Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5001/21. The contractual start date was in May 2013. The final report began editorial review in November 2016 and was accepted for publication in May 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Forsyth et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2017 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
Definition of older prisoners
The definition of an older person in prison is socially constructed. Wahidin et al. 1 noted that minimum cut-off ages as low as 45 years have been used in previous studies of older prisoners to obtain reasonable participant numbers. Both in the USA and the UK, the most frequently used minimum cut-off ages for defining ‘older’ prisoners are 50 or 55 years. 2,3 It is argued that 50 years old is an appropriate age at which to commence preventative health-care measures to reduce the financial burden and improve the health of older prisoners. 4 Furthermore, it has been suggested that prisoners aged ≥ 50 years have the physical appearance and health problems equivalent to those of a person aged 60 years living in the community. 4,5 The usefulness of providing minimum cut-off ages for defining older prisoners has been questioned. Yorston and Taylor6 emphasised the importance of considering levels of service need rather than simply referring to chronological age cut-off points when identifying older prisoners.
Studies exploring older prisoners’ health and social care needs have provided some supporting evidence to suggest that 50 years should be used as a minimum cut-off age to define older prisoners. A cross-sectional survey of older prisoners in the north-west of England found that prisoners aged 50–59 years have similar health and social care needs to those aged ≥ 60 years living in the community, thus suggesting it to be an appropriate cut-off point. 7 Fifty years is, therefore, the minimum cut-off age throughout the current study, unless otherwise indicated.
The increasing number of older prisoners
There has been a recent, considerable increase in the number of older prisoners across many developed countries, including the USA,8 Japan,9 Canada,10 Australia,11 France,12 England and Wales. 13 It is estimated that, by 2030, one-third of all prisoners in the USA will be ≥ 55 years old, equating to > 400,000 prisoners, a 4400% increase from 1980. 8
In England and Wales, people aged ≥ 50 years currently account for 15% of the prison population, with 12,577 in this age group in prison. 14 Those aged ≥ 60 years are the fastest growing age group in the prison estate and, strikingly, the number of prisoners aged ≥ 70 years old is projected to increase by 35% by 2020. 15
The rise in the number of older prisoners is a consequence of a number of factors. The increase is, in part, the result of an ageing population and increases in the number of older people committing crimes. 16 Importantly, it is also a consequence of changes to sentencing practices, with courts sentencing higher numbers of older people to increased periods of imprisonment. 17 The introduction of indeterminate sentences has also contributed to the increase. 18 Furthermore, enhanced forensic evidence and enhanced reporting resulted in greater numbers being convicted for crimes committed in previous decades. 19 In England and Wales, 42% of men in prison aged > 50 years have been convicted of sex offences, the most common offence for this group. 13
The policy context
There is no national strategy for the care of older prisoners, despite repeated recommendations. 19–22 However, prisoners should have access to the same quality and range of health services as they would receive in the community. 22,23 The formal process of passing on the responsibility of employing health-care staff and delivering health care from the prison service to the NHS was completed in 2006 and, since then, all NHS standards and policies apply in prison.
The most relevant NHS policy to older prisoners is the National Service Framework (NSF) for Older People. 24 This aimed to ensure ‘fair, high quality, integrated health- and social-care services for older people’ and outlined eight key standards for the NHS and partners in local authority and community sectors to meet. 24 The NSF incorporated a short paragraph concerning older adults’ care in prison, emphasising the need for collaborative working to support older offenders. Strikingly, Her Majesty’s Chief Inspector of Prisons (HMCIP)18 review of older prisoner care found that that many of the NSF standards were not being met in prison.
A wide range of definitions of social care are employed in the community. 25 Research conducted with staff working in prisons has suggested that there is a lack of agreement concerning this definition. 26 Some staff adopted broad definitions of social care that included assistance with finances, housing and employment, whereas others used narrower definitions, referring only to personal care concerns such as washing and dressing. Without clear agreement of what social care is, it is difficult to determine who is responsible for its provision to older prisoners. This lack of clarity has previously been acknowledged. 27,28 Where social care is provided, it has largely, and inappropriately, been seen as the sole responsibility of prison health-care services, as opposed to a wider multidisciplinary obligation. 18
In July 2012, the government published the white paper, ‘Caring for our future: reforming care and support’, which detailed the reform of adult social care in England and Wales. The white paper described a lack of clarity concerning responsibility for assessing and providing social care support to prisoners. 29 The resultant Care Act,30 introduced in 2014, clearly stipulated that the local authority where the prisoner resides was responsible for providing social care. The extent to which local authorities have become involved in the care of older prisoners and the form this has taken since the introduction of the 2014 Care Act is unknown. Cornish et al. 31 have recommended that a review of the implementation of the 2014 Care Act across the English and Welsh prison estate should be undertaken.
Health and social care needs
Physical health needs
Older prisoners have multifaceted health problems. 7,20,27,32,33 However, to date, only a small number of studies in the UK have identified older prisoners’ physical health status. Hayes et al. 7 found that 93% of their sample of older prisoners aged ≥ 50 years had some form of physical illness. In addition, Fazel et al. 34 identified that 85% of prisoners aged ≥ 60 years had one or more major illness reported in their medical notes.
Four studies have examined the physical health status of older prisoners in England and Wales since the 1980s. 7,27,32,35 These studies are summarised in Table 1. The prevalence rate for each illness varies between studies, reflecting the adoption of different assessment measures, and data collection and sampling methods. Kingston et al. 32 report considerably lower prevalence rates than the other studies, which is possibly a result of the low response rates (51%), indicating that those experiencing poorer health may have been less likely to participate. Excluding the Kingston et al. 32 study, the findings presented in Table 1 indicate that older prisoners have higher rates of genitourinary, haematological, audio/sensory, cardiovascular, respiratory and endocrine illnesses than reported figures from both their younger counterparts in prison38 and those aged ≥ 65 years living in the community. 39
| First author and year of publication | Measures | Age (years) | Sample size | Illnesses reported (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Central nervous system | Genitourinary | Haematological | Auditory/sensory | Cardiovascular | Musculoskeletal | Respiratory | Endocrine | Cancer | ||||
| Senior et al., 201327 | Note review | ≥ 60 | 100 | n/a | n/a | n/a | n/a | 38 | n/a | 33 | 19 | 3 |
| Hayes et al., 20127 | Burvill grid36 | ≥ 50 | 262 | 17 | 47 | 3 | 49 | 49 | 57 | 78 | 21 | n/a |
| aKingston et al., 201132 | Note review, SF-1237 | ≥ 50 | 237 | n/a | 6 (4) | 2 (1) | 9 (4) | 22 (18) | 23 (24) | 9 (8) | 5 (5) | 1 (2) |
| Fazel et al., 200134 | Burvill grid36 | ≥ 60 | 203 | n/a | 13 | 3 | 6 | 35 | 24 | 15 | 10 | n/a |
| Bridgewood et al., 199538 | Self-report | 18–49 | 992 | n/a | 1 | 0 | 4 | 3 | 16 | 15 | 2 | n/a |
| Prior, 199639 | Self-report | 65–74 | 16,443 | n/a | n/a | 1 | n/a | 29 | 25 | 12 | 9 | n/a |
There has been very little research regarding the extent to which older prisoners’ physical health needs are met. Fazel et al. 40 explored whether or not older prisoners received medication for their diagnosed health conditions. They found that 85% of prisoners with cardiovascular disease, 78% with endocrine disorders and 65% with musculoskeletal conditions recorded in their medical notes were prescribed medication for these issues. Hayes et al. 20 aimed to identify the met and unmet needs of older adults in prison through a cross-sectional survey. Physical health needs were the second most common type of perceived unmet need (n = 52, 33%). Senior et al. 27 also used the CANFOR to explore older prisoners’ needs on entry into prison and found that 22% (n = 22) reported unmet needs concerning their physical health. This percentage is lower than in the Hayes et al. 20 study and may reflect older prisoners prioritising other issues, rather than their physical health, immediately on entry into prison.
Mental health needs
There is a limited number of studies concerning the mental health of older prisoners. Reported overall rates of mental disorder among older prisoners vary from 50% to 61%. 8,32,35 The most commonly reported diagnosis within the three studies was depressive disorder (12–34%). Murdoch et al. 41 explored depression in elderly life-sentenced prisoners using the Geriatric Depression Scale (GDS) and reported that 48% scored within the mild depression range and 3% scored within the severe depression range. Senior et al. 27 also used the GDS to identify depression among older prisoners newly received into custody, reporting lower rates of mild depression (31%) but higher rates of severe depression (23%), suggesting that those newly received into prison are more likely to be suffering from severe depression than those at other points in their sentence. This supports previous research indicating that the initial entry period is particularly risky in terms of prisoners’ mental health. 42 Two studies27,40 have explored older prisoners’ treatment for depression. Fazel et al. 40 found that only 14% of the sample from their cross-sectional survey who had achieved caseness for depression were being treated with antidepressants. Similarly, the Senior et al. 27 study explored treatment for depression during the 4 weeks after prison entry, reporting that 17% of older prisoners who showed symptoms of depression were prescribed antidepressants. However, it is not known whether these symptoms of depression were a temporary result of prison entry or a longer-term illness. Furthermore, the extent to which other forms of treatment for depression were provided to participants was not explored. No research has explored other treatment options for older prisoners suffering from depression.
Research suggests that rates of personality disorder among older prisoners range from 20% to 30%. 7,35 Fazel et al. 40 also reported that 8% of their sample had an antisocial personality disorder, which is lower than reported among younger prisoners. 43 No research has been conducted regarding the specific treatment needs of older prisoners with personality disorders.
Dementia has been identified as a growing issue for prisons;43 however, very limited research has been conducted. It is argued that the highly structured routine of prison can mask symptoms of dementia. 43 However, it is estimated that between 1% and 2% of older prisoners experience dementia,32,35 similar to rates of dementia found in older people living in the community but much lower than rates among older people at different stages of the criminal justice system. 35 This suggests that either older people with dementia are successfully diverted from prison and/or individuals with dementia are less likely or able to commit crimes of a severe nature for which they become imprisoned. 35
One study has identified the extent to which older prisoners with psychiatric illness received appropriate medication. Fazel et al. 40 reported that 18% (n = 11) of older prisoners in their sample with any recorded psychiatric illness were receiving targeted medication. This was considerably lower than the number of older prisoners with any physical health problem receiving targeted medication, as previously discussed. Yorston44 has argued that there is a need for communication between old-age psychiatrists and forensic psychiatrists at local and national levels to prevent the needs of older mentally ill prisoners from being overlooked. Current mental health services for older prisoners are limited and inequitable to services provided in the community, with very few specialist old-age forensic psychiatry services. 44
Few studies have explored substance misuse among older prisoners in England and Wales. Fazel et al. 35 reported that 5% of their sample misused or were dependent on substances at the time of interview. However, the authors acknowledged that the study failed to examine lifetime substance misuse. Hayes et al. 7 found that 33% of their sample had lifetime substance misuse disorder. A greater number of older prisoners reported lifetime alcohol misuse (30%) than drug misuse (9%). This differs greatly from the younger prison population. Singleton et al. 45 found that 43% of the general prison population aged 16–64 years were drug dependent. In the USA, Arndt et al. 46 examined the prevalence of substance abuse among 10,652 offenders using data from interviews conducted on prison entry, and found that 71% of prisoners aged ≥ 55 years reported a substance misuse problem. They were more likely to abuse only alcohol than their younger counterparts, who were more likely to misuse alcohol and drugs. Many of the older prisoners had abused substances for > 40 years, but had never received treatment. There is a paucity of research evaluating older prisoners’ substance misuse treatment in England and Wales.
Social care needs
Older prisoners often have complex social care needs as a result of their multifaceted health needs and the ageing process. 18,19 Few studies have examined the social care needs of older prisoners, but evidence suggests that older prisoners experience a lack of appropriate support in this area. 19,28,47 Hayes et al. 20 conducted the most recent study regarding older prisoners’ social care needs, reporting that accommodation was the most commonly unmet need. Further evidence for a lack of appropriate and timely support with housing was provided by Senior et al. ,27 whose findings revealed that older prisoners were frequently unaware of where they were going to be living in the community in the months, weeks and even days prior to release. Without confirmation of accommodation on release, older prisoners felt unable to plan for other aspects of their resettlement into the community, such as health care or financial issues.
Older prisoners are required to negotiate narrow doorways and to walk long distances, often without handrails, while in prison. 47 Hayes et al. 7 found that over one-third of older prisoners in their sample had some level of functional need in activities of daily living (ADL), with 11% having personal care needs, in over half of whom they were unmet. A US study48 explored prison activities of daily living (PADL) in 120 female prisoners aged > 55 years. These included dropping to the floor for alarms, getting to the canteen for meals, hearing orders from staff and climbing on and off the top bunk. Over two-thirds (69%) reported impairment in PADL, whereas only 16% reported difficulties in standard ADL tasks. Consequently, the authors emphasised the importance of considering PADL when assessing older prisoners’ needs, rather than just the standard ADL. 48 Further research is required to establish the extent to which older prisoners demonstrate difficulties with PADL within the context of English and Welsh prisons.
Strikingly, there have been examples of other prisoners inappropriately providing personal care (such as washing, dressing and assistance with incontinence issues) to older prisoners as part of ‘buddy’ schemes. 19 This may be inappropriate because ‘buddies’ may not be adequately trained and may exploit others. However, some prisoners may have no choice but to receive this type of support, even though it is not in line with the principle of equivalence. However, there is no evidence to determine how widespread this practice is, nor what type or extent of training and support ‘buddies’ receive to undertake the role or to what extent they are vetted or supervised. There are occasions when buddy schemes may be appropriate, for example when the buddies of prisoners with mobility difficulties push wheelchairs, carry food trays and clean cells. However, such schemes are relatively rare and no published research has evaluated their effectiveness or appropriateness. 18,49
Limited research has considered older prisoners’ social support networks. In the Hayes et al. 27 study, nearly half of prisoners were imprisoned far from their home, making contact with social support networks difficult. A total of 40% received no visits at all. Furthermore, 20% rarely left their cell during opportunities for socialisation with other prisoners. Many older prisoners have elderly parents, siblings and friends who have difficulties travelling to visit them, and they may have been be disowned by their families, particularly if they have committed sexual offences. 18 The impact of this lack of social support networks for older prisoners has not been fully explored.
The care pathway
Assessment of need and care planning
Professionals conducting health and social care assessments with older people in the community face a number of challenges, namely the under-reporting of need, poor-quality tools, variations in assessments across professions and geographical areas and a lack of agreement among professionals working in different sectors. 50–53 The NSF for older people introduced processes to improve assessment procedures, most notably the introduction of the Single Assessment Process (SAP). 24 The aims of the SAP were to standardise assessments across different organisations and geographical areas, raise the standard of assessment, assist with information sharing, prevent duplication and ensure a comprehensive assessment of need. 24 Studies have suggested some improved identification of older adults’ health and social care needs; however, the extent to which these improvements are a result of the SAP is unknown. 50
Prisons are required to conduct health assessments for all new prisoners on reception into custody. 54 The current standardised reception health assessment tool, introduced in 2004, is designed to identify immediate health concerns, with a recommended second health screen conducted at a later date to allow prisoners to discuss their health needs in more depth. However, research suggests that there are low completion rates for the second, non-mandatory health screen. 55 A further criticism is that it is too often viewed as a one-off process, as opposed to a continuous pathway to care. 56 The tool does not investigate social care need.
The Department of Health57 guidance entitled A Pathway to Care for Older Prisoners: A Toolkit for Good Practice recommends the use of health and social care assessments specifically designed for older prisoners, with reassessments and revised care planning taking place at least every 6 months. There is no standardised older prisoner health and social care assessment in England and Wales; however, some establishments have developed their own. Cooney and Braggins58 reported that 40% of establishments in their survey had no specific assessments in place for older prisoners. Senior et al. 27 found that 81% had not established specialised assessments for older people on prison entry. The specialised assessments introduced in some establishments have not been evaluated, and anecdotal evidence suggests that they are not always delivered systematically to all prisoners. Consequently, in the majority of prisons, the identification of health-care need for older prisoners is largely dependent on information obtained by the generic screening instrument. 59 It is known that, if health issues are not identified at reception, they are unlikely to be detected throughout a person’s time in prison. 60
Health and social care services
There are limited examples of older prisoners being provided with additional specialised services; however, in general, they receive the same treatment as younger prisoners. The implications of being treated the same as younger prisoners have been discussed. 61 Crawley61 conducted interviews with those aged ≥ 65 years in two prisons where there were separate wings for older prisoners, and in two with no such separation. Sustained observations of prisoners’ daily life were also conducted. Crawley61 found that prison officers had to find a balance between consistency and flexibility when supporting older prisoners. She highlighted that ‘treating everyone the same does not always equate to equality’. Crawley61 used the term ‘institutionalised thoughtlessness’ to describe the ways in which ‘prison regimes simply roll on, with little reference to the needs and sensibilities of the old’. Examples included not being provided with sufficient time to move from one location to another or to complete specific activities, being provided with hard chairs and top bunks to sleep on, insufficient warm clothing in cold weather, queuing for long periods of time for medication, unavailability of grab rails in the showers and being unable to go outside for exercise because exercise areas lack seating or a readily accessible toilet. These examples suggest that older prisoners are being ‘doubly punished’ because, in addition to their loss of freedom, they experience inadequate care that is not equivalent to that in the community. 58
Release and resettlement
The post-release period poses particular risks for prisoners in terms of their physical and mental health. 62 Research has identified complex relationships between reoffending and nine key factors, namely education, employment, drug and alcohol misuse, attitudes and self-control, institutionalisation and life skills, housing, financial support and debt, family networks, and mental and physical health. 62 However, 42% of released prisoners are of no fixed abode, 50% have no general practitioner (GP), 50% reoffend within 2 years, debt problems for one-third worsened whilst in custody and 60% are unemployed. 63
Recent research conducted by Wilson64 has explored how prisoners with serious mental health illness seek help after leaving prison. In this study, 63% identified housing and 35% identified financial assistance as one of their two most important service needs; only 12% selected treatment services, thus emphasising the importance of meeting basic needs as well as providing treatment services on release from prison. Released prisoners are also at a greater risk of suicide than the general population, particularly in the first few weeks after their release. 65 Furthermore, discharged prisoners have an increased risk of drug overdose. 66 Consequently, it is essential that contact with care services is maintained on release from prison. 67,68 The National Association for the Care and Resettlement of Offenders recommends that the resettlement needs of every offender should be considered from the start of their prison sentence,69 although little is known regarding the extent to which this is realised because there is a paucity of research concerning discharge planning for prisoners. The UK government has argued that effective release planning is a key priority to reduce barriers to resettlement. 70 However, it has been argued that the current discharge planning process and a lack of effective multiagency working are current barriers to effective resettlement in the UK71 and the USA. 68
The HMCIP review of older prisoner care identified grave concerns that needs were not planned or provided for after release,18 based on identifying only four prisons in England and Wales that provided specific resettlement support for older prisoners. It repeated its previous recommendation72 that the specific resettlement needs of older prisoners should be accurately assessed and provided for on release. The Department of Health’s toolkit for good practice provided recommendations around preparing older prisoners for release and supporting their transition into the community. 73 The Department of Health stipulated that release planning should involve the conduction of a pre-release health and welfare assessment, a face-to-face assessment by a social worker, collaboration with external organisations and the organisation of a care package. This guidance also emphasised the importance of monitoring the progress of released prisoners to ensure that they have access to the appropriate services.
A limited number of studies have explored older prisoners’ concerns and issues about release prior to discharge. 74,75 Findings suggest that older prisoners struggle disproportionately with resettlement as a result of reduced support networks and their increased likelihood of health and mobility problems. In addition, older prisoners experience intense anxieties about their release, and inadequately understand the resettlement process. Key concerns include where they are going to live and how they will get there; their physical safety (for convicted sex offenders in particular); loss of personal possessions and support networks; and access to health-care support for chronic illness. Concerns prior to discharge are so intense that many feel that it would be better to stay in prison. In spite of these increased needs, older prisoners’ resettlement needs are often ignored; it has been suggested that this is because they are generally considered less of a risk75 and are less assertive than younger peers. 76
One study explored whether or not older prisoners’ fears about release became reality. Forsyth et al. 77 conducted interviews with older prisoners prior to and after release, and reported that older prisoners perceived release planning to be effectively non-existent. Those due to reside in Probation Approved Premises were very anxious about the prospect and were concerned about sharing accommodation with younger people who may abuse substances and be physically violent towards them. However, interviews with older prisoners after release revealed that the immediate health and social care needs of those housed in Probation Approved Premises were generally fairly well met. Many with complex social care needs were inappropriately housed; for example, some wheelchair users were housed in accommodation accessed by steps, meaning that they could not enter or exit the premises independently. Similarly, a lack of suitably adapted bathroom facilities compromised safety and independence in this aspect of self-care. It is possible that the Offender Rehabilitation Bill (2013–14)78 will improve this situation. The Bill proposed the introduction of 70 resettlement prisons, with offenders being sent to a prison close to their release destination at least 3 months prior to discharge. The extent to which this will improve release planning for all prisoners, including those in older age, is as yet unknown.
Rationale for the current study
In summary, there has been an increase in the number of older prisoners across developed countries, including England and Wales. Older prisoners have more health needs than younger prisoners and those of the same age living in the community. They also have a multitude of social care needs that are difficult to meet within the constraints of prison. There is no national strategy for older prisoners’ care, in spite of repeated calls for one to be developed. Consequently, the care of older prisoners is currently generally ad hoc and largely unco-ordinated. The Older prisoner Health and Social Care Assessment and Plan (OHSCAP) was developed through action research by prison staff, health-care staff and older prisoners themselves at one prison in England. It is a structured approach for identifying and managing the health and social care needs of older prisoners and consists of an assessment, care plan and review of these needs. During a pilot study (Service Delivery Organisation programme reference number 08/1809/23027) in the same prison, it was found to be both feasible and acceptable to patients, as well as being effective at reducing older prisoners’ unmet health and social care needs.
This study aimed to build on previous work by evaluating the effectiveness and acceptability of the OHSCAP in a larger-scale, randomised controlled trial (RCT).
The objectives of the study were to:
-
train prison staff to deliver the OHSCAP
-
implement the OHSCAP in a number of prisons in England
-
evaluate the efficacy of the OHSCAP in improving:
-
the meeting of older male prisoners’ health and social care needs (primary outcome)
-
health-related quality of life (HRQoL)
-
depressive symptoms
-
functional health and well-being and ADL.
-
-
assess the quality of care plans produced through the OHSCAP
-
explore the experiences of older prisoners receiving the OHSCAP, and staff involved in conducting the OHSCAP
-
evaluate the cost-effectiveness of the OHSCAP compared with treatment as usual (TAU).
Research questions
-
Does the use of the OHSCAP compared with TAU improve:
-
proportion of met health and social care needs
-
HRQoL
-
depressive symptoms
-
functional health and well-being and ADL
-
quality of health and social care planning
-
cost-effectiveness?
-
-
What are the facilitators of, and barriers to, the implementation and operation of the OHSCAP?
Hypotheses
Primary hypothesis
The OHSCAP will significantly increase the proportion of met health and social care needs 3 months after prison entry, compared with TAU controls.
Secondary hypothesis
Compared with TAU controls, the OHSCAP will significantly improve the following at 3 months after prison entry:
-
HRQoL
-
depression
-
functional health and well-being
-
quality of health and social care planning.
Chapter 2 Randomised controlled trial methodology
Study design
The study was designed to evaluate the OHSCAP. It consisted of a parallel two-group RCT with 1 : 1 individual participant allocation to either the OHSCAP intervention plus TAU (intervention group) or TAU alone (control group). The main trial was conducted alongside (1) an audit of the fidelity, and quality, of implementation of the OHSCAP (see Chapters 4 and 5), (2) economic evaluation examining the cost-effectiveness of providing the OHSCAP (see Chapters 8 and 9) and (3) a nested qualitative study to explore the views and experiences of participants and professionals involved in the study (see Chapters 6 and 7). The protocol containing trial design and methods protocol is included as Appendix 1.
Ethics approval
Ethics approval for the study was granted by the Research Ethics Committee for Wales in May 2013 (reference number 13/WA/0108). National Offender Management Service (NOMS) research approval was provided in July 2013 (reference number 2013-115). The trial was registered with the International Standard RCT Number ISRCTN11841493. Additionally, all required site-specific permissions and research governance approvals (research and development) were obtained from the relevant NHS trusts.
Changes to protocol
-
Increase in number of sites.
We closely monitored data collection to ensure that we would meet our targets. It became apparent that we needed to add further sites in order to meet the follow-up target of 392 participants. Additional sites were selected for pragmatic reasons while still ensuring that we had included a range of prison types. Consequently, the number of sites increased from 4 to 10. We are confident that the increase in number of sites had no impact on the overall study design.
-
Increase in baseline target.
As we progressed into the trial, it became apparent that our attrition rate was much higher than the expected 10%, at almost 20%. This was mainly because of retention issues in the local (remand) prison sites, where it proved to be harder than expected to identify individuals who would remain in custody for the 3-month follow-up period. As a result of this, we extended our recruitment period and increased our baseline recruitment target to a maximum of 502 participants at baseline, from the original target of 462.
-
Changes to assessment tools.
A number of changes were made to the assessment tools before data collection commenced. The SF-3679 was replaced by the Bristol Activities of Daily Living Scale (BADLS)80 because it was considered more appropriate for use in prison. The Client Service Receipt Inventory81 was replaced by the Secure Facilities Service Us Schedule (SF-SUS)82 for the same reason. We also added the following tools in order to describe the sample: the Operational Criteria Checklist for Psychotic and Affective Illness (OPCRIT),83 PriSnQuest84 and the Burvill grid. 36
Sites
The study aimed to recruit male prisoners aged ≥ 50 years. Originally, this recruitment was to be from four prison establishments in the north of England, but, as a result of recruitment difficulties, this was subsequently expanded to include a further six prison establishments. A range of prisons including open, training and high-security prisons were involved.
Participants
Inclusion criteria
To be eligible for inclusion, participants had to:
-
be aged ≥ 50 years
-
have a known release date (convicted) or likely release date (unconvicted) of at least 3 months after their prison entry date.
Exclusion criteria
The following individuals were excluded:
-
those who did not have the capacity to consent
-
those considered by prison or health-care staff not safe to interview alone as a result of their current risk assessment
-
those previously included in the study.
Procedure
Recruitment procedure
An administrator within each of the prisons identified potential participants who fulfilled the inclusion criteria. They did this by running a search on all prisoners newly received from court into their establishment on the prison computer system [Computer – National Offender Management Information System (C-NOMIS)]. An administrator was selected for this role because they did not need to access health information, but they did need to access sentence information. It would not have been appropriate for the members of staff delivering the OHSCAP to conduct the initial approach because this would have affected anonymity, and may have then had an impact on the support the TAU group received. The administrators were also required to inform potential participants of the proposed study. If the service user expressed an interest in learning more, the administrator requested their permission to pass their name on to a member of the research team. A researcher then arranged a time to talk to the potential participant to discuss the study further and ask them to consider participating in it.
Release dates for unconvicted prisoners were predicted using an adapted version of an algorithm developed for a previous study. 85 The algorithm and accompanying offence list is appended (see Appendix 2).
Consent
Informed consent was sought from all potential participants prior to taking part. Researchers explained the project, provided an information sheet and described the relevant ethical rights as part of the consent process. Sensitivity was shown to the high levels of learning difficulties and vulnerability in this population, with researchers reading and explaining the information sheet, when required, and remaining aware of the potential for any coercion.
All participants were informed that participation was voluntary and that they were free to withdraw at any point, with their decision to participate or otherwise having no bearing on the future care they received or their other legal rights.
Confidentiality
Participants were all informed of the arrangements to ensure confidentiality, including the limits of this, and data protection.
During the consent process, the limits of confidentiality were clearly outlined with participants. Participants were informed that all information disclosed during the research process was confidential unless (1) the information imparted revealed real risks of harm (e.g. self-harm, suicide, violence towards others) that needed to be acted on to safeguard the participant or others; and/or (2) the participant revealed criminal activity previously unknown to a relevant authority. This covered the potential for reporting previously undisclosed offending outside custody, or criminal offences committed while in prison including, but not limited to, illicit drug importation/use, importation or possession of other prohibited items (e.g. mobile phones), assaults on other prisoners and/or other criminal activity (e.g. continuing involvement with crime outside prison). How a required breach of confidentially would be dealt with depended on the circumstances. Risks of self-harm or suicide would involve the researcher either starting self-harm management processes [Assessment, Care in Custody and Teamwork (ACCT)] if the risk had not been previously identified, or liaising with staff directly to contribute to a person’s ongoing care under ACCT if the risk was already known. Reporting of previous/current criminal activity would be reported to the prison’s security department using routine procedures.
No circumstances arose that required a breach of confidentiality.
Each participant was allocated a unique participant identification number. This identifier was used to link participants’ study data with identifiable data, which were stored securely and separately.
Individuals lacking capacity
Researchers received training in assessing capacity using the two-stage process outlined in the Mental Capacity Act (2005). 86 If there was any indication that an individual lacked the capacity to consent, that individual was excluded from participation.
Randomisation
An individual-level randomised design was selected for two key reasons. First, it was anticipated that there would be minimal contamination because older prisoners are not usually systematically identified on entry into prison and, therefore, the older prisoner lead does not usually come into contact with the older prisoners unless specific issues arise. Second, a clustered or stepped-wedge design was considered; however, such designs would not have been feasible to implement because many more institutions would be required to participate, thus having an impact on cost and time.
Randomisation was undertaken by the Manchester Academic Health Science Centre Clinical Trials Unit (MAHSC-CTU). Participants were randomised to receive the OHSCAP or TAU. The MAHSC-CTU provided a telephone-based central randomisation service for the trial. The allocation method was minimisation with a random element using imbalance scores over the margins of two factors: institution and baseline number of unmet needs (0, 1, 2, 3, ≥ 4). With minimisation, the group allocated to the next participant is dependent on the characteristics of existing participants. 87 The aim is that the allocation of each participant should minimise the imbalance across groups. In order to achieve this, provisional imbalance scores were calculated (one for each trial arm assuming allocation of the case to that arm). The imbalance score was Sum (|n1 – n2|), where the sum is taken over the observed levels of each factor of the ‘case at hand’ and n1 and n2 are the accrued cases to date in the two trial arms for the given levels, including the provisional allocation. If the imbalance scores were tied, we considered imbalance in the totals in each arm without reference to the factors. Allocation was made to the arm that would yield lower imbalance with probability 0.75 or with probability 0.5 if scores were tied. This random allocation sequence was generated by David Ryder [statistician, Clinical Trials Unit (CTU)].
The procedures for randomisation were as follows. Once a participant had consented to participate and had been confirmed as eligible for the trial, and the baseline assessments were completed, contact was made with the MAHSC-CTU to be allocated a participant identification number and allocated to either the intervention or the TAU group. The following information was provided: a trial password (allocated by the project manager), the centre name, the participant’s initials and date of birth, and the caller’s name. A participant identification number was allocated immediately, followed by, via e-mail, the result of allocation to intervention or TAU.
Blinding
When possible, RCTs should be double blinded, that is, the participants and researchers should not be aware of which group they have been allocated to. 88 Participants unavoidably became aware of which group they had been allocated to when they received the intervention. Furthermore, the researchers did know which group some of the participants belonged to because 14 of the participants in the intervention group were invited to take part in qualitative semistructured interviews. Within the current study, however, quantitative data analysis was conducted blind. Identifying variables were removed by a statistician at the CTU before the data were provided to the researcher conducting the analysis.
Intervention
The OHSCAP was developed and implemented as part of a previous study funded by the National Institute for Health Research (NIHR) Service Delivery and Organisation programme. An action learning group (including prisoners, NHS staff and prison staff) at one prison in England developed the OHSCAP. 27
The OHSCAP is a structured approach for better identifying and managing the health and social care needs of older prisoners. The previous study showed that the OHSCAP was acceptable to prisoners and staff, could be integrated into current prison/health-care processes, assisted effective multiagency working, provided an opportunity for prisoners to raise concerns that would have otherwise gone unreported and could be successfully conducted by a prison officer.
The OHSCAP is paper based and information collected is uploaded onto existing prison, health and offender management computer programs. A copy of the OHSCAP is appended (within the OHSCAP manual; see Appendix 3). The first page of the OHSCAP includes instructions for completion and background information. A table for collecting basic demographic information including name, age, date of birth and NOMS number is also included. The OHSCAP consists of an assessment, a care plan and reviews of these.
The assessment includes a series of open questions to facilitate discussion, and is divided into three key parts, namely social, well-being and discharge planning. The social assessment includes open questions around relationships, activities and mobility. The well-being assessment includes exploratory questions around emotional well-being, physical well-being, and medications and treatment. A section for other concerns is also incorporated. The final section of the assessment includes open questions around discharge planning. A series of ‘trigger’ open questions are included for each of these sections. A place for the signatures of those conducting the assessment and the prisoner is also incorporated.
The care plan consists of a matrix with five columns. These are (1) issue raised from assessment, (2) aim of the proposed action, (3) action (including by whom and when), (4) date to be reviewed and rationale and (5) status of action.
The review section includes space for a date and details of the reviewer. It also takes the form of a matrix and includes the following columns: (1) progress since last review, (2) action planned and (3) next review with rationale.
The assessment is conducted approximately 1–2 weeks after an older prisoner enters prison. This was based on discussion in the action learning group around the wealth of information that is both asked of and provided to other prisoners, immediately after they arrive in prison, and around how prisoners are suffering from ‘entry shock’ and would find it difficult to cope with a further assessment during the initial entry period. In addition, it was felt that older prisoners require a period to settle into the prison in order to be able to identify their needs effectively. The older prisoner lead accesses the prison’s computer system, C-NOMIS, on a daily basis to identify any prisoners aged ≥ 50 years newly received from court into the prison, whose known release date (convicted prisoners) or likely release date (unconvicted), is at least 3 months after prison entry. The older prisoner lead conducts the assessment on a one-to-one basis with the older prisoner. The care plan is completed in conjunction with the older prisoner, who is provided with a copy of the OHSCAP. In addition, a summary of the OHSCAP is entered onto the prison computerised information system (C-NOMIS) and a copy of the OHSCAP is scanned onto the prison computerised clinical records (SystmOne; The Phoenix Partnership, Leeds, UK) and probation computer records (Offender Assessment System). The older prisoner lead conducts reviews as considered necessary and develops further action plans. Reviews of care plans involve ensuring that actions have been completed and pursuing these as necessary.
It was initially intended that the older prisoner leads, who are usually prison officers, would deliver the intervention. This followed the recommendation of an earlier action learning group comprising prisoners, NHS staff and prison staff at one particular prison who decided that they would be the most appropriate individuals to conduct the OHSCAP in their establishment. The previous study found that prisoners were happy to discuss their health and social care issues with prison officers. However, in 6 of the 10 sites in this study, health-care workers delivered the OHSCAP, as this was deemed by senior managers at the sites to be more appropriate or more achievable within their prison at the time the project was being set up. This was largely because of the benchmarking process that was taking place at the time, which was resulting in a reduction in prison officers and the loss of some roles, including the disability liaison officer (DLO) in some establishments. The DLO is responsible for supporting prisoners with disabilities. They assess the needs of disabled prisoners and try to ensure that adaptations are made when necessary. The DLO is often given the responsibility of supporting older prisoners as well. How they do this varies from prison to prison, but may include facilitating older prisoner groups. The OHSCAP facilitator received training before commencing this work.
Training
All of the OHSCAP facilitators were trained to deliver the OHSCAP, in line with the OHSCAP manual (see Appendix 3). Throughout the study, two training sessions were held at the University of Manchester, which were attended by facilitators from all study sites. Some of the facilitators attended both sessions and were able to share experiences and good practice, having already completed the OHSCAP process with some prisoner participants. Ongoing support was also offered by Dr Elizabeth Walsh, who has vast experience as a clinician within prison settings. She acted as a mentor to facilitators and was contactable by telephone and e-mail, should they have any questions or need any reassurance. Additional site-specific training sessions were provided at prisons that joined part-way through the study in an attempt to bolster recruitment.
Treatment as usual
Treatment as usual included the standard, non-age-specific health assessment carried out at prison entry. 59 Support provided as TAU varied from prison to prison, but included interventions such as older prisoner social groups, peer carers and healthy man checks. Ongoing assessments and interventions followed local procedures at each establishment. Previous research has indicated that the identification of health and social needs and subsequent care planning is generally ad hoc and inadequate. 55
Data collection and management
The following outcome measures were used at baseline and 3 months after prison entry.
Primary outcome measure
The primary outcome measure was the mean number of unmet health and social care needs at 3 months, as measured by the Camberwell Assessment of Need – Short Forensic Version (CANFOR). 89 CANFOR includes 25 domains, namely accommodation, food, looking after the living environment, self-care, daytime activities, physical health, psychotic symptoms, information about condition and treatment, psychological distress, safety to self, safety to others, alcohol, drugs, company, intimate relationships, sexual expression, childcare, basic education, telephone, transport, money, benefits, treatment and access to anti-recidivist interventions for sexual offending and arson. Participants are asked to identify if they have no need, a met need or an unmet need in each of these domains. The extended version of this tool incorporates the perspectives of carers or members of staff working with participants. The short version of the tool was selected because of previous difficulties experienced during the pilot study27 in identifying a member of staff who knew the older prisoner well enough to answer these questions. This was a particular challenge immediately after entry into the prison. A limitation of the tool is that it provides respondents only with an opportunity to state whether their needs in each domain are met or unmet, rather than any indication of the extent to which this is the case. Furthermore, it does not provide specific details about which areas of the domains are met/unmet. However, the CANFOR is the only validated tool available for assessing need among forensic populations. In addition, it has been successfully used in previous studies with older prisoners. 7,20,27
Secondary outcome measures
-
Functional health and well-being and ADL as measured by BADLS. 80 The BADLS measure incorporates the 20 domains of preparing food, eating, preparing drink, drinking, dressing, hygiene, teeth, bath/shower, toilet/commode, transfers, mobility, orientation (time), orientation (space), communications, telephone, housework/gardening, shopping, finances, games/hobbies and transport. The scale was originally designed for patients with dementia, but has recently been used with an older prisoner population. 7,20 Hayes et al. 7,20 omitted items 18 (money) and 20 (transport) because they are not relevant to prisoners, and more relevant versions of these items are covered in the CANFOR. 89 This approach was also adopted for the current study. Total scores were not used because this would affect the internal consistency of the measure. Items were, therefore, to be examined separately.
-
Depression as measured by the Geriatric Depression Scale – short form (GDS-15). 90 The GDS-15 contains 15 questions, which may be answered with ‘yes’ or ‘no’. Each item to which a response of ‘yes’ indicates depression generates a score of 1. A total scale score of ≥ 5 suggests mild depression, and guidelines suggest that further investigation is required, and a total score of ≥ 10 almost always indicates severe depression. The scale has been validated for use with older people and has been used with older prisoners in a previous study. 41 Murdoch et al. 41 adapted question 12 of the assessment from ‘Do you prefer to stay at home rather than go out and do new things?’ to ‘Do you go on association?’. Association refers to prisoners leaving their cells to mix with other prisoners and participate in games and/or other social events. The current study also made this alteration to the question to make it appropriate for prison use.
-
Health-related quality of life as measured by the EuroQoL-5 Dimensions, five-level version (EQ-5D-5L). 91 The EQ-5D-5L is a standardised assessment that has been widely adopted and validated in a variety of different populations. 92 The EQ-5D-5L encompasses the following five domains of health: mobility; ability to self-care; ability to undertake usual activities; pain/discomfort; and anxiety/depression. For each of these, five options are provided (e.g. no problem, slight problem, moderate problem, severe problem, unable). The EQ-5D-5L will be used because the current study is part of a broader study measuring the cost-effectiveness of the OHSCAP. The EQ-5D-5L is recommended by the National Institute for Health and Care Excellence (NICE) to enhance the comparability of different studies. 92 The visual analogue scale aspect of this tool was excluded to reduce participant burden, as this aspect of the tool is not widely used. This was administered face to face. The face-to-face version of this tool was not available when this research commenced.
-
Bespoke OHSCAP research tool. The extent to which specific health and social care needs had been addressed was measured by the bespoke OHSCAP tool specifically designed for the study. It has been necessary to design a specific tool because no standardised assessments will measure improvements in specific issues for older prisoners, such as hearing instructions, receiving information about their release or delays in receiving medication. The bespoke OHSCAP research tool is based around the three sections of the OHSCAP assessment, that is, physical health, well-being and discharge from prison. A number of specific topics are addressed in each of these sections. For each topic, participants are asked if they are experiencing difficulties, if they are receiving help and whether or not they have an unmet need in this area.
The following tools were also used at baseline to describe the sample.
-
PriSnQuest. 84 PriSnQuest consists of seven questions, each with yes or no responses. A score of three or more indicates that a further assessment for mental health is required. PriSnQuest has been selected because it has been developed from other standardised assessments, is widely used in prison and is short, reducing participant burden.
-
Burvill grid to measure physical health. 85 The Burvill grid was used to obtain data on the physical health of participants. The Burvill grid categorises physical disorders into different body systems. Each system is rated according to severity of the disorder (coded 0 = absent, 1 = mild, 2 = moderate, 3 = severe) and disability as a consequence of the disorder (coded 0 = none, 1 = little, 2 = some, 3 = great deal). Physical problems are also defined as acute or chronic. A disorder is considered chronic if it has been present for at least the previous 3 months. The Burvill grid has been used in previous studies of older prisoners. 20,35
All data were collected between 28 January 2014 and 6 April 2016.
Fidelity
The fidelity, and quality, of implementation of the OHSCAP were assessed using an audit tool specifically designed for this study (see Appendix 4 and Chapters 4 and 5).
Sample size
From our previous work (a cross-sectional study assessing the unmet needs of 100 older prisoners at baseline) the mean number of unmet needs was assumed to be 2.71 [standard deviation (SD) 2.65 unmet needs]. The distribution of unmet needs, ranging from 0 to 25, was unsurprisingly positively skewed, with a median number of unmet needs of 2. Although we did not have supporting data, we assumed that this distribution would be broadly similar at 3 months’ follow-up in the TAU group. The purpose of the current study was to see if the average number of unmet needs can be reduced with the OHSCAP intervention. For the study to be practice-changing, we believed that at least a 30% reduction, to a mean of 1.90 unmet needs, was required, and thus powered the study proposal accordingly [mean 1 = 2.71, mean 2 = 1.90 (= 0.7 × mean 1), common SD 2.65 unmet needs, implies n = 169 participants per group for 80% power in a two-tailed t-test at a 5% level of significance]. A 1 : 1 randomised trial employing a two-tailed t-test at the 5% level of significance would require 169 per group for 80% power if the true means are 2.71 and 1.90 unmet needs and the common SD is 2.65 unmet needs. As the distributions would be quite skewed, it was considered preferable at the planning stages to use a non-parametric Mann–Whitney U-test. The asymptotic relative efficiency of this test is at worst 0.864 compared with the t-test, and so a conservative approach is to inflate the proposed sample size accordingly, that is, 169/0.864 = 196 per group. Linear regression was used to analyse the primary outcome measure with bootstrapping to account for skewness, and adjust for minimisation factors (institution and baseline measures of unmet need). This allowed for a more sophisticated approach than would have been adopted if we had used the Mann–Whitney U-test as originally planned and, consequently, we will have > 80% power. The trial stopped when we achieved sufficient numbers at baseline to estimate that we would reach our follow-up target.
Statistical analysis
All analyses were carried out using the intention-to-treat principle with data from all participants included in the analysis, including those who did not complete the OHSCAP assessments.
Analysis was conducted in Statistical Product and Service Solutions, version 20 (SPSS Inc., Chicago, IL, USA). Descriptive statistics within each randomised group are presented for baseline values. These include counts and percentages for binary and categorical variables, and means and SDs, or medians with lower and upper quartiles, for continuous variables, along with minimum and maximum values and counts of missing values. There were no tests of statistical significance or confidence intervals (CIs) for differences between randomised groups on any baseline variable.
It was important to verify that the characteristics of participants that may influence the outcome were distributed evenly between groups at baseline, so that any difference in outcome could be attributed to the intervention. 93 The minimisation process used as part of the randomisation procedures ensured balance between the TAU and intervention groups. Prognostic variables are described for each of the groups to demonstrate that the randomisation procedure has been properly conducted. 93
Primary outcomes
The primary hypothesis for the change in the mean number of unmet needs, as measured by the CANFOR, was analysed using appropriate regression models. We adjusted for baseline characteristics used in the minimisation process, for example site and number of unmet needs at baseline. We used bootstrapping to account for the skewness in the outcome of the data. The 95% CIs were calculated around all key effect size measures and two-sided p-values were reported.
In addition to analysing the mean number of unmet needs, we used a Poisson model to analyse the data as counts.
The CANFOR was used because it was the most appropriate available tool for assessing unmet health and social care needs within the prison population. The research team were, however, aware that there were certain domains of the CANFOR that the OHSCAP specifically aimed to address and some domains of the CANFOR that the OHSCAP did not aim to address. The research team therefore felt that it would be useful to analyse the data separately for the specific domains of the CANFOR that were considered most relevant to the OHSCAP. The aim of this analysis was to gain a more detailed understanding of the specific domains of the CANFOR that the OHSCAP appeared to assist more with and of which domains the OHSCAP was less able to address.
Logistic regression was used to conduct this analysis, with adjustment for site and number of unmet needs at baseline. Table 2 shows the ratings the research team applied to each of the domains for relevance to the OHSCAP. The highest value is 3 and the lowest is 1.
| Domain number | Domain | Relevance |
|---|---|---|
| 1 | Accommodation | 3 |
| 2 | Food (meeting dietary needs) | 3 |
| 3 | Looking after living environment | 3 |
| 4 | Self-care | 3 |
| 5 | Daytime activities | 3 |
| 6 | Physical health | 3 |
| 7 | Psychotic symptoms | 3 |
| 8 | Information about conditions and treatment | 3 |
| 9 | Psychological stress | 3 |
| 10 | Safety to self | 3 |
| 11 | Safety to others | 2 |
| 12 | Alcohol | 2 |
| 13 | Drugs | 2 |
| 14 | Company | 3 |
| 15 | Intimate relationships | 1 |
| 16 | Sexual expression | 1 |
| 17 | Childcare | 1 |
| 18 | Basic education | 3 |
| 19 | Telephone | 3 |
| 20 | Transport | 1 |
| 21 | Money | 3 |
| 22 | Benefits | 2 |
| 23 | Treatment | 3 |
| 24 | Sexual offending | 2 |
| 25 | Arson | 1 |
Secondary outcomes
Similar approaches were adopted for the secondary outcomes, with the form of regression depending on the distribution of the particular outcome. Linear models were used for continuous outcomes, and logistic regression for binary outcomes. Bootstrapping was used only with linear regression. For each of the secondary outcome measures we adjusted for establishment at baseline and for that specific secondary outcome measure at baseline.
Missing data
Data completeness and accuracy were confirmed by the MAHSC-CTU during the data entry process. If, during the data collection and inputting processes, a field was found to have been left blank, the Data Manager at the CTU raised a query and the research team clarified whether the missing information could be obtained or confirmed that it was not available. This assisted in preventing unexplained missing data. The research team conducted further checks to ensure that the data were complete and accurate. Missing data were minimal and, therefore, it was not necessary to compute any missing data.
Database and data entry checks
All data entry checks were conducted by the CTU throughout the duration of the trial. Any missing or inconsistent data were clarified with sites through the data query/correction process. In line with the CTU’s policies, 100% of critical fields and 2% of non-critical fields were quality checked.
Harms reporting
Definitions
Adverse event
An adverse event (AE) was defined as any untoward medical occurrence, unintended disease or injury, or any untoward clinical signs (including an abnormal laboratory finding), in participants, whether or not related to any research procedures or to the intervention.
Seriousness
Any AE will be regarded as serious if it:
-
results in death
-
is life-threatening
-
requires hospitalisation or prolongation of existing hospitalisation
-
results in persistent or significant disability or incapacity
-
consists of a congenital anomaly or birth defect.
An AE meeting any one of these criteria was considered a serious adverse event (SAE).
Relationship
The expression ‘reasonable causal relationship’ means, in general, that there is evidence or argument to suggest a causal relationship. The research team assessed the causal relationship between reported events and trial participation according to the Consolidated Standards of Reporting Trials (CONSORT)65 guidance.
No harms were reported that were considered to be related to this trial.
Reporting serious adverse events
In this study, SAEs were reported to the Chief Investigator (JS), regardless of relatedness, within 24 hours of the principal investigator (or authorised delegate) becoming aware of the event. All SAEs deemed to have a causal relationship were reported to the Trial Steering Committee. Any non-serious AEs, regardless of relatedness, were not reported in this study.
Patient and public involvement
The current study is informed by a previous NIHR-funded study (Service Delivery and Organisation 08/1809/230). As part of the previous study, older prisoners at one prison in England designed the OHSCAP as active members of an action learning group. The OHSCAP was piloted as part of the current research. Prisoners successfully participated in the action learning group and have since reported that they valued the opportunity to be involved in shaping future services. The information the prisoners provided was extremely valuable, and informed the content, and format, of the OHSCAP, for example the specific inclusion of open questions to facilitate discussion. These discussions have also informed the development of the current study. Furthermore, Dr Stuart Ware is a co-applicant and Project Management Group member. Dr Ware is an ex-older prisoner and founder member of the Restore Support Network (RSN), a support network for older prisoners. His involvement has been highly valuable and an important mechanism for ensuring we have considered the needs of older prisoners throughout the current study. Additionally, we had two service user representatives sit on the independent Trial Steering Committee for this study.
Chapter 3 Randomised controlled trial results
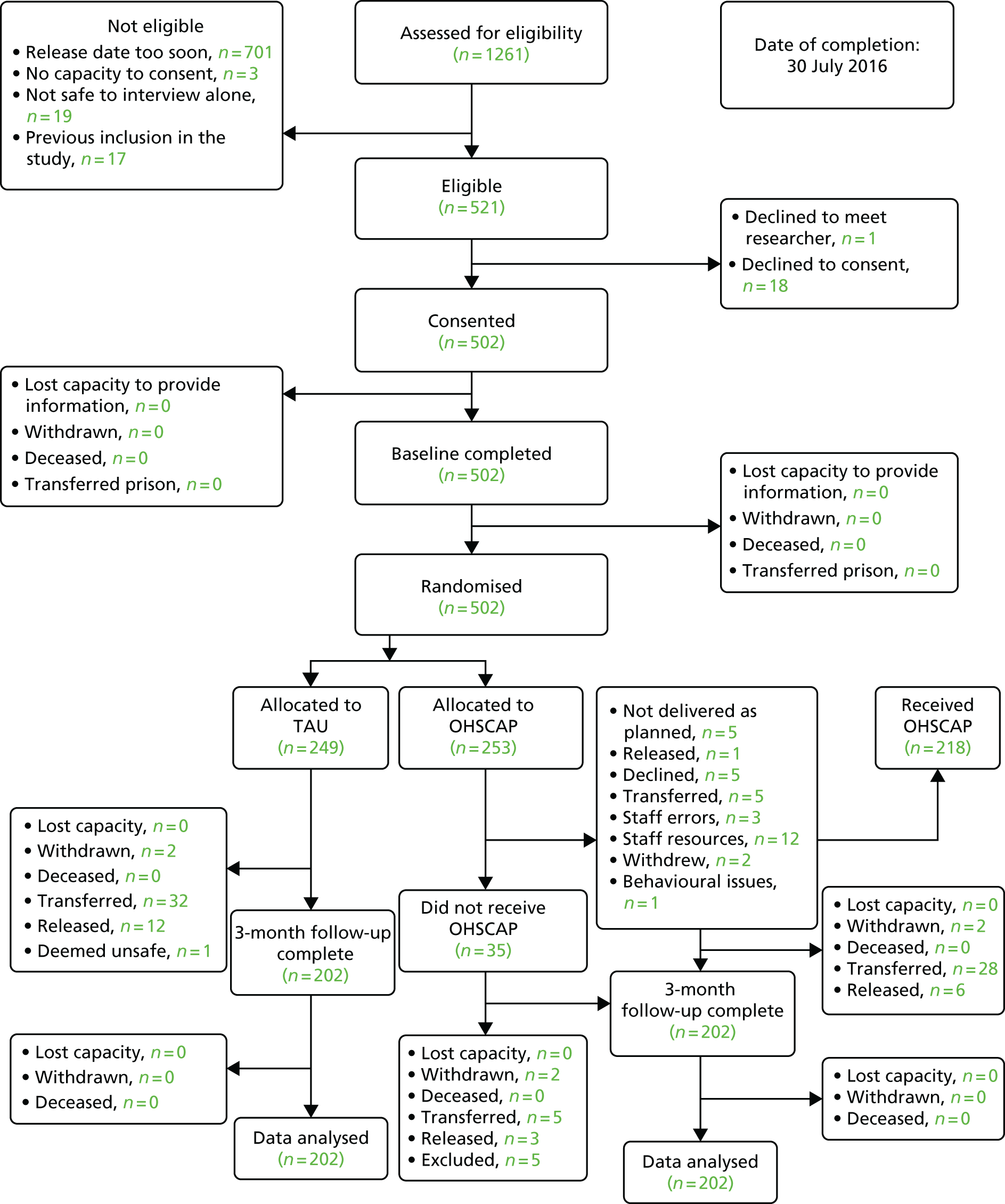
In total, 1261 older prisoners were screened for inclusion in the study. Of these, 521 were eligible for inclusion; informed consent was obtained and baseline assessments were conducted with 502 participants. The study CONSORT flow diagram detailing refusals, loss to follow up, etc., is given in Figure 1.
FIGURE 1.
The CONSORT flow diagram.
Baseline comparability
Table 3 displays a summary of the baseline demographics in order to describe the sample and illustrate the baseline comparability of the randomised groups.
| Demographic | Trial arm | All (N = 497) | |
|---|---|---|---|
| TAU (N = 249) | OHSCAP (N = 248) | ||
| Age (years), mean (SD) | 59 (7.8) | 57 (7.0) | 58 (7.4) |
| Age group (years), n (%) | |||
| 50–54 | 101 (41) | 118 (48) | 219 (44) |
| 55–59 | 56 (22) | 56 (23) | 112 (23) |
| 60–64 | 42 (17) | 35 (14) | 77 (16) |
| 65–69 | 18 (7) | 22 (9) | 40 (8) |
| 70–74 | 21 (8) | 8 (3) | 29 (6) |
| 75–79 | 8 (3) | 8 (3) | 16 (3) |
| 80–84 | 2 (1) | 0 (0) | 2 (0) |
| 85–89 | 1 (1) | 0 (0) | 1 (0) |
| Missing | 0 (0) | 1 (0) | 1 (0) |
| Establishment, n (%) | |||
| Establishment 1 (Local) | 52 (21) | 52 (21) | 104 (21) |
| Establishment 2 (Local) | 1 (0) | 3 (1) | 4 (1) |
| Establishment 3 (Local) | 57 (23) | 59 (24) | 116 (22) |
| Establishment 4 (High security) | 22 (9) | 26 (10) | 48 (10) |
| Establishment 5 (Open) | 46 (19) | 46 (18) | 92 (19) |
| Establishment 6 (Training) | 26 (10) | 22 (9) | 48 (10) |
| Establishment 7 (Open) | 12 (5) | 7 (3) | 19 (4) |
| Establishment 8 (Training) | 5 (2) | 6 (3) | 11 (2) |
| Establishment 9 (Training) | 11 (4) | 10 (4) | 21 (4) |
| Establishment 10 (Training) | 17 (7) | 17 (7) | 34 (7) |
| Ethnicity, n (%) | |||
| White British | 206 (85) | 226 (91) | 432 (87) |
| Other white | 9 (3) | 5 (2) | 14 (3) |
| White and black Caribbean | 2 (1) | 0 (0) | 2 (0) |
| Black Caribbean | 7 (3) | 0 (0) | 7 (1) |
| Other black | 7 (3) | 2 (1) | 9 (2) |
| Indian | 2 (1) | 2 (1) | 4 (1) |
| Pakistani | 6 (2) | 3 (1) | 9 (2) |
| Other Asian | 2 (1) | 1 (0) | 3 (1) |
| Other | 8 (3) | 7 (3) | 15 (3) |
| Missing | 0 (0) | 2 (1) | 2 (0) |
| Marital status, n (%) | |||
| Single | 82 (33) | 69 (28) | 151 (30) |
| Married (partner) | 97 (39) | 114 (46) | 211 (43) |
| Divorced | 40 (16) | 37 (15) | 77 (16) |
| Separated | 17 (7) | 15 (6) | 32 (6) |
| Widowed | 13 (5) | 12 (5) | 25 (5) |
| Missing | 0 (0) | 1 (0) | 1 (0) |
| Employment status, n (%) | |||
| Employed full-time | 80 (32) | 96 (39) | 176 (35) |
| Employed part-time | 9 (4) | 12 (5) | 21 (4) |
| Unemployed but casual work | 2 (1) | 3 (1) | 5 (1) |
| Unemployed | 40 (16) | 36 (14) | 76 (15) |
| Long-term sickness (on benefits) | 47 (19) | 40 (16) | 87 (18) |
| Long-term sickness (employed) | 11 (4) | 10 (4) | 21 (4) |
| Retired | 54 (21) | 38 (16) | 92 (19) |
| Carer | 4 (2) | 7 (3) | 11 (2) |
| Other | 2 (1) | 6 (2) | 8 (2) |
| Living circumstances, n (%) | |||
| Alone | 106 (43) | 93 (38) | 199 (40) |
| With spouse/partner/children | 49 (19) | 63 (25) | 112 (22) |
| With spouse/partner (no children) | 51 (21) | 52 (21) | 103 (21) |
| With children only | 15 (6) | 9 (4) | 24 (5) |
| With parents | 9 (4) | 11 (5) | 20 (4) |
| With other friends/family | 17 (7) | 16 (7) | 33 (7) |
| Probation approved premises | 2 (0) | 1 (0) | 3 (1) |
| Nursing home | 0 (0) | 1 (0) | 1 (0) |
| Other | 0 (0) | 1 (0) | 1 (0) |
| Missing | 0 (0) | 1 (0) | 1 (0) |
| Accommodation, n (%) | |||
| Homeless/no fixed abode | 7 (3) | 1 (0) | 8 (2) |
| Hostel | 4 (1) | 4 (2) | 8 (1) |
| House or flat | 225 (91) | 235 (95) | 460 (93) |
| Nursing home | 0 (0) | 1 (0) | 1 (0) |
| Sheltered accommodation | 4 (2) | 1 (0) | 5 (1) |
| Bungalow | 6 (2) | 1 (0) | 7 (1) |
| Other | 3 (1) | 5 (3) | 8 (2) |
| Main offence, n (%) | |||
| Violence against a person | 33 (13) | 29 (12) | 62 (12) |
| Sexual offence | 98 (39) | 109 (44) | 207 (42) |
| Robbery | 5 (2) | 7 (3) | 12 (2) |
| Burglary | 10 (4) | 9 (3) | 19 (4) |
| Theft and handling | 2 (1) | 8 (3) | 10 (2) |
| Fraud and forgery | 22 (9) | 21 (10) | 43 (9) |
| Drug offences | 52 (21) | 36 (14) | 88 (18) |
| Other | 24 (8) | 28 (11) | 52 (10) |
| Missing | 3 (1) | 1 (0) | 4 (1) |
| Prisoner status, n (%) | |||
| Remand | 41 (17) | 37 (15) | 78 (16) |
| Convicted, unsentenced | 13 (5) | 8 (3) | 21 (4) |
| Convicted, sentenced | 195 (78) | 203 (82) | 398 (80) |
| Participant has been in prison before, n (%) | |||
| Yes | 132 (53) | 123 (49) | 242 (48) |
| No | 117 (47) | 125 (51) | 255 (52) |
| Times been in prison before, mean (SD) | 5.23 (7.2) | 4.43 (6.7) | 4.82 (6.9) |
The sample were all male (100%) and the majority were white British (87%). The mean age of the sample was 58 years; 92 (33%) were aged ≥ 60 years, 43% were married or had a partner and 35% were employed full-time at the time of imprisonment. One hundred and ninety-nine (40%) were living alone and 460 (93%) were living in a house or flat before being sent to prison.
Sexual offences were the most common type of index offence (42%), followed by drug (18%) and violent offences (12%). Eighty per cent had been convicted and sentenced. Just over 50% had not been in prison before, and on average participants had been in prison five times previously. Forty per cent were residing on a general wing for convicted prisoners, 25% on an induction wing and 25% on a vulnerable prisoners unit. Prisoners are able to move from basic to standard, and then to enhanced, status if they obey prison rules and demonstrate good behaviour. These statuses have an impact on a number of prisoner entitlements including the number and length of weekly visits and the amount of money they are allowed to spend within the prison. The majority of participants were on a standard regime (66%), as opposed to having basic or enhanced status (Table 4).
| Criminogenic details | Trial arm | All (N = 497) | |
|---|---|---|---|
| TAU (N = 249) | OHSCAP (N = 248) | ||
| Type of wing, n (%) | |||
| Remand/induction | 58 (23) | 68 (27) | 126 (25) |
| Convicted | 100 (41) | 96 (39) | 196 (40) |
| Vulnerable prisoners unit | 60 (24) | 67 (27) | 127 (25) |
| Health care | 6 (2) | 3 (1) | 9 (2) |
| Category A/closed secure unit | 2 (1) | 1 (0) | 3 (1) |
| Segregation | 0 (0) | 1 (0) | 1 (0) |
| Detox and drug free | 7 (2) | 4 (2) | 11 (2) |
| Older person | 9 (4) | 6 (3) | 15 (3) |
| Other | 7 (3) | 2 (1) | 9 (2) |
| Current regime, n (%) | |||
| Basic | 6 (2) | 2 (1) | 8 (2) |
| Standard | 158 (64) | 172 (69) | 330 (66) |
| Enhanced | 85 (34) | 74 (30) | 159 (32) |
The majority scored < 3 on PriSnQuest (80%), indicating that they did not require any further mental health assessment at the time the interview was conducted. The most common mental illness was general anxiety disorder (6%, identified via OPCRIT). The mean number of body systems acutely affected, according to the BADLS, was 0.2, and the mean number chronically affected was 2.1 (Table 5).
| Mental and physical health measure | Trial arm | All (N = 497) | |
|---|---|---|---|
| TAU (N = 249) | OHSCAP (N = 248) | ||
| PriSnQuest score, n (%) | |||
| 3+ | 52 (21) | 46 (19) | 98 (20) |
| < 3 | 197 (79) | 202 (81) | 399 (80) |
| OPCRIT diagnosis, n (%) | |||
| Psychosis | 8 | 5 | 12 |
| Schizophrenia | 0 | 0 | 0 |
| Depression | 5 | 8 | 12 |
| Anxiety disorder | 17 | 16 | 33 |
| Personality disorder | 1 | 1 | 2 |
| Harmful use of drugs | 25 | 9 | 34 |
| Harmful use of alcohol | 11 | 15 | 26 |
| Other | 5 | 3 | 5 |
| Total acute severity score, mean (SD) | 0.3 (0.7) | 0.4 (0.9) | 0.3 (0.8) |
| Total chronic severity score, mean (SD) | 4.3 (3.3) | 3.5 (3.2) | 3.9 (3.3) |
| Total acute disability score, mean (SD) | 0.2 (0.7) | 0.2 (0.7) | 0.2 (0.7) |
| Total chronic disability score, mean (SD) | 3.7 (3.4) | 2.9 (2.97) | 3.2 (3.2) |
| Number of systems acutely affected, mean (SD) | 0.2 (0.4) | 0.2 (0.5) | 0.2 (0.4) |
| Number of systems chronically affected, mean (SD) | 2.3 (1.5) | 1.8 (1.4) | 2.1 (1.5) |
Primary outcome
The primary outcome was the total number of unmet needs as measured by the CANFOR (Table 6). The individual domains of the CANFOR that were considered most relevant and important were also examined individually (Tables 7 and 8). Logistic regression was conducted for the domains of the CANFOR that > 30 participants stated that they had an unmet need for. There were no significant differences between the two groups at 3 months’ follow-up (Table 7). When the log linear negative binominal regression model was run, the results were unchanged from the Poisson model.
| Unmet needs | Time point | Analysis | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | ||||||
| TAU (n = 249) | OHSCAP (n = 248) | TAU (n = 202) | OHSCAP (n = 202) | Odds ratio (95% CI) | p-value | N | |
| Total number of unmet needs,a mean (SD) | 2.84 (2.311) | 2.57 (1.978) | 2.06 (2.114) | 2.03 (2.066) | 0.088 (–0.276 to 0.449) | 0.621 | 404 |
| Total number of unmet needs (count using Poisson model) | – | – | – | – | –0.078 (–2.16 to 0.061) | 0.272 | 404 |
| Domain | Trial arm, n (%) | Analysis | |||
|---|---|---|---|---|---|
| TAU (N = 202) | OHSCAP (N = 202) | Odds ratio (95% CI) | p-value | N | |
| Psychological stress | |||||
| Met need | 26 (41) | 21 (40) | 1.104 (0.514 to 2.373) | 0.800 | 115 |
| Unmet need | 37 (59) | 31 (60) | |||
| Food | |||||
| Met need | 98 (52) | 110 (58) | 0.716 (0.456 to1.125) | 0.148 | 376 |
| Unmet need | 89 (48) | 79 (42) | |||
| Self-care | |||||
| Met need | 5 (23) | 3 (19) | 1.617 (0.289 to 9.048) | 0.584 | 38 |
| Unmet need | 17 (77) | 13 (81) | |||
| Daytime activities | |||||
| Met need | 100 (65) | 106 (67) | 0.924 (0.572 to 1.493) | 0.747 | 312 |
| Unmet need | 54 (35) | 52 (33) | |||
| Physical health | |||||
| Met need | 120 (72) | 103 (71) | 1.093 (0.659 to 1.812) | 0.731 | 312 |
| Unmet need | 46 (28) | 43 (29) | |||
| Information about conditions and treatment | |||||
| Met need | 5 (9) | 4 (6) | 1.344 (0.327 to 5.528) | 0.682 | 120 |
| Unmet need | 50 (91) | 61 (94) | |||
| Money | |||||
| Met need | 1 (5) | 2 (8) | 0.602 (0.047 to 7.715) | 0.696 | 47 |
| Unmet need | 21 (95) | 23 (92) | |||
| Domain | Trial arm, n (%) | N | |
|---|---|---|---|
| TAU (N = 202) | OHSCAP (N = 202) | ||
| Accommodation | |||
| Met need | 9 (56) | 6 (55) | 27 |
| Unmet need | 7 (44) | 5 (45) | |
| Looking after living environment | |||
| Met need | 13 (39) | 11 (31) | 69 |
| Unmet need | 20 (61) | 25 (69) | |
| Psychotic symptoms | |||
| Met need | 4 (67) | 2 (25) | 14 |
| Unmet need | 2 (33) | 6 (75) | |
| Safety to self | |||
| Met need | 3 (50) | 4 (36) | 17 |
| Unmet need | 3 (50) | 7 (64) | |
| Safety to others | |||
| Met need | 4 (67) | 1 (100) | 7 |
| Unmet need | 2 (33) | 0 (0) | |
| Alcohol | |||
| Met need | 5 (83) | 6 (67) | 15 |
| Unmet need | 1 (17) | 3 (33) | |
| Drugs | |||
| Met need | 10 (91) | 6 (86) | 18 |
| Unmet need | 1 (9) | 1 (14) | |
| Company | |||
| Met need | 1 (10) | 0 (0) | 15 |
| Unmet need | 9 (90) | 5 (100) | |
| Intimate relationships | |||
| Met need | 1 (13) | 1 (14) | 15 |
| Unmet need | 7 (87) | 6 (86) | |
| Basic education | |||
| Met need | 12 (75) | 13 (76) | 14 |
| Unmet need | 4 (25) | 4 (24) | |
| Telephone | |||
| Met need | 1 (9) | 1 (8) | 24 |
| Unmet need | 10 (91) | 12 (92) | |
| Benefits | |||
| Met need | 11 (52) | 9 (45) | 41 |
| Unmet need | 10 (48) | 11 (55) | |
| Treatment | |||
| Met need | 7 (41) | 4 (44) | 26 |
| Unmet need | 10 (59) | 5 (56) | |
| Sexual offending | |||
| Met need | 3 (75) | 2 (100) | 4 |
| Unmet need | 1 (25) | 0 (0) | |
Secondary outcome measures
In addition, at 3-month follow-up we collected data concerning ADL. None of the participants indicated that they experienced any problems with 10 out of the 19 of the domains of the BADLS at the 3-month follow-up. These domains were food, drink, drinking, dressing, teeth, orientation (space), communication, telephone, shopping/canteen and games/hobbies. The domains of the BADLS that a minority of participants experienced some difficulties with are detailed in Table 9.
| BADLS domain | Trial arm, n (%) | All (N = 404), n (%) | |
|---|---|---|---|
| TAU (N = 202) | OHSCAP (N = 202) | ||
| Eating | |||
| Needs to be fed | 1 (0) | 0 (0) | 1 (0) |
| Dressing | |||
| Unable/requires total dressing | 0 (0) | 1 (0) | 1 (0) |
| Hygiene | |||
| Unable/needs full assistance | 0 (0) | 1 (0) | 1 (0) |
| Bath/shower | |||
| Needs full assistance | 0 (0) | 1 (0) | 1 (0) |
| Toilet/commode | |||
| Taken and given assistance | 0 (0) | 1 (0) | 1 (0) |
| Incontinent urine or faeces | 1 (0) | 0 (0) | 1 (0) |
| Transfers | |||
| Gets in chair – needs help out | 1 (0) | 1 (0) | 2 (0) |
| Totally dependent | 0 (0) | 1 (0) | 1 (0) |
| Mobility | |||
| Walks with assistance | 7 (3) | 4 (2) | 11 (2) |
| Uses aids | 17 (8) | 8 (4) | 25 (5) |
| Unable to walk | 2 (1) | 2 (1) | 4 (1) |
| Orientation (time) | |||
| Unaware but unconcerned | 5 (2) | 3 (1) | 8 (2) |
| House (cell) work | |||
| Not to required standard | 1 (0) | 1 (0) | 1 (0) |
| Unable/unwilling to clean | |||
Data regarding depressive symptoms were also collected at the 3-month follow-up: 31% scored between 6 and 15, indicating that they were showing depressive symptoms. There were no statistical differences between the groups (Table 10).
| GDS at 3-month follow-up | Trial arm, n (%) | All (N = 404), n (%) | Analysis | |||
|---|---|---|---|---|---|---|
| TAU (N = 202) | OHSCAP (N = 202) | Odds ratio (95% CI) | p-value | N | ||
| 0–5 normal | 135 | 142 | 277 (69) | 1.033 (0.617 to 1.732) | 0.901 | 403 |
| 6–15 depressive symptoms | 67 | 59 | 126 (31) | |||
| Missing | 0 | 1 (0) | 1 (0) | |||
Additionally, we used a bespoke OHSCAP tool to measure the extent to which needs were met across 23 specific domains. For each domain, participants were asked to stipulate the extent to which their needs were met. The Likert scale included the following options: not at all, very little, somewhat, and to a great extent. For clarity, only responses for not at all and to a great extent are presented in Table 11. Needs that were more likely to be met were access to a GP on release, and collecting meals and showering while in prison (mean = 2.95, 2.87 and 2.84, respectively). Needs that were less likely to be met included information about release processes, sleep and boredom (mean = 1.98, 2.06 and 2.06, respectively). There was a statistically significant difference between groups for hearing instructions (p = 0.014, 95% CI –0.046 to 0.018).
| Health and social care need | Trial arm, n (%) | All (N = 404), n (%) | Analysis | ||||
|---|---|---|---|---|---|---|---|
| TAU (N = 202) | OHSCAP (N = 202) | Treatment effect | 95% CI | p-value | N | ||
| Telephoning family/friends | |||||||
| Not at all | 11 (5) | 13 (6) | 24 (6) | 0.013 | –0.424 to 0.429 | 0.952 | 391 |
| To a great extent | 166 (82) | 162 (80) | 328 (81) | ||||
| Mean (SD) | 2.69 (0.8) | 2.65 (0.86) | 2.67 (0.827) | ||||
| Missing | 6 (3) | 7 (3) | 13 (3) | ||||
| Receiving visits from family and friends | |||||||
| Not at all | 24 (12) | 20 (10) | 44 (11) | 0.083 | –0.115 to 0.285 | 0.430 | 384 |
| To a great extent | 133 (66) | 124 (61) | 287 (71) | ||||
| Mean (SD) | 2.35 (1.09) | 2.52 (1.01) | 2.43 (1.05) | ||||
| Missing | 12 (6) | 8 (4) | 20 (5) | ||||
| Giving/receiving letters to/from family/friends | |||||||
| Not at all | 12 (6) | 9 (4) | 4 (0) | 0.066 | –0.100 to 0.229 | 0.436 | 393 |
| To a great extent | 147 (73) | 155 (78) | 373 (94) | ||||
| Mean (SD) | 2.58 (0.87) | 2.66 (0.79) | 2.62 (0.830) | ||||
| Missing | 12 (6) | 12 (6) | 11 (3) | ||||
| Bullying by other prisoners | |||||||
| Not at all | 2 (1) | 2 (1) | 6 (1) | –0.022 | –0.111 to 0.062 | 0.628 | 392 |
| To a great extent | 188 (93) | 185 (92) | 370 (92) | ||||
| Mean (SD) | 2.93 (0.386) | 2.90 (0.44) | 2.91 (0.41) | ||||
| Missing | 6 (3) | 5 (2) | 12 (3) | ||||
| Mixing/socialising with other prisoners | |||||||
| Not at all | 3 (1) | 3 (1) | 6 (1) | 0.006 | –0.092 to 0.107 | 0.899 | 392 |
| To a great extent | 183 (92) | 187 (94) | 370 (92) | ||||
| Mean (SD) | 2.88 (0.51) | 2.89 (0.48) | 2.89 (0.50) | ||||
| Missing | 7 (3) | 5 (2) | 12 (3) | ||||
| Boredom | |||||||
| Not at all | 25 (12) | 27 (13) | 287 (71) | 0.039 | –0.160 to 0.224 | 0.682 | 384 |
| To a great extent | 96 (48) | 96 (48) | 45 (11) | ||||
| Mean (SD) | 2.04 (1.09) | 2.08 (1.08) | 2.06 (1.08) | ||||
| Missing | 4 (2) | 2 (1) | 20 (5) | ||||
| Lack of appropriate education | |||||||
| Not at all | 18 (9) | 22 (11) | 40 (10) | –0.107 | –0.318 to 0.079 | 0.294 | 375 |
| To a great extent | 140 (69) | 137 (69) | 277 (69) | ||||
| Mean (SD) | 2.51 (0.98) | 2.41 (1.05) | 2.46 (1.01) | ||||
| Missing | 18 (9) | 11 (5) | 29 (7) | ||||
| Lack of appropriate employment | |||||||
| Not at all | 20 (10) | 26 (13) | 46 (11) | –0.011 | –0.288 to 0.201 | 0.919 | 383 |
| To a great extent | 141 (71) | 140 (70) | 281 (70) | ||||
| Mean (SD) | 2.46 (1.02) | 2.41 (1.07) | 2.43 (1.05) | ||||
| Missing | 13 (6) | 8 (4) | 21 (5) | ||||
| Accessing parts of the prison | |||||||
| Not at all | 6 (3) | 4 (2) | 10 (2) | 0.005 | –0.136 to 0.156 | 0.956 | 393 |
| To a great extent | 181 (90) | 178 (88) | 359 (89) | ||||
| Mean (SD) | 2.54 (0.87) | 2.60 (0.88) | 2.57 (0.87) | ||||
| Missing | 6 (3) | 5 (2) | 11 (3) | ||||
| Collecting meals | |||||||
| Not at all | 9 (4) | 14 (7) | 23 (6) | 0.067 | –0.031 to 0.162 | 0.179 | 394 |
| To a great extent | 146 (73) | 156 (78) | 302 (75) | ||||
| Mean (SD) | 2.83 (0.58) | 2.92 (0.44) | 2.87 (0.52) | ||||
| Missing | 5 (2) | 5 (2) | 10 (2) | ||||
| Getting in and out of bed | |||||||
| Not at all | 3 (1) | 3 (1) | 6 (1) | –0.075 | –0.187 to 0.040 | 0.199 | 391 |
| To a great extent | 178 (89) | 187 (94) | 365 (91) | ||||
| Mean (SD) | 2.85 (0.53) | 2.79 (0.67) | 2.82 (0.61) | ||||
| Missing | 6 (3) | 7 (3) | 13 (3) | ||||
| Showering/washing | |||||||
| Not at all | 3 (1) | 8 (4) | 11 (3) | –0.011 | –0.114 to 0.085 | 0.819 | 392 |
| To a great extent | 177 (89) | 175 (87) | 352 (87) | ||||
| Mean (SD) | 2.84 (0.60) | 2.84 (0.55) | 2.84 (0.572) | ||||
| Missing | 7 (3) | 5 (2) | 12 (3) | ||||
| Feeling safe | |||||||
| Not at all | 10 (5) | 8 (4) | 18 (4) | 0.062 | –0.078 to 0.203 | 0.421 | 391 |
| To a great extent | 160 (79) | 170 (8) | 330 (82) | ||||
| Mean (SD) | 2.67 (0.8) | 2.74 (0.72) | 2.71 (0.76) | ||||
| Missing | 8 (4) | 5 (2) | 13 (3) | ||||
| Sleep | |||||||
| Not at all | 26 (13) | 29 (15) | 55 (14) | –0.052 | –0.247 to 0.160 | 0.590 | 396 |
| To a great extent | 103 (51) | 106 (52) | 209 (51) | ||||
| Mean (SD) | 2.07 (1.12) | 2.06 (1.14) | 2.06 (1.13) | ||||
| Missing | 5 (2) | 3 (2) | 8 (2) | ||||
| Stress | |||||||
| Not at all | 23 (11) | 29 (15) | 52 (13) | 0.029 | –0.182 to 0.211 | 0.774 | 394 |
| To a great extent | 38 (19) | 22 (11) | 60 (15) | ||||
| Mean (SD) | 2.04 (1.07) | 2.15 (1.11) | 2.09 (1.09) | ||||
| Missing | 6 (3) | 4 (2) | 10 (2) | ||||
| Glasses/contact lenses | |||||||
| Not at all | 20 (10) | 17 (9) | 37 (9) | 0.073 | –0.109 to 0.273 | 0.427 | 390 |
| To a great extent | 131 (66) | 141 (70) | 272 (68) | ||||
| Mean (SD) | 2.37 (1.02) | 2.47 (0.96) | 2.42 (0.2) | ||||
| Missing | 9 (4) | 5 (2) | 14 (3) | ||||
| Hearing instructions | |||||||
| Not at all | 12 (6) | 2 (1) | 14 (3) | 0.173 | 0.030 to 0.311 | 0.014 | 392 |
| To a great extent | 136 (67) | 149 (74) | 285 (71) | ||||
| Mean (SD) | 2.48 (0.90) | 2.67 (0.64) | 2.58 (0.78) | ||||
| Missing | 8 (4) | 4 (2) | 12 (3) | ||||
| Delays in receiving medication | |||||||
| Not at all | 10 (5) | 9 (4) | 19 (5) | –0.025 | 0.242 to 0.197 | 0.821 | 295 |
| To a great extent | 126 (63) | 116 (58) | 242 (59) | ||||
| Mean (SD) | 2.60 (0.87) | 2.59 (0.89) | 2.60 (0.88) | ||||
| Missing | 44 (22) | 57 (28) | 101 (25) | ||||
| Receiving appropriate medication | |||||||
| Not at all | 12 (6) | 10 (5) | 22 (5) | 0.071 | –0.139 to 0.269 | 0.490 | 303 |
| To a great extent | 127 (64) | 125 (62) | 252 (63) | ||||
| Mean (SD) | 2.59 (0.92) | 2.68 (0.85) | 2.63 (0.89) | ||||
| Missing | 45 (22) | 56 (28) | 101 (25) | ||||
| Finances | |||||||
| Not at all | 17 (8) | 13 (6) | 30 (7) | –0.22 | –0.229 to 0.173 | 0.846 | 346 |
| To a great extent | 130 (65) | 128 (64) | 258 (65) | ||||
| Mean (SD) | 2.49 (0.20) | 2.47 (0.96) | 2.48 (0.98) | ||||
| Missing | 31 (15) | 27 (13) | 58 (14) | ||||
| Accommodation | |||||||
| Not at all | 17 (8) | 5 (2) | 22 (5) | 0.160 | –0.041 to 0.338 | 0.102 | 333 |
| To a great extent | 130 (65) | 141 (70) | 271 (68) | ||||
| Mean (SD) | 2.51 (0.20) | 2.72 (0.73) | 2.61 (0.880) | ||||
| Missing | 35 (18) | 36 (18) | 71 (17) | ||||
| Information about release processes | |||||||
| Not at all | 12 (6) | 12 (6) | 24 (6) | 0.115 | –0.381 to 0.598 | 0.659 | 133 |
| To a great extent | 35 (17) | 35 (17) | 70 (17) | ||||
| Mean (SD) | 1.97 (1.24) | 21.99 (1.18) | 1.98 (1.20) | ||||
| Missing | 138 (69) | 133 (66) | 271 (68) | ||||
| Access to GP in the community | |||||||
| Not at all | 1 (0) | 0 (0) | 1 (0) | 0.20 | –0.092 to 0.154 | 0.760 | 173 |
| To a great extent | 83 (41) | 85 (42) | 168 (42) | ||||
| Mean (SD) | 2.95 (0.32) | 2.95 (0.26) | 2.95 (0.30) | ||||
| Missing | 117 (59) | 114 (57) | 231 (58) | ||||
| OHSCAP bespoke total | |||||||
| Mean (SD) | 60.15 (7.624) | 61.83 (6.546) | 60.97 (7.123) | –0.166 | –3.996 to 4.231 | 0.941 | 404 |
Losses to follow-up
Follow-up data collection was scheduled to take place at the 3-month follow-up. Data were collected for 404 participants at follow-up, a retention rate of 81%. The main reason for loss at follow-up was the prisoner’s transfer to another prison.
Chapter 4 Fidelity-of-implementation audit: methodology
Procedure
Following the completion of data collection and all OHSCAP assessments in all study sites, researchers contacted the OHSCAP lead at each site and requested anonymised photocopies of the assessments and care plans they had produced throughout the duration of the study. Once collated, the anonymised copies were audited by a trained reviewer, who remained independent of the research team.
Each OHSCAP was assessed using a bespoke pro forma designed to assess the quality of the assessment and care planning (see Appendix 4). The team have developed similar pro formas for other studies. 94,95 The independent reviewer was trained by the research team (who developed the audit tool), and 10%14 of the OHSCAPs audited were also audited by a researcher for the purposes of establishing inter-rater reliability. Inter-rater agreement was measured using Cohen’s kappa coefficient statistic, specifically in relation to the final section of the audit tool, which required a subjective judgement about the appropriateness of care plan actions. Cohen’s kappa (κ) is a measure of inter-rater agreement for categorical variables when there are two raters. The statistic accounts for chance agreement and produces an output figure ranging from –1.00 to 1.00, with the latter value representing perfect inter-rater agreement. Positive figures < 1.00 represent agreement that is better than chance, and the higher the figure, the stronger the agreement. Negative figures represent agreement below that expected by chance.
The audit process aimed to assess the fidelity-of-implementation of the OHSCAP process and the quality of care planning. The audit tool was broken down into three core sections: compliance fidelity, context fidelity and competence fidelity.
The compliance fidelity section assessed the extent to which key elements of the process were conducted as per training and the OHSCAP manual. This included, for example, how many days after prison entry the OHSCAP was completed (the target was 7–14 days), whether or not the care plan was copied to various electronic systems and paper records within the prison and whether or not reviews were completed according to schedule.
Context fidelity was assessed in relation to the extent to which each area of need was assessed and the level of detail of the information documented. Table 12 describes the definitions of each label.
| Not completed | Poor | Adequate | Good | No problem |
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 |
| Section not completed | Very brief notes made (e.g. majority of subquestions not answered) | Sufficient notes made (e.g. the majority of subquestions answered sufficiently) | Detailed notes made (e.g. all subquestions answered in detail) | Prisoner indicated that there was no problem in this area |
This section also included assessment of whether or not any outstanding needs were identified in each area and, if so, whether or not a corresponding action was documented in the subsequent care plan.
Finally, the section on competence fidelity sought to assess the quality of care planning, in terms of the extent to which care plan actions were an appropriate response to the outstanding needs identified. Table 13 describes the definition of each label.
| Not completed | Poor | Adequate | Good | No problem |
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 |
| Need raised not included in care plan, but need had arisen during assessment | Need raised dealt with to some extent, but detail lacking (e.g. aim, action or review date not set) | Need raised dealt with in detail (e.g. all sections complete) | Need raised appropriately dealt with in detail (e.g. all sections complete with specific details provided) | Prisoner stated that there were no needs that need to be addressed |
Sample
Overall, 220 OHSCAPs were completed, of which 150 (68.2%) were available for potential audit. Reasons for loss can be seen in Table 14.
| Site | OHSCAPs audited (%) | Reasons for audit failures |
|---|---|---|
| 1 | 83.9 | Nine lost |
| 2 | 2.3 | 42 lost (entire folder during office moves) |
| 3 | 91.1 | Four lost |
| 4 | 57.1 | Three lost |
| 5 | 0.0 | Two lost |
| 6 | 94.1 | One lost |
| 7 | 85.7 | One with every other page missing/incomplete |
| 8 | 60.0 | Two lost |
| 9 | 53.3 | Six lost, one incomplete as a result of participant incompliance |
| 10 | 100.0 | N/A |
Only one site was able to provide 100% of completed OHSCAP assessments to the research team for audit. In most sites, between 1 and 10 OHSCAP assessments were lost, with the exception of site 2, where an entire folder of filed assessments went missing during office moves. The prison health-care provider changed at this site and large volumes of paperwork were securely destroyed as part of the transition.
Assessments were audited from 9 of the 10 study sites. One site, from which only four participants were ever recruited, was unable to provide copies of the two OHSCAP assessments that it completed.
Chapter 5 Fidelity-of-implementation audit: results
Information sharing
Almost three-quarters (74%) of the OHSCAPs audited were completed by prison staff, with health-care staff completing the other 26%.
The OHSCAP training manual requires that copies of assessments and care plans are offered to the prisoner and are uploaded onto (1) the electronic clinical records system, (2) the C-NOMIS prison records system and (3) the probation service’s system and (4) placed in the prisoner’s core record. The losses prior to the audit process highlighted that OHSCAP facilitators often failed to copy the care plan to these other systems, as lost paper versions were not recoverable from other physical or electronic locations. Of the 150 audited, facilitators recorded that they had not copied the care plan to the prisoner or any of the various systems in the majority of cases (Figure 2).
FIGURE 2.
Copies/uploads of OHSCAPs as reported in audit.
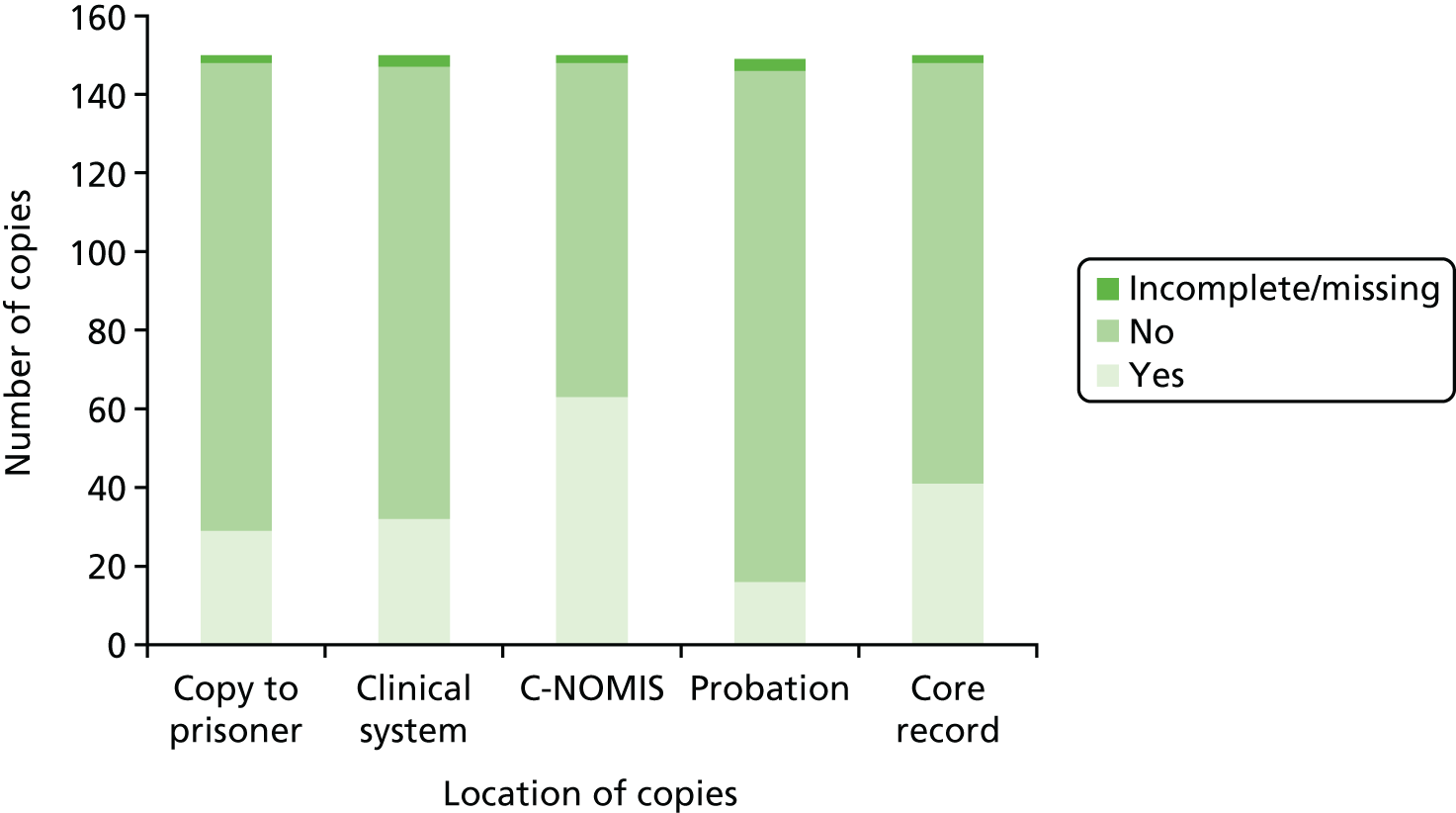
In many cases, facilitators did note on the OHSCAP assessment that the prisoner had been offered a copy of the assessment and care plan but did not wish to take a copy. This could be because participants did not want other prisoners to potentially have an opportunity to see the personal information it contained. During the training phase, it also became apparent that information sharing across the various systems was more common in some sites than others, and varied according to the role of the facilitator. For example, some of the prison officer facilitators reported that they did not have the facility to copy the care plan onto the health-care system and, likewise, some health-care staff reported difficulties in accessing prison and probation systems. These comments are supported by the audit findings, as health-care staff copied the care plan to the clinical system in a greater proportion of cases than prison staff and vice versa for the prison systems, while there was little difference between the groups in terms of providing the prisoner with a copy (Figure 3). It is standard practice that health-care staff have access to both health-care and prison systems, while, for reasons of medical confidentiality, prison officers are not permitted access to health-care systems. Therefore, prison officers could share the OHSCAP on the electronic clinical records system only with the help of a health-care colleague.
FIGURE 3.
Copies/uploads to prisoner and systems by facilitator role.
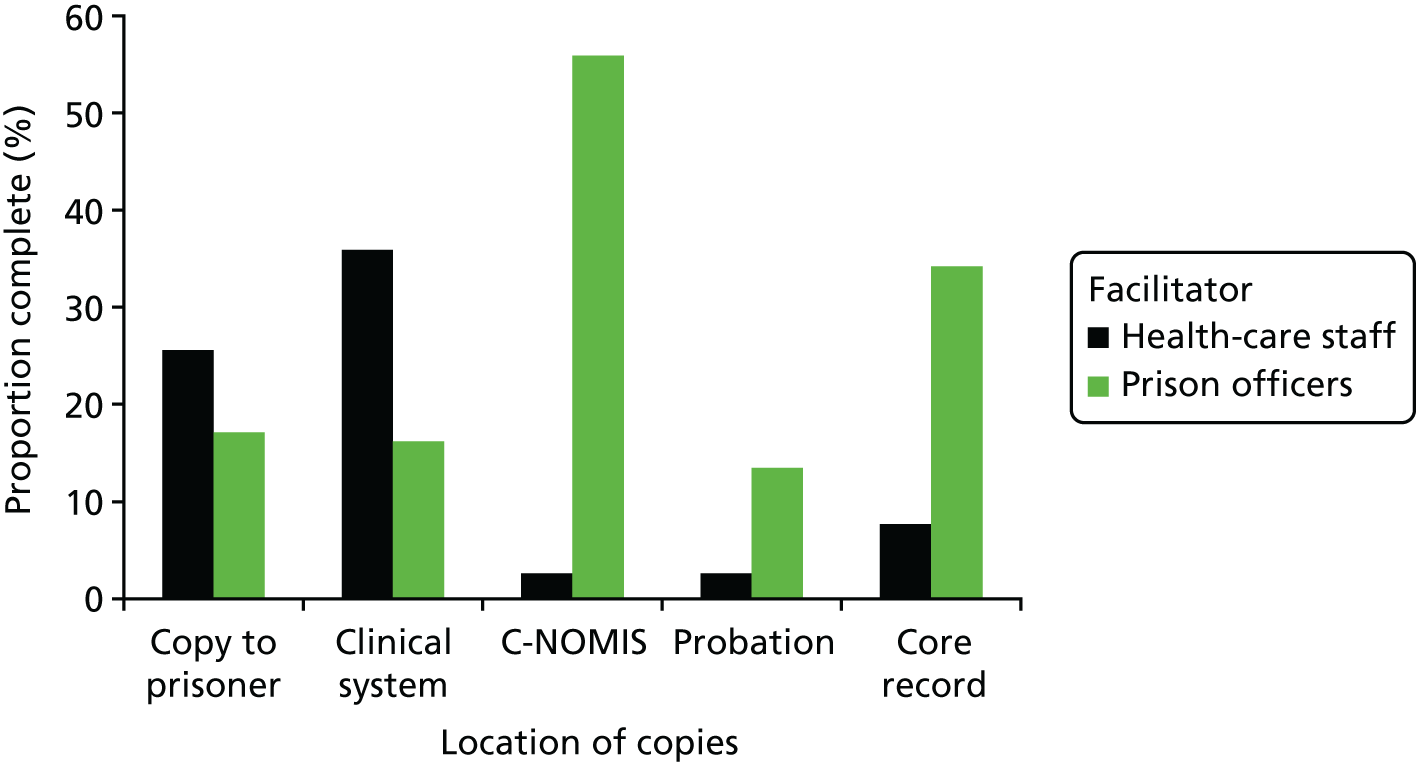
Completion of the assessment and care plan
The OHSCAPs were completed, on average, 20 days after arrival into the prison (mean 20.43 days, median 18 days). Time from arrival to completion of the OHSCAP ranged from 4 to 63 days. The OHSCAP manual stipulates that the assessment and care planning process should be completed 7–14 days after reception.
A care plan was generated following fewer than half of the assessments audited (65; 43.3%). During training sessions, researchers noted that health-care staff seemed more comfortable than prison officers with the concept of drawing up a care plan, as would perhaps be expected. However, in practice, the proportion of assessments that led to a care plan was largely similar, regardless of the role of the facilitator, with plans completed on 46.2% and 43.2% of cases for health-care staff and prison officers, respectively.
In two sites, where only a small number of participants were recruited to the study, all of the OHSCAP assessments that were audited resulted in care plans. In two other sites, 100% of those assessed did not receive a care plan. This may indicate that some individual facilitators were more comfortable with the care planning process than others, regardless of their role.
In the majority (69.2%) of assessments that resulted in a care plan, there was no clear reference to the prisoner having been involved in the development of the care plan. The OHSCAP manual stipulates that the care plan should be completed in conjunction with the prisoner, and stresses the importance of involving them in the care planning process. However, it should be noted that the reviewer was reliant on there being some explicit, written evidence of the prisoner’s involvement in the process, as they were not present during the care planning process. This finding could therefore reflect an issue with documenting prisoners’ involvement in the care planning process, rather than failure to actually involve them in the process in practice.
Reviews
The OHSCAP manual stipulates that each individual should be offered a review at least every 6 months, although the timing of review for each care plan action is left to the discretion of the OHSCAP facilitator. In theory, this should allow facilitators the flexibility to prioritise the most urgent actions, while providing additional time to deal with less-pressing issues. However, the evidence obtained from the audit process suggests that facilitators generally struggled to implement the review process as intended.
Of the assessments that resulted in care plans, only 22 (33.8%) were followed up with an initial review. Reviews were most often (26.2%) set for 5–12 weeks after the care plan was drawn up (Figure 4).
FIGURE 4.
Time planned between initial assessment and review.
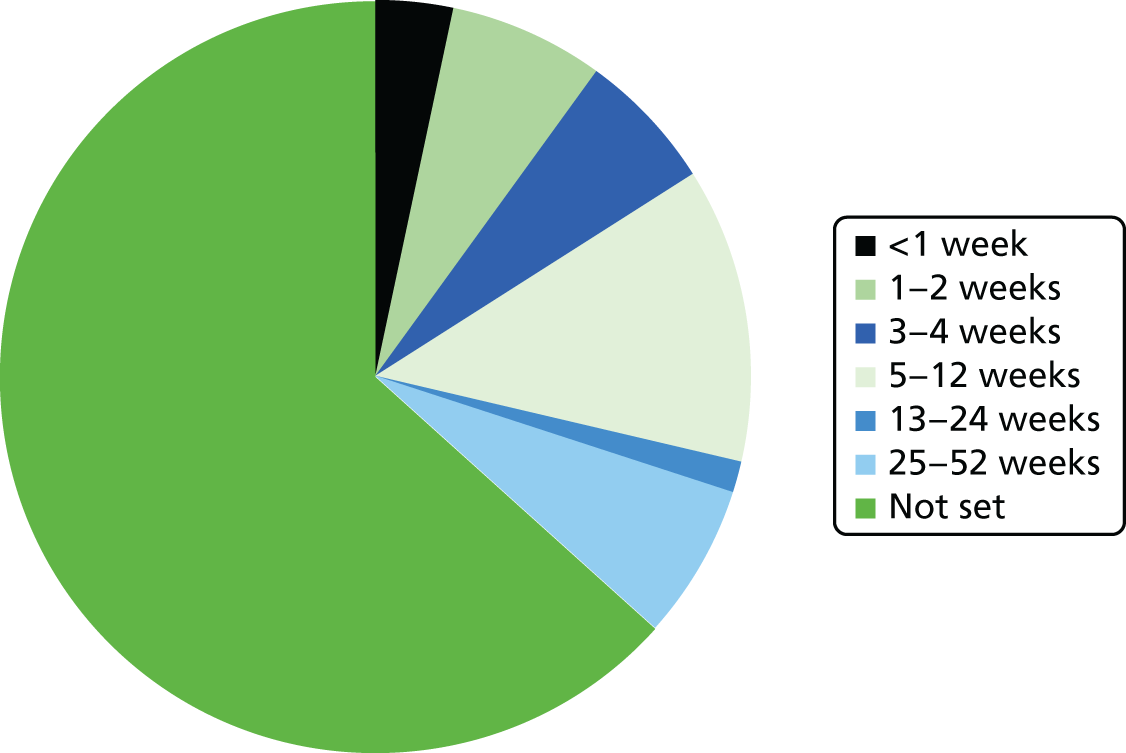
An initial review was set following 54 assessments (36% of the sample), but our auditor could find evidence of this having taken place in only 22 cases (14.7% of all OHSCAPs audited).
None of the reviews set for ≥ 13 weeks after the assessment was evidenced in the audit. This could indicate that some of the facilitators forgot to conduct reviews that they had set for the maximum of 6 months post assessment.
Figure 4 shows that, of the 22 facilitators who completed an initial review, only six set a second review. The second review was completed in all six cases, but only two were completed within the planned time frame. Only three third reviews were planned. All three were completed, but only one was completed on time.
Quality/extent of completion
The aim of this section was to assess the extent to which all questions and subquestions were addressed, and the level of detail of the information recorded. This could prove important at a later stage in terms of allowing another professional to be able to pick up the assessment and understand the prisoner’s needs.
As can be seen from Table 15, the majority of sections (relationships, activities, emotional well-being, medication and discharge planning) were most frequently assessed as being completed to a ‘good’ standard. Mobility and ‘other’ were most frequently considered to be ‘no problem’. However, the sections that were most likely to result in actual actions for prisoners and improve their outcomes (i.e. the care plan and the review) were most frequently rated as ‘not complete’.
| Area | Number of OHSCAPs completed | Completion score, n (%) | ||||
|---|---|---|---|---|---|---|
| Not complete | Poor | Adequate | Good | No problem | ||
| Relationships | 150 | 0 (0) | 15 (10) | 38 (25) | 83 (56) | 14 (9) |
| Activities | 150 | 0 (0) | 9 (6) | 55 (37) | 81 (54) | 5 (3) |
| Mobility | 150 | 0 (0) | 5 (3) | 31 (21) | 28 (19) | 86 (57) |
| Emotional well-being | 150 | 1 (1) | 30 (20) | 44 (29) | 61 (41) | 14 (9) |
| Physical well-being | 146 | 0 (0) | 25 (17) | 49 (33) | 40 (27) | 32 (21) |
| Medication | 146 | 0 (0) | 4 (3) | 33 (22) | 62 (41) | 47 (31) |
| Other | 146 | 0 (0) | 2 (1) | 4 (3) | 32 (21) | 108 (72) |
| Discharge planning | 146 | 6 (4) | 22 (15) | 44 (29) | 67 (45) | 7 (5) |
| Care plan | 144 | 81 (54) | 2 (1) | 3 (2) | 56 (37) | 2 (1) |
| Reviews | 142 | 68 (45) | 2 (1) | 20 (13) | 52 (35) | 52 (34)a |
Problem identification and response
In total, 194 problems were identified across all areas, but only 115 (59.3%) were translated into care plan actions. Proportionally, the areas where problems were least often addressed were discharge planning (35.7%), emotional well-being (41.2%) and mobility (51.6%). This is shown in Figure 5.
FIGURE 5.
Translation of identified problems into care plan actions by area of need.
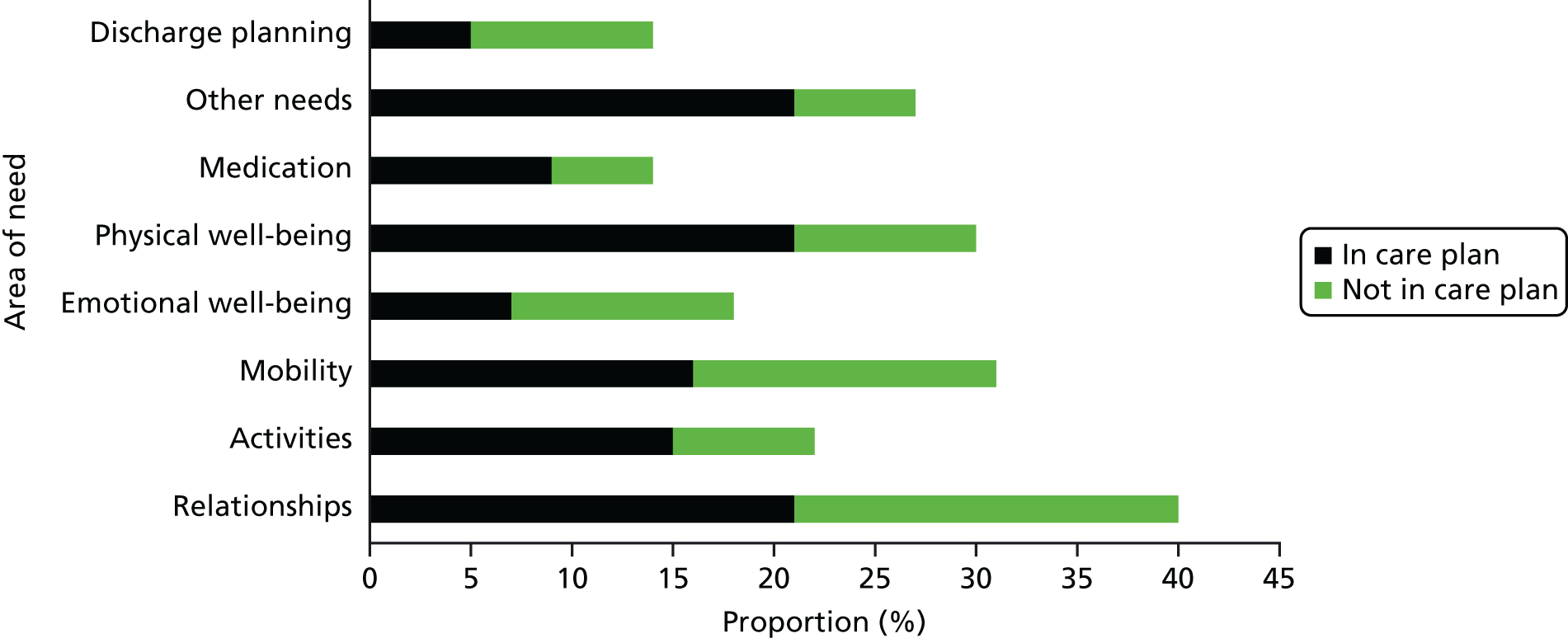
Relationships
In total, 40 problems were identified in this area, but only 21 (52.5%) were directly addressed in subsequent care plans.
Within the category of ‘other relationship needs’, issues identified included concerns for personal safety or family members, problems using prison telephones, financial difficulties, lost property and wanting transfers between wings or prisons. Only 16 out of 26 (61.5%) of these problems were addressed in care plans. Financial problems were the least likely to be addressed, with four out of five not translating into care plan actions. Two specific problems that were identified and not addressed are cause for particular concern. One assessment stated that the individual ‘doesn’t feel safe’ and another stated that the participant was ‘worried about children in general’, but neither of these problems led to actions in the subsequent care plan.
Activities
Across all subcategories, 21 problems relating to activities were identified. Of these, 15 (68.2%) resulted in a care plan action.
Mobility
Of the 31 mobility problems identified during the OHSCAP assessments, only 16 (51.6%) were actioned in the care plans that followed. Difficulties with getting in or out of bed were more often not addressed (63.6%) than any other type of problem within this category.
With regard to ‘other mobility needs’, a small majority (57.1%) were addressed in care plans, but difficulties that remained unaddressed included complaints of leg and back pain and swollen feet.
Emotional well-being
Only 7 of the 17 (41.2%) emotional well-being problems raised during assessment resulted in care plan actions. Difficulties sleeping were the most common type of problem reported (n = 7), and also the least often addressed (28.6%).
Half of the problems within the ‘other emotional well-being’ category were not addressed in care plans. These included reports of low mood, ‘concern regarding child contact’ and ‘lost mum and family doesn’t speak’.
Physical well-being
Within this category were five reports of difficulties with accessing health care, eight problems relating to glasses or contact lenses and 17 ‘other physical well-being’ concerns. With 70% of problems identified leading to a subsequent care plan action, physical well-being problems were addressed more often than any other type of problem. However, some concerning issues remained unaddressed despite the OHSCAP process, including five within the ‘other’ category relating to pain, a chest infection and a prisoner’s ventilator.
Medication
Over one-third (35.7%) of identified outstanding medication needs were not addressed through the care planning process. All of the issues that remained outstanding related to the appropriateness and/or timing of medication.
Discharge planning
The majority8,13 of problems in this area were not addressed during the OHSCAP care planning process. None of the identified financial concerns was actioned and only half of those relating to accommodation had corresponding actions in the subsequent care plan. ‘Other’ needs, including employment problems and concerns about relationships outside prison, were also apparently overlooked by facilitators.
Other needs
In total, 27 ‘other’ needs were highlighted in the final section of the OHSCAP assessment, and over 80% of these appeared in subsequent care plans. Problems relating to privileges, transfers, cell sharing and a request for suitable winter clothing were not explicitly addressed.
Actions taken according to facilitator role
Although there were no differences in the overall percentage of assessments that resulted in a care plan, notable differences can be seen according to facilitator role in terms of translating identified problems into care plan actions.
As can be seen in Figure 6, prison officer facilitators identified 157 problems in total, and addressed 83 (52.9%) of them during the care planning phase of the OHSCAP. Health-care staff facilitators identified only 37 problems, but went on to action 32 (86.5%) of them. The difference in the overall number of problems identified is likely to be a reflection of the number of OHSCAPs completed by each type of facilitator that were available for review. Only just over one-quarter of the OHSCAPs reviewed were completed by health-care staff. However, the vast difference in the proportion of problems that were addressed in care plans according to facilitator role is worthy of further consideration. It may be because of the familiarity of health-care staff with the care planning process or, to some extent, the type of problem encountered. Given that the OHSCAP is a health and social care planning tool, it may be that the health-care staff were better placed to address the majority of the issues raised.
FIGURE 6.
Needs translated into care plan actions by facilitator role.
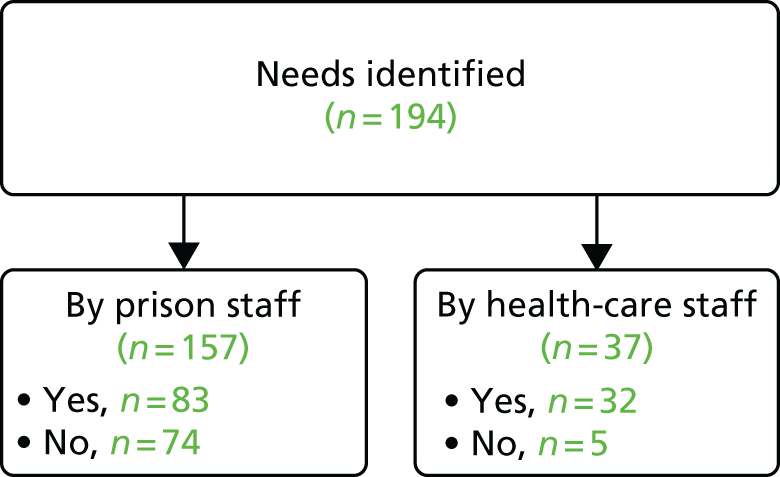
As can be seen from Table 16, the biggest differences between facilitators were in relation to emotional and physical well-being needs, which should be easier for health-care staff to address, given that this falls within the remit of their everyday role. Nevertheless, the reverse does not hold true in relation to prison officers and problems that could be considered more a part of their core role, with discharge planning being the area in which they least often addressed identified issues.
| Category | Facilitator role (%) | |
|---|---|---|
| Prison officers | Health-care staff | |
| Relationships | 54.1 | 33.3 |
| Mobility | 46.2 | 80.0 |
| Emotional well-being | 37.5 | 100.0a |
| Physical well-being | 57.9 | 91.0 |
| Medication | 50.0 | 83.3 |
| Discharge planning | 30.8 | 100.0a |
| Other | 71.4 | 100.0 |
These data may also support the impression that there were difficulties in partnership working, as well as in sharing information across disciplines. Theoretically, regardless of who facilitates the OHSCAP process, the built-in prompts for referrals within, and outside, the prison should mean that individuals’ problems are addressed by an appropriately qualified professional.
Referrals
As a result of the OHSCAPs reviewed, 36 (24%) individuals received a total of 48 referrals. Two individuals received three separate referrals, and eight were referred to more than one professional or team.
External
Only five external referrals were made across all of the 150 OHSCAPs and 65 care plans reviewed. One individual was put in touch with a solicitor, one with the probation service and three with housing support. No individual received multiple external referrals.
Internal
In total, 43 internal referrals were made. Table 17 shows them broken down by type.
| Referral type | Frequency |
|---|---|
| GP | 9 |
| Nurse | 3 |
| Psychiatrist | 1 |
| SMS/CARATs | 1 |
| Dentist | 2 |
| Optician | 4 |
| Other | 23 |
Within the ‘Other’ category, the most common referral was to a prison officer/wing staff (n = 6), followed by the equalities department, offender management unit and carers (presumably prisoner carers; n = 2). Other referrals documented included to reception, education, an anxiety group and remedial gym.
Referrals by facilitator role
Prison officer facilitators referred 23 individuals to 26 professionals. Only nine (34.6%) of these referrals were to health-care professionals. Health-care referrals were made by prison officers to a psychiatrist, GPs, opticians and the mental health in-reach team.
In contrast, health-care staff facilitators made 21 referrals in total for 13 individuals, with 15 (71.4%) of them being to health-care professionals. The ‘non-health-care’ referrals they made included education, the kitchen (participant’s workplace), the offender management unit and the gym.
Care plan actions
The number of needs identified within each care plan ranged from zero to six, with the mean and median being 2. Almost half (44.6%) of the OHSCAPs that resulted in a care plan only identified one need to be addressed.
Completion of the care planning section of the OHSCAP was generally poor, with either zero or one care plan action being allocated a member of staff to complete in over 70% of the care plans generated. Furthermore, in the vast majority (89.2%) of care plans, none of the care plan actions was time-limited, as no planned completion date was recorded. In all but nine (16.9%) of the 65 care plans reviewed, a review date was set against each individual care plan action generated. However, in 80% of these cases, no rationale was provided for the review date of any actions.
Encouragingly, in 149 of the 150 OHSCAPs reviewed, the auditor felt that sufficient information was documented for care to be continued effectively by a professional who had not been present during the assessment interview.
Inter-rater reliability
Inter-rater agreement was fair in relation to two areas of need (activities and physical well-being) and good in four of the other areas (Table 18; applying interpretations of Cohen’s kappa provided by Altman96).
In the final two areas of need, Cohen’s kappa could not be computed as a result of one of the raters’ responses being constant across all cases. Analysis of the percentage of cases’ scores on which raters agreed revealed that in relation to both areas of need, agreement was 86.7% (13 out of 15 cases).
| Area of need | κ | 95% CI | Significance |
|---|---|---|---|
| Relationships | 0.741 | 0.486 to 0.996 | 0.000** |
| Activities | 0.302 | 0.006 to 0.598 | 0.008* |
| Mobility | 0.643 | 0.018 to 1.268 | 0.001* |
| Emotional well-beinga | – | – | – |
| Physical well-being | 0.348 | 0.158 to 0.538 | 0.002* |
| Medication and treatmenta | – | – | – |
| Other issues | 0.648 | 0.360 to 0.936 | 0.000** |
| Discharge planning | 0.706 | 0.343 to 1.069 | 0.004* |
Summary
The audit of completed OHSCAP assessments and care plans highlighted several problems with completion of the document; although the assessment part of the document was often completed well, there were key problems with care planning and review processes and with information sharing. The evidence obtained during the audit process overwhelmingly suggests that the OHSCAP was not implemented as intended.
The OHSCAP assessments were completed later than recommended, meaning that prisoners had sometimes been in the establishment for almost 2 months before the assessment took place. The impact of the intervention is likely to be diminished when its delivery is significantly delayed, as prisoners may access the standard, albeit often slow, processes for resolving their problems instead.
The assessment section of the OHSCAP was completed to at least a satisfactory level in the majority of cases audited. However, despite outstanding needs being successfully identified, they were not consistently translated into appropriate care plan actions. Considerable differences were observed between facilitators according to their core role, with health-care staff demonstrating that they were more comfortable than their prison officer counterparts with the care planning process. When care plan actions were generated, they were not followed up with timely review in the majority of cases, or if they were, this was not documented in the paperwork. In either case, when needs are identified but no action is taken to resolve them, or no follow-up is completed to establish if the actions taken have been successful in addressing needs, any potential impact of the OHSCAP process is likely to be undermined.
There is a lack of evidence to suggest that participants were involved in the care planning process, despite the OHSCAP training manual highlighting the importance of this. However, it must be acknowledged that this finding may just reflect a lack of clear documentation of prisoner involvement rather than a lack of actual involvement in the process per se.
Finally, issues that indicated difficulties in collaborative working across disciplines within the prison study sites became apparent during the audit process. Facilitators clearly struggled to share copies of the assessment across health-care, prison and probation service systems. In addition, they made more referrals and resolved more unmet needs when the area of need fell within the remit of their core role, and very few external referrals were made. Within this context of individuals or teams in key roles working in isolation, it seems unlikely that the OHSCAP will realise its full potential as the multiagency, problem-solving approach it is intended to be.
Chapter 6 Qualitative methodology
Background
There has been an increase in awareness of the importance of qualitative research methods and process evaluation within RCTs seeking to assess the effectiveness of health and social care interventions. 97,98 When meaningfully integrated with quantitative data, nested qualitative studies can provide an in-depth understanding of the issues surrounding the intervention. For example, qualitative interviews can provide explanations for any differences in the quantitative data across sites. 97 Consequently, semistructured interviews with older prisoners who had received the intervention were conducted to gain an understanding of the facilitators and barriers involved in delivering the OHSCAP. It was essential to go beyond just developing a list of barriers and facilitators. It was necessary to ensure that an in-depth understanding of the social context and relationships affecting the successful implementation of the OHSCAP was obtained. 99 Process evaluation is essential for understanding and accurately documenting how interventions work in practice and understanding why certain aspects are effective or ineffective. 100
Sample
Semistructured interviews were held with staff delivering the intervention (seven health-care workers and five prison officers) to gain an understanding of the processes used. It was important to ensure that a range of roles were included. Additionally, a purposive sample of prisoner participants who had received the OHSCAP were interviewed (n = 14). Prisoners from all of the 10 sites were interviewed and attempts were made to include prisoners with a range of ages and health and social care needs.
Semistructured interviews
The interview guide format followed the OHSCAP process itself to ensure that all relevant issues were covered. For example, the interview guides covered the process of coming into prison, the OHSCAP assessment, the development of the care plan and any reviews that took place. When possible, the interviewer let the interviewee lead the discussion and the interview guide was used only as a prompt to ensure that key issues were discussed. In line with an inductive approach, further questions were added to the interview guide as key issues arose during the first few interviews. The interview guides are included in Appendix 6. An asterisk has been used within the interview guides to indicate when additional questions were added as a result of data generated from initial interviews. The qualitative interviews were conducted over a period of time when prisons were experiencing changes as a result of severe reductions in staff numbers. This constant revisiting of the interview guide was therefore essential.
Prisoners were interviewed between one and four times. We attempted to interview prisoners as soon as possible after they entered the prison, then immediately after they had received the initial OHSCAP and, when they remained in prison, we went back to interview them at key time points according to the nature of their health and social care needs (see Chapter 2, Procedure, Consent for details of the informed consent process).
All interviews with staff were audio recorded and lasted for approximately 1 hour. On three occasions, two staff interviewees from the same prison were interviewed in tandem, at their request. It was not possible to audio record interviews with 6 of the 14 prisoners as a result of security restrictions. In these instances, two researchers attended the interviews and, when possible, detailed notes were made. Initial interviews with prisoners lasted for around 1 hour; however, subsequent interviews were often much shorter as prisoners often reported that little had changed.
Data analysis
All interviews were analysed thematically. Thematic analysis was adopted because it is simple, flexible and has the ability to generate findings that are accessible to practitioners and policy-makers. 101 A framework method (a specific form of thematic analysis) was used. 102 The framework method produced a matrix of summarised data, which provided a structure to analyse and reduce the data. It also allowed systematic constant comparisons across cases to refine themes.
Gale et al. 102 proposed a seven-stage framework approach that was followed within this study. Stage 1 involved transcription of the data. Transcriptions were produced by professional transcribers for pragmatic reasons. Transcriptions were produced in vivo; however, the focus was on content rather than pauses and tone. During stage 2, the researchers conducting the analysis familiarised themselves with the whole interview. Coding commenced at stage 3 of the process, and the first few transcriptions were coded by two researchers. This involved applying a label that described the aspects of the transcripts that were considered to be important. Codes included behaviours, incidents, structures, values and emotions. The coding classifies the data so that they can be systematically compared. The coding was conducted using the computer software NVivo (version 10; QSR International, Warrington, UK) to assist with the organisation of the data. Stage 4 included developing a working analytical framework. After the initial few transcripts were coded, a set of codes were developed that were applied to the analysis of all subsequent transcripts. The constant comparison method was used to achieve this. Constant comparison methods involve both the fragmenting and the subsequent connecting of data. Data are coded and separated from their original interview transcript. Extracts are then compared and combined with other fragments until connections are made to help the researcher understand the overall picture of what the interviewee has said. Numerous adaptations were made to the analytical framework throughout the analysis process until no new themes emerged. An ‘other’ category was developed to include data that did not fit the analytic framework, and this was revisited a number of times. The analytical framework was then applied to all subsequent transcripts using the existing categories and codes during stage 5 of the analysis. During stage 6, framework matrices were developed in NVivo and data were charted into the matrices. This involved summarising the data by category for each transcript. It was important to try to achieve a balance between reducing the data and maintaining the meaning of the data. The chart will include references to illustrative quotations. The final stage, stage 7, is concerned with interpreting the data. Impressions, ideas, and early interpretations of the data will be noted throughout the data generation and analysis process. Analytical memos were written and discussed with the wider research team throughout the data collection and data analysis process.
A key benefit of this approach, in comparison to other forms of thematic analysis, is that the context of participants’ data is not lost. The framework approach is not limited to a particular epistemological, philosophical or theoretical approach, but is a flexible tool that can be utilised within many different types of qualitative studies. It was useful for this study because it allowed the inclusion of some key predefined themes and allowed others to be developed through the data. The research team wanted to ensure that they learned about the OHSCAP process and, therefore, included the predefined themes of facilitators and prisoner involvement. ‘Facilitators’ was included as a predefined theme because the use of prison officers in delivering health and social care initiatives was novel and it was important that we captured the acceptability of this. ‘Prisoner involvement’ was included because, within our previous work, this was considered to be an important aspect of the intervention.
Chapter 7 Qualitative findings
Semistructured interviews were held with staff delivering the OHSCAP, including prison officers (n = 5) and health-care staff (n = 7). All five prison officers were part of wider safer custody or diversity and equality teams. Three had the specific title of DLO. The health-care workers interviewed included health-care assistants (n = 3), general nurses (n = 2) and a mental health nurse (n = 1).
Additionally, semistructured interviews were held with 14 prisoner participants who had received the OHSCAP. The prisoner participants ranged in age from 50 to 69 years (mean = 58 years). Their index offences were sexual (n = 5), drugs (n = 5) and other (n = 4). The majority had been imprisoned between one and eight times previously (n = 11). Two of the prisoners had not been incarcerated previously and one had been imprisoned on > 10 previous occasions.
The findings from the semistructured interviews with staff who delivered the OHSCAP and prisoners who received it are discussed below. Illustrative quotes of broader themes are provided. Where possible, illustrative quotes from prison staff, health-care workers and prisoners themselves are presented.
Four superordinate themes emerged from the data, namely the broken prison system, rigid prison processes, prisoner and staff relationships and the OHSCAP procedure itself. A number of subthemes for each of these key themes are described (Figure 7).
FIGURE 7.
Overview of subordinate themes from qualitative interviews with prisoners and staff.
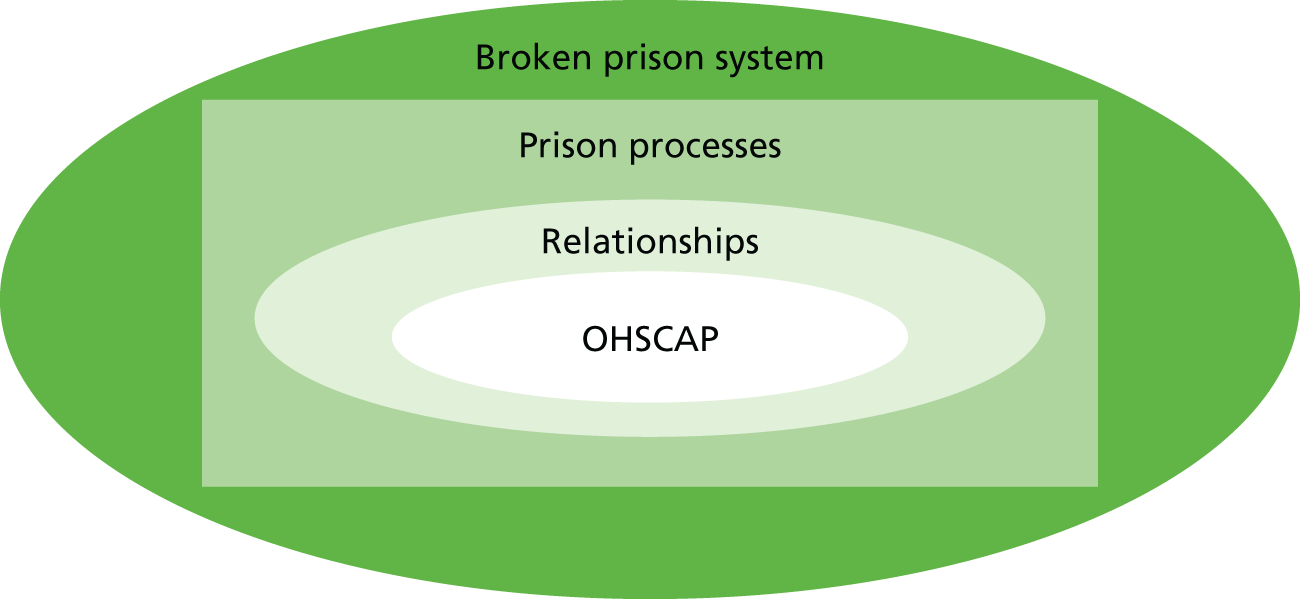
Theme 1: ‘broken’ prison system
The most recurring theme that emerged from the data was the perceived ‘broken prison system’. Participants reported that recent drastic reductions in the number of prison officers were causing serious concerns and having a detrimental impact on the functioning of the prison system. Participants explained that the staff reductions had occurred as a result of the ‘benchmarking’ programme. This initiative involved changing the prison regime in order to reduce staffing and associated costs. This was deemed, by both prison and health-care staff, to be having a negative impact on the care of prisoners of all ages. It was also causing serious problems for staff members, which are reflected in the following subthemes: staff shortages, job satisfaction and unmet basic needs.
Staff shortages
Prison officers described a staffing crisis across the prison estate. This was considered to have had an impact on day-to-day prison practices, as illustrated by this prison officer’s quotation:
The staffing levels are just ridiculous, to be honest, every day there’s a wing shut down because there’s no staff, prisoners are noticing it, prison officers are stressed, it’s dangerous at the minute, to be honest, the staffing levels.
Prison officer 3
All of the prison officers delivering the OHSCAP were based within wider safety custody and diversity teams. These teams conducted a variety of tasks to support prisoners. This included monitoring prisoners who were at risk of suicide and self-harm, resolving bullying issues and assessing the needs of prisoners with disabilities. The prison officers described how they were frequently redeployed to general wing security duties, resulting in them being unable to appropriately support vulnerable prisoners:
I’ve had probably 10 hours in my job this month in 23 days. Ten hours and you’re just playing catch-up all the time and that’s when you start missing things. I like. I love this job, or like/love. If I could do it properly but I don’t feel I can do my job properly. It’s redeployment, it just, it messes you up.
So how much notice would you get if you’re going to be redeployed?
About a minute.
Prisoners also discussed how a shortage of prison officers had an impact on the care they received and how implementing initiatives such as the OHSCAP were consequently given a low priority:
If it’s [implementing OHSCAP] relying on prison staff, they’re so short of staff, I think things like that would be bottom-drawer stuff.
Prisoner 4
There were also staff concerns across health-care departments within a number of the prison establishments involved in this study:
Well, when I first went one of the sisters was leaving, the other sister was on long-term sick. There was a couple of bank staff. We were working on, sort of, sometimes just on one nurse a shift with one HCA [health-care assistant], sometimes two nurses a shift and one HCA. And we had clinics all day and went to the emergencies, and it’s very poorly staffed.
Health-care worker 2
The staff shortages across health-care departments were considered by health-care staff to be a result of high sickness levels and also difficulties and delays in recruiting new staff:
They’ve shortlisted about three or four [health-care worker candidates] each time, there have been three sessions and not one’s turned up. Another one last week, last Monday, there were supposed to be four coming for band 5 nurses, no one showed up.
Health-care worker 10
Job satisfaction
Strikingly, 6 out of the 11 staff participants we interviewed were in the process of leaving their job role, three of whom were leaving the prison service altogether. Many referred to the current staffing crisis as an explanation for their departure. Staff members stated that there was low morale among the workforce as a result of the recent drastic reductions in staff numbers and the added pressures this placed on them. As one health-care assistant surmised:
I think we’ve got quite low morale haven’t we at the minute, in the health-care staff.
I’m totally disillusioned by it all.
And the prison staff aren’t happy, I think as well, ‘cause they’ve had a lot of changes so they’re feeling very negative about things, and it has a knock-on effect really doesn’t it?
Staff members stipulated that staff shortages were having a negative impact on their health. Prison officers and health-care staff described how staff shortages were causing high levels of stress among their colleagues, resulting in high levels of staff absence:
Staff are stressed, sickness has gone up massively. Plus you’re doing three people’s jobs instead of one person’s job and you can’t, it’s a lot to deal with, it’s a lot to deal with.
Prison officer 3
Prisoners had also noticed the high levels of stress among prison officers, and this led them to be less likely to request support or approach prison officers for advice. As one prisoner described:
On [A] wing I had a very hard bed, good for my back. It was a brand new mattress, downstairs but this one is very old. They don’t come in to ask how I am, they don’t care. If you ask too much, the officers go angry because they had too many people come asking, all complaining.
Prisoner 7
Some prison officers expressed concerns that the current prison environment was a dangerous place to work. Consequently, staff would prioritise remaining safe over meeting prisoners’ health and social care needs:
I think some people [prison officers] kind of come in and just think, as long as I go home at the end of the day safe then it’s alright.
Prison officer 8
Basic needs unmet
Both prisoners and staff described how current staff shortages were resulting in prisoners’ basic needs (such as access to showers, socialisation, etc.) frequently not being met:
Well, because we’ve put lots of security reports in, we’ve heard the prisoners saying that’s it going to go off soon because they’re always locked behind their doors because they’re getting back from work, they’re getting locked up, they’re not even able to have a shower, make a phone call, it’s all those little things that mean a lot to people. And if those things are taken away from them, I mean things like showers it’s a basic human right being able to wash especially if you’ve been in, say for example, the kitchen where it’s hot and sweaty all day and stuff.
Prison officer 3
One prisoner, who suffered from mobility difficulties, endorsed the prisoner officers’ perceptions. In this excerpt, he describes how a lack of available prison officers to take prisoners to a suitable, safe shower facility meant that they were unable to have their basic hygiene needs met:
I’m using wet wipes to shower still. There is a wet room on A wing and they [prison officers] say they’ll give me access but it’s when they’ve got time on their hands.
Prisoner 8
Theme 2: prison processes
Participants discussed how rigid prison processes impeded the meeting of older prisoners’ health and social care needs. Subthemes encompassed being process focused, the existence of prison and health-care ‘silos’, discontinuity of care and perceptions of service provision.
Process focused
Throughout the interviews, both prison and health-care staff focused on describing the processes they adhered to rather than addressing individuals’ needs. Frequently, staff would continue to refer back to the recognised process even if this was failing to meet prisoners’ needs. This appeared to be a survival tactic for dealing with the challenging prison environment. This focus on process is captured in the transcription of an interview with two health-care workers described below:
Yeah, some of the lads [prisoners] obviously didn’t have their medication when they first came in, but that’s because of processes that we’ve got, it can take up to 2 weeks.
They’re quite upset about it. But obviously it was sorted in the end. But I agree with them, why should they have to go without their medication basically. It’s been an ongoing issue for a long time.
Right, and is there anything you can do to speed things up?
It’s just the process.
I mean the process is the process.
One prisoner also described how prison staff focused on processes, stipulating:
They come out with pathways this and pathways that but I don’t think any of them could find a path up their own garden.
Prisoner 4
Applications, frequently referred to as ‘apps’, were described as the written process by which prisoners could access help or support while incarcerated. Prisoners detailed how officers often simply told them to complete an application for every aspect of support they required, without listening to their needs:
Oh yeah, ‘put an app in. See you in a week’. No one’s really interested.
Prisoner 9
Reflecting the quotation above, prisoners stated that they would frequently not get a response from an ‘app’ or would experience long delays:
I’ve gone into the office sometimes and said ‘how do I get . . . ?’ – ‘put in an app’. I put one in and I get no response.
Prisoner 4
Although there were, reportedly, ‘processes’ to manage and address prisoners’ health and social care needs, participants stipulated that the documented processes were often not adhered to in practice, as one health-care worker explained:
On the [staff] induction they actually told us about . . . well it sounded all wonderful, about how they were helped and how they were helped with housing and work, but what most of them say, the older ones [prisoners] that I’ve spoken to, it’s not true, it doesn’t happen. You’re just told where you’re going to go, you’re allocated somewhere far away from where you come from, away from any sort of family network.
Health-care worker 2
Prison and health-care ‘silos’
Staff members and prisoners considered prison issues and health-care issues to be very separate, and prison staff and health-care staff did not generally appear to work collaboratively to support older prisoners:
And one [prisoner] . . . he’d lived in children’s homes all his life and he’d had a girlfriend that had died and he had nothing to support him on the outside, and he really didn’t want to come out of prison. So I really didn’t know what to do about that. I didn’t have enough experience with the prison to know about that, and unless it’s a safety issue we’re not allowed to share that sort of information with the prison side of it.
Health-care worker 4
However, there was some evidence that the introduction of the OHSCAP had begun to support the development of positive working relationships between prison and health-care staff:
And it [attending the OHSCAP training] made it easier as well, to bridge the gap, when I’m going to get it on SystmOne; I can say, [health-care worker’s name], can you put this on SystmOne for me please; because I don’t really know many of the nurses very well, because I don’t work with them. I know their names, but I don’t really know them very well to talk to; so many people that work in there.
Prisoner officer 6
Both staff and prisoners stipulated that there was a lack of accountability for resolving prisoners’ social care needs, resulting in needs remaining unmet. For example, one health-care worker described the difficulties they experienced when trying to meet the prisoners’ needs identified during the OHSCAP, as a result of a lack of accountability:
There is a wheelchair based in the centre but the brake broke so we could not use it. You ask people to look into it and no one gets back to you.
Health-care worker 5
Discontinuity of care
Prisoners described their frustration at not being able to resolve their concerns in relation to both prison and health-care issues, as a result, at least partly, of inconsistent staffing:
You don’t see the same person [GP] more than once. It’s a lucky dip. You don’t know if you’re coming or going.
Prisoner 8
My problem is I have a bad leg, had an operation, pain all down the side, leg and back. I have been on the top bunk for one week. There is another cell empty, single one, so people say why don’t I ask for it but I don’t get the chance. I showed the officer here my letter [from the GP], but nothing happens. What happens here is you show one officer one day, then next day he’s not here, so you start again, explain again to another officer.
Prisoner 7
Perceptions of service provision
There were many examples of perceived poor service provision, including delays in seeing a GP and receiving medication; limited appropriate education opportunities; a failure to organise home leave (where applicable); being located far from family, impeding visiting opportunities; and a lack of input from offender managers and psychologists. Prison induction procedures were also deemed to be suboptimal by both prison staff and prisoners. An illustrative example of a quotation regarding the limited induction procedures is provided below:
It’s like being transported back to the dark ages sometimes. It’s helplessness. If you’re not depressed when you come in, you are when you get out. I feel like I’ve been fighting all the time. [During induction] they should tell you who you can see for help and how to access services. What they tell you [during induction] is very limited – ‘go to the kiosk . . . ask one of the cons [prisoners]’.
Prisoner 8
In addition, all prisoners should reportedly be allocated a personal officer. However, many had never met theirs:
I haven’t had a chance to speak to my case officer since I’ve been here. I saw him once after I searched him out but he’s been on another wing. His job as a personal officer is redundant, made redundant by their absence.
Prisoner 1
There were also some examples of what was perceived to be a good standard of health-care service provision, particularly in relation to prisoners with complex or serious health concerns:
I’ve never had so much health-care as I have in here. It’s been very good. They do look after you.
Prisoner 1
One prisoner felt it was unlikely that the OHSCAP facilitator would identify any health concerns that the health-care department had not previously detected:
The health-care department in here is very good. The health care up the top there is very good. They’re on top of everything. I don’t think [OHSCAP facilitator] would pick up much that they haven’t found before him.
Prisoner 9
Theme 3: prisoner and staff relationships
The relationships between staff and prisoners played a vital role in the functioning of the OHSCAP. Subthemes included a lack of interest in social care needs, supporting only ‘genuine’ issues and ‘walking on egg shells’.
Uninterested in social care needs
Prison officers inadvertently described how they did not believe that social care needs to be particularly important, as illustrated in the quotation below. Consequently, they were less interested in supporting prisoners with social care issues than they were with concerns that had more traditionally been considered to be the responsibility of prison officers:
Well, I just consider working on the wings like the actual bread and butter of the job, that’s why you join the job, to be on the wings and dealing with issues. But it’s not issues like ‘can I have a new flask because I can’t open mine properly’, or . . . you know, because we do get that; or, ‘can I have a sock aid to help me get my socks on because I can’t bend over properly’; it’s proper issues, like ‘I need to ring my mum because she’s not well’ and ‘I’ve got no money on my PIN [a person’s individual payphone accounts], can you sort this for me’; ‘I can’t get this person cleared for a visit, can you help me’; or just the general day-to-day of supervising the prisoners, making sure they’re not up to no good really.
Prison officer 6
Some prisoners described how they felt that prison officers lacked insight into the social care issues faced by older prisoners. For example, one prisoner described his experience of mandatory drug testing:
I have to stand up for an hour or so because the seat isn’t anywhere near the wall to lean back on. I’ve told them before that I need a seat to sit on but they won’t give me one.
Prisoner 5
One prisoner stipulated that officers failed to consider the varying nature of his illness but highlighted that, when officers were responsible for caring for fewer prisoners, they were able to better meet his needs:
I have ups and downs. They don’t understand that I can have good days and bad. I finally got to the library once and it’s caused me grief ever since. I’m being penalised for going to the library ‘cause they now expect me to be able to walk everywhere. On [other wing] they had more understanding, a smaller wing – they know you better.
Prisoner 8
Support for ‘genuine’ issues
There were many occasions when staff were reportedly supportive of prisoners’ needs. This appeared to happen only if staff perceived the need to be genuine and usually of a serious nature. For example, when prisoners were considered to be at risk of suicide or self-harm, there were examples of staff developing positive, supportive relationships with prisoners:
The officers are good. They’ve been coming to see if I’m ok because I’m on an ACCT, this is the system used to provide monitoring and support to those considered to be at risk of self-harm.
Prisoner 5
A further example was provided by one prisoner, who had reportedly been given Spice (a synthetic cannabinoid substance) unwittingly. He described how he had attempted suicide after this event but, after receiving support from officers, was no longer experiencing suicidal thoughts:
‘Cause some people were giving me Spice and I didn’t know what it was. People just gave me, like, a rollie [rolled-up cigarette] and I smoked them and I went under. I nearly died. And then tried to kill myself . . . Well . . . you’ve got to get on with them [prison officers], haven’t you. It’s where you live ‘til you get out. ‘Til you get out those gates you say to yourself, they’ve looked after me, do you know what I mean? Now if those officers weren’t here, you know, they’d turned their backs, I wouldn’t be sitting here now . . . Like, that SO’s [senior officer’s] done a lot for me.
Prisoner 14
‘Walking on egg shells’
Within open establishments, prisoners can walk around relatively freely within the confines of the prison, without being reliant on prison officers unlocking doors. Prisoners residing in open prisons may also be eligible for home leave. Both prisoners and prison officers described how prisoners housed in open prisons were ‘walking on egg shells’ as a result of not wanting to lose their right to home leave or be returned to closed conditions. This inability to raise concerns freely within open establishments was the most striking difference between sites in relation to how the OHSCAP works in practice. Within closed conditions, there are far more security restrictions and prisoners are locked in their cells or on a prison wing without freedom of movement for longer periods of time. These concerns prevented prisoners from raising any issues with staff:
And you’re then in a situation where you can’t create a fuss over it . . . Because anything that they give you can always be taken off you . . . I’ve done it [raise concerns] in the past . . . Doesn’t get you nowhere. Just another rod for your own back. That’s all’s it is.
Prisoner 9
One prison officer stated that this reluctance to raise concerns in open establishments was particularly pertinent to discussions around safety:
And the stupidest question of the lot [within the OHSCAP], is, do they feel safe? Because they’re always going to say, yes, I feel safe . . . Because if they don’t feel safe, they wouldn’t be in open conditions, they’d have to go back to closed conditions. Where they get protection. We don’t offer any protection.
Prison officer 1
Theme 4: the OHSCAP process
The final key theme referred to the specific details of the OHSCAP process itself. Subthemes comprised prison officers not being ideal facilitators, ‘going above and beyond’ and prisoner involvement.
Facilitators
A recurring theme was that it was perceived to be inappropriate that prison officers were OHSCAP facilitators. Over half of the participants expressed concerns about prison officers leading the process. Concerns were expressed about knowledge, trust and confidentiality:
At the end of the day, they’re still in uniform aren’t they? And she [prison officer] could go and say to another officer, ‘oh, he doesn’t like this place’, and all that, like, they do.
Prisoner 2
However, some prisoners did consider it acceptable for officers to deliver the OHSCAP:
It doesn’t matter who it is as long as I can speak to someone when I need to. I’ve nothing to hide about my health have I?
Prisoner 5
No real pattern could be identified regarding the characteristics of prisoners who considered it acceptable for prison officers to deliver the OHSCAP. Their perspective was influenced by a complex set of factors, including their previous experience of prison officers, the personalities of the prison officers in question and the nature of the prisoners’ health and social care needs. Some prisoner participants stipulated that they were able to build trust over time with prison officers:
I get on OK with the officers, I know them well.
Prisoner 5
Other prisoners felt that their experience of prison had taught them not to divulge information to prison officers:
In the days of old, I would have been very disquieted but after a while, you learn that some things are best kept under your hat. It’s not wise to blab everything the first time you see someone. I wouldn’t want to talk about personal things . . . not to an officer because I’ve seen officers elsewhere use knowledge and position to dehumanise or belittle prisoners in front of others.
Prisoner 4
Prison officers did not generally perceive there to be any concerns with them delivering the OHSCAP:
I’ve had no negative reactions to me being an officer.
Prison officer 1
Some prison officers lacked skills in conducting assessments. One prison officer described how she shadowed a colleague to support them conducting the OHSCAP (both members of staff had previously attended the training):
The actual assessment is really self-explanatory, the fact that you’ve done all the example questions; I mean I fly through them now. When I went with [prison officer colleague] and she said, ‘can I shadow you doing one’ . . . ‘No’, I was shadowing her, she said, ‘well, you can watch me because I’m nervous’, I don’t know how; I says, ‘it is easy’, you just ask all the questions that are on there; ‘oh, please, come with me’. And I could see that she was struggling, so every now and again I were jumping in; and afterwards she went, ‘oh, it’s just so easy for you, isn’t it, you could just do it straightaway’; I went, it’s not that, I says, I’ve done more than you, that’s all . . . But all I do is ask all the questions that are on there.
Prison officer 6
‘Above and beyond’
There were occasions when some OHSCAP facilitators clearly went ‘above and beyond’ what was normally expected of them in their role. For example, some officers created ‘distraction packs’ (paper packs including crosswords, word searches, etc.) to prevent boredom and potentially depressive symptoms. There were examples of health-care workers who were OHSCAP facilitators making GP appointments for prisoners on release and organising repeat prescriptions for older prisoners who were confused by the system. There was one example of a health-care worker telephoning the health-care department of the establishment where prisoners were previously held, in order to locate their glasses and have them sent to them to prevent them having to put in a new application with months of delays. One health-care worker described how she introduced an older prisoner to other prisoners in an attempt to make him less isolated:
I would introduce the chap so he could make friends. Especially on A wing, they all sit around in a group, you know, and I took him over and introduced him to people . . . I think it’s just . . . putting that foot forward, isn’t it, sometimes?
Health-care worker 3
These examples of going ‘above and beyond’ were reportedly relatively rare and the majority of identified needs would simply be fed back into the prison systems through the applications procedure, as previously discussed:
I didn’t find it [the OHSCAP] helpful because they didn’t go over anything more than you [the researcher]. It felt like a double-up. No useful information apart from saying I’d have to put ‘apps’ in. They [prison officers delivering the OHSCAP] didn’t say they could help with anything.
Prisoner 4
Frequently, prisoners reported being told that there was nothing that could be done to help them and nowhere to refer them to. This was particularly evident with financial and housing concerns:
I ended up passing him on to his solicitor, because there was nobody in the prison that can help him with that [housing]. Yeah, it’s a separate issue to the fact, completely separate to prison service, so there were nobody that could help him; I said, you’re going to have to get a solicitor to help you with it.
Prison officer 6
Prisoner involvement
There was an apparent lack of genuine prisoner involvement in developing the care plans. One prison officer described his attempt at involving prisoners in the development of the care plans. However, he appeared to have a lack of understanding of what genuine prisoner involvement would involve, and discussed how he simply informed prisoners what would happen instead of meaningfully collaborating with them to involve them in decisions:
I always tell him [prisoner] what we’re going to do, if he’s happy with what we’re going to do, and would he mind if we went ahead and did it. And that’s it [how they involved the prisoner in the development of care plans].
Prison officer 1
However, prisoners greatly appreciated the rare opportunity to talk to someone about their needs, even when little was done to try and address these needs. As one prisoner explained:
Blimey, after 15 years, someone is finally taking notice that I’m here.
Prisoner 4
The OHSCAP facilitators also recognised that prisoners appreciated the opportunity to be listened to. Prison officers described how the OHSCAP process became an isolation prevention tool:
So generally even if people didn’t have issues they’d still say it was nice to chat to somebody. I don’t know if it’s made that much difference to their needs, to what I could help them with, but in general as an isolation tool, I suppose, I think that’s been the positive things and being able to chat to them because it’s nice to chat to someone and then I’ve linked to others who maybe feel a bit isolated, can you ask one of the cleaners or a carer just regularly check up on him and that kind of stuff.
Prison officer 1
Comparisons of prisoner participants’ transcripts over time
Comparisons between prisoner participants’ earlier transcripts and those conducted at a later date revealed that little had changed. The majority reported that their health and social care needs remained unmet. Some had experienced new problems. The majority, however, had not seen the OHSCAP facilitator more than once to review the meeting of their health and social care needs:
I don’t remember the process anymore (OHSCAP) but it did just stop. No one came to see me again.
Prisoner 4
Some described how the issues raised at their initial OHSCAP session remained unmet:
I brought a [walking] stick in but wasn’t allowed it because it had a point. I asked [OHSCAP facilitator] when I saw her at visits last week if she could sort it or come out and measure me for a stick. She said she’d come to see me but hasn’t yet. That’s the only time I’ve seen her since the beginning.
Prisoner 5
Summary
The OHSCAP was being delivered within a prison system that was perceived by prisoners and staff to be in crisis. This acted as a fundamental barrier to the successful implementation of the OHSCAP. The ‘broken prison system’ was considered to be creating a multitude of pressures and the staff shortages were reportedly making initiatives, such as the OHSCAP, difficult to deliver and low priority. Rigid prison processes including a lack of real partnerships between prison and health-care staff impeded the OHSCAP process. Relationships between staff and prisoners were also crucial in determining whether or not meaningful discussions could be held to address older prisoners’ health and social care needs. Prison officers’ lack of insight and interest in the social care issues faced by older prisoners often hampered the process. There were, however, examples of support for what were considered to be ‘genuine issues’. Overall, prison officers were not considered to be ideal facilitators of the OHSCAP. Facilitators with appropriate knowledge and skills, who could prioritise the role, were lacking. There were examples of OHSCAP facilitators going beyond what is normally expected within their role in order to meet older prisoners’ needs, and prisoners greatly appreciated the experience of being listened to during the OHSCAP process.
Chapter 8 Cost-effectiveness methodology
Introduction
A within-trial cost–utility analysis of the OHSCAP compared with TAU was conducted as part of the trial. The economic evaluation presented in this chapter was conducted from the public sector perspective, incorporating costs borne by the NHS, personal and social services, criminal justice system and education authorities. This perspective is recommended by NICE for interventions with health and non-health outcomes in the public sector and other settings. 93 The economic analysis estimates the incremental cost-effectiveness of the OHSCAP compared with TAU to evaluate whether or not its implementation would represent a cost-effective use of resources at standard UK willingness-to-pay thresholds.
Methods
Outcome measures
The primary outcome measure for the economic evaluation was HRQoL, as measured by the EQ-5D-5L. 91 The EQ-5D-5L is a generic preference-based measure of HRQoL covering five domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. This new version was developed as a result of concerns over the original EQ-5D-5L’s lack of sensitivity to change, and consists of five severity levels for each domain: no, slight, moderate, severe and extreme problems. Participants’ responses were converted to a single index utility value based on preference weights obtained from an English general population sample. 103 These utility values facilitate the calculation of quality-adjusted life-years (QALYs), which form the outcome of the economic evaluation, using the area under the curve method.
The EQ-5D-5L was administered during interviews with participants, with the questions read out and responses recorded by the interviewer. There is a dearth of cost-effectiveness research in the prison setting and, to our knowledge, this study represents the first application of the EQ-5D-5L to a UK prison population. The number of missing EQ-5D-5L responses was therefore examined to assess the acceptability of the EQ-5D-5L to respondents. The strength of the correlation between the EQ-5D-5L and the primary outcome measure used in the trial, the number of unmet needs as assessed by the CANFOR, was also examined to assess the relevance of the EQ-5D-5L to the prison population.
Resource utilisation
Relevant resource use between baseline and follow-up was collected retrospectively using the SF-SUS. 104 The SF-SUS is an instrument designed specifically to collect individual-level resource-use data in secure facilities for the purpose of economic evaluations. Resource utilisation information was collected from a mixture of health-care files and participant recall. The instrument records itemised resource use in the categories detailed below. General prison accommodation and overhead costs were not included, as these are common to both arms of the trial and, therefore, do not affect the choice between OHSCAP and usual care. 105
External services used in secure facility
This comprised information on both contacts the individual had with external professionals and other community-based/visiting services received while inside the secure facility. The number of personal contacts with each service and, when relevant, the number of telephone calls and letters received were recorded. The services recorded were the following: Samaritans or Listeners, Citizens Advice Bureau, solicitor, barrister, legal advocate, social worker, care worker, organised prison visitors (National Association of Prison Visitors), older prisoner organisation, police officer and other.
Daily activities inside secure facility
This refers to group and other activities inside the secure facility. The name of the group or activity, the number of contacts over the study period and the average duration of each activity were recorded. The daily activities recorded were the following: therapeutic group, creative activity, work, education course, sports activity, older prisoner group and other.
Assessment, Care in Custody and Teamwork
Whether or not an individual was on an ACCT, and, if so, the start and end dates of this, were recorded.
Professional contacts inside secure facility
Information on one-to-one contacts with professionals inside the secure facility was recorded. The number of contacts with each professional and the average duration of these contacts was recorded. The professional contacts recorded were the following: GP/prison doctor, older prisoner lead nurse, practice/prison nurse, psychiatric nurse, psychiatrist, psychologist, counsellor/therapist, drug and alcohol treatment staff/Counselling, Assessment, Referral, Advice and Throughcare (CARAT) staff, dentist, optician, chiropodist, physiotherapist, chaplain and other.
Hospital contacts inside secure facility
Contacts with hospital services and visiting hospital specialists running outpatient clinics inside the secure facility were recorded. The number of contacts and the duration were recorded. The hospital contacts recorded were the following: inpatient stays and contacts with visiting specialists.
Medication
Information was collected covering all medication prescribed. The name of the medication, the daily dose and the number of days that the medication was prescribed during the study period were recorded.
Hospital contacts outside secure facility
Contact with hospital services outside the secure facility were recorded, for example inpatient stays, outpatient attendances, accident and emergency (A&E) attendances. The number of contacts and the length of any inpatient stays were collected.
Unit costs
Costs were calculated by multiplying resource use data by the relevant unit cost figures. All costs were valued in Great British pounds, according to the price year representing the mid-point of the trial (2014/15). Any unit costs not available for this price year were inflated to 2014/15 prices using the Retail Price Index. 106 This general inflation index was chosen as costs falling on multiple sectors were inflated. As the trial follow-up period was < 12 months, no discounting was required. Only resource utilisation falling under the public sector perspective was costed. Utilisation of services funded by charities is therefore presented descriptively, but not included in the cost calculations.
Unit costs data are not as readily available in the criminal justice field as in health care. Unit costs were therefore derived from a number of different sources, following the methodology used in the Personal Social Services Research Unit’s Unit Costs in Criminal Justice (PSSRU UCCJ) report when possible. 107 After consulting with offender health commissioners, the report concluded that once the associated security costs were removed, the cost per hour of health services delivered within the prison system would be the same as those delivered in the community. This assumption was therefore applied when prison-specific unit costs were not available.
The NHS health-care costs were estimated using the 2015 Personal Social Services Research Unit’s Unit Costs of Health and Social Care (PSSRU UCHSC)108 and NHS Reference Costs 2014–15. 109 To account for the fact that not all of NHS staff time is spent on direct patient contact, unit costs relating to the cost of face-to-face or direct patient contact were used when available. Unit costs for contacts with legal professionals were sourced from The Civil Legal Aid (Remuneration) Regulations 2013. 110 Prison-specific costs of education and contact with drug and alcohol staff and CARAT staff were available from the PSSRU UCCJ. 107 Unit costs of criminal justice staff were estimated based on the NOMS published pay scales,111 with the exception of the hourly costs of a police officer, which was sourced from available literature. 112 Unit costs of medications prescribed were derived from the British National Formulary. 113
Costs of the OHSCAP intervention
The costs of the OHSCAP intervention were estimated combining the cost of training staff to deliver the intervention, and the time spent by staff delivering the OHSCAP. Although the OHSCAP was intended to consist of an initial OHSCAP assessment and subsequent review, the intervention was not delivered to protocol and subsequent reviews were rarely undertaken in practice. The costs estimated in the cost-effectiveness analysis represent the resources involved in the OHSCAP as it was delivered, rather than those that would be needed if the intervention was delivered to protocol. The resources required for the performance of subsequent reviews were therefore not included in the cost calculations.
Cost-effectiveness analysis
The incremental cost-effectiveness ratio (ICER) was calculated, controlling for institution and the number of unmet needs at baseline as measured by the CANFOR, as these were the margins over which the minimisation was performed during randomisation. Age at randomisation was also controlled for, as age is known to have an impact on both costs and QALYs, along with baseline utility according to the recommendations of Manca et al. 114
The incremental cost of the OHSCAP over and above TAU was combined with the incremental effectiveness in terms of QALYs to compute the ICER. To account for the skewed nature typically displayed by cost data, both costs and QALYs were bootstrapped (pairwise bootstrapping with replacement using 10,000 replications) and these data were used to plot cost-effectiveness planes to illustrate the uncertainty around the point estimate of the ICER.
The primary cost-effectiveness analysis was performed on the full sample of participants for whom baseline data were collected, and multiple imputation was used to impute values for those lost to follow-up. A sensitivity analysis was performed estimating the cost-effectiveness of the OHSCAP using only the complete-case sample for which both baseline and follow-up data were available. The following baseline variables were used as predictors in the imputation analysis: establishment, age, number of unmet needs and EQ-5D-5L responses, with 50 imputations.
Chapter 9 Cost-effectiveness results
Resource utilisation and costs
The OHSCAP intervention
The resources required to deliver the OHSCAP comprised training sessions for staff on how to deliver the intervention, and an average of 40 minutes’ delivery per individual receiving the OHSCAP. The three main training sessions were delivered by a combination of project research staff and one prison officer, lasting 3 hours each. These sessions also involved some explanation of the research process, and, thus, if the OHSCAP were to be implemented, these would, in practice, be shorter. As the proportion of the session spent on training versus explanation of the research process was not recorded, the cost of training was based on the full 3-hour session. As additional sites were recruited to the trial, four informal training sessions were run by research staff to train additional staff members at these new sites.
The resources required for training and delivery of the OHSCAP are presented in Table 19. It was estimated that each OHSCAP delivered cost an average of £25.52 per prisoner, consisting of £16.42 for the costs of delivery and the remaining £9.10 for training costs.
| Cost and unit estimation | 2014/15 value | Notes |
|---|---|---|
| Formal OHSCAP training sessions | ||
| Training session 1 | ||
| Facilitating staff time | £144.21 per 3-hour session | Three-hour training session run by two university researchers (one associate professor and one research associate). Based on the mid-points of the University of Manchester bands 8 and 6 pay scales, respectively |
| Attending staff time | £513.36 per 3-hour session | Based on the attendance of four prison officers, one mental health nurse, one prison nurse and one health-care assistant. See Table 21 for the sources of staff unit costs |
| Total costs for session 1 | £657.57 | |
| Training session 2 | ||
| Facilitating staff time | £144.21 per 3-hour session | Three-hour training session run by two University researchers (one associate professor and one research associate). Based on the mid-points of the University of Manchester bands 8 and 6 pay scales, respectively |
| Attending staff time | £684.36 per 3-hour session | Based on the attendance of four prison officers, one older prisoner lead nurse, three health-care assistants and one prison nurse. See Table 21 for the sources of staff unit costs |
| Total costs for session 2 | £828.57 | |
| Training session 3 | ||
| Facilitating staff time | Three-hour training session run by one university researcher (research associate) and one prison officer. Based on the mid-point of the University of Manchester band 6 pay scale and prison officer (band 4 mid-point) taken from NICE draft guideline on mental health of adults in contact with the criminal justice system reference [1] below | |
| Attending staff time | Based on the attendance of seven prison officers and one health-care manager. Prison officer (band 4 mid-point) taken from NICE draft guideline on mental health of adults in contact with the criminal justice system.115 Health-care manager based on AFC band 7 mid-point, cost per working hour108 | |
| Total costs for session 3 | £645.15 | |
| Additional training was provided to some individuals on a more informal basis as new sites were added to the study | ||
| Informal training 1 | £26.91 | Thirty-minute informal training session by one research associate to train one mental health nurse. See Table 21 for the sources of staff unit costs |
| Informal training 2 | £35.16 | Thirty-minute informal training session by one research assistant to train one prison nurse and one health-care assistant. See Table 21 for the sources of staff unit costs |
| Informal training 3 | £17.66 | Thirty-minute informal training session by one research assistant to train one health-care assistant. See Table 21 for the sources of staff unit costs |
| Informal training 4 | £16.68 | Thirty-minute informal training session by one research assistant to train one prison officer. See Table 21 for the sources of staff unit costs |
| Overall for the OHSCAP | ||
| Total training costs | £2227.69 | |
| Delivering the OHSCAP: staff time | £16.42 per OHSCAP | Based on an average of 40 minutes to deliver the OHSCAP. Assumed that the OHSCAP was delivered by a mixture of prison officers, mental health nurses, prison nurses, health-care assistants and health-care managers based on the attendance composition of the training sessions |
| Average cost of the OHSCAP | £25.52 per prisoner receiving the OHSCAP | Based on the costs of training and delivery of 245 OHSCAPs during the study period |
Additional resource utilisation
In addition to the direct cost of providing the OHSCAP intervention, the economic analysis considered the wider resource utilisation of both the TAU and intervention arms. This information was available only for the complete-case sample. Of the 497 individuals in the trial at baseline, 404 were retained at follow-up and thus provided resource utilisation data. Table 20 provides the average resource utilisation for the complete-case sample over the trial period. Resource utilisation is presented separately by trial arm and summarised as the mean number of contacts with each service per individual.
| Type of service | Trial arm | |||
|---|---|---|---|---|
| TAU (n = 202) | OHSCAP (n = 202) | |||
| Mean number of times accessed | SD | Mean number of times accessed | SD | |
| External services used in secure facility | ||||
| Samaritans or Listeners (personal contact) | 0.83 | 7.07 | 0.34 | 2.33 |
| Samaritans or Listeners (telephone call) | 0 | 0 | 0.05 | 0.71 |
| Samaritans or Listeners (letter received) | 0 | 0 | 0 | 0 |
| Citizens Advice Bureau (personal contact) | 0.02 | 0.14 | 0.01 | 0.10 |
| Citizens Advice Bureau (telephone call) | 0 | 0 | 0 | 0 |
| Citizens Advice Bureau (letter received) | 0.00 | 0.00 | 0.00 | 0.00 |
| Solicitor/legal advocate (personal contact) | 0.67 | 1.58 | 0.79 | 1.58 |
| Solicitor/legal advocate (telephone call) | 1.00 | 3.37 | 1.62 | 9.14 |
| Solicitor/legal advocate (letter received) | 1.30 | 2.20 | 2.10 | 8.87 |
| Barrister (personal contact) | 0.18 | 0.55 | 0.23 | 0.76 |
| Barrister (telephone call) | 0.05 | 0.57 | 0.31 | 4.22 |
| Barrister (letter received) | 0.10 | 0.53 | 0.09 | 0.59 |
| Social worker (personal contact) | 0.02 | 0.20 | 0.00 | 0.07 |
| Social worker (telephone call) | 0 | 0 | 0 | 0 |
| Social worker (letter received) | 0.01 | 0.07 | 0.01 | 0.10 |
| Care worker (personal contact) | 0 | 0 | 0 | 0 |
| Care worker (telephone call) | 0 | 0 | 0 | 0 |
| Care worker (letter received) | 0 | 0 | 0 | 0 |
| Organised prison visitors (NAPV) (personal contact) | 0.14 | 1.21 | 0.04 | 0.44 |
| Organised prison visitors (NAPV) (telephone call) | 0.30 | 4.22 | 0 | 0 |
| Organised prison visitors (NAPV) (letter received) | 0.05 | 0.70 | 0.01 | 0.14 |
| Older prisoner organisation (personal contact) | 0 | 0 | 0.00 | 0.07 |
| Older prisoner organisation (telephone call) | 0 | 0 | 0 | 0 |
| Older prisoner organisation (letter received) | 0 | 0 | 0 | 0 |
| Probation officer (personal contact) | 0.34 | 0.83 | 0.17 | 0.44 |
| Probation officer (telephone call) | 0.44 | 1.72 | 0.29 | 1.52 |
| Probation officer (letter received) | 0.28 | 0.62 | 0.24 | 0.63 |
| Police officer (personal contact) | 0.02 | 0.18 | 0.05 | 0.25 |
| Police officer (telephone call) | 0 | 0 | 0 | 0 |
| Police officer (letter received) | 0 | 0 | 0.01 | 0.07 |
| Daily activities inside secure facility | ||||
| Therapeutic group | 2.30 | 11.53 | 0.96 | 3.94 |
| Creative activity | 4.33 | 20.06 | 1.94 | 11.37 |
| Work | 40.84 | 45.31 | 48.25 | 43.58 |
| Sports activity | 15.18 | 30.60 | 12.38 | 25.98 |
| Older prisoner group | 0.52 | 3.29 | 0.56 | 4.66 |
| Education course | 13.45 | 24.12 | 12.69 | 22.99 |
| ACCT | ||||
| On ACCT | 0.07 | 0.25 | 0.10 | 0.30 |
| Professional contacts inside secure facility | ||||
| GP | 2.15 | 2.07 | 2.16 | 2.26 |
| Older prisoner lead nurse | 0.15 | 0.42 | 0.75 | 1.81 |
| Practice or prison nurse | 5.09 | 7.97 | 5.39 | 9.26 |
| Psychiatric nurse | 0.98 | 2.27 | 0.72 | 1.87 |
| Psychiatrist | 0.13 | 0.55 | 0.05 | 0.32 |
| Psychologist | 0.00 | 0.07 | 0.03 | 0.42 |
| Counsellor/therapist | 0.04 | 0.36 | 0.05 | 0.45 |
| Drug alcohol staff/CARAT worker | 0.49 | 2.04 | 0.64 | 3.82 |
| Dentist | 0.25 | 0.76 | 0.32 | 0.75 |
| Optician | 0.28 | 0.47 | 0.27 | 0.49 |
| Chiropodist/podiatrist | 0.17 | 0.60 | 0.50 | 2.10 |
| Physiotherapist | 0.07 | 0.37 | 0.10 | 0.43 |
| Chaplain | 2.40 | 11.59 | 1.71 | 7.41 |
| Other (listed by five or more individuals in free-text section) | ||||
| Health-care assistant | 1.61 | 3.76 | 1.50 | 4.51 |
| Psychological well-being practitioner | 0.08 | 0.54 | 0.02 | 0.35 |
| Smoking cessation advisor | 0.15 | 0.71 | 0.10 | 0.64 |
| Health coach | 0.08 | 0.44 | 0.04 | 0.25 |
| Pharmacist | 0.03 | 0.18 | 0.09 | 0.40 |
| Pharmacy technician | 0.09 | 0.38 | 0.04 | 0.24 |
| Hospital contacts inside secure facility | ||||
| Inpatient stay (health-care wing) | 0.03 | 0.18 | 0.01 | 0.10 |
| Visiting specialist | 0.02 | 0.21 | 0.02 | 0.18 |
| Hospital contacts outside secure facility | ||||
| Inpatient days outside | 0.03 | 0.17 | 0.01 | 0.12 |
| Outpatient attendance | 0.19 | 0.39 | 0.16 | 0.37 |
| A&E attendance | 0.06 | 0.25 | 0.02 | 0.16 |
The number of missing data for each resource-use category was zero. This reflects the method of data collection, with resource use data being collected from a combination of health-care record examination and participant recall. Resource use was recorded as zero if there was no mention of the service being accessed in any prisoner records or if the participant did not report having accessed the service for categories obtained via participant recall. It is not possible to tell whether all of these values are true zeros or, in reality, they reflect missing information in the individuals’ records. It is possible that a prisoner accessed a service and this was not recorded, but there is no way to verify this information. There is, however, no reason to suggest that the level of missingness should vary by trial arm, and any missing data should, therefore, not bias the comparative results.
The data presented in Table 20 indicate that, although the prisoners in our sample are accessing a wide range of services and there is some variation in the use of each service category between the two trial arms, there is no systematic pattern of greater resource utilisation in one treatment group than in the other.
Of the external services utilised inside the secure facility, solicitors were the most commonly accessed. No prisoners in either treatment group accessed a care worker. The daily activity most frequently reported was work and the least frequently reported activity was participation in older prisoner group meetings. During the study period 7% of the TAU group and 10% of the OHSCAP group were placed on an ACCT. Practice and prison nurses were the most frequently accessed professionals inside the secure facility, followed by GPs. The professionals inside the secure facility who were least contacted by individuals in our sample were psychologists and counsellors/therapists. Three per cent of the control group were admitted to the health-care wing for an inpatient stay during the study, and 2% saw a visiting specialist within the secure facility. In the OHSCAP group, 1% of the sample were admitted to the health-care wing and 2% saw a visiting specialist. Although, wherever possible, health care is provided within the prisons, some individuals in our sample did leave the secure facility to receive health care. Among the TAU group, 3% were admitted to hospital as inpatients, 19% left the secure facility to attend outpatient appointments and 6% attended A&E departments. Within the OHSCAP arm, 1% were admitted to hospital outside the secure facility as inpatients, 16% attended outpatient appointments and 2% were taken to A&E.
To assign a monetary value to the resource utilisation consequences in both arms of the trial, unit costs were applied to each individual’s resource utilisation. Table 21 presents the unit cost figures used in the analysis.
| Item | Unit cost (£) | Unit | Source | Details |
|---|---|---|---|---|
| External services used in secure facility | ||||
| Solicitor/legal advocate (personal contact) | 44.97 | 45-minute contact | Civil Legal Aid (Remuneration) Regulations 2013110 | Hourly rates: controlled work |
| Solicitor/legal advocate (telephone call) | 3.56 | Per telephone call | Civil Legal Aid (Remuneration) Regulations 2013110 | Routine letters out and telephone calls |
| Solicitor/legal advocate (letter received) | 3.56 | Per letter | Civil Legal Aid (Remuneration) Regulations 2013110 | |
| Barrister (personal contact) | 115.30 | 45-minute contact | Civil Legal Aid (Remuneration) Regulations 2013110 | Junior counsel |
| Barrister (telephone call) | 3.56 | Per telephone call | Civil Legal Aid (Remuneration) Regulations 2013110 | Routine letters out and telephone calls |
| Barrister (letter received) | 3.56 | Per letter | Civil Legal Aid (Remuneration) Regulations 2013110 | |
| Social worker | 55.00 | 45-minute contact | PSSRU UCHSC108 | Social worker (adult services). Cost per hour of client-related work |
| Probation officer | 22.27 | 45-minute contact | Own calculations | Based on NOMS band 4 mid-point 37 hours including 17% unsociable hours. See Table 28, Appendix 5 for calculations |
| Police officer | 44.58 | 45-minute contact | Heslin et al., 2016112 | Police officer: cost per hour |
| Daily activities inside secure facility | ||||
| Therapeutic group | 4.78 | Per hour per attendee | Own calculations | Based on the assumption of one civilian instructor (grade 3) and one prison officer (grade 4) for each activity session. See Table 29, Appendix 5 for calculations |
| Creative activity | 3.19 | Per hour per attendee | ||
| Work | 1.37 | Per hour per attendee | ||
| Sports activity | 3.19 | Per hour per attendee | ||
| Older prisoner group | 3.19 | Per hour per attendee | ||
| Education course | 50.21 | Per hour per attendee | PSSRU UCCJ | Per hour of accredited learning delivered |
| ACCT | ||||
| ACCT | 72.12 | Per 24 hours | ||
| Professional contacts inside secure facility | ||||
| GP | 40.00 | Consultation | PSSRU UCHSC | GP consultation lasting 11.7 minutes |
| Older prisoner lead nurse | 81.00 | 1-hour appointment | PSSRU UCHSC | Advanced nurse. Cost per hour of client contact |
| Practice or prison nurse | 9.67 | 10-minute appointment | PSSRU UCHSC | Community nurse. Cost per hour of client contact |
| Psychiatric nurse | 33.50 | 30-minute appointment | PSSRU UCHSC | Nurse (mental health). Cost per hour of face-to-face contact |
| Psychiatrist | 80.25 | 45-minute appointment | PSSRU UCHSC | Consultant: psychiatric. Cost per contract hour |
| Psychologist | 26.00 | 30-minute appointment | PSSRU UCHSC | Clinical psychologist (AFC band 7). Cost per working hour |
| Counsellor/therapist | 44.00 | 1-hour appointment | PSSRU UCHSC | Clinical psychology trainee, counsellor (AFC band 6). Cost per working hour |
| Drug alcohol staff/CARAT worker | 28.68 | Per hour | PSSRU UCCJ | CARAT worker. Cost per hour |
| Dentist | 22.00 | 15-minute appointment | PSSRU UCHSC | NHS dentist (performer only). Cost per hour of patient contact |
| Optician | 25.00 | Per contact | Cost of a high-street eye test | |
| Chiropodist/podiatrist | 9.00 | 15-minute appointment | PSSRU UCHSC | Community chiropodist/podiatrist (AFC band 5). Cost per working hour |
| Physiotherapist | 18.00 | 30-minute appointment | PSSRU UCHSC | Physiotherapist (AFC band 5). Cost per working hour |
| Chaplain | 24.98 | Per hour | Own calculations | Based on NOMS band 5 mid-point 37 hours including 17% unsociable hours. See Table 30, Appendix 5 for calculations |
| Other | ||||
| Health-care assistant | 3.33 | 10-minute appointment | PSSRU UCHSC | Clinical support worker nursing (community) |
| Psychological well-being practitioner | 26.00 | 30-minute appointment | PSSRU UCHSC | AFC band 7. Cost per working hour |
| Smoking cessation advisor | 6.00 | 10-minute appointment | PSSRU UCHSC | AFC band 5. Cost per working hour |
| Health coach | 6.00 | 10-minute appointment | PSSRU UCHSC | AFC band 5. Cost per working hour |
| Pharmacist | 7.33 | Per contact | PSSRU UCHSC | Pharmacist (AFC band 6). Cost per working hour |
| Pharmacy technician | 4.83 | Per contact | PSSRU UCHSC | Pharmacy technician (AFC band 4). Cost per working hour |
| Hospital contacts inside secure facility | ||||
| Inpatient stay on health-care wing | ||||
| Short stay (< 10 days) | 608.00 | Per short stay | PSSRU UCHSC | Non-elective inpatient stay (short stay) |
| Long stay (> 10 days) | 2,863.00 | Per long stay | PSSRU UCHSC | Non-elective inpatient stay (long stay) |
| Visiting specialist | 82.00 | Per contact | PSSRU UCHSC | Prison health adult and elderly. Cost per care contact |
| Hospital contacts outside secure facility | ||||
| Inpatient stay | ||||
| Short stay (< 10 days) | 608.00 | Per stay | PSSRU UCHSC | |
| Bed watch | 432.72 | Per 24 hours | Own calculations | Assumed bed watch by one prison officer at £18.03 per hour. See Table 29, Appendix 5 for calculation of hourly cost of a prison officer |
| Escort to and from hospital | 216.36 | Per stay | Own calculations | Assumed three prison officers needed to escort a prisoner to and from hospital (one officer driving and two officers guarding); average duration of 4 hours. See Table 29, Appendix 5 for calculation of hourly cost of a prison officer |
| Outpatient attendance | ||||
| Attendance | 112.00 | Per attendance | PSSRU UCHSC | |
| Escort to and from hospital | 216.36 | Per attendance | Own calculations | Assumed three prison officers needed to escort a prisoner to and from hospital (one officer driving and two officers guarding); average duration of 4 hours. See Table 29, Appendix 5 for calculation of hourly cost of a prison officer |
| A&E attendance | ||||
| Attendance | 132.00 | NHS reference costs | ||
| Escort to and from hospital | 216.36 | Own calculations | Assumed three prison officers needed to escort a prisoner to and from hospital (one officer driving and two officers guarding); average duration of 4 hours. See Table 29, Appendix 5 for calculation of hourly cost of a prison officer | |
Table 22 multiplies the resource utilisation of the complete-case sample by the unit costs presented in Table 21 to obtain the average costs associated with the resource utilisation of individuals by trial arm. Only costs falling under the public sector perspective are included, with the services supplied by charitable organisations excluded from these calculations. The mean costs per individual are presented separately for each type of service used, in addition to the mean total costs for each resource use category, and the mean total costs of all services used.
| Type of service (personal contact unless otherwise specified) | Trial arm | |||
|---|---|---|---|---|
| TAU (n = 202) | OHSCAP (n = 202) | |||
| Mean cost (£) | SD | Mean cost (£) | SD | |
| External services used in secure facility | ||||
| Solicitor/legal advocate | 22.54 | 53.13 | 26.72 | 53.27 |
| Solicitor/legal advocate (telephone call) | 3.54 | 11.99 | 5.78 | 32.54 |
| Solicitor/legal advocate (letter received) | 4.64 | 7.83 | 7.47 | 31.59 |
| Barrister | 15.41 | 47.86 | 20.12 | 65.71 |
| Barrister (telephone call) | 0.19 | 2.02 | 1.09 | 15.03 |
| Barrister (letter received) | 0.35 | 1.88 | 0.33 | 2.09 |
| Social worker | 0.82 | 8.19 | 0.20 | 2.90 |
| Probation officer | 5.62 | 13.79 | 2.89 | 7.35 |
| Police officer | 1.10 | 8.25 | 2.43 | 11.07 |
| Mean total cost of external services in facility | 54.22 | 96.32 | 67.04 | 128.67 |
| Daily activities inside secure facility | ||||
| Therapeutic group | 20.14 | 108.39 | 9.90 | 47.26 |
| Creative activity | 32.58 | 157.75 | 11.95 | 80.79 |
| Work | 159.90 | 183.86 | 193.66 | 199.92 |
| Sports activity | 46.75 | 98.44 | 44.79 | 104.03 |
| Older prisoner group | 3.76 | 32.06 | 3.83 | 40.75 |
| Education course | 2018.70 | 3648.45 | 1881.16 | 3556.33 |
| Mean total cost of daily activities inside facility | 2281.85 | 3642.29 | 2145.28 | 3551.92 |
| ACCT | ||||
| ACCT | 81.40 | 486.19 | 136.39 | 737.65 |
| Professional contacts inside secure facility | ||||
| GP | 85.94 | 82.62 | 86.53 | 90.27 |
| Older prisoner lead nurse | 12.03 | 34.06 | 60.55 | 146.79 |
| Practice or prison nurse | 49.26 | 77.10 | 52.13 | 89.52 |
| Psychiatric nurse | 32.84 | 76.13 | 24.05 | 62.65 |
| Psychiatrist | 10.59 | 45.18 | 4.48 | 26.20 |
| Psychologist | 0.13 | 1.83 | 0.77 | 10.98 |
| Counsellor/therapist | 1.74 | 15.73 | 2.18 | 19.99 |
| Drug alcohol staff/CARAT worker | 0.00 | 0.00 | 0.00 | 0.00 |
| Dentist | 5.45 | 16.69 | 7.08 | 16.57 |
| Optician | 6.93 | 11.76 | 6.68 | 12.16 |
| Chiropodist/podiatrist | 1.56 | 5.42 | 4.50 | 18.90 |
| Physiotherapist | 1.34 | 6.70 | 1.78 | 7.83 |
| Chaplain | 67.13 | 317.84 | 31.49 | 102.92 |
| Other | ||||
| Health-care assistant | 5.36 | 12.52 | 5.01 | 15.02 |
| Psychological well-being practitioner | 2.19 | 13.91 | 0.64 | 9.15 |
| Smoking cessation advisor | 0.89 | 4.26 | 0.62 | 3.85 |
| Health coach | 0.50 | 2.66 | 0.27 | 1.50 |
| Pharmacist | 0.25 | 1.34 | 0.65 | 2.94 |
| Pharmacy technician | 0.43 | 1.82 | 0.19 | 1.16 |
| Mean total cost of professional contacts inside facility | 284.55 | 375.02 | 289.62 | 319.62 |
| Hospital contacts inside secure facility | ||||
| Inpatient stay on health-care wing | 65.72 | 405.33 | 17.18 | 205.72 |
| Visiting specialist | 2.03 | 17.23 | 2.03 | 15.17 |
| Mean total cost of hospital contacts inside facility | 67.75 | 408.24 | 19.21 | 206.11 |
| Hospital contacts outside secure facility | ||||
| Inpatient stay | 71.21 | 460.51 | 65.39 | 604.70 |
| Outpatient attendance | 183.69 | 1023.22 | 82.90 | 214.94 |
| A&E attendance | 27.59 | 117.15 | 12.07 | 87.76 |
| Mean total cost of hospital contacts outside secure facility | 282.49 | 1171.94 | 160.37 | 781.56 |
| Medication | 93.68 | 134.79 | 102.23 | 258.37 |
| OHSCAP | – | – | 25.52 | – |
| Mean total cost | 3145.94 | 3945.82 | 2945.65 | 3656.38 |
The most costly category of resource use was daily activities inside the secure facility, with these costs driven by the costs of education. These education costs were taken from the PSSRU UCCJ,107 based on information provided by The Skills Funding Agency, and include Offenders’ Learning and Skills Service overheads.
For individuals receiving TAU, mean costs were £54.22 for external services used inside the secure facility, £2281.85 for daily activities inside the secure facility, £81.40 for time spent on ACCT, £284.55 for professional contacts inside the secure facility, £67.75 for hospital contacts inside the secure facility, £282.49 for hospital contacts outside the secure facility and £93.68 for medications. The mean total cost for individuals in the TAU group was £3145.94 over the study period.
For individuals receiving the OHSCAP, in addition to the mean cost of £25.52 associated with the intervention, the mean costs were £67.04 for external services used inside the secure facility, £2145.28 for daily activities inside the secure facility, £136.39 for time spent on ACCT, £289.62 for professional contacts inside the secure facility, £19.21 for hospital contacts inside the facility, £160.37 for hospital contacts outside the secure facility and £102.23 for medications. The mean total cost for individuals receiving the OHSCAP was £2945.65 over the study period.
Outcomes
Descriptive statistics for the EQ-5D-5L responses of the full sample at baseline are shown in Table 23. The most frequently reported level, for all five of the domains, was ‘no problems’. Self-care was the domain for which most individuals reported having ‘no problems’ across both groups, followed by usual activities. In both the control and the OHSCAP group, pain/discomfort was the domain for which most individuals reported having problems. The mean utility score at baseline for the full sample of individuals enrolled in the trial was 0.830 among the control group and 0.855 in the group randomised to later receive the OHSCAP. There was, however, significant range in utility scores within both groups. Some individuals in the TAU group had negative EQ-5D-5L utility scores, indicating health states considered to be worse than the state of being dead. The level of missing responses to the EQ-5D-5L questions was zero, suggesting that participants found the questionnaire to be acceptable. The correlation coefficient between EQ-5D-5L utility scores and the number of unmet needs at baseline (as measured by the CANFOR) was –0.349, indicating a moderate correlation between the two measures. 116
| Response | TAU arm (N = 249) | OHSCAP arm (N = 248) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| EQ-5D-5L domain | ||||||||||
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | |
| No problems, n (%) | 162 (65.06) | 216 (86.75) | 206 (82.73) | 108 (43.37) | 150 (60.24) | 174 (70.16) | 226 (91.13) | 216 (87.10) | 121 (48.79) | 160 (64.52) |
| Slight problems, n (%) | 27 (10.84) | 18 (7.23) | 19 (7.63) | 40 (16.06) | 46 (18.47) | 23 (9.27) | 10 (4.03) | 11 (4.44) | 44 (17.74) | 42 (16.94) |
| Moderate problems, n (%) | 38 (15.26) | 9 (3.61) | 12 (4.82) | 70 (28.11) | 39 (15.66) | 30 (12.10) | 8 (3.23) | 8 (3.23) | 58 (23.39) | 35 (14.11) |
| Severe problems, n (%) | 20 (8.03) | 5 (2.01) | 11 (4.42) | 26 (10.44) | 12 (4.82) | 18 (7.26) | 1 (0.40) | 11 (4.43) | 24 (9.68) | 9 (3.63) |
| Extreme problems, n (%) | 2 (0.80) | 1 (0.40) | 1 (0.40) | 5 (2.01) | 2 (0.80) | 3 (1.21) | 3 (1.21) | 2 (0.81) | 1 (0.40) | 2 (0.81) |
| EQ-5D-5L utility score | ||||||||||
| Mean (SD) | 0.830 (0.200) | 0.855 (0.180) | ||||||||
| Range | –0.102 to 1.00 | 0.010–1.000 | ||||||||
The EQ-5D-5L responses for the complete-case sample at baseline and follow-up are presented in Table 24. The EQ-5D-5L responses for the complete-case sample are very similar to those of the full sample at baseline, and we fail to reject the null hypothesis that baseline EQ-5D-5L utility score is the same between those followed up and individuals lost to follow-up (p = 0.945). There is a difference in baseline utility between the treatment and control groups of 0.019, confirming the need to control for baseline utility in the analysis. The level of missing responses to the EQ-5D-5L questions among the full sample at follow-up was, again, zero, suggesting that participants found the questionnaire to be acceptable. The correlation coefficient between EQ-5D-5L utility scores and the number of unmet needs at follow-up as measured by the CANFOR was –0.426 among the complete-case sample, again indicating a moderate correlation between the two measures. 116
| Response | TAU arm (N = 202) | OHSCAP arm (N = 202) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| EQ-5D-5L domain | ||||||||||
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | |
| Baseline | ||||||||||
| No problems, n (%) | 133 (65.84) | 177 (87.62) | 166 (82.18) | 90 (44.55) | 122 (60.40) | 142 (70.30) | 185 (91.58) | 177 (87.62) | 90 (44.55) | 131 (64.85) |
| Slight problems, n (%) | 22 (10.89) | 15 (7.43) | 15 (7.43) | 34 (16.83) | 34 (16.83) | 17 (8.42) | 6 (2.97) | 11 (5.45) | 38 (18.81) | 32 (15.84) |
| Moderate problems, n (%) | 34 (16.83) | 5 (2.48) | 10 (4.95) | 53 (26.24) | 33 (16.34) | 26 (12.87) | 8 (3.96) | 6 (2.97) | 51 (25.25) | 31 (15.35) |
| Severe problems, n (%) | 11 (5.45) | 4 (1.98) | 10 (4.95) | 22 (10.89) | 11 (5.45) | 14 (6.93) | 1 (0.50) | 6 (2.97) | 22 (10.89) | 6 (2.97) |
| Extreme problems, n (%) | 2 (0.99) | 1 (0.50) | 1 (0.45) | 3 (1.49) | 2 (0.99) | 3 (1.49) | 2 (0.99) | 2 (0.99) | 1 (0.50) | 2 (0.99) |
| EQ-5D-5L utility score, mean | 0.833 | 0.852 | ||||||||
| (SD) | (0.197) | (0.181) | ||||||||
| Range | –0.102 to 1.000 | 0.010–1.000 | ||||||||
| Follow-up | ||||||||||
| No problems, n (%) | 145 (71.78) | 182 (90.10) | 169 (83.66) | 102 (50.50) | 133 (65.84) | 152 (75.25) | 186 (92.08) | 164 (81.19) | 99 (49.01) | 142 (70.30) |
| Slight problems, n (%) | 19 (9.41) | 6 (2.97) | 11 (5.45) | 46 (22.77) | 32 (15.84) | 15 (7.43) | 8 (3.96) | 15 (7.43) | 32 (15.84) | 23 (11.39) |
| Moderate problems, n (%) | 21 (10.40) | 11 (5.45) | 13 (6.44) | 42 (20.79) | 30 (14.85) | 24 (11.88) | 4 (1.98) | 14 (6.93) | 53 (26.24) | 28 (13.86) |
| Severe problems, n (%) | 15 (7.43) | 3 (1.49) | 8 (3.96) | 10 (4.95) | 5 (2.48) | 10 (4.95) | 4 (1.98) | 8 (3.96) | 14 (6.93) | 9 (4.46) |
| Extreme problems, n (%) | 2 (0.99) | 0 (0.00) | 1 (0.50) | 2 (0.99) | 2 (0.99) | 1 (0.50) | 0 (0.00) | 1 (0.50) | 4 (1.98) | 0 (0.00) |
| EQ-5D-5L utility score, mean | 0.867 | 0.866 | ||||||||
| (SD) | (0.172) | (0.182) | ||||||||
| Range | 0.174–1.000 | 0.021–1.000 | ||||||||
| QALYs, mean | 0.186 | 0.187 | ||||||||
| (SD) | (0.043) | (0.042) | ||||||||
| Days between baseline and follow-up EQ-5D-5L, mean (SD) | 80 (9.94) | 80 (8.74) | ||||||||
For the TAU group, the mean EQ-5D-5L utility score was 0.833 at baseline and 0.867 at follow-up in the complete-case sample. For the group receiving the OHSCAP, the mean baseline utility was 0.852 and the mean utility at follow-up was 0.866. Over the study period, the mean unadjusted QALY for the TAU group was 0.186 and for the OHSCAP group was 0.187. This indicated that there is no incremental effect of the OHSCAP over and above TAU in the unadjusted figures.
Cost-effectiveness analysis: full sample with imputation
Table 25 provides an adjusted estimate of the effect of the OHSCAP on the incremental costs and incremental QALYs over and above TAU, as estimated on the full sample with imputed cost and QALY values for those lost to follow-up. This analysis controls for age, baseline establishment and baseline utility.
| OHSCAP over TAU | Mean | Bootstrapped | |
|---|---|---|---|
| Standard error | 95% CIs | ||
| Incremental cost (£) | –115.27 | 290.27 | –684.19 to 453.64 |
| Incremental QALYs | –0.002 | 0.002 | –0.006 to 0.002 |
| ICER (£) | 54,487.24 | ||
The OHSCAP is associated with a mean incremental total cost reduction of –£115.27 (95% CI –£684.19 to £453.64). This suggests no significant difference in cost between the two arms of the trial. The incremental QALY associated with the OHSCAP is –0.002 (95% CI –0.006 to 0.002), indicating that there is also no significant difference in QALYs between the two groups.
Although there are no statistically significant differences in either costs or effects, the point estimate of the ICER is £54,487.24. The uncertainty around this estimate is represented in the cost-effectiveness plane in Figure 8. Figure 9 plots the 10,000 bootstrap replications of the incremental cost and QALY estimates associated with the OHSCAP. This illustrates the uncertainty around the point estimate of the ICER in probabilistic terms. The bootstrap results are clustered around the axes’ origin, with a tendency to fall to the west side of the cost axis, reflecting the point estimates of a very small but insignificant QALY loss and a small but insignificant reduction in costs.
FIGURE 8.
Cost-effectiveness plane: full sample with imputed values.
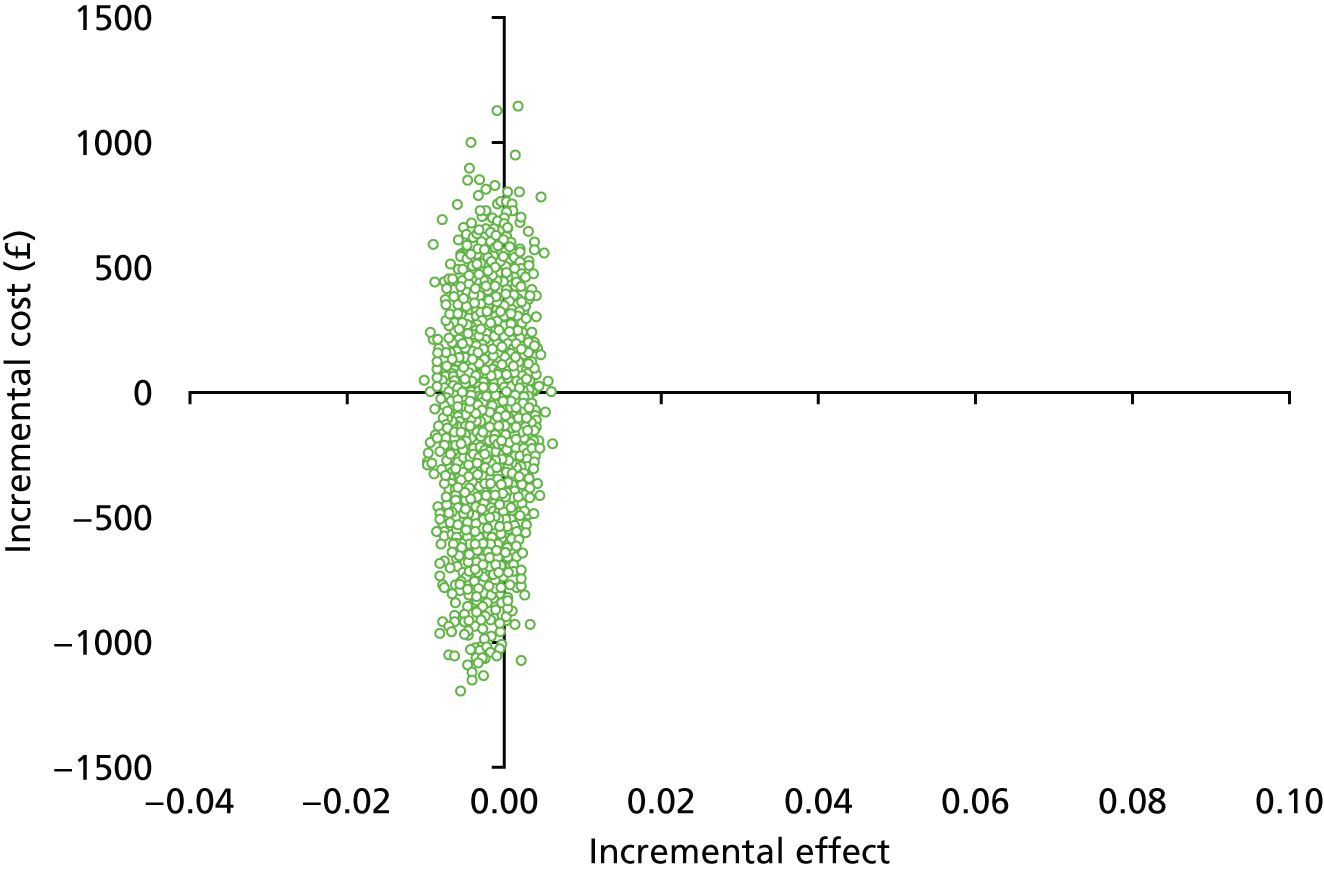
FIGURE 9.
Cost-effectiveness plane: complete-case sample.
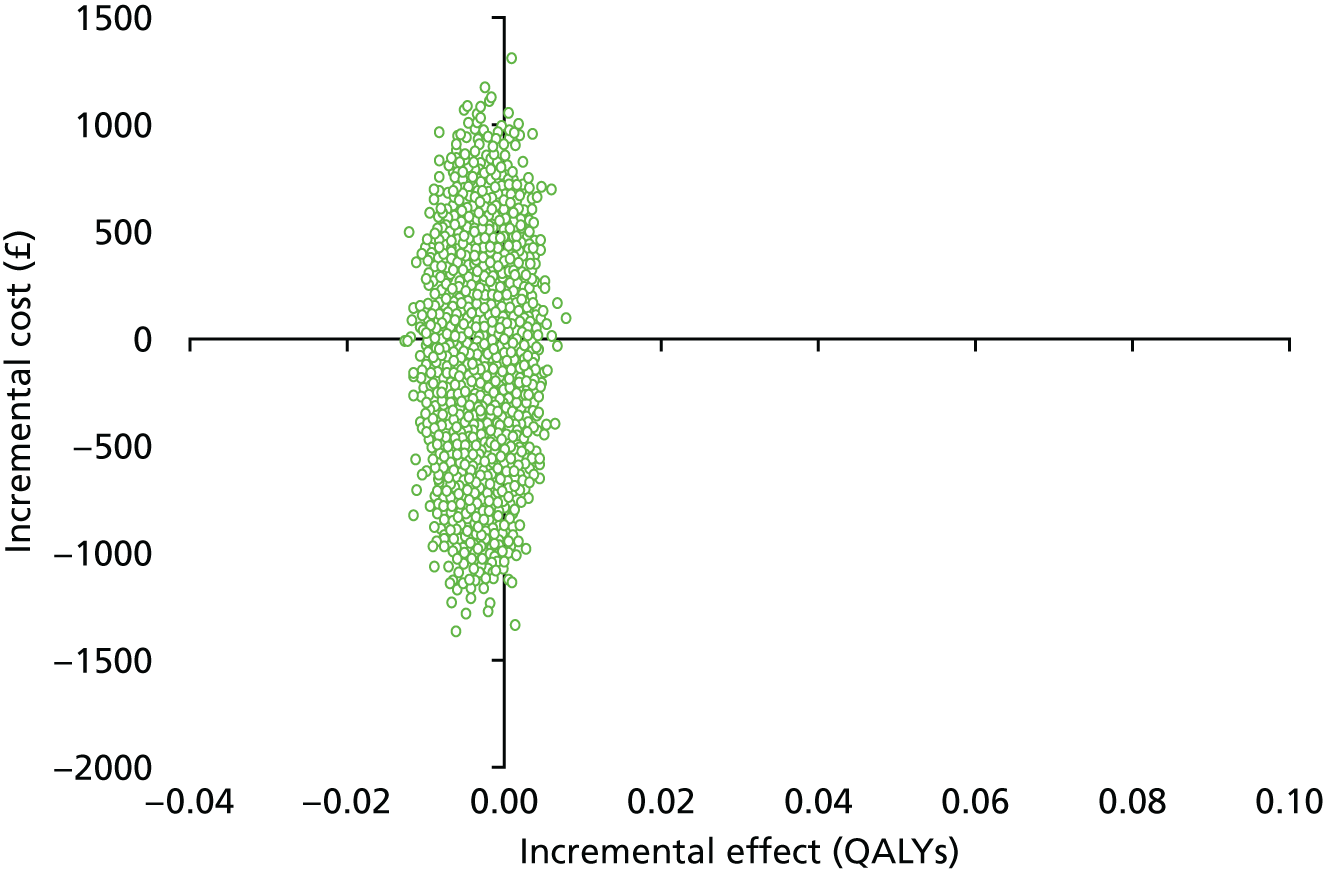
The cost-effectiveness plane illustrates the uncertainty in whether the OHSCAP will cost more or less than TAU. The OHSCAP had a lower cost than TAU in 65% of bootstrap replications. However, it also resulted in an incremental QALY loss in 83% of replications. This is reflected in the cost-effectiveness plane, with the majority of the bootstrap replications falling in the north-west and south-west quadrants.
Cost-effectiveness acceptability curves (CEACs) would normally be plotted at this point to further investigate the uncertainty around the ICER. The CEAC illustrates the probability that an intervention will be deemed cost-effective at given willingness-to-pay values for a QALY. However, the positive ICER produced for the OHSCAP is a function of negative point estimates of impacts on both costs and QALYs. The point estimates therefore suggest that the intervention has the potential to be cost saving, but at the expense of QALY loss. Although there is evidence that individuals value health gains and losses differently,117 CEACs are generated on the assumptions that QALYs gained and lost are of identical value. In the UK, the willingness-to-pay value for a QALY is known to be £20,000–30,000, but the willingness-to-accept value for a QALY lost is not known. CEACs were, therefore, not plotted.
Cost-effectiveness analysis: complete-case analysis
Table 26 provides an adjusted estimate of the effect of the OHSCAP on the incremental costs and incremental QALYS over and above TAU in the complete-case sample. This analysis controls for age, baseline establishment and baseline utility.
| OHSCAP over TAU | Mean | Boostrapped | |
|---|---|---|---|
| Standard error | 95% CIs | ||
| Incremental cost (£) | –81.35 | 361.57 | –790.02 to 627.31 |
| Incremental QALYs | –0.003 | 0.003 | –0.009 to 0.003 |
| ICER (£) | 30,948.74 | ||
The results of the cost-effectiveness analysis estimated on only the complete-case sample are very similar to those estimated on the full sample using imputed values. The OHSCAP is associated with a mean incremental total cost reduction of –£81.35 (95% CI –£790.02 to £627.31). This suggests no significant difference in cost between the two arms of the trial. The incremental QALY associated with the OHSCAP is –0.003 (95% CI –0.009 to 0.003), indicating that there is also no significant difference in QALYs between the two arms of the trial.
Although there are no statistically significant differences in either costs or effects, the point estimate of the ICER is £30,948.74. However, it is important to examine the uncertainty around this estimate. Figure 8 shows the cost-effectiveness plane that plots the 10,000 bootstrap replications of the costs and QALY estimates. This illustrates the uncertainty around the point estimate of the ICER in probabilistic terms.
The bootstrap results are clustered around the axes’ origin, with a tendency to fall to the west side of the cost axis, reflecting the point estimates of a very small but insignificant QALY loss and a small but insignificant reduction in costs. The OHSCAP had a lower cost than TAU in 58% of the bootstrap replications. However, it also resulted in an incremental QALY loss in 83% of replications. This is reflected in the cost-effectiveness plane, with the majority of the bootstrap replications, again, falling in the north-west and south-west quadrants.
A CEAC was, again, not plotted as a result of the negative point estimates on both costs and QALYs.
Summary of main findings
The within-trial cost-effectiveness analysis found no significant differences in either the costs or QALYs between the TAU and OHSCAP arms of the trial. Although the point estimates of the incremental cost of the OHSCAP showed a reduction of –£115.27 (95% CI –£684.19 to £453.64) associated with the intervention in the primary analysis, and –£81.35 (95% CI –£790.02 to £627.31) in the complete-case analysis, there is a high level of uncertainty around these estimates, as illustrated by the cost-effectiveness planes. There is also a high level of uncertainty around the point estimates of the impact of the OHSCAP on QALYs, which were estimated to be –0.002 (95% CI –0.006 to 0.002) in the primary analysis and –0.003 (95% CI –0.009 to 0.003) when estimated on the complete-case sample only. The average cost of delivering the OHSCAP per prisoner was estimated to be £25.52, comprising £16.42 for the costs of delivery and the remaining £9.10 for training costs.
Chapter 10 Discussion
Summary of findings
A wide range of prison types were included in the study, including open, training, remand and high-security prisons, thus ensuring generalisability of the findings to the wider older prisoner population in England and Wales. Additionally, the demographics of the sample were broadly in line with those of the total older prisoner population in England and Wales.
There were no significant differences in the number of unmet health and social care needs between those receiving the OHSCAP and those receiving TAU (95% CI –2.76 to 0.449; p = 0.621). There were no differences between the two groups with regard to depressive symptoms as measured by the GDS (95% CI 0.617 to 1.732; p = 901). There were insufficient numbers of participants experiencing problems with ADL (as measured by the BADLS) to conduct statistical tests. A bespoke tool, specifically designed for the study to measure whether or not the OHSCAP improved the meeting of very specific needs, revealed a statistically significant difference between the two groups in relation to how well hearing needs were met, with those needs better met in the OHSCAP group (95% CI 0.030 to 0.311; p = 0.014). There were no other significant differences.
A total of 150 OHSCAPs (assessments and care plans) were audited (68%). Considerable variability in the way in which the OHSCAP had been delivered was identified. Assessments were of a reasonable standard, but generally took place later than the target of 7–14 days after arrival, and the outstanding needs identified were not consistently translated into care plan actions. There was little evidence to suggest that prisoners had been involved in the care planning process. Where reviews were set, they were often not completed, or at least not documented. Therefore, the success of planned actions in addressing needs was unclear. All of these deviations from the training and the OHSCAP manual (see Appendix 3) are likely to have negatively affected the potential of the OHSCAP to have an impact on unmet needs.
Clear differences in the delivery of the OHSCAP were found and related to the core role of the facilitator. Health-care staff addressed a much greater proportion of the needs they identified through subsequent care planning than did prison officers. However, all facilitators had difficulty sharing documentation across the various information systems in use. Additionally, difficulties in resolving issues that did not fall within the remit of their everyday role were evident. Health-care staff made mostly health-care referrals to resolve health-care needs, and this trend was true, in reverse, for the prison officer facilitators. Overall, very few referrals to external agencies were made. This apparent inability to share information and successfully collaborate with partner agencies within, and outside, the prison was likely to have been a major barrier to the successful implementation of the OHSCAP.
Semistructured interviews were held with 12 members of staff who facilitated the OHSCAP (seven health-care workers and five prison officers). Fourteen prisoners who had received the OHSCAP were also interviewed, between two and four times each.
Prisoners and staff considered the prison system to be ‘broken’ as a result of a staffing crisis. This resulted in concerns for safety, basic needs remaining unmet and low levels of job satisfaction among staff. The implementation of the OHSCAP was further impeded by a tendency for both prison and health-care staff to focus on the implementation of core processes, as opposed to ensuring that outcomes were delivered and needs were met. Additionally, there was a reported lack of meaningful partnership working between prison and health-care staff, which had an impact on the quality of care received by prisoners.
The relationship between staff and prisoners was a further key factor in determining the success of the OHSCAP. Prison officers often did not recognise the value in ensuring that social care needs were met and, on occasion, lacked insight into older prisoner issues. When prison staff perceived concerns to be ‘genuine’, for example if a risk of suicide or self-harm was identified, they did offer valuable support to prisoners. Prisoners held within open prisons were reportedly less likely to raise issues because they were concerned that they might get returned to closed conditions if high support needs were identified.
The OHSCAP process itself was discussed during the interviews with prisoners and staff. In contrast to the pilot study, the majority of prisoners did not consider prison officers to be appropriate facilitators of the OHSCAP. This was related to issues of trust, confidentiality and concerns about the appropriateness of their knowledge and skills. However, some prisoners did find it acceptable for prison officers to act as facilitators. Prisoner views on this were based on a complex set of factors including the nature of their health and social care needs; their previous experiences, good or bad, with prison officers; and the personalities of the individual officers concerned. There were some examples of OHSCAP facilitators going above what would normally be expected of them in their core role in order to meet older prisoners’ health and social care needs. Furthermore, prisoners reported greatly valuing the OHSCAP experience as a rare opportunity for someone to take the time to listen to their concerns.
The ‘app’ process (the way in which prisoners can make applications for support through a paper-based system) is often prisoners’ only way to access services, but our findings show that it has limitations. For example, prisoners were reportedly repeatedly putting in ‘apps’ but were not receiving responses or were only receiving responses after considerable delays. In some instances it might be appropriate for OHSCAP facilitators to recommend that prisoners put an ‘app’ in (for example, if their request was straightforward and they had not previously put in an ‘app’ concerning the issue in question). However, some OHSCAP facilitators were asking prisoners to put in ‘apps’ simply because they did not consider the issue in question to be within their remit. For example, some prison officers facilitating the OHSCAP would simply tell prisoners that if they had a health-care issue they should put an ‘app’ in, because it was not their role to deal with health-care issues. However, if repeated ‘apps’ had been made to no avail, it may have been more appropriate for a prison officers to obtain some advice from a health-care member of staff and report back to the prisoner. Prison officers may have simply repeated the instruction to ‘put in an app’ because this is what they are used to doing on a daily basis, or because they may not have fully understood that the role of the OHSCAP facilitator was to co-ordinate the meeting of older prisoners’ health and social care needs.
The OHSCAP did not demonstrate convincing benefits in HRQoL over TAU, as no significant QALY gain was observed. There were also no significant differences in costs between delivering the OHSCAP and TAU. Although the point estimates showed a trend towards a reduction in both costs and QALYs associated with the OHSCAP, there is a high level of uncertainty around these estimates. This uncertainty is illustrated by the wide CIs around these estimates, and is displayed visually on the cost-effectiveness planes. This uncertainty is likely to be a result of the improper delivery of the OHSCAP intervention during the trial.
Limitations of the study
Randomised controlled trial
Limitations in relation to the trial include the possible impact of increasing the number of sites involved in the study and limitations of the outcome measures used. On balance, the impact of adding further sites on the trial processes was insignificant but the qualitative study revealed some potential issues with outcome measures.
The CANFOR was the tool used to measure the primary outcome. We found that, on average, prisoners had 2.05 unmet health and social care needs, as measured by the CANFOR. This accords with the findings of a previous study, using similar methodology, that reported an average of 2 unmet needs per older prisoner. 8 Senior et al. 28 reported a slightly higher figure of 2.74 unmet needs. However, participants in the Senior et al. study were newly received from court and it is therefore, perhaps, unsurprising that they had needs that the prison system had not yet had time to address, in contrast to those interviewed in later stages of their sentence (as in the current study and Hayes et al. 7
Some participants indicated that many of the discrete domain items were not applicable to their current situation in prison, or at all, given their age (e.g. childcare responsibilities). In addition, the CANFOR considered needs to be either met or unmet, but it is unlikely that some health and social care needs are ever fully met as they are ongoing and changeable in nature/severity. Findings from our previous research suggest that older prisoners are less likely than their younger counterparts to raise concerns27 and, consequently, participants in this study may not have always disclosed if they were experiencing unmet needs. In spite of the limitations of this tool, it was considered by the authors to be the best available tool for measuring health and social care needs within the prison setting and has been successfully used with this population in previous studies. 21,27
The GDS-15 was not designed for use in prison. However, the scale has been used with older prisoners in a previous study. 41 In that study, one question was adapted from ‘Do you prefer to stay at home rather than go out and do new things?’ to ‘Do you go on association?’ to better reflect prison life. We adopted the same approach. The current study found that 31% of participants had GDS-15 scores indicating symptoms of clinical depression. Previous studies have reported that the percentage of older prisoners experiencing depressive symptoms ranges from 12% to 56%. 7,27,32,35,41 However, the Murdoch et al. 41 study, reporting a rate of 51%, focused on life-sentenced prisoners, and the Senior et al. 27 study’s reported rate of 54% included only prisoners newly received from court. It is therefore, perhaps, to be expected that both of these figures are higher than those found in the current study because this study included participants with a wider range of prison sentence lengths and participants were at various stages of their sentence.
Very few ADL needs were identified using the BADLS. This tool has been used in previous older prisoner studies;7 however, it is designed for use with dementia patients and is perhaps not sensitive enough to identify ADL needs among either older adults not experiencing dementia or those living in a limiting institutional setting.
It was decided that a 3-month follow-up period should allow sufficient reasonable time for initial needs to be met. The CANFOR measures whether or not prisoners are receiving some assistance that is helping them. The research team perceived 3 months to be sufficient time for the prisoners to begin to get suitable help. We also wanted to minimise attrition.
It is possible that the OHSCAP may have initially helped to speed up the meeting of health and social care needs, but that, by 3 months, this had evened out between the two groups. Previous research has illustrated that early identification of mental health needs is important as issues are unlikely to be picked up later in custody. In order to address this early potential to meet needs and to establish whether or not more needs are eventually met with the OSCHAP, multiple follow-ups at 1, 3 and 6 months would be useful.
Audit
Unfortunately, not all of the completed OHSCAPs were available for audit. All of one site’s assessments were lost entirely, reportedly because documents were destroyed as part of the process of changing health-care provider. In another site, only 2% of documents were recoverable for audit. Unfortunately, the latter was the site where the greatest number of OHSCAP assessments had been completed by a health-care member of staff. The availability of these records would have enabled us to draw clear inferences about the impact of the facilitator’s core role on the OHSCAP process.
The original protocol specified that 10% of the OHSCAPs should be reviewed. The research team decided to review 100% of the audits. This decision was made because the number of sites involved in the RCT increased from 4 to 10 and we wanted to ensure that we had a clear understanding of how well OHSCAPs were completed at each site. The auditor was trained by the research team, independent of the trial. Some sections of the bespoke audit tool required a subjective judgement to be made; therefore, the judgement of one individual may not have been entirely reliable. However, 10% of the OHSCAPs were also reviewed by one of the researchers employed on the RCT, with good agreement between raters.
Regardless of which or how many individuals were involved in the audit process, the audits were based on the actual documented comments within the OHSCAP plans. Without being present for the assessment interview, it is not possible to know exactly what happened in practice and whether or not this is fully reflected in the documentation. For example, where ‘no issues’ was noted in relation to an entire area of need, the auditor could not possibly know whether or not a full and meaningful discussion had taken place in order to establish this. The same applies in relation to whether or not prisoners were actively involved in the care planning process. The auditor was able to establish only whether or not there was documented evidence of involvement, but this may not accurately reflect what happened in practice. Examination of the OHSCAPs and rating them in this way was a useful process that, with adaptation, is fit for purpose for other studies of this type to assess one aspect of fidelity.
Qualitative interviews
As a result of security restrictions, we were unable to audio record 6 out of the 14 prisoner participants’ qualitative interviews. In these circumstances, detailed notes were produced by an additional researcher in order to allow the first researcher to focus on the interview itself without distraction. These notes were typed up and analysed alongside the transcriptions. We were able to obtain very detailed notes, but obtaining audio recordings and transcribing them verbatim would likely have added greater richness to the data generated for these participants.
The research team decided to conduct interviews with prisoner participants on several occasions in order to capture rich data on progress with health and social care needs over time. One of the findings was that there was little further input from OHSCAP facilitators after initial assessment. Furthermore, as very few OHSCAP reviews took place, the additional interviews did not yield very rich data. Little had changed for the majority of participants between the initial and later interviews. Thus, through conducting a series of interviews with each individual, we were able to demonstrate that health and social care needs often remained unmet while new problems emerged.
The researcher who generated and analysed the majority of the qualitative data has undertaken research concerning the health and social care needs of older prisoners for the last 7 years. Her previous experience includes the study within which the OHSCAP was created and piloted, although she did not have direct involvement with the action learning group processes that created the OHSCAP itself. Her previous experience will, however, have had an impact on the way in which the interview content guides were designed, the issues she chose to focus on within interviews and the way in which she analysed the data. We aimed to reduce the potential impact that the researcher’s previous experience may have had on the findings by ensuring that a second researcher analysed a selection of transcriptions and assisted with the development of themes.
It is also important to consider the potential impact of the data being collected by three female researchers within a male-dominated environment, particularly as a large proportion of the prisoner participants were convicted of sexual offences. This could have led prisoner participants to be more or less open or truthful when discussing issues with female researchers, depending on broader influences on their personalities and their own views on their offending behaviour. It is possible that the research participants may have responded differently to a male researcher. Despite a shared view among researchers that prisoner participants were not always truthful about the type of offence they had committed, it was felt that prisoners did respond openly and honestly about their experience of health and social care within the prison.
Cost-effectiveness
Cost-effectiveness analyses are rarely performed in prisons in the UK. As part of the OHSCAP trial, we collected detailed individual-level data on prisoners’ resource utilisation over a number of different service categories. These data provide a snapshot of the service use within an under-researched area. There were some difficulties with accessing data on service usage from SystmOne. Common issues were the lack of documentation around length of contact and the professional role of the person involved, thus affecting basic pricing decisions. SystmOne has an option to add a symbol to indicate whether or not the comment being made was in relation to a face-to-face contact; however, this was sparsely used, making the process of service usage identification time-consuming, and reducing the reliability of the data.
Unit costs data are not as readily available in the criminal justice field as in health-care; thus, some of the unit costs applied were based on the best available information, but may not reflect the true cost of the resources utilised. In addition to the costs of the actual services assessed in secure facilities, prison officers are often required to escort prisoners to and from their cells to these services and no data were available on these additional security costs. Thus, it should be noted that the full cost of additional service use by prisoners is likely to be higher than presented here, as it would include additional security costs.
As part of the study, we collected EQ-5D-5L responses from participants. To our knowledge, this study represents the first application of the EQ-5D-5L to a UK prison population. There were no missing item responses at either baseline or follow-up for the EQ-5D-5L, indicating that the measure appears to be acceptable to the prison population. However, it was necessary to ask prisoners to specifically consider what their ‘usual activities’ in prison, as opposed to in the community, would be. EQ-5D-5L utility scores showed a moderate correlation to the number of unmet needs, as assessed by the CANFOR.
A cost-effectiveness analysis using the CANFOR was originally planned, but it was not undertaken as a result of the lack of impact on this primary outcome detected in the main analysis. As the OHSCAP was not implemented as planned, and found to have no impact on any outcomes or costs, further sensitivity analyses were felt to be futile.
Implications of the findings
Our findings illustrate that the OHSCAP did not contribute to prisoners’ health and social care needs being met any better than TAU. The main reason for this was that the OHSCAP was not implemented as planned. Staff and prisoners placed great emphasis on the current state of the prison system as ‘broken’ overall and, therefore, concluded that it was not possible to implement new initiatives. However, other contributory factors need to be considered.
The majority of prisoners perceived prison officers to be inappropriate facilitators of the OHSCAP. These findings are strikingly different from the pilot study, during which no concerns about prison officers being facilitators were raised. 27 In the pilot study, 24 prisoners aged ≥ 60 years received the OHSCAP. They were more likely to have been first-time offenders than the participants in the current study. It appears that the extent to which prisoners consider it acceptable for prison officers to deliver the OHSCAP is a result of a complex set of factors, such as the personality of the individual officer, the prisoners’ previous experiences with staff and the nature of their health and social care needs. Participants reported that prison officers often lacked insight into older prisoner issues. This has previously been described as ‘institutionalised thoughtlessness’ by Crawley,61 and defined as ‘the ways in which prison regimes (routines, rules, time-tables, etcetera) simply roll on with little reference to the needs and sensibilities of the old’. The findings from this research suggest that such thoughtlessness is still apparent in prisons in England and Wales. Including a wider range of participants in the current study than in the pilot has allowed us to establish that prison officers are not universally accepted facilitators of a health and social care initiative.
The audit revealed that the OHSCAP was not delivered as planned in several respects. In particular, it was delivered later than planned, reviews were not consistent and little prisoner involvement was evident. These failings were mainly linked to staff shortages and systemic pressures, but a consideration of the wider prison officer/staff role is required. The OHSCAP is much closer to the type of planning processes common in health-care settings rather than in the wider prison environment. The closest comparative process to the OHSCAP undertaken by prison officers is the ACCT process for those identified as at risk of self-harm and/or suicide. Similar failings have been found in regard to incomplete and inadequate care planning and a lack of robust review and follow-up processes within that system. 118 Perhaps this, along with our findings regarding the OHSCAP, highlights a fundamental issue around the prison officer role not always naturally or universally adapting to an overt caring function as required by the ACCT and the OHSCAP. A further similarity between the ACCT and the OHSCAP processes is that reviews were designed to be conducted at intervals that are appropriate to individuals’ needs, rather than at set intervals. Evidence suggests that prison staff find making decisions about when to conduct the ACCT reviews reactive to need rather than to a set timetable to be difficult; this appears to also be the case with the OHSCAP. 119
The ‘advantage’ the ACCT process has in terms of adherence to its requirements is that suicide prevention is seen as a core function of the prison system, and the understanding that ‘suicide is everyone’s concern’ has been embedded in everyday custodial care for a long period of time. Prisons are used to being judged by their abilities to prevent people taking their own lives, with frequent criticism of their failings forming part of an active media dialogue. In comparison, although increasing year on year, concern about and awareness of the problem of growing older in prison, and the needs of an increasingly frail prison population, has a much less established track record in terms of national policy and targeted implementation.
In addition, the ACCT process aimed to make suicide risk management more dynamic, especially on the part of prison discipline staff. Traditionally, discipline staff had been more used to focusing on observation rather than on interaction. It remains the case that prison staff are still not universally comfortable with undertaking an interventionist role in relation to prisoner well-being and mental health, with the latter very much regarded, still, as the domain of clinicians. This reluctance of not inconsiderable numbers of prison staff to readily adopt ‘caring’ roles was recognised in the government’s 2017 Prison and Courts Bill120 (now no longer to be progressed as a result of the early May 2017 general election), which included plans to create up to 2000 officer posts nationwide with specialist mental health training, offering an increased salary. Although more widespread mental health training for officers is positive in itself, the creation of specialist posts could potentially act to make ‘normal’ officers even less willing to undertake caring duties, especially if they are not paid a premium to do so, as others will be. These specialist officers could be the natural facilitators for a further trial of the OHSCAP, to see if fidelity is improved and whether or not that adherence translates to improved outcomes for individuals in terms of needs being better met, both when they are identified but also ongoing and when circumstances change.
The audit also revealed the apparent lack of individual engagement with prisoners during the OHSCAP process. Under previous models of custody, prison officers were named as personal officers for a small number of prisoners in their residential location, with the aim of allowing them to build constructive relationships designed to support prisoners in a range of aspects of their imprisonment, including desistance from crime, maintaining family contact, skills and vocational activity, and discharge planning. This model has not been operational for a number of years, but it is conceivable that aspects of the personal officer role and ethos may form part of the responsibilities of the new ‘specialist officer’ role currently being proposed. Again, it would be a retrograde step for the specialist role to effectively abdicate other officers from engaging with prisoners on this supportive level of basic human decency. For prisoners to benefit from any and all rehabilitative processes, whether designed to reduce offending, improve skills and education or to improve individual/public health outcomes, staff must seek to engage with prisoners as individuals, and offer suitable and targeted interventions. Individual needs, integrity and differences must be acknowledged within the operation of the institution as a whole. There is also a further step required, namely that of involving prisoners in planning their own care. The audit revealed little evidence of this. Engaging people in planning their own care needs has been shown to be efficacious in the community and should be encouraged in prisons.
The OHSCAP processes are designed to begin within the first 2 weeks of custody, but audit evidence showed that this was frequently delayed. The first days and weeks of imprisonment are stressful for all concerned and are a high-risk period for suicide. With that in mind, early assessment processes are important to identify and respond to a range of health and social care needs and risks, establish prisoners on appropriate care pathways and medication, and facilitate any referrals to external services. Previous research has shown that, if health needs are not picked up at reception or very quickly afterwards, they tend to remain unaddressed throughout someone’s whole sentence. 61 Our study showed that the OHSCAP was often delayed and thus decisions around a person’s care and safety (including appropriate location, access to prison facilities, suitable work/vocational activities and care needs around assistance needed for dressing, washing or mobilisation) could be being taken without the comprehensive information required to inform such decision-making, leaving the person potentially at risk or unable to maintain their care needs. We would argue that this is fundamental to the decency agenda and that an overall review of the processes and systems that operate during an early custody induction period needs to ensure that the most important processes are implemented early and inform the remaining processes. This may, again, lead back to the need to promote the importance and value of early health and social care assessment procedures as fundamental to all other aspects of safety custody, and for governors and senior health-care staff to ensure that there is protected and early time within regimes for such tasks.
The current study was conceived and in process at a time when the then coalition government introduced policies with the intention of reducing the full-time equivalence of staff across NOMS as a whole. Data collection itself was undertaken when the benchmarking process came into operation. 121 Benchmarking involved an attempt to reduce costs across the English and Welsh prison systems by decreasing the number of prison officers. These reductions were achieved through alterations to the prison regimes. According to the most recent figures, released by the Ministry of Justice on 10 November 2016, between March 2010 and September 2016, the number of operational prison officers of grades 3–5 in public sector prisons fell by 26.3% excluding structural changes (prison closures, movement between public/private operation). 121
This loss of prison officer numbers has been linked, by a range of media, political and societal informants, including the staff and prisoners who took part in this research, to a range of complex and inter-related negative outcomes. Between April 2015 and March 2016, self-inflicted deaths increased by 13% and self-harm incidents rose by 26%. 121 In addition, prisons have become increasingly violent places and, according to HMCIP, they are currently ‘unacceptably violent and dangerous’. 122 Overall, assaults increased by 34%, with assaults on staff and prisoners increasing by 43% and 32%, respectively, between April 2015 and March 2016. 121
Echoing the findings of our audit and interview data, HMCIP122 reported evidence of there being less time for meaningful interaction and, therefore, little action taken in response to prisoners’ complaints or requests for help. In addition, they found that previous progress made in terms of addressing equality and diversity issues had been undone as a result of cutbacks to resources.
Of particular concern in our study was the finding that areas of need that the Ministry of Justice123 and others31,77 have highlighted as key to reducing reoffending and ensuring the resettlement of prisoners into the community post release were the needs least often addressed by OHSCAP facilitators. For example, longstanding needs, in relation to discharge planning, emotional well-being and family relationships, were rarely actioned in subsequent care plans.
The House of Commons Justice Select Committee has stipulated that:124
The key explanatory factor for the obvious deterioration in standards over the last year is that a significant number of prisons have been operating at staffing levels below what is necessary to maintain reasonable, safe and rehabilitative regimes.
The detrimental impacts of these staff shortages were widely described by participants, both professionals and prisoners, during the qualitative interviews. In the same month that this report was finished (November 2016), a government white paper entitled Prison Safety and Reform acknowledged serious problems with the prison system and the need for change. 123 The paper proposes a number of changes to the prison system, including increasing staff-to-prisoner ratios through the recruitment of an additional 2500 prison officers. However, it should be acknowledged that the recruitment of a relatively small (in comparison with the overall reduction in the prison officer workforce since 2010) number of new recruits will, arguably, not compensate for the prison officers with considerable experience who have been lost since 2013.
Conducting randomised controlled trials in prison
Research in prison and, perhaps most acutely, the conduct of RCTs in prison, is challenging. Sometimes changes to the landscape may occur as a result of positive policy initiatives. For example, a RCT conducted by Abel et al. 119 among women who repeatedly self-harm was affected by the publication of the Corston Report on women’s imprisonment,118 which made numerous recommendations for a holistic person-centred approach to supporting female prisoners. Consequently, general improvements were made to support women in prison at risk of suicide and self-harm across England and Wales, and the impact of the Women Offenders’ Repeated Self-Harm Intervention Pilot could not easily be established. 119 However, other RCTs conducted by our research group have been affected in more negative ways. For example, the current study was affected by the loss of the dedicated time given to prison officers and others as older prisoner leads and/or DLOs, meaning that the individual role identified in the pilot study as core to the OHSCAP process simply no longer exists in many establishments. Where it does still exist, individuals within the role are often redeployed to other duties. Other trials into through-the-gate support to promote engagement with mental health services for people with serious and/or common mental health problems have been similarly negatively affected by reduced staff time and availability (Professor Pamela Taylor, Cardiff University, 2016, personal communication).
The quite dramatic shift in the prison landscape throughout this study illustrates the challenges of conducting a RCT in a real-life setting. It may have been possible to fund a designated role to deliver the OHSCAP for the duration of the trial, which may have reduced some of the problems with staffing shortages, but wider staff shortages would still have had an impact on the ability of the OHSCAP facilitator to make referrals to other services, etc. Furthermore, it is likely that such funding would not have been made available after the study ended, so the effectiveness of the OHSCAP would not have been evaluated within a real-life setting.
Chapter 11 Conclusion
The aim of the OHSCAP was to streamline current processes and create a more systematic approach to identifying and managing older prisoners’ health and social care needs. There were no statistically significant differences in unmet health and social care needs between the group of older prisoners who received the OHSCAP and those who received TAU. However, the results of the audit illustrate that the OHSCAP was fundamentally not delivered as intended. In summary, care plans were not produced in the majority of cases, identified needs were frequently not translated into actions, reviews were often not conducted and, when care plans were produced, they were not adequately shared among prison and health-care staff.
The qualitative interviews provided insight into why the OHSCAP was not delivered as intended. Most strikingly, the prison system was considered currently to be fundamentally ‘broken’, predominantly as a result of a drastic reduction in prison officers. To potentially add value, the OHSCAP is reliant on previously established prison processes being fully operational. However, data collection for this study commenced just as the recommendations from the benchmarking process were being implemented, which fundamentally resulted in drastic staff reductions across the prison estate, including all the study sites. Furthermore, the staff who were lost were commonly those with the most experience and knowledge. The loss of the discrete disability and liaison officer role across some establishments was particularly pertinent to this study, as the OHSCAP was initially designed to be completed by the prison officer who held that responsibility. The loss of this role did, however, provide opportunities to evaluate the acceptability of health-care workers and other prison staff members facilitating the OHSCAP.
The current staffing crisis is not the only explanation for why the OHSCAP was not successfully delivered. During qualitative interviews, staff reported that, on occasions, there was a lack of meaningful partnership working between prison and health-care staff to support the meeting of older prisoners’ needs. Both prison officers and health-care workers described a tendency to focus on processes rather than outcomes, alongside a lack of accountability for the meeting of prisoners’ needs. This was coupled with a perception that prison officers, on occasion, lacked insight into chronic conditions and older prisoner issues. Furthermore, social care concerns were often not fully understood or prioritised. A confounding factor was that, unlike in our pilot study, prisoners did not perceive prison officers to be ideal facilitators of the OHSCAP, because of issues of confidentiality and trust, and concerns about the appropriateness of their knowledge and skills. Older prisoners did, however, greatly appreciate what they described as a ‘rare’ opportunity to be listened to and there were positive examples of staff going beyond what was normally expected of them in their role to address older prisoners’ needs.
Implications for practice
-
Careful consideration should be given to who should facilitate initiatives for older prisoners, such as the OHSCAP, which involve multidisciplinary input. Prisoners did not deem it acceptable for prison officers to deliver the OHSCAP. This needs to be taken into consideration for any further exploratory work with this or similar tools. It may be possible if the intervention was delivered within a designated role with protected time, preventing routine redeployment to other wing duties. Facilitators should have knowledge and experience of, and interest in, older prisoner issues. Facilitators require skills in conducting assessments, case management and setting appropriate review periods.
-
Further work is required to assist in meaningful partnership working and information sharing between prison and health-care staff. Initiatives that would assist this process include joint training, designated ‘information sharing and collaboration leads’ within each relevant organisation and the development of clear policies to assist staff in understanding what can and cannot be appropriately shared, again centring on what social care is and why it is different from health care.
Implications for future research
-
To better reflect equivalency with the community and to improve the quantity, scope and targeting of services, further research should explore and identify the role that other prisoners and third-sector organisations (such as older adult specialist services) could play in identifying and appropriately addressing older prisoners’ health and social care needs.
-
The ways in which the 2014 Care Act30 and the recently announced prison reforms have been, and will continue to be, implemented across the English and Welsh prison estate need to be identified and gaps in services addressed. Furthermore, the implementation of the 2014 Care Act30 places new responsibilities on local authority adult social care departments. The way in which these responsibilities are discharged, particularly case finding, assessment and care co-ordination, needs further investigation.
-
A full training-needs assessment of the knowledge and skills of prison and health-care staff concerning older prisoner issues should be completed. This will provide a basis from which skills deficits can be clearly identified, and suitable training developed and implemented with the aim of improving individual care and making prisons more informed environments with regard to older people. Because prisons are unique, and discrete, environments that differ significantly from either home or other institutional settings in which older people are cared for, focused ethnography should be conducted to generate an understanding of the way in which the prison environment, prison staff and younger/age-matched peers interact with and affect/influence the day-to-day lives of older prisoners, particularly with regard to the meeting of social care needs.
-
Researchers conducting future RCTs in prison should carefully consider the balance between protecting the fidelity of initiatives being evaluated and ensuring that the research is conducted in a ‘real-life’ setting.
-
The conduct of this research highlights fundamental issues relevant to future research in particular, and to service improvement initiatives more generally in prisons and, by logical extension, the NHS, during times of public service cuts and austerity. This research was commissioned by NIHR at a time when the problems faced within prisons regarding the care of older people had clearly had an impact on regimes, gained recognition from managers, commissioners, civil servants and politicians, and become a routine consideration during inspections by Her Majesty’s Inspectorate of Prisons. We have discussed throughout this report the day-to-day negative impact that staff cuts and reduction of specialist officer roles were felt by participants to have had on our ability to trial the OHSCAP intervention, which maintained fidelity to the research protocol. This may, of course, be only a partial explanation for the failure of this intervention, but it is undoubtedly an important part of the overall problem. It became clear that, as a result of staff cuts and a number of other changes, frontline staff struggled to be mentally receptive or physically resourced to work with the research team.
-
When public finances are severely limited, any money spent needs to be spent efficiently. A major contribution to this is the conduct of high-quality research that identifies ‘what works’. For services to evolve positively and efficiently, institutions need to continue facilitating research as a valuable and valued contributor to high-quality, modern service provision. Active engagement of providers and decision-makers with research and the research community has the potential to improve services in both the short and the longer term.
Acknowledgements
Manchester Academic Health Science Centre Clinical Trials Unit
David Ryder (Statistician).
Anne Bowers (Data Management Lead).
Dr Heather Driscoll (Clinical Trials Project Manager).
Sally Falk (former Clinical Trials Project Manager).
Claire Goldrick (Senior Clinical Trials Data Manager).
Robert Peet (Data Officer).
Joe Wilson (Data Officer).
Other contributors
We would also like to thank the following individuals who contributed to the completion of the study and/or report:
Anya Francis (Research Assistant, formerly University of Manchester).
Dr Gavin Daker-White (Research Fellow, Qualitative Methods, University of Manchester).
Daisy Shaw (Student, Bachelor of Medicine, Bachelor of Surgery, University of Manchester).
Roxanne Todd (Research Assistant, University of Manchester).
Caroline Stevenson (Research Assistant, University of Manchester).
David While (former Statistician, University of Manchester).
Elaine Crawley (former Reader in Criminology, University of Salford).
Mark Harrison (Assistant Professor of Health Economics/Epidemiology, University of British Columbia).
Members of the OHSCAP study Trial Steering Committee
Louise Ridley (Chairperson, Northumbria University).
Charlotte Bilby (Northumbria University).
Paul Biddle (Northumbria University).
Dr Stuart Ware (Restore Support Network).
Dr Mary Piper (formerly Public Health England).
Dr Marian Peacock (Manchester Metropolitan University).
Dr Victoria Simm (Greater Manchester West NHS Foundation Trust).
Dr Harry Allen (Manchester Mental Health and Social Care Trust).
Natasha Peniston (Service User Representative).
David O’Brien (Service User Representative).
Professor Brian Francis (Lancaster University).
Carol Williams (HMP Risley).
Dr Iain Brew (formerly Leeds Community Healthcare NHS Foundation Trust).
Professor Jenny Shaw (University of Manchester).
Paul Goodridge (HMP Parc).
Mark Hopkins (HMP Risley).
Derek Athey (HMP Risley).
Paula Atherton (HMP Liverpool).
Dave Jones (Liverpool Community Health NHS Trust).
Jayne Swarbrick (HMP Wymott).
Natalie Hunt (HMP Wymott).
Contributions of authors
Mrs Katrina Forsyth (Research Associate) was involved in the design of the study, compiled the quantitative data for analysis, interpreted the findings of the quantitative analyses and carried out the transcription, coding and analysis of the qualitative data. She co-authored the background, methods, quantitative and qualitative analyses, discussion and conclusion chapters.
Mrs Laura Archer-Power (Research Associate) interpreted the findings of the fidelity-of-implementation audit and carried out the analysis of the audit data. She co-authored the audit and discussion chapters, and undertook the initial compilation and formatting of the final report.
Dr Jane Senior (Senior Research Fellow/Research Manager – Offender Health Research Network) was involved in the design of the study; provided clinical guidance on the interpretation of the findings and implications for service development; and was involved in revising the report and the final approval of the report to be published. She is a member of the Trial Steering Committee.
Ms Rachel Meacock (Research Fellow) was involved in the design of the study; conducted the economic evaluation of the intervention and co-authored the relevant chapters of the report; and was involved in revising the report and the final approval of the report to be published.
Dr Roger Webb (Reader in Mental Health Epidemiology) was involved in the design of the study; advice and supervision regarding the quantitative data analysis; and was involved in revising the report and the final approval of the report to be published.
Professor Richard Emsley (Professor of Medical Statistics) supervised the quantitative data analyses and reviewed/revised the quantitative results chapter.
Dr Dawn Edge (Senior Lecturer, Psychology) reviewed and revised the qualitative methodology and results chapters.
Dr Elizabeth Walsh (Honorary Senior Lecturer, Division of Psychology and Mental Health, University of Manchester) was responsible for training the OHSCAP facilitators and supporting them throughout OHSCAP delivery; design of the study; revising the report and the final approval of the report to be published.
Dr Stuart Ware (Chief Executive, Restore Support Network) was responsible for patient and public involvement throughout the study; co-ordinated input from the RSN regarding the design of study materials and final approval of the report to be published. He is a member of the Trial Steering Committee.
Professor David Challis (Director of Personal Social Services Research Unit and Associate Director of the NIHR School for Social Care Research) was involved in the design of the study, revising the report and the final approval of the report to be published.
Dr Adrian Hayes (Academic Clinical Fellow, University of Oxford and Oxford Health NHS Foundation Trust) was involved in the design of the study, revising the report and the final approval of the report to be published.
Dr Kate O’Hara (Former Research Assistant, University of Manchester) was involved in the design of the study, revising the report and the final approval of the report to be published.
Professor Alistair Burns (Professor of Old Age Psychiatry/National Clinical Director for Dementia and for Mental Health in Older People/Consultant Old Age Psychiatrist) was involved in the design of the study, revising the report and the final approval of the report to be published.
Professor Jenny Shaw (Professor of Forensic Psychiatry/Consultant Forensic Psychiatrist) was involved in the design of the study, overall interpretation of the findings and implications for service development and practice. She is a member of the Trial Steering Committee.
Data sharing statement
The data arising from this study are handled in strict accordance with the University of Manchester’s Data Protection Policy, which can be found at http://documents.manchester.ac.uk/display.aspx?DocID= 14914. Participant consent forms did not specifically refer to sharing of anonymised data with third parties and this factor would need to be explored. Any request for access will be referred to the University of Manchester Records Office for advice before disclosure. All enquiries and queries should submitted to the corresponding author for initial consideration.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Wahidin A, Aday R. The needs of older men and women in the criminal justice system: an international perspective. Prison Serv J 2005;160:13-2.
- Loeb SJ, Abudagga A. Health-related research on older inmates: an integrative review. Res Nurs Health 2006;29:556-65. https://doi.org/10.1002/nur.20177.
- Morton JB. An Administrative Overview of the Older Inmate 1992. www.ncjrs.gov/pdffiles1/Digitization/144056NCJRS.pdf (accessed 19 October 2017).
- Wahidin A. Ageing, Crime and Society. Oxford: Oxford University Press; 2005.
- Doing Time: The Experiences and Needs of Older People in Prison. A Prison Reform Trust Briefing. London: Prison Reform Trust; 2008.
- Yorston GA, Taylor PJ. Commentary: older offenders – no place to go?. J Am Acad Psychiatry Law 2006;34:333-7.
- Hayes AJ, Burns A, Turnbull P, Shaw JJ. The health and social needs of older male prisoners. Int J Geriatr Psychiatry 2012;27:1155-62. https://doi.org/10.1002/gps.3761.
- At America’s Expense: The Mass Incarceration of the Elderly. New York, NY: American Civil Liberties Union; 2012.
- Ministry of Justice . White Paper On Crime 2004: Treatment of Offenders 2004. http://hakusyo1.moj.go.jp/en/50/nfm/mokuji.html (accessed 14 June 2013).
- Uzoaba JHE. Managing Older Offenders: Where Do We Stand? (Report No. R-70). Ottawa, ON: Research Branch, Correlation Service of Canada; 1998.
- Grant A. Elderly inmates: issues for Australia. Aust Inst Criminol Trends Issues Crime Crim Justice 1999;115:1-6.
- Gautier S. Growing old and dying in prison. Soins Gerontol 2011;88:22-4.
- Offender Management Caseload Statistics 2013. London: Ministry of Justice; 2014.
- Offender Management Statistics Bulletin, England and Wales. London: Ministry of Justice; 2016.
- Prison Population Projections 2016–2021 England and Wales. London: Ministry of Justice; 2016.
- Howse K. Growing Old in Prison. A Scoping Study on Older Prisoners. London: Prison Reform Trust; 2003.
- Frazer L. Ageing Inside. Bristol: University of Bristol; 2003.
- Her Majesty’s Chief Inspector of Prisons . Older Prisoners in England and Wales: A Follow-up to the 2004 Thematic Review by HM Chief Inspector of Prisons 2008. www.justice.gov.uk/downloads/publications/inspectorate-reports/hmipris/thematic-reports-and-research-publications/older_prisoners_thematic-rps.pdf (accessed 2 March 2013).
- Ginn S. Elderly prisoners. BMJ 2012;345. https://doi.org/10.1136/bmj.e6263 (accessed 28 February 2013).
- Hayes AJ, Burns A, Turnbull P, Shaw JJ. Social and custodial needs of older adults in prison. Age Ageing 2013;42:589-93. https://doi.org/10.1093/ageing/aft066.
- Hayes AJ, Burns A, Shaw J. Health, Social and Custodial Needs of Older Men in Prison 2010.
- The Future Organisation of Prison Health Care. London: Department of Health; 1999.
- The Provision of Mental Health Care in Prisons. London: Prison Service; 1997.
- National Service Framework for Older People. London: Department of Health; 2001.
- Daly M, Lewis J. The concept of social care and the analysis of contemporary welfare states. Br J Sociol 2000;51:281-98. http://doi.wiley.com/10.1111/j.1468-4446.2000.00281.x.
- O’Hara K, Forsyth K, Senior J, Stevenson C, Hayes A, Challis D, et al. ‘Social Services will not touch us with a barge pole’: social care provision for older prisoners. J Forens Psychiatry Psychol 2015;26:275-81.
- Senior J, Forsyth KJ, Walsh E, O’Hara K, Stevenson C, Hayes AJ, et al. Health and social care services for older male adults in prison: the identification of current service provision and piloting of an assessment and care planning model. Heal Serv Deliv Res 2013;1:1-160. https://doi.org/10.3310/hsdr01050.
- Williams J. Social care and older prisoners. J Soc Work 2012;13:471-91. http://jsw.sagepub.com/content/early/2012/02/20/1468017311434886.full.pdf+html (accessed 19 October 2017).
- White Paper: Caring for Our Future; Reforming Care and Support (Cm 8378). London: Department of Health; 2012.
- Great Britain . Care Act 2014 c.23 n.d. www.legislation.gov.uk/ukpga/2014/23/contents (accessed 13 December 2017).
- Cornish N, Edgar K, Hewson A, Ware S. Social Care or Systematic Neglect? Older People on Release from Prison Prison Reform Trust and Restore Support Network. London: Prison Reform Trust; 2016.
- Kingston P, Le Mesurier N, Yorston G, Wardle S, Heath L. Psychiatric morbidity in older prisoners: unrecognized and undertreated. Int Psychogeriatr 2011;23:1354-60. https://doi.org/10.1017/S1041610211000378.
- Potter E, Cashin A, Chenoweth L, Jeon Y-H. The healthcare of older inmates in the correctional setting. Int J Prison Health 2007;3:204-13. https://doi.org/10.1080/17449200701520115.
- Fazel S, Hope T, O’Donnell I, Piper M, Jacoby R. Health of elderly male prisoners: worse than the general population, worse than younger prisoners. Age Ageing 2001;30:403-7. https://doi.org/10.1093/ageing/30.5.403.
- Fazel S, Hope T, O’Donnell I, Jacoby R. Hidden psychiatric morbidity in elderly prisoners. Br J Psychiatry 2001;179:535-9. https://doi.org/10.1192/bjp.179.6.535.
- Burvill PW, Mowry B, Hall WD. Quantification of physical illness in psychiatric research in the elderly. Int J Geriatr Psychiatry 1990;5:161-70. https://doi.org/10.1002/gps.930050304.
- Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:403-7. https://doi.org/10.1097/00005650-199603000-00003.
- Bridgewood A, Malbon G. Survey of Physical Health Needs of Prisoners. Survey of Physical Health of Prisoners. London: Office for National Statistics; 1995.
- Prior G, Prescott-Clarke P, Primatesta P. Health Survey for England 1996 Volume 1 Findings. London: HMSO; 1998.
- Fazel S, Hope T, O’Donnell I, Jacoby R. Unmet treatment needs of older prisoners: a primary care survey. Age Ageing 2004;33:396-8. https://doi.org/10.1093/ageing/afh113.
- Murdoch N, Morris P, Holmes C. Depression in elderly life sentence prisoners. Int J Geriatr Psychiatry 2008;23:957-62. https://doi.org/10.1002/gps.2017.
- Shaw J. Suicide by prisoners: national clinical survey. Br J Psychiatry 2004;184:263-7. https://doi.org/10.1192/bjp.184.3.263 (accessed 19 June 2013).
- Moll A. Losing Track of Time: Dementia and the Ageing Prison Population: Treatment Challenges and Examples of Good Practice. London: Mental Health Foundation; 2013.
- Yorston G. Aged and dangerous. Old-age forensic psychiatry. Br J Psychiatry 1999;174:193-5. https://doi.org/10.1192/bjp.174.3.193.
- Singleton N, Meltzer H, Gatward R. Psychiatric Morbidity Amongst Prisoners in England and Wales. London: Office for National Statistics; 1998.
- Arndt S, Turvey CL, Flaum M. Older offenders, substance abuse, and treatment. Am J Geriatr Psychiatry 2002;10:733-9. https://doi.org/10.1097/00019442-200211000-00012.
- Snyder C, van Wormer K, Chadha J, Jaggers JW. Older adult inmates: the challenge for social work. Soc Work 2009;54:117-24. https://doi.org/10.1093/sw/54.2.117.
- Williams BA, Lindquist K, Sudore RL, Strupp HM, Willmott DJ, Walter LC. Being old and doing time: functional impairment and adverse experiences of geriatric female prisoners. J Am Geriatr Soc 2006;54:702-7. https://doi.org/10.1111/j.1532-5415.2006.00662.x.
- Age UK . Older People in Prison. A Monitoring Guide for IMBs 2011. www.nicklemesurier.org/uploads/9/3/8/7/938735/id10735_imb_guide_older_people_in_prison_-_final_july_2011.pdf (accessed 16 April 2013).
- Clarkson P, Abendstern M, Sutcliffe C, Hughes J, Challis D. Reliability of needs assessments in the community care of older people: impact of the single assessment process in England. J Public Health 2009;31:521-9. https://doi.org/10.1093/pubmed/fdp035.
- Clarkson P, Abendstern M, Sutcliffe C, Hughes J, Challis D. The identification and detection of dementia and its correlates in a social services setting: impact of a national policy in England. Dementia 2012;11:617-32. https://doi.org/10.1177/1471301211421089.
- Stewart K, Challis D, Carpenter I, Dickinson E. Assessment approaches for older people receiving social care: content and coverage. Int J Geriatr Psychiatry 1999;14:147-56. https://doi.org/10.1002/(SICI)1099-1166(199902)14:2<147::AID-GPS901>3.0.CO;2-8.
- Worden A, Challis DJ, Pedersen I. The assessment of older people’s needs in care homes. Aging Ment Health 2006;10:549-57. https://doi.org/10.1080/13607860600637794.
- PSI 52/2010 Early Days in Custody. London: Her Majesty’s Prison Service; 2010.
- Shaw J, Senior J, Hassan L, King C, Mwasambili N, Lennox C. An Evaluation of the Reception Health Screening Process Used Within Prisons in England and Wales. Manchester: University of Manchester; 2009.
- Durcan G. From the Inside: Experiences of Prison Mental Health Care. London: Centre for Mental Health; 2008.
- A Pathway to Care for Older Offenders. A Toolkit for Good Practice. London: Department of Health; 2007.
- Cooney F, Braggins J. Good Practice with Older People in Prison – the Views of Prison Staff. London; 2010.
- Grubin D, Carson D, Parsons S. Report on New Reception Health Screening Arrangements: The Result of a Pilot Study in 10 Prisons. Newcastle: University of Newcastle; 2002.
- Birmingham L, Mason D, Grubin D. Health screening at first reception into prison. J Forensic Psychiatry 1997;8:435-9. https://doi.org/10.1080/09585189708412022.
- Crawley E. Institutional thoughtlessness in prisons and its impacts on the day-to-day prison lives of elderly men. J Contemp Crim Justice 2005;21:350-63. https://doi.org/10.1177/1043986205282018.
- Social Exclusion Unit . Reducing Re-Offending by Ex-Prisoners, HMG Cabinet Office – The Learning Journey 2002. www.thelearningjourney.co.uk/file.2007-10-01.1714894439/file_view (accessed 11 April 2013).
- Williamson M. Improving the Health and Social Outcomes of People Recently Released from Prisons in the UK: A Perspective from Primary Care. London: The Sainsburys Centre for Mental Health; 2006.
- Blank Wilson A. How people with serious mental illness seek help after leaving jail. Qual Health Res 2013;23:1575-90. https://doi.org/10.1177/1049732313508476.
- Pratt D, Piper M, Appleby L, Webb R, Shaw J. Suicide in recently released prisoners: a population-based cohort study. Lancet 2006;368:119-23. https://doi.org/10.1016/S0140-6736(06)69002-8.
- Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction 2008;103:251-5. https://doi.org/10.1111/j.1360-0443.2007.02081.x.
- Lennox C, Senior J, King C, Hassan L, Clayton R, Thornicroft G, et al. The management of released prisoners with severe and enduring mental illness. J Forens Psychiatry Psychol 2012;23:67-75. http://dx.doi.org/10.1080/14789949.2011.63492.
- Binswanger IA, Nowels C, Corsi KF, Long J, Booth RE, Kutner J, et al. ‘From the prison door right to the sidewalk, everything went downhill,’ a qualitative study of the health experiences of recently released inmates. Int J Law Psychiatry 2011;34:249-55. http://dx.doi.org/10.1016/j.ijlp.2011.07.002.
- Integrated Resettlement: Putting the Pieces Together. London: NACRO; 2005.
- Breaking the Cycle: Government Response. London: Ministry of Justice; 2011.
- Dyer W, Biddle P. Prison health discharge planning – evidence of an integrated care pathway or the end of the road?. Soc Policy Soc 2013;12:1-12. http://journals.cambridge.org/abstract_S1474746412000693 (accessed 11 April 2013).
- ‘No Problems - Old and Quiet’: Older Prisoners in England and Wales. A Thematic Review by HM Chief Inspector of Prisons. London: HMIP; 2004.
- Walsh E, Dilworth S, Freshwater D. Establishing Clinical Supervision in Prison Health Care Settings: Phase Three. Bournemouth: Department of Health; 2007.
- Crawley E, Sparks R. Is there life after imprisonment? How elderly men talk about imprisonment and release. Criminol Crim Justice 2006;6:63-82. https://doi.org/10.1177/1748895806060667.
- Davies M. The reintegration of elderly prisoners: an exploration of services provided in England and Wales. Internet J Criminol 2011. https://docs.wixstatic.com/ugd/b93dd4_f285f55736e54bb4a39b7a07379aad80.pdf (accessed 19 October 2017).
- Crawley E. Release and resettlement: the perspectives of older prisoners. CJM 2004;56:32-3. https://doi.org/10.1080/09627250408552945.
- Forsyth K, Senior J, Stevenson C, O’Hara K, Hayes A, Challis D, et al. ‘They just throw you out’: release planning for older prisoners. Ageing Soc 2014;35:2011-25. http://journals.cambridge.org/action/displayFulltext?type=1&fid=9315473&jid=ASO&volumeId=-1&issueId=-1&aid=9315449 (accessed 12 November 2014).
- Great Britain . Offender Rehabilitation Act 2014 c.11 n.d. www.legislation.gov.uk/ukpga/2014/11/contents/enacted/data/htm (accessed 18 October 2017).
- Ware JE, Snow KK, Kolinski M, Gandeck B. The SF-36 Health Survey. Boston, MA: The Health Institute, New England Medical Centre; 1993.
- Bucks R, Ashworth D, Wilcock G, Siegfried K. Assessment of Activities of Daily Living in Dementia: Development of the Bristol Activities of Daily Living Scale 1996. https://pdfs.semanticscholar.org/b96e/91b5ea2ca1ee24a6f80e5b75551fa624da29.pdf (accessed 19 October 2017).
- Chisholm D, Knapp MRJ, Knudsen HC, Amaddeo F, Gaite L, Van Wijngaarden B. Client socio-demographic and service receipt inventory – European version: development of an instrument for international research. Br J Psychiatry 2000;177:28-33. https://doi.org/10.1192/bjp.177.39.s28.
- Barrett B, Byford S. Collecting service use data for economic evaluation in DSPD populations: Development of the Secure Facilities Service Use Schedule. Br J Psychiatry 2007;190:s75-8. http://bjp.rcpsych.org/content/190/49/s75 (accessed 10 November 2016).
- Azevedo MH, Soares MJ, Coelho I, Dourado A, Valente J, Macedo A, et al. Using consensus OPCRIT diagnoses. An efficient procedure for best-estimate lifetime diagnoses. Br J Psychiatry 1999;175:154-7. https://doi.org/10.1192/bjp.175.2.154.
- Shaw J, Tomensen B, Creed F. A screening questionnaire for the detection of serious mental illness in the criminal justice system. Journal of Forensic Psychiatry &Amp; Psychology 2003;14:138-50. www.tandfonline.com/doi/pdf/10.1080/1478994031000077943 (accessed 19 October 2017).
- Shaw J, Thornicroft G, Marshall M, Senior J, King C, Hassan L. Trial Platform of Critical Time Intervention for Released Prisoners with Serious Mental Illness: A Report to the Medical Research Council. Manchester: University of Manchester; 2008.
- Great Britain . Mental Capacity Act 2005 c.9 n.d. www.legislation.gov.uk/ukpga/2005/9/contents (accessed 18 October 2017).
- Altman DG, Bland JM. Treatment allocation by minimisation. BMJ 2005;330. www.bmj.com/content/330/7495/843 (accessed 17 January 2014).
- Sibbald B, Roland M. Understanding controlled trials. Why are randomised controlled trials important?. BMJ 1998;316. https://doi.org/10.1136/bmj.316.7126.201.
- Thomas S, Harty MA, Parrott J, McCrone P, Slade M, Thornicroft G, et al. The Forensic CAN(CANFOR). A Needs Assessment for Forensic Mental Health Service Users. London: Gaskell; 2003.
- Sheikh RL, Yesavage JA. Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. Clin Gerontol 1986;5:165-73. https://doi.org/10.1300/J018v05n01_09.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136–011–9903-x.
- NICE Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Roberts C, Torgerson DJ. Understanding controlled trials: baseline imbalance in randomised controlled trials. BMJ 1999;319:185-5. https://doi.org/10.1136/bmj.319.7203.185 (accessed 17 January 2014).
- Rahman MS, Gupta S, Rodway C, Bickley H, While D, Windfuhr K, et al. Quality of Risk Assessment Prior to Fatal Outcomes in Mental Health Services – A Pilot Study. Manchester: University of Manchester; 2013.
- Shaw J, Senior J, Hayes AJ, Davies L, Appleby L. Evaluation of the Care of at Risk Prisoners Project. Manchester: University of Manchester; 2006.
- Altman D. Practical Statistics for Medical Research. London: Chapman & Hall; 1991.
- Lewin S, Glenton C, Oxman AD. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: methodological study. BMJ 2009;339.
- Donovan J, Mills N, Smith M, Brindle L, Jacoby A, Peters T, et al. Quality improvement report: improving design and conduct of randomised trials by embedding them in qualitative research: ProtecT (Prostate testing for cancer and Treatment) study. Commentary: presenting unbiased information to patients can be difficult. BMJ 2002;325:766-70. www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1124277&tool=pmcentrez&rendertype=abstract (accessed 8 April 2013).
- Checkland K, Harrison S, Marshall M. Is the metaphor of ‘barriers to change’ useful in understanding implementation? Evidence from general medical practice. J Health Serv Res Policy SAGE 2007;12:95-100. http://hsr.sagepub.com/content/12/2/95.abstract (accessed 20 December 2013).
- Guba E, Lincoln YS. Fourth Generation Evaluation. London: Sage; 1989.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471–2288–13–117.
- Devlin N, Shah K, Feng Y, Mulhern B, Van Hout B. Valuing Health-Related Quality of Life: An EQ-5D-5L Value Set for England. London: Office of Health Economics; 2016.
- Barrett B, Byford S. Collecting service use data for economic evaluation in DSPD populations: development of the Secure Facilities Service Use Schedule. Br J Psychiatry Suppl 2007;49:s75-8. https://doi.org/10.1192/bjp.190.5.s75.
- Drummond MF, Sculpher M, Claxton K, Stoddart G, Torrance G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Office for National Statistics . Consumer Price Inflation Dataset 2016. www.ons.gov.uk/economy/inflationandpriceindices/timeseries/chaw/mm23 (accessed 19 October 2017).
- Brookes N, Barrett B, Netten A, Knapp E. Unit Costs in Criminal Justice (UCCJ). Discussion Paper 2855 2013. www.pssru.ac.uk/pub/dp2855.pdf (accessed 19 October 2017).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- NHS Reference Costs 2014–15. London: Department of Health; 2015.
- Legal Aid Agency . The Civil Legal Aid (Remuneration) Regulations 2013. 422 2013. www.legislation.gov.uk/uksi/2013/422/pdfs/uksi_20130422_en.pdf (accessed 19 October 2017).
- NOMS . Pay Policy Manual 2012. www.justice.gov.uk/downloads/offenders/psipso/psi-2012/psi-28-2012-noms-pay-policy-manual.pdf (accessed 19 October 2017).
- Heslin M, Callaghan L, Packwood M, Badu V, Byford S. Decision analytic model exploring the cost and cost-offset implications of street triage. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015–009670.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2015.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- NICE National Guideline Alliance . Mental Health of Adults in Contact With the Criminal Justice System, Draft Guideline Version 2 2016. www.nice.org.uk/guidance/GID-CGWAVE0726/documents/draft-guideline (accessed 6 December 2017).
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Brighton: Psychology Press; 1988.
- O’Brien BJ, Gertsen K, Willan AR, Faulkner LA. Is there a kink in consumers’ threshold value for cost-effectiveness in health care?. Health Econ 2002;11:175-80. http://onlinelibrary.wiley.com/doi/10.1002/hec.655/abstract (accessed 10 November 2016).
- Corston J. The Corston Report: A Review of Women with Particular Vulnerabilities in the Criminal Justice System. London: Home Office; 2007.
- Walker T, Shaw J, Turpin C, Reid C, Abel K. The WORSHIP II study: a pilot of psychodynamic interpersonal therapy with women offenders who self-harm. J Forensic Psychiatr Psychol 2017;28:158-71. https://doi.org/10.1080/14789949.2017.1301529.
- Prisons and Courts Bill (HC Bill 170) n.d. https://publications.parliament.uk/pa/bills/cbill/2016-2017/0170/cbill_2016-20170170_en_1.htm (accessed 19 October 2017).
- Prison Reform Trust . Bromley Briefings Prison Factfile 2012 2012. www.prisonreformtrust.org.uk/Portals/0/Documents/FactfileJune2012.pdf (accessed 21 March 2013).
- HMCIP . HM Chief Inspector of Prisons for England and Wales Annual Report 2015–16 n.d. www.justiceinspectorates.gov.uk/hmiprisons/wp-content/uploads/sites/4/2016/07/HMIP-AR_2015-16_web.pdf (accessed 19 October 2017).
- Prison Safety and Reform. 2016.
- House of Commons . Justice Committee Prisoners: Planning and Policies Ninth Report of Session 2014–15 n.d. https://publications.parliament.uk/pa/cm201415/cmselect/cmjust/309/309.pdf (accessed 19 October 2017).
- Annual Report and Accounts 2012–2013. London: The Stationery Office; 2013.
Appendix 1 Case report forms
Baseline case report forms
Follow-up case report form (additional sections only)
Appendix 2 Offences algorithm and red flag list
FIGURE 10.
Offences algorithm for study inclusion.
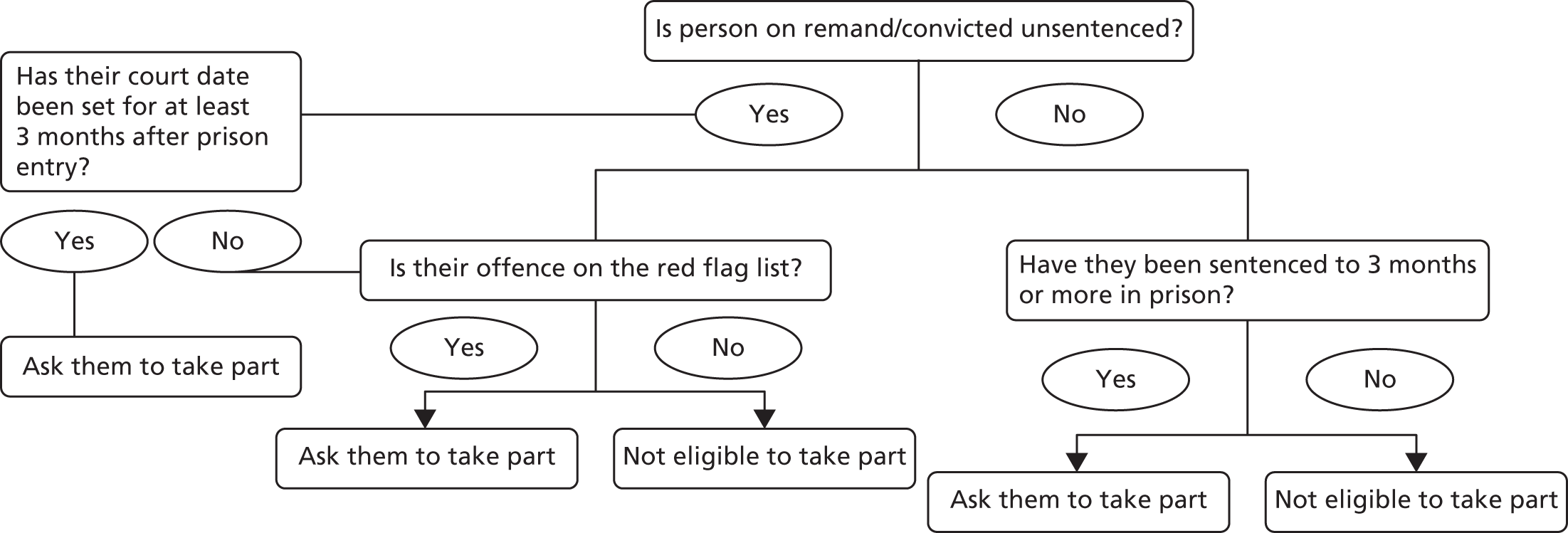
| Offence | Categories | Notes |
|---|---|---|
| Assault | ||
| GBH/wounded with intent | All | |
| GBH/unlawful wounding | 1 and 2 | |
| Racially/religiously aggravated GBH/unlawful wounding | 1 and 2 | |
| Assault occasioning ABH | 1 | |
| Attempted murder | ||
| Attempted murder | All | |
| Manslaughter by reason of provocation | All | |
| Burglary/theft/robbery offences | ||
| Aggravated burglary | n/a | |
| Domestic burglary | 1 | |
| Burglary | n/a | Goods at ≥ £20,000 |
| Theft | n/a | ≥ £125,000 |
| Theft | n/a | ≥ £2000 – high degree of trust breached |
| Robbery | All | |
| Drug offences | ||
| Importing/exporting class A drugs | 1–3 | |
| Importing/exporting class B drugs | 1–3 | For category 3 only if leading or significant role |
| Importing/exporting class C drugs | 1–3 | Category 1 – any role |
| Category 2 – leading or significant role | ||
| Category 3 – leading role | ||
| Supplying/offering to supply/possession with intent class A drugs | 1–4 | Not category 4 lesser role |
| Supplying/offering to supply/possession with intent class B drugs | 1–3 | Category 3 – leading and significant role only |
| Supplying/offering to supply/possession with intent class C drugs | 1–3 | Category 3 – leading role only |
| Production/cultivation class A | 1–4 | Category 4 – leading and significant role only |
| Production/cultivation class B | 1–3 | Category 3 – leading and significant role only |
| Production/cultivation class C | Category 2 – leading and significant role only | |
| Category 3 – leading role only | ||
| Permitting use on premises class A | 1 | |
| Permitting use on premises class B | 1 | |
| Causing death by driving | ||
| Causing death by dangerous driving | 1–3 | |
| Causing death by careless driving | Falling not far short of dangerous driving | |
| Fraud | ||
| Large-scale advance fee fraud or other confidence fraud involving the deliberate targeting of a large number of vulnerable victims | Any amount | |
| Lower-scale advance fee fraud or other confidence fraud characterised by a degree of planning and/or multiple transactions | Any amount | |
| Possessing, making or supplying articles for use in fraud | Article(s) intended for use in an extensive and skilfully planned fraud (making or adapting not just supplying) | |
| Banking and insurance fraud or obtaining credit through fraud | Fraudulent from the outset, professionally planned and either fraud carried out over a significant period of time or multiple frauds (any amount) | |
| Fraudulent from the outset and either fraud carried out over a significant period of time or multiple frauds (≥ £100,000) | ||
| Not fraudulent from the outset and either fraud carried out over a significant period of time or multiple frauds (≥ £100,000) | ||
| Benefit fraud | Fraudulent from the outset, professionally planned and either fraud carried out over a significant period of time or multiple frauds (any amount) | |
| Fraudulent from the outset and either fraud carried out over a significant period of time or multiple frauds (≥ £100,000) | ||
| Not fraudulent from the outset and either fraud carried out over a significant period of time or multiple frauds (≥ £100,000) | ||
| Revenue fraud | Fraudulent from the outset, professionally planned and either fraud carried out over a significant period of time or multiple frauds (any amount) | |
| Fraudulent from the outset and either fraud carried out over a significant period of time or multiple frauds (≥ £100,000) | ||
| Not fraudulent from the outset and either fraud carried out over a significant period of time or multiple frauds (≥ £100,000) | ||
| Sexual offences | ||
| Rape of an adult | ||
| Rape of a child < 13 years | ||
| Assault by penetration of a child < 13 years | ||
| Sexual assault | Unless no contact with genitalia | |
| Causing a person to engage in sexual activity without consent | Unless no contact with genitalia | |
| Causing or inciting a child < 13 years to engage in sexual activity | Unless no contact with genitalia | |
| Causing or inciting a person with a mental disorder impeding choice to engage in sexual activity | Unless no contact with genitalia | |
| Engaging in sexual activity in the presence of a child/person with a mental disorder impeding choice | Unless consensual sexual touching of naked body parts but not involving naked genitalia | |
| Causing a child/person with a metal disorder impeding choice to watch a sexual act | Unless images did not involve penetration | |
| Sexual activity with a child/causing or inciting a child to engage in sexual activity | Unless did not involve genitalia | |
| Sexual activity with a child family member/inciting a child family member to engage in sexual activity | Unless did not involve genitalia | |
| Abuse of trust: sexual activity with a child/causing or inciting a child to engage in sexual activity | Unless did not involve genitalia | |
| Abuse of trust: sexual activity in the presence of a child | Unless not involving naked genitalia | |
| Abuse of trust: causing a child to watch a sexual act | Unless images did not involve penetration | |
| Sexual activity with a person who has a mental disorder | Unless did not involve genitalia | |
| Care worker sexual activity with a person who has a mental disorder | Not if only naked contact | |
| Sexual activity in the presence of a person with a mental disorder | Not if not involving genitalia | |
| Causing or inciting a person with a mental disorder to watch a sexual act | Images did not involve penetration | |
| Sexual grooming | ||
| Trespass with intent to commit a sexual offence | ||
| Administering a substance with intent to commit a sexual offence | ||
| Prohibited adult sexual relationships: sex with an adult relative | ||
| Voyeurism | With aggregating factors | |
| Indecent images of children | Offender commissioned or encouraged the production of level 4 or 5 images | |
| Offender involved in the production of level 4 or 5 images | ||
| Level 4 or 5 images shown or distributed | ||
| Offender involved in the production of, or has traded in, material at levels 1–3 | ||
| Possession of a large quantity of level 4 or 5 material for personal use only | ||
| Large number of level 3 images shown or distributed | ||
| Paying for the sexual services of a child | ||
| Child prostitution or pornography | ||
| Controlling/causing/inciting prostitution for gain | Evidence of physical or mental coercion or offender closely involved in the victim’s prostitution | |
| Keeping a brothel for prostitution | Unless involvement of the offender was minimal | |
| Trafficking | ||
| Theft and burglary in a building other than a dwelling | ||
| Theft in breach of trust | Theft of £20,000 or more but less than £125,000 | |
| Theft of £2000 or more but less than £20,000 in breach of a high degree of trust | ||
| Theft in a dwelling | If vulnerable victim | |
| Theft from a person | If vulnerable victim | |
| Theft from a shop | Organised gang/group and intimidation or the use or threat of force (short of robbery) | |
| Burglary in a building other than a dwelling | Goods valued at ≥ £20,000 | |
Appendix 3 The OHSCAP manual
Reproduced with permission (Professor Jenny Shaw, Offender Health Research Network, 2017, personal communication).
Appendix 4 Fidelity-of-implementation audit scale
Appendix 5 Estimations of unit costs
| Cost and unit estimation | 2014/15 value | Notes |
|---|---|---|
| Wages/salary | £26,771 per year | Based on NOMS band 4 mid-point 37 hours including 17% unsociable hours. Inflated from 2012/13 figure of £25,389111 |
| Oncosts | £3694.40 per year | National Insurance; employer contribution of 13.8% |
| £4899.09 per year | Pension; employer contribution 18.3% (average of probation trusts local government pension scheme employer contributions ranged from 10.1% to 26.5%)125 | |
| Working time | 1587.97 hours per year | 225 working days minus 10.41 days sickness absence (average sick days across NOMS and probation trusts)125 |
| Unit cost per hour | £22.27 |
| Cost and unit estimation | 2014/15 value | Notes |
|---|---|---|
| Civilian instructor wages/salary | £17,925.36 per year | One civilian instructor employed to facilitate. Based on NOMS band 3 mid-point. Inflated from 2013/14 figure of £17,000111 |
| Civilian instructor oncosts | £2346.00 per year | National insurance, employer contribution of 13.8% |
| £3111.00 per year | Pension. Employer contribution 18.3% (average of probation trusts local government pension scheme employer contributions ranged from 10.1% to 26.5%)125 | |
| Working time | 1587.97 hours per year | 225 working days minus 10.41 days sickness absence (average sick days across NOMS and probation trusts)125 |
| Ratio of direct-to-indirect time on face-to-face contact | 1 : 1 | Assumed 50% of time is spent on face-to-face contact and 50% on other activities |
| Civilian instructor: cost per hour of direct contact time | £29.82 | |
| Prison officer cost per hour | £18.03 | Prison officer (band 4 mid-point). Taken from NICE draft guideline on Mental Health of Adults in Contact with the Criminal Justice System, Draft Guideline Version 2115 |
| Total staff costs per hour | £47.85 | Based on one civilian instructor and one prison officer for each daily activity session |
| Unit costs per hour of daily activity per attendee | Assumed average number of attenders per activity: | |
| Therapeutic group | £4.78 | 10 |
| Creative activity | £3.19 | 15 |
| Work | £1.37 | 35 |
| Sports activity | £3.19 | 15 |
| Older prisoners group | £3.19 | 10 |
| Cost and unit estimation | 2014/15 value | Notes |
|---|---|---|
| Wages/salary | £30,030.25 per year | Based on NOMS band 5 mid-point 37 hours including 17% unsociable hours. Inflated from 2012/13 figure of £25,389111 |
| Oncosts | £4144.17 per year | National Insurance; employer contribution of 13.8% |
| £5495.54 per year | Pension; employer contribution 18.3% (average of probation trusts local government pension scheme employer contributions ranged from 10.1% to 26.5%)125 | |
| Working time | 1587.97 hours per year | 225 working days minus 10.41 days sickness absence (average sick days across NOMS and probation trusts)125 |
| Unit cost per hour | £24.98 |
Appendix 6 Interview schedule: OHSCAP staff facilitators
Follow-up staff facilitator interview guide
Can you tell me a bit about your role at the prison?
-
Are you a member of the health-care or prison staff?
-
Could you tell me a little bit about the prison?
-
What role have you had supporting older prisoners?
-
How long have you worked in the prison service?
-
What do you like about working in the prison service?
-
What do you not like about working in the prison service?
-
How did you end up working in prison (motivations)?
-
How did you end up working with older prisoners/doing the OHSCAP?
Can you tell me what’s it’s like to work in prison?
-
What’s a typical day like for you?
What impact have recent changes (staff reductions/social care act) had on staff/prisoners/older prisoners?*
-
Prisoner–staff relationships*
-
Morale*
Overall, how have you found conducting the OHSCAP?
How did you find the training in the use of the OHSCAP?
-
What was useful?
-
What could be improved?
-
How well did it prepare you for delivering the OHSCAP?
How did the identification of older prisoner on entry into prison work?
-
What worked well?
-
What could be improved?
How have you found conducting the assessments?
-
Where did you generally see the prisoners?
-
How long did the conversations last?
-
What type of issues did you discuss?
-
To what extent did you feel prisoners were being open with you?
-
Go through an OHSCAP?
-
Can you give me any examples of when it worked well?
-
Any examples of when it did not work so well?
Can you tell me about making the care plans?
-
How did the care plans get decided upon?
-
What kind of actions did you generally come up with for the care plans?
-
What services did you make referrals to in the care plans?
-
To what extent were you able to involve older prisoners in the development?
Can you tell me about the reviews of the care plans?
-
How able did you feel to identify when reviews should be conducted?
-
How able were you to stick to the agreed review periods?
-
What did you discuss during the reviews?
-
In general, how often did the reviews take place?
-
Was this too often, not enough, about right?
-
What was useful about the reviews?
-
What aspects of the reviews could be improved?
How has the OHSCAP helped you to support older prisoners?
-
What was helpful?
-
What could be improved?
-
Multiagency working.
-
Speed of getting things done.
-
Has it helped particular groups more than others (ages, vulnerable prisoners, new to prison)?
How were the care plans shared?
-
Were the care plan uploaded on to prison, clinical/probation computer systems?
-
To what extent was sharing the care plans helpful?
-
Were there any problems identified with sharing the care plans? Please explain.
How well did conducting the assessment and reviews fit into your job role?
-
How much time did it take up?
-
How did it assist you in your role?
Could you tell me a little bit about what happened before the implementation of the OHSCAP to identify and manage older prisoners’ health and social care needs and what has changed?
-
How were older prisoners identified before the OHSCAP was implemented?
-
How were older prisoners’ health and social care needs identified and managed before the OHSCAP?
-
Have there been any spin off as a result of the OHSCAP?
Would you like to summarise what you feel are the key points to consider when delivering the OHSCAP? Is there anything else you would like to tell me?
*Indicates that the question was added after the first few interviews suggested that the issue was important and warranted further exploration.
Appendix 7 Interview schedules: intervention participants
Initial patient interview guide
The effectiveness of the OHSCAP: a randomised controlled trial – semistructured qualitative initial patient interview guide
Introduction
-
Name.
-
Research project overview.
-
Interview format.
-
Consent.
-
Confidentiality.
-
Audio recording/researcher notes.
-
Right to withdraw/refuse to answer questions.
-
Any questions before we start.
Background information
-
Could you tell me a little bit about yourself?
-
How old are you?
-
What wing are you based on?
-
How long have you been in prison for?
-
Have you any idea how long you are going to be here for at the moment?
-
Have you been in prison before this time? How many times?
-
Have you come straight into this prison from court?
Prison experience
-
Could you tell me about your experiences of prison so far?
-
What happened when you came in?
-
How did you feel when you first came in?
-
How was the journey here?
-
Where were you located when you arrived? How was that?
-
-
Health screening.
-
What happened at your health screening on reception?
-
How did you feel during your health screening?
-
What did you discuss at your health screening?
-
What happened as a result of your health screening?
-
-
Induction.
-
How did you learn about how the prison works/rules regimes/your rights?
-
Information booklets.
-
Peers.
-
Prison Officers, etc.
-
Induction session.
-
-
How helpful was the information provided?
-
Was anything missing?
-
How did you feel about the way the information was provided?
-
Problems/needs/concerns
-
Can you tell me about any problems or concerns you have experienced since arriving in prison?
-
Physical health (medication, treatment, access to health care).
-
Social care (accessing the prison, beds, meals, showering, toilet).
-
Mental health (depression, memory).
-
Emotional well-being (anxiety, stress, low mood, self-harm).
-
Problems on the wing (mixing with others, bullying, the regime, booking appointments).
-
Housing.
-
Finances (benefits, pensions, getting money in, telephone credit).
-
Employment.
-
Education.
-
Family and social networks (isolation, visits, elderly spouses/parents).
-
Feeling safe.
-
Preparation for release.
-
Help/support received
-
Can you tell me about the support/help you have received to date?
-
Who have you received help from?
-
Which members of staff have visited you? What happened?
-
Have you been called to health care? What happened?
-
How helpful has the help you have received been?
-
How would you describe your relationship with staff (health-care staff, prison officers, education, probation, third sector, Age UK, etc.)?*
-
To what extent do you feel able to discuss any issues or concerns with staff?*
-
How would you describe your relationships with other prisoners?*
-
Summary
-
Overall, what have been your main issues/concerns since you came in to prison?
-
Overall, how well do you feel your issues/concerns have been addressed?
-
What has been most helpful about the support you have received so far?
-
In what ways do you feel the support could be improved for people aged ≥ 50 years coming into prison?
-
That is all of my questions, is there anything else you would like to add about your experiences of prison so far?
Thank you and explanation of what happens next.
*Indicates that the question was added after the first few interviews suggested that the issue was important and warranted further exploration.
Follow-up patient interview guide
Semistructured qualitative follow-up patient interview guide
Introduction
-
Name.
-
Research project overview.
-
Interview format.
-
Consent.
-
Confidentiality.
-
Audio recording/researcher notes.
-
Right to withdraw/refuse to answer questions.
-
Any questions before we start.
Background update
-
How long have you been in this establishment for now?
-
Where are you located?
Progress since last visit
-
How have you been since I last saw you?
-
Last time I saw you mentioned that your were having difficulties with x, y and z, how are things now?
-
Have you received any help/support with these issues?
-
What type of help/support have you received?
-
Who has given you any help/support?
-
Officers.
-
Health-care staff.
-
Prisoners.
-
Other organisations.
-
-
Can you tell me about the support you received? What happened?
-
How helpful was this support?
-
Is there anything you still need support with?
OHSCAP
-
Can you tell me about when you saw (older prisoner lead) and completed the OHSCAP? (Show tool as prompt.)
-
Who completed the OHSCAP with you?
-
How did you find the person completing the OHSCAP?
-
Who do you feel should complete the OHSCAP with you? (A member of health-care staff, an officer, your personal officer, another prisoner, anyone else.)
-
Where did you see the older prisoner lead?
-
How long did the conversation last?
-
What did you discuss? (Physical health, emotional well-being, discharge from prison.)
-
How able were you to discuss these things openly/honestly?
-
How comfortable did you feel talking to them?
-
Did they take notes?
-
Was there anything that you feel they should have asked you about that they did not?
-
At what point do you feel you should be discussing your release from prison?
Care plan
-
Can you tell me about making the care plan?
-
How did the care plan get decided upon?
-
What kind of actions did you come up with for the care plan?
-
Were you referred to other services as a result of the care plan?
-
To what extent did you feel involved in the development of the care plan?
-
Were you offered a copy of your care plan?
-
Did you take a copy of the care plan? If not, why not?
Reviews
-
Can you tell me about the reviews of the care plan?
-
Did the older prisoner lead come back and see you to do a review?
-
How many times?
-
Was this what had been agreed?
-
What did you discuss during the reviews?
-
How often did the reviews take place?
-
Was this too often, not enough, about right?
-
How much had things moved forward since you last met?
-
What was useful about the reviews?
-
What aspects of the reviews could be improved?
Comparison to previous experience
-
Have you been in prison before? If so, how did you find your health and social care needs were met this time, compared with the previous time(s)?
-
How well do you feel your needs are being met in comparison to how they were met in the community?
Summary
-
Overall, how did you find meeting up with the older prisoner lead and receiving the OHSCAP?
-
In what ways did completing the OHSCAP help you? (Health needs, social care needs, time to talk, anxiety, depression, explaining how things worked.)
-
What aspects of the OHSCAP could be improved? How?
-
What support would be helpful to support people aged ≥ 50 years in prison?
-
I have finished my questions, is there anything else you would like to add about your experience of prison, the help you have received or your experience of the OHSCAP?
Appendix 8 Dissemination strategy
To date, a number of dissemination events have occurred/are planned.
-
In December 2016 an event was held (free of charge) and attended by around 150 prison-based managers and practitioners (prison and health staff) and third-sector/user carer representatives.
-
The research was presented at the Royal College of Psychiatrists Forensic Faculty conference (March 2017).
-
The findings will be presented at a forthcoming meeting of the Royal College of Psychiatrists Quality Network for Prison Mental Health Standards.
-
A seminar was organised on older people in prison for the annual International Association of Forensic Mental Health Services conference (June 2017).
-
We are working with serving and ex-prisoners to produce lay summaries of the research, which will be distributed in prison using the same methods used by publications such as Inside Times, the prisoners’ newspaper. We will circulate these out of custody via our/partner e-news/social media/website outlets.
-
We began, in June 2017, drafting academic papers relating to this work.
-
We are conducting further work into growing old in prison and have service user groups ongoing for that work, thus this work will continue to feature in, and inform, these groups.
List of abbreviations
- A&E
- accident and emergency
- ACCT
- Assessment, Care in Custody and Teamwork
- ADL
- activities of daily living
- AE
- adverse event
- BADLS
- Bristol Activities of Daily Living Scale
- CANFOR
- Camberwell Assessment of Need – Short Forensic Version
- CARAT
- Counselling, Assessment, Referral, Advice and Throughcare
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- C-NOMIS
- Computer – National Offender Management Information System
- CONSORT
- Consolidated Standards of Reporting Trials
- CTU
- Clinical Trials Unit
- DLO
- disability liaison officer
- EQ-5D-5L
- EuroQoL-5 Dimensions, five-level version
- GDS
- Geriatric Depression Scale
- GDS-15
- Geriatric Depression Scale – short form
- GP
- general practitioner
- HMCIP
- Her Majesty’s Chief Inspector of Prisons
- HRQoL
- health-related quality of life
- HSDR
- Health Services and Delivery Research
- ICER
- incremental cost-effectiveness ratio
- MAHSC-CTU
- Manchester Academic Health Science Centre Clinical Trials Unit
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NOMS
- National Offender Management Service
- NSF
- National Service Framework
- OHSCAP
- Older prisoner Health and Social Care Assessment and Plan
- OPCRIT
- Operational Criteria Checklist for Psychotic and Affective Illness
- PADL
- prison activities of daily living
- PSSRU UCCJ
- Personal Social Services Research Unit’s Unit Costs in Criminal Justice
- PSSRU UCHSC
- Personal Social Services Research Unit’s Unit Costs of Health and Social Care
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RSN
- Restore Support Network
- SAE
- serious adverse event
- SAP
- Single Assessment Process
- SD
- standard deviation
- SF-SUS
- Secure Facilities Service Use Schedule
- TAU
- treatment as usual