access to health care | Staff satisfaction | ||||
| Mannion and Davies,92 2008 | Discussion document | Payment schemes to enhance quality of health care | Discussion of evidence and long-term advantages and risks | System-based quality improvement | Resource use and cost |
| MacEntee et al.,87 2012 | Scoping review | Oral health care in long-term care | Narrative review, including grey literature on funding | Access to age-appropriate care | Resident satisfaction (oral health) |
| McCormack et al.,188 2010 | Evaluation | Development of person-centred practice | Data collected at three time points using person-centred care index | Relational approaches | Staff satisfaction |
| Co-design | |||||
| McDermott et al.,189 2012 | Interview study | GP decision-making | Interviewed 21 GPs, medicolegal issues around admission to hospital identified as an issue | Education and training | Hospitalisations |
| System-based quality improvement | |||||
| McDonald et al.,93 2007 | Ethnography | Impact of financial incentives | Interview-driven study with observation in two GP practices | System-based quality improvement | Staff satisfaction |
| Thematic analysis | |||||
| Moylan et al.,190 2008 | Retrospective cohort study | Residents’ medical needs in long-term care/palliative care needs | Survival analysis | Age-appropriate care | Hospitalisations |
| Mozley et al.,126 2007 | Feasibility study | Occupational therapy programme to reduce depression | Pre- and post-intervention assessment | Access to age-appropriate care | Staff satisfaction |
| Co-design | Resident health | ||||
| Nyman and Victor,191 2011 | Systematic review (supplement) | Falls prevention: the role of older people’s participation and engagement | Forty-one RCTs reviewed | Age-appropriate care | Medication |
| Nursing homes’ adherence to guidance | Education and training | Resident satisfaction | |||
| Staff satisfaction | |||||
| Ong et al.,192 2011 | Retrospective case analysis | Reasons for admission to hospital and resident mortality | Interviews/observation in eight care homes and review of acute hospital admissions from care homes to hospital | Age-appropriate care | Hospitalisations |
| Parsons et al.,193 2011 | Discussion of evidence (based on earlier review) | Medication management | Suggests some prompts/questions to inform prescribing practice | Education and training | Medication |
| Costs | |||||
| Quinn,194 2011 | Prospective study | Admissions to care homes from care homes | Matched care home residents with community dwelling. More readmissions for care home residents | System-based quality improvement | Hospitalisations |
| Robbins et al.,5 2013 | Qualitative/grounded theory | Health-care provision to care homes | Interviews with care home staff/GPs/community nurses | Relational approaches | Resident satisfaction |
| Staff satisfaction | |||||
| Roland and Paddison,95 2013 | Discussion and review of evidence | Impact of multimorbidity on clinical uncertainty and decision-making | Commentary on clinician judgement responsibility, use of incentives | Education and training | Staff satisfaction |
| Age-appropriate care | Resident satisfaction | ||||
| System-based quality improvement | |||||
| Sackley et al.,119 2006 | Feasibility trial | Occupational therapy intervention | Intervention delivered by OT to individual residents | Age-appropriate care | Resident satisfaction (self-care/mobility) |
| Outcomes self-care/mobility/deterioration/death | Education and training | ||||
| Sackley et al.,136 2009 | Cluster RCT | Impact of therapy intervention | 3-month occupational therapy and physiotherapy programme aimed to enhance mobility, independence and ADL and staff training | Age-appropriate care | Resident satisfaction (self-care, mood, mobility, ADL performance) |
| Education and training | |||||
| Schneider et al.,127 2007 | Feasibility study | OT provision to care homes | Client Service Receipt Invenory tool | System-based | Cost/resource use |
| Interviews with care home managers, supervisors, key workers and residents (see also Mozley et al.126 paper) | Education and training | Hospitalisations | |||
| Staff satisfaction | |||||
| Seymour et al.,69 2011 | Qualitative case studies and postal survey | Palliative care | Critique of range of services that are offered to care homes |
Education and training Relational approaches |
Cost/access to specialist services |
| Staff satisfaction | |||||
| Shah et al.,99 2012 | A comparison of prescribing quality in care homes vs. community using the THIN database and comparison with US data | Prescribing practice in care homes | Using Beers criteria, compared prescribing between community-dwelling older people and care home residents | System-based quality improvement | Medication |
| Laxatives, antidepressants, antibiotics and cardiovascular medication | |||||
| Potentially inappropriate medication | |||||
| Shah et al.,100 2011 | Secondary analysis, THIN primary care database | Quality indicators for chronic disease management | Reviewed characteristics of community-dwelling residents and those in care homes aged 65 to 104 years with at least 90 days with GP | System-based quality improvement | Access to health care of care home residents |
| South et al.,195 2009 | Letter reporting survey findings | Service provision to care homes | Surveyed GPs and community matrons in Leeds | Age-appropriate care | Out-of-hours care |
| System-based quality improvement | Staff satisfaction | ||||
| Sprakes and Tyrer,124 2010 | Case study | Tissue viability using education of care home staff using competency-based framework | Retrospective notes review | Access to age-appropriate care | Use of services (resource use) |
| System-based quality improvement | Hospitalisations | ||||
| Co-design | Staff satisfaction | ||||
| Szczepura et al.,27 2008 | Prospective study | Local authority care homes, 131 residents in four care homes | Staff interviews | Age-appropriate care | Costs |
| Team supporting in situ virtual beds to reduce need for transfer | Structured prospective data collection on resource use | Education and training | Hospitalisations | ||
| Relational working | Length of stay | ||||
| Szczepura et al.,196 2011 | Prospective study in 13 care homes to measure the incidence of medication administration errors in nursing and residential homes | Introduction of barcode medication administration system | Data collection in real time for 345 residents: observation | System-based quality improvement | Incidence of medication administration errors |
| Incidence and type of potential error over 3 months. Staff were surveyed prior to barcode medication administration | |||||
| Zermansky et al.,197 2006 | RCT | Medication review | Clinical medication review by a pharmacist with patient and clinical records | Access to health care | Medication changes/cost |
| System-based quality improvement | Hospital admissions | ||||
| Co-design | Access to health care |
Focus of research-based care home papers reviewed
| Research focus of papers reviewed with one or more outcomes of interest [medication use, use of out-of-hours services, hospital admissions (including emergency department attendances), length of hospital stay and user satisfaction] | Number of papers |
|---|---|
| Medication management | 11 |
| End-of-life care | 8 |
| Resident health promotion (e.g. nutrition, influenza prevention, tissue viability, oral health, functional improvement, dementia care, falls prevention) | 12 |
| Management of depression and related interventions | 10 |
| Pay for performance/audit | 4 |
| Interventions to promote health service use and integration of health and social care services in care homes, including specialist roles, and to reduce use of secondary care | 11 |
| Total | 56 |
Appendix 10 Resident characteristics at baseline by site and care home
| Baseline characteristic | Site | p-value for difference between sites | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||||||||||||
| Care homes | 1 | 2 | 3 | 4 | All | 1 | 2 | 3 | 4 | All | 1 | 2 | 3 | 4 | All | |
| Number of residents | 11 | 27 | 28 | 24 | 90 | 3 | 27 | 26 | 36 | 92 | 19 | 10 | 15 | 13 | 57 | |
| Sociodemographic characteristics | ||||||||||||||||
| Age (years) | 0.36 | |||||||||||||||
| Mean (SD) | 89 (5.1) | 85 (5.7) | 85 (7.5) | 85 (5.1) | 86 (6.2) | 84 (8.5) | 89 (5.5) | 85 (8.0) | 87 (5.9) | 87 (6.7) | 87 (9.0) | 88 (5.6) | 86 (5.3) | 85 (9.1) | 87 (7.6) | |
| Median | 91 | 86 | 87 | 85 | 87 | 84 | 89 | 86 | 86 | 87 | 89 | 88 | 87 | 88 | 88 | |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Gender | 0.38 | |||||||||||||||
| Female (%) | 100 | 63 | 71 | 75 | 73 | 67 | 81 | 69 | 58 | 68 | 95 | 70 | 80 | 61 | 79 | |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Ethnicity | – | |||||||||||||||
| White (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |
| Missing/NA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Self-payer | ||||||||||||||||
| Pays something 1 (%) | 36 | 78 | 14 | 21 | 38 | 33 | 70 | 68 | 54 | 61 | 58 | 60 | 27 | 15 | 42 | < 0.01 |
| Pays nothing 0 (%) | 64 | 22 | 86 | 79 | 62 | 67 | 30 | 32 | 46 | 39 | 42 | 40 | 73 | 85 | 58 | |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 26 | 4 | 3 | 10 | 0 | 0 | 27 | 0 | 7 | |
| Bed type | ||||||||||||||||
| Nursing (%) | 0 | 0 | 43 | 0 | 13 | 0 | 0 | 0 | 100 | 39 | 0 | 0 | 0 | 54 | 12 | < 0.01 |
| Non-nursing (%) | 100 | 100 | 57 | 100 | 87 | 100 | 100 | 100 | 0 | 61 | 100 | 100 | 100 | 46 | 88 | |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Comorbidities (number) | ||||||||||||||||
| Mean (SD) | 1.91 (2.07) | 1.37 (1.27) | 1.39 (1.10) | 1.25 (0.94) | 1.41 (1.26) | 0.3 (0.58) | 1.56 (1.25) | 0.77 (0.99) | 1.17 (0.97) | 1.14 (1.09) | 1.11 (0.99) | 1.10 (0.99) | 1.13 (0.91) | 1.62 (1.19) | 1.23 (1.02) | 0.27 |
| Median (range) | 1.00 (0–5) | 1.00 (0–5) | 2.00 (0–4) | 1.50 (0–3) | 1.00 (0–5) | 0.00 (0–1) | 2.00 (0–6) | 1.00 (0–4) | 1.00 (0–4) | 1.00 (0–6) | 1.00 (0–3) | 1.00 (0–3) | 1.00 (0–3) | 2.00 (0–3) | 1.00 (0–3) | |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Medication count (number) | ||||||||||||||||
| Mean (SD) | 6.81 (3.92) | 9.63 (3.41) | 6.86 (2.92) | 8.04 (3.32) | 8.00 (3.45) | 6.67 (1.53) | 6.68 (2.50) | 9.88 (4.15) | 7.62 (4.00) | 8.10 (3.86) | 8.37 (2.45) | 8.22 (2.86) | 9.27 (3.37) | 9.08 (4.01) | 8.75 (3.12) | 0.43 |
| Median (range) | 7.00 (1–14) | 10.0 (3–17) | 6.00 (2–15) | 7.00 (3–16) | 7.00 (1–17) | 7.00 (5–8) | 6.00 (2–12) | 9.00 (5–21) | 7.50 (2–20) | 8.00 (2–21) | 8.00 (4–13) | 7.00 (4–12) | 9.00 (4–17) | 9.00 (4–16) | 8.50 (4–17) | |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 30 | 0 | 11 | 13 | 0 | 10 | 0 | 0 | 2 | |
| Cognitive impairment 0/1 | ||||||||||||||||
| Without cognitive impairment (%) | 64 | 33 | 25 | 33 | 34 | 33 | 33 | 4 | 17 | 18 | 63 | 80 | 67 | 54 | 65 | < 0.01 |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| interRAI indicators | ||||||||||||||||
| sADLH | < 0.01 | |||||||||||||||
| Mean (SD) | 2.55 (1.75) | 2.22 (1.89) | 3.71 (1.61) | 3.41 (1.59) | 3.03 (1.80) | 1.67 (2.89) | 2.81 (1.75) | 2.96 (2.20) | 4.60 (1.09) | 3.51 (1.92) | 1.79 (1.72) | 2.30 (1.89) | 1.80 (2.04) | 2.46 (2.18) | 2.04 (1.92) | |
| Missing/NA (%) | 0 | 0 | 0 | 8 | 2 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | |
| sADLSF | < 0.01 | |||||||||||||||
| Mean (SD) | 6.82 (5.15) | 4.70 (4.59) | 8.96 (4.79) | 6.45 (3.60) | 6.76 (4.74) | 5.00 (8.66) | 5.81 (4.74) | 7.50 (6.28) | 11.94 (4.03) | 8.63 (5.72) | 3.47 (4.13) | 4.80 (4.66) | 3.60 (4.76) | 5.23 (5.17) | 4.14 (4.58) | |
| Missing/NA (%) | 0 | 0 | 0 | 8 | 2 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | |
| sCPS | < 0.01 | |||||||||||||||
| Mean (SD) | 2.27 (2.05) | 2.11 (1.87) | 2.86 (2.14) | 2.14 (1.28) | 2.37 (2.00) | 3.00 (3.00) | 2.22 (1.44) | 3.23 (1.86) | 3.78 (1.74) | 3.15 (1.83) | 0.89 (1.56) | 0.30 (0.48) | 0.57 (0.85) | 1.46 (1.76) | 0.84 (1.36) | |
| Missing/NA (%) | 0 | 0 | 0 | 8 | 2 | 0 | 15 | 0 | 11 | 9 | 0 | 0 | 7 | 0 | 2 | |
| Communication | < 0.01 | |||||||||||||||
| Mean (SD) | 0.91 (1.22) | 1.81 (2.02) | 3.11 (2.88) | 2.54 (2.32) | 2.30 (2.41) | 2.33 (4.04) | 2.20 (2.71) | 3.23 (3.04) | 5.15 (3.12) | 3.65 (3.22) | 0.74 (1.94) | 0.50 (1.27) | 0.40 (0.63) | 2.15 (2.70) | 0.93 (1.90) | |
| Missing/NA (%) | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 6 | 4 | 0 | 0 | 0 | 0 | 0 | |
| Pressure sores | 0.05 | |||||||||||||||
| Mean (SD) | 1.09 (1.04) | 1.41 (1.42) | 2.37 (1.57) | 2.32 (1.55) | 1.90 (1.53) | 1.67 (2.08) | 2.27 (1.71) | 1.75 (1.73) | 2.72 (1.28) | 2.25 (1.59) | 1.00 (1.41) | 1.90 (1.60) | 1.27 (1.39) | 2.55 (2.07) | 1.56 (1.66) | |
| Missing/NA (%) | 0 | 0 | 0 | 8 | 2 | 0 | 44 | 8 | 19 | 23 | 5 | 0 | 0 | 15 | 5 | |
| Pain 0/1 | 0.06 | |||||||||||||||
| Without pain (%) | 100 | 74 | 54 | 50 | 65 | 33 | 71 | 77 | 84 | 77 | 94 | 80 | 80 | 64 | 81 | |
| Missing/NA (%) | 0 | 0 | 0 | 8 | 2 | 0 | 22 | 0 | 11 | 11 | 5 | 0 | 0 | 0 | 5 | |
| Depression score | – | |||||||||||||||
| Mean (SD) | 0.60 (1.90) | 1.12 (1.67) | 0.93 (1.27) | 0.94 (1.55) | 0.93 (1.50) | 0.00 (–) | – (–) | 2.00 (–) | – | 1.00 (1.59) | 0.00 (0.00) | 0.00 (0.00) | – (–) | 0.00 (0.00) | 0.00 (0.00) | |
| Missing/NA (%) | 9.0 | 41.0 | 50.0 | 8 | 37.8 | 66.7 | 100 | 96.2 | 100 | 97.8 | 68.4 | 70.0 | 100 | 84.6 | 80.7 | |
Appendix 11 Univariate analyses undertaken during step 1 of Poisson regression
| Variable | Coefficient | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| sPURS | 0.08 | 0.03 | 2.49 | < 0.05 | 0.02 to 0.15 |
| sPAIN_1 | 0.40 | 0.12 | 3.32 | < 0.01 | 0.17 to 0.64 |
| Comorbidities | 0.15 | 0.04 | 3.49 | < 0.01 | 0.07 to 0.24 |
| Medication count | 0.07 | 0.01 | 4.76 | < 0.01 | 0.04 to 0.10 |
| Variable | Coefficient | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| sCPS | –0.13 | 0.06 | –2.10 | < 0.05 | –0.26 to –0.01 |
| Cognitive impairment | –0.77 | 0.23 | –3.42 | < 0.01 | –1.21 to –0.33 |
| Variable | Coefficient | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| sADLSF | 0.04 | 0.02 | 1.66 | < 0.10 | –0.01 to 0.08 |
| sPAIN_1 | 0.92 | 0.42 | 2.17 | < 0.05 | 0.09 to 1.74 |
| sPURS | 0.16 | 0.10 | 1.66 | < 0.10 | –0.03 to 0.35 |
| Comorbidities | 0.21 | 0.12 | 1.71 | < 0.10 | –0.03 to 0.46 |
| Variable | Coefficient | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| sADLSF | –0.06 | 0.03 | –2.02 | < 0.05 | –0.12 to –0.00 |
| sCPS | –0.42 | 0.12 | –3.50 | < 0.01 | –0.66 to –0.19 |
| sCOMM | –0.34 | 0.09 | –3.71 | < 0.01 | –0.52 to –0.16 |
| Cognitive impairment | –0.83 | 0.33 | –2.54 | < 0.05 | –1.48 to –0.19 |
| Comorbidities | 0.32 | 0.11 | 2.80 | < 0.01 | 0.10 to 0.54 |
| Medication count | 0.11 | 0.04 | 2.51 | < 0.05 | 0.02 to 0.20 |
| Variable | Coefficient | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| sADLSF | –0.04 | 0.03 | –1.70 | < 0.10 | –0.09 to 0.01 |
| sCPS | –0.16 | 0.07 | –2.13 | < 0.05 | –0.30 to –0.01 |
| sCOMM | –0.15 | 0.08 | –1.86 | < 0.10 | –0.31 to 0.01 |
| Variable | Coefficient | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| Medication count | 0.09 | 0.04 | 2.01 | < 0.05 | 0.00 to 0.17 |
| Variable | Coefficient | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| sCPS | –0.28 | 0.11 | –2.54 | < 0.05 | –0.49 to –0.06 |
| sCOMM | –0.21 | 0.08 | –2.68 | < 0.01 | –0.37 to –0.06 |
| Comorbidities | 0.39 | 0.15 | 2.59 | < 0.05 | 0.09 to 0.68 |
| Medication count | 0.11 | 0.06 | 1.74 | < 0.10 | –0.01 to 0.24 |
We also analysed total costs, entering each of the interRAI and derived variables separately. We noticed that total costs were skewed, so we applied a log-transformation and produced a normal distribution, which we analysed with a Gaussian distribution.
| Variable | Exp(B) | SE | z | p-value | 95% CI |
|---|---|---|---|---|---|
| sCPS | 0.92 | 0.04 | –1.77 | < 0.10 | 0.84 to 1.01 |
| sCOMM | 0.93 | 0.03 | –2.02 | < 0.05 | 0.87 to 1.00 |
| Comorbidities | 1.19 | 0.09 | 2.21 | < 0.05 | 1.02 to 1.39 |
| sPAIN_1 | 1.66 | 0.33 | 2.57 | < 0.05 | 1.13 to 2.43 |
| Medication count | 1.08 | 0.03 | 2.65 | < 0.01 | 1.02 to 1.14 |
Appendix 12 Multiple hospitalisations
Tables 44–46 give details of hospitalisations across the sites where residents had multiple admissions within the data collection time period.
| Resident | Total admissions | Admission 1: reason | Duration (nights) | Admission 2: reason | Duration (nights) | Admission 3: reason | Duration (nights) | Dementia | Other comorbidities | Loss to follow-up | Hospital or care home |
|---|---|---|---|---|---|---|---|---|---|---|---|
| S1CH2R09 | 2 | Breathing problems and infection | 26 | Breathing problems and infection (died) | 4 | No | IHD, angina, MI, prolapsed bowel | Yes (died) | Hospital | ||
| S1CH3NR07 | 2 | Unclear had conjunctivitis | 18 | No information but (died) | 2 | Yes | Glaucoma, tinnitus | Yes (died) | Hospital | ||
| S1CH2R21 | 3 | Blood in catheter | 1 | UTI | 1 | Severe UTI | 8 | Yes | Arthritis, UTI, Parkinson’s disease | Yes | Moved to nursing home |
| S1CH2R22 | 3 | SOB | 7 | Chest pain | 1 | Not recorded | 1 | Yes | Chest infection, asthma | No | N/A |
| S1CH3RR18 | 2 | Pyrexia | 1 | Vomiting | 1 | No | Depression, OA, hypertension | No | N/A |
| Resident | Total number of admissions | Admission 1: reason | Duration (nights) | Admission 2: reason | Duration (nights) | Dementia | Other comorbidities | Loss to follow-up | Hospital or care home |
|---|---|---|---|---|---|---|---|---|---|
| S2CH1R02 | 2 | No information | 1 | Fractured femur | 15 | Yes | None recorded | No | N/A |
| S2CH3R01 | 2 | Urinary retention | 3 | Effects of procedure | 1 | Yes | Depression, fibromyalgia, hypertension, BPH | No | N/A |
| Resident | Total number of admissions | Admission 1: reason | Duration (nights) | Admission 2: reason | Duration (nights) | Dementia | Other comorbidities | Loss to follow-up | Hospital or care home |
|---|---|---|---|---|---|---|---|---|---|
| S3CH2R01 | 2 | Fall | 1 | Mental health assessment | 47 | Yes (not formally) | Stroke, hemiplegia | Yes | Care home |
| S3CH1R06 | 2 | Refusing medication; staff told to call 999 | 26 | C. difficile; GP told staff to call 111, resident admitted | 14 | No | T2DM, stroke, hemiplegia, renal disease | Yes | Care home |
| S3CH1R18 | 2 | Possible infection | 14 | C. difficile | No information | Yes | Arthritis | Yes | Care home |
| S3CH1R09 | 2 | Abdominal pain | 7 | Rectal bleed (died) | 4 | Yes | T1DM, heart failure | Yes | Hospital |
| S3CH1R16 | 2 | Not known | 6 | Fall and fracture | 2 | Yes (not formally) | T2DM, hypertension | No | N/A |
Appendix 13 Single hospitalisations
Tables 47–49 give details of hospitalisations across the sites where residents had single admissions within the data collection time period.
| Resident | Total number of admissions | Admission 1: reason | Duration (nights) | Dementia | Other comorbidities | Loss to follow-up | Hospital or care home |
|---|---|---|---|---|---|---|---|
| S1CH1R02 | 1 | Fall and fracture | 28 | No | IHD, anaemia, arthritis | Yes | Moved to residential care home |
| Discharge to another care home that had a lift | |||||||
| S1CH2R05 | 1 | 999 paramedic admission for tachycardia and pyrexia | 7 | No | Arthritis, hypothyroidism, hiatus hernia, heart problem | No | N/A |
| S1CH3NR05 | 1 | Fall, fractured elbow or shoulder | 3 | Yes | Osteoporosis | No | N/A |
| S1CH1R05 | 1 | Fainted at outpatients appointment for eyes and was admitted | 2 | Yes | TIA, depression, angina, arthritis, leg ulcers, cataracts, T1DM, COPD, asthma | No | N/A |
| S1CH2R13 | 1 | Fall, no details | 2 | Yes | Diabetes mellitus, generalised cerebral atrophy | No | N/A |
| S1CH3RR04 | 1 | Catheter pulled out, UTI | 2 | Yes | Chest infection, UTI, glaucoma, BPH | No | N/A |
| S1CH3NR02 | 1 | No information | 1 | Yes | Stroke, cancer, DVT | No | N/A |
| S1CH3RR08 | 1 | For observation? TIA | 1 | Yes | Hypertension, diabetes mellitus, depression | No | N/A |
| S1CH4R06 | 1 | Fall and fracture | 1 | No | Emphysema, chest infection | Yes (died) | Hospital |
| Resident | Total number of admissions | Admission 1: reason | Duration (nights) | Dementia | Other comorbidities | Loss to follow-up | Hospital or care home |
|---|---|---|---|---|---|---|---|
| S2CH2R27 | 1 | Fractured pelvis | 25 | Yes | Hypercholesterolaemia, fracture | No | N/A |
| S2CH4R24 | 1 | Pneumonia | 8 | No | Hypertension, hip replacement, cervical myelopathy | No | N/A |
| S2CH2R05 | 1 | SOB, paramedic called | 7 | Yes | Anaemia, hypertension, cancer | No | N/A |
| S2CH2R02 | 1 | Pyrexia, shaking | 6 | Yes | Cancer, macular degeneration, hypertension | No | N/A |
| S2CH2R03 | 1 | Fall, cut head | 1 | Yes | Arthritis | No | N/A |
| S2CH2R11 | 1 | Chest pain | 1 | No | Blind, atrial fibrillation, aortic aneurysm | No | N/A |
| S2CH2R14 | 1 | Fall | 1 | Yes | Asthma, depression, hypertension | Yes (died) | Care home |
| S2CH3R02 | 1 | Infected toe for intravenous antibiotics? Infected bone | 1 | Yes | Arthritis | Yes (died) | Care home |
| S2CH3R08 | 1 | Fractured pelvis following fall | 1 | Yes | Hypertension, anaemia, cellulitis | No | N/A |
| Resident | Total number of admissions | Admission 1: reason | Duration (nights) | Dementia | Other comorbidities | Loss to follow-up | Hospital or care home |
|---|---|---|---|---|---|---|---|
| S3CH3R06 | 1 | Chest infection, SOB | 15 | No | Hyperthyroidism, renal failure, heart failure, glaucoma | Yes (died) | Care home |
| S3CH1R19 | 1 | Hypotension | 9 | No | Hypotension | No | N/A |
| S3CH3R09 | 1 | Urinary retention | 7 | Yes | Hemiplegia, stroke | No | N/A |
| S3CH3R10 | 1 | Fall, hip fracture | 6 | Yes | Heart failure | No | N/A |
| S3CH1R04 | 1 | SOB paramedic called ambulance admitted (died) | 6 | No | Arthritis, spondylitis | Yes (died) | Hospital |
| S3CH3R13 | 1 | No information | 3 | Yes | Stroke, asthma, anxiety, arthritis | No | N/A |
| S3CH2R07 | 1 | Respiratory arrest paramedics admitted with pneumonia (died) | 2 | Yes | T1DM | Yes (died) | Hospital |
| S3CH4R04 | 1 | Syncope, hypotension | 2 | No | Pneumonia, pleural effusion, arthritis | No | N/A |
| S3CH1R05 | 1 | Paramedic called following a fall, admitted | 1 | No | Schizophrenia | No | N/A |
Appendix 14 OPTIMAL film script: key messages
Main message: to achieve optimal health care for care home residents NHS services need to be care home-focused and based on an organisational structure that holds residents within the system of care, where the GP plays a known role and ongoing dementia expertise is integral to regular service provision (www.youtube.com/watch?v=aGY3-0QCMf8). Aspects of service provision that were key: teams/practitioners with responsibility for care homes where the role was endorsed and valued, care homes being seen as part of a network of care with linked systems of referral and time and space for NHS and care home staff to learn how to work together and align priorities and working practices.
| Key message | Submessage (question) | Data and key evidence for script |
|---|---|---|
| There are multiple ways that the NHS works with care homes | Unlikely that there is one right way of working with care homes but there are common features or aspects of how care home staff and NHS staff work together | Chapters 3 and 4 |
| Important that care home staff review how they work with NHS staff | ||
| Current situation ad hoc | ||
| Team working and joint visits from HCPs can increase residents’ access to the specialist care that they need within the care home setting | When HCPs with responsibilities for working with care homes see their work as valued and linked with other services, their priorities align with the priorities of the care home | Interviewer:Which of them work well and what is it exactly about them you feel that works well?S1CH2 care home staff focus group:I think they all work really well and I think depending on what services they are, I think they all do their job and help us out and everything else and they visit when required so I can’t complain that way and obviously every one of them services all link together and provide the overall care for the residents here and not one of them don’t do their job properly or help you out |
| Team working may circumvent the need for secondary care visits for residents | Example of two physiotherapists from different teams working together to assess a resident in the care home and prevent an outpatient visit | |
| The ability to co-ordinate residents’ care within the caseload of interconnected practitioners may militate against the need to involve other services in residents’ care such as out-of-hours services | Interviewer:OK. How do your visits work when you are at this care home, so this particular care home?S1CH1HP02, dementia team specialist nurse:Right, at this care home I’ll arrange an appointment as usual and I’ll either speak to the manager or a senior carer and we will discuss whatever plan we have put in place, if it’s being effective, I’ll go and talk to the patient. And then of course if the plan’s been effective and it’s useful and helping them we’ll continue with that and if not we’ll discuss how we can change and modify it. Then we’ll come back, talk to other members of the team for advice for us or we can refer to, because we’re a multidisciplinary team we’ve got physiotherapists, occupational therapists, support workers and so we can refer on if there’s any physiotherapy needs, occupational therapy needs, whatever, get support from support workers and we can do that so, and we’ve got consultant time as well, so that’s broadly how the visits work | |
| Dedicated care home services or the identification of a specified care home component within individual HCP roles may facilitate good rapport with care home staff and regular support with residents’ health care | Funding care home teams and GPs to work with care homes may facilitate co-operation, highlighting of best practice in care homes and finding shared health-care solutions | S1CH2HP03, occupational therapy rehabilitation team:. . . So you know, kind of educating staff on how to, you know, apply the sling on the stand aid more effectively and more efficiently. One of the carers in particular was excellent, because the person that I went, the resident had quite advanced dementia, and the carer was particularly good at communicating and putting the resident at ease. In that, in that case I did, I wrote an e-mail to the manager of care home 2 and complimented the particular carer, because she was very goodS1CH4HP02, specialist nurse care homes team:. . . It worked and it worked really well, the feedback was positive and then we rolled it out . . . But because we, because we go into the homes, then it’s not just a trainer delivering a training session, they could come back and say, ‘You know what you said on the course or could you explain more. I didn’t understand about this and can we go through it again?’ So, there’s open communication with them. And they, at that one (care home), they all, I’m always greeted with a smile, I’m always greeted with, ‘Oh really nice to see you again, where’ve you been?’ But it is a case of they feel confident that we have got a two-way communication and they feel that they can open up to me and I can open up to them as well and just to see that it is an open communication and that’s what works well there and . . . And the staff are consistent, which also works, where if you’ve got a place where they haven’t got consistent staff, then you’re sort of going over the same things all the time . . . |
| However, where multiple NHS services are visiting care homes and different practitioners’ roles were not known and understood by care home staff, this could be perceived as surveillance or covert quality monitoring | Different bodies. Different, you know, sometimes we can have three different professionals come in to see one person, you know and it’s a bit too much. I think care home life is like traffic, road traffic, everybody just coming and going, and demanding, and if you do not do this then the next thing you know you’re in safeguarding . . .S1CH1 care home manager | |
| Care home staff need explicit referral guidelines for NHS services together with opportunities for dialogue where they are uncertain | Established relationships between care home staff and HCPs facilitate direct referrals and can help to reinforce best practice | Interviewer:So how do they [care home staff] decide whether to contact you directly or the contact point or the GP?S3CH3HCP01, care home nurse specialist:Well, [laughs] . . . it’s regards preference on who’s on duty to be fair, I mean we, they have got information regarding the community matrons and almost like a spider diagram which would say that community matrons support a residential care homes and give us an idea of the sort of things that we would see for all the patients. Some carers [care home staff] would always call a doctor, where some more senior carer would call us direct, I think if I’ve got a relationship with the home, I’ve been going for a long time, they know me very well, then they’re more likely to call me direct and we’d go from there |
| Care home providers’ referral guidance needs to fit with NHS protocols | ||
| Care home-based training needs to include all care home staff working with residents, not just the carers | New care home staff in particular need support from NHS staff when working with residents | Interviewer:Yes, so they can sort of learn from each other’s experienceS3CH2HCP01, dietitian:Yeah . . . if there’s a care home that we know that the chef is really involved, we get them to come in and talk to the catering staff in other care homes . . . So some of our training is aimed at the care staff but some of it is aimed at the catering staff so that we can try to get things going that way . . .S2CH4HP01, palliative nurse specialist:Yeah, so I would say I always have contact with the care home staff. Many patients do not have full mental capacity so care home staff help with assessing of situation, feedback and education is given to the care home staff on drug management, symptom control, psychological and spiritual support. If a new member of staff is there, I try to encourage them to work alongside me so I’m teaching them how to manage without me . . . the ability of the staff to communicate well with families of patients and MDT |
| Working relationships between care home staff and HCPs need time to develop and establish | As relationships develop with HCPs, care home staff performance may also improve | District nurses, when I first came here in 2012 there was a fractured relationship . . . and the relationship then with the district nurses improved, because they could see the performance improving and the environment had improved and then they were coming on board with things to the point where we’ve got an excellent relationship with themS1CH3, care home manager |
| GPs need to play a central role in residents’ health care, but should work with care home schedules and staff working practices as far as possible to optimise working relationships | GP visits on request only were associated with low levels of care home staff satisfaction, poor working relationships and a lower quality of service for residents | Doctors just come strolling in like they’re god’s gift sometimes still and you know, they want to see the nurse and they want to know this and it doesn’t matter if it’s lunchtime, tablet time, you have to accommodate them and it is just sometimes you want to say hang on a minute . . .S3CH4, care home manager. . . Because sometimes they [GPs visiting on a resident-by-resident basis] want to assess them [residents] so quickly . . .S1CH4FG |
| Regular GP clinics were associated with higher levels of care home staff satisfaction with health care and fewer medication-related problems and more frequent medication reviews. When there was an opportunity to discuss care for all residents and not just individual residents’ health care | Monthly GP clinic is good because they are taking an interest in their well-being and their patients and they have check-ups every month, you might get somebody go for ages and be fine on the inside but when they come round and do checks [they find a health-care need] . . .S3CH4FG | |
| Dementia expertise needs to be integral to regular service provision, not part of a separate service | Care home staff need allocated time and resources to support residents with dementia | So the strategy is really sometimes it’s already in the care plan but what we find within the care home sometimes it’s written in the care plan but it’s not actually being implemented . . . so it’s really about occupying the patient, providing that facility, using distraction techniques, using other methods of music and getting to know the patient. So it’s really, it’s quite a challenge for the care homes because sometimes the staffing level is quite low so trying to provide some form of like complete care for, one-to-one type of care for a patient with dementia who’s quite distressed I think that’s where the challenging bits come and that’s where a lot of the time you find they will either use medication to just sort of help the situation at that moment rather than just looking at the whole, somebody just spending a bit of time, you know. Sometimes it takes more than just 10 minutes; really you’re talking about an hour or so with the patient just to sort of calm situationsS3CH1HCP03, dementia nurse specialist, p. 2 |
| HCPs need to liaise more closely with care home staff around dementia support with the resident rather than just focusing on assessment tools | Interviewer:You try a lot of things but they just don’t always work do they? And then Dementia Outreach come back and they try a different strategy but it doesn’t always workS1 FG p. 139:You know like you (specialist nurse) can’t just come in and like we say she’s got aggression when we’re changing her, all personal care, if she’s (specialist nurse) coming in on a morning and that, well really it’s absolutely fine, you know, that’s a good day. But then they need to do a few days in seeing this aggression that these people are giving . . .Interviewer:And was it helpful when they [the intensive mental health team] came out?S2CH4 FG p. 8:Not really because they’re all about, oh, looking on paperwork, what’s this resident been like . . . rather than go and look at the residents health, yeah, it’s only happened once, this has only happened once, yeah, but once is enough, yeah | |
| GPs and other NHS staff may benefit from more training and support in managing dementia-related behaviours to support residents and care home staff | Interviewer:You have described the challenges of working with care homes. Are there any issues in terms of resident health-care needs that you would say, is complex, and stretches you as a GP?S2GP8:I think physical violence is the biggest issue that I have to deal with and how to best manage thatWith people living with dementia?S2GP8:Yes, it can be very difficult to manage and to know what is best for the person and still think about the needs of the other residents. Symptoms of dementia that are not resolved. That has been an increasing area of my workS2GP7:I agree, that and safeguarding issues and deprivation of liberties, you can get drawn into that and that is quite difficult, who to work with and how to resolve it | |
| Care home staff play a vital role in managing and monitoring residents’ medication but may need further training and support in this area | What does ‘good’ look like for residents? | Example of a relative talking about care home staff effectively managing a complicated medication routine for the resident |
| When does it not work well for residents and relatives? | In general, residents and their relatives were satisfied with the health care they received, but medication was identified as a concern | |
| Example of residents waiting for medication | ||
| Example of the drawbacks of not involving family members in decisions to stop medication |
Format:
-
cartoon with actor voice-overs, building a script based upon the findings and the actual words that interviewees have said; being careful to be accurate to the research findings, but engaging through some level of humour
-
either a single cartoon or preferably a series of three or four ‘50-second films’? For example:
-
working with health professionals can be challenging (finish with reflective question of how can we make it better?)
-
sometimes we misunderstand each other (finish with reflective question of how can we make it better?)
-
when it works well, positive working relationships are the key to success (finish with reflective question of how can we make it better?)
-
there are some practical things that you can do to make a start (finish with reflective question of how can we make it better?).
-
Time frame and actions:
-
project manager and cartoon film-maker have been identified, to connect with a small group of local care home managers to touch base on concept and then to meet to be part of a script-reading exercise
-
research team to populate the table with data on key messages and quotations for the meeting with the project manager and the cartoon film-maker on 19 July
-
script to be drafted by mid-August, followed by script reading and then finalised for production (date to be confirmed)
-
cartoon to be produced by October 2016.
Glossary
Setting-specific definitions
The following are the definitions of a number of terms that are often used interchangeably. In this report care home is used as the overarching term for all residential care for older people with on-site care services. The key difference between settings is whether or not on-site nursing provision is available.
- Care home
- A residential setting where a number of older people live, and have access to on-site care services, for example meals and personal care (such as help with washing and eating). It may also provide nursing care. UK specific: a home registered as a care home will provide either personal care only – help with washing, dressing and giving medication – and/or care with on-site nursing. Colloquially, this is often expressed as a residential care home (i.e. no on-site nursing) or a nursing home. Some care homes are officially recognised as specialist providers, for example in dementia or palliative care.
- Long-term care facility
- Synonymous with a care home or residential aged care facilities, a residential setting that provides on-site care of services designed to meet a person’s health or personal care needs during a short or long period of time.
- Nursing home
- A home with registered nurses who can provide care for more complex health needs. UK specific: homes registered for nursing care may accept people who just have personal care needs but who may need nursing care in the future.
- Residential aged care facility
- A term used in Australia to describe a facility for older people that offers personal and/or nursing care, as well as accommodation. Synonymous with a care home in a UK context.
Other definitions
- Clinical Commissioning Groups
- Replaced primary care trusts in April 2013 as the commissioners of most services funded by the NHS in England.
- Horizontal integration
- Integrated care is about bringing together input, delivery, management and organisation of services related to diagnosis, treatment, care, rehabilitation and health promotion in order to improve services in relation to access, quality, user satisfaction and efficiency. Horizontal integration is about linking similar services that work around and for the patient. Vertical integration is about linking different levels of care like primary, secondary and tertiary care.
- Personalised care plans
- Implemented by general practitioner practices for the 2% most vulnerable patients on their list as part of the unplanned admissions Directed Enhanced Service contract worth £2.87 per patient. The personalised care plan is part of a proactive case-management approach for all patients on the register. It includes details of their medical history, current medication, preferred place of care and an agreed plan for escalating care, including crisis management, and can be shared with the multidisciplinary team and other relevant providers with the patient’s consent.
- Relational working
- Those activities and processes that emphasise shared decision-making, planning and learning, and continuity of contact between staff from different sectors. Thus relational working is achieved through a process of mutual recognition of different perspectives. This becomes a means to address the competing priorities, inequity of power and limited resources present when the NHS as a service and individual practitioners work with care homes. It recognises that care homes are distinctive cultural spaces that inform how health care is understood and prioritised. Froggatt and colleagues (Froggatt K, Hockley J, Parker D, Brazil K. A system lifeworld perspective on dying in long term care settings for older people: contested states in contested places. Health Place 2011;17:263–8) characterise relational working as an ambiguous position between medical and domestic domains of care.
Setting-specific definitions
The following are the definitions of a number of terms that are often used interchangeably. In this report care home is used as the overarching term for all residential care for older people with on-site care services. The key difference between settings is whether or not on-site nursing provision is available.
- Care home
- A residential setting where a number of older people live, and have access to on-site care services, for example meals and personal care (such as help with washing and eating). It may also provide nursing care. UK specific: a home registered as a care home will provide either personal care only – help with washing, dressing and giving medication – and/or care with on-site nursing. Colloquially, this is often expressed as a residential care home (i.e. no on-site nursing) or a nursing home. Some care homes are officially recognised as specialist providers, for example in dementia or palliative care.
- Long-term care facility
- Synonymous with a care home or residential aged care facilities, a residential setting that provides on-site care of services designed to meet a person’s health or personal care needs during a short or long period of time.
- Nursing home
- A home with registered nurses who can provide care for more complex health needs. UK specific: homes registered for nursing care may accept people who just have personal care needs but who may need nursing care in the future.
- Residential aged care facility
- A term used in Australia to describe a facility for older people that offers personal and/or nursing care, as well as accommodation. Synonymous with a care home in a UK context.
Other definitions
- Clinical Commissioning Groups
- Replaced primary care trusts in April 2013 as the commissioners of most services funded by the NHS in England.
- Horizontal integration
- Integrated care is about bringing together input, delivery, management and organisation of services related to diagnosis, treatment, care, rehabilitation and health promotion in order to improve services in relation to access, quality, user satisfaction and efficiency. Horizontal integration is about linking similar services that work around and for the patient. Vertical integration is about linking different levels of care like primary, secondary and tertiary care.
- Personalised care plans
- Implemented by general practitioner practices for the 2% most vulnerable patients on their list as part of the unplanned admissions Directed Enhanced Service contract worth £2.87 per patient. The personalised care plan is part of a proactive case-management approach for all patients on the register. It includes details of their medical history, current medication, preferred place of care and an agreed plan for escalating care, including crisis management, and can be shared with the multidisciplinary team and other relevant providers with the patient’s consent.
- Relational working
- Those activities and processes that emphasise shared decision-making, planning and learning, and continuity of contact between staff from different sectors. Thus relational working is achieved through a process of mutual recognition of different perspectives. This becomes a means to address the competing priorities, inequity of power and limited resources present when the NHS as a service and individual practitioners work with care homes. It recognises that care homes are distinctive cultural spaces that inform how health care is understood and prioritised. Froggatt and colleagues (Froggatt K, Hockley J, Parker D, Brazil K. A system lifeworld perspective on dying in long term care settings for older people: contested states in contested places. Health Place 2011;17:263–8) characterise relational working as an ambiguous position between medical and domestic domains of care.
List of abbreviations
- A&E
- accident and emergency
- ACB
- anticholinergic burden
- ADL
- activities of daily living
- ANOVA
- analysis of variance
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CMO
- context–mechanism–outcome
- CPN
- community psychiatric nurse
- CQC
- Care Quality Commission
- ENRICH
- Enabling Research in Care Homes
- GMS
- General Medical Services
- GP
- general practitioner
- HCP
- health-care professional
- interRAI
- international Resident Assessment Instrument
- LTCF
- long-term care facility
- MAR
- Medication Administration Record
- MDT
- multidisciplinary team
- PIR
- public involvement in research
- QOF
- Quality and Outcomes Framework
- sADLH
- interRAI – activities of daily living hierarchy scale
- sADLSF
- interRAI – short activities of daily living hierarchy scale
- sCOMM
- interRAI – communication scale
- sCPS
- interRAI – cognitive performance scale
- SD
- standard deviation
- sPAIN_1
- interRAI – clinical syndrome for pain
- sPURS
- interRAI – pressure ulcer risk scale
- SSC
- Study Steering Committee
