Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/114/17. The contractual start date was in June 2015. The final report began editorial review in September 2017 and was accepted for publication in February 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
All authors received grant support from the National Institute for Health Research (NIHR) for the conduct of this study, remuneration for employment from their employing institution and may be in receipt of other funding for non-commercial independent research outside the current work. Peter Griffiths is a member of the advisory group for NHS Improvement’s ongoing work on safe staffing in adult inpatient wards (unpaid). Chiara Dall’Ora received grants from the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC) Wessex to support her PhD. Anya De longh received personal fees for freelance work and employment outside the submitted work from Help & Care (Bournemouth, UK), Dorset HealthCare University NHS Foundation Trust, Health Education England/Skills for Health, University of Southampton, University of Cambridge, King’s College London, Queen Mary University London and the NIHR. Gary Smith receives non-financial support from non-commercial organisations: Resuscitation Council UK, Royal College of Physicians of London, International Society of Rapid Response Systems and the NIHR outside the submitted work. For some of the period of the research, Portsmouth Hospitals NHS Trust (PHT), which employed Paul Meredith, David Prytherch, Gary Smith, Nicola Sinden and Paul Schmidt, had a royalty agreement with The Learning Clinic Limited (now part of System C Healthcare Ltd, Maidstone, Kent) to pay for the use of PHT intellectual property within The Learning Clinic Limited’s Vitalpac system, which was used to collect the vital signs observations data used in the project. Until October 2015, the wives of David Prytherch and Gary Smith held minority shareholdings in The Learning Clinic Limited. Paul Schmidt held a personal shareholding prior to the commencement of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Griffiths et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Providing sufficient numbers of nurses to deliver safe care to patients in hospital wards has been a key concern in the NHS in recent years. The potential for inadequate nursing care to harm patients has been highlighted as an important factor in numerous reports on failings in hospitals worldwide, and low staffing levels are often implicated as a cause. 1–3 The findings of reports such as these three1–3 are consistent with a growing body of research that shows that hospitals with low levels of nurse staffing have more adverse patient outcomes and, in particular, more deaths. 4,5 Indeed, the importance of nursing care in shaping positive patient experiences and outcomes is widely recognised, if sometimes overlooked. 6 The current study explores the relationship between nurse staffing levels and the risk of patients dying, and explores whether or not one important aspect of nursing care – the timely and complete observation of vital signs to monitor progress and identify deterioration in a patient’s condition – may be influenced by staffing levels and, in turn, be part of the mechanism by which low staffing increases the risk of death.
The NHS faces pressure to maintain the quality and safety of care in hospitals, while also reducing costs. Investment in nurse staffing, specifically in registered nurses (RNs), is advocated by many professional bodies as a key strategy to maintain and enhance patient experience and safety. Indeed, several health services have introduced policies or legislation that mandate minimum nurse staffing levels. 7–10 However, in the face of absolute or relative resource constraints, such approaches are seen as, at best, blunt instruments with intrinsic inefficiencies. 11
In 2014, the National Institute for Health and Care Excellence (NICE), a public organisation with a statutory duty to advise on improving health and social care for England, produced guidelines on safe staffing in hospital wards. 12 While recognising the important role of nurse staffing, NICE also highlighted the limitations of current evidence to guide practice. It identified a need for more evidence from the UK and for indicators that more directly reflect safe nurse staffing. Although a number of economic studies have been performed, the evidence is inconsistent. Furthermore, no published peer-reviewed economic studies have been undertaken in the UK. 13,14 Although NICE commissioned an economic assessment15 that concluded that increased nursing skill mix was potentially cost-effective in relation to falls prevention, the analysis was based on a relatively old data set, which did not permit case-mix adjustment.
The lack of robust economic studies in the UK is a particularly significant issue because any economic conclusions are highly likely to be sensitive to local costs, including pay rates and the cost of treating adverse outcomes, which can vary substantially between countries. Furthermore, because the association between nurse staffing and patient outcomes has primarily been demonstrated by cross-sectional studies, the extent to which the observed associations demonstrate a causal relationship is still disputed. This further undermines confidence in the economic conclusions of these studies. 14
One challenge in assessing whether or not staffing levels are adequate has been that many of the potential indicators used in research (e.g. mortality rates, pressure ulcers, a ‘failure to rescue’ and so-called ‘never events’) focus on the worst possible, relatively rare, outcomes. They are often collated over a long period (e.g. annual mortality rates) and reviewed a long time after the care was provided. Nursing care is, at most, only a partial factor in causing variation.
Research that has established an association between nurse staffing levels and patient outcomes also identifies the ability of nurses to deliver care on time, and to do so completely, as a key factor in this relationship. 16–18 Missed care (i.e. when there are omissions in nursing care) or delayed care, if related to adverse outcomes and staffing levels, may have the potential to provide a more immediate indication of whether or not a unit is adequately staffed. 19
Missed opportunities to observe and act on patient deterioration have been implicated in preventable hospital deaths20,21 and studies have shown that low staffing levels are associated with nurse-reported missed care. 19,22 These studies provide partial confirmation of a possible causal pathway between low staffing and adverse patient outcomes. In addition, a small number of cross-sectional studies published during the current project have demonstrated that associations between low nurse staffing and adverse patient outcomes, including falls, patient experience and mortality, are mediated by nurses’ reports of missed care. 23–26 Although they provide more direct evidence of a causal pathway, these studies have, thus far, relied on intermittent, retrospective nurse reports of missed care, which must be regarded as subjective measures. Taken as a whole, these studies do suggest that care omissions may provide more direct indicators of nurse staffing adequacy, which are, in turn, related to important outcomes.
New approaches to research in this field create opportunities to address some of the limitations of existing studies and to begin to supplement the evidence identified by NICE. The use of clinical and workforce data collected in real time ‘at the bedside’ means that analyses need no longer be conducted using averages of staffing at a hospital level. Recently, a US study using longitudinal patient-level data showed that individual patients exposed to periods of low staffing subsequently experienced an increased risk of death. This study, therefore, provides more evidence for a causal relationship between staffing and patient outcomes than previous cross-sectional studies have. 27
The current study builds on these two emerging strands of research by considering both staffing levels experienced by individual patients and care delivered to patients. It examines the association between RN and health-care assistant (HCA) staffing levels, missed or delayed vital signs observations and mortality on general medical and surgical wards in a NHS acute hospital in England. For the first time, it uses objective measures of ‘missed care’ derived from a clinical information system used to record vital signs observations, and uses electronic rostering information to link staffing levels experienced by individual patients on wards to subsequent outcomes over time. The study models the costs and consequences of different staffing policies to achieve acceptable rates of observation, and assesses whether or not missed observations could be used as a leading indicator of nurse staffing adequacy by testing the extent to which missed observations mediate any relationship between staffing and outcomes.
Literature review
In this section, we provide a more detailed summary of some of the core research in the area. Because the literature is so extensive and has been reviewed previously, we do not aim to present a comprehensive systematic review of evidence relating nurse staffing and patient outcomes. Rather we aim to give a broad overview that reflects the ‘state of the art’ by relying on existing authoritative reviews where possible, including our own review originally undertaken for NICE and subsequently published with an extended methodological critique. 14 We adapted and developed the methods used in the NICE review to focus on addressing the link between nurse staffing levels and missed care, and between missed care and patient outcomes.
This section draws on comprehensive reviews of the literature based on searches and an original review undertaken for NICE with subsequent updates and additional analysis, which we later updated and expanded. 14 Some material in this section is based on analysis and reviews published as Recio-Saucedo et al. 28 This article is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text. Some material in this section is based on analysis and reviews published as Griffiths et al. 29 This article is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/.
The original search strategies and methods are reported in detail elsewhere. 28,30 The searches covered all major databases in the field [Cost-effectiveness Analysis Registry (CEA Registry), Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Database of Abstracts of Reviews of Effects (DARE), EconLit, EMBASE, Health Technology Assessment (HTA) database, MEDLINE, including MEDLINE In-Process & Other Non-Indexed Citations, NHS Economic Evaluation Database (NHS EED), Health Economic Evaluations Database (HEED), and databases of grey literature including the Health Management Information Consortiumm (HMIC) database and those held by NICE]. This was supplemented by extensive contacts with experts in the field to ensure comprehensive identification of literature reporting associations between nurse staffing and patient outcomes or care processes.
What follows is a narrative overview covering a range of questions. Our selection of material to demonstrate empirical associations between staffing and outcomes relies on existing high-quality reviews,4,13,14,31 with individual studies highlighted for illustrative purposes or because they represent significant developments since the reviews were published. For studies exploring the association between staffing and missed care, and those exploring the relationship between missed care and outcomes, we present a complete overview of empirical studies of association, with original searches and study selection undertaken up to June 2016 and supplementary searches undertaken to identify significant studies published subsequently (up to August 2017).
Nurse staffing levels and adverse outcomes
A large international body of evidence has explored links between low nurse staffing levels and adverse outcomes in hospitals, most notably mortality. One of the early seminal studies in the field, the Aiken et al. 32 study of 10,184 staff nurses and 232,342 surgical patients in 168 general hospitals in Pennsylvania, USA, found that for each additional patient cared for by one RN the odds of death among surgical patients increased by 7%.
This early study established a model of research that can be used to typify the field. It is dominated by large, cross-sectional studies with associations measured at the hospital level. Most evidence relates to RN staffing, with staffing levels drawn from a variety of sources but typically averaged to hospital level over an extended period of time. Most, but by no means all, of the evidence has originated in North America, although this limitation is fast being rectified, with major studies undertaken in countries including Australia,33 China,34 England35,36 and Thailand37 and across 12 European countries (Belgium, England, Finland, Germany, Greece, Ireland, the Netherlands, Norway, Poland, Spain, Sweden and Switzerland). 5,38 Generally, studies give little account of staffing levels in other professional groups, although mix within the wider nursing team (e.g. nursing assistants or the proportion of nurses with a degree qualification) has been considered in a number of them. 36,39 Some have demonstrated relationships between outcomes and nurse staffing levels while also considering or controlling for staffing by other groups, including doctors. 36,39
An early systematic review and meta-analysis by Kane et al. 4 found 101 studies published up to 2006, mainly from the USA. A meta-analysis based on 28 studies that reported adjusted odds ratios (ORs) showed a significant association with a range of adverse outcomes including mortality and infections (Table 1). The authors did, however, conclude that evidence for associations with outcomes that were regarded as potentially more sensitive to nursing, such as falls and pressure ulcers, was less consistent.
| Outcome | Studies (n) | OR (95% CI) |
|---|---|---|
| All patients | ||
| Mortality | 5 | 0.96 (0.94 to 0.98) |
| Hospital-acquired pneumonia | 4 | 0.81 (0.67 to 0.98) |
| Pulmonary failure | 5 | 0.94 (0.94 to 0.94) |
| Cardiopulmonary resuscitation | 5 | 0.72 (0.62 to 0.84) |
| Medical patients | ||
| Mortality | 6 | 0.94 (0.94 to 0.95) |
| Surgical patients | ||
| Mortality | 8 | 0.84 (0.80 to 0.89) |
| Failure to rescue | 5 | 0.84 (0.79 to 0.90) |
| Surgical wound infection | 1 | 0.15 (0.03 to 0.82) |
| Cardiopulmonary resuscitation | 1 | 0.72 (0.62 to 0.84) |
| Nosocomial bloodstream infection | 5 | 0.64 (0.46 to 0.89) |
| Relative change in length of stay | 3 | 0.69 (0.55 to 0.86) |
Although large cross-sectional studies have dominated the field, studies with a longitudinal element have also been undertaken. Kane et al. 4 concluded that overall results from cross-sectional studies were consistent with those from studies that considered temporality, although there was evidence that cross-sectional estimates were larger for failure to rescue. A direct comparison of estimates from longitudinal and cross-sectional analyses of the same data set found that cross-sectional estimates of associations between nurse staffing and patient experience were more often significant than longitudinal ones, although there was no clear pattern in relation to effect size. 40 A systematic review published in 201331 considered new studies in addition to those in the Kane et al. review. Of the 15 new studies considered, nine were classified as longitudinal. Although the review came to similar conclusions to Kane et al. ,4 the evidence from longitudinal studies was mixed, although these studies tended to consider changes in staffing over long time periods (typically from year to year), and so still made no direct link between patients and the staffing experienced.
Although most research has involved cross-sectional or longitudinal studies comparing year-on-year changes, one exception was a study undertaken in a single US hospital. This study measured exposure to periods of low staffing at the individual patient level for 197,961 admissions in 43 acute (adult) care units over 3 years. When patients were exposed to a shift in which the available nursing time was < 8 hours below the target (effectively one staff member short), the hazard of death was increased by 2% [hazard ratio (HR) 1.02]. 27 Although it was undertaken in only one hospital, this study is significant because it is the first large-scale study to show that the increased risk of death is directly associated with staffing experienced by that patient, making it far more likely that the observed association is causal.
The systematic review of evidence undertaken for NICE14 focused on 35 primary studies that had incorporated skill mix and measured staffing actually deployed on the relevant wards. The results of these studies confirmed the conclusions of other reviews in relation to RN staffing and/or measures of total nurse staffing. Although the evidence suggested that having more nurses was associated with lower rates of falls, findings for other outcomes, often regarded as nurse sensitive, were inconsistent. For example, 12 studies reported the association between staffing and pressure ulcers. Three studies found that higher staffing was significantly associated with lower rates of ulcers,41–43 but two found a significant association in the opposite direction, with units/hospitals with more staff having higher rates of pressure ulcers. 44,45
Skill mix and nursing assistants
The evidence review for NICE14 further explored the contribution of assistants or aides (also referred to as support workers) as part of the nursing team. Eight, mostly weak, studies gave no strong evidence of beneficial associations between nursing assistant staffing levels and patient safety. Studies found no association between assistant staffing level and mortality,46 failure to rescue,47 length of stay,46 venous thromboembolism48 or missed care. 19 However, higher assistant staffing was associated with higher rates of falls,43,49 pressure ulcers,50 readmission rates,51 medication errors50 and use of physical restraints43 and lower levels of patient satisfaction. 50 One study found that higher assistant staffing levels were associated with lower rates of pressure ulcers. 48 Subsequently, a cross-sectional study in 137 English hospital trusts36 found that higher levels of support worker staffing were associated with significant increases in mortality rates among medical patients when using whole Trust staffing figures, although the relationship was not observed in a subsample that looked at nursing assistants deployed on wards. A before-and-after study exploring the effect of introducing nursing assistants on acute care wards in Australia52 found mixed results but reached an overall conclusion that, for every 10% of extra time patients spent on wards using nursing assistants, the odds of developing a urinary tract infection or pneumonia increased by 1% and 2%, respectively.
The review also identified 22 studies reporting relationships between skill mix (typically, proportions of RNs to total nursing workforce) and outcomes. A number of these studies found an association between a nursing skill mix and a higher proportion of RNs and better outcomes including lower mortality or failure to rescue,53–55 lower rates of infections,44,55,56 falls,41,42,57,58 pressure ulcers42,48,55 and higher patient satisfaction. 59 The pattern of results is largely consistent, with the only significant contradictory evidence coming from one of the weaker studies that showed that a higher proportion of RNs was associated with a higher nurse-reported incidence of pneumonia. 60
Overall, there appears to be little evidence suggesting that adding nursing assistants makes a positive contribution to patient safety, although studies that report skill mix as a variable, rather than modelling the numbers in each group, risk confounding between absolute numbers and proportions. This is because skill mix can be lowered by both decreasing the number of RNs and increasing the number of assistants. So far, only one study19 has considered staffing levels by both staff groups as independent variables and modelled the interaction between the two in order to understand if the effect of adding care assistants is the same at all levels of RN staffing. Interestingly, this study found no effect from assistant staffing and no interaction between assistant staffing and RN staffing.
Economic evidence
A number of studies have explored the economic consequences of variation in nurse staffing by attempting to estimate the costs associated with staffing and the consequences, such as reduced length of stay or costs of treating complications. A review (up to 2013) found nine studies exploring either cost benefit or cost-effectiveness. 13 The conclusions varied depending on the costs considered, the context and the economic perspective taken (e.g. hospital vs. societal). In general, savings from better patient or system outcomes did not offset the costs to the hospital of increased nurse staffing. Using the studies considered in NICE’s evidence review,14 we estimated the cost per life saved, which varied hugely between studies. Cost per life saved in studies taking a hospital-cost perspective ranged from over US$9M61 to AU$62,522 (approximately US$46,000 at 2017 exchange rates). 45 Whereas studies that took a wider societal perspective suggested a net economic benefit from lost productivity avoided,61,62 only one scenario modelled in one study63 suggested a net cost saving to hospitals, which arose from increasing the proportion of RNs. A more recent study using longitudinal data over 4 years from 421 US hospitals confirms this analysis. 64 Increases in staffing were associated with increased costs, although the finding was not significant. Increasing the proportion of RNs in the licensed nursing workforce was associated with a net reduction in cost. The one UK study15 we identified, an economic assessment commissioned by NICE, estimated an incremental cost-effectiveness ratio for holding staffing levels constant and increasing skill mix by 10% (from 64% RN to 74%). The estimated costs were £1412 per fall averted and £128,779 per drug error avoided. This study did not explore associations with mortality.
Causation
Although all of the studies we reviewed here are observational, an assessment against the so-called Bradford Hill criteria65 largely supports the case that nurse staffing is related to mortality in a causal manner because of the overall consistency of results as shown in meta-analyses, the invariance of the conclusions to specific features of study design and features such as dose–response relationships. 4
Nonetheless, uncertainty remains. For outcomes most directly linked to nursing, such as pressure ulcers, inconsistency in evidence is likely to be a product of the challenges of recording outcomes in routine data, the possibility that higher staffing leads to higher detection for some outcomes and the lack of well-developed risk adjustment methods. 14 The Needleman et al. 27 study demonstrates that increased risk of mortality follows periods in which patients are exposed to nurse staffing below that deemed necessary, confirming the temporal order of events. However, the observed associations are typically small, making causal conclusions more difficult. Even assuming cause, the proportion of adverse events, such as mortality, that can be attributed to variation in nurse staffing is low. Kane et al. 4 estimated the proportion of deaths associated with variation in nurse staffing (as reported in Table 1) to be 4.2% for all patients at a hospital level, although estimates were higher for population subgroups (e.g. surgical patients, 16%) and outcomes (e.g. hospital-acquired pneumonia, 19%).
Since 2010, research has begun to focus on the mechanisms that must intervene between staffing levels and outcomes to cause the observed associations. It has been hypothesised that it is the nurses’ ability to monitor patients and initiate timely intervention in the face of deterioration that is the key mechanism linking nurse staffing levels to mortality. 17 In simple terms, there must be sufficient capacity in the workforce to maintain adequate surveillance in the face of numerous other demands on nurses’ time. Furthermore, if omissions in nursing care can be linked to important patient outcomes, not only does this provide support for a causal mechanism, it also generates a potential indicator of quality that is more directly linked to the nursing workforce and that can be observed and monitored without relying on the occurrence of rare and severe adverse outcomes. In one study,66 over 40% of variation in nurses’ ratings of care quality was associated with reports of care being left undone.
Missed nursing care
Although evidence for the association between nurse staffing levels and patient outcomes is considerable, and has been extensively reviewed, research on missed nursing care (variously referred to as ‘care left undone’, ‘missed care’ and ‘implicit rationing’) is more limited, in part because nursing activities can be difficult to measure and are often not routinely recorded in a useable format by health-care providers. 67 However, there is now a growing number of studies exploring the link between nurse staffing and missed care, and the subsequent impact on outcomes. We undertook an extensive database search using a core strategy for locating nurse-staffing research that we had developed previously. 30 We supplemented this with focused searches for terms related to missed care (‘missed nursing care’, ‘care rationing’, ‘care left undone’, ‘unfinished care’). We included any quantitative study reporting the association between any measure or report of missed nursing care and staffing levels, skill mix or patient outcomes. We found 18 papers reporting associations with staffing and 15 reporting associations with outcomes. Although we looked for studies with objective measures of missed care or measures recorded in routine clinical practice (e.g. omissions in drug administration), we could find none in which the specific omission of nursing care was reported separately. Instead, all reports relied on intermittent surveys primarily of nurses, or in some cases patients. All studies analysed data in a cross-sectional fashion, although, often, the temporal link between missed care and staffing was clear because it related to a specific shift. Searching was completed in September 2016. Subsequently, citation alerts were used to identify any significant new publications that might alter conclusions.
What care is missed?
In a large pan-European study,68 the frequency with which nurses reported that some care was left undone on the last shift ranged from 75% in England19 to 93% in Germany,69 with an overall estimate across 12 European countries of 88%, based on a survey of 31,627 nurses in 488 hospitals. 68 Studies from Korea, Kuwait and Switzerland also suggest that missed care is a frequent occurrence. 70–72 Although clinical care is less often reported as missed than aspects of planning, communication and psychosocial care, the rates of omission were still substantial. Although monitoring of vital signs was one of the least likely aspects to be reported as missed, omissions of care in this area were still relatively frequent, with up to 37% of nurses reporting some care missed on the last shift. 69
Association with staffing
Of the 18 studies, 15 found lower nurse staffing levels to be significantly associated with higher levels of missed nursing care. Two studies51,73 found no significant effects and one69 found mixed effects (Table 2). The magnitude of the effect varied across studies, but comparison was difficult because of the variety of measures used for staffing and for missed care. In the pan-European study,68 the odds of nurses leaving care undone were increased by 26% when nurses were caring for > 11.5 patients compared with when nurses were caring for ≤ 6 patients.
| Study | Country | Hospitals (n) | Unit type(s) | Participants | Sample size (n) | Higher nurse staffing associated with lower missed care? |
|---|---|---|---|---|---|---|
| Al-Kandari and Thomas, 200971 | Kuwait | 5 | Medical/surgery | RN | 780 | Yes |
| aAusserhofer et al., 201422 | Europe | 488 | Medical/surgery | RN | 33,659 | Yes |
| aBall et al., 201419 | England | 46 | Medical/surgery | RN | 2917 | Yes |
| aBall et al., 201674 | Sweden | 79 | Medical/surgery | RN | 10,174 | Yes |
| aBruyneel et al., 201524 | Europe | 217 | Medical/surgery | RN | 10,733 | Yes |
| Cho et al., 201575 | Korea | 1 | General hospital (NS) | RN | 232 | Yes |
| Cho et al., 201670 | Korea | 51 | General hospital (all) | RN | 3037 | Yes |
| Dabney and Kalisch, 201576 | USA | 2 | General hospital (NS) | Patient | 729 | Yes (some outcomes) |
| Friese et al., 201377 | USA | 9 | Oncology | RN and HCSW | 2318 | Yes |
| aGriffiths et al., 201468 | Europe | 488 | Medical/surgery | RN | 31,627 | Yes |
| Kalisch et al., 201178 | USA | 10 | General hospital (all) | RN and HCSW | 4086 | Yes |
| Kalisch et al., 201179 | USA | 10 | General hospital (all) | RN and HCSW | 4288 | Yes |
| Kalisch et al., 201373 | USA/Lebanon | 2 | Medical/surgery/ICU | RN | 747 | No |
| Orique et al., 201680 | USA | 1 | General hospital (all) | RN and HCSW | 169 | Yes |
| Palese et al., 201581 | Italy | 12 | Medical | RN and HCSW |
205 109 |
Yes |
| aSchubert et al., 201372 | Switzerland | 35 | Medical/surgery | RN | 1633 | Yes (someoutcomes) |
| Weiss et al., 201151 | USA | 4 | Medical/surgery | Patient | 1892 | No |
| aZander et al., 201469 | Germany | 49 | Medical/surgery | RN | 1511 | Mixed |
Of the 18 studies, the two using patient (as opposed to nurse) reports of missed care provided mixed results. RN hours per patient day (HPPD) were weakly correlated with patient reports of not receiving timely care, although not with overall patient reports of missed care. 76 A study focusing on discharge planning in four US hospitals51 found no significant association between non-overtime RN HPPD and patient-reported delivery of necessary discharge information.
Four studies explored associations between skill mix and missed care either directly or indirectly. The results suggest that adding support workers to the workforce does not generally reduce the level of missed nursing care and may even increase it where skill mix is diluted. Two studies19,74 found that greater numbers of support workers were not associated with reductions in the rate of care left undone, except with very high levels of support worker staffing in one study (fewer than four patients per support worker). Patient-reported timeliness of care was significantly correlated with increased RN skill mix in one study. 76 One study81 found that more daily care provided by support workers was associated with increased nurse-reported frequency of missed care [OR 1.04, 95% confidence interval (CI) 1.01 to 1.07].
Consequences of missed care
We found four studies reporting associations between missed care and patient mortality. Two studies found a significant association between levels of nurse-reported missed care and mortality23,82 and two did not. 67,83 Nurse reports of missing treatments and procedures were associated with hospital readmissions in one study. 84 Other studies have shown associations between nurse-reported missed care and falls,67,85 infections,60,67,85–87 pressure ulcers,85,86 pneumonia60 and medication administration errors,60,67 but several of these studies relied on nurse reports of adverse events and some studies found no significant associations between missed care and the rates of hospital-acquired pressure ulcers60,88 or urinary tract infections. 60 Four studies found nurse-reported missed care to be associated with significantly decreased patient satisfaction in hospitals24,85,89 and four found that nurses’ ratings of quality were higher when less care was reported as missed. 19,22,66,90
Does missed care mediate the relationship between nurse staffing levels and outcomes?
Although limited by reliance on nurse reports, the evidence for an association between nurse staffing levels and missed care is largely consistent. When staffing is lower, more care is reported as missed. The evidence for a link between these nurse reports of missed care and patient outcomes is less consistent, although the association between reports of missed care and more adverse perceptions of care by both patients and nurses seems clear. However, although the broad pattern of results supports a similar association with other outcomes, the evidence is more mixed. Crucially, if missed care is at least part of the mechanism through which low staffing affects patient outcomes, its role as a mediating variable needs to be directly tested.
In simple terms, it is proposed that the mechanism by which nurse staffing affects patient care is because necessary care is more often missed when staffing is low. Because this care is necessary to achieve desired patient outcomes (or to prevent adverse outcomes), outcomes are worse if more care is missed. Thus, missed care mediates the relationship between adverse outcomes and staffing. This is illustrated in Figure 1.
FIGURE 1.
Staffing: missed care outcome mediation model.
According to Baron and Kenny,91 if this is the case the following must apply:
-
There must be an association between staffing levels and the outcome. This is generally supported by the existing evidence.
-
There must be an association between staffing levels and missed care. Again, this is generally supported by the existing evidence.
-
There must be an association between missed care and outcomes. There is currently limited evidence to support this.
-
Finally, because the relationship between staffing and outcome is explained by the effect of staffing on missed care, the association between staffing and outcome is reduced when the outcome is regressed on staffing and missed care.
-
If the relationship is entirely explained by missed care (i.e. there is no other mechanism through which low staffing affects outcome), there is no residual association between staffing and outcome when both variables are included as independent variables in a regression analysis. Otherwise, the mediation is partial.
The final two points above illustrate that although existing evidence is largely consistent with mediation, this can be assessed directly only by modelling the relevant variables at the same time in a single study.
To date such analysis has been undertaken in four studies, demonstrating that missed care partially mediates observed relationships between staffing and patient satisfaction,24,26 falls25 and mortality. 23 However, although this provides general support for the mediation hypothesis, all of the studies relied on subjective reports of missed care, and only Kalisch et al. 25 focused specifically on the elements of care that were determined to be likely to affect the outcome (as opposed to a composite measure of all care missed). In relation to mortality, where evidence for the association between nurse staffing and outcomes is strongest, the support for missed care as a mediator is derived from a cross-sectional study (albeit a large multinational one) in which staffing levels and patient outcomes are measured at a hospital level, and both staffing levels and missed care are determined through a nurse survey, thus creating a risk of common method bias. 23
Case for the current study
With regard to the case for the current study, NICE guidance12 specifically highlights that:
There is a lack of evidence from UK data that allows the effects of actual nursing staff that are present . . . to be readily determined . . . There is a lack of good quality research on the . . . the indicators that are most sensitive to numbers of available registered nurses.
© NICE (2014) Safe Staffing for Nursing in Adult Inpatient Wards in Acute Hospitals. 12 Available from www.nice.org/uk/guidance/sg1 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this publication. The information provided by NICE was accurate at the time of publication of this report
More research is needed to develop direct and objective indicators of adequate staffing if any approach to determining nurse-staffing levels is to be properly validated.
Variation in nurse staffing levels in hospitals is associated with variation in death rates and in nurses’ reports of missed care. The current evidence is, with few exceptions, limited by:
-
use of nurse reports and intermittent surveys to assess missed care
-
cross-sectional studies
-
aggregated reports of staffing and outcome at unit or hospital level
-
inability to demonstrate temporal association.
Although there is a plausible theoretical mechanism that links nurse staffing levels to rates of death, so far there is limited evidence exploring whether or not surveillance of patients by nurses mediates the relationship. Furthermore, there is very limited evidence from the UK, and few UK-based economic analyses, which are crucial for evidence to inform policy-making. Only one US study27 has directly examined and demonstrated links between death rates and the staffing experienced by patients on a ward on a shift-by-shift basis. Finally, because deaths are rare and the contribution of nurse staffing to variation is small, death rates cannot be used as a specific indicator of nurse staffing adequacy. If the role of missed care (and, specifically, missed opportunities to undertake surveillance) can be established and measured through routinely collected data, it could provide a leading indicator of nursing service quality that is more sensitive and specific to variation in nurse staffing than are outcomes. A sensitive and specific indicator of nurse staffing adequacy could, in turn, provide a better guide to determining staffing requirements at a ward level. However, current measures of missed care are problematic because they rely on intermittent survey and a subjective report.
Aims and objectives
The monitoring of vital signs is a fundamental component of the ‘Chain of Prevention’, a structure that describes the interventions necessary to prevent patient deterioration. 92 This study examines whether and how variation in nurse staffing levels on general hospital wards are associated with omissions or delays in delivering necessary nursing care. Our specific focus is on monitoring and acting on vital signs, and whether or not variation in staffing levels and vital signs observations is associated with variation in patient death. Secondary outcomes explore the impact of staffing on cardiac arrest and unanticipated intensive care unit (ICU) admissions, timely nutritional risk assessment and an inferred ‘failure to respond’ to deterioration. The current study is the first to use objective measures of missed care to explore the relationship between staffing levels, missed care and adverse outcomes for patients.
Crucially, this study adds significantly to the body of evidence on associations between nurse staffing and outcomes because it:
-
determines whether or not variation in the presumed causal factor (nurse staffing) precedes the presumed effect (adverse outcomes)
-
explores an intervening care process (vital signs observation) that is a direct result of actions by nurses
-
provides evidence that is directly relevant to the UK context.
Thus, the study aims to provide a basis for identifying the nurse staffing levels and skill mix required to ensure adequate patient surveillance, and to assess whether rates of missed vital signs observations can be used to identify when or where care is falling below accepted standards and putting patients at risk.
To do this we:
-
modelled the relationship between the available nursing workforce (including hours of care by both RNs and HCAs per day or per shift), controlling for patient risk and ward-level factors (as appropriate), to identify the association between RN staffing levels and HCA staffing levels and:
-
hazard of death
-
ICU admission and cardiac arrest
-
length of stay
-
missed vital signs observations
-
timely response or resolution of deterioration
-
missed screening for nutritional risk
-
-
explored data to determine whether any relationships are linear or whether performance deteriorates beyond a threshold of staffing level, and whether or not relationships vary across ward types and by time of day
-
undertook secondary analyses to determine whether or not the use of bank and agency staff is related to adverse outcomes
-
undertook analysis to determine whether or not missed vital signs observations mediate any relationship between staffing and mortality
-
used coefficients from the regression models to identify staffing policies that are associated with desired outcomes and model the staffing costs associated with these policies.
Chapter 2 Methods
This is a retrospective, longitudinal observational study using routinely collected data from a single acute care NHS hospital to study the association between variation in nurse staffing, missed vital signs assessments and adverse events (including death). The study additionally considers associations between nurse staffing levels and nurses’ nutritional assessments, and between nurse staffing and length of stay.
In contrast to the majority of existing research, the study uses objective measures of nursing care delivery derived from clinical records and ward-level staffing data from an electronic rostering system to directly link outcomes to staffing levels experienced by the patient on every ward and for each day and nursing shift of their hospital stay.
Setting
The study was undertaken between April 2012 and March 2015 (3 years) using data from staff and patients admitted to all 32 adult medical and surgical wards (approximately 800 beds) of a large acute care general NHS hospital in the south of England. The hospital is located in an urban location on the outskirts of a city with a population of > 200,000 and provides acute services to approximately 650,000 people across a region that incorporates both urban and rural populations. Planned daytime staffing varies between wards, from eight patients per RN (identified as a risk threshold by NICE) to four or fewer patients per RN (reflecting recommended safe staffing levels from other countries). 93 These ratios suggest that the Trust is typical when compared with the range observed in England in our previous RN4CAST study. 94 Between 2012 and 2013, the hospital Trust had a hospital standardised mortality ratio (HSMR) of just under 100 and a Summary Hospital-level Mortality Indicator (SHMI; https://digital.nhs.uk/data-and-information/publications/clinical-indicators/shmi) of just over 100. Both of these indicators provide an estimate of the ratio of observed to expected mortality rates, based on well-developed risk adjustment models considering diagnosis, age, comorbidity and other factors. 95,96 A hospital Trust scoring 100 on either of these measures has exactly the number of deaths as predicted based on the underlying statistical model, which is calculated from admissions to all acute hospital trusts in England. For both of these indicators, the hospital was placed in the middle third of all English hospital trusts. ICU mortality, rates of cardiac arrest and survival after cardiac arrest are also close to national averages. Indicators of health for people living in this city are generally worse than the England average (NHS Health profile; www.gov.uk/government/collections/health-profiles), with approximately 20% of people living in areas categorised as among the 20% most deprived in England. The city has a diverse community, with approximately 14% coming from black and ethnic minorities. By contrast, the rural catchment area includes some of the least deprived areas of the country. Data on the hospital and local area are sourced from national reports of SHMI and HSMR, the hospital Trust website, Public Health England Health Profiles and local authority summaries of the Office for National Statistics data.
Data sources
We accessed data from 1 April 2012 to 31 March 2015 from a number of sources. More details of data fields are given in Appendix 1. All patient and staff data were pseudoanonymised.
Nurse staffing
Nurse staffing data were accessed from an electronic rostering system. The database contained records of shifts worked, location, hours (dates, start and end times), ward and grade for all nurses employed by the hospital. A second database recorded all bank (extracontractual work within the hospital by staff employed by the Trust) and agency shifts (shifts worked by staff employed through an external agency).
We considered shifts worked on adult medical and surgical wards including admissions units and care of older people. ICU staffing was not considered because the staffing levels differ fundamentally from those on general wards and vital signs are not recorded using the same electronic system as elsewhere in the hospital. We did not consider paediatric or maternity services for similar reasons.
A total of 764,008 shifts were recorded in the eRoster, of which 633,525 were rostered to permanent staff (RNs and HCAs) and 130,483 were rostered to temporary staff (RNs or HCAs employed via the bank or agency). The eRoster and bank and agency data were subject to extensive checks and validation by the Trust prior to transfer, as these are used as the source of data for payroll. Shifts with codes indicating sick leave or other absence, non-ward based or non-clinical roles (e.g. ward clerks) or study leave were removed prior to calculating ward staffing levels. A small number of shifts by staff working at an unknown grade (n = 1608) were also removed because the human resources department and senior nursing managers advised that these staff would be unlikely to have been clinical nursing staff.
We included all ward-based shifts (including supervisory hours) and calculated nursing hours based on the start and end times recorded in the eRoster. Although it might be of interest to explore whether or not supervisory hours made a distinct contribution to ward staffing levels, the coding used by the Trust meant that we could not reliably separate these from other hours worked on the ward.
In total, 538,238 shifts were classified as ‘worked’. There were periods when ward closures, mergers and moves created a mismatch between wards recorded for staff on the eRoster and those recorded on the patient administration system (PAS), resulting in ambiguity that meant that we could not reliably match records of staffing to patients. These periods were dropped from the study, resulting in a small reduction in both the available study days and the patient population.
Vital signs and other nutritional assessments
The hospital uses a handheld electronic system to record vital signs and some other nursing information. This is the Vitalpac system (System C Healthcare Ltd, Maidstone, Kent; formerly The Learning Clinic Limited). Vital signs observations and nutritional risk assessments, undertaken using the Malnutrition Universal Screening Tool (MUST) (see www.bapen.org.uk/screening-and-must/must/introducing-must), were derived from a database of records made using this system, where nurses record clinical data on handheld devices at the bedside. This system constitutes the only official record of observations that are maintained on the wards in the study, and the use of the system is mandated by Trust policy. The frequency of vital signs observations required is determined by a protocol based on the National Early Warning Score (NEWS). 97 NEWS uses parameters from vital signs observations to assign a score to the patient, with a higher score indicating a higher level of acuity and potential need for escalation of care. This in turn is used to identify the required frequency of vital signs observation, which identifies when the next observation is due. 97 In total, 3,702,717 sets of observations were extracted, of which 3,367,791 were complete.
Given that the Trust’s policy on recording nutritional assessments was implemented in early 2013, we used these data only from 1 April 2013. In total, we extracted 301,172 MUST assessments. As the policy requires that the first MUST score is recorded within 24 hours of admission, we considered MUST scores only in patients who had an initial stay of ≥ 24 hours on one of the study wards.
Patients
Patient data were extracted from the hospital’s PAS. These included patient demographic and diagnostic data, including reason for admission and comorbidities, which were used to control analyses for patient-level risk factors, and detail of transfers within the hospital, which were used to calculate length of stay and determine the wards where a patient received care. We also obtained records of cardiac arrests and unanticipated ICU admissions from the cardiac arrest audit and ICU WardWatcher (WardWatcher, Critical Care Audit Ltd, Yorkshire, UK) databases. Patient data were, in turn, used to estimate the number of new admissions to the ward for each day/nursing shift and the numbers of ‘patient hours’ per day or nursing shift. From 387,009 records in the PAS data set, 148,994 satisfied the following inclusion criteria: aged ≥ 16 years; discharge date after 1 April 2012; admission date before 31 March 2015; and admitted to a general medical/surgical ward. Patients aged 16 or 17 years were occasionally admitted to adult wards and were therefore included to allow accurate calculation of patient hours.
Data linkage/analytic sample
Our study required that these disparate data sources were linked for analysis purposes. Our primary approach to exploring staffing levels was based on the nursing HPPD. As the calculation of this variable was derived from nursing hours worked and the number of patients on that ward, we had to drop days from our study if we could not reliably match the two. From a theoretical maximum of 35,040 ward-days (365 days × 3 years × 32 wards), no patients were recorded on included wards on 1822 days owing to ward closures. Of the remaining 33,218 days, 2236 days (6.7%) were either dropped or unavailable for analysis. Reasons for the shortfall included days immediately preceding or following ward closure or opening where extremely low values for the patient population resulted in high nursing HPPD. In these cases, the relevant days were dropped from the study when the patient population fell below 25% of the median. In some cases we could not reliably match the ward codes used for patients with those used for staff. As an example, a ‘ward’ could move from one physical location to another (sometimes occupying part of another existing ward), resulting in the situation that patients were coded to the new ward, based on physical location, while the eRoster still recorded staff on the ‘old’ ward. Although the Trust provided some information on ward moves, and in some cases correct attributions could be made with confidence, there were periods of major reorganisation during which several moves happened simultaneously or we could not confidently reconcile patient and staff numbers.
The process of data linkage reduced our sample to 138,133 patients and 2,945,265 complete observations. We assessed 43,451 patient admissions for the presence and timeliness of their initial MUST assessments.
Outcomes
Patient-level outcomes
The primary patient outcome was in-hospital mortality, determined from the PAS.
For secondary outcomes, we also considered death in hospital within 30 days of admission and a composite adverse event outcome, defined as death, cardiac arrest or unplanned ICU admission. For this outcome, each patient was assigned the outcome based on the time of the first event to occur. Length of stay was calculated from the PAS, from first admission to hospital to discharge (or death) or transfer out of the hospital.
Omissions or delays in recording vital signs and other assessments
The protocol that determines the frequency of observations in the Trust is adapted from a national protocol based on the NEWS, which assigns scores to abnormal vital signs observations and then specifies the observation interval (see Appendix 2, Tables 22 and 23). For example, if a patient is assigned a NEWS of 7, the protocol requires a maximum interval between observations of 1 hour. This provides a clear basis on which to determine whether or not observations are completed and recorded in a timely fashion.
The primary outcome for this aspect of the study was missed vital signs observations. A ‘missed’ observation was assigned when a full set of vital signs observations was not recorded within the scheduled interval plus two-thirds of the interval (i.e. more than five-thirds of the scheduled interval). For example, if the next observation is scheduled to be in 1 hour, an observation is classified as missed after 1 hour and 40 minutes has elapsed, in effect when another set of observations is nearly due. Similarly, we classified observations as ‘late’ if the scheduled interval plus one-third of the interval had passed (i.e. more than four-thirds of the scheduled interval), and ‘not on time’ if not taken on or before the scheduled time.
Formally, we classified observations as:
-
on time: T ≤ T0 + I
-
not on time: T > T0 + I
-
late: T > T0 + (I × 4/3)
-
missed: T > T0 + (I × 5/3),
where T is the time of the observation, T0 is the time the previous observation was taken and I is the interval between observations determined by the observation taken at T0.
Our primary analysis considered a daily rate of missed observations. An observation was assigned to the time at which it was due, and rates of missed observations were determined using the total number of observations due during that period as the denominator. A similar approach was taken for ‘not on time’ and ‘late’ observations and for missed nutritional assessments. In addition to daily rates, we calculated missed observations within 6-hourly and hourly intervals to more closely match staffing to the rate of observations. In each case, the denominator was the number of observations due within the specified time period. As observation frequency is related to patient acuity, and, because the significance of missed or late observation may differ in different patient groups, we undertook subgroup analyses focusing only on patients classified as high or very high acuity (NEWS of ≥ 6). According to the current monitoring protocol, observations for these patients are scheduled every 4 hours or more frequently.
Although the focus of the study was the link between staffing levels, missed vital signs and mortality, we also took the opportunity to determine whether or not other electronically recorded assessments could be used to derive objective measures of missed care. Trust protocol specifies that nutritional assessments (MUST) be recorded in the Vitalpac system within 24 hours of admission for all patients; therefore, we were also able to determine whether or not these observations were undertaken within the time specified by the protocol.
Failure to respond
Timely observation is only the first step in preventing or mitigating the effects of patient deterioration. Consequently, we also calculated a variable which might be indicative of a wider failure to respond. According to the protocol, patients with a NEWS of > 7 are to be observed at least hourly and be seen by a doctor within 30 minutes (see Appendix 2). Based on this, we defined a variable indicating ‘failure to respond’ if a patient with a NEWS of ≥ 7 does not meet one of the following conditions within 4 hours:
-
a NEWS of < 7 recorded (indicating improvement)
-
admission to the ICU
-
indication that the patient has been placed on the end-of-life care pathway (flag in Vitalpac).
Similarly, a patient with a NEWS of ≥ 6 is to be observed at least every 4 hours and be seen by a doctor within 2 hours. Based on this, we defined a failure to respond indicator if the following did not occur within 16 hours:
-
a NEWS of < 6 recorded (indicating improvement)
-
admission to the ICU
-
indication that the patient has been placed on the end-of-life care pathway (flag in Vitalpac).
Staffing variables
Hours per patient day/shift/hour
Our primary approach to measuring staffing was to calculate care hours per patient day (CHPPD) (i.e. a 24-hour period starting at midnight) for RNs who are trained for a minimum of 3 years [Agenda for Change (www.nhsemployers.org/your-workforce/pay-and-reward/agenda-for-change) bands 5+], and unregistered HCAs with no standardised training requirement (Agenda for Change bands 2–4). For each ward, the nursing hours for each day were calculated from the eRoster with all hours between the shift start time and end time contributing (i.e. from midnight to midnight). In general, nurses would take a 1-hour break for every long shift worked (approximately 12.5 hours from start to finish), and so paid hours are approximately 8% less than the calculated HPPD (1 out of 12.5). These were summed for each ward for each day.
For each day, we also calculated ‘patient-days’, with 1 patient-day equivalent to one patient occupying one bed for 24 hours. The daily number of patient-days for each ward was calculated using the admission, discharge and transfer information during a 24-hour period (i.e. from midnight to midnight). For example, a patient occupying the bed for 12 hours would be assigned a value of 0.5 (patient hours ÷ 24). Consequently, patient-days represent the average number of occupied beds in a 24-hour period.
By combining these data with the staffing variables, we calculated RN HPPD and HCA HPPD as the sum of hours worked by each group divided by patient-days. Using the same approach, we were able to calculate hours provided by temporary nursing staff employed via the hospital’s bank or from an outside agency.
We also calculated staffing hours by shift and by hour. Shift patterns varied both within and between wards, with a mix of two ’12-hour’ shifts (day/night, each lasting 12.5 hours from start to finish) or a traditional three-shift system [with two 8-hour day shifts (early/late) and a 10-hour night shift] with other minor variations. Therefore, we divided the day into 6-hour period ‘pseudoshifts’ in an attempt to provide a degree of consistency that was congruent to major changes in staffing levels throughout the day:
-
from 01.00 to 07.00 ‘late night’
-
from 07.00 to 13.00 ‘early’
-
from 13.00 to 19.00 ‘late’
-
from 19.00 to 01.00 ‘twilight/night’.
Hereafter, for brevity, we refer to these four periods as ‘shifts’. For each shift we calculated hours of nursing per patient, taking the same approach to patient hours as for the day-level analysis (patient hours ÷ 4). Consequently, the shift-level staffing variable is on the same scale as the day-level variable, such that, if patient numbers were unchanged across each shift and staffing levels were constant, nursing hours per patient per shift = nursing HPPD. Finally, we took a similar approach to calculating staffing levels for each hour of the day.
For our analyses, we explored these variables in a number of ways. The Trust determined staffing establishments (target/planned staffing levels) for the wards using the Safer Nursing Care Tool,98 a validated acuity/dependency staffing tool endorsed by NICE. These establishments (planned staffing levels) varied by ward, reflecting variation in the typical staffing requirement. As patients experience care on different wards, this presents a challenge that makes it difficult to use absolute HPPD as a measure of staffing as the staffing required for each ward differed. Therefore, we determined days when staffing for each ward was low in terms of the following thresholds/approaches:
-
below the mean staffing for the ward (measured in HPPD or equivalent)
-
days when staffing fell below 80% of the mean
-
below the HPPD estimated from the establishment
-
HPPD below the mean.
We also considered the absolute HPPD relative to the mean: a patient who spends a day on a ward where mean staffing is 5 HPPD records a score of 0 for a day when staffing is at the mean level, a score of + 1 for a day when staffing is 6 HPPD and a score of – 1 on days when staffing is 4 HPPD, and so on.
When a patient was transferred during the day, we used staffing levels from the first ward of the day.
The information we received regarding establishments was provided in terms of nurse numbers on each shift, generally using a traditional early, late and night shift pattern, so calculating the established nursing HPPD required a number of assumptions to be made about shift patterns and overlaps. Therefore, we initially focused our analysis using thresholds on the mean staffing level because this required no assumptions on our part. However, mean staffing and established staffing were closely correlated (r = 0.97 for RN HPPD, r = 0.81 for HCA HPPD), with mean staffing levels for RN 6% lower than the HPPD estimated from the planned establishments, and mean staffing for HCA 12% higher than in planned establishments.
When exploring the association between staffing levels and rates of missed observations, we used absolute HPPD, as observations were clustered within wards and therefore ward differences in staffing levels could be accounted for within the statistical models directly.
Admissions per nurse
We calculated the ratio of admissions per nursing hour, to reflect the variation in patient turnover on wards, which also contributes to nurses’ workload. This variable was calculated by identifying the number of admissions to the ward (including transfers from other wards) in the time period and dividing by the number of nursing days or fractional days available during that period (i.e. nursing hours ÷ 24).
Patient acuity and risk
To account for patient-level variation in acuity and risk of death, we calculated two variables based on administrative data. Although the use of administrative data to assess outcomes, in particular risk-adjusted mortality, remains controversial, there is evidence that shows that routine administrative data performs well when compared with clinical data from a national speciality audit database. 99 The arguments against the use of routine administrative data to derive risk-adjusted mortality estimates have been extensively rehearsed in the literature. 100–104
The major criticisms are that:
-
the administrative data do not necessarily appropriately or completely describe the patient population
-
the process is perverted by the fact that the administrative data used to assign risk may also be used to determine payment
-
the risk generated can be ‘gamed’, for example by more extensive coding of comorbidities in those who die or by the use of codes indicating palliative care.
Such factors are likely to have more significance when comparing different hospitals, as practice between hospitals is likely to differ. They are less likely to have detrimental effect when used to examine performance through time in a single hospital (as in the current project), where one would expect coding practices to be (relatively) constant over time. However, inadequate coding could, of course, reduce the accuracy with which underlying risk is estimated. Crucially, there is no a priori reason to suppose that errors might be correlated with the independent variables of interest (i.e. staffing levels on wards) because coding is not undertaken on wards or by ward staff. Furthermore, our chosen approach combines the advantages of a nationally validated risk adjustment model using administrative data with additional risk adjustment using clinical data.
To account for patient-level risk factors, we also used diagnostic and demographic factors (including age and comorbidity) to calculate a predicted risk of death. To do this, we used coefficients derived from the nationally validated SHMI model. 96 We used the June 2015 model, which had been developed from national data for the previous 3 years, approximately coinciding with the study period. 105 This approach allowed us to apply robust estimates of risk associated with a wide range of diagnostic groups (including the effect of interaction between diagnosis and age/comorbidity/admission route) derived from a national population, whereas directly adjusting for mortality risk using the same factors and using only local data would inevitably mean that risks associated with some diagnoses could not be accurately estimated.
Given that the resulting SHMI risk score reflects the average risk for patients with a given diagnosis and comorbidities, we also used the patient’s first NEWS as a measure of their acuity on or near the point of admission. NEWS has been shown to be highly accurate in predicting death in hospital (area under the ROC curve for death within 24 hours of 0.89). 106 As this measure is taken at the beginning of the patient’s stay, it is largely independent of any effects that may result from variation in nurse staffing, whereas subsequent scores may be influenced by care received, including the effects of nurse staffing.
To control for variations in patient acuity on wards when assessing the association between missed observations and staffing, we also calculated the daily proportion of patient observations in categories indicating some higher degree of concern (i.e. NEWS of > 3).
Analysis
Staffing/outcomes
For all aspects of the analysis, we used multilevel/hierarchical mixed-effects regression models to explore the association between staffing levels and outcomes. In all models, outcomes were regressed onto independent variables for RN staffing levels and HCA staffing levels as the main variables of interest. For patient outcomes, models included independent variables controlling for patient condition and risk. All models also included variables to control for the number of admissions to the ward, also considered as a nursing workload variable (admissions per nurse). Patient outcomes were assessed at the patient level, with patients being exposed to varying staffing levels throughout their stay in hospital. These variables were typically expressed as a time-varying covariate representing the cumulative sum of staffing levels experienced up to that point in the stay. Given that patients could experience staffing on different wards, with different baseline staffing requirements, staffing variables for all patient-level analyses were normalised for each ward.
Missed observations were assessed at the ward level, with the rate of missed observations over a given time period (e.g. day, shift) regressed on staffing levels. For these models, absolute nurse staffing levels were used as predictors, with ward included as a random effect. Where appropriate, and possible, we explored for non-linear effects of staffing variables by including quadratic and cubic terms in models. We also tested for evidence of interactions between RN staffing and HCA staffing variables.
The modelling framework is described in more detail in the next section.
Modelling framework: patient outcomes
We used multilevel/hierarchical mixed-effects survival models to explore associations between nurse staffing and mortality/adverse events. We have repeated observations on the same patient because we observed them over a period of time from admission (i.e. onset of risk) until death/adverse event or discharge date. Covariates of interest (such as staffing levels) change over time and, thus, we had to specify a survival model able to account for repeated measurements and time-varying covariates, and unobserved patient-specific characteristics.
We defined a trivariate response (T0, T, d) where T0 is the starting time (i.e. admission date), T is the ending time and d is an indicator for death. Let us consider i = 1, . . ., I patients for which we have j = 1, . . ., Ti observations and let bi be unobservable patient-level random effects that are independent and identically distributed as a Gaussian distribution with zero mean and unknown variance.
A proportional hazard model was specified. The covariates have a multiplicative effect on the hazard function, for example:
for some baseline hazard function h0(tij). Here, a parametric (i.e. exponential) distribution is assumed for the baseline hazard function, selected as it provided a superior model fit to the Cox proportional hazards, for which no distribution is assumed. The resulting model leads to a likelihood function that is not closed and thus must be approximated. Here, the adaptive Gauss–Hermite quadrature method was employed.
Length of stay is measured on a continuous scale because day and time of admission and discharge for each patient are recorded. Thus, we are able to measure the time spent since admission, not only the ‘rounded’ number of days. Typically, modelling continuous outcomes call for the linear model (i.e. for a Gaussian distributed outcome). However, length of stay exhibits a right-skewed distribution with mode near zero and heavy tails. The Gaussian distribution says that values to the left and right of its mean are equally likely to be seen, by virtue of the symmetry inherent in the form of the probability density. Therefore, to better represent length of stay data features, the gamma distribution was used here [i.e. length of stay ∼ gamma(µ;σ2)]. The gamma distribution describes the probabilities with which a random variable Y takes on values, where Y can only be positive. More precisely, let yi be the length of stay for the ith patient, the probability density function for which is given by:
where Γ() is the so-called ‘gamma-function’. In the regression framework, the interest lies in modelling the expected value of the outcome, in this case µ. Here a log-linear model, based on the generalised linear model theory, is proposed. Formally:
where xi collects all patient-specific covariates.
Model variables
For all patient outcomes, we included as covariates the first NEWS, the mode of admission (emergency vs. elective) and a SHMI score indicating the patient’s underlying risk of death given their age, diagnosis and comorbidities [Charlson Comorbidity Index (CCI)]. 107 In addition, we included a random effect for ward, with each ward that a patient was admitted to during their stay assigned a dummy variable (0 or 1), with an additional dummy variable should the patient spend time on a ward where staffing data were unavailable.
The first focus of our analysis was to determine whether or not staffing has an effect on increasing death risk, taking into account the patient’s characteristics. In the core model, we included two time-varying variables measuring the daily exposure to both RN and HCA staffing levels. We extended this in a number of ways to investigate for the presence of further staff-related variables effects, for example by including different exposure variables and/or permanent compared with temporary staffing measures. In general, we considered the effect of RN and HCA staffing separately, reflecting the potentially distinct contribution of each staff group, but also allowing the possibility of staffing substitutions.
Following the approach taken by Needleman et al. 27 we generally restricted our analysis of the association between staffing levels and patient outcomes to consider the effect of staffing experienced over the first 5 days of the hospital stay. Thus, the analysis focused on the period of hospital stay when the patient is most likely to be acutely ill,27 while still including staffing levels experienced by the majority of patients for the majority of their stay (median stay is < 3 days).
Analyses were undertaken using the statistical software Stata®, release 14 (StataCorp LP, College Station, TX, USA).
Modelling framework: missed care
We used multilevel/hierarchical mixed-effects regression models to explore associations between nurse staffing and missed care in the hospital ward. Let y = (y11, y21, . . ., ytj, . . ., yT-1,J, yTJ) be the observed data vector that consists of clustered data, where ytj (t = 1 . . . T, j = 1 . . . J) denotes the number of missed observations on day t from ward j, and µtj is the expected count given the values of a number of explanatory variables (i.e. covariates) and a set of ward-specific random effects b = (b1, . . ., bj, . . ., bJ). Then µtj is necessarily a non-negative number, which could lead to difficulties if we considered using a linear model in this framework. Thus, as is often done when modelling counts in a regression framework, the natural logarithm is used as the function to link µtj with the covariates. For independent (i.e. not clustered) data, this leads to the Poisson regression model for the natural logarithm of the counts, log(µtj). In our setting, as we have clustered data (daily counts of missed care clustered in wards), mixed Poisson models are considered for the logarithm of µtj. When modelling at an hourly/shift level, we took an analogous approach with hours or shifts representing the level one unit nested within wards.
Using the logarithmic link function and P covariates x1, x2, . . ., xP, the model may be written as:
where bj is a random intercept following some known distribution and βs, p = 0, . . ., P, are the regression coefficients associated with the covariates xptj plus the intercept term. The term log(mtj) is included in the model as an offset to account for the total number of observations due at day t in ward j. The most commonly used estimation method for mixed Poisson models is the maximum likelihood. The marginal log likelihood for the considered mixed Poisson model can be written as:
where φ is the distribution of the random effects. The Gaussian distribution with zero mean and unknown variance (to be estimated with all other model parameters) is assumed for φ and the adaptive Gaussian quadrature is used to approximate the integral. A large number of quadrature points (e.g. 11) is used to approximate the likelihood because we have a high number of level 1 units and large intraclass correlations can be assumed.
To check the assumption that our counts of missed observations were adequately captured by the Poisson framework above, we examined the residuals visually for all models using quantile–quantile plots. For the ‘failure to respond’ analysis, we noted the presence of overdispersion and consequently refit a negative binomial model using the same logarithmic link function, although substantive conclusions were largely unaltered. Analyses were undertaken using the statistical software package R version 3.4.0 (The R Foundation for Statistical Computing, Vienna, Austria) using the lme4 and gamlss packages. 108–110
Other modelling considerations and planned subgroup analyses
Given that we were unable to access staffing data for medical teams (and other staff) that were comparable with those for nurse staffing, and indeed because medical staff are generally not clearly allocated to individual wards, it was not possible to directly consider staffing levels from other staff as a potential confounding variable in the analyses. However, we were able to consider this issue by exploring the effects of weekend admissions and stays over the weekend, when medical staffing is known to vary and is suspected to be related to variation in mortality. 111–114 Specifically, we looked to determine whether or not any observed relationships between nurse staffing levels and outcomes are attenuated when patient stays on weekend days are considered as covariates in the model, and also determine whether or not nurse staffing effects are limited to low staffing on night shifts (which might be confounded by low medical staffing at night).
Given that the likelihood and significance of missed observations for an individual may be related to the planned observation frequency, we undertook a subgroup analysis for the association between staffing and missed observations, considering only patients with a high NEWS (therefore requiring frequent observation). We explored for the effect of staffing at a given point in time on missed observations at later points in time, and, because observations are ‘missed’ over extended periods of time, we also explored the effects of the previous shift on subsequent missed observations. We undertook planned analyses on subgroups of wards (general medical, surgical and older people) and subgroups of patients (emergency admissions only).
In addition to assessing the magnitude and significance of the effects estimated for staffing variables in the models, we used the Akaike information criterion (AIC) and the Bayesian information criterion (BIC) to assess relative model fit, preferring models with lower values of AIC/BIC. The first one is known as an estimator of the Kullback–Leibler discrepancy between the data-generating model and the fitted model. The BIC provides an approximation of the Bayesian posterior probability of the candidate model. Compared with methods based on the likelihood ratio test between nested models, these criteria have the advantage of not requiring a bootstrap resampling procedure.
Mediation
Our approach to exploring mediation was based on that outlined by Baron and Kenny. 91 A mediator variable is a variable that accounts, in whole or in part, for the relationship between the independent and dependent variables. 115 First, we hypothesise that low staffing levels reduce the ability of nurses to undertake timely vital signs observations. Second, we hypothesise that timely vital signs observation is a mechanism by which nurses can reduce the risk of death. Thus, we hypothesise that the relationship between nurse staffing levels and mortality is mediated by timely vital signs observation.
If this is the case, there must be a significant relationship between the independent variable of interest (nurse staffing levels) and the dependent variable of mortality (after controlling for other confounders such as patient age and comorbidity). There must also be a significant relationship between the proposed mediator variable (vital signs observation) and the independent variable (staffing levels). Assuming this to be the case, when both the independent variable (staffing) and the mediator (vital signs observation) are included in the regression model, the relationship between the independent variable (staffing) and the dependent (mortality) is significantly reduced or, in the case of full mediation, eliminated. 116
Therefore, to be identified as a mediator, the missed observation variable must satisfy two conditions. First, it must be significantly correlated with the low staffing variable. Second, the missed observation variable must be significantly related with mortality, given that all other related factors are included in the model. If both conditions are satisfied, the variable will be included in the data set as a mediator.
A number of popular methods for the testing of an indirect effect have been proposed in the literature. 116–118 Here, the non-parametric bootstrap was used for inferences. A recommended method to test the hypothesis about a specific indirect effect is to calculate a CI for an indirect effect as the CI gives a range of plausible values for the indirect effect. 119 In general, as long as computing power is not an issue, CIs should be estimated via the bootstrap with > 1000 resamples, which is the used number of simulations in this analysis.
Economic analysis
The aim of the economic analysis was to identify the costs of variation in staffing levels and mixes, and their consequences in terms of reduced rates of missed observations and adverse events. We undertook extensive consultation among patients, the public and professional stakeholders to identify issues and select realistic scenarios to model, with a view to modelling the costs and consequences of staffing levels and skill mix that were associated with ‘acceptable’ levels of compliance with vital signs observations.
To ensure that they are based on an agreed methodology and are nationally representative, we used nationally validated reference and unit values to estimate costs, rather than local figures. For each cost, we determined an appropriate unit cost. We also estimated ‘high’ and ‘low’ costs to determine sensitivity to variation in costs and assumption. For RN staffing we used the unit cost of a band 5 nurse, and for HCA we used the unit cost of a band 2 nurse. For high estimates, we assumed a mix with the staffing band above (50 : 50) and included training costs, using estimates and calculated according to the methodology described in Curtis and Burns,120 although these costs are unlikely to fall directly on the employing trust. As no estimate for training costs is given for HCAs, we estimated these to be half the cost of RN training costs, which is a likely overestimate, although it may reflect the reality of a well-trained assistant workforce. For low estimates of staffing costs, we applied the NHS Improvement agency cap (155% of salary) applied to the hourly salary and applied on costs, but excluding estates and other overheads. We estimated the value of reduced length of stay using the NHS reference cost121 for excess bed-days, which provides a conservative estimate of potential savings from reduced stays. This assumes that no additional treatments costs are incurred associated with extended stays. High and low estimates of cost are taken from the upper/lower quartile estimates. All costs are based on 2015/16 estimates. 121 Sources of cost information are described in detail in Table 3.
| Costs | Resource | Cost basis | Cost (£) | Source |
|---|---|---|---|---|
| Hospital stay (per day) | Excess bed-day (non-elective) | Mean (lower/upper quartile) | 298 (215–357) | Department of Health and Social Care, 2016.121 Upper/lower quartiles estimated from data provided |
| RN hours | Employed/bank staff | Band 5 | 35 | Curtis and Burns, 2016120 |
| Band 6 | 44 | |||
| Agency | Band 5 | 20.34 | Monitor, 2015122 | |
| Band 6 | 25.38 | |||
| RN training | Estimated annual/hourly cost | £11,251 | 7.15 | Curtis and Burns, 2016120 |
| HCA hours | Employed/bank staff | Band 2 | 22 | Curtis and Burns, 2016120 |
| Band 3 | 28 | |||
| Agency | Band 2 | 12.78 | Monitor, 2015122 | |
| Band 3 | 14.27 | |||
| HCA training | Estimated at half of RN training cost | £5625.50 | 3.58 | Curtis and Burns, 2016120 |
The consequences of each scenario were estimated using coefficients from relevant regression models. For estimations involving mortality, we assumed that the HR approximated to a risk ratio, an assumption that is generally valid in the short run and when probabilities of events are small, which is the case with mortality in this study. 123,124 In each case, high and low estimates were based on the upper and lower 95% CIs. We estimated incremental costs and marginal gross costs per life saved associated with each staffing policy, based on staffing costs alone. Net costs were estimated by factoring in the value created by alterations in length of stay. Although reductions in length of stay do not automatically generate cost savings, the resource that is released is of value if it meets the needs of other patients who would otherwise not be able to avail themselves of a bed or of a service that would otherwise not be provided, or hospitals that would need additional bed capacity to meet patient need. Although in some cases fractional days of stay may not be of use, most of our patients were emergency admissions and so we assume that all reductions in stay have value.
Patient and public stakeholder consultations
We undertook a series of consultations with public, patient and clinical experts/stakeholders (including health services managers and ward-based nurses) to identify issues that should be considered when determining scenarios for economic models.
These included:
-
determining an acceptable level of vital signs observations compliance (completing a full set of observations in time)
-
acceptable ranges of skill mix, assuming that the results demonstrated some potential for substitution between HCA and RN.
The work was done in stages so that different groups were approached separately, thus providing the most conducive environment to engage in conversation and share views relevant to each individual group. We began with consultations with expert and professional groups to elucidate a concrete set of preliminary questions and scenarios that could be presented to other groups. Our approach, co-designed with our patient and public involvement representative/lay co-researcher (ADI), was intended to make the key issues to be discussed tangible for both a lay audience and general professional stakeholders such as staff nurses who might not consider themselves ‘experts’ in the specific topics. Thus, we began with consultations with health-care professionals through an online questionnaire and with members of the Study Advisory Group in order to identify preliminary indicators.
This led to the development of some preliminary propositions about skill mix and observation compliance that were used to structure future consultations.
In these consultations, each group was presented with an outline of the project and related research. Questions focused on:
-
current recommended skill mix and, specifically, whether or not the Royal College of Nursing’s125 recommendation of a minimum 65% RN should be regarded as an absolute minimum, and whether or not higher/lower thresholds should be considered
-
the acceptability of a target for compliance levels, using 90% as a starting point to stimulate discussion.
The ensuing responses were used to ‘sense check’ the propositions, to determine whether or not these scenarios made sense to participants and to capture alternative propositions that we might consider. The consultations included:
-
face-to-face engagement with patient and public representative groups
-
Experts by Experience patient groups – co-ordinated directly with members
-
Healthwatch Southampton – co-ordinated by a health community development worker
-
-
online consultation (link distributed at engagement events, to patient groups and on social media)
-
A total of 77 people provided partial responses to the questionnaire and 14 provided complete responses
-
-
face-to-face engagement with senior nursing and management forums
-
Wessex Directors of Nursing Network Meeting, December 2015 (directors of nursing/deputies from all regional NHS organisations; approximately 30 people attended)
-
Nursing and Midwifery Advisory Committee in the Portsmouth Hospital NHS Trust (ward managers and senior nurses; approximately 20 people attended)
-
Deteriorating patient group at Portsmouth Hospital (approximately 15 people attended)
-
-
hosting a Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) chat (@wenurses)
-
A total of 60 people participated in the Twitter chat.
-
Patient and public involvement
The project was developed with significant input from local public and patient groups that helped shape the original research focus, and with a ‘patient representative’ co-researcher (ADI) who was actively involved in day-to-day project activities including project management and discussion and interpretation of results. Perhaps the most central role of ‘involvement’ in this project was the role taken by ADI in the regular project management meetings, providing comment and contributing to all aspects of the project.
A key focus for patient and public involvement lay in the series of consultations/stakeholder engagement events designed to inform economic modelling. In all cases, the approach to these activities was co-designed with our patient co-researcher. In addition, we convened a ‘summit’ of patient, public and professional stakeholders in June 2017, at which we presented early results (co-facilitated by ADI). A second patient representative (MSW) was a member of our advisory group, which also included representatives from local Healthwatch groups and the Patient Association, and they also contributed to discussion and gave advice on the project. We are grateful to participants for the thoughtful contributions and discussion that have helped to inform final modelling decisions and aid our interpretation of findings.
Ethics approval
This project used patient and staff data that were not provided with explicit consent for research purposes. However, no data were used from which an individual’s identity could readily be determined. No sensitive data that might aid identification of individuals (e.g. postcode area) were transferred to the research team and all individual identifiers were pseudonymised, meaning that individuals could be linked across data sets but the research team had no way of linking to original identifiers in source files that contained personal information (e.g. names and addresses). Nonetheless, we took steps to minimise any residual risk arising from attempts to identify individuals from the data. Our report contains no ‘small numbers’ where a constellation of characteristics could be used to identify an individual by a process of elimination. Our data are housed on secure servers with access limited to members of the research team. All data transfers were made using fully encrypted files. The study was approved by the National Research Ethics Service, East Midlands – Northampton Committee (reference 15/EM/0099).
Chapter 3 Results: descriptive
Before considering the relationships between nurse staffing, missed care and patient mortality rates, this section provides a description of each of these key variables and the extent to which they vary between wards within the hospital.
Patients
The study sample comprised 138,133 patients who spent time on one of the 32 general wards of the hospital from April 2012 to March 2015. The majority (79%) were emergency admissions. The mean age was 67 years. Fourteen per cent were aged ≥ 85 years. While 50% had no comorbidities (CCI 0), the mean CCI was 6, with 35% of patients having a score of ≥ 5 (Table 4). Overall, 5662 patients died (4.1%).
| Patient characteristics | n (%)a | Mean (SD) | Median (range) |
|---|---|---|---|
| All patients | 138,133 (100) | ||
| Emergency admissions | 108,865 (79) | ||
| Elective | 29,268 (21) | ||
| Male | 64,596 (47) | ||
| Female | 73,537 (53) | ||
| Age | 62.93 (20.61) | 66.64 (16.03–106.14) | |
| < 65 | 64,984 (47) | ||
| 65–74 | 25,223 (18) | ||
| 75–85 | 28,316 (21) | ||
| > 85 | 19,610 (14) | ||
| Charlson Comorbidity Index | 6.08 (84.26) | 3 (0–98) | |
| CMI 0 | 68,682 (50) | ||
| CMI 1–2 | 231 (0.2) | ||
| CMI 3–4 | 20,385 (15) | ||
| CMI ≥ 5 | 48,663 (35) | ||
| SHMI risk | 0.06 (0.10) | 0.01 (0.00–0.85) | |
| First NEWS | 1.73 (2.03) | 1 (0–19) | |
| Low risk (NEWS ≤ 2) | 102,674 (74) | ||
| Medium risk (NEWS ≥ 3 and NEWS ≤ 5) | 27,409 (20) | ||
| High risk (NEWS ≥ 6) | 8050 (6) | ||
| Length of stay | 6.81 (12.63) | 2.73 (0.15–933.33) |
A total of 137 diagnostic groups were represented as the main diagnosis associated with the admission, based on the Clinical Classification Software groups used in calculating SHMI. 126 Pneumonia was the single most common diagnosis (4.2%), with the most common 15 diagnostic groups accounting for 38% of all admissions. The diagnostic group associated with most deaths was also pneumonia (21% of all deaths). For more detail, see Appendix 3, Table 24.
Staffing levels
Nursing hours per patient day
The average observed staffing level across all wards was 7.75 CHPPD, comprising 4.75 RN HPPD and 2.99 HCA HPPPD, with an average skill mix of 60% RN. Staffing levels varied considerably both between and within wards. Mean RN HPPD varied from 2.91 (medical respiratory ward 2) to 9.61 (medical renal high care). Skill mix (the proportion of RNs) varied from 86% (medical renal ward) to 46% (medical general ward 2). Within-ward variability was also high, with the average standard deviation (SD) representing 18% of the mean for RN HPPD, 29% of the mean of HCA HPPD, 10% of skill mix and 16% of total CHPPD. Figure 2 illustrates the variation of RN HPPD across wards. Ward labels and full data are given in Appendix 4, Tables 25 and 26.
FIGURE 2.
Mean RN HPPD by ward.
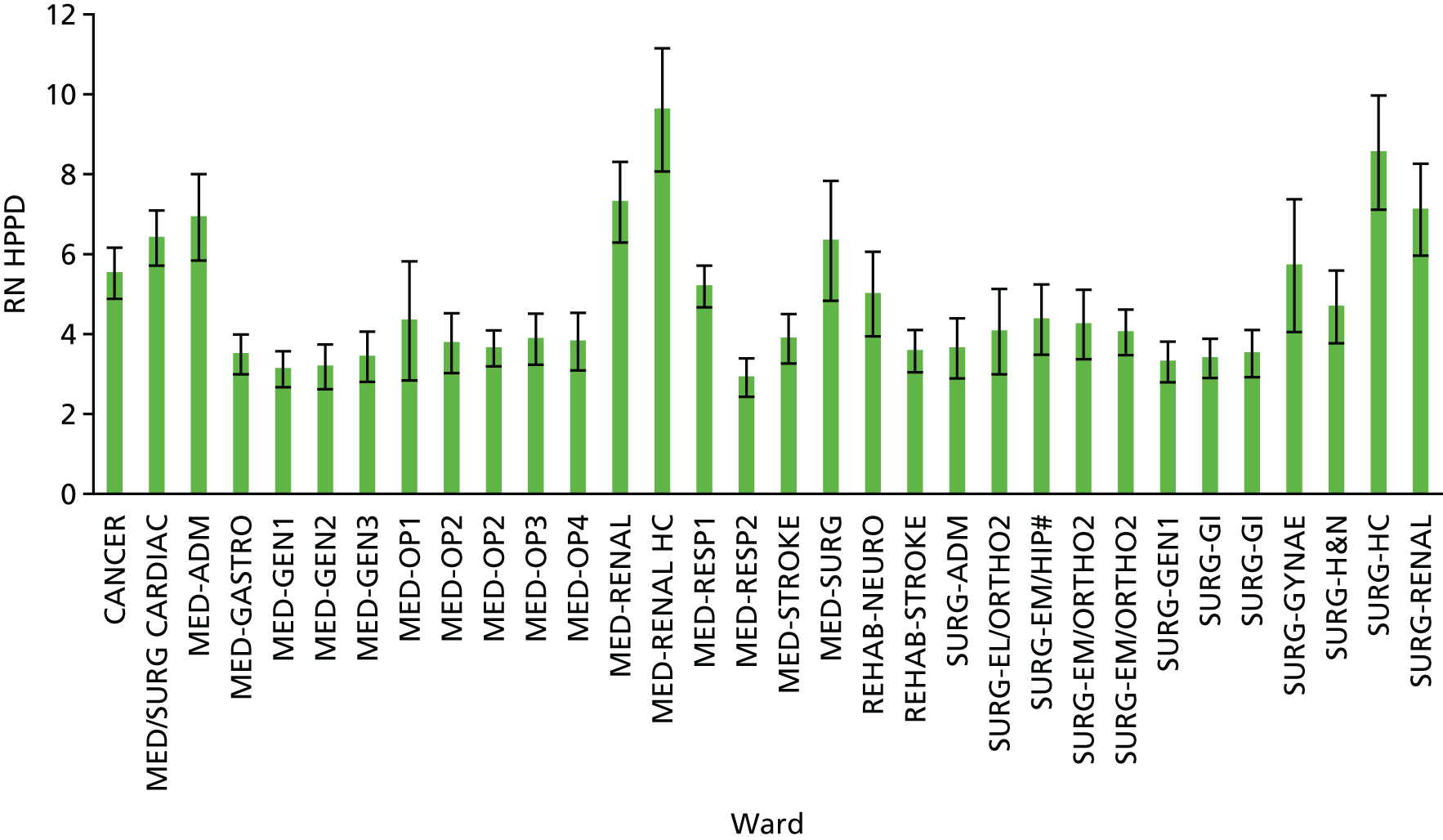
Although our estimated care hours were based on shift start and end time, and thus made no allowance for breaks (estimated as 8% of care hours), the average CHPPD across these wards falls at the low end of the range observed in the Carter Review of productivity in the NHS127 (where the range was from 6.3 to 15.48). After adjusting for breaks, the average CHPPD we observed was 7.13. The mean RN HPPD was approximately equivalent to a patient-to-nurse ratio of 5.5. This approximate patient-to-nurse ratio is based on the inverse of RN HPPD ÷ 24, which gives the nurse-to-patient ratio (after reducing hours to reflect approximately 8% of shift time as breaks). In the wards we studied, the average RN HPPD was lower by 8% at weekends than on weekdays. Reductions in RN hours at weekends were observed on all wards except surgical admissions, including those that handled exclusively emergency admissions (e.g. medical admissions, where weekend RN staffing was lower by 10%). There was no significant overall difference in HCA staffing levels between weekends and weekdays (mean difference 0.2%).
Mean RN HPPD was highly correlated with the estimated RN HPPD estimated from the planned establishment (Pearson’s r = 0.97), with average RN HPPD 95% of the establishment level. Similarly, mean HCA staffing was closely correlated with the establishment (Pearson’s r = 0.81), although there was more variation, with mean HCA staffing 115% of establishment.
The use of temporary staffing was common, with only 24% of the 30,980 ward days having no bank or agency RN staff and 13% having no bank or agency HCAs. However, the use of high numbers of temporary staff was relatively rare, with 4% of days having 1.5 temporary RN HPPD, although less so for HCAs, with 15% of days with ≥ 1.5 HCA HPPD (Figure 3). The use of temporary staff varied by ward, with one ward showing fewer than 1% of days with no temporary staff (see Appendix 4, Table 28).
FIGURE 3.
Days with temporary staffing.
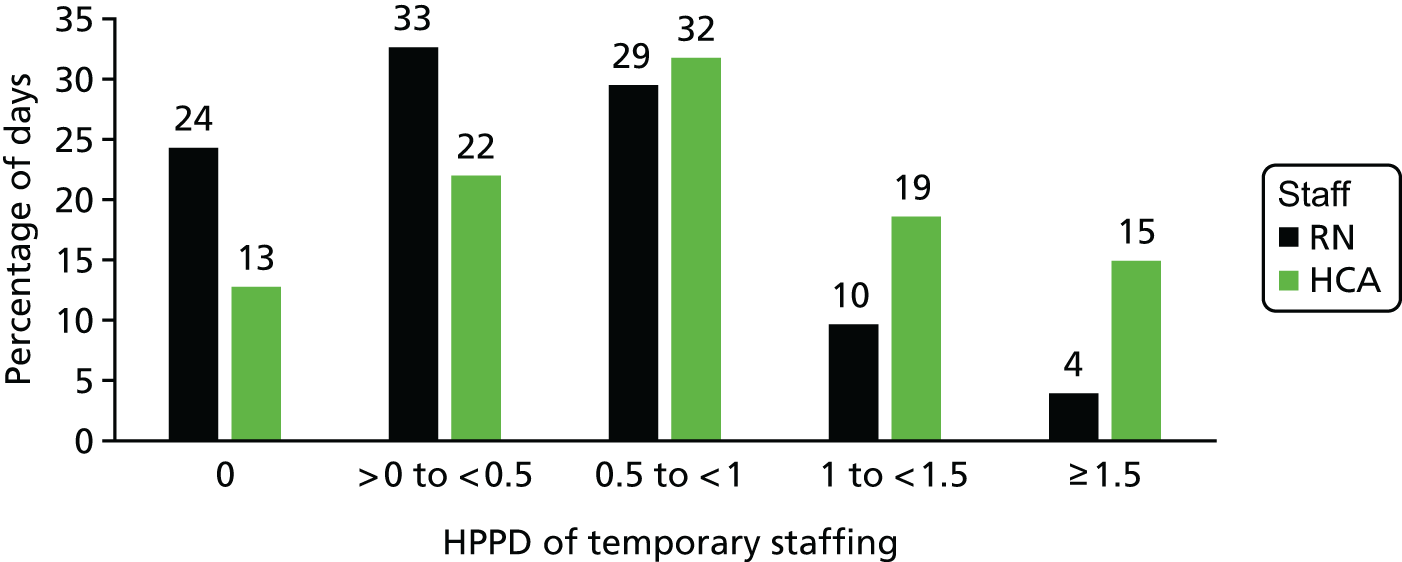
Exposure to low staffing levels
During a patient’s hospital stay, the median number of days of low staffing (below the mean of whichever ward they were on) was 2 (mean for low RN staffing 1.93; mean for low HCA staffing 1.94), with a mean cumulative shortfall of 0.39 RN hours per patient and 0.25 HCA hours per patient (see Appendix 4, Table 30). Out of a total of 30,980 ‘ward-days’, staffing fell below the mean HPPD on 54% of occasions for both RNs and HCAs. For RN HPPD, staffing was below the estimated establishment on 67% of days and fell below 80% of the mean on 10% of days. For HCA HPPD, staffing fell below establishment on 38% of days and below 80% of the mean on 19% of days (see Appendix 4, Table 29).
Admissions
Admissions per staff member varied between wards, ranging from 0.15 (rehabilitation-neurological) to 5.45 (surgical admissions) admissions per RN. On average, 1.4 patients were admitted per RN and 2.67 were admitted per HCA. Given that typical admissions will vary by ward, and ward establishments should be set to accommodate typical admission levels, we identified days when admissions per nurse exceeded 125% of the mean, reflecting a mismatch between demand and available staff, resulting from either a low number of staff or a high number of admissions. Overall, this occurred on around one-quarter of the days (27% for admissions per RN and 26% for admissions per HCA), with patients exposed to a mean of 0.88 days of high admissions per RN and 0.91 days of high admissions per HCA (see Appendix 4, Table 31).
Missed vital signs observations and nutritional assessments
Missed vital signs observations
In total, 2,869,963 complete sets of vital signs observations were available for the study from eligible wards and were matched to staffing data. Of these, 400,194 (14%) were taken significantly late (between one-third and two-thirds of the scheduled observation interval past time due) and 464,017 (16%) were classified as missed (more than two-thirds of the schedule observation period past time due). Rates of missed observations varied between ward, with the highest rates seen on the rehabilitation-neurological ward (45%) and the lowest on surgical/high care and admission wards (6%). Stroke rehabilitation and respiratory wards also showed high rates of missed observations (between 39% and 31%) (Figure 4).
FIGURE 4.
Percentage of observations missed by ward. See Appendix 4, Table 26 for a key to ward labels.

There are perceived problems with complying with observations scheduled by NEWS in respiratory patients because some patients have persistently high scores as a ‘norm’. 128 Although the two respiratory wards did have a high proportion of observations taken in patients with a NEWS of ≥ 6 (21% and 12%, compared with 6% overall), overall there was a low correlation between the proportion of observations required in high-acuity patients on the ward and the overall level of compliance on that ward (r = 0.24). Of all observations, 2,042,792 (71%) were taken for patients classified as ‘low-acuity’ based on their previous NEWS (NEWS of ≤ 3). Observations in high-acuity patients (NEWS of ≥ 6) accounted for 6% (184,628) of observations. Observations were more likely to be missed in patients classified as high acuity (44% missed) than in those classified as low acuity (9% missed). This pattern was observed on all wards, although the disparity was relatively small in some wards, particularly rehabilitation wards (see Appendix 4, Figure 14).
Who undertakes vital signs observations?
We scrutinised the observation records to determine which staff groups were recorded as taking vital signs observations. Practice appeared to vary by ward, with between 1% and 39% of all observations recorded as being taken by HCAs (see Appendix 4, Table 32). Overall, the average across all wards was 15%. This is likely to under-represent the proportion of ‘nursing’ observations taken by HCAs, as observations taken by other groups (including doctors) are also recorded. Although a sizeable majority of observations appeared to be taken by nursing staff, the lack of standardised coding for staff groups and the variety of groups listed (including a sizeable group of ‘unknown’) rendered more detailed analyses of these data impossible. However, while the proportion of observations recorded as taken by HCAs for high-acuity patients (NEWS of ≥ 6) is lower than for low-acuity patients (NEWS of 0–2), the difference is small (1.8%). The proportion of observations recorded by HCAs on a ward was not significantly associated with average RN HPPD (Pearson’s r = 0.19; p = 0.31) or skill mix (r = 0.25; p = 0.17).
Missed nutritional assessments
We scrutinised the Vitalpac data for other records of care whose completeness could be judged against a clear protocol that would define whether or not the required care was done on time. Although these care items would not necessarily fall on the causal path linking low staffing to mortality, there is an opportunity to explore whether or not these data might prove useful for assessing other aspects of care, and, specifically, to see whether or not there is evidence of associations between low staffing and omissions in other aspects of care. The clearest example of a policy that defined when an assessment was due (and therefore could be used to determine omissions) was the policy for nutritional screening using the MUST tool. Trust policy stated that a MUST assessment must be undertaken for every patient within 24 hours of admission to hospital.
We identified 43,451 instances where we could link staffing levels to a patient for whom a nutritional screening assessment was due within 24 hours of first admission. On 9312 (21%) occasions the assessment was recorded later than this or none was recorded. Compliance with the policy of assessment within 24 hours varied from 100% (rehabilitation-neurological ward) to 8% (surgical–gynaecology, admissions and medical/surgical wards) (see Appendix 4, Figure 14), although some wards had very few direct admissions and so were rarely required to undertake a patient’s first assessment.
Chapter 4 Results: overview
What follows is a series of analyses exploring many facets of the relationship between nurse staffing levels, patient outcomes and omissions in care. We begin by exploring the relationship between staffing levels that are encountered by individual patients during their hospital stay and the hazard of death; adverse events (death, cardiac arrest or unplanned ICU admission) and length of hospital stay.
In subsequent sections, we go on to explore the relationship between staffing on a ward and the levels of missed care, focusing primarily on levels of missed vital signs observations, but also considering a composite measure that might indicate a more general failure to respond to deterioration, and a measure of compliance with the Trust’s policy on nutritional screening.
Finally, we explore these relationships further to determine whether or not there is evidence that the omission of vital signs observations caused by low staffing might provide a mechanism by which low nurse staffing might be causally linked to increased rates of death. That is, we analyse the data to see if missed observations mediate any observed relationships between staffing and outcomes.
In Table 5 we outline the main sequence that we will follow in order to orient the reader by identifying the underlying questions driving the sequence of analyses.
| Results section | Main question | Approach |
|---|---|---|
| Staffing: patient outcomes | Is the risk of death increased when patients are exposed to days when staffing levels fall below the mean? | Survival models with cumulative exposure to days with staffing below ward mean |
| Are there different effects for low RN and HCA staffing? | Separate variables for each staff group | |
| Is any effect of low nurse staffing simply a general ‘weekend effect’, when staffing by other groups is also low? | Adding variables for weekend stay/admission | |
| What if we used different thresholds: lower than planned or very low (80% of the mean)? | Survival model with cumulative exposure to low staffing using other thresholds | |
| Is the amount of nurse staffing (absolute quantity) related to mortality? | Survival models with cumulative exposure to nursing hours relative to ward mean | |
| Is the relationship linear: does adding more staff have the same effect whatever the existing level? | Adding ‘non-linear’ (quadratic/cubic) terms to survival models | |
| Does the number of staff in one group alter the effects of the other? | Adding interaction terms to models | |
| What is the effect of the level of temporary staffing (bank and agency)? | Adding variables for temporary staff to models | |
| Are results similar when considering other adverse events (death, unplanned ICU admission and cardiac arrest)? | Survival models with alternative outcomes | |
| Staffing and missed care | Is the level of missed vital signs observations reduced on days when there are more nursing hours available? | Poisson regression models of relationship between HPPD and the rate of missed observations |
| Are there different effects for RN and HCA staffing? | Separate variables for each staff group | |
| Does the amount of one group of staff alter the effects of the other? | Interaction terms in the models | |
| Are the effects different for patients most at risk of deteriorating? | Exploration of subgroup of high-acuity patients | |
| Are the effects different on different types of wards? | Exploration of relationships on subgroups of wards | |
| Are similar relationships observed looking at staffing at shift/hourly levels? | Secondary analysis of staffing at shift/hourly level | |
| Is the relationship linear: does adding more staff have the same effect whatever the existing level? | Adding ‘non-linear’ (quadratic/cubic) terms to models | |
| Is there evidence of relationships between staffing levels and other ‘omissions’ in care? | Exploration of ‘failure to respond’ and missed nutritional assessment | |
| Mediation | Given the relationships found between staffing levels, mortality and missed vital signs observations, does low staff leading to increased ‘missed observations’ partially explain the effect of low staffing on risk of death? | Mediation analysis |
| Costs and consequences | Given the findings about links between RN and HCA staffing levels, risk of death and length of stay, what might happen if staffing levels were changed? | Economic cost–consequences model |
Chapter 5 Results: staffing – patient outcomes
Mortality
First, we consider a series of survival models considering different definitions of low staffing in order to explore the relationships between the staffing levels experienced by patients and their hazard of death. Given that mean staffing levels are empirically derived and correlate highly with the required hours per day estimated from the ward establishments, we use staffing below the mean of the ward the patient was on for each day as our starting point. For RN HPPD, this represents staffing marginally below the estimated establishment on most wards. We then consider alternative thresholds (i.e. staffing below 80% of the mean and staffing below the estimated establishment) and determine whether or not the effect of low staffing could be confounded with a more general ‘weekend’ effect.
We then move on to consider staffing as a continuous variable by focusing on the cumulative sum of nursing HPPD relative to ward means that the patient experiences. With these data, we explore further for evidence of non-linear associations and interactions between staff groups. Finally, we consider further the composition of the nursing staff by exploring whether or not the presence of temporary staff on the ward is associated with an increased risk of mortality.
Unless otherwise noted, all models consider the cumulative sum of staffing over the first 5 days. All models were controlled for patient characteristics and ward. Full models are presented in Appendix 5 or available on request. Unconditional coefficients for staffing outcomes associations (adjusting for ward only) are given in Appendix 5, Table 32.
Low staffing thresholds
For each day that a patient was on a ward with RN staffing below the mean for that ward, the hazard of death was increased by 3% (HR 1.03, 95% CI 1.01 to 1.06). Each day of exposure to HCA staffing below the mean was associated with a 4% increase in the hazard of death (HR 1.04, 95% CI 1.02 to 1.07). When patients were on wards where admissions per RN exceeded 125% of the mean for that ward, the hazard of death was increased by 5% (HR 1.05, 95% CI 1.01 to 1.09), although there was no association between admissions per HCA and hazard of death (HR 1, 95% CI 0.96 to 1.04) (Table 6).
| Staffing exposure (per day over first 5 days) | HR | p-value | 95% CI |
|---|---|---|---|
| Admissions per RN of > 125% of ward mean | 1.05 | 0.024 | 1.01 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.873 | 0.96 to 1.04 |
| RN staffing below ward mean | 1.03 | 0.009 | 1.01 to 1.06 |
| HCA staffing below ward mean | 1.04 | < 0.001 | 1.02 to 1.07 |
When considering only deaths within 30 days of admission, the model coefficients were almost identical. Similarly, restricting the model to emergency admissions only had no effect on the coefficients for the staffing variables (see Appendix 5, Tables 36 and 37). Considering staffing on all days of a patient’s stay showed significant adverse effects from low RN staffing only, although the coefficients were lower (HR 1.01 per day of low RN), which is probably a product of increased risk being primarily associated with days early in the stay (see Appendix 5, Table 38).
Patients admitted at the weekend experienced an increased hazard of death (HR 1.06), but the effect of low RN/HCA staffing was unchanged. When 1 or more days of a patient’s stay in hospital were over at a weekend, the hazard of death was reduced (HR 0.58) and the effect of low nurse staffing was marginally strengthened (each day of RN staffing below the mean, HR 1.04; HCA staffing below the mean, HR 1.05). As model fit was not clearly improved by including variables for weekend admissions/stay, we did not include these variables in other models (see Appendix 5, Tables 39 and 40).
Using alternative thresholds to define ‘low’ staffing provides somewhat contrasting results. For each day that RN HPPD fell below the estimated RN establishment, the hazard of death was increased by 9% (HR 1.09, 95% CI 1.06 to 1.11). However, the effect of HCA staffing below establishment was not statistically significant (HR 1.01, 95% CI 0.99 to 1.04; Table 7). There was no association between RN staffing below 80% of the ward mean and the hazard of death (HR 0.98, 95% CI 0.94 to 1.02), whereas HCA staffing below 80% of the ward mean was associated with an increased hazard of death (HR 1.04, 95% CI 1.01 to 1.07; see Table 7).
| Staffing exposure (per day over first 5 days) | HR | p-value | 95% CI |
|---|---|---|---|
| Estimated establishment as thresholda | |||
| RN staffing below establishment | 1.09 | < 0.001 | 1.06 to 1.11 |
| HCA staffing below establishment | 1.01 | 0.241 | 0.99 to 1.04 |
| Staffing below 80% of mean as thresholdb | |||
| RN staffing below 80% of ward mean | 0.98 | 0.314 | 0.94 to 1.02 |
| HCA staffing below 80% ward mean | 1.04 | 0.016 | 1.01 to 1.07 |
Although the models using the 80% threshold provide worse model fit (in terms of AIC and BIC), these results highlight the possibility that the staffing outcome relationships are non-linear, or that there could be interaction between the effects of RN and HCA staffing. We explore this further in the subsequent section.
Staffing levels
To further quantify the effect of variation in staffing levels, we explored the effects of absolute variations by calculating the cumulative sum of staffing in hours per patient relative to the mean for the ward for each patient for each of the first 5 days. This gives an indication of the average staffing experienced by the patient over these 5 days, relative to what was normal for each ward, effectively ‘standardising’ and allowing for variation in baseline staffing requirements.
Every additional RN hour was associated with a 3% reduction in the hazard of death (HR 0.97, 95% CI 0.94 to 1.00). However, additional HCA hours were not associated with a reduced hazard of death (HR 1.01, 95% CI 0.98 to 1.04; Table 8). Considering only hours below the mean provided similar estimates, with a 3% increase in the hazard of death for every RN hour below the mean, but no significant association with HCA HPPD (see Appendix 5, Table 44).
| Staffing exposure (per day over first 5 days) | HR | Standard error | p-value | 95% CI |
|---|---|---|---|---|
| Admissions per RN of > 125% of ward mean | 1.06 | 0.022 | 0.003 | 1.02 to 1.11 |
| Admissions per HCA of > 125% of ward mean | 1.02 | 0.020 | 0.238 | 0.98 to 1.06 |
| RN hours ± ward mean (cumulative sum) | 0.97 | 0.013 | 0.023 | 0.94 to 1.00 |
| HCA hours ± ward mean (cumulative sum) | 1.01 | 0.015 | 0.394 | 0.98 to 1.04 |
The pattern of results across different thresholds, and with staffing as a continuous variable, raised the possibility that the underlying relationship was non-linear, particularly in relation to HCA staffing levels. We explored this by introducing quadratic and cubic terms for the staffing variables (hours ± mean) into the models.
Introducing only quadratic terms left the linear coefficients unchanged, giving no indication of a non-linear effect (HR 1.00 for the quadratic term for both RN and HCA hours). Introducing a cubic term produced a significant quadratic coefficient for HCA hours and a near-significant coefficient for the cubic term. RN hours coefficients were non-significant, although the linear term was similar to the linear-only model. The plot of this model can be seen in Figure 5, with the full model in Appendix 5, Table 45.
FIGURE 5.
Care HPPD and hazard of death: non-linear effects.
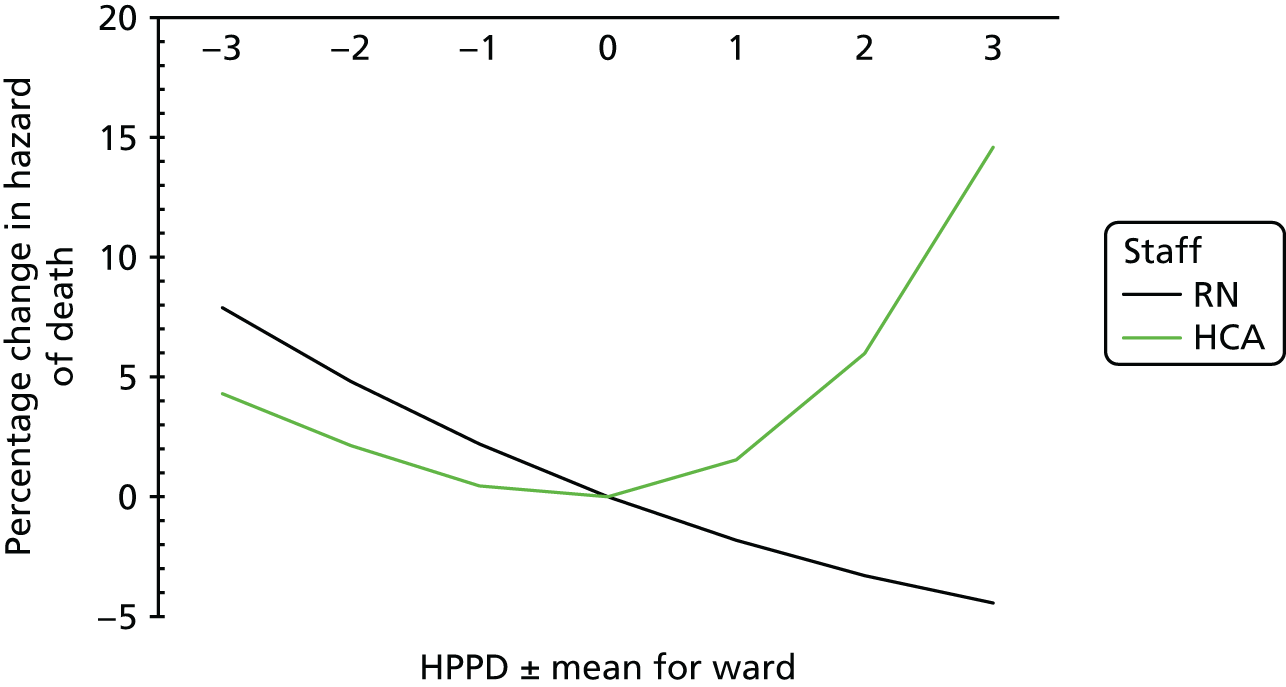
There was a slight tendency for the effect of RN staffing to reduce as staffing levels increased, but, as none of the non-linear terms was close to significance, a null hypothesis of linearity cannot be rejected. However, there seems to be some evidence that, as the cumulative level of HCA staffing (hours) experienced by a patient over the first 5 days of hospitalisation varies from the mean in either direction, the hazard of death may be increased. However, as these models do not give an improved fit in relation to the linear-only models (AIC 61920.19, BIC 62453.88), any conclusions about non-linear relationships must be made with caution.
We also considered whether there was evidence that variation in levels of HCA staffing could alter the ‘effectiveness’ of RN staffing (or vice versa) by introducing interaction terms into our models. There was no significant interaction between the cumulative sums of hours of RN staffing and HCA staffing for hazard of death. However, the interaction between these two cumulative sum variables gives no direct indication of how the staffing levels ‘on the day’ might interact, so we generated variables to indicates days of low RN staffing, low HCA staffing or both. This model provided no evidence of interaction with the sum of the coefficients for low staffing by one or the other group, yielding a combined HR very similar to that associated with low staffing by both (see Appendix 5, Table 46).
Temporary staffing
We considered the effect of temporary nurse staffing by adding a variable to indicate the number of CHPPD that were provided by temporary (bank or agency) staff. We considered three different thresholds for a ‘high’ level of temporary nurse staffing, and calculated a variable to reflect the cumulative sum of days the patient was exposed to temporary staffing above that threshold. In general, adding these variables for temporary staffing did not substantially alter the coefficients for other staffing variables, although levels of significance did alter. Temporary staffing was associated with significant increases in the hazard of death, particularly at higher levels (Table 9).
| Staffing exposure (per day over first 5 days) | Level of temporary staffing (HPPD) | |||
|---|---|---|---|---|
| Null model | > 0.5 hours | > 1 hour | > 1.5 hours | |
| Admissions per RN of > 125% of ward mean | 1.05 | 1.03 | 1.04 | 1.04 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 1.00 | 1.00 | 1.00 |
| RN staffing below ward mean | 1.03** | 1.02 | 1.03* | 1.03* |
| HCA staffing below ward mean | 1.04** | 1.05** | 1.05** | 1.05** |
| Days with temporary RN staffing | – | 0.99 | 1.03 | 1.12* |
| Days with temporary HCA staffing | – | 1.06** | 1.02 | 1.05** |
When patients experienced days with ≥ 1.5 HPPD of temporary RN staffing, the hazard of death was increased by 12% (HR 1.12, 95% CI 1.03 to 1.21). Exposure to lower levels of temporary RN staffing was not associated with significant increases in the hazard of death. Although the hazard of death was significantly increased with exposure to days with ≥ 30 minutes of temporary HCA staffing (HR 1.05), the trend was inconsistent across the different thresholds: exposure to days of ≥ 1.5 HPPD of temporary HCA staffing was associated with a similar increase in hazard of death (HR 1.04). There was no clear benefit in terms of improved model fit compared with models without the inclusion of temporary staffing (AIC was marginally lower and BIC was marginally higher) and, therefore, we did not routinely include this variable in other models.
Secondary outcomes
Adverse events
We calculated a composite outcome to identify patients who experienced a severe deterioration resulting in the first occurrence of any ICU admission, cardiac arrest or death. Every additional RN HPPD over the first 5 days was associated with a 2% decrease in the hazard of an adverse event (HR 0.98, 95% CI 0.96 to 0.99; Table 10).
| Staffing exposure (per day over first 5 days) | HR | Standard error | p-value | 95% CI |
|---|---|---|---|---|
| Admissions per RN of > 125% of ward mean | 1.04 | 0.020 | 0.034 | 1.00 to 1.08 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.020 | 0.873 | 0.97 to 1.04 |
| RN hours ± ward mean (cumulative sum) | 0.98 | 0.007 | 0.001 | 0.96 to 0.99 |
| HCA hours ± ward mean (cumulative sum) | 1.01 | 0.008 | 0.367 | 0.99 to 1.02 |
Length of stay
To explore the association between staffing levels and length of stay, we averaged staffing relative to the mean over the first 5 days of the patient’s hospital stay (Table 11).
| Staffing exposure (per day over first 5 days) | Coefficient | Standard error | p-value | 95% CI |
|---|---|---|---|---|
| RN hours ± ward mean (average) | –0.231 | 0.035 | < 0.001 | –0.30 to –0.16 |
| HCA hours ± ward mean (average) | 0.076 | 0.026 | 0.003 | 0.03 to 0.13 |
Higher RN staffing levels are associated with a small but significant reduction in length of stay. Every 1-hour increase in average RN HPPD was associated with a reduction in length of stay of 0.23 days (95% CI –0.30 to –0.13 days; p < 0.001). Additional hours of HCA staffing were associated with a small but significant increase in length of stay of 0.08 days (see Table 11). We tested for non-linear effects by considering quadratic terms. This was not significant for RN staffing. For HCA staffing, the quadratic terms were significant but had little impact on the overall relationship for a plausible range of values.
Summary and implications for remaining analyses
The analyses presented so far confirm a relationship between RN staffing levels and patient mortality. By taking a variety of perspectives on ‘low’ staffing, there is a largely consistent conclusion: when patients experience lower levels of RN staffing, there is an increased hazard of death. The relationship appears to be linear: the higher the average staffing levels experienced by the patient, relative to the mean for the current ward, the lower the hazard of death. The only clear exception to this conclusion comes when using a very low threshold to define low staffing; that is, when staffing falls below 80% of the mean. In this case, we have good reason to doubt the validity of staffing data as redeployment of staff from other wards to fill significant gaps is not recorded in our data sets. This is more likely to happen when staffing falls to extremely low levels. Mortality also appears to increase when admissions per RN exceed 125% of the mean for the ward. There is also evidence that increased adverse events are associated with lower RN staffing levels and that length of stay is reduced when patients experience higher staffing.
For HCA staffing the picture is substantially more ambiguous. Whereas previous research has found adverse outcomes to be associated with higher levels of HCA staffing, that is not clearly reflected here, although we did find a small negative effect on length of stay. On the other hand, there is no consistent picture of benefit. We did not see significant association between admissions per HCA and mortality. Days of low HCA staffing relative to the mean are associated with increased hazard, but there is no beneficial effect from cumulative hours and a possible non-linear effect whereby harm increases as hours of HCA staffing moves away from the mean in either direction. Although our analyses hint at potential non-linear effects and possible interactions with RN staffing levels, the nature of this relationship is not easy to resolve. Consequently, these potential effects and interactions will be explored further in subsequent analyses examining missed care to see if any light is shed on the matter.
Our secondary analyses identified that the nurse staffing effects we saw were independent of weekend effects (and so are unlikely to be confounded by low staffing from other groups) and also suggested that there were negative effects associated with days when temporary staffing levels were high.
Taking all this into account, we made a number of decisions to inform our basic approach to modelling in relation to missed care (e.g. observations, nutritional assessments and ‘failure to respond’). We dropped admissions per HCA from these models when preliminary testing confirmed that it was not a significant predictor in missed care models, just as it was not in survival models. However, our interest in a possible interaction led us to routinely include an interaction effect for the two main staffing variables (RN and HCA HHPD) because, unlike in the survival models, this variable reflected the interaction of staffing levels on a particular day or, indeed, shift.
Chapter 6 Results: staffing – missed care
In this section we explore the relationship between staffing on a ward and the levels of missed care, focusing primarily on levels of late or missed vital signs observations but also considering, as secondary measures, a composite measure that might indicate a more general failure to respond to deterioration and a measure of compliance with the Trust’s policy on nutritional screening. All models were controlled for ward (random effects), proportion of patients on the ward who were ‘unwell’ (NEWS of ≥ 3) and admissions per RN.
Vital signs observations
Table 12 gives the results of Poisson regression models examining the effect of staffing levels on missed and late observations in all patients and in those patients with a high NEWS (≥ 6). Higher RN and HCA HPPD were significantly associated with lower rates of missed observations. The effect of HCA staffing [incidence rate ratio (IRR) 0.95, 95% CI 0.95 to 0.96] was stronger than for RN staffing (IRR 0.98, 95% CI 0.98 to 0.99). More admissions per RN were associated with a significant increase in the rate of missed observations (IRR 1.01).
| Lateness category | Observations | |||||
|---|---|---|---|---|---|---|
| All | High-acuity patients (NEWS of ≥ 6) | |||||
| p-value | IRR | 95% CI | p-value | IRR | 95% CI | |
| Missed | ||||||
| RN HPPD | < 0.001 | 0.98 | 0.98 to 0.99 | < 0.001 | 0.98 | 0.97 to 0.99 |
| HCA HPPD | < 0.001 | 0.95 | 0.95 to 0.96 | 0.980 | 1.00 | 0.99 to 1.01 |
| Admissions per RN | < 0.001 | 1.01 | 1.01 to 1.01 | 0.591 | 1.00 | 0.99 to 1.01 |
| Proportion unwell | < 0.001 | 9.21 | 8.75 to 9.73 | < 0.001 | 1.63 | 1.47 to 1.81 |
| RN × HCA | < 0.001 | 1.01 | 1.01 to 1.01 | 0.223 | 1.00 | 0.99 to 1.00 |
| Late | ||||||
| RN HPPD | < 0.001 | 0.98 | 0.98 to 0.99 | 0.001 | 0.99 | 0.98 to 0.99 |
| HCA HPPD | < 0.001 | 0.98 | 0.98 to 0.98 | 0.734 | 1.00 | 0.99 to 1.01 |
| Admissions per RN | 0.012 | 1.00 | 1.00 to 1.01 | 0.342 | 1.00 | 0.99 to 1.00 |
| Proportion unwell | < 0.001 | 3.32 | 3.19 to 3.46 | < 0.001 | 1.58 | 1.44 to 1.74 |
| RN × HCA | < 0.001 | 1.01 | 1.00 to 1.01 | 0.710 | 1.00 | 1.00 to 1.00 |
There was a significant interaction between RN and HCA HPPD. The interaction is illustrated in Figure 6, which shows that the ‘beneficial’ effect of additional HCA hours exists only when RN HPPD is low. It is absent, and indeed associated with small increases in the rate of missed observations, when RN HPPD is ≥ 6.
FIGURE 6.
Interaction between HCA and RN HPPD: rate of missed observations.
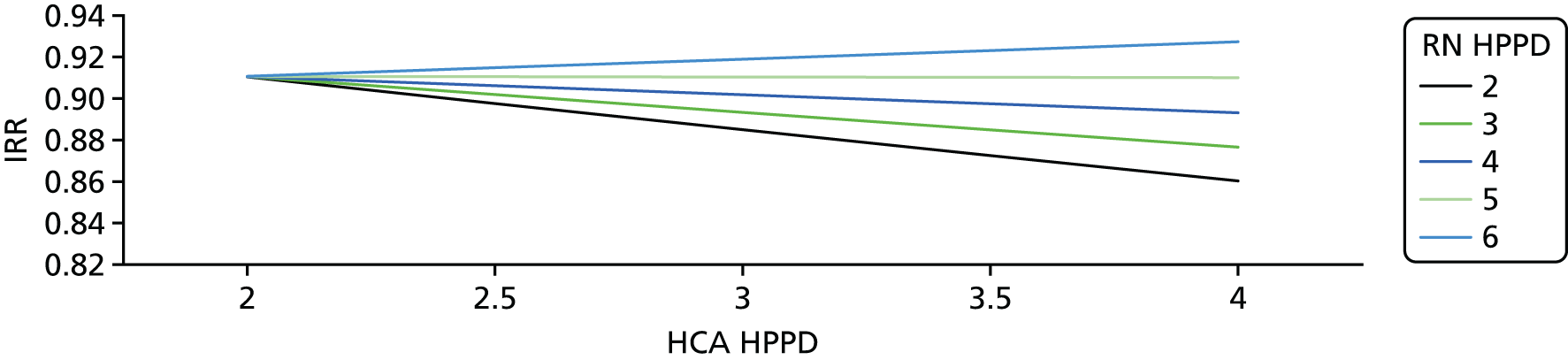
Results for late observations were similar, although there was no difference in effect between staffing groups (RN IRR 0.98; HCA IRR 0.98). Although highly significant (p < 0.01), the magnitude of the effects was small. For example, an additional HCA HPPD was associated with a reduction in the rate of missed observations of 5%. At the baseline rate of 16% missed observations, that equated to an absolute reduction of 0.8% associated with adding 1 HCA HPPD (from 16% to 15.2%).
In high-acuity patients, only RN HPPD was significantly associated with the rate of late observations (IRR 0.99) or missed observations (IRR 0.98). There were no significant interactions between RN and HCA staffing. The strongest effect was for missed observations (IRR 0.98). Although the effect size remained small, the rate of missed observations in this group of patients was high (44%) and the potential consequences of missed observations was greater. Nonetheless, an additional RN HPPD was associated only with a reduction in missed observations from 44% to 43%.
Ward subgroups
We explored ward subtypes focusing on older people, surgery and medicine (including all relevant specialties but excluding mixed medical/surgical, high dependency and admission units). Full results are reported in Appendix 5, Table 50.
Compared with the overall analysis, when analysing only medical wards the association between RN staffing levels and the overall rate of missed observations was stronger (IRR 0.94) and the association with HCA staffing levels was weaker (IRR 0.97). The findings for surgical wards were similar to the overall results: RN IRR per additional hour was 0.98 and HCA IRR per additional hour was 0.95. However, for care of older people wards, increased HCA HPPD was associated with lower rates of missed observations (IRR 0.91), but a higher level of RN staffing was associated with an increased rate of missed observations (IRR 1.06). In all cases there was a significant interaction between RN and HCA staffing. Plotting these interactions gave broadly similar results to that for the combined sample (Figure 7).
FIGURE 7.
Interaction of RN and HCA staffing in medical wards: missed high-acuity observations.
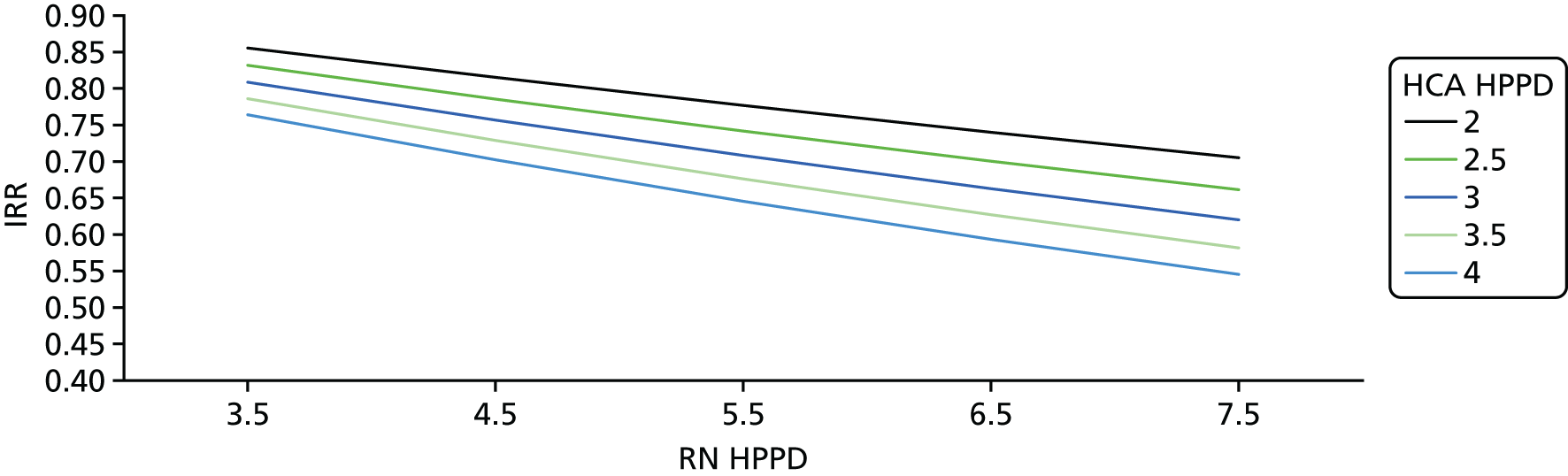
Focusing on high-acuity observations only in these subgroups yielded few significant results, although the pattern broadly mirrored that found in the combined sample. There were two exceptions: a significant interaction between RN and HCA staffing for medical wards and a significant reduction in the rate of missed observations in high-acuity patients associated with higher HCA HPPD in older people’s wards. Plotting the interaction effect for medical wards provided a ‘classic’ picture of HCA staff acting as labour complements by increasing the effect of RN staffing, while having no direct effect in isolation and not acting as a substitute for RN staffing (see Figure 7). The only evidence that HCAs might substitute for RNs in taking high-acuity observations came from care of older people wards, where HCA staffing was already high (average HCA HPPD of 3.93 hours vs. 2.85 hours in the surgical wards and 2.93 hours in the medical wards). The relatively small number of wards on a single site limited our ability to further explore these subgroups, although, among other issues, these findings do raise the possibility of non-linear effects; these will be explored further.
Shift and hourly level
We calculated separate models for the association between staffing levels and missed observations on four shifts (night, early, late and twilight). First, we considered associations with staffing levels at the time when the observation was due to occur. Given that observations are missed over a period of time rather than in a single moment, we also calculated models to explore the associations between missed observations and staffing on the previous shift and the subsequent shift.
There was evidence for associations between staffing and rates of missed observations on all shifts, which was broadly in line with the pattern observed at the day level. Although night RN and HCA HPPD were not significantly associated with the rate of missed observations on a night shift, the number of admissions per RN was. There was also evidence that the rate of missed observations on most shifts was significantly associated with staffing levels on both previous and subsequent shifts.
Focusing on observations in high-acuity patients, only a few associations were significant, although the pattern of results broadly resembles the results from a day-level analysis. Higher RN HPPD were associated with significant reductions in the rate of missed observations in high-acuity patients on early (IRR 0.99) and twilight (IRR 0.97) shifts. The non-significant relationships on night and late shifts were similar (IRR 0.99). HCA HPPD were associated with significantly higher missed observations in high-acuity patients on early shifts (IRR 1.02) and lower rates on a late shift (IRR 0.98). Missed observations on an early shift were significantly associated with RN HPPD on the previous shift (IRR 0.98) and the subsequent shift (IRR 0.98). See Appendix 5, Table 51, for full results.
We also analysed the association between staffing levels and missed observations at an hourly level. These models also included control for time of day. For models considering all observations, the direction and significance of the relationships were similar to the day-level analysis (RN HPPD IRR 0.98; HCA HPPD IRR 0.97; p < 0.01). For observations in high-acuity patients, the main effect relationships between staffing and the rate of missed observations were not significant, although event rates for many observation periods were very low.
Non-linear effects
We explored the potential for non-linear associations between HPPD and the rate of missed observations by including quadratic and cubic terms in the models for associations between staffing and missed observations at the day level. The full models are reported in Appendix 5, Table 52.
There was clear evidence for significant non-linear effects for both RN HPPD and HCA HPPD in relation to the overall rate of missed observations, with significant linear cubic and quadratic terms for both staff groups. For both RN and HCA HPPD, the incremental effects of adding staff diminish at higher staffing levels, with a clear indication that no further benefits are achieved by adding staff to increase HPPD above 7. The relationships are plotted in Figure 8.
FIGURE 8.
Non-linear associations between staffing and rates of missed observations.
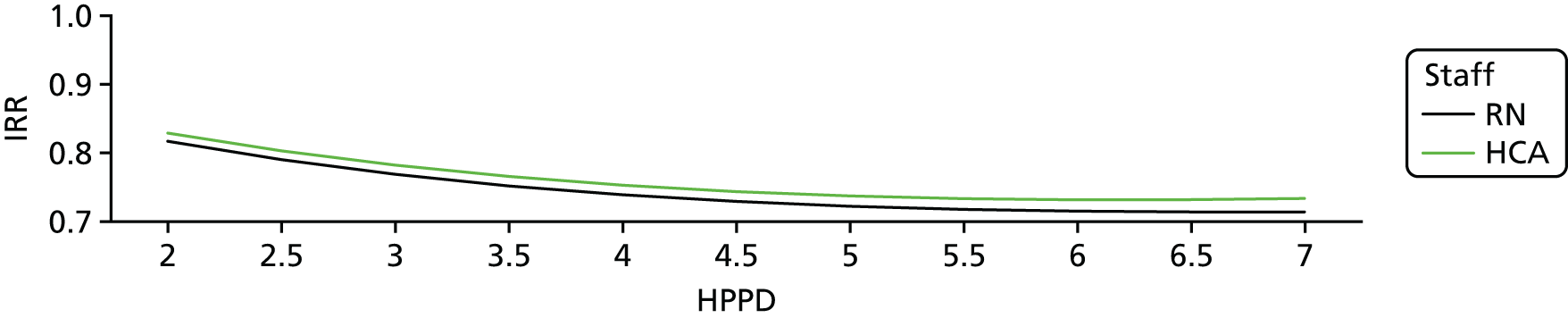
However, for observations in high-acuity patients only, there was no evidence of non-linear effects for RN HPPD, with incremental benefits continuing at higher staffing levels. However, significant quadratic effects suggest that increased HCA staffing is associated with increases in the rate of missed observations until its peak at approximately 3 HPPD, after which the effect of adding staff is to reduce the level of missed observations from this peak (Figure 9).
FIGURE 9.
Non-linear associations between staffing and rates of missed observations: high-acuity patients only.
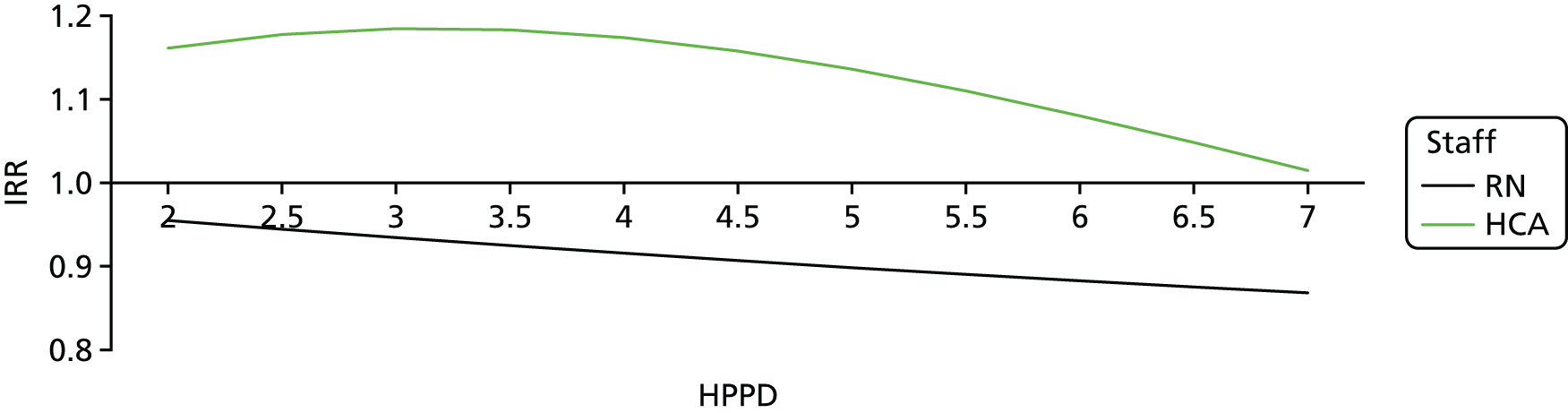
Although there was no significant interaction effect for RN and HCA HPPD in relation to missed observations in high-acuity patients, there was a significant interaction effect for the overall rate of missed observations. In very simple terms this showed that the incremental benefits of adding staff in one group was highly dependent on both the level of staffing by the other group and the base staffing level.
To further explore and clarify this complex relationship, we modelled the relationship as total CHPPD and skill mix, that is, the proportion of RN HPPD of all CHPPD, including non-linear terms (quadratic and cubic). These results do indeed shed light on the underlying relationship. There was a significant but non-linear association between total CHPPD and the rate of missed observations (see Appendix 5, Table 53). The effect of skill mix is not significant and there is no interaction between skill mix and staffing levels. The interaction between the two staffing levels observed in the previous models is a consequence of decreasing incremental effectiveness of adding more staff of any group, with no additional benefit once CHPPD reaches 10. The relationship is illustrated in Figure 10.
FIGURE 10.
Incremental effectiveness of 1 CHPPD at different staffing levels.
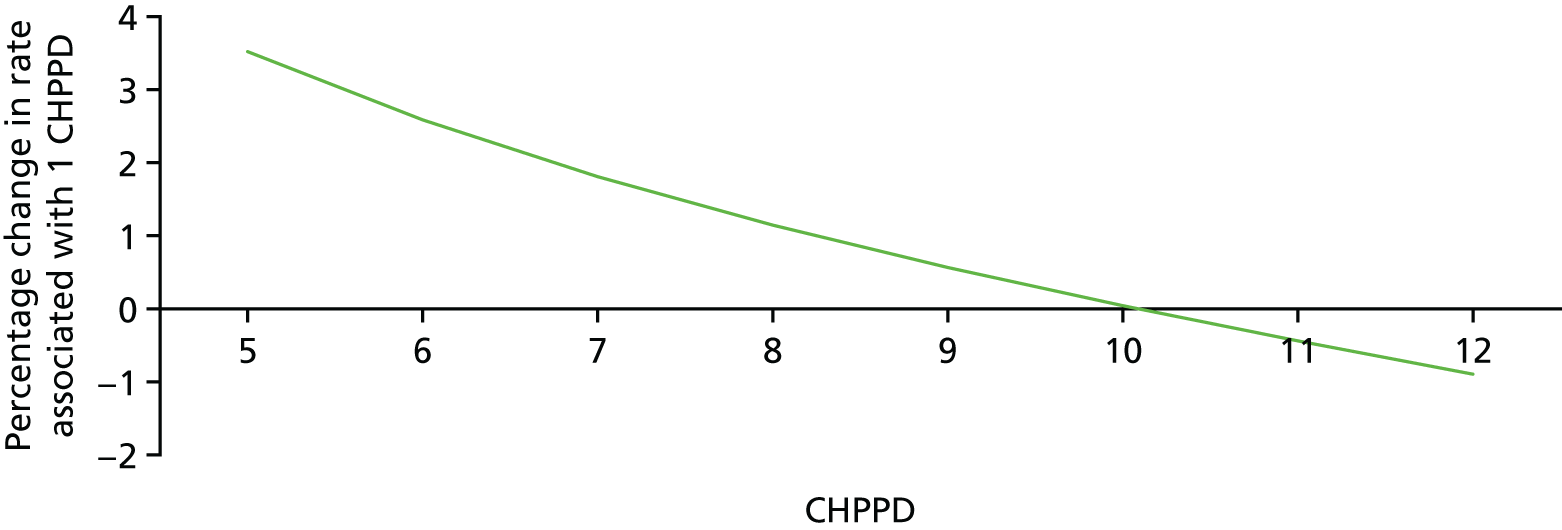
Secondary measures of missed care
Failure to respond
Timely observation is only the first step in preventing or mitigating the effects of deterioration and therefore we also calculated two variables that might be indicative of a wider failure to respond. Both of these variables were based on identifying patients with a high NEWS, indicating the need for intervention and identified in the response protocol as requiring review by a doctor. We then examined patient records and vital signs observations to determine evidence that a patient’s high NEWS was reduced or action taken (ICU admission or end-of-life care pathway) in a period determined as four times the response time identified in the protocol (4 hours for NEWS of ≥ 7; 16 hours for NEWS of ≥ 6). Where the outcome was not achieved, this might be indicative of a failure to properly respond to an identified deterioration. We calculated rates of response and determined associations with staffing levels.
‘Trigger’ events were common, with 189,123 NEWS of ≥ 6 and 114,504 NEWS of ≥ 7 events affecting 28,098 patients in total. At the lower threshold (NEWS of ≥ 6, response within 16 hours), the average level of response was 84%. For the higher threshold (NEWS of ≥ 7, response within 4 hours), rates of response were lower (50%). The death rate was high among affected patients, reflecting the high level of mortality predicted by these NEWSs (18% for those triggering a NEWS of ≥ 6; 23% for those triggering a NEWS of ≥ 7).
Neither RN HPPD nor HCA HPPD were significantly associated with rates of response for the lower threshold/longer response (NEWS of ≥ 6) criteria, but higher levels of RN HPPD were significantly associated with reductions in ‘failure to respond’ using the higher threshold/shorter response criteria (IRR 0.98, 95% CI 0.96 to 0.99; see Appendix 5, Table 54).
Nutritional risk assessments
Higher HCA HPPD were associated with significantly reduced rates of missed nutritional assessments in the first 24 hours of admission (OR 0.80). There was no significant main effect for RN HPPD, although higher admissions per RN were associated with significantly more missed assessments (OR 1.08), and the RN by HCA HPPD interaction was significant. This interaction suggested that associations between RN staffing levels and timely MUST assessments may exist when HCA staffing is low, but this association diminishes as HCA staffing levels increase (Table 13 and Figure 11).
| Variable | p-value | OR | 95% CI |
|---|---|---|---|
| RN HPPD | 0.107 | 0.97 | 0.94 to 1.01 |
| HCA HPPD | < 0.001 | 0.80 | 0.77 to 0.84 |
| Admissions per RN | 0.005 | 1.09 | 1.03 to 1.15 |
| RN × HCA | 0.011 | 0.97 | 0.95 to 0.99 |
FIGURE 11.
Interaction between RN and HCA HPPD and missed nutritional assessments.
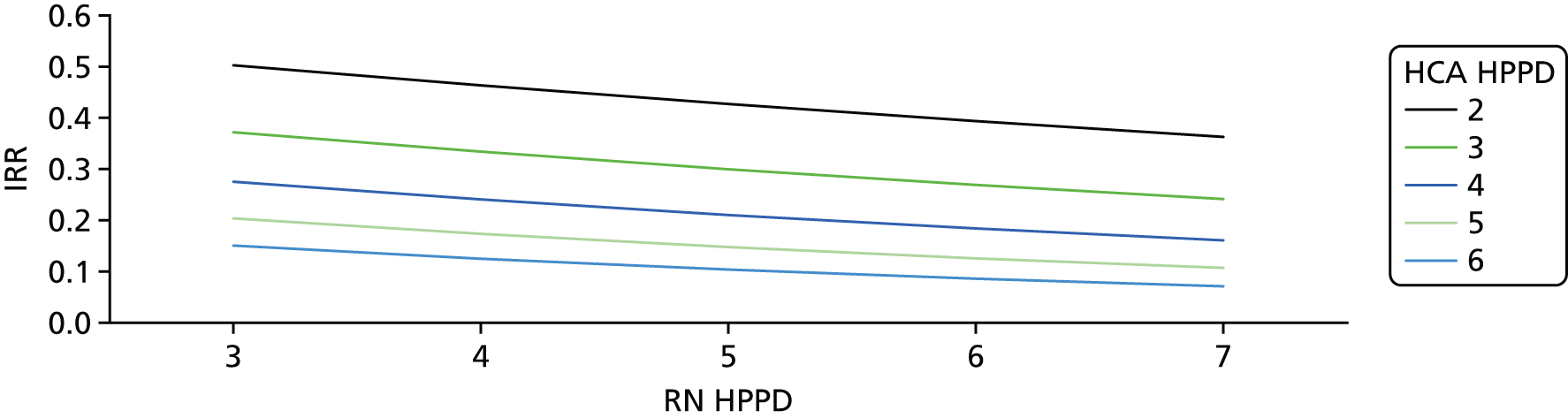
Summary and implications
In summary, these findings indicate that there is a relationship between staffing levels and missed vital signs observations. Lower staffing levels are associated with higher levels of missed observations. Overall, however, the relationship is not strong.
The contributions of each staff group appear to be initially perplexing, but the complex series of interactions and non-linear effects seem to resolve in a clear pattern: overall staff numbers are significantly associated with the overall compliance rate, whereas skill mix is not. There is a plausible dose–response relationship with diminishing returns from additional staff at high overall levels of staffing.
However, for observations in high-acuity patients, the conclusions are somewhat different. Higher RN staffing levels are associated with lower levels of missed observations. There is a dose–response relationship with no evidence that the relationship diminishes at higher staffing levels. However, the role of HCA staffing is less clear. There is some evidence that HCA staffing may complement RN staffing, strengthening the relationship between RN staffing and missed observations in some settings but not all. Direct evidence of benefit from additional HCA staffing is limited, although it may arise at high overall levels. Although the relationships may differ across ward types, which seems plausible, it is not clear whether this may simply reflect the different staffing patterns on those wards.
The weak associations combined with clear evidence of threshold effects make it clear that, even if causality were assumed, high levels of compliance cannot be achieved by increased staffing alone. For the overall rate, the thresholds suggest that the rate of missed observations might be halved (from 16% to 8%). Although the linear relationship observed between RN staffing and high-acuity observations does not point to diminishing returns from further increases in staffing, the high level of non-compliance observed (41%) means that, even if the linear relationship was maintained at all staffing levels, no likely ‘target’ level of compliance could be achieved with feasible increases in staffing levels.
The results from the MUST assessments suggest that HCA staffing might be the most important determinant of compliance with the routine assessment policy. The relationship between staffing levels compliance with the policy for routine assessment of MUST is much stronger than the relationship between staffing levels and missed vital signs observations, suggesting that it may be very sensitive to staffing levels. An overall picture emerges that suggests that HCA staffing levels may be significant in maintaining routine care processes (e.g. observations in primarily low-acuity patients), but that RN staffing is most significant for care of patients who are acutely ill. This is consistent with the results from patient outcomes. Although maintaining adequate HCA staffing appears to be important, the results focus attention on absolute RN staffing levels as the most significant element in maintaining patient safety.
Similarly to missed vital signs observations, our failure to respond indicator, suggested that RN staffing levels (but not HCAs) may be important for acutely ill patients. Although the significance of this outcome is uncertain, the association between staffing levels and patients experiencing a sustained level of acute illness (or death), in the absence of other evidence of response preceding it, does suggest that missed observations may have significance beyond simply complying with a process and may indicate a wider deficit in care. This paves the way to the final element of our analysis: to test the hypothesis that missed vital signs observations may indeed explain (in part) the association between low nurse staffing levels and increased risk of death.
Chapter 7 Mediation
Our analyses of the relationship between staffing levels and patient mortality provided evidence that lower RN staffing levels were associated with mortality. They provided less clear evidence in relation to HCA staffing levels and mortality, although there was evidence that HCA staffing levels below the ward mean were associated with increased mortality.
To be identified as a mediator, a variable must satisfy two conditions. First, the variable must be significantly correlated with the exposure to low staffing. We have seen that there is evidence for associations between staffing levels and rates of missed observations, and therefore this condition is satisfied. However, we are now faced with integrating the two modelling frameworks to assess the second condition: that the proposed mediator (i.e. missed observations) is associated with the outcome (i.e. mortality). This is challenging because the rate of missed observations varies depending on a patient’s acuity. Therefore, we restricted analysis only to those observations made in response to a NEWS of ≥ 6 (‘high-acuity observations’), which are likely to be those most critical in monitoring and preventing deterioration. We therefore calculated a dummy variable to indicate a day on which a high proportion of observations (above the mean) were missed, and a variable to indicate if any such observations were due. We included these variables in the survival model with high proportion of missed observations considered as a cumulative sum, in line with the modelling framework applied for staffing exposures.
Unsurprisingly, patients who were due high-acuity observations were at increased risk of death (HR 2.91). Crucially, patients who had a high proportion of missed observations were at a further increased risk, with a 34% increase in the hazard of death for every day on which a higher than average proportion of observations were missed (HR 1.34, 95% CI 1.30 to 1.39; Table 14). Clearly, the missed observations variable is significant. Hence, both conditions for possible mediation are satisfied and thus we proceed by including it as a potential mediator in the final models, testing the association between staffing and mortality.
| Variable | Mortality | Combined | ||||
|---|---|---|---|---|---|---|
| Missed care | Staffing | |||||
| HR | p-value | HR | p-value | HR | p-value | |
| Admissions per RN of > 125% of ward mean | – | – | 1.05 | 0.024 | 1.04 | 0.067 |
| Admissions per HCA of > 125% of ward mean | – | – | 1.00 | 0.873 | 1.00 | 0.834 |
| RN staffing below ward mean | – | – | 1.03 | 0.009 | 1.01 | 0.535 |
| HCA staffing below ward mean | – | – | 1.04 | < 0.001 | 1.02 | 0.038 |
| High proportion of observations missed (cumulative sum) | 1.34 | < 0.001 | – | – | 1.34 | < 0.001 |
| High-acuity observations due? | 2.91 | < 0.001 | – | – | 2.90 | < 0.001 |
First, we considered survival models where the staffing was measured in terms of days of low staffing (below the mean). When missed observations are included in this model, the effects of RN staffing (in terms of admissions per RN and days of staffing below the mean) are both reduced and become non-significant. Although the effect of exposure to low HCA staffing is reduced, it remains significant (see Table 14).
The estimated total effects can be split into direct (i.e. association between the exposure variables and death) and indirect effects (i.e. association between the exposure variables and death, mediated through the missed observation variable). With respect to low HCA staffing, both direct and indirect effects are significant, indicating partial but not complete mediation. With respect to low RN staffing, only the indirect effect is significant, suggesting complete mediation (Table 15).
| Model | Effect (95% CI) | ||
|---|---|---|---|
| Total | Indirect | Direct | |
| Staffing below mean | |||
| RN staffing below ward mean | 0.007 (–0.014 to 0.015) | 0.110 (0.08 to 0.013) | –0.120 (–0.023 to 0.003) |
| HCA staffing below ward mean | 0.023 (0.007 to 0.044) | 0.009 (0.007 to 0.012) | 0.014 (0.003 to 0.036) |
| Hours ± mean | |||
| RN hours ± ward mean | –0.034 (–0.051 to –0.022) | 0.001 (–0.001 to 0.001) | –0.034 (–0.051 to –0.022) |
| HCA hours ± ward mean | 0.019 (0.056 to –0.013) | –0.002 (0.001 to –0.003) | 0.021 (0.057 to –0.013) |
We then explored whether or not missed observations mediated the observed relationship between mortality and staffing hours ± ward mean. Including the potential mediator in the survival model in this case had little, if any, impact on the coefficients for the staffing variables (Table 16). Unsurprisingly, the test of mediation showed no evidence of an indirect effect for either RN hours or HCA hours, but there was a significant direct effect for RN hours (see Table 15).
| Variable | Mortality | Combined | ||||
|---|---|---|---|---|---|---|
| Missed care | Staffing | |||||
| HR | p-value | HR | p-value | HR | p-value | |
| Admissions per RN of > 125% of ward mean | – | – | 1.06 | 0.003 | 1.05 | 0.022 |
| Admissions per HCA of > 125% of ward mean | – | – | 1.02 | 0.238 | 1.01 | 0.778 |
| RN hours ± ward mean (cumulative sum) | – | – | 0.97 | 0.023 | 0.97 | 0.009 |
| HCA hours ± ward mean (cumulative sum) | – | – | 1.01 | 0.394 | 1.02 | 0.232 |
| High proportion of observations missed (cumulative sum) | 1.34 | < 0.001 | – | – | 1.34 | < 0.001 |
| High-acuity observations due? | 2.91 | < 0.001 | – | – | 2.91 | < 0.001 |
Chapter 8 Costs and consequences
In this section, we take results from our regression analyses to estimate the costs and consequences of a range of changes to staffing levels. In making these estimates, we are making assumptions that the relationships that we have seen are causal. For the sake of brevity, we will avoid issuing continual caveats along the lines of ‘. . . if the observed relationship were causal, a change in staffing would lead to . . .’. However, although the design of the study and the pattern of evidence give some confidence that the relationship is indeed a causal one, this caveat needs to be kept in mind. The issues will be discussed further and the analysis will take into account the potential sensitivity to changes in the effect size estimates.
In determining scenarios to be considered in economic models, we first needed to consider the implications of our primary analyses and the results of our stakeholder consultations. Our original intention had been to explore how variation in staffing levels and skill mix might influence vital signs compliance. Although there was some agreement among our stakeholders around achieving a 90% threshold as a scenario to be modelled (representing ‘satisfactory’ compliance with vital signs observations), there was a strong sense that anything short of 100% compliance was unsatisfactory. Although the parent Trust for the study sets an 80% threshold for compliance, there was little external support for this. There was a view from many that some observations matter more than others, which supports a focus on observations in high-risk groups. In relation to skill mix, there was support from the stakeholders for the relevance of the Royal College of Nursing standard of a minimum 65% of RNs on wards, but there was also a recognition that the required skill mix might vary by ward and, despite the RCN guidance being a recommended minimum, an indication that a lower skill mix should be considered, if only because of the challenges of recruiting RN staff. A low skill mix threshold of 50 : 50 was mentioned. A fuller account of the results of our consultations can be found in Appendix 6.
However, our results necessitated a revised approach. Although our findings do support a hypothesis that vital signs compliance may mediate the relationship between staffing and mortality that we observed, the mediation is partial. The significance of observations in low-acuity patients is unclear. In addition, although increased HCA staffing would deliver greater improvements at lower costs than increases in RN staffing, the benefits of these improvements are unclear, particularly when taking account of our findings on compliance with observations in high-acuity patients, mortality and length of stay. Furthermore, the presence of non-linear effects means that there are diminishing returns from increasing staffing above certain levels. In simple terms, our broad pattern of results render redundant a number of scenarios that we might otherwise have considered.
Although stakeholder consultation makes the desirability of a low rate of missed vital signs observations clear, we decided that this could not be a principle to guide economic modelling. Rather, we decided that the important focus was on the apparent direct consequences in terms of patient outcomes and resource use: mortality and length of stay. Changes in capacity to observe patients would be one mechanism through which changes would take effect, but observation compliance rates are not in themselves a primary goal to guide change. This is partly because strategies aimed at maximising compliance could, under some circumstances, lead to worse patient outcomes and, although we have seen some evidence that the relationship between RN staffing and mortality is mediated by missed vital signs, the evidence is ambiguous. Without pre-empting further discussion, it seems likely that there is not one single mechanism and so focusing on one mechanism alone may be counterproductive.
Broadly speaking, there are six possible strategies for changing staffing levels:
-
reduced HCA staffing
-
reduced RN staffing
-
reduced skill mix (staffing unchanged)
-
higher skill mix (staffing unchanged)
-
increased HCA staffing
-
increased RN staffing.
The relevant findings, implications for outcomes and resource use for each of these strategies are summarised in Table 17. Simple reductions in RN staffing levels would appear to be the least desirable option. Although staffing costs are reduced, the impact on the net cost is unclear because of increases in length of stay, and the risk of harm is clear because reduced RN staffing is associated with increased mortality. Reducing HCA staff levels would be associated with lower incremental cost savings (because salaries are lower), but the negative consequences for patients are less clear-cut, although it seems likely that capacity to deliver important care processes would be hindered and there is a risk of increased mortality. A reduction in skill mix (holding staff levels constant) would reduce staff costs and might deliver reduced rates of missed vital signs observations but, because lower RN staff levels are associated with increased mortality and length of stay, worse outcomes and additional costs of longer stay would probably occur.
| Factor | Outcomes | Costs and resource use | Conclusions |
|---|---|---|---|
| Reduced RN staffing | Higher rates of missed vital signs observations, increased mortality and increased length of stay | Reduction in costs because of reduced overall staffing. Potential cost increase through increase in length of stay | Unclear net reduction in costs, but likely to be negative consequences in both measured and unmeasured outcomes |
| Reduced HCA staffing | Potentially higher rates of missed vital signs and nutritional risk assessments (because HCA hours, which are associated with greater improvements than RN hours, are reduced). Potentially increased mortality | Reduction in costs because of reduced overall staffing. Potential cost reduction through reduction in length of stay | Net reduction in costs, but likely to be negative consequences in both measured and unmeasured outcomes |
| Reduced skill mix | Potentially lower rates of missed vital signs and nutritional risk assessments (because HCA hours, which are associated with greater improvements than RN hours, are increased). Potentially higher rates of missed vital signs observations in high-acuity patients because RN hours are reduced. Unclear impact on mortality rates but harm more likely than benefit | Reducing skill mix while maintaining existing staffing levels would reduce costs because HCAs are paid less. Length of stay could be increased because RN hours are lower and HCA hours are higher | Unclear net reduction in costs, but likely to be negative consequences in both measured and unmeasured outcomes |
| Higher skill mix | Potentially higher rates of missed vital signs and nutritional risk assessments (because HCA hours, which are associated with greater improvements than RN hours, are reduced). Potentially lower rates of missed vital signs observations in high-acuity patients because RN hours are increased. Lower rates of mortality because RN hours are increased | Increased costs because incremental costs of RN hours are higher, with potential cost savings through reduced length of stay | Net increase in costs uncertain with potential benefits |
| Higher HCA hours | Lower rates of missed vital signs and nutritional risk assessments. No change in vital signs observation rate in high-acuity patients. Unclear impact on mortality rates. Potentially marginally increased length of stay | Increased costs through additional net staff and potentially increased length of stay | Net increase in costs with uncertain benefits/harms |
| Higher RN hours | Lower rates of missed vital signs observations including in high-acuity patients. Reduced mortality rates. Reduced length of stay | Increased costs through additional net staff with potential cost savings through reduced length of stay | Net increase in costs uncertain with potential benefits |
Consequently, we modelled three scenarios:
-
Raise average RN staffing by 1 hour per patient per day.
-
Raise average RN staffing to reflect estimated establishment (net increase of 0.32 HPPD).
-
Alter staffing profile to reflect establishment (64%). This is essentially a skill mix change with an increase in RN staffing of 0.32 HPPD and a decrease in HCA resource of 0.3 HPPD.
To estimate net changes in staffing, we multiplied the change in HPPD (Δ HPPD) by the total number of patient days in the study (dividing by 3 to estimate annual figures). This gave the total addition (or reduction) in hours associated with each scenario. Costs were determined by multiplying hours by the hourly cost of staff (see Table 3), reduced by 8% to reflect unpaid breaks (1/12.5) during the shift.
The effect of staff change on length of stay was estimated by multiplying the number of patients by the average change in length of stay associated with each scenario (Δ HPPD × β) to determine the total number of days’ stay averted (or increased). Regression coefficients were derived from the relevant model (see Table 11). Costs were determined by multiplying the costs per day of stay by the number of days.
Finally, we estimated the impact of this change on mortality. As our survival models estimated the cumulative effect of exposure to variation in staffing, the effect of any change in staffing accumulates across the stay. That is to say, if average staffing levels are increased by 1 nurse HPPD, then a patient who stays for 5 days will experience an average increase of 5 nursing hours (1 hour per day). However, our models were based on the effect of exposures during the first 5 days of stay only and the distribution of stays was highly skewed towards shorter stays. Thus, we used the median number of days that patients were exposed to in the survival models as the multiplier in order to estimate the effect of the change on the hazard of death [HR = Exp (β × 1.93 × ΔHPPD)], which was, in turn, used as an estimate for the risk ratio – that is, the change in risk of death associated with the scenario. We then estimated the risk of death in the scenario by multiplying the observed risk by the HR and calculated the change in the number of deaths by subtracting the number of deaths expected in the scenario from the number of deaths observed. We estimated the additional change associated with a reduction in the frequency with which the rate of admissions per nurse exceeded the threshold of 125% of the current mean by estimating the reduction in frequency with which this occurred and used this to estimate the reduced risk of exposure to patients. We did not consider the effect of changes in HCA staffing on the death rate because the overall (linear) estimate of effect was non-significant and the effects of the changes were close to zero (< 0.1%) when estimated in the non-linear models.
High and low estimates were calculated by applying maximum and minimum estimates of effect (upper/lower 95% CIs) and high/low estimates of associated costs in such a way that the most pessimistic assumptions were combined (i.e. the lowest estimates of effect were combined with the highest estimates of costs for the high cost/minimum benefit estimate).
Table 18 shows the estimates of costs and consequences from the three staffing scenarios. All of these scenarios were associated with increases in staff costs. Increasing the average RN HPPD by 1 hour was associated with the greatest benefit but also with the highest costs. Assuming a median exposure to the higher staffing level of 1.93 days in the first 5 days, this scenario would be associated with an 8% reduction in the risk of death and a 0.23 day reduction in length of stay. This would result in £10.1M per year in increased staffing cost, with a gross cost per patient of £219 and a cost per life saved of £69,097. Factoring in cost savings from reduced length of stay leads to a net cost per patient of £150 and £47,376 per life saved. The annual costs/revenue for the Trust is approximately £500M, and therefore the gross cost of this strategy represents approximately 2% of the Trust budget.
Increasing RN staffing to reflect the establishment gives a 2% reduction in risk of death, with a similar cost per life saved and a gross cost per patient of £70 (net cost £40). Altering the staffing profile to reflect the estimated establishment staffing levels, effectively changing the staffing level and skill mix to reflect what is planned, yields a more favourable economic case. The estimated gross cost was £1.3M per year (0.3% of budget) at £26,351 per life saved or £28 per patient. The estimated net cost (factoring in savings from length of stay) was –£24,138 per year; therefore, the value of the hospital stays averted was greater than the costs of additional staff.
| Scenario | Best estimate | Low cost/maximum benefit | High cost/minimum benefits |
|---|---|---|---|
| Raise average RN HPPD by 1 hour | |||
| Percentage reduction in mortality rate (%) | 8 | 15 | 2 |
| Lives saved per year, n | 219 | 281 | 31 |
| Change in average length of stay (days) | –0.23 | –0.30 | –0.16 |
| Hospital bed-days saved (per year), n | 10,636 | 13,813 | 7367 |
| Staff cost per year (gross cost), £ | 10,096,620 | 9,094,747 | 13,431,390 |
| Staff cost per life saved (gross cost), £ | 69,097 | 32,318 | 426,687 |
| Staff cost per patient (gross cost), £ | 219 | 198 | 292 |
| Net cost per year, £ | 6,922,638 | 4,163,435 | 11,847,476 |
| Net cost per life saved, £ | 47,376 | 14,795 | 376,370 |
| Net cost per patient, £ | 150 | 90 | 257 |
| Raise average RN HPPD to establishment (0.31 HPPD) | |||
| Percentage reduction in mortality rate (%) | 2 | 4 | 0 |
| Lives saved per year, n | 50 | 96 | 11 |
| Change in average length of stay (days) | –0.07 | –0.10 | –0.05 |
| Hospital bed-days saved (per year), n | 3404 | 4420 | 2357 |
| Staff cost per year (gross cost), £ | 3,230,919 | 2,910,319 | 4,298,045 |
| Staff cost per life saved (gross cost), £ | 65,092 | 30,254 | 394,304 |
| Staff cost per patient (gross cost), £ | 70 | 63 | 93 |
| Net cost per year, £ | 2,215,244 | 1,332,299 | 3,791,192 |
| Net cost per life saved, £ | 44,630 | 13,850 | 347,806 |
| Net cost per patient, £ | 48 | 29 | 82 |
| Change skill mix to reflect establishment | |||
| Percentage reduction in mortality rate (%) | 2 | 4 | 0 |
| Lives saved per year, n | 50 | 96 | 11 |
| Change in average length of stay (days) | –0.10 | –0.14 | –0.06 |
| Hospital bed-days saved (per year), n | 4464 | 6234 | 2776 |
| Staff cost per year (gross), £ | 1,307,945 | 1,177,501 | 1,800,801 |
| Staff cost per life saved (gross), £ | 26,351 | 12,241 | 165,206 |
| Staff cost per patient (gross), £ | 28 | 26 | 39 |
| Net cost per year, £ | –24,138 | –1,048,000 | 1,203,963 |
| Net cost per life saved, £ | –486 | –10,894 | 110,452 |
| Net cost per patient, £ | –0.52 | –22.76 | 26.15 |
Although we do not know the long-term survival or quality of the lives potentially ‘saved’, the net cost per life saved in all scenarios has the potential to yield a cost per QALY that falls below generally accepted thresholds (e.g. £30,000 per QALY), with a relatively modest assumption that, on average, each life saved is associated with at least 1 QALY. This is an untested assumption but, given that the average age of this population is 62 years and that the average remaining life expectancy of a man aged 85 is 5.8 years, we would require very pessimistic assumptions about the quality and length of ‘lives saved’ to use an estimate of less than 1 QALY.
For the final scenario this also applies to the gross cost, with the negative net cost dominating conclusions based on this estimate. However, it was clear that these estimates are sensitive to the assumptions made, particularly about effectiveness where the extreme high and low estimate of costs/consequences is affected by pessimistic assumptions about the effect of nurse staffing levels on both length of stay and mortality. The extreme scenarios of high/low benefit are unlikely, but, nonetheless, the high cost–minimum benefit scenario (where all ‘worst case’ assumptions are compounded) indicates a need for careful consideration.
We further explored the ‘change skill mix to reflect establishment’ scenario by estimating the sensitivities of the gross and net cost per life saved to variation in each of the key parameters (rather than accumulating the extreme estimates from each). In each case, the pessimistic and optimistic assumptions are the same as applied above. Table 19 gives the results of the sensitivity analysis.
| Parameter | Gross (staff costs) (£) | Net (£) | ||
|---|---|---|---|---|
| Base estimate | 26,351 | –486 | ||
| Assumption | Optimistic | Pessimistic | Optimistic | Pessimistic |
| RN staff costs | 19,892 | 47,850 | –6945 | 21,013 |
| HCA staff costs | 14,781 | 30,182 | –12,056 | 3345 |
| Excess bed-day costs | 26,351 | 26,351 | –5755 | 7015 |
| RN HPPD on mortality | 15,627 | 61,548 | –1136 | –288 |
| Admissions per RN | 20,970 | 33,158 | –612 | –387 |
| RN HPPD on length of stay | 26,351 | 26,351 | –6598 | 5803 |
| HCA HPPD on length of stay | 26,351 | 26,351 | –5016 | 3372 |
In relation to gross costs of staffing changes, estimates are most sensitive to assumptions about RN staffing costs and, in particular, the effect of RN HPPD on mortality. Both pessimistic assumptions (high cost/low effectiveness) push estimated cost per life saved well above £30,000. In relation to net costs, the conclusion about savings is sensitive to assumptions, with most (but not all) pessimistic assumptions yielding a positive estimate of net cost per life saved. However, typically, these estimates are low (£7015 per life saved or less) with the exception of RN staff costs. The conclusion is highly sensitive to this assumption, with the pessimistic assumption giving an estimate of £21,013 per life saved.
Given that this is a single site study, it would seem unwise to base too much on these scenarios other than to consider the general direction of the findings. Although we have not specifically modelled them, all scenarios of a net increase in HCA staffing would give a net cost increase with no estimated benefit (however, that is not to say that such benefits may not arise in other outcomes). The search for cost-effectiveness should lie in the direction of increased skill mix. Given current issues of supply-side shortages of RNs, the implications of this finding will be considered further in the discussion. It is notable that the most favourable staffing solution considered is the one that is based on adhering to the Trust’s own establishment, derived using a tool that was endorsed by NICE; however, it should be noted that skill mix is left entirely to professional judgement when setting establishments using this tool.
Chapter 9 Discussion and conclusions
This study set out to examine whether variation in nurse staffing levels on general hospital wards is associated with omissions or delays in delivering necessary nursing care (focusing specifically on monitoring and acting on vital signs) and whether or not variation in staffing levels and vital signs observations is associated with variation in patient death. Monitoring vital signs has been put forward as a fundamental component of the ‘Chain of Prevention’, a structure that describes the interventions necessary to prevent patient deterioration. 92
This is the first study in the NHS to demonstrate a longitudinal association between nurse staffing levels and the risk of death for patients on general medical and surgical wards. It is only the second study worldwide to directly link patient-level staffing exposures to the risk of death. We are not aware of any other study that has used objective measures of missed care to explore the mechanism linking low RN staffing to increased death rate in hospital patients.
The key goals of the study were to:
-
determine whether or not the variation in the presumed causal factor (nurse staffing) precedes the presumed effect (adverse outcomes)
-
explore an intervening care process (vital signs observation) that is a direct result of actions by nurses
-
provide evidence on nurse staffing that is directly relevant to the UK context, including the likely costs and consequences of change.
This chapter starts with a summary of the key findings, before discussing the implications of each of these in turn, considering the limitations and ending with study conclusions.
Summary of results
Variation in nurse staffing levels as experienced by individual patients within hospital wards is associated with a subsequent variation in the risk of their dying and experiencing other adverse outcomes. We found similar associations with periods in which the number of admissions per nurse (turnover of patients) was high, and found that when patients spent time on wards where a high proportion of nursing hours were provided by temporary (bank and agency) staff, mortality was also increased. We found that variation in nurse staffing levels was also associated with variation in compliance with vital signs observations, scheduled according to a nationally recognised protocol based on patient acuity, timely response or resolution of acuity and compliance with a nutritional risk screening policy. We found some evidence that supported the role of missed vital signs observations mediating the association between low RN staffing and increased risk of death. In Table 20, the main results of the regression analyses are summarised showing relationships between staffing variables and outcomes that have been tested (including alternative approaches to defining staffing levels). We explored the effects of RN and HCA staffing, both independently and in interaction with each other, which revealed important differences in the effects associated with each group.
| Staff group measure | Death | Adverse events | Length of stay | Observations | ‘Failure to respond’ | Missed nutritional assessment | ||
|---|---|---|---|---|---|---|---|---|
| Missed | Missed in high-acuity patients | Late | ||||||
| RN | ||||||||
| Days below mean | ✓ | – | ||||||
| Days below establishment | ✓ | ✓ | ||||||
| Days below 80% of mean | – | – | ||||||
| Hours below mean | ✓ | ✓ | ||||||
| HPPD (total or ± mean) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – |
| Admissions per staff member | ✓ | ✓ | ✓ | ✓ | – | ✓ | – | ✓ |
| Temporary staffing | ✗ | |||||||
| Non-linear relationship | – | – | ✓ | – | ||||
| Interaction with HCA staff levels | – | ✓ | – (?) | ✓ | – | ✓ | ||
| HCA | ||||||||
| Days below mean | ✓ | – | ||||||
| Days below establishment | – | – | ||||||
| Days below 80% of mean | – | – | ||||||
| Hours below mean | – | – | ✓ | – | ✓ | – | ✓ | |
| HPPD (total or ± mean) | ? | ✓ | – | ✓ | ||||
| Admissions per staff member | – | – | ✓ | |||||
| Temporary staffing | ✗ | |||||||
| Non-linear relationship | ✓ | ✓ | ✓ | ✓ | ||||
| Interaction with RN staff levels | – | ✓ | – (?) | ✓ | – | ✓ | ||
| Care hours and skill mix | ||||||||
| Care hours | ✓ | – | ||||||
| Non-linear | ✓ | ✓ | ||||||
| Skill mix | – | ✓ | ||||||
When patients experienced lower RN staffing in the first 5 days of their hospital stay, the hazard of death was increased. The relationship between RN staffing levels, measured as cumulative hours per patient relative to the ward mean, appeared to be linear, with no evidence that benefits associated with increased staffing were reduced at higher staffing levels. Higher RN staffing was also associated with lower rates of adverse events and shorter hospital stays. This is the first study in the NHS to show that the risk of death is associated with, and preceded by, variation from the usual staffing level for a given ward.
There was some evidence that higher RN staffing was associated with lower levels of missed vital signs observations, including those taken in patients assessed as ‘high-acuity’ by the NEWS, and with higher rates of speedy resolution/response to acute deterioration (as measured by our ‘failure to respond’ variable), although the magnitude of the relationship was small. There was, however, no overall association between RN staffing levels and timely nutritional screening using the MUST assessment.
Health-care assistant staffing levels below the ward mean were associated with an increased hazard of death, but results were inconsistent. The relationship between HCA staffing levels and death appeared to be a non-linear one, with the hazard of death increasing when patients experienced either above- or below-average staffing.
Higher HCA staffing levels were associated with lower rates of missed observations and timely nutritional risk assessments, but not with lower failure to respond for patients who were acutely unwell. When considering observations of the most unwell patients (NEWS of ≥ 6), for whom regular and timely observations are likely to be most significant, there was little evidence for any direct association between HCA staffing levels and the rate of missed observations.
There was no evidence of an interaction between RN and HCA staffing levels in relation to mortality, observations in high-acuity patients or ‘failure to respond’, with the exception of high-acuity observations in medical wards where higher HCA staffing was associated with increased effectiveness of additional RN staff. However, there was a consistent interaction effect between RN and HCA staffing levels in relation to the overall rate of missed observations. The relationship also appeared to be non-linear. Further exploration of this finding suggested that the overall compliance rate is associated with the total number of staff (CHPPD) irrespective of skill mix, with a decreasing incremental effectiveness for additional staff at higher staffing levels.
A core purpose of this project was to further investigate the clinical significance of missed observations by determining whether or not they provided the ‘missing link’ between low staffing and increased mortality and could therefore be used more to guide staffing decisions. This study has confirmed this link between low staffing and mortality, using a design that establishes that it is the individual patient’s exposure to low staffing that is associated with worse outcomes and that these exposures precede the outcome. The study also showed that staffing levels were associated with the rate of missed observations in the same data set. Our analyses suggest that missed vital signs observations in high-acuity patients do indeed mediate the relationship between exposure to days of low RN staffing (below the mean) and mortality. However, when considering staffing as a continuous variable, the effect of RN staffing appears to be direct, with no evidence of mediation.
We modelled the costs and consequences of variations in staffing policies. Our original intention had been to use the relationship between staffing levels and missed care to model costs and consequences of staffing policies associated with acceptable levels of vital signs observations. However, the weak associations and non-linear relationships made it clear that the levels of compliance identified as ‘acceptable’ in our consultations with patients, public and professionals could not be achieved through changes in staffing levels alone. Instead, we used the findings outlined above, on the relationship between exposure to low staffing levels and adverse outcomes, to guide our selection of scenarios. Simple increases in average RN staffing levels by 1 RN HPPD were associated with an average increase of staff costs per patient of £219, at a total cost that would be approximately 2% of the hospital’s budget. The change would be associated with 219 fewer deaths per year and over 10,000 days’ reduction in bed utilisation, although the value of these days does not exceed the costs. As the staff deployed by the Trust did not match the planned staffing levels (with an overall lower skill mix because RN HPPD was slightly below the planned level and HCA HPPD was slightly above it), we modelled the costs and consequences of changing the workforce to match that plan (i.e. raising RN HPPD and decreasing HCA HPPD). This scenario would yield much more modest benefits in terms of reduction in deaths (50 per year) and bed-days (4464), but at a lower staff cost per patient (£28). The value of the bed-days saved would exceed the investment cost.
Discussion
Staffing levels and mortality
Although the association between nurse staffing levels and patient outcomes has been extensively studied, questions have remained about whether the observed associations were causal. 14 This study has addressed many of the shortcomings of previous research by directly linking patient outcomes to the level of staffing experienced by individual patients, showing that variation in a patient’s experience preceded their outcome and was associated with the staffing that they had directly experienced. The only comparable study of which we are aware is that by Needleman et al. 27 In a study of 197,861 patients in 42 units in a single US hospital, which was described as having low mortality for the case mix and high success in meeting planned staffing levels, the authors found that, for each shift that was ≥ 8 RN hours below target staffing, the hazard of death was increased by 2%. 27 High turnover shifts were associated with a 4% increase. Although the measurement units differ from those in our study, these findings are remarkably similar to ours.
Although there is considerable extrapolation involved, some idea of the comparability of the results in these two studies can be gained by identifying the shortfall from target RN staffing for our ‘days below the mean’ measure of exposure to low staffing, which was, on average, 0.32 HPPD below the target staffing level. On a ward with 30 patients, a day with staffing below this level would be ≥ 9.6 hours below target (HPPD × patients), and in our study this was associated with a 3% increase in the hazard of death. In common with the Needleman et al. study,27 we also found that mortality was increased during periods of high patient turnover relative to the norm for the ward and available RNs.
Studies that have directly linked outcomes to patient exposure to low staffing are rare, but Kuntz et al. 129 explored the effect of exposure to periods of high bed occupancy on mortality among 82,280 patients in 83 German hospitals. They demonstrated a tipping point, with mortality increase occurring when bed occupancy exceeded 92.5%, and no effect below this point. Until the tipping point is reached, the resources available, including staff, are able to absorb fluctuations in demand with no adverse effects. Once the tipping point is passed, the capacity to buffer is exceeded and so additional demand is associated with worse outcomes. 129
Although average occupancy for the Trust was close to or above this level for much of the current study, we did not observe a ‘tipping point’ in relation to the association between RN staffing levels and mortality. The relationship appeared to be linear. Other studies have observed non-linear relationships between nurse staffing levels and mortality. 130 However, the estimated non-linear relationships appear to be of the nature of a maximum benefit arising at staffing levels that are very high compared with those observed typically in the UK, rather than a ‘tipping point’ beyond which adverse outcomes occur. If there is indeed a tipping point, it may be that typical staffing levels observed in this study have already passed it, so there is no buffering effect to observe, and fluctuation in demand cannot be accommodated within the current capacity.
Few previous studies in this field have taken medical staffing levels into account, although a nurse staffing effect independent of medical staffing levels has been demonstrated in cross-sectional studies in the NHS and elsewhere. 36,39 Although we were unable to directly account for variation in medical staff levels in this study, the nature of the design means that it is not confounded by hospital-level correlations between medical and nursing staff sizes. Unless medical staffing variation is significantly correlated with ward-level nurse staffing levels, the relationships we observed are unlikely to be generated by variation in medical staff cover. We have managed to eliminate one significant source of correlation between medical and nurse staffing levels as an explanation of these results, given that the nurse staffing effect was independent of a ‘weekend’ effect.
Temporary staffing and flexible capacity
Our findings on the effects of temporary staffing are relevant to the issue of ‘buffering’ capacity and response to fluctuating demand. We found that, when temporary RN staffing was more than 1.5 HPPD, the hazard of death was substantially elevated. Clearly, the use of temporary staff is an important strategy for dealing with fluctuation in demand or imbalance between demand for and supply of staff caused by staff shortages. Current evidence around the effects of temporary nurse staffing is largely from the USA. A cross-sectional study131 in 665 US hospitals found that the use of agency supplemental nurses was associated with a 4% increase in the odds of death when controlling for staffing levels, but that the effect reduced and became non-significant when including a variable measuring the perceived quality of the nursing work environment. An earlier US study132 recorded similar findings in relation to nurse-reported adverse outcomes, such as job dissatisfaction and burnout, although nurses’ intention to leave the job was significantly associated with higher use of temporary staff even after adjustment for practice environment.
Although the design of our study is generally stronger than that of these cross-sectional studies, our study using routinely collected data was unable to control for nurse perceptions of the practice environment. However, this variable is generally considered to be a hospital characteristic and so the variation observed in our single-hospital study cannot be accounted for in this way. Furthermore, a nurse’s negative perception of the practice environment could itself be related to the use of temporary staff and so the extent to which this should be ‘controlled’ is unclear.
Other studies with an analysis at a unit level give results that are consistent with ours, albeit using other outcomes. We found that the modest use of temporary RN staff (below 0.5 or even 1 HPPD) was not associated with adverse outcomes. A study in 277 units in 142 US hospitals133 found that that the high use of temporary staff was associated with increased rates of falls and nurse injuries, but only where use of temporary staff exceeded 15% of the nursing workforce. While this study differentiated between internal and external temporary staff, the effects appeared to be associated with both groups.
Studies from both the UK and the USA indicate that, in general, wards that use more temporary nursing staff are more expensive to run than wards with primarily permanent nurses,134,135 although one study from the USA found that a modest use of supplemental (temporary) nurses (up to 0.2 nursing HPPD) was associated with slightly reduced total staffing costs. 136 Although our findings point to no harm from the modest use of temporary RNs, and even hint at a benefit because it maintains the overall staffing levels to meet patient need, our findings about the use of temporary HCA staffing suggest that there is risk in even relatively low levels (although it should be noted that 0.5 HPPD is a substantial proportion of the typical hours provided by HCAs). It is unclear whether or not the adverse effects are limited to external (agency) staff and whether or not strategies designed to mitigate the negative effects of temporary staffing (such as specially trained float pools) might be more effective.
Health-care assistant staffing levels
Previous research has provided a nearly uniformly negative conclusion in relation to staffing by assistant personnel. 14 Studies have made explicit conclusions that additional assistant staff have an adverse effect, irrespective of the level of RN staffing, because of the dilution of skill mix. 137 However, this may be an artefact that results from failing to examine the contribution of each staff group independently. Skill mix can be affected by changes in staffing levels by one group, or the other, or both, which is masked by a conclusion based on skill mix alone. One of the few studies to address each group separately, our cross-sectional study in English hospitals,36 in which HCA and RN staffing levels were modelled as independent effects, found that an apparent adverse association with higher HCA staffing at a hospital (trust) level was not present when looking at relationships with ward-based staffing. Where possible, in the current study, we attempted to model the effect of each group separately.
Although the relationship between lower RN staffing levels and increased mortality was generally clear, the relationship between HCA staffing levels and mortality was not. A large number of admissions per RN was associated with increased mortality, but we found no relationship between admissions per HCA and mortality. Although estimates of the additional time associated with admitting or discharging patients (likely to be highly correlated with admissions given high bed occupancy) have not been reported, admissions and discharges are widely recognised as significantly contributing to nursing workload; however, this is not recognised in workload measures based solely on patient census (e.g. HPPD). 138 However, as completing documentation and patient assessment for new admissions is primarily a RN role, the absence of a relationship with HCA staffing is unsurprising here given that we have formulated this as a ‘workload’ variable.
When patients experienced below-average HCA staffing, their risk of death was increased. However, when we modelled HCA HPPD relative to the mean as a continuous variable, we found no significant effect. The relationship was somewhat clarified by the significant non-linear relationship that showed mortality increasing as HCA HPPD deviated from the mean in either direction, suggesting that there is an appropriate and necessary level of HCA staffing that is close to current means or establishments.
To make sense of such a finding requires an exploration of possible mechanisms. The effect of low staffing seems to be potentially explained by mechanisms already articulated to explain associations between low staffing and adverse outcomes. In simple terms, there is insufficient capacity to deliver the required care completely and with quality. Low HCA assistant staffing may have direct effects or indirect effects by virtue of the absence of sufficient support for RN work. However, the mechanism by which a higher number of HCA hours per patient could increase the risk of death is less clear. One possible mechanism is through a combination of an increasing requirement for RN to delegate tasks to make full use of the capacity provided by additional HCA hours per patient, combined with an accompanying increase in the RN supervisory load. Recent research from the UK139 makes it clear that newly qualified RNs struggle to properly manage this process of delegation and supervision.
Low HCA staffing adversely affects mortality because the overall capacity to deliver work is low, with the negative effects arising partly because of the inability of HCAs to deliver their own work (demonstrated by the partial mediation of this relationship by missed vital signs observations), but also, potentially, by the effect this has on RNs’ ability to complete their own work.
However, when HCA HPPD is high, the amount of work that must be delegated to them in order to make use of available time is high. Even when the demand for supervision is balanced by RN capacity, this could result in inappropriate or ineffective delegation of tasks. When RN capacity is low, the ability to properly supervise the delegated work may also be compromised. Hypothetical configurations are illustrated in Table 21, with green and dark green indicating configurations in which the contribution of HCA HPPD could be negative – because of either the low capacity or the demands placed on RNs for delegation and supervision.
| High RN HPPD | Target RN HPPD | Low RN HPPD | |
|---|---|---|---|
| High HCA HPPD | Overall capacity high. Supervisory capacity balanced with demand but high demand for delegation | Overall capacity high. Supervisory capacity not balanced with demand (low skill mix) AND high demand for delegation | Overall capacity medium or low. Supervisory capacity not balanced with demand (low skill mix) AND high demand for delegation |
| Target HCA HPPD | Overall capacity high. Supervisory capacity exceeds demand (high skill mix), with expected demand for delegation | Overall capacity medium. Supervisory capacity balanced with demand, with expected demand for delegation | Overall capacity low. Supervisory capacity not balanced with demand (low skill mix) AND high demand for delegation |
| Low HCA HPPD | Overall capacity medium. Supervisory capacity exceeds demand (high skill mix), with low demand for delegation but low support | Overall capacity low. Supervisory capacity exceeds demand (high skill mix), with low demand for delegation but low support | Overall capacity very low. Supervisory capacity balanced with demand, with expected demand for delegation |
Clearly, this hypothetical mechanism requires further exploration, but it does provide a potential pathway whereby an apparent increase in the overall workforce capacity could have negative consequences. The use of non-registered assistants to undertake vital signs observations is one area where the effectiveness of the delegated work has been widely questioned. 140
Missed vital signs observations
The monitoring of vital signs is a fundamental component of the ‘Chain of Prevention’,92 a structure that describes the interventions necessary to identify and prevent avoidable patient deterioration (Figure 12).
The nursing roles in this ‘Chain of Prevention’17,18 and the extensive evidence of an association between nurses’ reports that they are unable to complete all necessary care and low staffing141 make the timely observation of vital signs a strong candidate mechanism through which low staffing may lead to adverse patient outcomes, including death. In this respect, this study breaks new ground in the use of objective measures of nurse behaviour in recording vital signs. Although many studies have shown that compliance with vital sign monitoring protocols is often poor,142 studies looking at nurse staffing have relied on nurse reports of missed care based on quite general questions.
As hypothesised, we found that the rate of missed and late vital signs observations increased when nurse staffing levels were lower. We also found some evidence that this relationship mediated the relationship between low RN staffing and mortality.
However, our findings were complex. We found that the total staff complement in terms of CHPPD (RN+HCA HPPD) was associated with the overall rate of missed observations, with no association between the rate of missed observations and skill mix (proportion of RN hours), whereas overall only RN HPPD were significantly associated with the rate of missed observations in a subgroup of observations in ‘high-acuity’ patients (NEWS of ≥ 6). The rate of missed observations in this group was, in turn, associated with increased mortality, and the association between mortality and exposure to days of RN staffing below the mean was mediated by missed observations.
The ‘Chain of Prevention’ highlights that there is more to preventing deterioration than simply complying with an observation protocol. Although it seems clear that assistant staff can be trained to take vital signs observations, concerns have been raised about their ability to appreciate the significance of these signs and initiate appropriate actions. 140 Our data suggest that on many wards a high proportion of vital signs observations are undertaken by HCAs. Anecdotal reports of device sharing and imprecision in the coding of staff in the system make it likely that our overall estimate of 15% of observations taken by HCAs is an underestimate, but even without this consideration there are several wards where over 30% of observations are taken by HCAs. Although some published accounts suggest that most observations are now taken by HCAs,143 our findings could provide some reassurance: sensitivity to RN staffing levels indicates that observations in high-acuity patients are RN work, although there appears to be little difference in the proportion of high- and low-acuity observations undertaken by HCAs. Nonetheless, these findings, combined with the association between HCA HPPD and nutritional screening and the association between RN staffing and rates of failure to respond, create a picture that is consistent with completion of ‘routine’ assessments being sensitive to HCA staffing, whereas acute care is more sensitive to RN staffing levels.
It is clear, however, that the mechanisms through which missed observations can translate into adverse outcomes (and the interaction between the staff groups in these mechanisms) are potentially complex. The relationship between exposure to days of low HCA staffing and mortality was only partially mediated by missed observations, and the relationship between RN hours and mortality was not mediated. Clearly, other causal mechanisms are at play that are not directly mediated through vital signs observations. In simple terms, the effect of low RN staffing appears to be mediated by missed observations, but other mechanisms related to the overall level of nursing care available are not.
Although overall HCA staffing was not related to missed observations in high-acuity patients, the ward subgroup analysis and exploration of non-linear relationships suggest that the pattern may change at higher staffing levels. Significant interaction between RN and HCA staffing levels on medical wards provides a clear picture of HCA staff acting as a labour complement144 in that the effect of an increase in HCA HPPD is to increase the incremental effect of RN HPPD in reducing the rate of missed observations. However, evidence elsewhere of this complementary relationship is scant, both in the current study and in others. 19,74
The extent to which the work of unregistered assistants does indeed complement that of RNs is a crucial issue in the face of developments in the NHS, where the creation of a new cadre of assistant personnel, the nursing associate, is explicitly based on their presumed ability to complement the work of RNs. 145 Although these new roles are by no means directly comparable with HCAs, they highlight that the potential for support staff to complement or substitute for the work of RNs is somewhat hypothetical and the nature and consequences of reconfigurations in nursing work in patient surveillance are not well understood.
Missed care as an indicator of nurse staffing adequacy
A core aim of this project was to explore the potential to use measures of missed care, and vital signs observation compliance in particular, as a direct indicator of staffing adequacy. Although the results of the study do provide support for the role that missed care may play in mediating the effect of nurse staffing levels on outcomes, two conclusions are clear. First, missed observations are not the only mechanism. This is perhaps an obvious conclusion as the recording of vital signs observations is a very partial measure of the completeness of the ‘Chain of Prevention’. However, the second conclusion is that the rate of missed vital signs observations is not a good indicator of staffing adequacy. Given that 16% of all observations were recorded as missed, it seems clear that most missed observations are attributable to factors other than overall staffing levels, as estimated relationships suggest that it is unlikely that staff increases are capable of reducing the rate to anywhere near zero, particularly for high-acuity observations.
Partial representation of the quality of the care delivered does not preclude missed care from providing a valid indicator, as long as it represents an important aspect of care. Vital signs observations are clearly important, and this study has demonstrated the potential utility of routine data systems to provide records of missed care. Our findings have also established that missed observations may be associated with important patient outcomes. Therefore, ‘missed observations’ meet some criteria for a good indicator. 146–148 Nonetheless, the rate of missed observations falls some way short of providing an ‘ideal’ indicator, particularly if focusing on the adequacy of nurse staffing.
The observed associations with nurse staffing, although statistically significant, were modest. Furthermore, it is unclear what the ‘correct’ level of compliance should be. Although our stakeholder consultation suggested that near 100% compliance is desirable, it is unclear whether or not this would represent a meaningful and important improvement in quality. Indeed, it is unclear if all non-compliance with the protocol should be construed as a failure of quality because the impact on patient outcome and the scientific basis of the particular observation regime are unclear. Current observation protocols are largely based on custom and practice, or on expert opinion. 142 The potential to alter clinical outcomes depends on the ability to detect and recognise an acute change in a patient’s physiology. Therefore, more frequent vital signs measurement and more complete observation sets should increase the probability that deterioration will be detected early, and some published research results support this. For example, an Australian study149 reported reductions in unplanned ICU admissions and hospital deaths when the vital sign measurement frequency increased from a mean of 3.4 to 4.5 times per day. A study from the Netherlands150 found that vital signs measured three times per day resulted in better detection of physiological abnormalities than a regime of taking observations only when ‘clinically indicated’. Belgian researchers151,152 reported that the use of a standard observation protocol, with observation frequency increasing according to an early warning score based on the observations, led to an increased frequency of recording vital signs, reduced hospital length of stay and mortality in postoperative patients and fewer serious adverse events for patients discharged from ICU.
However, other studies make it clear that the ideal observation frequency remains uncertain. A protocolised ‘once a day’ early-warning score assessment may be sufficient to screen for major adverse events in hospital populations,153 and research from Denmark found that for low-risk patients 8-hourly observations were no better than 12-hourly observations for reducing clinical deterioration. 154 Although a recent review of monitoring techniques found that continuous patient monitoring allowed earlier detection of deterioration in general ward patients than ‘usual care’, there was insufficient evidence of any impact on patient outcomes. 155
Therefore, although there is some evidence that increased frequency of observations may improve detection and patient outcomes, a finding supported by the results of this study, compliance with a specific regime cannot be said to be evidence based and it is not clear that outcomes continue to improve as observation frequency increases. Although under-observation can delay the opportunity to detect patient deterioration and initiate remedial treatment, over-observation uses valuable nursing resources that may be better deployed to other essential aspects of patient care and risks disturbing patients unnecessarily, with adverse consequences including interruption of sleep. 156 Although these results demonstrate that some non-compliance appears to have adverse consequences, much of it may not, with nurses exercising clinical judgement to prioritise observations on those most in need, or to prioritise other patient needs. The results of this and other studies suggest that these judgements may not always be correct, but the shortfall between current levels of compliance and that required by the observation regime is considerable. Moving to 100% compliance with the current regime may not be the best investment of nursing time.
Although changes in compliance rates within a ward might be influenced by staffing levels and thus act as a ‘red flag’ (as envisaged by NICE12), it is unlikely that missed observations can be directly used to guide staffing decisions. We have demonstrated that other measures of missed care can now be derived from routine data; these have also shown a degree of sensitivity to nurse staffing and so might prove useful in monitoring quality, although the relationship of these measures to patient outcome has not been established.
Determining safe staffing levels
Studies showing associations between nurse staffing levels and the quality or outcomes of care are not new. This study provides important confirmation of such associations in the English NHS and provides improved confidence that the observed relationship is likely to be a causal one. However, the relationships observed in this study have not, in themselves, provided a basis to model required staffing on different wards at different times of day.
The evidence base for current methods of matching the size and skill mix of the nursing workforce is extremely limited, particularly in terms of demonstrating that staffing matched to the calculated requirements delivers improved patient outcomes. 157 Our findings are all based on staffing levels relative to the norm for individual wards (either by directly deriving variables relative to the norm for our mortality analyses or by including a random effect with missed care clustered within wards for missed care analyses). Ward staffing levels in the Trust were determined using the Safer Nursing Care Tool,158 the only evidence-based tool that has received early endorsement from NICE. 98 Although mean staffing levels deviated somewhat from what was planned, there was a strong correlation between actual and planned staffing levels.
Although the results of this study give an indication that the level of HCA staffing that had been determined by the tool might be close to optimal, based on the non-linear relationship observed with mortality (where risk increased as staffing levels moved from observed mean levels in either direction), the level of RN staffing cannot be said to be optimal when improvements in outcomes are observed, as RN staffing levels increase above the mean in a linear fashion. However, these planned staffing levels are unlikely to reflect daily variation in need. Although our findings give some limited support to the tool, it remains unclear whether staffing solutions based on daily (or more frequent) measures taken with the tool provide an effective basis for determining adequate staffing, or whether routinely collected data such as NEWSs might have a role.
Economic and labour market considerations
Increased staffing levels, by necessity, lead to increased staff costs. Based on the data presented in this report, increases in HCA staffing would be associated with increased cost, but with either neutral or negative effects on outcomes. However, we found that increases in RN staffing were associated with improved outcomes, and, in some circumstances, the additional costs were more than offset by the value of hospital bed-days saved.
Our economic modelling suggests that, had the Trust been able to maintain its average staffing and skill mix at the levels identified using the Safer Nursing Care Tool, this would be associated with improved outcomes and reduced length of stay. This would involve small increases in RN staffing and a similar decrease in HCA staffing levels. Although changes to RN staffing leading to improved outcomes were associated with increased staff costs under all scenarios, the value of the decreased stay offsets the cost of additional staff in this scenario. This essentially involved a small increase in skill mix, moving close to the 65% level recommended as a minimum by the RCN,125 with little, if any, change in total CHPPD.
Although this change does not result in any direct cost savings for the Trust, given that the bed capacity released is likely to be used, the value of the resource that is released for use by other patients cannot be discounted. Our economic models assumed no additional treatment costs were associated with the increased stays and we costed them simply as ‘excess bed-days’. Even under this modest assumption, the findings are consistent with a positive return on investment. However, the absence of patient- or person-centred outcomes or quality-of-life data makes a comparison with returns from other investments challenging.
Our study places an emphasis on RN staffing levels and skill mix as the key variables associated with patient safety and, potentially, cost-effective care. Studies from the USA have come to similar conclusions; for example, a strategy of raising the proportion of RN in the licensed nursing workforce to the 75th percentile, observed in a sample of 799 US hospitals (94% RN), was the only strategy modelled to be associated with a net decrease in hospital costs. Although this finding is not directly comparable with ours, because it considered skill mix only within the licensed nursing team, these findings provide no encouragement for strategies that seek to maintain care hours by introducing less qualified/lower-skilled workforce roles, or for benchmarking systems such as the NHS CHPPD,127 which implicitly treats all members of the ward team as potentially equivalent.
Although these findings imply that there may be benefit in increasing RN staffing levels, there is clearly a major shortage in supply of RNs in the UK. This seems likely to be exacerbated by demographic change, the consequences of public sector pay restraint, wider labour market changes and long-term mismatch between the supply of and demand for RNs. 159 The solutions to these long-term problems are not all within the reach of a single trust. Although national pay frameworks prevent employers competing for scarce supply of nurses on the basis of remuneration, a trust still has the opportunity to present itself as a more attractive employer based on non-monetary benefits and the working environment on offer. In this context, there has been a recent resurgence in interest in the concept of ‘Magnet Hospitals’, a term initially coined to describe those hospitals whose work environments enabled them to attract and retain professional nurses. 160 Other research,38 linking higher staffing levels to higher job satisfaction, lower staff burnout and intention to remain with the current employer, suggests the potential for a virtuous cycle whereby higher staffing levels reduce nursing turnover and sickness absence linked to burnout and fatigue. However, this has yet to be tested with a prospective study.
Limitations
Although our study was able to overcome many limitations of previous research, it remains observational. Causal inference does not follow directly from the observed associations, although the design eliminates many plausible alternative explanations, therefore making a causal interpretation much more likely. We have not been able to observe the association between staffing by other groups and mortality, but our design makes it unlikely that such associations account for what we have observed. Although our analyses corrected for variation in the acuity of patients, and took into account the impact of patient turnover, unlike in the Needleman et al. 27 study we were not able to measure the nurse staffing level against the staffing requirement determined on a shift-by-shift basis; instead, we had to rely on ward means and establishment. Given that nursing establishments were not calculated directly in terms of care hours, we had to make a number of assumptions to estimate the planned HPPD, although the mean staff levels in the observed wards appeared to provide a good proxy for the established level as they correlated highly. Therefore, although these staffing levels reflect average need on the ward measured using a recognised staffing methodology, they do not reflect day-to-day variation. However, as it is probably the case that some of the variation in staffing that we have observed is an attempt to match this unobserved variation in need, the most likely effect of this is to attenuate any observed relationships.
This attenuation of the estimated effect of staffing is most notable in respect to our attempt to measure the effect of very low (below 80% of the mean) RN staffing. The staffing data we were able to access provided no record of internal redeployment of staff to make up staffing shortfalls, which is much more likely to happen when staffing is very low. Consequently, many of these apparently low-staffed shifts may have been covered by staff moved from other wards, therefore making estimates of effect at these extreme values unreliable at best. Given that absolute numbers of RN staff are larger than the numbers of HCA staff, it is likely that RN staffing is more affected by this issue than HCA staffing (e.g. moving one RN out of six may be more feasible than moving one HCA out of two). Again, the net effect of this is likely to attenuate observed relationships, as the donating ward would also have lower staff than it appeared.
Although we were able to make allowance for breaks, we were unable to determine if breaks were actually taken. Similarly, we could not measure unpaid overtime. Both missed breaks and unpaid overtime are frequently reported as a response to high work demands. 161,162 Both of these sources of unrecorded hours may provide an important buffering mechanism, reducing the potential harm that arises when patient needs exceed the apparent supply of staff to meet demand. However, the effect of this hidden work would be to attenuate (i.e. reduce the magnitude of) the relationship between patient outcomes and nurse staffing levels.
Our analysis made no distinction between bank and agency staff and did not permit the investigation of whether or not these temporary staff might be working paid overtime on their own ward. Therefore, our findings about adverse outcomes associated with high levels of temporary staffing could be conflating temporary staffing with overtime. Overtime has been associated with decreased quality of care and adverse outcomes for nurses, although the relationship with patient outcomes remains unclear. 68,163,164
Our measure of nursing activity in relation to the response to deterioration was limited. Although timely observations of vital signs is an essential element of nursing care, the ‘optimal’ observation frequency is unknown, creating some ambiguity about the significance of missed care. The data on who was taking observations were limited and, furthermore, it was not possible to determine what staff group was due to take scheduled observations. More significantly, although the missed care measured was directly relevant to the main outcome (mortality), it is not the only aspect of nursing care that might be important, and, in addition, mortality is not the only important patient outcome.
Our economic analysis was also based on a single outcome – mortality – which is unlikely to reflect the full ‘benefit’ that accrues to patients from nursing care. Our study was unable to undertake longer-term follow-up or to estimate QALYs for patients. We did not consider other patient- or person-centred outcomes that could also inform economic decision-making. Crucially, the validity of any economic conclusions is dependent on the strength of causal inference associated with the underlying study. Finally, our study was conducted in a single site. Although this is, in many ways, ‘typical’, caution must be used when applying these estimates of association elsewhere as they are based on staffing levels determined using a tool that allows considerable scope for professional judgement. Although our findings are consistent with much of the existing evidence base, and the qualitative conclusions about skill mix are robust to the estimates of effect of nurse staffing, nonetheless it must be remembered that these results are derived from a single study of a single site.
Conclusions
Although missed vital signs observations and other routine records of missed care may provide a tool for monitoring changes within wards, it is unlikely that they can be used to directly measure the safety of staffing. The results of this study emphasise and reiterate the potential benefits in terms of patient outcomes and use of scarce acute hospital beds that arise from RN staffing in acute-care hospitals. Although there is currently significant interest in exploring alternative approaches to supplying the care workforce, there is no evidence base associated with these new roles. The findings of this study, while showing the benefits associated with maintaining an adequate HCA workforce, do not support a case for reducing skill mix. The significance of efforts to increase the supply and retention of RNs is amplified by these findings.
Our findings show that patient outcomes and missed care were sensitive not only to RN and HCA HPPD, but also to days on which there were a large number of admissions per RN. This factor may be an important determinant of the RN staffing requirement on a ward, and days with unusually high turnover may require staff levels above that suggested by the patient census. The association between high levels of temporary staff and adverse outcomes suggests that the extent to which flexible staffing policies can effectively meet varying patient need may be limited, and, therefore, base staffing levels may need to be higher to accommodate variation.
A number of priorities for future research emerge from this study:
-
Replicate the current study across multiple sites.
-
Extend the economic analysis to consider cost per QALY and other measures of patient value.
Although this study suggests that an increase in skill mix may be a cost-neutral intervention, in common with other research, there remains much uncertainty because of sensitivity to assumptions made, which means that benefits and costs could be more or less than we have estimated. Furthermore, these results are from a single centre. Replication would allow us to make more precise estimates and to generalise with more confidence. Ideally, economic evaluation includes a measure that would allow a comparison between alternative options, and, certainly, focusing only on death means that the costs of nursing are being judged against a single outcome when the effects of variation in nurse staffing are likely to be experienced across multiple outcomes for both patients and health services. This is a high priority because the question of value in relation to investment in RNs remains unresolved at a policy level.
-
Validate existing and novel methods to determine ward-level staffing requirements, including an assessment of whether or not the use of such tools is associated with improved outcomes/experience.
A key motivation for this project was to determine whether or not missed care, and specifically missed vital signs observations derived from routine data, could be used as a leading indicator of staffing adequacy and could potentially guide staffing decisions at a ward level. The findings of the study have suggested that, while there may be a role for monitoring rates of missed vital signs, it is unlikely that missed vital signs observations can be used to directly determine nurse staffing adequacy. However, the problem of determining and verifying adequate nurse staffing levels remains. The evidence base for current tools in use is limited and no studies have evaluated the effectiveness or costs of using any existing tool.
-
Explore other measures of missed nursing care that can derive from routine data to provide a fuller picture of care delivery.
This study has provided some support for a proposed mechanism linking low staffing to patient outcomes. However, even in relation to acute deterioration and mortality, missed observations provide a very partial view of the care delivered by nurses. While nurse-reported missed care determined through surveys has strongly suggested that missed care might provide a more direct measure of nurse staffing adequacy than outcomes, surveys are unlikely to provide routine monitoring close to the point and time of care delivery. However, there are an increasing number of sources of routine records of complete and timely nursing care. If these can be validated as reflecting the quality of care, in part by establishing links to important person-centred or patient outcomes, it may be possible to develop responsive systems to monitor quality without introducing a significant additional burden of data collection. However, any such system would need to incorporate a range of validated indicators to reflect the diversity of nursing work.
-
Investigate the mechanism for the safe and effective use of assistant personnel within the nursing team.
Although previous research has suggested that reductions in skill mix have negative consequences for patient safety, this study has created a more nuanced picture. However, the findings have suggested that there may be an optimal level of assistant personnel that, when exceeded, produces adverse consequences. Although we have begun to consider the mechanisms of these adverse effects, further research should explore them directly and identify if there are mitigation strategies, especially given the introduction of new grades of nursing assistants/associates.
-
Further explore the association between temporary staff and outcomes and effective approaches to flexible staffing.
Previous research has given conflicting findings on the use of flexible staffing solutions based on deploying temporary staff. Although staff shortages may make using temporary staff necessary on occasion (and indeed frequently), these findings suggest that there may be negative consequences that persist after staffing shortfalls have been rectified. Given that this ‘risk’ has implications for a range of staffing decisions (including policies that attempt to minimise the base staffing requirement by flexibly deploying temporary staff and, hence, creating an apparent efficiency saving), this novel finding should be further explored and investigated in replication studies.
Acknowledgements
We would like to thank all the members of our advisory group:
-
Professor Carl May (chairperson), University of Southampton
-
Mark Stafford-Watson, NIHR CLAHRC Wessex (lay/patient/public representative)
-
Katherine Murphy, Patients’ Association
-
Steve Taylor, Healthwatch Hampshire
-
Dr Ruth May, Monitor/NHS Improvement
-
John de Pury, Universities UK
-
Dr Greta Westwood, Portsmouth Hospital NHS Trust
-
Dr Jeremy Jones, University of Southampton
-
Professor Anne Marie Rafferty, Florence Nightingale School of Nursing and Midwifery, King’s College London
-
Professor Mohammed A Mohammed, University of Bradford
-
Rosemary Chable, University Hospital Southampton
-
Mandy Odell, Royal Berkshire NHS Foundation Trust.
In particular, we wish to acknowledge the contribution of Mark Stafford-Watson, who was a lay member of our advisory group. Mark was generous in sharing his insights and experience of being a hospital patient. Sadly, Mark died before this report was completed. His contributions to this and other NIHR projects have been invaluable.
We would also like to thank Dr Greta Westwood, who facilitated our access to the Trust, all the staff in the Trust and other professional participants and members of the public, primarily from across the Wessex region, who provided practical assistance or took part in our consultation exercises.
Finally, we would especially like to thank and acknowledge the contribution of Ewa Crunden (Research Intern at the University of Southampton), who, despite not meeting all of the criteria for authorship, contributed to this report by preparing tables, drafting sections of the descriptive results and proofreading early drafts.
Contributions of authors
Peter Griffiths (Professor, Health Services Research) conceived and designed the study, interpreted data, and drafted and revised the final report.
Jane Ball (Principal Research Fellow) contributed to the design of the study and interpretation of data, commented on drafts and made significant revisions to the final report.
Karen Bloor (Professor of Health Economics and Policy) contributed to the design of the economic aspects of the study and interpretation of all data, commented on drafts and made significant revisions to the final report.
Dankmar Böhning (Professor, Medical Statistics) contributed to the design of the study, the statistical analysis plan and interpretation of data, supervised statistical analysis, and commented on drafts leading to significant revisions to the final report.
Jim Briggs (Professor, Informatics) contributed to the design of the study and interpretation of data, supervised the building of the project database, commented on drafts and made significant revisions to the final report.
Chiara Dall’Ora (Research Associate, Nursing) contributed to the acquisition of workforce data and ward profiles, contributed to the analysis and interpretation of data, commented on drafts and made significant revisions to the final report.
Anya De Iongh (independent PPI representative) contributed to the design of the study and interpretation of data, contributed to the design of stakeholder engagement to inform the economic modelling, commented on drafts and drafted the lay summary.
Jeremy Jones (Principal Research Fellow) contributed to the design of the economic aspects of the study and interpretation of the economic analysis and commented on drafts leading to revisions of the final report.
Caroline Kovacs (Research Associate, Health Informatics) contributed to the acquisition of data and drafting sections of the report relating to the use of routine data, and commented on drafts leading to revisions of the final report.
Antonello Maruotti (Research Fellow, Statistics) contributed to the design of the study, the statistical analysis plan and interpretation of data, undertook survival and mediation analysis and contributed to drafting the report.
Paul Meredith (Data Manager, Healthcare Research) contributed to the design of the study and led on the extraction of data from Trust systems, contributed to the interpretation of data and commented on drafts leading to revisions of the final report.
David Prytherch (Professor, Health Informatics) contributed to the design of the study and analysis/interpretation of data, and commented on drafts leading to revisions of the final report.
Alejandra Recio Saucedo (Research Fellow, Health Services Evaluation) was responsible for day to day project management, contributed to the acquisition of all data and drafting the report, including review of background literature, and contributed to the interpretation of data.
Oliver Redfern (Research Fellow, Health Informatics) built project database and undertook coding to extract analysis data sets, undertook statistical analysis for staffing/missed care relationships and contributed to drafting the report and interpreting all aspects of analysis.
Paul Schmidt (Consultant in Acute Medicine) contributed to the design of the study and interpretation of data, commented on drafts and made significant revisions to the final report.
Nicola Sinden (Lead Nurse for Workforce) contributed to the design of the study and acquisition of workforce data, commented on drafts and made significant revisions to the final report.
Gary Smith (Professor, Critical Care) contributed to the design of the study and interpretation of data, commented on drafts and made significant revisions to the final report.
Publications
Griffiths P, Ball J, Drennan J, Dall’Ora C, Jones J, Maruotti A, et al. Nurse staffing and patient outcomes: strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for NICE Safe Staffing guideline development. Int J Nurs Stud 2016;63:213–25.
Griffiths P, Recio Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, Smith GB, Ball J. The association between nurse staffing and omissions in nursing care: a systematic review. J Adv Nurs 2018;74:1474–87.
Recio-Saucedo A, Dall’Ora C, Maruotti A, Ball J, Briggs J, Meredith P, et al. What impact does nursing care left undone have on patient outcomes? Review of the literature. J Clin Nurs 2018;27:2248–59.
Griffiths P, Maruotti A, Recio Saucedo A, Redfern O, Ball J, Briggs J, et al. Nurse staffing, nursing assistants and hospital mortality: retrospective longitudinal observational study. BMJ Qual Saf 2018; in press.
Data-sharing statement
Owing to the nature of this study and the conditions attached to original data agreements, there are no data available for wider use. All queries should be submitted to the corresponding author in the first instance.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005–March 2009. London: The Stationery Office; 2010.
- Keogh B. Review into the Quality of Care and Treatment Provided by 14 Hospital Trusts in England: Overview Report. NHS; 2013.
- Marquez L. Nursing Shortage: How It May Affect You 2006. http://abcnews.go.com/WNT/Health/story?id=1529546 (accessed 1 June 2017).
- Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care 2007;45:1195-204. https://doi.org/10.1097/MLR.0b013e3181468ca3.
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 2014;383:1824-30. https://doi.org/10.1016/S0140-6736(13)62631-8.
- Lake ET, Germack HD, Viscardi MK. Missed nursing care is linked to patient satisfaction: a cross-sectional study of US hospitals. BMJ Qual Saf 2016;25:535-43. https://doi.org/10.1136/bmjqs-2015-003961.
- Avalere Health . Optimal Nurse Staffing to Improve Quality of Care and Patient Outcomes 2015. www.nursingworld.org/Avalere-WhitePaper-on-NurseStaffing (accessed 1 August 2017).
- Page A. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, DC: National Academies Press; 2004.
- Making Hospitals Safe for Patients and Nursing/Midwifery Staff Safe Staffing Levels and Skills Mix in South Australian Public Hospitals – Options for the Future. Ridleyton, SA: Australian Nursing and Midwifery Federation (SA Branch); 2012.
- Buchan J, Seccombe I. Safe Staffing Levels – A National Imperative: The UK Nursing Labour Market Review 2013. London: Royal College of Nursing; 2013.
- Buchan J. A certain ratio? The policy implications of minimum staffing ratios in nursing. J Health Serv Res Policy 2005;10:239-44. https://doi.org/10.1258/135581905774414204.
- Safe Staffing for Nursing in Adult Inpatient Wards in Acute Hospitals (Guidance). London: NICE; 2014.
- Twigg DE, Myers H, Duffield C, Giles M, Evans G. Is there an economic case for investing in nursing care – what does the literature tell us?. J Adv Nurs 2015;71:975-90. https://doi.org/10.1111/jan.12577.
- Griffiths P, Ball J, Drennan J, Dall’Ora C, Jones J, Maruotti A, et al. Nurse staffing and patient outcomes: Strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for Health and Care Excellence Safe Staffing guideline development. Int J Nurs Stud 2016;63:213-25. https://doi.org/10.1016/j.ijnurstu.2016.03.012.
- Cookson G, McGovern A. The Cost-Effectiveness of Nurse Staffing and Skill Mix on Nurse Sensitive Outcomes: A Report for the National Institute for Health and Care Excellence. Guildford: University of Surrey; 2014.
- Silber JH, Williams SV, Krakauer H, Schwartz JS. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Med Care 1992;30:615-29. https://doi.org/10.1097/00005650-199207000-00004.
- Clarke SP. Failure to rescue: lessons from missed opportunities in care. Nurs Inq 2004;11:67-71. https://doi.org/10.1111/j.1440-1800.2004.00210.x.
- Griffiths P, Jones S, Bottle A. Is ‘failure to rescue’ derived from administrative data in England a nurse sensitive patient safety indicator for surgical care? Observational study. Int J Nurs Stud 2013;50:292-300. https://doi.org/10.1016/j.ijnurstu.2012.10.016.
- Ball JE, Murrells T, Rafferty AM, Morrow E, Griffiths P. ‘Care left undone’ during nursing shifts: associations with workload and perceived quality of care. BMJ Qual Saf 2014;23:116-25. https://doi.org/10.1136/bmjqs-2012-001767.
- Luettel D, Beaumont K, Healey F. Recognising and Responding Appropriately to Early Signs of Deterioration in Hospitalised Patients. London: National Patient Safety Agency; 2007.
- Acutely Ill Patients in Hospital: Recognition of and Response to Acute Illness in Adults in Hospital (CG 50). London: NICE; 2007.
- Ausserhofer D, Zander B, Busse R, Schubert M, De Geest S, Rafferty AM, et al. Prevalence, patterns and predictors of nursing care left undone in European hospitals: results from the multicountry cross-sectional RN4CAST study. BMJ Qual Saf 2014;23:126-35. https://doi.org/10.1136/bmjqs-2013-002318.
- Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, Rafferty AM, et al. Post-operative mortality, missed care and nurse staffing in nine countries: a cross-sectional study. Int J Nurs Stud 2018;78:10-5. https://doi.org/10.1016/j.ijnurstu.2017.08.004.
- Bruyneel L, Li B, Ausserhofer D, Lesaffre E, Dumitrescu I, Smith H, et al. Organization of hospital nursing, provision of nursing care, and patient assessments of care in Europe. Med Care Res Rev 2015;72:643-4. https://doi.org/10.1177/1077558715589188.
- Kalisch BJ, Tschannen D, Lee KH. Missed nursing care, staffing, and patient falls. J Nurs Care Qual 2012;27:6-12. https://doi.org/10.1097/NCQ.0b013e318225aa23.
- Cho SH, Mark BA, Knafl G, Chang HE, Yoon HJ. Relationships between nurse staffing and patients’ experiences, and the mediating effects of missed nursing care. J Nurs Scholarsh 2017;49:347-55. https://doi.org/10.1111/jnu.12292.
- Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med 2011;364:1037-45. https://doi.org/10.1056/NEJMsa1001025.
- Recio-Saucedo A, Dall’Ora C, Maruotti A, Ball J, Briggs J, Meredith P, et al. What impact does nursing care left undone have on patient outcomes? Review of the literature. J Clin Nurs 2018;27:2248-59. https://doi.org/10.1111/jocn.14058.
- Griffiths P, Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, et al. The association between nurse staffing and omissions in nursing care: a systematic review. J Adv Nurs 2018;74:1474-87. https://doi.org/10.1111/jan.13564.
- Griffiths P, Ball J, Drennan J, James L, Jones J, Recio Saucedo A, et al. The Association Between Patient Safety Outcomes and Nurse/Healthcare Assistant Skill Mix and Staffing Levels and Factors that may Influence Staffing Requirements (NICE Evidence Review). Southampton: University of Southampton Centre for Innovation and Leadership in Health Sciences; 2014.
- Shekelle PG. Nurse-patient ratios as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:404-9. https://doi.org/10.7326/0003-4819-158-5-201303051-00007.
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002;288:1987-93. https://doi.org/10.1001/jama.288.16.1987.
- Twigg D, Duffield C, Bremner A, Rapley P, Finn J. The impact of the nursing hours per patient day (NHPPD) staffing method on patient outcomes: a retrospective analysis of patient and staffing data. Int J Nurs Stud 2011;48:540-8. https://doi.org/10.1016/j.ijnurstu.2010.07.013.
- You LM, Aiken LH, Sloane DM, Liu K, He GP, Hu Y, et al. Hospital nursing, care quality, and patient satisfaction: cross-sectional surveys of nurses and patients in hospitals in China and Europe. Int J Nurs Stud 2013;50:154-61. https://doi.org/10.1016/j.ijnurstu.2012.05.003.
- Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, et al. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int J Nurs Stud 2007;44:175-82. https://doi.org/10.1016/j.ijnurstu.2006.08.003.
- Griffiths P, Ball J, Murrells T, Jones S, Rafferty AM. Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: a cross-sectional study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-008751.
- Sasichay-Akkadechanunt T, Scalzi CC, Jawad AF. The relationship between nurse staffing and patient outcomes. J Nurs Adm 2003;33:478-85. https://doi.org/10.1097/00005110-200309000-00008.
- Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012;344. https://doi.org/10.1136/bmj.e1717.
- Bond CA, Raehl CL, Pitterle ME, Franke T. Health care professional staffing, hospital characteristics, and hospital mortality rates. Pharmacotherapy 1999;19:130-8. https://doi.org/10.1592/phco.19.3.130.30915.
- Martsolf GR, Gibson TB, Benevent R, Jiang HJ, Stocks C, Ehrlich ED, et al. An examination of hospital nurse staffing and patient experience with care: differences between cross-sectional and longitudinal estimates. Health Serv Res 2016;51:2221-41. https://doi.org/10.1111/1475-6773.12462.
- Donaldson N, Bolton LB, Aydin C, Brown D, Elashoff JD, Sandhu M. Impact of California’s licensed nurse-patient ratios on unit-level nurse staffing and patient outcomes. Policy Polit Nurs Pract 2005;6:198-210. https://doi.org/10.1177/1527154405280107.
- Duffield C, Diers D, O’Brien-Pallas L, Aisbett C, Roche M, King M, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl Nurs Res 2011;24:244-55. https://doi.org/10.1016/j.apnr.2009.12.004.
- Hart P, Davis N. Effects of nursing care and staff skill mix on patient outcomes within acute care nursing units. J Nurs Care Qual 2011;26:161-8. https://doi.org/10.1097/NCQ.0b013e3181efc9cb.
- Cho SH, Ketefian S, Barkauskas VH, Smith DG. The effects of nurse staffing on adverse events, morbidity, mortality, and medical costs. Nurs Res 2003;52:71-9. https://doi.org/10.1097/00006199-200303000-00003.
- Twigg DE, Geelhoed EA, Bremner AP, Duffield CM. The economic benefits of increased levels of nursing care in the hospital setting. J Adv Nurs 2013;69:2253-61. https://doi.org/10.1111/jan.12109.
- Unruh L, Joseph L, Strickland M. Nurse absenteeism and workload: negative effect on restraint use, incident reports and mortality. J Adv Nurs 2007;60:673-81. https://doi.org/10.1111/j.1365-2648.2007.04459.x.
- Park SH, Blegen MA, Spetz J, Chapman SA, De Groot H. Patient turnover and the relationship between nurse staffing and patient outcomes. Res Nurs Health 2012;35:277-88. https://doi.org/10.1002/nur.21474.
- Ibe T, Ishizaki T, Oku H, Ota K, Takabatake Y, Iseda A, et al. Predictors of pressure ulcer and physical restraint prevalence in Japanese acute care units. Jpn J Nurs Sci 2008;5:91-8. https://doi.org/10.1111/j.1742-7924.2008.00106.x.
- Lake ET, Shang J, Klaus S, Dunton NE. Patient falls: Association with hospital Magnet status and nursing unit staffing. Res Nurs Health 2010;33:413-25. https://doi.org/10.1002/nur.20399.
- Seago JA, Williamson A, Atwood C. Longitudinal analyses of nurse staffing and patient outcomes: more about failure to rescue. J Nurs Adm 2006;36:13-21. https://doi.org/10.1097/00005110-200601000-00005.
- Weiss ME, Yakusheva O, Bobay KL. Quality and cost analysis of nurse staffing, discharge preparation, and postdischarge utilization. Health Serv Res 2011;46:1473-94. https://doi.org/10.1111/j.1475-6773.2011.01267.x.
- Twigg DE, Myers H, Duffield C, Pugh JD, Gelder L, Roche M. The impact of adding assistants in nursing to acute care hospital ward nurse staffing on adverse patient outcomes: an analysis of administrative health data. Int J Nurs Stud 2016;63:189-200. https://doi.org/10.1016/j.ijnurstu.2016.09.008.
- Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giovannetti P. The impact of hospital nursing characteristics on 30-day mortality. Nurs Res 2005;54:74-8. https://doi.org/10.1097/00006199-200503000-00002.
- He J, Almenoff PL, Keighley J, Li YF. Impact of patient-level risk adjustment on the findings about nurse staffing and 30-day mortality in veterans affairs acute care hospitals. Nurs Res 2013;62:226-32. https://doi.org/10.1097/NNR.0b013e318295810c.
- Blegen MA, Goode CJ, Spetz J, Vaughn T, Park SH. Nurse staffing effects on patient outcomes: safety-net and non-safety-net hospitals. Med Care 2011;49:406-14. https://doi.org/10.1097/MLR.0b013e318202e129.
- McGillis Hall L, Doran D, Pink GH. Nurse staffing models, nursing hours, and patient safety outcomes. J Nurs Adm 2004;34:41-5. https://doi.org/10.1097/00005110-200401000-00009.
- Blegen MA, Vaughn T. A multisite study of nurse staffing and patient occurrences. Nurs Econ 1998;16:196-203.
- Patrician PA, Loan L, McCarthy M, Fridman M, Donaldson N, Bingham M, et al. The association of shift-level nurse staffing with adverse patient events. J Nurs Adm 2011;41:64-70. https://doi.org/10.1097/NNA.0b013e31820594bf.
- Potter P, Barr N, McSweeney M, Sledge J. Identifying nurse staffing and patient outcome relationships: a guide for change in care delivery. Nurs Econ 2003;21:158-66.
- Ausserhofer D, Schubert M, Desmedt M, Blegen MA, De Geest S, Schwendimann R. The association of patient safety climate and nurse-related organizational factors with selected patient outcomes: a cross-sectional survey. Int J Nurs Stud 2013;50:240-52. https://doi.org/10.1016/j.ijnurstu.2012.04.007.
- Dall TM, Chen YJ, Seifert RF, Maddox PJ, Hogan PF. The economic value of professional nursing. Med Care 2009;47:97-104. https://doi.org/10.1097/MLR.0b013e3181844da8.
- Shamliyan TA, Kane RL, Mueller C, Duval S, Wilt TJ. Cost savings associated with increased RN staffing in acute care hospitals: simulation exercise. Nurs Econ 2009;27:302-14.
- Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S. Nurse staffing in hospitals: is there a business case for quality?. Health Aff 2006;25:204-11. https://doi.org/10.1377/hlthaff.25.1.204.
- Martsolf GR, Auerbach D, Benevent R, Stocks C, Jiang HJ, Pearson ML, et al. Examining the value of inpatient nurse staffing: an assessment of quality and patient care costs. Med Care 2014;52:982-8. https://doi.org/10.1097/MLR.0000000000000248.
- Hill AB. The environment and disease: association or causation?. Proc R Soc Med 1965;58:295-300.
- Sochalski J. Is more better?: the relationship between nurse staffing and the quality of nursing care in hospitals. Med Care 2004;42:II67-73. https://doi.org/10.1097/01.mlr.0000109127.76128.aa.
- Lucero RJ, Lake ET, Aiken LH. Nursing care quality and adverse events in US hospitals. J Clin Nurs 2010;19:2185-95. https://doi.org/10.1111/j.1365-2702.2010.03250.x.
- Griffiths P, Dall’Ora C, Simon M, Ball J, Lindqvist R, Rafferty AM, et al. Nurses’ shift length and overtime working in 12 European countries: the association with perceived quality of care and patient safety. Med Care 2014;52:975-81. https://doi.org/10.1097/MLR.0000000000000233.
- Zander B, Dobler L, Bäumler M, Busse R. Nursing tasks left undone in German acute care hospitals – results from the international study RN4Cast. Gesundheitswesen 2014;76:727-34. https://doi.org/10.1055/s-0033-1364016.
- Cho E, Lee NJ, Kim EY, Kim S, Lee K, Park KO, et al. Nurse staffing level and overtime associated with patient safety, quality of care, and care left undone in hospitals: a cross-sectional study. Int J Nurs Stud 2016;60:263-71. https://doi.org/10.1016/j.ijnurstu.2016.05.009.
- Al-Kandari F, Thomas D. Factors contributing to nursing task incompletion as perceived by nurses working in Kuwait general hospitals. J Clin Nurs 2009;18:3430-40. https://doi.org/10.1111/j.1365-2702.2009.02795.x.
- Schubert M, Ausserhofer D, Desmedt M, Schwendimann R, Lesaffre E, Li B, et al. Levels and correlates of implicit rationing of nursing care in Swiss acute care hospitals – a cross sectional study. Int J Nurs Stud 2013;50:230-9. https://doi.org/10.1016/j.ijnurstu.2012.09.016.
- Kalisch BJ, Doumit M, Lee KH, Zein JE. Missed nursing care, level of staffing, and job satisfaction: Lebanon versus the United States. J Nurs Adm 2013;43:274-9. https://doi.org/10.1097/NNA.0b013e31828eebaa.
- Ball JE, Griffiths P, Rafferty AM, Lindqvist R, Murrells T, Tishelman C. A cross-sectional study of ‘care left undone’ on nursing shifts in hospitals. J Adv Nurs 2016;72:2086-97. https://doi.org/10.1111/jan.12976.
- Cho SH, Kim YS, Yeon KN, You SJ, Lee ID. Effects of increasing nurse staffing on missed nursing care. Int Nurs Rev 2015;62:267-74. https://doi.org/10.1111/inr.12173.
- Dabney BW, Kalisch BJ. Nurse staffing levels and patient-reported missed nursing care. J Nurs Care Qual 2015;30:306-12. https://doi.org/10.1097/NCQ.0000000000000123.
- Friese CR, Kalisch BJ, Lee KH. Patterns and correlates of missed nursing care in inpatient oncology units. Cancer Nurs 2013;36:E51-7. https://doi.org/10.1097/NCC.0b013e318275f552.
- Kalisch BJ, Tschannen D, Lee KH. Do staffing levels predict missed nursing care?. Int J Qual Health Care 2011;23:302-8. https://doi.org/10.1093/intqhc/mzr009.
- Kalisch BJ, Tschannen D, Lee H, Friese CR. Hospital variation in missed nursing care. Am J Med Qual 2011;26:291-9. https://doi.org/10.1177/1062860610395929.
- Orique SB, Patty CM, Woods E. Missed nursing care and unit-level nurse workload in the acute and post-acute settings. J Nurs Care Qual 2016;31:84-9. https://doi.org/10.1097/NCQ.0000000000000140.
- Palese A, Ambrosi E, Prosperi L, Guarnier A, Barelli P, Zambiasi P, et al. Missed nursing care and predicting factors in the Italian medical care setting. Intern Emerg Med 2015;10:693-702. https://doi.org/10.1007/s11739-015-1232-6.
- Schubert M, Clarke SP, Aiken LH, de Geest S. Associations between rationing of nursing care and inpatient mortality in Swiss hospitals. Int J Qual Health Care 2012;24:230-8. https://doi.org/10.1093/intqhc/mzs009.
- Ambrosi E, De Togni S, Guarnier A, Barelli P, Zambiasi P, Allegrini E, et al. In-hospital elderly mortality and associated factors in 12 Italian acute medical units: findings from an exploratory longitudinal study. Aging Clin Exp Res 2017;29:517-27. https://doi.org/10.1007/s40520-016-0576-8.
- Carthon JM, Lasater KB, Sloane DM, Kutney-Lee A. The quality of hospital work environments and missed nursing care is linked to heart failure readmissions: a cross-sectional study of US hospitals. BMJ Qual Saf 2015;24:255-63. https://doi.org/10.1136/bmjqs-2014-003346.
- Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care 2008;20:227-37. https://doi.org/10.1093/intqhc/mzn017.
- Schubert M, Clarke SP, Glass TR, Schaffert-Witvliet B, De Geest S. Identifying thresholds for relationships between impacts of rationing of nursing care and nurse- and patient-reported outcomes in Swiss hospitals: a correlational study. Int J Nurs Stud 2009;46:884-93. https://doi.org/10.1016/j.ijnurstu.2008.10.008.
- Nelson ST, Flynn L. Relationship between missed care and urinary tract infections in nursing homes. Geriatr Nurs 2015;36:126-30. https://doi.org/10.1016/j.gerinurse.2014.12.009.
- Thompson D. The Examination of Practice Environment, Burnout, and Missed Care on Pressure Ulcer Prevalence Rates Using a Complexity Science Framework 2014.
- Papastavrou E, Andreou P, Tsangari H, Merkouris A. Linking patient satisfaction with nursing care: the case of care rationing – a correlational study. BMC Nurs 2014;13. https://doi.org/10.1186/1472-6955-13-26.
- Zúñiga F, Ausserhofer D, Hamers JP, Engberg S, Simon M, Schwendimann R. Are staffing, work environment, work stressors, and rationing of care related to care workers’ perception of quality of care? A cross-sectional study. J Am Med Dir Assoc 2015;16:860-6. https://doi.org/10.1016/j.jamda.2015.04.012.
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173-82. https://doi.org/10.1037/0022-3514.51.6.1173.
- Smith GB. In-hospital cardiac arrest: is it time for an in-hospital ‘chain of prevention’?. Resuscitation 2010;81:1209-11. https://doi.org/10.1016/j.resuscitation.2010.04.017.
- Policy Briefing: Mandatory Nurse Staffing Levels. London: Royal College of Nursing; 2012.
- Ball J, Pike G, Griffiths P, Raffferty AM, Murrells T. RN4CAST Nurse Survey in England. London: King’s College London; 2012.
- Bottle A, Jarman B, Aylin P. Hospital standardized mortality ratios: sensitivity analyses on the impact of coding. Health Serv Res 2011;46:1741-61. https://doi.org/10.1111/j.1475-6773.2011.01295.x.
- Campbell MJ, Jacques RM, Fotheringham J, Maheswaran R, Nicholl J. Developing a summary hospital mortality index: retrospective analysis in English hospitals over five years. BMJ 2012;344. https://doi.org/10.1136/bmj.e1001.
- National Early Warning (NEWS). Standardising the Assessment of Acute-Illness Severity in the NHS. London: Royal College of Physicians; 2012.
- Safer Nursing Care Tool (SNCT): Statement of Endorsement. London: NICE; 2014.
- Aylin P, Lees T, Baker S, Prytherch D, Ashley S. Descriptive study comparing routine hospital administrative data with the Vascular Society of Great Britain and Ireland’s National Vascular Database. Eur J Vasc Endovasc Surg 2007;33:461-5. https://doi.org/10.1016/j.ejvs.2006.10.033.
- Hogan H, Zipfel R, Neuburger J, Hutchings A, Darzi A, Black N. Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ 2015;351. https://doi.org/10.1136/bmj.h3239.
- Mohammed MA, Deeks JJ, Girling A, Rudge G, Carmalt M, Stevens AJ, et al. Evidence of methodological bias in hospital standardised mortality ratios: retrospective database study of English hospitals. BMJ 2009;338. https://doi.org/10.1136/bmj.b780.
- Nicholl J. Case-mix adjustment in non-randomised observational evaluations: the constant risk fallacy. J Epidemiol Community Health 2007;61:1010-13. https://doi.org/10.1136/jech.2007.061747.
- Williams JG, Mann RY. Hospital episode statistics: time for clinicians to get involved?. Clin Med 2002;2:34-7. https://doi.org/10.7861/clinmedicine.2-1-34.
- Understanding HSMRs: A Toolkit on Hospital Standardised Mortality Ratios. London: Dr Foster Intelligence; 2011.
- Clinical Indicators Team . Summary Hospital-Level Mortality Indicator (SHMI): Deaths Associated With Hospitalisation. England July 2014–June 2015: Key Facts and Notes 2016.
- Prytherch DR, Smith GB, Schmidt PE, Featherstone PI. ViEWS – towards a national early warning score for detecting adult inpatient deterioration. Resuscitation 2010;81:932-7. https://doi.org/10.1016/j.resuscitation.2010.04.014.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. https://doi.org/10.1016/0021-9681(87)90171-8.
- R: A Language and Environment for Statistical Computing. Vienna: The R Foundation for Statistical Computing; 2017.
- Bates D, Machler M, Bolker BM, Walker SC. Fitting linear mixed-effects models using lme4. J Stat Softw 2015;67:1-48. https://doi.org/10.18637/jss.v067.i01.
- Stasinopoulos DM, Rigby RA. Generalized additive models for location scale and shape (GAMLSS) in R. J Stat Softw 2007;23:1-46. https://doi.org/10.18637/jss.v023.i07.
- Maggs F, Mallet M. Mortality in out-of-hours emergency medical admissions – more than just a weekend effect. J R Coll Physicians Edinb 2010;40:115-18. https://doi.org/10.4997/JRCPE.2010.205.
- Aldridge C, Bion J, Boyal A, Chen YF, Clancy M, Evans T, et al. Weekend specialist intensity and admission mortality in acute hospital trusts in England: a cross-sectional study. Lancet 2016;388:178-86. https://doi.org/10.1016/S0140-6736(16)30442-1.
- Aylin P, Yunus A, Bottle A, Majeed A, Bell D. Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 2010;19:213-17. https://doi.org/10.1136/qshc.2008.028639.
- Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 2001;345:663-8. https://doi.org/10.1056/NEJMsa003376.
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press; 2008.
- Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods 2010;15:309-34. https://doi.org/10.1037/a0020761.
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 2008;40:879-91. https://doi.org/10.3758/BRM.40.3.879.
- Tofighi D, MacKinnon DP. RMediation: an R package for mediation analysis confidence intervals. Behav Res Methods 2011;43:692-700. https://doi.org/10.3758/s13428-011-0076-x.
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002;7:83-104. https://doi.org/10.1037/1082-989X.7.1.83.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- Reference Costs 2015–2016. London: Department of Health and Social Care; 2016.
- Price Caps for Agency Staff Rules. London: NHS Trust Development Authority; 2015.
- Nurminen M. To use or not to use the odds ratio in epidemiologic analyses?. Eur J Epidemiol 1995;11:365-71. https://doi.org/10.1007/BF01721219.
- Stare J, Maucort-Boulch D. Odds ratio, hazard ratio and relative risk. Metodoloski Zvezki 2016;13.
- Guidance on Safe Nurse Staffing Levels in the UK. London: Royal College of Nursing; 2010.
- Summary Hospital-level Mortality Indicator (SHMI): Indicator Specification. n.d.
- Carter P. Operational Productivity and Performance in English NHS Acute Hospitals: Unwarranted Variations. London: Department of Health and Social Care; 2016.
- Eccles SR, Subbe C, Hancock D, Thompson N. M28 from NEWS to CREWS: the chronic respiratory early warning score for patients with chronic hypoxaemia. Thorax 2013;68. https://doi.org/10.1136/thoraxjnl-2013-204457.438.
- Kuntz L, Mennicken R, Scholtes S. Stress on the ward: evidence of safety tipping points in hospitals. Management Science 2014;61:754-71. https://doi.org/10.1287/mnsc.2014.1917.
- Kane RL, Shamliyan T, Mueller C, Duval S, Wilt TJ. Nurse staffing and quality of patient care. Evid Rep Technol Assess 2007;151:1-115.
- Aiken LH, Shang J, Xue Y, Sloane DM. Hospital use of agency-employed supplemental nurses and patient mortality and failure to rescue. Health Serv Res 2013;48:931-48. https://doi.org/10.1111/1475-6773.12018.
- Aiken LH, Xue Y, Clarke SP, Sloane DM. Supplemental nurse staffing in hospitals and quality of care. J Nurs Adm 2007;37:335-42. https://doi.org/10.1097/01.NNA.0000285119.53066.ae.
- Bae SH, Mark B, Fried B. Use of temporary nurses and nurse and patient safety outcomes in acute care hospital units. Health Care Manage Rev 2010;35:333-44. https://doi.org/10.1097/HMR.0b013e3181dac01c.
- Hurst K, Smith A. Temporary nursing staff – cost and quality issues. J Adv Nurs 2011;67:287-96. https://doi.org/10.1111/j.1365-2648.2010.05471.x.
- Bloom JR, Alexander JA, Nuchols BA. Nurse staffing patterns and hospital efficiency in the United States. Soc Sci Med 1997;44:147-55. https://doi.org/10.1016/S0277-9536(96)00063-9.
- Xue Y, Chappel AR, Freund DA, Aiken LH, Noyes K. Cost outcomes of supplemental nurse staffing in a large medical center. J Nurs Care Qual 2015;30:130-7. https://doi.org/10.1097/NCQ.0000000000000100.
- Aiken LH, Sloane D, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, et al. Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual Saf 2017;26:559-68. https://doi.org/10.1136/bmjqs-2016-005567.
- Myny D, Van Goubergen D, Gobert M, Vanderwee K, Van Hecke A, Defloor T. Non-direct patient care factors influencing nursing workload: a review of the literature. J Adv Nurs 2011;67:2109-29. https://doi.org/10.1111/j.1365-2648.2011.05689.x.
- Allan HT, Magnusson C, Evans K, Ball E, Westwood S, Curtis K, et al. Delegation and supervision of healthcare assistants’ work in the daily management of uncertainty and the unexpected in clinical practice: invisible learning among newly qualified nurses. Nurs Inq 2016;23:377-85. https://doi.org/10.1111/nin.12155.
- Mok WQ, Wang W, Liaw SY. Vital signs monitoring to detect patient deterioration: an integrative literature review. Int J Nurs Pract 2015;21:91-8. https://doi.org/10.1111/ijn.12329.
- Jones TL, Hamilton P, Murry N. Unfinished nursing care, missed care, and implicitly rationed care: state of the science review. Int J Nurs Stud 2015;52:1121-37. https://doi.org/10.1016/j.ijnurstu.2015.02.012.
- Smith GB, Recio Saucedo A, Griffiths P. The measurement frequency and completeness of vital signs in general hospital wards: an evidence free zone?. Int J Nurs Stud 2017;74:A1-4. https://doi.org/10.1016/j.ijnurstu.2017.07.001.
- James J, Butler-Williams C, Hunt J, Cox H. Vital signs for vital people: an exploratory study into the role of the Healthcare Assistant in recognising, recording and responding to the acutely ill patient in the general ward setting. J Nurs Manag 2010;18:548-55. https://doi.org/10.1111/j.1365-2834.2010.01086.x.
- Seidman LS. Complements and substitutes: the importance of minding p’s and q’s. Econ J 1989;56:183-90. https://doi.org/10.2307/1059065.
- Health Education England . Building Capacity to Care and Capability to Treat – A New Team Member for Health and Social Care: Consultation 2016. https://hee.nhs.uk/sites/default/files/documents/Nursing%20Associate%20consultation%20document.pdf (accessed 15 January 2018).
- Pencheon D. The Good Indicators Guide: Understanding How to Use and Choose Indicators 2008.
- Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care 2003;15:523-30. https://doi.org/10.1093/intqhc/mzg081.
- Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care 2003;15:i5-11. https://doi.org/10.1093/intqhc/mzg084.
- Mitchell IA, McKay H, Van Leuvan C, Berry R, McCutcheon C, Avard B, et al. A prospective controlled trial of the effect of a multi-faceted intervention on early recognition and intervention in deteriorating hospital patients. Resuscitation 2010;81:658-66. https://doi.org/10.1016/j.resuscitation.2010.03.001.
- Ludikhuize J, Borgert M, Binnekade J, Subbe C, Dongelmans D, Goossens A. Standardized measurement of the Modified Early Warning Score results in enhanced implementation of a Rapid Response System: a quasi-experimental study. Resuscitation 2014;85:676-82. https://doi.org/10.1016/j.resuscitation.2014.02.009.
- De Meester K, Haegdorens F, Monsieurs KG, Verpooten GA, Holvoet A, Van Bogaert P. Six-day postoperative impact of a standardized nurse observation and escalation protocol: a preintervention and postintervention study. J Crit Care 2013;28:1068-74. https://doi.org/10.1016/j.jcrc.2013.07.061.
- De Meester K, Das T, Hellemans K, Verbrugghe W, Jorens PG, Verpooten GA, et al. Impact of a standardized nurse observation protocol including MEWS after intensive care unit discharge. Resuscitation 2013;84:184-8. https://doi.org/10.1016/j.resuscitation.2012.06.017.
- van Galen LS, Dijkstra CC, Ludikhuize J, Kramer MH, Nanayakkara PW. A protocolised once a day Modified Early Warning Score (MEWS) measurement is an appropriate screening tool for major adverse events in a general hospital population. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0160811.
- Petersen JA, Antonsen K, Rasmussen LS. Frequency of early warning score assessment and clinical deterioration in hospitalized patients: a randomized trial. Resuscitation 2016;101:91-6. https://doi.org/10.1016/j.resuscitation.2016.02.003.
- Cardona-Morrell M, Prgomet M, Turner RM, Nicholson M, Hillman K. Effectiveness of continuous or intermittent vital signs monitoring in preventing adverse events on general wards: a systematic review and meta-analysis. Int J Clin Pract 2016;70:806-24. https://doi.org/10.1111/ijcp.12846.
- Griffiths P, Saucedo AR, Schmidt P, Smith G. Vital signs monitoring in hospitals at night. Nurs Times 2015;111:16-7.
- Fasoli DR, Haddock KS. Results of an integrative review of patient classification systems. Annu Rev Nurs Res 2010;28:295-316. https://doi.org/10.1891/0739-6686.28.295.
- Safer Nursing Care Tool Implementation Resource Pack. The Shelford Group; 2014.
- Buchan J, Seccombe I, Gershlick B, Charlesworth A. In Short Supply: Pay Policy and Nurse Numbers 2017.
- Mcclure ML, Poulin MA, Sovie MD, Wandelt MA. Magnet Hospitals: Attraction and Retention of Professional Nurses. Task Force on Nursing Practice in Hospitals. Kansas City, MO: American Nurses Association Publications; 1983.
- Wendsche J, Ghadiri A, Bengsch A, Wegge J. Antecedents and outcomes of nurses’ rest break organization: a scoping review. Int J Nurs Stud 2017;75:65-80. https://doi.org/10.1016/j.ijnurstu.2017.07.005.
- Harvey C, Thompson S, Pearson M, Willis E, Toffoli L. Missed nursing care as an ‘art form’: the contradictions of nurses as carers. Nurs Inq 2017;24. https://doi.org/10.1111/nin.12180.
- Bae SH, Fabry D. Assessing the relationships between nurse work hours/overtime and nurse and patient outcomes: systematic literature review. Nurs Outlook 2014;62:138-56. https://doi.org/10.1016/j.outlook.2013.10.009.
- Dall’Ora C, Griffiths P, Ball J, Simon M, Aiken LH. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: findings from a cross-sectional study of 12 European countries. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008331.
Appendix 1 Description of data sets accessed for the study
Data on patient observations and nursing assessments
Source: Vitalpac.
Patient observations (one record per observation set):
-
patient identification
-
nurse identification
-
nurse grade (derived category from Vitalpac free-text field)
-
timestamp
-
bed/bay/ward.
Plus for standard observation:
-
Early Warning Score (EWS) for complete and incomplete standard observations
-
flag for standard observation completeness
-
scheduled interval to next observation
-
risk category
-
timestamp of subsequent observation (a retrospective calculation not in the data source)
-
breached flag as defined for this site (this is a derivation, not from the data source).
Patient assessments/contacts (one row per contact):
-
patient identification
-
nurse identification
-
timestamp
-
bed/bay/ward.
Plus:
-
nutrition assessments (data from October 2012 onwards)
-
BMI
-
acutely ill and no intake flag
-
weight change
-
MUST score (not always available as dependent on recording of above components).
-
Patient observation status (recorded as a special kind of ‘partial’ observation):
-
patient identification
-
nurse identification
-
timestamp
-
bed/bay/ward
-
observation status (normal, partial or do not monitor/End of Life).
Administrative data
Data source: PAS.
-
Patient demographics (one row per patient).
-
Patient identification.
-
Date of birth (truncated to month to allow derivation of age at admission).
-
Sex.
Stay details (admission and discharge details as one record per stay, transfers as multiple records per stay):
-
patient identification
-
admission date/time
-
admission specialty
-
admission source (see NHS data dictionary for this and other ADT field descriptions and codes)
-
admission method
-
admission ward
-
discharge datetime
-
discharge specialty
-
discharge method
-
discharge destination
-
admission primary diagnosis group (CCS code – used by SHMI and HSMR)
-
discharge primary diagnosis group (CCS code)
-
CCI – calculated from secondary diagnoses on admission
-
Discharge Comorbidity Index – calculated from secondary diagnoses on discharge.
Transfer details (to include admission and discharge transfers with dummy codes for admission and discharge transfer attributes):
-
patient identification
-
transfer datetime
-
consultant from transfer
-
consultant to transfer
-
specialty from transfer
-
specialty to transfer
-
ward from transfer
-
ward to transfer.
Cardiac arrest data
Source: cardiac arrest audit database (one row per arrest).
-
Patient identification.
-
Arrest location/ward.
-
Arrest datetime.
-
Arrest outcome (return of spontaneous circulation > 20 minutes, yes/no).
Unanticipated intensive care unit admissions
Source: ICU WardWatcher (one row per unit admission).
-
Patient identification.
-
Unit admission datetime.
-
From ward.
-
Unit discharge datetime.
Workforce data
Source: eRoster.
Staff roster (one row per member of staff shift rostered and worked or rostered and absent):
-
ward
-
date
-
shift type [e.g. E (evening) or N (night) for worked shift; SK (Sick), SD (study day) and ML (maternity leave) for absence]
-
start time
-
end time
-
break duration
-
staff identification (surrogate for forename and surname)
-
grade
-
hours worked.
Bank/agency bookings (one row per shift booking):
-
location
-
reason
-
grade
-
shift date
-
shift day
-
shift type
-
requested start
-
requested end
-
actual worked hours
-
staff group
-
booking type
-
directorate
-
ward
-
assignment code
-
worked assignment code
-
reference
-
name identification.
Appendix 2 National Early Warning Score and Trust response protocol
| Observation | Score | ||||||
|---|---|---|---|---|---|---|---|
| 3 | 2 | 1 | 0 | 1 | 2 | 3 | |
| Pulse (beats per minute)a | – | ≤ 40 | 41–50 | 51–90 | 91–110 | 111–130 | ≥ 131 |
| Breathing rate (beats per minute)a | ≤ 8 | – | 9–11 | 12–20 | – | 21–24 | ≥ 25 |
| Temperature (°C)a | ≤ 35.0 | – | 35.1–36.0 | 36.1–38.0 | 38.1–39.0 | ≥ 39.1 | – |
| Systolic blood pressure (mmHg)a | ≤ 90 | 91–100 | 101–110 | 111–249 | ≥ 250 | – | – |
| SaO2 (%)a | ≤ 91 | 92–93 | 94–95 | ≥ 96 | – | – | – |
| Inspired O2 | – | – | – | Air | – | – | Any O2 |
| CNS (AVPU scale) | – | – | – | Alert (A) | – | – | Voice (V) |
| Pain (P) | |||||||
| Unresponsive (U) | |||||||
| NEWS | Risk category | Maximum interval between observations | Nurse actions | Doctor actions |
|---|---|---|---|---|
| 0–1 | Low | 6 hours/12 hours if stable for 6 hours | None specified – observations as per schedule | – |
| 2 | Low | 6 hours | None specified – observations as per schedule | – |
| 3–5 | Medium | 4 hours | Inform nurse in charge | – |
| < 6, but with one or more individual triggers | High | 4 hours | RN to inform doctor (FY2/SHO) | See patient within 2 hours |
| 6 | High | 4 hours | RN to inform doctor (FY2/SHO) | See patient within 2 hours |
| 7–8 | High | 1 hour | RN to inform doctor (FY2/SHO). Consider continuous monitoring | See patient within 30 minutes. Call SpR/outreach (after 8.30 PM SpR/ICU) |
| ≥ 9 | Critical | 30 minutes | RN to inform doctor (SpR). Consider continuous monitoring | See patient within 15 minutes. Call SpR/outreach (after 8.30 PM SpR/ICU) |
Appendix 3 Diagnostic groups
| SHMI group | Abbreviated SHMI label | Admissions, n (%) |
|---|---|---|
| 73 | Pneumonia | 5750 (4.2) |
| 114 | Arthritis and connective tissue disorders | 5403 (3.9) |
| 59 | Non-specific chest pain | 4500 (3.3) |
| 138 | Abdominal pain | 3811 (2.8) |
| 101 | Urinary tract infections | 3992 (2.9) |
| 82 | Influenza and other upper respiratory disease | 3555 (2.6) |
| 66 | Acute cerebrovascular disease | 3377 (2.4) |
| 75 | Chronic obstructive pulmonary disease and bronchiectasis | 3362 (2.4) |
| 113 | Other connective tissue disease | 3164 (2.3) |
| 105 | Inflammatory diseases of female pelvic organs and other female genital disorders | 2652 (1.9) |
| 92 | Biliary tract disease | 2799 (2.0) |
| 57 | Acute myocardial infarction | 2878 (2.1) |
| 52 | Headache and ear and sense organ disorders | 2627 (1.9) |
| 107 | Skin and subcutaneous tissue infections | 2454 (1.8) |
| 63 | Cardiac dysrhythmias | 2572 (1.9) |
| Other | 85,237 (61.7) | |
| Total | 138,133 (100) | |
| SHMI group | Abbreviated SHMI label | Admissions, n (%) | Deaths, n (%) |
|---|---|---|---|
| 73 | Pneumonia | 5750 (4.2) | 1188 (21.0) |
| 66 | Acute cerebrovascular disease | 3377 (2.4) | 454 (8.0) |
| 65 | Congestive heart failure | 1765 (1.3) | 277 (4.9) |
| 2 | Septicaemia, shock | 1424 (1.0) | 243 (4.3) |
| 75 | Chronic obstructive pulmonary disease and bronchiectasis | 3362 (2.4) | 174 (3.1) |
| 99 | Acute and unspecified renal failure | 1101 (0.8) | 170 (3.0) |
| 57 | Acute myocardial infarction | 2878 (2.1) | 143 (2.5) |
| 101 | Urinary tract infections | 3992 (2.9) | 158 (2.8) |
| 15 | Cancer of bronchus; lung | 479 (0.3) | 123 (2.2) |
| 96 | Gastrointestinal haemorrhage | 1991 (1.4) | 120 (2.1) |
| 77 | Aspiration pneumonitis; food/vomitus | 345 (0.2) | 108 (1.9) |
| 120 | Fracture of neck of femur (hip) | 2191 (1.6) | 97 (1.7) |
| 79 | Respiratory failure; insufficiency; arrest (adult) | 548 (0.4) | 87 (1.5) |
| 68 | Peripheral and visceral atherosclerosis | 773 (0.6) | 78 (1.4) |
| 83 | Intestinal infection | 2035 (1.5) | 76 (1.3) |
| Other | 106,122 (76.8) | 2166 (38.3) | |
| Total | 138,133 (100.0) | 5662 (100.0) | |
Appendix 4 Ward profiles and staffing levels
| Ward number | Ward label | Description | Number of beds |
|---|---|---|---|
| 21 | Cancer | Medical/radiotherapy haematology/oncology | 40 |
| 4 | Medical/surgery cardiac | Medical/surgical cardiac high care and step down | 23 |
| 30 | Med-adm | Medical – emergency admissions | 58 |
| 2 | Med-gastro | Medical – gastro and liver | 36 |
| 3 | Med-gen1 | Medical – general cardiac and gastro | 36 |
| 6 | Med-gen2 | Medical – general | 30 |
| 7 | Med-gen3 | Medical – general | 35 |
| 18 | Med-OP1 | Medical – older people | 30 |
| 22 | Med-OP2 | Medical – older people | 20 |
| 23 | Med-OP2 | Medical – older people | 29 |
| 24 | Med-OP3 | Medical – older people | 30 |
| 25 | Med-OP4 | Medical – older people | 21 |
| 28 | Med-renal | Medical – renal | 24 |
| 27 | Med-renal HC | Medical – renal high care/step down | 10 |
| 15 | Med-resp1 | Medical – respiratory high care and step down | 40 |
| 16 | Med-resp2 | Medical – respiratory | 36 |
| 20 | Med-stroke | Medical – acute stroke | 12 |
| 26 | Med-Surg | Medical/surgical elective and investigations | 13 |
| 17 | Rehab-neuro | Rehabilitation – neurological (working age) | 13 |
| 19 | Rehab-stroke | Rehabilitation – stroke (older people) | 26 |
| 31 | Surg-adm | Surgical – admissions | 28 |
| 9 | Surg-el/ortho2 | Surgical – elective orthopaedic | 36 |
| 10 | Surg-em/hip# | Surgical – fracture neck of femur/older people | 36 |
| 5 | Surg-em/ortho2 | Surgical – emergency orthopaedic (spinal) | 26 |
| 8 | Surg-em/ortho2 | Surgical – emergency orthopaedic (head injury) | 26 |
| 11 | Surg-gen1 | Surgical – general urology, vascular, plastic | 37 |
| 13 | Surg-GI | Surgical – general, upper GI | 30 |
| 14 | Surg-GI | Surgical – general, colorectal | 34 |
| 1 | Surg-gynae | Surgical – gynaecological | 22 |
| 12 | Surg-H&N | Surgical – head & neck | 21 |
| 32 | Surg-HC | Surgical – high care, step down/step up | 10 |
| 29 | Surg-renal | Surgical – renal transplant | 14 |
| Non-studya | |||
| Ward label | Days of staffing data | Staff | Total CHPPD | Skill mix | |||||
|---|---|---|---|---|---|---|---|---|---|
| RN HPPD | HCA HPPD | ||||||||
| Establishment | Mean (SD) | Establishment | Mean (SD) | Establishment | Mean (SD) | Establishment, % | Mean (SD), % | ||
| Cancer | 1095 | 5.49 | 5.52 (0.64) | 2.22 | 2.25 (0.30) | 7.71 | 8.58 (0.39) | 71 | 71 (3) |
| Med/surg cardiac | 1095 | 7.61 | 6.40 (0.69) | 0.78 | 1.40 (0.64) | 8.39 | 7.01 (0.89) | 91 | 82 (7) |
| Med-adm | 1095 | 7.19 | 6.92 (1.08) | 2.32 | 2.72 (0.58) | 9.51 | 6.05 (0.69) | 76 | 72 (3) |
| Med-gastro | 1095 | 3.73 | 3.49 (0.50) | 2.33 | 3.51 (0.89) | 6.06 | 7.80 (1.27) | 62 | 50 (7) |
| Med-gen1 | 1095 | 3.37 | 3.12 (0.45) | 2.67 | 2.92 (0.55) | 6.04 | 7.77 (0.74) | 56 | 52 (5) |
| Med-gen2 | 494 | 3.99 | 3.18 (0.56) | 3.17 | 3.78 (0.72) | 7.16 | 6.96 (1.00) | 56 | 46 (6) |
| Med-gen3 | 1046 | 3.94 | 3.43 (0.63) | 3.36 | 2.50 (0.59) | 7.30 | 5.93 (0.72) | 54 | 58 (6) |
| MED-OP1 | 1040 | 4.98 | 4.33 (1.49) | 3.89 | 4.22 (1.41) | 8.87 | 7.35 (1.51) | 56 | 51 (7) |
| MED-OP2 | 197 | 3.92 | 3.77 (0.75) | 3.92 | 4.21 (0.75) | 7.84 | 7.12 (0.88) | 50 | 47 (6) |
| MED-OP2 | 1095 | 3.55 | 3.64 (0.45) | 3.29 | 3.33 (0.48) | 6.84 | 8.30 (0.60) | 52 | 52 (5) |
| MED-OP3 | 1095 | 3.72 | 3.87 (0.64) | 3.44 | 3.56 (0.62) | 7.16 | 5.98 (0.82) | 52 | 52 (6) |
| MED-OP4 | 864 | 3.94 | 3.81 (0.72) | 3.55 | 4.32 (1.01) | 7.49 | 6.91 (1.51) | 53 | 47 (9) |
| Med-renal | 894 | 8.51 | 7.30 (1.01) | 1.39 | 1.91 (0.56) | 9.90 | 5.58 (0.74) | 86 | 79 (5) |
| Med-renal HC | 1095 | 10.76 | 9.61 (1.54) | 3.01 | 2.59 (0.95) | 13.77 | 5.88 (0.77) | 78 | 79 (7) |
| Med-resp1 | 854 | 5.05 | 5.19 (0.52) | 1.89 | 2.56 (0.46) | 6.94 | 7.74 (0.66) | 73 | 67 (5) |
| Med-resp2 | 1095 | 3.31 | 2.91 (0.48) | 2.62 | 2.95 (0.74) | 5.93 | 5.85 (0.91) | 56 | 50 (7) |
| Med-stroke | 1027 | 3.55 | 3.88 (0.62) | 3.31 | 3.36 (0.65) | 6.86 | 8.99 (0.86) | 52 | 54 (6) |
| Med-surg | 694 | 6.75 | 6.33 (1.50) | 2.95 | 2.79 (0.84) | 9.70 | 8.55 (0.95) | 70 | 70 (5) |
| Rehab-neuro | 1044 | 4.89 | 5.00 (1.06) | 3.49 | 3.99 (1.39) | 8.38 | 7.57 (1.31) | 58 | 56 (7) |
| Rehab-stroke | 794 | 3.86 | 3.57 (0.53) | 3.7 | 4.00 (0.47) | 7.56 | 7.25 (0.61) | 51 | 47 (5) |
| Surg-adm | 1095 | 4.1 | 3.64 (0.75) | 1.8 | 1.96 (0.55) | 5.90 | 7.77 (0.66) | 69 | 65 (7) |
| Surg-el/ortho2 | 1083 | 4.54 | 4.06 (1.07) | 2.36 | 3.06 (0.72) | 6.90 | 7.98 (0.85) | 66 | 57 (5) |
| Surg-em/hip# | 1095 | 4.09 | 4.36 (0.88) | 2.62 | 3.92 (0.99) | 6.71 | 6.98 (1.09) | 61 | 53 (5) |
| Surg-em/ortho2 | 1017 | 4.35 | 4.24 (0.87) | 3.31 | 3.53 (0.92) | 7.66 | 7.43 (1.28) | 57 | 55 (7) |
| Surg-em/ortho2 | 1047 | 4.36 | 4.04 (0.57) | 2.79 | 3.30 (0.68) | 7.15 | 8.14 (0.85) | 61 | 55 (6) |
| Surg-gen1 | 1095 | 4.27 | 3.30 (0.51) | 2.37 | 2.68 (0.42) | 6.64 | 9.12 (0.52) | 64 | 55 (5) |
| Surg-GI | 1095 | 3.56 | 3.39 (0.49) | 2.56 | 2.19 (0.34) | 6.12 | 12.20 (0.43) | 58 | 61 (5) |
| Surg-GI | 1095 | 3.6 | 3.51 (0.59) | 2.4 | 2.37 (0.39) | 6.00 | 9.22 (0.45) | 60 | 60 (5) |
| Surg-gynae | 874 | 4.48 | 5.71 (1.66) | 1.74 | 2.87 (1.01) | 6.22 | 9.40 (1.04) | 72 | 66 (7) |
| Surg-H&N | 1092 | 5.14 | 4.68 (0.91) | 2.48 | 2.24 (0.77) | 7.62 | 9.64 (0.92) | 67 | 68 (8) |
| Surg-HC | 1095 | 9.77 | 8.54 (1.43) | 1.7 | 2.27 (0.84) | 11.47 | 5.59 (1.17) | 85 | 79 (7) |
| Surg-renal | 494 | 7.95 | 7.11 (1.15) | 2.23 | 2.29 (0.69) | 10.18 | 10.81 (0.84) | 78 | 76 (6) |
| Mean | 968.13 | 5.07 | 4.75 (0.84) | 2.677 | 2.99 (0.72) | 7.75 | 7.73 (0.87) | 64 | 60 (6) |
| Ward | Days of data | Staff | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RN | HCA | ||||||||
| Number of days no temp RN (%) | Number of days ≥ 0.5 temp RN HPPD (%) | Number of days ≥ 1 temp RN HPPD (%) | Number of days ≥ 1.5 RN HPPD (%) | Number of days no temp HCA (%) | Number of days ≥ 0.5 temp HCA HPPD (%) | Number of days ≥ 1 temp HCA HPPD (%) | Number of days ≥ 1.5 temp HCA HPPD (%) | ||
| Cancer | 1095 | 39 (4) | 708 (65) | 237 (22) | 56 (5) | 92 (8) | 494 (45) | 68 (6) | 1 (0) |
| Med/surg cardiac | 1095 | 353 (32) | 427 (39) | 106 (10) | 24 (2) | 249 (23) | 581 (53) | 270 (25) | 102 (9) |
| Med-adm | 1095 | 80 (7) | 483 (44) | 64 (6) | 3 (0) | 20 (2) | 569 (52) | 93 (8) | 5 (0) |
| Med-gastro | 1095 | 73 (7) | 657 (60) | 223 (20) | 53 (5) | 4 (0) | 1014 (93) | 879 (80) | 657 (60) |
| Med-gen1 | 1095 | 281 (26) | 227 (21) | 18 (2) | 1 (0) | 23 (2) | 913 (83) | 528 (48) | 236 (22) |
| Med-gen2 | 494 | 21 (4) | 331 (67) | 109 (22) | 15 (3) | 10 (2) | 440 (89) | 340 (69) | 202 (41) |
| Med-gen3 | 1046 | 40 (4) | 682 (65) | 226 (22) | 42 (4) | 6 (1) | 861 (82) | 365 (35) | 111 (11) |
| MED-OP1 | 1040 | 109 (10) | 521 (50) | 153 (15) | 30 (3) | 114 (11) | 601 (58) | 245 (24) | 76 (7) |
| MED-OP2 | 197 | 1 (1) | 191 (97) | 159 (81) | 86 (44) | 0 (0) | 197 (100) | 181 (92) | 147 (75) |
| MED-OP2 | 1095 | 84 (8) | 521 (48) | 68 (6) | 4 (0) | 22 (2) | 844 (77) | 357 (33) | 128 (12) |
| MED-OP3 | 1095 | 66 (6) | 668 (61) | 239 (22) | 45 (4) | 25 (2) | 901 (82) | 546 (50) | 247 (23) |
| MED-OP4 | 864 | 96 (11) | 577 (67) | 213 (25) | 48 (6) | 37 (4) | 750 (87) | 602 (70) | 443 (51) |
| Med-renal | 894 | 286 (32) | 340 (38) | 97 (11) | 17 (2) | 143 (16) | 515 (58) | 144 (16) | 25 (3) |
| Med-renal HC | 1095 | 250 (23) | 825 (75) | 582 (53) | 371 (34) | 327 (30) | 747 (68) | 464 (42) | 168 (15) |
| Med-resp1 | 854 | 64 (7) | 383 (45) | 70 (8) | 6 (1) | 29 (3) | 675 (79) | 264 (31) | 37 (4) |
| Med-resp2 | 1095 | 241 (22) | 390 (36) | 56 (5) | 3 (0) | 15 (1) | 861 (79) | 469 (43) | 213 (19) |
| Med-stroke | 1027 | 120 (12) | 438 (43) | 65 (6) | 3 (0) | 14 (1) | 835 (81) | 382 (37) | 106 (10) |
| Med-surg | 694 | 305 (44) | 347 (50) | 247 (36) | 102 (15) | 188 (27) | 461 (66) | 306 (44) | 128 (18) |
| Rehab-neuro | 1044 | 330 (32) | 607 (58) | 208 (20) | 45 (4) | 163 (16) | 837 (80) | 553 (53) | 288 (28) |
| Rehab-stroke | 794 | 301 (38) | 223 (28) | 23 (3) | 0 (0) | 24 (3) | 630 (79) | 373 (47) | 142 (18) |
| Surg-adm | 1095 | 564 (52) | 178 (16) | 29 (3) | 2 (0) | 176 (16) | 449 (41) | 152 (14) | 38 (3) |
| Surg-el/ortho2 | 1083 | 341 (31) | 269 (25) | 36 (3) | 6 (1) | 228 (21) | 518 (48) | 179 (17) | 51 (5) |
| Surg-em/hip# | 1095 | 204 (19) | 459 (42) | 113 (10) | 15 (1) | 57 (5) | 771 (70) | 402 (37) | 160 (15) |
| Surg-em/ortho2 | 1017 | 468 (46) | 346 (34) | 134 (13) | 25 (2) | 329 (32) | 542 (53) | 297 (29) | 127 (12) |
| Surg-em/ortho2 | 1047 | 239 (23) | 476 (45) | 141 (13) | 19 (2) | 60 (6) | 806 (77) | 559 (53) | 301 (29) |
| Surg-gen1 | 1095 | 502 (46) | 98 (9) | 2 (0) | 0 (0) | 18 (2) | 742 (68) | 226 (21) | 37 (3) |
| Surg-GI | 1095 | 425 (39) | 204 (19) | 12 (1) | 0 (0) | 242 (22) | 441 (40) | 123 (11) | 21 (2) |
| Surg-GI | 1095 | 139 (13) | 404 (37) | 57 (5) | 0 (0) | 178 (16) | 305 (28) | 53 (5) | 8 (1) |
| Surg-gynae | 874 | 275 (31) | 430 (49) | 152 (17) | 46 (5) | 140 (16) | 667 (76) | 498 (57) | 276 (32) |
| Surg-H&N | 1092 | 530 (49) | 204 (19) | 43 (4) | 4 (0) | 240 (22) | 495 (45) | 149 (14) | 39 (4) |
| Surg-HC | 1095 | 599 (55) | 411 (38) | 145 (13) | 46 (4) | 762 (70) | 301 (27) | 98 (9) | 33 (3) |
| Surg-renal | 494 | 103 (21) | 316 (64) | 180 (36) | 100 (20) | 16 (3) | 454 (92) | 218 (44) | 72 (15) |
| ALL | 30,980 | 7529 (24) | 13,341 (43) | 4207 (14) | 1217 (4) | 3951 (13) | 20,217 (65) | 10,383 (34) | 4625 (15) |
| Ward | Days of staffing data | Staff | |||||
|---|---|---|---|---|---|---|---|
| RN | HCA | ||||||
| Number of days below establishment (%) | Number of days below mean (%) | Number of days below 80% of mean (%) | Number of days below establishment (%) | Number of days below mean (%) | Number of days below 80% of mean (%) | ||
| Cancer | 1095 | 540 (49) | 564 (52) | 30 (3) | 516 (47) | 569 (52) | 55 (5) |
| Med/surg cardiac | 1095 | 1040 (95) | 593 (54) | 26 (2) | 200 (18) | 605 (55) | 416 (38) |
| Med-adm | 1095 | 739 (67) | 611 (56) | 55 (5) | 274 (25) | 626 (57) | 162 (15) |
| Med-gastro | 1095 | 764 (70) | 565 (52) | 84 (8) | 110 (10) | 525 (48) | 266 (24) |
| Med-gen1 | 1095 | 819 (75) | 577 (53) | 75 (7) | 408 (37) | 612 (56) | 141 (13) |
| Med-gen2 | 494 | 460 (93) | 245 (50) | 62 (13) | 104 (21) | 260 (53) | 77 (16) |
| Med-gen3 | 1046 | 846 (81) | 512 (49) | 145 (14) | 963 (92) | 583 (56) | 193 (18) |
| MED-OP1 | 1040 | 865 (83) | 634 (61) | 176 (17) | 477 (46) | 582 (56) | 279 (27) |
| MED-OP2 | 197 | 123 (62) | 105 (53) | 24 (12) | 68 (35) | 106 (54) | 18 (9) |
| MED-OP2 | 1095 | 465 (42) | 557 (51) | 48 (4) | 513 (47) | 558 (51) | 92 (8) |
| MED-OP3 | 1095 | 439 (40) | 566 (52) | 108 (10) | 489 (45) | 580 (53) | 135 (12) |
| MED-OP4 | 864 | 521 (60) | 456 (53) | 122 (14) | 222 (26) | 419 (48) | 203 (23) |
| Med-renal | 894 | 797 (89) | 500 (56) | 40 (4) | 161 (18) | 459 (51) | 226 (25) |
| Med-renal HC | 1095 | 884 (81) | 576 (53) | 100 (9) | 855 (78) | 547 (50) | 246 (22) |
| Med-resp1 | 854 | 363 (43) | 441 (52) | 13 (2) | 39 (5) | 470 (55) | 102 (12) |
| Med-resp2 | 1095 | 877 (80) | 553 (51) | 122 (11) | 404 (37) | 614 (56) | 240 (22) |
| Med-stroke | 1027 | 309 (30) | 556 (54) | 86 (8) | 487 (47) | 520 (51) | 139 (14) |
| Med-surg | 694 | 475 (68) | 393 (57) | 125 (18) | 455 (66) | 405 (58) | 169 (24) |
| Rehab-neuro | 1044 | 517 (50) | 580 (56) | 129 (12) | 413 (40) | 576 (55) | 262 (25) |
| Rehab-stroke | 794 | 570 (72) | 435 (55) | 59 (7) | 195 (25) | 417 (53) | 24 (3) |
| Surg-adm | 1095 | 832 (76) | 597 (55) | 150 (14) | 472 (43) | 623 (57) | 258 (24) |
| Surg-el/ortho2 | 1083 | 809 (75) | 641 (59) | 218 (20) | 133 (12) | 615 (57) | 179 (17) |
| Surg-em/hip# | 1095 | 462 (42) | 619 (57) | 142 (13) | 25 (2) | 675 (62) | 203 (19) |
| Surg-em/ortho2 | 1017 | 619 (61) | 551 (54) | 117 (12) | 429 (42) | 524 (52) | 245 (24) |
| Surg-em/ortho2 | 1047 | 773 (74) | 563 (54) | 57 (5) | 240 (23) | 571 (55) | 156 (15) |
| Surg-gen1 | 1095 | 1050 (96) | 577 (53) | 86 (8) | 242 (22) | 579 (53) | 88 (8) |
| Surg-GI | 1095 | 721 (66) | 583 (53) | 70 (6) | 956 (87) | 540 (49) | 108 (10) |
| Surg-GI | 1095 | 622 (57) | 552 (50) | 130 (12) | 622 (57) | 590 (54) | 89 (8) |
| Surg-gynae | 874 | 187 (21) | 504 (58) | 212 (24) | 42 (5) | 495 (57) | 238 (27) |
| Surg-H&N | 1092 | 820 (75) | 604 (55) | 116 (11) | 688 (63) | 538 (49) | 290 (27) |
| Surg-HC | 1095 | 906 (83) | 575 (53) | 116 (11) | 315 (29) | 559 (51) | 368 (34) |
| Surg-renal | 494 | 401 (81) | 270 (55) | 34 (7) | 246 (50) | 264 (53) | 110 (22) |
| All | 30,980 | 20,615 (67) | 16,655 (54) | 3077 (10) | 11,763 (38) | 16,606 (54) | 5777 (19) |
| Staffing measure | Mode | Median | Mean | Minimum | Maximum |
|---|---|---|---|---|---|
| RN HPPD | |||||
| Days below mean | 0 | 2 | 1.93 | 0 | 5 |
| Days below 80% of mean | 0 | 0 | 0.35 | 0 | 5 |
| Days below establishment | 0 | 2 | 2.24 | 0 | 5 |
| Hours below mean (sum) | 0 | 0 | 0.39 | 0 | 36 |
| HCA HPPD | |||||
| Days below mean | 0 | 2 | 1.94 | 0 | 5 |
| Days below 80% of mean | 0 | 0 | 0.66 | 0 | 5 |
| Days below establishment | 0 | 1 | 1.11 | 0 | 5 |
| Hours below mean (sum) | 0 | 0 | 0.25 | 0 | 30 |
| Ward | Days of data (n) | Mean admission per RN (SD) | Number of days 25% above mean, n (%) | Mean admission per HCA (SD) | Number of days 25% above mean, n (%) |
|---|---|---|---|---|---|
| Cancer | 1095 | 0.78 (0.32) | 263 (24) | 1.94 (0.85) | 281 (26) |
| Med/surg cardiac | 1095 | 1.47 (0.64) | 300 (27) | 8.59 (6.33) | 285 (26) |
| Med-adm | 1095 | 3.44 (0.54) | 59 (5) | 8.89 (1.73) | 115 (11) |
| Med-gastro | 1095 | 1.70 (1.01) | 272 (25) | 1.79 (1.20) | 287 (26) |
| Med-gen1 | 1095 | 1.89 (0.78) | 281 (26) | 2.06 (0.91) | 280 (26) |
| Med-gen2 | 494 | 1.30 (0.76) | 143 (29) | 1.11 (0.67) | 142 (29) |
| Med-gen3 | 1046 | 0.92 (0.96) | 238 (23) | 1.31 (1.50) | 233 (22) |
| MED-OP1 | 1040 | 1.10 (0.56) | 275 (26) | 1.16 (0.64) | 284 (27) |
| MED-OP2 | 197 | 0.71 (0.67) | 63 (32) | 0.63 (0.58) | 58 (29) |
| MED-OP2 | 1095 | 0.58 (0.44) | 341 (31) | 0.65 (0.51) | 327 (30) |
| MED-OP3 | 1095 | 0.51 (0.36) | 344 (31) | 0.56 (0.40) | 352 (32) |
| MED-OP4 | 864 | 0.57 (0.60) | 252 (29) | 0.62 (2.90) | 198 (23) |
| Med-renal | 894 | 0.50 (0.29) | 273 (31) | 2.10 (1.52) | 250 (28) |
| Med-renal HC | 1095 | 0.41 (0.35) | 375 (34) | 1.75 (1.99) | 245 (22) |
| Med-resp1 | 854 | 1.19 (0.67) | 159 (19) | 2.48 (1.52) | 166 (19) |
| Med-resp2 | 1095 | 2.12 (1.23) | 225 (21) | 2.16 (1.26) | 260 (24) |
| Med-stroke | 1027 | 0.57 (0.45) | 303 (30) | 0.68 (0.53) | 295 (29) |
| Med-surg | 694 | 1.95 (1.06) | 204 (29) | 4.63 (2.75) | 197 (28) |
| Rehab-neuro | 1044 | 0.15 (0.29) | 308 (30) | 0.20 (0.38) | 308 (30) |
| Rehab-stroke | 794 | 0.4 (0.50) | 259 (33) | 0.37 (0.45) | 255 (32) |
| Surg-adm | 1095 | 5.45 (1.84) | 213 (19) | 10.41 (3.83) | 236 (22) |
| Surg-el/ortho2 | 1083 | 2.21 (1.46) | 413 (38) | 2.94 (1.99) | 412 (38) |
| Surg-em/hip# | 1095 | 1.56 (0.90) | 343 (31) | 1.78 (1.05) | 349 (32) |
| Surg-em/ortho2 | 1017 | 0.82 (0.60) | 318 (31) | 0.98 (0.75) | 301 (30) |
| Surg-em/ortho2 | 1047 | 1.07 (0.64) | 304 (29) | 1.34 (0.83) | 295 (28) |
| Surg-gen1 | 1095 | 1.88 (0.81) | 263 (24) | 2.30 (0.95) | 287 (26) |
| Surg-GI | 1095 | 2.06 (0.90) | 280 (26) | 3.26 (1.55) | 286 (26) |
| Surg-GI | 1095 | 1.45 (0.68) | 289 (26) | 2.18 (1.11) | 302 (28) |
| Surg-gynae | 874 | 2.26 (0.94) | 225 (26) | 4.69 (2.34) | 223 (26) |
| Surg-H&N | 1092 | 2.24 (0.91) | 289 (26) | 5.54 (4.25) | 249 (23) |
| Surg-HC | 1095 | 0.95 (0.51) | 342 (31) | 4.06 (3.17) | 271 (25) |
| Surg-renal | 494 | 0.72 (0.47) | 147 (30) | 2.42 (1.82) | 129 (26) |
| All (ward) | 968 | 1.40 (0.72) | 261 (27) | 2.67 (1.63) | 255 (26) |
FIGURE 13.
Relative frequency of missed observations by patient acuity, by ward.
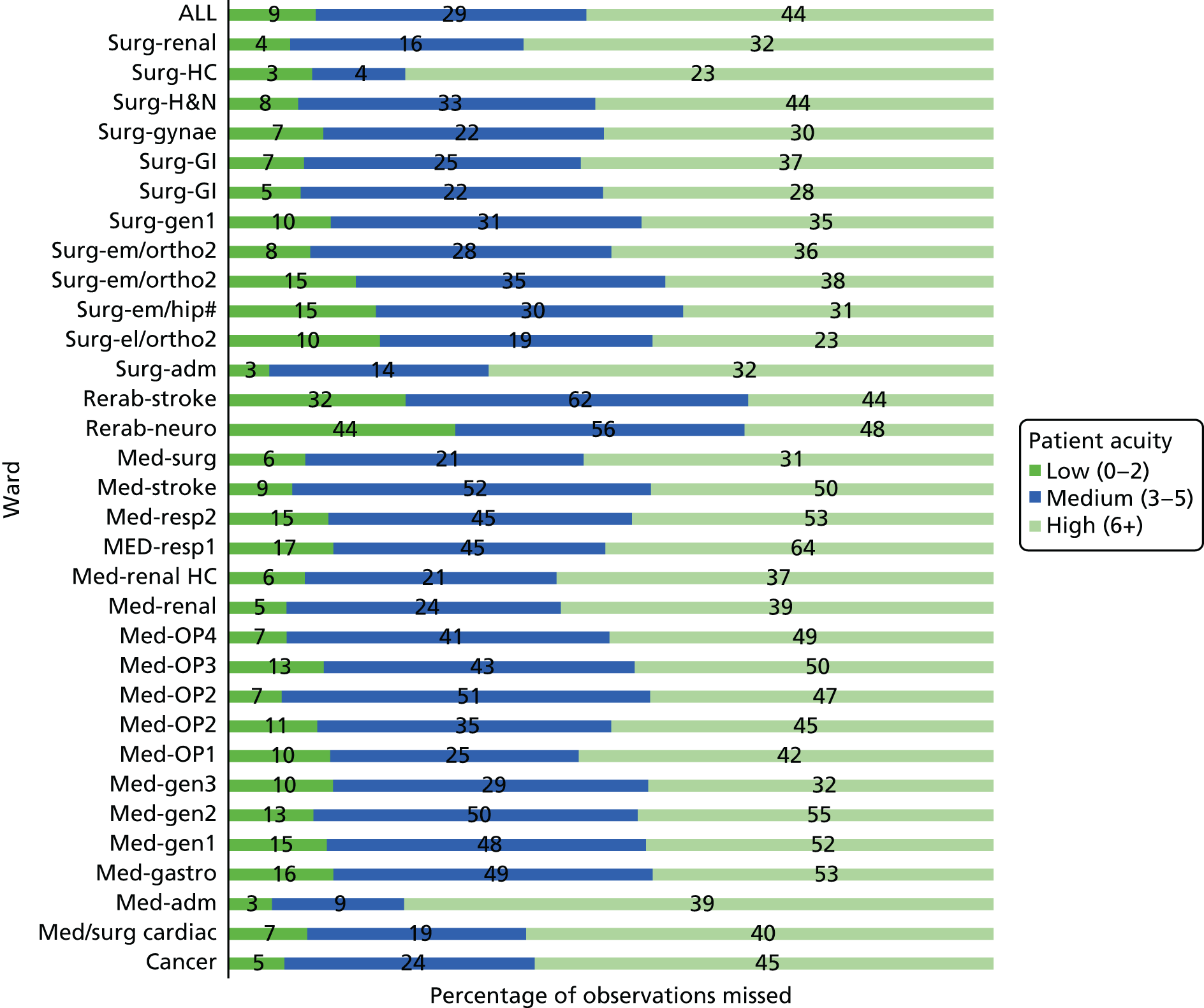
| Ward | Observations | ||
|---|---|---|---|
| All | High-acuity patients | Low-acuity patients | |
| Cancer | 7 | 8 | 7 |
| Med/surg cardiac | 6 | 5 | 6 |
| Med-adm | 7 | 8 | 6 |
| Med-gastro | 2 | 2 | 2 |
| Med-gen1 | 4 | 5 | 4 |
| Med-gen2 | 14 | 13 | 14 |
| Med-gen3 | 12 | 12 | 13 |
| MED-OP1 | 26 | 25 | 26 |
| MED-OP2 | 4 | 6 | 4 |
| MED-OP2 | 6 | 6 | 6 |
| MED-OP3 | 5 | 6 | 4 |
| MED-OP4 | 5 | 7 | 4 |
| Med-renal | 22 | 12 | 23 |
| Med-renal HC | 37 | 29 | 38 |
| Med-resp1 | 3 | 2 | 3 |
| Med-resp2 | 1 | 1 | 1 |
| Med-stroke | 18 | 15 | 18 |
| Med-surg | 15 | 18 | 15 |
| Rehab-neuro | 8 | 8 | 8 |
| Rehab-stroke | 39 | 36 | 40 |
| Surg-adm | 38 | 30 | 39 |
| Surg-el/ortho2 | 5 | 6 | 5 |
| Surg-em/hip# | 20 | 15 | 20 |
| Surg-em/ortho2 | 10 | 10 | 9 |
| Surg-em/ortho2 | 7 | 11 | 6 |
| Surg-gen1 | 21 | 26 | 20 |
| Surg-GI | 32 | 22 | 34 |
| Surg-GI | 33 | 25 | 35 |
| Surg-gynae | 9 | 10 | 8 |
| Surg-H&N | 37 | 29 | 39 |
| Surg-HC | 24 | 24 | 23 |
| Surg-renal | 19 | 13 | 20 |
| All | 15 | 14 | 16 |
FIGURE 14.
Nutritional risk assessments done within 24 hours of admission, by ward.
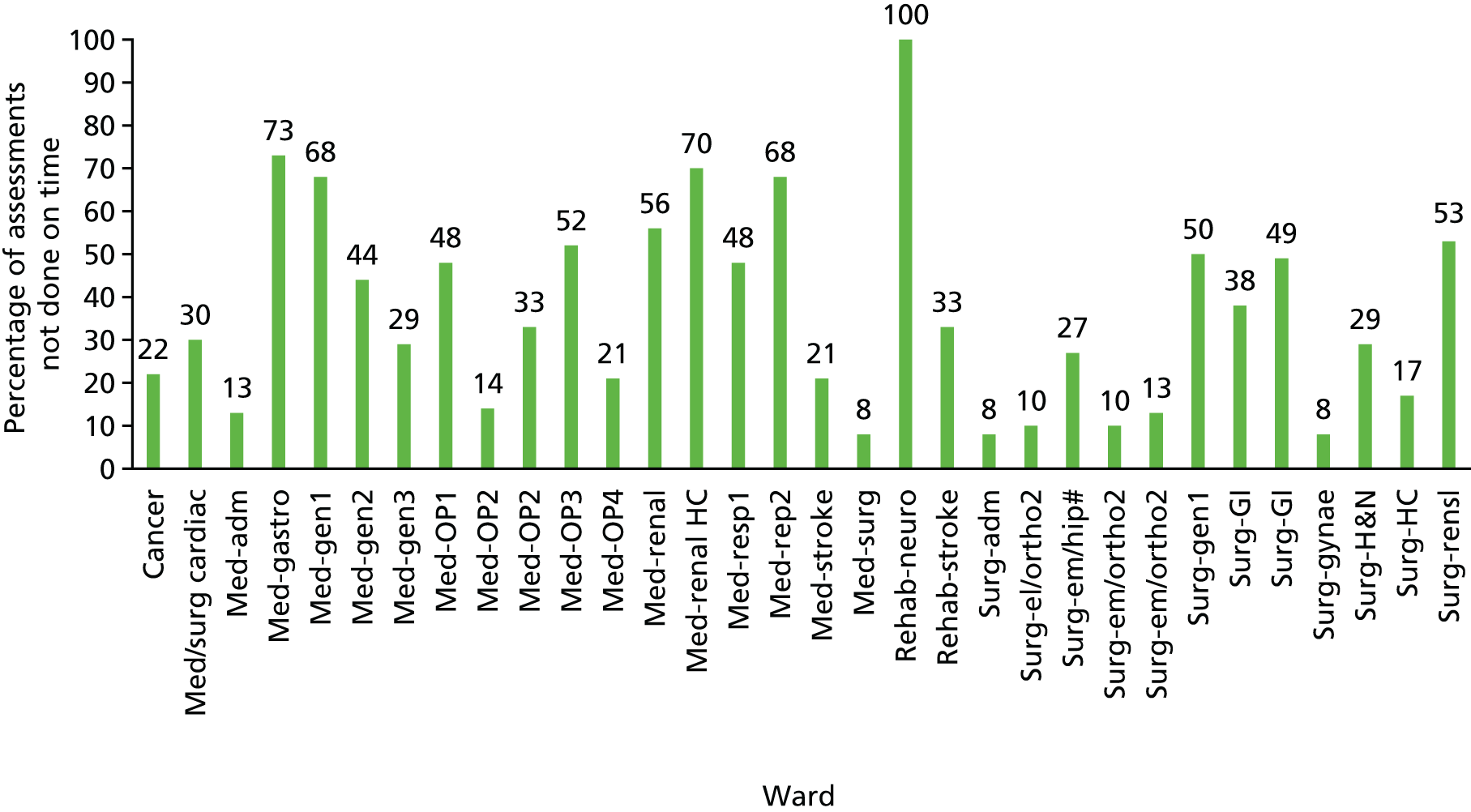
Appendix 5 Additional statistical models: results
All subsequent models include a random effect for ward–ward effects are not reported.
| Survival (death) | With ward effects | p-value | |
|---|---|---|---|
| HR | 95% CI | ||
| First NEWS | 1.30 | 1.28 to 1.31 | < 0.001 |
| SHMI risk score | 1.95 | 1.90 to 2.00 | < 0.001 |
| Emergency | 3.89 | 3.16 to 4.79 | < 0.001 |
| Admissions per RN of > 125% of ward mean | 1.06 | 1.04 to 1.08 | < 0.001 |
| Admissions per HCA of > 125% of ward mean | 1.06 | 1.04 to 1.08 | < 0.001 |
| RN staffing below ward mean | 1.07 | 1.04 to 1.10 | < 0.001 |
| HCA staffing below ward mean | 1.06 | 1.03 to 1.08 | < 0.001 |
| RN hours ± ward mean (cumulative sum) | 0.97 | 0.95 to 1.00 | 0.028 |
| HCA hours ± ward mean (cumulative sum) | 1.01 | 0.98 to 1.03 | 0.479 |
| RN hours below ward mean (cumulative sum) | 1.03 | 1.01 to 1.06 | 0.016 |
| HCA hours below ward mean (cumulative sum) | 1.01 | 0.98 to 1.04 | 0.440 |
| RN staffing below 80% of ward mean | 1.00 | 0.96 to 1.04 | 0.924 |
| HCA staffing below 80% of ward mean | 1.04 | 1.01 to 1.06 | 0.003 |
| RN staffing below establishment | 1.09 | 1.08 to 1.12 | < 0.001 |
| HCA staffing below establishment | 1.05 | 1.03 to 1.07 | < 0.001 |
| Temporary RN staffing above 30 minutes PPD | 1.02 | 1.00 to 1.04 | 0.016 |
| Temporary HCA staffing above 30 minutes PPD | 1.07 | 1.06 to 1.09 | < 0.001 |
| Temporary RN staffing above 1 HPPD | 1.01 | 0.98 to 1.04 | 0.356 |
| Temporary HCA staffing above 1 HPPD | 1.03 | 1.01 to 1.05 | 0.001 |
| Temporary RN staffing above 1.5 HPPD | 1.07 | 1.00 to 1.15 | 0.053 |
| Temporary HCA staffing above 1.5 HPPD | 1.05 | 1.02 to 1.07 | 0.001 |
| Missed observations | IRR | 95% CI | p-value |
|---|---|---|---|
| High acuity observations | |||
| RN HPPD | 0.98 | 0.97 to 0.99 | < 0.001 |
| HCA HPPD | 1.00 | 0.99 to 1.01 | 0.683 |
| Admissions per RN | 1.00 | 1.00 to 1.00 | 0.694 |
| Proportion unwell | 1.00 | 0.93 to 1.08 | 0.991 |
| RN × HCA | 1.00 | 0.93 to 1.08 | 0.991 |
| All observations | |||
| RN HPPD | 0.98 | 0.98 to 0.99 | < 0.001 |
| HCA HPPD | 0.96 | 0.95 to 0.96 | < 0.001 |
| Admissions per RN | 1.00 | 1.00 to 1.00 | 0.005 |
| Proportion unwell | 4.86 | 4.68 to 5.00 | < 0.001 |
| RN × HCA | 1.00 | 1.00 to 1.00 | < 0.001 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.25 |
| SHMI risk score | 1.82 | 0.025 | < 0.001 | 1.78 to 1.87 |
| Emergency | 1.11 | 0.124 | 0.365 | 0.89 to 1.38 |
| Admissions per RN of > 125% of ward mean | 1.05 | 0.023 | 0.024 | 1.01 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.873 | 0.96 to 1.04 |
| RN staffing below ward mean | 1.03 | 0.012 | 0.009 | 1.01 to 1.06 |
| HCA staffing below ward mean | 1.04 | 0.012 | < 0.001 | 1.02 to 1.07 |
| Ward dummy (surg-gynae is reference) | 1.00 | – | – | – |
| MED-GASTRO | 2.70 | 0.692 | < 0.001 | 1.64 to 4.47 |
| MED-GEN1 | 1.78 | 0.459 | 0.025 | 1.07 to 2.95 |
| MED/SURG CARDIAC | 2.17 | 0.565 | 0.003 | 1.30 to 3.61 |
| SURG-EM/ORTHO2 | 0.65 | 0.190 | 0.143 | 0.37 to 1.16 |
| MED-GEN2 | 1.13 | 0.311 | 0.656 | 0.66 to 1.94 |
| MED-GEN3 | 0.95 | 0.257 | 0.847 | 0.56 to 1.61 |
| SURG-EM/ORTHO2 | 0.83 | 0.246 | 0.528 | 0.46 to 1.48 |
| SURG-EL/ORTHO2 | 0.76 | 0.369 | 0.574 | 0.29 to 1.97 |
| SURG-EM/HIP# | 0.43 | 0.167 | 0.030 | 0.20 to 0.92 |
| SURG-GEN1 | 1.44 | 0.388 | 0.173 | 0.85 to 2.44 |
| SURG-H&N | 0.67 | 0.217 | 0.217 | 0.36 to 1.26 |
| SURG-GI | 1.34 | 0.368 | 0.288 | 0.78 to 2.29 |
| SURG-GI | 1.45 | 0.389 | 0.171 | 0.85 to 2.45 |
| MED-RESP1 | 2.80 | 0.704 | < 0.001 | 1.71 to 4.59 |
| MED-RESP2 | 2.34 | 0.592 | 0.001 | 1.43 to 3.84 |
| REHAB-NEURO | 0.04 | 0.040 | 0.002 | 0.01 to 0.29 |
| MED-OP1 | 2.55 | 0.649 | < 0.001 | 1.55 to 4.20 |
| REHAB-STROKE | 0.62 | 0.174 | 0.090 | 0.36 to 1.08 |
| MED-STROKE | 2.04 | 0.519 | 0.005 | 1.24 to 3.36 |
| CANCER | 2.66 | 0.673 | < 0.001 | 1.62 to 4.37 |
| MED-OP2 | 2.46 | 0.763 | 0.004 | 1.34 to 4.52 |
| MED-OP2 | 1.95 | 0.497 | 0.009 | 1.19 to 3.22 |
| MED-OP3 | 2.64 | 0.671 | < 0.001 | 1.61 to 4.35 |
| MED-OP4 | 2.02 | 0.530 | 0.007 | 1.21 to 3.38 |
| MED-SURG | 2.14 | 0.630 | 0.010 | 1.20 to 3.81 |
| MED-RENAL HC | 1.81 | 0.514 | 0.036 | 1.04 to 3.16 |
| MED-RENAL | 1.77 | 0.477 | 0.033 | 1.05 to 3.01 |
| SURG-RENAL | 1.21 | 0.386 | 0.549 | 0.65 to 2.26 |
| MED-ADM | 1.81 | 0.456 | 0.019 | 1.10 to 2.96 |
| NON STUDY | 1.41 | 0.357 | 0.180 | 0.85 to 2.31 |
| SURG-ADM | 2.96 | 0.774 | < 0.001 | 1.78 to 4.95 |
| SURG-HC | 2.36 | 0.695 | 0.004 | 1.32 to 4.20 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.26 | 0.007 | < 0.001 | 1.24 to 1.27 |
| SHMI risk score | 1.87 | 0.027 | < 0.001 | 1.81 to 1.92 |
| Emergency | 1.24 | 0.158 | 0.085 | 0.97 to 1.60 |
| Admissions per RN of > 125% of ward mean | 1.05 | 0.024 | 0.044 | 1.00 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.02 | 0.023 | 0.443 | 0.97 to 1.06 |
| RN staffing below ward mean | 1.03 | 0.013 | 0.014 | 1.01 to 1.06 |
| HCA staffing below ward mean | 1.04 | 0.013 | 0.001 | 1.02 to 1.07 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.25 |
| SHMI risk score | 1.82 | 0.025 | < 0.001 | 1.77 to 1.87 |
| Admissions per RN of > 125% of ward mean | 1.05 | 0.023 | 0.019 | 1.01 to 1.10 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.820 | 0.95 to 1.04 |
| RN staffing below ward mean | 1.03 | 0.012 | 0.015 | 1.01 to 1.05 |
| HCA staffing below ward mean | 1.04 | 0.012 | 0.001 | 1.02 to 1.07 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.25 | 0.007 | < 0.001 | 1.23 to 1.26 |
| SHMI risk score | 1.85 | 0.026 | < 0.001 | 1.80 to 1.90 |
| Emergency | 1.13 | 0.128 | 0.278 | 0.91 to 1.41 |
| RN staffing below ward mean | 1.01 | 0.003 | 0.013 | 1.00 to 1.01 |
| HCA staffing below ward mean | 1.00 | 0.003 | 0.135 | 1.00 to 1.01 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| Weekend admission | 1.06 | 0.035 | 0.096 | 0.99 to 1.13 |
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.25 |
| SHMI risk score | 1.82 | 0.025 | < 0.001 | 1.77 to 1.87 |
| Emergency | 1.10 | 0.123 | 0.416 | 0.88 to 1.37 |
| Admissions per RN of > 125% of ward mean | 1.05 | 0.023 | 0.027 | 1.01 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.897 | 0.96 to 1.04 |
| RN staffing below ward mean | 1.03 | 0.012 | 0.011 | 1.01 to 1.05 |
| HCA staffing below ward mean | 1.04 | 0.012 | < 0.001 | 1.02 to 1.07 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| Weekend stay | 0.58 | 0.020 | < 0.001 | 0.54 to 0.62 |
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.25 |
| SHMI risk score | 1.84 | 0.025 | < 0.001 | 1.79 to 1.89 |
| Emergency | 1.19 | 0.133 | 0.125 | 0.95 to 1.48 |
| Admissions per RN of > 125% of ward mean | 1.03 | 0.022 | 0.152 | 0.99 to 1.08 |
| Admissions per HCA of > 125% of ward mean | 0.99 | 0.021 | 0.517 | 0.95 to 1.03 |
| RN staffing below ward mean | 1.05 | 0.013 | < 0.001 | 1.03 to 1.08 |
| HCA staffing below ward mean | 1.04 | 0.012 | < 0.001 | 1.02 to 1.07 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.25 |
| SHMI risk score | 1.82 | 0.025 | < 0.001 | 1.78 to 1.87 |
| Emergency | 1.09 | 0.123 | 0.423 | 0.88 to 1.36 |
| Admissions per RN of > 125% of ward mean | 1.02 | 0.021 | 0.469 | 0.97 to 1.06 |
| Admissions per HCA of > 125% of ward mean | 1.03 | 0.022 | 0.224 | 0.98 to 1.07 |
| RN staffing below establishment | 1.09 | 0.012 | < 0.001 | 1.06 to 1.11 |
| HCA staffing below establishment | 1.01 | 0.013 | 0.241 | 0.99 to 1.04 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.22 to 1.25 |
| SHMI risk score | 1.82 | 0.024 | < 0.001 | 1.77 to 1.87 |
| Emergency | 1.14 | 0.128 | 0.235 | 0.92 to 1.42 |
| Admissions per RN of > 125% of ward mean | 1.07 | 0.023 | 0.001 | 1.03 to 1.12 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.840 | 0.96 to 1.05 |
| RN staffing below 80% of ward mean | 0.98 | 0.022 | 0.314 | 0.94 to 1.02 |
| HCA staffing below 80% of ward mean | 1.04 | 0.016 | 0.018 | 1.01 to 1.07 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.22 to 1.25 |
| SHMI risk score | 1.82 | 0.024 | < 0.001 | 1.77 to 1.87 |
| Emergency | 1.15 | 0.128 | 0.222 | 0.92 to 1.43 |
| Admissions per RN of > 125% of ward mean | 1.06 | 0.022 | 0.003 | 1.02 to 1.11 |
| Admissions per HCA of > 125% of ward mean | 1.02 | 0.020 | 0.238 | 0.98 to 1.06 |
| RN hours ± ward mean (cumulative sum) | 0.97 | 0.013 | 0.023 | 0.94 to 1.00 |
| HCA hours ± ward mean (cumulative sum) | 1.01 | 0.015 | 0.394 | 0.98 to 1.04 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.22 to 1.25 |
| SHMI risk score | 1.82 | 0.024 | < 0.001 | 1.77 to 1.87 |
| Emergency | 1.15 | 0.128 | 0.220 | 0.92 to 1.43 |
| Admissions per RN of > 125% of ward mean | 1.05 | 0.021 | 0.008 | 1.01 to 1.10 |
| Admissions per HCA of > 125% of ward mean | 1.03 | 0.019 | 0.091 | 0.99 to 1.07 |
| RN hours below ward mean (cumulative sum) | 1.03 | 0.016 | 0.046 | 1.00 to 1.06 |
| HCA hours below ward mean (cumulative sum) | 1.00 | 0.018 | 0.849 | 0.97 to 1.04 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.22 to 1.25 |
| SHMI risk score | 1.82 | 0.024 | < 0.001 | 1.77 to 1.87 |
| Emergency | 1.15 | 0.128 | 0.216 | 0.92 to 1.43 |
| Admissions per RN of > 125% of ward mean | 1.06 | 0.022 | 0.004 | 1.02 to 1.10 |
| Admissions per HCA of > 125% of ward mean | 1.02 | 0.020 | 0.265 | 0.98 to 1.06 |
| RN hours ± ward mean (cumulative sum) | 0.98 | 0.015 | 0.200 | 0.95 to 1.01 |
| RN hours ± ward mean squared | 1.00 | 0.003 | 0.621 | 0.99 to 1.01 |
| RN hours ± ward mean cubed | 1.00 | < 0.001 | 0.930 | 1.00 to 1.00 |
| HCA hours ± ward mean (cumulative sum) | 1.00 | 0.020 | 0.835 | 0.97 to 1.04 |
| HCA hours ± ward mean squared | 1.01 | 0.004 | 0.014 | 1.00 to 1.02 |
| HCA hours ± ward mean cubed | 1.00 | 0.001 | 0.061 | 1.00 to 1.00 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| Admissions per RN of > 125% of ward mean | 1.05 | 0.021 | 0.024 | 1.01 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.02 | 0.019 | 0.271 | 0.98 to 1.06 |
| HCA staffing below mean | 1.10 | 0.088 | 0.241 | 0.94 to 1.28 |
| RN staffing below mean | 1.17 | 0.086 | 0.032 | 1.01 to 1.35 |
| RN and HCA staffing below mean | 1.26 | 0.080 | < 0.001 | 1.12 to 1.43 |
| Staffing | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| ≥ 0.5 HPPD | ||||
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.26 |
| SHMI risk score | 1.82 | 0.025 | < 0.001 | 1.78 to 1.87 |
| Emergency | 1.08 | 0.122 | 0.475 | 0.87 to 1.35 |
| Admissions per RN of > 125% of ward mean | 1.03 | 0.023 | 0.124 | 0.99 to 1.08 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.854 | 0.96 to 1.05 |
| RN staffing below ward mean | 1.02 | 0.012 | 0.194 | 0.99 to 1.04 |
| HCA staffing below ward mean | 1.05 | 0.012 | < 0.001 | 1.02 to 1.07 |
| Days with ≥ 0.5 HPPD temporary RN staffing | 0.99 | 0.011 | 0.536 | 0.97 to 1.01 |
| Days with ≥ 0.5 HPPD temporary HCA staffing | 1.06 | 0.012 | < 0.001 | 1.03 to 1.08 |
| ≥ 1 HPPD | ||||
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.25 |
| SHMI risk score | 1.82 | 0.025 | < 0.001 | 1.78 to 1.87 |
| Emergency | 1.10 | 0.124 | 0.395 | 0.88 to 1.37 |
| Admissions per RN of > 125% of ward mean | 1.04 | 0.023 | 0.051 | 1.00 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.950 | 0.96 to 1.04 |
| RN staffing below ward mean | 1.03 | 0.012 | 0.018 | 1.00 to 1.05 |
| HCA staffing below ward mean | 1.05 | 0.013 | < 0.001 | 1.03 to 1.08 |
| Days with ≥ 1 HPPD temporary RN staffing | 1.03 | 0.018 | 0.149 | 0.99 to 1.06 |
| Days with ≥ 1 HPPD temporary HCA staffing | 1.02 | 0.012 | 0.051 | 1.00 to 1.05 |
| ≥ 1.5 HPPD | ||||
| NEWS on admission | 1.24 | 0.007 | < 0.001 | 1.23 to 1.25 |
| SHMI risk score | 1.82 | 0.025 | < 0.001 | 1.78 to 1.87 |
| Emergency | 1.10 | 0.124 | 0.390 | 0.88 to 1.37 |
| Admissions per RN of > 125% of ward mean | 1.04 | 0.023 | 0.055 | 1.00 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.988 | 0.96 to 1.04 |
| RN staffing below ward mean | 1.03 | 0.012 | 0.016 | 1.01 to 1.05 |
| HCA staffing below ward mean | 1.05 | 0.013 | < 0.001 | 1.03 to 1.08 |
| Days with ≥ 1.5 HPPD temporary RN staffing | 1.12 | 0.045 | 0.006 | 1.03 to 1.21 |
| Days with ≥ 1.5 HPPD temporary HCA staffing | 1.05 | 0.017 | 0.003 | 1.02 to 1.08 |
| HR | SE | p-value | 95% CI | |
|---|---|---|---|---|
| NEWS on admission | 1.23 | 0.006 | < 0.001 | 1.22 to 1.25 |
| SHMI risk score | 1.54 | 0.016 | < 0.001 | 1.51 to 1.57 |
| Emergency | 0.98 | 0.077 | 0.828 | 0.84 to 1.15 |
| Admissions per RN of > 125% of ward mean | 1.04 | 0.020 | 0.034 | 1.00 to 1.08 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.020 | 0.873 | 0.97 to 1.04 |
| RN hours ± ward mean (cumulative sum) | 0.98 | 0.007 | 0.001 | 0.96 to 0.99 |
| HCA hours ± ward mean (cumulative sum) | 1.01 | 0.008 | 0.367 | 0.99 to 1.02 |
| Coefficient | SE | p-value | 95% CI | |
|---|---|---|---|---|
| NEWS on admission | 0.037 | 0.002 | < 0.001 | 0.03 to 0.04 |
| SHMI risk score | 0.108 | 0.002 | < 0.001 | 0.11 to 0.11 |
| Elective (dummy) | –0.353 | 0.015 | < 0.001 | –0.38 to –0.32 |
| Admissions per RN of > 125% of ward mean (any) | 0.156 | 0.011 | < 0.001 | 0.14 to 0.18 |
| Admissions per HCA of > 125% of ward mean (any) | 0.148 | 0.011 | < 0.001 | 0.13 to 0.17 |
| RN hours ± ward mean (average) | –0.231 | 0.035 | < 0.001 | –0.30 to –0.16 |
| HCA hours ± ward mean (average) | 0.076 | 0.026 | 0.003 | 0.03 to 0.13 |
| Ward type | All missed observations | Missed observations in high-acuity patients (NEWS of ≥ 6) | ||||
|---|---|---|---|---|---|---|
| p-value | IRR | 95% CI | p-value | IRR | 95% CI | |
| Medical | ||||||
| Intercept | < 0.001 | 0.20 | 0.16 to 0.25 | < 0.001 | 0.46 | 0.39 to 0.55 |
| RN HPPD | < 0.001 | 0.94 | 0.93 to 0.95 | 0.356 | 0.99 | 0.96 to 1.01 |
| HCA HPPD | < 0.001 | 0.97 | 0.97 to 0.98 | 0.531 | 1.01 | 0.99 to 1.03 |
| Admissions per RN | < 0.001 | 1.01 | 1.01 to 1.02 | 0.806 | 1.00 | 0.98 to 1.01 |
| Proportion unwell | < 0.001 | 3.13 | 2.94 to 3.34 | 0.007 | 0.80 | 0.68 to 0.94 |
| RN × HCA | 0.015 | 0.99 | 0.99 to 1.00 | 0.040 | 0.98 | 0.97 to 1.00 |
| Surgical | ||||||
| (Intercept) | < 0.001 | 0.12 | 0.10 to 0.14 | < 0.001 | 0.33 | 0.30 to 0.37 |
| RN HPPD | < 0.001 | 0.98 | 0.98 to 0.99 | 0.082 | 0.97 | 0.94 to 1.00 |
| HCA HPPD | < 0.001 | 0.95 | 0.94 to 0.96 | 0.870 | 1.00 | 0.96 to 1.04 |
| Admissions per RN | 0.079 | 1.01 | 1.00 to 1.01 | 0.432 | 0.99 | 0.96 to 1.02 |
| Proportion unwell | < 0.001 | 4.32 | 4.02 to 4.64 | 0.051 | 0.76 | 0.58 to 1.00 |
| RN × HCA | < 0.001 | 1.01 | 1.01 to 1.01 | 0.375 | 0.99 | 0.97 to 1.01 |
| Older people | ||||||
| (Intercept) | < 0.001 | 0.17 | 0.16 to 0.19 | < 0.001 | 0.47 | 0.44 to 0.50 |
| RN HPPD | < 0.001 | 1.06 | 1.04 to 1.07 | 0.325 | 1.02 | 0.99 to 1.05 |
| HCA HPPD | < 0.001 | 0.91 | 0.90 to 0.92 | 0.002 | 0.96 | 0.94 to 0.99 |
| Admissions per RN | 0.023 | 1.02 | 1.00 to 1.04 | 0.234 | 1.03 | 0.98 to 1.07 |
| Proportion unwell | < 0.001 | 7.78 | 7.16 to 8.45 | 0.164 | 0.86 | 0.70 to 1.06 |
| RN × HCA | < 0.001 | 1.01 | 1.01 to 1.02 | 0.362 | 0.99 | 0.98 to 1.01 |
| Shift | All observations – lagged (previous shift staffing) | All observations | All observations – forward lagged (next shift staffing) | High-acuity observations – lagged (previous shift staffing) | High-acuity observations | High-acuity observations – forward lagged (next shift staffing) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p-value | IRR | p-value | IRR | p-value | IRR | p-value | IRR | p-value | IRR | p-value | IRR | |
| Late night (01.00–07.00) | ||||||||||||
| RN HPPD | 0.488 | 1.00 | 0.709 | 1.00 | < 0.001 | 1.01 | 0.563 | 1.00 | 0.145 | 0.99 | 0.063 | 1.01 |
| HCA HPPD | 0.001 | 0.99 | 0.612 | 1.00 | 0.257 | 1.00 | 0.183 | 1.01 | 0.173 | 1.01 | 0.090 | 1.02 |
| RN × HCA | 0.004 | 1.00 | < 0.001 | 1.01 | 0.028 | 1.00 | 0.573 | 1.00 | 0.737 | 1.00 | 0.054 | 0.99 |
| Early (07.00–13.00) | ||||||||||||
| RN HPPD | < 0.001 | 0.96 | < 0.001 | 0.98 | < 0.001 | 0.98 | 0.023 | 0.98 | 0.007 | 0.99 | 0.003 | 0.98 |
| HCA HPPD | < 0.001 | 0.98 | < 0.001 | 0.98 | < 0.001 | 0.98 | 0.545 | 1.00 | 0.013 | 1.02 | 0.037 | 1.02 |
| RN × HCA | 0.011 | 1.01 | < 0.001 | 1.01 | 0.119 | 1.00 | 0.149 | 0.99 | 0.692 | 1.00 | 0.509 | 1.00 |
| Late (13.00–19.00) | ||||||||||||
| RN HPPD | < 0.001 | 0.98 | 0.054 | 1.00 | < 0.001 | 0.96 | 0.211 | 0.99 | 0.184 | 0.99 | 0.102 | 0.99 |
| HCA HPPD | < 0.001 | 0.96 | < 0.001 | 0.95 | < 0.001 | 0.92 | 0.198 | 0.99 | 0.025 | 0.98 | 0.108 | 0.99 |
| RN × HCA | < 0.001 | 1.01 | < 0.001 | 1.01 | < 0.001 | 1.02 | 0.905 | 1.00 | 0.928 | 1.00 | 0.155 | 1.01 |
| Night (19.00–01.00) | ||||||||||||
| RN HPPD | 0.439 | 1.00 | 0.001 | 0.99 | 0.303 | 1.00 | 0.079 | 0.99 | 0.002 | 0.97 | 0.559 | 1.00 |
| HCA HPPD | < 0.001 | 0.97 | < 0.001 | 0.95 | < 0.001 | 0.96 | 0.231 | 0.99 | 0.956 | 1.00 | 0.386 | 1.01 |
| RN × HCA | < 0.001 | 1.01 | < 0.001 | 1.02 | < 0.001 | 1.01 | 0.381 | 1.00 | 0.238 | 1.00 | 0.668 | 1.00 |
| Variable | All missed observations | Missed observations in high-acuity patients (NEWS of ≥ 6) | ||||
|---|---|---|---|---|---|---|
| p-value | IRR | 95% CI | p-value | IRR | 95% CI | |
| Intercept | < 0.001 | 0.15 | 0.12 to 0.18 | < 0.001 | 0.39 | 0.36 to 0.43 |
| RN HPPD | < 0.001 | 0.88 | 0.86 to 0.90 | 0.506 | 0.98 | 0.91 to 1.05 |
| RN HPPD squared | < 0.001 | 1.02 | 1.01 to 1.02 | 0.935 | 1.00 | 0.99 to 1.01 |
| RN HPPD cubed | < 0.001 | 1.00 | 1.00 to 1.00 | 0.962 | 1.00 | 1.00 to 1.00 |
| HCA HPPD | < 0.001 | 0.89 | 0.87 to 0.91 | 0.001 | 1.12 | 1.05 to 1.20 |
| HCA HPPD squared | < 0.001 | 1.01 | 1.01 to 1.02 | 0.010 | 0.98 | 0.96 to 0.99 |
| HCA HPPD cubed | 0.002 | 1.00 | 1.00 to 1.00 | 0.185 | 1.00 | 1.00 to 1.00 |
| Admissions per RN | < 0.001 | 1.01 | 1.01 to 1.01 | 0.609 | 1.00 | 0.99 to 1.01 |
| Proportion unwell | < 0.001 | 4.83 | 4.67 to 4.99 | 0.838 | 1.01 | 0.93 to 1.09 |
| RN × HCA | < 0.001 | 1.01 | 1.01 to 1.01 | 0.086 | 1.00 | 0.99 to 1.00 |
| Variable | All observations | ||
|---|---|---|---|
| p-value | IRR | 95% CI | |
| CHPPD | < 0.001 | 0.86 | 0.84 to 0.87 |
| CHPPD squared | < 0.001 | 1.01 | 1.01 to 1.01 |
| CHPPD cubed | < 0.001 | 1.00 | 1.00 to 1.00 |
| Skill mix | 0.163 | 0.38 | 0.10 to 1.48 |
| Skill mix squared | 0.125 | 5.87 | 0.61 to 56.2 |
| Skill mix cubed | 0.147 | 0.41 | 0.12 to 1.37 |
| Admissions per nurse | < 0.001 | 1.01 | 1.01 to 1.01 |
| Proportion unwell | < 0.001 | 4.83 | 4.67 to 4.99 |
| Staff × skill mix | 0.494 | 0.99 | 0.97 to 1.01 |
| Variable | NEWS of ≥ 6 | NEWS of ≥ 7 | ||||
|---|---|---|---|---|---|---|
| p-value | IRR | 95% CI | p-value | IRR | 95% CI | |
| RN HPPD | 0.614 | 0.99 | 0.96 to 1.02 | 0.001 | 0.98 | 0.96 to 0.99 |
| HCA HPPD | 0.686 | 0.99 | 0.93 to 1.05 | 0.238 | 0.99 | 0.96 to 1.01 |
| Admissions per RN | 0.190 | 0.99 | 0.97 to 1.01 | 0.145 | 1.00 | 0.99 to 1.00 |
| Proportion unwell | < 0.001 | 4.29 | 3.67 to 5.02 | < 0.001 | 1.26 | 1.20 to 1.33 |
| RN × HCA | 0.802 | 1.00 | 0.99 to 1.01 | 0.563 | 1.00 | 1.00 to 1.01 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.12 | 0.007 | < 0.001 | 1.10 to 1.13 |
| SHMI risk score | 1.74 | 0.024 | < 0.001 | 1.70 to 1.79 |
| Emergency | 1.12 | 0.127 | 0.333 | 0.89 to 1.39 |
| High proportion of observations missed (cumulative sum) | 1.34 | 0.023 | < 0.001 | 1.30 to 1.39 |
| High-acuity observations due? | 2.91 | 0.125 | < 0.001 | 2.68 to 3.17 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.12 | 0.007 | < 0.001 | 1.10 to 1.13 |
| SHMI risk score | 1.75 | 0.024 | < 0.001 | 1.70 to 1.79 |
| Emergency | 1.10 | 0.125 | 0.403 | 0.88 to 1.38 |
| Admissions per RN of > 125% of ward mean | 1.04 | 0.023 | 0.067 | 1.00 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.00 | 0.022 | 0.834 | 0.95 to 1.04 |
| RN staffing below ward mean | 1.01 | 0.012 | 0.535 | 0.98 to 1.03 |
| HCA staffing below ward mean | 1.02 | 0.012 | 0.038 | 1.00 to 1.05 |
| High proportion of observations missed (cumulative sum) | 1.34 | 0.023 | < 0.001 | 1.29 to 1.38 |
| High-acuity observations due? | 2.90 | 0.124 | < 0.001 | 2.66 to 3.15 |
| Variable | HR | SE | p-value | 95% CI |
|---|---|---|---|---|
| NEWS on admission | 1.12 | 0.007 | < 0.001 | 1.10 to 1.13 |
| SHMI risk score | 1.74 | 0.024 | < 0.001 | 1.70 to 1.79 |
| Emergency | 1.12 | 0.127 | 0.336 | 0.89 to 1.39 |
| Admissions per RN of > 125% of ward mean | 1.05 | 0.022 | 0.022 | 1.01 to 1.09 |
| Admissions per HCA of > 125% of ward mean | 1.01 | 0.020 | 0.778 | 0.97 to 1.05 |
| RN hours ± ward mean (cumulative sum) | 0.97 | 0.013 | 0.009 | 0.94 to 0.99 |
| HCA hours ± ward mean (cumulative sum) | 1.02 | 0.015 | 0.232 | 0.99 to 1.05 |
| High proportion of observations missed (cumulative sum) | 1.34 | 0.023 | < 0.001 | 1.30 to 1.39 |
| High-acuity observations due? | 2.91 | 0.125 | < 0.001 | 2.67 to 3.16 |
Appendix 6 Patient and public stakeholder consultations
We undertook a series of consultations with public, patient and clinical experts/stakeholders (including health services managers and ward-based nurses) to identify issues that should be considered when determining scenarios for economic models.
These included:
-
determining an acceptable level of vital signs observations compliance (completing a full set of observations in time)
-
acceptable ranges of skill mix – assuming that the results demonstrated some potential for substitution between HCA and RN.
The work was done in stages so that different groups were approached separately, thus providing the most conducive environment to engage in conversation and share views relevant to each individual group. We began with consultations with expert and professional groups to elucidate a concrete set of preliminary questions and scenarios that could be presented to other groups. Our approach, co-designed with our patient and public involvement representative/lay co-researcher (ADI), was intended to make the key issues to be discussed tangible for a more lay audience including professional stakeholders, such as staff nurses, who might not identify themselves as ‘experts’ in the specific topics. Therefore, we began with consultations with health-care professionals through an online questionnaire, and with members of the study advisory group in order to identify preliminary indicators.
This led to the development of some preliminary propositions about skill mix and observation compliance that were used to structure future consultations.
In these consultations, each group was presented with an outline of the project and related research. Questions focused on:
-
current recommended skill mix and specifically whether the Royal College of Nursing’s recommendation of 65% RN should be regarded as an absolute minimum or if higher/lower thresholds should be considered
-
the acceptability of a target for compliance levels, using 90% as a starting point to stimulate discussion.
The ensuing responses were used to ‘sense check’ the propositions and to determine whether or not these scenarios made sense to participants, and to capture alternative propositions that we might consider. The consultations included:
-
face-to-face engagement with patient and public representative groups
-
Experts by Experience patient groups – co-ordinated directly with members
-
Healthwatch Southampton – co-ordinated by a health community development worker.
-
-
online consultation (link distributed at engagement events, in patient groups and over social media)
-
seventy-seven people provided partial responses to the questionnaire and 14 provided complete responses
-
-
face-to-face engagement with senior nursing and management forums
-
Wessex Directors of Nursing Network Meeting, December 2015 (directors of nursing/deputies from all regional NHS organisations – approximately 30 attendees)
-
Nursing and Midwifery Advisory Committee in Portsmouth Hospital NHS Trust (ward managers and senior nurses – approximately 20 attendees)
-
Deteriorating Patient Group at Portsmouth Hospital (approximately 15 attendees).
-
-
hosting a Twitter chat (@wenurses)
-
Twitter chat – 60 participants.
-
The groups consulted agreed on some points and differed on others. Senior nursing and management forums agreed that a skill mix level of < 65% RNs was not desirable. However, they also indicated that on some wards it was not possible to manage those levels, and felt that a skill mix of < 65% RN and < 35% HCAs may be necessary because of recruitment difficulties. They even considered that a 50 : 50 skill mix may be necessary. Some respondents to the online questionnaire agreed with the 65% RN: 35% HCA model suggested by the Royal College of Nursing; however, others did not agree, providing reasons such as ‘it depends on the type of ward, level of RN, patient acuity and patient dependency’. Respondents who suggested a lower skill mix offered a 60 : 40 or 50 : 50 skill mix. Patient groups agreed on some of the aspects raised by management groups on the skill mix question, indicating that ‘wards differ so much in their needs. A workforce more weighted towards fundamental care provision is obviously more essential on a care of older people ward than ITU’. Overall, the groups seemed to agree on issues about staffing: current guidelines are broadly relevant, but different settings may require higher or lower thresholds.
With regard to compliance of observations, management and patient groups agreed that the significance of compliance varies by patient, but there was a strong initial reaction that 100% compliance should be the target. However, it was noted that the local hospital audited against an 80% compliance threshold. Under further discussion, more uncertainty and recognition of exceptions emerged. Patient groups echoed these comments, indicating that ‘100% compliance is needed, because you can’t be sure a patient will not deteriorate; we do not accept 90% compliance with drugs for example; there is evidence, and it’s deemed to be needed so needs to be done’, while expressing that, with a target of 100%, there is a ‘risk of hitting the target, but missing the point’. A view emerged that a lower level of compliance might be acceptable for patients who were ‘ready for discharge’ or ‘not at high-risk stage of illness’. It was acknowledged that staff might legitimately ‘use professional judgement for deteriorating patients’, while at the same time it was generally acknowledged that higher thresholds of acceptable compliance should apply for ‘patients going through critical stages of illness’.
Feedback received from management groups included questions such as ‘what is the scientific basis for interval of observations?’ and ‘what does the data say regarding the associations between staffing, observations and patient mortality?’, suggesting that acceptable compliance may, to some extent, depend on the scientific credibility of any protocol that determines observation frequency.
List of abbreviations
- AIC
- Akaike information criterion
- BIC
- Bayesian information criterion
- CCI
- Charlson Comorbity Index
- CHPPD
- care hours per patient day
- CI
- confidence interval
- HCA
- health-care assistant
- HPPD
- hours per patient day
- HR
- hazard ratio
- HSMR
- hospital standardised mortality ratio
- ICU
- intensive care unit
- IRR
- incidence rate ratio
- MUST
- Malnutrition Universal Screening Tool
- NEWS
- National Early Warning Score
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- PAS
- patient administration system
- QALY
- quality-adjusted life-year
- RN
- registered nurse
- SD
- standard deviation
- SHMI
- Summary Hospital-level Mortality Indicator

