Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/77/25. The contractual start date was in July 2016. The final report began editorial review in August 2017 and was accepted for publication in January 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Greta Rait is a member of the Health Technology Assessment (HTA) Commissioning Board and HTA Mental Health Panel and Methods Group. Claire Goodman is a National Institute for Health Research (NIHR) senior investigator and a trustee of The Orders of St John Care Trust. Marie-Anne Durand reports personal fees from EBSCO Health and the ACCESS Community Health Network outside the submitted work. There are no other financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Bunn et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Introduction
Including the patient perspective is a central organising principle of integrated care. 1 Moreover, there is increasing recognition of the importance of strengthening relationships between patients, carers and practitioners,2,3 particularly for individuals most reliant on health and care services, such as people who are very old and those with long-term conditions (LTCs). 4,5 However, evaluations of the English integrated care pilots (ICPs) reported that patients were less satisfied with their involvement in decision-making about their care than prior to the instigation of the ICPs. 6 There is a need to establish the mechanisms that preserve and foster shared decision-making (SDM) between providers, patients and carers and ascertain how they achieve improvements in patient outcomes. 7,8
Shared decision-making
Shared decision-making involves patients and health and social care professionals (HSCPs) jointly selecting treatment, care and support packages to reflect, respect and accommodate the patient’s preferences, priorities and goals. 9,10 The phrase ‘sharing the decision’ was coined by Robert Veatch11 in an article exploring the ethics of patient–doctor interactions. The subject has gathered pace over the years and now includes the development, evaluation and implementation of patient decision aids (PDAs). 12 Stiggelbout et al. 13 show how differing philosophies, such as medical ethics and health services research, have contributed to the development of SDM. 13 The progression of these ideas is mapped out in Figure 1.
FIGURE 1.
The development of SDM. EBM, evidence-based medicine.

Towle and Godolphin19 identified eight essential elements of SDM:
-
develop a partnership with the patient
-
establish/review the patient’s preference for information, for example amount and format
-
establish/review the patient’s preferred role in decision-making
-
ascertain/respond to patients’ ideas, concerns and expectations
-
identify choices and evaluate the research evidence relating to the individual
-
present evidence and help the patient reflect on and assess the impact of alternative decisions
-
make/negotiate a decision in partnership and manage conflict
-
agree on an action plan and arrangements for follow-up.
Although the original underlying ethos for sharing decisions between patients and HSCPs is based on values, that is, people have the right to self-determination and autonomy, there is evidence that SDM can lead to better outcomes and care for people. 20 For example, patients who feel involved in the decision and in accord with the HSCP are less likely to need other services such as extra tests or referrals to other HSCPs. 21 More recently, SDM has been envisaged as being part of person- and family-centred care and integrated care,22–29 and linked with approaches such as care planning and the Year of Care. 30–33
Integrated care
For older people with complex health needs, which may arise as a result of dementia, frailty and multimorbidity, navigating health and social care can be difficult. 34 There is a high risk that they will experience poor continuity and fragmentation of care. 35,36 Approaches are needed that aim to address the complexity of life when living with, and managing, multiple LTCs (e.g. for older people with diabetes mellitus)37,38 or that recognise the need to consider the ability of patients and their families to attend to the demands of each condition. 39–41 Such approaches require the building of relationships, meaningful discussion and SDM between a range of different providers, patients and carers. 42 In addition, integrated care is seen as a way of reducing the costs of health and social care services1,43 by preventing duplication of services and reducing demand for acute hospital services. 44,45
Integrated care has been proposed as one solution to the fragmentation of care, and has been adopted in the UK46–49 and internationally. 45–50 Newer models of care have focused on whole-systems approaches to care delivery, particularly for those with LTCs and complex needs. 25–28,33,51,52 In England this includes initiatives such as the Year of Care,25 the House of Care26,27 and the vanguard sites of the Five Year Forward View. 8 In other parts of the UK, initiatives to increase integration (particularly of health and social care) have been in place for some time. 46 For example, in Scotland, integration authorities are now responsible for funding that was previously managed by NHS boards and local authorities. 49
The vanguard sites
In England, the Five Year Forward View8 set out new models of integrated care as part of a wider system change in the NHS; these reinforce the aim for ‘a more engaged relationship with patients, carers and citizens’ in order to promote well-being and prevent ill health. 8 Fifty vanguard sites are piloting integrated care with the aim of achieving personalised, well co-ordinated care for patients and addressing traditional divides between primary care, community services and hospitals. 8,53 Their remit is to find new ways to deliver care in line with the five models of care (Box 1) identified in the Five Year Forward View. 8 The models are underpinned by preparatory and exploratory work carried out in collaboration with National Voices. 54 Integrated Primary and Acute Care Systems (PACS) and multispeciality community provider (MCP) vanguards currently cover about 8% of England but are similar to the Sustainability and Transformation Plans (STPs) now being introduced across England. 55 STPs seek to implement the NHS Five Year Forward View by creating new accountable models of care provision. Some are using a MCP model; larger STPs are using the PACS model. 56 The MCP model involves creating integrated community-based multidisciplinary teams (MDTs), which are supported by other specialist disciplines and by care co-ordinators who help patients and families with multiple LTCs to access services in other health and social care settings. 56
-
Primary and acute care systems, which join up general practice, community, mental health and hospital services.
-
Multispeciality community providers, which move services out of hospitals and into the community.
-
Enhanced care in care homes, which improves services for older people, joining up their health, social care and rehabilitation.
-
Urgent and emergency care, which creates new approaches to improve service co-ordination and reduce emergency hospital admissions.
-
Acute care collaborations, which link hospitals to improve their clinical and financial viability.
Shared decision-making in an integrated care setting
Integrated care sites, such as vanguard sites, offer a particular challenge for SDM as decision-making has to be negotiated between, and communicated to, multiple HSCPs, as well as patients and their families. Decision-making becomes more complex for people with increasing frailty as the capacity to self-manage is affected by the cumulative effects of LTCs. The nature of decisions is complicated by resource availability, polypharmacy, decline in decision-making abilities and concordance, availability of support networks, suitability of treatment, safeguarding and the increased likelihood of depression. 39,57–59 The skills for sharing and discussing personal information with vulnerable patients and their families can be hard to embed in services.
Shared decision-making for older people with complex health and care needs
Older people with complex health and social care needs often rely on family members to negotiate access to care or to advocate for them. 5,60,61 Person-centred approaches and models, like the triangle of care,32 recognise the crucial role of families for quality and safety and encourage their routine involvement in decision-making, with agreement from the patient. 2,4 If the decision-making ability of an older person is significantly compromised, family members are able to act as proxies62,63 if they have legal power of attorney for health and welfare decisions, and they should also be consulted if not. Recently, discussion about continuity of care favours a coconstruction approach, with patients, families and professionals as active partners. 58,64,65 Although service providers recognise the contribution of family carers, this recognition does not always translate into their routine engagement in decision-making with or for older people with multiple, often interlinked, health conditions. 58
To develop an understanding of the realities of working in and across complex overlapping systems of care, it is necessary to synthesise evidence from diverse strands of research. 66,67 Similarly, the evidence demonstrating the effectiveness of interventions designed to promote SDM is drawn from a wide variety of research and practice. 68,69 Realist methodology allows the deconstruction of component theories underpinning different interventions and enables us to consider relevant contextual data to test our understanding of the applicability of different approaches for older people with multimorbidity. It also helps us to examine how SDM might achieve desired outcomes such as improvements in patient safety, clinical effectiveness, quality of life and patient experience7 within the context of integration, austerity measures, growing demand for health and social care and personalisation of care.
Aim and objectives
The overall aims of the synthesis were to:
-
identify key features or mechanisms of programmes and approaches that strengthen relationships between community HSCPs, patients with multiple health and care needs and their family carers
-
provide a context-relevant understanding of how models to facilitate SDM might work for older people with multiple health and care needs, and how they might be used to facilitate person-centred care (PCC) in collaborative models of health and social care.
The objectives were to:
-
identify how interventions, or elements of interventions, to promote SDM with older people with multiple long-term health and social care needs, and their family carers, are thought to work, on what outcomes and for whom they work (or why they do not work)
-
explore how models to facilitate SDM with older people with multiple health and social care needs might be incorporated into service delivery in collaborative models of care in order to achieve outcomes that reflect PCC
-
explore how different contexts support or inhibit participants’ responses to activities that support SDM in collaborative care models
-
inform the development of process and outcome measures to assess the impact of SDM and PCC in the vanguard sites
-
identify key areas for future research, including promising interventions that merit further evaluation.
Chapter 2 Methods
This chapter includes text from the protocol, which was published by Bunn et al. 70 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0.
We used an iterative three-stage approach that drew on the knowledge and networks of the research team and incorporated the views of stakeholders. Stakeholders are important in realist work because they articulate how different programmes are thought to operate and what needs to be present for change to occur. The realist synthesis focus is thus driven by ‘negotiation between stakeholders and reviewers’. 71 The review follows the Realist and Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) publication standards for realist synthesis,72 and is registered on the PROSPERO database (registration number CRD42016039013). 72,73 An overview of the study design is provided in Figure 2.
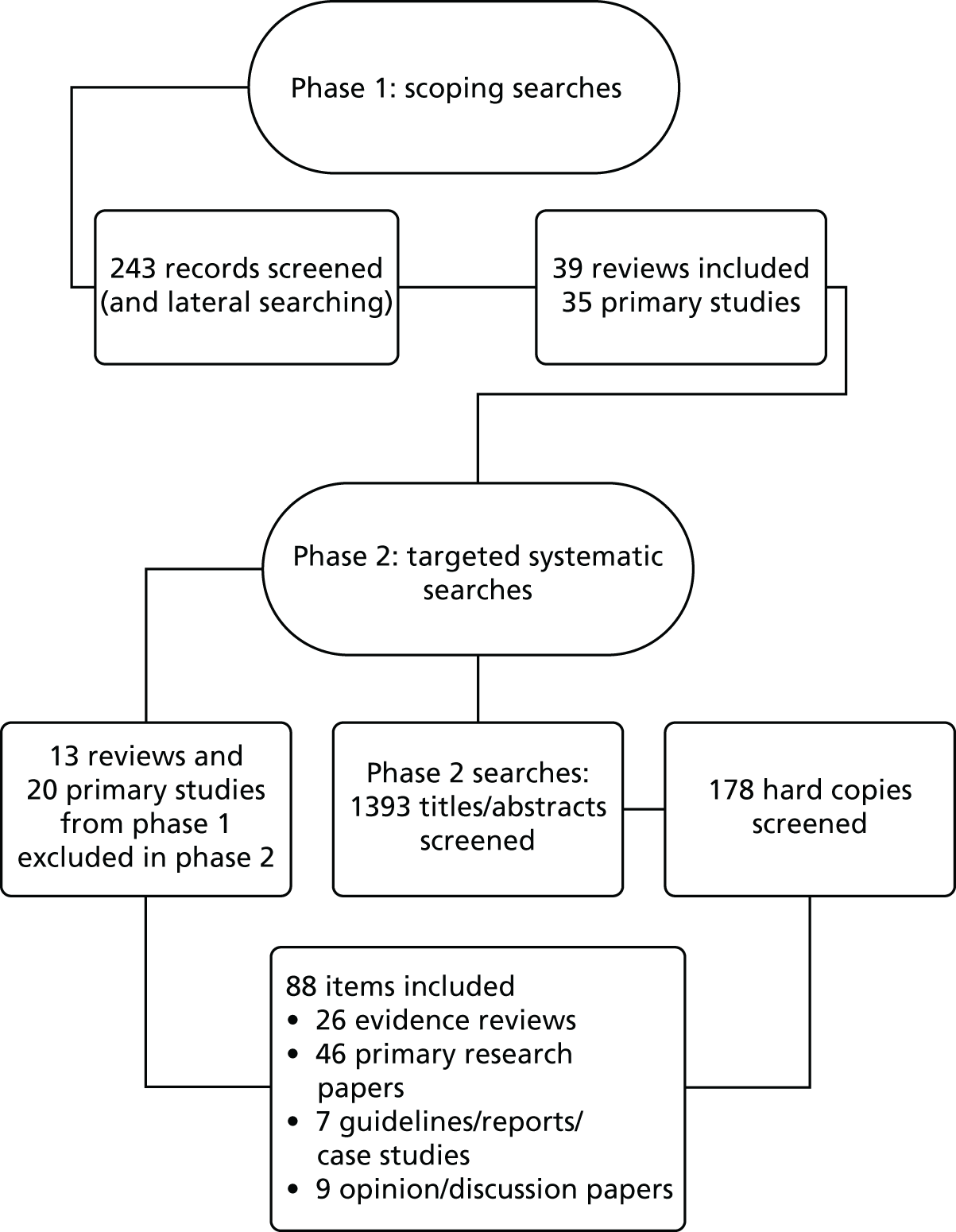
FIGURE 2.
Overview of study design.

Methodological approach
Realist synthesis is a systematic, iterative, theory-driven approach designed to make sense of diverse evidence about complex interventions applied in different settings. 72,74,75 Realist review assumes that there is more to reality than how we see it. There is an external reality or world that can be observed and measured, but how this reality is articulated and responded to is constantly being shaped by individuals’ perceptions and reasoning and/or dominant social and cultural mores. It is this interaction that creates particular responses, which in turn lead to observed outcomes. 76 The rationale for using a realist synthesis approach for this review was that interventions to promote SDM in older people with complex health and care needs are likely to be multicomponent and contingent on the behaviours and choices of those delivering and receiving the care.
A realist synthesis assumes a ‘generative’ approach to causation, that is, ‘to infer a causal outcome (O) between two events (X and Y), one needs to understand the underlying mechanism (M) that connects them and the context (C) in which the relationship occurs’. 77 It is typically used to understand complex interventions that ‘often have multiple components (which interact in non-linear ways) and outcomes (some intended and some not) and long pathways to the desired outcome(s)’. 72 Central to the realist review process is the development of programme theory, that is, what a programme or intervention comprises and how it is expected to work, which can then be tested and refined by reviewing the relevant evidence. 72 Key realist terms are defined in Box 2.
The ‘backdrop’ conditions (which may change over time), for example, the way systems are configured and to what extent they support SDM. Context can be broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism. 78
Mechanism (M)The generative force triggered in particular contexts that leads to outcomes. Often denotes the reasoning (cognitive or emotional) of the various ‘actors’, that is, older people with complex health and care needs, relatives and health-care professionals (HCPs). Mechanisms are linked to, but are not the same as, a service’s strategies or interventions. Identifying the mechanisms goes beyond describing what happened to theorising why it happened, for whom and under what circumstances. 79–81
Outcomes (O)A result of the interaction between a mechanism and the triggering context. These may include improved satisfaction with decisions or better adherence to treatment. 72
Programme theoryThose ideas about what needs to be changed or improved in order to facilitate SDM with older people with complex health and care needs, what needs to be in place to achieve improvement(s) and how programmes are believed to work. It specifies what is being investigated and the elements and scope of the review. Theories rather than ‘programmes’ are the basic unit of analysis. 82
Focus of the review
The synthesis focused on community-dwelling older people (aged ≥ 65 years) with complex health and care needs, for example people with frailty, multimorbidity, LTCs or dementia and those who require help with personal care. The rationale for focusing on this group was that these people often have experience of using many health and social care services, their needs change over time and/or suddenly (sometimes with progressive loss of cognitive and/or physical function), a family carer is frequently involved in their care and they are often at risk of exacerbation of their illness57 and death. In addition, many find it difficult to navigate complicated and under-resourced services and are particularly vulnerable to fragmented care. 35 Ideas around SDM were explored in Chapter 1. There are, however, other concepts (or mid-range theories) that emerged as important during the review process, for instance, ideas around person-centred approaches to care. In Table 1 we provide our working definition of SDM and other concepts that we feel are relevant to this review.
| Concept | How it is defined and operationalised in the review |
|---|---|
| SDM |
|
| Patient-centred care |
|
| Person-centred approaches | A person-centred approach puts people, families and communities at the heart of health, care and wellbeing. It means people feeling able to speak about what is important to them and the workforce listening and developing an understanding of what matters to people. It means working in a system in which people and staff feel in control, valued, motivated and supportedReproduced with permission from Skills for Care, Skills for Health292017Skills for Care, Skills for Health |
| Interprofessional working |
|
| Relational co-ordination |
|
| Continuity of care |
|
| Patient engagement |
|
| Patient activation |
Changes in the review process
As recommended in the RAMESES publication standards, changes in the review process are documented in Table 2.
| Protocol | Revisions/changes |
|---|---|
| We said that we would consult with up to 20 representatives in phase 1 | We conducted 13 stakeholder interviews in phase 1. As recruitment was proving difficult, the advisory group recommended that we focus on the literature review and complete stakeholder consultation once our programme theory was more established. We recruited fewer representatives from vanguard sites and from advocacy groups than hoped |
| We said that stakeholder interviews in phase 1 would initially be carried out by e-mail, followed by telephone or face-to-face interviews with a smaller sample of up to 10 participants purposively selected to reflect the original stakeholder groups | Several people were invited to respond by e-mail but no one did. Eight interviews (with 11 participants) were conducted face to face or by telephone |
| In the protocol we said that we would develop vignettes to use in stakeholder interviews | There was insufficient time to develop vignettes. Instead, the programme theory was used as a basis for the interviews in phase 3 |
Phase 1: defining scope and developing programme theories
In phase 1 we scoped the literature and consulted with stakeholders in order to develop candidate theories about why programmes that seek to promote SDM do, or do not, work. These two processes were conducted in parallel and were considered as independent ‘theory’-gleaning activities.
Scoping the literature
The scoping review of the literature sought to identify existing theories on how and why the involvement of patients and carers is thought to be important, how the existing theories are defined in the literature, how interventions on SDM are meant to work and on which outcomes and how SDM might work in professional settings. The starting point was systematic reviews of SDM and related topics (such as PCC). To identify relevant reviews we searched PubMed and The Cochrane Library using the following Medical Subject Heading (MeSH) terms: shared decision-making, patient participation, patient decision-making, decision support, decision aid, expert patient, proxy decision-making, collaborative care, co-construction, coproduction and minimally disruptive medicine. These terms were combined with methodological search terms for systematic reviews. In addition, we undertook keyword searches on Google Scholar (Google Inc., Mountain View, CA, USA) for both reviews and primary studies and looked for relevant papers published by key authors in the area, such as Elwyn and Légaré. Full details of the search strategy are provided in Appendix 1.
We identified 39 relevant reviews20,40,66–69,93–124 and 35 primary studies or discussion papers. 17,40,67,83,93–102,125–145 Information extracted from the reviews included study aims, types of participants, definition of SDM, outcomes measured, relevance to our target group and any theoretical assumptions made. The reviews allowed us to understand the range and approach of research on SDM but provided limited detail with which to develop our programme theory. Time limitations meant that we were unable to carry out detailed data extraction on all 35 primary studies in phase 1, but they were used to generate ideas about possible contexts and mechanisms.
Scoping interviews
We conducted face-to-face or telephone scoping interviews with 13 stakeholders (Table 3). In phase 1 the purpose of the consultation with stakeholders was to explore key assumptions about what needs to be in place for effective SDM within integrated care initiatives, identify relevant outcomes and clarify the focus and scope of the searches in phase 2. Interview participants were purposively sampled to include a range of programme stakeholders. 81 They were recruited as a result of the networks of the research team. Participants were given a copy of the study information sheet – this provided contact details for the research team and a consent form – which they were asked to read and sign. Ethics approval was obtained from the University of Hertfordshire Health and Human Sciences Ethics Committee with delegated authority (reference number CSK/SF/UH/02387). Interviews were guided by a topic guide, which was used to explore understanding and experiences of SDM, including what works well and what could be improved. Interview transcripts were read by one author (BR) and discussed with a second (FB). Data from the interviews were regularly reviewed (BR and FB) and the topic guide was adapted as our programme theory developed. 146 Interviews were audio-recorded and transcribed.
| Type of stakeholder | Phase (n) | |
|---|---|---|
| 1 | 2 | |
| Commissioners and managers from organisations initiating integrated care (e.g. vanguard sites) | 2 | |
| Providers of health and social care in community settings involved in initiatives to involve patients and their family carers in their care | 3 (2 GPs and 1 geriatrician) | 4 |
| Older people and family carers who have experience of multiple practitioners and services – recruited from the University of Hertfordshire Patient and Public Involvement in Research Group and the Social Care Workforce Research Unit’s User and Carer Group, which includes a diverse group of older people who are frail, and carers, from diverse backgrounds | 7 (3 older people and 4 family carers | 4 (1 older person and 3 family carers) |
| Advocacy and user/carer groups such as Age UK London, Carers UK, National Voices, Healthwatch and Greater London Forum for Older People | 1 | 3 |
| Total | 13 | 11 |
Initial programme theory
From the literature and from stakeholder transcripts, a series of seven explanatory accounts were built up that contained ‘if–then’ statements, which helped to specify context and mechanism. These ‘if–then’ statements were illustrated with supporting evidence from the interviews and literature. ‘If–then’ statements identify an intervention/activity linked to outcome(s) and contain references to contexts and mechanisms (although these may not be very explicit at this stage) and/or barriers and enablers (which can be both mechanism and context). 147 The ‘if–then’ statements provided a useful way of structuring our thinking. They also helped to focus the process of taking ideas and assumptions about how interventions work and testing them against the evidence that we found.
To refine the theory, the seven ‘if–then’ statements were discussed at a half-day workshop that was attended by eight members of the research team. To ensure transparency of approach and an audit trail, we transcribed recordings of group discussions and maintained structured field notes on suggestions and decision-making processes. Following this meeting the statements were revised and then presented to the Project Advisory Group (PAG) for further discussion. The PAG included experts in the field of older people’s health, primary care, patient involvement and realist methods. It also included members of the University of Hertfordshire Public Involvement in Research Group (PIRG) (experts by experience). The PAG suggested that some of the statements were too complex and needed to be disaggregated. It also introduced the concept of ‘fake versus real’ SDM, to indicate when SDM appeared to be conducted as a tick box exercise rather than as a real process for decision-making. As a result, the seven ‘if–then’ statements were reduced to five (Table 4).
| Title | If | Then | Outcome |
|---|---|---|---|
| Reflecting patient and carer values | If HCPs place less emphasis on ‘fixing people’ and more on patients’ goals and emotional, cultural and cognitive needs | Patients and their family carers will feel valued and listened to | Patients and their family carers will feel that they were involved in the decision and are satisfied with the outcome |
| Preparing (patients and carers) for the SDM encounter | If older people with complex health and social care needs are supported to participate in SDM (e.g. through education and information, the use of advocates or coaches, more focus on patient goals and values, good relationships with HCPs and appropriate decision aids that take account of multimorbidity) | Then patients and their family carers will feel empowered and will understand and value SDM | Patients and their family carers will be willing and able to participate in SDM |
| Sharing the communication of a decision | If HCPs are familiar with each other’s expertise, roles and responsibilities, and systems facilitate communication between individuals (including different HCPs and patients and carers) | Then professionals will work better together and are less likely to undermine each other | Once a decision has been made by the patient and a HCP it will be shared across the MDT/agencies |
| Fake vs. real SDM | If systems are organised to support and prioritise SDM (e.g. support from clinical leaders, regular measurement of patient outcomes, clear protocols around dealing with risk and uncertainty, appropriate information technology and longer appointments) | Then SDM is not just seen as a ‘tick box’ exercise by HSCPs | Real not fake SDM |
| Reducing the workload (for patients and carers) | If HCPs are able to use appropriate SDM techniques to regularly discuss the clinical value and effectiveness of proposed treatments or interventions | This will lead to a reduction in inappropriate clinical activity | Improved function or ability to enjoy life |
Phase 2: retrieval, review and synthesis
Selection criteria
In phase 2 we undertook systematic searches of the evidence to test and develop the theories identified in phase 1. The main inclusion criteria were as follows:
-
Community-dwelling older people with complex health and care needs, such as those with frailty, multimorbidity and/or dementia. The focus was on those aged ≥ 65 years, although for certain groups (e.g. minority ethnic groups and homeless people) younger participants (aged ≥ 55 years) could be included if the issues were similar.
-
Older people with complex health needs living in their own homes, in sheltered housing or in extra care housing (where people are very likely to still have the decision-making capacity to participate in SDM).
-
Studies of any intervention or strategy designed to promote the ongoing engagement of older people with complex health needs, and/or their family carers, in decision-making relating to their health or social care needs [e.g. decision aids, physician or patient coaching, education or training, personalised care planning (PCP) or joint goal-setting]. The focus was on complex decision-making and personal goals rather than studies focused on single issues (such as whether or not to have a hip replacement).
-
Studies of interprofessional SDM in which at least two health-care professionals (HCPs) collaborated to achieve SDM with the patient and/or family carer either concurrently or sequentially. 144
-
Studies that provided evidence relating to the implementation and uptake of interventions designed to promote SDM for older people with complex health needs.
Types of studies
The purpose of the searches was not to identify an exhaustive set of studies but rather to be able to reach conceptual saturation in which sufficient evidence was identified to meet the aims of the review. 148 A diversity of evidence provides an opportunity for richer data mining and theory development. Therefore, we included studies of any design including randomised controlled trials (RCTs), controlled studies, uncontrolled studies, interrupted time series studies, cost-effectiveness studies, process evaluations, surveys and qualitative studies of participants’ views and experiences of interventions. We also included grey literature, policy documents and information about locally implemented programmes in the UK. As is usual with a realist review, the process of identifying relevant information and deciding what to include was iterative, involving tracking backwards and forwards between the literature and our review questions. 149 As such, the identification of relevant literature carried on throughout the course of the review and some studies initially thought to be relevant were later excluded.
Outcomes
A main aim of the NHS Five Year Forward View8 is to tackle the gap between care and quality. Quality is seen in terms of patient safety, clinical effectiveness and patient experience. This definition of quality was used to guide the outcomes for this review, with a particular focus on the patient experience. However, part of the review process involved an iterative identification of outcomes that are important to stakeholders, that address patient and family involvement in care planning and decision-making and that have been reported in the literature. Potential outcomes included the following:
-
patient experience – participation in decision-making, improved match between chosen option and patient preferences, impact on the decision-making experience, quality of life and perceived burden of treatment
-
patient safety – access to appropriate care, prevention of adverse events such as falls, avoidable emergency admissions and substantiated abuse and/or neglect
-
clinical effectiveness – health-related outcomes (e.g. prevention of exacerbations of LTCs) and service use [e.g. unnecessary hospital admissions, unnecessary general practitioner (GP) visits].
Identification of studies
We used a range of search techniques to identify relevant English-language publications:
-
electronic databases such as PubMed, Scopus and The Cochrane Library [including Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effects (DARE) and Health Technology Assessment (HTA) database]
-
checking of reference lists from primary studies and systematic reviews
-
citation searches using the ‘cited by’ option in Scopus and Google Scholar and the ‘related articles’ option in PubMed (‘lateral searching’).
The searches were designed to reflect the five theory areas identified in phase 1 (see Table 4). For example, preparing for the SDM encounter (‘if–then’ statement 2) included searches around coaching, education and training and SDM for hard-to-engage groups. The latter (SDM for hard-to-engage groups) was built in because clinical members of the team (supported by stakeholder interviews) highlighted the difficulty that many people may have in engaging in SDM (e.g. those with chronic conditions and depression). Searches were conducted in December 2016. Two searches, interprofessional and reducing the workload, had date limits applied to the searches because literature in the area is relatively recent. Date limits and search terms used in PubMed are provided in Table 5. For full details of the searches see Appendix 1.
| Theory area | Search terms |
|---|---|
| 1. Reflecting patient and carer values |
No date limits: ((“shared decision making”) OR (“decision aid”) OR (“decision making”)) AND (((“goal setting”) OR (“person centred care”) OR (“person centered care”) OR (“personalised”) OR (“patient goals”) OR (“patient values”) OR (“patient preferences”) OR (personalised[Title] OR personalized[Title] OR (patient centred) AND Title OR (patient centered) AND Title OR (patient preference*) AND Title OR goals[Title] OR (goal setting) AND Title OR personalised[Title])) AND (old*[Title] OR aged[Title] OR elder*[Title] OR geriatric[Title] OR frail[Title] OR complex[Title] OR complex[Title] OR carer[Title] OR dementia[Title] OR alzheimer*[Title])) |
| 2. Preparing for the SDM encounter |
Coaching/advocacy (no date limits): (((“coaching”) OR (“advocacy”) OR (“advocate”) OR (advocate[Title/Abstract] OR advocacy[Title/Abstract] OR coach*[Title/Abstract]) OR (“coach”)) AND ((“shared decision making”) OR ((shared decision making) AND Title/Abstract OR SDM[Title/Abstract] OR decision[Title/Abstract]))) AND ((“frail elderly”) OR (“older person”) OR (“dementia”) OR (“elderly”) OR (old*[Title] OR elderly[Title] OR frail[Title] OR dementia[Title] OR alzheimer*[Title] OR aged[Title])) Education/training (no date limits): ((“shared decision making”) AND (education[Title] OR educate[Title] OR training[Title] OR guidance[Title] OR support[Title] OR information[Title] OR guide[Title] OR train[Title])) AND (old[Title] OR older[Title] OR elder*[Title] OR frail[Title] OR complex[Title] OR carer[Title] OR geriatric[Title] OR aged[Title] OR dementia[Title] OR alzheimer[Title]) ((“shared decision making”) AND (education[Title] OR educate[Title] OR training[Title] OR guidance[Title] OR support[Title] OR information[Title] OR guide[Title] OR train[Title])) AND (“primary care”) SDM for hard-to-engage groups (e.g. those with depression) (filters: published in the last 5 years): ‘Shared decision making’ OR ‘decision aid’ (both MeSH) OR (coproduction[Title/Abstract] OR co-productive[Title/Abstract] OR partnership[Title/Abstract] OR co-production[Title/Abstract] OR co-production[Title/Abstract]) AND ‘depression’ OR ‘mental health’ OR ‘mental illness’ (MesH) AND systematic review Shared decision making’ OR ‘decision aid’ (both MeSH) OR (coproduction[Title/Abstract] OR co-productive[Title/Abstract] OR partnership[Title/Abstract] OR co-production[Title/Abstract] OR co-production[Title/Abstract]) AND ‘depression’ OR ‘mental health’ OR ‘mental illness’ (MesH) AND ((“frail elderly”) OR (“older person”) OR (“dementia”) OR (“elderly”) OR (old*[Title] OR elderly[Title] OR frail[Title] OR dementia[Title] OR alzheimer*[Title] OR aged[Title])) |
| 3. Sharing the communication of a decision |
Interprofessional (limited to last 10 years): (((“interprofessionalism”) OR (“interprofessional”) OR (“interdisciplinary”) OR (“multidisciplinary”) OR (“coordinated”) OR (“cross discipline”) OR (“inter disciplinary”) OR (“integrated”)) AND ((“shared decision making”) OR (“decision aid”) OR (“decision making”))) AND (old*[Title] OR aged[Title] OR elder*[Title] OR geriatric[Title] OR frail[Title] OR complex[Title] OR complex[Title] OR carer[Title] OR dementia[Title] OR alzheimer*[Title]) “relational coordination” OR “relational coproduction” AND (old*[Title] OR aged[Title] OR elder*[Title] OR geriatric[Title] OR frail[Title] OR complex[Title] OR complex[Title] OR carer[Title] OR dementia[Title] OR alzheimer*[Title]) No date limits Relational competence (no date limits): Relational competence AND (promote[Title/Abstract] OR promotion[Title/Abstract] OR train*[Title/Abstract] OR increase[Title/Abstract] OR intervention[Title/Abstract] OR programme[Title/Abstract]) AND general OR community OR primary |
| 4. Fake vs. real SDM |
Draws on searches run for other theory areas (no date limits): Incentive (ti/ab) OR incentives (ti/ab) OR incentivisation [TI/AB] OR incentivization [TI/AB] AND “shared decision making” (MeSH) |
| 5. Reducing the workload (for patients and carers) |
Limited to last 5 years: (((“minimally disruptive medicine”) OR (“caregiver burden”) OR (“carer burden”) OR (“patient burden”) OR (“treatment burden”) OR (“quality of life”) OR (appropriate[Title] OR inappropriate[Title])) AND (“shared decision making”)) AND (old[Title/Abstract] OR older[Title/Abstract] OR aged[Title/Abstract] OR elderly[Title/Abstract] OR frail[Title/Abstract] OR carer[Title/Abstract] OR complex[Title/Abstract] OR geriatric[Title/Abstract] OR dementia[Title/Abstract] OR Alzheimer[Title/Abstract]) |
Screening and data extraction
Electronic search results were downloaded into bibliographic software and, when identified, duplicates were deleted. Documents from other sources were manually recorded in the same file. Two reviewers independently screened titles and abstracts for relevance. Full manuscripts of all potentially relevant citations were obtained and downloaded into Mendeley reference management and PDF (Portable Document Format) organisation software (Elsevier, Amsterdam, The Netherlands); all members of the research team had shared access to these manuscripts. Two reviewers screened full manuscripts for inclusion based on the relevance and rigour of the evidence, with disagreements resolved by discussion with a third team member.
Decisions on inclusion made at different points in time were recorded in a Microsoft Excel® (Windows® 10) spreadsheet (Microsoft Corporation, Redmond, WA, USA). Consistent with a realist synthesis approach, items were assessed for inclusion on the basis of whether or not they were considered ‘good enough and relevant enough’. 150,151 This was an iterative process that involved discussion between team members. ‘Good enough’ was based on the quality of evidence, for example was it of a sufficient standard for the type of research and were the claims made considered to be trustworthy. ‘Relevance’ related to whether or not the authors provided sufficient descriptive detail and/or theoretical discussion to contribute to the theories generated in phase 1. Poorly executed studies (low rigour) could still be included if the study was considered to contribute to understanding about how a programme was thought to work (high relevance).
A bespoke data extraction form was developed, piloted on five records and further refined as necessary. Once the final fields for data extraction were agreed, an electronic version was created in Microsoft Access® (Microsoft Corporation, Redmond, WA, USA). The data extraction form included fields relating to study aims, design and methods; the types of participants (e.g. older people, people with LTCs, HSCPs); outcomes; information relevant to the theory areas; and emerging context–mechanism–outcome (CMO) configurations. Data were extracted by one reviewer, with 20% of the manuscripts checked by a second reviewer. PDFs in Mendeley were also annotated and relevant sections highlighted. Data in a realist sense are not just restricted to the study results or outcomes measured but also include author explanations and discussions, which can provide a rich source of ‘data’ that make explicit how an intervention was thought to work or not.
Synthesis
The Access database was used to identify prominent recurrent patterns of contexts and outcomes (demi-regularities) in the data and the possible means (mechanisms) by which they occurred. 152 This process enabled iteration from plausible explanations to the uncovering of potential CMO configurations. An example of the development of one of the original ‘if–then’ statements into a preliminary CMO is given in Table 6. In total, this CMO went through six iterations before the final programme theory was developed. Although all of the theories were developed and refined as the review progressed, some, such as that presented in Table 6, remained similar to the original theory developed in phase 1. In contrast, statement 5 (reducing the workload) was not taken forward as a CMO. This was largely because it was not supported by the emerging evidence but also because it was felt to be too conceptually different from SDM.
| Original ‘if–then’ statement 1 (reflecting patient and carer values) | ‘If–then’ statement revised to a CMO (first draft of CMO) |
|---|---|
| If HCPs place less emphasis on ‘fixing people’ and more on patients’ goals and their emotional, cultural and cognitive needs | If HCPs are able to develop relationships with patients that allow them to understand their emotional, cultural and cognitive needs, and identify (and regularly assess) patient and carer goals (e.g. through continuity, appropriate communication skills, ability to factor in impact of previous experiences, less focus on biomedical targets) (context) |
| Then patients and their family carers will feel valued and listened to; they will feel that they were involved in the decision and will be satisfied with the outcome | Patients and their carers will feel valued and listened to, interested and involved in the decision and have trust in professionals (mechanism) |
| Leading to satisfaction with the decision (outcome) |
Data synthesis involved individual reflection and team discussion and was designed to (1) question the integrity of each theory, (2) adjudicate between competing theories, (3) consider the same theory in different settings and (4) compare the stated theory with practice experiences. Data from the studies or other evidence were then used to confirm, refute or refine the candidate theories. When theories failed to explain the data, alternative theories were sought.
Once the preliminary mapping of the evidence into tables was complete, the research team held a second workshop. This was attended by six members of the Research Management Group and one public and patient involvement (PPI) representative. This workshop was structured to include in-depth discussion of the findings and to develop and confirm the resultant hypotheses. As at the first workshop, we transcribed recordings of group discussions and took notes. This provided evidence of the reasoning processes and justification of inferential shifts. 74 Following the workshop the CMOs were revised (by FB, BR and CG) and circulated to all members of the research team for comments.
Phase 3: testing and refining programme theory/ies (validation)
To enhance the reliability of the resultant hypotheses and develop a final review narrative we tested the hypotheses and supporting evidence with interviews with a further 11 stakeholders. An interview schedule was developed based on the four CMOs and aimed to elicit stakeholders’ views on their meaningfulness, from both practice and service user/carer perspectives (see Appendix 3). The transcripts were read by one author (BR) and discussed with a second (FB). The interview data were used to test the CMOs. The final CMOs and the supporting evidence are presented in the next chapter.
Patient and public involvement
A well-established PIRG at the University of Hertfordshire trains and provides support to public members and has a broad membership of service users and carers. Two members of this group (Paul Millac and Marion Cowe) commented on the proposal and one (Paul Millac) was a co-applicant on the application. The review was also supported by the Social Care Workforce Research Unit User and Carer Group. Two members of this group (Jeanne Carlin and Jane Hopkins) were part of the PAG. Paul Millac attended our first project team workshop and Jane Hopkins attended the second. Our PPI members were therefore involved in shaping and refining our programme theory. As part of the realist review process, we also recruited additional service user representatives for stakeholder interviews.
Chapter 3 Results
This chapter includes text from Bunn et al. 208 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Description of included evidence
In phase 2 we included 88 items. These comprised 26 evidence reviews,20,66–69,93,94,103–121 46 primary research studies (48 papers),63,84,144,153–195,209 seven guidelines, cases studies or reports25,31,196–200 and nine discussion/opinion papers. 17,83,201–207 Of the 46 primary research papers 25 were qualitative studies, five were RCTs and the rest included a variety of study designs. Of the evidence reviews, 20 were systematic reviews,20,66–69,93,94,103,104,106–110,112,114,116–118,121 five were literature reviews105,111,115,119,120 and one was a realist synthesis. 113 The study selection process can be seen in Figure 3. Thirty-three papers from phase 1 were excluded at phase 2 because they were not considered to be of high enough rigour or relevance.
FIGURE 3.
Flow chart summarising study identification. Reproduced with permission from Bunn et al. 208 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
The included literature focused specifically either on SDM or on aspects of care, such as PCC or PCP, in which SDM plays an essential, if not specified, part with the patient or their proxy. We categorised the included reviews and other items on the basis of the focus of the paper. The numbers in each category can be seen in Table 7. Thirty-one primary studies and nine systematic reviews included HSCPs.
| Category | Number of | |
|---|---|---|
| Primary studies/itemsa | Systematic reviews | |
| Professionals views on SDM | 10 | 2 |
| Interprofessional SDM | 13 | 1 |
| Use of patient decision aids/tools | 13 | 10 |
| Patient engagement in SDM | 17 | 7 |
| Influences on SDM | 33 | 4 |
| Education/training HCPs | 13 | 4 |
| Patient/carer views/preferences/goals | 30 | 9 |
In total, 25 primary studies and four systematic reviews focused on older people or those with complex health and care needs. Of those, 19 focused on older people or had a population with a mean or median age of > 65 years, 9 specified that people had multimorbidities and 11 specified that they had a LTC (Table 8). Of these studies the majority were qualitative, surveys or uncontrolled evaluations. In other studies populations were younger, were health or care professionals or the population was not specified.
| Study author and date | Type of research | Mean or median age (years) | Specific condition | Older peoplea | Multimorbidity | LTC |
|---|---|---|---|---|---|---|
| Duquemin 201125 | Case study | Age not given | Diabetes mellitus | ✓ | ||
| Glenpark Medical Practice 201631 | Case study | Not specified | ✓ | ✓ | ||
| Health Foundation 2014198 | Case study | Not specified | Living in a care home | ✓ | ||
| Holmside Medical Group 2014200 | Case study | Not specified | ✓ | |||
| van Summeren et al. 2016192 | Mixed-methods pilot study | Mean age 83 | ✓ | ✓ | ||
| Fried et al. 2007169 | Observational | Mean 73 (SD 7) | ✓ | ✓ | ||
| Naik et al. 201663 | Observational | Mean age 65 | Cancer | ✓ | ||
| Bynum et al. 2014159 | Qualitative | Mean age 84 (range 80–93) | Relates to a variety of decisions (e.g. surgery, medication, diagnostic procedures) | ✓ | ||
| Groen-van de Ven et al. 2016172 | Qualitative | Mean age 80 (range 62–89) | Dementia | ✓ | ||
| Hart et al. 2016174 | Qualitative | Median age COPD 65.5, lung cancer screening 67 (range 48–83) | COPD and lung cancer screening | ✓ | ||
| Kuluski et al. 2013179 | Qualitative | Mean age 82.3 | ✓ | ✓ | ✓ | |
| Ladin et al. 2016180 | Qualitative | Mean age 76 | Receiving dialysis | ✓ | ||
| Mercer et al. 2016181 | Qualitative | Mean age 57 (range 42–67) | Economically deprived area | ✓ | ||
| Robben et al. 2012183 | Qualitative | Mean age 78.8 (range 65–90) | Frail older people | ✓ | ||
| Ruggiano et al. 2016184 | Qualitative | Mean age 76.9 (range 60–90) | ✓ | ✓ | ||
| Shay and Lafata 2014188 | Qualitative | Mean age 63 (SD 10.4) | ||||
| Sheaff et al. 2017189 | Qualitative | Mean age 78 | ✓ | ✓ | ✓ | |
| Wrede-Sach et al. 2013193 | Qualitative | 18 aged 70–80, 16 aged ≥ 80 | Living independently | ✓ | ||
| Blom et al. 2016155 | RCT | Median age 80 (range 77–83) | 3 + morbidities | ✓ | ✓ | ✓ |
| Hacking et al. 2013173 | RCT | Mean age: control 67.4, intervention 65.2 | Men with prostate cancer | |||
| Elliott et al. 2016113 | Realist review | Not specified | Older people (engagement in decision-making) | ✓ | ||
| Dardas et al. 2016165 | Survey | Median age 70 (range 65–92) | Orthopaedic clinic | ✓ | ||
| Cramm 2016162 | Survey | Mean age 69.9 (range 30–93) | COPD | ✓ | ✓ | |
| Gleason et al. 2016170 | Survey | Mean age 76 (SD 8) | ✓ | ✓ | ||
| Cramm 2014164 | Survey and qualitative | Mean 65.9 (range 20–93) | ✓ | ✓ | ||
| Austin et al. 2015103 | Systematic review | Not specified | Adults living with advanced or life-limiting diseases (including 2 on older people and 4 on dementia) | ✓ | ||
| Bratzke et al. 2015105 | Systematic review | Not specified | ✓ | |||
| Coulter et al. 201566 | Systematic review | Not specified | ✓ | |||
| van Weert et al. 2016121 | Systematic review | Not specified | ✓ |
Sixteen reviews were evaluating an intervention, such as decision aids or tools, coaching and interventions to increase or promote the adoption of SDM among HCPs. Nineteen of the other items described or evaluated an intervention. Interventions included care planning, training and education for professionals, the use of decision aids or integrated/collaborative care practices that involved SDM. More details of the reviews can be seen in Table 9 and of the other items (e.g. primary studies) in Table 10.
| Study author and year | Focus | Design/method | Description of intervention | Sample size | Type of participants |
|---|---|---|---|---|---|
| Austin et al. 2015103 | Decision tools | Systematic review | Decision aids | 17 RCTs | Adults with advanced or life-limiting diseases |
| Bélanger et al. 2011104 | Process of SDM in palliative care | Mixed-methods systematic review | NA | 37 studies (both quantitative and qualitative) | Palliative patients and their families |
| Bratzke et al. 2015105 | Process of priority-setting and decision-making | Narrative literature review | NA (but focused on studies of self-management) | 13 (mostly qualitative) | Adults with multimorbidity |
| Clayman et al. 2016106 | Patient participation in decision-making | Systematic review | Interventions to promote patient participation in decision-making | 116 studies | HCPs and a range of different patient groups and ages |
| Couët et al. 2015107 | Extent to which HCPs involve patients in decision-making | Systematic review | Use of the OPTION tool to facilitate SDM | 33 studies | HCPs and a range of different patient groups, ages and clinical contexts |
| Coulter et al. 201566 | PCP for adults with LTCs | Systematic review of RCTs | Involvement of patients in treatment and management decisions | 19 studies (10,856 participants) | Adults with LTCs |
| Coylewright et al. 2014108 | Decision aids | Patient-level MA of decision aid | Each RCT compared the use of a decision aid with UC | 7 RCTs | Adults: diabetes mellitus, chest pain, osteoporosis or MI |
| Doyle et al. 2013109 | Links between patient experience and clinical safety/effectiveness | Systematic review | NA | 55 studies (mixed) | Various |
| Durand et al. 201469 | SDM interventions for disadvantaged groups | Systematic review and MA | Interventions designed to engage disadvantaged patients in SDM | 19 studies | Socially disadvantaged groups |
| Dwamena et al. 2012110 | Promoting patient-centred approaches | Systematic review with MA | Interventions that promote patient-centred care in clinical consultations | 43 RCTs | HCPs including those in training. Patients, predominantly adults, with general medical problems |
| Dy and Purnell 2012111 | Quality of SDM | Literature review | NA | NA | Unclear |
| Edwards et al. 2009112 | Information exchange and SDM in health-care consultations | Systematic review (qualitative) | NA | 7 papers | HCPs and a variety of patient groups |
| Elliott et al. 2016113 | Engagement in health-care decision-making | Realist synthesis | Interventions to engage older adults in health-care decision-making | 213 papers | Older people and their caregivers |
| Elwyn et al. 2013114 | Patient-targeted decision support interventions | Systematic review with narrative synthesis | Brief tools for face-to-face encounters and more extensive tools such as booklets, videos or websites | 17 studies | HCPs in primary and secondary care |
| Fagerlin et al. 2013115 | The role of VCMs in decision aids | Evidence review and summary | Value clarification in decision aids | 61 studies (quantitative and qualitative) | Variety of patient groups |
| Joseph-Williams et al. 2014116 | Patient-reported barriers/facilitators of SDM | Systematic review with thematic synthesis | NA | 44 studies | Variety of patient groups |
| Land et al. 2017117 | Decision-making communication practices relevant to health-care outcomes | Systematic review of conversation analysis | NA | 28 papers | People consulting a HCP (face-to-face interactions) |
| Légaré et al. 200893 | HCP-perceived barriers and facilitators with regards to implementing SDM | Systematic review with content analysis | NA | 38 papers | The vast majority of participants (n = 3231) were physicians (89%) |
| Légaré et al. 201294 | Patients’ perceptions of the interventions designed to increase HCPs’ use of SDM | Systematic review of quantitative studies | Included educational material, educational meetings, audit and feedback, reminders and decision aids | 21 studies | HCPs |
| Légaré et al. 2014118 | Interventions to improve HCPs adoption of SDM | Systematic review and MA | Interventions to improve HCPs’ adoption of SDM | 38 RCTs, 1 non-randomised study | HCPs and patients. Most common conditions were cancer and CVD |
| Miller et al. 2014119 | Explore involvement of persons with dementia and their family carers in SDM | Literature review | NA – studies decision-making processes | 33 papers were included in the review | No specific details given |
| Shay and Lafata 201568 | SDM and patient outcomes | Systematic review | Studies that evaluated relationship between SDM and health outcome/s | 39 studies | Patient groups not specified |
| Sinnott et al. 201367 | GPs’ experiences of clinical management of multimorbidity | Systematic review of qualitative studies | NA | 10 studies (275 GPs) | GPs |
| Stacey et al. 2013120 | Coaching/guidance in the context of patient decision aids | Narrative review (not described as a systematic review) | Coaching and guidance for SDM | NA | NA |
| Stacey et al. 201420 | Decision aids for people facing treatment or screening decisions | Systematic review and MA | Decision aids | 115 studies | All patient groups |
| van Weert et al. 2016121 | Decision aids for treatment, screening or care decisions | Systematic review of RCTs and CCTs | Decision aids vs. usual care | Included 22 papers | Older people or their primary informal carers |
| Study author and year | Type of research | Description of intervention | Participants | Setting | Main focus |
|---|---|---|---|---|---|
| Agoritsas et al. 201583 | Discussion | Not appropriate | General population | Applies to all health-care settings | PDAs |
| Barrett et al. 2016203 | Discussion | Not appropriate | HCPs | Community | Communicating risk (regarding statins) |
| Belkora et al. 2008153 | Before/after | Pre-consultation coaching | People with cancer | Community | Identifying patient goals |
| Berger 2015202 | Discussion | Not appropriate | HCPs | Not appropriate | SDM and uncertainty |
| Berntsen et al. 2015154 | Review/content analysis | Not appropriate | General population | Variety | Patient goals |
| Blom et al. 2016155 | RCT | Proactive care planning | Older people | Primary care | Other |
| Bookey-Bassett et al. 2017156 | Concept analysis | Not appropriate | Older people | Community | Interprofessional SDM |
| Bridges et al. 2015157 | Qualitative | Not appropriate | HCPs | Secondary care – clinics | Influences on SDM, other |
| Bugge et al. 2006158 | Qualitative | Not appropriate | General population, HCPs | Community including outpatients | Barriers to SDM |
| Bynum et al. 2014159 | Qualitative | Not appropriate | Older people | Community | Patient/carer views or preferences |
| Chong et al. 2013160 | Qualitative | Not appropriate | HCPs | Primary and secondary care | Interprofessional SDM |
| Chong et al. 2013161 | Qualitative | Not appropriate | HSCPs (multidisciplinary) | Primary and secondary care | Interprofessional SDM |
| Clayman et al. 2016205 | Discussion | Not appropriate | Not appropriate | Not appropriate | Patient perspective of SDM |
| Col et al. 2011201 | Discussion | Not appropriate | HCPs | Primary care | Interprofessional SDM |
| Cooper et al. 2016206 | Discussion | Not appropriate | HCPs | Acute care | Goal concordance |
| Cramm 2012163 | Before/after | Chronic care model | HSCPs | Primary care | Service delivery for people with LTCs |
| Cramm 2014164 | Mixed methods | Chronic care model | Older people | Primary care | Service delivery for people with LTCs |
| Cramm 2016162 | Survey | Chronic care model | People with COPD (mostly older) | Community | Service delivery for people with LTCs |
| Dardas et al. 2016165 | Survey | Not appropriate | HCPs | Secondary care – orthopaedic clinic | Influences on SDM, patient/carer views or preferences |
| Diabetes UK et al. 201125 | Case studies | ‘Year of Care’ model | HCPs, people with diabetes mellitus | Primary care | PCC in LTCs |
| Durand et al. 2015166 | Documentary analysis | Not appropriate | Not applicable | Various | PDAs, incentives for SDM |
| Eaton et al. 2015204 | Discussion | Not appropriate | Not applicable | Community | PCC in LTCs |
| Edwards et al. 2004 | RCT | Training for GPs in SDM | GPs | Community, primary care | Education/training HCPs |
| Elwyn et al. 2004167 | RCT | Training for GPs in SDM | General population, HCPs (GPs) | Community | Education/training HCPs |
| Elwyn et al. 201217 | Discussion | Not appropriate | General population, HCPs | Any clinical consultation | Other, relationships |
| Farrelly et al. 2016168 | Qualitative | Joint care planning | People with mental health problems, HSCPs | Community | Care planning |
| Foot et al. 2014196 | Review for guideline | Not appropriate | Not applicable | Not appropriate | Influences on SDM, patient/carer views or preferences |
| Fried et al. 2007169 | Observational | Not appropriate | Older people with COPD, cancer or heart failure | Community | Influences on SDM |
| Gleason et al. 2016170 | Survey | Not appropriate | Older people with multimorbidities | Community | PDAs |
| Glenpark Medical Practice 201631 | Care study | The ‘Year of Care’ initiative | HCPs, people with LTCs | Inner city | PCC for people with LTCs |
| Gorin et al. 2017207 | Discussion | Not appropriate | Not applicable | Not appropriate | Clinical nudges |
| Grim et al. 2016171 | Qualitative | Not appropriate | People with mental health problems | Community | Influences on SDM |
| Groen-van de Ven et al. 2016172 | Qualitative | Not appropriate | People with dementia, informal and paid carers | Community | SDM for people with dementia |
| Hacking et al. 2013173 | RCT | Pre-consultation coaching | Men with prostate cancer | Community | Coaching |
| Hart et al. 2016174 | Qualitative | Not appropriate | Older people | Outpatient clinics | Use of PDA/tools |
| Health Foundation 2017198(also Baqir et al. 2016)191 | Case study | Multidisciplinary SDM | HSCPs, residents and family members | Care home | Interprofessional SDM |
| Herlitz et al. 2016175 | Qualitative | Not appropriate | Adolescents with diabetes mellitus | Diabetes melliuts clinic | Influences on SDM |
| Holmside Medical Group 2014200 | Case study | Holistic care for people with LTCs | HCPs | Primary care | Service organisation |
| Jones et al. 2011176 | Questionnaires | Tool for presenting risk | HCPs, people at risk of CVD | Clinics | Influences on SDM |
| Joseph-Williams et al. 2017177 | Qualitative | SDM training | HCPs | Primary care | Training for HCPs, implementation of SDM |
| Körner et al. 2013178 | Qualitative | Not appropriate | HCPs (multidisciplinary) | Primary and secondary care | Interprofessional SDM |
| Kuluski et al. 2013179 | Qualitative | Not appropriate | Older people (two or more LTC) | Urban community in ON, Canada | Identifying patient goals |
| Ladin et al. 2016180 | Qualitative | Not appropriate | Older people | Dialysis clinics | Interprofessional SDM |
| Légaré et al. 2011a144 | Qualitative | Not appropriate | HCPs (multidisciplinary) | Community | Influences on SDM, relationships |
| Légaré et al. 2011b209 | Qualitative | Not appropriate | General population | Community | Interprofessional SDM |
| Lown et al. 2011199 | Development of a model | Not appropriate | HCPs | Community or acute settings | Training for HCPs |
| Mercer 2016181 | Qualitative | Tool for providing PCC | Adults aged > 30 years with multimorbidity | Community | PCC |
| Naik et al. 201663 | Observational | Not appropriate | Cancer survivors with multimorbidities | Unsure | Patient/carer views or preferences |
| National Collaborating Centre for Primary Care 2009197 | Guideline | Not appropriate | Not applicable | Not appropriate | Medicines adherence |
| Politi and Street 2011182 | Development of a model | Not appropriate | Not applicable | Not appropriate | Collaborative decision-making |
| Robben et al. 2012183 | Qualitative | Not appropriate | Frail older people | Community | PDA |
| Ruggiano et al. 2016184 | Qualitative | Not appropriate | Older people | Community | HCPs views on SDM |
| Sanders et al. 2016185 | RCT | Training in SDM | GPs | Primary care | Training in SDM |
| Schaller et al. 2015186 and Schaller et al. 2016187 | Before/after | eHealth portal | Family caregivers | Memory clinic in secondary care | Patient/carer views or preferences |
| Schuling et al. 2012190 | Qualitative | Not appropriate | HCPs | Primary care | Patient engagement |
| Shay and Lafata 2014188 | Qualitative | Not appropriate | General population | Community | Identifying patient goals |
| Sheaff et al. 2017189 | Qualitative | Not appropriate | People aged ≥ 65 years, with at least two LTCs | Primary care | Patient electronic records and PCC |
| Tietbohl et al. 2015194 | Qualitative | Decision support intervention | HCPs | Community | PDA |
| van Summeren et al. 2016192 | Questionnaire | Outcome prioritisation tool | Frailty, multimorbidity | Primary care | Patient/carer views or preferences |
| Wrede-Sach et al. 2013193 | Qualitative | Not appropriate | Older people | Community | Older people’s experiences of SDM |
| Zoffmann et al. 2008195 | Qualitative | Not appropriate | PPl with diabetes mellitus and nurses | Community and acute | Interprofessional SDM |
Context–mechanism–outcome configurations
The theory development, refinement and testing process (see Chapter 2) led to the development of four CMO configurations, which are presented in Table 11. Together, these explanations or hypotheses constitute a programme theory about ‘what works’ (or ‘what might work’) to facilitate SDM for older people with multiple health and care needs or conditions, and how they might be applied within models of integrated working. These CMO configurations were developed and tested in stakeholder interviews and the SDM literature. In the following text, each CMO is discussed in more detail with supporting evidence from the literature. Supporting evidence from the stakeholder interviews can be seen in Table 12. More detail about the evidence supporting the CMOs can be seen in Report Supplementary Materials 1–4.
| Programme theory | Supporting evidence |
|---|---|
| CMO 1: systems that enable HSCPs to develop relationships with patients and carers, and with each other, and that allow them to understand and assess individual needs and patient and carer capacity to access and use care, will activate trust and engagement leading to better outcomes for patients and carers |
17,63,66–68,84,104,105,107,110,113,117–119,144,155–157,160,162–165,168,171,172,174,175,177–179,181–185,188,189,192,196–200,203 See Report Supplementary Material 1 |
| CMO 2: systems that are organised to support and prioritise SDM will lead to HSCPs feeling supported (and equipped) to engage in SDM, resulting in SDM becoming part of the culture of care |
17,25,31,66,67,107,110,157,162–165,167,168,177,182,183,185,189,200,202,203 See Report Supplementary Material 2 |
| CMO 3: people with complex health and care needs, and their family carers, are likely to need support, such as appropriate decision tools, and space and time to ask questions and discuss options, in order for them to be willing and able to participate in SDM |
25,31,69,103,108,112,115–117,120,121,153,158,159,165–167,170,171,173,175–177,180,186,187,192,196,197,200,204,207 See Report Supplementary Material 3 |
| CMO 4: a wider cultural change that includes SDM [e.g. family-centred approaches, changes in power dynamics and patients and carers taking (or sharing) responsibility for their health and the decisions that affect them], triggers the development of a shared expectation of (and familiarity with) SDM among patients, carers and HSCPs leading to improved patient outcomes |
25,31,103,104,107,114,116,118,120,164,168,177,200,202 See Report Supplementary Material 4 |
| Programme theory/supporting evidence | |
|---|---|
| CMO 1: reflecting patient and carer values | |
| Patient capacity to access and use care | It [refers to SDM] makes it easier to avoid situations where people either don’t understand what the medication that they’re being prescribed is for, when to take it, how to adjust it with other medication that they may be on, and so on. It can lead to . . . to a plan which is grounded in shared expectation.SH06 |
| Interprofessional approaches to PCC | So whether someone is seeing one clinician all of the time and over time making a number of decisions, or if they’re being seen in five different clinics over the course of whatever, the fact that that ethos of person-centeredness is embedded across that, you know, and their information shared and they build on it . . .SH15 |
| Patient feels involved and engaged | . . . when you’re offered an opportunity to discuss your own care you feel as proud as anything . . .SH02a |
| Patient-centred approaches | . . . he then saw where we were going with his treatment . . . he was an active participant whereas before he’d been very much, ‘No, I don’t want to do this, I don’t want to do that.SH10 |
| Goal-setting | I think the Year of Care Programme is another example of that, which was started in diabetes which focused on, you know, care and support planning, that’s how they framed it but essentially is about people making decisions together about what matters to them, setting their goals and then making decisions about what treatments and other things will support that.SH15 |
| Adherence | From the clinicians’ point of view, the benefits [refers to SDM] are that there’s an increased likelihood of adherence to clinical plans and to prescribed medicines. It leads to better use of resources . . .SH06 |
| Feeling valued | The consultant even phoned me at home and said, ‘This is what’s happening, this is what we need to do,’ so I was fully involved when my mum, you know, lost capacity for those few days, and I felt very valued . . .SH07a |
| Continuity: individual and system based | . . . when you’re talking about allowing them to develop the relationship, are we thinking about continuity over time or are we thinking that actually we’ve just got a system that supports person-centred care and that values that as part of any consultation.SH15 |
| CMO 2: systems to support SDM | |
| Risk | . . . on Monday that I had, a patient who has quite significant dementia who’s in her 90s, and there’s a lot of sort of indecisions about where, whether she should be at home, whether she should be in a care home or supported accommodation. There are clearly, you know, now some risk issues by her remaining at home on her own, but, you know, after a lot of sort of decision and discussion, I guess, you know, the decision was that it’s best, that’s where she was best to be even though we were all expecting some degree of risk . . .SH03. . . she said, ‘No, I don’t want to take any tablets, thank you very much. I know the risk.’ That’s fine . . .SH10 |
| System-based approaches | . . . we work with clinical colleagues here who do that [send results to patients before a consultation] in diabetes a lot and that works well and it just seems to make sense doesn’t it? You don’t go along to your bank manager and have a discussion about your bank account without knowing what your balance is . . .SH20. . . crucially, the patient is able to see the outcomes of all of those tests in advance of their care planning discussion, which means that they’re able to think about what that means for them, and a good care planning template will have on the front some free text boxes which ask questions like, ‘What’s most important to you to discuss in the care planning conversation?’ ‘Have there been any changes since we last spoke that you’d like to raise?’ ‘Do you have any questions?’ and so on, which means that the conversation, alongside taking into account the person’s clinical needs, also gives an invitation, I suppose, to the person, to feed in the other aspects of their life . . .SH06 |
| CMO 3: preparing for the SDM encounter | |
| Family involvement | So if you’re doing a care planning meeting with an older adult with multiple conditions that you give them a chance to have a think about it, often with their family member as well.SH10 |
| Choice | So it’s not about what people want, it’s about where there are options, understanding, so the patient and carers need to understand what the options are, you know, what the risks, the benefits, the consequences of the different options are and they need to understand what’s important to them in deciding between them.SH20 |
| Asking questions | . . . the provision of really high-quality information for people, we know that that makes a really significant contribution for people, increasing their confidence, potentially increasing their levels of literacy, in terms of their understanding of their condition and how it impacts on their life, but also being more confident to ask the questions that they need to from their clinicians, and to offering their own perspective . . .SH06. . . there was a video for patients and there was the ‘ask three questions’, materials that were used throughout . . . showing the video on, you know, in the waiting room in the GP’s surgery or whatever, that actually that had little or no impact on increasing the likelihood of patients asking those questions of their health care professional, but where it did have an impact is that it meant that the clinicians were much more likely to prompt patients around those questions.SH15 |
| Medical authority | . . . my parents, because they were both in their 90s when they died, they would assume somebody with, anyone medical had authority.SH17 |
| CMO 4: SDM as part of a wider cultural change | |
| Power differentials | . . . the power differentials are one of the bigger barriers to shared decision making and so it is about recognising, it’s a fairly simple thing to say, but recognising there are two experts, that the clinician who understands the options and the risks, the benefits, the consequences and so forth and the patient who understands what’s important to them.SH20 |
| Change | . . . how we have always framed, you know, our shared decision making and our self-management work is that this was part of essentially a transformational change . . .SH15 |
| Wider change | . . . there is no intervention that creates culture change, whatever it is, but it’s absolutely right that it has to happen and that happens because all sorts of different things get aligned if you like but that takes time and it has all the issues that you’ve already talked about around systems, skills, attitudes, education, training, patient roles, all of those things need to be aligned . . .SH20 |
| Changing attitudes | Yeah, so I think some of it will be attitude changes, I think some of it will be cultural. I think some of it will come, so we are seeing shifts within new care models to, you know.SH06 |
| Culture | . . . really good quality, shared decision-making, comes largely from the culture, and through communication and between clinical teams and people . . .SH06 |
| Patient responsibility | . . . changing attitudes and experiences of patients can be at times as much a barrier to shared decision-making as the attitudes of the clinicians.SH20 |
| Attitudes | . . . there are some really important attitudinal underpinnings that need to be addressed before you can even do the skills training . . .SH20 |
Context–mechanism–outcome 1: reflecting patient and carer values
Programme theory: systems that enable HSCPs to develop relationships with patients and carers, and with each other, and that allow them to understand and assess individual needs and patient and carer capacity to access and use care, will activate trust and engagement, leading to better outcomes for patients and carers.
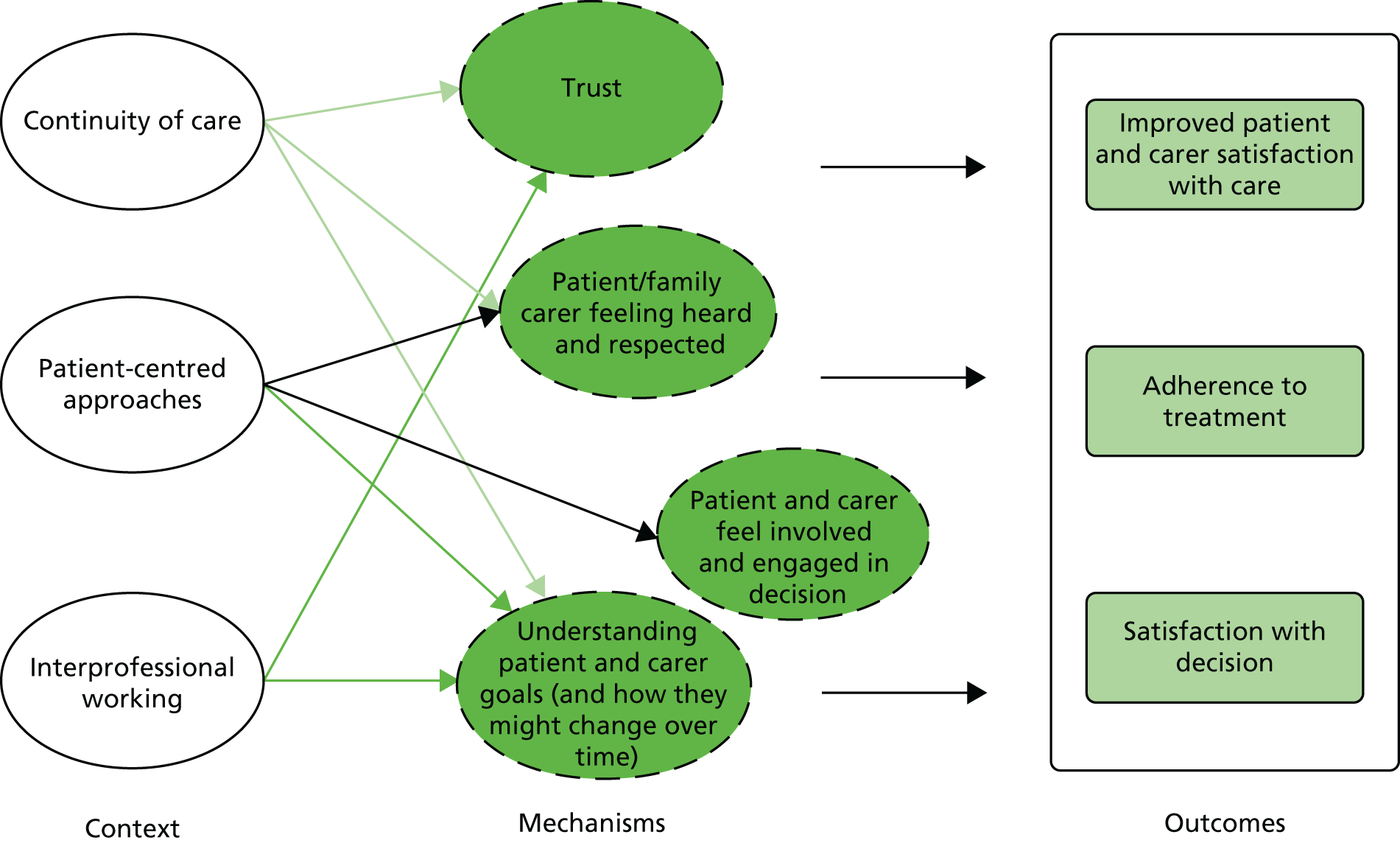
The components of this CMO can be seen in Figure 4. The figure illustrates the interaction between the contexts and mechanisms and the potential outcomes.
FIGURE 4.
Summary of CMO 1: reflecting patient and carer values.
Understanding the needs and priorities of service users
Many studies recognise the importance of considering patients’ and, when appropriate, family carers’ preferences and values in the decision-making process,63,105,113,119,203 not least because ‘decision-making is grounded in the personal and social context of an individual’s life’. 105 Despite this, the evidence shows that individual needs and circumstances of patients and their family carers are frequently not understood or taken into account. 107,157,179 In a systematic review observing the extent to which HCPs involve patients in decision-making across a range of clinical contexts, the least observed behaviours were those that involved enquiring about the patients’ preferences. 107 This implies that interventions aimed at improving the tailoring of care to patient preferences are needed. This is supported by the Making Good Decisions In Collaboration (MAGIC) study,177 a 3-year project to test and identify the best ways to embed SDM into routine primary and secondary care using quality improvement methods. In their training sessions, the researchers found that ‘the teams were generally already good at recognising options and discussing them with patients, but there was potential to improve their communication of risk and the task of exploring what matters to patients’177 (risk is discussed further in CMO 2). An observational study of people with cancer and multimorbidities suggests that it is more important for HCPs to consider values that are stable over time rather than goals and preferences that are more context or circumstance specific. 63 This of course assumes an ongoing and sustained relationship between service user/patient and provider.
Information-sharing difficulties and goal divergence may arise for any number of reasons. These include HSCPs having difficulty identifying and explaining patient preferences,68,104 differences in the way patients and clinicians interpret and frame the patient’s health problems,189 clinicians being reluctant to engage in SDM when the patient’s preferences are not in line with clinical guidelines185 or when there are concerns about safety or cognitive function. 179
There are also system-level barriers. A qualitative study in primary care in the UK investigated gaps between lay and medical discourse in care planning. 189 It suggests that electronic records ‘can marginalise aspects of care which lie beyond a biomedical focus or contractual requirements’. 189 Patients’ narratives could be misunderstood or reframed when they were formally recorded. A focus on a biomedical agenda was also identified in a qualitative study exploring the extent of PCC and SDM with adolescents with type 1 diabetes mellitus. 175 It found that when patients tried to raise themes or concerns of their own, they were often interrupted by professionals who were trying to restore a biomedical agenda. 175 The authors argue that health professionals concentrated on educating patients about biomedically optimal self-care rather than considering the patient’s preferences and how these might affect adherence.
Several studies explored interventions aimed at helping to identify patient and carer preferences. A qualitative study from the UK reported on the development of a primary care-based complex intervention for patients with multimorbidity. 181 The intervention involved establishing and maintaining therapeutic relationships with patients and a person-centred approach. Patients appreciated the time, being able to ask questions, being listened to and having their goals acknowledged. The intervention is due to be tested in a cluster RCT. A RCT conducted in the Netherlands155 evaluated the impact of proactive care planning and goal-orientated integrated care. Although GPs reported some improvements (e.g. a perception that there were fewer unexpected demands on care) there was no significant change in patient quality of life or functional status and only a small improvement in satisfaction levels. A pilot study tested the feasibility of a conversation tool for outcome prioritisation in medication reviews with older people. 192 The tool increased satisfaction with medication use and the authors contend that knowing the individual’s preferences appears to deepen the patient–doctor relationship. However, the mean consultation duration was 31 minutes, which, the authors caution, does not fit with routine medication reviews in family practice.
Developing relationships
Achieving SDM depends on building a good relationship in the clinical encounter. 17,113,182,194 The ability to build and maintain trusting relationships between HSCPs and patients/carers was seen as beneficial in the implementation of collaborative approaches by staff157 and patients/service users165,171,178,181,183,188 and was found to have an impact on patient and carer perceptions of the quality of care. 109,162,164 A systematic review109 found evidence of a positive association between the quality of clinician–patient communications and adherence to medical treatments. For example, the odds of patient adherence were higher when physicians had received communication training. 109 Longer consultations and physician verbal behaviour (such as exploring the impact of the condition or illness on the patient) have been shown to be associated with increased trust. 210
Trust is also facilitated by continuity of care. 68,113,174 However, a long-standing relationship with a clinician may lead a patient to assume that the clinician is aware of his or her values,159 whereas evidence suggests that there is often a mismatch between patients’ and clinicians’ views. For example, a qualitative study179 investigated alignment of goals between people with multimorbidity, their family carers and HCPs, and found that, although there were some common goals (such as maintaining independence), there was also a significant amount of goal divergence. This was particularly the case when patients had significant illness complexity, such as unstable/fluctuating health problems or cognitive decline, which posed immediate or anticipated threats to the safety of the patient or carer/caregiver. 179
The importance of ongoing relationships and the ability to reassess changing priorities were highlighted in several studies. They were particularly important for people with complex needs or dementia as ‘the dominant chronic illness shifts over time as conditions and treatments change, and re-prioritisation occurs’;105 decision-making responsibility may shift over time, from the person with dementia to the informal or family carer/caregiver. 172 A review to develop a communication model to enable greater understanding of patient-centred communication and decision-making says that communication about complex medical issues often occurs as ‘a series of conversations over time, with multiple clinicians involved.’182 In one review the authors suggested that a failure to identify an association between empirical measures of SDM and health outcomes is because most studies focus on a one-off encounter. 68 They added:
. . . one discussion between a clinician and patient may not lead to improved health outcomes. Instead, a long-standing relationship between a clinician and patient marked by patient-centred care and SDM may affect outcomes over time.
Shay et al. 68
Interprofessional working
Trust and partnership working between different HCPs were described as key to decision-making for older adults with complex needs. 156,161,172,178 Facilitators of relational coproduction and interprofessional working (see Table 1 for definitions) include familiarity with one another and a history of working together, mutual knowledge and understanding of disciplinary roles, trust and respect, a shared understanding of SDM and effective communication between individuals (including different HCPs and patients and carers). 84,162,199 However, few studies addressed an interprofessional approach to SDM, with most studies targeting a single professional group. 144 A systematic review118 of interventions to improve HCPs’ adoption of SDM found that only three studies targeted more than one HCP.
Légaré et al. 84,93,144 have published several qualitative or descriptive studies exploring interprofessionalism and SDM. They created a model to help health professionals envisage a common goal and enhance the contribution of different health professionals to SDM. 84,144 The model ‘factors in’ determinants at the individual or micro level such as patient priorities, and at the meso and macro health-care system levels. Meso-level considerations include the influence of individual team members’ professional roles and macro-level factors encompass health policies and social context. A decision coach who is trained to support the patient’s involvement in decision-making is seen as key to the process. They argued that by assigning particular tasks to specific members of the team the process can become more efficient. A UK initiative ‘The Year of Care’ also involved team members working together to facilitate decision-making. 25 The initiative (which was piloted in over 50 practices in England) first focused on people with diabetes mellitus. Care planning involved an initial consultation with a health-care assistant (HCA) to work out what the patient wanted to do and undertake weights and measurements; there was then a second consultation with a GP or specialist nurse to make a care plan. They reported improved patient experience and biomedical outcomes, although they suggested that it may take 3–5 years for improvements to biomedical outcomes to become apparent. 25
Several reports describe UK initiatives to promote interprofessional working and integrated care. For example, a case study of structured medication reviews in care homes, involving residents, family members, care home staff and HCPs provided qualitative evidence of the benefits of an interprofessional approach to decision-making:198
It used to be just the doctor and the pharmacist talking to each other. But actually having everybody round the table, it’s just wonderful. It’s a game changer in terms of the decisions you make.
Pharmacist
However, it was not always easy for GPs to attend these meetings. Evaluation of holistic primary care for people with multimorbidities reported an increase in patient satisfaction and engagement and fewer unplanned attendances at the practice (although how this was measured is not clear). The initiative involved cross-discipline training and the involvement of all clinical staff and the patient and their family in producing, monitoring and updating a care plan to focus on quality of life for the patient. 200
Patient/service user outcomes
In CMO 1 we suggested that resources such as a person-centred approach, continuity, good relationships between service users and providers and interprofessional collaboration in SDM lead to benefits such as improved adherence and greater patient satisfaction. A systematic review110 including 43 RCTs found that interventions to promote a patient-centred approach in clinical consultations generally had a positive effect on a range of measures, although the impact on satisfaction, behaviour and health status was mixed. Another review focused on PCP. 66 It reported improvements in some indicators of physical and psychological health status, and people’s capacity to self-manage their condition when in comparison with usual care. The impact was greater when the intervention was more comprehensive, intensive and better integrated into routine care. 66
Systematic reviews of SDM have identified positive benefits to patients and carers such as feeling more involved,117,119 an improved quality of life and reduced depression in carers,119 and improved affective cognitive outcomes for patients, such as enhanced satisfaction and reduced decisional conflict. 68 These impacts (particularly on patient/service user satisfaction) are echoed in many of the other studies we accessed. 109 There is also some evidence that SDM leads to better treatment adherence. 197 There is little evidence, however, to suggest that there is an association between empirical measures of SDM and health outcomes. 68
Context–mechanism–outcome 1: summary
The evidence shows how systems that enable HCPs to develop relationships with patients/service users and their family carers trigger feelings of trust, engagement and respect that can lead to improved outcomes such as patient and carer satisfaction with services and decisions. The quality of individual clinicians’ communication skills, and their ability to foster trusting relationships with older people and their families, is fundamental to SDM. In addition, there is also a need for systems that promote continuity of care both through ongoing relationships with one clinician (relationship continuity) and through system-based approaches that develops ways of working whereby the patient is linked to multiple professionals (management and informational continuity). SDM with older people with complex needs is likely to increase appointment length. Although it is thought to improve adherence to treatment regimens, there is currently little evidence to suggest a link to health outcomes or service use.
Context–mechanism–outcome 2: systems to support shared decision-making
Programme theory: systems that are organised to encourage and prioritise SDM will lead to HSCPs feeling supported (and equipped) to engage in SDM, resulting in SDM becoming part of the culture of care.
The premise of this CMO is that SDM may be conducted in a context in which it is not seen as a priority. Therefore, for older people with complex conditions SDM is hindered by the risk and uncertainty associated with complex conditions, and systems and structures that block communication between patients and the different professional groups involved in their care. The programme theory is explained in Figure 5.
FIGURE 5.
Summary of CMO 2: systems to support SDM.
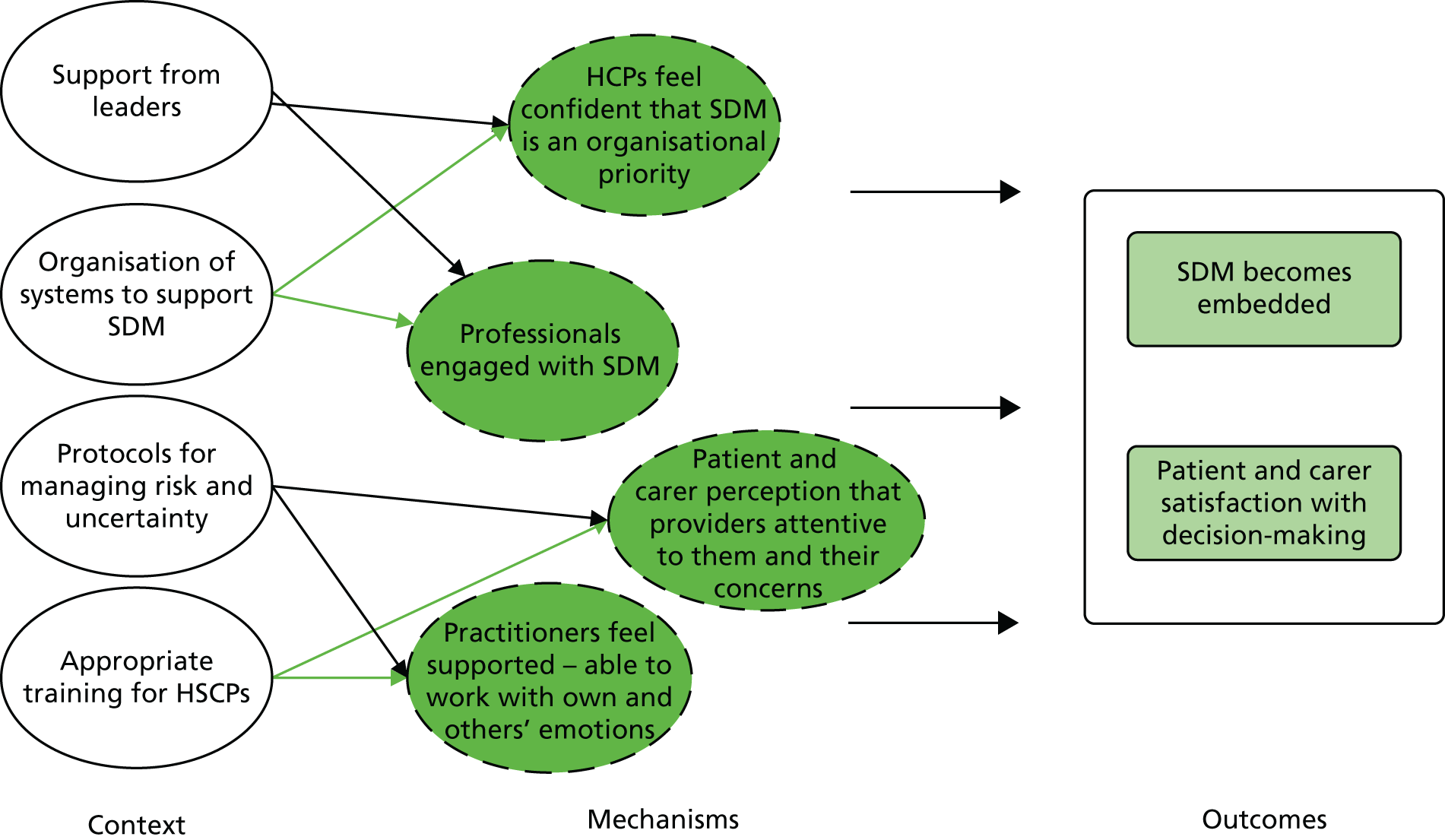
Organisation support
The MAGIC study177 supported the link between organisational buy-in (e.g. identifying SDM as an organisational priority) and an increase in HCP engagement with, and prioritisation of, SDM. It also affects patients’ perceptions that the health-care organisation and clinicians want them to be involved. 177 However, although SDM is a core part of policy in many countries, including the UK,211 at a service level, systems are not in place to incentivise or appropriately reward patient-centred practices and SDM. 17,177
Systems to support shared decision-making
In the UK, the Year of Care initiative aimed to improve care for people with LTCs. A report from one practice in North East England31 described the implementation of this initiative for people with multiple LTCs (the ages of participants were not specified). Although the report does not provide data on patient outcomes, the staff felt that it improved the quality of conversations with patients. The report documented key stages in the SDM process, such as preparatory work before the actual consultation with the GP, when relevant information about the patient is gathered by other members of the primary care team. Appointments are longer than normal, with the length of the appointment being adapted to reflect patient needs. In addition, all chronic disease monitoring is combined into one annual review, which involves a collaborative consultation, based on SDM and self-management support, via care planning. 31,200 A qualitative study on information sharing also supports the idea of looking at health as a whole rather than in a series of reviews focusing on specific chronic diseases. 189
In the Year of Care approach adopted by one practice in the UK,200 patients are sent relevant test results before the consultation. This is an increasingly common practice in the UK. We found no formal evaluations of this approach. Although a report from a GP practice in the UK said that despite concerns that such an approach would increase patient anxiety and generate more work for clinic staff, this has not been the case. It stated that ‘people are keen to have their own information and value the recognition that gives about their involvement’. 200
Managing risk and uncertainty
Several studies highlighted the way that perceptions of risk or uncertainty affect decision-making. A paper on collaborative decision-making concluded that the uncertainty that complicates medical decisions is rarely explicitly addressed in decision support tools or medical consultations. 182 One paper discussed the importance of addressing uncertainty in SDM and proposed an uncertainty toolbox that includes the principles of honesty, recognition of emotion, hope, support/co-ordination of care, willingness to readdress issues, respect for personal decisions and the acceptance that a lack of decision is possible. 202 A cluster RCT tested a SDM training programme for newly qualified GPs in the UK. The training involved two aspects: (1) SDM training and (2) training in risk communication. The authors stated that doctors’ confidence and satisfaction with the process were greater if they received the risk communication training before the SDM training. 167 However, the risk communication training was based on four discrete conditions and the study excluded people aged ≥ 75 years.
Training
The need for enhanced communication skills for clinicians was a common theme across the papers. 66,107,110,113,168 For example, a review of qualitative studies suggested that GPs need better communication skills, particularly when working with patients with complex needs. 68 A number of the included studies evaluated the impact of training for HCPs on SDM. A review of interventions for providers to promote a patient-centred approach (of which SDM was seen as an important component) in clinical consultations found ‘generally positive effects on a range of measures relating to clarifying patients’ concerns and beliefs; communicating about treatment options; levels of empathy; and patients’ perception of providers’ attentiveness to them and their concerns as well as their diseases’. 110 Short training (< 10 hours) was as successful as longer training. 110 Another review evaluating interventions to promote SDM found that interventions targeted at HCPs did lead to an improvement in SDM. Interventions that targeted professionals as well as patients were considered more effective than interventions that targeted only one of these groups. 118
A cluster RCT of a SDM training programme for newly qualified GPs in the UK found that, although training increased GPs’ SDM skills (measured on the option scale), there were no statistically significant changes in patient-focused outcomes. 167 The length of the consultation and being seen in a protected environment were linked to greater patient confidence in the decision and expectation to adhere to their chosen treatments. A more recent RCT of SDM training for GPs found that, although trained GPs exhibited less paternalistic decision-making, they were not judged (according to the control preference scale) to have engaged in SDM. 185 The study did not consider the impact on particular subgroups of patients such as older people or those with complex health needs.
In a discussion piece, Elwyn et al. 17 argued that the best way for clinicians to learn SDM skills is using simulations. This was supported by evidence from the MAGIC study in the UK. They reported that interactive skills training workshops based on a SDM model helped build coherence, improving skills and promoting positive attitudes. They added that role play-based training, which emphasised practical skills, worked better than theory-heavy presentations. It was also considered important that clinical teams were able to develop a shared understanding of how SDM might differ from their current practice. 177 The impact on patients was unclear as the authors reported that ‘we found it difficult to identify or develop suitable patient reported measures to capture experience of shared decision making’. 177
Context–mechanism–outcome 2: summary
There is evidence that organisational support, appropriate training for HCPs and system-based aspects, such as longer appointments, lead to HCPs feeling more supported and having the confidence to engage with SDM. It can also result in increased patient satisfaction with decision-making because they feel that service providers are attentive to them and their concerns. There is a lack of studies addressing interprofessional approaches to SDM or the training needs of providers other than doctors.
Context–mechanism–outcome 3: preparing patients, carers and health and social care professionals for the shared decision-making encounter
Programme theory: people with complex health and care needs, and their family carers, are likely to need support, such as appropriate decision tools and space and time to ask questions and discuss options, in order for them to be willing and able to participate in SDM.
Many patients, particularly those with complex needs and LTCs, are likely to find engaging in SDM difficult. Our CMO explores how interventions might provide resources that enable these barriers to be overcome. The programme theory is explained in Figure 6.
FIGURE 6.
Summary of CMO 3: preparing for the SDM encounter.
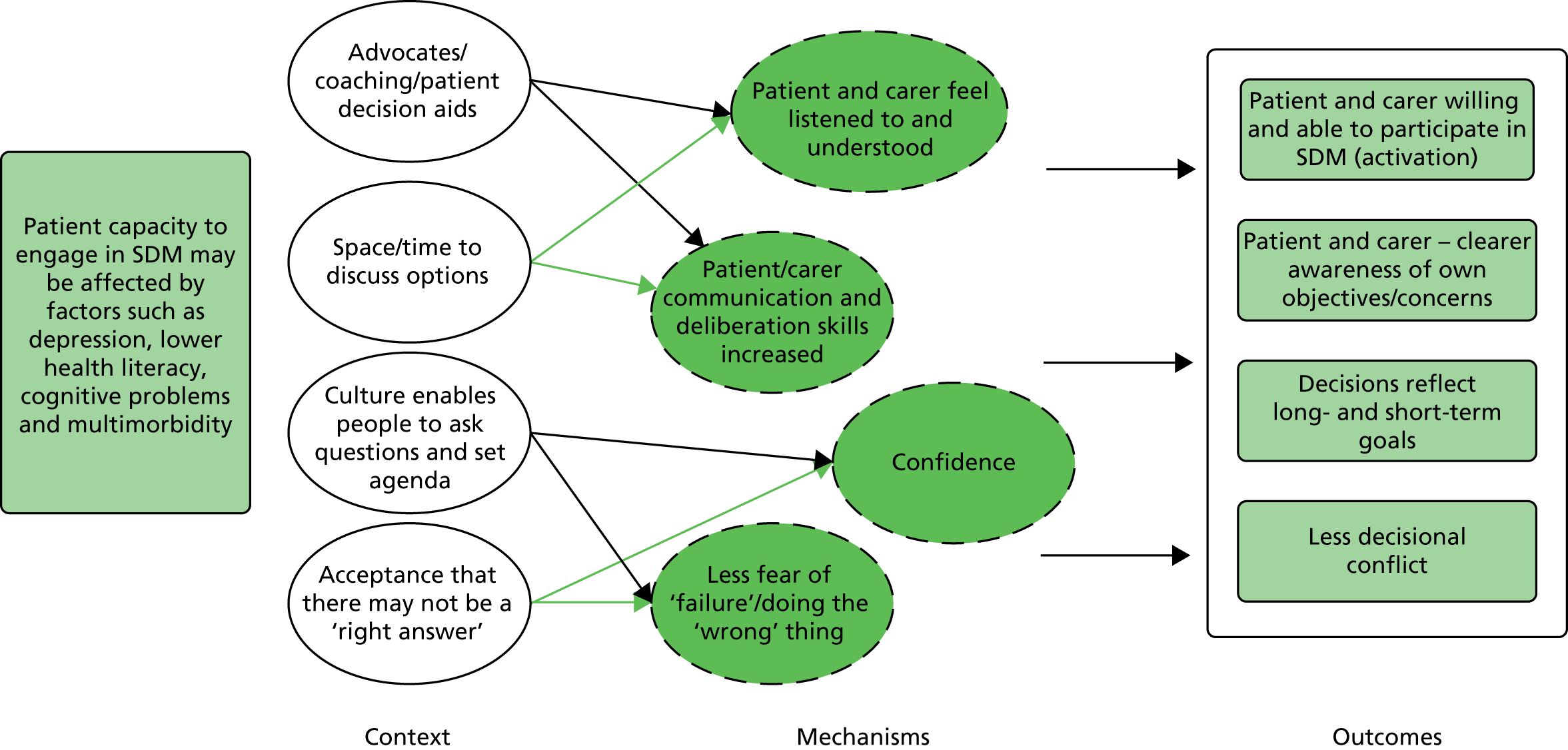
Decision aids
Much of the literature we found on preparing patients and carers relates to the use of PDAs (see Appendix 2 for more details of these studies). PDAs are tools designed to help people participate in decision-making about health-care options. They provide information on reasonable health-care options and are designed to help patients clarify and communicate the personal value they associate with different features of the options. 212 They differ from health education information because they focus specifically on the decision to be made. 20 Systematic reviews provide good evidence that PDAs can have a positive impact on patient knowledge, decisional conflict, informed choice, participation in SDM and decision self-efficacy,20,69,103,108,116,121 including for those who are socially disadvantaged. 69 Potential mechanisms relating to the likely benefits of decision aids include patients becoming more engaged,69 greater decisional self-efficacy,69 a greater feeling for patients that they are involved in decisions,167 and that ‘being offered the opportunity to prepare for a meeting is seen as an indicator of mutuality’. 171 However, those same systematic reviews provide little evidence that decision aids improve health outcomes or patient adherence.
Older age, depressive symptoms and difficulties with the activities of daily living are associated with decreased patient activation;170 interventions may therefore need to be tailored to older adults’ level of patient activation and address issues such as depression. 170 A review of decision aids for older people reported that they improve older adults’ knowledge, increase their risk perception, decrease decisional conflict and seem to enhance participation in SDM. 121 These findings were supported by a patient-level meta-analysis that looked at the impact of characteristics such as age on the efficacy of decision aids. 108 They found no difference, however, in concordance with chosen treatment. The authors highlighted several limitations of the current literature in this area; they found only one study108 in which the tool had specifically been designed for older people, most participants in the study were younger older people (≤ 70) rather than the oldest old (≥ 80) and tools were not tailored to the needs of people with multimorbidity. The authors argue that:
. . . it is doubtful whether it will ever be possible to provide relevant and evidence based information tailored to all possible combinations of comorbidities in a single decision aid. This indicates that decision aids for older adults might be most effective when combined with high quality patient-provider interaction during consultation, with personal tailoring of the decision aid to the individual persons’ context.
van Weert et al. 121
In contrast, most of the tools included in the review were designed to be used by the patient at home or in a research interview rather than as part of a routine consultation with a clinician.
Although decision aids are seen to have advantages, a number of studies also outlined potential problems with their use. In the MAGIC study177 the authors noted that a key finding of their programme was that ‘skills trump tools, and attitudes trump skills’. They argued that:
. . . there will never be decision support tools for every decision; nor will every patient find them acceptable or helpful. The skills to have different types of conversations with patients are paramount, with or without an available tool.
Joseph-Williams et al. 177
They concluded that short tools to use in the consultation are better than information sources used outside the consultation because they are better at facilitating discussion between the patient and clinician and are cheaper and easier to keep updated than an information source, such as a website. They cautioned, however, that there is a risk that brief decision aids may be used purely to enhance information transfer, rather than improving the way clinicians work with patients.
Another criticism of decision aids is that they do not address the essential first step of SDM, which is preparing for the encounter. 116 This includes perceiving the opportunity and personal ability to be involved, both of which were very important in our programme theory. A qualitative study with people with mental health problems suggested that ‘concrete aids for considering and contributing to the preparation of the decision-making occasion might reduce power differentials’. 171 However, in a systematic review of barriers and facilitators of SDM, Joseph-Williams et al. 116 argued that there is a need ‘to address the entry level factors to SDM, such as subjective norms and patients’ roles, before secondary process factors such as information provision and value clarification’. 116 In addition, several studies proposed that the provision of decision aids will not necessarily mean that they are used, or, if they are used, that they will lead to SDM. 114,166
Coaching
Another proposed way to help people in SDM is via coaching or facilitation. Studies on patients with cancer have found that when trained facilitators or navigators met with patients prior to their consultation with a clinician, there was improved self-efficacy and reduced decisional conflict. 153,173 However, one was a feasibility study173 and in the other rigour was low. 153 A systematic review of coaching or guidance as part of SDM concluded that the evidence supports the use of coaching or guidance to better guide patients in the process of thinking about a decision and in communicating their values/preferences with others. The mechanisms inferred from the paper are that if you improve patients’ deliberation and communication skills, this will lead to empowerment and thus patients will feel better supported. But the impact on other outcomes, such as participation in decision-making or satisfaction with the option chosen is mixed. 120 Moreover, the relevance of this review to our synthesis is only moderate as the studies mostly focused on single issues, such as screening.
Family-centred approaches
Research has underscored the importance of family-centred approaches for older people with complex needs. 58,213 However, similar to a previous realist review on engaging older adults in health-care decision-making,113 we found few studies that considered the involvement of family members and friends in SDM. A German pilot study reported on the development of a tailored e-health service for caregivers/carers of people living with dementia and HSCPs. 186,187 The aim of the tool was to facilitate communication between HCPs and informal carers and to empower the carers. Although not aimed at SDM, the intervention included an element related to preparation for doctors’ visits. The study suggested that such a tool might help informal carers to feel more prepared for doctors’ visits (e.g. identifying questions).
One initiative to make it easier for patients and their families to engage in evidence-based decision-making is ‘the three questions’ approach (AskShareKnow). 214 Patients are encouraged to ask the following: what are my options? What are the benefits and harms? And how likely are these?214 These questions have been shown to improve the information given by family physicians and increase physician facilitation of patient involvement. The authors considered the approach to be a potentially powerful intervention for affecting physician behaviour without affecting the length of the consultation. 214 It is possible that the approach may be less successful with adults with lower-than-general levels of literacy. 215
Permission/space to discuss options
Key to CMO 3 is that SDM is undertaken in a context in which HSCPs, patients and their families are able to discuss the value and effectiveness of proposed treatments and to set the agenda. A positive example of this comes from the Year of Care initiative, which described patients feeling free to ask questions, meaning that they feel that HCPs are interested in them as people and not just in the condition. The report added that the agenda-setting prompt had given patients permission to talk about things. 31 This ties in with a key part of our CMO: that interventions or programmes need to create a culture that enables people to ask questions without feeling judged. Longer consultations are linked to greater patient satisfaction and improved SDM,31,107,157,165,181,183,192 which is likely to be related to the opportunity for patients to ask questions and ‘feel listened to’. 165,181 Patients also want to feel respected. 178,188
However, there is evidence to suggest that clinicians’ attitudes act as a key facilitator or barrier to SDM. 116,177 A study of older people’s experiences of health-care decision-making found that participants often felt unable to make their needs heard because clinicians rushed them or ‘closed them down’. 159 A qualitative study of information exchange in consultations found that patients and HSCPs may not be able to reach a shared understanding because HCPs omitted relevant information or because patients often omitted relevant context or preferences during a consultation. 158 Older people may be reluctant to voice their concerns or openly disagree with a doctor but instead avoid conflict by choosing not to adhere to prescribed treatment. 159
Understanding that there is a choice
Studies have illustrated that the presentation of choices can substantially influence the decisions people make. For example, framing risk in survival rather than mortality terms increases the probability that patients will consent to an intervention. 207 Moreover, older people may not always be aware that there is a choice to be made. 159 A qualitative study with older people receiving dialysis found that patients were often unaware that dialysis initiation was voluntary and held mistaken beliefs about their prognosis. 180 Clinicians may find it difficult to present choices to patients because they are trained to display confidence to patients. Their own discomfort with uncertainty might lead them to engage in more paternalistic styles of decision communication. 182
In some instances, the choice being made may be constrained by resource limitations, health-care policies or evidence-based recommendations (such as guidelines). A qualitative systematic review of decision-making communication practices found that even when there is no alternative, exploring patients’ choices and reasons can validate the patients’ participation and mean that they have still ‘participated in the decision making process’. 117 They added that pursuing agreement without engaging with patients’ reasoning may be treated as coercive. This was echoed in a knowledge synthesis182 of medical decision making which concluded that:
Achieving shared mind will be more difficult when patient preferences are counter to the strongest clinical evidence. Under these circumstances, quality decision making will depend not only on clinician(s) and patient becoming aware of and understanding the other’s position, but also engaging in a dialogue to find common ground, identify and reconcile differences, and negotiate or compromise to reach a collaborative, agreed-upon decision.
Politi and Street182
The subject of coercion was also explored in a discussion paper that considered whether or not ‘clinical nudges’ are ever compatible with SDM. The authors argued that in instances in which patients do not have authentic preferences, clinicians are justified in using nudges in accordance with the best interest standard (e.g. the ethical requirement that people who care for others will do so in good faith, placing their assessment of that person’s best interests above their own). 207
Context–mechanism–outcome 3: summary
Older people with complex health needs are likely to need support to participate in SDM. Although the evidence suggested that interventions, such as decision aids and coaching, can improve involvement in SDM, the impact on adherence or health outcomes is not proven. Moreover, most tools were not designed (and have not been tested) for the oldest old. Evidence suggests that if tools are used they need to be brief, designed for use within a consultation and focused on facilitating discussion between the patient, family carer and HSCP. The right culture, that allows people time to ask questions and to discuss options, and staff with positive attitudes towards SDM are likely to be more important than tools for older people with complex health and care needs.
Context–mechanism–outcome 4: shared decision-making as part of a wider culture change
Programme theory: shared decision-making will only have a significant impact if it is part of a wider cultural change [e.g. family-centred approaches, changes in power dynamics and patients and carers taking (or sharing) responsibility for their health and the decisions that affect them], that triggers the development of a shared expectation of (and familiarity with) SDM among patients, carers and HSCPs.
The context for this CMO is the way current health and social care culture and norms, and power imbalances between HCPs and patients and their family carers, can act as barriers to SDM. Significant professional, patient and carer resources are needed to provide enough leverage to overcome those barriers and improve service user outcomes. CMOs 1–3 all feed into CMO 4. The programme theory is explained in Figure 7.
FIGURE 7.
Summary of CMO 4: SDM as part of a wider cultural change. Reproduced with permission from Bunn et al. 208 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
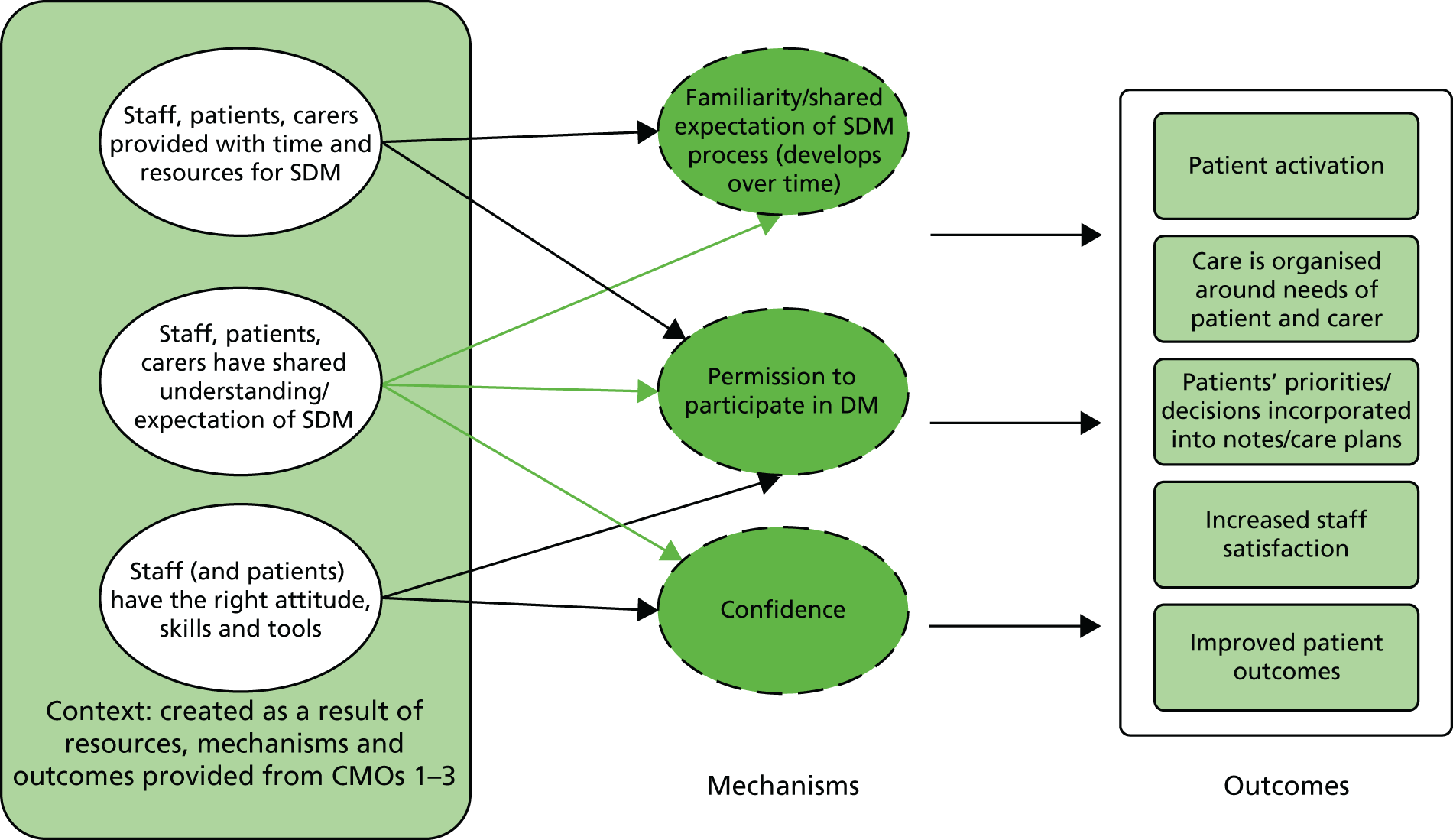
Time and resources
The programme theory outlined in CMOs 1–4 puts forward many barriers to SDM and it is clear that relying on individual clinicians or patients to implement SDM without system-based support is unlikely to be successful or sustainable. 114,116,118 Several of the papers we included have described system-based changes that involve person-centred, integrated approaches to people with LTCs,25,31,164,200 of which SDM is an integral part. A report describing the implementation of the Year of Care initiative in the UK suggested that valuing the development of staff is as important as valuing the expertise and lived experience of the patient. 31 This initiative reported increased staff and patient satisfaction. 25,31,200 One site reported that the quality outcomes framework (QOF) figures had not been negatively affected by the new ways of working. 200 Overall, it is suggested that similar initiatives (data not given) will take 2 or 3 years to make a difference to clinical outcomes as ‘habits of both patients and professionals die hard and engagement increases over a number of care planning cycles’. 200 This is reflected in our programme theory, which argues that familiarity and a shared expectation of new ways of working (which include SDM) are crucial, but these are likely to take time to develop.
Patient activation or engagement
The willingness or ability of patients to participate in SDM is a key contextual factor in our programme theory (see CMO 3). This is supported by the literature107 and also underscored by our interviews with stakeholders. In general, the consensus is that the majority of older people would wish to be involved in decision-making104 but in practice they are often not encouraged to participate in SDM. 104 Reasons for this include limited time, poor continuity of care, environmental conditions, organisational inertia, a biomedical focus, concern about disruption to routines, clinicians’ belief that they are already practising SDM and power imbalances. 114,116,168,202,216 Patients may feel unable rather than unwilling to share in decision-making. 116,177 Joseph-Williams et al. 177 suggested that, for older patients, their previous experiences are likely to give them an expectation of a paternalistic approach from clinicians. Although many SDM initiatives involve giving patients more information, this alone is not enough; patients need knowledge and power to participate in SDM. 102,116 A systematic review of patient-reported barriers to, and facilitators of, SDM suggested that power may be linked to perceptions of permission to participate in decision-making, perceived influence on decision-making, confidence in own knowledge and self-efficacy in SDM. 116
Outcomes
A systematic review of tools to promote SDM in serious illness suggested that decision aids have the potential to reduce health-care intensity and costs by decreasing unwanted major high-cost interventions or hospitalisations but that these outcomes have not been studied. 103 Another review suggested that as a result of SDM, patients tend to choose more conservative options. 20 One particular area in which there has been overlap between SDM and care for older adults with complex needs (which has a potential impact on resource use and patient outcomes) is around medication and, in particular, deprescribing. Deprescribing has been defined as ‘the process of withdrawal of an inappropriate medication, supervised by a health care professional with the goal of managing polypharmacy and improving outcomes’. 217 Inappropriate medication would include that which does not fit with the goals of treatment, does not align with patient values or is overly burdensome. 218 Although this was not the focus of our review, we did consider several studies that focused on deprescribing in a context of SDM. A project in care homes in the UK investigated structured pharmacy reviews for older adults. 198 The reviews, which involved the pharmacist, patient, family carer, GP and care home staff, significantly reduced unnecessary prescribing across care homes and reduced the risks of harm to residents caused by medication.
Context–mechanism–outcome 4: summary
We suggest that SDM is likely to be most effective when it involves service providers who have the right skills, attitudes and tools, working in systems that are structured to support service providers and users to engage in SDM. Key to this is a culture that involves person- (and family-) centred approaches. Although a shared expectation of, and familiarity with, the process is essential to its success, this is likely to take time to develop. The evidence indicates that such approaches may lead to improved service user and provider satisfaction with services and with the quality of decisions, but there is little research on the impact on health-related outcomes.
Chapter summary
The CMOs presented in this chapter are evidence-based statements that identify interventions, or elements of interventions, that are likely to promote SDM with older people with multiple long-term health and social care needs and their family carers. It identifies how they are thought to work, on what outcomes, and why, in some instances, they may not work. The CMOs are presented individually but in practice they are integrated and interactive. The implications of the results are explored further in the next chapter.
Chapter 4 Discussion
This chapter includes text from Bunn et al. 208 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
The overall aims of this study were to provide a context-relevant understanding of how models to facilitate SDM might work for older people with multiple health and care needs, and how they might be applied to integrated care models. We used an iterative three-stage approach that optimised the knowledge and networks of the research team and that was guided by the RAMESES criteria for realist review. 72 In this chapter we start by giving an overview of the findings and their implications. We then discuss the limitations of the study and conclude by outlining suggestions for practice and future research.
Summary of findings
There is a lack of evidence relating to older people with complex needs and SDM. Only 29 of the 88 included items were specifically focused on older people or people with multimorbidity or a LTC (see Table 2) Furthermore, the majority of these studies were qualitative or observational rather than quantitative evaluations of interventions. The rest of the evidence related to HSCPs (e.g. relating to training needs or attitudes towards SDM), younger populations or the ages of the participants was not specified. This evidence was included, however, because of the opportunities provided for transferable learning.
Despite the constraints of the current evidence base we were able to develop an explanatory account of what SDM should look like for older people with complex health and care needs. The theory draws on four CMO configurations that together provide an account of what needs to be in place for SDM to work for older people with complex needs (Table 13). The configurations highlight the importance of understanding patient and carer values, the organisation of systems to support SDM, the need to support and prepare patients and family carers to engage in SDM, and the need for wider cultural changes of which SDM is a part. The CMOs are grounded in evidence from the literature and stakeholder perspectives. Although designed to be specific to older people with complex needs, the CMOs are also likely to be relevant for other patient groups living with long-term and complex conditions.
| Name of CMO | Details of CMO |
|---|---|
| 1. Reflecting patient and carer values | Systems that enable HSCPs to develop relationships with patients and carers, and with each other, and that allow them to understand and assess individual needs and patient and carer capacity to access and use care, will activate trust and engagement leading to better outcomes for patients and carers |
| 2. Systems to support SDM | Systems that are organised to support and prioritise SDM will lead to HSCPs feeling supported (and equipped) to engage in SDM, resulting in SDM becoming part of the culture of care |
| 3. Preparing patients and family carers for SDM | People with complex health and care needs, and their family carers, are likely to need support, such as appropriate decision tools, and space and time to ask questions and discuss options, in order for them to be willing and able to participate in SDM |
| 4. Wider cultural changes that includes SDM | SDM as part of a wider cultural change [e.g. patient- or family-centred approaches, changes in power dynamics and patients and carers taking (or sharing) responsibility for their health and the decisions that affect them], that triggers the development of a shared expectation of (and familiarity with) SDM among patients, carers and HSCPs, leading to improved patient outcomes |
Key features of programmes
Context
The CMOs highlight several contextual factors that are likely to affect the success or otherwise of interventions or programmes to facilitate SDM with older people with complex health and care needs. These operate at individual, team and broader organisational levels (Figure 8):
-
At the macro or broader organisational level, a key context is to what extent systems legitimise and prioritise SDM for people with complex needs. Evidence from this review suggests that, for SDM to become embedded, there needs to be a level of organisational support that will trigger confidence in HSCPs that SDM is an organisational priority. 114,219
-
Meso-level factors relate to the way the team is organised and the extent to which services support and resource professionals, patients and family carers to have the time and skills necessary to be able to engage in SDM.
-
At the individual level, there are specific requirements needed of the workforce so that they can work in partnership with patients and family carers. For example, developmental needs around communication skills and how they define their role as a health or care professional working with and for older people over time. Maskrey and Gordon220 talk about the need for ‘a lifelong curriculum of learning’ in order to develop a shared understanding with patients.
FIGURE 8.
Summary of contextual factors at individual, team and system levels. IP, interprofessional working.
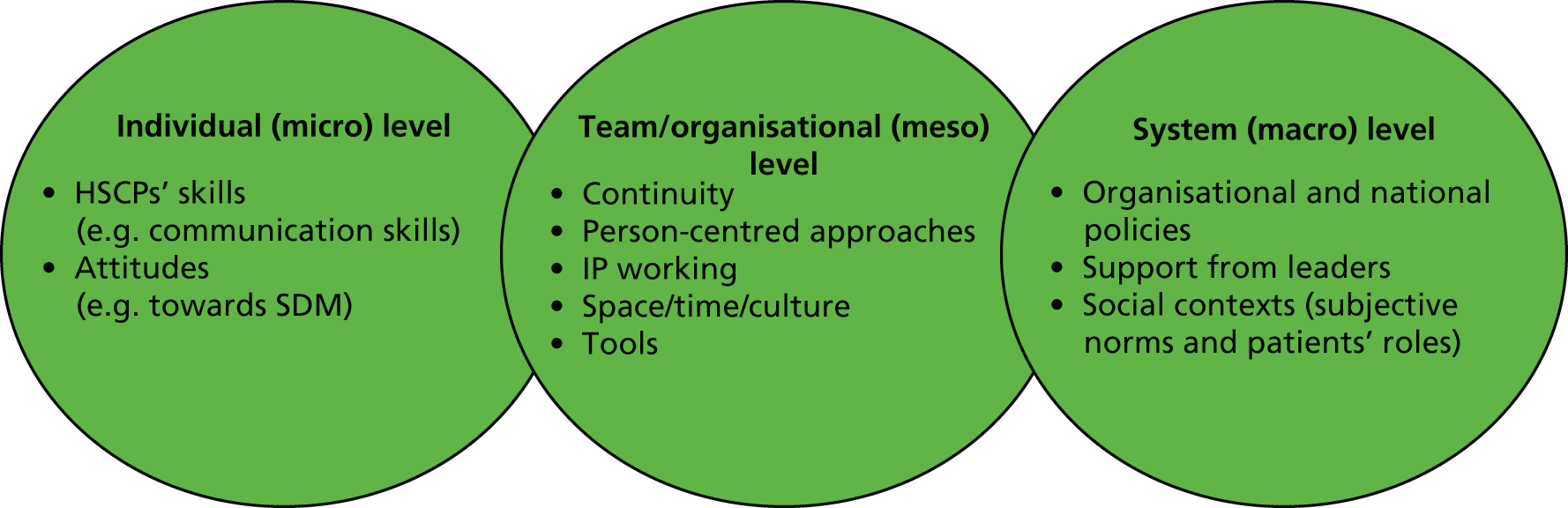
Mechanisms
A realist approach argues that exposing the resources and reasoning within mechanisms and their relationship to the context of their implementation is key to the evaluation of a complex programme of change. 221 Mechanisms are dynamic and may be interacting with each other;222 for example, in our programme theory, trust in HSCPs is likely to operate in parallel to patients and carers feeling heard and respected. In addition, what is seen as a mechanism or outcome, in one CMO, such as SDM becoming embedded, may, in turn, become a context in a subsequent CMO. 223
Our review suggests that interventions or programmes to promote SDM between HSCPs and older people with complex needs will have a greater chance of ‘working’, that is, engaging people in SDM and potentially improving satisfaction and health outcomes by paying attention to those activities or contexts that engender the following mechanisms:
-
Trust between patients, family carers and HSCPs.
The evidence60 suggests that relationship continuity (e.g. a continuous therapeutic relationship with one or more health professionals over time), is an important resource that engenders trust and the related mechanism of confidence in patients and family carers. This requires face-to-face contact to encourage the person to participate in SDM.
-
Trust between HSCPs.
Evidence84 shows that in order for HSCPs to take an interprofessional approach to SDM there needs to be trust and an understanding of each other’s roles.
-
Confidence.
Confidence is an important mechanism for HSCPs, patients and family carers. When HSCPs know that SDM is an organisational priority and that services are organised to facilitate person-centred approaches to care they are more likely to engage in SDM. For patients and carers, confidence might be engendered by interventions that increase their communication and deliberation skills (e.g. coaching, PDAs, longer appointments) and environments that mean that they are not afraid of ‘doing the wrong thing’ or being labelled difficult. 224 Confidence may then in turn become a context that enables people to persevere with SDM because they know that it is valued by those around them.
-
Respect.
Strategies to foster SDM are likely to be most effective when they are based on person-centred approaches that trigger a feeling in patients and family carers that they are respected, listened to and understood. 29,225 SDM is often conceptualised as an integral part of person-centred approaches to care;110 indeed, it has been described as the ‘pinnacle of person centred care’. 23 Respect among different HSCPs as well as between team members and the patient is also vital for interprofessional SDM. This includes a sharing of power among the team members so that all members can share knowledge and communicate effectively. 84
-
Familiarity/shared expectation.
We suggest that confidence is also related to all parties (HSCPs, patients, family carers) being familiar with the process of SDM and having a shared expectation of what this involves. Evidence (primarily from stakeholders) indicates that this may take time as both sets of actors have to assimilate the core assumptions of SDM and learn how to work together. 200
-
Permission to participate.
Programmes and strategies to promote SDM should also look to trigger a sense of permission so that all parties (patients, family carers and HSCPs) feel that they are able to participate in SDM. This may arise, for example, through knowing that SDM is an organisational priority.
Implications of the findings
Shared decision-making for older people with complex health and care needs
For those most reliant on health and social care support, such as older people living with frailty and/or severe disabilities arising from LTCs, decision-making may be particularly complex. It requires consideration of resource availability, the potential impacts of polypharmacy, the ability to obtain informed consent, the capacity of patients to attend to health-care demands, the support networks available, potential safeguarding issues and the appropriateness of individual treatments for people with multimorbidity. Initiatives to address these have focused on aspects of care such as interprofessional working,226 case management227,228 and the use of shared methods of assessment and planning (e.g. Comprehensive Geriatric Assessment). 229 All of these tend to be professionally initiated and directed. Although there is evidence230,231 that many older people and their family carers would like to be involved in decision-making, there is little evidence that relates specifically to SDM with older people with complex health needs. The overwhelming majority of the evidence on SDM relates to decisions about single conditions (e.g. prostate cancer or diabetes mellitus). It is more difficult to extrapolate this single condition-focused research to older people with multimorbidity. In addition, when older people are involved they are generally not the ‘oldest old’. 121 There is no consensus on how SDM should be structured or who should be involved, and few studies considered the involvement of family members in SDM when older people rely on them for ongoing support and care.
Person-centred approaches to health and care and consideration of the patient’s preferences and values is central to the SDM process. 29 For older people with complex needs, eliciting preferences is likely to involve regularly revisiting decisions as the dominant illness, and priorities, may shift over time. 105,172 However, the evidence suggests that doctors are better at recognising and discussing options than eliciting patient preferences (see CMO 1). This may reflect the fact that different HSCPs conceptualise PCC in different ways. 18,232 A review of literature on PCC suggests that, whereas the nursing literature tends to focus more on respecting patients’ values and beliefs in promoting PCC, the medical literature has devoted more attention to understanding the nature of the informed decision-making process between the doctor and the patient. 232 What is not explored in the literature is whether or not integrated care and interprofessional working might enable different members of the MDT to draw on the skills of others in order to promote effective person-centred approaches to SDM.
The quality of individual clinicians’ communication skills, and their ability to foster trusting relationships with older people and their families, is fundamental to SDM. In addition, there is also a need for systems that promote continuity of care. Continuity can be achieved through an ongoing relationship with one clinician (relationship continuity) or a system-based approach that develops ways of working whereby the patient is linked to multiple professionals (management and informational continuity). 60,233,234 The evidence would suggest that both need to be in place. Informational continuity is, however, often hindered by electronic systems not set up to record information relating to patient preferences and goals. For example, a study of record keeping in UK primary care found a gap between patients’ oral narratives and the way in which these are understood and recorded by clinicians. This suggests that universal adoption of electronic patient records in their present state will not alone achieve informational continuity between organisations. 189
Enabling older people to participate in shared decision-making
Context–mechanism–outcome 3 relates to the need to help prepare and support patients and their family carers to engage in SDM. This is likely to be particularly important for older people with complex needs, as older age, depression (which is often linked to LTCs) and difficulties with activities of daily living are associated with decreased patient activation. 170 The evidence highlights key contextual factors such as longer consultations, clinicians’ communication skills and a culture that allows people to ask questions without feeling judged. These are likely to lead to an increased ability and willingness to engage in decision-making through mechanisms such as feeling respected and understood.
Much of the literature on preparing patients and carers relates to the use of PDAs. Although there is some evidence that PDAs may enhance participation in SDM and decrease decisional conflict, very few studies include the oldest old, and tools are not designed for use with older people or those with multimorbidities. 121 Moreover, PDAs on their own are unlikely to address what Joseph-Williams et al. 116 calls the entry-level factors to SDM, such as subjective norms and patients’ roles. For older people, subjective norms235 may include the perception that there is a right and wrong decision, or that decisions should be made by doctors. HSCPs should actively consider the possibility that older people may be more hesitant than other age groups to express a wish that they feel is counter to that of the clinician,159 and that their attitude towards SDM may be affected by past experiences of a paternalistic approach from clinicians. 116
Patient decision aids for older people are likely to be most effective when used as part of face-to-face interactions, ongoing patient–clinician relationships and patient-centred approaches. 236 Hargraves and Montori237 argue that the real work of SDM is ‘collaborative deliberation in the face of uncertainty’237 which happens within the encounter between patients and doctors. Although this is a narrow conceptualisation of SDM, excluding family carers and other types of HSCPs, it does emphasise the importance of the conversation and the need to understand how factors such as decision aids, clinician skills, patient power and uncertain scientific evidence interact in the SDM encounter. 237
Shared decision-making and the new models of care
Many health-care systems, including the English NHS, are moving towards a more interprofessional health-care team-based approach. 8 In integrated care sites, decision-making and communication may need to be negotiated between, and communicated to, multiple HSCPs and personal assistants directly employed by care users, as well as patients and their family carers. Despite this, the vast majority of the SDM literature relates to encounters between a single clinician (usually a doctor) and a patient, and there is a lack of studies addressing interprofessional approaches to SDM. 118 In addition, when studies address the skills and attitudes needed for SDM, these focus almost exclusively on doctors. For interprofessional SDM to work, the development, and involvement, of all staff is important and power imbalances need to be addressed. 25 Doctors’ real and symbolic power is still strong and may be a barrier to interprofessional decision-making. 84
The literature does provide some examples of how decision-making might be negotiated between a patient and several clinicians. For example, a case study of medication reviews in care homes involved meetings between residents, family members, care home staff, a pharmacist and (when possible) a GP. 191 Another example of an interprofessional approach to care planning (which involves SDM) comes from the Year of Care initiative when care planning involved a first consultation with a HCA who helped the patient work out ‘what they want to do’ followed by a second consultation with a GP or specialist nurse to make a care plan. 25 Both reported positive outcomes.
Légaré et al. 84,144 have developed a model of interprofessional SDM, which incorporates the use of a decision coach who is trained to support the patient’s involvement in decision-making. They suggest that the decision coach could be a member of the team, such as a nurse or a therapist. A lack of time is a commonly cited barrier to SDM114,116 and the employment of members of the MDT as coaches could create more space and time for SDM. Although there is evidence to support the use of coaching to aid patients in the decision-making process, we found little evidence specific to older people with complex needs. In addition, the model proposed by Légaré et al. 84,144 does not appear to have been tested in practice; forward citation tracking from these papers suggests that the literature continues to be descriptive and explorative rather than describing the development and evaluation of interventions to promote interprofessional SDM. Although it is suggested that interprofessional approaches to SDM could improve quality of care by fostering continuity in the decision-making process, this has not yet been tested. 144
Shared decision-making and the reduction of unnecessary health services
There are several different paradigms underpinning SDM. 13 Imperatives behind SDM include policy drivers, moral arguments, the need to address uncertainty, the wish to deliver PCC and the potential for SDM to increase patient activation leading to improved self-management of LTCs and, in turn, improved health outcomes. There is also a suggestion that SDM can be used as a tool to reduce resource use or unnecessary treatment. 143 All of these assumptions are apparent in the literature although perhaps the strongest is that SDM (either on its own or as part of PCC) is morally right.
There was some evidence from the literature of a crossover between SDM and campaigns to reduce the use of harmful or unnecessary health services. For example, the Canadian initiative ‘choosing wisely’ includes in its framework the need for supporting SDM at the clinical level,238 and the promotion of better conversations between patients and physicians to facilitate informed decisions. 239 However, an evaluation of the ‘choosing wisely’ literature suggests that this does not meet criteria for SDM documentation because the patient materials presented imbalanced information and most did not provide an opportunity to clarify patient values and preferences. 145 It is also possible that if such approaches are seen by patients and family members as a way of rationing care or denying access to treatment, then it would be difficult to trigger the important mechanisms of trust and confidence needed for SDM.
Changing the culture
In CMO 4 we suggest that SDM needs to be situated in a context of wider changes in the culture and organisation of health-care systems. This CMO incorporates components from the previous CMOs, such as organisational resources (time and space), systems to support SDM and skills development through continuous practice development. These wider changes are important to trigger mechanisms such as familiarity and confidence. This familiarity, which develops over time, is necessary for both HCPs and patients and their families. It includes an understanding that patients and (when appropriate) their family carers have responsibility for their health and the decisions that affect them. Theories of organisational readiness for change in health-care settings suggest that, in order for change to occur, members of an organisation need to feel committed to implementing an organisational change and confident in their collective abilities to do so. 240,241 Such confidence is linked to an understanding of how to implement the change, having the available resources and current situational factors.
Clearly important to CMO 4 are person-centred approaches, and we suggest that desirable outcomes of a SDM approach would be that care is organised around the needs of the patient and family carer and that the patient’s priorities are incorporated into actions, notes and care plans. McCormack and McCane86 argue that PCC is about having a specific person-centred culture rather than PCC by itself, and that it should be practised by everyone in an organisation. He writes that ‘person-centredness can only happen if there is a person-centred culture in place in care settings that enables staff to experience person-centredness and work in a person-centred way’. 86 Person-centred SDM includes supporting patients so that ‘they feel capable of acquiring and understanding knowledge about the available options, and so that they value their personal knowledge contribution to SDM’. 116
Strengths and limitations
One of the main limitations of this review is the lack of evidence around interventions to promote SDM in older people with complex health and care needs. Evidence from stakeholders and from the literature suggests that older people with complex and competing health and care demands (and when depression is a common comorbidity) may need considerable support to enable them to engage in SDM. This can be exacerbated when there are issues such as deprivation, low health literacy or cognitive impairment. Although we found literature on interventions designed to improve patient involvement in decision-making (e.g. decision aids, coaching and care planning done over several consultations), there is a need for more work that specifically focuses on older people with complex needs. Models for health-care delivery often involve a variety of health and care professionals (such as nurses or HCAs providing some chronic illness management in primary care), whereas the majority of evidence concerns decision-making involving a single doctor and a patient. Although there is literature relating to interprofessional SDM, much of this is descriptive, for example, describing potential barriers to and facilitators of interprofessional SDM.
The outcomes specified in our protocol included patient experience, patient safety and clinical effectiveness. Outcomes reported in the studies, however, largely related to patient experience. There is good evidence that SDM has positive benefits for patients and carers such as feeling more involved, improved satisfaction and reduced decisional conflict. The evidence on the impact on adherence is mixed and there is little evidence to suggest an association between empirical measures of SDM and health outcomes. Moreover, little of this evidence is directly relevant to older people with complex needs or considers potential unintended consequences of SDM, such as the consolidation of health inequalities. 242,243 In addition, where SDM is part of a whole system change, such as in the vanguard sites, it is difficult to attribute particular outcomes to SDM.
In realist reviews the aim is not so much to summarise all the available evidence but rather to make sense of it. 244 Searching tends, therefore, to be iterative and ongoing throughout the review process with the aim of identifying sufficient sources for theory building and testing. To identify studies in phase 2 of our review, we did not undertake one overall search but instead conducted 11 separate searches that focused on aspects of the programme theory identified in phase 1. This was supported by extensive lateral searches, such as forward and backward citation tracking, and keyword searches on Google Scholar. Such lateral search techniques have been identified as particularly important for realist reviews. 245 Despite this extensive searching it is possible that we missed potentially relevant literature. However, the nature of realist methodology means that there is not a finite set of relevant papers to be found. Instead, the reviewer is able to take a more purposive approach to sampling that aims to reach conceptual saturation rather than identify an exhaustive set of documents. 148,149
The unit of analysis in realist methodology is the programme theory, or underpinning mechanism of action, rather than the intervention. 149 This meant that we were able to draw on a wider literature that provided opportunities for transferable learning, for example, studies involving people with LTCs or mental health problems. This enabled us to develop a theory-driven explanation, in the form of four CMO configurations that make up a programme theory, which can inform initiatives to promote SDM for older people with complex needs. However, although the ability to draw on a wider range of literature for realist reviews is an advantage, it does also raise the issue of when to stop searching. As already stated, this is largely based on judgements around theoretical saturation, but it is also influence by external factors, such as time and funding. 91
This review did not include formal assessment of the quality of included studies. This is because in realist reviews the traditional hierarchy of evidence is rejected in favour of an approach that prioritises the way studies contribute to the development of programme theory. For example:
Do the inferences made in a study gel with those from other studies?
Realist review is concerned with theoretical depth and transferability rather than with developing statements or recommendations that have statistical certainty about questions of effectiveness or cost-effectiveness (Pawson et al. 149). In line with this approach, we assessed evidence on how it contributed to our theory development. As part of our data extraction process, we assessed the relevance and rigour (was it ‘good enough’) of the evidence. 71,149 This included an appraisal of whether or not it provided valuable information, could be relied on and contributed to the review.
Older people with complex health and care needs are often reliant on others, typically family members, to advocate or negotiate access to care on their behalf. 58,213 Family members also often provide significant emotional and practical assistance. 58 Models, such as the triangle of care32 and person-centred approaches, recognise that families are often crucial allies for quality and safety. 2,32 Despite this, recent research has found that, although service providers recognise the contribution of family carers to the co-ordination and management of care, this does not translate into routine engagement of family carers in decision-making for people with dementia and comorbid conditions. 58,213 Although some of the literature we included in this review made reference to the involvement of family carers, we found no formal evaluations of such an approach.
Stakeholders are important in realist work and the realist synthesis focus is driven by ‘negotiation between stakeholders and reviewers’. 71 We had originally intended to interview up to 20 stakeholders in phase 1 and 10 in phase 3, but in the end, were only able to recruit a total of 21 stakeholders over both phases. This is fewer than we had intended but the stakeholder views were still important in clarifying the focus of the review and validating the programme theory. In addition, input from our advisory group and our PPI members helped to shape our programme theory.
Conclusions
Programmes that are likely to be successful in creating shared understanding and shared decision-making between service users and providers are those that create trust between those involved, that allow service users to feel that they are respected and understood and that engender confidence to engage in SDM. We suggest that confidence is likely to take time to develop as it is related to the development of a shared understanding and expectation of SDM between service users and service providers. The cultural shift that is needed to embed SDM in practice may require new ways of working for HSCPs and a shift away from a biomedical focus to a more person-centred ethos that goes beyond the individual patient encounter. To achieve this HSCPs are likely to need support, both in terms of the way services are organised and delivered and in terms of their own continuing professional development. This cultural shift also involves an expectation that patients and their family carers will take a greater responsibility for their health and the decisions that affect them, and they too may need support to engage in SDM. How this support might best be provided needs to be further explored, although face-to-face interactions and ongoing patient–professional relationships are clearly key. Support needs to ensure that well-meaning attempts to focus on patient goals do not increase health inequalities. 242
Models of SDM for older people with complex health and care needs should move away from thinking about SDM purely in terms of one encounter between a doctor and a patient. Rather, SDM should be conceptualised as a series of conversations that patients, and their family carers, may have with a variety of different health and care professionals. 68,144,182 Such an approach relies on continuity of care fostered through good relationships between service providers and users, and systems that facilitate the communication of information, including that about patient goals and preferences, between different health and care professionals.
The literature on SDM involving older people or those with complex needs is largely qualitative or descriptive and there are very few evaluations of interventions specifically designed to promote SDM with this group or with their family carers. This review suggests that there is need for further work to establish how organisational structures can be better aligned to the needs of older people with complex needs. This includes a need to define and evaluate the contribution that different members of the HSCP team can make to SDM for older people with complex health and care needs.
Implications for practice
The following implications for practice have emerged from the review.
Systems and culture
-
The evidence suggests that SDM is only likely to become embedded if it is regarded as an essential component of ‘good’ healthcare and is linked to a culture of person-centred approaches throughout an organisation.
-
The evidence suggests that a culture that allows people time to ask questions and to discuss options, and staff with positive attitudes towards SDM, are likely to be more important than decision support tools for older people with complex health and care needs.
-
The evidence suggests that there is a need for visible organisational support in order for SDM to become embedded. This includes visibility in internal policy documents, through financial and organisational support (e.g. enabling longer appointments when necessary, providing appropriate administrative support) and through the inclusion of SDM in continuing professional development.
-
The evidence suggests that systems that foster continuity of care both through ongoing relationships with one clinician (relationship continuity) and through system-based approaches that develop ways of working whereby the patient is linked to multiple professionals (management and informational continuity) are important for SDM.
-
It appears likely that in instances in which choices are constrained by resource limitations, health-care policies or evidence-based recommendations, it is still valuable to explore patients choices and reasons.
-
Although properly conducted SDM may increase the length of consultations (such as those in primary care), there is evidence to suggest that they may be ameliorated by involving other members of the MDT in the SDM process.
-
It is important that service providers and service users have shared expectations of, and familiarity with, SDM for it to become properly embedded. This is likely to take time to develop.
Education and training
-
Our findings suggest that SDM education and training should be focused on all members of the MDT and not just doctors or lead clinicians. It should be part of undergraduate training programmes but also part of ongoing professional development.
-
Evidence points to a need for SDM and communication skills training to include the task of exploring what matters to patients and how to elicit their goals and priorities.
-
SDM training should include information on risk communication.
Preparation for shared decision-making
-
Evidence suggests that many older people with complex health and care needs, particularly those with lower health literacy or conditions, such as depression, are likely to need support to take part in consultations involving SDM.
-
The evidence indicates that PDAs for older people with complex needs are likely to be most effective when used as part of a face-to-face interaction with a HCP, for example for facilitating discussion between the patient, family carer and HCP.
Suggestions for future research
Several potential areas for future research were identified by the review. These are listed in order of priority:
-
How can interventions be tailored to the SDM needs of older people with complex health and care needs and how effective are such approaches? For example, would longer consultations in primary care facilitate SDM and improve patient outcomes?
-
How can family members be involved in SDM and what is the impact of this? For example, what is the impact of making it the default option (with consent from the older person) to involve designated family members in consultations and discussions about treatment options? What models work best, what would be the uptake and how would it affect satisfaction and patient outcomes?
-
What service models are most likely to support SDM? For example, does moving away from disease-related checks in primary care to a more holistic and team-based regular review increase SDM and improve patient outcomes?
-
How can health and care professionals other than doctors be involved in SDM?
-
What is the impact of training members of the MDT to act as decision coaches for older people with complex health and care needs? Who should act as a coach and at what stage should coaching be provided?
-
What is happening in SDM conversations involving older people and how are PDAs being used and to what effect? Can modes of communication, other than face to face, be effective?
-
Can decision aids be developed for use with older people with multiple health and care needs? For example, rather than focusing on individual conditions, can SDM be used to look more generally at the overall treatment burden for the older person and their family members?
-
How can patient decisions, goals and preferences be best recorded and communicated between different team members in integrated care sites?
-
What would be the impact of overt discussions about prognosis? Would knowing more about an individual’s views about coming to the end of their life shape decisions?
-
How does working in a more patient-centred way, with a focus on SDM, affect health-care providers’ experience and satisfaction?
Acknowledgements
We would like to acknowledge the contribution of Ms Sue Davies who worked as a researcher on this project. We would like to thank our Project Advisory Group, Dr Geoff Wong (chairperson), Mrs Jane Hopkins, Mrs Jeanne Carlin and Ms Natalie Koussa; and PPI members Dr Paul Millac and Ms Marion Crowe for their support and guidance.
Contributions of authors
Professor Frances Bunn (Professor, Health and Complex Conditions) was the principal investigator, led the study, was involved in all aspects of the review process and was the lead author of this report.
Professor Claire Goodman (Professor, Health Services Research) was a co-applicant on the grant, was involved in study design, research team meetings and workshops, gave feedback between meetings and participated in the synthesis process and preparation of the final report.
Ms Bridget Russell (Research Assistant) assisted with project management, was involved in all aspects of the review process and participated in the preparation of the final report.
Professor Patricia Wilson (Professor, Primary and Community Care) was a co-applicant on the grant, was involved in review processes, attended research team meetings and workshops and participated in the preparation of the final report.
Professor Jill Manthorpe (Professor, Social Work) was a co-applicant on the grant, was involved in review processes, attended research team meetings and workshops and participated in the preparation of the final report.
Dr Greta Rait (Reader, Primary Care) was a co-applicant on the grant, was involved in study design, attended workshops and meetings, provided clinical expertise and participated in the preparation of the final report.
Dr Isabel Hodkinson (Tower Hamlets Clinical Commissioning Group) was a co-applicant on the grant, was involved in study design, attended workshops and meetings and provided clinical expertise.
Dr Marie-Anne Durand (Assistant Professor, Health Policy and Clinical Practice) was involved in review processes, provided expertise on SDM and participated in the preparation of the final report.
Data-sharing statement
All available data are contained in Report Supplementary Material 1–4 of the report. All queries should be submitted to the corresponding author.
Publication
Bunn F, Goodman C, Russell B, Wilson P, Manthorpe J, Rait G, Hodkinson I, Durand MA. Supporting shared decision making for older people with multiple health and social care needs: a realist synthesis. BMC Geriatrics 2018;18:165. URL: https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-018-0853-9
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Shaw S, Rosen R, Rumbold B. What Is Integrated Care? 2011. www.nuffieldtrust.org.uk/sites/files/nuffield/publication/what_is_integrated_care_research_report_june11.pdf (accessed 1 July 2017).
- Frampton S, Guastello S, Brady C, Hale M, Horowitz S, Bennett Smith S, et al. Patient-Centered Care: Improvement Guide 2008. www.patient-centeredcare.org (accessed on 1 May 2018).
- Jurgens FJ, Clissett P, Gladman JR, Harwood RH. Why are family carers of people with dementia dissatisfied with general hospital care? A qualitative study. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-57.
- Johnson B, Conway J, Edgman-Levitan S, Sodomka P, Schucter J, Ford D, et al. Partnering with Patients and Families To Design a Patient- and Family-Centered Health Care System: A Roadmap for the Future. A Work in Progress. Bethesda, MD: Institute for Family-Centered Care and Institute for Healthcare Improvement; 2008.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. https://doi.org/10.1186/1471-2288-6-35.
- National Evaluation of the Department of Health’s Integrated Care Pilots. Cambridge: RAND Europe; 2012.
- Goodman C, Drennan V, Manthorpe J, Gage H, Trivedi D, Shah D, et al. A Study of the Effectiveness of Inter-Professional Working for Community Dwelling Older People: Final Report – NIHR Service Delivery and Organisation Programme, 2011 2012.
- Five Year Forward View. Leeds: NHS England; 2014.
- Coulter A, Collins A. Making Shared Decision-making a Reality: No Decision About me, Without me. London: The King’s Fund; 2011.
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997;44:681-92. https://doi.org/10.1016/S0277-9536(96)00221-3.
- Veatch RM. Models for ethical medicine in a revolutionary age. What physician–patient roles foster the most ethical relationship?. Hastings Cent Rep 1972;2:5-7. https://doi.org/10.2307/3560825.
- Härter M, Moumjid N, Cornuz J, Elwyn G, van der Weijden T. Shared decision making in 2017: International accomplishments in policy, research and implementation. Z Evid Fortbild Qual Gesundhwes 2017;123–4:1-5. https://doi.org/10.1016/j.zefq.2017.05.024.
- Stiggelbout AM, Pieterse AH, De Haes JC. Shared decision making: concepts, evidence, and practice. Patient Educ Couns 2015;98:1172-9. https://doi.org/10.1016/j.pec.2015.06.022.
- Emanuel EJ, Emanuel LL. Four models of the physician–patient relationship. J Am Med Assoc 1992;267:2221-26. https://doi.org/10.1001/jama.1992.03480160079038.
- Wennberg JE, Barnes BA, Zubkoff M. Professional uncertainty and the problem of supplier-induced demand. Soc Sci Med 1982;16:811-24. https://doi.org/10.1016/0277-9536(82)90234-9.
- Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med 1999;49:651-61. https://doi.org/10.1016/S0277-9536(99)00145-8.
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012;27:1361-7. https://doi.org/10.1007/s11606-012-2077-6.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med 2000;51:1087-110. https://doi.org/10.1016/S0277-9536(00)00098-8.
- Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ 1999;319:766-71. https://doi.org/10.1136/bmj.319.7212.766.
- Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;4. https://doi.org/10.1002/14651858.CD001431.pub5.
- Elwyn G, Edwards A, Kinnersley P. Shared decision-making in primary care: the neglected second half of the consultation. Br J Gen Pract 1999;49:477-82.
- Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract 2000;50:892-9.
- Barry MJ, Edgman-Levitan S. Shared decision making – the pinnacle of patient-centered care. N Engl J Med 2012;366:780-1. https://doi.org/10.1056/NEJMp1109283.
- National Diabetes Support Team . Getting to Grips With the Year of Care: A Practical Guide 2008.
- Duquemin A. Year of Care Report of Findings from the Pilot Programme. Gateshead: Year of Care Partnerships; 2011.
- Taylor A. Building the House of Care: How Health Economies in Leeds and Somerset are Implementing a Coordinated Approach for People with Long-term Conditions. London: The Health Foundation; 2015.
- Coulter A, Kramer G, Warren T, Salisbury C. Building the House of Care for people with long-term conditions: the foundation of the House of Care framework. Br J Gen Pract 2016;66:e288-90. https://doi.org/10.3399/bjgp16X684745.
- Mathers N, Paynton D. Rhetoric and reality in person-centred care: introducing the House of Care framework. Br J Gen Pract 2016;66:12-3. https://doi.org/10.3399/bjgp16X683077.
- Person-centred Approaches: Empowering People in their Lives and Communities to Enable an Upgrade in Prevention, Wellbeing, Health, Care and Support. Leeds: Skills for Care, Skills for Health; 2017.
- Collaborative Care and Support Planning: Ready to be a Reality. London: Royal College of General Practitioners; 2014.
- The Glenpark Story: Implementing Care and Support Planning for People with Long Term Conditions. Gateshead: Year of Care Partnerships; 2016.
- Hannan R, Thompson R, Worthington A, Rooney P. The Triangle of Care. Carers Included: A Guide to Best Practice for Dementia Care. London: Carers Trust; 2013.
- The Year of Care Partnership Programme: Working Together for Better Healthcare and Self Care. Tyneside; 2014.
- Jamieson M, Grealish L, Brown J-A, Draper B. Carers: The navigators of the maze of care for people with dementia – a qualitative study. Dementia 2014;15:1112-23.
- Guthrie B, Saultz JW, Freeman GK, Haggerty JL. Continuity of care matters. BMJ 2008;337. https://doi.org/10.1136/bmj.a867.
- Sansoni J, Grootemaat P, Seraji M, Blanchard M, Snoek M. Targeting Integrated Care to those Most Likely to Need Frequent Health Care: A Review of Social and Clinical Risk Factors. Woollongong, NSW: Centre for Health Service Development, Australian Health Services Research Institute, University of Wollongong; 2015.
- Sinclair AJ, Hillson R, Bayer AJ. National Expert Working Group . Diabetes and dementia in older people: a Best Clinical Practice Statement by a multidisciplinary National Expert Working Group. Diabet Med 2014;31:1024-31. https://doi.org/10.1111/dme.12467.
- Sinclair A, Morley JE, Rodriguez-Mañas L, Paolisso G, Bayer T, Zeyfang A, et al. Diabetes mellitus in older people: position statement on behalf of the International Association of Gerontology and Geriatrics (IAGG), the European Diabetes Working Party for Older People (EDWPOP), and the International Task Force of Experts in Diabetes. J Am Med Dir Assoc 2012;13:497-502. https://doi.org/10.1016/j.jamda.2012.04.012.
- Leppin AL, Montori VM, Gionfriddo MR. Minimally disruptive medicine: a pragmatically comprehensive model for delivering care to patients with multiple chronic conditions. Healthcare 2015;3:50-63. https://doi.org/10.3390/healthcare3010050.
- Demain S, Gonçalves AC, Areia C, Oliveira R, Marcos AJ, Marques A, et al. Living with, managing and minimising treatment burden in long term conditions: a systematic review of qualitative research. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0125457.
- May C, Montori VM, Mair FS. We need minimally disruptive medicine. BMJ 2009;339. https://doi.org/10.1136/bmj.b2803.
- Ridgeway JL, Egginton JS, Tiedje K, Linzer M, Boehm D, Poplau S, et al. Factors that lessen the burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Prefer Adherence 2014;8:339-51. https://doi.org/10.2147/PPA.S58014.
- Integrated Care: Our Shared Commitment. London: Department of Health and Social Care; 2013.
- Next Steps on the NHS Five Year Forward View. Leeds: NHS England; 2017.
- Charles A. Developing Accountable Care Systems: Lessons from Canterbury, New Zealand. London: The King’s Fund; 2017.
- Ham C, Heenan D, Longley M, Steel DR. Integrated Care in Northern Ireland, Scotland and Wales: Lessons for England. London: The King’s Fund; 2013.
- Ham C. Next steps on the NHS five year forward view. BMJ 2017;357. https://doi.org/10.1136/bmj.j1678.
- A Framework for Delivering Integrated Health and Social Care for Older People with Complex Needs. Cardiff: Welsh Government; 2014.
- Health and Social Care Delivery Plan. Scottish Government; 2016.
- Goodwin N, Dixon A, Anderson G, Wodchis W. Providing Integrated Care for Older People with Complex Needs: Lessons from seven international case studies. London: The King’s Fund; 2014.
- Eaton S, Oliver L, Roberts S. House of care approach for patients with long term conditions works at the local level. BMJ 2013;347. https://doi.org/10.1136/bmj.f7359.
- Coulter A, Roberts S, Dixon A. Delivering Better Services for People with Long-term Conditions: Building the House of Care. London: The King’s Fund; 2013.
- Goodwin N, Smith J, Davies A, Perry C, Rosen R, Dixon A, et al. Integrated Care for Patients and Populations: Improving Outcomes by Working Together: A Report to the Department of Health and the NHS Future Forum. London: The King’s Fund and Nuffield Trust; 2012.
- National Voices . Six Principles for Engaging People and Communities 2016. www.nationalvoices.org.uk/publications/our-publications/six-principles-engaging-people-and-communities (accessed 3 August 2017).
- NHS England . Integrated Primary and Acute Care Systems (PACS) – Describing the Care Model and the Business Model 2016.
- The Multi-specialty Community Provider (MCP) Emerging Care Model and Contract Framework. Leeds: NHS England; 2016.
- Banerjee S. Multimorbidity – older adults need health care that can count past one. Lancet 2015;385:587-9. https://doi.org/10.1016/S0140-6736(14)61596-8.
- Bunn F, Burn A, Goodman C, Robinson L, Rait G, Norton S, et al. Comorbidity and dementia: a mixed method study on improving health care for people with dementia (CoDem). Health Serv Deliv Res 2016;4.
- Gagnon LM, Patten SB. Major depression and its association with long-term medical conditions. Can J Psychiatry 2002;47:149-52. https://doi.org/10.1177/070674370204700204.
- Freeman GK, Woloshynowych M, Baker R, Boulton M, Guthrie B, Car J, et al. Continuity of Care 2006: What Have We Learned Since 2000 and What Are Policy Imperatives Now? 2007. www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1609-138_V01.pdf (accessed 20 November 2017).
- Bunn F, Burn AM, Goodman C, Rait G, Norton S, Robinson L, et al. Comorbidity and dementia: a scoping review of the literature. BMC Med 2014;12. https://doi.org/10.1186/s12916-014-0192-4.
- Robinson L, Dickinson C, Rousseau N, Beyer F, Clark A, Hughes J, et al. A systematic review of the effectiveness of advance care planning interventions for people with cognitive impairment and dementia. Age Ageing 2012;41:263-9. https://doi.org/10.1093/ageing/afr148.
- Naik AD, Martin LA, Moye J, Karel MJ. Health values and treatment goals of older, multimorbid adults facing life-threatening illness. J Am Geriatr Soc 2016;64:625-31. https://doi.org/10.1111/jgs.14027.
- Heaton J, Corden A, Parker G. ‘Continuity of care’: a critical interpretive synthesis of how the concept was elaborated by a national research programme. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.794.
- Parker G, Corden A, Heaton J. Synthesis and Conceptual Analysis of the SDO Programme’s Research on Continuity of Care. York: Social Policy Research Unit, University of York; 2009.
- Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Syst Rev 2015;3. https://doi.org/10.1002/14651858.CD010523.pub2.
- Sinnott C, Mc Hugh S, Browne J, Bradley C. GPs’ perspectives on the management of patients with multimorbidity: systematic review and synthesis of qualitative research. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003610.
- Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making 2015;35:114-31. https://doi.org/10.1177/0272989X14551638.
- Durand MA, Carpenter L, Dolan H, Bravo P, Mann M, Bunn F, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0094670.
- Bunn F, Goodman C, Manthorpe J, Durand MA, Hodkinson I, Rait G, et al. Supporting shared decision-making for older people with multiple health and social care needs: a protocol for a realist synthesis to inform integrated care models. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014026.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-33.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Bunn F, Goodman C, Wilson P, Manthorpe J, Rait G, Hodgkinson I, et al. PROSPERO database. York: Centre for Reviews and Dissemination University of York; 2016.
- Pawson R. Evidence-based Policy: A Realist Perspective. London: Sage Publications Ltd; 2006.
- Realist Synthesis: An Introduction. Manchester: Economic and Social Research Council (ESRC) Research Methods Programme, University of Manchester; 2004.
- Pawson R, Greenhalgh J, Brennan C, Glidewell L. Do reviews of healthcare interventions teach us how to improve healthcare systems? The depth ontology of demand management. Soc Sci Med 2014;114:129-37. https://doi.org/10.1016/j.socscimed.2014.05.032.
- Kastner M, Estey E, Perrier L, Graham ID, Grimshaw J, Straus SE, et al. Understanding the relationship between the perceived characteristics of clinical practice guidelines and their uptake: protocol for a realist review. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-69.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. https://doi.org/10.1111/j.1468-0009.2012.00665.x.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage Publications Ltd; 2013.
- Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363-81. https://doi.org/10.1177/1098214010371972.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications Ltd; 1997.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Syntheses: Evolving Standards) project. Health Serv Deliv Res 2014;2.
- Agoritsas T, Heen AF, Brandt L, Alonso-Coello P, Kristiansen A, Akl EA, et al. Decision aids that really promote shared decision making: the pace quickens. BMJ 2015;350. https://doi.org/10.1136/bmj.g7624.
- Légaré F, Stacey D, Gagnon S, Dunn S, Pluye P, Frosch D, et al. Validating a conceptual model for an inter-professional approach to shared decision making: a mixed methods study. J Eval Clin Pract 2011;17:554-64. https://doi.org/10.1111/j.1365-2753.2010.01515.x.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academic Press; 2001.
- McCormack B, McCane T. Person-Centred Practice in Nursing and Health Care: Theory and Practice. Oxford: Wiley-Blackwell; 2016.
- D’Amour D, Ferrada-Videla M, San Martin Rodriguez L, Beaulieu MD. The conceptual basis for interprofessional collaboration: core concepts and theoretical frameworks. J Interprof Care 2005;19:116-31. https://doi.org/10.1080/13561820500082529.
- Légaré F, Stacey D, Graham ID, Elwyn G, Pluye P, Gagnon MP, et al. Advancing theories, models and measurement for an interprofessional approach to shared decision making in primary care: a study protocol. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-2.
- Gittell JH, Suchmann AL, Cameron K, Spreitzer G. Oxford Handbook of Positive Organizational Scholarship. Oxford: Oxford University Press; 2011.
- Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff 2013;32:223-31. https://doi.org/10.1377/hlthaff.2012.1133.
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005-26. https://doi.org/10.1111/j.1475-6773.2004.00269.x.
- Hibbard JH. Patient activation and the use of information to support informed health decisions. Patient Educ Couns 2017;100:5-7. https://doi.org/10.1016/j.pec.2016.07.006.
- Légaré F, Ratté S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns 2008;73:526-35. https://doi.org/10.1016/j.pec.2008.07.018.
- Légaré F, Turcotte S, Stacey D, Ratté S, Kryworuchko J, Graham ID. Patients’ perceptions of sharing in decisions: a systematic review of interventions to enhance shared decision making in routine clinical practice. Patient 2012;5:1-19. https://doi.org/10.2165/11592180-000000000-00000.
- Angel S, Frederiksen KN. Challenges in achieving patient participation: a review of how patient participation is addressed in empirical studies. Int J Nurs Stud 2015;52:1525-38. https://doi.org/10.1016/j.ijnurstu.2015.04.008.
- Clyne B, Bradley M, Hughes C, Fahey T, Lapane KL. Electronic prescribing and other forms of technology to reduce inappropriate medication use and polypharmacy in older people: a review of current evidence (provisional abstract). Clin Geriatr Med 2012;28:301-22. https://doi.org/10.1016/j.cger.2012.01.009.
- Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev 2010;1. https://doi.org/10.1002/14651858.CD007297.pub2.
- Holm AL, Berland AK, Severinsson E. Older patients’ involvement in shared decision-making – a systematic review. Open J Nurs 2016;6:170-85. https://doi.org/10.4236/ojn.2016.63018.
- Hyde C, Dunn KM, Higginbottom A, Chew-Graham CA. Process and impact of patient involvement in a systematic review of shared decision-making in primary care consultations. Health Expect 2017;20:298-30.
- Joosten EAG, DeFuentes-Merillas L, de Weert GH, Sensky T, van der Staak CPF, de Jong CAJ. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom 2008;77:219-26. https://doi.org/10.1159/000126073.
- Kogan AC, Wilber K, Mosqueda L. Person-centered care for older adults with chronic conditions and functional impairment: a systematic literature review. J Am Geriatr Soc 2016;64:e1-7. https://doi.org/10.1111/jgs.13873.
- Mavis B, Holmes Rovner M, Jorgenson S, Coffey J, Anand N, Bulica E, et al. Patient participation in clinical encounters: a systematic review to identify self-report measures. Health Expect 2015;18:1827-43. https://doi.org/10.1111/hex.12186.
- Austin CA, Mohottige D, Sudore RL, Smith AK, Hanson LC. Tools to promote shared decision making in serious illness: a systematic review. JAMA Intern Med 2015;175:1213-21. https://doi.org/10.1001/jamainternmed.2015.1679.
- Bélanger E, Rodríguez C, Groleau D. Shared decision-making in palliative care: a systematic mixed studies review using narrative synthesis. Palliat Med 2011;25:242-61. https://doi.org/10.1177/0269216310389348.
- Bratzke LC, Muehrer RJ, Kehl KA, Lee KS, Ward EC, Kwekkeboom KL. Self-management priority setting and decision-making in adults with multimorbidity: a narrative review of literature. Int J Nurs Stud 2015;52:744-55. https://doi.org/10.1016/j.ijnurstu.2014.10.010.
- Clayman ML, Bylund CL, Chewning B, Makoul G. The impact of patient participation in health decisions within medical encounters: a systematic review. Med Decis Making 2016;36:427-52. https://doi.org/10.1177/0272989X15613530.
- Couët N, Desroches S, Robitaille H, Vaillancourt H, Leblanc A, Turcotte S, et al. Assessments of the extent to which health-care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expect 2015;18:542-61. https://doi.org/10.1111/hex.12054.
- Coylewright M, Branda M, Inselman JW, Shah N, Hess E, LeBlanc A, et al. Impact of sociodemographic patient characteristics on the efficacy of decision AIDS: a patient-level meta-analysis of 7 randomized trials. Circ Cardiovasc Qual Outcomes 2014;7:360-7. https://doi.org/10.1161/HCQ.0000000000000006.
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-001570.
- Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD003267.pub2.
- Dy SM, Purnell TS. Key concepts relevant to quality of complex and shared decision-making in health care: a literature review. Soc Sci Med 2012;74:582-7. https://doi.org/10.1016/j.socscimed.2011.11.015.
- Edwards M, Davies M, Edwards A. What are the external influences on information exchange and shared decision-making in healthcare consultations: a meta-synthesis of the literature. Patient Educ Couns 2009;75:37-52. https://doi.org/10.1016/j.pec.2008.09.025.
- Elliott J, McNeil H, Ashbourne J, Huson K, Boscart V, Stolee P. Engaging older adults in health care decision-making: a realist synthesis. Patient 2016;9:383-93. https://doi.org/10.1007/s40271-016-0168-x.
- Elwyn G, Scholl I, Tietbohl C, Mann M, Edwards AG, Clay C, et al. ‘Many miles to go …’: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-S2-S14.
- Fagerlin A, Pignone M, Abhyankar P, Col N, Feldman-Stewart D, Gavaruzzi T, et al. Clarifying values: an updated review. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-S2-S8.
- Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns 2014;94:291-309. https://doi.org/10.1016/j.pec.2013.10.031.
- Land V, Parry R, Seymour J. Communication practices that encourage and constrain shared decision making in health-care encounters: systematic review of conversation analytic research. Health Expect 2017;20:1228-47. https://doi.org/10.1111/hex.12557.
- Légaré F, Stacey D, Turcotte S, Cossi MJ, Kryworuchko J, Graham ID, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev 2014;9. https://doi.org/10.1002/14651858.CD006732.pub3.
- Miller LM, Whitlatch CJ, Lyons KS. Shared decision-making in dementia: a review of patient and family carer involvement. Dementia 2014;15:1141-57. https://doi.org/10.1177/1471301214555542.
- Stacey D, Kryworuchko J, Belkora J, Davison BJ, Durand MA, Eden KB, et al. Coaching and guidance with patient decision aids: a review of theoretical and empirical evidence. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-S2-S11.
- van Weert JC, van Munster BC, Sanders R, Spijker R, Hooft L, Jansen J. Decision aids to help older people make health decisions: a systematic review and meta-analysis. BMC Med Inform Decis Mak 2016;16. https://doi.org/10.1186/s12911-016-0281-8.
- Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals’ perceptions. Implement Sci 2006;1.
- O’Connor AM, Bennett C, Stacey D, Barry MJ, Col NF, Eden KB, et al. Do patient decision aids meet effectiveness criteria of the international patient decision aid standards collaboration? A systematic review and meta-analysis. Med Decis Mak 2007;27:554-74.
- Thompson-Leduc P, Clayman ML, Turcotte S, Légaré F. Shared decision-making behaviours in health professionals: a systematic review of studies based on the Theory of Planned Behaviour. Health Expect 2015;18:754-7. https://doi.org/10.1111/hex.12176.
- Fraccaro P, Fraccaro P, Arguello Casteleiro M, Buchan I. Adoption of clinical decision support in multimorbidity: a systematic review. JMIR Med Informat 2015;3. https://doi.org/10.2196/medinform.3503.
- Hinsliff-Smith K, Feakes R, Whitworth G, Seymour J, Moghaddam N, Dening T, et al. What do we know about the application of the Mental Capacity Act (2005) in healthcare practice regarding decision-making for frail and older people? A systematic literature review. Health Soc Care Community 2017;25:295-308.
- Choosing Wisely. London: Academy of Medical Royal Colleges; 2015.
- Edwards A, Elwyn G, Hood K, Robling M, Atwell C, Holmes-Rovner M, et al. The development of COMRADE – a patient-based outcome measure to evaluate the effectiveness of risk communication and treatment decision making in consultations. Patient Educ Couns 2003;50:311-22. https://doi.org/10.1016/S0738-3991(03)00055-7.
- Edwards A, Elwyn G, Hood K, Atwell C, Robling M, Houston H, et al. Patient-based outcome results from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract 2004;21:347-54. https://doi.org/10.1093/fampra/cmh402.
- Elwyn G, Edwards A, Gwyn R, Grol R. Towards a feasible model for shared decision-making: focus group study with general practice registrars. BMJ 1999;319. https://doi.org/10.1136/bmj.319.7212.753.
- Elwyn G. Idealistic, impractical, impossible? Shared decision-making in the real world. Br J Gen Pract 2006;56:403-4.
- Elwyn G, Loyd A, May C, van der Wiejden T, Stiggelbout A, Edwards A, et al. Collaborative deliberation: a model for patient care. Patient Educa Couns 2014;97:158-64. https://doi.org/10.1016/j.pec.2014.07.027.
- Fried TR, Tinetti ME, Iannone L, O’Leary JR, Towle V, Van Ness PH. Health outcome prioritization as a tool for decision making among older persons with multiple chronic conditions. Arch Intern Med 2011;171:1854-6. https://doi.org/10.1001/archinternmed.2011.424.
- Légaré F, Politi MC, Drolet R, Desroches S, Stacey D, Bekker H. the SDM-CPD team . Training health professionals in shared decision-making: an international environmental scan. Patient Educ Couns 2012;88:159-6. https://doi.org/10.1016/j.pec.2012.01.002.
- Légaré F, Moumjid-Ferdjaoui N, Drolet R, Stacey D, Harter M, Bastian M, et al. Core competencies for shared decision making training programs: insights from an international, interdisciplinary working group. J Contin Educ Health Prof 2013;33:267-73. https://doi.org/10.1002/chp.21197.
- Légaré F, O’Connor A, Graham I, Wells G, Tremblay S. Impact of the Ottawa Decision Support Framework on the agreement and the difference between patients’ and physicians’ decisional conflict. Med Decis Making 2006;26:373-90. https://doi.org/10.1177/0272989X06290492.
- Légaré F, Stacey D, Briére N, Robitaille H, Lord MC, Desroches S, et al. An interprofessional approach to shared decision making: an exploratory case study with family caregivers of one IP home care team. BMC Geriatr 2014;14. https://doi.org/10.1186/1471-2318-14-83.
- Leng G. Shared Decision Making Collaborative: A Consensus Statement. London: National Institute for Health and Care Excellence; 2015.
- May CR, Eton DT, Boehmer K, Gallacher K, Hunt K, MacDonald S, et al. Rethinking the patient: using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-281.
- Muth C, van den Akker A, Blom JW, Mallen CD, Rochon J, Schellevis FG, et al. The Ariadne principles: how to handle multimorbidity in primary care consultations. BMC Med 2014;12. https://doi.org/10.1186/s12916-014-0223-1.
- Robben SHM, Heinen MM, Perry M, van Achterberg T, Olde Rikkert MG, Schers HJ, et al. First experiences with a two-step method for discussing goals with community-dwelling frail older people. Health Expect 2015;18:1559-66. https://doi.org/10.1111/hex.12145.
- Schulman-Green DJ, Naik AD, Bradley EH, McCorkle R, Bogardus ST. Goal setting as a shared decision-making strategy among clinicians and their older patients. Patient Educ Couns 2006;63:145-51.
- Jansen J, Naganathan V, Carter SM, McLachlan AJ, Nickel B, Irwig L, et al. Too much medicine in older people? Deprescribing through shared decision making. BMJ 2016;353. https://doi.org/10.1136/bmj.i2893.
- Légaré F, Stacey D, Pouliot S, Gauvin FP, Desroches S, Kryworuchko J, et al. Interprofessionalism and shared decision-making in primary care: a stepwise approach towards a new model. J Interprof Care 2011;25:18-25. https://doi.org/10.3109/13561820.2010.490502.
- Légaré F, Hébert J, Goh L, Lewis KB, Leiva Portocarrero ME, Robitaille H, et al. Do choosing wisely tools meet criteria for patient decision aids? A descriptive analysis of patient materials. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011918.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Pearson M, Brand SL, Quinn C, Shaw J, Maguire M, Michie S, et al. Using realist review to inform intervention development: methodological illustration and conceptual platform for collaborative care in offender mental health. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0321-2.
- Ford JA, Wong G, Jones AP, Steel N. Access to primary care for socioeconomically disadvantaged older people in rural areas: a realist review. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010652.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Pawson R. Evidence-based Policy: The Promise of ‘Realist Synthesis’. Evaluation 2002;8:340-58. http://evi.sagepub.com/cgi/doi/10.1177/135638902401462448 (accessed 2 May 2014).
- Rycroft-Malone J, Burton C, Hall B, McCormack B, Nutley S, Seddon D, et al. Improving skills and care standards in the support workforce for older people: a realist review. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005356.
- Wong G, Pawson R, Owen L. Policy guidance on threats to legislative interventions in public health: a realist synthesis. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-222.
- Belkora JK, Loth MK, Chen DF, Chen JY, Volz S, Esserman LJ. Monitoring the implementation of Consultation Planning, Recording, and Summarizing in a breast care center. Patient Educ Couns 2008;73:536-43. https://doi.org/10.1016/j.pec.2008.07.037.
- Berntsen GK, Gammon D, Steinsbekk A, Salamonsen A, Foss N, Ruland C, et al. How do we deal with multiple goals for care within an individual patient trajectory? A document content analysis of health service research papers on goals for care. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009403.
- Blom J, den Elzen W, van Houwelingen AH, Heijmans M, Stijnen T, Van den Hout W, et al. Effectiveness and cost-effectiveness of a proactive, goal-oriented, integrated care model in general practice for older people. A cluster randomised controlled trial: Integrated Systematic Care for older People – the ISCOPE study. Age Ageing 2016;45:30-41. https://doi.org/10.1093/ageing/afv174.
- Bookey-Bassett S, Markle-Reid M, Mckey CA, Akhtar-Danesh N. Understanding interprofessional collaboration in the context of chronic disease management for older adults living in communities: a concept analysis. J Adv Nurs 2017;73:71-84. https://doi.org/10.1111/jan.13162.
- Bridges J, Hughes J, Farrington N, Richardson A. Cancer treatment decision-making processes for older patients with complex needs: a qualitative study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009674.
- Bugge C, Entwistle VA, Watt IS. The significance for decision-making of information that is not exchanged by patients and health professionals during consultations. Soc Sci Med 2006;63:2065-78. https://doi.org/10.1016/j.socscimed.2006.05.010.
- Bynum JP, Barre L, Reed C, Passow H. Participation of very old adults in health care decisions. Med Decis Making 2014;34:216-30. https://doi.org/10.1177/0272989X13508008.
- Chong WW, Aslani P, Chen TF. Shared decision-making and interprofessional collaboration in mental healthcare: a qualitative study exploring perceptions of barriers and facilitators. J Interprof Care 2013;27:373-9. https://doi.org/10.3109/13561820.2013.785503.
- Chong WW, Aslani P, Chen TF. Multiple perspectives on shared decision-making and interprofessional collaboration in mental healthcare. J Interprof Care 2013;27:223-30. https://doi.org/10.3109/13561820.2013.767225.
- Cramm JM, Nieboer AP. The changing nature of chronic care and coproduction of care between primary care professionals and patients with COPD and their informal caregivers. Int J Chron Obstruct Pulmon Dis 2016;11:175-82. https://doi.org/10.2147/COPD.S94409.
- Cramm JM, Nieboer AP. In the Netherlands, rich interaction among professionals conducting disease management led to better chronic care. Health Aff 2012;31:2493-500. https://doi.org/10.1377/hlthaff.2011.1304.
- Cramm JM, Nieboer AP. A longitudinal study to identify the influence of quality of chronic care delivery on productive interactions between patients and (teams of) healthcare professionals within disease management programmes. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005914.
- Dardas AZ, Stockburger C, Boone S, An T, Calfee RP. Preferences for shared decision making in older adult patients with orthopedic hand conditions. J Hand Surg Am 2016;41:978-87. https://doi.org/10.1016/j.jhsa.2016.07.096.
- Durand M-A, Barr PJ, Walsh T, Elwyn G. Incentivizing shared decision making in the USA – where are we now?. Healthc (Amst) 2015;3:97-101. https://doi.org/10.1016/j.hjdsi.2014.10.008.
- Elwyn G, Edwards A, Hood K, Robling M, Atwell C, Russell I, et al. Achieving involvement: process outcomes from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract 2004;21:337-46. https://doi.org/10.1093/fampra/cmh401.
- Farrelly S, Lester H, Rose D, Birchwood M, Marshall M, Waheed W, et al. Barriers to shared decision making in mental health care: qualitative study of the Joint Crisis Plan for psychosis. Health Expect 2016;19:448-58. https://doi.org/10.1111/hex.12368.
- Fried TR, O’Leary J, Van Ness P, Fraenkel L. Inconsistency over time in the preferences of older persons with advanced illness for life-sustaining treatment. J Am Geriatr Soc 2007;55:1007-14. https://doi.org/10.1111/j.1532-5415.2007.01232.x.
- Gleason KT, Tanner EK, Boyd CM, Saczynski JS, Szanton SL. Factors associated with patient activation in an older adult population with functional difficulties. Patient Educ Couns 2016;99:1421-6. https://doi.org/10.1016/j.pec.2016.03.011.
- Grim K, Rosenberg D, Svedberg P, Schön UK. Shared decision-making in mental health care – a user perspective on decisional needs in community-based services. Int J Qual Stud Health Well-Being 2016;11. https://doi.org/10.3402/qhw.v11.30563.
- Groen-van de Ven L, Smits C, Span M, Jukema J, Coppoolse K, de Lange J, et al. The challenges of shared decision making in dementia care networks [published online ahead of print 9 September 2016]. Int Psychogeriatr 2016. www.cambridge.org/core/journals/international-psychogeriatrics/article/challenges-of-shared-decision-making-in-dementia-care-networks/78CBFC293C95644BC6A39B2E423EF32B (accessed 17 May 2018).
- Hacking B, Wallace L, Scott S, Kosmala-Anderson J, Belkora J, McNeill A. Testing the feasibility, acceptability and effectiveness of a ‘decision navigation’ intervention for early stage prostate cancer patients in Scotland – a randomised controlled trial. Psycho-Oncology 2013;22:1017-24. https://doi.org/10.1002/pon.3093.
- Hart JL, Pflug E, Madden V, Halpern SD. Thinking forward: future-oriented thinking among patients with tobacco-associated thoracic diseases and their surrogates. Am J Respir Crit Care Med 2016;193:321-9. https://doi.org/10.1164/rccm.201505-0882OC.
- Herlitz A, Munthe C, Törner M, Forsander G. The counseling, self-care, adherence approach to person-centered care and shared decision making: moral psychology, executive autonomy, and ethics in multi-dimensional care decisions. Health Commun 2016;31:964-73. https://doi.org/10.1080/10410236.2015.1025332.
- Jones JB, Bruce CA, Shah NR, Taylor WF, Stewart WF. Shared decision making: using health information technology to integrate patient choice into primary care. Transl Behav Med 2011;1:123-33. https://doi.org/10.1007/s13142-011-0023-5.
- Joseph-Williams N, Lloyd A, Edwards A, Stobbart L, Tomson D, Macphail S, et al. Implementing shared decision making in the NHS: lessons from the MAGIC programme. BMJ 2017;357. https://doi.org/10.1136/bmj.j1744.
- Körner M, Ehrhardt H, Steger AK. Designing an interprofessional training program for shared decision making. J Interprof Care 2013;27:146-54. https://doi.org/10.3109/13561820.2012.711786.
- Kuluski K, Gill A, Naganathan G, Upshur R, Jaakkimainen RL, Wodchis WP. A qualitative descriptive study on the alignment of care goals between older persons with multi-morbidities, their family physicians and informal caregivers. BMC Fam Pract 2013;14. https://doi.org/10.1186/1471-2296-14-133.
- Ladin K, Lin N, Hahn E, Zhang G, Koch-Weser S, Weiner DE. Engagement in decision-making and patient satisfaction: a qualitative study of older patients’ perceptions of dialysis initiation and modality decisions. Nephrol Dial Transplant 2016;8:1-8. https://doi.org/10.1093/ndt/gfw307.
- Mercer SW, O’Brien R, Fitzpatrick B, Higgins M, Guthrie B, Watt G, et al. The development and optimisation of a primary care-based whole system complex intervention (CARE Plus) for patients with multimorbidity living in areas of high socioeconomic deprivation. Chronic Illn 2016;12:165-81. https://doi.org/10.1177/1742395316644304.
- Politi MC, Street RL. The importance of communication in collaborative decision making: facilitating shared mind and the management of uncertainty. J Eval Clin Pract 2011;17:579-84. https://doi.org/10.1111/j.1365-2753.2010.01549.x.
- Robben S, van Kempen J, Heinen M, Zuidema S, Olde Rikkert M, Schers H, et al. Preferences for receiving information among frail older adults and their informal caregivers: a qualitative study. Fam Pract 2012;29:742-7. https://doi.org/10.1093/fampra/cms033.
- Ruggiano N, Whiteman K, Shtompel N. ‘If I don’t like the way I feel with a certain drug, I’ll tell them.’: older adults’ experiences with self-determination and health self-advocacy. J Appl Gerontol 2016;35:401-20. https://doi.org/10.1177/0733464814527513.
- Sanders AR, Bensing JM, Essed MA, Magnée T, de Wit NJ, Verhaak PF. Does training general practitioners result in more shared decision making during consultations?. Patient Educ Couns 2016;100:563-74. https://doi.org/10.1016/j.pec.2016.10.002.
- Schaller S, Marinova-Schmidt V, Setzer M, Kondylakis H, Griebel L, Sedlmayr M, et al. Usefulness of a tailored eHealth Service for informal caregivers and professionals in the dementia treatment and care setting: the eHealthMonitor Dementia Portal. JMIR Res Protoc 2016;5. https://doi.org/10.2196/resprot.4354.
- Schaller S, Marinova-Schmidt V, Gobin J, Criegee-Rieck M, Griebel L, Engel S, et al. Tailored e-Health services for the dementia care setting: a pilot study of ‘eHealthMonitor’. BMC Med Inform Decis Mak 2015;15. https://doi.org/10.1186/s12911-015-0182-2.
- Shay LA, Lafata JE. Understanding patient perceptions of shared decision making. Patient Educ Couns 2014;96:295-301. https://doi.org/10.1016/j.pec.2014.07.017.
- Sheaff R, Halliday J, Byng R, Øvretveit J, Exworthy M, Peckham S, et al. Bridging the discursive gap between lay and medical discourse in care coordination. Sociol Health Illn 2017;39:1019-34. https://doi.org/10.1111/1467-9566.12553.
- Schuling J, Gebben H, Veehof LJ, Haaijer-Ruskamp FM. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-56.
- Baqir W, Hughes J, Jones T, Barrett S, Desai N, Copeland R, et al. Impact of medication review, within a shared decision-making framework, on deprescribing in people living in care homes. Eur J Hosp Pharm 2016;24:30-3. https://doi.org/10.1136/ejhpharm-2016-000900.
- van Summeren JJ, Haaijer-Ruskamp FM, Schuling J. Eliciting preferences of multimorbid elderly adults in family practice using an outcome prioritization tool. J Am Geriatr Soc 2016;64:e143-8. https://doi.org/10.1111/jgs.14415.
- Wrede-Sach J, Voigt I, Diederichs-Egidi H, Hummers-Pradier E, Dierks ML, Junius-Walker U. Decision-making of older patients in context of the doctor–patient relationship: a typology ranging from ‘self-determined’ to ‘doctor-trusting’ patients. Int J Family Med 2013;2013. https://doi.org/10.1155/2013/478498.
- Tietbohl CK, Rendle KA, Halley MC, May SG, Lin GA, Frosch DL. Implementation of patient decision support interventions in primary care: the role of relational coordination. Med Decis Making 2015;35:987-98. https://doi.org/10.1177/0272989X15602886.
- Zoffmann V, Harder I, Kirkevold M. A person-centered communication and reflection model: sharing decision-making in chronic care. Qual Health Res 2008;18:670-85. https://doi.org/10.1177/1049732307311008.
- Foot C, Gilburt H, Dunn P, Jabbal J, Seale B, Goodrich J, et al. People in Control of their own Health and Care: The State of Involvement. London: The King’s Fund; 2014.
- Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence. London: Royal College of General Practitioners; 2009.
- The Power of People. London: The Health Foundation; n.d.
- Lown BA, Kryworuchko J, Bieber C, Lillie DM, Kelly C, Berger B, et al. Continuing professional development for interprofessional teams supporting patients in healthcare decision making. J Interprof Care 2011;25:401-8. https://doi.org/10.3109/13561820.2011.583563.
- The Holmside Story: Person Centred Primary Care. Care and Support Planning. Newcastle upon Tyne: Year of Care; 2014.
- Col N, Bozzuto L, Kirkegaard P, Koelewijn-van Loon M, Majeed H, Jen Ng C, et al. Interprofessional education about shared decision making for patients in primary care settings. J Interprof Care 2011;25:409-15. https://doi.org/10.3109/13561820.2011.619071.
- Berger Z. Navigating the unknown: shared decision-making in the face of uncertainty. J Gen Intern Med 2015;30:675-8. https://doi.org/10.1007/s11606-014-3074-8.
- Barrett B, Ricco J, Wallace M, Kiefer D, Rakel D. Communicating statin evidence to support shared decision-making. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0436-9.
- Eaton S, Roberts S, Turner B. Delivering person centred care in long term conditions. BMJ 2015;350. https://doi.org/10.1136/bmj.h181.
- Clayman ML, Gulbrandsen P, Morris MA. A patient in the clinic; a person in the world. Why shared decision making needs to center on the person rather than the medical encounter. Patient Educ Couns 2017;100:600-4. https://doi.org/10.1016/j.pec.2016.10.016.
- Cooper Z, Koritsanszky LA, Cauley CE, Frydman JL, Bernacki RE, Mosenthal AC, et al. Recommendations for best communication practices to facilitate goal-concordant care for seriously ill older patients with emergency surgical conditions. Ann Surg 2016;263:1-6. https://doi.org/10.1097/SLA.0000000000001491.
- Gorin M, Joffe S, Dickert N, Halpern S. Justifying clinical nudges. Hastings Cent Rep 2017;47:32-8. https://doi.org/10.1002/hast.688.
- Bunn F, Goodman C, Russell B, Wilson P, Manthorpe J, Rait G, et al. Supporting shared decision making for older people with multiple health and social care needs: a realist synthesis. BMC Geriatrics 2018;18. https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-018-0853-9.
- Légaré F, Stacey D, Forest PG, Coutu MF. Moving SDM forward in Canada: milestones, public involvement, and barriers that remain. Z Evid Fortbild Qual Gesundhwes 2011;105:245-53. https://doi.org/10.1016/j.zefq.2011.04.011.
- Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, McDaniel SH, et al. Patient trust: is it related to patient-centered behavior of primary care physicians?. Med Care 2004;42:1049-55. https://doi.org/10.1097/00005650-200411000-00003.
- The NHS Constitution. London: Department of Health and Social Care; 2015.
- International Patient Decision Aid Standards . What Are Patient Decision Aids? n.d. http://ipdas.ohri.ca/what.html (accessed 8 July 2017).
- Bunn F, Burn AM, Robinson L, Poole M, Rait G, Brayne C, et al. Healthcare organisation and delivery for people with dementia and comorbidity: a qualitative study exploring the views of patients, carers and professionals. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013067.
- Shepherd HL, Barratt A, Trevena LJ, McGeechan K, Carey K, Epstein RM, et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: a cross-over trial. Patient Educ Couns 2011;84:379-85. https://doi.org/10.1016/j.pec.2011.07.022.
- Muscat DM, Shepherd HL, Morony S, Smith SK, Dhillon HM, Trevena L, et al. Can adults with low literacy understand shared decision making questions? A qualitative investigation. Patient Educ Couns 2016;99:1796-802. https://doi.org/10.1016/j.pec.2016.05.008.
- Joseph-Williams N, Edwards A, Elwyn G. Power imbalance prevents shared decision making. BMJ 2014;348. https://doi.org/10.1136/bmj.g3178.
- Reeve E, Low L-F, Hilmer SN. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol 2015;80:1254-68.
- Reeve E, Thompson W, Farrell B. Deprescribing: a narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. Eur J Intern Med 2017;38:3-11. https://doi.org/10.1016/j.ejim.2016.12.021.
- Oostendorp LJ, Durand MA, Lloyd A, Elwyn G. Measuring organisational readiness for patient engagement (MORE): an international online Delphi consensus study. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0717-3.
- Maskrey N, Gordon A. Shared understanding with patients. JAMA Intern Med 2017;177:1247-8. https://doi.org/10.1001/jamainternmed.2017.1932.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Lacouture A, Breton E, Guichard A, Ridde V. The concept of mechanism from a realist approach: a scoping review to facilitate its operationalization in public health program evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0345-7.
- Jagosh J, Pluye P, Wong G, Cargo M, Salsberg J, Bush PL, et al. Critical reflections on realist review: insights from customizing the methodology to the needs of participatory research assessment. Res Synth Methods 2014;5:131-41. https://doi.org/10.1002/jrsm.1099.
- Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff 2012;31:1030-8. https://doi.org/10.1377/hlthaff.2011.0576.
- Da Silva D. Helping People Share Decision Making. London: The Health Foundation; 2012.
- Trivedi D, Goodman C, Gage H, Baron N, Scheibl F, Iliffe S, et al. The effectiveness of inter-professional working for older people living in the community: a systematic review. Health Soc Care Community 2013;21:113-28. https://doi.org/10.1111/j.1365-2524.2012.01067.x.
- Reilly S, Miranda-Castillo C, Malouf R, Hoe J, Toot S, Challis D, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev 2015;1. https://doi.org/10.1002/14651858.CD008345.pub2.
- Huntley AL, Thomas R, Mann M, Huws D, Elwyn G, Paranjothy S, et al. Is case management effective in reducing the risk of unplanned hospital admissions for older people? A systematic review and meta-analysis. Fam Pract 2013;30:266-75. https://doi.org/10.1093/fampra/cms081.
- Ellis G, Whitehead MA, O’Neill D, Langhorne P, Robinson D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev 2011;7. https://doi.org/10.1002/14651858.CD006211.pub2.
- Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: a systematic review. Patient Educ Couns 2012;86:9-18. https://doi.org/10.1016/j.pec.2011.02.004.
- Wolff JL, Boyd CM. A look at person-centered and family-centered care among older adults: results from a national survey. J Gen Intern Med 2015;30:1497-504. https://doi.org/10.1007/s11606-015-3359-6.
- Kitson A, Marshall A, Bassett K, Zeitz K. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs 2013;69:4-15. https://doi.org/10.1111/j.1365-2648.2012.06064.x.
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ 2003;327:1219-21. https://doi.org/10.1136/bmj.327.7425.1219.
- Parker G, Corden A, Heaton J. Experiences of and influences on continuity of care for service users and carers: synthesis of evidence from a research programme. Health Soc Care Community 2011;19:576-601. https://doi.org/10.1111/j.1365-2524.2011.01001.x.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Burton M, Kilner K, Wyld L, Lifford KJ, Gordon F, Allison A, et al. Information needs and decision-making preferences of older women offered a choice between surgery and primary endocrine therapy for early breast cancer. Psycho-Oncology 2017;26:2094-100. https://doi.org/10.1002/pon.4429.
- Hargraves I, Montori VM. Decision aids, empowerment, and shared decision making. BMJ 2014;349. https://doi.org/10.1136/bmj.g5811.
- Born KB, Coulter A, Han A, Ellen M, Peul W, Myres P, et al. Engaging patients and the public in Choosing Wisely. BMJ Qual Saf 2017;26:687-91. https://doi.org/10.1136/bmjqs-2017-006595.
- Wolfson D, Santa J, Slass L. Engaging physicians and consumers in conversations about treatment overuse and waste: a short history of the choosing wisely campaign. Acad Med 2014;89:990-5. https://doi.org/10.1097/ACM.0000000000000270.
- Weiner BJ. A theory of organizational readiness for change. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-67.
- Weiner BJ, Amick H, Lee SY. Conceptualization and measurement of organizational readiness for change: a review of the literature in health services research and other fields. Med Care Res Rev 2008;65:379-436. https://doi.org/10.1177/1077558708317802.
- Leduc C. Patient and Family Burden of Management: We Need New Knowledge n.d. www.patientlibrary.net/cgi-bin/library.cgi?page=Blog;prevref=;top=20 (accessed 17 August 2017).
- Katz JN. Patient preferences and health disparities. JAMA 2001;286:1506-9. https://doi.org/10.1001/jama.286.12.1506.
- Briscoe S. Literature Searching for Realist Reviews n.d. https://blogs.exeter.ac.uk/realisthive/2014/06/09/literature-searching-for-realist-reviews/ (accessed 19 November 2017).
- Booth A. Literature Searching for Realist Synthesis n.d. http://realistsearch.pbworks.com/w/page/88622804/FrontPage (accessed 19 November 2017).
- Pawson R. Assessing the Quality of Evidence in Evidence-based Policy: Why, How and When?. Manchester: Economic and Social Research Council (ESRC) Research Methods Program, University of Manchester; 2003.
Appendix 1 Details of search strategy
Phase 1 searches (scoping searches)
| Search | Query | Number of items found |
|---|---|---|
| #15 | Search (#14 AND #12) | 168 |
| #14 | Search (“shared decision making”[Title] OR “patient participation”[Title] OR “patient decision making”[Title] OR “decision support”[Title] OR “decision aid”[Title] OR SDM[Title]) | 5709 |
| #13 | Search (#6 AND #12) | 1339 |
| #12 | Search (#7 OR #8 OR #9 OR #10 OR #11) | 161,226 |
| #11 | Search “evidence synthesis” | 2207 |
| #10 | Search “narrative review” | 3566 |
| #9 | Search “meta synthesis” | 427 |
| #8 | Search “meta analysis” | 110,250 |
| #7 | Search “systematic review” | 77,243 |
| #6 | Search (#1 OR #2 OR #3 OR #4 OR #5) | 50,151 |
| #5 | Search “decision aid” | 1128 |
| #4 | Search “decision support” | 26,720 |
| #3 | Search “patient decision making” | 503 |
| #2 | Search “patient participation” | 20,987 |
| #1 | Search “shared decision making” | 3821 |
The Cochrane Library – searched on 25 July 2016 (no date restrictions)
| Search | Query | Number of items found |
|---|---|---|
| #16 | Search (#14 AND #15) | 75 |
| #15 | Search “systematic review” | 78,622 |
| #14 | Search (#6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13) | 2967 |
| #13 | Search “expert patient”[Title/Abstract] | 100 |
| #12 | Search (proxy[Title/Abstract] AND decision[Title/Abstract]) | 572 |
| #11 | Search proxy NEAR decision | 10 |
| #10 | Search “proxy decision making”[Title/Abstract] | 44 |
| #9 | Search “proxy decision making” | 44 |
| #8 | Search “collaborative care” | 1554 |
| #7 | Search “coconstruction” | 15 |
| #6 | Search “co production” | 724 |
| #3 | Search (#1 OR #2) | 15 |
| #2 | Search “minimally disruptive medicine”[Title/Abstract] | 14 |
| #1 | Search “minimally disruptive medicine” | 15 |
“shared decision making”:ti,ab,kw (Word variations have been searched) OR “patient participation” or “patient decision making”:ti,ab,kw (Word variations have been searched) OR “decision support” or “decision aid”:ti,ab,kw (Word variations have been searched)
Used just these terms for Cochrane Database of Systematic Reviews, but added terms below for Cochrane Central Register of Controlled Trials (CENTRAL):
AND
old or older or frail* or dement* or alzheimer* or complex or aged or elderly or geriatric:ti (Word variations have been searched)
Google Scholar (July/August 2016)
-
Search Google Scholar and Google (searches from 2000 onwards):
-
Shared decision making AND review
-
Patient participation AND review
-
Patient decision making AND review
-
Decision support AND review
-
Decision AID AND review
-
Health communication AND review
-
Informed decision making AND review.
-
Keyword searches for papers by key authors, such as Elwyn and Légaré.
Keyword searches for SDM and MDTs.
RESPOND phase 2 searches
Searches were focused on the five ‘if–then’ statements developed in phase 1.
Reflecting patient and carer values
PubMed: person-centred care – searched on 15 December 2016
Search strategy
((“shared decision making”) OR (“decision aid”) OR (“decision making”)) AND (((“goal setting”) OR (“person centred care”) OR (“person centered care”) OR (“personalised”) OR (“patient goals”) OR (“patient values”) OR (“patient preferences”) OR (personalised[Title] OR personalized[Title] OR (patient centred) AND Title OR (patient centered) AND Title OR (patient preference*) AND Title OR goals[Title] OR (goal setting) AND Title OR personalised[Title])) AND (old*[Title] OR aged[Title] OR elder*[Title] OR geriatric[Title] OR frail[Title] OR complex[Title] OR complex[Title] OR carer[Title] OR dementia[Title] OR alzheimer*[Title]))
Google Scholar
-
Shared decision making + patient values
-
House of Care
-
patient centred communication.
Preparing patients for the shared decision-making encounter
Coaching/advocacy – searched on 12 December 2016; no date restrictions
Search strategy
(((“coaching”) OR (“advocacy”) OR (“advocate”) OR (advocate[Title/Abstract] OR advocacy[Title/Abstract] OR coach*[Title/Abstract]) OR (“coach”)) AND ((“shared decision making”) OR ((shared decision making) AND Title/Abstract OR SDM[Title/Abstract] OR decision[Title/Abstract]))) AND ((“frail elderly”) OR (“older person”) OR (“dementia”) OR (“elderly”) OR (old*[Title] OR elderly[Title] OR frail[Title] OR dementia[Title] OR alzheimer*[Title] OR aged[Title]))
PubMed: education/training – searched on 13 December 2016; no date restrictions
Search strategy
-
Search 1 ((“shared decision making”) AND (education[Title] OR educate[Title] OR training[Title] OR guidance[Title] OR support[Title] OR information[Title] OR guide[Title] OR train[Title])) AND (old[Title] OR older[Title] OR elder*[Title] OR frail[Title] OR complex[Title] OR carer[Title] OR geriatric[Title] OR aged[Title] OR dementia[Title] OR alzheimer[Title])
-
Search 2 ((“shared decision making”) AND (education[Title] OR educate[Title] OR training[Title] OR guidance[Title] OR support[Title] OR information[Title] OR guide[Title] OR train[Title])) AND (“primary care”)
PubMed: shared decision-making for hard to engage groups (e.g. those with depression) – searched on 3 March 2017; date range 2012–17
Search strategy
-
‘Shared decision making’ OR ‘decision aid’ (both MeSH) OR (coproduction[Title/Abstract] OR co-productive[Title/Abstract] OR partnership[Title/Abstract] OR co-production[Title/Abstract] OR co-production[Title/Abstract]) AND ‘depression’ OR ‘mental health’ OR ‘mental illness’ (MeSH) AND systematic review Filters: published in the last 5 years
-
‘Shared decision making’ OR ‘decision aid’ (both MeSH) OR (coproduction[Title/Abstract] OR co-productive[Title/Abstract] OR partnership[Title/Abstract] OR co-production[Title/Abstract] OR co-production[Title/Abstract]) AND ‘depression’ OR ‘mental health’ OR ‘mental illness’ (MeSH) AND ((“frail elderly”) OR (“older person”) OR (“dementia”) OR (“elderly”) OR (old*[Title] OR elderly[Title] OR frail[Title] OR dementia[Title] OR alzheimer*[Title] OR aged[Title]))
Sharing the communication of a decision
PubMed: interprofessional – searched on 15 December 2016; date range 2006–16
Search strategy
(((“interprofessionalism”) OR (“interprofessional”) OR (“interdisciplinary”) OR (“multidisciplinary”) OR (“coordinated”) OR (“cross discipline”) OR (“inter disciplinary”) OR (“integrated”)) AND ((“shared decision making”) OR (“decision aid”) OR (“decision making”))) AND (old*[Title] OR aged[Title] OR elder*[Title] OR geriatric[Title] OR frail[Title] OR complex[Title] OR complex[Title] OR carer[Title] OR dementia[Title] OR alzheimer*[Title])
“relational coordination” OR “relational coproduction” AND (old*[Title] OR aged[Title] OR elder*[Title] OR geriatric[Title] OR frail[Title] OR complex[Title] OR complex[Title] OR carer[Title] OR dementia[Title] OR alzheimer*[Title]) (no date limits)
Relational competence: searched on 3 March 2017; no date restrictions
Search strategy
Relational competence AND (promote[Title/Abstract] OR promotion[Title/Abstract] OR train*[Title/Abstract] OR increase[Title/Abstract] OR intervention[Title/Abstract] OR programme[Title/Abstract]) AND general OR community OR primary
In addition, searches for papers by Légaré and colleagues who have written on the subject.
Google Scholar keyword searches
-
Shared decision making + interprofessional
-
Shared decision making + integrated
-
Relational coordination + integrated
-
Relational coordination + older
-
relational competence + shared decision making
Fake versus real shared decision-making
PubMed Search: incentives – searched on 13 December 2016; no date restrictions
Search strategy
Incentive (ti/ab) OR incentives (ti/ab) OR incentivisation [TI/AB] OR incentivization [TI/AB]
AND “shared decision making” (MeSH)
Plus keyword searches in Google Scholar
-
Shared decision making + incentivisation
-
Incentivizing shared decision making
Reducing the workload (no date restrictions)
PubMed: searched on 13 December 2016
Search strategy
(((“minimally disruptive medicine”) OR (“caregiver burden”) OR (“carer burden”) OR (“patient burden”) OR (“treatment burden”) OR (“quality of life”) OR (appropriate[Title] OR inappropriate[Title])) AND (“shared decision making”)) AND (old[Title/Abstract] OR older[Title/Abstract] OR aged[Title/Abstract] OR elderly[Title/Abstract] OR frail[Title/Abstract] OR carer[Title/Abstract] OR complex[Title/Abstract] OR geriatric[Title/Abstract] OR dementia[Title/Abstract] OR alzheimer[Title/Abstract])
Additional searches: in response to discussion with project team about areas where there appear to be gaps
PubMed: searched on 12 April 2017
Search strategy
#1 “Shared decision making” and preference* [TI/AB] OR goal* [TI/AB]
#2 “primary care” OR “general practice” or “community care”
#1 AND #2 – restricted to last 5 years
PubMed: searched on 18 April 2017
Search strategy
#1 shared decision making (MESH) and depression or depressed [TI/AB]
Scopus searches: searched on 19 April 2017
Search strategy
((TITLE-ABS-KEY(shared decision making) OR (decision aid)) AND (TITLE-ABS-KEY (patient goal*) OR (patient value*) OR (patient preference*) OR personalised OR personalized)) AND (TITLE-ABS-KEY(old*) OR (aged) OR (elder*) OR (geriatric) OR (frail*) OR (dementia) OR (alzheimers))) AND (TITLE-ABS-KEY(randomised) Or (randomized) OR (intervention) OR (controlled) OR (trial) OR (program*) OR (qualitative) OR (evaluation))) AND (TITLE-ABS-KEY(primary care) OR (community care) OR (general practice) OR (integrat*) OR (coach*) OR (interprof*) OR (multidisciplinary))) AND NOT ((cancer) OR (breast) OR (end of life) OR (palliative) OR (parent) OR (child*))
Appendix 2 Details of studies and reviews on the use of patient decision aids
| Author and date | Study design | Focus and participants | Positive impact/facilitators | No clear impact/negative impact/barriers |
|---|---|---|---|---|
| Austin et al. 2015103 | Systematic review (17 RCTs, includes two on older people, four dementia) | Decision aids for people with advanced and serious illness – most designed for use prior to consultation |
|
|
| Coylewright et al. 2014108 | Systematic review (7 RCTs) | Decision aid – diverse populations including diabetes mellitus, chest pain, osteoporosis or MI |
|
|
| Durand et al. 2015166 | Review |
Incentives for SDM All patient groups |
|
|
| Durand et al. 201469 | Systematic review (19 studies, 10 pooled in MA) | SDM interventions for socially disadvantaged groups |
|
|
| Edwards et al. 2004, Elwyn et al. 2004167 | Cluster RCT | Training GPs in SDM, and the use of simple risk communication aids in general practice |
|
|
| Fagerlin et al. 2013115 | Evidence review and expert consensus | The use of VCMs in patient decision aids |
|
|
| Grim et al. 2016171 | Qualitative (n = 22) | To investigate decisional and information needs in people with mental health issues |
|
|
| Jones et al. 2011176 | Questionnaires to assess patient experiences in RCT of SDM | Web-based decision aid for communicating risk to people with CVD |
|
|
| Joseph-Williams et al. 2014116 | Systematic review (44 studies, mainly qualitative and cross sectional) |
Patient-reported barriers to and facilitators of SDM All patient groups |
|
|
| Joseph-Williams et al. 2017177 | Qualitive | Embedding SDM in NHS – focus is on HCPs |
|
. . . skills trump tools, and attitudes trump skills
|
| National Collaborating Centre for Primary Care 2009197 | Guideline – based on review of evidence | How to involve adults and carers in decisions about prescribed medicine – all age groups, types of patients, any NHS setting |
|
|
| Stacey et al. 2014 | Systematic review | Decision aids – all patient groups, mainly one of decisions (e.g. screening) |
|
|
| van Summeren et al. 2016192 | Mixed-methods pilot study (n = 60 older people and 17 family practitioners) | Pilot study to test a conversation tool for medication review with older people and family practitioners |
|
|
| van Weert et al. 2016121 | Systematic review [22 RCTs, many of the studies focus on single issues (e.g. AF, diabetes mellitus)] | Decision aids for older adults |
|
|
Appendix 3 Schedules for stakeholder interviews phase 1
Programme intervention: How do we support shared decision-making for older people with multiple health and social care needs?
Preamble
We want to find out how we can improve the ways in which we involve older people, and their family carers, in decisions about their health and social care. We call this approach SDM. In particular, we want to find out how SDM can work in community settings where many different health and social care workers (such as GPs, nurses, social carers) may be involved in caring for the older person.
For this review we plan to use a research approach called realist synthesis. In realist synthesis the views of stakeholders (e.g. patients, carers, practitioners and policy makers) are very important in helping to guide the review process. There are three phases to the review.
In the current phase of the synthesis we are looking to find out what approaches are used to involve older people, and their family carers, in SDM and how these different approaches are thought to work.
Trigger questions
-
Are you familiar with the term SDM? What is your understanding of it?
-
What are the current problems and challenges facing older people with multiple health and social care needs and their families when they are trying to make decisions about their health and social care?
-
How should these issues be picked up within programmes to promote SDM or shared care planning?
-
-
Do you think current processes for making decisions about health care take into account patients’ values and preferences?
-
If yes, how? What are the facilitators?
-
If no, why not? What are the barriers?
-
-
For older people with multiple conditions there can be many HSCPs involved in their care; how can decisions be negotiated between, and communicated to, these different groups?
-
What skills/training do you think HSCPs require in order to able to share decision-making with older people and their families?
-
In your experience, do they have these skills?
-
If not, what changes are needed?
-
-
For you, what would be the components of an ‘ideal’ intervention or programme for promoting shared decision-making for older people with multiple health and social care needs?
Appendix 4 Interview schedule for phase 3
Service provider’s interview schedule
Context–mechanism–outcome 1: reflecting patient and carer values
Question: the evidence suggests that for SDM to happen it is very important that systems enable health and care professionals to develop relationships with patients and carers that allow them to understand patients’ and carers’ individual emotional, cultural and cognitive needs (e.g. person-centred approaches to care). Our hypothesis is that this will help patients and carers to feel valued, listened to and involved in the decision.
Do you have any examples where this has been done well?
If yes – why do you think it worked well? What needed to be in place? What were the outcomes?
Could follow up with prompts around:
-
continuity of care
-
effective communication skills (what would these look like)
-
less focus on biomedical targets.
Context–mechanism–outcome 2: systems to support shared decision-making
Question: the evidence suggests that systems need to be organised to support and prioritise SDM, for example via support from clinical leaders or commissioners.
Do you have any examples where this has been done well?
If yes – why do you think it worked well? What needed to be in place? What were the outcomes?
Could then go on to ask similar questions around:
-
systems and tools
-
longer appointments
-
training for health and care practitioners
-
systems to prepare patients for the consultation (e.g. getting results in advance).
Context–mechanism–outcome 3: preparing (patients, carers and health-care professionals) for the shared decision-making encounter
Question: one of the hypotheses is that some people will need more support that others to engage with SDM. This might be because of conditions such as depression, lower health literacy or cognitive problems.
Do you have any examples/thoughts of how people can be encouraged to participate in SDM?
If they give an example – why did it work? What needed to be in place?
This can be followed up with prompts around:
-
the use of advocates or coaches
-
decision aids that take account of multimorbidity
-
a culture of ‘no question is a silly question’.
Context–mechanism–outcome 4: shared decision-making as part of a wider culture change (the other context–mechanism–outcomes all lead to this one)
Question: our hypothesis is that SDM only becomes embedded if it is part of a wider culture change that involves practitioners letting go of the power in decision-making, and patients and carers taking (or sharing) responsibility for their health and the decisions which affect them.
We would be very interested in your thoughts on this.
Do you have experience or examples of where this has happened? How was it done? What needed to be in place?
List of abbreviations
- CMO
- context–mechanism–outcome
- GP
- general practitioner
- HCA
- health-care assistant
- HCP
- health-care professional
- HSCP
- health and social care professional
- ICP
- integrated care pilot
- LTC
- long-term condition
- MAGIC
- Making Good Decisions In Collaboration
- MCP
- multispeciality community provider
- MDT
- multidisciplinary team
- PACS
- Primary and Acute Care Systems
- PAG
- Project Advisory Group
- PCC
- person-centred care
- PCP
- personalised care planning
- PDA
- patient decision aid
- Portable Document Format
- PIRG
- Public Involvement in Research Group
- PPI
- public and patient involvement
- RAMESES
- Realist and Meta-narrative Evidence Syntheses: Evolving Standards
- RCT
- randomised controlled trial
- SDM
- shared decision-making
- STP
- Sustainability and Transformation Plan
