Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/136/104. The contractual start date was in December 2013. The final report began editorial review in December 2016 and was accepted for publication in May 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Storey et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
This report presents data and interpretations deriving from a National Institute for Health Research-funded study conducted from 1 November 2013 to 30 November 2016. The research was designed to shed light on the extent and nature of the mobilisation of clinical engagement and clinical leadership. The setting for this was mainly general practitioner (GP)-led Clinical Commissioning Groups (CCGs), but the issues and processes extend well beyond these. There were two interrelated foci: service redesign attempts as a function of clinical leadership; and CCGs as the institutional base for these efforts. CCGs were the promising, potentially enabling, platform from which would-be clinical leaders might launch their interventions. The main purpose of the research project was to understand how clinicians and others were able to use the opportunity presented by these new institutions to engage with, and indeed lead, the changes to service redesign which so many observers have insisted are fundamentally necessary for the survival of the NHS. Thus, three elements were in play at all times: the triangle of clinical leaders (the agents); the CCGs (the inner context operating within the wider context of other NHS institutions); and service redesign (the process and the potential outcome).
The project generated a unique collection of complementary data sets. These were generated through surveys, case studies, interviews, observations and analysis of documentation. The survey data results were also cross-correlated with NHS England (NHSE) ratings of CCGs. Although some of our findings confirm patterns already revealed by other research (such as the problems with widespread engagement of GPs), other findings which spell out the details of modes of clinical leadership in new service designs are unique and original. They add to the body of knowledge about service redesign in health by elaborating for the first time how this has been achieved within the commissioning domain.
The idea of ‘clinical leadership’ as something important and perhaps even vital in the modern health economy includes, but goes beyond, GPs and CCGs. There is now a much broader expectation that clinicians ‘step up’ to leadership beyond their immediate clinician-to-patient responsibility. As Lord Darzi expressed it:
Clinicians are expected to offer leadership . . . within the clinical team, to service lines, to departments, to organisations and ultimately the whole NHS. It requires a new obligation to step up, work with other leaders, both clinical and managerial, and change the system where this would benefit patients. 1
Thus, there is an ‘expectation’ and an ‘obligation’ that clinicians engage in leadership of the health service. CCGs are but one, albeit very important, example of just such an attempt to enact the expectation, obligation and opportunity. This study provides insight into the degree and the manner in which clinicians did, or did not, rise to the challenge and step up to meet the expectation described by Lord Darzi. The subsequent Lansley reforms in the 2012 legislation built on this same expectation. However, although this was the policy intent, the extent to which this expectation is actually shared and accepted by relevant agents is an empirical question.
The launch of CCGs gave clear institutional expression to the declared policy intent to enable clinical leadership. This was underpinned by a belief that clinicians, most especially GPs, would be able to understand patient priorities and would carry trust and credibility to a degree perhaps not achievable by managers acting alone. Expressed more succinctly, the idea was to put ‘GPs in charge’. All of these ideas were found in the Health and Social Care Act of 20122 and before that in the Public Health White Paper. Equity and Excellence: Liberating the NHS. 3 The Act came into operation on 1 April 2013. The original policy was for GP commissioning but, following the controversy which led to the pause in the progress of the legislation, other clinicians (such as nurses and secondary care doctors) were included in the groups and the name of the new local commission groups was changed accordingly. Our own focus on clinicians as potential leaders follows these developments, meaning that we also tracked the work of the wider group of clinicians. Although we found some nurses active in the leadership of service redesign, the main assumption among most actors in the system was that it was GPs who were the focus of attention and expectation.
From the outset, we anticipated that the policy landscape and the surrounding economic, social and political landscapes would continue to unfold and, in consequence, any response to the clinical leadership opportunities presented by CCGs would have to take those wider dynamic changes into account. There was the possibility that CCGs per se would not survive. This added an important strand to the unfolding drama. In this introduction we summarise the more important policy and contextual changes. These changes provide an important backcloth to the behaviours reported in the findings section (see Chapters 3–5) of this report.
The wider context and the policy intent
The basic policy shift, which abolished primary care trusts (PCTs) and strategic health authorities and introduced local commissioning groups led by GPs, can be seen to build on three ideas: (1) clinical leadership, (2) the use of CCGs as a platform which gave them commissioning powers and (3) the idea that these actors would use these powers to improve the quality and cost-effectiveness of the NHS and to redesign services (indeed ‘transform’ them) to make them better suited to local needs, in more effective and sustainable ways.
The policy, its ensuing reform and its legislative package was hugely controversial. The whole edifice could be seen as a massive experiment. Handing the purse strings to new groupings of GPs and disbanding existing structures came as a surprise; it had not featured in the Conservative Party Manifesto of 2010. It became mandatory for GP practices to be part of, and indeed members of, a CCG. Our research project was designed to target a set of questions which went to the heart of the package of reforms. In essence, the underlying aim was to assess how clinical leadership in and around CCGs would operate in practice. By ‘operate’ we mean what it would deliver and how it would produce any achieved outcome. In order to answer these questions, the research design was built, centrally, around a study of initiatives in specific service areas in order to map these in a manner which dug beneath the rhetoric of reform. These service areas were identified by the wide range of stakeholder informants at the scoping stage as the ones most critical to the future viability of the NHS. The service areas identified were redesigning urgent care, managing long-term conditions, care of the frail elderly and mental health.
Our central concern was how clinicians used, and were affected by, the institutional mechanisms. Lessons learned in manoeuvring through and around these carry a significance beyond the specifics of the CCG formation. The story is bigger than CCGs alone. A considerable amount of activity was initiated by clinical leaders who were not in a formal post within a CCG.
In 2012/13, the idea of facilitating clinical leadership through localised commissioning bodies was not entirely new. Former experiments included GP fundholding and related forms. As we and others anticipated, it was not long after the official launch of CCGs in April 2013 that other initiatives and other developments emerged – most notably, the NHSE-led ‘New Models of Care’ (URL: www.england.nhs.uk/ourwork/futurenhs/new-care-models/; accessed 25 October 2017). All CCGs have had to take note of, and respond in some way to, these policy thrusts. Inevitably, our research work in and around CCGs tracked these responses as they occurred in real time.
During the period since their inception, there appears to have been increasing oversight and monitoring of CCGs, most especially by NHSE and the Care Quality Commission (CQC). Some CCGs have been put into special measures, senior staff have been displaced and Ofsted-style ratings have been used to identify CCGs needing improvement or deemed to be in the ‘greatest need of improvement’ (URL: www.nhs.uk/service-search/scorecard/results/1173; accessed 25 October 2017). An interesting feature here is the way local commissioners are being held to account by central agencies in addition to the accountability to the local membership. In 2017, a number of CCG mergers were approved and further mergers leading to fewer and larger CCGs are likely to follow.
The requirement on local health economies to construct sustainability and transformation plans (STPs) also represents a game-changing initiative concerning the redesign of health and social care. Although the STPs require engagement by CCGs, local authorities (LAs) and provider trusts, there are concerns that these bodies, creations of the centre, may come to diminish the influence of CCGs. 4 A PricewaterhouseCooper report notes that the consequence of multiple initiatives has been a ‘complex middle ground’ of localism and central direction. 5
The plans focus on some common themes: reductions in secondary care provision, closure or redesignation of community hospitals and revamped primary care with larger practices. 6 The promotion of new models, which emphasises integration and collaboration, seems to point to a lower priority for competition and commissioning and a higher priority for planning and collaboration. Indeed, the NHS chief executive refers to the possibility of the ‘pooling of sovereignty to drive the changes’ planned by STPs between commissioners and provider organisations. 7 Such developments might suggest that there is increasing uncertainty whether or not CCGs will, in the future, be regarded as the natural leaders of change and service redesign or become subsidiary to the STP level.
These profound ongoing shifts in the wider context were very much borne in mind by the members of the research team as they progressed with the task of finding answers to the original set of research questions. Those questions were as follows.
Research questions
The overall aim was to assess and clarify the extent, nature and effectiveness of clinical engagement and leadership in the work of the CCGs. This was broken down into five main research questions.
-
What is the range of clinical engagement and clinical leadership modes being used in CCGs?
-
What is the extent and nature of the scope for clinical leadership and engagement in service redesign that is possible and facilitated by commissioning bodies, particularly the CCGs and the health and well-being boards (HWBs)?
-
What is the range of benefits being targeted through different kinds of clinical engagement and leadership?
-
What are the forces and factors that serve either to enable or block the achievement of benefits in different contexts, and how appropriate are different kinds of clinical engagement and leadership for achieving effective service design?
-
What can be learned from international practices of clinical leadership in service redesign in complex systems that will be of theoretical and practical value to CCGs and HWBs?
The case studies and the national surveys were used as means to generate relevant data to help answer these questions. Before we present the findings and our interpretations of those findings, it is necessary to:
-
summarise the state of knowledge about these questions as found in the existing literature
-
introduce the theoretical lens we used in undertaking the analysis found in later chapters
-
describe the research methods which we deployed in this study.
In seeking to answer the research questions we were of course aware that there were existing literatures relevant to aspects of the research agenda, most notably literatures concerning the policy context, previous initiatives prompting GP commissioning, clinical leadership more broadly and service redesign in health. Hence, before describing our research methods we now turn to an outline review of those literatures.
The policy context
Policies can be seen as ‘answers’ to actual or perceived challenges facing health and social care, hence we begin this section with a brief review of the literature on those challenges. The predominant perceived challenges during the course of this study (2013–16) was the fragmented health and social care system and the severe financial constraints.
The nature and scale of the challenges facing the NHS have been spelled out many times,8 and there have been many warnings about the non-sustainability of business as usual. Currently, capital budgets are being constrained. In this environment, the ambitious transformation plans which usually require funding may be hampered by lack of money. Failures in the joining up of fragmented services are widely seen as having an impact on care of the frail elderly in particular. 9 On the demand side, the growing ageing population with multiple morbidities and wider population ill-health associated with obesity, diabetes mellitus and other long-term conditions are well-recognised problems for which new approaches to health and social care and, indeed, wider and far-reaching ‘health of the public’ innovations will be required. 10
The fortunes of the health service and the adult social care service are intertwined. A CQC report on the state of play in 2015–16 revealed that, because of funding cuts in local government and rising demand, adult social care services were at a ‘tipping point’. 11
The responses to these challenges have been many. A common theme has been a call for a new focus on prevention, more self-care, integrated health and social care and more home-based care. 12
The main policy intervention, as far as the CCGs as institutions are concerned, was the Health and Social Care Act 20122 which established CCGs and abolished PCTs and strategic health authorities. This expressed the policy intent of an apparent devolution of power and accountability. The CCGs could be seen as the institutional expression of the policy thrust which put challenge, competition, choice and commissioning to the fore.
However, following the departure of Secretary of State for Health, Andrew Lansley, in 2012, the emphasis shifted. Following the publication of the Mid Staffordshire Report,13 patient safety, patient experience and quality of care came more to the fore and so too a fundamental shift in policy towards integrated care, community-based care and ‘new models’ which gave primacy to collaborative working and meeting the needs of patients. 14
Variability in policy and practice during the research period were all too evident. Local commissioning runs alongside more regional planning. Local initiatives are fuelled by short-term special funding such as the Prime Minister’s Challenge Fund, the Pioneers, the Vanguards, the new Care Models and the STPs. Among other things, this means that interpretation of the role of clinical leadership in CCGs, and indeed interpretations of the role of CCGs themselves, need to take account of multiple shifts in the wider landscape of health and social care.
During 2016, NHSE modified the basis of NHS planning, requiring STPs to be produced within 44 ‘footprints’. These STPs are intended to provide the local planning basis for moving towards the models for integrated service delivery outlined in the Five Year Forward View. 12 This has enforced some clustering of CCGs. Many CCGs now work closely with their neighbouring CCGs and some share an accountable officer and other members of a managerial team.
The Health and Social Care Act 20122 and the surrounding policies and initiatives set the scene for much of the debate. A critical juncture in the highly contested passage of the Bill was the ‘Pause’ and the work of the NHS Future Forum. This raised, and explored, many of the issues which are now being worked through in practice by the CCGs and their surrounding bodies. 15
The NHS Commissioning Board which became NHSE, was responsible for the authorisation of CCGs and continues to oversee, guide and influence them. 16 In Planning and Delivering Service Changes for Patients17 it stated that major service changes and reconfigurations must put patients and public first and must be clinically led. It is clear that at that time of inception, CCGs were seen as the critical instrument and agency for driving change. NHSE gave further guidance relating to clinical leadership:
Chairs, Accountable Officers, Chief Executives and Medical Directors from across the organisations involved in a service reconfiguration should exercise collective and personal leadership and accountability when considering the development of proposals for major service change. Front-line clinicians and other staff should also be involved in developing proposals and in their implementation.
NHSE17 (emphasis added in bold).
Expectations were thus set high. It sets out a process for the planning, development and implementation of major service redesigns.
In April 2014, NHSE published its plans for transforming primary care. 18 It urged a move ‘away from providing 20th century solutions that are based on a fix and treat model’. This reflects an emergent theme, which was then developed in the Five Year Forward View. 12 This set out the direction of travel to guide local decision-makers with a strong emphasis on joined-up, integrated care. Notably, there is not a lot of emphasis on CCGs as institutional leads in the Five Year Forward View, although there is this statement of intent:
Give GP-led Clinical Commissioning Groups (CCGs) more influence over the wider NHS budget, enabling a shift in investment from acute to primary and community services.
NHSE. 12
A growing policy emphasis is on general practice and the idea of an extended multidisciplinary team surrounding GPs. A key example is the General Practice Forward View. 19 This promised accelerated funding, an expanded workforce of GPs and a more diversified workforce mix surrounding GPs, practice infrastructure improvements and major programmes of care redesign. In 2016, NHSE and NHS Improvement published the NHS Operational Guidance for 2017/18 to 2018/19 under the title Delivering the Forward View. 20 This increases primary care allocations for general practice with recurrent funding to the General Practice Access Fund.
Ironically, despite the clear and emphatic policy intent, the continued influence of the acute sector continues to be felt. This was seen in relation to the STPs, with considerable influence allotted to acute sector leaders, and is seen also in the continued funding bias. There is also a continued high-demand pressure on hospitals.
Literature on Clinical Commissioning Groups
The literature on CCGs comprises reports on the predecessor bodies to the CCGs, which included early forms of GP fundholding and commissioning; literature on CCGs while they were in shadow form leading up to April 2013; and reports on the actual operation of CCGs since they became statutory bodies in April 2013.
Since the original purchaser–provider split in the NHS, introduced by the National Health Service and Community Care Act of 1990,21 there have been many variants of clinical commissioning. The GP fundholding scheme was voluntary and it allowed GP practices to take control of a budget for certain defined services along with funds for a practice management allowance. 22 The Act allowed for ‘fund-holding practices’, and there followed a series of pilots and experiments. Most notably, the pilots and experiments included GP commissioning using fundholding (from 1991), total purchasing (from 1995 to 1998), primary care groups (PCGs) (1999) and the authorisation of PCTs. Storey et al. 23 and Sheaff et al. 24 studied commissioning under PCTs; the latter research group also, to an extent, studied the transition into shadow CCGs and, in so doing, revealed a number of important features of the way it operated in England and to a degree in other countries.
The 23-year period from 1990 to 2013 included numerous pilots and new forms. There are many relevant lessons to be drawn from the experiments and from the related literature. This fact has been noted by some helpful meta-reviews by The King’s Fund,25–27 the Institute of Education, London,28 and by PRUComm (Policy Research Unit in Commissioning and the Healthcare System). 29
Most interpretations suggested that these early forms had modest impact, but that this stemmed more from the constraints placed on the experiments rather than from the concept itself.
Studies of CCGs in shadow form again reported much uncertainty around the link between the governance/assurance level and the operational level; about links with the wider GP membership; about how to resolve conflicts of interest; and about who could make decisions about what. 30 Other work drew lessons about the motivations of GPs, their levels of involvement, engagement and influence, and of leadership by clinicians under each of the previous schemes. A conclusion was that, on balance, the evidence of impact of clinical-led commissioning was ‘limited’. 29
NHS England/Ipsos MORI, The King’s Fund and the Nuffield Trust all produced reports on CCGs in their early statutory days. 31 The King’s Fund, in conjunction with the Nuffield Trust, reported on CCGs after 1 year of operation. The King’s Fund found that less than half of GPs judged that CCGs really reflected their views; nonetheless, GPs felt that they had more influence with CCGs than they had under the PCT regime. 32 Another Nuffield Trust report noted the flaw in attempting to commission secondary care effectively without also considering primary care. 33
The Nuffield Trust team noted the progress made by CCGs in involving GP members, yet, on the other hand, noted the threats to CCGs as much of the agenda, such as STPs and Vanguards, appeared to be being driven without regard to the supposed fundamental role for CCGs. 34
In summary, studies of CCGs and their predecessor bodies tended to find that, although there was much ‘in principle’ support for the general idea of clinical leadership through commissioning, the implementation of the idea across the land (apart from a few notable pioneering exceptions) had been limited in its realisation. These reports, although providing clear descriptions of aspects of governance and engagement, paid less focused attention to actual examples of service redesign activity by CCGs and the precise work of clinical leaders – themes that we address below.
Leadership, clinical leadership and engagement
The body of literature on leadership in the English NHS, and in health services more widely, reflects the themes and concerns across many industry sectors. 35 These include the distribution of leadership within organisations; adaptive leadership; concerns about heroic charismatic leadership styles and a search for more ‘authentic’ and ethical forms of leadership; collaborative and interorganisational leadership; and whole-system leadership.
The literature on leadership in health services and on clinical leadership is extensive and we have reviewed it fully elsewhere – most notably for the NHS Leadership Academy. 36 One of the dominant themes in that body of literature is the perceived need to shift towards a compassionate mode of leadership in keeping with the caring nature of the services provided in health. 37 Another strand of literature, highly relevant to our study, is that which investigates how health-care professionals respond to policies directed towards the design of a new workforce mix in order to facilitate access and make services more affordable. 38–41 Other literature has highlighted the merits of having medics, and clinicians more generally, involved in taking up leadership positions in health services and, relatedly, in investigating the required competences. 42,43
A National Institute for Health Research-funded project on medical leadership provided data on degrees of engagement by doctors in various trusts using the Medical Engagement Scale. This project showed, as with other studies, some considerable distance between many medics and the leadership teams. 44 This work also focused on acute, specialist and mental health trusts, all of which were characterised by professional bureaucracies. As explained, our prime focus was rather different, namely to trace the extent and nature of clinical leadership using the platform afforded by the CCGs. Thus, our prime focus was on active leadership of service redesign. Often this was undertaken by informal leaders, as well as those occupying formal roles within CCGs. Attempting to lead changes in service redesign across the complex boundaries in primary and secondary care is a very different challenge.
Another central theme in the literature has been the perceived tension between, on the one hand, professional autonomy and established notions of professional practice and, on the other, the cluster of notions attached to organisational practice. Hence, the various ways in which doctors have resisted managerial attempts at organisational change and re-engineering have been extensively researched and reported in the literature. Much of this research, however, has been located in acute hospital settings where issues of competing hierarchies are at stake. As our scoping research had indicated, the more salient issues in the context of CCGs were aspects of interorganisational leadership and interprofessional leadership.
Given that the policy thrust, as seen in The wider context and the policy intent, is ostensibly towards devolved leadership, then questions are inevitably raised as to where this leadership will be located and how it will be exercised in practice. Much of the leadership work seems to get done by combinations of managers and clinicians. Indeed, sometimes managers are clinicians who hold hybrid roles. Some researchers have emphasised and illustrated the pluralistic nature of organisational leadership. 45 This refers to tendencies in many organisations for leadership to be exercised by clusters of two or three players at the top (e.g. chief executive, a chief finance officer and a chief operating officer). Extending out from this are studies which point to much wider forms of distributed leadership throughout organisations. 46–48 Informal leadership seems to be an attractive idea for some clinicians and is associated with the identity formation of leaders who practise leadership and then reflect on that practice. 49
Alternatives to top-down, planned, transformational leadership approaches have been advocated, especially in health services. These leadership approaches include the idea of mobilising action in organisations through adaptive changes and ‘adaptive leadership’;50 other related approaches include ‘appreciative inquiry’ and similar modes of action research. 51 The adaptive leadership approach makes a distinction between ‘authority’ and ‘leadership’. Instead of seeking leaders who, supposedly, know all the answers and issue these from on high, advocates such as Heifetz50 contend that leaders should be encouraged and developed who can stimulate changes in attitudes, behaviours and values. This kind of leader mobilises people to solve problems. So, leadership in these terms is ‘adaptive work’ involving many people and, through exposing and confronting internal contradictions, allowing people to find new ways of thinking and behaving. 50 Thus, in place of the heroic leader model emerges an approach which views the organisation as a system. The associated skills can be learned and tools applied to nudge the system to adapt through mobilising the efforts of multiple people. 52 This requires processual and improvisational expertise. It involves experimentation, iteration and trialling rather than linear implementation of a top-down strategy.
Storey and Holti53 found that NHS structures and culture often present numerous barriers to the effectiveness of clinical leadership for improving service co-ordination and integration from within the acute sector. Despite the barriers, they also found cases where determined doctors and other clinicians persisted in their attempts to exert positive influence on reshaping service design and delivery. 54 Other studies of the roles of clinicians and others in bringing about complex service innovations support the view that there is a need for an effective alliance between clinicians and administrative managers. Complex service innovations, such as the establishment of a region-wide network of cancer services, seem to require a multilevel and multidisciplinary array of clinical and administrative leadership roles, sometimes referred to as a ‘leadership constellation’. 55,56 This idea is reflected in the role of ‘clinical communities’. 57,58
As the above analysis indicates, there is considerable overlap between the issues researched as part of understanding leadership in health and the related domain of understanding service redesign and change in health. It is towards this last domain that we now turn our attention.
Service redesign of health and social care
Most reports of actual attempts to bring about transformative change in health care have tended to focus on the acute sector. As largely hierarchical organisations these settings have lent themselves to exploration of redesign methods derived from the business literature including, for example, business process re-engineering. 59–63 The analysis of attempts to introduce radical redesign of processes in acute hospitals reveals the complexity of such attempts and the micro-political struggles involved. 59 Consent had to be won from clinicians, and this proved to be highly conditional. 40,64–66
Professional occupational groups lay claim to ‘jurisdictions’. 66 In particular, the jurisdictional claim embraces the classification and diagnosis of a problem, the power to reason about it and to take action in relation to the identified problem. Currie et al.,40 likewise, reveal the methods used by medics to maintain existing structures, building on previous work on professional defence routines. 66,67 They found that ‘In essence, the elite actors are engaging not simply in outright “change resistance” but more subtly in institutional work designed to shape the change trajectory to ensure continued professional dominance’. It is not only clinicians who engage in institutional work when creating new forms or shoring up old ones, managers in health service redesign attempts are also heavily involved. 68
Whether or not the same kind of analysis of professional jurisdictions made in these mainly acute contexts can be transferred to the primary care setting is an open question. This is especially so in the case of CCGs, where the core institution is ostensibly a ‘membership’ organisation.
The findings from research in the acute health-care setting reflect findings and theory from the wider organisational theory literature. 69 ‘New institutional theory’ places emphasis on the shaping power of existing institutional forms on human agency and the institutional ‘work’ undertaken by actors. Institutional work is found in everyday activities, which can be seen to serve underlying purposes. To use Lawrence and Suddaby’s70 categorisation, these purposes may be to ‘create, maintain and/or disrupt institutions’. We build on the institutional work perspective in our case studies.
It is important to note that attempts at exercising clinical leadership are located within existing institutional arrangements. Clinical leadership does not operate in a vacuum. Within the context of the NHS, a great deal of institution shaping and reshaping emanates from higher-level actors, most notably NHSE and political agents; these set the direction of travel and allocate resources (financial- and legitimacy-based resources). The very origins of CCGs themselves stemmed from this source, followed by the Five Year Forward View12 and the STPs. Each of these institutional shifts was built on the assumption of the need to relocate care from hospitals to community settings. During this journey there was a move from a reliance on commissioning in a competitive market environment to large-scale planning and collaboration. Recent literature has begun to question the validity of assumptions about savings and efficiency in the shift to community care. 71 Additional challenges relate to the leadership required to implement and deliver the broad policy ideas. Our research was directed at these forms of leadership.
Studies of successful leadership of service redesign72,73 point to lessons which include distributed change leadership from both formal clinical leaders and senior managers, credible opinion leaders at the level of senior clinicians in the services concerned and ‘willing workers’ – front-line clinicians prepared to embrace the new way of working. 73
Conclusions to the literature review and implications for a research agenda
From the research reports cited above, some common threads are evident. In CCGs, as with many other membership bodies, it evidently often proves difficult to fully engage the wider membership in any meaningful way. Furthermore, these studies find that the defence of professional autonomy often competes with attempts to ‘manage’ performance across primary care. (However, our case analysis in Chapter 4 reveals some successful examples.) The body of literature also indicates that the legacy effect of past experience with practice-based commissioning and similar initiatives tended to shape perceptions and responses to new arrangements; these often leaned towards the sceptical. There remains a significant gap between the ambitious agendas for change set out in key policy papers and the reality on the ground of actions taken, to date, by most CCGs.
Key themes emerging as requiring deeper understanding include:
-
the forms of influence that clinicians are actually achieving both as commissioners and providers under CCGs and associated arrangements
-
how leaders (managers and clinicians) are able to use the CCG as a platform and resource to bring about service redesign and, as a key part of this, the balance between formal and informal opportunities for leadership
-
the impact of these emerging forms of power and influence on the achievement of more integrated and effective forms of patient care.
Chapter 2 Project design and methodology
The findings presented and discussed in this report are derived from a number of data collection ‘windows’ into the work of CCGs, of clinical leaders and of other leaders in and around CCGs. The project proceeded through a series of sequential steps in five phases as mapped in the project Gantt chart (see Appendix 1). The five main phases were as follows:
-
An extended scoping study encompassing 15 CCGs spread across England.
-
Drawing on the results of this scoping work and on a review of the relevant literature, a national survey was designed and administered with the target population being all members of the governing boards of all 210 CCGs.
-
In-depth case studies in six CCGs. This work was designed to reveal details of the processes involved in seeking meaningful service redesign through the deployment of clinical leadership and the in-depth study of a number of specific examples of attempted service redesign within these cases; the method here was to study clinical leadership in action.
-
Drawing on the lessons learned from the case study work in phase 3, a second national survey was designed. Again, the target population was all the members of all CCG governing bodies (approximately 3100 people including accountable officers, chairpersons, GPs, secondary care doctors, nurses and lay members).
-
A set of international comparisons enabled by sharing our results with leading international experts in other relevant health economies. The health systems chosen were those where there seemed to be some likely comparative resonance and thus the opportunity to generate further insights through the use of the perspective allowed by these comparisons. The main comparative economies selected were Canada, Germany, the Netherlands, Sweden and the USA.
Phase 1
As part of the initial scoping work, studies were made of a relatively large sample of 15 CCGs and their associated hinterlands of HWBs, LAs and health-care providers. In this phase of the project, the research team were looking both outwards from focal CCGs and inwards from the perspectives of relevant others. This included gathering views from relevant stakeholder bodies such as NHSE, CQC, the Faculty of Medical Leadership and Management, the National Association of Primary Care, commissioning support units (CSUs), the London Office of CCGs, NHS clinical commissioners, clinical senates and local medical committees, LAs, HealthWatch, community services and acute hospitals (managers and consultants). We attended many relevant conferences such as Commissioning Live and workshops at The King’s Fund. Simultaneous with the work in the first phase we undertook a major literature review. This review, uniquely, not only embraced the literature on clinical leadership and leadership studies more generally, but reached out into related relevant literatures on CCGs and other earlier forms of local commissioning, and the literatures on service redesign and change in health services.
The scoping phase was used to allow insight into the varied types of CCGs and to gain a sense of the range of practice across the country. Interviews were conducted with accountable officers, chairpersons and a representative sample of CCG office holders, including various clinical leads, locality leads, GP governing board members, lay members, nurses, secondary care doctors and patient and public representatives. Interviews were also conducted with LAs and with members of HWBs. The aim at this stage was to gain a ‘rounded view’ of CCG activity. This phase of the study also included observational studies of CCG board meetings and of HWBs. These were used to gain a sense of the scope of ambition and insight into which agents were engaged in what kinds of service redesign.
The aim at this scoping stage was to capture and catalogue the range of issues. It was also designed to gain exposure to varied contexts across the country – allowing access to issues as experienced in inner and outer London, in Northern and Midland towns and cities, and in rural areas. Research team members used a common semistructured interview guide. Interviews were recorded and transcribed in most instances, depending on the wishes of the interviewees.
Phase 2
The findings from this pilot phase were used to help construct the questionnaire for the first national survey of all 210 CCGs (following a merger the total later became 209) across England. In turn, the responses from that survey helped inform the selection of six core cases that were targeted for in-depth research over the ensuing 2 years. The findings from these cases helped inform the design of the final national survey that was conducted in the third year of the project.
Phase 3
Central to the research design were the core cases studies. Theory building from multiple cases has many recognised benefits – as well as challenges. 74,75 Case studies enable exposure to rich data in their real-world contexts. The main case study work phase was informed by the initial scoping work and also by the results of the national survey. In the main in-depth case studies, the focus was sharpened more directly onto explorations of specific examples of service redesign and an identification of who did what in conceiving, planning, resourcing and driving the changes.
Hence, at this stage, the framing of a ‘case’ tended to settle more directly on these service redesign initiatives rather than the CCGs per se. So, although our point of entry was into six CCGs, the case analyses focused on eight specific service redesign attempts. Once again we used a common semistructured interview guide (see Appendix 4). We worked in fieldwork teams of two, sometimes three, researchers and, again, interviews were recorded when feasible and helpful. Interviews were supplemented with relevant documentary analysis and with observations of board meetings, programme board meetings and other events relevant to the particular service redesign.
Phase 4
Phase 4 was the second national survey. This included many questions which had been part of the first survey and, hence, comparisons over the intervening time period (nearly 2 years) were enabled. Additionally, by the time this second survey was being designed the project team had gained extensive knowledge from the main case studies and this allowed a number of new and more refined questions to be posed. The key questions in the 2016 survey included assessments of the perceived power and influence of CCGs relative to other bodies. This was important because these assessments of the CCG as a potential lever could be expected to shape expectations of these actors about how far they could use these institutions as a basis to bring about meaningful redesign. If the institutions were judged to be relatively powerless, then that would be reasonably expected to blunt and limit would-be leaders in seeking to harness the CCG as an agent for change. If, conversely, the CCGs were judged to be influential, then that could raise expectations about what could be done by making use of these institutions.
In a related set of questions we asked about the perceived influence of other relevant bodies such as NHSE (nationally and regionally), LAs, hospitals, other major provider organisations and clinical networks, and other bodies. If these other bodies were perceived as highly influential, then this might either inhibit or curb the scope for action by the CCG or it might at least indicate the need for collaborative relationships.
Other questions were asked about the degree of engagement by the wider GP membership in the affairs of the CCG. This area of questioning was designed to assess the breadth and depth of clinical engagement and leadership. Related questions were asked about the nature and degree of influence of clinical leadership in improving and redesigning services.
Phase 5
Phase 5 included a set of international comparisons. When we had collected and analysed the data from multiple sources we wanted to gain a richer perspective by examining the findings from an international comparative perspective. Part of the reasoning was to rise above parochial issues and to reassess the meaning of the findings by comparing how health-care managers and leaders in other countries were handling similar issues, even if their circumstances were not precisely the same. We also wanted to gain deeper insights into our own data and findings by exposing them to international expert teams and entering into question and answer mode with them.
We already had relevant international connections in our wider network and so we built on that basis while also inquiring about additional experts. Our initial idea had been to hold webinars for this purpose, but initial attempts made it apparent that it was difficult to gain full attendance at synchronous events across different time zones. Hence, we adapted the method by producing synoptic accounts of our findings and e-mailing them to our network of international experts. These accounts were accompanied by a structured set of questions, including questions about how similar issues, tensions and dilemmas were handled in their own settings. This proved to be an effective and efficient approach, and it triggered a constructive dialogue which was progressed iteratively. This process of international exchange allowed us deeper and more detached perspectives on the issues and findings.
Our theoretical perspective
Next we turn to an explanation of the underlying theoretic perspective that was used in this study as a means of understanding and interpreting the processes encountered in the field and in making sense of the data.
Our underlying interpretive lens is drawn from institutional theory. As the study unfolded, it became clear that the abundant initiatives and accounts we recorded about why the organisation of health and care had to be different (or why it needed in some aspects to be stable) were replays of some basic, fundamental narratives. Actors in the field (at multiple levels) were engaging in ‘institutional work’. 70,76 This work was and is designed to maintain and justify extant arrangements, to disrupt in part or whole those arrangements and/or to create new arrangements. 70,77
The unusually active state of this institutional work in the English NHS stemmed from ongoing prevalence of multiple and diverse ‘competing logics’. 78,79 The core prevailing logics were spelled out time and time again – in CCG strategy documents; in STPs and the workshops organised to prepare these plans; in NHSE statements and documents; and in our many interviews with actors at all levels and parts of the health service. A prevalent logic was the need to ‘integrate’ services across health and social care. This was the ‘dominant creative logic’ among persons seeking to disrupt extant systems and ways of working and to install new creative modes. The dominant logic, in the sense of extant practice, was fragmented organisations offering siloed services and based on an underlying notion of the value of ‘challenge and competition’. These competing logics coexisted as layers of statute and reform were laid on top of each other, pulling system actors in different directions. It was within this context that clinical leadership was being exercised or neglected. The question arises as to what form of institutional work clinicians are engaging in: are they, as some literature suggests, mainly seeking to ‘maintain’ and defend their privileged status?40 Or might we find cases where clinicians, as intended by the policy drive which established CCGs, undertake institutional work of a creative kind, which improves services for patients at scale and which deserves to be called active and constructive clinical leadership?
Despite the phenomenon of competing logics and the institutional work involved in creating, maintaining and disrupting institutions, the existence of ‘dominant logics’ has been widely noted. 80 The attachment to, and defence of, a dominant logic does not necessarily stem from a defence of self-interest. It has been noted that embedded actors often cleave to an institutional form because it has a taken-for-granted status that engenders a deep-seated belief in the necessity of the extant system. 81
The two national surveys
Using the findings from the pilot work, we constructed the first survey instrument for distribution to all members of the governing bodies of all 209 CCGs in England. A database of 3100 individual members of governing boards was constructed by tracking board papers and CCG websites. The questionnaires (see Appendix 3) were posted to this total population using their individual names and addresses. One postal reminder was then sent to those who had not responded and in that reminder letter an online version of the questionnaire was offered.
We calculated that a response of 340 would be required for 95% confidence intervals of reasonable width. For the first survey in 2014, there were 385 responses in total (12.42% of the total population of all CCG governing board members and 79% of all CCGs). For the second survey in 2016, there were 380 responses (12.26% of the total population of individuals and 77.5% of CCGs). The 18-month interval between the two surveys was designed to allow tracking of unfolding events and the maturation of the CCGs; thus, a longitudinal element was enabled.
We analysed key features of the non-responding CCGs, but there was no discernible pattern. They were distributed geographically and we could find no particular characteristic common features among the non-respondents that would distinguish them from those who did respond. In case of bias towards high-achieving CCGs, we compared our respondent CCGs with the profile of the 2016 NHSE ratings of CCGs. The resulting comparison is shown in Table 1.
| CCGs sampled | NHSE ratings profile 2015–16 (%) | |||
|---|---|---|---|---|
| Inadequate | Requires improvement | Good | Outstanding | |
| All NHSE CCGs | 12 | 44 | 39 | 5 |
| Our CCG sample | 12 | 41 | 41 | 6 |
The very close match suggests that respondents from struggling CCGs were just as willing to respond to the survey as those from high-performing CCGs.
The main in-depth case studies
Following the pilot case study phase and the first national survey, the focus of research work shifted to the six main case studies. The selection of these core cases was informed, as planned, by the results from the first national survey and was also shaped by our knowledge of activity across potential case sites. We wanted geographical coverage so we ensured that the cases included CCGs in London, the Midlands and the North, and we also ensured coverage of urban and rural settings. Of special importance was our knowledge of the degree of service redesign activity occurring in these settings. A random selection of cases might easily have resulted in six CCGs characterised by relatively little activity. In order for us to be able to tease out the elemental processes of clinical engagement and leadership in service redesign, it was important to ensure that some of the cases had strong prima facie indications that they would be able to offer opportunities for detailed study of substantial activity, but we avoided over-reliance on the feted cases that may have enjoyed unusual and exceptional support.
Within each CCG we selected for detailed study one, or in some cases two, specific service innovations in particular areas. These focused on care of the frail elderly (usually involving cross-boundary working designed to ‘integrate’ health and social care); innovations in urgent care (usually involving cross-boundary working with GPs, acute hospitals, the ambulance service and paramedics); and/or mental health.
Within these cases there were also many research choices to be made. We used both purposeful sampling and theoretical sampling to access the most appropriate informants.
Guidelines from Lincoln and Guba82 were followed regarding ‘purposeful sampling when selecting informants within the case studies’. First, we selected informants whom we expected would have the most relevant knowledge of the background issues affecting the CCG as a whole. This cluster was broadly common across the cases (accountable officer, CCG chairperson, clinical leads, and so on). However, in addition we were sensitive to the particularities of each service redesign attempt studied. Here we used onward referral – a snowball research technique – in order to include informed and diverse perspectives appropriate to the situation. For each service redesign attempt researched, a set of interviewees was agreed with a senior sponsor of the research collaboration within the CCG. The selection of each sample was guided by the need to include the actors who had played a key role in initiating, shaping and evaluating the course of the service redesign event. This typically meant that clinical leads, programme managers and project managers, as well as some of the clinicians, were involved. In several cases we were also able to include patient representatives who had been involved in the service innovation (e.g. through sitting on the relevant programme board). In recognition of the multilayered nature of health-care reform, it was necessary to look upwards and outwards to the wider context, including area, regional and national policies and institutions which had an impact on the service areas under focal scrutiny. Thus the institutional settings usually had fuzzy boundaries which extended across primary, secondary, administrative, regulatory, professional and educational institutions.
Theoretical sampling allows the clarification of the relationships among multiple constructs. 75 It allows the revelation of unusual phenomena of diverse kinds. We used this approach in order to identify further interviewees in each case, to ensure exposure to data from informants who could add to an accumulative and iterative body of knowledge about relevant issues. The range of informants evolved with the emergent theory. Themes were pursued until little additional insight (what has been termed ‘theoretical saturation’) was gained. 83
We used three main methods within the cases. First, we conducted pre-entry documentary analysis drawing on a wide range of sources. Second, we conducted face-to-face semistructured interviews. Third, we used non-participant observation. Although interviews can be a highly efficient and effective research tool, it is recognised that they also present the challenge that bias may arise because of the efforts of image-conscious informants. This challenge was mitigated through the use of multiple interviews among diverse informants who were likely to view the issues and events from different standpoints. 84
The mode of operation was for each case study to be conducted by two members of the research team, with one of them acting as the lead investigator and contact person for that site. Some of the interviews were conducted with both researchers present, other interviews with just one researcher. In the main, interviews were recorded and transcribed. The researchers drew on a semistandard interview schedule comprising semistructured interview questions. These had to be adapted to the varying situations including, for example, the subject of the service redesign under scrutiny and the role and vantage point of the interviewee. The semistructured interview schedule was adapted accordingly. Appendix 4 shows a typical example of one such interview guideline.
Case study data analysis
As mentioned, members of the research team worked in pairs for each main case study. These subteams undertook the first stage of each data analysis process. Following Miles et al. ,84 these first-level analyses were constructed by careful reading of each individual transcript and the development of codes for exploring, describing and ordering the data for an entire case. In this way a coherent narrative of the flow of events within each case could be constructed. This was combined with a descriptive account of the issues and challenges encountered by the actors involved. These first-level reports used a common framework: (1) context, (2) focus and narrative of the case, (3) clinical leadership themes emerging and (4) emerging ideas for cross-case comparisons. The first three sections of these initial draft reports were fed back to informants in the case studies concerned, as a way of validating the accuracy of the data collected and the descriptive interpretations made.
Next, the first-level case reports were discussed, in turn, at a monthly series of research team meetings. From these discussions emerged ideas for explanatory concepts that could be applied to understand differences and similarities in the nature of clinical leadership across the cases. This process of discussion, conceptualisation and comparison between the cases led to the development of the conceptual framework for analysing the cases set out at the beginning of Chapter 4. Once again, following guidelines from Miles et al. ,84 this conceptual framework was then used to develop explanatory codes for a second level of analysis of interview, observational and documentary data in each of the cases (Table 2). This second-level analysis was carried out by two members of the research team, who were also the main authors of this report. That analysis brings together the descriptive summary of events with an explanatory analysis of the forms of clinical leadership and their relationship to the achievements and difficulties encountered in bringing about service innovation. The analyses are compared and discussed further in Chapter 5.
| Interviewee role | Number of interviews |
|---|---|
| GP chairpersons, clinical leads, other GPs | 65 |
| CCG accountable officers and other managers | 36 |
| Nurses | 8 |
| Lay members | 7 |
| Acute sector doctors and managers, mental health | 25 |
| Community health managers and nurses | 10 |
| NHSE, CQC, NHS Improvement, CSU and other agencies | 10 |
| LA representatives, councillors, chief executives and directors, public health | 9 |
| Voluntary sector | 9 |
| GP practice managers | 7 |
| Patient representatives | 8 |
| Ambulance service, paramedics | 8 |
| Total | 202 |
Survey analysis
Results from the two national surveys were analysed in three main ways. First, the responses to each of the questions were gathered together and the results presented as tables and charts. Second, a number of cross-tabulations were made in order to investigate whether or not occupants of different roles answered questions in particular ways. Third, comparisons were made between our data and the ratings of CCGs made separately by NHSE. These correlations produced some very interesting findings.
A notable feature of the completed questionnaires were the free-form questions. These elicited fulsome, useful responses. As a result of the careful preparation of the questionnaires in conjunction with a range of informants from the scoping phase, respondents readily recognised the relevance of the issues being raised and were very keen to share their thoughts. In the next chapter, the statistical results stemming from the structured questions are presented and analysed along with the free-text responses.
Public and patient involvement
We sought to involve the public and patients as far as was feasible, relevant and practicable at all stages. In the first instance, a nationally renowned patient and public involvement (PPI) representative with very extensive experience of PPI was appointed as co-chairperson of the Project Steering Committee. This representative was involved in all aspects of the research from the initial design, the oversight of research instrument construction and the review of findings at all stages, to the discussions about the dissemination of findings. During the course of the project, PPI was used mainly in relation to the specific service redesign initiatives that were the focal component of this study. These initiatives often had PPI arrangements in place and we tapped into these rather than seek to set-up new arrangements. One extension of this approach was that a member of the project team sought permission to become an active participant member of a PPI group that was associated with one of the service redesign initiatives in the core case studies. Full ethics approval from the Research Ethics Committee overseeing the project was sought and full disclosure was made to members of the PPI group. Another dimension was that in the surveys and the case studies we took steps to find out how patients and the public had been involved in the redesign of services.
Chapter 3 Findings from the national surveys
Introduction
In order to gain a broad view of the state of play across all CCGs, a national survey was designed and administered in 2014 and again in 2016. The populations targeted were the members of the governing boards of all CCGs. This included chairpersons, accountable officers, finance directors, GP members (often these were clinical leads of particular service areas), other clinicians such as nurses and the secondary care doctor representatives, directors of public health and lay members.
The first survey gleaned 385 usable responses and these represented 12.42% of the total population of all CCG governing board members and 79% of all CCGs. For the second survey there were 380 responses, which represented 12.26% of the total population and 77.5% of all CCGs. The 18- to 19-month interval between the two surveys was designed to allow tracking of unfolding events in a time series and the possible maturation (or decline) of the CCGs.
The questionnaires in both phases contained many shared themes, but the 2016 questionnaire included additional questions which were derived from the case study work that had taken place during the intervening period. Patterns of responses were also correlated with a separate data set: the ratings allocated to CCGs by NHSE for 2015/16. In comparing our survey results with the NHSE data, we used the headline rating. We considered using the component ratings that were most relevant to our study (i.e. ‘Well-led’; ‘Finance and Planning’). However, we found such high correlations between these components and the headline rating that, in practice, the headline rating proved to be sufficient.
A number of core issues were investigated in both phases. The first of these was the respondents’ perceptions of the autonomy and influence of CCGs as institutions. This was assessed relative to other bodies such as NHSE, NHS Improvement and the CQC. In other words, the initial objective was to understand how important and influential the CCGs were in the wider scheme of the NHS. A second continuing theme was the relative influence of clinicians – most especially GPs – within the CCGs. This aspect was central to the project aim: do the CCGs in practice provide a platform for the meaningful exercise of clinical leadership? A third core question area was an examination of the nature of the contribution made by clinical leaders. Other more subsidiary questions covered in both surveys were: the degree of wider GP engagement; training and development offered to GP members of CCG boards; conflicts of interest; and assessments about the future role of CCGs.
The questionnaire was a combination of structured questions and a set of more open-ended questions with space for free-form answers. There was a very high response to the free-form questions – with 96% of respondents taking time to write in these sections. This was a strong indication of the extent to which respondents were engaged with the questionnaire and found it relevant and interesting. The respondents were keen to express their views and many did so with passion.
Copies of the questionnaire can be found in Appendix 3.
The profile of respondents
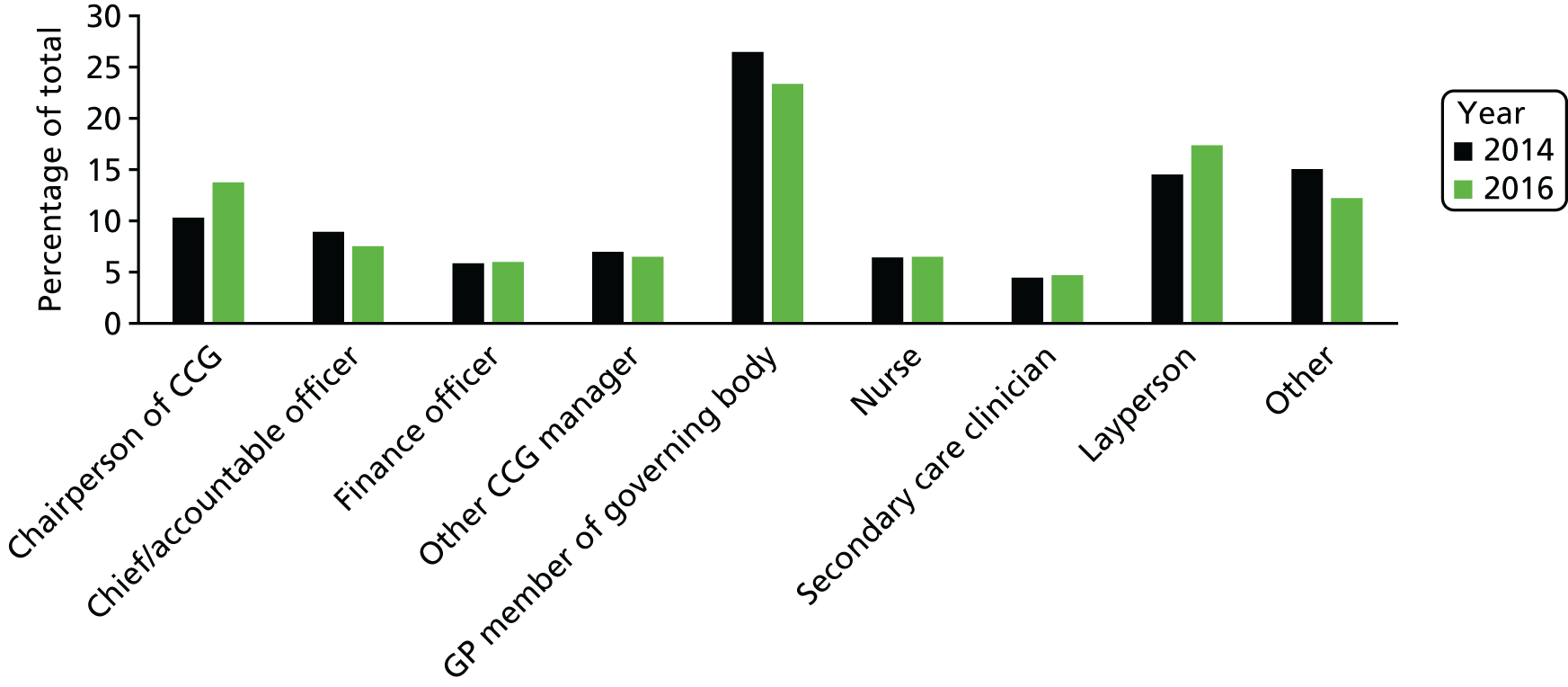
As can be seen from Figure 1, responses were received from all role categories with the numbers broadly reflecting the relative numbers sitting in these boards. Hence, GPs were the largest group of respondents.
FIGURE 1.
Roles of respondents.
The first thematic question examined was the perceived influence of CCGs. We wanted to understand what respondents thought was the scope to make a difference through these institutions.
Perceived influence of Clinical Commissioning Groups
The first main substantive question asked about the perceived influence of CCGs relative to other NHS organisations. The reason for asking about this was that the overall research question was essentially about the scope for leadership influence using CCGs as an institutional platform.
We asked board members to make a comparison of the perceived influence of their CCG relative to other bodies such as NHSE and NHS trusts. The form of the question asked for a rank ordering of the bodies most influential in shaping local health services. Figure 2 shows the results. Half of the respondents judged that their CCG was the most influential in this regard, and NHSE was ranked second. However, nearly half of the respondents did not rate their own CCG as the most influential. In the 2016 survey, some respondents under ‘other’ noted that Vanguards and STPs were emerging as influential in shaping local services.
FIGURE 2.
The relative influence of different institutions (2016).

It is clear from Figure 2 that ‘my CCG’ was seen as carrying the most influence. NHSE was seen as the next most influential institution in shaping service redesign and the growing importance of collaboration between CCGs is also indicated. However, the fact that nearly half of CCG board members themselves judged that their CCG did not exercise the most influence might be expected to be a potential curb on expectations about the exercise of leadership by CCG clinicians or other CCG players.
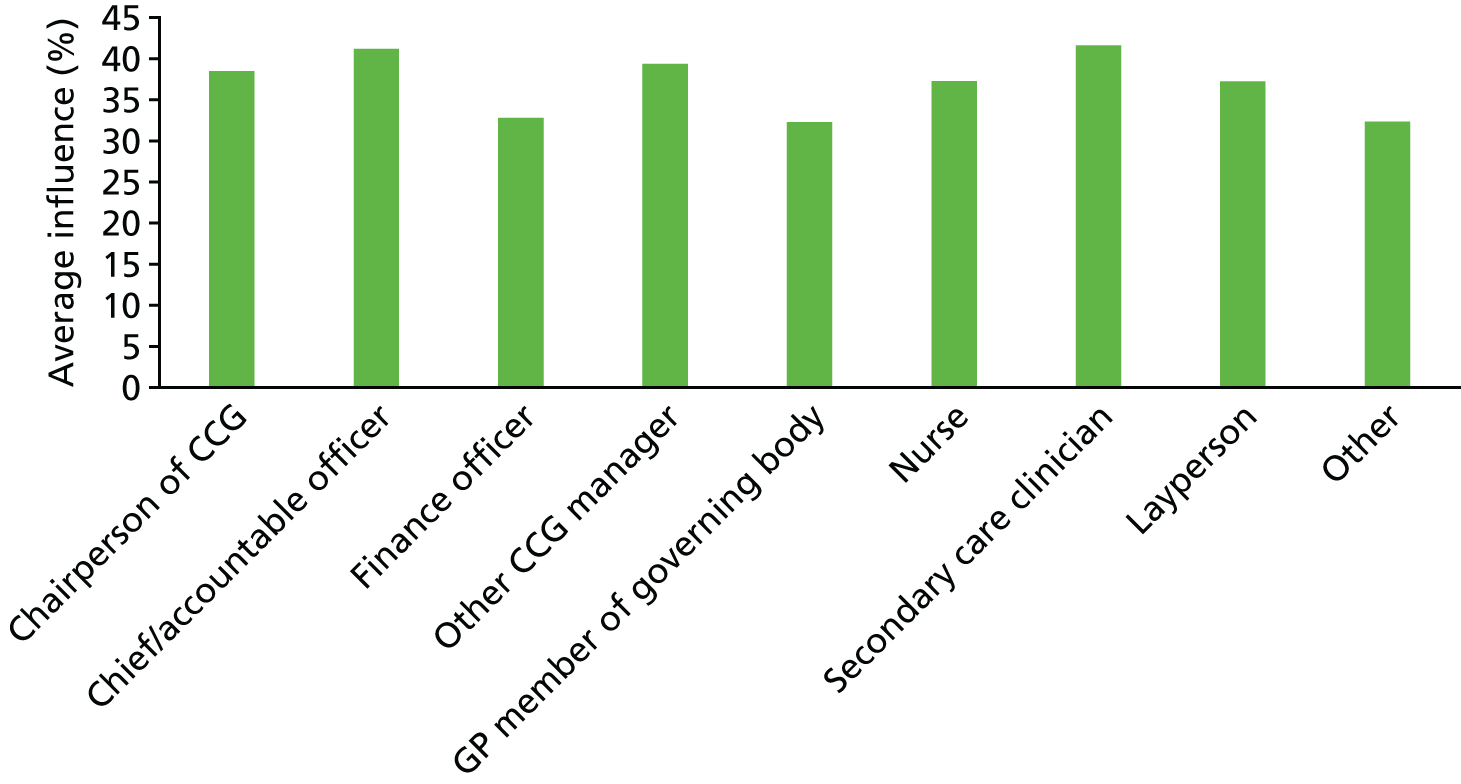
Would different role occupants have similar views? The data for the assessment of influence split by role holder are shown in Figure 3.
FIGURE 3.
Relative influence of different bodies as reported by different role holders.
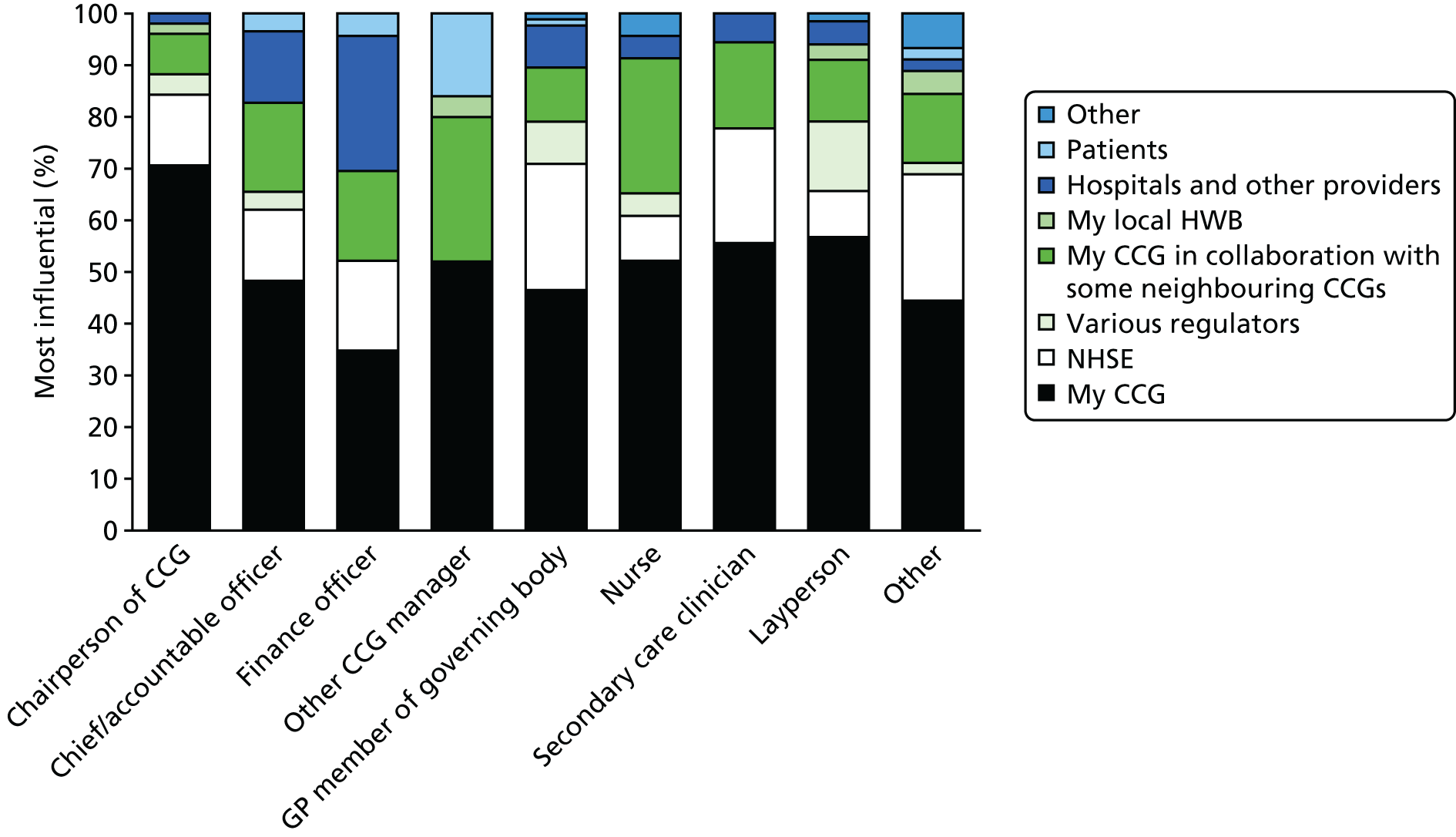
Notably, it was the chairpersons of CCGs who were most likely to perceive their CCGs as influential. However, other role holders, most notably finance directors, did not. Less than half of accountable officers perceived their CCG to be the most influential body in shaping services. This is an especially important finding because arguably, among all of the different role holders, one would expect the accountable officers to have the clearest line of sight on the various forces at play. It would suggest that the reality of CCG influence is rather less than was implied by the policy intent as it was described at the outset of this report.
Many GPs on CCG boards reported that they were disillusioned with their CCG experience. For example:
The CCG is becoming increasingly bureaucratic and much more like a PCT. We are increasingly subject to government directives and with short deadlines. There is no space for creative solutions from the CCG. I am angry and sad at the current state of CCGs.
GP member of governing body
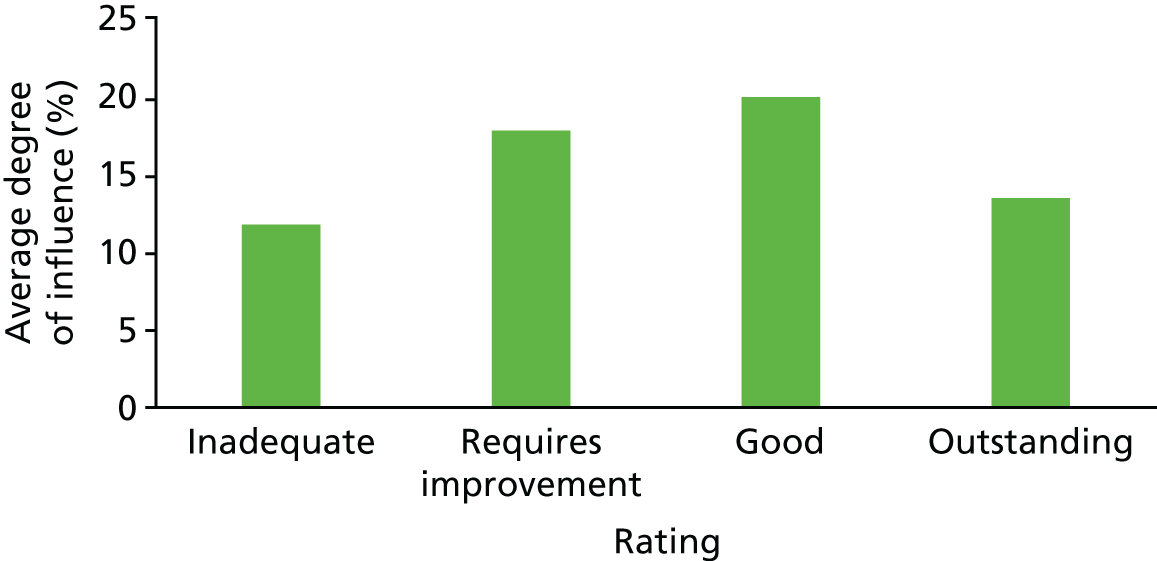
We then undertook a different analysis: the perceived relative influence of different bodies was correlated with the ratings of CCGs allocated by NHSE. The results are shown in Figure 4.
FIGURE 4.
The relative influence of different bodies (2016) by NHSE headline rating of the CCG.
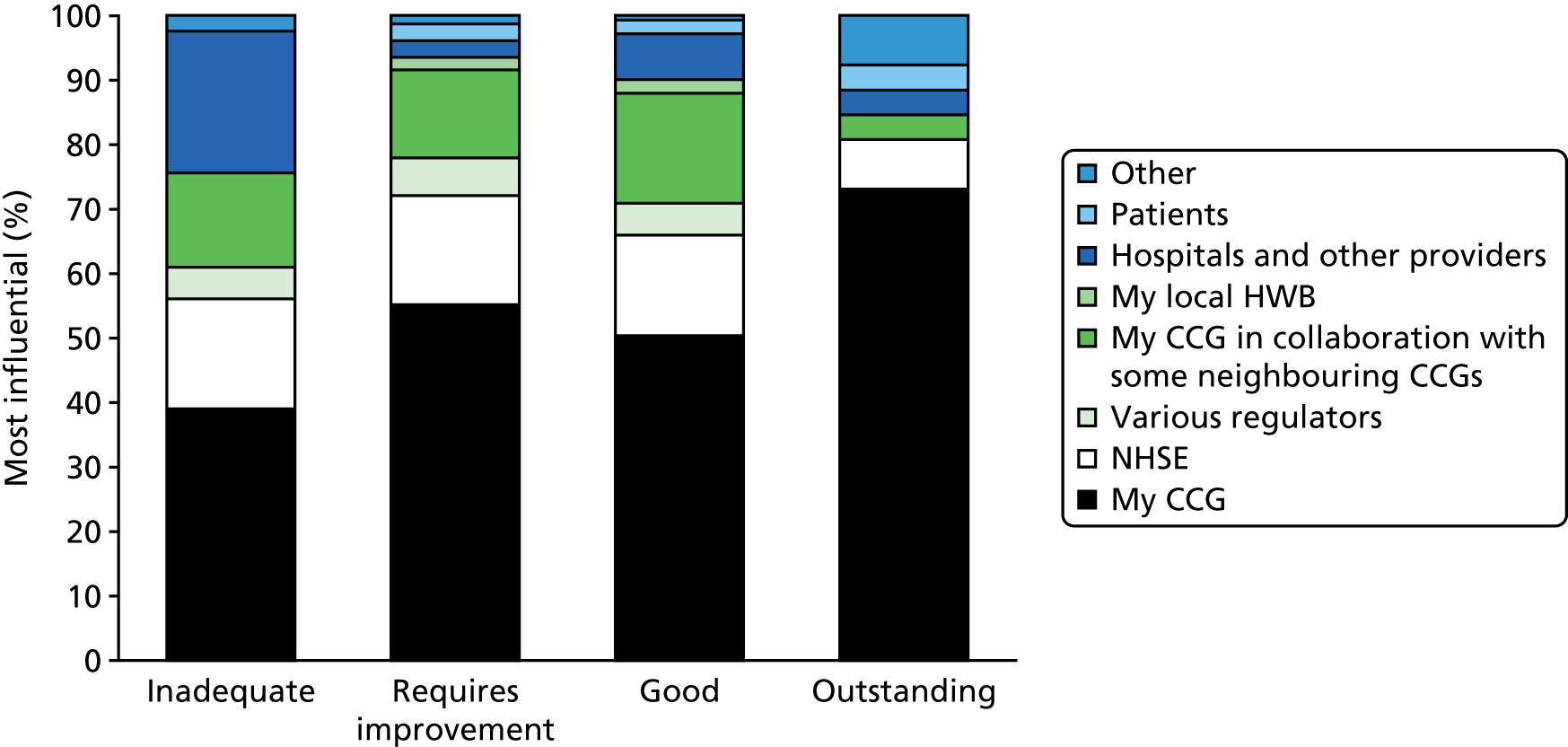
The notable finding is that respondents from CCGs rated as ‘inadequate’ were far less likely to rate their CCG as having influence. In contrast, respondents from CCGs rated as ‘outstanding’ were much more likely to perceive their CCG as influential. It may be that the pattern of institutional influence is reflected in performance. Alternatively, it may be that this pattern suggests the possibility of a self-fulfilling prophesy: those expecting low impact achieved just such; conversely, those assuming that they had influence were able to exercise it. There is an alternative explanation: the low and high performers sensed the state of play and disowned or owned responsibility accordingly.
Figure 5 shows comparative data for 2014/16 with regard to perceived influence on the design of services in the local health economy. (Respondents were asked to assign a percentage rating across the institutions listed, adding up to 100%.) The pattern remained fairly stable over the 2 years. ‘My CCG’ was seen as the most influential body, but there was a slight fall-off in this assessment in 2016. There certainly seemed to be no sense of a growing influence.
FIGURE 5.
Institutions influencing service redesign.
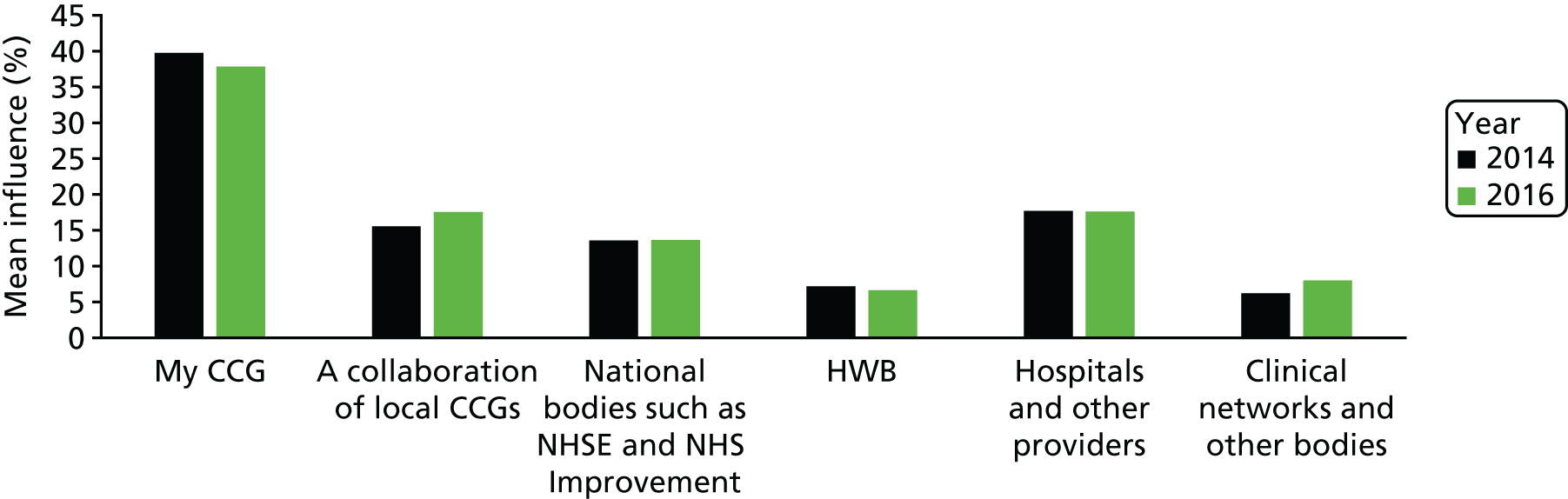
The largest group of respondents said that their own CCG was the major player (38% of influence in 2016). However, other bodies were also seen as important, and these included NHSE (14%) and local collaborations of CCGs (18%). There were significant differences in this assessment depending on the role of the respondent with regard to their views about NHSE and NHS Improvement. GP members of the governing bodies were most likely to perceive NHSE and NHS Improvement as influential.
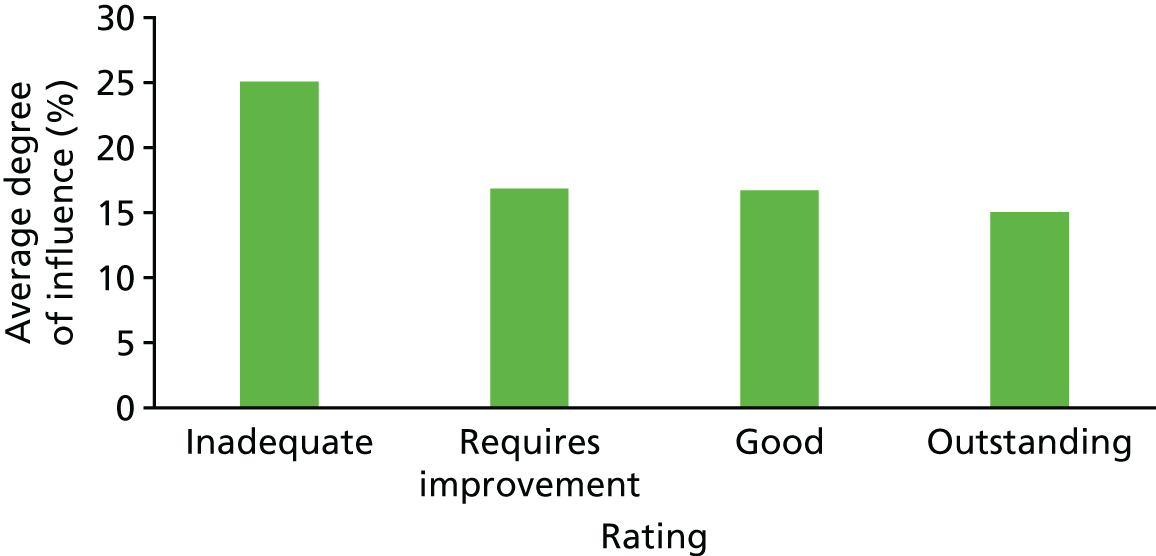
Next we looked at ratings of CCGs by perceived importance of collaboration among neighbouring CCGs. The results are shown in Figure 6.
FIGURE 6.
Rating of influence of a ‘collaboration of local CCGs’ by NHSE headline rating of CCG.
These results suggest that those respondents whose CCG was rated ‘good’ were those seeing collaboration with other CCGs as important, whereas those rated ‘inadequate’ tended to see it as less important. On the other hand, the ‘outstanding’ ones were seemingly able to be self-reliant. And perhaps they did not want to collaborate with others in case this affected their performance ratings. When asked to rate the influence exerted by hospitals and other providers, it tended to be respondents from CCGs rated as inadequate who were more likely to accord the highest influence to these bodies (Figure 7). This may reflect the reality of powerful local hospital trusts or it might reflect a lack of will or capability in tackling these providers.
FIGURE 7.
Rating of influence of ‘hospitals and other providers’ by headline rating of CCG.
The next section shifts focus from the influence of CGGs to an analysis of relative influence within them. Most especially, there was the contentious issue of whether managers or clinicians were exercising power and, relatedly, what influence, if any, other role holders such as the lay members, the secondary care doctors and the nurses had.
Influence within Clinical Commissioning Groups
Given that the policy intent, as shown in Chapter 1, was to create commissioning organisations led by clinicians – and most especially by GPs – we wanted to know whether or not these institutions had lived up to that aspiration. We began with a question which asked about the relative influence of different groups on the redesign of services. The four groups were managers, GPs, other clinicians excluding GPs and lay members. The results are shown in Figure 8.
FIGURE 8.
Influence of managers, GPs, other clinicians and lay members in the redesign of services.

In broad terms, managers and GPs were seen to be the most influential by far. In 2014, of the two, GPs were marginally ahead; however, by 2016 the rankings had reversed and managers were marginally ahead in terms of ranked influence. This is especially notable given that the majority of respondents were GPs. Other members of the governing bodies (including the lay members, secondary care doctors and nurses) were rated as far less influential.
Some answers from 2016 were then broken down to show how different kinds of respondents answered this question. The results are shown in Figures 9 and 10.
FIGURE 9.
Influence of managers, as reported by different role holders (2016).

FIGURE 10.
Influence of GPs as reported by different role holders (2016).
It was evident that finance officers tended to see managers as the most influential figures. GP members of governing boards and others (directors of public health and other managers) tended likewise to see managers as influential.
Next, we delved deeper into the perceived influence of GPs, as broken down by role of respondent. As the results in Figure 10 show, GP members of the boards were, ironically, the least convinced that they had much influence. It may be that other board members wished to maintain the official image of ‘GPs in charge’. Accountable officers, for example, may have wished to reflect the idea that they were the servants of a membership organisation.
We also wanted to know in what capacity GPs were acting when they influenced service redesign. Was it as official governing members, as clinical leads who did not have a seat on the governing body, as locality leads, or as leaders of GP federations? Figure 11 shows the results for both 2014 and 2016.
FIGURE 11.
Roles of GPs shaping service redesign (2014 and 2016 compared).
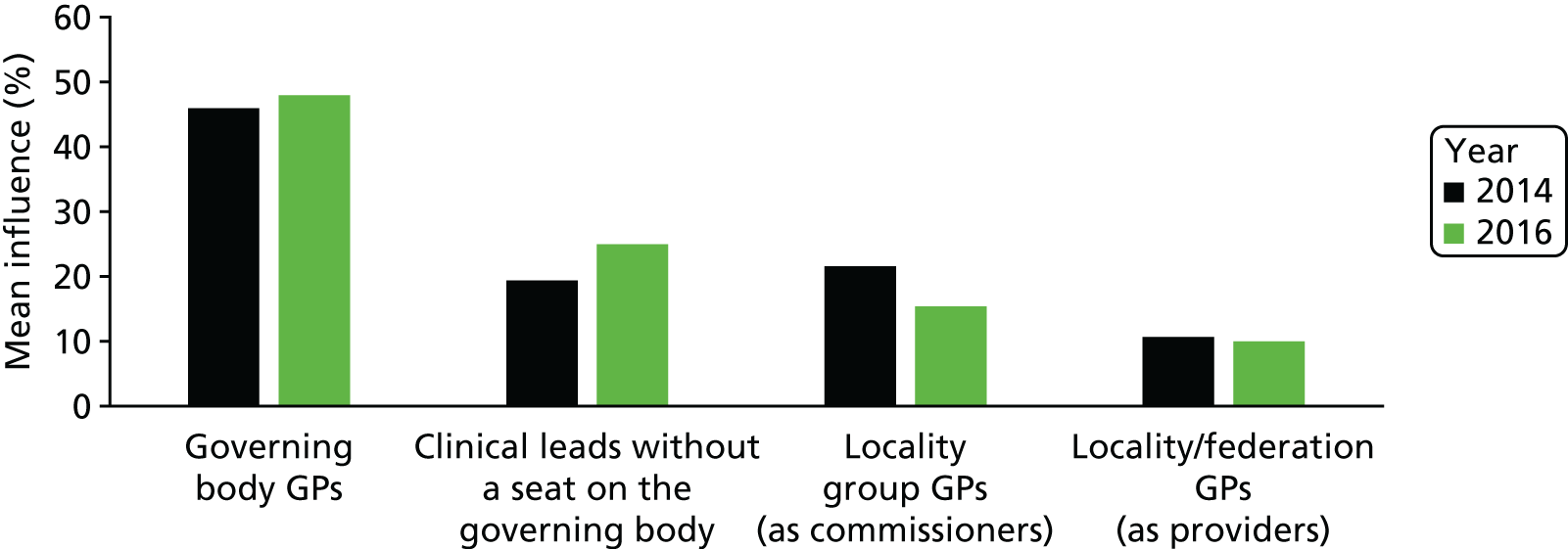
Perhaps not a surprise, given the role of many respondents, GPs sitting on the governing bodies were seen as the most influential of the GP categories. Of note also was that the perceived influence of locality-level commissioning GPs declined between 2014 and 2016.
A related question concerned who sets the compelling vision. Were GPs and other clinicians making a leadership contribution through envisaging alternative service provision or was this vital leadership role filled by others? Figure 12 shows the results.
FIGURE 12.
Who sets the compelling vision for service redesign?
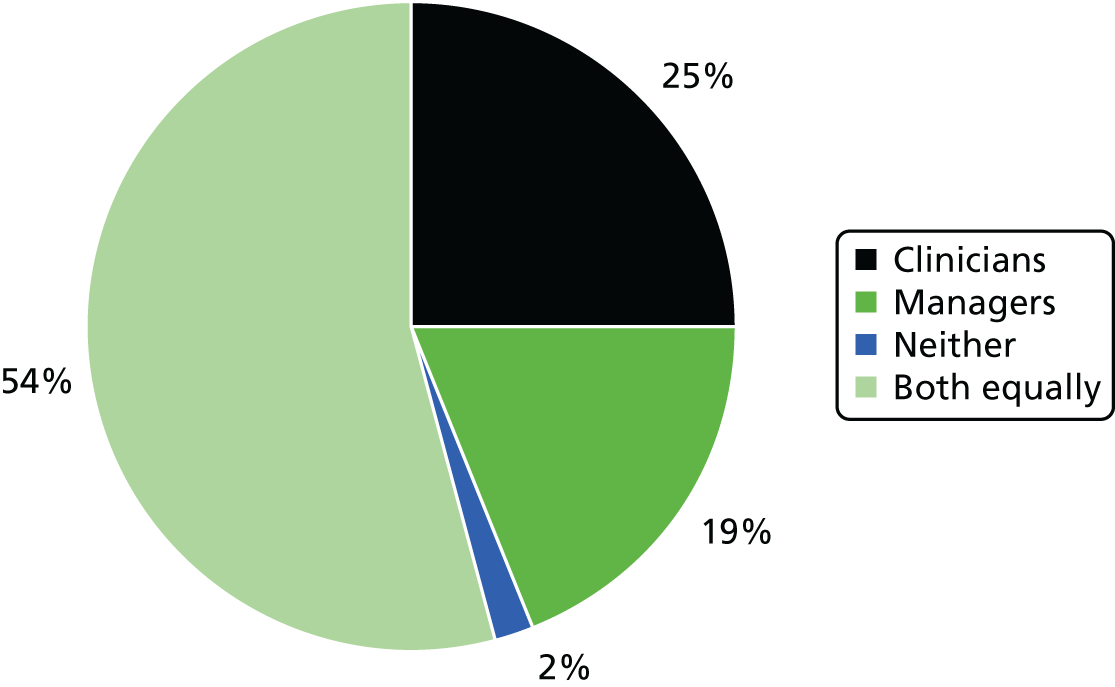
In 2014, the results for clinicians were the same (between 25% and 26% of respondents said that GPs set the compelling vision). The main difference between the two time periods was in the proportion of respondents who answered ‘neither’ to this question: 23% in 2014 but a mere 2% in 2016. At this later date the most common answer to the question ‘who sets the compelling vision?’ became ‘both equally’.
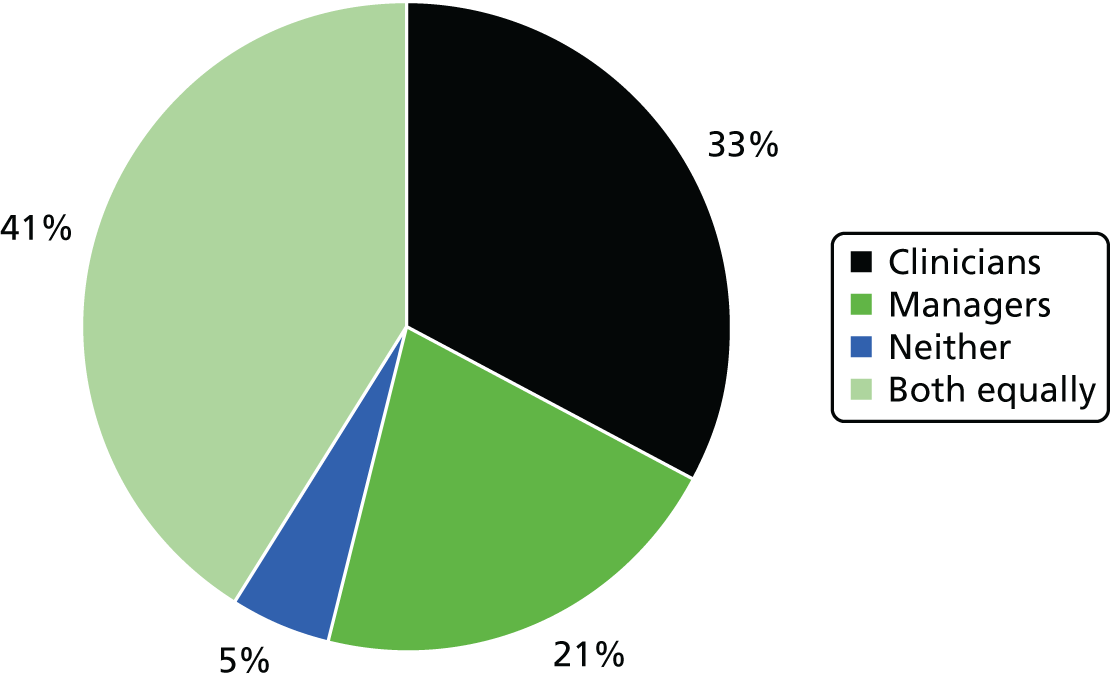
Figure 13 shows the breakdown by role of respondent to this same question. This shows that the nurses and accountable officers were most likely to say it was both equally, whereas more ‘independent’ observers (finance officers, secondary care doctors and laypersons) were more likely to name managers as key players in this regard. (Accountable officers once again played down their role.) No role group said that GPs were the ones mainly setting the compelling vision.
FIGURE 13.
Vision answers as reported by different role holders.

As shown in Figures 12 and 13, most respondents suggested that it was managers and clinicians equally who set out the compelling vision. These results suggest that the notion that GPs would be the visionaries and architects and that managers would play the role of delivery agents is not an accurate depiction of the reality in most cases. There is also more evidence here of dual leadership occurring – a particular type of distributed leadership.
We asked about communication with patients and the public, and the results are shown in Figure 14. For these stakeholders, managers acting alone or acting equally with clinicians account for 87.5% of this kind of communication. In their free-form answers, some respondents suggested that the role was mainly undertaken by managers, although clinicians might be ‘rolled out’ if some serious change was being proposed. Once again there was apparent progress between 2014 and 2016. In 2014, nearly one-quarter of respondents said that neither managers nor clinicians from the CCG were in communication with patients and the public, but in 2016 this fell to only 2%.
FIGURE 14.
Communication with patients and the public.

In a related question, we asked who provided the insights into public and patient needs. The results (shown in Figure 15) suggest that the largest part of this is done jointly with managers and clinicians, although 21% of respondents said that managers were mainly responsible for this activity.
FIGURE 15.
Who provides insight into patient needs?
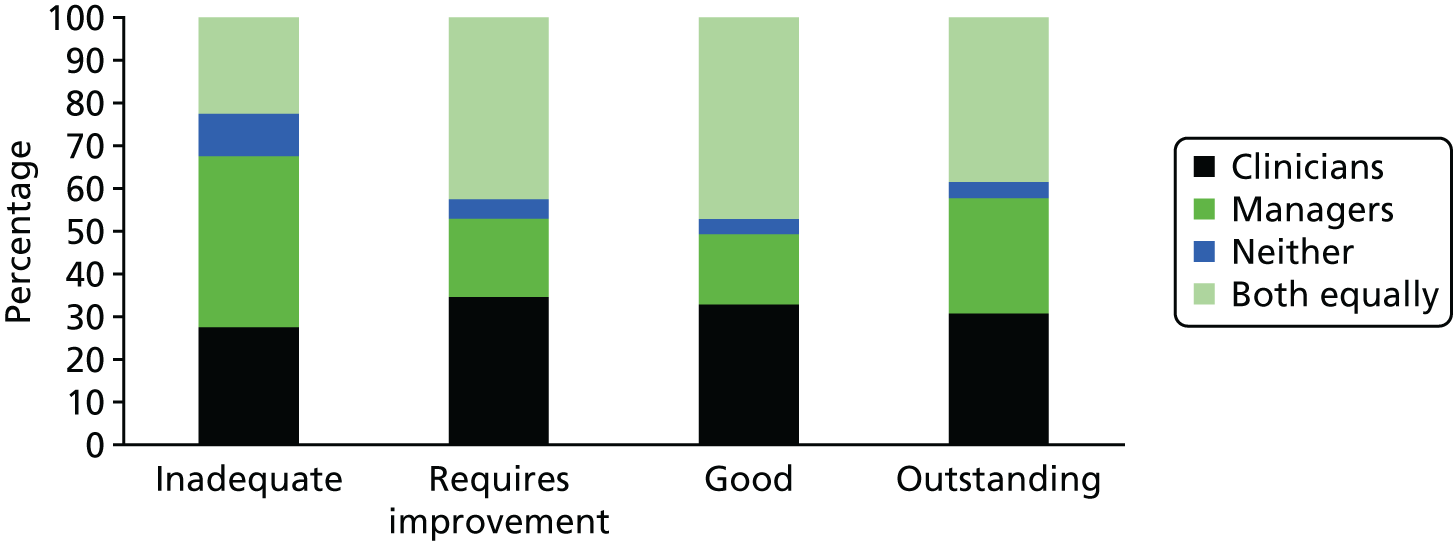
The main difference revealed in Figure 16 is that respondents from CCGs rated as ‘inadequate’ were most likely to say that managers provided most expert insight into patient and public need, and they tended to regard clinicians as less active in this regard.
FIGURE 16.
Who provides insights into patient needs? by headline rating of CCG
An increasingly important theme since the formation of CCGs as independent statutory bodies has been the growth of the idea that more collaboration is required – with other CCGs and with other stakeholders, such as social services and voluntary bodies. We asked about this next.
Building collaborations
The building of collaborations with providers and with other commissioners has increasingly become a vital activity for CCGs. Who would undertake this vital work? Figure 17 shows the results.
FIGURE 17.
Collaboration building.
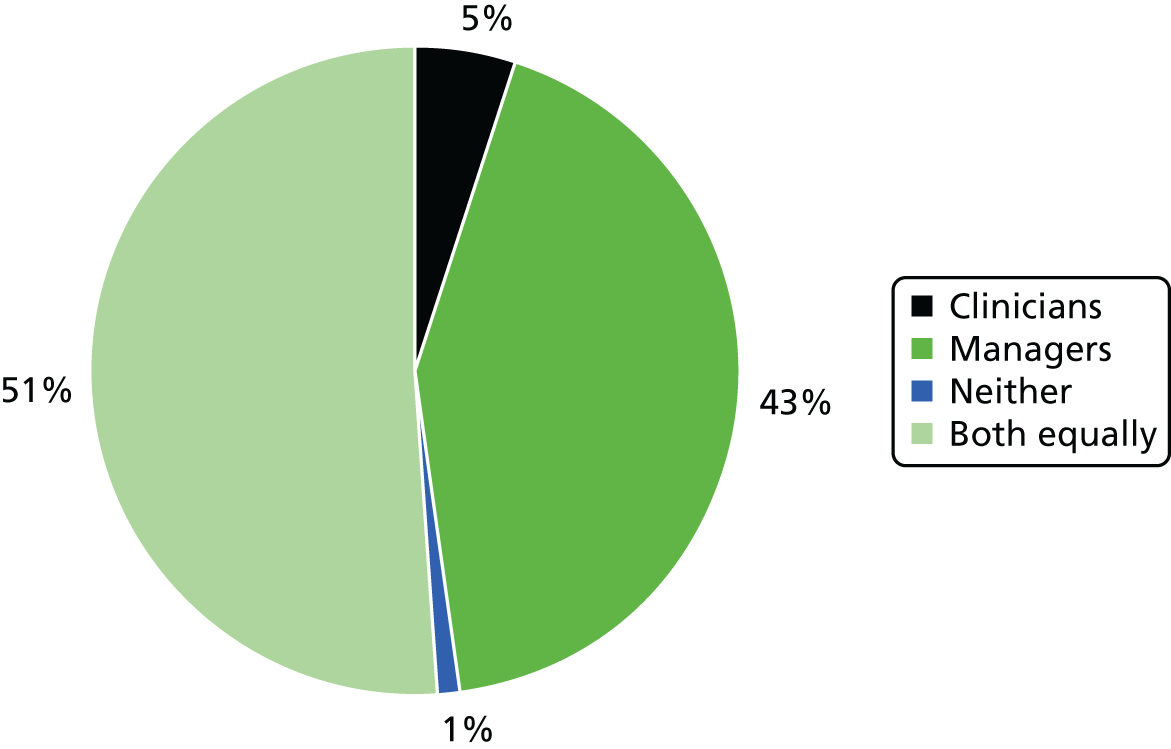
The results suggest that half the respondents saw managers and clinicians equally involved in this. However, a very significant proportion (43%) identified managers as leading on this, and only a very small proportion (5%) argued that clinicians led on this work.
Qualitative, free-form answers added some depth and flavour to the question of the kind of contribution being made by clinical leaders.
A central reason for much of the emphasis on clinical leadership, as we noted in the literature review, relates to the idea that clinicians have the potential to make a difference through a distinctive set of contributions. We asked for free-form response answers to the question ‘What distinctive contributions do clinicians make when clinical leadership works well?‘.
The answers clustered into eight main categories of types of response, as shown in the first column of Table 3. Text in the second column is verbatim responses. Fuller tables are shown in Appendix 6.
| Type of response | Example of verbatim response |
|---|---|
| Knowledge and understanding | Clinical knowledge; local knowledge; knowledge from front-line experience; professional knowledge |
| A more clinically informed view than managers could hope to offer | |
| They understand services much better than managers | |
| We understand the bigger picture | |
| Attention to detail: insight into small things that create large obstacles to good clinical care | |
| Knowledge of systems and advocate for patients | |
| Position/location in the system | They reflect and understand the realities of the ‘front line’ |
| Generalists, wide ranging | |
| Bring a ‘can do’ attitude | |
| Enthusiasm, practicality and prioritisation | |
| Better system overview than acute sector providers have | |
| They bring the voice of the front line | |
| Analytical and decision-making skills | Evidence based thinking |
| Sensible service design; . . . | |
| Understanding of the evidence and ability to describe what ‘good’ looks like | |
| Understanding of patient needs | |
| Expertise in care planning; | |
| Relationships and collaboration | Strategic clinical leadership influence and followed by all clinicians and officers |
| Experience and judgement | |
| Patient engagement and member engagement; . . . | |
| . . . collaborative instincts | |
| Challenge and independent views | Their challenges to plans proposed by others |
| Challenge the status quo | |
| Challenge potential inertia of consultant colleagues | |
| Brings healthy dose of challenge and always reminds staff of how it is in reality | |
| They influence provider clinicians to understand the need to change | |
| Trust, credibility and status | Important touchpoint with patient/public kudos and trust from the public |
| Momentum of purpose, authenticity, trust | |
| Patient focused, on quality issues and on problems with service | |
| Credibility, practical experience and local knowledge | |
| Independent: less wedded to organisations | |
| Communication and influence | Representing patient views; ability to communicate complex issues in plain English; . . . |
| Important in selling to colleagues and patients | |
| Influencing peers to change behaviour | |
| Evidence based mobilisation of clinical public support | |
| Communicate the vision to patients | |
| Common sense and pragmatism | Ensure things work in practice; . . . |
| Grounded; . . . | |
| They bring common sense | |
| They give a shrewd view on what will and won’t work | |
| Awareness of when systems don’t work and won’t work | |
| Sense check of management proposals | |
| Pragmatic | |
| Sensible pragmatic decisions that work in practice |
Although the form of the question asked for identification of the kinds of positive contributions that clinical leaders make, some respondents nonetheless used the space to express more critical views, such as ‘I’m not sure they do’.
As these reservations stem from governing board members with a close-up view of proceedings in CCGs, it is especially interesting to note the scepticism about the impact of clinical leadership.
These kinds of critical comments take us next to the question we asked about the ‘major obstacles to achieving clinical leadership in service redesign’.
Obstacles to achieving clinical leadership
This free-form question elicited many responses. The most commonly cited response was that GPs did not have the time to fulfil the role adequately. More than 92% of respondents gave this response. Respondents also took the opportunity to use this question to identify what they saw as the source of the failings and difficulties faced by CCGs. Hence, many GP respondents pointed to wider problems of the health service at large (such as fragmentation, complexity, political interference, bias towards the acute sector and the like). Some managerial respondents used the question to highlight shortcomings in the GP contribution (poor attendance, lack of system-wide understanding), whereas some GPs also pointed to managerial shortcomings. Answers are categorised in Figure 18.
FIGURE 18.
The main obstacles to clinical leadership in CCGs.
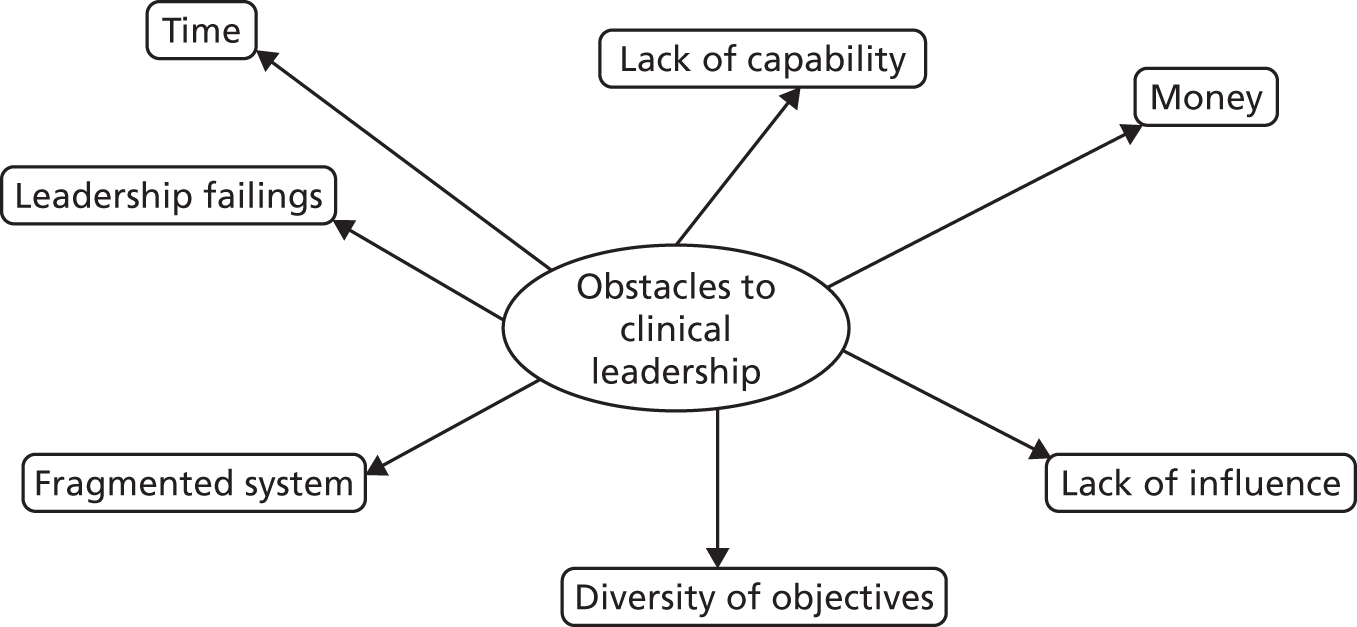
All types of respondents were ready to say that ‘lack of time’ was a major issue, but beyond that divisions opened up, with some managers suggesting that GPs lack the will and commitment to even want to devote time to CCG work and that there were shortcomings in capability.
Some GP respondents argued that the sources of the problem were deeper – that they extend to intractable system problems, such as fundamental diversity of objectives and lack of autonomy for the CCGs to influence the system because of the power and influence of bodies (such as NHSE, NHS Improvement) and the power of the acute hospitals – all of which impeded the plans of the CCGs. In other words, there was evidence of a perceived vicious circle. Yes, many GPs were reluctant to step forward to commit significant time and energy to the work of the CCGs, but they contended that this was because there was little incentive to do so, and indeed little point in so doing because bigger forces are stacked against this being a rational action. These perceptions led to a paradox of disengagement. This is shown in Figure 19.
FIGURE 19.
The vicious circle of lack of clinical engagement and leadership.
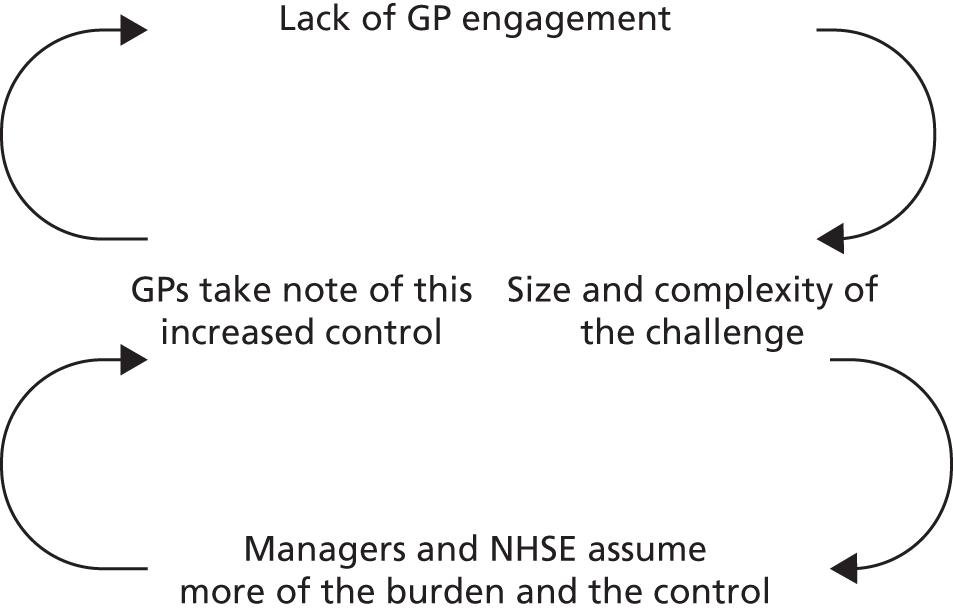
This paradox was a vicious circle which was mutually reinforcing. Talented, energetic, potential leaders were reluctant to step into active roles as leaders of service redesign on CCGs. Other system players, including managers and influential bodies (such as NHSE and NHS Improvement) judged that the problems facing the service were so large and urgent that they themselves needed to step in. This, in turn, further confirmed the suspicions of GPs and gave justification for limiting the amount of engagement; the one ramped up the perceived justification for the other. Further details can be found in Appendix 6.
We sought to gain an overall assessment of the influence of clinical leadership. Implicit in such a question could be perceived impact as well as an assessment of behaviour patterns on the governing bodies. The results are shown in Figure 20.
FIGURE 20.
Overall influence of clinical leadership.
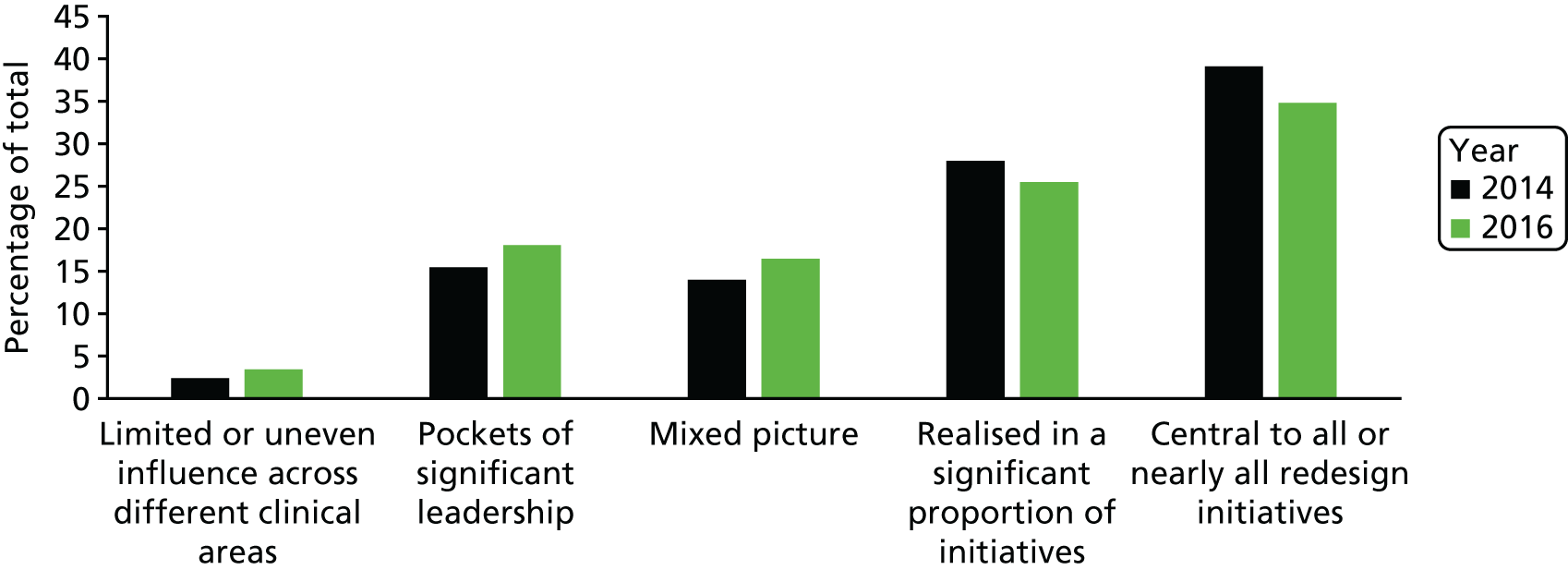
The results told an optimistic story. In both 2014 and 2016 the majority (68% in 2014 and 60% in 2016) of respondents leaned decisively towards the positive end of the spectrum; that is, they said that clinical leaders were central to all, or nearly all, redesign initiatives or to a significant proportion of these initiatives. This, in broad terms, might be seen as an overall endorsement of the idea of CCGs. The fall from 68% to 60% in just 2 years might, however, be seen as a matter of concern given the central nature of this question.
We dug deeper into this by disaggregating by role of respondent (Figure 21) and by the NHSE headline rating of the respondent’s CCG (Figure 22).
FIGURE 21.
Overall influence of clinical leadership as reported by different role holders.

FIGURE 22.
Overall influence of clinical leadership by headline rating of CCG.
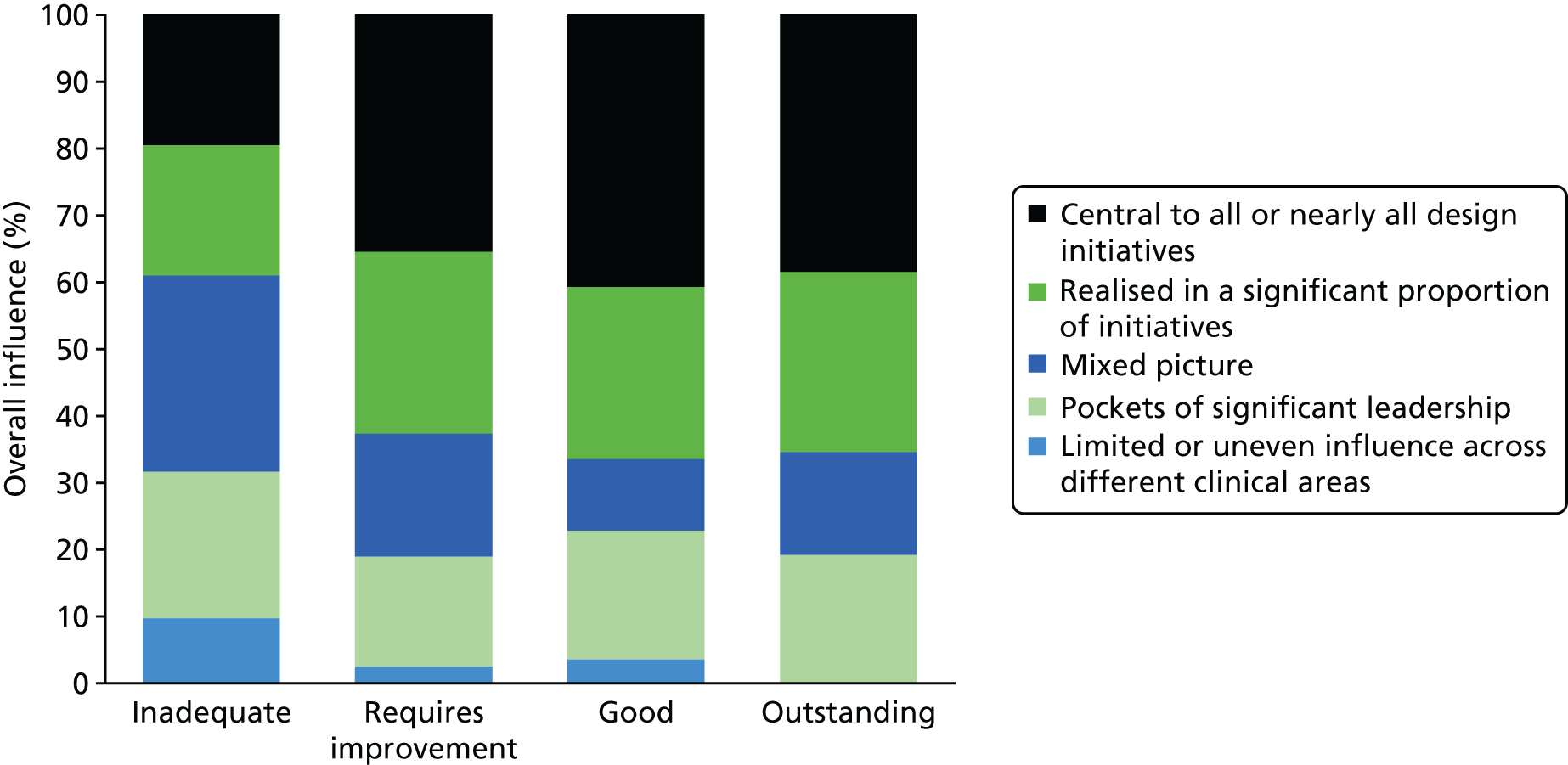
Significant differences were found. Most notably, finance officers tended to place much less importance on clinical leadership than did other role holders. GP members of governing bodies and managers (other than accountable officers) were also more circumspect about the role of clinical leaders in service redesign. The chairpersons and accountable officers on the other hand report that clinical leaders are central to nearly all design initiatives or at least involved in a significant proportion of initiatives.
As Figure 22 shows, respondents in CCGs rated as inadequate were the least likely to say that clinical leadership was significant in improving or redesigning services; and respondents from good and outstanding CCGs were most likely to say clinical leadership was central or influential in a significant proportion of initiatives. On the face of it, these findings are highly suggestive of the importance of the role of clinical leadership.
Examples of positive impacts by the Clinical Commissioning Groups
In the pilot phase in 2014 we had been somewhat surprised to hear the response from accountable officers and chairpersons that the main achievements had been to establish the CCGs and make appointments. In other words, they focused on process aspects and institution building. So, although at that time they were relatively new bodies, they had been in existence for around 2 years in statutory and shadow form and we were expecting to see some more substantial claims about new initiatives and their progress. Therefore, by the time of the survey in 2016, we expected to hear much more about meaningful impacts and service improvements.
The question was an open invitation to showcase the ‘best’, the most impressive impacts made by their CCGs. How did they measure up?
The resulting picture was very mixed. Some respondents struggled to cite any examples of significant impacts made by their CCG. Indeed, given that respondents were all serving members of CCG governing bodies, it was perhaps surprising to hear reports saying that there were ‘none’ (no impacts to report), ‘nil’ or ‘still waiting!’ However, these were not typical. Most respondents were able to list a few impacts, albeit often the claimed initiatives were in the early stages. For example, ‘We are designing a blueprint for primary care’, ‘Some service design’, ‘Raising awareness’, ‘Commissioning a local scan service’ and ‘Influencing the end-of-life care’. Others claim significant outcome-based impacts.
Most common were the modest claims, ‘Implementation of referral support website to improve communication and dissemination of projects and services to clinicians’.
Others were at an early stage and rather vague: ‘Plans for future changes to acute and primary care in a joined-up way’, ‘Bringing the future of primary care to the front of the agenda’ and ‘Looking at better working together with providers’.
The claimed impacts ranged across primary, secondary and community services. Judging by the number of ‘mentions’, CCG service redesign has been rather more directed at primary and community services than at secondary care. Notably, there was very little reference to the use of commissioning and decommissioning as tools for bringing about change. Another notable point is that impact is often perceived in process-improvement terms – such as building positive working relationships, engaging stakeholders and stimulating discussions.
As predicted by institutional theory, there appeared to be considerable evidence of imitation. CCGs form a loose community of practice, they have learned a common language, and their ambitions are, in part at least, formed by the wider institutional field. Hence, at a general level, there were very frequent mentions of ‘a shift of resources from acute to primary and secondary’; ‘bringing care closer to home’; and ‘reducing hospital admissions’. Other comments were responses to national initiatives: use of the Better Care Fund (BCF); co-commissioning. Conversely, some referred to initiatives being stopped by NHSE.
A straightforward frequency count of the most-mentioned impacts resulted in the following list of 10 in ranking order:
-
musculoskeletal service (MSK) moved from acute to community settings
-
mental health focus [e.g. Improving Access to Psychological Therapies (IAPT) self-referral]
-
improvements to frail elderly care and reduced emergency admissions
-
GP out of hours; federations and practice collaborations
-
urgent care and front door of accident and emergency (A&E)
-
redesign of rehabilitation/discharge
-
integrated care initiatives
-
implementation of a community-focused paediatric acute response team
-
stroke services improvement
-
redesign of community services.
Mentioned less frequently were any significant impacts on secondary care or much deployment of the power of commissioning and decommissioning. Indeed, it was also notable and curious that, given all of the talk about prime contractor arrangements and outcome-based commissioning, there was no mention of these in response to the question about the main impact of the CCG to date, or at least not directly. These forms of contracting were implicit in some of the responses about MSK and to a lesser extent in relation to changes in services for the frail elderly, but still there was no explicit mention. It might be suggested that this is because, even where arrangements had been made, it was rather too early to measure actual impact in terms of outcomes. However, that had not been a factor in many of the other responses, which were free in their references to ‘developing’ and ‘moving towards’. Fortunately, we had a specific question on prime contracting and outcomes-based commissioning. Despite the fact that, when asked the open question about ‘the difference made’ by their CCG, almost no one volunteered a reference to forging prime contractor arrangements or helping to design outcome-based commissioning and yet when asked directly about the importance of these, the majority of respondents (70%) said that they were ‘very important’. Indeed, many said that they were ‘vital’ and ‘absolutely necessary’.
Assessment of service redesign progress
The preliminary pilot work had alerted us to the need to distinguish between broad plans and actual activity. Hence, in the survey we asked a question which sought to tease out participants’ own assessments of impact. They were asked to respond to the statement ‘Plans for service redesign have far exceeded tangible changes to services’. Figure 23 shows the results.
FIGURE 23.
Plans vs. tangible achievements (1 = low agreement, 5 = high agreement).

Figure 23 shows that, even among those serving on boards, there is a widespread acceptance that their plans for service redesign ‘far exceeded’ what has been achieved in practice.
When participants were asked if ‘CCG achievements have more than matched expectations’, there was a very clear pattern. Respondents from CCGs rated as ‘outstanding’ agreed most strongly, whereas those from CCGs rated as ‘inadequate’ tended to report that achievements had not matched expectations. This might be as predicted. However, it does seem to indicate that CCG office holders had a pretty good sense of how well their organisations were performing.
Summary and conclusions
The two national surveys offered an opportunity to gain some overall impressions of these actors’ insights and assessments of some basic questions. The surveys revealed a mixed picture. There was evidence to support an optimistic view of the worth and importance of CCGs and of the role of clinical leaders, but there was also some evidence to support a more pessimistic view.
Indicators underpinning an optimistic assessment included the evidence that the majority of respondents said that ‘my CCG’ exercised more influence than the other bodies that were active in the area. Likewise, within CCGs, there were indicators of the influence exercised by GPs. They were assessed as broadly as influential as managers. Other data pointing towards an optimistic view can be found in assessments of who sets the compelling vision – a significant indicative role in the context of these bodies. The majority of respondents said it was set ‘equally by managers and clinicians’ and, among those who answered differently, clinicians were more likely than managers to be named as the vision setters. Moreover, this pattern represented a maturation of CCGs since 2014: the ‘both equally’ assessment increased from 33% to 54%. Trends in communication with secondary care clinicians and with patients and the public also offered grounds for optimism. The overall assessment of the influence of clinical leadership was that they were central to nearly all service redesigns (35%) or in a significant proportion of redesigns (25%). Taken together, this suggested that around 60% of respondents claimed a key role for clinical leadership in practice.
Positive assessments of CCG influence were more often made by chairpersons and accountable officers (i.e office holders whom one might well expect would champion CCGs and indeed remain optimistic about these institutions even in the face of challenges). In contrast, finance officers and GP board members were much less inclined to offer a positive assessment. Similarly, GPs on governing boards tended to be the least convinced that GPs were influential in the redesign of services. Moreover, GP respondents reported that practice workloads were impeding engagement with clinical leadership and that, as a result, engagement with CCGs was declining. One might expect that at least GPs on the CCG board would be the prime intermediaries and communicators with other primary care clinicians, but only 40% of CCG managers made this assessment, they suggested it was done either by managers or jointly with clinicians. In addition, as collaboration (with other commissioners and with providers) has become a bigger theme in recent years, one might look to the skills of clinicians in this regard. However, the data indicated that managers were felt to be more active in this – either on their own (43%) or conjointly with clinicians (51%) – but with only 5% saying that clinicians were the main builders of collaborations. On the overall assessment of the influence of clinical leadership on service redesign, this reduced somewhat (though not statistically significantly so) between 2014 and 2016. When asked if the plans for service redesign had ‘far exceeded’ tangible change, the majority (55%) agreed that they had.
Of note was that, although respondents many were highly doubtful about the future survival of CCGs, the majority expressed their strong conviction that commissioning and related devices, such as outcome-based commissioning, were approaches worth preserving. This finding might reflect the general orientation of those persons attracted to the work of the CCGs.
To gain further insight into the actual work of clinicians in service redesign using the CCG as a potential platform for action, it was necessary to delve deeper. For this purpose we used a case study methodology. We report on the results of the case study work in the next chapter.
Chapter 4 Findings from the case studies
In this chapter we present the findings from the six main CCG case studies. Their geographies covered the North, South and Midlands of England. Rural and urban areas were covered as well as a mix of deprived and affluent areas.
The case research complemented the survey findings reported in the previous chapter by adding insight into the ways in which clinical leadership for service redesign was practised using the CCG platform. Although the cases are based around CCGs, our prime unit of analysis when researching the cases on the ground were specific service redesign attempts taking place within these settings. One or, in some circumstances, two significant redesign instances were selected for study in each of the CCGs depending on local circumstances. This approach allowed us to move beyond abstract discussion of ‘leadership’ to a more grounded analysis of leadership in action.
Most of the research effort was directed at teasing out the origins, design and delivery of specified service redesign attempts. This allowed a focus on actor behaviours in relation to real events. The CCGs were researched as part of the context but the main focus was on the role played by clinicians and the extent to which this amounted to a process of leadership. As a result of the prime focus on acts of clinical leadership within specific service redesign attempts, we arrived at eight ‘cases’ (of leadership in service redesign), because in two of the CCGs we tracked change leadership across two different service areas.
We found initiatives were being launched above, below and around CCGs. ‘Above’ were regional groupings, ‘below’ were localities and ‘around’ were various forms of collaborations with neighbouring CCGs, LAs, provider institutions and other agencies (including voluntary sector bodies). Some of the initiatives studied involved a handful of collaborating managers and clinicians – often straddling primary care and other providers in secondary care, LAs and the voluntary sector. Sometimes these initiatives were sponsored by the CCG and allocated formally to one or more clinical leads. At other times the innovations were only loosely connected to the CCG and were driven by clinical leaders from other settings, such as GP federations. The case study narratives cover these different kinds of development. Each, in their different way, helps shed light on the contours and nature of the system – the role of the CCGs, the role of providers and the parts played by managers and clinicians.
Although many barriers and blockages were revealed, in what follows we place special emphasis on tracking and clarifying how some actors have shown themselves able to surmount – at least to some degree – these difficulties. Hence, these cases offer clues to the nature of clinical leadership and thus they point to lessons from which others can learn – whatever the particular institutional form might happen to be.
In order to facilitate cross-case comparisons, each case write-up is structured in accordance with a standard framework: the context within which the CCG operates; an account of the service redesign attempt being studied; emerging insights about clinical leadership; and the overall lessons and conclusions from the case. Systematic cross-case comparisons are made in the following chapter.
The analytical framework
Drawing on the findings from the 15 scoping CCGs in phase 1 and the findings from the two national surveys, we were aware that clinical leadership in service redesign was being enacted in different arenas. By ‘arenas’ we refer to the settings and domains where leadership is exercised. 85 This may be a physical space (such as a board room), but just as often it will be a social space (such as different communities of practice). These arenas may be temporary and sporadic or relatively stable. Crucially, in a health service context where there are multiple overlapping organisations and professional groups that periodically come together or are brought together, the arena is a realm of interaction. In the kinds of health service redesign attempts we were investigating, influence extended in varying degrees across organisational boundaries, across formal lines of authority and across looser informal groupings. Indeed, as CCGs are decidedly not conventional hierarchical organisations, exercising ‘leadership’ in and around them is of a very different order to that found in an organisation, such as an acute hospital or a public limited company.
In and around CCGs it appears that clinical leadership was located in each of our eight case studies in three main types of arena. One of these arenas was at the strategic, policy-making level, typically located at the CCG governing body, but sometimes also involving other strategic bodies above this level. A second was found in the setting of programme boards and similar bodies responsible within a CCG for the operational commissioning of particular groups of services. A third was in the delivery setting, where clinicians involved in providing innovative services worked on the operational and practice aspects. Figure 24 displays these types of arenas in a schematic way.
FIGURE 24.
Three arenas of clinical leadership.
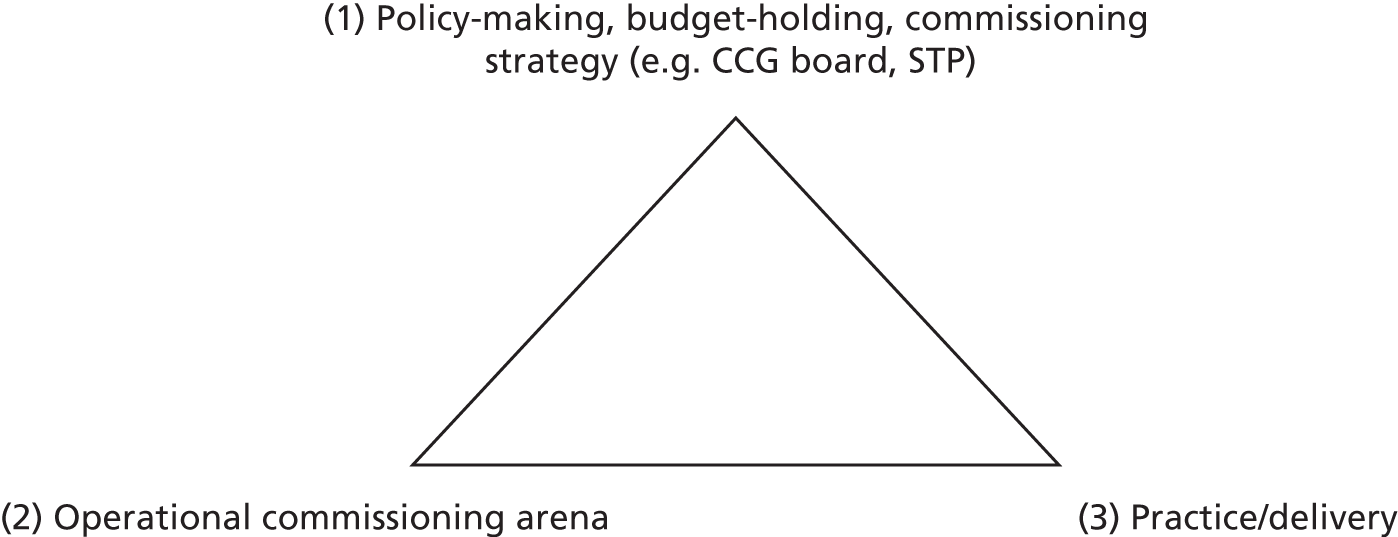
The depiction of three different kinds of arena as points of a triangle containing clinical leadership is intended to convey a richer understanding, beyond the idea that there is a hierarchy of clinical inputs corresponding to a hierarchy of NHS authority. Our cases demonstrate that clinical leadership is needed in each of these arenas, but that the system works in an interdependent way. The relationships between the arenas are constructed through a mix of collegial, professional network mechanisms and market relationships, as well as, indeed rather more than, through hierarchical command and control relationships.
The first arena for the potential exercise of clinical leadership (point 1 of the triangle in Figure 24) was concerned with the development of service priorities for the whole population living within a defined geography and with the strategic approach to meeting these priorities. In the original conception of CCGs, this strategic arena was the governing body of a CCG. This is where GPs and others were originally meant to be making a difference. They were to be allocated a budget to meet the needs of a population and expected to proceed with the whole commissioning cycle, including assessing need, reviewing service provision, deciding priorities, designing services, shaping the structure of supply, planning capacity and managing demand, managing performance and seeking public views. This cycle of activity was supposed to be ongoing. From the cases studies we found that practice was rarely quite so systematic. Opportunistic funding and, in some cases, financially straitened circumstances intervened.
We found that, in three of our eight cases, tasks in this strategic arena were undertaken by clusters of neighbouring CCGs acting in concert. In one case this was a collaboration between all CCGs active within a county-wide footprint. In another case the strategic work to redesign integrated services for the elderly and those with more severe long-term conditions was done at the level of a collaboration of four neighbouring CCGs working together with their LAs. Yet, in a third case the dominant strategic arena was a collaboration between the CCG and a coterminous LA. In all cases there was a drift towards, and pressure towards, shifting some strategic issues to a higher level, such as strategic reference groups and STPs.
Across all eight cases, we were able to track instances of the nature of clinical leadership within this kind of strategic arena. The normal key focus in these arenas was putting ‘the clinical case’ for major service development initiatives, such as an integrated care initiative or a primary care development initiative. Strategic clinical inputs of this nature can be seen as paving the way for further and rather different modes of clinical leadership needed to produce service redesign, in the second and third kinds of arena. At the same time, we found that this strategic level of commissioning leadership was perhaps less emphatically provided by clinicians than might have been expected from the original aspirations attached to CCGs. Professional managers, with support from CSUs, were likely to be attempting at least some of this.
The second arena (point 2 on the triangle) allowed the exercise of clinical leadership in the matters of operational commissioning. The cases showed that much of this work took place within ‘programme boards’. These bodies were allocated the responsibility for progressing tranches of work by the CCG, each typically concerning delivering services addressing broad categories of health need, such as mental health, urgent care, or care for the frail and elderly. The programme boards sought to bring together key stakeholders. Their remit was to review current provision and identify problems and gaps in that provision, to shape initiatives, develop detailed policies, recommended contracts and monitor performance. In the cases we followed, there was evidence of work within the tradition of collaborative supply chain activity; provider clinicians as well as GP commissioning leads for the area concerned were represented on these boards and were in a position to bring to the table both the legitimate concerns about viability being experienced by providers and ideas for how to deliver services more cost-effectively. Collaborative, clinically informed discussions about the best way of meeting needs could then provide the basis for formal contracts between the CCG and provider organisations, which the programme board would then monitor and manage.
The third arena (point 3 on the triangle) is where we found clinical leaders, usually based in provider organisations, engaging in what might be termed ‘implementation leadership’. It is also where we found much of the PPI taking place. The implementation and practice arena is hugely important because grand plans would count for little if GPs, community and acute clinicians failed to respond to and enact the new ways of working called for by their colleagues in commissioning roles. Indeed, all of our cases in some way illustrate that this work at the sharp end was where most work needed to be accomplished. In practice, the exercise of clinical leadership in this arena of delivery went well beyond ‘mere’ implementation of a new service specification. Although individual provider clinicians had key roles in fleshing out the detailed clinical practices, our cases also revealed the importance of new collaborative forums for working out operational detail in integrated services. We found fascinating examples of learning occurring between different acute providers. We also saw the creation of practice networks in primary care, where learning was shared between practices about how to improve services and standards. Peer pressure, peer-to-peer role modelling, the development of a shared moral ethos and mutual learning were all vital, especially in such instances. In some cases, this arena of service delivery leadership extended beyond primary and acute health service providers and took in additional service providers, such as adult social care, housing and employment support.
An essential point of Figure 24 is that clinical leadership is exercised in different arenas and depends on different capabilities. Clinical expertise and experience had important distinctive roles to play in each arena. However, there were also crucial interconnections, grounded in the nature of clinical expertise and experience. Clinical perspectives served as an important integrative mechanism. Clinicians with knowledge of the practical conditions for implementation were in some of our cases crucial in ‘selling’ big ideas within strategic arenas and making sure that operational commissioning took a viable form. Conversely, clinicians who had worked on developing service strategies to address the unmet health needs in the local population played key roles in convincing front-line staff of the underlying rationale and ethos of service innovation.
Introduction to the cases
Within the context of CCGs, our focus was on service redesign in selected areas: mental health, urgent care and integrated care (especially directed at the frail elderly). These tended to be areas of focal interest for a large number of CCGs. Sometimes the way they were framed and presented varied but the core issues were widespread. Hence, we found that many CCGs were working on various forms of extended general practice and this often included attempts to redesign the provision of services for people with long term-conditions and the frail elderly, and these initiatives often involved collaborative work with community services, social services and others. In four of the CCGs we focused on just one main service redesign attempt of this kind; however, in two of them, as there were significant service redesign attempts which matched our core areas of interest, we tracked two initiatives rather than one. Hence, in total, we studied eight service redesign ‘cases’ from the six CCGs. Table 4 shows an outline of the cases.
| Case profile | Case study | |||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |||
| 1 | 2 | 1 | 2 | |||||
| Location | London | London | Birmingham | Birmingham | Midlands | London | London | Greater Manchester |
| Urban/rural | Urban | Urban | Urban | Urban | Mainly rural | Urban | Urban | Part urban/rural |
| Service redesign focus | Mental health | Urgent care redesign | Extended general practice and primary care | Mental health and well-being | System-level redesign | Integrated care redesign | Urgent care redesign | Towards ACO |
| Levels and arenas | CCG board and programme board | Programme board and collaborative working with ambulance service | Locality-level activity as key | Practice-level activity as key | Emphasis on cross-CCG collaboration | GP-led collaboration across four neighbouring CCGs | CCG board led in collaboration with acute hospital services | Devolved plans for ACO from DevoManc |
Below we provide a first level of analysis of the cases; the following chapter provides a further analytical discussion of the insights into the nature of clinical leadership emerging from a comparison across the cases.
Case A: innovating in mental health and urgent care
Case A was one of the inner-London CCGs. The CCG leadership team had been successful in making innovative use of non-recurrent central funding and it had a track record of piloting new models of service delivery. The CCG case analysis below is divided into two parts reflecting two different service redesign initiatives. The first (case A1) focuses on a mental health redesign initiative and the second (case A2) on an urgent care redesign initiative.
Case A1: innovating in mental health services through establishing provider alliances
There was clear unmet need in mental health provision, but alongside this was fragmented provision with a range of different statutory and voluntary sector providers treating different levels of severity in Child and Adolescent Mental Health Services (CAMHS) and offering psychological therapies for adults (PTA). It was in this context that a particular GP who occupied a clinical lead role in the CCG began to design a new approach to all these services by taking a collaborative approach with a range of service providers.
This case reveals the power of distributed leadership when used in combination with an initial vision, top-down determination and associated funding activity. Following the launch of the collaborative alliances the leadership and ownership was transferred, in the main to the collaborating partners.
Initiation of mental health provider alliances
The mental health programme board of the CCG worked with existing mental health providers in the statutory and voluntary sectors to form a set of alliances. These were seen as having the potential to offer a more co-ordinated and holistic approach.
The CCG’s mental health programme board clinical chairperson (a GP) worked with the transformation director to develop the alliance concept. They drew on non-recurrent funding and convened meetings of diverse current providers to form shadow alliance boards. They challenged these boards to identify a number of objectives and discrete projects that would contribute to better integration over a funding period. A proportion of the funding was earmarked as dependent on successful progress, providing a basis for further funding of activities.
Three alliances were established:
-
psychological therapies alliance – formed of seven member organisations – this included a major acute mental health trust; a mental health service provider offering mainly talking therapies for mild-to-moderate mental health issues using the IAPT national funding programme; a provider operating from within an acute medical trust; a specialist primary care therapy service; three voluntary sector organisations providing therapy; and a voluntary sector body specialising in matching people with volunteer activities available across the borough
-
dementia – this comprised three member organisations, which were an acute medical trust; an acute mental health trust; and a voluntary sector organisation providing support and activities in the community
-
CAMHS – this comprised three member organisations, which were an acute mental health trust; a ‘first steps’ child and family psychology provider operating from within the children’s division of the acute medical trust; and a voluntary sector provider specialising in creative therapies.
As is evident from the listing of the various alliance member bodies, the CCG had within its territory a very complex array of mental health services. Each of the new alliances was steered by an alliance provider board. Each of these had a senior clinical and managerial representative from each provider. In addition, there were CCG representatives in the form of the mental health programme director and transformation director. Each alliance met monthly and were, from time to time, attended by the CCG mental health programme board clinical chairperson. Governance came from the represented bodies, but the initial impetus and vision came from the clinical leadership from within the CCG.
Implementation
Over a 15-month period, each of the three provider alliances completed a number of collaborative projects, which were formulated and agreed during the first quarter of alliance activity.
The psychological therapies alliance worked on an improved system for managing referrals. It also worked on joint projects with the third sector concerned with improving access for particular ethnic groups and with preparation for employment.
The dementia alliance worked on reminiscence pods, awareness training and treatments for improving cognitive abilities. It also designed an improved navigation procedure.
The CAMHS worked on more consistent use of clinical outcome measures, clarifying referral pathways, and offering targeted training and professional development workshops. This alliance also designed a new common triage system.
The three initiatives were viewed as successful, at least to the extent that they merited continued support. Clinical leadership within the programme board, an operational commissioning arena, supported by a dedicated manager, was seen as effective in bringing some order and coherence to a complicated set of activities and services which had grown in a disorderly manner and which resulted in overlap and duplication. At the same time, leadership within this operational commissioning arena needed to be matched by clinical leadership within various provider bodies involved in implementing alliance working.
Achievements reported
From the interviews with participants across the alliance membership, it was evident that the alliance initiative was viewed in a highly positive manner. As a result of participating in collaborative projects, service providers reported a greater openness to understanding each other’s services and expertise and were much more willing to co-operate with each other. Statutory and third-sector providers that had not previously worked together reported much improved working relationships and understanding of each other’s services.
There was enthusiasm across the alliance members offering PTA and psychological therapies for children and adolescents for the ‘complex cases referrals’ meetings that became established within each of these alliances. Here, clinicians from different providers brought cases they felt the need to be referred on elsewhere. These meetings were seen as producing rich professional discussion that would not otherwise have happened and a greater sense of connection between clinicians in different services. Clinicians reported much greater confidence in referring patients on now that they understand better how colleagues elsewhere work. One participant observed:
. . . it doesn’t feel such an unknown anymore or kind of, ‘I’m sending you off, but I don’t know if they’re going to look after you like I did . . .
Clinical psychologist
Alliance activities were widely felt to have built confidence for further collaboration. Clinicians in different settings had overwhelmingly positive experiences on collaborative projects and felt that they had a realistic understanding of each other’s capabilities – both strengths and weaknesses – which provided a basis for further joint working. The collection of outcome measures for these pilots contributed to this sense of achievement.
Challenges encountered
Some board members in all three alliances expressed concerns about the short-term focus. Delivery of the specific projects detailed in the alliance specifications was supposed to happen in just 15 months. This short-term focus was experienced as sapping energy from thinking about how longer-term and deeper collaboration could further overall service delivery and pursuit of alliance objectives.
However, this view was often held alongside a seemingly contradictory perspective that the achievements of these limited collaborative projects had built trust and confidence between alliance members and stimulated their appetite for further collaboration. There was also recognition that the CCG had a legitimate role in asserting the kinds of areas and priorities for collaboration that are most important for service users in the longer term.
Clinical leadership across different arenas
Interviews revealed the exercise of clinical leadership in a number of ways across the different kinds of arena identified in Figure 24.
The initial basis for the alliances was established by a leadership dyad at the apex of the CCG, operating within an operational commissioning arena, a programme board. This consisted of the GP clinical chairperson of the mental health programme board and her managerial counterpart, the mental health programme director. The clinical chairperson articulated the objectives and mechanisms of the alliances in terms of providers working out together how best to meet the needs of their user population rather than each provider defensively retreating to the scope and categories of patients specified in their existing provider contracts. This articulation also included members of the alliance taking mutual responsibility for managing each other’s performance, rather than seeing this as something that happened bilaterally between each provider and the CCG. As the CCG clinical lead stated:
Our mantra as commissioners is assess and then treat, because for years as a GP I watched how patients get bounced around. Oh, it’s not for our service, oh, just too bad for us, oh, not bad enough for us . . . what we’ve said, and I go on about, is the John Lewis model . . . if somebody comes in this door and asks and this is not the right department, they get shown to the right department . . . for me, it’s that very basic visceral thought about what an alliance is and that should be, on a clinical level, all the people trusting each other’s assessments, having very good working relationships . . .
CCG clinical lead
The CCG GP clinical leader had a vision of how the complex array of mental health services could work better and had a theory of how to bring this about. But the development of the theory and its realisation was then to be handed over to the alliance members. The main function of the theorising on the part of the GP clinical chairperson can therefore be seen as holding out a vision of how services could work together differently, without specifying detailed mechanisms for how to achieve this: the provider organisations in the alliance should take responsibility for meeting the adaptive challenge.
The strategic commissioning arena relevant to this initiative was that of the CCG governing body. The mental health clinical lead was also a member of this board and obtained backing from this board. In terms of institutional work, clinical leadership in this arena can be seen as involving advocacy and achieving the vesting of resources and responsibilities in alliance working.
Clinical leadership and institutional work also took place in the operational delivery arenas as senior provider clinicians shaped the actual practices of working in alliance mode. Without exception, providers saw the work of the alliances as improving collaboration between the separately commissioned services, but they wished to maintain the distinct identities, competencies and the connections that each separate provider workforce draws on:
The model of separate organisations forming an alliance I’m for. But the model of separate organisations all coming under one host organisation and being subsumed, I am not for . . .
Clinical psychologist
An underlying tension derived from the different professional ethos of providers that are closer to the medical model associated with psychiatry as opposed to clinical psychology or family therapy which work with a more socially based therapeutic approach. Staff in each provider preferred to continue to manage the professional tensions and syntheses they already knew, rather than be cast into more direct interaction with clinical and managerial traditions they knew less well.
A key element of leadership among senior provider clinicians working in operational commisioning arena was in reconciling commitment to collaborative working within the alliance with continued efforts to develop the distinctive capabilities, ethos and, indeed, funding of their ‘home’ organisation and service. This was a form of institutional work: developing the interfaces between the patterns of service activities offered by each alliance member.
This institutional work involved the development of a normative network of clinicians across each alliance. We have already described how clinicians cohered around the shared articulation of providing a more integrated experience for service users. The development of this normative commitment was fuelled to a considerable extent by the dissatisfaction of many clinicians with the kind of contract-driven performance management they experienced in their ‘home’ services, where their performance was scrutinised by the CCG in terms of metrics (e.g. numbers of people receiving and completing programmes of therapy of defined length and recovery rates based on user-assessed clinical outcome measures).
The institutional ‘interface work’ of provider clinicians within the alliances can be understood as involving a reinterpretation and blurring of these apparently neatly defined categories of severity, of ways of measuring progress with the improvement of symptoms. Rather than seeking to define new ways of treating mental illness, these clinicians were involved in advocating and developing new ways of blending or combining existing definitions. Clinicians held that the degree of need of particular people was difficult to assess at the outset and often proved difficult to match with a particular ‘mild to moderate’ or even ‘severe mental illness’ categorisation of services. As one interviewee observed:
. . . to get into any one of the teams or the wards, you’re not IAPT . . . you’re ill, you’re really ill. But then . . . people might be getting better. And I really think this is one of the problems with the whole PbR [payment by results] system is that somebody could drop down to the wrong cluster, and then you begin to get worried about how long you can continue to see them for . . . The other sort of confusing thing about clients is that sometimes you feel that they’re very cut off from their difficulties. And so it’s difficult to know where to cluster them . . .
Senior clinical psychologist
This meant that a key feature of an effective system of provision was finding ways of combining different therapeutic approaches and helping users manage transitions between them.
A further manifestation of this clinical leadership work of undoing existing definitions of users and services took the form of what was described as ‘pushing back’ on the commissioners. Alliance members said that they needed to articulate the need for the most effective intervention models for the clientele being seen, for example making the case for models that go beyond the six-session brief therapy model as the standard, given the complexity and severity of many cases. There was thus a degree of ‘reverse leadership’ with the institutional work of theorising and design coming from ‘below’.
There was also evidence of productive tension between the clinical leadership perspectives of commissioners and providers. Although both groups embraced the overall goals of providing seamless and comprehensive services for users, commissioners tended to emphasise the collective responsibility of providers to fill gaps by working creatively with existing resources, whereas providers emphasised the responsibilities of commissioners to fill specifically identified gaps. A feature of clinical leadership on both sides was the willingness to work through such tensions.
Case A2: innovating in urgent care – a combined general practitioner and paramedic service
Across the country as a whole, urgent and emergency care has been a recognised problem across the health service for some time. There has been rising demand and the service has found it difficult to cope with the numbers and the expense. A consistent case has been made for the need to reduce the numbers attending A&E departments. Many different ideas have been put forward about how to resolve the problem. In this case study we focus on one specific innovation which seeks to tackle the issue. It is a study of leadership from the CCG in the redesign of one focused aspect of urgent care. It involved stakeholders from the ambulance service as well as local GPs.
Leadership at the initiation stage
This urgent care initiative emerged from discussions at the CCG urgent care programme board. This was chaired by a GP, from the CCG governing body, and its deputy chairperson was the clinical lead consultant in emergency medicine from the acute hospital. The board included a range of other clinicians: a senior nurse from the acute hospital emergency department; senior paramedics from the regional ambulance trust; and senior GPs from an urgent primary care centre co-located with the acute hospital emergency department and from the out-of-hours GP provider. Its membership also included a patient representative and managers from the CCG and from the various providers involved in urgent and emergency care.
The idea was to set up a ‘blue light’ car operated by the ambulance trust but crewed by a paramedic and a GP. This in effect meant that selected 999 calls were allocated to primary care. The idea emerged from the urgent care programme board. Further theorising work for this initiative was undertaken by a senior paramedic (employed by the ambulance service), in conjunction with the clinical lead from the emergency department of the local hospital.
They were aware that paramedics often felt frustrated in their attempts to keep patients from being conveyed to hospital because they could not find a way to refer effectively to any local services which could provide care to patients at home.
Shortly after the production of an initial scoping document, the ambulance trust manager invited the GP chairperson of the urgent care board to go on an ambulance shift to see the kinds of cases that ambulances are called to and to assess for herself how a GP within an ambulance crew could intervene to treat patients at home and avoid the need to carry them to A&E. That GP-led alternative service was at the heart of the idea.
The main target group from the outset was elderly people with complex conditions and multiple medications. Ambulance crews often did not feel confident that they could leave such patients at home, and so they tended to play safe and transfer such cases to A&E. However, with a GP as a member of a paramedic crew, it was judged that they would have the professional knowledge and skills to make an informed assessment and to allow some immediate treatment decisions to be made. These GP crew members would also be able to directly refer patients rapidly to other services that could provide care at home. These wider services included a multidisciplinary, first-response duty team, specialist teams for respiratory conditions and heart failure and out-of-hours community nurses who can deal with dressings and catheter problems.
Such services meant that many patients can receive the same treatment at home as they would in hospital, without having all their home-based care plans cancelled and their independence undermined. Paramedics are typically less familiar with the well-developed range of home-oriented care services in the borough, and in any case may not have the experience to refer patients to them in the same rapid manner as a GP.
The wider context of establishing the pilot is that, across London, ambulance crews were perceived as commonly experiencing difficulty in getting support from primary care when they encountered a patient whom they judged could be cared for outside of hospital. They sometimes conveyed patients to hospital in the full knowledge that it would be better not to. There was a perceived culture of believing that GPs would not respond, even within normal surgery hours, based on reports of a few bad experiences that circulated widely. Furthermore, ambulance trust managers wanted to increase awareness among GPs of the range of help that their paramedics can offer, beyond carrying patients to hospital.
Implementation: activities and achievements
The service consisted of a car operating from late afternoon into the early hours of the morning, crewed from a roster of four GPs and four paramedics. Several aspects of the new service were developed incrementally in the context of its practical operation. The incremental nature of the initiative reflects the kind of ‘adaptive leadership’ we discussed in Chapter 1.
Leadership, in this phase, came from the clinical lead GP from the out-of-hours service, working with the four paramedics, the ambulance area manager – also a paramedic – and the ambulance trust medical director responsible for clinical governance. This grouping worked on defining operational issues, such as clinical record keeping, activity monitoring and clinical governance, particularly the circumstances in which the GP or paramedic had lead responsibility for a patient. This group developed and documented a range of clinical procedures appropriate for a GP–paramedic team, including taking urine and blood samples and getting results from the hospital laboratory during the same shift, if this was relevant to immediate treatment. Otherwise, tests were followed up by the patient’s own GP the next day.
Calls for the new service initially came through one of two routes. First, other ambulance crews or ‘first-response’ cars who attended a patient and assessed them as appropriate for the new service could make a request to the ambulance control room. A second route came via direct allocation by the control room based on their initial call triage. After a few months into the trial a third route for jobs emerged when crews on the service were concerned that they were not getting enough appropriate calls. The GP lead and paramedic crew members realised that they could use their own mobile visual display of the ambulance trust’s computerised job tracker system to view annotated details and locations of jobs currently awaiting dispatch, and from this self-identify appropriate jobs in a proactive rather than reactive manner.
Interviewees cited the achievements of the pilot service as the proven value of the GP–paramedic service; that unnecessary hospital admissions were being avoided; that the regular ambulance resource had been kept available for other jobs; shared knowledge was enhanced; and skills upgraded.
Challenges encountered
There was debate as to where the boundary should lie between patients who have a clear need of the combined skills of the paramedic and GP and those who perhaps could call the out-of-hours GP. Some argued the case that there are patients with long-term conditions, or their carers, who become panicked at a particular event or symptom and feel disempowered to use their usual coping strategies. They may also have felt that their GP has not been responsive in some way. Such people call ambulances in desperation.
The case for continuing the service after the pilot period was widely linked to increasing the number of suitable jobs each shift. By the end of the pilot period, the service was attending an average of around five patients per 12-hour shift. The CCG wanted this to be six or seven; the typical attendance for other ambulances and first-response cars was around 12 per shift. Although it was recognised by both the CCG and the ambulance trust that the service attendances were likely to take longer than regular emergency calls involving conveyance to hospital because of the treatment and possible onward referrals involved, there was acceptance that the number of jobs per shift needed to be greater.
As a result of shortages of paramedics, the ambulance service and CCG agreed to take forward a modified version of the service which consists of a GP accompanied by a driver. This now operates from the local ambulance garage so that links with paramedics and other ambulance crew are maintained.
Clinical leadership across different arenas
Two kinds of clinical leadership were found to be important in this case:
-
within an operational commissioning arena in the form of the urgent care programme board, there was leadership from a CCG GP, supported by a managerial programme director
-
leadership from provider–clinician members of the programme board, in particular emergency medicine doctors and paramedics in defining novel service solutions within an operational delivery arena.
The CCG urgent care lead GP and corresponding programme director were able to carry the case for funding this initiative to the strategic commissioning arena of the CCG governing body. This institutional work of achieving the vesting of resources in a new initiative was vital.
Characteristics of clinical leadership for service redesign with this Clinical Commissioning Group
Together, these two cases illustrate the distinctive roles of clinical leadership in first articulating the conception of a new approach to service delivery and then defining the operational realities of the new service. They show that the former aspect of clinical leadership can take place effectively in an arena such as a CCG programme board with operational responsibility for commissioning. The operational realities then need to be worked out in more practical detail by lead front-line clinicians in provider organisations. This second mode of leadership is of an adaptive kind. There is a need to bring the learning from operational experience with the new arrangement back into the commissioning arena. This can be seen as a further integrative element of clinical leadership, spanning the commissioning and provider roles.
Case B: redesigning general practice and primary care
This CCG is located in a part of Birmingham where the health of the population is generally worse than the England average. The CCG, which formed the site of this case study, derived its GP practices from three different former PCTs. The associated variability in practice and expectation is an important element in the case narrative. The CCG inherited huge variation in standards and coverage of care across its patch. The potential for GP practices that were to become unhappy with attempts at reform to renounce membership and join another CCG is also a significant feature. Loss of GP practices meant loss of income for the CCG. This was a very large CCG with > 100 GP practices and, as such, it saw a need to allow the localities a greater degree of influence than was often the case in other CCGs.
Focus and theme of the case: the primary care improvement programme
The research in this CCG focused on a major attempt that was made to redesign primary care across the whole patch. The particular focus of that initiative were the services provided by GP surgeries. The programme is of special interest here because it represents a service redesign initiative driven at the CCG strategic level and it used the official channels of the CCG.
The problems to be tackled included unacceptable variation in the range and quality of care offered in GP practices across the CCG. There was also a lack of uniformity in the pattern of payments: practices were paid at differential rates for the same kind of work. It was the chairperson of the CCG and the accountable officer (both GPs) acting in concert who took the lead in identifying these issues as a priority. It is noteworthy that at the time (2014–15) many other CCGs were not viewing GP services and primary care as a main concern. It may be speculated that it was the ‘new broom’ aspect – with new leaders of a new territory – which allowed and prompted this dispassionate appraisal of these primary care services. Conversely, those CCGs with established teams of people who had a long history of working together in, for example, the previous PCTs may have been less inclined to make such a new determined effort. (Conversely, the benefits deriving from long-established working relationships were noted by others in different circumstances.)
The service redesign solution was a three-step approach to reform. The first step was a baseline which all the practices were required to meet. This was a mandatory requirement to remain a member of this CCG. The second step was to standardise the local enhanced services offer. This meant that practices (in cluster form if necessary) were asked to improve their range of services so as to meet an acceptable standard. This started out as a voluntary exercise but increasingly became a requirement. The third step was a higher level of innovation in services offered. The CCG used a budget provided from the centre, which was geared towards care for the elderly, to invite bids for new enhanced services in this area.
We first describe the primary care improvement programme (a pseudonym of the title actually used by this CCG) as it was presented in official terms. We then present an analysis of how the programme was received and understood by multiple agents, including some of the designers of the programme and those who were the recipients.
The official picture
The main initiative driven by this CCG was a service improvement programme designed to make a step change in the quality of primary care. The key declared objective was to:
Reduce the level of variation in general practice and bring all practices up to the same standards of primary care. Through [primary care improvement programme] we will ensure there is universal coverage of services across our member practices and that these services are available for all patients, regardless of where they live.
Case B: CCG policy document
Attention focused on holistic care, integrated care, long-term conditions management and better care for the elderly and vulnerable. The constituent elements of the new model of primary care included universal coverage of some basic service standards across the whole CCG population; an overarching framework that allowed the freedom to identify creative solutions for how patients receive their care while ensuring accountability for care remains with practices; delivery of a patient-centred and integrated approach to improving primary care management of long-term conditions; and an up-skilled general practice workforce to deliver services that had previously been provided by secondary/community providers.
This was a 3-year programme which commenced even before the CCG was formally and officially invited to become involved in primary care co-commissioning. It required an investment of approximately £25M. Integration, access to mental health services and a transformation of urgent care were all elements of the total package of reform.
The programme rationale noted that the previous scheme of enhanced service contracts had ‘not delivered improvements’. Interviewees told us that this was because the previous scheme had been ‘too transactional’ and was based on process measures which were too mechanistic. The new plan from the top leadership duo was for a more integrated system built around general practices. This included new models of care with GPs and others working in new ways with support from secondary care, while also bringing in associated community services, community nursing and district nursing. Supporting elements included data sharing and use of the BCF to integrate social care. The problems of pressures on general practice, fragmentation and lack of a universal and equitable service provision were further reasons justifying action.
In exchange for extra funding and support, the GP practices in the CCG were expected to offer care closer to home, delivering a wider range of tests and investigations in primary care settings, such as electrocardiography, spirometry and insulin initiation. These steps were expected to reduce referrals to secondary care. Each service area, such as diabetes care, chronic obstructive pulmonary disease and asthma, had an associated set of target outcomes. For example, the plan stated that 90% of patients with type 2 diabetes should be managed outside the acute trust. The plans also included a place for appraisal of practices in relation to their conformance.
None of these interventions was without controversy. A number of GPs were very reluctant to accept the changes. The leadership skills of the CCG chairperson and accountable officer were very necessary. They undertook institutional work in conceptualising the required nature of the changes and in the creation of new institutional forms in place of long-standing and embedded institutional practices, which tended to emphasise and privilege professional autonomy.
The programme included some elements of PPI and, as was indicated in the survey results, clinicians are sometimes leaders of this process, as in this case. Part of this was through ongoing channels, as in the cases of respiratory and mental health, but in addition there were some special stakeholder consultation events. These included talks with the Patients Council and other patient participation groups. The part played by clinicians as front communicators was seen as very important in this context.
We encountered similar service redesign programmes in other CCGs, albeit rather less well elaborated and systemic than in this case. In the next section we analyse how various actors sought to lead these initiatives and how actors on the receiving end experienced them and how they responded.
Findings from the interviews and observations
The focus of attention for this CCG was without doubt on primary care itself. This large measure was because the CCG realised it was inheriting disparate systems and an uneven scope of services across practices as well as uneven levels of quality of service. The incoming leaders of this CCG held no attachment to the inherited systems and felt an urgent and pressing need to resolve the evident issues in primary care provision across its territory. Unevenness in the quality and range of primary care services across the different GP practices was the stated reason for a call to action. This point of focus is interesting because, at the time of its commencement, this initiative preceded the co-commissioning of primary care. In the many cases where CCGs largely represented pre-existing teams and localities, this prompt for change may not have been felt.
The initiative was widely viewed as having merit, but it was the availability of special funding which prompted the move to action:
We had funding available. What did we want practices to do? It was really interesting. So, people were throwing in ideas. It’s something that I never saw happen in PCT days where there would always be a specific problem to solve. This was a general performance approach and people were throwing in lots of ideas. I genuinely believe it ended up being the most successful piece of quality improvement I’ve ever seen.
GP governing body
The leadership was identified, by numerous informants, as essentially stemming from three persons at the head of the CCG: the accountable officer, the chairperson and the deputy accountable offer. All three were GPs. As a team they carried a great deal of credibility. One issue was that they all came from larger and more successful practices, and some of the smaller, less successful, practices at times felt that their situation was not so well understood. Nonetheless, there was little doubt from the interviewing across the wide range of informants that this CCG was seen as ‘clinically led’.
The number of accountable officers who are GPs has been in steady decline across the country. In this case it was argued:
A GP accountable officer carries more credibility with the clinicians. However, I think the clinicians in those roles find it quite tough sometimes because it is not something that clinicians are trained for.
A governing board member
The resistance from some of the smaller practices to the raised expectations for higher standards across all GP practices was seen by the proponents of change as defensive and a desire to continue with long-standing ways of working. The fact that the changes were being driven by fellow clinicians made it difficult for the resisters to argue that the initiative was a political or bureaucratic attack on the profession. Instead, the point of contention was that the clinicians who were leading the changes were somehow ‘different’ in that they came from more privileged, better-resourced and larger practices and, as a result, were insufficiently aware of the challenges faced by smaller practices in difficult areas.
There was an also an additional view that those GPs who had accepted leadership roles, either at locality level or at the CCG, were in danger of switching their identity and their allegiances from being first and foremost ‘a working GP’ to a rather different stance of being ‘leader–manager–clinician’. Some of the ‘ordinary’ GPs who were interviewed made the point that these role holders were in danger of losing touch with the day-to-day demands of the work in general practice. Notably, even some of the interviews at CCG level also accepted that there was a challenge in this regard. They normally expressed this by saying that such a shift in perspective might arise if the clinical leader ‘stayed in the role too long’. Moreover, they accepted that as a result of the innovation in primary care, the role of the locality leads had undergone a shift in nature. As one GP who sat on the CCG board commented:
I think that these roles [the locality leads] have emerged into being roles that are less clinical and more performance and operational orientated. I commend the people who have taken those roles on, they are doing a difficult job. It is also worth noting that these roles are still emerging, in terms of capability and conduct.
A governing board member (emphasis added in bold)
As a result of the drive to push through the primary care improvement programme, the nature of the leadership adopted was seen by some informants as essentially ‘directive’. The baseline level of the improvement programme (i.e. the absolute minimum, must-have scope of services and the quality-assurance measures) was mandatory. The time when mere transparent comparative measures and implicit peer pressure was judged as a sufficient ‘nudge’ for practices to be persuaded to come up to the mark was gone. To remain a member practice of this CCG it was necessary to conform to a formal service-level agreement.
The second level of the improvement programme (the offer of a range of extended services, such as electrocardiography, spirometry and diabetes treatment) was semi-mandatory in the sense that, although individual practices did not necessarily have to provide these themselves, they had to do so in partnership with other practices. This opened the way to a third level, which was to encourage bids for innovative services. These tended to involve some transfer of work from the acute providers into general practice. This was optional, but peer pressure and demonstration was helping to drive up standards all round – with a few exceptions of around half a dozen practices which were seen as needing more direct attention. In this sense, the case illustrates a step-by-step approach. To some degree the initiative has characteristics of being mainly a service quality improvement programme, but in other ways it has some features of a service redesign. The crucial point in terms of our analytical framework is that institutional work was being done which was creating a new set of working norms. This was effected through two main arenas of clinical leadership: the central CCG based around three GPs as core leaders and out in the localities where GP leaders had adapted their role from being primarily representatives of those localities and as prime channels of communication up and down the chain, to a new role of determined drivers of change insisting that the new standards of service were being developed and delivered. This also meant, as we saw in the previous quotation, that a more ‘performance management’ element was being introduced into the primary care arena.
Given the nature of the service redesign initiative, performance management was a key element. The CCG had its own system of assurance visits. It wanted to be sure that its payments were being matched by the required services being offered. The CQC was seen to be an additional quality control and the CCG welcomed and used that extra leverage.
There were some concerns about conflicts of interest. This was seen most clearly with regard to the expanded services (at levels 2 and 3). These services were offered by local provider groups – sometimes known as delivery units. These local units were the same bodies as the commissioning locality bodies. Hence, the local network lead (a commissioning role) would often be the person leading the design of the expanded service (a provider role). Meetings of these locality groups were often divided into two parts so that both roles could be addressed at the same meeting with the same personnel. As one CCG manager observed:
Conflicts of interest are huge at the moment, and it does concern me. I think whether you have real or perceived conflicts of interest you need to have a policy and a strategy for dealing with that. So I think what [this CCG] has done with their GPs is really good but the mechanism by which it’s been done could be challenged: was there a tender process? You know, why did the CCG support one organisation and nobody else? So there is that kind of challenge that would be legitimate, I don’t think you’d have many other providers coming forward to do it but the process needs to be quite transparent and clear, doesn’t it?
CCG manager
Part of the issue was seen as the urgency of the problem to be solved:
I think there’s been a rush and so it has been poorly planned at times. Desperation even, we are in a really tough economic climate, we’ve got to transform radically, quickly and at scale. So you’ve just got to get on with it and not have the barriers in place, which I think in one sense is a good thing, we’ve got to get rid of barriers. But on the other hand, you’ve got to have assurance and safeguards in the system and that’s been developed subsequently to new models emerging and I think it should have been done beforehand.
Regional-level player view
A related view came from a secondary care doctor:
I think that, generally, clinical leadership has to be system wide, it has to be unconflicted and, I would say, mostly void of commissioning or provider responsibility. I think that’s where I see myself sitting and I am seen as a fairly impartial voice, but I think at CCG level it’s really tough for the clinical leaders to be seen as impartial system leaders because they are not, because the system is designed in order to prevent that. I think it’s good to have clinical leadership in the system, there is no doubt that is the right thing to do. I think real clinicians have the interests of patients and populations at heart but all we sometimes see emerging is clinicians who get into those roles who suddenly have the interests of their organisations at heart, rather than the patients and populations.
Secondary care doctor
There was uncertainty about the sustainability of these arrangements. In general, it was believed that the direction of travel was towards the provider role. Indeed, a popular interpretation was that the primary care improvement programme, through its challenges and demands, had stimulated a new provider landscape in general practice and that the logical outcome would be the creation of accountable care organisations (ACOs).
The concerns about conflicts of interest and the related concerns about whether or not there was appropriate open tendering to allow potential alternative providers the chance to come forward reflect, in large measure, the wider institutional field prevailing at the time. The logic of open competition and challenge sat alongside an alternative logic based on the idea of improving services, although more effective collaboration among current providers. The institutional field altered during 2016–17 in that the erstwhile emphasis on the competition/challenge logic has been subsumed in favour of the planning and collaboration logic, as seen in the support for STP from the centre and the altered stance from NHS Improvement.
The lessons about the process of change include a view that the CCGs offered a mechanism to exert peer pressure more effectively. There was regular reference to some version of the 20–60–20 rule. The first category were those GPs and related professionals keen to effect a change to a better service. The second category were those seen as willing to be persuaded if the transitionary complications could be resolved. The third category were seen as laggards and even ‘troublesome’.
The membership nature of the CCGs meant that the process of change had to be handled cautiously, although at the same time it also could be used to lever change if the middle group could be persuaded to agree. The membership character also meant that malcontents could ‘jump ship’ if they were dissatisfied. They might negotiate transfer to another CCG. In one respect the CCG leadership welcomed this safety valve, it offered a means to be free of troublesome members. However, on the other hand, it came at a cost, as loss of these practices meant a reduced income stream for the CCG.
There was a view that, although the CCG was undoubtedly doing a valuable job through its single-minded commitment to primary care improvement and that the CCGs were an effective mechanism to enable that to occur, there were limits to this tool. The wider challenge was seen as a fragmented system with perverse incentives and vested interests which would resist these kinds of interventions beyond a certain point. This need was identified prior to the STPs. One of the interviewees on the periphery of this CCG made this point:
The NHS is so fragmented in terms of regulation, accountability and the rest, it needs to be unified. We have taken steps to bring together our clinical leaders across the [region] from both CCGs and providers. It also includes things like clinical networks, clinical reference groups, Health Education England, academic health science networks, Public Health England. All those bits that have been so fragmented. I’m trying to pull that together.
A regional stakeholder
That task was made extra difficult by the lack of coherence of the various bodies, as one informant said, ‘there is serious lack of co-terminosity’. That aspect has arguably been party addressed by the STP initiative. The need for such changes were being identified by the actors in this case. A further example of this prescience was the informant who argued:
I think that the new models of care aspire towards becoming ACOs, and to me it doesn’t matter from which direction you tackle that. So, whether you have MCPs [multispecialty community providers] or PACS [primary and acute care system] it doesn’t matter, often they are going be ACOs anyway. There is a lot of support for MCPs in the system whereas people often feel quite threatened by the PACS model. The initiative to generate primary care provider organisations is sensible. However, it is worth noting that the PACS model, with a hospital base, has the advantage of a better resourced and professional management structure and capability.
Secondary care clinical lead
The new models of care were generally welcomed by all those whom we interviewed. They were regarded as mechanisms which could help resolve many of the issues associated with the CCG initiatives taken to date as discussed earlier. The level 3 element of the programme, which involved innovations which could transfer appropriate services from hospitals to primary care, was recognised as precarious. Where clinicians talked to clinicians (GPs to consultants), it was argued that they could often identify areas of agreement about which services could be transferred. The consultants were pleased to be rid of much of the high-volume routine work. However, there was the question of the implications on the income flow into the hospitals and the means by which funds would be transferred to match changes in activity. The finance managers were cautious but, given the penalties imposed for breaches of performance targets, they too could be persuaded to relinquish some of this kind of work. The scheme’s funding was based, at the higher levels, on a matching fall in activity and cost in secondary care. The money to primary care was paid upfront. At the time of our research at this site there was huge uncertainty whether or not the corresponding alterations to activity in the acute sector were happening. There was no doubt, however, that general practice across the CCG had been improved even though there was more to do. A few general practices decided to transfer to a neighbouring CCG in order to avoid the change programme.
Summary: clinical leadership across different arenas
Clinical leadership was present in this case in the form of a determined push by a close group of three GPs at the summit of the CCG to reform primary care as a whole and general practice in particular. This leadership was enacted in all three arenas outlined in the analytical framework presented at the start of this chapter (see The analytical framework and Figure 24). The strategic planning was undertaken in the arena of the CCG central governing body. The operational activity was undertaken in the programme board for primary care and in the locality groups. The third arena for institutional work was at the practice level; here, the distributed clinical leadership was of a more variable nature and some GP practices moved ahead in delivering the primary care improvement programme much more fully and rapidly than others.
Notably, the kind of institutional work being undertaken by the leaders in this CCG was bounded by the institutional reach which they judged they could attain. They challenged existing practices, prescribed new versions of acceptable practice and set new levels of attainment. This required a complex mix of joint problem identification, joint problem-solving, visioning, contingent reward and, ultimately, prescription and monitoring.
Case C: redesigning early intervention services for mental health
Focus and narrative of the case
This CCG sought to transform mental health services through the design and launch of a ‘hub and spoke’ model of mental health provision. The hub component was a ‘well-being hub’ which operated under the broad umbrella of a mental health service in which intended service users were those with mild and moderate mental health issues. Many of these service users were often experiencing one or more other difficulties in life, such as family or financial problems. The prime purpose of the well-being hub was to bring a number of services together so that complex social, as well as mental well-being, issues could be tackled in a holistic manner. It provided the more established treatments, such as counselling and cognitive–behavioural therapy, and it also offered services such as employment support and chaplaincy. As a ‘hub’, it operated a triage system that was able to refer patients out to one or more local ‘spoke’ services. There was a single initial point of contact and a central database of patients’ records, administered centrally by the hub. The records were selectively shared with the spokes so that the patient did not need to undergo multiple assessments.
The initiation of this project was widely attributed to a single individual: a respected GP with a long-standing interest in mental health and also the CCG’s current clinical lead for the area. A senior manager described this leader as ‘driven and passionate’. Another interviewee connected to the hub identified ‘a strong sense of moral responsibility’, while also highlighting the leader’s networking skills and persuasiveness. One key figure from the third sector, a chief executive of one of the hub’s spokes and also on its board, corroborates these observations in describing how:
You couldn’t fail to be, you know, swept along by what he was saying about the need for this service, about the solutions, about the options, and about what works.
Third sector chief executive
According to this testimony, the clinical leader in this case appears to have undertaken institutional work which cuts across a number of the categories in Lawrence and Suddaby’s classification. 70 This work included ‘disrupting’ prevailing institutional arrangements, ‘theorising’ alternative vision and ‘creating’ a new set of institutional arrangements. These were accomplished in a manner which engaged, indeed ‘swept along’, the diverse players in the wider system.
Reports relating to the start and the background of this service redesign initiative for mental health care often mentioned the clinical lead’s personal professional history in the area of mental health, as he had a significant role leading mental health during the days of PCTs. In other words, prior reputation added to the credibility of the clinical leader’s suggestions. Yet, at the same time, his known history included a willingness to step aside on grounds of principle when he dissented from a course of action. It was reported that he had resigned from his PCT role because he was ‘disillusioned with the role’. It was stated that ‘working with the mental health trust around contract management – it was just not [his] thing’. As a result, he did not simply crossover from the PCT to the CCG as mental health lead during primary care’s restructure, but stood for the role relatively recently when he ‘just got absolutely fed up with waiting for the system to catch up with him and he saw the opportunity offered by the CCG’.
Interestingly, this reveals the mixed opinions about the way this individual operates as a clinical commissioner. One senior manager, working specifically in mental health (and with the counterpart clinical leads in neighbouring CCGs), described how this clinical lead had the critical combination of:
Understanding the commissioning process and being respectful of that process and understanding that there are steps that we need to take to make sure that we don’t leave ourselves exposed, organisationally, to be challenged.
Manager
In other words, this clinical leader had won the respect of managers through a demonstrated knowledge and understanding of commissioning and the risks and pitfalls associated with it. Managers made the point that passion, although important, on its own is not enough; the leadership that they observed on the basis of this example requires credibility won through awareness of the complexities surrounding mental health services that cut across multiple providers and agencies.
Despite the deep knowledge demonstrated by this clinical leader, the point was also made that, even in such a case, management support was crucial if real change was to occur. Partnership between manager and clinician was frequently reported as being required and indeed as being indispensable. Although the clinical lead brought forth the ideas and passion, the registrar followed up expressions of interest to attract ‘spokes’ into the hub arrangement, developed a business case for the CCG to pilot the model and helped to figure out how to construct an evidence base which would justify the ongoing funding and support for the new model.
Networking and relationships were a significant part of the hub’s foundation and continued survival. The clinical lead explained how he:
Just pulled loads of people in, people that I’ve known for ages, like the third sector organisations, people from the children’s mental health services, adult mental health services, from the police, from, anyone who was interested and wanted to be involved.
This quotation illustrates the power of an extended network around the clinical leader – a form of social capital. He described himself as playing a ‘facilitative’ role, one of ‘co-ordination, linking people together and getting them to find out what could be done’. This personal account was echoed by our other informants.
Turning passionate leadership and supportive relationships into something tangible required resources. Here, the localism of the CCG proved critical. Presenting the specific needs of the local population for the hub and testifying to both the collaboration of local practices as well as the need for funding, one long-standing GP said:
We felt that the needs of our patients were unique, they were a very transient, mobile population, quite deprived – we service three big council estates . . . So we started talking about this a good 10 years ago. A few models were set up, and at least twice, I think, we got together to work out some kind of a working model but on both occasions, due to commissioning failures, to funding failures and for other reasons, things fell apart. It was very difficult to untangle the money that was actually in the community.
The locality networks were given a pot of money by the CCG:
To spend on what they want to do as long as they can account for it. They can spend it on running their network or doing local network projects or whatever else they see fit to make the new model work.
CCG manager
From the CCG’s perspective, ‘the way [the clinical lead] really got it going was by influencing his fellow GPs in his network to support it’. Once this was established, the CCG’s role was to ‘provide fire cover for this commissioning and growth of new services in the communities’ (CCG manager).
A small amount of funding was allocated to a third sector organisation, which administered the city’s mental health consortium, to cover the construction of the database and the processing of applications from potential spoke services (with members of the mental health consortium being automatically eligible). Part of the funding was also reserved for two research projects: one to help capture and structurally develop the model as it progressed, effectively articulating the ‘proof of concept’; and a second to evaluate the hub against outcomes at a later date. The hub began operation as a 2-year pilot with 14 spoke services, the majority of which were working on the basis of goodwill, subsidising their participation through their patchwork of other funding because of their belief in the project and their hope that a successful pilot phase would lead to the hub becoming a formally commissioned service. This way of working illustrates the power of goodwill once the disparate organisations were convinced of the value of the new arrangements.
Patients were signposted to the hub by GPs from six GP practices. Users could also self-refer if they lived in the locality. Once initial contact was made with the hub they then underwent a triage process. This triage service was staffed on an alternating basis by individuals from one of the five spoke services. That there were five spoke services sharing the triage function (1 day a week each) was a result of the lack of funding and the abundance of goodwill to make the model work. It was argued that in an ideal world, a fully costed and commissioned service would have one central point of contact that would manage the patient’s data and journey, seamlessly, around the spoke services.
In the live pilot, not everything went smoothly. There were disruptions in the sharing of data between spokes and inconsistencies in their approach to triage. Although initially seen as ‘teething problems’, this data entry and management at the point of triage and subsequently (once the patient had been referred to and used a spoke service) was actually critical because completion of the hub’s well-being measurement tool at both these points would serve to provide data on the services’ outcomes. These data were important because they were used to evaluate the success of the arrangement and, ultimately, whether or not it could be justifiably commissioned on a continuing basis.
It was reported that the registrar’s completion of her training and her departure from the CCG around the middle of the hub’s first pilot year was a significant loss to the project because it undermined the daily driving force and compromised operational oversight. It was argued that, since her departure ‘things seem to have just got all snagged up in CCG governance issues’. This indicates that, running alongside powerful clinical leadership in terms of vision, plans and advocacy, if a new service is to be maintained over the long run it also requires efficient and competent administrative and managerial support services.
One of the organisations which offered one of the spoke services (the main mental health trust) eventually exhausted its goodwill and it withdrew its service. The IAPT service provided by the mental health foundation trust provided the hub’s triage function 1 day a week and, being the main provider for popular therapies, such as counselling and cognitive–behavioural therapy, it received the vast majority of the hub’s referrals. It was stated that the lack of funding was an obvious hindrance. However, additionally, the oversight and measurement regime proved to be too demanding. A manager in that service told us:
I can’t train 100 staff in another set of outcome measures. We just don’t have the resources, or the need, to do that, and, you know, we’ve got so many outcome measures and targets that we’ve got to fulfil anyway. It was just impossible to make sure that every patient that came from the Hub . . . given that we were the largest receiver of referrals, had these outcome measures used on them, pre and post treatment, by us. We just couldn’t do it as a service. We couldn’t include more outcome measures, when we’ve already got so many that are mandatory. So that was why we pulled out.
Mental health trust manager
Though this was a setback to the hub’s development, it is worth noting that its inclusion in the model was questioned by some at the outset because it effectively went against the grain of the idea of the hub. The point was to provide an alternative, even preventative, and holistic service for well-being, rather than treatment for mental health issues per se. In addition, from a strict commissioning perspective, its inclusion as a spoke was problematic if the hub was deemed successful enough to be a commissionable service because it could be viewed as a competitor. Providing a strategic overview to the complexity of commissioning here, senior interviewee concluded that ‘it may be a good thing [that the mental health trust pulled out]’ because the essential concept of the new service ‘was a completely different thing to [traditional] mental health services’.
The CCG was widely seen to have been supportive of the hub throughout its development. Indeed, as our study at this site was concluding in late 2016, further funding was agreed to keep the service operating. In fact, there was an upgrade in that the central triage was to be staffed by a qualified psychotherapist.
Summary: clinical leadership across different arenas
The idea of the hub was to bring together a diverse range of scattered, fragmented partial services. The new service was to be more holistic, more person centred and more widely cast to include well-being and sustainable living. The idea was to move away from an overt medicalised approach to mental health problems.
Clinical leadership was present in this case in the form of a credible, knowledgeable and committed leader operating in the operational arena who was able to harness the power of his diverse network and, as a consequence of that, to win support from the CCG strategic level. Yet even with a credible leader and widespread support there were significant institutional challenges.
Although the creative institutional work was seen to be efficient and effective, there was the legacy effect of the extant services to be taken into account. There was pressure on the clinical lead not to ‘destabilise’ the system too much. The CCG was working across a spectrum of services that they could influence through clinical commissioning. Even within mental health, other developments were taking place which the CCG saw as equally important. One of these focused on CAMHS, which was being extended beyond the normal age range to take in young adults up to the age of 25 years, whereas previously patients would transfer into adult mental health services at either 16 or 18 years of age, depending on their position in other services (social services or educational services). This was ground-breaking work, and some in the CCGs regarded this as the main ‘flagship’ service redesign. It demonstrates the difficulty faced by clinical commissioners trying to look after whole health economies within a transactional framework. It is a stark example of coexisting competing logics. The institutional work of the CCG’s actors was complicated by the need to operate with these competing logics in mind.
Case D: system and multilevel redesign
Case D illustrates many important aspects of the current reality of the leadership of multilevel service redesign attempts in the English NHS. The unit of analysis in this case was the area which became the new STP footprint. It comprised six CCGs, a county council, a city council and a collection of acute hospital trusts and community trusts. They are analysed as one unit here because these particular CCGs had made strenuous efforts to work together and indeed had been prompted to do so.
They all operated within one large, mainly rural, county and had worked together in pairs, in triads and indeed across all six CCGs. Case D covers a population of approximately 1 million people. The health system in the region is in deficit and it is considered not sustainable without radical reform. The context is also one of major change to hospital services following the dissolution of one of its hospital trusts and there were difficulties in recruiting clinical staff in both primary and secondary care.
The health economy so defined was identified as one of the 11 national challenged economies. There was a £140M deficit (2015/16), that is 7% of the funding available. It was forecast that if no change was made this would increase to £240M (11%) per annum over the next 5 years with an accumulated deficit of > £1B. The extent and severity of the challenges helps explain why these neighbouring CCGs were impelled to work together beyond the norm for CCGs nationally. The analysis that follows works through service redesign attempts at different levels and in different arenas starting with GP practices and moving up through localities, the CCG level and then the supra-CCG level.
Practice level
We investigated, in some depth, an example of very active service redesign activity originating within one general practice but extending into a multipractice initiative. Ironically, the context was one of general conservativism. For example, one interviewee observed:
Practices see themselves as individual businesses just getting on with the job. In the main they just follow the traditional model which is, you know, well, just what general practice was 20 years ago. But there’s one practice that has been more innovative about looking at what they do . . . behind that sits a very big issue of property and surgery ownership. As an individual practice over a number of years they have redesigned the way they work, redesigned their staffing structures, and redesigned the way that they do things.
GP locality lead and CCG board representative
The ‘unique’ practice innovator case was led by a highly entrepreneurial GP from his own practice base. The emphasis on concerted action led to the formation of a GP federation. This GP, with close colleagues, bid successfully to be a rapid test site for the ‘primary care home’ initiative. This initiative was launched by the National Association of Primary Care.
As a rapid test pilot site, the Case D group of GP practices is designing and trialling a new enhanced primary care service based around a ‘complete clinical community’. This includes an integrated primary, secondary and social care workforce providing more personalised and better-co-ordinated care closer to home. The initiative is designed to pilot and test a different and expanded mode of primary care. It includes a new workforce profile, less dependent on GPs, with an expanded array of services supported by new and enhanced training and development for the wide array of roles.
This initiative works to a model devised at national level but the detailed design and implementation is dependent on local initiative and activity by local leaders. Realising the concept and making it work is also dependent on a number of bodies, including educational and training bodies, such as Health Education England, working through community education provider networks.
The new model is designed to galvanise primary care, community health and social care professionals to work in partnership with specialists so as to provide out-of-hospital care in a holistic way. It has similarities with the multispecialty community provider (MCP) model as described in the Five Year Forward View. 12
The model is based around new workforce roles (such as physician associates and health-care assistants) leading to a new ‘community workforce’. Physician associates take postgraduate training under the supervision of a doctor, so as to equip the role holder with the skills to take medical histories, perform examinations, diagnose illnesses, analyse test results and develop management plans. The emergent model in the organisation we studied also had a focus on ‘urgent care practitioners’ and a further focus on the redesign of the nursing workforce, both new roles designed to fill urgent care gaps. The urgent care practitioners have a nursing or paramedic background. Accreditation and assurance is being arranged through existing Nursing and Midwifery Council and the Health and Care Professions Council regulatory bodies. Just one of the implementation leadership complexities includes the issue of indemnity. Steps were being taken to enable this to be covered by an existing provider who would also provide the necessary supervision. A further important element is an increased use of telemedicine and information technology allowing diagnostic tests without GP presence.
As all of the above indicates, the redesign of primary care services in the GP practices that we studied required many complex interlocking aspects: reimagining the nature of primary care in relation to other services, such as community care, social care and secondary care; redesigning the workforce to match the new service profile; arranging the necessary training, supervisory and indemnity arrangements; and designing and operationalising the required technology support.
Few GPs were in a position to take the lead on such an ambitious agenda. It required imagination, creativity, funding and persistence to even get such a package launched. It also required networking skills to bring on board not only fellow professionals, but also professionals from related but separate disciplines.
In the case we studied, the GP leaders had also to negotiate with the CCG in order to gain some assurance of ongoing support and eventual ongoing funding for the new model of primary care. This was not an easy task. The CCG leaders had their own priorities and they were reluctant to devolve funding to the local leaders of this initiative. At the time of the study, although there was ‘in principle’ support, the question of the devolved budget, which the local GPs said was necessary for them to act in an entrepreneurial way, remained open and uncertain. This provided a stark example of clinical leaders needing to exercise unusual levels of capacity in managing ambiguity and uncertainty. Not all of those who were taking a leadership role in this venture displayed the same level of tenacity in the face of setbacks. Some were inclined to step back and revert to business as usual (that is to retreat to their normal clinical role) when faced with lack of support, but one or two were very different in that they showed persistence and determination to continue in the face of adversity.
Locality level
The locality level was the sublevel of the CCG where groups of practices came together to share experiences and to act as a communication channel with the CCG. It was a potential arena for the exercise of clinical leadership. As we will see, the kind of leadership that was exercised here was what might be termed ‘implementation leadership’, but we found this to be very patchy across the different localities.
Although some informants suggested the locality level was where most GPs actually ‘engaged’ with the CCG, there was little hard evidence that any significant service changes have been triggered at this level. We interviewed a number of locality directors; the quotation below captures the essence of what most of them were saying:
Well, with the locality structure, and indeed the reason why I’ve stayed involved in this sort of stuff, is really there, partly, to protect the interests of [name of locality]; there needed to be a person and a group to bang the drum for [this locality]. So part of the [rationale] is to represent the local practices, with me as a sort of figurehead to feed things in, and represent the locality at CCG level. And indeed for me to represent CCGs in the bigger picture at locality and practice level.
Locality director (emphasis added in bold)
Locality working is not new. In some ways it could be argued that the influence of the locality level has decreased in this county, rather than increased, with the emergence of CCGs. This point is suggested by another locality director:
The locality has no dedicated support staff. In the past it existed as an entity, as part of a primary care trust and at that time it was seen as a meaningful organisation that had staff of its own and a programme of work.
Locality director
A practice nurse who was interviewed endorsed this view. She observed that activity at locality level had limited impact. She remarked ‘there have been some good ideas but they don’t seem to add up to anything’. She described how wound care at locality level could have been integrated with district nursing, but ‘a year later we are still talking about it’.
An influential manager working across three of the CCGs noted:
My concerns about locality working is that localities can become a bit anarchic if you let them go off. You have to keep them corporate as well as giving them some freedom. I don’t think they should have all the freedom because we need to have a grip on the corporate message and things like that so it’s a really fine balance. Because we don’t want them to go off and develop services that we don’t need or that we can’t pay for.
CCG manager
In summary, the localities (as a subsidiary level of the CCGs) are often where ordinary GPs have most direct contact with the CCG, but this is not a level where service redesign or clinical leadership had occurred to any significant degree. The exercise of clinical leadership was concentrated elsewhere.
Clinical Commissioning Group level
This section includes the initiatives pursued both by individual CCGs and CCGs working in concert with others. There were instances in this arena of the CCG boards of some bold and significant service redesign plans and attempts. These included some unusually large outcome-based contracts which handed significant areas of service provision to new-entrant provider organisations, as well as other bold moves to reconfigure services across the county. The radical nature of these moves could be regarded as proportional to the exceptional nature of the challenges in this health economy. The extent of the ‘challenge’ (some informants talked of crisis conditions) seemed to impel the degree of response. The national centre was taking a very direct and active interest and local leadership in the form of the senior managers were thus empowered to take the lead in an assertive way. This meant that some of the more emergent, bottom-up, clinician-led approaches to service redesign found in other cases were rather crowded out in this case, as the top-down plans were prioritised.
There was substantial evidence in the interviews to testify that management in this case area was more influential than clinicians. Furthermore, it was clear that getting the finances back under control was regarded as a priority in this health economy. This may have contributed to the control taken by, and acceded to, professional managers. As a GP board member argued:
Managers are in charge, and everything is driven by [them]. I think because it’s been going on for such a long time you can see the disengagement by the GPs. You come to a stage where you think, there is no point me saying anything or talking about anything when the management’s going to do what they have to do . . . the financial recovery plan governs everything.
Another assessment was:
A lot of people are disillusioned and they don’t want to get involved. I mean, they’ve advertised so many times for governing body members because we need more clinicians.
GP member of CCG governing body
This problem of a depleted clinical leadership pipeline was frequently noted in this case, as indeed in others, but to a lesser extent than in this case.
The Clinical Commissioning Groups in relation to other bodies
The rise of an influential GP federation was seen to implicate all the GPs as having a conflict of interest; this too was used to justify further tilting the balance of influence in management’s direction.
A CCG chairperson argued that a lot of time had been spent on aligning practices and getting them engaged.
We’ve had external consultants who came in and produced a fairly critical report about how the local organisations failed to work co-operatively. And so, out of that came a plan to try and do everything just once rather than six times and we’re sort of starting to try and do that. Although that’s actually just throwing up issues of how you make six autonomous organisations in terms of the six CCGs agree on things and whether that just slows down the sort of decision making and also how it works in terms of the governance of the organisations.
This chairperson then described priority actions by this CCG:
So, we have a primary care strategy which is divided into six work streams . . . There’s a stream around urgent care and one around the structure of primary care, and meds [medications] management, etc.
However, tellingly, he then goes on to describe how the local federation has won funding which enables them to set another primary care agenda:
Within the organisation there’s different thinking in different places. My thinking, as the director of primary care, is in a slightly different place from other managers within the organisation and some of the clinical leads. So, I think part of the challenge is to try and get some corporate thinking around this. Our local federation has worked with another provider and secured a very large fund bid. So that feels like that’s been sort of parachuted in above us. The challenge for us is sustainability and what this does in terms of our CCG operational plan and so on.
This interview extract reveals starkly the tension between multiple logics and multiple agents. The CCG representative here makes clear the view from the CCG that the primary care redesign initiative that was described in Practice level and Locality level was seen by the CCG leaders as, in a way, imposed on them uninvited, ‘sort of parachuted in above us’. He states that this short-term funded initiative, which was parachuted in, presented a challenge that needed to be counterbalanced with ‘some corporate thinking’. Thus, not all clinically led innovations – even those that brought in extra funding – were necessarily welcomed and celebrated. The service redesign initiatives, which were led using a different arena from the official CCGs, had the potential to compete with, and complicate, the CCGs’ own plans. In this instance, the federation’s initiative appeared to disrupt the ongoing CCGs’ primary care operational plan.
It was interesting to note that, from a CCG perspective, the authority of the GP federation and its use of due process could be questioned:
There is a suspicion around whether there’s equity in terms of the involvement of different practices and the rewards to different practices. You know, I guess like any sort of new organisation, it doesn’t have complete engagement from practices and some people are suspicious that this is just a vehicle to take over their businesses.
GP CCG board member
To add to the uncertainty, there were other initiatives and proposals, including some from the secondary care providers, which also had the potential to compete and vie with the CCG’s own plans:
At the moment the noise has been very much around the sort of multispecialty provider, this [pan-county] bid seems to be the biggest thing around. There has been talk by the local acute provider about moving into primary care services. There is a plan to put in a bid around urgent care which will be provider driven. Again we need to assess how all this fits within our own wider plan.
CCG chairperson
These observations from the chairperson of one of the more influential CCGs in the county raises questions about the difficulties in aligning the plurality of initiatives being encouraged and launched in different arenas. Hence, once again we see the complexities of leadership in practice when the context is given proper consideration.
The state of uncertainty about who is driving change, using what model and with what end point in mind, is reflected further in the next extract from the interviews:
As a CCG we don’t have sort of end point in mind, we just sort of follow the models [from the Five Year Forward View]. I think we’re fairly neutral on which model. I think we’re just wanting to see a development and an evolution. I suspect it will sort of be a natural move in one direction or the other.
Senior CCG official
This quotation is very revealing. It suggests a ‘neutral’ stance regarding the big service redesign questions and suggests the lack of an overarching strategy despite the extent of the challenges as already described. The admissions from the CCGs that they lack the wherewithal to tackle the fundamental redesign of health-care systems which the Vanguards are seeking to deliver was made apparent by the individual CCGs in this case. Nonetheless, the extent of the arm’s-length, detached stance which is signalled by the above interview extract is still surprising. More than 3 years into the CCG experiment, it indicates the extent and nature of CCG ambitions. Given such a context it can be readily seen that, on the one hand, there is an apparent open space and scope for ambitious clinical leaders to ‘step up’ and offer creative solutions but, on the other hand, if and when they do, the context is such that there is so much contestation and uncertainty that to make any service redesign endure is highly problematical.
We can elaborate on this important point by providing an illustration of just such a bottom-up, GP-led service redesign that was initially supported and then unsupported. We were informed of a new dementia service which located more care in GP practices and which therefore allowed patients to be treated locally rather than having to travel to the mental health trust. The redesign involved employment of care facilitators. Funding came jointly from the CCG and the mental health trust. However, despite apparent success and positive feedback, the initiative was ended and dementia services were taken away from primary care and returned solely into the hands of the acute sector, the mental health trust. Some GPs claimed that this resulted from pressure from the mental health trust which the CCG was unable to resist given its parlous financial state and the power of the trust.
As interviewees noted, the federation had, so far, remained on the periphery of the core GP business of the General Medical Services and Personal Medical Services contracts. One CCG board member observed, ‘the practices at the moment don’t particularly see it as a mechanism to provide, you know, their core services. So it hasn’t got into the sort of real federation working which would be sort of the front-line main contracts’. However, he noted that the access to extended hours work could catalyse a change as it creates a new workforce which would share information and patients across practices.
Activity and clinical leadership at a neighbouring CCG were even less developed. Practice in this particular CCG reflected that found in many others which we encountered at the scoping phase of the study where little advantage was being taken of the CCG institution as a platform for change. Instead, it was treated as just another administrative unit. Thus, even the accountable officer made the assessment that:
The function of the CCG to date, by and large, has been to fulfil statutory duties. In the early days of the CCG there were a large number of high-level strategies written around a number of things . . . those haven’t really been delivered . . . They’ve stayed at strategic level rather than developed into operational level. And the financial crisis has crept up on the CCG . . . about 18 months ago, it really hit, and since then that’s been the total focus of the organisation. So everything for the last year has been driven by the financial position in the CCG. It seems like we’ve been blinded by the headlights.
Accountable officer
This CCG is now in the hands of a managerial team which also manages two other CCGs. As a result, a similar situation prevails across this cluster of three CCGs:
There’s a much tighter grip on the finances but with regards to service redesigning, I can’t see much instance of that happening or having happened to date. A lot of stuff’s been talked about, but if you said give me some examples of that, I would find it much more difficult.
CCG chairperson
Asked if the CCG had taken a serious look at the organisation of primary care and general practice, the response was an emphatic ‘no’. The informant was asked, ‘So what has the CCG done then? If it’s not been looking at secondary care, and it’s not been looking at primary care and general practice, what has it been doing?’ The answer:
Well . . . as I said, it set out as a new organisation. It has to build itself and embed itself. It did a lot of work around high-level strategy. And then the finances got out of control. And then since then it’s been, been the overwhelming challenge. So that’s basically what it’s done.
CCG chairperson
Thus, in these instances, the work of the agents – managers and clinical leaders – in these new bodies was focused primarily on institution building. This included appointing chairpersons, accountable officers and other key figures plus the wider representation for the governing body. A practice nurse representative on this CCG likewise confirmed that assessment. When asked if the CCG had achieved much, she replied ‘No, I have to say, sadly. Sad to be part of it and have to say that’. A GP likewise observed, ‘ever since we became a CCG we have been firefighting, we have a historic debt, it’s frustrating, we haven’t made the progress I would like to have seen . . . we have been assured out of existence by the NHSE regional team’.
What these data suggest is that simply providing a new institutional platform with a general direction to allow GPs and other clinicians to ‘step up’ and lead the required service redesign is evidently not sufficient. Lack of resources and continued assertive intervention from the national centre had, in these cases, crowded out the hoped-for local leadership. The prime arena of the CCG, despite its statutory backing, was not enough in these cases to prompt the emergence of effective clinical leadership. In response to this increasingly evident lacuna, the national-level authority, in the shape of NHSE, initially encouraged much more cross-CCG collaboration and then moved more radically to offer firmer guidance in the shape of the models of collaboration outlined in the Five Year Forward View12 and then even more forthrightly with the creation (indeed imposition) of the STPs.
However, not all of the six CCGS in the county were quite so passive and reactive. Despite the financial and other challenges, some local leaders were able to use the new institutions as a means of devising local solutions. The CCG chairperson of one of the CCGs said that his GPs were ‘just going to get on with it’ and attempt transformation, especially of community services. He said he wanted to re-engineer the use of their two community hospitals. His vision was to transform their use from being ‘dumping grounds for the acute trusts’ to being sites for new outpatient work run by primary care including diagnostics instead of consultant led, to stop our patients leaking into secondary care’.
However, one of the hybrid clinical managers working across three of the CCGs reported:
There is a definite lack of clinical leadership and engagement in practices in [this CCG]. There’s a lot of distrust. There’s concerns about mismanagement, poor communication. So that’s what I’m focusing on: building relationships, making sure we’re open and transparent, we need to build a bit of confidence in the management team because I think that’s partly why they haven’t been able to make change happen. The clinical leaders are hidden. They haven’t been attending meetings. Goodness knows where they are. So that’s my priority.
Hybrid manager across three CCGs
Thus, overall, the picture that emerged from the CCG level (the apex of Figure 24) in case D was that, in a number of CCGs, the senior teams (managers, clinicians and hybrids) had failed to utilise the privileged statutory positon, resources and power of the CCG board-level arena as a means to bring about a redesign of local services in the way that had been hoped by the national policy-makers. However, other teams had used the same arena to make a difference both in reforming primary care and in reimagining the roles of acute and community services. Increasingly, these more innovative teams were given power by NHSE to take over the agenda-setting for the more passive CCGs.
Sustainability and transformation plan level
As momentum built behind STPs from mid-2016, all actors involved in any significant service redesign attempts had to consider how these would align with the emerging STP systems architecture. This process – occurring over a relatively short period of less than 12 months – revealed a great deal about the multilevel power dynamics in service redesign. We observed meetings as NHSE-funded management consultants facilitated the process of exploring and choosing between a number of ‘system architecture options’. Six main options were presented. They represented a spectrum offering varying degrees of integration across the system: from a loose association of providers and commissioners at one end, to a unified ACO at the other.
The loose end of the spectrum was based on what was termed the ‘status quo’ (i.e. with > 20 localities/hubs based on population sizes of between 10,000 to 50,000, continuing to operate alongside existing acute hospital providers, a mental health provider and a social care provider). The hubs would offer co-ordinated out-of-hours primary care services. The middling options were essentially variants of a new service architecture based on between one and three overarching MCPs catering for populations of approximately 500,000 with a set of localities/hubs or primary care homes sitting beneath them looking after populations of around 30,000 to 50,000.
Notably, most of the options assumed the continuing separation of acute hospital services on the one hand and primary/community care on the other. The subvariants essentially amounted to options relating to the number (and hence size) of the constituent MCPs and hubs. Our informants (clinical leaders and managers at CCG level) reported that they felt this exercise was taking place to a large extent beyond their sphere of influence. Nonetheless, a number of clinical leaders interviewed were keen to work within the templates offered by MCPs and the primary care home locality/hub models.
Thus, there were tendencies acting to pull the CCGs in two different directions: (1) the high-level STP work, which is driving strategy across much larger populations and (2) the considerable activity from below, such as that triggered by the Vanguards with MCPs. These and the acute-led services are heading towards ACOs. These bodies, if fully launched, lead to questions about the continued role for the CCGs.
Summary: clinical leadership across different arenas
Case D was instructive in revealing the scattered and tremendously varied nature of clinical leadership in and around CCGs. The local context in this case was of a financially challenged health economy with additional problems arising because of the difficulties in recruiting and retaining clinical staff in the primary care and acute sectors alike. Leaders of the CCGs, both mangers and clinicians, found that they spent a great deal of time doing what they described as ‘firefighting’. The extent and nature of the challenges also mean that these CCGs were being pressed to work together so as to begin to tackle system-wide issues. Thus, single CCGs were found not to be powerful platforms for change in this area.
The case reveals that, when a health system is under challenge, the scope for decisive leadership of service redesign is very much dependent on the power exercised by national bodies – most notably NHSE and the Department of Health – but also by the regulators such as NHS Improvement and the CQC. Hence, clinicians, even if willing to make a difference through adopting a leadership role, need to take account of the scope for action given, the ongoing and planned activity at any or all of these levels and forms. A clinician who wants to make a contribution faces uncertainty about what level and in what setting to make that contribution.
Some of the most impressive service redesign initiatives that we tracked in this case were time bound and contingent on special temporary funding. Pilots are to be evaluated, and hence ongoing sustained funding may not be forthcoming. An optimistic interpretation would be that the wide variation allows for multiple and diverse experiments, with bottom-up initiatives being encouraged. A more pessimistic interpretation is that the duplication and complexity crowds out creative action by clinicians and facilitates waste and duplication. We found both opportunity and constraint. The instances of the exercise of clinical leadership within these were all the more interesting.
Case D exposed the very mixed use of the strategic CCG-level arena by clinical leaders. In those instances where this opportunity had not been utilised, the main reasons offered were the financial challenges, which led to firefighting and perceived uncertainty about the scope for action given the extent of activity and review coming from other quarters – especially from the NHSE. The most impressive and far-reaching examples of clinical leadership in this case were found in the operational and practice arenas, where some entrepreneurial GPs had seized the opportunity to tackle specific service problems, such as dementia care and other forms of long-term condition management. They used their knowledge and their networks to offer more patient-oriented services at lower cost than was charged by the acute trusts (both mental health and general hospital trusts). However, even in these instances, these local leaders found that they were at the mercy of the precarious ongoing support from the CCG as holders of the purse strings. They discovered that funding could be withdrawn if other considerations and priorities arose – such as the pressure on the CCG not to ‘destabilise’ significant local provider organisations.
Case E: redesigning integrated care and urgent care
This case study was carried out in one of the London CCGs. It is located in a densely populated, inner-city area. Its geography was coterminous with its local borough council. The CCG remains in financial balance despite the pressures of supporting one of the most financially challenged acute trusts in the country.
This case study focuses on two key service redesign initiatives: integrated care and urgent care. Both provide useful insights into the origins, nature and outcomes of clinical leadership.
Case E1: the integrated care initiative
The cluster of initiatives designed to integrate care was manifest primarily in a large-scale programme carried out in partnership with neighbouring boroughs. There was a strong philosophical and normative base to the clinical leadership advocating integrated care, manifested within the strategic arena of the CCG governing body.
The institutional work of advocating and vesting resources in integrated care spanned wider strategic arenas in addition to the CCG. The regional integrated care programme was one of the largest integrated care transformation initiatives in the country. The programme involved all of the relevant health and social care organisations in this part of London (three CCGs, one acute provider, two mental health and community providers, all general practices and three LAs) across the area served by the acute provider.
The integrated care programme aims to ensure consistency and efficiency across physical health, mental health and social care. Interventions focus primarily on the top 20% of patients most at risk of hospital admission, a group responsible for approximately 80% of the activity and costs across health and social care in all three boroughs. The work targets the population in a phased approach, beginning with those at very high risk of hospital admission (the top 2% of people at highest risk), and working downwards to cover the full 20% over a 5-year period.
The programme is supported by a programme management office. There are workstreams on contracting and reimbursement, informatics and information technology, and evaluation. The programme management office also supports the local implementation of integrated care within the three localities. Integrated care boards within each CCG are responsible for the operational design and commissioning of their local programmes. Members of these boards include health service commissioners, LA representatives, public health representatives, voluntary and community sector representatives, and representatives from the locality’s provider organisations, including senior clinicians.
The three lead CCGs work in partnership, but also retain a high degree of autonomy within the wider programme. This has implications for the case study CCG, which informants claimed to be the most mature of the partners, particularly in terms of the emphasis placed on clinical leadership. CCG informants reported that they felt constrained by the slower pace of change in the other two areas.
Clinical leadership across different arenas
The chairperson of the CCG, the lead for the GP network, the local medical committee representative and the named CCG integrated care lead were widely seen as each having a particularly important role in advocating for integrated care not only in strategic arenas, but also to their colleagues involved in delivering primary care. They were perceived to be dedicated to ‘selling’ the benefits to colleagues and framing a range of local activities as being part of a wider intent to reduce fragmented care for patients.
However, there was evidence of a disconnect between the clinical leadership and institutional work of advocating and resourcing integrated care in strategic arenas and the level of engagement of many of the front-line clinical staff with delivering the various aspects of the programme.
There was one clinically led fundamental challenge to the integrated care programme, when a respected GP questioned the evidence base for focusing on unplanned hospital admissions. This can be seen as an instance of counter-implementation leadership, whereby a provider clinician actively opposes implementation of the new service model. The GP complained that if reducing unplanned admissions to hospital was a key rationale for the programme (which at a national level it is) then, on the basis of past evidence, the programme was probably doomed to failure. Instead, he felt that the CCG should be focusing on evidence-based, disease-focused interventions to manage the rising demand for hospital care, specifically by greater use of statins to reduce cholesterol and more effective management of atrial fibrillation. The GP arranged a meeting of key clinicians to discuss the issue and he gained some support from colleagues, although not enough to derail the wider integrated care programme.
Case E2: urgent care
The urgent care work in this case aimed to produce a single point of access for patients rather than the current array, which included a hospital A&E department, two walk-in centres, NHS 111 as an urgent telephone consultation and triage service, a GP out-of-hours service, a number of minor injuries centres and an urgent care centre. The ends or break clauses of the contracts for these commissioned services were aligned by the CCG in a way that enabled a system-level review of provision, its overlaps and its variation in per head/per visit cost. The plan was to use this to retender all urgent care services and achieve a more coherent and cost-effective result. This review involved a number of different partners, including the clinical leads of these services, A&E staff, the lead for extended GP hours (which is being funded nationally), and also a number of staff from the local CSU and a senior CCG manager responsible for urgent care. The review was carried out through a series of workshops facilitated by the CSU. In terms of Figure 24, the review can be seen as taking place in an operational commissioning arena, with commissioners and providers coming together to consider the future pattern of services. It remained in progress at the end of our fieldwork period.
There were a number of important local contextual factors affecting this urgent care review. First, and the biggest issue for the CCG, was the rapid increase in the population and the potential impact of this increase on future demand for urgent care services. A second factor was the co-location in the local acute hospital of traditional A&E services alongside some of the newer community-led services. This arrangement carried the potential for novel ideas in the way services were provided. Third, the distribution of urgent care services across the CCG area was at the time asymmetrical, and the desire to distribute all kinds of urgent care services evenly across this geography created logistical, estates and financial challenges for the CCG. Finally, the role of general practice in providing emergency services changed as the review was being carried out, most notably because local practices were awarded funding from the Prime Minister’s Access Fund to create four locality hubs open from 08.00 to 20.00 hours on weekdays and weekends as well as a virtual hub for web-based self-care and online consultations. This initiative raised the profile of urgent care redesign led by GPs, many of whom had been arguing that general practice should be the first port of call for patients requiring urgent care services.
Some provider clinicians felt their services to be under threat. Others complained of a lack of clarity about how differing costs between the various existing out-of-hours or urgent care providers would be rationalised and how the pressure on the local A&E service would be solved. As the review progressed there was a growing consensus that a single point of access using a telephone or online service was desirable, with patients triaged to the most appropriate service for their needs. Some provider clinicians expressed concern that this would not, however, meet the expectation of many service users for a ‘walk-in’ service as the first point of access.
Clearly, in this case, clinical leadership in the operational commissioning arena took the form of combining advocacy for more integrated and patient-centred services with arguing for the preservation of existing clinical services and the capabilities they had developed. The relatively early stage of service redesign in this case meant that there was no opportunity for us to study clinical leadership in operational delivery arenas – the initiative was not yet entering the stage of implementation.
Features of clinical leadership from these two cases
These two cases illustrate a well-developed pattern of clinical leadership in strategic and operational commissioning arenas, with mechanisms put in place to engage with clinicians in operational delivery roles. Although the latter mechanisms appear to have been problematic, this CCG illustrates some key features of clinical leadership in commissioning. These are now described.
Collaboration between clinical and non-clinical leaders
The working relationships between clinicians and managers working within both strategic and operational commissioning arenas in this case study were built on high levels of trust and mutual respect. Clinical leadership was seen as not just desirable but a core defining characteristic of what made the CCG successful. A strong emphasis was placed on face-to-face meetings, and the conversational style in these meetings was informal and friendly. This enabled significant challenges and passionate debates to be voiced in ways that were usually not perceived to be threatening.
The non-clinical managers were clear and explicit about what the clinical leaders on the CCG board brought to the conversation:
So I think they are [the clinicians on the board] quite good at going back to the fundamental principles and, again, a lot of our GPs on our board often remind us about, so what’s the evidence base? What are the outcomes that we’re expecting to get? How do we demonstrate value for money? And actually, bring an added level of vigour and rigour in relation to that process.
Senior manager
They also spoke explicitly about the ways in which clinical leaders had more traction with their colleagues than non-clinical managers. They tended to be effective at turning what might be perceived to be a managerial issue (such as a budget overspend) into a clinical one.
Challenging established assumptions
Many of the GPs in leadership roles in strategic and operational commissioning roles in this CCG had a long history of anti-establishment radicalism. They used this identity to differentiate themselves and thereby to create a strong ethos of common cause based on consistent principles. It appeared that they actually enjoyed challenging governmental authority and NHS bureaucracy. They enjoyed challenging what one informant called ‘corporate guff’. There was some evidence that clinicians were encouraging their managerial colleagues to also push back on directives from NHSE, empowering them to do what they thought was right rather than what they were told they must do.
They had started to question the medicalisation of the health service and were beginning to have discussions about how they might influence the broader determinants of health. A number of references were made to clinicians’ roles in ‘blurring the boundaries’ between what traditionally happened in primary care and other sectors. The clinical leaders in the locality were much less interested in defining detailed care processes than they perceived non-clinical managers had been in the past, placing a strong emphasis on outcomes and leaving clinical teams to determine how to deliver them.
Both the clinical and non-clinical leaders saw merit in the development of local networks of practices as ways to engage clinicians. The ‘offer’ to clinicians was better managerial support – a decentralisation of the CCG management resource, but the ‘ask’ was greater professional ownership of performance. Radical changes in ways of managing unacceptable performance and incentivising collective behaviours were introduced:
You cannot federate unless you really seriously tackle the very poor performance . . . because if you’re asking people . . . you know, if people’s income is going to depend on the performance of their peer network, you have to at least be in with a fighting chance, and if you have a total rotten apple in the barrel, it’s just not fair.
GP
In another example of professionally led challenge, clinicians countered the threatened withdrawal of the Minimum Practice Income Guarantee funding for struggling practices, launching a high-profile public campaign to highlight the problems of government policy in this area, and this appeared to have been successful in securing additional resources.
Working across boundaries
The emphasis of this case study on urgent care and integrated care demonstrated the CCG’s commitment to ‘working across boundaries’, a term used by several informants as an organising principle for the CCG. Indeed, the number of partnership-related initiatives in the CCG suggested a strong commitment to looking outside the boundaries of the CCG and of primary care. Much of this approach was driven by a strong clinical voice, supported by a robust strategy developed in partnership with non-clinical managers:
I think what would be very powerful . . . would be [local acute provider] saying, we want to help you deliver some efficiencies and some financial efficiencies. We want to reduce our bed base, we want to get people out of hospital, but we can only do it if your primary care is up to scratch and you deliver it for us.
Senior manager
Engaging general practitioners as Clinical Commissioning Group members
What came across strongly from the interviews was a very purposeful and planned approach to engagement of GPs as CCG members:
We need to manage members politically, and we need to shape members’ expectations . . . there has to be a purpose behind engagement. And everyone’s just too busy for engagement for engagement’s sake.
GP lead on CCG
In addition, a strong emphasis was placed on open communication so that clinicians were less likely to be in a position to complain that they did not know what was going on:
I think in every case when we’ve had an opportunity to talk it through . . . our strategy, this is our approach and . . . we haven’t been trying to do things in a Machiavellian way, which of course I think tends to worry people. We’ve been open about how we do business.
Senior manager
The CCG valued a widespread and inclusive leadership model, promoting leadership roles and behaviours widely. The CCG chairperson claimed that ‘50% of clinicians have leadership roles’, although the shift from disease-based to comorbidity group-based leaders might reduce the total number of clinicians in leadership positions. Leadership roles among clinicians were therefore the norm, rather than the exception, and it is possible that this may be helpful in removing any suggestion of elitism among those who are appointed to formal leadership roles.
There was a dominant historical narrative relating to sustained and coherent change over decades (‘we got rid of our most poorly performing practices 15 years ago and that was key to our success now’), irrespective of political drivers and NHS structures. Several informants described how their model of change would be difficult to replicate in other parts of the country which did not have a long history of focused effort. (Yet, as Case B revealed, there is an argument for a clean slate so that previous mistakes and compromises can be swept away.) In the present case there was the advantage that a consistent pattern of strong clinical leadership had demonstrated its ability to operate across diverse and changing organisational forms.
Strong leadership training and talent management programmes were in place and there was a willingness to invest in sending selected staff on expensive training courses outside the CCG as well as developing their own local leadership training (at the time of writing the CCG was considering establishing a ‘staff college’ for leadership development). Some clinicians placed much higher value on ‘learning by doing’ and creating ‘an environment in which young leaders can make mistakes and learn’. New clinical leadership roles, when advertised, were usually competitive despite the pressures of clinical workload in most practices, although there was some suggestion that this might be changing more recently.
Summary: clinical leadership across different arenas in the two cases
The integrated care programme provided a particularly good insight into the challenges of clinical leadership. On the one hand, it was a vehicle for a number of innovative work streams led and owned by clinicians, such as pathway development, care planning and out-of-hospital care initiatives. Clinical leaders played prominent roles in strategic arenas, articulating the concept and moral ethos of a new or improved service. This led to programme-level work in further articulating the new service and establishing a framework for bringing providers on board. However, on the other hand, clinicians involved in delivery appear not to have adequately understood the integrated care model being advocated. There was evidence that the overall planning and delivery of the programme was more top down in nature and more influenced by a managerial ethos from outside the CCG than clinically led from within.
In the urgent care case, there was similar evidence of a lack of connection between the clinically led strategic ethos of the CCG and clinical leadership in delivery of service redesign. Provider clinicians continued to query the concept of the single point of entry for urgent and emergency care.
The CCG has made a strategic, long-term and focused investment in promoting clinical leadership. Successive generations of local leaders over a period of at least two decades have developed a vision of integrated health care, promoted a set of values, driven up standards in primary care and launched a series of service redesign initiatives, promoting clinical engagement. The espoused belief is that, once clinicians believe that they really are responsible for what happens and have some authority, then they appear to be more willing to work through the challenges of leading in a complex and demanding environment. Being a leader then becomes part of their professional identity and something of which they are proud. Alongside this apparently positive dynamic, however, there appears to be a reality that this virtuous cycle of strengthening clinical engagement has not penetrated service redesign practice. In both cases studied, this remained vulnerable to a conflicting dynamic whereby clinicians perceived initiatives as issuing from a distant managerial authority and failing to connect with the realities of delivering effective care and maintaining the staffing and capabilities to do so.
Case F: towards an accountable care organisation
This case (named here ‘Northern Borough’) was selected for two reasons. The first was based on demographic and geographical criteria; the second reason was to illustrate important policy developments taking place jointly in health and social care. The CCG selected was one of the 12 CCGs in Greater Manchester [i.e. it was part of Manchester Devolution (‘DevoManc’)].
The case study CCG with its coterminous borough council has a population of > 228,000. Much of the population is located in areas of high density and relatively poor housing. Both the CCG and council have to deal with large disparities in economic, social and health indicators and situations.
There are three elements of the context which are particularly striking in this case and which affect the opportunities and challenges for clinical leadership.
First, many clinicians and managers and other actors in the wider network have been employed within the region for many years and have a close identity with the place.
Second, DevoManc is having a major impact on health and social care and has required considerable strategic attention from both the CCG and the LA as they work with their counterparts across the region to develop the strategic agenda, the new governance arrangements and the financial arrangements. The CCG leaders in this context have been able to use these developments and opportunities to accelerate ideas about the development of an ACO. However, on the other hand, so much activity at a higher level has tended to remove some of the local ownership and accountability for driving change.
Third, the devolution agenda mandates each of the boroughs to produce a locality plan, which has encouraged closer working between a number of agencies, including health, the LA, the fire and rescue service, Greater Manchester Police and housing associations. The LA in Northern Borough is one which had already developed a strong strategy based on ‘place making’ (an approach to public services well rehearsed in local government in the previous decade) and it has been active in working with the CCG to develop a joint approach. The ACO initiative is able to build on these place-based foundations. The devolution agenda has also led to a leadership development programme across the combined authority, strengthening cross-sectoral and place-based leadership. These are fertile conditions for the ACO initiative.
There is a huge challenge because the budgetary forecast under devolution is less than current spend and so it will leave health and social care with a major financial deficit within 5 years. There are considerable pressures to find ways of integrating services across geographical boundaries, across service sectors (e.g. health and LA), and with system improvements (e.g. improving housing will affect the health side of the budget substantially). Northern Borough with its poor health indicators could be particularly at risk in this.
Clinical leadership in strategic arenas
A powerful force within the CCG is the accountable officer, a GP who is also chief clinical officer. It was noted by several interviewees that this leader was brought up in the local area and was committed to it. He was full of ideas, plans, initiatives and actions which aim to address the poor health of the local population. Supporting this GP leader was a managing director, a quiet strategic thinker with a strong focus on health care.
The GP accountable officer and the managing director worked closely together with a high level of trust. They had occupied similar roles in the former PCT. They referred to each other’s work regularly. Together they focused their leadership on the institutional work of advocating collaboration with agencies, such as social care and housing, relevant to the wider agenda of improving population health.
At a macro level, beyond specific service initiatives, was a concern in the CCG to ensure that primary care services helped both with the preventative agenda and also with ensuring that patients were treated at scale – one of the clinical directors was appointed to lead on this. On the prevention (or mitigation) front, an initiative between the CCG, the LA and the local housing association had led to a ‘Warm Homes’ initiative. This involved the pooling of some of the budgets across these three organisations to help with insulation and heating measures; advice on energy use, switching tariffs and obtaining pre-payment meters. This is an example of partnership working on health and well-being in the locality and the CCG say that this has helped with respiratory illnesses and also for frail elderly patients in particular.
There were elements of a wider commitment to better primary care. This sought to place patients at the centre of such care and to reduce dependence on secondary care. Patient care management was an objective. Nonetheless, although the formal plans pointed to such a strategy, many of the people we interviewed indicated that the central thrust of activity was coming from the devolution agenda. These elements came together in the initiative to set up an ‘accountable managed care organisation’.
The accountable managed care organisation
The impetus within the CCG to develop the ACO had taken on added vigour because of the Five Year Forward View12 and the new models of care. In addition, the Greater Manchester devolution plan, as noted, required each district to produce a locality plan, and this was seen to be an opportunity to promote the ACO. As the emphasis moved towards the idea of increased joint working and accountability between the CCG and the LA, the idea transitioned into an ‘accountable managed care organisation’ in recognition of the joint governance concerns.
This may be seen as an example of leadership making use of a ‘policy window’ to push forward plans which had been hatching for some time.
A document from Northern Borough’s locality plan noted that:
Simply put, an accountable care organisation is an alliance . . . where all members in the ACO share the risk and assume accountability for the resources spent caring for a population and for the quality of that care.
The goal is to engage and regulate providers in a way that encourages them to work together, to pay providers in a way that does not encourage supplier induced demand, and to create a balanced system of commissioned services and suppliers that can be rewarded for providing high quality care.
Originally, these ideas for an ACO were about creating a legal structure to provide integrated care that includes GPs (and GP practices), other primary care clinicians and, potentially, over time, other types of NHS physicians and social care professionals, with its own in-house management support systems. However, the structure would not include hospitals, thus giving the ACO a strong primary care and public health focus.
Two events shaped the interest in this institutional structure further. The devolution agenda brought this to the foreground, making possible arguments for an ACO and also showing that, unless Northern Borough moved proactively and quickly, devolution could have risks in terms of financial share and reputation. Second, the developing partnership with the LA had helped to enlarge the conception of what the ACO would and could be.
There is now a leadership board that brings together the key players across the locality. They posed the question to their colleagues:
Are you a team of leaders that come together every now and then and talk about specific issues or are you a strategic leadership team for a place?
Initially, this idea was slow to get traction but:
The CCG has been really strong on that. Not just sitting in the health and well-being space . . . but bringing it into the broader team arena.
The LA recognised that nearly £2B of annual public sector spend is on various aspects of health and well-being. It recognised that:
We need an increasingly strong relationship with the CCG . . . Actually, can you sustain two separate commissioners? What’s the point of that? . . . So our single accountable care, health and care organisation, we’re not at the moment saying a new separate entity. But it could be.
The closer involvement of the LA in the ACO has led to a greater emphasis on the governance arrangements. At the time of the research the ACO details were still being worked through.
The pattern of clinical leadership across different arenas
The overall focus is on a profound transformation of the institutions involved in managing the health of the population, as well as on the redesign of particular services. This is reflected in our finding that clinical leadership was most strongly present in various strategic arenas, where clinicians are involved in formulating ideas and theories about new ways of promoting health in collaboration with other agencies. Given this focus on establishing collaborations across traditional agency and professional boundaries, it is important to capture the complexity of the interconnected strategic arenas that clinical leaders worked within. This is shown in Figure 25.
FIGURE 25.
Strategic arenas of leadership in case F.
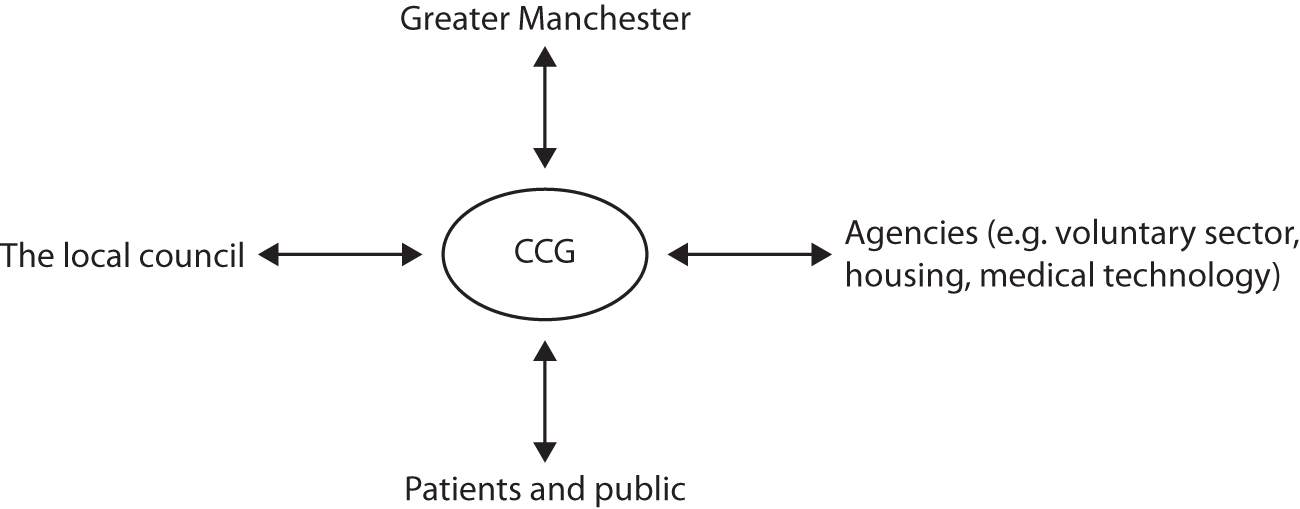
Leadership is part of the mobilising of attention, resources and commitment to particular plans and values within those arenas.
Figure 25 shows how the clinical and managerial leaders of the CCG were working jointly on conceptualising new kinds of services and mechanisms for delivering better health for the population, building collaborations simultaneously in a number of different directions.
The thought leadership exercised by the GP accountable officer jointly with the managing director drew on long experience of the locality combined with an international and entrepreneurial outlook, to create new visions, values and activities for the CCG. Clinical experience and judgement combined with managerial skills to create a view of health which was innovative and integrative.
Our interviews suggested that this visionary leadership was exercised strongly in strategic arenas. However, its connection with operational commissioning and delivery was, as yet, partial.
The Warm Homes scheme provided an example where thinking and acting holistically had achieved implementation. However, this implementation did not need to involve clinicians, as the scheme involved improving homes. More generally, we found that clinicians often understood that an ACO was in the process of being created. However, they appeared to see little connection between the ACO and the day-to-day improvement of the services they were working on. They appeared to be more embedded in their specialisms and were making incremental progress on service redesign.
Overall, the arena of patient services was dwarfed by the enormity of the DevoManc initiative, which was changing on an almost daily basis during the case study. The DevoManc initiative occupied a lot of the attention of the clinical and managerial leaders in this case study.
Devolution creates a lot to play for political positioning and reputation, budget surpluses or deficits, the quality and standards which will be applied across the combined authority and the governance levers open to the CCGs across Manchester and the LAs across Manchester. If poorly designed, devolution could lead to worsening services. However, if well designed it could create an integrated system across health and social care, bring in extra investment to the city region and improve the lives, the longevity and the health and well-being of local populations and patients.
To engage with devolution required local NHS leaders to work closely with the local authority. The circumstances were fortunate here because such collaboration had occurred for some considerable time in this borough, commencing even before the formation of the CCG. It had been initiated by the Northern Borough council, with its bigger vision of place leadership. The council has acted as a convener, not only of health partnerships, but of partnerships with other relevant sectors, such as housing, the voluntary sector, fire and police. The successful experience of Warm Homes inspired greater confidence to work together further. It appeared to be the council which has steered and opened up the debate about joint governance of the ACO. The clinical leadership of the CCG has embraced this partnership. However, engagement in the political processes of the council (HWB, Health Scrutiny) has perhaps been more statutory than enthusiastic.
The final arena is working with other stakeholders, such as the voluntary sector, the universities, and so on. This arena is rather diverse, and stronger relationships have been fostered with some more than others. The outward-facing and entrepreneurial nature of the CCG has meant a series of connections where the leadership can see key priorities which are relevant to it (e.g. around innovation and service improvement). However, the relationship with the voluntary sector is still being worked on. The voluntary sector is very complex and there are many layers, they tend to work directly with individual GP practices rather than with the CCG as a whole.
Examining leadership in terms of the competing demands of different arenas, one can see that the pull is towards devolution, and towards the council in particular.
Chapter 5 Cross-case findings and comparisons
In this chapter we seek to integrate the findings from across each of the cases. The focus is on clarifying and interpreting the part that clinicians, both in CCG roles and elsewhere, played in designing and improving services. By comparing the cases, we build up a picture of the different patterns in which clinicians engaged in leadership of service redesign across the three arenas identified in Figure 24. We examine the impact of these different patterns of leadership activity found across the cases, in particular when effective service redesign appears to be taking place and when blockages or barriers have been encountered. We also explore what helped, or conversely hindered, the emergence of more or less effective patterns of clinical leadership.
Patterns of clinical leadership
In some of the cases, the three arenas could be regarded as operating in harmony – consistent with a logical division of labour governed by the guiding hand of the CCG. However, this was not always the case. Hence, we first of all discuss four of our cases, which can be seen as enacting variations on the theme of a coherent and productive pattern of leadership. Our analysis brings out how various strands of institutional work, needed to achieve service redesign, were performed by clinicians across the three kinds of arena. We then turn to four cases that show problematic features in terms of the degree of coherence between different arenas. Progress was stalled because of the gaps in requisite institutional work in one or more arenas. Our analysis of both sets of cases brings out how achieving coherence or productive interplay between the work going on in each arena was a pervasive challenge, with various dynamics triggering and blocking change at each level.
Turning first to the cases exhibiting coherence (Table 5), a point emerging is that, although clinicians made key leadership inputs in each of the three arenas, there was some variety in the flow of activity.
| Arena | Case study: clinical leadership activities | |||
|---|---|---|---|---|
| Case A1: innovating in mental health services | Case A2: innovating in urgent care | Case B: redesigning general practice and primary care | Case C: redesigning early intervention services for mental health | |
| Strategic commissioning and budget holding | CCG board approves funding for this initiative instigated at programme board level | CCG board encourages urgent care programme board to make use of non-current funding opportunity from NHSE | GP triumvirate on governing body leads formulation of new standards of primary care combined with additional services | CCG board approves funding for this locally initiated service innovation |
| Operational commissioning, monitoring and evaluation | GP chairperson of mental health programme board works with managerial counterpart to challenge existing statutory and voluntary sector providers to form alliances and holds them to achieving patient-focused integration | GP chairperson of urgent care programme board asks for ideas as to how to reduce A&E attendances and hospital admissions: proposal for a joint GP/paramedic emergency vehicle emerges from clinical debate on programme board | CCG establishes co-commissioning of primary care and performance management systems, including inspections, opportunities for practices to bid to deliver additional integrated care services | Activist GP with lead responsibility for clinical area (mental health) makes case for funding a pilot well-being hub |
| Operational delivery and shaping of practice | Provider clinicians develop interfaces between existing services, reinterpreting established service definitions and build normative networks committed to more integrated working | GPs from out-of-hours service and paramedics from ambulance trust define the service and develop it in practice as a pilot, building normative commitment among crews and colleagues | Locality GPs act as local commissioners and provider leads for additional services previously delivered by acute providers, drawing on GP practices and other community health service organisations | GP advocate for well-being services drew on established relationships with six neighbouring practices and voluntary sector providers and built a steering group, funded initially from CCG locality discretionary budget |
The cases illustrating coherence between arenas
In cases A1 and A2, service redesign was instigated within an operational commissioning arena, working within an overall commissioning strategy set by the higher-level CCG governing body, which subsequently gave its approval to the emergent plans. For case A1, the articulation and fundamental theorising of the initiative – establishing mental health provider alliances – originated in discussions between the GP clinical chairperson and the programme director for the mental health programme board. Detailed proposals were then put before the programme board and passed to the CCG governing body for the approval of vesting of resources. The programme board then authorised the convening of shadow provider alliances, where provider clinicians took the opportunity offered of working on operational detail, in particular a reworking of interfaces between different mental health services. This was associated with the development of normative networks among provider staff, carrying and strengthening the moral ethos of working in alliances, with its central notion of a more integrated patient experience. This moral ethos can be seen as originating, along with the articulation of the alliance concept, from the GP chairperson of the mental health programme board and the programme director. This experience of a first phase of alliance working then fed back to further institutional work at the programme board, clarifying and strengthening the rationale for providers to work in alliances, leading to the vesting of resources in a further phase of the alliances.
In case A2, the urgent care programme board was itself the origin of the concept of the innovative service. The GP clinical chairperson and the programme director used this forum to agree new service designs jointly with clinician representatives from provider organisations. This programme board then engaged providers to work on defining the operational detail on a pilot service and a subsequent evaluation of this clinically led shaping of practice led to a revised version of the service being shaped by the programme board. The defining of operational detail was accompanied by the development of a normative network of provider staff carrying the moral ethos of the initiative first developed within the programme board.
Case B offers a different pattern. Here, the idea and associated moral ethos of devising, and then implementing, a new set of primary care standards originated with a triumvirate of GPs in the most senior positions on the CCG governing body. These three GPs steered the governing body to establish a programme for co-commissioning primary care (with NHSE), which developed the standards for core and additional services and implemented them, leading to further engagement of locality GPs and community health services during implementation. So, in this case, the articulation of the service innovation and its ethos occurred at the level of the CCG governing body. However, the programme arena and locality delivery level were again characterised by the involvement of clinicians in both developing the operational detail and persuading colleagues about the value of engaging with the new standards and building a normative network carrying the underlying moral ethos of improving population health.
Case C offers yet a further variation on how coherence and productive interplay can be achieved in clinical leadership across the three arenas in Figure 24. Here, the service innovation concept and moral ethos emerged from a history of collaborative relationships between a GP innovator, passionate about improving early intervention in mental health conditions, his six neighbouring practices and a number of voluntary sector organisations. This activist GP established his own role within the CCG as mental health lead and worked with the governing body to vest resources in an innovative pilot scheme. In effect, he persuaded the CCG to establish a new programme arena focused on mental health and well-being, which could then authorise the development of operational practices and further strengthen the associated normative network.
Together these four cases illustrate how clinical leadership is involved in all three kinds of arenas – strategic commissioning, operational commissioning and operational delivery – in order to create innovative services. This is a finding of some importance in that it moves beyond a simplistic idea that ‘putting GPs in charge of CCGs’ is the same as unleashing the clinical leadership needed to change services. Being ‘in charge’ means providing the conditions for the clinical voice to be heard and effective in three different kinds of arena, each with a distinctive role to play, and none of them consisting only of CCG staff.
However, there appears to be no simple top-down or bottom-up flow that characterises the way that these arenas function effectively. They each appear to have a crucial function in producing service innovation and a particular associated role for clinical leadership, but the way these intertwine can vary.
-
Strategic commissioning arenas are where clinical leaders can articulate a new service concept with a powerful rationale and moral ethos that can then be presented to a CCG governing body or other budget-holding body in order to achieve the vesting of resources.
-
Operational commissioning arenas, such as a programme board, are where clinical leaders in commissioning roles can further develop the concept and associated moral ethos and at the same time bring a nucleus of provider clinicians into the process of developing the operational detail, thereby extending the normative network carrying the rationale and ethos.
-
Operational delivery arenas are where provider clinicians go about the institutional work of defining ways of working and discovering the shifts in professional identities and commitments needed to bring new models of care delivery to life. This is bound up with further extending the normative network of staff committed to working in the new way.
A key element of the variety across the cases reflects the way in which the articulation of a new service concept can arise in any of the three arenas. Although institutional work always needs to be done at the strategic level in order to achieve the vesting of resources in new ways, clinically led ideas for service redesign can apparently arise in delivery or practice arenas, at programme board level, or at the level of the CCG governing body. The four cases in Table 5 also each illustrate the role of clinical leaders in engaging across the three arenas, making sure that each plays its role while engaging appropriately with the other two.
The cases illustrating a disconnect between arenas
Turning now to the four cases, each one illustrates a form of disconnect in the way that the three arenas of clinical leadership function as a system. In case D, the strategic work of the six CCGs attempting to reconfigure services across an entire county was, at the time of data gathering, decoupled from the initiatives arising from groups of GP practices. Although there was mutual awareness of an underlying ethos of improving and making use of primary care staffing and moving appropriate activity out of acute hospitals, there appears to have been something of a vacuum in terms of operational commissioning forums that could harness and encourage initiatives emerging at the level of primary care practice. The GP federation can be seen as attempting to fill this space, but without achieving solid cohesion with strategic plans which remained at an early and unclear stage. The GP federation further found CCGs reluctant to vest resources in its plans for integrated care and began to look to other national sources of authorisation and funding, which further undermined system coherence. This case can be characterised as one where a clear service concept and moral ethos emerged at the operational level, but failed to find backing in the strategic and operational commissioning arenas – the degree of turmoil in these arenas was too great.
Cases E1, E2 and F can be seen as providing a mirror image to the pattern of case D. In each of these, clinical leaders played prominent roles in strategic arenas, articulating the concept and moral ethos of a new or improved service. This led to programme-level work in further articulating the new service and establishing a framework for bringing providers on board. However, in each case the transmission of the concept and moral ethos to operational provider staff was weaker. In case E1, provider clinicians appear not to have fully understood the new integrated care model. In case E2, provider clinicians continued to query the concept of the single point of entry for urgent and emergency care. In case F, provider staff had little contact with, or even knowledge of, the ACO concept that was being developed within an innovative and highly collaborative strategic arena.
Factors shaping clinical leadership
Tables 6–8 summarise what was has been achieved through the exercise of clinical leadership across the three arenas in our eight cases, dividing them into the same two groups as above. The tables summarise the factors that were found to help or hinder forms of clinical leadership capable of bringing about service innovations.
We have already seen that the coherence of implementation of service redesign was greater in the four cases in Table 5, and this is reflected in the specificity of the achievements documented. The achievements shown emphasise service outcomes, whereas those in Table 6 mostly emphasise service arrangements that have yet to deliver improved outcomes. However, Tables 5 and 6 emphasise that both groups of four cases involved clinicians grappling with both favourable and unfavourable conditions as they engaged with the challenges of service redesign.
| Arena | Case study: clinical leadership activities | |||
|---|---|---|---|---|
| Case D: system and multilevel redesign | Case E1: redesigning integrated care | Case E2: redesigning urgent care | Case F: towards an accountable managed care organisation | |
| Strategic commissioning and budget holding | Six CCGs working together across a county to address existing poor performance and financial shortfalls. In parallel, finance-led CCG-level initiatives, with strong influence from NHSE | GPs in formal lead roles shape aspirations for integrated care service redesign across a formal collaboration between four CCGs and LAs | CCG establishes review of urgent-care services, given inconsistent facilities and services across its area and increasing demand | Devolved locality plans for city-wide integration of health and social care under development, with the LA and CCG discussing the form of a health and social care ACO |
| Operational commissioning, monitoring and evaluation | GP federation supports establishment of a local pilot integrating primary care across practices with community services, with support from NHSE rather than the CCGs | GPs in formal lead roles shape nature and objectives of integrated care programme, and communicate these to GP community | Clinical leads of a GP out-of-hours centre, an urgent-care centre, a walk-in centre, A&E and GP extended hours explore models for consistent access to urgent care | Specific collaborative projects between CCG and LA (e.g. BCF and Warm Homes scheme), where health funds contribute to improving homes and advising residents |
| Operational delivery and shaping of practice | GP practice-led initiatives for sharing capacity across a locality and integrating with community services and community hospitals run by primary care staff, supported by GP federation and to an extent by CCGs | GPs in practice networks call for more focus on operational detail and education of different staff groups. Community services struggle to understand the new models of integrated care | Working party of GPs and acute A&E clinicians agree on telephone access as first point of contact with urgent care: working party designs protocols. Some GPs continue to advocate extended-hour GP services as first port of call | GPs and acute providers involved in specific and relatively narrow scope improvements to existing services. As yet, little engagement or involvement in the conception of the ACO |
Tables 7 and 8 highlight the following key enablers of effective clinical leadership for service redesign.
| Achievements, facilitating factors and challenges | Case study: clinical leadership activities | |||
|---|---|---|---|---|
| Case A1: innovating in mental health services | Case A2: innovating in urgent care | Case B: redesigning general practice and primary care | Case C: redesigning early intervention services for mental health | |
| Key achievements | Fewer failed referrals and re-referrals; improved understanding and exchange between clinicians in different provider organisations | Improved understanding and knowledge exchange between GPs and paramedics; reductions in A&E attendance and admissions | Improved and more consistent primary care standards | New patterns of referral for less severe mental health conditions; more people referred to non-statutory well-being services |
| Factors facilitating clinical lead | Commissioning clinical leader keen to encourage provider clinical leadership; some established provider clinical networks, with provider clinicians keen to extend these where they were previously weak | Commissioning clinical and managerial leadership keen to encourage clinically led provider initiatives; culture of clinically led debate on programme board | Highly credible GP triumvirate established themselves at head of CCG; active persuasion of GPs across localities that new standards are needed, leading to widespread recognition of the need for consistency of primary care | GP leader mobilised established relationships with voluntary sector providers; also drew on extensive past experience of making use of local NHS funding opportunities to initiate pilot |
| Challenges facing clinical leadership | Maintaining existing provider identities while encouraging greater professional exchange; moving from short-term collaborative projects with limited scope to deeper collaboration | Shortages of paramedics made ambulance trust unwilling to continue the pilot arrangement, leading to modified crew model of GP and ambulance driver following the initial pilot | Unresolved issues about the impact of enhanced primary care services on viability of the acute sector; difficulties realising savings in secondary care; achieving sufficient influence on the whole system of care as a result of the lack of co-terminosity | Securing continued funding, reconciling commissioning procedures with the need for continued funding of an activist consortium; separating out the statutory IAPT provider from the well-being hub; achieving roll out of the hub model to neighbouring CCGs |
| Achievements, facilitating factors and challenges | Case study: clinical leadership activities | |||
|---|---|---|---|---|
| Case D: system and multilevel redesign | Case E1: redesigning integrated care | Case E2: redesigning urgent care | Case F: towards an accountable managed care organisation | |
| Key achievements | Primary care networks, integrating GP practices with some specialist clinics, have emerged in a few localities | Large-scale programme for integrated care, with services to support self-care, care co-ordination and appropriate discharge from hospital. Clearly argued and widely disseminated strategic rationale for this | Principle of first-line access to urgent care by telephone agreed | Productive relationship with LA, including 800 homes benefiting from Warm Homes scheme, attracting £1M external investment; well positioned in reputation and relationship terms for the emerging new structures at regional level |
| Factors facilitating clinical lead | Some GPs have history of collaborating to address issues arising from poor performance of local acute sector | Shared history among GPs of collaborating to improve health of a disadvantaged locality; culture of independence from national NHS direction; good relations between GPs and acute sector clinicians | Clinicians in various services have previous experience of defending the future of their services while responding to the need for rationalisation and integration | Established partnership at senior level between GP chairperson and strategic manager; established collaboration between CCG, LA and other public agencies |
| Challenges facing clinical leadership | CCG clinical leads experience disempowerment in terms of influencing emerging service models, squeezed between initiatives emerging from GP practice grouping and larger-scale STPs | Lack of understanding at practice level of how new models of care should function; some confusion as a result of multiple initiatives coming from highly committed and ambitious strategic leaders | Some providers involved are reluctant to move a service model where their service would no longer be first point of call. Concerns for the future viability of some services are not fully addressed | Clarifying the scope, boundaries and governance mechanisms for an ACO covering primary care and community services; bringing operational clinical leadership into implementation of the ACO |
The first key enabler concerns the nature of the clinical leadership itself – in the sense of what it is that clinicians see themselves as providing leadership about. For service redesign to be effective, it needs to be based not only on a technical rationale as to how new arrangements will improve health outcomes, but also a moral ethos that appeals to clinicians’ sense of occupational identity. Throughout all of our cases, clinical leadership can be seen as closely bound to aspirations to improve health outcomes and the experience of patients. Variously the benefits being sought include:
-
improving the quality and consistency of primary care, thereby decreasing the burden on acute care
-
improving understanding of patient preferences and needs, and communication between service providers and patients
-
achieving simpler patient journeys and better integration of care both within the health service and with other partners
-
improving efficiency and reducing wasted resources
-
improving system resilience and delivery.
Such benefits provide the core of a set of values that clinicians in both commissioning and providing roles have used to spread awareness of and commitment to new models of service provision.
We have seen that, in a number of our cases, this moral ethos has become powerfully enshrined within a ‘programme’ arena. When this happens, it is also more likely to be influential within the operational delivery arenas. More generally, a convincing moral ethos can itself serve as a mechanism for binding together the inter-related leadership work that needs to take place within each of the three arenas we have identified.
A second key feature of effective leadership for service innovation was a recognition, by those involved, that there are likely to be successive rounds of defining the nature of the new services and the skills involved. This defining work often involves rethinking the interfaces between previously overdefined and separate services that have become established under a contract-driven and somewhat adversarial model of commissioning. It also requires an interplay over time between the arenas of operational commissioning and operational delivery, as the requirements and performance potential of new service models become clearer. This sort of progressive defining and refining of service models, with clinical input on both the commissioning and provider side, is more likely to occur effectively under pilot arrangements, where competitive, market-driven aspects of commissioning are put in abeyance for a period or where system-driven co-production is emphasised (as in case F). More generally, our cases suggest that achieving effective clinical input requires commissioners to find ways of providing reassurance that they understand how change can be managed collaboratively across the system, rather than competitively, with providers cast as winners or losers. Issues of continued viability of particular provider organisations may need to be faced, but this is more likely to be done effectively if commissioners join providers in thinking through what a viable future might look like for them.
A closely related factor that supported the development of clinical leadership across the three arenas was the presence of established formal and/or informal clinical networks. Innovation in primary care in case C built on established relationships between many practices and active locality structures. Innovation in the alliances in case A1 built on established relations between acute providers. Even in the less developed cases, such as case E1, achievements have built on existing relationships.
Finally, Table 8 suggests a number of reasons why achieving coherence in clinical leadership across the three arenas may be difficult.
Elaborate and far-reaching service redesigns over a wide geography can preoccupy clinical leaders when creating plans in strategic and operational commissioning arenas (points 1 and 2 in Figure 24). This sometimes detracts from the development of operational detail. It may also deflect effort away from building normative networks among front-line provider staff (cases E1 and F).
Additionally, committed normative networks may emerge within providers, particularly among GPs who have been inspired by the aspirations of CCGs, but perhaps found that the realities of opportunities for influence have not lived up to their expectations. Such situations can lead to confusion and something of a vacuum at the operational commissioning level (point 2, see Figure 24), as delivery leaders recruit different NHS strategic initiatives to serve their purposes (case D).
Notably, in case D, innovations in primary care were driven not by GPs as commissioners using the CCG as the lever, but rather by GPs as providers using GP federations as the vehicle for change. There were service innovations built around telephone triage, new workforce designs, self-care, targeted work with the frail elderly using specialist teams of GPs with special interest, pharmacists and specialist nurses. Some of the major clinical innovators involved in these initiatives were of the view that the CCGs were simply not delivering and the service and the patient simply could not wait for them. Thus, they said, the provider side needed to get on with the redesign and present it to the commissioners as a new offer. Although these initiatives were undoubtedly examples of clinically led service redesign, they were often stymied by the lack of a receptive and sufficiently resourced operational commissioning forum to consider them.
Conclusions
This chapter has analysed the role of clinical leadership in our eight cases in terms of three arenas, concerned with strategic commissioning, operational commissioning and operational service delivery. We have also made a distinction between the leadership work of instigating service redesign and that of implementing new models or concepts of service delivery. In addition, we examined the range of ways that these activities can take place across the three arenas. A number of key points are worth bringing out by way of conclusion to our comparison of the eight cases.
First, the leadership work of crafting operational detail is bound up with the operational delivery arena – without leadership work within this arena, operational solidity is unlikely to emerge. However, this institutional work of defining operational detail requires interchange with the operational commissioning arena, so that the staff and other resources or delivery are appropriate and also so that there can be iterative refinement of the overall concept and its ethos.
Second, and perhaps more surprising, the leadership work of envisaging and articulating new service concepts can begin in any of the three arenas and often involves individuals who can move adroitly between them. We saw new service concepts being taken up to the strategic arena by clinicians who were also engaged in committed work in operational arenas, as well as cases where clinicians working mainly in strategic arenas formulated big ideas and found formal and informal ways of shaping powerfully the activities of colleagues in the other two kinds of arena.
Above all, our analysis brings out the key role played by operational commissioning arenas for steering service innovation. Arenas such as programme boards appear to offer a forum where clinical leaders in CCG commissioning roles and in provider roles come together to integrate the institutional work of creating new models of service delivery. In order to do this, they can be seen as bringing clinical expertise and experience to bear in reconciling a number of perspectives which are potentially in conflict with one another. These include:
-
thinking differently about what established clinical professions do, in the context of services designed to address the needs of members of the public in a holistic way; tackling identified public health challenges rather than providing a service as defined by established clinical specialisms
-
developing new or modified professional identities and skills sets; clinical leaders in commissioning and provider roles became engaged in practical debate about the skills and sense of priorities of particular clinical roles
-
preserving and enhancing the expertise base of established clinical workforces; in some of our cases, provider clinical leaders took up a key role of working out how the expertise they represented could continue to be useful and relevant in a new service delivery model
-
identifying where national-level funding schemes offer opportunities or incentives for investments in new models of service; in some cases, the work of making sense of, and capitalising fully on, a plethora of national initiatives and sources of funding demanded a great deal of attention
-
preserving the income streams of established clinical provider organisations; in a number of cases both commissioners and providers found themselves dealing with complexity around whether or not to continue to support an established provider or advocate it be replaced by something different that might serve public health needs better.
Grappling with these tensions involves much more than mediating between a managerial and a clinical perspective, which is one established notion of the work of clinical leadership. Our analysis of the work of programme boards suggests that clinicians and non-clinicians on such boards find themselves mediating between a variety of different managerial perspectives (e.g. looking at the best use of limited commissioning funds alongside how to preserve the viability of provider organisations), as well as simultaneously mediating between a variety of clinical perspectives (how to understand the future role of GPs or clinical psychologists from a provider perspective and how to reconcile such provider perspectives with an understanding of emerging public health needs which do not fit well with existing services or specialisms).
One of the key lessons from our cases is the function of programme boards in providing a kind of adaptive leadership forum where complex dilemmas can be tackled through a process of dialogue, guided by an ethos of commitment to public health. Solutions to such dilemmas need to be discovered rather than imposed.
This role of programme boards is particularly significant given the fact that, as we will see in the next chapter, these kinds of arenas do not exist in some health-care systems abroad. Although the original conception of CCGs emphasised the importance of their governing bodies as the place where the clinical voice would direct commissioning strategy, our cases demonstrate that this depends on carefully constructed operational commissioning forums, such as programme boards. In order to achieve this, we saw commissioners in these operational commissioning arenas finding ways to set aside models of market-based commissioning and instead seeking collaboration with providers to establish pilot arrangements for new models of care. These attempts frequently seemed to rely on using non-recurrent funding.
The fundamental work of achieving effective service innovation involves work occurring across the operational commissioning and operational delivery arenas. One constant leadership task addressed within strategic commissioning areas is the authorisation and vesting of resources in the other two arenas. In some cases, the work of making sense of, and capitalising fully on, a plethora of national initiatives and sources of funding demanded a great deal of attention.
The findings make clear that the integration of clinical leadership across the three arenas can be an uneven and lengthy process. This has important implications for the speed of progress in service innovation that policy-makers should expect.
Chapter 6 Discussion
In this chapter we situate our findings in relation to existing bodies of knowledge and we seek to show how this study contributes to existing knowledge.
As noted in Chapter 1, an ‘expectation’ has been established that clinicians should ‘step up’ and engage in leadership of the health service. CCGs are just one example, albeit a very important one, of just such an attempt to enact the expectation, obligation and opportunity. With the launch of the National Improvement and Leadership Development Board in 2016, that general expectation of a diffuse and widespread responsibility for leadership and development has been renewed and intensified. 86
The aim of this research project was to clarify the extent, nature and effectiveness of clinical leadership in and around CCGs. Implicit within this is the related question of whether or not CCGs have provided an appropriate platform for the exercise of clinical leadership.
This chapter is structured in five parts, each of which addresses findings in relation to the main research questions.
Modes of clinical engagement and clinical leadership
The first research question asked about the range of clinical engagement and clinical leadership modes being used in CCGs. One kind of answer to this question was given in the survey results chapter (see Chapter 3), the case study chapter (see Chapter 4) and the cross-case comparisons chapter (see Chapter 5). Engagement ranged from minimal to extensive. A significant proportion of GPs chose not to engage with their CCG. This tendency of disengagement grew slightly between 2014 and 2016. Yet, on the other hand, the research also uncovered some clinicians who were very active in the process of leadership of service redesign.
As noted in Chapter 5, this institutional work took place in three main arenas: strategic commissioning at CCG board level; operational commissioning at programme board level; and practical implementation work at service delivery level. Across the cases we tracked and clarified the key achievements, the factors which facilitated clinical leadership in these instances and the challenges which they had to overcome. As shown, the main instances were found in extended service and raised standards in primary care; new designs in integrated care, especially for the frail elderly; innovations in urgent care, which offered alternatives to A&E; and new service offers in mental health.
Given the relative autonomy inherent in the professional work of doctors, there was normally an understanding that some degree of persuasion would be required in order to switch patterns of service organisation and provision. ‘Leadership’ therefore was often seen to require communication of the need for change, a visualisation of the possible solutions to the identified problems and a roadmap of how to move towards the desired destination. Doctors tended to demand ‘evidence’ for each of the three steps. The various ways in which this game was played provided the drama that unfolded in each case. Above all, our cases all suggested that ‘evidence’ and rational persuasion was not enough by itself. Leadership for service innovation also involved the building of a network of clinicians who shared an ethical or moral commitment to a new model of more integrated service provision. Although this is perhaps not in itself surprising, our cases are revealing in the variety of ways these ‘normative networks’ came to be constructed.
The literature on this subject comprises a mix of prescriptive and descriptive approaches. A number of writers have advocated proceeding in a collaborative, consensual and adaptive way. 42,50,52 As Spurgeon et al. state in their book on medical leadership:
We favour a model of shared or distributed leadership . . . this is about the quality of interaction rather than formal positions and is evaluated by how well people work together. It is where everyone is engaged in acts of leadership, where communication and making sense of conflict ensure that the process is democratic, honest and ethical [and] based on evidence and professional judgement
Spurgeon et al. (pp. 6–7)42
Descriptive accounts often show situations where the predominant pattern is rather different. Detailed research of change in health-care settings reveals the influence of leadership by two or three at the strategic apex. 56,87 This phenomenon, in earlier literature, was referred to as the work of a ‘dominant coalition’. 88 Evidence from our case studies showed that such coalitions were very much in operation in CCGs. In one of the cases (case B), the three at the top were all GPs (the chairperson, the accountable officer and the vice chairperson). In other cases (e.g. case E), the dominant coalition comprised a GP chairperson and a manager occupying the accountable officer position, working in tandem. Even in the cases cited, implementation of new service modes required more plural forms of engaged leadership. In case B, for example, the required reforms to primary care required a sufficient critical mass of willing implementers for peer pressure to have an impact on those GPs seeking to hold on to the status quo.
These issues concerning stability and change in organisations have a significant presence in the literature. The tendency for organisations which operate in a shared environment to adopt similar practices has been noted by organisational researchers. 89,90 Hence, there tends to be a propensity for organisations to replicate known and accepted ‘recipes’. This may be because it is easier to maintain legitimacy this way and because it can be easier to mimic existing practices. 89 However, the more that persistence and stability is explained, the harder it is to explain change. Those changes that do take place may themselves be characterised by a certain conformity – conformity, that is, to an accepted model of change. It is the cases of divergence from existing institutions and institutionally promoted templates for change that are harder to explain. 69
The case studies revealed two types of change: conformist innovation (that which followed templates and guidance from the centre) and deviant innovation (that which diverged from directions set by the institutional status quo). The latter may require actors to distance themselves from accepted norms. In such cases, the role of ‘enabling actors’ and their location in an institutional field assume importance. 67,90 Actors at the margins, for example, who have less invested in the status quo, may be prompted to initiate such action. However, on the other hand, they are less likely to have the resources to make a major impact. Disruption may occur to the role divisions (jurisdictions) of organisations (e.g. the boundaries between primary care and secondary care) and/or between the jurisdictional boundaries of professional groups. In the NHS, actors/change agents are likely to be interfacing with, and having an impact on, both of these. Resistance to change may come from both of these interests.
Evidence from our cases suggests that disruption and the imagining of new forms of service was additionally complicated by the fact that in the NHS it is far from a simple matter to map which actors are more embedded in the status quo and which have a greater stake in challenging it. National policies and strategies emanating from senior levels in NHSE profoundly challenge the status quo in terms of the boundaries between primary and acute care. At the same time, front-line clinicians in district general hospitals are often the most passionate advocates of shoring up the status quo in terms of what happens in the acute sector. So, new models of service delivery can come both from apparently entrenched senior actors (such as those instances in cases B, E and F where the top two or three provided the vision and the impetus) and from more marginal actors (as in cases C and D where enthusiastic GPs with no formal place in the CCG hierarchy used their local knowledge to drive a path for change). Neither one could be said to be inherently superior. They each faced challenges. The former approach needed to win local commitment. The latter, ground-up approach, needed to win resources and support from above.
The coexistence of competing logics opens up space for disruptive challenge and for the creation of new forms. Insofar as elements of competition have been allowed, there has been scope for new service forms to be introduced by ‘new entrants’, such as new primary care provider groups run by GPs. Their position in the field means that they can deploy resources based on expertise and local knowledge and can, credibly, bid for contracts from commissioners of a kind which represent new modes of service provision. These new elements may include improved access, extended hours, multidisciplinary teams and an extended range of services in community settings. And all at potentially lower cost.
Our cases revealed instances where clinical leaders within CCGs (e.g. nominated clinical leads for specified service areas, GP chairpersons or GP accountable officers) drove change very much in line with approved models approved by NHSE. In these cases, leaders could deploy the allocated resources (managerial and financial) to deliver the plan. (Persuading all members to fall in line was not always so straightforward.) These instances could be seen as conformist innovation. Indeed, to ‘do nothing’ – to merely persist with established legacy behaviours – could be regarded as somewhat deviant. However, given the complexity of the NHS, matters were not always quite so simple. Our cases revealed numerous examples of leadership of service redesign where the challenges were more complicated. ‘Grass-roots’ innovation by enthusiastic locality groups or pioneering specialists had to negotiate the complex web of interest groups that might favour existing arrangements. The CCG might itself support the status quo because unpicking the tangled web of payments, contracts and systems maintenance appeared too daunting and they saw themselves as having more pressing immediate priorities.
Commissioning as a platform for clinical leadership
The second question asked about the extent and nature of the scope for clinical leadership and engagement in service redesign that is possible and facilitated by commissioning bodies. This question places the focus on the enabling conditions. The HWB aspect is the easiest to answer. These bodies rarely played a significant part. Nor did clinicians engage in any meaningful way with these bodies. Representatives from CCGs at HWBs tended to be accountable officers and/or chairpersons. Of more direct interest was the role of the CCGs themselves. There were two key aspects to this. The first of these was within the CCGs: how much influence were clinicians able to exercise? The second aspect was the power and influence of CCGs as institutions: what weight did they carry among the many other players in the landscape? Were they able to make a difference?
In formal terms, CCGs are membership organisations; nominally GPs are ‘in charge’. In reality, it is a much more complicated picture. There were a significant number of cases where managers acted as the most influential players. However, this was by no means a universal phenomenon. Our data point to cases where GPs exercised extensive influence over the strategic direction of the CCG as a whole and significant influence within specific service areas. In some of the cases this was because influential clinical figures took up roles as chairpersons or accountable officers and steered the CCG in a particular strategic direction. The case studies which focused on reform of primary care, for example, illustrated how leading clinician managers occupying hybrid roles pursued the kinds of changes which reflected the visions set out in Liberating the NHS3 and those wanted by NHSE. The puzzle is why there were not more cases of this kind. The answer stems not only from the expected difficulties in carrying along the GP membership but, additionally, from the complex interplay of diverse institutions each with their power basis and each part of a wider web of services underpinned by payment mechanisms, which were found to be difficult to unravel.
The scope for service redesign using the mechanism of these local commissioning groups was thus checked by numerous sources of inertia. Agents rooted in institutions can be expected to conform to the rules of those institutions; yet, as individual actors, they also have scope for the exercise of agency. This duality has been termed the ‘paradox of embedded agency’. 91 Explanations of why one or the other side of this paradox is enacted may be facilitated by referring to a mix of the individual actors’ location within the various institutions (organisational and professional), as indicated by Battilana,67 and also by the orientations and values of the individual actors.
Regarding the influence of CCGs as institutions in a competitive institutional landscape, the picture is again mixed. We found examples where CCGs were marginal, peripheral players.
The benefits being sought from clinical leadership
The third question asked about the range of benefits being targeted through different kinds of clinical engagement and leadership. The most straightforward answer to this is that there was very evident commonality in the declared objectives of the would-be service redesigners. Integration of service was the big theme and care closer to home and away from secondary care was another.
The findings suggest that the creation of CCGs did, to an extent, enable and prompt increased, and more potent, clinical leadership. As shown in the main body of the findings in this report, there were numerous examples of clinicians – along with managers – engaging seriously with service redesign and making a real difference to practice and to outcomes. However, this proved to be very irregular and uneven. Nor, after > 3 years of operation, did clinical leadership using the CCG platform, nor indeed CCGs themselves, live up, overall, to the level of expectation generated around the time of their inception. Part of the reason for this contingent and conditional performance was the degree of extraordinary turmoil in the wider context. The nationally driven agenda moved on. This piece of institutional work had to compete with other, newer, initiatives.
The research evidence, drawn from both the surveys and the case studies, revealed a number of weaknesses in the concept of GP-led commissioning groups. Insufficient numbers of GPs were willing to step forward to take up commissioning roles. There was regular reference to the paucity of the ‘leadership pipeline’. In addition, with regard to those GPs in such roles, there was concern about the amount and quality of training and development.
During the course of the study it was evident that GPs were showing more enthusiasm for leadership of the new provider bodies, such as the federations and the extended care delivery bodies. Hence, our work shows that clinical leadership seeks out spaces of influence almost regardless of the particular institutional arrangements. This is highly relevant because it means the findings in this report are likely to be generalisable beyond the life of CCGs. The findings point to the ways in which clinicians cope with, and shape, institutional change.
A further weakness stemmed from the size and limited influence of the CCGs. They were seen to be too many and too small. In the latter stages of the study it was evident that many CCGs were seeking to work collaboratively with their neighbouring CCGs and were taking steps to establish arrangements for a single shared accountable officer and a common commissioning body. The results of the second national survey showed that large numbers of governing board members did not expect their individual CCG to survive in the long term. The large acute providers continued to exercise considerable influence and the CCGs found it difficult to reshape the scope of services they offered – either because they were but one of a number of small commissioners or, conversely, because as a main commissioner they could not be seen to ‘destabilise’ their local secondary provider.
The construct of ‘leadership’ is just one lens through which the challenges and operation of the health system can be analysed and understood. A systems perspective would direct attention to issues of equilibrium and disequilibrium, interdependencies and adaptation in response to resource shifts. Similarly, changes in service models can be attributed to knowledge flows and power distribution. Important agents in both respects are the management consultancies. The large international firms enable and impel knowledge shifts in an important, but relatively hidden, way. The firms work behind the scenes and reference to their influence is rarely made in board papers and related strategy documents. Moreover, the firms work at multiple levels: simultaneously at national level (shaping policy changes) and at regional and local levels (including work with individual service providers and individual commissioning organisations). Enactment and delivery of their models normally depends on co-operation and engagement with clinical practitioners and indeed with managers. However, whereas managers can comparatively more easily be directed to conform with a policy shift, clinical professionals with their elements of autonomy, ethical codes and specialist knowledge require more subtle handling. Thus, enlisting local clinicians to the task of mobilising effort and making ideas work in practice is a vital requirement. The twin tasks of legitimising the direction of travel and the destination while also demonstrating how it can work in practice (implementation work) are crucial requirements. These tasks can merit the label leadership.
Enablers and barriers
The fourth question concerned the forces and factors that serve to either enable or block the achievement of benefits in different contexts and how appropriate are different kinds of clinical engagement and leadership for achieving effective service design. In this report the enablers were shown to be strong working relationships between key figures in and beyond the CCG – most especially when there was a clinical chairperson and an accountable officer working to a common agenda with a relationship based on trust and mutual respect. Intriguingly, prior working could operate in contradictory ways. In some of our cases, the CCG leaders had a long history of working with each other and they built on that track record. Yet, that was not always a positive. In other cases, where CCGs emerged from diverse groups and the organisation was thus starting anew, the incoming leaders reported that they could introduce a new broom with no regard to any previous compromises. The blockers were found to be many: complacency; lack of vision; lack of resources; feelings of disempowerment in the face of dominant providers; and new initiatives from above seemingly taking over the agenda for change. As our survey data clearly showed, the CCGs rated by NHSE as ‘inadequate’ or ‘requiring improvement’ were also those where respondents felt they had less influence – both as individuals and as organisations.
International comparisons
Finally, the fifth question was about the resonance, relevance and learning across health systems in different countries. To answer this question we shared our findings with expert scholars in a range of countries and sought their responses. Even though CCGs are unique, the underlying issues examined in this project found resonance in other systems. Below we give some examples.
The Quebec health system in Canada had sought to address similar challenges of an ageing population and the need for long-term care with new institutions – Health and Social Services Centres. These were designed to integrate acute, community and home care. Similar to the UK NHS, it tried to shift from a service-based approach to a population-based approach. It was found, as in our study, that actors at managerial level were needed to do the kind of ‘institutional work’ we discussed in order to translate grand policy into meaningful action. There, too, the ambiguities, contradictions and gaps had to be attended to by skilful agents. They too had to undertake structural, conceptual, operational and relational work to engage front-line staff in effective implementation. However, managers were expected to take on much of this work and there was rather less of an expectation that it would be done by clinicians.
Our colleagues in Germany and the Netherlands observed that our CCGs are somewhat similar (in some respects) to ‘practice networks’ in Germany and to ‘care groups’ in the Netherlands – both are organisations with 50–150 GPs which represent and put forward the GP voice in negotiations with health insurers and the provincial governments which, in a sense, ‘commission’ health provision. The groups are not vested with the same statutory power to act as commissioners as in England, but they do put forward a collective viewpoint. Germany and the Netherlands both have complex health-care systems with distributed decision-making in which health insurers have an important role. The German insurance groups monitored activities, payments and performance. GPs (and their organisations) negotiate with multiple health insurers, who may arrange different services in addition to the standard package. Some GPs have organised themselves in networks (Germany) or care groups (the Netherlands) for these negotiations. In Germany, health care is largely shaped in the various Bundesländer, so policy-making is at least at two levels: state and country. Our triangle of arenas of practice find resonance at the practice level and to some extent at the policy level, but our second arena (programmes of commissioning) was of course absent.
We asked about lessons for the UK. We were told that, in the Netherlands, health-care costs exploded after market principles were introduced in health care in 2006. The cost increases slowed down in 2011 after maximum budgets were reinforced for hospitals and budgets for home care were cut substantially a few years later. Both developments were unrelated to GP care but they increase pressure on GPs. GPs are well established in the system but perceive increased administrative control on their practice in recent years. In 2015, a large majority of GPs revolted against health insurers and the ministry of health because of the high administrative workload and unequal position in negotiations with health insurers.
Another expert in the Dutch system noted that some experiments in the Netherlands had resonance with our study. He noted some regional collaborations between hospitals and GP practices. These are often located near a hospital emergency room and in some cases even shared an entrance. They are funded by the local insurer (there are four large insurers that represent 90% of all patients and traditionally ‘own’ certain regions).
It might be argued that, in the light of our findings, the CCGs have a de facto role somewhat similar to these practice networks and care groups. In reality, their market power is limited and their role vis-à-vis NHSE could be seen as subsidiary and circumscribed. Using this analogy, the relationship between CCGs and NHSE could be likened to ‘care groups’ interfacing with a proxy insurer. Aspects of planning, allocated budgets and quasi-market principles are all in play. Similarly, in the Netherlands, the same debate about the relative merits of market versus co-operation/collaboration could be found.
In Sweden, GP groups were reported as jointly developing new models of care with hospitals. However, with regard to primary care services, these experiments tend to be limited to a few of the larger practices acting alone and the population coverage and scale are small compared with some of the initiatives in the UK. In the USA, we were told, despite the high-profile cases such as Kaiser Permanente, the dominant model is of professionally managed organisations and systems without any expectation that GPs would be in a position to lead significant changes. From that perspective, the English CCG experiment simply looks too radical.
These international examples reflect GPs acting in groups and engaging in service redesign, albeit as partner providers rather than commissioners. This is a pattern increasing in importance in England and may reflect a shift in emphasis and role for local GP groups here.
Chapter 7 Conclusions
In this final chapter we summarise the key findings and discuss the implications for practitioners and researchers. We also include some guidance based on the findings.
Findings
We summarise first the main findings relating to CCGs, then, second, the main findings relating to clinical leadership in and around CCGs.
Findings relating to Clinical Commissioning Groups
-
The extent of activity and the extent of impact across different CCGs was tremendously varied. Some seized the opportunity for radical innovations, while others were relatively passive.
-
CCGs were constrained to varying extents by other agencies in the institutional field. They faced uncertainties about their autonomy, their power and their futures.
-
CCGs found that they had to navigate between competing institutional logics (most notably between using commissioning powers to benefit from competition vs. using collaborative planning and integration).
-
Some CCGs focused on using their commissioning powers and entered into extensive design of new and substantial outcome-based contracts (mainly in the fields of muscular skeletal and frail elderly care); others concentrated on collaborative working with existing providers in pursuit of new patterns of care.
-
Policy initiatives at supra-CCG levels (most notably, the Five Year Forward View12 and its associated new models of care and the STPs) were increasingly relocating much of the inventiveness away from CCGs into other hands.
-
CCGs were increasingly sharing management teams, resources and plans with their neighbouring CCGs.
-
In a significant number of cases, non-clinical managers rather than clinicians exercised the most influence; in other cases, hybrid manager–clinicians exercised influence.
-
Despite the many challenges and limitations, we describe cases where GPs were encouraged by the climate of devolved leadership to seize the opportunity to redesign primary care by extending the reach and the quality of general practice.
Findings relating to clinical leadership in and around Clinical Commissioning Groups
-
Clinical leadership in and around CCGs is different in nature from that found in hospital settings where professional bureaucracies are entrenched. In the CCG context, cross-boundary intercession and negotiation across professional groups and across organisational boundaries is required.
-
This requires different sets of capabilities; these were found to hinge around cross-boundary relationship building.
-
Clinical leadership was most effective when it joined up practice across three arenas: the strategic apex of CCGs; programme boards; and the arena of practical service delivery.
-
The CCG board provided the legitimacy for strategic change; the programme boards worked through the competing logics of markets, hierarchy and networks; the practice arena allowed for the exercise of clinical leadership in practical problem-solving, detailed learning and routinisation of new ways of working at a common-sense everyday level.
-
The imagining and articulation of a new service concept can arise in any of these arenas. However, effective and sustained service redesign required matching, mutually reinforcing and commensurate action across all three arenas.
-
The programme board level of clinical leadership had a key role in resolving a variety of tensions between different clinical perspectives. Clinical and managerial leaders in this kind of board also played a vital role in mediating between managerial and clinical perspectives.
-
Effective clinical leadership in CCGs involves successive rounds of defining the nature of the new services and the skills involved. This defining work involves rethinking the interfaces between previously overdefined and separate services that have become established under a contract-driven, and somewhat adversarial, model of commissioning.
-
Achieving effective clinical input requires commissioners to provide reassurance to multiple agents that they understand how change can be managed collaboratively across the system. Issues of continued viability of particular provider organisations may need to be faced, but this is more likely to be done effectively if commissioners join providers in thinking through what a viable future might look like for them.
-
Service redesign worked best when clinical leaders and managers worked in tandem.
-
Most respondents suggested that it was managers and clinicians equally who set out the compelling vision. These results suggest that the notion that GPs would be the visionaries and architects, and that managers would play the role of delivery agents, is generally not an accurate depiction of the reality.
-
Managers acting alone, or acting equally with clinicians, account for 87.5% of the communication with patients and public.
-
Respondents from CCGs rated as ‘inadequate’ by the CQC were most likely to say that managers provided most of the insight into patient and public need and they tended to regard clinicians as less active in this regard.
-
Half of the respondents saw managers and clinicians as equally involved in forging collaborations with neighbouring CCGs and other major players. However, a very significant proportion (43%) identified managers as leading on this and only a very small proportion (5%) argued that clinicians led on this work.
The findings in context
The research took place during a period of unusual turmoil in the NHS – even when judged by its own standards in this regard. The period began with the extraordinary launch of the new local commissioning organisations as part of the extensive reforms as legislated by the Health and Social Care Act 2012. 2 It became clear during the course of the project that the activist agents we were studying were, to a large degree, seeking to compensate for, and work around, the resulting fragmentation. It is no coincidence that a great deal of the effort that we witnessed during the period of the project (2013–16) was, and is, directed at attempts to bring about integration. The Five Year Forward View12 and the associated Vanguards and then the STPs are all signals of this centre-led drive for integration. At grass-roots level, our core case studies tell the story of local efforts to pursue a similar set of objectives. Top down and bottom up, the attempted innovations seek to overcome the self-inflicted legacy of structures and systems put in place by previous organisational service designers. Despite being located in a particular point of time of institutional change, we suggest that our findings have wider generalisability, beyond the life and fortunes of CCGs. In part this is because many clinical leaders were already grappling with institutional structures which may, in time, replace CCGs and in part because our research shows how clinicians are leading, shaping or ignoring institutional change and this has wider resonance beyond the particular institutional features.
The critical view of CCGs is that there are too many of them and they are too small to make a difference. There is a strong perception that the expectation level at their launch has not been matched by their performance and delivery. In particular, in the current cash-strapped environment, criticisms are being heard that the costs of running small-scale commissioning organisations does not provide value for money. Whether or not it has been a lack of ambition and/or imagination, a lack of capacity or capability, or simply the insurmountable problems of moving an embedded system with powerful interests, the evidence of differential impact across these 200 plus bodies with their elaborate constitutions and governance procedures appears limited. Thus, there are many who look to, or expect, the erosion or even demise of CCGs.
There are counterviews. What would/will be lost if they were indeed abolished or allowed to wither on the vine? As our evidence shows, these clinical groups have encouraged many local GPs to take a serious interest in the organisation of health care and well-being which extends beyond the narrow confines of their own surgeries. CCGs have encouraged, galvanised and enabled a blossoming of some notable improvements in service redesign, led by active GPs. If CCGs were abolished there is a risk of the loss of this kind of positive engagement, and a risk too of resentment if a top-down, target-driven regime took their place. CCGs have offered a platform which has promoted some notable primary care-led innovation; given greater prominence to primary care; and, in turn, promoted the wider perspective of well-being as well as health. The holistic aspects of health are recognised in primary care and the risk management character of general practice is enabled. So, too, local knowledge and patient voices are facilitated. Peer pressure has in many areas – as noted in or case studies – raised the quality of general practice. If CCGs were removed from the scene there would also be the risk of inducing disillusion about yet more structural change and an attendant risk of a new perceived remoteness and bureaucracy in health governance and management. A shift from small-scale locally responsive commissioning back to a larger-scale, more centralised approach may not be without its own attendant complications. Arguably, the real source of the problem is not the nature of the commissioning body but the inherited rigid payment systems with their perverse incentives. Underlying all of this is the wider question of the competing logics we have tracked throughout the analysis: quasi-market competition on the one hand and planning and collaboration on the other.
Our survey data revealed the multiple indicators which can support both a pessimistic and an optimistic view. Evidence in Chapter 3 revealed that less than half of accountable officers and less than half of GPs on governing boards judged that their CCG was the most influential body in shaping local health services. This may reflect both the inbuilt power of the hospital sector as well as the level of intervention by NHSE and other central bodies that also have responsibilities. Inside the CCGs, respondents were just as likely to judge managers as being the most influential as to judge clinicians as wielding the influence. In terms of who set the compelling vision, 25% attributed this to clinicians compared with 19% to managers; however, the majority (54%) judged both to be equal. Broadly similar patterns were found too in relation to understanding public and patient needs. On a positive note, the majority of respondents in both 2014 and 2016 judged the overall influence of clinical leadership as significant or central. However, when asked whether or not plans for service redesign had ‘far exceeded’ tangible, achieved change, the majority (55%) agreed that they had.
The case studies tell the story of local efforts to respond to the challenges and the prompts. In many of the cases it was evident that much of the urgent drive for service redesign came from both ‘below’ the CCG level and from ‘above’ it. The level above was typified by the STPs of which footprints normally incorporate a dozen or so CCGs and of which governance teams included LAs, acute provider trusts as well as CCGs. Notably, the STP agendas and plans were guided by NHSE. The level ‘below’ included most notably the ‘localities’ or ‘hubs’ of half a dozen or so GP practices with populations of approximately 30,000–50,000 patients that, through concerted action, could offer better access and more extended services. Moreover, these localities tended to chime with the STP delivery plans. In such an emergent landscape, the individual CCGs were the bodies which began to seem out of place.
Although clinical leadership was thus as likely to be found above, below and around CCGs, it could be argued that it was the allocation of commissioning power to these statutory GP groups that gave the legitimacy and impetus for experimentation and innovation in service redesign with GPs in a leading role. Hence, although clinical commissioning may not have operated in the precise way it was expected to do so, with CCGs efficiently working through the commissioning cycle and making rational, lucid, allocative decisions using decommissioning and commissioning in a fully coherent manner, the edifice that was built enabled other more varied activity to take place and this is of wider significance.
The attempted enactment of clinical leadership practice was complex because it was necessary to look to see what was happening at the next level above, the level below and indeed in a sideways direction in order to calculate the implications for any proposed action. Because of the fragmentation in the NHS, most of the leadership of service redesign initiatives we studied traversed several units of providers, commissioners and partners. The skills required to build collaborative relations across complex networks were of a different order than the skills needed to lead within a contained service unit. Part of the challenge was the degree of turbulence in the system. To be sure, the climate of multiple initiatives encouraged experimentation; but, conversely, the relative lack of stability and the pace of change (in diverse directions) meant that the agents we studied had to cope with the extra uncertainty surrounding priorities, funding flows and patient flows.
The research findings reveal the many attempts to reform general practice and primary care. This involved larger practices or groups of practices, extended services and extended teams with mixed skills, and a shift in emphasis from commissioning to new forms of leadership and governance of provider organisations.
The examples of more far-reaching local action were normally those prompted by and legitimated by higher-level policy shifts. The higher-level sponsorship offered outline-approved ‘models’ and a degree of ‘air cover’. However, notably, even such national-level sponsorship was not enough to ensure a smooth passage for local reforms. As noted, one of our cases offered up the example of a very active local clinical leader who even secured the ‘in principle’ backing of the prime minister. Yet, even this piece of collaboration building was not enough to overcome local opposition.
Limitations
The research underpinning this report included a vast array of investigative activities across a very large number of CCGs. Nonetheless, such is the variety and complexity of the work of CCGs that it is difficult for any report to claim to fully capture and reflect the full ‘reality’ of CCG work and the leadership attempts therein. The six CCG cases are not necessarily reflective of the 2009 CCGs in England. That said, the detailed cases were not intended to be a representative sample of all CCGs. Indeed, as mentioned, they were selected through theoretical sampling and there was a bias towards CGGs where there was some evidence of meaningful activity. The wider survey, which covered all CCGs, allows a broader picture and much of the evidence from that source pointed to numerous instances where there has been much less activity than we record in our cases. So our casework is not statistically representative of CCGs, but it does help reveal the pattern of activities and factors which allow GPs to make a substantive difference – if they are minded to do so.
Implications for practising clinicians, managers and other local actors
The main practical implications to be drawn from this research project are as follows.
-
Managers and clinicians alike seeking to drive service change using CCGs need to attend to the alignment of work in the identified different arenas if their innovations are to be effective and sustainable.
-
Practitioners need to recognise that they are operating in a very different institutional field from that which pertained when CCGs were launched. Past assumptions about power and influence may not be valid. Major new initiatives emanating from national level, such as STPs, Vanguards and the promotion of ACOs, signal that the role of CCGs has been diminished. Work needs to be done in this fourth arena.
-
Practitioners in and around CCGs should seek to capture, preserve and build on the best examples of what has been achieved, while also learning about the processes which brought these about. The lessons will be useful in new contexts even if CCGs do not survive or become much reduced in their role.
-
Process innovators need to recognise that managers and clinicians are both required to work in tandem in order to make service redesigns stick.
-
The survey revealed that many individuals currently serving on CCG boards are heavily inclined towards the power of commissioning and contracting; the emergent emphasis on integrated services and collaborative working means that new attention has to be directed to the rather different ways of working and the associated sets of competences.
-
Clinicians with influential roles within strategic commissioning arenas – most especially on CCG boards – should see their role as making decisions to vest resources in new models of care that meet population health needs more effectively. Learning from the cases suggests that initiatives work best when there is commensurate supportive activity under way in operational planning and practice delivery arenas. Most crucially, clinical leaders on the commissioning side of programme boards need to make sure they engage creatively with influential GPs and acute provider clinical leads who are involved in creating the operational detail of new or improved services.
-
Clinical leaders responsible for implementing new service concepts need to ensure that they are engaged in building normative networks of clinical colleagues committed to the new way of working.
Service redesign is not an end in itself; rather, it should be a response to identified problems and opportunities for service improvement. Actors in the current system are under time pressure and so it is especially important that they are able to direct their energies in effective ways. Exercises in establishing common purpose and reanalyses of the state of the system can be useful but they can also be excessive. Launching reviews and initiatives was experienced by some as too easy and too frequent. The early stages of projects and programmes are the easy part; follow-through and the realisation of effective impacts are the difficult parts. The problem of the plethora of initiatives is not resolved simply by producing documents claiming alignment with other ongoing programmes and projects.
Implications for future research
When writing the proposal for this research project we stated that even if CCGs did not survive there was merit in studying how managers and clinicians would behave under these kinds of regime. We regarded it then, as we do now, as a valuable opportunity to take advantage of a bold, large-scale, natural experiment. No other system has given GPs such extensive commissioning powers. There was potential for radical change and we wanted to explore how these newly privileged actors would undertake the institutional work of disruption and rebuilding that lay in prospect.
In practice, we found that action, in the main, did not match initial expectations or plans. Institutional stickiness in the wider system alongside competing logics and forces meant that attempts at radical change were often blocked. Yet, as shown, we did identify and classify many rich instances of clinical leadership in three main arenas: the strategic, the operational level of programme boards and the practice level of service delivery. The research agenda emerging from this work relates most obviously to how the newly emergent bodies such as the STPs and the extended primary care formations and ACOs, will operate, and with what impact.
However, in addition, the other implication for future research is to delve deeper into the forms of clinical leadership which we identified. These operated in different arenas and they seem capable of recurring with, or without, altered forms of commissioning and collaborative planning in health care in the future. Whatever institutional form health-care governance and management may take in the future, many of the processes we uncovered and the capabilities inherent within them will resurface. Future research therefore can usefully focus on these enduring elements: how normative commitment is constructed; how front-line clinicians are engaged; how alliances across professional groups and organisations are built; how existing provider identities are handled while encouraging greater professional exchange in the interests of patients and public.
Another theme for future research that emerges from this work is how the established institutional hierarchies (most notably the acute hospitals, especially when they are foundation trusts with budgets to defend and targets to meet, plus also the general practices) will meet on the common ground of shared population-based health and well-being as the supposed priorities, when they continue to feel the tug of professional identity, professional jurisdictions, institutional survival and shortage of resources. The bases of negotiated order, whether or not contractual and/or relational, will need exploring.
Acknowledgements
We are grateful to members of our Study Steering Committee who were helpful from start to finish. The members were Professor Steve Field, Chief Inspector of General Practice at the CQC; Margaret Goose, a former lay member of the Council of the Royal College of Physicians and Chairperson of their Patient and Carer Involvement Steering Group; Dr Mark Ashworth, GP and Clinical Senior Lecturer, King’s College London; and Dr Louise Restrick, Consultant Physician, Whittington Health NHS Trust.
We also acknowledge the support of our Advisory Group: Dr Andrew Spooner, GP and Governing Board member of South Cheshire CCG; Dr Stephen Richards, a practising GP and currently Regional GP Advisor for the CQC for London, formerly Chief Executive of Oxfordshire Clinical Commissioning Group; Paul Haigh, Chief Officer, City & Hackney CCG; Peter Kohn, Director of the Office of London CCGs; and Professor Ewan Ferlie, King’s College London.
Our sincere thanks are also due to our international panel of experts who helped us think through the wider meaning of the findings in relation to similar issues in other health systems and other countries. In particular, we acknowledge the help of John Ovretveit, Stockholm, Sweden; Hub Wollersheim, the Netherlands; Frede Olesen, Peter Vedsted, Flemming Bro and Mogens Vestergaard from Denmark; Michel Wensing, Heidelberg University Hospital, Germany; Charles Heckscher and Susan Jackson, Rutgers University, New York, NY, USA; Jean-Louis Denis, Montreal, QC, Canada; Tom Kochan, Massachusetts Institute of Technology, Cambridge, MA, USA; and Barbara Kellerman, Harvard University, Cambridge, MA, USA.
We are also grateful to the many individuals and groups who helped make this research possible. This includes the hundreds of respondents from CCG governing boards who completed the national surveys, which produced the data for the charts and tables in Chapter 3. We are grateful also to the clinicians and managers who agreed to be interviewed about their work, which produced the data for the case study analyses in Chapters 4 and 5. In addition, acknowledgement is due to informants from outside CCGs, including patients and public representatives, ambulance service staff, LA officials and elected members, doctors and managers from the acute sector, and persons from all relevant surrounding bodies such as CSUs, STPs and regulatory bodies.
Contributions of authors
John Storey (Professor of Management) conceived and designed the study, conducted interviews, designed the national surveys, synthesised the results and authored the final report.
Richard Holti (Senior Lecturer in Human Resource Management) helped design the study, conducted interviews, helped design the national surveys, synthesised the results and authored the final report.
Jean Hartley (Professor in Public Leadership) helped design the study, conducted interviews, helped design the national surveys, synthesised the results and contributed to the final report.
Martin Marshall (Professor of Healthcare Improvement) helped design the study, conducted interviews, helped design the national surveys, synthesised the results and contributed to the final report.
Tatum Matharu (Research Fellow) conducted interviews, helped design and administer the national surveys, synthesised the results and contributed to the final report.
Data sharing statement
All available data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Darzi L. High Quality Care for All: NHS Next Stage Review, Final Report. London: Department of Health; 2008.
- Health and Social Care Act 2012. London: HMSO; 2012.
- Public Health White Paper. Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Engaging Local People: A Guide for Local Areas Developing Sustainability and Transformation Plans. London: NHS England; 2016.
- Redrawing the Health and Social Care Architecture: Exploring the Role of National Bodies in Enabling and Supporting the Delivery of Local Health and Care Services. London: PricewaterhouseCoopers; 2016.
- Edwards N. Sustainability and Transformation Plans: What we Know so Far. London: The Nuffield Trust; 2016.
- Williams D. NHS England Leader’s Decisions Not Consistent With NHS Values 2016. www.hsj.co.uk/workforce/exclusive-nhs-england-leaders-decisions-not-consistent-with-values/7020837.article (accessed 1 November 2017).
- The 2015 Challenge Declaration. London: NHS Confederation; 2014.
- Growing Older in the UK: A Series of Expert-Authored Briefing Papers on Ageing and Health. London: British Medical Association; 2016.
- Improving the Health of the Public by 2040. London: The Academy of Medical Sciences; 2016.
- The State of Health Care and Adult Social Care in England 2015–2016. London: Care Quality Commission; 2016.
- Five Year Forward View. London: NHS England; 2014.
- Francis R. Final Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. HC 947. London: The Stationery Office; 2013.
- Klein R, Exworthy M, Mannion R, Powell M. Dismantling the NHS? Evaluating the Impact of Health Reforms. Bristol: Policy Press; 2016.
- Field S. NHS Future Forum: Recommendations. London: Department of Health; 2011.
- Managing Conflicts of Interest: Guidance for Clinical Commissioning Groups. London: NHS England; 2013.
- Planning and Delivering Service Changes for Patients. Leeds: NHS England Strategy Unit; 2013.
- Transforming Primary Care. London: NHS England; 2014.
- General Practice Forward View. London: NHS England; 2016.
- Delivering the Forward View: NHS Operational Planning Guidance for 2017/18 and 2018/19. London: NHS England and NHS Improvement; 2016.
- National Health Service and Community Care Act of 1990. London: The Stationery Office; 1990.
- Moon G, Mohan J, Twigg L, McGrath K, Pollock A. Catching waves: the historical geography of the general practice fundholding initiative in England and Wales. Soc Sci Med 2002;55:2201-13. https://doi.org/10.1016/S0277-9536(01)00365-3.
- Storey J, Holti R, Winchester N, Green R, Salaman G, Bate P. The Intended and Unintended Outcomes of New Governance Arrangements Within the NHS. Southampton: National Institute for Health Research Service Delivery and Organisation; 2010.
- Sheaff R, Charles N, Mahon A, Chambers N, Morando V, Exworthy M, et al. NHS commissioning practice and health system governance: a mixed-methods realistic evaluation. Health Serv Deliv Res 2015;3.
- Clinical Commissioning: What Can We Learn from Previous Commissioning Models?. London: The King’s Fund; 2012.
- Le Grand J, May N, Mulligan JA. Learning from the NHS Internal Market: A Review of the Evidence. London: The King’s Fund; 1998.
- Mays N. The Purchasing of Health Care by Primary Care Organizations: An Evaluation and Guide to Future Policy. Buckingham: Open University Press; 2001.
- Newman M, Bangpan M, Kalra N, Mays N. Commissioning in Health, Education and Social Care: Models, Research Bibliography and In-Depth Review of Joint Commissioning Between Health and Social Care Agencies. London: Institute of Education; 2012.
- Miller R, Peckham S, Checkland C, Coleman A. Clinical Engagement in Primary Care-Led Commissioning: A Review of the Evidence. London: PRUComm; 2012.
- Checkland K, Coleman A, Segar J, McDermott I. Exploring the Early Workings of Emerging Clinical Commissioning Groups: Final Report. London: PRUComm; 2012.
- Ipsos MORI. CCG 360 Degree Stakeholder Survey. London: Ipsos MORI; 2014.
- Robertson R, Holder H, Bennett L. CCGs One Year On: Member Engagement and Primary Care Development. London: The King’s Fund and The Nuffield Trust; 2014.
- Smith J, Holder H. Securing the Future of General Practice: New Models of Primary Care. London: The Nuffield Trust; 2013.
- Robertson R, Holder H, Ross S, Naylor C, Machaqueiro S. Clinical Commissioning: GPs in Charge?. London: The King’s Fund and The Nuffield Trust; 2016.
- Storey J, Storey J. Leadership in Organizations: Current Issues and Key Trends. London: Routledge; 2016.
- Storey J, Holti R. Towards a New Model of Leadership for the NHS. London: NHS National Leadership Academy; 2013.
- West M, Lyubovnikova J, Eckert R, Denis J. Collective leadership for cultures of high quality health care. J Organ Eff 2014;1:240-60. https://doi.org/10.1108/JOEPP-07-2014-0039.
- Bourgeault IV, Mulvale G. Collaborative healthcare teams in Canada and the US: confronting the structural embeddedness of medical dominance. Health Sociol Rev 2006;15:481-95. https://doi.org/10.5172/hesr.2006.15.5.481.
- Coombs M, Ersser SJ. Medical hegemony in decision-making – a barrier to interdisciplinary working in intensive care?. J Adv Nurs 2004;46:245-52. https://doi.org/10.1111/j.1365-2648.2004.02984.x.
- Currie G, Lockett A, Finn R, Martin G, Waring J. Institutional work to maintain professional power: recreating the model of medical professionalism. Organ Stud 2012;33:937-62. https://doi.org/10.1177/0170840612445116.
- Sanders T, Harrison S. Professional legitimacy claims in the multidisciplinary workplace: the case of heart failure care. Sociol Health Illn 2008;30:289-308. https://doi.org/10.1111/j.1467-9566.2007.01052.x.
- Spurgeon P, Clark J, Ham C. Medical Leadership: From the Dark Side to Centre Stage. Oxford: Radcliffe Press; 2011.
- Ham C, Dickinson H. Engaging Doctors in Leadership: What We Can Learn from International Practice and Research. London: NHS Institute for Innovation and Improvement; 2008.
- Dickinson H, Ham C, Snelling I, Spurgeon P. Are We Nearly There Yet? Models of Medical Leadership: An Exploratory Study. London: National Institute for Health Research Service Delivery and Organisation; 2013.
- Denis JL, Storey J, Hartley J, Denis JL, ‘t Hart P, Ulrich D. The Routledge Companion to Leadership. New York, NY: Routledge; 2016.
- Currie G, Lockett A, Suhomlinova O. The institutionalization of distributed leadership: a ‘catch-22’ in English public services. Hum Relat 2009;62:1735-61. https://doi.org/10.1177/0018726709346378.
- Gronn P. Distributed leadership as a unit of analysis. Leadersh Q 2002;13:423-51. https://doi.org/10.1016/S1048-9843(02)00120-0.
- Spillane JP. Distributed Leadership. San Francisco, CA: Jossey Bass; 2006.
- Ibarra H. Act Like a Leader, Think Like a Leader. Cambridge, MA: Harvard Business Review Press; 2015.
- Heifetz R. Leadership Without Easy Answers. Cambridge, MA: Harvard University Press; 1994.
- Sharpe C, Dewar B, Barrie K. Forming New Futures Through Appreciative Inquiry. Glasgow: Iriss; 2016.
- Heifetz R, Grashow A, Linsky M. The Practice of Adaptive Leadership: Tools and Techniques for Changing your Organization and Your World. Boston, MA: Harvard Business School Press; 2009.
- Storey J, Holti R. Possibilities and Pitfalls for Clinical Leadership in Improving Service Quality, Innovation and Productivity. Southampton: National Institute for Health Research Service Delivery and Organisation; 2012.
- Storey J, Holti R, Storey J, Hartley J, Denis JL, ‘t Hart P, et al. The Routledge Companion to Leadership. New York, NY: Routledge; 2016.
- Touati N, Roberge D, Denis JL, Cazale L, Pineault R, Tremblay D. Clinical leaders at the forefront of change in health-care systems: advantages and issues. Lessons learned from the evaluation of the implementation of an integrated oncological services network. Health Serv Manage Res 2006;19:105-22. https://doi.org/10.1258/095148406776829068.
- Denis JL, Lamothe L, Langley A. The dynamics of collective leadership and strategic change in pluralistic organizations. Acad Manage J 2001;44:809-37. https://doi.org/10.2307/3069417.
- Aveling E, Martin GP, Armstrong N, Banerjee J, Dixon-Woods M. Quality improvement through clinical communities: eight lessons for practice. J Health Organ Manag 2012;26:158-74. https://doi.org/10.1108/14777261211230754.
- Using Clinical Communities to Improve Quality. London: The Health Foundation; 2012.
- McNulty T, Ferlie E. Reengineering Health Care: The Complexities of Organizational Transformation. Oxford: Oxford University Press; 2002.
- Packwood T. Good medicine: a case study of BPR in a hospital. Policy Polit 1998;26:401-15. https://doi.org/10.1332/030557398782106970.
- Guthrie B, Davies, H, Greig G. Delivering Healthcare Through Managed Clinical Networks (MCNs): Lessons From the North. Southampton: National Institute for Health Research Service Delivery and Organisation; 2010.
- Guthrie J. The joys of a health service driven by Toyota. Financial Times 2006.
- Radnor Z, Walshe K, Harvey G, Jas P. Connecting Knowledge and Performance in Public Services. Cambridge: Cambridge University Press; 2010.
- Dent M, Bourgeault IV, Denis JL, Kuhlman E. The Routledge Companion to Professions and Professionalism. London: Routledge; 2016.
- Saks M. The Routledge Companion to Professions and Professionalism. London: Routledge; 2016.
- Abbott A. The System of Professions: An Essay on the Division of Expert Labour. Chicago, IL: University of Chicago Press; 1988.
- Battilana J. The enabling role of social position in diverging from the institutional status quo: evidence from the UK NHS. Organ Sci 2011;22:817-34. https://doi.org/10.1287/orsc.1100.0574.
- Cloutier C, Denis JL, Langley A, Lamothe L. Agency at the managerial interface: public sector reform as institutional work. J Public Adm Res Theory 2016;26:259-76. https://doi.org/10.1093/jopart/muv009.
- Greenwood R, Hinings CR. Understanding radical organisational change: bringing together the old and new institutionalism. Acad Manage Rev 1996;21:1022-54.
- Lawrence T, Suddaby R, Clegg S, Hardy C, Lawrence T, Nord WR. Handbook of Organization Studies. London: Sage; 2006.
- Imison C, Curry N, Holder H, Castle-Clarke S, Nimmons D, Appleby J. Shifting the Balance of Care: Great Expectations. London: The Nuffield Trust; 2017.
- Greenhalgh T, Humphrey C, Hughes J, Macfarlane F, Butler C, Pawson R. How do you modernize a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009;87:391-416. https://doi.org/10.1111/j.1468-0009.2009.00562.x.
- Fitzgerald L, Ferlie E, Addicott R, Baeza J, Buchanan D, Gerry M. Clin Manage 2007;15:61-74.
- Eisenhardt KM. Building theory from cases. Acad Manage R 1989;14:532-50.
- Eisenhardt KM, Graebner ME. Theory building from cases: opportunities and challenges. Acad Manage J 2007;50:25-32. https://doi.org/10.5465/AMJ.2007.24160888.
- Lawrence T, Suddaby R, Leca B. Institutional work: refocusing institutional studies of organizations. J Manage Inq 2011;20:52-8. https://doi.org/10.1177/1056492610387222.
- Lawrence T, Suddaby R, Leca B. Institutional Work: Actors and Agency in Institutional Studies of Organizations. Cambridge: Cambridge University Press; 2009.
- Reay T, Hinings CR. Managing the rivalry of competing institutional logics. Organ Stud 2009;30:629-52. https://doi.org/10.1177/0170840609104803.
- Thornton PH, Ocasio W, Lounsbury M. The Institutional Logics Perspective: A New Approach to Culture, Structure and Process. Oxford: Oxford University Press; 2012.
- Heracleous L. A tale of three discourses: the dominant, the strategic and the marginalized. J Manage Stud 2006;43:1059-87. https://doi.org/10.1111/j.1467-6486.2006.00629.x.
- Kellog K. Challenging Operations: Medical Reform and Resistance in Surgery. Chicago, IL: University of Chicago Press; 2011.
- Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage; 1985.
- Glaser B, Strauss A. The Discovery of Grounded Theory. Chicago, IL: Aldine; 1967.
- Miles MB, Huberman M, Saldaña J. Qualitative Methods: A Sourcebook. London: Sage; 2013.
- Hartley J, Benington J, Bryman A, Collinson D, Jackson B, Grint K, et al. Sage Handbook of Leadership. London: Sage; 2011.
- Developing People – Improving Care: A National Framework for Action on Improvement and Leadership Development in NHS-Funded Services. London: National Improvement and Leadership Development Board; 2016.
- Denis JL, Langley A, Cazale L. Leadership and strategic change under conditions of ambiguity. Organ Stud 1996;17:673-99. https://doi.org/10.1177/017084069601700406.
- Cyert RM, March JG. A Behavioural Theory of the Firm. Englewood Cliffs, NJ: Prentice Hall; 1963.
- DiMaggio P, Powell WW, Powell WW, DiMaggio P. The New Institutionalism in Organisational Analysis. Chicago, IL: University of Chicago Press; 1991.
- Greenwood R, Suddaby R. Institutional entrepreneurship by elite firms in mature fields: the big five accounting firms. Acad Manage J 2006;49:2748-62. https://doi.org/10.5465/AMJ.2006.20785498.
- Seo MG, Creed W. Institutional contradictions, praxis, and institutional change: a dialectical perspective. Acad Manage R 2002;27:222-47.
Appendix 1 Gantt chart
Appendix 2 Additional figures and tables from the postal survey
General practitioner members of the governing bodies tended to see NHSE and other national bodies as influential (Figure 26).
FIGURE 26.
Influence of the national bodies.
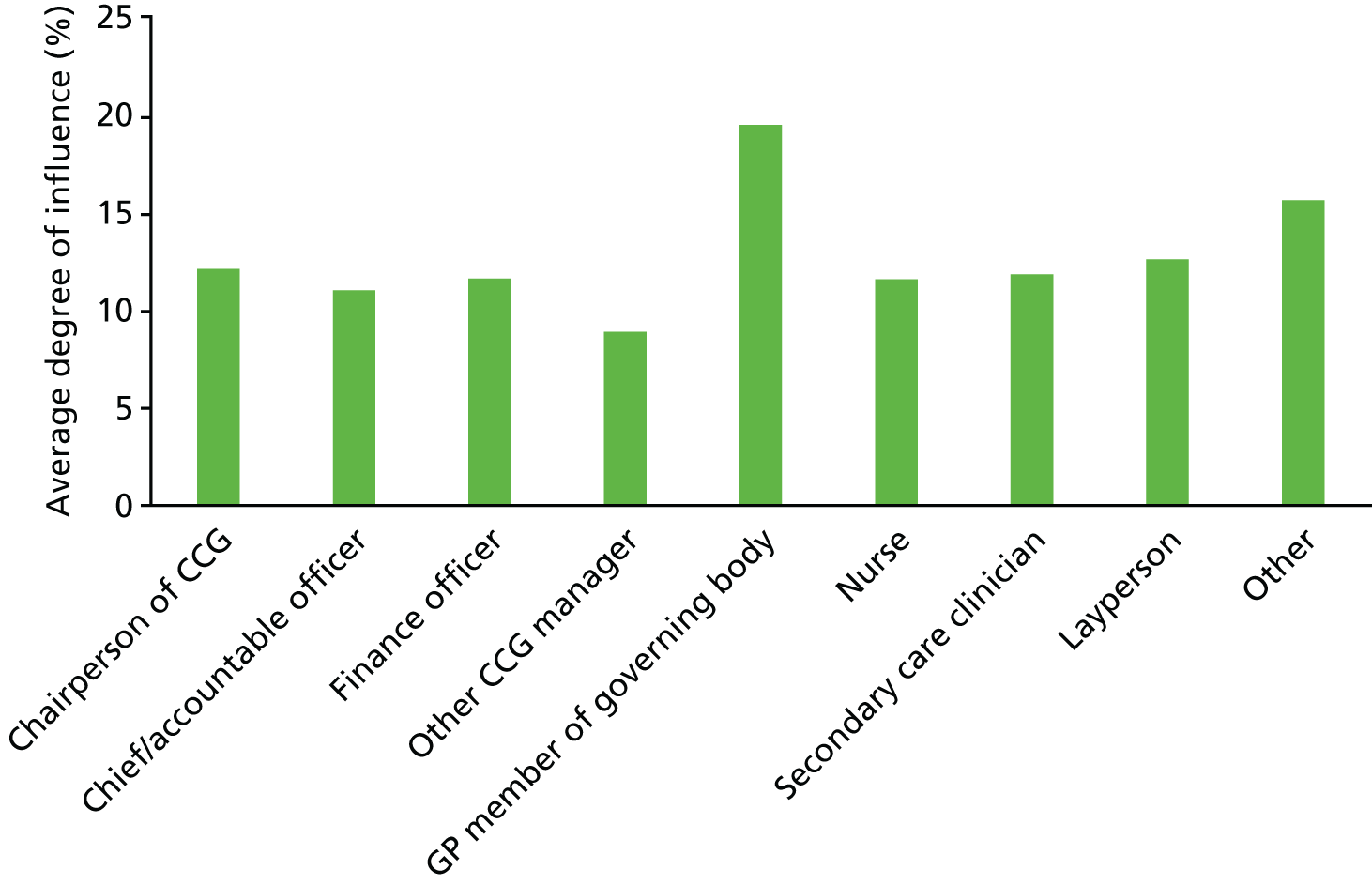
Training and development
Respondents were presented with a scale from minimal to major training and development provision. The average (mode) answer in 2016 was ‘an uneven pattern, some have some have not’. Only 8% of respondents reported that there had been major initiatives to provide training and development (Figure 27).
FIGURE 27.
How much training and development have clinical leaders received?
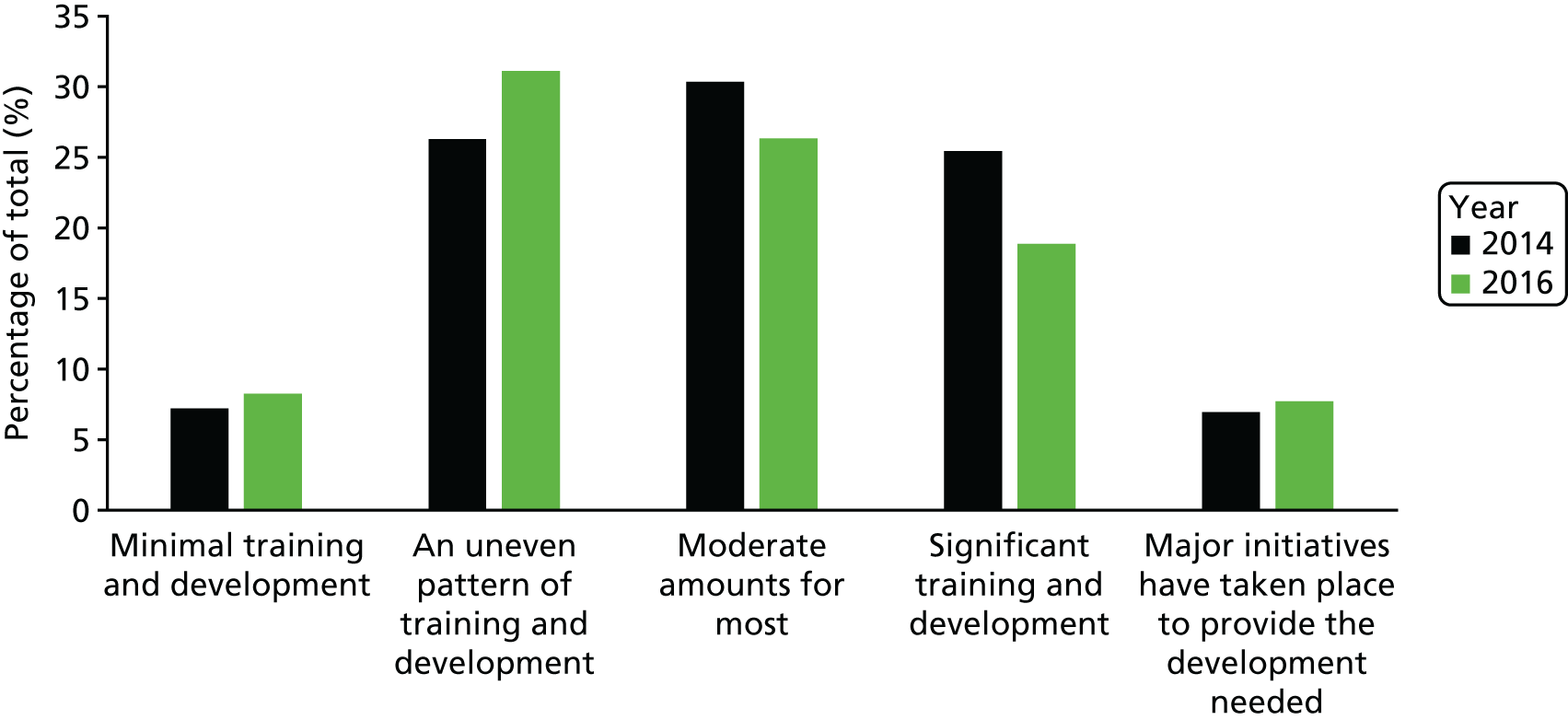
Figure 28 suggests, however, that there has been a decline in GP engagement with leadership in and around CCGs.
FIGURE 28.
Trends in GP engagement and leadership (1 = low agreement, 5 = high agreement).
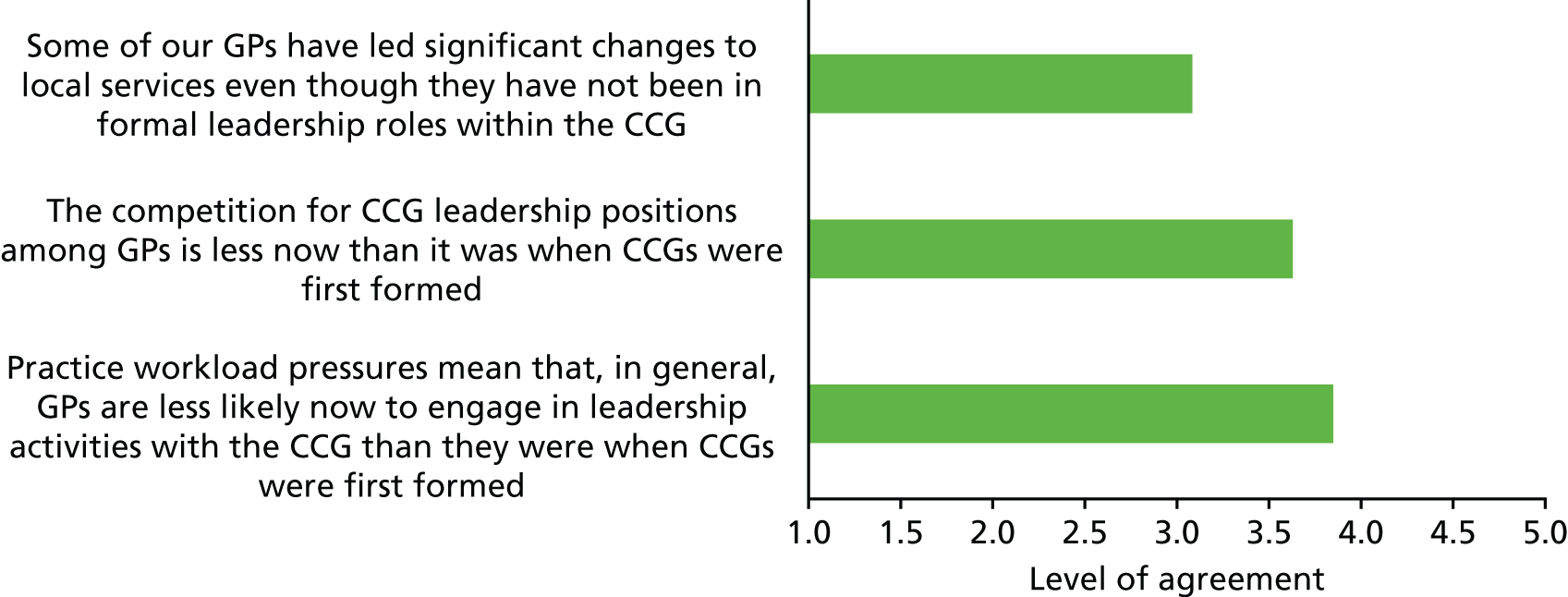
Once again we see the mixed nature of the picture. Whereas previous charts (e.g. Figure 20) have shown reason for an optimistic picture of clinical leadership in and around CCGs, Figure 28 shows a degree of pessimism. There was an overall view that GPs are now less engaged in leadership than they were previously.
Yet, when faced with the statement that ‘achievements of my CCG to date have more than matched expectations at the time of authorisation’, respondents, on average, agreed (3.4 on a 5-point scale, with 5 being high agreement).
There was broad agreement that, increasingly, service redesign is being tackled above the CCG level and that co-ordinated commissioning across multiple CCGs was increasingly common.
Appendix 3 Postal questionnaire

Appendix 4 Specimen interview guide
Data gathering for main cases
There are two sets of topics to be covered in our data gathering.
The first set relates to relevant contextual issues (the kind of challenges faced by the CCG and the way it is currently organised, such as the extent of collaboration with other CCGs and the level of influence and engagement by clinicians in general terms).
The second set relates to investigation of particular service redesign initiatives. In this second set, some typical questions are also set out that might be used in interviewing key actors. Data will also typically be gathered through analysing documents (e.g. of relevant programme boards), and observing relevant meetings. Two project team members per case.
Context topics
There is a set of issues that we need to be informed about. Data can be gathered through a variety of means: board papers, interviews with CCG executives and other key actors, observing meetings. The following list is a guide to topics that need to be covered.
-
In what service areas, and how, has the CCG actually had most impact? Where has the CCG made a difference (overall)? What is the degree of influence locally? System integrator/leader?
-
Current main developments/issues (e.g. co-commissioning, federations, outcome-based commissioning).
-
Legacy effects (e.g. of former PCT).
-
Local challenges (e.g. nature of local health economy and of providers).
-
Impact on primary, secondary, community services, integration.
-
Where is the leadership located (i.e. CCG board, HWB, localities or at another level such as CCG collaborations)?
-
What does the leadership look like? Is it realised through one particular individual, a particular set of people (how many/who) or is it more evenly spread?
-
Relevant issues/influence of key surrounding institutions: NHSE, Monitor/NHS Improvement, CQC, LA.
-
Engagement of GPs/members.
Particular service redesign initiative
Key topics
What was the perceived need for change or the problem to be fixed? Who identified this and how was it brought to institutional attention?
How were proposals for redesign developed, by whom and what was the content of these proposals?
What is the role in these proposals of ideas of integrated care or improving value? How far did/do the new service redesigns challenge existing models of clinical work or clinical organisations, as opposed to enhance what is already there?
Who was involved, in which kinds of ways, in getting agreement and implementing change?
What various stances and positions did different actors or agencies adopt? What blockages or setbacks were encountered? Which kinds of leadership, demonstrated by whom, were involved in achieving progress?
What has happened in terms of results achieved – service redesign implemented and/or health outcomes? What reflections or views do various parties have on success/compromise/what next?
Overall, what was revealed about clinical leadership and engagement by the change attempt? What has been revealed about the possibilities for more far-reaching service redesigns, particularly those that embody ideas of value-based care?
Some specifics
-
What do you see as the key service redesign initiatives that have taken place recently in your area? How did these come about? Who or what drove them?
-
What has happened to date and who (clinical and non-clinical) has been involved?
-
What kinds of measures of success are relevant to these initiatives and is there, at this point, evidence that the new or changed form of services provides better care?
-
What has made success achieved to date possible and what issues or blocks to progress have had to be overcome?
-
Who has provided what kinds of leadership to make these initiatives work?
-
What are possible next steps? Who is driving or leading on them? What challenges are likely to be involved?
-
Who else might it be worth talking to in order to gain further perspectives on this? What issues from your perspective would it be useful to focus on and understand better?
Specifics for the service change interviews
-
With respect to service change, how did this come to be a priority?
-
Who helped raise it up the agenda? Link with national agendas?
-
What are its key features? (For example, target group, size of budget.)
-
Build detailed chronology – when did it start and what milestone? What happened and when and why?
-
What obstacles were faced and how were/are these (being) overcome?
-
What role did clinical leaders play in these service changes?
-
What role was played by managers in the service changes?
Appendix 5 A note on the analysis of statistical data
Findings from the two surveys were presented in charts chosen according to the nature of the questions involved. Charts were produced using Microsoft Excel® (2010; Microsoft Corporation, Redmond, WA, USA).
The process for considering whether or not to investigate further particular relationships between responses on specific questions and the respondent’s role, or between question responses and NHSE ratings of their CCG, was as follows. Overall significance tests were performed for the association between the response and role (or rating), using Fisher’s exact test when the specific question had categorical responses and the Kruskal–Wallis test and/or one-way analysis of variance when the response was ordinal or on an interval scale. For the Kruskal–Wallis test, a randomisation procedure was used to calculate p-values because of the preponderance of ties. The analysis of variance results were taken into account only when residual plots indicated that the analysis of variance model was adequate. Questions where the p-value for the association was < 0.05 were shortlisted for further investigation. However, because of the multiple testing of many specific questions, attention concentrated on associations with smaller p-values. Not all such associations were reported on in Chapter 3, with a subjective choice being made depending on the statistical strength of the association and on its salience in the context of the study. Statistical calculations were performed using the R statistical programming language (version 3.1.2; The R Foundation for Statistical Computing, Vienna, Austria).
Appendix 6 Tables with verbatim quotes
Analysis of free-form answers in the postal questionnaires (Tables 9–11).
| Dimension | Verbatim response |
|---|---|
| Knowledge and understanding | Clinical knowledge; local knowledge; knowledge from front line experience; professional knowledge |
| A more clinically informed view than managers could hope to offer | |
| They understand services much better than managers | |
| We understand the bigger picture | |
| Attention to detail: insight into small things that create large obstacles to good clinical care | |
| Knowledge of systems and advocate for patients | |
| Position/location in the system | They reflect and understand the realities of the ‘front line’ |
| Generalists, wide-ranging | |
| Bring a ‘can do’ attitude | |
| Enthusiasm, practicality and prioritisation | |
| Better system overview than acute sector providers have | |
| Able to understand the problems of implementation at ground level | |
| Less constrained than managers | |
| A counter voice to finance imperatives | |
| They bring the voice of the front line | |
| Analytical and decision-making skills | Evidence based thinking |
| Sensible service design; . . . | |
| Understanding of the evidence and ability to describe what ‘good’ looks like | |
| Understanding of patient needs | |
| Expertise in care planning; . . . | |
| Patient centred, patient focused | |
| Outcome focused | |
| Clarity and structure, practical patient focus | |
| Clear evidence-based thinking. Clear understanding of what is needed to maximise the potential for front-line staff to work effectively together in the interest of their patients | |
| They have an understanding of resources | |
| Clear insight into the operational implications of challenges to services and service redesign | |
| Rapid option appraisal | |
| Relationships and collaboration | Strategic clinical leadership influence and followed by all clinicians and officers |
| Experience and judgment | |
| Patient engagement and member engagement; . . . | |
| . . . collaborative instincts | |
| Challenge and independent views | Their challenges to plans proposed by others |
| Challenge the status quo | |
| Challenge potential inertia of consultant colleagues | |
| Brings healthy dose of challenge and always reminds staff of how it is in reality | |
| They influence provider clinicians to understand the need to change | |
| Trust, credibility and status | Important touchpoint with patient/public kudos and trust form the public |
| Momentum of purpose, authenticity, trust | |
| Patient focused, on quality issues and on problems with service | |
| Credibility, practical experience and local knowledge | |
| Independent: less wedded to organisations | |
| Insight and understanding of realities | |
| Insight to what works/doesn’t work in a clinical sense – a reality check | |
| Ensure safety | |
| Communication and influence | Representing patient views; ability to communicate complex issues in plain English; . . . |
| Important in selling to colleagues and patients | |
| Influencing peers to change behaviour | |
| Evidence based mobilisation of clinical public support | |
| Communicate the vision to patients | |
| Engagement with clinicians to implement change with credibility | |
| Peer to peer discussions and influence | |
| They take other clinicians with them and patients as well |
| Dimension | Verbatim response |
|---|---|
| Lack of time/practice workload | Not enough GPs; increasingly have to devote time to direct patient care as fellow GPs leave |
| Inability to attend all meetings and planning sessions due to practice commitments | |
| Recruitment and dedicated time | |
| No paid time in job plans to do it | |
| Reducing number of clinicians willing to take leadership roles | |
| Providers’ financial constraints | |
| The pressure of doing the day job at the same time | |
| Pressure from clinical practice | |
| Recruitment difficulties | |
| Ageing GP population | |
| Lack of capability and experience | Poor commissioning support |
| Lack of project management skills in CCGs | |
| Managing a £1.2 billion budget is beyond the skill of clinicians | |
| In a CCG with three localities the default position is competition | |
| Lack of understanding of commissioning | |
| No knowledge of how to be a director of a board | |
| There are not many visionary GPs – they struggle to think bigger than a practice | |
| Clinicians are not usually organisational leaders and they have not usually been involved previously in major change programmes | |
| Often unclear decision making | |
| Lack of engagement with other professionals | |
| Inability of managers to ask focused questions rather than open-ended questions | |
| Managerial manipulation of the status quo | |
| Lack of trust between managers and clinicians | |
| Money | Finance; there is simply not enough money |
| Finances, every time we set up pilots without sustainability of funding | |
| Misaligning of incentives | |
| Government not matching input to expectation | |
| Constant policy change from centre, not being able to invest our plans in long term initiatives | |
| Lack of influence/lack of autonomy | Gaining approval from NHS England |
| NHSE | |
| The status quo; . . . | |
| Agenda driven by managers | |
| Over managers | |
| Over secondary care | |
| Tiers and tiers of bureaucracy | |
| NHSE! | |
| Inexperience of GPs in large organisations. Consultants are much more used to this environment | |
| Management blocking clinical change become of worry of loss of trust income. | |
| The clinical leadership is often sessional – lack of continuality, e.g. Mon, Thurs and Fri but not every day | |
| Therefore decisions move on at pace without clinical leadership input | |
| External factors which overrule us | |
| Meddling by non-clinical led organisations such as NHSE and local authorities | |
| Diversity of goals | Different views of what services should look like |
| Be clear about the rationale/case for change | |
| Pre-conceived ideas of what should happen | |
| Politics and the political cycle | |
| I have to question redesign as a concept: I would expect providers to drive service redesign (though with some collaboration with commissioners) | |
| NHS England’s relentless drive to increase expectation without expanding resource | |
| Attempting complete redesign rather than frequent small steps | |
| Conflict of interests among GP as care providers | |
| Pressure to bail-out hospitals | |
| Fragmented system with diverse goals | Too many providers; . . . |
| Too complex a system to unravel | |
| Failure of the acute hospital to deliver on promised service transformation | |
| Failure of county council to engage as no incentive to work outside their government targets | |
| NHS structures and organisational boundaries | |
| Historic provider/commissioner conflict | |
| System disintegration | |
| Too many meetings | |
| Influence of NHS Improvement and acute providers in maintaining their power | |
| Leadership failings | Lack of willingness to accept leadership role in convincing peers to change rather than simply reflecting existing willingness |
| Lack of belief that they can make a difference | |
| Lack of interest | |
| Lack of engagement from some members | |
| GPs have other interests and few incentives to change | |
| Not enough GP’s interested in leadership to spread the workload | |
| Demands of clinical time result in lack of proper engagement by secondary clinicians | |
| Lack of commitment | |
| Attendance issues |
| Type of leadership | Examples of types of leadership |
|---|---|
| System leadership | Vanguard projects |
| Development of ACO | |
| Early development of place-based care | |
| Stopping the local health economy from collapsing completely | |
| Raising awareness and prevention of health equalities | |
| Built a vision for transformation | |
| Service redesign | Changes to MSK services |
| Procuring an excellent MSK service which has reduced secondary care use and operations | |
| Community MSK services/physiotherapy | |
| Mental health redesign/talking therapies | |
| Redesign of urgent care | |
| Primary care commissioning | |
| Pathway redesign | |
| Redesign of frail and elderly services | |
| New models of primary care developing | |
| A new pathway for diabetics | |
| Community Respiratory Service | |
| Diabetic services – taken five separate providers and commissioned as whole programme budget – outcomes were below average now above national average | |
| Value-based commissioning for diabetes | |
| Out of hospital teams to lessen pressure on acute admissions | |
| New co-ordination centre | |
| Focus on self-care | |
| Integration: cross-boundary working | Developing an integrated community service across health and social care |
| New models of care | |
| A new integrated care team | |
| ‘Better Together Programme’, strategic alliance and new primary care strategy | |
| IT [information technology] sharing patient records with acute trust | |
| Joint planning with primary and secondary care services | |
| Multidisciplinary Team (MTD) working across traditional boundaries | |
| Commissioning integrated neighbourhood teams | |
| Re-shaping of maternity and paediatric services across NW [north-west] London | |
| Organisational development/softer skills impacts | Motivating an over-burdened workforce |
| We have a well-developed plan for closing the financial gap | |
| Built good working relationships across the system | |
| Starting to implement AQP [any qualified provider] | |
| Engagement | |
| Built good working relationships | |
| Stimulate positive discussions about the future | |
| Patient relations and customer service excellence | |
| CCG scope and nature of activities | Co-commissioning of primary care |
| GP practices appraisal | |
| Financial balance | |
| Excellent engagement with all CCG practices | |
| Established four neighbourhoods within the CCG and support them to work for themselves in shaping neighbourhood-level innovations | |
| Development of neighbourhood teams that are almost MCPs | |
| Implementation of referral support website to improve communication and dissemination of projects and services to clinicians | |
| Holding the secondary care provider to account | |
| Supporting GP federation and GPs | |
| An improved understanding of services | |
| Clinical leaders standing up and leading public consultations | |
| Our last public consultation was successful | |
| Quality initiatives | Referral management processes put into place |
| Improved elective referrals | |
| The ‘Way to Well-Being’ project: provision of patient mentors and coaches | |
| Prevention | |
| Impact on secondary care | Building relationships with hospital provider with a clear clinical focus |
| Reduction in mortality in local providers | |
| Utilising Right Care/Commissioning for Value | |
| Working relationships with the acute hospital are more constructive then they have been for up to 10 years | |
| Partnership work with ‘Keogh’ trust to raise standards of care for local community | |
| Primary care improvements | Weekend GP opening |
| GP practices working together | |
| GP access | |
| 18 practices doing 7 day GP services with others keen to join | |
| Making primary care an exciting and attractive area of work | |
| Better management of long term conditions by practices | |
| GP hubs and integrated care teams in the hubs | |
| Locality – integrated hubs operational | |
| Financial package to prevent practice closures | |
| A supportive practice programme | |
| Achieving GP federations | |
| GP quality contract – good uptake and engagement by practices | |
| Social prescribing | |
| Primary care-extended access | |
| Identifying ‘carers’ champions’ in all practices investing in community navigators’ who can signpost access to voluntary/local authority support services | |
| Multi-disciplinary teams delivering home first, hospital care at home | |
| Designing a blue print for primary care | |
| Community services | Vision that has been developed to change community services |
| (Plans for) a care co-ordination centre | |
| Community services: CVD, COPD and diabetics | |
| Re-procurement of community services using a collaborative partnership model | |
| No impact or very little | None |
| Lack of input from FT [foundation trust] secondary care consultants | |
| Still waiting . . . | |
| We’ve spent a year in recovery and are only now in a position to start making a real difference (assuming we can maintain the recovery momentum) | |
| NIL |
Prime contractor arrangement and outcome-based commissioning
Table 12 shows a brief overview of the answers with percentages rounded to the nearest 5%.
| Type of response | Response as percentage |
|---|---|
| Absolutely vital, very important | 70 |
| I remain hopeful | |
| Quite important | 5 |
| No idea/I just don’t know; what do these terms mean? | 10 |
| Other responses | |
| Less important than a year ago – STPs now setting a new agenda; . . . | 15 |
| Not important | |
| Good in principle but highly complex in practice | |
| Everyone is talking about it but nothing happening on my patch | |
| Contracts don’t drive change | |
| Would be better to move to a MCP | |
| A fad/flavour of the month | |
| It’s the wrong way to go | |
The answers to this question suggested some fundamental differences in the beliefs and perspectives held by those who hold positions on CCGs. As Table 12 shows, the majority leaned towards a view that commissioning through the use of contracts with clearer specification of outcomes was the surest way to proceed. Even where it was not currently in place, these respondents ‘remained hopeful’ and were committed to the general principle and logic. A surprisingly high number of CCG board members (10%) admitted that they did not know what the terms meant. Another significant group (around 15%) comprised persons opposed to these contracting approaches in principle and/or viewed them as too complicated, impractical and overhyped. A significant number of these sceptics were more attracted to what they saw as emerging models such as MCPs and the STPs, which gave hints that they leaned more towards planning and collaboration rather than completion and contracts. Other responses were:
I think this will take longer than 2–3 years to have an impact. It is difficult to get good reliable outcome measures in a number of areas.
I think the major issue will be that acute providers will have a disproportionate influence, and too much effort will be spent on managing this.
Prime contractor arrangements could be hugely important due to the risk around sustainability of individual providers and the blurring of responsibilities for sector based activity (i.e. acute, community, primary care). They will only work, however, if there is a strong and sustainable provider in the economy who can lead on them.
Wait to see, the power still seems to be with providers, and will continue to be so while the reorganisations are targeted at commissioners for political expediency.
Other respondents suggested the potential value of outcome-based commissioning:
It is very important. We need to move away from activity commissioning as this generates unsustainable levels of often ineffective activity – ‘failure demand’. Creative solutions will require a focus on the patient and their desired outcomes.
The current PbR [payment by results] framework and mechanism is a significant limiting factor on real transformation of service delivery.
Need to be realistic and flexible about commissioning for outcomes. This will require a review of the ‘payment systems’ and needs to be focussed around integration and must be a collective responsibility.
The future of Clinical Commissioning Groups
Finally, the survey asked an open-ended question inviting these CCG board members to share their expectations about the future of their CCGs and CCGs in general.
The notable feature arising from answers to this telling question is that the vast majority of respondents (65%) judged that CCGs – the organisations on which they were serving and devoting considerable amounts of their time – will not survive. Others (30%) expressed huge uncertainty about the future. Only a small minority of respondents said that they expected CCGs to continue. This is a surprising finding given the roles of these respondents. This was not a survey of GPs in general or of nurses and others of the > 1.2 million NHS workforce, but the select few who had stepped up to the task of leading these organisations and who had invested their energies into them. If only to help resolve tensions arising from cognitive dissonance, one might reasonably have expected a more optimistic and positive assessment of the future of the CCGs from this population group.
Of those large numbers who expected the demise of their institutions, there was a divide between those who viewed this eventuality as regrettable and those who judged it appropriate. Among the latter was the view that the clinical leadership role had not been sufficiently defined and grown, ‘Too much money spent on paying clinicians to do pure management roles’ and ‘It’s a flawed model’. However, others lamented the decline, ‘If they were allowed to commission services locally and in the best interest of patients then the mid- to long-term future could be significant!’
To some extent, the vicious circle described above was again at play. The perceived neglect of CCGs and the huge emphasis on STPs and devolution of health and care to LA areas perhaps not surprisingly had its consequences, for example as expressed in the answer ‘There is complete apathy among GPs; our morale is very low’. The CCGs were ‘Unlikely to survive due to lack of clinical engagement’.
There was a sense that CCGs were the wrong size – too small for core purposes but too large for local delivery – hence the phrase ‘A change to localised MCPs on the one hand and more centralised contracting arrangements on the other’. There was a view that they would ‘Merge then fold’.
Nor is it only a question of size and footprint. Questions were also raised about the continuing rationale. Some detected a ‘Blurring of the provider/commissioner split’.
This was associated also with the view that ‘I sense the centre has given up on CCGs’ and that ‘NHSE ignores CCGs most of the time anyway’. These responses, and others shown in Table 13, suggest that the future for CCGs was felt to be uncertain among many of the senior players who are needed to make them work.
| Category of expected change | Verbatim answer |
|---|---|
| Mergers | They will merge into Area Health Authority type bodies |
| Will be fewer of them | |
| Mergers of CCGs are inevitable current cost pressures could stop them functioning | |
| Move to bigger organisations | |
| There is a continual push now to work as STP | |
| Mergers and driving the QIPP programme | |
| There are too many commissioners and providers; perhaps STP footprints will be the next experiment in organisational form | |
| I think STPs will swallow up individual CCGs | |
| Mergers with each other and local government | |
| Create collaborative commissioning of public services – to which CCG will be part of wider structures | |
| Merge then fold | |
| Joint bodies of local authority social care and local health commissioning | |
| Will be abolished, replaced or downgraded | ACOs will replace them |
| I think they will be forced to cease | |
| A limited future | |
| STPs will give the power to providers | |
| Reorganisation, health and social care integration | |
| Reducing influence – trapped between growth in strength of federation/GP at scale and central dictate | |
| No long term future in current small configurations | |
| We are currently moving towards becoming an ‘accountable care organisation’ | |
| Impact will be progressively diluted | |
| Too small without additional management funding | |
| No future at sub-STP level | |
| I doubt there is a medium to long term future | |
| Falling influence and ability to redesign in view of falling funding | |
| With the new STP’s, CCGs will become bodies that implement rather than dictate compared to pre-STP’s | |
| Already been made unstable by imposition of STP’s; my concern is the current structure under threat, which will alienate GP board members | |
| Government will abolish us | |
| Closure | |
| Not sure CCGs are going to survive | |
| They will prove unworkable; a disastrous case of the Lansley reforms | |
| I think we are close to the end of CCGs as we know them today | |
| They will be replaced by something else | |
| I think we are close to the end of CCGs | |
| A change to localised MCPs and more centralised contracting arrangements | |
| There is clearly a return to regional management | |
| Clinicians’ role | In the last year it feels like clinicians increasingly disregarded, more production of policies |
| Complete apathy of GPs. Our morale is very low | |
| Clinical leadership will become clinical responsibility/accountability not leadership | |
| Too small, too much duplication, too much money spent on paying clinicians to do pure management roles | |
| Clinical engagement will reduce further | |
| Availability of GPs to provide clinical leadership uncertain | |
| Unlikely to survive due to lack of clinical engagement | |
| I think rationalisation is positive but also a shame as clinician–managerial relationship teams have matured to a point where I expect our CCGs to be considerably more effective going forward | |
| Uncertainty | Unsure because of devolution |
| Likely to change at some point | |
| Expect another reorganisation in due course | |
| Very uncertain | |
| Further change. Who knows? | |
| Only relevant up to next election in May 2020 | |
| Unsure | |
| Who knows? | |
| Threatened by funding and recruitment gaps as well as totally unacceptable QIPP | |
| Would be good if NHS England could back off a bit and let them get on with it | |
| I hope that in the transition to more centralised control that patient-focused clinical leadership isn’t lost | |
| The principle is great but the financial cost of maintaining 200+ CCGs is diverting funds from front-line clinical/health/care services | |
| Role will change | Shift to retain strategic commissioning only |
| Increasing alliance/collaboration and possibly an end to CCGs as entitles, but not clinical and commissioning as a method |
List of abbreviations
- A&E
- accident and emergency
- ACO
- accountable care organisation
- BCF
- Better Care Fund
- CAMHS
- Child and Adolescent Mental Health Services
- CCG
- Clinical Commissioning Group
- CQC
- Care Quality Commission
- CSU
- commissioning support unit
- DevoManc
- Manchester Devolution
- GP
- general practitioner
- HWB
- health and well-being board
- IAPT
- Improving Access to Psychological Therapies
- LA
- local authority
- MCP
- multispecialty community provider
- MSK
- musculoskeletal service
- NHSE
- NHS England
- PCT
- primary care trust
- PPI
- patient and public involvement
- PTA
- psychological therapies for adults
- STP
- sustainability and transformation plan
