Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/209/53. The contractual start date was in May 2014. The final report began editorial review in October 2016 and was accepted for publication in August 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Kinderman et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Scientific background
Dementia in society
There are currently > 850,000 people living with a diagnosis of dementia in the UK. 1 As well as the biological changes associated with a dementia process, which can lead to a range of cognitive difficulties, dementia is associated with numerous psychological and social consequences. Sixty-one per cent of people living with dementia have reported feeling anxious or depressed, 40% have reported feeling lonely and just over one-third do not feel part of their community. 1 This poses a major threat to the quality of life of a large number of people in our society and is in direct conflict with the National Dementia Strategy, the aim of which is to help people with dementia to ‘live well with dementia’. 2 The cost of dementia to the UK each year is estimated to be £26B. 3 We live in an ageing population and the issues associated with dementia will continue to increase. The status quo is unsustainable. Providing good-quality care to people with dementia will continue to be a concern over the coming years.
In 2007, the Alzheimer’s Society published Dementia UK. 4 This report stated that:
Dementia must be made a publicly stated national health and social care priority. This must be reflected in plans for service development and public spending.
In 2009, Living Well With Dementia: A National Dementia Strategy2 was published, outlining the government’s plan for providing quality services in dementia care. Dementia has been highlighted as a government priority. In 2015, the prime minister launched a programme of work5 that aims to deliver major improvements in dementia care and research by 2020. The focus of this is improving the services provided for people with dementia, with the view that England could become the best country in the world for dementia care and support, for people with dementia, their carers and families to live, and for undertaking research into dementia.
Dementia is widely feared in society6 and, traditionally, people with dementia have been among the most devalued, experiencing the double stigma of old age and cognitive impairment. Kitwood7 suggested that personhood (i.e. the state of being a person) is bestowed on us by the treatment of others. The stigma and misperceptions surrounding dementia and the resulting reactions of people towards those living with dementia have led to care practices that can undermine the humanity and personhood of an individual with dementia. 7 The literature highlights issues such as removing all choice and personal autonomy from people with dementia,8 restraint, and restrictions on ‘wandering’. It is clear that there are occasions when human rights for people with dementia are unnecessarily limited and their application is not routinely considered in clinical decision-making. 9 It is essential that approaches are adopted that maintain the humanity of an individual and challenge the stigma associated with dementia that people often report feeling.
Human rights
Human rights are brought into UK law through the Human Rights Act. 10 They represent the fundamental ways in which a person can expect to be treated simply by virtue of being human. Although human rights are based on values held for centuries, they became formalised following the atrocities of the second world war, in particular the Holocaust. It was acknowledged that human beings can inflict dreadful suffering on each other and that explicit statements on our rights as human citizens were required. The articles of the Human Rights Act are broad-ranging, covering physical, psychological and social issues, and they represent the minimum standard of treatment that we should expect. Table 1 outlines the articles of the Human Rights Act.
| Part I | The convention rights and freedoms |
| Article 2 | The right to life |
| Article 3 | The right not to be tortured or treated in an inhuman or degrading way |
| Article 4 | The right to be free from slavery or forced labour |
| Article 5 | The right to liberty and security |
| Article 6 | The right to a fair trial |
| Article 7 | The right to no punishment without law |
| Article 8 | The right to respect for private and family life, home and correspondence |
| Article 9 | The right to freedom of thought, conscience and religion |
| Article 10 | The right to freedom of expression |
| Article 11 | The right to freedom of assembly and association |
| Article 12 | The right to marry and found a family |
| Article 14 | The right not to be discriminated against in relation to any of the rights contained in the European Convention |
| Protocol 1: Article 1 | The right to peaceful enjoyment of possessions |
| Protocol 1: Article 2 | The right to education |
| Protocol 1: Article 3 | The right to free elections |
| Protocol 13: Article 1 | Abolition of the death penalty |
The United Nations adopted the Universal Declaration of Human Rights in 1948. 11 The European Convention on Human Rights,12 created in 1950 by the Council of Europe, was the first post-war attempt to unify Europe and institutionalise the shared values of democracy, human rights and the rule of law. The UK was among the first states to ratify the Convention and British jurists were highly influential in its design. The Human Rights Act10 incorporates most of the Convention rights into UK law. It came into force across the UK in October 2000.
Human rights law, including the rights composing the Human Rights Act, can be understood through the FREDA (Fairness, Respect, Equality, Dignity and Autonomy) principles. 13 The FREDA principles are not law in and of themselves. They are the values that run through the rights protected by the Human Rights Act and are at the heart of high-quality health and social care.
Human rights in health care
Where, after all, do human rights begin? In small places, close to home – so close and so small that they cannot be seen on any map of the world. Yet they are the world of the individual person . . .
Eleanor Roosevelt, 195814
Human rights are diagnosis neutral and compel us to treat everyone as human beings regardless of the difficulties they may be experiencing. They also recognise, however, that, in certain complex cases, a balance may need to be struck in order to meet competing rights of different individuals or to protect an individual from unwarranted risk, and rights may need to be limited. A human rights based approach describes the process of using the articles of the Human Rights Act in a very practical way to influence daily life. 15 A human rights based approach to care both allows for that balance to be considered and provides a lens through which such difficult decisions can be made. Failure to take the human rights of the service user into account can also lead to legal suits that impose an additional financial burden and undermine public confidence in services. 16,17 The NHS Constitution for England states that the NHS:
. . . has a duty to each and every individual that it serves and must respect their human rights.
Not only is it unlawful for NHS organisations to work in a way that is incompatible with human rights, but the application of a human rights based approach establishes minimum standards of care that help to safeguard individuals, particularly those who are vulnerable. They also remind us that individuals require a great deal more than safeguarding in order to maintain their self-respect and sense of dignity. The culture of organisations has led, on occasion, to staff delivering task-orientated, risk-averse care that fails to consider the human rights of an individual. 16 Human rights, in this context, can therefore be viewed as codifications of how relationships can be understood and the social obligations we hold as human beings. 19
The Human Rights Act10 is law; however, in health-care settings, it needs to be translated into a clear set of principles that guide everyday practice, bridging the gap between the legal system and good-quality health care. 20 Human Rights in Healthcare21 achieves this translation by outlining the key ingredients of a human rights based approach. An alternative but similar construction is found within the PANEL principles. 8 The PANEL principles are participation, accountability, non-discriminatory, empowerment and legality, and these are defined more fully in Table 2. They represent the guiding principles for organisations to follow to maximise the chances of the services they deliver aligning with a human rights based approach.
| PANEL principle | Description |
|---|---|
| Participation | To ensure that all stakeholders are meaningfully engaged in the service |
| Accountability | To ensure that there is clear accountability and transparency to services being provided |
| Non-discriminatory | To ensure that particular attention is paid to vulnerable groups |
| Empowerment | To ensure the empowerment of all stakeholder groups |
| Legality | Looking at things through a human rights lens and ensuring that all actions taken are legal |
Making the link between law and ethical practice is not the only step required. There is also a need to translate the concepts of a human rights based approach into practical strategies that can facilitate the everyday decision-making of staff; in other words, there is a need to make ‘choices guided by values’22 and by the more practical elements of a human rights based approach, such as proportionality (i.e. responding to situations in a way that is appropriate in magnitude and degree), the fit with other legal frameworks such as the Mental Health Act23 and Mental Capacity Act,24 proactive strategies (predicting responses to events through knowledge of the person and responding before a negative event occurs) and balancing rights and risks to make sensible decisions.
The disability model of dementia
Discussions around dementia and the difficulties it causes to individuals have historically been dominated by a medicalised notion of dementia, in which there is no cure and nothing can be done other than watch the person decline. 25 More recent social movements to recognise dementia as a disability26 have opened up opportunities to frame dementia within a rights based approach. The United Nations’ Convention on the Rights of Persons with Disabilities27 aims to ensure that, ultimately, people living with a disability do not experience discrimination and that their rights are maintained and promoted. The UK has ratified the Convention, which means that all UK laws and policies should be compliant with it. 28 As a result, people living with dementia should be able to utilise the Convention to protect and promote their rights.
Human rights and dementia
Although there is still limited empirical work being carried out specifically in the area of dementia and human rights, the last few years have seen an expansion of this topic as an area of focus. Several charters of human rights have been produced29,30 that aim to influence policy related to dementia. Literature also exists considering some of the major issues that may threaten an individual’s human rights. Laird31 has provided examples of how fundamental human rights can be violated in health-care settings:
[S]ituations cited by British Institute of Human Rights include failure to change soiled bed sheets, neglect leading to pressure ulcer development, not helping people to eat when they are too frail to eat themselves, excessive force used to restrain people and washing or dressing people without regard to dignity.
Laird,31 p. 6
It is notable, however, that the majority of publications are focused at a policy level32 or are discussion papers reviewing a concept33 as opposed to attempts to apply a human rights based approach in practice and evaluate its effectiveness. In 2016, Dementia Alliance International launched The Human Rights of People Living with Dementia: From Rhetoric to Reality. 34 Although this was a move to ensure that people living with dementia are aware of their rights, it stopped short of outlining the specific applications of a human rights based approach. In addition, the Dementia Engagement and Empowerment Project (DEEP) has worked alongside people with dementia to produce Our Dementia, Our Rights. 35 Although this was a real attempt to raise the issue of rights in the collective minds of society, and to produce a document in an accessible format, it did not evaluate the impact that the practical application of human rights law could have on the day-to-day lives of people living with dementia.
Since the work of Tom Kitwood,7 it has been widely accepted that person-centred principles are important in the provision of high-quality dementia care. These principles have, however, been criticised for being vague and difficult to research and enforce. 36 There are high levels of congruence between the fundamental principles of person-centred care and a human rights based approach, such as empowerment and inclusion. 37 A human rights based approach gives backbone and a legal framework to person-centred principles,37 potentially making them clearer to operationalise and more accessible to rigorous research.
Human rights training
Although there are various models of training to promote human rights awareness,38 there is limited evidence of their efficacy in terms of behavioural change. 39 These models include:
-
values and awareness model – this focuses on transmitting basic knowledge of human rights
-
accountability model – this assumes that participants will already be involved in the protection of individual and group rights and focuses on professional responsibility in relation to this
-
transformational model – this is geared towards empowering individuals who have previously experienced human rights abuses to both recognise human rights abuses and commit to their prevention.
The suggested common themes in these models are fostering and enhancing leadership, coalition and alliance development and personal empowerment. 38
Attitudinal change for staff through human rights awareness training may be more effective when there is emphasis on staff’s emotional responses and defences and the impact of organisational culture. 39 Reflections on rights awareness training in both dementia and intellectual disabilities services suggests that change might be achieved through placing ethical decision-making centrally. This has been termed ‘dilemma-based learning’. 37
Human rights evaluation
The need to evaluate human rights initiatives is often overlooked and there is no real consensus about how to evaluate them. 40 It has been argued that the evaluation of human rights based approaches is problematic for a number of reasons, including a belief that legal concepts should be monitored rather than evaluated, a fear that evaluation will lead to legal ramifications and a distaste for quantifying the extent of human misery and abuse when rights are not being upheld. 37
Donald40 provides a clear framework for evaluating human rights based approaches in health-care services. This framework encourages the exploration of human rights knowledge and understanding; skills in applying human rights based approaches; attitudes, perspectives and values; and, ultimately, the outcome and impact of applying the approach for the realisation of human rights. There is an argument that this is more palatable, as it allows researchers to directly assess the process and impact of the human rights based approaches rather than attempting to quantify abuses.
Rationale for research
Cultures of care
It may be comforting to assume that the human rights of the most vulnerable people in our society are routinely upheld and promoted by those tasked with caring for them. Unfortunately, the sad truth is that this is not always the case. The Francis report,41 arising from the lack of care provided at Mid-Staffordshire NHS Foundation Trust, highlighted the importance of creating the:
. . . right culture of care . . .
to ensure that people are treated in ways that promote dignity and respect.
The Care Quality Commission (CQC) routinely uncovers practices that threaten the human rights of people living with dementia. For example, in one care home, inspectors noted that many residents stayed in bed all day for no apparent reason. When the inspectors questioned staff about this practice, they were told, ‘One side [of the house] we get up Monday, Wednesday and Friday. The other side we get up Tuesday, Thursday, Saturday’. 42 This is obviously unacceptable and in direct conflict with the principles of the Human Rights Act. 10
When considering the moral imperative we all hold to protect the vulnerable, it has been highlighted that ‘compassion is the basis for all morality’. 43 If we want to develop cultures of care in which person-centred care is a reality, then it has been suggested that ‘the NHS must be a fertile soil for meaningful caring relationships’. 44 The work of Buber and Smith45 encouraged viewing relationships as ‘I-Thou’, thereby engaging on a human-to-human level with the people we provide care and support for, as opposed to ‘I-It’, which adopts a detached task-orientated approach whereby people are viewed as jobs to be done and tasks to be completed. It has been suggested that, in many care settings, ‘the gap between the rhetoric and the reality remains uncomfortably wide’46 when we are considering models of person-centred care. There is no obligation to carry out person-centred care other than knowing that it is the right thing to do. With their statutory weight, human rights approaches can strengthen person-centred approaches47 and maximise the chances that they will be adopted.
Training and care
The training currently given to care providers does not automatically feel congruent with the aim of producing compassionate, person-centred cultures of care. It is recognised that there are major failings in the training of staff who provide care, particularly those who work in the care home sector. The CQC found that, of those care homes told to improve after a visit, 71% had significant training gaps, with dementia care, safeguarding and the Mental Capacity Act faring worst. 48 This is particularly worrying given that > 70% of people who are residents of care homes are living with dementia,1 and that the very fact that a person resides in a care home increases the chances that there will be queries about their capacity.
In providing training we are assuming that we are equipping people to make complex clinical decisions on a day-to-day basis. In reality we are often training people to become task orientated and driven. Models of training that include real-life situations tend to produce better outcomes with more emotional attachment to them. 37
Care planning
The availability of a good-quality person-centred care plan does not automatically ensure that good-quality person-centred care is provided, but it does provide a template by which the standard of care can be judged. In 2017, NHS England stated that:
. . . care planning is a crucial element in delivering improved care for people living with dementia.
The National Institute for Health and Care Excellence (NICE)’s50 quality standard statement 4 for dementia requires that each person has a personalised care plan. There are models of good-quality care planning, such as enhanced care planning, but these are often not adopted. Traditional care planning approaches adopted in NHS services, such as the care programme approach (CPA), do not always lend themselves to the full involvement of people living with dementia because of the somewhat restrictive nature of their content and a focus on risk assessment. 51 It has been suggested that the CPA maintains:
. . . a system which too often defines people by their diagnosis and medication . . .
and
. . . finds it difficult to recognise the whole person and the unique individual . . .
Any model of quality dementia care recognises the centrality and importance of an in-depth knowledge of the person, their wishes and their preferences in providing support that is person centred and, therefore, is more likely to uphold their human rights. 53 It follows, therefore, that a good-quality care plan should be a vehicle for collating this detailed knowledge about a person and their care.
Decision-making in care settings
It is recognised that ‘making decisions that concern people’s health and quality of life creates complex ethical dilemmas, and one has to choose among alternatives’. 54 This can lead to decisions that have an impact on an individual’s human rights. For example, Robinson et al. 9 explored the area of balancing risks and rights in relation to wandering. They highlighted that staff often act in particular ways, such as having a locked-door policy, because they are worried about being viewed as negligent. The implementation of a human rights based approach may provide staff with a more comprehensive and robust framework in which decisions can be made, drawing on human rights principles, particularly proportionality, least restrictive practice and proactive strategies, rather than relying on the most risk-adverse approach. 37
Rationale
We are existing in systems where the care provided to some of the most vulnerable people in society is failing to meet their complex needs. Additionally, we are not equipping our workforces to meet these needs because of woeful lack of investment in their development.
This project will build on the existing literature exploring how the human rights of people living with dementia can be undermined and unnecessarily restricted within traditional models of care but expand the focus to look at an operationalised model of providing care that embeds a human rights based approach. The proposed intervention aimed to put human rights at the heart of care planning and service delivery. A human rights based approach was chosen as the appropriate focus for this project because not only does the NHS have a legal requirement to uphold the human rights of service users, but it is recognised that quality care is both person centred and respectful of an individual’s human rights. 55
Embedding a human rights based approach through the application of the ‘Getting It Right’ assessment tool56 and training package aimed to maximise quality of life and well-being for people with dementia and provide a framework for staff to make decisions about care within a human rights based approach, using the principles of proportionality, proactive strategies, positive risk-taking and use of least restrictive practices.
Conceptual framework
The underlying conceptual framework for the study was that the introduction of a human rights based approach to health care would lead to improvements in the well-being of people with dementia and the care they receive. This is summarised in Figure 1, which highlights how the outcome measures used allowed the exploration of these areas and the links between them. Specifically, the Quality of Life in Alzheimer’s Disease (QOL-AD)57 allowed a measurement of changes in subjective well-being but did not explain why these changes had taken place. The care plan audit measured the documented standard of care that a person should be receiving and also tapped into increases in human rights based language, etc., which would suggest that the human rights based nature of the intervention had an effect over and above simply providing generic training. However, care plans do not capture the actual care that is delivered and how it affects well-being. Dementia care mapping (DCM) was used to explore whether or not care provided on a unit changed and the effect that this had on the well-being of service users on the unit.
FIGURE 1.
Conceptual framework for the study. QOL-AD, Quality of Life in Alzheimer’s Disease.
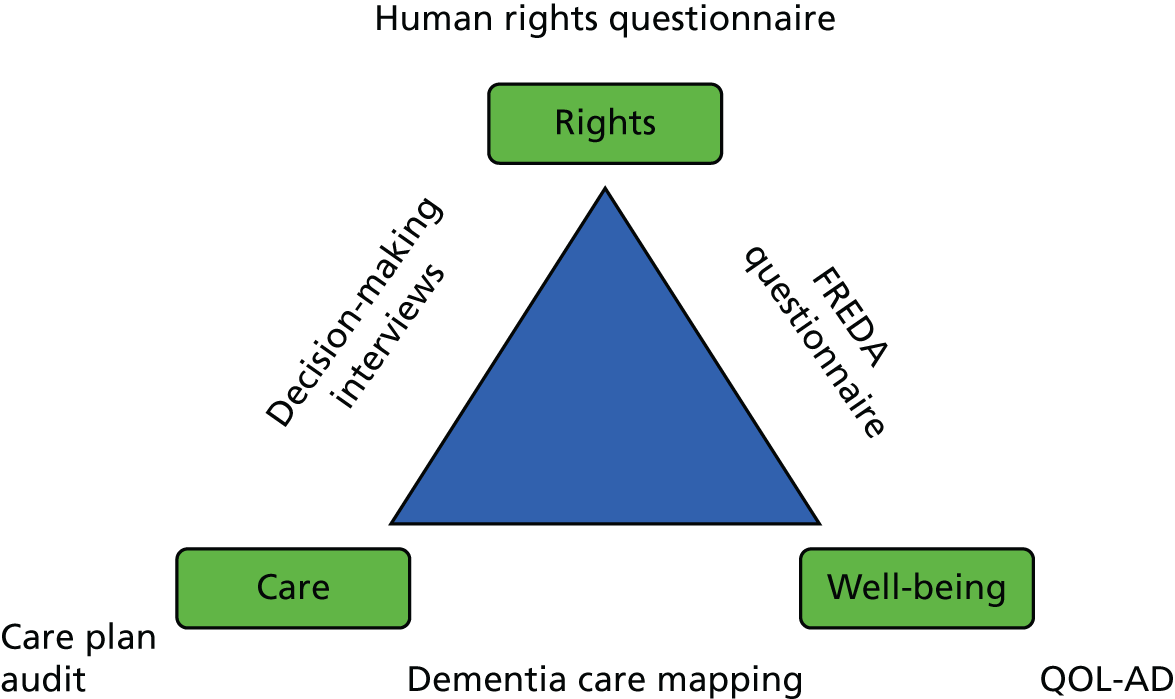
The completion of human rights knowledge and attitude questionnaires measured changes in these areas pre and post training but did not look at the impact that these had on staff in their everyday working lives and how they affected service user well-being. Staff interviews were conducted to explore whether or not the introduction of a human rights based approach led to differences in decision-making processes when considering care issues. Similarly, the FREDA-based questionnaire was included to allow the team to explore whether or not service users felt that their human rights were respected more after the intervention.
Aims and objectives
Aim
To establish whether or not the application of a human rights based approach to health care leads to significant improvements in the care and well-being of people with dementia in hospital inpatient and care home settings.
Specific objectives
-
To investigate whether or not the application of a human rights based approach to health care, as opposed to treatment as usual, leads to significant improvements in the quality of life of people with dementia in hospital inpatient and care home settings, as measured by scores on the QOL-AD scale. 57
-
To explore whether or not training on the application of a human rights based approach to health care leads to identifiable improvements in the quality of staff decision-making, as measured by vignette-based interviews with staff.
-
To explore whether training in the application of a human rights based approach to health care, and the use of the ‘Getting It Right’ assessment tool,56 as opposed to the standard care planning procedure, leads to identifiable improvements in the person-centred quality of service users’ care plans, as measured by care plan audits.
-
To explore whether the application of a human rights based approach to health care leads to changes in the well-being of family carers of people with dementia who are in hospital inpatient and care home settings, as measured by the Warwick–Edinburgh Mental Well-Being Scale (WEMWBS)58 and the Zarit Burden Interview (ZBI). 59
-
To validate a novel human rights and well-being questionnaire for dementia inpatient care.
-
To explore the costs and consequences of human rights training for staff looking after people with dementia in hospital and care home settings in terms of patient-reported well-being, care plan development, staff stress, family member well-being and overall quality of care, compared with usual patient management.
Chapter 2 Trial design and methods
Study design
The study was designed to evaluate whether or not the application of a novel human rights based intervention could improve the standard of care delivered in dementia inpatient wards and care home settings as opposed to treatment as usual.
The research employed a cluster randomised design to compare the impact of implementing the intervention (i.e. the training package, the ‘Getting It Right’ assessment tool56 and booster sessions) at 10 intervention sites with 10 control sites. The control sites continued with treatment as usual. No active placebo was indicated. It was acknowledged that there may have been significant variation in what constituted treatment as usual across the sites involved in the study.
Data collection points were at baseline (see randomisation) and at 4 months post intervention. Training was delivered at the intervention sites and booster sessions were given over a 3-month period post training.
Intervention package
The intervention package being applied was a novel human rights based intervention package that had previously been piloted within the host trust (Mersey Care NHS Foundation Trust). It consisted of three linked elements.
-
A one-day training package delivered to staff from the intervention unit at a time and place that was convenient to the site. The training was delivered by co-applicant Sarah Butchard, who jointly developed the intervention package and is an experienced clinical psychologist and senior clinical teacher. It was based on dilemma-based learning, utilising clinical scenarios that commonly occur in dementia services. It incorporated both direct learning about a human rights based approach and its utility in dementia and the practical application of the human rights based assessment tool (‘Getting It Right’56).
-
The completion of ‘Getting It Right’56 (see Appendix 1), which was based on person-centred principles and on the learning from enhanced care planning. 53 The aim of using the tool was to build up a person-centred care plan that was explicitly linked to the FREDA principles. Each unit was given multiple copies of the assessment tool following the training and requested to complete the assessment with both new and existing residents on the unit. There was no stipulation made as to how many assessments needed to be competed at each unit. It was emphasised that any member of staff, not just those who were qualified, could complete the assessment with residents, and that it was more important that it was completed by someone who had a good relationship with that resident.
-
Monthly booster sessions were delivered by Sarah Butchard to address issues arising from the application of the assessment tool. Three booster sessions were offered, one per month, following the training. These adopted a consultation model and allowed staff to reflect on any difficulties they had in applying the assessment tool.
Ethics approval and research governance
A protocol was submitted for ethics consideration to the National Research Ethics Service committee North West – Haydock (reference number 14/NW/1117) in June 2014 and it was approved in August 2014. No requests for alterations were made before approval was granted. For participating NHS sites, approval was also sought from the relevant NHS trust research and development department.
The trial was registered with the International Standard Randomised Controlled Trial Register Number (ISRCTN) Registry under the reference number ISRCTN94553028 (www.isrctn.com/ISRCTN94553028).
Patient and public involvement
Ensuring that people living with dementia were meaningfully involved in all aspects of the study was seen as essential because of the congruence of this with the key aims of the project: to ensure dignity and respect while remembering that the individuality of human needs does not diminish with the passage of time or diagnosis.
People living with dementia and their carers were included in all stages of the study; they were fully involved in the development of both the assessment tool and the FREDA-based questionnaire [IDEA (Identity, Dignity, Equality and Autonomy)] through a series of focus groups and consultation exercises.
Two people living with dementia and a carer were key members of the Trial Steering Committee (TSC) and contributed fully to these meetings throughout the study, advising on its smooth and ethical running.
Alongside this, a patient and public involvement (PPI) reference group was set up that included service users, carers and other interested stakeholders. This group worked on the wider issues having an impact on, and evolving from, the research, such as the perception of human rights among people living with dementia.
People living with dementia and carers also co-facilitated the post-study interviews with staff who had completed training to examine views on acceptability.
The group was consulted about the results of the study and their comments have been incorporated into the discussion.
Participants
The populations to be investigated during this study were people living with dementia, their carers and the staff of NHS inpatient dementia wards and care homes. All of the people living with dementia were either an existing resident of or a new admission to the ward or care home. ‘Carers’ in this context referred to family members, or significant others, of the people living with dementia. People living with dementia did not need to have a carer in order to be involved in the study.
Inclusion/exclusion criteria
The inclusion criteria were broad and are outlined below in relation to both sites (clusters) and individual participants at these sites.
Clusters
All inpatient ward sites were NHS dementia specific. Care homes were included if caring for people with dementia was a part of the facility’s core business and if they currently had enough residents with dementia to fulfil the requirements of the study.
Individuals within clusters
The main inclusion criterion for individuals within the cluster was having a diagnosis of dementia. Although issues such as age, severity of dementia and length of time at the setting were recorded, they were not inclusion/exclusion criteria. The main exclusion criterion for an individual was not having the capacity to consent and having no proxy available to support them in this.
Setting
The research was conducted in dementia inpatient wards within NHS trusts and in care homes. Table 3 shows the sites that participated in the study and their basic characteristics.
| Site | NHS trust or care home | Intervention or control | Number of beds | Total number of staff | Number of day staff | Average number of staff on shift |
|---|---|---|---|---|---|---|
| Dale Park | Care home | Intervention | 44 | 38 | 38 | 7 |
| Redholme Memory Care | Care home | Control | 55 | 47 | 35 | 9 |
| Abbotsbury | Care home | Intervention | 20 | 23 | 19 | 5 |
| Finch Manor | Care home | Intervention | 89 | 85 | 51 | 18 |
| Avalon | Care home | Control | 20 | 31 | 19 | 5 |
| Acacia Court | Care home | Control | 26 | 16 | 16 | 5 |
| Irwell Ward | NHS trust | Control | 17 | 43 | 33 | 6 |
| Meadowbank Ward | NHS trust | Intervention | 13 | 45 | 23 | 9 |
| Tudorbank | Care home | Control | 46 | 34 | 24 | 7 |
| Greenacres | Care home | Intervention | 41 | 38 | 20 | 5 |
| Cherry Ward | NHS trust | Intervention | 11 | 37 | 23 | 8 |
| Whiston & Halton Wards | NHS trust | Control | 20 | 50 | 35 | 6 |
| Leigh Ward | NHS trust | Control | 23 | 36 | 24 | 6 |
| Hollins Park | NHS trust | Intervention | 18 | 32 | 21 | 6 |
| Larkhill Hall | Care home | Intervention | 66 | 63 | 37 | 11 |
| Cressington Court | Care home | Control | 56 | 59 | 32 | 9 |
| Macclesfield | NHS trust | Intervention | 15 | 47 | 43 | 7 |
| The Harbour | NHS trust | Control | 36 | 91 | 73 | 10 |
| Thomas Leigh | Care home | Control | 19 | 40 | 13 | 4 |
| St Luke’s | Care home | Intervention | 56 | 78 | 51 | 22 |
Although the initial aim was to recruit 10 NHS wards and 10 care homes, practicalities resulted in eight NHS wards and 12 care homes being recruited. In reality, however, far more people living with dementia are care home residents than are admitted to specialist dementia wards. It is estimated that one-third of people with dementia live in care homes. 60 It is harder to obtain specific figures on those accessing specialist dementia wards, but figures for the local regions where the study was carried out suggest that only 1.5% of people living with dementia will need support on a specialist dementia inpatient ward. 61 It is, therefore, reasonable that more care homes than wards were included if the figures are to represent the population of people living with dementia.
Sample size
The sample size was based on the primary outcome measure, the QOL-AD scale,57 and on conservative figures on several parameters.
Effect size
The literature indicated that previous similar research yielded effect sizes of 0.6. 62 It is necessary to be more conservative given practical experience, and hence an effect size of 0.5 was used when calculating the sample size.
Intraclass correlation coefficient
Other trials utilising the QOL-AD scale have applied an intraclass correlation coefficient (ICC) of 0.02 based on pilot work. 63 As this was a different intervention and the difference between groups/clusters was the important aspect, we chose to apply a more conservative ICC of 0.05.
Sample size
The sample size was calculated based on detecting an effect size of 0.5 in the QOL-AD scale57 using a two-sided t-test. To achieve 80% power with a significance level of 0.05, and an ICC of 0.05, a sample size of 10 clusters with 11 individuals per group was required. Based on prior research, a retention rate of 77%64 was accounted for, which required a sample size of 10 clusters with 14 individuals per group. This resulted in a total sample of 280 participants.
Family carer well-being was explored via the WEMWBS. 58 The study had aimed to recruit a family caregiver for each participant but it was acknowledged that, in reality, this would not be possible. The sample size for this group was therefore dictated by the number of participants who had a family carer willing to take part in the trial. Vignette-based staff interviews were developed to explore the decision-making strategies employed. The aim was to recruit 50% of staff at each site. Similarly, as the care plan audit was designed specifically for this trial, a more pragmatic approach to sample size was taken. A sample was taken of 50% of all care plans at a particular site.
Recruitment procedure
Initial expressions of interest to be involved in the study were invited from local NHS trusts and care homes via existing networks and contacts. A decision was made to recruit initially within the north-west of England owing to logistical and financial constraints.
The research team also worked closely with the National Institute for Health Research (NIHR) ENRICH (Enabling Research in Care Homes) programme to identify care homes that identified themselves as willing to participate in research and to support care homes in being involved in the study. Initially all care homes in the north-west area that had been identified as research ready were approached and invited to take part in the study.
Characteristics of sites
The sites recruited varied in terms of their size, current levels of occupation and proportion of residents living with dementia. Table 4 outlines these characteristics at both baseline and follow-up. It is evident from these figures that even if a care home was not branded as exclusively for people living with dementia, a high proportion of residents were living with this condition.
| Site | Time point | Number of | ||
|---|---|---|---|---|
| Beds | Service users | Service users with dementia | ||
| Redholme Memory Care | Baseline | 55 | 48 | 48 |
| Follow-up | 55 | 50 | 50 | |
| Irwell Ward | Baseline | 17 | 13 | 12 |
| Follow-up | 17 | 12 | 11 | |
| Dale Park | Baseline | 44 | 42 | 41 |
| Follow-up | 44 | 42 | 41 | |
| Acacia Court | Baseline | 26 | 23 | 23 |
| Follow-up | 26 | 24 | 24 | |
| Abbotsbury | Baseline | 20 | 18 | 13 |
| Follow-up | 20 | 18 | 15 | |
| Avalon | Baseline | 20 | 18 | 18 |
| Follow-up | 20 | 19 | 18 | |
| Tudor Bank | Baseline | 46 | 37 | 16 |
| Follow-up | 46 | 40 | 20 | |
| Greenacres | Baseline | 41 | 39 | 13 |
| Follow-up | 41 | 32 | 8 | |
| Meadowbank Ward | Baseline | 13 | 12 | 12 |
| Follow-up | 13 | 13 | 13 | |
| Cherry Ward | Baseline | 11 | 11 | 11 |
| Follow-up | 11 | 11 | 11 | |
| Hollins Park | Baseline | 18 | 11 | 11 |
| Follow-up | 18 | 14 | 13 | |
| Leigh Ward | Baseline | 23 | 19 | 16 |
| Follow-up | 23 | 19 | 11 | |
| Larkhill Hall | Baseline | 66 | 60 | 44 |
| Follow-up | 66 | 66 | 46 | |
| Cressington Court | Baseline | 56 | 44 | 32 |
| Follow-up | 56 | 40 | 31 | |
| Whiston & Halton Wards | Baseline | 20 | 18 | 18 |
| Follow-up | 20 | 18 | 13 | |
| Macclesfield | Baseline | 15 | 11 | 11 |
| Follow-up | 15 | 11 | 11 | |
| Finch Manor | Baseline | 89 | 72 | 55 |
| Follow-up | 89 | 71 | 55 | |
| Thomas Leigh | Baseline | 20 | 18 | 18 |
| Follow-up | 19 | 18 | 18 | |
| St Luke’s | Baseline | 56 | 54 | 54 |
| Follow-up | 56 | 50 | 50 | |
| The Harbour | Baseline | 36 | 28 | 28 |
| Follow-up | 36 | 29 | 28 | |
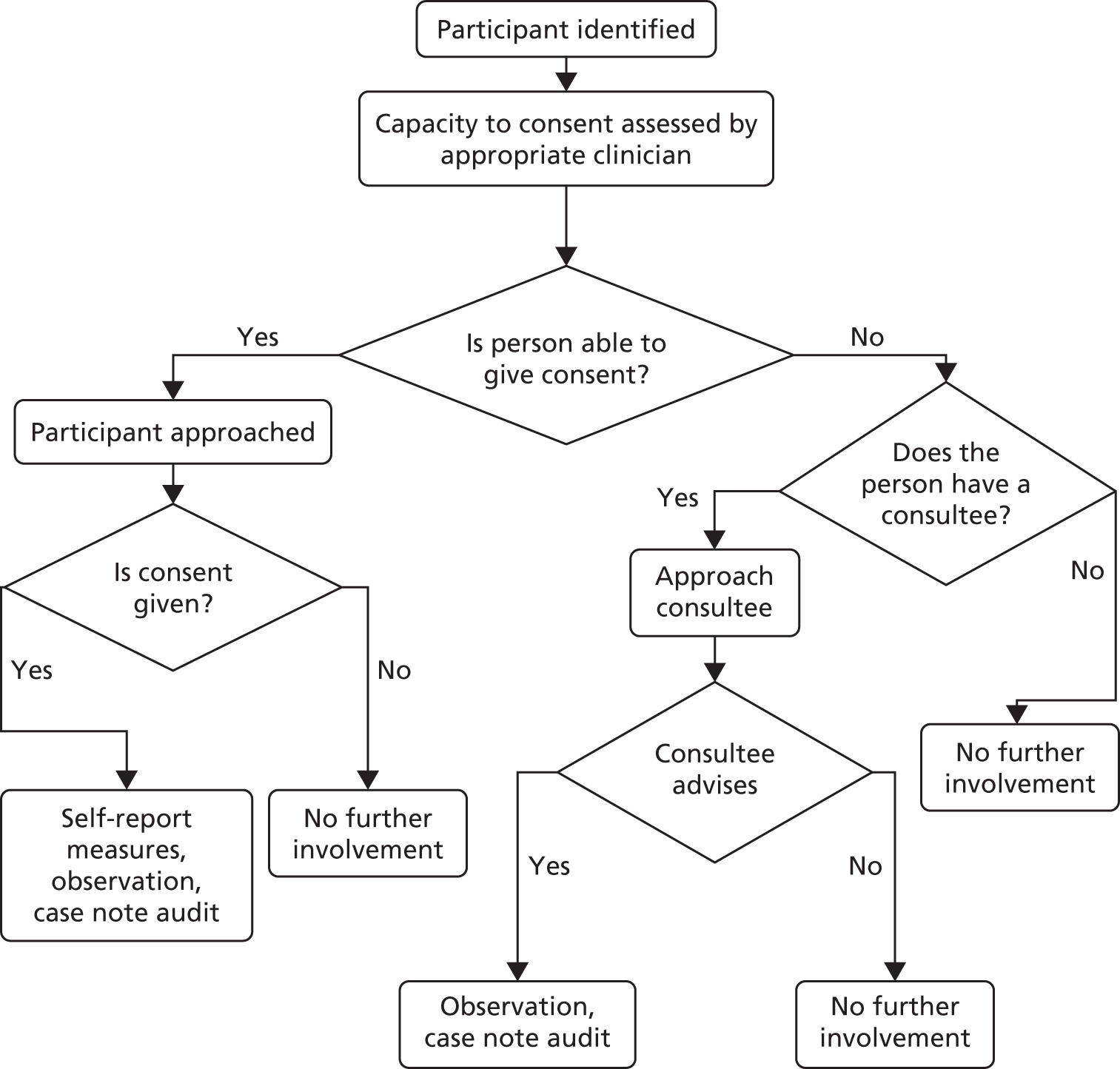
Informed consent
Obtaining informed consent is always an ethical dilemma when working in dementia care, and particularly when working with people in the later stages of dementia. The very fact that people are living in care homes or on a dementia ward means that they are likely to be in the later stages. The team acknowledged that people in the later stages, and particularly those without carers, are vulnerable to potential abuses of rights, and, therefore, it was important that they were included in the study. Every attempt was made to obtain informed consent from every potential participant, in line with the Mental Capacity Act. 24 Experienced clinical staff assessed the capacity of each potential participant, in line with best practice in research governance and the recommendations of the Mental Capacity Act,24 and individuals gave (or withheld) consent if they were able to do this themselves. If a person was not able to give informed consent, they were not asked to complete the self-report measures. Although the QOL-AD scale57 was chosen specifically because it is claimed to be suitable for people in the later stages of dementia, it was felt reasonable to assume that if a person was unable to give informed consent, then completion of the measure would be too cognitively complex for them. There was no reason for people without a family caregiver to be excluded from the study if they were able to give informed consent to participate.
When possible, when a person was unable to give consent, and therefore unable to complete the self-report measures, someone (either a family carer or a staff member) was invited to complete a proxy QOL-AD scale.
If a person was unable to give informed consent, and so they were not included in the self-report element of the study, they could still be included in DCM in cases when a nominated consultee could be identified. When it was not possible to identify a nominated consultee, or if the consultee advised against including the individual in the study, the person was not included in any aspect of the research. Informed consent was sought at both baseline and follow-up. Figure 2 presents a flow chart outlining these issues.
FIGURE 2.
Flow chart to illustrate the process of consent and participation.
Ethics arrangements
Both research assistants had regular contact with other members of the research team and were encouraged to share any concerns that they encountered during data collection. In addition, a TSC and a Data Monitoring and Ethics Committee (DMEC) were established, and these met regularly. Any serious concerns and issues that may have reached the threshold of a serious adverse event were taken to the TSC and/or the DMEC, as appropriate, and discussed thoroughly. Minutes of these meeting were kept and shared with NIHR. No reportable serious adverse events were identified during the study. Issues that were discussed with the committees as potential difficulties included changes to the protocol (which are outlined later in this report) and concerns about quality of care.
Randomisation
The randomisation of clusters was achieved by secure web access to the remote randomisation system at North Wales Organisation for Randomised Trials in Health (NWORTH) (https://nworth.bangor.ac.uk/randomisation/), Bangor University, using a dynamic adaptive randomisation algorithm. 65 The randomisation was performed by dynamic allocation to protect against subversion while ensuring that the trial maintained good balance to the allocation ratio of 1 : 1 across the trial. The complete list randomisation system was used and, therefore, there was an exact allocation of the sites to groups. No stratification variables were used for randomisation.
It is recognised that randomisation would usually take place after baseline measures were completed to avoid any bias generated by participants knowing which group they were in. In this study, however, it was not possible to do this. Site staff needed to know in advance when their training would take place so that practical arrangements could be made for staff to attend the training (e.g. ensuring that the site had adequate staff cover). Similarly, if baseline measures were completed too far in advance of the training, then there was a risk that factors other than the intervention would influence any changes identified. For this reason, sites were randomised before the baseline measures were collected. To minimise the effects of allocation to group before baseline measures were taken, the information given about the exact nature of the training provided, particularly its focus on human rights, was revealed only to those staff who needed to know it for planning (e.g. ward managers).
Allocation concealment
A web-based system was used to cluster randomise each recruited site. A complete-list randomisation was used, meaning that an even number of sites were entered into the system and allocated, at random, half to the usual-care group and half to the training group. The result was not seen until the allocation process was complete, and it was seen only by those who had access to the system. It was also possible to provide a blinded allocation report for the people who needed to be blinded to group allocations; groups were named group 1 and group 2 rather than control and intervention.
Implementation
Following recruitment, the web-based system generated the random allocation sequence. Sites were enrolled by the trial team, specifically the trial manager, Sarah Butchard, after which the web-based system completed the assignment of sites to the control or intervention group. If a service user was willing and able to consent to participate in the study, then they were included. Consent was obtained directly from the service user if possible; if this was not possible, then a proxy, usually a member of staff, was asked to provide consent on the service user’s behalf.
Blinding
Service users, research assistants who were collecting the data and the trial statistician were blinded. Service users received daily care and did not know whether or not staff had received the training. Staff members were obviously unblinded at follow-up as they knew whether or not the unit had received the training. Research assistants attended the sites to complete assessments and did not know to which group a site had been assigned. The trial statistician was able to see the data labelled as group 1 and group 2. The unblinding of the trial results occurred at a results meeting attended by members of the independent monitoring committees.
Data collection and management
The primary and secondary outcome measures were completed at baseline and then at 4 months after baseline. Figure 3 outlines the data collected at each time point. All measures were completed by two research assistants, who spent a week at each unit completing measures at each time point.
FIGURE 3.
Flow chart to illustrate the process of data collection. ASCOT, Adult Social Care Outcomes Toolkit; EQ-5D, EuroQol-5 Dimensions.
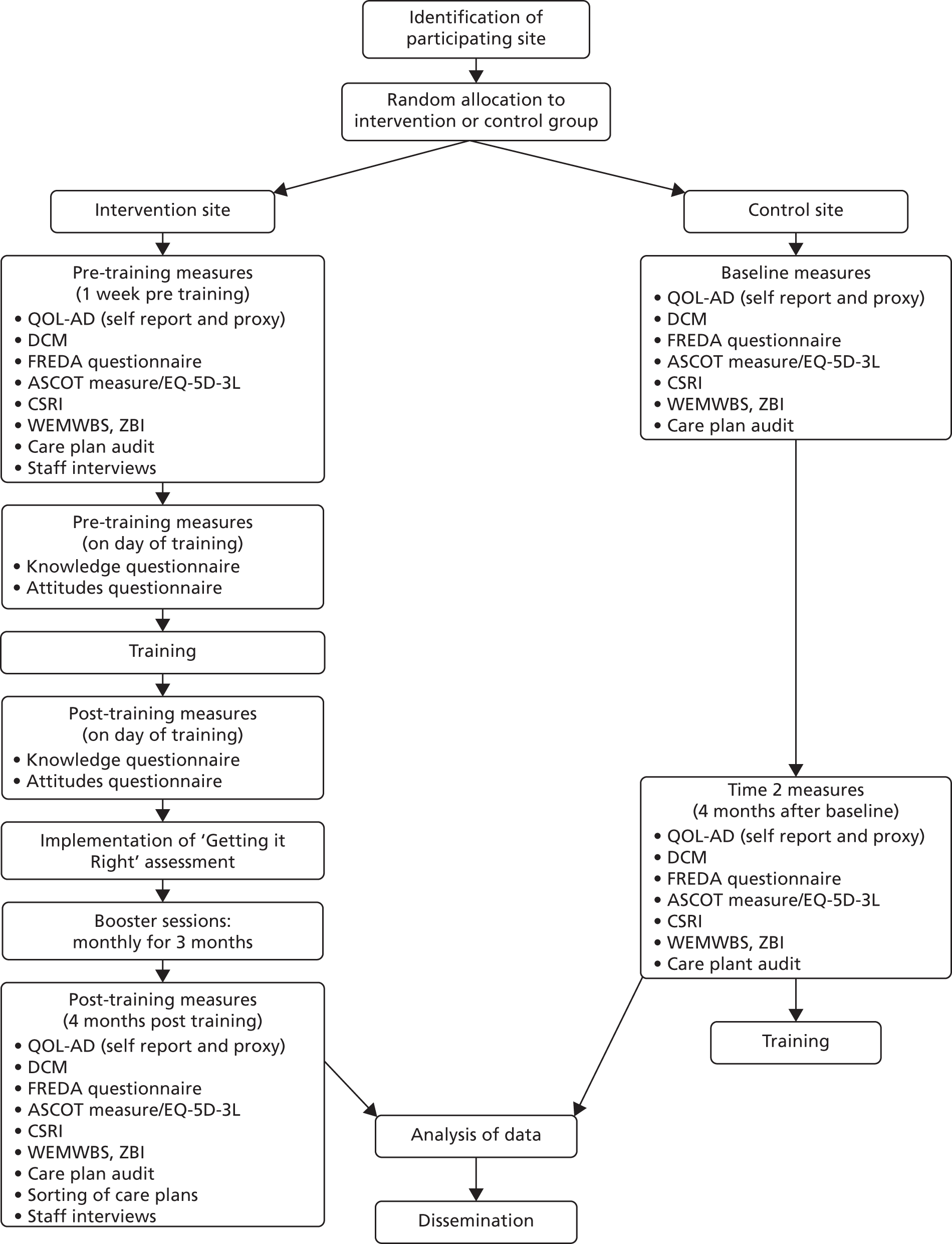
Dementia care mapping was completed first at each site to reduce the chances of the research assistants becoming unblinded at follow-up, as it was less likely that they would come across the assessment tools during this process. Table 5 shows the breakdown of tasks at each site.
| Day | Planned activities |
|---|---|
| 1 | DCM |
| 2 | Care plan audits |
| 3 |
Self-report/proxy measures Staff interviews |
| 4 |
Self-report/proxy measures Staff interviews |
| 5 |
Self-report/proxy measures Staff interviews |
All of the research data were collected on paper at the sites, and these were considered to be the source data. The data were then stored at the University of Liverpool for entry into the electronic system. These source data relevant to the participants’ outcome measures were managed through MACRO, an electronic data-capture system provided by NWORTH. MACRO 4.2 (Elsevier, London, UK; www.elsevier.com/solutions/macro) was used from 18 April 2015 to 15 December 2015, and MACRO 4.4 was used from 15 December 2015 onwards. MACRO meets regulatory compliance for the designing of electronic case report forms, data entry, data monitoring and data exporting, as well as good practice guidelines. MACRO has built-in systems for an audit trail and quality assurance.
A step-by-step cleaning process was implemented for the trial data, which was outlined in the data management plan written for the study. A random sample of 5% of the case report forms at each time point was selected for source data verification. This essentially involved cross-checking the data held in MACRO with the paper source data. If the percentage error rate for each site was > 2%, further checking was initiated based on this finding. A further 10% of randomly chosen case report forms could be checked, or if a systematic error was found with a particular item, then detailed checking of that item would be completed.
Further screening of the data was completed at all time points to identify outliers of potential errors.
Development of the intervention
The intervention for this trial was the introduction of a novel human rights based assessment tool, ‘Getting It Right’,56 into dementia wards and care homes. This tool was rooted in the principles of person-centred care and was specifically developed by Mersey Care NHS Foundation Trust to improve the person-centred nature of care plans and to ensure that the human rights of the service user were considered. Following human rights training by the British Institute of Human Rights, the assessment tool56 was developed by a project team at Mersey Care NHS Foundation Trust, which consisted of service user representatives, carers, researchers and staff from disciplines including nursing, clinical psychology, occupational therapy and psychiatry.
The tool was designed to be completed by a staff member and the service user collaboratively and, thus, encouraged both parties to consider the human rights that should be recognised during the service user’s stay in care. More specifically, the tool maps these human rights onto a wide range of areas of care, including preferences of food and drink, preferred name and access of visitors. The function of the tool was to generate a person-centred care plan that would maximise the person’s quality of life while they were on the unit and help to ensure that their human rights were acknowledged and upheld. The staff member was supported by a complementary manual and the end product was a care plan that could be kept by the service user as well as serving as the basis for the subsequent care that the person would receive. The tool was designed to be user friendly, with bold print, pictorial representations and clear, colour-coded sections.
To aid the implementation of the assessment tool, a staff training package was also developed. This took the form of one-day training, split between providing a general introduction to human rights and their relation to health care, and providing advice and instructions on how to correctly administer the tool. The training package utilised ‘dilemma-based learning’37 and included a specially designed and commissioned DVD (digital versatile disc) containing dramatised care-based scenarios that encourage interactive learning of human rights based approaches when making clinical decisions. During the training, participants were prompted to engage in discussions about how they would respond to clinical situations using a human rights-focused approach. As such, the training was framed as adopting the values and awareness model of human rights training. 38
The training was designed to be delivered to all grades and professions of care unit staff. This was the model used in the pilot phase when staff attending training encompassed a range of both (e.g. ward manager, registered nurses, support workers, domestic staff, occupational therapists and physiotherapists). The key issue was that training was provided to the team as a whole, in line with evidence that this increases discussion of the issues and allows staff to support each other in embedding the training into practice.
Following the initial training, each site was also offered three monthly booster sessions to help build their confidence in embedding the approach.
The ‘Getting It Right’ tool56 and associated training package were piloted within Mersey Care NHS Foundation Trust, and underwent an evaluation using a number of outcome measures: a specifically designed audit tool, vignette-based semistructured interviews, and human rights knowledge and attitude questionnaires.
Outcome measures
Primary outcome measure
Service user well-being
The primary outcome measure used in the research was the QOL-AD57 scale to assess the subjective well-being of the person with dementia. The European consensus on outcome measures for psychosocial intervention research in dementia care66 states that the QOL-AD scale is the measure of choice when looking at quality of life, as it is brief, has demonstrated sensitivity to psychosocial intervention, correlates with health-utility measures and can be used by people with Mini Mental State Examination (MMSE) scores of as low as 3.
The QOL-AD proxy version was also used with both staff and family caregivers to elicit the views of those supporting the person living with dementia.
Secondary outcome measures
Family carer well-being
It is recognised that caring for someone with dementia can be stressful. 67 Family carer well-being was therefore also assessed to explore whether or not it was improved by the application of a human rights based approach on a unit. This was assessed using the WEMWBS,58 and the ZBI59 explored carers’ perceptions of caring responsibilities.
Standard of care
A care plan audit was conducted at each site to provide a measure of the documented plan of care for each service user. An audit tool was specifically designed for the study, which was based on the gold standards of person-centred care in dementia care settings as outlined in the enriched care planning for people with dementia model53 and with a human rights based focus. The aim was to establish whether or not human rights based training is an explanatory variable for any changes in care and well-being observed over and above a standard training package, as the tool allowed the presence of human rights based language and concepts in care plans to be directly assessed.
The standard of care provided at the site and its link to well-being was assessed via DCM,68 an observational assessment yielding quantitative measures of well-being and ill-being for an individual with dementia.
Staff decision-making
Decision-making was explored through vignette-based interviews at the participating sites with staff of various grades. It was felt that this qualitative element of the study served several purposes. It provided an outcome in its own right, in that it explored how staff make decisions in difficult complex situations. The interviews also aimed to provide more information on the mediators of any effect observed, as questions were asked directly about decision-making and what assists with this. If the intervention was successful, then more human rights based language and a clearer framework for decision-making would be seen in the post-intervention interviews.
Knowledge of human rights
To assess knowledge acquisition during the training, pre- and post-training measures of human rights knowledge were collected via a human rights knowledge questionnaire, as recommended by A Guide to Evaluating Human Rights Based Interventions in Health and Social Care. 40 These data were collected on the day of the training. A human rights attitudes questionnaire was also used to look at changes in attitudes both pre and post training. Again, data from this were collected on the day of training.
Health economics
The trial also conducted a cost–consequences analysis, in which the consequences included patient-reported health-related quality of life [EuroQol-5 Dimensions, three-level version (EQ-5D-3L)], patient-reported well-being (QOL-AD57), family member well-being (WEMWBS58 and ZBI59) and overall quality of care [Adult Social Care Outcomes Toolkit (ASCOT69) and CSRI].
Development of outcome measures specific to the study
Care plan audit tool
A care plan audit tool was developed specifically for the study as there was no existing measure available that would capture the information required, namely the person-centred nature of the care plan and specific references to human rights language. The audit tool was based on the gold standards of person-centred dementia care as laid out in Enriched Care Planning for People with Dementia: A Good Practice Guide to Delivering Person-centred Care,53 a document derived from Kitwood’s principles of person-centred care. 7
The audit tool employed a ‘tick-box’ format, which meant that data could be expressed as a percentage as well as a raw number for both baseline and follow-up, and then compared formally. There is, however, also the capability to capture more qualitative data, which would allow for reflection on the person-centred nature of care plans and the inclusion of human rights based language in these. If the intervention was successful, it would be expected that care plans post training would be more person centred and include more human rights based language.
Vignette-based interviews
Interview schedules were developed by combining the areas of enhanced care planning from Kitwood’s model of dementia care7 and the human rights considered most relevant to health care. Ten vignettes were constructed that, between them, covered all relevant areas using examples from clinical practice. Using hypothetical examples such as these avoided asking directly about care provision, which may not lead to responses that reflect true practice owing to demand characteristics and staff concerns about the perceived potential repercussions of their responses.
Knowledge and attitudes questionnaires
The human rights knowledge and attitudes questionnaires were adapted from the original learning disabilities questionnaires outlined in A Guide to Evaluating Human Rights Based Interventions in Health and Social Care. 40
Issues of specificity
It is important that the outcome measures utilised allowed exploration of the specificity of the intervention in improving care and well-being over and above the application of general training. This has been addressed in a number of ways.
-
The care plan audit measured the documented standard of care that a person should be receiving but also tapped into increases in human rights based language and concepts that would suggest that the human rights based nature of the intervention had an effect over and above simply providing generic training.
-
The completion of human rights knowledge and attitude questionnaires measured changes in these areas pre and post training but did not look at the impact that this had on staff in their everyday working lives and how it affected service user well-being.
-
Staff interviews were conducted to explore whether or not the introduction of a human rights based approach leads to differences in their decision-making processes when considering care issues. Again, this would be evaluated through the identification of key phrases and concepts in the transcripts that would specifically indicate that a human rights based approach had a direct influence on daily decision-making.
-
The FREDA-based questionnaire enabled the team to explore whether or not service users felt that their human rights were respected and upheld more after the intervention.
Taken together, these elements allowed an evaluation of the proposal that the human rights based approach outlined had benefits that would not be seen by generic training.
Development of the FREDA assessment tool
Although there is recognition that violations of human rights can occur in health-care settings, little has been done to attempt to quantify the extent to which this occurs. To this end, work was undertaken to develop and begin validating a questionnaire measure based on the FREDA principles in order to assess how well individuals subjectively experience their human rights as being upheld.
The FREDA principles have been used elsewhere in health care to aid individuals’ understanding of their human rights. 70 However, the validity of these constructs has not been empirically tested. Therefore, the initial stage of this tool development was to consult with service users and their carers.
Items for the FREDA questionnaire were first generated from focus groups with people living with dementia and their carers. Participants came to one of two focus groups to discuss the care that they had received in relation to their human rights. The main aim of the focus groups was to investigate whether or not the FREDA principles adequately covered areas relevant to dementia care, along with eliciting examples of when such principles were valued or disregarded. All participants consented to the data generated by the focus groups being used in relation to the development of the human rights agenda.
People in the later stages of dementia are often excluded from consultation because of the increased communication and comprehension difficulties that can arise as the condition progresses. Given that this measure would be exploring the potential violations of an individual’s rights, it felt important that this group of people who may be vulnerable to having their human rights undermined were included in the consultation. A method developed by Kate Allen71 was utilised, which involves showing the person living with dementia a picture of an unknown person and asking them to reflect on how that person would feel in a particular situation and what advice they would give them. It is suggested that this elicits more information than asking direct questions about the treatment that they have received. This method was used on a dementia inpatient ward within Mersey Care NHS Foundation Trust and the information elicited was incorporated into the data collected from the focus groups.
Following the focus groups and ward interviews, the information was themed and statements were developed that reflected these themes. Grouping these statements together revealed four overarching themes: identity, dignity, empowerment and autonomy. The developing questionnaire was, therefore, named the IDEA questionnaire.
This resulting questionnaire was piloted with a group of people living with dementia in the community. As a result of this piloting phase, some changes were made to the structure and phrasing of items on the measure (e.g. removing any double negatives from the questions).
Changes to protocol
Despite the suggestion that the QOL-AD scale is suitable for people whose MMSE scores would imply that they have severe symptoms of dementia, in practice it became evident very quickly that there were limited numbers of people living with dementia on the inpatient wards and care homes who were able to complete the self-report version of the measure. Although every effort was made to identify and recruit all service users at each site who could complete this, it was also necessary to utilise proxy reports for those people who could not complete the questionnaire themselves. In these cases, a family caregiver was first sought, and, if none was identified, then a member of staff was asked to complete the proxy version. In total, 357 proxy measures were completed and, of these, 345 were completed by staff members.
Although the initial aim was to recruit 50% of staff from each site for an interview, it soon became apparent that this would not be practical. At each site a percentage of staff worked only night shifts and there were also many staff who were not available during the data collection week owing to annual leave, rota patterns, and so on. Therefore, a more pragmatic approach was taken and eight staff members per site were recruited to take part in the decision-making interviews.
Although it had been envisaged initially that booster sessions would last 2 hours, this was not practical when visiting the sites. In general, managers were not happy to release staff for this length of additional time and chose to speak directly to the team members themselves rather than involving other members of staff. Many of the booster sessions were refused.
It was proposed that the Alzheimer’s Disease Assessment Scale – Cognitive subscale (ADAS-Cog) be used to compare the cognitive abilities of people living in care homes with those of people on NHS wards. In practice, the majority of people living with dementia were unable to complete the assessment and, in addition, a large number of people refused to complete it. Given the small numbers collected, it was not possible to make a comparison between the groups. For this reason, no attempts were made to complete the scale at follow-up.
Fewer carers than expected were recruited to the study. The research assistants were surprised that many of the care home residents did not have visitors, and often when visitors were present they did not want to complete questionnaires as they felt that this would interrupt their time with the resident. As a result, the numbers of questionnaires completed were not large enough to allow meaningful comparisons to be made.
Statistical analysis
Missing data
There are two types of missing data possible in this data set: missing items within questionnaires at a time point and missing measures at a time point.
In the case of items missing within a questionnaire, the following approach was taken. If a missing value rule existed for a questionnaire, then this was utilised. Over and above this, if ≤ 25% of the items in a questionnaire were missing, then these were replaced with a pro-rated individual item score.
It was expected that there would be participants missing at follow-up who were present at baseline and vice versa and so the analysis model was influenced by this. The data were assessed for differences between those present at both baseline and follow-up and those present only at baseline for possible predictors to be included in the sensitivity models.
Baseline characteristics
Participant demographics, including age and gender, were reported, and split by allocated group, for baseline and follow-up. The type of dementia patients were living with was also included, when appropriate. There was no statistical comparison of the data for the two groups.
Interim analyses
No interim analyses were planned or scheduled to be completed. During the trial, no additional analyses were identified or requested by the DMEC.
Primary effectiveness analyses
The original model of analysis was planned to be a multilevel analysis of covariance model. Owing to the very nature of the wards and care homes, it was understandable that, for a number of reasons, participants present at baseline might not be present at follow-up. Therefore, a linear mixed model was used to assess the effect of time (baseline or follow-up) and group (control or intervention) and interaction of time and allocated group. The model also included site as a random effect. The main effect of interest was the group effect.
As it became evident that the ability to collect self-report data on the primary outcome measure was limited, proxy data were collected in the absence of self-report data. An additional term (self-report vs. proxy) was added to the model to assess the importance of this difference. If it was found that this term was significant, then separate analyses of self-report and proxy data were completed. This understandably affects the number of data available for the analysis and would have implications for the power of the study. The alternative was to include a self-report versus proxy and condition (group) interaction. This assesses whether or not there is a consistent difference between self-report and proxy data in both groups. The former model of analysis was chosen to allow simpler, more intuitive understanding of the data. Either way, the power of the models that could be applied would have been affected by the implications of using a mixture of proxy and self-report data.
Secondary effectiveness analyses
A linear mixed model was applied for all secondary outcome measures when appropriate. For the knowledge and attitudes questionnaire, data were collected pre and post training for the intervention group and only at baseline for the control group. This precluded the use of the linear mixed model to establish a group effect, and therefore a paired sample t-test was used to establish whether or not there was a difference in score before and after training.
Additional analyses
As indicated the significance of covariates, age, gender, DCM score, dementia type and whether or not the person had a carer were investigated by adding these to the linear mixed model.
It was also noted that one site had a different follow-up time from the other sites, with only 11 weeks in follow-up rather than the established 16 weeks. This nuance was investigated by allowing the time variable to vary for this site.
Economic analyses
Based on the Medical Research Council’s guidelines for the evaluation of complex interventions,72 our standard operating procedure for economic evaluation alongside pragmatic randomised controlled trials (RCTs) and experience in the conduct of economic evaluation alongside trials of psychosocial interventions in dementia care,63,73 we, from a public sector, multiagency perspective:74–79
-
fully costed the human rights staff training programme, distinguishing between set-up/training costs and running costs, with the former amortised over 3 years
-
collected service use data using an adapted Client Service Receipt Inventory, which recorded participants’ frequency of contacts with hospital services and selected community-based services at baseline and follow-up; participants’ medication usage was also recorded and service use was costed using national unit costs for the price year 2014–1580,81
-
conducted a cost–consequences analysis in which the consequences included patient-reported well-being (QOL-AD57), family member well-being (WEMWBS58 and ZBI59) and overall quality of care (ASCOT).
The EQ-5D-3L was included for participants with mild to moderate dementia to allow comparison with other published studies, and with previous trials, but a cost–consequences approach rather than cost–utility analysis was undertaken because of the range of relevant outcomes spanning the person with dementia, their family members, hospital and care home staff and objective measures of care quality.
Dementia care mapping
Dementia care mapping is an observational tool. A trained observer (mapper) records the behaviours of several participants for a specified amount of time (in this case 6 hours) to gain an insight into participants’ day-to-day experience. Owing to ethical reasons, observations can take place only in communal areas. After a 5-minute period, the mapper records a Behaviour Category Code that indicates what the individual was doing. Alongside this, a mood and engagement (ME) value is recorded, indicating how engaged the individual was and if their mood was positive or negative. Table 6 summarises the definitions of each score for ME.
| Mood | ME value | Engagement |
|---|---|---|
| Very happy, cheerful. Very high positive mood | +5 | Very absorbed, deeply engrossed/engaged |
| Content, happy, relaxed. Considerable positive mood | +3 | Concentrating but distractible. Considerable engagement |
| Neutral. Absence of overt signs of positive or negative mood | +1 | Alert and focused on surroundings. Brief or intermittent engagement |
| Small signs of negative mood | –1 | Withdrawn and out of contact |
| Considerable signs of negative mood | –3 | |
| Very distressed. Very great signs of negative mood | –5 |
Dementia care mapping is an established approach that looks at person-centred care in practice. This measure was completed for all sites at both baseline and follow-up. The study focused on one aspect of DCM that records the ME levels of up to eight participants living with dementia within a 6-hour time frame. The ME score for each unit at both baseline and follow-up were recorded and compared to look for changes in the quality of care provided.
Qualitative analysis
There were two sets of data in the study that were analysed qualitatively. These were the staff decision-making interviews and the post-study interviews with intervention sites. Both sets of data were analysed using thematic analysis as outlined by Braun and Clarke. 83 Thematic analysis is a method for identifying, analysing and reporting patterns (themes) within data. At its most basic, it organises and describes the data set in rich detail. In reality, however, it frequently goes further and interprets various aspects of the research topic. 84 Table 7 outlines the stages of thematic analysis proposed by Braun and Clarke. 83
| Phase | Description of the process |
|---|---|
| 1. Familiarising yourself with your data | Transcribing data (if necessary), reading and re-reading the data, noting down initial ideas |
| 2. Generating initial codes | Coding interesting features of the data in a systematic fashion across the entire data set, collating data relevant to each code |
| 3. Searching for themes | Collating codes into potential themes, gathering all data relevant to each potential theme |
| 4. Reviewing themes | Checking if the themes work in relation to the coded extracts (level 1) and the entire data set (level 2), generating a thematic ‘map’ of the analysis |
| 5. Defining and naming themes | Ongoing analysis to refine the specifics of each theme, and the overall story the analysis tells, generating clear definitions and names for each theme |
| 6. Producing the report | The final opportunity for analysis. Selection of vivid, compelling extract examples, final analysis of selected extracts, relating back of the analysis to the research question and literature, producing a scholarly report of the analysis |
Staff interviews
Data from the staff decision-making interviews were initially analysed as one data set using thematic analysis, as outlined by Braun and Clarke. 83 An inductive, or ‘bottom-up’, approach85 to data analysis was taken. An inductive approach assumes that the themes are derived directly from the data86 as opposed to imposing the data onto a pre-existing model.
From this analysis, themes were identified related to staff decision-making strategies. Themes were not combined as fully as they would usually be in thematic analysis, as it was felt important to identify specific, rather than general, decision-making strategies in this context. The interviews were then reanalysed to identify the frequency with which these strategies were discussed in each group (i.e. intervention baseline, intervention follow-up, control baseline and control follow-up).
Post-training interviews
Semistructured interviews were conducted with staff at intervention sites on an opportunistic basis. This included managerial staff, members of staff who attended training and those who did not attend training. The interviews were completed by a research assistant and a member of the PPI reference group. Interviews were recorded, transcribed and inductively, then subsequently deductively, analysed using thematic analysis. Each site was individually analysed to identify the main themes from each site. The main theme of management style was then deductively analysed using Bass and Avolio87 characteristics of active/transformational and passive/transactional management styles to identify descriptions of these characteristics within each site and how these affect descriptions of the relationships that service users and family members have with staff. Some sites were unable to accommodate the interviews owing to changes in management and lack of staffing.
Chapter 3 Trial results
Flow of participants in the trial
Sites
In total, 50 sites were contacted and offered the opportunity to be involved in the study (care homes, n = 34; NHS wards, n = 16). Twenty-eight sites declined to participate, and so 22 were randomised to either the intervention or the control arm. Between randomisation and data collection, two sites opted out of the study as they no longer wanted to be involved. These sites had previously been randomised and they withdrew because of a change of management. Of these sites, one had been randomised to the control arm and one had been randomised to the intervention arm. During data collection, two of the intervention sites did not complete training; therefore, they were classed as intent to treat (their data were still included in the intervention group’s analysis). The reason given for not completing the training at both sites was that there was not enough time or resources to release staff to attend the training. One of these sites accepted a ‘booster’ session and wanted to use the ‘Getting It Right’ assessment tool. 56 The recruitment of sites to the study is outlined in Figure 4.
FIGURE 4.
Number of sites approached to take part in and recruited to the study.
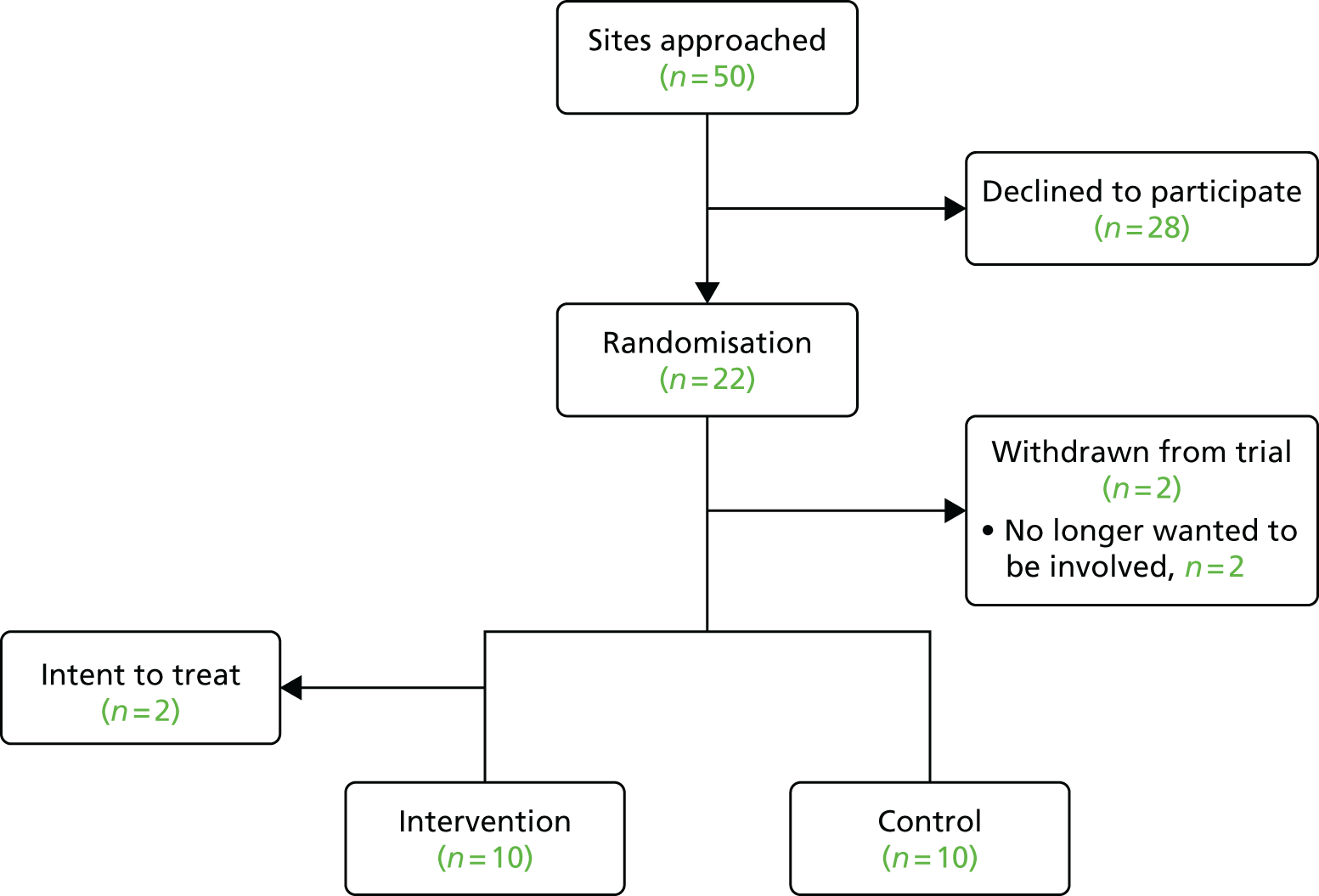
Overall recruitment
In total, the study recruited 439 people living with dementia, with 213 in the intervention arm and 226 in the control arm. These people may have completed self-report measures, had proxy measures completed, been observed in DCM or been involved in the care plan audit. They may have completed one, or more than one, element of the study. Table 8 summarises the number of aspects of the study that participants were involved in.
| Aspects (n) | |||||
|---|---|---|---|---|---|
| Baseline | Follow-up | ||||
| 1 | 2 | 3 | 1 | 2 | 3 |
| 93 | 124 | 115 | 80 | 122 | 120 |
New participants were able to be recruited at follow-up. Sites rather than participants were randomised to receive control or intervention, and participants did not receive control or intervention. This was an expected feature of recruitment, as it is was possible that participants would not be at the same site from baseline to follow-up. Recruitment from each site, for baseline and follow-up, was based on the individuals present at the time of the visits. In addition, 245 staff members were recruited to the study.
Staff completing the training
The aim was to recruit as many staff as possible from each intervention site to the training day. In practice, this was extremely difficult, and site managers reported this to be the case even when multiple training days were offered. Table 9 summarises the number of staff trained at each intervention site and the number of booster sessions that each site accepted during the intervention (i.e. the 3 months following the training).
| Site | Day staff at site (n) | Staff trained (n) | Proportion of staff trained (%) | Booster sessions (n) |
|---|---|---|---|---|
| A | 38 | 8 | 21.1 | 3 |
| B | 51 | 22 | 43.1 | 2 |
| C | 23 | 6 | 26.1 | 2 |
| D | 20 | 6 | 30.0 | 2 |
| E | 23 | 6 | 26.1 | 3 |
| F | 21 | 11 | 52.4 | 2 |
| G | 37 | 7 | 18.9 | 2 |
| H | 43 | 5 | 11.6 | 1 |
| I | 19 | 0 | 0 | 1 |
| J | 51 | 0 | 0 | 0 |
If the two sites that did not engage with the training are excluded, then an average of 8.88 staff per unit were trained, which equates to 28.7% of staff being trained. There was a large range in the proportion of staff trained at a particular site (11.6–52.4%).
It was initially envisaged that the booster sessions would take place every month and last 1–2 hours, and that staff who had either attended the training or who had not been able to attend the training but were completing the assessment tool could share their experiences, and that any difficulties or concerns could be addressed. This was to be similar to a consultation-style session and to be supportive in nature. In reality, only two sites accepted all three booster sessions offered. Booster sessions were most often rejected because of lack of time. They were also often not utilised in the way that was initially expected. In the majority of the sessions, the team member met with the manager of the unit alone, and the manager reflected on the assessment tool. This did not meet the aims of allowing the staff to explore difficulties that were arising and to cement the learning from the training session.
Service users completing the primary outcome measure
One hundred and forty-nine service users were able to self-complete the primary outcome (QOL-AD57) and a further 256 proxies were recruited to complete it. Figure 5 outlines the flow of participants completing the QOL-AD at each time point.
FIGURE 5.
Time points and number of service users/proxies completing the QOL-AD. a, Some participants completed only the baseline QOL-AD, some participants completed only the follow-up QOL-AD and some completed both the baseline and follow-up QOL-AD.

The most common reasons for not completing the follow-up visit after completing the baseline visit were death and being discharged from the care home or hospital ward. Differences in demographics and outcome results were tested for between the groups who died and those who did not die, and between the groups who were discharged and those who were not discharged.
The mean age of the participants who died (87.0 years, standard deviation (SD) 7.4 years] was significantly higher than the age of participants who did not die [81.4 years, SD 7.6 years; t(320) = –2.867; p = 0.004]. The QOL-AD score of participants who died (28.93, SD 5.35) was significantly lower than the QOL-AD score of the participants who did not die [32.85, SD 7.21; t(242) = 2.002; p = 0.046].
The mean age of the participants who were discharged (78.4 years, SD 7.7 years) was significantly lower than the age of those who were not discharged [82.5 years, SD 7.4 years; t(320) = 3.840; p < 0.001]. There was a significant difference in the proportion of men and women in the not-discharged and discharged groups [χ(1) = 9.219; p = 0.002]. The reason for this is that the group who were not discharged had a higher proportion of women (63.0%) than men (37.0%), whereas the discharged group had a higher proportion of men (58.1%) than women (41.9%).
Staff interviews
A total of 245 staff members were interviewed during the study: 101 members of staff completed an interview at baseline only, 88 members of staff completed an interview at follow-up only and 56 members of staff completed interviews at both time points. This yielded a total of 301 interviews. Table 10 summarises the number of interviews completed by staff at both baseline and follow-up in the control and intervention groups.
| Group | Time point (n) | Total (n) | |
|---|---|---|---|
| Baseline | Follow-up | ||
| Control | 77 | 70 | 147 |
| Intervention | 79 | 75 | 154 |
| Total | 156 | 145 | 301 |
Care plan audits
At each site, 50% of eligible service users were randomly selected to participate in the care plan audit aspect of the study. Figure 6 outlines the number of service users involved in the care plan audits at each time point, while Table 11 summarises the reasons that care plans were not selected for audit.
FIGURE 6.
Time points and number of service users involved in care plan audits.
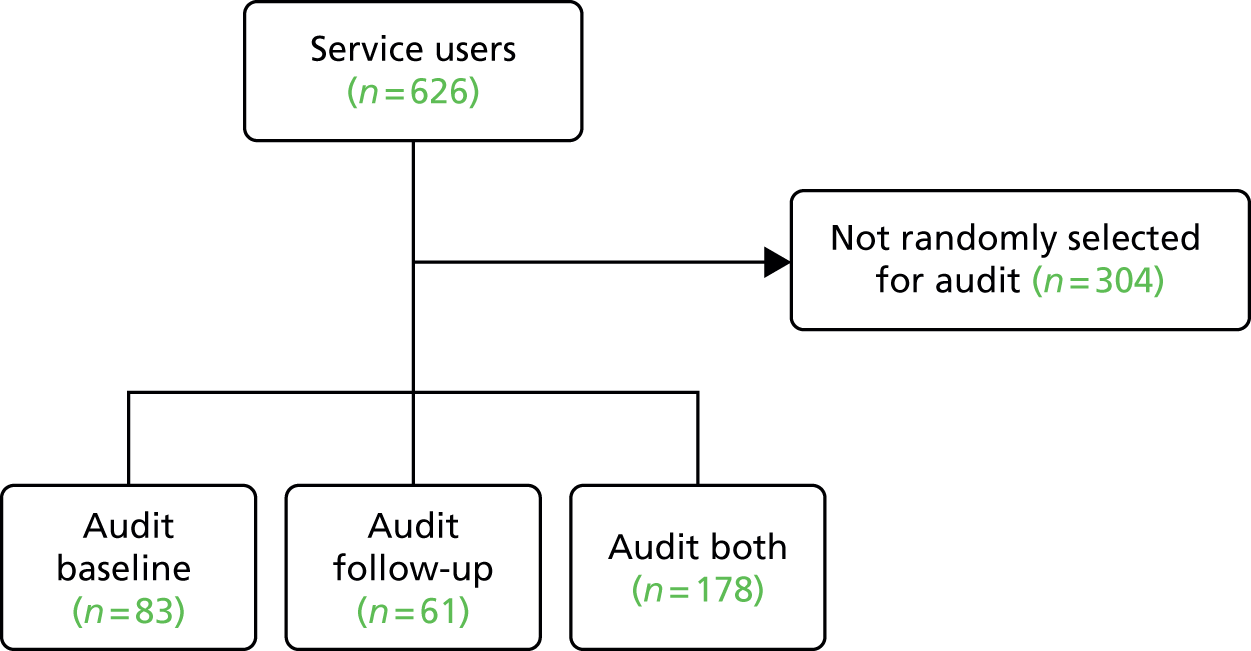
| Reason | Total (n) |
|---|---|
| At baseline | |
| Not randomised for selection | 242 |
| New service user at follow-up | 125 |
| Declined | 1 |
| In hospital | 1 |
| Not available | 1 |
| At follow-up | |
| Not randomised for selection | 236 |
| Declined | 12 |
| In hospital | 3 |
| Not available | 1 |
| Service user died | 48 |
| Service user discharged | 93 |
| Not appropriate | 4 |
Dementia care mapping
At each site, eight service users were randomly selected to participate in DCM. Figure 7 shows the number of potential participants and those involved at each time point.
FIGURE 7.
Time points and number of service users completing DCM.
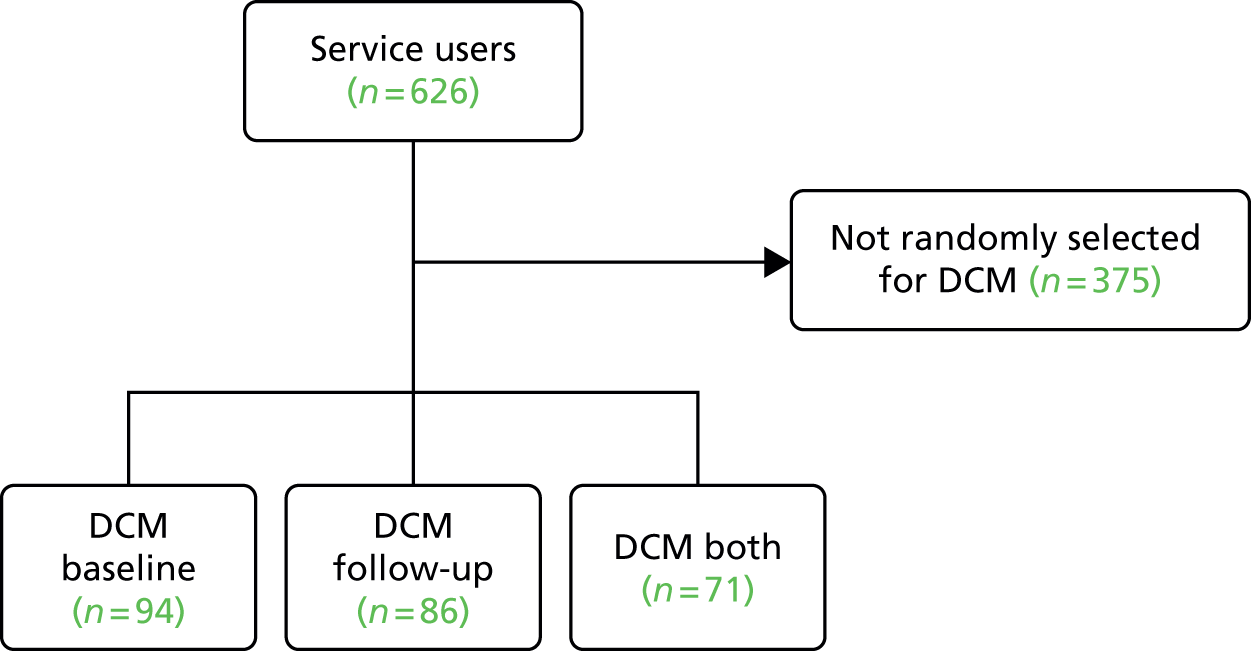
Maintenance of ‘blind’ assessments
Although the intention was that the attending researchers would not be aware of a site’s allocation while they were completing the assessments, in some cases this was unavoidable. Unblinding occurred three times at baseline and four times at follow-up, so in total seven sites were not blinded to the researchers by completion of the assessments. Table 12 summarises the reasons why researchers became unblinded to group allocation and when this unblinding process took place.
| Reasons | Total (n) | Time point at baseline or follow-up | Intervention or control |
|---|---|---|---|
| Baseline | |||
| Manager spoke about training | 1 | Day 5 | Intervention |
| Human rights training was scheduled on staff rota | 1 | Day 5 | Intervention |
| Informed by research team | 1 | Before collecting any data | Control |
| Follow-up | |||
| Manager asked when they would receive training | 1 | Before collecting any data | Control |
| ‘Getting It Right’ toolkit56 was present in care plans | 2 | Day 1 | Both intervention |
| Informed by staff during interviews | 1 | Day 5 | Intervention |
Characteristics of the samples at each time point
Tables 13 and 14 give the baseline and follow-up characteristics (age, gender and type of dementia), respectively, for each of the allocated groups.
| Characteristic | Group, n (%) | Total, N (%) | |
|---|---|---|---|
| Control | Intervention | ||
| Age (years) | |||
| Mean (SD) | 81.2 (8.0) | 82.2 (7.3) | 81.7 (7.7) |
| Gender | |||
| Female | 93 (57.1) | 103 (60.9) | 196 (59.0) |
| Male | 70 (42.9) | 66 (39.1) | 136 (41.0) |
| Type of dementia | |||
| Alzheimer’s disease | 55 (33.7) | 67 (39.6) | 122 (36.7) |
| Vascular dementia | 46 (28.2) | 45 (26.6) | 91 (27.4) |
| Dementia with Lewy bodies | 7 (4.3) | 2 (1.2) | 9 (2.7) |
| Mixed | 19 (11.7) | 14 (8.3) | 33 (9.9) |
| Frontotemporal dementia | 2 (1.2) | 0 (0.0) | 2 (0.6) |
| Other | 29 (17.8) | 41 (24.3) | 70 (21.1) |
| Missing | 5 (3.1) | 0 (0.0) | 5 (1.5) |
| Characteristic | Group, n (%) | Total, N (%) | |
|---|---|---|---|
| Control | Intervention | ||
| Age (years) | |||
| Mean (SD) | 81.1 (8.0) | 82.0 (7.6) | 81.5 (7.8) |
| Gender | |||
| Female | 120 (53.8) | 127 (59.6) | 247 (56.7) |
| Male | 103 (46.2) | 86 (40.4) | 189 (43.3) |
| Type of dementia | |||
| Alzheimer’s disease | 77 (34.5) | 85 (39.9) | 162 (37.2) |
| Vascular dementia | 61 (27.4) | 50 (23.5) | 111 (25.5) |
| Dementia with Lewy bodies | 8 (3.6) | 4 (1.9) | 12 (2.8) |
| Mixed | 30 (13.5) | 15 (7.0) | 45 (10.3) |
| Frontotemporal dementia | 3 (1.3) | 0 (0.0) | 3 (0.7) |
| Other | 38 (17.0) | 59 (27.7) | 97 (22.6) |
| Missing | 6 (2.7) | 0 (0.0) | 6 (1.4) |
Combining the diagnostic categories of ‘Alzheimer’s disease’ and ‘other’ would yield figures (baseline, 57.8%; follow-up, 59.8%) that are more in keeping with national prevalence figures for Alzheimer’s disease, which suggest that 62% of people living with dementia are living with Alzheimer’s disease-type dementia. 1
Table 15 gives the characteristics of the staff recruited to the study in both the control and the intervention groups. The groups appeared to be similar in their characteristics, and the key features are that the majority of the staff members involved were white British and female. There were far more unqualified than qualified staff recruited to the study.
| Characteristic | Group, n (%) | Total, N (%) | |
|---|---|---|---|
| Control | Intervention | ||
| Age (years) | |||
| Mean (SD) | 39.3 (12.3) | 39.5 (12.0) | 39.1 (12.6) |
| Gender | |||
| Female | 94 (76.4) | 100 (80.6) | 194 (78.5) |
| Male | 29 (23.6) | 24 (19.4) | 53 (21.5) |
| Ethnicity | |||
| White/white British | 104 (83.9) | 113 (91.1) | 217 (87.5) |
| Black/black British | 5 (4.0) | 0 (0.0) | 5 (2.0) |
| Asian/Asian British | 6 (4.8) | 1 (0.8) | 7 (2.8) |
| Mixed | 3 (2.4) | 1 (0.8) | 4 (1.6) |
| Other | 4 (3.2) | 4 (3.2) | 8 (3.2) |
| Missing | 2 (1.6) | 5 (4.0) | 7 (2.8) |
| Qualified member of staff? | |||
| Yes | 21 (16.9) | 19 (15.3) | 40 (16.1) |
| No | 102 (82.3) | 103 (83.1) | 205 (82.7) |
| Missing | 3 (0.8) | 2 (1.6) | 3 (1.2) |
See Appendix 2 for a full list of roles of the staff interviewed for the study.
Primary analysis of outcomes
The primary intention-to-treat analysis did not demonstrate any evidence of a difference between the treatment groups. The primary model fitted was as described, with the model fitted using self-report/proxy, time point, allocated group and the interaction of time and allocated group as fixed effects and site as a random effect. Table 16 shows the mean values for the control and intervention group scores on the QOL-AD57 (both self-report and proxy) at both baseline and follow-up.
| Time point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| Baseline | 117 | 14.08 | 51.00 | 32.12 (6.96) |
| Follow-up | 146 | 13.00 | 46.09 | 31.98 (6.69) |
| Baseline self-report | 58 | 26.00 | 51.00 | 35.79 (5.70) |
| Follow-up self-report | 55 | 22.75 | 44.91 | 35.14 (5.67) |
| Baseline proxy | 59 | 14.08 | 41.17 | 28.51 (6.19) |
| Follow-up proxy | 91 | 13.00 | 46.09 | 30.07 (6.56) |
| Intervention | ||||
| Baseline | 127 | 15.00 | 48.75 | 33.09 (7.34) |
| Follow-up | 127 | 16.55 | 45.00 | 32.99 (6.38) |
| Baseline self-report | 45 | 26.00 | 48.75 | 37.56 (5.03) |
| Follow-up self-report | 38 | 23.83 | 45.00 | 35.61 (5.49) |
| Baseline proxy | 82 | 15.00 | 47.67 | 30.63 (7.27) |
| Follow-up proxy | 89 | 16.55 | 42.55 | 31.87 (6.43) |
| Total | ||||
| Baseline | 244 | 14.08 | 51.00 | 32.62 (7.16) |
| Follow-up | 273 | 13.00 | 46.09 | 32.45 (6.56) |
| Did not complete | ||||
| Baseline | 67 | N/A | N/A | N/A |
| Follow-up | 148 | N/A | N/A | N/A |
There are higher numbers of proxy measures completed at follow-up than at baseline because proxy measures were not introduced until several sites had been completed at baseline. Table 17 summarises the QOL-AD scores for carer proxy (in this context referring to those measures completed by carers about the person living with dementia as opposed to the proxy measures reported in Table 16, which were on behalf of the person living with dementia).
| Time point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| Baseline | 27 | 14.18 | 46.58 | 35.60 (7.46) |
| Follow-up | 31 | 21.00 | 45.50 | 35.33 (6.98) |
| Intervention | ||||
| Baseline | 19 | 17.73 | 42.55 | 32.33 (6.41) |
| Follow-up | 13 | 17.00 | 39.00 | 33.01 (5.76) |
| Total | ||||
| Baseline | 46 | 14.18 | 46.58 | 34.25 (7.16) |
| Follow-up | 44 | 17.00 | 45.50 | 34.65 (6.67) |
| Did not complete | ||||
| Baseline | 276 | N/A | N/A | N/A |
| Follow-up | 379 | N/A | N/A | N/A |
As previously mentioned, it was harder than expected to recruit carers to the study. Of the measures completed, seven were completed by family carers and 61 were completed by professional carers.
Table 18 shows the mean IDEA questionnaire scores for both the control and the intervention groups. It can be seen from the figures that only small numbers of these questionnaires were completed as they appeared to be too cognitively complex for most of the participants. All proxy measures of the IDEA questionnaire were completed by family carers as it was not felt appropriate to ask staff to comment on whether or not they were upholding a resident’s human rights. The range of possible scores on the IDEA questionnaire was 29–87. A higher score on the IDEA questionnaire reflects less satisfaction with human rights. The IDEA questionnaire is included in Appendix 3.
| Time point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| Baseline | 42 | 29.00 | 63.37 | 36.81 (6.41) |
| Follow-up | 25 | 29.00 | 56.79 | 39.13 (7.02) |
| Baseline self-report | 40 | 29.00 | 63.37 | 36.90 (6.42) |
| Follow-up self-report | 21 | 29.00 | 56.79 | 38.88 (6.89) |
| Baseline proxy | 2 | 29.00 | 41.00 | 35.00 (8.49) |
| Follow-up proxy | 4 | 33.14 | 53.00 | 40.48 (8.66) |
| Intervention | ||||
| Baseline | 28 | 29.00 | 53.17 | 35.33 (6.01) |
| Follow-up | 17 | 29.00 | 54.22 | 36.41 (7.01) |
| Baseline self-report | 27 | 29.00 | 53.17 | 35.37 (6.12) |
| Follow-up self-report | 15 | 29.00 | 54.22 | 35.91 (6.92) |
| Baseline proxy | 1 | 34.37 | 34.37 | 34.37 (N/A) |
| Follow-up proxy | 2 | 33.64 | 46.65 | 40.15 (9.20) |
| Total | ||||
| Baseline | 70 | 29.00 | 37.00 | 36.22 (6.25) |
| Follow-up | 42 | 29.00 | 56.79 | 38.03 (7.06) |
| Did not complete | ||||
| Baseline | 260 | N/A | N/A | N/A |
| Follow-up | 391 | N/A | N/A | N/A |
Table 19 shows the mean scores on the care plan audit for both the control and the intervention groups at both baseline and follow-up. The minimum possible score on the care plan audit was 0 and the maximum was 86. A higher score implies a more detailed, person-centred care plan. The care plan audit tool is included in Appendix 3.
| Time point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| Baseline | 107 | 24.00 | 60.00 | 41.69 (7.24) |
| Follow-up | 136 | 21.00 | 63.00 | 44.38 (8.01) |
| Intervention | ||||
| Baseline | 112 | 24.00 | 59.00 | 43.82 (6.58) |
| Follow-up | 127 | 27.00 | 61.00 | 47.20 (6.43) |
| Total | ||||
| Baseline | 243 | 21.00 | 63.00 | 43.19 (7.78) |
| Follow-up | 239 | 24.00 | 61.00 | 45.62 (6.70) |
Table 20 summarises the mean values on the knowledge questionnaire for both the control and the intervention groups at both baseline and follow-up. The maximum possible score on the knowledge questionnaire was 13 and the minimum was 0. Follow-up measures were not completed with the control group. A copy of the knowledge questionnaire is included in Appendix 3.
| Time point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| Baseline | 32 | 6.00 | 11.00 | 9.00 (1.34) |
| Follow-up | N/A | N/A | N/A | N/A |
| Intervention | ||||
| Baseline | 36 | 5.00 | 12.00 | 9.31 (1.41) |
| Follow-up | 43 | 6.00 | 13.00 | 11.40 (1.58) |
| Total | ||||
| Baseline | 68 | 5.00 | 12.00 | 9.16 (1.38) |
| Follow-up | 43 | 6.00 | 13.00 | 11.40 (1.58) |
Table 21 shows the mean scores for each group on the attitudes questionnaire. The minimum possible score on the attitude questionnaire was 12 and the maximum was 60. Follow-up measures were not completed in the control group. A copy of the attitude questionnaire is included in Appendix 3.
| Time point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| Baseline | 41 | 40.00 | 60.00 | 51.24 (5.18) |
| Follow-up | N/A | N/A | N/A | N/A |
| Intervention | ||||
| Baseline | 58 | 40.00 | 60.00 | 49.78 (4.32) |
| Follow-up | 57 | 44.00 | 60.00 | 53.02 (4.11) |
| Total | ||||
| Baseline | 99 | 40.00 | 60.00 | 50.38 (4.73) |
| Follow-up | 57 | 44.00 | 60.00 | 53.02 (4.11) |
When the full data set was examined for the QOL-AD,57 the additional covariate included for self-report/proxy was statistically significant, indicating that there was a difference between the data collected by self-report and those collected by proxy. Therefore, as per the analysis plan, the data have also been split to investigate the models on the self-report and proxy data separately.
There was no indication that the interaction between time and allocated group was significant.
All outcomes were assessed for normality within the model fitting; the data for the proxy QOL-AD exhibited some trends towards non-normality and a cubic transformation was applied. Tables 22 and 23 summarise these data.
| Source | Numerator df | Denominator df | F | p-value |
|---|---|---|---|---|
| Complete data set | ||||
| Intercept | 1 | 16.22 | 7136.13 | < 0.001 |
| Status QOL-AD | 1 | 295.29 | 77.20 | < 0.001 |
| Time | 1 | 274.35 | 0.09 | 0.761 |
| Group | 1 | 16.51 | 3.63 | 0.074 |
| Time × Group | 1 | 266.73 | 0.001 | 0.980 |
| Self-report data | ||||
| Intercept | 1 | 14.67 | 3692.15 | < 0.001 |
| Time | 1 | 73.02 | 1.10 | 0.297 |
| Group | 1 | 14.88 | 0.23 | 0.641 |
| Time × Group | 1 | 74.90 | 0.04 | 0.836 |
| Proxy data | ||||
| Intercept | 1 | 13.04 | 4596.29 | < 0.001 |
| Time | 1 | 177.18 | 1.90 | 0.170 |
| Group | 1 | 13.53 | 4.35 | 0.056 |
| Time × Group | 1 | 181.67 | 0.02 | 0.886 |
| Source | Mean difference | df | SE | 95% CI | Effect size |
|---|---|---|---|---|---|
| Complete data set | |||||
| Group | 1.48 | 16.505 | 0.655 | –0.28 to 3.24 | 0.03 |
| Self-report data | |||||
| Group | 0.449 | 14.879 | 0.664 | –2.15 to 3.05 | 0.10 |
| Proxy data | |||||
| Group | 1.785 | 17.678 | 0.548 | –0.33 to 3.90 | 0.14 |
Secondary outcome measures
There was no evidence of a significant difference for the allocated group for either of these outcomes. The IDEA questionnaire scores demonstrated trends towards non-normality, and a square root transformation was applied to rectify this. There was no indication that time and allocated group were significant; this is displayed in Table 24.
| Measure | Mean difference | df | F | p-value | SE | 95% CI | Effect size |
|---|---|---|---|---|---|---|---|
| Carer QOL-AD | |||||||
| Group | 11.576 | 6.440 | 1.850 | 0.219 | 31.587 to 38.814 | 0.04 | |
| IDEA questionnaire | |||||||
| Group | –0.002 | 9.758 | 1.130 | 0.313 | 34.492 to 39.288 | –0.08 | |
| Care plan audit | |||||||
| Group | 1.960 | 18.138 | 1.149 | 0.298 | 1.041 | 42.580 to 46.930 | 0.12 |
For the care plan audit there was a significant effect of time [F(1,220.19) = 22.093; p < 0.001].
Owing to the limited number of family carers present providing data for the IDEA proxy questionnaire, the WEMWBS58 and the ZBI,59 it was not possible to analyse these with any stability using a linear mixed model. Descriptive statistics have been included in Appendix 2.
There was a statistically significant difference in both the knowledge [t(30) = –7.02; p < 0.001] and the attitudes questionnaires [t(55) = –53.87; p < 0.001] demonstrating an increase in both immediately post training. These figures are summarised in Table 25. The difference between the intervention and control group at baseline was also assessed and no statistically significant difference was seen [knowledge, t(66) = –0.914, p = 0.364; attitude, t(97) = 1.532; p = 0.129]. Given the short time span and no control data over the same period, these results must be interpreted carefully, but there is some evidence of an improvement in these domains post training.
| Measure | Paired differences | t | df | Significance (two-tailed) | ||
|---|---|---|---|---|---|---|
| Mean (SD) | Standard error of the mean | 95% CI of the difference | ||||
| Human rights attitude questionnaire baseline – human rights attitude questionnaire follow-up | –3.00 (3.82) | 0.51 | –4.02 to –1.98 | –5.87 | 55 | < 0.001 |
| Human rights knowledge questionnaire baseline – human rights knowledge questionnaire follow-up | –2.13 (1.69) | 0.30 | –2.75 to –1.51 | –7.02 | 30 | < 0.001 |
Additional analyses
Additional covariates
The additional covariates included in the linear mixed models were age, gender, DCM, dementia type and whether or not a person had a carer (Carer _ YN).
For the QOL-AD measure,57 none of these covariates was statistically significant. For the IDEA questionnaire, there was an indication that gender was statistically significant [F(1,70.43) = 5.96; p = 0.02]. The results of all these models are given in Appendix 2.
For the CPA, the additional covariate added into the model was the completion of the QOL-AD57 (self-reported, not completed and proxy completed). This was statistically significant, indicating that there were differences in the CPA scores.
Variation of follow up
One of the sites had only an 11-week follow-up period rather than the 16-week period stipulated. Allowing the time difference to feature in the linear mixed model by adjusting the time variables to have three levels (baseline, 11-week follow-up and 16-week follow-up) did not change any of the statistical interpretation of the models. Therefore, it was deemed that there was no impact of this difference in follow-up time on the outcomes observed.
Intraclass correlation coefficient
The ICC was calculated for the QOL-AD. The difference between pre and post results was calculated first. Then the variance component was calculated with site as a random effect. Using this method, the ICC was found to be 0.09.
Dementia care mapping
At each site, the ME scores for participants were grouped together to give an overall score at baseline and follow-up. The scores were then separated into intervention and control, and an overall average of the ME scores was calculated. The results of the mapping exercise are displayed in Table 26.
| Group | ME score | Time point (%) | |
|---|---|---|---|
| Baseline | Follow-up | ||
| Intervention | +5 | 0.8 | 0 |
| +3 | 39.3 | 29.3 | |
| +1 | 57.8 | 69.5 | |
| –1 | 1.8 | 1.1 | |
| –3 | 0.3 | 0.1 | |
| –5 | 0 | 0 | |
| Control | +5 | 1.4 | 0.1 |
| +3 | 34.1 | 28 | |
| +1 | 62 | 69 | |
| –1 | 2 | 2.5 | |
| –3 | 0.5 | 0.4 | |
| –5 | 0 | 0 | |
In accordance with one of the study objectives, it was hypothesised that an increase in ME scores would be seen at sites where training had been delivered. However, Table 26 highlights that, regardless of whether sites were intervention or control, there was no improvement in ME scores. In addition, for the majority of sites there was a decrease from baseline to follow-up.
Health economics
Outcome measures
Descriptive statistics for the outcome measures are shown in Table 27 for baseline and Table 28 for follow-up. As can be seen, completion rates of the carer measures (ZBI59 and WEMWBS58) were low, precluding any further analysis.
| Measure | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| ASCOT total | 45 | 0.22 | 1.00 | 0.8396 (0.16536) |
| ASCOT proxy total | 60 | 0.46 | 1.00 | 0.7848 (0.15177) |
| EQ-VAS | 40 | 50.0 | 100.0 | 75.350 (15.8802) |
| EQ-5D-3L total | 56 | –0.016 | 1.000 | 0.72641 (0.265127) |
| EQ-VAS proxy | 93 | 10.0 | 100.0 | 61.452 (22.4768) |
| EQ-5D-3L proxy total | 95 | –0.349 | 1.000 | 0.35873 (0.329315) |
| WEMWBS total | 3 | 41.0 | 47.0 | 44.000 (3.0000) |
| ZBI total | 3 | 28.000 | 37.000 | 33.03333 (4.593836) |
| Intervention | ||||
| ASCOT total | 40 | 0.74 | 1.00 | 0.8870 (0.09504) |
| ASCOT proxy total | 87 | 0.16 | 1.00 | 0.8182 (0.18658) |
| EQ-VAS | 31 | 50.0 | 100.0 | 81.935 (17.4010) |
| EQ-5D-3L total | 45 | –0.043 | 1.000 | 0.76378 (0.271051) |
| EQ-VAS proxy | 109 | 5.0 | 100.0 | 63.789 (17.6363) |
| EQ-5D-3L proxy total | 107 | –0.371 | 1.000 | 0.34907 (0.345178) |
| WEMWBS total | 3 | 48.0 | 52.0 | 50.333 (2.0817) |
| ZBI total | 3 | 8.381 | 34.000 | 19.71429 (13.062209) |
| Measure | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Control | ||||
| ASCOT total | 43 | 0.24 | 1.00 | 0.8451 (0.1712) |
| ASCOT proxy total | 88 | 0.2 | 1.0 | 0.793 (0.170) |
| EQ-VAS | 38 | 20.0 | 100.0 | 74.868 (21.701) |
| EQ-5D-3L total | 53 | –0.016 | 1.000 | 0.74428 (0.25537) |
| EQ-VAS proxy | 128 | 10.0 | 100.0 | 59.414 (21.136) |
| EQ-5D-3L proxy total | 128 | –0.536 | 1.000 | 0.34233 (0.34451) |
| WEMWBS total | 0 | |||
| ZBI total | 0 | |||
| Intervention | ||||
| ASCOT total | 27 | 0.09 | 1.00 | 0.8522 (0.1990) |
| ASCOT proxy total | 88 | 0.4 | 1.0 | 0.824 (0.161) |
| EQ-VAS | 24 | 0.0 | 100.0 | 73.125 (28.239) |
| EQ-5D-3L total | 33 | –0.077 | 1.000 | 0.66467 (0.32191) |
| EQ-VAS proxy | 108 | 10.0 | 100.0 | 61.861 (17.540) |
| EQ-5D-3L proxy total | 105 | –0.429 | 1.000 | 0.42918 (0.32765) |
| WEMWBS total | 2 | 38.0 | 48.0 | 43.000 (7.071) |
| ZBI total | 2 | 10.000 | 30.381 | 20.19048 (14.41151) |
The mean EQ-5D-3L self-report score at baseline was 0.74 (SD 0.267), which is similar to the mean UK population score of 0.78 (SD 0.26) for the age group of 65–74 years. We note that proxy scoring of the EQ-5D-3L was much lower (mean 0.35, SD 0.337), which is a similar finding to other studies involving proxy reporting for people with dementia. 63 The lower proxy scores of the EQ-5D-3L were driven by lower ratings in the self-care item.
Service use
Most health and social care contacts at both baseline and follow-up were home visits. The mean number of contacts was highest for general practitioners (GPs) and community nurses. A more detailed breakdown of the community- and hospital-based services used during a 4-month period is available in Appendix 2.
Medication
At baseline, medication records were collected for 254 participants. Medications were categorised by British National Formulary therapeutic class, obtained from Prescription Cost Analysis88 data, and are shown in Table 29. The most frequently prescribed category of medication was for the central nervous system, which includes dementia medication, analgesics, antidepressants and hypnotics and anxiolytics. A total of 101 out of the 254 participants for whom information was available were prescribed a dementia drug. Eight of these people were prescribed more than one dementia drug.
| Category of medication | Prescriptions (n) | |
|---|---|---|
| Baseline | Follow-up | |
| Anaesthesia | 5 | 1 |
| Cardiovascular system | 377 | 337 |
| Central nervous system | 722 | 651 |
| Ear, nose and oropharynx | 3 | 1 |
| Endocrine system | 105 | 102 |
| Eye | 29 | 17 |
| Gastrointestinal system | 297 | 266 |
| Infections | 29 | 25 |
| Malignant disease and immunosuppression | 1 | 5 |
| Musculoskeletal and joint diseases | 19 | 13 |
| Nutrition and blood | 211 | 156 |
| Obstetrics, gynaecology and urinary tract disorders | 16 | 10 |
| Respiratory system | 57 | 31 |
| Skin | 32 | 8 |
| No medication | 7 | 6 |
| Sterile water | 1 | 0 |
| Total | 1911 | 1602 |
A more detailed breakdown of the medications prescribed is available in Appendix 2.
Cost of the intervention
There were no intervention design costs as the intervention was developed before this study took place. Nine training sessions were delivered on site to staff. Staff who received training at hospital sites ranged from NHS band 3 support workers to NHS band 7 ward managers. Staff who received training at care home sites ranged from care home managers to care home assistants. Each training session lasted 5 hours and was delivered by a NHS band 8a trainer. Sites were given two copies of the training manual and 12 copies of response booklets. In total, 71 members of staff were trained at a cost of £7157, or £101 per staff member. The intervention costs are summarised in Table 30.
| Site | Type of cost (£) | Number of staff trained | Cost per staff member trained (£) | ||||
|---|---|---|---|---|---|---|---|
| Staff time | Trainer’s travel | Training materials | Administration | Total | |||
| 901 | 473.35 | 44.58 | 43.46 | 29.83 | 591.22 | 8 | 73.90 |
| 904 | 880.10 | 19.81 | 43.46 | 29.83 | 973.20 | 11 | 88.47 |
| 904 (second visit) | 880.10 | 19.81 | 43.46 | 29.72 | 973.09 | 11 | 88.46 |
| 910 | 591.25 | 24.77 | 43.46 | 44.58 | 704.06 | 6 | 117.34 |
| 912 | 564.00 | 14.86 | 43.46 | 14.92 | 637.24 | 6 | 106.21 |
| 913 | 684.85 | 44.58 | 43.46 | 44.58 | 817.47 | 6 | 136.25 |
| 916 | 1040.25 | 29.72 | 43.46 | 29.72 | 1143.15 | 11 | 103.92 |
| 917 | 507.45 | 19.81 | 43.46 | 14.92 | 585.64 | 7 | 83.66 |
| 919 | 584.90 | 59.44 | 43.46 | 44.58 | 732.38 | 5 | 146.48 |
| Total | 6206.25 | 277.39 | 391.14 | 282.67 | 7157.45 | 71 | 100.81 |
Qualitative results
Staff decision-making interviews
The thematic analysis identified 21 themes from the combined data set (301 interviews). The interviews were then reanalysed to identify the frequency of each decision-making strategy within the data and for each group (i.e. control baseline, control follow-up, intervention baseline and intervention follow-up). This information is shown in Table 31.
| Theme | Group (n) | |||
|---|---|---|---|---|
| Control | Intervention | |||
| Baseline | Follow-up | Baseline | Follow-up | |
| Teamwork/talking to other staff | 228 | 185 | 225 | 241 |
| Hierarchical decision-making | 191 | 222 | 192 | 147 |
| Previous experience | 87 | 83 | 66 | 45 |
| Speak to the family | 84 | 95 | 104 | 124 |
| Knowledge of the person | 69 | 65 | 86 | 89 |
| Using pre-existing documents | 68 | 75 | 98 | 84 |
| ‘It’s in their best interests’ | 67 | 60 | 57 | 61 |
| Using legislation (e.g. DOLS, Mental Capacity Act) | 65 | 49 | 42 | 52 |
| Observe/monitor | 64 | 44 | 44 | 57 |
| Common sense | 58 | 81 | 65 | 27 |
| Training | 58 | 47 | 29 | 28 |
| Share information | 28 | 33 | 20 | 33 |
| Speak to the person | 24 | 69 | 40 | 48 |
| Empathy | 21 | 21 | 14 | 22 |
| Human rights | 25 | 17 | 20 | 49 |
| Policy and procedure | 19 | 26 | 28 | 18 |
| It’s not my job | 19 | 22 | 20 | 12 |
| Fear | 16 | 19 | 10 | 1 |
| Person-centred care | 15 | 19 | 15 | 43 |
| Follow the rules | 9 | 10 | 15 | 4 |
| Total | 1223 | 1245 | 1190 | 1183 |
There were similar total numbers of decision-making strategies in each group. Table 31 shows that the most common theme in all groups, with the exception of the control group at follow-up, in relation to decision-making strategies was working as a team or consulting with other staff. The most common strategy described in the control group was hierarchical decision-making, whereby responsibility for making a decision was passed to another member of staff who was considered to be in a higher position and therefore more able to decide. It can be noted, however, that there was a drop in the reliance on hierarchical decision-making in the intervention group (although it remained the second most popular strategy in this group).
Although there are some variations in decision-making strategies across the groups, and it is acknowledged that any conclusions drawn would need to be cautious, it does appear that there are some differences in the intervention group at follow-up. Staff in this group were less likely to cite common sense as a strategy that they would employ to help them make decisions, whereas this strategy actually increased in the control group. The intervention group was also less likely to cite fear, the need to follow rules and ‘it’s not my job’ as methods by which they made a decision. The intervention group was also more likely to explicitly mention human rights (such as dignity, respect and positive risk-taking) and person-centred care. It is perhaps not surprising that the intervention group was more likely to mention specific human rights based approaches, given the training that they had undertaken and their knowledge by this time that the site was involved in a human rights study. Given that it has been suggested that person-centred principles are closely linked to the key elements of a human rights based approach,37 it is interesting to note that there was also more discussion of person-centred principles in the intervention group at follow-up, despite the principles not having been explicitly taught in the training.
Follow-up interviews
Follow-up interviews were offered to all intervention sites that completed the training. Some sites were unable to accommodate the interviews because of changes in management and lack of staffing. In total, six of the eight sites that completed training completed interviews designed to look at acceptability and effectiveness of the intervention. Interviews were conducted on an opportunistic basis and included staff who had attended the training, staff who had not attended the training and, when possible, the unit manager. The interviews were completed by a research assistant (not the same research assistant who had visited the site to collect data) and a member of the PPI reference group, who was either a person living with dementia or a carer.
On average, four staff per site were interviewed. Of the eight sites that had completed the intervention, four had a new manager by the time of these interviews. Table 32 shows the staff who were interviewed at each site and the percentage of staff trained who remained at the site at this point (approximately 6–10 months after the intervention). Sites here are listed as 1, 2, 3, etc., so that they are not identifiable. Given that the information gathered at individual sites is later linked to management styles, it was felt important to preserve the sites’ anonymity.
| Site (n) | Staff interviewed | Attended training | Did not attend training | Manager interviewed | Staff trained still at site (%) | Manager still in post |
|---|---|---|---|---|---|---|
| 1 | 4 | 4 | 0 | No | Unknown | Yes |
| 2 | 4 | 4 | 0 | Yes | 86 | Yes |
| 3 | 4 | 1 | 3 | Yes | 67 | No |
| 4 | 3 | 1 | 2 | No | Unknown | No |
| 5 | 6 | 3 | 3 | Yes | 100 | Yes |
| 6 | 3 | 1 | 2 | No | Unknown | No |
Three themes were derived from the data on the use and acceptability of the intervention. It is fully acknowledged that the questions posed to staff guided them to discuss the acceptability and effectiveness of the intervention and that the themes generated are therefore not surprising. The overarching themes and subthemes related to acceptability and effectiveness are summarised in Table 33 and described in more detail below.
| Theme | Subtheme |
|---|---|
| Accessibility of the intervention | Simple |
| Time-consuming | |
| Similar to current practice | |
| Management support | |
| Benefits to the residents | Increased knowledge about residents |
| Improved care plans | |
| Increased trust between service users and staff | |
| Benefits to staff | Access to training |
| Increased knowledge about residents | |
| Feeling like they were behaving in a less institutionalised way | |
| Changed thinking |
Accessibility of the intervention
In general, staff found the training and the assessment tool extremely simple and understandable:
The tutor lady was fab. Simple.
The information that was given. The way it was laid out as well. It was explained simply in layman’s terms. The way we understand it. When someone comes in and talks to you the likes of solicitors they talk and I go listen just tell me as it is and that is what was good about the kit. It was in our terms. There was no complex words. Nothing that we didn’t understand.
It was noted that the ‘Getting It Right’ assessment tool56 could be time-consuming to complete, and this had implications for its completion:
. . . it is such a busy unit. It is hectic to try and fit the extra stuff in.
However, there was also a sense that completing the tool was worth the effort:
It does take quite a bit of time to gather all the information from the individual. Learning about the individual and what they like especially if they can’t always tell you. And meeting family members and being able to have those conversations because sometimes they just want to off load what they have been going through. So it is quite timely but that is fine because it is so worthwhile because it allows you to collect so much data basically off the patient about what is important and how we are going to make their stay better that it is worth while taking the time over it.
Some sites reported that they felt that the intervention was similar to their current practice, particularly in terms of life story work, which was routinely carried out:
We were partly doing it anyway and this was just a slight improvement on what we were already doing.
Both positive and negative comments were made about the level of management support for the intervention and the impact that this had on its application:
But I am the one who gave the staff the support and said how are you getting on, have you been through it? We supported each other.
No, they just got put in the office and we never got around to it.
Benefits to the residents
There were several potential benefits to residents identified in the interviews. It was recognised that the completion of the ‘Getting It Right’ assessment tool56 ensured that more information was readily available about each resident and that this had an impact on residents’ care and treatment. Interviewees also emphasised the positive involvement of the family in gathering this information:
Because you are asking the family as well they are surprised at oh how do you know that about me. So they’re I feel that they are more involved. Rather than just plodding along everyday it is making them feel involved as well. You are all working collectively then. All singing under the same umbrella. If you talk about something individual to them. It makes them think more as well. It makes them feel more important knowing their background.
Similarly, staff highlighted that the completion of the assessment tool improved care plans and that this translated into more individualised care:
I went through the care plan in great depth and found out bits and pieces and I spoke to the family to find out more and got bits. We got books and music because we found out things this lady used to do. I do find some people do sit and do not talk as such where I am happy to just sit and talk and eventually she will talk back.
This continued even when the staff members were no longer directly using the assessment tool:
. . . when the staff are formulating care plans the information is there. We got given your care plans but we don’t have that paperwork here but now the content of the care plans reflect that information. There is a lot more information. A lot more making sure we have background information. They get more involved with family and friends to get as much information about that individual.
There was also a sense that completing the assessment tool and gathering the information increased trust between residents and staff:
The main things is that the service users trust you. Because they are frightened. Dementia is a frightening thing. So they have got to have trust and if people can come along and say this is Jack he likes this he likes that without having to explain to 24 different staff. I think it helps build trust and it helps build that professionalism that they feel they can trust you. That they are not every 5 minutes having to explain who they are. Makes them feel understood and cared for.
In turn, this facilitated a more empathic approach to care:
The books that we filled in we have used them on a daily basis. Use them to support people. I feel like I can empathise more. We have one lady who has bad dementia and we understand what she needs and what she wants. She folds tissues up and she thinks that is money. [We] understand why they do something that might seem strange to us. She just folds them up and she has them in her handbag she gives them to you. And you take them off her and she feels 1000 times better.
Benefits to staff
It could be seen as concerning that staff felt that this training, which was not designed to be core training in dementia care, was filling a need for training for members of staff, particularly those who were unqualified:
The support workers do not often get training and they feel that they have benefitted from the training. It has made them think about things.
This resulted in many staff being extremely positive about the training they received:
I just remember it all being really exciting. I was buzzing.
And the impact it had on them and their ability to do their job:
And it did make a massive difference to our job. A massive difference.
Staff highlighted that getting to know residents better, and having a greater understanding of their past, helped them become closer to the residents and, in turn, improved their working lives:
Like one guy who absolutely loves chatting and he will chat to you all day long. The minute you mention [name] his eyes just light up. Because that is all he knows and remembers. So we have got history on the computer, so we have looked up things that involve him. You know reading into things like that so you can talk to him properly and his eyes light up, it is amazing. Going back like more like information more than anything else, getting more background on them and their interests. It has had a big impact on myself.
One lady we have got different pictures in her room now, because I found out a lot more about her . . . That made me feel so happy though because I felt so much closer to her.
Staff commented that the training in particular had changed the way that they thought about situations and encouraged them to think of things through a human rights lens, considering each person as a human being with rights:
I just think that people think they know the Human Rights Act but it is in terms of their own situation, rather than how it translates to everyone else because I have never [experienced it] . . . it is always a given the right to have a choice and all those things but it is not necessarily so. And I think that institutions and care staff tend to think that they are the rules and if you live in a particular place meal times have always got to be on time and if you don’t want what is on the menu you don’t eat and it still goes on. If you don’t eat it you won’t have anything else. Well that is not right. It certainly shouldn’t be like that today. So with this training it makes staff realise we are only part of a bigger world and everyone has got a right.
This also led to a more compassionate approach among staff, and recognition of potential ‘mistakes’ they may make, by helping them to understand the reasons behind behaviour:
I think people’s attitudes changed during the training. People should only be vilified if they know what they are doing is wrong. Sometimes people come working in a place like this and they have got no experience and they do just see tasks. They do just see 18 baths or 18 toilets. That is all they see. They focus on that and it is easy to forget the person. I just think that with this it – makes you think what have I done? I have done that in the past. Would I do it again? No. Because I have seen it from a different perspective.
This resulted in staff feeling like they were behaving in a less institutionalised way and responding more to the needs of the person living with dementia. In this way, the training and adoption of the approach provided freedom to act in way that the staff fundamentally felt was right but that had previously been criticised:
In a way it has taken pressure off. In as much that nobody expects everybody to be in their clothes by 10 o’clock. If they are not in their clothes by 10 a.m. there is a blooming good reason for it. And people go along with that. You know it is less of an institutionalised way. Because it is about what fits in with the service user, not what fits in with the programme on the ward. There is more awareness and like I say it has created a bit more freedom for us.
Suggestions for improvements
During the interviews, staff were also asked to suggest improvements to the approach. The following suggestions were made:
-
training more staff from each unit so that knowledge could be shared and the whole team could appreciate the approach
-
providing more booster sessions to cement learning
-
digitalising the ‘Getting It Right’ assessment tool56 to make it easier to use.
Management style
As management support was such a key feature in many of the interviews, the data gathered were subsequently analysed using a deductive approach and mapped on to the characteristics from Bass and Avolio’s87 management style. It is acknowledged that the information gathered in this way was not specifically about management style and any conclusions made are tentative.
Bass and Avolio87,89 describe transactional leadership as a relationship in which both the leader and follower are working to meet their own self-interests. In this type of leadership, the leader gives clear direction as to what the follower must do in order to be rewarded. Whereas transformational leadership is described as moving beyond pure self-interest. In this style of leadership, the leader works to enhance motivation towards a shared vision. The model breaks down each leadership style into different characteristics. Transformational leadership comprises intellectual stimulation, individualised consideration, charisma and inspiration. By comparison, transactional leadership comprises leadership styles such as passive management by exception (i.e. waiting for problems to arise before taking corrective action), active management by exception (i.e. monitoring performance and taking corrective action if the follower fails to meet standards), laissez-faire and contingent reward. Table 34 outlines the characteristics associated with both transformational and transactional leadership styles.
| Leadership style | Characteristics |
|---|---|
| Transformational leadership | Intellectual stimulation |
| Individualised consideration | |
| Charisma and inspiration | |
| Transactional leadership | Passive management by exception |
| Active management by exception | |
| Laissez-faire | |
| Contingent reward |
It has been suggested that a transformational management style can enhance commitment, involvement, loyalty and performance and help individuals deal with stress. 90 In contrast, a transactional management style is likely to induce stress in staff.
When the data from the interviews were deductively analysed in line with the management styles outlined above, certain patterns were noted. At sites 2 and 5, more codes were identified that related to a transformational management style, and to two characteristics in particular: intellectual stimulation and individual consideration.
Intellectual stimulation refers to a managerial style whereby the manager encourages their staff to behave in creative ways, generating novel solutions for old problems. It is suggested that this leads to a working environment that values people questioning their own assumptions and those of the organisation and tolerates differences in views and opinions. 89 Four codes appearing to relate to intellectual stimulation were identified in the interviews.
-
Managers actively seeking ways in which the team can improve:
We heard about the study from another care home that is actually a dementia care home and we sort of asked could we join. We were desperate to be involved.
-
Managers being open to criticism:
If I have got problems in my home can you tell me. If you can do something better that is great. It affects everybody.
-
Managers showing evidence of problem-solving and adapting the human rights based approach and the ‘Getting It Right’ toolkits:
They still use the books, but the pages have been printed and put on the walls in the bedroom. This makes them much easier to use for staff and patients.
-
Managers actively disseminating information about a human rights based approach:
Well basically we just got an e-mail saying listen, we are going to start trying this, see if it works, see if it is helpful and they brought in the paperwork and went through it with us and we just started implementing it on the ward.
Individual consideration is characterised as helping others to develop, letting others know how they are doing and giving personal attention to those who seem rejected. Two codes were identified that related to this aspect of transformational style.
-
Managers being active in motivating staff to attend training and to utilise the assessment toolkits:
But I am the one who gave the staff the support and said ‘how are you getting on? Have you been through it?’ We supported each other. Do you understand it? I think at first they said we just have to concentrate on the red things and that was it, you can leave the others. And I said it is not that you can leave them it is just that initially when they come into the building, they are the things you need to give them, safe care but everything is important. And they were like OK we will carry on doing it. But we worked together with that one. I was integral. I am really lucky with my staff.
-
‘Understanding staff’ and their motivations:
For them to have volunteered for it, nobody ever volunteers for training. They would be reluctant at first. If I hadn’t driven it, would they have done it, probably not? I do that with any of the training because if you didn’t they would say if you can’t be bothered they can’t be bothered. Put it that way. I do think someone has to give them that drive. If you explain it to them they are like OK.
At sites 1 and 3, there were more codes relating to a transactional management style. These mainly fit into the laissez-fare style of management, although one code fits into the passive management by exception category.
Laissez-faire describes a manager who is content to continue functioning in the way the organisation has worked: someone who does not encourage staff to develop, embraces the status quo and asks no more of staff than what is essential. Four codes relating to a laissez-faire style of management were identified in the interviews.
-
Lack of management support and encouragement:
I think it covered every aspect but I don’t think we have enough support and staffing levels. A lot of staff on the floors.
-
Failure in communication between past and present management. The following quotation was from a new manager who had not been in position when the study took place at their unit:
I only heard about the study from this evaluation.
-
Failure to communicate to staff:
No they just got put in the office and we never got round to it. I don’t know where they are because our manager has left.
-
Using a lack of resources as a reason not to make changes:
Always resources stop me from doing these things. You always want more than what you have got. I don’t feel as though profit and care are good bedfellows really. When certain things are counted and continent aids are counted that does not lead to respect or rights. That is a major issue.
Passive management by exception is described as dealing with an issue only if it arises. It describes a manager who is happy if staff are meeting agreed standards as long as things are working and as long as individuals know the standards. One code was identified that related to this style of management.
-
Passive support:
We didn’t use it but I can’t see what would prevent us. I was wanting to have a word with the manager about it rather than just go ahead off my own back. I would rather ask, check with the manager to check that it is OK.
At sites where there were more descriptions of managers being active or transformational in adopting a human rights based approach, staff described utilising the ‘Getting It Right’ toolkits and they felt generally more supported and understood and experienced the worth of prioritising them to provide person-centred care. Staff provided examples of service users’ improved well-being, and of engagement and increased trust with services users and their families.
At sites that had more themes related to transactional management, there was a smaller degree of uptake of the approach. Although staff reported that they were excited about the approach (‘I just remember it all being really exciting. I was buzzing’), a lack of management support meant that the approach was not applied: ‘No they just got put in the office and we never got round to it’.
Chapter 4 Discussion and conclusions
Summary of findings
The findings of the study are very clear. There was no evidence that introducing this human rights based approach improved the well-being of people with dementia or the quality of care in dementia inpatient wards or care homes. The delivery of the training had the desired effect in that it significantly increased both knowledge about human rights and positive attitudes towards human rights. Similarly, there was a shift in decision-making strategies in the intervention group at follow-up, with this group relying less on ‘common sense’ to make decisions and talking more explicitly about using human rights concepts, such as dignity, respect, least restrictive practice, positive risk-taking, and person-centred care, to influence choices. However, neither of these factors translated into an increase in quality of care or in the reported well-being of people living with dementia.
There was an improvement in the quality of care plans at follow-up, but group was not a factor (i.e. there were improvements in both the control and the intervention group). This suggests that it was the process of care plans being monitored, rather than the intervention, that had an impact on the quality of care plans. Similarly, as there was no difference in care provided or reported well-being as a result of improved care plans, it could be inferred that what people are getting better at is writing person-centred care plans as opposed to delivering person-centred care. People who completed the QOL-AD57 had significantly better care plans than people who did not. This was most apparent when the QOL-AD had been completed by a proxy. Those who did not have a QOL-AD completed had the lowest-quality care plans. Although research has previously been carried out into how a good-quality care plan can improve the care people receive,91 there is limited work on what influences the development of a good-quality plan. In this situation, it may be that the process of completing a QOL-AD about an individual prompted the staff member to update that person’s care plan with the relevant information. If so, it would highlight the importance of staff feeling responsible for getting to know specific residents in order to enable them to develop good-quality care plans. At some sites there has been a move away from people having a key worker to acknowledging that all staff need to be able to interact with all residents, but this may be diluting feelings of responsibility for care planning.
Men reported significantly higher numbers of human rights violations on the IDEA questionnaire. Given the numbers collected and the fact that there appeared to be a floor effect on the questionnaire (with most participants reporting no or extremely limited human rights violations), it may be that this is not really a clinically significant finding. However, it could reflect several of the characteristics of care settings that were identified in this study. During the interviews, staff were asked to identify issues that they found challenging in their daily work, and the most common theme related to aggression and challenging behaviour. Although aggression and challenging behaviour do not apply only to men, these issues were identified as particular to male service users. Trying to manage this difficult situation, which many staff report feeling unequipped to deal with, may result in practices that could undermine an individual’s human rights, such as restraint, seclusion and an over-reliance on medication. 92 Similarly, it was clear from the demographics that the majority of staff providing care were female (67.4%). This may have had an impact on issues of privacy and dignity in relation to issues such as personal care.
Comparison with pilot
The approach was initially piloted on Acorn ward in Mersey Care NHS Foundation Trust. It was adopted well and has been used by that site since 2012. During a recent visit,93 the CQC praised the approach, stating that:
we saw that this had an impact on the frontline, with the implementation of a Human Rights Based Approach. This involved the development of a person centred assessment tool, which incorporated the values of Human Rights law.
and it was highlighted as an area of good practice (p. 15). During data collection, the ‘Getting It Right’ assessment tool56 was observed to be used in control care homes because it had been implemented on the pilot inpatient wards and then shared with these care homes when the people were discharged.
Reflection was therefore needed as to why uptake and adoption was so positive at the pilot site and yet was more difficult at intervention sites. It seems that there are several factors that may have contributed to this difference. Staff members from the pilot ward were involved in the study from its outset, including the design of the assessment tool and training package. As a result, they may have felt more ownership for the approach and engaged with it more fully. All staff on the ward were trained in the approach together as there was trust investment to support this and backfill was provided while the training took place. Staff in the current study suggested that it would have been better if more staff from each unit were trained as it would have increased support and understanding. There was more support available during the pilot from a number of sources: the ward manager was fully supportive of the approach, advocated for it and allowed staff the time to complete the assessment tools; the trust board was keen to see a human rights approach adopted and provided support in thinking about how this approach may replace other documentation; the ward identified a lead person to ensure that the assessment tools were completed and this person oversaw its application; and the trainers were readily available to address any questions or queries as they were at the same base. All of these factors may have contributed to better adoption at the pilot site.
Generalisability
The baseline comparability of the two groups was good and the characteristics reflected national statistics for people living with dementia. As such, it is likely that a representative sample of the population of people living with dementia was recruited to the study. This would allow some degree of generalisability. There are, however, a number of factors that could affect this.
Although units were recruited from across the north-west of England, which is a relatively diverse area in relation to cultural and socioeconomic variables, the participants involved in the study were less diverse, particularly in terms of ethnicity. Although there are no definitive figures on the ethnicity of the unit residents, the research assistants felt that they were overwhelmingly white British or white Irish. Similarly, the vast majority of the staff (87.5%) were white British. This is unlikely to represent the general care home and inpatient population across the country.
It was acknowledged that sites varied considerably in what they would consider ‘treatment as usual’. Differences were observed in the extent to which sites adopted the human rights based approach and applied it to their work. There appeared to be some common themes that accounted for differences in uptake, such as management style, but there are also likely to be idiosyncratic reasons. As such, it could be concluded that it may be more useful to consider each site individually and to tailor training and support to a site’s particular requirements, as happened initially at the pilot site. This, of course, would have implications for the cost-effectiveness of interventions.
Appropriateness of outcome measures
Well-being measures
As in previous studies,94 QOL-AD scores were lower when the measure was completed by a proxy than when it was completed by the person living with dementia. Previous studies have shown that agreement between proxy and self-report on the QOL-AD is higher when examining observable functions such as physical health and disability and relatively poorer for more subjective measures. It has also been shown that disagreement between proxy report and self-report increases as the severity of dementia increases. 95 This is interesting in the context of this study, as many of the people involved will have been living with severe dementia. Similarly, previous work has found that whereas care home residents’-reported QOL-AD scores correlate highly with levels of depression, carer-completed reports on the same measure correlate highly with levels of dependence and behavioural issues. 96 Therefore, as dementia progresses and people living with it become more dependent, proxies would see those living with dementia as having a lower quality of life, whereas there is evidence that levels of depression decrease as severe dementia progresses97 and so these same people living with dementia may rate their subjective quality of life higher.
In this study, self-reported quality of life, as measured by the EQ-5D-3L, was just as high as the reported norms of people of a similar age without dementia. This again challenges the assumption that living with dementia has a negative impact on self-reported quality of life. It is often assumed that the reason for a difference between self-report and proxy report measures is that people with dementia lack the required insight into the impact of their condition to be able to accurately report on their quality of life, but it is of course possible that proxies are unable to imagine what it is like to live with dementia, particularly in the later stages, and as such may assume that the quality of life will be poor. This may not be the reality for the person living with dementia. As such, it is possible that the self-report and proxy report versions of the same measure are actually measuring different concepts. Pickard and Knight98 identify two distinct proxy perspectives. The ‘proxy-patient’ perspective requires proxies to project themselves into the patient’s internal state, whereas the ‘proxy-proxy’ perspective is based on the proxy’s judgement. The authors found that there tends to be less discrepancy between self-report and proxy report when a proxy is explicitly asked to adopt a proxy-patient perspective. There is also evidence that a proxy’s own quality of life has an impact on their judgement. 99 It could, therefore, be questioned whether or not it is appropriate to use proxy measures to capture the subjective well-being of people living with severe dementia.
Although it has been suggested that the QOL-AD57 can be usefully completed with some people with a MMSE score of as low as 3100 (although it was originally suggested to be valid for use with people with MMSE scores of > 1057), it quickly became obvious that the majority of people living with dementia in the care homes and wards visited were unable to complete the measure, even with assistance from skilled clinicians. Of course, this does not mean that information about quality of life cannot be elicited from people with more severe dementia101 or that the team did not think that this was important. Indeed, processes undertaken to elicit information from people in the later stages of dementia were described earlier in this report (see Development of the FREDA assessment tool). 71 Rather, the use of the QOL-AD and the heavy reliance on proxy measures would raise the question of whether or not it was an appropriate measure to use in this context. It may have been more useful to interview residents about their experiences of quality of life to elicit their views in a more naturalistic way.
Figure 8 summarises the domains of well-being covered by the QOL-AD. 57 Given the items included in the measure, it is worth considering why an intervention would be expected to bring about change in these domains. The current intervention under investigation, even if successful, is not likely to change a person’s financial issues, their ability to do things around the house (although a person-centred approach may encourage people to do more) or their marriage.
FIGURE 8.
The constructs included in the QOL-AD.
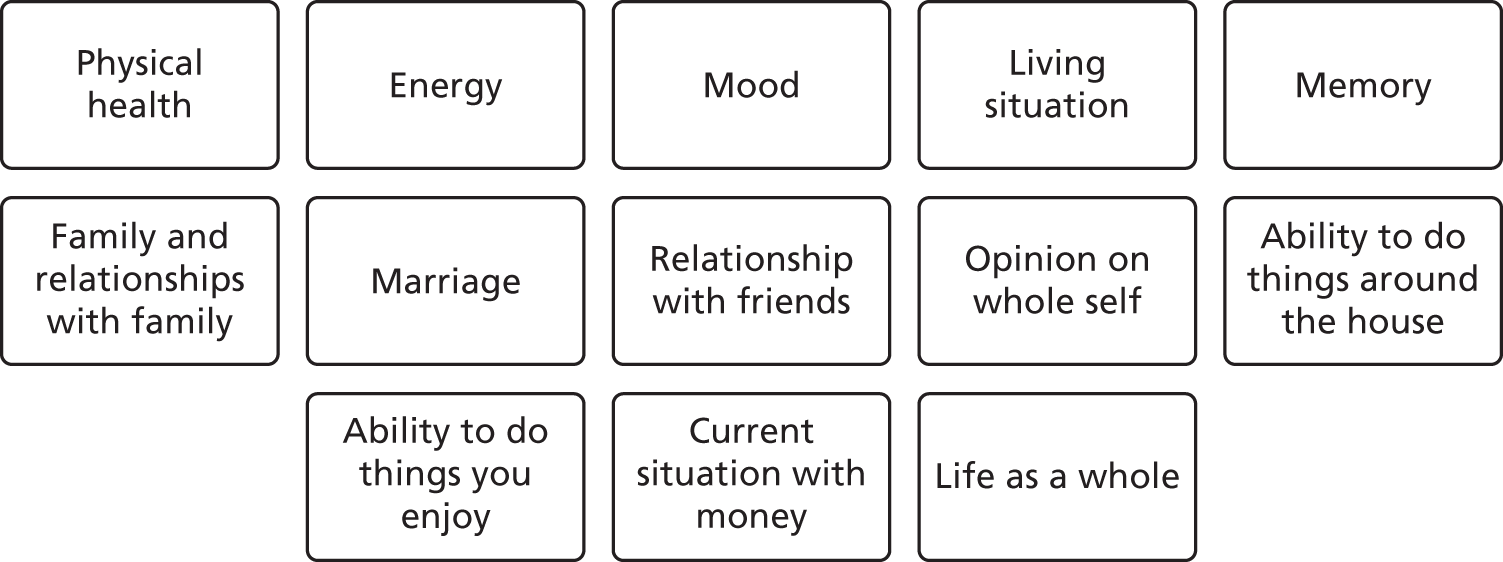
It may be more useful to look at other concepts that have been shown to have links to subjective well-being in dementia. Studies have indicated that care home residents with greater perceived control (e.g. regarding decisions about food, social activities, daily routines, privacy and sense of self) experienced significantly greater psychological well-being. 102 Similarly, a study of care home residents in Singapore identified five predictors of quality of life in this population:103 comfort, dignity, food enjoyment, autonomy and security. Taken together, this evidence would suggest that a more innovative measure, designed to tap into concepts that actually matter to people living with dementia, is needed if we are to accurately capture the subjective quality of life of people living with dementia, particularly those with more severe dementia.
Dementia care mapping
Dementia care mapping was utilised to observe the care provided at each unit. In particular, the ME scores from each unit were compared at baseline and at follow-up to uncover any differences in care following the intervention. However, it is important to be cautious about how much can be extrapolated from the overall ME scores. Although DCM was originally created as a clinical tool to help improve the quality of care in clinical settings, it has been used effectively in a number of research studies to gain a more objective measure of service user well-being. 104 There are potentially a number of factors, over and above the hypothesis of no change to care, that could have accounted for no change or a decrease in ME scores.
It was apparent that at baseline the majority of staff were not aware that the research was being carried out; therefore, at this time several staff initially believed that they were being observed and were uncertain about the motives of the research assistants. As a result, levels of engagement with service users may have been influenced and potentially increased, particularly given that there was a clear finding within the study that care plans improved when people felt that they were being monitored. Generally, at sites at follow-up, staff appeared to be more relaxed and it was felt that the behaviours observed were potentially a more accurate representation of the day-to-day care being provided. Given this finding, it could have been useful to complete a pre-baseline set of measures to allow the staff to become accustomed to being observed. This would, of course, have had financial and time implications for the completion of the research.
Between baseline and follow-up, there were a large number of service users who had been discharged or had died, which, at times, resulted in a different service user being observed at follow-up. According to the Bradford Dementia Group,105 it is difficult to see change at separate time points when observing different people, and therefore any changes that were hypothesised to occur at intervention sites may not be reflected in the overall ME scores.
Throughout the study, it was noted that there was a large turnover of staff at sites from baseline to follow-up. For a number of sites, there was a larger proportion of agency staff being employed at follow-up than at baseline. Although the use of agency staff is beneficial for meeting the desired staffing levels, it does not necessarily result in continuity of care for service users. A lack of consistent staff could potentially be unsettling for some service users,106 and this could be a reason why ME scores decreased at particular sites at follow-up. In addition, at some sites agency staff were not being used and hence staffing levels were extremely low. This is highly likely to have had an impact on ME scores, as staff members were able to meet only the basic care needs of service users.
In some sites in particular, the environment could have had an adverse impact on ME scores. More specifically, the layout of the communal areas where mapping took place was not ideal. At times, individuals could not be observed, which meant that they were given a behaviour category code of Q (quit: individual was not in mapping area) for a number of time frames. At these particular sites, there may have been several observations that could not be reported, and, owing to this, the overall ME scores for these sites may not be a true representation as behaviours and levels of engagement could have been missed. This was, of course, true at both time points.
A general observation made during DCM was that, at follow-up, some service users’ cognitive abilities had declined, and in some instances their physical health had deteriorated. This could result in individuals not being able to participate or have difficulty participating in behaviours that generate higher ME scores. This may account for no change or a decrease in the overall ME scores obtained. However, given the client group involved this would not be unexpected after a 4-month follow-up.
During DCM, the team observed a number of representatives from external organisations facilitating various activities with service users. At one site in particular it was noted that, at baseline, activities took place throughout the day, but at follow-up this did not occur. As activities can potentially have a positive influence on an individual’s ME score, this may account for the decrease in ME scores at this site.
For these reasons, it is important to think about the scores obtained during DCM in context rather than in isolation.
Strengths
Recruitment
The study recruited more participants than had been originally planned. Although initially it was feared that the recruitment rate of people living with dementia might be low because many might not be able to complete the self-report measures, the introduction of proxy report measures ensured that a high proportion of people at each site could be included in the study. Research assistants strove to recruit as many people as possible at each site and the only reasons that they did not recruit everyone at each site were lack of consent, the person not being available during the data collection period, the person not having a dementia diagnosis and time pressures on staff to complete proxy measures (see Figure 5). It was considered important that as many people as possible at each site were given the opportunity to be involved in the study. Similarly, as it could not be known until analysis whether or not there were significant differences between proxy and self-report scores on the QOL-AD;57 therefore, it was important to obtain as many of each category of questionnaire as possible. It was felt that the development of good working relationships at each site between the research assistants and the staff at the unit contributed considerably to the high recruitment figures. Reflection by the TSC and in research team meetings focused on how important it was that the research assistants had previous experience working in dementia care settings, as this allowed the development of a trusting working relationship with staff at the care homes that was built on mutual respect and understanding.
Study design
The study involved a rigorous investigation of the intervention that allowed clear claims about its effectiveness and utility to be made. Without a rigorous framework for evaluation and a clear conceptual framework (outlined in Figure 1), claims about effectiveness could have been made without giving consideration to the impact on well-being of the people living with dementia. It would have been possible to say that training improved knowledge and attitudes, changed decision-making strategies and, without considering a control group, improved care plans. Without looking at the elements of care and well-being, it could have been concluded that the intervention was a success. The translation to improvements in care and well-being is not always considered in such approaches. 107
Patient and public involvement
There were high levels of engagement with people living with dementia and carers in all aspects of the study through the PPI work, and their contributions both guided the study and influenced its direction. In total, 79 people living with dementia or carers gave input into some element of the study design, delivery or the subsequent public engagement work. The involvement of people living with dementia and those who support them was felt to be paramount in this study because of its congruence with the underlying principles of a human rights based approach to care. PPI is concerned with a shift to carrying out research and development with or by members of the public and service users rather than on or for them simply as participants. 108 This helps to uphold and promote the rights of each person to have ‘a right to voice’, with suppression or denial of that voice being a potential violation of rights. 109 Similarly, the nature of this study and the fact that it was funded by NIHR makes this even more important,110,111 as it could be considered a core democratic principle that:
. . . people who are affected by research have a right to have a say in what and how publicly funded research is undertaken.
Alzheimer Europe recently issued a position paper112 regarding involving people with dementia in research through PPI. In this paper the authors recommend that people living with dementia be involved in all aspects of research, including the initial generation of research ideas. An important output from this study is the development of a PPI reference group comprising people living with dementia and carers who have developed an interest in promoting the area of human rights in dementia. Although the group’s initial role was to support the current study, the members felt that it was of utmost importance that the output would be accessible information that increased public awareness about the human rights of people living with dementia and how easily these can be undermined in society. This PPI reference group will continue to exist after this study ends and will form the basis for the development of further research in the area.
Innovative methods
Innovative methods were used throughout the study to try to ensure that information was elicited in ways that would be as ecologically valid as possible. It has previously been discussed in this report (see Development of the FREDA assessment tool) that every effort was made to include people living with later stages of dementia in the development of the assessment tool. 71
A key element of the study was the exploration of staff decision-making strategies. To assess this, staff were provided with clinical vignettes that were designed specifically for this study and that combined potential human rights violations with person-centred principles. Vignettes have long been used to investigate a number of phenomena in the social, behavioural and health sciences. 113 In this study, staff were read a number of clinical vignettes and asked what they would do in each particular situation. On each occasion they were asked supplementary questions of ‘how would you come to that decision?’ and ‘what would help you in coming to that decision?’ It was felt that asking staff to reflect directly on their own experiences and how they make decisions may feel threatening to many. Similarly, it is often unethical or impossible to assess clinical decision-making experimentally with real clinicians and service users in health-care settings. Therefore, although vignette designs may be an alternative method for investigating how health clinicians make decisions that affect service user care, it has been questioned whether or not a written stimulus, and a participant’s responses to it, can accurately represent certain aspects of what happens in the real world. It has been suggested that three conceptually distinct, but functionally inter-related, factors contribute to validity. 114
-
Vignettes must simulate aspects of real-world scenarios and bear some resemblance to situations encountered by the participant (construct validity).
-
Vignettes, and the differences between vignettes, elicit some kind of effect that is hypothesised to exist independently in the real world (internal validity: the degree to which changes in the dependent variable can be accurately attributed to changes in the independent variable).
-
Vignette studies should produce results that generalise to real-world situations encountered by the participants and others like them (external validity).
It is important to note that vignettes are not intended to recreate real-world situations. 113,115,116 Rather, they are designed to ‘approximate, isolate, manipulate, and measure key aspects of the decision-making processes that individuals use in real world situations’. 116 Similarly, participants’ behaviour in a vignette study is not intended to be interpreted as representative of their behaviour in the real world, but rather viewed as strong predictors or proxies for such behaviour. 115,116 It is, therefore, more useful to think about whether or not the mental and behavioural processes used in responding to the vignettes are activated in a way similar to the manner in which these processes are used in real life.
In considering these factors, the vignettes used in this study were developed collaboratively with staff working in dementia care settings so that they accurately reflected clinical situations that may be encountered on a regular basis. The vignettes were refined during the pilot phase of the study and they elicited a wide range of distinct responses that reflected a variety of decision-making strategies. It cannot be claimed, however, that the responses reflected proxies to behaviour, as little, or no, behavioural change was noted as a result of the intervention despite changes in decision-making strategies.
National dementia initiatives
The approach was also congruent with a number of national initiatives related to dementia. There is a clear commitment to reducing the prescription of antipsychotic medication to people with dementia. 92 The principles of a human rights based approach, particularly proportionality, least restrictive practice and proactive strategies together with a detailed understanding of the person with dementia, through a person-centred care plan, are key in finding alternatives to antipsychotic prescribing in challenging behaviour. A key to managing challenging behaviour is the understanding of the need being expressed through this behaviour. 117 An in-depth knowledge of the person is obviously essential in helping formulate this. It was proposed that the application of this approach would lead to more detailed person-centred care plans that allow a more detailed knowledge of the person.
The National Institute for Health and Care Excellence (NICE),50 in its quality standard for dementia, states that:
People with dementia have an assessment and an ongoing personalised care plan, agreed across health and social care that identifies a named care coordinator and addresses their individual needs.
The proposed intervention, if applied, would clearly address this issue.
Many of the concepts covered in the ‘Getting It Right’ assessment tool56 map directly onto the standards of the Quality Network for Older Adults Mental Health Services118 and allow wards to meet the required standards more readily. It was hoped, therefore, that the approach may be acceptable to sites as it would help them to meet other requirements.
Limitations
Effectiveness and acceptability of the intervention
Despite staff and managers stating that they found the approach useful and simple to use – ‘It was explained simply in layman’s terms’ – there was limited uptake of the approach in practice. It was hard to get staff to attend the booster sessions and releasing staff for training seemed extremely difficult. Although NHS wards were harder to recruit, once recruited they had clear mechanisms in place to enable staff to attend the training day. In contrast, care homes were relatively easier to recruit but were often unable to protect the time required for staff to attend the training. There were multiple occasions when the trainer would visit a care home to find that no staff had been given dedicated time to attend the training and so staff were taken off active duty to attend, resulting in additional pressure on the other staff who had to cover their work. The fact that 2 out of 10 intervention sites were unable to undertake the training in the required time frame, despite having prior knowledge of the requirements, demonstrates the difficulties or level of willingness sites had in releasing staff for training and development. Similarly, several staff from care homes reported attending the training on their days off as they were interested in the topic but had not been given the time to attend during working hours. Although this shows a positive commitment from these staff, it calls into question the commitment of those care homes to the approach.
Although it was initially envisaged that as many staff as possible would be trained at each site, in reality only 8.88 members of staff (28.7%) at each site were recruited to the training. The proportion of staff trained at each site ranged widely, between 11.6% and 52.4%. Similarly, the protocol suggested that three ‘booster sessions’, which were designed to support the implementation of a human rights based approach, should be delivered to each site. In reality, this was not possible. There is obviously a major difference between training the majority of staff at each site and facilitating booster sessions to embed the approach (the expectation), and training an average of 28.7% of the staff with minimal follow-up (the reality). However, staff who had attended training were positive about it, and felt that it was tailored to their needs and had an impact on their ability to complete their job successfully: ‘The tutor lady was fab. Simple’. Given the reluctance of sites to engage with the training and booster sessions, it is interesting that a theme from interviews with staff in the intervention sites was that they would have liked more training, training for more staff and more booster sessions.
There was also evidence that the ‘Getting It Right’ assessment tool56 was not routinely completed at participating sites. When it was used, however, it was considered to be helpful (‘the training and the handouts and the paperwork that they gave us has definitely helped’) and it had a positive impact on the work people were carrying out. Unfortunately, there was no mechanism within the study to specify the number of assessments that needed to be completed at each unit, and in hindsight this may have improved the completion rate.
These somewhat mixed findings about the acceptability and effectiveness of the intervention seem to reflect the finding that uptake varied across sites and that a number of factors influenced uptake. However, it was clear that the majority of staff enjoyed the training and felt that it was targeted at a level appropriate to their skills and knowledge. They also valued the ‘Getting It Right’ assessment tool,56 but a variety of factors meant that they were not always able to use it in their setting.
Ultimately, despite positive reports from staff about the approach, there was also evidence of difficulty engaging teams with the training, problems getting staff to attend follow-up sessions, limited use of the assessment tool and the approach having no impact on the care and well-being of people living with dementia. Therefore, the intervention could not be concluded to be effective. This will be considered when offering training to the control sites (in line with the original protocol) and different models will be considered.
A further limitation of the study related to the intervention was the lack of any fidelity assessment. No attempts were made to assess whether or not residents found the application of the ‘Getting It Right’ assessment tool56 useful. The study may have been improved by adding this to the evaluation framework.
On reflection, the evaluation mechanism used to assess the effectiveness of the intervention was completed with a population once removed from the direct intervention. Although staff received the human rights training, completed the assessment tool and attended the booster sessions, the primary outcome measure (QOL-AD57) was completed with the residents at each unit. The team still maintain that it was of utmost importance that the well-being of people living with dementia, who were of course the recipients of the care from staff who had received the intervention, was assessed. Without improvements to the care and well-being of people living with dementia, there is little use in applying the intervention. However, as discussed in Appropriateness of outcome measures, Well-being measures, it may have been more useful to consider other ways of measuring the impact of the intervention on people living with dementia.
Treatment as usual
There was considerable variation in the baseline treatment and care at each individual site. Different sites adopted different models of care and completed different documentation that formed the basis of the care plan. There was no way to standardise the baseline care provided across the sites. In addition, and as previously discussed, on occasion, external events may have had an impact on the recorded standard of care at different time points. For example, at one site an orchestra was visiting during baseline data collection, which could have increased the well-being scores of residents and, therefore, skewed the baseline results.
Although the RCT is widely considered the gold standard for evaluating new interventions, some questions have been raised about its efficacy in dementia studies. It is recognised that promoting change in people living with dementia is very difficult and, as a result, many interventions targeting behavioural or psychological change are found to be ineffective in RCTs,119 even when qualitative evidence related to the same intervention is overwhelmingly positive. 63 If we add high levels of variation of treatment as usual to the picture, then these issues will be compounded further. There is perhaps a need to seek alternative ways of effectively and rigorously evaluating the impact of interventions targeting the well-being of people living with dementia.
Measurement of cognitive abilities
There were difficulties with the completion of the ADAS-Cog,120 which resulted in fewer people than expected being able to complete the measure. As a result, there was no conclusive way to ensure that the severity of dementia was comparable between hospital wards and care homes.
The ADAS-Cog is generally recommended as a useful tool to assess cognitive functioning in dementia trials66 and it is especially useful for determining the extent of cognitive decline, which can help to evaluate which stage of Alzheimer’s disease a person is experiencing. Similarly, the ADAS-Cog is often used in clinical trials because it can determine incremental improvements or declines in cognitive functioning. Despite this, it is a time-consuming assessment to complete (up to 45 minutes per person) and in reality the majority of participants refused to complete it. On reflection, the use of a briefer screening assessment, such as the MMSE or Addenbrooks Cognitive Examination, might have yielded more useful results. Although these measures are less detailed than the ADAS-Cog, there is a greater chance that people would have engaged with them and, therefore, that some level of comparison could have been made.
Blinding
Despite the intention that the research assistants collecting the data would have remained blinded, this did not occur at 7 out of the 20 sites. It is acknowledged that this could have biased the data collection but, given the results, which suggest that there was no difference in care and well-being, it perhaps becomes less important. It is also important to note that as staff acted as proxies for service users when no care was available (i.e. the majority of cases), staff who had attended the training were also unblinded and this may have influenced their responses to the follow-up questionnaires.
High staff turnover
There were high levels of staff and management turnaround at several of the intervention sites, as illustrated in Table 35. Additionally, at follow-up, four of the eight intervention sites that had completed training had new managers. Table 35 also shows that at a number of sites staff had not been replaced, meaning that the remaining staff members were under additional pressure. Conversely, at some sites there were additional new staff at follow-up, meaning that the staff team was larger than at baseline. Obviously, none of these staff would have been trained in a human rights based approach and would therefore have reduced the proportion of staff trained in the approach at these sites. These factors are likely to have had implications for the continuation of the intervention at each site. Given that, on average, < 30% of staff at each site were trained, high staff turnover will make it even less likely that a critical mass of staff will be present to implement the intervention.
| Site | Total staff (n) | |
|---|---|---|
| Left before follow-up | New at follow-up | |
| A | 7 | 7 |
| B | 8 | 3 |
| C | 8 | 2 |
| D | 0 | 2 |
| E | 4 | 2 |
| F | 2 | 2 |
| G | 5 | 8 |
| H | 4 | 2 |
| I | 5 | 8 |
| J | 2 | 2 |
| K | 4 | 7 |
| L | 1 | 3 |
| M | 3 | 2 |
| N | 2 | 0 |
| O | 9 | 8 |
| P | 7 | 5 |
| Q | 0 | 2 |
| R | 0 | 4 |
| S | 2 | 1 |
| T | 3 | 3 |
It is estimated that > 40% of care home staff leave their job within a year of taking up post and 60% leave within 2 years. 121 Crucially for those in care, the level of staff turnover can be a matter of life or death. 122 The CQC has noted a statistical link between those care homes with increased rates of staff turnover and notifications of death and has suggested that:
too many changes in staff may result in gaps in care.
It has been proposed that high levels of staff turnover make it impossible to adhere to the principles of continuity of care that NICE highlights as being of utmost importance. 122
Recruiting carers
There were major problems with the recruitment of informal carers to the study. It was initially expected that, when possible, a carer would be recruited for each participant. This goal was not achieved by a long way. The research assistants reported that many residents had no visitors at all, and, of those who did, their visitors were reluctant to complete measures. It has been estimated that 85% of care home residents have no visitors. 124 Although this figure may be an overestimation in reality,124 it does suggest that there is a shift in the relationship of carer and person receiving care when the recipient enters a care setting. The term ‘couplehood’ is used to refer to the shared identity and experiences that a couple have that help to reinforce their sense of themselves as a couple. 125 It could be hypothesised that the transition from living together at home to living apart, with one half of the couple in a care setting, may have an impact on couplehood as there may be reduced opportunities for new shared experiences. This could usefully be explored in further research.
Given that difficulty recruiting carers is commonly reported in dementia studies, this raises questions about the most appropriate way to engage them in research.
Use of proxy measures
Because participants with dementia found it difficult to complete the self-report version of the QOL-AD,57 it was necessary to also seek proxy completion of the measure. As in previous studies, significantly lower scores were found from proxy report than from self-report. As a result, it was necessary to analyse the data from the proxy and self-report measures separately, which resulted in smaller numbers for each group than would have been possible had the group been able to be analysed as a whole. The issues related to the use of proxy measures are described in detail in Appropriateness of outcome measures, Well-being measures.
The issue of proxy completion was compounded by a lack of visitors, which required staff to complete proxy measures for residents.
Interpretation
Theory of planned behaviour
A major finding of the study is that although the intervention has changed the knowledge staff have about human rights, the attitudes that they hold and their reasoning about decision-making in relation to clinical care, it has not altered their behaviour when delivering care. The theory of planned behaviour126 (Figure 9) may provide some insights into this finding. This theory proposes that the chances of an individual behaving in a particular way is influenced by their attitude towards the topic, their perceptions of other people’s (their peers’) attitudes to the issue and their perceived level of control over the situation.
FIGURE 9.
Theory of planned behaviour.
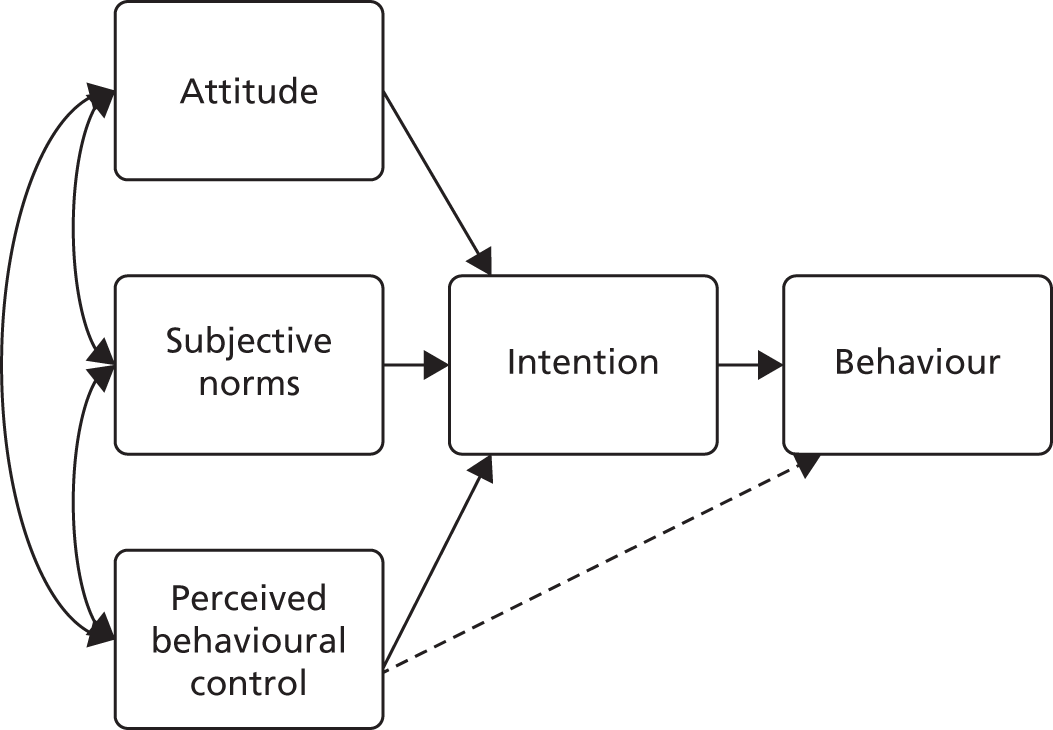
Although the current intervention may change an individual’s attitude to human rights (as demonstrated by significant changes in the attitudes questionnaire scores) and their intention to behave in a way more congruent with a human rights based approach (as evidenced by improvements in care plans and different decision-making strategies), the actual behaviour, as measured by DCM, remains unchanged. The theory of planned behaviour would suggest that this discrepancy between actual and intended behaviour may be accounted for by considering staff’s perceived level of control and perception of others’ views about human rights. Although the current study did not directly collect information on these areas, some tentative conclusions could be drawn from the available data.
Although the initial intention was to train as many staff as possible in a human rights based approach, practicalities meant that an average of < 30% of staff at each site were trained. Similarly, there was limited uptake of the booster sessions that would have provided staff, both trained and untrained in the approach, with the opportunity to discuss the application of a human rights based approach to care. As a result, there may have been fewer opportunities for staff members to assess their peers’ attitudes to and understanding of such an approach. This is further backed up by information from the follow-up interviews at intervention sites, in which staff suggested that having more opportunities to discuss the approach with other staff at the unit may have been helpful in applying it.
It has been hypothesised that perceived control relies on two elements: locus of control and self-efficacy. Whereas locus of control refers to a person’s beliefs around whether people in general can achieve positive outcomes and avoid bad outcomes through their own actions or whether external factors control these outcomes, self-efficacy refers to the perception that a person themselves has the skills and abilities to enact effective responses. A common theme across all groups, derived from the staff decision-making interviews, was the use of hierarchical decision-making. This implied that staff felt a lack of control in making autonomous clinical decisions and instead relied on seeking consent to act in a particular way from others, which may, in turn, have led to staff feeling that they lacked the self-efficacy to bring about change. Similarly, the follow-up interviews at intervention sites highlighted that staff applied the model more effectively at units where managers encouraged them to be independent thinkers and adopted a more transformational approach to leadership.
Given that a key finding of many care home studies is a lack of uptake of new interventions, future research could explicitly use the theory of planned behaviour to investigate human rights based approaches and their application.
Management style
The results of the follow-up interviews demonstrated the importance of management style in maximising the chances of this intervention being adopted at any particular site. Although there is insufficient evidence to make wide-ranging claims about this element of the study, initial findings showed that sites with a more transformational manager were more likely to adopt the approach and think of ways to adapt it, whereas sites with a more transactional manager were less likely to adopt the approach and more likely to dismiss its relevance. 90 It is perhaps not completely surprising that management style has such an impact on uptake given that hierarchical decision-making was one of the most popular decision-making strategies. If managers are not supportive and other staff look to them to make decisions, then the approach will not be adopted.
An issue highlighted in the study was that there was a high level of turnover of managers at the units. By the time of the follow-up interviews, half of the sites at which the intervention was delivered had new managers, and there was evidence of poor communication between past and current management: ‘I only heard about the study from this evaluation’. There is recognition that care homes that provide person-centred, high-quality care tend to have managers who focus on leadership rather than just management127 and that emotional intelligence is the key to good-quality care. 128 A Joseph Rowntree Foundation report129 exploring ways of improving the quality of care in care homes highlighted management as a key driver in developing and implementing improvements. The report proposed that a change culture must start with managers who are willing to embrace change (in this study the transformational managers) and that these managers must empower staff to participate in decision-making about both clinical care and the more organisational aspects of the unit. This fits well with the finding that staff felt reluctant to make decisions independently and instead sought advice from more senior colleagues. Linking to the theory of planned behaviour, it would appear that managers are key in enabling staff to feel that they have behavioural control over any initiatives and facilitating staff ability to implement these independently. This maximises the chances that initiatives will actually be implemented.
Given these findings, it would seem vital that managers with the correct skills and the ability to develop effective teams are recruited to these important positions. There has been a move within the NHS and other services to utilise values-based recruitment. 130 Values-based recruitment aims to select candidates for roles based on their individual values and behaviours and how closely these align with those of the organisation. It may be that selecting managers based on their values, particularly those related to an ethos of person-centred care, may improve the care provided at a unit.
Cultures of care
Culture has been defined as ‘the basic assumptions, values and norms shared by and influencing how members of an organisation behave and interact’. 131 Too often, substandard care is accepted and unquestioned. It is expected that quality of life will be low in care homes and that little else is aimed for. This can lead to care that is task orientated and driven by goals and objectives rather than by resident-orientated factors. 129 It is notoriously difficult to change cultures of care and, although many initiatives are introduced, a culture of care continues to exist that falls short of the optimal standards.
It is unacceptable that the culture of care in care homes remains substandard and unable to meet the basic needs of the people to whom it applies. A recent UNISON report132 found that < 20% of care home staff who responded to their questionnaire felt that they had enough time to provide care that upheld the dignity and individuality of residents. This led to residents not receiving treatment such as assistance to go to the toilet, efficient monitoring of their condition and meeting of personal care needs, and 88% of workers reported that they did not have time for a conversation with their residents.
A large-scale study looking at what constitutes an excellent culture in care homes (Care Home Organisations Implementing Cultures for Excellence – CHOICE)133 identified seven factors that contribute to a positive culture in care homes:
-
shared purpose in providing the best person-centred care
-
a sense of community between all involved in the care home
-
managers ensure that external pressures do not have a negative impact on service delivery
-
staff are empowered to take responsibility for residents’ well-being by active management processes
-
openness to change for the benefit of residents
-
using the care home environment to the benefit of residents
-
person-centred activity and engagement is integral to care work.
Again, these factors mirror those of this report in that they highlight the importance of cementing person-centred practice in care, not just talking about it; the centrality of management in ensuring that staff are empowered to take responsibility for their own practice and are protected from external pressures that may have an adverse impact on their ability to provide the best-quality care; and the necessity of cohesion among staff and managers in developing a positive culture at the unit.
This study aimed to utilise a human rights based approach to bring about cultural change. Previous work by the Equality and Human Rights Commission found that public authorities continued to lack a culture of respect for human rights, despite some examples of good practice. 134 They identified a number of barriers that they suggested could contribute to this finding. These included ‘initiative overload’, 135 with staff feeling that there is always something new to implement; a lack of autonomy among staff; the hierarchical and target-driven nature of health-care settings;136 and a low awareness of human rights among staff, service users and members of the public. It has been suggested that the use of human rights language in conversations with organisations, staff and members of the public is ineffective because of this lack of awareness. 137 In contrast to this belief, the current study has demonstrated that training could raise awareness of human rights, improve attitudes towards human rights and, in the context of decision-making, change staff’s use of language about human rights.
The CQC has integrated the FREDA principles into the inspection framework. When rights are fully integrated into policy and practice within services, the impact has been anecdotally described as:
. . . a magnet pulling services in the direction that best supports the dignity, respect, equality and autonomy of those that use them.
This study does not endorse this finding. Instead, it suggests that although a human rights based intervention can change knowledge, attitudes and decision-making, it does not influence care delivery.
Training
The findings of this study call into question the efficacy of training as a medium for improving care and changing culture. Although the training appears to significantly increase knowledge about human rights and positive attitudes towards human rights immediately following the training, it does not translate into improvements to care practices and in the reported well-being of people living with dementia.
There is a current government mandate through Health Education England to provide effective, relevant dementia education and training for the entire workforce. 138 However, it is recognised that there is limited evidence about what effective dementia training and education for this diverse workforce looks like. 139
It seems important to consider what any training programme is aiming to achieve. Kirkpatrick’s model for the evaluation of learning140 identifies four levels for evaluating the efficacy of training.
-
Level 1: reaction – learners’ reaction to and satisfaction with the programme.
-
Level 2: learning – the extent to which learning has occurred included increasing knowledge, skills, confidence and attitude change.
-
Level 3: behaviour – the extent to which staff behaviour or practice have changed and whether or not participants are applying their learning in practice.
-
Level 4: results – examines what results have occurred because of the training, in this case the impact on people living with dementia.
The remit of this study was to train staff in a human rights based approach, with the aim of assisting staff to make decisions in complex clinical situations. It also trained staff in a new way of care planning and provided them with a tool to complete more person-centred assessments. What it did not do explicitly was teach people the skills to behave in a more person-centred way. Given that there are low levels of knowledge of more basic issues related to dementia observed, could we have expected people to make this transition independently? There was low uptake of the booster sessions, but, even if the uptake had been higher, the sessions would not have been detailed enough to fulfil this role. To start meeting these goals, we would be looking at a far more intensive model of coaching and consultation; there are examples of this such as the Newcastle model of challenging behaviour,141 but they are far more time and labour intensive and, therefore, are likely to also have financial consequences.
Preliminary results from What Works in Dementia Training and Education? A Critical Interpretive Synthesis of the Evidence139 suggest that there are a number of elements that contribute to training to bring about changes to people living with dementia. These are that the training:
-
uses face-to-face delivery, discussion and activities that support the application of learning to practice
-
is delivered by an experienced trainer
-
is > 1 hour in duration
-
is designed for a specific service setting
-
provides training on a structured tool or delivery manual that assists the application of learning in practice.
This study utilised all aspects of this framework but failed to embed the approach into care. Given the results from this study it would be useful to add that management support is also required both to attend the training and, more importantly, to apply the approach to clinical situations.
Patient and public involvement
A key element of the study has been the involvement of people living with dementia and those who support them. Not only was this congruent with the theoretical underpinning of the study by promoting participation and accountability, it was also essential in gaining a meaningful understanding of what human rights means to this group of people in the context of living with dementia. Much work has been undertaken over recent years to build rights based approaches into policy26,29,30,32,34,35 but this work has focused less on the practical application of these approaches to the everyday lives of people living with dementia. Without this focus, there is a danger that human rights based approaches will suffer the same fate as person-centred care, whereby ‘the gap between the rhetoric and the reality remains uncomfortably wide’. 46
From the outset, the PPI reference group felt that it was essential to engage with the realities of applying a human rights based approach to dementia care. A series of focus groups involving both people living with dementia and carers were held during the study, with the aim of eliciting information about the relevance of human rights to people living with dementia. In total, 79 people attended these groups; some continued as part of the PPI reference group, while others attended just one or more focus groups. Some focus groups were linked to other existing networks, such as the local memory group and service user forum, to hear from a wider range of voices than might otherwise have been accessed. No existing human rights models were presented to the groups; instead, they were asked to reflect on, and explore, elements of their experiences that had had a positive and negative impact on their sense of well-being as individuals living with dementia.
This information was collated and a thematic analysis83 was undertaken to identify themes within the wide data set. These themes were then shared with the PPI reference group and translated into statements, directly relevant to dementia care, that reflected the rights of people living with dementia. These statements are presented in Table 36. Subsequently, human rights informed models were considered and the group felt that the statements fitted most comfortably into the FREDA framework. A notable exception, raised in all of the focus groups, was the importance of preserving identity in dementia. This theme highlighted the importance of preserving elements of identity in the face of changing abilities. It is recognised that although dementia can pose a threat to an individual’s sense of identity, there is clear evidence of the persistence of self-identity throughout the course of the condition. 142 A social constructionalist model of self-identity143 would posit that the interactions between the person living with dementia and other individuals are key in upholding the self-identity of the person living with dementia. If we view human rights as concepts that are universal to us purely because we are human, then an argument could be made for actively promoting identity in dementia as a fundamental right. To this end, we included identity in the FREDA framework when considering dementia.
| FREDA principle | Statement |
|---|---|
| Fairness | Do not make assumptions about me |
| Give me time and space | |
| Do not exclude me because of my dementia | |
| Respect | Listen to me |
| Find out who’s important to me | |
| Make a positive effort to get to know me | |
| Speak to me | |
| Look at me when you speak to me | |
| Identity | Respect my intelligence |
| Recognise my skills and talents | |
| Respect my choices about how I want to live my life | |
| Let me live my life | |
| Equality | Give me input into the care I receive |
| Respect my culture, race and religion | |
| I have the right to intimate relationships | |
| I have the right to vote | |
| Dignity | Do not embarrass me |
| Ask my opinion | |
| Do not patronise me | |
| If you are helping me, explain what you are doing to me | |
| Autonomy | Allow me to express my views |
| Respect my personal freedom | |
| Give me the freedom to do what I want, which may include taking risks | |
| Provide assistance to make decisions for myself | |
| Take my significant others into account | |
| Give me advice but do not try to control me |
It was felt that these statements, linked to an already well-recognised and respected human rights framework, made a good start in defining what human rights mean, on a day-to-day basis, to people living with dementia. The FREDA principles have usefully been applied in other health-care settings, including with people living with an intellectual disability. 144 Defining the issues related to the systematic and subtle ways in which human rights can be threatened in dementia care is, of course, a useful endeavour, but if this information is not shared in a way that is accessible to many people it will not influence the treatment that people receive. The PPI group is currently working with filmmakers to produce a series of short films that will represent these principles and their interpretation in an engaging way.
Language
It was considered important that all language used in this report was in line with the underlying principles of the study, namely upholding the human rights of people living with dementia. To this end, every effort was made to adhere to the language guidance provided by DEEP, which was compiled by people living with dementia. 145
Implications for health care
The findings of this study have a number of implications for both the current provision of health care and future developments.
There is a tendency within health and social care for training to be used as a primary mechanism for bringing about sustained change in care settings. Current initiatives, such as the requirement for all staff working in health care to have a basic level of dementia awareness,138 are, in theory, clearly beneficial to the population and aim to promote ‘positive outcomes for people living with dementia, their families and carers’. 138 In practice, however, these training initiatives are often delivered online, with little opportunity given for discussion or debate of the issues raised, and the extent to which these actually have an impact on the lives of service users and carers is unclear. Health Education England states that it:
exists for one reason only: to support the delivery of excellent healthcare and health improvement to the patients and public of England by ensuring that the workforce of today and tomorrow has the right numbers, skills, values and behaviours, at the right time and in the right place.
Training is one vehicle for such changes, but the findings of this study imply that although training may increase knowledge and attitudes about a topic, and may even change the way people discuss the topic and intend to act, it results in little change to actual behaviours.
Many models of learning suggest that simply imparting information is not enough to bring about cultural and organisational change. Bloom’s taxonomy147 outlines the stages of learning that culminate in all stakeholders creating a better culture together. This requires more than direct learning and learners instead need to be active participants in the process: first remembering the information, and then understanding it and critically analysing it, before being supported to apply it and then synthesising it with their current knowledge and practice to create new cultures within organisations. This process is obviously more complex, time-consuming and costly than providing an online or 1-day training package and expecting staff to utilise it.
One finding from this study was that although staff members found the approach to be useful and simple, they did not independently apply it. The theory of planned behaviour, when applied in this situation, would suggest that further opportunities to discuss the topic and enabling staff to feeling empowered to make independent decisions may improve the chances that this initiative will be adopted. These findings could be useful beyond the confines of this study, as they suggest that, if training is to be embedded in practice, there need to be opportunities for staff to consult on and debate the issues involved, as well as a freedom for them to act independently in ways that are congruent with the approach. Obviously this would require a shift in both the methods through which training is delivered and the follow-up support required.
The King’s Fund suggests that a major reform of the health and social care system is required to make it fit for purpose for the future. 148 They identify three challenges to innovative change in NHS systems: system inertia, whereby systems are stuck doing things in ways that they have always done them; the complexity of NHS systems where interactions cannot always be predicted; and risk adversity within the NHS. All three barriers were encountered in the current study and have been discussed. The King’s Fund claims that, as in social enterprises, the answer comes in part from engaging with staff at all levels to empower them to make changes to their organisation. Related to this is seeking to build a social movement for change in which innovation occurs by harnessing the creativity, energy and commitment of the workforce. These suggestions are in line with a human rights based approach to care that recognises the participation of, and aims to empower, all stakeholders.
A human rights based approach would also include people living with dementia and their carers as important stakeholders in this process. The inclusion in this study of a wider reference group of people living with dementia and carers has highlighted the importance of their involvement in all aspects of service delivery. There can be multiple benefits of services engaging with service users and carers. DEEP has produced Making an Impact Together,149 which encourages people with dementia to work together to ensure that they receive quality services, but also outlines the benefits to the services. Service user groups often have a lot more freedom to highlight areas in which change is needed and to push for this change to happen.
One clear finding was that, in both the intervention and the control groups, care plans had improved by the follow-up data collection point. One interpretation of this could be that it is the process of being monitored that leads to improvements. There has long been a tension related to human rights between clinicians who feel that the most effective way to encourage staff to engage with human rights is through supporting them to apply them, and human rights advocacy bodies (e.g. the British Institute of Human Rights) that propose human rights to be a legal framework against which people should be monitored. 37 This finding would seem to suggest that the latter is more effective in this case and imply that the most effective way to bring about change may be to set clear standards for services related to human rights against which those services are then monitored.
To bring about innovative change within systems, however, effective management and leadership is vital. In this study it was observed that when managers were more open to change and willing to let their staff act more independently, there was greater uptake of the approach. The issue of values-based recruitment for ensuring that managers who are willing to foster cultures where change can take place are recruited has been discussed in Management style. The findings would suggest that any new approaches should target management in the first instance to help ascertain what would work in their unit. This is the approach that will be adopted in the control sites that are still to receive training.
Although this study concluded that this human rights based intervention was not effective in bringing about behavioural changes that resulted in the improved care and well-being of people living with dementia, this does not of course imply that the human rights of people living with dementia are not important. As outlined above, barriers to the adoption of human rights approaches have been noted, including a lack of awareness of human rights and a reluctance to engage with the concept. This study has clearly demonstrated that staff will engage with the concepts of human rights and identify them as useful in the work they do. Addressing the cultural issues described above may pave the way for a more explicitly human rights based approach to be adopted.
A final point relates to the current systems of measurement and data capture in health services. Although it is acknowledged that outcome measures are essential in ensuring that high-quality services are being delivered, the current study and previous high-profile studies63 call into question the effectiveness of the current measures in capturing a true reflection of well-being and quality of life for those living with dementia. Services may want to spend more time focusing on the elements of a person’s life on which they feel the specific interventions will actually have an impact and then finding ways to capture those data effectively.
Future research implications
Some areas for future research and investigation have arisen from this study.
As discussed in detail above, there were concerns about the suitability of the outcome measures used in this study. The utility of the QOL-AD as an appropriate measure of change following the implementation of this intervention was questioned, and a review of the concepts contained in the measure suggested that many interventions currently delivered would not be likely to make a change. Given that there is a clear, and welcomed, mandate to further develop research that explores the most effective ways to promote well-being and deliver high-quality care, it is vital that effective measurement tools are available that will accurately capture change. This study would suggest that this should be a research priority. Without appropriate measures, a lack of clarity will continue over the most appropriate ways to support people living with dementia, particularly those living with the later stages. Related to this issue, however, there appears to be a lack of research focused on fully understanding what contributes to quality of life in the later stages of dementia, and many assumptions are made about this. To develop meaningful evaluation tools, it will first be vital to fully understand the factors that contribute to quality of life in the later stages of dementia.
It was clear from this study that engaging carers in research is extremely difficult. More work must be carried out to ensure that carers are given every opportunity to engage with research and to have their voices heard. The PPI reference group suggested that the most effective way to help informal carers see the benefits of research for both themselves and those they care for would be to have the research promoted by people living with dementia and other informal carers who have been involved in the research process previously. Members of the PPI group were keen to take on these roles in the future.
A fuller understanding is needed of why interventions are not routinely applied when they are reported qualitatively as being effective and acceptable to services. Two further research focuses can be drawn from this:
-
explicitly applying the theory of planned behaviour to human rights based approaches to look at whether or not altering a person’s perceived control over the situation improves the uptake of the intervention
-
working directly with managers to understand the impact management style has on the application of a human rights based approach (and other novel approaches to care).
At the outset, this study worked from the premise that the human rights of people living with dementia would be the same as those of everyone else because human rights are fundamental principles that apply simply because we are human beings. However, public engagement throughout the study highlighted that the understanding of rights may be subtly different when dementia is involved. One area that consistently arose was the centrality of identity in preserving and promoting the rights of people living with dementia. Similarly, there were numerous fascinating debates in the sessions about the changing nature of autonomy and the relative importance, or not, of individual autonomy as a concept. Both of these areas could warrant further research to investigate their role in the quality of life and well-being of people living with dementia.
The IDEA questionnaire was developed as a way of trying to capture the extent to which people living with dementia felt that their human rights were being upheld. It was developed collaboratively with people living with dementia, staff and carers, but all of the people living with dementia who took part were at earlier stages of the condition. Within the study, the IDEA questionnaire was not found to be an effective tool as it tended towards a floor effect, with the majority of people stating that they had experienced no violations of their rights. The questionnaire was also too complex for people in the later stages of dementia to complete effectively. More work is needed to ascertain whether or not this tool would be effective for use with people in the earlier stages of dementia. It is also essential that work is undertaken to find ways to capture the extent to which people in the later stages of dementia feel that their human rights are upheld.
Conclusions
The findings of this study did not support the hypothesis that increasing staff knowledge and attitudes towards human rights leads to improvements in the care and well-being of people living with dementia. It does not, of course, imply that the issues of human rights are not important for this group of people. People in the later stages of dementia remain some of the most vulnerable in our society and, unfortunately, reports of human rights abuses continue. There remains a need to find a way to ensure that the human rights of people with dementia are both respected and promoted.
The study highlighted some of the difficulties that exist within health and social care systems. The care and support that people received was inconsistent and failed to meet the standards we might expect for some of the most vulnerable in our society. Person-centred care was not routine and there were many examples of institutionalised behaviours. Human rights was a concept that was alien to staff and it was not routinely considered during the provision of care. Staff did not feel empowered to act independently to support people in their units and the management support that was provided was variable. To provide quality care that is person centred and respects the rights of people with dementia, it is essential that the cultures in which care is delivered are suitable. The results of this study, taken together, give some indication of the factors that may influence the development of these cultures of care. These include:
-
managers who lead and are willing to adopt an innovative approach to change
-
all staff feeling empowered to make decisions and to act in ways that they see as appropriate
-
a shift away from training that has awareness raising as its only aim
-
a tolerance of risk
-
full involvement of service users in service development and delivery
-
entire sites adopting new cultures
-
monitoring of progress in relation to human rights based targets.
These factors link well with the PANEL principles, which form the basis of a human rights based approach to care. They encourage the active participation of all stakeholders, including managers, staff and service users. They highlight the importance of all levels of staff being accountable for their own actions as opposed to always deferring to more senior colleagues. They actively promote the voices of vulnerable groups, in this case people living with dementia, in ensuring that practices are non-discriminatory. They seek to empower all staff regardless of grade and to empower service users to take control of their own services, and they provide a clear framework through adherence to human rights principle to ensure that all decisions taken are legal.
Overall, the study was hopeful in identifying that the majority of staff caring for people living with dementia were keen to explore how a human rights based approach to care could improve the lives of people living with dementia. In reality, however, these same individuals worked in cultures and organisations that did not explicitly promote person-centred care and the promotion of human rights. It is the challenge of those in positions of relative power to ensure that meaningful change is made that will allow the enthusiasm of care staff to translate into more effective and compassionate caring relationships with those they support.
Acknowledgements
We would like to thank the external members of the TSC for their advice and support during the project: Professor Dawn Brooker (University of Worcester), Mr Thomas Dunne (service user), Ms Gina Shaw (service user), Mr Graham Garvin (carer), Mrs Anna Gaughan (Life Story Network Community Interest Company), Mr Toby Williamson (Mental Health Foundation) and Dr Matthew Tedford (Royal Liverpool and Broadgreen University Hospitals NHS Trust). Our thanks also go to the DMEC comprising Dr Jane Simpson (Lancaster University), Dr Rebecca Walwyn (Research Design Service, Yorkshire and the Humber), Dr Steven Lane (Research Design Service North West) and Ms Julie Morton (University of Salford). The team would also like to thank Ella Perry (Mersey Care NHS Foundation Trust), who completed the interviews at sites following the end of the study and worked on the interpretation and reporting of these results.
We are grateful to the participants, wards and care homes that supported this study and gave their time so generously. We would also like to offer our appreciation to the members of the Service User Reference Forum, who supported the study and acted as an external reference group for service user and carer issues.
Particular thanks are given to Jill Pendleton (Mersey Care NHS Foundation Trust), who was a driving force in the initial development of applying a human rights based approach to dementia care, co-authored the ‘Getting It Right’ assessment tool with Sarah Butchard and provided advice and support throughout the process.
Contributions of authors
Peter Kinderman (Professor of Clinical Psychology) acted as principal investigator on the study, and led the team in study design, grant application and management, and recruitment. He shared responsibilities with Sarah Butchard for the supervision of research assistants, and with other members of the team in data collection, the interpretation of findings and the drafting of the final report.
Sarah Butchard (Clinical Psychologist) conceived, planned and designed the study. She acted as the trial manager and co-ordinated the running of the study, delivered the intervention, interpreted the qualitative elements of the study and led on the writing of the final report.
Ashley J Bruen (Research Assistant) completed data collection and interpretation of the DCM findings and drafted elements of the final report.
Abbie Wall (Research Assistant) completed data collection and interpretation of the DCM findings and drafted elements of the final report.
Nia Goulden (Trial Statistician) developed the statistical analysis plan, undertook the statistical analysis, aided interpretation of the results and drafted sections of the final report.
Zoe Hoare (Principal Statistician) gave input into the design and methodology of the study, designed the randomisation system, oversaw the development of the statistical analysis plan and subsequent analysis, and had input into the interpretation of the results and the presentation of the final report.
Carys Jones (Research Officer, Health Economics) was involved in design, analysis, the interpretation of findings, and the writing and review of the report.
Rhiannon Edwards (Professor of Health Economics) was involved in design, the interpretation of findings, and the writing and review of the report.
Data sharing statement
All available data can be obtained from the corresponding author once they have been fully anonymised and checked.
This statement confirms that the report contains no defamatory material or brand names. The identity of all individuals has been protected throughout the report.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Dementia 2014: Opportunity for Change. London: Alzheimer’s Society; 2014.
- Living Well With Dementia: A National Dementia Strategy. London: Department of Health and Social Care; 2009.
- Prince M, Knapp M, Guerchet M, McCrone P, Prina M, Comas-Herrera A, et al. Dementia UK: Update. London: Alzheimer’s Society; 2014.
- Dementia UK. London: Alzheimer’s Society; 2007.
- Prime Minister’s Challenge on Dementia 2020. London: Department of Health and Social Care; 2015.
- Saga Home Care . Are You Worried About Dementia? 2012. https://yougov.co.uk/news/2012/05/22/are-you-worried-about-dementia/ (accessed 8 August 2017).
- Kitwood T. On Being a Person. Dementia Reconsidered: The Person Comes First. London: Open University Press; 1997.
- Human Rights in a Health Care Setting: Making it Work – An Evaluation of a Human Rights-based Approach at The State Hospital. Glasgow: Scottish Human Rights Commission; 2009.
- Robinson L, Hutchings D, Corner L, Finch T, Hughes J, Brittain K, et al. Balancing rights and risks: conflicting perspectives in the management of wandering in dementia. Health Risk Soc 2007;9:389-406. https://doi.org/10.1080/13698570701612774.
- Human Rights Act 1998. London: The Stationery Office; 1998.
- UN General Assembly . Universal Declaration of Human Rights 1948. www.refworld.org/docid/3ae6b3712c.html (accessed 8 August 2017).
- European Convention on Human Rights. Strasbourg: Council of Europe; 2010.
- Curtice MJ, Exworthy T. FREDA: a human rights-based approach to healthcare. BJPsych Bull 2010;34:150-6. https://doi.org/10.1192/pb.bp.108.024083.
- ‘The Great Question’: Remarks Delivered at the United Nations in New York, March 27 1958. New York, NY: United Nations; 1958.
- Nyamu-Musembi C, Cornwall A. What is the ‘Rights Based Approach’ All About? Perspectives from International Development Agencies. Brighton: Institute of Development Studies; 2004.
- Equality and Human Rights Commission . Close to Home: An Inquiry into Older People and Human Rights in Home Care 2011. www.equalityhumanrights.com/sites/default/files/close_to_home.pdf (accessed 15 August 2017).
- Transforming Care: A National Response to Winterbourne View Hospital. London: The Stationery Office; 2012.
- The NHS Constitution for England. London: Department of Health and Social Care; 2012.
- Kinderman P. A Human Rights Commission Structure, Functions and Powers (Consultation; Joint House of Commons House of Lords Committee on Human Rights. Leicester: British Psychological Society; 2004.
- Roberts A, Townsend S, Morris J, Rushbrooke E, Greenhill B, Whitehead R, et al. Treat me right, treat me equal: using national policy and legislation to create positive changes in local health services for people with intellectual disabilities. J Appl Res Intellect 2013;26:14-25. https://doi.org/10.1111/jar.12009.
- Human Rights in Healthcare. London: The Stationery Office; 2008.
- Casali GL, Day GE. Treating an unhealthy organisational culture: the implications of the Bundaberg Hospital Inquiry for managerial ethical decision making. Aust Health Rev 2010;34:73-9. https://doi.org/10.1071/AH09543.
- Mental Health Act. London: The Stationery Office; 1983.
- Mental Capacity Act. London: The Stationery Office; 2005.
- Guleria R, Curtice M. Dementia, Rights, and the Social Model of Disability. London: Royal College of Psychiatrists; 2016.
- Dementia, Rights, and the Social Model of Disability. London: Mental Health Foundation; 2015.
- United Nations . Convention on the Rights of Persons With Disabilities 2006. www.un.org/disabilities/documents/convention/convoptprot-e.pdf (accessed 15 August 2017).
- UN Convention on the Rights of Persons with Disabilities: Initial Report on How the UK is Implementing it. London: Office for Disability Issues; 2011.
- A Charter of Rights for People with Dementia. Dublin: The Alzheimer Society of Ireland; 2016.
- Charter of Rights for People with Dementia and their Carers in Scotland. Edinburgh: Alzheimer Scotland; 2009.
- Laird S. Projects put human rights at the heart of good practice: service providers adopting a rights-based approach to care are seeing a change in culture. Nursing Older People 2010;22:6-7. https://doi.org/10.7748/nop.22.3.6.s10.
- Ensuring a Human Rights Based Approach for People Living with Dementia. Geneva: World Health Organization; 2015.
- Innes A, Kelly F, Dincarslan O. Care home design for people with dementia: what do people with dementia and their family carers value?. Aging Ment Health 2011;15:548-56. https://doi.org/10.1080/13607863.2011.556601.
- The Human Rights of People Living with Dementia: From Rhetoric to Reality. Ankeny, IA: Dementia Alliance International; 2016.
- Hare P. Our Dementia: Our Rights 2016. http://dementiawithoutwalls.org.uk/wp-content/uploads/2016/10/Our-dementia-Our-rights-booklet.pdf (accessed 15 August 2017).
- O’Connor D, Phinney A, Smith A, Small J, Purves B, Perry J, et al. Personhood in dementia care: developing a research agenda for broadening the vision. Dementia 2007;6:121-42. https://doi.org/10.1177/1471301207075648.
- Butchard S, Greenhill B. Giving clinical psychology a backbone. Clin Psychol Forum 2015;276.
- Tibbits F. Understanding what we do: emerging models for human rights education. Int Rev Educ 2002;48:159-71. https://doi.org/10.1023/A:1020338300881.
- Redman M, Taylor E, Furlong R, Carney G, Greenhill B. Human rights training: impact on attitudes and knowledge. Tizard Learning Disability Review 2012;17:80-7. https://doi.org/10.1108/13595471211218811.
- Donald A. A Guide to Evaluating Human Rights-Based Interventions in Health and Social Care. London: Human Rights and Social Justice Research Institute, Metropolitan University; n.d.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Nursing Times . CQC Uncovers Staffing Problems at Care Homes Rated ‘Inadequate’ 2016. www.nursingtimes.net/news/reviews-and-reports/cqc-uncovers-staffing-issues-at-inadequate-care-homes/7009773.article (accessed 15 August 2017).
- Comte-Sponville A. A Short Treatise On Great Virtues: The Uses of Philosophy in Everyday Life. London: William Heinemann; 2000.
- McCrae N. Person-centred care: rhetoric and reality in a public healthcare system. Br J Nurs 2017;22:1125-8. https://doi.org/10.12968/bjon.2013.22.19.1125.
- Buber M, Smith RG. I and Thou. Edinburgh: T & T Clark; 1937.
- Mathers N, Paynton D. Rhetoric and reality in person-centred care: introducing the House of Care framework. Br J Gen Pract 2016;66:12-3. https://doi.org/10.3399/bjgp16X683077.
- Mansell J, Beadle-Brown J. Person centred planning or person centred action? Policy and practice in intellectual disability services. J Appl Res Intellect 2004;17:1-9. https://doi.org/10.1111/j.1468-3148.2004.00175.x.
- Poor Training of Care Home Staff Leaving Residents at Risk, Investigation Finds. London: Community Care; 2015.
- NHS England Dementia: Good Care Planning – Information for Primary Care Providers and Commissioners. Leeds: NHS England; 2017.
- Dementia Support in Health and Social Care. London: NICE; 2010.
- Langdon J, Lindow V. Living with Risk. Mental Health Service User Involvement in Risk Assessment and Management. Bristol: Policy Press; 2004.
- Gould D. Service Users’ Experiences of Recovery Under the 2008 Care Programme Approach: A Research Study. London: National Survivor User Network; 2012.
- May H, Edwards P, Brooker D. Enriched Care Planning for People with Dementia: A Good Practice Guide to Delivering Person-centred Care. London: Jessica Kingsley Publishers; 2009.
- Zarit S, Goodman C. Decision making and dementia. Am J Alzheimers Dis 1990;5:22-8. https://doi.org/10.1177/153331759000500508.
- Age UK . Delivering Dignity: Securing Dignity in Care for Older People in Hospitals and Care Homes. A Report for Consultation 2012. www.ageuk.org.uk/Global/Delivering%20Dignity%20Report.pdf?dtrk=true (accessed 15 August 2017).
- Butchard S, Pendleton J. Getting it Right: A Human Rights Based Assessment for People with Dementia. Liverpool: Mersey Care NHS Foundation Trust; 2012.
- Logsdon RG, Gibbons LE, McCurry SM, Teri L. Quality of life in Alzheimer’s disease: patient and caregiver reports. J Ment Health Aging 1999;5:21-32. https://doi.org/10.1186/1477-7525-1-11.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 1980;20:649-55. https://doi.org/10.1093/geront/20.6.649.
- Dementia: A State of the Nation Report on Dementia Care and Support in England. London: Department of Health and Social Care; 2013.
- More Community Services for West Lancashire Dementia Patients. Ormskirk: West Lancashire Clinical Commissioning Group; 2013.
- Selwood A, Thorgrimsen L, Orrell M. Quality of life in dementia – a one-year follow-up study. Int J Geriatr Psychiatry 2005;20:232-7. https://doi.org/10.1002/gps.1271.
- Woods RT, Bruce E, Edwards RT, Elvish R, Hoare Z, Hounsome B, et al. REMCARE: reminiscence groups for people with dementia and their family caregivers – effectiveness and cost-effectiveness pragmatic multicentre randomised trial. Health Technol Assess 2012;16. https://doi.org/10.3310/hta16480.
- Hoe J, Hancock G, Livingston G, Woods B, Challis D, Orrell M. Changes in the quality of life of people with dementia living in care homes. Alzheimer Dis Assoc Disord 2009;23:285-90. https://doi.org/10.1097/WAD.0b013e318194fc1e.
- Russell D, Hoare ZS, Whitaker R, Whitaker CJ, Russell IT. Generalized method for adaptive randomization in clinical trials. Stat Med 2011;30:922-34. https://doi.org/10.1002/sim.4175.
- Moniz-Cook E, Vernooij-Dassen M, Woods R, Verhey F, Chattat R, Vugt MD, et al. A European consensus on outcome measures for psychosocial intervention research in dementia care. Aging Ment Health 2008;12:14-29. https://doi.org/10.1080/13607860801919850.
- Miller LA, Mioshi E, Savage S, Lah S, Hodges JR, Piguet O. Identifying cognitive and demographic variables that contribute to carer burden in dementia. Dement Geriatr Cogn Disord 2013;36:43-9. https://doi.org/10.1159/000347146.
- Brooker D, Surr C. Dementia Care Mapping: Principles and Practice. Bradford: Bradford Dementia Group, University of Bradford; 2005.
- Netten A, Burge P, Malley J, Potoglou D, Towers A, Brazier J, et al. Outcomes of social care for adults: developing a preference-weighted measure . Health Technol Assess 2012;16:1-165. https://doi.org/10.3310/hta16160.
- Curtice M. Article 8 of the Human Rights Act 1998: implications for clinical practice. Adv Psychiatr Treat 2009;15:23-31. https://doi.org/10.1192/apt.bp.107.005462.
- Allen K. Drawing out views on services: ways of getting started. J Dement Care 2001;9:23-5.
- Health Services and Public Health Research Board. A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health. London: Medical Research Council; 2000.
- Hounsome N, Orrell M, Edwards RT. EQ-5D as a quality of life measure in people with dementia and their carers: evidence and key issues. Value Health 2011;14:390-9. https://doi.org/10.1016/j.jval.2010.08.002.
- Edwards RT, Hounsome B, Linck P, Russell IT. Economic evaluation alongside pragmatic randomised trials: developing a standard operating procedure for clinical trials units. Trials 2008;9. https://doi.org/10.1186/1745-6215-9-64.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2014.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Brazier J. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2007.
- Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996.
- A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health. London: Medical Research Council; 2008.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- NHS Reference Costs. London: Department of Health and Social Care; 2015.
- DCM8 User’s Manual. Bradford: School of Dementia Studies, University of Bradford; 2016.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998.
- Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval 2006;27:237-46. https://doi.org/10.1177/1098214005283748.
- Patton MQ. Qualitative Evaluation and Research Methods. Thousand Oaks, CA: Sage; 1990.
- Bass BM, Avolio BJ. Full Range Leadership Development – Manual for the Multifactor Leadership Questionnaire. Redwood City, CA: Mind Garden; 1997.
- NHS Digital . Prescription Cost Analysis, England 2015 n.d. https://digital.nhs.uk/catalogue/PUB20200 (accessed 22 January 2018).
- Bass BM, Avolio BJ. MLQ: Multifactor Leadership Questionnaire. Menlo Park, CA: Mind Garden; 2000.
- Bass BM. Transformational Leadership: Industrial, Military, and Educational Impact. Mahwah, NJ: Erlbaum; 1998.
- Brooker D, Latham I. Person-centred Dementia Care: Making Services Better with the VIPS Framework. London: Jessica Kingsley Publishers; 2016.
- The Use of Antipsychotic Medication for People with Dementia: Time for Action. London: Department of Health and Social Care; 2009.
- Mersey Care NHS Foundation Trust CQC Inspection Report. Newcastle upon Tyne: CQC; 2015.
- Rand S, Caiels J. Using Proxies to Assess Quality of Life: A Review of the Issues and Challenges. Canterbury: Quality and Outcome of Person-centred Care Policy Research Unit; 2015.
- Novella JL, Jochum C, Jolly D, Morrone I, Ankri J, Bureau F, et al. Agreement between patients’ and proxies’ reports of quality of life in Alzheimer’s disease. Qual Life Res 2001;10:443-52. https://doi.org/10.1023/A:1012522013817.
- Hoe J, Hancock G, Livingston G, Orrell M. Quality of life of people with dementia in residential care homes. Br J Psychiatry 2006;188:460-4. https://doi.org/10.1192/bjp.bp.104.007658.
- Camozzato A, Roriz-Filho JS, Cruz IR, Chaves MLF, Roriz-Cruz M, Abdel-Rahman E. Depression in the Elderly. Hauppauge, NY: Nova Science Publishers; 2012.
- Pickard AS, Knight SJ. Proxy evaluation of health-related quality of life: a conceptual framework for understanding multiple proxy perspectives. Med Care 2005;43:493-9. https://doi.org/10.1097/01.mlr.0000160419.27642.a8.
- Huang HL, Chang MY, Tang JS, Chiu YC, Weng LC. Determinants of the discrepancy in patient- and caregiver-rated quality of life for persons with dementia. J Clin Nurs 2009;18:3107-18. https://doi.org/10.1111/j.1365-2702.2008.02537.x.
- Thorgrimsen L, Selwood A, Spector A, Royan L, de Madariaga Lopez M, Woods RT, et al. Whose quality of life is it anyway? The validity and reliability of the Quality of Life-Alzheimer’s Disease (QoL-AD) scale. Alzheimer Dis Assoc Disord 2003;17:201-8. https://doi.org/10.1097/00002093-200310000-00002.
- Mozley CG, Huxley P, Sutcliffe C, Bagley H, Burns A, Challis D, et al. ‘Not knowing where I am doesn’t mean I don’t know what I like’: cognitive impairment and quality of life responses in elderly people. Int J Geriatr Psychiatry 1999;14:776-83. https://doi.org/10.1002/(SICI)1099-1166(199909)14:9<776::AID-GPS13>3.0.CO;2-C.
- Mahan TL. Perceived Control in Older Adults Living in Long-Term Care Facilities. Dissertation Abstracts International: Section B: The Sciences and Engineering 2010;66.
- Wang P, Yap P, Koh G, Chong JA, Davies LJ, Dalakoti M, et al. Quality of life and related factors of nursing home residents in Singapore. Health Qual Life Out 2016;14. https://doi.org/10.1186/s12955-016-0503-x.
- Fossey J, Lee L, Ballard C. Dementia Care Mapping as a research tool for measuring quality of life in care settings: psychometric properties. Int J Geriatr Psychiatry 2002;17:1064-70. https://doi.org/10.1002/gps.708.
- Dementia Care Mapping Process and Application. Bradford: Bradford Dementia Group; 2014.
- Persistent Challenges to Providing Quality Care: An RCN Report on the Views and Experiences of Frontline Nursing Staff in Care Homes in England. London: Royal College of Nursing; 2012.
- Surr CA, Smith SJ, Crossland J, Robins J. Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: a repeated measures study. Int J Nurs Stud 2016;53:144-51. https://doi.org/10.1016/j.ijnurstu.2015.09.009.
- INVOLVE . What Is Public Involvement in Research? 2012. www.hra.nhs.uk/resources/public-involvement-research/ (accessed 15 August 2017).
- Swain J, Heyman B, Gillman M. Public research, private concerns: ethical issues in the use of open-ended interviews with people who have learning difficulties. Disabil Soc 1998;13:21-36. https://doi.org/10.1080/09687599826894.
- Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research. Eastleigh: INVOLVE; 2012.
- Tarpey M, Bite S. Public Involvement in Research Applications to the National Research Ethics Service: Comparative Analysis of 2010 and 2012 Data. Eastleigh: INVOLVE; 2014.
- Gove D, Diaz-Ponce A, Georges J, Moniz-Cook E, Mountain G, Chattat R, et al. European Working Group of People with Dementia . Alzheimer Europe’s position on involving people with dementia in research through PPI (patient and public involvement). Aging Ment Health 2017;17:1-7. https://doi.org/10.1080/13607863.2017.1317334.
- Alexander CS, Becker HJ. The use of vignettes in survey research. Public Opin Quart 1978;42:93-104. https://doi.org/10.1086/268432.
- Finger MS, Rand KL, Roberts MC, Ilardi SS. Handbook of Research Methods in Clinical Psychology. Malden, MA: Blackwell Publishing; 2005.
- Wallander L. Measuring social workers’ judgments: why and how to use the factorial survey approach in the study of professional judgments. J Soc Work 2012;12:364-84. https://doi.org/10.1177/1468017310387463.
- Evans SC, Roberts MC, Keeley JW, Blossom JB, Amaro CM, Garcia AM, et al. Vignette methodologies for studying clinicians’ decision-making: validity, utility, and application in ICD-11 field studies. Int J Clin Health Psych 2015;15:160-70. https://doi.org/10.1016/j.ijchp.2014.12.001.
- James IA. Understanding Behaviour in Dementia that Challenges: A Guide to Assessment and Treatment. London: Jessica Kingsley Publishers; 2011.
- Standards for Acute Inpatient Services for Older People – 3rd Edition. London: Royal College of Psychiatrists; 2014.
- Cohen-Mansfield J, Buckwalter K, Beattie E, Rose K, Neville C, Kolanowski A. Expanded review criteria: the case of nonpharmacological interventions in dementia. J Alzheimers Dis 2014;41:15-28. https://doi.org/10.3233/JAD-132357.
- Rosen WF, Mohs RC, Davis KL. A new rating scale for Alzheimer’s disease. Am J Psychiatry 1984;141:1356-64. https://doi.org/10.1176/ajp.141.11.1356.
- Nursing Times . Concerns Over High Staff Turnover in Care Homes n.d. www.nursingtimes.net/concerns-over-high-staff-turnover-in-care-homes/1806216.fullarticle (accessed 15 August 2017).
- Franklin B. The Future Care Workforce 2014. www.ilcuk.org.uk/images/uploads/publication-pdfs/Future_Care_Workforce_Report.pdf (accessed 15 August 2017).
- The State of Health Care and Adult Social Care in England in 2013/14. Newcastle upon Tyne: CQC; 2013.
- Redlanders in Service . Visiting the Lonely Ones Makes Rounds of Nursing Homes n.d. www.redlandsdailyfacts.com/general-news/20130801/redlanders-in-service-visiting-the-lonely-ones-makes-rounds-of-nursing-homes (accessed 15 August 2017).
- Molyneaux V, Butchard S, Simpson J, Murray C. The co-construction of couplehood in dementia. Dementia 2012;11:483-502. https://doi.org/10.1177/1471301211421070.
- Ajzen I, Kuhl J, Beckmann J. Action Control: From Cognition to Behavior. Berlin: Springer-Verlag; 1985.
- Sheard D. Steering Cultural Change Matters in Dementia Care Homes: Commissioning Briefing Booklet. Brighton: Dementia Care Matters; 2013.
- Sheard D. Bringing relationships into the heart of dementia care. J Dement Care 2004;12:22-4.
- Improving Care in Residential Care Homes: A Literature Review. York: Joseph Rowntree Foundation; 2008.
- Values Based Recruitment Framework. Leeds: Health Education England; 2016.
- Sehein EH. Organizational Culture and Leadership: A Dynamic View. San Francisco, CA: Jossey-Bass; 1985.
- UNISON . Residential Care Worker Survey and Residential Care Charter Executive Summary 2017. www.unison.org.uk/content/uploads/2017/06/residential-care-summary.pdf (accessed 15 August 2017).
- Killett A, Bowes A, Brooker D, Burns D, Kelly F, La Fontaine J, et al. What Makes a Real Difference to Resident Experience? Digging Deep into Care Home Culture: The CHOICE (Care Home Organisations Implementing Cultures of Excellence) Research Report. Cambridge: Cambridge University Press; 2013.
- Donald A, Watson J, McClean N, Leach P, Eschment J. Human Rights in Britain Since the Human Rights Act 1998: A Critical Review. Manchester: Equality and Human Rights Commission; 2009.
- Kinderman P, Butler F. Implementing a Human Rights Approach Within Public Services: An Outline Psychological Perspective. London: Department for Constitutional Affairs; 2006.
- Matthews L, Sanz R. Older People and Human Rights. London: Age UK/British Institute of Human Rights; 2011.
- Prepared to Care. Challenging the Dementia Skills Gap. London: The Stationery Office; 2009.
- Dementia Core Skills Education and Training Framework. Leeds: Health Education England; 2015.
- Surr C, Gates C, Irving D. What Works in Dementia Training and Education? A Critical Interpretive Synthesis of the Evidence. Leeds: Leeds Beckett University; 2017.
- Kirkpatrick DL. Evaluating Training Programs: The Four Levels. San Francisco, CA: Berrett-Koehler; 1984.
- James I. Understanding Behaviour in Dementia That Challenges: A Guide to Assessment and Treatment (Bradford Dementia Group Good Practice Guides). London: Jessica Kingsley Publishers; 2011.
- Caddell LS, Clare L. The impact of dementia on self and identity: a systematic review. Clin Psychol Rev 2010;30:113-26. https://doi.org/10.1016/j.cpr.2009.10.003.
- Sabat SR, Harre R. The construction and deconstruction of self in Alzheimer’s disease. Ageing Soc 1992;12:443-61. https://doi.org/10.1017/S0144686X00005262.
- Roberts A, Greenhill B, Talbot A. Standing up for my human rights: a group’s journey beyond consultation towards co-production. Br J Learn Dis 2011;40:292-301. https://doi.org/10.1111/j.1468-3156.2011.00711.x.
- Dementia Engagement and Empowerment Project . Dementia Words Matter: Guidelines on Language About Dementia n.d. http://dementiavoices.org.uk/wp-content/uploads/2015/03/DEEP-Guide-Language.pdf (accessed 15 August 2017).
- Health Education England n.d. https://hee.nhs.uk/ (accessed 15 August 2017).
- Bloom BS. Taxonomy of Educational Objectives, Handbook I: The Cognitive Domain. New York, NY: David McKay Co., Inc.; 1956.
- Transforming the Delivery of Health and Social Care: The Case for Fundamental Change. London: The King’s Fund; 2012.
- Innovations in Dementia . Making an Impact Together 2015. https://dementiawithoutwalls.org.uk/wp-content/uploads/2016/10/Making-An-Impact-Together.pdf (accessed 15 August 2017).
- Curtis L. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
Appendix 1 ’Getting it Right’ assessment tool

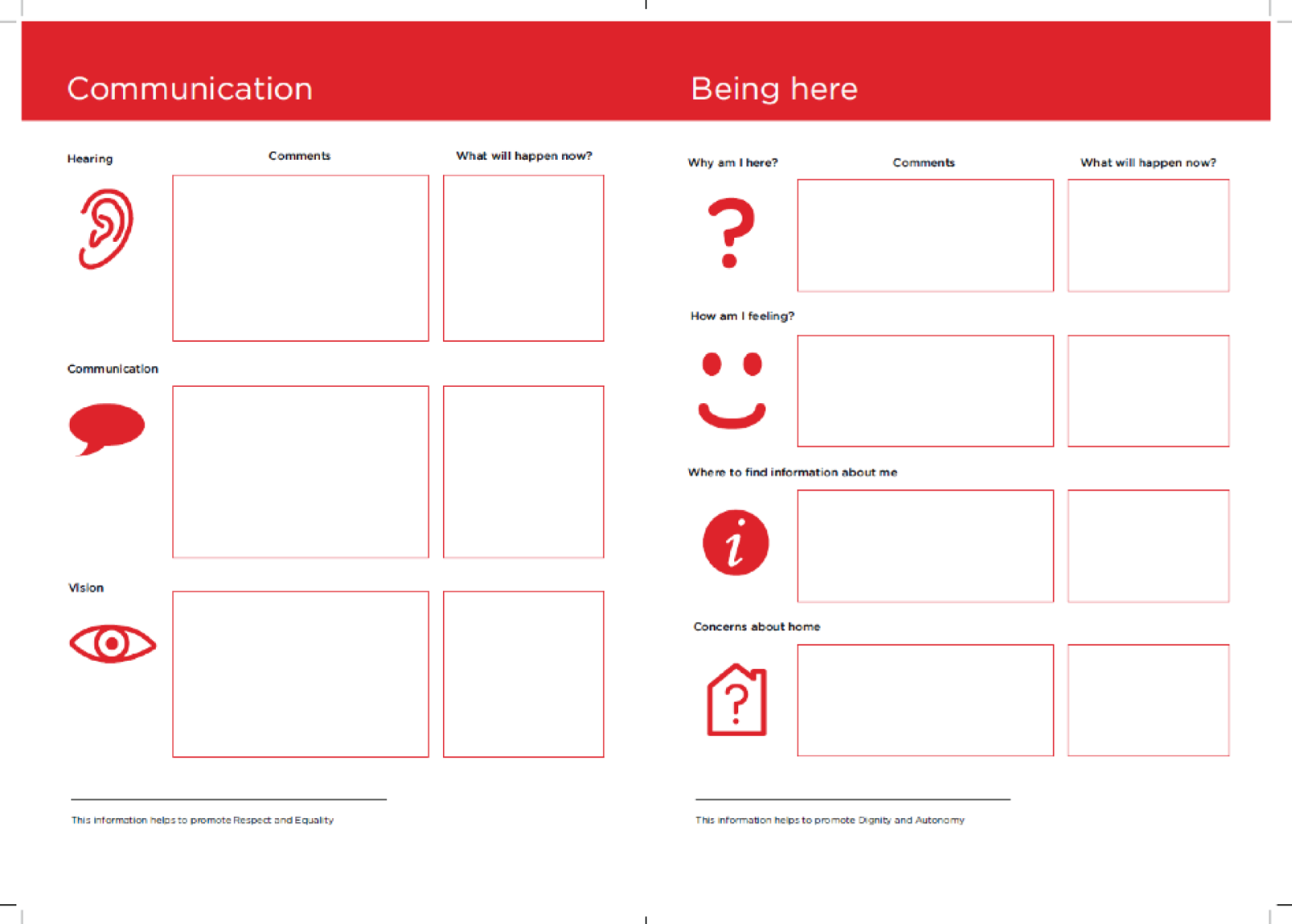

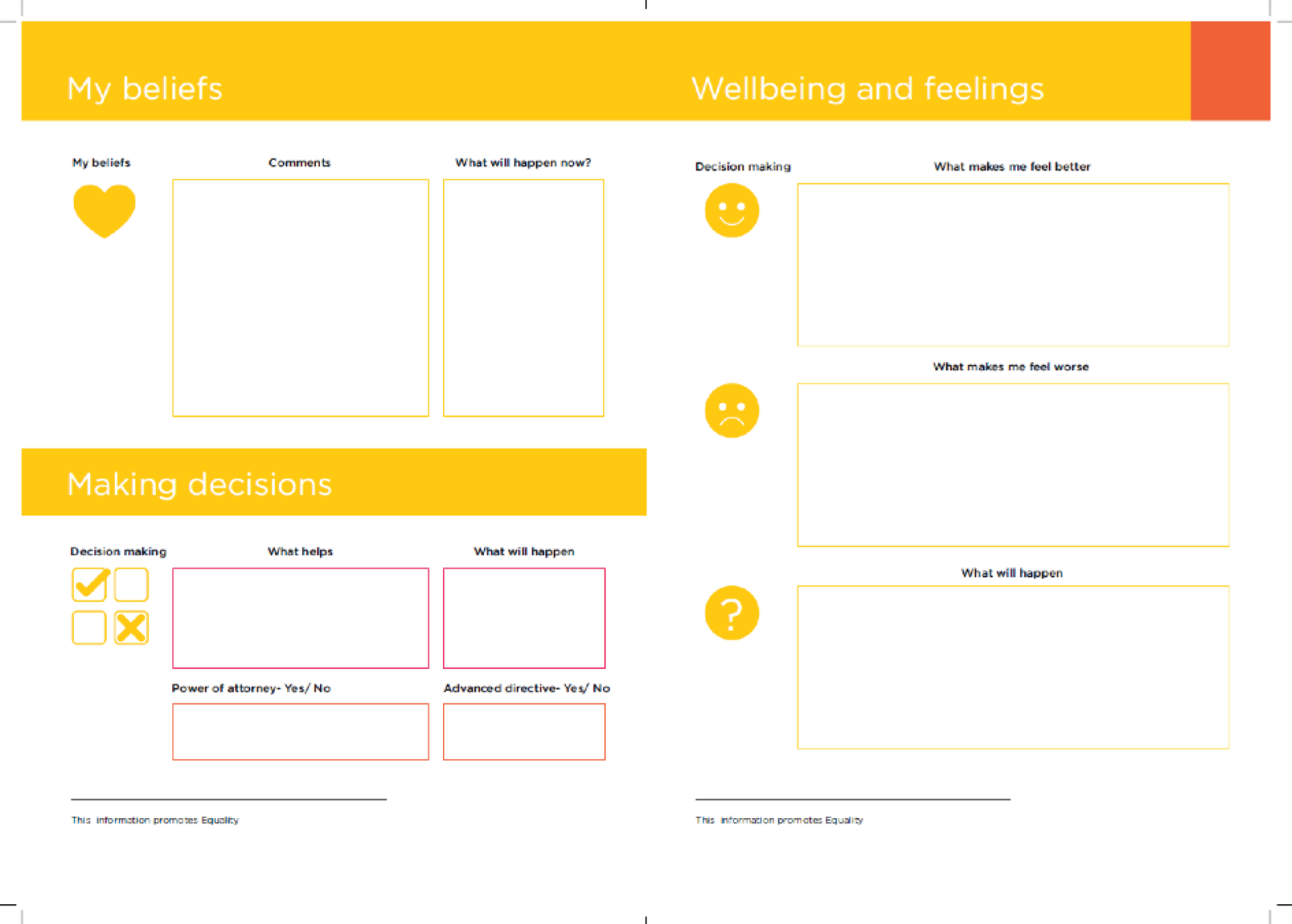
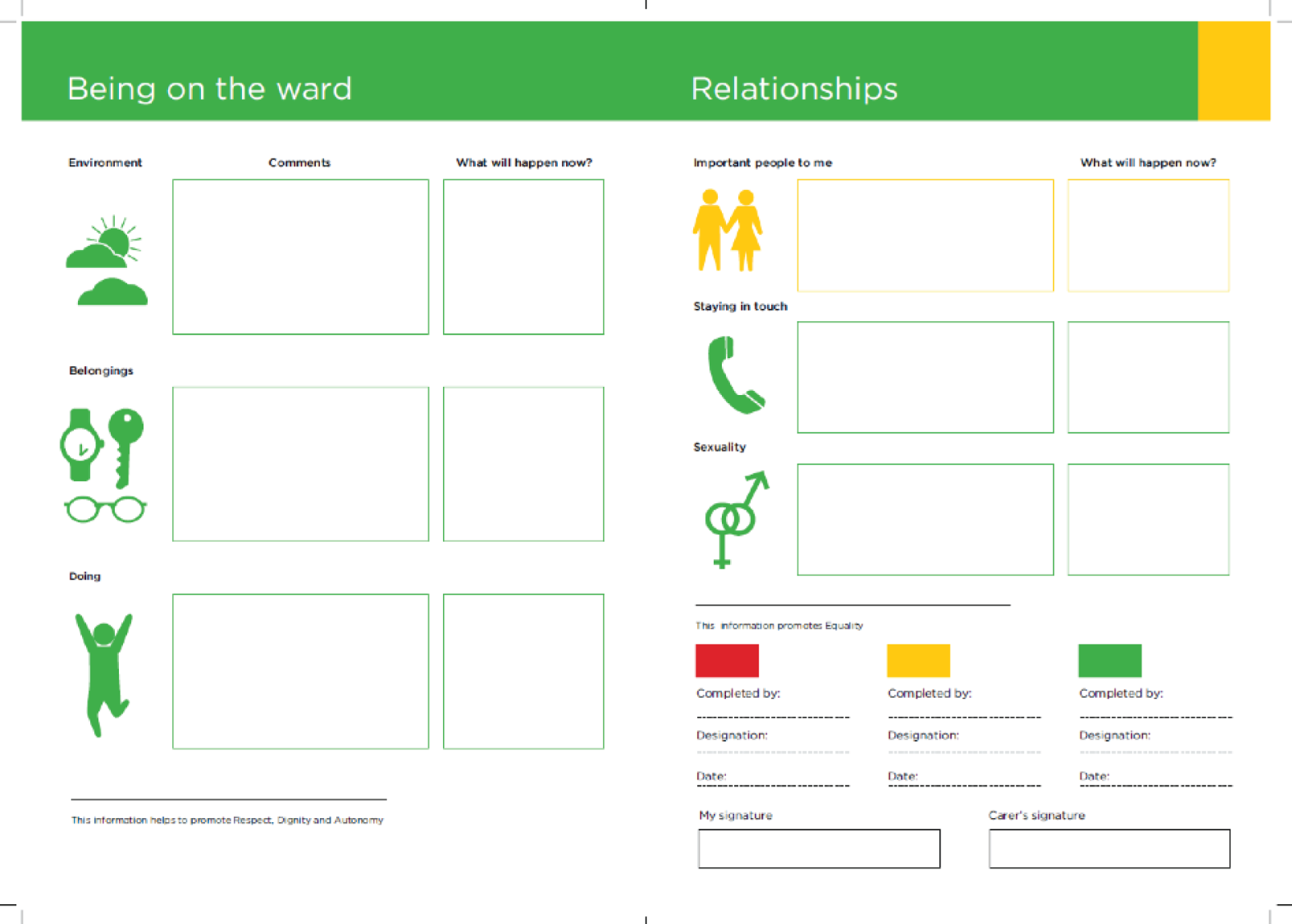
Appendix 2 Supplementary tables
Service use
| Job title | Group, n (%) | |
|---|---|---|
| Control | Intervention | |
| Acting senior carer | 1 (0.8) | |
| Activities co-ordinator | 2 (1.6) | |
| Activity co-ordinator | 2 (1.6) | 1 (0.8) |
| Apprentice clinical support worker | 1 (0.8) | |
| Assistant practitioner | 2 (1.6) | |
| Assistant support worker | 1 (0.8) | |
| Care assistant | 18 (14.5) | 27 (21.8) |
| Care assistant and acting senior | 1 (0.8) | |
| Care assistant/driver | 1 (0.8) | |
| Care home manager | 1 (0.8) | |
| Care worker | 2 (1.6) | 2 (1.6) |
| Carer | 3 (2.4) | 6 (4.8) |
| Clinical lead | 2 (1.6) | |
| Clinical specialist physiotherapist | 1 (0.8) | |
| Clinical support worker | 19 (15.3) | |
| Deputy manager | 2 (1.6) | |
| Deputy ward manager | 1 (0.8) | 1 (0.8) |
| Domestic | 1 (0.8) | |
| Gardener/domestic | 1 (0.8) | |
| General nurse | 2 (1.6) | |
| Health-care assistant | 42 (33.9) | 8 (6.5) |
| Health-care assistant: training to be assistant practitioner | 1 (0.8) | |
| Health-care support worker | 1 (0.8) | |
| Housekeeper/carer | 1 (0.8) | |
| Health support worker | 1 (0.8) | |
| Hotel services manager | 1 (0.8) | |
| Kitchen assistant | 1 (0.8) | |
| Maintenance lead | 1 (0.8) | |
| Manager | 1 (0.8) | |
| Mental health nurse | 1 (0.8) | |
| Nurse | 6 (4.8) | 3 (2.4) |
| Nurse practitioner | 2 (1.6) | |
| Nursing assistant | 2 (1.6) | 1 (0.8) |
| Occupational therapist | 2 (1.6) | |
| Occupational therapist assistant | 1 (0.8) | 1 (0.8) |
| Occupational therapist assistant/care assistant | 1 (0.8) | |
| Physical health nurse | 1 (0.8) | |
| Physiotherapist | 1 (0.8) | |
| Physiotherapy assistant | 1 (0.8) | |
| Registered manager | 1 (0.8) | |
| Registered mental health nurse | 2 (1.6) | 1 (0.8) |
| Senior care assistant | 2 (1.6) | 6 (4.8) |
| Senior carer | 4 (3.2) | 3 (2.4) |
| Senior health-care assistant | 1 (0.8) | |
| Senior unit manager | 1 (0.8) | |
| Staff nurse | 3 (2.4) | 4 (3.2) |
| Supervised practice nurse | 2 (1.6) | |
| Supervised practitioner nurse | 1 (0.8) | |
| Supervisor | 1 (0.8) | |
| Support worker | 8 (6.5) | 13 (10.5) |
| Team leader | 2 (1.6) | 1 (0.8) |
| Trainee assistant practitioner | 1 (0.8) | 1 (0.8) |
| Unit manager | 1 (0.8) | |
| Unit manager/nurse | 1 (0.8) | |
| Ward manager | 2 (1.6) | |
| Total | 124 (100.0) | 124 (100.0) |
| Assessment point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Group 1 | ||||
| Pre | 8 | 13.67 | 46.33 | 31.17 (10.52) |
| Post | 1 | 27.33 | 27.33 | 27.33 (N/A) |
| Group 2 | ||||
| Pre | 5 | 16.33 | 44.33 | 29.53 (11.97) |
| Post | 0 | N/A | N/A | N/A |
| Total | ||||
| Pre | 13 | 13.67 | 46.33 | 30.54 (10.63) |
| Post | 1 | 27.33 | 27.33 | 27.33 (N/A) |
| Did not complete | ||||
| Pre | 319 | N/A | N/A | N/A |
| Post | 435 | N/A | N/A | N/A |
| Assessment point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Group 1 | ||||
| Pre | 3 | 31.00 | 37.00 | 34.00 (3.00) |
| Post | N/A | N/A | N/A | N/A |
| Group 2 | ||||
| Pre | 2 | 29.00 | 33.14 | 31.07 (2.93) |
| Post | 2 | 36.00 | 41.00 | 38.50 (3.54) |
| Total | ||||
| Pre | 5 | 29.00 | 37.00 | 32.83 (3.04) |
| Post | 2 | 36.00 | 41.00 | 38.50 (3.54) |
| Did not complete | ||||
| Pre | 318 | N/A | N/A | N/A |
| Post | 421 | N/A | N/A | N/A |
| Assessment point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Group 1 | ||||
| Pre | 3 | 41.00 | 47.00 | 44.00 (3.00) |
| Post | 0 | N/A | N/A | N/A |
| Group 2 | ||||
| Pre | 3 | 48.00 | 52.00 | 50.33 (2.08) |
| Post | 2 | 38.00 | 48.00 | 43.00 (7.07) |
| Total | ||||
| Pre | 6 | 41.00 | 52.00 | 47.17 (4.17) |
| Post | 2 | 38.00 | 48.00 | 43.00 (7.07) |
| Did not complete | ||||
| Pre | 317 | N/A | N/A | N/A |
| Post | 421 | N/A | N/A | N/A |
| Assessment point | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| Group 1 | ||||
| Pre | 3 | 28.00 | 37.00 | 33.03 (4.59) |
| Post | 0 | N/A | N/A | N/A |
| Group 2 | ||||
| Pre | 3 | 8.38 | 34.00 | 19.71 (13.06) |
| Post | 2 | 10.00 | 30.38 | 20.19 (14.41) |
| Total | ||||
| Pre | 6 | 8.38 | 37.00 | 26.37 (11.40) |
| Post | 2 | 10.00 | 30.38 | 20.19 (14.41) |
| Did not complete | ||||
| Pre | 317 | N/A | N/A | N/A |
| Post | 421 | N/A | N/A | N/A |
| Outcome measure | n | Minimum | Maximum | Mean (SD) |
|---|---|---|---|---|
| T1 ASCOT total | 85 | 0.22 | 1.0 | 0.86 (0.14) |
| T2 ASCOT total | 70 | 0.09 | 1.0 | 0.85 (0.18) |
| T2 ASCOT proxy total | 147 | 0.16 | 1.0 | 0.81 (0.17) |
| T2 ASCOT proxy total | 176 | 0.2 | 1.0 | 0.81 (0.17) |
| T1 EQ-VAS | 71 | 50.0 | 100.0 | 78.23 (16.77) |
| T2 EQ-VAS | 62 | 0.0 | 100.0 | 74.19 (24.23) |
| T1 EQ-VAS proxy | 202 | 5.0 | 100.0 | 62.71 (19.99) |
| T2 EQ-VAS proxy | 236 | 10.0 | 100.0 | 60.53 (19.57) |
| T1 EQ-5D-3L total | 101 | –0.043 | 1.0 | 0.743 (0.27) |
| T2 EQ-5D-3L total | 86 | –0.077 | 1.0 | 0.714 (0.28) |
| T1 EQ-5D-3L proxy total | 202 | –0.371 | 1.0 | 0.35 (0.34) |
| T2 EQ-5D-3L proxy total | 233 | –0.536 | 1.0 | 0.381 (0.34) |
| T1 QOL-AD total | 103 | 26.00 | 51.00 | 36.56 (5.46) |
| T2 QOL-AD total | 93 | 22.75 | 45.00 | 35.33 (5.57) |
| T1 QOL-AD proxy total | 183 | 14.08 | 47.67 | 30.89 (7.27) |
| T2 QOL-AD proxy total | 224 | 13.00 | 46.09 | 31.69 (6.72) |
| T1 WEMWBS total | 6 | 41.0 | 52.0 | 47.17 (4.17) |
| T2 WEMWBS total | 2 | 38.0 | 48.0 | 43.00 (7.07) |
| T1 ZBI total | 6 | 8.381 | 37.00 | 26.37 (11.40) |
| T2 ZBI total | 2 | 10.00 | 30.38 | 20.19 (14.41) |
| Service accessed | Time point | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | ||||||||
| Minimum | Maximum | Mean | SD | Minimum | Maximum | Mean | SD | ||
| Alternative therapist | 0 | 1 | 0.01 | 0.076 | – | – | – | – | |
| Care manager | 0 | 2 | 0.01 | 0.152 | – | – | – | – | |
| Community nurse | 0 | 14 | 0.69 | 1.909 | 0 | 8 | 0.67 | 1.351 | |
| CPN | 0 | 10 | 0.20 | 0.885 | 0 | 3 | 0.19 | 0.500 | |
| Dentist | 0 | 2 | 0.06 | 0.268 | 0 | 2 | 0.03 | 0.200 | |
| Dietician | 0 | 2 | 0.17 | 0.447 | 0 | 3 | 0.18 | 0.515 | |
| GP | 0 | 6 | 0.84 | 1.138 | 0 | 5 | 0.94 | 1.066 | |
| Mental health team worker | 0 | 1 | 0.03 | 0.184 | 0 | 1 | 0.02 | 0.131 | |
| Optician | 0 | 2 | 0.18 | 0.429 | 0 | 2 | 0.15 | 0.370 | |
| Occupational therapist | 0 | 1 | 0.01 | 0.076 | 0 | 1 | 0.02 | 0.151 | |
| Physiotherapist | 0 | 4 | 0.08 | 0.433 | 0 | 5 | 0.08 | 0.446 | |
| Practice nurse | 0 | 1 | 0.03 | 0.184 | 0 | 1 | 0.02 | 0.151 | |
| Psychiatrist | 0 | 4 | 0.12 | 0.521 | 0 | 2 | 0.16 | 0.410 | |
| Social worker | 0 | 2 | 0.10 | 0.369 | 0 | 3 | 0.08 | 0.375 | |
| Chiropodist | 0 | 2 | 0.40 | 0.598 | 0 | 3 | 0.38 | 0.736 | |
| A&E visits | 0 | 23 | 0.23 | 1.800 | 0 | 29 | 0.57 | 2.940 | |
| Inpatient nights | 0 | 35 | 0.42 | 3.074 | 0 | 33 | 0.44 | 2.995 | |
| Outpatient visits | 0 | 3 | 0.06 | 0.300 | 0 | 2 | 0.09 | 0.311 | |
Service use data was collected using an adapted CSRI, which recorded participants’ frequency of contacts with hospital services and selected community-based services at T1 and T2. Participants’ medication usage was also recorded. Service use was costed using national unit costs for the price year 2014–15. 80,81
| Service accessed | Time point | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | |||||||
| Minimum (£) | Maximum (£) | Mean (£) | SD | Minimum (£) | Maximum (£) | Mean (£) | SD | |
| Alternative therapist | 0.0 | 17.0 | 0.10 | 1.2962 | – | – | – | – |
| Care manager | 0.0 | 78.0 | 0.45 | 5.9474 | – | – | – | – |
| Community nurse | 0.0 | 938.0 | 45.97 | 127.8901 | 0.0 | 536.0 | 44.80 | 90.5172 |
| CPN | 0.0 | 750.0 | 15.26 | 66.3617 | 0.0 | 225.0 | 14.39 | 37.4643 |
| Dentist | 0.0 | 178.0 | 5.69 | 23.8662 | 0.0 | 178.0 | 2.59 | 17.8191 |
| Dietician | 0.0 | 76.0 | 6.41 | 16.9719 | 0.0 | 114.0 | 6.85 | 19.5828 |
| GP | 0.0 | 270.0 | 37.67 | 51.2088 | 0.0 | 225.0 | 42.12 | 47.9675 |
| Mental health team worker | 0.0 | 42.0 | 1.47 | 7.7289 | 0.0 | 42.0 | 0.73 | 5.5143 |
| Optician | 0.0 | 42.0 | 3.79 | 9.0007 | 0.0 | 42.0 | 3.05 | 7.7628 |
| Occupational therapist | 0.0 | 44.0 | 0.26 | 3.3550 | 0.0 | 44.0 | 1.02 | 6.6508 |
| Physiotherapist | 0.0 | 152.0 | 2.87 | 16.4429 | 0.0 | 190.0 | 2.87 | 16.9487 |
| Practice nurse | 0.0 | 56.0 | 1.95 | 10.3052 | 0.0 | 56.0 | 1.30 | 8.4647 |
| Psychiatrist | 0.0 | 556.0 | 16.91 | 72.4343 | 0.0 | 278.0 | 21.82 | 57.0064 |
| Social worker | 0.0 | 158.0 | 7.81 | 29.1737 | 0.0 | 237.0 | 5.971 | 29.6069 |
| Chiropodist | 0.0 | 62.0 | 12.26 | 18.5328 | 0.0 | 93.0 | 11.90 | 22.8215 |
| A&E visits | 0.0 | 2461.0 | 24.26 | 192.6203 | 0.0 | 3103.0 | 60.97 | 314.5914 |
| Inpatient | 0.0 | 13,930.0 | 168.92 | 1223.5115 | 0.0 | 13,134.0 | 173.55 | 1192.1741 |
| Outpatient | 0.0 | 372.0 | 7.21 | 37.2346 | 0.0 | 248.0 | 11.54 | 38.5317 |
| Total | 0.0 | 13,930.0 | 349.28 | 1254.3541 | 0.0 | 13735.0 | 405.46 | 1292.1842 |
| Service accessed | Time point | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | |||||||
| Minimum | Maximum | Mean | SD | Minimum | Maximum | Mean | SD | |
| Alternative therapist | 0 | 1 | 0.01 | 0.115 | – | – | – | – |
| Care manager | – | – | – | – | – | – | – | – |
| Community nurse | 0 | 3 | 0.25 | 0.676 | 0 | 4 | 0.46 | 0.930 |
| Community psychiatric nurse | 0 | 2 | 0.12 | 0.364 | 0 | 2 | 0.30 | 0.589 |
| Dentist | 0 | 1 | 0.01 | 0.115 | – | 2 | 0.03 | 0.229 |
| Dietician | 0 | 2 | 0.12 | 0.364 | 0 | 2 | 0.13 | 0.442 |
| GP | 0 | 6 | 0.66 | 1.114 | 0 | 4 | 0.76 | 0.922 |
| Mental health team worker | 0 | 1 | 0.03 | 0.161 | – | – | – | – |
| Optician | 0 | 1 | 0.08 | 0.271 | 0 | 1 | 0.16 | 0.367 |
| Occupational therapist | – | – | – | – | – | – | – | – |
| Physiotherapist | 0 | 4 | 0.14 | 0.605 | 0 | 5 | 0.14 | 0.647 |
| Practice nurse | 0 | 1 | 0.04 | 0.196 | 0 | 1 | 0.03 | 0.161 |
| Psychiatrist | 0 | 3 | 0.17 | 0.575 | 0 | 2 | 0.24 | 0.513 |
| Social worker | 0 | 2 | 0.12 | 0.431 | 0 | 3 | 0.08 | 0.392 |
| Chiropodist | 0 | 2 | 0.17 | 0.413 | 0 | 1 | 0.21 | 0.410 |
| A&E visits | 0 | 23 | 0.34 | 2.641 | 0 | 14 | 0.42 | 1.995 |
| Inpatient nights | 0 | 35 | 0.64 | 4.304 | 0 | 14 | 0.46 | 2.346 |
| Outpatient visits | 0 | 1 | 0.03 | 0.161 | 0 | 2 | 0.13 | 0.377 |
| Service accessed | Time point | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | |||||||
| Minimum (£) | Maximum (£) | Mean (£) | SD | Minimum (£) | Maximum (£) | Mean (£) | SD | |
| Alternative therapist | 0.0 | 17.0 | 0.22 | 1.9500 | – | – | – | – |
| Care manager | – | – | – | – | – | – | – | – |
| Community nurse | 0.0 | 201.0 | 16.75 | 45.2767 | 0.0 | 268.0 | 30.86 | 62.3168 |
| Community psychiatric nurse | 0.0 | 150.0 | 8.88 | 27.2959 | 0.0 | 150.0 | 22.70 | 44.1923 |
| Dentist | 0.0 | 89.0 | 1.17 | 10.2090 | 0.0 | 178.0 | 2.34 | 20.4180 |
| Dietician | 0.0 | 76.0 | 4.50 | 13.8299 | 0.0 | 76.0 | 5.00 | 16.8143 |
| GP | 0.0 | 270.0 | 29.61 | 50.1382 | 0.0 | 180.0 | 34.34 | 41.4837 |
| Mental health team worker | 0.0 | 42.0 | 1.11 | 6.7677 | 0.0 | – | – | – |
| Optician | 0.0 | 21.0 | 1.66 | 5.7004 | 0.0 | 21.0 | 3.32 | 7.7084 |
| Occupational therapist | – | – | – | – | 0.0 | – | – | – |
| Physiotherapist | 0.0 | 152.0 | 5.50 | 22.9716 | 0.0 | 190.0 | 5.50 | 24.5908 |
| Practice nurse | 0.0 | 56.0 | 2.21 | 10.9767 | 0.0 | 56.0 | 1.47 | 9.0236 |
| Psychiatrist | 0.0 | 417.0 | 23.78 | 79.8919 | 0.0 | 278.0 | 32.92 | 71.3055 |
| Social worker | 0.0 | 158.0 | 9.36 | 34.0516 | 0.0 | 237.0 | 6.24 | 30.9700 |
| Chiropodist | 0.0 | 62.0 | 5.30 | 12.7948 | 0.0 | 31.0 | 6.53 | 12.7221 |
| A&E visits | 0.0 | 2461.0 | 36.61 | 282.5841 | 0.0 | 1498.0 | 45.05 | 213.4737 |
| Inpatient | 0.0 | 13930.0 | 256.61 | 1713.0393 | 0.0 | 5572.0 | 183.29 | 933.8243 |
| Outpatient | 0.0 | 124.0 | 3.26 | 19.9809 | 0.0 | 248.0 | 16.32 | 46.8018 |
| Total | 0.0 | 13930.0 | 399.61 | 1727.8158 | 0.0 | 6764.0 | 395.87 | 1042.8599 |
| Service accessed | Time point | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | |||||||
| Minimum | Maximum | Mean | SD | Minimum | Maximum | Mean | SD | |
| Alternative therapist | – | – | – | – | – | – | – | – |
| Care manager | 0 | 2 | 0.02 | 0.204 | – | – | – | – |
| Community nurse | 0 | 14 | 1.03 | 2.434 | 0 | 8 | 0.83 | 1.594 |
| Community psychiatric nurse | 0 | 10 | 0.27 | 1.138 | 0 | 3 | 0.10 | 0.397 |
| Dentist | 0 | 2 | 0.10 | 0.340 | 0 | 1 | 0.03 | 0.175 |
| Dietician | 0 | 2 | 0.21 | 0.501 | 0 | 3 | 0.22 | 0.566 |
| GP | 0 | 5 | 0.98 | 1.142 | 0 | 5 | 1.07 | 1.154 |
| Mental health team worker | 0 | 1 | 0.04 | 0.201 | 0 | 1 | 0.03 | 0.175 |
| Optician | 0 | 2 | 0.26 | 0.508 | 0 | 2 | 0.14 | 0.373 |
| Occupational therapist | 0 | 1 | 0.01 | 0.102 | 0 | 1 | 0.04 | 0.201 |
| Physiotherapist | 0 | 2 | 0.02 | 0.204 | 0 | 1 | 0.02 | 0.144 |
| Practice nurse | 0 | 1 | 0.03 | 0.175 | 0 | 1 | 0.02 | 0.144 |
| Psychiatrist | 0 | 4 | 0.08 | 0.474 | 0 | 1 | 0.09 | 0.293 |
| Social worker | 0 | 2 | 0.08 | 0.313 | 0 | 3 | 0.07 | 0.363 |
| Chiropodist | 0 | 2 | 0.57 | 0.661 | 0 | 3 | 0.52 | 0.894 |
| A&E visits | 0 | 4 | 0.14 | 0.555 | 0 | 29 | 0.69 | 3.519 |
| Inpatient nights | 0 | 11 | 0.25 | 1.522 | 0 | 33 | 0.42 | 3.436 |
| Outpatient visits | 0 | 3 | 0.08 | 0.375 | 0 | 1 | 0.06 | 0.243 |
| Service accessed | Time point | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | |||||||
| Minimum (£) | Maximum (£) | Mean (£) | SD | Minimum (£) | Maximum (£) | Mean (£) | SD | |
| Alternative therapist | – | – | – | – | – | – | – | – |
| Care manager | 0.0 | 78.0 | 0.81 | 7.9608 | – | – | – | – |
| Community nurse | 0.0 | 938.0 | 69.09 | 163.0914 | 0.0 | 536.0 | 55.83 | 106.7878 |
| Community psychiatric nurse | 0.0 | 750.0 | 20.31 | 85.3254 | 0.0 | 225.0 | 7.81 | 29.7606 |
| Dentist | 0.0 | 178.0 | 9.27 | 30.2274 | 0.0 | 89.0 | 2.78 | 15.5666 |
| Dietician | 0.0 | 76.0 | 7.92 | 19.0333 | 0.0 | 114.0 | 8.31 | 21.4983 |
| GP | 0.0 | 225.0 | 44.06 | 51.4030 | 0.0 | 225.0 | 48.28 | 51.9252 |
| Mental health team worker | 0.0 | 42.0 | 1.75 | 8.4368 | 0.0 | 42.0 | 1.31 | 7.3461 |
| Optician | 0.0 | 42.0 | 5.47 | 10.6622 | 0.0 | 42.0 | 2.84 | 7.8396 |
| Occupational therapist | – | 44.0 | 0.46 | 4.4907 | 0.0 | 44.0 | 1.83 | 8.8385 |
| Physiotherapist | 0.0 | 76.0 | 0.79 | 7.7567 | 0.0 | 38.0 | 0.79 | 5.4559 |
| Practice nurse | 0.0 | 56.0 | 1.75 | 9.7947 | 0.0 | 56.0 | 1.17 | 8.0402 |
| Psychiatrist | 0.0 | 556.0 | 11.58 | 65.8692 | 0.0 | 139.0 | 13.03 | 40.7285 |
| Social worker | 0.0 | 158.0 | 6.58 | 24.7619 | 0.0 | 237.0 | 5.76 | 28.6444 |
| Chiropodist | 0.0 | 62.0 | 17.76 | 20.4866 | 0.0 | 93.0 | 16.15 | 27.7196 |
| A&E visits | 0.0 | 428.0 | 14.49 | 59.3619 | 0.0 | 3103.0 | 73.56 | 376.5659 |
| Inpatient nights | 0.0 | 4378.0 | 99.50 | 605.6652 | 0.0 | 13,134.0 | 165.83 | 1367.3781 |
| Outpatient | 0.0 | 372.0 | 10.33 | 46.4547 | 0.0 | 124.0 | 7.75 | 30.1732 |
| Total | 0.0 | 4901.0 | 309.44 | 686.7635 | 0.0 | 13,735.0 | 413.05 | 1465.1972 |
| Community services | Sum of other visits | |
|---|---|---|
| Clinic | Home | |
| Visit 1 | ||
| Anticoagulation service | 0 | 3 |
| Audiology | 2 | 1 |
| Cardiology | 0 | 1 |
| Care home liaison | 0 | 4 |
| COPD nurse | 0 | 1 |
| Diabetes nurse | 0 | 1 |
| DWP | 0 | 1 |
| Eye clinic | 1 | 0 |
| Falls team | 0 | 1 |
| Geriatric consultant | 0 | 1 |
| Health-care assistant | 0 | 1 |
| Memory clinic | 6 | 4 |
| Pharmacist | 0 | 1 |
| Phlebotomist | 0 | 10 |
| Solicitor | 0 | 1 |
| Speech and language | 1 | 16 |
| Urologist | 1 | 0 |
| Warfarin nurse | 0 | 1 |
| Equipment/wheelchair services | 0 | 5 |
| Visit 2 | ||
| Anticoagulation service | 0 | 2 |
| Audiology | 0 | 1 |
| Care home liaison | 0 | 7 |
| Community liaison | 0 | 1 |
| Community matron | 0 | 4 |
| Consultant geriatrician | 0 | 1 |
| Dermatologist | 1 | 0 |
| Diabetes nurse | 0 | 3 |
| Falls team | 0 | 8 |
| Health-care assistant | 0 | 2 |
| Memory clinic | 0 | 3 |
| Parkinson’s nurse | 0 | 1 |
| Pension advisor | 0 | 1 |
| Pharmacist | 0 | 5 |
| Phlebotomist | 0 | 12 |
| Solicitor | 0 | 2 |
| Speech and language | 2 | 7 |
| Stoma nurse | 0 | 1 |
| Warfarin nurse | 0 | 2 |
| Equipment/wheelchair services | 0 | 1 |
| Item | Unit | Cost (£) | Source/notes |
|---|---|---|---|
| District/community nurse | Per hour | 67 | Community nurse home visit, including qualification and travel costs (Unit Costs of Health and Social Care 2015,80 p. 169) |
| GP | Per visit | 45 | Per contact lasting on average 11.7 minutes. Includes qualification costs and direct care staff costs (Unit Costs of Health and Social Care 2015,80 p. 177) |
| Community mental health team worker | Per hour | 42 | (CMHT) for older people with mental health problems (Unit Costs of Health and Social Care 2015,80 p. 199) |
| Community psychiatric nurse | Per hour | 75 | Nurse, mental health, per hour of face-to-face contact (Unit Costs of Health and Social Care 2015,80 p. 170) |
| Practice nurse | Per hour | 56 | Assumed home visit is the same as clinic visit. Per hour of face-to-face contact, including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 174) |
| Psychiatrist | Per hour | 139 | Consultant: psychiatric cost per hour of face-to-face patient contact, including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 237) |
| NHS physiotherapist | Per hour | 38 | Per physiotherapist hour, including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 217) |
| NHS occupational therapist | Per hour | 44 | NHS community occupational therapist, including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 191) |
| NHS chiropodist/podiatrist | Per hour | 31 | Assumed home visit and clinic visit the same. Per hour, community chiropodist (Unit Costs of Health and Social Care 2013,150 p. 178), inflated to 2015 prices using the Bank of England calculator |
| NHS dietician | Per hour | 38 | Per hour, hospital-based dietician including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 220) |
| NHS optician | Per contact | 21 | NHS sight test fee for Optometrists and Ophthalmic Medical Practitioners (URL: www.fodo.com/resource-categories/nhs-sight-test-fees; accessed 8 March 2018) |
| NHS dentist | Per hour | 89 | NHS dentist-performer only, including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 180) |
| Social worker | Per hour | 79 | Per hour of face-to-face contact (adult services), including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 188) |
| Care manager | Per hour | 39 | Per hour, including qualification costs (Unit Costs of Health and Social Care 2015,80 p. 193) |
| Alternative therapist | Per hour | 17 | Taken as mid-point of NHS pay band 5, including National Insurance and pension |
| A&E | Per visit | 107 | NHS Reference Costs,81 T01NA, type 1 non-admitted, VB09Z, emergency medicine, category 1 investigation with category 1–2 treatment |
| Inpatient services | Per night | 398 | NHS Reference Costs,81 nonEI, HE11H, hip fracture without interventions, with a CC score of 0–3 |
| Outpatient services | Per visit | 124 | NHS Reference Costs,81 WF01A non-admitted face-to-face attendance, follow-up, general surgery 100 |
| Type of medication | n |
|---|---|
| Anaesthesia | |
| General | 1 |
| Local | 4 |
| Cardiovascular system | |
| Anticoagulants and protamine | 22 |
| Antiplatelet drugs | 83 |
| Beta-adrenoceptor blocking drugs | 42 |
| Diuretics | 55 |
| Hypertension and heart failure | 42 |
| Lipid-regulating drugs | 78 |
| Nitrates, calcium channel blockers and other antianginal drugs | 42 |
| Positive inotropic drugs | 13 |
| Central nervous system | |
| Analgesics | 171 |
| Antidepressant drugs | 147 |
| Antiepileptics | 30 |
| Drugs for dementia | 113 |
| Drugs used in nausea and vertigo | 9 |
| Drugs used in Parkinsonism/related disorders | 8 |
| Drugs used in psychoses and related disorders | 92 |
| Drugs used in substance dependence | 2 |
| Hypnotics and anxiolytics | 150 |
| Ear, nose and oropharynx | |
| Drugs acting on the nose | 1 |
| Drugs acting on the oropharynx | 1 |
| Other appliances | 1 |
| Endocrine system | |
| Corticosteroids (endocrine) | 12 |
| Drugs affecting bone metabolism | 25 |
| Drugs used in diabetes | 34 |
| Sex hormones | 3 |
| Thyroid and antithyroid drugs | 31 |
| Eye | |
| Anti-infective eye preparations | 8 |
| Miscellaneous ophthalmic preparations | 6 |
| Treatment of glaucoma | 15 |
| Gastrointestinal system | |
| Acute diarrhoea | 4 |
| Antisecretory drugs and mucosal protectants | 96 |
| Antispasmodics and other drugs altering gut motility | 5 |
| Chronic bowel disorders | 2 |
| Dyspepsia and gastro-oesophageal reflux disease | 6 |
| Laxatives | 184 |
| Infections | |
| Antibacterial drugs | 23 |
| Antifungal drugs | 2 |
| Antiprotozoal drugs | 4 |
| Malignant disease and immunosuppression | |
| Sex hormones and antagonists in malignant disease | 1 |
| Musculoskeletal and joint diseases | |
| Drugs used in neuromuscular disorders | 5 |
| Drugs used in rheumatic diseases and gout | 11 |
| Soft-tissue disorders and topical pain relief | 3 |
| Nutrition and blood | |
| Anaemias and other blood disorders | 62 |
| Base/dil susp agents/stabilisers | 3 |
| Minerals | 7 |
| Oral nutrition | 42 |
| Vitamins | 97 |
| Obstetrics, gynaecology and urinary tract disorders | |
| Drugs for genito urinary disorders | 16 |
| Respiratory system | |
| Antihistamines, hyposensitisation and allergic emergencies | 15 |
| Bronchodilators | 28 |
| Corticosteroids (respiratory) | 11 |
| Cough preparations | 1 |
| Mucolytics | 2 |
| Skin | |
| Anti-infective skin preparations | 2 |
| Emollient and barrier preparations | 7 |
| Emollients | 4 |
| Preparations for eczema and psoriasis | 2 |
| Skin cleansers, antiseptics and desloughing agents | 6 |
| Skin fillers and protectives | 6 |
| Sunscreens and camouflagers | 1 |
| Topical corticosteroids | 4 |
| No medication | |
| No medication | 7 |
| Sterile water | |
| Waters | 1 |
| Grand total | 1911 |
Appendix 3 Outcome measures
List of abbreviations
- ADAS-Cog
- Alzheimer’s Disease Assessment Scale – Cognitive subscale
- ASCOT
- Adult Social Care Outcomes Toolkit
- CPA
- care programme approach
- CQC
- Care Quality Commission
- DCM
- dementia care mapping
- DEEP
- Dementia Engagement and Empowerment Project
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- FREDA
- Fairness, Respect, Equality, Dignity and Autonomy
- GP
- general practitioner
- ICC
- intraclass correlation coefficient
- IDEA
- Identity, Dignity, Equality and Autonomy
- ISRCTN
- International Standard Randomised Controlled Trial Number
- ME
- mood and engagement
- MMSE
- Mini Mental State Examination
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NWORTH
- North Wales Organisation for Randomised Trials in Health
- PANEL
- participation, accountability, non-discriminatory, empowerment and legality
- PPI
- patient and public involvement
- QOL-AD
- Quality of Life in Alzheimer’s Disease
- RCT
- randomised controlled trial
- SD
- standard deviation
- TSC
- Trial Steering Committee
- WEMWBS
- Warwick–Edinburgh Mental Well-Being Scale
- ZBI
- Zarit Burden Interview
