Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/33/16. The contractual start date was in April 2015. The final report began editorial review in January 2017 and was accepted for publication in June 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Maxwell et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction, background and aims
Introduction
Over 15M people in the UK (2M in Scotland) report living with a long-term condition (LTC), with an estimated 6.5M people living with more than one condition. These numbers are projected to keep rising over the next decade. 1 A 2012 study of multimorbidity found that 42.2% of all patients in the UK had one or more morbidities. 2 People with LTCs account for 50% of general practitioner (GP) appointments (80% in Scotland), 70% of inpatient bed-days and 70% of the total health and care spending in England. 1 People with multiple morbidities use more health-care resources, including hospital beds. 3 Improving the management of LTCs has the potential to both reduce hospital-bed occupancy and improve the quality of life for this group of patients. 4
Those living in a deprived area are more than twice as likely to have a LTC as those living in more affluent areas. People with LTCs are also more likely to be disadvantaged across a range of social indicators. 5 Living with these conditions can result in additional acute and chronic stress, increasing the risk of anxiety and depression, which can, in turn, further affect their physical health and capacity for self-care.
Chronic physical illnesses are associated with increased prevalence of depression. 6 Until recently, expert guidelines recommended screening for depression in patients with diabetes mellitus (DM) and coronary heart disease (CHD); however, research found only little or no impact of screening on the recognition of depression in these patients. 7–9 Screening was mostly carried out by nurses, without training, as part of annual LTC reviews. Research has highlighted problems with nurse engagement in ‘screening’ and how the ‘tick-box’ approach of the Quality and Outcomes Framework (QOF) might have led to the underdetection of depression in patients with LTCs. 10 Previous studies have also found that practice nurses (PNs) recognised only 16% of psychologically distressed patients attending their clinics. 11
It is well accepted that deprivation and physical and mental health are closely linked, with an understanding that a broad range of stressors, more common in deprived communities, can have a negative impact on the physical and mental health of individuals. A recent study showed that the onset of multimorbidity occurred 10–15 years earlier in people living in the most deprived areas than in those living in the most affluent areas, with socioeconomic deprivation particularly associated with multimorbidity that included mental health disorders (coexistence of physical and mental health disorders). The presence of a mental health disorder increased as the number of physical morbidities increased, and was much greater in more deprived people than in less deprived people. 2 Broader social and economic conditions influence both the incidence of, and success in treating, many conditions,12 including patient engagement in self-care practices that are essential for managing LTCs.
Engaging in health-promoting behaviour and self-care practices can be limited or even impossible when adverse social circumstances intervene. Attention to these circumstances (often patient-identified priorities) could lead to improvements in patients’ abilities to subsequently engage in self-care and achieve benefits. The Department of Health has long anticipated that, with increased self-care practices, there would be a corresponding reduction in the use of health-care resources, better quality of life and reduced mortality. The current mechanisms within the NHS for encouraging self-care practices might better acknowledge or be responsive to the barriers that are created through many patients’ disadvantaged lives. This often includes reduced health literacy, which will require a different type of input if self-care behaviours are to be understood and accommodated within difficult lives. Again, attention to recognising and addressing these broader needs and organising responses (which other sectors are better positioned to meet) will ensure the more efficient use of NHS resources. Such an approach is endorsed by the Royal College of General Practitioners (RCGP) in its report The 2022 GP: A Vision for General Practice in the Future NHS,13 in which one of the first recommendations is about strengthening links between general practice and communities.
Supporting People with Long Term Conditions4 based its improvement programme on models from the USA (Kaiser Permanente, Pfizer and Evercare). These models are based on nurses acting as case managers who have a key role in co-ordinating services from other health and social care providers. 14 However, in primary care in the UK, this ideal has moved little beyond nurses conducting annual health checks that meet the requirements of the QOF. The RCGP promotes care planning,15 but acknowledges that coexisting mental and social circumstances may prevent such approaches. The RCGP response to QOF indicators for depression noted that ‘a holistic assessment should be part of the routine management of any patient with a LTC’. There are few validated tools for such assessment, especially for use by nurses. The development of interventions for primary care that encourage holistic assessment and action to address complex health and social needs is urgently required.
Depression screening in LTCs has now been removed from the QOF, but patient and carer groups have argued that this will serve only to remove the imperative to include assessing mental health needs in LTCs. The National Institute for Health and Care Excellence (NICE) now recommends that a biopsychosocial assessment is carried out, but only for patients newly diagnosed with depression, and it provides little guidance on how this should be addressed and no imperative to act on this assessment. 16
The Patient Centred Assessment Method (PCAM) tool has been developed to enable a broad assessment of needs alongside an assessment of how urgent these health or care needs are. The PCAM tool aims to help to identify and address patient biopsychosocial needs and to promote action based on the severity of these needs, including broader social problems that often lead to or exacerbate poor mental health, which can, in turn, have an impact on physical health and the patient’s ability to perform self-care. The tool encourages linking with other sectors to more appropriately address these problems for patients and to access alternative types of resources. The PCAM tool also encourages new ways of working that enhance opportunities for health promotion, even in those with few current health or social problems, to maintain healthy behaviour. It is anticipated that this will lead to improved quality of life for patients and better patient–professional interactions and relationships.
The PCAM tool is an adapted version of the Minnesota Complexity Assessment Method (MCAM), which was derived from the INTERMED (a method to assess health service needs). 17–19 The PCAM has previously been evaluated in anticipatory (Keep Well) health check clinics, which were initiated by the Scottish Government for early identification of LTCs, or risk of LTCs, in those aged 40–64 years and living in deprived communities in Scotland. 20 In an additional small-scale evaluation of the potential of the PCAM tool for use in highly vulnerable populations it was shown that the tool was perceived as having strong advantages in better managing the needs of homeless and travelling populations. 20 If the PCAM tool is shown to improve the care of people living in highly deprived communities, it could have real advantages for addressing health inequalities. The PCAM tool may also provide a more systematic approach for primary care in responding to the NICE and RCGP recommendations for biopsychosocial assessment of patients with LTCs and/or depression.
There is strong potential for the PCAM tool to make a real difference to the quality of care delivered in primary care to patients living with LTCs. The PCAM tool aims to encourage nurses to address more than just the physical care needs of their patients, or at least to determine these needs for others to address. By addressing these needs, patients could be better positioned to engage with health promotion and self-care advice and should also see improvements in their physical and mental well-being. There is also a strong potential for the PCAM tool to result in a greater range of services and support being enlisted in the care and support of those with LTCs, and especially for those patients from disadvantaged communities. This has the potential to reduce the burden on the NHS as the main or sole provider of care and support for many of these patients, who often end up with repeat hospitalisations and high levels of primary care use.
However, to date, the PCAM tool has not been evaluated for use by primary care PNs, and its potential value for addressing mental well-being in patients with LTCs has not been assessed, nor has it been subject to clinical trial to determine its impact on nurse behaviour and patient outcomes.
This research aimed to determine whether or not the PCAM tool can be used by primary care PNs to engage in holistic assessment of patients’ needs in those with LTCs, and particularly for those with multiple and complex needs. This tool encourages action to be taken based on the severity and urgency of the patient’s situation. Its use encourages a dialogue between the health-care practitioner and the patient, which serves to draw on practitioner skills, or even re-skill the practitioner in providing patient-centred holistic care, as opposed to the ‘de-skilling’ that has been reported by nurses through the tick-box mechanisms to improve quality of care. 10 It is hoped that future demonstration of the efficacy of the PCAM tool will transform how primary care engages with patients and their needs. It is also hoped that it will result in greater integration of health and social care needs and the co-ordination of meeting these needs, and that use of the PCAM tool can result in greater use of community and voluntary sector resources, as was demonstrated in the Keep Well evaluation in Scotland. The proposed PCAM tool can support making and strengthening such links, as it encourages nurses’ signposting to local (non-medical) resources. Such actions have the potential to reduce the current burden on ‘NHS-only’ use of services in the management of LTCs.
This research also aimed to determine whether or not a future full-scale randomised controlled trial (RCT) is feasible and whether or not the methods proposed for such a trial are acceptable, with the aim of developing a research protocol and application for funding for such a trial.
Aims
-
To assess the acceptability and implementation requirements of the PCAM tool for use in UK primary care, particularly in the context of PN-led annual reviews for people with LTCs.
-
To examine fidelity of the use of the PCAM tool by PNs in routine annual reviews of LTCs.
-
To assess the feasibility of conducting a full-scale trial of the effectiveness of the PCAM tool based on two potential units of analysis, namely intermediate-level nurse behaviour and longer-term patient well-being.
Research questions
Overall, this study sought to answer the following two main questions:
-
Is it feasible and acceptable to use the PCAM tool in primary care nurse-led annual reviews for those with LTCs?
-
Is it feasible and acceptable to run a cluster randomised trial of the PCAM intervention in primary care?
The pilot trial aimed to answer the following questions:
-
Can we recruit practices and nurses to take part in the study and retain them?
-
Can the practices and nurses implement study procedures correctly?
-
Are patients willing to complete questionnaires/outcome measures?
-
How many missing data are there, and does this relate to nurse- or patient-level follow-up?
-
What estimates of effect size, variance and likely intracluster correlation coefficient (ICC) should be used to inform the sample size of the full study? Should the unit of analysis be at the nurse or patient level, or is it feasible or necessary to include both?
Objectives
-
To conduct focus groups with primary care staff and patients with LTCs to assess acceptability and implementation requirements.
-
To conduct a cluster RCT in eight practices and with 16 nurses to test the acceptability and feasibility of running a full-scale trial of the PCAM tool in primary care.
-
To examine the fidelity of nurse use of the PCAM tool via a sample of audio-recorded consultations before and during implementation.
-
To explore nurse and patient perceptions of using the PCAM tool in annual reviews for LTCs.
-
To conduct a process evaluation to identify possible contextual influences on study implementation.
Structure of the report
The research is reported as five related research studies (studies A to E). Chapter 2 provides an overview of the overarching study design and conceptual framework for the research, and the general methodological approach to each of the individual studies. Chapter 2 also reports on the general management and conduct of the research, including ethics approval and patient and public involvement (PPI). Chapters 3–7 report on each of the separate studies (A–E), including their methods, findings/results and a discussion of the findings and conclusions. Chapter 8 presents on overall discussion, including the strengths and limitations of our work, a reflection on our PPI and summary conclusions and recommendations.
Chapter 2 Overview of study design, methodology and general management
Design
This study included a:
-
qualitative study of GP, PN and patient views of the acceptability and implementation requirements of the PCAM tool
-
feasibility study for a cluster RCT to test the acceptability and feasibility of conducting a future effectiveness trial
-
qualitative comparison of audio-recorded nurse consultations before and during the use of the PCAM tool to assess the fidelity of its use by nurses
-
qualitative study of nurse and patient perceptions of using the PCAM tool in assessments of patients with LTCs
-
qualitative process evaluation of the implementation of the PCAM tool and the trial implementation processes.
The feasibility cluster RCT contains the potential for two units of analysis, namely nurses (changes in nurse behaviour and consultation feedback on nurses’ behaviour) and patients (patient well-being and quality-of-life outcomes).
Methodology
Study A: acceptability and implementation requirements of the Patient Centred Assessment Method
The PCAM [formerly known as the Minnesota and Edinburgh Complexity Assessment Method (MECAM)] tool was derived from ‘INTERMED’, which was developed for use in acute settings. The INTERMED assessed biopsychosocial aspects of the patient and how they related to the health-care system, which, taken together, reflect ‘case complexity’. 17–19 The purpose of the PCAM tool was to provide a practical but systematic vocabulary and action-based evaluation system that could be applied to a primary care setting to improve the care, and self-care, of patients with multiple (complex) needs. An early version, the MCAM, was developed in the USA for use by clinical teams (doctors and nurses) for the case management of patients with medically unexplained symptoms. 19 Although the conceptual basis for assessing complexity has been established via the INTERMED and MCAM, further adaptation and validation was required for use in a UK health context. This has been undertaken by the current team in the context of adapting it for use in Keep Well health screening consultations. This resulted in the development of the PCAM, as an adapted version of the MECAM, for use in the UK. It was successfully implemented and evaluated with seven Keep Well nurses, and was shown to increase non-medical referrals, especially to psychological, social and lifestyle referrals. 20 Use of the PCAM tool was embedded into the Keep Well assessment by NHS Lanarkshire and was reported by the service lead to be making ‘a real difference’ to nurse engagement with the mental and social well-being of patients. The PCAM tool is also in use in the USA, where it is undergoing further testing.
It was therefore a reasonable theoretical assumption that the PCAM tool could be of value for primary care nurse engagement with the mental and social well-being of their patients with LTCs who are at higher risk of poor mental health and social problems. However, the ‘Keep Well’ context is not entirely comparable to routine primary care. ‘Keep Well’ services involved anticipatory health checks among ‘at-risk’ populations, with more time available at each consultation. The PCAM intervention had not been reviewed by GPs or PNs, and neither had its usability and acceptability been evaluated in primary care. Furthermore, there had been no patient input to the use of the PCAM tool. This initial study aimed to assess its ‘face validity’, acceptability and implementation requirements for use with PNs and their patients with LTCs. We would also gain qualitative knowledge surrounding primary care professionals’ views and readiness to conduct biopsychosocial assessments, and whether or not this tool could prove useful to GPs in their management of depression.
This study of ‘face validity’, acceptability and feasibility of primary care nurse use of the PCAM tool was conducted via focus groups with primary care practice teams. The inclusion of different members of the practice team was important, given the role of primary care nurses as ‘employees’ of the practice, whose work is determined by the practice (GP partners). The use of the PCAM tool also requires that other appropriate professionals may need to be called on if the nurse has identified areas of need, especially urgent needs. As the PCAM tool should facilitate nurse assessment and signposting to other professionals, including GP colleagues, ‘how’ the PCAM tool would work at a practice level was also important. In addition, as the role of practice managers (PMs) in implementing new initiatives in primary care was also taken into account, these members of staff were also included in the focus group study in assessing the feasibility, acceptability and implementation requirements for the use of the PCAM tool.
The discussion of the implementation of the PCAM tool at a practice level, as well as nurse use of the tool, and the discussion of adaptations that might be needed at a practice level (e.g. more time for nurse consultations in the early stages of use) made the focus group methodology and the inclusion of the primary care team appropriate.
Study B: feasibility study of a cluster randomised controlled trial of using the Patient Centred Assessment Method intervention in primary care nurse assessments of patients with long-term conditions
A feasibility study aims to assess the acceptability and practicality of a proposed project, and whether or not an intervention should be recommended for efficacy testing. 21 This feasibility study sought to assess the feasibility of the intervention for use in primary care, test the methods and protocol for a future trial of the PCAM intervention and consider whether or not it should be recommended for efficacy testing. This also included assessing which outcomes were feasible to collect and which outcomes may perform better or be more likely to detect change or improvement as a result of the intervention.
The recruitment of practices, and nurses within these practices, raised the possibility for two levels of clustering (practice and nurse level), and the question of whether or not a matched pairs design would be possible or more appropriate. There was the possibility that there would be more variation between nurses than between practices, and the decision to randomise at the level of practices was somewhat pragmatic; it was intended to reduce the number of practices needed to recruit sufficient nurses and to minimise nurse contamination caused by exposure to the PCAM tool of the nurses randomised to care as usual (CAU), if other nurses in the practice were using the PCAM tool. However, this feasibility study also had an added complexity in that there were two levels of outcome that were being observed: change at the level of the PN and change at the level of the patient. Therefore, nurses would also be included as a unit of analysis, and we determined patient recruitment to enable this. Although the overall design of the feasibility trial is complex (with baseline and follow-up being conducted both before and after randomisation of practices), this was necessary to observe changes at both the nurse level (where patients are also evaluating nurses’ caring behaviour) and the patient level.
A matched pairs design is used to explicitly control for confounding variables to eliminate the bias of these variables. We could have aimed to match nurses based on criteria likely to influence their delivery of the PCAM. However, besides assumptions of nurse experience being important, we do not currently empirically know which nurse characteristics should be included in any block allocation of pairs. We thought about which factors could be confounding and, therefore, included nurse demographic and clinical experience data alongside (patient-reported) caring behaviour as the most likely explanatory variables we could control for in a future matched pairs design. However, if we had paired nurses in this current study, we would have needed to recruit all nurses from different practices, as we could not have nurses from the same practice being paired to receive training or no training; the potential for nurse contamination was too great. This would have increased the overall number of practices required. Our chosen design of a cluster randomised trial with the practice as the unit of cluster would enable us to decide whether or not nurse variables are a significant bias that would necessitate a matched pairs design for a full trial.
Randomisation of matched pairs at the patient level (even if we also knew the likely confounding variables at this stage) would require PCAM-trained and untrained nurses to exist within the same practice and risk contamination, or for patients from one practice to be sent to another practice for their LTC consultation. Apart from the inconvenience to patients, it is likely that caring for another practice’s patients would result in changes in nurse behaviour. It would also add significantly to the complexity, costs (researcher input for patient consent to randomisation and a lengthy recruitment process) and ethical concerns of this study. A design based solely on patient outcomes would not allow for studying any changes or impact on nurse behaviour.
We aimed to conduct a feasibility study (not a pilot of ‘fixed’ trial methods) and hoped to use our findings to determine the best outcomes and units of analysis, and to determine whether our ‘efficient’ design (based on ease of recruitment of practice, nurses and patients) was robust or if confounding variables would need to be controlled for in future randomisation processes.
Studies or trials of complex interventions also allow for the inclusion of more than one primary outcome. A feasibility study can help to determine which outcomes are more likely to be able to detect sufficient levels of change, and the degree of change observed can help to determine the likely numbers needed in a full trial to detect a sufficient level of change. This study was set up to include the collection of potential measures of change in nurse behaviour, as well as the collection of a set of measures relating to outcomes for patients. Nurse behaviour change was measured in several ways: patient assessment of the nurses’ consultation skills, as measured by the Patient Enabled Instrument (PEI)22 and Consultation and Relational Empathy (CARE)23 measure; changes in nurse confidence with mental health, as measured by the Depression Attitude Questionnaire (DAQ);24 changes in nurse consulting behaviour, as observed before and during the PCAM intervention via the recorded and coded consultations with patients; and changes in nurse referral patterns collected before and during the PCAM intervention.
Patient assessment of nurse consultation skills (measured by the PEI and the CARE measure) can be measured only post consultation; therefore, this necessitated obtaining baseline scores for all nurses before they were randomised to the PCAM intervention or CAU and after randomisation. This then resulted in two cohorts of patients being recruited at baseline and after randomisation. The longer-term outcomes for patients following their consultation were also followed up for all nurses at baseline and post randomisation. The inclusion of nurse baseline assessment added to the complexity of the design of this study, but this serves to demonstrate the need for alternative trial methods when multilevel interventions are delivered in complex care settings such as primary care.
Patient outcomes were assessed by the General Health Questionnaire (GHQ),25 the Short Form questionnaire-12 items (SF-12)26 and the Warwick–Edinburgh Mental Well-Being Scale (WEMWBS)27 immediately post consultation and at the 8-week follow-up.
Study C: fidelity of use of the Patient Centred Assessment Method by nurses
Taking an approach based on the early work of Engel,28 the aim of the PCAM is to encourage more holistic consultations by primary care professionals (in this study, PNs) and to ensure that nurses pay attention to a broader range of the biopsychosocial needs of patients. This is done within a patient-centred framework and a chronic disease management model.
There have been many theories and models derived from the analysis of structures, processes and outcomes occurring during traditional medical consultations. 29–32 More recently, these have included the role of the patient in health-care provision, with the aim of improving quality outcomes for patients. 33,34 However, the majority of ‘consultation’ work in primary care has been focused on the interaction between the patient and the GP, with little attention to nurse consultations. More recently, with attention to changing roles in primary care, such as the ‘nurse practitioner’, there has been some discussion around which of the existing (medical) consultation models might apply to primary care nursing. 35–37
In a similar vein, there are validated coding tools for assessing communication skills and empathy in medical consultations, such as the Verona Coding definitions of Emotional Sequences,38,39 a consensus-based system for coding patient expressions of emotional distress in medical consultations, defined as cues or concerns, and the Roter Interaction Analysis System40,41 as a method for coding medical dialogue. However, these would not meet the needs of this study in assessing whether or not nurses were implementing the PCAM tool as intended, which should be assessed by determining whether or not nurses did indeed explore the biopsychosocial needs of patients and whether or not they did this in a patient-centred conversation, as opposed to a ‘tick-box’ exercise. The study therefore required the development of a bespoke coding frame, and one that could be applied systematically by more than one researcher to recorded transcripts of nurse–patient interactions.
We developed a coding system for classifying conversation segments according to whether or not they address any of the domains/items within the PCAM tool (and which ones are discussed), whether or not they identify or acknowledge needs against each of the domains and whether or not they discuss potential actions against each of the domains. This coding frame was then applied to recorded consultations with a sample of nurse–patient interactions that occurred both before and after the nurses were trained in the use of the PCAM tool in order to understand whether or not they were already consulting in a way that helped to address biopsychosocial needs or if there had indeed been a change in their behaviour following training and use of the PCAM tool. The specific coding system and the analysis of recorded consultations is reported in Chapter 5.
Study D: nurse and patient perceptions of using the Patient Centred Assessment Method in long-term condition annual reviews
In assessing the acceptability and feasibility of using the PCAM tool in primary care, it was important to gain some perspectives from nurses and their patients following nurse use of the PCAM tool in patient consultations. All nurses who were allocated to receive the PCAM intervention were invited to participate in a qualitative interview of their experiences of its use. For those patients recruited by nurses to complete outcome-based questionnaires, the follow-up questionnaire contained an invitation for patients to also participate in a follow-up interview if they wished. Individual interviews were chosen because the numbers involved were small (maximum of eight nurses and two patients per nurse), and individual rather than ‘group’ experiences were important to capture at this stage. Patients were asked about their own personal experience of the consultation and any advice or actions that the nurse had initiated at this consultation.
Study E: process evaluation
A qualitative process evaluation was conducted in order to identify possible contextual influences on both the implementation of the PCAM and the feasibility trial, and to identify any barriers to PCAM use or implementation of trial processes. This consisted of data from the early focus groups with practices and patients on the acceptability and feasibility of use of the PCAM, researcher field notes of meetings and discussions with staff and any comments made to the research team or reported by practice staff from patients during implementation, data from the final interviews with practice staff and patients, and open-ended questions on staff and patient questionnaires. The process evaluation was based on the Medical Research Council (MRC) guidance for best practice and its key components as identified by Moore et al. 42 (Figure 1).
FIGURE 1.
Key functions of a process evaluation. Based on Moore et al. 42 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
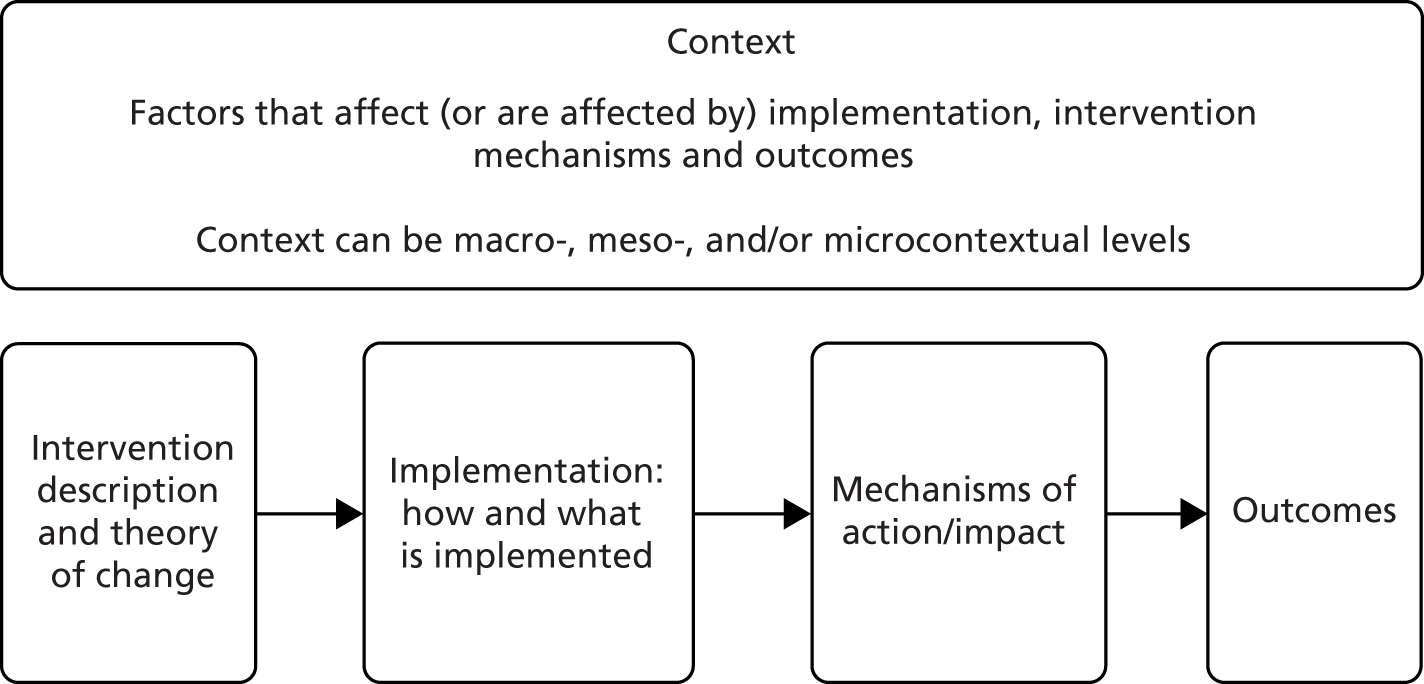
The process evaluation aimed to gather knowledge around the implementation or use of the PCAM tool in primary care as well as around the implementation of the proposed trial methods in each of the different practice settings. The intervention description and its causal assumptions are described in The Patient Centred Assessment Method: intervention description. This will be reflected on in Chapter 7, in which the data on context, implementation and mechanisms of impact are described, including how these differed across sites.
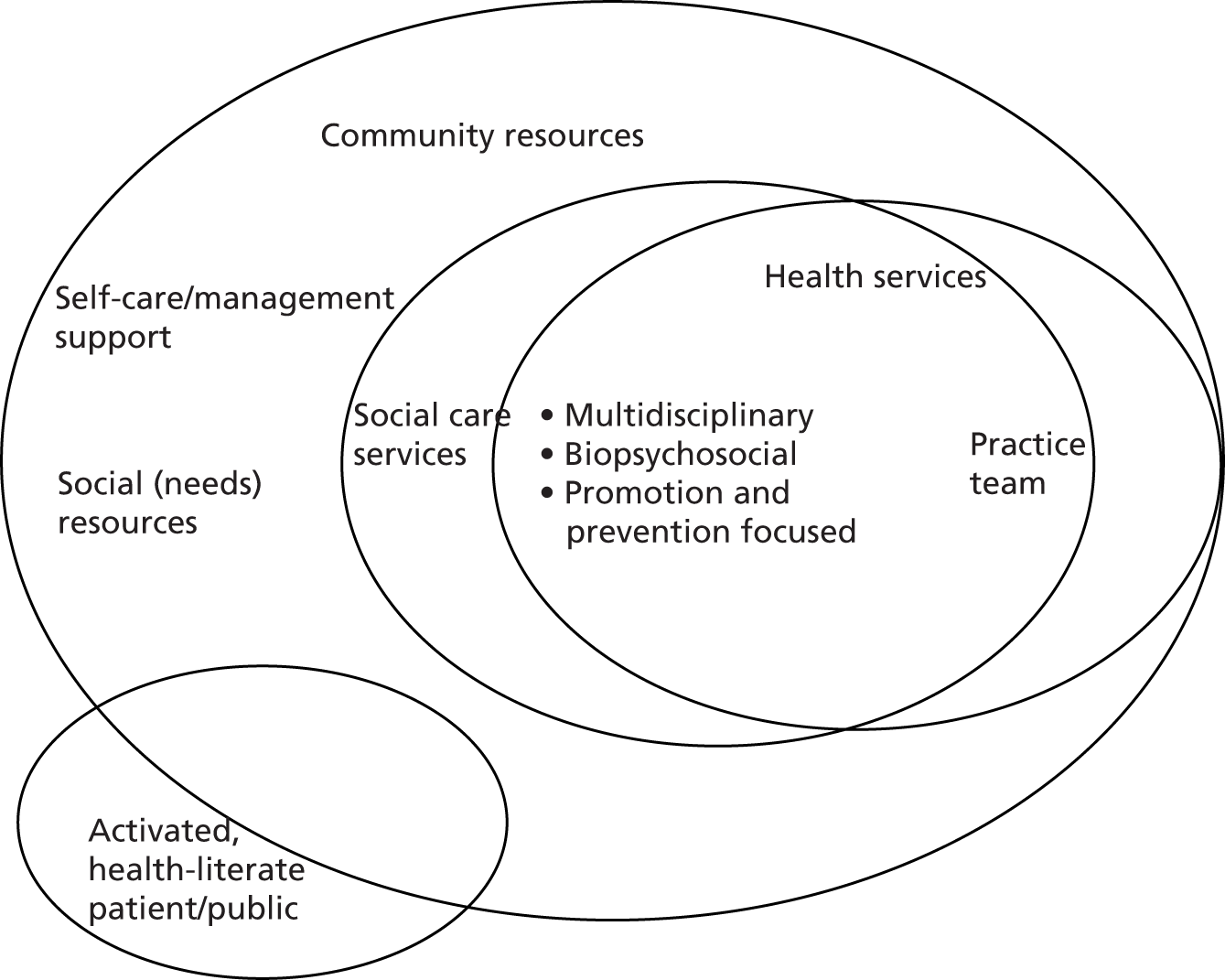
Theoretical/conceptual framework
The conceptual models used to consider how to address LTCs were influenced by the chronic care model (CCM)43 (Figure 2); however, the CCM has been criticised for failing to articulate, in greater detail, what the community resources aspect of the model could consist of. 44,45 Although the CCM provides a comprehensive and well-tested model, it suggests that the ‘informed, activated patient’ somehow sits outside the broader social influences of the community and health system. However, research on LTCs shows a compelling link with broader social determinants of health,2 and it could be useful to find a way to make these social determinants and patient experiences more central to the conceptual model. This would re-emphasise the role of broader social determinants not as outside influences on the interactions between patients and providers, but as a key part of patients’ overall experience of becoming unwell and living with a LTC. Finding ways to facilitate productive interactions throughout all levels of the patient/ provider experience then becomes the methodological challenge of adapting the CCM to a model that integrates the social determinants of health that are so central to the experience of patients living with LTCs. This research would test the role of the PCAM tool in furthering the conceptual frameworks used to understand the care and experience of patients living with LTCs.
FIGURE 2.
A model for chronic care management.
The Patient Centred Assessment Method: intervention description
The PCAM aims to provide a systematic language for the integrated assessment of a broad range of physical, mental well-being and social needs. It is also ‘action oriented’, so that if needs are identified – even if these extend the professional boundaries of providing physical health care – they will be acted on at some level. It is an intervention that fits with the CCM for the improvement of chronic illness care in that it is intended to link the health system with community supports, encourage and support self-management approaches, specifically encourage more productive (nurse) interactions with patients that should lead to more motivated patients, facilitate decision support (by nurses) to improve the care of patients and encourage a proactive practice team.
The ‘PCAM intervention’ being implemented in this feasibility study is fully described using the Template for Intervention Description and Replication (TIDieR) checklist46 (see Appendix 1). It consists of three elements:
-
the PCAM assessment tool
-
a half-day (or equivalent length) training course to support the use of the PCAM tool
-
a resource pack with locally relevant and operational services to support needs identified during the nurse–patient interaction using the PCAM tool.
Following a half-day of training in use of the PCAM tool, nurses were encouraged to use the PCAM tool with 10 patients to gain confidence in its use before starting the formal implementation phase. Intervention sites were supported by the project team to assist with embedding the PCAM tool into routine practice and to support clinic participation in the research study.
The Patient Centred Assessment Method tool
The PCAM tool involves nurses making an assessment of their patient in each of the following domains:
-
health and well-being (covering physical health needs, the impact of physical health on mental health, lifestyle behaviours, mental well-being)
-
social environment (covering home safety and stability, daily activities, social networks and financial resources)
-
health literacy and communication (covering understanding of symptoms, self-care and healthy behaviour and how engaged the patient is in discussions)
-
service co-ordination (how comprehensively, and efficiently, health and social care services currently meet patient needs).
These then lead to action-oriented tasks to deal with the identified problem, which may include referral or signposting to other professionals or agencies. The PCAM tool is provided in Appendix 2.
Patient Centred Assessment Method training
The training was designed to give nurses an understanding of the social determinants of health and how social factors can influence morbidity and mortality. They also learned about the comorbidity of physical and mental ill health, building a picture of why it is important to conduct biopsychosocial assessment and address broader health needs. They were then introduced to the PCAM tool and discussed ways in which knowledge of patients’ circumstances can be elicited as part of a conversation (not a tick-box exercise), and in a naturalistic way that builds on their communication skills. For more detailed information about the PCAM training, see Appendix 3.
Patient Centred Assessment Method resource pack
The PCAM resource pack is a list of local, regional or national groups, organisations and information sources for use by PNs as potential signposting/referral opportunities for patients with LTCs.
Referral and signposting opportunities presented within the resource packs were those covering psychosocial problems within the PCAM domains. For more detailed information about the PCAM resource pack, see Appendix 4.
Control or ‘care as usual’
Nurses in control or CAU practices delivered CAU to their patients. Until April 2016 in Scotland, this was guided by the requirements of the QOF for LTCs, such as DM and CHD. During the development of this study and its funding, the QOF requirement for screening for mental health problems in LTCs was removed, but nurses could still, and indeed were encouraged by NICE guidelines to, include some attention to mental health and well-being in their annual assessments. Normal referral systems or pathways of care would be maintained for patients in the CAU practices.
Research ethics
A favourable ethics opinion for the overall study was granted by the West of Scotland Research Ethics Committee [reference number 14/WS/1161; Integrated Research Application System (IRAS) 168310]. Individual site approvals were then obtained from NHS Greater Glasgow and Clyde (NHS GGC), NHS Forth Valley (NHS FV) and NHS Grampian. All changes to the protocol were reported to the Research Ethics Service and approved as minor amendments.
We ensured that all accompanying documentation sent to the NHS Ethics Committee was produced in partnership with the Health and Social Care Alliance Scotland (the ALLIANCE), which represents nearly 400 bodies and individuals working to make the lives of people with LTCs and disabilities, and the lives of unpaid carers, better. More than three-quarters of its member organisations are voluntary groups that support or represent disabled people, people living with LTCs and unpaid carers. We also recruited two PPI representatives early in this process to enable them to contribute to all study documentation prepared for the NHS Ethics Committee (letters of invitation, information and consent forms, etc.). These PPI representatives also served on our project management group (PMG) throughout the study.
Patient and public involvement
Our aims for PPI were to conduct research with members of the public, taking on board their expert advice in the design and conduct of our study, especially in relation to the presentation of our study and its materials to our patient/public/carer audience (through commenting on, and developing, research materials); ensuring continued input to the conduct of the research as members of a project steering group; and ensuring that our dissemination strategy and our key messages were clear and targeted appropriately for patient/public/carer audiences. This would ensure that the language and content of information provided were appropriate and accessible (e.g. in questionnaires and patient/participant information leaflets); the methods proposed for the study were more acceptable and sensitive to the situations of potential research participants; and our research would capture outcomes that are important to the public, and we would ensure that the findings of our research were accessible to the public. This amounted to three levels of public involvement (out of a possible six) endorsed by the National Institute for Health Research (NIHR), namely as joint grant holders or co-applicants on a research project, as members of a project advisory or steering group and commenting on and developing patient information leaflets or other research materials. However, we also included a further level around enhancing dissemination activity and outputs, especially for public audiences.
Patient and public involvement in preparing this application was provided via the ALLIANCE. The ALLIANCE is the national third-sector intermediary for a range of health and social care organisations. It has over 1700 members, including large, national support providers, as well as small, local volunteer-led groups and people who are disabled, living with LTCs or providing unpaid care. The ALLIANCE’s vision is for a Scotland where people of all ages who are disabled or living with LTCs, and unpaid carers, have a strong voice and enjoy their right to live well, as equal and active citizens, free from discrimination, with support and services that put them at the centre. Our key contact within the ALLIANCE was a full partner on this project and also shared the protocol with ALLIANCE members. They commented on the proposal during its development and specifically on issues of recruitment of patients, and the feasibility of patient data collection processes. They also provided current experiences of members of their health assessments in primary care to inform the feasibility and applicability of the research.
Three patient representatives were recruited to the study on a formal basis; two attended all PMG meetings and another commented on all documentation provided to the Study Steering Committee (SSC). One member of the PMG was already known to the project team from PPI in a previous study led by the RCGP. The second member of the PMG was recruited via an e-mail from NHS FV to its PPI advisors, and the PPI member recruited to the SSC was recruited in the same way. All PPI members were offered support to participate by the ALLIANCE, but no PPI member requested such support, and most were experienced as PPI representatives or felt that they had sufficient life experience to confidently participate and contribute.
The ALLIANCE representative (CH) attended all PMG meetings and was available for emotional support in relation to the PPI’s project advisory role if required. In the event that there was any concern for the health and well-being of our PPI members, we also had a GP team member (SM) who could provide some initial advice, with the proviso that they then contact their own GP. Neither Christine Hoy nor Stewart Mercer was called on to act in these capacities.
We used the NIHR cost calculator for public involvement, in conjunction with advice from the ALLIANCE about appropriate levels and methods of remuneration for patient/public involvement, to ensure that we had the funds to support this.
Project management
Margaret Maxwell was responsible for overall project delivery and worked on a day-to-day basis as required with the project manager (CH) and the two part-time research assistants (RAs).
Carina Hibberd was project manager and supervised the two part-time RAs on a day-to-day basis and conducted fieldwork alongside the RAs as required, as well as being responsible for adapting and delivering the training to nurses.
There were weekly meetings between Margaret Maxwell, Carina Hibberd and the RAs to report on study progress and timelines, and to deal with any immediate problems. Nadine Dougall and Rebekah Pratt also attended these meetings, as required, to ensure that preparation for data collection and subsequent data management and analysis were robust. Video and telephone conferencing was available to minimise time and travel when attendance was required.
Formal PMG meetings were held with all co-applicants and other members of our PMG, including our patient/carer representatives. These included a feedback report on study progress and discussion of any problems/issues arising.
An independent SSC was established with four members: Professor Brian McKinstry (University of Edinburgh, Professor of Primary Care and practising GP) to chair the committee; Dr Ruth Jepson (University of Edinburgh, Senior Scientific Advisor, Scottish Collaboration for Public Health Research and Policy); Dr Dorothy Horsburgh (Edinburgh Napier University, Senior Lecturer, nurse and specialist in LTCs); and one PPI member. Dr Horsburgh retired during the study and was replaced by Dr Debbie Baldie of Queen Margaret University. Observers such as a sponsor representative, a representative of the Scottish Primary Care Research Network (SPCRN) and any members of the research team could be invited at the request of the chairperson.
Formal SSC meetings (n = 4) were held in Edinburgh and consisted of a feedback presentation and supporting documentation, including any ethics amendments and their outcomes, interim reports to the funder (NIHR) and minutes of the PMG.
Analytical framework
Quantitative analysis
The primary outcome of the pilot trial was to determine recruitment and retention rates of PNs, and the recruitment of patients and data completion for a future cluster RCT. We also wanted to establish which nurse- and patient-level measures should constitute primary and secondary outcomes for a future cluster RCT and, hopefully, use this knowledge to determine sample size for a future trial. The study combined data collection for nurses and patients as two separate units of analysis. One of the criteria for continuation to a full-scale trial would be to determine if the number of nurses required for a cluster RCT was feasible and within reasonable cost boundaries. Such a design would also need to be sufficiently powered at the patient level, thereby testing the impact of the PCAM tool on both nurse behaviour and patient outcomes.
The characteristics of the nurses and patient groups and their related outcome measures were summarised using descriptive analysis. The related outcome measures were summarised using descriptive analysis together with estimates of precision, and any relevant change scores. Some modifications were made to the statistical analysis plan that was created at the time of requesting funding for the study. Since then, there has been a shift in expert guidance advising against all formal significance testing for pilot and feasibility study outcome measures, as these are not powered to detect statistical significance. Therefore, formal significance testing was omitted, as was the use of the multiple regression modelling approach. The focus of the analysis centred on the recruitment, data completion and attrition rates, and making use of descriptive analysis to summarise the data. The PEI and CARE measures were analysed at the nurse level and the 12-item General Health Questionnaire (GHQ-12), SF-12 and WEMWBS were analysed at the patient level. Both units of analysis were summarised between randomisation groups, using means and standard deviations, or medians and interquartile ranges, together with change scores estimated with their 95% confidence intervals (CIs). The number of practices recruited and the number of nurses recruited were less than planned, and this also ruled against the use of formal regression models to explore the influence of covariates on outcome measures. In addition, as the number of clusters was so low, and as some of the follow-up data were missing, the estimation of the ICC for the outcome measures was not appropriate.
Data management and quality assurance
All paper questionnaire forms were pseudonymised and double locked. Digital data were stored on a shared, password-secured folder on the University of Stirling intranet. Questionnaire data were managed using Microsoft Access® 2007 (Microsoft Corporation, Redmond, WA, USA). The front end of the database was designed to simplify data entry and quality checking. Data were entered and quality checked (paper to digital) by a different member of the research team. This was completed for each form before follow-ups were posted. Digital data were regularly quality checked and an audit trail maintained.
Following acceptance of the study final report to the funder, identifiable patient contact details (used for focus groups and interviews) were destroyed. At this point, practices were also asked to destroy any identifiable lists of patients approached for the study. All digital and paper data have been archived and managed in accordance with the NHS Ethics Committee, research and development and University of Stirling policies.
Qualitative analysis
Qualitative data analysis of focus groups and interviews followed the social constructivist version of grounded theory, through which themes and subthemes were identified in the data. 47,48 The social constructivist approach is an iterative process of review that allows for the incorporation of existing knowledge and literature that can be drawn upon in the analysis process. 47,48 NVivo 11 (QSR International, Melbourne, VIC, Australia) software was used to help facilitate the interviews. In an iterative process, all focus group transcripts and interview transcripts were reviewed by multiple team members to identify key themes in relation to our research questions. These themes were discussed and amended until a core set was agreed for use as a final coding frame, which was systematically applied to all data. The research team met throughout the analysis process to review the emerging themes and discuss areas of agreement or divergence until consensus was reached. Additional details on the qualitative data analysis are included in Chapters 3 and 6.
The analysis was specifically intended to identify barriers to, and facilitators of, adoption/use, and was informed by the normalisation process theory (NPT). 49 The NPT offers an explanation of the work of implementation, embedding and integration, and specifically focuses on the contribution of individuals and groups as agents of change. The NPT helps to explain how practices can become embedded in organisational and professional contexts. There are four generative mechanisms to help explain how change can be adopted and embedded: coherence (sense-making), cognitive participation, collective action and reflexive monitoring. The production and reproduction of a practice requires continuous investment by agents (in this case, PNs) over time. NPT mechanisms are constrained (or aided) by the operation of norms (notions of how beliefs, behaviours and actions should be accomplished) and conventions (how beliefs, behaviours and actions are practically accomplished).
The NPT generative mechanisms and their constructs have provided a framework for analysis of the qualitative data, to help understand and think through implementation problems and to help identify techniques to solve them. This was drawn on at the start of the project, using the focus group data, to help shape improvements to the implementation process and the training materials. Researcher field notes and post-implementation interviews were then also subsequently used to identify further barriers to, and facilitators of, adoption.
Analysis of audio-recorded consultations
The analysis of audio-recordings consisted of classifying conversation segments according to whether they attended to physical health, mental well-being or social elements of care. The range of social circumstances attended to were also identified. The PCAM tool should encourage a conversation flow that attends to well-being and social circumstances throughout the consultations (not leaving it until the end, when time may be limited). The analysis, therefore, also included attention to when conversation segments appeared in the consultation. Attending to a mix of physical health, mental well-being and discussion of social circumstances through the consultation, and discussing a range of social circumstances, was considered to be maintaining fidelity to the PCAM tool. It could be the case that nurses were already familiar with a patient’s social circumstances, but they would still be expected to enquire about these – to ask how patients were getting on or about any change in circumstances. A list of codes by which to classify segments, based on the domains within the PCAM tool, was developed by the research team and consistently applied to all consultation recordings before and after nurse training in the use of the PCAM tool.
Integration and synthesis of data sets
Overall, the qualitative and quantitative analysis aimed to determine whether or not and how a future cluster trial should proceed. This included assessing whether or not recruitment, retention and data collection were achieved to a sufficient level, and whether or not the outcomes used were sensitive enough to detect change (at what level and for whom), as well as identifying any key methodological issues in converting from a feasibility or pilot trial to a full-scale trial, as established by Shanyinde et al. 50 We used a tool known as ‘A process for Decision-making after Pilot and feasibility Trials’ (ADePT). 51 The ways in which researchers decide to respond to the results of feasibility work may have significant repercussions for both the nature and degree of tension between internal and external validity in a definitive trial. The ADePT decision aid is described and reported alongside the process evaluation in Chapter 7.
Chapter 3 Study A: acceptability and implementation requirements of the Patient Centred Assessment Method
Methods
Introduction
Embedded in the overall PCAM study, this first project was designed as a qualitative study of GP practice staff, including PNs, and patient views of the acceptability and implementation requirements of the PCAM. The project aimed to elicit views on the PCAM approach as a model for conducting reviews of patients with LTCs and to identify barriers to, and facilitators of, the implementation of the PCAM tool in practice.
Recruitment and sample
Sample 1: professional staff groups
The target for this study was to conduct four focus groups, each comprising between five and eight GPs/PNs. The inclusion criteria specified that we would aim to recruit medium-sized or large GP practices (with over four partners or list sizes above 3500 patients) based in NHS GGC or NHS FV. This was to reflect the majority of practices across Scotland.
The SPCRN facilitated recruitment of GP practices for participation in the focus groups. The SPCRN selected practices from its database reflecting the same demographic mix as for the pilot trial participants, but, to avoid contamination, these were a separate set of practices from those in the feasibility trial. The SPCRN sent out 89 e-mails inviting PMs in eligible practices to participate. A minimum of 1 week after invitation letters were sent, research staff followed up by contacting 43 practices by telephone to invite their practices to participate.
Participants signed consent forms prior to the start of the focus group discussion. Participants were given a paper copy of the presentation slides for reference at the start of the focus groups. Each focus group was recorded and transcribed verbatim.
Sample 2: patients
The target was to conduct two focus groups comprising 8–10 patients per group of mixed age/sex, and which reflected the social demographics of participating practices. Patients were eligible for inclusion if they were aged over 18 years, registered with the GP practice, living with a LTC [mainly DM, CHD or chronic obstructive pulmonary disease (COPD)] and required a long-term review.
Patient recruitment was facilitated by the SPCRN. With the approval of participating GP practices, the SPCRN extracted and numbered patient lists using inclusion criteria. GPs reviewed lists to exclude anyone who would have difficulty travelling to the practice or participating in a focus group (e.g. owing to cognitive or communication impairment). Eligible patients were sampled based on multiples of 5 (number 5, 10, 15, etc.). Letters of invitation were sent by the GP practice in batches of 10 until sufficient opt-in responses were received. In NHS FV, 50 letters of invitation were sent from one practice and, similarly, in NHS GGC, 100 letters of invitation were sent from one practice. Patients opted in to the focus groups via a prepaid reply slip, text, telephone or e-mail, and were then contacted by researchers to confirm attendance and to inform them about focus group arrangements.
All focus group participants signed consent forms before the start of the focus group discussion. Participants were given a paper copy of the presentation slides for reference at the start of the focus group discussions. All patient participants were given a £10 gift voucher after the focus group and travel costs were reimbursed. Each focus group discussion was recorded and transcribed verbatim.
Ethics considerations
Participants were asked at the start of each focus group discussion to not mention the names of staff or non-participants, and to respect the confidentiality of other participants. Researchers also informed patients that if they raised any questions in relation to their personal health issues during the focus group discussion, researchers could not respond to these and they were, therefore, advised to contact their GP.
Data collection
All focus groups were conducted using topic guides as a framework for discussions. Professional groups aimed to address the implementation of the PCAM tool within annual reviews of patients with the LTCs specified, along with determining any potential barriers to the use of the model and how these could be overcome. As the NPT was used as an analytic framework, the topic guides aimed to identify whether or not, and in what ways, nurses and other practice staff considered the PCAM to differ from existing ways of working; whether or not nurses and GPs could come to a collective agreement on the purpose of the PCAM; how practice staff understood what the PCAM required each of them to do; whether or not nurses and other practice staff constructed a potential value for the PCAM in the context of annual reviews; and whether or not nurses and other practice staff believed that the PCAM was an appropriate part of their work. Practical issues relating to the implementation of the embedded feasibility RCT and the PCAM in general were discussed to allow consideration to be given to how the individual requirements of different practices might be taken into account. This included discussion of what training may be needed to enable the use of the PCAM and how this could be delivered.
Patient focus groups aimed to discuss how wider psychosocial factors impacted on patients’ health and also how their LTC(s) affected their lives. Topics for discussion included what support patients needed to manage their conditions and whether or not primary care practitioners should play a role in helping them to manage life difficulties that might, potentially, have an impact on their health. The PCAM was then explained to patients and they were invited to discuss whether or not it was acceptable to them and whether or not they considered it useful in relation to their care. Patients were asked how PNs might best raise sensitive or difficult issues with them, and they were also asked about any potential barriers that nurses may experience in using the PCAM.
Data analysis
Data analysis involved constant comparison of key ideas/themes emerging from multiple staff reviews of focus group transcripts. Carina Hibberd, Eileen Calveley and Patricia Aitchison reviewed and compared patient and staff focus group transcripts as they became available. Use of the constant comparative technique within the ‘framework’ method enabled the identification of emergent themes for exploration in subsequent focus groups. 52
Data sources (focus group transcripts) were imported into an NVivo 11 database, which was then used for data management and the facilitation of analysis. Data from staff and patient focus groups were organised separately within the database. Only designated members of the research team had access to the database.
Carina Hibberd, Patricia Aitchison and Rebekah Pratt conducted initial, independent thematic analyses of focus group transcripts to devise a coding frame that was then discussed in detail by the wider analysis group (CH, PA, RP, EC and MM). Where required, analytical codes were amended at this stage by Rebekah Pratt, and descriptors were created to avoid duplication or lack of clarity in meaning. Rebekah Pratt recoded the entire data set based on the amended codes.
From this thematic analysis, a higher-level theory-driven analysis was conducted to organise coded data into more helpful explanatory themes, with attention given to reflecting on these explanations for participation, engagement, adoption and adaptation in line with NPT constructs. For the purposes of this report, the key elements of analysis that are relevant to the acceptability and feasibility of using the PCAM tool in primary care-led annual reviews for LTCs, and for answering questions on the feasibility of a cluster RCT, are presented. The theory-driven NPT analysis will be presented in a future publication.
Findings
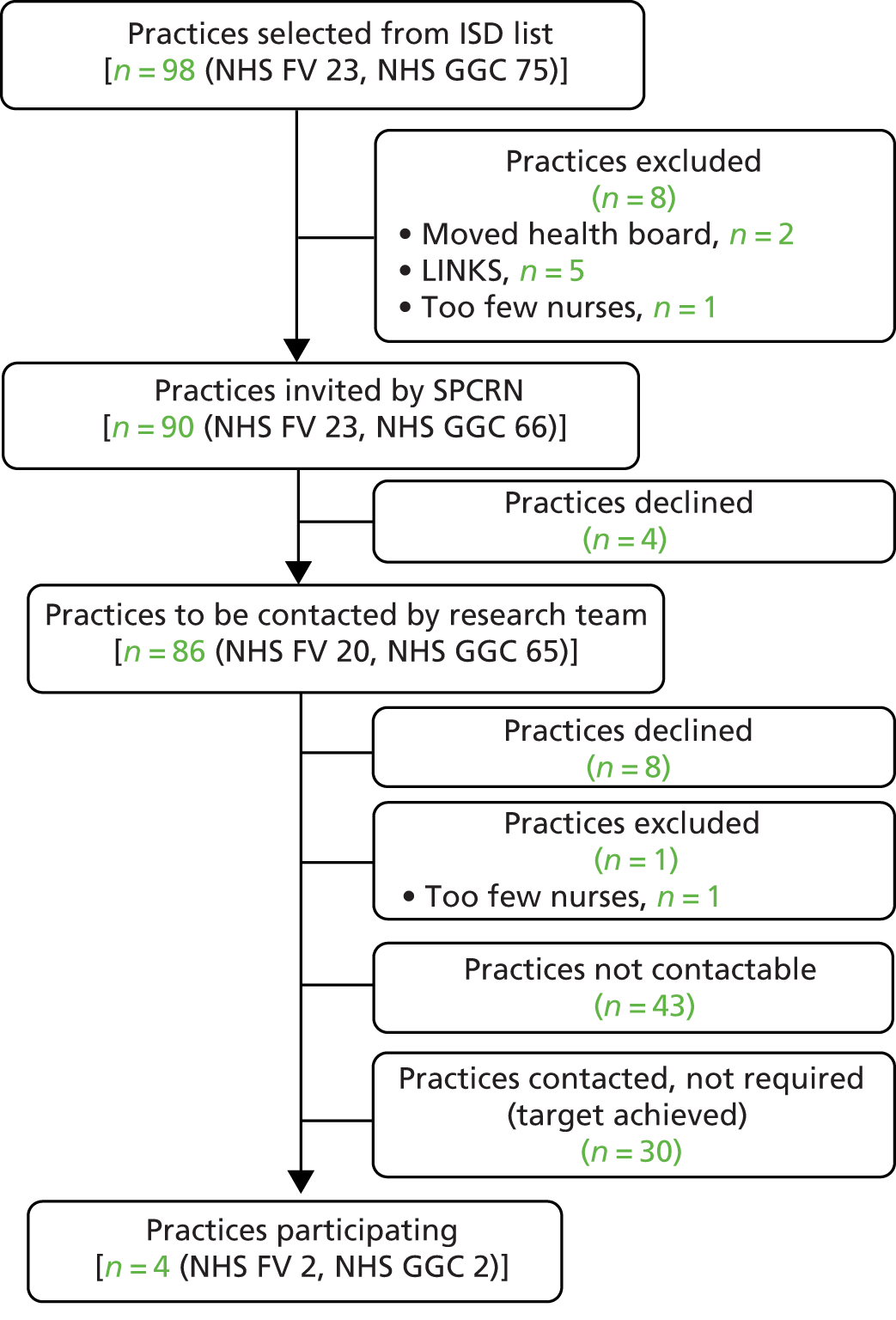
Recruitment of practices
Figure 3 shows the number of GP practices contacted and subsequently recruited for focus group participation. Four practices agreed to take part in focus groups following telephone contact by researchers, two practices within NHS FV and two practices within NHS GGC. Our recruitment target for the number of focus groups was met.
FIGURE 3.
The recruitment of practices to the focus group study. ISD, Information Services Division of National Services Scotland; LINKS, National Links Worker Programme (funded by the Scottish Government to make links between people and their communities through their GP practice).
Recruitment to staff focus groups
Sixteen health-care staff participated in the four focus groups. Participating health-care staff included PNs (n = 7), GPs (n = 3), PMs (n = 3), assistant PMs (n = 1) and administrative/reception staff (n = 2). The duration of staff focus group sessions ranged between 47 and 72 minutes. The four staff focus group sessions were held in the GP practice.
Recruitment to patient focus groups
Two of the four participating GP practices agreed to host a patient focus group. A total of 27 patients returned a note of interest, of whom one could not be directly contacted, seven declined or could not attend, two agreed but did not attend and 17 attended and consented. As intended, patient focus groups included a mix of age groups and sex, and reflected the social demographics of participating practices (Table 1).
| Participants and demographics | Sex (n) | |
|---|---|---|
| Male (N = 7) | Female (N = 10) | |
| Age (years) range | 66–83 | 47–83 |
| Employment status | ||
| Retired | 5 | 6 |
| Paid/self-employed | 1 | 1 |
| Housewife/husband | 1 | 1 |
| Voluntary work | – | 1 |
| No data (long-term sickness) | – | 1 |
| LTCa | ||
| DM (type 1) | 1 | 1 |
| DM (type 2) | 3 | 6 |
| CHD | 5 | 5 |
| COPD | 2 | 2 |
One patient focus group was held in the GP practice, and one patient focus group was held in a local community centre because of limited meeting space in the GP practice. The duration of each patient focus group was 105 minutes.
Patient perceptions of living with a chronic illness
Participants described the struggle of coming to terms with living with a chronic illness. Some described a tension between rejecting their diagnosis and accepting the limitations of their condition, and how that had an impact on their ability to manage their condition. Some had been told that they had DM, but felt that being asymptomatic made it hard to believe that they really did have the condition. Some described spending time, even years, in denial about their condition. This rejection of their condition led to avoidance of doctors, being scared of coming to the clinic, not taking medications and not looking after their health. One participant reflected on rejecting her condition after a negative experience with her GP, and is now facing serious kidney damage.
Participants also reflected on the process of coming to terms with their condition, often describing a period of surprise followed by learning how to adjust and adapt to managing their condition. Some noted that there could be experiences that had a negative impact on their confidence, which may take some time to rebuild. Some described a longer process of having to come to terms with more than one condition, which may lead to more complications and care in managing their health.
During the focus group session, participants shared with each other the many limiting aspects of living with their particular condition. Some were feeling generally well, but others were navigating more complex medical needs, such as surgery and therapies. Many reflected on various losses, such as limiting their food or activities. Participants also described feeling the need to just carry on and make the best of their situation. Some felt that they should be grateful and took comfort in feeling that things could be worse:
But other than that I’m just quite happy, jog along, but every day’s a different day of course you just . . . what I can do today, I’m fine if I can, well tomorrow, but tomorrow doesn’t come, but I just suit myself how I jog along kinda thing, but as I say I can’t complain when I listen to what other people have got, you know, but I’ve enough to be going on with quite honestly [laugh]!
Patient 14
In relation to managing physical aspects of a chronic condition, participants described a period of learning about their condition, mostly through medical appointments and the development of systems to keep track of timing medications. However, participants described their challenges as not just being related to the management of their condition, but also dealing with limitations in daily life more broadly. A small number of participants in the focus groups described very positive, and even life-changing, experiences of taking part in exercise courses (as suggested by their nurse). These participants felt that exercise had led to positive changes in weight, wellness and mood:
So I went on that course and it was 12 visits to the course over a few weeks/few months, and I found that’s been a great help. What it’s actually done to me is it’s not only helped my COPD, it’s helped me mentally because I’m quite a shy person and I want to help myself but I can’t, I want people to help me but because my wife looks after my every need, but it’s to force me to get my a*** off my chair and go and do something.
Patient 34
Participants talked about how difficult it could be to make changes in their lifestyles, even when they knew that it would help with their health. They felt that changing habits around eating required constant attention and monitoring. Some felt that it was hard to ask for help with changes, partly because it took away feelings of independence. Some participants described how they also needed to manage their mental health, as there were difficult days of feeling down or not coping, and a tendency towards self-isolation:
You want to stay in and put a blanket round you but you’ve just got to kinda’ motivate yourself.
Patient 32
Although learning about their condition and how to manage it was a process participants went through, they also described the impact of their condition more widely, in terms of challenges with daily activities and lifestyle adjustments. In this sense, PCAM-related topics are consistent with the broad range of concerns that patients have about their condition.
Professional and patient views on acceptability of Patient Centred Assessment Method topic areas
Professional and patient participants were asked to reflect on how they would feel about a broader range of biopsychosocial questions, as is reflected on the PCAM assessment, being discussed in consultations relating to LTCs. To a certain extent, patient participants felt that their nurses already asked a broad range of questions about how they were and, in particular, participants felt that district nurses might observe more social and environmental aspects of a patient’s life on home visits. There was a wide range of opinions on how participants felt about the potential of being asked about biopsychosocial aspects of their health. Professional participants also reflected on this wide variety of opinions, with some participants much more familiar or comfortable than others with asking patients about the broader context of their lives. In Mental health, Health literacy and Social environment and finances, we discuss responses to these potential discussions for patient and professional respondents by general topic area.
Mental health
There was a general agreement among patient participants that nurses should, and already do, ask questions about mental health in the context of talking about the patient’s LTC. Participants talked about not necessarily always choosing to be open about their mental health, but most seemed to welcome the opportunity to talk about how they were feeling and how they were coping with their condition. There was a good level of awareness that living with a LTC could lead to depression or anxiety, and it was seen as appropriate for the nurse to ask questions about this:
Well she just kinda’ pops it into the conversation, you know, ‘how are you feeling, you’re not depressed or you’re not this . . . you know, different things, ‘are you coping with everything?’ and it’s normally yes but, you know, different people react different to it.
Patient 16
Professional participants were in agreement that discussions about mental health were an expected part of the consultation with patients with LTCs. The professional participants were able to describe the tools they used to assess mental health, and the value of the inclusion of mental health screening on the templates they follow for conducting reviews with patients. Some described conducting these questions routinely as part of their standard care:
I’ve usually asked them before they even reach their bottom on the seat really, it’s just a kind of introductory type of question isn’t it?
Professional staff participant 7
Some professional participants described some reluctance to talk about mental health with patients for fear that it would mean running out of time to do the other standardised review tasks. There were also concerns that the standard screening tools were not as easy to use with non-English-speaking patients. Professionals also shared how few of them had been able to participate in mental health training opportunities. In general, however, the conversations on mental health were described as valuable for supporting the patient in managing their condition, and may open up a broader discussion about the kind of support a patient could have in dealing with the challenges they face:
And you know they’re down and depressed and getting isolated and that’s only going to make their physical condition worse, but there’s just lots of things are kinda outwith so you’ve just maybe got to look at another way of ‘well who’s with you?’ or getting somebody else in and getting the family members are handy. For highlighting really if they’re to go and get support.
Professional staff participant 2
In summary, both patient and professional participants expressed that being comfortable with discussions about mental health was an important part of receiving care for a LTC. Patient participants were comfortable with having these conversations with the nurses, and the professional participants saw it as an important part of the care they provided.
Health literacy
Patient participants were asked how they would feel if they were asked questions about their health literacy. It was seen as appropriate that the nurse would check in about how patients wanted information and help to support them in finding better ways to get information. In general, participants described issues with retaining information, as a result of feeling ‘foggy’, difficulties concentrating or failing to remember things as well as they might have in the past. Standard written information, such as leaflets, was not seen as desirable, but being able to have information or a summary about what happened in the consultation with the doctor or nurse written down was viewed as potentially very useful:
I used to think I had a really good . . . I don’t mean a long-term memory, but I used to think I had a better memory and I was able to absorb things and retain them, but I just put it down to getting old and too many things in my head and whatever, but I’ve never even heard that before that it can affect your concentration.
Patient 31
The professional participants also highlighted the challenge of health literacy and, just like the patient participant group, they highlighted a lack of comprehension of information by patients. One professional focus group noted that their practice area had patients for whom English was a second language, which made some work challenging. One group also noted the difficulties in working with people with learning difficulties, although it was felt that there might then be a carer involved to help support communication. Generally, though, professional participants did not commonly or actively identify literacy problems in their patient populations, and when they did, it was a challenge to get assistance:
I’ve only ever referred for literacy once in I think the whole time and I phoned to where it was supposed to be referred to and it was impossible to get in touch with them but that was a wee while ago and she felt ‘no wait, leave it just now’ but maybe it’s changed, maybe it’s easier to get that referral done now, but the referral contact number that we were given at that time it didn’t actually work.
Professional staff participant 4
What was more commonly mentioned by professional participants was the need to repeat information to patients, and patients’ limited ability to recall or comprehend the information. Professional participants described their frustration at the time spent sharing information repeatedly. Some felt that it was likely that patients were just overwhelmed or overloaded with information, and some felt that patients were failing to pay attention or were not listening:
We’ll maybe explain it to them and they’ll be ‘OK, OK’ and then they go off and you think they’ve not really listened, you can tell they’re not sure, they phone back and we’ll say just make an appointment with the doctor.
Professional staff participant 10
In summary, health literacy is an area of concern for patient and professional participants. The patient participants described their frustration at a lapse in memory or comprehension. Professional participants noted a lack of information retention. Both felt that it was an important area, yet there was no discussion of patients and professionals communicating together about this topic together. As a result, some professionals may assume that patients are not listening, while some patients may be reluctant to share, unprompted, that they are having cognitive challenges. This suggested that this area of the PCAM tool could be particularly useful and seems like an acceptable area of discussion for consultations.
Social environment and finances
There was a lively exchange between patient focus group participants about the appropriateness of nurses asking questions about their patients’ social environments. It was certainly seen, by this group of participants, as something that PNs mostly do not discuss, although some felt that district nurses might be more likely to do so. Some felt that such questions should be asked of patients only if the nurses had a reason to be concerned about the patient. Some participants felt quite strongly that it was not the role of the nurse to ask questions about their patient’s social environment, while others felt that anything that might have an impact on their health should be discussed with the nurse, including information about their social environment:
I think what you’ve got to be very careful about as well as far as nurses are concerned, they’re not social workers, they’re nurses, you know, there’s only a certain amount, just what we were talking about earlier on there, there’s only a certain amount of things that we talk to nurses about and social environment, what your background is about your next door neighbour and that sort of thing, it’s not things that you would come and talk to your nurse about.
No, no that’s right. These are things that you talk to a social worker or the police or whatever, so we’ve got to be very careful that we don’t sort of categorise them in the social, because they’ve got enough on their plate without being social workers as well.
But some of these things can affect your health.
Yeah I know but how d’you reach that, I mean, d’you go and sit with a nurse and turn round and say ‘look, my next door neighbour’s giving me a lot of hassle’ you wouldn’t say that.
But it would make you ill that.
Yeah but you don’t say that to your nurse.
But that’s you giving the nurse the whole picture, if you tell her things like that you’re giving her the whole picture.
Patient focus group 1005
The professional participants reflected a similar split in opinion. Some professional participants felt that they would actively discourage any discussion of non-clinical topics with patients, and felt that the population they served would find it inappropriate or unnecessary to talk about their broader social environment. It was also true, however, that such participants came from a small community in which there was a sense that the professional would know if there were broader issues going on for their patient. However, in the same focus group, a colleague reflected that asking questions systemically could lead to finding hidden challenges for patients, and considered that it would be useful for uncovering important issues:
I suppose though, if it [PCAM] becomes standard and these are standard questions and that’s what you ask everybody, then you are going to find the person that is being abused or is struggling and things, because if you just presume that just cause you live in a nice posh house or something that your life’s all rosy, then I suppose that’s what you’re trying to find is the people who there’s something that they’re never going to tell you unless you maybe just manage to ask the right question at the right time, isn’t it?
Professional staff participant 30
Some professional participants described the challenge of dealing with these issues for patients as being very much part of their daily practice, as these issues were seen to be very relevant for their patient population. Dealing with these issues clinically, while feeling unsupported, was felt to be a source of strain and burnout for professionals. As in the patient focus group, some participants felt that these questions should be asked by social workers and not nurses:
No, I think it should be clinical and I think that that is what’s causing the burnout with GPs and nurses, I think it’s what’s causing the waiting list really long to get appointments and I think we need more social workers there that can really help.
Professional staff participant 272
Some participants felt that it was appropriate for nurses to ask questions about the social environment, and that they should be asking these questions. The issues in the social environment were seen as impactful on the health of patients. When nurses supported asking such questions, participants described having an approach in which the nurse was seen as having a role as a connector to other services and help, and was not identifying these issues in order to fix them directly, but to use their role as a conduit to connecting patients to more appropriate help:
I think you can’t be everything to everybody, so I think you have to maybe identify it that I’m not the best person to address these things and it’s just passing on and I can certainly . . . I’m in a position that I can hopefully find out who’s going to be the most appropriate for them and get them on board for their benefit.
Professional staff participant 2
When specifically asked if nurses should ask questions about patients’ finances, the patient and professional participants were again split in their views. Some felt that such topics were taboo and not appropriate for discussion, and others expressed support for the need to ask about financial strain, particularly for older patients, who might be facing financial hardship. Some professional participants had experienced asking such questions under Keep Well, and had found that being able to connect people to financial counselling was a valuable resource.
In summary, patients and professional participants are concerned about the impact of the social environment and circumstances of patients, and see it as important. There is no clear agreement on the acceptability of discussions about the social environment and finances in patient and nurse consultations. Although there is general recognition of the impact of the social environment for the practice population, the perceived availability of resources (or lack of resources) that professionals can connect patients to is likely to be a driver in whether or not and how these issues are discussed and addressed.
Patient views on the Patient Centred Assessment Method implementation in long-term condition annual reviews
Patient and professional participants were asked to describe the ways in which conversations about their broader biopsychosocial experience would fit into the current relationship between nurse and patient, and into the current delivery of care for patients living with LTCs, particularly in relation to annual reviews.
For patients, contact with primary care was described as usually being in the form of doctor visits, nurse visits or condition-specific nurse-led clinics. Patients also described having their annual review, in which there were checks of their health, including a check of their feet and eyes for those with DM. There was a mix of views on whether or not the care being provided was sufficient. Some participants, particularly those who had been fairly recently diagnosed with their condition, felt that there should be more careful monitoring of how they were managing their health. Others appeared very satisfied with the amount of care they received, and described having useful referrals put in place for things like exercise. Some participants seemed to be much more proactive than others at connecting to their GP surgery and asking for the help they needed, whereas others were hoping that there would be more outreach to them as a patient, to check on how they were managing their condition.
Participants were asked to describe their experience of engaging with primary care in relation to managing their LTC. In general, participants spoke about valuing their doctors and felt pleased with the care they provided overall. It was particularly valued when it was possible to have continuity in care, and when patients felt that they had enough time to talk about their health concerns with the doctor and that they were treated as an individual and with compassion. There was some discussion for this group of participants about how the role of the doctor has changed over their lifetimes, and those changes were generally seen as leading to less personally connected relationships with the doctor:
I think one of the things that used to happen that doesn’t happen now is that you don’t see the same doctor all the time, you know, whereas in the old days when you paid half a crown the doctor would say ‘oh aye your grandmother, aye yes you may have the same, I’ll keep an eye’, they knew about you personally and your relations and everything, but nowadays it’s . . . well most of them only work three days a week.
Patient 19
Some described feeling that the doctor was the authority figure in the clinic, the one that makes key decisions about medication and care, or who might express concerns about how the patient is managing their condition. Those participants who had talked about rejecting their diagnosis also described avoiding the doctor to avoid such interactions, even if they knew it might have negative consequences. Nurses were described as having more personal relationships with patients, with more time to spend with them during regular reviews and check-ups. The relationship was described as one in which there was more accessibility, time and generally more supportive care. Nurses were also described as suggesting activities such as exercise or weight loss, rather than being medication focused. The nurse was described as less of an authority figure than the doctor, but still as an authority figure to be respected and listened to:
Yeah, my wife turns round and tells me to go on a diet and I go ‘aye OK’, you know, a nurse tells me to go on a diet ‘aye, yeah’ ‘oh you’re losing weight!’ and you turn round and say to your wife . . . I don’t know, ‘go on the scales’ ‘no’, but if your nurse turns round and tells you to do it you’ll do it!
Patient 34
In addition to the areas of discussion that might be presented by the PCAM tool, the participants reflected on how, in their view, asking such questions related to how they see the role of the nurse. Some participants felt that nurses might not have the skills and training required to ask such questions of their patients and, in that sense, it was asking nurses to go beyond their current role. However, participants were more concerned with protecting nurses from being overcommitted by being asked to do another task on top of an already significant range of responsibilities. There were concerns that nurses needed to have their time somewhat protected, and the boundaries of their role more clearly defined.
There was also discussion in the focus groups about the role of nurses and what they would do with information gathered with a tool such as the PCAM. There was a sense, for some participants, that nurses should be distinguished from social workers, and not ask questions that would be more typically asked by a social worker, who was seen as more likely to act on any concerns identified by these questions. For these participants, there were concerns about nurses asking about things they might not be able to provide assistance with. Other participants saw nurses as being appropriate to talk to about any issue that might have an impact on health, and those participants tended to see the nurse as a resource who could refer a patient to a social worker, or other services, as required:
She’s not got that teaching, she’s not got that know all but she could refer you, say to you ‘right you are, we are lucky to have a social worker who’s available at certain times in the month or certain times in the year that you can maybe go and have a private conversation with’ and you don’t have to tell anybody, it’s just an appointment from A to B and that’s it. And then you would come in here as if you’re coming in for a normal appointment and speak to a social worker privately.
Patient 34
In summary, when patient participants felt that it was appropriate to be asked the PCAM-related questions, they felt that the nurse was an appropriate role for leading that conversation. It was felt that nurses could connect patients to resources as needed, and that the supportive relationship with the nurse was conducive to talking about these topics. For those who did not feel that it was acceptable to be asked the PCAM questions, they did not feel that it was appropriate for the nurse to ask such questions, and tended to see it as a social worker role.
Professionals’ views on the Patient Centred Assessment Method implementation
Professional participants were asked to explore how the PCAM assessment might fit in with their usual work of caring for patients with LTCs. Their input reflects the split in opinion about the acceptability of the the PCAM tool, with a variety of views about the potential impact of implementation. In The Patient Centred Assessment Method in the consultation, Relationships with patients and The connection to resources, we discuss their views in relation to the consultation itself, their relationship with patients, their approach to care and the availability of resources.
The Patient Centred Assessment Method in the consultation
Professional participants were concerned that the PCAM would be difficult to fit into the consultation because of time constraints. Participants felt that the annual reviews were often quite time-consuming and covered a lot of different topics, and including PCAM questions might add additional work and time into the consultation:
I think it would be a lot of work, you know, to try and think about all the things . . . very often I run late anyway, don’t I!
Professional staff participant 28
One focus group offered a counter-view, however, and indicated that time was not a barrier for consultations, as they had a structure that allowed for longer appointment times. That practice’s approach encouraged matching a patient to a longer time if needed, and talking about the impact of broader life challenges was seen as an appropriate reason to allow for a longer consultation:
Cause you do know the patients and you know the ones that are coming in that are going to take a bit longer, that are going to chat about things if their life’s a bit rubbish just now or whatever, I would give them . . . I would add on an extra 10 minutes if you see somebody coming in that’s got a lot of problems.
Professional staff participant 3
In summary, the participants’ concern about time reflected how their practice was currently organised. The majority of practices had set consultation times and felt that additional topics and questions would be a strain. One practice setting already had an approach that was inclusive of having longer consultations if needed and saw the PCAM-related topics as justifiable reasons for using longer times.
Relationship with patients
Professional participants described the value and importance of their relationship with patients. Some described having developed relationships with patients over many years of care, and having a good knowledge of their patients’ lives. For those professionals who were not inclined to see the PCAM as clinically relevant, there was a concern that asking PCAM-related questions might have a negative impact on that relationship with the patient. Some professional participants expressed resentment for when patients tried to raise issues that they felt were relevant, such as concerns about their home environment, if the professional did not see it as relevant. When this happened, participants described patients as being time wasters or as trying to dominate the consultation:
Very often they will tell you and very often they try and dominate the consultation with that, so clearly that’s very important to them, but that isn’t why they’re there to speak to me if you like, so I have to get through other things as well and try and, yeah, flag other people up to help.
Professional staff participant 28
Some professional participants expressed frustration at patients not following their instructions or contradicting them when talking to the doctor. There was a feeling expressed by some participants that there was an agenda for the reviews set by the nurse and that the patients’ role was to stick with that agenda, regardless of their own concerns. Participants in one focus group provided a different perspective, as they had a practice-wide approach that was about the patient setting the consultation agenda, which may include addressing broader social determinants of health. For those professional participants, the relationship the nurse may have with a patient was seen as creating a safe place for patients to express broader concerns, and the nurse’s role was to listen to the patient and prioritise what they might want to work on:
So it’s all about them setting the agenda and then the cycle of change and identifying what they, you know, there might be they’re smokers, they drink to excess, their diet’s rubbish and they don’t exercise and they’ve got money worries, but you know, then they are majorly stressed out, ‘by the way I’m suicidal now’! So we went through things, I was in a group, and we had different ways of assessing, you know, so you’d a sheet with the six pictures and the automatic will, ‘OK you’ve kinda said oh gosh I should do this, that and the next thing, what d’you feel, what kinda jumps out at you?’ you know, you’ve got the money worries one so you’ll get there but that could be causing them all sorts of stress or they’re not eating so it cascades back, like you say, to the disease management and vice versa.
Professional staff participant 2
In summary, the relationship between the nurse and the patient was highly valued. The professionals’ perspective on how consultations should be conducted influenced the view on how the PCAM tool could be implemented. Some felt that the relationship supported the inclusion of PCAM-related questions, and that was consistent with a patient-led agenda. Others felt that the nurse should set the agenda and lead the consultation, including avoiding non-clinical topics; those participants were more likely to feel that the PCAM questions should not be asked or that they could have a negative impact on the nurse–patient relationship.
The connection to resources
Professional participants described a wide range of resources they accessed, or connected patients to, which would address non-clinical concerns. These included local community centres, social work, counselling, drug and alcohol services, healthy lifestyle referrals and online support. Participants also described the work that went into identifying and maintaining accurate lists of information as being challenging. There was variation in how well each practice setting was connected to local agencies or how much information they felt they had available. Some described how access to certain agencies or link workers had been reduced because of cuts to funding, which was a source of disappointment. Overall, having access to resources or information was seen as an important part of feeling that it was feasible to ask the PCAM-related questions.
The professional participants’ views about when or how to access resources seemed to differ on the basis of what they felt was clinically relevant and what they felt were appropriate courses of action. Some felt that the consultation agenda should focus on clinical issues that could be addressed through the patient following the nurse’s guidance. That guidance might be on clinical issues, such as smoking cessation, diet and exercise. Participants expressed frustration when this guidance was not followed, with some expressing disappointment that patients were not following the suggested course of action. Other participants described their role as not being there to offer solutions for clinical issues, but as a support for the patient to address what was relevant to them, clinical or non-clinical. In this sense, they saw their role as helping to connect patients to a broader range of resources and supports, with the view that it would ultimately help the patient to address their LTC. These professional participants were clear that their role was not to work out the solutions for patients, but to help support the patient in identifying their own priorities and understanding how to address them:
But yeah it is that whole thing about when patients come in, you know, you do want to utilise your listening skills and everything and you want to let them, cause quite often that’s what they are wanting to do, it’s not that they’re wanting particularly you to solve problems and that’s where I try and encourage maybe utilising these services our counselling or whatever where they maybe can just get a chance to sit with somebody, with a psychologist or a counsellor and they can just talk for an hour or whatever and sort out their own problems because, I mean, I would love to be able to do that but just wouldn’t be able to.
Professional staff participant 4
In summary, resources to support the areas of a patient’s life that are identified as being a challenge for patients by the PCAM tool are essential to support PCAM implementation. However, the approach of the nurse is of equal importance. The PCAM implementation may be more likely to be successful in settings where the nurse values the non-clinical aspects of the patient’s experience, alongside the clinical aspects of care. It seems clear that it would be useful to emphasise in the PCAM implementation that the role of the nurse is to connect patients to resources, rather than to fix problems.
Conclusions
The PCAM-related topics are consistent with the broad range of concerns that patients have about their condition. Both patient and professional participants were comfortable with discussions about mental health being an important part of receiving care for a LTC. Health literacy was an important area, yet there was no discussion of patients and professionals communicating about this topic together. This suggests that this area of the PCAM tool could be particularly useful to include, but mechanisms for facilitating discussion on health literacy may need more attention.
Many patient participants felt that it was appropriate to be asked PCAM-related questions, and that the nurse was an appropriate person for leading that conversation. Nurses could connect patients to resources as needed, and a supportive relationship with the nurse was conducive to talking about these topics. However, some patients did reflect that tackling areas such as patients’ social circumstances was more appropriate to social worker roles.
There was an expectation that the PCAM tool would require additional time within a consultation, but this was not seen as a barrier by all practices. The nurse–patient relationship was used as a justification by some professionals to engage with the PCAM domains (to enhance the relationship), but was also used by others to justify not encroaching on the private lives of patients. The views of nurses on who should control and set the agenda for consultations were an indicator of their willingness to go beyond the physical health needs of patients, with those who were more willing to be led by patients’ needs also being open to addressing the wider psychosocial needs of patients.
Resources to support the areas of a patient’s life that are identified as being a challenge for the patient by the PCAM tool are essential to support the PCAM implementation. Nurses accepted that their role can be one of connecting patients to resources, rather than being there to fix problems. As such, the PCAM could be a useful tool in this expanded role, without extending the boundaries that nurses considered to be appropriate.
Chapter 4 Study B: feasibility study of a cluster randomised controlled trial of using the Patient Centred Assessment Method intervention in primary care nurse assessments of patients with long-term conditions
Methods
Design
The feasibility RCT element of the PCAM study used a cluster RCT design to assess the acceptability and feasibility of conducting a full-scale trial of effectiveness. With the GP practice as the unit of cluster, it considered pre- and post-implementation outcomes for two units of analysis, that is, nurse and patient levels.
At the nurse level, the RCT collected baseline data of nurse behaviour for all nurses in order to consider whether or not change had occurred in both the control and intervention arms. This was followed up after completion of phase 2. At the patient level, patients were asked to complete baseline data and data at 8 weeks’ follow-up in both phases of the trial, with a separate cohort of patients in phase 2.
Randomisation was conducted by the study statistician at the end of phase 1 data collection and independently of the broader research team. The decision was recorded, and practices were then informed of their allocation by Carina Hibberd.
Practice recruitment
The feasibility RCT aimed to recruit eight medium-sized to large GP practices in three locations, FV, Grampian and GGC, through the SPCRN’s research register. Practices were eligible for inclusion if they were medium-sized to large (four or more GP partners or a practice population of > 3500) and able to recruit two nurses who deliver annual reviews for patients with LTCs (DM – type 1 or 2, CHD or COPD). In addition, GGC practices were selected from the ‘Deep End’ cohort in order to compare practices in the most deprived city areas of Scotland with those in communities of more mixed affluence, which are generally smaller. Practices that had been approached in the focus group stage of the study were not approached in this stage.
The SPCRN initially issued e-mails, which included invitations and study information sheets, in batches of eight, to practices on their register that met the inclusion criteria. The first batch of invitations was sent to PMs in May 2015. The e-mails were followed up with telephone calls from the researchers to PMs to confirm receipt and interest in participating. If a PM did not recall receiving the invitation e-mail but expressed interest in the trial, the SPCRN was asked to resend the invitation either by e-mail or by post.
As there was insufficient interest from practices, a minor ethics amendment was made to permit direct contact with PNs and to include smaller practices with only one PN. Letter invitations were sent directly to PNs in practices already contacted (that had not yet declined) and to PNs in a further batch of practices. Researchers followed up the written invitations with telephone calls directly to PNs. Simultaneously, an open invitation to participate was issued in the Scottish Practice Nurse Association e-newsletter.
Following the completion of baseline recruitment, the five practices participating in both stages were randomised to the PCAM or CAU arms in a 2 : 1 ratio. This resulted in three practices being placed in the PCAM arm and two in the CAU arm for the second phase of research.
Patient recruitment
Participating PNs were each asked to identify up to 30 consecutive patients attending a review for one or more of the eligible LTCs, which were COPD, CHD and DM (type 1 or 2). PNs were able to exclude patients if the study was contraindicated as a result of a physical/mental health impairment or a cognitive or communication impairment, or if personal or family circumstances might have a serious impact on the patient’s physical or mental well-being. Potentially eligible patients could also be excluded if they did not attend the review and if NHS organisational or nursing time constraints interfered with the normal running of the clinics. PNs continued to recruit patients until they were informed by the research team that at least 10 questionnaires had been received or, in the later stages of the study, until data collection was terminated as a result of time constraints. This process was repeated with new patients post randomisation.
Outcome measures
Nurse-level outcomes were measured at the start of phase 1 and the end of phase 2 by:
-
the number and range of referrals and signposting to GPs, repeat appointments with the PN and/or other services aligned with PCAM domains in the two stages of the trial, recorded on a nurse consultation form
-
the DAQ24
-
a bespoke questionnaire regarding confidence in asking about mental health issues.
Patient-level outcomes were measured by the:
The questionnaire at the 8-week follow-up repeated these measures, with the exception of the CARE measure, and also asked patients whether or not they had taken up any signposting or referral advice, and their views on the outcomes of doing this or reasons for not taking these up.
Nurses also recorded demographic information about patients on the nurse consultation form, with postcodes being retained in the practice for collection by the SPCRN, which then matched these with Scottish Index of Multiple Deprivation (SIMD) code data and returned the SIMD codes matched to patient identification numbers to the research team.
Serious adverse events were monitored for each participant until the date of their follow-up.
Outcome data were summarised by descriptive analysis at baseline, at follow-up and, where relevant, between study arms. Continuous outcome data were assessed for ‘normality’, and parametric and non-parametric summary estimates were used, depending on the underlying data distributions. Data completion rates were estimated on demographics and outcome measures for each stage of the study. Change scores were estimated between arms, as to assess whether or not these were in the expected direction of effect; these are presented with their 95% CIs. No formal significance testing was done, as this study was not powered to detect differences between any groups.
Materials
Each participating PN was given a document case with 30 study packs, each marked with a unique patient identification number. Study packs contained a patient information pack, a patient questionnaire (with a prepaid envelope) and a nurse consultation form, all marked with the corresponding patient identification number. Standard operating procedures, a flow chart of the study process and a short suggested script for introducing the study to patients were also included in the document case. Post randomisation, study packs for practices in the PCAM arm of the trial also included a PCAM form in phase 2.
Practices randomised to the PCAM arm of the trial were also given a bespoke resources pack, containing contact names, brief information and numbers for local and national support organisations relating to the PCAM domains and to the specific LTCs. These were presented in an A4 slim file folder, with an index for the 8–10 pages of information. Space was also left for the practice to add any further resources. The pack was also made available electronically. See Appendix 5 for further information about the design and content of the resource packs.
Practice implementation of phase 1
Consenting PNs were given a 1-hour training session on the research processes and procedures. This included an explanation of the background to the PCAM approach and the current research study; an introduction to the standard operating procedures; a discussion on the practice’s preferred approach to patient recruitment; and administrative procedures. PMs or lead PNs were also invited to participate in this session.
Practices were asked to identify suitable recruitment periods. These could be either specific clinics, in which a number of patients with a particular condition were seen on the same day, or ad hoc review of patients during a specified period of time. Researchers offered to be present in the clinics on specified recruitment days to provide support to staff and to assist patients with questionnaire completion. This offer was accepted by all practices for the first recruitment session. Thereafter, this varied, with two practices requesting support throughout phase 1, while others had occasional visits to help with administration and address any issues.
Implementation of patient recruitment and follow-up
Patients were recalled for their routine LTC review through participating practices’ normal procedures. On attending, patients were given an information pack by their PN and an opportunity to ask questions about the trial at the start of their review at each stage of the trial. During phase 1, the review was conducted as normal and the patient was asked if they were willing to complete the patient questionnaire at the end. Nurses noted patient age, sex and postcode for all patients on the nurse consultation form, along with the patient’s inclusion status. For patients who accepted the questionnaire, the length of the consultation and all referrals or signposting to the GP, and repeat appointments with the PN and/or to other services were noted. The patient’s contact details were placed on the individual study pack and noted on a study recruitment clinic sheet, both of which remained in the practice before being destroyed at the end of the study.
Patients who accepted the questionnaire were offered the opportunity to complete it before leaving the practice, and either placed it in a ballot box or, where the practice and the patient so requested, completed it with support from the researcher on site. Alternatively, patients could complete the questionnaire later and return it by post in a prepaid envelope. If the questionnaire had not been received 2 weeks after the appointment, a reminder was sent out via the practice, using the study identification number to match reminders and patients.
Eight weeks after the initial review, patients were sent a follow-up questionnaire via the practice, again using the study identification number to match these with the correct patient. Patients returned the questionnaire by post to the research team. If the questionnaire had not been received 2 weeks after being sent, a reminder was sent out via the practice.
Following randomisation, CAU practices repeated the process set out in phase 1. Practices randomised to the PCAM arm underwent the training intervention, described in Chapter 2, Patient Centred Assessment Method training, and Appendix 2. After practising the PCAM approach on between 5 and 10 patients, study nurses repeated the recruitment process set out in phase 1, but using the PCAM approach with patients. In addition to the existing data completion, PNs were asked to note the patient’s status within each domain by circling the appropriate text on the PCAM tool.
Following completion of data collection, postcode data were collected by the SPCRN and used to identify the SIMD 2016 Datazone code for each unique patient identification number. The code (but not the postcode) for each identification number was then passed to the research team.
Findings
No adverse events, serious or otherwise, were reported. This was verbally checked by researchers to ensure that this was not as a result of missed reporting.
Figure 4 presents the Consolidated Standards of Reporting Trials (CONSORT) flow chart for PN recruitment to the feasibility trial, Figure 5 presents the CONSORT flow chart of nurse involvement and Figure 6 presents the CONSORT flow chart for patient recruitment to phases 1 and 2.
FIGURE 4.
Flow chart of practice recruitment to the feasibility trial. a, The initial recruitment strategy gave slow results, so practices which had not responded were reinvited using a new strategy, together with unsampled practices. Thus, the greyed-out boxes only show a transitional exclusion and addition, and should not be considered in the final numbers. ISD, Information Services Division of National Services Scotland; SPNA, Scottish Practice Nurses Association.
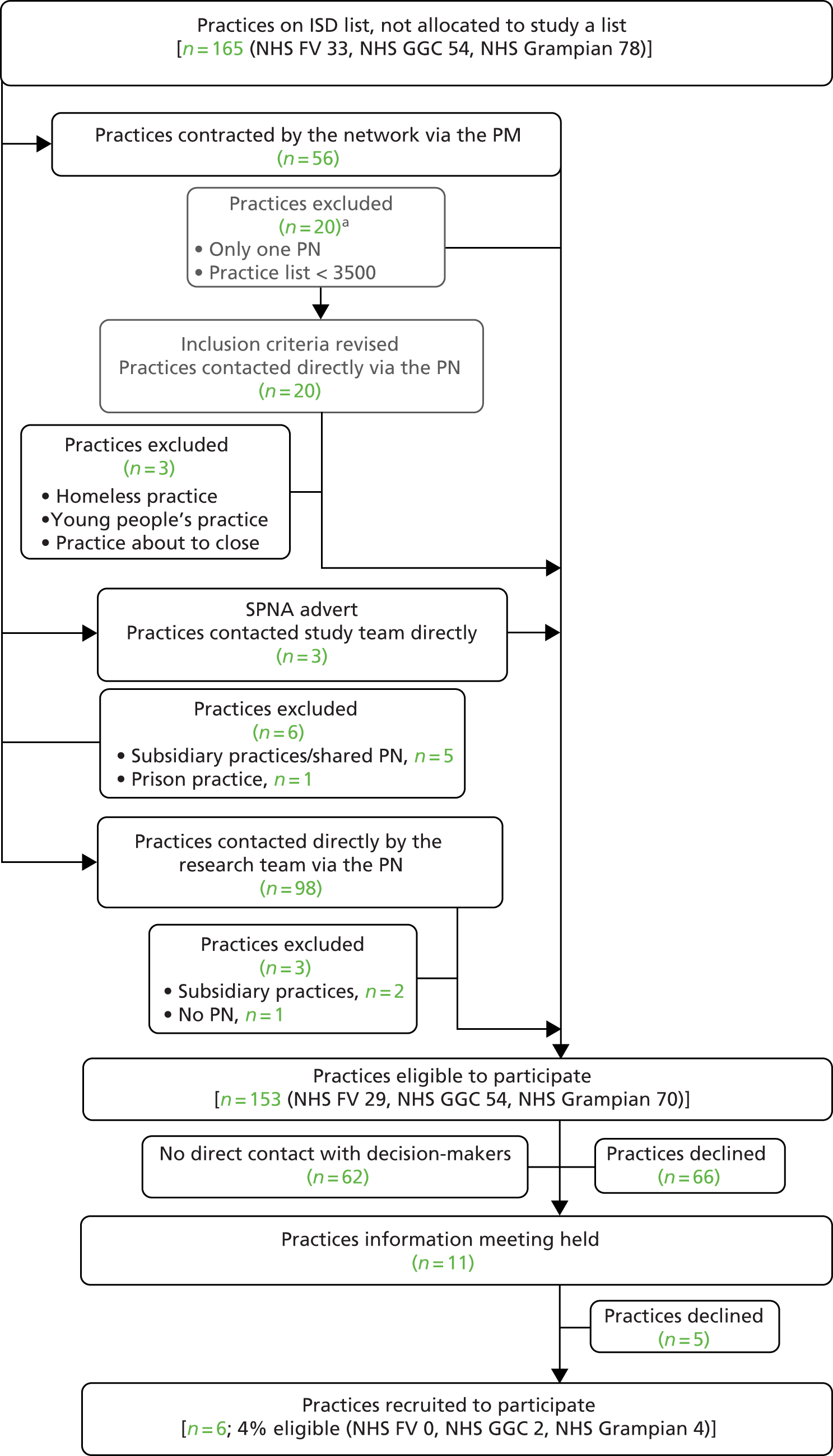
FIGURE 5.
Flow chart of nurse involvement in the feasibility trial.
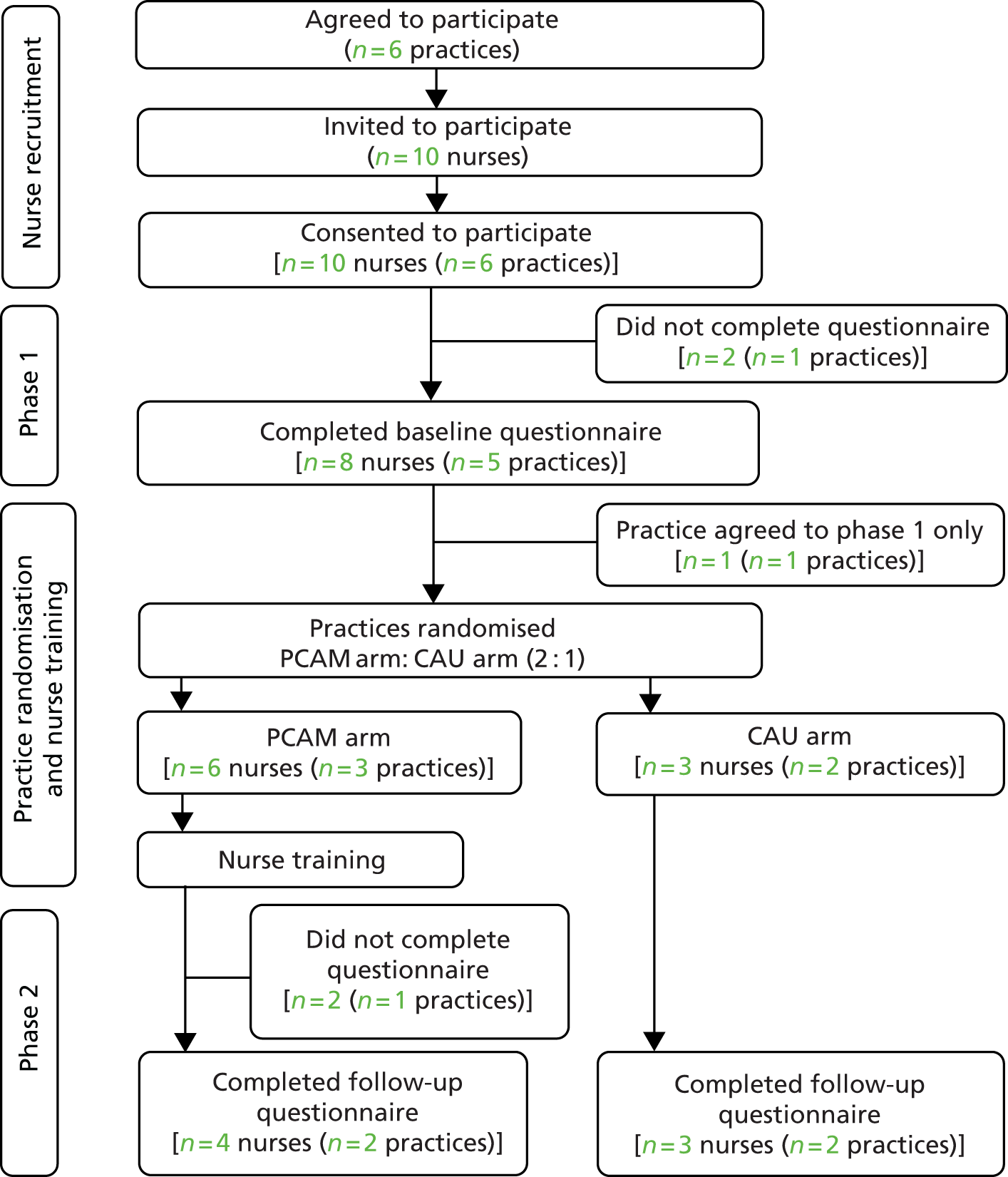
FIGURE 6.
Flow chart of patient involvement in the feasibility trial. (a) Phase 1; and (b) phase 2.
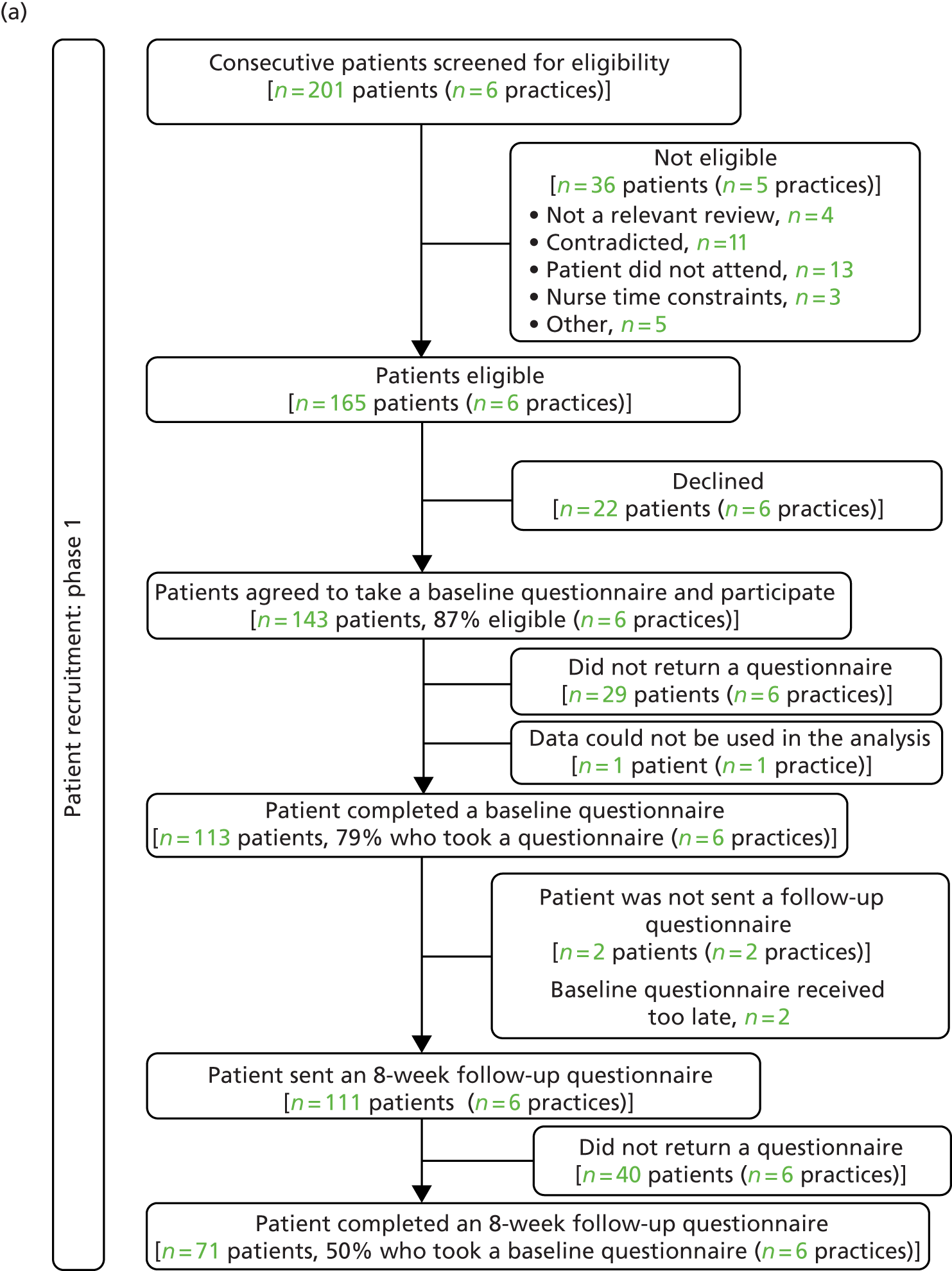
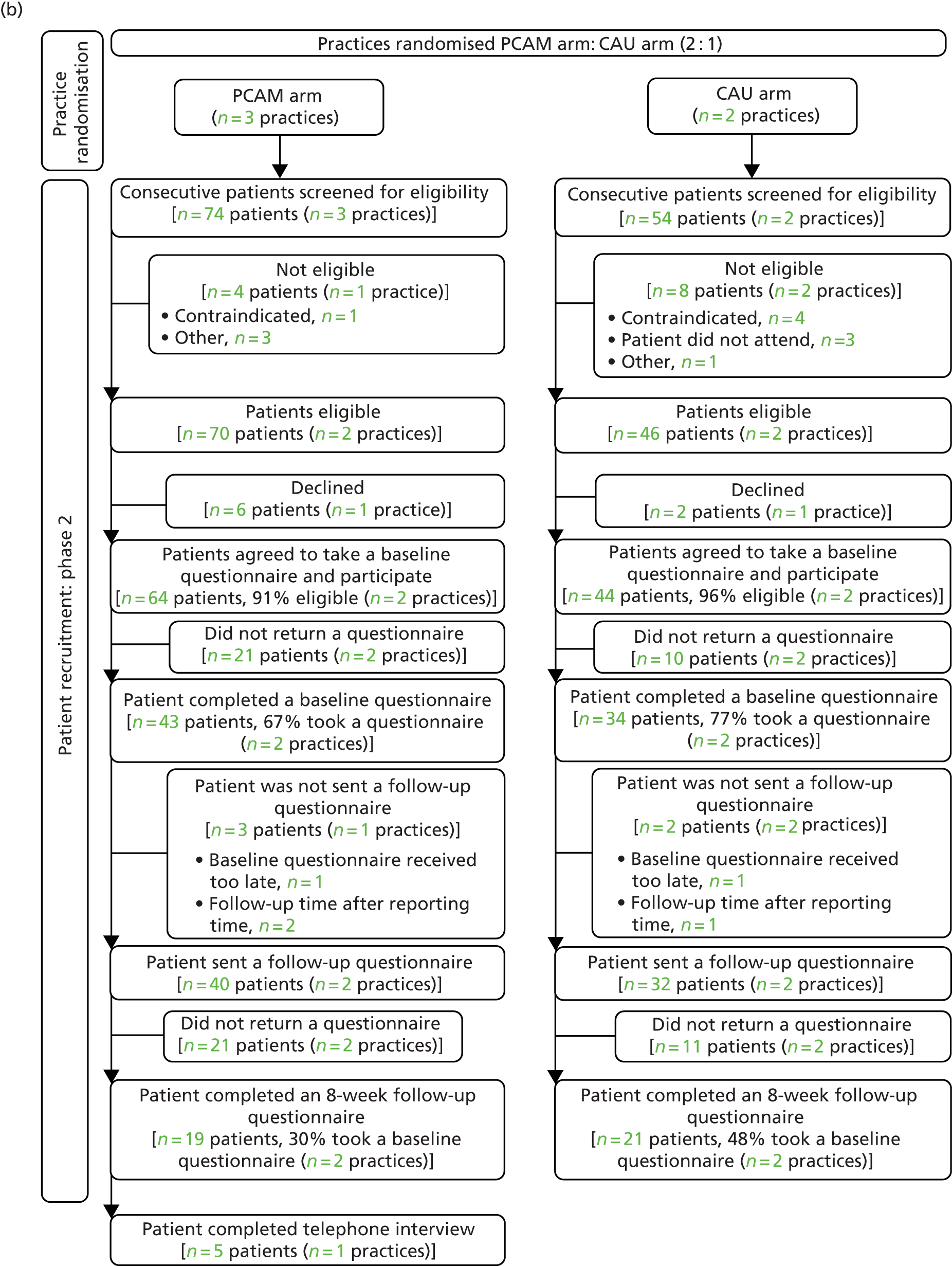
Using the combination of recruitment approaches outlined previously, 156 GP practices were contacted directly and a further three responded to the e-newsletter article. Of the practices with which telephone contact was made or which responded to the SPCRN or the PCAM research team directly, 68 declined, and the reasons for declining are summarised in Figure 7.
FIGURE 7.
Practice-reported reasons for declining to participate.
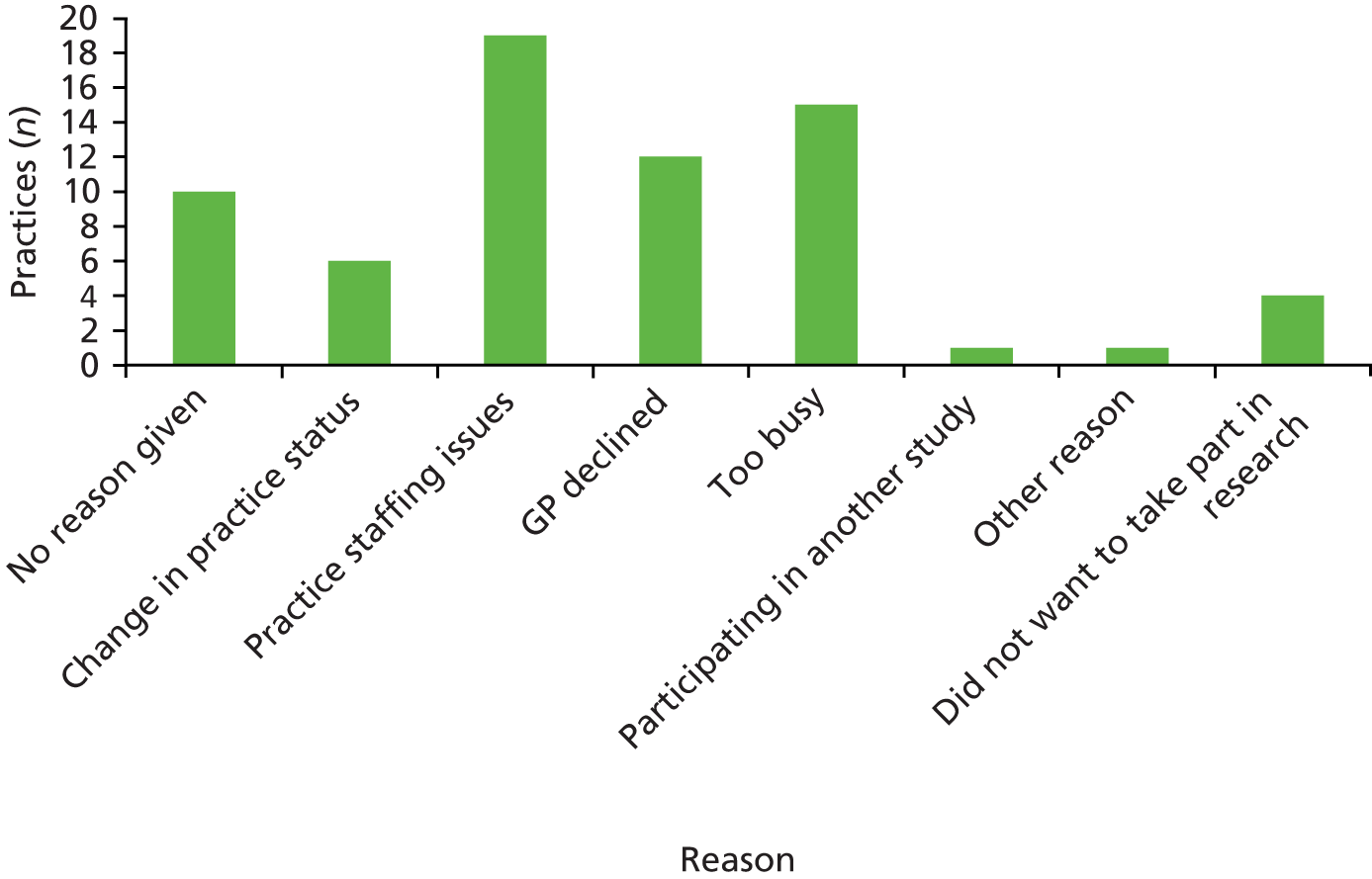
Fourteen practices expressed interest in participating in the study. Of these, eight practices concluded that they would not be able to participate because of existing commitments or time constraints. A further five practices accepted the invitation to participate in both phases of the study, and one to participate in phase 1 only, as a result of planned extended leave. Of the six participating practices, two had only one PN each. Four were located in the NHS Grampian area and two in NHS GGC. No practices were recruited in NHS FV.
Patient participant information
Ten nurses from six practices assessed a total of 329 patients in review consultations, of whom 113 and 77 participated in phases 1 and 2, respectively. Patients in phases 1 and 2 are different and are unpaired. Phase 1 is a baseline review of patient data prior to randomisation and phase 2; both phases had both pre- (baseline, T0) and post-intervention (follow-up, T1) data collection. Randomisation was to the PCAM arm (which included nurse training and nurse use of the PCAM tool and an accompanying resource pack) or the CAU arm.
Table 2 reports on the numbers of patient participants per practice. Only four of the six practices managed to complete phase 2 data collection (reasons for this are described in Chapter 7). This explains the reduced numbers of patient participants in phase 2. Some practices involved only one nurse (practices H and K), whereas others involved two nurses in data collection (practices E, F, G and J). Each nurse was asked to recruit 10 patients with completed questionnaires in each phase; this was achieved by all nurses in phase 1 and by six nurses in phase 2; however, only one nurse who participated in phase 2 failed to recruit the 10 patients required. This suggests that patient recruitment is achievable using the methods proposed in this feasibility trial. Some nurses recruited more than 10 patients, as their recruitment accumulated while patients delayed returning baseline questionnaires for a few weeks.
| GP practice | Phase, number of participants | |
|---|---|---|
| 1 | 2 | |
| E | 20 | 13 |
| F | 27 | 23 |
| G | 23 | 30 |
| H | 13 | 11 |
| J | 20 | – |
| K | 10 | – |
| Total | 113 | 77 |
Table 3 shows the comparison of the patient participants in phase 1 with those in phase 2, and reveals small differences between the two samples. There was a higher proportion of males in both phases, and this increased slightly in phase 2. The sample was entirely/predominantly white in both phases. Slightly higher proportions of participants were in paid employment in phase 2, but slightly more also reported caring responsibilities. There were slightly more participants cohabiting and fewer living alone in phase 2, with more home owners and fewer participants reporting living in rented accommodation. It is not known whether or not the small differences in patient demographics are random, or if these are attributable to some bias in the nurse selection of patients to approach to take part.
| Demographic characteristics | Phase, n (%) | |
|---|---|---|
| 1 (maximum N = 113) | 2 (maximum N = 77) | |
| Age (years) | n = 111 | n = 77 |
| Mean (SD) | 67.7 (10.2) | 68.1 (9.2) |
| Sex | n = 112 | n = 77 |
| Male | 67 (59.8) | 49 (63.6) |
| Female | 45 (40.1) | 28 (36.3) |
| Ethnicity | n = 111 | n = 76 |
| White | 111 (100) | 72 (94.7) |
| Non-white | 0 (0.0) | 4 (5.3) |
| Education | n = 109 | n = 73 |
| HE/FE/higher school level | 32 (29.4) | 23 (31.5) |
| Attainment at age 16 years | 77 (70.6) | 50 (68.5) |
| Employment | n = 113 | n = 77 |
| In paid employment | 23 (20.4) | 18 (23.4) |
| Not in paid employment | 90 (79.7) | 59 (76.6) |
| Ill health stopping work | n = 94 | n = 60 |
| No | 73 (77.7) | 48 (80.0) |
| Yes | 21 (22.3) | 12 (20.0) |
| Caring responsibilities | n = 110 | n = 71 |
| No | 102 (92.7) | 63 (88.7) |
| Yes | 8 (7.3) | 8 (11.3) |
| Living arrangements | n = 110 | n = 71 |
| Living alone | 32 (29.1) | 17 (23.9) |
| Cohabiting | 78 (70.9) | 54 (76.1) |
| Home ownership | n = 110 | n = 71 |
| Owned | 75 (68.2) | 52 (73.2) |
| Rented | 35 (31.8) | 19 (26.8) |
Table 4 compares the characteristics of patients in phase 2 by randomisation group (PCAM vs. CAU). A total of 43 patients were recruited by the nurses in practices allocated to the PCAM arm, and 34 patients were recruited by nurses in practices allocated to deliver CAU. The randomised samples differed in their ratio of males to females, with a higher proportion of females in the PCAM arm. The PCAM arm participants were slightly better educated and more likely to be in paid employment, but also more likely to be living alone and in rented accommodation. The PCAM arm had, on average, much higher mean deprivation decile scores than the CAU arm, which means that PCAM arm participants were living in more affluent areas. This may have been attributable to high recruitment in one PCAM practice in a relatively affluent area.
| Demographic characteristics | Trial arm, n (%) | |
|---|---|---|
| PCAM (maximum N = 43) | CAU (maximum N = 34) | |
| Age (years) | n = 43 | n = 34 |
| Mean (SD) | 68.72 (9.20) | 67.4 (9.20) |
| Sex | n = 43 | n = 34 |
| Male | 25 (58.1) | 24 (70.6) |
| Female | 18 (41.9) | 10 (29.4) |
| Ethnicity | n = 43 | n = 33 |
| White | 43 (100) | 29 (87.9) |
| Non-white | 0 (0.0) | 4 (12.1) |
| Education | n = 40 | n = 33 |
| HE/FE/higher school level | 15 (37.5) | 8 (24.2) |
| Attainment up to age 16 years | 25 (62.5) | 25 (75.8) |
| Employment | n = 43 | n = 34 |
| In paid employment | 11 (25.6) | 7 (20.6) |
| Not in paid employment | 32 (74.4) | 27 (79.4) |
| Ill health stopping work | n = 37 | n = 23 |
| No | 29 (78.4) | 19 (82.6) |
| Yes | 8 (21.6) | 4 (17.4) |
| Caring responsibilities | n = 41 | n = 30 |
| No | 36 (87.8) | 27 (90.0) |
| Yes | 5 (12.2) | 3 (10.0) |
| Living arrangements | n = 41 | n = 30 |
| Living alone | 13 (31.7) | 4 (13.3) |
| Cohabiting | 28 (68.3) | 26 (86.7) |
| Home ownership | n = 41 | n = 30 |
| Owned | 27 (65.9) | 25 (83.3) |
| Rented | 14 (34.2) | 5 (16.7) |
| SIMD | n = 42 | n = 34 |
| Mean (SD) | 7.10 (3.02) | 4.47 (3.10) |
Table 5 shows the self-reported health conditions of patients recruited to both phases. Although there are differences in the proportions having particular conditions, the overall levels of multimorbidity are similar across samples. Table 6 compares the same patient self-reported health conditions for patients in phase 2 by randomisation group (PCAM vs. CAU). There was a higher proportion of patients reporting higher levels of multimorbidity in the PCAM cohort.
| Diagnosed with conditiona | Phase, n (%) | |
|---|---|---|
| 1 (N = 113) | 2 (N = 77) | |
| High blood pressure | 73 (64.6) | 48 (62.3) |
| Arthritis | 33 (29.2) | 27 (35.1) |
| Asthma | 20 (17.7) | 18 (23.4) |
| Stroke | 6 (5.3) | 5 (6.5) |
| Back pain | 34 (30.1) | 23 (29.9) |
| DM | 67 (59.3) | 56 (72.7) |
| Thyroid disease | 12 (10.6) | 11 (14.3) |
| Angina/heart attack | 31 (27.4) | 18 (23.4) |
| Eczema/psoriasis | 3 (2.7) | 4 (5.2) |
| Cancer | 9 (8.0) | 11 (14.3) |
| Heart failure | 7 (6.2) | 5 (6.5) |
| Liver disease | 6 (5.3) | 1 (1.3) |
| IBS | 11 (9.7) | 6 (7.8) |
| Anxiety/depression | 26 (23.0) | 15 (19.5) |
| Kidney disease | 4 (3.5) | 3 (3.9) |
| Migraine | 3 (2.7) | 7 (9.1) |
| COPDb | 15 (13.3) | 14 (18.2) |
| Other | 18 (15.9) | 4 (5.2) |
| Multimorbidity | ||
| 0 | 2 (1.8) | 0 (0) |
| 1 | 15 (13.3) | 10 (13.0) |
| 2 | 24 (21.2) | 17 (22.1) |
| ≥ 3 | 72 (63.7) | 50 (64.9) |
| Diagnosed with conditiona | Trial arm, n (%) | |
|---|---|---|
| PCAM (N = 43) | CAU (N = 34) | |
| High blood pressure | 30 (69.8) | 18 (52.9) |
| Arthritis | 17 (39.5) | 10 (29.4) |
| Asthma | 8 (18.6) | 10 (29.4) |
| Stroke | 3 (7.0) | 2 (5.9) |
| Back pain | 12 (27.9) | 11 (32.4) |
| DM | 38 (88.4) | 18 (52.9) |
| Thyroid disease | 8 (18.6) | 3 (8.8) |
| Angina/heart attack | 9 (20.9) | 9 (26.5) |
| Eczema/psoriasis | 3 (7.0) | 1 (2.9) |
| Cancer | 8 (18.6) | 3 (8.8) |
| Heart failure | 2 (4.7) | 3 (8.8) |
| Liver disease | 1 (2.3) | 0 (0) |
| IBS | 3 (7.0) | 3 (8.8) |
| Anxiety/depression | 9 (20.9) | 6 (17.7) |
| Kidney disease | 1 (2.3) | 2 (5.9) |
| Migraine | 4 (9.3) | 3 (8.8) |
| COPD | 4 (9.3) | 10 (29.4) |
| Other | 2 (4.7) | 2 (5.9) |
| Multimorbidity | ||
| 0 | 0 (0) | 0 (0) |
| 1 | 3 (7.0) | 7 (20.6) |
| 2 | 9 (20.9) | 8 (23.5) |
| ≥ 3 | 31 (72.1) | 19 (55.9) |
Additional data on the SIMD for the sample are included in additional tables (see Appendix 6, Tables 10 and 11). Patient-reported outcome data (Appendix 6, Tables 13–19) are also presented. This feasibility study was not powered to detect any significant changes in outcomes; its purpose was to estimate data completion rates, including completion rates for different outcome measures. However, if possible, some indication of whether or not an outcome measure was likely to be able to detect any change as a result of the PCAM intervention was also of interest.
Patients were asked to self-complete questions that were similar to, or reflected the main domains of, the PCAM tool, to see how they might assess themselves in relation to biopsychosocial concerns: these data are reported in Appendix 6, Tables 12 and 13. Table 7 shows the patient-reported biopsychosocial concerns (reflecting the PCAM domains) for participants in both phase 1 and phase 2, and Table 8 shows the same data for participants in phase 2 by randomisation group of PCAM or CAU. Data completion for these sets of questions was around 94%. Participants were most concerned about their health, followed by their lifestyle and their finances. Problems with daily activities and concerns about their social networks were also reported. Participants recruited by nurses in practices allocated to the PCAM arm had higher levels of concerns about daily activities, social networks and finances. However, as these data were collected after their annual review using the PCAM tool, the patients’ perceptions of their problems may have been affected by the discussion.
| GP practice | Phase, number of participants | |
|---|---|---|
| 1 | 2 | |
| E | 2 | 2 |
| F | 2 | 2 |
| G | 2 | 2 |
| H | 1 | 1 |
| J | – | 2 |
| K | 1 | – |
| Total | 8 | 9 |
| Demographic and clinical data | Trial arm | |
|---|---|---|
| PCAM (N = 4) | CAU (N = 3) | |
| Age (years) | ||
| Mean (SD) | 48.00 (5.48) | 53.67 (4.04) |
| Median (IQR) | 47.5 (44–52) | 53 (50–58) |
| Sex, n (%) | ||
| Male | 1 (25.0) | 0 (0) |
| Female | 3 (75.0) | 3 (100) |
| Years qualified | ||
| Mean (SD) | 21.00 (8.08) | 33.67 (5.03) |
| Median (IQR) | 23 (15–27) | 33 (29–39) |
| Training in mental health, n (%) | ||
| None | 1 (25.0) | 1 (33.0) |
| Yes, in the past year | 0 (0.0) | 0 (0) |
| Yes, in the past 5 years | 2 (50.0) | 1 (33.0) |
| Yes, > 5 years ago | 0 (0.0) | 1 (33.0) |
| Previous use of screening tools, n (%) | ||
| HADS | 1 (25.0) | 3 (100) |
| PHQ-9 | 2 (50.0) | 2 (66.7) |
| PHQ-2 | 0 (0) | 0 (0) |
| BDI | 0 (0) | 1 (33.3) |
| EPDS | 0 (0) | 0 (0) |
| GAD-7 | 0 (0) | 1 (33.3) |
| Other | 1 (12.5) | 0 (0) |
| No previous use | 1 (25.0) | 0 (0) |
In Appendix 6, Tables 14 and 15 show patient-reported outcomes from the CARE measure, which rates patient perceptions of health-care professional’s empathy during consultations. There were no apparent differences across phases or between PCAM and CAU cohorts.
In Appendix 6, Tables 16 and 17 report on the WEMWBS, PEI and GHQ patient-reported outcomes. The percentages of participants completing follow-up outcome measures in phase 2 T1 are reduced because of the dropout rate of practice E. There was no apparent difference between measures on rates of completion. Although the study was not powered to observe any differences in outcomes, Table 17 in Appendix 6 presents an analysis of the outcome scores by randomised group. On the WEMWBS, the scores show a small reduction at follow-up (indicating worse mental well-being), but these are further reduced in the CAU arm. On the PEI, in which scores were also reduced in both trial arms, there was also a larger reduction observed in the CAU arm. On the GHQ, in which reduced scores indicate an improvement in psychological morbidity, reductions were observed in both trial arms, with a larger reduction being observed in the PCAM arm. This might only very tentatively indicate that the PCAM tool might be likely to achieve more positive outcomes for patients than CAU, but this would require further testing on a larger sample.
In Appendix 6, Tables 18 and 19 report on summary scores and subscales of the SF-12 for patient participants across phases and for phase 2 by randomised group. There were no differences observed between participants in phases 1 and 2, and no differences between PCAM and CAU cohorts from baseline to follow-up.
Nurse participation information
In total, 10 nurses provided data (Table 7), of whom seven participated from practices E, F, G and H in both phases, and had paired data available to summarise (Table 8). Practices E, G and J were randomised to the PCAM arm, and practices F and H were randomised to CAU. Practice K was enrolled but not randomised, and no phase 2 data were available. Practice J was enrolled, with two nurses recruited; however, no nurse data were provided.
Nurse demographic and professional experience data were collected to indicate feasibility of data collection, and to test heterogeneity, which would affect a full trial. Table 8 shows the demographics of the nurse participants. Nurses in both arms were of a similar age group and sex (mostly female). The CAU nurses had been qualified for slightly longer, and those in the PCAM arm were more likely to have had some training in mental health in the past 5 years. Most nurses had used the Hospital Anxiety and Depression Scale (HADS) or the Patient Health Questionnaire – 9 (PHQ-9) depression screening tools.
Additional nurse outcome data are presented Appendix 6, Tables 20–25, comparing nurses by randomisation group: PCAM versus CAU; however, numbers are too small to draw any conclusions from these data beyond completion rates. In Appendix 6, Table 20 presents data on nurses’ responses to statements on how confident or skilled they felt in dealing with depression by randomisation group (PCAM versus CAU). Appendix 6, Table 21 presents data on nurses’ responses to statements on ‘the most effective treatment for depression is . . .’ by randomisation group (PCAM versus CAU) and Tables 22 and 23 in Appendix 6 present data on nurse confidence in raising and dealing with mental health issues and nurse confidence in raising and dealing with social issues, respectively. In these respects, the data show some slight improvements in nurses in the PCAM arm compared with the CAU nurses. This is the only discernible finding from these nurse outcome data. Table 24 in Appendix 6 presents nurse responses to questions about their perceptions of the care they deliver to patients and how patient centred they feel they are. Finally, Table 25 in Appendix 6, presents nurse responses to the DAQ.
Conclusion
The feasibility trial aimed to address the following questions:
-
Can we recruit and retain practices and nurses to take part in the study?
This study has shown substantial difficulties in recruitment of practices (and, therefore, nurses) and significant retention problems for practices/nurses, which would indicate that any study would need to over-recruit the required number of practices and nurses by about one-third to account for potential practice/nurse attrition.
-
Can they implement study procedures correctly?
This study has shown that practices, nurses and patient participants can implement study procedures. However, this required support to practices in both phases of data collection. Any future study would need to stagger practice participation to allow for the attendance of researchers during data collection phases. This was difficult, as practices/nurses could not always predict or plan data collection, as unforeseen problems, such as staff absences, could cancel any such plans. The time frames for data collection would need to be extended in any future trial to avoid attrition, especially in phase 2, when significant delays occur.
-
Are patients willing to complete questionnaires/outcome measures?
This study has shown that patient numbers can be achieved by nurses who remain in the study and that patients are willing to complete questionnaires to an acceptable level. The loss of patients at follow-up was impacted, to some degree, by practice problems in sending out follow-up questionnaires and the timetable for the study being significantly delayed so that phase 2 follow-up data collection was curtailed. Phase 2 data collection for patients may require additional efforts to achieve levels beyond 50% retention.
-
How many missing data are there and does this relate to nurse- or patient-level follow-up?
Missing data were primarily attributable to nurse retention, which then impacted on patient recruitment and follow-up. As reported in Practice recruitment and Findings, difficulties in recruitment of practices incurred delays to starting phase 2 data collection for many practices, which resulted in a loss to follow-up in phase 2. Nurses were more reluctant to complete questionnaires, but patient completion of all questionnaires was very high. Nurses were reluctant to engage in having their consultations recorded and, therefore, the study of fidelity was difficult to achieve. This will require alternative methods to assess fidelity or achieve an understanding of how to overcome barriers to nurse recording of consultations.
-
What estimates of effect size, variance and likely ICC should be used to inform the sample size of the full study? Should the unit of analysis be at the nurse level or the patient level, or is it feasible or necessary to include both?
There were insufficient data from the limited number of practices and PNs to determine effect sizes or ICCs. The failure to recruit and retain sufficient practices leads to the conclusion that a full-scale cluster randomised trial would not be recommended as feasible without significant effort and resources, and would therefore not be a cost-effective endeavour at this time.
Chapter 5 Study C: fidelity of the use of the Patient Centred Assessment Method by nurses
Methods
Introduction
This observational study, embedded within the wider PCAM study, used audio-recordings of PNs’ reviews with patients with LTCs to gather data to assess how nurses use the PCAM tool and whether or not their practice had changed, following training in using the PCAM approach.
Sample and recruitment
All eight PNs participating in the study were invited to give consent to two or three consultations per nurse being recorded, both before and after PCAM training was completed, if the practice was randomised to the PCAM intervention group. Following completion of baseline data collection, each of these nurses was asked to approach up to five consecutive patients before and after the PCAM training to invite them to have their consultation audio-recorded.
Data collection
A digital audio-recorder was placed in the consulting room by the PN before each consultation, in a position adjacent to where the majority of the discussion would be taking place, but also where it would allow data from discussions in other areas of the room to be recorded. Patients were offered a letter of invitation and an information pack on the study by the PN before being asked to give informed consent. The nurse allocated each recording a unique identification number, which was also given to the patient in case they wished to withdraw consent. Patients were informed that they could withdraw consent to the use of the recording at any time. Nurses noted the patient’s participant number and their own identification number at the start of the recording. Nurses were asked to follow standard operating procedures, including noting the time of any breaks in the recording and when it resumed, if appropriate. A researcher collected the recorders from the practice either when recordings were completed or when the time allocated for this stage came to an end. Recordings were transcribed and anonymised.
Data analysis
Each audio-recording was listened to by two researchers, and analysed to note the time point when conversation segments relating to each PCAM domain appeared in the consultation. Any disagreements were discussed and consensus reached. Timelines of the sequence in which each domain appeared in each consultation were then constructed and used to compare the order and frequency of their occurrence before and after training in the use of the PCAM tool. The content of the discussions on mental well-being, social environment and health literacy was further analysed by two researchers to assess any changes in questioning styles or depth of exploration and consensus reached on any disagreement in interpretation. The range of lifestyle behaviours and social circumstances discussed was also considered. Non-specific greetings and enquiries (e.g. ‘How are you?’) were coded as ‘general’.
Findings
Four of the six nurses randomised to the PCAM arm agreed to do the audio-recordings. Two nurses recruited two patients at each stage, but, of the remaining two nurses, only one recruited a single patient within the time frame given for this stage of the study, giving a sample of nine patients (five before and four after PCAM introduction).
Nurses approached only a small number of patients, but then reported that all patients who were approached agreed to participate. Patients ranged in age from 55 to 84 years, with a mean age of 72 years. Five patients were male and four patients were female.
Figures 8 and 9 present the pre- and post-consultation content and timeline analyses. Blocks represent the start of a discussion rather than the duration.
FIGURE 8.
Pretraining consultation content and timeline analysis. The following key describes the content of each consultation segment that relates to the PCAM domains: DA, daily activities; Gen, general; HE, home environment; HL, health literacy; LB, lifestyle behaviour; MW, mental well-being; OS, other services; PH, physical health and SN, social network.
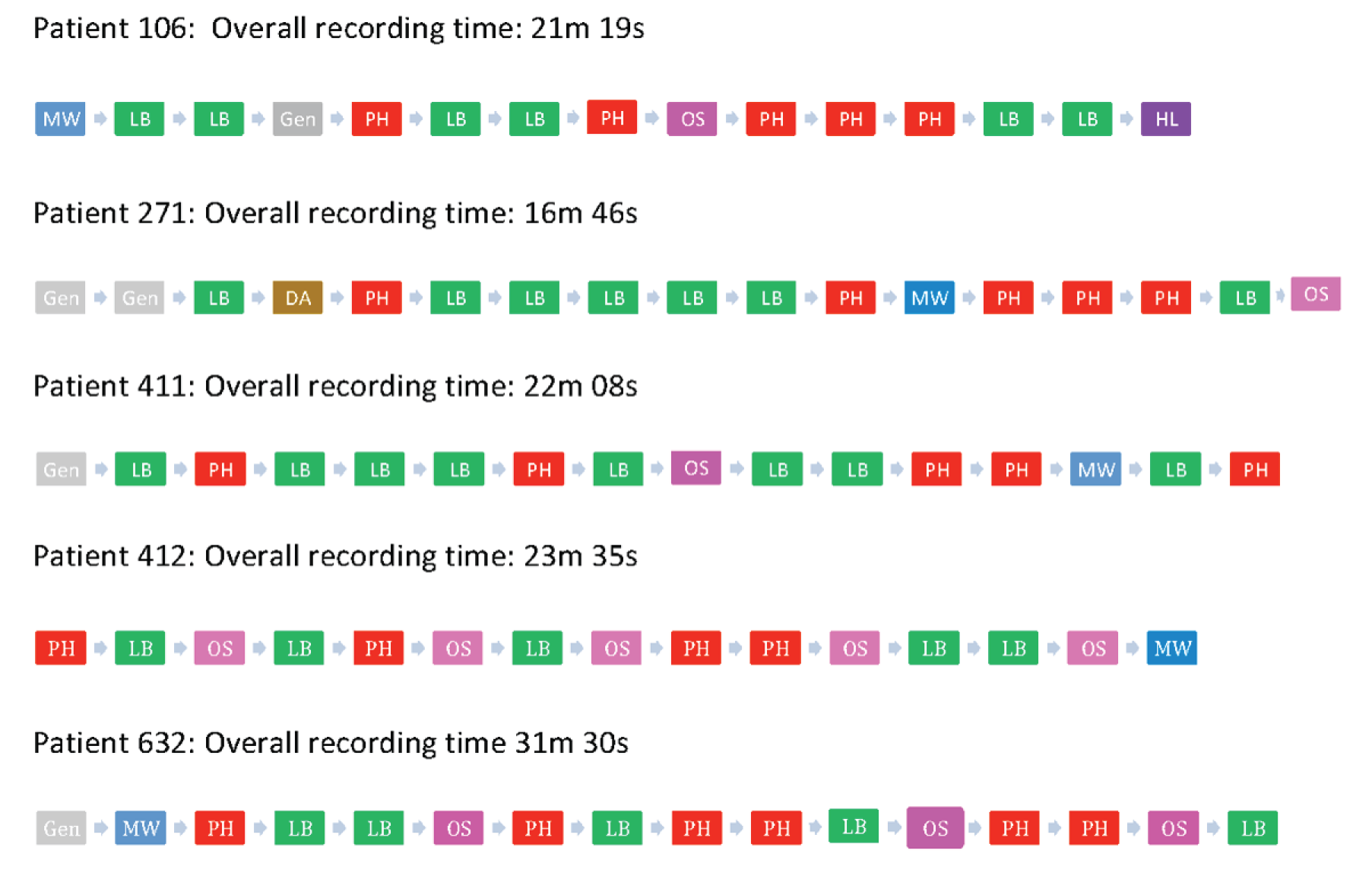
FIGURE 9.
Post-training consultation content and timeline analysis. The following key describes the content of each consultation segment that relates to the PCAM domains: DA, daily activities; Gen, general; HE, home environment; HL, health literacy; LB, lifestyle behaviour; MW, mental well-being; OS, other services; PH, physical health and SN, social network.
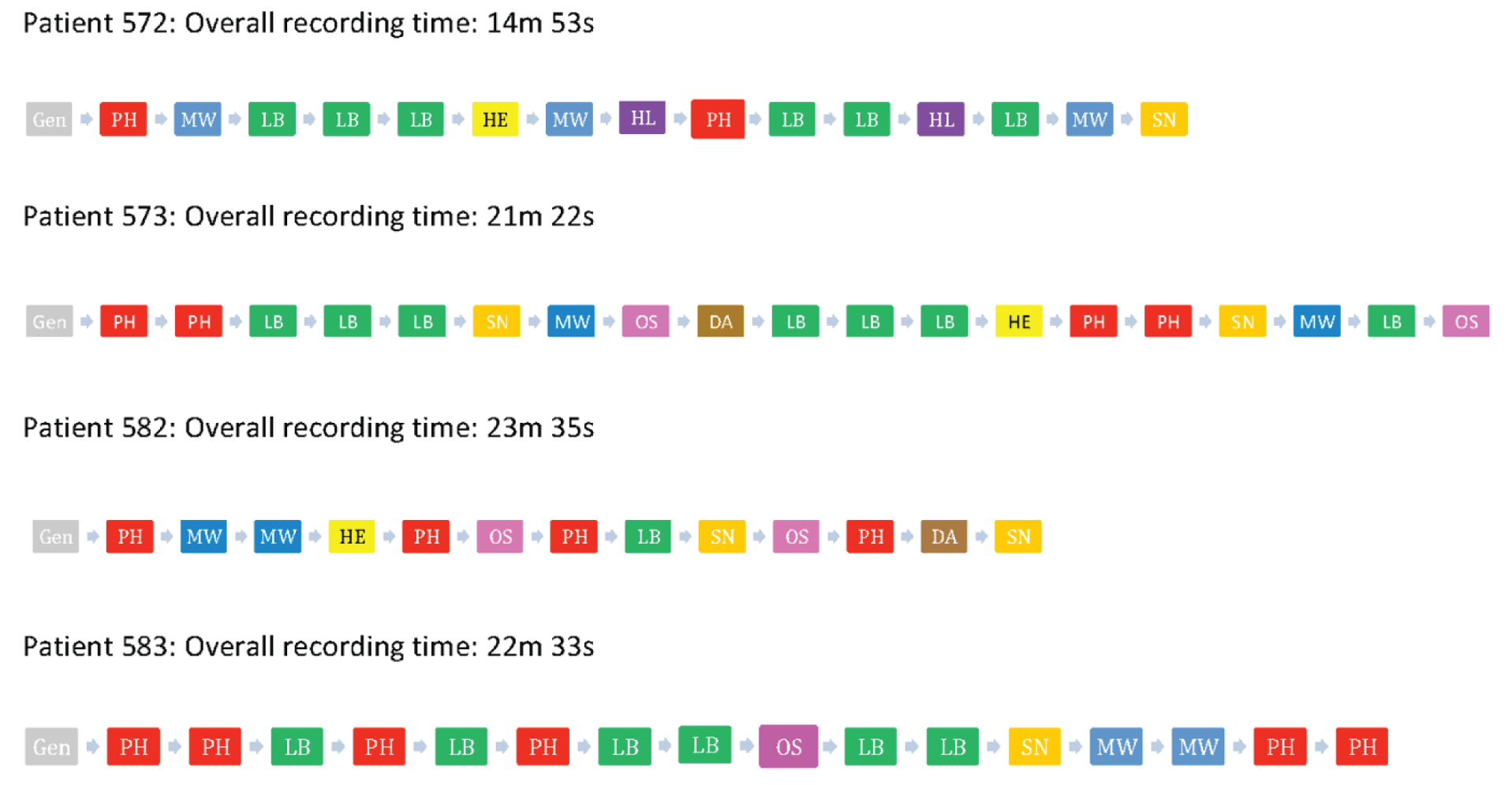
Pretraining consultations
Four of the pretraining consultations were DM reviews. One consultation (632) was a COPD review. The average duration of pretraining consultations was 23 minutes and 4 seconds. PNs started their pretraining consultations with brief introductory questions around general health and well-being, typically ‘How are you?’ or a variation of this.
In pretraining consultations there was a strong focus on physical health and lifestyle behaviour domains, which were discussed from the start and throughout consultations within the context of physical health checks conducted by the PN (e.g. blood pressure, weight and urine testing) and within the context of the communication of blood test results. Questions and discussions about lifestyle behaviours, particularly diet, exercise and smoking, were touched on when these were identified as negatively or positively impacting on physical health symptoms or issues, for example, the impact of diet on blood sugar levels or the impact of smoking on lung function.
During pretraining consultations, exploration of the impact of physical, lifestyle or other concerns for the patients’ mental well-being was not particularly evident. Opportunities to pick up on cues associated with mental well-being raised by patients were sometimes missed or avoided. For example, patient 412 mentioned irregular sleeping patterns, but this was not explored further by the PN within the context of lifestyle behaviour and a possible relationship to mental well-being. At the start of consultation 106, the PN made an early enquiry about whether or not the patient was shocked at a recent diagnosis of DM, but did not explore the patient’s own emotional responses further when the patient responded with a brief account of their family history of DM. Slightly later in this consultation, the PN asked, ‘And how d’you feel in yourself?’, but although the patient replied, ‘much better’, the patient’s additional comment about recent tiredness, possibly as a result of business at work, was not explored further. At the start of consultation 632, the patient mentioned being stressed, but this comment was light-heartedly deflected by the PN, as illustrated by the following quotation:
. . . you’re generally keeping quite well yeah?
Bit stressed.
And it’d be quite fine if we’d treatment for that wouldn’t it!
Mh mmm.
So, breathing-wise, chest-wise, any issues, any coughs at all?
Consultation 632
Other enquiries around the domain of mental well-being were touched on, usually towards the end of consultations; however, these enquiries were limited in scope/depth, drawn back into relating patients’ well-being to physical health issues or too vague, as illustrated by the following quotations:
Is there anything that’s concerning you at all [patient’s name] [PN pauses slightly] . . . about your diabetes?
Consultation 106
Anything that is worrying or concerning you Mr . . .?
No, not a thing. I feel good.
Good.
I feel quite fit.
Uh huh. Do you have any oily fish in your diet?
Consultation 271
So, on a whole, are you happy enough with things just now?
Consultation 411
Everything else alright with you?
Consultation 412
Within the DM reviews, references to other services and support for patients were limited to enquiries about whether or not patients had attended DM-related eye tests or podiatry appointments, or brief discussions about future review appointments. No referrals or signpostings were made during these pretraining consultations. During the COPD review, the PN signposted the patient to a range of smoking cessation services, and to the GP in relation to a foot problem, which presented as a barrier to exercise.
Attention to social environment domains did not feature within pretraining consultations, with the exception of one consultation (271), in which the PN enquired about a patient’s holidays and daily gardening activity.
Post-training consultations
All post-training consultations were DM reviews. The average duration of post-training consultations was 20 minutes and 59 seconds. Post-training consultations began similarly, with general introductory enquiries by PNs about the patients’ overall health or well-being.
Figure 2 shows that, post training, physical health and lifestyle domains featured at frequencies similar to pretraining consultations, again within the context of PNs conducting review tests and providing feedback on blood tests.
There was more evidence of attention being given to the impact of physical, lifestyle or other concerns on patients’ mental well-being during post-training consultations, with enquiries about this domain beginning as early as 1 minute and 50 seconds (23G561). Only in one consultation (583) was enquiry about mental well-being left until towards the end of the conversation.
Markedly, PNs’ enquiries about mental well-being were more explicit in post-training consultations. For example, during consultation 572, the PN began with a general question, ‘. . . how are you feeling?’, which elicited a response about physical symptoms, but she followed this up with two clearly worded questions about mental well-being: ‘And how are you feeling in yourself with all of this going on, I mean emotionally?’ and ‘Does your mood ever dip or d’you ever feel that you’re struggling emotionally with what’s been going on?’. The patient’s response to the second question, ‘No, no, no, definitely not’, indicated that he had understood the question, and the PN then moved on to talk about the patient’s home environment and activities. Another example of explicit wording of questions relating to mental well-being occurred in consultation 573, in which the PN asked, ‘And how are you feeling in yourself, . . . mood-wise and things?’ and, later in the same consultation, ‘Is there anything that’s worrying you or anything that’s concerning you at the moment that we can help you with?’. It was evident from consultation transcripts that even PNs who knew a patient very well were not precluded from asking specifically about mental well-being.
Not all patient cues around mental well-being were addressed fully by PNs. For example, during consultation 582, the PN began the consultation with a general question, ‘How have you been since we last saw you?’, leading to the patient’s detailed reporting of current physical health issues negatively affecting daily activities. The expressed negative impact of these issues on how the patient felt was not immediately probed more fully, but the PN then enquired more broadly about the patient’s well-being by asking, ‘So, other than the . . . problem, how’s things been otherwise, health wise, mobility wise, life’.
In contrast to pretraining consultations, the domain of social environment was attended to more fully post training. This domain was introduced and interwoven as review tests were being conducted. The introduction and conversation about aspects of social environment began as early as 3–5 minutes into consultations and continued at various points until the end of the consultation, usually in a relaxed conversational style. During consultations, a range of social environment subdomains, including home environment, daily activities and social network, were addressed. Examples of the types of questions asked by PNs included:
And how’s your mobility around the house with using the stairs and things. Do you have any concerns there?
PN (consultation 572)
And are you getting out and about . . .?
PN (consultation 573)
Do you manage at home? Do you manage to do all your jobs around the house?
PN (consultation 582)
And do you still work or are you retired now?
PN (consultation 583)
Occasionally, opportunities were not taken to probe further about a patient’s social circumstances. For example, during consultation 582, the patient mentioned that she did not have much contact with her daughter, who lived locally, but the PN did not explore this relationship in more detail or ask, in the absence of family support, what other regular social contact and support the patient had.
The domain of financial resources was not touched on by PNs in any of the post-training consultations.
In common with pretraining consultations, references to other services and support for patients were again limited to enquiries about whether or not patients had attended DM-related eye tests or chiropody appointments, or brief discussions about future review appointments. One exception to this was a PN’s conversation with a patient (573) about attendance at weekly/respite care services. No referrals or signpostings were made during post-training consultations.
Conclusion
The domains of physical health and lifestyle behaviours were attended to with, more or less, equal frequency in pre- and post-training consultations. Although the domain of mental health was touched on in pretraining consultations, this tended to be done very briefly, and there was limited or no probing. Post training, the PNs introduced the domain earlier and more explicitly. They made specific reference to asking about patients’ feelings and moods.
The domain of social environment was attended to more fully in post-training consultations, particularly enquiries about patients’ home environments and social networks. Aspects of patients’ social environment domains were not always probed fully and there was no reference at all to financial resources. This perhaps reflects PNs’ sensitivity and apprehension about broaching this topic, as expressed during the staff focus groups.
Overall, there was evidence of fidelity to the PCAM tool during post-training consultations. Although pre- and post-training consultations were of similar durations, this did not prevent PNs introducing and discussing PCAM domains, usually by weaving these into the consultation in a relaxed way, while conducting other review tasks.
Chapter 6 Study D: nurse and patient perceptions of using the Patient Centred Assessment Method
Methods
At the conclusion of phase 2 data collection, semistructured telephone interviews were conducted with PNs and nurse management staff involved in the implementation of the study in the practices randomised to the PCAM arm of the feasibility RCT. The interviews aimed to gather information on the experience of taking part in the study and of delivering the PCAM intervention, to assess the acceptability and feasibility of both the research methods used and the PCAM tool. Data were collected and analysed using the same stages as for study A, and have also contributed to the overall theoretically informed NPT analysis being written up for publication.
Semistructured telephone interviews were also held with a self-selecting sample of patients in the PCAM arm of the trial who had returned questionnaires. Interviews aimed to assess their views on the use of the PCAM tool in their review, and to gather further information on the outcome of any referrals or signposting made in the review. Patient interviews were analysed using thematic analysis.
Sample and recruitment
Practice nurses
All PCAM-arm PNs were asked to take part in interviews. Owing to the low number of participating practices, all nurses consenting to participate were interviewed. In addition, PMs in two sites, and the lead PN in a further site who had contributed to the implementation of the research, were also invited and, subsequently, consented to take part in interviews.
Patients
An invitation to take part in a telephone interview was sent to all patients who had completed a baseline questionnaire. The invitation was included in the envelope containing their follow-up questionnaire. Patients wishing to take part in an interview provided their name and contact details on a form and returned this to the research team, together with a consent form, in a prepaid envelope. A researcher then contacted the patient to explain the purpose of the interview in more detail and arrange a suitable time for the interview. Verbal consent was further confirmed at the start of the audio-recording of the interviews. All consenting patients were interviewed and blinded to allocation.
Procedure
Nurses and other practice staff were interviewed by a member of the research team who had not been involved in supporting them during the data collection phase. Interviews were conducted by telephone and were audio-recorded. The audio-recording was unsuccessful for one interview, and for this interview, written notes were used to summarise the key points made.
Practice nurses and staff were asked for their views on the importance of psychosocial issues to their patients’ health and well-being, along with the relevance of assessing these in a nurse-led LTC review. The experience of taking part in the training, and whether or not it adequately explained the purpose of the PCAM tool and prepared staff for its implementation, was explored, along with a discussion of perceptions of using the PCAM tool. Reasons for taking part in the study, views on whether or not the PCAM was an appropriate tool for nurse-led annual reviews and how the tool was used in a typical consultation were considered. Support within the practice and any impact on patient interaction and assessment of patient needs, particularly mental well-being, were discussed, as well as perceptions and use of the resource pack. The integration of the resource pack and other PCAM-related issues with normal clinical practices were also explored. Future use of the PCAM and factors that would be needed for its widespread use were considered. Throughout the discussion, any barriers and facilitators encountered were probed.
Interviews with patients considered issues that were discussed in their consultation, and whether or not they were aware that the nurse was using the PCAM tool. Patients were asked about their awareness of nurse attention to wider aspects of their overall well-being, and what their views were on this wider discussion. Patients were also asked if they had received any health promotion and lifestyle advice or had been referred or signposted to other services. Their views on any referrals or advice offered were sought.
Findings
Study D aimed to gather nurse and patient views on the use of the PCAM tool in their LTC reviews. Six patients and six nurses were interviewed. Nurse participants were asked about their experience of learning how to use the PCAM tool and integrating it into their consultations. Patient participants were asked about their experience of their last review. Given that the PCAM tool is a guide for the nurse, it may not have always been apparent to the patient how the tool was being used, so questions focused on the consultation in general, and the patient’s experience of their review.
Patient perception of the Patient Centred Assessment Method
Not all patient participants in this sample noticed any overtly discernible difference in their annual review post PCAM implementation. However, some patients did report being asked more questions or finding out more about their health condition. Given that the PCAM tool is not a survey, or something administered to patients, it was not necessarily expected that the patients would notice the presence of the PCAM itself; however, patients did describe talking with their nurse about their lives and their broader concerns during reviews, and described welcoming these conversations with their nurse. Participants also described feeling listened to and feeling that the nurse was trying to address the concerns raised by the patient:
And I do remember that the time before I was quite upset because it was . . . it was just about a year to when my husband died and things were just making me upset. So we talked quite a bit in June about how I was feeling compared to the time before and she listened quite a lot to me and asked if she could do anything more for me because she thought maybe if I went to see a dietitian, but I couldn’t fit a dietitian into my life just now [laugh]! So she was trying hard to try and help with the problems that she thought I was having.
Patient interview, participant 422
Patient participants described the consultations as being conversational in style. This confirms that the PCAM tool was implemented as intended, as a guide for conversations with patients rather than as a tick-box tool:
Yeah. it’s more as a chat than, you know, sort of ticking a box, you know, she more sort of generally just chats and tries to get you to communicate.
Patient interview, participant 449
Because the PCAM tool is delivered conversationally, participants were asked how they felt about being asked questions about the broader context of their lives within the review. Overall, participants seemed happy to be asked questions, and the questions had helped participants to share some of the challenges and struggles they were facing in their lives with their nurse:
It doesn’t bother me, I’m quite happy to answer any questions like that. I mean, I had a difficult time when my husband died because he didn’t have enough insurance and it was something that had never crossed our minds, I don’t know why, I mean, we are, we were older, . . . so it just never crossed our minds. I have insurance as well so since then I’ve actually looked to see I have enough to cover [laugh], so things like that. Yeah, I wouldn’t hide anything from any questions that she asked, I’d be quite truthful in answering questions and that.
Patient interview, participant 422
Participants talked about trusting that their nurse would have a reason behind the questions they asked, and that it helped to promote a good relationship with the nurse when there was an opportunity to talk more broadly about their lives. Some described feeling that, if the nurse felt that it was relevant to their care to ask a broader question about their lives, it would be acceptable to them:
I think she could basically ask anything she wants if she thinks it’s relevant and it may have an effect on people, it must have an effect on people.
Patient interview, participant 449
Once information was shared with the nurse, patient participants talked about appreciating being given information or resources to help with addressing those concerns. Examples of information shared with patients included referrals to clinics for additional services, information about walking groups and referrals to dietitians. Not all participants felt that they wanted to act on these referrals at that point in time, but described appreciating having the option available to them. One patient participant described sharing their concerns with the nurse as beneficial in its own right, regardless of whether or not they proceeded to access the support suggested by the nurse:
But yes, in a way it is very nice to chat with somebody, even if they just want to talk about your health or a health problem or something, that alone can make you feel better I think.
Patient interview, participant 457
In summary, PCAM implementation did not have a negative or obstructive impact on the consultation. The use of the PCAM tool to guide the consultation appeared to be seamlessly integrated into the consultation from the patient’s point of view.
Nurse perception of the Patient Centred Assessment Method
Nurse participants had a very different experience of using the PCAM tool in consultations, as it was integrating a new approach to consultations for them. So while patient participants were generally unaware of the influence of the PCAM, the nurse participants were able to describe their experience of the PCAM in greater detail.
Preparation for Patient Centred Assessment Method consultations
The PCAM training provided by the research team was generally sufficient for the nurse participants. There was a mix of presentations and cases to consider in the training; however, some nurse participants felt that having more emphasis on role playing would be helpful for learning how to integrate the PCAM into the consultation:
I would say a bit more hands on. For example, a bit of role play, a bit more role play, you know, pretend I’m the patient, you know, let’s go through the PCAM toolkit, use that just to get a feel for how it works. Whereas the presentations were a bit wordy, but not overly, not overly so.
Nurse interview, participant 745
Including information on the use of the PCAM tool and evidence for the tool was described as important in the training. It allowed participants to think through any reservations they had about the value of a PCAM-based consultation and, accordingly, address any scepticism:
Well to start with, I can’t deny that I was a bit sceptical. There was nothing I wasn’t aware of, but it was useful to get the paper evidence and then hearing it being confirmed.
Nurse interview, participant 178
In addition to role playing, and useful presentations, participants spoke of the value of having time to explore the PCAM tool in relation to their own patients and real clinical cases. This allowed for a deeper consideration of how to apply the PCAM and how best to integrate it with their own patient population:
Yeah and one thing that was quite good, well we actually had enough time where we could obviously chat things through and we spoke about our own patients, possibly what would be even more helpful is, like, when you’re on the spot you’re trying to think of your own patients relate them to, but even for the training if you had some case studies as well.
Nurse interview, participant 275
In summary, a multifaceted approach to training, which integrated key information, role playing and opportunities to apply the training to real consultations, was useful for nurse participants.
Use of the Patient Centred Assessment Method in consultations
The general implementation of the PCAM tool into the consultations appeared to have gone well and without many challenges. Some described that it took a little time and practice to fully integrate the PCAM tool into their consultation in a way that felt naturalistic:
Now, yes, now. I’m not saying . . . at the beginning you were still sort of stuttering your way through it, you know, you were sort of finding your feet, you know, but now you keep all the sort . . . when they’re coming in for the review obviously you’re talking about health and well-being anyway, you know, but in the cases of maybe social environment and things like that, you know, it’s something you would never have brought up before but now when someone mentions ‘oh my father’s . . .’ ‘oh, so what like is it at home?’ you know, your window’s there then, you know.
Nurse interview, participant 41
Some nurse participants described the PCAM as being a close fit with their current practice-wide approach, and for those participants it was straightforward to include the PCAM tool, and it was described as helping to formalise the consultation. For other participants, the PCAM was a change in their consultation style, as it raised topics that had not necessarily been part of their annual review previously:
In the way that it’s delivered. Before PCAM we just . . . we didn’t concentrate on the sort of social aspects, the financial, the mental health, you know, that sort of thing, it was just mostly the lifestyle of ‘do you smoke, do you drink, how’s your diet, how would you describe your diet to me, do you exercise?’ you know, and then you would pick the whole of that and you would make your plan accordingly to that. But now you’re just . . . what’s the word I’m looking for . . . you’re just doing your consultation so different from what you did before you did the study, you know.
Nurse interview, participant 41
Participants talked about how certain domains took a little more practice and review to include in their consultation style than others. Some were struggling to ask questions around mental health, and others mentioned that it felt awkward getting used to asking questions about finances:
The only thing was the financial one I found a bit . . . yeah I wasn’t so sure about that one, just how to word that and to come out with that. Again there were certain people that are more than happy to sort of divulge things without you asking too much, and others that it just seemed completely inappropriate to be asking about their financial situation.
Nurse interview, participant 177
Interestingly, this project was happening alongside another initiative, House of Care (HoC), in some of the practices. The two initiatives were viewed by participants as being consistent with each other, with a focus on broadening the consultation to consider the context of patients’ lives more fully. Some had incorporated the PCAM into their HoC activities, and described using the PCAM as a tool to help achieve their HoC goals. Several participants reflected that they found the PCAM to have better utility than HoC in their setting, as they found that the PCAM allowed for deeper conversations with patients about their concerns than the approach suggested under HoC:
Yeah it turned out because I honestly thought the House of Care was going to be the answer and everybody was so excited about getting on and starting this House of Care and we were doing PCAM starting at the same time, and because House of Care is such a big thing and it’s so widely known, PCAM’s got kinda ‘oh well, yeah we’re doing this as well’ and very quickly, within a few months, we thought ‘wait a minute, this PCAM is better’ [laugh] and that’s the way it was, uh huh. To be honest we didn’t think it was going to be as successful as it was, we thought it would be House of Care would’ve been, you know, and it just wasn’t.
Nurse Interview, participant 745
Overall, it appears that the PCAM tool was fairly easily integrated into consultations, although some participants reflected that the process of integration took some time and support.
Relationship with patients
The nurse participants in this study all described the use of the PCAM as a positive influence on the quality of the relationships they have with patients. The PCAM consultation was described as improving trust and communication with the patient, which was seen to allow for more open communication about what was happening in the patient’s life that might be having an impact on their LTC. The PCAM was seen as providing a tool to help guide and encourage that open communication, and for some nurse participants, it had challenged their assumptions about which patients might be facing difficulties, particularly as they came to learn that some patients who they had assumed were coping, were not. The PCAM tool also helped to guide discussions for patients who might have been typically unforthcoming or hesitant to share their concerns:
I guess people, I think once they start to open up to you about something that’s troubling them and they get a trust there, they will tell you quite a lot, so that’s a good thing, but then there’s others that you know that there’s things troubling them and you can’t get that out of them. I can’t think of anything that completely surprised or shocked me when we were doing it, but yeah people are maybe more open than before, don’t know.
Nurse interview, participant 177
In study A’s findings, we noted that focusing on clinical care alone seemed to lead to some professional participants making negative attributions about patients’ participation in their LTC care. Participants were sometimes frustrated, with a perception that patients were not paying attention or not following recommendations. In this post-implementation sample, nurse participants described how the PCAM helped to offer insights into why patients might not be following their recommendations, and this appeared to help promote empathy for the patient and a greater understanding of their circumstances:
PCAM’s just taken it that step further, as in really homing in if the patient says no to one thing, how you can get back to it and get a bit deeper again, you know, they’re not just there about their chronic disease, it’s things that they reveal once they start down these conversations, it’s things that you think well no wonder they can’t look after their respiratory or their diabetes or their cardiovascular conditions because they’re so stressed about whatever else is going on in their life.
Nurse interview, participant 745
When nurse participants were able to find out about issues they had not known their patient was facing, and to find ways to work with that patient to connect them to resources or troubleshoot problems, they reported satisfaction in feeling that it improved the quality of the care they could provide. The PCAM was described as having an impact on their practice by uncovering hidden concerns, and then offering an opportunity to support patients in relation to those concerns. This was seen to be more holistic care, which appeared to resonate well for the participants:
I would say it’s . . . a way of caring for patients, looking after their needs, not just their health, their immediate health needs, it’s looking after their social needs as well. It’s having a much more holistic approach. Health and social well-being, they affect each other, you know, if one’s not right the other’s not right. So if your health’s poorly, your social well-being will be poorly, if your social well-being’s poorly your health won’t be 100%. And to look at them as two separate issues is not the way forward, you have to look at it as a holistic . . . you know, you have to look at it all together. If you’re caring for that patient you want to care for the whole . . . quite often someone, especially with anxiety, stress, you have to find out what that problem is, why are they anxious, what are they stressed about? If you can sort that out or help them, you know, even to help them manage their own needs and give them some kind of direction, that has a huge impact on their health.
Nurse interview, participant 745
In addition, the nurse participants described times when the PCAM identified needs that the nurse could not address, even though they make onwards referrals. However, the participants described the value in knowing information about the patient that might influence the care they provided to the patient, by being sensitive to the context of that individual and their challenges. In this sense, the PCAM was seen as helping the PN to avoid making suggestions that the patient might not be able to act on:
It’s a concern that you may not be able to help. There’s nothing in the PCAM that isn’t going to affect their health. It’s fair enough to at least be looking at the overall picture and how it’s affecting their condition, because there are so many that can have a knock on effect. It’s not as simple as just telling them what to do when you realise the things that might make that difficult for them.
Nurse interview, participant 178
In summary, the PCAM appears to help support a positive patient–nurse relationship by increasing the quality and openness of communication, and the understanding of the patient’s life. The nurse participants perceived this to be beneficial for both the patient and the nurse, in relation to both the quality of the relationship and the quality of the care provided.
Signposting
As part of its participation in the project, each practice was given a locally relevant collection of resources to which they could direct patients in response to any concerns raised by the various PCAM topic areas. The resource pack provided by the research team was very well received by the nurse participants. Some of the participants knew their local agencies and resources well, and did not find that the pack offered new information, although the convenience of it being provided in a folder was appreciated. Some nurse participants had not known of the local resources provided in the folder and were very pleased to have that information made available to them. Some participants expressed concern that they were unlikely to have the time and capacity to update the information following the conclusion of the project. One practice had integrated their own resources with the PCAM team-provided resources, and was actively working to update the information on an ongoing basis:
Well we’ve decided what we’ll do is that I’ll be responsible for that, so the first time the nurses go to access a service and it’s not available or they can’t get through on the phone, they’ll let me know, I will chase it up to see if the service is no longer available. If it’s not available anymore I’ll take it out the folder. Or if any information’s changed I’ll put the new information in.
Nurse interview, participant 745
Nurse participants described routinely connecting patients to resources and onward referrals, and finding the process of doing so very valuable. Some had extended the use of the pack to patients who might be new to the practice as a way of helping them to learn what was available in the area:
I’ve used the signposting and that on many occasions and not just for people with long-term conditions, I’ve also . . . I see every new patient who joins the practice and we’re getting quite a lot from Europe, Africa, Asia and some of the signposting when they come in, you know, they’re asking you and you’re giving them . . . you know, information about of the pack as well.
Nurse interview, participant 41
Participants also talked about copying and sharing the resource pack across the practice, and with colleagues who were not part of the research, as it was found to be of benefit for other staff to also be able to access:
It was very easy. The format means it’s easy to keep with you and find things. We were just saying that it would be good to copy it and let other staff in the practice use it too. We’ve been able to think about what else we can put in it and who can keep an eye on it.
Nurse interview, participant 178
Overall, there was a sense that the nurses found the resource pack very useful and had been active in signposting patients to various supports. This seemed to be accompanied by an approach of helping patients to access support for themselves and to address what their own priorities were, rather than focusing on fixing clinical issues:
For patients to take the responsibility of looking after themselves with support from us and the better we can support them then hopefully the easier they will find it to take on the responsibility for their own health. That’s a huge thing.
Nurse interview, participant 177
Some described feedback from patients themselves on the use of signposting, when patients were generally pleased to have been put in touch with resources in their local community:
Oh yes there’s been many. I’ve had patients coming in and saying to (the nurse) thank you very much for getting me in contact with whatever group, this is what’s happened’ and positive things.
Nurse interview, participant 745
Intended future use of the Patient Centred Assessment Method
Participants were asked to reflect on their intentions around integrating PCAM-based consultations into their ongoing practice, beyond the course of the research project. Some participants described being very keen to continue to use the PCAM consultation approach, and had already extended the practice to other patient groups in their clinic:
We don’t only use it in CHD, diabetes, COPD, we use it in everything from our asthma patients . . . we use it in every sort of . . . even our hypertensive patients we use it, you know, we’re using it . . . well, me and my fellow nurse we’re both incorporating it into our daily tasks if you get what I mean.
Nurse interview, participant 41
Some participants were more reserved, describing an intention to use the approach in informal ways by incorporating the questions and approach into their consultations in an ongoing manner:
I think certainly to a certain extent there will be bits that I use on it in my annual reviews, I’ll certainly use the pack and I might refer to the sort of outline of questions just for guidance.
Nurse interview, participant 177
No participant in their feedback stated that they were opposed to using the PCAM in the future or made any comments indicating that they would be avoiding using the PCAM. Long-term adoption of the PCAM appears likely for some of the nurse participants in this research, beyond the research project itself.
Conclusion
The PCAM implementation did not have a negative or obstructive impact on the consultation. The use of the PCAM to guide the consultation appeared to be seamlessly integrated into the consultation from the patient’s point of view. There was some indication that a small number of patients may have been aware of more discussion about their lives and their broader concerns.
The PCAM training was acceptable, but required a multifaceted approach to training that integrated key information/knowledge, role playing and opportunities to apply the training to real consultations. Future training delivery will require the incorporation of these different aspects, and in a way that is flexible with nurse availability and workload.
Overall, it appears that the PCAM was fairly easily integrated into consultation, although some participants reflected that the process of integration took some time and support, which will need to be taken into account in future training and support.
The PCAM appears to help support a positive patient–nurse relationship by increasing the quality and openness of communication, and the understanding of the patient’s life. The nurse participants perceived this to be beneficial for both the patient and the nurse, in relation to both the quality of the relationship and the quality of the care provided.
Resource packs were seen as integral to using the PCAM, and practices engaged with these resources, often to the extent of taking ownership of their continuing development. However, for some practices, this could be seen as a future problem (how to keep these resources up to date) that could have an impact on their use of the PCAM.
Long-term adoption of the PCAM was seen as feasible and possible by some nurses, which indicates overall potential for the acceptability and feasibility of the PCAM for use in primary care nurse-led consultations.
Chapter 7 Study E: process evaluation
Methods
The process evaluation aimed to reflect on two issues: the implementation of the PCAM in PN consultations and the implementation of the feasibility trial methods. The data used for the overall evaluation comprised:
-
contributions from study A focus groups with practices and patients on the acceptability and feasibility of the use of the PCAM, and any early reflections on barriers to using the PCAM in PN consultations
-
researcher field notes of meetings and discussions with staff
-
any comments to the research team or reported by practice staff from patients during implementation
-
data from study D, the final interviews with practice staff and patients
-
data from open-ended questions on staff and patient questionnaires collected as part of study B.
The methods for studies A, B and D have been reported elsewhere. The collection of study field notes was seen as a fundamental part of the process evaluation and was ongoing throughout the study. Each study researcher kept their own logbook of visits and contacts with practices and any reported incidents/problems, actions or comments associated with the study. The two researchers (EC and PA) had the most contact with practices, and each had more of a relationship with particular practices, thereby building rapport with practice staff and facilitating catch-up telephone or e-mail conversations between practice visits. However, this relationship was not exclusive to a single researcher and, therefore, all researchers, including Carina Hibberd, had some familiarity with all practices.
The research team met regularly to discuss any incidents/problems, actions or comments from each site in order to compare notes and reflect on observations. This alerted each practice contact to possible similar problems or allowed reflection on possible solutions based on experiences within other practices. The research team had more in-depth contact with those allocated to the PCAM intervention because of their involvement in training and responding to queries concerning the PCAM, and the need to obtain feedback on nurses’ experience of using the PCAM. However, close contact was still required with CAU practices to ensure that data collection was still being achieved.
The process evaluation was based on the MRC’s guidance for best practice and its key components, as identified by Moore et al. 42 (see Figure 1). This model was helpful in guiding the areas of knowledge needed for the process evaluation, but was also helpful in the analysis stage in pulling together knowledge from across the relevant data sets to articulate the context, implementation and mechanisms of impact within and across practices.
Field note analysis
The analysis of study A, B and D data sets has been described elsewhere in this report. The contributions of each of these data sets to the process analysis were initially discussed by several members of the research team (MM, CH, EC, PA, RP), and key relevant points for the implementation of both the PCAM and trial methods were agreed and summarised in accordance with the key components in the Moore et al. 42 model. The field note data were extracted from researcher logbooks into summary tables for each practice, one table reflecting on the trial process (for all six practices) and one table reflecting on the PCAM implementation (for three practices). Each researcher (EC, PA and CH) added their separate field notes on each practice into the summary tables and each researcher contribution was colour coded in case any further discussion was needed across the team. The summary tables were organised around the Moore et al. 42 MRC model. For implementation of the PCAM, this included:
-
training and support
-
broader multidisciplinary team (MDT) involvement
-
the review/patient consultation
-
resources.
For trial implementation this included:
-
training and support for data collection
-
broader practice involvement
-
patient conversations about the study.
Within each of these broad areas, the researchers then grouped their field note data around topics of context, fidelity to study intentions, dose (in relation to trial training or intervention training), adaptations, reach (who did nurses include/exclude), unanticipated consequences and participant responses/interactions with the study. The research team then collectively reflected on these processes to determine key learning points for the implementation of the PCAM and the implementation of the trial.
The extraction tables were constructed as a ‘best fit’ for enabling all researchers to input their knowledge on a single practice in relation to use of the PCAM or trial implementation. If time had allowed, we would have attempted to populate these tables, and followed this with a review of how best the broad areas and their topics consistently captured and described all the necessary detail, with a further iteration of the tables for final population/data extraction. Not all topics were populated across all practices, and some duplication of information occurred across categories, for example, some reflections on participant responses to/interactions with the study could also populate the topic of adaptations. Regardless of where information was collated on these extraction tables, the research team were confident that the ‘important knowledge’ they had collected in their field notes had been conveyed to the data tables and that this knowledge had contributed to the key learning points for the study. This method of analysis of multiple researcher field note data was novel and could be refined for further studies.
From feasibility to full-scale trial: using the ADePT decision aid to help identify protocol changes
The true value of any feasibility study is to identify and/or address any threats to internal or external validity that may have an impact on a full-scale trial. However, very few feasibility studies assess this in any systematic way. We chose to reflect on our study and its process evaluation with reference to ADePT,51 to identify protocol modifications for a full-scale study. The ADePT algorithm seeks to encourage systematic identification and appraisal of problems and potential solutions, improve transparency of decision-making processes and reveal tensions that exist between choices that lead to a pragmatic versus explanatory trial. The algorithm draws on Shanyinde et al. ’s framework50 of 14 questions for feasibility/pilot studies to consider (Box 1).
-
Did the feasibility/pilot study allow a sample size calculation for the main trial?
-
What factors influenced eligibility and what proportion of those approached were eligible?
-
Was recruitment successful?
-
Did eligible participants consent?
-
Were participants successfully randomised and did randomisation yield equality in groups?
-
Were blinding procedures adequate?
-
Did participants adhere to the intervention?
-
Was the intervention acceptable to the participants?
-
Was it possible to calculate intervention costs and duration?
-
Were outcome assessments completed?
-
Were the outcomes measured those that were the most appropriate outcomes?
-
Was retention to the study good?
-
Were the logistics of running a multicentre trial assessed?
-
Did all components of the protocol work together?
We identified the following areas as relevant to this feasibility trial: sample size, eligibility, recruitment, consent, randomisation, adherence/fidelity of intervention, acceptability of intervention, selection of appropriate outcomes, completion of outcomes, retention and logistics of multicentre sites and whether or not all components of the protocol worked. In evaluating the feasibility trial and its methods, several of the methodological issues identified by Shanyinde50 have been addressed elsewhere. Chapter 4 has addressed the quantitative findings in relation to sample, eligibility, recruitment, consent, randomisation and outcomes; Chapter 5 has addressed some aspects of adherence and fidelity to the PCAM intervention; and Chapters 3 and 6 have explored the acceptability of the PCAM intervention. The following analysis will focus on:
-
retention
-
study logistics in the multicentre sites
-
where any adaptations to protocol were identified
-
any unintended consequences
-
whether or not components of the protocol worked together.
We then reflect on any identified issues using the ADePT algorithm to ‘problem solve’ and evaluate solutions for both trial and ‘real-world’ contexts. ADePT encourages assessment of problems into the following ‘problem types’: type A is an issue likely only to be a problem for the trial (unlikely to be a problem in the real world); type B is an issue likely to be a problem for both the trial and the real world; and type C is an issue likely only to be a problem for the real world. Solutions are developed in line with whether or not there is a need to change aspects of the intervention, the trial design or the context. Solutions (single or multiple) can then be reflected on for the likelihood of their feasibility or effectiveness in a trial and/or the real world (depending on the type of problem).
Findings
The findings will first be presented for the process evaluation of the implementation of the PCAM by PNs, followed by the findings of the process evaluation of the feasibility trial and its methods. The findings of the process evaluation of the implementation of the PCAM are presented as a collective analysis for all three PCAM practices because the majority of issues (contextual, implementation and mechanisms of impact) were common across all practices.
Implementation of the Patient Centred Assessment Method in primary care nurse consultations for long-term conditions
Context
There were some overarching contextual issues that were relevant to all practices. The removal of the QOF in Scotland from April 2016 resulted in a lack of certainty around funding for primary care support for people with LTCs and what practices would be expected to achieve. For some practices, this appeared to be creating an organisational limbo. This could either support practice engagement, with the PCAM being seen as providing an interim way forward, or acting as a barrier to adoption, if practices interpreted the removal of the QOF as meaning that they were no longer required to focus on LTCs. In one practice, the PM hoped that the PCAM might be a useful way to identify and manage lifestyle behaviours, which is likely to be a future priority for LTC management in primary care.
Some practices already had some of their own initiatives in place, which were seen as overlapping with the PCAM goals; for example, practice E had already developed a holistic programme for patients with COPD. This same practice also began to use HoC between phases 1 and 2 of the feasibility study.
There was also ‘training fatigue’ in some practices. In one practice, the PN had just completed holistic needs assessment (HNA) training, 1 day per month for 6 months, and an asthma course over a 3-year period. There were also concerns about accessing future training as NHS support was reduced and GPs could no longer be compensated for allocating training time. Despite this, nurses frequently changed their opinion of the benefits of the PCAM training after putting it into practice. Some nurses were confident that they were conducting person-centred reviews already, but became aware that they could improve on existing practice to the benefit of the patient.
Implementation
In relation to training and support to implement the PCAM tool, practices tended to find difficulty in allocating the full block of time required to the training, as a result of other demands and heavy workloads. The disadvantage of attempting to condense all training into a 3.5-hour single session meant that little training in actually using the PCAM had been delivered and, therefore, further training had to be included at a later date. In some practices, both the initial and a subsequently organised training session had to be curtailed as a result of more urgent practice business. To some extent, the need to adapt the training to circumstances became an advantage, as it allowed nurses to reflect on the rationale and then refocus on the practical aspects of delivery at a later session. It became apparent that nurses need to experience short-term indicators of patient benefit over a range of issues to engage fully with the PCAM.
There was some enthusiasm for broader MDT involvement. The GPs had been enthusiastic about the PCAM at the outset and had initially planned to attend the training. Following good reviews from the first PN about using the PCAM approach, one practice began to discuss whether or not it could also be used, to some extent, by GPs. Issues that arose from the PCAM were discussed at MDT case meetings in one practice. This potentially acted to reinforce the embedding of the PCAM.
In terms of thinking about using the PCAM in consultations, nurses were often considering its application to the most complex cases in primary care and how they would cope with addressing these complex issues all at once. The worst-case scenario or ‘can of worms’ was the default case they envisaged. When asked for examples of patients for role playing, PNs tended to come up with highly complex scenarios, with issues beyond the scope of the PCAM. There was less reflection of its use for less highly complex cases in which less urgent/severe problems could still be addressed to the benefit of patients. However, one practice had also begun to use a HoC approach by the second phase of the study, prompting reflections on the two different approaches. In that practice, it was felt that the PCAM offered a tangible way of supporting patients, which complemented other approaches, and was revealing relevant and important patient issues.
During an initial presentation of the PCAM study, one PN recounted that, as a Keep Well practice, PNs were already inviting patients to talk about well-being issues and that it was difficult to contain and manage these types of discussions within an appointment time limit. Concerns about issues being raised that could not be addressed through known resources contributed to this, and the resource pack element of the PCAM was welcomed, as it increased confidence in being able to offer some potential solutions.
In training, several reminders to use the resource packs were needed during role plays. However, once PNs began to use the resource packs they praised the relevance of its contents and ease of use. There were many local suggestions for how to improve the resource packs and how they could or would take these forward once the PCAM study had ended. Most wanted a version they could control so that a practice could adapt it in the future. One practice reported that they were copying the resource packs for GPs to also use in consultations. One key concern was about keeping it up to date, and discussion is needed on creating a practice ‘champion’ to add and amend details on a regular basis.
The completion of the PCAM on paper was sometimes seen as an added burden, as it did not fit with the on-screen completion of other data collected during an annual review. This could feel like having multiple tasks to achieve in a consultation and the storage of additional paperwork then has to be considered.
Mechanisms of impact
There is no doubt that having the support of enthusiastic, research- and psychosocial needs-focused GPs helped to promote study adoption. Practice interest and attention to psychosocial needs was very common in practices in the most deprived areas. However, even in less deprived practices, having one enthusiast for supporting psychosocial needs in the practice could help push others into trying the PCAM.
The consideration of evidence within the process evaluation suggests that the PCAM is more likely to be feasible under the following conditions:
-
when nurses consider the asking of these questions to be part of the role of nursing
-
when nurses view their role as facilitating links to information or resources that can address concerns (rather than feeling that they have to address the concerns themselves)
-
when nurses have the information about resources available to them
-
when there is a whole-practice commitment to the approach, although in some large nurse-led units, this may be less important.
Nurses in some areas acknowledged that they were less confident in discussing the ‘financial resources’ domain with patients. Being aware of this was often helpful in opening discussion with nurses about potential benefits to their practice. A full explanation of each of the domains allowed nurses to consider cases in which touching on an issue might be of value, and increased interest in using the PCAM.
The MDT meetings provided an opportunity for the PCAM to be used and discussed, and this helped practices to see the overall value to patients and PNs in using the PCAM. When this happened, nurses commented that it might then encourage the practice to continue to use the PCAM.
The resource pack for facilitating signposting and referral was influential in securing practice participation, as it acted as an incentive; it provided nurses with a resource that they already recognised they needed, but did not have available in an easily accessible and LTC-focused format. The low-technology aspect of the paper-based version did appeal to users. It also helped to allay PNs’ fears of not knowing what to do if patients raised psychosocial issues, as they always had a potential solution for each of the PCAM domains. Maintaining this resource would be integral to maintaining use of the PCAM.
Some PNs reported that patient reluctance to take up referrals may limit the potential impact of the PCAM, reflecting that, in their view, patients were resistant to referrals because of real/perceived barriers, such as the cost and time of travel, shift patterns at work or childcare issues. However, it was recognised that such issues are not limited to the PCAM.
Key learning for implementation of the Patient Centred Assessment Method
Training in the use of the Patient Centred Assessment Method
-
There needs to be flexibility in how training and support is delivered. Brief training, followed by nurse reflection on the PCAM, alongside testing small areas of the PCAM and building up to its full use, can be interspersed with training/support sessions as nurses become more familiar and confident with the process or need to come back and ask questions.
-
Training needs to include more on boundaries and how to deal with complex issues over a number of reviews. There is a need to further emphasise where the PCAM fits into the ‘pyramid of psychological need’. 53 When this was emphasised in later training sessions, it helped the PNs to see that the PCAM, like most other approaches, was not designed to solve all problems.
-
Training needs to place more emphasis on helping nurses to practise completion of the PCAM tool and to see the benefits of the tool as a record of the consultation and any proposed actions.
Clarity of practice nurses’ role
-
Nurses do want a ‘magic wand’. Sometimes they do not broach an issue because they feel that they cannot help. Nurses need to be clear about their role in terms of signposting and referral, and have readily accessible resources to facilitate this.
Resource pack
-
Practices need to identify a resource ‘champion’ who can keep the resource list up to date. In some cases, the PM saw this as a role they could fulfil.
Integrating the Patient Centred Assessment Method with practice systems
-
If the PCAM could be appended to the practice electronic record system for completion and storage, it may help to embed this within annual reviews and streamline the process. This would overcome problems of storage and could facilitate MDT access to the PCAM data, and actions being initiated by the practice. This would also allow any change and progress to be monitored.
Implementation of the feasibility trial
This analysis will focus on retention and study logistics in the multicentre sites and where any adaptations to protocol were identified.
Recruitment and retention of practices
Many of the reasons for non-recruitment have been presented in Chapter 4, and the same issues were also often responsible for nurse dropout. Although reported at a practice level, it was common across all practices for staffing issues, such as sickness absence or recruitment difficulties, to be a prime reason for not participating in the study or to result in delays in participating and implementing the PCAM. Even PMs felt that they lacked capacity to engage with the PCAM study when their practice had staff shortages.
One PN had always indicated that the practice was not available to complete phase 2 data collection because of the uncertainty of future staffing levels in the practice beyond the summer of 2016; therefore, this practice was not included in the randomisation process. However, another practice failed to complete phase 2 data collection, initially because of staff sickness, and then subsequently because of additional pressures on practice resources, including the flu vaccination programme timing as well as perceived general under-resourcing. Every effort was made to accommodate postponement of phase 2 data collection and follow-up interviews, even up to and beyond the end date for the study, but, as each deadline for data collection approached, the practice reported that it would be unable to prioritise this within its current workload. The PCAM study and its data collection could not be prioritised over other practice issues; however, this practice has also indicated that it will continue to use the PCAM post study.
Some practices expressed interest in participating on the basis of enthusiastic PNs who had received communication about the study and, in follow-up calls, were able to make the autonomous decision as to whether or not they wanted to learn more about the study. However, individual practice circumstances affected PNs’ ability to follow up this type of contact, particularly whether or not the practice, as a whole, felt that it could accommodate additional demands on resources. In some practices, GPs or PMs expressed concern that participation in research, even for quality improvement, would have a negative impact on workloads and place PNs under too much pressure.
Having someone in the practice who was enthusiastic about participation and who understood the need to comply with study requirements made a big difference to completion rates. Nurses with an advanced level of nurse training and, previous research experience, and who were proactive in their local PN network had a greater understanding of the need to work within time scales and the study protocol.
Having the support of the PM was helpful for implementing trial processes and data collection. In some cases, the PM was proactive about identifying potential study recruits attending clinics; however, their absence from the practice for annual or sick leave had an impact on patient recruitment, particularly in phase 2. For privacy reasons, reception staff could not always reveal to the study team that the PM was absent and, therefore, contact with practices was hampered on occasion.
This would indicate that any future study involving two phases of data collection would need to over-recruit practices to account for such attrition.
Patient recruitment
The intention to recruit eligible patients by approaching consecutive patients attending for their LTC annual review was affected by a number of factors. PNs were keen to recruit ‘good patients’ who would be more likely to comply with questionnaire completion or who could complete questionnaires unaided, and comments in clinics, such as, ‘put them in. They’ll be good’, were made. Where such views were expressed, researchers were able to emphasise the importance of adhering to research protocol in patient recruitment. Researchers are not aware of any instances where fidelity to the patient recruitment protocol was breached and, in one case, a 100% recruitment rate from consecutive patients was directly observed by the researcher in the clinic.
Practices were variable in how much they could accommodate patient completion of questionnaires. One practice was able to provide a dedicated room for patients, but this could also depend on how busy the practice was, with Monday mornings proving more busy and noisy than other days.
Fidelity to the patient recruitment protocol was reported to have been greatly enhanced by the availability of researcher support within clinics. However, in some practices, the opportunities for researchers to attend clinics dealing with multiple annual reviews were limited, as there was no condition-specific clinic, and annual reviews of individuals were interspersed with regular check-ups or other nurse consultations. This made the process of recruiting ‘consecutive patients’ very difficult, and staff were more likely to have difficulties in remembering to recruit patients.
Researcher support (being a presence in the practice to answer patient queries concerning questionnaires) was offered in phase 2. Some PNs accepted this offer, whereas others were confident enough to undertake patient recruitment without a researcher being present. However, for some nurses, the number of patient-completed questionnaires was lower in phase 2 than in phase 1. The possible benefits of the presence of a researcher were emphasised at the end of the study by nurse 042, who thought, with hindsight, that recruitment and data accuracy might have been better.
An early request from PNs for guidance on how to introduce the study to patients led to the development of a suggested introductory script that PNs could use. PNs were free to use their own words and some chose to do this; however, the researcher noted that this resulted in some aspects of the study being missed from nurses’ introductory statements. A ‘pathway’ template was also added to the training materials to clarify the recruitment process. The responsiveness of the research team to any small problems the PNs identified was commented on by nurses, and may have helped in maintaining participation by practice staff. Explaining the study and answering patient questions were reported as the main demands on time associated with the study.
Practice organisation of LTC annual reviews was variable. In one practice, appointments were made via an annual recall automated process and arranged by the PM and reception team, with patients telephoning the practice to confirm attendance. PNs did not know who was on their list until the day of the appointment, and there were no condition-specific clinics. In other practices, some condition-specific LTC annual reviews (usually for DM) were held on the same day every week, but for other conditions (COPD) they were held on ad hoc days. In this practice, different LTCs also received different appointment times (40 minutes for DM and only 15 minutes for COPD) and, therefore, there were implications for including some LTCs in the study, as additional consulting time was required.
However, some practices were willing to alter clinic patterns or nurse duties to facilitate study completion rates. For example, in one practice, nurses managed separate LTCs, and the nurse responsible for COPD patients was worried that she may not be able to recruit sufficient numbers. The PM offered to add CHD patients to her clinic list during the study.
Fidelity study
Any future trial may also want to evaluate fidelity to the intervention. The method of recording and coding PN consultations would seem an appropriate way to do this. Chapter 5 has reported that this method appears to be able to determine changes in nurse behaviour within the consultation when using the PCAM. However, this study did not recruit sufficient nurses to make a definitive conclusion because, although willing to participate in the feasibility trial, some declined to have their consultations recorded. Even some who agreed to record consultations found it difficult to achieve sufficient numbers of recordings. Their reasons for non-participation and poor completion may be the same: general perceptions that patients would not agree to this. In the PCAM practice that did not consent to having any consultations recorded, both the PNs and the PM held this view.
Key learning
Some basic research principles may need to be included in trial processes training, especially explaining reasons for research processes in order to avoid selection bias in patient recruitment. There may be merit in the development of a short training session on research processes that could contribute to nurses’ continuing professional development training.
The PM role can be very important in helping to facilitate patient recruitment processes, especially for establishing practice processes for identifying ‘consecutive patients’, or temporarily changing practice processes to accommodate study requirements. Early trial discussions should include the PM, and practice-specific standard operating procedures could be agreed with PMs. PMs could help with the following processes:
-
grouping appointments for specific days to facilitate researcher attendance on recruitment days
-
allocating extra time for recruitment clinics, especially during the PCAM stage
-
addressing PN concerns where they can
-
making arrangements for patient information packs to be given out within the practice, by either reception staff or nurses
-
flagging potentially eligible PCAM patients in PNs’ daily list.
Researcher support of data collection in practices is needed for both phase 1 and 2 data collection, at least for the initial few days. There is a need for a system of administrative data review in the early stages of the process with a researcher present, and throughout the recruitment phase, to ensure that protocols are adhered to. However, because of the ad hoc nature of booking LTC annual reviews in some practices, there is a conflict between being able to provide support for the research process and conducting research within budget constraints.
There is a need to establish particular times when other issues/seasonal workloads may make the implementation of the study difficult.
Further research is required to explore PN reluctance to audio-record their consultations and how this might be overcome in future fidelity studies, or indeed, other studies of the work of primary care nurses in managing LTCs.
Review of problems and solutions using the ADePT
Table 9 below sets out the problems identified within this feasibility study, the proposed solutions to these problems and an evaluation of the proposed solutions based on the AdePT decision aid.
| Problem type | Problem | Solution(s) | Could the solution/strategy be effective and feasible? For the trial or the real world? | Evaluation of solutions |
|---|---|---|---|---|
| Type B | Practice recruitment | Develop more efforts to access PNs directly | Dependent on how autonomous nurses are within individual practices | Exploratory work would be needed |
| Feasible, but effectiveness not able to be demonstrated at this stage | ||||
| Type A | Practice recruitment | Over-recruit to study to allow for practice attrition | Effective for managing attrition | Would be necessary for any future trial |
| Feasibility unknown in current climate of primary care | ||||
| Type B | Nurse retention | Back-fill of posts so that study time is fully supported | Feasibility unknown, as primary care practices in Scotland already report a crisis in nurse recruitment | Exploratory work would be needed |
| Effectiveness unknown at this stage | ||||
| Type B | Nurse retention | Cultivating a practice/local champion to motivate and support nurses | Feasible, as some PNs or PMs acted in this role | Recommended solution |
| Effective in maintaining participation in the study | ||||
| Type A | Nurse recruitment of patients | Change practice processes to run sufficient LTC batch clinics | Feasible, as this was done in some practices | Recommended solution |
| Effective, as this was done in some practices and helped to achieve recruitment targets more easily | ||||
| May be more difficult in some practices or require more set-up time | ||||
| Type A | Patient follow-up | Telephone completion | Feasible, but would require telephone contact details to be provided on the first questionnaire | Recommended solution |
| Effective in other studies | ||||
| Participants could opt in to either paper or telephone | ||||
| Type A | Patient follow-up | Reduce questionnaire burden | Feasible | Recommended solution |
| Effectiveness unknown | ||||
| Type A | Patient follow-up | Incentive scheme such as prize raffle or voucher for all | Feasible | Recommended solution |
| Effective in other studies | ||||
| Type B | Training attendance/completion | Discussion of training delivery and tailoring of how this will work for each practice | Feasible, as this was necessary for the feasibility study | Recommended solution |
| Effective, but can lead to omitting important elements if future sessions not guaranteed |
Conclusion
The current context of primary care in Scotland may have made the implementation of the PCAM and the feasibility trial more difficult, as practices found it difficult all round to find the time to engage with the overall study requirements. It required a great degree of flexibility in both the PCAM implementation and implementation of trial methods, but more so with the implementation of the PCAM.
The training in the use of the PCAM has to be flexible to fit in with limited practice time, and a model of training and reflexive practice, followed by more training or individual practice-level support would work best.
When nurses did use the PCAM, there was general support for its value, and this grew with additional time to use the PCAM in consultations. The resource pack is an integral part of the PCAM intervention, but practices that engage with using the PCAM need to find dedicated time for keeping this resource live. There were no existing mechanisms for doing this at a local level that delivered the bespoke resource pack provided by the study team to facilitate the PCAM implementation.
The PCAM was acceptable to PNs and wider members of the practice team (such as PMs and GPs) where they had any contact with the PCAM nurses or the study. It was feasible to use in primary care with the right level of support for its implementation and use.
The trial methods were generally acceptable and feasible; however, the crucial aspect of practice and nurse recruitment was the most problematic, and in a small feasibility study of this size, we failed to recruit sufficient numbers. The process evaluation of necessary adaptations to trial methods as the study was rolled out has identified lessons learned and the need to minimise nurse involvement in data collection. This would require researcher support in at least two clinics, in both phases of data collection in each practice, with further support needed if processes were still not able to be adhered to. Practices that did not run clinics dealing with consecutive LTC annual reviews may need to be excluded, or a system developed to help remind nurses to recruit such patients.
The main problem of practice recruitment to the feasibility study may be viewed as a type A problem – a problem for the trial. However, given the overall problems of time commitment to training and the general crisis that primary care finds itself in with staff shortages, PCAM participation and adoption might also be a problem for the real world.
Chapter 8 Discussion
Introduction
This research aimed to determine whether or not the PCAM tool could be used by PNs to engage in holistic assessment of needs in patients with LTCs, and particularly for those with multiple and complex needs. The PCAM tool encourages action to be taken based on the severity and urgency of the patient’s situation. Its use is also aimed at encouraging a dialogue between the health-care practitioner and the patient, which serves to re-skill the practitioner in providing patient-centred holistic care, as opposed to the de-skilling that has been reported by nurses through the ‘tick-box’ mechanisms to improve quality of care. The PCAM should help to identify and address some of the broader social problems that often lead to or exacerbate poor mental health, which can, in turn, have an impact on physical health and the patient’s ability to self-care. It aims to encourage health-care practitioners to think about and make links with other sectors to more appropriately address these problems for patients, and to access alternative types of resources. The PCAM also aims to encourage new ways of working that enhance opportunities for health promotion, even in those with few current health or social problems, to maintain healthy behaviour. This should lead to improved quality of life for patients and better patient–professional interactions and relationships.
The findings from studies A, C, D and E would indicate that the PCAM tool can be used by PNs and that it did indeed encourage nurses to address some of the broader social needs of patients in their annual review consultations. Even when some nurses perceived that they already worked in a holistic way, they subsequently reported that use of the PCAM had highlighted to themselves that they did not always do this as well as they had previously thought, and that there were also some areas (such as mental well-being and finance) that they had not previously been addressing, and the PCAM had encouraged them to do so. In a very limited number of recorded consultations, the post-PCAM consultations did show some changes in nurse behaviour in line with what the PCAM would aim to achieve; nurses engaged in approaching a broader range of biopsychosocial problems when using the PCAM and these were more likely to be addressed throughout the consultation, rather than as a list of questions at the end. All practices reported that they would continue to use the PCAM, and one thought it was a better mechanism for addressing the care of those with LTCs than other initiatives in Scotland.
This study was not powered to determine any impact on nurse or patient behaviour or outcomes; however, the preliminary data show that the use of the PCAM may influence nurse referral patterns, with fewer referrals to GPs and more referrals to social care/community-based resources. There are some very tentative data showing that the PCAM might be likely to achieve more positive outcomes for patients than CAU, but this would require further testing on a larger sample. There were also tentative findings that the PCAM may lead to improvements in how well the PN could empathise with their patients, which may lead to reduced levels of frustration with patients who struggle to follow self-care recommendations.
The research also aimed to test the feasibility of running a cluster randomised trial in primary care. The difficulty in recruiting primary care practices in Scotland, and the number of practices approached to obtain the six that agreed to take part, led to the conclusion that it would not be feasible to run a large-scale cluster randomised trial in the current climate of primary care in Scotland. If practice interest and support could be generated, it would be possible to engage nurses in such a trial, although they would also require more support in any data collection activity. The inevitable crises that can happen in primary care, coupled with the small numbers of staff involved (most practices have only one or two nurses), mean that it can be difficult even for the most motivated of practices to guarantee participation when staff shortages (from illness or other reasons) occur. There are also many times when practice priorities have to come before research needs, such as annual mass vaccination programmes or clearing backlogs of annual check-ups. The difficulties in primary care in Scotland have been highlighted in a recent Audit Scotland review,54 which highlights problems with GP and nurse recruitment. The one health board area from which we did not recruit any practices to the feasibility trial is reported to have the highest GP vacancy rates outside the three island boards. The number of practices taken over by health boards in Scotland (mainly as a result of recruitment problems) has been steadily increasing since 2013. The Audit Scotland report also highlighted high levels of sickness absence in the NHS in Scotland, with major challenges for the future of the NHS workforce, particularly in the primary and community care setting, in which one in every two nurses is aged ≥ 50 years.
Patient recruitment was more feasible within this study design. Nurses were asked to only hand out study packs to patients with minimal advice. The patients were asked to complete questionnaires and return these before leaving the surgery or by post. Patients who completed questionnaires then received another questionnaire by post at 8 weeks. The aim was to obtain 10 completed questionnaires per nurse. Overall, patient recruitment and follow-up (retention) was acceptable, but was much lower in the phase 2 follow-up. However, in this study, this was affected by the delayed timeline of the study, meaning that some follow-up questionnaires were not issued by practices, as the study had ended.
There was significant nurse reluctance to have their consultations recorded. This was reported by nurses as a perceived problem in obtaining patient consent, which resulted in some nurses refusing to undertake this part of the study. Even nurses who did consent to taking part were reluctant to approach patients and did not recruit many, even though they reported that all patients who were approached consented to their consultation being recorded. This would indicate that it is a nurse issue and not a patient issue. However, any future study of fidelity would have to involve a different methodological approach or an understanding of nurse reluctance that could then be addressed.
The Patient Centred Assessment Method versus other tools or interventions to promote holistic assessment
We believe that we have already made strong arguments that nurse use of depression screening tools has been ineffective and may have led to underdetection of mental health issues in patients with LTCs. However, as with the existence of the INTERMED, there are some other tools that may be considered as promoting holistic assessment, and it is important to reflect on the PCAM in relation to these other tools.
We found reference to the use of the Family Nurse Partnership Tool55 among adults with learning disability and, although it includes attention to social circumstances, it also includes using a battery of other mental health assessment tools that we did not find appropriate for PNs. We are not aware that this approach has either been specifically designed for use in primary care or tested for use in primary care, whereas the PCAM tool has been specifically designed for use in primary care.
Tools such as the Cardinal Needs Schedule,56 the Camberwell Assessment of Needs57 and the Nursing Needs Assessment Tool58 are specifically focused on psychiatric or older people’s needs and, for some, readiness for discharge. None of these was deemed appropriate for the purpose of PN assessment of biopsychosocial needs in primary care settings.
The HNA by MacMillan59 provides details of what a HNA and care plan should include for cancer patients, but does not provide training and skills to accompany this, and it directs practitioners to use patient-completed ‘tick-box’ assessment tools such as the Distress Thermometer, the Concerns Check List and the Sheffield Profile for Assessment and Referral to Care, which they would then discuss with patients. This process is more burdensome than the ‘tick-box’ screening associated with QOF, which nurses did not engage with or adhere to well. The HNA has not been fully evaluated in any clinical trials and has not been developed for use in primary care by patients with LTCs.
Other initiatives to promote care co-ordination for people with long-term conditions
The HoC60 is a system-wide approach to improving care for people with LTCs. This initiative has been rolled out in NHS England and now also in Scotland. Figure 10 is a composite of models used to describe the HoC. The key approach of the HoC is to enable grass roots localities to build and develop their own ‘houses’ collaboratively with people and local communities. It requires enthusiastic clinical leadership supported by administrators and policy-makers. It is an approach that aligns with locality working and with health and social integration.
FIGURE 10.
A composite version of the HoC model.
However, it is not clear what this means for practitioners at the level of the consultation and face-to-face interactions, other than that these should encompass patient-centred co-ordinated care. The HoC relies on many parts of the system (of health and social care professionals) working together, and it is less clear how non-medical support (formal and informal) will be included and accessed within the consultation to support patient self-management and address other identified needs.
There was one practice in our study that was involved in HoC Scotland and, although this was seen as complementary to the PCAM study, the PNs reported that, for them, the PCAM had more relevance for influencing their direct patient care interactions and they ‘preferred’ to work with the PCAM going forward to address the needs of patients with LTCs.
The Links Worker Programme61 in Scotland is a Scottish Government-funded programme aiming to mitigate the impact of the social determinants of health in people who live in areas of high socioeconomic deprivation. Its basis is the inclusion of a new specialist role, the community links worker, in primary care teams. Links workers have a third-sector or community development background and work with patients to identify goals that they want to achieve, and then facilitate links with resources or organisations which can help to support patients’ needs and goals. They undertake some of the signposting and community referral tasks that the PCAM was asking of primary care nurses, but can go further in facilitating access for patients to these suggested signposting or referral options. Similarly to the goals of nurse use of the PCAM with patients, the rationale for links workers is that, if individuals feel supported in their lives, then they are more likely to respond to information on ways to improve their health and to live well. If these people were to be successfully supported sooner rather than later, then there is a potential that their risk of developing LTCs would be reduced, or further complications delayed or prevented if they have already contracted long-term illness(es).
The PCAM is probably most similar to the Links Worker model in its aims. The Links Worker Programme commenced during the PCAM study and its evaluation is still under way. Therefore, the evidence base for the Links Worker Programme is still unclear. However, there is still a need in primary care for nurses (and GPs) who see the majority of patients with LTCs to be able to feel confident in determining whether or not patients have any problems that could be dealt with by the links worker. The completion of the PCAM tool in annual reviews could act as a facilitator for referral to those in links worker-type roles, who could then facilitate access to community-based resources. The two initiatives are more compatible than incompatible, and could strengthen the identification of needs and communication between the primary care team and the links worker. It is also unclear who will fund, and whether or not they will fund, the continuation of the links worker roles in Scotland, and these are not available across the UK. Therefore, the PCAM may still be the best method available for the promotion of biopsychosocial assessment in primary care and, with the development of a locally derived resource pack, could also be the best-available method for facilitating access to a broader range of psychosocial supports.
In conclusion, we believe that the PCAM is uniquely developed for primary care and we are not aware of directly comparable assessment tools that have been prepared for and tested in primary care.
The PCAM provides a comprehensive and practical approach via the three components of training, the PCAM tool and the resource toolkit. Other initiatives like HoC lack an easily understood and easy-to-use practical tool. The use of the PCAM by primary care nurses as a decision aid for referral to links-type roles in primary care would work really well. Links-type roles could also make use of the PCAM itself. The PCAM could serve as a systematic way of recording needs and actions to be shared across the primary care team (GPs, nurses, links or other social care roles).
Patient and public involvement
One of the key benefits of including PPI in clinical trials and on trial design is that they are likely to make studies more feasible, at least in terms of patient recruitment.
Research has shown that trials with higher levels of PPI are four times more likely to recruit to target. 62 Use of patient and public representatives can help reflect on whether or not a recruitment strategy will work, how it could be made easier for patients to participate in, how burdensome various elements of the study might be on participants and innovative ways of retaining participant interest in studies for follow-up completion. These can help to identify necessary adjustments to improve recruitment and retention.
The PPI partners in this study did indeed help to shape the recruitment strategy for patients, which was to opt in to either a focus group study or involved opting in to completing questionnaires and a possible interview. The burden on participants with LTCs was carefully considered by our PPI team in the light of this being a ‘feasibility’ study and the need to include a wider range of ‘outcomes’ to establish which ones worked best in terms of acceptability and completion rates. The outcomes needed to include measures of physical health, mental health and social needs. We also required information on actions undertaken by nurses (advice, referrals, signposting) and on whether or not patients had taken up this advice, referral or signposting to services. The complexity of the study design, and its attempt to gather multiple outcomes at both the nurse level and the patient level, was not lost on our PPI members, as we worked together to gather the required knowledge in the most efficient manner. This was probably helped by the degree of knowledge of research that our PPI members had and their enthusiasm for the study.
However, patient recruitment was not the problem in this study, and our PPI members were often as frustrated as the research team at the lack of recruitment of practices. They contributed to the many discussions throughout the study on how to address this and were reassured that the team had tried all possible avenues within the time scale available to achieve practice recruitment and retention.
In reflecting on our PPI as a team, we thought it best to allow our PPI members to write their own contributions to this. We asked them to reflect on their experience of working with us and whether or not we could have done anything differently to enable their participation in the study. Their responses are included in the following two subsections.
My experience and comments on the Patient Centred Assessment Method process; by patient representative 1
As a patient representative I appreciate the requirement and desirability for academia to be sometimes balanced by a lay point of view and if not present the journey from concept to publication may not be as comprehensive as it could be.
I sit as a patient representative (I prefer the term representative patient) on several committees and research groups so feel qualified to state that my experience with this feasibility study was one of the best in terms of support, inclusiveness, consideration and birthday cakes.
The panel made an effort to explain any terms or acronyms I or my fellow PR [patient representative] were unfamiliar with and always listened to our viewpoints and took the time to solicit our thoughts.
As to the actual content of the study I share the disappointment on the paucity of the total numbers of patients and practices involved but strongly believe that this holistic approach will show many benefits.
My particular thanks must go to Professor Maxwell, Dr Carina Hibberd and Ms Nadine Dougall.
My experience and comments on the Patient Centred Assessment Method process; by patient representative 2
As a sufferer from a sluggish (not to say absent) NHS protocol in dealing with anxiety issues caused by the diagnosis of a cardiac problem, I joined the Living Better Project Steering Committee which was an RCGP-led study aiming to improve the care of people with LTCs in primary care, hoping for procedural improvement . Unfortunately the results of the research resulting from the Living Better project did not translate into the hoped for improved protocol to establish a route to identify co-lateral problems which frequently resulted alongside a chronic disease diagnosis. But, in PCAM, I saw an opportunity to introduce a method to improve this situation within the existing structure.
Encouraged to be involved from the start in discussing the initial documentation and to join the Steering Committee by the key researchers it has been a pleasure to be involved with and to follow the development of this ambitious project. Always encouraged to participate fully in committee discussions and to contribute ideas throughout, and to feel free to criticise, my lay colleague and I were kept involved in all of the developing problems by the project leaders as well as in the successes. Our involvement in the discussion of the final report has also been thorough.
The infectious enthusiasm of the researchers and their stoicism when things were difficult have been singular.
There is no doubt in my mind that, in PCAM, there is the germ of an idea which will become part of NHS protocol in the years to come.
Strengths and limitations
The strength of this study is that it was designed as a feasibility study that has fully tested practice, nurse and patient recruitment and retention. The combination of the five studies, which all contribute to the overall aims of the study, means that, often, multiple sources of information could be used to contribute to overall study findings. For example, studies A, C and D contributed to the acceptability and feasibility of using the PCAM in primary care nurse-led annual reviews, as well as the overall process evaluation (study E).
Practices were recruited from very different areas of Scotland, for example from NHS GGC, which has the highest proportion of deprived practices in Scotland, and from NHS Grampian, which has small urban towns and rural areas.
There is no doubt that the recruitment and retention figures are a big limitation for this study; however, this was what the study was designed to test, so it is a finding rather than a limitation in this case. The lack of nurse participation in study C is probably one of the most disappointing aspects, because it resulted in very few consultation recordings, and yet, these showed great promise in demonstrating that the PCAM may actually achieve its goals of changing nurse behaviour in consultations.
The fact that researchers delivered training as well as being involved in study data collection may have introduced some bias into practices allocated to the PCAM arm; nurses may have felt that they had to be positive about the PCAM with the researcher with whom they had developed a relationship over time. However, interviews with PCAM PNs at the end of the study were conducted by the researcher with whom practices had had the least or no contact.
Some differences between phases 1 and 2, and between the PCAM and CAU patient populations, may indicate that there is some nurse bias in selection of patients for inclusion in the study. This may have been as a result of learning which patients were more likely to accept or decline to complete questionnaires.
Conclusions
The PCAM has been uniquely adapted for use in primary care and there are no other directly comparable assessment tools that have been developed for and tested in primary care. The PCAM provides a comprehensive and practical approach to assessing biopsychosocial needs in patients with LTCs, including multimorbidity. The PCAM intervention consists of three components: a tailored and flexibly delivered training package; the PCAM tool; and a locally based resource toolkit.
The PCAM has been shown to be feasible and acceptable for use in primary care in the UK, and shows that it does indeed have the potential to change the ways in which nurses engage with patients with LTCs, in the context of LTC reviews, which results in more attention to the mental well-being and social care needs of patients. The PCAM is more likely to be feasible when nurses see the asking of these questions as part of the role of nursing, view their role as facilitating links to information or resources that can address concerns (rather than feeling that they have to address the concerns themselves) and have the information about resources available to them, and there is a whole-practice commitment to the approach. Any future study of implementing or testing the PCAM in primary care would require these conditions to be met.
Training in the use of the PCAM has to be flexible to fit in with limited practice time, and also requires the inclusion of reflective practice. The resource toolkit is also an integral part of the PCAM intervention and practices need to find dedicated time to keep this resource live, potentially reinforcing local connections at the same time.
A cluster RCT would be theoretically possible at a practice-site level; however, given the above conditions, this would be resource intensive and may require a different approach to working with practices to establish their ‘state of readiness’ (such as an improvement methodology), and a different research design to evaluate adoption and impact. In addition, the efforts required to recruit to a primary care-based cluster randomised trial, and the current ‘crisis’ climate of primary care that seems to prevent many practices from engaging with research even when ‘interested’, would further indicate that a full cluster trial is not feasible or in any way cost-effective at this time.
Recommendations
The PCAM intervention warrants further exploration as an effective mechanism for improving the quality of care for people with LTCs in primary care, particularly in the holistic review of patient needs by primary care nurses.
In particular, research is needed to evaluate whether or not the PCAM has an impact on patient outcomes. The new GP (quality) clusters that are emerging across the UK, and currently being developed across Scotland, may offer an opportunity to engage clusters of practices in implementing the PCAM, which could then be tested in a pragmatic before-and-after effectiveness study. The use of a stepped-wedge design could still allow for randomisation (to start time for implementing the PCAM), and for baseline and post-implementation outcomes to be robustly collected.
Further research should also be conducted to confirm nurse fidelity to the intervention, as well as further testing of whether or not the PCAM has changed nurse behaviour as intended, by applying the methodological techniques developed during this study. Further developing the training and use of audio-recording consultations may help to improve discussion of social issues, such as housing, finance and relationships, and of health literacy. In addition, the patients’ perspective in terms of the impact of PCAM methods, and patient expectations on disclosure, should be further explored. There has been very little research into nurse consultations in primary care, despite their increasing role in managing LTCs; this study has provided a basis for conducting future work in this area.
Future studies also require the use of evidence-based improvement methodologies for at-scale implementation, such as evaluating GP practices’ readiness for change, practice commitment to the approach and nurse acceptance of their role in asking such questions and in making the required links with others in managing their patients’ needs. Active GP/practice support for use of the PCAM (and the initial investment of time for training and familiarisation) can help nurses to adopt and embed it.
In addition to these known improvement mechanisms, implementation would also require that practices have access and develop closer links to community-based resources, which would form part of their locally derived and locally owned resource toolkit.
Nurses require training to encourage them to address all domains of the PCAM and to become confident in its use. This is best delivered through an initial brief training session, followed by some time for nurses to apply the PCAM in practice and to build confidence in addressing all domains of the PCAM. Some mechanism for supporting nurses while they develop their skills and confidence is recommended, such as follow-up by the trainer or peer support/sharing of knowledge. Training needs and delivery formats can and should be tailored to practice- or nurse-based needs, and this is important for initial buy-in and securing precious time.
Nurses should be encouraged to use the PCAM across the whole range of patients they see (not just highly complex cases), when less urgent/severe problems could still be addressed to the benefit of patients, and to enhance promotion and prevention opportunities.
The increasing role that nurses play in managing LTCs in primary care means that more effort needs to be directed towards understanding how they deliver care and what opportunities there are for enhancing self-care. However, future research in this area will always be hampered, unless there are better ways of accessing, engaging and retaining primary care nurses in research. Some exploratory research should be conducted to understand how to better access, engage and retain primary care nurses in research.
Acknowledgements
We must start by giving our thanks to the patients and staff of participating practices, and to staff who considered participation, but found that other pressures prevented their active involvement. We cannot name them for reasons of confidentiality.
We would also like to thank our PPI and health-care/scientific partners, who contributed to the development and conduct of the study.
Study Management Group (additional to authors): Lucy Clancy (NHS GGC), Chris MacNamee (PPI), Graham Bell (PPI) and Dr Alison Hinds (SPCRN).
Study Steering Committee: Professor Brian McKinstry (chairperson) (University of Edinburgh); Dr Ruth Jepson (University of Edinburgh), Dr Edward Duncan (University of Stirling), Dr Deborah Baldie (NHS Tayside) and Mr Patrick McGuire (PPI).
Thanks also go to other regional members of the SPCRN for their help in recruitment and data collection tasks within practices.
Finally, we would like to thank NIHR for supporting this work.
Contributions of authors
Professor Margaret Maxwell is lead author of the report and, as such, substantially wrote the report (specifically Chapters 1, 2, 4, 7 and 8), as well as editing contributions to all other chapters. She was principal investigator of the study.
Dr Carina Hibberd was responsible for co-ordinating contributions to the report and its timely production and editing, as well as taking lead responsibility for Chapter 4. She also project-managed the PCAM study, co-ordinating recruitment, data collection, data management and the development and delivery of PCAM training.
Ms Patricia Aitchison took lead responsibility for Chapter 5, as well as contributing to methodological sections in Chapters 3 and 5–7. She was also responsible for study recruitment, data collection and qualitative data coding and analysis.
Ms Eileen Calveley took lead responsibility for Chapter 6, as well as contributing to methodological sections in Chapters 3 and 5–7. She was also responsible for study recruitment, data collection, and qualitative data coding and analysis.
Dr Rebekah Pratt took lead responsibility for qualitative data analysis and writing up of the qualitative analysis in Chapters 3 and 6. She also contributed to the development of the PCAM training and advised on implementation, recruitment and retention issues, as well as contributing to the overall editing of the document.
Ms Nadine Dougall was the statistician in the study and was responsible for the analysis presented in Chapter 4 and tables in the appendices. She also advised on study outcomes and data management.
Ms Christine Hoy read and edited the report, taking lead responsibility for the plain English summary and PPI contributions. She made particular contributions to the development of the resource packs and specifically to Chapter 8, the discussion on other initiatives in the field of LTC management.
Professor Stewart Mercer read and edited the report. He made particular contributions to the recruitment methods, and methods for evaluating fidelity and assessing the content of consultations, and specifically to Chapter 8, the discussion on other initiatives in the field of LTC management.
Dr Isobel Cameron read and edited the report. She advised on study methods and outcomes and facilitated recruitment and study implementation in one of the study sites.
Data sharing statement
Data sharing will be fully open to all collaborators in this study, in line with any EU and other regulations, including ethics approvals. Access to anonymised data by other external agents will be available on request from the study principal investigator, in accordance with ethics permissions and consents by the research participants.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Department of Health . Improving the Health and Well-Being of People With Long Term Conditions 2010. www.yearofcare.co.uk/sites/default/files/pdfs/dh_improving%20the%20h&wb%20of%20people%20with%20LTCs.pdf (accessed Jan 2018).
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43. https://doi.org/10.1016/S0140-6736(12)60240-2.
- Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract 2011;28:516-23. https://doi.org/10.1093/fampra/cmr013.
- Department of Health . Supporting People With Long Term Conditions. An NHS and Social Care Model to Support Local Innovation and Integration 2005. http://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4100252 (accessed 1 December 2016).
- Better Health, Better Care. Edinburgh: Audit Scotland; 2007.
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med 2004;66:802-13. https://doi.org/10.1097/01.psy.0000146332.53619.b2.
- Thombs BD, Ziegelstein RC. Depression screening in primary care: why the Canadian task force on preventive health care did the right thing. Can J Psychiatry 2013;58:692-6. https://doi.org/10.1177/070674371305801207.
- Subramanian DN, Hopayian K. An audit of the first year of screening for depression in patients with diabetes and ischaemic heart disease under the Quality and Outcomes Framework. Qual Prim Care 2008;16:341-4.
- Burton C, Simpson C, Anderson N. Diagnosis and treatment of depression following routine screening in patients with coronary heart disease or diabetes: a database cohort study. Psychol Med 2013;43:529-37. https://doi.org/10.1017/S0033291712001481.
- Maxwell M, Harris F, Hibberd C, Donaghy E, Pratt R, Williams C, et al. A qualitative study of primary care professionals’ views of case finding for depression in patients with diabetes or coronary heart disease in the UK. BMC Fam Pract 2013;14. https://doi.org/10.1186/1471–2296–14–46.
- Plummer SE, Gournay K, Goldberg D, Ritter SA, Mann AH, Blizard R. Detection of psychological distress by practice nurses in general practice. Psychol Med 2000;30:1233-7. https://doi.org/10.1017/S0033291799002597.
- Wilkinson RG, Pickett K. The Spirit Level: Why More Equal Societies Almost Always do Better. London: Penguin Books Ltd; 2010.
- The 2022 GP: A Vision for General Practice in the Future NHS. London: RCGP; 2013.
- Singh D, Ham C. Improving Care for People with Long Term Conditions: A Review of UK and International Frameworks. Birmingham: NHS Institute for Innovation and Improvement; 2006.
- Care Planning: Improving the Lives of People with Long Term Conditions. London: RCGP; 2007.
- Howe A. NICE Consultation on Potential New Indicators for 2013/14 Quality and Outcomes Framework. London: RCGP; 2012.
- de Jonge P, Huyse FJ, Stiefel FC, Slaets JP, Gans RO. INTERMED – a clinical instrument for biopsychosocial assessment. Psychosomatics 2001;42:106-9. https://doi.org/10.1176/appi.psy.42.2.106.
- de Jonge P, Huyse FJ, Slaets JP, Söllner W, Stiefel FC. Operationalization of biopsychosocial case complexity in general health care: the INTERMED project. Aust N Z J Psychiatry 2005;39:795-9. https://doi.org/10.1080/j.1440-1614.2005.01684.x.
- Peek CJ, Baird MA, Coleman E. Primary care for patient complexity, not only disease. Fam Syst Health 2009;27:287-302. https://doi.org/10.1037/a0018048.
- Maxwell M, Hibberd C, Pratt R, Cameron I, Mercer S. Development and Initial Validation of the Minnesota Edinburgh Complexity Assessment Method (MECAM) for Use Within the Keep Well Health Check. Edinburgh: NHS Scotland; 2012.
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med 2009;36:452-7. https://doi.org/10.1016/j.amepre.2009.02.002.
- Howie JG, Heaney DJ, Maxwell M, Walker JJ. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998;15:165-71. https://doi.org/10.1093/fampra/15.2.165.
- Mercer SW, Maxwell M, Heaney D, Watt GC. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract 2004;21:699-705. https://doi.org/10.1093/fampra/cmh621.
- Botega N, Mann A, Blizard R, Wilkinson G. General practitioners and depression-first use of the depression attitude questionnaire. Int J Methods Psychiatr Res 1992;2:169-80.
- A Users’ Guide to the General Health Questionnaire. Slough: NFER-Nelson; 1988.
- Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. https://doi.org/10.1097/00005650-199603000-00003.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Engel GL. The clinical application of the biopsychosocial model. J Med Philos 1981;6:101-23. https://doi.org/10.1093/jmp/6.2.101.
- Byrne PS, Long B. Doctors Talking to Patients. London: Her Majesty’s Stationery Office; 1976.
- Stott NC, Davis RH. The exceptional potential in each primary care consultation. J R Coll Gen Pract 1979;29:201-5.
- Pendelton D, Schofield T, Tate P, Havelock P. The Consultation: An Approach to Learning and Teaching. Oxford: Oxford University Press; 1984.
- Neighbour R. The Inner Consultation. Lancaster: N/ITO Press; 1987.
- Kurtz SM, Silverman JD. The Calgary-Cambridge Referenced Observation Guides: an aid to defining the curriculum and organizing the teaching in communication training programmes. Med Educ 1996;30:83-9. https://doi.org/10.1111/j.1365-2923.1996.tb00724.x.
- Pendleton D, Schofield T, Tate P, Havelock P. The New Consultation. Oxford: Oxford University Press; 2003.
- Duffin C. Nurse consultation style is becoming more ‘medical’. Nurs Stand 2001;15. https://doi.org/10.7748/ns.15.48.9.s27.
- Duxbury J, Walsh M. Nurse Practitioners: Clinical Skills and Professional Issues. Edinburgh: Butterworth-Heinemann; 2002.
- Smith S. Nurse practitioner consultations: communicating with style and expertise. Primary Health Care 2004;14:37-41. https://doi.org/10.7748/phc2004.12.14.10.37.c473.
- Zimmermann C, Del Piccolo L, Bensing J, Bergvik S, De Haes H, Eide H, et al. Coding patient emotional cues and concerns in medical consultations: the Verona coding definitions of emotional sequences (VR-CoDES). Patient Educ Couns 2011;82:141-8. https://doi.org/10.1016/j.pec.2010.03.017.
- Del Piccolo L, de Haes H, Heaven C, Jansen J, Verheul W, Bensing J, et al. Development of the Verona coding definitions of emotional sequences to code health providers’ responses (VR-CoDES-P) to patient cues and concerns. Patient Educ Couns 2011;82:149-55. https://doi.org/10.1016/j.pec.2010.02.024.
- Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns 2002;46:243-51. https://doi.org/10.1016/S0738-3991(02)00012-5.
- Roter DL, Stewart M, Putnam SM, Lipkin M, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA 1997;277:350-6. https://doi.org/10.1001/jama.1997.03540280088045.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Wagner EH. Chronic disease management: what will it take to improve care for chronic illness?. Eff Clin Pract 1998;1:2-4.
- Abrams LS, Dornig K, Curran L. Barriers to service use for postpartum depression symptoms among low-income ethnic minority mothers in the United States. Qual Health Res 2009;19:535-51. https://doi.org/10.1177/1049732309332794.
- Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention?. Milbank Q 2001;79:579-612. https://doi.org/10.1111/1468-0009.00222.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. Gesundheitswesen 2016;78:175-88. https://doi.org/10.1055/s-0036-1586630.
- Morse JM, Stern PN, Corbin J, Bowers B, Clarke AE, Charmaz K. Developing Grounded Theory: The Second Generation (Developing Qualitative Inquiry). Walnut Creek, CA: Left Coast Press; 2009.
- Charmaz K. Constructing Grounded Theory. London: Sage; 2014.
- May C, Murray E, Finch T, Mair F, Treweek SA, Ballini L, et al. Normalization Process Theory On-Line User’s Manual and Toolkit 2010. www.normalizationprocess.org/npt-toolkit (accessed 25 February 2013).
- Shanyinde M, Pickering RM, Weatherall M. Questions asked and answered in pilot and feasibility randomized controlled trials. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-117.
- Bugge C, Williams B, Hagen S, Logan J, Glazener C, Pringle S, et al. A process for Decision-making after Pilot and feasibility Trials (ADePT): development following a feasibility study of a complex intervention for pelvic organ prolapse. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-353.
- Ritchie J, Spencer L, O’Connor W. Carrying Out Qualitative Analysis. London: Sage; 2003.
- Fellow-Smith E, Moss-Morris R, Tylee A, Fossey M, Cohen A, Nixon T. Investing in Emotional and Psychological Wellbeing for Patients with Long-term Conditions. London: NHS Confederation; 2012.
- NHS in Scotland 2016. Edinburgh: Auditor General; 2016.
- The Family Nurse Partnership Programme: Information Leaflet. London; 2012.
- Marshall M, Hogg LI, Gath DH, Lockwood A. The Cardinal Needs Schedule – a modified version of the MRC Needs for Care Assessment Schedule. Psychol Med 1995;25:605-17. https://doi.org/10.1017/S0033291700033511.
- Slade M. CAN: Camberwell Assessment of Need: A Comprehensive Needs Assessment Tool for People with Severe Mental Illness. London: Royal College of Psychiatrists; 1999.
- Slater P, McCormack B. Determining older people’s needs for care by Registered Nurses: the Nursing Needs Assessment Tool. J Adv Nurs 2005;52:601-8. https://doi.org/10.1111/j.1365-2648.2005.03641.x.
- Henry R, Hartley B, Simpson M, Doyle N. The development and evaluation of a holistic needs assessment and care planning learning package targeted at cancer nurses in the UK. Ecancermedicalscience 2014;8. https://doi.org/10.3332/ecancer.2014.416.
- Coulter A, Kramer G, Warren T, Salisbury C. Building the House of Care for people with long-term conditions: the foundation of the House of Care framework. Br J Gen Pract 2016;66:e288-90. https://doi.org/10.3399/bjgp16X684745.
- Health and Social Care Alliance Scotland . National Links Worker Programme n.d. www.alliance-scotland.org.uk/what-we-do/our-work/primary-care/national-links-worker-programme/ (accessed 5 December 2016).
- National Institute for Health Research . Clinical Trials Toolkit: Trial Planning and Design 2016. www.ct-toolkit.ac.uk/routemap/trial-planning-and-design (accessed 5 December 2016).
- McCluskey S, Heywood S, Fitzgerald N. How Healthcare Professionals in Scotland Develop their Communication Skills, Attitudes and Behaviours. An Independent Report for NHS Education for Scotland. Glasgow: Create Consultancy Ltd; 2011.
- Making it Easy, A Health Literacy Plan for Scotland. Edinburgh: Scottish Government; 2014.
- Good Mental Health For All. Edinburgh: NHS Health Scotland; 2016.
- Ware JE, Kosinski M, Keller SD. How to Score the SF-12 Physical and Mental Health Summary Scales. Boston, MA: The Health Institute, New England Medical Center; 1998.
- Bruun NH. SF12: Stata Module to Validate SF12 Input and Calculate SF12 Version 2 t Scores. Aarhus: Aarhus University; n.d.
Appendix 1 The TIDieR (Template for Intervention Description and Replication) checklist
Item 1: brief name
Patient Centred Assessment Method: improving nurse-led biopsychosocial assessment of patients with LTCs and comorbid mental health needs.
Item 2: why? (Rationale, theory or goal of the elements essential to the intervention)
The PCAM tool has been developed to enable broad assessment of the biopsychosocial needs of patients with LTCs in primary care, and to promote action based on the severity and urgency of needs. The PCAM tool aims to help identify and address some of the broader social problems that often lead to or exacerbate poor mental health, which can, in turn, have an impact on physical health and the patient’s ability to self-care. It encourages linking with other sectors to more appropriately address these problems for patients and to access alternative types of resources. The PCAM also encourages new ways of working that enhance opportunities for health promotion, even in those with few current health or social problems, to maintain healthy behaviour. This will, hopefully, lead to improved quality of life for patients and better patient/professional interactions and relationships.
Nurses need to be supported in such tasks and, therefore, the PCAM intervention consists of three essential elements:
-
Training in the importance of addressing biopsychosocial needs and the evidence supporting this, as well as training in how to implement the PCAM within the context of LTC management in primary care.
-
The PCAM tool to support systematic assessment of needs based on the domains of:
-
health and well-being (covering physical health needs, impact of physical health on mental health, lifestyle behaviours, mental well-being)
-
social environment (covering home safety and stability, daily activities, social networks; financial resources)
-
health literacy and communication (covering understanding of symptoms, self-care and healthy behaviour, how engaged patient is in discussions).
-
-
A locally derived resource pack that includes options for signposting or referral to other agencies in response to identified needs.
Item 3: what? (Materials used in the intervention, including those provided to participants or used in intervention delivery or in training of intervention providers)
The PCAM tool is available at www.pcamonline.org.
The PCAM training was based upon learning from the Keep Well MECAM study and was informed by How Healthcare Professionals in Scotland Develop Their Communication Skills, Attitudes and Behaviours. 63
The aim was to provide:
-
up-to-date evidence of the bidirectional links between biological and psychosocial domains in LTCs
-
evidence that was relevant to nurses and their patients’ experience
-
an understanding of the face validity (to date) of the PCAM tool
-
an understanding of each of the PCAM domains, items and responses
-
confidence in delivering the PCAM in a person-responsive, conversational style throughout a review
-
an understanding of the involvement required for the broader practice team
-
familiarity with the resource list and what might be required to maintain it in the long term.
In order to do this:
-
nurses were asked to provide anonymous case studies
-
evidence was presented for each of the LTCs under consideration
-
nurses were asked to share and reflect on the evidence and their case study patients. Each case was discussed in terms of suitability and application of the PCAM tool
-
nurses were provided with some examples as to how the PCAM items may be introduced and discussed, and then invited to role play
-
each nurse was encouraged to practice the PCAM with around 10 patients. For the sake of the study, these did not always have to be LTC patients. In order to build experience and confidence, it was suggested that they begin with just a few domains. They should reflect on each experience and discuss with colleagues as required
-
a researcher was attached to the practice and provided support in one additional face-to-face session, online and by telephone.
In addition, the nursing team were provided with:
-
hard copies of the presentation slides
-
a copy of Making it Easy, a Health Literacy Plan for Scotland64
-
a copy of Good Mental Health For All. 65
Adaptations
Initially, the training was developed as a half-day meeting with a brief face-to-face follow-up after nurses had practised using the PCAM tool with 10 patients.
However, after the first session it became apparent that nurses:
-
would be unlikely to be able to dedicate a full unbroken half-day
-
may benefit from focusing the evidence further on their own experience
-
may benefit from time to reflect on the evidence and the PCAM introduction, and some distance in time before trying to integrate it into their practice.
In order to respond to this, the training was adapted over the course of the study:
-
advance creation and sending of three case studies each
-
2.5-hour information session
-
1.5-hour self-study and reflection with resources
-
1.5-hour face-to-face practical session with a researcher
-
self-reflective practice with 10 patients
-
quick review with researcher (face-to-face or telephone).
The PCAM resource packs were organised in discrete sections based on the PCAM domains, with relevant service areas included for each domain:
-
health and well-being: physical health support
-
allied health professionals
-
smoking cessation
-
addiction services
-
NHS weight management service
-
-
health and well-being: mental well-being and social isolation support
-
mental well-being national resources
-
mental well-being local resources
-
voluntary befriending services
-
-
health and well-being: lifestyle/social activities
-
physical activities
-
social activities
-
weight management support
-
-
social environment/employment, care and support
-
money, employment, debt and benefit advice
-
domestic abuse services
-
carer support
-
-
social environment/housing and home safety
-
housing and home safety
-
transport services
-
-
health literacy and communication
-
literacy support
-
English for speakers of other languages
-
culturally sensitive support
-
support for sensory impairments.
-
An additional two sections comprised information relating to:
-
condition-specific support
-
COPD
-
CHD
-
DM
-
-
useful websites for further information.
Within each section, information comprised national resources [e.g. nationally available resources such as Citizens Advice or A Local Information System for Scotland (ALISS) database] and local or regional resources specific to each GP practice location.
Information about each resource comprised:
-
name of resource (e.g. group/organisation/website title)
-
short description of resource
-
geographic area covered
-
resource telephone/e-mail
-
website address (as appropriate)
-
opening hours (as appropriate)
-
contact name (If available).
Each section was printed on plain white paper and placed together in clip file with a front index for ease of use.
To make the pack usable for nurses, the lists of resources were not exhaustive, but were targeted. In addition, the low-technology approach was somewhat influenced by the feasibility nature of the research, but was appreciated by nurses.
Copies of example resource packs are available on request from: pcam@stir.ac.uk.
Item 4: what? (Procedures, activities and/or processes used in the intervention, including any enabling or support activities)
In addition to the PCAM tool training and its required adaptations, researcher support was available to practices during the period of the study if required. However, this was in line with the ‘adapted’ training.
However, the support of a PM was helpful in some circumstances for enabling scheduling of time for training.
Item 5: who provided each aspect of the intervention?
Training was delivered by the research team, led by Carina Hibberd (who developed the training resources for the Keep Well study as well as the adapted training for this study in collaboration with RP). Carina Hibberd has a PhD in biological sciences, in exploring and understanding the links between physical and emotional responses. Each session was delivered by Carina Hibberd and another researcher (EC or PA, both of whom had received 5 hours of training, in a train-the-trainer model, from Carina Hibberd).
Training covered use of the PCAM tool and nurses received copies of the PCAM at this stage.
Patricia Aitchison developed the bespoke resource packs for each practice; however, these were then reviewed by local PMs and PNs who were encouraged to add and amend these resources as local knowledge emerged. Patricia Aitchison has been engaged in primary care research for over a decade.
Item 6: how? The modes of delivery (face to face or by some other mechanism, such as internet or telephone) of the intervention and whether it was provided individually or in a group
The PCAM training was delivered face to face, but with the option of either a face-to-face follow-up/review session or a telephone session. Training was provided both individually (when single PNs were involved) or in small groups where more than one PN was involved. The adaptability of delivery of training is an essential feature for making this implementable in primary care.
Practice nurses were then to use the PCAM tool and resource pack in their routine delivery of annual individual face-to-face health checks for patients with LTCs (such as CHD, DM, COPD).
Item 7: where? Type(s) of location(s) where the intervention occurred, including any necessary infrastructure or relevant features
The PCAM intervention was implemented in primary care practices by PNs. This involved practices with one or more PN. Practices were located in two health board areas of Scotland, covering both highly deprived urban and less deprived small town/semirural locations.
Practice nurses then used the PCAM tool and the resource packs in their routine delivery of annual individual face-to-face health checks for patients with LTCs (such as CHD, DM, COPD).
Item 8: when and how much? The number of times the intervention was delivered and over what period of time, including the number of sessions, their schedule and their duration, intensity or dose
Practices (and PNs) varied in the number of visits they required to introduce the overall study to them, from one to three. However, these visits included introducing the PCAM tool, as well as introducing the feasibility trial, and the number of visits/sessions required to introduce the PCAM intervention cannot be separated out.
The training intervention received by nurses and its duration and number of sessions has been reported under Item 3 above.
Nurses were then requested to practise using the tool on up to 10 patients to familiarise themselves with the PCAM delivery. Nurses could be flexible in how they did this.
Practice nurse delivery of the PCAM tool with patients consisted of using the tool throughout the annual LTC review of a patient. PN-delivered annual reviews for LTCs vary in the time allocated and this intervention is designed to be implemented into usual care delivery.
Item 9: tailoring – if the intervention was planned to be personalised, titrated or adapted, then describe what, why, when, and how
Interventions that require substantial ‘work’ by health-care professionals have to be pragmatic to fit with available resources. This is especially so when an intervention aims to change practitioner behaviour/outcomes as well as patient behaviour or outcomes.
The ‘planned’ training delivery was more about convenience for the training team in delivering the training, in one visit, to the maximum number of nurses possible. However, after the first training session in one practice, it became apparent that training delivery would have to be tailored to suit individual practice needs. The content of the training was also adapted in response to early nurse feedback in order to maximise learning in the limited time available. The essential element of learning why it is important to conduct a biopsychosocial assessment, and how to use the PCAM tool to facilitate this, was still delivered to all PNs.
There was still some attempt in our adaptations to ensure that nurses had received equivalent training intensity and follow-up support.
When the PCAM tool is being used in LTC annual reviews, the delivery of this is very much dependent on the individual circumstances of the patient, and also with individual practice procedures for patient follow-up if required.
Item 10: modifications – if the intervention was modified during the course of the study, describe the changes (what, why, when and how)
It was planned that the PCAM tool used in the study should be open to adaptation in response to management and steering group partners, and to focus group and feasibility RCT findings. However, it was important that it did not change during the feasibility RCT and that it remained congruent with the US version. The following changes were all made before the feasibility RCT:
-
For clarity, abbreviations were expanded.
-
The word ‘client’ was changed to ‘patient’ to reflect the health-care context.
-
Smoking was added to the list of lifestyle behaviours to be considered.
-
The phrase ‘functions’ was replaced with ‘activities’. This was consistent with the rest of the document and International Classification of Functioning, Disability and Health (ICF) wording.
-
The financial resources guide was rephrased from ‘ability to afford all medical care’ to ‘ability to afford all required care and medical costs or ability to live well’ to reflect both the US and UK health-care systems and to include non-medical costs, which can also influence self-care and well-being.
-
The Actions section was reformatted to prevent confusion with the traffic-light coding from above.
The modification to the training intervention and delivery has been reported under Item 3 above.
The resource packs were designed to be an evolving resource and to encourage local ownership of the resource for ongoing use. Some practices added new resources to these packs or deleted services if they no longer operated.
Item 11: how well (planned) – describe how, by whom and if any strategies were used to maintain or improve fidelity
The inclusion of a ‘trial period’ in which nurses would practise using the PCAM tool was to allow the training to be put into practice, and for nurses to gain confidence in using the PCAM tool and its training. Nurses were then allowed to discuss any queries or issues with the researcher/trainer before using the PCAM tool in phase 2 of the study.
Intervention fidelity was studied using a sample of recorded nurse-led annual reviews before and after training in the use of the PCAM tool was delivered. This was to assess how nurses conducted their annual reviews before and after PCAM introduction, specifically, whether or not nurses already conducted a biopsychosocial assessment in the annual review of patients with LTCs and, if so, what domains (as specified in the PCAM) did they cover and whether or not the PCAM made any difference to their delivery of a biopsychosocial assessment, and what domains of the PCAM tool they were covering in this assessment.
Nurses approached patients to get consent to record the consultation for up to five patients before and five patients after the introduction of the PCAM tool. Recordings were then transcribed and analysed, by Patricia Aitchison and Eileen Calveley, based on a predefined template that sought to categorise interactions based on the PCAM domains and to note when these occurred within the consultation.
There was some reluctance by nurses to approach patients to have their consultations recorded; nurses reported this as ‘patients will not want to do this’ and, therefore, some nurses declined to participate in this aspect of the study, thereby limiting the data available in this study on the assessment of fidelity.
Item 12: how well (actual) – the extent to which the intervention was delivered as planned
The adapted training was delivered to all practices but in ways that fitted with practice resources and organisational needs.
The PCAM intervention was used by all PCAM-trained nurses and the analysis of the small number of recorded consultations indicates that nurses are including more domains of the PCAM tool in their annual assessments than they did prior to the introduction of the PCAM tool.
The resource packs were found to be helpful by PNs and other members of the primary care team, but there was concern about who would keep this resource up to date beyond the study. The resource pack is an integral part of the PCAM intervention and, without it, PNs would perceive an added burden to using the PCAM if they had to find sources of help themselves, or they would perceive using the PCAM as ‘a worry’ if they could not then offer some immediate referral or signposting when problems were raised.
Appendix 2 Patient Centred Assessment Method tool
© Maxwell, Hibberd, Pratt, Peek and Baird 2013. PCAM may not be copied or shared with any third party without inclusion of the copyright declaration. There are no licence costs for the use of PCAM and the developers are committed to PCAM being freely available to use. www.pcamonline.org
Appendix 3 Patient Centred Assessment Method training outline
Initial plan
The original training plan was based on learning from the Keep Well MECAM study, and was informed by How Healthcare Professionals in Scotland Develop Their Communication Skills, Attitudes and Behaviours. 63
The aim was to provide:
-
up-to-date evidence of the bidirectional links between biological and psychosocial domains in LTCs
-
evidence that was relevant to nurses and their patients’ experience
-
an understanding of the face validity (to date) of the PCAM tool
-
an understanding of each of the PCAM domains, items and responses
-
confidence in delivering the PCAM tool in a person-responsive, conversational style throughout a review
-
an understanding of the involvement required for the broader practice team
-
familiarity with the resource list and what may be required to maintain it in the long term.
In order to do this:
-
nurses were asked to provide anonymous case studies
-
evidence was presented for each of the LTCs under consideration
-
nurses were ask to share and reflect on the evidence and their case study patients. Each case was discussed in terms of suitability and application of the PCAM tool
-
nurses were provided with some examples as to how the PCAM tool items may be introduced and discussed, and then invited to role play
-
each nurse was encouraged to practise the PCAM tool with around 10 patients. For the sake of the study, these did not always have to be LTC patients. In order to build experience and confidence, it was suggested that they begin with just a few domains. They should reflect on each experience and discuss with colleagues as required
-
a researcher was attached to the practice and provided support in one additional face-to-face session, online and by telephone.
In addition, the nursing team were provided with:
Adaptations
Initially, the training was developed as a half-day meeting, with a brief face-to-face follow-up after nurses had practised using the PCAM tool with the 10 patients.
However, after the first session, it became apparent that nurses:
-
would be unlikely to be able to dedicate a full unbroken half-day
-
may benefit from focusing the evidence further upon their own experience.
-
may benefit from time to reflect on the evidence and the PCAM tool introduction, and some distance in time before trying to integrate it into their practice.
In order to respond to this, the training was adapted over the course of the study:
-
advance creation and sending of three case studies each
-
2.5-hour information session
-
1.5-hour self-study and reflection with resources
-
1.5-hour face-to-face practical session with a researcher
-
own practice with 10 patients
-
quick review with researcher (face to face or telephone).
Appendix 4 Patient Centred Assessment Method resource pack outline
Patient Centred Assessment Method resource packs: purpose, design and use
What is a Patient Centred Assessment Method resource pack?
A list of local, regional or national groups/organisations/information sources for use by PNs as potential signposting/referral opportunities for patients with LTCs taking part in the PCAM study (intervention only).
Purpose of the resource pack
To aid PNs’ signposting and referral of patients to other professionals or organisations.
Design principles
-
Reference was to be made to ALISS, which is a search and collaboration resource tool for health and well-being resources in Scotland. It is used to collect, organise and share links to community support. ALISS is funded by the Scottish Government and is delivered by the ALLIANCE.
-
Referral and signposting opportunities presented within the resource packs were to be those covering psychosocial problems within the PCAM domains.
-
PNs were to be a part of the design process by accessing their knowledge about the range of local supports available to patients.
-
The format of the pack was aimed to make it as easy as possible for nurses to access and provide information for patients. Wherever possible, relevant leaflets were available.
Design stages
Preparation of the PCAM resource packs began following the randomisation of GP practices. Resource packs were prepared for only the three practices randomised to the intervention arm of the feasibility trial.
Following randomisation, two researchers were allocated the relevant GP practice locations for initial preparation of the resource packs.
Stage 1: internet search
An internet search was structured and conducted using key search terms:
-
condition-specific descriptions (CHD, DM, COPD, LTCs)
-
PCAM domain headings (e.g. mental well-being, employment support, financial resources)
-
geographic location of the practices.
A range of search engines and directories were identified:
-
ALISS
-
NHS national and local search engines (e.g. Grampian Care Data)
-
statutory agencies’ web-based directories (e.g. Aberdeen City Council Community Contacts and Neighbourhoods directory)
-
third-sector community directories (e.g. Infobase, Glasgow Council for the Voluntary Sector)
-
other relevant websites.
Stage 2: data checking and verification
Where required, primary search results were checked to ensure that information about resources, for example, organisations’ contact details, locations and opening times, was current and accurate. Most frequently, researchers verified information by either contacting organisations by telephone/e-mail or speaking to staff with knowledge of local services in the relevant GP practice.
In one area, the researcher contacted and met with two local staff from the local authority’s community learning and development service. These staff helped the researcher to check and supplement the resource pack contents for that area.
Stage 3: draft preparation of resource pack
Draft PCAM resource packs were prepared using the information gathered from the primary search results. Information was organised in discrete sections, structured using the six principal PCAM domains:
-
health and well-being: physical health support
-
allied health professionals
-
smoking cessation
-
addiction services
-
NHS weight management service
-
-
health and well-being: mental well-being and social isolation support
-
mental well-being national resources
-
mental well-being local resources
-
voluntary befriending services
-
-
health and well-being: lifestyle/social activities
-
physical activities
-
social activities
-
weight management support
-
-
social environment/employment, care and support
-
money, employment, debt and benefit advice
-
domestic abuse services
-
carer support
-
-
social environment/housing and home safety
-
housing and home safety
-
transport services
-
-
health literacy and communication
-
literacy support
-
English for speakers of other languages
-
culturally sensitive support
-
support for sensory impairments.
-
An additional two sections comprised information relating to:
-
condition-specific support
-
COPD
-
CHD
-
DM
-
-
useful websites for further information.
Within each section, information comprised national resources (e.g. nationally available resources such as Citizens Advice or the ALISS database) and local or regional resources specific to each GP practice location.
Information about each resource comprised:
-
name of resource (e.g. group/organisation/website title)
-
short description of resource
-
geographic area covered
-
resource telephone/e-mail
-
website address (as appropriate)
-
opening hours (as appropriate)
-
contact name (if available).
Each section was printed on plain white paper and placed together in a clip file with a front index for ease of use.
To make the pack usable for nurses, the lists of resources were not exhaustive, but were targeted. In addition, the low-technology approach was somewhat influenced by the feasibility nature of the research, but was appreciated by nurses.
Stage 4: presentation of draft resource packs to practice nurses
Each PN was given a copy of the draft resource pack at their PCAM training session. The purpose and design strategy of the packs was explained by the researchers. PNs were invited to examine the resource packs during and after the training and to participate in the further design of the packs by (1) informing researchers of any inaccurate/outdated information and (2) supplementing the contents by contributing their knowledge of other resources, particularly local resources, that had not been found during the primary search. Space was left within each section for PNs to insert additional information as required.
In one practice, a PN supplemented her PCAM resource pack with information from Keep Well resources that had been compiled by another PN within the practice.
Patient Centred Assessment Method resource packs: an evolving resource
During and after the PCAM training session, researchers talked through with PNs the ongoing, evolving nature of the resource packs and issues relating to keeping packs relevant and up to date. PNs expressed concerns about the time commitment that would be required to regularly update information. Researchers suggested that, perhaps, this was a role that could be adopted by a member of the wider GP practice team.
The compilation of the resource packs also provided potential for establishing broader relationships between GP practices and local community services. For example, the community learning and development service staff who met with the researcher in one of the GP practice areas indicated their interest in the PCAM tool and identified the potential for establishing closer links with the GP practice to share information about local services for patients. The researcher passed details of these staff on to the PM.
Appendix 5 Wider resource use
Nurse advice/referral and signposting monitoring
Practice nurses were asked to record the actions of each annual review in terms of the advice, signpostings and referrals they made for patients. This also included whether or not they were perceived as ‘accepted’ by the patient or declined by the patient. Advice, referral or signposting was recorded across a range of possible options that reflected both statutory and third-sector resources, but have been grouped in the analysis below as signposting/referral to a PN or GP for a physical health issue, signposting/referral to a PN or GP for a mental health issue and advice/signposting/referral to broader community-based resources. A single patient could have multiple advice/signposting/referral actions recorded. The data include patients who attended their annual review and were deemed eligible for inclusion in the study, and agreed to nurses completing anonymised information about their consultation, and to also taking a questionnaire, but who did not subsequently return their baseline questionnaire. Although practices were not yet randomised to the PCAM in phase 1, for the purposes of this analysis it is being made clear which arm practices were subsequently allocated to, in order to compare pre- and post-referral/signposting patterns for PCAM and CAU nurses.
Results
Figure 11 is based on a count of the number of times any advice, signposting or referral actions were recorded by the nurse, and is presented as a percentage of the annual reviews conducted during the period of the study.
FIGURE 11.
Nurse advice/signposting/referral patterns by study phase and by subsequent randomisation group: PCAM vs. CAU.
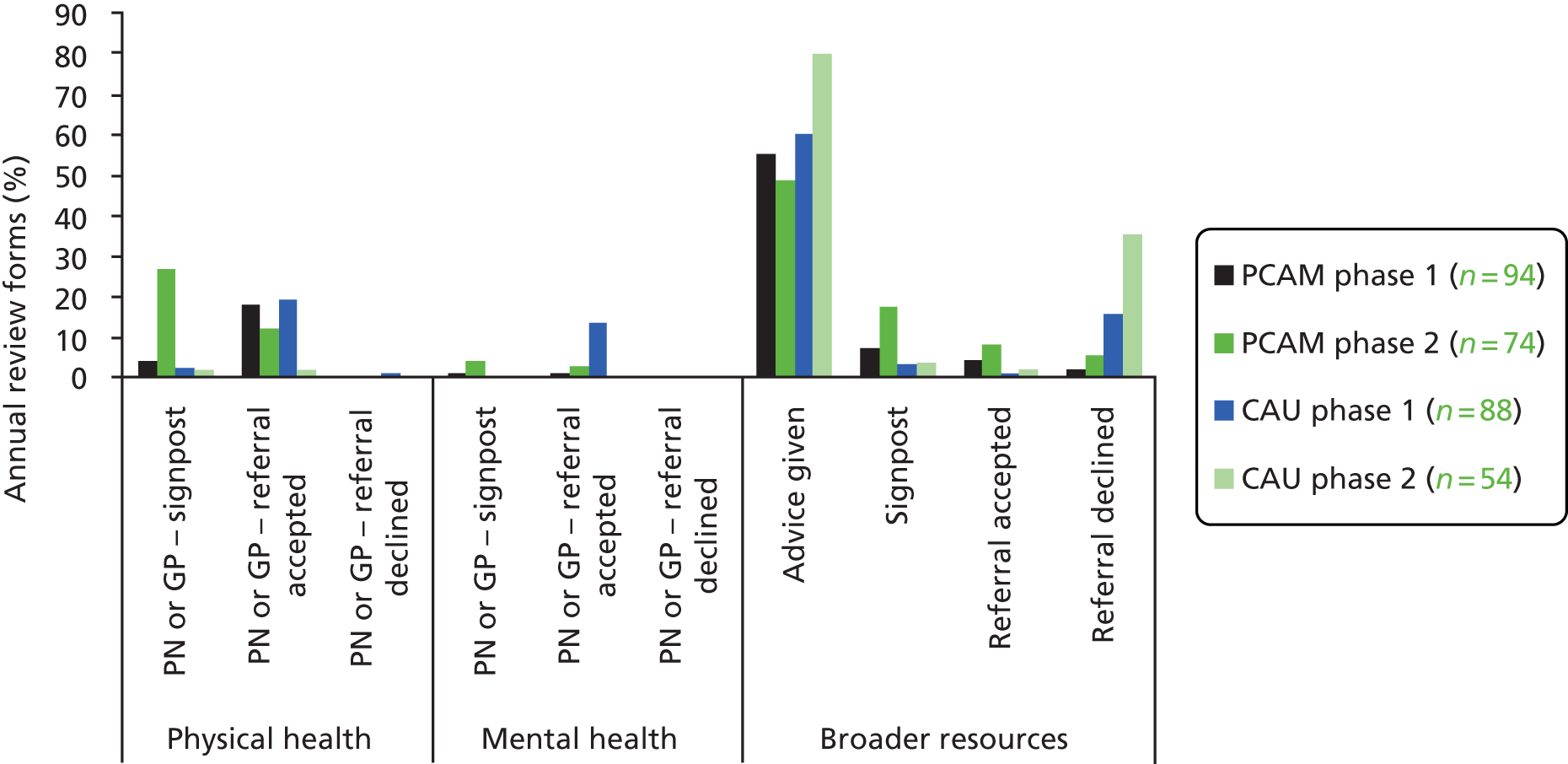
Discussion
The analysis of nurse advice/signposting/referral behaviours could indicate the nurses in the PCAM group using their PCAM resource packs in phase 2 with a more proactive, person-centred review style. However, there are several cautions to the data. For most resources, the number of actions was very low. In addition, without access to the review (e.g. audio-recording or routine data) we cannot be certain of the validity of the data. Researchers did directly ask PNs about the general validity (did the record reflect what happened) and there was no indication that records were not valid. However, one PN interview suggested extensive use of referral and signposting that was not reflected in these data. That nurse had been extremely busy and had acknowledged that record-keeping had been difficult.
One PN in the CAU group felt that discussion and advice were the only proactive options open to her, as she had tried on several occasions before to refer her patients over a long period of time. It should be remembered that annual reviews sit with ongoing care, and priorities have to be made for one episode out of many. Therefore, all possible actions cannot be made at one episode.
Appendix 6 Patient and nurse outcome tables
| SIMD decile | Frequency | Percentage | Cumulative percentage |
|---|---|---|---|
| 1 | 5 | 11.90 | 11.90 |
| 2 | 2 | 4.76 | 16.67 |
| 3 | 1 | 2.38 | 19.05 |
| 6 | 5 | 11.90 | 30.95 |
| 7 | 3 | 7.14 | 38.10 |
| 8 | 7 | 16.67 | 54.76 |
| 9 | 11 | 26.19 | 80.95 |
| 10 | 8 | 19.05 | 100.00 |
| Total | 42 | 100.00 |
| SIMD decile | Frequency | Percentage | Cumulative percentage |
|---|---|---|---|
| 1 | 7 | 20.59 | 20.59 |
| 2 | 8 | 23.53 | 44.12 |
| 3 | 1 | 2.94 | 47.06 |
| 4 | 3 | 8.82 | 55.88 |
| 5 | 2 | 5.88 | 61.76 |
| 6 | 2 | 5.88 | 67.65 |
| 7 | 3 | 8.82 | 76.47 |
| 8 | 1 | 2.94 | 79.41 |
| 9 | 7 | 20.59 | 100.00 |
| Total | 34 | 100.00 |
| PCAM domains | Phase, n (%) | |
|---|---|---|
| 1 (maximum N = 113) | 2 (maximum N = 77) | |
| Concerns about health | n = 113 | n = 76 |
| No | 53 (46.9) | 38 (50.0) |
| Yes | 60 (53.1) | 38 (50.0) |
| Concerns about lifestyle | n = 109 | n = 75 |
| No | 85 (78.0) | 54 (72.0) |
| Yes | 24 (22.0) | 21 (28.0) |
| Concerns about home life | n = 110 | n = 73 |
| No | 102 (92.7) | 72 (98.6) |
| Yes | 8 (7.3) | 1 (1.4) |
| Concerns about daily activities | n = 108 | n = 73 |
| No | 91 (84.3) | 60 (82.2) |
| Yes | 17 (15.7) | 13 (17.8) |
| Concerns about social network | n = 108 | n = 75 |
| No | 97 (89.8) | 62 (82.7) |
| Yes | 11 (10.2) | 13 (17.3) |
| Concerns about finances | n = 108 | n = 75 |
| No | 86 (79.6) | 57 (76.0) |
| Yes | 22 (20.4) | 18 (24.0) |
| PCAM domains | Phase 2 randomisation group, n (%) | |
|---|---|---|
| PCAM (maximum N = 43) | CAU (maximum N = 34) | |
| Concerns about health | n = 43 | n = 33 |
| No | 21 (48.8) | 17 (51.5) |
| Yes | 22 (51.2) | 16 (48.5) |
| Concerns about lifestyle | n = 42 | n = 33 |
| No | 29 (69.1) | 25 (75.8) |
| Yes | 13 (31.0) | 8 (24.2) |
| Concerns about home life | n = 41 | n = 32 |
| No | 40 (97.6) | 32 (100.0) |
| Yes | 1 (2.4) | 0 (0.0) |
| Concerns about daily activities | n = 42 | n = 31 |
| No | 31 (73.8) | 29 (93.6) |
| Yes | 11 (26.2) | 2 (6.5) |
| Concerns about social network | n = 42 | n = 33 |
| No | 32 (76.2) | 30 (90.9) |
| Yes | 10 (23.8) | 3 (9.1) |
| Concerns about finances | n = 42 | n = 33 |
| No | 30 (71.4) | 27 (81.8) |
| Yes | 12 (28.6) | 6 (18.2) |
| CARE measure | Phase | |
|---|---|---|
| 1 | 2 | |
| Data collected n/N (%) | 108/113 (95.6) | 74/77 (96.1) |
| Median score (IQR) | 48.9 (41–50) | 47 (41–50) |
| Mean score (SD) | 45.70 (5.39) | 44.6 (6.52) |
| CARE measure | Phase 2 randomisation group | |
|---|---|---|
| PCAM | CAU | |
| Data collected n/N (%) | 41/43 (95.3) | 33/34 (97.1) |
| Median score (IQR) | 45 (42–50) | 50 (40–50) |
| Mean score (SD) | 43.7 (7.03) | 45.8 (5.72) |
| Measures | Phase | |||
|---|---|---|---|---|
| 1 | 2 | |||
| T0 | T1 | T0 | T1 | |
| WEMWEBS | ||||
| Data collected n/N (%) | 109/113 (96.5) | 65/113 (57.5) | 67/77 (87.0) | 36/77 (46.8) |
| Median score (IQR) | 51 (42–60) | 54 (43–59) | 52 (42–60) | 49 (42–58.5) |
| Mean score (SD) | 50.28 (11.8) | 50.48 (12.88) | 50.55 (11.60) | 49.47 (11.77) |
| PEI | ||||
| Data collected n/N (%) | 108/113 (95.6) | 71/113 (62.8) | 72/77 (93.5) | 40/77 (51.9) |
| Median score (IQR) | 5 (0–8) | 9 (6–12) | 5.5 (0.5–10.5) | 9 (6–13.5) |
| Mean score (SD) | 4.98 (4.28) | 10.15 (4.12) | 5.47 (4.65) | 9.58 (4.79) |
| GHQ-12 | ||||
| Data collected n/N (%) | 111/113 (98.2) | 67/113 (59.3) | 75/77 (97.4) | 36/77 (46.8) |
| Median score (IQR) | 9 (7–14) | 8 (60–14) | 10 (7–12) | 8.5 (6–12) |
| Mean score (SD) | 11.14 (6.15) | 10.79 (6.62) | 11.07 (6.00) | 9.53 (4.19s) |
| Measures | Phase 2 randomisation group | |||
|---|---|---|---|---|
| PCAM | CAU | |||
| T0 | T1 | T0 | T1 | |
| WEMWEBS | ||||
| Data collected n/N (%) | 38/43 (88.4) | 17/43 (32.6) | 29/34 (85.3) | 19/34 (44.2) |
| Median score (IQR) | 48 (40–56) | 48 (40–56) | 56 (43–61) | 51 (45–60) |
| Mean score (SD) | 48.61 (12.46) | 47.53 (13.47) | 53.10 (10.00) | 51.21 (10.05) |
| WEMWBS | ||||
| Change score (95% CI) | –1.07 (–8.55 to 6.40) | –1.89 (–7.85 to 4.06) | ||
| PEI | ||||
| Data collected n/N (%) | 41/43 (95.3) | 16/43 (37.2) | 31/34 (91.2) | 19/34 (55.9) |
| Median score (IQR) | 5 (1–9) | 5 (0–7.5) | 6 (0–11) | 3 (0–9) |
| Mean score (SD) | 5.34 (4.68) | 4.31 (3.66) | 5.65 (4.69) | 4.42 (4.66) |
| PEI | ||||
| Change score (95% CI) | –1.03 (–3.64 to 1.59) | –1.22 (–3.96 to 1.52) | ||
| GHQ-12 | ||||
| Data collected n/N (%) | 42/43 (97.7) | 17/43 (39.5) | 33/34 (97.1) | 19/34 (55.9) |
| Median score (IQR) | 11 (7–13) | 8 (7–12) | 9 (6–12) | 10 (6–12) |
| Mean score (SD) | 11.81 (6.73) | 9.82 (4.88) | 10.12 (4.86) | 9.26 (3.59) |
| GHQ-12 | ||||
| Change score (95% CI) | –1.99 (–5.59 to 1.62) | –0.86 (–3.43 to 1.71) | ||
| SF-12 summary domains | Phase, n; mean score (SD) | |||
|---|---|---|---|---|
| 1 | 2 | |||
| T0 (N = 113) | T1 (N = 113) | T0 (N = 77) | T1 (N = 77) | |
| Mental health summary | 101; 49.73 (11.28) | 60; 48.73 (11.82) | 73; 48.94 (10.89) | 35; 48.84 (10.75) |
| Physical health summary | 101; 39.00 (11.68) | 60; 40.40 (12.49) | 73; 39.37 (12.51) | 35; 40.13 (13.14) |
| Physical function | 111; 40.45 (12.61) | 66; 40.98 (13.15) | 76; 41.66 (12.75) | 38; 41.77 (13.82) |
| Role physical | 109; 42.55 (11.56) | 64; 42.56 (12.99) | 74; 41.49 (12.78) | 37; 43.85 (13.29) |
| Pain | 111; 41.84 (13.38) | 67; 45.12 (13.69) | 75; 42.63 (14.83) | 38; 40.82 (15.06) |
| General health | 110; 39.08 (11.65) | 67; 39.46 (12.06) | 76; 38.10 (11.46) | 38; 38.84 (11.77) |
| Vitality | 109; 45.16 (11.24) | 67; 46.10 (11.83) | 76; 45.63 (11.30) | 36; 47.47 (10.62) |
| Social function | 111; 45.65 (12.93) | 66; 44.63 (14.81) | 76; 45.81 (13.53) | 38; 45.41 (13.24) |
| Role emotional | 106; 45.16 (12.74) | 66; 43.46 (13.85) | 73; 42.75 (13.23) | 38; 42.98 (13.71) |
| Mental health | 108; 50.04 (10.92) | 67; 50.44 (11.73) | 76; 50.99 (11.42) | 36; 50.49 (11.64) |
| Proportion of SF-12 completed | ||||
| Summary scales | ≥ 89.4% | ≥ 53.1% | ≥ 94.5% | ≥ 45.5% |
| SF-12 summary domains | Phase 2 randomisation group, n; mean score (SD) | |||
|---|---|---|---|---|
| PCAM | CAU | |||
| T0 (N = 43) | T1 (N = 43) | T0 (N = 34) | T1 (N = 34) | |
| Mental health summary | 40; 47.66 (11.97) | 17; 49.00 (11.19) | 33; 50.50 (9.35) | 18; 48.69 (10.64) |
| Change score (95% CI) | 1.34 (–5.48 to 8.16) | –0.31 (–7.82 to 7.20) | ||
| Physical health summary | 40; 41.16 (11.76) | 17; 41.10 (13.44) | 33; 37.20 (13.21) | 18; 39.21 (13.17) |
| Change score (95% CI) | –0.06 (–7.18 to 7.06) | 2.01 (–5.76 to 9.78) | ||
| Physical function | 43; 43.28 (12.76) | 18; 44.06 (12.92) | 33; 39.55 (12.61) | 20; 39.72 (14.61) |
| Change score (95% CI) | 0.78 (–6.41 to 7.97) | 0.17 (–7.45 to 7.79) | ||
| Role physical | 41; 43.24 (11.90) | 18; 45.66 (13.24) | 33; 39.31 (13.66) | 19; 42.14 (13.46) |
| Change score (95% CI) | 2.42 (–4.55 to 9.39) | 2.83 (–5.03 to 10.69) | ||
| Pain | 42; 42.40 (15.14) | 18; 39.33 (15.06) | 33; 42.93 (14.64) | 20; 42.16 (15.33) |
| Change score (95% CI) | –3.07 (–11.59 to 5.45) | –0.77 (–9.25 to 7.71) | ||
| General health | 43; 38.42 (11.68) | 18; 38.63 (11.84) | 33; 37.68 (11.32) | 20; 39.03 (12.02) |
| Change score (95% CI) | 0.21 (–6.38 to 6.80) | 1.35 (–5.24 to 7.94) | ||
| Vitality | 43; 45.18 (11.43) | 17; 46.56 (9.99) | 33; 46.22 (11.28) | 19; 48.28 (11.36) |
| Change score (95% CI) | 1.38 (–4.96 to 7.72) | 2.06 (–4.48 to 8.60) | ||
| Social function | 43; 46.70 (13.67) | 18; 45.91 (14.06) | 33; 44.63 (13.47) | 20; 44.96 (12.80) |
| Change score (95% CI) | –0.79 (–8.53 to 6.95) | 0.33 (–7.19 to 7.85) | ||
| Role emotional | 40; 42.66 (14.43) | 18; 45.21 (13.35) | 33; 42.86 (11.85) | 20; 40.98 (14.06) |
| Change score (95% CI) | 2.55 (–5.47 to 10.57) | –1.88 (–9.12 to 5.36) | ||
| Mental health | 43; 49.66 (11.92) | 17; 49.48 (12.40) | 33; 52.72 (10.66) | 19; 51.39 (11.18) |
| Change score (95% CI) | 0.32 (–6.59 to 7.23) | -–1.33 (–7.61 to 4.95) | ||
| Proportion of SF-12 completed | ||||
| Summary scales | ≥ 93.0% | ≥ 39.5% | ≥ 97.1% | ≥ 52.9% |
| Statement | Randomisation group, n of responses (%) | |||
|---|---|---|---|---|
| PCAM (N = 4) | CAU (N = 3) | |||
| Disagree or neutral | Agree | Disagree or neutral | Agree | |
| I have the skills necessary to address depression | ||||
| Baseline | 2 (50.0) | 2 (50.0) | 0 (0) | 3 (100) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100) |
| I do not have time to adequately address depression | ||||
| Baseline | 1 (25.0) | 3 (75.0) | 2 (66.7) | 1 (33.3) |
| Follow-up | 1 (25.0) | 3 (75.0) | 2 (66.7) | 1 (33.3) |
| Feeling down is a normal part of life | ||||
| Baseline | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Follow-up | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Most depression improves without treatment | ||||
| Baseline | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Follow-up | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Patients respond negatively when asked about mood | ||||
| Baseline | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Follow-up | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Patients tell me if they want to discuss low mood | ||||
| Baseline | 2 (50.0) | 2 (50.0) | 2 (66.7) | 1 (33.3) |
| Follow-up | 2 (50.0) | 2 (50.0) | 2 (66.7) | 1 (33.3) |
| Prefer to leave discussion about depression until a good relationship is established with patients | ||||
| Baseline | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Follow-up | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Feel confident in my knowledge of potential treatments or interventions for depression | ||||
| Baseline | 1 (100.0) | 0 (0) | 1 (33.3) | 2 (66.7) |
| Follow-up | 3 (75.0) | 1 (25.0) | 2 (66.7) | 1 (33.3) |
| Statement | Randomisation group, n of responses (%) | |||
|---|---|---|---|---|
| PCAM (N = 4) | CAU (N = 3) | |||
| Disagree or neutral | Agree | Disagree or neutral | Agree | |
| To understand the patient’s childhood | ||||
| Baseline | 3 (75.0) | 1 (25.0) | 3 (100.0) | 0 (0) |
| Follow-up | 3 (75.0) | 1 (25.0) | 3 (100.0) | 0 (0) |
| To have someone to talk to about their problems | ||||
| Baseline | 2 (50.0) | 2 (50.0) | 0 (0) | 3 (100.0) |
| Follow-up | 2 (50.0) | 2 (50.0) | 0 (0) | 3 (100.0) |
| Changing unhelpful thoughts and behaviours | ||||
| Baseline | 2 (50.0) | 2 (50.0) | 1 (33.3) | 2 (66.7) |
| Follow-up | 2 (50.0) | 2 (50.0) | 1 (33.3) | 2 (66.7) |
| Antidepressant medication | ||||
| Baseline | 4 (100.0) | 0 (0) | 2 (66.7) | 1 (33.3) |
| Follow-up | 2 (50.0) | 2 (50.0) | 2 (66.7) | 1 (33.3) |
| Mental well-being, statement | Randomisation group, n of responses (%) | |||
|---|---|---|---|---|
| PCAM (N = 4) | CAU (N = 3) | |||
| Disagree or neutral | Agree | Disagree or neutral | Agree | |
| I am aware of mental well-being issues generally for patients | ||||
| Baseline | 2 (50.0) | 2 (50.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 1 (33.3) | 2 (66.7) |
| I am confident in raising mental well-being issues with patients | ||||
| Baseline | 2 (50.0) | 2 (50.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 1 (33.3) | 2 (66.7) |
| I am willing to raise mental well-being issues with patients | ||||
| Baseline | 1 (25.0) | 3 (75.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| I am able to raise mental well-being issues with patients | ||||
| Baseline | 1 (25.0) | 3 (75.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Social issues, statement | Randomisation group, n of responses (%) | |||
|---|---|---|---|---|
| PCAM (N = 4) | CAU (N = 3) | |||
| Disagree or neutral | Agree | Disagree or neutral | Agree | |
| I am aware of social issues generally for patients | ||||
| Baseline | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 1 (33.3) | 2 (66.7) |
| I am confident in raising social issues with patients | ||||
| Baseline | 1 (25.0) | 3 (75.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 1 (33.3) | 2 (66.7) |
| I am willing to raise social issues with patients | ||||
| Baseline | 1 (25.0) | 3 (75.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| I am able to raise social issues with patients | ||||
| Baseline | 1 (25.0) | 3 (75.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Care, statement | Randomisation group, n of responses (%) | |||
|---|---|---|---|---|
| PCAM (N = 4) | CAU (N = 3) | |||
| Disagree or neutral | Agree | Disagree or neutral | Agree | |
| I consistently conduct a patient-centred health check | ||||
| Baseline | 1 (25.0) | 3 (75.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| I am able to provide patients with the care/services they need | ||||
| Baseline | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| I provide effective care for patients | ||||
| Baseline | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Patients are able to discuss their concerns with me | ||||
| Baseline | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Follow-up | 0 (0) | 4 (100.0) | 0 (0) | 3 (100.0) |
| Statement | Randomisation group, mean change in score (SD) | |
|---|---|---|
| PCAM (N = 4) | CAU (N = 3) | |
| 1. During the last 5 years I have seen an increase in the number of patients presenting with depressive symptoms | ||
| Baseline T0 | 3.75 (0.50) | 2.67 (1.15) |
| Follow-up T1 | 4.25 (0.50) | 3.33 (1.53) |
| Change (95% CI) | 0.50 (–0.41 to 1.42) | 0.67 (–0.77 to 2.1) |
| 2. The majority of depression seen in general practice originates from patients’ recent misfortunes | ||
| Baseline T0 | 2.75 (0.96) | 3.67 (0.58) |
| Follow-up T1 | 2.25 (0.96) | 2.67 (1.53) |
| Change (95% CI) | –0.5 (–2.55 to 1.55) | –1.0 (–5.30 to 3.30) |
| 3. Most depressive disorders seen in general practice improve without medication | ||
| Baseline T0 | 2.25 (0.50) | 3.00 (0.00) |
| Follow-up T1 | 2.25 (0.96) | 2.67 (1.53) |
| Change (95% CI) | 0.0 (–1.30 to 1.30) | –0.33 (–4.13 to 3.46) |
| 4. An underlying biochemical abnormality is the basis of severe cases of depression | ||
| Baseline T0 | 3.25 (0.96) | 2.67 (0.58) |
| Follow-up T1 | 2.75 (1.26) | 2.33 (1.15) |
| Change (95% CI) | –0.5 (–3.26 to 2.26) | –0.33 (–4.13 to 3.46) |
| 5. It is difficult to differentiate between whether patients are presenting with unhappiness or a clinical depressive disorder that needs treatment | ||
| Baseline T0 | 3.50 (0.58) | 2.33 (0.58) |
| Follow-up T1 | 2.00 (0.82) | 3.00 (1.73) |
| Change (95% CI) | –1.5 (–3.55 to 0.55) | 0.67 (–3.13 to 4.46) |
| 6. It is possible to distinguish two main groups of depression: one psychological in origin and the other caused by biochemical mechanisms | ||
| Baseline T0 | 3.00 (0.82) | 3.67 (0.58) |
| Follow-up T1 | 3.00 (0.82) | 3.00 (0.00) |
| Change (95% CI) | 0.0 (–2.60 to 2.60) | –0.67 (–2.10 to 0.77) |
| 7. Becoming depressed is a way that people with poor stamina deal with life difficulties | ||
| Baseline T0 | 1.75 (0.96) | 2.33 (0.58) |
| Follow-up T1 | 3.00 (1.83) | 1.33 (0.58) |
| Change (95% CI) | 1.25 (–1.76 to 4.26) | –1.00 (–3.48 to 1.48) |
| 8. Depressed patients are more likely to have experienced deprivation in early life than other people | ||
| Baseline T0 | 3.00 (1.41) | 2.33 (1.53) |
| Follow-up T1 | 2.50 (1.53) | 2.33 (1.53) |
| Change (95% CI) | –0.50 (–3.55 to 2.55) | 0.00 (0 to 0) |
| 9. I feel comfortable in dealing with depressed patients’ needs | ||
| Baseline T0 | 3.25 (0.96) | 3.00 (1.73) |
| Follow-up T1 | 2.75 (0.96) | 4.00 (0.0) |
| Change (95% CI) | –0.5 (–2.55 to 1.55) | 1.00 (–3.30 to 5.30) |
| 10. Depression reflects a characteristic response in patients that is not amenable to change | ||
| Baseline T0 | 2.00 (0.82) | 2.33 (0.58) |
| Follow-up T1 | 2.00 (1.41) | 2.00 (0.00) |
| Change (95% CI) | 0.0 (–1.30 to 1.30) | –0.33 (–1.77 to 1.10) |
| 11. Becoming depressed is a natural part of being old | ||
| Baseline T0 | 1.50 (0.58) | 1.33 (0.58) |
| Follow-up T1 | 1.50 (0.58) | 1.33 (0.58) |
| Change (95% CI) | 0.0 (0 to 0) | 0.0 (0 to 0) |
| 12. A PN could be a useful person to support depressed patients | ||
| Baseline T0 | 4.25 (0.96) | 4.33 (1.15) |
| Follow-up T1 | 4.50 (0.58) | 4.00 (0.00) |
| Change (95% CI) | 0.25 (–1.27 to 1.77) | –0.33 (–3.20 to 2.54) |
| 13. Working with depressed patients is heavy going | ||
| Baseline T0 | 2.50 (1.29) | 3.00 (1.00) |
| Follow-up T1 | 2.75 (0.96) | 3.67 (0.58) |
| Change (95% CI) | 0.25 (–1.27 to 1.77) | 0.67 (–2.20 to 3.54) |
| 14. There is little to be offered to those depressed patients who do not respond to what GPs do | ||
| Baseline T0 | 2.25 (1.26) | 1.67 (0.58) |
| Follow-up T1 | 1.25 (0.50) | 3.33 (1.53) |
| Change (95% CI) | –1.00 (–3.25 to 1.25) | 1.67 (–3.50 to 6.84) |
| 15. It is rewarding to spend time looking after depressed patients | ||
| Baseline T0 | 4.00 (0.82) | 3.33 (2.08) |
| Follow-up T1 | 3.5 (0.58) | 3.33 (0.58) |
| Change (95% CI) | –0.50 (–2.09 to 1.09) | 0.00 (–4.30 to 4.30) |
| 16. Psychotherapy tends to be unsuccessful with depressed patients | ||
| Baseline T0 | 2.25 (0.96) | 2.33 (1.15) |
| Follow-up T1 | 2.00 (0.82) | 2.67 (0.58) |
| Change (95% CI) | –0.25 (–1.77 to 1.27) | 0.33 (–1.10 to 1.77) |
| 17. If depressed patients need antidepressants, they are better off with a psychiatrist than with a GP | ||
| Baseline T0 | 2.25 (0.96) | 2.67 (1.15) |
| Follow-up T1 | 2.00 (0.82) | 3.00 (1.00) |
| Change (95% CI) | –0.25 (–1.05 to 0.55) | 0.33 (–1.10 to 1.77) |
| 18. Antidepressants usually produce a satisfactory result in the treatment of depressed patients in general practice | ||
| Baseline T0 | 3.00 (1.41) | 3.67 (0.58) |
| Follow-up T1 | 2.50 (1.00) | 2.67 (0.58) |
| Change (95% CI) | –0.50 (–1.42 to 0.42) | –1.00 (–3.48 to 1.48) |
| 19. Psychotherapy for depressed patients should be left to a specialist | ||
| Baseline T0 | 3.50 (0.58) | 4.00 (1.00) |
| Follow-up T1 | 2.75 (0.50) | 4.33 (0.58) |
| Change (95% CI) | –0.75 (–2.27 to 0.77) | 0.33 (–3.46 to 4.13) |
| 20. If psychotherapy was freely available, this would be more beneficial than antidepressants for most depressed patients | ||
| Baseline T0 | 3.25 (0.96) | 3.67 (0.58) |
| Follow-up T1 | 3.50 (0.58) | 4.00 (1.00) |
| Change (95% CI) | 0.25 (–1.27 to 1.77) | 0.33 (–1.10 to 1.77) |
Appendix 7 Scottish Primary Care Research Network letter on practice recruitment
Appendix 8 Project timeline
Glossary
- A process for DEcision-making after Pilot and feasibility Trials
- An algorithm for summarising the lessons learned from pilot and feasibility trials in terms of trial and real-world implementation issues.
- Biopsychosocial
- An approach that values considering the integration of biological, psychological and social factors as influencing the health and well-being of individuals.
- Carer
- Anyone who cares, unpaid, for a friend or family member who, as a result of illness (including mental ill health), disability or an addiction, cannot cope without their support.
- Chronic care model
- A model that consists of many components of various disease management schemes. The chronic care model summarises the basic elements for improving care in health systems at the community, organisation, practice and patient levels. The model is attributed to a team led by Edward Wagner, in the USA, in the 1990s.
- Cluster randomised controlled trial
- A type of clinical trial in which groups of participants, as opposed to individuals, are randomised. These ‘groups’ can be groups of people (e.g. general practitioners or physiotherapists) or groups of places/settings (e.g. general practices or NHS wards).
- Community mental health team
- A team of health-care professionals that provides assessment, care and treatment for people living in the community who have one or more severe mental illnesses. It usually comprises a multidisciplinary team of community psychiatric nurses, social workers, health-care support workers, psychiatrists, psychologists and occupational therapists.
- Feasibility trial
- A study that aims to assess the practicality of a proposed study (can it be done?) and to identify any problems or issues. A ‘feasibility trial’ aims to assess the practicality of running a trial by looking at specific aspects of the design of the proposed full study to demonstrate its practicality and identify areas where amendments or adjustments are required.
- General Practitioners at the Deep End
- A group of 100 general practices that serve the most socioeconomically disadvantaged communities throughout Scotland.
- Health literacy
- This is about people having enough knowledge, understanding, skills and confidence to use health information, to be active partners in their care and to navigate the health and social care systems.
- House of Care
- An approach to supporting the care of patients with long-term conditions by providing toolkits, information and resources to encourage closer working between professionals, organisations and communities.
- INTERMED
- An observer-rated instrument used as a method of assessing and integrating biological, psychological, social, and health-care-related aspects of disease. This clinical instrument was developed by Huyse et al. (Huyse FJ, Lyons JS, Stiefel FC, Slaets JP, de Jonge P, Fink P, et al. ‘INTERMED’: a method to assess health service needs. I. Development and reliability. Gen Hosp Psychiatry 1999;21:39–48) and further developed by de Jonge et al. (de Jonge P, Huyse FJ, Stiefel FC, Slaets JP, Gans RO. INTERMED – a clinical instrument for biopsychosocial assessment. Psychosomatics 2001;42:106–9) for use in hospital settings to identify complex patients at admission, and is used for early integral case management.
- Keep Well
- An initiative launched in October 2006 as part of the Scottish Government’s 2005 health policy, ‘Delivering for health’. It aims to increase the rate of health improvement in deprived communities by enhancing primary care services to deliver anticipatory care. In the Keep Well programme, individuals aged between 40 and 64 years living in areas of high deprivation are invited to attend a health check. The checks include screening for cardiovascular disease and its main risk factors, such as high blood pressure and cholesterol level, smoking and diet, as well as discussions around wider life circumstances, such as employment and literacy.
- Links worker
- An individual who provides support, sometimes in a general practice setting, to people who require help to improve their circumstances, health and well-being. This may be provided through supportive conversations and assistance to identify and access helpful connections and appropriate resources.
- Local health board
- In Scotland, any one of the 14 regional NHS boards that are responsible for the protection and improvement of their population’s health and for the delivery of front-line health-care services.
- Long-term conditions
- Health conditions that last for 1 year or longer, and which have an impact on a person’s life and may require ongoing care and support. The definition does not relate to any one condition, care group or age category. Examples of long-term conditions are diabetes mellitus, coronary heart disease, chronic obstructive pulmonary disease, arthritis and multiple sclerosis, among many others.
- Morbidity
- A way to describe how often a particular disease or condition occurs in a population, and commonly the impact of its presence in an individual.
- Multimorbidity
- The presence of two or more illnesses or conditions in a population or an individual.
- Normalisation process theory
- A sociological toolkit that can be used to understand the dynamics of implementing, embedding and integrating some new technology or complex intervention. It is mainly applied to understanding how new technologies or interventions are taken up or adopted in health-care settings by health-care professionals and/or patients. It was developed by May et al. [May C, Murray E, Finch T, Mair F, Treweek SA, Ballini L, et al. Normalization Process Theory On-line User’s Manual and Toolkit. 2010. URL: www.normalizationprocess.org/npt-toolkit (accessed 25 February 2013)], and continues to be researched and revised.
- NVivo
- A software program that supports qualitative and mixed-methods research. It is designed to help organise, analyse and find insights in unstructured or qualitative data, such as interviews, open-ended survey responses, articles, social media and web content.
- Patient-centred care
- A term with many definitions, but which usually means care that puts patients at the centre and gives them the opportunity to make informed decisions about their care and treatment in partnership with their health and social care practitioners.
- Patient outcome measures
- Tools and measures that patients can complete that help to measure their experience of their illness. Examples include the 12-item General Health Questionnaire (GHQ-12) or the Patient Health Questionnaire – 9 (PHQ-9), which are patient-completed forms that assess the patient’s general health status (GHQ-12) or mental health status (PHQ-9).
- Quality and Outcomes Framework
- The annual reward and incentive programme detailing general practice achievement results. It rewards practices for the provision of high-quality care and helps standardise improvement in the delivery of primary medical services. It is a voluntary process for all surgeries in England and was introduced as part of the general practitioner contract in 2004. The indicators for the Quality and Outcomes Framework change annually, with new measures and indicators being introduced or retired. General practices in Scotland ceased to use the Quality and Outcomes Framework on 1 April 2016.
- Scottish Index of Multiple Deprivation
- A tool that provides a standardised way to describe the extent of deprivation in any one Scottish residential area, and which allows for the comparison of levels of deprivation between areas.
- Scottish Mental Health Research Network
- A network set up in 2009 and funded by the Chief Scientist Office in Scotland to provide support to improve the quality and quantity of research conducted in Scotland, including through increasing the number of people participating in mental health research, and to promote excellence in mental health clinical research in Scotland.
- Scottish Primary Care Research Network
- A network set up in 2002 and funded by the Chief Scientist Office in Scotland to co-ordinate national research activity in primary care in Scotland and to increase the amount of research relevant to patient care undertaken in a primary care setting.
- Service user
- Someone who uses health and social care services, or who is a potential user of health and social care services.
List of abbreviations
- ADePT
- A process for Decision-making after Pilot and feasibility Trials
- ALISS
- A Local Information System for Scotland
- ALLIANCE
- Health and Social Care Alliance Scotland
- CARE
- Consultation and Relational Empathy
- CAU
- care as usual
- CCM
- chronic care model
- CHD
- coronary heart disease
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- COPD
- chronic obstructive pulmonary disease
- DAQ
- Depression Attitude Questionnaire
- DM
- diabetes mellitus
- GHQ
- General Health Questionnaire
- GHQ-12
- 12-item General Health Questionnaire
- GP
- general practitioner
- HNA
- holistic needs assessment
- HoC
- House of Care
- ICC
- intracluster correlation coefficient
- LTC
- long-term condition
- MCAM
- Minnesota Complexity Assessment Method
- MDT
- multidisciplinary team
- MECAM
- Minnesota and Edinburgh Complexity Assessment Method
- MRC
- Medical Research Council
- NHS FV
- NHS Forth Valley
- NHS GGC
- NHS Greater Glasgow and Clyde
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- PCAM
- Patient Centred Assessment Method
- PEI
- Patient Enablement Instrument
- PM
- practice manager
- PMG
- project management group
- PN
- practice nurse
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- RA
- research assistant
- RCGP
- Royal College of General Practitioners
- RCT
- randomised controlled trial
- SF-12
- Short Form questionnaire-12 items
- SIMD
- Scottish Index of Multiple Deprivation
- SPCRN
- Scottish Primary Care Research Network
- SSC
- Study Steering Committee
- TIDieR
- Template for Intervention Description and Replication
- WEMWBS
- Warwick–Edinburgh Mental Well-Being Scale
