Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5002/01. The contractual start date was in September 2013. The final report began editorial review in December 2016 and was accepted for publication in August 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Sophie Staniszewska is a member of the National Institute for Health Research (NIHR) Evaluation, Trials and Studies Coordinating Centre Patient and Public Involvement Reference Group and is Associate to Professor Kate Seers (NIHR Health Services and Delivery Research Commissioning Board).
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Currie et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Conceptual problem
The research study was commissioned by the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme, under its knowledge mobilisation theme, following a number of other studies commissioned under the same theme in recent years. Such studies tend to empirically focus on the organisational level of knowledge mobilisation. Analysis and research-informed suggestions tend to lean towards the panacea of knowledge brokering (see, for example, a previous NIHR HSDR study by the same principal investigator, GC, 09/1002/051). Although knowledge brokering was proposed as a solution, Graeme Currie and colleagues criticised the concept and practice because it fails to account for the capacity of the organisation to mobilise knowledge. In this study, we extend the knowledge-brokering solution by accounting for the contextual intricacies that affect knowledge mobilisation. We enhance the evidence base for effectively mobilising knowledge through a system level of analysis regarding capacity to mobilise knowledge (e.g. of a complete commissioning network, which encompasses health-care providers and other organisations supplying commissioning intelligence). ‘Absorptive capacity’ (ACAP) represents such a concept, which can be applied at the health-care system level of analysis. 2 ACAP maps on to the term ‘critical review capacity’, and can be applied to consider the empirical case of health-care commissioning networks. In so doing, our study addresses a need for the development of a model of ACAP that is more tailored to health care, a need that was encompassed within the original NIHR HSDR call for commissioned studies. 3
We highlight studies of ACAP in health care that are already published. 4–6 We seek to develop a model of knowledge mobilisation focused on ACAP of health-care commissioning networks, but one that is more widely transferable across the health-care system. Within our study, we draw on a more generic literature to set out some of the expected characteristics of health care that affect dimensions of ACAP and its antecedent combinative capabilities. 7–13 We then consider distinctive features of the health-care context that may affect ACAP.
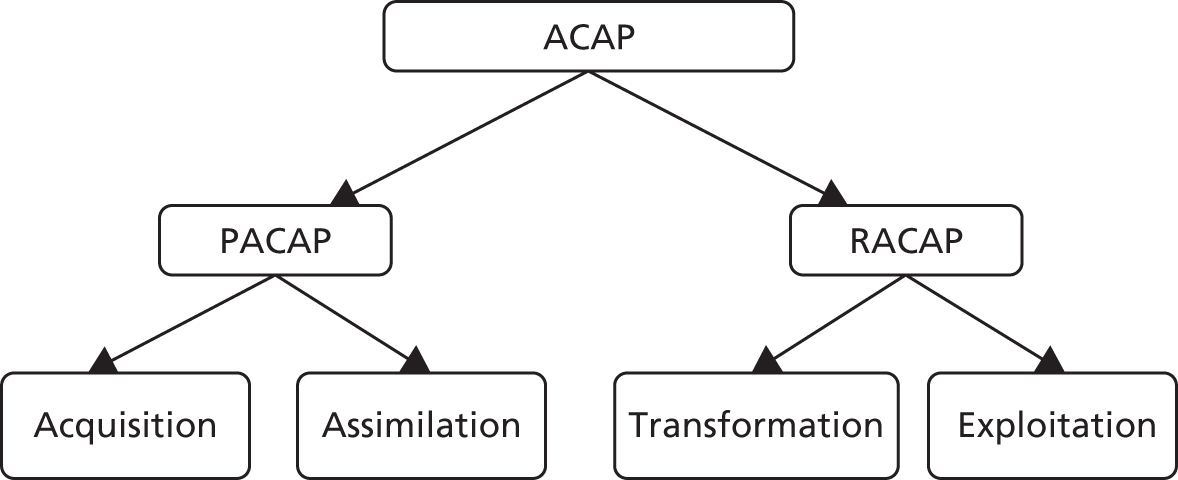
Applying the concept of ACAP, we argue that knowledge mobilisation occurs within overlapping processes, which can be conceptualised as acquisition, assimilation, transformation and exploitation of knowledge. These processes are influenced by combinative capabilities: systems capabilities, socialisation capabilities and co-ordination capabilities. Systems capabilities, such as targets and incentives and standardised data sets, can limit the type of knowledge acquired and used to guide service interventions. Socialisation capabilities, represented by professional and organisational cultures and associated professional–managerial relations, can limit knowledge mobilisation across occupational groups. Co-ordination capabilities can overcome the barriers of systems and socialisation capabilities, encouraging more flexible approaches to the four stages of knowledge mobilisation. In particular, this study highlights the importance of general practitioner (GP) involvement, patient and public involvement (PPI), business intelligence (BI) and social integration mechanisms, which further enhance knowledge mobilisation in health-care settings.
Practical problem
Our study provides help with the challenge the NHS faces in the wake of recent structural reform, but also supports the long-standing concern of policy-makers and research institutions, including NIHR, about the ability of the NHS to translate different types of evidence into transformative action for service development.
With respect to the long-standing translation challenge for the NHS, the development and validation of an ACAP model contextualised for the health-care system offers considerable promise to address knowledge mobilisation at the levels of individual, group and organisational behaviour, as well as systems-level behaviour. Particularly in financially parsimonious times, Quality, Innovation, Productivity and Prevention (QIPP) gains are likely to be realised through better mobilisation of existing knowledge from both formal and local informal sources, rather than necessarily generating new knowledge. A model of ACAP contextualised for the case of the health-care system will guide action regarding how this might be realised. The case of intervention to reduce potentially avoidable elderly admissions into hospitals represents an exemplary tracer study revealing lessons for other complex areas.
Recent government policy in England emphasises that services in the NHS can be improved through the increased involvement of clinicians and service users at local levels. These policy developments have resulted in the creation of Clinical Commissioning Groups (CCGs), devolving financial decision-making and commissioning of services to clinicians based in general practice, and thereby giving them greater freedom to respond to the needs of local client groups. 14,15 Our study is particularly timely in the face of NHS commissioning reforms, but we note that knowledge mobilisation in commissioning is a long-standing concern evident in previous primary care trust (PCT) arrangements, and is likely to extend to any other commissioning structures and processes in the future. In short, our study is intended to produce and disseminate analytical lessons regarding the enhancement of critical review capacity beyond current arrangements, and with a focus on the wider commissioning network, not merely on CCGs as organisational entities. Our analytical lessons also extend beyond the tracer study of elderly care. We suggest that the challenge of commissioning high-quality elderly care in a productive but preventative way is exemplary of a more general challenge of commissioning complex care, which often encompasses more than a single disease pathway and crosses boundaries within and outside the NHS.
With respect to current structural reform, should CCG-led commissioning networks fail to develop critical review capacity (which our study conceives as ACAP) for commissioning, structural reform is unlikely to succeed. Commissioning networks developing critical review capacity depends on enhancing antecedents for ACAP, that is, understanding how combinative capabilities of the commissioning network affects ACAP. We emphasise that our study is concerned not just with CCGs, which represent the centrepiece organisations in current reforms, but with the commissioning network as a whole, inclusive of a wide range of organisations. So, if CCGs were to be supplanted in a future round of structural reform, our focus on the commissioning network as a whole means that our study still holds practical relevance. Our stance regarding the wider commissioning network, rather than focusing on CCGs alone, is supported by Swan et al. ,16 who, in their study of previous commissioning arrangements, highlight the multilevel interdependencies around commissioning that mean that any commissioning organisations, such as CCGs, need to build effective relationships with, for example, the NHS Commissioning Board, including their local area teams; GPs and their practices; public health; local authorities; commissioning support units (CSUs); acute hospitals and other providers, such as community health, mental health and care homes providers; and other bodies that may provide commissioning intelligence, such as out-of-hours services, emergency services, the Care Quality Commission and Healthwatch England.
Research examining critical review capacity related to the new commissioning arrangements is scarce as a result of how new the organisational networks are. Limited research that does examine new commissioning networks highlights a need to increase critical review capacity for evidence-based decision-making through not just acquiring knowledge, but also using that knowledge. 17
Specifically, CCGs struggle to commission effective, targeted interventions for reducing potentially avoidable elderly care hospital admissions. Our study will indirectly reduce some of the uncertainty that hospitals face and that manifests itself in crises such as a lack of hospital beds in winter, as commissioning networks improve their ability to mobilise knowledge to commission interventions to prevent potentially avoidable elderly care admissions to hospital.
Regarding patient benefit, there is strong evidence that patient/carer experience of care and clinical outcome improves through being kept out of hospital. For the NHS, potentially avoidable admissions prove to be difficult and costly to manage. Frail elderly admissions, many of which can safely be avoided, are both clinically and economically deleterious. 18,19 Noting considerable variation in admissions, it is estimated that bringing provision up to best practice in England could result in savings of £132M,20 and a reduction of 7000 beds. 17 Proactive integrated care can reduce the proportion of frail elderly patients who go to hospitals. 21,22 Good care is diligent care that recognises and responds to signs of deterioration in early stages. Social support in the community is also important for people with both physical and mental impairment, with approximately half of all elderly patient admissions fulfilling the criteria for dementia. 23 Evidence might be used to commission community care that is sensitive to clinical pathways, recognises that most people have comorbidity and reduces potentially avoidable admissions of older patients. 19,24
Taking account of the above, we empirically focus on the service domain of elderly care, specifically a tracer study of capacity to mobilise knowledge to reduce otherwise avoidable admissions into hospital. This, as highlighted above, is particularly relevant to the case of ‘frail’ older people, a population group that our research sought to focus on in interviews with key stakeholders in CCG-led commissioning networks. However, as evident in empirical material, there is some slippage in our characterisation of the group we seek to reduce avoidable admissions of. This reflects the varied capacity of our 13 comparative cases of commissioning networks to acquire and use knowledge for intervention targeted at frail elderly patients rather than the larger, more general, group of older patients (over-65s who are not ‘frail’). We apologise in advance for what might appear to be imprecision, but argue that it derives from empirical data that we wanted to use effectively.
In considering a commissioning network’s acquisition and use of evidence, it is not our intention to set priorities for CCGs or to say how different sources of evidence (e.g. academic research, voluntary sector, PPI, GPs’ experiential knowledge and BI) might be combined. We suggest that different forms of evidence should be deemed to be of different levels of importance depending on the decision to be made, but nevertheless do not go about assessing this. What we would say is that ‘effective’ commissioning demands that CCGs acquire and use pluralist types of evidence in making decisions about service interventions. We stress that, although it is one thing to acquire evidence, such as that about the patient experience, it is another thing to use such evidence. Effective commissioning demands both acquisition and use.
Research question
Our conceptual contribution is the development of a model of ACAP encompassing its four dimensions (acquisition, assimilation, transformation and exploitation) and its three antecedent combinative capabilities (co-ordination, systems and socialisation), which are applicable to a wide range of health-care organisations. Our overarching empirical research question (RQ) is: how can we enhance ACAP of CCG-led commissioning networks in health care to inform decisions to reduce potentially avoidable elderly care acute hospital admissions?
Aims
The aims of this study are to:
-
develop a conceptual model of ACAP and an associated ACAP tool that are contextualised to the health-care case and are of practical use across the health-care system
-
enhance the critical review capacity (conceived as ACAP) of CCG-led commissioning networks in commissioning interventions to reduce potentially avoidable admissions of elderly people into acute hospitals, and other complex commissioning domains.
Objectives
The objectives of this study are to:
-
assess the development of critical review capacity, conceived as ACAP, of the new CCG-led commissioning networks
-
enhance the development of critical review capacity, conceived as ACAP, of the new CCG-led commissioning networks
-
support the acquisition and utilisation of patient experience knowledge to enhance the critical review capacity, conceived as ACAP, of commissioning networks
-
develop and provide face validation for a self-reflection ACAP tool for use by CCG-led commissioning networks and other health-care organisations, to enhance their critical review capacity
-
bridge the gap between potential and realised critical review capacity or ACAP of CCG-led commissioning networks.
Our study is formative, not merely summative. Following staged analysis, we intervene to enhance the critical review capacity of commissioning networks in a staged process throughout the study. In particular, we feed back to participating CCG-led commissioning networks in real time, and we develop the ACAP tool across the necessary wide range of health-care organisations to ensure its applicability beyond commissioning networks.
Research methods
We adopt mixed methods (mainly semistructured interviews, but also PPI focus groups, observation, secondary data and, in the future following validation, the ACAP psychometric tool) to examine comparative cases of commissioning networks regarding external and internal contingencies around their critical review capacity and to conceptualise critical review capacity as ACAP. See Chapter 3 for more detail.
Study governance
A strategic advisory group governed the study (meeting four times throughout the course of the study). Alongside this strategic advisory group, a distinctive PPI group was formed, which met regularly (also meeting four times throughout the course of the study). Our thanks go to Tony Sargeant (Chairperson of the strategic advisory group and PPI group) and his colleagues, who, beyond providing the necessary governance for our study, provided invaluable advice that shaped our empirical endeavour and, in particular, helped develop and provide face validation for the ACAP tool. The PPI group’s reflections on our study and its findings are presented in Chapter 10.
Structure of the report
We commence with a literature review, which outlines and critiques the ACAP concept before discussing its recent application to health care (see Chapter 2). Following this, we outline our research design (see Chapter 3). We then set out our empirical findings across five chapters: constraints of socialisation and systems capabilities (see Chapter 4), GP involvement (see Chapter 5), PPI (see Chapter 6), BI (see Chapter 7) and social integration (see Chapter 8). This is followed by a chapter that discusses the development of the ACAP tool, exhibits its dimensions and suggests how it might best be used (see Chapter 9). We then present our PPI group’s reflections on our study and its findings (see Chapter 10). Finally, we have a concluding discussion, within which we highlight our contribution to cumulative knowledge, practical implications, transferability of findings and further research (see Chapter 11).
Chapter 2 Absorptive capacity and clinical commissioning
Our literature review is not ‘systematic’ in the way that other epistemic communities, such as clinical science, might expect. Rather, it is one that is more selective, focusing on the focal empirical organisation of commissioning organisations and the mobilisation of knowledge within their decision-making, specifically the theoretical concept framing the analysis (ACAP). As set out below, commissioning organisations, particularly CCGs, enjoy very limited coverage in academic literature as they are relatively new organisations. Meanwhile, regarding ACAP, we focused on higher-quality journals in business and management regarding its generic model, and when considering its application to health-care settings, again, we note a very limited coverage.
Introduction
Recent reforms in NHS England have seen the introduction of CCGs, which lead commissioning networks, replacing the previous commissioning structures of PCTs (see Timmins25 for an in-depth overview of the policy progression from PCTs to CCGs). It is proposed that CCGs will increase positive clinical outcomes, financial management and service effectiveness through the creation, assimilation and exploitation of existing clinical guidelines and new innovations. 15,26,27 For these processes to take place, CCGs will need to critically review the external information they receive before assimilating, transforming and exploiting this knowledge through their commissioning decisions.
Given that CCGs are new organisations, literature on their critical review capacity for intelligent commissioning is sparse. Nevertheless, early scoping studies highlight the weak critical review capacity among CCGs,17 which was also apparent in their predecessors, PCTs. 16,28 One study produced a live simulation with a number of new CCGs to explore how they would adapt to some of the challenges they may face in the next few years. 17 The results indicated some areas of concern as GPs leading the groups struggled to work in a proactive, innovative way, acknowledging that they were overwhelmed by transactional demands that reduced their critical review capacity. These concerns have been echoed more recently, as researchers question whether or not commissioning reforms have actually led to increased performance and quality in health-care delivery. 29
Studies highlight that the quality of services delivered by health-care organisations is improved when the organisational capacity for learning and integration of diverse sources of knowledge is developed. 30–32 Recently, academic studies have highlighted how the concept of ACAP,2 derived from private sector settings, can be applied to health-care organisations to address how they might enhance service interventions by improving their critical review capacity. 3–5,33,34 In this chapter, we outline the concept of ACAP, which describes an organisation’s ability to acquire, assimilate, transform and exploit knowledge from the environment, improving competitive advantage2,13 in the context of CCGs. We highlight that the realisation of an organisation’s critical review capacity comes from reducing the variance between its potential absorptive capacity (PACAP) and its realised absorptive capacity (RACAP). Following this, we explore the antecedents to ACAP, known as combinative capabilities, highlighting how they can enhance or stymie the critical review capacity of organisations. 9–12 Finally, we highlight the importance of four co-ordination capabilities for enhancing the critical review capacity of CCGs.
Absorptive capacity
The concept of ACAP was first coined by Cohen and Levinthal2 to describe an organisation’s ‘ability to identify, assimilate, and exploit knowledge from the environment’. Lane et al. 9 hail ACAP as ‘one of the most important constructs to emerge in organisational research in recent decades’. Since its inception, ACAP has been seen as a core element of increasing critical review capacity, but the dynamics of enhancing ACAP are theoretically underdeveloped. 6,9
In this study, we adopt Zahra and George’s13 conceptual framework of ACAP, which characterises four activities of pulling in external knowledge that are crucial for the development of ACAP: (1) identifying and accessing relevant knowledge through acquisition processes; (2) analysing and interpreting this knowledge through assimilation; (3) integrating existing knowledge with the newly assimilated knowledge through transformation; and (4) refining and developing existing organisational routines and behaviours through exploitation of the transformed knowledge.
We recognise that health care represents a distinctive environment compared with private sector research and development (R&D) contexts in which much of the empirical work around ACAP has taken place. This renders some of the dimensions of the ACAP literature less relevant to health care, but, at the same time, brings others to the forefront. 5 In particular, in application of ACAP theory to literature, it is important to recognise two interacting and complementary elements: PACAP, the ability to acquire and assimilate knowledge; and RACAP, the ability to put newly acquired knowledge into action within the organisation through transformation and exploitation (as outlined in Figure 1). It is the variance between PACAP and RACAP that accounts for performance differences among organisations, with a decrease in variance crucial to enhancing ACAP. 13 In the following section, we discuss PACAP and RACAP in the context of CCGs.
Potential absorptive capacity
Zahra and George13 conceptualise an organisation’s PACAP as its ability to acquire and assimilate diverse sources of knowledge. The role of CCGs is to use external knowledge and guidance to identify areas for improvement in services and to base commissioning decisions on this knowledge. 35 Acquiring information is the first step in the critical review process and is suggested to result in better commissioning outcomes. 36,37
Knowledge is expected to be acquired from central institutions, such as the National Institute for Health and Care Excellence (NICE), which provides standardised advice and clinical guidelines about service provision and prescribing practices. 27 Exposure to these guidelines aims to reduce clinical variation and ensure that quality improvement decisions are embedded in the processes of CCGs. 27,35 However, it is important to acknowledge that these guidelines are not necessarily objects to be immediately internalised by professionals, but rather information processes that can be interpreted and translated to suit the organisational context. 38
The need for substantial infrastructure to assist in the acquisition of this information has been demonstrated in the USA, where clinical commissioners rely heavily on information technology (IT) and management systems to guide their critical decision-making. 39 The first challenge in increasing the effectiveness of CCGs, therefore, needs to focus on a more systematic mechanism for the diffusion of NICE clinical guidelines. 27 This has been recognised in government policy, and national efforts are under way to increase the scope of central knowledge acquisition by CCGs. 15,27
The second element of PACAP, assimilation, will rely on the skills and combined knowledge of the CCG. To become authorised, CCGs needed to fulfil certain criteria pertaining to a mix of professionals and stakeholder engagement, strong conformity to central governance and financial performance measures, collaborative working with other CCGs, and demonstrable strong leadership. 15 A mix of professional skills and knowledge should therefore be embedded in the organisation from conception, increasing the capacity for assimilation of external knowledge. This is the fundamental premise of CCGs, and providing a central role for clinicians in decision-making is crucial as they can assimilate their expert knowledge in response to the needs of their service users. 14,15 Decisions relating to managerial or financial information may be harder for clinicians to assimilate, highlighting the importance of managerial expertise as a component of the board and of increased training for clinicians. 26,39
Initial consideration of the PACAP of CCGs suggests that it should be realised provided that the infrastructure and support systems are in place to increase the acquisition of central guidance and the assimilation of managerial or financial information. The interventions required to increase PACAP are relatively structural, taking the form of BI functions, which we discuss later.
Realised absorptive capacity
Realised absorptive capacity refers to the transformation and exploitation processes of an organisation. 13 In order to effectively transform assimilated knowledge into commissioning decisions, CCGs need to engage in processes demonstrated by effective corporate boards, in particular constructive conflict, which encourages open discussion and sharing of ideas. 40–42 Previous studies on innovation adoption in health care have demonstrated these processes occurring with positive outcomes, but have acknowledged that these groups are usually uniprofessional. 38,43 As previously acknowledged, CCGs are required to represent multiple professional skills and knowledge bases. 15 Although this will increase the potential for constructive conflict and subsequently enhance the critical review capacity of these groups, there is also the increased potential for destructive, emotional conflict as a result of professional stereotypes and social hierarchies, leading to a reduction in performance and a lack of candid discussion. 41,44
The highly professionalised context of CCGs will compound the potential for destructive conflict as a result of existing professional hierarchies and existing board behaviours, undermining ACAP. Professional bureaucracies are characterised by the formal knowledge and power of highly trained experts and represent an institution in which knowledge is individualistic, hierarchical and separated into functional specialties. 45 In these contexts, the sharing of information across functional boundaries among professionals is limited, and the powerful status of expert professionals can inhibit knowledge sharing and transfer with non-experts, even when the group itself exhibits goal congruence. 45,46 This has been shown in similar medical groups in the USA, where a key element of effective groups was the ability to reconcile business goals and needs with the commissioning of high-quality health care. 39 How clinical and non-clinical members of CCGs will reach these decisions is, as yet, unclear.
The final element of ACAP, exploitation, will be influenced by the professionalised context of the wider institution, which will have an impact on the extent to which decisions made by commissioning groups can be diffused into the organisational network. Growth and development of tacit knowledge results from building on existing social relationships. In this way, what an organisation has done before will predict what it will do in the future. 47 Context is a major determinant of capacity for knowledge exchange and assimilation, and deeply ingrained existing organisational structure and social networks will have developed institutionalised channels of communication. 48 Encouraging innovation, rather than institutionalised routines and behaviours, is particularly difficult because the collective mindset of organisational members presents significant barriers to change and adaptation, resulting in the ‘non-spread’ of innovations, a problem associated with highly professionalised contexts, and one that has been acknowledged as an issue within the NHS. 43,49
Within health-care organisations, academic commentators highlight that acquisition of external knowledge is less of a problem than actual use (i.e. assimilation, transformation and exploitation) of that evidence to drive quality improvement. 3–5,33 It is the RACAP of CCGs that needs to be addressed to enhance critical review capacity. The existing institutional and professional hierarchies, behaviours and cultures will influence the potential for constructive conflict, information sharing and subsequent comprehensive decision-making. Candid discussion and equal power distribution may not be possible, undermining the potential for critical reviewing capacity as more powerful CCG members take the lead. These existing cultural and social mechanisms are also reflected in the problems encountered when exploiting the clinical decisions within the larger organisation. Knowledge and innovations will be shared and diffused throughout existing institutionalised channels of communication and will have to be internalised into the existing organisational behaviour to have an impact. This can be difficult in a heavily institutionalised context.
Reducing the variance between potential absorptive capacity and realised absorptive capacity: the influence of combinative capabilities
It would appear from the literature review that any interventions aimed at increasing the effectiveness of CCGs need to be focused on increasing RACAP. The ability to transform and exploit knowledge throughout the organisational network, and to implement innovations and recommendations, is a fundamental need for CCGs. Consequently, when considering critical review capacity in health care, there is a need for research into how organisational antecedents affect ACAP, which takes into account organisational context, the role of individuals and groups, and associated power and politics. 8,9,12,13 This requires more focus on social mechanisms, as the CCG will need to develop the ability to share and transform information and knowledge to make critical decisions. The difficulties associated with knowledge sharing and transfer cannot be resolved through redesign of governance structure because of the socially embedded nature of tacit knowledge, which is a key element of critical decision-making in social contexts. 50
Although existing research into ACAP has engendered deeper understanding of the organisational conditions that have an impact on organisational knowledge processes, literature in this theoretical domain remains focused on knowledge acquisition, rather than its use,6 and there is a lack of detailed understanding of the antecedent capabilities for enhancing ACAP, and in particular of reducing the variance between PACAP and RACAP. 8,11 What is clear is that there are antecedents to ACAP, specifically known as combinative capabilities. 10,12 As noted previously, health-care organisations represent a distinctive context compared with private sector R&D contexts, in which much of the empirical work around ACAP has taken place, and, as such, combinative capabilities will influence the four ACAP mechanisms in health-care organisations in a particular way. 5 Van den Bosch et al. 11 distinguish three types of combinative capabilities that influence ACAP: socialisation capabilities, system capabilities and co-ordination capabilities. In the following section we discuss these capabilities in the context of CCGs.
Socialisation capabilities
Socialisation capabilities refer to an organisation’s ability to produce a shared ideology and develop a distinct group identity. The social processes associated with this capability are often seen as most influential in the development of ACAP within professional organisations. 6,13 Health-care organisations exemplify the professional bureaucracy archetype,51 within which professional organisation is likely to represent a key influence on socialisation capability, limiting ACAP as described in the following paragraphs.
External knowledge interacts with strong organisational cultures and structures, so that socialisation capability within health-care organisations restricts the development of ACAP. 11 Thus, power and status linked to professional roles are likely to have an impact on health-care organisations’ ability to exploit new knowledge. 3,33 For example, Berta et al. 4 note the role of doctors in subverting an organisation’s learning capacity in relation to the adoption of new clinical guidelines into practice, based on formal evidence. Similarly, Ferlie et al. 49 note that deeply ingrained organisational structures and social networks within health-care organisations engender institutionalised epistemic communities of professional practice, which exist in silos, relatively decoupled from one another. This may have an impact on socialisation capabilities, as professional training and early career experience may engender a custodial role orientation whereby professionals orientate narrowly towards their peers, rather than across the health-care delivery system. 52
This stymies the search for external knowledge that lies outside current ways of thinking among powerful professional groups. The shared culture or ideologies represented by socialisation capabilities enables the transformation and exploitation of new knowledge, but those same cultures may represent a ‘mental prison’ that limits the potential of absorption of external knowledge, particularly when that knowledge may contradict shared beliefs. 10 The implication is that employees need to be exposed to diverse knowledge sources, but transformation and exploitation of this knowledge will be enhanced only when it complements existing knowledge sources. 13
Further to this, knowledge is more likely to be transferred and shared within organisations, rather than with external stakeholders, as they have shared experiences in terms of expertise and training in addition to a shared collective identity. 12 Finally, there is considerable but variable agency for actors to influence knowledge acquisition, assimilation, transformation and exploitation. 4 In particular, powerful groups of actors may influence knowledge absorption processes to achieve their goals. 5,10
Systems capabilities
System capabilities refer to formal knowledge exchange mechanisms such as written policies, procedures and manuals that are explicitly designed to facilitate the transfer of codified knowledge. 11 The primary virtue of systems capabilities is that they provide a memory for staff handling routine situations in an organisation, with the result that staff can react quickly, increasing the efficiency of knowledge exploitation. For example, within health-care contexts, admissions data or other patient information may be collected and collated in certain ways to comply with the demands of external agencies and legal requirements regarding sharing of data. Such data may (or may not) prove useful for CCGs to monitor trends, such as the local patterns of GP referrals of older people into hospitals, potentially allowing CCGs to distinguish between necessary and avoidable admissions. Alternatively, systems capabilities may take the form of clinical guidelines, such as those set by NICE, or mandatory priority setting by top-down government initiatives, such as the continuing influence of the National Commissioning Board over CCGs. System capabilities such as pre-existing policy in the realm of organisational incentives, legislation and system-level dissemination mechanisms or initiatives, which afford access to external resources and influencers, formalise but narrow knowledge acquisition and assimilation and, at the same time, restrict exploratory learning, innovation and transformation. 4
Health-care organisations are subject to New Public Management reform that frames performance through financial incentives and regulation. Encompassed within systems capabilities, such government policy affords access to external resources, and directs and formalises acquisition and assimilation of knowledge. However, it narrows the search for new external knowledge and the scope for processing of that knowledge, as managers in health-care organisations ‘gameplay’ to ensure compliance with policy requirements around their governance. 31,53 Pulling in external knowledge within health-care organisations towards quality improvement appears to be particularly directed towards compliance with government regulation and performance management54 in a way that is likely to limit the search and utilisation of external evidence, limiting the level of ACAP.
Co-ordination capabilities
Co-ordination capabilities refer to lateral forms of communication or structures, such as education and training, job rotation, cross-functional interfaces and distinct liaison roles. In contrast to socialisation and systems capabilities, co-ordination capabilities increase the scope of external knowledge acquired and assimilated, and may also engender greater organisational flexibility regarding subsequent transformation and exploitation of knowledge (subsequently reducing the variance between PACAP and RACAP). Hence, to enhance ACAP, managers might attend to organisational mechanisms associated with co-ordination capability. 8,11 The aim for organisational managers, in developing co-ordination capabilities, is to establish ties with external sources of new knowledge (enhancing acquisition and assimilation) and to support this through establishing dense networks of ties within the organisation (enhancing transformation and exploitation). 8 Thus, organisation managers might seek to enhance ‘social integration mechanisms’, such as boundary-spanning or liaison mechanisms and roles and communities of practice, and seek to decentralise authority and decision-making. 2,9,12 For example (as discussed in General practitioner involvement), within CCGs, the increased involvement of GPs within the commissioning structures might act as a co-ordination capability, as doctors have been noted as holding a mediating role in communication (or lack of) across jurisdictional boundaries. 4
Co-ordination capabilities could be a mechanism that facilitates mediation between the effects of socialisation and systems capabilities. This is particularly evident in professionalised organisations, as co-ordination capabilities facilitate development and dissemination of internal knowledge, which is commonly tacit, as well as external, codified knowledge. 33 This enhances ACAP by ensuring that external knowledge is effectively combined with prior knowledge held by front-line clinicians, informing the commissioning and delivery of health care.
Co-ordination capabilities in commissioning
Identifying and enhancing co-ordination capabilities is particularly important in complex organisational settings, such as health care, ‘where . . . the ability to engage in flexible, knowledge exchange and generation across hierarchy and function – are essential to organisational performance’. 33 However, as noted previously, the influence of intraorganisational dynamics on co-ordination capabilities has received little attention in the existing literature, within both health care and the wider body of organisational research. 12 Although dimensions of co-ordination capability have been identified within health-care settings,3,4,32 there is a lack of understanding of how such co-ordination capabilities work to enhance ACAP, and how development of co-ordination capabilities might be supported. Drawing on the ACAP literature outlined above, it appears that there are key elements of co-ordination capabilities that could be drawn on to improve the critical review capacity of CCGs: information support systems, social integration mechanisms, clinical participation in decision-making, appropriate leadership and, more generally, social relations with diverse group inside and outside the organisation. 33 In the specific context of CCGs, we conceptualise these co-ordination capabilities as four mechanisms: GP involvement, PPI, BI functions and social integration mechanisms.
General practitioner involvement
The policy emphasis on the need for medical involvement in organisational decision-making and commissioning relies on influence through formal managerial roles. 14,55,56 Structurally positioned across managerial and professional boundaries, doctors occupying these spaces take on leadership roles over their ‘rank and file’ colleagues who are not involved in organisational decision-making. 57 Those doctors discharging medical responsibilities alongside a managerial role are seen as crucial drivers of policy-led change in health-care organisations, and they are expected to proactively steer their professional colleagues towards organisational aims. 58
Doctors involved in organisational management can, arguably, exert influence outwards to control external forces intruding on the profession, while, at the same time, enjoying influence and control over their colleagues. 59,60 As a result, policy aspirations assume that doctors in formal management roles should be able to influence organisational decision-making, as they occupy an established, powerful role and voice within a dominant coalition with general managers, controlling health services. 61–63 Consequently, medical involvement in decision-making should act as a co-ordination capability, as doctors are able to acquire, assimilate and transform information from different sources and in different ways from general managers, overcoming issues of systems and socialisation capabilities.
However, doctors involved in management represent both the professional agenda and its disciplining by a managerial one, resulting in a lack of credibility with their rank and file professional peers, or a lack of influence over managerial decision-making. As such, managerial and professional aims may not be aligned as doctors enact medical management roles, with consequent deleterious effects on rank and file doctors’ involvement in organisational decision-making. 64 Furthermore, medical managers are seen as encouraging the ‘colonisation’ of managerial priorities in professional practice, standards and discourse. 59,65–68 Rank and file doctors may prove resistant to such soft governance mechanisms, again with deleterious effects on their involvement in organisational decision-making. 62 Even where studies show that formal involvement of doctors in decision-making results in better organisational performance, such as those set within the US health-care system,55,56 exactly how they influence decision-making is unclear. 63
The studies cited in the preceding paragraphs characterise doctors involved in organisational decision-making as a homogeneous group: a substratum of the profession ascending into formalised medical management roles, exerting influence over rank and file peers. This represents an oversimplification of doctors’ involvement in organisational decision-making and neglects a consideration of differences between forms of medical influence. 59,64 The potential emergence of doctors who influence organisational decision-making from outside formalised managerial roles (i.e. those who do not occupy a formal position spanning medical and managerial perspectives, but nevertheless engage with managerial decision-making) is neglected in both policy and research. 69,70 This is problematic, and results in policy approaches to organisational improvement that do not consider the potential benefits offered by involving doctors through alternative, non-formal, arrangements.
In the context of CCGs, the involvement of GPs in formal commissioning roles is crucial. 14 Commissioning organisations in England are multidisciplinary, yet GPs arguably exert the most power and influence, reinforced by their increasing fiscal responsibilities and involvement in commissioning. 71,72 However, not all GPs are engaged in formal roles, resulting in intraprofessional variation, as some focus on clinical, rather than managerial, interests, whereas others take on a unique level of responsibility for strategic decision-making through commissioning leadership roles. 67,73 Further to this, a recent report by Robertson et al. 29 highlighted that increased GP involvement in commissioning has not necessarily been translated into improvements in health-care delivery. They highlight dwindling levels of GP engagement in formal commissioning roles, and advocate the need to develop new roles for GPs that allow them to maximise their potential contribution to CCG decision-making processes without needing to withdraw from clinical work.
In summary, although GP involvement should, theoretically, act as a co-ordination capability to enhance critical review capacity of CCGs, recent work suggests that this potential is not being realised. 17 More research is needed into exactly how doctors influence organisational decision-making,63 with a specific focus on the challenges faced when co-opting GPs into formal commissioning roles in CCGs. 29
Patient and public involvement
Patient and public involvement is a global priority in health-care settings and is assumed to empower communities, improve service decisions, provide democratic accountability and contribute to higher-quality services. 74,75 Despite the benefits of PPI for health and social care services,76 much existing research suggests that, although there is strong policy support, its potential contribution is stymied by contested terminology, limitations in the underpinning evidence base, different attitudes to PPI and variable attempts at implementation. 77,78 Commentators note the impact of professional hierarchies on the translation of PPI policy into practice in public sector organisations,79–81 but neglect the impact of managerial influences on PPI. 82 This is surprising, considering that recent research highlights how PPI representatives attempt to increase their influence by working more closely with managers,83 suggesting that changes in managerial context may represent a means by which to enhance involvement.
In NHS England, PPI is reflected in policy advocating patient choice and shared decision-making, from the individual level of care to the development and improvement of health services. 84,85 The importance of PPI in CCGs is also reflected in the central focus on the involvement of service users in commissioning decisions, driving patient-focused decision-making that is theoretically autonomous from top-down control.
The new commissioning arrangements, in particular the renewed focus on public and clinical involvement, distinguish CCGs from their commissioning predecessors, which were criticised for being managerially focused with limited, tokenistic engagement with the public. 86,87 This is reflected in the new legal requirements for commissioning organisations to engage with the public at multiple stages of the commissioning process. 88 However, reflecting other policies relating to PPI, the interpretation of what PPI ‘is’, or how the public should be integrated into commissioning decisions, is vague. Commentators suggest that this ambiguity is key to CCGs, as they theoretically have more flexibility and autonomy from top-down control, creating contexts that have the potential to develop PPI according to their local needs and organisational cultures. 89 CCGs, therefore, offer insight into the varying ways that policy will be interpreted and implemented within the commissioning context.
Patient and public involvement should act as a co-ordination capability in a similar way to GP involvement, overcoming limitations of systems capabilities by broadening the scope of information being acquired, assimilated and transformed into service design. However, although patient involvement is a key policy imperative, making the vision of fully integrated PPI in commissioning has historically been challenging. 90 Although CCGs go some way towards improving previous commissioning systems, commissioners are still criticised for a lack of progress in fully involving the public in decisions about their own health and service provision. 91 In particular, researchers note how, when commissioners are preoccupied with meeting immediate performance management demands, or responding to centrally determined policy mandates, the patient voice is the first to be sidelined and ignored during commissioning processes. 17
Business intelligence
The third co-ordination capability alluded to in the literature relates to the BI functions available to CCGs. In policy, BI comes from CSUs, which were set up to provide IT, human resources and strategic BI support to CCGs. 92 CSUs arguably provide transactional information (such as admissions details from secondary care, and insight into spending in the regional area) as well as more transformational insights, such as intelligence around service redesign. As such, BI functions act as a potential co-ordination capability by mediating limitations of systems capabilities, as discussed in Chapter 7.
Initially, CCGs were able to decide whether or not to retain BI services in-house, encouraging relational interactions with commissioners and operating under the umbrella of the NHS Commissioning Board. 93 However, from 2016, policy mandates that CSUs become independent businesses to introduce competition into the market and encourage more strategic BI offerings to CCGs. Policy-makers suggest that the potential added value of outsourcing BI functions results from the fact that their services are bought in by CCGs in a competitive market, encouraging CSUs to move beyond the limitations of transactional information provision and towards more strategic approaches to health-care improvement. 94
However, the success of CSUs working in transformative partnership with CCGs is ambiguous and requires further research. First, policy notes that CSUs vary in size, capacity, capability and commercial skills. 93 This is also the case for CCGs, meaning that there will be variation between cases in both the way they engage with CSUs (i.e. in-house or outsourced) and the way they are able to transform the information from CSUs into service design at a local level. Associated with this variation is a concern that CCGs initially lacked the understanding required to be ‘intelligent customers’, and were unsure of how to use CSUs to enhance their critical review capacity. 93
Second, in the context of this study, NHS England has considerable influence over CSUs and the subsequent monitoring and guiding of activities of CCGs. Rather than encouraging truly transformational BI through relational interactions with CCGs, this close link with NHS England may reduce BI to transactional interactions with CCGs, which we noted previously as a limitation of CCG systems capabilities. 54 As a consequence, Petsoulas et al. 95 note that CCGs may be distrustful of CSUs, as they resent being required to outsource business functions that previously existed in-house. Therefore, whether or not a competitive market for CSUs will encourage more strategic, transformative relationships between commissioners and CSUs, rather than perpetuating fragmented, transactional interactions driven by central performance management systems, remains to be seen.
Social integration
There is a distinct imperative, both in policy and in research literature, for health and social care provision to be better co-ordinated. 96,97 When CCGs first began operating, social integration was promoted through health and well-being boards. 88 However, these boards were quickly criticised for excluding local organisations and leaders central to care integration, and focusing more on politically driven issues of public health rather than acting as an integration mechanism. 98
In response to the criticism of the perceived failure of health and well-being boards, pooled budgets, in the form of the Better Care Fund, were set up to encourage the development of integrated care teams, with a focus on reducing emergency admissions to hospital. 99 Integrated care teams work by taking a joined-up approach to complex, holistic care for patients who often have comorbidity. 19,24 It is crucial to strengthen integrated community care, through intelligent commissioning, so that care is holistic and sensitive to patient need, and there is strong evidence that integrated care teams can reduce the proportion of elderly patients being admitted into acute hospitals. 21,22 It is estimated that integrating health and social care could result in savings of £132M,20 and a reduction of 7000 beds. 17
In addition to the importance of integrating health and social care, close working with the voluntary sector is increasingly noted in policy as a crucial element of social integration mechanisms. 100 A report for NHS England highlights the potential benefits of engaging voluntary organisations in both the commissioning and provision of complex service arrangements. 101 Voluntary organisations are able to work with health and social care providers, often crossing institutional barriers, which can enhance patient outcomes, particularly for frail or vulnerable patients. 102,103 However, despite the potential benefits of engaging with voluntary sector organisations, research into how commissioning organisations engage with the third sector during commissioning processes is unclear and requires further exploration.
Despite a policy focus on the need for integrated health and social care,88,100 and increased involvement of the voluntary sector,101 the outcomes of integrated teams in practice are ambiguous. 104 Addicott105 notes two key approaches to facilitating social integration attempts: relational (nurturing trust and building relationships between providers) and transactional (holding providers to account for outcomes, streamlining patient care and facilitating the flow of money between providers). However, socialisation and systems capabilities, in the form of funding, governance, accountability and information systems, act as a limiting influence on the ability of service integration. 96 Social integration mechanisms, although noted as potential mechanisms through which to overcome these limitations, are seen as complex and often risky for commissioners, reducing the appetite for true social integration in a number of CCGs. 17,105
Conclusions
Absorptive capacity is a theoretical concept that can be used to explore critical review capacity in organisations. 2 Of particular importance is the consideration of variance between PACAP (acquisition and assimilation) and RACAP (transformation and exploitation), an area that has been highlighted for future research. 8 Although the majority of research concerning ACAP is limited to the private sector, in this chapter we reported the potential benefits when applied to the health-care context of CCGs, outlining previous research that suggests that health-care organisations might apply ACAP concepts to enhance service interventions by improving their critical review capacity. 3–5,33
In particular, we highlighted the important, yet underdeveloped, effect of combinative capabilities on the reduction in variance between PACAP and RACAP. Indeed, Van den Bosch et al. 11 call for future research to assess not just ACAP stages but how combinative capabilities affect the acquisition, absorption and use of new knowledge for improved organisational performance. The literature suggests that systems and socialisation capabilities act to reduce ACAP in a more pronounced way in health-care organisations. 8 This highlights the need for health-care organisations to develop co-ordination capabilities to offset the effects of systems and socialisation capabilities so that their ACAP is enhanced.
The four co-ordination capabilities that are identified as important in the context of CCGs are GP involvement, PPI, BI functions and social integration mechanisms. Each of these co-ordination capabilities has the potential to mediate some of the barriers of systems and socialisation capabilities, which characterise complex organisational contexts. However, although policy identifies the development of these four elements as a priority for CCGs, the extent to which each is able to reduce the variation between CCG PACAP and RACAP, enhancing critical review capacity, is unclear.
Chapter 3 Research design
Introduction
To explore how CCGs can enhance their critical review capacity for intelligent commissioning, we followed a tracer study:106 that of commissioning interventions to reduce avoidable admissions of older persons into hospitals. For the NHS, potentially avoidable admissions prove difficult and costly to manage. Frail elderly admissions, many of which can safely be avoided, are both clinically and economically deleterious. 17–20 Avoiding admissions is a matter of improving care in the community, which is particularly important for people with both physical and mental impairment, with approximately half of all elderly patient admissions fulfilling the criteria for dementia. 23
Elderly care admission avoidance was therefore chosen as a tracer study owing to its central importance, particularly in the face of the austere financial climate facing health care. As such, the study contributes to system transformation that takes costs out of hospitals, and links to local transformational efforts around QIPP, a significant part of which focuses on system improvement and cost reduction in elderly care. Our study aims to reduce some of the uncertainty that hospitals face and that manifests itself in crises, such as a lack of hospital beds in winter, as CCGs improve their ability to anticipate fluctuations in demand and commission interventions to prevent potentially avoidable elderly care admissions to hospital. Improvement in organisational and clinical outcomes is enhanced by our consideration of joint commissioning across health and social care, noted as particularly challenging,96,105 with Swan et al. ’s16 2012 study of PCTs further highlighting complex, multilevel interdependencies in commissioning decisions across organisations. Practically, we suggest that the relationship between CCGs and acute hospitals may be prone to tension in this area as productivity gains ensue through transfer of care outside hospitals, so, in this regard, the tracer is interesting.
Further to the theoretical reasoning for selecting elderly care admission avoidance as the tracer study, the issue was viewed as a particularly pressing issue by the CCG leads whom we interviewed in an exploratory study. However, the results from this study are not limited to care of older people, as application of the ACAP concept allows theoretical generalisation to other commissioning domains. 107 In other words, although we focus specifically on commissioning processes related to elderly care, the underpinning processes and findings are generalisable to a broad range of commissioning issues.
Our overarching RQ is as follows: how can we enhance ACAP of CCG-led commissioning networks in health care to inform decisions to reduce potentially avoidable elderly care acute hospital admissions? This breaks down into three linked RQs:
-
How do CCG external relationships and system antecedents to new commissioning arrangements affect CCG critical review capacity?
-
What features of CCG organisational context (i.e. internal capacity) affect CCG critical review capacity?
-
How do we reduce the variation between PACAP and RACAP?
Case studies
We follow a comparative case study approach,108 focusing on 13 CCGs in NHS England, allowing generation of more robust analysis, alert to contextual contingencies, when considering the antecedents of critical review capacity. Case study research involves a multilevel approach to the understanding of in-depth, dynamic settings, and can expand knowledge of individual, group, organisational and social phenomenon by allowing researchers to examine real-life events in a rich, holistic context. 107 Case study research does not attempt to select statistically representative samples, instead focusing on events or programmes that provide a unique conceptual insight into a theoretical framework at different levels of analysis. 107,109,110 Interviewing participants from different hierarchical levels and organisational positions will provide different perspectives on phenomenon, an essential element of multiple case research. 111,112
Case study research explains processes such as how we enhance CCG critical review capacity. Comparative case analysis allows generation of more robust analysis, particularly when concerned with drawing out contingencies, such as those external and internal contingencies framing CCG critical review capacity. 111 Comparative case analysis also accommodates heterogeneity of CCGs, and our study sites are representative of heterogeneity nationally.
The eventual sample of 13 CCG-led commissioning networks is representative of their characteristics (Table 1); however, we faced a considerable challenge in accessing empirical sites, that is, we approached many more potential empirical cases. Commonly, we experienced some interest and an invitation to discuss our study with a key stakeholder, often the chief operating officer, but were then passed down the CCG organisation to a GP commissioning lead or commissioning manager. Beyond the chief operating officer, other stakeholders sought to translate our research intent towards something else of more operational priority (at which point we politely disengaged). Our overall impression was that CCGs remained rather passive about developing their critical review capacity, even though, in our eyes, this was necessary to achieve their strategic remit set out by policy-makers.
| CCG characteristics | CCG A | CCG B | CCG C | CCG D | CCG E | CCG F | CCG G | CCG H | CCG I | CCG J | CCG K | CCG L | CCG M |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subject of specific focus | Integrated teams | Integrated teams | Patient involvement | Patient involvement | BI | Integrated teams | Patient involvement | Integrated teams | GP involvement | Voluntary sector/integrated teams | Integrated teams | GP involvement | BI |
| Population served | 93,000 | 128,000 | 128,000 | 270,000 | 897,300 | 239,550 | 327,754 | 167,800 | 270,000 | 167,000 | 108,300 | 428,100 | 8.3M |
| Area | Urban | Mixed | Mixed | Rural | Rural | Mixed | Mixed | Rural | Rural | Rural | Mixed | Rural | Urban |
| Budget (£) | 145,500 | 200,843 | 200,000 | 410,889 | 1,461,432 | 125,950 | 549,310 | 289,615 | 410,000 | 289,615 | 4.3B | 738,514 | 10B |
However, once we negotiated access to our 13 empirical cases, we asked each CCG to suggest a commissioning issue related to elderly care admission avoidance that was currently important in their organisation. The focus of each case fell broadly into the four categories of co-ordination capabilities highlighted in the literature review (see Chapter 2): GP involvement, PPI, BI functions and social integration. The demographic spread of each CCG, and their specific commissioning focus discussed during interviews, is outlined in Table 1.
Interviews
Comparative case studies were underpinned by qualitative fieldwork, with data gathering mainly via 159 semistructured interviews,113 most of which were conducted by the fieldworker (research fellow employed on the study), with the principal investigator for the study conducting a smaller number to ‘keep in touch’ with the primary data. Interview schedules were informed by themes generated from the literature review, which was thematic and followed narrative models. 114 In-depth interviews allow researchers to understand how the respondent views the world without researcher preconceptions being imposed on them, and to generate rich data with minimal researcher reactivity. 115,116 Individual interviews allow an insight into how large-scale transformations are experienced and are affected by the interactions of individuals, and they focus on how these interactions are embedded in the social and cultural context. 117 Semistructured interviews offer a much richer account of how the interviewees’ experiences, knowledge, ideas and impressions are considered and documented. Interviewees are less constrained by the researchers’ pre-understanding and there is space for the negotiation of meanings, so some level of mutual understanding is reached. 118
Our sample of interviewees from the 13 CCG-led commissioning networks represented stakeholders who were seen to be central to the commissioning process, and in many cases carried some ‘managerial’ responsibility for commissioning. We also engaged with ‘lay members’ of the CCG, individuals without clinical backgrounds who participated in PPI groups, or who acted in a lay member capacity on the CCG governing body. With assistance from the relevant CCG chief operating officer in exploratory interviews designed to engage CCGs in our study, we identified some respondents a priori, and then followed a snowball sampling pattern119 until the themes emerging from interviews were theoretically saturated. To ensure that the extended commissioning network was considered, interviews were not limited to those working within CCGs but also encompassed those working in hospitals, in addition to public health and local government professionals concerned with provision and commissioning of older people’s care. Further to this, to reflect the ongoing politicised nature and top-down control that remains within health-care contexts, we interviewed six NHS England staff, including three of the NHS Commissioning Board local area team leads linked to our focal CCG empirical cases. After we obtained ethics approval from local NHS research ethics committees and R&D departments, a total of 159 participants were interviewed (Table 2).
| Occupation/organisation | CCG A | CCG B | CCG C | CCG D | CCG E | CCG F | CCG G | CCG H | CCG I | CCG J | CCG K | CCG L | CCG M | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinician (GP or nurse) | 2 | 2 | 2 | 1 | 2 | 3 | 4 | 3 | 2 | 4 | 3 | 8 | 0 | 36 |
| CCG managerial staff (finance, strategy, governance, etc.) | 3 | 2 | 3 | 2 | 10 | 3 | 2 | 3 | 2 | 4 | 7 | 7 | 12 | 60 |
| Secondary care provider | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 4 | 1 | 0 | 12 |
| Tertiary care provider | 1 | 1 | 1 | 0 | 1 | 1 | 3 | 3 | 0 | 4 | 0 | 0 | 0 | 15 |
| Local authority | 1 | 0 | 1 | 0 | 0 | 2 | 2 | 3 | 0 | 2 | 2 | 0 | 0 | 13 |
| PPI representative | 2 | 3 | 2 | 2 | 3 | 0 | 4 | 0 | 1 | 0 | 0 | 0 | 0 | 17 |
| NHS England representative | 1 | 3 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| Total | 10 | 12 | 11 | 6 | 17 | 10 | 17 | 12 | 6 | 14 | 16 | 16 | 12 | 159 |
Within each CCG network, we undertook semistructured interviews and asked respondents to describe the commissioning process, focusing on the four processes encompassed within knowledge mobilisation, embedded in an organisation’s ACAP (acquisition, assimilation, transformation and exploitation), and their antecedents or combinative capabilities. We did not directly invoke technical terms such as ACAP and capabilities, but asked more general questions, such as the following: ‘How do you acquire data and information about elderly care hospital admissions?’; ‘How do you use such data and information?’; ‘What are the barriers to using data and information?’; and ‘How are these barriers mediated?’. Participants were also encouraged to speak freely about their experiences of commissioning processes, and interview themes were guided by issues arising during the conversation.
As we gathered data, we sought to collect rival explanations for the phenomena reported, in a spirit of scepticism about reporting of events and actions. We sought to collect discrepant evidence to develop a plausible rival description of events and activities. In short, we sought to challenge our explanation of knowledge mobilisation by CCG-led commissioning networks as one focused on ACAP. There were specific explanations of poor use of knowledge mobilisation by CCG networks. More generally, top-down policy pressures, power differentials with large acute providers and bureaucratic tendencies of CCG employees converged, meaning that knowledge mobilisation was poor. Theoretically, the concept of ACAP provides an explanation for poor knowledge mobilisation.
Patient and public involvement during the study
Although the overarching study was concerned with enhancing decision-making processes for commissioning organisations, specifically related to interventions to reduce avoidable admissions of older people into hospital, we were also interested in PPI in CCG networks. Although only three of our networks explicitly asked us to explore PPI, it was a central component of our interview schedule at each site. Over the course of the study, distinct variations in managerial interventions shaping PPI involvement were noted, leading to different outcomes for PPI influence on service development at each site. Although all commissioning networks had formalised structures for public engagement, the managerial influences on PPI varied immensely (this is discussed in detail in Chapter 6).
In addition to questions relating to ACAP, as outlined above, we also asked interviewees to describe how information or opinions were acquired from the public and through what structures this took place; how feedback was used with other forms of data to determine the needs of the local community; how information from PPI was used to design services; and what the influences on PPI were. In addition, when possible, the research team intended to attended public engagement forums or meetings at each site. This was limited, in most cases, by managerial reluctance for us to observe meetings and, for this reason, was restricted to six observations of PPI meetings occurring over three sites (those specifically interested in their public engagement). Extensive hand-written field notes were taken during observations and used to supplement analysis of themes related to PPI.
In addition to the focus on PPI during research, the research group itself had a strong PPI focus. The study advisory board, which meets yearly, is chaired by Tony Sargeant, patient involvement champion. In addition to the research staff on the board, Andrew Entwistle, lay specialist in patient involvement, and Graham Martin, academic specialist in patient involvement, were key members of the study advisory board. This group was heavily involved in the design of the study, the ongoing planning and response to themes emerging, the analysis of the findings and the dissemination plans for the findings. Further to this, Tony and Andrew also sat on the study PPI group. This group met at least twice a year to receive regular study updates from the research team and to triangulate study analysis. They offered insight into the direction of research and highlighted issues that the research team may not have isolated as influences on critical review capacity in CCGs. Finally, the PPI group were also involved in the dissemination of research. Crucially, the ACAP psychometric tool was coproduced between the researchers and PPI group in an iterative manner (see Chapter 10 for further details). Their meetings were audio-recorded by Sophie Staniszweska (co-investigator), who continues to work with the group to produce some user-led publications or study outputs.
Analysis
Semistructured interviews lasted between 45 minutes and 1 hour and were audio-recorded and transcribed. Initial coding was carried out by one member of the research team (research fellow) following template analysis. Coding was then discussed with the principal investigator, with the research fellow and principal investigator jointly engaging in further rounds of coding as we moved towards more abstracted theoretical themes. Coded material was organised in a hierarchical manner to provide general, parallel and subcategory codes to allow analysis at different levels of specificity. This allowed a flexible and adaptive approach to research analysis, with some a priori codes drawn from literature review, but with the detail of these and how they inter-related induced from analysis of the data. 120,121 Observational field notes and documentary evidence from the CCG networks helped generate early contextual understanding of empirical sites,122 but the data presented draws solely on interview transcripts. Coding was facilitated through the use of the software program NVivo 11 (QSR International, Warrington, UK), which produced a more rigorous and transparent approach to data analysis. 123
We checked our emerging analysis with the study PPI group, research team and study advisory board, and through iterative feedback with each CCG site, to inductively identify how the four co-ordination capabilities (GP involvement, PPI, social integration and BI functions) were evident in interview transcripts. This was then refined by coding for examples of the three combinative capabilities: barriers of systems capabilities, barriers of socialisation capabilities and co-ordination capabilities as a mediator. An example of the coding structure is presented in Table 3. Following this, we present the findings of each of these co-ordination capabilities in detail.
| CCG characteristic | Systems | Socialisation | Co-ordination |
|---|---|---|---|
| GP involvement | Trying to find out what the CCG wanted of us and whether I thought that was what I could deliver for them . . . To be honest, there was quite a lot of uncertainty about what they wanted me to do here . . . they didn’t seem to know what to do with me at firstCCG L, interview 4 | There is still a problem for them in that there are still people in the system who are old PCT SHA staff so still see themselves as the old PCT SHA sort of ‘You’ll do what I say’ type, but I actually think that’s probably improvingCCG H, interview 4 | If you get buy-in from the GPs it’s a lot easier to get the service running. And they can tell you whether it will work or not, where the problems might be. So that’s always importantCCG I, interview 3 |
| BI | We no longer have that data coming directly to us, therefore we have to access it from the CSU, the Clinical Support Unit, and quite often we have sort of . . . Prior to my coming here there was a list of data which it was agreed we would have access to regularly. My understanding is that we are not always being given access to the data that we require from the CSU and I’m not entirely sure why that is. I’m actually waiting for a phone call. Someone was supposed to phone me yesterday so we’d have the conversation about what’s happening. Our access to data is currently quite limitedCCG M, interview 5 | I think it’s very easy to become just an analyst where you’re just this is the process, there’s the number, churn the numbers out, give them an overarching this is how we’ve got to the numbers, but then to understand the question that they’ve asked in the first place you probably need to be there to react to what they react to when they see that number in front of themCCG M, interview 9 | They started from the fact that they’ve got a single acute provider working across two sites with basically unsustainable services, in their view, into the long term because of insufficient capacity. So they wanted to run a reconfiguration programme to design a new clinical model for that patch and then out of that clinical model to run all the processes necessary to try to identify a preferred option for reshaping their hospital system . . . now we’re helping them design their primary care strategy, their community services strategy and helping them properly work out what the implications are for primary care, community care, social care, mental health services of their intended shift of activity out of the acute sector, which is the bit that everyone struggles to doCCG M, interview 12 |
| Integrated teams | I think we’re quite advanced in recording of information, but generally community services are quite poor at really understanding what their services are and what they cost and how they’re deliveredCCG G, interview 10 | It was complicated before the reforms; now it is just . . . it’s unworkable and we’re seeing this with cancer, we’re seeing it with specialised commissioning, we’re seeing it with general practice. It’s just bonkers the current system. Fragmentation along relatively arbitrary lines denies the complex interrelationships between the components of delivery of good care. The fragmentation between health and social care was bad enough and now we’ve broken health care up you’ve probably got seven different players pulling bits of the service in different directions to meet their own requirements and of course the person who gets left in the gap is the patientCCG J, interview 7 | So the idea of the [integrated team] is to be multiprofessional. So you’ve got clinicians, commissioners, service providers, researchers . . . Not the voluntary sector if I’m honest, although we’ve got good contacts building with the voluntary sector, but we’ve got representation from all those groups, so when the team discuss a problem you’ve got all those voices around the table which I think is what makes it quite uniqueCCG K, interview 5 |
| PPI | Our patients have been telling us, if people had had their ears open, that care was unsatisfactory for a long time, but we’ve chosen or not been able to for various reasons to listen to and respond to thatCCG C, interview 8 | There’s no culture within the health service’s or GPs’ way of looking at the world that has a link with local communities apart from say the GP. They don’t go out. There’s no outreach and that sort of thing. So there’s not a culture first of all, but I think they would like there to be one. You see, I think they would like there to be, but at the moment I can only see it as something that they aren’t giving enough priority toCCG G, interview 2 | That’s where I think our biggest influence can be. We think out of the box. We’re not restrained and tied and if somebody says ‘Oh, you can’t do that.’ ‘Why?’ We won’t accept the restraints. ‘Oh, you can’t do that because of such and such.’ ‘Well let’s change it then.’ And people are saying ‘We haven’t looked at it like that. We haven’t thought about it like that,’ but as lay people we will and I think that is the best thingCCG A, interview 7 |
Limitations
A common criticism of case studies, even when there as many as we sampled, is their uniqueness and their ‘generalisability’. Although we attempted to elicit a representative sample of CCG-led commissioning networks for study, they proved difficult to access and many of the initial agreements for access fell through as key personnel acting as gatekeepers changed, as we were passed on to other staff who were to operationalise the study and as staff in CCGs came under increasing work pressures. Therefore, some readers might judge our sample of case studies as less representative along other dimensions of commissioning networks; for example, given the empirical tracer of elderly care, we might have sampled for population demographics. Nevertheless, we have attempted to generate transferable lessons for other commissioning networks through theoretical analysis, drawing on dimensions of ACAP to highlight factors influencing knowledge mobilisation.
Similarly, as revealed in our table of interviewees, although managerial staff engaged with our research, accessing GPs proved more challenging. Of all commissioning stakeholders, they are subject to the greatest work pressures, particularly when they undertake hybrid roles combining commissioning and clinical responsibilities. We thank those GPs in particular who gave up their valuable time to participate in our study. However, given the variable influence of different groups of GPs revealed within our empirical analysis, we encourage others to engage in more specific study of GP involvement in commissioning to ascertain if this has spread beyond a narrow cadre of GPs who engaged similarly with previous arrangements under PCTs.
At the inception of our study, CCGs were fledgling organisations. As highlighted in empirical analysis, the development of social and organisational relationships across the commissioning network takes time. Our study only partially revealed this given the limited time period over which we undertook data collection. Others may follow our study, perhaps revealing the development of critical review capacity of CCGs as their relationships developed across the commissioning network.
Chapter 4 Constraints of systems and socialisation capabilities
As outlined in our literature review, systems capabilities (e.g. targets and incentives and standardised data collection systems) and socialisation capabilities (e.g. professional and organisational cultures and associated managerial–professional relations) are assumed to stymie the ACAP of organisations. Our analysis clearly confirms this, as set out below. We focus on CCGs A to C as exemplary of the common systems and socialisation capabilities faced by all CCGs.
Systems capabilities
Systems capabilities differed slightly between CCGs in terms of the IT systems used to gather information, but all had access to similar data sets, guided by the same centrally determined governance structures:
We have our own information . . . what patients have gone to hospital, what’s happened to them. Also we have a lot of information for secondary care. We can look at trends, emergency admission trends, elective admission trends. For long-wait domains we actually have an absolutely granular understanding of waiting lists to make sure we’re going to hit key targets.
CCG B, interview 1
The thorough nature of secondary care data sets was frequently acknowledged as enabling them to be particularly strong sources from which to acquire information. However, the ease with which CCGs could assimilate and transform these data into commissioning decisions was not as clear. Many respondents voiced concerns about their ability to use the information to fully guide their decision-making:
There’s an awful lot of data out there, but it never really comes back as intelligence and I see quite a lot of leaps of faith in terms of data to conclusions.
CCG C, interview 4
This problem was also articulated by a manager from another CCG, who noted ‘we are awash with data, but probably not awash with information’ (CCG B, interview 2). One reason for this barrier to assimilating the data was related to the centrally predetermined nature of the information, which was not always meaningful in terms of its representation of the CCGs’ local population needs:
It’s not geared up around us as a CCG. It’s not really meaningful for us in terms of making decisions.
CCG C, interview 3
This was further illuminated by respondents who acknowledged the benefits of using local information to commission in response to patient needs, but also reported barriers to doing so. For example, one GP commissioner was clear on the need for CCGs to commission according to local need:
You can’t use national statistics to drive what we’re doing locally because our patients have different needs and we need to build data up from the ground asking ‘Well, what do we need for our patients? How should that look? How will it serve them best from a clinical perspective?’.
CCG A, interview 7
However, that same GP commissioner subsequently described the problems in accessing that information:
So one of the barriers we’ve met right now is we’re trying to get the data for local patients and it seems to be a nightmare trying to get the data. All sorts of people hold this data and say ‘Oh well, for governance issues you can’t have this and you can have this. You can have the regional data, but not the local data’.
CCG A, interview 8
In addition to the concerns about the local responsiveness of data, there was a sense of distinct lack of information from community or tertiary services. This was a particular problem for commissioners attempting to reduce potentially avoidable elderly care admissions into hospital by ensuring comprehensive community care. Although secondary care providers could generate information about admissions, interventions and discharges, community services could only provide vague metrics that were not always seen as helpful for the commissioning process:
But for us as commissioners even if we have the data, we need to know is that a good thing or a bad thing? Well I’ve no idea. It doesn’t mean anything. We have information about different services provided . . . but the information is fundamentally a garbage metric whichever way you look at it.
CCG B, interview 1
Subsequently, the systems capabilities of CCGs were undermined by their reliance on data sets that did not provide comprehensive information about their service provision. This was also compounded by continuing central control, which could undermine the ability to commission according to local needs, as CCGs also needed to conform to centrally set priorities:
The National Commissioning Board have started saying ‘These are your targets. You’ve got to do this. This is how you will do it’, and they’re starting to be very prescriptive.
CCG C, interview 7
However, despite the problems undermining the systems capabilities of CCGs, it was evident that there were also mechanisms in place to mediate these problems and enhance their capabilities. Most notable was the integration of clinical knowledge, through GP involvement, into the system:
They’re watching us really closely, but it does also still feel like we are in control . . . we listen to them, of course we do . . . but we’ve still got to use our patient data and everything that we know about them to drive intervention.
CCG A, interview 5
This was also acknowledged by a member of the management structure, who reported that the gaps in information with regard to service provision were less important when commissioning decisions were guided by the tacit knowledge of clinicians. This increased their systems capabilities and, subsequently. their commissioning capacity:
If I’m being honest, there’s probably some retro fitting of that information to the things that the GPs want to do. So kind of regardless of all of that analysis, from the experience of the GPs in their consulting room the key issue is with the elderly and we need to be more integrated.
CCG C, interview 1
Therefore, the involvement of clinicians within the data acquisition process could mediate the problems encountered as a result of their limited systems capabilities. However, unleashing the potential of that information also relied on CCG socialisation capabilities.
Socialisation capabilities
Socialisation capabilities mediate the extent to which CCGs are receptive to new forms of knowledge or information. The importance of developing a shared identity and common vision was repeatedly noted by respondents:
You’ve got to get people to own the problem and feel like it’s theirs . . . It’s one of those things where you need to take the time to build the relationships because you’ll get the payback if you do.
CCG C, interview 6
However, this is problematic as CCGs are highly professionalised contexts with two distinct cadres: managerial staff and professional staff (GPs). Although they are often referred to as new organisational forms, they are based on pre-existing organisations that have historical footprints. Indeed, the way many CCGs were set up created the potential for repetition of institutionalised behaviour, as managers were recruited straight from pre-existing structures:
We had a chief exec[utive] at the time and his view was that he didn’t like uncertainty, so when the policy about CCG creation came out he wanted to very quickly move towards new CCG structures. So basically he approached the old practitioner-based commissioning clusters which were there before and they were largely on the old footprint of the previous PCTs . . . and said ‘Right OK, you need to find yourself a chief officer and then that person needs to get some structures in and then we’ll transfer people from the PCT into these structures. Get on and do it’.
CCG B, interview 2
The direct transfer of management staff between old and new structures was seen to exacerbate institutionalised behaviours, with some GPs reporting that, on occasion, managerial behaviours had been reminiscent of previous organisational structures:
Initially I think some of the key managers didn’t really get what we were trying to do . . . For example, one of the CCG managers came up with an idea and just e-mailed all the GPs saying ‘This is what we’re going to do’, and we said ‘Hold on a minute! Where’s the discussion about this? You’ve not even asked what we think.’. So it then actually went back a good three or four steps to engage with GPs, engage with nurses, engage with the stakeholder reference group, then bring it to the governing body to have a further discussion before we went ‘Yes, this is now going to happen.’. Because in the old days that’s all we used to get – the PCT e-mailed round going ‘You’re going to do this’.
CCG A, interview 6
The institutionalised behaviours linked to the previous organisational forms were seen to undermine CCG capabilities, as the GPs sometimes reported a sense that managerial staff had different priorities to them, generating an organisational divide:
I think a lot of clinicians are a bit dismissive of managers . . . the perception is that nurses and doctors in hospitals are the heroes and managers are sort of boo, hiss, pantomime villains and that we shouldn’t have any managers . . . the sense of putting patients first is very important. We don’t tend to lose ourselves in sort of targets and things as I think some managers do.
CCG C, interview 7
This exacerbated tensions between managers and GPs, and was reported by managerial staff as well as by clinicians:
There’s tensions that are starting to come out between the managers and the clinicians . . . I think they do think as managers we sit there twiddling our thumbs quite a lot of the time and there is a tendency to sometimes feel like they’re trying to run it like a practice, and I don’t think they really know what clinical leadership means . . . doctors’ egos still get in the way to be perfectly honest . . . There’s no sense of ‘we’re a team’.
CCG C, interview 2
The interaction between managers and GPs, and the perceived obstructiveness of both groups, had a negative impact on the cohesiveness of the CCG. Generating a sense of being a ‘team’ was acknowledged as something that was going to take some time, particularly in CCG C, which had encountered some divisions between its managerial and GP staff (as outlined above):
It’s a lot of hard work to build a Board, to build the cohesion, the understanding between people, the mutual support and the mutual challenge within that so you build a team and building a team is not something you do overnight and we’re only just embarking on that process.
CCG C, interview 9
However, CCG B seemed to have overcome the majority of tensions between the different groups by investing time in CCG team development and setting a joint direction:
We’ve got a really good governing body. We’ve really gelled together as a team. That’s really important. We get on well, but we also get the job done . . . There’s clearly a culture here. There’s very much a ‘yes we can do, we do want to change, we want to be different’ culture from the top down and I think that’s clearly what makes a difference if you’ve got an inclusive management style.
CCG B, interview 8
Despite this, influences on socialisation capabilities were not limited to the immediate CCG context, but extended to the wider network. Our informants perceived that secondary care providers may not be working towards the same vision. This may have been the case with other network partners as well, but the large size and influence of secondary care meant that discussions about these relationships often came to the fore during interviews:
The acute services have this huge gravity which pulls in commissioning thinking . . . The Trust has a contract of more than £600M so that’s six times [our] entire commissioning budget, so it’s a vast organisation and a very powerful, huge power in the marketplace.
CCG A, interview 3
This power differential was problematic, as there were few ways for small CCGs to negotiate with the larger organisations, meaning that they could sometimes be at a disadvantage:
Sometimes you feel that actually it’s the tail wagging the dog really rather than us as commissioners going out to providers and saying ‘We want you to provide this service’.
CCG C, interview 1
The awareness of this power differential was enhanced by uncertainty around the motives of secondary care providers, and their desire to truly work in partnership with the CCGs:
Don’t go in a hospital. That doesn’t sit with the financial structure of [the secondary care hospital] and you’ve got that contention. So if I was on that side of the fence I’d be doing everything I could to keep patients in longer, get more money . . . there is this tension between primary care and secondary care . . . there’s a lot of doubt and a lot of speculation that secondary care is manipulating to their advantage.
CCG A, interview 9
Socialisation capabilities across different organisational sectors were often undermined as a result of a sense that there may be different priorities or ways of working, which could be detrimental:
Everybody talks the same language, but do they see the outcomes of dealing with those issues the same way? My personal view is I don’t think they do. I think that whilst everybody would agree that keeping somebody supported in their home for longer is a self-evident benefit for a patient, a service user, how that translates into money moving round the system is a different and knottier issue that people don’t want to face up to.
CCG B, interview 2
However, as mentioned previously, individuals from a common professional background may often share common ideals as an aspect of their professional identity. Within our CCGs, despite the managerial concern that secondary care providers and CCGs may have different priorities in terms of funding outcomes, GPs in CCGs and clinicians in other organisations may work effectively together because of their professional background. This was acknowledged by a public health doctor discussing his relationship with medical colleagues in other organisations:
We do have the same broad shared values because we’ve been through the same training, we’ve been through the same processes, we understand where each other are coming from. Even if we’re not totally lined up I think that we are much more comfortable with each other than is always the case with managerial colleagues.
CCG C, interview 10
Once again, despite the issues that may undermine the socialisation capabilities of CCGs and their wider networks, the engagement of clinicians in the CCG may mediate these problems. Being able to harness this potential contribution is, in turn, related to the development of CCG co-ordination capabilities, as we discuss in the next sections below.
Chapter 5 General practitioner involvement
As noted in the literature review, CCGs were set up with an increased focus on the involvement of GPs in commissioning decisions. GP involvement was noted across all 13 cases in varying degrees and in multiple roles. We consider GP involvement as a co-ordination capability, and organise the responses of GPs into three groups: formal commissioning roles, informal commissioning interactions and non-commissioning GPs. The third group, those based entirely in practice without involvement or influence among the commissioning organisation or their professional group, are not considered in detail in this chapter, but their interview responses are still presented. This group represents the ‘rank and file’ professionals, who the GPs involved in commissioning attempt to influence in their roles.
Formal commissioning roles
General practitioners who were engaged in formal roles within the commissioning organisation suggested that their practice-based knowledge about the patient population enabled them to improve commissioning processes. By framing themselves as representing the needs of patients, or the voice of other clinicians, they highlighted their influence over management decisions through the provision of clinical leadership:
I give clinical leadership to try and make sure the decisions we make are made clinically, not just in terms of finances or things, but actually putting patients at the centre of what we are trying to achieve for them.
CCG D, interview 5
Describing themselves as clinical leaders, the GPs drew on their professional standing to influence commissioning decisions. In particular, their expert claims enabled them to elevate themselves over general managers, who were unable to draw on similar practice-based knowledge to enhance their influence:
The commissioners are not clinical and they may think something’s a good idea, but actually in practice having that clinical background just helps you know that it would be useful or it wouldn’t be useful. So that’s a more important insight.
CCG K, interview 14
It was acknowledged by general managers that GP involvement was an important element within the commissioning organisation. The general managers indicated that the expert knowledge held by GPs about their patient population was one of the main influences on strategic decision-making for clinical services.
In particular, formalised GP involvement acted as a co-ordination capability as GPs drew on tacit, or professional, knowledge and experience to enhance critical review capacity. As outlined previously, standardised data sets or systems of reporting may not represent a full picture from which to make commissioning decisions. By acquiring tacit knowledge from GPs, assimilation processes were enhanced as standardised data could be contextualised with professional understanding, overcoming limitations of systems capabilities:
What we’re currently finding is that CCGs often tend to pick on one particular piece of evidence, primarily data, that seems to drive decisions more than anything else . . . the commissioners are pretty good at using data and they love numbers and they love looking at activity and costs, but where the gaps are more around the research evidence, so what we’re saying to commissioners is ‘It’s all very well looking at the data, that’s fine, but we need you to have a much richer, rounder picture of what’s out there to inform your decisions’ . . . that’s where the GPs come in.
CCG L, interview 15
For example, the involvement of GPs as a co-ordination capability was particularly highlighted in examples in which standardised acquisition systems, such as risk profiling tools for patients at risk of admission, were not perceived as comprehensive. Involving GPs in further identification of ‘at risk’ patients subsequently enhanced the scope of knowledge available to guide decisions:
My experience is that the people that it [existing standardised systems] throw up are not all of the people that we need to discuss. So the GPs will bring up other people that haven’t been thrown up by the risk profiling system which they know are ongoing cases that we’re all involved with and we know are possibly at more risk of going into hospital than others. They don’t come up in the system but the GP knows about them.
CCG G, interview 3
Further to their potential as a co-ordination capability to mediate systems limitations, GPs in formal commissioning roles also acted as a conduit between non-commissioning GPs and the commissioning organisation. This conduit role facilitated the flow of information both to and from rank and file GPs. Suggesting that they were able to influence their peers, commissioning GPs took ownership of the profession, referring to ‘my GPs’ and setting themselves apart as leaders of the group:
I’ll e-mail my GP constituents about what’s coming up on the agenda, particularly the things I think they’ll want to make their views known on . . . I’ll say ‘Well actually, I’ve spoken to or communicated with my GPs and what they would like to make known is that they don’t think it’ll work for this reason’, or ‘They think more funding should be given to that’.
CCG B, interview 3
Commissioning GPs consequently worked to mediate barriers of socialisation capabilities, working to communicate clinician opinion to the commissioners, but also attempting to facilitate the uptake of commissioning decisions in practice, to reduce the potential of professional resistance. Through their conduit role, they used their professional background to influence other GPs to align with commissioning priorities:
I try and explain to them about the cost involved and the reasons we should change, and GPs want to be in line with their peers so they usually make the change if you explain it peer to peer.
CCG F, interview 7
Furthermore, in addition to enhancing critical review processes by engaging their clinical peers in the design and delivery of services, GP commissioners were able to overcome the barriers of socialisation capabilities evident in interactions with other stakeholders such as secondary care. Negotiations with secondary care partners were noted by general managers as potentially inhibitory during the negotiations of services:
For me to go in as a manager and try and argue a case with a dozen clinical directors, with the best motivation all I can do is argue the numbers, the philosophy, present a management argument to why we should do this or we should do that . . . they don’t see that as credible.
CCG B, interview 3
In these circumstances, the influence of power differentials between professional groups, representing socialisation capabilities, could be inhibitory. CCGs are commonly small organisations that are seen as less influential than hospitals, the latter being dominated by powerful groups of doctors who have been accustomed to patterns of resource allocation around which they resist any change, whatever the ‘evidence’ might suggest. However, those interviewed once again noted that the involvement of GPs had the potential to mediate limitations of socialisation capabilities. The involvement of GPs acted as a co-ordination capability by encouraging integrated working with clinicians in secondary care organisations and involving them in service design discussions:
When we involved GPs, we saw negotiation moved away quite dramatically from the old-style negotiation which was all about finance and activity to a discussion that focused on quality outcomes and patient pathways . . . the GPs were able to bring a level of reasonableness into that room with their medical colleagues that had previously not been there, with hospital doctors viewing us managers with some suspicion. GPs brought in the perspective of a practitioner dealing with patients on a day-to-day basis, which hospital doctors accepted and which really altered the dynamic in the room.
CCG B, interview 10
However, although GPs in formal commissioning roles suggested that they were able to influence both commissioners and professional colleagues because of their professional background, there were indications that co-option into a formal managerial role had the potential to undermine influence with their rank and file peers. Reducing clinical time to accommodate the demands of their commissioning role led to concerns about their credibility with peers:
Once you become a full-time commissioner, or say just do 1 day a week, you start to lose a bit of your clinical credibility . . . People say ‘Well he only does a day a week, what does he know?’.
CCG A, interview 4
Reflecting concerns that colleagues may perceive them as ‘bloody managers’ (CCG B, interview 1), comments from non-commissioning GPs suggested that the close association with general management of formal commissioning GPs undermined their influence within the profession, subsequently reducing their potential to encourage uptake of commissioning decisions:
Some of them don’t really know what it’s like working day in day out. They go and sit at a desk all day and say they’re representing me, but I’m the one seeing patients all day . . . I don’t care that the CCG has decided this or decided that, it makes little difference to me.
CCG I, interview 9
The extent to which GPs in commissioning roles had continuing influence among their non-commissioning colleagues was thus questionable. Although they could act as a co-ordination capability to some extent, presenting themselves as professional leaders who represent the voice of the patients and of other clinicians, responses from non-commissioning GPs suggested that they were not fully able to overcome socialisation barriers. Commissioning GPs suggested that their influence lay in their ability to act in a formal two-way conduit role, to communicate both to and from the commissioning organisation, influencing both managers and practitioners. However, although their claims of influencing strategy within the commissioning organisation were reflected by comments from general managers, their association with managerial structures and priorities had the potential to undermine their claims as professional leaders, reducing influence among non-commissioning peers.
Practice-based general practitioners in informal roles
In addition to GPs taking on a formal role within commissioning organisations, we identified a group that was actively engaged with commissioning organisations, but did not occupy a formal commissioning role. These GPs worked full time in practice, but frequently communicated information to the commissioning organisation through informal structures:
When I want to voice my opinion about something I usually go round [the formal GP commissioner] and just ring someone higher up, the chief operating officer or the head of urgent care commissioning or whoever it may be. They know me, I’m fairly well-known in the area, and I tell them what I think the issues are and what they should be doing.
CCG F, interview 14
In other words, there was another group of GPs attempting to establish themselves as professional leaders. They presented the front-line, real-time experience of the patient population to managers in the commissioning organisation, in order to influence commissioning decisions:
Rather than the very high level it’s actually ‘What does this actually mean in practice?’ and sort of brings a flavour of the situations that I encounter on a daily basis . . . that voice saying ‘Actually is that really going to work? Is that really how it happens in GP practice?’.
CCG D, interview 3
General practitioners who were engaging informally with the CCG attempted to position themselves as professional leaders, suggesting that they had more influence within the profession than formal commissioning GPs, as those working in formalised roles no longer represented the reality of rank and file professionals:
All the clinical commissioning leads are really well embedded into their roles and sometimes you need somebody to be a critical friend saying ‘Actually is that really what happens?’ . . . You just need to be that person to say ‘But is that really the right thing to be doing?’.
CCG D, interview 10
As such, informal GPs were better placed to overcome the challenges of socialisation capabilities faced by formal commissioning GPs, as outlined above. However, although those informally engaged aggrandised their position by highlighting their distance from the formal organisational management, their influence over managerial decision-making was subsequently reduced. As they did not occupy formal positions, they were unable to attend meetings in which strategic decisions were made, and their contribution was limited to the informal communications with commissioners outlined previously. Conversely, formal commissioning GPs were able to attend formal meetings as part of their role. Consequently, GPs who were engaged informally in commissioning reported less influence over managerial strategies than they might have liked:
I wouldn’t say I feel hugely influential . . . I speak to the commissioners fairly regularly, they ask my opinion and I don’t hesitate to ring them if I think they need to be approaching things differently. But I think the difficult part is not being able to attend meetings . . . I can’t be that person sitting there going ‘What about this?’ when decisions are made.
CCG G, interview 6
Although these GPs were able to communicate their ideas to the commissioning organisation, and were actively engaged in doing so, their influence over managerial decision-making was undermined by their lack of a formal role. However, despite their lack of influence within the commissioning organisation, informally engaged GPs suggested that they enjoyed having more influence among their professional peers. To this end, they positioned themselves as professional leaders among rank and file GPs, communicating the opinions of the professional community to commissioners. Further to this, as a result of their high levels of credibility because of their full-time practice-based roles, they were able to encourage and influence their peers to engage with commissioning decisions:
I think the fact that I’m a full-time clinician helps from a couple of aspects. I think it helps practices understand that there is value to these decisions, but also that clinicians just approach things in a slightly different way. I have more sway than the commissioners, my colleagues listen to me.
CCG A, interview 16
Their full-time position in practice, combined with their informal relationship with the commissioning organisation, afforded them more influence with their peers than formal commissioning GPs:
At the end of the day I’m going to be the one actually using these services every day, or being asked to do whatever they’ve decided. So I have influence in practice which is relevant, and I communicate back to the commissioners about how those things are working, or how they are viewed by other GPs.
CCG C, interview 2
Indeed, during interviews, in contrast to the self-aggrandising narrative of the formal commissioning GPs to communicate their professional influence, it was their rank and file peers who identified the practice-based GPs as leaders of the profession:
One of the partners here is very engaged with the CCG, he doesn’t work there but he’s always e-mailing them, phoning them, pinning them down about things . . . I trust him more to tell them how it is, not to worry about whether it fits with their priorities. I’m sure the others [formal hybrids] do that as well at the beginning, but they must naturally get sucked into the CCG mindset.
CCG H, interview 8
The comments from rank and file GPs suggest that, rather than identifying themselves as professional leaders, those who engaged informally with the CCG were seen by their colleagues as professional leaders, and were more successful in overcoming limitations of socialisation capabilities. Although their lack of formal managerial involvement detracted from their ability to directly influence commissioning decisions, it facilitated their influence within their professional group.
Complementing roles to protect professional influence
In the sections above, we outlined variations in influence in a non-homogeneous professional group. Differentiating between formal and informal commissioning roles, the findings indicated that neither group had influence across both managerial and professional groups. GPs in formal roles acted primarily to overcome systems limitations, drawing on tacit knowledge to enhance commissioning decisions. However, their co-option into managerial roles undermined their influence among non-hybrid peers. For GPs engaging in informal roles, a lack of co-option restricted their ability to influence decision-making processes in the commissioning organisation. However, they were more able to act in a co-ordination capability to overcome socialisation capabilities by influencing their non-commissioning peers.
Exploring how hybrids mediated the limitations of their influence in different spheres, both formal and informal GPs indicated that they worked together to ensure that there was continued professional influence over managerial decisions. For example, an informal commissioning GP noted how a balance between formal and informal roles maintained a focus on the needs of patients:
There are a few clinicians who have devoted much more to this, but then they’re not doing very much clinical practice at all . . . but I think hopefully in our area we’ve actually quite a good balance between those who are dedicated to it full time and those who come in on a more limited, informal basis like myself. And we work together for the good of the patients.
CCG H, interview 8
Both groups of GPs discussed episodes during which they worked together to enhance or protect the status and influence of the profession as a collective. During interviews, both groups noted examples of when they had worked together, drawing on either the managerial influence of formal GPs or the professional influence of those in informal roles. For example, one formal commissioning GP highlighted how they were able to use their understanding of managerial structures within the organisation to maximise the influence of the profession as a collective:
I know how the system works. I think I’ve used that to my benefit, to the benefit of colleagues and their patients by knowing who to go to when something doesn’t work . . . And so now the GPs might phone me and I know that if I make a couple of phone calls I can escalate that to the right contracts manager who can then put pressure on the provider to make those services easier [to access]. So there are lots of things like that where me having the commissioning knowledge and my colleagues in practice can come together to do good things.
CCG A, interview 4
Similarly, GPs engaging informally noted how they were able to act as mid-level brokers or mediators between the commissioners and their rank and file peers. In particular, one informal GP who enjoyed high levels of influence within their professional community, and who regularly engaged with the commissioning organisation, was able to communicate information and feedback across professional and managerial boundaries during a service dispute between GPs and the managerial staff at the organisation:
I knew the [commissioner] to talk to, so I had a word with them and made it clear what the GPs were concerned about, what they could do, and then I fed that back to my colleagues . . . at the moment I feel I’ve done my initial bit which is be the middle man and mediator with it . . . I’m not tied into the CCG, so I feel a bit more of a free agent to move between the two groups. I actively stay out of the formal commissioning part, and that means I’m not seen as such by my colleagues.
CCG D, interview 10
The GP in this case highlighted how they actively chose to remain in full-time practice, rather than taking on a formal hybrid role. In doing so, they were able to achieve influence by selectively engaging with managerial structures and commissioners without being co-opted.
Although the two groups of GPs used their professional or managerial influence in different ways, they were aware of the need to remain as two distinct groups, rather than diluting the formal or informal nature of their role to make the group more homogeneous. Both formal and informal roles were seen as fundamental to the ability of the profession as a collective to influence service change:
I take the view that my [GP] colleagues want to be left alone to get on and do their day job . . . I don’t expect all of them to be involved in service redesign because not everyone wants to do that . . . So I don’t expect them to be experts on that and how could they be? That’s a job that I take on to do for the CCG. And I’ll work closely with my peers who are influential in practice and that’s how we can achieve change.
CCG G, interview 10
At the same time, all of those who were interviewed suggested that their professional collegiality, and commitment to buffering professionalism from managerial influence, encouraged both groups of GPs to work together to retain professional control:
I feel that now, if we work together, we do have a genuine chance to possibly change the way the system works.
CCG A, interview 4
By working together in formal and informal roles, GPs could use their influence to achieve change within the commissioning organisation. For example, one informally engaged GP discussed a new service that had been designed and set up in collaboration with commissioning peers, and the resulting positive feedback from rank and file GPs:
Initially there was a lot of scepticism . . . But I worked very closely with [formal GP commissioner] and they pulled strings in the CCG . . . and I worked very closely with my colleagues in practice, so now I’ve had a lot of my colleagues say ‘well, it actually sounds like you’re doing something rather than just sitting round a table and talking endlessly about things and not actually making any changes.’ So we’re now actually in the roll-out of that project and both the commissioners and the GPs are on board with it.
CCG K, interview 5
Ultimately, through collaboration, the two groups co-opted managerial processes, drawing on peer influence to encourage commissioning decisions that were aligned with the values of the collective profession, rather than driven by managerial demands. Although formal GPs actively took on commissioning roles, they combined their managerial knowledge of the commissioning organisation with the practical experience and influence of those in informal roles to enhance professional practices and protect professional jurisdiction. In doing so, they buffered the professional group from control by general commissioning managers.
In conclusion, by working together, GPs in both formal and informal roles were able to co-optate managerial processes and maintain a form of professional resistance to managerial infringement.
Conclusions
General practitioner involvement acted as a co-ordination capability in two ways. First, by drawing on tacit or professional knowledge, GPs could enhance critical review capacity by overcoming systems limitations. Second, they engaged in clinical leadership to mediate socialisation limitations by using their professional background to influence peers in both primary and secondary care. This enhanced service design and delivery, and reduced the potential for professional resistance. There were variations in the way GPs engaged with the CCG, as some took on formal roles and others engaged more informally. Although formal GP commissioners had more influence over commissioning decisions, they may have limited capacity to overcome socialisation capabilities, because of their proximity to formal managerial roles. Those in informal roles had more influence over their peers, but faced inherent challenges as a result of the time limitations of their involvement and maintaining a clinical practice. However, we also noted how these two groups worked together to protect professional jurisdiction and ensure continued influence over commissioning decisions. We highlight the importance of this non-homogeneous professional group, and do not suggest that all GPs need to become formally engaged in CCGs, as their clinical practice is an important element of their professional influence. Commissioning organisations should be aware of the need to balance formal and informal engagement with GPs to maximise their potential as a co-ordination capability.
Chapter 6 Patient and public involvement
Patient and public involvement is a legal requirement of UK commissioning groups. However, the extent to which PPI is used within the commissioning process is variable. All cases in our study noted that they acquired external information through standardised PPI mechanisms. However, the way in which PPI was subsequently used to enhance critical review capacity varied between CCGs. As noted previously in Patient and public involvement during the study, only three of our CCG cases asked us to focus specifically on the way in which they engaged with PPI during commissioning. These three cases illuminated different approaches to PPI, which were reflected across all 13 cases. We present the findings from the three cases to further illustrate the potential for PPI, and highlight how it is limited in CCGs.
Clinical Commissioning Group D: rational ideologies of managerial control
The following extract is from field notes taken at the second PPI group meeting attended by the research team:
The group was asked by the lay chair to identify what they feel their contribution to the CCG should represent. There was a lot of confusion amongst members about their potential contribution . . . The chair had difficulty keeping the group on point . . . Two general managers attended the meeting, and they were responsible for setting the agenda. By the end of the meeting the managers had taken over the running of the session to ensure all the agenda items were discussed in a more structured manner.
Field notes, 11 February 2014
This observation of the PPI group at this site highlights two influences on PPI: (1) confusion among public representatives about their role and potential contribution to the organisation and (2) the dominance of managerial control over the group. The management team took over the running of the PPI meeting as the group was not seen to be conforming to the agenda predetermined by the managers. When interviewed about the PPI group, a general manager said:
It is hard work . . . We’ve spent countless hours doing terms of reference, loads of time explaining what their role is . . . they don’t necessarily understand how the NHS works so that’s part of the problem . . . people’s understanding of the health system is actually really quite minimal and they don’t understand all the interorganisational arrangements.
General manager, interview 5
The perception on behalf of the management team, reflected above, seemed to be that the PPI group was not informed enough about the NHS to contribute meaningfully about decisions made by the commissioning organisation. Indeed, the manager notes how they spent time ‘explaining what their role is’ to the group, limiting PPI contribution to a managerially determined role, rather than encouraging the group to determine a role for themselves. This represents a limitation of socialisation capabilities. In addition, the perception that they had ‘minimal’ understanding of the issues in the health service often led to derisive comments from managers during discussions about PPI:
They’ll randomly e-mail me going ‘oh [manager’s name], have you seen this thing about telehealth?’ and I’m like ‘oh god.’ . . . they don’t understand the priorities or the organisation, so it’s really difficult to manage them.
General manager, interview 7
Again, the suggestion above is that the PPI group needs to be managed. Managers, therefore, did not accommodate PPI contributions outside those considered to be in line with managerially defined organisational priorities. The influence of the hierarchical organisational context in encouraging rational ideologies of control was illuminated by many of the managers interviewed, who suggested that they often limited PPI to smaller, peripheral discussions, rather than involvement in strategic decision-making. Consequently, there was relative diminishing potential for the PPI group to influence decision-making processes and act as a co-ordination capability to enhance critical review capacity. This sentiment was also voiced by doctors involved in the commissioning organisation, suggesting that the hierarchical organisational context encouraged rational ideologies of control across professional groups as well as managers:
I think them feeling involved is probably the best that we can do. They don’t necessarily have all the information or the knowledge and experience to make the decisions that we would make as health professionals and they do make some really valid points but it’s really peripheral stuff to be honest.
General practitioner, interview 9
Consequently, PPI involvement in decision-making processes was marginalised, and the management team characterised PPI in a way that suggested that they did not see much strategic value in any PPI contribution:
They want better plates or something ridiculous . . . But then again, you see, if you’re a member of the public and you know nothing, like a lot of them don’t really about how the NHS works, then why shouldn’t they bring these things up? It’s not really that helpful for us though, it doesn’t change the way we work.
General manager, interview 3
As noted by the manager interviewed above, PPI contributions were not considered to be changing organisational processes. During interviews, none of the managers or PPI representatives could give examples of the way in which ideas from the PPI groups influenced development of services, demonstrating that, in this case, PPI was not working as a co-ordination capability. In addition, there was little capacity for new ideas to be generated from the PPI groups, as the management team set the agenda, constraining PPI contributions to managerially determined issues. As such, the potential for new, or different, ideas to emerge from the PPI group was limited:
There aren’t many things that come up that don’t really fit with the main themes because we set the agenda to make sure that what they’re discussing fits with the main themes.
General manager, interview 3
On the one hand, organisational managers were aware of the need to engage in PPI in line with national policy. However, their interpretation of policy led them to engage in rational ideologies of control, which constrained the PPI group, allowing them to contribute only through formally determined, and managerially led, discussions. For many PPI representatives, the lack of flexibility for their involvement led to feelings of frustration and questions about their potential for strategic influence:
It’s difficult to see how you make a difference really. I think a lot of the time the managers just sit there and nod their heads, they don’t hear us. And we’re not supposed to talk about a lot of things, just stick to the agenda or you get into trouble!
PPI representative, interview 10
However, the chairperson of the group, who also represented the PPI group as a lay representative of the commissioning board, described how he felt that he was involved in strategic-level discussions. An experienced manager in the private sector, he had been appointed as chairperson of the group by commissioning managers, who identified him as ‘our champion for public and patient involvement’ (general manager: interview 1). As such, the chairperson felt that he could use his professional background, and the influence afforded to him by his managerially appointed position, to contribute to managerial decisions:
I have some skills from a professional management point of view . . . So as a non-exec[utive] sitting on the board I’m able to say ‘Well, why do you do it that way? Have you thought of . . . ?’ So I’m able to put constructive challenge into the system.
Lay member, interview 2
Therefore, by drawing on previous experience of management within different organisational contexts, the PPI representative achieved more strategic influence by working within a managerially framed role. However, he was also aware that, to retain this influence and his position given to him by managers, he had to behave in a way that aligned with managerial interests or accepted behaviours, influencing the way he communicated information from other PPI representatives to commissioning managers. In this way, he could be seen to replicate forms of rational control over his PPI group members, replicating the barriers of socialisation capabilities:
If I go to that board with a proposal which is unrealistic, then I’ve failed . . . I have to go back to the [PPI group] and say is ‘It’s all very well coming up with these ideas. How do we fund it?’ They have a responsibility as well. They can’t just say ‘We want a cancer consultant on our doorstep every day of the week’ like sometimes they do . . . So if I take it into the board I have to make sure it is credible. If it’s not, then I’m going to get thrown out and rightly so. I’ll have a fight and I won’t be taken seriously.
Lay member, interview 2
CCG D represents an organisational context in which the potential of PPI to act as a co-ordination capability is undermined by socialisation capabilities. Specifically, rational ideologies of managerial control undermined opportunities for PPI. An organisational context, which did not prioritise the potential for PPI outside formal structures, meant that managers set the agenda to limit PPI contributions to peripheral issues, rather than allowing strategic decision-making processes. Consequently, there were no examples of the PPI group influencing the commissioning organisation at a strategic level. Although the managerially appointed chairperson of the group felt that he had influence, this was related to his ability to work in a way that was consistent with managerial expectations, as a result of his professional background and previous experience, and having a position bestowed on him by the commissioning managers. The need to act in a way that was aligned with managerial interest, through channels determined by rational ideologies of control, subsequently influenced the type of information the lay member communicated between the PPI group and the management team, as the chairperson himself replicated forms of managerial dominance and reinforced socialisation barriers.
Clinical Commissioning Group G: increasing recognition of the potential of public involvement
In CCG G, characterising their attitude towards PPI as a ‘supportive culture’, managers were keen to communicate the importance of PPI within the organisation, highlighting that their organisational context encouraged and recognised potential benefits of PPI in service design and delivery:
If we actually end up designing services or commissioning services that have got strong, local backing it’s going to make it 10 times easier to actually put those services in place because you can say ‘well actually, we’ve got the backing of the general public here and this has all been informed.’. Yes, we’ve been influenced by our clinicians and the GPs, but particularly the public.
General manager, interview 7
However, although all managers claimed that they valued PPI, some voiced concerns over the level of understanding of PPI representatives about the commissioning organisation, and the context of the wider health system. Similar to CCG D, some managers acknowledged that a lack of awareness of the wider organisational landscape could limit PPI:
What’s practically quite hard is having to go over things that we’ve already talked about, and so something maybe you talked about 3 weeks ago you then spend half the meeting going through it again. It’s quite time-consuming and can be quite frustrating.
General manager, interview 13
Despite what was characterised as a more supportive managerial culture, managers once again resorted to rational ideologies of control, and limited PPI to topics or contributions determined by the management team. However, the chief executive of this organisation suggested that a need for control was not because of a reluctance to involve the public in strategic decisions, but was about identifying the most relevant opportunities for involvement, arguably enhancing their contribution towards decision-making:
There is always a line to be drawn between what is operational detail that we sort out every day, kind of day-to-day stuff, and what is really important, relevant stuff that the public ought to know about . . . So sometimes it’s not conducive to ask them about it.
Chief executive, interview 11
Although managers acknowledged that their dominance could limit the potential of PPI as a co-ordination capability, trying to focus the contribution by involving PPI representatives in ‘relevant’ discussions, they suggested their organisational culture was one that valued PPI. Diverging from the findings in CCG D, in which organisational approaches to control trivialised PPI and led to concerns from PPI representatives that they had no real involvement, PPI representatives in CCG G seemed more satisfied with their contribution. In particular, they suggested that they were able to challenge managerial decisions and overcome limitations of systems capabilities by raising issues outside the managerially determined agenda:
I think they’ve realised that we are a real asset so, you know, I think we’ve got a good working relationship . . . they’re very welcoming and, you know, we can be very challenging and raise some really difficult questions, but then they do try and seek the answers. We can ask about anything really.
PPI representative, interview 4
However, despite positive attitudes towards PPI in CCG G, which might have engendered more normative forms of control, the way in which PPI influenced structure and recruitment to the PPI group was tightly controlled by commissioning managers and, as such, represents a further limitation of socialisation capabilities. PPI representatives were not able to offer contributions to the commissioners outside the boundaries of managerially controlled mechanisms for involvement:
I was appointed by the commissioners to the committee . . . So the public interact with [PPI] committee; the [PPI] committee collates the information and then we transmit this in one way or another to the clinical commissioning group.
PPI representative, interview 2
This was particularly frustrating for one PPI representative, who acknowledged that the organisational context was supportive of PPI when occurring within controlled strictures, but questioned the extent to which he could contribute to wider issues:
They didn’t discourage me from doing research, but they couldn’t say if a layman like myself could carry out something . . . so now as an active member, quite active and outspoken, I’m still feeling somewhat tagged on . . . Are we really important or is it all window dressing? I’m allowed to have an opinion but only on topics they allow me to. So I just wonder what my contribution is.
PPI representative, interview 1
Therefore, although more anecdotally committed to PPI than CCG D, PPI was still influenced by socialisation capabilities, limiting involvement to a small number of preselected topics. Although some PPI representatives were satisfied with their involvement, perceiving the organisational context as one that supported and valued PPI, others felt limited in their contribution. For this reason, although the managers in this organisation attempted to enhance PPI, facilitating involvement where it could have the most impact, inhibitory socialisation capabilities in the form of managerial dominance had the potential to exclude PPI representatives from involvement in more strategic issues. This led to some members feeling ‘tagged on’ and not integral to the commissioning process, and undermined their potential as a co-ordination capability.
Clinical Commissioning Group C: the potential of normative control
Clinical Commissioning Group C is notable because of the different approach to the implementation of PPI policy taken by the management team. At this site, the managerial culture encouraged a more normative approach to the organisation and control of the PPI group. Managers were significantly less controlling in a formal sense and described themselves as holding a greater commitment towards the diverse viewpoints that PPI potentially brought into decision-making. They thus claimed a ‘hands-off’ approach to PPI.
The management team was not actively involved in the development of agenda or running of meetings, and the PPI group had a small budget provided by the commissioning organisation, which they could use for their own purposes (such as room bookings, transport and small research projects). In addition, the PPI group members elected a chairperson and determined the group recruitment strategy independently of managerial control:
We decided to try and have a representative body and my original thought was that we’d have a group with one representative from each of the patient participation groups and any special interest groups would bring in a representative . . . The other thing we did, we decided that if people showed a strong enough interest then we’d take on a few independent members.
PPI representative, interview 2
Despite the apparent lack of direct involvement from the commissioning managers, the PPI representatives reported excellent relationships with management. Some representatives had been involved under previous organisational structures and noted the difference under the new commissioning arrangements:
[Previous organisations] were very much management led . . . they tended to do things on business lines rather than on patient-need lines . . . everything was organised because that seemed like the right way to make it easy for somebody who was organising it rather than ‘what actually are we trying to get out of this? What does the patient really need?’ . . . So I have seen a major shift.
PPI representative, interview 1
Rather than determining the topics the PPI group should be involved in, the management staff allowed the group to discuss issues they felt were important. This encouraged the generation of new ideas for service development:
We don’t tell the PPI group what to discuss, they come up with the ideas and set their own agenda, arrange their own meetings. And sometimes they’re used as a sounding board, so they will often come up with ideas, very good ideas which we will use in commissioning design.
General manager, interview 7
During interviews, managers noted that their normative approaches to control – claiming that they set aside organisational hierarchy and encouraged a collaborative ethos – not only enhanced the PPI contribution, but developed a sense of organisational belonging or ownership among PPI representatives. This subsequently influenced the implementation of the services in a wider public setting:
If you use patients to help in the design you may still end up with the same result, but because you’ve taken patients along with you they will go out and defend it themselves . . . at a public meeting somebody was having a go at our CCG over something and one of the guys from the patient group stood up and defended it because he’d been in on the inside and said ‘you’ve totally got this wrong. They’re doing it this way.’. So it shows it does work.
General manager, interview 13
In contrast to CCGs D and G, both managers and PPI representatives interviewed in this case could give explicit examples of episodes when PPI had influenced service design or had been clearly involved in strategic decision-making processes. In other words, PPI, in this case, acted as a co-ordination capability to overcome limitations of socialisation capabilities, enhancing the critical review capacity of the CCG. As noted above, this also encouraged a sense of organisational commitment and ownership of services, and instilled a feeling among PPI representatives that they were able to contribute at all levels of commissioning processes. This was reflected in an example from one of the PPI representatives who was concerned with the local ambulance service and, as a result, undertook their own research, independent of the commissioning organisation. After developing a paper and arguing a case for change in the way services were being delivered, the PPI representative distributed it to the PPI group, the board of the commissioning organisation and the board of the local ambulance service:
I sent a paper off to the chief executives because I’ve been concerned about the lack of data transparency from the ambulance service . . . So I wrote a paper and it’s very challenging potentially . . . I’ve pursued it, asked questions.
PPI representative, interview 10
The above example illustrates how a more collaborative ethos towards PPI encouraged representatives to become more actively involved in strategic issues outside formalised, managerially determined roles, overcoming socialisation limitations. As a result, there evolve ideas or opinions that may not otherwise have been facilitated, enhancing the critical review capacity of the CCG. A second example of the positive influence of PPI was illustrated in the design for a respiratory [chronic obstructive pulmonary disorder (COPD)] service:
One of the chief executives came to me and said they’d been looking at the plans I’d sent them for a project on COPD, and they wanted my input in developing the service . . . it’s now showing something like a 17% reduction in unplanned admissions. Well, if you add up £3000 or £4000 a time that’s a lot of money we’re saving . . . So the patients are benefiting and the CCG are benefiting because the patients are benefiting.
PPI representative, interview 4
By having the confidence (and managerial encouragement) to send ideas or project proposals that may not be managerial priorities to the management team of the organisation, PPI encouraged the development of a new service, subsequently resulting in patient benefit and cost savings. If the PPI representative, in this case, had been constrained by socialisation capabilities, such as those reflected in CCGs D and G, which were characterised by rational control, it is unlikely that the service would have been developed, as it was not part of the immediate managerial agenda.
Public involvement representatives in CCG C seemed aware that their potential influence within the CCG was not reflective of the types of involvement in other areas. As a result, some members within the PPI group were reluctant to work with other ‘less credible’ PPI groups in case this undermined their influence. This aversion to actions that may reduce their level of influence within the commissioning process was noted in field notes during a discussion at a PPI group meeting about the potential for collaboration with a neighbouring organisation:
[Discussion about collaboration with neighbouring organisation]. Everyone becomes very animated and derogatory about the PPI rep[resentative]s in neighbouring area. Many people appear concerned that the other group have less ‘credibility’ as patient representatives, and that they do not take their role as seriously. A number of people suggest that they are ‘not the same as us’ and ‘don’t know how to work with their CCG in the best way’. Someone says they are just ‘yes men’ and will not challenge managers.
Field notes, 9 November 2013
The PPI group seemed aware that its influence came from its ability to work alongside commissioning managers but remain outside managerially determined roles. Working in an organisation with a more normative approach from managers towards their contribution did not require PPI representatives to work within rationally controlled involvement structures, and afforded them freedom to think more innovatively about service design as they were not constrained to managerial priorities or visions. The distinction with the neighbouring group was that it was seen as being particularly influenced by a more hierarchical structure that privileged managerial priorities:
In [the other organisation] they’re appointed by management . . . The thing is when you suggest something the people from [the other organisation] will put all the obstacles in the way and the people from here will say ‘well why can’t we do it? What’s stopping us?’ . . . You see, I wouldn’t hear ‘we can’t do that’ from us, but I would from them.
PPI representative, interview 6
The PPI representatives were aware of the unique freedom afforded to them by the commissioning management team, enhancing their influence and potential contribution. Their aversion to working with managerially controlled groups was a result of concerns that they may find their influence lessened by increased pressure to conform to managerial priorities. However, the PPI group were also keen to help educate others and encourage them to work independently of managerial agenda. This was highlighted during interviews by an awareness of their role in developing influential PPI representatives for the future:
I’ve been to meetings and I’ve asked questions and I’ve heard somebody say afterwards ‘he shouldn’t have asked that question. He knew the answer.’ Yes, I did know the answer, but half of the people there didn’t which is why I asked the question and they wouldn’t have known to ask the question . . . So that’s where I see my role. I see my role now bringing those people along, helping them along so we’ve got some people who can question things in the future.
PPI representative, interview 10
In conclusion, CCG C illustrates the potential for PPI to act as a co-ordination capability when it is subject to normative, rather than rational, ideologies of control, meaning that it is not constrained by socialisation capabilities, and is capable of realising the aims of PPI policy. By being able to work outside rationally controlled roles, while maintaining supportive relationships with commissioning managers as a result of normative control, PPI representatives could inform commissioning processes at a strategic level and had a clear influence on the development of services. In addition to encouraging organisational commitment, and ownership of services within the wider public, normative control of the PPI group enhanced the ability of the commissioning organisation to design responsive services, resulting in positive outcomes such as the COPD service.
Conclusion
Public involvement is a legal requirement of CCGs and was shown in varying levels across all 13 cases, but notably in three situations. We identified that rational, managerial control inhibits the potential of PPI as a co-ordination capability by restricting involvement to managerially determined topics and areas. Most CCGs were increasingly aware of the need for ‘genuine’ PPI, but socialisation capabilities again undermined the potential of true engagement. One CCG took a more normative approach to PPI, indicating an approach that enhanced the potential of PPI as a co-ordination capability, resulting in positive outcomes in the design and delivery of services.
Chapter 7 Business intelligence
Business intelligence functions relate to the units set up to facilitate integration of diverse forms of knowledge from multiple sources. With the exception of one of our cases, BI was provided by CSUs. BI units generally acted as a co-ordination capability by encouraging the acquisition and assimilation of multiple types of information:
So a lot of the work I’ve been doing has been feeding directly into the urgent care partnership board; so that is hospital but also community services, social care. We build a dashboard around that urgent care system so we can see the pressure building as it does month on month. So it’s about sharing that sort of information so the level of understanding is increased so everyone’s then working to the same agenda, or they understand that it’s not just the acute hospital that suffers increased pressure in the winter; community services do, primary care do. Everyone’s experiencing the same thing, but actually what you’re trying to understand is it’s a whole-system capacity issue.
CCG F, interview 7
Encouraging the integration of information from partner organisations and disparate data sets enabled BI units to provide a more contextual understanding of the entire health-care system, overcoming barriers of systems and socialisation capabilities. However, although this is generally how BI units functioned, it is important to note that BI occurred at two different levels among CCGs, using different mechanisms to enhance critical review capacity. The first, an embedded or ‘in-house’ team, worked in the same location as the CCGs, and was seen as part of the commissioning organisation. The second level was an external model, whereby CSUs, distinct from CCGs, provided intelligence services at a cost to multiple CCGs. In the second BI formation, the relationship was based on a consultancy model, rather than the embedded team who were seen as part of the commissioning organisation. We now consider each of these BI types and their mediating influence on systems and socialisation limitations.
Embedded business intelligence teams
As noted, embedded BI teams were situated within the CCGs, rather than offering BI services from outside the organisation. One of our cases (CCG E) had integrated its BI unit into the commissioning organisation, rather than contracting with an external CSU, resulting in a BI team that was fully embedded in the CCG. This was rare, and not seen in our other cases. Most commonly, CSUs were contracted to provide both embedded staff, who worked at CCG offices, and services from staff who worked externally to the CCG at CSU headquarters.
In both BI formations, interactions between embedded BI staff and commissioners were relational, rather than contract-based and transactional. The embedded teams were able to draw on social resources to overcome limitations of socialisation capabilities by being seen as ‘one of the team’, and working together with the commissioners towards a shared end goal:
And I thought driving down here today that’s what makes us different, is we are in-house and we are a team from that point of view and we have the same ethos. We’ve built our vision together, we’ve built our strategic core principles together. All of those things actually we are in us. That’s not a service we buy.
CCG E, interview 15
For embedded BI teams, their physical location within CCGs, rather than working remotely, was also seen as facilitating their assimilation processes:
It’s more reactive I think and you can overhear things and be involved in more things if you’re on the ground with the people who are making the decisions. I think if we were a central team rather than an embedded team you’d find you’d just get asked for a number and then they would go away and do it, whereas this is more they’ll ask you for a number but then you can add more understanding to what that number represents.
CCG M, interview 4
The local knowledge of embedded BI teams was a crucial mechanism, which allowed them to act as a co-ordination capability. By drawing on prior relational experience with both commissioners and providers, embedded BI teams were able to overcome some of the limitations of systems capabilities:
You’re getting local knowledge, which is actually priceless when you’re doing the kind of work we’re doing. We’re dealing with large data sets and we know the ins and outs. Because we’ve worked for so many years with our local hospitals we know the ins and outs of their data . . . having the local, in-house knowledge is very valuable. It stops people from going off on a bit of a whim redesigning pathways, which perhaps don’t need to be redesigned because there are no savings there to be had anyway.
CCG E, interview 14
The local knowledge of those working within the BI unit encouraged lateral communication between the BI unit and the commissioners, preventing ‘people from going off on a bit of a whim redesigning pathways’. Embedded BI teams also overcame systems limitations by giving meaning to the ‘pure numbers’, as described in the following quotation. Rather than providing decontextualised information, local BI teams could tailor information to local need, enabling commissioners to analyse and apply information to the situation at hand:
If I was just asking somebody for activity data relating to a particular service who didn’t know the area then I’d probably get exactly what I asked for. If I ask for that here I’ll get additional information and insight around ‘but these used to be coded differently. This time around . . . ’ or ‘there’s been a change in the contract here,’ or ‘when we talk to the provider about this we know they’re coding it in a particular way’, and that really, really helps when we try to describe an implementation or try to work out what the benefit of doing something is. It’s more than the pure numbers. So that’s really good and it helps because it’s individuals who understand the locality and we have a relationship with.
CCG E, interview 16
In particular, the relational nature of interactions between embedded teams and commissioners was beneficial in encouraging the engagement of GPs in commissioning discussions. Developing relational interactions with GPs was seen in some cases as reducing the potential for professional resistance, as embedded BI staff were able to respond to immediate concerns of local clinicians, rather than being viewed as detached or separate from the needs of clinicians:
A lot of the things I’d picked up from being in the GP meetings allowed me to feed into that some of the issues and concerns that GPs were having on a local level and concerns on specific projects that are coming up where the GPs are going ‘well, we’ve tried this four times before and it hasn’t worked. Why are we trying it again?’. So that side of things . . . I like to get as much information as possible to try and add more value to everything that we’re trying to do because it’s very easy to just give somebody a number and say ‘well this is what it is’, and I think you need to have an understanding of why they’re asking the question and what impact it’s going to have on everyone around.
CCG M, interview 5
In addition to a potential reduction in professional resistance, embedded BI teams were better situated to involve clinicians in the assimilation and understanding of standardised data sets. By working closely with the BI team, clinicians could use tacit knowledge to influence service design and provision:
I think it was eye-opening to him what we could do with the data, and how we could build a service out of that, and it was eye-opening to us because I wouldn’t have known ‘golly, if we did that and that we can actually inform better practice.’. And that’s all about if you inform better practice you’re keeping people out of hospital.
CCG E, interview 5
However, although the embedded team was well positioned, as a co-ordination capability, to mediate socialisation barriers, there were concerns that its ability to provide timely, locally appropriate information to commissioners was limited by systems capabilities. In particular, restricted access to patient information was seen as a barrier undermining the embedded BI team’s critical review capacity:
So from April 2013 we were not allowed to see patient-identifiable data any more and the primary care data that we used to be able to access was turned off . . . Now if we can’t extract the primary care data to be able to say who’s [turning up] at the GPs with different long-term conditions and how they’re being managed at the GP surgery and all we’re seeing is the secondary care element of that when they’re going through as an emergency admission, what we haven’t got any idea of is what’s happening to them in primary care, or even then when they step down and go into social care we don’t have any of that data. So that to me is the massive gap that is missing in the data that we’re doing.
CCG M, interview 1
Further to this, the embedded teams voiced concerns that the detail of data they were acquiring, even from secondary care providers, was not comprehensive enough to fully answer questions from their CCGs:
Some of the data that we get is very difficult to scrutinise . . . It’s a very aggregated data set so it’s very difficult to try and actually drill down into that data to see whether you really think there’s anything wrong . . . we can’t drill down.
CCG M, interview 2
A second limitation to the critical review potential of the embedded teams was their capacity to respond to ad hoc, time-sensitive requests for information from commissioners. As noted earlier, the strength of the embedded team lay in their relational, rather than transactional, interactions with the commissioning team. However, this could also be problematic, as embedded BI teams tended to be small and limited in their capacity. As a result, high levels of demand and fragmented requests for information could undermine the critical review capacity of the CCGs:
I do think we have a strategy as a CCG, but our approach to achieving that is a bit scattergun and we get flavours of the months . . . It just feels probably we’re trying to fight too many battles at the same time and perhaps because of that it’s difficult to succeed or understand any of them because you can’t focus on them for long enough. We’ve become the bottleneck really and it’s an uncomfortable position to be in when you know you want to support them all . . . we’ve got no kind of defence mechanism or control mechanism for workload . . . we’re just sort of at the whim of who needs what and often it’s very urgent.
CCG E, interview 3
In addition, embedded BI units reported little or no influence on exploitation processes. This seemed to be related to the limitations of systems capabilities, in particular the underdeveloped nature of data sources relating to evaluation of services, undermining the ability of the BI unit to integrate evaluation data into ongoing commissioning decisions. A particular challenge related to how they might measure the effect of absence of the service intervention they had commissioned to reduce avoidable admissions of older people into hospital:
I think some of the difficulty is capturing what doesn’t happen. Sometimes you will put in a service to prevent avoidable hospital admissions or perhaps deterioration in the health of an older person that might eventually lead to admission. However, there’s a real dilemma about how you evidence the impact of the new service, what would have happened if it wasn’t there. Our data management systems aren’t sophisticated enough for this.
CCG G, interview 2
Finally, it was of concern, even where BI was in-house, when commissioners were asked the question about evaluation of interventions designed to reduce unnecessary admissions of older people to hospital, that they admitted an absence of such a feedback loop:
So how is the virtual older persons’ wards intervention working to reduce admissions?
We don’t gather data about that. Maybe we should evaluate though since I guess we don’t know whether to continue or decommission it.
CCG I, interview 2
In conclusion, embedded BI units are able to draw on relational interactions to overcome socialisation capabilities, and incorporate local or tacit knowledge to mediate the barriers of systems capabilities. Thus, the embedded BI unit can be conceptualised as a co-ordination capability of the CCG. The unit is embedded in the organisation and can contextualise the information acquired. The unit has the right people generating the right knowledge at the right time. However, critical review capacity could be enhanced if the exploitation of information could be improved. More research is needed into the most effective way to enhance this co-ordination capability with a view to improving exploitation of information and knowledge, and subsequent improvement of critical review capacity. In addition, it is important to note that the level of embeddedness varied among CCGs. Some units operated purely in-house, whereas others were employed by external CSUs but physically worked within CCG headquarters. Therefore, there may be national variation depending on CCG structure.
External business intelligence teams
Centralised BI teams were external organisations to the CCGs, denoted as CSUs. Offering BI based on more of a consultancy model, CCGs bought services from CSU teams to varying degrees. At a basic level, external BI could offer similar services to those seen with the embedded teams. However, their potential as a co-ordination capability lay in their ability to offer a more systems-level overview in response to information requests. This was facilitated by their ability to view data from across a regional area, rather than a local CCG area:
The benefit obviously of being a CSU is that we’ve got access to everybody’s data . . . You know, if you’ve got an embedded analyst that’s employed by the CCG they can obviously only see their own data, the CCG data. The benefit with the business intelligence department here is that we can benchmark. We’ve got full access to all the secondary care data for their own CCG plus these 23 other CCGs that allows us to be able to point out where they’re very different or where stuff’s costing more than what other CCGs are paying.
CCG M, interview 1
External BI units could subsequently enhance critical review capacity by linking multiple data sets to provide cross-comparisons of assimilated data from different CCGs across a regional area:
So it’ll be can we do some benchmarking and have a look at our ACS [Adults and Community Services] conditions for our over-75s, for instance. How do we compare to other CCGs? How do we compare over time? Are we getting better or are we getting worse? What would be the benefit to the CCG if we managed to reduce our admission rates compared to the best in our patch or whatever? Things like that trying to quantify potential cost savings and potential admission reductions.
CCG M, interview 2
By using multiple information sources to contextualise the acquired information, the external BI units facilitated the generation of a systems-level overview for CCG performance. This provided CCGs with a more comprehensive ‘picture’ of the flow of patients throughout the entire system:
You can actually follow whole person pathways. So you can look at how people come into the system, how they leave the system and each of the points along that . . . and then there’s an understanding of the demographic characteristics of those, so what’s the age, gender, some kind of social marketing data, characteristics of these cost groups and why they’re different whilst looking at the services that make up those groups . . . So we’ve been creating baselines for people so they understand how people kind of work within that system . . . So if you looked at reducing things like delayed discharge in hospital you can actually see where those people go to now, so you might be able to model whether that would have an impact on things like intermediate care from the community, re-ablement from social care and whether it actually has a perverse effect and increases permanent admissions to residential nursing homes.
CCG M, interview 10
An integrated perspective, overcoming systems limitations, was particularly important when considering the interplay between health and social care, the data systems of which are disjointed:
There’s a lot of activity going on out there and there’s a lot of disjointed information systems I suppose across the NHS, so for me it’d be picking all those flows up, centralising those flows and then working with CCGs to say what’s really going on, what’s really happening to patients around the system . . . So it’s having the capacity to pick that up and look at it as a holistic view from a pathway angle and then obviously help to commission better services for patients.
CCG M, interview 5
In addition, although embedded teams suggested that systems limitations could undermine their potential to act as a co-ordination capability, the external BI team noted fewer limitations. To overcome the barriers to using data systems, the external team acquired information from more diverse sources or used the data in more creative ways:
I know people often feel that absence of data or poor data quality are obstacles, that they can’t address the particular question they’re interested in. My perspective has always been slightly different. I just think that you’ve got a question, you’ve got to make that decision. You deploy whatever data you’ve possibly got at that time in whatever form you’ve got it to answer that question as best you can. There’s no point just shrugging and saying you can’t do anything . . . we have to go with what we’ve got really and part of our job is knowing how to make best use of the data sets that we already have, thinking of different creative ways of using the data to answer the questions they’ve got and knowing which fields or records we should just ignore because we know the data quality’s not sufficiently robust.
CCG M, interview 11
For example, one member of an external BI unit noted how they acquired information from another external organisation to consider the impact of weather on increases in urgent care provision, adding an extra dimension of insight to a question from a CCG:
You know, there’s lots of other stuff out there that’s accessible to anyone that you can just download, so depending on what question we’re going to answer we’ll decide how we might provide evidence for it and then go out to look for the various data sets that we might need. So for example, when we were looking at some of the unexpected increases in urgent care provision, one of the hypotheses was that it had been a particularly bad winter in terms of being really cold that winter or really wet, so we’d go out and perhaps get some data from the Met Office to try and substantiate that claim or disprove it and those sorts of things.
CCG M, interview 8
In particular, the strength of the external teams lay in their ability to provide more in-depth analytical responses to complex questions from CCGs:
So it’s the questions that are much more difficult to answer, so things like ‘what are the impacts of doing X on Y? What’s the likely demand on our services in the future? How has this service done compared to another service in another area?’ or ‘What is the evidence for this service to change?’. It’s kind of those more difficult questions which can’t necessarily be done with routine processing of data and reporting on routine data. We often have to link data and we have to provide a variety of different perspectives on a particular service or clinical area.
CCG M, interview 9
For example, an external BI team member outlined how they were working with one CCG to consider the impacts of service redesign:
They started from the fact that they’ve got a single acute provider working across two sites with basically unsustainable services, in their view, into the long term because of insufficient capacity. So they wanted to run a reconfiguration programme to design a new clinical model for that patch and then out of that clinical model to run all the processes necessary to try to identify a preferred option for reshaping their hospital system.
CCG M, interview 12
However, the external teams noted that their co-ordination capabilities could be undermined by the attitudes of CCGs themselves. They voiced frustrations that the products they provided to CCGs were not being used, limiting their impact on the critical review capacity of the CCG:
I suspect one of the difficulties we have is once we’ve done a piece of work making sure that that work is taken forward and used. Because we don’t work for them or we’re not embedded with them we’ll do a piece of work and then hand it over and then that’s the end of our involvement and it’s difficult for us to be involved with those projects on a longer term.
CCG M, interview 5
The working relationship between external BI staff and the CCG could negatively influence the way the BI unit was able to affect CCG critical review capacity, and prevented it from being fully integrated into decisions about evaluating services:
I probably would say it’s this lack of trust and respect from the CCGs . . . It just feels like actually no one respects our opinion when we give it to them. You know, ‘you asked us to do a piece of work. We explained to you in detail why it’s not a good piece of work to do and why it’s not useful and how it’ll actually probably muddy the waters more than it will help’, and then you still end up doing it. It makes the working relationship between CCGs and the CSU quite difficult I think.
CCG M, interview 2
Problematically, this tension could be related to the system pressures faced by CCGs, which are not focused on long-term evaluation of projects because of immediate demands for service provision and cost reductions:
I think there is a lack of strategic planning at the CCGs. I think we show the commissioning cycle in terms of being able to evaluate need and you do something about that, you commission services differently and then you evaluate that, but I’m not sure that that happens . . . What they’re bothered about is actually implementing these schemes and doing that commissioning, but what they don’t think is ‘how am I actually going to evaluate whether that’s working or not?’.
CCG M, interview 1
In conclusion, the external BI teams, acting in a consultancy capacity, were able to provide a co-ordination capability by drawing together multiple, diverse information sources to provide strategic insight to CCGs, beyond standardised data reporting. However, at times there was a lack of engagement between the CCGs and the external BI teams. This could undermine critical review capacity, as a result of the influence of socialisation capabilities. On many occasions, exploitation processes within CCGs were seen as underdeveloped, and evaluation of services was a secondary consideration in many cases.
Conclusion
Business intelligence units, in general, have the potential to enhance the critical review capacity of CCGs by acting as a co-ordination capability. However, they operate at two distinct levels: embedded teams and external teams. Although embedded teams were able to overcome socialisation limitations by interacting with commissioners on a relational basis and using local knowledge to enhance assimilation and transformation of knowledge, they reported restrictions of systems capabilities. Conversely, external BI teams were better equipped to overcome systems limitations, but were influenced by socialisation barriers as they were perceived as being ‘outside’ the CCG. Exploitation processes of BI teams were underdeveloped at both levels.
Chapter 8 Social integration
One of the main themes to emerge during analysis was the importance of social integration in enhancing critical review capacity. A key area of exploration in four of the CCG cases, social integration acted as a co-ordination capability in two ways: first, by developing transactional relationships by integrating health and social care strategy and funding and, second, by developing relational interactions by creating boundary-spanning roles that reached into external organisations, such as the voluntary sector.
Sharing strategy: bridging health and social care
Integrated teams, particularly those that straddled health and social care, were the focus of four of the CCG cases, but were represented in some form across all 13 CCG networks. Spanning two or more organisations, integrated roles were designed to acquire and integrate information from disparate information systems, overcoming systems capabilities. In particular, barriers between health and social care information systems were identified as limitations of knowledge acquisition and sharing among CCGs, and integrated roles were perceived as a way to overcome these barriers:
It has specifically improved communication a lot between social services and health I think. Because we both have two different computer systems we don’t talk to each.
CCG H, interview 1
This integration was seen as key for commissioners attempting to design services, as integrating perspectives and demands from multiple organisations could be seen as problematic:
It’s challenging to get that shared interpretation of what the information actually means for actual service design because clearly there are different interpretations you can apply to the same information. From a commissioner perspective, we will see a problem or challenge from one particular perspective, but health-care providers will see a very different challenge, and so we will support different service interventions.
CCG D, interview 12
By facilitating the acquisition of diverse sources of information, integrated roles enhanced the assimilation and transformation of multiple forms of knowledge, enhancing critical review capacity of the CCG. This could enhance the commissioning process and have a positive influence on patient care, acting as a co-ordination capability. This was particularly the case for complex care provision for older people, who were often admitted to hospital in the absence of effective collaboration across health and social care organisations. Integrated care teams encouraged knowledge mobilisation across sector boundaries, enhancing service provision:
It [an integrated health and social care pathway] represents a smoother pathway for the patient. In the past the older patient would have been taken into hospital, the patient discharged, and community social care teams have little contact with what’s going on. The older patient may then be subsequently re-admitted to hospital because the social care support wasn’t there. Because we’re integrated now we can see two sides, the need for social care, as well as health care, for the patient, and so prevent readmission.
CCG F, interview 5
In particular, being able to take a wide view of the patient case enabled integrated teams to move past some of the potential challenges of systems capabilities, such as distinct funding streams for social and health care, which complicates elderly care provision:
I think obviously the funding bit, social care funding and health funding. They’ve both got their pots and they both want to protect their money and ‘no, that’s not my job, that’s health.’ ‘No, that’s not us, that’s social care.’. I’ve really just been, you know, in the middle saying ‘the person needs care. Let’s put it in and fight about it later . . . Let’s just get this care in. It’s Friday afternoon. Let’s argue about it next week’, which is how I think it’s got to work. There’s got to be somebody to draw the line, hasn’t there? I know there’s cuts and problems with funding, but the patients have got to have the care, haven’t they?
CCG H, interview 9
In one of our cases, the CCG had almost fully integrated its resources with those of the local authority. Working in the same location, sharing staff in hybrid roles (those who were employed 50% by the CCG and 50% by the local authority) and combining budgets for health and social care were seen as key mechanisms through which the CCG provided a more joined-up approach to service design:
I think I’m very, very pleased to have found that [the] CCG is able to work so closely with [the] borough council to the extent that we’re actually based in council buildings as you can see. That was never the case in the days of PCTs. There was a lot of suspicion between the two, but now they work hand in hand. That I think facilitates what you’re talking about – being able to bring in social care so that we can give people a package of care that’s not fragmented.
CCG F, interview 10
Integrating teams created a more relational approach to joined-up commissioning between commissioners and the local authority, rather than a transactional approach in which funding was a major barrier. In addition, an integrated approach positively affected the alignment of other stakeholders. For example, as a result of close working relationships between the CCG and the local authority, commissioners reported that the secondary care organisation was more ‘in line’ with the shared vision of the commissioning network:
To actually make all the changes that we’re going to make it’s required a lot of engagement between clinicians and directors of both CCG and the borough council and secondary care and that’s only happened because the CCG and the borough council work very closely together and there’s no suspicion anymore, so everyone’s pushing in the same direction and because of that I think that secondary care feel that . . . so you can actually get people in a room that actually will agree to things more readily.
CCG F, interview 10
The integrated teams acted as a co-ordination capability for the CCG network by encouraging the sharing of information and resources across boundaries, mediating the barriers of systems and socialisation capabilities. Although this facilitated commissioning decisions, the more important impact of integration was seen in the transformation of service decisions, having a positive impact on complex patient care:
I had a 100-year-old lady this week . . . I think third case of pneumonia, doctors wanted to admit her. She didn’t want to be admitted. She wanted to stay at home. In anybody’s eyes that’s a health need because there was a hospital admission . . . The matron phoned me up and said ‘what can we do? What can you do? Do you think we ought to put care at home in?’ but when I looked at the situation . . . I could have gone to the care at home team and put a team in to support her at home, but actually she was having agency care. Really good package, carers she trusted. They all really cared for her. You know, they were first name. Really good and it worked really well. So instead of taking them out and ‘it’s a health need. Let’s put health in to do it’, I left them in, looked at the contingency [fund], we had some money in the contingency, increased the care visits so they could spend a lot of time with her. So perhaps if that was cut and dried I should have used health because that was a health need, but I used social services because that was for her . . . So I think there’s ways to work round things.
CCG J, interview 9
Boundary spanning: engaging with the voluntary sector
One CCG case we explored had an integrated team that worked to mediate systems barriers between health and social care, but also encouraged integration from external providers, most notably the voluntary sector. In particular, the integrated team used voluntary services to enhance acquisition of information about complex patients, influencing transformation into better services for patients:
We’ve been dealing with cases over the last 2 or 3 days in fact where volunteers obviously are our eyes and ears into some of these people as well, which is very useful and also because they go in once or maybe twice a week and they’ll sometimes see things that even if that person’s having a daily care package people don’t always see. So the volunteers can feed that back to the [integrated team] who will have a good helicopter view of the services they need.
CCG J, interview 2
The integrated teams gave a number of examples of when they had engaged with voluntary services to provide patients with services not covered by health or social care teams, or to extend the services available. The following illustrates the importance of these services:
One of the nurses, she’d been out to a gentleman . . . He’s got a leg wound and it’s got maggots in it. So she’d come back to the office to me and said ‘oh, can we get some care in there because this gentleman’s really in a state? There’s flies everywhere in the house, it’s a tip. You know, he’s not managing, he’s not coping. Can we get some care?’. I said ‘OK. . . . He’s back on his feet, care’s ended, nursing needs have ended, he’s fine’ . . . So that was a joint effort by all – social services, the nursing team and the voluntary service. All three involved there.
CCG J, interview 10
In the example above, the integrated team acted as a co-ordination capability, bringing together health services, social services and the voluntary sector. However, by engaging with the voluntary sector at an early stage, the integrated team limited the number of services required by the patient. The volunteer was able to engage with the family to improve the patient’s standard of living, resulting in a better health outcome, removing the need for a social services care package and potentially avoiding a crisis situation that could have resulted in an urgent care admission. Other examples of volunteer involvement also noted the importance of creating a safer living environment for preventing accidents, ill health or urgent admissions:
I mean just decluttering somebody’s house – the impact that has on unplanned hospital admission is immense because if somebody doesn’t fall over they don’t end up sat waiting for the ambulance service to come and get them for 7 hours, they don’t end up queuing up at A&E [accident and emergency], they don’t end up in hospital, they then don’t end up stuck there for 3 weeks because social care can’t pick up what their needs are. Just through simply having somebody spending an hour chatting to them about making their house a bit safer.
CCG J, interview 2
A further benefit of engaging with the voluntary sector prior to admissions was an awareness of the potential of voluntary services in facilitating discharge from hospital after an admission:
If somebody is admitted in an unplanned way into hospital it means that the social care system for that person at home has to change in order for them to come out of hospital and the complexities around doing that are just immense. The other side to it is also about trying to understand what we can do to better support people that are making a planned admission to hospital so that discharges aren’t delayed, so that people make a sustainable return home . . . What we can do is just make sure we’ve got a volunteer going in working with the patient to prepare their home – so sort out any trip hazards, make sure they’ve got kind of heat and light available when they come home, make sure they’ve got basic groceries, have got contact lists, all those sorts of things – and that volunteer will then work with the patient to get them into hospital and work with the patient when they come home from hospital so that that whole pathway is delivered more effectively.
CCG J, interview 3
In other examples, voluntary services were used for more-relational interventions, such as befriending, to prevent social isolation. In many cases, the integrated team worked as a co-ordination capability to facilitate the involvement of volunteers and to integrate them with the health or social care services also being provided, to develop a more holistic package of care:
One was for a befriender for a lady who’s housebound, had recently been bereaved and was very, very withdrawn and desperately needed friends. No family, no children, her husband had obviously died and she was really quite sad. The nurses couldn’t do anything to help really. They’d done their piece as far as medical, so they sort of said to me and at the same time it was discussed at the risk profiling as well for this lady what can we do, so I said ‘well, I can ask [voluntary organisation] if they have a befriender’.
CCG J, interview 5
The above examples illustrate instances in which voluntary services have been used as an extension of, or have been integrated with, statutory health and social care services. Facilitated by the integrated teams, which co-ordinate the interaction of all three organisations, involving volunteers in this way has the potential to improve quality of life for patients. In some circumstances, this can be identified through improved health outcomes or a reduction in health and social care services, or through more-relational interventions such as befriending or social activities.
A word of warning: ‘patching’ health and social care
Although integrated teams were a key co-ordination capability for CCGs in encouraging the integration of knowledge, but also in ensuring comprehensive packages of care for older people, we also uncovered examples of situations in which voluntary services had been used to ‘patch’ gaps in health and social care. In some cases, illustrated in the following quote, this was because of limitations of funding or responsibility for the patient:
Not long after I started I had a case with a lady . . . I think she was due to go in for some surgery and she needed an MRSA [meticillin-resistant Staphylococcus aureus] wash each day and she could do a certain percentage of her body but she couldn’t do her back. So that was basically all it was and health-care were saying ‘it’s not us, it’s not a health need, it’s a social care need.’. Social care were saying ‘no, it’s not us, it’s a health need’, and this went on for a couple of hours and then in the end I just sort of went back to her and I said ‘Look, we’re having a bit of difficulty getting somebody in to you. Would you be prepared to pay, you know, it could be £5 each day for the next week for somebody to come in from a voluntary organisation and support you with this?’.
CCG J, interview 4
Although voluntary services could be effective in preventing patients from falling through the ‘gaps’ in service provision, there were also examples of situations in which they were used because of lack of capacity within the health and social care systems. Owing to pressures on, particularly, social care, there were examples of voluntary services being used instead of statutory services:
So we use them mainly because social services are so stacked up accepting our referrals that we’ve used the [voluntary organisation] more because they’re an agency that can . . . They can do kind of everything in one visit. They can spend up to 2 hours with somebody. I mean this is something which in the past social care were able to do . . . but now as everything is moving so quickly and everyone’s got so many patients there’s not enough time.
CCG J, interview 5
We do not suggest that voluntary organisations should not be ‘patching’ health and social care services, as they can play an important role in crossing organisational jurisdictions to stop patients falling through gaps. However, there were examples of voluntary services being used to fulfil gaps in services as a result of a lack of capacity within health and social care teams. The use of voluntary services in this way can be beneficial to patients, preventing crisis admissions and enabling them to remain at home, but it should be negotiated carefully.
Conclusion
Integrated teams acted as a co-ordination capability in two ways. First, they encouraged the integration of knowledge from two (previously disparate) data systems. By integrating health and social care information, hybrid roles could develop transactional relationships to overcome systems limitations and positively influence the commissioning process and patient services. Second, by taking an overview of the wider context, integrated teams developed relational roles that encouraged the acquisition of external information, such as from the voluntary sector. This could then be used to further enhance the commissioning process and facilitate the delivery of comprehensive care to complex elderly patients.
Chapter 9 The absorptive capacity tool
Introduction
Based on the qualitative study and extensive literature research, we designed a self-development tool for CCGs and their partner organisations. The tool has been constructed in line with recommendations for a high-standard psychometric tool. 124,125 It has been cocreated with members of the PPI and pilot tested with a volunteering CCG to enhance face validity and applicability. The next step is to provide evidence for construct and criterion validity, which involves collecting data from CCGs and testing the psychometric properties of the tool.
The self-development tool captures ACAP, which is the mechanism linking combinative capabilities of ACAP (antecedents to ACAP, including system capability, co-ordination capability and socialisation capability) and its outcomes for the CCGs. The tool focuses on how different parties in a commissioning process acquire and use knowledge, and how they collaborate within CCGs and across partners to make decisions.
The aim of the tool is to provide CCGs with information on their commissioning processes, which can help to improve their decision-making. The self-development tool offers the following benefits: first, CCGs interested in improving their decision-making processes can do so with the help of a structured tool, which provides specific feedback on a number of vital aspects of the decision-making process. The feedback provides an evidence base for participating CCGs, facilitating discussion and communication with different stakeholders in a targeted way. Second, over time, data collected with the tool form an anonymous database. This will provide statistical norms and benchmarks with which CCGs can compare their scores, so that they can identify their specific strengths and potential areas for improvement. Third, CCGs will be able to identify how the commissioning process is perceived from the perspectives of different stakeholders.
The self-development tool comprises a 15-minute online survey, available to all CCGs and their partner organisations free of charge. A participating CCG will invite all individuals working directly for it, as well as its partners. The more individuals who complete the tool, the more detailed the feedback will be, providing a more valid evidence base for the CCG to work with. An anonymised report is generated from the responses, which includes a summary of the main constructs and feedback on the average scores, alongside recommendations on how to improve (see An example of a Clinical Commissioning Group report). Over time, with increasing CCGs participating, the database built will provide norms and standards, which provides a basis for comparison.
The RQs guiding the tool development are the same as those for the qualitative study. Our overarching RQ is as follows: how can we enhance ACAP of CCG-led commissioning networks in health care to inform decisions to reduce potentially avoidable elderly care acute hospital admissions? This breaks down into three linked RQs:
-
How do CCG external relationships and system antecedents to new commissioning arrangements affect CCG critical review capacity?
-
What features of CCG organisational context (i.e. internal capacity) affect CCG critical review capacity?
-
How do we reduce the variation between PACAP and RACAP?
Theoretical justification and brief overview of constructs
This section discusses the constructs in the tool and provides the rationales to include them. As shown in Figure 2, the tool consists of the four elements of PACAP and RACAP (acquisition, assimilation, transformation and exploitation), linking relevant antecedents (organised into three categories: socialisation capability, system capability and co-ordination capability) with a number of commissioning outcomes of ACAP following QIPP (including commissioning-related criteria such as the perceived quality of the commissioning, as well as organisational outcomes such as innovation, productivity and prevention). Most of the variables are assessed with respect to one particular exemplary commissioning process, which is hereafter referred to as the commissioning of Project X, whereas the remaining variables are about the CCG in general.
FIGURE 2.
Overview of the framework.

In the following section we provide a brief explanation for each group of variables. An extensive description of the development of all variables, including their theoretical and empirical origins, can be found in Appendix 1. Table 4 summarises the variables and items of the tool.
| Concepts | Constructs | Items | Sources |
|---|---|---|---|
| Socialisation capability | Individual knowledge sharing |
|
van den Hooff and Huysman126 (2009) |
| Group knowledge sharing |
|
Faraj and Sproull127 (2000) | |
| Trust (in CCG colleagues) |
|
de Jong and Elfring128 (2010) | |
| Trust between CCG and partners |
|
Poppo et al.129 (2008) | |
| Trust in CCG managers |
|
Mayer and Gavin130 (2005) | |
| Organisational commitment |
|
Conway et al.131 (2014) | |
| Identification |
|
Mael and Ashforth132 (1992) | |
| Team reflexivity |
|
de Jong and Elfring128 (2010) | |
| Emotion | Angry, frustrated, disappointed, anxious, fed up, let down, happy, surprised, excited, proud, satisfied, pleased | Van Katwyk et al.133 (2000) | |
| Taking charge |
|
Morrison and Phelps134 (1999) | |
| Voice |
|
Van Dyne and LePine135 (1998) | |
| Being heard |
|
New scale | |
| Influence | Managers, doctors, nurses, local authority, PPI | New scale | |
| System capability | Rules, procedures and knowledge-sharing platform |
|
|
| Feedback seeking |
|
Schippers et al.136 (2007) | |
| Organisational and team infrastructure |
|
New scale | |
| Co-ordination capability | Cross-functional interaction |
|
New scale |
| Participative leadership |
|
Arnold et al.137 (2000) | |
| ACAP | Acquisition |
|
Flatten et al.138 (2011) |
| Assimilation |
|
||
| Transformation |
|
||
| Exploitation |
|
||
| Outcome of commissioning | Innovativeness of CCGs |
|
Wang139 (2008) |
| Quality of decisions |
|
Bresman140 (2010) | |
| Acceptability of the outcome | Considering the resources available, how acceptable was the outcome of the commissioning of Project X? | Added with suggestions from PPI group |
Antecedents of absorptive capacity
Socialisation capability
Socialisation capability refers to an organisation’s vision to produce a shared ideology and develop of a distinct group identity, and focus on the connectedness of different professionals. 13,141 A shared ideology is achieved through ‘congruence of values, needs, and beliefs among individuals within units’, whereas connectedness of different staff groups encouraged trust and communication, as well as knowledge sharing in the organisation. 8 We view socialisation capabilities as a cornerstone for ACAP, laying the psychological and social foundation for individuals to constructively interact and share information with each other. We therefore capture a range of concepts, including attitudes towards colleagues and the CCG (trust in colleagues and in CCG managers, and trust between a CCG and its partners; affective commitment towards the CCG; and identification with the CCG), emotional responses as vital indicators of the experience of the functioning of the commissioning process, and individual and team behaviours directly underlying ACAP (knowledge sharing, group knowledge sharing, team reflexivity, taking charge, voice, being heard and group influence). See Table 4 for a summary.
System capability
System capability refers to the existence and making use of knowledge-sharing platforms such as organisational and team infrastructures and formal knowledge exchange mechanisms including written policies, procedures and manuals that are explicitly designed to facilitate the transfer of codified knowledge. 4,8,11 We assess the existence and use of organisational and team infrastructure, the existence and use of rules and procedures and the CCGs feedback-seeking behaviours (see Table 4).
Co-ordination capability
Co-ordination capability refers to ‘knowledge exchange across disciplinary and hierarchical boundaries’ and normally includes job rotation and cross-functional interaction and participation in decision-making. 8 Job rotation is not identified as a characteristic of CCGs from the qualitative study and hence was excluded from the tool. However, cross-functional interaction and leadership were identified as important functions of co-ordination capability in the interviews. We capture interactions across knowledge and hierarchical boundaries as well as the extent and quality of participative leadership from both the individuals’ and managers’ perspectives.
Absorptive capacity
As outlined in Chapter 2, Absorptive capacity, we adopt Zahra and George’s13 conceptual framework of ACAP, which characterises four activities: (1) identifying and accessing relevant knowledge through acquisition processes; (2) analysing and interpreting this knowledge through assimilation; (3) integrating existing knowledge with the newly assimilated knowledge through transformation; and (4) refining and developing existing organisational routines and behaviours through exploitation of the transformed knowledge.
The scale items of ACAP are adapted from Flatten et al. 138 Comparing across different existing ACAP scales,142–144 the one developed by Flatten et al. fits with the CCG context most closely. 138 However, Flatten et al. 138 focus on collective ACAP. In this study, we adapt the items to assess individual ACAP. The rationale to assess individual ACAP is twofold. First, our qualitative study suggests that people working in CCGs might not be familiar with each other’s work, and, therefore, collective-level ACAP might not capture a full picture. Second, individual ACAP is in line with other individual-level constructs measured in this study. The scales for each element of ACAP were adjusted accordingly.
Outcomes of absorptive capacity
This element of the tool aims to understand how ACAP and its antecedents relate to a range of outcomes, both related to the end result of the commissioning process as well as wider outcomes for the CCG. We based the outcomes of ACAP on the QIPP model proposed by the UK Department of Health and Social Care. We adapt the QIPP model and assess innovativeness of CCGs and the quality and productivity of commissioning to fit the CCG context.
Methods
The development of the tool started after the qualitative part of the study finished and all executive reports were submitted. We developed the tool in three iterative steps in collaboration with PPI. The fourth step of the tool development, the rigorous psychometric testing of it, lies outside the scope of this bid and is currently under way.
-
Development of the theoretically guided model, including antecedents, ACAP and consequences, based on previous theory and research as well as the results of the qualitative study (in close collaboration with PPI).
-
Operationalisation of all three elements of the model (antecedents, ACAP and consequences). We developed items following our theoretical assumptions and by drawing heavily on existing measures, amending and extending those based on the results from the qualitative data.
-
Revising and editing items based on feedback from members of PPI, members of a CCG, academic experts and conferences. The tool was refined with comments from the PPI group and conferences attended, before sending out for piloting in one participating CCG. The role and involvement of the PPI is described in depth in Chapter 10.
-
Psychometric testing (outside the scope of this project): we are recruiting CCGs for participation to collect sufficient data to rigorously test the psychometric properties of the tool and to amend where appropriate.
The final version of the self-development tool consists of an online survey, which takes ≈15 minutes to complete. The survey should be self-explanatory and the first page explains what the survey is about and how to complete it. It also asks for respondents’ consent, guaranteeing confidentiality. Ethics approval to pilot the tool and to gather data in the future was sought and granted by the University of Warwick and the Biomedical & Scientific Research Ethics Committee.
During the period of development, we presented the tool in several conferences for feedback and to advocate its future dissemination. The conferences and events included Commissioning LIVE London (2 March 2017, London), Improving the Capabilities of NHS Organisations to Use Evidence Workshop (2 May 2017, Warwick) and Health Service Research UK (6/7 July 2017, Nottingham). As a result, we were in conversation with a number of CCGs about the tool and advocated the publicity of the tool. We have also been in conversation with NHS England about the potential dissemination of the tool.
We have also been in contact with CCGs for pilot sites, raising the awareness of the tool. All CCGs that we approached were sent an information sheet (see Appendix 2) and consent form (see Appendix 3), introducing the tool and guaranteeing the confidentiality of participants. Participants and CCG anonymity will be maintained at all times during the dissemination of the research findings.
An example of a Clinical Commissioning Group report
This section shows results from our pilot CCG and its partner organisations as an example of the nature of evidence that CCGs can receive from the tool. It is important to note that the psychometric testing of the tool is still outstanding, hence this chapter exemplifies what the tool will be able to demonstrate (1) once a database has been built and (2) when a representative number of CCGs participate. The data analysis again follows the conceptual framework depicted in Figure 2 and provides means and standard deviations (SDs) of combinative capabilities, ACAP and outcome of commissioning. The mean is the central or typical value in a particular set of data, whereas the SD shows how much respondents differ from the mean value of the group, that is, the average score of respondents in this group. A mean score of three signifies the scale’s conceptual midpoint. A low SD suggests that respondents’ views are close to the mean of the data set, whereas a high SD indicates that respondents’ views are scattered. Once the data set has been built, we will be able to integrate and compare CCGs’ scores with the population norms.
We present the results of each category in radar charts for easier comparison, and means and SDs are summarised in Table 5. Owing to the small sample size of our pilot study, we are unable to provide significance testing to demonstrate differences between groups or variables. Hence, when describing a variable as higher, lower, less likely, etc., this does not indicate statistical significance and is merely descriptive at this point.
| Constructs | CCG staff, mean | CCG staff, SD | Partner, mean | Partner, SD |
|---|---|---|---|---|
| Socialisation | ||||
| Individual knowledge sharing | 4.28 | 0.74 | 3.78 | 0.64 |
| Group knowledge sharing | 3.67 | 0.85 | 3.57 | 0.87 |
| Trust (in colleagues) | 3.64 | 1.15 | 3.87 | 0.75 |
| Trust in CCG managers | 4.19 | 0.70 | 3.97 | 1.22 |
| Organisational commitment | 4.13 | 0.91 | ||
| Identification | 4.19 | 0.66 | ||
| Team reflexivity | 3.65 | 1.01 | 4.06 | 1.20 |
| Emotion | See Figure 6 | See Figure 7 | ||
| Taking charge | 3.19 | 1.03 | ||
| Voice | 3.75 | 0.81 | ||
| Being heard (my voice) | 3.92 | 0.87 | 3.43 | 0.92 |
| Being heard (my group) | 3.43 | 0.92 | ||
| System capability | ||||
| Rules, procedures, knowledge-sharing platform | 3.42 | 1.53 | 3.63 | 1.20 |
| Feedback seeking | 3.20 | 1.43 | 3.20 | 1.27 |
| Organisational and team infrastructure | 4.05 | 0.81 | ||
| Co-ordination capability | ||||
| Cross-functional interaction | 4.35 | 0.67 | ||
| Participative leadership | 4.35 | 0.71 | ||
| ACAP | ||||
| Acquisition | 4.03 | 0.68 | ||
| Assimilation | 3.71 | 0.77 | ||
| Transformation | 4.13 | 0.67 | ||
| Exploitation | 3.71 | 0.74 | ||
| Outcome of commissioning | ||||
| Innovativeness of CCG | 3.92 | 0.90 | 4.23 | 0.94 |
| Quality of decision | 3.58 | 1.05 | 3.77 | 1.20 |
| Use of resources | 3.69 | 1.27 | 3.65 | 1.00 |
| Acceptability of outcome | 2.45 | 1.42 | 2.65 | 0.92 |
Table 5 is exemplary of what a report back to the CCG might consist of; however, the very low number of participants in this pilot group does not allow for indicative assumptions.
Socialisation capability
As shown in Figure 3, we grouped all constructs from socialisation capability except trust and emotion in one radar chart for easy comparison. The results show that CCG staff perceive themselves to strongly identify with, and to be committed to, the CCG, sharing knowledge among themselves as individuals. They also report feeling heard and voicing issues, but may feel less comfortable with taking charge during the commissioning process. Nevertheless, a high SD of the construct ‘taking charge’ shows great variation in individuals’ responses (see Table 5 and Figure 3).
FIGURE 3.
Socialisation capability (CCG staff, mean): range from 1 (strongly disagree) to 5 (strongly agree). KS, knowledge sharing.

We also assessed some constructs of socialisation capability that are related to the commissioning work with the CCG (see Table 5 and Figure 4). Both the mean and SD of the construct ‘being heard’ are lower than for other constructs, suggesting that partners believe that the CCG disengages with comments and feedback from partners.
FIGURE 4.
Socialisation capability (partner, mean): range from 1 (strongly disagree) to 5 (strongly agree). KS, knowledge sharing.

The results show that ‘trust in partner that should have worked with more closely’ is relatively low compared with ‘trust in partner most crucial to outcome’, ‘trust in CCG managers’ and ‘trust in CCG colleagues’ (Figure 5); however, a high SD of this variable (see Table 5) shows that respondents’ views on this matter varied quite significantly. Moreover, a low SD (see Table 5) of ‘trust in CCG managers’ suggests that most CCG staff have quite a high level of trust in CCG managers.
FIGURE 5.
Trust (CCG staff, mean): range from 1 (strongly disagree) to 5 (strongly agree).

We also assessed 12 emotions related to the decision-making process of both CCG staff and partners in the survey (six positive and six negative emotions). Emotions are a good indicator of the decision-making process. As presented in Figure 6 and Table 5, the data show that CCG staff mostly show positive emotions and occasionally feel angry and surprised during the commissioning process. Interestingly, SD of emotion shows that CCG staff vary significantly in the frequency of negative emotions they experience.
FIGURE 6.
Emotion (CCG staff, mean): range from 1 (never) to 5 (very frequently).
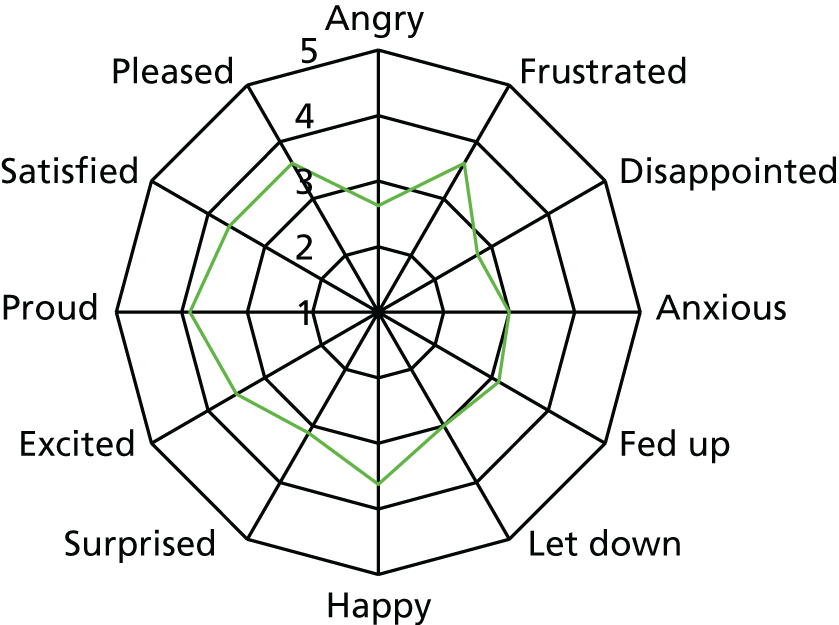
Our data show that positive emotions experienced by partners are in a similar pattern to CCG staff; however, partners experience fewer negative emotions than CCG staff (Figure 7). Nevertheless, the high SD of negative emotions such as ‘angry’, ‘frustrated’ and ‘fed up’ suggests that some partners experienced these three emotions frequently or very frequently during the commissioning process (see Table 5).
FIGURE 7.
Emotion (partner, mean): range from 1 (never) to 5 (very frequently).

System capability
System capability includes the following three constructs: knowledge-sharing platform, feedback seeking and organisation/team infrastructure. As shown in Figure 8 and Table 5, the relative high mean and low SD of the construct ‘organisation/team infrastructure’ suggests that most respondents believe that there is adequate and sound organisation/team infrastructure in place. Meanwhile, the low mean and high SD of the variable ‘feedback seeking’ show that respondents vary significantly in their views of how frequently CCGs seek feedback from partners and customers.
FIGURE 8.
System capability (CCG staff, mean): range from 1 (never) to 5 (very frequently). KS, knowledge sharing.

Co-ordination capability
There are two constructs, cross-functional interaction and participative leadership, in co-ordination capability. Figure 9 and Table 5 draw the mean and SD of these two constructs. The high mean and low SD of both constructs suggest that most respondents are quite confident that (1) the CCG general manager shows the characteristics of participative leadership and (2) there are cross-functional interactions within the CCG.
FIGURE 9.
Co-ordination capability (CCG staff, mean): range from 1 (never) to 5 (very frequently).

Absorptive capacity
The data in Figure 10 show that the pilot CCG frequently engaged in acquisition and transformation, with slightly lower frequency in assimilation and exploitation. Moreover, low SD across all four elements of ACAP shows that responses from CCG staff are close to the mean values, that is, they are frequently engaged in the four elements of ACAP (see Table 5).
FIGURE 10.
Absorptive capacity (CCG staff, mean): range from 1 (never) to 5 (very frequently).
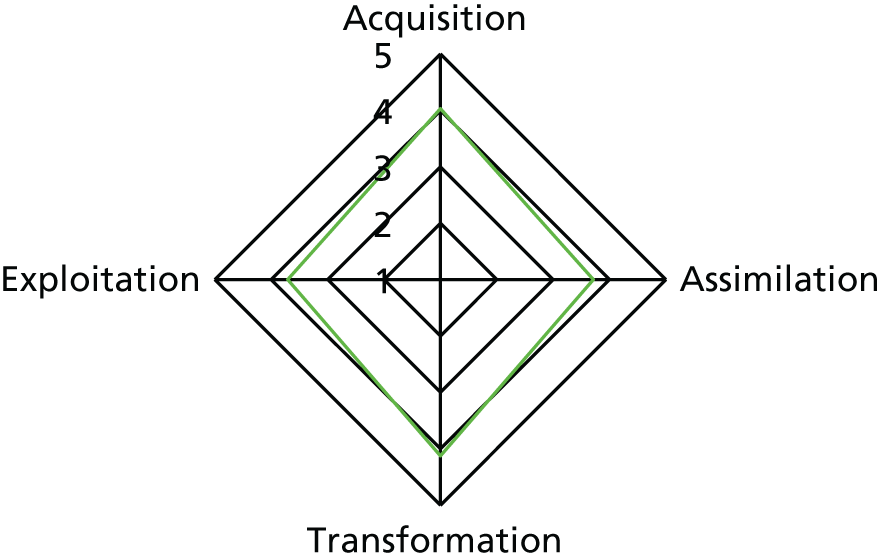
Outcome of commissioning
Outcome of commissioning includes the following four constructs: CCG innovativeness, quality of decision, use of resources and acceptability of outcome. As shown in Figure 11, innovativeness, quality of decision and use of resources were rated highly. Yet most respondents rated the acceptability of outcome as low, and its high SD shows great variance in responses in rating this construct (see Table 5). This result raises the question of why the acceptability of the outcome is rated so low. As a consequence of this result, we have added an open comment box to the tool, asking participants to clarify.
FIGURE 11.
Outcome of commissioning (CCG staff, mean): range from 1 (poor) to 5 (excellent).
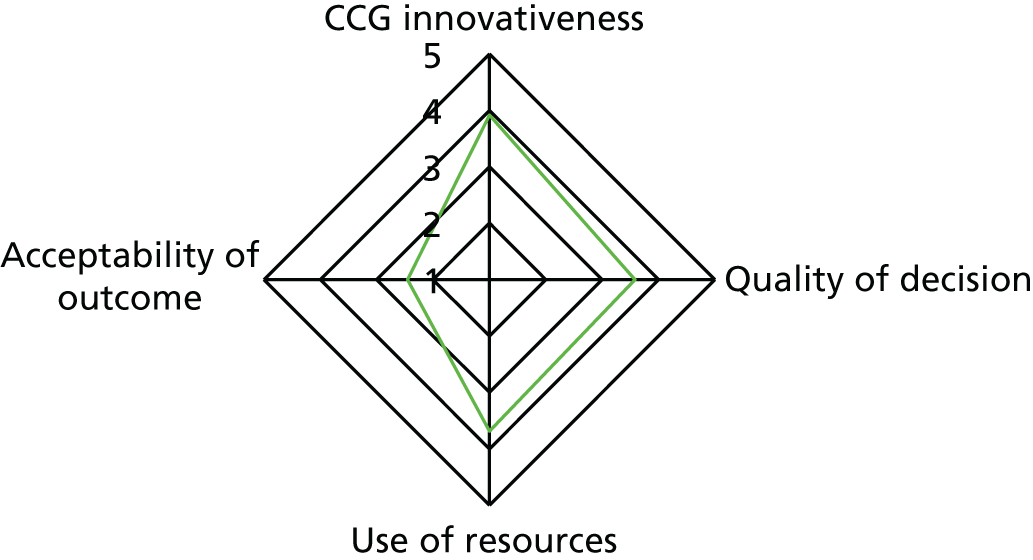
Similar results are shown in the partner survey, that is, most respondents rated the acceptability of outcome as low (Figure 12); however, the relative low SD of acceptability of outcome from partners suggest that partners’ answers to this question are quite close to each other, that is, low acceptability of outcome (see Table 5).
FIGURE 12.
Outcome of commissioning (partner, mean): range from 1 (poor) to 5 (excellent).
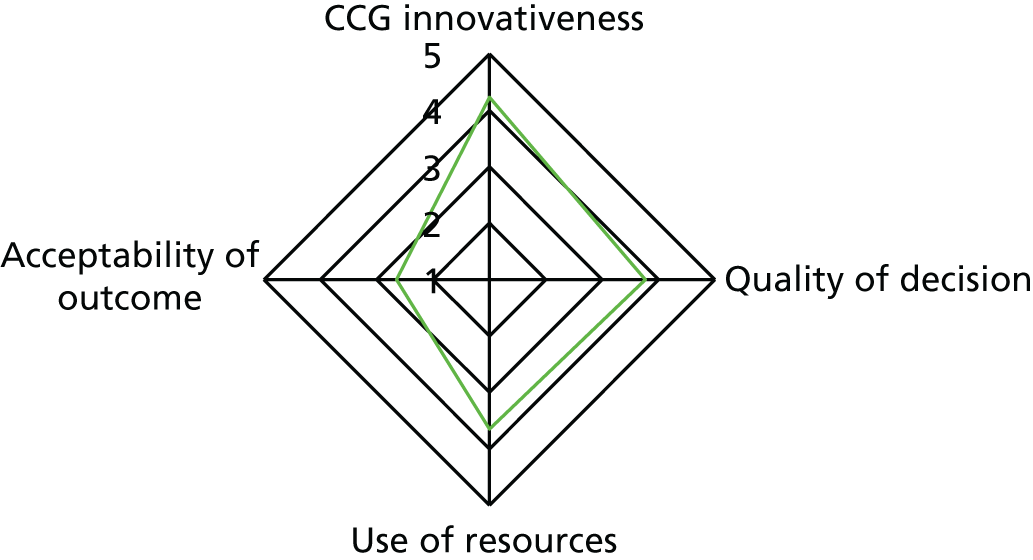
To sum up, this section analyses responses from both partners and CCG staff on the following aspects: socialisation capability (with a special focus on trust and emotion), co-ordination capability, system capability, the four elements of ACAP and outcome of commissioning. Nevertheless, the analysis should be interpreted in light of the limited number of respondents in this pilot group (10 partners and 8 CCG staff), as the high SD of certain constructs might be a result of the limited number of informants taking part in the survey.
Dissemination of the tool
We plan to disseminate our research in the following ways. First, we have obtained an Economic and Social Research Council acceleration grant to disseminate our research and enable evidence use in health-care commissioning together with another NIHR-funded research project at Warwick Business School. The objective of the grant is to convert academic findings of the two research projects into practice and make the evidence more accessible to practitioners. In doing so, we build an online professional development platform, which offers integrated resources for better commissioning decision-making. Specifically, the online development platform includes, but is not limited to, the self-development tool, case studies of the two studies, discussion boards, a process roadmap and links to relevant resources and blogs.
Moreover, NIHR Collaborations in Leadership for Applied Health Research and Care (CLAHRC) West Midlands (WM) and East Midlands (EM) (a translational health research initiative funded by NIHR) could be utilised to disseminate the tool, given the close relationship with NIHR CLAHRC WM and EM via steering group members. A possible way to engage might be to raise awareness of the tool in their newsletters and invite friendly CCGs from the WM and EM to participate in the self-development tool and write testimonials about the usefulness of it.
Chapter 10 Reflections of the patient and public involvement group
Introduction
This chapter reports on the PPI undertaken in this study within work package 3, focuses on the discussions of the PPI reference group and explores the nature of their contribution to the study.
The importance of PPI in research is briefly introduced in the context of the wider PPI evidence base. The reporting of PPI within this chapter is guided by the Guidance for Reporting Involvement of Patients and Public (GRIPP) 2 Short Form checklist to ensure that important aspects of PPI are considered. 145 Thus, the chapter includes aims, methods, results, discussion in relation to outcomes and discussion in relation to critical reflection from the study of what went well and what went less well.
Background
Patient and public involvement has become a key activity in health research and health-care settings nationally and internationally. Ideally, PPI is undertaken ‘with’ or ‘by’ patients or members of the public, rather than ‘to’, ‘about’ or ‘for’ them. It can mean patients becoming members of the research team, or part of reference groups, involved in key discussions and decisions and sharing their unique knowledge, expertise and perspective. For example, patients may be involved in identifying key RQs, planning study designs, selecting appropriate outcome measures, collecting data, analysing and interpreting data and disseminating and implementing results. The intention of PPI is to prioritise and create research that is relevant, acceptable and appropriate from the patient or public perspective. 146–148 It may be more likely to be implemented, creating greater impact on health and well-being, particularly if patients also have an active role in implementation. 149 PPI can also help to avoid waste in research by ensuring that it focuses on issues of importance and benefit for patients,150 so maximising the potential for democratic accountability to the wider public, who fund a significant proportion of research.
Patient and public involvement evidence base
The underpinning evidence base of PPI has evolved over the last decade, although significant challenges remain with conceptualisation, definition and poor-quality reporting. 77,78,148 Key systematic reviews have identified the beneficial impacts of PPI on research, researchers, patient and communities in health research and health services. 76,146 For example, impacts on research include the identification of patient-relevant topics, the grounding of studies in the day-to-day reality of patient experience, enhancing the relevance and appropriateness of studies and the identification of patient-important outcome measures. 146 For patients, benefits included being listened to, feeling empowered, increased confidence and self-worth and enhanced skills for self-management. 146 PPI can empower communities, improve service decisions, provide democratic accountability and contribute to higher-quality services. 74,75
At an individual level, patients involved in research can benefit in a number of ways that can also improve their experience of care and potentially benefit the provision of services. 91,151,152 People’s knowledge, gained through their experience of health and social care and research, is vital to developing the treatments, interventions and services required to tackle the health needs and priorities of the population.
Capturing involvement, contribution and impact
Understanding the contribution or impact of involvement in health research is important to the development of the PPI evidence base. Reviews have attempted to bring together evidence about the contribution or impact of involvement. 76,146 The poor reporting of impact identified from these reviews by Staniszewska et al. 148 has led to a greater focus on exploring the contribution that patients and the public make to research. In studies that include a reference group such as this one, this provides the opportunity to identify the nature of PPI contribution, which is the focus of this chapter.
Patient and public involvement in developing the concept
Although PPI has developed in the context of clinical and health services research, there has been less exploration of PPI within organisational studies. In relation to the PPI reference group, this conceptualisation is extended and the role of the reference group was in reviewing and considering study results, and developing a perspective on how effectively they perceived PPI to have been operationalised within commissioning, or how effectively PPI has contributed to critical review capacity within commissioning. Based on its perspectives of the study data, the PPI reference group also contributed to the development of the psychometric tool aimed to enhance the ACAP of commissioning groups.
The PPI evidence base does not always differentiate between the types of patients involved in studies, who are often poorly described. 148 This study included individuals with a wide range of experiences and expertise. Their contribution to the study included a public or citizen perspective but, importantly, was informed by patient and carer experiences.
The aims of patient and public involvement within this study
The aims of PPI within this study were to:
-
provide the critical review capacity in relation to study results, specifically to discuss emerging findings
-
develop understanding of the potential for PPI to contribute to organisational studies in health care
-
contribute to the development of the ACAP tool
-
identify the impacts of PPI in the study.
Methods
Establishing the patient and public involvement reference group
Patient and public involvement reference groups are a common and useful way of involving patients in research studies. They enable the creation of knowledge spaces where different forms of discussion and expertise can be shared and integrated. They aim for an embedded form of involvement during the course of a study, and can provide flexibility about contact points to ensure that meetings happen at the most appropriate times for the research process. They also provide a structure for contact by e-mail between meetings. NIHR INVOLVE [www.invo.org.uk (accessed 1 March 2017)] guidance states that ethics approval is not required for PPI in research, recognising that participants are not involved as research subjects, but as collaborators, contributing their expertise to different aspects of the research process.
An advert for group members was circulated via the University/User Teaching and Research Action Partnership (UNTRAP) (Warwick University PPI network) and via contacts and networks related to PPI and commissioning. The intention was to recruit public members who were aware of commissioning, understood the wider context, had experiences as patients or carers and could offer a diverse range of perspectives. Thus, the emphasis was on members of the public rather than patients, although members of the reference group had experience of both.
As the study aims and methods had already been agreed on prior to the establishment of the group, more active involvement was anticipated in discussions about the data, data analysis, interpretation and synthesis of data and in the drawing together of study findings within a wider context. A collaborative approach to PPI in this study was adopted, working with the reference group at key points as the study progressed, although the limitations of full collaboration when only using a reference group model are acknowledged, in terms of more-limited opportunities for contribution when compared with patient partners as members of a research team. 76 We utilised INVOLVE ways of working, which emphasise listening and collaborative communication.
Public involvement reference group
A reference group was established following telephone discussions with each potential member to establish suitability and interest. The reference group was made up of eight members of the public, although membership changed over time as individual circumstances changed. Members of the reference group had a range of backgrounds, including a nurse with a NHS background and others involved in midwifery, health visiting, caring, health strategy, research science in other areas, health research experience, business experience, clinical commissioning experience and experience with charitable organisations. A key focus was on enhancing the diversity within the group to include a broad range of perspectives. At each meeting, the research team presented progress, key issues or aspects of the data or the analysis that required discussion. The reference group met regularly during the study with e-mail contact between meetings. The group also interacted virtually, particularly when commenting on the developing ACAP tool. The group commented on the psychometric tool by e-mail or in the comments section as they completed the tool. The reference group was to be paid at the UNTRAP (University of Warwick PPI Network) rate of £20 per hour.
Capturing the contribution of the public involvement reference group
In order to develop our understanding of the contribution of the reference group, both within this study and more widely in terms of contributing to the evidence base of PPI, the members of the reference group agreed that the meetings could be recorded to ensure that their contribution was fully understood and we worked with them in reporting these contributions in peer-reviewed publications. This is particularly important in developing our understanding of the contribution of a reference group to organisational studies.
The transcripts from the reference group were reviewed to identify the nature of the contributions. The intention was not to analyse these discussions as data, but to review them in order to better understand the nature of public discussions in the context of the study focus. The reference group was supportive of this approach as it wanted to better understand its contribution to the study. Anonymised quotes from the reference group meetings are used to provide insight into the depths of the discussion.
Reference group discussions
Introduction
The intention of the reference group meetings was to provide a deliberative knowledge space, an opportunity for the research team to discuss findings with the reference group and to attempt coproduction of new knowledge. Researchers leading work packages were present during the discussion and provided important information about the study in their presentations, thus enabling members of the group to ask questions and to develop the clarity they require in order to contribute.
The members of the reference group had a wide range of experience and expertise, beyond what can be collected as research data. This included commissioning experience, PPI in research, PPI in service development and delivery and experience of the challenge of diversity and equality in PPI. This experience and the wider experiential knowledge of the reference group was vital in considering and reviewing study findings. Thus, the group members provided a rich, insightful perspective on the study, its methods, results, outcomes and wider implementation of the ACAP tool. Their broad experience of services from a range of different standpoints provided deep insights into the way in which data reflected the reality of current practice. In many respects, many of the group’s discussions reflected the concept of community validity,148 a wider context, based on knowledge, practice and a public perspective. Moreover, the group provided important review capacity in their interpretation of the data emerging from case studies. Using INVOLVE ways of working provided an effective context for ensuring good communication. The reference group was facilitated by Sophie Staniszewska, with research team members present during the meetings to ensure full discussion.
The first section reports the wider contextual issues that the reference group discussed, and the second section focuses on the development of the ACAP tool.
Contextual issues in commissioning
The reference group discussed a range of broader contextual issues of relevance to commissioning, thus demonstrating their valuable collective insights. The discussions demonstrate the experiential knowledge that reference group members brought to the study, based on a wide range of expertise, experience and insight. The reference group drew on this individual and collective perspective in discussing all aspects of the study, but it was particularly valuable in discussing the development of the ACAP tool, presented in the next main section.
Although the focus of the reference group was on all aspects of study data, it was particularly interested in PPI within the commissioning process. It noted the challenges that still exist within CCGs’ understandings of PPI and its implementation, particularly when perceived as a very different way of working:
I’ve worked for many years in community engagement, patient involvement and equality and diversity and I have constant battles with the organisations I’ve been in that even though the organisation may have declared a commitment to patient involvement it doesn’t actually happen in practice. It’s not because people conceptually don’t get it, although some don’t, and it’s not because they deliberately resist it, but sometimes the whole idea of it seems huge.
Meeting 1, p. 18
Such broader insights provided a valuable space for the research team to discuss study results from the first phase of case studies. Insights from the reference group provided both challenges to and explanations of the results of data analysis, helping the research team to understand why PPI may be difficult to operationalise within a CCG setting.
In discussing the case study data, the reference group noted that PPI within commissioning seemed limited, which created concerns and reinforced the need for the ACAP tool to include aspects of PPI in ways that would enable the CCGs to develop more appropriate PPI practice:
I mean I agree that there has to be a role because I think one of the things that comes out of the material that we’ve certainly looked at so far is that most of the requirements or the interests relating to patient public input seems to me in most of the places you’ve looked at to be either marginalised or certainly not looked at as if it’s anything essential to the issue. But I think from our point of view I do think we have to find a way of identifying and defining very clearly what we mean by, if you like, what I would call the public interest and where that’s located within CCG networks.
Meeting 3, p. 6
The process and purpose of commissioning
The reference group discussed the process and purpose of commissioning more broadly, with a particular focus on its contribution to creating patient benefit. The reference group wanted to ensure that the research team was mindful of this ambition in analysing study results. It was also within this context that the reference group considered the ACAP tool, discussing how it would provide CCGs with critical self-evaluation capacity, but with the ultimate ambition always in mind: that of creating better outcomes for patients through high-quality commissioning:
I think is to start out saying very clearly [that] the point of having CCGs was to improve the commissioning in the interests of . . . for patient benefit. And then where this project stands in terms of saying, well to do this we have to look at how do they gather, use, transform information, maybe with some . . . I mean maybe you can find some anecdotes which indicate how by better information the patient outcomes are better. I think that has to be the starting point. I think if you start out saying we’re doing some, you know, methodological exercise to validate something then nobody will be the slightest bit interested.
Meeting 2, p. 6
What’s the outcome? So back to your question I think, what the end-user or the public can judge is the outcome of this process. So maybe not necessarily the process but the quality of it or what comes out of it and that takes us back to the question of what are the criteria by which we know that a CCG has done a good job. How would I as an end-user know that this CCG has done an excellent job, a mediocre job or a bad job?
Meeting 3, p. 7
The reference group recognised the importance of responsiveness in commissioning and the significant cultural changes needed to deliver services with flexibility, responding to patient need, which the reference group regarded as being of key significance. It commented that such system responsiveness to need could mean less reliance on data to be used at one time point in the commissioning process:
I think it’s about commissioning more flexible services so less reliance on data. You know, society’s changing very rapidly, but you’ve got the flexibility in services to respond to those changes and they’ve got a degree of autonomy and latitude in the decisions they make.
There’s a cultural shift needed in the country because we’ve still got that GP–hospital axis fixed in our heads and what’s trying to happen is that we move services closer to the community, that we devolve decision-making more locally, that we get a range of services like response and reablement teams and that sort of thing.
The reference group did not underestimate the challenges in delivering such cultural change in service responsiveness within commissioning, but underlined the need for the research team to adopt a broader view of how commissioning operated, which accounted for the key focus on patient need.
The reference group also included its perspective on decommissioning of services, particularly in relation to the types of information used for such decisions as legal aspects of service change:
One point I’d like to raise with that question around scaling up or decommission services is that in many instances services are decommissioned without relevant information actually being used and also meeting legal obligations as well. I mean I mentioned earlier about if a public authority intends to decommission a service, then basically they’re supposed to use information to be able to ensure that they’re going to sort of mitigate the impact of that on protected characteristics, but generally a quality impact assessment isn’t actually undertaken. A decision is just basically made on cost. So I’d like to see how we can put that in somewhere if it’s possible because that’s a legal obligation, not carry out and report the impact, but to use relevant information to review or enable that decision.
Meeting 3, p. 36
Generating public interest in commissioning
The reference group discussed the importance of commissioners engaging with their different publics, but recognised that this might be challenging because as an activity commissioning is one step removed from more direct patient experience:
I mean, yes, you’re right, it’s very difficult to get people interested in commissioning; it’s very difficult to get patient/public involvement in that whole set of processes that precede the delivery of a service because it’s the service and how people experience the service which they can feel comfortable quite often without relating to. But that whole process that leads up to it is difficult.
Meeting 2, p. 4
In discussing the diversity of publics, the reference group recognised the importance of including groups whose poor experiences can motivate them to get involved in commissioning:
In [location] for example there’s a very active group of people in say the South Asian community and some of those people are actually involved because there’s a whole history of problematic issues around service delivery for South Asian people. Some, very few have got an interest in that.
Meeting 1, p. 4
In generating interest in involvement, the reference group also recognised the need for early embedding of patient perspectives in the commissioning process and not just as a consultation activity at the end, recognising the significance of commissioning as an activity in delivering high-quality care:
Yes, I’m intrigued [talking together], because it’s commissioning and everybody’s connected at some point and affected by it.
I think you’re right. I mean I’ve sat on many user and other groups; coming along at the, you know, sort of the last consultation on something and expecting to have an influence is a waste of time.
Meeting 2, p. 32
Understanding who contributes to commissioning
In discussing PPI in commissioning, the reference group discussed the types of individuals and organisations who may be best placed to contribute to discussions about commissioning within CCGs, and whether this should be the patient who experiences a service or the organisation that might represent their views:
I think what you might have to do is to take a step back from that to those groups involved in the service user movement that start out from a position in which they have an interest in the way in which services are commissioned, not necessarily the people who directly experience those services, but the organisations. So I’m thinking, you know, there are lots of organisations; we’re concerned mainly with older people and, you know, there’s lots of organisations that are concerned, or subsets of organisations are concerned.
Meeting 2, p. 4
The range of relevant types of organisation was discussed by the reference group:
One point I wanted to raise was around how they actually get information from the voluntary, community and charitable organisations. Some of them might fit into the category of providers, but some not.
Meeting 3, p. 19
The reference group recognised the importance of community leaders in commissioning as well as the critical role of carers in providing observations that contribute important knowledge:
I call them mediators, because you know, we have to be realistic about in some parts there is a realistic political issue, you know, about what are perceived to be if you like, white or non-ethnic organisations approaching other people. And I think you’re right, those people can be seen as mediators.
Meeting 2, p. 7
Can we stop talking about patients and call it patients and carers, because the carers have other observations which might be valuable and they do tend to get lost.
As the ACAP tool developed, the reference group identified a narrow group of stakeholders who filled in the questionnaire (the tool):
I noticed that the questionnaire is directed to certain groups or members within the CCG network, and I don’t see there any reference to any patient public members who for example might be part of an executive committee, and who actually could be parts of the consideration etc., on a decision of the kind that you’ve illustrated. So I’m just asking how is that going to be treated, because I think there are two issues. One is we need to know what impact if any people with some responsibility for PPI have actually had in commissioning process, but secondly there are certain legal obligations on CCGs to actually do that.
Meeting 4, p. 4
The reference group recognised that certain skill sets were required for effective PPI in commissioning:
I think therefore, I think [name] is right in that there’s a certain knowledge, experience and skill set which you need to be able to contribute to that effectively, and it doesn’t always match I don’t think with the groups that are involved in . . . I mean some will, but some won’t.
The location of power in decision-making and commissioning
A key theme that emerged across many reference group discussions was the location of power within decision-making in CCGs, particularly in relation to the role of PPI. In reviewing the emerging themes from the case studies presented in the meetings, members of the reference group reflected on the extent to which case study data indicated consultative or collaborative involvement within CCGs, expressing their concerns about the passive approach to PPI:
I’m wondering if I’ve missed the point because all of these quotes are still the ‘to’ model and not the ‘with’ model. So we’re still talking about systems applying interventions to patients. It’s not patient centred at all and I’m not hearing anything in the text that you’ve chosen that has any support for a perspective.
Meeting 1, p. 13
In response to this discussion, researchers commented that, with the exception of a small number of case studies, data from case studies indicated relatively limited PPI in commissioning and, as suggested by the reference group, reflected a system-based perspective rather than a patient-based perspective.
The reference group challenged the current approaches and argued for a change in the location of power for the patients, public and organisations involved in commissioning:
I think there’s a cultural shift needed in organisations about the degree of autonomy people have at different levels and that flows through into the relationship you have with the voluntary sector, a more mature understanding of the role that the voluntary sector have and the fact it shouldn’t be on the cheap because I think there’s a lot of that attitude.
Meeting 1, p. 20
The reference group reflected on the location and exercise of power within current commissioning. Concern was expressed about the reality of commissioning and the limited opportunities this may represent for PPI to have a significant impact on decision-making:
I just think in terms of individuals within CCGs it’s the commissioning managers that actually have the power. And when I say ‘the power’ – because they’ll be the ones who are actually given responsibility for redesigning a service or coming up with what a new service should actually look like and it’s about how they then engage with patients and members of the wider public to form that service to be something that meets needs in that local area. You know, one of the issues that I often see is that you don’t necessarily get that engagement. You have somebody who’s been given a deadline to, say for example, redesign a service and they sit at their desk and they write that document and then present it.
Meeting 3, p. 11
This prompted further discussions among the reference group about how the ACAP tool will tap into the decision-making process, in order for a CCG to review its capacity in relation to PPI:
Or is it a serious question within the tool? How far have you balanced these views in this process?
Meeting 3, p. 13
The reference group was very aware of the potential for PPI to operate weakly within commissioning. Models of good practice were discussed, particularly as case study data had been limited in demonstrating strong, effective PPI. The reference group has a very clear concept of effective PPI and its impact:
Yeah. I think that happens quite a lot when you’ve got a serious PPI consultation. You actually change your views about who you’re talking to and what you’re talking about and I think that might be true of providers as well. I’m less experienced in that area, but I think that might be true.
Meeting 3, p. 35
In developing the ACAP tool, the reference group felt the tool should consider power and other forms of influence:
Power and influence is really important conception, because a lot of the absorptive capacity literature ignores power and politics. And we know in health care it’s absolutely rife, so you know, just let’s make sure that you pick up on that.
Meeting 4, p. 20
The nature of evidence, knowledge and insight for commissioning
Commissioning depends on a range of evidence, knowledge and insight and the reference group discussed different aspects of this. They understood and valued a range of different forms of evidence and knowledge. However, they were concerned that some forms of knowledge may be less valued in commissioning, particularly patient experience data and how they are used to inform service provision:
All that data’s collected around accountability and financial accountability. It’s not collected around the patient experience. I don’t see the evidence for that.
Meeting 1, p. 29
But can I just say I work with a hospital trust which routinely collects from bedside electronic devices, sort of touch-screen devices all over the place, quite a bit of information from patients about all kinds of dimensions of the patient experience. What I found quite interesting is that that information has just simply not appeared anywhere in my local Clinical Commissioning Group’s decisions and so I have to ask the question ‘So you say you’re interested about patient experience?’. Now yeah, you can raise the question . . . so the only place that it ever appears is in the PPI report from the relevant hospital trust.
Meeting 1, p. 29
In addition to content of evidence or knowledge for commissioning, the reference group was concerned about the impact on aggregating data in different ways. They were concerned that the depth and granularity of individual patient experience could easily be lost:
I’ve found in patient reference groups – you’ve got a small group of people sometimes that are pitching at the strategic level. You know, they want to get in there and they want to find out where the money’s going and who’s making these decisions, whereas other people are concerned about what colour the reception area in the GP practice is, and often those people are drowned out, but that atomised, individual perception of my pathway and where it’s going right and where it’s going wrong when aggregated out could give you very rich information; and often those stories are lost in sort of statutory data sets and often there’s a cycle to those, so it’s only on a 3- or 4-month cycle that you’re getting a pattern come through that you can actually start to interrogate and look at closely and it’ll be 2 years down the line before you can do anything effective really.
Meeting 1, p. 30
Identifying key questions for commissioning
The reference group identified that a key challenge for CCGs was asking key questions that direct the appropriate use of evidence and knowledge. Without these key questions, decisions may not be focused on issues of importance to patients, unless there is strong PPI:
The ability to ask the key question and that’s where your data comes in. You know, the key question centres around the information that you develop from your data and it seems to me that there’s . . . What I don’t understand and have never understood all the time I’ve been thinking about PPI is how you sift patient involvement into something that is a key question as opposed to a trivial question. I’ll illustrate. A patient reference group in a local GP surgery that I know about is very exercised by the appointment system and some of the stuff I know about that practice I think the appointment system is the patient experience of a subgroup who are very concerned that they can go and they’ve hijacked that agenda, but at the same time there are other patients in that group who are asking some really important questions around provision of services at that GP practice and for me it’s how you capture and identify the key question because that is where the challenge arises and that’s what our real involvement is – is to challenge the service to say ‘this is the question that is the important one that you need to be thinking about’.
Meeting 1, p. 24
Identifying missing evidence
The reference group was able to identify areas in which data appeared to be missing within the case studies. One key area appeared to be the relatively limited PPI undertaken within many CCGs, which made the identification of good practice for the study more challenging. The reference group felt that this was an area in which its collective knowledge of standard and practice expertise would be valuable, particularly as it was concerned that such missing data may have an impact on the content of the ACAP tool, leading to the omission of key aspects of PPI (meeting 1, p. 8). As a result of this discussion, the reference group discussed the need for the ACAP tool to differentiate between CCGs that embraced PPI and those that did not:
How much of this depends on the willingness or desire of the people in a professional capacity to involve, say, PPI for instance? It may be that they don’t realise the full implications of their role as a doctor of saying patients are patients, I’m not sure they understand . . . in other words, there must be a difference in the performance between those who are open-minded and are willing to try and those who [don’t].
Meeting 2, p. 16
The reference group also questioned the capacity of CCGs to be able to reflect effectively on the quality of their PPI, which is particularly pertinent because of the variable efforts of delivering PPI within CCGs in the study. They also questioned whether or not those with excellent PPI would be able to recognise it, if it was truly embedded:
Can you have situations where you’ve got excellent PPI, but nobody there knows they’ve got excellent, it’s just because it’s second nature to them the way they’re going to work, they don’t know it’s good, it’s just the way they do things?
Meeting 2, p. 19
The capacity of the CCG to be a lone self-reflector was queried by the reference group, which highlighted the need for evaluation from partner organisations as part of a wider approach to assessing their effectiveness:
Can I just raise some issues about some of the evaluative terms here . . . I read this and I feel uneasy about the whole . . . so for example, if you say this is able to be effectively applied . . . well, what is effectively, I mean, and you know, who are you to judge whether you’re effective or not. So I just wonder how . . . and you can go through it, are able to exploit partners on it. Well so you may say, but the partner might have a better judgement of whether you can exploit it or not.
Meeting 2, p. 28
Data collection systems and data quality
The reference group reflected on the nature and type of data collection undertaken by CCGs, reflecting its knowledge of data use within commissioning:
Yeah and that’s just one example. So there’s a whole range of ways in which they can gather that information. You may have the local voluntary organisation anyway that kind of supports, infrastructure organisation from the voluntary sector in each city . . .
Meeting 3, p. 21
The reference group raised concerns about the breadth and reach of CCGs in relation to their capacity to find the information in order to make good decisions. The reference group reflected on the need for CCGs to prioritise certain forms of knowledge to make decisions:
What we’ve got is front-line knowledge that needs to be pushed upwards for service delivery rather than relying on a systems perspective and statutory data.
Meeting 1, p. 18
The reference group understood the different systems that might operate in commissioning and how the focus on a systems approach might be limiting a more patient-centred approach:
I’m really, really concerned that this is getting embedded in a systems perspective and that you’re describing three systems here – a volunteer system, the health-care system and social care system – whereas if you suddenly looked at that anecdote as patient-centred care then your perspective changes completely. And your comments about data keep us in the systems paradigm and that anecdote is crying out for a paradigm shift.
The reference group also discussed the quality of data that CCGs may be working with and was concerned with how this could be evaluated. For example, the ACAP tool could ask about aspects of quality, such as ensuring that the most-recent guidance is being used:
‘Are you using the most up-to-date guidelines? Are you using the most up-to-date formularies?’ You know, the basic structural stuff.
Meeting 3, p. 15
In summary, the discussions between the reference group and the study research team provided invaluable opportunities for the research team to explore the case study data and the wider context of commissioning, and to work with the reference group to interpret it and to consider its implications for the development of the ACAP tool.
Developing the absorptive capacity tool
The reference group drew on its discussions about the case studies and its wider contextual knowledge and expertise to inform discussions about the development of the ACAP tool:
I mean for me the strength of the group is around, particularly for the next phase, is ensuring that tool that is developed has that sort of relevance, has that acceptability and is appropriate for CCGs, but has that built-in patient/public element within it, which is very easy for it not to have if a group like this isn’t involved.
The group acknowledged that the research bid had set the aims, which could not be changed at this point, but it wanted to test the rationale for the development of the ACAP tool.
Concepts and conceptual frameworks
The reference group was interested in the concepts and frameworks that influenced research thinking in the study, particularly in relation to tool development.
The reference group highlighted the importance of tacit models that may underpin tool development and the need for the research team to be clear about what was influencing their thinking and to understand how this may manifest itself in tool construction:
I think the problem is that in asking the question, who do you send it to, you’re already driving this tool down the direction of being a model and setting up suggested ways of running your consultations around your CCG community and I’m not sure that you actually want to do that because I think . . . quite different models out there, because different areas need to respond differently to their population needs. That’s the strength of local commissioning.
In discussing the development of the ACAP tool, the reference group noted the challenge of the language used when discussing conceptual frameworks such as ACAP, which were acknowledged as potential barriers to a full discussion, prompting the research team to explain concepts in more accessible ways:
Could I ask . . . can I come up, or no, can you come up with a more friendly word . . . I get stuck somehow on this conceptual work, you’ve said it so many times. It would be nice if when you say conceptual framework, if there was a buzzier, more easily understandable word for people like me, or perhaps even people in your questions. You actually put it very well about what concept means.
Meeting 2, p. 12
In considering the nature of the tool, the reference group queried exactly what was meant by information (that would provide the content for tool dimensions and items) and the importance of ensuring that aspects relevant to patients were captured within the dimensions and items included in the tool:
There’s a big debate then in what do we mean by information? . . . Certainly from my point of view what we’re interested, or what we think we can contribute, mine is this, that whatever the shape of that tool happens to be, whatever the dimensions, the wider dimensions happen to be, I would like to feel that we can feel reasonably satisfied that in its various forms the patient interest is going to be captured.
Meeting 2, p. 13
In discussing the content of the tool and its aims, the group drew on their wider knowledge about commissioning and the current standards to consider potential tool content:
We need to perhaps cover the domain three of the World Commissioning Standards has a list of statements about what world class, whatever that might mean, world class commission would look like. And it gives a series of statements about the things that would be involved in it.
Identifying dimensions
Following discussions in which the research team explained key concepts such as ACAP, the reference group was able to discuss and engage with the conceptual framework and dimensions of ACAP and the developing ACAP tool. These explanations and discussions were vital in ensuring deliberative discussion that supported explanation of key concepts:
I think if I provide a bit of context for assimilation. The assimilation dimension is important for the reason that there’s a path dependency. So you tend to rely on the same sources of data all the time and just stick to it and ignore sources of data that you may not normally tackle, particularly new insights and assimilations about that. Often the new insights they’ll not appear for you’ll sideline them . . . and that’s what this dimension’s trying to get at.
Meeting 3, p. 24
The reference group was able to test this conceptual framework through its discussions, and apply it to the developing ACAP tool, often questioning the way the tool tapped into a dimension of the overarching concept or dimension of ACAP:
Yeah, I think the key thing about acquisition [dimensions of ACAP] if we’re looking at it in this context is precisely how open are you, it seems to me, receiving and being aware of information that could be of use to you. That’s about it, isn’t it? That’s what we’re really saying, isn’t it, however you phrase it. That’s not very well phrased, but isn’t that what acquisition is about? ‘Are you open or are you closed?’ I guess is what we’re really wanting to know.
Meeting 3, p. 23
In reviewing the dimensions, tacit models were clarified, and the adequacy of the item in successfully capturing the intended concept was reviewed:
Your subdimension is develop a shared vision, but your verb is ‘discuss’ and there’s a big leap between developing a shared vision and discussing. That question doesn’t capture the subdimension for me.
Meeting 3, p. 26
The reference group looked for evidence of how key dimensions of ACAP were represented and operationalised in the ACAP tool:
Well, it’s about exploitation. So what do you make with the information that you have acquired, assimilated, transformed? Has it taken you a step further? And for that you need to take into account both positive and negative feedback on the process, on the [XXXX], on the weighting, on whatever it is.
Meeting 3, p. 35
The reference group discussions ranged across topic areas they would expect to see in the ACAP tool. They were interested in areas that had not been identified by the research team and raised them for discussion:
Being totally cynical on this first item, you’ve put a further category ‘from literature data’, but a further category that’s missing for me . . . If this tool’s going to be used in a specific commissioning area rather than a generic commissioning area, one category that’s missing in acquisition is ‘how far are you doing what you should be doing?’.
Meeting 3, p. 15
Discussions about dimensions and items sometimes led to changes in the ACAP tool, which the team was able to discuss with the reference group. See Chapter 9 for more details.
Development of items
The reference group discussed the specific questions that would be used by those completing the ACAP tool. The nature of specific questions in relation to the underpinning aim was scrutinised by the group, which provided some important challenges for the way CCGs may be operating based on their past experience:
So how do you ask the question ‘How do we bury information in this organisation?’.
Meeting 3, p. 24
The reference group was able to review the ACAP tool for understandability:
I don’t understand the question.
Meeting 3, p. 28
What do you mean by comprehensible data?
Meeting 3, p. 30
The reference group was able to identify redundant or less-helpful questions. For example:
My view is that actually the critical questions there are 4, 5 and 6. I don’t really see how you could actually assess that in any useful way, but the critical one is ‘how frequently do you scale up, decommission and review services based on information?’ and then I think the question of whether you improve your information collection. So my own feeling would be that some of those other questions are really redundant or not very useful questions to ask and maybe 4, 5 and 6 may be expanded a little bit in some way.
Meeting 3, p. 36
During discussions about the ACAP tool dimensions and items, members of the reference group discussed the possibility that, even when information is collected from patients, it may not be used to aid decision-making. The reference group discussed how item wording might need to be changed to account for this possibility:
That presumably must mean that professionals don’t take notice of what the PPIs are saying. When you say deaf ears presumably you’re meaning that the information that the PPIs give isn’t taken notice of or isn’t incorporated for whatever reason.
Meeting 3, p. 34
So even if it’s asked and provided, it still doesn’t influence the decision-making process. But yes, that one has to be rephrased.
Meeting 3, p. 34
As the ACAP tool developed, the PPI reference group was involved in reviewing each of the developing items, particularly focusing on item meaning, understandability, flow of questions and whether or not they tapped into key concepts of interest:
Is there a specific reason for question . . . for the order of the questions there, or is that just how it’s been written down? Question 9 seemed to me to be sitting more naturally next to question 12.
Meeting 4, p. 17
We have no power questions in here at all, do you?
Meeting 4, p. 17
Reference group members also identified items that they felt were important, based on previous discussion within the group:
You’ve asked how far we modify our objectives in light of change of circumstance. Can we ask how far we modified our behaviour in the light of changing circumstances? In other words it’s flexible organisation.
Meeting 4, p. 28
Selection of response options
In addition to discussing the content of the ACAP tool, the reference group also discussed the response options that were suitable for different items:
The answer therefore to my question is in that column the metric is frequency because . . . and there’s the reference. This makes it a very nice evidence base and if I’m looking at the tool and I want to believe in this tool that’s something I would look for. So you’ve defended that metric there, but I’d like to see a metric against everything that you ask because I’d like to see defence of the metric for how often, how long, how deep or whatever you’re using within that question.
Meeting 3, p. 16
Clarifying the intention behind the question was important in ensuring appropriate response options for the reference group:
This question here, ‘how frequently does your CCG involve other external providers in service design?’. If you just take what happens today, what is the range? Is it a lot or just some specific ones that they’re experienced with?
Meeting 3, p. 32
I know what’s bothering me because I’ve suddenly realised that I actually want to put different words in there. It’s not how frequent but how common is it for you to do this. In other words, never . . .
Meeting 3, p. 32
The reference group challenged the team on some of their response options and offered solutions to the challenges they identified:
So could we get around that by having plenty of open-ended boxes where we say, and now can you please explain everything [unclear at 00:27:39]. If you feel that you have not been heard in a process you might actually put down a few notes and say, yes you know, we did contribute but we weren’t heard, or something . . .
Meeting 4, p. 8
The reference group discussed the weighting of the tool and was keen to ensure that the PPI element within it was reflected appropriately within the number and nature of items:
The problem with a psychometric type approach too is that you don’t get the necessary weightings in there sometimes. PPI is something that’s always under weighted and is always tokenistic or very frequently tokenistic and so is it possible to reflect that at this?
Meeting 1, p. 9
The reference group discussed the way in which the ACAP tool would capture key concepts. For example, one member of the reference group highlighted the need to reconsider the concept of frequency in the way the questions were asked and in the response options:
Well, I would say the frequency isn’t as relevant as what you actually do with it.
Meeting 3, p. 15
So if that’s in the next dimension . . . But I’m not sure if here how frequently is . . . I wouldn’t call that necessarily critical. I mean you’ve got to interact some time, so it could be, you know, ‘Do you? Do you do it?’ without necessarily being too bothered about how frequently you do it.
Meeting 3, p. 15
That’s a data analysis issue though, isn’t it, because I picked up a more generic issue about Tony’s point which is that there should be a metric on there. Is frequency the right metric? You say no, it’s not necessary and it’s possible that frequency is actually a metric that is observed, but actually it’s the back-room conversation when everybody leaves. It’s the quality of the conversation, not the frequency in which that happens.
Meeting 3, p. 15
Practical utility of the ACAP tool
The reference group was interested in many aspects of the ACAP tool in terms of its practical utility in enabling CCGs to enhance their ACAP. The group discussed the way in which the ACAP tool would be used, who should complete it, how it should be completed and who would be seen as stakeholders in the process:
What I was going to say is I think one thing we must do very early is to nail very precisely what we mean by the stakeholder interest groups and client and who we mean by end-user.
Meeting 3, p. 6
The importance of third-party groups, which emerged from the discussion, was in their significant and unique perspectives on commissioning that the research team needed to consider:
So that also then takes us out into I think a third group of, if you like, public interest stakeholders not as individuals, but of groups that would be working or supposed to be working with the CCG to look at its absorptive capacity. And again just based on my own experience, in Bury, which I’m familiar with, we had and we still have a protocol in operation in which the CCG agrees to share and collect information from Health Watch, for example, and possibly other bodies.
Meeting 3, p. 7
Members of the reference group were aware that knowing who was involved in CCG business was not necessarily the same as knowing who has influenced decision-making:
I think it would be. Actually I asked at one time through our CCG as part of its audit on decision-making, to actually do precisely that. When we got committee papers back I asked, could they please just list who has been part of this decision-making process. I didn’t get anywhere on that.
The reference group was interested in whether or not, in addition to its use as a self-development tool, CCGs would be able to use the tool to benchmark against each other as a way of enhancing the quality of the commissioning process:
So would they be able to see . . . how would they be able to compare their CCG to [another] . . . yeah, but how useful is it not be able to compare sort of like with like, if you see . . . do you know what I mean? If you’ve got a CCG in say [X], could they not compare somehow with a similar sort of CCG in a different part of the country say with a similar population?
Meeting 1/2
Will CCGs be benchmarked? In other words, it almost looks as though everyone measures everything in the States [USA], performance and impact and all that sort of stuff, and if they measure themselves using this tool, CCGs, that then has a potential to benchmark where different CCGs are measured.
Meeting 3, p. 2
The reference group understood that patients experiencing the service would not be completing the tool, but they still queried the extent to which patient perspectives would be understood by those completing the tool:
Do the managers understand what patient voice is?
Meeting 1/2
The reference group sought clarity and reassurance in relation to its generalisability to areas not included in the development of the tool. This prompted discussions that helped clarify the way in which the research team approached generalisability, and how it would be generalised to other settings was discussed with the research team:
Can I just have a point of clarity? So is it just focused on unplanned, elderly care admissions or not?
The reference group was interested in how well the ACAP tool could capture voices that are rarely heard:
If we go back to the first part, about the people whose voices we may not hear in this, which was the first part, that’s a different . . . that isn’t so much picked up in the questions, it’s the way we distribute this questionnaire isn’t it?
The discussions with the PPI advisory group also provided a source of encouragement for the research team as they recognised how the instrument had developed over time:
Well I don’t know how other people think, but I’m liking the shape of this questionnaire. I’m understanding it’s much progressed from the last version isn’t it?
Meeting 4, p. 19
Creating wider impact of the ACAP tool
When the reference group discussed the development of the ACAP tool, there was significant interest in creating wider impact through the use of the tool. The reference group suggested additional activities, for example considering how other organisations might use the tool:
I’m just wondering if . . . do you think, [name], that organisations like Health Watch might use something like this to almost review capacity locally, how things are working?
Reflection on process
We have included two researcher reflections and two public member reflections on the PPI in the study.
Researcher reflections
It would have been paradoxical for the research study to focus upon the acquisition and use of PPI and patient experience evidence by CCG-led commissioning networks, and then not apply this principle to our own research efforts. However, encompassing PPI within a study that is focused upon an organisational issue about mobilising knowledge for commissioning, rather than informing service improvement around a clinical condition, is challenging. It requires a different set of criteria than that commonly applied to the selection of PPI representatives. Indeed, the issue of representativeness becomes less important compared the expertise and articulacy of PPI representatives. Given the ‘back stage’ role that CCGs play in the delivery of health care, and that, in essence we were examining a matter of strategy, we carefully selected PPI representatives that had experience of, and understood strategic decision-making within a complex system of interdependent organisations. Their contribution was one that provided ‘grit in the oyster’ for our analysis of knowledge mobilisation. Their influence extended beyond analysis of use of PPI and patient experience for commissioning decisions, to inform our broader analysis of the way that CCGs were working, such as GP involvement and use of their knowledge in decision-making. Specifically, PPI representatives helped detail our psychometric tool to enhance its face validity with potential users of the tool; e.g. CCG commissioning managers. Given our difficulties in gaining traction upon CCGs to influence their use of knowledge, PPI representatives are likely to prove particularly useful in diffusing our research more widely beyond those CCGs participating in our study. These efforts are ongoing.
Here is my observation: I am a research fellow for the ACAP project since November 2015. I found that the research team and PPI gelled well throughout the project. PPI members have been really helpful with their abundant experience and in-depth knowledge about the actual commissioning world. As a matter of fact, a few items in the self-development tool were inspired by these discussions. The PPI members were also helpful in pointing out any management language in the tool and suggesting terms that are understandable to practitioners.
Public reflections
I am a carer involved in health-care research at various universities. I have been a member of the ACAP steering group since the start of the research. The subject matter was new to me and I found parts technically challenging. However, this was largely resolved by the fully democratic management under the guidance of the chair and active listening by the rest of the steering group. I felt comfortable about asking questions and that I was listened to as an equal with the academics and received clear explanations. I now know more about the process of knowledge transfer, hence stimulating ideas how to implement the findings into health-care management. This project is an example of how PPI should contribute and, in my opinion, sets a ‘gold standard’.
I felt that the process was very inclusive and that we were listened to not spoken at. It was not a tokenistic process on the part of the researchers. The varied backgrounds of the PPI members was valuable. I felt that my time was well spent, comments taken on board and I feel that we contributed fully to the report and the development of the tool.
Discussion
The PPI in this study aimed to provide the critical review capacity in relation to study results, specifically to discuss emerging findings. The reference group provided an effective context in which to discuss how commissioning was operating, to create new challenges and to discuss the validity of identified barriers. As such, they provided a form of community validity. The study also aimed to develop understanding of the potential for PPI to contribute to organisational studies in health care. The contribution and impact clearly demonstrate the significant potential for PPI to grow in such studies. A key area of contribution was the development of the ACAP tool, particularly in relation to the dimensions and items, in addition to the practical utility. The research team will be working with the reference group to publish the PPI aspects of the study.
Chapter 11 Conclusion
We set out to explore how a health-care commissioning organisation might enhance its critical review capacity, so that it uses relevant knowledge to inform decision-making about what might constitute an effective service intervention. Theoretically, we took inspiration from recent calls for its application to health-care settings, and applied the concept of ACAP to examine commissioning decisions to address a health policy problem of global significance, reducing needless admissions of older patients into hospitals.
Our application of the concept of ACAP highlights that there are four stages of mobilisation of knowledge relevant to commissioning decisions: acquisition, assimilation, transformation and exploitation. Each stage is interdependent on others; for example, if an organisation merely acquires and assimilates relevant knowledge, then PACAP is not realised, or vice versa, and if an organisation is effective at transforming and exploiting knowledge, this is of little use if it does not effectively acquire and assimilate knowledge in the first place. Thus, a commissioning organisation must attend to all four stages of knowledge mobilisation in order to enhance its ACAP.
The literature about ACAP highlights that each of these stages of knowledge mobilisation are underpinned by antecedents, labelled combinative capabilities, specifically systems, socialisation and co-ordination capabilities. To support knowledge mobilisation across all four stages requires that commissioning organisations attend to combinative capabilities, but with the awareness that each of the combinative capabilities plays out differently at each stage of knowledge mobilisation.
Regarding knowledge mobilisation across all four stages, on the one hand, our study suggested that ‘hard data’ were relatively easily acquired by commissioning organisations; indeed such data might be described as plentiful. On the other hand, although data were plentiful, it could prove difficult for the commissioning organisation to access data filed in other parts of the health and social care system, such as hospital data or social services data relevant to the care of older people. Such problems are a consequence of systems capabilities, for example if policy dictated that providers of health care be separated from commissioners of that health care, if there was competition between providers or if different sectors of care (acute care, primary care, mental health care and social care) were decoupled, rather than integrated, which was a particularly significant issue for the care of older people who suffer from long-term conditions and comorbidities. The overall effect is that data held by one organisation might not easily be shared with others. Thus, there was a need for the commissioning organisation to develop co-ordination capability at this stage of knowledge mobilisation to ensure that it acquired the relevant range of data across health and social care agencies, based on which it could intelligently commission. To address this challenge, co-ordination capability was provided by BI units, mainly external to the commissioning organisations (CSUs in NHS England), but in one case it was situated within the commissioning organisation. Data analysts within CSUs proved to be important brokers for the commissioning organisation to develop a relationship with the necessary range of health and social care providers so that the former could acquire hard data important to making decisions about appropriate service interventions in order to reduce needless admissions of older people to hospitals.
More than data acquisition, concern was raised about the assimilation of hard data with other sources of knowledge, such as local population need and patient experience. In this case, co-ordination capability was provided through the engagement of GPs and their role in blending hard data with local knowledge about the patient population and the latter’s experiences. Professional, tacit knowledge was acquired from GPs to supplement the hard data acquired from information systems, enabling CCGs to more appropriately guide commissioning decisions about local population needs, taking account of patient experiences. Although the influence of tacit professional knowledge within decision-making processes has been explored before,4,114,153,154 our results illuminate the benefits of clinician involvement as a co-ordination capability to mediate system capabilities at a commissioning level, and subsequently enhance PACAP of commissioning organisations. We also highlight that assimilation was better supported in the case of the commissioning organisation, where the BI unit was ‘in-house’ rather that externally situated. This meant that data analysts were closer to both managers requesting data and clinicians delivering front-line care, and could better present data in an intelligent form. We highlight the fact that this ran rather counter to encouragement by policy-makers in NHS England for commissioning organisations to outsource the BI function. Perhaps more disappointing for policy-makers who encourage PPI in health-care decision-making, the inclusion of patients and carers was relatively absent as a significant influence within most of our commissioning organisations, as discussed further below.
Moving beyond acquisition and assimilation of knowledge to consider subsequent stages of ACAP, our study highlights power differentials that existed between different organisations and service providers. This was particularly the case with ‘large’ (in employment terms) and powerful (in historical and professional terms) secondary care providers, which were reported as having the potential to undermine the commissioning influence of the ‘smaller’ and less powerful organisation that commonly constituted CCGs. This proved obstructive to transformative learning, and subsequently meant that PACAP went unrealised.
Professional power had an impact on the relationship between commissioning organisations, which are managerially dominated and located in primary care, and hospitals, many of which in our study might deliver tertiary care, and were dominated by specialist doctors. Thus, we see socialisation capability inhibit the ACAP of commission organisations, which are located in a system of interdependent organisations, but in which it is of lower status. To mediate socialisation capability, strong engagement by commissioning organisations with GPs represented co-ordination capability that supported all stages of ACAP. Although not all the entrenched barriers could be overcome through GP engagement, difficult negotiations with secondary care were facilitated by involving medical professionals in discussions, rather than limiting them to managerial interactions. Our respondents noted that decisions were being made faster than under previous systems, with a strong focus on clinical outcomes and service quality. Although there have been concerns that an orientation towards professional peers may prevent knowledge mobilisation, it may be that in circumstances like this professional engagement could have more positive influence in acquiring and assimilating knowledge, particularly across organisational boundaries. 52 In this study, we suggest that GP engagement, and a strong focus on high-quality patient services, provides the ‘grit in the oyster’ for enhancing co-ordination capabilities to facilitate transformative learning.
However, the same professional engagement that provided an ‘acceptable face’ and enhanced co-ordination capabilities could also undermine the RACAP of CCGs. Pre-existing, institutionalised behaviours, which represent socialisation capabilities, could have a negative influence on the ability to exploit knowledge in commissioning decisions. The health-care context is one in which professional hierarchies, silos and power differentials are well documented, and in which resistance from professional groups as a result of institutionalised behaviour can prevent the exploitation of new knowledge. 4,11 Our findings reflected an ingrained level of distrust between clinicians and managers, which was resolved to some extent but which could still have a negative influence on the commissioning process. The socialisation capabilities of CCGs need to be mediated if CCGs are to successfully exploit knowledge and overcome professional or organisational barriers, something that will not be achieved until all the actors involved are able to develop a shared sense of group identity and purpose. 8
Although the mediation of socialisation capabilities is problematic for CCGs, and the primary differential between their PACAP and RACAP, our study provides insight into another potential solution in the form of increased service user involvement, which is likely to enhance the co-ordination capability of CCGs. Patient experience and opinions are increasingly important in modern health-care contexts,3 something that was advocated by our respondents. However, despite this acknowledgement, service users appeared to be the least involved group during knowledge acquisition, assimilation and transformation. A focus on high-quality patient care and outcomes has been identified as a key element to enhance health-care knowledge-brokering processes, with Currie and White52 stating ‘when held together with the glue of a focus on patients, this provided a powerful driver for collaboration’. A focus on patient involvement and high-quality service provision may therefore help to mediate some of the potential conflicts that exist between professional groups, mediating socialisation capabilities and increasing RACAP.
In summary, our study identified four co-ordination capabilities: GP involvement, PPI, BI and social integration mechanisms. How such co-ordination capabilities play out is summarised in Figure 13. The figure shows the deleterious effect of targets and incentives and standardised data collection systems (i.e. systems capabilities) on the critical review capacity of CCG-led commissioning networks. Targets and incentives narrow the commissioning network’s acquisition of knowledge, whereas standardised data, although acquired, remain insufficiently contextualised to inform decision-making. Meanwhile, socialisation capabilities, in the form of organisational and professional cultures, mean that some types of knowledge are privileged for use in decision-making, with knowledge use further compromised by different perspectives of managers and professionals. This contributes towards the gap between PACAP and RACAP. The gap between PACAP and RACAP is mediated by the development of co-ordination capabilities in the form of BI (internal and external functions), GP involvement, PPI, and social integration in which health care, social care and voluntary organisations come together in real time to deliver services. The latter, although crucial to bridging the PACAP–RACAP gap, has proved to be slow to develop, and remains poor in places, particularly PPI.
FIGURE 13.
The ACAP model in commissioning.
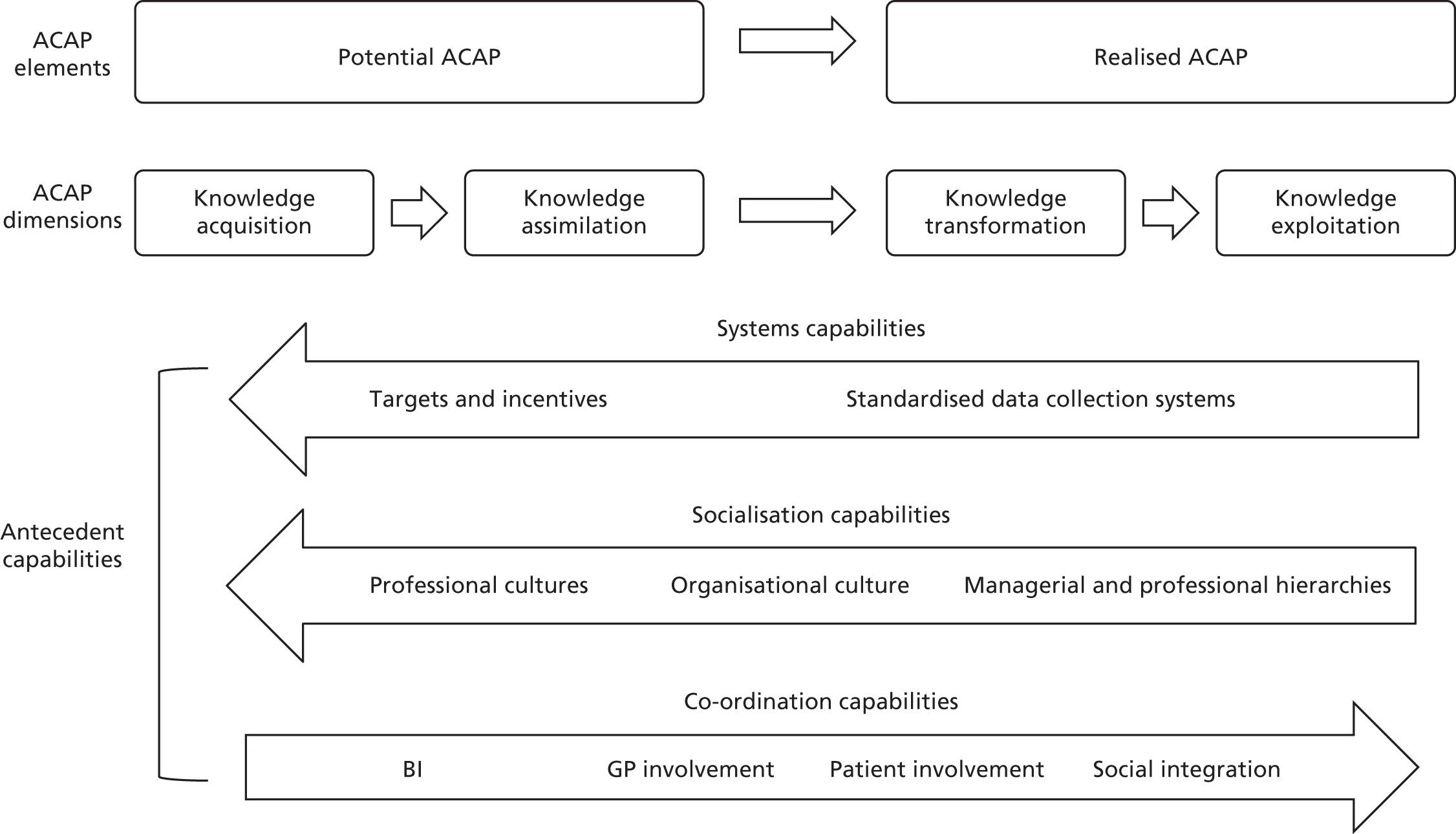
The model outlines how evidence and knowledge take the form of information from a diverse range of sources, including research, patient involvement and clinician and managerial knowledge. Facilitating, or inhibiting, knowledge mobilisation are the three combinative capabilities: systems, socialisation and co-ordination capabilities, which are antecedents to the four overlapping processes of knowledge mobilisation that underpin ACAP. However, socialisation and systems capabilities have the potential to inhibit ACAP, limiting the breadth and type of information acquired and used to guide service decisions. The four types of co-ordination capability identified in this study – GP involvement, PPI, BI and social integration mechanisms – work to overcome the limitations of systems and socialisation capabilities. In particular, the co-ordination capabilities have the potential to enhance exploitation processes, an area that is underdeveloped in health-care organisations. Enhancing exploitation encourages the scaling of service intervention in response to knowledge mobilisation of information from a wide range of sources, and is an area in which health-care organisations should seek to develop their capacity, improving decision-making and quality of services.
Implications for practice
We have noted that our study of CCG-led commissioning networks has taken place soon after their inception. In part, this might explain why their critical review capacity for knowledge mobilisation (in our conceptual terms, ACAP) is not well developed. Over time, we might expect relationships with key stakeholders, such as GPs, PPI representatives and CSUs, to further develop to the benefit of critical review capacity for knowledge mobilisation. During the study period, however, CCGs exhibited less concern about their lack of critical review capacity than we might have expected (as evident in challenges we experienced in accessing CCGs described in our research design). To encourage CCG-led commissioning networks to take their critical review capacity more seriously, as a first practical implication, we offer our psychometric ACAP tool in the hope that this encourages CCG-led commissioning networks to develop their critical review capacity, not just regarding our tracer study domain but more generally across all service domains. The tool is orientated towards bridging the gap between their PACAP and RACAP, so that the knowledge acquired and assimilated by commissioning networks is transformed and exploited, and consequently evidence-based service interventions are scaled up.
In our original protocol, our fourth RQ was ‘How can we ensure that PACAP is realised in commissioning networks?’. We suggest that our original use of the word ‘ensure’ was overoptimistic; the study shows how multiple factors influence the exploitation of new knowledge, and makes a range of suggestions about how the likelihood of transformation and exploitation could be increased, as described in the following paragraphs.
Policy-makers’ influence on the ACAP of CCG-led commissioning networks most obviously lies with influence on their systems capabilities. Policy-makers mandate the performance and incentive structures to which CCG-led commissioning networks respond. In some respects, policy-makers can be seen to support ACAP through, for example, requirements that CCG-led commissioning networks encompass PPI. However, policy requirement is one thing, its implementation is another. PPI was patchy across the CCG-led commissioning networks that participated in our study. Similarly, GP involvement was not as it might be. The relative absence of both across our CCG-led commissioning networks had deleterious effects on ACAP. CCG-led commissioning networks appeared to be more orientated towards what might be regarded as transactional mode with providers regarding contracting. They were thus concerned with monitoring contracts rather than with behaving in a more strategic way towards use of evidence in re-engineering services. Any vision of ‘world-class commissioning’ from policy-makers appears to be slow to realise. Policy-makers might attend to such matters.
In part, the above might link to socialisation capabilities, specifically the managerial cadre employed by CCGs, which appears wedded to its traditional bureaucratic orientation. We caution that this is merely a tentative suggestion derived from impressions during fieldwork, which might be followed up in further research. Nevertheless, to realise policy aspirations for evidence-based commissioning might require greater sophistication on the part of managers. In particular, managers might reflect on their involvement of GPs, who may be decoupled from their practice-based colleagues, and thus need to consider how commissioning-based GPs and their practice-based peers might be better linked to engender co-ordination capability that enhances ACAP.
Alongside this, CCG-led commissioning networks themselves might enhance their ACAP, not only through co-ordination capabilities, such as more effective PPI and GP involvement in their commissioning, but through better use of and interaction with those providing BI, either internal or external (CSUs) to the CCG. Admittedly, our study was limited, but it is striking that ACAP was enhanced when the BI function was ‘in-house’. In this case, interactions between data analysts and commissioners were relational rather than transactional, the former leading to enhanced service from the BI function to commissioners, as they understood the data needs of commissioners in real time. The challenge for CCG-led commissioning networks that rely on external CSUs is to replicate this relationship.
Better relationships across the network of service providers and commissioners are certainly a significant factor in enhancing ACAP. Often, the problem is that different perspectives need to be bridged, for example between health and social care, so that they collaborate more effectively. Voluntary sector organisations help provide the necessary social integration to support this. More generally, shared strategies and mental models of care across organisations, managers and professionals from different providers and commissioners enhance the ACAP of the CCG-led commissioning network.
Suggestions to reduce potentially avoidable elderly care admissions to hospitals
Regarding our specific tracer study, patient/carer experience of care and clinical outcome improves through being kept out of hospital. For the NHS, potentially avoidable admissions prove to be difficult and costly to manage. Our study has four implications of importance for our specific tracer study, each of which result in research-informed suggestions:
-
The evidence here suggests that commissioning networks may want to consider developing proactive integrated care to reduce the proportion of frail elderly patients who go to hospitals, for example by improving care and social support in the community. Given this, many of our empirical cases focused on integrated commissioning teams, and specifically how those managers and professionals from health and social care came together to share and use evidence across organisational boundaries to inform commissioning decisions.
-
Research-informed suggestion 1: may want to consider the development of integrated teams comprising health and social care professionals facilitated mobilisation of both formal knowledge (held in different information systems) and informal knowledge (about local populations/patients and services).
-
Research-informed suggestion 2: where integrated teams are absent, may want to consider drawing on one of our specific empirical cases, voluntary organisations can act as the conduit for mobilising knowledge about the local elderly population/patient and services offered across sectoral boundaries.
-
-
One might expect that ‘strategic’ commissioning may want to consider involving CCGs pulling in data about current and prospective population demographics and service demand to reconfigure services to reduce potentially avoidable elderly admissions to hospitals. In light of this prospect, two of our empirical cases focused specifically on BI functions: one on CSUs and the other on an internal BI function within a CCG that made limited use of the CSU but faced a rapidly expanding ageing population. Regarding the first of these, it is rather worrying that our study found that the CCG-led commissioning network and CSU were working together less effectively than policy-makers might anticipate. The specialist (e.g. focused on elderly care) and strategic (population-level data and service benchmarked across CCGs) input that CSUs provided, and the support they offered in pathway redesign, was not taken advantage of by CCGs. The CSUs report that their ability to monitor contracts between commissioners and providers is given primacy by CCGs, rather than the latter pulling in the expertise of CSUs to examine and respond to data about flows of older patients, with the purpose of making strategic decisions about interventions to prevent potentially avoidable elderly care admissions to hospitals. Furthermore, there is an absence of feedback loops to show whether or not those interventions that are commissioned to reduce potentially avoidable admissions are effective. Hence, CCG-led commissioning networks cannot judge whether to decommission these or scale them up. In short, BI is less sophisticated than it should be for supporting decision-making in the domain of elderly care to prevent potentially avoidable admissions to hospitals. CCG-led commissioning networks might attend to the BI challenge as an imperative. The second empirical case, which encompassed a well-developed internal BI function, similarly, did not make the most of its potential. On the one hand, the internal BI function appeared to access locally acquired data and make this available to commissioning managers in the realm of elderly care, but, again, policy and other performance pressures led to a more transactional, and less strategic, use of these data than was otherwise ideal. The end result in both CCGs was that any opportunity for reconfiguration of pathways to reduce potentially avoidable elderly care admissions was lost.
-
Research-informed suggestion 3: CCGs may want to consider utilising strategic capabilities within BI functions, particularly within CSUs, more effectively, to reconfigure pathways for elderly care to reduce potentially avoidable hospital admissions.
-
-
The variable involvement of GPs in commissioning decisions is concerning. There seems to be a decoupling of GPs within their professional ranks that causes local knowledge about the elderly population and service offerings held by front-line GPs to inform commissioning decisions less than might be expected. In negotiating access to CCGs, and identifying relevant service innovations designed to reduce potentially avoidable elderly care admissions, commissioning managers often exhibited a lack of knowledge about what was happening in primary care settings. Our analysis suggests that GPs who are formally involved in commissioning roles may not sufficiently act as a conduit to implement innovations developed by their professional colleagues to inform commissioning decisions. It seems that they remain distant from some of their professional colleagues. Of course, it may be that professional colleagues do not engage with the GP leads for commissioning, and relationships may take time to develop around the new commission structures.
-
Research-informed suggestion 4: it could be considered that the knowledge held by front-line GPs about local population and service offerings in primary care be acquired and used, with those GPs who are formally involved in commissioning decisions enacting their roles to ensure that this takes place.
-
-
Patient and public involvement in commissioning was less developed than might be expected. This represents a concern applicable to all service domains, but reveals itself as particularly significant regarding the involvement and influence of older people and/or their carers. Again, we highlight a proviso that relationships may take time to develop so that PPI is enacted, and we note that our study focused on ‘early days’ in the new commissioning arrangements. Our study reveals, however, that it may want to be considered that PPI should not be driven by managers, but cultivated so that it is allowed to emerge rather than be forced by managerial dictate.
-
Research-informed suggestion 5: PPI in commissioning requires particular support, as it relates to elderly care and the specific issue of how to develop proactive, integrated care that prevents potentially avoidable elderly admissions to hospitals.
-
Transferability of analysis
Although we highlight specific implications for elderly care above, we note that this is a tracer study designed to surface issues, lessons and a self-development tool for allowing commissioning networks to use different evidence across all service domains. In these terms, our study indirectly affects improved service and potential reconfiguration of pathways; that is, our intention is to directly affect the use of evidence rather than the service outcome itself. Nevertheless, our study, which provides insight into the application of ACAP, is particularly relevant to current health-care settings. Health-care settings globally are subject to financial parsimony, and, as such, need to be smarter about knowledge mobilisation, in particular how acquired knowledge informs the planning of, and funding for, service interventions, not least given burgeoning demands as a result of the increasing demands from older patients on hospital services (e.g. in NHS England, ≈50% of hospital beds may be occupied by older patients). For example, a health-care organisation may invest significant resources in IT capacity to acquire information, but if this information is not then used intelligently to inform service development, investments will merely result in PACAP, rather than RACAP,13 without patient, financial or competitive advantage. To emphasise, we note that our analysis is not limited to commissioning the care of older people, as application of the ACAP concept allows theoretical generalisation to other domains of health care, both the delivery and commissioning of services, and indeed other public services characterised by professional organisation and central government intervention. 108
Further research
Finally, in terms of further research, co-ordination capabilities within health-care organisations have been identified within the literature, as represented by the following: the development of learning relationships through the establishment of internal and external networks, staff development and training, appropriate leadership, organisational strategy, investment in information support systems, participation in decision-making and, more generally, social relations inside and outside the organisation. 33,34 Although our empirical study has highlighted professional involvement, client involvement and integrated service delivery models, others may wish to examine possibilities offered by other forms of co-ordination capability.
We have noted that our study took place at the early stages of development of CCG-led commissioning networks. We suggested that relationships to allow GP involvement and PPI to flourish would take time to develop, although we noted that front-line GPs seemed to be disengaging with the new commissioning structures and processes. In short, there is a temporal dimension that is relatively absent in our analysis, but that further study might examine. As CCGs developed, were some of our concerns addressed, particularly those about GP involvement and PPI?
Acknowledgements
Contributions of authors
Graeme Currie led the research and writing of the report.
Charlotte Croft and Yaru Chen carried out fieldwork and cowrote the report.
Tina Kiefer led the development of the psychometric tool derived from fieldwork.
Sophie Staniszewska led development for the governance of PPI.
Richard J Lilford provided methodological advice for fieldwork and the psychometric tool, contributed to the analysis of empirical findings and checked and edited the final report.
Publication
Croft C, Currie G, Staniszewska S. Moving from rational to normative ideologies of control over public involvement: a case of continued managerial dominance. Soc Sci Med 2016;162:124–32.
Data sharing statement
Owing to the nature of this study, the type of data collected and the conditions attached to ethics approval, there are no data available for wider use. The empirical sections of the report contain a rich section of primary data quotations across all 12 comparative cases. All queries should be submitted to the corresponding author in the first instance.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Currie G, Burgess N, White L, Lockett A, Galdman J, Waring J. A qualitative study of the knowledge brokering role of middle level managers in service innovation: managing the translation gap in patient safety for older persons’ care. Health Serv Deliv Res 2014;2. https://www.ncbi.nlm.nih.gov/books/NBK260045.
- Cohen W, Levinthal D. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q 1990;35:128-52. https://doi.org/10.2307/2393553.
- Ferlie E, Crilly T, Jashapara A, Peckham A. Knowledge mobilisation in healthcare: a critical review of health sector and generic management literature. Soc Sci Med 2012;74:1297-304. https://doi.org/10.1016/j.socscimed.2011.11.042.
- Berta W, Teare GF, Gilbart E, Ginsburg LS, Lemieux-Charles L, Davis D, et al. Spanning the know–do gap: understanding knowledge application and capacity in long-term care homes. Soc Sci Med 2010;70:1326-34. https://doi.org/10.1016/j.socscimed.2009.11.028.
- Smith M, Prieto IM. Easterby . Dynamic capabilities and knowledge management: an integrative role for learning?. Br J Manag 2008;19:235-49. https://doi.org/10.1111/j.1467-8551.2007.00543.x.
- Hotho JJ, Becker-Ritterspach F, Saka-Helmhout A. Enriching absorptive capacity through social interaction. Br J Manag 2012;23:383-401.
- Cepeda-Carrion G, Cegarra-Navarro JG, Jimenez-Jimenez D. The effect of absorptive capacity on innovativeness: context and information systems capability as catalysts. Br J Manag 2012;23:110-29.
- Jansen JJ, Van den Bosch FA, Volberda HW. Managing potential and realized absorptive capacity: how do organizational antecedents matter?. Acad Manage J 2005;48:999-1015. https://doi.org/10.5465/AMJ.2005.19573106.
- Lane P, Koka B, Pathak S. The reification of absorptive capacity: a critical review and rejuvination of the construct. Acad Manage Rev 2006;31:833-63. https://doi.org/10.5465/AMR.2006.22527456.
- Todorova G, Durisin B. Absorptive capacity: valuing a reconceptualization. Acad Manage Rev 2007;32:774-86. https://doi.org/10.5465/AMR.2007.25275513.
- Van den Bosch FA, Volberda HW, De Boer M. Coevolution of firm absorptive capacity and knowledge environment: organizational forms and combinative capabilities. Organ Sci 1999;10:551-68. https://doi.org/10.1287/orsc.10.5.551.
- Volberda HW, Foss NJ, Lyles MA. Absorbing the concept of absorptive capacity: how to realize its potential in the organization field. Organ Sci 2010;21:931-51. https://doi.org/10.1287/orsc.1090.0503.
- Zahra S, George G. Absorptive capacity: a review, reconceptualization, and extension. Acad Manage Rev 2002;27:185-203.
- Clinical Commissioning: Our Vision for Practice Based Commissioning. London: Department of Health and Social Care; 2009.
- Developing Clinical Commissioning Groups: Towards Authorisation. London: Department of Health and Social Care; 2011.
- Swan J, Clarke A, Nicolini D, Powell J, Scarborough H, Roginski C, et al. Evidence in Management Decisions (EMD) – advancing knowledge utilization in healthcare management. Southampton: Service Delivery and Organisation Programme; 2012.
- Imison C, Curry N, McShane M. Commissioning for the Future: Learning from a Simulation of the Health System in 2013/2014. London: The King’s Fund; 2011.
- Benefits Realisation: Assessing the Evidence for the Cost Benefit and Cost Effectiveness of Integrated Health and Social Care. London: Turning Point; 2010.
- Windle K, Wagland R, Forder J, D’Amico F, Jansen D, Wistow G, et al. Unit Costs of Health and Social Care. Canterbury: University of Kent; 2009.
- Joining Up Health and Social Care: Improving Value for Money Across the Interface. London: Audit Commission; 2011.
- Lyon D, Miller J, Pine K. The Castlefields integrated care model: the evidence summarised. J Integrated Care 2006;14:7-12. https://doi.org/10.1108/14769018200600003.
- Keating P, Sealy A, Dempsey L, Slater B. Reducing unplanned hospital admissions and hospital bed days in the over 65 age group: results from a pilot study. J Integrated Care 2008;16:3-8. https://doi.org/10.1108/14769018200800002.
- Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009;195:61-6. https://doi.org/10.1192/bjp.bp.108.055335.
- Europe R, Young E. National Evaluation of the Department of Health’s Integrated Care Pilots. Cambridge: RAND Europe; 2012.
- Timmins N. Never Again?, Or, The Story of the Health and Social Care Act 2012: A Moderne [sic] Drama in Five Incompleted Acts. London: The King’s Fund; 2012.
- Mannion R. General practitioner-led commissioning in the NHS: progress, prospects and pitfalls. Br Med Bull 2011;97:7-15. https://doi.org/10.1093/bmb/ldq042.
- Innovation Health and Wealth, Accelerating Adoption and Diffusion in the NHS. London: Department of Health and Social Care; 2011.
- Smith J, Regen E, Shapiro J, Baines D. National evaluation of general practitioner commissioning pilots: lessons for primary care groups. Br J Gen Pract 2000;50:469-72.
- Robertson R, Holder H, Ross S, Naylor C, Machaqueiro S. Clinical Commissioning: GPs in Charge?. London: The King’s Fund; 2016.
- Damanpour F, Schneider M. Characteristics of innovation and innovation adoption in public organizations: assessing the role of managers. J Public Adm Res Theory 2009;19:495-522. https://doi.org/10.1093/jopart/mun021.
- Moynihan DP, Landuyt N. How do public organizations learn? Bridging cultural and structural perspectives. Public Adm Rev 2009;69:1097-105. https://doi.org/10.1111/j.1540-6210.2009.02067.x.
- Salge TO, Vera A. Hospital innovativeness and organizational performance: evidence from English public acute care. Health Care Manage Rev 2009;34:54-67. https://doi.org/10.1097/01.HMR.0000342978.84307.80.
- Harvey G, Skelcher C, Spencer E, Jas P, Walshe K. Absorptive capacity in a non-market environment. Public Manage Rev 2009;12:77-9. https://doi.org/10.1080/14719030902817923.
- Walshe K, Smith L. The NHS Management Workforce. London: The King’s Fund; 2011.
- Goodwin N, Dixon A, Poole T, Raleigh V. Improving the Quality of Care in General Practice. London: The King’s Fund; 2011.
- Fabrizio KR. Absorptive capacity and the search for innovation. Res Policy 2009;38:255-67. https://doi.org/10.1016/j.respol.2008.10.023.
- Smith J, Mays N, Dixon J, Goodwin N, Lewis R, McClelland S, et al. A Review of the Effectiveness of Primary Care-led Commissioning and its Place in the NHS. London: The Health Foundation; 2004.
- Kitson A. Knowledge translation and guidelines: a transfer, translation or transformation process?. Int J Evid Based Healthc 2009;7:124-39. https://doi.org/10.1111/j.1744-1609.2009.00130.x.
- Thorlby R, Rosen R, Smith J. GP Commissioning: Insights from Medical Groups in the United States. London: The Nuffield Trust; 2011.
- van Ees H, van der Laan G, Postma TJBM. Effective board behavior in the Netherlands. Euro Manage J 2008;26:84-93. https://doi.org/10.1016/j.emj.2008.01.002.
- Pelled L, Eisenhardt K, Xin K. Exploring the black box: an analysis of work group diversity, conflict and performance. Adm Sci Q 1999;44:1-28. https://doi.org/10.2307/2667029.
- Finkelstein S, Mooney A. Not the usual suspects: how to use board process to make boards better. Acad of Manage Exec 2003;17:101-13. https://doi.org/10.5465/AME.2003.10025204.
- Fitzgerald L, Ferlie E, Hawkins C. Innovation in healthcare: how does credible evidence influence professionals?. Health Soc Care Community 2003;11:219-28. https://doi.org/10.1046/j.1365-2524.2003.00426.x.
- Forbes D, Milliken F. Cognition and corporate governance: understanding boards of directors as strategic decision-making groups. Acad Manage Rev 1998;24:489-505.
- Lam A. Tacit knowledge, organizational learning and societal institutions: an integrated framework. Organ Stud 2000;21:487-513. https://doi.org/10.1177/0170840600213001.
- Grant R. Toward a knowledge-based theory of the firm. Strat Manage J 1996;17:109-22. https://doi.org/10.1002/smj.4250171110.
- Kogut B, Zander U. Knowledge of the firm, combinative capabilities, and the replication of technology. Organ Sci 1992;3:383-97. https://doi.org/10.1287/orsc.3.3.383.
- Contandriopoulos D, Lemire M, Denis JL, Tremblay E. Knowledge exchange processes in organizations and policy arenas: a narrative systematic review of the literature. Milbank Q 2010;88:444-83. https://doi.org/10.1111/j.1468-0009.2010.00608.x.
- Ferlie E, Fitzgerald L, Wood M, Hawkins C. The nonspread of innovations: the mediating role of professionals. Acad Manage J 2005;48:117-34. https://doi.org/10.5465/AMJ.2005.15993150.
- Lam A. Embedded firms, embedded knowledge: problems of collaboration and knowledge transfer in global cooperative ventures. Organ Stud 1997;18:973-96. https://doi.org/10.1177/017084069701800604.
- Mintzberg H. The Structuring of Organization: A Synthesis of the Research. Englewood Cliffs, NJ: Prentice-Hall; 1979.
- Currie G, White L. Inter-professional barriers and knowledge brokering in an organizational context: the case of healthcare. Organ Stud 2012;33:1333-61. https://doi.org/10.1177/0170840612457617.
- Moynihan DP, Hawes DP. Responsiveness to reform values: the influence of the environment on performance information use. Public Adm Rev 2012;72:S95-S105. https://doi.org/10.1111/j.1540-6210.2012.02653.x.
- Nicolini D, Waring J, Mengis J. Policy and practice in the use of root cause analysis to investigate clinical adverse events: mind the gap. Soc Sci Med 2011;73:217-25. https://doi.org/10.1016/j.socscimed.2011.05.010.
- Ham C, Zollinger-Read P. What are the lessons from the USA for clinical commissioning groups in the English National Health Service?. Lancet 2012;379:189-91. https://doi.org/10.1016/S0140-6736(11)61088-X.
- Shortell SM, Addicott R, Walsh N, Ham C. Accountable Care Organisations in the United States and England: Testing, Evaluating and Learning What Works. London: The King’s Fund; 2014.
- Friedson E. The reorganization of the medical profession. Med Care Rev 1985;42:11-35. https://doi.org/10.1177/107755878504200103.
- Llewellyn S. ‘Two-way windows’: clinicians as medical managers. Organ Stud 2001;22:593-62. https://doi.org/10.1177/0170840601224003.
- McDonald R, Checkland K, Harrison S, Coleman A. Rethinking collegiality: restratification in English general medical practice 2004–8. Soc Sci Med 2009;68:1199-205. https://doi.org/10.1016/j.socscimed.2009.01.042.
- Hunter DJ. Doctors as managers: poachers turned gamekeepers?. Soc Sci Med 1992;35:557-66. https://doi.org/10.1016/0277-9536(92)90349-U.
- Noordegraaf M, Van Der Meulen M. Professional power play: organizing management in health care. Public Adm 2008;86:1055-69. https://doi.org/10.1111/j.1467-9299.2008.00746.x.
- Sheaff R, Smith K, Dickson M. Is GP restratification beginning in England?. Soc Policy Adm 2002;36:765-79. https://doi.org/10.1111/1467-9515.00316.
- Veronesi G, Kirkpatrick I, Vallascas F. Clinicians on the board: what difference does it make?. Soc Sci Med 2013;77:147-55. https://doi.org/10.1016/j.socscimed.2012.11.019.
- McGivern G, Currie G, Ferlie E, Fitzgerald L, Waring J. Hybrid manager–professionals’ identity work: the maintenance and hybridization of medical professionalism in managerial contexts. Public Adm 2015;93:412-32. https://doi.org/10.1111/padm.12119.
- Courpasson D. Managerial strategies of domination. Power in soft bureaucracies. Organ Stud 2000;21:141-61. https://doi.org/10.1177/0170840600211001.
- Kitchener M. The ‘bureaucratization’ of professional roles: the case of clinical directors in UK hospitals. Organization 2000;7:129-54. https://doi.org/10.1177/135050840071007.
- Moffatt F, Martin P, Timmons S. Constructing notions of healthcare productivity: the call for a new professionalism?. Sociol Health Illn 2014;36:686-702. https://doi.org/10.1111/1467-9566.12093.
- Tummers L, Steijn B, Bekkers V. Explaining the willingness of public professionals to implement public policies: content, context, and personality characteristics. Public Adm 2012;90:716-36. https://doi.org/10.1111/j.1467-9299.2011.02016.x.
- Currie G, Croft C. Examining hybrid nurse managers as a case of identity transition in healthcare: developing a balanced research agenda. Work Employ Soc 2015;29:855-65. https://doi.org/10.1177/0950017015572581.
- Waring J. Restratification, hybridity and professional elites: questions of power, identity and relational contingency at the points of ‘professional–organisational intersection’. Sociol Compass 2014;8:688-704. https://doi.org/10.1111/soc4.12178.
- Charles-Jones H, Latimer J, May C. Transforming general practice: the redistribution of medical work in primary care. Sociol Health Illn 2003;25:71-92. https://doi.org/10.1111/1467-9566.t01-1-00325.
- Jones L, Green J. Shifting discourses of professionalism: a case study of general practitioners in the United Kingdom. Sociol Health Illn 2006;28:927-50. https://doi.org/10.1111/j.1467-9566.2006.00513.x.
- Numerato D, Salvatore D, Fattore G. The impact of management on medical professionalism: a review. Sociol Health Illn 2012;34:626-44. https://doi.org/10.1111/j.1467-9566.2011.01393.x.
- Barnes M, Newman J, Knops A, Sullivan H. Constituting ‘the public’ in public participation. Public Adm 2003;81:379-99. https://doi.org/10.1111/1467-9299.00352.
- Gustafsson U, Driver S. Parents, power and public participation: Sure Start, an experiment in New Labour governance. Soc Policy Adm 2005;39:528-43. https://doi.org/10.1111/j.1467-9515.2005.00454.x.
- Mockford C, Staniszewska S, Griffiths F, Herron-Marx S. The impact of patient and public involvement on UK NHS health care: a systematic review. Int J Qual Health Care 2012;24:28-3. https://doi.org/10.1093/intqhc/mzr066.
- Baggott R. A funny thing happened on the way to the forum? Reforming patient and public involvement in the NHS in England. Public Adm 2005;83:533-51. https://doi.org/10.1111/j.0033-3298.2005.00461.x.
- Contandriopoulos D. A sociological perspective on public participation in health care. Soc Sci Med 2004;58:321-30. https://doi.org/10.1016/S0277-9536(03)00164-3.
- Boivin A, Lehoux P, Burgers J, Grol R. What are the key ingredients for effective public involvement in health care improvement and policy decisions? A randomized trial process evaluation. Milbank Q 2014;92:319-50. https://doi.org/10.1111/1468-0009.12060.
- Litva A, Coast J, Donovan J, Eyles J, Shepherd M, Tacchi J, et al. ‘The public is too subjective’: public involvement at different levels of health-care decision making. Soc Sci Med 2002;54:1825-37. https://doi.org/10.1016/S0277-9536(01)00151-4.
- Rutter D, Manley C, Weaver T, Crawford MJ, Fulop N. Patients or partners? Case studies of user involvement in the planning and delivery of adult mental health services in London. Soc Sci Med 2004;58:1973-84. https://doi.org/10.1016/S0277-9536(03)00401-5.
- Renedo A, Marston CA, Spyridonidis D, Barlow J. Patient and public involvement in healthcare quality improvement: how organizations can help patients and professionals to collaborate. Public Manage Rev 2015;17:17-34. https://doi.org/10.1080/14719037.2014.881535.
- El Enany N, Currie G, Lockett A. A paradox in healthcare service development: professionalization of service users. Soc Sci Med 2013;80:24-30. https://doi.org/10.1016/j.socscimed.2013.01.004.
- Equity and Excellence: Liberating the NHS. London: Department of Health and Social Care; 2010.
- Everyone Counts: Planning for Patients 2013/14. London: Her Majesty’s Stationery Office; 2013.
- Callaghan G, Wistow G. Publics, patients, citizens, consumers? Power and decision making in primary health care. Public Adm 2006;84:583-601. https://doi.org/10.1111/j.1467-9299.2006.00603.x.
- Martin GP. The third sector, user involvement and public service reform: a case study in the co-governance of health service provision. Public Adm 2011;89:909-32. https://doi.org/10.1111/j.1467-9299.2011.01910.x.
- Great Britain . Health and Social Care Act 2014. www.legislation.gov.uk/ukdsi/2014/9780111117613 (accessed 24 March 2015).
- Hudson B. Public and patient engagement in commissioning in the English NHS: an idea whose time has come?. Public Manage Rev 2014;17:1-16. https://doi.org/10.1080/14719037.2014.881534.
- Coulter A, Collins A. Making Shared Decision-making a Reality: No Decision About Me, Without Me. London: The King’s Fund; 2011.
- Foot C, Gilburt H, Dunn P, Jabbal J, Seale B, Goodrich J, et al. People in Control of their Own Health and Care. The State of Involvement. London: The King’s Fund; 2014.
- Developing Commissioning Support: Towards Service Excellence. London: NHS Commissioning Board; 2012.
- Towards Commissioning Excellence: Developing a Strategy for Commissioning Support Services. London: NHS England; 2013.
- Commissioning Support Units. London: NHS England; 2016.
- Petsoulas C, Allen P, Checkland K, Coleman A, Segar J, Peckham S, et al. Views of NHS commissioners on commissioning support provision. Evidence from a qualitative study examining the early development of clinical commissioning groups in England. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005970.
- Humphries R, Wenzel L. Options for Integrated Commissioning: Beyond Barker. London: The King’s Fund; 2015.
- Integrated Care and Support: Our Shared Commitment. London: National Collaboration for Integrated Care and Support; 2013.
- Humphries R, Galea A. Health and Wellbeing Boards: One Year On. London: The King’s Fund; 2013.
- Curry N, Ham C. Clinical and Service Integration: The Route to Improved Outcomes. London: The King’s Fund; 2010.
- Joint Review of Partnerships and Investment in Voluntary, Community and Social Enterprise Organisations in the Health and Care Sector. London: Her Majesty’s Stationery Office; 2016.
- Holder H. Role of the Voluntary Sector in Providing Commissioning Support. London: Nuffield Trust; 2013.
- Addicott R. Working Together to Deliver the Mandate. London: The King’s Fund; 2013.
- Grant C, Goodenough T, Harvey I, Hine C. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. BMJ 2000;320:419-23. https://doi.org/10.1136/bmj.320.7232.419.
- Brown L, Tucker C, Domokos T. Evaluating the impact of integrated health and social care teams on older people living in the community. Health Soc Care Community 2003;11:85-94. https://doi.org/10.1046/j.1365-2524.2003.00409.x.
- Addicott R. Commissioning and Contracting for Integrated Care. London: The King’s Fund; 2014.
- Hornby P, Symon G, Cassel C, Symon G. Qualitative Methods in Organizational Research: A Practical Guide. London: Sage; 1994.
- Yin R. Case Study Research: Design and Methods. London: Sage; 2003.
- Eisenhardt K. Building theories from case study research. Acad Manage Rev 1989;14:532-50.
- Siggelkow N. Persuasion with case studies. Acad Manage J 2007;50:20-4. https://doi.org/10.5465/AMJ.2007.24160882.
- Curtis S, Gesler W, Smith G, Washburn S. Approaches to sampling and case selection in qualitative research: examples in the geography of health. Soc Sci Med 2000;50:1001-14. https://doi.org/10.1016/S0277-9536(99)00350-0.
- Eisenhardt K, Graebner M. Theory building from cases: opportunities and challenges. Acad Manage J 2007;50:25-32. https://doi.org/10.5465/AMJ.2007.24160888.
- Gobo G, Seale C, Gobo G, Gubrium J, Silverman D. Qualitative Research in Practice. 2007.
- Kvale S, Brinkmann S. Interviews: Learning the Craft of Qualitative Research Interviewing. Thousand Oaks, CA: Sage Publications; 2009.
- Greenhalgh T, Wieringa S. Is it time to drop the ‘knowledge translation’ metaphor? A critical literature review. J R Soc Med 2011;104:501-9. https://doi.org/10.1258/jrsm.2011.110285.
- Bryman A. The debate about quantitative and qualitative research: a question of method or epistemology?. Br J Sociol 1984;35:75-92. https://doi.org/10.2307/590553.
- Parry KW. Grounded theory and social process: a new direction for leadership research. Leadersh Q 1998;9:85-105. https://doi.org/10.1016/S1048-9843(98)90043-1.
- Gerson K, Horowitz R, May T. Qualitative Research in Action. London: Sage; 2002.
- Alvesson M. Leadership studies: from procedure and abstraction to reflexivity and situation. Leadersh Q 1996;7:455-85. https://doi.org/10.1016/S1048-9843(96)90002-8.
- Biernacki P, Waldorf D. Snowball sampling: problems and techniques of chain referral sampling. Sociol Methods Res 1981;19:141-63. https://doi.org/10.1177/004912418101000205.
- King N, Symon G, Cassell C. Qualitative Methods and Analysis in Organizational Research: A Practical Guide. London: Sage; 1998.
- Gibbs G. Analysing Qualitative Data. London: Sage; 2007.
- Silverman D, Denzin NK, Lincoln YS. Collecting and Interpreting Qualitative Materials. London: Sage; 2003.
- Bringer J, Johnston L, Brackenrisge C. Maximising transparency in a doctoral thesis: the complexities of writing about the use of QSR*NVivo within a grounded theory study. Qual Res 2004;4:247-65. https://doi.org/10.1177/1468794104044434.
- Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol 2003;88:879-903. https://doi.org/10.1037/0021-9010.88.5.879.
- Hinkin TR. A brief tutorial on the development of measures for use in survey questionnaires. Organ Res Methods 1998;1:104-21. https://doi.org/10.1177/109442819800100106.
- van den Hooff B, Huysman M. Managing knowledge sharing: emergent and engineering approaches. Info Manage 2009;46:1-8. https://doi.org/10.1016/j.im.2008.09.002.
- Faraj S, Sproull L. Coordinating expertise in software development teams. Manage Sci 2000;46:1554-68. https://doi.org/10.1287/mnsc.46.12.1554.12072.
- De Jong BA, Elfring T. How does trust affect the performance of ongoing teams? The mediating role of reflexivity, monitoring, and effort. Acad Manage J 2010;53:535-49. https://doi.org/10.5465/AMJ.2010.51468649.
- Poppo L, Zhou KZ, Ryu S. Alternative origins to interorganizational trust: an interdependence perspective on the shadow of the past and the shadow of the future. Organ Sci 2008;19:39-55. https://doi.org/10.1287/orsc.1070.0281.
- Mayer RC, Gavin MB. Trust in management and performance: who minds the shop while the employees watch the boss?. Acad Manage J 2005;48:874-88. https://doi.org/10.5465/AMJ.2005.18803928.
- Conway N, Kiefer T, Hartley J, Briner RB. Doing more with less? Employee reactions to psychological contract breach via target similarity or spillover during public sector organizational change. Br J Manag 2014;25:737-54. https://doi.org/10.1111/1467-8551.12041.
- Mael F, Ashforth BE. Alumni and their alma mater: a partial test of the reformulated model of organizational identification. J Organ Behav 1992;13:103-23. https://doi.org/10.1002/job.4030130202.
- Van Katwyk PT, Fox S, Spector PE, Kelloway EK. Using the Job-related Affective Well-being Scale (JAWS) to investigate affective responses to work stressors. J Occup Health Psychol 2000;5:219-30. https://doi.org/10.1037/1076-8998.5.2.219.
- Morrison EW, Phelps C. Taking charge: extra-role efforts to initiate workplace change. Acad Manage J 1999;42:403-19. https://doi.org/10.2307/257011.
- Van Dyne L, LePine JA. Helping and voice extra-role behaviors: evidence of construct and predictive validity. Acad Manage J 1998;41:108-19. https://doi.org/10.2307/256902.
- Schippers MC, Den Hartog DN, Koopman PL. Reflexivity in teams: a measure and correlates. Appl Psychol 2007;56:189-211. https://doi.org/10.1111/j.1464-0597.2006.00250.x.
- Arnold JA, Arad S, Rhoades JA, Drasgow F. The empowering leadership questionnaire: the construction and validation of a new scale for measuring leader behaviors. J Organ Behav 2000;21:249-69. https://doi.org/10.1002/(SICI)1099-1379(200005)21:3<249::AID-JOB10>3.0.CO;2-#.
- Flatten TC, Engelen A, Zahra SA, Brettel M. A measure of absorptive capacity: scale development and validation. Eur Manage J 2011;29:98-116. https://doi.org/10.1016/j.emj.2010.11.002.
- Wang CL. Entrepreneurial orientation, learning orientation, and firm performance. Entrepreneurship Theory and Practice 2008;32:635-56. https://doi.org/10.1111/j.1540-6520.2008.00246.x.
- Bresman H. External learning activities and team performance: a multimethod field study. Organ Sci 2010;21:81-96. https://doi.org/10.1287/orsc.1080.0413.
- Hotho JJ, Becker-Ritterspach F, Saka-Helmhout A. Enriching absorptive capacity through social interaction. Br J Manag 2012;23:383-401.
- Camison C, Fores B. Knowledge absorptive capacity: new insights for its conceptualization and measurement. J Bus Res 2010;63:707-15. https://doi.org/10.1016/j.jbusres.2009.04.022.
- Jimenez-Barrionuevo MM, Garcia-Morales VJ, Molina LM. Validation of an instrument to measure absorptive capacity. Technovation 2011;31:190-202. https://doi.org/10.1016/j.technovation.2010.12.002.
- Jiménez-Castillo D, Sánchez-Pérez M. Nurturing employee market knowledge absorptive capacity through unified internal communication and integrated information technology. Info Manage 2013;50:76-8. https://doi.org/10.1016/j.im.2013.01.001.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, . GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involve Engage 2017;3.
- Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient 2014;7:387-95. https://doi.org/10.1007/s40271-014-0065-0.
- Staniszewska S, Denegri S. Patient and public involvement in research: future challenges. Evid Based Nurs 2013;16. https://doi.org/10.1136/eb-2013-101406.
- Staniszewska S, Brett J, Mockford C, Barber R. The GRIPP checklist: strengthening the quality and transparency of reporting for patient and public involvement in research. Int J Technol Assess Health Care 2011;27:391-9. https://doi.org/10.1017/S0266462311000481.
- Coulter A, Collins A. Making Shared Decision-making a Reality. London: The King’s Fund; 2011.
- Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Obstet Gynecol 2009;114:1341-5. https://doi.org/10.1097/AOG.0b013e3181c3020d.
- Coulter A. Engaging Patients in Healthcare. Maidenhead: McGraw Hill/Open University Press; 2011.
- Robert G, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences. Oxford: Oxford University Press; 2013.
- Gabbay J, le May A. Evidence based guidelines or collectively constructed ‘mindlines?’ Ethnographic study of knowledge management in primary care. BMJ 2004;329. https://doi.org/10.1136/bmj.329.7473.1013.
- Greenhalgh J, Flynn R, Long AF, Tyson S. Tacit and encoded knowledge in the use of standardised outcome measures in multidisciplinary team decision making: a case study of in-patient neurorehabilitation. Soc Sci Med 2008;67:183-94. https://doi.org/10.1016/j.socscimed.2008.03.006.
- Rousseau DM, Sitkin SB, Burt RS, Camerer C. Not so different after all: a cross-discipline view of trust. Acad Manage Rev 1998;23:393-404. https://doi.org/10.5465/AMR.1998.926617.
- Möllering G. The nature of trust: from Georg Simmel to a theory of expectation, interpretation and suspension. Sociology 2001;35:403-20. https://doi.org/10.1177/S0038038501000190.
- Grant AM, Gino F, Hofmann DA. Reversing the extraverted leadership advantage: the role of employee proactivity. Acad Manage J 2011;54:528-50. https://doi.org/10.5465/AMJ.2011.61968043.
- Burries ER, Detert JR, Romney AC. Speaking up vs. being heard: the disagreement around and outcomes of employee voice. Organ Sci 2013;24:22-38. https://doi.org/10.1287/orsc.1110.0732.
- West MA, Beyerlein MM, Johnson DA, Beyerlein ST. Advances in Interdisciplinary Studies of Work Teams. Stamford, CT: JAI Press; 2000.
- Meyer JP, Allen NJ, Smith CA. Commitment to organizations and occupations: extension and test of a three-component conceptualization. J Applied Psychol 1993;78:538-51. https://doi.org/10.1037/0021-9010.78.4.538.
- Grandey AA, Barling A, Cooper C. Handbook of Organisational Behaviour. London: Sage Publications; 2008.
- Kiefer T, Hartley J, Conway N, Briner RB. Feeling the squeeze: public employees’ experiences of cutback- and innovation-related organizational changes following a national announcement of budget reductions. J Public Adm Res Theory 2015;25:1279-305. https://doi.org/10.1093/jopart/muu042.
- Barton A, Mulley G. History of the development of geriatric medicine in the UK. Postgrad Med J 2003;79:229-34. https://doi.org/10.1136/pmj.79.930.229.
- Oborn E, Dawson S. Learning across communities of practice: an examination of multidisciplinary work. Br J Manag 2010;21:843-58. https://doi.org/10.1111/j.1467-8551.2009.00684.x.
- Currie G, Burgess N, Hayton JC. HR practices and knowledge brokering by hybrid middle managers in hospital settings: the influence of professional hierarchy. Hum Res Manage 2015;54:793-812. https://doi.org/10.1002/hrm.21709.
Appendix 1 Description of variables in the tool
We describe the development and items of each variable in the tool, following the three elements: antecedents (capabilities), ACAP and outcomes (see Figure 2).
Socialisation capability
Trust in Clinical Commissioning Group colleagues
Trust is an individual-level construct in this research and assesses the trust in other CCG colleagues who were involved in the commissioning process in question. We adopt the trust definition given by de Jong and Elfring,128 that is, the ‘psychological state of individuals involving confident, positive expectations about the actions of another’. Following previous scholars, trust, in this research, captures two main elements: ‘positive expectations’ and ‘suspension of uncertainty’. 128,155,156 Positive expectation is assessed by items 1, 2, 5, 6 and 7, which are related to whose interest people take into account when making decisions. Suspension of uncertainty is assessed through items 3 and 4. We assess trust in CCG colleagues specifically here, as individuals working in the CCG might also work at another practice or health-care organisation, and the aim is to assess the ACAP of CCGs in particular.
The first four items in the construct of trust in CCG colleagues are adapted from de Jong and Elfring:128 ‘they helped me if I had difficulties with my CCG-related job’, ‘they took my interests into account’, ‘they kept me informed’ and ‘they kept their word’. The last three items, ‘they had the best interest of service users at heart’, ‘they had the best interest of their own practice/organisation at heart’ and ‘they had the best interest of their professional group at heart’, have been developed based on the results of the qualitative study.
Trust between Clinical Commissioning Groups and their partners
Interorganisational trust is also assessed to capture the status quo of the relationships with partner organisations. We first ask respondents to list the partner that their CCG worked with most frequently, the partner that was the most crucial to the outcome and the partner that, in hindsight, they should have worked more closely with during the commissioning of Project X, and why they listed the three partners. Then, we use a three-item comparative scale to assess the trust between the CCG and their partners, comparing the partner that was most crucial to the outcome with the partner that the CCG should have worked with more closely. The rationale for comparison is that we predict variation in the trust between these two partners and the CCG. The three items are adapted from the five-item interorganisational trust scale developed by Poppo et al. :129 ‘the relationship with this partner was mutually trusting’, ‘this partner kept their promises to our CCG’ and ‘our CCG was sure what this partner said was true’.
Trust in Clinical Commissioning Group managers
To assess trust in CCG managers, we adapt the trust scale from Mayer and Gavin,130 which is developed to measure the trust between employees and managers specifically. Considering the CCG context, we use a short version of their 10-item scale, including ‘I wish I had more influence over the manager’s decision’, ‘I share my opinion about sensitive issues with the manager even if my opinion may be unpopular’, ‘if the CCG manager asks why a problem happened, I speak freely even if I am partly to blame’ and ‘my manager and I have mutual trust’.
Taking charge
Taking charge focuses on proactive improvement at one’s organisation or work unit in terms of work structures, policies and procedures134,157 and, therefore, is likely to affect how the organisation acquires and shares information. We measure taking charge using four of the eight items developed by Morrison and Phelps:134 ‘I tried to bring about improved procedures’, ‘I tried to correct a faulty procedure or practice’, ‘I tried to eliminate redundant or unnecessary procedures’ and ‘I tried to change rules, procedures and policies that were non-productive or counterproductive’. The other four items were dropped as they do not fit the context.
Voice
Voice is ‘making innovative suggestions for change and recommending modifications to standard procedures even when others disagree’, a concept indicating the degree to which individuals speak up with useful suggestions. 135,157 Previous scholars examine the possible link between voice and organisational outcome, and reveal that voice can improve employees’ overall performance and organisational performance. 135,157,158 Based on the context, we use three items for voice based on the four-item scale developed by Grant et al. :157 ‘I spoke up with ideas for changes in work procedures of the CCG’, ‘I communicated opinions about CCG-related work issues to others even if my opinions differed or others disagreed’ and ‘I developed and made recommendations on CCG-related work issues’.
Being heard
We also sought advice from a PPI group, involving participants in commenting and critiquing the tool. The notion of being heard was considered relevant during the PPI meeting, particularly for some partners of CCGs. Being heard is linked to voice and is a necessary prerequisite for having an impact on organisational performance, and what’s been voiced needs to be actively taken on board by managers to have an impact on organisational outcome. 158 A three-item scale was developed to capture the sentiment of being heard: ‘my voice was heard by the CCG general manager’, ‘my voice had influence over commissioning decision’ and ‘my voice should have had more influence’.
Knowledge sharing
Knowledge sharing in this study refers to the exchange of both tacit and explicit knowledge related to the commissioning of Project X. 126 We assess knowledge sharing from both the individual and group level. Group knowledge sharing involves interaction and communication among team members regarding the commissioning process in questions. 127
The four-item scale for individual knowledge sharing is adapted from van den Hooff and Huysman:126 ‘I was kept informed of what my CCG colleagues knew about the Commissioning Project X’, ‘When I needed certain information about Commissioning Project X, I asked my CCG colleagues’, ‘I informed my CCG colleagues of what I was working on related to Commissioning Project X’ and ‘When I learnt something new related to Commissioning Project X, I made sure my CCG colleagues learnt about it too’.
The three items for group knowledge sharing are adapted from the four-item scale developed by Faraj and Sproull:127 ‘CCG colleagues shared relevant information or knowledge with one another’, ‘if a colleague in the CCG had some relevant information or knowledge, he or she was not likely to tell the others about it’ and ‘CCG colleagues provided each other with hard-to-find relevant information or knowledge’. The fourth item, ‘there is virtually no exchange of information, knowledge, or sharing of skills among members’, is excluded, partly because we are constrained by time and space, and also because this item assesses the same aspect of knowledge sharing as item 1.
Team reflexivity
Team reflexivity assesses how frequently team members reflect on their work in relation to processes, structures and objectives and modify them accordingly. 128,159 Scholars find that team reflexivity affects intrateam trust and team performance, as team reflexivity helps to find problems in work processes, structures and objectives, and seeks improvement at the same time. 136 De Jong and Elfring128 also point out the potential positive relationship between trust and team performance. To measure team reflexivity, we use a five-item scale from de Jong and Elfring,128 such as ‘the CCG reviewed the feasibility of our objectives’, ‘the CCG discussed the methods used to get the job done’ and ‘the CCG discussed whether we were working effectively together’.
Organisational commitment
Organisational commitment describes ‘the degree to which an individual feels attached to the organisation’. 131,160 We focus on affective commitment, adopting a four-item scale from Conway et al. 131 that has the following items: ‘I do not feel a strong sense of belonging to my CCG’, ‘I do not feel personally attached to my CCG’, ‘working at my CCG has a great deal of personal meaning to me’ and ‘I really feel that problems faced by my CCG are also my problems’.
Organisational identification
Organisational identification is defined as ‘a perceived oneness with an organisation and the experience of the organisation’s success and failures as one’s own’. 132 Identification is measured with a four-item scale: ‘when someone criticises the CCG, it feels like a personal insult’, ‘I am very interested in what others think about my CCG’, ‘when I talk about this CCG, I usually say “we” rather than “they” and ‘when someone praises the CCG, it feels like a personal compliment’. 132
Emotion
Emotional experiences in relation to the job are known to affect a range of relevant employee attitudes and behaviours, including decision-making, knowledge sharing and commitment. 161 We identify 12 different types of emotional reactions to the commissioning process during the qualitative study: angry, frustrated, disappointed, anxious, fed up, let down, happy, surprised, excited, proud, satisfied and pleased. We aim to assess the frequency of each emotion during the commissioning process of Project X. Our emotion scale of six positive and six negative items is a short version of the job-related affective well-being scale developed by Von Katwyk et al. ,133 which includes a 30-item scale assessing a wide range of positive and negative emotional responses with different levels of intensity. 133,162
Group influence
We develop the group influence construct to assess the level of influence of different groups involved in the commissioning of Project X, including managers, doctors, nurses, local authority and PPI. The rationale to incorporate the construct, group influence, is the different roles that the aforementioned groups could play in the decision-making process. The health-care sector is known for multiple professionals working together, and there is distinction between the status of different actors such as doctors, nurses and managers. 163,164 For example, existing literatures show that nurses struggle to diffuse their knowledge upwards and outwards to doctors and managers. 165 Thus, different professionals in CCGs might have a different level of influence on the decision-making of the commissioning of Project X.
System capability
Organisational and team infrastructure
The five-item scale to assess organisational and team infrastructure is developed based on the results of the qualitative study. Items 1 and 4 assess whether or not there is organisational and team infrastructure in place to help communication among different stakeholders in commissioning decision-making: ‘an efficient IT system is in place to help our decision-making’ and ‘community and other public sector events are held to help with our decision-making’. Items 2, 3 and 5 assess whether or not people use the existing organisational and team infrastructure: ‘we involve end-users to inform our decision-making’, ‘I am required to attend meetings/events where end-users are involved’ and ‘I am required to attend community and other public sector events’.
Rules, procedures and knowledge-sharing platform
The scale items for rules and procedures are developed from the qualitative research. They capture the extent to which participants utilise existing procedures or structures in the commissioning process. There are three items in this construct: ‘I used the IT system in place’, ‘I actively participated in meetings where end-users were involved’ and ‘I actively participated in public and community events’.
Feedback seeking
Feedback seeking is ‘getting information on how far one is from the (performance) goal’. 136 Thus, feedback-seeking behaviour serves as an information- and knowledge-obtaining system. We adapt three items from the five-item scale developed by Schippers et al. 136 to assess feedback-seeking behaviours in CCGs, and the other two items were disregarded given the context of CCGs. The three items are: ‘the CCG checked how satisfied partners were with the commissioning process’, ‘the CCG asked for feedback from internal and external customers on the result’ and ‘the CCG checked how well we performed as a team’. The first item is asked three times with regard to the three partners that CCGs stated at the beginning of the survey.
Co-ordination capability
Cross-functional interaction
We developed a five-item scale for the construct of cross-functional interaction based on the qualitative study and with respect to the cross-functional interactions discussed by other scholars. 8 The main aim of cross-functional interaction is to break knowledge boundaries across different units and hierarchies within the organisation. 2,8,9 The five items are ‘I know the functions of other colleagues in my CCG’, ‘people in my CCG know each other’s job/function’, ‘I regularly have interactions with other colleagues in my CCG’, ‘people in my CCG regularly have interactions with each other’ and ‘we hardly ever meet other colleagues in my CCG’.
Participative leadership
Participative leadership is assessed from both the employee’s viewpoint and the manager’s viewpoint. The construct is adapted from Arnold et al. 137 and includes six items. The following are the items for participative leadership from the employee’s viewpoint: ‘the CCG general manager encouraged us to express ideas/suggestions’, ‘the CCG general manager listened to our ideas and suggestions’, ‘the CCG general manager used our suggestions to make decisions’, ‘the CCG general manager gave us a chance to voice our opinions’, ‘the CCG general manager considered our ideas when he/she disagreed with them’ and ‘the CCG general manager made decisions that were based only on his/her own ideas’.
Absorptive capacity
Acquisition
Acquisition consists of four items: ‘I searched for relevant information’, ‘I acquired relevant information’, ‘I used the standardised national statistics for information’ and ‘I identified gaps in existing information’. Items 1 and 2 are adapted from Flatten et al. 138 Items 3 and 4 are based on the results of the qualitative part of this study with the advice from the PPI group.
Assimilation
Assimilation is also assessed with four items: ‘I communicated ideas across the CCG’, ‘I appreciated support from other colleagues in the CCG to solve problems’, ‘I communicated knowledge I obtained promptly to all other colleagues in the CCG’ and ‘I met other colleagues in the CCG periodically to interchange new developments, problems and achievements’.
Transformation
Transformation is also assessed with four items: ‘I used collected information’, ‘I prepared new knowledge for future use’, ‘I linked existing knowledge with new insights’ and ‘I applied new knowledge in my practical work’.
Exploitation
Exploitation is assessed with three items: ‘I supported the development of new practice/technologies in the CCG’, ‘I incorporated feedback in my CCG work’ and ‘when a new idea met resistance within the CCG, I put in a great deal of effort to guarantee the idea was brought to fruition’.
Outcomes of absorptive capacity
Innovativeness of Clinical Commissioning Groups
To assess the innovativeness of CCGs, we use the three-item scale developed by Wang:139 ‘the CCG adopted new way of doing things from other CCGs’, ‘the CCG tried new ways of doing things and sought unusual, novel solutions’ and ‘the CCG encouraged people to think and behave in original and novel ways’.
Quality and productivity
The quality scale is adapted from Bresman,140 and we ask respondents to rate different aspects of the quality of the commissioning process of the commissioning Project that include the following: ‘the decision of what services were needed’, ‘ensuring needed services were provided’ and ‘comparing to other CCGs that you are familiar with’. We measured the productivity of CCGs by assessing their ‘use of resources’ and ‘ability to meet objectives’.
Acceptability of the outcome
Finally, we ask respondents the acceptability of the commissioning outcome, which is assessed with a single item: ‘considering the resources available, how acceptable was the outcome of the commissioning of Project X?’. This single-item construct is added with the suggestions of the PPI group.
Appendix 2 Participant information sheet
Appendix 3 Consent form
Appendix 4 Meeting agendas and notes
Appendix 5 Survey questions for partners of Clinical Commissioning Groups
Appendix 6 Survey questions for Clinical Commissioning Group staff
List of abbreviations
- ACAP
- absorptive capacity
- BI
- business intelligence
- CCG
- Clinical Commissioning Group
- CLAHRC
- Collaborations in Leadership for Applied Health Research and Care
- COPD
- chronic obstructive pulmonary disorder
- CSU
- commissioning support unit
- EM
- East Midlands
- GP
- general practitioner
- HSDR
- Health Services and Delivery Research
- IT
- information technology
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PACAP
- potential absorptive capacity
- PCT
- primary care trust
- PPI
- patient and public involvement
- QIPP
- Quality, Innovation, Productivity and Prevention
- R&D
- research and development
- RACAP
- realised absorptive capacity
- RQ
- research question
- SD
- standard deviation
- UNTRAP
- University/User Teaching and Research Action Partnership
- WM
- West Midlands