Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/177/13. The contractual start date was in September 2014. The final report began editorial review in December 2017 and was accepted for publication in July 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Tessa Crilly is a member of the National Institute for Health Research Journals Library Editorial Group. Iestyn Williams is a member of the Health Services and Delivery Research Prioritisation Commissioning Panel.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Davidson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction and context
The evolution and diversification of community hospitals in England has not been matched by research on such institutions. There is no consistent definition and little is known of the numbers of community hospitals, their distribution and the services and facilities they offer. Although two parallel National Institute for Health Research (NIHR)-funded projects have explored the nature and scope of service provision models of community hospitals and international comparisons1 and the efficiency and effectiveness of community hospitals,2 the primary aim of this study was to provide a comprehensive analysis of their profile, characteristics, patient experience and community value.
In this introductory chapter, we briefly describe the origins and development of community hospitals in England, before setting out the policy context and providing a brief summary of previous research about the role and function of community hospitals, patient experience and their community engagement and value. A formal review of the evidence was funded as part of the NIHR 12/177 call on research into community hospitals (see Pitchforth et al. 1) and so was beyond the remit of this study.
Community hospital development
Community hospitals [previously known as ‘cottage hospitals’ or ‘general practitioner (GP) hospitals’] have been part of the landscape for health care in England since 1859, evolving to offer local health-care services and accessible facilities to support patients and their families and enable patients to return home (and to work) as soon as possible. 3 The cottage hospital model was widely emulated: within a period of 30 years, more than 240 were established. 4 By 1895, only three counties in England had not developed one.
Loudon’s research5 illustrated that all cottage hospitals opened with inpatient beds for the sick and injured and a room for operating. However, over the decades, their services and facilities evolved in parallel with medical and nursing developments. The visionary report by Lord Dawson in 19216 saw such hospitals as part of a wider move to population health, playing a role in integrated service hierarchies by providing facilities in which GPs and interdisciplinary teams could work together to offer preventative and curative medicine.
In 1948, cottage hospitals were transferred to the NHS. Traditions of voluntary support and local involvement were maintained with the formation of local hospital Leagues of Friends, with a national association being established in 1949 [URL: www.attend.org.uk/about-us/national-association-of-leagues-of-friends (accessed 8 October 2018)]. There was little change in the number of cottage hospitals between 1948 and 1960, and they remained largely outside government attention.
Government policy
In 1962, the Hospital Plan7 heralded the centralisation of services, threatening many cottage/GP hospitals with closure. In practice, the plan’s proposed closures were pursued only partially and more positive alternative futures were envisaged for cottage hospitals. Through the work of Rue and Bennett,8,9 the concept of the ‘community hospital’ emerged, signifying co-location of GP practices and hospital facilities and facilitating integration of GPs and consultants. 10 National policy identified the need to strengthen the role of the family doctor and community hospital services, recognising their role, particularly in post-acute care, but also in integrated health provision. 11
Over the following 20 years, community hospitals barely featured in central policy or local plans12 until the government’s strategy document Opportunities in Intermediate Care,13 in which the role of community hospitals was conceptualised as providing either ‘substitutional’ care as an alternative to a general hospital or ‘complex care in the community’. Six years later, Keeping the NHS Local: A New Direction of Travel14 emphasised that community hospitals could:
provide a more integrated range of modern services at the heart of the local community.
Keeping the NHS local: A New Direction of Travel,14 p. 4.
In 2006, Our Health, Our Care, Our Say15 gave further impetus to the idea, calling for a shift of resources from secondary care to the community in order to prevent unnecessary acute admissions. The potential for outpatient clinics to take place in community settings and better use of community hospital services and intermediate care facilitating admission prevention were key themes in this shift of services and financial resources. In 2008, there was further policy encouragement16 for primary and community services to play a vital role in meeting the policy aim of care closer to home.
However, there was no explicit national strategy for community hospitals in England. This contrasted with the prioritisation of such facilities in Scotland. 17 In England, devolved responsibility as part of the NHS Five Year Forward View18 and sustainability and transformation plans (STPs) within 44 health and social care ‘footprints’ have led to proposals for a fundamental reconfiguration of services. The configurations being proposed, and, in some areas, being implemented, are a combination of:
-
community hospitals with beds – these are either existing community hospitals or community wards created in general hospitals, which are expected to serve an area wider than their immediate local population
-
community hubs – community hospitals without beds, being redeveloped with a role wider than health and social care to incorporate health promotion, well-being and welfare and involving the voluntary as well as the statutory sectors.
In some locations, reconfiguration has led to the threatened closure of community hospitals and significant planned reductions in the number of community hospital beds. Elsewhere, there has been an investment in community hospitals. Neither investment in nor closure of community hospitals has been informed by authoritative guidance. 19
Given their history, strong local support from GPs and communities as well as a continued policy focus on care closer to home, important questions are being asked about the role, function and value of community hospitals. In order to inform such discussions, it is important to define, map and profile the characteristics of community hospitals in England, examine patient experience and explore their support from, and value to, local communities.
Research on community hospitals
The effect of this history of evolution and diversification, exacerbated by the twists and turns of English health-care policy, has been to make classification, and, therefore, assessment, of the role and value of community hospitals far from straightforward. We lack a universally accepted definition of a community hospital. Although Ritchie and Robinson20 point to numerous descriptive studies indicating a distinct and important role within health-care delivery, they nevertheless conclude that definitive evidence is lacking.
The most positive assessments, such as those by Seamark et al. ,21 highlight characteristics such as links with local communities, GP involvement, multidisciplinary rehabilitation services and diagnostic facilities, which suggest that community hospitals should have a significant role in the evolution of intermediate care. This notion is echoed by Heaney et al. 22
Internationally, a similar picture has been observed, for example by Pitchforth et al. 1 They echo British work in concluding that community hospitals defy ‘the formulation of a single, overarching definition’ (p. 47) (contains information licensed under the Non-Commercial Government Licence v2.0).
Overall, although these studies have identified several features that seem common to many community hospitals, an agreed definition remains elusive. Nevertheless, they provide a starting point for a ‘working definition’:
-
A hospital with < 100 beds serving a local population of up to 100,000, providing direct access to GPs and local community staff.
-
Typically GP-led or nurse-led with medical support from local GPs.
-
Services provided are likely to include inpatient care for older people, rehabilitation and maternity services, outpatient clinics and day care as well as minor injury and illness units, diagnostics and day surgery. The hospital may also be a base for the provision of outreach services by multidisciplinary teams (MDT).
-
Will not have a 24-hour accident and emergency (A&E) department nor provide complex surgery. In addition, a specialist hospital (e.g. a children’s hospital, a hospice or a specialist mental health or learning disability hospital) would not be classified as a community hospital.
Recognising these gaps, the aim of our first work package was to undertake a national mapping study to identify, locate and yield a set of characteristics to develop a definition and typology and, thereby, address the question: what is a community hospital?
Research on patient experience of community hospitals
There is a notable lack of systematic and in-depth research into patient experience in community hospitals. There are few high-quality and/or multicentre studies, with most being adjunct to research that is primarily focused on aspects of care delivery and largely based on experiences of inpatient services, with a tendency to rely on survey methods focusing on satisfaction rather than on more qualitative approaches to explore patient experience.
The literature contains three broad themes relating to patients’ experiences of community hospitals: (1) environment and facilities, (2) delivery of care and (3) staff.
Environment and facilities
Many previous studies of community hospitals focused on the functional aspects of care, asking patients to give feedback on, for example, access to services, the quality and range of facilities and equipment, the environment and atmosphere, and levels of cleanliness.
Patients in these studies valued a close proximity to family and friends when using community hospitals, as well as the opportunity to interact with patients from the same geographical location,23–26 the homely and friendly atmosphere,24–26 the orientation to older people,27 the level of cleanliness,24,25,28 the availability of single-room accommodation,23,24,29 and the quality, choice and presentation of food. 23,24,29,30 However, some patients felt that community hospitals could be noisy environments23,26 and others reported long periods of boredom. 23,25,31 Few studies appeared to go on to explore how these environmental factors affected patients’ experiences of care.
Delivery of care
Several studies also focus on the technical aspects of care. Community hospital inpatients were often satisfied with their care, comparing this favourably with experiences in acute care,24,32 and valuing greater continuity of care,24,25 information sharing23,26,33,34 and the potential for longer lengths of stay. 26,29,31,35 However, rehabilitation and ongoing needs were reported as not always being met on discharge. 31
Staff
A subset of these studies also focus on the more relational aspects of care. Community hospital staff were often perceived more positively than those at district general hospitals (DGHs); they were experienced as being kind, caring, friendly, knowledgeable and committed to seeing people as individuals. 23–26,29,32 However, at times, patients lacked confidence in the technical skills of some staff,25 preferring to go to an acute hospital when requiring more complex medical expertise. 26
Notwithstanding these insights, the evidence base remains underdeveloped and focuses primarily on the functional and technical aspects of care. Bridges et al. 35 argue that patients’ and relatives’ narratives rarely focus on the functional or technical aspects of care. Instead, they often relate to the more relational and interpersonal aspects of their experience. Similarly, our previous research into older peoples’ experience of moving across service boundaries36 found that, although health and social care services often focus on the physical aspects of transition (e.g. relocating from one setting to another), older people tended to talk about transition in terms of the psychological (e.g. changes in their identity or sense of self) and social (e.g. changes in their relationships with partners, family and friends) impacts.
These insights from, and gaps within, the existing research, combined with a concern for what matters to patients and how that is understood and represented, shaped the aim and methodological approach of work package 2, which addresses the question: what are patients’ experiences of community hospitals?
Research on community engagement and value
Community hospitals are often known to, and are valued by, their communities37 and can play an important part in responding to the health and social care needs of local (often rural) populations. It has been suggested that support for, and satisfaction with, community hospitals by the public has been considerable,38 and this has been echoed by the GP population in such areas. 39,40 However, Heaney et al. 22 identify a striking lack of research into the wider role that community hospitals may play in the communities in which they are located. We suggest that there is a similar dearth of research on the role that communities play in supporting community hospitals.
Forms and levels of voluntary and community support
A key gap in the literature is empirical analysis of voluntary and community support for community hospitals in England. Hospital Leagues of Friends (the main conduit of such support) have been the subject of only one published UK academic study. 41 Existing national survey evidence does not allow for the identification of health-related voluntary activity in anything but the most general terms. 42
Broader research on engagement with other health settings gives an indication of the significance of voluntary support in the field. Naylor et al. 42 estimate that approximately 2.9 million people regularly volunteer for the health sector as a whole in England. The study by Galea et al. 43 of NHS acute trusts in England found that, on average, they involve 471 volunteers, making a total of 78,000 people who together contribute a total of 13 million hours per year. Volunteers undertake a considerable range of roles – as many as 100 – within NHS hospitals. 44 Naylor et al. 42 note that volunteers are increasingly involved in both strategic roles and roles that involve direct patient contact.
Previous studies of voluntary income for the NHS or other specific subsectors of health care45 have focused on relatively large organisations or have used data at the level of District Health Authorities, meaning that levels of support for individual institutions cannot be identified. 46
Engagement patterns and variations
Evidence on specific patterns of engagement within community hospitals is very limited. Historical evidence of voluntary income for the pre-NHS period hospitals, however, suggests that considerable variations may well persist. 47,48 More generally, national surveys of volunteering show that rates and levels of volunteering differ by socioeconomic status, employment status, age, strength of religious affiliation, ethnicity, disability and region. 49 Mohan and Bulloch50 report strong social and geographical gradients in voluntary activity and identify a ‘civic core’ delivering the bulk of voluntary effort. Prosperous, well-educated, middle-aged population groups dominate the civic core. 51 These studies suggest that voluntary support for community hospitals might be expected to vary between and within communities. Such national samples, however, cannot provide detail on voluntarism in individual types of organisation (such as community hospitals) and on the nature of voluntary activities within them.
The outcomes and impact of voluntary support
Describing different forms of voluntary support or counting the numbers of volunteers or the levels of voluntary income raised will give a measure of activity, but not of difference made. It is also important to consider the outcomes of such activities, such as contribution to patient experience and/or the quality of services in the hospital. This moves us to a level of considering and assessing impact and value. Direct or intended outcomes, for example, may include enhanced patient experience. Indirect, or unintended, outcomes include whether or not community engagement has wider spillover for the community in the form of raised levels of social capital, for example (elsewhere we refer to this as latent value). Unfortunately, capturing outcomes, impact or value is by no means simple. Although some elements lend themselves to quantification (e.g. funds raised, numbers of volunteers recruited), others are harder to identify and rely on self-reports by stakeholders, who may not be without their own interests and biases.
A small number of studies have considered the outcomes of certain forms of community engagement for hospitals and for the wider health-care system. There have, for example, been some attempts to measure the financial value of volunteering to individual hospitals, although with considerable limitations. 52,53 The qualitative research of Naylor et al. 42 with volunteers, patients, commissioners and service providers, and the Mundle et al. 54 review of literature on volunteering in health and social care both found that volunteers have a positive impact on health and social care systems in a number of ways. Identified impacts included improving the experience of care and support, strengthening the relationships between services and community, improving public health and supporting integrated care. The findings of another study, however, somewhat contradicted this: Milton et al. 55 found no existing evidence of positive impact on population health or quality of health services and failed to identify any studies that had attempted to determine the impact of community engagement on wider health outcomes.
There is even less evidence of the impact of such activities in community hospitals (or health-care services more generally) on the wider community. Indeed, there is very little evidence of the outcomes of volunteering on communities more generally, beyond general suggestions that volunteering contributes to community-level social capital development, which, in turn, contributes to community vitality, sustainability and resilience. 56 None of these focus specifically on the outcomes and impact of voluntary support in/through community hospitals.
Finally, distributional effects require attention. As noted above, underlying theories of voluntary action predict that its distribution (whether expressed in terms of funding or volunteering) will reflect variations between communities in resources, the availability of leadership and the idiosyncratic preferences of donors, rather than a needs-based allocation of resources. 57,58 How these processes work out is a contingent matter. Voluntary effort and charitable giving are known to be capricious and unpredictable. Salamon59 articulates four weaknesses: (1) philanthropic insufficiency (and variability), (2) paternalism, (3) amateurism and (4) parochialism. As levels of forms of voluntary action in community hospitals are likely to vary, so too are its outcomes.
The social value of community hospitals
Although it is often assumed that community hospitals are important to their local communities, the specifics of this relationship are under-researched. There have been many assertions recently about the concept of ‘social value’, particularly in relation to public service reforms and following the Public Services (Social Value) Act 2012,60 which enjoined commissioners of public services to take account of ‘economic, social and environmental wellbeing’ when placing public service contracts. With an increasing emphasis on outcomes-based commissioning, a consideration for the social value of a service offered the potential to move beyond purely financial considerations. As Dayson61 notes, however, ‘what constitutes social value and how to measure it is contested’. Citing Phills et al. ,62 Dayson goes on to suggest that ‘social value can be described as the benefits created for society through efforts to address social needs and problems’; these benefits, or values, may be economic, social or environmental and may be experienced by certain individuals, groups of individuals or society as a whole. 63 Social value is not exclusively associated with a particular organisational form, but there has been a strong association with voluntary organisations through the suggestion that the voluntarism and pro-social motivations for behaviour within such organisations add value to their activities.
There is little existing evidence on the social value of community hospitals to the communities in which they are based. More generally, however, wider literature points to the significance of hospitals and other institutions to communities, and rural communities in particular, as a source of collective identity and in contributing to a sense of place. 57–59,64 Research from New Zealand65 found small hospitals to be a source of civic pride and security and a symbol of legitimacy. Jones66 proposes Giddens’s67 concept of ‘ontological security’ as a way of understanding the ‘deep sense of reassurance’ that hospitals contribute to the communities in which they exist.
Developing these ideas further, Prior et al. 68 presented a typology (subsequently further developed by Farmer et al. 64) of the ‘added-value’ contributions of health services to remote rural communities at institutional and individual level, incorporating economic, social and human capital.
History provides a guide as to why such community attachment is important. In the pre-NHS era, although competition between doctors in a crowded medical marketplace also drove innovation, many hospital foundations were originally motivated by community needs, and the memorialisation of those fallen in war was also significant. Thus, symbolic value was inbuilt from the outset. Nationalisation did not quell the fires of attachment, with many Leagues of Friends established within a few years of the establishment of the NHS in 1948. The flames of community resistance were fanned by proposals for centralisation, as described by Mohan’s69 analysis of the 1962 Hospital Plan for England and Wales and the associated resistance to closures; it is hardly surprising that when hospitals had been established largely by local voluntary effort, proposals to remove them by the state would be fiercely resisted.
Broader social changes may plausibly be said to be associated with attachment to local hospitals: as the fabric of communities thins out (e.g. through closures of major employers) and as community ties are weakened (e.g. by longer commuting patterns) then mobilisation for remaining institutions becomes more important; international studies confirm this, particularly within the context of hospital closures. 70
In response to gaps in the knowledge of the role that voluntary and community action plays in supporting community hospitals, and that community hospitals play in their local communities, the aim of work package 3 was to undertake robust and systematic quantitative and qualitative research to address the research question: what does the community do for its community hospital, and what does the community hospital do for its community?
Summary
Community hospitals have been a part of the health-care landscape in England since the mid-nineteenth century. Over time, they have evolved into a diverse set of institutions, which some have suggested defy a single overarching definition. Although community hospitals are generally recognised as playing an important role in our health-care system, particularly through the provision of intermediate care, the evidence base to support their development is relatively weak. The lack of a universally accepted definition makes any measurement and assessment difficult; to date, we know little about their profile and characteristics, for example. Although existing evidence generally suggests positive patient experience, there is a tendency for this to rely on small-scale or functionally focused studies. Despite historic indications of strong levels of community support, there is very little evidence of how communities support community hospitals today and what value community hospitals represent to these communities. This study sets out to address these gaps in evidence by exploring the profile, characteristics, patient (and carer) experience, community engagement and value of community hospitals.
Having introduced the study and framed it within the existing literature, we move now to Chapter 2, which sets out the aims, objectives and research questions in more detail, followed by a full discussion of the approaches adopted in addressing them. In Chapter 3, the findings from the national mapping exercise locating, profiling and defining community hospitals are presented. In Chapter 4, we revisit our emerging definition in the light of qualitative findings from our nine case studies. Chapter 5 sets out the findings relating to patient and carer experiences, and Chapters 6 and 7 explore community engagement and value, respectively. Finally, Chapter 8 distils the findings from across the different research elements and relates them back to the existing literature to provide a new understanding of the profile, patient experience, community engagement and value of community hospitals.
Chapter 2 Research objectives, questions and methodology
In the light of the unfolding policy context and gaps within the existing literature outlined in Chapter 1, and informed by conversations with key stakeholders (see Patient and public involvement), this study aimed to provide a comprehensive analysis of the profile, characteristics, patient and carer experience and community engagement and value of community hospitals in contrasting local contexts. The specific objectives were to:
-
construct a national database and develop a typology of community hospitals
-
explore and understand the nature and extent of patients’ and carers’ experiences of community hospital care and services
-
investigate the value of the interdependent relationship between community hospitals and their communities through in-depth case studies of community value (qualitative study) and analysis of Charity Commission data (quantitative study).
In meeting these aims and objectives, the study addressed three overarching research questions (each with an associated set of more specific subquestions as summarised in Table 1):
-
What is a community hospital?
In addressing this question, we drew on existing definitions and conceptualisations of ‘community hospitals’ as outlined in Chapter 1, Research on community hospitals. Although our emphasis here was primarily empirical and descriptive, we were nevertheless guided by, and sought to contribute to, theoretical debates on definitions of community hospitals and their place within wider health and care systems, drawing on concepts of rural health care, chronic disease and complex care burden, integrated care and clinical leadership.
-
What are patients’ (and carers’) experiences of community hospitals?
This element of the study was designed to contribute to the conceptualisation of the distinctive elements of community hospitals as understood through the ‘lived experiences’ of patients, rather than just satisfaction ratings. Here, we were influenced by prior analysis of the functional, technical and relational components of patient experience (e.g. environment and facilities, delivery of care, staff) alongside a more theoretical interest in the interpersonal, psychological and social dimensions of patient experience.
Very early on in our study, through conversations with patient and public involvement (PPI) stakeholders, we recognised the importance of exploring and understanding the experience not only of patients but also of family carers, and hence we extended our initial question to include both patients’ and carers’ experiences.
-
What does the community do for its community hospital, and what does the community hospital do for its community?
In addressing this question, we drew on notions of voluntarism and participation and brought together thinking from the separate bodies of literature on volunteering, philanthropy and co-production. This led us to question not just the level of voluntary support for community hospitals but also the different forms it took, how this varies between and within communities, how it is encouraged, organised and managed, and what difference it makes (outcomes). We also drew on notions of social value, including existing typologies, that encouraged us to question different forms of value (e.g. economic, social, human, symbolic) and different stakeholder groups (e.g. staff, patients, communities).
| Objective (work package) | Research question | Subquestions | Research phase | Data collection |
|---|---|---|---|---|
| 1. To construct a national database and develop a typology of community hospitals | What is a community hospital? |
|
National mapping |
|
| 2. To explore and understand the nature and extent of patients’ experiences of community hospital care and services | What are patients’ and carers’ experiences of community hospitals? |
|
Case studies |
|
| 3. To investigate the value of the interdependent relationship between hospitals and their communities | What does the community do for its hospital and what does the community hospital do for its community? |
|
Charity Commission data analysis |
|
|
Case studies |
|
Given the diversity of the questions, we do not set out to provide an over-riding hypothesis or unified theoretical framework for the study as a whole. Instead, these concepts, frameworks and debates served as ‘sensitising categories’, shaping our approach to study design as well as data collection and analysis. 71 We return to these in Chapter 8 and augment them with new concepts that emerged from our analysis.
In addressing these diverse questions, we adopted a multimethod approach with a convergent design. Quantitative methods were employed to provide breadth of understanding relating to the questions concerning ‘what’, ‘where’ and ‘how much’, whereas qualitative methods provided depth of understanding, particularly in relation to questions of ‘how’, ‘why’ and ‘to what effect’.
The research was conducted in three distinct (although temporally overlapping) phases, each with a number of different associated elements and research methods: (1) mapping (database construction and analysis through data set reconciliation and verification), (2) qualitative case studies (semistructured interviews, discovery interviews, focus groups) and (3) quantitative analysis of charity commission data. Table 1 summarises the study objectives, questions and research methods. Each of the three phases of research are discussed in turn through the following sections of this chapter, before the final sections discuss data integration, PPI and ethics.
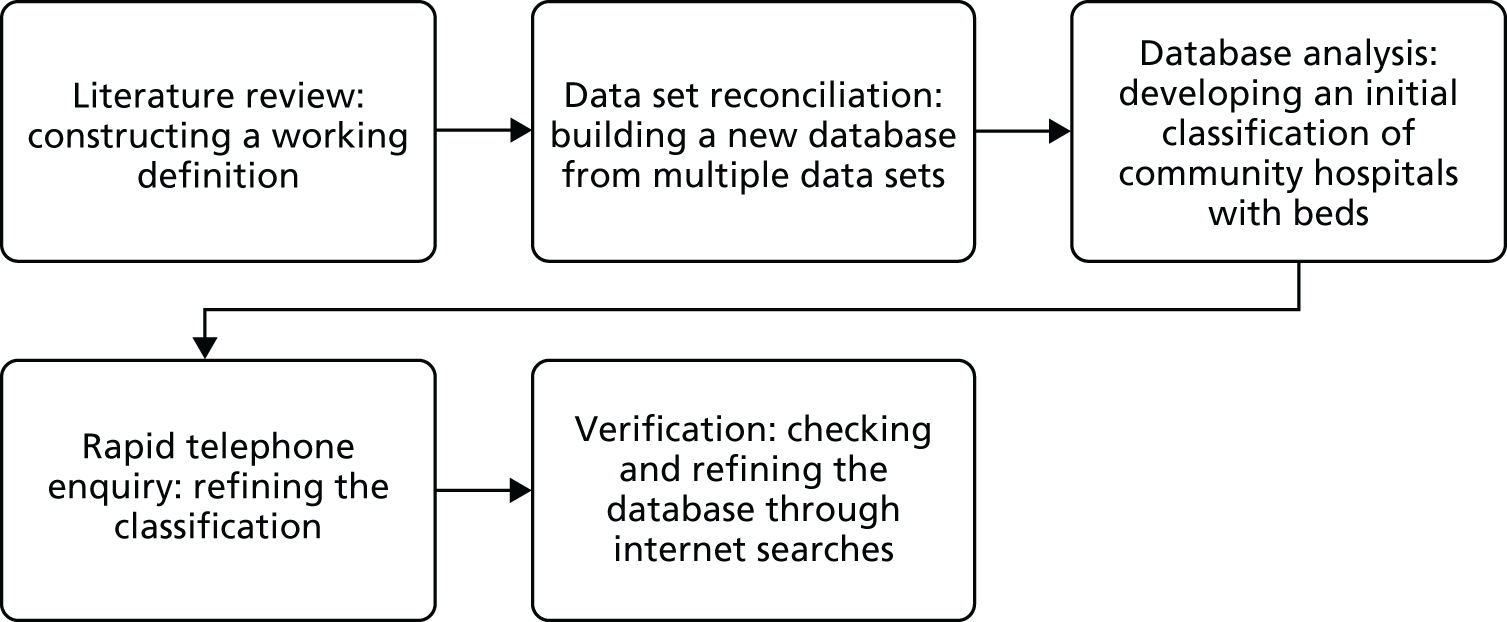
Phase 1: mapping and profiling community hospitals
Phase 1 of the research involved a national mapping exercise to address the first study question ‘what is a community hospital?’. It aimed to map the number and location of all hospitals in England to then provide a profile and definition of community hospitals. A database of characteristics would enable the profiling of community hospitals, inform a typology and support a sampling strategy for subsequent case studies. Data were collected from all four UK countries but, in accordance with the brief of the study, this report focuses on England. Reference is made to Scotland’s data as they were important in developing the methodology. The structure of the mapping comprised five elements:
-
literature review – constructing a working definition: (see Chapter 1)
-
data set reconciliation – building a new database from multiple data sets
-
database analysis – developing an initial classification of community hospitals with beds
-
rapid telephone enquiry – refining the classification
-
verification – checking and refining the database through internet searches.
The flow of activities is depicted in Figure 1.
FIGURE 1.
Structure of the national mapping exercise.
Literature review: constructing a working definition
We developed a working definition of a community hospital as drawn from the literature (and as outlined in Chapter 1):
-
A hospital with < 100 beds serving a local population of up to 100,000 and providing direct access to GPs and local community staff.
-
Typically GP led, or nurse led with medical support from local GPs.
-
Services provided are likely to include inpatient care for older people, rehabilitation and maternity services, outpatient clinics and day care as well as minor injury and illness units, diagnostics and day surgery. The hospital may also be a base for the provision of outreach services by MDTs.
-
Will not have a 24-hour A&E nor provide complex surgery. In addition, a specialist hospital (e.g. a children’s hospital, a hospice or a specialist mental health or learning disability hospital) would not be classified as a community hospital.
The initial enquiry was framed around a ‘classic’ community hospital. The term was drawn directly from the Community Hospital Association 2008 classification,72 describing classic community hospitals as ‘local community hospitals with inpatient facilities’ (i.e. with beds) and as distinct from community care resource centres (without beds), community care homes (integrated health and social care campus) or rehabilitation units. Although the term ‘classic’ was initially helpful in setting the boundaries of the study, it presented ongoing problems, such as whether it described all community hospitals with beds or a subset within that. Throughout the study, therefore, we have adopted the term ‘community hospital’ and omitted the adjective ‘classic’. Our focus, however, has remained on community hospitals with beds.
Data reconciliation: building a new database from multiple data sets
There was no up-to-date comprehensive database of community hospitals in England. The NHS Benchmarking Network [URL: www.nhsbenchmarking.nhs.uk (accessed 8 October 2018)] membership database was not comprehensive and could not be used to populate our hospital-level database because the data were anonymised. For this reason, one of our first tasks was to compile a new database, by bringing together existing health-care data sets, each of which provided different fields of information needed to test our working definition and to map and profile community hospitals.
Two types of data sets were collected. Centrally available data sets formed the starting point for the mapping study, providing codified data (see Appendix 1). As none of these centrally available data sets provided a comprehensive picture, it was necessary to supplement them through extensive internet searching and by talking to people in the field, as well as drawing on the expertise of research team members.
The base year for major data sets was 2012/13. Data were difficult to access, not comprehensive and spread across a greater number of sources. Four data sets were used:
-
Community Hospital Association databases of community hospitals (one from 2008 and another from 2013)
-
Patient-Led Assessments of the Care Environment (PLACE) 2013 [replacing the former Patient Environment Action Team programme]
-
Estates database – Estates Returns Information Collection (ERIC) 2012
-
NHS Digital activity by site of treatment 2012/13.
Barriers to obtaining site and activity data included (1) specific difficulties in the period 2012/13 when primary care trusts (PCTs) were being disbanded and clinical commissioning groups (CCGs) were being established (with effect from 31 March 2013) and (2) processes and caution in NHS Digital associated with releasing patient-sensitive data (even though we had not requested patient-based data). Quality problems were associated with the ‘location of treatment’ code, which was central to our enquiry identifying community hospitals but did not appear to be well used in England, leading to examples of missing data and inconsistent labels (described under reconciliation and duplication). The code also lacked stability as it changed with each new NHS reconfiguration in England.
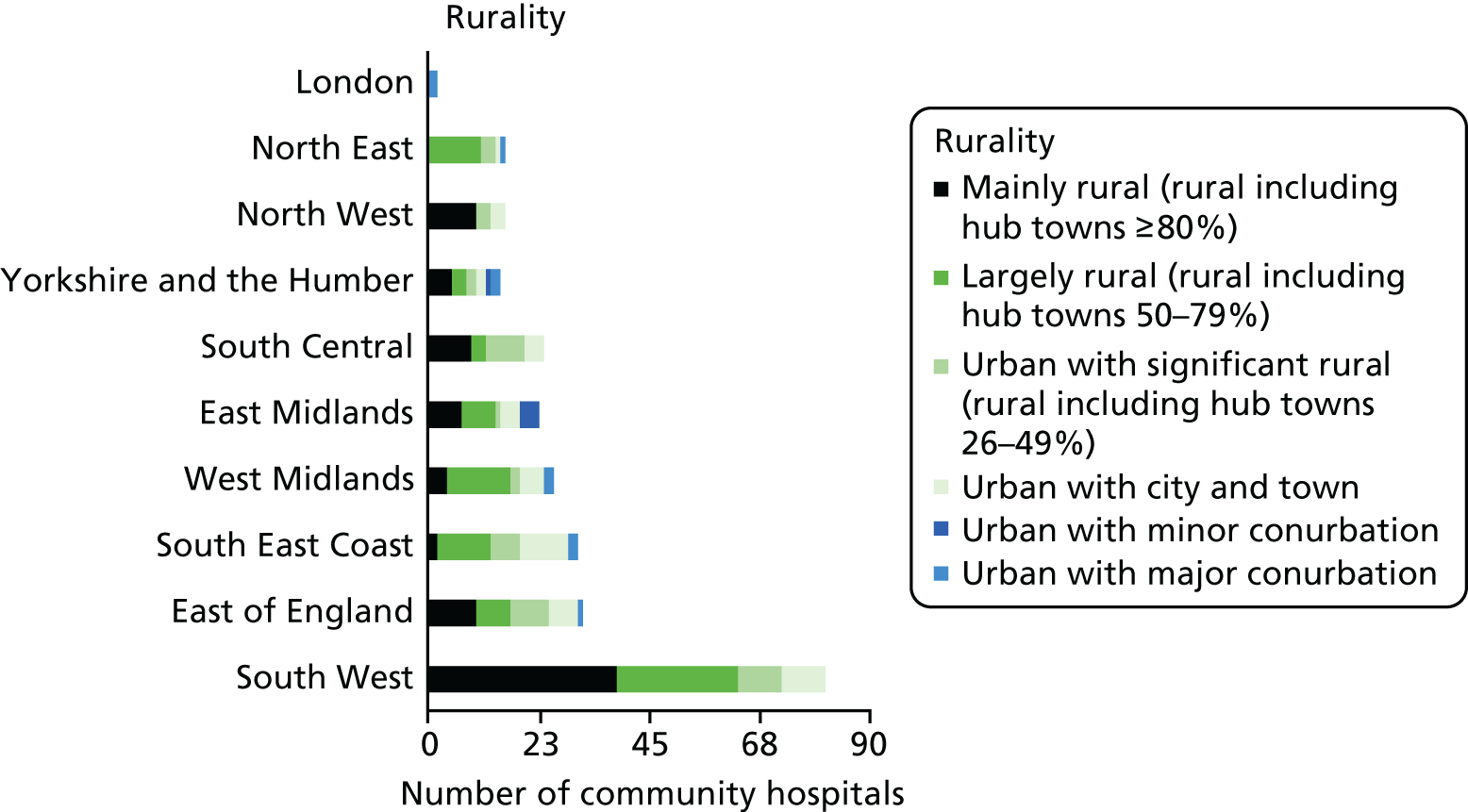
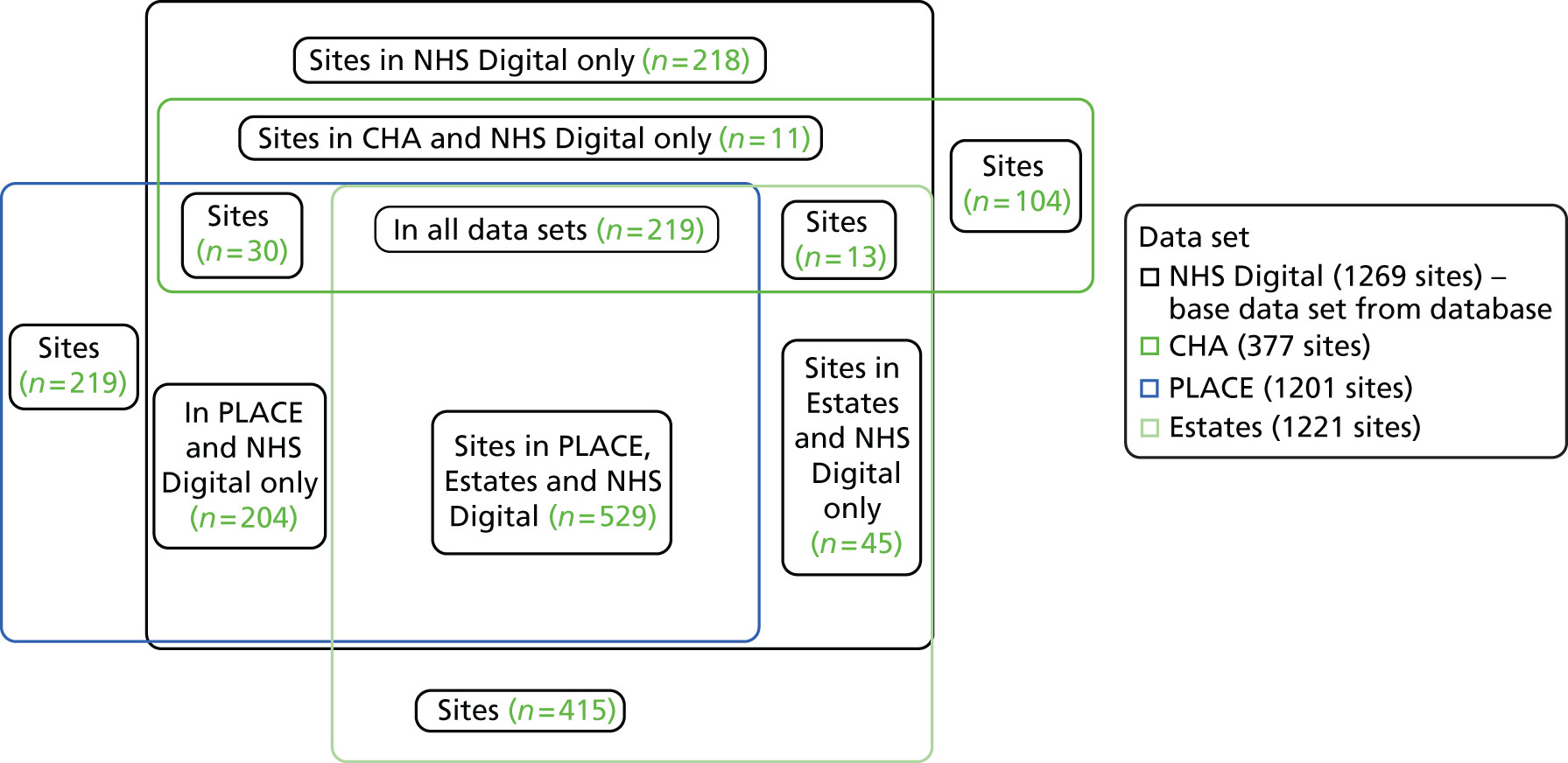
The core data set for England, supplied by NHS Digital, was a list of all hospitals in England, based on ‘site of treatment code.’ Figure 2 shows the relationship between national data sets.
FIGURE 2.
The relationship between four England data sets. CHA, Community Hospitals Associations.
The new database, populated through our reconciliation of these various data sets, provided a census of community hospitals at 2012/13, which was updated to August 2015 (e.g. when a hospital closed and then redeveloped, formed a new hospital replacing two old community hospitals, closed beds on a temporary basis and changed its name).
Database analysis: developing an initial classification of community hospitals with beds
Although the focus of this report is on England, it is important to mention our work on mapping community hospitals in Scotland, as this was instrumental in developing our approach to classifying data for England. Data sets on community hospitals in Scotland [Information Services Division (ISD) and government community hospital data sets: community hospital, general hospital, long-stay/psychiatric hospital, small long-stay hospital] were both more accessible and more comprehensive, lending themselves to early analysis (see Appendix 2).
An initial classification of hospitals in England was developed, informed by categories set out by Estates (community hospital, general acute hospital, long-stay hospital, multiservice hospital, short-term non-acute hospital, specialist hospital, support facility, treatment centre) and PLACE (acute/specialist, community, mental health only, mixed acute and mental health/mental health, treatment centre). It was combined with specialty classifications based mainly on NHS Digital inpatient activity data and developed further through analysis of Community Hospitals Association (CHA) data and discussions within the study team (Table 2).
| Classification | |
|---|---|
| Based mainly on inpatient specialtya | Based on the percentage of the hospital’s total occupied bed-days |
| Acute hospital | < 8% general practice with spread of consultant specialties |
| Small general hospital | 0% general practice with spread of consultant specialties, but < 100 beds |
| General medicine | > 75% general medicine with limited other specialties |
| GP | 80% + general practice specialty |
| GP with other specialties | > 1.9% and < 80% general practice specialty with psychiatry, rehabilitation, general medicine |
| Geriatric medicine | 0% general practice specialty with ≥ 85% geriatric medicine |
| Geriatric mixed specialties | 0% general practice specialty with geriatric medicine, general medicine and psychiatry representing the bulk of occupied beds |
| Geriatric psychiatric | 0% general practice specialty (> 80% geriatric psychiatry) |
| Rehabilitation hospital | Rehabilitation and nursing episode represent ≥ 90% of inpatient specialty (rehabilitation is a specialty label that is applied to two different types of hospital. At a general level it describes hospitals that provide rehabilitation for patients discharged from hospital to enable them to become fit to go home. At a specialist level, it describes facilities treating neurological or musculoskeletal impairment) |
| Learning disabilities | ≥ 90% learning disabilities and mental health (ex-Older Adults Mental Health) specialty |
| Mental health | 0% general practice with geriatric, adolescent, general mental health, learning difficulties, rehabilitation and community medicine representing the bulk of occupied bed-days |
| Hospice | Palliative medicine |
| Specialist | Maternity, children and cancer |
| Surgical | Independent hospital specialising in surgery (mainly trauma and orthopaedic) |
| No beds | No occupied bed-days recorded by NHS Digital, even though fieldwork suggested that beds did exist |
Rapid telephone enquiry: refining the classification
Analysis of the Scotland data suggested that the code ‘GP specialty’ was a defining feature of community hospitals, but early analysis of the England data showed that this was less transferable. If we relied on GP specialty coding alone, many known community hospitals would be excluded from our database: not all community hospital inpatient beds in England were coded to GPs.
A short piece of empirical data collection was undertaken to understand the link between the specialty codes and practice and to test the working definition (based on the literature and on the Scottish data) that community hospitals were predominantly GP led. A telephone questionnaire was designed by the study team (see Appendix 3) and piloted through the CHA.
Seven hospitals from five specialty category codes (≥ 80% GP, < 80% GP and mixed specialties, general medicine, geriatric medicine, geriatric mixed specialties) were randomly selected. The test sample of 35 was reduced by four as a result of closure or conversion to nursing homes. The research team called the hospitals to gain contact details of the matron or ward manager (n = 20; the small sample size highlighting the difficulty of identifying leadership, especially when the community hospital is represented by a single ward), e-mailed the questionnaire, conducted telephone interviews with staff to complete the questionnaire (taking 10–20 minutes each), transcribed notes and returned the completed questionnaire to respondents (n = 12). Analysis of these telephone interviews gave us confidence in the specialty coding, while also confirming the need to be more expansive in our working definitions and categorisations.
Verification: checking and refining the database through internet searches
The mapping enquiry was finalised through five iterations of searching and checking. The CHA consulted its database and membership list (from both 2008 and 2013). A full internet search took place at two points, in February 2015 and August 2015, taking account of hospital closures and changes of function up to 2014/15, with further validation and amendments up to August 2015. By the end of the study, the 2012/13 data set, based on the NHS Digital Spine using ‘site of treatment code’, had been validated through a check of every potential community hospital. A total of 366 sites were examined through web-based and telephone enquiries, including 60 that were not present on the NHS Digital database (see Appendix 4 for the list of community hospitals with beds).
Phase 2: case studies
In order to explore patient and carer experience of community hospitals and aspects of community engagement and value, we undertook qualitative case studies. Although the initial aim of the case studies was to address the second and third research questions, the findings also enabled new insights into the first study question of ‘what is a community hospital’.
The decision to adopt a comparative case study design73 across multiple community hospital sites was influenced by three factors. First, given the gaps in the literature highlighted in Chapter 1, it would be useful to uncover different aspects of the patient experience, community engagement and value of community hospitals and enable the identification and analysis of common themes (looking for similarities, differences and patterns) both within and across cases. 74–76 Second, it provides a suitable way of ‘exemplifying’ sites,77 given the variety of ownership models and locations. Third, it is useful in enabling an examination of ‘complex social phenomena’,78 and, in particular, the social, functional, interpersonal and psychological factors that shape patient experiences, as well as those that influence community engagement and value. Below, we summarise the approach to case study selection for work packages 2 and 3, before moving on to discuss the research elements used.
Selection of case study sites
In selecting case study sites, we adopted a ‘realist’ approach to sampling,79 moving back and forth between categories identified from the literature as being important for patient experience and community value and our learning about the characteristics of community hospitals identified from the mapping exercise. In order to reflect the diversity of community hospitals (highlighted in the literature and mapping), we selected cases in contrasting locations with different numbers of beds, ranges of services, ownership/provision and levels of voluntary income and deprivation.
To allow for a particular focus on variations in voluntary support for community hospitals, hinted at through the national mapping exercise and identified as a particular gap in the existing literature, we selected pairs of hospitals across four Clinical Commissioning Group (CCG) areas with contrasting levels of voluntary income but similar levels of deprivation. This would allow for a good comparison within and between cases (e.g. why two community hospitals within one CCG area, with similar levels of deprivation, have contrasting levels of voluntary support, given that previous research has tended to suggest a strong negative correlation between deprivation and voluntary activity).
Using these criteria, we selected eight case studies of hospitals of different sizes, ages and service profiles located across England (although mostly concentrated in the south, reflecting the national pattern of community hospital development; see Figure 7) in areas of contrasting levels of deprivation. Six of the buildings were owned by, and their main inpatient service was provided by, the NHS. Two were owned by the NHS but their main inpatient services were provided by a community interest company (CIC). We added a ninth case study, owned by a charity, to increase diversity in terms of ownership/provision (as there were very few examples of independently owned community hospitals, it was not possible to identify a matched pair). Table 3 provides a summary of the nine case studies selected, according to the data that were available from the mapping exercise. Fuller qualitative descriptions are provided in Chapter 4 and Appendix 5.
| Geography | Reference | Owner (main provider) | Urban rural codea | Available beds, n | Time period (% m2) | MSOA IMDb | Average voluntary income in past 5 years (£) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre 1948 | 1948–64 | 1965–84 | 1985–2004 | 2005–13 | |||||||
| South | CH1 | NHS (NHS) | 2 | 19 | – | 9 | 4 | 76 | 11 | 27.48 | 19,680.53 |
| CH2 | NHS (NHS) | 1 | 37 | – | – | – | – | 100 | 28.7 | 86,699.93 | |
| CH3 | NHS (CIC) | 3 | 33 | – | – | – | – | – | 4.68 | 97,641.65 | |
| CH4 | NHS (CIC) | 3 | 31 | – | – | – | – | – | 3.01 | 21,571.90 | |
| CH5 | NHS (NHS) | 2 | 19 | 100 | – | – | – | – | 14.78 | 55,398.18 | |
| CH6 | NHS (NHS) | 3 | 22 | 32 | – | 32 | 36 | – | 12.84 | 102,957.30 | |
| CH7 | Charity (NHS) | 2 | 13 | – | – | – | 100 | – | 33.04 | 423,521.20 | |
| North | CH8 | NHS (NHS) | 1 | 9 | – | – | 59 | 42 | – | 21.21 | 1370.79 |
| CH9 | NHS (NHS) | 1 | 28 | – | – | 90 | 10 | – | 19.04 | 23,817.45 | |
Case study data collection
The case studies involved seven research elements, as summarised in Table 4. All elements were conducted over five visits to each case study. Across all case study sites and research methods, 241 people participated in the study through interviews and 130 people participated through 22 focus groups; a small number of people who participated in individual interviews also participated in focus groups (see Appendix 6 for full details).
| Method | Focus (respondent) | Focus (theme) | Numbers |
|---|---|---|---|
| Scoping |
|
|
|
| LRG |
|
|
|
| Semistructured interviews |
|
|
|
| Discovery interviews |
|
|
|
| Semistructured interviews |
|
|
|
| Focus groups |
|
|
|
| Telephone interviews |
|
|
|
Scoping
Scoping visits were made to each of the case studies in order to build relationships with key stakeholders (primarily matrons and chairpersons of Leagues of Friends), gather background information on the hospitals and local communities, identify potential study participants and collect key documents and data. Documents selected included hospital histories, annual reports, local service information (when available) and media coverage. Reviewing these helped to provide a basic understanding of the cases prior to the main fieldwork visits and added to our profiling of each of the case study hospitals.
We also aimed to gather hospital-level data from patient-reported experience measures (PREMs)80 and the revised Friends and Family Test (FFT). 81 However, none of the case study community hospitals collected PREMs data, as this had only recently been required of community providers. Although all sites collected FFT scores, we were able to access data for only seven of the nine case studies because, in the remaining two cases, the trust compiled data at trust rather than hospital level and it was not possible to disaggregate the data. Furthermore, the FFT data were not strictly comparable as some scores covered inpatient care only, whereas others covered both inpatient and outpatient care.
Local reference group
We established a local reference group (LRG) in each of our case studies to bring local people together to steer, support and inform the research at the local level. These LRGs comprised key members of hospital staff, the League of Friends, volunteers and local voluntary and community groups, some of whom had also been patients and/or carers. Their role was to help build a picture of the local context to inform subsequent data collection elements, build support for the study within the local community and reflect on emerging findings and their implications for local practice. There were two LRG meetings per case study during the local fieldwork stage: one at the start of the fieldwork period (which focused on mapping the community hospital services and community links) and one at the end (which focused on discussing the emerging findings and their potential implications). The first LRG meeting for CH3 and CH4 was joint (for convenience) but the second meeting was separate. Following completion of the fieldwork and analysis, each LRG received a report of the findings relating to their specific case study (i.e. alongside this national report, we produced nine local reports).
Semistructured interviews with staff, volunteers and community representatives
We conducted semistructured interviews with staff (n = 89 staff across the nine cases), community stakeholders (n = 20) and volunteers (n = 35). Although most of the interviews were with single respondents, some were with two or, very occasionally, three people (depending on respondent preferences). Respondents were selected through purposive sampling79 guided by the scoping visits, the initial LRG and snowballing. Each of the interviews explored the profile of the hospital and the local context, perceptions of patient and carer experience, and community engagement and value. The emphasis placed on the different sets of questions, however, varied between the groups of respondents (e.g. more time was spent on community engagement and value within the community stakeholder interviews, although we still asked questions relating to hospital profile and perceptions of patient/carer experience). Interviews were nearly all conducted face to face, although a small number were conducted via telephone, at respondent preference. Interviews with staff, volunteers and stakeholders lasted, on average, 60 minutes. All were digitally recorded and later transcribed verbatim.
Discovery interviews with patients
Rather than focusing on satisfaction levels, or other quantifiable measures of experience, the study was concerned with exploring the lived experience of being a patient using community hospital services. Lessons from previous studies show that gathering experiences in the form of stories enhances their power and richness,36 so we selected an experience-centred interview method82 that drew on the principles of narrative approaches83 and, particularly, discovery interviewing. 84 Narrative approaches invite respondents to tell their stories uninterrupted, rather than respond to predetermined questions, giving control to the ‘storyteller’. This approach can elicit richer and more complete accounts than other methods85,86 because reflection enables respondents to contextualise, and connect to, different aspects of their experiences. Discovery interviewing helps to capture patients’ experiences of health care when there may be pathways or clinical interventions central to patient experience. 87 As such, after a general opening question, our interviews focused around a very open question inviting respondents to tell their story of being a patient at the community hospital. We followed this by asking respondents to consider a visual representation we had developed of factors found in previous research to have shaped patient experience, to prompt people’s memories and thoughts (see Appendix 7 for an example of the discovery interview).
Our aim was to interview six patients from each case study. Our final sample across all sites was 60 patients. The small sample size reflected the in-depth nature of the interviews. We sought, as far as possible, to select patients with a mix of demographics (particularly in terms of gender), care pathways (particularly in terms of step up/step down) and services used (inpatient/outpatient). Potential participants were identified by the hospital matron and/or lead clinician and/or service leads. Each was written to by the hospital with a request to participate in the study and was sent an information sheet and an opt-in consent form. Patients who were willing to participate sent their replies directly to the study team. Written consent was provided prior to the commencement of the interview. In line with the Mental Capacity Act 2005 Code of Practice,88 we made provision for the appointment of consultees when potential respondents lacked the capacity to consent to participation in the study, although this was not utilised.
Although many of our respondents were current inpatients, we also spoke to some inpatients who had been recently discharged and to outpatients from a range of different clinics. Outpatients who agreed to participate tended to be those using services several times a week (e.g. renal patients) or over a longer period of time (e.g. those with chronic conditions), rather than one-off users. Interviews with patients lasted between 30 and 90 minutes, were digitally recorded (in all cases except for two because of respondent preference/requirements) and transcribed verbatim. At the end of the interviews, we asked respondents to complete a short pro forma to gather basic demographic and service information for analysis purposes.
Semistructured interviews with carers
Semistructured interviews were conducted with carers in order to explore their experience of using the community hospital as a carer of an inpatient. Our aim was to interview three carers per case study; in total we spoke to 28 carers across the nine sites. Carers were either related to, or close friends of, patients (either current or recent) at the hospital. In most cases, we interviewed carers of patients who had also been interviewed, but in some cases carers were not directly linked to patients involved in the study (indeed, some carers were reflecting on the experience of caring for a patient who had recently died).
The main focus of the interviews was on the experience of being a carer of someone at the hospital, with our initial question reflecting the narrative approach adopted for patients by asking respondents to tell us their story of using the hospital. In addition, as the respondents were typically local residents, we also asked questions about their perceptions of patient experience, about local support for, and engagement with, the hospital and of value. Interviews with carers lasted, on average, 60 minutes. All were digitally recorded and later transcribed verbatim.
Focus groups
We conducted focus groups with members of MDTs, volunteers and community stakeholders. Although we had anticipated conducting each of the three focus groups in each of the case study sites, this was not always possible owing to practical reasons; for example, in some of the case study sites there were very few volunteers, making it difficult to organise a focus group. We ran focus groups with MDTs in eight of the nine case studies, involving a total of 43 respondents; with volunteers in six of the case studies, involving a total of 33 respondents; and with community stakeholders in eight of the cases, involving 54 respondents. Individual focus group respondents were selected through purposive sampling. We worked with LRGs and other key contacts to identify potential participants, each of whom was written to and asked to participate.
The focus groups complemented the interviews, enabling the inclusion of a wider range of perspectives in the study and, in particular, allowing us to observe the emergence of discussion, consensus and dissonance among groups of participants. They lasted, on average, 90 minutes and were digitally recorded and transcribed in full.
Telephone interviews with managers and commissioners
We conducted telephone interviews to explore the views of senior managers of provider organisations and commissioners of community hospitals. The nine case studies were based in five CCG areas where the main inpatient services were provided by four NHS trusts and one integrated health and social care CIC. Our aim was to interview one respondent from each of the providers and CCGs. In total, we spoke to five provider and four CCG representatives. The interviews explored the strategic context for the community hospitals involved in the study, alongside the perceptions of these senior stakeholders of patient experience and the value of community hospitals. The interviews lasted, on average, 60 minutes and were digitally recorded and later transcribed in full.
Qualitative case study data analysis
We adopted a thematic approach to qualitative data analysis, aided by the use of NVivo 11 (QSR International, Warrington, UK) for data management and exploration. Our approach was both inductive, with themes emerging from the data, and deductive, framed by our research questions and ongoing reading of the literature. Initial themes and codes were developed after three members of the team (AEP, DD and NLM), who collectively had been responsible for the case study data collection, reviewed the transcripts. The emerging themes, codes and associated findings were discussed at wider study team meetings, at the LRG meetings for individual case studies and at annual learning events that brought together participants from across the case studies. A refined coding frame was then tested by the same three members of the research team each coding a sample of transcripts; this led to a further refinement of the codes, while also helping to ensure that each of the researchers was adopting a similar approach.
In this report, we focus in particular on across-case comparisons, highlighting themes that emerged across the case studies, emphasising key points of similarity and difference between the cases, as relevant. In addition, we have produced individual reports for each of the local case study sites that have shared findings from our within-case analysis, as relevant for each individual hospital. Comparative analysis, including of the paired cases, will be developed further in future research articles, in which a focus on more specific aspects of the study will allow more space for presentation of such work.
Throughout the analysis, unique identifiers were used for the transcripts/respondents to help ensure confidentiality and anonymity. Sites were assigned a number (e.g. CH1) and respondents given a letter: patient (P), family carer (CA), staff (S), volunteer (V), community stakeholder (CY) and senior manager or commissioner (T), with sequential numbering, date of interview and initials of researcher added to provide an audit trail. This basic coding method is used throughout the report (e.g. CH1, S01 represents the first staff member to be interviewed at the first community hospital case study site). It is worth noting, however, that, although respondents were identified by a key characteristic (e.g. patient or staff) and their transcripts labelled as such, the boundaries between these categories were not discrete: many community stakeholders, for example, had also been patients or carers, and many staff were also members of the local community.
Phase 3: quantitative analysis of Charity Commission data
Collating data on charitable finance and volunteering support
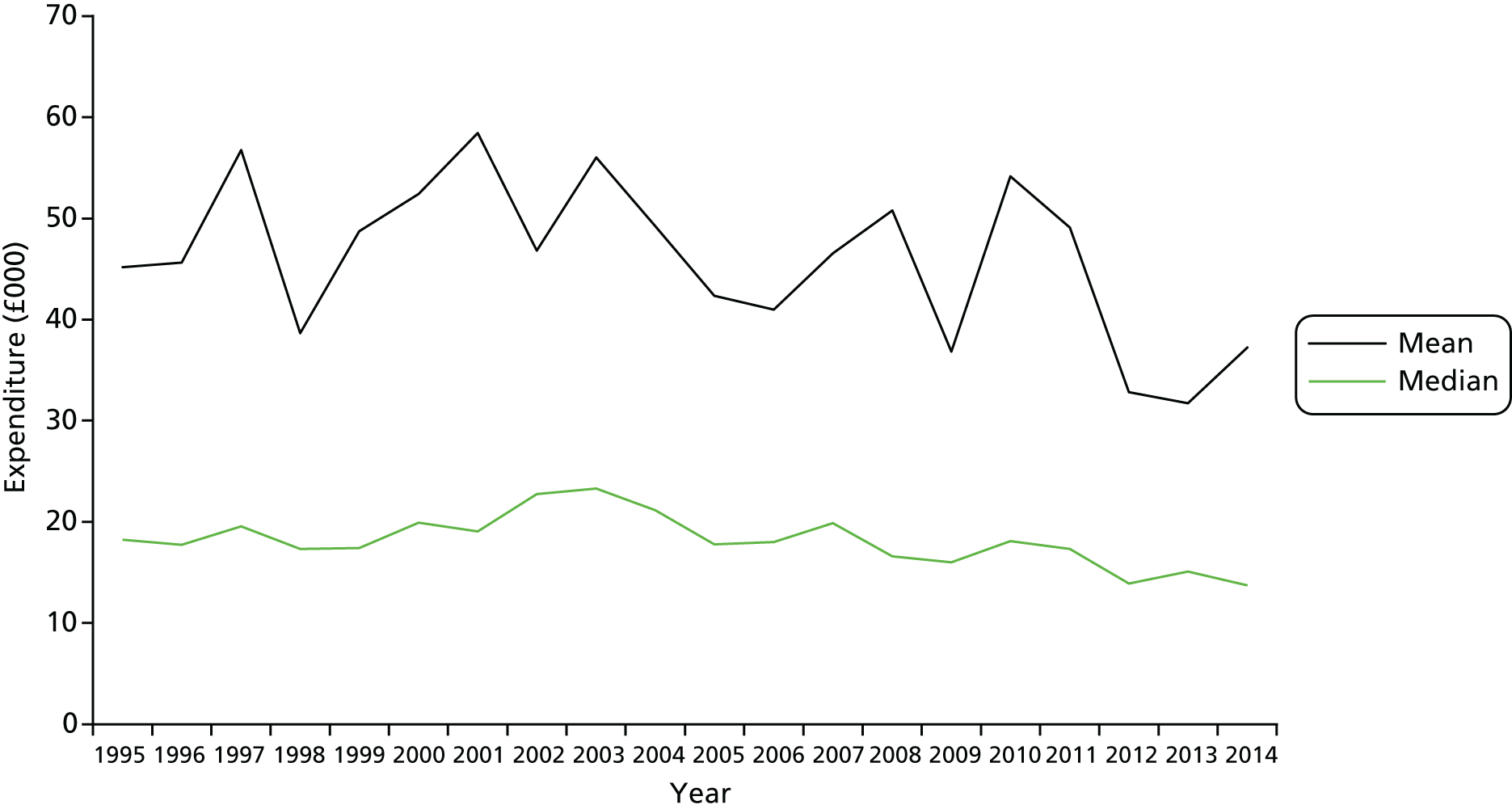
The third phase of our research involved the quantitative analysis of data from the Charity Commission on voluntary income and volunteering for community hospitals across England. The aim of this activity was to examine charitable financial and volunteering support for community hospitals by investigating:
-
variations in the likelihood that hospitals receive support through a formal organisational structure such as a League of Friends, and if so, variations in its scale (in financial terms) between communities
-
uses of the funds raised (e.g. capital development, equipment, patient amenities).
We captured financial and volunteering data for registered charities from the Charity Commission (the Commission). The Commission holds details of organisations that have been recognised as charitable in law and that hold most of their assets in England, or have all or the majority of their trustees normally resident in England, or are companies incorporated in England. The data are described more fully in Appendix 9.
Subject to a small number of exceptions, all charities in England with incomes of > £5000 must register with the Commission and submit financial statements consisting of trustees’ annual reports (returns) and annual accounts. The accounts of those charities whose income or expenditure exceeds a threshold of £25,000 are made available on the Commission’s website. 89 Charities that have income and expenditure of < £5000 a year have (since 2009) been exempted from the need to register. We identified 274 hospitals in England that satisfied the inclusion criteria for this research project (Figure 3). We used the Charity Commission’s data to identify charities that support each of these hospitals, matching by name or through examining lists of charities registered in the locality where the hospital is based.
FIGURE 3.
Community hospital and charities sampling frame.
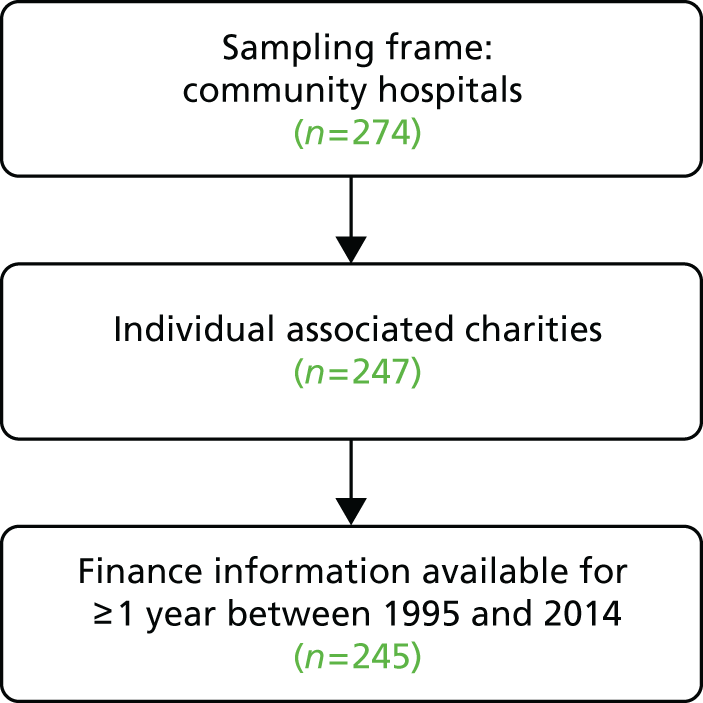
We also directly approached eight non-registered charities (usually those with an income of < £5000 a year) that were known to have been established to support specific community hospitals, but received no usable data relating to them. Four hospitals in our data set were registered as charities themselves but were excluded from the analysis because they are exceptional cases of charitable action.
We found that 247 of these charities were registered in their own right (labelled ‘individual associated charities’ in Figure 3). The remainder were what is known as ‘linked’ charities, that is, entities associated with larger charitable organisations serving a NHS trust comprising several institutions. These ‘linked’ charities were excluded because it was not possible to disaggregate the support they provide to individual components of the trust. Financial information was available for the period from 1995 to 2014 (only small numbers of observations were available for years prior to that because digitisation of the register began only in the early 1990s).
Measurements
Financial information for at least 1 year between 1995 and 2014 was available for 245 charities in England, and this information formed the final sample for this part of the study. The number of non-zero financial reports to the Commission in each year ranged from 181 (1996) to 226 (2007). The data, covering the period to 2014, were the latest available at the time of analysis (2016). See Appendix 9 for full details of available charity reports by year. All financial information in this paper is presented at constant 2014 prices.
Using the Charity Commission website, we obtained copies of these accounts for those selected charities whose expenditure or income exceeded £25,000 in any one year. This gave data covering 358 separate financial years; the number of accounts available is shown in Table 5.
| Year | Number of accounts |
|---|---|
| 2008 | 91 |
| 2009 | 55 |
| 2010 | 49 |
| 2011 | 52 |
| 2012 | 41 |
| 2013 | 70 |
We focused on the period from 2008 to 2013, when between 41 and 91 charities of interest generated at least one such financial return. Numbers vary because an individual charity may or may not exceed the £25,000 threshold at which its accounts are presented via the Charity Commission’s website, depending on fluctuations in its finances.
Charity accounts aggregate income and expenditure figures into a small number of general categories. These provide relatively little detail on income and expenditure and may even aggregate quite different sources of expenditure within the same funding stream. As such, to probe income sources and the application of expenditure in more detail, data were captured from the notes to the accounts of these charities. The extensive income data that were generated (21,733 items) were categorised to provide useful insights into sources of income. Classifying the expenditure of charities was not undertaken because of the complexity of the data and the limits to the usefulness of such an exercise. Appendix 9 provides further details of the extraction, classification and analysis of income and expenditure data.
Contribution: number of volunteers and estimates of input
The Charity Commission guidelines90 require charities to record their best estimates of the number of individual UK volunteers involved in the charity during the financial year, excluding trustees (see Appendix 9).
Before 2013, data on volunteer numbers were often sparse, but, since that date, efforts have been made to gather more detailed information. Approximately 73,000 charities had supplied between one and three non-zero returns of their volunteer counts in the three years between 2013 and 2015, including > 90% of our charities. We calculated the average number of volunteers for the period in question. To provide an upper-bound estimate, we also take the maximum value returned for each charity.
Volunteer hours were estimated using regular survey data (Home Office Citizenship Survey, 2001–10; Community Life survey, 2012 onwards). We take the average number of hours per week reported by those who say they have given unpaid help to organisations during the previous year. This is approximately 2.2 hours. This is a minimum estimate and it may be that the actual numbers are larger than these survey data would imply. If we make the assumption that these are probably fairly regular volunteers, a higher figure of 3.05 hours per week is given if we take the average number of hours reported by those who say they volunteer either at least once a week or more frequently, or at least monthly but less frequently than once a week.
There are no studies that would tell us with any certainty whether or not volunteers in these kinds of organisations put in more or fewer hours than the volunteering population generally. We then multiply these two estimates of time inputs by the average and maximum volunteer numbers, respectively, to give the number of hours contributed by volunteers over the course of the year (assuming 46 weeks of volunteering a year). These can be converted to full-time equivalent numbers by dividing by 37.5 (hours per working week) and 46 (weeks per working year).
Opinions differ on the best method for calculating a cash equivalent for the value of volunteer labour. The lowest is to use the national minimum wage; others might include an estimate of the replacement cost (i.e. what it would cost the organisation to employ people to do the same tasks if they had to pay them), but this assumes knowledge of the tasks being undertaken. The national minimum wage for the period for which we have the most comprehensive volunteering data (2013–15) was £6.50 per hour. 91
Data convergence and integration
Although the quantitative (phases 1 and 3) and qualitative (phase 2) data were collected separately, they could nevertheless be considered ‘integrated’ because the different research elements were explicitly related to each other within a single study and in such a way ‘as to be mutually illuminating, thereby producing findings that are greater than the sum of the parts’. 92 Data triangulation, convergence and integration occurred in a number of different ways, at different stages of the research.
In phase 1 of the research, a revised definition and set of characteristics captured within the database was used to support development of a typology and informed the case study sampling for phase 2. For phase 3, the database informed the sample of charities selected for analysing voluntary income and volunteering data and providing additional data fields to be linked to the Charity Commission data.
Although the national quantitative data provided breadth to the study, these were limited and left questions unanswered. The local qualitative data brought depth to the question ‘what is a community hospital’, by helping to build a picture of the history, context and change over time. Qualitative interviews in work packages 2 and 3 were conducted concurrently, and triangulation of data between stakeholder, volunteer, staff, carer and patient interviews helped validate findings and strengthen our understanding of patient and carer experiences and community engagement and value.
In addition, the combination of researchers working on more than one work package, reflexive team meetings and the involvement of different representations in the team [CHA, University of Birmingham and Crystal Blue Consulting (London, UK)] allowed for healthy dialogue, debate and analysis. Emerging findings from each phase of the research were, for example, shared through internal working papers and discussed regularly at whole project team meetings.
Patient and public involvement
Our commitment to PPI ensured that patients, carers and the public were involved in this study before and during its conduct. PPI involvement in the study design was facilitated by one of the researchers (HT), who first consulted with 10 PPI members of the Swanage Health Forum, representing the League of Friends; a GP practice Patient Participation Group; Swanage Carers; Partnership for Older People’s Programme; Wayfinders; the Senior Forum; the Health and Wellbeing Board; Cancare; a public Governor for Dorset Healthcare NHS Trust; and a retired GP. This group provided an endorsement of the study’s proposed focus and methodology.
At the national level, 13 board members of CHA (four GPs, six nurses, two managers and one League of Friends member) co-produced the initial research proposal. Two members then became part of the study steering group, which met regularly throughout the study, supported the development of research materials and supporting documentation, helped facilitate access to potential case studies, contributed to the local and national reports and reviewed several drafts. We also engaged with approximately 100 delegates at three CHA annual conferences (presentations and workshops focused on working with findings) that included not only practitioners but members of community hospital Leagues of Friends.
In addition, a cross-study steering group, chaired by Professor Sir Lewis Ritchie, University of Aberdeen, provided guidance across all three Health Services and Delivery Research community hospital studies, with representation from the CHA, Attend (National League of Friends) and the Patients Association, alongside the three study teams. The steering group met seven times over the period of this study, offering opportunities to share findings and explore experiences between the studies.
As described in Local reference group, at the local level we established LRGs within each of our case study sites to bring local people together (hospital staff, volunteers and community members, a number of whom were patients and/or carers) to steer, support and inform the case study research. To facilitate cross-case learning, we brought together representatives from each of the LRGs three times to share experiences, identify best practice and network. Event themes reflected each of the three research questions, and the days offered time for case study representatives to work together, share across sites, hear from national experts, contribute to the ongoing development of the study and reflect on emerging findings and their implications.
Ethics approval
Ethics approval was provided by the University of Birmingham, in line with the Department of Health and Social Care’s Research Governance Framework, for work package 1 (national mapping) and elements of work package 3 (quantitative charitable finance and volunteering support data). The university also provided sponsorship for the whole study. The qualitative case studies required full ethics review through the National Research Ethics Service as they involved interviews with patients and carers and interviews and focus groups with NHS staff, volunteers and community stakeholders. The Wales Research Ethics Committee 6 reviewed this research and provided a favourable ethics opinion (study reference number: 16/WA/0021).
Summary
Informed by key stakeholder engagement and a review of the policy context and existing literature, this study explored the profile, characteristics, patient and carer experience, community engagement and value of community hospitals in England through a multimethod approach. The research was conducted in three overlapping phases – mapping, case studies and Charity Commission data analysis – that, together, involved a range of qualitative and quantitative methods. Data for each phase were collected and analysed separately but iteratively, with emerging findings discussed regularly through a range of mechanisms, including whole project team meetings and internal working papers. We involved key national and local stakeholders throughout the study, from design, through to data collection and analysis, and reporting and dissemination.
Having framed the study (see Chapter 1) and described our research methodology (see Chapter 2), we now move on to share the findings. Chapters 3–7 describe the findings emerging from different elements of the study, and Chapter 8 brings those findings together and discusses them in relation to the wider literature and their significance for knowledge and practice.
Chapter 3 Defining and mapping community hospitals: the national picture
This chapter addresses our first research question, ‘what is a community hospital?’, by reporting the findings of the national mapping work that identified, located and profiled the characteristics of community hospitals (see Chapter 2, Phase 1: mapping and profiling community hospitals). This chapter also shows how the working definition of community hospitals has been modified in response to findings and draws a typology from distinguishing characteristics.
Set of community hospitals
The mapping study produced a set of 296 hospitals as of August 2015. The set comprised 267 hospitals that could be linked to 2012/13 NHS Digital data (groups A–C in Table 6), lending themselves to further analysis, and an additional 29 hospitals (shown as group D) that were not visible on national data sets (PLACE, ERIC or NHS Digital), thought to be because NHS trusts reported activity on an aggregated basis without specifying every site of treatment in detail.
| Group | Inpatient specialty/type | Number of hospitals |
|---|---|---|
| A | > 80% GP (predominantly GP) | 92 |
| < 80% GP and mixed specialties (GP plus consultant) | 34 | |
| Group A subtotal | 126 | |
| B | Consultant (predominantly general medicine) | 26 |
| Geriatric medicine (consultant – predominantly consultant physician for older people) | 55 | |
| Geriatric mixed specialties (consultants – mixed consultants for older people) | 26 | |
| Group B subtotal | 107 | |
| C | Rehabilitation | 10 |
| Geriatric psychiatric | 3 | |
| Mental health | 2 | |
| Specialist | 8 | |
| Bed data missing (on NHS Digital) | 8 | |
| Small general hospital | 3 | |
| Group C subtotal | 34 | |
| Total community hospitals on NHS Digital (2012/13) | 267 | |
| D | Named, but no NHS Digital data available (updated to August 2015) | 29 |
| Total | 296 | |
Groups A–C are categorised by inpatient activity specialties: 126 hospitals identified with GP activity (group A); 107 hospitals where patients were coded to consultant-led inpatient specialties of general medicine, geriatric medicine and geriatric mixed specialties (group B); and 34 hospitals (group C) included through a case-by-case examination (telephone and internet), guided by the CHA database and the criterion of providing inpatient care without 24/7 medical presence. Group D has also been generated from information contained in the CHA database: a set of 60 hospital names was explored and 29 hospitals were entered onto the list (following an internet search and telephone enquiry).
In terms of replicability of methods, the results suggest that approximately 80% of the set (groups A and B) are identifiable as community hospitals based on their inpatient specialty mix (GP, general medicine, care of the elderly), whereas 20% (groups C and D) have a more complex identity in which perception of community hospital status (based on long history) is influential. For further information see Report Supplementary Material 1, supplied separately as an output to the study, the CHA’s website,93 which continues to be updated, and Report Supplementary Materials 2–4.
Refining the classifications
Our working definition, linking (classic) community hospitals to primary care, had led to categorisation of hospitals based on inpatient specialty. We found in England, however, that GP utilisation of beds occurred in only 126 hospitals (group A), whereas we might have expected to find at least 200 community hospitals based on other inventories (236 in PLACE; 200 in Estates; 247 classic community hospitals in CHA 2013). The working definition was, therefore, too narrow.
The research team voiced concerns about the validity, meaning and accuracy of specialty codes attached to patients, which appeared to reflect clinical authority of either GP or consultant with no reference to the reality of widespread nurse leadership. To address this, a rapid enquiry into the clinical leadership of community hospitals, using a telephone questionnaire (see Chapter 2, Rapid telephone enquiry: refining the classification) was undertaken. Nurse managers of 12 community hospitals responded and were interviewed in a sample that included four mainly GP hospitals (≥ 80% general practice specialty), five hospitals with mixed general practice and geriatric medicine or general medicine and three hospitals that are entirely geriatric medicine or general medicine. This was supplemented by direct enquiry with two NHS trusts covering 15 community hospitals in which activity was coded to general physicians or geriatricians.
Findings from the rapid enquiry cast light on the role of clinical leaders and changes to the relationship between community hospitals and the acute sector; these are summarised in Box 1.
The hospitals ranged in size from 12 to 28 beds.
Describe the bedsMost beds functioned as step-down beds (i.e. referred from the acute unit), even where beds were coded 100% to GPs. Patients referred from the community (step up) were outnumbered by those being discharged from acute wards (step down).
Who refers patients to community beds?Referrals mainly came from the acute hospital (estimated at 65–75%), irrespective of GP/consultant coding.
Who has authority to admit to community hospital beds?The ward itself (directly managed by the nurse in charge) admitted the patient. Responses revealed a movement towards using a single point of access or central admission point for a cluster of community hospitals in a county. The practice enabled acute hospitals to discharge to the next available bed, even though it might not be the bed nearest to the patient’s home. Growing patient acuity, combined with a trend to receive non-local patients, was leading GPs to become less involved. The ward manager/matron/senior nurse admitted the patient in accordance with predetermined admission criteria.
Who can veto admission to community beds?The ward (managed by the nurse) could veto admission but it was a rare occurrence.
Who has clinical responsibility for the beds once the patients are admitted?Clinical responsibility was broadly aligned with the specialty coding, described as being with the GP (daily or twice-weekly visits), consultant (weekly round) or with advanced nurse practitioners in some places who could prescribe. Clinical responsibility and day-to-day management were separate features (e.g. a secondary care physician may retain formal clinical responsibility but delegate day-to-day management to a nurse or GP). In other instances, clinical responsibility could be transferred from secondary care to the GP on admission to the hospital. (Direct enquiry: in the NHS trusts covering 15 hospitals where patients were coded to general medicine/geriatrics, clinical responsibility lay with the acute consultant physician, although GPs in some cases would oversee the patient’s daily care. One trust had a contract with the acute hospital to provide a consultant-led service in small hospitals where GPs had withdrawn from being the lead clinicians.)
Who can discharge from the community hospital beds?Patients needed to be assessed as being medically fit and therapy fit, requiring a multidisciplinary approach. Authority was attributed either to the lead medic or to the lead nurse who co-ordinated the multidisciplinary assessments.
Do you have on-site medical cover 24/7?Medical staff were not on site overnight in any of the sample hospitals.
How would you describe out-of-hours medical cover?GPs usually provided out-of-hours cover. If a patient were to become acutely unwell, then the community hospital would ring 999 for transfer to the acute hospital.
What is your core population for the community beds?The concept of a local hospital for local people was being eroded in some areas by county-wide admissions arrangements for subacute (step-down) patients. (Step-up care referrals continued to be directed to the local community hospital, but, overall, appeared to be outnumbered by step-down referrals that may cover a broader area.)
Broadening the inclusion criteria for group B
Findings from the rapid enquiry supported the conclusion that:
-
community hospitals had no medical presence overnight, and that the matron or ward manager (sister) was the most senior clinical presence 24/7
-
referrals could come from the community but, in practice, mainly came from the acute hospital (i.e. step down)
-
admissions practices indicated a loosening of the ‘local’ role of community hospitals where patients were discharged from acute wards to the next available bed across a group of community hospitals.
The distinction between GP specialty code and consultant geriatrician/physician code was not arbitrary and seemed to indicate a level of formal clinical responsibility for the patient. However, the coding said little about the patient. The case mix and function of community hospitals appeared to be the same for patients whether they were coded to GP or to consultant physicians/geriatrics. The patient mix was reported to be increasingly frail older people with complex needs.
In summary, these findings supported the use of specialty codes as a means of categorising hospitals within national data sets (when combined with size), but needed to be broadened out from GP specialism to include secondary care physician utilisation.
Triangulation
We acknowledge the limitation of overinterpreting output from a small sample within a narrow timescale. Case study data enabled triangulation (see Chapter 4).
In addition, findings from the NHS Benchmarking 2014/1594 data set were consistent with our rapid enquiry:
-
clinical leadership – 40% (63 out of 158) sites described themselves as nurse led
-
source of referral – 64% of admissions were recorded as coming from the acute hospital, more than twice as many as from the patient’s home (Table 7).
| Time period | Admission source (%) | |||||
|---|---|---|---|---|---|---|
| Home | Place of care | A&E | Acute hospital | Other | Total | |
| 2014/15 | 30 | 1 | 3 | 64 | 2 | 100 |
Comparing hospital types
The working definition prompted comparison of inpatient metrics (e.g. specialism, bed utilisation), population characteristics (e.g. rurality) and service provision [e.g. minor injury units (MIUs), outpatient clinics, day cases). Table 8 sets these characteristics in the context of all hospital types in England. Each column can be interpreted as the percentage of hospitals that possess the field characteristic. Community hospitals in England are distinctive through the contribution of GPs, rurality and size in terms of bed numbers (they are typically smaller than acute and small general hospitals: approximately 70% have ≤ 30 beds).
| Hospital type | Characteristic, % of hospitals | |||||||
|---|---|---|---|---|---|---|---|---|
| Has GP specialty | ≤ 30 beds | Occupancy > 85% | ALOS ≤ 30 days | Is rural (ONS category ≤ 2) | Has A&E/MIU | Has outpatient clinics | Has day cases | |
| Acute | 0.1 | – | 0.7 | 1.0 | 0.1 | 1.0 | 1.0 | 1.0 |
| Small general hospital | 0.2 | 0.1 | 0.2 | 1.0 | 0.4 | 0.9 | 1.0 | 1.0 |
| Community hospital | 0.6 | 0.7 | 0.6 | 0.7 | 0.6 | 0.5 | 0.8 | 0.3 |
| Geriatric psychiatric | – | 0.7 | 0.7 | – | 0.1 | – | 0.5 | 0.0 |
| Learning disabilities | 0.0 | 0.9 | 0.7 | 0.3 | 0.2 | – | 0.3 | 0.0 |
| Mental health | 0.0 | 0.6 | 0.8 | 0.1 | 0.1 | 0.0 | 0.4 | 0.0 |
| Rehabilitation | – | 0.5 | 0.4 | 0.5 | 0.2 | – | 0.3 | – |
| Specialist | – | 0.5 | 0.3 | 0.9 | 0.1 | 0.1 | 0.9 | 0.8 |
| Surgical | – | 0.9 | 0.0 | 1.0 | 0.1 | 0.0 | 1.0 | 1.0 |
| Care/nursing home | 0.2 | 1.0 | 0.5 | 0.5 | 0.3 | – | 0.2 | – |
| Hospice | – | 1.0 | 0.2 | 0.8 | – | – | 0.3 | 0.1 |
Size of community hospitals
The median number of available beds was 23 (Figure 4), the interquartile range was 15–38 and the mean number of available beds was 30, skewed by a small number of larger hospitals (10% with 60–142 beds). Size proved to be an indicative rather than a limiting criterion because three hospitals had > 100 beds (see Figure 4) (Table 9).
FIGURE 4.
Cumulative frequency distribution of available beds per community hospital (based on NHS Digital data 2012/13 updated to 2015).
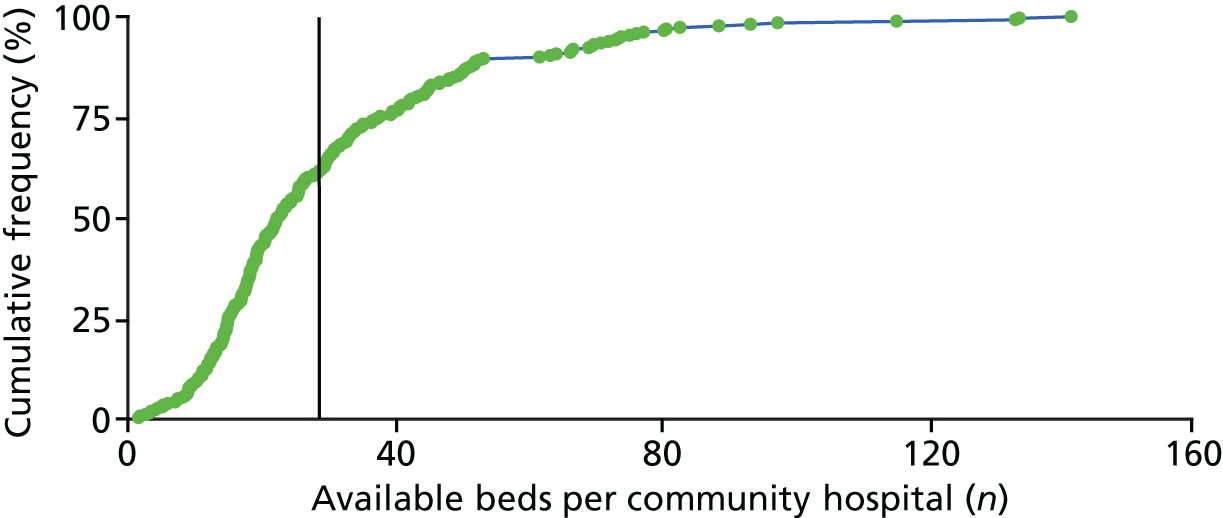
| Group | Community hospital type | Number of | Average number of | % of beds occupied | |||
|---|---|---|---|---|---|---|---|
| Community hospitals in group | Available beds | Occupied beds (NHS Digital) | Available beds | Occupied beds | |||
| A | GP – predominantly | 92 | 1827 | 1586 | 19.9 | 17.2 | 87 |
| A | GP plus consultant | 34 | 1142 | 996 | 33.6 | 29.3 | 87 |
| Group A total | 126 | 2969 | 2582 | 23.6 | 20.5 | 87 | |
| B | Consultant – predominantly general medicine | 26 | 680 | 592 | 26.2 | 22.8 | 87 |
| B | Consultant – predominantly consultant physician for older people | 55 | 1739 | 1519 | 31.6 | 27.6 | 87 |
| B | Consultants – mixed consultants for older people | 26 | 1400 | 1248 | 53.8 | 48.0 | 89 |
| Group B total | 107 | 3819 | 3358 | 35.7 | 31.4 | 88 | |
| C | Rehabilitation | 10 | 283 | 255 | 28.3 | 25.5 | 90 |
| C | Geriatric psychiatric | 3 | 150 | 124 | 409.9 | 41.4 | 83 |
| C | Mental health | 2 | 71 | 66 | 35.3 | 33.1 | 94 |
| C | Small general hospital | 3 | 234 | 190 | 77.9 | 63.4 | 81 |
| C | Specialist | 8 | 235 | 209 | 29.3 | 26.2 | 89 |
| C | Bed data missing (NHS Digital) | 8 | – | – | – | – | – |
| Group C total | 34 | 971 | 845 | 37.4 | 32.5 | 87 | |
| Community hospitals (visible on NHS Digital) | 267 | 7759 | 6786 | 30.0 | 26.2 | 87 | |
| D | No data on NHS Digital | 29 | – | – | – | – | – |
| Grand total | 296a | ||||||
Revised definition: ‘small hospital, usually with 30 or fewer beds’.
Average length of stay
The set of 259 hospitals (267 minus eight hospitals with missing bed data) had a median average length of stay (ALOS) of 24 days and a mean ALOS of 27 days, with interquartile range of 18–31 days. Table 10 indicates convergence within groups A and B towards 23 and 27 days mean ALOS, respectively. Group C is much more variable, particularly within the geriatric psychiatric and rehabilitation categories. Figure 5 [excluding three outliers (i.e. one rehabilitation unit and two geriatric psychiatric units, which each have an ALOS of > 100 days)] shows distribution of ALOS across community hospitals, indicating that 70% of community hospitals have an ALOS of < 30 days.
| Group | Specialty classification | Mean ALOS per hospital (days) |
|---|---|---|
| A | GP – predominantly | 22.1 |
| GP plus consultant | 25.0 | |
| Total | 22.9 | |
| B | Consultant – predominantly consultant physician for older people | 27.0 |
| Consultant – predominantly general medicine | 24.4 | |
| Consultants – mixed consultants for older people | 28.8 | |
| Total | 26.8 | |
| C | Geriatric psychiatric | 200.8 |
| Mental health | 17.4 | |
| Rehabilitation | 42.7 | |
| Small general hospital | 5.7 | |
| Specialist | 21.8 | |
| Total (excluding eight hospitals with missing bed data) | 48.3 | |
| Grand total | 27.1 | |
FIGURE 5.
Cumulative frequency distribution of ALOS in community hospitals (based on NHS Digital data 2012/13 updated to 2015).
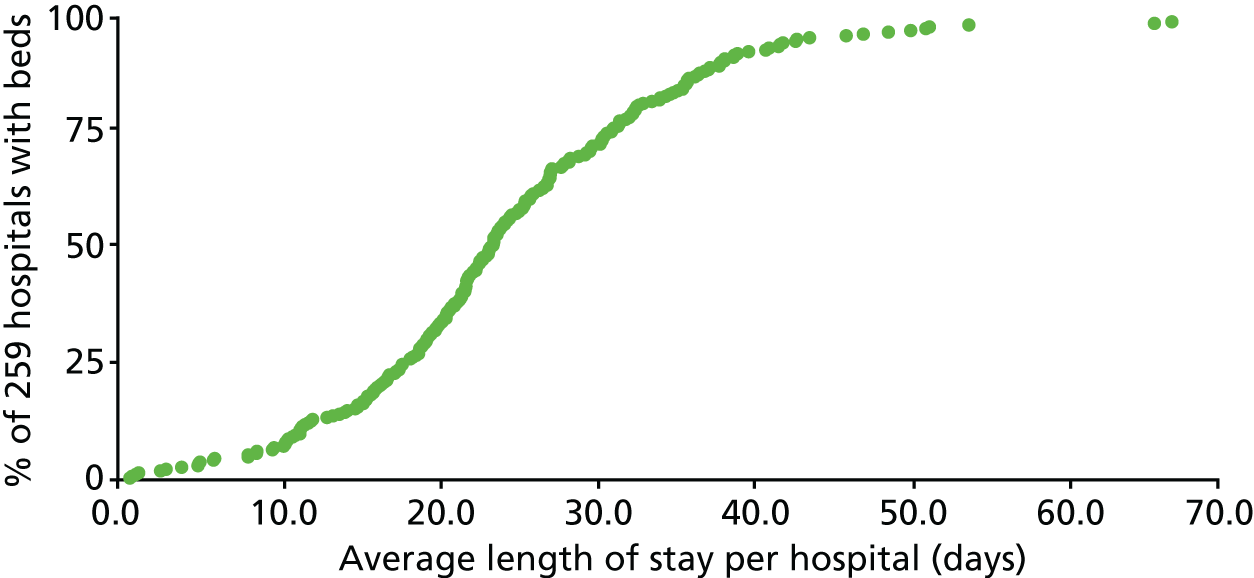
Revised definition: ‘average length of stay typically fewer than 30 days.’
Population characteristics
Rurality
In England, 85% of the land is rural but 82% of the population live in urban areas (settlements of > 10,000 people), with 18% in rural areas [i.e. in smaller towns (< 10,000 people), villages, hamlets or isolated dwellings]. 95 Three-fifths (62%) of the set of 267 community hospitals serve a rural population (categories 1 and 2 in Table 11), with a further 16% in ‘urban areas with significant rural’, leaving 22% of sites in fully urban areas. Figure 6 shows a high concentration in the rural South-West Peninsula and the south-east and clusters in, for example, the Cotswolds, Peak District and parts of East Anglia. Figure 7 depicts the geographical spread, based on Strategic Health Authority boundaries that were extant in 2012/13.
| Code | Description | Number of community hospitals | Percentage of community hospitals |
|---|---|---|---|
| 1 | Mainly rural (rural including hub towns ≥ 80%) | 86 | 32 |
| 2 | Largely rural (rural including hub towns 50–79%) | 80 | 30 |
| 3 | Urban with significant rural (rural including hub towns 26–49%) | 42 | 16 |
| 4 | Urban with city and town | 44 | 16 |
| 5 | Urban with minor conurbation | 5 | 2 |
| 6 | Urban with major conurbation | 10 | 4 |
| Total | 267 | 100 | |
FIGURE 6.
Location of the 267 community hospitals in England (2012/13). Source: My Maps data © 2015 Google.
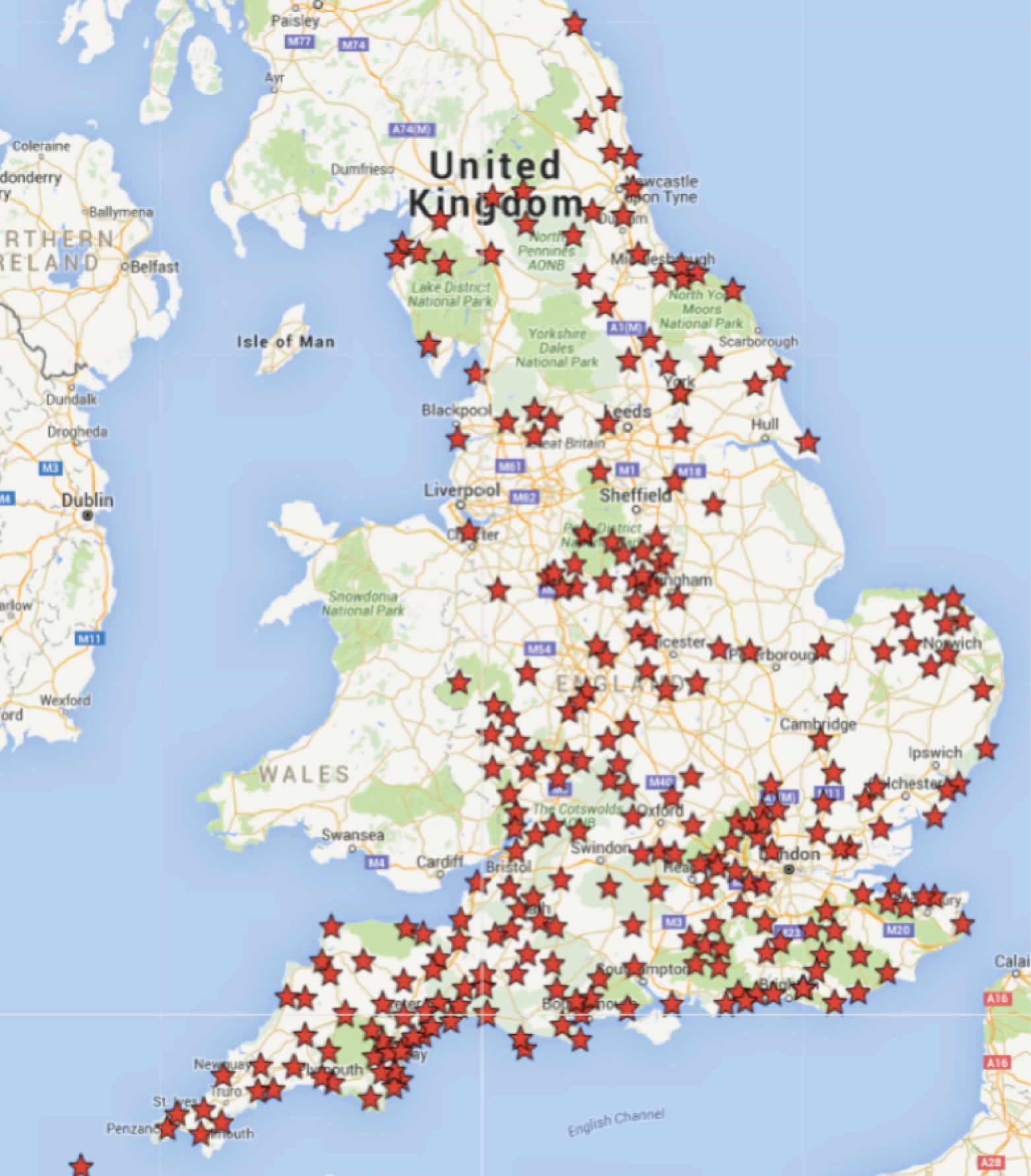
Revised definition: ‘typically serving a rural population.’
Deprivation
Community hospitals serve populations that are relatively privileged according to the Index of Multiple Deprivation (IMD). 96 In England, scores range from 0.5 to 92.1 between the most and least deprived neighbourhoods (at lower-layer super output area level). The range is narrower because of offsetting high/low variations when aggregated to CCG level (i.e. from 5.6 to 47.8) (Table 12). Among the 91 CCGs that have a community hospital, the average IMD score is 16.62, which is significantly lower than the average of 25.11 among 117 CCGs with no community hospital (p < 0.00000, analysis of variance).
| IMD score | England CCG | With community hospital CCG | No community hospital CCG | Community hospital MSOA |
|---|---|---|---|---|
| Mean | 21.97447 | 17.89527 | 25.14719 | 17.81189 |
| Median | 20.78831 | 16.62413 | 25.11411 | 15.40211 |
| Minimum | 5.67958 | 5.67958 | 7.955736 | 1.930938 |
| Maximum | 47.76322 | 40.97243 | 47.76322 | 71.93618 |
| Count | 208a | 91a | 117 | 267 |
At the middle super output area level, representing the local community hospital demographics, Figure 8 shows that 30% of community hospitals are located in areas scoring an IMD of ≤ 10, whereas only 6% of hospitals are in the most deprived areas scoring ≥ 40. The deprivation scores are consistent with the rural–urban spread of community hospitals described above.
FIGURE 8.
The IMD scores (MSOA) for 267 community hospitals. MSOA, middle super output area.
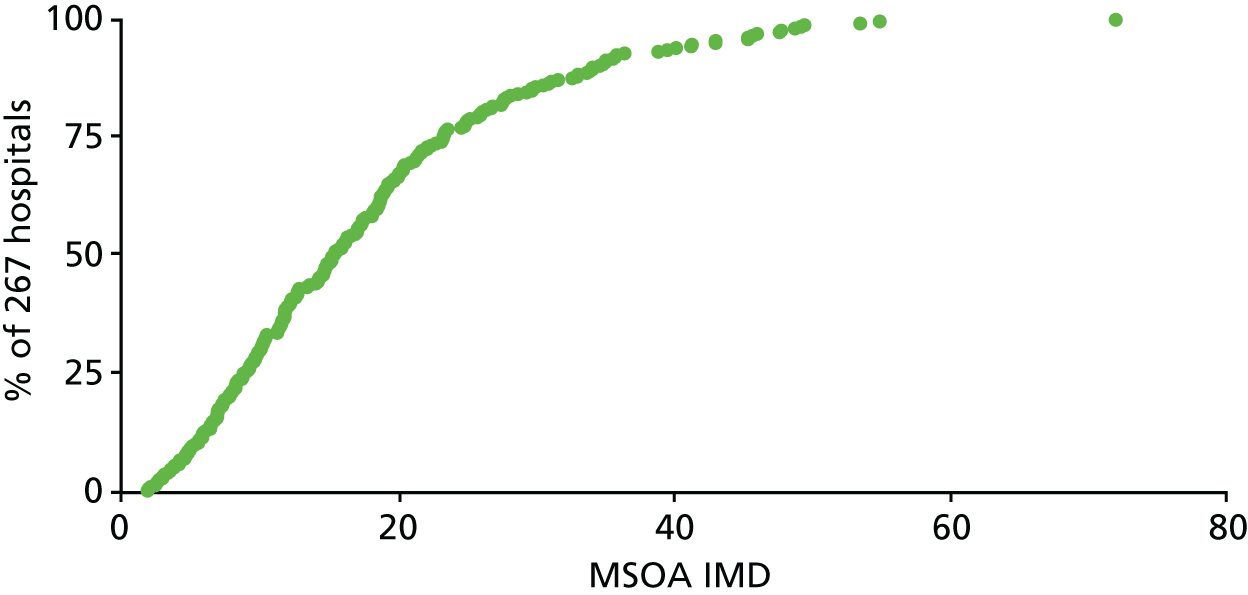
Localness
The working definition characteristic of hospitals ‘serving local populations of less than 100,000’ has been considered in the light of (1) available population data and (2) insights gained through the rapid qualitative enquiry.
Mapping community hospitals to 91 CCGs shows that concentration varies between 20 community hospitals in a CCG (equating to 30,000 population per hospital) and 40 CCGs that contain a single community hospital (Figure 9). As it happens, 267 hospitals in 91 CCGs cover a population of 26 million, averaging a population of 100,000 per hospital. But, overall, the data do not tell us very much.
FIGURE 9.
Concentration of 267 community hospitals across 91 CCGs.

Evidence from the rapid qualitative exercise suggested that the concept of localness was being eroded when community hospitals received inpatients on a county-wide basis and GPs stepped back as the patients were no longer ‘theirs’.
Revised definition: reference to population size and localness has been omitted.
Clinical features
Evidence drawn from the qualitative enquiry triangulated with 2014 NHS Benchmarking Survey findings94 was helpful in clarifying some of the clinical features that are particular to community hospitals:
-
Doctors on site.
Community hospitals do not have a medical presence overnight (except where the community hospital is situated in a larger general acute setting). Nurses provide overnight clinical presence. Hospitals are supported by out-of-hours medical cover, often provided by GPs.
-
Clinical leadership.
Clinical leadership of community hospitals on a daily basis is delegated to nursing staff, and community hospitals are often described as being ‘nurse led’. All patients are under the charge of a doctor who bears ultimate clinical responsibility, either in secondary care (consultant) or in primary care (GP).
-
Inpatient function.
Inpatient function is a pre-set boundary feature used to define community hospitals in this mapping study. In principle, patients may come from either the community or the acute sector, even though the proportions may vary from year to year. The step-up or step-down referral routes span the integrated care spectrum between primary care and secondary care (in which ‘integrated care is the delivering of services across primary and secondary care, mental and physical health and health and social care’). 97
Revised definition: expanded to include these characteristics.
Range of services
The focus on inpatient beds throughout this work package has been necessary for methodological reasons. However, community hospitals provide a wide range of ambulatory services (described in more detail in case study sites and addressed in Developing a typology of community hospitals) with an average of 11 outpatient specialties per site. For every one inpatient discharged, there are 1.4 day cases and nine new outpatients (Table 13).
| Service | Number across all hospitals (n = 267) | Average per hospital |
|---|---|---|
| Inpatient discharges | 101,169 | 379 |
| Day case (Finished Admissions Episodes) | 141,438 | 530 |
| Outpatients first attends | 884,127 | 3311 |
| Outpatients follow-up attends | 1,916,809 | 7179 |
| Total outpatient attends | 2,800,936 | 10,490 |
The working definition has also identified functions that do not belong to a community hospital (e.g. A&E and complex surgery, hospice or mental health admissions).
Revised definition: no change to working definition.
Revised definition
The mapping study took the working definition as a starting point, tested it against data and generated revisions. Table 14 brings together the final definition of a community hospital.
| Characteristic | Definition |
|---|---|
| Metrics | |
| Size | A small hospital, usually with ≤ 30 beds |
| ALOS | Typically < 30 days |
| Population served | Typically serving a rural population |
| Clinical features | |
| Doctors on site | Community hospitals do not have 24/7 on-site medical cover |
| Clinical leadership | May be GP led or nurse led with medical support from local GPs or consultant physicians and geriatricians |
| Inpatient function | The main inpatient function of community hospitals is to provide intermediate care for frail older patients with complex needs or chronic long-term conditions who are referred for step-up (from community) or step-down (from acute hospital) care |
| Range of services | |
| Generalist range of services | Services provided are mostly generalist and are likely to include inpatient care for older people, rehabilitation, some palliative care, outpatient clinics and day care. Some provide maternity services, minor injury and illness units, diagnostics and day surgery |
| Multidisciplinary working | They also often provide a base for multidisciplinary health and social care community health-care outreach teams |
| Services not included | A community hospital will not have a 24-hour A&E department nor provide complex surgery; specialist hospitals (e.g. children’s hospital, a hospice or mental health or learning disability hospital) would not be classified as community hospitals |
Trends
The mapping study was scoped as a snapshot or census (based on 2012/13 data and brought up to date to August 2015 based on telephone enquiries and internet searches). In 2008, the CHA reported72 that there were 296 classic community hospitals (i.e. hospitals with beds) in England. The number, and broad geographical distribution, has remained consistent. Table 15 includes the 267 hospitals visible through NHS Digital data, plus 29 named hospitals from CHA sources. The data show that the number of ‘classic’ community hospitals (hospitals with beds) remained stable between 2008 and 2015. We do not know, however, how the bed complement has changed, nor do the figures show how community hospital numbers have changed through closures during the period since the fieldwork in 2015.
| Strategic Health Authoritya | Number of community hospitals in 2008 | Percentage of community hospitals in 2008 | Number of community hospitals after mapping (2012/13 updated at 2015) | Percentage of community hospitals after mapping |
|---|---|---|---|---|
| South West | 80 | 27 | 82 | 28 |
| East of England | 35 | 12 | 40 | 14 |
| South Central | 34 | 11 | 25 | 8 |
| South East Coast | 34 | 11 | 35 | 12 |
| East Midlands | 29 | 10 | 26 | 9 |
| North West | 22 | 7 | 20 | 7 |
| West Midlands | 22 | 7 | 27 | 9 |
| Yorkshire and The Humber | 18 | 6 | 21 | 7 |
| North East | 17 | 6 | 16 | 5 |
| London | 5 | 2 | 4 | 1 |
| Total | 296 | 100 | 296 | 100 |
Developing a typology of community hospitals
After defining the set of community hospitals as distinct from other hospital types, we sought to develop a typology of community hospitals with beds, drawing on literature and expertise within the research team and from our engagement activities with community hospital stakeholders.
In accordance with our protocol, as only one literature review had been funded across the three studies, we shared findings with the Nolte study team98 and drew on its work to inform our typology development; a high level of consistency emerged. The Nolte study took as its working definition of community hospitals ‘those (1) providing a range of services to a local community; (2) being led by community-based health professionals; and (3) providing inpatient beds’,1 (contains information licensed under the Non-Commercial Government Licence v2.0) but recognised that they provide a wide range of services which produced ‘. . . an inherently variable model of service delivery . . .’. 98
They conceptualised the function of community hospitals as occupying ‘the space between, and to some extent encompassing, primary care services, care and nursing home services, and acute hospital care’1 (contains information licensed under the Non-Commercial Government Licence v2.0) (Figure 10) and reflecting ‘. . . the needs of a local population and the availability of other health services as well as the interests of local practitioners . . .’1 (contains information licensed under the Non-Commercial Government Licence v2.0). This conceptualisation is consistent with the primary–secondary care clinician involvement identified through our mapping work. The space between primary and secondary care spans the intermediate care spectrum.
FIGURE 10.
The nature and scope of services provided by community hospitals. Reproduced from Pitchforth et al. 1 Contains information licensed under the Non-Commercial Government Licence v2.0.
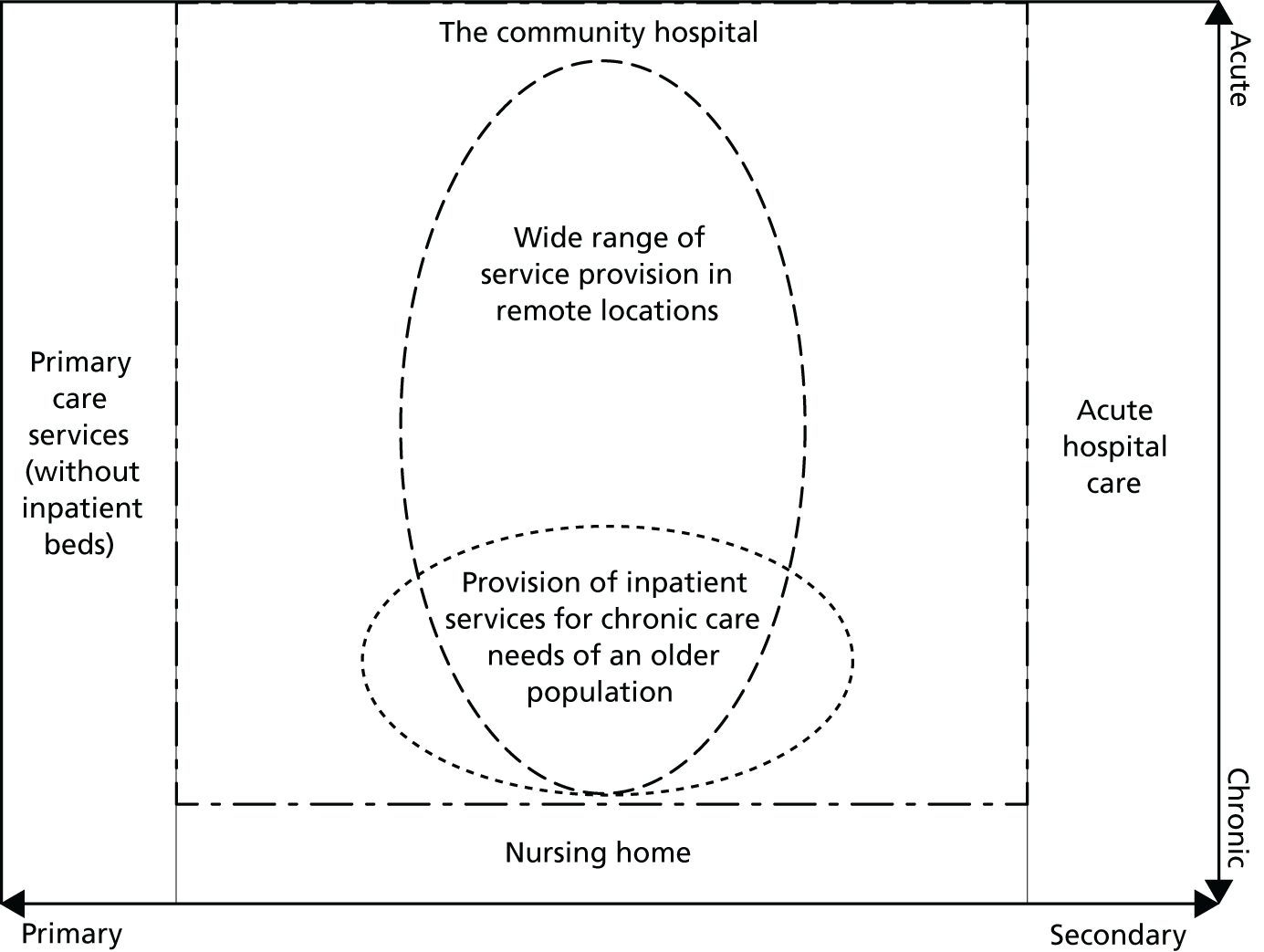
The literature, combined with our stakeholder engagement activities, suggested that one of the key aspects that distinguished community hospitals from each other was their orientation to primary and/or secondary care.
Community hospitals provide diverse services that can be classified along a spectrum with (1) core community hospital provision extended by services orientated to (2) primary/community care and (3) acute care.
-
Core community hospital services, identified with the historic purpose of community hospitals,99 comprise inpatient beds, outpatient clinics and, in some hospitals, minor injuries/urgent care. (Table 8 shows that 80% of the set of community hospitals provide outpatient services and 50% provide MIU). Services may vary in extent and orientation, with some being more community orientated (step-up beds, community-led clinics and a minor injuries and ailments service) or acute orientated (step-down beds, consultant-led clinics and an urgent care unit).
-
Primary/community care-orientated services are likely to be extensions of a GP practice and sited within a community base. Table 16 provides examples of such services.
-
Acute-orientated services are those that might otherwise have been provided in an acute hospital but that have been moved out into the community. Typically, these services are provided as an outreach function to general hospitals and are supported by specialist practitioners. Table 17 provides examples of such services.
| Function | Service examples |
|---|---|
| Rehabilitation/therapy | Physiotherapy, muscular-skeletal therapy, occupational therapy, speech and language therapy, podiatry/chiropody, dietetics |
| Non-consultant clinics | Tissue viability/leg ulcer, continence, falls clinic, audiology, diabetes, sexual health, bereavement support, etc. |
| Day service | Day hospital, day centre, day assessment – for older people, for people with long-term conditions and for those at end of life |
| Community teams | Integrated care for older people, rapid response team, mental health team, Macmillan Team, etc. |
| Third-sector/voluntary organisations | Patient information and resources, complementary therapies, befriending, transport schemes, help in the home |
| Function | Service examples |
|---|---|
| Surgery | Operations and procedures including endoscopy, gastroscopy, cataracts |
| Ambulatory care | Blood transfusions, venesections, intravenous therapies, chemotherapy, renal dialysis, stoma service, etc. |
| Diagnostic | X-ray, ultrasound, DEXA scanner, CT, MRI, phlebotomy, ECG |
The bridge between primary/community and acute care spans the intermediate care spectrum. 100 Figure 11 presents a colour-coded schema indicating how a hospital’s service may be weighted towards either end of the spectrum, depending on service intensity. The extent, frequency and level of service may be calculated based on measures such as the number of beds, number of clinics and hours per week that services such as diagnostics and rehabilitation therapies are available. This schema enables community hospitals to locate themselves within a frame of reference that has been found (among stakeholders) to be realistic and have intuitive appeal. Further detail is available in Report Supplementary Material 5.
FIGURE 11.
A typology of community hospital orientation. a, Not all community hospitals provide all three core services.
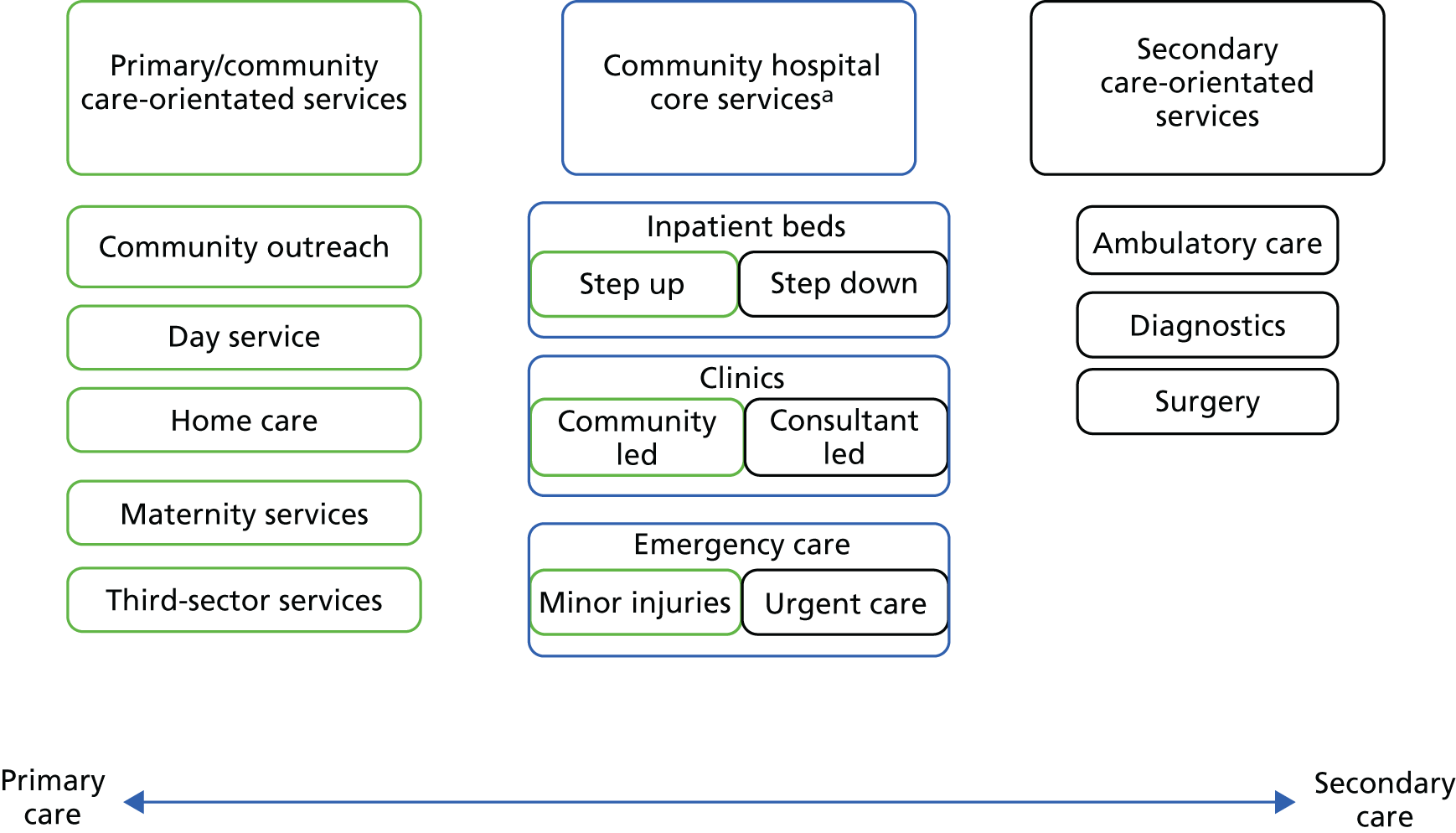
Summary
Findings from this work package add to the understanding of ‘what is a community hospital?’. For the first time, a set of 296 hospitals in England (at 2012/13 updated to 2015) has been identified on the basis of explicit criteria, distinguishing community hospitals from other types, mainly driven by centrally available data and metrics, such as size and rurality. This study provides a baseline for observing future changes in hospital and bed volume.
National data sources were sense checked against other evidence bases, including local practitioner knowledge. The criteria have been encapsulated into a definition that features some change from the reference working definition, removing assumptions of localness, small population base and primary care leadership, and modifying others.
A typology (see Figure 11) has been developed that allows community hospitals to locate themselves along a spectrum of intermediate care provision, distinguishing between primary/community care and acute care orientation. The relationship between community hospitals and other parts of the health system appeared to be shifting, raising questions about how services are commissioned across dispersed geographical areas for consideration in the case studies. These themes are explored in subsequent chapters.
Clinical leadership, involving the role of GPs, nurses and secondary care consultants, has emerged as a complex and changing area, which was further highlighted through our case studies, as discussed in the Chapter 4, and remains worthy of further research.
Chapter 4 Understanding community hospitals: dynamic local contexts
Chapter 3 provided a national profile and revised working definition of community hospitals. In this chapter, we develop this further by describing the nine case study hospitals, identifying their defining features and exploring the changes and developments affecting them. In so doing, we add an inductive, qualitative component to our hitherto primarily deductive and quantitative account of ‘what is a community hospital?’. This chapter reports from case study interviews with commissioners, staff, patients, carers, volunteers and community members. Findings directly relating to patient experience, community engagement or value are reported in subsequent chapters.
Introducing the case studies
In this section, we provide a summary of the case study hospitals (see Appendix 5 for further details). Together, they demonstrate the diversity of community hospitals, while also indicating points of commonality. The descriptions in Box 2 represent a snapshot during fieldwork; some have subsequently experienced significant change.
A classic community hospital providing ‘cradle-to-grave’ services through 18 inpatient beds, a MIU, maternity unit, renal unit, X-ray and extensive outpatient clinics. It is situated in a middle-sized market town in the rural south. The hospital has its origins as a Victorian workhouse, but was rebuilt on an adjacent site in the 1990s. The main provider is a NHS (acute and community) health-care trust, which also owns the property. GPs from the adjacent surgery provide the medical cover. It has a reinvigorated League of Friends, but below average voluntary income levels. Since the fieldwork finished, the main provider and ownership have changed, and inpatient services have been unexpectedly closed.
CH2A large community hospital providing 32 beds, maternity, day surgery, diagnostics and an extensive range of outpatient services. It is situated in a large market town in the rural south. There has been a hospital in the town since the mid-1850s, with the current building opening on a new site in the mid-2000s, funded through a private finance initiative. The main provider is a NHS acute trust (under transition during fieldwork), with several other providers also on site. Medical cover is provided by both local GPs and trust doctors. It has an active League of Friends, with above average voluntary income levels.
CH3A classic community hospital providing ‘cradle-to-grave’ services that include 28 beds, MIU, maternity and extensive outpatient clinics. It is situated in spacious surrounds, in an ex-mining village in the rural south. The early development of the hospital is closely tied to the mining community, with community links further strengthened through its designation as a memorial hospital. It was rebuilt in the 1990s with community support. It is owned by NHS Property Services and the main provider is an integrated health and social care CIC. In-house doctors provide medical cover. It has a committed League of Friends with high levels of voluntary income and extensive support. Following fieldwork, there was a change of provider to a private sector organisation.
CH4Provides 31 beds (eight of which are designated stroke beds), a mental health inpatient facility and various outpatient clinics. It is situated in a small city, with a rural hinterland. It originated as a workhouse and was the site of the city’s main general hospital before losing many of its services in the 1990s. Some questioned its designation as a community hospital. It is currently owned by NHS Property Services and the main provider is an integrated health and social care CIC. In-house doctors provide medical cover with advanced nurse practitioner support. There is no League of Friends, with the group having folded following the retirement of previous committee members. Following fieldwork, there was a change of provider to a private sector organisation.
CH5A classic community hospital providing 14 beds, a MIU, X-ray, a day care centre, and extensive outpatient clinics. It is situated in beautiful surrounds on the edge of a medium-sized market town in the rural south. It has its origins as a cottage hospital built in the late 1800s, but was rebuilt as a war memorial in the early 1930s, with land and bricks donated by the local community. It is currently owned by NHS Property Services, with the main provider being a NHS community health-care trust. Various other providers also operate on site. Medical cover is provided by an in-house doctor. Staff recruitment has been an issue, at times leading to temporary bed and other service closures. It has an active League of Friends with healthy levels of voluntary income, although membership has been declining. As the fieldwork came to an end, consultations were underway regarding the development of a new GP surgery with implications for the hospital’s future.
CH6A small community hospital with its services limited to 22 inpatient beds and outpatient physiotherapy services. It is situated on the edge of a village in the semirural south. It was built in the 1870s with the support of a local benefactor. Its main services are provided by a NHS community health-care trust that also owns the property. Medical cover is provided by local GPs. Staff recruitment has been an issue. It has an active League of Friends, although their activities are increasingly focused on initiatives outside the hospital itself.
CH7A relatively small hospital with 14 inpatient beds and a range of community and outpatient services. It is situated within a developing ‘health campus’ that contains a GP surgery and sheltered housing, with plans for further development. It is situated in a small, vibrant coastal town in the rural south. The hospital originated in the late 1910s as a war memorial. In the early 1990s it was closed by the NHS against considerable public protest. Following considerable fundraising efforts, the community established a charity to buy, rebuild and reopen the hospital. It is currently owned by the community-led charity, with the main services provided by a NHS acute and community health-care trust and medical cover provided by local GPs. The League of Friends merged with the charity, which together represent significant voluntary (time and money) support.
CH8A relatively small community hospital with nine beds and a limited range of community and outpatient services. It also houses the GP surgery. It is situated within a small, isolated town in the rural north, which has experienced decline. It is a relatively new hospital, having been built in the mid-1970s on land donated by a local benefactor. The property is currently owned by a NHS community and mental health foundation trust, which also provides the main services, and GPs provide medical cover with advanced nurse practitioner support. In the early 2000s, the community launched a vigorous and successful campaign to ‘save’ the hospital in the face of (perceived) threats to its future. The campaign led to a new partnership between commissioners, providers and community, and the repositioning of the hospital at the centre of an integrated care community. Although community support is strong and active, the League of Friends is relatively small with low levels of voluntary income.
CH9A relatively large community hospital providing ‘cradle-to-grave’ services including 24 beds, MIU, X-ray, clinical decisions unit, day hospice, and an extensive range of community services and outpatient clinics. It is situated in a large-ish market town in the rural north. The hospital has its origins as a cottage hospital founded in the late 1890s, but was rebuilt on a new site in the 1980s. It is currently owned and its main services are provided by a NHS community and mental health foundation trust; the trust employs salaried doctors to provide in-house medical cover. Its League of Friends has average levels of voluntary income, and its volunteers are particularly active in supporting the day hospice.
Revisiting our national definition of community hospitals
In this section, we revisit the working definition of community hospitals identified through the national mapping (see Chapter 3), highlighting any significant local variations and changes within these dimensions.
Small, usually ≤ 30 beds
Smallness was confirmed as one of the defining features of community hospitals, and was a significant factor in shaping patient experience (see Chapter 5). The bedded capacity of the case studies ranged from 9 to 32, although this fluctuated depending on commissioning decisions and availability of staff. At least two of the case study hospitals had recently closed a number of their beds because of a lack of qualified nursing staff.
Furthermore, the future of community hospital beds was the subject of intense debate locally: ‘beds are absolutely a touchstone issue for the public’ (CHs 8&9, T02). Many respondents argued passionately that community hospital beds continue to provide an important role in acute admission avoidance, step-down rehabilitation and end-of-life care. Some respondents (most often commissioners and senior managers), however, questioned the need for and/or affordability of community hospital beds, suggesting that patients could be better cared for either in their own home or (less often) in acute hospitals. Many, from both sides of the argument, questioned how a ‘new model’ of care at home would be supported considering the significant reductions to social care budgets and problems associated with delivering care across dispersed rural communities.
Typically serving a rural population
The case studies reinforced the significance of ‘rurality’ as a defining feature of community hospitals, although not all community hospitals are in rural locations: one of our case studies was in a city (although situated within a largely rural area). Regardless of their official classification (three of the case studies were classified as semirural, and six were identified as rural), all but the city-based community hospital were described by respondents as being ‘rural’ and (relatively) ‘isolated’ or ‘peripheral’, because they were far from any major centre of population, on the border of two or more counties, or on the coast. Rurality was associated with poor transport links, particularly public transport, which meant that accessing centralised services could be difficult:
Rurality is quite a burden actually. A lot of our patients aren’t as rich as city dwellers and transport is a huge issue really.
CH1, S03
Rurality and isolation were, however, acknowledged to be relative concepts. For two communities, each based 20 miles from their nearest acute hospital, this might represent 30 minutes of travel time for one, and 1 hour of travel time for the other; for an older person reliant on public transport this might represent a significant, challenging journey, whereas for a younger person with access to a car it might not seem far at all. Alongside accessing acute services, respondents identified poor rural transport as exacerbating the challenges of organising care packages to enable patient discharge.
The rural locations of community hospitals were also perceived to exacerbate recruitment challenges, because of poor accessibility and (generally) high housing costs. Recruitment challenges extended from qualified nursing staff to other professions: the inability to recruit a radiologist in one hospital, for example, had resulted in the X-ray facility being closed for several months. In a couple of cases, a number of recruitment issues had, at certain times, coincided to create a particularly challenging, risky, environment. Additional features of rural communities, including a limited and declining range of services, limited employment opportunities and relatively high levels of social capital and volunteering, influenced the function, use and value of community hospitals (see Chapters 5–7).
The one city-based community hospital case study appeared distinct from the others in a number of ways, most notably its lack of active community engagement (see Chapter 6), but also in some aspects of patient experience. As the only city-based hospital within the sample, however, it was not possible to conclude on the significance of this over other influential factors. It had also, for example, changed its function and service mix considerably over time from a workhouse to a DGH to a community hospital. Indeed, some respondents questioned whether or not this case study should be considered a ‘community hospital’ (see Chapter 7).
Without 24/7 medical cover
The mapping work established that community hospitals are distinguished from other hospitals by not having 24/7 medical cover, and this was reflected in the case studies. However, the case studies highlighted variability in the level of cover provided. Although there was clear guidance on the ratio of nursing staff to patients, this was not the case for GPs/doctors and there was considerable variation in the number of hours of medical cover provided. In one case study, the local GP surgery was reportedly contracted to provide just 0.5 hours a day (although in practice it provided more), whereas others had the equivalent of more than one full-time doctor. The difference could not be accounted for by bed numbers alone. Getting the level and type of medical cover ‘right’ was a challenge identified by a number of respondents: too little medical cover could leave patients at risk and contributed to GPs’ reluctance to continue providing cover.
General practitioner or nurse led
The involvement of GPs has historically been a defining feature of community hospitals. The mapping indicated a shift in GP leadership, the extent and significance of which was highlighted in the case studies. Although GPs have traditionally provided medical cover for community hospitals, we identified two distinct medical models:
-
general practitioner – in which either one specific GP from a local practice or a number of GPs from one or more practices were responsible for providing medical cover through a service level agreement for a specified number of hours per week
-
in-house doctor(s) – salaried doctor(s) employed directly by the trust to work specifically within the hospital.
Overall, there appears to have been a shift away from the first model towards the second. The withdrawal of GPs in a number of community hospitals has been influenced by a number of factors including the increasing acuity of community hospital patients, referrals being drawn from an increasingly wide geographical area and frustrations from GPs who have had admission rights withdrawn and/or find it increasingly difficult to step up their own patients into community hospital beds because of pressures from the acute hospital for step-down beds. The burden on those GPs who remain involved can be considerable:
It was just like looking after our patients but now we don’t know them so it’s changed [. . .] I mean, certainly we have found with our new young GP he could not cope with it, trying to do rounds here at 10 p.m.. It’s not good for the patients either but it’s not good for him and the worry is that if it does not change, you know, as we sort of retire, are they actually going to be able to stick with it?
CH7, S08
Despite these challenges, it was felt that the majority of the GPs interviewed were committed to their local community hospitals and recognised their value in the (rural) health-care system. Regardless of GP involvement and the medical model in operation, in practice, patient care at each of the hospitals was best described as nurse led, with nurses being the constant presence and medical staff providing a service on a sessional basis.
Main inpatient function is to provide step-up and step-down care
The case studies reflected the findings of the national mapping: that community hospitals provide a mix of step-up and step-down care. However, there was a strong suggestion that they are increasingly likely to be operating as step-down facilities (as extensions of acute hospitals), reducing the capacity to provide step-up care.
Increasing pressure from acute hospitals to discharge patients to community hospital beds was seen to have contributed to this general shift in the ratio of step-up to step-down patients. In turn, step-down patients were seen to be contributing to high occupancy rates, an increasing acuity of patients and longer lengths of stay. Together this meant that it was hard to ringfence beds for step-up patients, leaving GPs and residents frustrated when beds were not available for direct admissions, which could in turn contribute to more people going directly to A&E/acute hospitals:
But I think if we looked at figures for the last 6 months, we’d find that the step ups are very reduced, and that’s due to our pressure in the acute, which feeds down to us. They have been on level 4 all summer, which is a high level of crisis [. . .] So that means that they over-ride our ability to be able to keep [. . .] step-up beds because they are just filled [. . .] and we have also been running on almost 100% occupancy constantly for the last 6 months, so, literally, the beds are not cooling before another patient arrives.
CH9, S10
Increased pressure to step down patients also meant that patients were increasingly likely to come from outside the local area. Although this was mentioned in all but one of the case study sites, it was particularly extreme in two cases where a minority of the inpatients at the time of our visits were ‘local’.
The balance of step up and step down was seen as a ‘real battle of philosophies’, raising fundamental questions about the function of community hospitals and whether or not this was shifting from rehabilitation towards subacute care:
It is rehabilitation in one aspect, but it is also semiacute care, hospital care, that we are providing and that is a significant change that we have seen. People before just came for rehab[ilitaion], but now people are coming because they are unwell and we are looking after them and getting them better.
CH9, S01
Many respondents expressed a desire for a higher number of step-up referrals and for community hospitals to play a greater role in acute admission avoidance and broader prevention work.
For frail older patients
Community hospital inpatients were typically described as being ‘very elderly, very frail, multiple comorbidities . . .’, increasingly including patients with dementia, and often with a range of other associated health and social care issues. The ability to provide generalist, holistic care to address these multiple issues was identified as an important and valued aspect of patient experience (see Chapter 5). However, the increasing age and frailty of patients combined with the shift from step-up to step-down care also meant that community hospitals were caring for patients who are increasingly unwell; the level of acuity on many wards was reported to have risen considerably.
The increasing acuity of patients presented a number of challenges for community hospitals, not least relating to the level of medical cover available and the skills of nursing staff. This could result in patients being bounced back to the acute hospital when it became apparent that they were too poorly to be looked after within a community hospital. Some staff talked about being given misleading or incomplete information about prospective patients that could lead to inappropriate admissions:
So, we’ve had patients come over and within a few hours they are back at the [acute] because again they are just not well or they’ll tell us that they are walking and they can transfer with one, they arrive and they cannot walk.
CH7 S09
Although inpatients in all the case studies were typically older, frail and increasingly acute, the age range of all patients varied across the hospitals, influenced by the range of services that were provided, with the presence of a maternity unit and MIU in particular broadening the age and demographic mix of hospital service users.
With an average length of stay typically < 30 days
Considerable developments have taken place over the past decade or so to reduce the ALOSs of community hospitals to typically < 30 days. However, these efforts were being countered by the increasing acuity of patients.
An even more significant challenge to reducing lengths of stay was the (lack of) availability of care packages to enable timely discharge. Underinvestment in community and social services and a lack of domiciliary care services and nursing homes in rural areas were identified as significant contributory factors. It was suggested that a significant proportion of patients within some community hospitals ‘do not need to be there’ but could not be discharged because ‘there are not enough care packages available’. This led some to suggest that community hospitals had become ‘waiting rooms for social services’.
Likely to include rehabilitation and palliative inpatient care and a range of additional services
The main function of the case study hospitals’ inpatient services is rehabilitation, with each contributing to post-acute discharge and acute admission avoidance. In addition, all play an important role in providing end-of-life care. There were, however, differences as to the emphasis placed on these different roles. The provision of generalist intermediary care was a key feature and value of community hospitals:
Well, for me it bridges the gap between traditional general practice and the large secondary care hospital, and that is increasingly important with our patient demographic and rising age of our patients.
CH1, S06
There was considerable variation, however, in the range of services provided. Despite providing 22 beds, for example, one hospital offered very few other services beyond a few outpatient physiotherapy and antenatal clinics. This is in contrast to four hospitals that were typically described as providing ‘cradle-to-grave’ services in that, alongside the beds, they provided maternity services, a MIU, X-ray, and a wide range of outpatient and community services. Thus, the case studies occupied different positions along the intermediate care spectrum identified through our mapping work (see Chapter 3). Although some were firmly positioned in the middle of the intermediate care spectrum, others had additional services that led them towards a primary/community care orientation, whereas still others tended towards the acute orientation end of the spectrum.
These differences in function, service mix and orientation were influenced by a number of factors, including commissioning context, provider characteristics, local ecology of related health and social care services, size and range of services, medical model, patterns of recruitment, community support and transport infrastructure.
Additional key features of community hospitals
Interviews and focus groups carried out in the nine case study sites uncovered further features that appeared to be characteristic of community hospitals. These are described below.
Historically embedded
The case study hospitals were of different ages and had different origins, ranging from six that dated back to the 1800s to one that was built in 1975. All but one were in operation prior to the establishment of the NHS. Two had their origins as workhouses, one was built as a First World War memorial and two more became memorial sites. Three started as cottage hospitals founded and run by members of the local community; the early history of one was strongly tied to the local mining community. Most (if not all) had benefited from significant voluntary contributions from either an individual local benefactor or more widespread local investment to get them started – even the newest was built on a plot of land donated by a local resident. The different historic origins and development trajectories of the hospitals influenced contemporary patient experience (see Chapter 5), engagement (see Chapter 6) and value (see Chapter 7).
Operating with complex models of ownership and provision
Although all hospitals were incorporated into the NHS in the 1940s, the current ownership, commissioning and provision of community hospitals were diverse and complex. At the time of the research, one of the hospitals had been (re)built as a Private Finance Initiative, one was owned and had been rebuilt by a local charity, the others were owned either by NHS Property Services Ltd (London, UK) or by a local provider NHS trust. Regardless of legal ownership, many communities (including patients and staff) perceived the hospitals to be theirs (see Chapters 5 and 7).
The commissioning context was also significant. Different commissioners viewed community hospitals, their value and position in the health-care system differently. For some, community hospitals appeared to be ‘key’ to supporting ‘the wider health community’ with an ‘integral role in our discharge and admission avoidance approach’ (CHs 3&4, T02). For others, they appeared more marginal or unaffordable.
Other aspects of context were also influential: some were in Success Regime areas, one was in a vanguard area, one was entering a period of consultation regarding its future, and all were implicated in developing STPs. This complex local policy landscape, combined with a lack of national community hospital policy, was adding to the variation across community hospitals.
There was also variation in the ‘main providers’ (defined here as those responsible for inpatient services) of community hospital services. The main services in two of the hospitals were provided by a CIC that encompassed both health and social care (the contract was awarded to a private provider shortly after our fieldwork at this site). In the others, main inpatient services were provided by NHS trusts, but each trust differed in terms of its focus and its provision of community, acute, mental health and/or social services. In each of the case study sites, the main provider was just one of a number of statutory, voluntary and private providers within the hospital, although the significance of the main provider varied. In one hospital, we identified over 10 providers.
The increasing number and diversity of providers operating services within a single community hospital site was identified as a significant, if not unique, feature of contemporary community hospitals. It was suggested that the lack of a single organisation or person responsible for overseeing each community hospital as a whole exacerbated challenges of integrated working across a multiprovider site. Without any overall control, multiple providers, it was suggested, could lead to fragmentation:
. . . we would love to feed in and out for staff training into different departments, but we’re a different organisation, so what would have been simple within our organisation becomes complex and you have to get a set of special agreements [. . .] we have different induction, you know, different training, different management responsibility, governance. I mean it just goes on and on really. It’s a very peculiar invisible barrier, which the NHS is full of invisible barriers.
CH2, S10
Providing a base for rewarding, integrated and multidisciplinary work
Despite current concerns about fragmentation of providers, community hospitals were more generally seen as important sites for the increasing integration of health and social care across statutory, voluntary and private providers. This was particularly so for those whose main (inpatient) services were provided by an integrated provider and/or where health and social care services were co-located and/or where a single manager had responsibility for health and social care teams.
Significant challenges to integration were noted however, particularly because of pressures on social care budgets. A number of our respondents reported a recent reduction in the presence of social workers at the hospitals and a more general reduction in the capacity of social care teams to support patients.
Multidisciplinary working was also identified as a distinguishing feature and strength of community hospitals and as contributing to the high levels of staff satisfaction we observed. One respondent suggested that this was facilitated through more equal power dynamics between disciplines:
So it’s very different here from when I used to work in an acute hospital many years ago. The doctors there were very much in charge, very much, ‘right, that person can go home tomorrow’. And you’d be scrabbling around trying to get what they need to go home. Whereas here we are having these discussions, aren’t we, about ‘they are well but, OK, they cannot do this, they cannot do the stairs, they have not got their care in place’. And the doctors understand that here.
CH3, S03, focus group (FG)
There were, however, different dimensions to this, and some exceptions. In most cases, it was suggested that there was a strong MDT working across ward-based nursing and therapy teams. This was facilitated by a range of mechanisms (e.g. case meetings, ward meetings, shared notes), teams being permanently based within the hospital and being jointly managed. There was less consensus on the effectiveness of multidisciplinary working across hospital and community teams and across community and acute hospitals.
Constantly evolving in response to external demands
A number of respondents suggested that, as a result of historic evolution, subsequent diversity and ongoing contemporary change, there was a lack of clarity regarding what community hospitals are and what they do. This lack of clarity, it was suggested, left community hospitals vulnerable to questions regarding their relevance and value. Indeed, the current financial, policy and commissioning context, combined with recent changes within community hospitals, had contributed to considerable debate about their future role and function.
It was suggested that, over time, a lack of strategic planning had meant that community hospitals had evolved in different directions: that many had ‘morphed and changed organically’ and that this had ‘contributed to an identity crisis for the [community] hospitals’. Although this ability to adapt was seen as a strength and a sign of resilience, some argued that for the potential of community hospitals to be realised a more strategic approach was needed:
But, of course, we do need to think more strategically. My concern is that, if you like, [this community] hospital at the moment is in the same position, nobody is thinking strategically about it [. . .] But if [this community] hospital could make up its mind about where it needs to be, I think then it could be very much more successful than it is.
CH2, V03
A ‘strategic vision’ was more evident in two of our case studies: in one case a charity owned the hospital and was working hard to develop and deliver its vision of the community hospital in the centre of a health campus, and in the other case a crisis had brought commissioners, providers and the community together to think creatively about the hospital’s future role in the local population’s health care.
Discussions regarding the future of community hospitals centred on their potential as ‘hubs’ for a wider range of health and social care, public and voluntary sector services: ‘a real heart of health and well-being of the community’. Community hospital ‘hubs’, it was suggested, could play a role not only in step-up or step-down care but also in prevention.
Although there was a consensus and enthusiasm regarding the potential for community hospitals to develop as hubs, there was less agreement regarding the provision of beds within them (as discussed above). Although patients, carers and communities generally agreed that inpatient beds should remain a feature of community hospitals with an expanded range of services, commissioners and senior trust staff were more likely to question this. They tended to see ‘hubs’ without beds replacing community hospitals with beds. Any mention of removing beds was strongly opposed by local community members, with a belief that only financial imperatives were driving such decisions, regardless of patient experience and community value:
The line behind all this is the philosophy that the whole driving force is money and the patient is very much far down the list. It is all about money, and not about the patient.
CH5, V03, FG
In some areas, a counter-argument put forward was that communities were not fully informed about either the safety of community hospital beds or the wider context within which they operate:
So I think those people that speak very strongly about community hospitals, the League of Friends and things have got, they might not necessarily see the bigger picture so yeah they will fight very strongly for their community hospital and may not also understand where it fits in into the bigger jigsaw and actually may not be aware of some of its limitations.
CH9, S05
The ability of all stakeholders to influence strategic decisions regarding the future of community hospitals was questioned by community stakeholders in many of the case studies (see Chapter 6).
Summary
Community hospitals are a diverse set of institutions, each rooted in its own historical, geographical, commissioning, service and social context and each having evolved over time. Although change is nothing new to community hospitals, the current pace and scale of change was seen to be exceptional. Increasing pressure from acute hospitals, moves towards step-down care, increasing acuity of patients, moves away from serving only local patients, withdrawal of GPs and growing financial and policy pressures raising questions over the future of community hospital beds were all identified as significant developments that, together, contributed to a sense that ‘community hospitals have changed tremendously’.
Community hospitals remain, however, small, predominantly rural, hospitals that are historically embedded within their communities, operating complex models of ownership and provision without 24/7 medical cover. They are GP and/or nurse led, provide integrated, multidisciplinary, step-down and (limited) step-up inpatient care for frail, older and increasingly acute patients, with a variable range of additional services across a spectrum of generalist intermediate care, with some orientated towards either the primary or secondary end of that spectrum.
Community hospitals are sites of considerable, but different, expectations – from commissioners, staff, patients, family carers, community members – but without any consensus on how those expectations should play out and often without any clear leadership and governance structure at the individual hospital level to enable those decisions to be made. Subsequent chapters will illustrate how many of these issues play out in complex ways to influence patient and carer experience, community engagement and community value.
Chapter 5 Patients’ and carers’ experiences: a human kind of care
In this chapter, we explore patients’ and family carers’ experiences of community hospital care and services. Drawing predominantly on patient narratives and carer interviews, we explore how people describe their experiences of community hospital services, care and treatment, and examine the factors that shape or influence those experiences. When relevant, we integrate accounts from interviews with staff, volunteers and community members of their perceptions of patient and carer experiences. The emphasis within our analysis and reporting within this chapter is on the themes that emerged from the interviews: on what featured most strongly in patients’ and carers’ stories of their experience of community hospitals, rather than on predetermined categories. In Chapter 8, we link these findings back to existing literature, including that on the danger of context-bound research, and propose new categories for evaluating patient experience.
Experiences reported are primarily about inpatient services, with some reflections on outpatient clinics, MIU, maternity services and specialist tertiary services. Narratives reflect the experiences of patients and family carers, with staff, volunteers and community stakeholders also included, both for triangulation and because many had used the services themselves, had family members who used services or, through their work or volunteering in community hospitals, had observed or received feedback on patient and carer experiences. Findings are clustered into three overarching themes that are central to what we have identified as distinguishing features of community hospital services and care: (1) it is and is not a hospital (care closer to home), (2) it is a whole experience (personalised, holistic care) and (3) it is a huge life event (support through transitions). These themes reflect patient and carer narratives, which bring together the relational – interpersonal, social and psychological – aspects of their experiences (themes we return to more explicitly in Chapter 8). This contrasts with previous studies that more typically focus on the functional and technical aspects of care.
It is and is not a hospital: care closer to home
Many patients, carers, staff and others talked about community hospitals as not really being like a hospital, describing its location, outlook, facilities and atmosphere as being different from previous experiences of acute care. In this way, patients and carers experienced community hospitals as being and providing ‘care closer to home’ in ways that went way beyond physical proximity, convenience or physical environment.
It is just different
It is unique [. . .] you go out into the day room and you look across those fields, you know, it’s bright and airy and there’s no sort of closed corners or anything. It doesn’t feel like a hospital, does it.
CH6, S05
‘It’s different’ was a frequent response when patients and carers (and indeed staff) were asked to reflect on their experiences of the community hospital, with participants often distinguishing the atmosphere and environment in community hospitals particularly when compared with that in acute care. A difference in ‘pace’ was frequently cited, with a more relaxed environment, less pressure on staff, more time to pay attention to individuals/the whole person (see below) and a strong sense of feeling less anonymous:
The whole thing was so much nicer and easier rather than if she’d have gone into the [acute hospital]. She’d have just been one more elderly person in a great big ward.
CH1, P06
Carers also frequently mentioned differences in the environment and atmosphere, describing community hospitals as cleaner, tidier, more peaceful, quieter and calmer than acute hospital wards: they were more like home than hospital.
Other differences were the outlook and access to gardens, which staff and/or volunteers often facilitated; this made a real difference and lifted patients’ spirits:
I don’t have any children, my dog is my world, and it was possible when I asked the nurses that my parents brought my little dog to the garden outside so that I would be able to see her, which I wouldn’t have got at another hospital.
CH9, P03
Some people talked about the physical size of most community hospitals as being different, particularly in contrast to acute hospitals. Community hospitals were less intimidating, and this, it was suggested, was particularly valued by patients who were older, frail, and confused, or when they were dying:
She was by far and away happier with those visits to [this community hospital] and I think that’s all about the fact that it’s a small community and much less daunting, particularly people who get, and often the case, get a bit confused towards the end of their lives.
CH1, CY04 FG
Others talked about how a ‘community-based’ hospital felt different because of its location and because of a greater chance of being known by staff (we return to this theme in It is known to me):
Because it’s a small community and it’s quite an old-fashioned community here, everybody knows everybody, it’s one of those sorts of places, people know the staff and most of them are very local.
CH8, CA01
In MIUs and clinics, differences related to the design of reception areas and meeting familiar faces, as well as to the environment, waiting times and staff attention:
I think the longest wait I’ve had [. . .] I probably waited best part of an hour but you know, pleasant surroundings, water to drink, loos to go to if necessary, plenty of magazines around and the attention when I get it is faultless, as far as I’m concerned.
CH1, P01
As many people attended clinics on a regular basis, however, ‘familiarity’ sometimes made it difficult for staff to get on with their work:
They stay there talking and it’s like ‘I really need to see the other patient behind you’.
CH1, S04
They recognised, however, that this was a distinguishing feature of working in a community hospital:
You probably know them far more than what you would do if you worked in an acute hospital.
CH1, S04
However, not all patients thought that community hospitals were all that different from acute hospitals in all respects, and not all found all aspects of the environment positive. Issues such as night-time noise from doors or a sluice disturbed some people’s sleep. Some also felt isolated in single rooms and missed the social interaction of multibedded bays, whereas others commented on clinics not being as friendly. Some staff suggested that younger people sometimes associated the hospital atmosphere with an ‘old people’s home’ and felt alienated because of their age.
Like home from home
Many patients and carers directly used the term ‘home’ or ‘homely’ to describe their community hospital, with familiarity, relationships and proximity to their own home contributing to them feeling ‘at’ home. The notion of home also emerged when community hospitals were compared with acute hospitals, with the smallness of the hospital making it feel very much like a ‘family home’. Some Leagues of Friends deliberately invested in more homely design and furnishings, contributing to the creation of a less clinical environment:
I think they felt it was like home. And I think when we designed the hospital and furnished the hospital, we particularly wanted to make it slightly less clinical, you know, so a home from home type of place, you know, that people did feel comfortable in.
CH3, CY02
Staff and community stakeholders recalled with amusement how two community hospitals were locally referred to as the ‘Hilton.’ They associated this with the quality of the food, how patients felt cared for, and the comfortable facilities, such as single rooms and en-suite bathrooms being a ‘luxury’, as well as the way staff responded to calls:
If you needed someone . . . you rang a bell and the response was always immediate, absolutely immediate.
CH1, P03
However, feeling too much at home could have its downsides. Some staff thought that patients expected to be looked after and could end up a little too comfortable, citing times when inpatients did not want to go home:
And then you get some of them, you say they’ve got to go home, they have a little fall so they do not have to go home! They do not fall enough to hurt themselves, but just enough to give them a shock so they will not send them home that day.
CH6, S03
This was mirrored by some patients talking about how they could ‘live here quite happily’ (CH7, P07). However, staff understood that people’s reluctance might be an expression of their fear of social isolation and the lack of similar comforts and levels of support at home:
And then they don’t relish the thought necessarily of going home where they might be isolated or maybe not have all the same services in place or not get that same level of comfort [. . .] and then when it comes closer to that discharge, all of a sudden it’s, ‘Oh, I’m going to be on my own’.
CH7, S04
It is convenient
Being local and accessible (physically closer to home) was also key to patient and carer experiences. Patients and carers valued having a local hospital that they felt was much more convenient than other forms of service delivery, with less distance to travel, ease of parking and less waiting:
It saves us all going in there [acute] and using our money and fuel to get there and parking there and waiting there.
CH1, P06
Convenience was important for both inpatients (and their carers) and outpatients, particularly those who had to attend the hospital regularly for relatively small procedures:
I think convenience does come a lot into it . . . with the ageing population, and having to travel so far, to say it will take 2 minutes to get somewhere for a blood test or it’s going to take you half a day, to go in and, all that sort of thing.
CH2, S10
Being so conveniently located often enabled family members to visit daily, several times a day for some, which was particularly valued. Flexible visiting hours were also seen as convenient and helped both working visitors and older visitors who found driving stressful:
Here, they’re convenient hours because they are 3 till 5, which is better. To me those are better hours [. . .] I can’t travel at night because the lights [. . .] especially through these lanes, they affect me [. . .] It’s hard to judge. It’s a strain. And that affects a lot of people.
CH8, CA02
Weekend services and later opening times for urgent care also provided convenience for the whole family, and a range of local clinics provided easy access:
You can self-refer here for physio[therapist] treatment where normally you would have to go to your doctor, then you have to wait for appointments [. . .] it’s very, very good in the fact that it is almost like a drop-in centre for that.
CH8, CA03
At times, the idea of the convenience of local services appeared to mean more than practicality, encompassing other important social and emotional aspects, such as enabling someone to maintain their independence and dignity through being self-reliant in terms of getting to and from the hospital:
That was that much more convenient and in fact I can drive myself here [. . .] to do it here again makes a big difference in the life of somebody of my age [89 years] and ability to get around and that sort of thing.
CH1, P01
However, the location of a community hospital was not always convenient for everyone. Some of our case studies were located just outside a village or town, making them seem slightly isolated. Moreover, some inpatients who had been referred in to the community hospital from outside the local area talked about feeling a long way from home, even when care was experienced as good. Poor public transport made it difficult for those living outside the immediate area to get to community hospitals when they could not drive:
If you don’t drive, I am afraid the bus, public transport, is appalling. We had one woman whose husband was in here, and sadly she passed away not long ago, but he was in here for quite some time. She would visit every day, she came on the bus. And it took her 1 hour from [town], each way, and of course if you miss one bus, you are in dire straits.
CH5, V01
As an increasing proportion of inpatients within community hospitals are stepped down from acute services (rather than stepped up from the community) and come from outside the local, immediate area, this is likely to become an increasing concern for community hospital patients. This meant that some people had to take taxis, a considerable cost for those living on pensions, or rely on family members to transport them; at times, this meant carers and other family members making big sacrifices:
Yes, well I’ve had to rely on my daughter [to take me to visit my husband in hospital] because I don’t drive and she actually gave up her job because she was going to have like a few months off knowing probably this would be more care.
CH1, CA03
For some, their frustration with the lack of public transport in rural areas was closely linked to their experience of having to drive long journeys to acute hospitals for some clinics, which heightened their concern that community hospitals remain part of local service provision:
It’s a 60-mile round trip for me [to acute], and at 80 years old you do not want to be [. . .] in the winter, driving 60 miles. So when they said she was coming [to the local hospital] I thought, ‘Fine.’ And I thought then, well this is what it should be all about. They should not be trying to put patients away from their families, you should try and consolidate them.
CH2, CA01
It is less stressful and more reassuring
For a number of people, going into hospital itself was experienced as stressful, perhaps because of the anxiety about their illness. Being able to attend a small, local hospital where they were known appeared to relieve this stress: ‘you do not get tensed up about coming here.’ Some patients experienced such a ‘fear’ of hospitals in general that the only way they would be persuaded to accept treatment was by going into a local community hospital:
[This] lady, absolutely epitomises why we need to be here. This is a lady with white coat syndrome, terrified of acute admission, terrified of attending appointments.
CH7, S05 FG
For some ‘fear’ seemed to be linked to separation from what was known and familiar: ‘because they are torn away from everything and everyone.’ For others, anxiety was about hospital size, impersonal surroundings and not knowing anyone there. Being ‘closer to home’, in all the different ways described above (i.e. not just physically), helped to ease these kinds of fears and anxieties for patients attending community hospitals.
Stress and worry were quite often talked about by family members, with the term ‘lifesaver’ used to convey the relief families felt by being able to access local services and receive good care for their loved ones:
It totally saved my life. Without [community hospital] I really don’t know what we’d have done because I was in a total mess with [name] care and, as I’ve said before, I just did not know what to do.
CH3, CA01
For carers, it was reassuring to know that their relatives were being cared for well and nearby, particularly when they were unable to do it themselves and when they were at the end of their tether. When patients were admitted to hospital, carers were concerned about ensuring that their needs were understood and taken care of properly, particularly when relatives could not communicate for themselves. In this context, finding a community hospital where a relative could receive good care provided palpable reassurance for one carer and perhaps shared her burden for a short while, as she had never had more than 1 hour off from caring for her husband:
I just knew that he was safe and for me that was huge. I was trying to work, I was trying to sort out what I was going to do with him, I was trying to sort out my father’s palliative care [. . .] They just seemed to understand here that that’s what we needed . . . I am on my own, I don’t have a support network apart from through the NHS and I haven’t got a clue what I’d have done. I think I would have probably ended up taking him off the bridge or something because there was not anywhere to go. I even went away for a weekend while he was here and left them to it; I had not been away for more than an hour.
CH3, CA01
It is known to me
Local community hospitals often engendered a deep sense of ownership and connectedness, because they were embedded in community history, civic pride, family values and personal significance: ‘I was born on this land here where the hospital is now sited [. . .] and I’ve lived here ever since’ (CH1, P02) (see Chapter 7). This ‘known-ness’ was fundamental to many people’s experiences of community hospital inpatient care, because it was experienced as less anonymous, more understood, more personalised and connected. A staff member, who also used the community hospital as a patient – as did her family – illustrated this fundamental ‘known-ness’:
I suppose for me it’s where I come to work but it’s also my community hospital. This is where I come to use maternity services, we have used outpatient physio[therapy], we have seen consultants here. Used it for lots of reasons so it’s my hospital to come to as well as my place of work. So yeah, it feels like another home and it’s like a good place to come to.
CH3, S03 FG
Knowing others in the local community was a factor that shaped people’s experience of hospital, and this offered a safety blanket at times: ‘my taxi driver always took me indoors [after hospital visits] and checked that there was no sign of break-ins’ (CH2, P07). This safety blanket included staff using personal connections to reassure relatives unable to visit locally: ‘she will report back to a relative [. . .] whose mother is in here’ (CH7, P05). It also included helping ease the anxiety of patients going into an acute hospital that was not local, by community hospital staff asking staff they knew working at the acute hospital to look out for a patient and facilitate a more personal connection:
There is a sister there [in acute] that’s a very good friend of mine [. . .] I will ring her and say, ‘Just say [to the patient] you know [me] very well.’ [. . .] that makes their hospital stay a lot easier knowing that the people who are working there know us.
CH2, CY03
Knowing the community hospital and its staff was often associated with ‘family’ and, in part, this was because of to local families using the community hospital over generations:
That’s because they know us and the wider community now, as their families all know what [the hospital] does and that makes it quite settling for them.
CH3, S01
When patients were not placed in a familiar local hospital, the emotional impact of being away from family and home could be profound. For one patient returning to their local community hospital after a period in an acute hospital, the experience was transformational. His daughter recalled how he had been at the time:
Then dad was transferred to [unfamiliar, acute hospital] and while he was there his mood changed, it was very low mood but as soon as he realised that he would be able to come back to [this community hospital] his mood completely lifted and he came back [. . .] a completely different person [. . .] because he’s a local person and the staff are local and I would add that into the equation, you know [. . .] they recognise dad and dad’s been able to talk to them but dad’s also been able to have his family around more often.
CH3, V03 FG
Familiarity between staff and patients also had practical benefits for patients regularly using the hospital, as both could refer back to recent treatments and this helped to avoid patients having to repeat information about themselves – it helped facilitate continuity of care (see below). Knowledge of patients’ histories also seemed vital when staff needed to understand and appropriately assess patients’ needs:
This is a lady terrified of acute admission, terrified of attending appointments, has struggled and struggled and struggled until basically she’s reached the point of inability to cope and had to concede – her circumstances have forced the situation [. . .] And they [acute hospital] would not have known any of that historical, vitally important [information].
CH7, S05 FG
A low staff turnover (in some of the case studies) meant that patients also had more time to get to know staff: ‘they get to know our nurses because we have such a stable workforce’ (CH3, S01). This stability helped when caring for patients with impaired capacity and offered comfort to relatives:
Yeah because with dementia that’s the thing, they need something fairly stable, don’t they?
CH1, CA03
In contrast, when a local inpatient stay was not possible, the lack of familiarity could cause distress for patients and anguish for relatives:
He was absolutely miserable in [the acute hospital], really miserable [. . .] I can only think because it wasn’t [the local community hospital], because we have been here over the years for minor things with the kids, you know [. . .] we have been here since 1958, but we know everybody and we know all the doctors, you see, that’s what’s so lovely really.
CH5, CA02
Patients visiting outpatient clinics became well known to clinic staff and this regular contact facilitated social connections: ‘They are almost part of the family . . . you do get to know them and that’s really nice’ (CH1, S04). Again, descriptors relating to home and family were prevalent in patients’ and carers’ narratives. Patients knowing each other also presented an opportunity that staff deliberately exploited for patients’ benefit: ‘you know, those two ladies are really sociable let’s get those two in a room together’ (CH1, S01). One man who attended a clinic twice weekly fondly described his experience:
Well, they’re just all so nice, you know [. . .] they are like friends, really, you know. I’ve known them, as I say, for 4 years now, and, you know, they’ll chat and tell you all about their families, what they are up to, holidays and all that sort of thing, and it’s like a sort of social event, really, coming in [laughs].
CH1, P01
For most people, being known was a positive factor. However, for patients and staff, this occasionally presented personal and professional challenges. For patients, being known could mean that ‘everyone knows everyone else’s business’ (CH1, P06). For nursing and therapy staff, knowing patients personally required professional vigilance at all times:
Well, because it’s a small town as well [. . .] a lot of people who work here could obviously know a lot of the people who’s coming in. But you have to remain obviously very professional about that. And staff do know, you know nothing should be talked about.
CH1, S07 FG
This sense of ‘known-ness’, however, was being challenged. Health system changes (referrals taken from a wider geographical patch) meant that the ‘localness’ of inpatients had decreased. Not being known by the doctor or nurses also meant that patients’ expertise and knowledge of their disease was difficult to exercise and was frustrating:
They are given the charts by the doctor and it tells them what insulin, when they can give it, how much to give and, of course, the doctor that is covering this area isn’t obviously known to Dad, Dad does not know him, so obviously they are just going on the basis that the patient is here and that is the insulin they have to have, blah blah blah. Obviously Dad being quite knowledgeable about his diabetes, it is frustrating for him.
CH6, CA01
It is a ‘whole’ experience: personalised, holistic care
A key theme for patients and families was their sense of a ‘whole’ experience; the way in which staff provided sensitive, personalised and holistic care to patients, involved their families and worked together to enable people to recover and return home. Many respondents suggested that one of the key differences between acute hospitals and community hospitals is that acute hospitals treat specific medical problems, whereas community hospitals take care of the whole person. Both are important and valued, but serve distinct purposes and use different models of care to meet these purposes.
Staff personally care about me
For people using inpatient facilities and their families, experiences of community hospital care were greatly influenced by the way staff cared for them. Frequently, patients talked about them as ‘welcoming’, warm and attentive:
That’s from everybody, from the auxiliaries to the nursing staff, to the sisters, they all have such a wonderful manner with them and attentive.
CH8, CA03
One patient shared her experience of being admitted to a community hospital late at night and how staff had welcomed her, anticipating her anxiety and need to be settled in quickly:
They were totally welcoming and you felt that everything was prepared and ready [. . .] they had already realised that I needed something to settle and tea and coffee was offered almost immediately. And within half an hour I felt, ‘Thank god for that’, relaxation, that having built yourself up to think, ‘I’m not sure what’s going to happen.
CH7, P05
Some family members talked about how staff related to patients as if they were their own relative: ‘and it’s almost like they are part of their family, the way they look after them’ (CH9, CA03). Patients noticed staff showing genuine concern. They also talked about how staff made them feel welcome, and they never felt in the way:
You never thought that you were taking their time up or getting in their way. Never felt like you were an inconvenience or anything like that.
CH8, CA01
One patient explained how personalised her day-to-day experience had been, and how staff did not take their knowledge of her needs for granted:
And I had the same thing every morning so (laughing) it wasn’t as if they needed to ask every morning, now would you like your white toast with no butter and just marmalade? Yes, please. Black tea? Yes, please. And they would remember.
CH1, P03
At times, providing care meant that staff would have more intimate interactions with patients, particularly around helping with personal care, which some patients could find embarrassing. However, patients talked about the sensitivity with which nurses conducted themselves and how this enabled them to retain some dignity and privacy:
It was difficult at times for me, especially toilet-wise and that sort of thing. I was embarrassed as I’m sure anybody would be but they have never complained. Never a complaint. They wash you and clean you and make you feel whole again, time after time. Time after time.
CH8, P01
For family carers, the dignity and respect given to their older relatives were enormously important:
The respect and dignity they gave to my grandma was a huge thing for my mum and my aunty [. . .] But I feel the respect that’s shown to patients on the ward is – you cannot compare it to anywhere.
CH9, S04
Paying attention to privacy and dignity was important to staff because that is how they wanted to work:
I sometimes think it’s the simple things, isn’t it? People being treated with respect, not just they are old and ill, you know. The staff showing a bit of kindness and consideration. I think things like that are important. You know, it’s awful if you have been in hospital if you get a snappy nurse, you think, ‘Hmm, I don’t want to be here anyway,’ you know. Doesn’t make it nice, does it?
CH9, S07
Alongside nurses, the friendliness and personal contact from domestic and catering staff was also valued:
They all know all the patients and you can hear them in the kitchen when they’re dishing out the lunches and things. They are really caring about who they are giving it to.
CH3, S04
Being offered a choice around food was also a feature of the personalised care provided, and in community hospitals with their own kitchens, patients particularly valued the food being ‘cooked on site’ and personally served to them: ‘they serve it up in front of you’. They also appreciated being offered daily choice and having their individual needs catered for:
I even asked the other day if we could have a jacket potato if we wanted one. She said if you want one, we’ll do one for you. I think you would not get that in a bigger, not in, like, the [acute]. There’s too many people, isn’t there? But in a place like this, I think you’re an individual in a way.
CH3, P03
Most patients and carers spoke positively about staff and the personalised care they received, and it was fairly rare to hear otherwise. However, there were a few instances mentioned. In one community hospital, an outpatient talked about how, previously, there were more staff who took the time to greet him personally. He felt that this was no longer the case because staff were busy and just seemed to get on with their jobs:
You go there nowadays and you are just a person within a building. The staff just walking by don’t acknowledge patients. They don’t say, ‘Are you OK there? Are you in the right place?’ Or just, ‘Good morning, lovely day.’ None of that [. . .] The older hospital, I think, was more personalised because people recognised you from going there.
CH3, P01
They do whatever wants doing
Well, I think it’s the quality and the tenderness of the nursing care, it’s having a medical expertise on tap and an independent assessment will be made of their needs in social services support to get their care package in, home visits if necessary. The sort of link between the hospital environment and the home environment, the discharge planning is a big part of it.
CH5, S14
The ethos of community hospitals seemed to be about, as one patient put it, ‘whatever wants doing’. Indeed, providing holistic care was seen as a distinguishing feature when compared with acute hospital care: ‘[in acute hospitals] it’s really just a snapshot of the person in that situation by the bed. It’s not the whole picture’ (CH2, S14). Specialist expertise, time and a non-clinical approach were all used to put this ethos into practice:
You go to a local community hospital and you see a specialist nurse who’s maybe not in a uniform, and who has time to sit down and have a conversation with you.
CH4, S09
For patients, a major benefit of this ethos and practice was having all their needs assessed and treated, rather than staff dealing only with the presenting problem. Staff carried out comprehensive needs assessments – ‘we look at the whole person’ – which were seen to be particularly relevant for older people with a number of underlying conditions. There were numerous examples of staff identifying and addressing issues that had not been picked up during patients’ admissions to acute care, and this holistic, ‘generalist’ approach (rather than a disease-specific or single-issue approach) was thought to be an important feature of patients’ experiences of community hospital. The thoroughness of this holistic approach was recognised by patients:
They find out all sorts of thing about you when you come in. [laughing] Because they’ve found now that I’ve got trouble with my heart.
CH3, P03
Assessments were multidisciplinary and addressed a number of needs, such a person’s physical health, medication, cognition, mobility, living situation and social support needs. This was done alongside patients’ personal wishes and expectations of themselves. Although some of the case study sites provided some specialist mental health services, we saw little explicit evidence of mental health needs, for example anxiety and depression, being considered as part of the overall needs assessment (beyond cognitive functioning), or of mental health being seen as integral to inpatient care practice. This is discussed in more detail in It is a huge life event: psychological transitions.
However, when undertaking an assessment, staff did recognise the importance of involving family members and worked to build a good relationship with them, arranging meetings at the beginning and over the duration of the stay, to inform and involve them in what was likely to happen:
We involve families from day one, as soon as we meet them we give them ideas of what the procedures are and how long we expect their family to be here, so people have a broad outline of what we’re gonna be doing.
CH3, S01
Ongoing multidisciplinary support together with home visits, and close work with patients and their families, all enabled staff to put together tailored packages of care: ‘we all work together to make sure that the package of care is the correct package of care’ (CH2, S07 and S08). They also focused on supporting a person’s discharge home and enabling them to remain there safely: ‘we make sure the discharge is very safe and we build up a relationship with the patient and their families.’ (CH3, S01).
The first practical step towards going home was planning for discharge, with staff across a number of disciplines focusing on helping people return home:
I work very, very closely with [. . .] the nurses on the ward, the doctors, physiotherapists, occupational therapists, social services to look at what that person is going to need, if anything, when they go home.
CH2, S05
Home visits supported this and were seen as a feature of community hospital care: ‘You’re more likely to do home visits or environmental visits which potentially you would not do within [acute] so much’ (CH1, S07, FG). This provided an important opportunity to glean more information about the person in their home context. One patient talked about her home visit and how staff assessed, supported and encouraged her to understand how well she could cope at home:
Well, the home visit was about 3 or 4 days [. . .] before I was discharged [. . .] I did walk up the steps . . . they measured the height of the loo and looked at the shower and the kitchen and had me walking with the Zimmer [. . .] so they then had me going round the kitchen, furniture walking, they called it. [laughing] They had me getting onto and off the bed with a piece of kit, which you’ve probably come across, called a leg lifter [. . .] a magic piece of kit. It is so simple, but so helpful when you are first doing those sort of movements [. . .] and again, it was a confidence booster [. . .] you’d got someone there to see how you coped with it and offer you advice on how to do it differently, if there was a better way of doing it.
CH1, P03
There were times when patients’ and carers’ expectations of treatment differed from that provided, often in relation to physiotherapy. At times, this was because patients did not recognise the ‘informal’ physiotherapy being undertaken by nurses. One member of staff described how patients can be left disappointed:
Well, patients often are shocked that they’re not having ‘formal’ physio[therapy]. They are led to believe when they are at the [acute] that they are going to come for intensive rehabilitation and they do not recognise this is intensive rehabilitation. And they are bitterly disappointed.
CH4, S06
Staff members also described how expectations may be built up when people are being discharged from acute hospital, and insufficient staffing meant that they were not able to always meet these expectations:
It depends how it’s been sold to them at say the [acute] if they are coming across. They, you know, whoever’s told them they have got to move on [. . .] they might have said, ‘oh, you can go there and have intense physio[therapy]’ [. . .] actually you cannot. There’s not enough staff.
CH3, S03 FG
In addition to insufficient staffing, the inexperience of some nursing staff in working with people with complex needs meant that, at times, multidisciplinary care planning was not followed, and this could concern family members:
I think some of the nurses there maybe don’t have the support, the training, the skills that they need to deal with the more complex service users, and so they get impatient with them or they do not follow the protocol. I’ve certainly had that from family members where they said, ‘The physio[therapist] has said they need to transfer like this or they need to be doing this but the nurses did it all wrong.’ So I think there maybe are some issues.
CH4, S07 FG
They help me to recover and return home
[They] give them the best opportunity they can to return home, if that’s where they want to go, and to stay at home. It’s a stepping stone back to try and get a bit of normality in their lives, really.
CH4, S09
The approach to ‘rehabilitation’ across community hospitals was usually informed by patients’ personal goals as well as what they needed to get around their home as part of their daily living. For staff, this started with focusing on short-term goals:
It’s a little more goal orientated for us [. . .] all they want to do is be able to walk down to the bottom of their garden and get to their greenhouse. So we pick up that individual personal goal that needs to be achieved for them to get home or to get back to their baseline.
CH1, S07 FG
When setting goals, staff talked about the need for realism as well as recognising a person’s potential: ‘Look at the bigger picture all the time [. . .] maybe they can and it’s giving them that opportunity to be able to do that’ (CH1, S05). A major part of their rehabilitation work was also to encourage patients who, for one reason or other, may have stopped doing things for themselves:
As soon as they come into hospital, they just stop, and I think a big part of particularly here – I couldn’t say for other community hospitals but I would imagine it is – is stopping that. Is bringing that back and saying, ‘Actually, you can brush your own teeth . . .’.
CH2, S05
Once agreed, staff worked together with patients and their families to implement a care plan. Treatment and care varied depending on individual need but often involved a brief period of recovery before starting regular physiotherapy to build their confidence around balance and walking, practising daily living with occupational therapy support (e.g. being in a kitchen) and preparing (home visits) for going home. As time spent in hospital could last several weeks, a relationship between visiting relatives and staff often developed over this time.
For carers, being included, involved and informed seemed paramount. One woman recalled how staff had quickly got to know her husband and her, and how they had kept her informed about his health when she visited. She went on to explain how important proactive communication was, particularly when caring for people with dementia, suggesting that staff had a double task in such circumstances:
If you have someone with dementia, you are really dealing with two people, you are dealing with the person with dementia and their carer. You need to care for one and you need to communicate with the other.
CH3, CA01
During inpatient stays, staff worked progressively to improve people’s physical health and strengthen their mobility, recognising the multiple comorbidities that patients had to contend with during recovery:
So they are very elderly, very frail, multiple comorbidities, and it can be everything from a routine hip replacement or planned bowel surgery or something and recovery from that, because they are frail it’s taking longer, to a fall at home, not found for 3 days, people with UTIs [urinary tract infections] or chest infections and they just lose the power of their legs and get very confused. So not only do they have to get over that illness, they have then got to regain their strength and their confidence in order to hopefully get back home.
CH1, S01
The degree of complexity varied, and for some patients their recovery was more straightforward. A woman who spent 3 weeks in her local community hospital recovering from surgery after having badly broken her pelvis illustrates how staff had steadily supported her physical rehabilitation through praise and encouragement:
From the moment I got here they made me feel as though they were here to make me better and they were here to help me progress forward; it’s not, ‘Oh, you’re here. You can just sit and do nothing.’ ‘Oh, you’re here; we want you there’. ‘You can have that but we want to take your commode away; you’re not going to have it there all the time.’ ‘You will hop down there.’ ‘If you’re capable you will go and have your own shower and wash your hair and do all those sorts of things.’ And each day they praise you for achieving something new, I mean stupid little things like I can now stand on one leg and clean my teeth with the basin which for the first bit, because I could not have it hanging there, I could not do [. . .] that was another achievement one day. And I think it doesn’t matter whether it’s me or anybody else, they are looking for you to achieve one little thing, maybe not every day, but every time you achieve something you get the feeling that they are pleased for you, and I think that’s vital and that again is the building of the confidence for people to go home.
CH7, P05
She stressed the importance of building people’s confidence when sharing a story about another patient to highlight just how frightened people can become:
Daphne was absolutely furious, the whole thing was a disaster. By the time she was leaving, she was the most jolly soul. She was here a fortnight and [. . .] every time she walked past there was a joke, she was smiling, she couldn’t wait to go home, she felt confident in herself; and that purely because they’d had time to bring her from being an angry old lady, probably very frightened I should imagine, to being somebody who was confident to go home again.
CH5, P05
Recovering from illness or a fall sufficiently well to return home could take many weeks, with ‘formal’ rehabilitation activities taking up only part of each day. This meant that time, and what to do with it, became a significant feature of daily inpatient life. Patients commented on the lack of social stimulation: ‘[it’s] pretty boring laying [sic.] here all day’. Carers also noticed this, particularly when their relatives were recovering:
When Dad was poorly, when he felt really poorly, it was OK because he was sleeping a lot but as soon as he started to pick up he felt bored . . . I think once you’re getting better there does not seem to be very much [. . .] what’s the word I’m looking for [. . .] yes, [to] keep them stimulated.
CH9, CA05
They also noticed that some of the dedicated facilities lacked atmosphere and appeared underused:
It’s a big room but it’s [. . .] hardly anybody uses it. Another chap next door to my dad had gone through to watch the television because he was aware that other people in his room did not want to, but he said, ‘I didn’t like it in there, I felt completely on my own’. There was nobody else there apart from him, he’d been wheeled through sitting there, in a cold-ish room, just because it was big and just on his own but nobody else there.
CH8, CA03
The lack of ‘things to do’ was observed across a number of case study sites, raising a question as to whether or not more could be done to support social interaction between patients. Staff accounted for the lack of social stimulation in different ways. In one community hospital, they suggested that activities were limited because patients were quite unwell, whereas others indicated that staff shortages might be a reason. However, this varied within and between hospitals and there were also some good examples of social stimulation supported by volunteers as well as examples of excellent staff support. The same carer who spoke about the cold and empty day room also recalled how an occupational therapist had provided some ‘brilliant’ stimulation for her mum:
One of the occupational staff members – she was brilliant with Mum. She would go and sit in. And we even had her singing at one point, my mum, in the hospital. She actually could sing, but she couldn’t speak.
CH8, CA03
At times, the social interactions between patients also provided stimulation and helped people to forget about their health or mobility difficulties:
And it was brilliant because, you know, we’re social animals, and that also is part of your recovery, I think. And I laughed my way out of hospital there, you know, because they were such [. . .] I mean, there were two, a couple of youngish girls there who were not very well actually, but their sense of humour was just amazing, you forgot about yourself, you know.
CH5, CA02
Despite lots of positives, discharge could often be a source of tension between staff, patients and family carers. Sometimes this was because patients did not wish to return home because of the pending social isolation and having to take care of themselves, or because their families needed a break or the patient did not have family support. At other times, pressure from acute hospitals to take people who no longer needed acute care (step down) meant that staff had to juggle priorities and this pressure then could be transferred to family carers, who would find themselves responsible for caring for their relatives before they felt able to cope:
The pressure came because the [acute hospital] was on black so they were under pressure for beds here [. . .] but I knew that if I didn’t stand my ground that we were totally out on a limb. He was in hospital, I knew that he was being cared for, but as soon as I allowed him to be discharged, then I was on my own, so that was really difficult. I sat in meetings with five or six people just saying ‘No’.
CH3, CA01
Delayed discharges were often attributable to cuts in social care and this had a major impact on family members:
I found the social services side of it very hard really and not really kept in the loop. It was almost like they’re really under pressure to find places but there are not places for somebody with as much going on as my father had at the end, if you will. Yes, I found that quite hard and it becomes distressing, especially for my mother.
CH9, CA03
There were also many accounts of patients not being able to return home, either because their home was no longer suitable or because a person needed more care than their partner was able to provide. At times like these, when staff had had done as much as they could and going home was no longer an option, this had to be discussed with patients and their families. The impact of this is discussed in the next section.
It is a huge life event: psychological transitions
There’s a big psychological transition, isn’t there? [. . .] it is a huge life event for people [. . .] and it is a shock.
CH6, V06
For a number of older people, the accident or illness leading to their admission to a community hospital often triggered a major life event. These accidents and illnesses took place at a time in their lives when they often had multiple comorbidities or had experienced a sequence of illnesses, were no longer able to fully manage at home or were experiencing the loss of friends and partners of a similar age.
The practical and physical adjustments they needed to make were considerable. But more profoundly, not being able to return to the family home (often where a person had lived for decades) was emotionally traumatic and a major psychological undertaking, requiring time to come to terms with such life changes. Below is one person’s story from the many we listened to that profoundly illustrates the shock and enormity of such life changes and psychological transitions:
It’s a bit raw because my husband has just died [. . .] [crying] [. . .] We were married for 56 years. But everything has gone wrong in the last 6 months, really. One thing to another. I discovered I had breast cancer and I’m having sort of treatment for that, well not treatment, a pill for that, and they are hoping to do something with it at the end of the month, but I had all this to contend with that I could not cope with that [her husband’s care and death] as well really . . . Had so much going on [. . .] And now from here I think I’m going to go into a care home because I can’t look after myself, really. My two daughters have got their careers and their families, they have both got houses with stairs and things that would not suit me, so we are looking around at the moment to see what’s what, which is a shame because we have got a lovely bungalow, but there you go. It’s what’s safest for me, really, in the long run. So hopefully we’ll get something within the next few weeks because I’ve been in here 6 or 7 weeks now . . . This has all happened within 6 months, all at the same time. Luckily I had the girls because they looked after him really because he was looking after me until he got lung cancer [. . .]. Just after Christmas he was diagnosed and he died in April [. . .] I do not feel as though I’ve had time to grieve properly.
CH6, P05
Emotional responses to such ‘life events’ differed from person to person. Some were able to remain positive and many of those we interviewed presented an outward stoicism. However, stoicism can conceal the significant emotional impact of changes experienced in such a short period of time, such as anxiety or depression. Given the number of people interviewed who were experiencing life transitions and appeared shaken by those events or who were anxious about an unknown future, we were surprised to see little explicit evidence of mental health needs being integral to inpatient care practice.
Staff in a small number of hospitals mentioned the importance of working with anxiety. In one, this related to maternity services and younger women. In the other, looking for and working with anxiety and depression was more integral to the care provided. However, this was only because a senior staff member who had previously worked in mental health services had used her knowledge and experience to integrate mental health into their assessments:
Certainly when I’m assessing them on the ward, I’m looking for mental health problems, a lot of elderly people have depression or anxiety [. . .] or they can start having problems and we pick up on that fairly quickly.
CH8, S06
However, despite her observation that ‘a lot of places that do physical health acknowledge that elderly people can get depressed and anxious’ (CH8, S06), assessments and focused work on anxiety and depression did not appear to be formalised in some case studies, and responses such as ‘we do not provide counselling here’, when we asked about supporting people’s psychological transitions, suggested that this was not always properly understood. There were many examples of staff supporting patients to recover physically, and build their confidence, and a few examples of recognising patients’ anxieties. One physiotherapist focused on keeping patients’ spirits up:
If we can make it fun, it does make a difference. I’d rather be doing something if I was in hospital, than sitting in a chair thinking about myself, thinking, oh dear, I’ve got to go home, I’ve got to do this, that and the other.
CH6, S05
Similarly, a volunteer chatted about the outside world to bring ‘a little light relief’ and reassurance:
So I do think we bring a little bit of the outside world in, a little bit of light relief as well perhaps. ‘I saw so and so on the television the other day,’ ‘Oh that’s a lovely programme,’ just anything like that. ‘Have you seen the paper?’ [. . .] it does not have to be heavy, it can just be that light relief . . . and sometimes it’s a bit of reassurance.
CH6, V06
Although both of these approaches are important strategies in the care and recovery of older people, they appeared to be about distracting people from their general anxieties and concerns. When caring for older people who, as a result of an accident or illness, were facing a major life change, such as giving up driving, no longer being able to walk or having to sell their home and go into care, and with all the emotional and physical upheaval that inevitably follows, we would argue that there is a need for a greater focus on people’s psychological, emotional and mental health, alongside their physical health.
Factors influencing variations in patient and carer experiences
Although patients and family carers were overwhelmingly positive about their experiences of community hospitals, there were some variations. Variations in patient and carer experiences within the same community hospitals were reported above. Here, we highlight four inter-related factors that appeared particularly influential in the variations in patient experience between community hospitals.
-
Staff shortages: inpatients across almost all the hospitals talked about the ‘busyness’ of doctors, nurses and therapy staff, with patients in some hospitals observing and commenting on staff shortages and, in particular, the impact when being treated or cared for by unfamiliar clinical staff, which was more likely when locum doctors or agency nurses were used. Although the impact of staff shortages was apparent across all case studies, they were experienced more frequently in smaller and more isolated community hospitals. It is possible that hospitals with a greater range of services (and wider group of staff) had more flexibility in covering issues such as staff sickness and annual leave, even if there were similar shortages.
-
Community involvement: the extent and nature of community involvement could also make a difference in patient experience across hospitals. Although all benefited from enhanced facilities, patients and carers in hospitals where there were active volunteers on the wards were more likely to talk about additional benefits, such as providing a distraction from illness, reducing anxiety, alleviating boredom, running errands and providing transport. We also observed some indirect benefits to patient experience, with volunteers in some hospitals counteracting staff shortages by helping with non-clinical tasks while also contributing to staff feeling valued. This seemed to generate a greater sense of purpose and connectedness in staff that, in turn, positively affected patients and carers. Examples of when active community involvement made a difference were through school visits, informal apprenticeships, community choirs and present giving at Christmas and commemoration services.
-
General practitioner medical support: another influencing factor seemed to be whether or not patients were treated by their own GP. When community hospital inpatients were treated by their own GP, they talked about good medical care more often and felt that there was better clinical continuity through knowledge of their medical history and social contexts. They also felt a more sensitive and personalised approach was offered including, for example, reviewing medication and checking for underlying issues. There was also better institutional continuity through communication between the hospital and surgery. However, the positive effects on patient experience associated with GP-led services were countered in some hospitals by their limited presence relative to those with in-house doctors who generally provided a greater level of cover.
-
Greater range of services, equipment and clinical skills: there were also differences in patients’ experiences for those being treated in a hospital providing a greater range of services. There was, for example, more ability to self-refer or drop in to clinics or to have minor injuries attended to out of normal working hours and far greater convenience when having to attend clinics regularly. A key issue that was reported by many patients across hospitals with fewer services beyond inpatient beds was the ‘ping-pong’ experience of having to go for diagnostic treatments or specific interventions (for example, for intravenous antibiotics or X-ray). For those hospitals that were able to provide such services on site, there was reduced stress (travelling, parking, waiting) for patients and carers, as well as a freeing up of staff resources (accompanying patients on such visits could take a full day). In addition, hospitals with better integrated community support meant that patients experienced a greater continuity of care between hospital and home, and social as well as health needs were picked up.
Summary
When asked to describe their experiences of community hospitals, patients and carers talked about such services as ‘being different’, their location as generally more convenient and the atmosphere as more homely and relaxed, less stressful or daunting and more reassuring. Taken together, these different aspects contributed to community hospitals feeling ‘closer to home’, not just in a physical sense but also in a social, emotional and psychological sense. This contributed significantly to patients’ (and family carers’) experiences of community hospitals, eased anxiety and helped to facilitate both independence and connectedness to family and community. However, not all patients felt the same: not all found the environment positive or staff friendly and younger people felt alienated because of their age; community hospitals could be seen as places used only by older people.
Having a range of services situated locally was hugely important to patients and meant far more than expediency, with less stress and travel time cited as major factors when patients had to attend clinics. In addition, a deep sense of ownership and connectedness, because community hospitals were embedded in local communities, appeared to be fundamental to many people’s experiences of community hospital care. Patients and staff often knew each other, and this appeared to render inpatient experiences less anonymous, more understood, and more personalised and connected. However, with patients increasingly being referred from a wider geographical patch, community hospitals were becoming less local, and, when patients were not placed in a familiar local hospital, the emotional impact of being away from family could be profound.
With an ethos of holistic care and a focus on supporting people to recover and return home when possible, patients benefited from a generalist multidisciplinary approach to assessment and care delivery. This ensured that underlying health conditions, not picked up by acute hospitals, were assessed and treatment, care and support for physical, cognitive and social needs, alongside their personal expectations and family involvement, were provided. Staff worked progressively to improve inpatients’ physical health only and mobility, as well as build their confidence through praise and encouragement. Patients observed less pressure on staff, so received more attention, and the individualised focus made them feel less anonymous and more cared for. However, a lack of social stimulation was observed across a number of case study sites and little formal assessment and work with anxiety and depression in some case studies raised a question as to whether or not this was a gap.
Familiarity with the hospital and staff offered relief and reassurance, as did being included, involved and informed. Knowing that loved ones were being cared for well, particularly when they were unable to do it themselves, was a lifesaver. However, tensions could emerge between staff and family carers on discharge, particularly when families or partners were not able to cope or when discharge was delayed because of cuts in social care.
Although many patients and carers had similar experiences, there were also some differences. Family carers worried about relatives admitted to hospital and experienced a considerable amount of stress as a result of carrying the burden of responsibility for their care and well-being. Having a hospital locally situated eased this stress, because they could more easily make frequent visits (which helps with recovery), which saved a considerable amount of their time, particularly if they were also working or caring for their own family; family carers’ time appeared to be taken for granted by the NHS.
Overall, patients and family carers were overwhelmingly positive about their experiences of community hospital treatment, care and support. The holistic approach, personalised care, close involvement of families and relationships between patients and staff, their families and the wider community were intrinsic factors in patients’ and carers’ experiences. Nevertheless, there were some variations in patient experiences between community hospitals, mainly related to staff shortages, levels of community involvement, GP medical support and access to a greater range of services.
We cannot conclude this chapter without also discussing the relationship between what matters to patients and their family carers, how it is represented in the literature and how we have attempted to represent it in this report. Through use of discovery interviews,85 an experienced-centred method, we were able to draw out not only what happened, but also how those experiences made patients and family carers feel about community hospital care. In doing so, the language used (e.g. ‘it’s home from home’, ‘they do whatever wants doing’) differs from that used in previous research (e.g. ‘access to services’, ‘comprehensive holistic care), reflecting an experience-centred voice (as opposed to a policy, commissioning or service improvement agenda) and capturing ‘meaning’ in the stories told. We return to this in Chapter 8 in our discussion of a new model to understand community hospital care.
Chapter 6 Community engagement: passionate support
In this chapter, we explore the different ways in which communities engage with and support their hospitals, addressing the first part of our third research question, ‘what do communities do for their community hospitals?’. We draw on both national quantitative data from Charity Commission reports and qualitative data from our nine case studies (see Chapter 2). The main vehicle for community engagement in community hospitals was Leagues of Friends and, as such, we pay particular attention to their role.
We identify and discuss four forms of support that communities provide for their hospital (giving time, raising money, providing services, giving voice), the levels at which they occur and how this varies. Although we discuss each of these different forms of support separately, they are not mutually exclusive: volunteers, for example, often undertake fundraising and co-production activities. We then consider how levels of voluntary and community support in general varied between and within our cases, before exploring what difference such activities make to the different stakeholders involved.
Giving time
Levels of volunteering
Returns to the Charity Commission suggest that, on average, Leagues of Friends involve 24 volunteers: an estimated total of 5880 volunteers across the 245 community hospitals that we identified as having such a group. Depending on assumptions made about the average hours contributed each week (see Chapter 2), this equates to between 1.4 and 2.5 full-time equivalent personnel or a financial input of £15,600–28,500 per hospital, or £3.8–6.9M across England. These figures are likely to be underestimates: they exclude trustees and are unlikely to include those who volunteer outside the League of Friends, and the calculations use national averages for volunteer hours and the minimum national hourly wages (see Chapter 2).
Among the 197 community hospital League of Friends that reported volunteer numbers to the Charity Commission, the range was from 2 to 162 volunteers. Among our case studies, one currently had no League of Friends and only ‘one or two’ volunteers involved directly on the wards; Charity Commission returns for the others gave figures of between 6 and 33 volunteers (although our qualitative findings reinforce the view that these are likely to be underestimates).
Volunteering roles and activities
Volunteers from our case studies undertook a range of roles as summarised in Table 18.
| Categories | Examples of volunteer activities/roles |
|---|---|
| Campaigning and advocacy |
|
| Governance, leadership and management |
|
| Fundraising |
|
| Administrative assistance |
|
| Service delivery |
|
| Facilities |
|
| Patient well-being |
|
In some of our case studies, volunteering roles were limited to fundraising, with very few volunteer roles within the hospital itself. In others, we found a greater range and mix. There was a clear consensus that volunteers could not get involved in medical or personal care or access confidential data and that they were there to complement paid staff. There was far less consensus on the actual roles that they could undertake.
Regulations regarding health and safety and confidentiality were the most commonly cited restrictions on volunteer involvement, but these seemed to be interpreted differently in different hospitals. In some, they were seen as reasons not to involve volunteers, in others they were seen to represent a set of training requirements or a need for expectation management, but it was emphasised that any risks could easily be managed:
I think the majority of people are absolutely safe and would not bring risk into a community hospital . . . These are intelligent people who’ve retired often, who’ve got intellect and skills that they want to do something.
CH1, S08
The range of roles and activities that volunteers could undertake was perceived to be limited by the capacity of patients to engage with them and the capacity of staff to support or facilitate volunteering. Some staff only ‘wanted them to do things that weren’t generating more work for us’ (CH3, S03, FG). It was also reported that some patients and/or their families raised concerns about the involvement of volunteers in their care, necessitating communication regarding the distinction between staff and volunteers.
It was suggested that these factors combined to limit the breadth of volunteer involvement in community hospitals. These constraints contributed to a perception among a number of respondents that community hospitals were putting ‘barriers up where they don’t exist’ and were not always making the most of (potential) ‘untapped resource’ available to them.
Volunteering co-ordination and support
Much of the volunteering within community hospitals was organised through the League of Friends. In some hospitals, a specific League of Friends committee member had been allocated the role of volunteer co-ordinator, with responsibility for recruiting and supporting volunteers. In others, there was less explicit consideration of the need for volunteer co-ordination.
Members of the community could also volunteer directly with the hospital, with their input co-ordinated by a member of staff or by a voluntary service manager (VSM), or equivalent, working at trust level across a number of sites. In some of our case study hospitals, the trust VSM was a regular presence and significant influence, but in most they appeared remote, both geographically and practically. In one hospital, a close link had been forged with external volunteer support agencies. Increasing involvement of trusts in volunteering at community hospitals was sometimes considered as a more bureaucratic approach through, for example, the introduction of additional paperwork, health checks and training, which was welcomed by some but not by all. In some of the case studies, there was tacit acceptance of the place of the volunteer; in others, volunteering, and wider community engagement, was actively encouraged and ‘nurtured’:
We actively encourage our League of Friends to come in whenever they want. And I attend everything they do as well [. . .] If anyone ever asks to come here, to provide any kind of service, we do actively encourage that and we want people to be involved with us.
CH3, S01
Overall, despite a general acknowledgement of the need to nurture volunteering and the value of doing so, examples of a more considered or strategic approach to volunteer co-ordination and development were limited (see Naylor et al. 42 for similar findings regarding volunteering in acute hospitals).
Patterns of volunteering: diversity, recruitment, retention and commitment
There are no quantitative data available on who volunteers in community hospitals. Our case studies, however, suggest that the majority of volunteers were retired, female, white and middle class. In part, this reflects the characteristics of the communities within which many community hospitals are located. Although not dominated by current or retired hospital (and other health/social care) staff, their involvement was also notable. It was not unusual for League of Friends committee members to be well into their 80s, with a majority aged> 65 years of age. This was identified as a challenge for future sustainability:
. . . look at the average age of people who are running it. I mean, we fear for the future because you know . . . 60 plus is quite young actually . . .
CH3, CY01, FG
In one case study hospital, the League of Friends had ceased to operate as previous volunteers retired and they had been unable to recruit new members to take over. Difficulties in recruiting younger people (particularly to committee roles) was attributed to the busy lives that younger people led, the types of activities they do/do not engage in and also the (lack of) relevance of the community hospital services to them.
Overall, although there were generally high levels of latent support for community hospitals (demonstrated, for example, through membership), it was difficult to convert this into active, and particularly regular, volunteer engagement:
I think that a lot of people would go up in arms if it was closed but whether they’d be willing to do anything about it to help, I don’t know. There seems to be a little core of people who would but I’m not sure that that spreads right out across the community.
CH9, CA05
These challenges were exacerbated by a reliance on recruitment through the personal and social networks of those already involved. There was limited evidence of wider, more active or formal forms of volunteer recruitment and a general acknowledgement that they did not quite know how to reach out and engage a wider range of people.
There were, however, exceptions: in one case study, the League of Friends, and volunteering within the hospital more generally, had been reinvigorated following the recruitment of a new chairperson. A number of the case studies involved some young people as volunteers through student placements, through Girl Guides or school groups, or through tailored fundraising activities. One hospital had employed a fundraiser with responsibility for building community support, and it was suggested that this had allowed them to focus attention on diversifying engagement. Together, such examples suggested that concerted efforts to broaden engagement could pay off.
Once involved, volunteers tended to stay involved for considerable periods of time. It was not uncommon for League of Friends committee members to have been involved for well over 20 years or for volunteering to span generations:
Her mother did the library trolley for 40 years and when the hospital closed that was it, she was in her 80s by then. When it opened again, she said, ‘Well darling, I’ll buy a new trolley and perhaps you’d do it instead now’ and darling did, she’s done it ever since [. . .] and that means going and changing the books once a fortnight.
CH7, V04
Regular volunteers often contributed considerable amounts of time, often ‘doing something’ most days of the week. One volunteer respondent had worked at the hospital 6 days a week, 1.5 hours a day, for over 10 years. For some, it was ‘more like being at work’. This level of commitment contributed to a risk of burn-out and, once involved, some volunteers found it hard to say no:
It was much more than we ever expected it to be and, to be quite honest, if I knew 2 years ago that I would be involved in so much I don’t know if I would have done it, because I probably have an average of five health meetings a week.
CH8, V01
Such intense forms of engagement occasionally also represented a challenge for hospital staff. Some volunteers were reported to have ‘gone beyond the boundaries’ of acceptable behaviour (e.g. walking through wards with apparently little concern for patient privacy) because of an overfamiliarity and sense of entitlement that came through their intensive involvement. This is the terrain of the Lampard Inquiry101 into the implications for hospital governance of allowing prominent fundraisers undue influence.
Beyond this relatively small group of very active volunteers, a wider group provided a regular but more limited input and a wider group still helped out on an occasional basis, particularly to support specific fundraising events.
A much larger group of people provided more passive support: they paid their membership fees, made donations and turned up to events but did not help with the organising. This ‘really strong network of supporters’ was typified by one respondent as providing ‘quiet support and acceptance’ and characterised as an ‘important and valued feature of community hospitals’, although the challenge of converting it into more active engagement was recognised:
Bearing in mind we have a catchment area of 70,000 people, very, very few people turn up [to support League of Friends events]. It’s not part of the culture, if you like.
CH2, V03
Overall, respondents in most of our case studies reported widespread community support for the hospital, although there was a clear pyramid of involvement, from a relatively small number of active and regular volunteers to a much wider group providing more passive support in the form of membership or event attendance. The limitations of our research (see Chapters 2 and 8), however, meant that we did not reach beyond those who had some connection to or interest in the hospital.
Raising money
Levels of charitable income
Communities also support their hospitals through giving money. In 2014, on average, community hospital Leagues of Friends generated an income of £45,387 (Figure 12). This figure is influenced by a small number of very large outliers. The median is £15,632. In addition, some community hospitals benefit from income generated through donations made to NHS trusts; these additional funds were particularly significant in three of our case studies. As discussed in Chapter 2, however, our quantitative data are confined to income generated through Leagues of Friends.
FIGURE 12.
League of Friends income distribution in 2014. Notes: solid line, mean (£45,387); dashed line, median (£15,632).
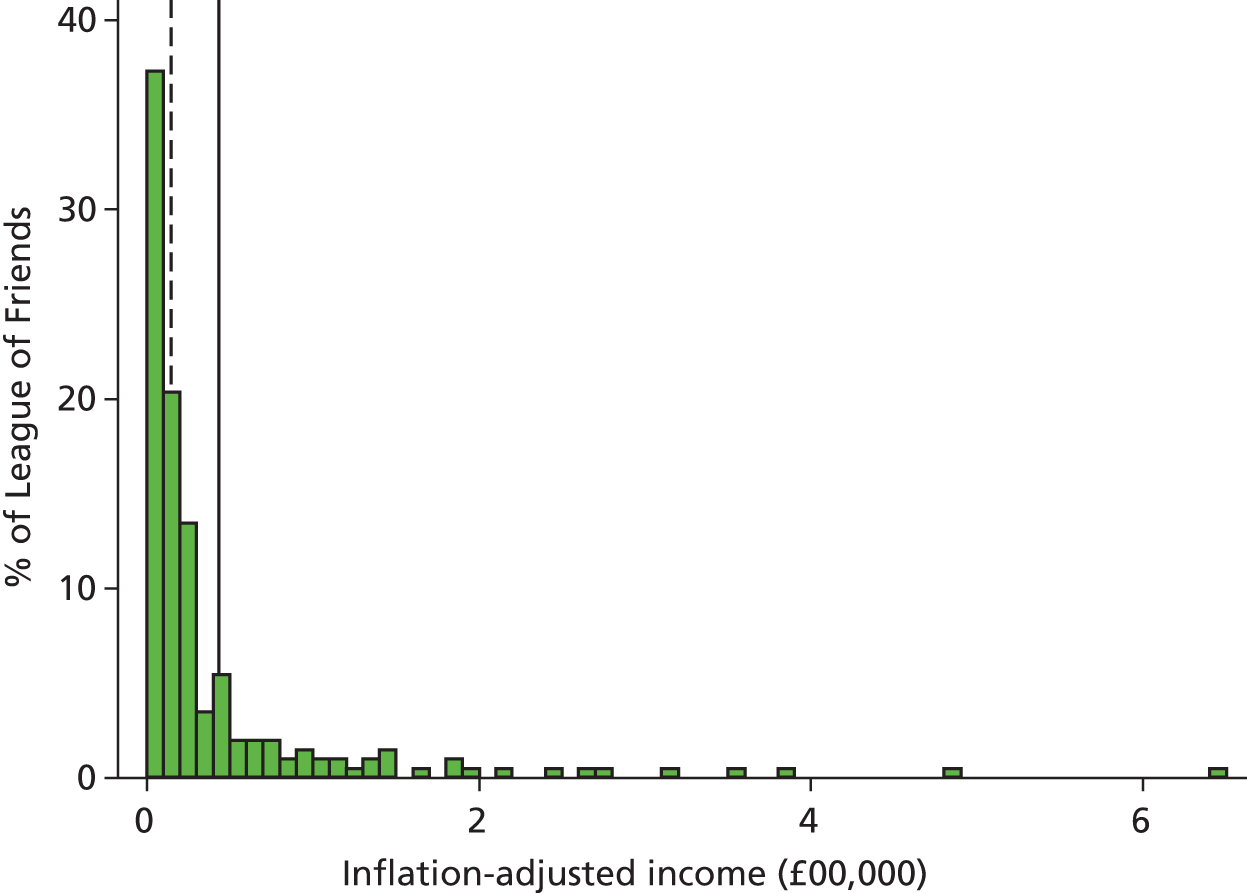
Two indicators of the relative significance of this source of funding can be given. First, 40% of the Leagues of Friends in our sample were among the top 100 charities in their local authorities in terms of income; in three local authorities, they were among the top 10. Second, our analysis suggests that Leagues of Friends are likely to be among the largest and most stable charities in many of the communities within which they are based (e.g. around 40% of them made non-zero returns to the Charity Commission in every financial year from 1995 to 2014, compared with a national proportion of approximately 10%). This is important in terms of the wider social contribution made by community hospitals. The stability of the institution, its visibility and presence provide a base for various forms of participation.
Sources of income
Leagues of Friends, and other charities involved in supporting community hospitals, engage in a range of activities to generate their income, including domino nights, car boot sales, fêtes, fashion shows, charity shops, providing day care services and (very rarely) significant property investment portfolios. Table 19 presents an overview of income sources, derived from charity accounts from Leagues of Friends with an income or expenditure of > £25,000 in any given year (reflected in annual variations of the number of observations).
| Income | Year | Total | |||||
|---|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | ||
| Mean voluntary (£) | 72,316 | 73,298 | 80,453 | 59,036 | 61,461 | 65,637 | 70,942 |
| Percentage of total income | 76 | 88 | 81 | 82 | 63 | 73 | 77 |
| Mean charitable activities (£) | 9455 | 1929 | 4181 | 3047 | 11,545 | 6082 | 7541 |
| Percentage of total income | 10 | 2 | 4 | 4 | 12 | 7 | 8 |
| Mean generating funds (£) | 12,830 | 7612 | 14,547 | 9696 | 24,737 | 18,231 | 13,880 |
| Percentage of total income | 14 | 9 | 15 | 14 | 25 | 20 | 15 |
| Average total income (£) | 94,601 | 82,839 | 99,181 | 71,779 | 97,743 | 89,950 | 92,363 |
| Number of charity accounts | 91 | 55 | 49 | 52 | 41 | 70 | 366 |
Over a 5-year period (2008–13), three-quarters (77%) of Leagues of Friends’ income was ‘voluntary income’ generated through gifts, donations, legacies, grants, membership subscriptions and sponsorships (see Table 19). More than half of ‘voluntary income’ (indeed, two-fifths of all income) came from legacies. Legacies were more significant for community hospital Leagues of Friends than for other charities. One-sixth (15%) of income was from ‘activities for generating funds’, such as jumble sales, lotteries and charity shops. Less than one-tenth was raised through ‘charitable activities’, such as trading goods and services. In this regard the Leagues of Friends are fairly typical of local charitable organisations. They do not rely on statutory funding or on contracts. These forms of fundraising are an outcome of, and contribute to the formation of social capital through, active fundraising efforts.
Variations in income levels
Although the mean income for League of Friends in 2014 was £45,387, the median was £15,632, suggesting considerable variation. Most (65%, n = 130) Leagues of Friends had an income of < £25,000 a year, around 35% (n = 70) had an income of between £25,000 and £499,000 and only one had an income of > £500,000. We observed occasional years in which income exceeded £1M, generally associated with ad hoc inflows, such as large legacies.
Figure 13 shows how average levels of income vary over time. The trend is now downwards: League of Friends’ incomes have been declining since 1995. The decline was most pronounced in 2011 and 2012, but showed signs of recovery in 2013 and 2014.
To test whether or not temporal changes were statistically significant, we conducted a fixed-effects regression analysis, entering a constant term and year as the only predictors, in order to compare income with that of a base category (income in 1995). The graph suggests that, in general, the average and median income that Leagues of Friends have received yearly was on the rise until the mid-2000s but since then it has declined. Our analysis suggests 2 peak years of income: 2000, when annual income significantly (at p < 0.01) exceeded the income in the base year for comparison (1995), for the first time, by £22,304, and in 2006, when the annual income exceeded the income in 1995 by £15,454 (p < 0.05). The decline in income was statistically significant (p < 0.05) in 2 years: 2011 and 2012. Then, charities received £18,820 and £18,197, respectively, less than in 1995. In other words, these results indicate that 2011 and 2012 were the years when, for the first time, charity income dropped substantially from the income level of 1995. The analysis also indicates that the decline in income in general has been statistically significant (b = –901.29, p < 0.01). This means that, since 1995, the charitable income of Leagues of Friends has declined on average by approximately £901 a year.
Notwithstanding this finding, there was little evidence among our case studies of concern over declining levels of income, although some Leagues of Friends felt that they had relatively low levels of income compared with others nearby: ‘others experiencing the converse of this’ (CH3, V01). The receipt of significant legacies was seen by some to offset the need to fundraise.
Some had limited their fundraising activities, recognising a potential crowding out of other local charities, had continued to run fundraising activities but had shared the proceeds with other related charities or were holding key fundraising events every other year, with another charity running theirs on the alternate years, so that ‘not one [charity] is hogging all of it’.
Although declining income was not identified as a current issue, some did question the future sustainability of income levels. Where inpatients were increasingly drawn from outside the local area and/or where the range of services had declined, this would weaken the local base on which the hospital had relied, reducing the League of Friends’ membership base.
Furthermore, concerns were raised with regard to declining membership levels. This would be reflected in declining income, but was seen more as a concerning indicator of a reduction in engagement with the hospital in general. Declining membership was also linked to the current economic conditions and to questions over the relevance of community hospital services to some community members. Although some of our case studies seemed resigned to declining membership, others had been working to address it.
Expenditure
Expenditure has also declined, but less sharply than income. Since 1995, the Leagues of Friends have, in most years, received more than they have spent, indicating that they have been building reserves. The exceptions from this trend are the years 1997 and 2011, when an average Leagues of Friends group spent more than it received. Overall, within the data set that we have, it appears that in 2011 their funding position was at its weakest since 1995: income was at its lowest and expenditure was relatively high, exceeding income (Figure 14).
Underneath these national trends in levels of expenditure, the case studies enable a more textured account of expenditure. Table 20 summarises the key categories of expenditure found in the case studies. The nature of the data means that we have not had the scope to quantify this in detail.
| Categories of expenditure | Examples from our case studies |
|---|---|
| Buildings |
|
| Equipment |
|
| Staff time |
|
| Staff development |
|
| Patient ‘comforts’ |
|
The boundaries between what were and were not considered appropriate forms of expenditure varied between hospitals and over time, with a particular concern for where the boundary should be drawn between voluntary and statutory responsibility.
How these were defined did not follow a hard and fast rule, raising wider issues of policy. Some adopted a clear demarcation, avoiding anything that they felt was the preserve of statutory responsibility (e.g. buildings, equipment). But we also found examples of support being extended to other health services connected to the hospital (e.g. district nurses), to individual patients and carers (e.g. to purchase equipment in patients’ homes to enable discharge) and beyond. One League of Friends had changed its constitution, responding to the increasing use of inpatient beds for non-local residents, which the League of Friends felt had resulted in it becoming less relevant to the local community:
. . . we felt that focusing solely on the hospital was no longer a proper use of the funds that came in because people were giving it for something that didn’t really exist any more.
CH6, V01
In general, the boundaries defining appropriate/inappropriate expenditure were becoming greyer as hospitals/NHS trusts faced considerable financial challenges. Covering staff costs was a clear example: one League of Friends was paying for a chaplain (after the trust ‘dispensed’ with the service) and a gardener and had funded the extension of the minor injury unit opening hours. Such decisions often came with reservations:
We are supposed to help the hospital for extras. This was how it started off. It has got to be very much more mainstream now because of lack of funds.
CH9, V01
A more specific concern regarding expenditure arose in a number of case studies in which uncertainty regarding the future of the hospital contributed to hesitancy to invest. One example given involved the restriction of fundraising in response to uncertainty about the hospital’s future:
[W]e talked to the NHS about building a public walkway between the ward and the day centre and we would happily pay for, and they absolutely point blank refused to consider it [. . .] Because it’s their building. Possibly because they might have been in the back of their mind thinking ‘we are going to be closing it anyway’, we don’t know.
CH5, V02
Concerns were also raised regarding the ownership of community hospitals, with a suggestion that some Leagues of Friends were less willing to commit to expenditure relating to refurbishment if the building had come into the ownership of NHS Property Company as opposed to an individual trust. The challenges of allocating resources to a growing number of providers within individual community hospitals were also highlighted:
But now you are dealing with five or six different providers, you are beginning to think, well, where is the benefit of this property, or this equipment? Where even now, every piece of equipment we buy we do get a signature from someone in charge of that department saying that it still continues to belong to the League of Friends, because you find that you brought it and it has gone and been used in another hospital, because of this change.
CH2, V01
More specific still were discussions around the processes for approving and enacting expenditure and the subsequent utilisation and sustainability of any items purchased. Criticisms were made of inappropriate or unsustainable purchases illustrative of broader weaknesses of charitable giving: philanthropic particularism, devoting resources to items that did not really meet community needs. These frustrations were balanced against the overall contribution that such expenditure made to the hospitals.
Providing services
Beyond the direct input of Leagues of Friends and individual volunteers described above, various community and voluntary groups also contributed to community hospitals. In the case studies, such groups provide some direct form of patient care either during their time in hospital, including taking patients out for the day, or on discharge (e.g. Age UK, Red Cross, Motor Neurone Disease Association, Stroke Association, hospices, alms-houses, counselling services, depression and anxiety services, singing and other therapeutic activity groups). They also provided support for families and carers of hospital patients (e.g. carers’ association, bereavement groups) or more general support for the hospital (e.g. schools, Rotary club, local businesses, supermarkets, sports and social clubs). Some of these services were free to the hospitals, some were paid for, and some were delivered by paid staff, some by volunteers.
We found some examples of voluntary and community groups, or members of staff from them, being co-located within the hospital. Two hospitals provided office space for local charities: one had a worker from the Stroke Association sitting alongside the community stroke team and one hosted a centre that brought together a group of local charities all providing well-being services. This sharing of resources and assets was seen to provide important mutual benefits (see below and Chapter 7).
Some voluntary and community groups had ‘grown out of’ the hospital or the League of Friends. For example, in one hospital, a befriending service had been set up by a member of the League of Friends initially to support patients from the hospital returning home, but had since been extended to support older people within the community more generally. In another, a day care centre had been established (outside the hospital grounds) by members of the League of Friends to provide a local facility.
The extent to which the community hospitals interacted with such voluntary and community organisations varied considerably. Extensive links seemed to be associated with facilitation of networking initiatives through Councils for Voluntary Service (or their equivalent). The general perception was that more could be done to strengthen the links between the community hospital and local voluntary and community groups and that community assets were being underutilised. Some identified the barrier of a lack of knowledge or capacity among hospital staff to identify and build relationships with relevant organisations.
Giving voice
Leagues of Friends in particular, but also other community groups and individuals, were increasingly drawn into discussions about the future of those hospitals or wider local health-care services. This happened at different levels.
Communication
An important role for the League of Friends was to provide a communication channel between the hospital and its community. This could take the form of raising the profile of the hospital and providing feedback on services. Members of the League of Friends were well placed to do this:
Every member [of the League of Friends] has neighbours, friends, all the organisations they go to, they go out to lunch, they meet people, and we will then feed anything back to the trust that has gone wrong, particularly now we’ve got a governor because they are able and the trust are actually very, very open with us.
CH9, V01
For some Leagues of Friends, providing a communication channel and profile raising had become explicit aims with a set of specific associated activities, ranging from running social media campaigns through to providing signage and leafleting local residents to encourage correct MIU usage and organising events. Two hospitals, for example, had reintroduced fêtes with the specific aim of helping to raise the profile of the hospital. One was thinking of establishing a network of ambassadors: volunteers living within the surrounding villages who would have a specific remit to raise the profile of the hospital. For others, such outcomes were more of a coincidental outcome of other (fundraising) activities that they were undertaking, although one might argue that, even if unintended, the latent benefits of voluntary action are evident (see below for further discussion on outcomes).
Consultation
A number of the case study sites had active consultations running at the time of the research, with particular implications for the future of community hospital beds. Most had prior experience of such processes. Leagues of Friends had come, by design or default, to represent the ‘voice of the community’ in many such consultation processes. This was not always a role they had anticipated, or had the capacity to fulfil, and some were more comfortable with it than others. One League of Friends chairperson admitted that, although they could act as a conduit of opinions between the community and NHS management:
I did not feel like I was representing the whole of [the] community. It did not feel quite right. And cynically it felt like it was going through a process and whatever we said did not actually make any [. . .] difference in the long run.
CH1, V04
Considerable frustration was expressed about such consultations, focusing on poor processes (e.g. lengthy documents, technical language, onerous schedules), lack of timely communication, uneven engagement (e.g. consultations failed to engage the range of groups within the local population) and an apparent inability to influence outcomes. Often, consultations were dismissed as token exercises, with a perception of decisions having been made prior to opinions being sought.
Trusts and CCGs recognised the importance of consultation, particularly given the attachment that many people had to their local hospital. It was suggested that communities would react more ‘reasonably’ to the changes that CCGs felt needed to be made if they had been involved in the decisions and understood the context behind them. Some commissioners, however, also expressed their own frustrations about the consultation processes, suggesting that:
However much you do, it’s never enough and some people will always feel that they have, in some way, been excluded. I’ve kind of grown tired actually of looking people in the eye and saying, ‘You know what? I’m here to listen. We have not already decided and you can believe us or not on that but I’d like to hear your views’.
CH8&9, T02
Co-production
Moving beyond periodic consultation exercises, examples of sustained patient and/or wider community involvement in the ongoing design and delivery of community hospitals was also limited (with two notable exceptions – see below). Indeed, considerable frustration was expressed by some respondents that they had no guaranteed and ongoing place in governance processes: ‘decisions are made by the hospital without really engaging with the community’ (CH2, CY04, FG).
Strong feelings were expressed particularly in relation to times of threat to the hospital or its services, affecting three of the case studies during the research. Most had experienced threats at least once, often more, in the past: one had ‘fought many battles over the years’ to save the hospital.
There was a discussion in interviews and focus groups about the most appropriate mechanism or body to ensure that the ‘voice of the community’ was heard. Protest, or ‘ginger’, groups had been established in at least two of the case study communities during previous moments of threat; they could, it was suggested, be more overtly oppositional. In both existing cases, the group had continued to operate beyond the specific crisis that they were established to fight. Although it was suggested that both took a more strategic view than the League of Friends, there was no clear mechanism for these groups to influence decisions beyond moments of crisis. In the other case, however, the group (seen as ‘the community’) had become an established part of a partnership of health and social care commissioners and providers in the local area. Both were set up in response to an initial perceived threat to the future of the community hospitals but had broadened their remit considerably, placing the community hospital at the centre of wider population health plans.
In addition, in some of our cases, community members had opportunities to influence decisions through the appointment of key individuals, often a key member of the League of Friends, to governance positions within health-care trusts.
The general view, however, appeared to be that opportunities for and the abilities of communities to have a say in key decisions regarding community hospitals were limited:
There is no local input at all and I think there should be. You call it a LRG: I would love to have a small LRG and that would at least – not run the hospital – but at least be able to have a say and it could be listened to.
CH1, V01
Underlying some of these tensions was a perception among many respondents that the communities ‘owned’ their hospital (see Chapter 7) and were therefore entitled to have a say in its governance. As actual ownership and associated governance and decision-making structures were perceived to have become more remote and fragmented, communities felt that they had less ability to influence decisions. The ‘community hospital’ was not always managed or governed as a single entity, but as a series of services, each of which might be the responsibility of a different provider.
One of the case studies had, however, addressed this issue directly. When the hospital was closed by the NHS, they raised the funds to buy it, establishing a charity to own and run the hospital, leasing the space to a local health-care trust, which then provided services. They said:
That’s where owning the building came in, because if we owned the building then we had a bit of a say in how it was all maintained. The NHS does the actual caring but we can back it up.
CH7, CY08, FG
Factors influencing variations in community support
Looking across these different, individual forms of support, we identified several factors as influencing variations in community support for community hospitals.
Deprivation/privilege
When reflecting on differences in levels of community support, respondents tended to initially suggest that they could be explained by variations in prosperity/deprivation. Analysis of the Charity Commission data89 on League of Friends income, however, shows that the size of income was not significantly related to the level of deprivation in the area [t-test: F(3,3) = 1.94, p = 0.12]. These results are likely to be influenced by the low variability in the level of deprivation across community hospital Leagues of Friends, given that most community hospitals were located in more prosperous areas, but do, nevertheless, suggest that other factors are contributing to these variations.
Geography, rurality and community
With a small number of cases, generalisation is difficult, but the level of engagement and support provided to community hospitals appeared to be influenced by a range of geographical factors including its degree of rurality and isolation. Respondents highlighted long travel times to acute hospitals, poor public transport, the lack of other services, the stability of the local population and the strength of community belonging and resilience as being features of rural or more isolated areas that strengthened the support for the community hospital. The one case study with no League of Friends and very limited community engagement was based in a city, close to the centre, and surrounded by housing. The most frequent interaction hospital staff had with residents was complaining about car parking: ‘So there doesn’t seem to be any great relationship at all to be honest’ (CH4, S03).
The precise location of hospital sites in relation to the centres of population was felt likely to influence local commitment. Visible locations in centres of populations were thought likely to facilitate engagement, in contrast to peripheral sites.
The presence, or otherwise, of other health organisations, charities and community groups within the local area was thought to influence engagement with the hospital in a number of ways, including acting as a source of competition for people’s time and money. More generally, however, it was suggested that hospitals located within communities that had a vibrant mix of voluntary and community groups were likely to have higher levels of engagement. This is consistent with wider arguments about collective efficiency: in some circumstances, voluntary sector diversity has been associated with wider community initiatives.
History
The history of the hospital and the community also shaped engagement. Two case studies were war memorial hospitals that were positively associated with community engagement:
. . . I think the history of the community, with this being a memorial site, I think people within the community have generations of people using their bare hands to build the hospital. So there’s a lot of history and passion in that sense.
CH5, S02
This provided a sense of ownership and also temporal connection to one’s ancestors. For the two case studies that had their origins as workhouses, the legacy was less clear, and one respondent said:
That was the workhouse and it’s got a whole different persona really, it’s got a whole different stigma attached to it.
CH3, S01
This folk memory is interesting given that workhouses were abolished in 1948. It seemed to affect engagement in one community more than another, suggesting the interaction of other factors.
Related to the historic origins of the hospital was the sense of ownership: ‘local people feel this is really their hospital’ (see Chapter 7). Those with a strong sense of ownership of the hospital were more likely, it was suggested, to actively support it:
Well I think it’s because the community built the hospital, I think they significantly put finance in for it, that they owned it, they made it their responsibility and I think that that has been passed from generation to generation. You know, from my great-grandparents right through to me, that this is our local community hospital and we are proud of that.
CH3, S01
Threats to the survival of the hospital were identified as being linked to variations in levels of support. When communities had to fight for the survival of the hospital, or services within it, levels of engagement and support often peaked. One of the case studies, however, suggested that persistent threats to the future of the hospital had ‘caused unsettlement to the community’ that, over time, was weakening support for the hospital.
Range of services
The range of services available within the community hospital, and, subsequently, the numbers and types of patients using those services, was also influential: ‘if it can provide care and service for the whole community, it will have more community support’ (CH7, S11). Particularly influential was the provision of maternity services, end-of-life care and MIUs, through increasing the relevance of the hospital among a broader range of people. In one of the case studies, it was suggested that a narrowing of services, to little more than inpatient beds, coupled with those beds serving an ever-widening geographical area, contributed to a perception that ‘it’s not the community hospital anymore and, therefore, getting support is not easy’ (CH6, V01).
The outcomes and impact of community engagement and support
In this remaining section, we present findings on the impact that these different forms of engagement make when considered together. Distilling the contribution of communities to their hospitals was difficult: it was often a taken-for-granted part of hospital and community life with rarely any attempt to assess its wider impact. Overall, however, some suggested that community engagement was ‘key to the community hospital’: it was what makes a hospital a ‘community hospital’, and community hospitals would be a ‘totally different place’ without it.
Enhancing hospital sustainability and utilisation
Community engagement had, in some cases, kept community hospitals or, more frequently, specific services open. Indeed, this engagement may be an important factor in the apparent resilience of community hospitals (at least, until recently), as suggested through the stability in their numbers as reported in Chapter 3. This was particularly evident in one of the case studies when the hospital had been closed by the NHS but was subsequently reopened after the community raised the money to buy and run it, as has been noted elsewhere. 102
The significance of community engagement to retaining hospitals and/or specific hospital services was thought likely to increase in the future as the pressures on NHS budgets heightened. The challenges that this may raise in terms of equality of access to health-care services was recognised by some respondents; although the sums are small relative to NHS budgets, there are considerable variations between hospitals.
Community engagement had also contributed to service utilisation in some community hospitals, generally through raising awareness of the hospital and the facilities available there through fundraising activities, or more specifically through running campaigns to improve utilisation of specific services.
The impact of the community on the hospital was, however, far less significant in some cases. In one case study, for example, it was suggested that if the community did not get involved, no-one would really notice, although ‘some of the trimmings might disappear round the edges’. In addition, a tendency towards resisting change was seen by some to be a significant downside of community engagement, potentially preventing important improvements to service delivery.
Contributing to patient and carer experience
Community engagement was seen to affect patient (and carer) experience in a number of ways. Enhancements to the appearance of and equipment within hospitals were agreed to contribute to patient experience and were characterised as ‘the cherry on the cake’, giving them the ‘extra bits which the hospital won’t or cannot afford’, and contributing to the ‘happy atmosphere’ found in most of the case studies.
It was suggested that the physical presence of volunteers in the hospital and onto the wards could ease anxieties about hospitalisation contributing to the ‘known-ness’ and feelings of being ‘closer to home’, reported as key facets of patient experience (see Chapter 5). Intergenerational connections, facilitated through, for example, school children coming into the wards at Christmas, were an additional, beneficial aspect of this and one that patients responded to particularly enthusiastically.
It was suggested that some patients found it easier to talk to volunteers, ‘someone out of uniform’, than to staff or even family members, and this could be an important form of therapy: volunteers could help to tackle isolation, loneliness and boredom, and, more generally, by helping to ‘lift people’s spirits’ and ‘making them happy’.
Community engagement could also be beneficial at the point of discharge, helping to enhance the transition from hospital to home. Relationships with third-sector organisations were seen to be particularly important here, as they could fulfil an important function in enabling safe discharge through, for example, providing befriending services or day care facilities. Leagues of Friends funding had also been used in some hospitals to buy ‘little gadgets and bits and pieces that are making the patients’ discharge and safety better’ (CH5, S11).
Boosting staff morale
Community engagement also had an effect on staff experience: feeling supported and valued by the community was important and, for some, contributed to a distinction between the experience of working in a community hospital and an acute hospital. Community engagement could help boost staff morale as a demonstration of appreciation:
I think the staff feel the benefit of a bit of community involvement, I think they feel supported by the community I would say [. . .] well, I think it’s an encouragement, isn’t it, that they are doing a good job and sort of a morale booster.
CH1, S06
Experiences were not, however, universally positive. Building and supporting community engagement takes time and energy, and some staff reported having to ‘pick up’ tasks when volunteers had not turned up or had not done a job effectively. Some staff also found that community engagement could create expectations that they found hard to manage, such as expectations regarding access to the building (volunteers thinking they had ‘free rein’ of the hospital) and regarding care: that those who actively supported the hospital had a right to be treated there. Some staff felt that they had compromised themselves in bowing to the pressure of such expectations.
Enhancing volunteer well-being
Engaging with the hospital was also found to have outcomes for the volunteers themselves. For some, getting involved in the hospital/League of Friends represented a replacement for paid work: it had eased the transition into retirement, giving them something to do, a structure to their day and a source of satisfaction, identity, pride and status. This was a particular theme for those who were retiring from nursing, enabling them to continue a life-long commitment to health and care. For a small number of respondents, volunteering at the hospital was an alternative to paid work, which they were unable to sustain for varying reasons.
The social interaction and physical and mental activity associated with volunteering at or for the hospital was also important for some, particularly older, respondents. As one respondent said of volunteering for the League of Friends: ‘for me it is like playing bridge: a challenge which I like’ (CH6, V2); another said: ‘I think it’s better than any medicine really.’
However, active engagement in the hospital can encroach on personal and family time and can be experienced as stressful and tiring, particularly for ageing respondents with health problems: ‘eventually you start to run out of steam, or you have a health problem, and it’s very difficult’ (CH6, V03). Equally, when not being well utilised or supported, volunteering was, for some, at times boring or frustrating. Once involved, however, it could be hard to give up: ‘it’s hard to get off the crazy train . . . My husband says he’s going to divorce me if I take anything else on!’ (CH8, V01). For some, there was then a risk of burn-out.
Community life
Beyond the hospital and the individuals involved in supporting it, community engagement was seen to have a positive impact on community life in general. The activities involved in supporting community hospitals, described in the sections above, were building (and were often reliant on) social interaction, networks and trust. Fundraising events in particular, both small (e.g. bingo) and large (e.g. fêtes), were highlighted as important functions in the social calendar of the community by bringing people together and tackling social isolation. This was seen as particularly important for older people within the community, with the additional benefit that an absence at a regular bingo night, for example, would be noted and followed up to check on the person’s well-being. Part of the value of the community hospital to the community, which the following chapters go on to discuss, comes through the engagement and community action that it engenders.
Summary
Communities do a lot to support their hospitals. This takes a number of different forms, including community members giving their time as volunteers to raise funds, provide a range of services to patients and their families and seek to influence decisions about the development of services.
There are, however, considerable variations in support both within and across communities and over time. Although overall support for community hospitals is generally widespread within communities, active, regular engagement is often limited to a relatively small and select group of predominantly older, female middle-class community members. The potential to do more to enable and support active community engagement was recognised, but often without any clear strategy or investment in doing so.
Between communities, variations were not easily explained by levels of deprivation/privilege alone, but instead were influenced by a range of interacting factors including geography, history, service mix and organisation/management. Over time, the general trend appears to be one of decline, particularly in terms of levels of voluntary income and membership. Some of the wider developments affecting community hospitals, such as the shift towards more step-down and less step-up care, and the associated loosening of the geographical boundaries from which inpatients were drawn, seemed to be influential here alongside broader societal shifts.
Together, these different forms of community support were felt to lead to a range of outcomes for the different stakeholders involved, contributing to hospital utilisation and sustainability (arguably contributing to the apparent resilience of community hospitals), patient and carer experience, staff morale, volunteer well-being and community life. Positive outcomes cannot, however, be assumed or taken for granted. Overall, it was suggested that community engagement was key to community hospitals: it is at least part of what makes a community hospital a community hospital. This is something we shall return to in more detail in Chapter 8, after first exploring what community hospitals do for their communities.
Chapter 7 Perceptions of social value: reassurance and pride
Introduction
In this chapter, we explore perceptions of the social value of community hospitals to the communities where they are situated in order to address the second part of our third study question: ‘what do community hospitals do for their communities’. We draw on the broad framing of social value, which (as argued in Chapter 1) goes beyond the direct (or instrumental) benefits of a hospital for the community to include broader considerations of latent (symbolic) benefits including those related to well-being. We draw on qualitative data from our nine case study hospitals.
Most of the respondents from our case study hospitals were emphatic about their value. It was suggested that the presence of a community hospital was ‘a Godsend’ (CH1, CY05), ’a local treasure’ (CH3, V01), ‘means so much’ (CH5, V03 FG), ‘absolutely crucial’ (CH7, CY08, FG), ‘invaluable’ (CH8, CA01) and ‘just vital’ (CH9, V01).
It was acknowledged that value was unlikely to be ‘reflected in the spreadsheet’; instead, it was to be found in a range of softer, less tangible contributions to economic and social well-being. It should be remembered that this research was limited to those who had some kind of connection to the hospital or at least a key role within the local community (see Chapters 2 and 8); in other words, we would expect a predisposition to affirm the hospitals’ value. We have previously made distinctions between direct and latent benefits of community support, so we pursue that here, beginning with the instrumental (direct) benefits/value of community hospitals and then considering their latent (indirect or unintended) benefit/value.
Direct, instrumental value
Local services
Community hospitals were valued as providers of ‘an essential service’ that was perceived as being ‘desperately’ needed. The instrumental value of community hospitals as providers of a range of local and accessible health (and often social) care services was invariably cited first by respondents, but was seen as going beyond the individual patient and carer experience reported in Chapter 4 (and, therefore, not repeated here). As summarised by one respondent: ‘there’s a lot of that social value that can be added from us being closer to home’ (CH4, S01). The value of providing local health-care services was heightened, it was suggested, in more remote, rural areas and for older people, people with learning disabilities or mental ill health, those with degenerative long-term conditions and those at the end of life. This is an argument for decentralisation and accessibility of health care rather than for the precise form through which services are delivered.
This was argued in psychological terms, somewhat overlapping with the symbolic benefits of the institution (see Institutional presence, identity and belonging), such as the deep feeling of reassurance and safety it provided for many community members. The following words were used regularly in discussions regarding the value of the hospital to respondents: ‘security’, ‘life line’, ‘peace of mind’, ‘a safety value’, ‘confidence’, ‘comfort’, ‘reassurance’, ‘safe haven’, ‘sanctuary’, ‘arm around the shoulder’. The presence of a hospital provided this sense of security, irrespective of actual or potential use by individual respondents: ‘it’s a safety blanket basically’. This was felt to have additional associated tangible benefits, including enabling older people to stay in their own homes for longer as they felt confident in the knowledge that a hospital was close by should they need it.
There was a suggestion that the depth of reassurance and security provided was enhanced through the historic continuity of a hospital within its community. The converse of the security provided by the presence of the hospital was a fear of its closure:
You’d say ‘thank God it’s there’, because, I mean, you never know when these things are going to happen . . . you know they’re always here and you just pop up, even though you’ve got to be prepared to wait. But it’s like a lifeline really. I couldn’t imagine if it closed. Well, I think everybody would die overnight. They’d be terrified of this place closing.
CH1, CA01
Local economy and employment
Community hospitals also had a more direct economic value as local employers, providing opportunities in places where ‘most of the work had dried up’. This points to perceptions of economic vulnerability because of the decline of other sources of employment associated with rural areas. In terms of staff numbers, community hospitals are small or medium-sized enterprises.
Looking beyond numbers, community hospitals were seen to provide valuable, convenient, high-quality, satisfying employment (although it is important to note that it was also often pressured, stressful and sometimes isolating). Many of the staff to whom we spoke, from hotel staff to assistants, therapists, nurses and doctors, were passionate about their community hospitals: ‘it has been my career and I have loved it. I have been here all this time and I love this place to pieces’ (CH5, S04). The scale and local orientation of community hospitals were compared favourably with those of acute hospitals, with one respondent suggesting that working in a community hospital was ‘what nursing is all about – it’s about proper hand holding, it’s about what every nurse in her heart should be able to do still and some people forget about’ (CH6, S01).
The value attached to the work was intensified for those working close to home. Not only were staff more likely to know each other and their patients outside work, they were also likely to be users of the hospital services themselves. This heightened their attachment to the hospital, contributing to a sense of wanting to work hard to provide the best possible service, to the point where ‘. . . we then do the extra mile [sic.]: we will put in extra shifts, we will stay after shifts . . .’. As one respondent put it:
. . . it is pride in what you provide, because you are walking, you are bumping into people on the street that know that is where you work and you want them to be pleased [. . .] it is providing a service for locals that they are proud of and you are proud of.
CH7, S11
Economic contributions extended beyond employment and had a positive impact on the wider economy and ‘economic well-being . . . people going to a MIU and coming away are at work quicker’. Particular mention was made of their contribution to agriculture (relatively high-risk work with a need to return to work quickly) and tourism (reassurance for visitors). Historical research suggests that such instrumental motivations were certainly in the minds of hospital founders. It was also suggested that having a community hospital may attract people to move into an area, and as one respondent stated: ‘one of the things that drew us here was the hospital’.
Social economy and community ecology
The presence of a community hospital also has an impact on the wider social economy and the network of voluntary and community groups operating in the area. The most visible manifestation of a contribution to social value was that community hospitals provided a base for the activities of community organisations. As well as many instances of free use of hospital space for meetings, examples included a community hospital kitchen providing catering services for a local charity, a charity worker being co-located with a community team within a community hospital and charities being physically based on hospital premises. Institutional presence was crucial to one community transport organisation because the hospital staff supported it through holding keys for drivers out of office hours; this enabled the organisation to extend it services: ‘for our user groups to have access to the buses 24 hours a day, 7 days a week, 365 days a year’ (CH4, CY03).
It may be stretching the evidence to suggest that without the presence of the hospital these activities would not take place, but, by being focused on the institution, they facilitate the strengthening of social networks, and if the hospital was not there, groups would have to find alternative, and potentially more expensive, places to meet.
Indirect, latent value
Assets and ownership
When asked about the value of hospitals to the communities within which they were based, many respondents argued that it was a ‘key community resource’ or ‘a huge asset’. Such views were underpinned by a strong sense of ownership of community hospitals by their communities, regardless of formal legal ownership. Here, respondents drew on repositories of knowledge concerning community initiative in establishing the hospital, the symbolism of institutions whose physical presence memorialised those fallen in war and a sense that the hospital united all members of the community, particularly by bridging generational gaps. The following is illustrative of such views, with a respondent explaining that support for the hospital was:
. . . because the community built the hospital for themselves. I think all that time ago, I think they significantly put finances in for it, they owned it, they made it their responsibility and I think that that has been passed from generation to generation. You know, from my great-grandparents right through to me, that this is our local community hospital and we are proud of that, and that we each should support it.
CH3, S01
It was also associated with a sense of entitlement among some community members to have a say in how the hospital was run, with one respondent claiming that some elderly residents were unaware that the hospital had been transferred to public ownership on establishment of the NHS, so that:
. . . they still have that firm belief – ‘this is our hospital. We don’t want to lose it. We get a choice’. And they should get a choice because it is their community hospital, whether they own the building or not any more it makes no difference. It is their community hospital and it’s so evident[ly] the feeling of everybody in the community, even young people.
CH5, S05
It does seem implausible that someone interviewed in 2016 would have been unaware for seven decades that the hospital was no longer in voluntary hands, and perhaps what is being referred to here accords more with the lack of awareness of recent organisational change in the NHS:
I thought that we owned the land? And I thought they owned the . . .
No, it was taken over, the whole thing, in 1948, it became government property and it was in the local administration’s management. But about a year ago, this trust was set up called NHS Property [Company], that own all NHS property.
Even though the [local community] residents raised the money in the First World War for the hospital to be . . .?
That doesn’t wash.
CH5, V03, FG
However, there was also evidence that a sense of community ownership had survived shifts in legal ownership, not to mention the many changes in service providers and workers:
So, the ownership by League of Friends and local population is, you know, I always say they’re the ones that kind of own the hospital in a sense. I always do the analogy of a football club in that the manager can change, the players change, the stadium changes, the board has taken over but the fans stay . . . committed to the club even though everything else changes . . .
CH1 and 2, T02
The issue of ownership, however, became contentious when the community hospital was under threat of closure or significant change. In some of the hospitals, recent changes, including changes in ownership, provider, services and/or patient mix, which the community themselves felt they had little control over (see Chapter 7), had contributed to an erosion of the sense of community ownership and value:
So what I’m saying is, if you are interested in the connection between the village and the surroundings and the hospital, then the emotion connection is very much diminishing [. . .] It’s because it is not a cottage hospital any more.
CH5, V01
Institutional presence, identity and belonging
Beyond the instrumental and social value of providing local health-care services, however, community hospitals had important cultural and symbolic value. It was suggested that they embodied and were a visible demonstration of shared, communal values:
It’s a site of remembrance and it’s a site of sort of practical help for the community in helping its most vulnerable members, people who are injured and who are sick.
CH5, S14
They provided a common point of reference and a physical site through which individuals, families, groups and organisations came together:
It’s one of the central points that makes up the town and the community. And also gives us a very essential, local feeling. It’s part of the glue that makes up the whole community.
CH1, P06
At least one of the hospitals, for example, holds an annual World War memorial service, bringing together patients, staff, the church and other members of the community: an important symbolic and social event. When combined with the fundraising activities organised by the League of Friends, some hospitals become important facilitators of routine social interaction, ‘contributing to the social life’, within their communities.
Thus, they ranked alongside other important local institutions (almost regardless of the specific services they provided), such as churches, schools, banks and libraries. They were focal points within their communities and their presence was seen as an indicator of the viability of the community:
. . . it’s a very important pillar, along with, say, the bank and the building society and everything else that goes with it. It’s a good thing for morale, I think, for the area to have such an organisation.
CH8, CY03 FG
This was particularly so in rural, isolated communities and/or communities that had experienced economic decline and an associated loss of services:
And people are, you know, they are very emotionally attached to it because they see pubs closing and they see shops closing and I think to close hospital beds, they see it as a nail in the coffin.
CH9, S08
For these reasons, many respondents had strong emotional attachments to their community hospitals and even stronger emotional responses to any threat to their future. Words such as ‘pride’, ‘love’, ‘hope’, ‘trust’, ‘passion’, ‘anguish’, ‘anger’, ‘sadness’, ‘distress’ and ‘fury’ were frequently used.
One respondent went as far as to say: ‘I cannot really put it into words really. I would fight to the death for it. I would’ (CH8, CA03). Such emotional responses were reflective of the significant ways in which hospitals were valued for their contribution to a collective sense of identity, to a sense of place and belonging: not only could they provide an important service, they could ‘define the community’.
Again, this was particularly so, it was suggested, for more isolated rural communities and those that had experienced decline, where any remaining ‘pockets of ownership mean an awful lot’. In such contexts they were, it was suggested, fundamental to ‘a sense of place’. This could, on occasion, be mobilised in service of the collective goal of retaining the hospital. In one community in particular, the previous loss of several services added to a conviction that they must fight to save the hospital when it was threatened with closure: ‘that was the last straw’. Fighting a successful battle to retain the hospital (even though some questioned whether or not it was ever actually under threat) had the dual benefits of maintaining local health-care services while also boosting local ‘civic pride’ and feelings of ‘resilience and autonomy’.
Variations in value
Although a majority of our respondents from the case study locations were passionate about the value of their hospitals, not everyone felt the same. Indeed, one might suggest that it is precisely because many community hospitals are long-established parts of the social fabric that their presence and contribution goes unmarked and unquestioned. Even among those who, when prompted, placed a relatively high value on the contribution of community hospitals to their communities, they received little regular active thought or attention:
I think we take it for granted, we’ve always had a hospital. We had one in town before this one was built. So I just think we take it for granted [. . .] I expect it to be here.
CH2, V04, FG
Many respondents suggested that it was not until a hospital, or its services, were under threat that its value to the community was recognised. Indeed, it was suggested that many residents may have little knowledge of their community hospital:
. . . I think sometimes they see this thing up the hill and they don’t really know what it is for. Local people do not tend to ask the question. It is a bit like, I suppose, if you have a sofa in your front room and you do not know what it is, nobody says ‘what is that?’, it’s kind of a bit like that, nobody actually asks the obvious question ‘what is that hospital for?’.
CH7, S10
In addition, although generalisations from nine case studies must be made with caution, we argue that there was evidence of variations in the degree of attachment to hospitals between communities.
First, inaccessibility and distance from, or a lack of, other services were felt to amplify the value of community hospitals and our perception was that attachment to the hospitals was greatest in the more remote rural communities. However, we had only one truly urban case study, which also generated mixed opinions because of folk memories of its origins as a workhouse and its subsequent rise and fall from DGH status/service mix.
Second, the origins of the hospital appeared to influence the extent of support for it. Those that were founded by the community as a war memorial or that developed in association with the mining industry had a particularly deep significance to their local communities. For those that had originated as workhouses, the connection with the community was less straightforward. Memories were very persistent, with one staff member strongly arguing that patients were reluctant to be admitted to a particular hospital ’because their parents [. . .] very much still had that working memory of it being a workhouse. So I think it’s been disadvantaged from that point of view’ (CH4, S10).
Third, the range of services provided by a community hospital affected the extent to which the community valued it. Generally speaking, the greater range of services provided, and thus the wider the potential user group, the higher the local estimation of value. However, this was not a simple linear relationship: one of the case study hospitals was very small and provided relatively few services but was deeply valued. In any event, the nature of the hospitals, the services they provided and the communities they served were always in flux. This could weaken the sense of local identification with the hospital. In one case, as inpatients at one hospital came to be drawn from a wider geographical area, respondents questioned whether or not it should still be termed a ‘community’ hospital because ‘the emotional connection [was] diminishing.’ As one respondent said: ‘it’s not really a local facility for the local community. It’s an intermediate care unit and just happens to be situated in [this village]’ (CH6, S06). In another case study, for similar reasons, the description of the hospital as a ‘community hospital’ was questioned: ‘we are just a hospital in an area really’. The relationship was a purely functional one.
Finally, community hospitals meant more to some people than to others: there were variations within communities. The value of community hospitals was particularly significant for older residents and those with long-term, chronic conditions, mainly because of the relevance of the services to them but also in part because of their greater historic connection to them through long residence and awareness of treatment provided to previous generations. There were suggestions that those people who had recently moved into areas were less attached and saw less value in the hospital compared with longer-term residents, although, as noted above, we also heard that community hospitals could attract people to move into the area.
Summary
Community hospitals can fulfil a number of important functions within the communities where they are situated that go well beyond health care. They can represent significant community assets, with an associated strong sense of community ownership. Their provision of local, accessible health (and often social) care services has an important instrumental value, particularly in more remote rural communities, many of which have suffered from a decline in other services. Through providing local services, they are also providing highly valued local employment and adding to the local economy both directly and indirectly. Their value, however, often goes beyond the practical: they can have deep emotional, social, cultural and symbolic significance, contributing to a sense of community identity, pride, belonging, security and reassurance.
However, some developments were beginning to change perceptions of the value of some community hospitals to their communities, including any narrowing of the range of services provided and/or changes in the accessibility of inpatient beds for local people associated with a shift towards step-down provision and the widening of the hospital catchment area (see Chapter 4). A combination of these factors left some respondents questioning if certain hospitals could still be considered community hospitals if they did not meet the needs of all members of the local community. Such developments could be seen to be exacerbating the differences within communities as they become increasingly seen as a service for older people.
Although acknowledging the variability and, indeed, the limitations of our research, which meant that we did not include the views of many people who had no connection to the hospital, many of our respondents argued passionately about the practical, economic, social, human, cultural and symbolic value of community hospitals (we develop these concepts further in Chapter 8). They were less convinced, however, that those in a position to make decisions would attend to such arguments. There were strong arguments against a financially driven logic promulgated by:
. . . some people – not in this community but outside – who regard whether there’s a community hospital or not as clearly a financial matter. Sorry, they’re wrong. This is a social facility that needs to be kept up and whether it makes money or not is slightly irrelevant – all this has got to be as efficient as possible but [. . .] it will save money if you concentrate more activities here. They may not be the cheapest ways of doing things, but socially and [. . .] ecologically they are the best way of doing it.
CH5, CY01, FG
Our respondents were generally sceptical about the ability of these arguments to influence decisions within the current funding context of the NHS.
Chapter 8 Discussion and conclusions: the meaning of community hospitals
The study sought to provide a comprehensive profile and analysis of the characteristics, patient experience and community value of community hospitals. In this chapter, we discuss and conclude findings from across the different elements of the study that, together, addressed this central aim. In doing so, we provide new understandings of these different aspects of community hospitals that we suggest go beyond the questions of what a community hospital is, and how it is experienced, supported and valued, to make a significant and original contribution to understandings of what community hospitals mean.
What is a community hospital?
Community hospitals have evolved over time to become a diverse set of institutions that present a challenge to any attempt to define, categorise or map them. Our initial attempts to develop a definition based on a comparison of inpatient metrics, population characteristics and service provision found that community hospitals were distinct from other types of hospitals through the contribution of GPs and rurality and were typically smaller than acute and DGHs. Beyond these aspects, however, we were not able to identify a definitive set of metrics to determine what should and should not be considered a community hospital. Instead, it was necessary to combine these top-down data with experiential, ‘bottom up’, evidence gathered from community hospital leaders and websites. Bringing these sources together enabled the development of a more comprehensive and inclusive set of defining characteristics, retaining and revising some features identified within earlier definitions12,20–22,103,104 (e.g. size, rurality, length of stay, GP leadership), removing others (e.g. population size, localness) and adding new ones (e.g. lack of 24/7 onsite medical cover).
Based on this definition, we identified 296 community hospitals in England in 2015. These hospitals were within a database containing details of each hospital against multiple criteria and were placed on the Community Hospital Association’s website [URL: www.communityhospitals.org.uk/birmingham-university.html (accessed 22 July 2015)]. The overall number of community hospitals remained constant since they were last mapped in 2008,72 suggesting resilience within this sector; however, closures and new entrants mean that the make-up of the list shows some differences.
The majority of the community hospitals that we identified were concentrated within rural areas, located in relatively privileged communities, with a bias towards the south of England. This uneven distribution reflects, in part at least, the voluntary nature of their origins and their largely organic evolution.
This definition was taken a step further through the development of a typology, developed through our reading of the literature, analysis of data and conversations with key stakeholders, that recognised community hospitals as operating on a spectrum of intermediate care provision. Core community hospital services were identified as inpatient beds, outpatient clinics and (in half of all community hospitals) MIUs. Alongside these core services, some community hospitals were more orientated towards primary care provision, with others orientated more towards acute care provision.
Implicit within the methodological challenges associated with defining and mapping community hospitals (discussed in Chapter 2), yet somewhat obscured within the results, is the more dynamic reality of community hospitals at the local level. The apparent stability in the total number of community hospitals (until 2015 at least), for example, tells us something about their apparent resilience, but little about the changes that have taken place within them. The mapping alone could not track the declining number of inpatient and maternity beds nor the shifting relationship between community hospitals and other parts of the health-care system, as demonstrated through a reduction in GP involvement, an increase in step-down care and the growing acuity and geographical spread of inpatients. Adding findings from our qualitative case studies to those from our quantitative definitional and mapping work provided a fuller answer to the question ‘what is a community hospital?’. Table 21 summarises what we have come to understand, through the integration of our quantitative and qualitative research findings, as the common characteristics of community hospitals.
| Characteristics | Definition |
|---|---|
| Small | Usually with ≤ 30 beds. The ‘smallness’ of a community hospital is an important feature of patient experience |
| Historically embedded within and valued by its local, typically rural, community | The history and rural geography of a community hospital is significant for its role, function, patient experience, community engagement and value |
| Operating with a complex model of ownership and provision | Regardless of legal ownership, communities feel ownership of community hospitals. Services are provided by a range of different organisations, leading to concerns about fragmentation when there is no governance or management structure responsible for individual, whole, community hospitals |
| Providing a (valued) relational model of care | Patients and carers experience a relational, human, kind of care, facilitated through the relationships between not just patients and staff, but patients, staff, families and communities and between these people and their environment |
| Based on integrated, multidisciplinary working | Integration and MDT working is facilitated through the co-location of multiple primary, secondary, community and voluntary health and social care teams and services |
| Without 24/7 medical cover | Community hospitals do not have 24/7 onsite medical cover and are reliant on nursing staff and on-call doctors outside core hours. The exact medical model operating, and extent of cover, varies considerably |
| Led by GPs, in-house doctors, and nurses | Historically, GPs have been an integral part of community hospital provision and their involvement remains significant. GP involvement has, however, reduced considerably, while the in-house employment of doctors has grown. In practice, most are led by nurses |
| Providing step-down and step-up care for frail, older (and increasingly acute) inpatients | The balance in provision of step-up and step-down inpatient care has shifted towards the latter, while at the same time the age, frailty and acuity of patients have also increased. This has implications for patient experience and community value |
| With an ALOS of typically < 30 days | Average lengths of stay are typically < 30 days (often much shorter) but are currently being challenged by pressures from acute hospitals to admit and from insufficient social care provision, which delays discharge |
| With a range of additional local, intermediate and generalist care services, on a spectrum from primary to acute care orientations | The range of services varies along a spectrum of intermediate care, from those which are more primary care orientated to those which are more acute orientated, and is significant for patient experience, community engagement and value. Those with ‘cradle-to-grave’ provision are highly prized |
| Constantly evolving in response to external demands | Community hospitals are constantly evolving, often in response to external – local and national – demands, which has contributed to the diversity of the network. Policy-makers, commissioners, staff, patients and family carers and communities have considerable but often different demands and aspirations for the role and function of community hospitals. Currently, although there is general enthusiasm across the board for the expansion of community hospitals as ‘hubs’ of integrated care, the future of beds is contested. The ability of each group to influence outcomes varies considerably |
Community hospitals are diverse and dynamic, but they are united by these common characteristics. Although previous studies have offered various definitions, they were rarely rigorously tested against an analysis of their characteristics; this study has provided a robust list of defining characteristics along with a typology to differentiate among community hospitals and a definitive database on how many community hospitals with beds there are, where they are and what they do.
What are patients’ and carers’ experiences of community hospitals?
Patients and family carers were overwhelmingly positive in ratings of their experiences of community hospital care, support and treatment, thus echoing findings of earlier studies (e.g. Small et al. 24). Although we did not set out to make comparisons, many respondents contrasted their experience of community hospitals with that of acute hospitals. Comparisons were favourable (see Green et al. ,32 Small et al. 24 and Lappegard and Hjortdahl105 for similar findings), although both were recognised as fulfilling valued, but distinct, functions. Respondents frequently told us that acute hospitals were where you would want to go to treat a specific medical condition, and community hospitals were where you would want to go to get (physically, emotionally and socially) better.
We identified three sets of factors highlighted as being key to patient and carer experiences of community hospitals, as distinct from other types of hospitals:
-
Closeness to home – this encompassed many different functional, interpersonal, social and psychological dimensions, including patients and carers experiencing their locations as more convenient and accessible; their environment and atmosphere as more familiar, homely and relaxed, less stressful and daunting, and more reassuring; and the relationships that they fostered between patients and staff, and between patients, their families and communities, as transformational.
-
Personalised and holistic – closely associated with the elements described above, community hospitals were recognised as providing personalised care. Moreover, a key element of the patient experience was their provision of holistic care. Both were facilitated through community hospitals’ valuable range of co-located, integrated, intermediate services; their fostering of MDT working and, more specifically, of a work ethic that encouraged staff (from different disciplines) to look beyond their professional boundaries to go the extra mile and take care of all the diverse needs any individual patient may present with, while also involving and informing carers.
-
Supporting difficult psychological transitions – for many older people, the accident or illness leading to their admission to a community hospital often triggered a major life event, which was emotionally traumatic and a major psychological undertaking, requiring time to come to terms with such life changes. Trappes-Lomaz and Hawton31 suggest that ‘failure to understand patients motivations or their social and psychological realities will risk undermining the rehabilitation process’. Community hospitals were responding in different ways to the demands placed on them through supporting patients through these transitions.
Although this study did not look at outcomes, together these different dimensions of patient experience appeared to help reduce stress among patients and carers and were perceived to aid recovery or, where relevant, to facilitate a ‘better death’. Although there were many examples of staff supporting patients to build their confidence, and a few examples of staff recognising patients’ general anxieties and concerns, we observed little formal assessment and work with anxiety and depression. When caring for older people who, as a result of an accident or illness, were facing a major life change, we would argue that there is a need for a greater focus on people’s psychological, emotional and mental health, alongside their physical health.
Cutting across these different accounts of patient and carer experience are four key dimensions to patient and carer experiences of community hospitals (functional, interpersonal, social and psychological) that we detail below. Previous studies have tended to focus on just two dimensions, the functional and relational (e.g. Glenn and Cornwell106 and Doyle et al. 107), conflating relational and psychological aspects of care and missing the social. Our study suggests that these should be separately analysed as part of the unique patient experience of community hospitals.
-
Functional, particularly environmental, features of community hospitals were fundamental to patient and family carer experiences, resonating with the findings of earlier studies (e.g. Small et al. ,24 Payne et al. 25 and Lappegard and Hjortdahl26). These included their accessible locations, small size, often pleasant surroundings, interiors designed to look more like home, ‘home-cooked’ food and (generally) quiet and less frenetic atmosphere. These environmental, or functional, features were part of what made community hospitals feel ‘closer to home’. Being ‘closer to home’ increased the accessibility of community hospitals and went beyond convenience, through reducing the stress of travelling long distances or finding parking, through enabling frequent visits by family and friends and through representing an environment that was familiar, known, reassuring and nurturing, particularly for local patients and their families.
-
Interpersonal aspects of care also featured strongly in patients’ and carers’ narrative accounts – relationships between staff, patients and family carers were central to experiences of using community hospitals and so too were relationships between patients and the wider community. Patients highlighted the warm and welcoming staff, being looked after personally with sensitivity and respect, staff and volunteers spending time with them, being listened to, keeping their spirits up and time taken to care for the whole person, including multiple medical and social conditions. Instead of the depersonalizing patient experience associated with larger hospitals, reports of a much more ‘connected and reciprocal’ relationship between patients and staff were common; this is exactly what Bridges et al. 35 argue that we need more of.
-
Social aspects of patient experience were also highlighted, particularly the importance of having family and friends close by so that they could visit often – keeping families and communities together. The importance of the hospital being local, and community based, was stressed in terms of patients being known to staff and maintaining social connections during periods of hospital treatment, rather than being distanced and isolated. Social interactions between patients featured less in narrative accounts, but were facilitated to varying degrees in different hospitals through the utilisation of communal spaces for group dining and activity sessions and through the involvement of volunteers. For some, not enough was done to encourage activity and alleviate boredom (see Small et al. ,23 Payne et al. 25 and Trappes-Lomax and Hawton31 for similar findings).
-
Psychological aspects of patient experience were often wrapped up in their accounts of feeling less anonymous and frightened within their community hospital than they would in an acute setting and feeling more confident and hopeful, while also coming to terms with loss and change. Similarly, among family carers, the reassurance and reduction of stress associated with patients being cared for, often by people they knew, within a familiar, local community hospital were significant factors. On the other hand, this aspect also captured the shock and enormity of life events and psychological transitions that frequently coincided with patients’ use of community hospitals. Although community hospitals were generally seen to build patients’ confidence and physical health, a greater focus on psychological, emotional and mental health was needed.
When considered together, these four elements point to community hospitals as providing a relational (more human, caring, attentive), rather than transactional, model of care. Personal, reciprocal relationships between not just staff and patients, but between staff, patients, their families (predominantly referred to as carers within this report) and the wider community, and between all these people, the hospital services and their environments, were intrinsic factors in patients’ and carers’ experiences. This often contrasted strongly with patients’ and carers’ accounts of their previous experience of acute services. This relational model of care was facilitated through a closeness to home and community, for patients, their families and staff; the co-location and integration of a range of intermediate, generalist and personalised services; the small size, familiar and homely environment of community hospitals; and, as we shall discuss in more detail in the next section, their connection to and integration with the local community.
However, this highly valued relational model of care cannot be assumed or taken for granted. Although it was evident in all of the case studies, there were variations, moderated by a number of external and internal factors. Some of the developments currently affecting community hospitals, as outlined above (and in more detail in Chapter 4), were thought to pose a particular challenge to some of these highly regarded aspects of patient experience. In some, for example, the functional aspects of patient experience were challenged as facilities became dated, services were cut back or inpatients were drawn from an increasingly wide geographical area, meaning that community hospitals were no longer always local, convenient or easily accessible to all. The widening of geographical boundaries, and associated shifts towards greater provision of step-down care for increasingly elderly and acute patients, also had implications in some hospitals for the maintenance of the social and interpersonal aspects of care. In others, the interpersonal aspects were challenged by pressures on staff, exacerbated by recruitment challenges and a withdrawal of GPs from community hospital medical provision.
What does the community do for its community hospital, and what does the community hospital do for its community?
Community hospitals have a strong history of community engagement and support, often starting with raising funds to buy the land and build the hospital,108 but until now there have been few attempts to empirically explore what communities do for their hospitals or vice versa. Whereas previous studies of community or voluntary support for, and engagement with, health-care institutions more generally have tended to focus on one particular form of support (e.g. volunteering, philanthropy or co-production), we looked more broadly at the different forms of support that were provided, to what level and to what effect. We found that communities support their hospitals in four key ways:
-
Giving time – volunteering was commonplace across community hospitals, particularly through the League of Friends, with each involving, on average, 24 volunteers, equating to between 1.4 and 2.5 full-time equivalent personnel per hospital. Volunteers undertook a range of roles, from fundraising through to befriending, campaigning and governance. Their efforts were mostly encouraged, co-ordinated and supported through Leagues of Friends, although in some community hospitals there was a significant amount of volunteering that took placed outside the League of Friends co-ordinated and managed by individual members of staff.
-
Raising money – community hospitals have been supported by financial donations and fundraising efforts within their local communities throughout their history. In 2014, on average, community hospital Leagues of Friends generated an income of £45,387 (median £15,632). Two-fifths of all income came from legacies, with the rest coming from a variety of activities ranging from domino nights, fêtes, running charity shops and providing day care services. Expenditure focused on supporting the hospital, patients and staff in a range of different ways, from providing patient comforts through to purchasing equipment, major building work and paying for staff time.
-
Providing services – the study shows that voluntary and community groups contribute to community hospitals through the provision of a wide range of services and activities, both within and outside the hospitals, for patients, their families or for the hospital in general. Some, however, thought that more could be done to further enhance partnership working between community hospitals and local voluntary and community groups.
-
Giving voice – despite a long history of involvement in community hospitals and active information and communication exchange through the Leagues of Friends, the mechanisms for and the depth to which communities are involved in decisions regarding their ongoing delivery and strategic future are generally limited. Overall, regular, ongoing engagement would likely be positioned towards the lower ends of the various spectra of participation (e.g. Arnstein109): although information sharing and general communication was commonplace, engaging in consultations was periodic (and often frustrating) and meaningful redistribution of power through co-production relatively rare. Communities’ extensive voluntary support bought them no ongoing or privileged influence on decision-making, just as was the case in the pre-NHS voluntary hospitals. 69 This generated considerable frustration. These findings sit in tension with the strong sense of ownership that communities feel towards their hospitals.
Underlying these headline findings, we found considerable variations in the support that communities provided their community hospitals with. In line with wider studies on voluntary action, we found variations on three key lines:
-
Variations between community hospitals – there were considerable variations in the levels and forms of voluntary support between community hospitals. Whereas one of the case studies involved dozens of volunteers, for example, in a wide range of roles, another involved only one or two in a very limited capacity. Similarly, in common with many wider findings on philanthropy, this work reveals considerable variation in levels of charitable income between community hospitals. These variations were not easily explained in terms of, for example, community-level prosperity alone, but instead were influenced by the interaction of a range of factors that went beyond demographics to include the history of the hospital, of the community’s engagement with it, of local geographical characteristics including rurality and isolation and the range of services provided by the hospital.
-
Variations within communities – within-community variations were particularly notable in terms of regular, active volunteer involvement (including engagement in co-production activities). We found a tendency to rely on a small group of highly committed volunteers, many of whom had been involved for years. Although a wider group of community members offered more occasional support, the more active, regular volunteers were predominantly drawn from older age groups and were often women, with challenges identified in recruiting newer, more diverse participants. This raised concerns about future sustainability of involvement, particularly given that we also found that younger demographic groups identify less strongly with community hospitals. 110 We agree with the conclusion of Munoz et al. 51 that ‘harnessing more local volunteers . . . is more complex than governments assume’: we found a general lack of ‘investment’ in their recruitment, co-ordination or support outside that provided by Leagues of Friends or individual staff. Such investment is needed to sustain and support voluntary action, especially in an era of heightened expectations about the recruitment and conduct of volunteers.
-
Variations over time – we observed variations over time, particularly concerning voluntary income but also in membership and general patterns of engagement. Quantitative trend data were available only for voluntary income: since 1995, this suggests a steady decline in Leagues of Friends income, thus reflecting Clifford’s111 findings on charity finances that identify several groups of charities for whom levels of resources have declined from the mid-1990s. However, we found little concern among the case studies regarding declining income. Instead, we heard more concerns about expenditure: spending money when the future of hospitals, their services or ownership were uncertain and/or about shifting boundaries between statutory and voluntary responsibility. We also found evidence that some of the hospitals continued to accrue funding even when they reduced their fundraising efforts because of, for example, concerns about the future of the hospital or so as to not overly dominate local fundraising endeavours. More generally, we heard that community support and engagement fluctuates over time in response to wider developments, such as policy and commissioning decisions, with activity (e.g. membership) peaks associated with services being perceived to be under threat, as well as to more local developments, such as changing personnel (hospital or League of Friends), that can serve to either encourage or discourage engagement.
These findings reflect broader thinking about the limitations of philanthropic effort, that is the variations in supply and the inability to match provision and need in a systematic manner. 59
Through these different forms of engagement, communities provide significant support (and, on occasion, challenge) to their community hospitals, leading to various outcomes for the different stakeholders involved:
-
Patient experience – communities can positively affect patient experience, reflecting findings from Hotchkiss et al. ,53 Naylor et al. ,42 and Kang and Hasnain-Wynia. 112
-
Service enhancement, utilisation and sustainability – they can also positively contribute to community hospital services by adding capacity, enhancing facilities and boosting staff morale, reflecting Mundle et al. 54 on the impact of volunteering in health services. They can also contribute to the resilience of community hospitals, through communication and promotional activities boosting utilisation and their campaigning, protesting and fundraising sustaining services that had been under threat of closure.
-
Well-being and social capital – at the same time, although quantification is difficult (and beyond the scope of this project) and the evidence does not unequivocally state that volunteering always generates wider public benefits, in line with wider volunteering literature,113 we found that individual supporters (especially volunteers) and communities more generally can themselves benefit through, for example, the development of skills, networks, trust and reciprocity.
In doing so, the voluntary support that communities provide to their community hospitals adds to and, indeed, is an integral part of the social value of community hospitals, as we discuss further below.
None of these forms and levels of engagement, or their positive outcomes, however, can be taken for granted. The study suggests that a lack of appropriate support for volunteering, for example, may lead to volunteers doing too much and risking burn-out, reducing the benefit to patients and putting a strain on relationships with paid staff. Recruiting new, younger volunteers can be difficult, while membership and voluntary income levels are both on the decline, and concerns about the appropriate role for voluntary support within statutory services were expressed. Furthermore, echoing research elsewhere,51,114 there are capricious variations in the extent of voluntary support that cannot be simply explained by any one factor. Converting the extensive passive support found across communities into more regular, active engagement requires investment of time, energy, enthusiasm and, inevitably, money.
The other half of our question (‘what do community hospitals do for their communities?’) addressed an evidence gap in relation to the social value of community hospitals. 22,64 This study suggests that community hospitals can fulfil a number of important functions for the communities in which they are embedded and can provide significant added value. Community hospitals can represent a significant community asset, with an associated strong sense of community ownership. Their provision of local, accessible health and social care services has an important practical social and symbolic significance, particularly in the more isolated rural communities, and, as established institutions known to generations of the same family, they are integral to a sense of community identity, pride, belonging, reassurance and security. The engagement of communities in the community hospitals, as discussed above, is an important element of their added social value.
Adapting and expanding the framework devised by Prior et al. 68 and developed by Farmer et al. ,64 we found that the ‘social value’ of community hospitals, at collective (family, community) and individual (patient, carer, staff, volunteer, resident) level, can be disaggregated into six distinct forms of value that, together, can be conceptualised as ‘community value’. The study was not designed to measure any of these quantitatively, but interviewees identified each to be significant and important:
-
Instrumental – through the provision of local, accessible, integrated, intermediate health and social care services, associated with highly regarded patient experience.
-
Economic – through the provision of local, high-quality, valued jobs, the reduction of travel costs associated with accessing more distant health-care services and through the encouragement and support of agriculture, tourism and in-migration and the viability of other services.
-
Social – through the development of networks of interaction, trust and reciprocity, built directly through the services provided by the community hospital and indirectly through the community engagement activities that support it.
-
Human – through the creation of jobs and volunteering opportunities for local people that involve skills development and utilisation and can enhance confidence, morale and well-being (of staff, volunteers and patients).
-
Cultural – community hospitals can have cultural value, through contributing to a sense of individual (especially for staff and volunteers) and collective identity, feelings of belonging and civic pride and a collective sense of place (see James,115 Farmer et al. ,64 Gesler116 and Kearns and Joseph117 for similar findings).
-
Symbolic – as a symbol of vitality and viability of the community (see Liu et al. 70 and Lepnurm and Lepnurm118), community hospitals contribute to perceptions of resilience and autonomy. More profoundly, they can provide a sense of security and safety individually, for patients and their families, and collectively for the wider community, thus supporting Jones’s66 suggestion that hospitals might contribute a deep sense of reassurance to the communities in which they exist. This symbolic value is absent from previous frameworks, although referred to within wider discussion. 64,68
Overall, community hospitals are an important community asset. Their value comes not only directly and indirectly from their physical presence and service provision but also through the different forms of engagement that they inspire: the process of actively supporting community hospitals (e.g. through volunteering and fundraising) further enhances their value. Although previous studies have suggested a link between the history of place, hospital, health and community through the study of individual cases (e.g. Andrews and Kearns119) or in other countries (e.g. James115), this study is the first to demonstrate these findings across multiple community hospitals in England.
What does ‘community hospital’ mean?
Although we started by posing the question ‘what is a community hospital?’, this question has developed to become ‘what do community hospitals mean?’. This enables us to capture the depth of feelings and significance often expressed by the patients and carers who use them, the staff who work in them and the individuals and communities who support and value them – among whom there is much crossover. It is only by combining the understandings that emerge from addressing each of the three individual study questions, and seeing the connections between them, that we come to new insights into the meaning of community hospitals. As Higgins120 suggested, small (community) hospitals mean more to communities than simply a place to receive health care. We highlight three particular, inter-related, meanings.
-
Community hospitals mean locally embedded, integrated, intermediate, generalist care (see also Heaney et al. 22 and Pitchforth et al. 1) that brings together not just primary, secondary and community health care and health and social care, but also statutory provision with voluntary and community ‘provision’ within one accessible location. The existing and potential significance of community hospitals as sites of integrated intermediate care was widely recognised, with considerable enthusiasm for further expansion of the range of services they provide as ‘hubs’ at the heart of their communities.
-
Community hospitals mean embedded, relational care. The relational model of care, which we outlined above, stems from the embeddedness of community hospitals within their local health-care systems and, more fundamentally, within the histories, cultures and social networks of the communities and places within which they are anchored (Figure 15). Understanding the significance of the interdependent, reciprocal or mutually reinforcing and beneficial relationships between individual patients and families, their hospitals and their communities is an important step forward in recognising not just what community hospitals are, but also how they are experienced and valued and what they mean. Through actively supporting their hospitals, for example, community members can help boost staff morale, which, in turn, can have a positive influence on patient and care experience, which, in turn, can help boost active community support.
-
Community hospitals mean a deep sense of reassurance and of ontological security,67 as Jones66 suggested they might. This reassurance comes, in part, from the physical presence of a community hospital, which acts as a visible expression of both historic and contemporary collective care and identity, but also from the different forms of interaction with it and the sense of ownership that this inspires. It extends beyond individual patients and their families to staff and, significantly, to the communities in which they are based, and it connects together the different forms of value that community hospitals represent to these different stakeholders.
FIGURE 15.
An embedded, relational model of care.
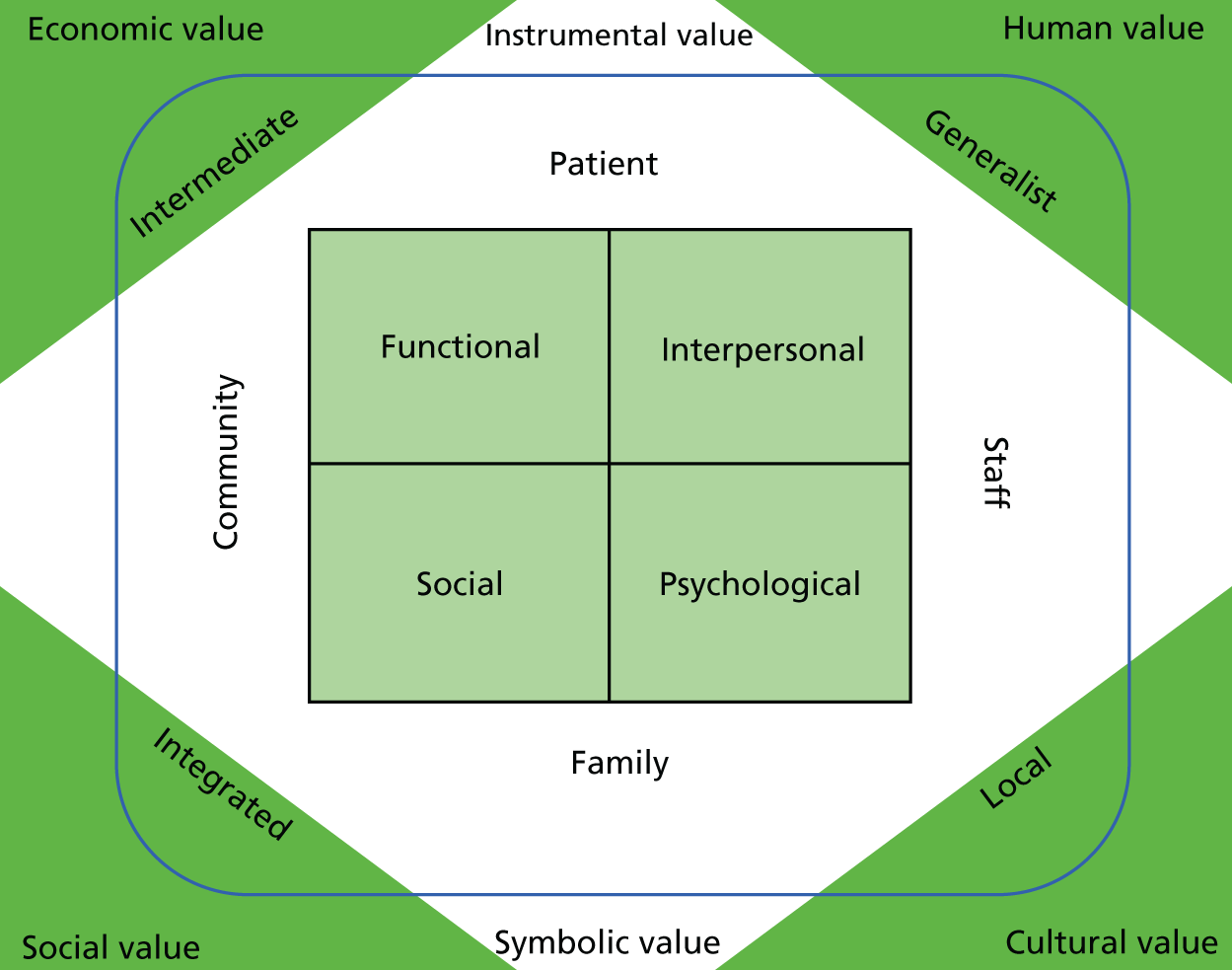
These meanings, however, vary between communities. Community hospitals, for example, vary not just in their orientation towards primary or acute care, but also in their embeddedness within the communities within which they are situated. Both orientations make a difference to patient experience, community engagement, value and meaning. If, for example, community hospitals become disconnected from their communities, not only do they risk losing out on the direct benefits of community engagement, but they also risk weakening the relational model of care that currently defines them, reducing their community value.
Meanings also vary within communities, influenced by factors such as age, health, duration of residence and personal connection. In general, community hospitals mean more to those who have direct contact with them than to those who do not: whether as patients, family or friends of patients, staff, volunteers or more distant supporters. For many community members, they may become aware of their local hospital only during moments of crisis. Furthermore, despite the significant value and meaning that community hospitals represent for their communities in general, this translates into regular, active and sustained engagement for only a relatively small and selective group of people.
There is also variation over time. This research has highlighted the dynamic nature of community hospitals (see also Pitchforth et al. 1 and Heaney et al. 22) and their susceptibility to change as a result of both internal and external developments that have contributed to their current diversity and, arguably, to their agility and resilience. These changes potentially shift the meaning of community hospitals.
The current context of austerity, an ageing population and increasing pressures on health-care services overall, combined with a lack of national strategy for community hospitals, are putting them under pressure and pulling them in different directions without any clear steering mechanisms. The withdrawal of GPs, the shift towards step-down care, the delivery of services to a wider geographical area, the associated increasing acuity of inpatients and questions over the future of community hospital beds are particularly visible demonstrations of these pressures. Together, they have the potential to shift not just the characteristics, function and patient experience of community hospitals, but also their community value and meaning. We found examples among the case studies when the hospitals had changed/were changing to such an extent that community members felt that they were no longer providing local services for local people by local people, which in turn led them to withdraw their active support and, in turn, led them to question whether or not they could still be considered ‘community hospitals’. Their meaning had been lost: they were no longer embedded, relational or reassuring, but were simply intermediate care units based in the local area.
Within this challenging context, questions arise as to how both patient (and carer) experience and community value are taken into account when making decisions regarding the future of community hospitals. Harlock121 identified the challenge of embedding social value in commissioning processes in general. Many of this study’s respondents, outside the commissioning process, argued strongly that neither community value nor patient experience was taken fully into account and that, instead, cost was the over-riding consideration. It was felt that patient experience could be dismissed as undiscerningly positive and community value dismissed as an innate resistance to change and/or a naive understanding of the cost and value of community hospitals.
Implicit within these discussions is an inherent tension within community hospitals: they are not bounded entities with discrete, matching ownership, management and governance structures to steer and direct them. Although communities, and indeed many patients and staff, feel a strong sense of ownership towards community hospitals as whole entities, they rarely retain legal ownership or have a significant say in their strategic direction through formal governance or management structures. Furthermore, with the relatively recent proliferation of providers operating within them (stemming from the 2012 Health and Social Care Act),122 there is a lack of ‘overall control’ for individual community hospitals as whole entities rather than as collections of services, the management and governance mechanisms for which extend beyond either hospital or community. This seems a unique and particularly challenging feature of the community hospital sector.
There have been threats to these institutions in the past. The Ministry of Health’s 1962 Hospital Plan7 proposed the closure of numerous community hospitals, but a combination of community opposition, changing views as to the nature of general hospital provision and economic circumstances meant that many survived and new visions came to be articulated of the contribution that community hospitals might make. Within the current context of STPs (now Sustainability and Transformation Partnerships), there is a concern that the localised approach to their development may obscure their combined effect on community hospitals across the country, limiting the potential for local voices to be heard at national level. 19 The attractiveness of proposals for new models of care focused on supporting patients in their own home, while also making financial savings elsewhere in the system, is likely to sideline the potential role for community hospitals to provide a range of services ‘closer to home’ (in the different ways that we have demonstrated this to represent), let alone their wider social value. A lack of authoritative guidance for the NHS as a whole,19 combined with a lack of hospital-level governance and management mechanisms that involve local stakeholders, could leave individual community hospitals vulnerable to financially driven decision-making processes. Although some areas have recognised and reinforced the role of community hospitals within their STPs, many appear to be looking to reduce provision and/or to move away from a model of community hospitals with inpatient beds to one of community hubs with an extending range of services but often no inpatient beds. Although an expansion of services is likely to be welcomed by many communities, a closure of beds or a threat to their community hospital is not.
Evidence from elsewhere suggests that community hospital closure can be a ‘critical incident’ for rural communities,123 mobilising extensive support120 motivated by a desire to preserve and protect the hospital. This can represent both significant challenges for commissioners and providers and a significant opportunity. It offers the potential to harness the passion and pride that communities feel towards their hospitals and build on the highly valued embedded, relational model of care experienced by patients. It provides an opportunity to realise the potential identified by Pitchforth et al. 1 for community hospitals to assume a more strategic role in health-care delivery locally, providing care closer to people’s homes or, more ambitiously, as recognised by at least one case study, to put community hospitals at the heart of new models of population-based health and social care.
Key contributions
For all the longstanding (and sometimes controversial) debates that there have been around the role and future of community hospitals in England, it is remarkable that, until now, we have lacked:
-
a widely accepted definition of community hospitals and a definitive understanding of the number, location and services provided
-
a detailed understanding of patient experience
-
an understanding of the relationship between community hospitals and their local communities.
At a time when many areas are disinvesting in community hospitals (particularly in bed-based services), but when others are investing in an expansion of such services, it is difficult to see how either of these directions of travel can be evidence based given the very limited nature of current knowledge. That we know so little about such a longstanding feature of the NHS (and pre-NHS health care) is perhaps itself a symbol of neglect, and remains a significant concern given current debates about the future of a number of community hospitals, and the very strong public reactions that these debates provoke, in a challenging policy context.
Against this background, we believe that this study is the most detailed, comprehensive and robust analysis of the characteristics and value of community hospitals that there has been for many years (perhaps even in the history of the NHS), with the subsequent data shared with community hospitals themselves and made publicly available as a resource for the CHA, local services, commissioners and policy-makers alike. In particular we have:
-
Developed a new typology of community hospitals and produced a publicly available database of current community hospitals, their size and location, their services and key activity data. As described in Chapters 2 and 3, this has significant advantages compared with previous attempts to capture such information, producing the most comprehensive and detailed data ever compiled. This was significantly aided by the ability to combine the experience of working with national data sets with the detailed local knowledge of the CHA (essentially, a ‘top down’ and a ‘bottom up’ way of understanding the nature of community hospital services). This process has revised previous assumptions around localness, small population base and primary care leadership and contributed to a new typology for understanding the orientation of community hospitals.
-
Generated in-depth data on patient experience that contrast strongly with participants’ prior experience of acute care. This not only fills a significant gap in the literature but has also enabled us to propose a new model for analysing patient experience based on the functional, social, psychological and interpersonal aspects of care and to conceptualise community hospitals as providing embedded, relational care.
-
Produced unique insights and data into community engagement and community value, combining the best of the health services management and voluntary sector research expertise of the current team. Such data are patchy/rare for most health services, but are almost non-existent for community hospitals. This has allowed us to understand the breadth, depth and variability of community engagement and to adapt and extend the framework proposed by Prior et al. 68 and Farmer et al. 64 to consider the contribution of community hospitals in terms of the economic, social, human, cultural instrumental and symbolic value that they represent at individual and collective levels. Asking what a hospital does for its community and what a community does for its hospital are highly significant questions in the current context (both academically and in policy terms), and it seems remarkable that such questions have rarely been explored in depth before.
-
Moved beyond discussions of what community hospitals ‘are’ or ‘do’ to more fundamental questions about what they ‘mean’; this is significant academically, but also in terms of current debates about the configuration of health services in a challenging financial context and, particularly, how concerns for patient experience and community value are taken into consideration, alongside the domination of cost efficiencies.
Limitations of the study
The mapping exercise within work package 1 was limited to those community hospitals with beds. This is consistent with our provisional and final definition, but we are aware that others might wish to include some other local sites under the umbrella of community hospitals. Furthermore, the cross-sectional nature of the mapping exercise combined with time delays within our data collection and analysis of the NHS Digital database (which was collected in 2012/13 and validated against data current at 2015) means that our finalised list will subsequently have become outdated following hospital closures and other changes to hospital function.
The site of treatment code used to identify community hospitals within the NHS Digital data is not stable or complete: it is organisation based and changes each time the NHS restructures. The need to investigate 60 potential sites that were not visible in the NHS Digital data set highlights the limitation of site of treatment code, which, in a minority of cases (< 10%), may be set at a level that is more aggregated than community hospital (e.g. trust level).
The investigation of patient experience (work package 2) was intended to include an equal sample of inpatients and outpatients/clinic patients, but this did not prove possible, with the resulting patient sample skewed towards inpatients. As such, the experiences we report are more reflective of inpatients than of all patients and this is reflected in the presentation and analysis of results.
In analysing data on the uses of funds raised by the communities for their hospitals, there are limitations to the Charity Commission data. Only in those cases in which a League of Friends (or its equivalent) has an income of > £25,000 do we have any detail at all about expenditure beyond an aggregate figure, and variations in recording of this between hospitals, plus the degree of generality of the terms used in accounts (e.g. terms, such as ‘charitable activities’, with no further detail), limit what we can say. We also lack information that would help us understand the financial position of charities in more depth, such as their reserves.
In exploring questions of community engagement and value, the case studies were limited by the focus on respondents who had some form of connection with the hospital, or who at least had a significant role within the local community. Practical limitations meant that we were unable to extend our sample to general members of the public with no connection to or involvement in the hospital at all.
Implications
Implications for system planning (i.e. sustainability and transformation plans)
Adopting a localised approach to health service planning, for example through STPs, offers considerable potential for devolved decision-making, but carries strategic risk. There is a danger that the combined impact of proposed changes to community hospitals across the country may be obscured. This risk is heightened by the notable lack of any national policy for community hospitals.
This study has highlighted both the diversity of community hospitals but also their points of commonality, including the role they play in providing local, accessible, intermediate health care; the valued embedded, relational model of care that they provide; and the significant community value they represent. Questions have been raised, however, as to the power of existing evidence of either patient experience or community value to temper financial rationales that are perceived to be dominating discussions about the future of community hospitals. Unduly privileging financial imperatives risks underestimating or undermining other forms of value. Future plans should be based on a sophisticated analysis of not just the economic costs and benefits of community hospitals, but also their community value, which encompasses individual, collective, instrumental, economic, social, human, cultural and symbolic costs and benefits.
The feelings of ownership that communities often have over their community hospitals suggest considerable potential, and, indeed, expectation, if not obligation, to involve them in the design and delivery of services. Existing consultation mechanisms often appear insufficient, leading to frustration on both sides, and meaningful coproduction was the exception rather than the rule. There is a tension between the scale at which communities appear to want to engage, making decisions about ‘their’ community hospital or ‘their’ community’s health care, and the scale at which engagement activities are currently often focused (i.e. at a wider geographical or system level).
The attraction of new models of care focused on supporting patients in their own home (increased financial savings and clinical safety) appears to underestimate both the lack of social care funding available to facilitate this strategic change and the lack of alternative community bed provision (e.g. nursing homes, residential care homes and hospices) for people unable to return home after an acute inpatient admission. Community hospital beds continue to play an important part not only in step-down care, but also in acute admission avoidance (step up) and effective generalist provision for addressing the multiple comorbidities prevalent in older people. The potential to expand their role in both acute attendance avoidance and broad preventative agendas appears significant.
The increasing pressure on acute hospitals and the growing acuity of patients is presenting a number of challenges for community hospitals (including the level of medical cover available, skills of nursing staff, longer lengths of stay, more pressure to discharge). There is some evidence that this is resulting in inappropriate referrals and patients being bounced back to acute hospitals or staying in community hospitals for longer than would otherwise be necessary. When combined with pressures on social care that are having an adverse effect on community hospital discharges, the process is acting as an ineffective shifting of the (acute hospital beds) problem.
Implications for community hospitals
Community hospitals provide a distinctive and valued model of care that is both relational and embedded. They are flexible and agile in their response to changing demands and are generally supported and valued by the communities from which they originate, within which they are based, from which they draw their staff and to which they provide service and care. Although the mapping work undertaken through this study has provided greater clarity on the characteristics of community hospitals, it is these deeper points of distinction that were highlighted by respondents and stand out as being worthy of particular emphasis.
Community hospitals, however, are changing and are already diverse. Although the story of community hospitals has always been one of evolution, the pace and scale of the changes they are currently experiencing, including the withdrawal of GPs, the fragmentation of provision, the shift towards step-down care, the associated increasing acuity and decreasing localness of inpatients, the questions being raised in some areas of the future of inpatient beds and the wider financial and demographic pressures, could represent a significant cross roads. The erosion of community hospital-level management and governance structures represents a particular challenge for navigating these complex external developments at the local level and reduces the potential for both integrated working and patient or community involvement in service design or delivery.
Community hospitals provide an embedded, relational model of care within which the functional, social, interpersonal and psychological aspects of patient experience are all integral. Each of these aspects requires attention, not least because each can be moderated by external and internal factors that may undermine the overall model of care. A particular challenge identified was attending to patients’ psychological health. Although patients were generally far less anxious about attending a community hospital than an acute hospital, admission to hospital was often associated with a significant life transition, potentially generating anxiety and depression, yet clinical attention to psychological, emotional and mental health needs was not consistent and represents an area to be addressed.
Communities do a lot to support their hospitals, and the contribution of volunteers and voluntary income can have a significant impact. There are, however, considerable variations in support both across and within communities and over time. Although support for community hospitals is generally widespread, active, regular engagement is often limited to a relatively small and select group of community members and voluntary income (and membership) is on the decline. The potential to do more to enable and support active community engagement was recognised, but often without any clear idea of how to do so. Converting the more widespread, yet more passive, support into more regular, active engagement – beyond moments of crisis – requires time, energy, enthusiasm and, inevitably, money. The case studies suggest that mobilisation is difficult, but that in the right circumstances it can be achieved. This may mean more actively supporting Leagues of Friends in their efforts; it may mean developing a range of structures to facilitate and support wider forms of engagement.
In addition to the above implications for community hospitals as a whole, each of the participating case study community hospitals has received an individual presentation and report of the findings specific to their hospital within which specific implications for each were discussed.
Implications for patients, carers, communities and Leagues of Friends
Community hospitals are widely valued by patients, their families and communities. They are, however, changing, at the same time as communities are also changing, and their contribution to community life can change over time. In particular, a number of current developments are beginning to change perceptions of the value of some community hospitals to their communities. Although much of this may feel out of the control of individual patients, their families or community members, there is evidence from this study that when communities engage in supporting their hospitals not just through practical voluntary action but also through strategic action within decision-making processes, the value of community hospitals can be not only retained but enhanced.
Leagues of Friends make a significant and valued contribution to the hospitals they support and their wider communities. The individuals involved make considerable personal investments, demonstrating significant commitment and loyalty, often over generations. The challenge of maintaining membership and broadening active engagement, particularly among younger generations, was, however, widely recognised. Getting new people involved may require new ways of thinking and working, both in terms of finding new ways to ask a more diverse range of people to get involved and new activities to involve them in.
Concerns were expressed that the understanding that has informed community fundraising for the NHS for most of its history, namely that funds raised be dedicated to supporting patient and staff amenities or comforts, was in danger of being breached. For instance, we found examples of the use of charitable income to employ staff or purchase equipment for clinical use. Even though the sums involved were generally not large, this raises issues of equity and, more broadly, the appropriate balance between statutory responsibility and voluntary initiative.
Recommendations for future research
-
Compare and contrast patient experience and outcome of those supported in acute hospitals, in community hospitals and in their own home. This is particularly important in the current context with the drive for new models of care that look to optimise the level of home-based care.
-
Longitudinal studies of community engagement (including historic) with local health services, how this varies between different types of service provision (e.g. acute, community), how it is changing over time, how the boundary between statutory and voluntary support is shifting and the implications of all of this.
-
Longitudinal research with community hospitals to explore the ways in which they are evolving, particularly the change in clinical leadership and practice associated with the withdrawal of GPs, but also the development of hubs without beds and the effect of such changes on patient experience, community engagement and value.
-
An international comparative study on inpatient case mix in community hospitals, examining levels of dependency, acuity and complexity to establish reasons for admission, diagnosis, outcome and discharge destination.
Acknowledgements
We would like to thank a number of people who contributed to the successful completion of this study. We would like to thank all of our study respondents who contributed to this study through participating in interviews, focus groups, site visits and responding to requests for information. Their willingness to engage with us and their openness to the study provided effective and easy access to others across the nine community hospitals. Particular thanks goes to matrons/ward sisters and the League of Friends members who co-ordinated research activities for us, organised LRGs and participated in annual learning events. We would also like to thank the CHA Board, Research Committee and members for coproducing the research application and documentation and responding to and verifying emerging findings; Helen Tucker and Jan Marriott (CHA, England) for providing important suggestions and offering feedback at every stage of the application, design and execution of the study, as well as on draft chapters of the final report; Dr David Seamark for providing clinical advice throughout this study; all members of the cross-project steering group, chaired by Professor Sir Lewis Ritchie (University of Aberdeen); Satnam Virdee (Research Associate) for case study scoping visits and patient experience evidence synthesis; and Rachel Posaner (Head) and Emma Green (Librarian) of the Health Services Management Centre Library, who conducted literature searches for Chapter 1 and set up the EndNote [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] file for final report references.
Contributions of authors
Deborah Davidson co-conceived the study with Professor Glasby and drafted the protocol. She was responsible for day-to-day programme and budget management and research partner co-ordination, contributed to overall study design and case study sampling, and undertook case study field work across all nine case studies for work packages 2 and 3. She also contributed to coding, synthesis and drafting of the final report and provided inputs to annual learning events and study presentations/workshops.
Angela Ellis Paine co-designed work packages 2 and 3 and drafted the case study research instruments, sampling frame and community engagement and value evidence synthesis. She led on five case studies and undertook case study field work across all nine case studies for work packages 2 and 3, led on the formation of LRGs, the design and delivery of the annual learning events and qualitative data coding. She significantly contributed to the synthesis and drafting of this final report, as well as local case study reports.
Jon Glasby was principal investigator and provided intellectual oversight for the whole study, programme management and delivery oversight. He contributed to the overall study design, synthesis and the final report. He also provided inputs to annual learning events and study presentations/workshops.
Iestyn Williams provided intellectual support to the study and contributed to the study design, work packages 2 and 3 (qualitative studies), the synthesis and the final report.
Helen Tucker provided advice and support regarding contemporary and historical knowledge of community hospitals, and national and local liaison. She contributed to work package 1 through validating national data on community hospitals with CHA data, undertaking a rapid synthesis of the national and international literature on definitions and drafting a typology of community hospital service orientation. She also contributed to work packages 2 and 3 (qualitative studies) through local liaison (helped with ease of case study recruitment) and offered important suggestions and feedback on study sampling, design and execution. She contributed to the final report and provided specific inputs to team meetings (updates on community hospital, such as briefing papers on developments, innovations and closures), annual learning events and study presentations/workshops.
Tessa Crilly was responsible for the mapping study design and implementation, data generation for case study sampling and analysis, interpretation and reporting of results. She contributed to the final report.
John Crilly contributed to the design, analysis and interpretation of results for work package 1, retrieving and reconciling three national data sets (Scotland, Wales and Northern Ireland), reconciling four England data sets and analysing national data to generate a database and directory of community hospitals in England. He contributed to the interpretation of results in work package 1 and clarification of work package 1 data for the final report.
Nick Le Mesurier led on four case studies and undertook case study field work across all nine case studies for work packages 2 and 3. He contributed to coding, synthesis and local reports. He also provided inputs to annual learning events and study presentations/workshops.
John Mohan contributed to study design in relation to literature on voluntary action and charitable giving. He constructed the databases on the activities and resources of registered charities that underpinned the relevant sections of this report, oversaw the capture of data on hospital finances and accounts, directed analyses by Daiga Kamerade and contributed to quantitative analyses. He contributed to relevant sections of the final report.
Daiga Kamerade examined the financial and volunteer support that local community groups and organisations provide to community hospitals and how that support varies between communities and community hospitals. Her contribution was to develop an analytical strategy, link financial data from the Charity Commission Charity Register and from the organisations themselves with relevant indicators from various databases, and to conduct data analysis.
David Seamark provided expert knowledge in relation to clinical and medical practices in community hospitals. He also contributed to the study through local liaison and offering important suggestions and feedback on study design and execution, as well as on drafts of the final report.
Jan Marriott provided advice and support regarding community hospitals’ history, knowledge, and national and local liaison, and contributed to the study through offering important suggestions and feedback on study design and execution, as well as on drafts of the final report.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration in the first instance. Access to available anonymised data may be granted following review.
Qualitative transcripts: all respondents consented to making anonymised transcripts accessible; however, appropriate preparation of these will require discussion with the study team prior to release.
Charity Commission data: links to the data discussed are provided in Appendix 9 of this report.
NHS Benchmarking 2014/15 data set: anonymised data can be obtained via a data-sharing agreement with NHS Benchmarking [www.nhsbenchmarking.nhs.uk/contact/ (accessed 8 October 2018)].
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Pitchforth E, Nolte E, Corbett J, Miani C, Winpenny E, van Teijlingen E, et al. Community hospitals and their services in the NHS: identifying transferable learning from international developments – scoping review, systematic review, country reports and case studies. Health Serv Deliv Res 2017;5.
- Young J, Smith A, Tucker H, Longo R, Eardley H, Godfrey M, et al. A study to understand and optimise community hospital ward care in the NHS. Health Serv Deliv Res 2019.
- Willavoys D, Crowther A. The Hospitals and Medical Practices of Tewkesbury. Tewkesbury: Tewkesbury Hospital Leaflet; 2013.
- Swete H. The Handy Book of Cottage Hospitals. London: Hamilton Adams; 1870.
- Loudon IS. The contribution of general practitioner hospitals. J R Coll Gen Pract 1972;22:220-6.
- Consultative Council on Medical and Allied Services, Interim Report: Future Provision of Medical and Allied Services. London: HSMO; 1920.
- A Hospital Plan for England and Wales. London: HMSO; 1962.
- Bennett AE. Evaluating the role of the community hospital. Br Med Bull 1974;30:223-7. https://doi.org/10.1093/oxfordjournals.bmb.a071205.
- Rue R, Bennett AE. Community Hospitals: Progress in Development and Evaluation. Oxford: Oxford Regional Hospital Board; 1974.
- Rickard JH. Cost-Effectiveness Analysis of the Oxford Community Hospital Programme. Oxford: University of Oxford; 1976.
- Community Hospitals: Their Role and Development in the National Health Service. London: HMSO; 1974.
- Tucker H. Community hospitals. Progress of a concept of care. Health Serv J 1987;97:244-5.
- Hadridge P. Opportunities in Intermediate Care: Summary Report from the Anglia and Oxford Intermediate Care Project. London: DH NHS Publication; 1997.
- Keeping the NHS Local: A New Direction of Travel. London: HMSO; 2003.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: HMSO; 2006.
- Delivering Care Closer to Home: Meeting the Challenge. London: HMSO; 2008.
- Community Hospitals Strategy Refresh. Edinburgh: Scottish Government; 2012.
- Five Year Forward View. London: HMSO; 2014.
- Seamark D, Tucker H, Penwarden H. England must support its community hospitals. BMJ 2016;354. https://doi.org/10.1136/bmj.i3933.
- Ritchie LD, Robinson K. Community hospitals: new wine in old bottles?. Br J Gen Pract 1998;48:1039-40.
- Seamark D, Moore B, Tucker H, Church J, Seamark C. Community hospitals for the new millennium. Br J Gen Pract 2001;51:125-7.
- Heaney D, Black C, O’Donnell CA, Stark C, van Teijlingen E. Community hospitals – the place of local service provision in a modernising NHS: an integrative thematic literature review. BMC Public Health 2006;6. https://doi.org/10.1186/1471-2458-6-309.
- Small N, Green J, Spink J, Forster A, Young J. Post-acute rehabilitation care for older people in community hospitals and general hospitals – philosophies of care and patients’ and caregivers’ reported experiences: a qualitative study. Disabil Rehabil 2009;31:1862-72. https://doi.org/10.1080/09638280902847002.
- Small N, Green J, Spink J, Forster A, Lowson K, Young J. The patient experience of community hospital – the process of care as a determinant of satisfaction. J Eval Clin Pract 2007;13:95-101. https://doi.org/10.1111/j.1365-2753.2006.00653.x.
- Payne S, Hawker S, Kerr C, Seamark D, Roberts H, Jarrett N, et al. Experiences of end-of-life care in community hospitals. Health Soc Care Community 2007;15:494-501. https://doi.org/10.1111/j.1365-2524.2007.00714.x.
- Lappegard Ø, Hjortdahl P. Perceived quality of an alternative to acute hospitalization: an analytical study at a community hospital in Hallingdal, Norway. Soc Sci Med 2014;119:27-35. https://doi.org/10.1016/j.socscimed.2014.08.014.
- King G, Farmer J. What older people want: evidence from a study of remote Scottish communities. Rural Remote Health 2009;9.
- Boston NK, Boynton PM, Hood S. An inner city GP unit versus conventional care for elderly patients: prospective comparison of health functioning, use of services and patient satisfaction. Fam Pract 2001;18:141-8. https://doi.org/10.1093/fampra/18.2.141.
- Green J, Forster A, Young J, Small N, Spink J. Older people’s care experience in community and general hospitals: a comparative study. Nurs Older People 2008;20:33-9. https://doi.org/10.7748/nop2008.07.20.6.33.c6617.
- Clegg A. Older South Asian patient and carer perceptions of culturally sensitive care in a community hospital setting. J Clin Nurs 2003;12:283-90. https://doi.org/10.1046/j.1365-2702.2003.00724.x.
- Trappes-Lomax T, Hawton A. The user voice: older people’s experiences of reablement and rehabilitation. J Integr Care 2012;20:181-94. https://doi.org/10.1108/14769011211237528.
- Green J, Young J, Forster A, Mallinder K, Bogle S, Lowson K, et al. Effects of locality based community hospital care on independence in older people needing rehabilitation: randomised controlled trial. BMJ 2005;331:317-22. https://doi.org/10.1136/bmj.38498.387569.8F.
- Safety First: A Report for Patients, Clinicians and Healthcare. London: Department of Health and Social Care; 2006.
- Baker R, Sanderson-Mann J, Longworth S, Cox R, Gillies C. Randomised controlled trial to compare GP-run orthopaedic clinics based in hospital out-patient departments and general practices. Br J Gen Pract 2005;55:912-7.
- Bridges J, Flatley M, Meyer J. Older people’s and relatives’ experiences in acute care settings: systematic review and synthesis of qualitative studies. Int J Nurs Stud 2010;47:89-107. https://doi.org/10.1016/j.ijnurstu.2009.09.009.
- Ellins J, Glasby J, Tanner D, McIver S, Davidson D, Littlechild R, et al. Understanding and Improving Transitions of Older People: A User and Carer Centred Approach. Southampton: National Institute for Health Research Service Delivery and Organisation Programme; 2012.
- Tucker H, Meads G, Meads T. Trust in Experience. Abingdon: Radcliffe Medical Press; 2001.
- Hine C, Wood VA, Taylor S, Charny M. Do community hospitals reduce the use of district general hospital inpatient beds?. J R Soc Med 1996;89:681-7. https://doi.org/10.1177/014107689608901207.
- General Practitioner Hospitals: Report of a Working Party Appointed by the Council of the Royal College of General Practitioners – Occasional Paper 23. London: Royal College of General Practitioners; 1983.
- Community Hospitals: Preparing for the Future – Occasional Paper 43. London: Royal College of General Practitioners and Association of GP Community Hospitals; 1990.
- Cooney E. The Leagues of Hospital Friends. Public Administration 1960;38:263-72. https://doi.org/10.1111/j.1467-9299.1960.tb01266.x.
- Naylor C, Mundle C, Weaks L, Buck D. Volunteering in Health and Care: Securing a Sustainable Future. London: The King’s Fund; 2013.
- Galea A, Naylor C, Buck D, Weaks L. Volunteering in Acute Trusts in England: Understanding the Scale and Impact. London: The King’s Fund; 2013.
- Hawkins S, Restall M. Volunteers Across the NHS: Improving the Patient Experience and Creating a Patient-Led Service. London: Volunteering England; 2006.
- Mocroft I, Pharoah C. Coming Full Circle: Charitable Funds in London’s Health. London: The King’s Fund; 2001.
- Lattimer M. The Gift of Health. London: Directory of Social Change; 1996.
- Mohan J. Voluntarism, municipalism and welfare: the geography of hospital utilization in England in the 1930s. Trans Inst Br Geogr 2003;28:55-74. https://doi.org/10.1111/1475-5661.00077.
- Mohan J, Gorsky M, Sheard S. Financing British Medicine. London: Routledge; 2006.
- The National Council for Voluntary Organisations UK Civil Society Almanac . UK Civil Society Almanac 2015 Volunteer Profiles 2015. https://data.ncvo.org.uk/a/almanac15/volunteer-profiles/ (accessed 24 February 2016).
- Mohan J, Bulloch C. Is There a British ‘Civic Core’? Evidence From the Citizenship Survey. Working Paper 73. Birmingham: Third Sector Research Centre, University of Birmingham; 2012.
- Munoz S-A, Farmer J, Warburton J, Hall J. Involving older people in service co-production: is there an untapped pool of potential participants?. J Rural Stud 2014;34:212-2. https://doi.org/10.1016/j.jrurstud.2014.02.001.
- Handy F, Srinivassan N. The demand for volunteer labor: a study of hospital volunteers. Nonprofit Volunt Sect Q 2005;34:491-509. https://doi.org/10.1177/0899764005278037.
- Hotchkiss R, Unruh L, Fottler M. The role, measurement and impact of volunteerism in hospitals. Nonprofit and Voluntary Sector Management 2014;43:1111-128. https://doi.org/10.1177/0899764014549057.
- Mundle C, Naylor C, Buck D. Volunteering in Health and Care in England. London: The King’s Fund; 2012.
- Milton B, Attree P, French B, Povall S, Whitehead M, Papay J. The impact of community engagement on health and social care outcomes: a systematic review. Commun Dev J 2011;47:316-34. https://doi.org/10.1093/cdj/bsr043.
- Kamerāde D. Third Sector Impacts on Human Resources and Community, TSRC Working Paper 134. Birmingham: Third Sector Research Centre; 2015.
- Weisbrod B, Phelps ES. Altruism, Morality, and Economic Theory. New York, NY: Russell Sage Foundation; 1975.
- Hansmann H. The role of nonprofit enterprise. Yale Law J 1980;89:835-901. https://doi.org/10.2307/796089.
- Salamon L. Partners in public service: government-nonprofit relations in the modern welfare state. AJS 1996;101:1451-53.
- Public Services (Social Value) Act 2012. London: The Stationery Office; 2012.
- Dayson C. Evaluating social innovations and their contribution to social value: the benefits of a ‘blended value’ approach. Policy and Politics 2017;45:395-41. https://doi.org/10.1332/030557316X14564838832035.
- Phills JA, Deiglmeier K, Miller DT. Rediscovering social innovation. Stanford Soc Innov Rev 2008;6:34-43.
- Teasdale S, Alcock P, Smith G. Legislating for the Big Society? The case of the Public Services (Social Value) Bill. Public Money Manag 2012;32:201-8. https://doi.org/10.1080/09540962.2012.676277.
- Farmer J, Prior M, Taylor J. A theory of how rural health services contribute to community sustainability. Soc Sci Med 2012;75:1903-11. https://doi.org/10.1016/j.socscimed.2012.06.035.
- Barnett R, Barnett P. ‘If you want to sit on your butts you’ll get nothing!’ Community activism in response to threats of rural hospital closure in southern New Zealand. Health Place 2003;9:59-71. https://doi.org/10.1016/S1353-8292(02)00019-9.
- Jones L. What does a hospital mean?. J Health Serv Res Policy 2015;20:254-6. https://doi.org/10.1177/1355819615585893.
- Giddens A. Modernity and Self-Identity: Self and Society in the Late Modern Age. Stanford, NJ: Stanford University Press; 1991.
- Prior M, Farmer J, Godden DJ, Taylor J. More than health: the added value of health services in remote Scotland and Australia. Health Place 2010;16:1136-44. https://doi.org/10.1016/j.healthplace.2010.07.005.
- Mohan J. Planning, Markets and Hospitals. London: Routledge; 2002.
- Liu L, Hader J, Brossart B, White R, Lewis S. Impact of rural hospital closures in Saskatchewan, Canada. Soc Sci Med 2001;52:1793-804. https://doi.org/10.1016/S0277-9536(00)00298-7.
- Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. London: Transaction Publishers; 2006.
- Tucker H, Moore B, Jones S, Marriott J. Profiling Community Hospitals in England 1998–2008. Community Hospitals Association: Department of Health and Community Health Partnership 2008.
- Kaarbo J, Beasley RK. A practical guide to the comparative case study method in political psychology. Polit Psychol 1999;20:369-91. https://doi.org/10.1111/0162-895X.00149.
- Lincoln YS, Guba EG. Naturalistic Inquiry. London: Sage; 1985.
- Ovretveit J. Comparative and Cross-Cultural Health Research: A Practical Guide. Abingdon: Radcliffe Medical Press; 1998.
- Yin R. Case-Study Research Design and Methods. Beverley Hills, CA: Sage; 1984.
- Bryman A. Social Research Methods. Oxford: Oxford University Press; 2004.
- Yin RK. Case Study Research: Design and Methods. London: Sage; 2009.
- Emmel N. Sampling and Choosing Cases in Qualitative Research: A Realist Approach. London: Sage; 2013.
- Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health C 2002;14:353-8. https://doi.org/10.1093/intqhc/14.5.353.
- Friends and Family Test. London: NHS England; 2014.
- Patterson W. Strategic Narrative: New Perspectives on the Power of Stories. Oxford: Lexington; 2002.
- Andrews M, Squire C, Tamboukou M. Doing Narrative Research. London: Sage; 2008.
- Bridges J, Gray W, Box G, Machin S. Discovery interviews: a mechanism for user involvement. Int J Older People Nurs 2008;3:206-10. https://doi.org/10.1111/j.1748-3743.2008.00128.x.
- Riessman C, Quinney L. Narrative in social work: a critical review. Qual Soc Work 2010;4:391-412. https://doi.org/10.1177/1473325005058643.
- Elliott J, Elliott J. Using Narrative in Social Research: Qualitative and Quantitative Approaches. Thousand Oaks, CA: Sage; 2011.
- Learning from Patient and Carer Experience: A Guide to Using Discovery Interviews to Improve Care. Leicester: NHS Modernisation Agency; 2004.
- Mental Capacity Act 2005 Code of Practice. London: The Stationery Office; 2007.
- Charity Commission Returns, England and Wales. London: Charity Commission for England and Wales; 2015.
- Annual Return 2014 Guidance Notes. London: Charity Commission; 2014.
- UK Government . National Minimum Wage and National Living Wage Rates n.d. www.gov.uk/national-minimum-wage-rates (accessed 30 October 2018).
- Wooley C. Meeting the mixed method challenge of integration in a sociological study of structure and agency. J Mix Methods Res 2009;3:7-25. https://doi.org/10.1177/1558689808325774.
- Progress and Reports. n.d.
- 2014/15 Dataset. Manchester: NHS Benchmarking Network; n.d.
- Rural Classifications. Newport: Office for National Statistics; 2011.
- The English Indices of Deprivation. London: Department for Communities and Local Government; 2010.
- National Collaboration for Integrated Care and Support . Integrated Care and Support: Our Shared Commitment 2013. www.gov.uk/government/uploads/system/uploads/attachment_data/file/198748/DEFINITIVE_FINAL_VERSION_Integrated_Care_and_Support_-_Our_Shared_Commitment_2013-05-13.pdf (accessed 26 October 2017).
- Winpenny EM, Corbett J, Miani C, King S, Pitchforth E, Ling T, et al. Community hospitals in selected high income countries: a scoping review of approaches and models. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2463.
- Emrys-Roberts M. Cottage Hospitals 1859–1990: Arrival, Survival and Revival. Dorset: Tern Publications; 1991.
- Intermediate Care Including Reablement Guideline [NG74]. London: NICE; 2017.
- Lampard K, Marsden E. Themes and Lessons Learnt from NHS Investigations into Matters Relating to Jimmy Savile: Independent Report for the Secretary of State for Health 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/407209/KL_lessons_learned_report_FINAL.pdf (accessed 29 October 2018).
- Mohan J, Gorsky M. Don’t Look Back? Voluntary and Charitable Finance of Hospitals in Britain, Past and Present. London: Office of Health Economics; 2001.
- Tucker H. The Role and Function of Community Hospitals: King’s Fund Project Paper Number 70. London: King Edward’s Hospital Fund for London; 1987.
- Ritchie L. Community Hospitals in Scotland: Promoting Progress. Aberdeen: University of Aberdeen; 1996.
- Lappegard Ø, Hjortdahl P. Acute admissions to a community hospital - health consequences: a randomized controlled trial in Hallingdal, Norway. BMC Fam Pract 2014;15. https://doi.org/10.1186/s12875-014-0198-1.
- Glenn R, Cornwell J. What Matters to Patients?: Policy Recommendations. Coventry: NHS Institute; 2011.
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-001570.
- Hall J. From cottage to community hospitals: Watlington Cottage Hospital and its regional context, 1874–2000. Local Popul Stud 2012;88:33-49.
- Arnstein SR. A ladder of citizen participation. J Am Plann Assoc 1969;35:216-24. https://doi.org/10.1080/01944366908977225.
- Lindsey R, Mohan J. Continuity and Change in Voluntary Action. Bristol: Policy Press; 2018.
- Clifford D. Charitable organisations, the great recession and the age of austerity: longitudinal evidence for England and Wales. J Soc Policy 2017;46:1-30. https://doi.org/10.1017/S0047279416000325.
- Kang R, Hasnain-Wynia R. Hospital commitment to community orientation and its association with quality of care and patient experience. J Healthc Manag 2013;58:277-88. https://doi.org/10.1097/00115514-201307000-00007.
- De Wit A, Bekkers R, Karamat Ali D, Verkaik D. Welfare Impacts of Participation. Deliverable 3.3 of the Project: ‘Impact of the Third Sector as Social Innovation’ (ITSSOIN), European Commission – 7th Framework Programme. Brussels: European Commission, DG; 2015.
- Wilson J, Musick M. The contribution of social resources to volunteering. Soc Sci Q 1998;79:799-814.
- James AM. Closing rural hospitals in Saskatchewan: on the road to wellness?. Soc Sci Med 1999;49:1021-34. https://doi.org/10.1016/S0277-9536(99)00180-X.
- Gesler WM. Therapeutic landscapes: medical issues in light of the new cultural geography. Soc Sci Med 1992;34:735-46. https://doi.org/10.1016/0277-9536(92)90360-3.
- Kearns R, Joseph A. Restructuring health and rural communities in New Zealand. Prog Hum Geo 1997;21:18-32. https://doi.org/10.1191/030913297666611118.
- Lepnurm R, Lepnurm MK. The closure of rural hospitals in Saskatchewan: method or madness?. Soc Sci Med 2001;52:1689-707. https://doi.org/10.1016/S0277-9536(00)00283-5.
- Andrews GJ, Kearns RA. Everyday health histories and the making of place: the case of an English coastal town. Soc Sci Med 2005;60:2697-713. https://doi.org/10.1016/j.socscimed.2004.11.004.
- Higgins J. The Future of Small Hospitals in Britain. Southampton: Institute for Health Policy Studies, University of Southampton; 1993.
- Harlock J. From Outcomes-Based Commissioning to Social Value? Implications for Performance Managing the Third Sector. Third Sector Research Centre Working Paper 123. Birmingham: Third Sector Research Centre; 2014.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Petrucka PM, Wagner PS. Community perception of rural hospital conversion/closure: re-conceptualising as a critical incident. Aust J Rural Health 2003;11:249-53. https://doi.org/10.1111/j.1440-1584.2003.tb00546.x.
- Information Services Division Scotland . File Listings 2013 n.d. www.isdscotland.org/Health-Topics/Finance/Costs/File-Listings-2013.asp (accessed 1 November 2014).
- Office for National Statistics . RPIJ All Items Retail Price Jevons: Percentage Change over 12 Months n.d. www.ons.gov.uk/economy/inflationandpriceindices/timeseries/kvr9 (accessed 13 November 2018).
- Guidance to Help to Complete the Annual Return for 2015. London: Charity Commission; 2015.
Appendix 1 Data sets used for England analysis
| Number | Name | Content | Raw data issues | Data source |
|---|---|---|---|---|
| Main databases | ||||
| 1a | CHA 2008 | List of 339 sites (296 community hospitals) as of 2008 with name, address, attributes | Query completeness and whether or not up to date | CHA |
| 1b | CHA 2013 | Updated version of CHA 2008, 20 sites added and some closures marked | Query completeness and whether or not hospital activity was changed | CHA |
| 2 | Estates 2012/13 | List of NHS sites, name, ERIC code, lead organisation, available beds, occupied beds, square footage and utilities | 1586 ‘sites’. Only 49% matched other data sets, plus a number of ‘aggregate’ sites | http://hefs.hscic.gov.uk/ERIC.asp. Data files at 19 November 2014 |
| 3 | PLACE 2012/13 | List of NHS/independent sites, name, site code, lead organisation, wards, beds, performance indicators | 1355 ‘sites’. 72% matched other data sets | http://hefs.hscic.gov.uk/PLACE.asp. Data files at 21 November 2014 |
| 4 | NHS Digital 2012/13 |
Data by ‘site of treatment code’ admissions, day cases, ALOS, inpatient discharges, inpatient occupied bed-days by specialty Outpatient attends by specialty Data by trust – A&E attends |
1754 ‘sites’. 782 matched Estates list, 982 matched PLACE list | NHS Digital reference number: NIC-283421-C9X8C. Downloaded 14 November 2014 |
| Supplemented by | ||||
| 5 | NHS Digital postcodes | A list of NHS/independent sites with addresses and postcodes | http://systems.hscic.gov.uk/data/ods/datadownloads/index | |
| 6 | NHS Choices A&E | List of NHS A&E sites at hospital level | NHS Choices | |
| 7 | National statistics postcodes A | All postcodes with local authorities, wards, PCTs, SHAs, LSOA, MSOA urban/rural indicator (2011 Census) | ONS website NSPLC01_May_2014 and NSPLC_May_2014 (13 October 2014 and 23 July 2015) | |
| 8 | National statistics postcodes B | As above but with CCGs | ONS website NSPLC01_May_2014 and NSPLC_May_2014 (13 October 2014 and 23 July 2015) | |
| 9 | NHS staff staffing team | Number of ward nurses FTE on duty actual/planned | Incomplete as some hospitals missing | Safe staffing England NHS England – england.safestaffing@Nhs.net |
| 10 | Care/nursing homes (beds) by CCG | Nursing homes mapped to postcodes and GP practices 2012/13 | CQC 2012/13 database, ONS 2013 | |
Appendix 2 Mapping community hospitals in Scotland
The mapping process for Scotland informed the England study, the main focus of our enquiry. There are two existing views on the number of community hospitals in Scotland. The first, using ISD’s Cost Book 2012/13,124 listed 63 community hospitals (62 plus Uist and Barra Hospital, Western Isles) within 228 short-stay hospitals.
The second, based on the Scottish Government’s 2012 report Community Hospitals Strategy Refresh,17 listed 96 community hospitals, 11 of which have since closed or been reconfigured to outpatient-only treatment centres, leaving a total of 85 community hospitals. Merging the two lists produced a set of 88 hospitals.
An analysis of inpatient activity by specialty showed the link with primary care to be a dominant characteristic: 87% (55 out of 63) of ISD community hospitals and 73% (64 out of 88) of the bigger ISD/Scottish Government grouping of community hospitals had a GP inpatient specialism, with two-thirds (43 out of 63) of ISD and half (46 out of 88) of ISD/Scottish Government community hospitals showing > 80% inpatient activity coded to GPs.
This is shown in Table 22.
| ISD category | Number of hospitals | Total number of hospitals (ISD/Scottish Government) | ||
|---|---|---|---|---|
| > 80% general practice | < 80% general practice | 0% general practice (100% other) | ||
| Community hospitals | 43 | 12 | 8 | 63 |
| General hospitals | 1 | 1 | 2 | 4 |
| Long-stay/psychiatric hospitals | 0 | 3 | 9 | 12 |
| Small long-stay hospitals | 2 | 2 | 5 | 9 |
| Total number of hospitals | 46 | 18 | 24 | 88 |
| Percentage | 52 | 21 | 27 | 100 |
Appendix 3 Telephone questionnaire (rapid enquiry)
Appendix 4 Summary of hospitals named in mapping study (2012/13 data updated in 2015)
| Number | Name | Trust |
|---|---|---|
| 1 | ABINGDON COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 2 | ACCRINGTON VICTORIA HOSPITAL | East Lancashire PCT, 18 |
| 3 | ALDEBURGH HOSPITAL | Suffolk Community Healthcare |
| 4 | ALDERNEY HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 5 | ALFRED BEAN HOSPITAL | HUMBER NHS FOUNDATION TRUST |
| 6 | ALNWICK INFIRMARY | NORTHUMBRIA HEALTHCARE NHS FOUNDATION TRUST |
| 7 | ALTON COMMUNITY HOSPITAL | SOUTHERN HEALTH NHS FOUNDATION TRUST |
| 8 | AMERSHAM HOSPITAL | BUCKINGHAMSHIRE HEALTHCARE NHS TRUST |
| 9 | ANDOVER WAR MEMORIAL HOSPITAL | HAMPSHIRE HOSPITALS NHS FOUNDATION TRUST |
| 10 | ARCHWAYS INTERMEDIATE CARE UNIT | YORK TEACHING HOSPITAL NHS FOUNDATION TRUST |
| 11 | ARUNDEL AND DISTRICT HOSPITAL | SUSSEX COMMUNITY NHS TRUST |
| 12 | ASHBURTON AND BUCKFASTLEIGH HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 13 | ASHBY DIST HOSP WARD | Leicestershire County and Rutland |
| 14 | ASHFIELD COMMUNITY HOSPITAL | NOTTINGHAMSHIRE HEALTHCARE NHS TRUST |
| 15 | ASHFORD HOSPITAL | ASHFORD AND ST PETER’S HOSPITALS NHS FOUNDATION TRUST |
| 16 | AXMINSTER HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 17 | BABINGTON HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 18 | BECCLES HOSPITAL | Great Yarmouth and Waveney |
| 19 | BENJAMIN COURT | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 20 | BERWICK INFIRMARY | NORTHUMBRIA HEALTHCARE NHS FOUNDATION TRUST |
| 21 | BEXHILL HOSPITAL | EAST SUSSEX HEALTHCARE NHS TRUST |
| 22 | BICESTER COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 23 | BIDEFORD HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 24 | BILLERICAY COMMUNITY HOSPITAL (Mayflower CH) | NORTH EAST LONDON NHS FOUNDATION TRUST |
| 25 | BISHOPS CASTLE HOSPITAL | SHROPSHIRE COMMUNITY HEALTH NHS TRUST |
| 26 | BLANDFORD COMMUNITY HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 27 | BLYTH COMMUNITY HOSPITAL | NORTHUMBRIA HEALTHCARE NHS FOUNDATION TRUST |
| 28 | BODMIN COMMUNITY HOSPITAL | Peninsula Community Health C.I.C |
| 29 | BOGNOR REGIS WAR MEMORIAL HOSPITAL | SUSSEX COMMUNITY NHS TRUST |
| 30 | BOLSOVER HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 31 | BOVEY TRACEY HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 32 | BRADWELL HOSPITAL (PCT HQ) | STAFFORDSHIRE AND STOKE ON TRENT PARTNERSHIP NHS TRUST |
| 33 | BRAINTREE COMMUNITY HOSPITAL | |
| 34 | BRAMPTON HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 35 | BRENTWOOD COMMUNITY HOSPITAL | BASILDON AND THURROCK UNIVERSITY HOSPITALS NHS FOUNDATION TRUST |
| 36 | BRIDGNORTH HOSPITAL | SHROPSHIRE COMMUNITY HEALTH NHS TRUST |
| 37 | BRIDGWATER HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 38 | BRIDLINGTON & DISTRICT HOSPITAL | YORK TEACHING HOSPITAL NHS FOUNDATION TRUST |
| 39 | BRIDPORT COMMUNITY HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 40 | BRIXHAM HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 41 | BROMYARD COMMUNITY HOSPITAL | WYE VALLEY NHS TRUST |
| 42 | BROOKFIELDS HOSPITAL | CAMBRIDGESHIRE COMMUNITY SERVICES NHS TRUST |
| 43 | BUCKINGHAM HOSPITAL | BUCKINGHAMSHIRE HEALTHCARE NHS TRUST |
| 44 | BUDLEIGH SALTERTON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 45 | BURNHAM ON SEA WAR MEMORIAL HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 46 | BUXTON HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 47 | CAMBOURNE REDRUTH COMMUNITY HOSPITAL | Peninsula Community Health CIC |
| 48 | CARTER BEQUEST PRIMARY CARE HOSPITAL | SOUTH TEES HOSPITALS NHS FOUNDATION TRUST |
| 49 | CAVENDISH HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 50 | CHARD HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 51 | CHASE COMMUNITY HOSPITAL | SOUTHERN HEALTH NHS FOUNDATION TRUST |
| 52 | CHEADLE HOSPITAL | NORTH STAFFORDSHIRE COMBINED HEALTHCARE NHS TRUST |
| 53 | CHESTER LE STREET HOSPITAL | COUNTY DURHAM AND DARLINGTON NHS FOUNDATION TRUST |
| 54 | CHIPPENHAM COMMUNITY HOSPITAL | GREAT WESTERN HOSPITALS NHS FOUNDATION TRUST |
| 55 | CHIPPING NORTON COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 56 | CIRENCESTER HOSPITAL | GLOUCESTERSHIRE HOSPITALS NHS FOUNDATION TRUST |
| 57 | CLACTON AND DISTRICT HOSPITAL | NORTH ESSEX PARTNERSHIP UNIVERSITY NHS FOUNDATION TRUST |
| 58 | CLAY CROSS HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 59 | CLEVEDON HOSPITAL | North Somerset PCT, 14 |
| 60 | CLIFTON HOSPITAL | BLACKPOOL TEACHING HOSPITALS NHS FOUNDATION TRUST |
| 61 | CLITHEROE COMMUNITY HOSPITAL | East Lancashire PCT, 18 |
| 62 | COALVILLE HOSP WARDS | Leicestershire County and Rutland |
| 63 | COCKERMOUTH HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 64 | CRANMER HOUSE | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 65 | CRAWLEY HOSPITAL | SUSSEX COMMUNITY NHS TRUST |
| 66 | CREDITON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 67 | CREWKERNE HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 68 | CROWBOROUGH WAR MEMORIAL HOSPITAL | EAST SUSSEX HEALTHCARE NHS TRUST |
| 69 | DARTMOUTH HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 70 | DAWLISH HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 71 | DENE BARTON COMMUNITY UNIT | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 72 | DEREHAM HOSPITAL | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 73 | DIDCOT COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 74 | DILKE MEMORIAL HOSPITAL | Gloucestershire PCT, 15 |
| 75 | DONCASTER – ST MARY’S INTERMEDIATE CARE | ROTHERHAM DONCASTER AND SOUTH HUMBER NHS FOUNDATION TRUST |
| 76 | DORKING GENERAL HOSPITAL | |
| 77 | ECCLESHILL NHS TREATMENT CENTRE | Care UK |
| 78 | ECH – EAST CLEVELAND HOSPITAL | SOUTH TEES HOSPITALS NHS FOUNDATION TRUST |
| 79 | EDENBRIDGE HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 80 | EDGWARE COMMUNITY HOSPITAL | BARNET AND CHASE FARM HOSPITALS NHS TRUST |
| 81 | EDWARD HAIN COMMUNITY HOSPITAL | Peninsula Community Health CIC |
| 82 | ELLEN BADGER HOSPITAL | SOUTH WARWICKSHIRE NHS FOUNDATION TRUST |
| 83 | ELLESMERE PORT HOSPITAL | COUNTESS OF CHESTER HOSPITAL NHS FOUNDATION TRUST |
| 84 | EVESHAM COMMUNITY HOSPITAL | WORCESTERSHIRE HEALTH AND CARE NHS TRUST |
| 85 | EXMOUTH HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 86 | FALMOUTH HOSPITAL | Peninsula Community Health CIC |
| 87 | FARNHAM HOSPITAL & CENTRE FOR HEALTH | Surrey PCT, 10 |
| 88 | FAVERSHAM COTTAGE HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 89 | FEILDING PALMER WARD | Leicestershire County and Rutland |
| 90 | FELIXSTOWE HOSPITAL | Suffolk PCT, 5 |
| 91 | FIRWOOD | EAST SUSSEX HEALTHCARE NHS TRUST |
| 92 | FORDINGBRIDGE | SOUTHERN HEALTH NHS FOUNDATION TRUST |
| 93 | FOWEY HOSPITAL | Peninsula Community Health C.I.C |
| 94 | FRIARY HOSPITAL | SOUTH TEES HOSPITALS NHS FOUNDATION TRUST |
| 95 | FROME COMMUNITY HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 96 | GOSPORT WAR MEMORIAL HOSPITAL | SOUTHERN HEALTH NHS FOUNDATION TRUST |
| 97 | GOSSOMS END ELDERLY CARE UNIT | HERTFORDSHIRE COMMUNITY NHS TRUST |
| 98 | GUISBOROUGH GENERAL HOSPITAL | SOUTH TEES HOSPITALS NHS FOUNDATION TRUST |
| 99 | H & B HOSPITAL WARDS | Leicestershire County and Rutland |
| 100 | Halstead Community Hospital | Central Essex Community Services |
| 101 | HALTWHISTLE WAR MEMORIAL HOSPITAL | NORTHUMBRIA HEALTHCARE NHS FOUNDATION TRUST |
| 102 | HARPENDEN MEMORIAL HOSPITAL | HERTFORDSHIRE PARTNERSHIP UNIVERSITY NHS FOUNDATION TRUST |
| 103 | HASLEMERE AND DISTRICT HOSPITAL OPD | Surrey PCT, 10 |
| 104 | HAWKHURST COTTAGE HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 105 | HAYWOOD HOSPITAL | STAFFORDSHIRE AND STOKE ON TRENT PARTNERSHIP NHS TRUST |
| 106 | HEANOR MEMORIAL HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 107 | HELSTON COMMUNITY HOSPITAL | ROYAL CORNWALL HOSPITALS NHS TRUST |
| 108 | HEMEL HEMPSTEAD HOSPITAL | WEST HERTFORDSHIRE HOSPITALS NHS TRUST |
| 109 | HERTFORDSHIRE & ESSEX HOSPITAL | HERTFORDSHIRE COMMUNITY NHS TRUST |
| 110 | HILLSIDE INTERMEDIATE CARE UNIT | WYE VALLEY NHS TRUST |
| 111 | HITCHIN HOSPITAL | HERTFORDSHIRE COMMUNITY NHS TRUST |
| 112 | HOLME VALLEY MEMORIAL HOSPITAL | Kirklees PCT, 2 |
| 113 | HOLSWORTHY HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 114 | HONITON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 115 | HORSHAM HOSPITAL | SUSSEX PARTNERSHIP NHS FOUNDATION TRUST |
| 116 | ILFRACOMBE | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 117 | ILKESTON COMMUNITY HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 118 | JOHN COUPLAND HOSPITAL | LINCOLNSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 119 | KELLING HOSPITAL | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 120 | KESWICK HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 121 | LAMBERT MEMORIAL COMMUNITY HOSPITAL | SOUTH TEES HOSPITALS NHS FOUNDATION TRUST |
| 122 | LANGLEY HOUSE | HERTFORDSHIRE COMMUNITY NHS TRUST |
| 123 | LAUNCESTON GENERAL HOSPITAL | Peninsula Community Health CIC |
| 124 | LEDBURY COMMUNITY HOSPITAL | Herefordshire PCT, 15 |
| 125 | LEEK MOORLANDS HOSPITAL | North Staffordshire PCT, 16 |
| 126 | LEOMINSTER COMMUNITY HOSPITAL | WYE VALLEY NHS TRUST |
| 127 | LEWES VICTORIA HOSPITAL | EAST SUSSEX HEALTHCARE NHS TRUST |
| 128 | LINGS BAR HOSPITAL | NOTTINGHAMSHIRE HEALTHCARE NHS TRUST |
| 129 | LISKEARD COMMUNITY HOSPITAL | Peninsula Community Health CIC |
| 130 | LONDON ROAD COMMUNITY HOSPITAL | DERBY HOSPITALS NHS FOUNDATION TRUST |
| 131 | LONGRIDGE COMMUNITY HOSPITAL | LANCASHIRE CARE NHS FOUNDATION TRUST |
| 132 | LONGTON HOSPITAL | Stoke on Trent PCT, |
| 133 | LUDLOW HOSPITAL | SHROPSHIRE COMMUNITY HEALTH NHS TRUST |
| 134 | LYDNEY HOSPITAL SITE | GLOUCESTERSHIRE HOSPITALS NHS FOUNDATION TRUST |
| 135 | LYMINGTON NEW FOREST HOSPITAL | SOUTHERN HEALTH NHS FOUNDATION TRUST |
| 136 | MALTON COMMUNITY HOSPITAL | YORK TEACHING HOSPITAL NHS FOUNDATION TRUST |
| 137 | MALVERN COMMUNITY HOSPITAL | WORCESTERSHIRE HEALTH AND CARE NHS TRUST |
| 138 | MANSFIELD COMMUNITY HOSPITAL | NOTTINGHAMSHIRE HEALTHCARE NHS TRUST |
| 139 | MARLOW HOSPITAL | BUCKINGHAMSHIRE HEALTHCARE NHS TRUST |
| 140 | MARYPORT HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 141 | MEADOW LODGE | EAST SUSSEX HEALTHCARE NHS TRUST |
| 142 | MIDHURST COMMUNITY HOSPITAL | WESTERN SUSSEX HOSPITALS NHS FOUNDATION TRUST |
| 143 | MILLOM HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 144 | MINEHEAD COMMUNITY HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 145 | MORETONHAMPSTEAD HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 146 | MOSELEY HALL HOSPITAL | BIRMINGHAM COMMUNITY HEALTHCARE NHS TRUST |
| 147 | NEWHOLME HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 148 | NEWQUAY HOSPITAL | Peninsula Community Health CIC |
| 149 | NEWTON ABBOT COMMUNITY HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 150 | NORTH CAMBRIDGESHIRE HOSPITAL | CAMBRIDGESHIRE COMMUNITY SERVICES NHS TRUST |
| 151 | NORTH COTSWOLD HOSPITAL- (Moerton Marsh CH) | Gloucestershire PCT, 15 |
| 152 | NORTH WALSHAM HOSPITAL | NORFOLK AND NORWICH UNIVERSITY HOSPITALS NHS FOUNDATION TRUST |
| 153 | NORWICH COMMUNITY HOSPITAL | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 154 | OGDEN COURT | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 155 | OKEHAMPTON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 156 | OTTERY ST MARY HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 157 | PAIGNTON HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 158 | PALMER COMMUNITY HOSPITAL | SOUTH TYNESIDE NHS FOUNDATION TRUST |
| 159 | PAULTON MEMORIAL HOSPITAL | GREAT WESTERN HOSPITALS NHS FOUNDATION TRUST |
| 160 | PENDLE COMMUNITY HOSPITAL | EAST LANCASHIRE HOSPITALS NHS TRUST |
| 161 | PENRITH HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 162 | PERSHORE HOSPITAL | WORCESTERSHIRE HEALTH AND CARE NHS TRUST |
| 163 | PETERSFIELD HOSPITAL | SOUTHERN HEALTH NHS FOUNDATION TRUST |
| 164 | PLYMOUTH COMMUNITY HEALTHCARE (CIC) | Plymouth Community Healthcare (CIC) |
| 165 | POLTAIR HOSPITAL | Peninsula Community Health CIC |
| 166 | PORTLAND HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 167 | PRINCESS OF WALES HOSPITAL (Cambridge) | CAMBRIDGESHIRE COMMUNITY SERVICES NHS TRUST |
| 168 | PRINCESS OF WALES HOSPITAL (Worcestershire) | WORCESTERSHIRE HEALTH AND CARE NHS TRUST |
| 169 | QUEEN VICTORIA HOSPITAL (Morecambe) | UNIVERSITY HOSPITALS OF MORECAMBE BAY NHS FOUNDATION TRUST |
| 170 | QUEEN VICTORIA MEMORIAL HOSPITAL (Hertfordshire) | HERTFORDSHIRE COMMUNITY NHS TRUST |
| 171 | QUEEN VICTORIA MEMORIAL HOSPITAL (Kent) | KENT COMMUNITY HEALTH NHS TRUST |
| 172 | REDCAR PRIMARY CARE HOSPITAL | SOUTH TEES HOSPITALS NHS FOUNDATION TRUST |
| 173 | RICHARDSON HOSPITAL | COUNTY DURHAM AND DARLINGTON NHS FOUNDATION TRUST |
| 174 | RIPLEY HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 175 | RIPON AND DISTRICT COMMUNITY HOSPITAL | HARROGATE AND DISTRICT NHS FOUNDATION TRUST |
| 176 | RMH RUTLAND WARD | LEICESTERSHIRE PARTNERSHIP NHS TRUST |
| 177 | ROMSEY HOSPITAL | SOUTHERN HEALTH NHS FOUNDATION TRUST |
| 178 | ROSS ON WYE COMMUNITY HOSPITAL | WYE VALLEY NHS TRUST |
| 179 | ROTHBURY COMMUNITY HOSPITAL | NORTHUMBRIA HEALTHCARE NHS FOUNDATION TRUST |
| 180 | ROYAL LEAMINGTON SPA REHABILITATION HOSPITAL | SOUTH WARWICKSHIRE NHS FOUNDATION TRUST |
| 181 | RUTH LANCASTER JAMES HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 182 | RYE MEMORIAL CARE CENTRE | EAST SUSSEX HEALTHCARE NHS TRUST |
| 183 | SAFFRON WALDEN HOSPITAL | SOUTH ESSEX PARTNERSHIP UNIVERSITY NHS FOUNDATION TRUST |
| 184 | SALVINGTON LODGE | SUSSEX COMMUNITY NHS TRUST |
| 185 | SAMUEL JOHNSON COMMUNITY HOSPITAL | BURTON HOSPITALS NHS FOUNDATION TRUST |
| 186 | SAVERNAKE HOSPITAL | GREAT WESTERN HOSPITALS NHS FOUNDATION TRUST |
| 187 | SEATON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 188 | SEDGEFIELD COMMUNITY HOSPITAL | COUNTY DURHAM AND DARLINGTON NHS FOUNDATION TRUST |
| 189 | SEVENOAKS HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 190 | SHEPPY COMMUNITY HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 191 | SHEPTON MALLET COMMUNITY HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 192 | SHOTLEY BRIDGE HOSPITAL SITE | COUNTY DURHAM AND DARLINGTON NHS FOUNDATION TRUST |
| 193 | SIDMOUTH HOSPITAL | ROYAL DEVON AND EXETER NHS FOUNDATION TRUST |
| 194 | SIR ROBERT PEEL HOSPITAL | BURTON HOSPITALS NHS FOUNDATION TRUST |
| 195 | SITTINGBOURNE MEMORIAL HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 196 | SOUTH BRISTOL COMMUNITY HOSPITAL | UNIVERSITY HOSPITALS BRISTOL NHS FOUNDATION TRUST |
| 197 | SOUTH HAMS HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 198 | SOUTH MOLTON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 199 | SOUTH PETHERTON HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 200 | SOUTHLANDS HOSPITAL | WESTERN SUSSEX HOSPITALS NHS FOUNDATION TRUST |
| 201 | ST ALBANS CITY HOSPITAL | WEST HERTFORDSHIRE HOSPITALS NHS TRUST |
| 202 | ST AUSTELL COMMUNITY HOSPITAL | Peninsula Community Health CIC |
| 203 | ST BARNABAS HOSPITAL | Peninsula Community Health CIC |
| 204 | ST BARTHOLOMEW’S HOSPITAL (ROCHESTER) | |
| 205 | ST LEONARDS COMMUNITY HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 206 | ST LUKE’S HOSPITAL (Leicester) | Leicestershire County and Rutland |
| 207 | ST MARGARET’S HOSPITAL EPPING | NORTH ESSEX PARTNERSHIP UNIVERSITY NHS FOUNDATION TRUST |
| 208 | ST MARKS HOSPITAL (Berks) | BERKSHIRE HEALTHCARE NHS FOUNDATION TRUST |
| 209 | ST MARTINS HOSPITAL (ind) | |
| 210 | ST MARY’S HOSPITAL (Cornwall) | Peninsula Community Health CIC |
| 211 | ST MICHAELS HOSPITAL (Norfolk) | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 212 | ST MONICAS HOSPITAL | YORK TEACHING HOSPITAL NHS FOUNDATION TRUST |
| 213 | ST OSWALD’S | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 214 | ST PETER’S HOSPITAL (Essex) | MID ESSEX HOSPITAL SERVICES NHS TRUST |
| 215 | STAMFORD & RUTLAND HOSPITAL | PETERBOROUGH AND STAMFORD HOSPITALS NHS FOUNDATION TRUST |
| 216 | STRATFORD HOSPITAL | SOUTH WARWICKSHIRE NHS FOUNDATION TRUST |
| 217 | STRATTON HOSPITAL | Peninsula Community Health CIC |
| 218 | STROUD GENERAL HOSPITAL | GLOUCESTERSHIRE HOSPITALS NHS FOUNDATION TRUST |
| 219 | SWAFFHAM COMMUNITY HOSPITAL | NORFOLK COMMUNITY HEALTH AND CARE NHS TRUST |
| 220 | SWANAGE COMMUNTIY HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 221 | TAVISTOCK HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 222 | TEDDINGTON MEMORIAL HOSPITAL | HOUNSLOW AND RICHMOND COMMUNITY HEALTHCARE NHS TRUST |
| 223 | TEIGNMOUTH HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 224 | TENBURY COMMUNITY HOSPITAL | WORCESTERSHIRE HEALTH AND CARE NHS TRUST |
| 225 | TEWKESBURY GENERAL HOSPITAL | GLOUCESTERSHIRE HOSPITALS NHS FOUNDATION TRUST |
| 226 | THAME HOSPITAL | BUCKINGHAMSHIRE HEALTHCARE NHS TRUST |
| 227 | THE FRYATT HOSPITAL AND MAYFLOWER MEDICAL CENTRE | North East Essex PCT |
| 228 | THE NEW SELBY WAR MEMORIAL HOSPITAL | YORK TEACHING HOSPITAL NHS FOUNDATION TRUST |
| 229 | THORNBURY HOSPITAL (Bristol) | NORTH BRISTOL NHS TRUST |
| 230 | TIVERTON AND DISTRICT HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 231 | TONBRIDGE COTTAGE HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 232 | TORRINGTON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 233 | TOTNES HOSPITAL | TORBAY AND SOUTHERN DEVON HEALTH AND CARE NHS TRUST |
| 234 | TOWNLANDS COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 235 | UCKFIELD HOSPITAL | EAST SUSSEX HEALTHCARE NHS TRUST |
| 236 | UPTON HOSPITAL | BERKSHIRE HEALTHCARE NHS FOUNDATION TRUST |
| 237 | VALE COMMUNITY HOSPITAL | Gloucestershire PCT, 15 |
| 238 | VICTORIA HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 239 | VICTORIA HOSPITAL W’BORNE | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 240 | WALLINGFORD COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 241 | WANTAGE COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 242 | WAREHAM COMMUNITY HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 243 | WARMINSTER COMMUNITY HOSPITAL | GREAT WESTERN HOSPITALS NHS FOUNDATION TRUST |
| 244 | WEARDALE HOSPITAL | COUNTY DURHAM AND DARLINGTON NHS FOUNDATION TRUST |
| 245 | WELLINGTON & DISTRICT COTTAGE HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 246 | WEST BERKSHIRE COMMUNITY HOSPITAL | ROYAL BERKSHIRE NHS FOUNDATION TRUST |
| 247 | WEST HEATH HOSPITAL | BIRMINGHAM COMMUNITY HEALTHCARE NHS TRUST |
| 248 | WEST MENDIP COMMUNITY HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 249 | WESTHAVEN HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 250 | WESTMINSTER MEMORIAL HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 251 | WHALTON UNIT | NORTHUMBRIA HEALTHCARE NHS FOUNDATION TRUST |
| 252 | WHIPTON HOSPITAL | NORTHERN DEVON HEALTHCARE NHS TRUST |
| 253 | WHITBY COMMUNITY HOSPITAL | YORK TEACHING HOSPITAL NHS FOUNDATION TRUST |
| 254 | WHITCHURCH HOSPITAL | SHROPSHIRE COMMUNITY HEALTH NHS TRUST |
| 255 | WHITE CROSS REHABILITATION HOSPITAL | YORK TEACHING HOSPITAL NHS FOUNDATION TRUST |
| 256 | WHITSTABLE & TANKERTON HOSPITAL | KENT COMMUNITY HEALTH NHS TRUST |
| 257 | WHITWORTH HOSPITAL | DERBYSHIRE COMMUNITY HEALTH SERVICES NHS TRUST |
| 258 | WIGTON HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 259 | WILLITON HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 260 | WINCANTON COMMUNITY HOSPITAL | SOMERSET PARTNERSHIP NHS FOUNDATION TRUST |
| 261 | WITHERNSEA HOSPITAL | HUMBER NHS FOUNDATION TRUST |
| 262 | WITNEY COMMUNITY HOSPITAL | OXFORD HEALTH NHS FOUNDATION TRUST |
| 263 | WOKING COMMUNITY HOSPITAL | Surrey PCT, 10 |
| 264 | WOKINGHAM COMMUNITY HOSPITAL | BERKSHIRE HEALTHCARE NHS FOUNDATION TRUST |
| 265 | WORKINGTON COMMUNITY HOSPITAL | CUMBRIA PARTNERSHIP NHS FOUNDATION TRUST |
| 266 | YEATMAN HOSPITAL | DORSET HEALTHCARE UNIVERSITY NHS FOUNDATION TRUST |
| 267 | ZACHARY MERTON HOSPITAL | SUSSEX COMMUNITY NHS TRUST |
| 268 | Southwold & District Hospital | East Coast Community Health Care |
| 269 | Newmarket Hospital | Serco Ltd |
| 270 | Tarporley War Memorial Hospital | Tarporley War Memorial Charity |
| 271 | All Hallows Hospital | All Hallows Healthcare Trust |
| 272 | Archer Unit | South Essex Partnership University NHS Foundation Trust (SEPT) |
| 273 | Bluebird Lodge | Serco |
| 274 | Peterborough City Care Centre | Suffolk Community Healthcare |
| 275 | Newton Community Hospital | Bridgewater Community Healthcare NHS Foundation Trust |
| 276 | Biggleswade Hospital | South Essex Partnership University NHS Foundation Trust (SEPT) |
| 277 | Castleberg Hospital | Airedale NHS Foundation Trust |
| 278 | Patrick Stead Hospital Halesworth | East Coast Community Health Care |
| 279 | Congleton War Memorial Hospital | East Cheshire NHS Trust |
| 280 | Corby Community Hospital | Northamptonshire Healthcare NHS Foundation Trust |
| 281 | Danetre Hospital | Northampton General Hospital NHS Trust |
| 282 | Finchley Memorial Hospital | Central London Community Healthcare NHS Trust |
| 283 | Bealey Community Hospital | Pennine Care NHS Foundation Trust |
| 284 | Caterham Dene Hospital | First Community Health and care |
| 285 | East Riding Community Hospital | Humber NHS Foundation Trust |
| 286 | Fleet Community Hospital | Southern Health NHS Foundation Trust |
| 287 | Skegness Hospital | Lincolnshire Community Health Services NHs Trust |
| 288 | Livingstone Hospital | Kent Community Health NHS Foundation Trust |
| 289 | Eccleshill Community Hospital | Bradford Teaching Hospitals NHS Foundation Trust |
| 290 | Eltham Community Hospital | Oxleas NHS Foundation Trust |
| 291 | Gravesend Community Hospital | Kent Community Health NHS Foundation Trust |
| 292 | Molesey CH | CSH Surrey |
| 293 | Norman Power Intermediate Care Unit | Birmingham Community Healthcare NHS Trust |
| 294 | St Helen’s Rehabilitation Hospital | York Teaching Hospital NHS Foundation Trust |
| 295 | Westbourne Green Community Hospital | Bradford Teaching Hospitals NHS Foundation Trust |
| 296 | Westwood Park | Bradford Teaching Hospitals NHS Foundation Trust |
Appendix 5 Profiles of the nine case study sites
| Community hospital 1 | Community hospital 2 | Community hospital 3 |
|---|---|---|
|
|
|
| Community hospital 4 | Community hospital 5 | Community hospital 6 |
|
|
|
| Community hospital 7 | Community hospital 8 | Community hospital 9 |
|
|
|
Appendix 6 Number of case study participants interviewed, by category/group
| Participants | Analysis coding | Interviews (n) | Focus groups (n) |
|---|---|---|---|
| Patients | P | 60 | |
| Carers | CA | 28 | |
| TREXs | T | 9 | |
| Volunteers | V | 35 | 33 |
| Community stakeholders | CY | 20 | 54 |
| Staff | S | 89 | 43 |
| Totals | 241 | 130 | |
| Overall total | 371a | ||
| Focus groups | Analysis coding | Community hospital, n | Total, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| Volunteers | V, FG | 4 | 4 | 2 | 0 | 11 | 0 | 9 | 3 | 0 | 33 (25.4) |
| Community stakeholders | CY, FG | 15 | 9 | 5 | 2 | 4 | 0 | 5 | 9 | 5 | 54 (41.5) |
| Staff | S, FG | 4 | 9 | 3 | 2 | 7 | 3 | 7 | 0 | 8 | 43 (33.1) |
| Overall total | 130 | ||||||||||
| Interviews with | Community hospital, n | Total, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| Patients | 6 | 8 | 5 | 9 | 7 | 7 | 7 | 6 | 5 | 60 (25.9) |
| Carers | 3 | 2 | 3 | 2 | 5 | 2 | 3 | 3 | 5 | 28 (12.1) |
| Volunteers | 6 | 3 | 3 | 0 | 2 | 6 | 8 | 4 | 3 | 35 (15.1) |
| Community stakeholders | 5 | 3 | 1 | 2 | 1 | 1 | 5 | 2 | 0 | 20 (8.6) |
| Staff | 9 | 13 | 3 | 9 | 13 | 5 | 10 | 15 | 12 | 89 (38.4) |
| Overall total | 232 | |||||||||
| Interviews with | CCG patch, n | Total, n | ||||||||
| A | B | C | D | E | ||||||
| Commissioners | 1 | 1 | 1 | 0 | 1 | 4 | ||||
| Senior Managers | 1 | 1 | 1 | 1 | 1 | 5 | ||||
| Overall total | 9 | |||||||||
| Total number of participants of focus groups and interviews | 371 | |||||||||
Appendix 7 Example of discovery interview
Appendix 8 Coding frame
| Name | Description |
|---|---|
| Contextualising | Descriptions of the case study community hospitals |
| History | Descriptions of the general history of the hospital |
| Geography | Discussions relating to the significance of the geographical location of the hospital e.g. rurality, distance from a DGH, close to border of county. N.B. might be a lot of double coding with later ‘community description’ child node |
| Policy and commissioning context | Discussions of the national and local policy, systems, commissioning and provider context affecting the case study community hospitals (e.g. STPs, Success Regimes, CCG positions) |
| Function | Narratives relating to the roles and functions of the case study community hospital (e.g. rehabilitation, subacute, end of life, and their relationships with/distinction from primary and acute care), source of referrals, balance of step up and step down |
| Service provision | Details about the case study hospitals (e.g. ownership of services and building, number of beds, range of services, range of providers, ALOS) |
| GPs and medical model | Narratives describing and reflecting on the medical models within the community hospitals and how this is changing (e.g. role of GPs). Note: code everything relating to role of GPs here – although won’t fit here within report |
| Staffing | Details of the staffing structure and roles within the case study hospitals and general issues relating to recruitment and retention. Not about individual career trajectories or experience of working in the hospital |
| Systems integration | Narratives relating to place of hospital within wider health system/ecology, including issues of integration or fragmentation – across providers, services, teams, MDT care agencies, hospices, etc. Includes descriptions of the models of integration and reflections on them. Does not include reflections on how this affects patient experience |
| Patients | Narratives relating to who the patients are within each of the case study hospitals (e.g. age, acuity, frailty, local), including how this is changing |
| Utilisation | Narratives relating to levels of use and utilisation of the hospital and services provided |
| Evolving | Discussions of the ways in which the community hospitals have or have not changed in the relatively recent past, and how they are changing/likely to change in the near future, in terms of the services they provide and their function – what they do and how they do it. Note: change in relation to patient experience or community support, etc. or much longer-term history |
| Working | Parent node bringing together all codes relating to staff experience of working in community hospitals |
| Leadership and co-ordination | Narratives relating to leadership and co-ordination within the hospital – including individuals reflecting on their leadership position |
| Nature of work | Descriptions and discussions relating to respondents and/or general career of nursing and other staff within the community hospitals (not GPs), including the local (or otherwise) nature of work and the significance of this, and issues of stress, overwork, unclear boundaries |
| Meaning and purpose of work | Discussions relating to the experience and meaning of work in the community hospital (e.g. that it is meaningful, second home, second family, high levels of autonomy, commitment, duty, sense of purpose, achievement and satisfaction). Would include reflections on feeling part of a team, sense of well-being for staff, etc. Note that there will be some double-coding here with value nodes |
| Experiencing | Parent node for all child nodes relating to patient and carer experience of using the community hospital |
| Assessment | Assessments of the overall or general quality of the patient experience (e.g. cannot fault it, excellent care) or any reference to patient experience data |
| Local and accessible | Reflections on the local and accessible nature of the community hospital and how it affects patient and carer experience, and how this is changing, including car parking |
| Personal and known | Narratives relating to experiencing community hospitals as both personal/personalised, including narratives relating to familiarity with the services, hospital or staff, knowing/being known/getting to know, flexibility, etc. |
| Holistic | Narratives relating to the ways in which community hospitals are providing holistic care (e.g. looking beyond individual conditions, being able to care for social as well as medical needs) |
| Atmosphere | Narratives relating, broadly speaking, to the atmosphere within the hospital and how this affects patient and carer experience (e.g. discussions of it being small, homely, friendly, pleasant, noisy, busy, relaxed, quiet, calm, welcoming) |
| Pace | Narratives relating in different ways to the pace of work and of life within community hospitals (e.g. time for staff to care, but also time for patients to get bored) |
| Dignity and respect | Narratives relating to dignity, respect, privacy, etc. |
| Environment and facilities | Narratives relating to the physical environment – inside and outside – and the facilities, including single rooms, small wards, cleanliness, food, outside areas and view, etc. |
| Continuity | Narratives relating to how patients and carers experience continuity and integration e.g. between GP and community hospital, between acute and community hospital, community hospital and home and across different teams (e.g. nursing and therapy, health and social care) |
| Confidence | Experience or care inspires and builds confidence in patients and families, also includes having confidence in the service/staff |
| Informing and involving | Whether or not how and when patients and carers are informed and included in decisions about their care, including when admitted into hospital and during discharge planning, etc. – and how they feel about this (e.g. comprehensive, poor, made to feel part of the ward, made to feel welcome) |
| Social interaction and stimulation | Narratives relating to interactions among patients, between patients and staff/volunteers and between patients and their families. Also discussions relating to and reflections on activity and stimulation experienced by patients |
| Reflections on staff | Patients’ and carers’ reflections on how they experience the staff within the hospitals – their relationships to/with them, staff attitudes, behaviours, skills, capabilities, capacities and characters, etc. |
| Treatment, care and support | Narratives relating to the particular forms of care, treatment and support that the patients have received, including services used and care and therapies received – what and how |
| Journey and transition | Narratives that relate to patients’ journeys to and from the hospital (how they came to be there) and particularly the significance of being at points of transition (patients and carers). This may include the stories of individual patient journeys and conditions, as well as reflections directly relating to the experience of using community hospitals at points of transition |
| Varied | Narratives reflecting on the varied or variable nature of patient and carer experience (e.g. as a result of patients’ condition/personalities), namely patient, carer and staff talking about whether all patients have the same experience or if it varies depending on who the patients are, etc. |
| Acute comparisons | Specific comparisons made between patient experience within acute hospitals and community hospitals. N.B. there may be a lot of double coding here |
| Valuing | Parent node bringing together all codes relating to the social or community value of community hospitals. Relating to the question of what community hospitals do for their community |
| Community descriptions | Narratives relating to the character of the towns/villages/communities within which the case study hospitals are based, including population, levels of deprivation, rurality, isolation, change, services, social activities, etc. |
| Known and everyday life | Narratives relating to whether or how community hospitals and their services are known and/or taken for granted, or seen as part of everyday life, perhaps until threatened, and the significance of this. Includes reflections on the extent to which the services are/are not known about |
| Value as positional | Narratives relating to the positional nature of value (i.e. when respondents have talked about the fact that how you view the value of the hospital depends on who you are or your position within the community and in relation to the hospital) |
| Local service(s) | Reflections on the value of the hospital as a local service and as a hub for local services |
| Asset and ownership | Narratives reflecting view of the hospital as a community asset – both real and symbolic. Include within this reflection on ownership – (e.g. it belongs to the community . . .) – and how this might be threatened |
| Security | Discussions reflecting community hospital as a source of security, safety, reassurance to carers and within the community. N.B. above and beyond individual patients feeling reassured by care provided, which would be coded in patient experience – and how this might be threatened (e.g. through closure of beds) |
| Social capital and interaction | Hospital as locus for social interaction, either directly on site or through League of Friends activities, etc. (e.g. bingo drives) |
| Position and status | Providing a social position and source of identity for both staff and volunteers/League of Friends members within the community |
| Quality employment | Providing quality local employment for individual members of the community working in the hospital, with high levels of autonomy, commitment and satisfaction, meaning – more than a job |
| Economy | Role of hospital as local employer, but also wider economic impact of hospital (e.g. in relation to farming and tourism) |
| Intergenerational connections | Reflections of significance as a point of intergenerational connections – cradle-to-grave provision, different generations using the hospital, supporting/volunteering/contributing to the hospital, working in the hospital |
| Engaging | Parent node for all child nodes relating to the ways in which communities/volunteers/fund raisers, etc. Engage and support the community hospitals |
| Scale and type | Narratives relating to the scale, types and models of community/voluntary engagement within the hospitals, both historic and currently (e.g. levels of voluntary income, of volunteering, connections with voluntary/community organisations, patient participation). Also include narratives relating to wider more general support from the community for the hospital through things like attending events |
| Mobilisation | Who, why and how people engage in the hospital – including the role of the trust, hospital, League of Friends, individual staff members and wider organisations, such as Councils for Voluntary Service, in promoting, encouraging and facilitating involvement – now and in the past |
| Leading and organising | Ways in which voluntary engagement is led, organised, managed and supported within the hospital – including role of the trust, hospital/staff, League of Friends, other organisations |
| Limits and tensions | Narratives relating to the limits to voluntary engagement either from the individual perspective (e.g. ‘young people don’t have the time’) or from the institutional perspective (e.g. ‘volunteers are not allowed to do that’). In addition, any narratives relating to any tensions within or related to voluntary support (e.g. where/where not to spend voluntary income, relationships between staff and volunteers) |
| Variation | Reflections on the differences in levels of engagement/support across hospitals and what factors may underlie these |
| Outcomes | Reflections on the contributions that volunteers/voluntary engagement make to the hospital (e.g. money and equipment, improving physical spaces, awareness of hospital and/or services, patient experience, staff morale, networking, campaigning and advocacy) |
| Respondent details | Bucket node for respondent personal backgrounds |
Appendix 9 Financial and volunteering data for registered charities
Charity Commission Register data
Given that the Register of Charities is not a widely used source in the field of health services research, in this appendix we describe the information available from it regarding the number of volunteers who support charities linked with the hospitals, and regarding the amounts of money those charities raise.
The Charity Commission Register maintained by the Charity Commission holds details of organisations that have been recognised as charitable in law, that hold most of their assets in England and/or Wales, or have all or the majority of their trustees normally resident in England and/or Wales, or are companies incorporated in England or Wales.
The information from the Commission is available publicly at the following location: http://data.charitycommission.gov.uk/ (accessed 20 June 2015). The data used in this study included annual return headline financial figures for all registered charities that included start and end dates of the financial period, total income and spending for this period and number of volunteers (discussed in more detail below). Historic financial data covering the period from 1995 onwards are available through the following data set deposited by the Third Sector Research Centre at the UK data service [URL: http://reshare.ukdataservice.ac.uk/850933/ (accessed 20 April 2016)]. This collection refers to a ‘financial history’ file that incorporates the results of extensive work done by the Third Sector Research Centre in conjunction with the National Council for Voluntary Organisations (NCVO) to clean up and merge old versions of data from the Charity Commission register from the early 1990s onwards. Typically, that file contains between 70,000 and 130,000 non-zero financial returns from charities in any given year. We updated it with data from 2013 and 2014. In total, there are some 3 million financial records for English and Welsh charities covering the past 20 years. Notwithstanding this extensive prior work on the quality of the data, manual checks were carried out for all unusual entries (e.g. very large values, relatively large/small values in comparison to values reported in previous financial period or to values reported by other charities).
There were some advantages and challenges of using Charity Commission data. Almost all charities in England and Wales are required to register and to submit financial statements consisting of trustees’ annual reports (returns) and annual accounts. As most community hospital charities are registered, they are required by law to publish their annual reports every year. As such, the Charity Commission register data present a nationally representative census of registered community hospital charities in England and Wales. Charities with incomes of > £5000 a year must submit their annual reports to the Commission; for those whose income or expenditure exceeds a threshold of £25,000, the Commission makes these accounts available on its website. In the cases of charities that are very small, that is those whose income and expenditure are < £5000 a year, they have (since 2009) been exempted from the need to register and submit the accounts; we sought copies of their accounts directly from the charities themselves. In practice, this does not affect many of the charities studied in this work, because their median expenditure is around £15,000.
Sample
Community hospitals were identified as described in detail in this report, providing a list of 274 hospitals in England and 21 in Wales. We then identified those charities that provided charitable and voluntary support to those organisations. In the majority of cases, these are individual entities often including the phrase ‘league of friends’ or similar in their title. Community hospitals in England may also receive financial support from the NHS trusts’ charitable funds (in England). However, these trust-wide charities usually cover large geographical areas, such as a multisite trust across a whole city or county. It is impossible to identify from these charities the voluntary resources that go to support a particular community hospital. We therefore excluded such institutions from consideration.
To locate non-registered charities (usually those with an income of < £5000 a year) and to link them to community hospitals, we employed two methods. First, we involved Attend, a national charity that supports voluntary organisations promoting healthy communities. Second, we contacted community hospitals on our list and enquired as to whether or not they have a supporting charity and, if so, what were its contact details.
We approached eight non-registered organisations with an income of < £5000 a year directly for copies of their annual reports in order to capture data from them. However, two of these did not have up-to-date contact details and only two of the remaining six charities responded to our request. We therefore did not use these data in our analysis.
In one case, one charity supported three local community hospitals. To avoid counting its financial contribution three times, it was linked to just one of those hospitals and, therefore, included in our sample only once.
As a result, financial information for at least 1 year between 1995 and 2014 was available for 245 charities in England and that formed the final sample for this part of the analysis. The number of non-zero financial reports to the Commission in this period ranged from 181 to 226; note that the data for the 1990s are known to be incomplete because of problems with the old electronic media from which they were recovered, and there is no definitive backup of the data. The data from 1997 onwards are available for a broadly stable population of organisations. The 2014 data were those available at the time of analysis (2016): there is a time lag in the availability of data as a result of the processes of (1) charities themselves producing their annual accounts, (2) the Charity Commission then processing returns and adding them to their database and (3) the supply of the data to researchers and its integration into their own databases.
| Year | Number of available annual reports |
|---|---|
| 1995 | 197 |
| 1996 | 181 |
| 1997 | 205 |
| 1998 | 219 |
| 1999 | 220 |
| 2000 | 215 |
| 2001 | 217 |
| 2002 | 218 |
| 2003 | 220 |
| 2004 | 224 |
| 2005 | 219 |
| 2006 | 215 |
| 2007 | 226 |
| 2008 | 225 |
| 2009 | 223 |
| 2010 | 220 |
| 2011 | 217 |
| 2012 | 222 |
| 2013 | 215 |
| 2014 | 201 |
Measurements
Financial contribution: total income and total expenditure
All financial figures for 1995–2013 were adjusted for inflation using the Office for National Statistics’ annual retail price index;125 therefore, all financial information is presented at constant 2014 prices.
Detail of income and expenditure
Charities’ accounts are published on the Charity Commission website, typically for the preceding 5 or 6 financial years, if their income or expenditure exceeds a threshold of £25,000. Using this, we obtained copies of these accounts covering 397 separate financial years; after the exclusion of Wales, the number of accounts available are presented in Table 24.
| Year | Accounts | ||
|---|---|---|---|
| Number | Percentage | Cumulative percentage | |
| 2008 | 91 | 24.86 | 27.05 |
| 2009 | 55 | 15.03 | 42.08 |
| 2010 | 49 | 13.39 | 55.46 |
| 2011 | 52 | 14.21 | 69.67 |
| 2012 | 41 | 11.20 | 80.87 |
| 2013 | 70 | 19.13 | 100.00 |
We have focused on the period 2008–13, for which between 41 and 91 charities of interest generated at least one such financial return. This variation is for two reasons: individual hospitals may or may not reach the threshold of £25,000 in any given year and, even if they do, they may not always submit copies of their accounts as requested. Capturing more recent financial data was not possible for a further reason, namely that there is usually a delay between a charity submitting its reports and accounts and the material being processed and published by the Charity Commission.
Charity accounts provide relatively little detail on income and expenditure and may even aggregate what are quite different sources of expenditure within the same funding stream. For example, a health charity may record, under the general heading of ‘income from charitable activities’, both fees paid by individuals themselves directly (e.g. for private consultations or treatment) and payments made under contract by a CCG. Technically, both payments to the charity are for services rendered; substantively, the two are distinct.
In order to probe income sources and the application of expenditure in more detail, data from the notes to these charities’ accounts were captured by the Centre for Data Digitisation and Analysis at Queen’s University Belfast. This generated 21,773 items of data, or an average of 54.9 items per set of accounts captured. The data are characterised by a text description of either the income source (e.g. ‘legacy from estate of J. Smith’; ‘proceeds of hospital fête’) or the expenditure (e.g. ‘purchase of television for ward X’, ‘costs of running hospital fête’). In order to get beneath the rather aggregated categories used by the Charity Commission, these items were classified by our research partners, the NCVO, using established automated Bayesian matching techniques. These procedures scan the text and compare it with previously captured data (with some 10 years’ experience of classifying approximately half a million lines of text data per annum, the library of text against which new data are being compared is very comprehensive). The aim is to identify the most plausible match.
The data provide useful insights, although it can be argued that each set of charity accounts is unique, because there are variations between accountants in the interpretation of the financial data available to them. Indeed, we ourselves encountered exactly this problem when comparing presentation of financial information in two of our case study sites. Although broadly comparable in terms of levels of expenditure, one charity presents a great deal of detail for relatively small amounts of expenditure, whereas the other aggregates most of the charitable expenditure into a small number of categories.
Classifying the expenditure of charities has not been attempted because it is time-consuming, and not very informative. Some 6700 lines of expenditure are recorded in our data and, of these, there are nearly 2000 unique descriptions of the subject of the transaction, and nearly two-thirds of these occur fewer than five times. The items that occur most frequently include general categories, such as ‘direct charitable expenditure’ or just ‘expenditure’. Neither is particularly informative.
Volunteer contribution: number of volunteers and estimates of volunteer input
According to the Commission’s guidelines126 for reporting the number of volunteers, charities must provide their best estimate of the numbers of volunteers involved in their activities via their annual returns. There may be differences between charities in how they define a volunteer, but they are commonly understood to encompass people who contribute to the charity’s objectives in a voluntary and unpaid capacity (though legitimate expenses may be paid). The decision on who to count as volunteers is left to the discretion of the trustees of the charity
Prior to 2013, data on numbers of volunteers were often sparse, but since that date, efforts have been made to gather more detailed information. We have data for 106,000 charities; these were derived from over 320,000 separate returns, some of which went back a number of years. However, approximately 73,000 charities had supplied between one and three non-zero returns of the counts of their volunteers in the 3 years between 2013 and 2015. We summed the total for each charity and divided it by the number of years for which we have a return. Thus, a charity with 175 volunteers, which had made five financial returns, will be regarded as having, on average, 35 volunteers. To provide an upper-bound estimate we also calculated the maximum value returned for each charity over the period in question. The data on volunteer numbers for community-related League of Friends are significantly more comprehensive than for the charity population as a whole. We have numbers of volunteers for nearly 90% of these entities compared with approximately 64% for charities generally.
Volunteer hours were estimated using regular survey data (Home Office Citizenship Survey, 2001–2010; Community Life survey, 2012 onwards). We take the average number of hours per week reported by those who say they have given unpaid help to organisations during the previous year. This is approximately 2.2 hours. This is a minimum estimate and it may be that the actual numbers are larger than this would imply. If we make the assumption that these are probably fairly regular volunteers, a higher figure of 3.05 hours per week is given if we take the average number of hours reported by those who say they volunteer either at least once a week or more frequently, or at least monthly but less frequently than once a week.
There are no studies that would tell us with any certainty whether or not volunteers in these kinds of organisations put in more, or fewer, hours than the volunteering population generally. Two widely quoted studies (Galea et al. 43 and Naylor et al. 42), which estimate that there are around 3 million volunteers in health and social care, do not allow any inferences to be drawn about the settings in which such health-related volunteering takes place.
We then multiplied these two estimates of time inputs by the average and maximum volunteer numbers, respectively, to give the number of hours contributed by volunteers over the course of the year (assuming 46 weeks’ volunteering). These can be converted to full-time equivalent numbers by dividing back by 37.5 and 46.
Opinions differ on the best method for calculating a cash equivalent for the value of volunteer labour. The lowest is to use the national minimum wage; others might include an estimate of the replacement cost (i.e. what it would cost the organisation to employ people to do the same tasks if they had to pay them), but this assumes knowledge of the tasks being undertaken. The national minimum wage for the period for which we have the most comprehensive volunteering data (2013–15) was £6.50. 91
Glossary
- Sustainability and transformation plans
- Place-based plans developed by NHS organisations and local authorities in England around the future of health and care services in their area. For more details see www.kingsfund.org.uk/topics/integrated-care/sustainability-transformation-plans-explained (accessed 28 November 2017).
List of abbreviations
- A&E
- accident and emergency
- ALOS
- average length of stay
- CA
- family carer
- CCG
- Clinical Commissioning Group
- CH
- community hospital
- CHA
- Community Hospitals Association
- CIC
- community interest company
- CY
- community stakeholder
- DGH
- district general hospital
- ERIC
- Estates Returns Information Collection
- FFT
- Friends and Family Test
- FG
- focus group
- GP
- general practitioner
- IMD
- Index of Multiple Deprivation
- ISD
- Information Services Division
- LRG
- local reference group
- MDT
- multidisciplinary team
- MIU
- minor injury unit
- NCVO
- National Council for Voluntary Organisations
- NIHR
- National Institute for Health Research
- P
- patient
- PCT
- primary care trust
- PLACE
- Patient-Led Assessments of the Care Environment
- PPI
- patient and public involvement
- PREM
- patient-reported experience measure
- S
- staff
- STP
- sustainability and transformation plan
- T
- senior manager and commissioners
- V
- volunteer
- VSM
- voluntary service manager