Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/54/75. The contractual start date was in January 2015. The final report began editorial review in May 2017 and was accepted for publication in March 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Aloysius Niroshan Siriwardena reports grants from the National Institute for Health Research, the Medical Research Council, the Falck Foundation, the British Heart Foundation, the Health Foundation and the Wellcome Trust outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by O’Cathain et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
The ambulance service in England
Eleven regional ambulance services provide emergency and urgent care to the population of England. In 2015/16 these services responded to almost 11 million calls at a cost of £1.78B. 1 Ten of these services respond to > 99% of calls. These services are working under increasing pressure, with demand rising at a faster rate than growth in resources. 1
Most calls are made by members of the public calling for themselves or on behalf of others, using the emergency number 999. Some calls are referred directly to the emergency ambulance service from the urgent helpline NHS 111 and some are made by health-care professionals on behalf of patients.
The types of responses made to calls
When patients call 999 for an ambulance, some calls end in telephone advice, some patients are sent an ambulance and are discharged at scene, some are conveyed to an emergency department, and some are conveyed to alternative services such as minor injury units and hospices. ‘Non-conveyance’ is a term used to describe a 999 call to the ambulance service that results in a decision not to transport the patient to a health-care facility. It includes calls ending in telephone advice only without the dispatch of an ambulance, and calls ending in discharge at scene, whereby an ambulance 999 call results in a face-to-face assessment of a patient by an ambulance crew at the scene without onward transport to a health-care facility. A more specific definition of non-conveyance is ‘non-conveyance to an emergency department’. By this definition, calls ending in transport to a health-care facility other than an emergency department are also viewed as non-conveyance. At the start of this study the focus was on the three types of non-conveyance to an emergency department: telephone advice only, discharge at scene and transport to an alternative to an emergency department. Ambulance services in England have developed terminology for different ambulance response types. This terminology is discussed in more detail in Chapter 2, Terminology and definitions.
Measuring performance of the ambulance service
The performance of ambulance services is measured by a set of Ambulance Quality Indicators (AQIs), which are published monthly by NHS England. 2 A key performance indicator is the proportion of life-threatening and serious calls responded to within a particular timeframe, referred to as ‘response-time targets’. Targets are set and ambulance services can be penalised financially for not meeting these targets. There are also four AQIs on different types of non-conveyance to emergency departments:
-
of the calls that receive a telephone or face-to-face response, the proportion resolved by telephone advice (‘Hear and Treat’)
-
of the calls that receive a face-to-face response from the ambulance service, the proportion managed without the need for transport to Type 1 and Type 2 accident and emergency (A&E) services
-
of the patients making emergency calls that are closed with telephone advice, the proportion with recontact via 999 within 24 hours
-
of the patients treated and discharged on scene, the proportion with recontact via 999 within 24 hours.
Benefits of non-conveyance
There are three potential benefits of non-conveyance. First, non-conveyance may offer the most appropriate response to patients’ needs. Second, emergency departments are under increasing pressure. If ambulance services can deal with patients safely and appropriately without conveyance to emergency departments then this can reduce pressure on this key service within the emergency and urgent care system. Non-conveyance to emergency departments may also affect emergency admissions; research has shown that potentially avoidable admission rates were lower in areas with higher rates of ambulance non-conveyance. 3 Third, non-conveyance can benefit the performance and sustainability of ambulance services. With ambulance services dealing with increasing demand without a similar increase in resources,1 ending low-acuity calls with telephone advice may reduce demand for ambulance journeys; discharging patients at scene may reduce the wastage of ambulance crew time if there is a need to queue outside emergency departments. Saving time and resources in this way may allow ambulance services to respond more quickly to life-threatening situations. NHS England proposed a shift within the NHS to offer care closer to patients’ homes. 4 The ambulance service in England is fulfilling this remit by dealing with a large proportion of patients by not conveying them to an emergency department unless necessary.
Variation in non-conveyance rates in England
Rates of non-conveyance have increased over time in England. Between January 2013 and December 2016 published AQIs showed that, across England, rates of calls ending in telephone advice almost doubled from 6% to 11%, and rates of patients sent an ambulance and not conveyed to an emergency department increased slightly from 35% to 38%. Non-conveyance rates have always varied between ambulance services. For the 10 large ambulance services at the end of 2016, the rate of calls ending in telephone advice varied between 5% and 17%, the rate of calls sent an ambulance but not conveyed to an emergency department varied between 23% and 51%, and overall non-conveyance rates varied between 40% and 68%. The total non-conveyance rate is not an AQI and is reported here as a crude addition to the two non-conveyance rates of each ambulance service to show that the variation between ambulance services is not explained simply by ambulance services undertaking different types of non-conveyance.
Patients’ views of non-conveyance
Patients’ views of non-conveyance in national surveys in England have generally been positive. In January 2017, 94% of patients discharged at scene recommended the service to family or friends; however, caution is needed around generalisability because the number of responses compared with numbers eligible to respond was small (311 out of a total of 213,792). 5 In 2013/14, patients who did not receive a face-to-face visit from the ambulance service were asked if they agreed with the advice given. A total of 72% said that they agreed with the advice ‘completely’, 15% agreed ‘to some extent’ and 13% said that they did not agree with the advice. 6 This was a much more reliable source of patients’ views, with a response rate of 55% from 2900 patients whose calls had ended with a call-handler or a clinician offering advice over the telephone.
Researchers have also measured patients’ views of non-conveyance using surveys, showing that 90% who received a telephone intervention were satisfied,7 and 75% of patients transferred from the ambulance service to a national telephone helpline NHS Direct were satisfied, although this was lower than for patients who were not transferred. 8 A survey of people attending emergency departments by ambulance in the USA identified that patients were willing to be transported to alternative places. 9
Patients’ views of non-conveyance have also been explored using qualitative research. Patients have been positive about not being conveyed to an emergency department. 10 A sample of ambulance service users that included patients who were offered telephone advice and patients who were discharged at scene identified positive experiences of feeling reassured by the service offered. 11 Focus groups with users of the ambulance service, exploring decision-making and safety, identified perceptions of the importance of including patients and their families in decision-making about non-conveyance as key, because they may have strong views about not wanting to go to hospital that differ from clinical views. Patients and their families also expressed concerns that the risks of telephone triage should be addressed by training staff in communication, and that a lack of awareness of the range of options used by ambulance services might lead to patients expecting conveyance to emergency departments. 12 Within this research there was a sense that patients and their families were happy to have non-conveyance as an option and even preferred it in some situations. This preference for non-conveyance was also found in a qualitative study of patients who called the ambulance service for primary care conditions because they wanted to be treated at home; this was in contrast to calling their general practitioner (GP), who they felt would be likely to send them to hospital. 13 A qualitative interview study of patients in Australia who were not transported to hospital identified high levels of satisfaction and found that some patients chose to stay at home against the clinical advice of paramedics. Reasons for this included that they had only wanted advice when they called the ambulance service, their symptoms had resolved, they did not want to wait at an emergency department, or did not want a fuss made. 14
Although there is patient support generally for non-conveyance in the research literature, it is worth noting that not all patients’ views of non-conveyance are positive. Some patients call the ambulance service for transport to an emergency department and may not want telephone advice only or to be discharged at scene.
Paramedics’ views of non-conveyance
The decision to discharge a patient at scene is complex and can be affected by a range of factors, including the high demand for ambulance services, priorities around performance management, access to care options as an alternative to the emergency department, risk tolerance when the least risky option is conveyance to an emergency department, the level of training paramedics receive, and the quality of communication and feedback for paramedics who often make non-conveyance decisions in isolation. 12 Paramedics work with the fear of litigation and can perceive a lack of support from management for their non-conveyance decisions if adverse events occur. 15 Negotiating the balance between patient safety and patient choice, together with paramedics’ own fears of litigation, can result in conveyance to an emergency department as a precaution. 16 In the past, crew members have not always completed documentation around non-conveyance because they did not perceive it to be important. 17
International perspective
Non-conveyance is undertaken in many countries around the world. 18 In the past, non-conveyance rates have been identified as varying between 23% and 33% internationally. 19 However, rates can be lower; for example, only 11.5% of incidents in 2012/13 in a region in Australia did not result in transport to hospital. 14 A recent systematic review of non-conveyance for falls in older people identified 12 studies showing that the rate varied between 11% and 56% in different studies. 20 Telephone advice by a clinician can be offered in different countries and is sometimes called ‘secondary telephone triage’. For example, 1 in 10 calls to the ambulance service in a region in Australia was dealt with by telephone. 21
Non-conveyance for specific health problems
Some research on non-conveyance has focused on the specific reasons for calling the ambulance service. Researchers have tended to study falls because this is the most common reason for calls to an ambulance service that end in non-conveyance. 20 There are interventions to facilitate discharge at scene by referring patients directly to falls services: a recent randomised controlled trial of paramedics using computerised clinical decision support when attending older people who had fallen showed an increase in referral to a falls service but no difference in non-conveyance rates. 22 In recent years researchers have started to study other health conditions or reasons for calling the ambulance service that result in non-conveyance. A study of hypoglycaemic emergencies showed that most patients stayed at home after attendance by an ambulance and a small number suffered a repeat episode within a short time period. 23 In contrast, three-quarters of calls for people with suspected seizures – a large number of which were likely to be epileptic seizures – ended in transport to hospital. 24
Respiratory problems have been identified as a common reason for calling an ambulance service in the USA, where 12% of encounters have been categorised as ‘respiratory distress’. 25 Although research studies have described the epidemiology and outcomes of ambulance service users with respiratory distress,25–28 they have focused on patients who are transported to emergency departments rather than those not conveyed. We could find only one study of non-conveyance of patients with breathing difficulties that focused on the impact of advanced paramedics on this condition. 29
Determinants of non-conveyance
No research explaining why different ambulance services have different rates of non-conveyance was found. However, there is evidence about the determinants of some types of non-conveyance internationally. 19,30 The evidence base tends to focus on patients discharged at scene19,30 and determinants can differ between countries. 19 An epidemiological study of non-conveyance in one ambulance service in the UK in 2000 at a time when 17% of patients were not conveyed found that 34% were falls, mainly in elderly people. A well-researched determinant of discharge at scene is the skill level of the attending ambulance crew. A systematic review and meta-analysis identified that paramedics with extended skills had higher non-conveyance rates than conventional paramedics, although concerns were expressed about whether all potential confounders were adjusted for within analyses of individual studies. 31
Safety and appropriateness of non-conveyance
Although some interventions to increase non-conveyance rates have been found to be effective without compromising safety,32 evidence reviews have identified some concerns about the safety of discharge at scene. 19,20 Event rates have been found to vary by staff skill-mix. For example, patients who had fallen and who were attended by advanced paramedics had lower emergency department attendance rates and hospital admission rates than those attended by paramedics. 20 A meta-analysis of the appropriateness of discharge at scene by staff skill-mix for all types of calls was equivocal. 31
A recent review of patient safety in the ambulance service is an excellent source of evidence for the safety of non-conveyance. 33 The authors concluded that the evidence base on the safety of telephone advice, discharge at scene and use of alternative pathways to emergency departments is mixed and that further research is needed. In contrast, a systematic review of telephone advice by ambulance services concluded that it was safe but that there is a need to understand its effect on demand for ambulance services. 34
The types of events measured to assess the safety and appropriateness of non-conveyance include additional calls to the ambulance service, emergency department attendance, primary care contacts, hospital admission and mortality. 20,35 There appears to be no consensus on the time period of measurement of subsequent events, which has varied considerably in different studies, for example, 48 hours, 7 days, 14 days or 28 days. 19,20,35,36
An important contextual issue when considering the safety and appropriateness of non-conveyance is that decisions around non-conveyance are negotiated between paramedics, patients and their families. 37 Patients may choose to stay at home against clinical advice and, therefore, subsequent events may not be the responsibility of the ambulance service. 14 Indeed, a national audit of recontacts with the ambulance service within 24 hours revealed that over half of patients were documented as having refused to travel. 38
Non-conveyance in the wider health system
In England, Clinical Commissioning Groups (CCGs) are required to ensure that high-quality services are available for the health needs of the geographical populations they serve. CCGs commission a range of health services for their populations. Therefore, each CCG geographical area can have different configurations of health and social care services. Each of the 10 large regional ambulance services in England serves the populations of between 12 and 33 CCGs. Each ambulance service is commissioned by a lead commissioner on behalf of all the CCGs within the ambulance service region. 39 Non-conveyance rates may be influenced by these commissioners in two ways. First, they may take different approaches to commissioning non-conveyance. Second, they may take different approaches to configuring the range of health and social services within their health system that can offer alternatives to an emergency department when the ambulance service would like to non-convey.
Research gaps
Research is needed to understand the determinants of non-conveyance rates and of variation in non-conveyance rates between ambulance services. Non-conveyance rates vary so much between ambulance services in England that a study is necessary to identify the reasons for this. Because of the way in which services are commissioned and provided in England, and the geographical variation in provision within regions served by ambulance services, a consideration of variation within ambulance services is also important. The emphasis on discharge at scene in the evidence base suggests that there is a need to consider the provision of telephone advice only as well as discharge at scene. Because of the mixed conclusions from the evidence base on safety and appropriateness, there is a need for further research on this aspect of non-conveyance. Finally, the emphasis on falls in the evidence base means that there is also a need to consider non-conveyance for other health conditions or reasons for calling an ambulance service. Respiratory problems are a good focus because they make up a reasonable proportion of calls to the ambulance service and there is no evidence about the non-conveyance of patients who call an ambulance service for this reason.
Chapter 2 Aims and methods
Aims and objectives
The aim of the study was to explore reasons for variation in non-conveyance rates between and within ambulance services.
The objectives were to:
-
explore the perceptions of ambulance service managers, paramedics and commissioners of factors affecting variation in different types of non-conveyance
-
identify the determinants of variation between ambulance services for different types of non-conveyance
-
explore the variation in different types of non-conveyance within ambulance services
-
explore variation in the provision of telephone advice only in detail within three ambulance services
-
identify the determinants of variation between services in rates of 24-hour recontact with the ambulance service after non-conveyance
-
assess the safety and appropriateness of non-conveyance in one ambulance service
-
identify the determinants of variation when the reason for calling is ‘breathing problems’.
Setting
The research was located in 10 of the 11 regional ambulance services in England serving > 99% of the population of England. The ambulance service for the Isle of Wight was excluded because of its relatively small size.
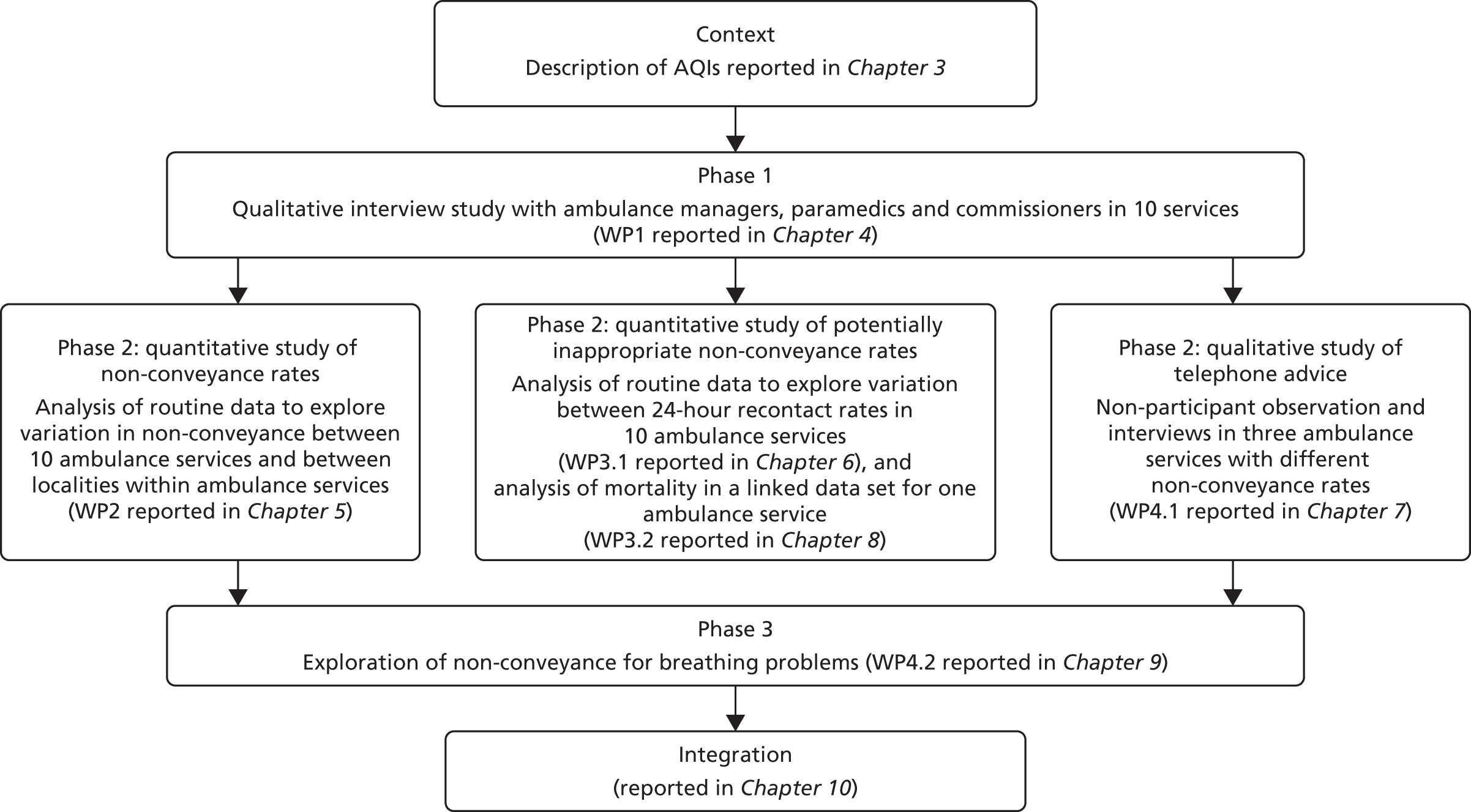
Design
The design was a phased sequential mixed methods study with five work packages (WPs) (Figure 1). In preparation for the study we described the variation in non-conveyance AQIs between ambulance services over time. In Phase 1 we undertook a qualitative interview study of managers, paramedics and commissioners from each ambulance service (WP1) in the research proposal. In Phase 2 we analysed 1 month of routine data from each ambulance service (WP2 and WP3.1), analysed a linked data set to explore safety and appropriateness (WP3.2), and undertook a qualitative study using non-participant observation and staff interviews in three ambulance services with different published rates of telephone advice only (WP4.1). In Phase 3 we conducted a substudy of non-conveyance for patients calling the ambulance service with ‘breathing problems’ (WP4.2). The detailed methods of each component are described in later chapters.
FIGURE 1.
Mixed methods study design.
Conceptual framework
It is important to publish variation in health care, to identify causes of variation and to encourage actions to deal with it. 40 Appleby’s framework of factors affecting variation in health care shaped the data collection and analysis within our study. 40 It helped us to consider the wide range of factors that might affect variation in non-conveyance rates between ambulance services so we could explore them in WP1 and test them in WP2. Factors within Appleby’s framework address the demand (e.g. population morbidity, commissioning practices) and supply (e.g. service configuration, clinical decision-making) of health care. From our literature review (see Chapter 1, Determinants of non-conveyance), we expected demand factors, such as patient age and reason for calling, and supply factors, such as the skill-mix of attending crew, to explain some variation in rates of discharge at scene. We expected ambulance services with a higher proportion of older patients calling about falls to have higher non-conveyance rates because older people and falls are more likely to be non-conveyed. We expected ambulance services with larger proportions of advanced paramedics in their workforce to have higher non-conveyance rates because these paramedics would have more training to make the clinical decisions required to discharge patients at scene. From our interviews with ambulance staff in WP1 we expected to identify a list of factors affecting non-conveyance rates at a patient, crew and organisational level, and an understanding of how these factors affected non-conveyance rates, in order to test them in WP2 and WP3.
A further conceptual framework was used for the study, namely ‘unwarranted variation in health care’,41,42 whereby some variation may be warranted owing to patient need or preference and some may be unwarranted. Unwarranted variation can be related to variation in evidence-based practice, variation in preferences held by key stakeholders, and variation in the supply of types of resource. For example, variation in non-conveyance rates between ambulance services caused by variation in the supply of advanced paramedics would be considered unwarranted. This concept shaped our analyses of variation in non-conveyance rates between ambulance services when we adjusted for differences in case mix between ambulance services (warranted variation) before testing whether or not differences in the workforce configuration (unwarranted variation) explained variation between ambulance services.
Finally, we distinguished variation that was likely to be modifiable by ambulance services from variation that was likely to be outside the control of ambulance services so that we could consider the implications of our findings for ambulance services. For example, workforce configuration is largely modifiable by ambulance services (although some aspects such as national training schemes may not be modifiable by them), whereas the availability of services in the wider emergency and urgent care system is outside the control of ambulance services.
Integration of work packages
Attention to integration is important within mixed methods studies so that the whole is more than the sum of the parts. 43 Integration occurred in a number of ways:
-
It was built in to the sequential design of the study. The main role of the qualitative interviews in WP1 was to identify potential determinants of variation in non-conveyance and how these affected non-conveyance rates. We were then able to test some of these in the quantitative analyses in WP2 and WP3 for which data were available. We also analysed the qualitative interviews in WP1 by ambulance service – treating each ambulance service as a ‘case’ – to identify organisational characteristics of ambulance services for testing as factors in WP2 and WP3.
-
We triangulated findings from the qualitative and quantitative WPs. After analysis of all WPs, integration of findings from all WPs occurred using an adapted triangulation protocol. 43,44 The qualitative interviews in WP1 helped to draw attention to potential factors affecting non-conveyance that were not tested quantitatively, and helped to identify how factors affected non-conveyance or how factors tested in the quantitative study might not capture the complexity of an issue. Thus, the qualitative interviews often facilitated interpretation of some of the quantitative findings. This integration is reported in Chapter 10. The report discussion in Chapter 11 is based on insights from Chapter 10. This integration also resulted in the reporting of some findings from the WP1 qualitative study alongside findings from the WP2 and WP3 quantitative WPs in Chapters 5–7 because they related to the content of these chapters.
-
We brought together all the potential factors affecting non-conveyance within a conceptual framework constructed from all WPs of the study. 40 This is reported in Chapter 10.
-
We undertook a multiple case study analysis in Chapter 10 by summarising findings about each ambulance service in a matrix and considering patterns across cases with different rates of non-conveyance. 45
Presentation of findings
Mixed methods research can be reported in different ways. 46 One approach is to report each WP in separate chapters and then present an integration chapter towards the end of the report. Another approach is to identify themes (usually related to research questions) and present each theme in a chapter, integrating qualitative and quantitative data or findings within each chapter. The first approach was undertaken here because each WP addressed different research questions. However, a small number of themes from the qualitative research in WP1 were highly relevant to findings in the quantitative WP2, WP3 and WP4.2. Because of this, small amounts of qualitative research are reported in largely quantitative report chapters (see Chapter 5, Results, Chapter 6, Results, Chapter 7, Findings, and Chapter 9, Findings). The presentation of findings is summarised in Figure 1.
Patient and public involvement
A patient and public involvement (PPI) representative (MM) was a co-applicant and she attended monthly project management meetings. Enid Hirst, who is a long-standing member of the Sheffield Emergency Care Forum, joined the Project Advisory Group which met four times over the project. A PPI group was established for the project. PPI members from the field of emergency and urgent care from three ambulance services met together three times a year to discuss planned data collection, emerging findings, interpretation and dissemination. The impact of PPI on the research is summarised in Chapter 11, Discussion.
Ethics and approvals
We obtained approval from the National Research Ethics Service Committee North West – Greater Manchester West (REC reference number 14/NW/1388).
We sought guidance from the Confidentiality Advisory Group of the Health Research Authority for the reuse of the linked data set created as part of the Pre-Hospital Outcomes for Evidence Based Evaluation (PhOEBE) study. As the subset of data used in the variation in ambulance non-conveyance (VAN) project was pseudonymised and there were no other identifiable data being used within the study, we were advised that an application to the Confidentiality Advisory Group was not necessary. We obtained permission to reuse the linked data set created as part of the PhOEBE study through NHS Digital’s Data Access Request Service.
Project Advisory Group
The Project Advisory Group was chaired by Professor Tom Quinn, a leading researcher in pre-hospital care. Members included Liz Harris (a paramedic), Mark Docherty (a director at an ambulance service) and Enid Hirst (a PPI representative).
Terminology and definitions
International differences in terminology
Terminology relevant to this topic differs by country. Ambulance service provision (the term used in this report) is also known as Emergency Medical Services or pre-hospital care internationally. In the UK, ambulance services are known as Ambulance NHS Trusts. Non-conveyance (the term used in this report) may be called non-transport in other countries. Telephone advice (the term used in this report) can be known as secondary telephone triage whereby patients are triaged over the telephone by a clinician after their initial triage by a call-handler. Different terms can be used to describe staff working in ambulance services. We use the term ‘call-handler’ for staff taking initial 999 calls, ‘clinicians’ for staff offering telephone advice in the clinical hub of an ambulance service, and ‘crew members’ or ‘paramedics’ for staff making decisions to discharge patients at scene or convey them to a health-care facility.
Variation in definitions used by ambulance services, national quality indicators and this study
‘Hear and Treat’ is a term used in England to describe a key type of non-conveyance, whereby a call-handler triages patients to receive advice from a clinician working within the ambulance service dispatch centre, sometimes called a clinical hub. The clinician may give information or advice to self-manage or make a formal referral to an alternative service (this last option can be called ‘Hear, Treat and Refer’.) Clinicians may also return calls for the dispatch of an ambulance if they decide that this is necessary, resulting in conveyance to an emergency department or an alternative service. The AQI definition in England for ‘Hear and Treat’ is ‘Of calls that receive a telephone or face-to-face response, proportion resolved by telephone advice (Hear and Treat)’. This includes calls ending in telephone advice by call-handlers as well as clinicians. In this study we use the terms ‘calls ending in telephone advice’ or ‘telephone advice only’, which are similar to the AQI definition. We do not use the term ‘Hear and Treat’ because it has a variety of meanings. ‘Telephone advice only’ calls in our study include whatever ambulance services included in their AQIs. They include calls for which an ambulance was not dispatched either by call-handlers or by clinicians in the clinical hub. Our attempts to identify calls ending in telephone advice by clinicians only, and to consider variation between ambulance services for rates of these calls, were not successful (see Chapter 5, Methods).
‘See and Treat’ is a term used in England to describe a key type of non-conveyance. Ambulance services dispatch an ambulance and attending crew members may discharge patients at scene with treatment, information or advice, or formally refer patients to another service. In such cases, patients are not conveyed anywhere by ambulance. The related AQI is ‘Of calls that receive a face-to-face response from the ambulance service, proportion managed without need for transport to Type 1 and Type 2 A&E’. This includes ‘See, Treat and Convey Elsewhere’ calls, which may end in transport by ambulance to a range of services other than an emergency department. In practice, ambulance services calculate this AQI based on calls for which an ambulance is dispatched but the patient is not transported to a hospital with an emergency department. People who are not conveyed because they have died are included in this indicator because they have not been conveyed to an emergency department by an ambulance. In our study we successfully distinguished patients discharged at scene from those transported to alternative services and label these ‘discharged at scene’ rather than ‘See and Treat’. These ‘discharged at scene’ patients include those who are referred to alternative health and social care services but not transported to them.
In our original research proposal we planned to explore the separate group of patients to whom an ambulance is dispatched and who conveyed to a service other than an emergency department. We were interested in these ‘See, Treat and Convey Elsewhere’ responses because of the potential benefits of not conveying patients to emergency departments, and because conveyance to lower acuity services such as minor injury units and urgent care centres posed a potential risk to patient safety. We were able to identify these calls but also learnt enough about the mix of patients within this type of ‘conveyance but not to an emergency department’ to stop at a descriptive analysis (see Chapter 5, Results).
Finally, some paramedics have advanced skills that allow them to administer a wider range of medications, undertake more advanced assessment and diagnosis, and deliver a wider range of treatments than paramedics. They have a number of labels within England and internationally. In this report we call them ‘advanced paramedics’.
Definitions of terms used are summarised in the Glossary.
Contextual factors potentially affecting non-conveyance over the study period
Over the time of the study, AQIs changed for some ambulance services. We considered this in our analyses and interpretation of findings. In January 2015, the Secretary of State for Health approved a trial of Dispatch on Disposition within the NHS England Ambulance Response Programme, allowing up to three additional minutes for making a dispatch decision with the intention that this could allow ambulance call-handlers more time to assess the clinical situation and determine the type of response needed. This started in two ambulance services in February 2015 and in October 2015 was extended to an additional four ambulance services. This had the potential to affect telephone-advice-only rates as ambulances were not sent early in the call process. This contextual change occurred after the time period covered by our routine data (November 2014).
Changes to the planned research
Most of the study was delivered as planned. However, it was not possible to deliver everything set out in the original proposal. Changes are summarised in Appendix 1.
Anonymity
We aimed to maintain anonymity of interviewees in the qualitative WPs of the study (WP1 and WP4.1). The best way of doing this was to report quantitative as well as qualitative findings for ambulance services labelled A to J. Because some ambulance services have very high or very low rates of non-conveyance, it is possible to identify them from the quantitative findings. To make the identification of services and individuals more difficult, we sometimes exclude labels for ambulance services from figures and quotations within the report, or use ‘H’ or ‘L’ to indicate high or low rates of a factor rather than give the actual rate. We also use different labels for quotations from the qualitative research at different times in the report, sometimes using the service the interviewee worked in and sometimes using the interviewee’s role. Although this looks like inconsistent labelling, it has been undertaken deliberately to preserve anonymity.
Chapter 3 Description of variation in non-conveyance rates measured by Ambulance Quality Indicators
Background
Ambulance Quality Indicators are published monthly for each of the 11 ambulance services in England. 2 Four of these AQIs relate to non-conveyance:
-
Of calls that receive a telephone or face-to-face response, the proportion resolved by telephone advice. This excludes calls that have been passed from NHS 111.
-
Of calls that receive a face-to-face response from the ambulance service, the proportion managed without the need for transport to Type 1 and Type 2 emergency departments. This includes face-to-face responses as a result of NHS 111 calls. Calls not transported to hospitals with Type 1 and 2 emergency departments are included, that is, patients discharged at scene and those conveyed to other health-care facilities (sometimes called ‘See and Convey Elsewhere’).
-
Of emergency calls closed with telephone advice, the proportion recontacting the same ambulance service via 999 within 24 hours. This excludes calls that have been passed from NHS 111.
-
Of patients treated and discharged on scene, the proportion recontacting same ambulance service via 999 within 24 hours. This excludes calls that have been passed from NHS 111.
Variation in non-conveyance Ambulance Quality Indicators over time
According to the published AQI data, the proportion of calls ending in telephone advice doubled to 10% and the proportion of calls sent an ambulance and not conveyed to an emergency department in England steadily increased to 38% between 2011 and 2016 (Figure 2). Twenty-four-hour recontact rates with the ambulance service decreased over time to 6% for calls ending in telephone advice and remained stable at around 5% for calls sent an ambulance but not conveyed to an emergency department.
FIGURE 2.
Variation in AQIs over time. a, Definitions of AQIs change in May 2013.
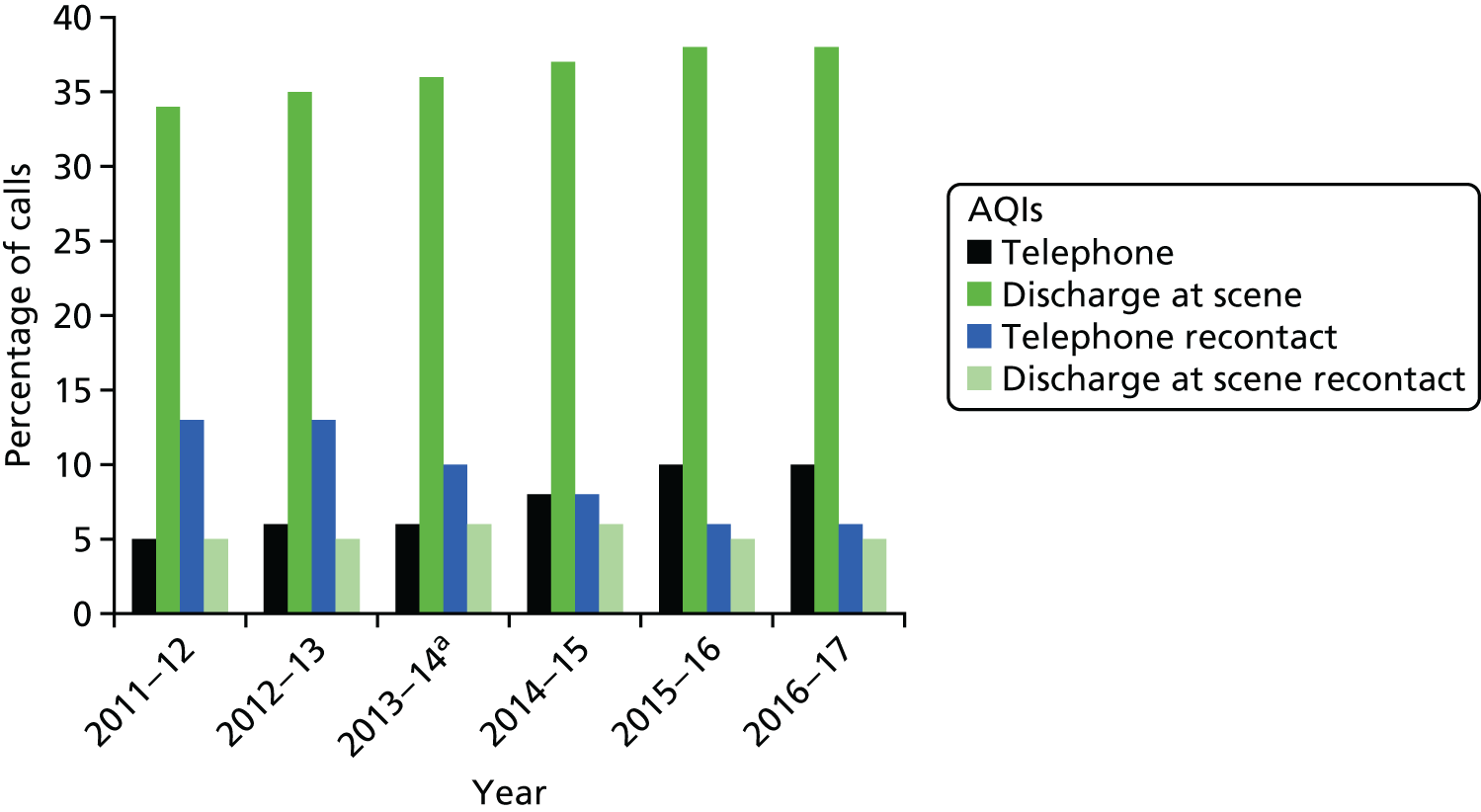
We considered seasonal variation in AQIs for England (not displayed here). The only seasonal effect noticeable in monthly data was a small peak in activity for the proportion of patients not conveyed to an emergency department during December of each year.
Variation in Ambulance Quality Indicators between ambulance services
There are 11 regional ambulance services providing care to the population of England. We decided to exclude one ambulance service offering provision to the small population of the Isle of Wight because of the relatively small number of calls it responds to compared with the other ambulance services (e.g. in September 2016, 1768 calls compared with 19,908 calls in the next largest service).
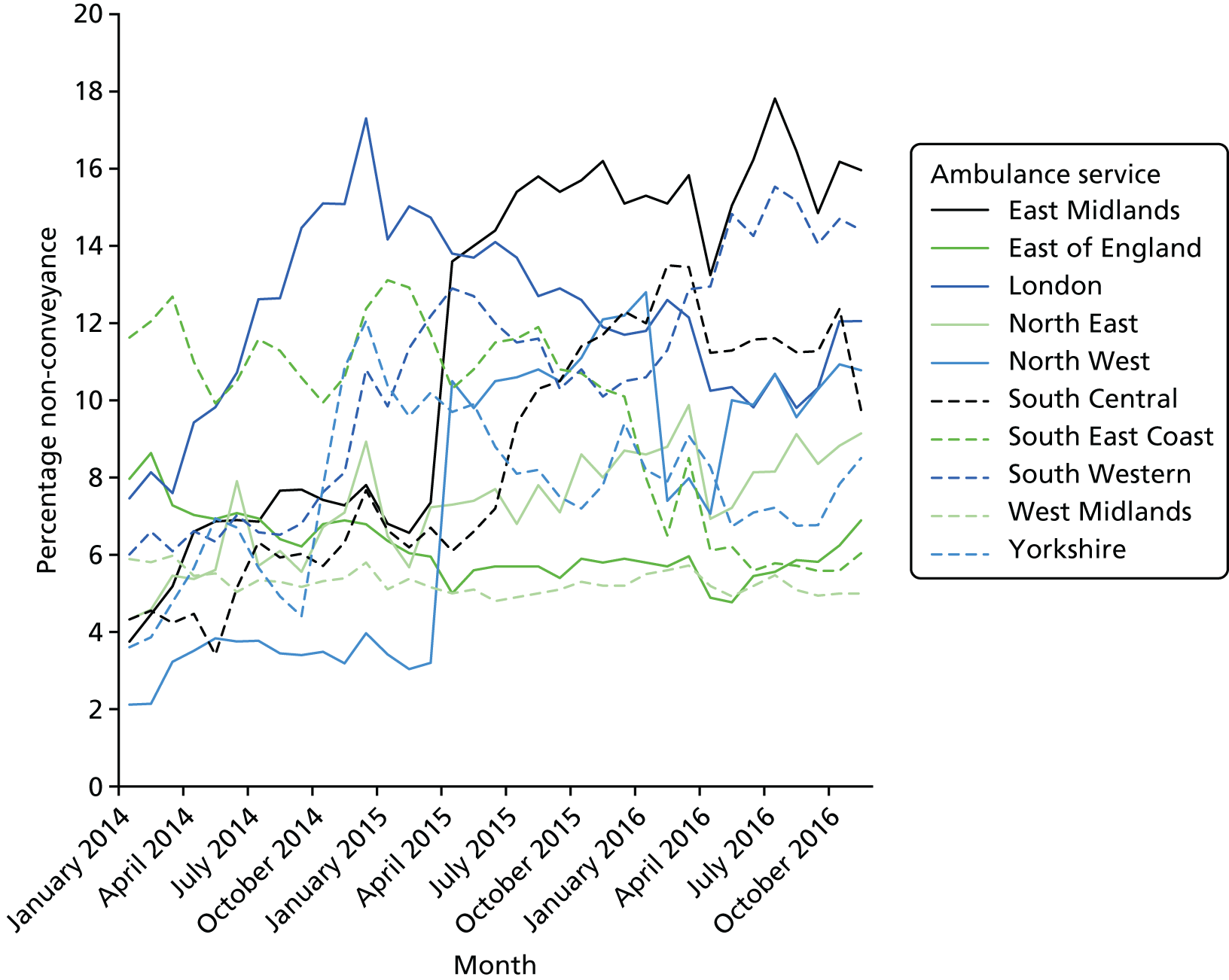
Non-conveyance rates
Variation between ambulance services for the rate of calls ending in telephone advice was threefold in November 2014 when the data for WP2 were obtained (Figure 3). The level of variation between services was similar over time, although the ranking of services was not consistent over time. There were a number of sudden shifts in rates for individual services, in particular for the Yorkshire Ambulance Service, North West Ambulance Service and East Midlands Ambulance Service. We know through another research study that in April 2015 the North West Ambulance Service stopped following national guidance and started to include hoax calls and calls closed by call-handlers (Janette Turner, University of Sheffield, 2017, personal communication). Although our analysis in WP2 was based on data prior to these sudden shifts, this indicates that individual ambulances services can change the way they calculate AQIs, which may not necessarily reflect their rate of non-conveyance.
FIGURE 3.
Variation between 10 large regional ambulance services in England: AQI percentage of calls ending in telephone advice.
Variation between ambulance services for the rate of patients receiving an ambulance but not being conveyed to an emergency department was twofold in November 2014 when the data for WP2 were obtained (Figure 4). These calls were largely made up of patients who were discharged at scene. The variation between services was reasonably consistent over time, with services largely maintaining the same rank over time. One ambulance service had a much higher rate than the others and one had a much lower rate than the others throughout 2014. There were some sudden shifts in the AQIs for some services. This could indicate a change in the way an AQI was calculated by a particular ambulance service or a change in non-conveyance rates. Sudden shifts are likely to be related to changes in calculations, whereas slow shifts over time are more likely to be related to changes in practice. South East Coast Ambulance and North West ambulance services had sudden shifts in rates, suggesting that rates were calculated differently over this time period.
FIGURE 4.
Variation between 10 large regional ambulance services in England: AQI percentage of calls ending in non-conveyance to emergency department (most of these are discharge at scene).
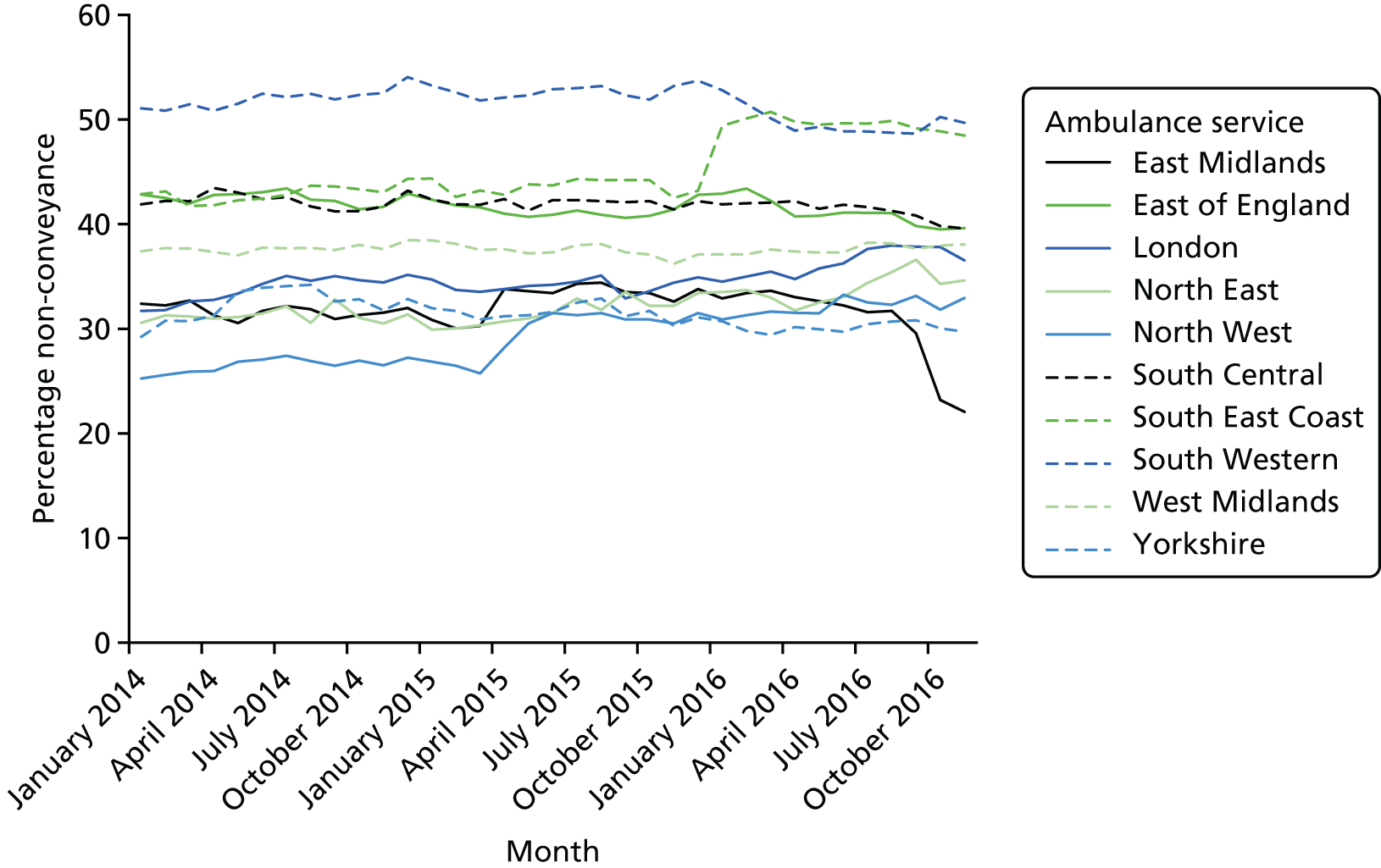
Variation in total non-conveyance was calculated crudely by adding the two AQIs together, namely the percentage of telephone advice calls and the percentage of non-conveyance to an emergency department. A graph similar to those in Figures 3 and 4 was constructed and this is displayed in Appendix 2. It shows that there was a twofold difference in total non-conveyance rates between services over time, with one service having a consistently higher rate than others over time.
Recontact rates
Variation in recontact rates for the two types of non-conveyance are shown in Appendix 3. There was fivefold variation between ambulance services in recontact rates for calls ending in telephone advice. One service had a consistently high recontact rate and another had a consistently low recontact rate. There was twofold variation between ambulance services for recontact rates when an ambulance was dispatched but patients were not conveyed to an emergency department.
Relationship between non-conveyance and recontact rates
It was not the case that services with high non-conveyance rates also had high recontact rates. For example, in November 2014 when the data for WP2 were obtained, the service with the highest AQI rate for telephone advice had a 3% recontact rate compared with an 11% recontact rate for the service with the lowest AQI. The services with the highest and lowest AQI rates of non-conveyance to an emergency department once an ambulance had been sent had the same recontact rate of 6%.
Discussion
Summary of findings
Ambulance Quality Indicators showed considerable variation between ambulance services in both non-conveyance rates and recontact rates within 24 hours of non-conveyance. Sudden shifts in monthly AQIs for specific services raised concerns about the extent to which AQIs represent the actual non-conveyance rate within an ambulance service, particularly for calls ending in telephone advice.
Implications for the empirical study
-
AQI non-conveyance rates changed over time for individual services so we documented when data collection occurred for different WPs of the study and the AQIs for that time period to help interpret the findings:
-
April–December 2015 (WP1 interviews in Chapter 4)
-
November 2014 (WP2 routine data in Chapters 5 and 6)
-
January–June 2013 (WP3.1 linked data in Chapter 7)
-
November 2015–September 2016 (WP4.1 observations and interviews reported in Chapter 8)
-
-
We needed to select a month of ambulance service routine data to analyse for WP2 and WP3.1. At the start of the study in January 2015 we decided to select the latest month available. However, we avoided December 2014 because of small peaks in published AQI non-conveyance rates in December each year. We selected November 2014 instead.
-
One of the 11 services is very small so the study focused on the 10 larger services in England only. Including the small service would introduce uncertainty related to small numbers in the quantitative analyses in WP2 and WP3.1.
-
Sudden changes in monthly rates for individual ambulance services raised concerns about the AQI data, particularly for rates of calls ending in telephone advice.
Chapter 4 A qualitative interview study of stakeholders’ perceptions of non-conveyance (Work Package 1)
Background
The aim of this WP was to explore stakeholders’ perceptions of different types of non-conveyance and potentially inappropriate non-conveyance. These interviews were a source of perceptions of factors affecting non-conveyance rates generally, and perceptions of non-conveyance within each of the ambulance services.
Methods
Design
We undertook a qualitative interview study with three key stakeholder groups: (1) ambulance service managers, (2) paramedics and (3) commissioners. We selected these three groups because ambulance service managers can shape strategic decisions that affect non-conveyance at an organisational level, such as workforce configuration or investment in staff training; paramedics make daily decisions about whether or not to convey patients and can offer views on patient characteristics, workforce practices and organisational factors affecting non-conveyance; and commissioners can encourage ambulance services to undertake non-conveyance by setting targets for non-conveyance rates within contracts and offering additional investment for non-conveyance initiatives. We supplemented these interviews with documentary analysis and sent a request to each ambulance service for information about resources within each organisation.
Data collection and sampling for the interviews
We undertook semistructured interviews with staff and commissioners from all 10 ambulance services. Our intention was to undertake around five interviews per service with staff in the following roles:
-
ambulance service managers – a manager who dealt with non-conveyance and a director-level member of staff to address operational and strategic levels of the organisation
-
paramedics – an advanced paramedic and an entry-grade paramedic with no less than 1 year’s experience post qualification to include different levels of expertise
-
commissioners – the ambulance service lead commissioner
We identified a local collaborator in each service who helped to identify relevant staff for interview. In addition, managers or team leaders sent out recruitment e-mails and the study information to their teams to recruit paramedics. We contacted the relevant CCG for each ambulance service to request an interview with the ambulance service lead commissioner. Each potential interviewee was contacted by e-mail and formally invited to take part in the study. Non-responders to our initial invitation were contacted again within 1 month.
Following receipt of written informed consent, we undertook semistructured interviews mainly by telephone, although a small number of early interviews were undertaken face to face while we tested out the topic guide. One researcher undertook all the interviews. 18 The interviewer was blind to the non-conveyance and recontact rates of the interviewee’s organisation throughout data collection. The same topic guide was used for all participants and was developed based on our research objectives and discussion at our project management group. The topic guide covered perceptions of factors that affected non-conveyance at a local level, and those that were perceived to have an impact on appropriateness of ambulance non-conveyance (see Appendix 4). Interviews were digitally recorded and lasted between 40 and 90 minutes.
Data collection using documents
Prior to starting our research, we identified a number of organisational factors that might explain variation in non-conveyance rates. We were interested in organisational responsibilities and resources such as whether the ambulance service was a provider of the NHS 111 telephone service, and numbers of advanced paramedic and clinical hub staff. While analysing WP1 interviews we identified further organisational issues that we wished to measure for use in our quantitative analysis of variation in WP2 and WP3. We had intended to collect information from services using a pro forma. In practice we identified information from each ambulance service’s annual report where possible (for the period 2014–15),47–56 and where information was missing we sought to identify it from our study contact at each ambulance service. We sought information for 2014 because our quantitative data in WP2 and WP3 were for November 2014 (see Chapter 5). We identified the following characteristics as being of potential interest: population size, geographical size, software used, whether or not the ambulance service was a provider of NHS 111, the number of ‘advanced paramedics’, staff skill-mix, staff turnover, sickness absence rates, income, type of contract with commissioners, system complexity (number of CCGs/NHS acute trusts), and numbers of complaints/serious events.
We had concerns about the consistency of the information collected from documents and our contacts. When the recent National Audit Office (NAO) report was published we chose to use the information within it about individual ambulance services instead,1 with the proviso that the data were for the later period (2015–16) rather than for 2014.
Analysis
We transcribed the digital recordings of interviews verbatim. A researcher checked each transcript for accuracy by listening to the recording and correcting mistakes or filling in gaps where possible. We analysed all interviews using framework analysis. 57 First, we familiarised ourselves with the interviews by reading a sample of transcripts. Second, we developed a thematic framework based on our research questions, the topic guide and reading a sample of transcripts (EK, LBE). The thematic framework consisted of descriptive rather than conceptual themes, including types of non-conveyance, views of rates, calculation of rates, national drivers, local drivers, organisational drivers, collaborative working, workforce issues (skill-mix, culture, working patterns), triage software, patient characteristics, defining and measuring appropriate non-conveyance, commissioning, and respiratory problems. Third, we coded all transcripts to the framework, adding further emergent themes and subthemes throughout the process of coding transcripts. Three researchers undertook the coding (LBE, FF, and NA) using the qualitative software package NVivo (QSR International, Warrington, UK). Lindsey Bishop-Edwards led the process, working closely with Nisar Ahmed and Flavia Saraiva Leao Fernandes to ensure consistency of coding.
One researcher (EK) led the analysis supported by Lindsey Bishop-Edwards. Emma Knowles read extracts of transcripts within a theme within each service. She analysed the overarching theme and documented the variation in perceptions within each ambulance service, discussing findings with Lindsey Bishop-Edwards and Alicia O’Cathain. She repeated this for further themes, considering the connections between themes and refining the thematic framework by collapsing some themes together (e.g. the themes of ‘collaborative working’ and ‘the emergency and urgent care system’ were so interrelated that these were brought together).
The focus of the study was variation between ambulance services. A key difference between our analysis and the analysis for a standard qualitative interview study was the additional process of treating ambulance services as cases within the analysis, which resulted in the need to analyse and present data by ambulance service for use in the quantitative analysis in WP2 and WP3 and in the multiple case study comparison in Chapter 10. 45 A matrix was developed with ambulance services as columns and themes and subthemes as rows. Emma Knowles summarised variation in perceptions about a theme or subtheme on this matrix to allow the team to consider patterns of themes within and across ambulance services. This was undertaken blind to the non-conveyance rates. When this matrix was complete, the AQI non-conveyance rates at the time of the interviews were added to the matrix to consider patterns by non-conveyance rates. We then added data to this matrix from our documentary analysis/the NAO report1 for use in an analysis reported in Chapter 10.
Findings
Sample description
We planned to interview around 50 stakeholders. We formally invited 80 individuals to be interviewed, and undertook 50 interviews with those who consented. The main type of stakeholder who did not agree to interview was paramedics (see Appendix 5). On average we interviewed five members of staff working in, or commissioning, each of the ambulance services, ranging between four and seven participants per service. A complete range of stakeholders was obtained in eight services. Of the remaining two services, we were unable to include one of the two managers and one of two paramedics. The digital recording of one interview (a paramedic) was of such poor quality that we were unable to transcribe it and therefore did not include this in our analysis. In total, 49 of the interviews undertaken were analysed.
Interviewees identified a range of factors that they perceived to affect non-conveyance. These are summarised in Table 1. Factors that we could measure in WP2 (see Chapter 5) are simply listed here. Factors that could not be measured, and instances in which there was evidence of variation in perceptions between ambulance services, are detailed in this chapter.
| Level of factor | Factor | Details of how the factor affects non-conveyance | Tested in WP2 |
|---|---|---|---|
| Patient | Age | Children and elderly people were discussed. Non-conveyance is lower for children because of the need to offer reassurance to parents. Mixed views on elderly people depending on complexity of health problems and social support | Yes |
| Deprivation | People from deprived areas more likely to want to go to hospital, to have to go to hospital because of higher levels of morbidity, or not to be registered with a GP so use ambulance service as primary care, leading to lower non-conveyance rates | Yes | |
| Rurality | People in rural areas do not want to go to hospital because of long distances so non-conveyance rates are higher. People living near hospitals prefer to be conveyed because it is easier than alternatives. Easier for ambulance services to convey if a hospital is nearby, leading to lower non-conveyance rates in urban areas | Yes | |
| Language barriers | Demand for ambulance services higher when patients have difficulty speaking English because they do not use alternative services. No mention of effect on non-conveyance | Yes | |
| Living alone | People who are lonely may be frequent callers to the ambulance service. Elderly fallers with no social support will be conveyed. So, if patients live alone, may have lower non-conveyance rates | Yes | |
| Poor housing | People living in chaotic situations less likely to be left at home so lower non-conveyance rates | Yes | |
| Suffering from long-term illness | People with mental health problems and diabetes mellitus can be frequent callers. Unclear effect on non-conveyance rates | Yes | |
| Expectations | See Chapter 4, Findings | No | |
| Call | Reason for calling | Falls, mental health problems and long-term conditions discussed, but these have an unclear effect on non-conveyance rates | Yes |
| Source of call | NHS 111 discussed, but has an unclear effect on non-conveyance rates | Yes | |
| Day/time of call | Family and some services not available out of hours, so non-conveyance rates lower out of hours | Yes | |
| Organisational | Triage system used | NHS Pathways described as risk averse, but has an unclear effect on non-conveyance rates | Yes |
| Motivation to undertake non-conveyance | See Chapter 4, Findings | Yes | |
| Stability | See Chapter 4, Findings | Yes | |
| Skill mix of workforce | See Chapter 4, Findings | Yes | |
| Experience of clinical decision-maker | See Chapter 4, Findings | No | |
| Support for workforce | See Chapter 4, Findings | Yes | |
| Emergency and urgent care system | Connectivity with other services in the system | See Chapter 4, Findings | Yes |
| Availability and accessibility of onward referral services | See Chapter 4, Findings | Yes | |
| Pressure at emergency departments (i.e. long handover times) | See Chapter 4, Findings | No | |
| Complexity of system | See Chapter 4, Findings | Yes | |
| National | Training of paramedics | See Chapter 4, Findings | No |
| Response-time targets | See Chapter 4, Findings | No | |
| Commissioning | See Chapter 4, Findings | Yes |
Patient-level factors: patients’ expectations
Some interviewees – mainly paramedics and managers – perceived that a range of patient characteristics influenced decision-making for non-conveyance (see Table 1), with no discernible variation in perceptions across the 10 ambulance services. A key issue, which we were unable to test in WP2 (see Chapter 5), was patients’ and their families’ expectations that an ambulance would be dispatched and patients transported to hospital. Interviewees described trying to persuade patients calling for an ambulance to seek help from other services, or make their own way to an emergency department, and noted the problem of formal complaints arising when patients did not have their wishes met:
[. . .] some people ring an ambulance and they want an ambulance and they want to go to hospital [. . .] so when you’ve assessed them and done everything and said actually, you don’t actually need to go [to an emergency department], you can go to your GP or your walk-in centre or something, some of them are a little bit off, put out a little bit, you know, well ‘I was wanting to go to hospital’. Some people that it doesn’t matter, how hard you try to explain to them that they don’t need to go to hospital [. . .] they insist that they want to go to hospital [. . .] then you’ve got, you’ve got no alternative choice, you know they have to go.
Paramedic, interviewee 41
For patients who had prior experience of non-conveyance, interviewees perceived that patients were receptive to discharge at scene and welcomed the tasks that paramedics undertook on their behalf, such as arranging a GP appointment. One interviewee expressed the concern that the popularity of discharge at scene with patients might lead to supply-induced demand from people who did not need an ambulance:
I think the patients see that they’re getting a lot within the [non-conveyance] encounter. Obviously they get more assessments than they’d get at a GP practice and they get it all in one go whereas a GP practice might bring you back for your 12-lead ECG [electrocardiogram] the next day or oxygen saturations or blood glucose test thing. Those are all sorts of things that they’d send a patient away for, then do at a later date unless they are critically ill. I think some of our ‘See and Treat’ activity going up isn’t due to us being able to deliver higher levels of care [. . .] they were never appropriate for an ambulance service.
Manager, interviewee 37
There was some suggestion that expectations differed by patient characteristics. Patients living in rural areas were described as being more receptive to discharge at scene than those in urban areas, because of the inconvenience of travelling a long distance to an emergency department and arranging their return home from that hospital facility. This was in contrast to patients living in areas of social deprivation whom interviewees perceived as more likely to expect transport to an emergency department:
[. . .] two hospitals, one is about 37 miles in one direction, and the other is about 30-something miles in the other direction, so there’s quite long distances involved. So actually people would prefer to be treated at home. There’s an expectation ‘well I only live down the road from the hospital so you’re going to take me there aren’t you’ there is the opposite here. So, you know, there is a difference in expectations.
Paramedic, interviewee 17
[patients from] socially deprived areas tend to have much more comorbidities and are generally more complex patients. But also, quite often there is an expectation that they just want to go to hospital. It’s important that you discuss with the patient [what their] ideas, concerns and expectations are, and why it would be appropriate for them not necessarily to go to hospital.
Paramedic, interviewee 26
Organisational-level factors
Motivation to undertake discharge at scene
There was considerable variation in the way that interviewees within different ambulance services described their organisation’s approach to non-conveyance, from embracing it through to viewing it as extremely risky. Interviewees in most services discussed the need to change the culture both within their service and nationally from a service that transported all patients to an emergency department to one that focused on providing care closer to home. This appeared to be particularly high on the agenda of interviewees in one service (Service C), with interviewees expressing a strong belief in non-conveyance and describing actively pursuing a goal to improve or sustain non-conveyance rates within their organisation. This service appeared to be embracing non-conveyance across the whole organisation, with interviewees in both managerial and paramedic roles highlighting a ‘whole organisation’ approach to non-conveyance. Indeed, it was the only service in which the paramedics we interviewed offered positive views of the organisational support they received for non-conveyance. Interviewees in this service also described a historical commitment to non-conveyance, viewing it as part of the established culture within that service:
[. . .] back in 2006 we were leaving, looking at leaving more asthmatic patients at home, which no one else agreed with but actually that’s been a mainstay of what we’ve done and I think we’ve just had that culture a lot longer because staff back, almost a decade ago, were leaving people at home. Whereas in some services their non-conveyance rates are awful and I think their staff have still got to get their head around that’s what their job is.
Service C, interviewee 4
[. . .] across the Trust, trying to reduce non-conveyance rates, and it’s in our strategy as well, reducing conveyance rates now by 10% over the next 5 years and we’re all part of that and staff are aware of that and obviously working towards it.
Service C, interviewee 2
Interviewees within another service (Service I) also described their organisation as embracing non-conveyance but did so in terms of a recent development over the past few years and as an aspiration for the future. Both a paramedic and manager described a drive towards optimising non-conveyance in terms of vehicles, patients, equipment, service models, education and skills in the control room of this service:
[. . .] it’s growing in aspiration. See and Treat as a service is growing in aspiration and the infrastructure around to make that happen.
Service I, interviewee 21
Interviewees from other services either talked about the influence of organisational commitment to non-conveyance generally rather than specifically within their service (Services E and G) or expressed less enthusiasm regarding their organisation’s motivation to undertake non-conveyance (Services A, B, D, H), describing the organisation as having other priorities, or staff as being resistant or fearful of the risks involved:
[. . .] there’s a resistance within the organisation to change. It’s literally bizarre. They’re under pressure but they’re looking, they’re pushing in the wrong ways to get what they want really. They push a target of getting an ambulance to a scene but they don’t look at what happens when someone gets there, what’s the decision-making around what happens next.
Service A, interviewee 17
[. . .] even some of the team leaders that I know, their idea is ‘I’ve taken the majority of my patients to hospital, I’ve still got my job’, you know [. . .]
Service H, interviewee 44
Interviewees in one service (Service F) appeared to discuss non-conveyance differently from those in the other services because the discussion was largely about the risks of non-conveyance. In particular, one manager did not want to increase non-conveyance rates because of the risks involved to ambulance crews if something went wrong. The commissioner also viewed non-conveyance as a low priority within this ambulance service and a paramedic described it as a ‘new concept’ within this service:
The CCGs and the GPs, and everybody else hate us, because, we, I won’t release the crews to just leave people at home and make a call to a GP receptionist to say I’ve left this person at home because that crew member themself doesn’t realise what he’s doing there, he’s putting himself in the coroner’s court in a non-defendable position, so unless it’s a safe structured handover recorded and shared I won’t let it happen. The fact that it does happen all over the place is another matter and I’ll, when I go round other ambulance services I do think that this point is sometimes missed.
Service F, interviewee 39
Motivation for providing telephone advice
In two services (Services C and H) there was a significant amount of discussion in relation to telephone advice. Interviewees spoke enthusiastically about the provision of telephone advice as a specialist service and perceived this initiative to be working well within their organisations. In Service C, interviewees attributed some of their success to being part of a pilot service offering longer telephone time for triage prior to dispatching an ambulance; they felt that this was increasing their rates of calls ending in telephone advice. In both services managers discussed a historical and continuing strategic vision to increase telephone advice rates through significant investment of resources in the clinical hub. One interviewee discussed a potential negative consequence of the success of their telephone advice strategy, namely supply-induced demand, with an increase in ambulance service callers seeking telephone advice:
[. . .] we have had people calling up specifically asking to speak to the clinical hub after previously being handled very well which is obviously doing the paradoxical thing of increasing the call rate, which is not something we were particularly after.
Service H, interviewee 45
In contrast, in one service (Service E) there appeared to be a lack of motivation to focus resources on telephone advice within the service. A manager described how the service had opted for a minimal number of clinicians undertaking telephone advice, and noted that non-clinical staff were undertaking telephone advice decision-making. Another interviewee in this service appeared to suggest that telephone advice was not necessarily what patients wanted and would inevitably increase the workload for the service:
[. . .] with ‘Hear and Treat’, how many complaints do you want to deal with, what’s your appetite for dealing with high level of complaints? So very simply, the more non-conveyance you do the [more] dissatisfaction you will have. People have phoned 999, they didn’t phone 999 for a chat, they phoned 999 with an expectation that an ambulance was going to appear, otherwise you would have rung 111 for a chat.
Service E, interviewee 32
A negative view of telephone advice was also apparent among interviewees in Service A on account of the risks involved in making an assessment without being able to see a patient. In Service G there appeared to be some tension between the ambulance service and the commissioner regarding the provision of telephone advice. In comparing their telephone advice rates with those of other ambulance services, Service G interviewees felt that they could increase their telephone advice activity but this was dependent on additional funding from the commissioners. The ambulance service and commissioner were currently ‘in mediation’, with the commissioner suggesting that they did not have the resources to offer additional funding.
Organisational stability and workforce challenges
Interviewees described different organisational contexts at the time of the interviews. Some services appeared to be stable, with no significant restructuring within the service. However, interviewees in four services (Services A, H, I and J) reported current or recent operational restructure. Interviewees did not expand on how this might affect non-conveyance rates, but it is possible that the ability to innovate or address a range of organisational priorities might be affected by these changes. In addition, although interviewees from all services expressed concern about the recruitment and retention of paramedics, interviewees in three services (Services A, G and H) reported significant problems with recruitment and staff shortages, which they perceived to have a negative impact on the organisation’s ability to undertake discharge at scene:
[. . .] it’s been a difficult year last year because we were in such a difficult situation. We were very much around response and all of our focus was around increasing [staff] numbers and getting the response right in the first instance, so, in fairness we were not necessarily, necessarily entertaining anything that took paramedics away from core frontline business.
Service A, interviewee 5
[. . .] front line ambulance staff are leaving their job in droves [. . .]
Service H, interviewee 44
I’ll say it again, we’re [paramedics] chasing our tails all day long just, looking for pathways that sometimes aren’t there. We’re short-staffed, we’re busy. We’re getting fatigued and tired. I don’t know the answers but in terms of non-conveyance, I think there needs to be more done
Service G, interviewee 29
Skill-mix within a service
Interviewees described how the composition of ambulance crews could differ and how this could affect non-conveyance rates. Advanced paramedics were viewed as having more confidence to discharge at scene than paramedics, and paramedics were viewed as having more confidence than crews without paramedics. Therefore, the skill-mix distribution within an ambulance service could affect its discharge-at-scene rate:
[it is] widely known, we’ve been particularly challenged by a shortage of senior clinicians, that is, paramedics. Paramedic numbers have been very low, and that will affect the decision-making of the clinicians and their confidence level. The more senior clinician you get on the ‘See and Treat’, the face-to-face element, arguably the more confidence they’ll have to make a decision not to convey, whereas if you’re running a number of non-paramedic-based ambulances, so emergency medical technicians, or student ambulance paramedics, or emergency care assistants, anything lower, generally the lower the grade the more likely the conveyance rates will be affected.
Service A, interviewee 5
Interviewees described skill-mix as being related to experience as well as to training, and some interviewees had concerns that ambulance crews with little experience or training could make non-conveyance decisions that might affect patient safety:
[We have an] incredibly young and inexperienced workforce, some of whom do a less than thorough patient assessment, leaving patients at home when it’s not safe to do so.
Service A, interviewee 16
[. . .] if they’re responding, then you need to make sure that they’ve got the appropriate trained paramedic within that skill-mix to undertake discharge at scene safely.
Service A, interviewee 23
The role of advanced paramedics
There was evidence of considerable variation in how interviewees in different ambulance services described the role of advanced paramedics in relation to their contribution to non-conveyance. In some services there was consensus among the interviewees that the advanced paramedic was an established role within the service and was perceived to be a valued resource in reducing conveyance to the emergency department (Services C, D and G). In these services, paramedics spoke positively about being able to access these practitioners and refer patients to them, and also described them as a support mechanism for seeking advice to facilitate their own decision-making regarding non-conveyance. Interviewees in these services wanted to expand this part of the workforce because of its perceived value. In contrast, interviewees in other services described limited implementation of these roles, or a recent renewed focus on them, which implied that they had possibly been neglected within the organisation in the past (Services A, E, H and J). Reasons for limited implementation of these roles included a need to focus resources elsewhere in the service or a lack of interest at an organisational level:
It’s a bit of a ‘dying on the vine’ situation. Yes we have ECPs [emergency care practitioners], a small number that were from the prerequisite arrangements. I’ll never get rid of them, but I’m not, we haven’t trained ECPs here since [a number of years].
Service E, interviewee 32
[. . .] the ECP system fell over a long time ago in [PLACE], and they never really reimplemented it in any sense.
Service H, interviewee 45
Renewed focus on advanced paramedics within an ambulance service appeared to be led by a change in key ambulance personnel management, with the employment of a new manager who valued these practitioners and their contribution to non-conveyance rates. Services viewed these practitioners differently, with some services described by interviewees as not integrating the role within the ambulance service workforce (Service D), not supporting the role (Service E), or perceiving that the role did not positively affect non-conveyance (Service H). There was also evidence that some services used these practitioners differently (e.g. some used them to target specific calls, which were perceived to have the potential for discharge at scene):
There’s no point in sending an advanced paramedic practitioner [to] the patient [that] needs transporting, but on those urgent care presentations there’s a lot more opportunity to ‘See and Treat’.
Service J, interviewee 40
Length of service of crew members
Although some interviewees expressed concerns that a lack of experience in the job could lead crew members to make unsafe decisions around non-conveyance, on the whole, interviewees perceived that paramedics who had undertaken their training more recently were more likely to consider non-conveyance as an option for a patient. Although there was no discernible variation between the views expressed by interviewees from different ambulance services, it is possible that the distribution of experience of a service’s workforce could have an impact on non-conveyance rates, whereby a ‘younger’ workforce might deliver higher rates:
[. . .] but it’s again a cultural thing, so the older staff, they join the service and everyone went to hospital, the younger staff, we have a different perspective on it which becomes apparent when you’re at jobs sometimes and the [older] crew that turns up just say ‘right, in the back of the ambulance’ irrespective of whether or not you’re halfway through an assessment.
Service H, interviewee 45
Organisational support for the workforce
Although there was a perception that ambulance crews followed protocols and policies, including formal pathways of care, when making non-conveyance decisions, many interviewees described the importance of the confidence of paramedics when deciding to discharge at scene. Indeed, one interviewee identified paramedic confidence as the most important factor affecting the decision to discharge patients at scene. Interviewees described how confidence could be improved through experience in the role, training to extend skills, mentoring in non-conveyance, the ability to discuss potential cases for non-conveyance with clinicians in the clinical hub, and being part of an organisation that was supportive of their workforce. Interviewees discussed how supportive they felt that their organisation would be if something went wrong after a decision to discharge at scene. Senior managers described the importance of supporting their workforce and understanding that a decision not to convey can be the right decision at the time, even if it appears not to be at a later stage:
I say, eradicate the fear of, the blame culture [. . .] being supportive then obviously that will then increase individuals’ confidence and ability to increase non-conveyance.
Service C, interviewee 2
[. . .] probably the most important one is the support for staff. So if we’re encouraging the staff to non-convey it’s making sure we’re supporting them in that decision and if it does go wrong, making sure again that we understand the reason why it’s gone wrong, but again continue to support the staff because they’ve probably made the right decision in the first place.
Service G, interviewee 30
In contrast with the views of these managers, paramedics in some services openly described a fear of retribution if things went wrong (Services B, D, E, G, H and J):
[. . .] generally people saying ‘it’s not our job to be discharging people’. I’m seeing ‘we’re not doctors’. [Workforce] concerned about potentially getting the sack if they were to leave somebody at home, and quoting that ‘the service would never back us up’.
Service H, interviewee 44
Indeed, in some services senior managers described how supportive they were of the workforce when things go wrong, but the paramedics interviewed expressed the opposite view (Services E, G, H and J). A senior manager in one service ascribed this to organisational memory whereby an historical case of disciplinary action is remembered by the workforce and shapes their current actions.
Skill-set in the clinical hub
There was much discussion about the necessary skill-set required in the clinical hub to optimise the provision of telephone advice. Providing telephone advice was perceived to be a specialism, beyond that of the basic training of paramedics. There was a perception that the provision of telephone advice historically had been by staff who were no longer physically able to work ‘on the road’, and that these staff did not necessarily have the skills to be effective in providing telephone advice. The provision of specially trained paramedics working alongside other clinicians such as mental health specialists, midwives and GPs within a clinical hub to undertake more complex assessment was described as a more modern approach. Most services appeared to have established specialised multidisciplinary teams to provide telephone advice, but had perhaps implemented this to varying degrees:
I actually think that ‘Hear and Treat’ is a specialism, and I think there is, there is much scope in developing people, because ‘Hear and Treat’ is, is inherently risky and it does take a certain specialism to do that because, you know, it’s not, it’s not for everybody, and, you know, we, we had, we’ve had incidences where a paramedic can no longer deliver their service on the road due to capability or an injury and they say well, come in [. . .] and do some ‘Hear and Treat’, and they, they hate it, it’s just not for them, so, it isn’t for everybody [. . .] there’s really subtle nuances that you have to listen to what people are saying and, and almost read between the lines when you can’t see someone you have to really pay attention to what they’re saying and how they’re saying it [. . .] if you’re nervous about making decisions about, you know, discharging someone over the telephone then you should, you know, it doesn’t matter how much you teach someone they’re not going to have that confidence to do good ‘Hear and Treat’.
Service A, interviewee 16
[. . .] mental health nurses, when, when we brought those in, were just far more competent at resolving complex mental health care needs than paramedics were, just because the nature of their world, so it allows that knowledge to flourish when they are working, sitting side by side in different disciplines.
Service H, interviewee 49
The wider emergency and urgent care system
A consistent message across all ambulance services and stakeholders was the importance of the wider emergency and urgent care system as an enabler of non-conveyance:
[. . .] there’s lots of expectation on ambulance services to single-handedly reduce conveyance to [an emergency department] but, we can, a lot of that is, the success is down to the buy-in from the local health community in terms, if they’ve not got the alternative pathway we can’t use it.
Service C, interviewee 4
Interviewees talked about the importance of the system in relation to connectivity with the ambulance service (how easily the ambulance service can access another health or social-care service), provision (the availability of alternative services or pathways), pressure (high demand or a lack of resource within the system), complexity (numbers of CCGs or consistency between CCGs) and the level of integration with NHS 111.
Connectivity with the wider system
Interviewees in one service (Service C) shared consistently positive views about the connections between their ambulance service and services in the wider emergency and urgent care system. They described an initiative that linked ambulance crews with other services necessary for non-conveyance rather than relied on the crews attempting to locate and contact services themselves. This initiative was perceived as successful and as operating differently from other models across the country because it took some of the responsibility for discharge at scene off the ambulance crew. In contrast, another service described a similar initiative as a barrier to non-conveyance because it was not consistently provided across their region and thus caused more rather than less work for ambulance crews:
[. . .] some [models in other ambulance services] don’t clinically take on the patient. They just say ‘oh you need to phone such and such and refer them there’. With our [model] you basically hand [the patient] over and one of their clinicians [will] take responsibility for the patient [. . .] and they sort everything else out behind the scenes.
Service C, interviewee 4
[. . .] each one of the commissioners [CCGs] puts in what they call an SPA [single point of access], a single point of access. Some of them put in several single points of access, which in itself is a bit of an oxymoron because it’s not single point, it’s several points of access, and so what we’ve done is then created another obstacle that a crew has to navigate before they can pass this job on.
Service B, interviewee 43
In other services (Services A, B, D, E, F and I) interviewees perceived that relationships with key services in the wider system were poor because they could not access these services, could not access services reliably when needed in relation to non-conveyance decisions, could not access services with ease, or were not confident in the quality of the service to which they wanted to refer patients. These services included primary care in or out of hours, community services, falls services, minor injury units and urgent care centres. Variation in service provision in different geographical areas within their region, or within the same service over time, created a burden for crew members and the sheer effort of making contact with a necessary service could result in a decision to convey to an emergency department because this was the easiest option:
[the] minor injury unit is one of the, probably the main places for ‘See and Convey Elsewhere’ and that’s where we really do have this difficulty about ‘will they be open, have they got the right skill on, is their X-ray working today’. Every minor injury unit deals with a different case mix. Very difficult to persuade the ambulance crews to go to that place.
Service I, interviewee 11
[. . .] they go to a [patient who has had a] fall in [PLACE A], and [the crew] might be very familiar with the falls service that’s back in [PLACE B], but now they’re in [PLACE A] it’s all completely different, the criteria’s different, they haven’t a clue, so they’re left with the decision ‘well, I haven’t a clue what’s going on here so do you know what, I’m just going to take them to the [emergency department]’.
Service B, interviewee 43
Patchy provision of services across the system
Interviewees in one service (Service C) described good provision of services across the health-care system and the region covered by the ambulance service. They considered themselves to be in a fortunate position to have a range of pathways available to them and had a sense that a wide range of services were receptive to working with them. In contrast, interviewees in two services (Services A and I) described a distinct lack of services in their wider health-care system that could facilitate non-conveyance in their region. In most other services (Services B, D, E, F, G, H and J) interviewees provided a mixture of positive and negative views, or described variability in the provision of services in different geographical areas of the region served by the ambulance service:
I think it’s fair to say, very few options available to us in as far as referral pathways.
Service A, interviewee 15
There are some areas which have got really good pathways, so where you’ve got direct access to GPs, direct access to minor injuries units, direct access to walk-on admission on to certain wards for certain clinicians. But then in other areas, actually the only place you’ve got is the emergency department, so the GPs won’t take a referral from the paramedics [. . .] so you’ll get a minor injuries unit, often called a walk-in centre, and often the reason why we call it a walk-in centre is they don’t take stretcher patients. So they have a perception that if you’re an ambulance, the patient must be on a stretcher, therefore, they won’t accept you.
Service D, interviewee 20
Services under pressure
Interviewees highlighted how pressure at their acute trusts, specifically their local emergency departments, affected non-conveyance. Problems with long handover times at some emergency departments, and criticism by clinical staff in emergency departments about the inappropriateness of conveyance of some patients, could be an incentive to increase non-conveyance rates for ambulance crews. These could also be an incentive for the ambulance service to generally increase their focus on non-conveyance:
[. . .] some hospitals have a big problem with hospital handover delay and [local Acute Trust] are desperately trying to get that reduced and improved, but what all the hospitals are saying, ‘well if you didn’t bring all these wrong patients to us, you know, we wouldn’t have these delays, it’s all your fault’. It doesn’t quite get like that, but it does get sometimes a little heated, so, some of that pressure to reduce conveyance is very much from a hospital end.
Service I, interviewee 11
[. . .] the [local] health system is in extreme difficulty, under a huge amount of pressure. We’ve seen huge increases in demand, longer bed stays, the acute trust in [locality area] are struggling [. . .] We’ve got a couple of the acute trusts that take this in the way that it’s meant, the worst performers in the country particularly around hospital handover time because of the pressure they’ve got with their throughput [. . .] So, the focus very much this year is around reducing those levels of activity and where can we impact on appropriate non-conveyance to try and alleviate the pressures on the system on the whole.
Service A, interviewee 5
Complexity of the system
Ambulance services covered between 12 and 33 CCGs within their region. Ambulance service managers and paramedics described how each CCG could have different priorities in terms of non-conveyance, creating complexity in terms of a single ambulance service having to deal with multiple commissioners. The complexity also arose from each CCG area having different services operating in different ways. Ambulance service interviewees discussed how CCGs could facilitate non-conveyance by working together to standardise services across CCGs and increase connectivity between the ambulance service and other services in the system.
NHS 111
Ambulance services had different relationships with NHS 111. Some of them ran NHS 111 for the whole of their population or for some localities within it, whereas other ambulance services had no leadership of NHS 111. There was a perception that NHS 111 had increased demand for ambulance services because it was a risk-averse service that requests the unnecessary dispatch of ambulances:
Obviously the introduction of 111 has been a really big thing. It happened locally, I think last year when it was extremely busy in the area anyway, and then we’re getting this influx of 111 red calls for patients say with a chest pain, that they might have had for 3 or 4 days [. . .] I think you automatically, you get a 111 red call, and then you think well already your mood is lowered just because it’s got those symbols, the three 1s and then a red call.
Paramedic, interviewee 29
The number of low-acuity jobs that we get called to has gone up dramatically since 111 [. . .] our ‘Hear and Treat’ clinicians within the ambulance service wouldn’t retriage something that had been triaged by a 111 clinician, but quite often they haven’t been triaged by 111 clinician, they’ve been triaged by the system, by the Pathways system and therefore there isn’t any clinical input into the decision to send an ambulance at all, and obviously we can’t then regrade that.
Paramedic, interviewee 17
Interviewees within different services discussed initiatives to integrate 999 and NHS 111 calls in some way, for example, by having dual-trained 999/111 call-handlers and putting more clinicians in the NHS 111 control room to reduce the inappropriate dispatch of ambulances (Services D and J).
National-level factors
Training of paramedics
One commissioner interviewee saw their local ambulance service struggle to engage with new initiatives for non-conveyance because they could not recruit new staff to deliver them. They identified the national shortage of paramedics as a barrier to increasing non-conveyance rates, and noted that national funding is required to train these health professionals.
Response-time targets
A key performance indicator for ambulance services historically, and at the time of the study, was the percentage of potentially life-threatening calls attended to within a particular time frame. Interviewees within ambulance services viewed these ‘response-time targets’ as their key priority. Only one ambulance service was meeting its targets at the time of our study, and the push for better performance against these targets, rather than increases in non-conveyance rates, was paramount for some services:
[. . .] so therefore we focus on hitting our performance targets at the expense of virtually everything else, because if we don’t hit our performance total targets, we then become not viable as an organisation, and we’d either get split up and merged with other trusts, or be taken over, lock, stock or privatised or whatever doomsday scenario you want to think.
Senior manager, interviewee 43
Interviewees in one service (Service C) described non-conveyance only as a way of helping to meet these targets. Interviewees from other services either held response-time targets and non-conveyance as dual priorities or viewed a focus on non-conveyance initiatives to be a distraction from meeting their targets:
[. . .] so, in fairness, we were not necessarily entertaining anything that took paramedics away from core frontline business. So CCGs wanted to talk to us about an [advanced paramedic]-led response car that deal only with lower acuity calls, only responded to those to look at admission avoidance. We were not entertaining that throughout last year because of the position that we found ourselves in, and that was accepted by the CCGs.
Senior manager, interviewee 5
Commissioning ambulance services
Commissioning can be viewed as a local endeavour because it is provided by local CCGs across England. However, the commissioning structure introduced for ambulance services was established at a national level so is included in the theme of national-level factors affecting non-conveyance. The structure introduced nationally was that a lead commissioner would commission on behalf of the multiple CCGs served by each ambulance service. This makes commissioning ambulance services more complex than the usual single CCG/single service provider relationship. The relationship is a triad rather than a dyad: the local CCGs, the ambulance service, and either a lead commissioner or a commissioning support unit is responsible for negotiation between these two parties. In theory the lead commissioner was supposed to identify a unified strategy from the 12–33 CCGs within an ambulance service region and then present this to the ambulance service, monitor progress on the strategy and feed back to the CCGs. In practice, commissioners described the challenge of getting a large number of CCGs to agree on a set of commissioning intentions and noted the inability to present a unified strategy to the ambulance service. There could be tensions between lead commissioners/commissioning support units and some of the CCGs they worked on behalf of, with CCGs bypassing their lead commissioners to negotiate and monitor contracts directly with their ambulance service. This could lead to a lack of trust between the lead commissioner and the CCGs. There could also be a lack of trust between the commissioners and the ambulance service, with tense relationships and the need to have formal mediation to get the contract signed. One lead commissioner/commissioning support unit identified their role as being that of a mediator between the CCG and ambulance service rather than a leader.
Variation in approaches to commissioning
When interviewees described their commissioning, considerable variation was apparent in terms of whether there was a lead commissioner model operating in practice or a commissioning support unit involved, or whether commissioning took place directly with individual CCGs. The types of contracts also varied; some commissioners used block contracts and some used tariffs. It was unclear which approach facilitated increases in non-conveyance, but one senior manager described how their service was not incentivised to discharge at scene in their tariff contract because payment for non-conveyance and conveyance was so similar. Regardless of the model of commissioning, both commissioners and ambulance service managers perceived that the actions of local commissioners affected non-conveyance rates:
[. . .] some of it is about the way we commission them, and what we have enabled them to do [. . .]
Commissioner, interviewee 13
[. . .] I think [commissioning is] fundamental, I think it’s pivotal to improving and increasing non-conveyance [. . .]
Commissioner, interviewee 19
The importance of a collaborative relationship
The difficulty of managing the triad relationship between lead commissioners, CCGs and ambulance services was apparent but some ambulance services and their commissioners managed it by having CCGs work together in localities or divisions, by establishing a board to bring all CCGs together or by making other efforts to work collaboratively. All parties felt that a collaborative approach was ideal and were pleased when they achieved this:
I’ve had an argument about the money inevitably, and you have the nuances, the priorities within it, or a particular area wants to push something faster than another area or do something slightly different. But the negotiation and the facilitation is around making it consistent enough, and manageable enough for [the ambulance service] to operate as one organisation, while making it feel local enough and integrated enough that a CCG is still also getting what they need for their patient. And that’s the tension and the challenge all the time.
Commissioner, interviewee 11
We have been blessed in the past with [PLACE] specifically [CCG] has been very, very innovative and supportive, and previously it’s delivered different approach to things. They have been hugely supportive in supporting us as a local ambulance service in developing new models of care, and interestingly [. . .] we as partners come regularly together to try and look at different ways of doing things collectively.
Senior manager, interviewee 16
[. . .] it’s becoming more collaborative. Some places are already there and are working really closely together and that’s possibly one of the reasons why there are variations in conveyance rates. So those areas that have already been working together to find solutions to the challenges, others I think are working together better and are now starting to, we’re starting to see some of the benefits in that close working relationship.
Commissioner, interviewee 19
The commissioning patchwork quilt
The difficulty of identifying a single strategy for all the CCGs within an ambulance service region could result in local negotiations between single CCGs or a small set of CCGs, leading to different provision of non-conveyance initiatives in ambulance service localities. In one ambulance service there were two contracts with different commissioners because the lead commissioner could not broker a single contract. In another, three geographical areas had their own different contracts with the same ambulance service. This increased the workload of ambulance services because of the need to negotiate with a number of commissioners at the same time. The picture emerging from the interviewees’ descriptions was that of a patchwork quilt of different strategies for non-conveyance in different localities, based not necessarily on patient need but on commissioner preference and the ability of the provider to offer them:
[. . .] there’s obviously different models that are being run throughout the respective counties and trying to look at [. . .] where there’s potential for some of the CCGs to get together, we do find that the ones that work better are ones where they’re sharing with a number of CCGs the infrastructure and the particular scheme.
Commissioner, interviewee 38
The patchwork quilt image that emerged was related not only to the different non-conveyance strategies within ambulance services but also to the different availability and accessibility of services in different CCGs, so that ambulance crews struggled to know whether and how to use alternatives to conveyance to an emergency department. In theory, ambulance services made use of the Directory of Services provided by commissioners to communicate where and when which services were available within a CCG, but some ambulance service interviewees felt that this was not updated enough to be fully useful:
[. . .] my biggest frustration is that each commissioner, all [number] of them, only worry about their square few miles, and just simply do not give a monkeys what happens a mile over the border.
Senior manager, interviewee 43
Aligning goals and financial incentives
Commissioners and ambulance managers wanted to have aligned goals around non-conveyance:
I think they have very similar priorities, there’s not a massive difference between what we’re both trying to achieve because the more efficiently the ambulance trust can use its resource for what it needs to use it, the better for them and, by default if they are able to treat more patients either by phone or in the home, it releases the pressure on the acute trusts, so for those commissioners who do acute commissioning it helps them as well.
Commissioner, interviewee 7
However, both parties did not necessarily feel that goals were aligned or that incentives existed for non-conveyance. For one ambulance service, the commissioner wanted more innovation and more detailed business cases for initiatives to increase non-conveyance. In another, the managers wanted discharge at scene to be incentivised financially but the commissioner did not agree. In contrast, contracts were used to promote increases in non-conveyance in another ambulance service:
[. . .] that we’ve got some very good commissioners [. . .] support the provision of our service. They understand that to build the ‘Hear and Treat’ back up they have to state that a certain amount of money from their contract will go into ‘Hear and Treat’.
Senior manager, interviewee 16
Variation between ambulance services
Qualitative findings based on stakeholders’ perceptions of each ambulance service were summarised and displayed in a table ready for quantitative testing in WP2 and WP3 (Table 2). Ambulance service-specific data displayed in the 2017 NAO report were extracted into the same table (see Table 2) for testing in WP2 and WP3. 1
| Factor | Aspect of factor | Service | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | ||
| Non-conveyance at time of interviews | Total | M | L | H | L | M | L | M | L | H | L |
| Telephone | L | H | M | L | L | M | M | M | M | L | |
| Discharge at scene | M | L | H | L | L | L | M | L | M | L | |
| Organisational | Operational stability of service (WP1) | Operational restructure and problems with staffing | No change reported | No change reported | Focus on paramedic recruitment | No change reported | No change reported | Staff shortages | Operational restructure and problems with staff retention | Operational restructure | Operational management restructure |
| Organisation motivation to undertake non-conveyance (WP1) | Recent motivation but inconsistent views | Possible lack of motivation | Active and established | Inconsistent views | No view expressed | Risk aversion at a senior level | No view expressed | Inconsistent views | Recent motivation | Inconsistent views | |
| Commissioner describes work to understand gaps in non-conveyance | Commissioner view – negative | Commissioner view – negative | Commissioner view – negative | Commissioner view – positive | |||||||
| Workforce | Advanced paramedics and practitioners (WP1) | Limited implementation | Limited discussion | An established and valued resource for non-conveyance | A valued resource, but possibly a lack of integration within workforce | Limited implementation and a lack of support for the role | Limited discussion | An established and valued resource for non-conveyance | Limited implementation and some negative perceptions of impact on non-conveyance | Limited discussion | A recent development |
| Fear of retribution (paramedic perception WP1) | Low levels of fear | Evident | No evidence | Evident | Evident | No evidence | Evident | Evident | No evidence | Evident | |
| Wider health-care system factors | System provision | Lacking | Inconsistent views | Good | Inconsistent views | Inconsistent views | Inconsistent views | Inconsistent views | Inconsistent views | Lacking | Inconsistent views |
| System connectivity | Lacking | Lacking | Connected | Lacking | Lacking | Lacking | Inconsistent views | Inconsistent views | Lacking | Inconsistent views | |
| System pressure | Pressured | No discussion | No discussion | Inconsistent views | Some mention of pressure | Some mention of pressure | Some mention of pressure | Some mention of pressure | Some mention of pressure | No discussion | |
| Complexity | Few CCGs | Many CCGs | Many CCGs | Few CCGs | |||||||
| Commissioning | Close working, CCGs pay or innovation | Work together but non-conveyance is not incentivised | Commissioners invest in non-conveyance | Disagreements about non-conveyance | Collaborative but locality-specific | Collaborative but no incentive to undertake non-conveyance | Tensions | Good relationship | Tensions | Collaborative but locality-specific | |
| Telephone advice | Perception of telephone advice provision | A sense that they could do better | Limited, recent focus | Enthusiasm and a view that they were doing well | A recent focus | Negative view | Limited, but positive view | Tension. A sense that they could do better | Enthusiasm and a view that they were doing well | A recent focus | Limited, but negative view. A recent focus? |
| From NAO report1 | Cost per call | L | H | H | L | ||||||
| Cost per face-to-face interaction | H | H | L | H | L | ||||||
| Performance against response-time target ‘Red 1’ | H | ||||||||||
| Staff absence rate | L | H | |||||||||
| Frontline staff advanced practitioners | H | H | H | ||||||||
| Income per head of population – not standardised for population age distribution (NAO) | L | L | H | L | |||||||
Discussion
Summary of findings
There were a large number of factors perceived by stakeholders to influence non-conveyance rates. The factors operated at different levels: patient, call, organisation, the wider emergency and urgent care system, and national. A key finding was the variation in the degree of motivation among senior managers to undertake non-conveyance, with some services actively embracing non-conveyance and others more concerned about the risks than the opportunities. It is possible that this motivation could affect other organisational-level factors, such as how advanced paramedics were used within a service. There was also variation in the way interviewees in different ambulance services talked about their wider emergency and urgent care system. Some systems were perceived to be under pressure, complex or lacking in service provision, all of which acted as barriers to non-conveyance.
Context of other research
Our findings are in line with recent evidence of the complexity for ambulance services of collaborating with so many stakeholders across the geographical areas that they serve. 1 Operational challenges were evident in some services, with interviewees reporting problems with staffing levels. Again, ambulance staff recruitment and retention has been reported as a problem elsewhere. 1 In our study, low staffing levels were perceived to be problematic for undertaking non-conveyance. Some paramedics did not feel supported within their organisation, and this is likely to have an impact on how they practice and the level of decision-making they are prepared to take. Staff satisfaction in the ambulance service, as reported in the NHS staff survey, is poor in comparison to that of other staff in the NHS. 58 Ambulance services also have higher sickness absence rates than other NHS organisations.
Strengths and limitations
This is the first study to take such a comprehensive national view of non-conveyance, drawing on the perceptions of key stakeholders. The inclusion of paramedics of different grades offers further insight into the complexity of decision-making facing ambulance crews that has been noted in other studies. 3,12 This WP had two limitations. First, we analysed the perceptions of a few individuals in relation to each ambulance service to identify organisational characteristics for testing in the quantitative analysis in WP2 and WP3 and for further exploration in the chapter on integration (see Chapter 10). We took care not to be swayed by an individual’s very negative or very positive view of non-conveyance within their organisation. This resulted in us not categorising many services for which mixed or unclear views were apparent. Perceptions are very important; nevertheless, perceptions are not objective measures of organisational practice or priorities. Second, individual paramedics were identified for interview by managers employed by each ambulance service. Therefore, there could have been bias in our sample, with the selection of paramedics made based on the viewpoint that the organisation wished to portray within the study. Although this might have occurred, we reflected throughout data collection and analysis on the amount of ‘account-giving’ within our full data set, whereby individuals wished to convince us of their positions as ‘good commissioners’, ‘good ambulance managers’ or ‘good paramedics’. There is no doubt that some of this occurs within any qualitative interview study. However, overall we felt that interviewees talked to us in an open and informative way, expressing both positive and negative views about non-conveyance within their organisations.
Implications for work packages 2, 3 and 4
Interviewees in WP1 identified a range of factors affecting variation in non-conveyance rates. We considered where to find quantitative data to measure the effect of these factors. Quantitative data were available for some patient characteristics from census data and ambulance service routine data, and for some call characteristics and ambulance processes from ambulance service routine data. Organisational-level data were available from two sources. The first was the qualitative interviews undertaken in WP1 from which we summarised interviewees’ perceptions for each organisation and coded ambulances services as 1, 2 or 3 for a range of factors. The second source was the 2017 NAO report. 1 A number of processes were summarised in the NAO report and showed variation between ambulance services. Despite not being raised in the WP1 interviews, these variables had the potential to affect non-conveyance rates (e.g. income per head of population and staff absence rates).
Factors identified in WP1 as affecting non-conveyance rates (see Tables 1 and 2) and factors identified as varying between ambulance services from the NAO report were tested in WP2 and WP3 to try to explain variation in non-conveyance rates as well as potentially inappropriate non-conveyance rates between ambulance services.
Additional findings from WP1 relating to inappropriate non-conveyance and non-conveyance for breathing problems are reported in Chapters 6, 7 and 9 reporting WP3 and WP4.2.
Chapter 5 Characteristics affecting variation in non-conveyance rates: analysis of routine data (work package 2)
Background
The aim was to explain the amount of variation in non-conveyance rates between ambulance services. We also investigated variation within ambulance services because while working with ambulance service staff to design the study, key personnel identified within-service variation as considerable. We sought individual-level data from ambulance services rather than aggregated AQI data to address these aims.
This chapter is based largely on routine data collected by ambulance services and the methods reported below focus on the data collection. We also include a small number of themes from the qualitative research from WP1 reported in Chapter 4 and refer the reader back to Chapter 4, Methods, where the methods of this qualitative research are detailed.
Methods
Data request from the ambulance services
We requested 1 month’s worth of routine computer-aided dispatch (CAD) data from each of the 10 large ambulance services in England. The study started in January 2015 and we requested data for November 2014 because it was the last full month for which data were available and November is not an unusual month for non-conveyance historically (see Chapter 3). The data specification form is displayed in Appendix 6.
Ideally, we would have requested these data after undertaking the qualitative interview study in WP1 so that we could request data on factors identified by stakeholders as being important to non-conveyance. However, we knew that obtaining and cleaning this type of routine data is time-consuming so we requested them before we started WP1. When services sent the data, we compared them with AQIs published for that month and worked closely with analysts at each service to reconcile differences between the data and the AQIs. We also requested all CAD data for that month so that we could apply the national guidance on calculating AQIs in a standardised way to the CAD data by applying standard definitions of specific types of non-conveyance.
We intended to link patient-level characteristics available from the 2011 census59 to each call by using the postal sector of the incident and the online census tool to relate this to deprivation and rurality indices from the latest census. Postal sector required special agreements from national information governance structures because they are considered to be identifiable data. As an alternative, we requested that services attach the lower layer super output area (LSOA) of the incident for each call to allow us to link calls with geospatial census data that might explain variation in non-conveyance rates. The Office for National Statistics (ONS) created the current set of LSOAs from 2011 census data59 such that England is entirely covered by a set of non-intersecting geographical areas, all of which have similar population sizes and internally homogeneous populations (assessed on a variety of census measures). LSOAs are the smallest geographical unit for which certain census data are available. They consist of clusters of adjacent areas with a mean population size of around 1600 people (in 2011). We then used the LSOA to link 2011 census data to each call. One service (Service H) could supply only 2001 census-based LSOAs, which we mapped to the most likely 2011 LSOA using population size. 59 The census variables that we linked to the ambulance routine data were informed by early WP1 interviews. These factors were related to the area from which the call was made to the ambulance service rather than to the individual patient.
Data obtained
We obtained data related to our specification from all 10 services. However, one service could not provide data on skill-mix (Service J), one service could not reconcile the differences between AQIs and the data sent (Service C), and one service engaged in a limited way with our team to reconcile differences, which could not therefore be explained (Service H). When we received the data, a team member (TS) checked it against published AQIs. When Tony Stone found disparities he worked with analysts at Business Intelligence/Data Analytics Teams at each ambulance service to resolve differences or explain why they had occurred. The amount of time spent reconciling the data with AQIs was considerable and we paid ambulance services for this. Most services could not fulfil our full specification in terms of providing data on calls sent to clinicians in clinical hubs, free-text on breathing problems and the full CAD data set. Therefore, it was not possible to undertake some of the analyses that we had planned.
Each ambulance service used one of two types of call assessment/triage systems to prioritise calls [Medical Priority Dispatch System (MPDS) and NHS Pathways]; one service used both systems for different localities but the calls associated with each triage system could not be distinguished and the service was categorised as using MPDS in our analyses. These triage systems categorised the reason for the call differently. Services also used different CAD systems, which had different labels for skill-mix and resource/type of ambulance sent. We established a working group of clinicians and experts within our team and a research paramedic from East Midlands Ambulance Service to develop common categories for these variables. We applied the common categories for reason of call to the data from each service. For skill-mix and resource we requested that each service link their specific codes to the common categories.
Some of the variables had limitations, as follows:
-
Age – we had to analyse this as a categorical variable because call handlers can sometimes enter only an approximate age for a patient when a caller is unsure of this information.
-
Age – telephone advice only is not advised for infants aged 0–2 years in some ambulance services so this age group was identified separately for the analysis.
-
Age – ’0’ was used to indicate a baby and to indicate a missing value in some services. We included 0 as a baby.
-
Reason for call – this was missing for a considerable proportion of calls, namely calls transferred from NHS 111, calls from health-care professionals, ‘running calls’ reported by ambulance crews on their way to another job, and calls from other emergency services such as police. Calls in which new information comes to light before an ambulance arrives at the scene may result in an upgrade or downgrade of the reason for the call; this was categorised as ‘upgrade’ or ‘downgrade’ rather than a specified reason for call.
-
Type of caller – two services had very small percentages of calls from health-care professionals.
-
Skill-mix – the skill-mix variable was based on the most senior crew member attending the scene. Analysts from the ambulance services were concerned that data on crew members could be incomplete and out of date and might not reflect who made the decision to non-convey. In addition, the most senior clinician might not be on scene but in the control room giving advice to the on-scene clinician. We had data for on-scene skill-mix only. We developed the common categories of doctor, advanced paramedic or nurse, paramedic, emergency medicine technician (can do basic life support, not registered), co-responding role (student paramedic, emergency care assistant, community first responder), and other (specialist roles, e.g. disasters). Owing to small numbers in some categories, these were collapsed to ‘advanced paramedic or nurse’, ‘paramedic’ and ‘other’ for the analysis.
-
Resource sent – different types of vehicles are sent to the scene and this might have an impact on conveyance. We developed the common categories of air ambulance, dual-crewed ambulance (emergency transport vehicle), single-manned vehicle (which can sometimes convey), other conveying vehicle, and non-conveying vehicle (e.g. bike, motorbike, other). We decided not to use this variable in the analysis because it was not raised by interviewees in WP1.
-
LSOA – any census variable linked to a call was for the area in which the call was made. The census variables were small area-level characteristics acting as proxies for patient-level characteristics. In addition, the incident may have occurred in a public place, or at the homes of friends or family members rather than a patient’s home.
-
Calls sent to a clinician – we wanted to identify calls ending in telephone advice that had been sent through to the clinical hub for management by a clinician so that we could compare the rates of these types of telephone advice calls between services. Six services provided the data with the proviso that they were not accurate. In three services all or most of calls categorised as ending in telephone advice were coded as managed by a clinician: in one no calls were coded in this way, and in the other two around half of calls were coded in this way. We had no confidence in these data so did not use them within the analysis.
Analysis
Descriptive analysis of different types of non-conveyance
A descriptive analysis was undertaken, comparing calls resulting in different types of non-conveyance with those transported to a hospital with an emergency department. The denominator for this descriptive analysis was all calls.
Focus on two types of non-conveyance only
We attempted to explain variation between ambulance services in rates of telephone advice and in rates of discharge at scene only. We did not undertake the analysis for patients conveyed to facilities other than hospitals with emergency departments because they included such a mix of acuities, for example low-acuity calls taken to minor injury units, end-of-life calls taken to hospices and high-acuity calls taken to specialist tertiary care (e.g. patients with suspected stroke taken to a hyper-acute stroke unit).
Explaining variation between ambulance services
We started the analysis by investigating variation in the rates of discharge at scene between ambulance services using mixed-effects logistic regression models with ambulance services as a random intercept. The denominator for this analysis was all calls attended by an ambulance, that is, calls ending in telephone advice only were excluded from the denominator. We undertook this analysis first because discharge at scene accounts for the majority of non-conveyance. The first stage of the analysis was to investigate which patient-level variables (age, sex, time of call, source of call, type of caller, condition, urgency level and skill-mix and those based on LSOA urban/rural location, deprivation, and the percentage of the population with a severe long-term illness) were statistically associated with non-conveyance. At this stage, type of caller was removed from the analysis because there were no data available on this variable for Service E and no health-care professional calls recorded for Service I. The skill-mix variable was also missing for one of the ambulance services (Service J) but as this was considered to be a potentially important factor in non-conveyance we conducted the analysis on the nine ambulance services that provided skill-mix (the primary analysis) and then refitted the final models on data from all 10 ambulance services with the skill-mix variable excluded (sensitivity analysis). Using a likelihood ratio test, all single variables that were significantly related to the outcome at a p-value of < 0.1 were entered into the multivariable model building analysis. We then used a backward elimination strategy with variables removed at a p-value of > 0.05 to identify the subset of variables that independently predicted the outcome. As a final check, all variables excluded in the first stage of model selection were added to the model to see if they became important in the presence of others. First-order interactions between predictor variables were investigated but owing to the large sample size we found statistically significant interactions with small effects that made the models difficult to interpret. As a result, we made the decision to remove all interactions from the models. The set of patient-level variables from this analysis was used for all other regressions.
The next stage of the analysis was to consider ambulance service-level variables. We investigated adding each ambulance service-level variable to the model with patient-level variables. All ambulance service-level variables from either the model with case-mix included or excluded with a p-value of < 0.1 were entered into the next stage of analysis. All of these variables were added to the model and backward elimination was used to remove ambulance service-level variables with a p-value of > 0.05.
Variability between ambulance services was assessed visually using caterpillar plots (see Figures 6 and 7). These plots show the conditional modes of the random effects (ambulance service) from the fitted models presented as odds ratios and 95% confidence intervals. Vertical dotted lines represent the mean odds of non-conveyance across ambulance services and allow the population-level average response to be compared to the individual ambulance service response. These odds ratios were plotted for (1) the null model or intercept-only model (i.e. the model with no patient- or ambulance service-level variables), (2) the model with patient-level variables only and (3) the model with all levels of variables. By comparing these plots it is possible to see how variability between random intercepts (ambulance services) is reduced as different levels of variables are added.
The approach used to investigate variation in discharge-at-scene rates was repeated for telephone-advice-only rates. The denominator for the telephone advice analysis was all calls. For this analysis, urgency level, skill-mix and source of call were excluded because they were not relevant to these types of calls: most telephone-advice-only calls are not emergencies, there was little or no skill-mix data available, and calls from NHS 111 are not supposed to be retriaged by clinicians in ambulance services. All mixed-effects models were fitted in the statistical software R (The R Foundation for Statistical Computing, Vienna, Austria) using the lme4 library. 60
Exploring variation within ambulance services
For exploring variation within ambulance services we used 150 upper-tier local authorities (counties) as localities because not all services supplied divisions or localities as requested. The Isles of Scilly were combined with Cornwall; the City of London was combined with Westminster. Two different statistical approaches were used for this analysis.
For the first approach we fitted mixed-effects logistic regression models with counties as a random intercept. These models included the same patient-level variables as selected during the variation between ambulance services analysis. The odds ratios of the random intercepts were displayed using caterpillar plots and the counties were coloured by ambulance service. An additional analysis investigated differences in the rankings of counties between ambulance services using a Kruskal–Wallis test.
For the second approach we fitted fixed-effect logistic regression models to calculate standardised non-conveyance rates using direct risk standardisation. 61 This approach to standardisation uses the predicted probability or risk of non-conveyance from the logistic regression and assigns them to a risk category. The risk categories for each county are then standardised using weights defined from the superset of all counties. This produces a standardised rate of non-conveyance per 100 incidents or calls. The direct risk standardised rate for each county was then displayed using funnel plots. 62 Funnel plots display the number of incidents or calls against the standardised rates with 95% and 99.8% limits (or 2 and 3 standard deviations). They are normally used to identify outlying institutions or services but in this case we use them to display variation within and between ambulance services.
Presentation of results
The quantitative results from the analysis are presented in this chapter. In addition, findings from the qualitative study in WP1 relating to calculations of rates of non-conveyance are presented here.
Results
Reconciling computer-aided dispatch data with published Ambulance Quality Indictors
In the AQIs, 537,046 calls received a telephone or face-to-face response from one of the 10 large ambulance services in England in November 2014. In our data set, we had 638,254 calls; these included calls from NHS 111, which were not included in the AQIs. We had 93,900 calls from NHS 111 in our data set and 544,354 calls from 999. That is, we had slightly more 999 calls than included in the AQIs. Some ambulance services matched the AQI data closely when responding to our data request but there were large disparities for telephone advice rates for Service H (see Appendix 7).
Applying national guidance for Ambulance Quality Indictor calculations to our data set
During our conversations with analysts in ambulance services we learnt that some services had not followed national guidance for calculating AQIs in terms of inclusion and exclusion of NHS 111 calls and calls from health-care professionals. We applied the guidance to their data to calculate what we termed ‘standardised AQIs’. Applying standardised definitions of AQIs changed the non-conveyance rates for some ambulances services but did not reduce variation between ambulance services. Figure 5 shows the variation in published AQIs for ambulance services A–J (first columns of graphs), variation in AQIs based on the November 2014 data sent to us by services (middle columns of graphs), and variation in AQIs based on the application of national guidance on calculating AQIs applied to the November 2014 data sent to us by services (final columns of graphs). The bold horizontal line on each graph in Figure 5 is the mean of the 10 ambulance services. The similarity of the graphs in each row for each of the four AQIs suggests that variation between ambulance services was not simply related to these differences in interpretation of the national guidance. However, even when services followed guidance it was apparent from our consideration of the data that the range of ways in which calls can end in practice is complex and calculations were open to subjective opinions about the inclusion, exclusion and categorisation of calls (e.g. cancelled calls, standing down an ambulance and definitions of calls ending in telephone advice). Therefore, Figure 5 does not indicate that variation was not explained by differences in calculations between ambulance services.
FIGURE 5.
Comparison of published AQIs by source (see ‘published’ column), AQIs based on the November 2014 data provided to this study by services (see ‘service data’ column), and AQIs calculated using national guidance on the November 2014 data provided by services to this study (see ‘standardised’ column). The horizontal black lines indicate the mean of the 10 ambulance services. (a) The proportion of calls closed by telephone service; (b) the proportion of incidents managed without the need for transport to A&E department; (c) the proportion of patients who recontacted following discharge of care, by telephone within 24 hours; and (d) the proportion of patients who recontacted following treatment and discharge at the scene, within 24 hours.
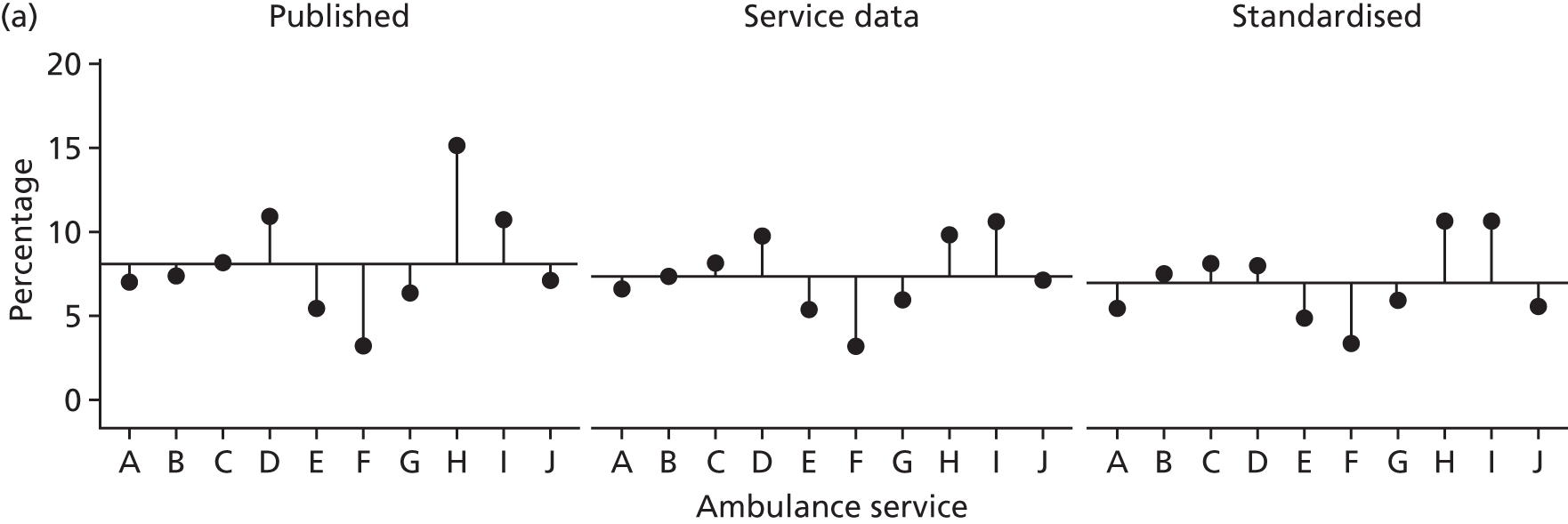
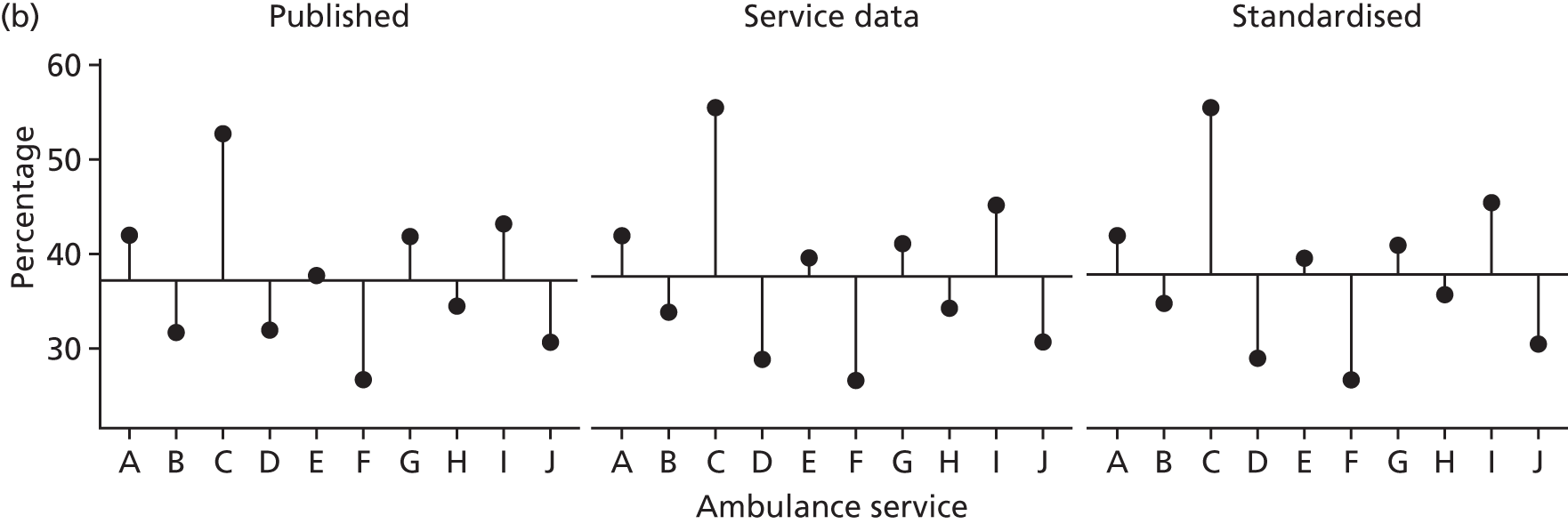


Deaths
Some people are not conveyed to an emergency department because they are pronounced dead when the ambulance crew arrives or die while the crew is present. These deaths are included in the AQIs and it would be helpful to consider variation with them removed. However, it was not possible to remove all of them consistently from our data set. Deaths are coded differently by the two triage systems, MPDS and NHS Pathways, and can be coded under a variety of headings. Therefore, attempting to remove deaths would have introduced variation between ambulance services into our data set. In WP3.2 (see Chapter 7) deaths could be identified with confidence for a single service: 3% (2099/63,852) of non-conveyed patients in this ambulance service were pronounced dead at scene, indicating the size of the contribution of death to non-conveyance rates.
Description of patient-level factors affecting non-conveyance
Ambulance quality indictor definitions require that NHS 111 and health-care professional calls are included or excluded from certain calculations. We included calls from all sources in our analyses to measure the effect of a range of factors on non-conveyance rates. The description below is based on all calls.
A total of 41% of all calls resulted in non-conveyance to a hospital with an emergency department (Table 3). Most of these were discharged at scene after attendance by an ambulance (29% of all calls). Smaller percentages were seen for calls ending in telephone advice (7%) or the conveying of the patient to an alternative service (4%). Services alternative to an emergency department included a mix of facilities. Names of services rather than types of service were documented in our data set so it was difficult to know what some of these services were. They included walk-in centres/urgent care centres/minor injury units, GP out-of-hours services, different types of hospitals (such as maternity, cancer, psychiatric, hospice/cancer, major trauma with specialist care available), and ‘home’ if an incident occurred elsewhere and a patient was transported to their home. Rates of all non-conveyance to a hospital with an emergency department varied between services, from 28% to 59% (see Appendix 7).
| Characteristic | Type of non-conveyance, % (n) | All calls (N = 615,815) | |||
|---|---|---|---|---|---|
| Telephone advice (N = 40,679) | Discharged at scene (N = 182,479) | Conveyed elsewhere (N = 28,519) | Conveyed to emergency department (N = 364,138) | ||
| Patient characteristics | |||||
| Age (years) | |||||
| 0–2 | 6.6 (1738) | 20.8 (5473) | 4.7 (1229) | 67.9 (17,867) | 26,307 |
| 3–10 | 8.5 (1450) | 24.9 (4242) | 4.1 (693) | 62.3 (10,671) | 17,056 |
| 11–20 | 8.3 (3320) | 29.1 (11,611) | 4.4 (1750) | 58.2 (23,197) | 39,878 |
| 21–30 | 9.5 (5931) | 30.0 (18,688) | 6.2 (3875) | 54.3 (33,874) | 62,368 |
| 31–40 | 8.7 (4227) | 28.4 (13,834) | 5.8 (2838) | 57.1 (27,857) | 48,756 |
| 41–50 | 6.9 (3659) | 27.0 (14,249) | 4.2 (2204) | 61.9 (32,703) | 52,815 |
| 51–60 | 6.2 (3154) | 26.3 (13,339) | 4.6 (2355) | 62.9 (31,917) | 50,765 |
| 61–70 | 5.5 (3205) | 25.9 (15,048) | 4.8 (2772) | 63.8 (37,135) | 58,160 |
| 71–80 | 4.7 (3841) | 27.3 (22,243) | 4.6 (3752) | 63.4 (51,650) | 81,486 |
| 81–90 | 4.5 (4408) | 32.0 (31,544) | 3.7 (3639) | 59.9 (59,032) | 98,623 |
| > 91 | 3.7 (1264) | 36.9 (12,479) | 3.1 (1057) | 56.2 (18,975) | 33,775 |
| Sex | |||||
| Male | 6.6 (18,044) | 28.0 (76,465) | 4.2 (11,536) | 61.1 (166,855) | 272,900 |
| Female | 6.5 (19,696) | 29.5 (89,870) | 4.7 (14,267) | 59.3 (180,699) | 304,532 |
| Area-level characteristics | |||||
| IMD quintile | |||||
| 1 (least deprived) | 6.1 (4757) | 32.1 (25,012) | 3.8 (2940) | 58.0 (45,238) | 77,947 |
| 2 | 6.2 (5938) | 31.3 (29,856) | 4.5 (4304) | 57.9 (55,198) | 95,296 |
| 3 | 6.5 (7345) | 31.2 (35,164) | 4.7 (5274) | 57.7 (65,101) | 112,884 |
| 4 | 6.9 (9602) | 29.2 (40,453) | 5.0 (6985) | 58.8 (81,422) | 138,462 |
| 5 (most deprived) | 6.7 (11,319) | 27.7 (46,588) | 4.6 (7730) | 61.0 (102,811) | 168,448 |
| Rural/urban | |||||
| Urban | 6.7 (34,485) | 29.2 (150,978) | 4.8 (24,587) | 59.3 (306,476) | 516,526 |
| Rural | 5.9 (4476) | 34.1 (26,095) | 3.5 (2646) | 56.6 (43,294) | 76,511 |
| Percentage of patients with no heating at home | |||||
| 1 (lowest) | 6.1 (7406) | 29.1 (35,055) | 4.3 (5146) | 60.5 (73,004) | 120,611 |
| 2 | 6.3 (7602) | 30.1 (36,144) | 4.2 (5059) | 59.3 (71,249) | 120,054 |
| 3 | 6.9 (8219) | 29.9 (35,536) | 4.8 (4646) | 58.4 (69,347) | 118,748 |
| 4 | 6.7 (7978) | 29.7 (35,174) | 5.1 (6070) | 58.5 (69,263) | 118,485 |
| 5 (highest) | 6.7 (7756) | 30.5 (35,164) | 4.6 (5312) | 58.1 (66,907) | 115,139 |
| Percentage of patients for whom English is not first language | |||||
| 1 (lowest) | 5.3 (6166) | 29.9 (34,850) | 3.7 (4281) | 61.1 (71,223) | 116,520 |
| 2 | 5.8 (6748) | 31.6 (37,021) | 3.9 (4511) | 58.7 (68,702) | 116,982 |
| 3 | 5.9 (6960) | 31.6 (37,218) | 4.3 (5044) | 58.3 (68,682) | 117,904 |
| 4 | 7.0 (8358) | 29.9 (35,752) | 4.7 (5595) | 58.5 (70,057) | 119,762 |
| 5 (highest) | 8.8 (10,729) | 26.4 (32,232) | 6.4 (7802) | 58.3 (71,106) | 121,869 |
| Percentage of patients living alone | |||||
| 1 (lowest) | 6.8 (8148) | 28.9 (34,636) | 4.6 (5545) | 59.7 (71,501) | 119,830 |
| 2 | 6.6 (7850) | 29.9 (35,312) | 4.2 (5009) | 59.3 (70,124) | 118,295 |
| 3 | 6.3 (7453) | 29.9 (35,209) | 4.7 (5501) | 59.1 (69,600) | 117,763 |
| 4 | 6.4 (7637) | 29.6 (35,110) | 4.5 (5376) | 59.4 (70,396) | 118,519 |
| 5 (highest) | 6.6 (7873) | 31.0 (36,806) | 4.9 (5802) | 57.4 (68,149) | 118,630 |
| Percentage of patients with a severe long-term illness | |||||
| 1 (lowest) | 7.8 (9339) | 31.0 (37,044) | 4.8 (5742) | 56.4 (67,493) | 119,618 |
| 2 | 7.1 (8356) | 30.0 (35,509) | 4.7 (5535) | 58.3 (69,017) | 118,417 |
| 3 | 6.6 (7820) | 30.3 (35,880) | 4.6 (5502) | 58.4 (69,196) | 118,398 |
| 4 | 6.2 (7289) | 30.0 (35,353) | 4.2 (4939) | 59.6 (70,074) | 117,655 |
| 5 (highest) | 5.2 (6157) | 28.0 (33,287) | 4.6 (5515) | 62.2 (73,990) | 118,949 |
| Call characteristics | |||||
| Time of call | |||||
| Out of hours | 7.2 (29,132) | 31.2 (126,798) | 4.0 (16,370) | 57.7 (234,608) | 406,908 |
| In hours | 5.5 (11,547) | 26.7 (55,681) | 5.8 (12,149) | 62.0 (129,530) | 208,907 |
| Source of call | |||||
| 999 | 7.2 (38,146) | 29.0 (154,027) | 4.8 (25,734) | 59.0 (313,384) | 531,291 |
| NHS 111 | 3.0 (2533) | 33.7 (28,452) | 3.3 (2785) | 60.0 (50,754) | 84,524 |
| Type of caller | |||||
| HCP | 0.7 (296) | 6.7 (3031) | 17.5 (7860) | 75.1 (33,718) | 44,905 |
| Patient | 7.4 (36,878) | 30.8 (153,853) | 3.9 (19,218) | 57.9 (289,104) | 499,053 |
| Reason for call | |||||
| Abdominal pain | 25.9 (3269) | 18.2 (2299) | 2.2 (283) | 53.6 (6771) | 12,622 |
| Breathing | 3.5 (1681) | 26.6 (12,698) | 2.8 (1323) | 67.1 (32,035) | 47,737 |
| Suspected cardiovascular problems | 2.7 (1727) | 22.0 (14,102) | 3.6 (2308) | 71.7 (45,851) | 63,988 |
| Falls | 4.2 (2764) | 42.5 (28,092) | 2.5 (1630) | 50.8 (33,589) | 66,075 |
| Fitting | 2.7 (500) | 28.5 (5317) | 2.3 (430) | 66.5 (12,401) | 18,648 |
| Injury | 8.7 (5647) | 30.9 (20,201) | 3.6 (2347) | 56.8 (37,084) | 65,279 |
| Psychiatric problems | 9.4 (1144) | 33.3 (4048) | 5.1 (615) | 52.2 (6341) | 12,148 |
| Person sick or unconscious | 12.9 (8544) | 29.1 (19,245) | 2.6 (1713) | 55.4 (36,699) | 66,201 |
| Other | 9.0 (7367) | 33.2 (27,169) | 5.2 (4292) | 52.5 (42,968) | 81,796 |
| Ambulance processes | |||||
| Triage system | |||||
| MPDS | 6.5 (26,660) | 27.9 (113,912) | 5.2 (21,120) | 60.4 (247,100) | 408,792 |
| NHS Pathways | 6.8 (14,019) | 33.1 (68,567) | 3.6 (7399) | 56.5 (117,038) | 207,023 |
| Urgency level allocated | |||||
| Red 1 (high) | 0.5 (66) | 41.4 (5799) | 3.2 (452) | 54.9 (7677) | 13,994 |
| Red 2 | 0.5 (1328) | 26.1 (64,261) | 4.4 (10,927) | 68.9 (169,439) | 245,955 |
| Green 1 | 3.2 (869) | 26.9 (7328) | 2.7 (731) | 67.2 (18,307) | 27,235 |
| Green 2 | 2.1 (4531) | 36.8 (77,799) | 3.7 (7823) | 57.4 (121,544) | 211,697 |
| Green 3 | 16.8 (3986) | 31.3 (7415) | 2.9 (698) | 49.0 (11,626) | 23,725 |
| Green 463 | 26.6 (22,896) | 23.0 (19,842) | 9.1 (7879) | 41.3 (35,542) | 86,159 |
| Highest skill level | |||||
| Advanced | 1.9 (604) | 43.9 (14,287) | 3.7 (1197) | 50.6 (16,463) | 32,551 |
| Paramedic | 0.7 (2882) | 31.3 (131,058) | 4.4 (18,268) | 63.7 (266,956) | 419,164 |
| Other | 1.7 (1254) | 29.4 (22,150) | 6.8 (5159) | 62.1 (46,885) | 75,448 |
Patient characteristics
There were differences for some of the eight patient characteristics tested (see Table 3).
For calls ending in telephone advice, rates were higher for younger people (6–9% in patients aged < 60 years compared with 4–5% in those aged > 60 years), people for whom English was not a first language (9% vs. 5%) and people living in areas with lower prevalence of severe long-term illness (8% vs. 5%).
For discharge at scene after attendance by an ambulance, rates based on all calls were higher for very old people (37% for people aged > 90 years compared with 21% for those aged < 2 years) and higher in affluent areas (32% vs. 28%), in rural areas (34% vs. 29%) and in areas in which there were low numbers of people for whom English is not a first language (≥ 30% vs. 26%).
There were no important differences for patients transported elsewhere.
For non-conveyance overall (defined as all calls following which a patient was not conveyed to an emergency department), there were differences in terms of age extremes: very old people aged > 90 years were more likely to be non-conveyed (44%) and children aged 0–2 years were less likely to be non-conveyed (32%). Non-conveyance overall was higher in areas with lower prevalence of severe long-term illness than in areas with higher prevalence (44% vs. 38%).
Call characteristics
For calls ending in telephone advice, rates were higher if patients called 999 rather than NHS 111 (7% vs. 3%) because services are not supposed to retriage NHS 111 calls. Rates were also higher for calls made by patients rather than by health-care professionals (7% vs. 1%) and for some reasons for making the call, for example abdominal pain compared with a cardiovascular problem (26% vs. 3%).
Discharge at scene rates, based on all calls, were higher if calls were made out of hours (31% vs. 27%), came from NHS 111 rather than 999 (34% vs. 29%), were made by patients rather than health-care professionals (31% vs. 7%) and were made for particular reasons, for example falls compared with abdominal pain (42% vs. 18%).
Rates of conveyance elsewhere, based on all calls, were higher if a health-care professional rather than a patient called (18% vs. 4%).
Rates of non-conveyance overall differed by time of call, who made the call and the reason for the call (see Table 3). Rates were higher for calls made out of normal working hours (42% vs. 38%), calls made by patients rather than health-care professionals (42% vs. 25%), and for falls (49%) and psychiatric problems (48%) compared with cardiovascular (28%) and breathing problems (33%).
Ambulance processes
Rates of calls ending in telephone advice differed by urgency level, with higher rates for low urgency calls than for high urgency calls (27% vs. 0.5%). Rates of discharge at scene were higher for the NHS Pathways triage system than for MPDS (33% vs. 28%), for high-urgency calls than for low-urgency calls (41% vs. 23% – because deaths are likely to be included in ‘Red 1’ calls) and for advanced paramedics than for paramedics (44% vs. 31%). Rates of transport elsewhere were higher for low-urgency calls (9% vs. 2%). Rates of non-conveyance overall were higher for low-urgency calls than for high-urgency calls (59% vs. 31%) and for calls attended by an advanced paramedic than for calls attended by a paramedic (49% vs. 36%).
Explaining variation between ambulance services
Focus on telephone advice and discharge at scene only
Further analysis was not undertaken for patients conveyed elsewhere because the proportion of calls with this end point was small and it included such a diverse mix of low-acuity services (such as minor injury units), high-acuity services (such as specialist services) and end-of-life services (such as hospices) that it would be impossible to draw conclusions from any analysis.
Adjusting for patient-level variables in the regressions
Patient-level variables in the telephone-advice-only regression were age, sex, time of call, condition, living in an area with a different percentage of long-term conditions and living in an area with a different percentage of deprivation.
Patient-level variables in the final discharge at scene regression were age, sex, time of call, condition, urgency level of call, source of call, highest level skill-mix of attending crew, living in an area with a different percentage of long-term conditions and living in an area with a different percentage of deprivation.
Explaining variation between services: telephone advice only
There were no skill-mix data available for telephone-advice-only calls so the primary analysis was undertaken on all 10 ambulance services (see Appendix 8). The denominator was all calls. There was considerable variation between ambulance services in terms of their telephone-advice-only rates (between ambulance service variance = 0.0991; Figure 6a). When patient-level variables were tested, this variation between ambulance services remained (variance = 0.1214; Figure 6b), even though telephone-advice-only rates varied by some patient characteristics (see Appendix 8). When ambulance service-level variables were tested, none explained the variation between ambulance services. Therefore, the variation in telephone advice rates between ambulance services could not be explained.
FIGURE 6.
Variation in telephone-advice-only rates between ambulance services explained in regression (based on 10 ambulance services, including calls from NHS 111). (a) Null model; and (b) model with patient-level variables.

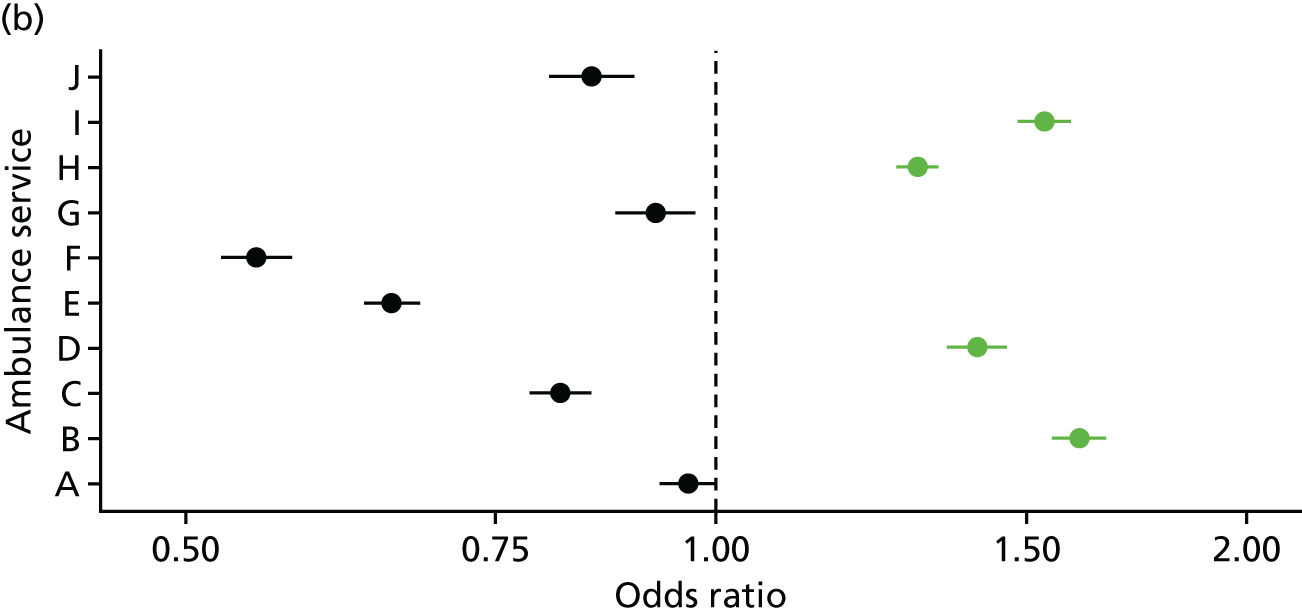
Explaining variation between services: discharge at scene
Only nine ambulance services provided skill-mix data in terms of the type of crew attending individual calls. The primary analysis was undertaken on these nine services (see Appendix 9). The denominator was all calls attended by an ambulance. There was considerable variation between ambulance services for their discharge-at-scene rates (between ambulance service variance = 0.1206; Figure 7a). When patient-level variables were tested, this variation between ambulance services remained (variance = 0.1142; Figure 7b) even though discharge-at-scene rates varied by some patient-level variables (see Appendix 9). When ambulance service-level variables were tested, variation in discharge-at-scene rates reduced considerably (variance = 0.0095; Figure 7c). Variation between ambulance services was explained by three ambulance service-level variables after adjustment for patient-level variables:
-
Ambulance services with higher proportions of calls attended by advanced paramedics had higher discharge-at-scene rates [odds ratio 1.05, 95% confidence interval (CI) 1.04 to 1.07], taking into account that patient-level data showed that advanced paramedics had a higher discharge-at-scene rate than paramedics (odds ratio 1.38, 95% CI 1.34 to 1.42).
-
Ambulance services for which interviewees in WP1 described the management as risk averse to non-conveyance had lower discharge-at-scene rates (odds ratio 0.78, 95% CI 0.61 to 0.98).
-
Ambulance services for which interviewees in WP1 described advanced paramedics as an established and valued part of the workforce had higher discharge-at-scene rates (odds ratio 1.82, 95% CI 1.31 to 2.34).
A secondary analysis was undertaken by excluding skill-mix variables from the ambulance routine data and thereby including all 10 ambulance services. This regression failed to explain variation between ambulance services (see Appendix 10), although the odds ratios of variables were very similar to those in the regression that included skill-mix.
FIGURE 7.
Variation in discharge-at-scene rates between ambulances services explained in regression (based on nine ambulance services with skill-mix data, including calls from NHS 111). (a) Null model; (b) model with patient-level variables; and (c) model with patient and ambulance service-level variables. Black dots, odds ratio of < 1; green dots, odds ratio of > 1.
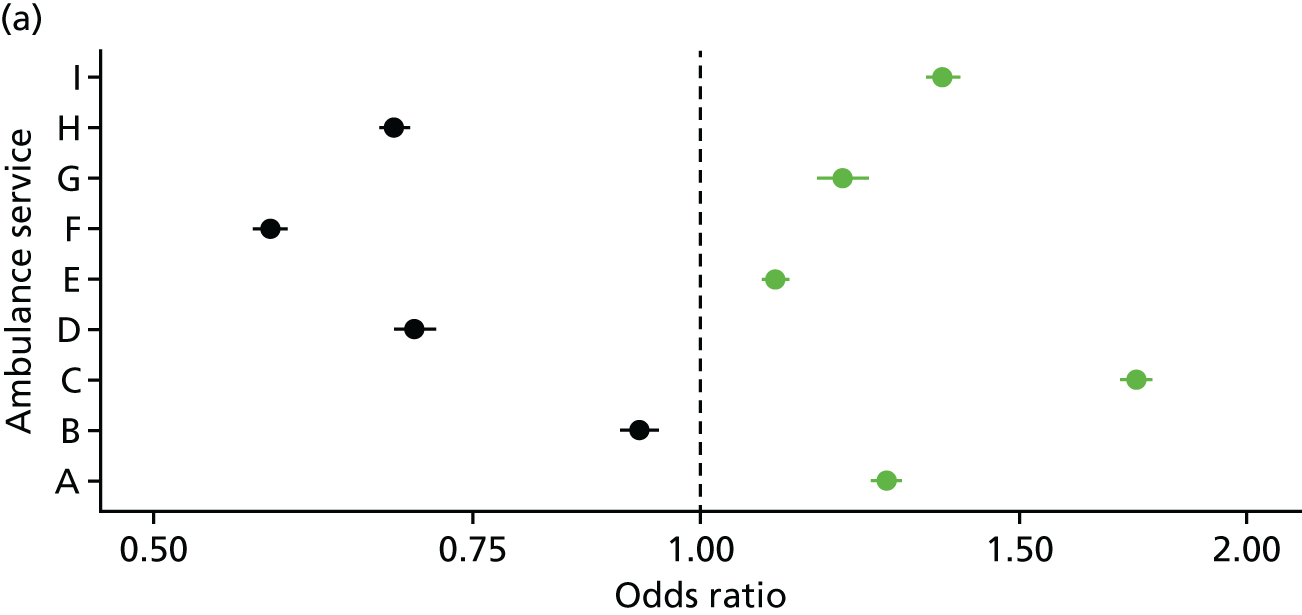

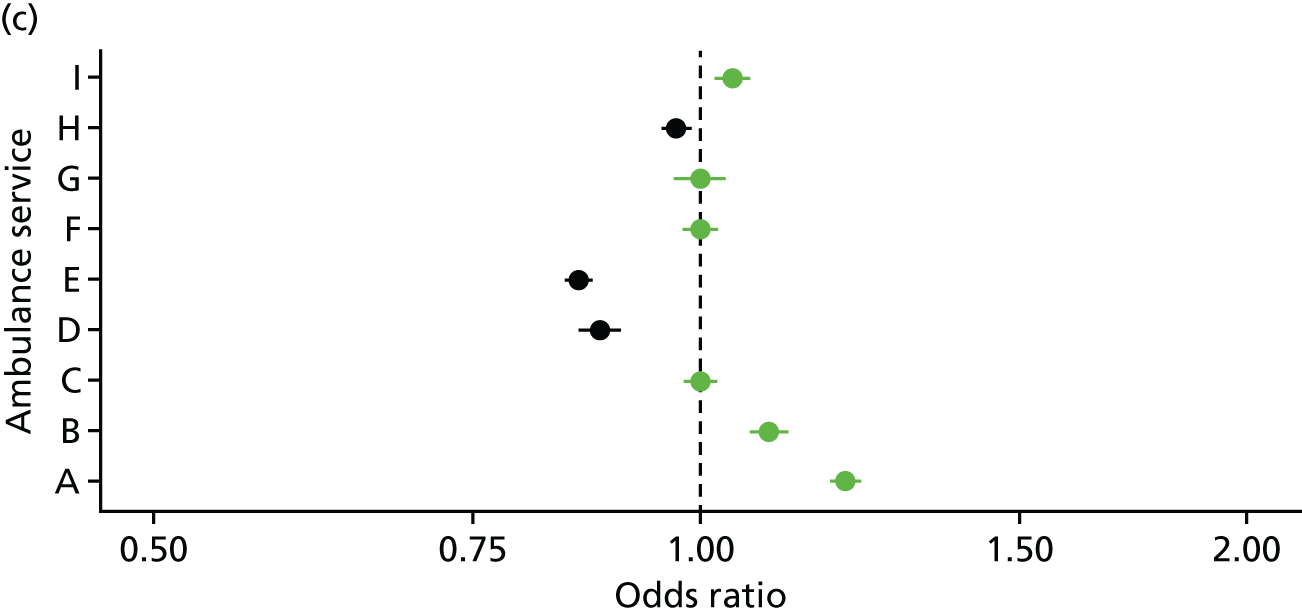
Exploring variation within ambulance services: telephone advice
Telephone-advice-only rates for localities within ambulance services, adjusted for patient-level variables, are displayed in Figure 8. The denominator was all calls. The localities for each ambulance service have the same colour dot. This shows that there is variation in telephone-advice-only rates within ambulance services but that the variation between ambulance services is larger than the variation within ambulance services (Kruskal–Wallis test p < 0.001). A caterpillar plot showed the same pattern (see Appendix 11).
FIGURE 8.
Telephone-advice-only rates for localities within ambulance services, adjusted for patient-level variables (all 10 services, including calls from NHS 111).
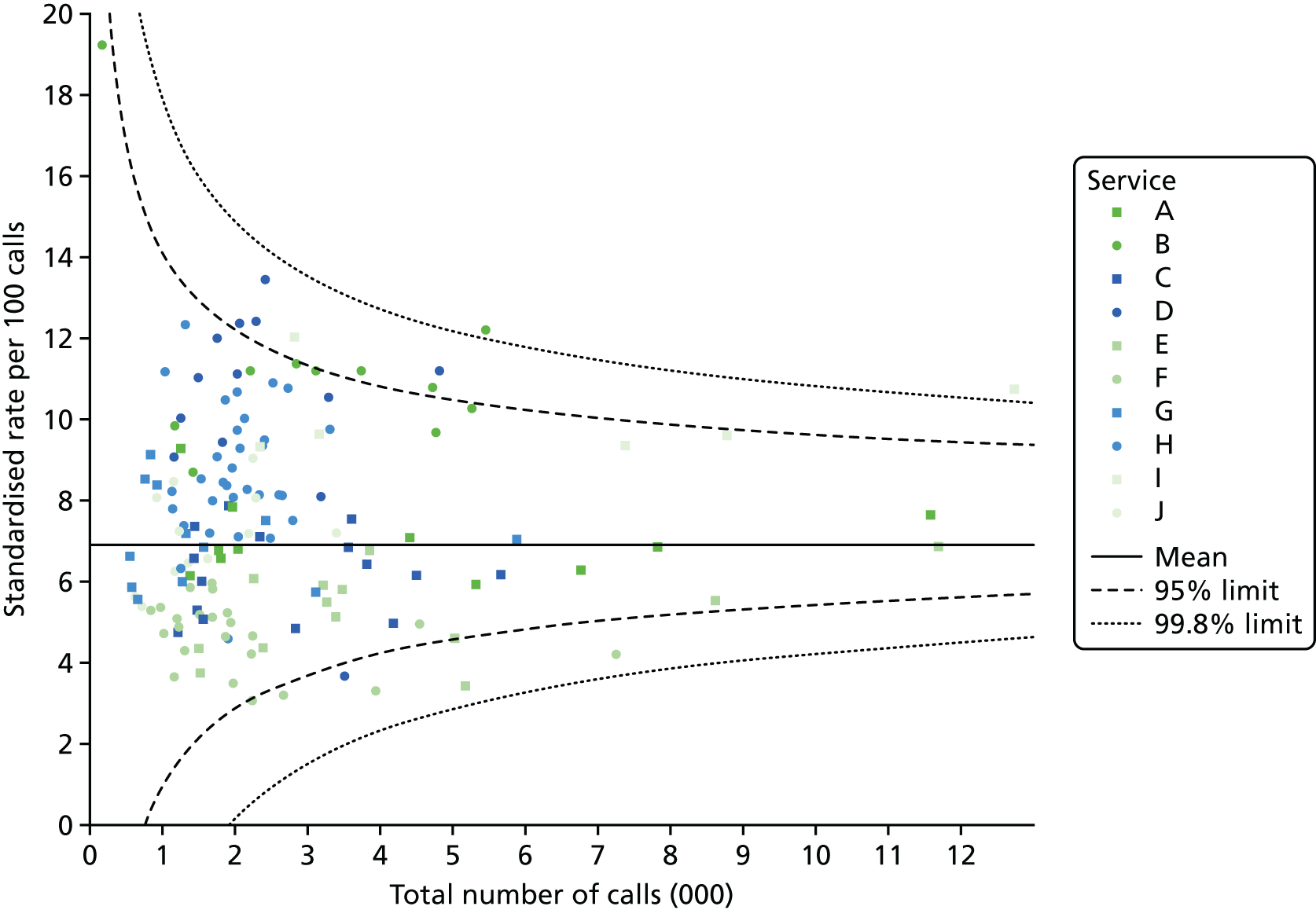
Exploring variation within ambulance services: discharge at scene
Discharge at scene rates for localities within ambulance services, adjusted for patient-level variables, are displayed in Figure 9. The denominator was all calls attended by an ambulance. The localities for each ambulance service have the same colour dot. This shows that there is variation in discharge-at-scene rates within ambulance services but that the variation between ambulance services is larger than the variation within ambulance services (Kruskal–Wallis test p < 0.001). A similar graph for all 10 services, not adjusted for skill-mix, showed the same pattern (not shown). A caterpillar plot showed the same pattern (see Appendix 11).
FIGURE 9.
Discharge at scene rates for localities within ambulance services, adjusted for patient-level variables (nine ambulance services only because adjusted for skill-mix, including calls from NHS 111).
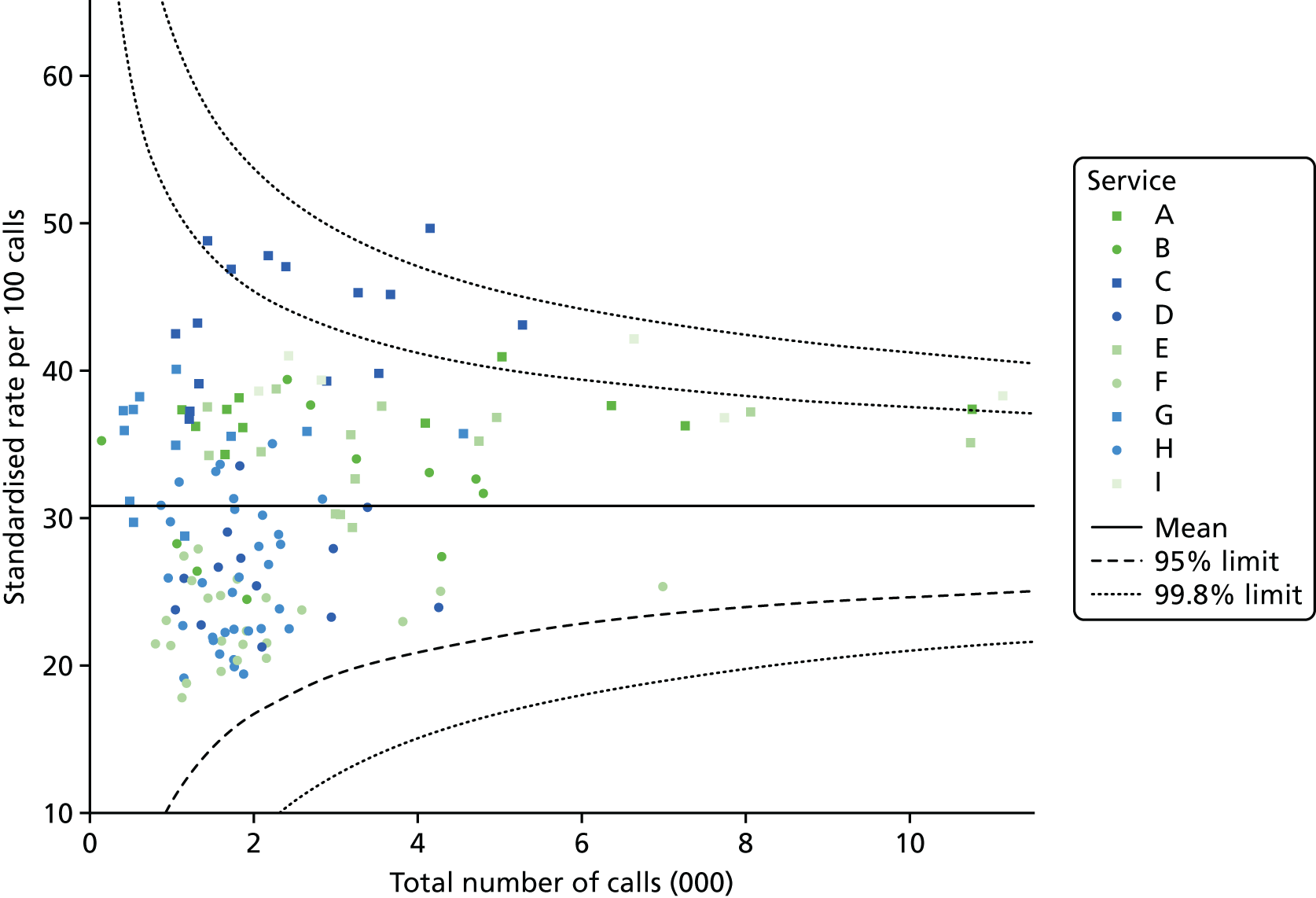
Interviewees’ views of measures of non-conveyance
Inconsistencies in the coding of data
Some interviewees from WP1 (see Chapter 4) suggested that it was not helpful to compare non-conveyance rates between ambulance services because there were inconsistencies in how each service calculated their non-conveyance rates. For example, a senior manager in one service felt that the AQI guidelines, particularly in relation to calls ending in telephone advice, were open to interpretation and was not confident of the accuracy of this AQI for different services:
We take the very hard-core approach to this, ‘this is what the handbook says’, and we do an exact interpretation of it, whereas it’s very easy for others to give slightly different interpretations and there’s no one who enforces that, so you could pretty much make, measure what you wanted within reason and report it as that stat.
Senior manager, interviewee 4
Range of ‘telephone advice’ calls
During WP1 interviews, the interviewer used the definition of telephone advice as calls receiving further triage by a clinician over the telephone, resulting in advice or onward referral to another service without a face-to-face assessment of the patient. However, paramedics described examples of calls that might be categorised as ending in telephone advice but for which crews attended the patient in person, namely crew on the scene and referral to a GP out-of-hours service to call the patient at home, or crew on the scene and referral of the patient back to 999 for telephone advice from the clinician in the clinical hub.
Discussion
Summary of findings
We could not eliminate variation in calculations of different types of non-conveyance between ambulance services. Only a small amount of variation in non-conveyance rates between services was explained by patient-level variables, most of which were non-modifiable by ambulance services. Variation in telephone-advice-only rates between ambulance services could not be explained. However, a considerable amount of variation in discharge-at-scene rates was explained by three ambulance service-level variables: ambulance services with a higher proportion of calls attended by advanced paramedics, or that reported valuing advanced paramedics for non-conveyance, had higher discharge-at-scene rates; ambulance services reporting risk-averse views of non-conveyance among managers had lower rates of discharge at scene. There was variation in non-conveyance rates within ambulance services but this was smaller than variation between services.
Putting the findings in context
Similarly to our study, ambulance service personnel expressed concerns about inconsistencies in calculations of ‘Hear and Treat’ AQIs in the recent NAO report. 1 A secondary triage service in an Australian ambulance service found that abdominal and back pain were the most common problems dealt with by telephone,21 which aligns with our finding that calls for abdominal pain were more likely to end in telephone advice than other conditions. Population rates of secondary triage have been found to be higher for deprived communities21 but we did not consider population rates in our study. Similarly to our study, in a systematic review and meta-analysis, advanced paramedics have been shown to discharge at scene more than conventional crews,31 although the odds ratio was considerably larger than our study (10.5 vs. 1.4, respectively). We found no other research explaining variation between ambulance services.
Strengths and limitations
This is the first large study attempting to explain variation between different ambulance services. The data set was large and we were able to test a wide range of variables. There were five limitations. First, there were 2 days of industrial dispute in November 2014 when some ambulance staff were on strike. Even given this, November 2014 did not appear to be unusual in any way when compared with previous and future months in AQI statistics. Second, we were unable to construct a data set that eliminated differences in calculations of different types of non-conveyance by ambulance services. Third, data were missing for some factors for some services and we undertook a complete case analysis. Fourth, there may have been differences in interpretation of the term ‘advanced paramedic’ by the different ambulance services. Fifth, some of the ambulance service-level variables tested were derived from the WP1 qualitative interviews. It is possible that knowledge of their ambulance service AQIs and ranking compared with other ambulance services may have led some interviewees to describe their service in a particular way. It is also possible that our coding of qualitative interview data was influenced by our knowledge of the AQIs for each ambulance service. To guard against this, Emma Knowles and Lindsey Bishop-Edwards were blinded to the AQIs until the coding of qualitative findings was complete.
Implications
A large amount of variation between ambulance services in telephone-advice-only rates remained unexplained at the end of this analysis. This variation could be explained by variables that we did not test. For example, in WP1 patient expectations were identified as affecting non-conveyance rates but have not been tested here. However, we would be surprised if this variable explained variation between services because of the range of case-mix variables we tested, some of which are likely to be related to patient expectations. Variation could also be explained by differences in the way telephone-advice-only calls are identified by different ambulance services, an issue we could not test for in this study. A considerable amount of variation between discharge-at-scene rates was explained by factors potentially modifiable by ambulance services: the numbers of advanced paramedics in their service, how these advanced paramedics were used, and whether non-conveyance was seen as an opportunity or a risk by management.
Chapter 6 Potentially inappropriate non-conveyance: variation between ambulance services in 24-hour recontact rates with the ambulance service (work package 3.1)
Background
Each ambulance service calculates the proportion of callers recontacting their service within 24 hours of any call that ended in non-conveyance. As reported earlier (see Chapter 5), these recontacts are based on calls from people of the same sex and postal address as the original call. Therefore, they may not be true recontacts. In addition, it is possible that people call the ambulance service within 24 hours for a problem unrelated to the original call.
According to the national AQIs, the proportion of recontacts for calls ending in telephone advice has been decreasing over the years, from 8% at the time of data collection for this study (November 2014) to 6% in recent months (December 2016); see Appendix 3. The proportion of recontacts for patients who receive an ambulance response but are not conveyed to an emergency department has remained steady, at around 5% over this time.
This chapter is based largely on routine data collected by ambulance services and the methods reported below focus on this data collection. We also include a small number of themes related to recontacts with the ambulance service from the WP1 qualitative research reported in Chapter 4 and refer the reader back to the Methods section, in which the methods of this qualitative research are detailed.
Methods
We obtained data on recontacts for all 10 ambulance services. We had concerns about the quality of the data for three services (C, H and I) because analysts at those services could not give us a data set that matched published AQIs (see Appendix 7). In addition, we did not have sufficient detail within our data to check the consistency of the way these rates were calculated by each ambulance service. Most services provided recontact data only for calls sourced from 999 rather than NHS 111 because the AQIs exclude NHS 111 calls. Therefore, we excluded NHS 111 calls from the analysis.
The analysis was similar to that described in Chapter 5 for WP2. We describe how recontact rates for telephone advice only and discharge at scene varied by patient-level variables. In these analyses we compared the characteristics of the original calls that had resulted in recontacts with original calls that had not resulted in recontacts. We then undertook logistic regression to test different patient-level and ambulance service-level variables to determine factors explaining variation in recontact rates between ambulance services.
We asked interviewees in WP1 about recontact rates and AQIs measuring recontact rates and these findings are reported here.
Results
Description of patient-level factors affecting non-conveyance
The recontact rate was 8.8% (3300/37,435) for calls ending in telephone advice and 5.1% (7690/152,106) for patients discharged at scene. This compared with the national AQIs of 8.1% (3737/46,355) and 5.5% (8997/163,205) respectively during that month.
Calls ending in telephone advice were more likely to result in a recontact if they were about older people (recontact rate of > 10% for > 40-year-olds compared with < 5% for < 10-year-olds), from areas with low levels of English not being the first language (12% vs. 6%), from areas with high levels of severe long-term illness (12% vs. 7%), for calls about psychiatric problems and abdominal pain (> 11%), and for low urgency calls (> 11%) (Table 4).
| Characteristic | Telephone advice (N = 37,435), % (n/N) | Discharged at scene (N = 152,106), % (n/N) |
|---|---|---|
| Patient characteristics | ||
| Age (years) | ||
| 0–2 | 3.7 (60/1614) | 2.4 (90/3706) |
| 3–10 | 4.6 (62/1339) | 2.2 (64/2914) |
| 11–20 | 5.7 (175/3073) | 2.6 (250/9654) |
| 21–30 | 7.4 (406/5517) | 3.3 (499/15,253) |
| 31–40 | 8.3 (331/3968) | 4.0 (457/11,517) |
| 41–50 | 10.4 (358/3429) | 4.8 (568/11,841) |
| 51–60 | 11.6 (343/2951) | 5.8 (651/11,147) |
| 61–70 | 12.8 (377/2943) | 5.7 (725/12,730) |
| 71–80 | 12.1 (433/3566) | 6.2 (1194/19,149) |
| 81–90 | 12.1 (503/4172) | 6.7 (1832/27,534) |
| > 91 | 10.5 (125/1195) | 6.7 (743/11,032) |
| Sex | ||
| Male | 8.4 (1421/16,940) | 5.1 (3359/66,276) |
| Female | 9.9 (1805/18,184) | 5.2 (3904/74,625) |
| Area-level characteristics | ||
| IMD quintile | ||
| 1 (least deprived) | 8.7 (380/4346) | 5.0 (989/19,973) |
| 2 | 8.9 (479/5380) | 4.8 (1170/24,470) |
| 3 | 9.2 (615/6712) | 5.1 (1489/29,180) |
| 4 | 8.7 (766/8830) | 5.4 (1853/34,250) |
| 5 (most deprived) | 9.0 (958/10,595) | 5.0 (1988/39,641) |
| Rural/urban | ||
| Urban | 8.6 (2743/31,847) | 5.2 (6516/126,191) |
| Rural | 11.3 (455/4016) | 4.6 (973/21,323) |
| Percentage of patients for whom English is not a first language | ||
| 1 (lowest) | 11.9 (667/5619) | 5.0 (1439/28,613) |
| 2 | 11.0 (662/6034) | 5.2 (1578/30,172) |
| 3 | 9.3 (588/6317) | 5.5 (1662/30,337) |
| 4 | 8.4 (641/7645) | 5.3 (1582/29,862) |
| 5 (highest) | 6.2 (640/10,245) | 4.3 (1228/28,530) |
| Percentage of patients living alone | ||
| 1 (lowest) | 7.6 (568/7479) | 4.6 (1282/27,824) |
| 2 | 9.7 (686/7106) | 5.1 (1468/28,716) |
| 3 | 9.2 (630/6811) | 5.4 (1576/29,121) |
| 4 | 9.4 (665/7086) | 5.1 (1512/29,404) |
| 5 (highest) | 8.8 (649/7381) | 5.1 (1651/32,449) |
| Percentage of patients with a severe long-term illness | ||
| 1 (lowest) | 6.6 (571/8692) | 4.6 (1389/30,360) |
| 2 | 7.7 (587/7021) | 4.4 (1299/29,363) |
| 3 | 9.3 (672/7205) | 5.2 (1551/29,839) |
| 4 | 10.4 (697/6705) | 5.5 (1649/29,735) |
| 5 (highest) | 11.9 (671/5653) | 5.7 (1601/28,217) |
| Call characteristics | ||
| Time of call | ||
| Out of hours | 8.9 (2362/26,489) | 5.2 (5331/101,765) |
| In hours | 8.6 (938/10,946) | 4.7 (2359/50,341) |
| Type of caller | ||
| HCP | 2.4 (7/292) | 2.9 (85/2935) |
| Patient | 8.6 (2905/33,886) | 5.0 (6427/128,046) |
| Reason for call | ||
| Abdominal pain | 11.4 (369/3230) | 6.8 (139/2040) |
| Breathing | 8.2 (134/1633) | 6.1 (734/12,004) |
| Suspected cardiovascular problems | 7.9 (132/1668) | 4.9 (662/13,379) |
| Falls | 8.3 (227/2740) | 6.1 (1684/27,411) |
| Fitting | 5.8 (29/499) | 5.3 (278/5239) |
| Injury | 6.8 (374/5516) | 3.7 (741/19,859) |
| Psychiatric problems | 12.8 (138/1076) | 6.1 (239/3912) |
| Person sick or unconscious | 10.1 (844/8372) | 4.9 (891/18,269) |
| Other | 11.4 (820/7176) | 4.7 (1232/26,202) |
| Ambulance processes | ||
| Triage system | ||
| MPDS | 8.5 (2134/25,018) | 4.8 (4675/98,319) |
| NHS Pathways | 9.4 (1166/12,417) | 5.6 (3015/53,787) |
| Urgency level | ||
| Red 1 (high) | 0.0 (0/62) | 2.1 (112/5400) |
| Red 2 | 2.6 (32/1242) | 5.0 (2657/52,771) |
| Green 1 | 3.0 (25/846) | 3.8 (258/6874) |
| Green 2 | 2.4 (88/3721) | 5.2 (3274/62,655) |
| Green 3 | 11.0 (437/3966) | 5.0 (355/7169) |
| Green 4 | 11.0 (2394/21,758) | 6.0 (1034/17,202) |
| Highest skill level | ||
| Advanced | Missing | 4.6 (546/11,755) |
| Paramedic | Missing | 5.0 (5486/110,592) |
| Other | Missing | 5.2 (944/18,142) |
For discharge at scene, there was little variation in recontact rates by characteristics. The largest difference was a higher recontact rate for older people (6% in > 50-year-olds compared with 2% for < 10-year-olds) (see Table 4). There was no evidence of differences by skill-mix.
Explaining variation between ambulance services
Explaining variation between services: telephone advice only
There was considerable variation between ambulance services in recontact rates for calls ending in telephone advice (variance = 0.0790; Figure 10a). This variation was not explained by patient-level variables (variance = 0.0534; Figure 10b). All the variation was explained by ambulance service-level variables after adjustment for patient-level variables (variance < 0.0001; Figure 10c). The regression details are shown in Appendix 12. In summary, the ambulance-service-level variables explaining variation were:
-
Recontact rates were higher in ambulance services covering a large number (odds ratio 1.22, 95% CI 1.06,1.40) or a small number of CCGs (odds ratio 1.41, 95% CI 1.19 to 1.67).
-
Recontact rates were higher for which the perception of telephone advice provision within an ambulance service reported by our interviewees in WP1 was negative (odds ratio 1.36, 95% CI 1.20 to 1.53).
-
Recontact rates were lower in ambulance services for which the cost per call reported in the NAO report1 was high (odds ratio 0.76, 95% CI 0.66 to 0.87).
FIGURE 10.
Variation in recontact rates with ambulance service after telephone advice only between ambulance services explained in regression (based on 10 ambulance services, excludes calls from NHS 111). (a) Null model; (b) model with patient-level variables; and (c) model with patient- and ambulance service-level variables.
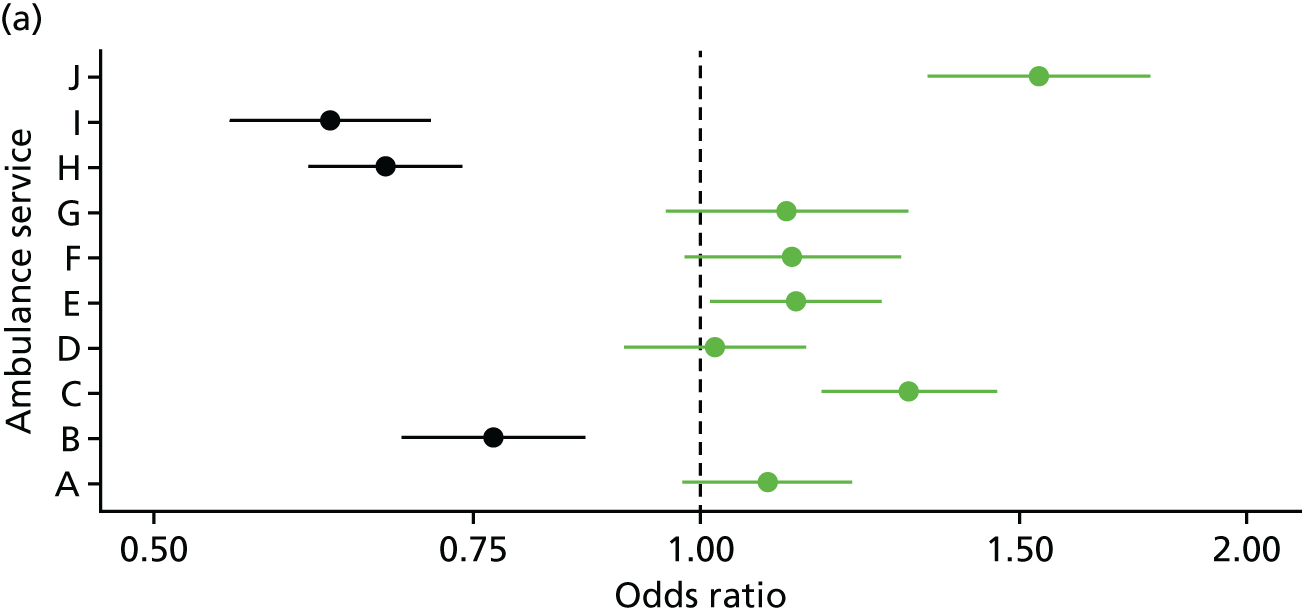
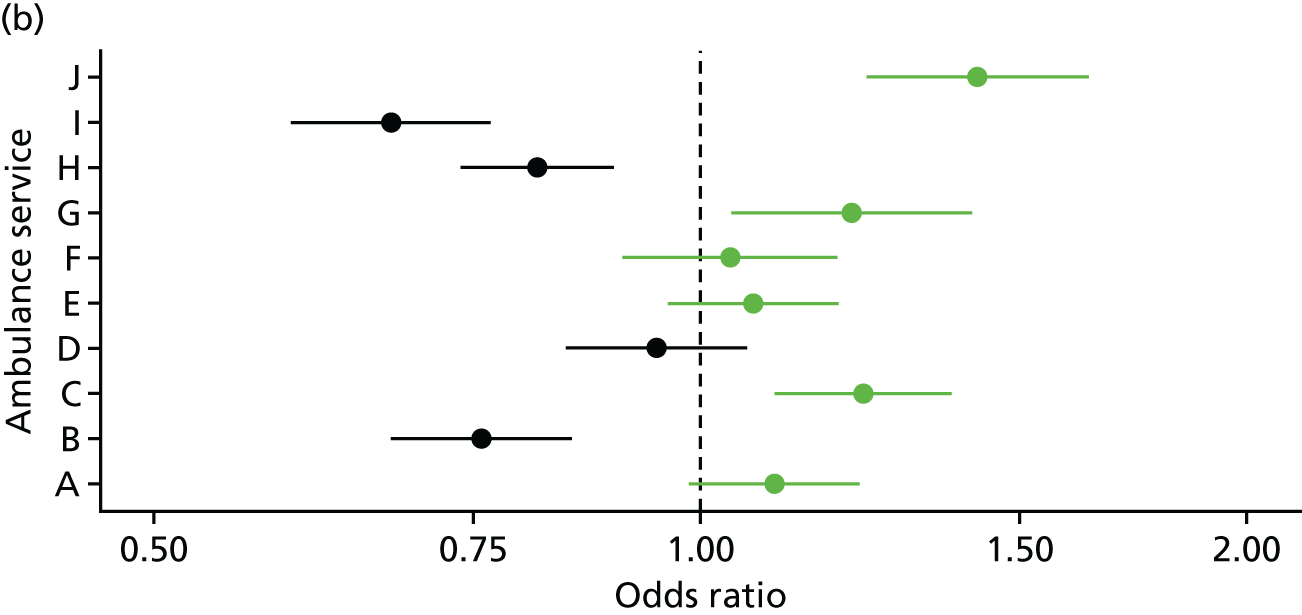
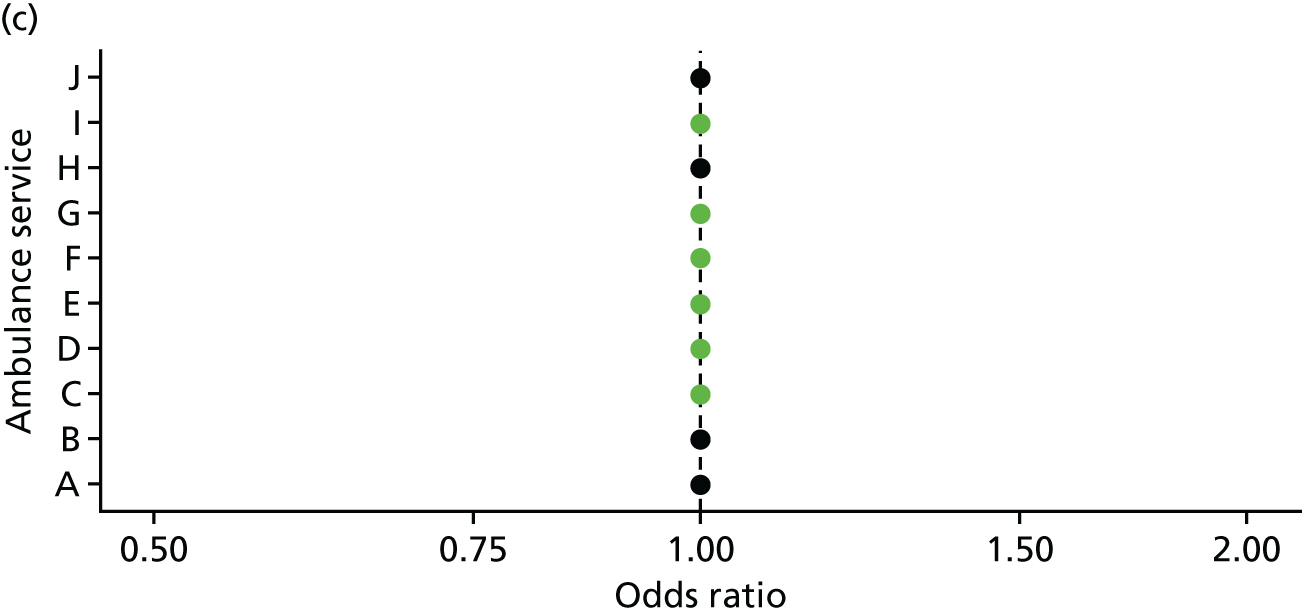
Explaining variation between services: discharge at scene
As in Chapter 5, skill-mix data were not available for one ambulance service. The primary analysis was undertaken on the nine ambulance services with skill-mix data. There was considerable variation between ambulance services in recontact rates for calls ending in discharge at scene (variation = 0.0181; Figure 11a). This variation was not explained by patient-level variables (variance = 0.0285; see Figure 11b). All the variation was explained by ambulance service-level variables after adjustment for patient-level variables (variance = 0.0004; Figure 11c). The regression details are shown in Appendix 13. In summary, the ambulance service-level variables explaining variation were:
-
Recontact rates were higher in services for which advanced paramedics were reported in the WP1 interviews as being more established (odds ratio 1.16, 95% CI 1.06 to 1.28) and lower in services for which there was reported limited use of advanced paramedics (odds ratio 0.87, 95% CI 0.79 to 0.96). This took into account that, for patient-level data, advanced paramedics had the same recontact rates as paramedics (odds ratio 0.95, 95% CI 0.86 to 1.04).
-
Recontact rates were higher in services for which the NAO reported high levels of advanced practitioners within frontline staff (odds ratio 1.38, 95% CI 1.27 to 1.51).
The results were similar when all 10 services were included and skill-mix variables excluded, although some variables were not statistically significant and less variation was explained (see Appendix 14).
FIGURE 11.
Variation in recontact rates for discharge at scene between ambulance services explained in regression (based on 9 ambulance services with skill-mix data, excludes calls from NHS 111). (a) Null model; (b) model with patient-level variables; and (c) model with patient- and ambulance service-level variables.

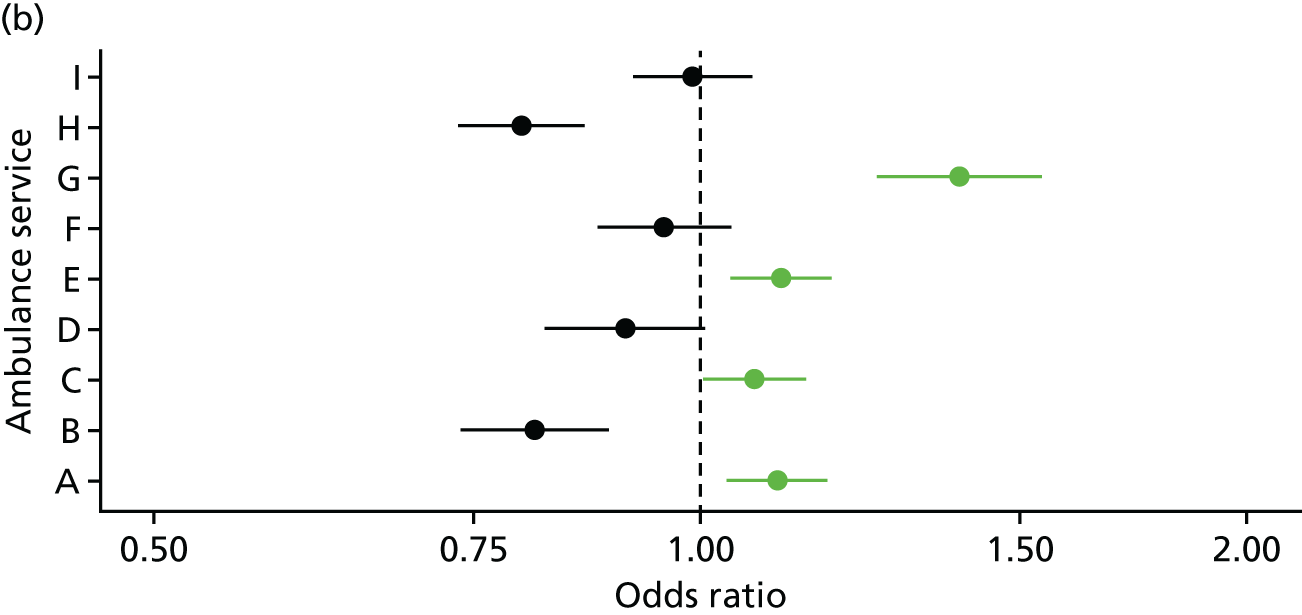
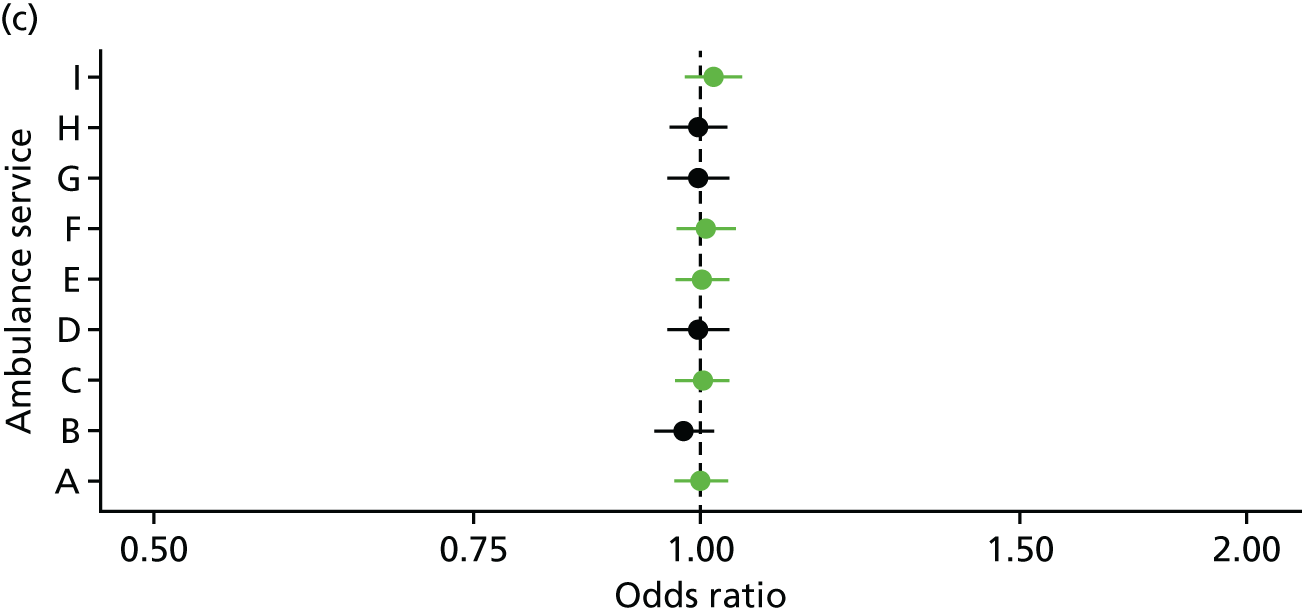
Ambulance Quality Indicators on recontacts: a problematic measure
During the WP1 interviews (see Chapter 4), some ambulance managers described the two AQIs on recontact rates as a useful source of information because they were indicators of quality and safety, or because they allowed ambulance services to benchmark their performance against that of other ambulance services. For more managers in the sample these indicators lacked credibility because of concerns that actual recontacts were not measured but rather that a proxy was used (recontacts were based on anyone of the same sex calling from the same postcode rather than the same patient calling again about the same issue). Ambulance managers wanted a more reliable approach to measurement using NHS Number to identify genuine recontacts. They also expressed concern about what exactly these measures indicated. The AQIs might include very different issues such as unsafe practices, the fact that the right decision had been made at the time but that some patients’ health had deteriorated over time, or that patient dissatisfaction with the decision not to send an ambulance or transport them to hospital was the cause of the recontact. One manager was concerned that these indicators included frequent callers who called the ambulance service multiple times each week when they did not need an ambulance and that this resulted in difficulty understanding the level of recontacts indicating potential problems.
A useful source of information for commissioners
During the WP1 interviews, commissioners of ambulance services were interested in the monthly data on recontact rates. Both managers and commissioners described having discussions about them, with one manager perceiving that they were ‘held to account’ by commissioners for performance measured by these AQIs. Commissioners described the indicators as useful for a broad overview, allowing them to compare their ambulance service with others, look out for increasing rates, or look for differences by localities within the ambulance service geography (these ambulance services must have produced this small area analysis for the commissioners). Like ambulance managers, some commissioners expressed concerns about the credibility of the data and the importance of the serious incident data to identify inappropriate non-conveyance (see Chapter 7).
Discussion
Summary of findings
Variation in 24-hour recontact rates for both telephone advice only and discharge at scene were explained by ambulance service-level variables. Recontact rates for telephone advice were higher for ambulance services for which interviewees in WP1 reported negative perceptions of telephone advice, higher for ambulance services with both small and large numbers of CCGs, and lower for services for which the cost per call was high. Recontact rates were higher for ambulance services reporting established advanced paramedics in WP1 interviews, and a high proportion of advanced practitioners in frontline staff. At a patient level, recontact rates for discharge at scene were similar for advanced paramedics and paramedics. Ambulance managers had some reservations about the way the recontact AQIs were calculated and how to interpret them, but some reported using the data with commissioners to consider variation between services and variation over time.
Strengths and limitations
A strength of this analysis is that it brings together recontact data on all ambulance services and identifies factors explaining variation in recontact rates between ambulance services within 24 hours of non-conveyance. A limitation is that we could not reconcile our data set with published AQIs for three services and this suggests variation in the calculation of recontact rates by ambulance services.
Implications
Some findings make sense but others do not. For example, higher rates of recontact for telephone-advice-only calls in ambulance services for which WP1 interviewees expressed negative perceptions of telephone advice makes sense, although there is uncertainty about the direction of this relationship because the perception of interviewees may have been based on knowledge of these recontact rates (see Chapter 5, Discussion). We can find no possible explanation for the finding that recontact rates were higher for ambulance services with both small and large numbers of CCGs. Most confusing of all is the finding that advanced paramedics have the same recontact rates as paramedics for individual patients but that ambulance services with established advanced paramedics have higher recontact rates. Concerns expressed by ambulance service interviewees in WP1 about the recontact data, and the lack of coherence of findings, suggest that caution should be exercised when interpreting the findings of this analysis.
Chapter 7 Potentially inappropriate non-conveyance: emergency department attendance, hospital admission and mortality within 3 days of non-conveyance (work package 3.2)
Background
Safety is an important consideration for decisions about, and outcomes of, non-conveyance. 33 Patients who are not conveyed to a hospital – either an emergency department or specialist services – may recontact the ambulance service, may end up in an emergency department or hospital bed, or may die. There are challenges to researching this issue. A decision not to convey may have been appropriate at the time at which it was made, or it may have been inappropriate and jeopardised patient safety. Attempting to distinguish ‘unsurprising’ subsequent events (such as patients in an end-of-life situation dying) from potentially inappropriate subsequent events (such as a child with a fever being hospitalised) is difficult. The situation is further complicated by some non-conveyance decisions being made independently by patients against clinical advice.
Some researchers have used an expert panel to assess the appropriateness of non-conveyance decisions. 31 This approach is time-consuming and limited to an assessment of small numbers of calls. An alternative approach, which is useful for large numbers of calls, is to identify subsequent events using linkage of routinely available data from ambulance services, Hospital Episode Statistics (HES) and the ONS. A limitation of this approach is the lack of detail about individual cases to allow assessment of appropriateness of the decision not to convey. We took advantage of a linked data set from an ongoing National Institute for Health Research-funded study aiming to build predictive models for ambulance outcomes (see www.sheffield.ac.uk/scharr/sections/hsr/mcru/phoebe) to explore what we label ‘potentially inappropriate’ non-conveyance in recognition of the challenges in determining appropriateness of decisions. The original plan was to use linked data for two ambulance services and to compare subsequent event rates for patients who were not conveyed. In practice the data for one service only was available. This was not a great loss because the data for the second service were for one locality only within the service.
This WP describes the frequency of different types of subsequent events for calls to a single ambulance service, and describes variation by patient characteristics. Event rates identified through this process indicate potentially inappropriate non-conveyance only. Detailed investigations of each case would be necessary to identify inappropriate or unsafe non-conveyance decisions.
This chapter is based largely on a data set linking routine ambulance service data with mortality and subsequent service use data for one ambulance service only. Our intention had been to undertake this analysis for two ambulance services and to consider variation between those services but the linked data could not be obtained for one service (see Appendix 1). The findings presented here are, therefore, descriptive, displaying subsequent event rates for one service rather than explaining variation in these rates between services. We also include a small number of themes from the qualitative research from WP1 reported in Chapter 4 and refer the reader back to the Methods section, in which the methods of this qualitative research are detailed. During interviews in WP1 we explored interviewees’ views on definitions and meanings of inappropriate non-conveyance and this is reported below (see Findings).
Methods
Obtaining and linking data
Data for the 6-month period of January–June 2013 were obtained from one ambulance service. In order to create a clinically meaningful data set, exclusions were applied to the sample: attendances with no electronic Patient Report Form (ePRF), which documents details for calls attended by an ambulance crew; inter-hospital transfers; calls passed to other ambulance services; and duplicate calls for the same incident. An ePRF is never available for calls ending in telephone advice so these calls were included using information in CAD. A narrower definition of calls ending in telephone advice was applied within the PhOEBE study than in AQIs. This definition focused on calls that received input from a clinician: ‘Hear and Treat by Nurse Triage’, ‘Refer and Treat – Nurse Triage referred to other provider’, or ‘Nurse Agreed Plan’. Calls that were dealt with by a call-handler only were not included: ‘Automatically Closed Call’ or ‘Dealt with by NHS Direct’; these accounted for around 5000 calls in that period. The size of the sample we received was 51% of the total number of calls reported in AQIs by that ambulance service during January–June 2013. This was due to the exclusions applied and the fact that AQIs are a call-based data set, whereas our study data set was an individual patient-based data set.
Data linkage was undertaken by NHS Digital, using their data linking algorithm based on NHS number, date of birth, postcode and sex. If NHS number was not available, NHS Digital’s NHS number tracing service looked up NHS numbers using date of birth and patient name. NHS Digital undertook linkage of the calls in the ambulance service data to HES and ONS data to identify whether or not, and, if so, when, patients attended an emergency department, were admitted to hospital, or died. A total of 83% (154,927/187,426) of the patients in the sample were successfully traced; unsuccessful traces were attributable to missing or incomplete patient identifier data from CAD/the ePRF. Unsuccessful traces could not be linked to subsequent health-care information. Subsequent recontacts with the ambulance data were identifiable using a unique HES identification (ID) number generated for each patient. All relevant permissions were obtained for this linkage and for reuse of the data within our study.
Events within a specific time period
There is no consensus on the time period for measuring subsequent events after non-conveyance. Using a short time period may miss events attributable to the decision not to convey, and using a long time period may lead to the inclusion of events that are not attributable to the non-conveyance decision. As described in Chapter 1, researchers have tended to use a range of time periods. In the qualitative interviews in WP1 we sought the views of the ambulance service staff about the most appropriate time period to measure but no clear picture emerged. Interviewees who answered this question said that it depended on the context. We selected 3 days as the primary analysis because events are likely to be attributable to the decision not to convey. We report events up to 1 week to allow comparison of event rates with other studies. Date rather than exact time of hospital admission and death is documented in HES and ONS data. Therefore, 3 days is not 72 hours after the original call but somewhere between 48 and 96 hours. For consistency, we report events within 3 days for ambulance recontact and emergency department attendance (where time of event is recorded).
Recontact with the same ambulance service and Ambulance Quality Indicators
It was possible to identify the recontacts that the same patient had with the same ambulance service. This calculation was superior to that used to calculate AQI recontact rates for which recontact rates are based on whether a call was received from someone of the same sex at the same postcode within 24 hours.
Removal of deaths at scene and end-of-life deaths
Ambulance Quality Indicators and our analysis of CAD data in WP2 include people who are found dead on arrival of the ambulance or who die while the crew is in attendance. We were able to identify these deaths and remove them from the analysis here. In addition, we wanted to identify events that were not expected to occur, so a medical practitioner co-applicant (NS) identified International Statistical Classification of Diseases and Related Health Problems, 10th Revision codes of deaths associated with end-of-life care and we removed these patients prior to analysis.
Perceptions of inappropriateness
In the qualitative interviews in WP1 we sought the views of the ambulance service staff about inappropriate non-conveyance and these views are reported in this chapter.
Analysis
The analysis was descriptive. We undertook the following:
-
Compared the characteristics of patients with linked data with patients with unlinked data to consider bias in our sample.
-
Calculated the different event rates for telephone advice only and discharge at scene separately.
-
Performed a sensitivity analysis. For the sensitivity analysis we included unlinked calls in the denominator, excluded very elderly people who we assumed were very ill and likely to have subsequent events, excluded deaths in very elderly people, and excluded frequent callers. Ambulance services have their own definition of frequent callers but we chose to use our definition because of the complex relationship between calls and recontacts in our data set; we removed anyone who had called the service more than six times in the 6-month period of routine data included here.
Findings
Our included calls compared with Ambulance Quality Indicators
The AQIs for the 6-month period for this ambulance service were based on around 16,000 calls ending in telephone advice and 94,000 calls not conveyed to a hospital with an emergency department. Our PhOEBE data set included a smaller number of calls than this (approximately 11,000 and 51,000 calls, respectively) because of the narrower definition of telephone advice used and the inclusion criterion of the need for an ePRF.
Ability to link data
A total of 24% (2521/10634) of calls receiving telephone advice only were linked. Eighty-five per cent (43,108/50,894) of calls discharged at scene were linked (see the flow diagram of included calls in Appendix 15).
There was bias in the linkage process. The quality of data on identifiers for patients attended by an ambulance was better than for patients who received telephone advice only. During this time period, date of birth was not routinely recorded on the CAD system and we failed to link any data for telephone-advice-only calls because this linkage relied on information within CAD. To facilitate linkage, an information analyst at the ambulance service searched for previous and future attendance by an ambulance for all our telephone-advice-only calls to locate the necessary identifiers for linkage. This meant that patients with a history of calling the ambulance service were more likely to be linked for our telephone-advice-only analysis. Therefore, they were more likely to be ill and potentially more likely to have events after their original non-conveyance than those we failed to link.
There was little evidence of differences between patients with linked and unlinked data for those discharged at scene (see Appendix 16). However, there were differences for patients receiving telephone advice only whereby patients with linked data were older than patients with non-linked data (see Appendix 16). Because of the bias within the telephone-advice-only sample, we report event rates for this group with linked calls as a denominator and also all calls (linked and not linked) as a denominator. This offers what are likely to be maximum and minimum event rates for telephone advice only.
Event rates
For telephone advice only, the minimum recontact rate with the ambulance service within 3 days was 7.6%; the minimum emergency department attendance rate within 3 days was 6.2%; the minimum hospital admission rate within 3 days was 2.6%; and the minimum mortality rate within 3 days was 0.06% (6/10,627) (Table 5).
| Time frame (days) | Telephone advice only | Discharged at scene, n (%) | Total, N (%) | |
|---|---|---|---|---|
| Linked calls only as denominator, n (%) | All calls as denominator (%) | |||
| Time to first recontact | ||||
| 0 | 468 (18.6) | 4.4 | 1110 (2.6) | 1578 (3.5) |
| 1 | 202 (8.0) | 1.9 | 1427 (3.3) | 1629 (3.6) |
| 2 | 88 (3.5) | 0.8 | 769 (1.8) | 857 (1.9) |
| 3 | 51 (2.0) | 0.5 | 555 (1.3) | 606 (1.3) |
| 4–7 | 129 (5.1) | 1.2 | 1290 (3.0) | 1419 (3.1) |
| No recontact | 1576 (62.7) | 37,645 (88.0) | 39,221 (86.6) | |
| Time to first emergency department attendance | ||||
| 0 | 357 (14.2) | 3.4 | 2188 (5.1) | 2454 (5.6) |
| 1 | 173 (6.9) | 1.6 | 1702 (4.0) | 1875 (4.1) |
| 2 | 85 (3.4) | 0.8 | 877 (2.1) | 962 (2.1) |
| 3 | 49 (1.9) | 0.5 | 645 (1.5) | 694 (1.5) |
| 4–7 | 127 (5.1) | 1.2 | 1464 (3.4) | 1591 (3.5) |
| No recontact | 1723 (68.5) | 35,920 (83.9) | 37,643 (83.1) | |
| Time to first hospital admission | ||||
| 0 | 112 (4.5) | 1.0 | 685 (1.6) | 797 (1.8) |
| 1 | 109 (4.3) | 1.0 | 1179 (2.8) | 1288 (2.8) |
| 2 | 32 (1.3) | 0.3 | 600 (1.4) | 632 (1.4) |
| 3 | 28 (1.1) | 0.3 | 431 (1.0) | 459 (1.0) |
| 4–7 | 73 (2.9) | 0.7 | 1073 (2.5) | 1146 (2.5) |
| No recontact | 2160 (85.9) | 38,828 (90.7) | 40,988 (90.5) | |
| Time to death | ||||
| 0 | 1 (0.04) | 0.01 | 28 (0.07) | 29 (0.06) |
| 1 | 3 (0.12) | 0.03 | 36 (0.08) | 39 (0.09) |
| 2 | 1 (0.04) | 0.01 | 35 (0.08) | 36 (0.08) |
| 3 | 1 (0.04) | 0.01 | 30 (0.07) | 31 (0.07) |
| 4–7 | 4 (0.16) | 0.04 | 100 (0.23) | 104 (0.23) |
| Did not die | 2504 (99.60) | 42,567 (99.46) | 45,071 (99.47) | |
| Total, N (%) | 2514 (100.0) | 10,627 (100.0) | 42,796 (100.0) | 45,310 (100.0) |
For discharge at scene, the recontact rate with the ambulance service within 3 days was 9.0%; the emergency department attendance rate within 3 days was 12.6%; the hospital admission rate within 3 days was 6.8%; and the mortality rate within 3 days was 0.30% (129/42 796) (see Table 5).
Using an alternative way of expressing the mortality rate, around one person died within 3 days for every 1000 people given telephone advice only and around three people died within 3 days for every 1000 people discharged at scene.
Description of patients having events
A description of patients having different types of events is provided in Appendix 17. For example, a large percentage of patients discharged at scene who subsequently died within 3 days of the original call were aged 81–90 years [42% (54/129)] or > 90 years [12% (16/129)]. This linked data set did not include information on skill-mix, so differences in event rates by crew type could not be calculated.
Sensitivity analysis
The sensitivity analysis showed that the event rates for telephone advice were sensitive to the denominator used and exclusion of frequent callers (see Appendix 18). The event rates for discharge at scene were stable.
Comparison of recontact rates with Ambulance Quality Indicators
The monthly AQIs measure recontact with the ambulance service within 24 hours of the original call. They varied between 3% and 7% per month for this service over this 6-month time period for telephone advice only, averaging around 5%. For incidents in which patients were not conveyed to a hospital with an emergency department, including incidents in which patients were conveyed elsewhere, the AQIs were between 6% and 7%, averaging around 6%. The equivalent statistics in our linked data set were 8% (telephone) and 9% (discharge at scene). The patients included in our data set and the AQIs differed: our calculations were based on 1 day rather than 24 hours, we excluded the small percentage of patients who were dead but categorised as discharged at scene, we excluded patients conveyed elsewhere and we excluded telephone advice calls ended by call-handlers. Nonetheless, the recontact rates we found were of a similar order to those reported in the AQIs.
Timing of recontacts with the ambulance service
The exact timing of recontacts with the ambulance service was available. Timing was plotted by hour after the original call (see Appendix 19). Recontacts for calls ending in telephone advice were usually made within 2 hours of the original call. Recontacts after discharge at scene were usually made within 4 hours of the original call. This suggests that patient expectations for an ambulance, and for transport to an emergency department, rather than changing circumstances, were likely to play a part in some recontacts.
Ambulance staff views of inappropriate non-conveyance
Ambulance staff interviewed in WP1 commented on the utility of AQIs for 24-hour recontact rates with the ambulance service. They also discussed the importance of safety, the challenges of interpreting rates of subsequent events post non-conveyance, alternative approaches to assessing appropriateness, the importance of paramedics learning from their practice, and the need for data on subsequent events:
Patient safety paramount
Managers and commissioners discussed the importance of patient safety and used descriptions of inappropriate events that aligned with those used in this chapter: attendance at an emergency department, hospital admission and death. Paramedics discussed in detail the importance of patient safety when making decisions about discharge at scene.
I think the word I would choose would be safe, it should all be about patient safety, patient safety focused because you’re right, anyone can non-convey a patient, anyone anywhere can leave someone at home, that’s very straightforward, and we tend to talk a lot about non-conveyance but people don’t use the word safe non-conveyance. So for me, appropriate conveyance just revolves around patient safety above everything else, that was the safest thing for that individual.
Paramedic, interviewee 28
Paramedics described being able to refer patients to a service that would contact the patient within 24 hours and follow up on why they had fallen or help them manage their hypoglycaemic control, for example, as helping them to discharge at scene.
Expected subsequent events
Managers and paramedics perceived that some patients wanted to be conveyed to hospital regardless of the outcome of their clinical assessment and that efforts to convince patients to stay at home or use a different service were not welcomed in these circumstances. They also pointed out that some patients were told over the telephone to make their own way to an emergency department if they wanted to attend. Thus, some subsequent events were not attributable to poor ambulance processes and indeed were part of the response offered by the ambulance service to some patients who did not need an ambulance to transport them to an emergency department. Interviewees identified unexpected events as signs of inappropriate non-conveyance.
Alternative ways of assessing appropriateness
Ambulance service managers perceived that it was difficult to assess the appropriateness of non-conveyance. They used alternatives to the AQIs, in particular formal complaints and reports on serious incidents. Managers felt that it was important to look beyond the monthly AQIs and drill down into detail on the appropriateness of non-conveyance. They talked about wanting to do this by investigating case reports, or by looking at AQIs by locality and skill-mix, but not having the resources to do so or having other priorities. Managers in some services described participating in an across-service audit, or having regular or one-off audits, which helped them to explore the appropriateness of non-conveyance, for example, interviews with patients and audits of cases with feedback to the paramedic involved when problems were identified. One service bought data to link with their own data and assessed hospital admission rates for their conveyed patients so that they could reflect on the appropriateness of their conveyance using admission rates (high hospital admission rates were viewed as an indicator of appropriate decisions to convey).
Need for feedback to paramedics as part of positive learning culture
Only one of the paramedics interviewed knew how the appropriateness of non-conveyance decisions was assessed by their organisation. Paramedics at all grades expressed a desire for feedback about their decision-making concerning discharge at scene and referral to other services to help to understand how to make better decisions. They wanted individual feedback on their practice, either through a formal system whereby a team leader assessed their decision-making or through information about which patients had been admitted to hospital in the days since they had assessed them. They wanted feedback about decisions that were assessed as appropriate as well as those assessed as problematic because they felt that they heard about only problematic cases (e.g. a complaint) or heard about cases by accident if a colleague visited a patient later the same day. They felt that this feedback was important for their personal practice:
I think it would be nice to know, say for example you were keeping 100 people out of hospital every week or something, if 99 of them were going in the day later, you’re obviously not really being as useful as you could be. [. . .] The quality of the decision so not just thinking about if it’s a really wrong decision, but I guess it would be good to have feedback on where it’s, how it’s working, or what happened to somebody.
Paramedic, interviewee 14
Even when managers described special audits occurring within their organisations, paramedics described hearing the outcome of only those cases highlighted as problematic. Thus, even when information about good practice existed, it did not appear to be communicated to individual paramedics involved in the audited cases.
Getting the balance right
Because some patients want to be conveyed, some interviewees discussed the fine balance between increasing non-conveyance rates while keeping complaints and recontacts rates low. They discussed how paramedics working to maximise non-conveyance when this was clinically appropriate might receive more complaints than paramedics providing people with their wish to be conveyed to hospital. One paramedic discussed tensions between different departments in their organisation, whereby one department appeared to want more non-conveyance and the other less non-conveyance, because of this tension between non-conveyance and complaints. A senior manager at one service was very sensitive to the numbers of complaints about their organisation because these could make the ambulance service look poor to external assessors or result in actions by the Executive Board, which might have detrimental effects on the organisation.
Another issue concerning balance was highlighted by commissioners, that is, the appropriateness of some calls to the ambulance service in the first place. If this was improved then commissioners described how ambulance services might see a reduction in non-conveyance rates, that is, they considered the need for non-conveyance to be driven partly by patients calling an ambulance service when this was not clinically necessary.
A desire to understand the risks associated with the range of responses made by ambulance services
There was an appetite among the ambulance staff we interviewed for information about the risks of conveyance and non-conveyance:
So we know that patients going into hospital, it has a risk of hospital acquired infections, mortality rates, for certain groups, particularly the elderly. It’s higher when you go to hospital at particular times of the day or night. But equally, that doesn’t mean that not taking them to hospital is the right thing. And we just assumed, and everybody’s pushing rates of non-conveyance that have no evidence base to them at all. And one of my, one of my questions would be, what is the mortality from patients who don’t get conveyed to hospital? What’s the morbidity? What’s the length of stay for somebody who has their admission delayed by 3 days because they weren’t conveyed on the first episode? [. . .] I think we get pushed into non-conveyance because people think it’s the right thing for the system. There are clearly occasions when it is in the best interest of the patient, but equally I think there are occasions where it is not clear that it is in the best interests of the patient, and I suppose in that situation, what is the right thing to do?
Senior manager, interviewee 20
Discussion
Summary of findings
Linkage for patients discharged at scene where an ePRF was available was high. A minority of patients had subsequent events within 3 days that might indicate inappropriate non-conveyance. Linkage for patients offered clinical advice by telephone was poor; a minority of patients had subsequent events within 3 days. It is difficult to comment on the acceptability of these rates without comparing them with event rates in other services.
Context of evidence base
The rates of subsequent events reported here can be placed in two contexts. The first of these would be in relation to the rates found by other ambulance services in other studies and countries. Because of the range of ways in which researchers have measured rates of subsequent events, we have summarised these rates from other studies in Appendix 20. Comparison is challenging because researchers used different approaches to identify events (e.g. data linkage, record review, routine data analysis), measured rates over different time periods (e.g. 24 hours, 48 hours, 72 hours, 1 week, 28 days), focused on specific conditions (e.g. falls) or specific groups (e.g. paediatric), included specific types of practitioners (e.g. advanced paramedics only), or excluded certain types of patients (e.g. excluded people who refused to travel). Rates are likely to vary by these factors. For example, patients seen by advanced paramedics had lower emergency department attendance rates and hospital admission rates than patients seen by paramedics. 20 It is also the case that rates are likely to vary by case-mix. Second, we can place the findings in the context of rates for similar services such as emergency department discharge.
Telephone advice
Comparing findings from our study with those from others is not straightforward because our data are about calls ending in telephone advice, whereas published studies focus on secondary triage services, which include calls sent an ambulance as well as ending in telephone advice. 21,34 For example, one secondary triage service of low-acuity calls in Australia referred 68% to an emergency department and 28% of total cases went there by ambulance. 21 The conclusion from a systematic review of secondary triage services – similar to clinical hubs in our study – is that they have been shown to be safe but that further research is needed to determine safety owing to small sample sizes and variation between systems. 34 Concerns have also been expressed about using hospital admission rates and attendance at emergency departments as indicators of lack of appropriateness or safety because some people may need to go to hospital but not need an ambulance. Instead, expert panels are considered a more useful approach by which to determine appropriateness. For example, one study found only 1% of cases in which a panel of experts believed that an ambulance should have been sent. 64 This rate was similar in other studies. 34
An alternative comparison is a survey of patients who were offered telephone advice from ambulance services. 6 Eight per cent contacted the ambulance service once within 7 days, 4% contacted the service twice, and 3% called the ambulance service three or more times. A problem with relying on surveys is that people will not respond if they have died or been admitted to hospital for a serious illness.
Discharge at scene
Focusing on studies that measured events within 3 days or 72 hours, attendance at an emergency department varied, with findings of 8%,65 12% and 15%,29 and 19%66 compared with 13% in our study. Hospital admission was somewhat higher than was found in our study, at 9% and 13% 29 and 10%66 compared with 6% in our study. Death rates were 0.3% of people dying during hospital admission,65 which was similar to our rate of 0.3%. In England and Wales all incidents related to patient death in the ambulance service were analysed. The rate was one safety incident-related death per 168,000 calls received,67 or around 50 per year in England. Most of these were due to delayed response rather than non-conveyance.
A comparison with death rates of patients discharged from emergency departments in the USA shows that the rate of 1.2 per 1000 within 1 week of discharge was lower than our rate of 5.4 per 1000 within 1 week of discharge at scene. 68 The higher rate in our study may be explained by the severity level of illness of patients calling an ambulance compared with those patients attending emergency departments.
Strengths and limitations
A strength of this study is that it was a large study of a wide range of subsequent events post non-conveyance. There were five limitations. First, linkage was poor for telephone-advice-only calls and these findings need to be considered with caution. Second, it was unlikely that we removed all calls from patients dying with end-of-life conditions and some of the deaths and admissions may have been expected. Third, our time period for measuring an event was calculated using date rather than time of event, so is not directly comparable to studies using time of event. Fourth, comparing like-for-like was not possible when placing our event rates in the context of other research because of the wide range of factors that may affect rates. Fifth, if non-conveyance facilitates the capacity of ambulance services to send ambulances to critically ill patients quickly, then the true picture of safety and appropriateness can be gauged only by also considering adverse events attributable to ambulances not responding to some events quickly enough. 67
Implications
Given that ambulance staff are making decisions in situations in which health status can change quickly, that some decisions to discharge at scene are due to the strong preferences of patients and their families, and that the sample is likely to include people in an end-of-life phase, the event rates found here were not large. It is certainly not the case that these non-conveyance decisions simply delay use of emergency departments and hospital beds, because the majority of patients did not have a subsequent event within 3 days of the non-conveyance decision.
Chapter 8 Exploring variation in telephone advice in depth in three ambulance services: non-participant observation and interviews (work package 4.1)
Background
Around 1 in 10 calls to ambulance services in England end in telephone advice, without the dispatch of an ambulance (see Chapter 3). These calls may be dealt with by clinicians in a clinical hub; this is known as secondary triage internationally. A systematic review of secondary triage concluded that telephone advice is a safe alternative for patients categorised as low priority by the initial triage process but recommended the need to understand the impact on demand for ambulance service care. 34 The review authors point out that the effectiveness of secondary triage is limited by the range of options available to clinicians and suggest that the availability of alternative options may also affect the level of recontacts following telephone advice. AQIs for ambulance services show variation between organisations in the rate of calls ending in telephone advice and in the recontact rates with the ambulance service within 24 hours (see Chapter 3). We aimed to explore organisational variation in the provision of telephone advice within clinical hubs in three ambulance services.
Methods
Study sample
Telephone advice involving clinician assessment is a two-stage process provided within the ambulance service Emergency Operations Centre. Initial assessment (triage) of 999 calls is conducted by non-clinical call-handlers (variously called call-takers, emergency medical dispatchers and emergency medical advisors) to triage calls for an ambulance response and identify calls potentially suitable for telephone advice. These calls are passed for secondary assessment (secondary triage) by clinicians who are usually paramedics but can also be trained in a range of clinical disciplines including nursing, mental health and midwifery. Callers dealt with by clinicians may be given self-care advice; they may be advised to contact, be referred to or have appointments arranged with other health professionals/services; or an ambulance may be dispatched.
Using monthly AQIs we selected three ambulance services showing variation in the rate of calls ending in telephone advice and in recontact rates. This selection was made based on the average of the 3 months of August–October 2014 to allow sufficient time for the research permissions process. One ambulance service had a low rate of calls closed with telephone advice but one of the highest recontact rates (Service E). One service had a high telephone advice rate but one of the lowest recontact rates (Service H). These two services were selected to represent the extremes of variation for our study. An additional service offering further contrast was selected on the basis of having average rates of both telephone advice and recontact (Service B). At the time of data collection for this component of the study (November 2015–September 2016), the AQI data were different for some of these services: Service E still had a low rate of telephone advice and high recontact rate; Service H had an average telephone advice rate but the recontact rate remained low; and Service B had a high telephone advice rate and a low recontact rate.
Data collection
Observation
In each of the three services we conducted non-participant observation around two key processes: making the decision to offer telephone advice and offering telephone advice. Ambulance services can have more than one Emergency Operations Centre. In one Emergency Operations Centre of each service we observed the processes involved in both initial triage and secondary triage. We considered the interaction between the caller and the ambulance staff members, and the interactions between staff, including in cases in which referrals were made that involved contact with other health and social care staff. The observation of staff in their ‘natural’ work environment combined with interviews (see below) to explore the observed behaviour helped to gain an understanding of staff actions and decisions in relation to telephone advice. The actions of health-care professionals have been examined previously using observation in similar settings;69–71 these insights could not be obtained by other methods. 72
The initial stage of this work entailed 1 day of familiarisation for the researcher with the Emergency Operations Centre setting in two services (B and E) to identify a broad framework for the data collection. Following this, five shifts of 8 hours on different days and times were arranged with each service via the appropriate Emergency Operations Centre contact. For all services, a standard initial request was made for shifts, including 1 week day, 1 weekend day and a Friday or Saturday night. Once these shifts had been completed and the researcher had asked during the observation about which additional days and times might be useful to observe, the remaining two shifts were arranged. Appendix 21 gives details of the months, days and times of the observation shifts. In total, data collection entailed 120 hours of observation across the three services and involved 20 call-handlers and 27 clinicians. Table 6 shows the staff roles for observation and interview participants per service.
| Rates and staff type | Service B | Service E | Service H | |||
|---|---|---|---|---|---|---|
| At time of selection: rate and recontact rate | MM | LH | HL | |||
| During data collection: rate and recontact rate | HL | LH | ML | |||
| Staff role | Interview | Observation | Interview | Observation | Interview | Observation |
| Call-handler | 3 | 7 | 2 | 8 | 2 | 5 |
| Clinician | 3 | 8 | 3 | 7 | 4 | 12 |
| Clinician manager | 1 | – | 1 | – | 1 | – |
Data collection included some observation of call-handlers but was predominantly focused on clinicians or team leaders who were undertaking secondary triage. Some observed individuals were selected by the shift leader but many were opportunistic during the session. All individuals who were observed were informed about the study, provided with study information leaflets and invited to complete a consent form. No individuals refused observation. Handwritten observation notes were taken throughout the sessions and any information provided verbally by staff was also noted.
Interviews
In addition to observation, semistructured telephone interviews were conducted with call-handlers, clinicians and clinician managers to understand how they manage telephone advice calls and minimise recontact rates. These included an exploration of the issues identified from the observations. The three services were asked for volunteers to participate in the telephone interviews. Each service was asked for three call-handlers, three clinicians and one clinician manager. Potential volunteers were identified by a team leader or manager. All volunteers subsequently had private contact with the researcher who ensured that they were willing to take part. Of the three services, one completed a full range of interviews, and the remaining two completed all with the exception of one call-handler per service. At that stage it was considered that data obtained in relation to call-handlers’ practices were sufficient and, therefore, did not warrant the additional time required to conduct these two interviews. All interviewees were informed about the study, provided with study information leaflets and invited to complete a consent form. Overall, 20 interviews were completed.
The telephone interviews were audio-recorded. The same topic guide was used for all participants (see Appendix 22). Following observation, an additional question regarding the interaction between call-handlers and clinicians was added to call-handler interviews.
The same researcher (LBE) conducted all data collection and was blind to the AQI data for the services visited throughout all observations and interviews.
Data analysis
Observation notes and researcher reflections were recorded using handwritten notes and transcribed into electronic format suitable for analysis after each observation shift. Interviews were digitally recorded and transcribed verbatim. Transcripts were checked for accuracy. The data were analysed using a framework approach57 supported by the use of NVivo qualitative data analysis software. The coding was undertaken by three researchers (LBE coded the observations and NA and ROH coded the interviews). The coding frames developed for both the observation and interview data were reviewed, checked and discussed with a senior researcher (ROH) and the themes were refined and developed through a number of iterations. The data were analysed by Rachel O’Hara. The observation data were analysed first, followed by the interview data and, finally, the data were analysed per service. The emerging findings were discussed at various stages with the study management team and PPI group. Lindsey Bishop-Edwards was blind to the AQI data for services throughout the coding. Rachel O’Hara was aware of the AQIs throughout the analysis.
Presentation of findings
Findings from the non-participant observation and interview data collection have been combined. Differences and similarities across the three participating ambulance services are addressed to explore organisational variation in the provision of telephone advice.
Findings
An analysis of data from the observations and interviews identified a number of areas of variation as well as consistency in relation to the provision of telephone advice. These findings emerged as eight inter-related aspects of telephone advice: (1) the role of secondary triage, (2) the workforce, (3) the triage process, (4) the type of work undertaken, (5) telephone advice options relating to the wider system of care, (6) work in times of high demand, (7) patient factors, and (8) organisational factors.
Role of telephone advice: appropriate response or demand management tool?
We explored the perceived role of telephone advice within each of the participating services to understand how this might have an impact on any variations in practice. There was considerable consensus of opinion across participants in the three services regarding the perceived purpose of telephone advice. Key aspects were identified as being telephone triage of patients identified as lower risk/non-emergency; referral of patients to the most appropriate care; signposting patients to the right resource; providing self-care advice; and reducing demand for emergency ambulances, and to a lesser extent, reducing demand on emergency departments:
An ambulance isn’t always the right response for somebody just because they’re unwell [. . .] or taking them to [an emergency department] isn’t always the best thing because obviously that then overloads that, as an emergency service which [the emergency department] really is. And it just causes this massive imbalance that they can’t respond to effectively and it then means that people that genuinely need it aren’t getting the help they need in the right time.
Service E, interviewee 53
I think it’s basically to filter out the calls that don’t warrant an emergency ambulance and to pass them to other pathways.
Service B, interviewee 61
In Services B and H, demand management in relation to the increasing number of emergency calls appeared to be a greater consideration in the provision of telephone advice:
Demand was quickly outweighing supply with regards to ambulances etc. so something had to be done.
Service H, interviewee 65
Clinicians and call-handlers identified an additional aspect of secondary triage as identifying calls that needed an ambulance. Indeed, this was observed on a number of occasions in all services. As identified here by one of the clinicians in Service E, risk management was identified as a key consideration:
I think ‘Hear and Treat’ does work as far as we’re concerned, based on our patients that we do get. As I say, we’re a unit that’s very risk averse. We will send [an ambulance] where there is any query.
Service E, interviewee 70
Some clinicians regarded the organisational rationale for telephone advice as being more aligned with organisational performance and achieving targets for ambulance response times (i.e. demand management). This view was more prominent in Services B and H and is illustrated in the two quotations below. The clinician in Service H appeared to be more accepting of this as a valid aspect of telephone advice that was not at odds with delivering appropriate care for patients:
I think the ambulance [service] have a different view, I think it’s relating to targets.
Service B, interviewee 59
It’s also to minimise the impact on front line motor crews, and to increase their productivity.
Service H, interviewee 64
Clinicians advocated communication of telephone advice response options as an opportunity to educate callers and explain why an ambulance response was not appropriate in this instance, as well as offering information on alterative options to calling 999. Call-handlers also appeared to have a role in this regard, as they often needed to explain to callers why they would be receiving a clinician call-back rather than an ambulance response:
I’m happy when I don’t have to send an ambulance and I can give them health advice on what they should be doing because this, it’s all about education, it’s all about making sure that people know the correct reasons for calling 999, so we educate that way as well.
Service B, interviewee 63
Related to this issue of telephone advice as a demand management tool was the concern voiced by some clinicians and managers that delivering high-quality telephone advice might encourage patients to call 999 for non-emergency health problems in the future:
You would like to think that you are educating them that on this instance you didn’t need to call us, you could have got this service from 111. But because we are very proactive and we will do the best for our patients and we’ll have arranged something such as a district nurse, then some people will call back because we did that so well.
Service E, interviewee 70
Workforce
Skill-mix
The skill-mix of staff involved in telephone advice varied across the three services, with Services B and H appearing to have a larger variety of skill-mix. Service E had only paramedics in the clinician team, whereas Service B used paramedics, nurses and midwives (the midwives were not observed); and Service H employed paramedics, nurses and part-time mental health nurses who also worked in a mental health role outside the ambulance service.
Reason for being in this clinical role
Service H appeared to have a higher concentration of paramedics who had chosen to work in telephone advice, and all appeared to enjoy the role. Both Services B and E had a mix of paramedics who were doing telephone triage either because they are no longer able to work ‘on the road’ for health reasons or through choice. Those who had chosen to do the role viewed it more favourably:
I know some people have gone up there because of health reasons and hate it; I can quite honestly say I quite enjoy it.
Service E, interviewee 51
Each of the services appeared to recognise the value of staff making a conscious choice to do telephone advice and now required staff to apply for the role. Interviewees at Service H described a detailed selection process that seeks to assess the necessary skills for the unique demands of triaging patients over the telephone rather than face to face:
We can chose our staff now, it used to be, I think it used to a bit of a ‘if you’re off sick you can come here and do it’, but actually it’s a bit more of a privilege [. . .] we won’t accept just anyone now. And you have to go through an assessment process to do this, even if you are a practising paramedic on the road.
Service H, interviewee 56
Training
All staff (call-handlers and clinicians) had received training before starting in their role, including how to use the various triage systems. Service H appeared to place the greatest emphasis on paramedics remaining fully operational and doing at least one shift a month ‘on the road’, although some staff talked of doing more than this. A manager stated:
We are very insistent that people still remain fully operational, and update, upkeep their clinical skill.
Service H, interviewee 65
In Services B and E some of the staff members who were fit enough spent a minimal amount of time ‘on the road’. Clinicians in Service E talked of a lack of ongoing training and referred to ‘people going nowhere’, whereas in Service H the telephone advice role was referred to as a career development path. Workload was mentioned as a barrier to ongoing training in Service B.
Risk tolerance
Clinicians across all services were conscious of their professional responsibility as clinicians and the potential risk that telephone triage posed for them personally:
Each patient you hear, you are clinically responsible, you are not there just to divert ambulances. As an ultimate goal you are there to give that patient the most appropriate care each time.
Service H, interviewee 62
In Service E the clinicians talked more about the risk associated with telephone advice, referring to the triage system and colleagues as risk averse.
Morale
Clinicians identified the unrelenting demand in Service B as affecting morale and the ability to work effectively. Despite the availability of funding for additional clinicians in Service B, there were concerns that new recruits would only offset the high numbers of experienced staff leaving the organisation:
When I first started with the ambulance service on the assessment team, it wasn’t that busy. There were times when, you know, you could take time to look at emails or update yourself on something that you weren’t sure about, and now it just seems to be solidly one call after the other, without any break in-between, and, you know, that can be for a whole 12 hours [. . .] so it can be a bit demoralising at times, in fact a lot, a lot of the time it can be demoralising.
Service B, interviewee 63
In contrast, some of the clinicians in Service E were demotivated by the constraints on what they are allowed to do, feeling that there were restrictions on their ability to use their skills; one even suggested that their skills might be better used working from a GP surgery. In contrast, clinicians in Service H appeared generally satisfied with what they were doing.
The triage process
The process of triage – both initial triage by call-handlers and secondary triage by clinicians – is very detailed and can vary according to the level of demand. Coverage of this process here will necessarily focus on key aspects that are relevant rather than providing a detailed account of the process operating in each service. Initial triage of 999 calls is conducted by call-handlers who identify and prioritise calls as either life-threatening conditions that require an immediate emergency ambulance response or conditions that are not life-threatening. More serious non-life threatening conditions are allocated a lower priority ambulance response but for other conditions a non-ambulance response may be more suitable, for example referral to GP, pharmacy, minor injuries unit, urgent care centre or attendance by community services. The general process of call-handler and clinician triage was broadly similar across the three services, although variation was apparent in relation to the specific practices around triaging patients and delivering telephone advice.
Initial triage by call-handlers
In all three services, triage software provides the call-handler with scripted questions to elicit patient information in a systematic way. On the basis of this information calls are prioritised and allocated resources according to the severity of the patient’s condition. Non-emergency calls are then transferred to the clinician team, which undertakes further assessment to determine whether to allocate an ambulance response or an appropriate alternative. The caller is advised that, based on the information they have given, an ambulance will not be sent but they will be contacted by a clinician as quickly as possible for further assessment. Callers are asked to keep their telephone line available and are advised to call back if the condition changes.
A key variation in call-handler triage process related to the triage software used. In Services B and E call-handlers used MPDS to assess 999 calls, whereas in Service E the call-handlers used NHS Pathways. The NHS Pathways system provides self-referral advice for selected low-priority calls. This essentially means that the call-handlers are delivering telephone advice that results in the call being closed without an ambulance response. However, call-handlers can use their discretion when they are concerned about the appropriateness of the triage outcome for that particular patient and can pass on the call for clinician attention:
Sometimes you’ll have a call and from what they tell you it comes out as a non-ambulance disposition. You tell them to go away and take two paracetamol, but you do have occasions when you think, you know what, I’m really not happy with that, and we do have the option [. . .] not to give them the non-ambulance disposition [. . .] so in cases where we don’t think ‘Hear and Treat’ is appropriate there is a fall-back scenario.
Service E, interviewee 60
In Services E and H interviewees described how an ambulance could arrive on scene before the triage is completed, preventing closure of calls with telephone advice; this was observed happening in Service E. This was more likely to occur when the demand for ambulances was not very high or when the service was well staffed. Service E had joined the national pilot that extended the time for the initial triage (this commenced after the observation visits were completed). It was anticipated that this would allow more time to assess the suitability of telephone advice response options.
Secondary clinician triage
Clinicians also used triage software to support their decision-making. Unlike the call-handlers, they appeared to have greater discretion to exercise their clinical knowledge and judgement regarding appropriate response options for patients. The triage software available to clinicians was different in all three services.
All clinicians also have access to the national Directory of Services, which is populated with details of local services to support the delivery of suitable telephone advice. This is integrated with the NHS Pathways system. Clinicians in all three services indicated that the Directory of Services has the potential to be a useful tool but experienced frustration with regard to the time taken to access information and problems with keeping the information up to date. One clinician, observed in Service E, could not find information on the patient’s GP surgery on the Pathways system. Variations in terminology could also make searching for information time-consuming. Interviewees described how delays in accessing information and services increased the likelihood of having to send an ambulance.
Clinicians in each service also had their own local sources of information, for example, a local directory providing phone numbers for each region (Service B), which was subject to the same issue of out-of-date contact details; an intranet page (Service E); and an ambulance service ‘app’ (Service H) for accessing and sharing clinical or other relevant information. Given the scope for clinician discretion in decisions even when using these systems, it was not clear how the different systems might affect the advice provided. It may be that individual knowledge, skills and experience have more influence on variations in telephone advice than the different software.
Clinicians in Service H can access patient information when it has been registered by the GP and when the patient gives consent; this was described as helpful for elderly patients. They can also stop the dispatch of an ambulance to a call they are triaging to avoid the problem of the ambulance arriving before triage is complete. In Service B one of the call-handlers commented that if it looks like an ambulance will arrive within 8 minutes, the clinician may not accept the call for triage.
Type of work: managing a variety of tasks as well as telephone advice
Welfare calls
Each service operated differently in terms of the varying tasks clinicians were expected to do as well as offering telephone advice. Additional roles included calls to check on patients when an ambulance has been delayed and to upgrade the call response if necessary (referred to as ‘welfare calls’ in Services B and E), assisting with advice over the telephone to ambulance crews (e.g. assessment of possible overdose) and passing information to GPs. In contrast, in Service H the clinicians were dedicated to offering telephone advice rather than juggling various roles. In Service H tasks such as communicating with GPs and ambulance crews and managing call-handler queries were generally dealt with by more senior clinicians such as team leaders.
Service B appeared to experience the greatest challenge in managing various roles. In Service B, clinicians were often engaged in other tasks and they spoke negatively about the impact of ‘welfare calls’ in particular on their ability to undertake assessment for telephone advice during times of high demand. Clinicians in Service E engaged in welfare calls and the communication of information to GPs and advice to ambulance crews, but, as demand for dealing with potential telephone advice calls did not appear to be as high as in Service B and H, staff did not appear to experience the sense of role conflict that was very apparent in Service B:
Our main priority is still the low category 999, that is our main function. All the other things, Toxbase enquiries, crew enquiries, call assessors, those are sort of add-ons.
Service E, interviewee 69
Proactive downgrading of calls
In Services B and H clinicians could listen in to calls being assessed by call-handlers. They could intercept calls that they could deal with straight away, including serious, but less immediately time-critical calls (e.g. ‘Red 2’) that could sometimes be downgraded to a lower priority response. This not only freed up call-handlers to deal with more incoming 999 calls but could also reduce the demand for an immediate ambulance response. In contrast, the option to downgrade calls was no longer possible in Service E. During the observations in this service one of the clinicians expressed frustration at this change and commented that it was ‘totally appropriate’ to assess and downgrade these calls. They added that, as a consequence, there was not much to do in their role, describing it as ‘boring’ and stating that they used to like the job but now did not.
The effect of very high demand for an ambulance on the triage process
Each of the services have resource escalation procedures that specify the actions required to mitigate the impact of increased demand on patient care. When demand levels are very high the lowest priority calls are given a self-referral response. A standard script is delivered either by the call-handler or by recorded message (to free up the call-handler), explaining that the ambulance service is currently experiencing very high demand and based on the information given they will not be sending an ambulance. Callers are advised to contact other services (e.g. GP, NHS 111, minor injury unit or emergency department). This does not apply to vulnerable patients including the very young, the elderly and elderly patients who have fallen and are on the floor. Depending on the level of escalation, these calls are passed to the clinician team, team-leader or duty manager to check and close the call. The call-handler can exercise their discretion and identify concerns about the response allocated to specific calls for the attention of the clinicians.
Demand levels in Services B and H were very high on a number of occasions during the observations and this had an impact on call-handler and clinician activity. In Service E high demand appeared to have more of an impact on call-handlers than clinicians. On the whole, clinicians in Service E were observed to be less busy than in the other two services. The following quotation from a clinician also points to the view that they are generally sufficiently resourced to meet demand:
As the day progresses, and perceived demand increases, then staffing levels increase. Until we get to sort of 11 o’clock at night and 2 o’clock in the morning, where demand in theory should start to wane, then we are left with, the manning should be, again two people at each site. Some days it can go to just one person, and in those instances yes demand can outstrip the ability to do the ‘Hear and Treat’. But generally if we’re fully staffed, there is two staff both sites 24/7 with an incremental number of staff coming in across the busy period.
Service E, interviewee 70
In Service H the activity of clinicians was less affected by high demand. In Service B clinicians identified very high demand as an ongoing problem that affected the delivery of telephone advice. Several calls were observed being allocated a ‘no send’ script after call-handler triage. When concerns were raised about some of the ‘no send’ outcomes, they were passed for clinician assessment. For the clinicians, the impact of this ongoing high demand on their ability to deliver telephone advice was a source of frustration, whereby a significant amount of their time was spent doing ‘welfare calls’ for delayed ambulances, rather than telephone advice:
I think it is sheer volume of workload, because we’re having to do welfare calls as opposed to ‘Hear and Treat’ [. . .] that now seems to be taking over at least 50% of our role. We allocate at least two, three or four people every day, every shift to purely be doing nothing but welfare calls, which means those three or four clinicians aren’t hearing and treating, they aren’t, they aren’t doing the job properly, they’re just literally ringing up saying sorry.
Service B, interviewee 61
Although it might be expected that this would reduce the scope for the delivery of telephone advice that results in closing calls without dispatching an ambulance, a number of instances were observed in which an ambulance response was cancelled as the caller or patient decided to use their own transport to get to a hospital.
In all three services, clinicians were expected to call back patients within 1 hour to conduct their assessment. This could be time-consuming, involving a number of call attempts, and when contact with the caller was not possible within this time frame, the call would be upgraded for an ambulance response. In Service B, in which clinicians were busy dealing with welfare calls, this could limit their ability to conduct timely call-backs. One of the clinicians suggested that additional staff could help to address this problem.
Patient factors
Reasons for calling an ambulance
Table 7 identifies the main presenting health problems for a sample of the calls observed during secondary triage by clinicians. This is not a reliable comparison, as not all details were accessible to the researcher and it was a relatively small number of calls observed. The main observation to make here is that across the services there was a broad consistency in terms of the type of issues being considered for a telephone advice response. In Service H the higher number of mental health calls reflects the presence of mental health nurses to assess these calls. The lack of welfare calls in this service reflects the focus of the clinicians on telephone advice only.
| Service B (n) | Service E (n) | Service H (n) |
|---|---|---|
|
Mental health (2) Overdose/Alcohol related (5) Diarrhoea/vomiting/abdominal/nausea (8) Fall (9) Multiple issues (1) Numbness in arm/leg (1) Bleeding (2) Burn (1) Back pain (1) Animal bite (1) Welfare calls observed (12) |
Mental health (1) Overdose/alcohol related (1) Diarrhoea/vomiting/abdominal/nausea (4) Fall (3) Urinary tract infection/issue (1) Multiple issues (3) Diabetic (3) Back pain (1) Eye problem (1) Breathing (1) Rash (1) Welfare calls observed (4) |
Mental health (10) Overdose/alcohol related (3) Diarrhoea/vomiting/abdominal/nausea (2) Fall (3) Urinary tract infection/issue (2) Multiple issues (1) Pain in leg (1) Cough/sore throat (1) Prank (1) Poorly person (2) Diabetic (1) Frequent caller (1) Kidney stones (1) Numbness in arm/leg (1) Welfare calls observed (0) |
| Total = 31 | Total = 20 | Total = 30 |
Interviewees identified a number of challenges in connection with the following issues: falls; mental health; social problems; mental capacity; and communication difficulties. Although an ambulance response and conveyance to an emergency department might not be the most appropriate option for these calls, they were described as often ending up requiring an ambulance response. For example, a lot of calls are received in relation to elderly people who have fallen and these often do not require an emergency ambulance response. Callers include paid carers, residential homes and ‘lifeline’ services to pick up patients who had fallen and for whom there were ‘no lift’ policies in place and/or concerns over injuries. Ambulance service staff blamed a lack of awareness of local falls services and a lack of communication about these services to staff within these organisations. Staff across all three services identified calls related to mental health problems as particularly challenging with regard to their skills and response options. These calls were described as very time-consuming. Only Service H employed specialist mental health clinicians for triaging patients and liaison with mental health services.
Patients’ expectations of receiving an ambulance
There was a consensus of opinion among our interviewees that the public expectation of an ambulance response when calling 999 was a significant barrier to offering telephone advice, with both call-handlers and clinicians encountering resistance to their advice to seek alternative sources of care. One member of staff had experienced the younger adult population as more ‘forceful and demanding, and want that ambulance’. This is where the skill of call-handlers and clinicians was important in reassuring patients that an alternative response was appropriate and safe:
We have what we call appropriate care pathways which we use, anything from a GP referral to a social worker, to mental health pathways [. . .] but, the thing that can affect this are primarily the patient’s/caller’s unwillingness to accept the process [. . .] that we’re laying out for them. That sometimes is hard. We also have, we refer to a taxi service which we use, that generally is well received because we pay for it.
Service H, interviewee 65
In some instances it was not possible to convince the caller regarding an alternative response and the clinician therefore dispatched an ambulance. Dissatisfaction with being offered telephone advice was identified as prompting callers to recontact the service in order to secure an ambulance response:
A lot of people do phone back, particularly, we get a lot of repeat callers who tend to phone and phone and phone and phone. You find people with the expectation of an ambulance will phone back: ‘I phone 999, I will, I should have an ambulance, therefore you’ve told me, right, the clinician’s going to phone me back or whatever, but actually, I want an ambulance’. So they will then, and sometimes they phone within moments of you putting the phone down.
Service E, interviewee 53
Interviewees partly blamed a lack of understanding of the existence of alternative services and felt that there is a need for greater public education to improve awareness. They felt that there is a common myth that patients will get seen quicker at the emergency department if they arrive by ambulance. Advice from other services (e.g. NHS 111, GPs) to call 999 was also identified as a factor and potentially more challenging in terms of delivering telephone advice as it established an expectation of an ambulance response.
Availability of telephone advice response options in wider emergency and urgent care system
Variation was observed in relation to telephone advice response options in each of the three services. All services offered self-care advice and recommended self-referral to other services including daytime GP or an out-of-hours service, NHS 111, walk-in centres, urgent care centres, minor injury units or emergency departments as appropriate. This advice could include details of the location of services. A common problem concerned the variability of response options available within each ambulance service, whereby interviewees described some areas as having quite a lot of resources but others as having less. There was also inconsistency in referral criteria and how services were accessed. Where the referral process took a long time, it could result in the call being upgraded to a full emergency response, particularly when the patient had deteriorated.
Taxis and passenger transport options
One specific option in Service H that was not offered by the other two ambulance services was a taxi to transport patients to other services such as the emergency department. This was intended for patients who were assessed as not requiring ambulance transport and unable to self-transport. Services E and H also used the organisation’s non-emergency passenger transport service for transporting lower priority 999 calls. The following is an example of when a taxi was used:
Call back to young adult experiencing pain in leg, ongoing problem, 111 advised to call 999. [. . .] Patient says he can’t get public transport or walk to hospital, clear desire for ambulance. Able to get into car and agrees to taxi. Hospital has an urgent care centre. Kept screen up re taxi until it reports call complete.
Service H, observation 2
General practitioner appointments
Clinicians in each of the services reported making GP appointments for patients. This worked well in some instances with very co-operative GPs but it could also be a time-consuming process to find the correct contact information and to communicate directly with the practice. Service E had access to a direct referral system for inner city GPs in one area where they have a number to contact the surgery directly and speak to the duty doctor without having to go through reception:
That’s [GP direct number] very good because, again patients will have dialled 999, GPs are very rarely aware of how many times people are actually ringing 999 up. So if it is suitable for them to see the GP, we can actually speak to a GP and say ‘look we think Mabel’s got a UTI [urinary tract infection] can you go out and treat it appropriately’. And they’ve been very receptive towards it.
Service E, interviewee 70
Burden of contacting other services
In Service B, to make a GP appointment for patients, clinicians had to contact the individual patient’s GP directly by telephone and to access a GP ‘out of hours’ they had to make a request via the NHS 111 system. Clinicians were expecting the introduction of a system to facilitate direct booking of appointments online, which had been delayed as a result of technical system conflicts. Service H could access out-of-hours GP providers in one area via NHS 111. Clinicians could speak directly to the service provider and try to get a referral over the telephone; alternatively they could request a GP referral via NHS 111. One of the clinicians in Service H reported that some GPs require an on-scene assessment before they will accept a direct referral. From our observations, referring to other health-care professionals (e.g. GPs) and NHS 111 was at times a frustrating cyclical process whereby patients were referred back to the ambulance service despite a triage recommendation that an ambulance was not appropriate.
Mental health services
Calls related to mental health problems were regarded as a significant challenge for telephone advice across all of the services because of the limited mental health services to which clinicians have access. Accessing crisis care was regarded as very difficult and time-consuming. In the previous year, Service H had introduced mental health nurses in the clinical hub and it was reported that they had been very effective in reducing ambulance responses because they knew the available pathways and contacts in order to gain access. Both Services B and E had access to ‘street triage’ cars operated by paramedics and mental health workers with police support to assist in managing patients experiencing a mental health crisis. However, these did not operate in all areas covered by the ambulance services and had other limitations in terms of the times at which they were available and the patients that they could assist.
District nurses
Clinicians in all services could access district nurses but it was not always easy to access them out of hours. Similar issues were observed to those affecting access to GPs whereby clinicians had to contact the district nurses via the GP surgery:
We are lucky, we have lots of referral pathways, but having 24-hour referral pathways is a different matter, particularly patients who might require something in the middle of the night [. . .] An example would be a blocked catheter and we don’t have enough district nurses, or we don’t have a rapid response team that can go round to the patient’s house to deal, so that patient has to wait for an ambulance.
Service H, interviewee 56
Special response teams
Service H clinicians had access to advanced paramedics in cars, with 2–3 available during the day and at night. In Service B clinicians had access to clinician response teams that included an ‘out-of-hours’ GP and advanced paramedics in cars who could attend patients at home. Staff spoke favourably of advanced paramedics but there were concerns that this already limited resource was diminishing further as staff were leaving to work in other parts of the NHS for higher pay:
Some of the pathways we’ve got do work very effectively. We’ve got a team of ECPs, emergency care practitioners, if we ring them up and say we’ve got a patient whose got a chest infection [. . .] they go and they’re there within an hour, and they’re brilliant, that type of thing works really, really well. We pass it on, the communication is excellent, the service is excellent and we’ve very rarely get any call backs from them to say ‘no actually we’ve got here and we do require an admission, we need an ambulance’. Very rare, so they’re, that works really, really well.
Service B, interviewee 61
In Service E it was reported that the advanced paramedic car service had stopped and there would be no training of new advanced paramedics.
Falls services
In Service B, falls services were available, for elderly patients who fall over at home, and could be contacted directly to assess and lift patients following a fall. They could also assess the need for further equipment or action to reduce likelihood of further falls. When available, these services were regarded as a valuable resource. Service H clinicians could request a falls assessment car; the assessments were conducted by a paramedic for falls for which there was no injury. It was stated that this was available in one area only within the ambulance service region.
Organisational factors
Performance targets and feedback
Service B was perceived by clinicians as being very target driven. Some of the clinicians referred to an expectation to complete a fixed number of telephone advice calls per hour and considered this unrealistic in the context of current demand. One of the clinicians viewed this target as a team rather than individual expectation and therefore felt less pressure to achieve it:
Basically we’ve now had funding on the basis we will try and guarantee that we will do six calls an hour per clinician, and because things have changed and because of the sheer volume, that’s no longer the case, we can’t perform to that standard.
Service B, interviewee 61
Clinicians in Service H also felt under pressure owing to service demands but not in relation to specific targets. In contrast, Service E clinicians did not appear to feel under pressure in relation to performance demands, despite the recent introduction of feedback on call percentages. It was stated that the amount of telephone advice was not as high as the organisation would like and described it as a ‘work in progress’:
It’s not target based at all, if we have a good day of ‘Hear and Treat’, then we’ve had a good day. But nobody will come over to us and say you’ve fallen below 5%.
Service E, interviewee 70
Audits of calls were carried out by all three organisations; clinicians in Services B and H spoke more positively about the feedback they received:
You get the feedback from your audit, so you might get a positive audit saying, you know, very compassionate, very reassuring, an excellent job, that’s me knowing that I’m doing my job properly, and, you know, if I done the right thing for that patient, that, I’m happy with that.
Service B, interviewee 59
Organisational support
Some of the staff in Services B and E expressed negative views about the management in their organisations; specifically, some clinicians lacked confidence that they would be supported in the event of a negative incident associated with telephone advice. In comparison, Service H staff appeared to view their management more positively:
It’s a lot of rhetoric and speak that you would be supported, but I am not confident that that would be the case.
Service E, interviewee 51
Communication within the organisation
Staff in Services B and E expressed dissatisfaction regarding organisational communication, in particular a lack of open communication about problems and how they were being addressed. Interviewees in Service B described a system whereby new procedures or new policies are communicated on a single day each week to reduce overload; however, one of the clinicians highlighted a lack of communication about a new falls service that they could have been using.
The work environment
Seating arrangements for staff varied in each site and could contribute to the level of interaction between staff. Clinicians in Services B and E were in closer proximity to call-handlers than in Service H. In Service H clinicians were completely separate from call-handlers. Some staff in Service B felt that the noisy environment could make it difficult to hear callers, which could give the impression that clinicians were not listening; this was also a safety issue if information was missed owing to difficulty hearing:
It’s very noisy around you, which I’ve questioned the safety element of. You’re trying to conduct a triage and you’re struggling to hear what’s going on on the other end of the phone because of the noise around you.
Service B, interviewee 58
Based on impressions gained during the observation visits, Service B appeared to have a relaxed feeling overall and a less formal feel than the other two services. However, over time a more chaotic feel emerged as it became busier. Despite this, clinicians generally engaged very well with callers in a manner that would engender confidence in their assessment. The environment in Service E felt calm and professional overall. Staff seemed relaxed and confident. The clinicians were often observed unoccupied and not very busy with calls. Some variation was observed in relation to staff interaction with callers, whereby clinicians who expressed enthusiasm for the role appeared to communicate more confidently than clinicians who seemed more indifferent about their role. Service H was generally quieter earlier in the day and became busier as the day progressed. The staff seemed professional and confident about their approach to delivering telephone advice. They communicated with callers in a way that would engender confidence.
Discussion
Summary of findings
A summary of variation between services and the possible direction of effect of factors on rates of telephone advice and recontact rates are displayed in Table 8. It is noticeable that Service E appears to be very different from the other two services, with fewer factors that might increase rates of telephone advice and more factors that might keep rates low. This is consistent with it having consistently low rates in the AQIs. There are differences between Services B and H, with Service B having more factors that might keep rates low. The change in AQIs for these two services over the time of the study makes it difficult to relate these findings to the AQIs. The only thing we can say with any confidence is that we would expect higher rates in these services than in Service E given our observations and interviews, and this is apparent in the AQIs.
| Rate | Service B | Service E | Service H |
|---|---|---|---|
| Rate of telephone advice at time of selection (and data collection) | M(H) | L(L) | H(M) |
| May increase rate |
|
|
|
| May decrease rate |
|
|
|
| Unknown |
|
|
|
| Recontact rate at time of selection (and data collection) | M(L) | H(H) | L(L) |
| May increase rate |
|
||
| May decrease rate |
|
||
| Unknown |
|
|
|
We identified few factors that might affect recontact rates but we did identify two factors and they aligned with the different rates in that the more risk-averse service (Service E) had high recontact rates and the service with more response options that patients were likely to be satisfied with had low recontact rates (Service H). The effect of whether staff engaged solely or largely with telephone advice rather than other tasks was unclear to us because this would depend on how calls related to other tasks were coded by each service.
Context of other research
The findings highlight a range of areas of variation in the delivery of telephone advice across the three ambulance services. Although the triage process appeared to be broadly similar, there were some specific differences in practice in terms of the system triage tools used, the staff involved, the type of work they did, and response options offered to patients. This is similar to variation in the organisation and delivery of NHS 111 across five different sites. 70
One aspect of variation concerned the degree of alignment of this type of non-conveyance with either demand management or risk management. The former was more a feature in Services B and H, with the latter being very prominent in Service E. This has the potential to influence both the amount of telephone advice given and recontacts in 24 hours. In Service E, staff were more likely to view their role as ensuring that anyone who might need an ambulance got one, whereas staff in Services B and H focused on only offering an ambulance to people who needed one so that ambulances were available for critical cases.
It was expected and observed that call-handlers have a role in the identification of potential calls for telephone advice. However, the findings also showed that non-clinical call-handlers deliver telephone advice and do not simply pass calls to clinicians for secondary triage. In all three services, telephone advice responses were delivered at the initial triage stage. The circumstances when this is permitted and who actually closes the call varied across the services. Similarly, non-clinical staff in NHS 111 also undertake call assessments and have different levels of autonomy according to the organisations they work in. 70
The most notable variation in relation to skill-mix concerned the availability of mental health nurses in Service H. Patients experiencing a mental health crisis were identified by staff as particularly challenging to deal with. Therefore, the experience and professional links that these specialist nurses brought appeared to offer the potential for better care and outcomes that did not involve an ambulance response or referral to an emergency department. The three services also had different sets of alternative response options for delivering telephone advice, with Service H having a greater variety of alternatives to an emergency ambulance. A systematic review of secondary triage indicated that its effectiveness is limited by the range of options available to clinicians and suggests that the availability of alternative options may also reduce the level of recontacts following telephone advice only. 34 Access to a range of alternative options would therefore appear to be an important factor in the delivery of telephone advice and minimising recontacts. To this end, the NHS England document Transforming Urgent and Emergency Care Services in England. Clinical Models for Ambulance Services, designed to help Urgent and Emergency Care Networks (UECNs) commission ambulance services, states that ‘clinicians working in the 999 system – through “Hear and Treat” or “See and Treat” models – should have unrestricted referral rights to all other services in the UECN, including social care services.’73 However, it appears that there is still some way to go to achieve this given the current inconsistency in access to services.
Ambulance service staff talked about caller expectation as a challenge in delivering telephone advice, as the ability to communicate confidently is important to convey why an alternative to an ambulance may be better. A 2013/14 survey of 999 callers in England who had been classified as receiving telephone advice (‘Hear and Treat’) found that the majority of respondents were positive about their experiences of initial call-handler triage and their interaction with the second person they spoke to (presumably clinicians conducting further assessment). 6
Some ambulance service staff expressed reservations that delivering high-quality telephone advice might promote 999 as the first place to call for similar non-emergency health problems in the future. This concern was also stated in a paper detailing a similar secondary telephone triage service for ambulance service patients in Australia21 in which the authors commented that recruiting a new ‘customer base’ for the ambulance service through the provision of telephone advice needs to be considered against its impact on managing existing demand. A number of staff across the three services referred to a need for public education to reduce 999 calls related to minor health problems. Some clinicians advocated communicating educational information to callers when conveying telephone advice.
Strengths and limitations
A key strength of this study was the use of non-participant observation to explore the processes involved in delivering telephone advice. The observation of staff in their ‘natural’ work environment combined with semistructured interviews has enabled us to gain an understanding of organisational variation in the provision of telephone advice within three ambulance services. Although there have been a number of studies using observation to explore the actions of health-care professionals in similar settings,69–71 we are not aware of any other study examining telephone advice in response to 999 calls and specifically focusing on variation. The participation of three ambulance services allowed the comparison of practices across three organisations with recorded variation in the amount of telephone advice and recontacts. The same researcher conducted all data collection with support from members of the study team. Data were presented to the team at various stages for feedback.
In terms of limitations, this was a relatively small-scale study comprising five observation shifts and a small number of interviews at each site. Although this provided a considerable number of qualitative data, it does to some extent represent a ‘snapshot’ of what was happening on the particular occasions that the services were observed. We attempted to capture potential variation across times of the day and days of the week, but there may have been variations over time that we did not capture. For the interview data, participants were either self-selected or had been invited by their manager. Although the interviewees provided a range of views and insights, we acknowledge that these do not necessarily reflect all staff views. Although we have used AQI data to identify participating ambulance services on the basis of recorded variation in the amount of telephone advice and recontacts, we cannot verify that these data have been recorded consistently by services (see Chapter 5) and therefore offer a cautious approach to relating variation in the AQI data with variation in processes across the three services. Finally, it was not possible to identify how NHS 111 affected telephone advice in response to 999 calls and whether this was another source of variation depending on how effective NHS 111 services are at diverting low-acuity calls away from ambulance services.
Implications
The aim of this WP was to explore organisational variation in the provision of telephone advice within clinical hubs. The findings provide insights on the complexity of the process and key areas of variation across the three participating ambulance services. We have considered the potential impact of these variations in practice on rates of telephone advice and recontacts as measured by AQIs. However, having confidence in the accuracy of rates of telephone advice is needed to establish the extent to which the various factors are related to these outcomes in order to understand what model of telephone advice works best for different outcomes.
Variation was identified in relation to the staff involved in telephone advice and highlights the need to consider the specific workforce requirements (staff numbers and skill-mix) for telephone advice to meet the needs of the local population. For example, although staff in all three services identified patients experiencing a mental health crisis as particularly challenging, only one service had mental health clinicians to manage these calls at the time of our research. The issue of variation in response options also seems worthy of attention at the commissioning level; this has already been identified in other research as a key factor influencing the effectiveness of telephone advice and reducing recontacts.
Finally, it is worth considering the role of telephone advice in relation to the wider emergency and urgent care system. Advice to attend an emergency department using their own transport, or transport there by taxi, are potential outcomes from telephone advice. Findings from WP3.2 (see Chapter 7) indicate that hospital admission within 1 day of receiving telephone advice occurred for approximately 2% of calls (see Table 5). Thus, although telephone advice reduces demand for ambulances, some patients may still be admitted that day and it is possible that an ambulance response with discharge at scene may have prevented this.
Chapter 9 Variation in non-conveyance of patients with breathing problems (work package 4.2)
Background
Previous research around non-conveyance for specific health problems has tended to focus on falls because they are the most common reason for calls to the ambulance service that end in non-conveyance. The plan was to explore the non-conveyance of patients with respiratory problems. Perceptions of factors affecting non-conveyance of patients with respiratory problems were explored in the WP1 qualitative interviews. In our analysis of CAD data in WP2 and WP3.1, the relevant code within the triage software is ‘breathing problems’. This is a broad category and includes both cardiac and respiratory conditions. 74 We intended to use both free-text and subcategories within the ‘breathing problems’ reason for the call category to identify calls for respiratory problems and for different types of respiratory problems. Our attempts to distinguish respiratory problems from other types of breathing problems were not successful (see Methods) so we changed the focus of this WP to an exploration of ‘breathing problems’ rather than ‘respiratory problems’. WP3.2 and WP4.1 also focused on breathing problems rather than respiratory problems.
Methods
In the WP1 qualitative interviews we asked ambulance staff to discuss non-conveyance for respiratory problems. This was part of a much wider interview and yielded a small number of data from each of the ambulance staff interviews; few commissioners discussed respiratory problems specifically. In the WP2 analysis of CAD data, 11% (47,737/434,494) of calls from the 10 services were for breathing problems (1681 patients received telephone advice only and 12,698 patients were discharged at scene). As part of the WP2 data specification we requested free-text data from each ambulance service on the reason for the call, with the intention of identifying respiratory conditions in the ‘breathing problems’ category. We could obtain a free-text description of the reason for the call from only two services. The vast majority of free text was generic description, such as ‘shortness of breath’ or ‘difficulty in breathing’, with very few specific descriptions of respiratory problems such as chronic obstructive pulmonary disease (COPD) and asthma. We explored the feasibility of obtaining more detailed data on the reason for the call from two services with different triage systems, using codes embedded within the triage systems. These coding systems were established for triage purposes rather than research analysis and we struggled to identify respiratory problems from these data. We therefore had to focus the quantitative analyses in WP2 and WP3 on the reason for the call being ‘breathing problems’ rather than the underlying condition of ‘respiratory problems’. We repeated our statistical analyses for WP2 and WP3 for the category of calls for ‘breathing problems’. In WP4.1, few data from the non-participant observation and interviews in three ambulance services focused on breathing or respiratory problems.
We analysed the limited amount of qualitative data specific to respiratory problems, undertook a descriptive analysis of the quantitative data on breathing problems and repeated the quantitative analysis of variation between ambulance services. We did not undertake an analysis of variation within ambulance services owing to small numbers.
Findings
Not a reason for calling that raises concerns
During qualitative interviews in WP1 and WP4.1 ambulance staff identified health conditions or reasons for calling for an ambulance that resulted in unnecessary conveyance to emergency departments. Respiratory problems were not mentioned as a condition about which staff had particular concerns. In WP1 interviewees frequently raised concerns about the unnecessary conveyance of people with mental health problems.
Initial call: taking the patient’s word
During observation and interviews within three ambulance services offering telephone advice (WP4.1), some call-handlers making initial triage decisions and their managers discussed the challenge of assessing breathing problems during the initial call. They described having to make a triage decision based on patients’ views of their breathing difficulties rather than their own perceptions of patients’ breathing based on listening to patients. They found the short length of time available to make a triage decision problematic and were frustrated at having to send an ambulance to patients who might not need one:
[. . .] they may be having breathing problems, but they are completing sentences, they’re not fighting desperately for every breath. But then they may still receive an ambulance anyway. It’s hard to know until you get to the end of the assessment [. . .] these things like the breathing problem, where I mentioned, somebody says ‘yeah it’s getting worse in the last hour’, we can’t, if they said that is the case, even if they’re breathing really, really well on the phone, we cannot go against what they’ve told [us].
Call-handler, interviewee 53 from WP4.1
Non-conveyance for breathing problems versus other reasons for calling an ambulance
When the reason for the call was available in the CAD data in WP2, 11% (47,737/434,494) of calls from the 10 services were for breathing problems. Breathing problems had lower levels of non-conveyance than all other reasons for calling combined (χ2 = 2190, df = 3, p < 0.001): 3.5% compared with 8.0% for calls ending in telephone advice and 27% compared with 31% for patients discharged at scene. It was the sixth most common reason (5%) for telephone advice after being sick or unconscious (26%), having an injury (17%), having abdominal pain (10%), having had a fall (9%) and having cardiovascular problems (5%). It was the fifth most common reason (10%) for discharge at scene after reported falls (21%), an injury (15%), being sick or unconscious (14%) and having cardiovascular problems (11%).
Types of respiratory conditions not conveyed
During WP1 qualitative interviews, ambulance staff mainly discussed discharge at scene of patients with exacerbations of COPD. Asthma was sometimes mentioned, with staff describing how nebulisers could usually be used to sort out problems without the need for conveyance to an emergency department.
Initiatives to facilitate non-conveyance: pathways and individual care packages
Staff in some services in the WP1 qualitative interviews described specific services that could increase rates of discharge at scene or conveyance to alternative services for people with chronic respiratory conditions. In particular, ambulance crews could convey or refer directly to respiratory clinics or specialist services, or they could access patients’ individual care packages. The latter option enabled access to clinical information for a specific patient to allow staff to judge what was clinically normal for the patient, and also allowed staff the opportunity to discuss care with a community matron or specialist nurse to support their decision-making.
Staff often described these referral and information-sharing initiatives as specific to some localities rather than something that was available across the whole ambulance service region. Some paramedics also described informal pathways in their locality, built up through historical relationships with local services rather than through formal agreements. Their descriptions of helpful initiatives that facilitated non-conveyance for people with chronic respiratory problems included having proactive staff in services in the wider emergency and urgent care system and having services that were easy to access, responsive and able to instil confidence in crew members that patients would receive timely and quality care if not conveyed to an emergency department. If these characteristics were not present then interviewees described how paramedics would cease to use available initiatives for referral or conveyance to alternative services and simply convey patients to an emergency department.
Variation between ambulance services
Variation in perceptions of interviewees in work package 1
In WP1 qualitative interviews, staff at two services consistently described the existence of pathways or individual care packages across large parts of their ambulance service region that could specifically help with the non-conveyance of patients with respiratory problems (Services G and I). In particular, staff at one of these services described an information system that ensured the availability of a large number of individual care plans to ambulance crews (Service I). Staff in most other services described initiatives to facilitate non-conveyance in this group inconsistently, or described them as being localised or non-existent (Services A, B, E, F, H and J). There was insufficient information within interviews to classify perceptions of services to facilitate non-conveyance for respiratory problems in the two remaining ambulance services (Services C and D).
Explaining variation in non-conveyance rates between ambulance services
Telephone-advice-only rates were lower for older people (patient aged > 60 years), for calls made in hours, and for ambulance services in which interviewees in WP1 perceived that managers were risk averse to non-conveyance (odds ratio 0.05, 95%CI 0.01 to 0.19). The patient-level variables did not change the variance between ambulance services (null model variance = 1.131, patient-level model variance = 1.1500). The ambulance service-level variables explained only a small amount of variation between ambulance services (variance = 0.3859); see Appendix 23.
Discharge at scene rates for the nine ambulance services with skill-mix data were higher for any patient aged > 2 years, males, low-urgency calls, calls made to NHS 111, calls attended by advanced paramedics, and calls made to ambulance services in which interviewees in WP1 reported that advanced paramedics were established in their service (odds ratio 1.94, 95% CI 1.21 to 3.10). Rates were lower for calls made in hours and to ambulance services with a larger number of CCGs (odds ratio 0.51, 95% CI 0.37 to 0.70). The patient-level variables did not change the variance between ambulance services (null model variance = 0.2256, patient-level variance = 0.2203). The ambulance service-level variables explained a large amount of the variation between ambulance services (variance 0.0374); see Appendix 24.
Explaining variation in 24-hour recontact rates between ambulance services
Numbers of recontacts for telephone advice only for breathing problems were too small to undertake a regression. For discharge at scene, recontact rates were higher for older people (aged > 40 years) and for services for which the NAO documented a high proportion of frontline staff as advanced practitioners (odds ratio 1.41, 95% CI 1.11 to 1.79). As was the case for all conditions reported in Chapter 6, there was no difference in recontact rates between advance paramedics and paramedics. These variables explained much of the variation between ambulance services (null model variance = 0.0488, patient-level model variance = 0.0410, ambulance service-level model variance = 0.0122); see Appendix 25.
Safety and appropriateness of discharge at scene
In WP3 the linked data set for a single ambulance service showed that 12% (5316/45,310) of calls were made for breathing problems, similar to the 11% found in WP2 for all 10 ambulance services.
Three days after discharge at scene, there was some evidence that more patients had events after non-conveyance than patients for all other conditions:
-
12% (607/5083) of patients with breathing problems recontacted the ambulance service compared with 9% for all other conditions (p < 0.001);
-
13% (678/5083) of patients with breathing problems attended an emergency department compared with 13% for all other conditions (p = 0.137);
-
9% (437/5083) of patients with breathing problems were admitted to hospital compared with 6% for all other conditions (p < 0.001);
-
0.77% (39/5083) of patients with breathing problems died compared with 0.30% for all other conditions (p < 0.001).
Caution is required when interpreting the p-values because small differences have small p-values when numbers are so large.
Patients who died within 3 days were all > 40 years of age. A total of 54% (21/39) of deaths were in patients aged > 80 years.
Discussion
Summary of findings in the context of other research
Breathing problems were a common reason for calling an ambulance service (11% of calls). This was similar in the USA, where 12% of emergency medical services encounters have been categorised as occurring in response to respiratory distress. 25 Patients were less likely to be non-conveyed and more likely to have subsequent events within 3 days of non-conveyance than patients calling with all other conditions. Factors explaining variation between ambulance services were similar to those found for all conditions reported in Chapters 5 and 6, although the complexity of the emergency and urgent care system in terms of serving large numbers of CCGs resulted in lower discharge-at-scene rates for breathing problems. Internationally, a small number of research studies have been undertaken to describe the epidemiology and outcomes of ambulance service users with respiratory distress or breathing problems. 25–28 As stated in the introduction to this report, these studies focused on patients who were transported to emergency departments rather than those who were not conveyed. A study of the impact of advanced paramedics on admission rates of people calling 999 with breathing difficulties identified a hospital admission rate of 15% (18/119) within 72 hours for those attended by an advanced paramedic. This was higher than the rate found in our study, in which the admission rate was 9% for patients discharged at scene.
Strengths and limitations
We could find no research focusing specifically on non-conveyance of people calling an ambulance service with breathing problems, so this study is a unique contribution to the evidence base. During the qualitative WPs of our study, staff had little to say about this reason for calling; thus, the data are sparse and do not offer the ‘thick’ description associated with high-quality qualitative research. Routine data held in CAD systems did not have sufficient detail to allow an analysis of non-conveyance for respiratory problems or specific types of respiratory problems, such as COPD. Clinical data collected by ambulance crew attending a scene or collected within triage software used in clinical hubs in which telephone advice is offered, would be needed to identify patients with respiratory problems who are not conveyed to an emergency department. The quantitative data reported here for ‘breathing problems’ comprise calls for a range of health conditions with breathing problems, including cardiac-related conditions.
Implications
Although it is interesting to consider the specific reasons for calling an ambulance service, and although non-conveyance rates differ by reason for the call, there was nothing particularly distinct about the non-conveyance of patients calling with breathing problems. Indeed, ambulance staff expressed concerns about other reasons for calling, particularly people calling with psychiatric problems, rather than concerns about the conveyance of people with COPD or asthma. These concerns were not about people with COPD who also had anxiety and depression75 but rather about users of mental health services who were suffering crises.
Our respiratory physician co-author was surprised by these findings, expecting to see much higher levels of non-conveyance for breathing problems than identified here. He viewed these findings from the perspective of a physician working with people with COPD in the community when, in practice, the category studied here included a range of conditions. Nonetheless, he expected to see higher levels of non-conveyance given national guidelines around home care and alternative care options for people with COPD and asthma. His personal experience of developing local community initiatives for managing chronic respiratory conditions was that the ambulance service was not part of their multiagency working and that there was opportunity to expand the use of care at home through working closely with the ambulance service. It would be worthwhile undertaking additional research on identifying and evaluating ways of increasing appropriate non-conveyance for chronic respiratory conditions given that this patient group is likely to make up a significant proportion of callers to the ambulance service.
Chapter 10 Integration of findings
Background
Attention to integration is important within mixed methods studies so that the whole is more than the sum of the parts. 76 The mixed methods design of this study was sequential, with the qualitative interview study in WP1 informing the factors tested in the quantitative analyses on determinants of variation in non-conveyance in WP2 and the variation in potentially inappropriate non-conveyance in WP3.1. Summaries of findings from WP1 for each ambulance service were used to construct ambulance service-level variables for testing in the regression in WP2 and WP3.1. This design-related integration has been reported in earlier chapters. Additional integration of findings from all the WPs is considered in this chapter. The role of triangulation of qualitative methods has been explored in the pre-hospital care setting,77 some of which is relevant to combining qualitative and quantitative methods in this study.
Methods
We undertook two approaches to integrating findings in this chapter. First, we used an adapted Triangulation Protocol to display all the findings from the different WPs on the same page and consider where they converged, complemented or explained each other, where they disagreed or where there was unexpected silence from some WPs. 43 Second, we constructed a framework of potential causes of variation in non-conveyance based on Appleby’s framework of causes of variation in health care;40 we drew on findings from all WPs to construct this framework and to highlight statistically significant factors affecting variation in this study. The benefit of using Appleby’s framework was that it helped to identify factors that were not measured in our study or that were not identified as important.
Findings
The adapted triangulation protocol is displayed in Table 9. The findings from each WP tended to converge or complement each other. There were no surprising silences or disagreements. This protocol was used to contribute to the conclusions drawn from the study (see Chapter 11) and from the conceptual framework of factors affecting variation in non-conveyance (Figure 12).
| Factor | Different aspects of factor | WP | Conclusions | ||||
|---|---|---|---|---|---|---|---|
| WP1: qualitative interview study | WP2: analysis of routine data on rates of non-conveyance from 10 ambulance services | WP3.1: analysis of 24-hour recontact rates from 10 ambulance services | WP3.2: analysis of data from one ambulance service linked to mortality and subsequent service use | WP4.1: qualitative study of telephone advice only in three ambulance services | |||
| Data inaccuracy | AQIs lack credibility for some managers owing to concerns about the proxy nature of recontact calculations and inaccuracies in calculations of telephone advice rates |
CAD systems vary by ambulance service CAD data are complex with multiple possible interpretations of some call types used in the AQIs Variation in ability of ambulance services to replicate AQI data Some ambulance services were not following national AQI guidance but this had little effect on variation between services Historical graphs of AQIs by ambulance service show sudden changes, particularly increases, for some services, which suggest changes in how rates have been calculated in some services over time. This is apparent for both types of non-conveyance but there is a change in ranking of services for telephone advice |
Three services were largely unable to replicate published AQIs Some sudden changes for some ambulance services in AQIs over time, suggesting some changes in the way in which some services calculated these rates |
The 24-hour recontact rate with the ambulance service for one service based on linked data were of a similar order to the published AQIs. There were differences in inclusion criteria so the comparison was not like-for-like |
A large number of ambulance processes observed varied by ambulance service, suggesting that variation in non-conveyance for telephone advice rates could be expected Conclusions drawn from observation of three clinical hubs matched the general ranking of the AQIs for those services. However, AQIs changed over time in two services and it was not possible to relate our findings to those AQIs |
Although there are differences in the way in which services calculated AQIs, and the research team was unable to measure the size of the differences, it is unlikely that all the variation is explained by data inaccuracy There was some evidence that inaccuracies were more likely for telephone advice than for discharge at scene There are likely to be differences in rates of telephone advice between services but AQIs may not accurately portray these differences |
|
| Random variation | No comment | Display of published AQIs over time shows consistency of ranking of ambulance services for discharge at scene but changes in ranking for telephone advice only | Ranking of services in published AQIs over time pretty stable | No comment | No comment |
Numbers are large for each ambulance service and rankings of services were similar over time for discharge at scene There was more movement of rates for telephone advice only but this is probably due to changes in calculation algorithms rather than random variation There is likely to be random variation and this must be considered at all times. However, this is highly unlikely to be the only cause of variation between services |
|
| Patients’ characteristics | Patients’ expectations | Staff perceptions that patients’ expectations that they will receive an ambulance or to be transported can be strong and lead to conveyance when it is not clinically necessary | Patients’ expectations were not measured directly. However, factors such as social deprivation, which may be related to expectations, were tested. These had little effect on non-conveyance rates | Not measured | Recontacts with the ambulance service within 24 hours are likely to be affected by patients’ expectations because a large proportion of recontacts occur within 4 hours of the original call | Observation within three clinical hubs identified the effect of patients’ expectations on telephone advice only. Some patients wanted a lift to the emergency department. Services dealt with this expectation differently – one offered a paid taxi, whereas staff at another service spent time persuading patients not to make use of an ambulance | Patients’ expectations likely to be an important factor but unlikely to be a key factor in terms of explaining variation between services. However, how different services handle these expectations could affect variation between services |
| Morbidity | No comment |
The percentage of severe long-term illness in the area in which the call was made, reason for calling and the level of urgency assigned to a call were tested. The last of these factors was highly associated with non-conveyance rates for telephone advice but these factors did not account for the variation between ambulance services Deaths are counted as ‘discharge at scene’ and contribute to rates Although the percentage of long-term illness was in the final regression, the gradient was not consistent, leaving a question about how to interpret this finding |
Same as WP2 | No comment | The types of patients passed through to the clinical hub may depend on the variety of skill-mix there | This explained some variation in non-conveyance rates but was not a key factor in terms of explaining variation between ambulance services | |
| Demographic composition of calls (age, deprivation, ethnicity) | Age, deprivation, rurality, language, reason for call | Rates varied by age, sex, social deprivation and reason for call. Effect of a factor dependent on type of non-conveyance. These did not account for the variation between ambulance services | Rates varied by age, social deprivation and reason for the call | Older people had higher rates of subsequent events | No comment | This was not a key factor in terms of explaining variation between ambulance services. Indeed, differences in case-mix explained a very small amount of variation between services | |
| Rurality | Some perceptions that people in rural areas were more amenable to non-conveyance than those in urban areas | Tested urban/rural area from which call was made. Discharge at scene rates were higher in rural areas but the ‘urban/rural’ factor did not make an independent contribution to the final regression | No differences for discharge at scene. Not in final regression | No comment | No comment |
This was not a key factor in terms of explaining variation between ambulance services This was a surprising finding in WP2 because WP1 findings indicated that rural areas would have considerably higher rates of non-conveyance because of the distance to emergency departments; rates were only slightly higher |
|
| Commissioning priorities |
Variation in approaches to commissioning between ambulance services Variation in relationship between commissioner and service: collaborative or dysfunctional Variation in perceived support of commissioner for non-conveyance initiatives Variation could operate at an ambulance service, locality or CCG level |
WP1 summaries of commissioning for each ambulance service did not explain variation between services Variation in non-conveyance rates within ambulance services was evident and this could signify the effect of differences in commissioning from different CCGs. It could also signify the effect of differences in connectivity with local emergency and urgent care systems Variation within ambulance services existed but did not explain the variation between ambulance services |
No effect | No comment | No comment | There was variation in commissioning processes between ambulance services. Differences in commissioning processes did not explain the differences in non-conveyance rates between ambulance services. The effect might be apparent through variation in non-conveyance within ambulance services | |
| Call characteristics | Time of day | A perception that alternatives to the emergency department are limited during the out-of-hours period | Discharge at scene rates were higher out of hours | Same as WP2 | No comment | No comment | Non-conveyance rates were higher out of hours |
| NHS 111 |
A perception that the introduction of NHS 111 has led to an increase in low-acuity demand for the ambulance service Some services may be integrating NHS 111 and 999 more than others? |
Calls from NHS 111 were more likely to be discharged at scene than calls from 999. Not in final regression | NHS 111 calls were not included in analysis | No comment | Not possible to understand effect of NHS 111. Findings raised issues in researchers’ minds about case-mix. If NHS 111 is used extensively by the population then fewer calls that are suitable for telephone advice will go to 999. If lots of NHS 111 calls are referred to the ambulance service then discharge-at-scene rates can be higher because these are low-acuity calls |
Uncertainty about what conclusions to draw about NHS 111. Further research is needed NHS 111 has the ability to filter out many of the potential ‘telephone advice’ calls that the ambulance service currently receives High population use of NHS 111 could lead to higher discharge-at-scene rates Integration between NHS 111 and 999 call-handling services may affect telephone advice only? |
|
| Workforce | Shortages | Concerns expressed about recruitment and retention but perceptions of problematic shortages in some services more acute | No comment | No comment | No comment | No comment | Differences in staffing rates could affect non-conveyance rates between ambulance services but we did not measure this |
| Advanced paramedics/skill-mix: numbers | Advanced paramedics can discharge more patients at the scene because of higher confidence levels |
Advanced paramedics had higher discharge-at-scene rates Ambulance services with higher proportions of calls attended by advanced paramedics had higher discharge-at-scene rates |
No differences in recontact rates by skill-mix | Skill-mix not measured | Different clinical hubs had different skill-mix | An influential part of the workforce in relation to non-conveyance and variation between ambulance services | |
| Advanced paramedics/skill-mix: how the workforce is used? | Variation in the use and perceived value to non-conveyance of advanced paramedics. Established and valued in some services and not in others | How the advanced paramedic workforce was used explained variation between services. If established and valued, higher discharge-at-scene rates were seen | Ambulance services with established advanced paramedics had higher recontact rates | No skill-mix data | There was evidence that staff did different types of work in each hub (e.g. welfare calls vs. telephone advice) | It is not simply the numbers of advanced paramedics but how they are used and valued that explains variation between ambulance services | |
| Staff morale and support for staff | Variation in the perceptions of paramedics feeling supported by their organisation when ‘things go wrong’ | Did not explain differences | Did not explain differences | No comment | Staff morale appeared to differ by clinical hub | Poor morale or fear of retribution if something goes wrong may have a detrimental effect on non-conveyance but no evidence was found that the variation in this between services explained the variation in non-conveyance rates | |
| Length of service | Newly trained paramedics see non-conveyance as part of their job | No comment | No comment | No comment | No comment | Insufficient evidence to bring this out in the discussion | |
| Software | No strong perceptions |
Variation in triage software used Some difference in rates depending on triage software used but did not remain in the regression Different CAD systems used |
No differences | Only one service included in analysis so only one example of triage software | Different triage software used in each of three services |
We did not measure the effect of all the different types of software used by ambulance services There is considerable variation in all the different types of software ambulance services use (e.g. CAD, dispatch, triage) It is possible that triage systems affect non-conveyance rates but we could test the effect of the dispatch software only |
|
| Organisational level | Stability | Although some services appeared to be operating in a period of stability, others had experienced recent operational restructure | No effect | No effect | No comment | No comment | Ambulance services experiencing restructure may have struggled to invest resources into increasing non-conveyance. Conversely, operational restructure may offer opportunities to introduce non-conveyance initiatives. Does not appear to be an important variable here |
| Motivation to undertake non-conveyance | Variation in motivation to undertake non-conveyance apparent at extremes of rates. A service with a high rate appeared to have a long-established culture, which promoted non-conveyance. A service with a low rate had management that was risk averse about discharge at scene | Services with risk-averse management had lower rates of discharge at scene | No effect | No comment |
The workforce in one of the services reported higher levels of motivation for telephone advice than in the other two services. This service had a higher rate of telephone advice Services motivated to undertake non-conveyance by different things (e.g. demand management or risk management) |
There were differences in how management in each ambulance service, or commissioners, talked about non-conveyance – why they did it and how risky they thought it was Services with low rates appeared to discuss non-conveyance as a risky thing to do |
|
| Wider emergency and urgent care health system | Provision of services |
A perception that the provision of alternative services (to the emergency department) in the emergency and urgent care system was a facilitator of non-conveyance Variation in perceptions of the provision of services in different localities |
No effect between ambulance services Rates varied within ambulance services, possibly showing the effect of provision of services in different CCGs |
No effect | No comment | A perception that the provision of alternative services (to the emergency department) in the emergency and urgent care system was a facilitator of non-conveyance | Good provision of services in the wider system perceived to facilitate non-conveyance but no statistical support for this |
| Connectivity with services | Variation in how well connected interviewees felt the ambulance service was to the wider system. However, in the main there was felt to be a lack of connectivity | No effect | No effect | No comment | No comment | Connectivity could facilitate non-conveyance but no statistical support for this | |
| Pressure in the system | Some perceptions of pressures within the wider system for the majority of services | No comment | No comment | No comment | No comment | This could affect non-conveyance in different ways. If other services are under pressure then demand for ambulance services may increase. If acute trusts are under pressure with long handover times then this may increase non-conveyance to avoid the emergency department. Few data to discuss this | |
| Complexity of the system |
Ambulance services had to work with multiple CCGs and each CCG had a different approach to commissioning, made different investments in non-conveyance and supported different configurations of services within their CCG area There was a perception that complex systems were a barrier to non-conveyance |
Number of CCGs varied within each ambulance service so some services had less complexity in terms of numbers of areas to work with in their region No effect |
Recontact rates were higher for services with small and large numbers of CCGs | No comment | No comment | This is a potential barrier to non-conveyance. The more complex the system (i.e. the more CCGs located within the geographical boundary of the ambulance service, or the more CCGs that operate independently) the harder ambulance services have to work to make connections around the system and deliver non-conveyance. However, there was no evidence of this in the regression and the relationship with recontact rates was not easily explained | |
| National | Response-time targets | The pressure to meet response-time targets was considerable and the main priority for some ambulance services. For others, response-time targets and non-conveyance were priorities of similar importance | See motivation to undertake non-conveyance | No comment | No comment | No comment | This is a key priority shaping the actions of ambulance services. See motivation to undertake non-conveyance |
| Volume of calls | Concerns about increasing demand | No comment | No comment | No comment | Services operated a different ways when under pressure. Clinical hub staff in some areas did welfare calls or downgraded some calls after intervention | High volume of calls may increase or decrease rates of non-conveyance. Not tested | |
| Safety and appropriateness |
Safety was important to staff There was a perception that recontact AQIs do not necessarily communicate inappropriateness |
No comment | Factors affecting 24-hour recontacts with the ambulance service offered a confusing picture whereby how advanced paramedics were used and the proportion of advanced practitioners within frontline staff increased recontact rates for discharge at scene even though advanced paramedics and paramedics had the same recontact rates |
Most non-conveyed calls did not result in subsequent events such as mortality, hospital admission and attendance at emergency departments within 3 days A considerable proportion of recontacts occur within a few hours, suggesting patient dissatisfaction with the decision |
Some services use the option of a taxi for telephone advice only, which might reduce recontact rates |
No evidence of lack of safety Perhaps measure of recontact with ambulance service includes many things, including patient dissatisfaction with a non-conveyance decision |
|
FIGURE 12.
Framework of factors affecting VAN rates (dark green circles identify statistically significant factors in the final regressions).

Discussion
The process of bringing findings together highlighted key points for the discussion and drew attention to areas in which there was uncertainty. There was considerable overlap between our framework of factors affecting variation in non-conveyance and Appleby’s framework of causes of variation in health care. 40 Demand factors were very similar, with the exception of the role of ‘GP decisions’. GPs were important to non-conveyance but in terms of being part of the supply of care, as one of many services in the wider emergency and urgent care system. Health-care professionals called ambulance services directly but these calls made up a small minority of all calls. Supply factors were quite different from Appleby’s framework. We did not find much mention of clinical issues in our study so did not include clinical guidelines in our framework, even though some guidelines are used by paramedics when making decisions about non-conveyance. The supply side of our framework was much more varied than Appleby’s and included the effect of the wider emergency and urgent care system; this highlighted the extent to which non-conveyance is dependent on other services and not simply on the ambulance service.
Chapter 11 Discussion
Summary of findings
Non-conveyance rates differ by ambulance service. We found that some variation was due to differences in the ways in which these rates were calculated by individual services. Rates for calls ending in telephone advice appeared to be particularly susceptible to calculation differences. Only a small amount of variation between ambulance services was explained by differences in case-mix that were non-modifiable by ambulance services. Variation in telephone-advice-only rates between ambulance services could not be explained in the statistical regression. However, our qualitative research in three ambulance services with different rates showed large variation in many practices and processes, including the motivation of staff delivering the service. Staff in the two services with higher rates were motivated by the desire to send ambulances only to patients who needed them, whereas staff in the service with the lower rate were motivated by the need to manage risk if an ambulance was not sent. Variation in discharge-at-scene rates was explained by ambulance service-level factors related to the workforce and the degree of motivation to undertake non-conveyance. Ambulance services with higher proportions of calls attended by advanced paramedics, and for which interviewees from an ambulance service described advanced paramedics as an established and valued part of the workforce, had higher discharge-at-scene rates. Ambulance services from which interviewees described senior management as risk averse about non-conveyance had lower rates of discharge at scene. Factors explaining differences in 24-hour recontact rates between ambulance services for both types of non-conveyance offered a confusing picture. For discharge at scene, where interviewees described their service as one in which advanced paramedics were established and valued and a higher proportion of frontline staff were advanced practitioners, recontact rates were higher, even though advanced paramedics and paramedics had similar recontact rates. A small minority of patients called the ambulance service, attended an emergency department or were admitted to hospital within 3 days of their non-conveyance. Finally, the qualitative research identified factors perceived to affect non-conveyance, which were not modifiable by ambulance services, namely attributes of the wider emergency and urgent care system in which ambulance services operated. Although these did not explain variation between ambulance services in the regressions, it is possible that they affect variation in rates within ambulance services. In summary, variation between ambulance services appeared to be largely unwarranted and modifiable by ambulance services.
The wider evidence base
Findings from each chapter have been discussed in the context of related research. Although there is an evidence base on non-conveyance, the evidence on variation in non-conveyance is limited. A recent publication on ambulance services in England, which focused partly on non-conveyance and variation between services, identified similar issues to our research. 1 The only issues that differed were the NAO’s emphasis on the problem with the recruitment and retention of paramedics that is likely to limit the ability of services to expand non-conveyance in the future, and the external barrier of lack of availability of services in the wider emergency and urgent care system, which limits the referral options for non-conveyance. The NAO report is likely to have placed more emphasis on these issues owing to its focus on non-conveyance for ambulance services in general and our focus on variation between ambulance services.
Recent reports on the ambulance service in England have identified the context in which ambulance services have increased their non-conveyance rates over the years, that is, one of higher demand for life-threatening as well as less urgent problems; of resources and workforce not increasing at the rate of demand; of delays in handovers at emergency departments, rates of which may differ by ambulance service region; and of worsening performance in terms of meeting response-time targets. 1,78 Although some of these issues were raised in our qualitative research, it is worth considering our findings within this wider context.
Causes of variation in non-conveyance between ambulance services were similar to those identified by Appleby’s framework of causes of variation in health care. 40 Our framework included factors specific to the ambulance service and was more complex than Appleby’s. Organisational factors contributed to the variation that we found. We have tried to avoid using the term ‘organisational culture’ because of the difficulties in defining this within the academic study of organisations. 79 Instead, we have focused on aspects of the organisation that affect performance in terms of non-conveyance rates.
Policy questions
Is there an optimal rate for non-conveyance?
The recent NAO report suggests that there is a need to identify an optimal rate for non-conveyance. 1 Our study has not identified an optimal rate; this would require a consideration of the safety and cost-effectiveness of different rates of non-conveyance based on a stable case-mix and we have not done this. However, the AQIs show that it is possible to achieve a rate of 10% of calls ending in telephone advice and 35% of calls ending in discharge at scene or conveyance to an alternative service. Some services may be achieving this by including types of calls that policy-makers may not define as non-conveyance. Some services have put considerable effort into increasing their non-conveyance rates and have achieved these, or higher, rates. Policy-makers cannot necessarily expect the rate to continue to increase in the future. Increases in rates will depend on the following:
-
How non-conveyance in current performance indicators is counted – calls ending in telephone advice in current published indicators include calls referred to the clinical hub, calls terminated by call-handlers and, for some ambulance services, a mix of other calls such as hoax calls. Non-conveyance could be defined based only on calls sent to a clinical hub that end in telephone advice, which would reduce current rates in AQIs. If all ambulance services adhered to guidance by including only real calls for an ambulance that are ended by either call-handlers or clinicians, then this would reduce current rates in AQIs for some ambulance services. If people who have died prior to the ambulance arriving or while the crew are on scene are removed from AQIs then current rates would reduce.
-
Changes in the urgency levels of calls to the ambulance service – demand for the ambulance service has increased over recent years. NHS 111’s direct referrals to the ambulance service have been identified as contributing to this increase in an evaluation of NHS 111 pilots. 80 This relatively new service in the emergency and urgent care system is likely to have changed the urgency levels of cases attended by an ambulance and, therefore, to have increased the potential for discharge at scene. Other changes in case-mix in the future may affect the potential for ambulance services to increase non-conveyance: increases in low-acuity calls will increase the opportunity for telephone advice and discharge at scene.
-
The actions ambulance services are allowed to take in response to low-urgency calls – if ambulance services are allowed to retriage referrals from NHS 111, or if ambulance service call-handlers are allowed to refer low-urgency callers to NHS 111,8 then the potential for non-conveyance by ambulance service clinicians will decrease. These actions may be a more appropriate response to some calls than clinical input by an ambulance service either by telephone or face to face.
-
The investment services make in non-conveyance processes – investment can include numbers of staff, types of staff, the education of staff, the training offered to staff, how staff are valued within their workplace, and the types of work that staff are asked to undertake. This investment may be helped or hindered by commissioners’ views of the importance of different type of non-conveyance.
-
The changing characteristics of the wider emergency and urgent care system – if other services in the emergency and urgent care system, such as emergency departments, acute hospital beds, social services or daytime general practice, are under pressure, then demand for ambulance services may increase, or the ability of ambulance service clinicians to discharge at the scene in the confidence that the patient will have contact with another appropriate service may be reduced. Conversely, pressure at emergency departments with long handover times may increase discharge-at-scene rates.
Should NHS 111 clinical advice and 999 telephone advice in clinical hubs merge?
One can argue that NHS 111 calls referred to a clinician within that service and 999 low-urgency calls sent to a clinical hub for telephone advice could be the same types of calls, which are simply being dealt with by two different services. Having two separate pathways to this telephone advice is essential because having both NHS 111 and 999 allows patients to self-triage their problem as urgent or emergency, which, in the main, they do very well. However, some patients understandably do not self-triage appropriately and, therefore, the relationship between NHS 111 clinical telephone advice and ambulance service clinical telephone advice needs careful consideration, especially given that ambulance services provide NHS 111 in large areas of England. In 2016/17 three ambulance services provided NHS 111 to all their population and a further six provided it to part of their populations. In some ambulance services, there is co-location of NHS 111 and clinical hub clinicians but this does not mean that there is integrated working. There was some evidence within our WP1 interviews that some services were moving towards aspects of integrated working, but there is an opportunity to consider integrating staff and practices in ways that might increase efficiency. Furthermore, other aspects of the relationship between ambulance services and NHS 111 could be reviewed in terms of the ability of the two services to refer to the other. There is the option that ambulance service call-handlers triage directly to NHS 111. This was evaluated when NHS Direct was in operation. 8 It had some problems in terms of a proportion of calls being sent back to the ambulance service, which was less than ideal, as some patients could have felt like they were being bounced around the emergency and urgent care system. 76 However, additional assessments of this practice, with evaluation, would be useful.
Is non-conveyance cost-effective?
We have not undertaken an economic analysis of non-conveyance. A recent systematic review of secondary telephone triage identified that this was an important thing to do. 21 The recent NAO report estimated that ambulance trusts potentially saved themselves £74M and emergency departments £63M in 2015/16 by increasing non-conveyance rates compared with rates recorded in 2011/12. 1 The report points out that this could be an underestimate because it did not include hospital admissions in this calculation, and non-conveyance to emergency departments is associated with lower emergency admission rates. 3 However, the authors also point out that they did not include the additional costs of community services that ambulance services may refer to as part of the non-conveyance decision. 1 Nor did they consider that it may take more time to treat a patient at home than convey them to an emergency department in some circumstances (low-urgency calls took 88 minutes to deal with in 2015/16 compared with 75 minutes in 2011/12). 1 It is also the case that a proportion of patients subsequently get an ambulance or attend an emergency department after the original decision to non-convey (see Chapter 7). Finally, the high quality of the advice provided to patients during ambulance service non-conveyance may result in supply-induced demand, encouraging patients to use the service in preference to alternatives. 13 This is related to the issue of recursivity in urgent care provision whereby how services act encourages future patient demand. 81 In summary, the economics of non-conveyance are complicated but should be addressed in future studies.
Is supply-induced demand likely?
The possibility that supply-induced demand is contributing to increases in demand for ambulance services should be seriously considered. It was a concern raised by interviewees in our study and has been raised as a concern about secondary triage services internationally. 21
How can risks be balanced?
There are a number of risks related to non-conveyance. First, there is a risk that an ambulance service might not be able to meet demand unless non-conveyance is an option. Second, there is a risk that ambulances may not be able to make timely responses to life-threatening conditions because they are responding to low-acuity patients. Third, there is a risk that a patient may die or experience a permanent adverse event as a result of a decision not to convey. Fourth, there is a risk that ambulance crews may be disciplined or lose their jobs if something goes wrong after a decision not to convey. This can lead to ‘disproportionate risk aversion’, as identified in a study of decision-making at transition points in the ambulance service. 12 Fifth, there is a risk that an ambulance service may face a loss of reputation if it receives large numbers of patient complaints about decisions not to convey. There is no right balance of risks; the balance is open to debate and discussion between policy-makers, commissioners, national patient groups such as Healthwatch, and senior managers and frontline staff in ambulance services is necessary.
Strengths and limitations
The strengths and limitations of different WPs have been discussed in earlier chapters. Here, we address some overarching issues for the whole study. This is one of the first research studies in the world to take such an extensive view of variation in ambulance service non-conveyance. A major strength of the study is that the 10 large ambulance services in England agreed to participate in the research and provided the relevant data. There were four limitations:
-
We were unable to obtain data items that might have helped us to offer more standardisation of calculations of non-conveyance rates between ambulance services. In addition, ambulance services can make a large range of responses to calls that are not easily categorised in terms of non-conveyance (e.g. an ambulance that arrives on scene while a patient is receiving telephone advice). How the full range of responses is dealt with in each ambulance service for data items contributing to numerators and denominators of rates can affect reported non-conveyance rates. Therefore, some variation between services within our data set in WP2 and WP3 may have been attributable to differences in the ways in which services calculated the variables we requested.
-
We identified ambulance service-level variables to test in regressions within WP2 and WP3.1 based on staff perceptions of non-conveyance within their service from qualitative interviews in WP1. Staff may have been selected for interview to offer a positive view of non-conveyance within their organisation, staff may have acquired beliefs about non-conveyance in their service shaped by their position in the ranking of ambulance service non-conveyance rates, and perceptions may have been shaped by the personality traits of interviewees (e.g. some individuals may offer a more negative view of the same organisation than others). We paid attention to these issues during our qualitative analysis. Related to this, variables from WP1 were developed for testing in WP3 by researchers blinded to non-conveyance rates for individual services. However, it is possible that blinding was not 100% reliable because these researchers worked within a team in which members knew the ranking of ambulance services. We paid considerable attention to the maintenance of blinding throughout the study.
-
Contextual changes occurred over the time of our study that may have affected different ambulance services at different times. A key contextual change was the introduction of the Ambulance Response Programme during the course of our study, whereby some ambulance services participated in a pilot study that allows call-handlers up to 4 minutes to make a decision on the most appropriate response to a call (in contrast to the existing 1 minute). The intention of this scheme is to improve the efficiency of resource use by allocating resources based on clinical need, and to increase the potential for offering telephone advice rather dispatching an ambulance. This did not affect our quantitative analyses but could have influenced some of the views expressed by interviewees in WP1, as well as the observations in WP4.1.
-
We did not understand the effect of all the factors that we explored in the study. We were left with considerable uncertainty about the relationship between NHS 111 and non-conveyance rates in ambulance services. The way in which NHS 111 operates, and the way in which the ambulance service responds to NHS 111 calls, may affect non-conveyance rates, particularly for telephone advice. However, we did not have sufficient qualitative or quantitative data to understand this relationship in enough depth.
Generalisability, transferability and reflexivity
Emergency Medical Systems or ambulance services vary internationally. The findings here are relevant to England. Policy-makers, service providers and researchers in other countries will have to consider similarities and differences between their system and the system researched here when considering the transferability of findings.
Our team comprised researchers with many years of experience in emergency and urgent care research, patients, paramedics and members of a body for ambulance service leaders. We have tried to take a respectful approach to services working under challenging circumstances while also identifying areas with the potential for improvement.
Patient and public involvement
As well as having PPI members as part of the project team and Project Advisory Group, patients and members of the public working with three ambulance services or research teams engaged with emergency and urgent care came together to form a VAN project PPI group. Although members associated with one of the ambulance services had to drop out over time, the two established PPI groups worked together successfully for the duration of this project. The PPI members helped to interpret the findings of the study and develop a strategy for disseminating the findings to a non-academic audience. The group met on five occasions and were also present at the final project management meeting at which the findings from each WP were presented. The group met for a final meeting after the submission of this report to finalise the plans for PPI-led dissemination.
During the PPI meetings, members of the research team presented emerging findings from each WP. PPI members’ discussions affected the research in numerous ways, including the following:
-
PPI members were interested in variation in total non-conveyance rates as well as the different types of non-conveyance. We included graphs of total non-conveyance in our presentations to show that variation existed at this level as well as at the level of different types of non-conveyance.
-
The appropriateness of non-conveyance was very important to the PPI group. This was a key component of our study.
-
Our study focused on NHS staff views and analysis of routine data. PPI members felt that patients’ perceptions were missing from our study. They understood that we had not been funded to include patients’ perceptions but wanted us to place our findings alongside other research focusing on patients’ views. We included a review of literature of patients’ views in the introduction to the study. We highlight the need to focus on patients’ views of non-conveyance in our recommendations for future research.
-
PPI members were keen to promote patient education about how best to use the ambulance service.
Conclusions
Variation in non-conveyance rates between ambulance services in England could be reduced by addressing variation in the availability of advanced paramedics and how they are used within services and in the perceptions of the risks associated with non-conveyance within ambulance service management.
Implications
Non-conveyance occurs in a context in which ambulance services are judged largely by their ability to meet response-time targets as demand for their service increases. Non-conveyance is a relatively new activity in the history of ambulance provision, which requires ambulance services to shift their focus from transporting emergency cases to hospital to managing emergency and urgent care cases in a way that is much more aligned to providing care appropriate to clinical need. Many processes vary between ambulance services, which may contribute to unwarranted variation in non-conveyance rates. These processes include the standardisation of CAD systems, triage software, skill-mix labels, how different grades of paramedics are used in practice, and how ambulance services are commissioned in practice. We have identified that workforce configuration, how advanced paramedics are used and management motivation to undertake non-conveyance were key issues that ambulance services can address to reduce variation in non-conveyance rates between ambulance services. There are a number of implications in light of this.
Formalising definitions of non-conveyance
When policy-makers and researchers assess non-conveyance rates for ambulance services they may wrongly interpret these rates, especially for calls ending in telephone advice. It is easy to interpret published AQIs as rates of patients offered advice over the telephone by clinicians when in practice this includes an array of reasons for the call ending without an ambulance being dispatched. The evidence suggests that policy-makers might benefit from considering what they wish to see measured and putting in place plans to produce AQIs that can measure this. There remains concern about the validity of the data used to calculate AQIs, especially for calls ending in telephone advice. Real variation between services, and especially variation in calls receiving clinical advice that end in telephone advice, could easily be larger or smaller than rates reported in AQIs. A first step to better understand the important aspect of clinical telephone advice by ambulance services is to investigate the development of new indicators that separate out what might be called ‘true hear and treat’ from calls dealt with by call-handlers or calls that should simply never be classified as ending in telephone advice, such as hoax calls. Improving the accuracy of the AQIs, and monitoring adherence to the guidance for calculating AQIs, would help ambulance services to consider real differences between themselves and other services.
Reducing variation so that all ambulance services offer the optimum rate of non-conveyance
It is possible that the ambulance service with the highest rate of non-conveyance at the time of the research did not have the optimal rate of non-conveyance. Establishing what the optimal rate is requires modelling of the cost-effectiveness, and safety and appropriateness, of different rates of non-conveyance. Some approaches to non-conveyance may not be cost-effective, may result in increased mortality or increased severity of illness, or may simply delay conveyance. This study did not set out to establish the ‘right’ rate of non-conveyance and cannot shed light on this issue. A further research study is required to address this, which repeats the linked data analysis undertaken here for one service only for all ambulance services in England and considers the relationship between mortality and subsequent service use for different rates of non-conveyance. A future study would also be necessary to identify the cost-effectiveness of different approaches to non-conveyance.
How to reduce variation
The variation in overall rates of non-conveyance mainly concerned the small number of ambulance services with extreme rates, namely one service with a relatively high rate of discharge at scene and some with relatively low rates of discharge at scene. There was no indication that the high rate was problematic (although safety was not measured for this service and a limited measure of appropriateness was considered). There was evidence of opportunities to increase the discharge-at-scene rate for ambulance services with lower rates. Some of this unwarranted variation lay within the control of the ambulance service and was determined by their workforce policies and motivation to undertake discharge at scene. National policies cannot be the cause of variation because some ambulance services achieved high non-conveyance rates with these policies in operation. However, a change in policies – in particular response-time targets – may help services with low rates to prioritise investment in non-conveyance. A key issue is the considerable amount of variation in ambulance processes in terms of CAD systems, triage software for dispatch, triage software by telephone or face-to-face clinical input, paramedic nomenclature, and how staff with different skills are used. Much of this variation is not necessary and standardisation of these processes could contribute to reductions in the variation in outcomes such as non-conveyance.
Recommendations for future research
We recommend that researchers:
-
Create a linked data set for all ambulance services in the UK, linking routine ambulance service data with HES and ONS data on emergency department attendances, hospital admissions and mortality to compare the safety and appropriateness of different non-conveyance rates in operation in different ambulances services.
-
Measure the cost-effectiveness of undertaking telephone advice within clinical hubs and undertaking discharge at scene.
-
Seek patients’ and their families’ views of non-conveyance, including in episodes in which patients experience subsequent events, such as hospital admission, within 3 days. During this research, consideration can be given to the need for, and consequences of, educating the public about when to call 999 and about different types of non-conveyance.
-
Undertake more national research on the ambulance service because this is a large and important service in NHS emergency and urgent health-care provision.
-
Establish a national PPI group for ambulance research to facilitate national research on ambulance services.
Acknowledgements
Contributions of authors
Professor Alicia O’Cathain (Professor of Health Services Research) led the study, led the analysis of routine data, led the analysis of data on breathing problems and wrote the first draft of the report, with the exception of Chapters 4 and 8.
Dr Emma Knowles (Senior Research Fellow in Emergency and Urgent Care) was the project manager, led the qualitative interview study in WP1 and wrote Chapter 4.
Ms Lindsey Bishop-Edwards (Research Associate in Emergency and Urgent Care) undertook all non-participant observations and interviews, and contributed to analysing the qualitative data.
Ms Joanne Coster (Research Fellow in Emergency and Urgent Care) led the data linkage of routine data for measuring events after non-conveyance for WP3.2 reported in Chapter 7.
Ms Annabel Crum (Data Support Manager in Emergency and Urgent Care) managed and prepared the linked data for WP3.2.
Dr Richard Jacques (Lecturer in Statistics) analysed the quantitative data.
Ms Cathryn James (Paramedic, Association of Ambulance Chief Executives) attended project meetings and advised on accessing data, the interpretation of data and the dissemination of findings.
Dr Rod Lawson (Respiratory Physician) advised about the breathing problems analysis in WP4.2.
Mrs Maggie Marsh (PPI representative) attended project meetings and advised on the interpretation of data and the dissemination of findings.
Dr Rachel O’Hara (Senior Lecturer, Occupational Psychologist) led the study of telephone advice in three ambulances services (WP4.1) and wrote Chapter 8.
Professor Aloysius Niroshan Siriwardena (Professor of Primary and Pre-Hospital Health Care) attended project meetings and advised on accessing data, the interpretation of data and the dissemination of findings.
Mr Tony Stone (Data Management Support Officer in Emergency and Urgent Care) managed and prepared the routine data from ambulance services in WP2, WP3.1 and WP4.2.
Ms Janette Turner (Reader in Emergency and Urgent Care) attended project meetings and advised on accessing data, the interpretation of data and the dissemination of findings.
Professor Julia Williams (Professor of Paramedic Science) advised on accessing data, the interpretation of data and the dissemination of findings.
Acknowledgements of external help
Members of the National Ambulance Research Steering Group, the National Ambulance Information Group and Research & Development Managers helped to ensure that the study was successfully completed in all 10 ambulance services in England.
We would like to thank the managers and clinicians in the ambulance services, and commissioners of ambulance services, for participating in interviews. We are very grateful to them for giving their time and views while working under considerable pressure to deliver and commission health care. We have not named them here to maintain anonymity.
The study relied on working closely with staff in Business Intelligence/Data Analytics Teams within each ambulance service. We are grateful to Darren Coxon, James Hill and Martin Sheehan (East Midlands Ambulance Service NHS Trust); Jonathan Barwick (East of England Ambulance Service NHS Trust); Anthony Buckler and Michael Damiani (London Ambulance Service NHS Trust); Tobias Lightfoot (North East Ambulance Service NHS Foundation Trust); Emma Thompson and Paul Wickstead (North West Ambulance Service NHS Trust); Mark Green (South Central Ambulance Service NHS Foundation Trust); Tushar Mody (South East Coast Ambulance Service NHS Foundation Trust); Rhys Hancock and Richard Wortham (South Western Ambulance Service NHS Foundation Trust); Andrew Barlow (West Midland Ambulance Service NHS Foundation Trust); and Russel Danby and Phillipa Wood (Yorkshire Ambulance Service NHS Trust).
We are also grateful to:
The Project Advisory Group – Professor Tom Quinn (Chairperson, Associate Dean for Research and Innovation, Kingston University and St George’s Hospital, University of London), Liz Harris (Paramedic, Yorkshire Ambulance Service), Mark Docherty (Director of Clinical Commissioning, West Midlands Ambulance Service) and Enid Hirst (PPI representative, Sheffield Emergency Care Forum).
The PPI Group established for the study – Linda Abouzeid, Amanda Brewster, Beryl Darlison, Rosemary Harper, Enid Hirst, Maggie Marsh, Gordon McGhee, Pauline Mountain, Mo Reece, Jim Reece, Brian Russell and Lissie Wilkins.
Nisar Ahmed and Flavia Saraiva Leao Fernandes for contributing to the coding of the qualitative data.
Richard Campbell for administrative support.
Disclaimer
HES data were made available by NHS Digital (copyright © 2016, reused with permission of The Health & Social Care Information Centre. All rights reserved).
Data sharing statement
There are no data available for further access or sharing owing to the nature of the study. The data collected for the qualitative study are not suitable for sharing beyond that contained within the report. The routine data were supplied by the Ambulance Trusts under strict conditions and usage agreements that prohibits further sharing. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- NHS Ambulance Service. London: National Audit Office; 2017.
- Ambulance Quality Indicators. Redditch: NHS England; 2017.
- O’Cathain A, Knowles E, Turner J, Hirst E, Goodacre S, Nicholl J. Explaining variation in emergency admissions: a mixed-methods study of emergency and urgent care systems. Health Serv Deliv Res 2014;2.
- High Quality Care for all, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England – Urgent and Emergency Care Review End of Phase 1 Report. 2013.
- Friends and Family Test Data. Redditch: NHS England; 2017.
- Ambulance Survey of ‘Hear and Treat’ Callers 2013/14. Newcastle upon Tyne: Care Quality Commission; 2017.
- Smith WR, Culley L, Plorde M, Murray JA, Hearne T, Goldberg P, et al. Emergency medical services telephone referral program: an alternative approach to nonurgent 911 calls. Prehosp Emerg Care 2001;5:174-80. https://doi.org/10.1080/10903120190940092.
- Turner J, Snooks H, Youren A, Dixon S, Fall D, Gaze S, et al. The Costs and Benefits of Managing Some Low Priority 999 Ambulance Calls by NHS Direct Nurse Advisers. Report for the National Institute for Health Research Service Delivery and Organisation programme. Southampton: National Institute for Health Research; 2006.
- Jones CM, Wasserman EB, Li T, Shah MN. Acceptability of Alternatives to Traditional Emergency Care: Patient Characteristics, Alternate Transport Modes, and Alternate Destinations. Prehosp Emerg Care 2015;19:516-23. https://doi.org/10.3109/10903127.2015.1025156.
- Machen I, Dickinson A, Williams J, Widiatmoko D, Kendall S. Nurses and paramedics in partnership: perceptions of a new response to low-priority ambulance calls. Accid Emerg Nurs 2007;15:185-92. https://doi.org/10.1016/j.aaen.2007.09.001.
- Togher FJ, O’Cathain A, Phung VH, Turner J, Siriwardena AN. Reassurance as a key outcome valued by emergency ambulance service users: a qualitative interview study. Health Expect 2015;18:2951-61. https://doi.org/10.1111/hex.12279.
- O’Hara R, Johnson M, Hirst E, Weyman A, Shaw D, Mortimer P, et al. A qualitative study of decision-making and safety in ambulance service transitions. Health Serv Deliv Res 2014;2.
- Booker MJ, Simmonds RL, Purdy S. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emerg Med J 2014;31:448-52. https://doi.org/10.1136/emermed-2012-202124.
- Keene T, Davis M, Brook C. Characteristics and outcomes of patients assessed by paramedics and not transported to hospital: A pilot study. Aust J Paramed 2015;12.
- Colver KA. Ambulance Service Treat and Refer Guidelines: A Qualitative Investigation into the Use of Treat and Refer Guidelines by Ambulance Clinicians 2012. https://dspace.stir.ac.uk/bitstream/1893/11298/1/Keith%20Colver_Treat%20and%20Refer_%20MPhil%20Thesis_FINAL.pdf (accessed 24 April 2018).
- Burrell L, Noble A, Ridsdale L. Decision-making by ambulance clinicians in London when managing patients with epilepsy: a qualitative study. Emerg Med J 2012;30:236-40. https://doi.org/10.1136/emermed-2011-200388.
- Porter A, Snooks H, Youren A, Gaze S, Whitfield R, Rapport F, et al. ‘Covering our backs’: ambulance crews’ attitudes towards clinical documentation when emergency (999) patients are not conveyed to hospital. Emerg Med J 2008;25:292-5. https://doi.org/10.1136/emj.2007.050443.
- Hjälte L, Suserud BO, Herlitz J, Karlberg I. Why are people without medical needs transported by ambulance? A study of indications for pre-hospital care. Eur J Emerg Med 2007;14:151-6. https://doi.org/10.1097/MEJ.0b013e3280146508.
- Snooks HA, Dale J, Hartley-Sharpe C, Halter M. On-scene alternatives for emergency ambulance crews attending patients who do not need to travel to the accident and emergency department: a review of the literature. Emerg Med J 2004;21:212-15. https://doi.org/10.1136/emj.2003.005199.
- Mikolaizak AS, Simpson PM, Tiedemann A, Lord SR, Close JC. Systematic review of non-transportation rates and outcomes for older people who have fallen after ambulance service call-out. Australas J Ageing 2013;32:147-57. https://doi.org/10.1111/ajag.12023.
- Eastwood K, Morgans A, Smith K, Hodgkinson A, Becker G, Stoelwinder J. A novel approach for managing the growing demand for ambulance services by low-acuity patients. Aust Health Rev 2016;40:378-84. https://doi.org/10.1071/AH15134.
- Snooks HA, Carter B, Dale J, Foster T, Humphreys I, Logan PA, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1): cluster randomised trial of computerised clinical decision support for paramedics. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0106436.
- Fitzpatrick D. Hypoglycaemic Emergencies Attended by the Scottish Ambulance Service: A Multiple Methods Investigation 2015. https://dspace.stir.ac.uk/handle/1893/21854?mode=full#.Wt9NO3rwaUk (accessed 24 April 2018).
- Dickson JM, Taylor LH, Shewan J, Baldwin T, Grünewald RA, Reuber M. Cross-sectional study of the prehospital management of adult patients with a suspected seizure (EPIC1). BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010573.
- Prekker ME, Feemster LC, Hough CL, Carlbom D, Crothers K, Au DH, et al. The epidemiology and outcome of prehospital respiratory distress. Acad Emerg Med 2014;21:543-50. https://doi.org/10.1111/acem.12380.
- Mercer MP, Mahadevan SV, Pirrotta E, Ramana Rao GV, Sistla S, Nampelly B, et al. Epidemiology of shortness of breath in prehospital patients in Andhra Pradesh, India. J Emerg Med 2015;49:448-54. https://doi.org/10.1016/j.jemermed.2015.02.041.
- Kelly AM, Holdgate A, Keijzers G, Klim S, Graham CA, Craig S, et al. Epidemiology, prehospital care and outcomes of patients arriving by ambulance with dyspnoea: an observational study. Scand J Trauma Resusc Emerg Med 2016;24. https://doi.org/10.1186/s13049-016-0305-5.
- Smith SM, Mitchell C, Bowler SD, Heneghan C, Perera R. The health behaviour and clinical characteristics of ambulance users with acute asthma. Emerg Med J 2009;26:187-92. https://doi.org/10.1136/emj.2008.059188.
- Gray JT, Walker A. Avoiding admissions from the ambulance service: a review of elderly patients with falls and patients with breathing difficulties seen by emergency care practitioners in South Yorkshire. Emerg Med J 2008;25:168-71. https://doi.org/10.1136/emj.2007.050732.
- Marks PJ, Daniel TD, Afolabi O, Spiers G, Nguyen-Van-Tam JS. Emergency (999) calls to the ambulance service that do not result in the patient being transported to hospital: an epidemiological study. Emerg Med J 2002;19:449-52. https://doi.org/10.1136/emj.19.5.449.
- Tohira H, Williams TA, Jacobs I, Bremner A, Finn J. The impact of new prehospital practitioners on ambulance transportation to the emergency department: a systematic review and meta-analysis. Emerg Med J 2014;31:e88-94. https://doi.org/10.1136/emermed-2013-202976.
- Mason S, Knowles E, Colwell B, Dixon S, Wardrope J, Gorringe R, et al. Effectiveness of paramedic practitioners in attending 999 calls from elderly people in the community: cluster randomised controlled trial. BMJ 2007;335. https://doi.org/10.1136/bmj.39343.649097.55.
- Fisher JD, Freeman K, Clarke A, Spurgeon P, Smyth M, Perkins GD, et al. Patient safety in ambulance services: a scoping review. Health Serv Deliv Res 2015;3.
- Eastwood K, Morgans A, Smith K, Stoelwinder J. Secondary triage in prehospital emergency ambulance services: a systematic review. Emerg Med J 2015;32:486-92. https://doi.org/10.1136/emermed-2013-203120.
- Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung WY. Towards primary care for non-serious 999 callers: results of a controlled study of ‘Treat and Refer’ protocols for ambulance crews. Qual Saf Health Care 2004;13:435-43. https://doi.org/10.1136/qshc.2003.007658.
- Kahalé J, Osmond MH, Nesbitt L, Stiell IG. What are the characteristics and outcomes of nontransported pediatric patients?. Prehosp Emerg Care 2006;10:28-34. https://doi.org/10.1080/10903120500373322.
- Shaw D, Dyas JV, Middlemass J, Spaight A, Briggs M, Christopher S, et al. Are they really refusing to travel? A qualitative study of prehospital records. BMC Emerg Med 2006;6. https://doi.org/10.1186/1471-227X-6-8.
- National Ambulance Non-Conveyance Audit (NANA) Report. London: National Ambulance Service Clinical Quality Group; 2013.
- Developing an Ambulance Commissioning Strategy: Five Year Forward View and Beyond. London: National Ambulance Commissioners Network, NHS Clinical Commissioners; 2015.
- Appleby J, Raleigh V, Frosini F, Bevan G, Gao H, Lyscom T. Variations in Health Care. The Good, the Bad and the Inexplicable. London: The King’s Fund; 2011.
- Wennberg JE. Time to tackle unwarranted variations in practice. BMJ 2011;342. https://doi.org/10.1136/bmj.d1513.
- Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ 2002;325:961-4. https://doi.org/10.1136/bmj.325.7370.961.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res 2006;16:377-94. https://doi.org/10.1177/1049732305285708.
- Yin RK. Case Study Research: Design and Methods. London: Sage; 2013.
- O’Cathain A, Andrew S, Halcomb EJ. Mixed Methods Research for Nursing and the Health Sciences. Chichester: John Wiley & Sons; 2009.
- Annual Report 2014/15. Melbourn: East of England Ambulance Service NHS Trust; 2015.
- Annual Report 2014/2015. Nottingham: East Midlands Ambulance Service NHS Trust; 2015.
- Annual Report 2014/15. London: London Ambulance Service NHS Trust; 2015.
- Annual Report & Accounts for the Period 1 April 2014–31 March 2015. Newcastle upon Tyne: North East Ambulance Service NHS Foundation Trust; 2015.
- Annual Report 2014/2015. Bolton: North West Ambulance Service NHS Trust; 2015.
- Annual Report & Accounts 2014/15. Bicester: South Central Ambulance Service NHS Foundation Trust; 2015.
- Annual Report and Accounts 1 April 2014–31 March 2015. Banstead: South East Coast Ambulance Service NHS Foundation Trust; 2015.
- Annual Report and Accounts 1 April 2014–31 March 2015. Exeter: South Western Ambulance Service NHS Foundation Trust; 2015.
- Annual Report and Accounts 1st April 2014–31st March 2015. Brierley Hill: West Midlands Ambulance Service NHS Foundation Trust; 2015.
- Annual Report and Financial Summary 2014–15. Wakefield: Yorkshire Ambulance Service NHS Trust; 2015.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2013.
- NHS Staff Survey 2017. Oxford: NHS Survey Coordination Centre; 2017.
- Office for National Statistics . 2011 Census n.d. www.ons.gov.uk/census/2011census (accessed 22 May 2018).
- Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw 2015;67:1-48. www.jstatsoft.org/v067/i01 (accessed 24 April 2018).
- Nicholl J, Jacques RM, Campbell MJ. Direct risk standardisation: a new method for comparing casemix adjusted event rates using complex models. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-133.
- Spiegelhalter DJ. Funnel plots for comparing institutional performance. Stat Med 2005;24:1185-202. https://doi.org/10.1002/sim.1970.
- Sandelowski M. Combining qualitative and quantitative sampling, data collection, and analysis techniques in mixed-method studies. Res Nurs Health 2000;23:246-55. https://doi.org/10.1002/1098-240X(200006)23:3<246::AID-NUR9>3.0.CO;2-H.
- Dale J, Williams S, Foster T, Higgins J, Snooks H, Crouch R, et al. Safety of telephone consultation for ‘non-serious’ emergency ambulance service patients. Qual Saf Health Care 2004;13:363-73. https://doi.org/10.1136/qshc.2003.008003.
- Anderson S, Høgskilde PD, Wetterslev J, Bredgaard M, Møller JT, Dahl JB, et al. Appropriateness of leaving emergency medical service treated hypoglycemic patients at home: a retrospective study. Acta Anaesthesiol Scand 2002;46:464-8. https://doi.org/10.1034/j.1399-6576.2002.460424.x.
- Magnusson C, Källenius C, Knutsson S, Herlitz J, Axelsson C. Pre-hospital assessment by a single responder: The Swedish ambulance nurse in a new role: A pilot study. Int Emerg Nurs 2016;26:32-7. https://doi.org/10.1016/j.ienj.2015.09.001.
- Yardley IE, Donaldson LJ. Deaths following prehospital safety incidents: an analysis of a national database. Emerg Med J 2016;33:716-21. https://doi.org/10.1136/emermed-2015-204724.
- Obermeyer Z, Cohn B, Wilson M, Jena AB, Cutler DM. Early death after discharge from emergency departments: analysis of national US insurance claims data. BMJ 2017;356. https://doi.org/10.1136/bmj.j239.
- Pope C, Halford S, Turnbull J, Prichard J, Calestani M, May C. Using computer decision support systems in NHS emergency and urgent care: ethnographic study using normalisation process theory. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-111.
- Turnbull J, Halford S, Jones J, May C, Pope C, Prichard JS, et al. The work, workforce, technology and organisational implications of the ‘111’ single point of access telephone number for urgent (non-emergency) care: a mixed-methods case study. Health Serv Deliv Res 2014;2.
- McCann L, Granter E, Hyde P, Hassard J. Still blue-collar after all these years? An ethnography of the professionalization of emergency ambulance work. J Manage Stud 2013;50:750-76. https://doi.org/10.1111/joms.12009.
- Walshe C, Ewing G, Griffiths J. Using observation as a data collection method to help understand patient and professional roles and actions in palliative care settings. Palliat Med 2012;26:1048-54. https://doi.org/10.1177/0269216311432897.
- Transforming Urgent and Emergency Care Services in England. Clinical Models for Ambulance Services. London: Urgent and Emergency Care Review Programme Team; 2015.
- Clawson J, Barron T, Scott G, Siriwardena AN, Patterson B, Olola C. Medical Priority Dispatch System breathing problems protocol key question combinations are associated with patient acuity. Prehosp Disaster Med 2012;27:375-80. https://doi.org/10.1017/S1049023X1200101X.
- Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis 2014;9:315-30. https://doi.org/10.2147/COPD.S53255.
- O’Cathain A, Coleman P, Nicholl J. Characteristics of the emergency and urgent care system important to patients: a qualitative study. J Health Serv Res Policy 2008;13:19-25. https://doi.org/10.1258/jhsrp.2007.007097.
- Johnson M, O’Hara R, Hirst E, Weyman A, Turner J, Mason S, et al. Multiple triangulation and collaborative research using qualitative methods to explore decision making in pre-hospital emergency care. BMC Med Res Methodol 2017;17. https://doi.org/10.1186/s12874-017-0290-z.
- Appleby J, Dayan M. Nuffield Winter Insight Briefing 3: The Ambulance Service. London: Nuffield Trust; 2017.
- Scott T, Mannion R, Marshall M, Davies H. Does organisational culture influence health care performance? A review of the evidence. J Health Serv Res Policy 2003;8:105-17. https://doi.org/10.1258/135581903321466085.
- Turner J, Nicholl J, Mason S, O’Keeffe C, Anderson J. Whole System Solutions for Emergency and Urgent Care. Sheffield: ScHARR, University of Sheffield; 2014.
- Hunter C, Chew-Graham C, Langer S, Stenhoff A, Drinkwater J, Guthrie E, et al. A qualitative study of patient choices in using emergency health care for long-term conditions: the importance of candidacy and recursivity. Patient Educ Couns 2013;93:335-41. https://doi.org/10.1016/j.pec.2013.06.001.
- Tohira H, Fatovich D, Williams TA, Bremner A, Arendts G, Rogers IR, et al. Which patients should be transported to the emergency department? A perpetual prehospital dilemma. Emerg Med Australas 2016;28:647-53. https://doi.org/10.1111/1742-6723.12662.
- Jensen JL, Travers AH, Bardua DJ, Dobson T, Cox B, McVey J, et al. Transport outcomes and dispatch determinants in a paramedic long-term care program: a pilot study. CJEM 2013;15:206-13. https://doi.org/10.2310/8000.2012.120965.
- Al-Sulaiti M, Snooks H, Porter A. Non-conveyance of 999 callers: early findings related subsequent health services callers. Emerg Med J 2009;26. https://doi.org/10.1136/emj.2009.075416h.
Appendix 1 Summary of differences between planned and actual study
| Planned | Change | Reason |
|---|---|---|
| Focus on variation between 11 ambulance services | 10 large ambulance services only | One ambulance service is very small compared with the others (1768 calls in September 2016 compared with 19,908 calls in the next largest service). Owing to the degree of uncertainty that these small numbers would introduce in our quantitative analyses we approached the 10 large services in England, all of which participated in the study |
| WP2: routine CAD data from each ambulance service for 1 month including ambulance type and crew type |
Crew type available for nine services only Data on ambulance type/resource not used |
We were aware that the ambulance and crew type data were held separately from the CAD system data and that it might not be possible to link them. One ambulance service could not deliver data on the skill-mix of staff responding to patients We did not test ‘resource sent’ because this was not raised by interviewees in WP1 |
| WP2: link census data to calls using postcode | Linked census data using LSOA | Permissions to use postcode were time-consuming to pursue and likely to delay the study so we opted for LSOA, which did not require extra permissions |
| WP2 and WP3.1: analyse CAD data for three types of non-conveyance: ‘Hear and Treat’, ‘See and Treat’, and ‘See and Convey Elsewhere’ | All analyses not undertaken for ‘See and Convey Elsewhere’ | Proportion of calls resulting in ‘See and Convey Elsewhere’ was small and included a mix of low-acuity services (such as minor injury units) high-acuity services (such as specialist services) and end-of-life services (such as hospices). This diversity would make it impossible to draw conclusions from any analysis |
| WP3.2: linked data set for two ambulance services to explore events after non-conveyance | Data obtained for one service only | Data from the second service were obtained for one locality only. Delays in ambulance service delivery of data precluded their use in the analysis |
| WP4.2: analysis of all data sets for respiratory problems | Routine data in CAD identify ‘breathing problems’, which include conditions other than respiratory ones. The focus of this WP changed to breathing problems | Attempts to use subcodes and free text to identify respiratory problems were not successful because most ambulance services could not supply these data; where they were supplied we could not fully understand the coding systems |
Appendix 2 Total non-conveyance rates by ambulance services over time (based on adding telephone advice only and discharge-at-scene rates reported in ambulance quality indicators)
FIGURE 13.
Variation between 10 large regional ambulance services in England. Total non-conveyance = AQI telephone advice + AQI non-conveyance to emergency department.
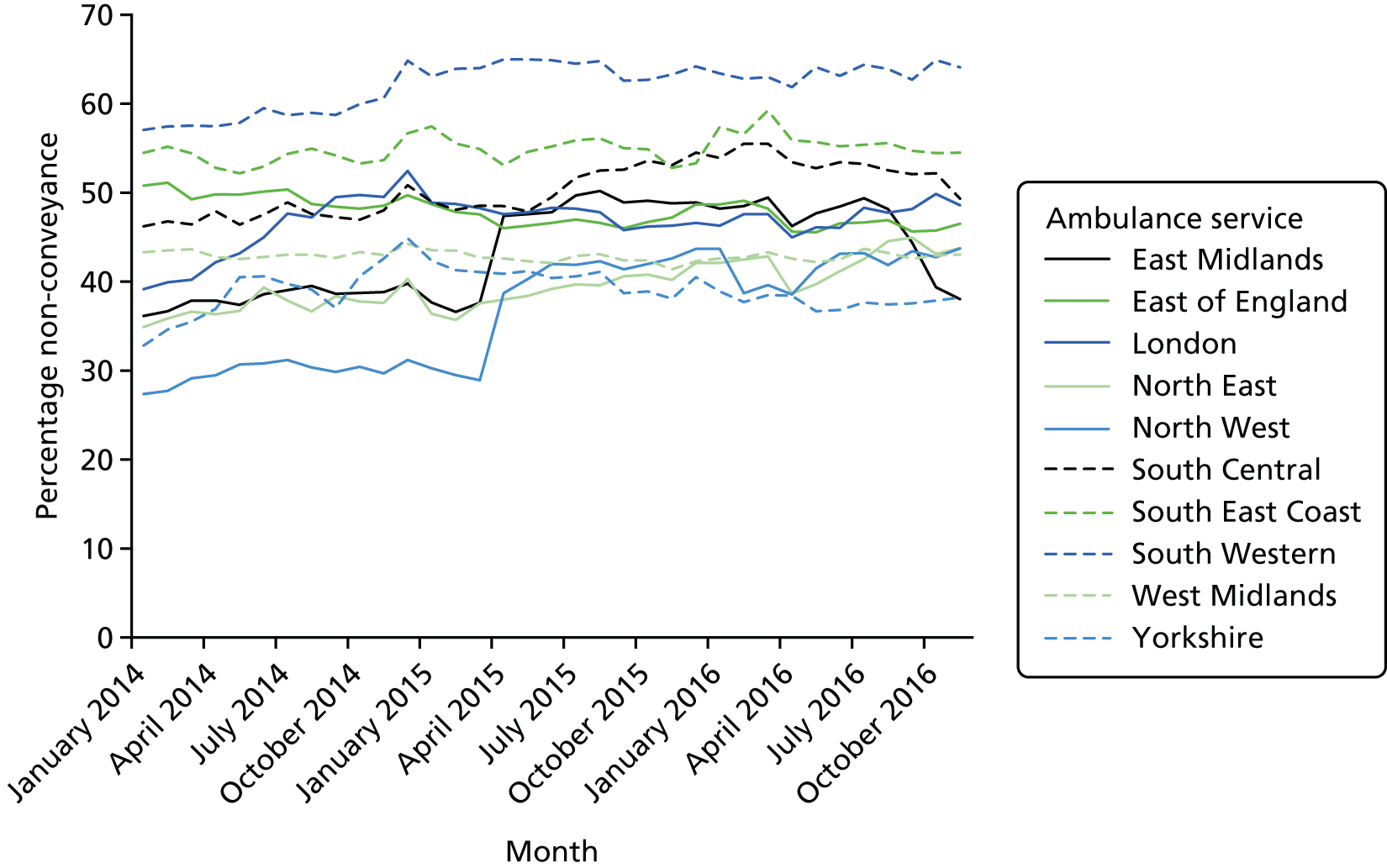
Appendix 3 Recontact rates by ambulance service over time (based on ambulance quality indicator data)
FIGURE 14.
Variation between 10 large regional ambulance services in England: AQI percentage of recontact rates for calls ending in telephone advice.
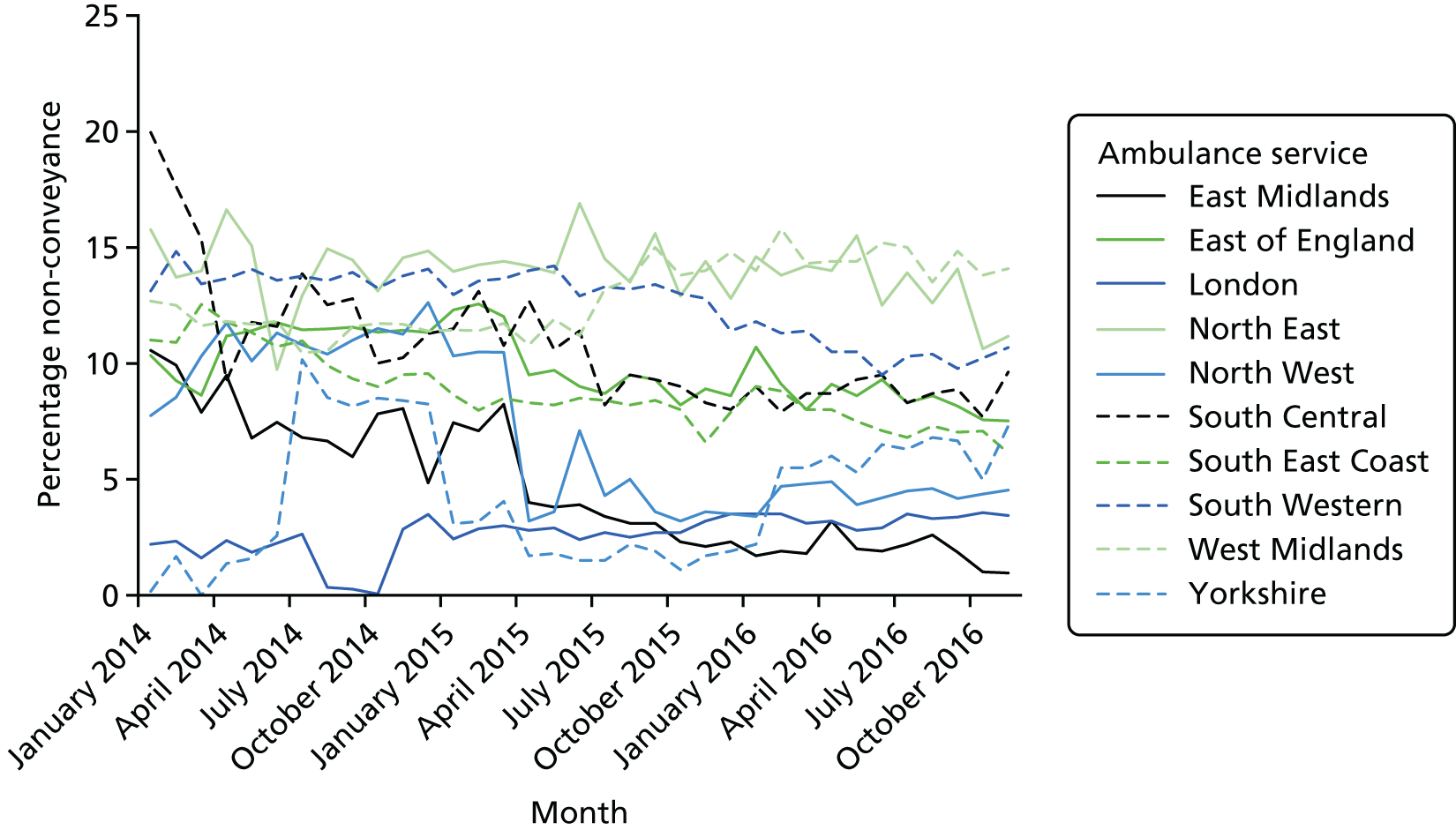
FIGURE 15.
Variation between 10 large regional ambulance services in England: AQI percentage of recontact rates for calls ending in non-conveyance to hospitals with an emergency department.
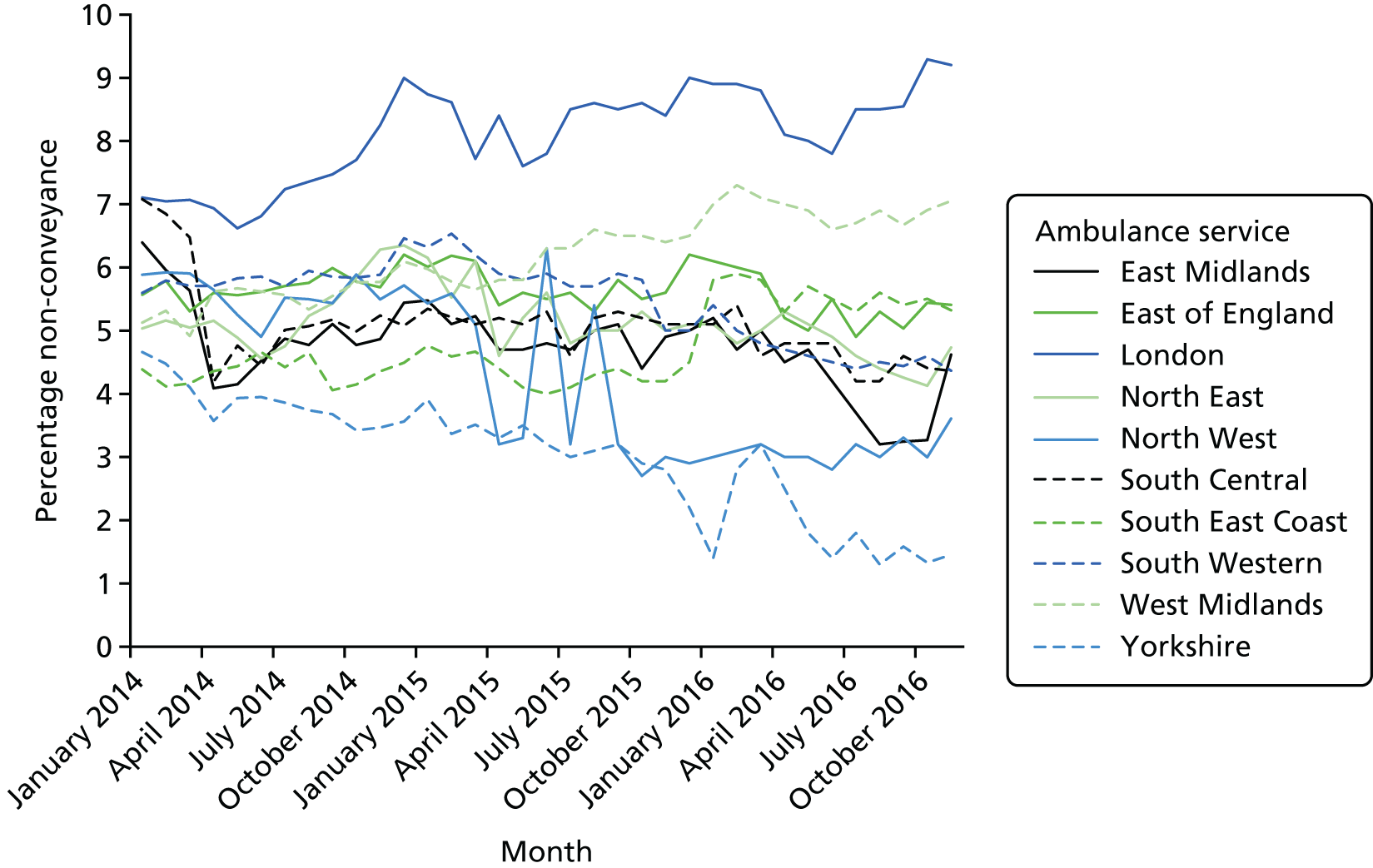
Appendix 4 Topic guide used in work package 1 interviews
Study ID
Site ID
Date of interview
Consent form signed
Thank you for agreeing to take part in this interview. The interview should take less than an hour to complete. The focus of the interview is on non-conveyance (meaning the 3 types – state). Do you have any questions before we begin? Can you confirm that you are happy for the interview to be recorded?
-
It will help to have some background information:
Paramedic
-
How long have you been a paramedic?
-
How long have you worked in this ambulance service?
-
Have you worked for any other ambulance services? (which ones)
-
What Band are you?
-
Tell me about your education/training/specialisms.
Commissioner
-
How long have you been a commissioner for this ambulance service?
-
Have you commissioned any other ambulance services?
-
Are you a lead commissioner/Commissioning Support Unit?
Manager
-
What is your role?
-
How long have you worked for this ambulance service?
-
Have you worked for any other ambulance services? (which ones)
-
There is a large amount of variation in non-conveyance rates between ambulance services in England. Why do you think this is?
-
Now I’d like you to focus at a local level. Thinking about [name of ambulance service], what factors affect ‘non-conveyance to an emergency department’ in your ambulance service? (Commissioners: what approach does your service take to non-conveyance in the following areas . . .?) *Ask if variation is seasonal/demand driven*
-
‘Hear and Treat’ (both sending to clinician and telephone advice only)
-
‘See and Treat’
-
‘See and Convey Elsewhere’.
Prompt if the interviewee does not volunteer the following factors:
-
population factors (e.g. socioeconomic status, ethnicity, morbidity, living alone)
-
geographical factors (e.g. urban/rural)
-
patient factors (e.g. preferences, expectations)
-
crew factors (e.g. training, decision tools)
-
locality factors (e.g. services available in each locality, time of call)
-
organisational factors (e.g. policies)
-
resources (e.g. money, types of ambulances, staffing)
-
commissioning factors
-
national factors (e.g. promotion of non-conveyance).
-
Respiratory problems are the second largest clinical problem for ‘See and Treat’ after falls. Can you tell me how respiratory problems are managed regarding non-conveyance?
-
How might you define ‘appropriate non-conveyance’ in your ambulance service? i.e. recontacting ambulance service within 24 hours
-
What factors affect the appropriateness of non-conveyance within your ambulance service? Can you tell me if and how this is monitored/measured?
-
What is the thing in your ambulance service (or the wider emergency and urgent care system) that contributes the most to appropriate non-conveyance?
-
What is the thing in your ambulance service that could work better in terms of appropriate non-conveyance?
Note – for 6 and 7 – explore if these things are outside the control of the ambulance service (i.e. system factors)
-
In an ideal world, what solutions could be put in place to increase appropriate non-conveyance in your ambulance service? Which one could have most impact? Realistically, what could be done to make a difference?
-
We will be looking at mortality rates, hospital admissions and attendance at emergency departments at 24 hours after an emergency call, 72 hours and 1 week after an emergency call for all three types of non-conveyance. In your view, which of these time points is most appropriate for associating any of these events with the ambulance service? Note – are there any differences between the three types of non-conveyance?
-
Is there anything else that you’d like to say about non-conveyance rates?
-
Given what we have spoken about today, is there anyone else within your ambulance service we should talk to regarding non-conveyance?
The study is due to be completed in February 2017. If you would like to see a summary of the findings I would be happy to forward them on to you. Would you like me to do this?
Thank you for your time.
Appendix 5 Numbers of stakeholders approached and interviewed for qualitative interviews (work package 1)
| Service | Stakeholders approached and interviewed (n) | |||||
|---|---|---|---|---|---|---|
| Managers approached | Managers interviewed | Paramedics approached | Paramedics interviewed | Commissioners intervieweda | Interviews included in the analysis | |
| A | 4 | 4 | 5 | 2 | 1 | 7 |
| B | 3 | 1 | 5 | 1b | 1 | 3 |
| C | 2 | 2 | 4 | 2 | 1 | 5 |
| D | 2 | 2 | 3 | 2 | 1 | 5 |
| E | 2 | 2 | 2 | 2 | 1 | 5 |
| F | 5 | 2 | 5 | 2 | 1 | 5 |
| G | 2 | 2 | 4 | 1 | 1 | 4 |
| H | 2 | 2 | 2 | 2 | 1 | 5 |
| I | 2 | 2 | 5 | 2 | 1 | 5 |
| J | 2 | 2 | 9 | 2 | 1 | 5 |
| Total | 26 | 21 | 44 | 18 | 10 | 49 |
Appendix 6 Data specification form used in work package 2
Variation in ambulance non-conveyance
We need routine data from each ambulance service in England to:
-
identify the determinants of variation between and within ambulance services for three different types of non-conveyance to an emergency department: ‘Hear and Treat’ (resolved by telephone advice), ‘See and Treat’ (discharged after treatment at the scene or onward referral to an alternative care pathway) and ‘See and Convey Elsewhere’ (a patient journey to a destination other than Type 1 or 2 A&E)
-
identify the determinants of variation between and within ambulance services in recontact rates for three different types of non-conveyance
-
understand variation between and within ambulance services in three different types of non-conveyance rates for respiratory problems.
Data specification:
-
AQI validated data – all emergency calls that receive a telephone or face-to-face response from the ambulance service. Please follow the guidance on calculating AQIs.
-
One month only. The month is November 2014. We have selected this month so that we do not include data when some services were involved in the pilot of 2-minute calls. We have also avoided holiday months when some areas can see a large influx of holiday-makers. We are aware of the industrial action that took place in this month.
-
Single incident per row. For example, if multiple vehicles are sent then all vehicle information is given on the same row as all the other variables. Some ambulance services have sent us data in this format already but you may find it easier to send resource data (see table) on multiple lines.
-
We would like the following variables (see table). We cannot ask for named variables from CAD because we know that different ambulance services use different CAD systems (e.g. C3). Can you give the label of the variable you have used from your CAD system below please?
| Variable we want | Response code | Explanation | Name of variable from your system |
|---|---|---|---|
| Anonymous ID | We want a unique indicator of each patient/incident in the data set | ||
| Age of patient | We understand that this is based on caller report and may not be accurate. We do NOT want date of birth | ||
| Sex of patient |
1 = male 2 = female |
||
| Locality | We know that ambulance services code to different localities/divisions/patches such as counties. We would like the localities that you use (if you use any). If you do not have localities specific to your service, just leave this blank. We ask for CCG and LSOA later | ||
| CCG | Some ambulance services code which CCG the call/incident belongs to. If you do this please add CCG | ||
| Time of call | |||
| Day of call |
1 = Monday 2 = Tuesday 3 = Wednesday 4 = Thursday 5 = Friday 6 = Saturday 7 = Sunday |
This is to help us to calculate calls that are in or out-of-hours (where in hours is 08.00–18.00 Monday to Friday) | |
| Urgency level | Red 1, etc., using standard codes | ||
| Response time | In seconds | We are aware that response times can be calculated in different ways. Please use definition for AQI | |
| Outcome of incident |
1 = resolved by telephone advice 2 = discharged after treatment at the scene or onward referral to an alternative care pathway 3 = a patient journey to a destination other than Type 1 or 2 A&E 4 = taken to Type 1 or 2 A&E |
We would like you to use the definitions used in the AQI calculations: emergency calls closed with telephone advice; patients treated and discharged on scene, etc. We know that to calculate rates of ‘Hear and Treat’ you exclude NHS 111 calls but for ‘See and Treat’/‘See and Convey Elsewhere’ you include NHS 111 calls We know that you combine 2 and 3 for the AQI but would like these to be separated for our study We know that there is no definitive list of hospitals with Type 1 and 2 A&E services. If you have a list that you use for hospitals relevant to your service can you send it to us? |
|
| Source of call |
1 = NHS 111 2 = other |
||
|
Was the call reviewed by a clinician/doctor (hear-and-treat service) regardless of final outcome of call? Outcome of call with clinician |
1 = yes 2 = no 1 = conveyance to Type 1 or 2 A&E 2 = resolved by telephone advice 3 = advice to attend Type 1 or 2 A&E 4 = other |
If possible we want variables relating to whether or not a caller is referred to speak to a clinician for advice, and the outcome of that advice. We understand that this may not be possible. If this is not possible, can we have free-text variables related to this? Please include stop codes to give us extra information on this |
|
| Place of conveyance | We want to know where patients are conveyed. We know that there will be missing values. If this is only in free text this is fine | ||
| Reason for the call |
MPDS chief complaint dispatch code or NHS Pathways symptom group discriminator We also want the free text for the chief complaint/group discriminator We are aware that this may be available only in free text and that it may not be possible for NHS Pathways |
||
| Type of response (e.g. solo responder in car or dual-crewed ambulance) |
All vehicles that turn up on scene (not stood down). We recognise that this may not be robust. We want to see the timing of arrivals of each response type. You may wish to supply this as separate file linked by incident ID Please indicate which vehicle conveyed the patient |
||
| Skill-mix attending the incident (e.g. paramedic qualification or emergency care assistant) |
Ultimately we are looking for the highest level of skill of those attending. We shall find a way of determining this based on the data you give us about the last documented qualification of each crew member who attended the incident You may wish to supply this is a separate file linked by incident ID |
||
| Recontact with 999 within 24 hours of ‘Hear and Treat’ |
1 = original call that had a recontact 2 = recontact call 3 = no |
AQI definition of calls closed with telephone advice where recontact occurs within 24 hours | |
| Recontact with 999 within 24 hours of ‘See and Treat’ |
1 = original call that had a recontact 2 = recontact call 3 = no |
AQI definition of patients treated and discharged on scene where recontact occurs within 24 hours | |
| Recontact with 999 within 24 hours of ‘See and Convey Elsewhere’ |
1 = original call that had a recontact 2 = recontact call 3 = no |
Not part of AQI so only if this is possible using a new query | |
| LSOA |
The 2011 census-derived output area boundaries (as opposed to the 2001 census-derived output area boundaries). 59 This is a census area code that includes a number of postcodes. We have attached a file from the NHS Postcode Directory called grid.csva that links postcodes to LSOAs so you can use your postcodes to identify the LSOA relevant to each incident postcode. Postcode = pcd2 in column 1 and LSOA = LSOA11 in column 40. You can also attach postcode to CCG in column 18 This is a really important variable for us because it allows us to link census data to each call/incident (e.g. deprivation). We know that postcode is for the place of the call/incident and not for the residence of the patient. We do NOT want postcode so please delete this from the data set |
Validation: we would like a download of the CAD data set from November 2014 with LSOA (2011 census-derived boundaries) attached and name, address and postcode removed. This will allow us to see what is included and excluded from the AQI data set so that we can interpret our findings correctly.
Deadline: end of October 2015 to receive first attempt at data set (all data sets we have received have had some problems that need investigating). End of November 2015 to receive final data set.
Appendix 7 Description of routine data by ambulance service
| Ambulance service | Telephone advice denominator | Telephone advice numerator | Not transported to emergency department denominator | Not transported to emergency department numerator | Telephone advice recontacts denominator | Telephone advice recontacts numerator | Not transported to emergency department recontacts denominator | Not transported to emergency department recontacts numerator |
|---|---|---|---|---|---|---|---|---|
| A | 0 | < 5 | < 1 | < 1 | < 5 | < 5 | < 5 | < 1 |
| B | 0 | 0 | 0 | < 10 | 0 | 0 | < 10 | 0 |
| C | < 10 | < 10 | < 5 | < 20 | < 10 | < 20 | < 20 | < 30 |
| D | < 10 | < 5 | < 5 | < 20 | < 5 | 0 | < 5 | < 5 |
| E | < 1 | < 1 | 0 | < 5 | < 1 | < 1 | < 1 | < 5 |
| F | < 1 | < 1 | < 1 | < 1 | < 1 | < 5 | < 1 | < 5 |
| G | < 1 | < 10 | < 1 | < 5 | < 10 | < 20 | < 1 | < 5 |
| H | < 10 | < 50 | < 1 | < 5 | < 50 | < 10 | < 40 | < 10 |
| I | < 1 | < 1 | < 1 | < 10 | < 1 | < 50 | < 1 | < 20 |
| J | < 1 | < 1 | < 1 | < 1 | < 1 | < 1 | < 1 | 0 |
| Ambulance service | Outcome, n (%) | Total number of outcomes, N | |||
|---|---|---|---|---|---|
| Telephone advice | Discharged at scene | Conveyed elsewhere | Conveyed to emergency department | ||
| A | 3237 (5.1) | 22,784 (36) | 1192 (1.9) | 36,069 (57.0) | 63,282 |
| B | 3912 (7.3) | 16,224 (30.2) | 567 (1.1) | 33,041 (61.5) | 53,744 |
| C | 4034 (8.1) | 23,285 (46.5) | 2207 (4.4) | 20,526 (41.0) | 50,052 |
| D | 3931 (6.3) | 13,493 (21.5) | 4738 (7.6) | 40,580 (64.7) | 62,742 |
| E | 3505 (4.9) | 25,595 (35.6) | 1441 (2.0) | 41,316 (57.5) | 71,857 |
| F | 2378 (2.8) | 16,948 (19.8) | 4852 (5.7) | 61,332 (71.7) | 85,510 |
| G | 2353 (5.4) | 15,476 (35.3) | 0 (0.0) | 25,967 (59.3) | 43,796 |
| H | 9168 (9.8) | 21,178 (22.7) | 7564 (8.1) | 55,552 (59.2) | 93,462 |
| I | 6512 (10.6) | 20,809 (33.8) | 4024 (6.5) | 30,156 (49.0) | 61,501 |
| J | 1649 (5.5) | 6687 (22.4) | 1934 (6.5) | 19,599 (65.6) | 29,869 |
| Total | 40,679 (6.6) | 182,479 (29.6) | 28,519 (4.6) | 251,677 (40.9) | 615,815 |
FIGURE 16.
Percentage of calls by outcome for each ambulance service in the routine data set. ED, emergency department.
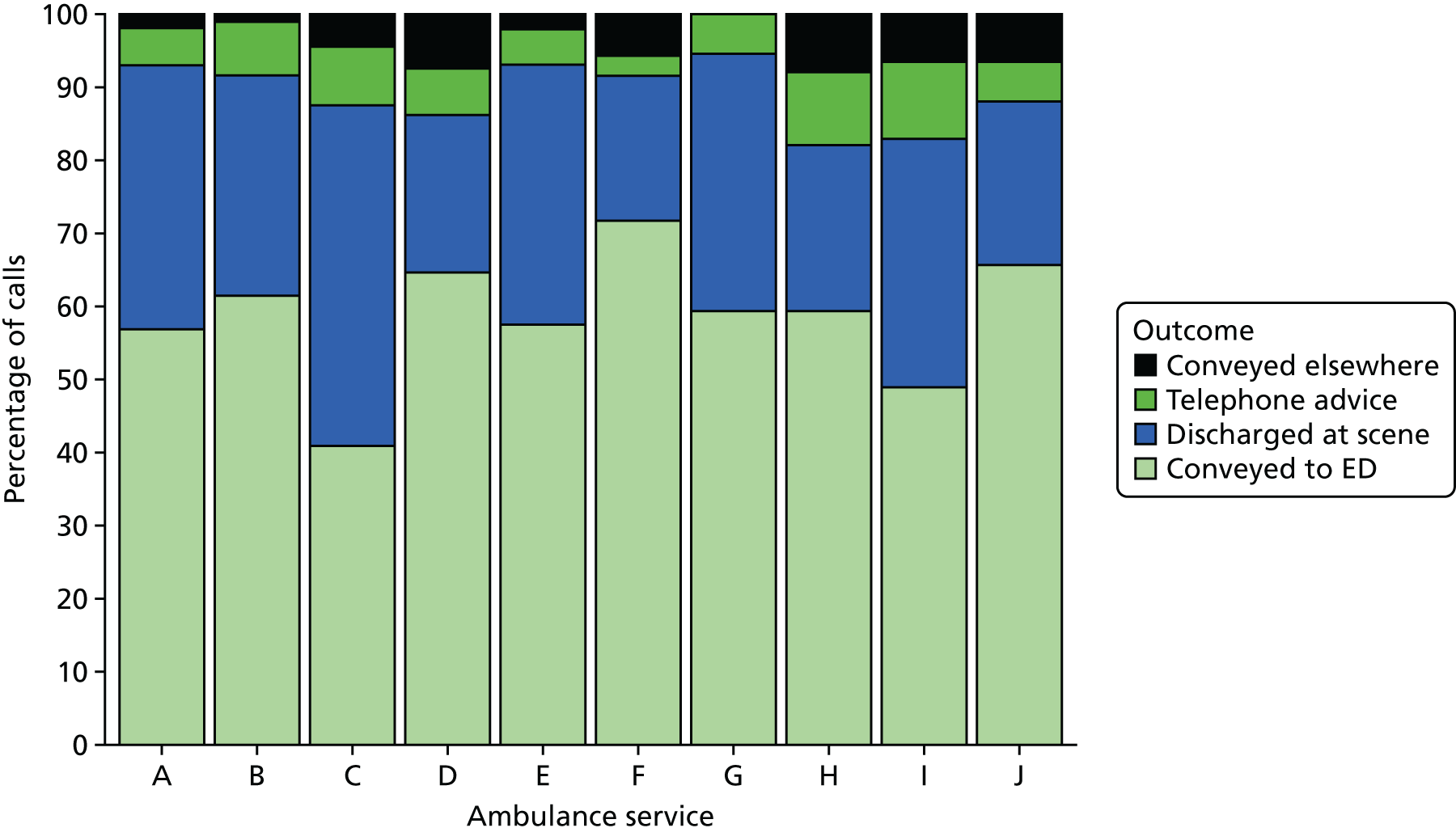
FIGURE 17.
Number of calls by outcome for each ambulance service in the routine data set. ED, emergency department.

Appendix 8 Regression for telephone-advice-only rates (based on 10 services, including calls from NHS 111)
| Variables | Model 1 | ||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Patient-level variables | |||
| Age (years) | |||
| 0–2 | 1 | – | – |
| 3–10 | 1.22 | 1.12 to 1.32 | < 0.001 |
| 11–20 | 0.81 | 0.75 to 0.86 | < 0.001 |
| 21–30 | 0.93 | 0.87 to 0.99 | 0.019 |
| 31–40 | 0.91 | 0.85 to 0.97 | 0.004 |
| 41–50 | 0.78 | 0.73 to 0.84 | < 0.001 |
| 51–60 | 0.77 | 0.72 to 0.82 | < 0.001 |
| 61–70 | 0.70 | 0.65 to 0.75 | < 0.001 |
| 71–80 | 0.70 | 0.56 to 0.64 | < 0.001 |
| 81–90 | 0.61 | 0.53 to 0.60 | < 0.001 |
| > 90 | 0.45 | 0.41 to 0.49 | < 0.001 |
| Sex | |||
| Female | 1 | ||
| Male | 1.02 | 1.00 to 1.05 | 0.100 |
| Call variables | |||
| Time of call | |||
| Out of hours | 1 | ||
| In hours | 0.81 | 0.79 to 0.83 | < 0.001 |
| Reason for call | |||
| Falls | 1 | – | – |
| Abdominal pain | 7.36 | 6.94 to 7.80 | < 0.001 |
| Breathing problems | 0.69 | 0.64 to 0.73 | < 0.001 |
| Cardiovascular problems | 0.55 | 0.52 to 0.59 | < 0.001 |
| Fitting | 0.48 | 0.43 to 0.53 | < 0.001 |
| Injury | 1.89 | 1.80 to 1.99 | < 0.001 |
| Psychiatric problems | 1.86 | 1.72 to 2.02 | < 0.001 |
| Person sick or unconscious | 2.93 | 2.79 to 3.07 | < 0.001 |
| Other | 2.18 | 2.07 to 2.29 | < 0.001 |
| Patient-level variables (LSOA based) | |||
| Long-term condition quintile | |||
| Q1 (lowest) | 1 | ||
| Q2 | 0.97 | 0.94 to 1.01 | 0.176 |
| Q3 | 0.96 | 0.92 to 1.00 | 0.034 |
| Q4 | 0.96 | 0.92 to 1.01 | 0.093 |
| Q5 (highest) | 0.89 | 0.85 to 0.93 | < 0.001 |
| IMD quintile | |||
| Q5 (least deprived) | 1 | ||
| Q4 | 1.02 | 0.97 to 1.07 | 0.493 |
| Q3 | 1.01 | 0.96 to 1.06 | 0.692 |
| Q2 | 1.01 | 0.96 to 1.06 | 0.714 |
| Q1 (most deprived) | 1.11 | 1.06 to 1.17 | < 0.001 |
Appendix 9 Regressions for discharge at scene (including skill-mix, so based on nine services, and including calls from NHS 111)
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 1.35 | 1.27 to 1.44 | < 0.001 | 1.35 | 1.27 to 1.44 | < 0.001 |
| 11–20 | 1.66 | 1.58 to 1.75 | < 0.001 | 1.66 | 1.58 to 1.75 | < 0.001 |
| 21–30 | 1.91 | 1.82 to 2.00 | < 0.001 | 1.91 | 1.82 to 2.00 | < 0.001 |
| 31–40 | 1.76 | 1.68 to 1.85 | < 0.001 | 1.76 | 1.68 to 1.84 | < 0.001 |
| 41–50 | 1.63 | 1.55 to 1.71 | < 0.001 | 1.63 | 1.55 to 1.71 | < 0.001 |
| 51–60 | 1.60 | 1.52 to 1.68 | < 0.001 | 1.60 | 1.52 to 1.68 | < 0.001 |
| 61–70 | 1.52 | 1.45 to 1.60 | < 0.001 | 1.52 | 1.45 to 1.60 | < 0.001 |
| 71–80 | 1.54 | 1.47 to 1.62 | < 0.001 | 1.54 | 1.47 to 1.62 | < 0.001 |
| 81–90 | 1.75 | 1.67 to 1.83 | < 0.001 | 1.75 | 1.67 to 1.83 | < 0.001 |
| > 90 | 1.99 | 1.89 to 2.09 | < 0.001 | 1.99 | 1.89 to 2.09 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 1.02 | 1.00 to 1.03 | 0.034 | 1.02 | 1.00 to 1.03 | 0.034 |
| Call variables | ||||||
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.87 | 0.85 to 0.88 | < 0.001 | 0.87 | 0.85 to 0.88 | < 0.001 |
| Reason for call | ||||||
| Falls | 1 | – | – | 1 | – | – |
| Abdominal pain | 0.34 | 0.32 to 0.36 | < 0.001 | 0.34 | 0.32 to 0.36 | < 0.001 |
| Breathing problems | 0.62 | 0.60 to 0.63 | < 0.001 | 0.62 | 0.60 to 0.63 | < 0.001 |
| Cardiovascular problems | 0.46 | 0.45 to 0.48 | < 0.001 | 0.46 | 0.45 to 0.48 | < 0.001 |
| Fitting | 0.64 | 0.62 to 0.67 | < 0.001 | 0.64 | 0.62 to 0.67 | < 0.001 |
| Injury | 0.55 | 0.54 to 0.57 | < 0.001 | 0.55 | 0.54 to 0.57 | < 0.001 |
| Psychiatric problems | 0.74 | 0.71 to 0.78 | < 0.001 | 0.74 | 0.71 to 0.78 | < 0.001 |
| Person sick or unconscious | 0.71 | 0.69 to 0.72 | < 0.001 | 0.71 | 0.69 to 0.72 | < 0.001 |
| Other | 0.77 | 0.75 to 0.80 | < 0.001 | 0.77 | 0.75 to 0.80 | < 0.001 |
| Urgency level | ||||||
| Red 1 & 2 | 1 | – | – | 1 | – | – |
| Green 1 & 2 | 1.25 | 1.23 to 1.27 | < 0.001 | 1.25 | 1.23 to 1.27 | < 0.001 |
| Green 3 & 4 | 1.90 | 1.85 to 1.95 | < 0.001 | 1.90 | 1.86 to 1.95 | < 0.001 |
| Origin of call | ||||||
| 999 | 1 | – | – | 1 | – | – |
| NHS 111 | 1.46 | 1.38 to 1.53 | < 0.001 | 1.46 | 1.38 to 1.53 | < 0.001 |
| Skill-mix | ||||||
| Paramedic | 1 | – | – | 1 | – | – |
| Advanced paramedic | 1.38 | 1.35 to 1.42 | < 0.001 | 1.38 | 1.34 to 1.42 | < 0.001 |
| Other | 0.96 | 0.94 to 0.99 | 0.003 | 0.96 | 0.94 to 0.99 | 0.002 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 0.95 | 0.93 to 0.97 | < 0.001 | 0.95 | 0.93 to 0.97 | < 0.001 |
| Q3 | 0.99 | 0.96 to 1.01 | 0.307 | 0.99 | 0.96 to 1.01 | 0.301 |
| Q4 | 0.97 | 0.95 to 1.00 | 0.041 | 0.97 | 0.95 to 1.00 | 0.039 |
| Q5 (highest) | 1.01 | 0.98 to 1.04 | 0.361 | 1.01 | 0.98 to 1.04 | 0.368 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 1.02 | 0.99 to 1.04 | 0.265 | 1.02 | 0.99 to 1.04 | 0.265 |
| Q3 | 1.04 | 1.02 to 1.07 | 0.002 | 1.04 | 1.02 to 1.07 | 0.002 |
| Q2 | 1.05 | 1.02 to 1.08 | 0.001 | 1.05 | 1.02 to 1.08 | 0.001 |
| Q1 (most deprived) | 1.05 | 1.02 to 1.08 | 0.002 | 1.05 | 1.02 to 1.08 | 0.002 |
| Ambulance service-level variables | ||||||
| Percentage of calls with advanced paramedic | – | – | – | 1.05 | 1.04 to 1.07 | < 0.001 |
| Organisational motivation | ||||||
| Lack/no view/recent | – | – | – | 1 | – | – |
| Active and established | – | – | – | 0.80 | 0.58 to 1.11 | 0.176 |
| Risk aversion | – | – | – | 0.78 | 0.61 to 0.98 | 0.036 |
| Workforce advanced paramedics | ||||||
| No evidence | – | – | – | 1 | – | – |
| Limited | – | – | – | 1.06 | 0.91 to 1.24 | < 0.001 |
| Established | – | – | – | 1.82 | 1.31 to 2.34 | < 0.001 |
Appendix 10 Regressions for discharge at scene (without skill-mix, so based on 10 services, including calls from NHS 111)
| Variables | Model 3 | Model 4 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 1.35 | 1.27 to 1.43 | < 0.001 | 1.35 | 1.27 to 1.43 | < 0.001 |
| 11–20 | 1.66 | 1.58 to 1.74 | < 0.001 | 1.66 | 1.58 to 1.74 | < 0.001 |
| 21–30 | 1.89 | 1.81 to 1.98 | < 0.001 | 1.89 | 1.81 to 1.98 | < 0.001 |
| 31–40 | 1.75 | 1.67 to 1.83 | < 0.001 | 1.75 | 1.67 to 1.83 | < 0.001 |
| 41–50 | 1.62 | 1.55 to 1.70 | < 0.001 | 1.62 | 1.55 to 1.70 | < 0.001 |
| 51–60 | 1.58 | 1.51 to 1.66 | < 0.001 | 1.58 | 1.51 to 1.66 | < 0.001 |
| 61–70 | 1.50 | 1.44 to 1.58 | < 0.001 | 1.50 | 1.44 to 1.58 | < 0.001 |
| 71–80 | 1.52 | 1.45 to 1.59 | < 0.001 | 1.52 | 1.45 to 1.59 | < 0.001 |
| 81–90 | 1.73 | 1.66 to 1.81 | < 0.001 | 1.73 | 1.66 to 1.81 | < 0.001 |
| > 90 | 1.97 | 1.87 to 2.07 | < 0.001 | 1.97 | 1.87 to 2.07 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 1.01 | 1.00 to 1.03 | 0.065 | 1.01 | 1.00 to 1.03 | 0.064 |
| Call variables | ||||||
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.87 | 0.86 to 0.88 | < 0.001 | 0.87 | 0.86 to 0.88 | < 0.001 |
| Reason for call | ||||||
| Falls | 1 | – | – | 1 | – | – |
| Abdominal pain | 0.34 | 0.32 to 0.36 | < 0.001 | 0.34 | 0.32 to 0.36 | < 0.001 |
| Breathing problems | 0.62 | 0.60 to 0.63 | < 0.001 | 0.62 | 0.60 to 0.63 | < 0.001 |
| Cardiovascular problems | 0.46 | 0.45 to 0.47 | < 0.001 | 0.46 | 0.45 to 0.47 | < 0.001 |
| Fitting | 0.65 | 0.62 to 0.67 | < 0.001 | 0.65 | 0.62 to 0.67 | < 0.001 |
| Injury | 0.56 | 0.55 to 0.58 | < 0.001 | 0.56 | 0.55 to 0.58 | < 0.001 |
| Psychiatric problems | 0.74 | 0.70 to 0.77 | < 0.001 | 0.74 | 0.70 to 0.77 | < 0.001 |
| Person sick or unconscious | 0.70 | 0.68 to 0.72 | < 0.001 | 0.70 | 0.68 to 0.72 | < 0.001 |
| Other | 0.74 | 0.73 to 0.76 | < 0.001 | 0.74 | 0.73 to 0.76 | < 0.001 |
| Urgency level | ||||||
| Red 1 & 2 | 1 | – | – | 1 | – | – |
| Green 1 & 2 | 1.24 | 1.22 to 1.26 | < 0.001 | 1.24 | 1.22 to 1.26 | < 0.001 |
| Green 3 & 4 | 1.87 | 1.82 to 1.91 | < 0.001 | 1.87 | 1.82 to 1.91 | < 0.001 |
| Origin of call | ||||||
| 999 | 1 | – | – | 1 | – | – |
| NHS 111 | 1.43 | 1.37 to 1.50 | < 0.001 | 1.43 | 1.37 to 1.50 | < 0.001 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 0.95 | 0.93 to 0.98 | < 0.001 | 0.95 | 0.93 to 0.98 | < 0.001 |
| Q3 | 0.98 | 0.96 to 1.01 | 0.161 | 0.98 | 0.96 to 1.01 | 0.162 |
| Q4 | 0.97 | 0.95 to 1.00 | 0.047 | 0.97 | 0.95 to 1.00 | 0.048 |
| Q5 (highest) | 1.00 | 0.98 to 1.03 | 0.803 | 1.00 | 0.98 to 1.03 | 0.798 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 1.02 | 1.00 to 1.05 | 0.111 | 1.02 | 0.99 to 1.05 | 0.111 |
| Q3 | 1.05 | 1.03 to 1.08 | < 0.001 | 1.05 | 1.03 to 1.08 | < 0.001 |
| Q2 | 1.05 | 1.03 to 1.08 | < 0.001 | 1.05 | 1.03 to 1.08 | < 0.001 |
| Q1 (most deprived) | 1.05 | 1.02 to 1.08 | < 0.001 | 1.05 | 1.02 to 1.08 | < 0.001 |
| Ambulance service-level variables | ||||||
| Organisational motivation | ||||||
| Lack/no view/recent | – | – | – | 1 | – | – |
| Active and established | – | – | – | 1.38 | 0.64 to 2.97 | 0.407 |
| Risk aversion | – | – | – | 0.70 | 0.39 to 1.29 | 0.255 |
| Workforce advanced paramedics | ||||||
| No evidence | – | – | – | 1 | – | 1 |
| Limited | – | – | – | 1.19 | 0.75 to 1.87 | 0.460 |
| Established | – | – | – | 1.52 | 0.81 to 2.84 | 0.191 |
FIGURE 18.
Variation in discharge-at-scene rates between ambulance services explained in regression (based on 10 ambulance services without skill-mix data, including calls from NHS 111). (a) Null model; (b) model with patient-level variables; and (c) model with patient- and ambulance service-level variables.

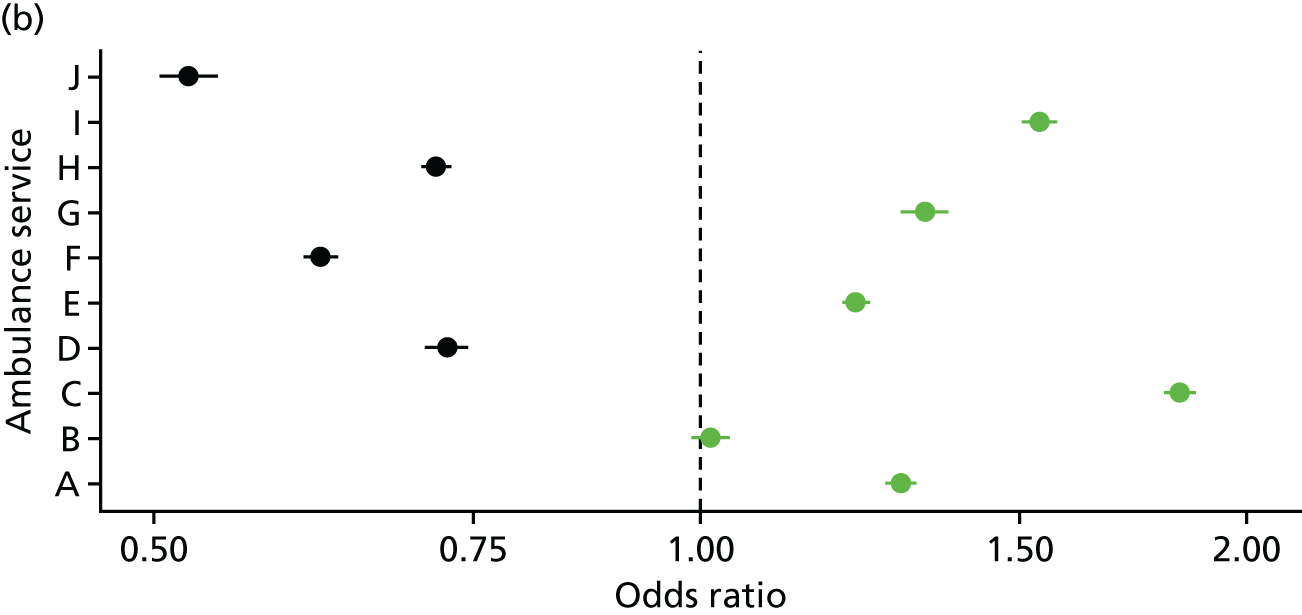
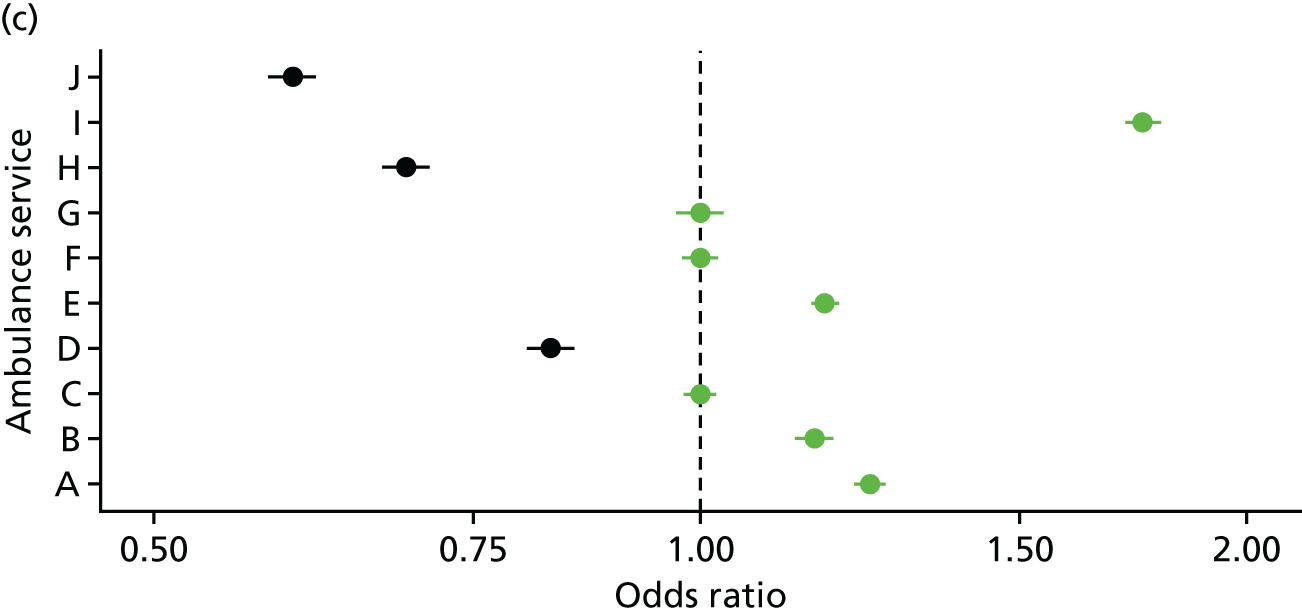
Appendix 11 Caterpillar plots for non-conveyance rates
FIGURE 19.
Telephone-advice-only rates by localities within ambulance services, adjusted for patient-level variables (based on 10 ambulance services, including calls from NHS 111).
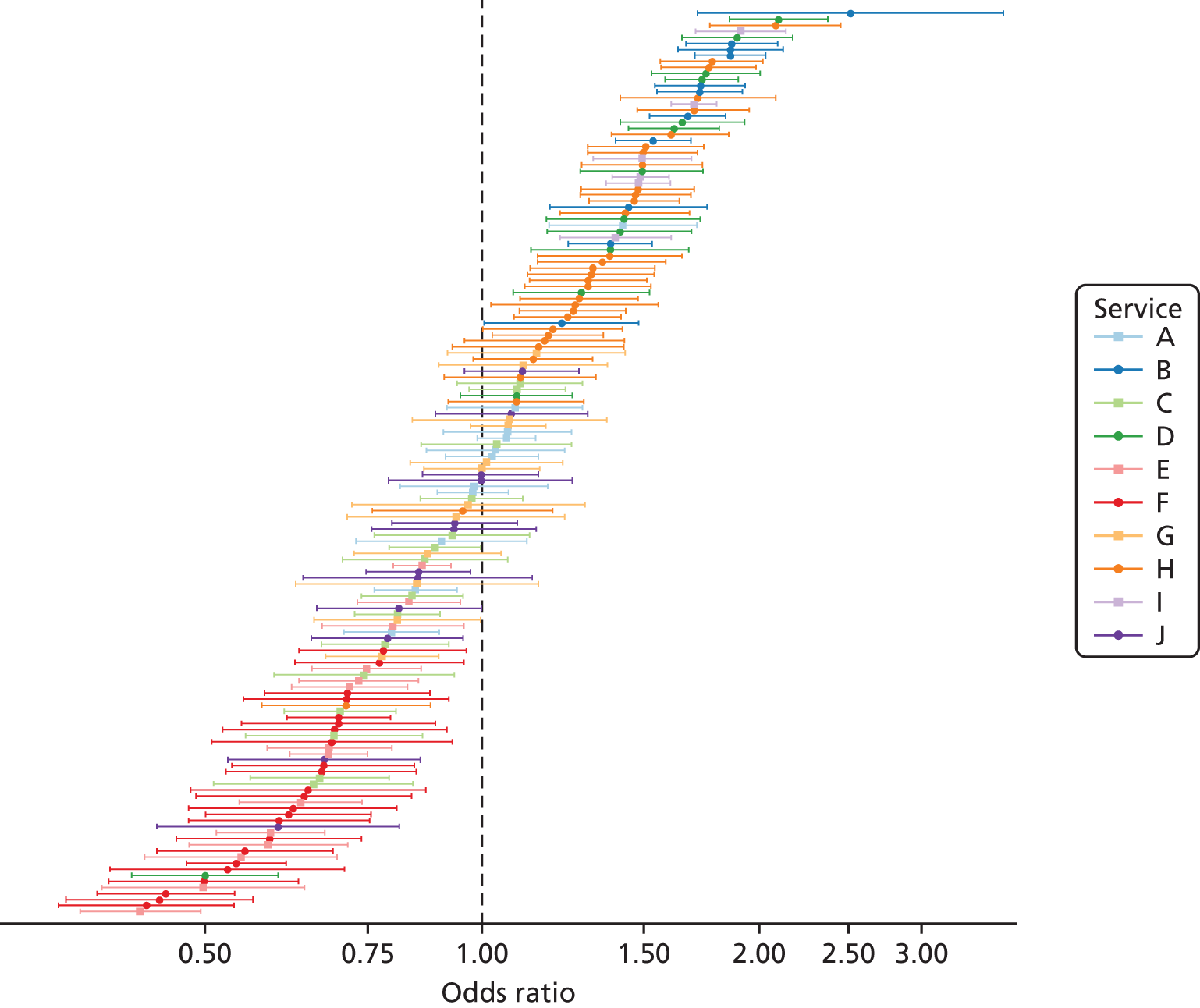
FIGURE 20.
Discharge at scene rates by localities within ambulance services, adjusted for patient-level variables, with skill-mix (based on nine ambulance services, including calls from NHS 111).
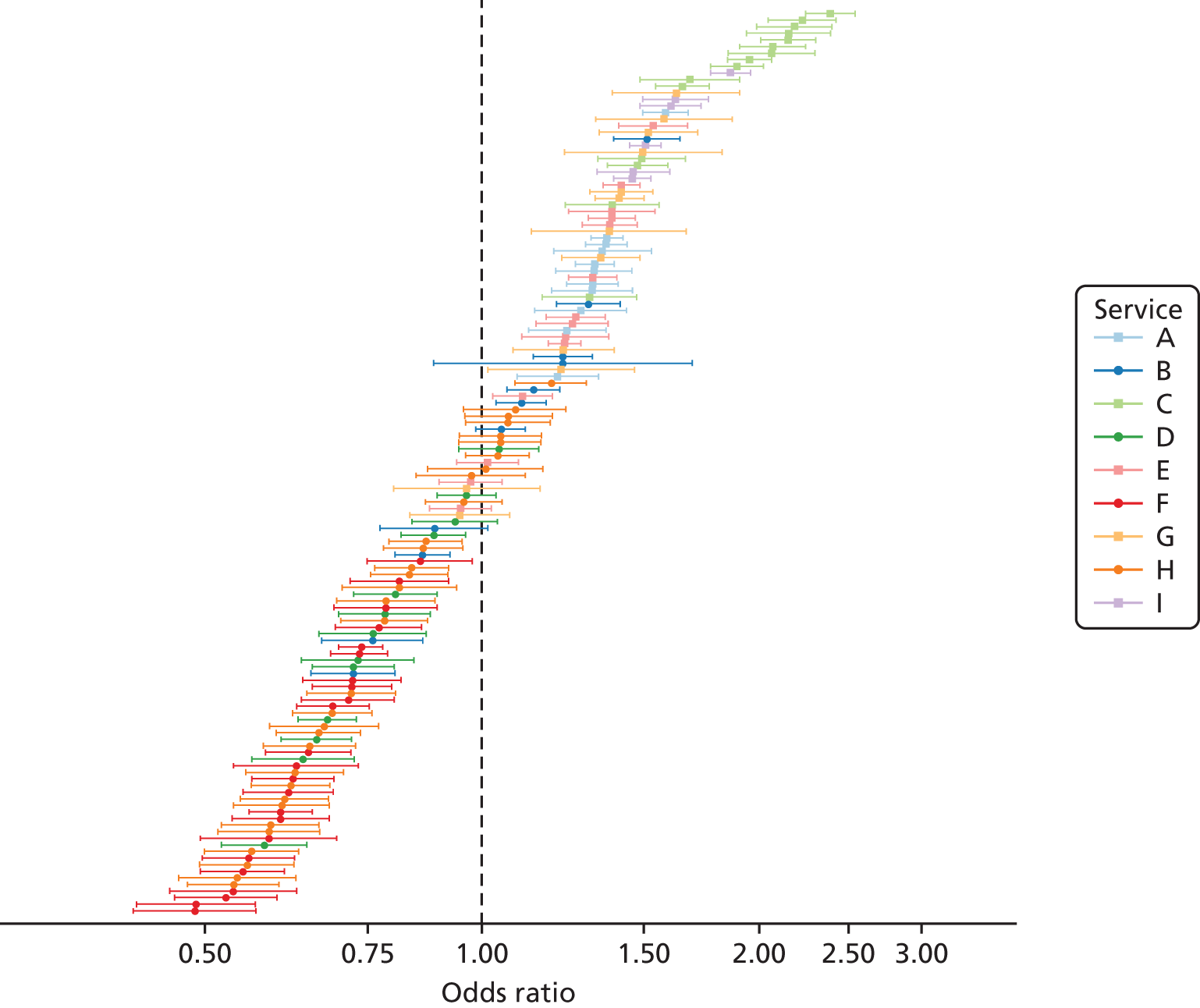
Appendix 12 Regressions for recontact rates after telephone advice (excluding calls from NHS 111)
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 1.27 | 0.87 to 1.86 | 0.221 | 1.27 | 0.87 to 1.87 | 0.221 |
| 11–20 | 1.69 | 1.23 to 2.33 | 0.001 | 1.70 | 1.24 to 2.35 | 0.001 |
| 21–30 | 2.18 | 1.62 to 2.93 | < 0.001 | 2.19 | 1.63 to 2.95 | < 0.001 |
| 31–40 | 2.44 | 1.81 to 3.30 | < 0.001 | 2.47 | 1.82 to 3.33 | < 0.001 |
| 41–50 | 2.99 | 2.21 to 4.03 | < 0.001 | 3.01 | 2.23 to 4.06 | < 0.001 |
| 51–60 | 3.48 | 2.58 to 4.70 | < 0.001 | 3.51 | 2.60 to 4.74 | < 0.001 |
| 61–70 | 3.70 | 2.74 to 4.99 | < 0.001 | 3.74 | 2.77 to 5.04 | < 0.001 |
| 71–80 | 3.42 | 2.55 to 4.60 | < 0.001 | 3.45 | 2.57 to 4.64 | < 0.001 |
| 81–90 | 3.30 | 2.46 to 4.42 | < 0.001 | 3.32 | 2.47 to 4.46 | < 0.001 |
| > 90 | 3.02 | 2.15 to 4.24 | < 0.001 | 3.05 | 2.17 to 4.28 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 1.13 | 1.04 to 1.22 | 0.003 | 1.13 | 1.04 to 1.22 | 0.003 |
| Call variables | ||||||
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.97 | 0.89 to 1.05 | 0.456 | 0.97 | 0.89 to 1.05 | 0.448 |
| Reason for call | ||||||
| Falls | 1 | – | – | 1 | – | – |
| Abdominal pain | 1.48 | 1.24 to 1.78 | < 0.001 | 1.49 | 1.25 to 1.79 | < 0.001 |
| Breathing problems | 1.11 | 0.88 to 1.40 | 0.383 | 1.12 | 0.89 to 1.41 | 0.330 |
| Cardiovascular problems | 1.10 | 0.87 to 1.39 | 0.424 | 1.12 | 0.89 to 1.42 | 0.327 |
| Fitting | 0.97 | 0.64 to 1.47 | 0.888 | 0.97 | 0.64 to 1.46 | 0.880 |
| Injury | 0.96 | 0.80 to 1.15 | 0.669 | 0.98 | 0.82 to 1.18 | 0.856 |
| Psychiatric problems | 1.85 | 1.46 to 2.35 | < 0.001 | 1.90 | 1.50 to 2.41 | < 0.001 |
| Person sick or unconscious | 1.30 | 1.11 to 1.52 | 0.001 | 1.31 | 1.12 to 1.54 | 0.001 |
| Other | 1.31 | 1.11 to 1.55 | 0.002 | 1.33 | 1.13 to 1.57 | 0.001 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 1.11 | 0.97 to 1.26 | 0.115 | 1.10 | 0.97 to 1.26 | 0.136 |
| Q3 | 1.25 | 1.09 to 1.42 | 0.001 | 1.23 | 1.08 to 1.42 | 0.002 |
| Q4 | 1.32 | 1.15 to 1.52 | < 0.001 | 1.31 | 1.14 to 1.51 | < 0.001 |
| Q5 (highest) | 1.39 | 1.19 to 1.62 | < 0.001 | 1.37 | 1.17 to 1.61 | < 0.001 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 0.96 | 0.83 to 1.12 | 0.641 | 0.96 | 0.82 to 1.12 | 0.593 |
| Q3 | 1.00 | 0.86 to 1.16 | 0.990 | 1.00 | 0.86 to 1.16 | 0.972 |
| Q2 | 0.98 | 0.85 to 1.15 | 0.842 | 0.98 | 0.84 to 1.14 | 0.804 |
| Q1 (most deprived) | 0.93 | 0.79 to 1.09 | 0.355 | 0.93 | 0.79 to 1.09 | 0.359 |
| Ambulance service-level variables | ||||||
| Complexity | ||||||
| Average CCGs | – | – | – | 1 | – | – |
| Many CCGs | – | – | – | 1.22 | 1.06 to 1.40 | 0.005 |
| Few CCGs | – | – | – | 1.41 | 1.19 to 1.67 | < 0.001 |
| NOA cost per call | ||||||
| Average | – | – | – | 1 | – | – |
| Low | – | – | – | 0.93 | 0.80 to 1.07 | 0.323 |
| High | – | – | – | 0.76 | 0.66 to 0.87 | < 0.001 |
| Perception of telephone advice provision | ||||||
| Limited | – | – | – | 1 | – | – |
| Negative | – | – | – | 1.36 | 1.20 to 1.53 | < 0.001 |
| Positive | – | – | – | 1.04 | 0.88 to 1.22 | 0.655 |
Appendix 13 Regressions for recontact rates after discharge at scene (including skill-mix, based on nine services, excluding calls from NHS 111)
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 0.89 | 0.61 to 1.29 | 0.530 | 0.88 | 0.61 to 1.28 | 0.506 |
| 11–20 | 1.07 | 0.81 to 1.42 | 0.637 | 1.07 | 0.80 to 1.42 | 0.656 |
| 21–30 | 1.30 | 1.00 to 1.70 | 0.052 | 1.30 | 1.00 to 1.70 | 0.053 |
| 31–40 | 1.73 | 1.33 to 2.27 | < 0.001 | 1.73 | 1.32 to 2.26 | < 0.001 |
| 41–50 | 2.10 | 1.61 to 2.73 | < 0.001 | 2.09 | 1.61 to 2.72 | < 0.001 |
| 51–60 | 2.70 | 2.08 to 3.51 | < 0.001 | 2.69 | 2.08 to 3.49 | < 0.001 |
| 61–70 | 2.65 | 2.04 to 3.44 | < 0.001 | 2.64 | 2.04 to 3.42 | < 0.001 |
| 71–80 | 2.92 | 2.26 to 3.77 | < 0.001 | 2.92 | 2.26 to 3.76 | < 0.001 |
| 81–90 | 3.26 | 2.53 to 4.20 | < 0.001 | 3.25 | 2.53 to 4.19 | < 0.001 |
| > 90 | 3.29 | 2.53 to 4.27 | < 0.001 | 3.29 | 2.54 to 4.27 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 0.97 | 0.92 to 1.03 | 0.326 | 0.97 | 0.92 to 1.03 | 0.325 |
| Call variables | ||||||
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.88 | 0.83 to 0.93 | < 0.001 | 0.88 | 0.83 to 0.93 | < 0.001 |
| Reason for call | ||||||
| Falls | 1 | – | – | 1 | – | – |
| Abdominal pain | 1.45 | 1.20 to 1.76 | < 0.001 | 1.46 | 1.20 to 1.77 | < 0.001 |
| Breathing problems | 1.37 | 1.23 to 1.52 | < 0.001 | 1.37 | 1.23 to 1.51 | < 0.001 |
| Cardiovascular problems | 1.08 | 0.97 to 1.20 | 0.184 | 1.08 | 0.97 to 1.20 | 0.173 |
| Fitting | 1.47 | 1.27 to 1.71 | < 0.001 | 1.48 | 1.27 to 1.71 | < 0.001 |
| Injury | 0.89 | 0.80 to 0.99 | 0.029 | 0.89 | 0.80 to 0.99 | 0.029 |
| Psychiatric problems | 1.67 | 1.43 to 1.96 | < 0.001 | 1.68 | 1.43 to 1.97 | < 0.001 |
| Person sick or unconscious | 1.09 | 1.00 to 1.20 | 0.046 | 1.10 | 1.00 to 1.20 | 0.042 |
| Other | 0.84 | 0.77 to 0.93 | < 0.001 | 0.84 | 0.76 to 0.92 | < 0.001 |
| Urgency level | ||||||
| Red 1 & 2 | 1 | – | – | 1 | – | – |
| Green 1 & 2 | 1.08 | 1.01 to 1.16 | 0.021 | 1.09 | 1.01 to 1.16 | 0.018 |
| Green 3 & 4 | 1.20 | 1.10 to 1.31 | < 0.001 | 1.20 | 1.10 to 1.31 | < 0.001 |
| Skill-mix | ||||||
| Paramedic | 1 | – | – | 1 | – | – |
| Advanced paramedic | 0.94 | 0.84 to 1.03 | 0.187 | 0.95 | 0.86 to 1.04 | 0.270 |
| Other | 0.99 | 0.91 to 1.07 | 0.757 | 0.99 | 0.91 to 1.07 | 0.802 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 0.87 | 0.79 to 0.95 | 0.002 | 0.87 | 0.79 to 0.95 | 0.002 |
| Q3 | 0.96 | 0.87 to 1.05 | 0.341 | 0.96 | 0.87 to 1.05 | 0.340 |
| Q4 | 1.02 | 0.93 to 1.12 | 0.713 | 1.02 | 0.93 to 1.12 | 0.691 |
| Q5 (highest) | 0.99 | 0.90 to 1.10 | 0.899 | 1.00 | 0.90 to 1.10 | 0.960 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 1.04 | 0.94 to 1.15 | 0.400 | 1.04 | 0.94 to 1.15 | 0.403 |
| Q3 | 1.13 | 1.02 to 1.25 | 0.017 | 1.13 | 1.02 to 1.25 | 0.017 |
| Q2 | 1.27 | 1.15 to 1.40 | < 0.001 | 1.27 | 1.14 to 1.40 | < 0.001 |
| Q1 (most deprived) | 1.18 | 1.06 to 1.32 | 0.002 | 1.18 | 1.06 to 1.32 | 0.003 |
| Ambulance service-level variables | ||||||
| Workforce advanced paramedics | ||||||
| No Evidence | – | – | – | 1 | – | – |
| Limited | – | – | – | 0.87 | 0.79 to 0.96 | 0.005 |
| Established | – | – | – | 1.16 | 1.06 to 1.28 | 0.001 |
| NAO frontline staff advanced practitioners | ||||||
| Average | – | – | – | 1 | – | – |
| High | – | – | – | 1.38 | 1.27 to 1.51 | < 0.001 |
Appendix 14 Regressions for recontact rates after discharge at scene (no skill-mix, based on 10 services, excluding calls from NHS 111)
| Variables | Model 3 | Model 4 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 0.99 | 0.70 to 1.41 | 0.970 | 0.99 | 0.70 to 1.41 | 0.969 |
| 11–20 | 1.13 | 0.86 to 1.49 | 0.385 | 1.13 | 0.85 to 1.49 | 0.381 |
| 21–30 | 1.42 | 1.09 to 1.83 | 0.009 | 1.42 | 1.09 to 1.84 | 0.009 |
| 31–40 | 1.84 | 1.41 to 2.39 | < 0.001 | 1.84 | 1.42 to 2.39 | < 0.001 |
| 41–50 | 2.22 | 1.72 to 2.88 | < 0.001 | 2.22 | 1.72 to 2.88 | < 0.001 |
| 51–60 | 2.77 | 2.15 to 3.58 | < 0.001 | 2.78 | 2.15 to 3.58 | < 0.001 |
| 61–70 | 2.74 | 2.12 to 3.53 | < 0.001 | 2.74 | 2.12 to 3.53 | < 0.001 |
| 71–80 | 3.04 | 2.37 to 3.90 | < 0.001 | 3.04 | 2.37 to 3.90 | < 0.001 |
| 81–90 | 3.43 | 2.68 to 4.39 | < 0.001 | 3.43 | 2.68 to 4.39 | < 0.001 |
| > 90 | 3.42 | 2.65 to 4.43 | < 0.001 | 3.43 | 2.66 to 4.42 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 0.97 | 0.92 to 1.02 | 0.251 | 0.97 | 0.92 to 1.02 | 0.250 |
| Call characteristics | ||||||
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.88 | 0.83 to 0.93 | < 0.001 | 0.88 | 0.83 to 0.93 | < 0.001 |
| Reason for call | ||||||
| Falls | 1 | – | – | 1 | – | – |
| Abdominal pain | 1.44 | 1.19 to 1.73 | < 0.001 | 1.44 | 1.19 to 1.73 | < 0.001 |
| Breathing problems | 1.38 | 1.25 to 1.52 | < 0.001 | 1.38 | 1.25 to 1.52 | < 0.001 |
| Cardiovascular problems | 1.06 | 0.95 to 1.18 | 0.288 | 1.06 | 0.95 to 1.18 | 0.290 |
| Fitting | 1.46 | 1.27 to 1.69 | < 0.001 | 1.46 | 1.27 to 1.69 | < 0.001 |
| Injury | 0.89 | 0.81 to 0.98 | 0.019 | 0.89 | 0.81 to 0.98 | 0.020 |
| Psychiatric problems | 1.62 | 1.39 to 1.90 | < 0.001 | 1.62 | 1.39 to 1.90 | < 0.001 |
| Person sick or unconscious | 1.10 | 1.00 to 1.20 | 0.044 | 1.10 | 1.00 to 1.20 | 0.043 |
| Other | 0.86 | 0.79 to 0.94 | 0.001 | 0.86 | 0.79 to 0.99 | 0.001 |
| Urgency level | ||||||
| Red 1 & 2 | 1 | – | – | 1 | – | – |
| Green 1 & 2 | 1.09 | 1.02 to 1.16 | 0.008 | 1.09 | 1.02 to 1.16 | 0.009 |
| Green 3 & 4 | 1.20 | 1.10 to 1.30 | < 0.001 | 1.20 | 1.10 to 1.30 | < 0.001 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 0.88 | 0.81 to 0.96 | 0.005 | 0.88 | 0.81 to 0.96 | 0.005 |
| Q3 | 0.97 | 0.89 to 1.06 | 0.520 | 0.97 | 0.89 to 1.06 | 0.518 |
| Q4 | 1.03 | 0.94 to 1.13 | 0.546 | 1.03 | 0.94 to 1.13 | 0.545 |
| Q5 (highest) | 1.01 | 0.91 to 1.11 | 0.911 | 1.01 | 0.91 to 1.11 | 0.892 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 1.02 | 0.92 to 1.12 | 0.750 | 1.02 | 0.92 to 1.12 | 0.730 |
| Q3 | 1.10 | 1.00 to 1.21 | 0.042 | 1.11 | 1.01 to 1.22 | 0.039 |
| Q2 | 1.23 | 1.11 to 1.35 | < 0.001 | 1.23 | 1.12 to 1.35 | < 0.001 |
| Q1 (most deprived) | 1.17 | 1.05 to 1.30 | < 0.001 | 1.17 | 1.06 to 1.30 | < 0.001 |
| Ambulance service-level variables | ||||||
| Workforce advanced paramedics | ||||||
| No evidence | – | – | – | 1 | – | – |
| Limited | – | – | – | 0.76 | 0.55 to 1.06 | 0.104 |
| Established | – | – | – | 1.04 | 0.75 to 1.44 | 0.780 |
| NAO frontline staff advanced practitioners | ||||||
| Average | – | – | – | 1 | – | – |
| High | – | – | – | 1.42 | 1.04 to 1.95 | 0.027 |
FIGURE 21.
Variation in recontact rates after discharge at scene (no skill mix, based on 10 services, excluding calls from NHS 111). (a) Null model; (b) model with patient-level variables; and (c) model with patient- and ambulance service-level variables.
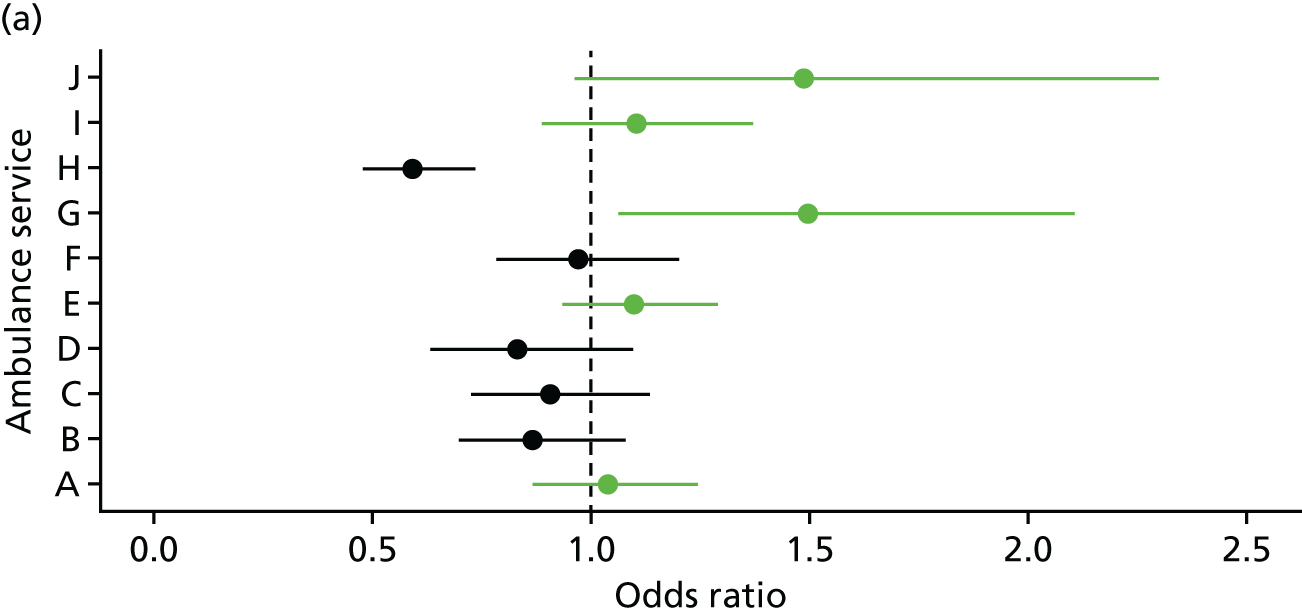

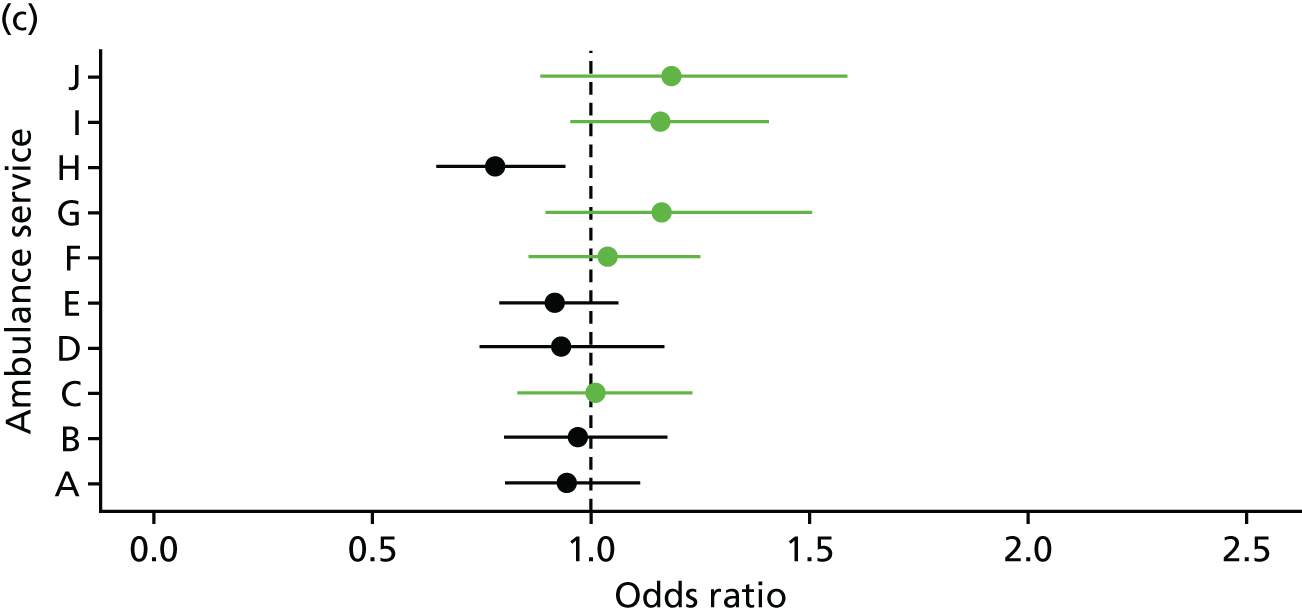
Appendix 15 Flow diagram for inclusion of calls in analysis of events after non-conveyance (work package 3.2)
FIGURE 22.
Flow diagram for inclusion of calls in analysis of events after non-conveyance (WP3.2). ED, emergency department.

Appendix 16 Comparison of characteristics of linked calls with calls that were not linked in work package 3.2
| Variables | Call characteristic, n (%) | |||
|---|---|---|---|---|
| Telephone advice only | Discharged at scene | |||
| Linked | No link | Linked | No link | |
| Age (years) | ||||
| 0–2 | 58 (2.3) | 576 (7.1) | 610 (1.4) | 148 (1.9) |
| 3–10 | 29 (1.2) | 490 (6.0) | 1169 (2.7) | 209 (2.7) |
| 11–20 | 90 (3.6) | 1095 (13.5) | 2219 (5.2) | 732 (9.4) |
| 21–40 | 421 (16.7) | 2465 (30.4) | 6998 (16.4) | 2452 (31.5) |
| 41–60 | 637 (25.3) | 1457 (18.0) | 7917 (18.5) | 1513 (19.4) |
| 61–80 | 762 (30.3) | 1204 (14.8) | 11,105 (25.9) | 1235 (15.9) |
| 81–90 | 402 (16.0) | 564 (7.0) | 9,137 (21.4) | 915 (11.8) |
| > 90 | 101 (4.0) | 141 (1.7) | 3,631 (8.5) | 446 (5.7) |
| Missing | 14 (0.6) | 121 (1.5) | 10 (0.02) | 136 (1.7) |
| Sex | ||||
| Female | 1504 (59.8) | 4386 (54.1) | 23,946 (56.0) | 3733 (47.9) |
| Male | 1010 (40.2) | 3665 (45.2) | 18,189 (42.5) | 3802 (48.8) |
| Missing | 0 (0.0) | 62 (0.8) | 661 (1.5) | 251 (3.2) |
| Time of call | ||||
| In hours | 712 (28.3) | 2365 (29.3) | 13,733 (32.1) | 2512 (32.3) |
| Out of hours | 1802 (71.7) | 5748 (70.8) | 29,063 (67.9) | 5274 (67.7) |
| Reason for call | ||||
| Abdominal pain | 465 (18.5) | 1229 (15.1) | 576 (1.3) | 111 (1.4) |
| Breathing problems | 233 (9.3) | 532 (6.6) | 5083 (11.9) | 824 (10.6) |
| Cardiovascular problems | 101 (4.0) | 334 (4.1) | 6014 (14.1) | 1015 (13.0) |
| Falls | 108 (4.8) | 461 (5.7) | 9785 (22.9) | 1246 (16.0) |
| Fitting | 19 (0.8) | 56 (0.7) | 1840 (4.3) | 461 (5.9) |
| Injury | 254 (10.1) | 1379 (17.0) | 3702 (8.7) | 1099 (14.1) |
| Other condition | 301 (12.0) | 1189 (14.7) | 3458 (8.1) | 958 (12.3) |
| Psychiatric problems | 105 (4.2) | 177 (2.2) | 605 (1.4) | 189 (2.4) |
| Person sick | 765 (30.4) | 2112 (26.0) | 3412 (8.0) | 546 (7.0) |
| Person unconscious | 65 (2.6) | 382 (4.7) | 2969 (6.9) | 727 (9.3) |
| Missing | 98 (3.9) | 262 (3.2) | 5352 (12.5) | 610 (7.8) |
| Location | ||||
| Rural | 383 (15.2) | 1302 (16.0) | 8407 (19.6) | 1278 (16.4) |
| Urban | 2131 (84.8) | 6808 (83.9) | 34,369 (80.3) | 6499 (83.5) |
| Missing | 0 (0.0) | * (***) | 20 (0.001) | 9 (0.1) |
| IMD quintile | ||||
| 1 (least deprived) | 208 (8.3) | 822 (10.1) | 5982 (14.0) | 821 (10.5) |
| 2 | 527 (21.0) | 1302 (16.0) | 7495 (17.5) | 1135 (14.6) |
| 3 | 409 (16.3) | 1231 (15.2) | 7781 (18.2) | 1277 (16.4) |
| 4 | 493 (19.6) | 1926 (23.7) | 9480 (22.2) | 1904 (24.5) |
| 5 (most deprived) | 877 (34.9) | 2829 (24.9) | 12,038 (28.1) | 2640 (33.9) |
| Missing | 0 (0.0) | * (***) | 20 (0.001) | 9 (0.1) |
| Total | 2514 (100.0) | 8113 (100.0) | 42,796 (100.0) | 7786 (100.0) |
Appendix 17 Patient and call characteristics of events within 3 days in work package 3.2
| Variable | Telephone advice only | Discharged at scene | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Ambulance recontact, n (%) | ED attendance, n (%) | Hospital admission, n (%) | Died, n (%) | N | Ambulance recontact, n (%) | ED attendance, n (%) | Hospital admission, n (%) | Died, n (%) | |
| Age (years) | ||||||||||
| 0–2 | 58 | 7 (12.1) | 14 (24.1) | * (***) | 0 (0.0) | 610 | 12 (2.0) | 151 (24.8) | 37 (6.1) | 0 (0.0) |
| 3–10 | 29 | * (***) | * (***) | 0 (0.0) | 0 (0.0) | 1169 | 22 (1.9) | 175 (15.0) | 32 (2.7) | 0 (0.0) |
| 11–20 | 90 | 15 (16.7) | 20 (22.2) | 6 (6.7) | 0 (0.0) | 2219 | 46 (2.1) | 268 (12.1) | 51 (2.3) | 0 (0.0) |
| 21–40 | 421 | 132 (31.4) | 146 (34.7) | 49 (11.6) | 0 (0.0) | 6998 | 379 (5.4) | 847 (12.1) | 224 (3.2) | * (***) |
| 41–60 | 637 | 248 (38.9) | 185 (29.0) | 57 (8.9) | * (***) | 7917 | 751 (9.5) | 994 (12.6) | 428 (5.4) | 13 (0.16) |
| 61–80 | 792 | 289 (37.9) | 183 (24.0) | 89 (11.7) | * (***) | 11,105 | 1232 (11.1) | 1479 (13.3) | 1006 (9.1) | 44 (0.40) |
| 81–90 | 402 | 84 (20.9) | 82 (20.4) | 60 (14.9) | * (***) | 9137 | 1063 (11.6) | 1147 (12.6) | 853 (9.3) | 54 (0.59) |
| > 90 | 101 | 28 (27.7) | 25 (24.8) | 16 (15.8) | 0 (0.0) | 3631 | 355 (9.8) | 350 (9.6) | 264 (7.3) | 16 (0.44) |
| Missing | 14 | 5 (35.7) | 5 (35.7) | 0 (0.0) | 0 (0.0) | 10 | * (***) | * (***) | 0 (0.0) | 0 (0.0) |
| Sex | ||||||||||
| Female | 1504 | 562 (37.4) | 418 (27.8) | 158 (10.5) | * (***) | 23,946 | 2134 (8.9) | 2886 (12.1) | 1600 (6.7) | 56 (0.23) |
| Male | 1010 | 247 (24.5) | 246 (24.4) | 123 (12.2) | * (***) | 18,189 | 1713 (9.4) | 2448 (13.5) | 1287 (7.1) | 72 (0.40) |
| Missing | 0 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 661 | 14 (2.1) | 78 (11.8) | 8 (1.2) | * (***) |
| Time of calla | ||||||||||
| In hours | 712 | 230 (32.3) | 191 (26.8) | 83 (11.7) | 0 (0.0) | 13,733 | 1172 (8.5) | 1716 (12.5) | 925 (6.7) | 40 (0.19) |
| Out of hours | 1802 | 579 (32.1) | 473 (26.2) | 198 (11.0) | 6 (0.33) | 29,063 | 2689 (9.3) | 3696 (12.7) | 1970 (6.8) | 89 (0.31) |
| Reason for call | ||||||||||
| Abdominal pain | 465 | 220 (47.3) | 144 (31.0) | 53 (11.4) | * (***) | 576 | 54 (9.4) | 97 (16.8) | 50 (8.7) | * (***) |
| Breathing problems | 233 | 73 (31.3) | 61 (26.2) | 40 (17.2) | * (***) | 5083 | 607 (11.9) | 678 (13.3) | 437 (8.6) | 39 (0.77) |
| Cardiovascular problems | 101 | 38 (37.6) | 28 (27.7) | 9 (8.9) | 0 (0.0) | 6014 | 462 (7.7) | 669 (11.1) | 352 (5.9) | 12 (0.20) |
| Falls | 108 | 29 (26.9) | 27 (25.0) | 12 (11.1) | 0 (0.0) | 9785 | 1090 (11.1) | 1231 (12.6) | 796 (8.1) | 19 (0.19) |
| Fitting | 19 | * (***) | 7 (36.8) | * (***) | 0 (0.0) | 1840 | 195 (10.6) | 230 (12.5) | 95 (5.2) | * (***) |
| Injury | 254 | 72 (28.3) | 79 (31.1) | 25 (9.8) | 0 (0.0) | 3702 | 178 (4.8) | 634 (17.1) | 158 (4.3) | * (***) |
| Other condition | 301 | 78 (25.9) | 89 (29.6) | 33 (11.0) | 0 (0.0) | 3458 | 268 (7.8) | 336 (9.7) | 174 (5.0) | 10 (0.29) |
| Psychiatric problems | 105 | 39 (37.1) | 32 (30.5) | 14 (13.3) | 0 (0.0) | 605 | 74 (12.2) | 106 (17.5) | 43 (7.1) | * (***) |
| Person sick | 765 | 217 (28.4) | 161 (21.0) | 78 (10.2) | * (***) | 3412 | 413 (12.1) | 487 (14.3) | 304 (8.9) | 9 (0.26) |
| Person unconscious | 65 | 14 (21.5) | 12 (18.5) | * (***) | * (***) | 2969 | 189 (6.4) | 283 (9.5) | 147 (5.0) | 9 (0.30) |
| Missing | 98 | 24 (24.5) | 24 (24.5) | 13 (13.3) | 0 (0.0) | 5352 | 331 (6.2) | 661 (12.4) | 339 (6.3) | 19 (0.36) |
| Location | ||||||||||
| Rural | 383 | 101 (26.4) | 95 (24.8) | 52 (13.6) | 0 (0.0) | 8407 | 724 (8.6) | 1063 (12.6) | 603 (7.2) | 34 (0.40) |
| Urban | 2131 | 708 (33.2) | 569 (26.7) | 229 (10.7) | 6 (0.28) | 34,369 | 3137 (9.1) | 4348 (12.7) | 2292 (6.7) | 95 (0.28) |
| Missing | 0 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 20 | 0 (0.0) | * (***) | 0 (0.0) | 0 (0.0) |
| IMD quintile | ||||||||||
| 1 (least deprived) | 208 | 51 (24.5) | 52 (25.0) | 32 (15.4) | 0 (0.0) | 5982 | 454 (7.6) | 759 (12.2) | 425 (7.1) | 18 (0.30) |
| 2 | 527 | 248 (47.1) | 135 (25.6) | 58 (11.0) | 0 (0.0) | 7495 | 594 (7.9) | 867 (11.6) | 501 (6.7) | 22 (0.29) |
| 3 | 409 | 112 (27.4) | 113 (27.6) | 58 (14.2) | 0 (0.0) | 7781 | 670 (8.6) | 963 (12.4) | 540 (6.9) | 29 (0.37) |
| 4 | 493 | 94 (19.1) | 104 (21.1) | 45 (9.1) | * (***) | 9480 | 857 (9.0) | 1205 (12.7) | 648 (6.9) | 21 (0.22) |
| 5 (most deprived) | 877 | 304 (34.7) | 260 (29.6) | 88 (10.0) | * (***) | 12,038 | 1286 (10.7) | 1617 (13.4) | 781 (6.5) | 39 (0.32) |
| Missing | 0 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 20 | 0 (0.0) | * (***) | 0 (0.0) | 0 (0.0) |
| Total | 2514 | 809 (32.2) | 664 (26.4) | 281 (11.2) | 6 (0.2) | 42,796 | 3861 (9.0) | 5412 (12.6) | 2895 (6.8) | 129 (0.3) |
Appendix 18 Sensitivity analysis for events within 3 days of non-conveyance in work package 3.2
| Non-conveyance type | Variables, n (%) | ||||
|---|---|---|---|---|---|
| Telephone advice only | Linked calls (N = 2514) | Linked plus not linked calls (N = 10,627) | Remove patients aged > 90 years (N = 2413) | Remove deaths in patients aged > 90 years (N = 2514) | Remove frequent callers (N = 1770)a |
| Ambulance recontact | 809 (32.2) | 809 (7.6) | 781 (32.4) | 809 (32.2) | 337 (19.0) |
| ED attendance | 664 (26.4) | 664 (6.2) | 639 (26.5) | 664 (26.4) | 387 (21.9) |
| Hospital admission | 281 (11.2) | 281 (2.6) | 265 (11.0) | 281 (11.2) | 206 (11.6) |
| Death | 6 (0.24) | 6 (0.06) | 6 (0.25) | 6 (0.24) | 6 (0.34) |
| Discharged at scene | Linked calls (N = 42,796) | Linked plus not linked calls (N = 50,582) | Remove patients aged > 90 years (N = 39,165) | Remove deaths in patients aged > 90 years (N = 42,780) | Remove frequent callers (N = 39,087)a |
| Ambulance recontact | 3861 (9.0) | 3861 (7.6) | 3506 (9.0) | 3857 (9.0) | 2427 (6.2) |
| ED attendance | 5412 (12.6) | 5412 (10.7) | 5062 (12.9) | 5409 (12.6) | 4525 (11.6) |
| Hospital admission | 2895 (6.8) | 2895 (5.7) | 2631 (6.7) | 2892 (6.8) | 2422 (6.2) |
| Death | 129 (0.30) | 129 (0.26) | 113 (0.29) | 113 (0.26) | 127 (0.32) |
Appendix 19 Numbers of hours at which recontact with an ambulance service is made after original call in work package 3.2
FIGURE 23.
Numbers of hours at which recontact with an ambulance service is made after original call in WP3.2 (a) ‘Hear and Treat’; and (b) ‘See and Treat’.
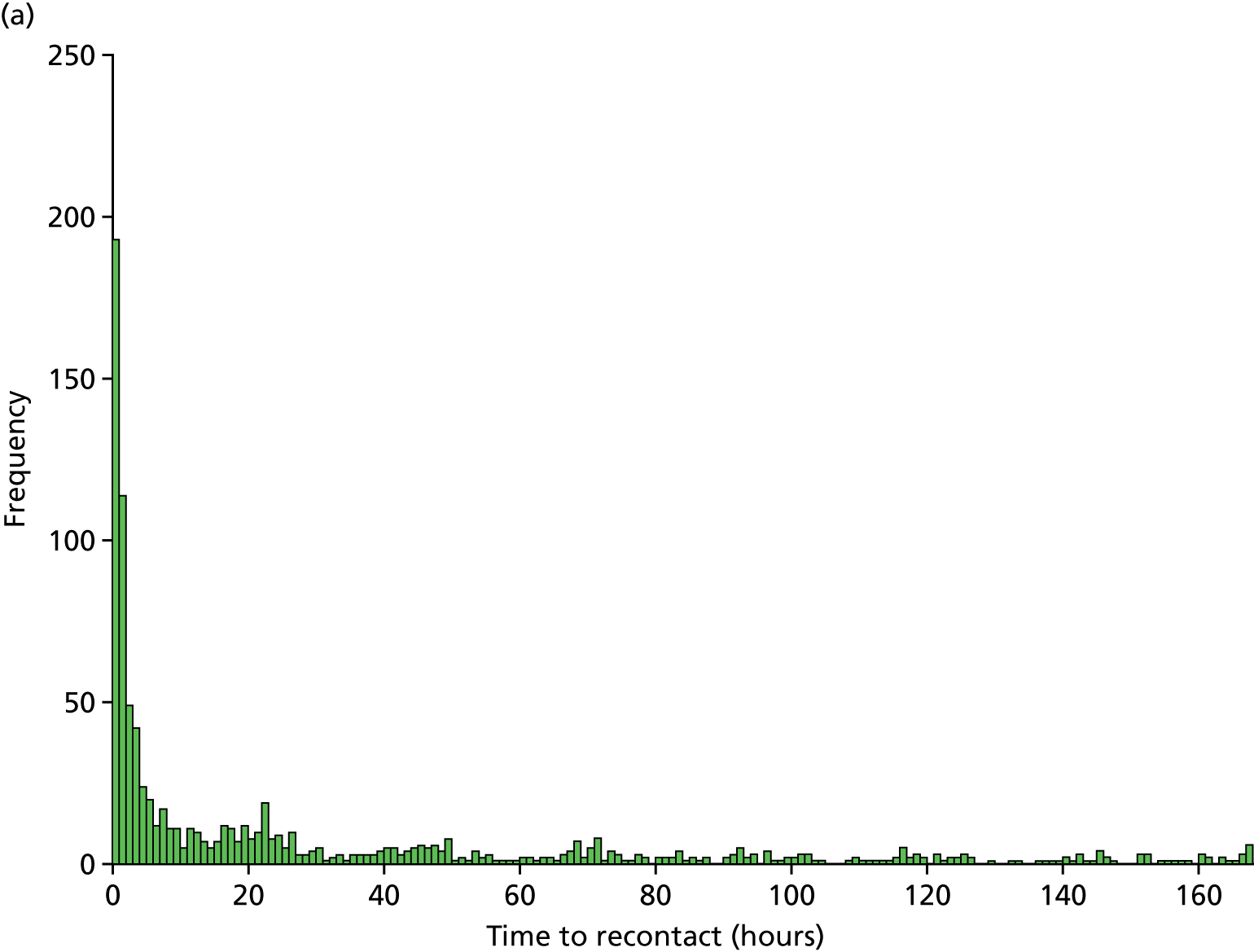
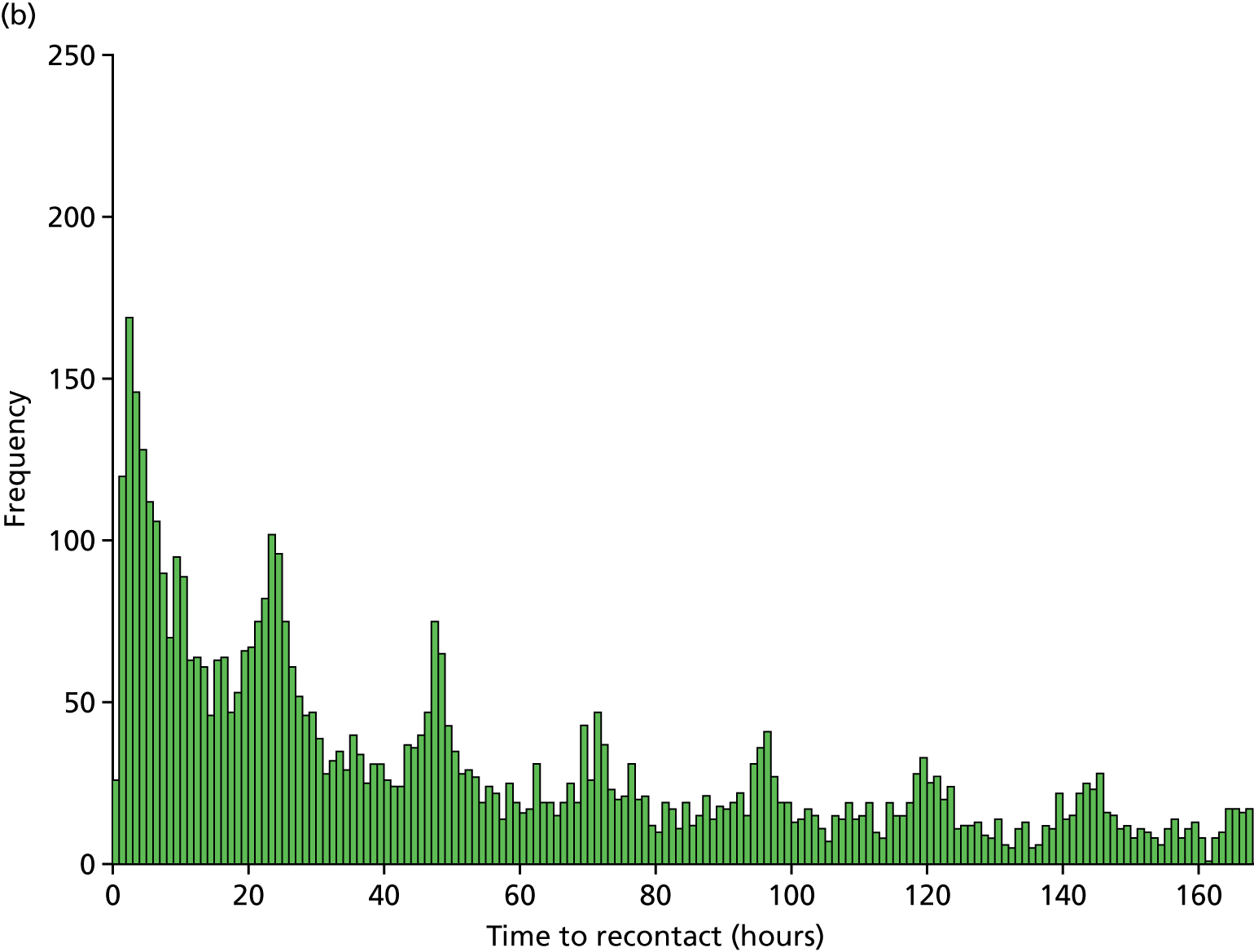
Appendix 20 Data extraction from literature reporting events following non-conveyance in ambulance services
| Study (first author, year, country) | Study type (original research/systematic review) | Type of non-conveyance assessed (e.g. telephone advice, non-transport | Sample size | Sample (inclusion/exclusion criteria) | Skill mix | Rate of recontacts/subsequent health-care events | Measurement details12 | Quality concerns | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ambulance | Emergency department | Admission | Death | ||||||||
| VAN analysis, 2017, UK | Analysis using routine linked data | TA; NT |
2514/10,634 TA; 42,796/50,894 NT |
Excludes dead on scene; end-of-life care; non-traced cases | N/A |
TA: NT: 3861/42,796 (9.0%) |
TA: NT: 5412/42796 (12.6%) |
TA: 2.5–10.5% NT: 694/42,796 (6.3%) |
TA: 0.06 –0.04% NT: 129/42,796 (0.3%) | 3 days (day of call is day 0) | Telephone advice only data sample bias owing to low match rate (24%). Minimum threshold assumes all non-traced cases had zero recontacts |
| Fisher, 2015, UK33 | Systematic and documentary review | TA; NT | 40 papers included | Various, paper-specific exclusions | Various paper-specific skill-mix | Mixed evidence around patient safety of NT interventions and decision-making. For example, some studies looking at patients with hypoglycaemic episodes show they can be treated safely at home, whereas others report recontacts with ambulance and other services | N/A | Research generally poor quality. More detail required to thoroughly evaluate safety and effectiveness of NT decisions | |||
| Mason, 2007, UK32 | Cluster randomised controlled trial | NT | I: 1549; C: 1469 | Includes patients aged ≥ 60 years who made calls between 08.00 and 20.00 from a Sheffield postcode | Paramedic practitioners | Not measured | I: 970/1549 (62.6%); C: 1286/1469 (87.5%) | I: 626/1549 (40.4%); C: 683/1469 (46.5%) | Not measured | Within 28 days | Potential clustering at practitioner level; May have limited generalisability owing to study location |
| Snooks, 2004, UK19 | Routine data analysis | NT | 194 patients left at home (175 participated owing to opt-outs and incomplete data) | Includes people aged ≥ 65 years who had fallen in catchment area of study hospitals | Standard paramedic and emergency medical technician staffed vehicles | 83/175 (47.5%) | 42/175 (24%) | 11/175 (6.3%) | 4/175 (2.3%) | Within 2 weeks | Did not assess appropriateness of NT decisions |
| Kahalé, 2006, Canada36 | Prospective cohort study | NT | 345 NT patients | Children aged < 16 years assessed by paramedics but NT | Paramedics | Not reported | 51/345 (14.8%) | (8.7) | 0/345 (0%) | Within 48 hours of the call | Single city evaluation |
| Tohira, 2016, Australia82 | Prospective cohort study | NT | 10,204 patients discharged on scene | Included lower-acuity patients (triage level 3, 4 or 5) attended by paramedics within a metropolitan area. Patients aged < 14 years excluded | Paramedics | 742/10204 (7.3%) | 524/10204 (5.1%) | 365/10204 (3.6%) | 19/10204 (0.19%) | Within 24 hours | Aim of study was accuracy of paramedic decision-making. Only 11.5% were identified as suitable for care in community. Hospital admission includes admission to short-stay units. Findings may not be generalisable to paramedics who have received extended training |
| Jensen, 2013, Canada83 | Observational pilot study. Routine data analysis | NT | 238 calls ECP: 88/140 discharged on-scene; EP: 21/98 discharged on-scene | Included: people with long-term care condition. Excluded: people living in assisted units; or long-term condition facility employees | ECP: (59%), Emergency paramedics: (41%) | ECP: 9/98 (6.4%) | Not reported | Not reported | Not reported | Within 48 hours | Recontacts were for a related clinical reason (determined by study team consensus). LTC patients are a vulnerable group and may suffer from multiple conditions, including dementia. ECPs were assigned to calls differently from EPs owing to some callers specifically requesting ECP services. Overall, the number of NTs is small. Repeat emergency calls were not always indicative of inappropriate decisions related to the first call |
| Magnusson, 2016, Sweden66 | Record review | NT | 529 patients assessed; 200 left at home | Includes calls assigned to emergency nurse (low-priority cases) | Nurse-manned single responder | Not reported | 38/200 (19%) | 20/200 (10%) | Not reported | 72 hours | NT patients were significantly younger than transported patients |
| Al-Sulaiti, 2009, Wales,84 | Data linkage | NT | 734 non-conveyed patients | Not stated | Not stated | Not reported | 24 hours: 73/734 (10%); 7 days 95/734 (13%) | 24 hours: 51/734 (7%); 7 days 59/734 (8%) | 24 hours: 0/734 (0%); 7 days 7/734 (1%) | 24 hours; 7 days; 1 month; 3 months; 6 months | Also reports GP out of hours and GP contacts. Numbers are calculated from percentage and denominator. Conference abstract |
| Gray, 2008, UK29 | Data linking | NT | 119 people with breathing difficulties and 171 EFs | People with breathing difficulties and patients aged ≥ 65 years who have fallen | ECP | Not reported |
72 hours BD: 18/119 (15%); EF: 21/171 (12.3%) Further events 28 days BD: 19/119 (16%); EF: 19/171 (11.1%) |
72 hours BD: 15/119 (12.6%); EF: 16/171 (9.4%) Further events 28 days BD: 13/119 (10.9%); EF: 13/171 (7.6%) |
Not reported | Within 72 hours and 28 days of initial incident | All admissions were included, even if for different presenting complaints. Cases were matched through searching ED admissions at the nearest ED. It is possible that callers could have attended other EDs outside the study area |
| Anderson, Denmark, 200265 | Data linking | NT | 968/1148 patients assessed by MICU | Hypoglycaemic patients | MICU | 29/968 (3%) seen again by MICU | 76/968 (7.9%) seen by either ED or hospital | 3/968 (0.3%) (died during admission) | 72 hours | 31 patients expressed a preference to stay at home | |
| Mikolaizak, 201320 | Systematic review | NT | 12 included studies | Older people aged > 60 years and older people with falls | Various, paper-specific skill-mix | Up to 49% of NT people who have fallen had unplanned health-care contacts within 28 days | Within 28 days of initial incident | Follow-up periods of included studies varied from 1 to 12 months. Little evidence on effectiveness of alternative models of care. Ambulance systems of included studies operationally and clinically heterogeneous | |||
| Eastwood, 2016, Australia21 | Systematic review | TA | 7 articles/reports included | Patients categorised as low-acuity. Various, paper-specific exclusions | Various, paper-specific skill-mix | Low incidence of adverse events. Nearly one-third of patients were recommended self/home care and the remainder were referred to other (non-ambulance) health-care professionals | Not applicable | Use of different secondary triage algorithms. Most studies had small sample sizes. In some studies the hours of operation were limited to OOH. Different studies used different final disposition categories | |||
| Fitzpatrick, 2015, Scotland23 | Systematic review | NT | 23 papers included | Patients with hypoglycaemia signs and symptoms | Various, paper-specific skill-mix | Post-hypoglycaemic patients treated in the prehospital environment have a 2–7% risk of experiencing a RHE within 48 hours | 48 hours | Lack of high-quality research in this area | |||
Appendix 21 Details of observation data collection months, days and times in work package 4.1
| Service/visit numbera | Month | Day | Time (8 hours) |
|---|---|---|---|
| B, 1 | November | Weekend | Day/early |
| B, 2 | January | Weekend | Night |
| B, 3 | January | Weekday | Day/early |
| B, 4 | March | Weekday | Day/early |
| B, 5 | March | Weekday | Day/early |
| E, 1 | January | Weekday | Day/early |
| E, 2 | February | Weekday | Day |
| E, 3 | February | Weekday | Evening |
| E, 4 | February | Weekend | Night |
| E, 5 | March | Weekday | Day/early |
| H, 1 | April | Weekday | Night |
| H, 2 | May | Weekday | Day/early |
| H, 3 | May | Weekend | Day/early |
| H, 4 | August | Weekday | Evening |
| H, 5 | August | Weekday | Evening |
Appendix 22 Variation in ‘Hear and Treat’: topic guide used in work package 4.1
Variation in ‘Hear and Treat’: topic guide
Thank you for agreeing to take part with this interview. The interview should take less than an hour to complete. Do you have any questions before we begin? Can you confirm that you are happy for the interview to be recorded?
-
Can you describe your role and how you are involved in ‘Hear and Treat’?
-
What do you consider to be the role of ‘Hear and Treat’ (in your ambulance service)
-
What factors affect the provision of ‘Hear and Treat’ in your ambulance service?
Prompt if the interviewee does not volunteer the following factors:
Population factors [e.g. conditions, socioeconomic status, ethnicity, morbidity, geography (urban/rural)].
Staff (e.g. who offers advice, training and skills, communication).
Locality factors (e.g. services/care pathways available in each locality).
Organisational factors (e.g. work environment, commissioner or service decisions about priorities, targets, protocols).
National (e.g. funding, targets).
-
What factors affect the appropriateness of ‘Hear and Treat’ decisions? Does this result in recontacts?
-
What works well in your ambulance service for ensuring appropriate ‘Hear and Treat’ (decisions)?
-
What does not work well in your ambulance service for ensuring appropriate ‘Hear and Treat’ (decisions?)?
-
What solutions could be put in place to improve ‘Hear and Treat’? Which one could have most impact on the amount of ‘Hear and Treat’ cases being done?
-
Is there anything else that you’d like to say about ‘Hear and Treat’?
The study is due to be completed in February 2017. If you would like to see a summary of the findings I would be happy to forward them on to you. Would you like me to do this?
Thank you for your time.
Appendix 23 Explaining variation in telephone-advice-only rates for breathing problems
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 0.96 | 0.75 to 1.23 | 0.750 | 0.96 | 0.75 to 1.23 | 0.755 |
| 11–20 | 1.02 | 0.79 to 1.31 | 0.886 | 1.02 | 0.79 to 1.31 | 0.887 |
| 21–30 | 1.18 | 0.95 to 1.47 | 0.138 | 1.18 | 0.95 to 1.48 | 0.136 |
| 31–40 | 1.59 | 1.28 to 1.97 | < 0.001 | 1.59 | 1.28 to 1.97 | < 0.001 |
| 41–50 | 1.12 | 0.90 to 1.40 | 0.320 | 1.12 | 0.90 to 1.40 | 0.319 |
| 51–60 | 0.90 | 0.72 to 1.13 | 0.382 | 0.90 | 0.72 to 1.14 | 0.386 |
| 61–70 | 0.61 | 0.48 to 0.77 | < 0.001 | 0.61 | 0.48 to 0.77 | < 0.001 |
| 71–80 | 0.71 | 0.58 to 0.87 | < 0.001 | 0.71 | 0.58 to 0.87 | 0.001 |
| 81–90 | 0.62 | 0.51 to 0.77 | < 0.001 | 0.63 | 0.51 to 0.77 | < 0.001 |
| > 90 | 0.53 | 0.39 to 0.73 | < 0.001 | 0.53 | 0.39 to 0.73 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 1.02 | 0.92 to 1.13 | 0.697 | 1.02 | 0.92 to 1.13 | 0.699 |
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.80 | 0.71 to 0.90 | < 0.001 | 0.80 | 0.71 to 0.90 | < 0.001 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 0.96 | 0.82 to 1.11 | 0.568 | 0.96 | 0.82 to 1.11 | 0.564 |
| Q3 | 0.84 | 0.71 to 0.99 | 0.043 | 0.84 | 0.71 to 0.99 | 0.043 |
| Q4 | 1.05 | 0.88 to 1.25 | 0.581 | 1.05 | 0.88 to 1.25 | 0.579 |
| Q5 (highest) | 0.76 | 0.61 to 0.95 | 0.016 | 0.77 | 0.62 to 0.96 | 0.018 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 0.94 | 0.77 to 1.15 | 0.545 | 0.94 | 0.77 to 1.15 | 0.533 |
| Q3 | 0.84 | 0.69 to 1.02 | 0.085 | 0.84 | 0.69 to 1.02 | 0.081 |
| Q2 | 0.99 | 0.82 to 1.20 | 0.932 | 0.99 | 0.82 to 1.20 | 0.916 |
| Q1 (most deprived) | 0.88 | 0.72 to 1.09 | 0.247 | 0.88 | 0.72 to 1.09 | 0.237 |
| Ambulance service-level variables | ||||||
| Organisational motivation: lack/no view/recent | – | – | – | 1 | – | – |
| Organisational motivation: active and established | – | – | – | 0.82 | 0.22 to 3.02 | 0.762 |
| Organisational motivation: risk aversion | – | – | – | 0.05 | 0.01 to 0.19 | < 0.001 |
FIGURE 24.
Telephone-advice-only rates for breathing problems. (a) Null model; (b) model with patient-level variables; and (c) model with patient- and ambulance service-level variables.
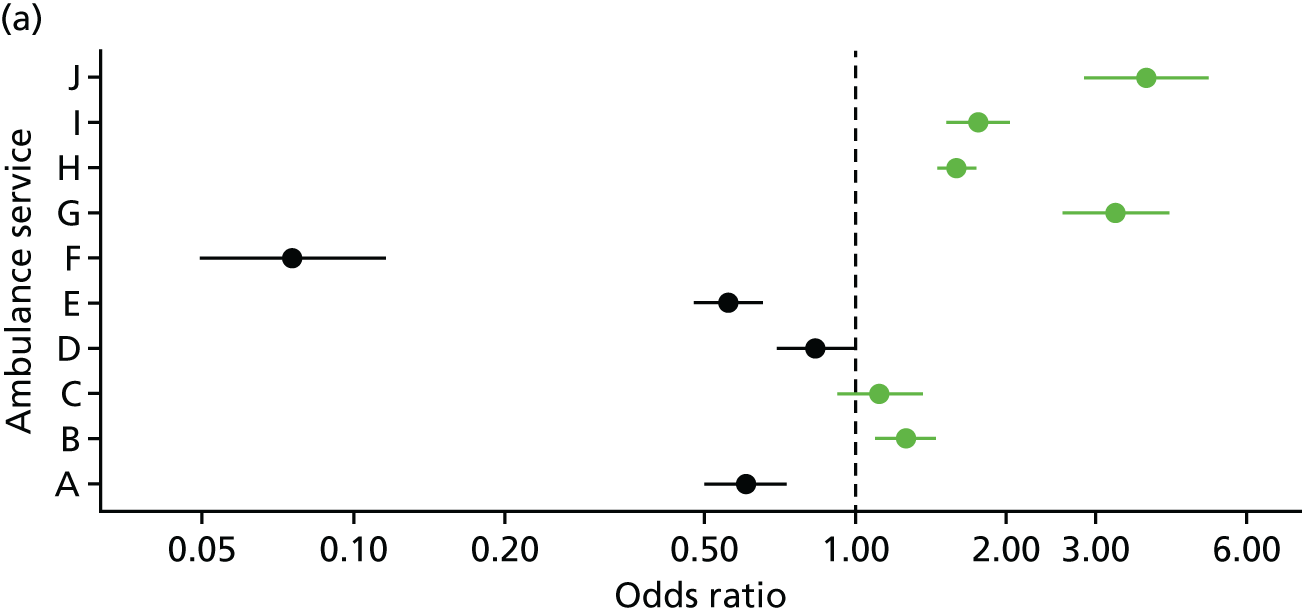
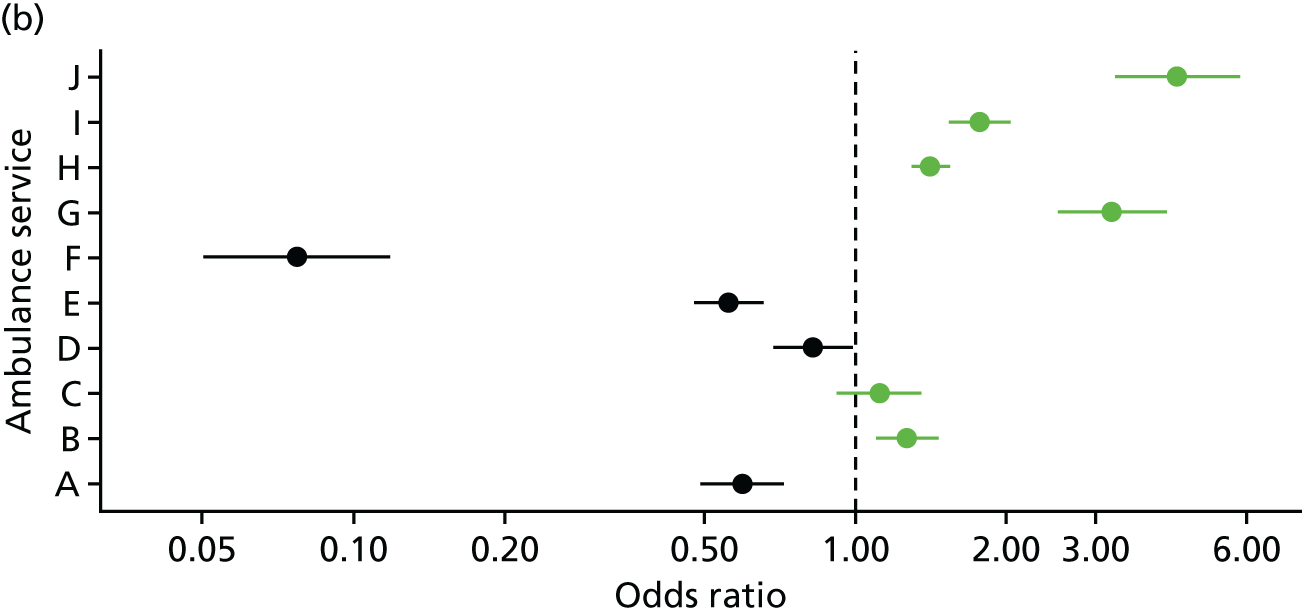

Appendix 24 Explaining variation in discharge-at-scene rates for breathing problems (with skill-mix, nine services, including NHS 111)
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 1.45 | 1.28 to 1.65 | < 0.001 | 1.45 | 1.28 to 1.65 | < 0.001 |
| 11–20 | 3.93 | 3.49 to 4.43 | < 0.001 | 3.94 | 3.49 to 4.44 | < 0.001 |
| 21–30 | 3.91 | 3.50 to 4.37 | < 0.001 | 3.91 | 3.50 to 4.38 | < 0.001 |
| 31–40 | 3.15 | 2.80 to 3.54 | < 0.001 | 3.15 | 2.81 to 3.55 | < 0.001 |
| 41–50 | 2.37 | 2.11 to 2.66 | < 0.001 | 2.37 | 2.11 to 2.66 | < 0.001 |
| 51–60 | 2.12 | 1.90 to 2.37 | < 0.001 | 2.12 | 1.90 to 2.37 | < 0.001 |
| 61–70 | 1.80 | 1.62 to 2.00 | < 0.001 | 1.80 | 1.62 to 2.00 | < 0.001 |
| 71–80 | 1.76 | 1.59 to 1.94 | < 0.001 | 1.76 | 1.59 to 1.94 | < 0.001 |
| 81–90 | 1.89 | 1.71 to 2.08 | < 0.001 | 1.89 | 1.71 to 2.09 | < 0.001 |
| > 90 | 2.06 | 1.82 to 2.34 | < 0.001 | 2.06 | 1.82 to 2.34 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 1.15 | 1.10 to 1.20 | < 0.001 | 1.15 | 1.10 to 1.20 | < 0.001 |
| Call variables | ||||||
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.86 | 0.82 to 0.90 | < 0.001 | 0.86 | 0.82 to 0.90 | < 0.001 |
| Urgency level | ||||||
| Red 1 & 2 | 1 | – | – | 1 | – | – |
| Green 1 & 2 | 1.34 | 1.26 to 1.42 | < 0.001 | 1.33 | 1.26 to 1.42 | < 0.001 |
| Green 3 & 4 | 1.60 | 1.46 to 1.74 | < 0.001 | 1.60 | 1.46 to 1.74 | < 0.001 |
| Origin of call | ||||||
| 999 | 1 | – | – | 1 | – | – |
| NHS 111 | 1.51 | 1.33 to 1.71 | < 0.001 | 1.51 | 1.33 to 1.58 | < 0.001 |
| Skill-mix | ||||||
| Paramedic | 1 | – | – | 1 | – | – |
| Advanced paramedic | 1.45 | 1.33 to 1.57 | < 0.001 | 1.45 | 1.33 to 1.58 | < 0.001 |
| Other | 1.00 | 0.93 to 1.08 | 0.909 | 1.00 | 1.46 to 1.74 | 0.984 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 0.90 | 0.83 to 0.96 | 0.004 | 0.90 | 0.83 to 0.96 | 0.004 |
| Q3 | 0.92 | 0.85 to 0.99 | 0.027 | 0.92 | 0.85 to 0.99 | 0.027 |
| Q4 | 0.95 | 0.88 to 1.03 | 0.219 | 0.95 | 0.88 to 1.03 | 0.213 |
| Q5 (highest) | 1.00 | 0.92 to 1.09 | 0.988 | 1.00 | 0.92 to 1.09 | 0.994 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 1.07 | 0.98 to 1.17 | 0.136 | 1.07 | 0.98 to 1.17 | 0.136 |
| Q3 | 1.02 | 0.93 to 1.11 | 0.728 | 1.02 | 0.93 to 1.11 | 0.725 |
| Q2 | 1.01 | 0.92 to 1.10 | 0.897 | 1.01 | 0.93 to 1.10 | 0.892 |
| Q1 (most deprived) | 1.03 | 0.94 to 1.13 | 0.576 | 1.03 | 0.94 to 1.12 | 0.583 |
| Ambulance service-level variables | ||||||
| Workforce advanced paramedics | ||||||
| No evidence | – | – | – | 1 | – | – |
| Limited | – | – | – | 1.30 | 0.97 to 1.75 | 0.076 |
| Established | – | – | – | 1.94 | 1.21 to 3.10 | 0.006 |
| Complexity | ||||||
| Average CCGs | – | – | – | 1 | – | – |
| Many CCGs | – | – | – | 0.51 | 0.37 to 0.70 | < 0.001 |
| Few CCGs | – | – | – | 1.06 | 0.60 to 1.88 | 0.847 |
FIGURE 25.
Variation in discharge-at-scene rates for breathing problems. (a) Null model; (b) model with patient-level variables; and (c) model with patient- and ambulance service-level variables.
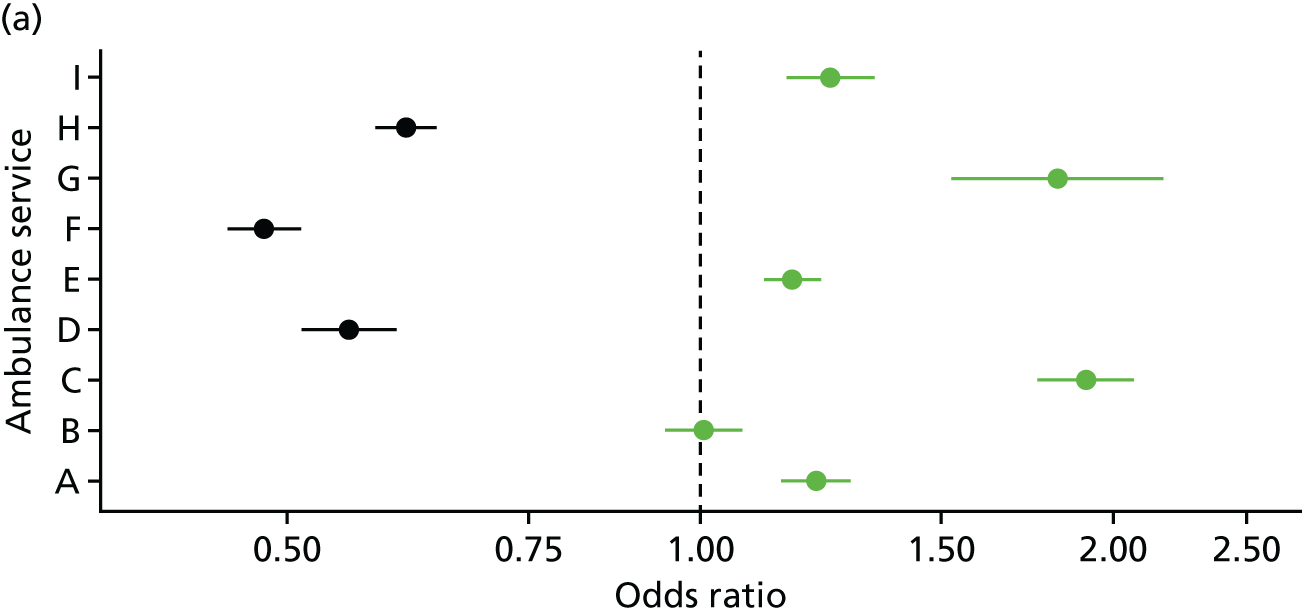
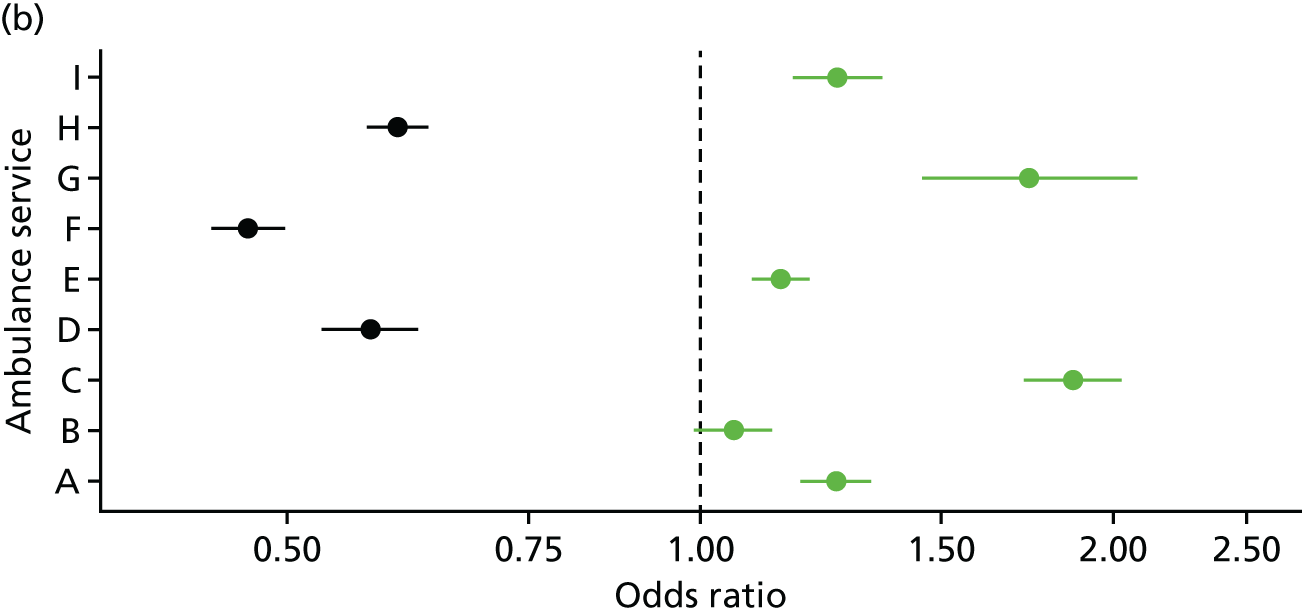
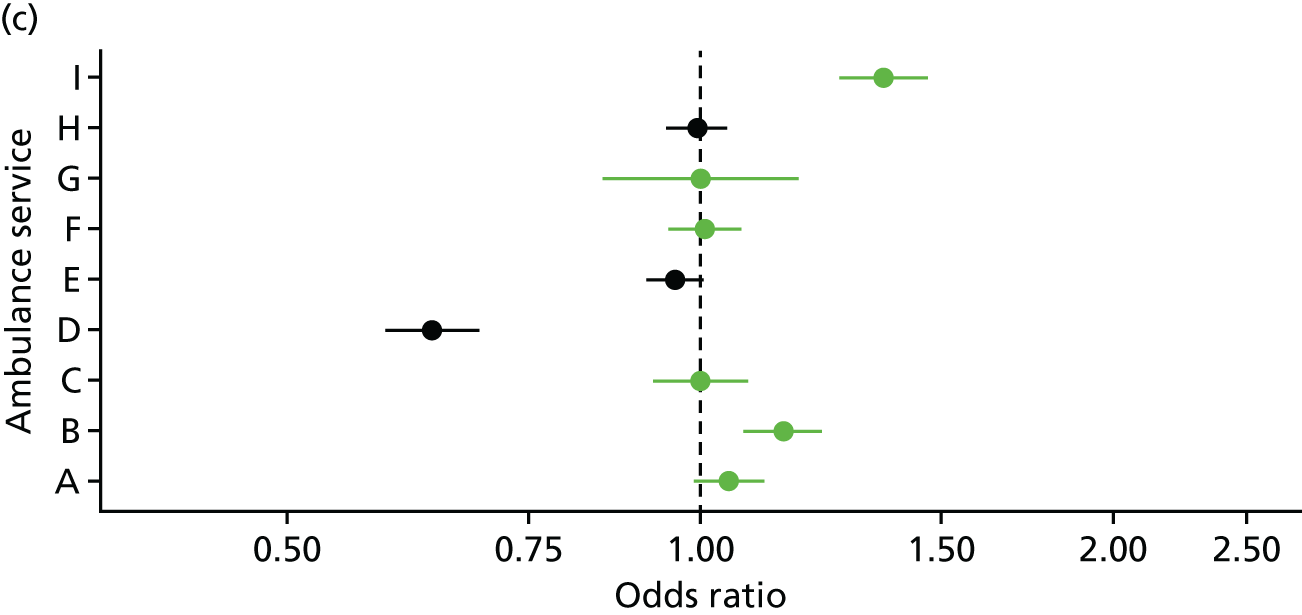
Appendix 25 Explaining variation in 24-hour recontact rates for discharge at scene for breathing problems (with skill-mix, nine services, excludes NHS 111 calls)
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Patient-level variables | ||||||
| Age (years) | ||||||
| 0–2 | 1 | – | – | 1 | – | – |
| 3–10 | 0.54 | 0.23 to 1.25 | 0.151 | 0.54 | 0.23 to 1.25 | 0.148 |
| 11–20 | 0.92 | 0.49 to 1.74 | 0.805 | 0.93 | 0.49 to 1.75 | 0.826 |
| 21–30 | 1.29 | 0.73 to 2.27 | 0.384 | 1.30 | 0.74 to 2.29 | 0.367 |
| 31–40 | 0.96 | 0.51 to 1.81 | 0.896 | 0.96 | 0.51 to 1.82 | 0.908 |
| 41–50 | 2.32 | 1.34 to 4.02 | 0.003 | 2.35 | 1.36 to 4.06 | 0.002 |
| 51–60 | 3.12 | 1.84 to 5.29 | < 0.001 | 3.15 | 1.86 to 5.33 | < 0.001 |
| 61–70 | 3.63 | 2.18 to 6.06 | < 0.001 | 3.68 | 2.21 to 6.13 | < 0.001 |
| 71–80 | 3.18 | 1.92 to 5.26 | < 0.001 | 3.20 | 1.94 to 5.30 | < 0.001 |
| 81–90 | 3.40 | 2.06 to 5.63 | < 0.001 | 3.45 | 2.09 to 5.70 | < 0.001 |
| > 90 | 3.22 | 1.84 to 5.63 | < 0.001 | 3.26 | 1.86 to 5.69 | < 0.001 |
| Sex | ||||||
| Female | 1 | – | – | 1 | – | – |
| Male | 0.97 | 0.83 to 1.14 | 0.736 | 0.97 | 0.83 to 1.14 | 0.734 |
| Call variables | ||||||
| Time of call | ||||||
| Out of hours | 1 | – | – | 1 | – | – |
| In hours | 0.86 | 0.72 to 1.03 | 0.096 | 0.86 | 0.72 to 1.03 | 0.093 |
| Urgency level | ||||||
| Red 1 & 2 | 1 | – | – | 1 | – | – |
| Green 1 & 2 | 1.01 | 0.83 to 1.23 | 0.932 | 1.01 | 0.83 to 1.24 | 0.912 |
| Green 3 & 4 | 0.95 | 0.70 to 1.29 | 0.749 | 0.95 | 0.70 to 1.28 | 0.733 |
| Skill-mix | ||||||
| Paramedic | 1 | – | – | 1 | – | – |
| Advanced paramedic | 1.02 | 0.77 to 1.24 | 0.902 | 1.03 | 0.78 to 1.36 | 0.814 |
| Other | 1.06 | 0.83 to 1.26 | 0.654 | 1.07 | 0.83 to 1.37 | 0.605 |
| Patient-level variables (LSOA based) | ||||||
| Long-term condition quintile | ||||||
| Q1 (lowest) | 1 | – | – | 1 | – | – |
| Q2 | 0.85 | 0.65 to 1.13 | 0.273 | 0.86 | 0.65 to 1.13 | 0.281 |
| Q3 | 0.96 | 0.73 to 1.27 | 0.799 | 0.97 | 0.74 to 1.28 | 0.855 |
| Q4 | 0.95 | 0.71 to 1.27 | 0.734 | 0.97 | 0.73 to 1.29 | 0.831 |
| Q5 (highest) | 0.81 | 0.59 to 1.12 | 0.199 | 0.84 | 0.61 to 1.16 | 0.288 |
| IMD quintile | ||||||
| Q5 (least deprived) | 1 | – | – | 1 | – | – |
| Q4 | 1.09 | 0.79 to 1.50 | 0.610 | 1.08 | 0.78 to 1.49 | 0.653 |
| Q3 | 1.11 | 0.81 to 1.54 | 0.510 | 1.09 | 0.79 to 1.51 | 0.583 |
| Q2 | 1.17 | 0.85 to 1.62 | 0.334 | 1.14 | 0.83 to 1.58 | 0.422 |
| Q1 (most deprived) | 1.42 | 1.02 to 1.98 | 0.039 | 1.37 | 0.98 to 1.92 | 0.064 |
| Ambulance service-level variables | ||||||
| NAO frontline staff advanced practitioners: average | – | – | – | 1 | – | – |
| NAO frontline staff advanced practitioners: high | – | – | – | 1.41 | 1.11 to 1.79 | 0.005 |
FIGURE 26.
Variation in 24-hour recontact rates for discharge at scene for breathing problems. (a) Null model; (b) model with patient-level variables; and (c) model with patient- and ambulance service-level variables.

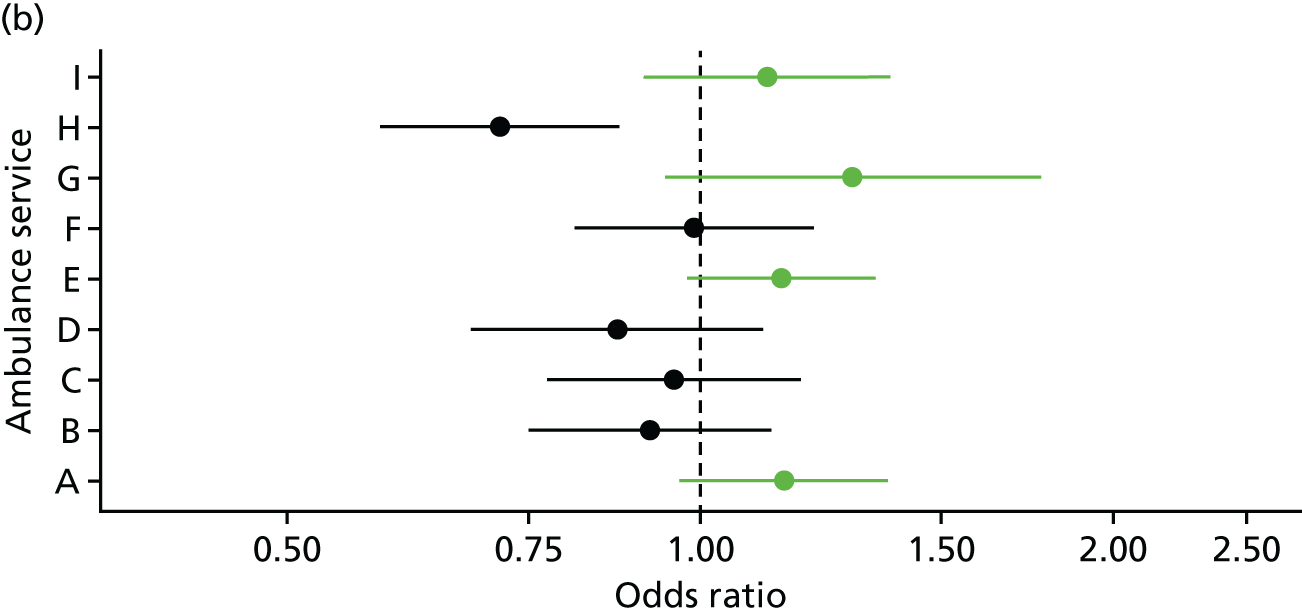

Glossary
- Advanced paramedic
- A term used here to describe paramedics who have expanded their scope of practice beyond their initial training. These paramedics have advanced skills that allow them to administer a wider range of medications, undertake more advanced assessment and diagnosis, and deliver a wider range of treatments than paramedics. Ambulance services in England use a range of labels for these types of staff, including ‘emergency care practitioner’. The types and numbers of calls that advanced paramedics attend may vary by ambulance service, the types of calls they are dispatched to may vary, and some advanced paramedics may focus on critical care, which often requires conveyance to hospital.
- Call-handler
- A term used here to describe those staff providing the first point of contact for a caller dialling the 999 ambulance service. A call-handler documents the reason for the call and uses triage software to decide on the response needed. Ambulance services in England use a range of labels for these staff, including ‘emergency medical dispatchers’ or ‘emergency call advisors’.
- Clinical hub
- The clinical hub is based in the Emergency Operations Centre and refers to a range of clinicians who provide enhanced clinical support to call-handlers and patients following an ambulance 999 call. They decide when calls can end in telephone advice only. These clinicians may have paramedic or other clinical backgrounds (e.g. nurse, midwife). Not all ambulance services in England describe their clinical staff as working in a clinical hub.
- Discharge at scene
- A term used here to describe an ambulance 999 call that results in a face-to-face assessment of a patient by an ambulance crew at the scene without transport to a health-care facility. This includes cases in which patients are referred to health and social care services such as a falls service. This term is used instead of ‘See and Treat’ for international relevance.
- Emergency Operations Centre
- The physical facilities housing the call-handlers who dispatch ambulances and the clinical staff who offer telephone advice.
- Hear and Treat
- A term used in England to describe a range of telephone responses to 999 ambulance calls whereby an ambulance is not sent to a patient. The alternative term ‘telephone advice only’ is used in this report for international relevance.
- NHS 111
- A national telephone-based service in England offering urgent health-care advice, operating 24 hours a day, 365 days a year.
- Non-conveyance
- A term used to describe a 999 call to the ambulance service that results in a decision not to transport the patient to a health-care facility. A more specific type of non-conveyance is ‘non-conveyance to an emergency department’, which includes ‘Hear and Treat’, ‘See and Treat’ and ‘See and Convey Elsewhere’.
- See and Convey Elsewhere
- A term used in England to describe an ambulance 999 call that results in a face-to-face assessment of a patient by an ambulance crew at the scene and onward transport to a health-care facility that is not an emergency department.
- See and Treat
- A term used in England to describe an ambulance 999 call that results in a face-to-face assessment of a patient by an ambulance crew at the scene and no onward transport to a health-care facility.
- Telephone advice only
- An alternative term for ‘Hear and Treat’ that may have more international relevance. This term is used to describe calls sent to clinicians within the ambulance service and ending without dispatch of an ambulance. It also includes some calls ended by call-handlers.
List of abbreviations
- A&E
- accident and emergency
- AQI
- Ambulance Quality Indicator
- CAD
- computer-aided dispatch
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- COPD
- chronic obstructive pulmonary disease
- ECP
- emergency care practitioner
- ePRF
- Electronic Patient Report Form
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- ID
- identification
- LSOA
- lower layer super output area
- MPDS
- Medical Priority Dispatch System
- NAO
- National Audit Office
- ONS
- Office for National Statistics
- PhOEBE
- Pre-Hospital Outcomes for Evidence Based Evaluation
- PPI
- patient and public involvement
- UECN
- Urgent and Emergency Care Network
- VAN
- variation in ambulance non-conveyance
- WP
- work package
