Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/178/18. The contractual start date was in May 2014. The final report began editorial review in November 2017 and was accepted for publication in April 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Hogan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Introduction
The nature of the problem and policy responses
Despite national guidance,1 regional collaborations2 and additional resources to facilitate change over the last two decades,3 data from the National Cardiac Arrest Audit (NCAA) show that a fourfold variation in in-hospital cardiac arrest (IHCA) incidence and survival exists between hospitals in England (D.A. Harrison, Intensive Care National Audit & Research Centre, 2013, personal communication). It is estimated that resuscitation teams are called to between one and five IHCAs per 1000 hospital admissions, equivalent to around 20,000 IHCAs in NHS hospitals in England each year, with survival to discharge around 15%. 4,5 Although unexpected cardiac arrests are relatively rare, with any ward likely to see only one or two cases per year,6 they may signal a failure to manage antecedent events. Reviews of these patients have shown that many exhibit clear signs of deterioration (physiological changes or level of consciousness) for up to 8 hours beforehand. 7,8 This is despite a further 100,000 ward patients being visited annually by outreach teams with advanced critical care skills because of concerns for their clinical state. One-third of these patients will have died within 30 days of this contact, indicating the high-risk nature of their conditions. 9 Unchecked deterioration, even if not leading to death, is costly for both patients and the NHS, creating a need for extra treatment, prolonging lengths of stay and increasing risk of exposure to hazards, such as drug side effects and hospital-acquired infections.
Since the late 1990s, evidence has been emerging that has demonstrated that patients admitted to the intensive care unit (ICU) from the ward have a worse outcome than those coming straight from the operating theatre or the emergency department. 10,11 Furthermore, up to 25% of ICU patients die following discharge from the ICU. These findings were seen as an indication of the suboptimal care of critically ill patients on the wards. The Department of Health and Social Care (DHSC)’s review of critical care provision in 200012 reported that problems existed with the skills and knowledge of ward staff and their access to advice and support in the care of acutely ill patients. These problems were compounded by increasing workload pressures. In 2005, the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report An Acute Problem?13 found that in many hospitals, junior doctors continued to be largely responsible for providing emergency care on the ward, with inadequate consultant input, and that communication failures between teams contributed to delays in escalating care to a higher level. The report estimated that 21% of admissions to the ICU from general wards could have been avoided with better care. A further NCEPOD report based on a review of a sample of deaths associated with IHCAs14 found that a lack of early assessment by consultants, inadequate management and monitoring plans, a lack of decision-making around appropriate ceilings of care or suitability for resuscitation and failure to escalate care in response to deterioration continued to contribute to these events.
Other far-reaching changes affecting hospitals in recent years have challenged the pace of improvement in the quality of care of acutely ill patients. Most significantly, the implementation of the European Working Time Directive15 has led to a reduction in the number of hours that junior doctors are able to work. There have been concerns that senior doctor coverage has not expanded to adequately fill the gap. The introduction of shift systems as part of these changes has also had an impact on teamwork and continuity of care. 16 Difficulties recruiting and retaining both medical and nursing staff and the increasing use of agency staff and health-care assistants (HCAs) to deliver key clinical activities has further exacerbated the situation. 17–19 As the elderly population expands, many of whom are living with multiple long-standing illnesses, there is mounting pressure on hospital beds. This leads to some patients being cared for on wards that are not suitable to meet their needs and growing numbers of acutely ill patients being cared for on the wards as they wait for a bed to become available in the ICU. 20,21
In response, the DHSC’s 2000 report Comprehensive Critical Care12 set out a strategy to provide an integrated hospital-wide approach to critical illness, in effect breaking down the walls between ICUs and the wards, thus ensuring wider access to critical care expertise through support and collaboration. This policy led to the introduction of nurse-led critical care outreach teams (CCOTs). 22 The task of these teams was to strengthen critical care skills amongst ward staff and provide support to ward staff in managing patient deterioration. In doing so, it was hoped that unplanned ICU admissions would be reduced and that there would be better outcomes for patients discharged from the ICU to the wards. They were also to have a role in promoting the uptake of track-and-trigger systems (TTSs), scoring systems based on physiological measures to detect patients at risk and trigger appropriate responses. 23 In 2007, the National Institute for Health and Care Excellence (NICE) issued guidance on the care of the acutely ill patients, reiterating the need for CCOTs and the widespread use of TTSs. 24
With recent evidence that failure to recognise and respond to deteriorating patients accounts for around one-third of avoidable mortality within hospitals,25,26 this issue has continued to be prioritised in efforts to improve patient safety across the NHS. 27 Recent initiatives include the promotion of the situation, background, assessment, recommendation (SBAR) tool by the NHS Institute for Innovation and Improvement. 28 This is one of a number of structured handover tools designed to improve the quality of communication of urgent patient information among clinicians. A national, standardised TTS [the National Early Warning Score (NEWS)] was introduced by the Royal College of Physicians (RCP) in 2012. 29 The RCP and the NCEPOD have called for consultant assessment shortly after admission and adherence to policies related to treatment limitation and ‘do not attempt cardiopulmonary resuscitation’ (DNACPR) decisions to ensure that cardiopulmonary resuscitation (CPR) is not undertaken on those patients unlikely to benefit. 14,30
Interventions aimed at identifying and responding to patient deterioration
DeVita et al. 31 developed the concept of the rapid response system composed of two parts. The afferent arm is focused on the recognition of patient deterioration through the collection and interpretation of abnormal physiological parameters and triggering an appropriate response to that deterioration. The efferent arm brings staff with critical care skills to the patient’s bedside in a timely way. This system requires knowledgable staff, who understand the implication of any changes in a patient’s level of consciousness or physiological status, to accurately convey that concern to secure the appropriate response. Ensuring an effective system requires ongoing monitoring of performance and improvement activities when failures are detected. 31 Staff education, TTSs, tools for structured communication between staff and rapid response teams (RRTs), an international generic term for critical care-trained response teams that incorporates UK outreach teams, are the four key interventions that need to be in place to identify and respond to deterioration.
Life-support training, which focuses on preparing staff to deal with cardiopulmonary arrest, is mandatory for most NHS clinical staff,32 but formal courses that take a wider perspective on the knowledge and skills needed to identify patient deterioration and provide early intervention are also widely available. 33 Research has suggested that such training can influence detection of deterioration,34 early management by ward staff35 and the likelihood of calling for help if needed. 36
Track-and-trigger systems are based on the association between abnormal physiological findings, poor outcomes and the fact that early intervention can prevent serious consequences, such as cardiac arrest. 37 Such systems let staff ‘track’ a range of physiological parameters including respiratory rate, blood oxygen levels, temperature, blood pressure and heart rate to create scores. These scores then ‘trigger’ specific actions, which might include increased frequency of monitoring or a request for further support. They are seen as an effective way of monitoring the condition of acutely ill patients and their increase in use over the past 20 years has seen a large and diverse number of tools in use across the NHS. 38 Addressing concerns around the lack of consistency across hospitals, and even within hospitals,39 the NEWS has been accepted across the country since 2013, following evaluations that showed that it performed at least as well as, and often better than, the scoring systems already in place. 40 Hospitals are increasingly adopting electronic TTSs to replace paper-based systems. Electronic systems can be designed to counter known problems with paper-based TTSs by mandating entry of a full set of patient observations, accurately calculating scores and automatically sending an alert to an appropriate responder when a particular score threshold is met. 41,42 Many of these recently introduced electronic TTSs use the NEWS as the system for score calculation.
Clinician-to-clinician handovers represent a high-risk area for patient safety if key information about a patient’s risk of deterioration is omitted. 43 There are a number of standardised communication tools, the use of which is designed to increase the effectiveness of communication between clinicians, especially when information has to be passed between different professional groups. 28 A RCP survey in 2010 identified a range of tools in place across NHS hospitals, with some hospitals not using any. 44 SBAR, originally designed for use in the military, organises the information to be transferred into four parts: (1) situation – a description of what is happening now and where, (2) background – the patient’s past medical history, (3) assessment – an overview of the patient’s current condition including physiological measures and (4) recommendation – what help is needed and when. 45 This has become the main tool promoted for use in the NHS. 28
The trend for establishing designated RRTs began in Australia in the 1990s as an expansion of the role of the cardiac arrest team, following the recognition that earlier interventions could improve patient outcomes. 46 Subsequent to the publication in 2000 of Comprehensive Critical Care,12 funding was made available in England to establish CCOTs, the majority of which were nurse led. This was followed by the establishment of RRTs in Scandinavian countries and the USA. 31 The roles of these teams and their composition varied within and across countries, often in response to organisational needs. 47 In Australia, Sweden, Denmark and the Netherlands, the majority of teams called to attend patients actively deteriorating on the wards are doctor led and in the USA they may be nurse or doctor led. 48
NHS acute hospital trusts in England have a number of teams that respond to emergencies. Some have a doctor-led medical emergency team (MET) that attends sudden and overwhelming clinical events (e.g. massive gastrointestinal bleeding or an epileptic seizure), a doctor-led resuscitation cardiac team for cardiopulmonary arrests and a nurse-led outreach team responding to ward patients at earlier stages of deterioration. Unlike outreach teams that have staff members permanently allocated to the team, METs and resuscitation teams tend to be formed from ‘on-call’ staff who come together as a team on a particular day or weekend as part of their ‘on-call’ duties.
In general, the METs and resuscitation teams could be described as reactive to adverse events, such as acute collapse or IHCA. Following the original objectives set out for these teams, nurse-led outreach teams usually play both a proactive role in preventing deterioration (through education and support of ward staff, promoting the use of TTSs and actively identifying high-risk cases) and a reactive role by attending to deteriorating patients when alerted by ward staff. By intervening at an earlier stage of deterioration, evidence suggests that outreach teams are likely to have a greater impact on reducing cardiac arrests and unplanned admissions to the ICU. 49 Given that deterioration in some ward patients may indicate proximity to the natural end of their lives, part of this impact may be attributable to the opportunity it provides team members to interact with patients and their relatives to identify goals of care. As a consequence, treatment limits can be agreed, preventing patients from receiving inappropriate CPR when it is felt it would provide little benefit. 50 International evidence is emerging that this is an expanding role for both doctor-led and nurse-led RRTs. 51,52 In view of the fact that no recommendations were made as to the structure of CCOTs in Comprehensive Critical Care53 it is not surprising that wide variation in service models have been reported across hospitals. Some teams play a larger role in the implementation of TTSs and the education of ward staff, whereas others spend a greater proportion of their time providing clinical care for patients on the ward.
The relationship between interventions and outcomes
Despite concerted national efforts to address the issue of ‘failure to rescue’ deteriorating patients, variation in IHCA rates and survival persists. This suggests that either the effectiveness of these recommended interventions is not as great as anticipated or problems with implementation limit their effect. At face value, a rapid response system would seem to be an appropriate intervention to address delayed response to deterioration. However, its components are each complex interventions in themselves, and implementation may not lead to the predicted outcome because of the possibility of unanticipated consequences. 54 This is evident from the inconsistent findings of evaluations of even the most scrutinised interventions, such as RRT (both doctor led and nurse led), with the early promising results from single-site studies not replicated in larger trials. 55,56 The growing literature on complex interventions also points to the importance of implementation fidelity if such interventions are to achieve predicted outcomes in different settings. 54,56 Variation, such as in outreach team composition or roles, the proportion of patients they are called to see, the levels of uptake of TTSs and the process of making DNACPR decisions will lead to differences in outcomes. 53 The importance of implementation fidelity is apparent in one local collaborative (University College London Partners Deteriorating Patient Collaborative) that reported significant reductions in IHCA incidence through the introduction of standardised approaches to the management of acutely ill patient across the patient pathway in 13 hospitals (J Welch, University College London, 2013, personal communication).
Subbe and Welch57 have described a ‘chain of survival’ for the deteriorating patient. The chain relies on ‘high-quality recording of physiological signs; the education and mind-set of staff at the bedside to recognize pathological patterns; the reporting of abnormality to the response team; a timely and appropriate response by the latter’. 57 This model highlights the point that the impact of any one intervention is limited by any weaknesses at other points in the chain. For instance, TTSs rely on staff having the ability to effectively escalate concerns to avoid the TTS score being limited simply to monitoring a patient’s decline. Thus, the effectiveness of any intervention instituted to detect or respond to deterioration will, to some extent, depend on the thoroughness with which other interventions have been implemented. These interventions exist within a particular context that may also act as a barrier or facilitator to their effectiveness.
Attempts to estimate the impact of staff education, TTSs, tools for structured communication between staff, and outreach teams on IHCA rates and survival are complicated by the fact that a number of other mechanisms may affect these outcomes. For example, IHCA rates are also sensitive to changes in case mix. Older patients with multiple comorbidities are more likely have unshockable cardiac rhythms if they arrest, which increases the risk of death. 58 More older patients in the pool of those eligible for resuscitation will potentially reduce rates of IHCA survival. At the same time, more attention is being paid to improving end-of-life care and promoting early decision-making around goals of care and treatment limitations. 59 The appropriate use of DNACPR decisions to avoid futile resuscitation attempts is part of this effort. This will remove from the pool of patients who receive CPR those who are likely to have the poorest outcomes and potentially improve survival. In the UK, suitability for CPR is a clinical decision usually made by a patient’s consultant. National guidance exists to ensure good practice in this area and this is regularly updated to incorporate statutory or legal changes, such as the High Court ruling (‘the Tracey case’)60 in 2014, that ensured that patients in the UK must be consulted and informed of DNACPR decisions. 61 Little information is available about changes in rates of DNACPR decisions across the NHS over the recent years. Although an ageing population and improved practice in this area may have led to increased use, these increases may have been countered to some extent by the reluctance of consultants to discuss end-of-life issues with patients or relatives or by increasing pressure from families to continue active treatment. 62
The CPR process, both intra-arrest and post arrest, affects survival. 63 Standardisation of training, emergency calling systems and equipment have combined with improved management of arrest and post-arrest care to increase survival. The faster the response, the more likely a patient will still be in a shockable rhythm, such as ventricular fibrillation, when the resuscitation team arrives and this carries an improved survival rate. 6
Given that the use of different configurations of preventative interventions is well-established across the NHS, it has not been possible to evaluate the impact of each component using experimentation [i.e. a randomised controlled trial (RCT)]. However, the opportunity of natural experimentation, which exploits variation in health care, exists. 64 When combined with assessment of implementation fidelity,65 to determine which aspects of an intervention have been delivered, it will be possible to gain a better understanding of the association between different arrangements of interventions and IHCA incidence and survival. This study set out to test several hypotheses in order to make recommendations for best practice likely to have an impact on levels of avoidable serious harm and mortality. The hypotheses tested were as follows:
-
TTSs (in combination with structured handover and education) will reduce IHCA rates by identifying deteriorating patients earlier while there is greater opportunity of reducing their risk of arresting.
-
TTSs (in combination with structured handover and education) will have no association with survival following a cardiac arrest. It would be expected that the afferent (trigger) arm of the rapid response system would have little impact on survival compared with the efferent (response) arm.
-
Outreach teams will reduce IHCA rates by reducing the risk of deteriorating patients arresting more than traditional patterns of response, such as ward-based staff.
-
Outreach teams will increase survival following a cardiac arrest by increasing the application of treatment limitation orders, such as DNACPR decisions in deteriorating patients at high risk of an unsuccessful resuscitation.
Aim
This research aimed to use the principles of natural experimentation to identify which packages of interventions aimed at detection and management of patient deterioration in acute hospitals are associated with the lowest rate of IHCA when resuscitation attempts are made and with best short- and long-term survival, and in doing so identify models of care that are likely to have the most impact on decreasing avoidable mortality.
Objectives
-
To design a typology of interventions based on previous research and an understanding of how interventions are implemented in practice.
-
To determine the association between different arrangements of interventions and rates of IHCA when resuscitation attempts are made and short- and long-term survival.
-
To identify service features associated with the lowest rates of IHCA when a resuscitation attempt was made and best short- and long-term survival, and to disseminate the findings across the NHS to guide service design.
Methodological overview
Theoretical framework
The design of the study drew on three theoretical approaches. The first is natural experimentation, an approach that exploits variation in health-care service provision and outcomes to determine associations between different service models and those outcomes. 64 It is particularly useful when a range of services are already in place and it has become impossible to undertake randomised trials to determine which have the best outcomes. 66 Second, Rogers’67 ‘theory of diffusion transfer’ postulates that developing effective interventions is only the first step in improving outcomes. Aside from dissemination and adoption, interventions need to be implemented effectively and then sustained. The literature on complex interventions in health care indicates that implementation is a key determinant of discrepancies between expected and observed outcomes. 54 To address this, the third theory we employed was that of implementation fidelity (the degree to which programmes are implemented as intended68), which has received relatively little attention to date. 69 To identify how interventions were implemented in practice we used Carroll et al. ’s65 conceptual framework for implementation fidelity. The framework defines adherence in terms of intervention content, coverage, frequency of use and duration, all of which are influenced by four contextual moderators: (1) intervention complexity, (2) facilitation strategies, (3) quality of delivery and (4) staff engagement. Through understanding how interventions have been implemented in practice, we were able to go beyond what systems hospitals reported they have in place and identify key differences in how these interventions have developed and are currently organised and run. This information was used to support the development of our major quantitative analyses focused on associations between intervention types and outcomes and to determine explanatory factors for our findings.
Definitions
Our outcome measures, IHCA rates and survival, were obtained from NCAA. This was the first major study to be able to use data collected by this audit, which started in 2009 and was a collaboration between the Intensive Care National Audit & Research Centre (ICNARC) and the Resuscitation Council (UK). 61 The audit is now receiving reports from > 80% of hospitals in England, representative of the range of hospitals found in the NHS. The audit definitions70 for the outcomes were as follows:
-
IHCA – all individuals, including neonates, who receive either chest compressions or defibrillation by a hospital-based resuscitation team in response to a 2222 call.
-
Return of spontaneous circulation for > 20 minutes – all individuals receiving either chest compressions or defibrillation by a hospital-based resuscitation team who have a return of spontaneous circulation after a cardiopulmonary arrest for > 20 minutes. (Return of spontaneous circulation implies that the patient’s heart has begun to beat on its own again. This is a measure of short-term survival.)
-
Survival to hospital discharge – all individuals receiving either chest compressions or defibrillation by a hospital-based resuscitation team who are alive at the time of discharge from hospital. This is a measure of intermediate-term survival.
We also measured longer-term survival including survival to 30 and 90 days post admission.
The NCAA audit, focusing only on those arrests that elicit a resuscitation team visit, provides an objective count of the majority of arrests, apart from those occurring in patients with DNACPR decisions in place and those occurring on coronary care units (CCU), high-dependency units (HDU) and ICUs where a resuscitation team is unlikely to be called. However, practice does vary across NCAA hospitals as to exactly which IHCA data are submitted, and 16.8% of the inpatient arrests in the audit do originate from CCUs (9.9%), HDUs (1.6%) and ICUs (5.3%), plus another 7.4% from theatres or imaging departments.
Work packages
The research was divided into four work packages:
Work package 1 – systematic literature review of evaluative studies of interventions designed to decrease the incidence of and improve outcomes from IHCAs.
-
Research questions:
-
What was the scientific evidence for interventions designed to decrease the incidence of and improve outcomes following IHCA?
-
What are the essential components of effective interventions and key contextual factors that influence their impact (effectiveness)?
-
Work package 2 – developing and piloting a questionnaire for assessing the use of interventions designed to identify and respond to deteriorating patients in acute hospitals based on the combined findings from work package 1 and qualitative work in a sample hospitals.
-
Research question:
-
How were interventions aimed at deteriorating patients implemented in practice (how did the organisation and contextual moderating factors vary across hospitals)?
-
Work package 3 – national survey of hospitals.
-
Research question:
-
How much current variation was there in types of intervention across hospitals taking part in the NCAA and how had these changed over time?
-
Work package 4 – evaluating the impact of interventions through interrupted time-series and difference-in-difference approaches.
-
Research question:
-
How was variation in interventions associated with variation in IHCA incidence and outcomes found in the NCAA?
-
Linkage across work packages
The principle of natural experimentation is to observe associations between differing arrangements of services and outcomes. To understand variation in service provision for deteriorating patients, we initially planned to summarise the policy drivers leading to the introduction or spread of the interventions and supplement this with a review of the evidence of effectiveness of interventions in relation to our outcomes of interest (IHCA and survival). From this review, we extracted the key components for each intervention that might be linked to positive outcomes to produce a typology.
Having established key components for each intervention, the next stage was to undertake qualitative semistructured interviews with frontline clinical staff and managers to understand how the services are being implemented on the ground in the NHS, how this implementation varies from the evidence-based typology and the nature of any contextual factors that might be acting as important barriers and facilitators to implementation.
Combining the findings from the literature review and the qualitative work enabled key variations in services across England, and other factors in the hospital environment that are potentially having an impact on patient outcomes, to inform the design of a questionnaire survey. The survey was the main mechanism through which we identified the current range of variation in services for deteriorating patients in NCAA hospitals and explored how these have changed over time.
The final stage saw the hospitals grouped by their differences in key service features, cross-sectionally and across time and patient-level outcome data for each hospital examined. In this way, we were able to establish the relationship between different service configurations and outcomes, and determine which variants produce the best outcomes.
Ethics approval
Research ethics approval and local NHS research and development (NHS R&D) approval were sought to cover the qualitative interviews with staff. These approvals were gained using standard procedures. Consultation with our local NHS R&D lead indicated that approval would not be necessary for each of the NCAA hospitals taking part in the survey.
Patient and public involvement
The two patient representatives on the Steering Group (SG) were able to provide a unique perspective on the context and interventions employed in the care of acutely ill patients, either through their own direct experience or that of a close relative. One patient representative, who lost her partner to a cardiac arrest, was also the patient representative on the NCAA SG and was familiar with the aims and the development of this audit since its introduction. The other representative had been an inpatient for an acute illness managed on both the ward and in the ICU. Their combined experience helped us to identify important aspects of care for acutely ill patients from the patient’s perspective, which supported the development of our understanding and typology of interventions.
Our representatives contributed to the development of the proposal and the lay summary for the final report. They were helpful in identifying some of the likely impacts of the study findings and advising on the best ways to communicate these findings to the general public prior to dissemination activities.
To facilitate the patient representatives’ involvement in the management of the research, Dr Catherine Carver, our research fellow, provided support by clarifying any issues prior to the SG meetings and providing an opportunity for debriefing afterwards.
Issues faced
In the first year of the study we were delayed by 4 months owing to a combination of factors, including an initial delay in recruitment of the research fellow, the length of time it took to process NHS R&D approvals for the semistructured interviews and delays in getting permissions from the research ethics council and the Health Research Authority’s Confidentiality Advisory Group to access linked data. In the second year, a further delay of 12 months was encountered while we waited to receive the complete linked data set necessary for final analysis from NHS Digital.
Chapter 2 Systematic literature review of evaluative studies of interventions designed to decrease the incidence of, and improve outcomes from, in-hospital cardiac arrests
Parts of this chapter have been reproduced with permission from Hogan et al. 71 Republished with permission of MA Healthcare Limited, from Effectiveness of ways to improve detection and rescue of deteriorating patients, Hogan H, Carver C, Zipfel R, Hutchings A, Welch J, Harrison D, Black N, British Journal of Hospital Medicine, vol. 78, 2017; permission conveyed through the Copyright Clearance Center, Inc.
Introduction
Health-care organisations have adopted a multifaceted approach to identifying and responding to deteriorating patients on hospital wards following recommendations made by national bodies. 24,27 The four main categories of interventions include RRTs (doctor or nurse led), TTSs, education programmes for doctors and nurses and standardised approaches to patient handover. The international generic term ‘RRT’ is used to cover the range of different models for designated teams of clinicians who rapidly respond to deterioration. These interventions tackle different elements of what Subbe and Welch57 have described as a ‘chain of survival’ for the deteriorating patient, which includes the need for accurate recording of physiological measures, a considered judgement of their meaning that derives a timely response and rapid delivery of the required escalation in care to the bedside. As a consequence of this interlinkage, the effectiveness of any of the four categories of intervention will, to some extent, depend on the thoroughness with which the other three categories have been implemented. Previous reviews of the literature have usually focused on one or two of the categories in the chain of survival. In contrast, our aim was to consider the evidence of the effectiveness of all four categories as a way of gauging the likely impact each might have on the other. We considered effectiveness in four ways: (1) outcome (preventing cardiac arrests, hospital deaths and adverse events), (2) use of hospital beds (reducing unplanned admissions to critical care units and lengths of stay), (3) vital sign recording and (4) improving staff confidence, communication and satisfaction.
Aim and objectives
Our aim was to derive an overview of the evidence of the effectiveness of all four categories of intervention that make up the ‘chain of survival’ (RRTs, TTSs, structured handover tools and continuing education) and to develop a typology for each based on the elements that were found to be linked to effectiveness.
Methods
Given the broad scope of the review, it was not possible to undertake a Cochrane-style systematic review for each intervention. Our method was pragmatic and adapted to the time and resources available. For each intervention, we initially looked for the latest rigorous systematic review published since 2010. Having scrutinised these reviews, we supplemented the findings with primary research studies that had been published more recently (i.e. since the end of the search period of each review) or studies previously overlooked.
Scope and search strategy for systematic reviews
Initial scoping searches were used to find the latest high-quality systematic review of each of the four categories of intervention to use as the foundation for our search strategy (see Appendix 1). A de novo search strategy was created for additional primary research published since the last high-quality systematic review. Underpinning these searches were four distinct population, intervention, comparison, outcome questions (Table 1), each tailored to the nature of the intervention and the available evidence.
| Topic | Population | Intervention | Comparison | Outcome |
|---|---|---|---|---|
| RRT | Adult inpatients on general medical or surgical wards | Introduction of a RRT (a team that responds to calls for help managing deteriorating patients) | Current or historic comparison group | Any that evaluate effectiveness of the intervention |
| TTS | Adult inpatients on general medical or surgical wards |
|
Current or historic comparison group | Any that evaluate effectiveness of the intervention |
| Standardised handover tool | Qualified doctors and nurses working on adult general medical or surgical wards in hospitals | Introduction of a standardised tool to structure communication during intrahospital handover of patient information (e.g. standardised handover sheets) | Current or historic comparison group | Any that evaluate effectiveness of the intervention |
| Continuing education | Qualified doctors and nurses working on adult general medical or surgical wards in hospitals | Implementation of an educational intervention aimed at improving the subject’s identification and management of deteriorating adult inpatients not being managed in critical care areas | Current or historic comparison group | Any that evaluate effectiveness of the intervention |
Inclusion criteria common to all four interventions were (1) the implementation of a new intervention in the adult general inpatient environment, (2) interventional or observational studies with a comparison group, or a review of such studies, and (3) the assessment of outcomes. Intervention-unique criteria were also applied, for instance single parameter TTSs were excluded as they are not recommended by NICE and are therefore less likely to be used in modern clinical practice.
For all interventions, we excluded studies that were (1) entirely retrospective, (2) had no comparison group, (3) performed no statistical tests, (4) had an abstract only or (5) were already incorporated in a selected review paper. There were also exclusion criteria specific to each intervention, as listed in Table 2.
| Intervention | Exclusion criteria |
|---|---|
| RRT |
|
| TTS |
|
| Standardised handover tools |
|
| Continuing education |
|
The strategies were finalised following consultation with a university librarian who was knowledgeable in search techniques for systematic reviews.
Searches were run in EMBASE and MEDLINE in October 2014 and updated in September 2017, with the expectation that this approach would capture the majority of studies of interest. A combination of Boolean operators, truncations, key words and Medical Subject Heading (MeSH) or Emtree terms were used (see Appendix 2). Results were limited to the English language and by date.
The sensitivity of each search was verified by checking its ability to find key papers identified during the scoping searches.
Selection strategy
Following removal of duplicate papers, they were divided between reviewers (CC, RZ and HH) for single title and abstract sifting. If a reviewer was uncertain about including a paper, a second reviewer’s judgement was sought and a consensus reached. The same process was applied to the full-text articles that remained after the initial sift. A detailed breakdown of each sift can be found in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-style flow diagrams in Appendix 3.
Data extraction and quality assessment
Data items based on the Cochrane Handbook for Systematic Reviews of Interventions72 were extracted from each review (see Appendix 4). For published systematic reviews that had a broader focus, we restricted our data extraction to the primary research studies cited that were relevant for our aim. The number of included papers is indicated in the first column of each of the summary tables. The exclusion criteria were specific to each of the four categories of intervention (see Table 2).
The quality of each systematic review and primary research paper was assessed by a single reviewer using the NICE methodology checklists used in Clinical Guideline 5024 (CG50) (see Appendix 4). Primary research papers were assessed for selection bias, attrition bias, performance bias and detection bias (see Appendix 4). All papers were then allocated an overall rating based on the study type and quality assessment, founded on the system used by NICE in CG5024 (Table 3). This resulted in all systematic reviews being rated 2++. Most primary studies were rated 2– except for four73–76 rated 1– and two rated 2+. 77,78 The detailed tables containing extracted data are presented as Report Supplementary Materials 1–8.
| Rating | Evidence |
|---|---|
| 1 ++ | High-quality meta-analyses, systematic reviews of RCTs or RCTs rated as having a very low risk of bias |
| 1 + | Well-conducted meta-analyses, systematic reviews of RCTs or RCTs rated as having a low risk of bias |
| 1 – | Meta-analyses, systematic reviews of RCTs or RCTs rated as having a high risk of bias |
| 2 ++ | High-quality systematic reviews of case–control or cohort studies |
| High-quality case–control or cohort studies rated as having a very low risk of confounding, bias or chance and a high probability that the relationship is causal | |
| 2 + | Well-conducted case–control or cohort studies rated as having a low risk of confounding, bias or chance and a moderate probability that the relationship is causal |
| 2 – | Case–control or cohort studies rated as having a high risk of confounding, bias or chance and a significant risk that the relationship is not causal |
| 3 | Non-analytic studies (for example, case reports or case series) |
| 4 | Expert opinion, formal consensus |
Data synthesis and analysis
Given the heterogeneity of the studies, it was not possible to undertake a statistical summary; therefore, a narrative summary was undertaken. This started with tabulation of the study descriptions to identify commonalities and differences across the studies, along with consideration as to the weight of the evidence for each study based on the study design. This synthesis was summarised in tables reporting study outcomes throughout this report.
Findings
Rapid response teams
Six systematic reviews incorporated relevant studies from Australia, North America and Europe, from 1950 to 2015 (Tables 4 and 5). The reviews combined evaluations of both medically led and nurse-led teams, with studies focused on the latter being in the minority.
| First author and year of study, search period (number of studies) | Setting | Intervention | Main results |
|---|---|---|---|
| NICE 2007,24 2004–6 (n = 20) | Hospital patients | RRT | Cardiac arrest rate: unchanged (cluster RCT), decreased (5 out of 8 before-and-after studies) |
| Unplanned ICU admissions: unchanged (cluster RCT), decreased (3 out of 4 before-and-after studies) | |||
| Hospital mortality: unchanged (cluster RCT), decreased [OR 0.52 (RCT)], decreased (4 out of 9 before-and-after studies) | |||
| Chan 2010,56 1950–2008 (n = 11) | Inpatients (adults) | RRT | Cardiac arrest rate: decreased in non-ICU patients (RR 0.66; 21.1% reduction in high-quality studies) |
| Hospital mortality: unchanged (RR 0.96) | |||
| Massey 2010,84 1995–2008 (n = 8) | Inpatients (adults) | Rapid response system | Cardiac arrest rate: decreased (13–50%) in 5 studies |
| Unplanned ICU admissions: decreased (45% vs. 29%) (one study) | |||
| Hospital mortality: decreased in three studies | |||
| McNeill 2013,48 1996–2012 (n = 20) | Inpatients (adults) | METs (doctor led) | Cardiac arrest rate: decreased (14 studies) |
| Unplanned ICU admission: decreased (14 studies) | |||
| Hospital mortality: decreased (14 studies) | |||
| McNeill 2013,48 1996–2012 (n = 23) | Inpatients (adults) | Non-doctor-led RRT | UK:
|
Australia:
|
|||
USA:
|
|||
| Winters 2013,79 2000–2012 (n = 28) | Inpatients (adults) | RRT | Cardiac arrest rate: decreased in non-ICU patients (12 out of 20 studies) |
| Hospital mortality: decreased (7 out of 18 studies) | |||
| Maharaj 2015,47 1990–2013 (n = 29) | Inpatients (adults and children) | RRT | Cardiac arrest rate: decreased in non-ICU patients (13 out of 18 studies) |
| Hospital mortality: decreased (9 out of 20 studies) | |||
| No significant effect on ICU admissions |
| First author and year of study, design | Setting (number of patients) | Intervention | Comparison periods | Results |
|---|---|---|---|---|
| Rothschild 2008,77 controlled before-and-after study | Tertiary care academic medical centre, USA (n = 9519) | MET | Introduced in four wards over a 6-month period and compared with preceding 6-months and with six control wards | Cardiac arrest rate: unchanged |
| Unplanned ICU admission: increased (2% vs. 3.1%); no change on control wards | ||||
| Hospital mortality: unchanged | ||||
| Mean LOS: decreased (3.78 days vs. 3.46 days) | ||||
| Ludikhuize 2015,80 uncontrolled before-and-after study | 12 Dutch hospitals (two wards in each hospital) (n = 166,569) | EWS, SBAR and RRT | 5 months pre-implementation, 7 months implementing MEWS/SBAR, 12 months implementing RRT, 5 months post implementation | Decrease in cardiac arrests (OR 0.6) |
| Decrease hospital mortality (OR 0.8) | ||||
| No change in unplanned ICU admissions | ||||
| Pirret 2015,81 uncontrolled before-and-after study | Single New Zealand city tertiary referral centre (n = 96,645) | Nurse-led RRT. MET already in place | 12 months pre-implementation, 36 months implementation, 12 months post implementation | Decrease in cardiac arrests |
| Decrease in ICU admissions | ||||
| No change in MET activations | ||||
| Jeddian 2016,76 stepped wedge cluster randomised trial | Single Iranian teaching hospital (n = 21,029) | Rapid response system (outreach team, EWS and education) | – | No significant difference in cardiac arrest, hospital mortality or admissions to ICU |
The first review contained two RCTs and 16 uncontrolled before-and-after studies. 24 One RCT was a large cluster trial of a medically led RRT alongside the use of an early warning score (EWS) and an education intervention. 82 They found no statistically significant impact on the cardiac arrest rate, unplanned ICU admissions or hospital mortality. In contrast, a smaller RCT83 reported a significant reduction in hospital mortality. The review authors suggested intervention variability as one possible explanation for the result in the larger cluster RCT because, although the calling criteria were uniform, the RRT makeup was not. In addition, they noted that the sample size was potentially inadequate. The results of the 16 uncontrolled before-and-after studies were mixed. Although a majority found a significant decrease in cardiac arrest rate and unplanned ICU admissions, less than half found a significant reduction in hospital mortality.
Chan et al. 56 also found no overall effect on hospital mortality in their meta-analysis of 11 mixed-quality studies, but they did find a 34% reduction in rates of cardiac arrest outside ICUs (although less impressive in the high-quality studies). A reduction in cardiac arrest rate was also reported by Massey et al. 84 Five out of eight studies (all single-centre observational studies) reported a significant reduction in arrests, ranging from 13% to 50%. Unlike the earlier reviews, four of the studies also reported a reduction in hospital mortality. Despite this, the authors concluded that, overall, the evidence for the effectiveness of the RRT was inconclusive, suggesting underuse of the teams as a possible explanatory factor.
McNeill and Bryden48 tackled the issue of intervention heterogeneity by dividing their review into teams that were medically led (20 studies) and those that were not (23 studies). They reported that METs reduced cardiac arrest rates and hospital mortality and, in addition, unplanned ICU admissions decreased. The evidence on hospital length of stay (LOS) and ICU mortality was unclear. The evidence for non-doctor-led teams was not as strong. Across 17 uncontrolled before-and-after studies, eight found reductions in cardiac arrests, five in mortality and one in ICU admissions. Three interrupted time-series studies found a reduction in cardiac arrest rates but no impact on mortality. A single-site, stepped-wedge RCT83 did show a significant reduction in mortality (48%) but validity was weakened by randomisation of only 2903 out of 7450 patients declared as eligible.
A systematic review by Winters et al. 79 reported a reduction in cardiac arrests and hospital mortality, although the latter was statistically significant in only seven studies, Maharaj et al. 47 conducted a meta-analysis of 29 studies that reported a decrease in cardiac arrest rates and in mortality. The authors found considerable heterogeneity for both outcomes, reflecting the variation in results across the included studies. Only three of the included studies were non-doctor led.
Four additional studies (one stepped-wedge RCT, one controlled and two uncontrolled before-and-after study) not included in the six reviews are some of the largest reported. Two studies evaluated medically led teams,77,80 and two evaluated nurse-led teams. 76,81 All studies also introduced either a NEWS or altered the escalation criteria for an existing scoring system. Both of the uncontrolled before-and-after studies reported a reduction in cardiac arrest rates and one also found a reduction in mortality. In contrast, both the RCT and controlled before-and-after study reported no change in cardiac arrest rates or hospital mortality, which they attributed to underuse of the RRT. 76,77
Track-and-trigger systems
There were three systematic reviews, starting with NICE in 2007,24 which included five studies83,85–88 of introducing aggregate weighted scoring systems (Tables 6 and 7). The one RCT reported a significant reduction in hospital mortality (but in combination with a RRT and continuing education). 83 One small, single-site before-and-after study confirmed a reduction in mortality but without a concurrent RRT,88 another reported no impact on mortality. 86 Only one of the three studies that assessed unplanned admission to critical care found a reduction,86–88 and only one of four studies83,86–88 (a RCT) reported a reduction in LOS. 83
| First author and year of study, search period (number of studies) | Setting and participants | Intervention | Main results (p < 0.05) |
|---|---|---|---|
| NICE 200724 1990–2006 (n = 5) | Hospital patients (inpatients, emergency department and those in transition) | TTS (physiological parameters and neurological state). Three studies also introduced rapid response systems | Cardiac arrest rate: unchanged |
| Unplanned admission to ICU: decreased in one out of three studies (58% vs. 43%) as did ICU readmissions (5.1% vs. 3.3%) | |||
| Hospital mortality: decreased in one RCT (OR 0.52) and one before-and-after study (5.8% vs. 3%), unchanged in one before-and-after study | |||
| Hospital and ICU LOS: decreased (hazard ratio: 0.90) | |||
| McNeill 201348 1996–2012 (n = 4) | Inpatients (adults) | EWS (aggregate weighted scoring system) | Cardiac arrest rate: decreased |
| Unplanned ICU admissions: decreased | |||
| Hospital mortality: decreased | |||
| Mean ICU and hospital LOS: unchanged | |||
| Alam 201489 up until 2013 (n = 7) | Inpatients and emergency departments (adults) | EWSs | Vital sign recording: increased in one study (7.0% vs. 75.6%) |
| Cardiac arrest rate: decreased in one study, increased in one study (0.6% vs. 2.3%) | |||
| Unplanned ICU admission: decreased in one study (11% vs. 5%) but HDU admission rate increased (14% vs. 21%) | |||
| Hospital mortality: decreased in two studies (5.8% vs. 3%; 1.4% vs. 1.2%), unchanged in three studies | |||
| Mean LOS: unchanged |
| First author and year of study, design | Setting (number of patients) | Intervention | Comparison periods | Results |
|---|---|---|---|---|
| Odell 2007,90 uncontrolled before-and-after study | Two UK hospitals – adults (n = 2638) | Reading-MEWS (one hospital also had a CCOT) | 1 year before and 4 years after | Respiratory rate recording: increased each year (6.0% vs. 16.8%, 57.2%, 70.0%, 77.9%). Increased more in the hospital with a CCOT (9.8% vs. 28.9%, 70.3%, 83.8%, 87.7%) |
| Bellomo 2012,93 uncontrolled before-and-after study |
Hospitals in the USA (n = 5), Sweden (n = 2), UK (n = 1), Netherlands (n = 1) and Australia (n = 1) (n = 18,305) |
Paper TTS converted to electronic version | 3 months before and 3 months after | Cardiac arrest rate: unchanged |
| Hospital mortality: unchanged | ||||
| RRT calls: unchanged; proportion for respiratory problems increased (21% vs. 31%) | ||||
| Number of abnormal physiological criteria present at time of RRT call: decreased | ||||
| Proportion of RRT calls resulting in transfer: unchanged (41% vs. 49%) – except in the USA (54% vs. 69%) | ||||
| Mean hospital LOS: decreased (4 days vs. 3 days) | ||||
| De Meester 2013,91 uncontrolled before-and-after study | One general hospital in Belgium – post-operative adults (n = 4247) | MEWS | 4 months before and 4 months after | Vital sign recording (mean number of vital signs measured for observation episode): increased 1.81 vs. 2.45, greatest during night shifts (1.94 vs. 3.37) |
| Increase in: oxygen saturation (27%), GCS (23%), respiratory rate (17%) | ||||
| Decrease in: temperature (68% vs. 63%), pulse rate (54% vs. 49%) | ||||
| Hospital mortality: decreased (19% vs. 4%; RRR 73.7%) | ||||
| Reoperation rate: decreased (141% vs. 78%; RRR 30.9%) | ||||
| Mean LOS: decreased (4.55 days vs. 4.11 days) | ||||
| Hammond 2013,92 uncontrolled before-and-after study | Tertiary referral hospital in Australia – post-ICU adults (n = 139) | MEWS | 1 month before and 1 month after | Vital sign recording in unplanned ICU admissions: full set increased (44.0%), urine output increased (26.9%) |
| Vital sign recording in 24 hours post ICU: full set increased (210%), urine output increased (103%) | ||||
| McDonnell 2013,94 uncontrolled before-and-after study | District general hospital in England. Survey of 213 nurses and 15 interviews | Locally devised TTS | 2 weeks before and 6 weeks after | Number of staff concerns: decreased (4.3 vs. 3.7) for ‘lack of prior specific experience’ and ‘keeping calm’ |
| Staff ability: increased (experience 7.5 vs. 8.1; knowledge 7.3 vs. 8.0) | ||||
| Staff confidence: increased – recognise deterioration (7.5 vs. 8.2), when to contact (8.8 vs. 9.0), who to contact (8.9 vs. 9.2), report abnormal observations (9.0 vs. 9.3), ask senior staff to come (9.3 vs. 9.4) | ||||
| Kyriacos 2015,75 cluster RCT | Single large public hospital in South Africa – surgical adults (n = 114) | MEWS and education programme | No change in nurse response to deterioration (repeat vital signs or call for help) | |
| Increased recording of respiratory rate and recordings of all seven parameters | ||||
| O’Connell 2016,78 interrupted time-series analysis | Single Australian tertiary hospital (n = 855,870) | TTS | 6 years before and 18 months after | Pre-chart RRT calls were increasing while ICU admissions from the ward, deaths and cardiac arrests were decreasing |
| Post-chart RRT calls and ICU admissions initially increased by 82% and 41%, respectively, before becoming constant | ||||
| Trends in the cardiac arrest rate and hospital mortality did not change |
A 2013 review by McNeill and Bryden48 reported decreases in cardiac arrest rates, unplanned ICU admissions and hospital mortality. In addition, they concluded that TTSs improved documentation of vital signs. This was based primarily on a before-and-after study that replaced a single parameter score with an aggregate scoring system plus an education programme. This review found that LOS was unchanged. The latest review, a 2014 study by Alam et al. ,89 was limited to studies of poor methodological quality, with heterogeneous study populations. The impact on cardiac arrest was inconsistent and of six papers assessing mortality, only two reported a reduction. One study reported decreased unplanned ICU admissions but increased HDU admissions.
We identified seven additional studies (five uncontrolled before-and-after studies, one interrupted time-series and one cluster RCT) of which four assessed a form of Modified Early Warning Score (MEWS). 75,90–92 One cluster RCT and three before-and-after studies reported improved recording of one or more vital signs. 75,90–92 De Meester et al. 91 also reported decreased hospital mortality, incidence of reoperation and LOS, but there were no changes in trends for cardiac arrest rates and hospital mortality found in the interrupted time-series study. 78
Less encouraging were the results of a large multinational before-and-after study that examined the introduction of electronic vital signs monitors. 93 The monitors used in every site were the same, but the warning score and escalation were based on each hospital’s pre-existing policy. There was no impact on cardiac arrest rates, frequency of RRT calls or hospital mortality. There was some international variation: US hospitals reported a decrease in LOS and an increase in the proportion of RRT call patients transferred to a greater-acuity ward. This suggested that caution is needed when transferring results between countries. These findings were echoed in the 2016 Australian interrupted time-series study. 78
McDonnell et al. 94 focused on the impact of introduction of a TSS on the knowledge and confidence of nurses. There were improvements in the number of staff concerns, reported levels of experience and knowledge, and staff confidence in recognising deterioration, reporting abnormal observations and in knowing who and when to contact for help. However, these improvements were small and the improvements were greater among non-registered nurses. In addition, confidence in asking senior staff to attend, a key part of the chain of survival, did not increase.
Standardised handover tool
The majority of studies in the four systematic reviews found that handover tools were associated with an improvement in at least one outcome (Tables 8 and 9). 95–98 Examples of improvements included decreases in the number of dropped tasks, the number of omissions, the number of preventable adverse events and LOS. However, there were also a small number of studies that reported an increase in the number of unexpected changes in care and the number of errors attributed to handover. 110,111 The most common benefit in the Robertson et al. 96 review was improved information transfer. Few studies considered outcomes, but four found a decreased LOS and two reported a decrease in adverse events.
| First author and year of study, search period (number of studies) | Setting | Intervention | Main results |
|---|---|---|---|
| Foster 201295 up until 2010 (n = 7) | Hospital clinical staff | Standardised handover forms | Interventions required, dropped tasks, preventable adverse events, mean LOS: decreased (at least one of these measures decreased in six studies) |
| Outcomes: improved (3 out of 4 studies) | |||
| Dropped tasks, time to first intervention, ‘undesirable actions’, deviations from expected care, medical errors, adverse drug events: unchanged (no significant changes in one or more of these measures in three studies) | |||
| Unexpected changes in care: increased (OR 7.16) (one study) | |||
| Errors attributed to handover: increased (OR 7.68) (one study) | |||
| Robertson 201496 2002–12 (n = 17) | Hospital clinical staff | Mnemonics, minimum data sets, standard operating procedures, IT | Information transfer: improved (10 studies) |
| Adverse events: decreased by 12% (one study) | |||
| Mean LOS: decreased (one study) | |||
| Pucher 201597 up until 2013 (n = 11, all adults) | Hospital clinical staff (surgery) | Prompt tools (pro formas and checklists) mainly used in the context of daily hand offs | Decreased omissions (six studies) |
| Decreased task errors (three studies) | |||
| Decreased time for handover (two studies) | |||
| Decreased mean LOS (one study) | |||
| Davis 201598 2008–14 (n = 37) | Doctors | Electronic tools to support physician-to-physician hand offs | Improved content (16 studies) |
| Decreased omissions (nine studies) | |||
| Increase self-reported quality of handover (six studies) | |||
| Decreased time for handover (six studies) | |||
| Increase in perception that patient safety is improved (five studies) | |||
| Decreased telephone calls between staff and increased weekend discharges (one study) | |||
| Decreased median LOS (one study) | |||
| Decreased unexpected events (two studies) |
| First author and year of study, design | Setting, type of clinicians (number of clinicians) | Intervention | Comparisons | Results |
|---|---|---|---|---|
| Payne 2012,99 controlled trial | Three teaching hospitals in the USA, medical residents (n = 124–251) | Structured web-based handover application (WardManager, Washington, DC, USA) | Part 1: four teams (intervention) vs. eight teams (controls) | Part 1
|
| Part 2: intervention hospital vs. two control hospitals | Part 2
|
|||
| Moseley 2012,100 uncontrolled before-and-after study | Neurology department in the USA, medical residents (n = 20–33) | SBAR | 2 weeks before and 3 weeks after implementation | Overall level of satisfaction (on a 10-point scale): increased (6.2 vs. 7.4) |
| All important data being transmitted: increased (49% vs. 80%) | ||||
| Sharing test results with patients: increased (69% vs. 95%) | ||||
| Night staff update electronic service list: increased (45% vs. 75%) | ||||
| Other 12 criteria: no improvement | ||||
| Ahmed 2012,101 uncontrolled before-and-after study | Acute surgical admission unit in the UK, junior doctors (n = unknown) | Computerised structured template | 4 weeks before and 4 weeks after | Improvement in transfer of data on: date of birth (91% vs. 98%), hospital number (61% vs. 85%), history (91% vs. 97%), past medical history (28% vs. 48%), diagnosis (37% vs. 50%), management plan (82% vs. 94%) and senior review (2% vs. 91%) |
| No change in data on ward location or investigations | ||||
| De Meester 2013,102 uncontrolled before-and-after study | Tertiary referral hospital in Belgium, nurses (n = 425) | SBAR | 9 months before and 9 months after | Documentation of four SBAR elements: increased (4% vs. 35%) |
| Communication score: increased (58 vs. 64) | ||||
| Unplanned ICU admissions: increased (13.1 vs. 14.8/1000 admissions) | ||||
| Unexpected deaths: decreased (0.99 vs. 0.34/1000 admissions) | ||||
| Number of cardiac arrest team calls: unchanged | ||||
| Yazici 2013,103 uncontrolled before-and-after study | Teaching hospital in the USA, medical residents (n = 48) | Standardised handover tool (Mercy 10-D, Mercy Hospital and Medical Center, Chicago, IL, USA) | Before and 3 and 9 months after | Frequency of morning handover: increased (59% vs. 89%) |
| Overnight events that should have been communicated during handover: decreased (84% vs. 50%) | ||||
| Uncertainty about decisions because of poor handover: decreased (72% vs. 37%) | ||||
| Graham 2013,104 uncontrolled before-and-after study | Teaching hospital in the USA, medical interns (n = 39) | Electronic handover template | 3 months before and 3 months after (following 9-month implementation period) | Written handover quality: improved (5 out of 6 measures) |
| Spoken handover quality: improved (4 out of 10 measures) | ||||
| Critical data omissions: decreased (23 vs. 0) | ||||
| Adverse events (including near misses): unchanged | ||||
| Content of sign-out documents: improved (3 out of 5 measures) | ||||
| Connor 2013,105 uncontrolled before-and-after study | Military medical centre in the USA, medical residents (n = 15) | Structured mnemonic (IMOUTA) | 6 weeks before and 6 weeks after | Knowledge of patient diagnoses: improved (3.96 vs. 4.60) |
| Knowledge of hospital course: improved (3.49 vs. 4.69) | ||||
| Knowledge of active concerns: improved (3.49 vs. 4.69) | ||||
| Knowledge of treatment plans: improved (3.44 vs. 4.60) | ||||
| Overall helpfulness: improved (3.62 vs. 4.71) | ||||
| Cornell 2013,106 uncontrolled before-and-after study | Suburban hospital in the USA, nurses (n = 75) | SBAR (initially paper, then electronic) | Before and 1 month after | Time to complete shift report: unchanged |
| Proportion of time on shift report tasks: increased with electronic version (54.6% vs. 66.4%) | ||||
| Proportion of time on spoken report: increased with electronic version (29.5% vs. 42.1%) | ||||
| Younan 2013,107 uncontrolled before-and-after study | Hospital in Lebanon, nurses (n = 32) | Standardised handover tool | 1 month before and 6 months after | Omissions: decreased (18 out of 36 measures) including risk for fall (24% vs. 8%), pain status (10% vs. 1%), abnormal laboratory results (90% vs. 48%), abnormal radiology results (74% vs. 30%), isolation precautions (100% vs. 65%), level of consciousness (100% vs. 65%), fall risk (95% vs. 65%) and pressure ulcer risk (95% vs. 65%) |
| Interruptions of handovers: decreased (2.17 vs. 1.26) | ||||
| Gonzalo 2014,108 uncontrolled before-and-after study | Tertiary-care hospital in the USA, medical residents (n = unknown) | Standardised electronic tool (eSignout) | 3 weeks before and 12 months after | Spoken communication: improved, including being complete and helpful (3.13 vs. 3.44) |
| Communication of ‘results of completed studies/consults: decreased (4.1 vs. 3.9) | ||||
| Eight other communication measures: unchanged, including provisional diagnosis, vital signs on arrival and on transfer/trigger criteria at time of transfer | ||||
| Gagnier 2016,109 uncontrolled before-and-after study | Tertiary-care hospital in the USA, orthopaedic residents (n = 127 patients) | Hand off checklist | 1 month before and 1 year after | Decrease in adverse events (8%) |
| No significant change in LOS |
In the 11 additional studies identified, three used the SBAR approach: Cornell et al. 106 found no significant difference in the time taken to complete shift reports, although there was an increase in the percentage of time spent on shift report tasks; Moseley et al. 100 found no improvement in 12 out of 16 measures, although medical residents reported an improvement in whether or not all the important data were transmitted during sign-out; and De Meester et al. 102 reported an increase in the number of unplanned ICU admissions and a decrease in hospital deaths (although concurrent educational interventions may have contributed).
Of the other eight studies, five tested a bespoke electronic handover tool. In the only study to use a parallel control group, users were more likely to report inclusion of key patient information and to be confident about the quality of the handover they received. 99 Ahmed et al. 101 also found an improvement in data transfer, the biggest improvement being the recording of senior review. Similarly, Graham et al. 104 reported improvements in the quality of written accounts of five out of six measures. Yazici et al. 103 noted an improvement in five quality markers, but this was sustained to 9 months for only three of them. Gonzalo et al. 108 also found limited benefits after 12 months, with no improvement in eight measures of communication and a worsening in communication of results of completed studies/consults.
The other three studies were of non-electronic handover approaches. One reported improvements in all self-reported measures of knowledge (patient diagnoses, hospital course, active concerns and treatment plans), as well in the overall helpfulness of the handover. 105 Another found that the proportion of missing data decreased for 18 out of the 36 criteria, including fall risk, pain status and home medication. 107 The third reported an 8% decrease in adverse events and a decrease in LOS across an orthopaedic service. 109
Continuing education
The systematic review by Liaw et al. 112 included three before-and-after evaluations113–115 of educational programmes aimed at doctors and nurses (Tables 10 and 11). One reported improved confidence across several measures, including recognising critical illness, keeping patients alive, remembering essential life-saving procedures and seeking out senior staff for help. 113 Of the other two studies, one reported no change in mortality or staff awareness of patients at risk on general wards 5–9 months post intervention,114 whereas the other reported a reduction in unplanned admissions to ICU and in hospital deaths. 115 However, in the latter, the educational intervention was accompanied by greater use of a MET review, more vital signs documentation and a new TTS. Connell et al. 116 included 13 studies evaluating the impact of educational programmes on doctors and nurses and all except one study showed either a change in behaviour or increased knowledge and confidence post training. This review also included the before-and-after study by Fuhrmann et al. 114 showing no change in hospital mortality.
| First author and year of study, search period (number of studies) | Setting, participants | Intervention | Main results |
|---|---|---|---|
| Liaw 2011,112 2000–10 (n = 3) | Hospital wards, doctors and nurses | ALERT™: ABCDE approach, team problem-solving skills, communication skills, ethics of acute care | ALERT™
|
MFS
|
|||
| Multiprofessional Full-scale Simulation (MFS): recognition of deterioration, criteria of abnormal physiological signs, ABCDE, teamwork and communication skills including SBAR | COMPASS
|
||
| COMPASS: physiology, MEWS, SBAR, management plan and teamwork | |||
| Connell 2016,116 2002–14 (n = 13) | Inpatients and qualified health professionals | Seven educational programmes blended classroom teaching with simulation, five were classroom only | Increased knowledge or confidence found in seven studies |
| Improved skills or behaviour change found in eight studies | |||
| Hospital mortality measured in one study: no change | |||
| MET activations increased in one study |
| First author and year of study, design | Setting, type of clinicians (number of clinicians) | Intervention | Comparison period | Results |
|---|---|---|---|---|
| Kinsman 2012,117 interrupted time-series analysis | Rural hospital in Australia, nurses (n = 34) | Programme (FIRST2ACT) for detection and management of clinical deterioration | 2 weeks before and 8 weeks after | Unsatisfactory pain score charting: decreased (–0.179) |
| Unsatisfactory frequency of observations: decreased (–0.112) | ||||
| Observation frequency: improved in medical but not in surgical patients | ||||
| Administration of oxygen therapy: unchanged | ||||
| Schubert 2012,118 uncontrolled before-and-after study | University medical centre in the USA, nurses (n = 58) | Deteriorating patient simulation scenario with a high-fidelity mannequin | Before, immediately after and 2 weeks after | Failure to rescue knowledge: increased by 0.73 points (immediately after) and by 1.76 points (after 2 weeks) |
| Critical thinking: improved (immediately after) but no difference at 2 weeks | ||||
| Laiw 2016,74 RCT | Single acute-care tertiary hospital, registered nurses (n = 70) | E-RAPIDS Rescuing A Patient In Deteriorating Situations web-based training programme including multimedia modalities | – | Increased knowledge of deteriorating patient and appropriate response |
| Increased monitoring of pulse (74.3% vs. 37.5%) and respiratory rate (48.2% vs. 25%) compared with controls | ||||
| Johnston 2016,73 RCT | Single UK teaching hospital, junior doctors (n = 36) | Educational intervention (small group teaching session on assessment of acute illness including training in SBAR) | – | Better scores on assessment, communication, non-technical skills and detection of medical error when undertaking two scenarios involving simulated patients requiring escalation of care |
A subsequent interrupted time-series analysis observed reductions in unsatisfactory pain score charting and observations (in medical, but not surgical patients) following an educational intervention. 117 A before-and after study found nurses’ knowledge of failure to rescue events increased after they were exposed to a deteriorating patient simulation scenario with a high-fidelity mannequin. 118 Of the three most recent studies, two were RCTs that evaluated a web-based training programme focused on improving the care of acutely ill patients74,119 and one was a small group teaching session. 73 Liaw et al. 74 looked at the impact of a web-based tool on qualified nurses in Singapore and found changes in knowledge and increased monitoring of both heart rate and respiratory rate. Johnston et al. 73 found improved assessment, communication and non-technical skills, along with improved identification of errors.
Discussion
Main findings
Of the four interventions, the strongest evidence for impact on IHCA rates and survival exists for RRTs in which studies tended to have larger sample sizes and be focused on a smaller number of patient outcomes. There is evidence that RRTs reduce cardiac arrest rates and, to a lesser extent, mortality. The evidence was weaker for nurse-led teams. The introduction of TTSs has also been shown to be effective in improving the recording of one or more vital signs, although the sustainability of the impact is unclear, as is the impact on patient outcomes.
Studies evaluating standardised handover tools, which have been weaker methodologically, have mostly reported improvements, in particular in information transfer. Whether or not this translates into better patient outcomes is not known; despite the majority of studies showing a positive benefit, most of the studies were of poor quality and were small, uncontrolled before-and-after studies. 95–98,100–109
Continuing education is the most challenging of the four interventions to assess in terms of the quality and quantity of evidence available. There is some evidence of improved knowledge and self-reported confidence in a range of skills, as well as in process measures, such as frequency of observations, but the evidence for improved patient outcomes is weak.
Limitations
As other reviews of these topics have found,24,47,48,56,79,84,89,95–98,112,116 there is a mixed picture with regard to study results in all four interventions. There are a number of possible explanations for this. First, there is considerable diversity in the details of the interventions being employed within each category: RRTs varied in their calling criteria, composition and the hours they covered; TTSs varied in the parameters they included, the thresholds for activation and the responses they triggered; continuing education interventions had different curricula and teaching methods; and structured handover tools varied in the information being conveyed.
Second, in many studies the use of concurrent interventions creates a challenge; for instance, implementation of RRTs was associated with the introduction of new TTSs. Such an approach is pragmatic from the perspective of service providers as it tackles several aspects of the chain of survival at once; however, it’s difficult to attribute impact to any one of the interventions as each may have contributed all or nothing to the result.
Third, there was variation in the way interventions were implemented. For instance, Simmes et al. 120 reported that their MET was not consulted prior to a serious adverse event in 50% of cases, even though abnormal vital signs were observed and should have been activated. A study of the same team would have returned different results had it been consulted 100% of the time. Many factors may have modulated the implementation of the interventions. Some studies had educational packages to accompany the roll-out of their RRTs or TTSs, while others made no mention of this. In addition, the enthusiasm and teaching aptitude of the trainers in the educational interventions will likely have been key to their success or failure. Participants will have also influenced implementation; for example, 50% of the learners in Schubert’s118 study had just finished a night shift when they started the course, which could easily have affected their motivation and capacity to learn. There are also broader contextual factors at play, such as the support of hospital managers for the intervention or the financial support for its roll-out. Another potential moderating factor is the country the intervention was set in. Most of the studies took place in Australia, the UK and the USA, which have different health-care systems with different staffing, working hours and access to ICU beds. Evidence to support the idea that the country of use could be introducing variability in results comes from Bellomo et al. ’s93 study of electronic TTSs in Australia, the USA and Europe. They found that the American hospitals produced significantly different results on several key outcomes, including hospital LOS and the percentage of patients transferred to a greater-acuity ward following the RRT being called.
Fourth, the majority of studies used an uncontrolled before-and-after design. There is, therefore, the risk of confounding affecting the results. The majority of these studies provided no reassurance that confounding had been adequately taken into account.
It is also possible that our own methodological approach, such as restricting searches to just two databases (MEDLINE and EMBASE), may have led to the exclusion of some relevant research studies. However, the impact was mitigated by using the most recent rigorous published systematic literature review as a foundation for our review across three out of the four interventions.
Implications
Although the existing literature provides a fairly consistent picture of the benefits of each of the four types of intervention, larger studies conducted over a longer period of time, to allow the intervention to become established and to assess sustainability, are needed. A core set of outcomes based on the chain of survival should be agreed and applied to improve interstudy comparability. There is also a need to define precisely what intervention is being evaluated to facilitate meaningful pooling of the evidence. For instance, RRTs could be described in terms of four dimensions: (1) team makeup, (2) hours of operation, (3) services provided and (4) ICU admission rights. This would reduce the problem of variability when synthesising results from different studies and would allow meaningful comparisons and conclusions to be drawn. Finally, it is unlikely that any single intervention would perform in the same way when put in place in hospitals with different cultures or resources for the intervention’s roll-out. This interplay between context and the success or failure of these interventions has not been addressed sufficiently. Given the heterogeneity of the interventions and the contexts in which they were implemented, plus the fact that many studies did not provide an adequate level of detail of either the intervention or the context, it was not possible to create a typology based on this literature alone. This required qualitative work within NHS hospitals, the findings from which are presented in the following chapter.
Chapter 3 A qualitative study of staff perspectives on measures to prevent patient deterioration
Introduction
The aim of the qualitative study was to explore how outreach teams, TTSs, standardised handover tools and education initiatives had been implemented in acute hospitals and to gather staff perspectives on key factors that had been important in the effectiveness of that implementation.
Carroll et al. 65 have highlighted that patient outcomes may be influenced by both the way services are implemented and the context in which that implementation takes place. Understanding the organisation of services and barriers to and facilitators of implementation will assist in the interpretation of any associations between service configurations and trends in IHCA and mortality over time. Opinions of a wide range of hospital staff across both clinical and management roles were sought to create a rich picture of current practice. The objectives of this qualitative investigation were to:
-
inform the quantitative survey design through the documentation of variations in structures of services that aim to prevent IHCAs in hospitals across England
-
explore staff perspectives of barriers to and facilitators of implementing good care of deteriorating patients that might contribute to variations in IHCAs across hospitals.
Methods
Study setting
The semistructured interviews were conducted in NHS acute hospital trusts.
Sample
Purposive sampling was used to identify a range of hospitals of different size, location, teaching status and foundation versus non-foundation status in order to maximise the likelihood of understanding the full range of interventions that have been used and the ways in which they have (or have not) been implemented. The principal investigator contacted 13 trusts across England, who SG members knew to have a diverse range of services, and invited them to take part in the study (Table 12). A senior clinician at each trust was asked to identify up to five staff as key personnel involved in deteriorating patient care. Potential interviewees were sought at different levels throughout the trust, encompassing strategic-level staff (e.g. medical directors), staff involved in planning patient care (e.g. consultants in the ICU), members of outreach teams and ward-based clinical staff (junior doctors and nurses) involved in day-to-day patient care and monitoring.
| Hospital trust | Number of staff interviewed |
|---|---|
| Mid Essex Hospital Services NHS Trust | 4 |
| University College London Hospitals NHS Foundation Trust | 6 |
| Royal Free NHS Foundation Trust | 5 |
| Basildon and Thurrock University Hospitals NHS Foundation Trust | 5 |
| West Hertfordshire Hospitals NHS Trust | 5 |
| Homerton University Hospitals NHS Foundation Trust | 5 |
| County Durham and Darlington NHS Foundation Trust | 5 |
| South Tees Hospitals NHS Foundation Trust | 7 |
| Barking, Havering and Redbridge University Hospitals Trust | 5 |
| University Hospitals Bristol NHS Foundation Trust | 4 |
| The Whittington Hospital NHS Trust | 2 |
| Buckingham Healthcare NHS Trust | 5 |
| North Middlesex University Hospital NHS Trust | 2 |
| Total | 60 |
After securing NHS R&D approval, those members of staff identified were approached via e-mail to take part in an interview. All interviews were conducted by members of the research team (CC, RZ and HH), the majority being face to face and 15% being via telephone. Prior to interviews, written consent was obtained after fully informing participants of the objectives of the study and providing an information sheet. Interviewees were assured that neither their name nor hospital would be recognisable in the presentation of any analyses. In total, 60 people agreed to be interviewed (Table 13). Interviews lasted between 20 and 90 minutes, depending on staff time available, and were recorded as detailed field notes with accompanying audio-recording. Interviews followed a topic guide developed before and during pilot interviews.
| Staff role | Number of staff interviewed |
|---|---|
| ICU consultant | 8 |
| Anaesthetic consultant | 4 |
| Nurse consultant | 3 |
| Other medical consultant | 4 |
| Outreach team lead | 8 |
| Outreach team nurse | 7 |
| Ward nurse | 6 |
| Medical director | 2 |
| Resuscitation officer/manager | 6 |
| Foundation year doctor | 4 |
| Medical registrar | 3 |
| Quality nurse/manager | 3 |
| Clinical site manager | 2 |
| Total | 60 |
Topic guide
The topic guide was developed based on the findings from the literature review, as well as on issues related to implementation identified from descriptive papers in the field, recommendations in guidelines and the expertise of the Project Management Group (PMG) and other contacts. Carroll et al. ’s65 framework for implementation fidelity guided the design of questions focused on how far actual interventions adhered to their intended designs. Box 1 shows an example of how the guide was applied in practice to one such intervention: the outreach team.
The interviews principally assessed service configurations for TTSs (e.g. the NEWS), outreach teams, handover procedures and practices, education provision and any contextual factors such as leadership and management, organisational culture, staff engagement and communication, strategic goals and resourcing, monitoring, and evaluation affecting those services. In addition, other important moderating factors, such as changes in end-of-life care practices, (e.g. use of DNACPRs) were covered. The topic guides for interviews with outreach team staff and strategic-level staff are found in Report Supplementary Material 9 and Report Supplementary Material 10. Questions also evolved based on topics raised through the course of the interviews. The questions asked varied by interviewee depending on their area of expertise; for example, strategic staff were more likely to know about quality improvement incentives, such as the Commissioning for Quality and Innovation (CQUIN) payments scheme.
Content of intervention: what are the objectives? Are there standards and protocols? What is the structure of the team? What are the team processes including triggering?
Frequency: how often is the team called and to which wards?
Duration: when was the team implemented? How was it implemented (in stages or full roll-out)?
Coverage: what are the hours of operation?
Context factorsFacilitation strategies: what is the nature of training and organisational support given to the outreach team?
Quality of delivery: are there monitoring and feedback mechanisms in place?
Participant responsiveness: how are the outreach team regarded by ward staff? Do ward staff feel supported? How do ward staff respond to visits? What are staff attitudes to escalating care?
Data analysis
All interviews were typed up as in-depth field notes. An initial thematic analysis was undertaken to group the data by broad themes, concepts and emergent categories. 121 A further in-depth thematic analysis of the data was undertaken to classify the findings into pragmatic categories, which were used to produce the main findings, after discussion with key members of the research team.
Findings
Deteriorating patients in context
‘Deteriorating patients’ were characterised as patients with worsening physiological measures (e.g. blood pressure, heart rate, temperature or respiratory rate) who were in need of escalation to a higher level of care to prevent adverse outcomes. Generally, interviewees reported that deterioration is identified through observations of physiological measures and their appropriate interpretation. In the last decade, much work has been undertaken to improve the care of acutely ill patients in hospital in order to prevent deterioration and adverse outcomes. Interviewees were familiar with local and national initiatives aimed at improving the care of hospitalised patients, such as the implementation of a NEWS, funding for outreach teams/specialist nurses, sepsis action plans or CQUIN payments. Some interviewees stated that a great deal of work had been carried out in the preceding 5 years and improvements in care had been observed, but acknowledged that more work is needed in the future.
Service configurations
Track-and-trigger systems
Overview of systems in place
The majority of trusts used the NEWS to monitor hospital patients’ physiological condition. Interviewees often highlighted that adaptations had been made to this system across adult, paediatric, maternity and accident and emergency patients. Some hospitals had modified the NEWS to include additional physiological measurements. Some additions were applied universally across the hospital, such as pain measurements, oxygen saturation and urine output. Others were used only in specific wards or groups of patients, for example the inclusion of the Glasgow Coma Scale for use in neuroscience service wards or fluid balance measurements for use in a cardiothoracic ward. The NEWS was felt to represent a ‘baseline scoring system’ in terms of the range of observations that should be collected and the inclusion of additional parameters seen as ‘good practice’. These adaptations were seen as an attempt to improve the NEWS so that more acutely ill patients could be identified at earlier stages of deterioration. In contrast, some trusts had made changes to the trigger or calling criteria when it was felt that the tool was oversensitive and leading to an unmanageable workload for first responders.
A small number of trusts elected to use a scoring system other than the NEWS. Differences between these scores and the NEWS included additional measures (similar to additions to the NEWS, but often more extensive), a different colour coding system to indicate when an escalation should occur and different criteria/triggers/levels for escalation.
Benefits of track-and-trigger systems
Interviewees felt that research evidence suggested that TTSs were effective in identifying deteriorating patients. The simple design of the NEWS made it easier to use for HCAs and student nurses, requiring minimal training and supervision. This allowed routine observations to be delegated to these staff, freeing up time for registered nurses to continue with other tasks or more complex patient care. Standardisation enabled all staff across the NHS to be familiar with a single tool and decreased the length of time required to train new or bank staff when they began working in a new ward or hospital. Some ward nurses felt that track and trigger tools empowered them to call a doctor if concerned about a patient by providing evidence that something was wrong.
Limitations of track-and-trigger systems
Several interviewees raised concerns about using a TTS in practice. Simple operational issues, such as adding up the scores correctly, even with the aid of colour coding, were reported, as were incomplete observations; some nurses anecdotally reported that student nurses or HCAs were not always aware that the form had to be fully completed before adding up the scores, leading to possible missed escalations. It was generally felt that these issues could be easily rectified through training if time and resources permitted, or through the implementation of electronic systems that automatically calculated scores.
A further frequently voiced criticism was that these scores were not a substitute for experience and familiarity with an individual patient’s context when making decisions about escalation. It was felt that some staff, particularly HCAs, did not have the experience to put the findings from observations in context, especially when confronted with a patient who was ill despite having scores outside the alerting range. A small number of interviewees linked this to a wider problem of the ‘deskilling’ of the NHS workforce, meaning that there were proportionally more ‘less-skilled’ staff in patient caring roles than previously. They saw the introduction of a ‘one-size-fits-all’ TTS as a mechanism to cope with this, but one that did not really address the core issues of the skills deficit on the wards.
Interviewees acknowledged that the changeover to the NEWS had not been an easy process, taking up to 2 years to be fully implemented in many places. The transition, which was often led by the outreach team during the course of their usual duties, had involved negotiations with different wards, trial periods with subsequent changes and significant training for staff. Trialling modifications and rolling out these changes was as lengthy and as difficult a process as the original roll-out of the NEWS had been.
Another key criticism levelled at the NEWS was its lack of sensitivity for detecting early deterioration and deterioration in certain patient groups. On the other hand, some interviewees complained that it was oversensitive and resulted in unnecessary escalations. These differing perceptions were dependent on the context in which the interviewee worked (e.g. general or specialist wards) and their personal experience of using the NEWS. A unifying theme was the need to combine calculation of the NEWS with assessment of the patient’s clinical context by an experienced health-care professional. Those trusts that had chosen to use alternative scores cited a range of criticisms including that the switch would be too onerous given that there was another scoring system already embedded; that evidence in favour of the NEWS being more effective than the existing scoring was lacking; the risk of adverse events during transition; the NEWS had been trialled but was found to be either too sensitive or not sensitive enough; the risk of an unmanageable staff workload and consequent desensitisation to alarms and failure to respond to triggering patients; and the score was too generic for use in certain specialties or in particular patients.
Electronic systems
Electronic versions of the NEWS, which had been or were in the process of being rolled out to wards in some hospitals, were viewed as important mechanisms in improvement of care around deteriorating patients. In those hospitals that used electronic systems, the response was positive amongst both the ward teams completing the observations and the outreach team members responding to calls. Benefits cited included removing barriers to escalation and decreasing the possibility of ‘human error’, as calculation of scores and triggering a response were done automatically. Moreover, omissions of certain observations were decreased as the electronic systems forced staff to enter a full set of observations. The positive response to using electronic technology to complete the NEWS was not without teething problems during its roll-out, with electronic NEWSs experiencing some of the same issues as paper NEWSs including issues of sensitivity and additional issues, such as the need to help staff get over their fears of new technology, as well as the requirement to update and maintain hardware and software systems (which was usually contracted out to a specialist company). Interviewees felt that further digitisation, such as electronic patient records or Wi-Fi access throughout the hospital to enable tablets to be used to collect observations, would make their jobs easier and free up time for patient care.
Outreach teams
Overview of outreach teams
Some hospitals reported a different local name for their nurse-led outreach team including patient-at-risk and resuscitation teams (PARRTs), patient emergency response and resuscitation teams (PERRT), patient acute response teams (PARTs) and trigger and response teams (TARTs). Common to all teams was the dedicated funding of members and training in early resuscitation interventions and advanced life support. Team member composition, team skills and team working patterns varied across hospitals. Some teams were 24/7, whereas others were operational only in the daytime (Monday to Friday or 7 days a week). Most teams comprised multiple nurses at various seniority bands and were led by a senior nurse or nurse consultant. Consultant physicians were often members of the team, but in an advisory and time-limited capacity, rather than attending calls. Their input could be called on when assistance was required to secure an ICU bed for a patient. Some teams had expanded to include allied health professionals, such as physiotherapists, and others included HCAs.
Achieving the core objectives of rescuing deteriorating patients and reducing admissions to critical care involved a number of functions such as offering advice, information and guidance to ward staff on patients they are worried about; managing transitions between critical care and the wards; responding to calls generated by the TTS; liaising with clinicians and families regarding appropriate DNACPR implementation; auditing IHCAs and TTS performance; and education in deteriorating patient prevention.
Benefits of nurse-led outreach teams
Several interviewees made the argument that the evidence base in support of outreach teams was not strong but, overwhelmingly, staff who worked at a hospital with an outreach team in place felt that the service they provided was beneficial as an intervention to manage deteriorating patients. Comments were made as to the lack of barriers to calling out the team or just calling them to ask for advice at an earlier stage. Team members identified being able to see the ‘bigger picture’ as a major benefit, meaning they could effectively identify patients at risk and communicate information about these patients to a variety of interested parties who may not necessarily communicate otherwise. This ‘overview’ function also meant that teams had useful insider knowledge of how wards were performing across the hospital and where patients at risk were located. They were viewed as a rich source of local information through their knowledge of which wards were well stocked with particular equipment or where a nurse with a particular specialist skill could be found.
They also offered a route to timely and appropriate care, whether through advising on end-of-life care and placing DNACPR decisions or arranging admission to the ICU from the ward. Outreach team leaders often stated that their staff were of a high quality and were carefully selected to fit this type of role. They were seen as a resource of experience and could proactively identify and respond to deteriorating patients who may get missed during admissions, on busy wards or by junior staff. A key function that team members themselves and other staff often cited was that they were an educational resource and that visiting the wards was a training opportunity for ward staff. In many hospitals, they had also been instrumental in leading on the NEWS implementation and providing the education and support to staff to ensure that the tool was used properly.
Good relationships facilitated both the team being alerted early by ward staff when there were concerns about a patient and the ability to engage ward staff in informal education. Good communication skills may have been one reason for the expansion of the outreach team role into end-of-life care planning.
Barriers to outreach teams’ effective functioning
Generally, trust-level support for outreach teams was good; however, inadequate funding was perceived to be an issue and had prevented team expansion in some cases. It was sometimes a challenge to recruit suitably qualified staff to the team. Outreach staff reported that, as a consequence, there was less time available for education and training, with some feeling that this training role had been scaled back in recent years as clinical duties increased. This was compounded by the time pressure also felt by ward staff. Some outreach interviewees remarked that ward staff viewed calling outreach to assess a patient as a chance to leave that patient and catch up on other tasks, rather than staying at the bedside and taking up the learning opportunity.
Demand for clinical intervention from the outreach team time was reported to be increasing and in some places teams were struggling to meet this demand, especially overnight. There were complaints that during these hours they were increasingly being used as an inappropriate substitute for junior doctors. Paradoxically, although some trusts were keen to extend outreach hours to meet overnight demand, other teams were not able to gain support from the trust to provide 24-hour cover. Sometimes this reluctance was based on the fact that cardiac arrest audit data had not shown a higher frequency of arrests at night or weekends. Coverage was also affected by not all team members being equally qualified, for instance some may not be independent prescribers, leading to ‘patchy’ functioning at times.
In some hospitals, outreach teams were not able to directly refer patients to the ICU; this had to be done consultant to consultant. Not being able to make direct referrals was seen as a barrier to providing timely care for deteriorating patients by some staff. Others felt that the negative impact of such service organisation could be mitigated by good relations between outreach and consultants, which led to prompt transfer once the outreach recommendation was made.
Hospitals without an outreach team
Some hospitals did not have a dedicated outreach team. The lack of evidence for the effectiveness of outreach teams, trouble recruiting suitable staff and a desire that ward staff continue to be able to act appropriately to manage deteriorating patients were given as reasons. One hospital reported that their outreach team existed in name only, being unable to provide any service owing to a lack of staff. Such staff shortages were caused by trust deliberations on whether or not to continue their funding, which subsequently resulted in team members leaving and not being replaced.
Handover procedures
Overview
Situation, background, assessment, recommendation was reported as the main handover tool used in acute NHS hospitals. It is designed to structure the flow of information between clinicians such that important clinical details about patients are unlikely to be missed. Descriptions of the tool and its use were included in many of the formal education courses covering the care of acutely ill patients provided for doctors and nurses. Trusts also used a range of ‘advertising’ approaches (banners, posters, key cards, screen savers and stickers on telephones) to remind staff to use it and to raise levels of awareness of the tool.
Advantages of situation, background, assessment, recommendation
Interviewees generally felt that SBAR was an effective method of transferring information and some hospitals had even made its use compulsory when calling the outreach team. The tool was also said to act as a familiar prompt in stressful situations and helped to avoid miscommunication by providing clear information to the team member taking over the patient’s care. A small number of hospitals had introduced an electronic version. This was characterised as being easy to use and had additional functionality, such as the ability to look over past handover communications. It also allowed prioritisation of handover time for face-to-face discussion of complex cases, with information about simpler cases being shared solely electronically.
Barriers to use of situation, background, assessment, recommendation
Barriers to using SBAR included ward staff feeling that this structured approach was unnecessary and the discomfort experienced when using such a formal communication style in front of patients, especially if information being communicated is perceived as sensitive. Moreover, nurses not trained within the NHS did not have training in the method. Some staff admitted that although knowledge of the tool was high in the trust, it was rarely used in practice.
Education and training
Overview of training programmes in place
Apart from basic life-support training, which remains mandatory for all clinical staff, formal training programmes, such as the ALERTTM (Acute Life-Threatening Events Recognition and Treatment) course (Queen Alexandra Hospital, Portsmouth, UK; see www.porthosp.nhs.uk/departments/alert/alert.htm), which focuses on providing care for acutely ill patients, and NEWS training courses are commonly available to staff. Some interviewees highlighted that these training methods might become redundant as education around the acutely ill patient was increasingly being provided at an earlier stage of training.
Training in acute care for ward staff has an increasing ‘real-world’ emphasis and can include learning from case record review, safety huddles and improving communication skills around end-of-life care. In some hospitals, a dedicated nurse is assigned the role of ‘educator’ and visits all wards to complete the required training. Others were using e-learning to increase access to courses. Alongside these approaches, senior ward nurses will undertake teaching at the patient bedside. Training in the recognition of acute illness and deterioration, the use of TTSs and in DNACPR processes ‘on the job’ was felt to be an important part of increasing the skills of junior staff. However, opportunities for bedside learning were felt to have lessened because of the workload experienced on the ward and staff shortages.
Outreach team members were often involved in teaching on formal courses, alongside their role in providing informal training, to accompany the roll-out of new e-observation technology, SBAR and modifications to the DNACPR process. Training for outreach team members beyond advanced life-support skills has not been mandated to date. However, some external formal educational course is usually undertaken in the form of a module or whole Masters course at a university, the latter being required to achieve advanced nurse practitioner status.
Benefits of education and training programmes
Interviewees valued bedside teaching, especially when provided by outreach teams, as a way of improving their knowledge in identifying and responding to deteriorating patients. This was felt to add value to the outreach team ward visit. Some interviewees spoke of the role that education and training can have in empowering nurses to speak to clinicians about the need for a DNACPR decision to be put in place and how it helped overcome challenges of communication across different disciplines and seniorities.
Barriers to effective education and training
Some interviewees were sceptical of the value of formal courses. Staff shortages and high staff turnover were felt to be detrimental to maintaining a suitably trained workforce. Outreach team members also described the difficulty of maintaining the role of educator while at the same time being increasingly called on to fill other roles, such as providing overnight cover in place of junior doctors. There was often not enough time left for this function before moving on to the next call. Some senior ward staff worried that there was such a prioritisation of risk assessments and paperwork that they could not spend as much time as they wanted on teaching at the bedside.
Training in communication around end-of-life decisions was seen as very important and a key enabler in starting conversations with patients and carers. It was felt that this was an area where trusts should be expanding their provision.
Other moderating factors
‘Do not attempt cardiopulmonary resuscitation’ decisions
Effective end-of-life planning and appropriate use of DNACPR decisions were viewed as vital in order to avoid a patient receiving inappropriate CPR. Interviewees felt that implementation of DNACPR decisions were appropriate in circumstances where the patient was at the end of their life or would not benefit from active resuscitation. Overall, the majority of interviewees were positive about how such orders were being used in practice within their trusts. They felt that use had been increasing appropriately given the increasing number of frail, multimorbid, elderly patients being admitted to hospital. An increasing proportion of patients have a DNACPR in place on admission, either implemented in a community setting or from a previous admission.
Increased awareness and confidence among staff as a result of training had been a facilitator of increasing DNACPR use. The fact that orders could be retained across admissions was also felt to streamline the process and protect patients from unwanted or unnecessary interventions. The process was further simplified when the same form was used across a region. However, problems could still arise if the form was not with the patient at the time of admission.
In the majority of cases, consultant decisions to implement DNACPR decisions were mostly accepted by families. This acceptance was seen as a result of good communication between front-line staff and patients and their families. Fostering such relationships enabled an honest dialogue about end-of-life issues and the wishes of patients and their relatives. Patients and relatives were often more open-minded than expected about engaging in these discussions. Some interviewees acknowledged that communication was easier when the patient was elderly and their current condition made the decision more straightforward. Discussions were more difficult in other patients in whom the balance between benefiting or not benefiting from resuscitation was less clear.
Treatment escalation plans (TEPs) were also viewed as an important mechanism for avoiding inappropriate resuscitation attempts, especially if implemented early in the care pathway and by the clinical team that knows the patient best. Formal TEP usage varied across hospitals, and interviewees at some hospitals reported that this approach had only recently been introduced or that use was very patchy. TEP agreements were sometimes viewed as of secondary importance to DNACPR decisions. It was felt that their use would increase once consistent implementation of DNACPR decisions were achieved. In addition, there had been a lot more focus on DNACPR policy and process nationally, which had tended to overshadow the TEP process. Some hospitals are implementing a combined DNACPR/TEP policy reflecting the intertwined nature of the processes.
Although the patient’s own consultant is responsible for completing a DNACPR decision, members of outreach teams are becoming increasingly involved in end-of-life decision-making, including providing a second opinion to a consultant about whether or not to put an order in place. If a DNACPR is not already in place when outreach teams are called to see deteriorating patients on the ward, team members are often the first staff to formally recognise that the patient might be reaching the end of their life and initiate discussions with the patient and their relatives regarding their wishes for further treatment. Some interviewees highlighted that some consultants were more hesitant than others to take steps to implement DNACPR decisions because of either individual or medical speciality culture, or preference. It was reported that as a result of the 2014 judgement made in the Tracey case,60 which required clinicians to inform patients and relatives when DNACPR decisions were put in place, some consultants had become more reluctant to make DNACPR decisions. The situation was compounded by the perception that trust-level support for decisions that go against family wishes might not be forthcoming. Some outreach team members felt that some of the responsibility for starting discussions with patients and relatives about DNACPR decisions was being left to them. Although some still viewed DNACPR decisions as being the sole responsibility of the patient’s consultant, others felt that this expansion of the team’s original remit was a natural evolution.
Quality assessment and improvement
Outreach staff are involved in the initiation of quality assessment and improvement activities around the care of acutely ill patients. This role reflects their system-wide overview providing opportunities to both identify problems that put safety at risk on the wards and communicate the need for action to clinicians and managers. They described playing a major role in key initiatives, such as the roll-out of the NEWS, which required bringing both nurses and doctors on board at an early stage and providing ongoing educational support. Many teams still organise ward audits to monitor subsequent performance. They were also often the initiators of case record reviews of patients experiencing IHCAs. Such audits are an important way of identifying areas requiring improvement. The teams also drew in new ideas through involvement in regional or national networks. A number of trusts saw investment in the team as one approach to increasing capacity for quality improvement across wards.
Ward-level audit and feedback of the quality of recorded observations and the appropriateness of the triggering/response to those observations was now common practice. Results were used to identify variations in practice and target educational interventions. In some trusts, the mechanisms for turning the findings into actionable learning and improvement were not always effective, with delays in feedback or failure to provide training. Some interviewees were able to point to improvements that had been made based on the findings from case record reviews of patients experiencing IHCAs; however, others questioned the utility of the process given that these records do not always provide enough detail to pinpoint where problems lay. In some hospitals, the scope of the audits had broadened to look at cases of missed deterioration rescued before an arrest. Often, particularly committed individuals or the patient safety team were responsible for ensuring 100% of cardiac arrests were entered into the review.
In addition, many hospitals were taking part in the NCAA, with information on cardiac arrests generating a resuscitation team response generally collected by trust resuscitation officers. Some interviewees were sceptical about the quality of their own data or the data of other hospitals in the audit and wondered if changes in cardiac arrest rates or outcomes really reflected safety improvements or just the idiosyncrasies of the data collection. Some interviewees stated that, as a result, they only looked at their own data trends. Others complained about a lack of dissemination of the audit findings within their organisation.
Some interviewees were concerned that adverse events linked to missed patient deterioration and IHCAs went unreported because of the prevailing organisational culture. Although most staff were made aware of the adverse event-reporting system at induction, there were reports that culture on the wards discouraged reporting. Additional barriers included access to paper or electronic forms, lack of time and responsibility falling only to the team leader. On the contrary, some trusts had established a positive reporting culture and actively encouraged all staff, no matter what level, to raise concerns, and this approach was felt to have increased the frequency of incident reporting.
High-level support and leadership
Support at board level was an important enabler for improvements in deteriorating patient care. How support was provided varied between trusts. Some interviewees stated that it was dependent on key members of the hospital board (e.g. chief executive, medical director or chief nurse) being motivated to improve deteriorating patient care and influencing the acceptance of new interventions or changes in organisational culture that might allow these interventions to thrive. This included providing financial support to enable the development and growth of outreach teams. On the other hand, in some trusts where investment in staff or new interventions was closely linked to an ability to show value, there had been difficulty in making progress. Outreach staff felt that it was difficult to produce this evidence and, in particular, evidence showing the value of teams, and they felt frustrated that this approach held back funding.
Some interviewees felt that the inclusion of a consultant as a member of the outreach team lent ‘credibility’ and helped to promote visibility within trusts. Very supportive trusts were characterised as being flexible, allowing freedom to frontline staff to implement changes on their wards or within their teams and to experiment within the boundaries of good care. This approach had led to improvements such as redesign of DNACPR forms. Some outreach teams had a large degree of control over who might be recruited to their team and were able to veto applicants without the requisite skills.
Discussion
We interviewed 60 key members of NHS staff across 13 acute hospital trusts, operating over a varity of levels and grades, about TTSs, outreach teams, handover procedures, education and training and factors that affect their use. Our results highlight how multiple interventions function within a complex environment.
Our interviewees reported that use of the NEWS, either paper or electronic, is now widespread, with very few trusts using alternative systems. On the whole, it has been well received and is seen as straightforward to use and the standard tool is helpful in an environment where staff turnover is high. As reported previously,42,122 TTSs enabled staff to feel more confident in contacting the doctor about a patient because they were able to provide objective evidence to accompany their concerns. The utility of the NEWS across the whole spectrum of patients found in a typical trust was questioned, both from the point of view of the scope of the physiological measures included and its under/oversensitivity in particular groups. Many clinicians viewed it as a basic building block and had added additional measures when they felt that the additions added value. These alterations of a validated tool may threaten its reliability. 123 Perhaps more alarming are reports of alteration of calling criteria to reduce the tool sensitivity in trusts where there is a sense of not being able to cope with the consequent workload for responders.
Track-and-trigger systems have facilitated the transfer of the observation tasks from nurses to less-skilled HCAs. 124 We found concerns about HCAs’ lack of clinical assessment skills to put scores into context, along with incomplete observations or inaccurate scoring, as underlying reasons for failing to trigger an appropriate response. The MERIT (Medical Early Response, Intervention and Therapy)82 study had found that inaccurate completion of the TTS was one of the reasons for the suboptimal level of RRT deployment. A 2015 systematic review125 highlighted the importance of clinical intuition in the recognition of deterioration: how nurses use intuition in conjunction with the scoring systems in judging when to trigger an escalation of care. This review highlighted 37 different signs and symptoms, aside from standard measures, that were used to trigger escalation of care, which were categorised into 10 general indicators: (1) change in respiration, (2) change in circulation, (3) rigors, (4) change in mentation, (5) agitation, (6) pain, (7) unexpected trajectory, (8) patient indicating that they are feeling unwell, (9) subjective nurse observation and (10) nurse convinced that something is wrong without a rationale.
Although there was apparent homogeneity amongst outreach teams in terms of delivering their key objectives of educating ward staff, following up ICU discharges and responding to requests to attend patients who show signs of deterioration on the ward, there was substantial variation in team composition, roles, skill distribution and hours of coverage. This variation had been observed in a previous evaluation,126 and is not surprising given that no service model was stipulated when recommendation for implementation was made. 12 Ward staff reported that the presence of an outreach team had a beneficial impact on the management of deteriorating patients. Qualitative findings from interviews and focus group discussions with nurses show that this support is provided through education, ease of access to advice and the ability to marshal critical care skills to the bedside when needed. 127,128 Benin et al. 129 also highlight the increased sense of morale and empowerment in ward nurses who know that they have access to expert help via a single telephone call, and the positive effect of outreach in reducing neglect of non-acutely ill patients during emergencies by allowing redistribution of ward staff. However, we found that outreach team members felt that there was a loss of opportunity to educate ward staff either because those staff saw the arrival of the outreach team as an opportunity to go off and do other work, or the team themselves were under time pressure to move on to their next referral.
Studies130–132 have explored potential barriers to ward staff calling outreach teams in order to determine why a delay in response to deterioration occurs. These suggest distinct intraprofessional clinical decision-making pathways and, where the outreach team is doctor led, interprofessional communication barriers. 130–132 Shearer et al. 132 also state that, despite an organisational commitment to outreach, clinical staff act on local cultural rules within the clinical environment, which are usually not explicit. 132 Our ward-based interviewees reported few barriers to calling the team and this extended to seeking advice about patients at earlier stages of concern.
There is a dearth of peer-reviewed academic literature that captures the impact of ‘on the job’ or informal learning, but this mode of knowledge and skills transfer was seen as critical in promoting clinical awareness of signs of deterioration and increasing confidence in initial management. NICE guidance24 stresses the importance of workplace-based education for nurses to acquire skills in assessment and response to the acutely ill patients. The role of senior ward and outreach nursing staff in this educational provision was highlighted along with how time pressures curtailed opportunities for teaching. Formal classroom-based training programmes, such as the multiprofessional ALERT™ course, are still run and a range of modes of delivery are available for courses to make these more accessible. E-learning or online modules are also an increasingly popular method of delivering education programmes to hospital staff. 133 Recent literature has predominantly focused on human patient simulation programmes, which allow learners to develop, refine and apply knowledge and skills in a realistic clinical situation. 134,135 Its rise in popularity may be because of the known importance of practical experience in education programmes focusing on acute care and the potential for this teaching to be limited on busy wards. 136
Effective communication between health-care professionals was universally acknowledged as being highly pertinent to the safe management of acutely ill patients. Modern health care is delivered by teams rather than individuals and requires the co-operation of health-care professionals from multiple disciplines. Psychological barriers, such as professional silos and hierarchies, and organisational barriers, such as geographically distributed teams, can increase the chance of communication failures. 137 Such failures in communication lead directly to compromised patient care, staff distress, tension and inefficiency and make a substantial contribution to medical error. 137–141 Although interviewees reported awareness of the utility of formal handover tools, such as SBAR, in increasing the safety of handover, and that much effort was put into promoting its use, many conceded that it was not always used in practice. A 2016 study by Bauer142 highlighted that progress is still required in this area. He found that in some settings just over half of the time no handover took place, and of those that did take place one-third were interrupted and one-third failed to hand over key information, such as the patient’s age, responsible consultant and recent operations or procedures, all of which potentially compromised future management. Smith et al. 143 highlight that different expectations on content and timing of information transfer amongst staff may lead to incomplete handovers, especially within time-pressured and event-driven environments. McElroy et al. 144 also found that ambiguous roles and conflicting expectations of team members during the handover can increase the risk of patient harm.
Changes in the frequency of DNACPR use is likely to be one mechanism by which interventions aimed at identifying and responding to patient deterioration are associated with reduced IHCAs and improved outcomes. Appropriate DNACPR decisions have increasingly been advocated as an important component of good-quality patient care, protecting patients from invasive treatments that have little or no chance of success. 59 Despite the availability of national guidance, trust-wide resuscitation policies and standardised DNACPR forms, inconsistencies in decision-making, communication and documentation still occur and lead to misunderstandings about what DNACPR means and a failure to ensure adequate planning of treatment escalation. 145,146 A recent systematic review147 of the barriers and facilitators surrounding DNACPR use found that a lack of clear documentation resulted in a breakdown in communications within health teams, which led to poor patient care. Interviewees in the current study highlighted that some progress had been made in the co-ordination of documentation with the advent of community DNACPR forms that spanned community and hospital settings. Furthermore, experienced outreach staff or trained ward nurses had confidence to start conversations about end-of-life needs with patients and their families, but complained that doctors did not necessarily fulfil their responsibility to discuss these issues with patients in a timely manner. A survey of clinicians across Europe148 showed that many are hesitant to initiate conversations about DNACPR decisions owing to concerns about causing distress to the patient or for fear of complaints. The impact of the Tracey case60 is likely to have exacerbated this reluctance for some. Outreach teams are increasingly finding themselves in positions where they are ‘diagnosing dying’ because this has not been tackled at an earlier stage of the admission. 149 Some members found this a natural extension of their role.
The lack of availability of resources, particularly of adequately trained and experienced ward staff, was seen as an important barrier to improving the quality of care that patients received on the wards. Odell et al. 124 found that inadequate staffing levels created excessive workloads and led to failures to identify deteriorating patients. These issues are compounded by the increasing delegation of routine nursing tasks to less qualified staff who lack the clinical experience to set a patient’s condition in a clinical context. 42 In some organisations, outreach teams are struggling to justify ongoing funding or expansion despite their capacity to act as co-ordinators of care across the different professional groups and, also, as antennae for system failures that, when communicated back to managers, can promote change. Outreach teams’ work is intimately involved with improving patient safety, with many teams having played a crucial role in the roll-out of the NEWS or the delivery of training in the care of acutely ill patients and end-of-life decision-making. Trust-board understanding of the issues that drive poor performance on the wards combined with support for frontline staff to both raise patient safety concerns and get involved in implementing new approaches to tackle these issues was felt to be essential for making further progress.
Strengths and limitations
The study had a large sample size and included staff with a range of professional roles who were closely associated with delivering care to acutely ill patients. We were therefore able to ensure that we captured information on how services for deteriorating patients varied within and across trusts and to gather as wide a range of views on contextual facilitators and barriers as possible. The hospital sites were also varied in terms of geographical location, size and teaching status.
The study has several limitations. Interview data were primarily collected to inform survey development rather than as an in-depth qualitative study, with interviews typed up as field notes as opposed to being transcribed verbatim. As interviewees were informed about the purpose of the interviews this may have led to an element of social desirability bias in some responses, but generally we found that staff were more than willing to tell us about the problems they faced in implementing services. Only one researcher, who had not collected the original data, undertook the analysis. As a consequence, there is a risk that interpretation of these data does not wholly capture the meaning intended by the interviewees. However, the findings were circulated to experts in the area for external validation. Furthermore, the need to cover a number of different interventions and contextual factors that might affect their effectiveness did not allow in-depth questioning to better establish deeper beliefs and attitudes. In addition, any references made to changes over time will be subject to the accuracy of recall.
Implications
Given that our literature review did not provide a clear steer as regards the composition of effective interventions to detect and respond to patient deterioration, semistructured interviews with hospital staff were required to explore how these interventions have developed on the ground. We found that the majority of hospitals had adopted the NEWS. Such standardisation has the potential to improve outcomes as staff across the NHS become familiar with its use. However, key contextual factors that may prevent attainment of these outcomes were reported by staff, including the delegation of observations to less-qualified nursing staff and the modification of the tool to address concerns about its sensitivity in certain subgroups of patients. Outreach teams are a much less standardised intervention, with different levels of skill across the team, hours of coverage and autonomy. Their ability to work system-wide on improving the care of acutely ill patients through educating ward staff to care for such patients and ensuring correct use of tools, such as the NEWS, is limited by increasing hands-on clinical demands and, in some cases, under-resourcing. Handover tools and formal educational courses covering acute care are also becoming increasingly standardised. Most hospitals report promoting the SBAR tool and have ALERT™ or similar courses. However, neither of these things is a guarantee that improved communication or clinical skills are seen in practice. The effectiveness of these interventions will also depend on how long they have been running, the degree of educational support and promotion of staff engagement, and ongoing quality assurance. Members of the outreach team are often charged with these duties but may face challenges in finding the time to undertake them. Fulfilment of this role is more likely if there is board-level prioritisation and support.
Although these interventions have been implemented, other changes in the system have occurred that modify their impact. The increasing emphasis on improved end-of-life planning and protection of patients from interventions that may be of little benefit to them, such as resuscitation, has resulted in improved awareness of the need for timely DNACPR decisions. Outreach teams have gradually become more involved in this decision-making. Removing substantial numbers of patients who are likely to have poor outcomes from CPR might be expected to reduce cardiac arrest rates and improve survival.
Our analysis identified key intervention components to explore further in the survey. These elements included the range of TTSs in use, their spread across wards, the main groups using them and how well they were completed; the composition of outreach teams, their roles and autonomy, their involvement in education and the impact of work pressures; the types of handover tools in use and approaches to promoting use; and contextual factors affecting both interventions and outcomes, such as the implementation of DNACPR decisions. Our findings indicated that formal education courses did not vary substantially across hospitals; therefore, no candidate questions on these interventions were put forward for the survey.
Chapter 4 Organisational survey of hospitals
Introduction
The aim of the survey was to map service configurations in NCAA hospitals with the intention of understanding changes in interventions over time and characterising variation in intensity of services. Intensity is expressed through features such as the hours of cover provided, or the breadth of roles and responsibilities held by the outreach team, or introduction of an electronic TTS in all wards.
Methods
Pilot survey
An initial consultation with staff at the ICNARC was undertaken to determine the design features of previous surveys that they felt had resulted in a good response rate. Examples of other surveys that investigated NHS service configurations were also reviewed.
The semistructured interviews reported in Chapter 3 helped hone questions related to each intervention, serving to clarify how they have been implemented (e.g. structure, staffing, coverage, etc.). Contextual questions critical to the delivery of services were based on responses from interviewees as to which factors were most important in the delivery of their services such as any governance arrangements, communication processes, resources, etc. A list of candidate questions was collated and circulated to the PMG and SG for initial comment. Subsequently, each question was analysed by the PMG according to a range of criteria, including the amount of likely variation between hospitals, overlap with similar questions, the likelihood that answers would be available from respondents and the extent to which questions capture the intensity of service provision. Redundant questions were discarded. The survey was piloted with six clinical staff in different hospitals to test face and content validity after which revisions were made to ensure any ambiguity was removed from the questions and that instructions were clear. Questions related to formal educational courses were dropped as they did not provide enough variation in response between respondents.
Sampling frame
The NCAA staff sent the questionnaire to their lead clinical contact (usually the lead resuscitation officer) at each participating acute general hospital (excluding specialty hospitals). These contacts were asked to complete all questions within their remit and then forward the survey to another member of staff best placed to complete other questions. We suggested that this would probably be the lead for the outreach team.
Survey design
The survey comprised mainly closed questions, but space was left for comments that allowed respondents to provide textual clarifications. It was divided into sections covering the following areas:
-
detection of deteriorating patients – type of TTS in use, ward coverage and compliance and staff groups responsible for taking observations
-
response to deteriorating patients (focused on RRTs that have designated team members who respond to deterioration on the ward and not teams that respond to emergency/2222/cardiac arrest calls. The generic term RRT was used in this section instead of outreach team because we wished to capture all teams fulfilling this role if a hospital had more than one and because some hospitals call their outreach teams by different names) – RRT composition, roles, hours of coverage, calling frequency of various staff groups and level of demand on the service
-
ceilings of care – use of TEPs and DNACPR
-
handover – handover tools in use and methods to promote use
-
contextual factors – use of overspill wards and agency staff
-
data collected for NCAA – estimates of how many cardiac arrests were submitted to the audit and interventions to improve case ascertainment.
It was created in SurveyMonkey (SurveyMonkey Inc., Palo Alto, CA, USA) to allow electronic data entry but a Microsoft Word (Microsoft Corporation, Redmond, WA, USA) version was also available on request (see Report Supplementary Material 11). A survey guide (see Report Supplementary Material 12) was sent out with the initial mailing and this contained an e-mail and telephone number should respondents have queries not addressed by the guide.
Data collection
A personalised e-mail was sent to each NCAA contact containing the link to the questionnaire on SurveyMonkey accompanied by the guide and the date of the first deadline, which was in 4 weeks’ time. For each of the first 4 weeks, those that had completed the survey were entered into a prize draw for a £50 gift token. Follow-up e-mails were sent weekly to non-respondents for the first 4 weeks up to the deadline and then weekly for a further month. One reminder e-mail came with an endorsement letter from the chair of the Resuscitation Council. From this point on, non-respondents were followed up individually by e-mail and telephone. Messages advertising the survey were circulated in the National Outreach Forum Newsletter and through the personal contacts of the SG. If no contact could be made with a hospital, an e-mail was sent to the medical director asking for help with facilitating a response.
Using best practice in maximising responses, we expected to achieve a response rate of 80%. This target response rate was based on experience from surveys administered by ICNARC in two of their earlier National Institute for Health Research-funded studies. The Critical Care Outreach Services survey (SDO/74/2004)150 achieved a response rate of 80% and the Critical Care Modernisation survey (SDO 08/1604/133)3 achieved a response rate of 84%. These high rates reflected the long-standing relationship between ICNARC and the hospitals participating in its various audit programmes.
To increase the validity of questionnaire responses, follow-up telephone calls were made to seek clarification if responses were unclear.
Data analysis
Survey responses were exported from SurveyMonkey to a Microsoft Excel® 2016 spreadsheet (Microsoft Corporation, Redmond, WA, USA) for checking and cleaning. Data were then imported into Stata® version14 (StrataCorp LP, College Station, TX, USA). Continuous variables were categorised and reported as percentages. Differences in hospitals’ current provision of care were illustrated using bar and pie charts. Changes in hospitals’ historic provision of TTSs and outreach were plotted graphically by quarter to illustrate trends in these variables between 2009 and 2015.
Findings
Response rate
The survey was sent to 171 acute general hospitals taking part in NCAA and 139 responded (81.2%). The non-respondents did not differ from the respondents in terms of location and length of time in NCAA. There was a low response to the questions about the use of overflow wards and agency staff, and those that did respond indicated that their answers were their own estimates. It was decided to drop these questions from the analysis.
Characteristics of hospital interventions
Track-and-trigger systems
The majority of NCAA hospitals operated a paper-based TTS in 2009 (94.1%) (Figure 1). These were a range of systems including the MEWS and a hospital’s own scoring systems. The NEWS was introduced in late 2012. Following its introduction there was a decline in the use of other paper-based systems and by the end of 2015, 48.7% of hospitals indicated use of a paper-based NEWS.
Only a handful of hospitals had an electronic system in 2009 (1.7%), but this had grown to 29.4% in 2015; the majority of these systems are also based on the NEWS (67.5%).
Over the index period (2009–15), 21.8% of hospitals made no changes in their TTSs, 58.8% made one change, 18.5% made two changes and 0.8% made three changes. A total of 11.8% of hospitals reported operating dual systems at some point over this time period.
FIGURE 1.
Changes over time in TTSs (2009–15). q, quarter.
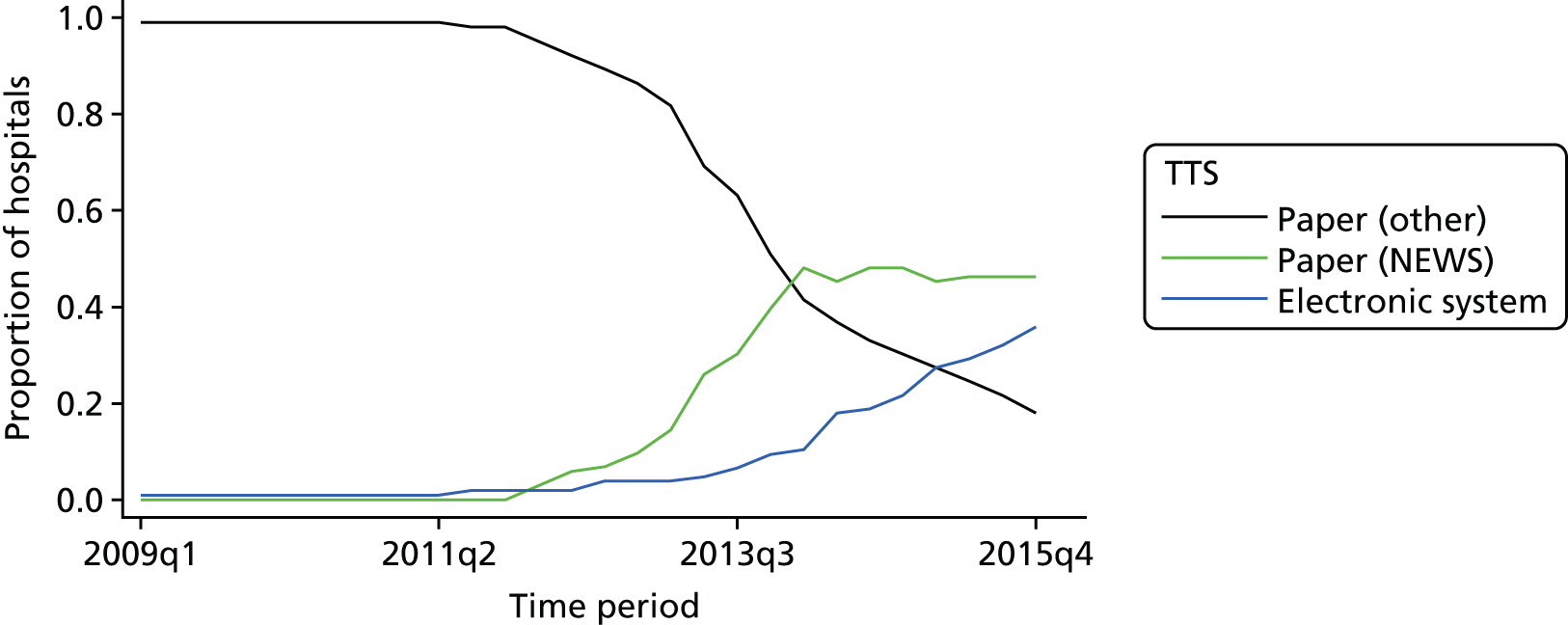
Compliance, a composite variable comprising full and accurate completion of observations on the TTS and escalation of patients in line with local policy, has shown a gradual increase in both reporting within hospitals (from 65.5% to 85.7%) and the proportion of hospitals reporting compliance rates of > 90% (from 15.1% to 41.2%), with an accompanying fall off in rates of compliance below the level of 75% (from 18.5% to 9.2%) (Figure 2).
FIGURE 2.
Compliance with TTSs between 2009 and 2015. q, quarter.
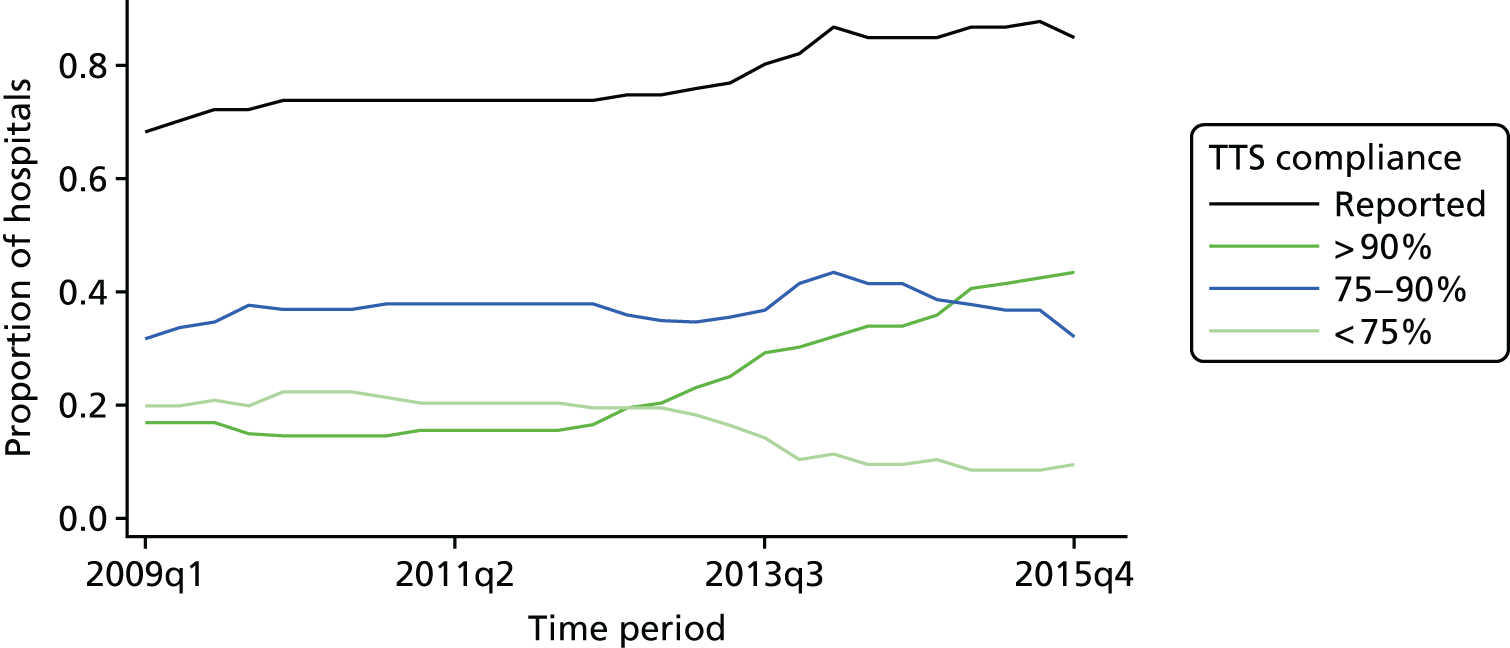
Hospitals were asked to provide a breakdown by estimated percentage of which professional groupings (registered nurse, student nurse, HCA) predominantly take observations on the wards and complete the TTS. The predominant group was the one that took at least 10% more of the observations than the next highest group. The mixed category was allocated if the difference in proportions taking observations was < 10%. Figure 3 shows the predominant staff group completing the TTS across responding hospitals.
FIGURE 3.
Dominant professional groups taking observations in 2015.
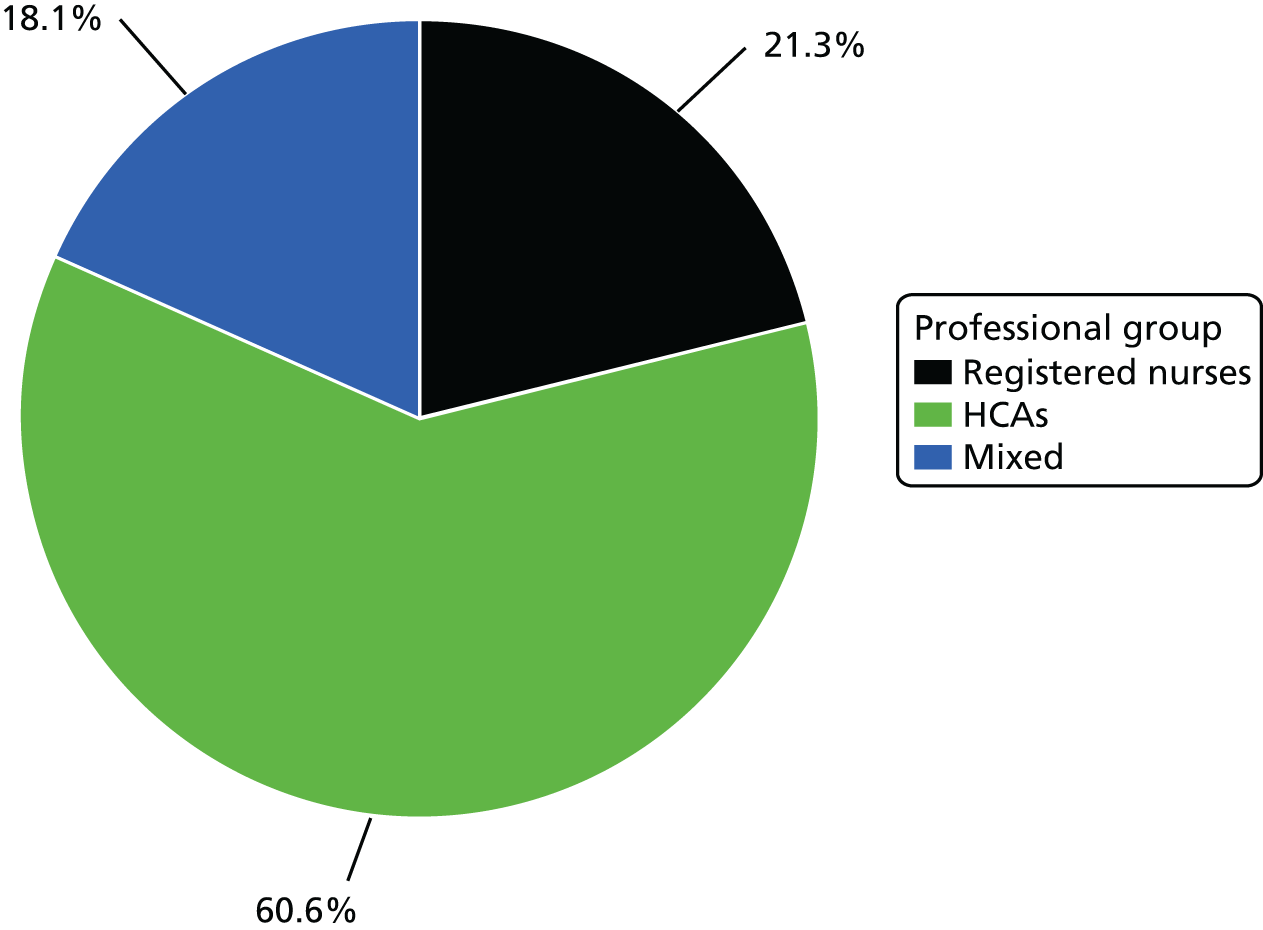
Outreach teams
Over the 5-year study period, there was a trend towards hospitals setting up outreach teams and increasing the hours that the team covered (Figure 4). The number of hospitals without outreach fell from 26.1% to 17.6%; those providing only a Monday to Friday service fell from 16.8% to 5.0%. There was a slight increase in teams that covered 7 days per week, but daytime shifts only, from 32.8% to 38.7%, but the largest increase was in the proportion of teams that were offering a 24/7 service, which increased from 24.4% to 38.7% over the study period.
FIGURE 4.
Outreach team coverage from 2009 to 2015. q, quarter.
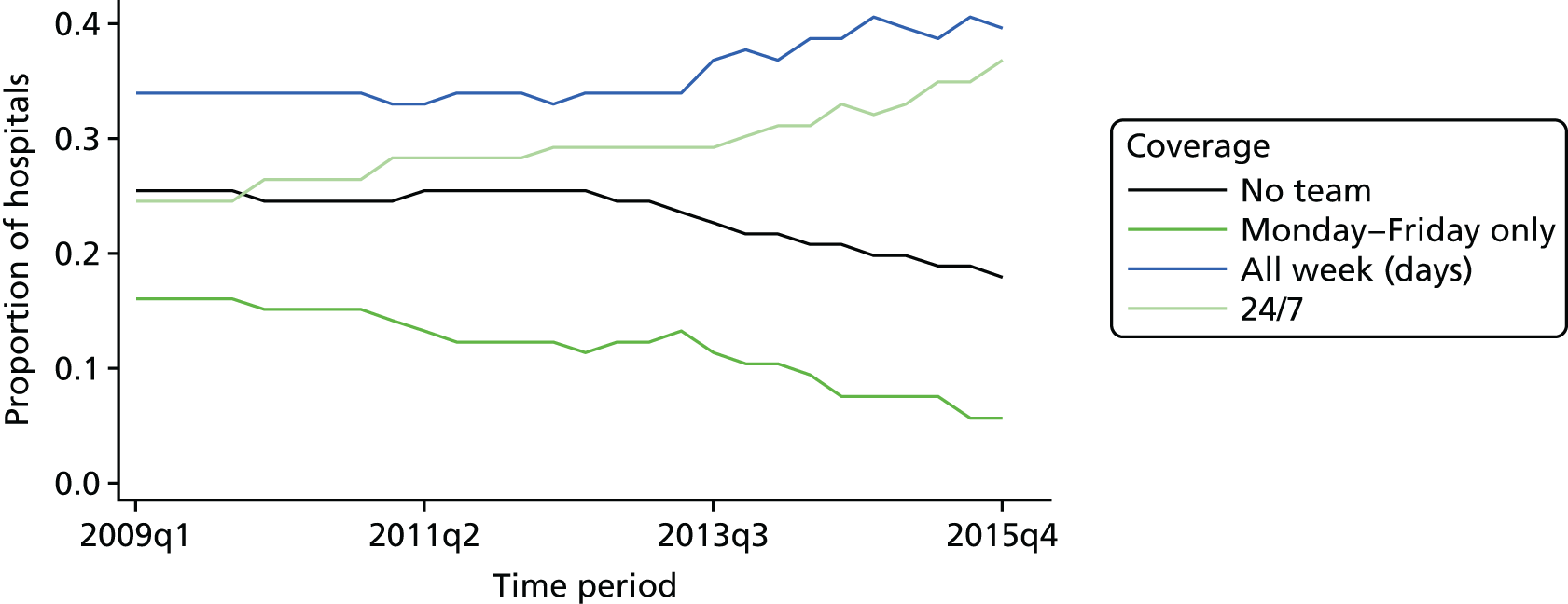
Outreach teams were typically composed of a mixture of grade 6 and 7 nurses, and 43.7% of teams included a grade 8 nurse. Only 4% of outreach teams had doctors with protected clinical time dedicated to the team. A total of 20% had input from a consultant, usually from the ICU, who mainly had an administrative and training role for one or two sessions per week. The most common additional team members in the 16.6% of outreach teams that included other health professionals were physiotherapists.
Nearly all of the teams provided step-down care for patients who had recently been transferred from the ICU to the wards (97.3%), as well as undertaking assessment of deteriorating patients on the ward, which included taking arterial blood gases (95.5%) (Figure 5). Most teams also played a role in end-of-life decision-making and the consideration of DNACPR decisions (92%). Two-thirds of teams reported involvement in the monitoring of patients for acute kidney injury (64.9%). Just under half of teams had capacity for independent prescribing on the team (48.6%). A total of 51.9% of teams had some protected time for teaching or quality improvement hours timetabled into their monthly schedule; 14.8% had > 10 hours.
FIGURE 5.
Roles of outreach teams in 2015. AKI, acute kidney injury.
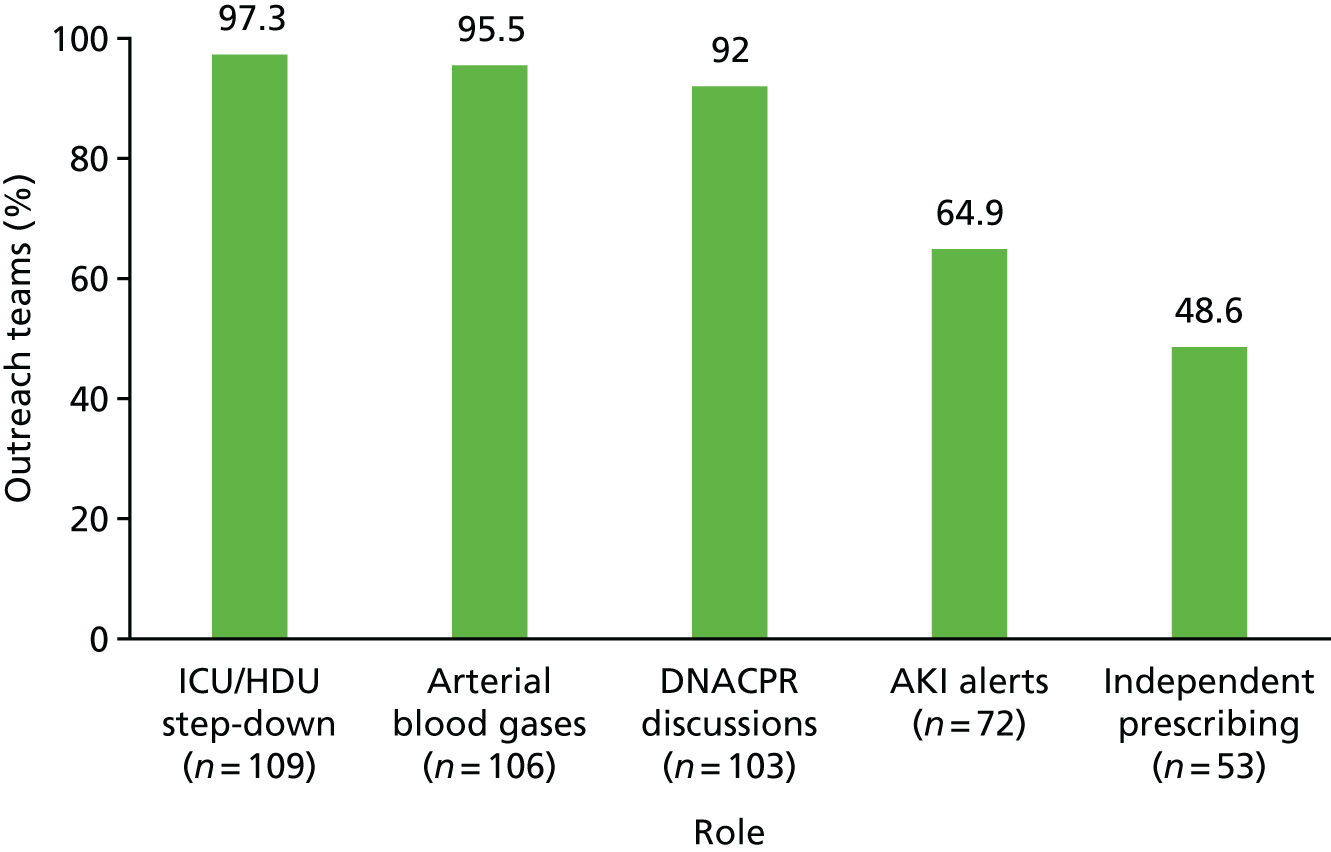
Liaising with an ICU consultant (44.3%) or the patient’s own consultant (31%) were the main referral routes that teams used when arranging an admission to the ICU (Figure 6). A minority of teams (7.3%) could make direct referrals.
FIGURE 6.
Primary referral routes into the ICU used by outreach teams in 2015.
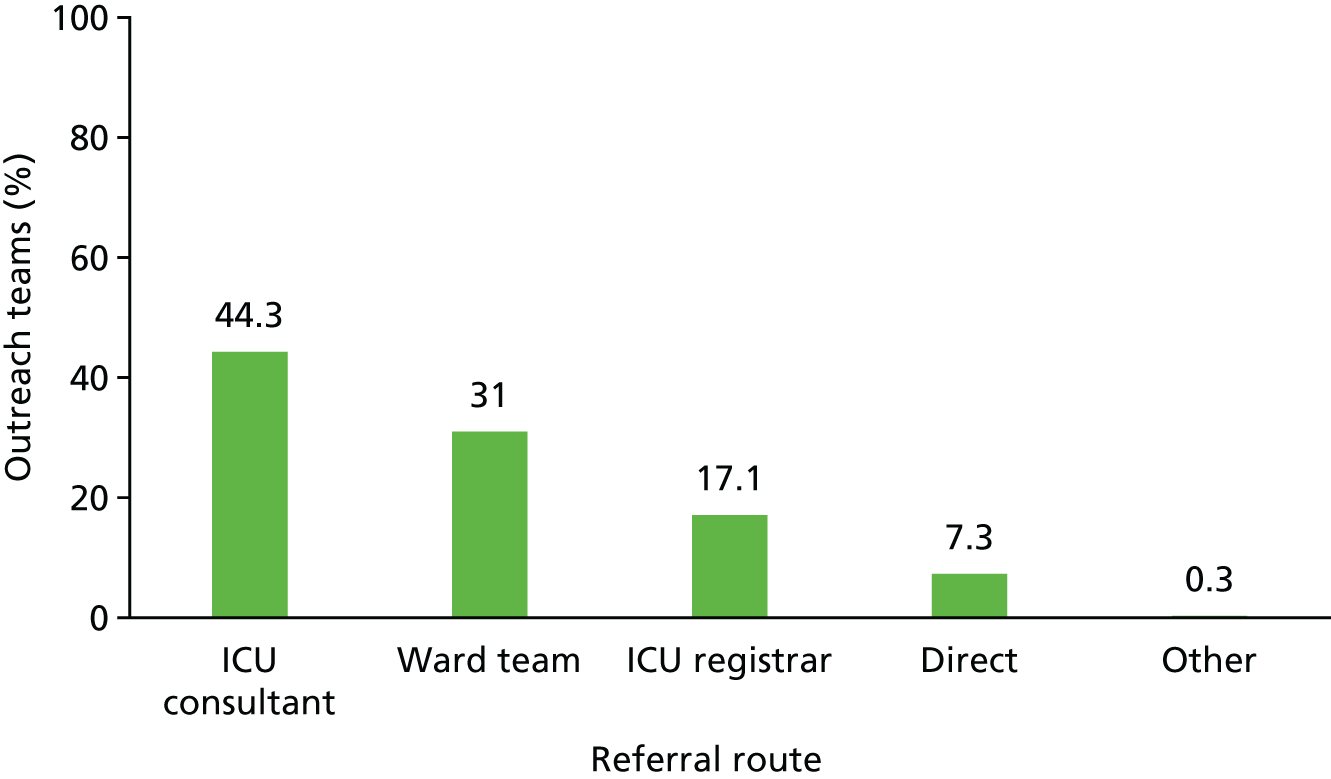
Nearly all of the teams reported that the staff who made the most requests to outreach were registered nurses (99%) and junior doctors (77%). Half of the teams also identified other doctors, including consultants, as frequent callers (45.7%) (Figure 7).
FIGURE 7.
Staff members who made calls to the outreach team in 2015.
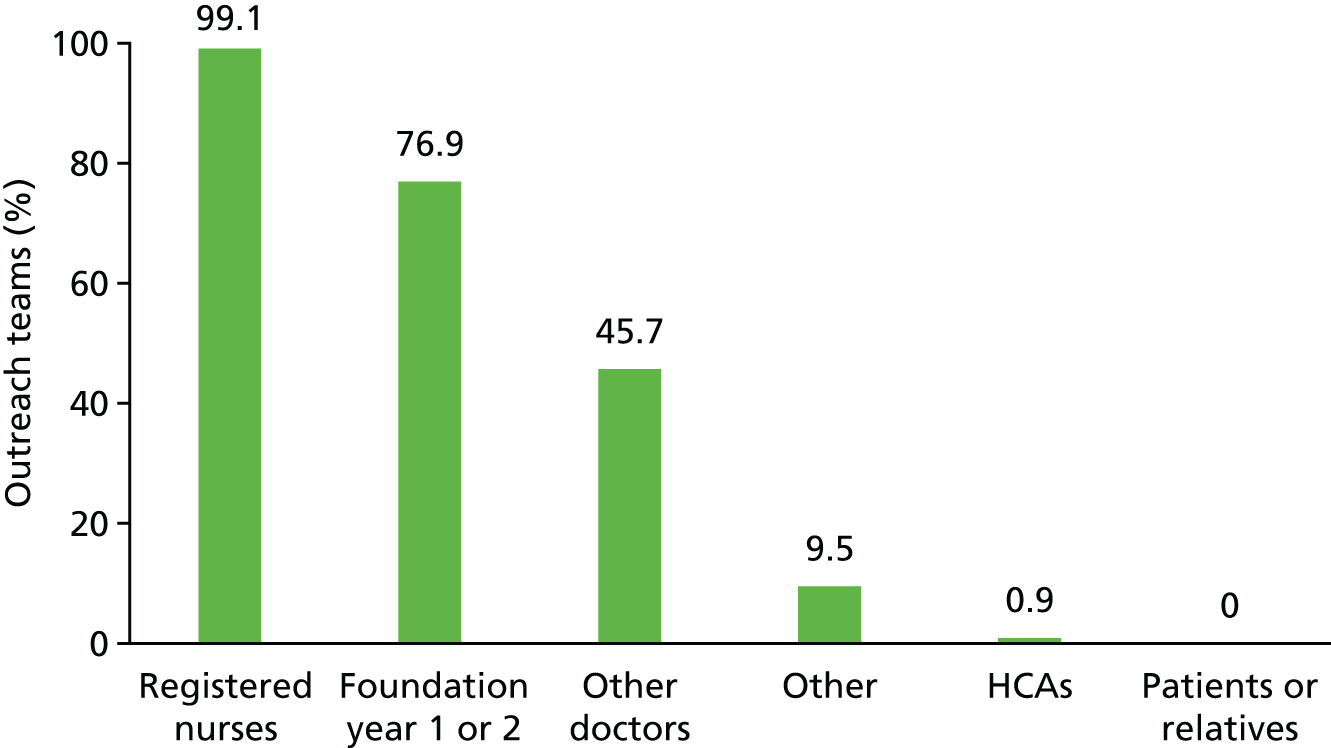
When outreach teams were asked whether or not demand regularly exceeds supply across the week, as an assessment of strain on the system, nearly two-thirds responded that this was the case for both weekday (60%) and weekend (58%) shifts (Figure 8). A total of 57.6% of hospitals with outreach teams said that normal service was suspended on ≥ 14 days across the previous year, and that this was usually because of inadequate staffing levels.
FIGURE 8.
Reporting of demand regularly exceeding supply across the week in 2015.
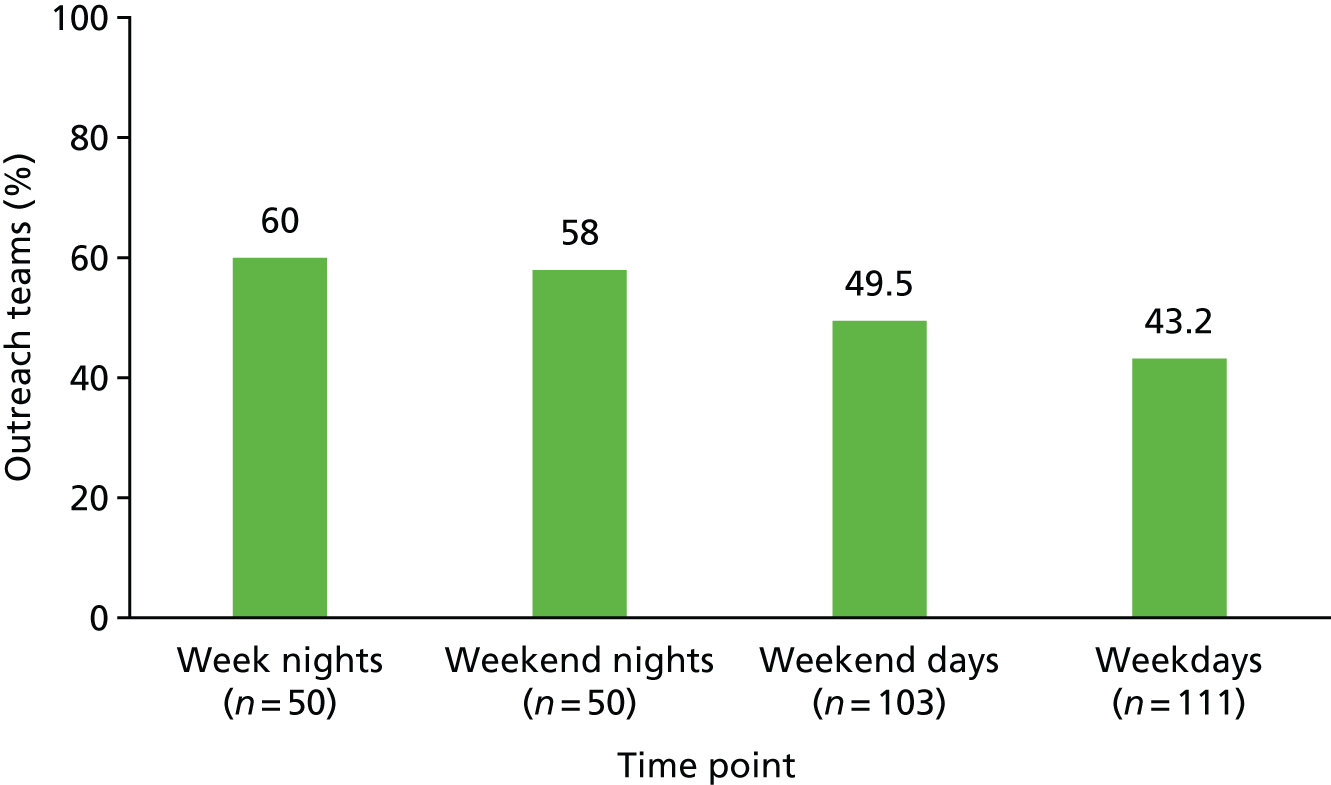
Handover systems
A total of 87.7% of hospitals reported using SBAR as their main standardised communication tool. A range of approaches to promote and encourage its use were reported, the most popular being training courses (96.1%), mention at staff induction (84.7%) and integration into local policy (77.7%) (Figure 9).
FIGURE 9.
Approaches used by hospitals to promote the use of the SBAR communication tool in 2015.
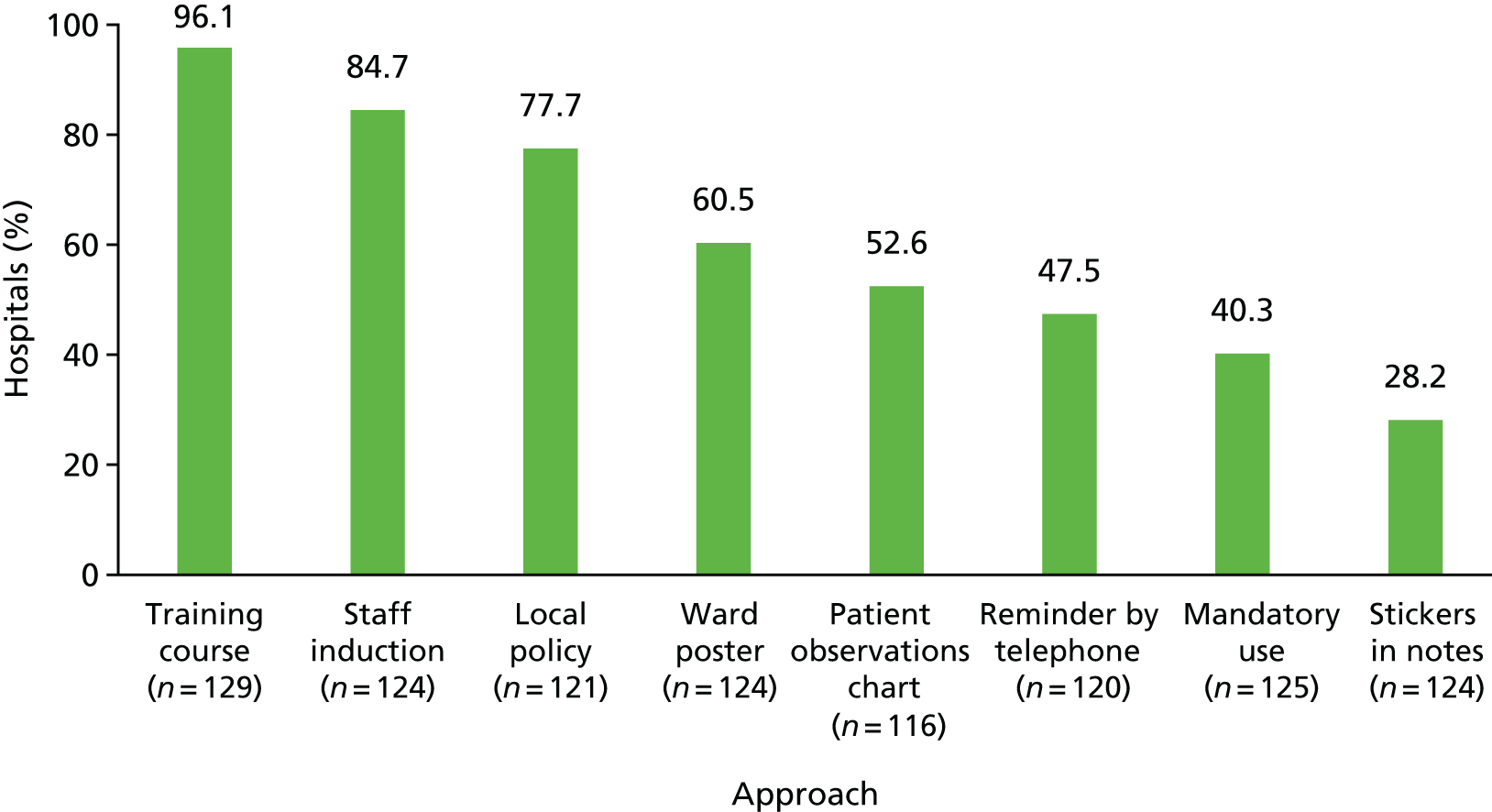
Contextual factors
Two-thirds of hospitals reported reviewing the case records of > 80% of patients who experienced an IHCA in an effort to learn from the care that these patients had received.
Efforts to ensure that patients who are unlikely to benefit from CPR do not under go CPR still appear to have some way to go, with reports of only half of those eligible patients actually having a plan in place that outlines appropriate levels of intervention in the case of deterioration (TEPs) (Figure 10). Moreover, half of the survey respondents estimated that > 50% of their patients who experience an IHCA should have had a DNACPR decision in place before the arrest occurred (Figure 11).
FIGURE 10.
An estimate of the percentage of patients eligible for a TEP who actually had one in place in 2015.
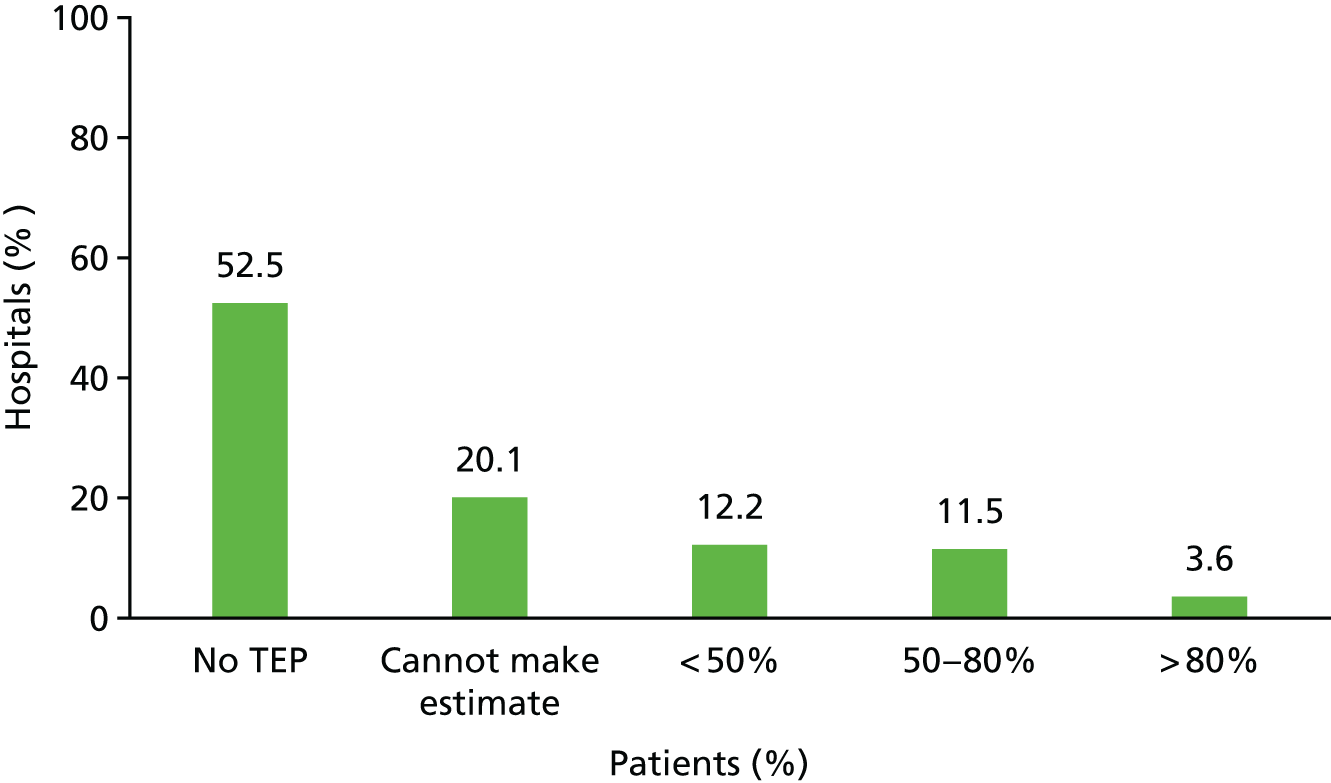
FIGURE 11.
An estimate of the percentage of patients experiencing an IHCA who should have had a DNACPR decision in place in 2015.
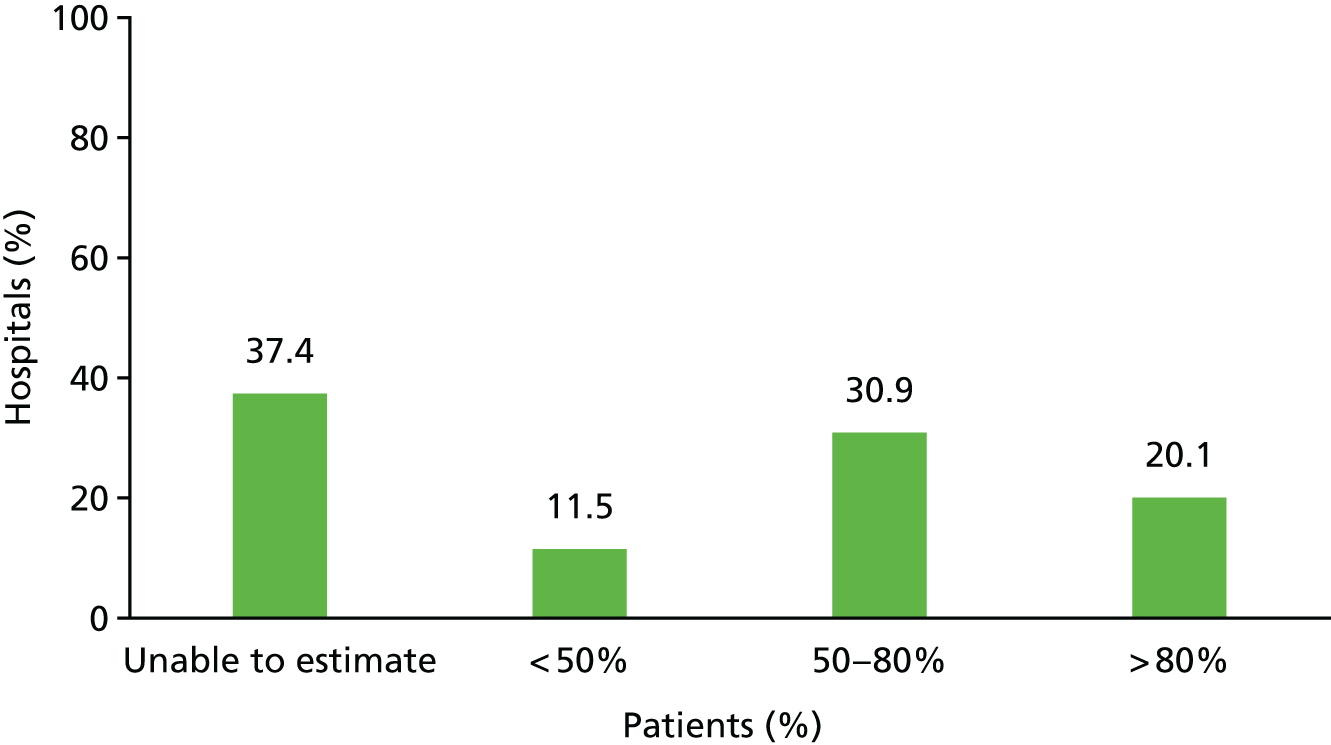
Discussion
Since its recommendation by the RCP in 2012,29 our survey showed that the NEWS has been adopted by 70% of responding hospitals, either in paper or electronic form. This standard approach replaces many other systems that were in place. 39 Investment in electronic systems may be an attempt to address a gap in the chain of prevention where, despite observations being taken, there is a failure to trigger a response because of inaccurate scoring or the failure to appreciate the need for escalation. 42,151
One benefit of standardisation is the ability to delegate the task of physiological monitoring to less-skilled staff. In 2015, 60% of hospitals reported that HCAs were the main group taking observations. However, this may have implications for the recognition of deterioration if these staff do not have adequate clinical knowledge and experience to also take into account the patient’s overall condition. 53,56
The largest temporal shift for outreach teams was to 24/7 coverage. One-quarter of hospitals had this level of coverage in 2009, rising to just under 40% in 2015, with a converse decline in the proportion of hospitals with a weekday, daytime service only. In 2015, only 17% of hospitals reported having no team, which was down from the 27% reported in a 2007 survey. 53 This may reflect the gradual build-up of evidence supporting the association between such teams and reduced cardiac arrests and, possibly, mortality. 47 Alternatively, these teams may be seen as less costly alternatives to out-of-hours medical staffing. The absence of senior medical staffing out of hours might account for the high demand that teams experience at these times and the frequency of calls from junior doctors. In addition, as the ICU works at full capacity for longer stretches of the year, increasing numbers of critically ill patients are having to be managed on the wards as they wait for admission. 152,153 Outreach teams are one way to deliver the necessary critical care to these patients. The variability in the composition of outreach teams, reported previously, is still evident for both seniority of nursing team members and presence of medical staff. 53
The consistency found across roles, with nearly all teams engaging in skilled procedures needed for the care of acutely ill patients, such as taking arterial blood gases and the step-down care of patients discharged from the ICU onto the ward, reflects the founding principles for such teams outlined in Comprehensive Critical Care. 12 However, there was evidence of variation across teams in terms of team composition and skill mix. Although outreach teams increasingly have a range of skills that allow team members to work autonomously, this is an area that is still developing, as demonstrated by only half the teams having members who are independent prescribers and < 10% of teams being able to secure direct admission to the ICU. These shortfalls may be detrimental to patient care if inconsistencies in skill levels among different team members or a lack of authority to secure an ICU admission delays adequate clinical intervention. 154 Only half of the teams had dedicated time for education or quality improvement activities; a role most likely to contribute to improving the care of acutely ill patients hospital-wide.
Outreach team involvement in end-of-life decisions implies that such decision-making is still being conducted too near the point of death. The fact that local audits of patients who suffer a cardiac arrest reveal a failure to apply TEPs or DNACPR decisions amongst many eligible patients acts as confirmation of this. Further progress on timely end-of-life planning appears necessary despite recent attempts to promote better practice. 59 Our findings echo previous research. 51,155
The majority of hospitals now report that they have introduced the SBAR tool and have employed a raft of activities to try to embed it, from training programmes to multiple reminders. However, these interventions may not necessarily lead to its widespread use in practice.
Strengths and limitations
The number of hospitals in the NCAA has been growing steadily since its inception, and around 70% of English NHS acute hospitals were participating in the audit in 2015 when we conducted our survey; the response rate of 81% suggests that our findings are representative of English acute hospitals. There are a number of limitations that need to be considered. We were unable to determine if survey respondents differed from non-respondents for any characteristics other than geographical location and the length of time they had participated in the NCAA. Non-responding hospitals may have differed systematically with regard to the intensity of their interventions. The survey was limited in size to promote a good response rate. It was therefore not possible to explore all aspects of the interventions and the contextual factors that have influenced their implementation. For example, we did not collect data on the ‘dose’ of outreach teams, a factor that may be an important element of team effectiveness. 47,156 We also did not gather information on other differences in service configuration that may determine effectiveness, for instance what response systems were being used in hospitals that reported having no outreach team. This limitation might have had a greater impact on findings for outreach teams than those for TTSs. Moreover, respondents found some of the contextual questions hard to answer because of a lack of direct access to the required information. This led to more missing data for these questions. We required staff to report on changes across a 5-year period, which opens up the possibility of recall bias. For organisations with significant staff turnover, some respondents may not have been working at the hospital when changes were initiated. This bias was potentially reinforced by our limiting of respondents to two staff, neither of whom were front line or ward based, who may have held different perspectives.
Implications
The survey builds on the findings of the qualitative interviews by providing a time-based perspective. Across the NCAA hospitals, we see a substantial change in the organisation of interventions designed to identify and respond to deteriorating patients over the last 5 years. Most of these changes have been driven by national policy and clinical guidelines, which set out standards for improving the care of acutely ill patients despite a conflicting evidence base. There is evidence of increasing standardisation in the detection arm of the rapid response system with the introduction and spread of the NEWS. The SBAR tool has also been widely adopted across hospitals to promote a standardised approach to the communication of key information about patients causing concern between clinical staff. The response arm is still showing considerable variability despite trends towards increasing outreach team coverage.
The changes in interventions over time seen in NCAA hospitals can be used to group hospitals with similar characteristics and then to look at the impact of such changes on patient outcomes using an interrupted time-series analysis. This approach is described in the following chapter.
Chapter 5 Quantitative study: evaluating the impact of interventions
Introduction
Since 2009, the NCAA has been collecting data on IHCAs that involved a resuscitation team being called. Prior to its inception, there was no objective way of determining if cardiac arrests had occurred other than by searching medical records, which were often unreliable or lacking in detail. The availability of audit data on the case mix and short-term survival for IHCAs provides an opportunity to evaluate the impact of interventions aimed at recognising and rescuing deteriorating patients. Linkage to other data, such as the Office for National Statistics (ONS) mortality and Hospital Episode Statistics (HES) hospital admissions, allows the impact of interventions for survival following hospital discharge to be evaluated.
The previous section reports the findings from the survey of NCAA hospitals and describes differences in the ways that interventions for recognising and rescuing deteriorating patients are provided. The majority of the survey questions focused on the provision of services currently in place at hospitals. Hospitals were also asked to provide responses on how care has been provided since 2009 for two interventions: TTS and RRT. The variation observed between hospitals and, more importantly, between changes in provision in hospitals provides an opportunity to examine the impact of different provisions of TTSs and outreach teams. Data from the organisational survey on how services are currently provided by hospitals were used to capture and summarise differences between hospitals in three areas: (1) the outreach team, (2) handover systems and (3) contextual factors. A count of positive responses to five questions on the outreach team, eight questions on handover systems and six contextual questions was used to indicate the intensity of interventions currently in place in hospitals.
The objectives of the quantitative study were to:
-
describe overall trends in IHCAs, survival of patients with an IHCA and hospital survival of all patients, in hospitals participating in the NCAA
-
evaluate the impact of an electronic (vs. paper-based) TTS on the rate of IHCAs, survival of patients with an IHCA and hospital survival of all patients
-
evaluate the impact of a NEWS or NEWS-based (vs. non-NEWS) TTS on the rate of IHCAs, survival of patients with an IHCA and hospital survival of all patients
-
evaluate the impact of an outreach team (compared with no outreach team) on the rate of IHCAs, survival of patients with an IHCA and hospital survival of all patients
-
evaluate the impact of three summary measures of care intensity (outreach team, handover systems, contextual factors) on the rate of IHCAs, survival of patients with an IHCA and hospital survival of all patients.
Methods
Five data sources were linked to create two data sets. A data set of all hospital admissions was used to examine survival of all hospital admissions and rates of IHCAs. A smaller data set of IHCAs was used to examine survival of patients included in the NCAA. Descriptive analysis was used to examine trends in IHCA rates and survival. The impact of TTSs, outreach and summary measures of care intensity on IHCA rates is evaluated using case mix-adjusted Poisson regression models, and the impact on survival is evaluated using case mix-adjusted Poisson and logistic regression models.
Data sources
Five data sources were used for the analyses:
-
The organisational survey of NCAA hospitals – data on the systems that hospitals have in place to identify and care for deteriorating patients as described in Chapter 4. Data from this source are linked to other data sources by hospital and by time period (quarter).
-
The NCAA data on IHCAs – data on IHCAs collected in the NCAA and including dates, times and locations of IHCAs, sociodemographic data and outcomes. Data are recorded for each arrest and are linked by hospital, patient and time period to other data sources.
-
Hospital Episode Statistics episodes for patients in the NCAA – data describing episodes of admitted patient care for patients in the NCAA were provided by NHS Digital. 157 Linkage of NCAA and HES data was undertaken by NHS Digital based on personal data provided by the NCAA. Unique encrypted patient identifiers for successfully matched patients were provided to allow patient-level linkage to other data sources. An additional year of data prior to the start of the NCAA was requested to allow measurement of comorbidity using a modified version of the Charlson Comorbidity Index. 158 Linkage to other data sources was by hospital, time period and patient.
-
Hospital Episode Statistics for patients admitted to hospitals participating in the NCAA – a second, larger data set of HES episodes of admitted patient care was provided by NHS Digital157 to allow the number of hospital admissions by quarter to be calculated for each NCAA hospital. Owing to the huge volume of admissions and episodes since 2008/09, these data were restricted to episodes for ordinary admissions to NHS trusts with hospitals participating in the NCAA. These data therefore excluded certain types of admissions such as day cases, regular attenders and some maternity admissions. An additional prior year of data for each trust was provided to allow measurement of comorbidity. Linkage to other data sources was by hospital, time period and patient.
-
Office for National Statistics mortality data159 – these data were provided by NHS Digital to allow measurement of 30- and 90-day mortality following IHCAs. Data were linked to other data sources by patient.
Data from the NCAA and the smaller HES data set (NCAA patients only) were linked to identify the HES episode that included the IHCA and, if different, the first episode of the hospital admission that includes the episode with the IHCA. The location and time of day of the arrest was used to determine if IHCAs occurring on the date of admission could be treated as post admission. Any IHCAs located in emergency departments were not linked. Some admissions with IHCAs involve transfers between hospitals in the same NHS trust; these admissions were attributed to the hospital where the IHCA took place. If an admission involved multiple IHCAs in different hospitals, then the admission was split to create a separate ‘admission’ for each hospital.
Inclusion criteria and data linkage
The eligibility of hospitals was first determined by identifying those hospitals that had completed the survey and those hospitals participating in the NCAA. A hospital was deemed to have completed the survey if responses were provided for a minimum of four consecutive quarters for three measures. The measures were the hours covered by the outreach team (no team, Monday to Friday days only, Monday to Sunday days only or full 24/7 coverage), the use of TTSs (no system, NEWS/NEWS-based) and the type of TTS (paper-based or electronic). A hospital was eligible if a minimum of three consecutive quarters of participation in NCAA coincided with complete survey data for those quarters. Participation in the NCAA was deemed to start from the first complete quarter of data collection.
Eligible hospitals were linked to data on hospital admissions from HES in order to identify all the ordinary admissions by hospital and by quarter and to derive the denominator for estimating IHCAs. Linking by hospital involved identifying hospitals from five character provider codes and site of treatment in HES. Relevant codes were identified from the linked NCAA and HES episode data and the database of NHS organisation codes. The proportion of missing or generic codes were reviewed for each hospital; NHS trusts or time periods where admissions could not be reliably attributed to a NCAA hospital were excluded. The number of admissions by quarter for each hospital was derived using the episode end date of the first episode in the admission. These were reviewed and explanations sought (HES data quality notes, hospital restructuring) for substantial changes in order to identify and exclude periods of under-reported hospital activity.
An additional criterion for including hospitals or specific time periods for hospitals was a requirement that there should be a minimum of two eligible quarters of data before and after any quarter that includes a change in one of the variables of interest, for example when a hospital switches from a paper-based to an electronic TTS. Quarters were dropped until this criterion was met.
The application of the above criteria identified the hospitals and time periods that were eligible for analysis and created a data set of survey variables and individual hospital admissions linked by hospital and by quarter. Data on IHCAs were then linked to hospital admissions using the unique episode key for the first episode of an admission in the previously linked NCAA and HES data. IHCAs were ineligible for linkage and inclusion if the IHCA (or the first IHCA in a series) occurred in the emergency department, the IHCA was a visitor or staff member rather than a patient at the time of arrest or no matching ordinary hospital admission was identified. Multiple IHCAs within an admission were dealt with by retaining NCAA case mix and outcome data for the first IHCA and creating a new variable for the number of IHCAs for each hospital admission.
Identification of variables for case mix and outcomes
Case mix for all hospital admissions included sociodemographic and clinical variables from HES. Sociodemographic characteristics comprised age group (in 10-year age bands), sex, ethnicity (white, black/black British, Asian/Asian British, any other and missing/not reported) and deprivation decile group using the Index of Multiple Deprivation. 160 Other case mix variables comprised emergency/non-emergency admission and main reason for diagnosis (circulatory, respiratory, pregnancy-related or other). Comorbidity was also captured using a modified Charlson Comorbidity Index score derived from the index admission and prior hospital admissions. A hospital-level variables, based on the proportion of admissions with a main diagnosis of atherosclerotic heart disease (International Classification of Diseases, Tenth Revision, code I259),161 was used to capture the extent of specialisation of cardiac services among individual NHS trusts and hospitals.
Case mix for analysis of survival of IHCAs also used variables collected in the NCAA. These were the length of hospital stay prior to the 2222 call, the location of the cardiac arrest, the presenting or first documented rhythm and the reason for admission to hospital. In addition, case mix used the interactions between the location of the cardiac arrest and the presenting rhythm.
The outcome for the analysis of IHCA rates was the count of eligible IHCAs occurring during the hospital admission. Survival for all hospital admissions was defined as being discharged alive from that hospital admission. Survival following IHCA was measured in three ways. Survival for 20 minutes was defined as the return of a spontaneous circulation that was sustained for > 20 minutes in a patient who was attended by the hospital-based resuscitation team (or equivalent) and who received chest compression(s) and/or defibrillation in response to the 2222 call. Survival from the date of IHCA to 30 and 90 days was identified using date of death from ONS mortality data and last known date alive was identified using HES admissions data.
Derivation of intervention variables
The organisational survey collected quarterly data on TTSs and outreach from 2009 to 2015 to capture changes in provision within hospitals as well as differences between hospitals. Three primary variables were derived from these data:
-
Use of NEWS/NEWS-based TTSs or non-NEWS TTSs – all hospitals reported using some form of TTS. Any TTS defined as NEWS, based on NEWS or locally modified NEWS was included as a NEWS/NEWS-based TTS. All other TTSs were included as non-NEWS TTSs.
-
Paper TTSs or electronic TTSs – all hospitals indicated if their TTS was paper-based or electronic. Hospitals that used both paper and electronic TTSs, for example, during a period of transition to an electronic TTS, were categorised according to the predominant system in the relevant quarter.
-
No outreach team, non-24/7 outreach team or 24/7 outreach team – the survey of hospitals captured historic information on whether or not a hospital had an outreach team and if it operated during the week, at the weekend and during the night. Few hospitals had an outreach team that did not operate at the weekend so three categories of outreach were defined. An outreach team was categorised as 24/7 if it operated on days and nights for 7 days a week. All other outreach teams were categorised as non-24/7 RRTs.
Three secondary variables describing a hospital’s current (at the time of survey in 2015) systems were derived from survey data. These variables do not vary with time, and so are able to capture only those differences between hospitals:
-
Outreach team features: this variable was scored between 0 and 5 based on positive responses to the following – (1) the outreach team included at least three core functions from ICU/HDU step-down care, independent non-medical prescribing, obtaining and interpreting arterial blood gases, and initiating DNACPR discussions with the clinical team and responding to acute kidney injury alerts, (2) the outreach team made direct admission to the ICU, (3) no temporary outreach team suspension in the last year, (4) demand for outreach was not regularly exceeded and (5) doctor or minimum of 10% senior nurse membership of the outreach team. A score of zero was recorded if there was no outreach team.
-
Handover system features: this variable was scored between 0 and 8 based on positive responses to the following – (1) staff induction explicitly advised on handover tool use, (2) posters on wards to encourage use, (3) use is mandatory for calls to the outreach team, (4) tool reminder notices are adjacent to telephones, (5) a written local policy advises on use, (6) use of tool is explicitly mentioned on patient observation charts, (7) stickers exist for use in patients’ notes and (8) staff training courses advise on use.
-
Contextual factors: this variable was scored between 0 and 6 based on positive responses to the following – (1) formal written TEPs are used, (2) at least 50% of patients eligible for a TEP had one in place, (3) IHCAs are subject to case record review, (4) at least 90% of case records are reviewed, (5) < 50% of IHCAs were judged as unsuitable for resuscitation after the event (should have had a DNACPR in place) and (6) < 20% of IHCAs were judged as unsuitable for resuscitation after the event (should have had a DNACPR in place).
Analysis
Descriptive analysis was used to show the distribution and changes in the provision of TTSs and outreach teams in hospitals included in the analysis, and the clinical and sociodemographic characteristics of hospital admissions and patients who have an IHCA. Annual trends in IHCA rates and survival were estimated using Poisson regression and logistic regression, respectively, with hospitals included as random effects and adjustment for case mix and seasonality.
Poisson regression was used to evaluate the impact of interventions on rates of IHCAs. The outcome was the count of IHCAs in the hospital admission. The majority of patients had no IHCA, whereas some had multiple IHCAs during their hospital stay. Hospitals were fitted as random effects. All models were adjusted for case mix from HES.
The analysis was conducted in four stages: (1) examining individual interventions in separate case mix-adjusted analyses of all hospitals, (2) examining a combination in interventions in a case mix-adjusted analysis of all hospitals; (3) examining individual and combined interventions in a case mix-adjusted analysis restricted to those hospitals that reported a change in the intervention during the study and (4) examining the impact of the three secondary variables.
In the first stage of the analysis, each intervention was evaluated individually after adjusting for case mix, temporal trend and seasonality. Two alternative ways of modelling the impact of interventions were specified: (1) a difference in levels and (2) a difference in slopes. 162 The intervention was included as a dummy variable to test for a difference in levels. Intervention–time (quarter) interactions were used to test for a difference in slopes.
Figure 12 shows how the two approaches (i.e. a difference in levels or in slopes) are modelled in hospitals that have a change an intervention during the study (e.g. changing from a non-NEWS to NEWS TTS). In these hospitals, the approaches are, in essence, interrupted time-series. A difference in levels models an immediate change in outcome following a change in an intervention. A difference in slopes models a change in an outcome’s trend over time following a change in an intervention and is the same as fitting a linear spline.
FIGURE 12.
Illustration of alternative approaches to modelling the impact of an intervention in a hospital reporting a change in the intervention. (a) Difference in level; and (b) difference in slope.
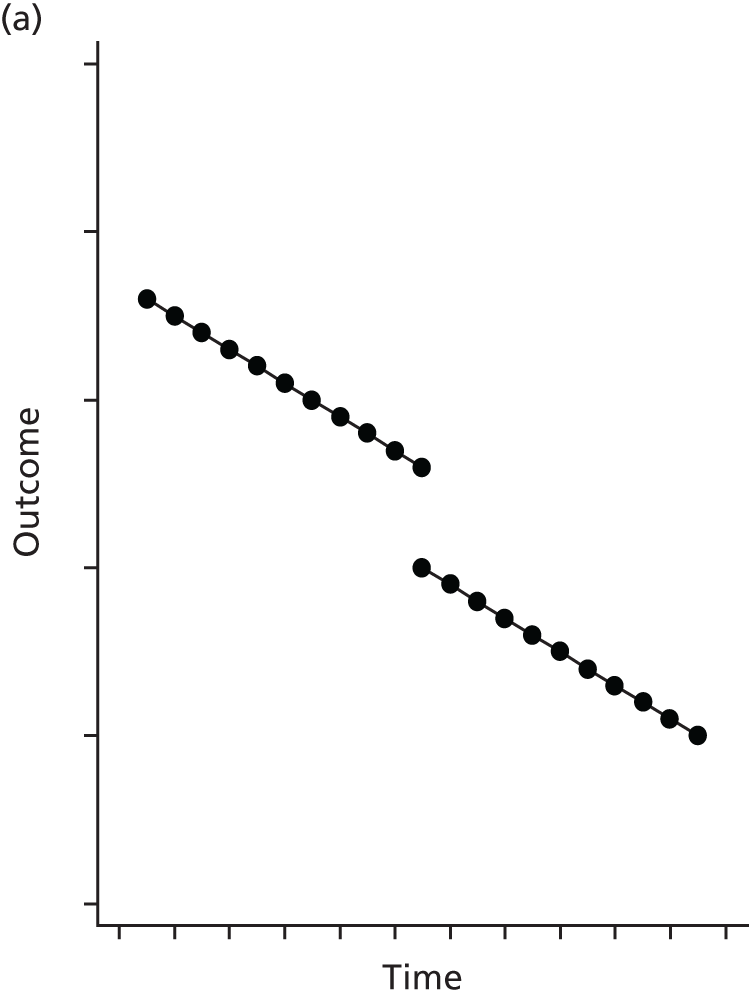
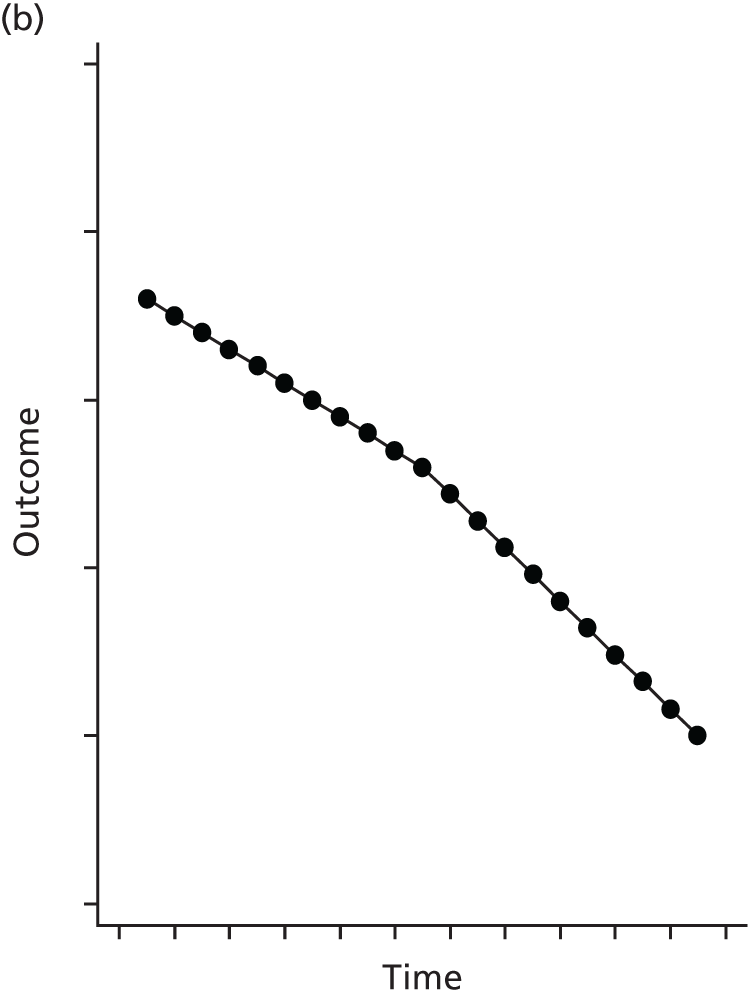
Figure 13 shows how the two approaches are modelled in hospitals that have no change in the intervention during the study (e.g. hospitals that only had a NEWS TTS or only had a non-NEWS TTS). A difference in levels models the average difference in outcome between hospitals with a NEWS TTS compared to those with a non-NEWS TTS. A difference in slopes models the average trend or slope in the outcome in hospitals with a NEWS TTS compared with the average slope in hospitals with a non-NEWS TTS.
FIGURE 13.
Illustration of alternative approaches to modelling the impact of an intervention in hospitals reporting no change in the intervention. (a) Difference in level; and (b) difference in slope.
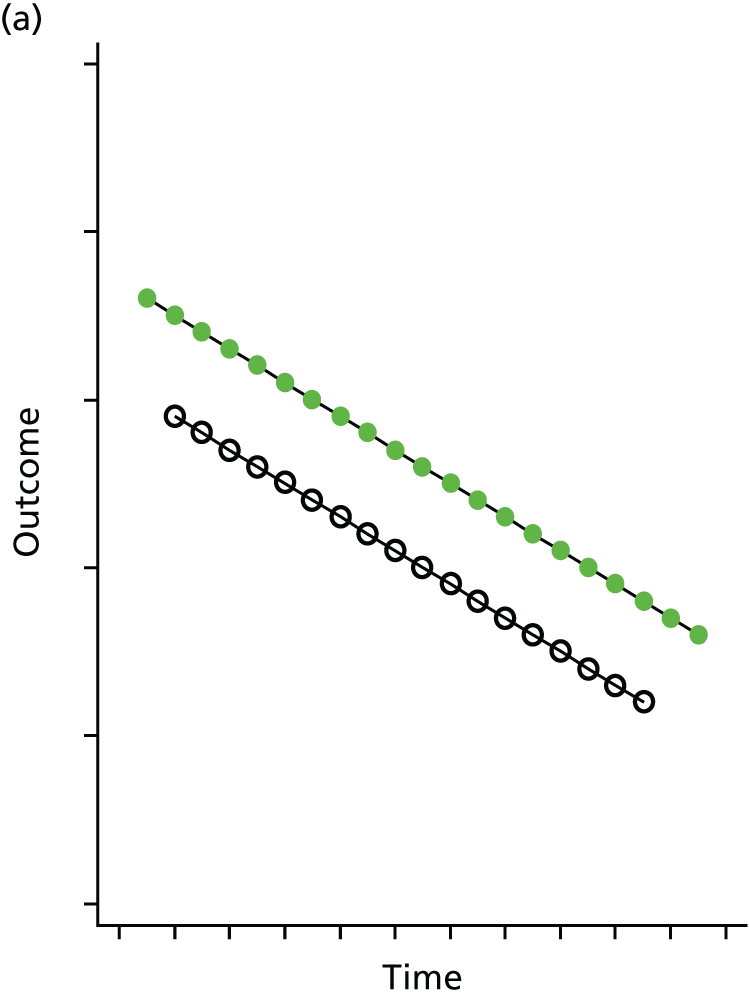
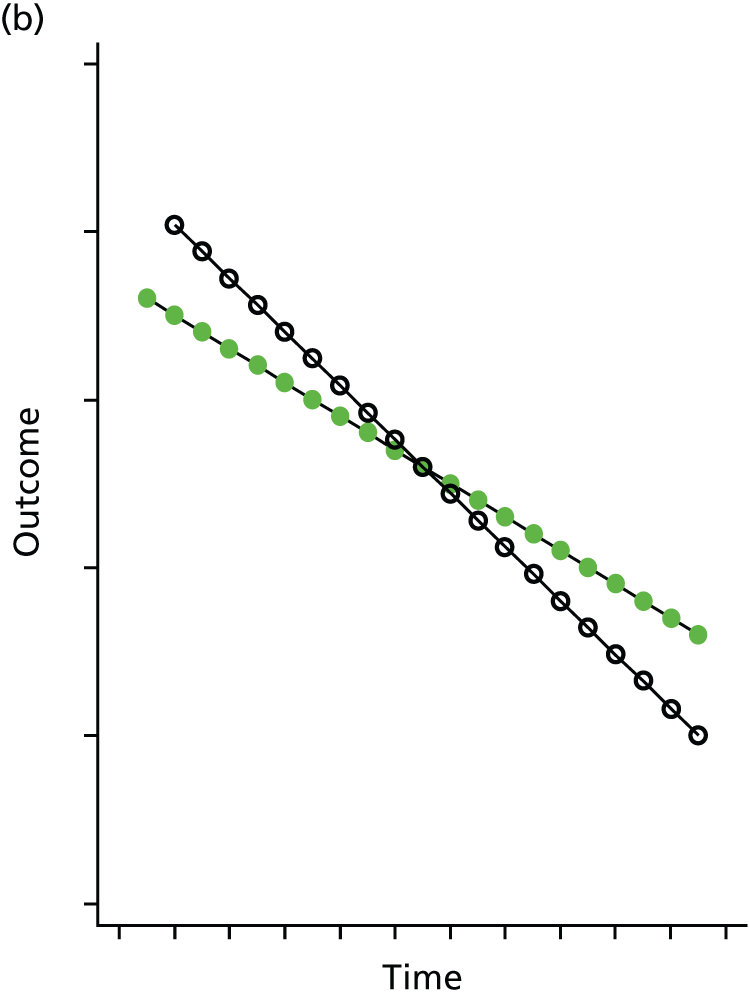
An analysis of all 106 hospitals using either a difference-in-levels approach or a difference-in-slopes approach will therefore combine the effects of within-hospital differences (as shown in the relevant graph in Figure 12) and between-hospital differences (as shown in Figure 13) in the intervention. Thus, six separate models were used to estimate the individual impact of the three interventions (NEWS/non-NEWS TTS, paper/electronic TTS, and outreach team) using the two approaches (difference in levels, difference in slopes). To examine a difference in levels, the incidence rate ratios (IRRs) for the difference in levels were estimated with 95% confidence intervals (CIs). To examine a difference in slopes, the IRRs and 95% CIs were estimated for the slope for each category of an intervention (e.g. for paper TTS and for electronic TTS). IRRs and CIs were annualised to show the average yearly change in rates, and p-values were calculated to test for evidence for a difference in slopes. All models were adjusted for case mix, quarterly trend and seasonality, with hospitals included as random effects.
The second stage of the analysis involved selecting interventions and approaches for inclusion in a model that combined different interventions. Inclusion required evidence for an association between intervention and outcome at a p-value of < 0.1 from the first stage of the analysis. IRRs and 95% CIs were estimated after value of adjusting for other interventions included in the model, case mix, quarterly trend and seasonality, with hospitals included as random effects.
The third stage was to repeat the first two stages, after restricting the hospitals in the analyses to those that reported a change in intervention during the study, for example a hospital that switched from a paper to an electronic TTS. This was done to provide some assurance that any impact of an intervention observed in an analysis of all hospitals was also observed if restricted to those hospitals that reported a change in that intervention. The final stage of analysis involved examining the impact of the three secondary variables (outreach features, handover features and contextual factors) on IHCA rates. These were examined individually in case mix-adjusted models, with IRRs and 95% CIs estimated for a 1-point increase in the count. All analyses were repeated after restricting IHCAs to those occurring on wards. This was done to examine the sensitivity of the results using rates of ward-based IHCAs as the outcome, rather than all IHCAs in admitted patients attended by the resuscitation team regardless of the location of the arrest.
Poisson regression was also used to examine the impact of interventions on hospital survival for all hospital admission. An identical four-stage modelling approach was used, with adjustment for case mix, temporal trends and seasonality. Hospitals were modelled as random effects.
Logistic regression was used to examine the impact of interventions on four measures of IHCA survival: (1) return of a spontaneous circulation of > 20 minutes, (2) hospital survival (survival to discharge), (3) 30-day survival and (4) 90-day survival. Again, the four-stage modelling approach was used. Case mix also included variables from NCAA: the length of hospital stay prior to the 2222 call, the location of the cardiac arrest, the presenting or first documented rhythm and the reason for admission to hospital. In addition, case mix used the interactions between the location of the cardiac arrest and the presenting rhythm. Hospitals were included as random effects and the impact of interventions was measured as odds ratios (ORs) with 95% CIs.
Findings
Descriptive analysis
There were 106 hospitals eligible for analysis. The number of quarters of eligible data from the hospitals ranged from 3 to 22 between the final (October–December) quarter of 2009 and the first (January–March) quarter of 2015. The data for analysis comprised 13,059,865 hospital admissions from HES linked with 32,364 patients having 34,202 IHCAs from the NCAA database.
Table 14 shows the characteristics of all patients admitted to 106 hospitals included in the analysis, and the characteristics of those patients who had an IHCA. An IHCA was more likely in older male patients who have greater comorbidity and who entered hospital as an emergency admission. The mean age of IHCAs changed little over time, whereas there was a small increase in the mean age of all admissions. Trends in case mix of IHCAs over time indicated a small reduction in the proportion of females and the proportion of emergency admission compared with trends in all admissions.
| Patient characteristic | Admission | |
|---|---|---|
| IHCAs (N = 32,820) | All admissions (N = 13,059,865) | |
| Age category (years) | ||
| < 65, n (%) | 6557 (20.0) | 7,558,437 (57.9) |
| 65–74, n (%) | 6844 (20.9) | 1,953,500 (15.0) |
| 75–84, n (%) | 11,050 (33.7) | 2,127,250 (16.3) |
| ≥ 85, n (%) | 8368 (25.5) | 1,420,677 (10.9) |
| Missing, n | 1 | 1 |
| Annual trend in mean age (in years) | +0.003 | +0.362 |
| Sex | ||
| Male, n (%) | 18,807 (57.3) | 5,276,200 (40.4) |
| Female, n (%) | 14,013 (42.7) | 7,783,187 (59.6) |
| Missing, n (%) | 0 | 478 |
| Annual trend in proportion female (%) | –0.62 | –0.12 |
| Ethnicity | ||
| White, n (%) | 28,407 (86.6) | 10,922,469 (83.6) |
| Asian/Asian British, n (%) | 1230 (3.8) | 620,412 (4.8) |
| Black/black British, n (%) | 512 (1.6) | 314,316 (2.4) |
| Any other ethnic group, n (%) | 397 (1.2) | 276,563 (2.1) |
| Not stated or missing, n (%) | 2274 (6.9) | 926,105 (7.1) |
| Annual trend in proportion non-white | +0.19% | +0.10% |
| Deprivation (index of multiple deprivation by decile) | ||
| Least deprived 10%, n (%) | 2607 (8.0) | 1,048,095 (8.1) |
| Less deprived 10–20%, n (%) | 2775 (8.5) | 1,123,433 (8.7) |
| Less deprived 20–30%, n (%) | 3129 (9.6) | 1,204,167 (9.3) |
| Less deprived 30–40%, n (%) | 3342 (10.2) | 1,282,332 (9.0) |
| Less deprived 40–50%, n (%) | 3386 (10.4) | 1,272,685 (9.8) |
| More deprived 40–50%, n (%) | 3401 (10.4) | 1,263,100 (9.8) |
| More deprived 30–40%, n (%) | 3481 (10.6) | 1,328,799 (10.3) |
| More deprived 20–30%%, n (%) | 3347 (10.2) | 1,360,653 (10.5) |
| More deprived 10–20%, n (%) | 3400 (10.4) | 1,431,102 (11.1) |
| Most deprived 10%, n (%) | 3848 (11.8) | 1,637,906 (12.7) |
| Missing, n | 104 | 107,593 |
| Annual trend in mean decile group | –0.008 | –0.012 |
| Charlson Comorbidity Index | ||
| No comorbidity, n (%) | 6138 (18.7) | 6,636,490 (50.8) |
| One comorbidity, n (%) | 10,061 (30.7) | 3,382,501 (25.9) |
| Two comorbidities, n (%) | 8542 (26.0) | 1,811,933 (13.9) |
| Three or more comorbidities, n (%) | 8079 (24.6) | 1,228,941 (9.4) |
| Missing, n (%) | 0 (0) | 0 (0) |
| Annual trend in mean index score (0–3) | +0.038 | +0.037 |
| Admission method | ||
| Non-emergency, n (%) | 3275 (10.0) | 4,561,122 (34.9) |
| Emergency, n (%) | 29,380 (90.0) | 8,498,578 (65.1) |
| Missing, n | 165 | 165 |
| Annual trend in proportion emergency (%) | –0.69 | 0.00 |
The majority of the 32,820 IHCAs occurred on wards (21,595; 65.8%). Other locations included CCUs (10.3%), emergency admissions units (10.0%), critical care units (4.7%) and cardiac catheter laboratories (2.6%).
Figure 14 shows a general downward trend in the rate of IHCAs over time, with evidence of seasonality (higher rates in October to December and January to March quarters). Table 15 indicates a reduction of 6.4% per year once case mix and seasonality are allowed for. Note that some fluctuation in earlier quarters is attributable to there being fewer data and fewer hospitals from this time period.
FIGURE 14.
Trends in the crude rate of IHCAs attended by the resuscitation team in 13 million hospital admissions. q, quarter.
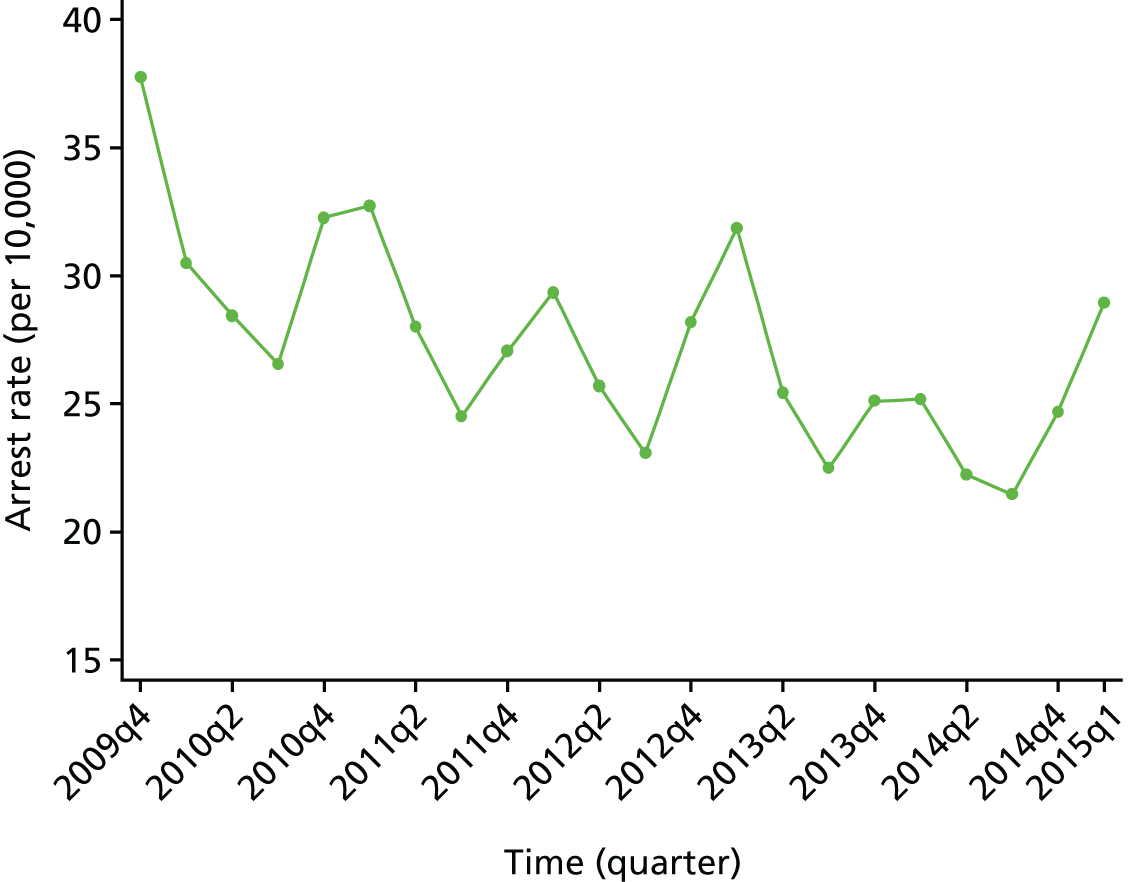
| All admissions | Adjusted annual trend (95% CI) | |
|---|---|---|
| Seasonal | Case mix | |
| IHCA rates: IRR | 0.954 (0.946 to 0.962) | 0.936 (0.927 to 0.944) |
| Hospital survival: OR | 1.032 (1.016 to 1.048) | 1.053 (1.043 to 1.064) |
| IHCAs attended by resuscitation team | ||
| 20-minute survival: OR | 1.060 (1.041 to 1.080) | 1.070 (1.049 to 1.091) |
| Hospital survival: OR | 1.028 (1.004 to 1.053) | 1.048 (1.020 to 1.077) |
| 30-day survival: OR | 1.028 (1.004 to 1.053) | 1.051 (1.022 to 1.080) |
| 90-day survival: OR | 1.025 (1.000 to 1.051) | 1.048 (1.019 to 1.079) |
Hospital survival (discharge alive) for all hospital admissions is over 95% (Figure 15). The odds of survival is increased by 5.3% per year (see Table 14) between 2009 and 2015. Hospital survival for admitted patients who had IHCAs also rose, with an increase in the odds of survival of 4.8% per year (Table 15).
FIGURE 15.
Trends in hospital survival for all hospital admissions and for IHCAs attended by the resuscitation team. q, quarter.

Just under half of patients with IHCAs survived to 20 minutes (return of a spontaneous circulation of > 20 minutes) and the odds of surviving to 20 minutes increased, on average, by 7.0% per year after allowing for differences in case mix (Figure 16 and see Table 15). Similarly, the odds of surviving to 30 or 90 days increased, on average, by around 5% per year.
FIGURE 16.
Trends in survival at 20 minutes, and 30 and 90 days in IHCAs attended by the resuscitation team. q, quarter.

Association between interventions and in-hospital cardiac arrests
All hospitals in the analysis used some form of TTS. The majority (81%) operated a paper-based system throughout the study. A total of 18 (17%) hospitals switched from a paper system to an electronic system, and two hospitals operated an electronic system throughout the study.
During the study period, almost half of the hospitals changed to a NEWS or NEWS-based TTS from a non-NEWS system. There were 22 hospitals with no outreach team throughout the study and five that introduced a team during the study period. There were 29 hospitals with 24/7 outreach teams throughout the study and six hospitals that increased the hours of the outreach team to 24/7 during the study (Table 16).
| TTS | Number of hospitals (%) |
|---|---|
| Paper only | 86 (81) |
| Electronic only | 2 (2) |
| Switched from paper to electronic | 18 (17) |
| Non-NEWS only | 42 (40) |
| NEWS or NEWS-based only | 12 (11) |
| Switched from non-NEWS to NEWS/NEWS-based | 52 (49) |
| Outreach team | |
| No team | 22 (21) |
| Non-24/7 team | 41 (39) |
| 24/7 team | 29 (27) |
| Changed from no team to non-24/7 team | 5 (5) |
| Changed from non-24/7 team to 24/7 team | 6 (6) |
The secondary variables of interest were outreach features, handover system features and contextual factors. There were 29 hospitals (including 22 with no outreach team) that reported no features. The median number of outreach features was one (interquartile range 0–3) and only one hospital reported all five. The median number of handover features was five (interquartile range 3–6), with a maximum of seven of eight features. The median number of contextual factors reported as positive was three (interquartile range 1–3), with 16 hospitals reporting none and only one hospital reporting all six.
Table 17 shows the associations between interventions and IHCAs in 13 million hospital admissions after adjusting for case mix, time trends and seasonality. There was evidence that use of a NEWS or NEWS-based TTS was associated with a lower rate of IHCAs compared with a non-NEWS TTS (IRR 0.925; p < 0.001). There was no evidence for a difference in annual trends in IHCA rates between NEWS/NEWS-based TTSs and non-NEWS TTSs (p = 0.193 for a difference in slopes). There was also evidence that an electronic TTS was associated with a lower rate of IHCAs compared with a paper TTS (IRR 0.923; p = 0.005). There was no evidence for a difference in annual trends between an electronic TTS and a paper TTS (p = 0.217 for a difference in slopes). There was no evidence that the rate of IHCAs differed for a non-24/7 outreach team compared with no outreach team (IRR 0.976; p = 0.554) or for a 24/7 outreach team compared with a non-24/7 outreach team (IRR 1.039; p = 0.305). There was evidence that annual trends in IHCA rates differed. The greatest reduction was observed for non-24/7 outreach teams (IRR 0.932 or 6.8% reduction in rate of IHCAs per year), which represented a difference in slopes in comparison with no outreach (p = 0.008) and with a 24/7 outreach (p = 0.035).
| Intervention | Intervention, case mix-adjusted IRR (95% CI) | |
|---|---|---|
| Individual | Combined | |
| TTS | ||
| Non-NEWS | Reference | Reference |
| NEWS/NEWS-based | 0.925 (0.890 to 0.961) | 0.916 (0.882 to 0.952) |
| p-value for difference in levels | p < 0.001 | p < 0.001 |
| Annual trend: non-NEWS | 0.941 (0.931 to 0.950) | – |
| Annual trend: NEWS/NEWS-based | 0.921 (0.897 to 0.947) | – |
| p-value for difference in slopes | p = 0.193 | – |
| Paper | Reference | Reference |
| Electronic | 0.923 (0.873 to 0.976) | 0.924 (0.873 to 0.977) |
| p-value for difference in levels | p = 0.005 | p = 0.006 |
| Annual trend: paper | 0.939 (0.930 to 0.948) | – |
| Annual trend: electronic | 0.916 (0.882 to 0.950) | – |
| p-value for difference in slopes | p = 0.217 | – |
| Outreach team | ||
| Non-24/7 outreach team (compared with no outreach team) | 0.976 (0.902 to 1.057) | – |
| p-value for difference in levels | p = 0.554 | – |
| 24/7 outreach team (compared with non-24/7 outreach team) | 1.039 (0.966 to 1.119) | – |
| p-value for difference in levels | p = 0.305 | – |
| Annual trend: no outreach team | 0.961 (0.945 to 0.978) | 0.970 (0.954 to 0.987) |
| Annual trend: non-24/7 outreach team | 0.932 (0.918 to 0.945) | 0.951 (0.936 to 0.966) |
| Annual trend: 24/7 outreach team | 0.952 (0.939 to 0.966) | 0.967 (0.953 to 0.982) |
| p-values for difference in slopes | – | – |
| Non-24/7 outreach team vs. no outreach team | p = 0.008 | p = 0.091 |
| 24/7 outreach team vs. non-24/7 outreach team | p = 0.035 | p = 0.099 |
The three variables with evidence for an association were included in a single model in the next stage of the analysis (see Table 17). The lower IHCA rate associated with a NEWS or NEWS-based TTS remained (IRR 0.916; p < 0.001) after adjusting for the other two variables. Similarly, the lower IHCA rate associated with an electronic TTS also remained (IRR 0.924; p = 0.006) after adjusting for the other two variables. There was weaker evidence that the downward trend in the IHCA rate with a non-24/7 outreach team was greater than for no outreach team (p = 0.091) and for a 24/7 outreach team (p = 0.099).
The third stage of the analysis involved restricting the sample of hospitals to those hospitals that changed intervention during the study (Table 18). There were 52 hospitals that switched from a non-NEWS to a NEWS TTS, 18 that switched from a paper to an electronic TTS and 11 that changed their outreach team (five from no outreach team to a non-24/7 outreach team, and six from a non-24/7 to 24/7 outreach team). In the 52 hospitals that changed to a NEWS/NEWS-based TTS, there remained evidence for a lower rate of IHCAs after switching to a NEWS/NEWS-based TTS (IRR 0.904, p < 0.00, after adjusting for the other two variables). Similarly, in the 18 hospitals that changed to an electronic TTS there was still evidence for a lower rate of IHCAs after switching (IRR 0.884, p = 0.001, after adjustment for the other two variables). However, evidence for a difference in slopes associated with the outreach team was not observed in an analysis restricted to the 11 hospitals that reported a change in their outreach team. There was no longer any evidence for a stronger downward trend in the IHCA rate with a non-24/7 outreach team; the IRR for the annual trend in IHCA rates for a non-24/7 outreach team (IRR 0.969) indicated a smaller downward trend than for no outreach team (IRR 0.936, p = 0.360 for a difference in slopes) and a 24/7 outreach team (IRR 0.936, p = 0.426), although neither difference was statistically significant.
| Intervention | Intervention, case mix-adjusted IRR (95% CI) | |
|---|---|---|
| Individual | Combined | |
| TTS | ||
| Hospitals changing from non-NEWS to NEWS/NEWS-based TTS (n = 52) | ||
| Non-NEWS | Reference | Reference |
| NEWS/NEWS-based | 0.946 (0.898 to 0.995) | 0.904 (0.863 to 0.948) |
| p-value for difference in levels | p = 0.033 | p < 0.001 |
| Hospitals changing from paper to electronic TTS (n = 18) | ||
| Paper | Reference | Reference |
| Electronic | 0.934 (0.857 to 1.016) | 0.884 (0.822 to 0.950) |
| p-value for difference in levels | p = 0.113 | p = 0.001 |
| Outreach team | ||
| Hospitals changing outreach team (n = 11) | ||
| Annual trend: no outreach team | 0.931 (0.890 to 0.975) | 0.936 (0.893 to 0.980) |
| Annual trend: non-24/7 team | 0.953 (0.91 to 0.995) | 0.969 (0.913 to 1.029) |
| Annual trend: 24/7 team | 0.929 (0.878 to 0.984) | 0.936 (0.882 to 0.992) |
| p-values for difference in slopes | – | – |
| Non-24/7 vs. no team | p = 0.505 | p = 0.360 |
| 24/7 team vs. non-24/7 team | p = 0.541 | p = 0.426 |
The final stage of the analysis was to examine the impact of the three secondary variables measuring outreach team features, handover features and contextual factors. These variables were added to the case mix-adjusted model that included the two statistically significant variables from Table 17 (NEWS/NEWS-based or non-NEWS TTS; paper or electronic TTS). There was no evidence for any association when each of the three secondary variables were included on their own or when all three were included in the same model (Table 19).
| Variable | Intervention, case mix-adjusted IRR (95% CI) | |
|---|---|---|
| Individual | Combined | |
| Outreach team features (per additional feature) | 0.992 (0.958 to 1.028) | 0.995 (0.95 to 1.031) |
| p = 0.668 | p = 0.790 | |
| Handover features (per additional feature) | 0.982 (0.957 to 1.008) | 0.983 (0.962 to 1.023) |
| p = 0.184 | p = 0.213 | |
| Contextual factors (per additional factor) | 0.988 (0.959 to 1.019) | 0.992 (0.959 to 1.019) |
| p = 0.451 | p = 0.602 | |
Sensitivity analysis was conducted to restrict the outcome (rate of IHCAs attended by the resuscitation team for all admitted patients) to IHCAs occurring on the ward. The restricted analysis produced similar results for TTSs to those shown in Table 17. In the analysis of combined interventions, the IRR for the impact of a NEWS/NEWS-based TTS was 0.901 (95% CI 0.858 to 0.944; p < 0.001), a marginally larger effect than the 0.916 shown in Table 17. The IRR for the impact of an electronic TTS was 0.869 (95% CI 0.809 to 0.933; p < 0.001), indicating a larger effect than the 0.924 in shown in Table 16.
The change in slopes for the impact of outreach team was also retained in the model, with IRRs for annual trends of 0.997 (95% CI 0.976 to 1.017) for no outreach, 0.951 (95% CI 0.936 to 0.966) for non-24/7 outreach and 0.957 (95% CI 0.940 to 0.975) for 24/7 outreach. Comparison of trends in the sensitivity analysis showed evidence for a decline in IHCAs with non-24/7 outreach compared with no outreach (p = 0.001 for difference in slopes), a difference which is less apparent in Table 17 (p = 0.091).
The impact of restricting the primary analysis to those hospitals that changed intervention during the study is shown in Table 18 and indicated consistent results for TTSs, but not for outreach. Similar results were produced by restricting the sensitivity analysis to those hospitals that changed intervention. Evidence of effects were observed for NEWS/NEWS-based TTSs in the 52 hospitals that changed to NEWS: IRR 0.895 (95% CI 0.844 to 0.949; p < 0.001). In the 18 hospitals that changed to an electronic TTS, the IRR was 0.845 (95% CI 0.764 to 0.934; p = 0.001). In common with the primary analysis, the apparent evidence for a difference in slopes for outreach was no longer observed in the 11 hospitals that changed their outreach during the study. As with the primary analysis, the IRR for no outreach strengthened to 0.935, and the IRR for non-24/7 outreach weakened to 1.021 (p = 0.068 for difference in slopes).
Association between interventions and survival in all hospital admissions
Table 20 shows the impact of interventions on the survival of 13 million hospital admissions to 106 hospitals after adjusting for case mix, time trends and seasonality. There was no evidence that use of a NEWS or NEWS-based TTS was associated with better survival compared with a non-NEWS TTS (IRR 0.9998; p = 0.838). There was evidence for a difference in annual trends in survival between NEWS/NEWS-based TTSs and non-NEWS TTSs (p = 0.012 for a difference in slopes), with a stronger trend observed with non-NEWS TTSs. There was no evidence that survival was improved with an electronic TTS (IRR 1.0010; p = 0.400), but there was evidence that the trend in improvement was stronger with a paper TTS (p = 0.013 for a difference in slopes). There was some evidence that the survival rate differed for a non-24/7 outreach team compared with no outreach team (IRR 0.9983; p = 0.056), but no difference between a 24/7 outreach team compared with a non-24/7 outreach team (IRR 0.9995; p = 0.525). There was no evidence that annual trends in survival rates differed (non-24/7 outreach team vs. no outreach team p = 0.394 and 24/7 outreach team vs. non-24/7 outreach team p = 0.270 for difference in slopes).
| Intervention | Intervention, case mix-adjusted IRR (95% CI) | |
|---|---|---|
| Individual | Combined | |
| TTS | ||
| Non-NEWS | Reference | Reference |
| NEWS/NEWS-based | 0.9998 (0.9983 to 1.0014) | – |
| p-value for difference in levels | p = 0.838 | – |
| Annual trend: non-NEWS | 1.0016 (1.0012 to 1.0024) | 1.0016 (1.0004 to 1.0024) |
| Annual trend: NEWS/NEWS-based | 1.0004 (0.9992 to 1.0012) | 1.0000 (0.9992 to 1.0012) |
| p-value for difference in slopes | p = 0.012 | p = 0.122 |
| Paper | Reference | Reference |
| Electronic | 1.0010 (0.9987 to 1.0032) | – |
| p-value for difference in levels | p = 0.400 | – |
| Annual trend: paper | 1.0016 (1.0012 to 1.0020) | 1.0004 (0.9992 to 1.0016) |
| Annual trend: electronic | 0.9996 (0.9984 to 1.0012) | 0.9996 (0.9960 to 1.0008) |
| p-value for difference in slopes | p = 0.013 | p = 0.361 |
| Outreach team | ||
| Non-24/7 outreach team (compared with no outreach team) | 0.9983 (0.9966 to 1.0000) | 0.9936 (0.9869 to 1.0008) |
| p-value for difference in levels | p = 0.056 | p = 0.083 |
| 24/7 outreach team (compared with non-24/7 outreach team) | 0.9995 (0.9980 to 1.0010) | 0.9995 (0.9979 to 1.0010) |
| p-value for difference in levels | p = 0.525 | p = 0.500 |
| Annual trend: no outreach team | 1.0004 (1.0000 to 1.0012) | – |
| Annual trend: non-24/7 outreach team | 1.0004 (0.9996 to 1.0008) | – |
| Annual trend: 24/7 outreach team | 1.0008 (1.0000 to 1.0016) | – |
| p-value for difference in slopes | – | – |
| Non-24/7 outreach team vs. no outreach team | p = 0.394 | – |
| 24/7 outreach team vs. non-24/7 outreach team | p = 0.270 | – |
The three variables with evidence for an association were included in a single model in the next stage of the analysis (see Table 20). The impact on trends in the survival rate associated with a NEWS or NEWS-based TTS was no longer statistically significant (p = 0.122) after adjusting for the other two variables. Similarly, the change in trend associated with an electronic TTS was also no longer statistically significant (p = 0.361). There was suggestive evidence (p = 0.083) that a non-24/7 outreach team was associated with a lower rate of survival than no outreach team.
In the third stage of the analysis, the three variables included in the combined analysis in Table 20 were examined in the restricted samples of hospitals that changed intervention during the study. The results in Table 21 show no evidence of any statistically significant association for any of the interventions in these groups of hospitals.
| Intervention | Intervention, case mix-adjusted IRR (95% CI) | |
|---|---|---|
| Individual | Combined | |
| TTS | ||
| Hospitals changing from non-NEWS to NEWS/NEWS-based TTS (n = 52) | ||
| Annual trend: non-NEWS | 1.0008 (0.9984 to 1.0032) | 1.0006 (0.9982 to 1.0030) |
| Annual trend: NEWS/NEWS-based | 1.0004 (0.9980 to 1.0024) | 1.0004 (0.9982 to 1.0027) |
| p-value for difference in slopes | p = 0.682 | p = 0.865 |
| Hospitals changing from paper to electronic TTS (n = 18) | ||
| Annual trend: paper | 0.9984 (0.9936 to 1.0028) | 0.9978 (0.9927 to 1.0029) |
| Annual trend: electronic | 0.9976 (0.9932 to 1.0016) | 0.9982 (0.9940 to 1.0025) |
| p-value for difference in slopes | p = 0.688 | p = 0.858 |
| Outreach team | ||
| Hospitals changing outreach team (n = 11) | ||
| Non-24/7 outreach team (compared with no outreach team) | 0.9986 (0.9942 to 1.0030) | 0.9979 (0.9931 to 1.0028) |
| p-value for difference in levels | p = 0.532 | p = 0.408 |
| 24/7 outreach team (compared with non-24/7 outreach team) | 1.0012 (0.9965 to 1.0058) | 1.0016 (0.9965 to 1.0068) |
| p-value for difference in levels | p = 0.621 | p = 0.532 |
In the final stage of the analysis, shown in Table 22, the inclusion of the three secondary variables found no evidence for any difference in survival with respect to outreach team features (p = 0.374), handover features (p = 0.315) and contextual factors (p = 0.214). Including all three together in the same model made little difference.
| Variable | Intervention, case mix-adjusted IRR (95% CI) | |
|---|---|---|
| Individual | Combined | |
| Outreach team features (per additional feature) | 1.0002 (0.9998 to 1.0006) | 1.0002 (0.9998 to 1.0006) |
| p = 0.374 | p = 0.342 | |
| Handover features (per additional feature) | 0.9998 (0.9993 to 1.0002) | 0.9997 (0.9992 to 1.0002) |
| p = 0.315 | p = 0.185 | |
| Contextual factors (per additional factor) | 1.0004 (0.9998 to 1.0010) | 1.0004 (0.9998 to 1.0011) |
| p = 0.214 | p = 0.150 | |
Association between interventions and survival in in-hospital cardiac arrests
The analysis of survival in the 32,820 IHCAs attended by the resuscitation team in 106 hospitals is shown in Table 23. For the first outcome, the return of a spontaneous circulation that was sustained for > 20 minutes, there was no evidence that either a NEWS/NEWS-based or electronic TTS was associated with a difference in survival or a difference in trends. Similar results were found for hospital survival, survival to 30 days and survival to 90 days. For outreach, there was no evidence for a difference in the odds of survival (difference in levels) in any of the four survival outcomes. However, there was some evidence that the annual trend in odds of survival for 20 minutes was greater with a non-24/7 outreach team (OR 1.059, 95% CI 1.028 to 1.091) than it was for no outreach team (OR 0.992, 95% CI 0.959 to 1.026; difference in slopes p = 0.013). However, this difference was not observed in the other three outcomes.
| Intervention | Survival, case mix-adjusted OR (95% CI) | |||
|---|---|---|---|---|
| 20 minutes | Hospital | 30 days | 90 days | |
| TTS | ||||
| Non-NEWS | Reference | Reference | Reference | Reference |
| NEWS/NEWS-based | 1.019 (0.940 to 1.104) | 1.042 (0.935 to 1.160) | 1.046 (0.939 to 1.164) | 1.038 (0.929 to 1.160) |
| p-value for difference in levels | p = 0.655 | p = 0.457 | p = 0.414 | p = 0.507 |
| Annual trend: non-NEWS | 1.055 (1.031 to 1.080) | 1.046 (1.013 to 1.081) | 1.050 (1.016 to 1.084) | 1.043 (1.009 to 1.079) |
| Annual: NEWS/NEWS-based | 1.096 (1.040 to 1.156) | 1.024 (0.957 to 1.095) | 1.022 (0.955 to 1.093) | 1.024 (0.955 to 1.098) |
| p-value for difference in slopes | p = 0.237 | p = 0.602 | p = 0.518 | p = 0.673 |
| Paper | Reference | Reference | Reference | Reference |
| Electronic | 0.995 (0.885 to 1.119) | 1.055 (0.908 to 1.226) | 1.088 (0.936 to 1.263) | 1.072 (0.918 to 1.251) |
| p-value for difference in levels | p = 0.934 | p = 0.485 | p = 0.272 | p = 0.381 |
| Annual trend: paper | 1.070 (1.047 to 1.092) | 1.049 (1.019 to 1.080) | 1.047 (1.017 to 1.078) | 1.046 (1.015 to 1.078) |
| Annual trend: electronic | 1.043 (0.971 to 1.120) | 0.978 (0.892 to 1.073) | 1.004 (0.914 to 1.102) | 1.009 (0.917 to 1.110) |
| p-value for difference in slopes | p = 0.521 | p = 0.180 | p = 0.420 | p = 0.500 |
| Outreach team | ||||
| Non-24/7 outreach team (compared with no outreach team) | 0.996 (0.905 to 1.202) | 1.008 (0.868 to 1.171) | 0.985 (0.846 to 1.147) | 1.022 (0.878 to 1.190) |
| p-value for difference in levels | p = 0.949 | p = 0.914 | p = 0.848 | p = 0.778 |
| 24/7 outreach team (compared with non-24/7 outreach team) | 1.081 (0.965 to 1.211) | 1.014 (0.883 to 1.163) | 1.068 (0.928 to 1.230) | 1.005 (0.874 to 1.155) |
| p-value for difference in levels | p = 0.176 | p = 0.847 | p = 0.357 | p = 0.946 |
| Annual trend: no team | 0.992 (0.959 to 1.026) | 0.996 (0.954 to 1.041) | 1.007 (0.964 to 1.052) | 1.004 (0.960 to 1.051) |
| Annual trend: non-24/7 team | 1.059 (1.028 to 1.091) | 1.002 (0.965 to 1.040) | 1.007 (0.970 to 1.046) | 1.008 (0.970 to 1.049) |
| Annual trend: 24/7 team | 1.029 (0.998 to 1.060) | 1.047 (1.006 to 1.091) | 1.037 (0.996 to 1.080) | 1.036 (0.993 to 1.080) |
| p-values for difference in slopes | – | – | – | – |
| Non-24/7 team vs. no team | p = 0.013 | p = 0.879 | p = 0.999 | p = 0.908 |
| 24/7 team vs. non-24/7 team | p = 0.218 | p = 0.169 | p = 0.364 | p = 0.430 |
The second stage of the analysis involved examining the impact of the different trends in the return of a spontaneous circulation that was sustained for > 20 minutes in the restricted sample of 11 hospitals that changed their outreach provision during the study. The results were broadly consistent with those in Table 23, with a downward trend in those hospitals with no outreach team (OR 0.971, 95% CI 0.899 to 1.050) and an upward trend in those hospitals with a non-24/7 outreach team (OR 1.095, 95% CI 1.002 to 1.197). The statistical significance for the difference in slopes was p = 0.091. There was little evidence that the trend for 24/7 outreach (OR 0.985, 95% CI 0.890 to 1.091) differed from the trend for non-24/7 outreach (difference in slopes p = 0.204).
However, investigation of the impact of outreach in the 11 hospitals in terms of a change in levels (as opposed to a change in slopes) showed a reduction in survival following a change from no outreach team to a non-24/7 outreach team. This was observed for all measures of survival: 20-minutes survival OR 0.831 (95% CI 0.693 to 0.996; p = 0.045), hospital survival OR 0.687 (95% CI 0.540 to 0.874; p = 0.002), 30-day survival OR 0.664 (95% CI 0.522 to 0.846; p = 0.001) and 90-day survival OR 0.674 (95% CI 0.524 to 0.866; p = 0.002). There was no evidence for any difference in hospitals changing to 24/7 outreach from non-24/7 outreach. There was also evidence that the case mix of IHCAs changed following the introduction of outreach. The odds of a non-shockable IHCA increased in hospitals switching from no outreach team to a non-24/7 outreach team: OR 1.315 (95% CI 1.092 to 1.583; p = 0.004) after adjusting for all other case mix variables, excluding presenting rhythm.
Finally, both approaches (difference in levels and difference in slopes) were modelled together to examine the impact of outreach on the four measures of survival. No statistically significant associations were observed for an impact of outreach on any outcome (all p > 0.1). The magnitude of associations observed in previous analyses was also reduced. These findings support the general results in Table 23 that indicate a lack of evidence for an impact of TTSs or outreach on survival of IHCAs. The apparent better trend for improvement in 20-minute survival with non-24/7 outreach (see Table 23) was not supported in further analysis of the 11 hospitals that changed their outreach provision.
Secondary variables were examined in a case mix-adjusted analysis with no other interventions included (Table 24). There was some limited evidence that more outreach team features were associated with increased odds of 20-minute survival and hospital survival but this was not statistically significant at p < 0.05. There was no evidence that the number of handover features or the number of contextual factors were associated with differences in any of the four measures of survival.
| Variable | Survival, case mix-adjusted OR (95% CI) | |||
|---|---|---|---|---|
| 20 minutes | Hospital | 30 days | 90 days | |
| Outreach team features (per additional feature)a | 1.039 (0.995 to 1.086) | 1.054 (0.997 to 1.115) | 1.039 (0.980 to 1.101) | 1.042 (0.983 to 1.105) |
| p = 0.085 | p = 0.062 | p = 0.201 | p = 0.169 | |
| Handover features (per additional feature) | 1.025 (0.995 to 1.056) | 1.026 (0.991 to 1.062) | 1.016 (0.981 to 1.053) | 1.020 (0.985 to 1.056) |
| p = 0.101 | p = 0.141 | p = 0.379 | p = 0.268 | |
| Contextual factors (per additional factor) | 0.983 (0.950 to 1.017) | 0.982 (0.944 to 1.022) | 0.981 (0.942 to 1.021) | 0.990 (0.951 to 1.031) |
| p = 0.321 | p = 0.379 | p = 0.342 | p = 0.627 | |
Sensitivity analysis restricted to the smaller sample of 21,595 IHCAs attended by the resuscitation team that occurred on wards produced similar results to those from the primary analysis in Table 23. The ORs for NEWS/NEWS-based TTSs were larger but remained statistically non-significant for all survival outcomes. Survival was marginally better with NEWS/NEWS-based TTSs modelled as a difference in levels (ORs 1.028–1.105, p-values 0.182–0.574). The sensitivity analysis of annual trends also mirrored the primary analysis and produced results that marginally favoured NEWS for 20-minute survival (p = 0.055) and non-NEWS for other measures of survival (p = 0.178–0.495). Sensitivity analysis applied to electronic TTSs also produced similar results to those in Table 23. No statistically significant ORs were observed for a difference in levels (p-values 0.263–0.721) or a difference in slopes (p-values 0.425–0.914).
The primary analysis of survival indicated evidence for a difference in slopes (p = 0.013) favouring non-24/7 outreach (OR 1.059) compared with no outreach (OR 0.992). The sensitivity analysis produced similar results [OR 1.057 (non-24/7 outreach) and 0.992 (no outreach); p = 0.042]. No other comparisons of outreach were statistically significant in the sensitivity analysis (p-values 0.459–0.889).
The sensitivity analysis did produce different results to the analysis of secondary variables on survival shown in Table 24. This is most marked for the impact of outreach team features, with evidence for improved survival for all survival outcomes (Table 25). There is also some evidence that additional handover features are also associated with better odds of 20-minute survival. No significant results were observed for an association with contextual factors.
| Variable | Survival, case mix-adjusted OR (95% CI) | |||
|---|---|---|---|---|
| 20 minutes | Hospital | 30 days | 90 days | |
| Outreach team features (per additional feature)a | 1.060 (1.014 to 1.107) | 1.109 (1.047 to 1.174) | 1.104 (1.041 to 1.171) | 1.100 (1.037 to 1.168) |
| p = 0.010 | p < 0.001 | p = 0.001 | p = 0.002 | |
| Handover features (per additional feature) | 1.040 (1.008 to 1.074) | 1.034 (0.991 to 1.080) | 1.018 (0.974 to 1.065) | 1.022 (0.977 to 1.069) |
| p = 0.014 | p = 0.125 | p = 0.428 | p = 0.349 | |
| Contextual factors (per additional factor) | 0.988 (0.953 to 1.024) | 0.995 (0.949 to 1.044) | 0.992 (0.944 to 1.043) | 1.006 (0.958 to 1.058) |
| p = 0.508 | p = 0.842 | p = 0.759 | p = 0.803 | |
Discussion
Between 2009 and 2015 there was a downward trend in the rate of IHCAs attended by the resuscitation team, improvement in the survival of IHCA patients and improved survival across all patients admitted to hospital, whatever their diagnosis. There were only minor changes in the case mix of patients who experienced IHCAs over that period. The quantitative analysis of 106 hospitals sought to attribute improvements in IHCA rates and survival to differences in the provision of TTSs and outreach.
All hospitals used a TTS. The use of a NEWS or NEWS-based TTS, when compared with a non-NEWS TTS, was associated with an additional reduction above pre-existing trends of 8.4% in the rate of IHCAs. The use of an electronic TTS, compared with a paper TTS, was also associated with an additional reduction above pre-existing trends of 7.6% in the rate of IHCAs. Restricting IHCAs to ward-based arrests increased the reduction to 9.9% for NEWS or NEWS-based TTSs and to 13.1% for electronic TTSs. There was no evidence of an association between the type of TTS and survival of all hospital admissions, or on any of the measures of survival of patients who had an IHCA.
There was no evidence of an association between the type of outreach (none, a non-24/7 team or a 24/7 team) and the rate of IHCAs. There was also little evidence for an association between outreach and overall hospital survival or survival after IHCA in the analysis of all 106 hospitals. An apparent trend for improved short-term survival when going from no team to a non-24/7 outreach team was not supported by further analysis of the 11 hospitals that changed their outreach provision. When the analysis was restricted to ward-based IHCAs only, there was significant association between the 2015 cross-sectional variable outreach team features (reflecting intensity of implementation through team composition, function, autonomy and ability to meet demand) and both short-term (return of a spontaneous circulation for > 20 minutes and survival at hospital discharge) and longer term (30-day and 90-day) IHCA survival. This was also true for the handover variable (reflecting intensity of handover tool promotion) and short-term IHCA survival (return of a spontaneous circulation for > 20 minutes).
Strengths and limitations
This was a large study that included 106 hospitals with > 32,000 IHCAs in > 13 million hospital admissions. Potential confounding factors have been controlled for by adjustment for case mix, and temporal trends and seasonal differences have also been controlled for. The approach to the analysis investigated the consistency of results between the larger sample of 106 hospitals and the smaller groups of hospitals that changed their TTS or outreach provision during the study to ensure that findings are robust. This approach, together with the modelling of hospitals as random effects, provides some protection against unmeasured hospital-level confounding factors. However, there remains the possibility of residual confounding because of incomplete adjustment for patient case mix and other hospital factors that are time varying.
The study also relied on the accurate measurement of the interventions in the hospitals and the specification of the type of impact (difference in levels and difference in slopes) that these interventions might have. Mis-specification in either would generally reduce the study’s ability to detect a true impact of an intervention. The focus on three primary interventions reduced the risk of statistically significant findings arising by chance. However, the limited number of hospitals that changed their TTS and outreach provision during the study meant that the study lacked power to examine interactions between interventions and their impact on IHCA rates and survival. Under-reporting of attended cardiac arrests to NCAA will also reduce the power of the study to detect changes in outcomes. Our survey found that 13% of hospitals reported a case ascertainment of < 90%.
Chapter 6 Discussion
Overview of findings
Objective 1: to design a typology of interventions based on previous research and an understanding of how interventions are implemented in England
Given the heterogeneity of the interventions and the contexts in which they were implemented, plus the fact that many studies did not provide an adequate level of detail of either the intervention or the context, it was not possible to create a typology of interventions designed to recognise and respond to patient deterioration based on this literature. Deeper understanding of how interventions were being implemented in practice was derived from qualitative work within NHS hospitals which, in turn, informed the information gathered by the survey.
Track-and-trigger systems
Internationally, the introduction of TTSs has been shown to be effective in improving the recording of one or more vital signs, although the impact on patient outcomes is less clear. Following the introduction of a single, standard tool, NEWS, by the RCP in late 2012, there has been a gradual uptake across the NHS, and by the end of 2015, paper-based NEWS had replaced a number of other paper-based TTSs, with nearly 50% of NCAA hospitals reporting its use. In addition, a substantial increase in the use of electronic TTSs was seen from 2013 onwards, reaching almost 30% in 2015. Two-thirds of electronic TTSs were also based on the NEWS.
This widespread adoption of the NEWS by the NHS has been regarded positively, increasing familiarity amongst clinical staff and increasing the safety of delegation of the task of taking observations to HCAs. Having objective information about a patient’s condition has empowered nurses and strengthened their confidence in knowing when to call for help. However, local modifications, missed observations, miscalculations of scores and a lack of clinical experience amongst those taking observations were all seen as threats to the effectiveness of the tool in identifying and responding to at-risk patients. Electronic systems that necessitated entry of a full set of observations, automatically calculating the patient’s EWS and directly alerting the appropriate responder, were felt to overcome the main limits of the paper-based system. Those hospitals that were yet to adopt the NEWS usually had a well-established TTS in place and were concerned that there was not an adequate evidence base to justify the change, the workload implications of the change or the degree of risk to which the organisation might be exposed during the upheaval.
Outreach teams
Following the publication of the DHSC’s strategy to provide an integrated hospital-wide approach to critical illness in 2000,12 there has been a gradual adoption of nurse-led RRTs, commonly known as outreach teams, across the NHS. Accumulating evidence from before-and-after studies indicate that RRTs reduce cardiac arrest rates and, to a lesser extent, mortality. 47 Although a few studies with a more robust design (three interrupted time-series and one RCT) show a reduction in the incidence of cardiac arrests,163–165 only one study shows that this translates into a fall in hospital-wide mortality. 83 Furthermore, the majority of the evidence comes from countries where RRTs have been doctor led rather than nurse led. By 2015, 83% of NCAA hospitals reported having an outreach team, with a trend towards increasing hours since 2009 (24/7 team coverage rose from 25% to 40%).
The overarching roles (clinical care for critically ill patients on the ward, end-of-life decision-making and education and quality assurance) for outreach teams were similar across the hospitals. However, there was little uniformity in terms of team composition (nursing grade or inclusion of allied health professionals), hours of coverage, level of autonomy (in areas such as prescribing or arranging admissions to the ICU) or proportion of time devoted to education or improvement activities. Teams’ involvement in end-of-life discussions, combined with increased awareness and use of DNACPR decisions or treatment limitation plans across the NHS, were felt to have reduced the number of inappropriate resuscitation attempts by excluding patients who were likely to have a poor outcome. However, some staff reported that external factors, such as the impact of the Tracey case,60 had countered some of this progress.
A common theme was the role of outreach in monitoring and improving the care of acutely ill patients across the hospital through provision of training and quality assurance/improvement activities related to TTSs, and by identifying gaps in capacity on the wards. Increasing workload, driven by the need to substitute for experienced ward nurses and junior doctors, threatened this hospital-wide role, particularly reducing opportunities for educating ward staff around the care of acute illness. A board-level champion could ensure that the team retained a broad role. On the other hand, limited resources stifled team growth, particularly where team members had difficulty convincing their organisation that there was a problem that required addressing, such as increasing rates of out-of-hours cardiac arrests.
Structured handover tools
Poor communication of vital patient information across different professional groups can lead to delays in tackling patient deterioration. 140 Evidence suggests that handover tools lead to improvements in information transfer and fewer omissions. The SBAR tool was first adapted for use in health care in the USA and then advocated for use in the NHS in 2012 by the NHS Institute for Innovation and Improvement. 28 A total of 87.7% of NCAA hospitals reported its introduction by 2015, along with a variety of promotional activities from education to visual reminders. We were unable to determine actual frequency of use; however, nursing staff expressed reluctance to use it as it felt an unnatural way to communicate, especially in front of patients.
Educational interventions
A range of educational interventions, including both formal classroom sessions and simulation-based training, have been shown to improve doctors’ and nurses’ confidence and knowledge when caring for acutely ill patients. The impact on patient outcomes has rarely been considered. The majority of hospitals ran formal courses directed at improving ward-based management of acutely ill patients, such as the multiprofessional ALERT™ course. It was felt that these courses would become increasingly redundant because the content was gradually being included in undergraduate medical and nursing courses. Much value was placed on ward-based teaching in which junior staff could learn while providing care to patients. Despite education having an important role in empowering nurses to raise concerns with medical teams, time for ward-based teaching was often limited by ongoing workload demands.
Across the constituent interventions making up the rapid response system, increasing uniformity had developed in the afferent (trigger) arm with 70% of NCAA hospitals implementing either paper-based or electronic NEWS by 2015, and nearly 90% reporting that SBAR was the main standardised communication tool in use. The efferent (response) arm shows more variability in organisation. Hospitals exhibited differing levels of service intensity based on elements of Carroll’s model of implementation fidelity,65 such as intervention content or coverage. This is particularly seen in the configuration of TTSs or outreach. A hospital providing a 24/7 outreach team or one with an electronic TTS has more intense service provision than a hospital with daytime-only outreach services or using paper-based NEWS. Key contextual factors were changing in the environments in which rapid response systems were functioning, particularly the increasing awareness of the need for improved end-of-life planning. This was affecting familiarity and use of DNACPR decisions and the number of patients with a poor prognosis of surviving CPR who might end up receiving it. However, influences, such as the legal requirement for patients and relatives to be informed when a DNACPR decision is put in place (as a result of the 2014 Tracey case legal ruling60) or the lack of support clinicians felt from their organisations when initiating a DNACPR decision against relatives’ wishes, made the overall impact of such changes difficult to establish. There was still a sense that some appropriate patients did not have treatment limitations in place, leading to futile resuscitation attempts.
Objective 2: to determine the association between different arrangements of interventions and in-hospital cardiac arrest incidence and outcomes
-
Across 106 NCAA hospitals there was a reduction in IHCA rates of 6.4% per year and increased hospital survival after arrest rates of 4.8% per year.
-
Use of the NEWS was associated with an additional 8.4% lower rate of IHCAs compared with pre-existing trends, and the introduction of an electronic TTSs was associated with an additional 7.6% reduction compared with pre-existing trends. Restricting the analysis to ward-based arrests lowered rates by 9.9% and 13.1% for NEWS and electronic TTSs, respectively.
-
This study was not adequately powered to test the interaction between NEWS and electronic TTS interventions to determine if their individual associations with IHCAs were additive.
-
Outreach teams, either non-24/7 or 24/7, were not associated with a reduction in IHCA rates.
-
Neither NEWS nor electronic TTSs were associated with additional reductions in short (return of a spontaneous circulation for > 20 minutes), medium (survival to discharge) or longer-term (30- or 90-day) survival following an IHCA.
-
Overall, outreach teams had no impact on short- or long-term survival over time.
-
When analysis was restricted to ward-based IHCAs in 2015, increased intensity of outreach team implementation was associated with both better short- and long-term IHCA survival. Increased intensity of promotion of handover tools was associated with better short-term survival.
Objective 3: to identify service features associated with the lowest in-hospital cardiac arrest incidence and best outcomes
Our study set out to test a number of hypotheses of how interventions designed to detect and respond to patient deterioration on the ward might have an impact on the rate of IHCAs for which a resuscitation attempt was made and on the short- and longer-term survival of those patients. Continuing education interventions were dropped from this analysis after findings from the qualitative interviews and piloting of the survey suggested that there would be limited variability in provision across NCAA hospitals and across our index years. Following the survey, structured handover was also dropped from the time-series analysis as SBAR was in place in around 90% of hospitals. The hypotheses were revised to reflect the focus of the analysis on TTSs and outreach teams.
The use of TTSs will reduce IHCA rate by identifying deteriorating patients earlier while there is greater opportunity of reducing their risk of arresting.
Both NEWSs and electronic TTSs were associated with reductions in IHCA rates compared with pre-existing trends, but we were unable to confirm whether or not these separate associations were additive. This observation may be due to these two tools enabling the early identification of deteriorating patients. It has been established that physiological changes in heart rate, blood pressure, respiration rate and oxygen saturations precede most cardiac arrests and that these measures can predict cardiac arrest, admission to the ICU and mortality. 7,140 The TTSs promote the monitoring of physiological parameters, the calculation of risk-based scores based on these observations and provide graded guidance on action at particular score thresholds. A reduction in cardiac arrests may result from enabling ward staff to make early, simple interventions known to be effective in reversing deterioration, such as providing oxygen to a patient35,166 or by empowering the sharing of concerns about patients with appropriate responders. Such action may lead to an increase in the number of patients transferred to the ICU. The TTS is a system-wide intervention that has the potential to improve the performance of the afferent (trigger) arm of the rapid response system across the whole hospital. Introduction of the NEWS has standardised the TTSs used in the NHS and reduces some of the barriers to effectiveness found in previous studies, including unfamiliarity with the scoring system or response algorithm. 41 The introduction of an electronic TTS would be expected to counter known problems with paper-based TTSs, such as failure to undertake all required observations, miscalculation or the reluctance of ward staff to trigger the appropriate responses. 41,42
However, there may be other indirect mechanisms by which NEWSs and electronic TTSs may influence IHCA rates: they may change the number of patients who are eligible for resuscitation by encouraging ward staff to engage in the process of making DNACPR/end-of-life decisions as a result of recorded deterioration. Our study does not allow us to ascertain easily the contribution of such indirect mechanisms to the lowering of the IHCA rates. An analysis of changes in case mix between 2009 and 2015 in those patients undergoing resuscitation did not show any major differences across the years that might imply a substantial shift in the numbers of patients with poorer health becoming ineligible for resuscitation through the implementation of DNACPR decisions. Both direct and indirect mechanisms represent good care as long as they are appropriate responses for individual deteriorating patients.
-
The use of TTSs will have no association with survival following an IHCA.
Our findings that indicate no association between TTSs and either short- or long-term IHCA survival support this hypothesis. This finding was not unexpected given that the response arm of the rapid response system and intra- and post-cardiac arrest care are likely to have a greater influence. 63
-
Outreach teams will reduce IHCA rates by reducing the risk of deteriorating patients arresting more than traditional patterns of response from ward staff.
Our findings do not support this hypothesis. We found no association between either non-24/7 or 24/7 outreach teams and cardiac arrest rates. It had been expected that, through delivery of their key objectives of strengthening critical care skills amongst ward staff, supporting ward staff in the management of acutely ill patients and promoting the uptake of TTSs,12 outreach teams would be associated with a reduction in IHCA rates, with the greatest impact seen in hospitals with the most intensive services. Our findings may reflect that outreach teams form only part of the efferent or response arm of the rapid response system and that their individual effect cannot be separated from other response mechanisms, or that it does not particularly matter how the response is provided as long as the afferent arm is effective at identifying patients at risk and ensuring that the response is timely. Outreach teams may be making a greater contribution to the functioning of the afferent arm rather than the efferent arm through their education and support activities related to TTS implementation. However, the fact that configurations and roles of teams are still as variable as described in the findings of a previous national survey53 would also limit the strength of association found between these teams and IHCA rates at a hospital level. Furthermore, the nature of the introduction of the intervention across hospitals also affects the strength of association with outcomes. The faster and more widespread introduction of the NEWS provides a stronger signal compared with the more gradual transition to fully operational outreach teams, many of which were adaptions of local arrangements already in place.
These findings are not consistent with those from the majority of studies evaluating RRTs, which have found reductions in cardiac arrest rates. 47 However, given that the organisation and implementation of teams in these studies is heterogeneous and that their introduction is invariably associated with the simultaneous introduction of a TTS or a revision of the TTS response criteria, it is possible that the implementation of TTSs represent an alternative mechanism by which this effect on arrest rates is achieved. The evidence for nurse-led teams (as opposed to doctor-led teams) is mixed, with only half of the studies showing a positive association with IHCAs. 48 Most studies of RRT have an uncontrolled before-and-after design. The small number with more robust designs have shown a mixed picture with half of the studies showing a reduction in cardiac arrests (all nurse-led teams)163–165 and the other half showing no reduction. 76,77,82 None of these studies showed any change in hospital mortality. The largest of these, the MERIT study,82 was a cluster randomised trial of doctor-led RRTs in Australia that found no impact; however, there were major design limitations, not least the low number of team activations triggered (30%) despite a larger group of patients having clearly fulfilled the calling criteria.
-
Outreach teams will increase survival following a cardiac arrest by increasing the application of treatment limitation decisions, such as DNACPR, in deteriorating patients at a high risk of an unsuccessful resuscitation.
Our findings from the time-series analysis did not support this hypothesis. We found that the presence of an outreach team was not associated with a change in short- or longer-term survival of patients who have had an arrest. In addition, there was no association found between outreach team presence and hospital survival. However, there was an association between increasing intensity of outreach team provision in 2015, as reflected by the team composition, roles, autonomy and ability to meet demand, and both short- and long-term survival. By playing a role in end-of-life care and the implementation of DNACPR decisions in patients for whom CPR would be futile, outreach teams can reduce the number of patients with the highest risk of death undergoing CPR. 50
Strengths and limitations
Evaluating the impact of complex health service interventions that have developed organically, are not protocol driven and show marked heterogeneity is a challenge, especially once these services are already established across the country. Such a scenario precludes a RCT design. An observational study is the only option for studying these interventions at scale and the robustness of the approach is strengthened when, as in this case, it utilises large data sets collected from across many organisations in the analysis (106 acute hospitals covering a total of 13 million admissions).
This natural experiment exploited the variation that exists between established services and changes in service configurations over time to determine the association between those services and patient outcomes of interest. It also optimised the use of available data without the costs of bespoke data collection. The interrupted time-series design controlled for longer-term trends, which is not possible with simple before-and-after studies.
This was the first study to use data from the NCAA database linked to HES and ONS data. This audit collects data on patients who have chest compressions or defibrillation in hospital following an emergency call. The NCAA is a high-quality database and has inbuilt mechanisms to ensure accurate data entry. This is the only source of routinely collected information on IHCAs available in England. Prior to the audit, recording of these arrests happened in clinical records and was rarely collated across organisations. Focusing only on those arrests that elicit a resuscitation team visit (based on the 2222 call) provides an objective count of the majority of arrests. We do not believe that the audit misses many other IHCAs (that do not generate a 2222 call), other than those occurring in patients with DNACPR decisions in place and those occurring on CCUs, HDUs and ICUs where a resuscitation team is unlikely to be called. Given the different reporting practices amongst NCAA hospitals, around 60% of arrests in the audit are ward based, with the remainder occurring in settings such as HDUs, radiology departments or operating theatres. As these are areas in which the interventions under examination in the study are less likely to have an impact, we also conducted a sensitivity analysis to determine the association between the interventions and ward-only IHCAs. The number of hospitals in the audit has been growing steadily since its inception and around 70% of English NHS acute hospitals were participating in 2015 at the time of our organisational survey. The response rate of 81% suggests that our findings are representative of English acute hospitals.
Inevitably, there are limitations to our approach that might have introduced bias. For the organisational survey, we were unable to determine if survey responders differed from non-responders for any characteristics other than geographical location and the length of time they had participated in the NCAA. Non-responding hospitals may have differed systematically with regard to the intensity of their interventions. The survey was limited in size to promote a good response rate. It was therefore not possible to explore all aspects of the interventions and the contextual factors that have influenced their implementation. For example, we did not collect data on the ‘dose’ of outreach, a factor that may be an important element of team effectiveness. 47,156
Furthermore, we did not gather information on other differences in service configuration that may determine effectiveness, for instance, what response systems were being used in hospitals that reported having no outreach team. This limitation might have had a greater impact on findings for outreach teams compared with those for TTSs. Respondents found some of the contextual questions hard to answer because of a lack of direct access to the required information. This led to more missing data for these questions. We had to simplify the reporting of organisational arrangements for the analyses; for example, for outreach teams, a non-24/7 team could include teams that cover 09.00–17.00, 08.00–20.00, weekdays only or weekdays and weekends. It was also difficult to elicit variation in handover tools or formal education courses, limiting our ability to include these interventions in the time-series analyses. The time-dependent data collected in the survey required respondents’ recall, which had the potential to lead to inaccuracies. In addition, there is under-reporting of attended cardiac arrests to the NCAA. In our survey, 22% of hospitals reported a case ascertainment of < 90%.
For interventions showing marked heterogeneity, such as outreach teams, it is likely that only a relatively strong association between the intervention and the outcome will be detectable. Given that observational methods cannot determine causality, it does not follow that a lack of association indicates that a particular intervention is ineffective; it may instead reflect that either the impact is too weak to detect or that the mechanism of action for the intervention is via an alternative pathway that does not change the outcome under study. As the rapid response system is a complex system with interdependent components, it may be artificial to look at the impact of individual interventions rather than looking at outcomes for the system as a whole.
One possible source of confounding when estimating the association between interventions and both cardiac arrest rates and survival will be changes in the proportions of patients with DNACPR decisions over time. Such changes could lead to both fewer cardiac arrests and better survival because of alteration in the case mix of attended arrests and is likely to account for some of the pre-existing improvement in cardiac arrest rates and survival that we found. Five NCAA Trusts across England, who had undertaken audits of DNACPR decisions across time, reported rates of DNACPR decisions of around 85–89% in patients who die. Over the 2009–15 period, three hospitals showed no change in these rates, one showed a decline (10%) and one showed an increase (15%). These findings indicate that some NCAA hospitals may have been seeing changes in levels of DNACPR decision-making during the study period. However, investigation of trends in case mix amongst those that experienced an IHCA during the study period showed only minor changes across sex and in the proportions of emergency versus elective patients, which suggests that any major effect related to increasing the use of DNACPR decisions was unlikely. A lack of data on rates of DNACPR decisions prevented us from further establishing the degree to which changes in the use of these decisions was influencing outcomes.
Another hypothesis from our findings is that TTSs do little to prevent deterioration in patients already at high risk of a poor outcome and that when these patients go on to have an IHCA they usually die once transferred to the ICU. These arrests would generally not feature in the NCAA audit. If this were the case, it would be possible to detect a lowering of NCAA IHCA rates, while at the same time finding no overall improvement in hospital mortality. Given the complex range of factors that drive ICU admissions, we were not able to determine the degree to which this alternative explanation might be driving the observed findings.
Implications for policy and practice
Pre-existing trends across NCAA hospitals indicate decreasing rates of IHCA and increasing rates of survival. The introduction of the NEWS and of electronic TTSs has been associated with a decrease in IHCAs requiring resuscitation over and above the pre-existing declining trend. However, there was no association with survival of such patients and on overall hospital mortality. These findings suggest that improvements in the afferent arm of the rapid response system, through increased standardisation and systems that both facilitate correct score calculation and automate the triggering of a response, may have the greatest potential to reduce avoidable mortality associated with a failure to recognise and respond to deteriorating patients on the ward. This is consistent with findings from Australia. 50
Our findings suggest that implementation of TTSs is not without difficulties. There are risks associated with the transition from a well-embedded system to a new and unfamiliar one. TTSs may encourage staff to prioritise scores over clinical intuition, leading to late responses in some cases. 167 There may also be issues with a lack of sensitivity in particular patient subgroups. 168 Despite reports of modifications to the NEWS by individual hospitals to address the latter, the observed positive impact on cardiac arrest rates indicates that sufficient fidelity to purpose has survived such changes. Future development of electronic TTSs to include laboratory results may allow earlier intervention before physiological instability happens. 169
The lack of evidence of a statistically significant improvement in either IHCA rates or survival for outreach teams across time should not be interpreted as evidence of ineffectiveness. It is possible that outreach does in fact contribute to trends in IHCA reduction through provision of support for TTSs. Our findings do not provide a clear picture on the best configuration for responding to deterioration. It may not matter how the response is provided, including whether or not it is formalised as a team, as long as it is prompt at reversing patient decline. The association between implementation intensity and short- and longer-term survival following an IHCA suggests that the outreach team’s impact on end-of-life planning may be affected by team capacity.
It could be argued that changes in cardiac arrest rates, survival and overall hospital mortality over time are not the best outcome measures to evaluate outreach-team impact. A mature team can only review between 2% and 8% of hospital admissions,170,171 many of which were not destined to go on to have an IHCA. 172 Outreach activities, such as clarification of goals of care or empowering ward staff to continue with the course of action already embarked on,51,127 contribute to improving the quality of care for patients who are acutely unwell, but such benefits may not be captured by the metrics considered in this study. A recently introduced audit tool, Multi-disciplinary Audit Evaluating Outcomes of Rapid Response (MAELOR),127 advocates the assessment of the proportion of positive and negative interventions undertaken 24 hours after the initial team call out. These interventions relate to the following outcomes: transfer to the ICU (timely or delayed), alive on ward (TTS no longer triggering or still triggering) and deceased (was on terminal care pathway/with DNACPR decision or following cardiopulmonary arrest). 127
It has been proposed that IHCA rates could be a useful indicator of the quality of care for acutely ill patients on hospital wards. 63 The NCAA audit captures only those events that result in an emergency call and consequent chest compressions or a defibrillation attempt by the resuscitation team. It excludes arrests occurring in an ICU or a CCU to which the hospital resuscitation team is not usually called. Around two-thirds of the arrests in the audit are ward-based. 6 The NCAA, which now covers around 70% of acute hospitals in England, indicates that these arrests are rare and becoming rarer, with the average hospital seeing around 50 IHCAs associated with resuscitation each year. 6,32 With such small numbers, the likelihood of chance variation over time and between hospitals is quite high. Apart from chance, variation in IHCAs between hospitals reflects an interplay between case mix, interventions that alter the number of patients eligible for resuscitation, and prevention of deterioration. Differences in case mix can be adjusted for using a variety of approaches, but there will always be residual unadjusted differences, particularly in relation to the severity of patients’ diseases. Currently, the scale of impact of changes in the use of DNACPR decisions on the number of patients undergoing CPR is unknown. Teasing out the contribution of hospital factors, such as changes in end-of-life care, from the impact of interventions preventing deterioration are difficult without more detailed data.
Implications for research
There are several fruitful avenues that might be pursued in future research. First, a study to assess the potential impact of outreach teams at a hospital and patient level would be helpful in understanding the factors that might enable such teams to have a greater impact and would help identify the best models for this service. Qualitative research looking at organisational and delivery factors (input and process factors), including aspects such as leadership, relationship with ward staff, attitudes and beliefs, and substitution for medical staff, will help elucidate barriers to and enablers of effective outreach services. In turn, this work would support development of process indicators to determine if an outreach team is working well, which could be used in further quantitative evaluations. Both the implementation period and dose of the intervention would need to be adequate. Consideration of a wider range of outcome measures could be part of this research.
Second, it is not clear what impact modifications to the NEWS have on the tool’s sensitivity and specificity, and a ward-based study could clarify this. Third, a greater understanding of the impact of different elements of the NEWS (such as complete observation sets, correct calculation of scores or automatic escalation) on outcomes would help determine the degree of added value that electronic tools might bring to reducing IHCAs compared with paper-based TTSs. This should be accompanied by an economic evaluation of electronic NEWS to determine the full range of costs associated with any better outcomes.
Finally, it would also be useful to establish the best approach to collecting data on the implementation and impact of treatment limitation plans and DNACPR decisions.
Conclusions
Since 2012, there has been widespread adoption of a standard EWS (NEWS) across NHS hospitals and an increase in the use of electronic monitoring systems. Both interventions were associated with reductions in IHCA rates that were additional to pre-existing declining trends. It is likely that positive associations between the NEWS, electronic TTSs and IHCAs may be related to a variety of mechanisms including early identification of patient deterioration and institution of treatment on the wards, timely transfer to the ICU if required and implementation of DNACPR decisions when appropriate. Further research is required to establish the impact of these different mechanisms on patient outcomes. The majority of NHS hospitals have outreach teams in place with similar overarching roles of supporting care for acutely ill patients on the wards, engaging in end-of-life decision-making and education and quality assurance. However, the teams remain heterogeneous in staff composition, coverage and autonomy. There was no association between outreach team implementation and IHCA rates and survival over time. This may be a result of how the teams have been introduced in hospitals, their heterogeneity or the fact that they do not have a direct impact on the study outcomes. The association between team intensity and improved IHCA survival may indicate that teams with more capacity are more likely to engage in DNACPR decision-making. Further research is required to determine the impact of outreach teams on hospitals and individual patients.
The findings suggest a stronger association between the afferent arm of the rapid response system and IHCA rates, and that configuration of the efferent response arm may be less important as long the response is timely. The use of IHCA rates as an indicator of the quality of care of acutely ill patients on hospital wards is challenging because of the rarity of the event, the need for case mix adjustment to make fair comparisons and the challenge of determining the impact of key confounders, such as changing DNACPR decision rates.
Acknowledgements
We are extremely grateful to the NHS staff who took part in the qualitative interviews and the organisational survey and to the National Outreach Forum who publicised the survey. The support of staff from the ICNARC and the NCAA was invaluable in conducting this research. Ms Rebecca Zipfel (Research Assistant, London School of Hygiene & Tropical Medicine) contributed to the literature review and undertook qualitative interviews, Ms Laura Doubleday (Research Assistant, London School of Hygiene & Tropical Medicine) and Ms Katie Ferguson (Public Health Speciality Registrar, London School of Hygiene & Tropical Medicine) actively followed up survey responses to ensure a good response rate.
We would like to thank all the members of our SG for their expert contributions and, in particular, our patient representatives. The members of the SG were Mrs Viv Cummin (patient representative), Mr Chris Whitman (patient representative), Professor Jerry Nolan (Consultant In Anaesthesia And Intensive Care Medicine, Royal United Hospital, Bath; Honorary Senior Lecturer, University of Bath; Chair of the Research Subcommittee of the Resuscitation Council UK), Professor Kathy Rowan (Director Of Scientific And Strategic Development, ICNARC), Dr Martin Kuper (Consultant In Intensive Care Medicine And Anaesthesia, Department of Anaesthesia; Medical Director, Homerton University Hospital NHS Foundation Trust), Dr Steve Harris (Consultant In Intensive Care Medicine And Anaesthesia, Department of Anaesthesia, University College London Hospitals NHS Foundation Trust) and Ms Anne Schlattl (Consultant Nurse For Acute Care, University College London Hospitals NHS Foundation Trust).
Contributions of authors
Dr Helen Hogan (Associate Professor of Public Health, London School of Hygiene & Tropical Medicine) was principal investigator and responsible for the design and conduct of the study and is lead author of the report.
Mr Andrew Hutchings (Assistant Professor, London School of Hygiene & Tropical Medicine) was a co-applicant and member of the study management group, led on the design and conduct of the quantitative analysis and was a co-author of the report.
Mr Jerome Wulff (Statistician, ICNARC) was a member of the study management group, undertook the quantitative analysis and was a co-author of the report.
Dr Catherine Carver (Research Fellow, London School of Hygiene & Tropical Medicine) was a member of the study management group and led on the qualitative interviews, literature review, design and implementation of the organisational survey and was a co-author of the report.
Ms Elizabeth Holdsworth (Research Fellow, London School of Hygiene & Tropical Medicine) was a member of the study management group and led on the analysis of the qualitative interview, analysis of the organisational survey and was a co-author of the report.
Mr John Welch (Consultant Nurse for Critical Care Outreach, University College London Hospitals NHS Foundation Trust) was a co-applicant and member of the study management group, contributed to the design and analysis of the study and overall interpretation of findings and was a co-author of the report.
Dr David Harrison (Senior Statistician, ICNARC) was a co-applicant and member of the study management group, contributed to the design and analysis of the quantitative work package and overall interpretation of findings and was a co-author of the report.
Professor Sir Nick Black (Professor of Health Services Research, London School of Hygiene & Tropical Medicine) was a co-applicant and member of the study management group, had the original idea for the study, contributed to the design, analysis and overall interpretation of findings and was a co-author of the report.
Publication
Hogan H, Carver C, Zipfel R, Hutchings A, Welch J, Harrison D, Black N. Effectiveness of ways to improve detection and rescue of deteriorating patients. Br J Hosp Med 2017;78:150–9.
Data-sharing statement
This study utilised a linked NCAA–HES–ONS data set that cannot be disseminated further because of conditions attached to initial release to the authors. All queries should be submitted to the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Reducing Avoidable Deaths (Medical Directors). London: Department of Health and Social Care; 2007.
- Benning A, Ghaleb M, Suokas A, Dixon-Woods M, Dawson J, Barber N, et al. Large scale organisational intervention to improve patient safety in four UK hospitals: mixed method evaluation. BMJ 2011;342. https://doi.org/10.1136/bmj.d195.
- Hutchings A, Durand M, Grieve R, Harrison D, Green J, Cairns J, et al. Evaluation of the Modernisation of Adult Critical Care Services in England. Research Report. London: National Institute for Health Research, Service Delivery and Organisation Programme; 2009.
- Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med 2007;33:237-45. https://doi.org/10.1007/s00134-006-0326-z.
- Roberts D, Hirschman D, Scheltema K. Adult and pediatric CPR: attitudes and expectations of health professionals and laypersons. Am J Emerg Med 2000;18:465-8. https://doi.org/10.1053/ajem.2000.7338.
- Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation 2014;85:987-92. https://doi.org/10.1016/j.resuscitation.2014.04.002.
- Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest 1990;98:1388-92. https://doi.org/10.1378/chest.98.6.1388.
- Smith AF, Wood J. Can some in-hospital cardio-respiratory arrests be prevented? A prospective survey. Resuscitation 1998;37:133-7. https://doi.org/10.1016/S0300-9572(98)00056-2.
- Tirkkonen J, Tamminen T, Skrifvars MB. Outcome of adult patients attended by rapid response teams: a systematic review of the literature. Resuscitation 2017;112:43-52. https://doi.org/10.1016/j.resuscitation.2016.12.023.
- McQuillan P, Pilkington S, Allan A, Taylor B, Short A, Morgan G, et al. Confidential inquiry into quality of care before admission to intensive care. BMJ 1998;316:1853-8. https://doi.org/10.1136/bmj.316.7148.1853.
- Goldhill DR, White SA, Sumner A. Physiological values and procedures in the 24 h before ICU admission from the ward. Anaesthesia 1999;54:529-34. https://doi.org/10.1046/j.1365-2044.1999.00837.x.
- Comprehensive Critical Care: A Review of Adult Critical Care Services. London: Department of Health and Social Care; 2000.
- An Acute Problem?. London: National Confidential Enquiry into Patient Outcome and Death; 2005.
- Time to Intervene? A Review of Patients Who Underwent Cardiopulmonary Resuscitation as a Result of In-Hospital Cardiorespiratory Arrest. London: National Confidential Enquiry into Patient Outcome and Death; 2012.
- Cresswell B, Marron C, Hawkins W, Harrison E, Fitzgerald E, Roon A. Optimising Working Hours to Provide Quality in Training and Patient Safety. A Position Statement by the Association of Surgeons in Training. London: Association of Surgeons in Training; 2009.
- The Implementation of the Working Time Directive, and Its Impact on the NHS and Health Professionals: Report of the Independent Working Time Regulations. London: Royal College of Surgeons; 2014.
- Addicott R, Maguire D, Honeyman M, Jabbal J. Workforce Planning in the NHS. London: The King’s Fund; 2015.
- Buchan J, Seccombe I, Gershlick B, Charlesworth A. In Short Supply: Pay Policy and Nurse Numbers. Workforce Profile and Trends in the English NHS. London: Health Foundation; 2017.
- Aiken LH, Sloane D, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, et al. Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual Saf 2017;26:559-68. https://doi.org/10.1136/bmjqs-2016-005567.
- State of the Health System. Beds in the NHS: England. London: British Medical Association; 2017.
- Harris S, Singer M, Rowan K, Sanderson C. Delay to admission to critical care and mortality among deteriorating ward patients in UK hospitals: a multicentre, prospective, observational cohort study. Lancet 2015;385. https://doi.org/10.1016/S0140-6736(15)60355-5.
- Bright D, Walker W, Bion J. Clinical review: Outreach – a strategy for improving the care of the acutely ill hospitalized patient. Crit Care 2004;8:33-40. https://doi.org/10.1186/cc2377.
- McArthur-Rouse F. Critical care outreach services and early warning scoring systems: a review of the literature. J Adv Nurs 2001;36:696-704. https://doi.org/10.1046/j.1365-2648.2001.02020.x.
- Acutely Ill Patients in Hospital: Recognition of and Response to Acute Illness in Adults in Hospital. NICE Clinical Guideline CG50. London: National Institute for Health and Care Excellence; 2007.
- Hogan H, Healey F, Neale G, Thomson R, Vincent C, Black N. Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual Saf 2012;21:737-45. https://doi.org/10.1136/bmjqs-2011-001159.
- Donaldson LJ, Panesar SS, Darzi A. Patient-safety-related hospital deaths in England: thematic analysis of incidents reported to a national database, 2010–2012. PLOS Med 2014;11. https://doi.org/10.1371/journal.pmed.1001667.
- Recognising and Responding Appropriately to Early Signs of Deterioration in Hospitalised Patients. London: National Patient Safety Agency; 2007.
- Quality and Service Improvement Tools: SBAR Situation, Background, Assessment, Recommendation. London: NHS Institute for Innovation and Improvement; 2012.
- National Early Warning Score (NEWS): Standardising the Assessment of Acute Illness Severity in the NHS – Report of a Working Party. London: Royal College of Physicians; 2012.
- An Evaluation of Consultant Input into Acute Medical Admissions Management in England. Report of Hospital Service Patterns Versus Clinical Outcomes in England. London: Royal College of Physicians; 2012.
- DeVita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med 2006;34:2463-78. https://doi.org/10.1097/01.CCM.0000235743.38172.6E.
- Spearpoint KG, Gruber PC, Brett SJ. Impact of the Immediate Life Support course on the incidence and outcome of in-hospital cardiac arrest calls: an observational study over 6 years. Resuscitation 2009;80:638-43. https://doi.org/10.1016/j.resuscitation.2009.03.002.
- Smith GB, Poplett N. Impact of attending a 1-day multi-professional course (ALERT) on the knowledge of acute care in trainee doctors. Resuscitation 2004;61:117-22. https://doi.org/10.1016/j.resuscitation.2004.01.003.
- Theilen U, Leonard P, Jones P, Ardill R, Weitz J, Agrawal D, et al. Regular in situ simulation training of paediatric medical emergency team improves hospital response to deteriorating patients. Resuscitation 2013;84:218-22. https://doi.org/10.1016/j.resuscitation.2012.06.027.
- Campello G, Granja C, Carvalho F, Dias C, Azevedo LF, Costa-Pereira A. Immediate and long-term impact of medical emergency teams on cardiac arrest prevalence and mortality: a plea for periodic basic life-support training programs. Crit Care Med 2009;37:3054-61. https://doi.org/10.1097/CCM.0b013e3181b02183.
- DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL. Medical Emergency Response Improvement Team (MERIT) . Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care 2004;13:251-4. https://doi.org/10.1136/qhc.13.4.251.
- Kause J, Smith G, Prytherch D, Parr M, Flabouris A, Hillman K. Intensive Care Society (UK) . A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom – the ACADEMIA study. Resuscitation 2004;62:275-82. https://doi.org/10.1016/j.resuscitation.2004.05.016.
- Smith GB, Prytherch DR, Schmidt PE, Featherstone PI. Review and performance evaluation of aggregate weighted ‘track and trigger’ systems. Resuscitation 2008;77:170-9. https://doi.org/10.1016/j.resuscitation.2007.12.004.
- Patterson C, Maclean F, Bell C, Mukherjee E, Bryan L, Woodcock T, et al. Early warning systems in the UK: variation in content and implementation strategy has implications for a NHS early warning system. Clin Med 2011;11:424-7. https://doi.org/10.7861/clinmedicine.11-5-424.
- Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013;84:465-70. https://doi.org/10.1016/j.resuscitation.2012.12.016.
- Johnston M, Arora S, King D, Stroman L, Darzi A. Escalation of care and failure to rescue: a multicenter, multiprofessional qualitative study. Surgery 2014;155:989-94. https://doi.org/10.1016/j.surg.2014.01.016.
- Mackintosh N, Rainey H, Sandall J. Understanding how rapid response systems may improve safety for the acutely ill patient: learning from the frontline. BMJ Qual Saf 2012;21:135-44. https://doi.org/10.1136/bmjqs-2011-000147.
- Starmer AJ, Sectish TC, Simon DW, Keohane C, McSweeney ME, Chung EY, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA 2013;310:2262-70. https://doi.org/10.1001/jama.2013.281961.
- Acute Care Toolkit 1: Handover. London: Royal College of Physicians; 2011.
- Thomas CM, Bertram E, Johnson D. The SBAR communication technique: teaching nursing students professional communication skills. Nurse Educ 2009;34:176-80. https://doi.org/10.1097/NNE.0b013e3181aaba54.
- Lee A, Bishop G, Hillman KM, Daffurn K. The Medical Emergency Team. Anaesth Intensive Care 1995;23:183-6.
- Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care 2015;19. https://doi.org/10.1186/s13054-015-0973-y.
- McNeill G, Bryden D. Do either early warning systems or emergency response teams improve hospital patient survival? A systematic review. Resuscitation 2013;84:1652-67. https://doi.org/10.1016/j.resuscitation.2013.08.006.
- Chen J, Ou L, Hillman KM, Flabouris A, Bellomo R, Hollis SJ, et al. Cardiopulmonary arrest and mortality trends, and their association with rapid response system expansion. Med J Aust 2014;201:167-70. https://doi.org/10.5694/mja14.00019.
- Jones D, Moran J, Winters B, Welch J. The rapid response system and end-of-life care. Curr Opin Crit Care 2013;19:616-23. https://doi.org/10.1097/MCC.0b013e3283636be2.
- Jones DA, Bagshaw SM, Barrett J, Bellomo R, Bhatia G, Bucknall TK, et al. The role of the medical emergency team in end-of-life care: a multicenter, prospective, observational study. Crit Care Med 2012;40:98-103. https://doi.org/10.1097/CCM.0b013e31822e9d50.
- Pattison N, O’Gara G, Wigmore T. Negotiating transitions: involvement of critical care outreach teams in end-of-life decision making. Am J Crit Care 2015;24:232-40. https://doi.org/10.4037/ajcc2015715.
- McDonnell A, Esmonde L, Morgan R, Brown R, Bray K, Parry G, et al. The provision of critical care outreach services in England: findings from a national survey. J Crit Care 2007;22:212-18. https://doi.org/10.1016/j.jcrc.2007.02.002.
- Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Esmonde L, McDonnell A, Ball C, Waskett C, Morgan R, Rashidian A, et al. Investigating the effectiveness of critical care outreach services: a systematic review. Intensive Care Med 2006;32:1713-21. https://doi.org/10.1007/s00134-006-0380-6.
- Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med 2010;170:18-26. https://doi.org/10.1001/archinternmed.2009.424.
- Subbe C, Welch J. Failure to rescue: using rapid response systems to improve care of the deteriorating patient in hospital. Clinical Risk 2013;19:6-11. https://doi.org/10.1177/1356262213486451.
- Chan PS, Spertus JA, Krumholz HM, Berg RA, Li Y, Sasson C, et al. A validated prediction tool for initial survivors of in-hospital cardiac arrest. Arch Intern Med 2012;172:947-53. https://doi.org/10.1001/archinternmed.2012.2050.
- Decisions Relating to Cardiopulmonary Resuscitation: Guidance from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing, 3rd Edition (1st revision). London: Resuscitation Council; 2016.
- Court of Appeal . Tracey V CUH NHS Trust and Secretary of State for Health. EWCA Civ 822 2014. https://www.judiciary.uk/wp-content/uploads/2014/06/tracey-approved.pdf (accessed 16 September 2017).
- National Cardiac Arrest Audit: Recruitment Pack – Overview Information. London: Resuscitation Council (UK) and Intensive Care National Audit & Research Centre; 2012.
- Hartin J, Walker J. Rapid response systems supporting end of life care: time for a new approach. Br J Hosp Med 2017;78:160-4. https://doi.org/10.12968/hmed.2017.78.3.160.
- Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW, et al. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation 2013;127:1538-63. https://doi.org/10.1161/CIR.0b013e31828b2770.
- Using Natural Experiments to Evaluate Population Health Interventions: Guidance for Producers and Users of Evidence. London: Medical Research Council; 2011.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2. https://doi.org/10.1186/1748-5908-2-40.
- Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ 1996;312:1215-18. https://doi.org/10.1136/bmj.312.7040.1215.
- Rogers E. Diffusion of Innovations. New York, NY: Free Press; 1995.
- Dusenbury L, Brannigan R, Falco M, Hansen WB. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res 2003;18:237-56. https://doi.org/10.1093/her/18.2.237.
- Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F, Peacok R. How to Spread Good Ideas: A Systematic Review of Literature on Diffusion, Dissemination and Sustainability of Innovations in Health Service Delivery and Organisation. London: National Co-ordinating Centre for Service Delivery and Organisation; 2004.
- National Cardiac Arrest Audit Data Collection Manual V1.3. London: Intensive Care National Audit & Research Centre; 2016.
- Hogan H, Carver C, Zipfel R, Hutchings A, Welch J, Harrison D, et al. Effectiveness of ways to improve detection and rescue of deteriorating patients. Br J Hosp Med 2017;78:150-9. https://doi.org/10.12968/hmed.2017.78.3.150.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) 2011. http://handbook.cochrane.org (accessed 21 January 2017).
- Johnston MJ, Arora S, Pucher PH, McCartan N, Reissis Y, Chana P, et al. Improving escalation of care: a double-blinded randomized controlled trial. Ann Surg 2016;263:421-6. https://doi.org/10.1097/SLA.0000000000001543.
- Liaw SY, Wong LF, Ang SB, Ho JT, Siau C, Ang EN. Strengthening the afferent limb of rapid response systems: an educational intervention using web-based learning for early recognition and responding to deteriorating patients. BMJ Qual Saf 2016;25:448-56. https://doi.org/10.1136/bmjqs-2015-004073.
- Kyriacos U, Jelsma J, James M, Jordan S. Early warning scoring systems versus standard observations charts for wards in South Africa: a cluster randomized controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0624-2.
- Jeddian A, Hemming K, Lindenmeyer A, Rashidian A, Sayadi L, Jafari N, et al. Evaluation of a critical care outreach service in a middle-income country: a stepped wedge cluster randomized trial and nested qualitative study. J Crit Care 2016;36:212-17. https://doi.org/10.1016/j.jcrc.2016.07.018.
- Rothschild JM, Woolf S, Finn KM, Friedberg MW, Lemay C, Furbush KA, et al. A controlled trial of a rapid response system in an academic medical center. Jt Comm J Qual Patient Saf 2008;34:417-25. https://doi.org/10.1016/S1553-7250(08)34052-5.
- O’Connell A, Flabouris A, Kim SW, Horwood C, Hakendorf P, Thompson CH. A newly designed observation and response chart’s effect upon adverse inpatient outcomes and rapid response team activity. Intern Med J 2016;46:909-16. https://doi.org/10.1111/imj.13137.
- Winters BD, Weaver SJ, Pfoh ER, Yang T, Cuong J, Dy SM. Rapid-response systems as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:417-25. https://doi.org/10.7326/0003-4819-158-5-201303051-00009.
- Ludikhuize J, Brunsveld-Reinders AH, Dijkgraaf MG, Smorenburg SM, de Rooij SE, Adams R, et al. Outcomes associated with the nationwide introduction of rapid response systems in the Netherlands. Crit Care Med 2015;43:2544-51. https://doi.org/10.1097/CCM.0000000000001272.
- Pirret AM, Takerei SF, Kazula LM. The effectiveness of a patient at risk team comprised of predominantly ward experienced nurses: a before and after study. Intensive Crit Care Nurs 2015;31:133-40. https://doi.org/10.1016/j.iccn.2014.10.005.
- Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet 2005;365:2091-7. https://doi.org/10.1016/S0140-6736(05)66733-5.
- Priestley G, Watson W, Rashidian A, Mozley C, Russell D, Wilson J, et al. Introducing Critical Care Outreach: a ward-randomised trial of phased introduction in a general hospital. Intensive Care Med 2004;30:1398-404. https://doi.org/10.1007/s00134-004-2268-7.
- Massey D, Aitken LM, Chaboyer W. Literature review: do rapid response systems reduce the incidence of major adverse events in the deteriorating ward patient?. J Clin Nurs 2010;19:3260-73. https://doi.org/10.1111/j.1365-2702.2010.03394.x.
- Odell M, Forster A, Rudman K, Bass F. The critical care outreach service and the early warning system on surgical wards. Nurs Crit Care 2002;7:132-5.
- Subbe CP, Davies RG, Williams E, Rutherford P, Gemmell L. Effect of introducing the Modified Early Warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia 2003;58:797-802.
- Pittard AJ. Out of our reach? Assessing the impact of introducing a critical care outreach service. Anaesthesia 2003;58:882-5.
- Paterson R, MacLeod DC, Thetford D, Beattie A, Graham C, Lam S, et al. Prediction of in-hospital mortality and length of stay using an early warning scoring system: clinical audit. Clin Med 2006;6:281-4.
- Alam N, Hobbelink EL, van Tienhoven AJ, van de Ven PM, Jansma EP, Nanayakkara PW. The impact of the use of the Early Warning Score (EWS) on patient outcomes: a systematic review. Resuscitation 2014;85:587-94. https://doi.org/10.1016/j.resuscitation.2014.01.013.
- Odell M, Rechner IJ, Kapila A, Even T, Oliver D, Davies CW, et al. The effect of a critical care outreach service and an early warning scoring system on respiratory rate recording on the general wards. Resuscitation 2007;74:470-5. https://doi.org/10.1016/j.resuscitation.2007.01.035.
- De Meester K, Haegdorens F, Monsieurs KG, Verpooten GA, Holvoet A, Van Bogaert P. Six-day postoperative impact of a standardized nurse observation and escalation protocol: a preintervention and postintervention study. J Crit Care 2013;28:1068-74. https://doi.org/10.1016/j.jcrc.2013.07.061.
- Hammond NE, Spooner AJ, Barnett AG, Corley A, Brown P, Fraser JF. The effect of implementing a modified early warning scoring (MEWS) system on the adequacy of vital sign documentation. Aust Crit Care 2013;26:18-22. https://doi.org/10.1016/j.aucc.2012.05.001.
- Bellomo R, Ackerman M, Bailey M, Beale R, Clancy G, Danesh V, et al. A controlled trial of electronic automated advisory vital signs monitoring in general hospital wards. Crit Care Med 2012;40:2349-61. https://doi.org/10.1097/CCM.0b013e318255d9a0.
- McDonnell A, Tod A, Bray K, Bainbridge D, Adsetts D, Walters S. A before and after study assessing the impact of a new model for recognizing and responding to early signs of deterioration in an acute hospital. J Adv Nurs 2013;69:41-52. https://doi.org/10.1111/j.1365-2648.2012.05986.x.
- Foster S, Manser T. The effects of patient handoff characteristics on subsequent care: a systematic review and areas for future research. Acad Med 2012;87:1105-24. https://doi.org/10.1097/ACM.0b013e31825cfa69.
- Robertson ER, Morgan L, Bird S, Catchpole K, McCulloch P. Interventions employed to improve intrahospital handover: a systematic review. BMJ Qual Saf 2014;23:600-7. https://doi.org/10.1136/bmjqs-2013-002309.
- Pucher PH, Johnston MJ, Aggarwal R, Arora S, Darzi A. Effectiveness of interventions to improve patient handover in surgery: a systematic review. Surgery 2015;158:85-9. https://doi.org/10.1016/j.surg.2015.02.017.
- Davis J, Riesenberg LA, Mardis M, Donnelly J, Benningfield B, Youngstrom M, et al. Evaluating outcomes of electronic tools supporting physician shift-to-shift handoffs: a systematic review. J Grad Med Educ 2015;7:174-80. https://doi.org/10.4300/JGME-D-14-00205.1.
- Payne CE, Stein JM, Leong T, Dressler DD. Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Qual Saf 2012;21:925-32. https://doi.org/10.1136/bmjqs-2011-000308.
- Moseley BD, Smith JH, Diaz-Medina GE, Paz Soldan MM, Wicklund M, Dhamija R, et al. Standardized sign-out improves completeness and perceived accuracy of inpatient neurology handoffs. Neurology 2012;79:1060-4. https://doi.org/10.1212/WNL.0b013e318265a698.
- Ahmed J, Mehmood S, Rehman S, Ilyas C, Khan LU. Impact of a structured template and staff training on compliance and quality of clinical handover. Int J Surg 2012;10:571-4. https://doi.org/10.1016/j.ijsu.2012.09.001.
- De Meester K, Verspuy M, Monsieurs KG, Van Bogaert P. SBAR improves nurse–physician communication and reduces unexpected death: a pre and post intervention study. Resuscitation 2013;84:1192-6. https://doi.org/10.1016/j.resuscitation.2013.03.016.
- Yazici C, Abdelmalak H, Gupta S, Shmagel A, Albaddawi E, Tsang V, et al. Sustainability and effectiveness of a quality improvement project to improve handoffs to night float residents in an internal medicine residency program. J Grad Med Educ 2013;5:303-8. https://doi.org/10.4300/JGME-D-12-00175.1.
- Graham KL, Marcantonio ER, Huang GC, Yang J, Davis RB, Smith CC. Effect of a systems intervention on the quality and safety of patient handoffs in an internal medicine residency program. J Gen Intern Med 2013;28:986-93. https://doi.org/10.1007/s11606-013-2391-7.
- Connor MP, Bush AC, Brennan J. IMOUTA: a proposal for patient care handoffs. Laryngoscope 2013;123:2649-53. https://doi.org/10.1002/lary.24118.
- Cornell P, Gervis MT, Yates L, Vardaman JM. Improving shift report focus and consistency with the situation, background, assessment, recommendation protocol. J Nurs Adm 2013;43:422-8. https://doi.org/10.1097/NNA.0b013e31829d6303.
- Younan LA, Fralic MF. Using ‘best-fit’ interventions to improve the nursing intershift handoff process at a medical center in Lebanon. Jt Comm J Qual Patient Saf 2013;39:460-7. https://doi.org/10.1016/S1553-7250(13)39059-X.
- Gonzalo JD, Yang JJ, Stuckey HL, Fischer CM, Sanchez LD, Herzig SJ. Patient care transitions from the emergency department to the medicine ward: evaluation of a standardized electronic signout tool. Int J Qual Health Care 2014;26:337-47. https://doi.org/10.1093/intqhc/mzu040.
- Gagnier JJ, Derosier JM, Maratt JD, Hake ME, Bagian JP. Development, implementation and evaluation of a patient handoff tool to improve safety in orthopaedic surgery. Int J Qual Health Care 2016;28:363-70. https://doi.org/10.1093/intqhc/mzw031.
- Flanagan ME, Patterson ES, Frankel RM, Doebbeling BN. Evaluation of a physician informatics tool to improve patient handoffs. J Am Med Inform Assoc 2009;16:509-15. https://doi.org/10.1197/jamia.M2892.
- Nabors C, Peterson SJ, Lee WN, Mumtaz A, Shah T, Sule S, et al. Experience with faculty supervision of an electronic resident sign-out system. Am J Med 2010;123:376-81. https://doi.org/10.1016/j.amjmed.2009.12.010.
- Liaw SY, Scherpbier A, Klainin-Yobas P, Rethans JJ. A review of educational strategies to improve nurses’ roles in recognizing and responding to deteriorating patients. Int Nurs Rev 2011;58:296-303. https://doi.org/10.1111/j.1466-7657.2011.00915.x.
- Featherstone P, Smith GB, Linnell M, Easton S, Osgood VM. Impact of a one-day inter-professional course (ALERT) on attitudes and confidence in managing critically ill adult patients. Resuscitation 2005;65:329-36. https://doi.org/10.1016/j.resuscitation.2004.12.011.
- Fuhrmann L, Østergaard D, Lippert A, Perner A. A multi-professional full-scale simulation course in the recognition and management of deteriorating hospital patients. Resuscitation 2009;80:669-73. https://doi.org/10.1016/j.resuscitation.2009.03.013.
- Mitchell IA, McKay H, Van Leuvan C, Berry R, McCutcheon C, Avard B, et al. A prospective controlled trial of the effect of a multi-faceted intervention on early recognition and intervention in deteriorating hospital patients. Resuscitation 2010;81:658-66. https://doi.org/10.1016/j.resuscitation.2010.03.001.
- Connell CJ, Endacott R, Jackman JA, Kiprillis NR, Sparkes LM, Cooper SJ. The effectiveness of education in the recognition and management of deteriorating patients: a systematic review. Nurse Educ Today 2016;44:133-45. https://doi.org/10.1016/j.nedt.2016.06.001.
- Kinsman L, Buykx P, Cant R, Champion R, Cooper S, Endacott R, et al. The FIRST2ACT simulation program improves nursing practice in a rural Australian hospital. Aust J Rural Health 2012;20:270-4. https://doi.org/10.1111/j.1440-1584.2012.01296.x.
- Schubert CR. Effect of simulation on nursing knowledge and critical thinking in failure to rescue events. J Contin Educ Nurs 2012;43:467-71. https://doi.org/10.3928/00220124-20120904-27.
- Liaw SY, Chng DYJ, Wong LF, Ho JTY, Mordiffi SZ, Cooper S, et al. The impact of a web-based educational program on the recognition and management of deteriorating patients. J Clin Nurs 2017;26:4848-56. https://doi.org/10.1111/jocn.13955.
- Simmes F, Schoonhoven L, Mintjes J, Fikkers BG, van der Hoeven JG. Effects of a rapid response system on quality of life: a prospective cohort study in surgical patients before and after implementing a rapid response system. Health Qual Life Outcomes 2013;11. https://doi.org/10.1186/1477-7525-11-74.
- Braun V, Clarke V. What can ‘thematic analysis’ offer health and wellbeing researchers?. Int J Qual Stud Health Well-Being 2014;9. https://doi.org/10.3402/qhw.v9.26152.
- Donohue LA, Endacott R. Track, trigger and teamwork: communication of deterioration in acute medical and surgical wards. Intensive Crit Care Nurs 2010;26:10-7. https://doi.org/10.1016/j.iccn.2009.10.006.
- Gao H, McDonnell A, Harrison DA, Moore T, Adam S, Daly K, et al. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med 2007;33:667-79. https://doi.org/10.1007/s00134-007-0532-3.
- Odell M, Victor C, Oliver D. Nurses’ role in detecting deterioration in ward patients: systematic literature review. J Adv Nurs 2009;65:1992-2006. https://doi.org/10.1111/j.1365-2648.2009.05109.x.
- Douw G, Schoonhoven L, Holwerda T, Huisman-de Waal G, van Zanten AR, van Achterberg T, et al. Nurses’ worry or concern and early recognition of deteriorating patients on general wards in acute care hospitals: a systematic review. Crit Care 2015;19. https://doi.org/10.1186/s13054-015-0950-5.
- Rowan K. Evaluation of Outreach Services in Critical Care. London: National Institute for Health Research, Service Delivery and Outcomes Research; 2004.
- Pattison N, Eastham E. Critical care outreach referrals: a mixed-method investigative study of outcomes and experiences. Nurs Crit Care 2012;17:71-82. https://doi.org/10.1111/j.1478-5153.2011.00464.x.
- Stafseth SK, Grønbeck S, Lien T, Randen I, Lerdal A. The experiences of nurses implementing the Modified Early Warning Score and a 24-hour on-call Mobile Intensive Care Nurse: an exploratory study. Intensive Crit Care Nurs 2016;34:25-33. https://doi.org/10.1016/j.iccn.2015.07.008.
- Benin AL, Borgstrom CP, Jenq GY, Roumanis SA, Horwitz LI. Defining impact of a rapid response team: qualitative study with nurses, physicians and hospital administrators. BMJ Qual Saf 2012;21:391-8. https://doi.org/10.1136/bmjqs-2011-000390.
- Alshehri B. Medical-surgical nurses’ experiences of calling a rapid response team in a hospital setting: a literature review. Middle East J Nurs 2015;9:3-23. https://doi.org/10.5742/MEJN.2015.92660.
- Kitto S, Marshall SD, McMillan SE, Shearer B, Buist M, Grant R, et al. Rapid response systems and collective (in)competence: an exploratory analysis of intraprofessional and interprofessional activation factors. J Interprof Care 2015;29:340-6. https://doi.org/10.3109/13561820.2014.984021.
- Shearer B, Marshall S, Buist MD, Finnigan M, Kitto S, Hore T, et al. What stops hospital clinical staff from following protocols? An analysis of the incidence and factors behind the failure of bedside clinical staff to activate the rapid response system in a multi-campus Australian metropolitan healthcare service. BMJ Qual Saf 2012;21:569-75. https://doi.org/10.1136/bmjqs-2011-000692.
- Wakefield AB, Carlisle C, Hall AG, Attree MJ. The expectations and experiences of blended learning approaches to patient safety education. Nurse Educ Pract 2008;8:54-61. https://doi.org/10.1016/j.nepr.2007.04.007.
- Durham CA, Hughes R. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality (USA); 2008.
- Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, et al. Training and simulation for patient safety. Qual Saf Health Care 2010;19:i34-43. https://doi.org/10.1136/qshc.2009.038562.
- Naeem N. Beyond the intensive care unit: a review of interventions aimed at anticipating and preventing in-hospital cardiopulmonary arrest. Resuscitation 2007;73:491-2. https://doi.org/10.1016/j.resuscitation.2007.01.037.
- Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J 2014;90:149-54. https://doi.org/10.1136/postgradmedj-2012-131168.
- Lingard L, Espin S, Whyte S, Regehr G, Baker GR, Reznick R, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care 2004;13:330-4. https://doi.org/10.1136/qshc.2003.008425.
- Pronovost P, Berenholtz S, Dorman T, Lipsett PA, Simmonds T, Haraden C. Improving communication in the ICU using daily goals. J Crit Care 2003;18:71-5. https://doi.org/10.1053/jcrc.2003.50008.
- Alvarez G, Coiera E. Interdisciplinary communication: an uncharted source of medical error?. J Crit Care 2006;21:236-42. https://doi.org/10.1016/j.jcrc.2006.02.004.
- Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med 2004;79:186-94. https://doi.org/10.1097/00001888-200402000-00019.
- Bauer NJ. Improving patient safety in cardiothoracic surgery: an audit of surgical handover in a tertiary center. Adv Med Educ Pract 2016;7:309-10. https://doi.org/10.2147/AMEP.S107189.
- Smith AF, Pope C, Goodwin D, Mort M. Interprofessional handover and patient safety in anaesthesia: observational study of handovers in the recovery room. Br J Anaesth 2008;101:332-7. https://doi.org/10.1093/bja/aen168.
- McElroy LM, Macapagal KR, Collins KM, Abecassis MM, Holl JL, Ladner DP, et al. Clinician perceptions of operating room to intensive care unit handoffs and implications for patient safety: a qualitative study. Am J Surg 2015;210:629-35. https://doi.org/10.1016/j.amjsurg.2015.05.008.
- Cohn S, Fritz ZBM, Frankau JM, Laroche CM, Fuld JP. Do not attempt cardiopulmonary resuscitation orders in acute medical settings: a qualitative study. QJM 2013;106:165-77. https://doi.org/10.1093/qjmed/hcs222.
- Fritz Z, Slowther A-M, Perkins GD. Resuscitation policy should focus on the patient, not the decision. BMJ 2017;356. https://doi.org/10.1136/bmj.j813.
- Mockford C, Fritz Z, George R, Court R, Grove A, Clarke B, et al. Do not attempt cardiopulmonary resuscitation (DNACPR) orders: a systematic review of the barriers and facilitators of decision-making and implementation. Resuscitation 2015;88:99-113. https://doi.org/10.1016/j.resuscitation.2014.11.016.
- Mentzelopoulos SD, Bossaert L, Raffay V, Askitopoulou H, Perkins GD, Greif R, et al. A survey of key opinion leaders on ethical resuscitation practices in 31 European Countries. Resuscitation 2016;100:11-7. https://doi.org/10.1016/j.resuscitation.2015.12.010.
- Jones DA, McIntyre T, Baldwin I, Mercer I, Kattula A, Bellomo R. The medical emergency team and end-of-life care: a pilot study. Crit Care Resusc 2007;9:151-6.
- Adam S, Ball C, Bray K, Baker-McLearn D, Carmel S, Daly K, et al. Evaluation of Outreach Services in Critical Care. London: National Institute for Health Research Service Delivery Organisation Programme; 2004.
- Subbe CP, Gao H, Harrison DA. Reproducibility of physiological track-and-trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med 2007;33:619-24. https://doi.org/10.1007/s00134-006-0516-8.
- Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet 2010;376:1339-46. https://doi.org/10.1016/S0140-6736(10)60446-1.
- Vincent JL. Forgoing life support in western European intensive care units: the results of an ethical questionnaire. Crit Care Med 1999;27:1626-33. https://doi.org/10.1097/00003246-199908000-00042.
- Leach LS, Mayo AM. Rapid response teams: qualitative analysis of their effectiveness. Am J Crit Care 2013;22:198-210. https://doi.org/10.4037/ajcc2013990.
- Sulistio M, Franco M, Vo A, Poon P, William L. Hospital rapid response team and patients with life-limiting illness: a multicentre retrospective cohort study. Palliat Med 2015;29:302-9. https://doi.org/10.1177/0269216314560802.
- Jones D, Bellomo R, Bates S, Warrillow S, Goldsmith D, Hart G, et al. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care 2005;9:R808-15. https://doi.org/10.1186/cc3906.
- NHS Digital . Hospital Episode Statistics, Admitted Patient Care, England 2009 10–2014 15 n.d. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity (accessed 15 December 2017).
- Armitage JN, van der Meulen JH. Royal College of Surgeons Co-morbidity Consensus Group . Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg 2010;97:772-81. https://doi.org/10.1002/bjs.6930.
- Linked HES–ONS Data. Leeds: NHS Digital; n.d.
- Department for Communities and Local Government . The English Indices of Deprivation 2015. Statistical Release. Department for Communities and Local Government 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015_-_Statistical_Release.pdf (accessed 11 September 2017).
- International Classification of Diseases and Related Health Problems Tenth Revision, Volume 2. Geneva: WHO; 2011.
- Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 2017;46:348-55. https://doi.org/10.1093/ije/dyw098.
- Gao H, Harrison DA, Parry GJ, Daly K, Subbe CP, Rowan K. The impact of the introduction of critical care outreach services in England: a multicentre interrupted time-series analysis. Crit Care 2007;11. https://doi.org/10.1186/cc6163.
- Jolley J, Bendyk H, Holaday B, Lombardozzi KA, Harmon C. Rapid response teams: do they make a difference?. Dimens Crit Care Nurs 2007;26:253-60. https://doi.org/10.1097/01.DCC.0000297401.67854.78.
- Rothberg MB, Belforti R, Fitzgerald J, Friderici J, Keyes M. Four years’ experience with a hospitalist-led medical emergency team: an interrupted time series. J Hosp Med 2012;7:98-103. https://doi.org/10.1002/jhm.953.
- Flabouris A, Chen J, Hillman K, Bellomo R, Finfer S. MERIT study investigators from the Simpson Centre and the ANZICs Clinical Trials Group . Timing and interventions of emergency teams during the MERIT study. Resuscitation 2010;81:25-30. https://doi.org/10.1016/j.resuscitation.2009.09.025.
- Chen J, Hillman K, Bellomo R, Flabouris A, Finfer S, Cretikos M. MERIT Study Investigators for the Simpson Centre . The impact of introducing medical emergency team system on the documentations of vital signs. Resuscitation 2009;80:35-43. https://doi.org/10.1016/j.resuscitation.2008.10.009.
- Khan N, Carle C. Should the national early warning score be adopted throughout the NHS?. Br J Hosp Med 2014;75. https://doi.org/10.12968/hmed.2014.75.8.478.
- Huh JW, Lim CM, Koh Y, Lee J, Jung YK, Seo HS, et al. Activation of a medical emergency team using an electronic medical recording-based screening system*. Crit Care Med 2014;42:801-8. https://doi.org/10.1097/CCM.0000000000000031.
- Jones D, Bellomo R, DeVita MA. Effectiveness of the medical emergency team: the importance of dose. Crit Care 2009;13. https://doi.org/10.1186/cc7996.
- Jones D. The epidemiology of adult rapid response team patients in Australia. Anaesth Intensive Care 2014;42:213-19.
- Tirkkonen J, Setälä P, Hoppu S. Characteristics and outcome of rapid response team patients ≥ 75 years old: a prospective observational cohort study. Scand J Trauma Resusc Emerg Med 2017;25. https://doi.org/10.1186/s13049-017-0423-8.
Appendix 1 High-quality review papers used as foundation for the search strategy
| Topic | Original systematic review | Original search start | Original search end | Our search start date | Our search end date |
|---|---|---|---|---|---|
| Rapid response schemes | NICE CG5024 | January 2004 | December 2006 | December 2006 | 21 October 2014 |
| EWS | NICE CG5024 | November 2004 | October 2006 | October 2006 | 21 October 2014 |
| Standardised handover tool | Robertson et al. 201496 | January 2002 | July 2012 | July 2012 | 21 October 2014 |
| Continuing education | None found | – | – | January 1990 | 21 October 2014 |
Appendix 2 Search strategies
Rapid response schemes
The search strategies were modified versions of those used by NICE in CG50. 24
Date range searched: December 2006 onwards.
Date searched: 21 October 2014.
MEDLINE
Search strategy
-
exp Critical care/
-
Critical care$.tw.
-
exp *Intensive Care Units/
-
intensive care$.tw.
-
((critical$or acute$or sever$or sudden$or unexpected$) adj2 ill$).tw.
-
(patient$adj2 deterior$).tw.
-
(risk$adj2 deterior$).tw.
-
critical illness/
-
(clinical$adj2 deterior$).tw.
-
Heart Arrest/ep, mo, pc [Epidemiology, Mortality, Prevention & Control]
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10
-
exp patient care team/
-
outreach.tw.
-
patient at risk$.tw.
-
patient care team$.tw.
-
hospital emergency team$.tw.
-
12 or 13 or 14 or 15 or 16
-
11 and 17
-
rapid response team$.tw.
-
medical emergency team$.tw.
-
Hospital Rapid Response Team/
-
rapid response system$.tw.
-
(outreach adj (service$or team$)).tw.
-
19 or 20 or 21 or 22 or 23
-
18 or 24
-
200612$.ed.
-
2007$.ed.
-
2008$.ed.
-
2009$.ed.
-
2010$.ed.
-
2011$.ed.
-
2012$.ed.
-
2013$.ed.
-
2014$.ed.
-
or/26–34
-
25 and 35
-
limit 36 to english language
EMBASE
Search strategy
-
deterioration/
-
general condition deterioration/
-
poor general condition/
-
Critical care$.tw.
-
exp *Intensive Care Units/
-
intensive care$.tw.
-
((critical$or acute$or sever$or sudden$or unexpected$) adj2 ill$).tw.
-
(patient$adj2 deterior$).tw.
-
(risk$adj2 deterior$).tw.
-
critical illness/
-
(clinical$adj2 deterior$).tw.
-
Heart Arrest/ep, pc
-
or/1–12
-
outreach.tw.
-
patient at risk$.tw.
-
patient care team$.tw.
-
hospital emergency team$.tw.
-
or/14–17
-
13 and 18
-
rapid response team$.tw.
-
medical emergency team$.tw.
-
Rapid Response Team/
-
rapid response system$.tw.
-
(outreach adj (service$or team$)).tw.
-
20 or 21 or 22 or 23 or 24
-
19 or 25
-
limit 26 to dd=20061201–20141021
-
limit 27 to english language
Early warning scores
The search strategies were modified versions of those used by NICE in CG50. 24
Date range searched: 31 October 2006 onwards.
Date searched: 21 October 2014.
MEDLINE
Search strategy
-
*Health Status Indicators/
-
exp *Severity of Illness Index/
-
*Risk Assessment/
-
severity of illness ind$.tw.
-
health status ind$.tw.
-
risk assess$.tw.
-
early warning.tw.
-
(warning adj2 (scor$or system$)).tw.
-
(track and trigger).tw.
-
((trigger or calling) adj5 criteria).tw.
-
*Point-of-care Systems/
-
point of care system$.tw.
-
serious$ill$.tw.
-
or/1–13
-
exp *Critical Care/
-
critical care.tw.
-
intensive care.tw.
-
exp *Intensive Care Units/
-
Hospital Rapid Response Team/
-
rapid response system$.tw.
-
rapid response team$.tw.
-
medical emergency team$.tw.
-
hospital emergency team$.tw.
-
exp *Patient Care team/
-
patient care team$.tw.
-
patient at risk$.tw.
-
(outreach adj (service$or team$)).tw.
-
shock team$.tw.
-
*critical illness/
-
((critical$or acute$or sever$or sudden$or unexpected$) adj2 ill$).tw.
-
(patient$adj2 deterior$).tw.
-
(risk$adj2 deterior$).tw.
-
Heart arrest/ep, mo, pc
-
or/15–33
-
14 and 34
-
200611$.ed.
-
200612$.ed.
-
2007$.ed.
-
2008$.ed.
-
2009$.ed.
-
2010$.ed.
-
2011$.ed.
-
2012$.ed.
-
2013$.ed.
-
2014$.ed.
-
or/36–45
-
35 and 46
-
limit 47 to english language
EMBASE
Search strategy
-
exp *Health Status Indicator/
-
*Risk Assessment/
-
severity of illness ind$.tw.
-
health status ind$.tw.
-
risk assess$.tw.
-
early warning.tw.
-
(warning adj2 (scor$or system$)).tw.
-
(track and trigger).tw.
-
((trigger or calling) adj5 criteria).tw.
-
*scoring system/
-
point of care system$.tw.
-
serious$ill$.tw.
-
or/1–12
-
deterioration/or general condition deterioration/or poor general condition/
-
critical care.tw.
-
intensive care.tw.
-
exp *Intensive Care Units/
-
Rapid Response Team/
-
rapid response system$.tw.
-
rapid response team$.tw.
-
medical emergency team$.tw.
-
hospital emergency team$.tw.
-
patient care team$.tw.
-
patient at risk$.tw.
-
(outreach adj (service$or team$)).tw.
-
shock team$.tw.
-
*critical illness/
-
((critical$or acute$or sever$or sudden$or unexpected$) adj2 ill$).tw.
-
(patient$adj2 deterior$).tw.
-
(risk$adj2 deterior$).tw.
-
Heart arrest/ep, pc
-
or/14–31
-
13 and 32
-
limit 33 to dd=20061031–20141021
-
limit 34 to english language
Standardised handover tools
The search strategies were modified versions of those used by Robertson et al. 96
Date range searched: July 2012 onwards.
Date searched: 21 October 2014.
MEDLINE
Search strategy
-
patient handoff/
-
handover?.tw.
-
hand-over?.tw.
-
handoff?.tw.
-
hand-off?.tw.
-
signout?.tw.
-
sign-out?.tw.
-
patient transfer/
-
patient transfer$.tw.
-
intrahospital transfer$.tw.
-
intra-hospital transfer$.tw.
-
intrahospital transport$.tw.
-
intra-hospital transport$.tw.
-
shift to shift.tw.
-
intershift.tw.
-
inter-shift.tw.
-
or/1–16
-
quality improvement/
-
intervention*.tw.
-
(improv* and quality).tw.
-
(improv* and safety).tw.
-
strateg*.tw.
-
tool$.tw.
-
training.tw.
-
instrument$.tw.
-
standardi*.tw.
-
mneumonic$.tw.
-
or/18–27
-
17 and 28
-
SBAR.tw.
-
ISBAR.tw.
-
30 or 31
-
29 or 32
-
201207$.ed.
-
201208$.ed.
-
201209$.ed.
-
201210$.ed.
-
201211$.ed.
-
201212$.ed.
-
2013$.ed.
-
2014$.ed.
-
or/34–41
-
33 and 42
-
limit 43 to english language
EMBASE
Search strategy
-
clinical handover/
-
handover?.tw.
-
hand-over?.tw.
-
handoff?.tw.
-
hand-off?.tw.
-
signout?.tw.
-
sign-out?.tw.
-
patient transport/
-
patient transfer$.tw.
-
intrahospital transfer$.tw.
-
intra-hospital transfer$.tw.
-
intrahospital transport$.tw.
-
intra-hospital transport$.tw.
-
shift to shift.tw.
-
intershift.tw.
-
inter-shift.tw.
-
or/1–16
-
quality improvement/
-
intervention*.tw.
-
(improv* and quality).tw.
-
(improv* and safety).tw.
-
strateg*.tw.
-
tool$.tw.
-
training.tw.
-
instrument$.tw.
-
standardi*.tw.
-
mneumonic$.tw.
-
or/18–27
-
17 and 28
-
SBAR.tw.
-
ISBAR.tw.
-
30 or 31
-
29 or 32
-
limit 33 to dd=20120701–20141021
-
limit 34 to english language
Continuing education
Date range searched: 1990 onwards.
Date searched: 21 October 2014.
MEDLINE
Search strategy
-
exp Critical care/
-
Critical care$.tw.
-
((critical$or acute$or sever$or sudden$or unexpected$) adj2 ill$).tw.
-
(patient$adj2 deterior$).tw.
-
(risk$adj2 deterior$).tw.
-
(clinical$adj2 deterior$).tw.
-
critical illness/
-
or/1–7
-
*education, continuing/or *education, medical, continuing/or *education, nursing, continuing/or *education, professional, retraining/or *education, medical/or *education, nursing/
-
medical education.tw.
-
nurs$education.tw.
-
exp *teaching/
-
exp *inservice training/
-
or/9–13
-
immediate life support$.tw.
-
Life Support Care/ed
-
Advanced Cardiac Life Support/ed
-
or/15–17
-
Heart arrest/ep, mo, pc
-
8 or 19
-
20 and 14
-
21 or 18
-
limit 22 to yr=‘1990 -Current’
-
limit 23 to english language
EMBASE
Search strategy
-
deterioration/or general condition deterioration/or poor general condition/
-
Critical care$.tw.
-
Advanced Cardiac Life Support$.tw.
-
((critical$or acute$or sever$or sudden$or unexpected$) adj2 ill$).tw.
-
(patient$adj2 deterior$).tw.
-
(risk$adj2 deterior$).tw.
-
(clinical$adj2 deterior$).tw.
-
critical illness/
-
Heart arrest/ep, pc
-
or/1–9
-
*continuing education/or *vocational education/or *medical education/or *interdisciplinary education/or *nursing education/
-
medical education.tw.
-
nurs$education.tw.
-
exp *teaching/
-
exp *in service training/
-
or/11–15
-
immediate life support$.tw.
-
10 and 16
-
17 or 18
-
limit 19 to yr=‘1990 -Current’
-
limit 20 to english language
Appendix 3 The PRISMA-style flow diagrams
Rapid response schemes
FIGURE 17.
Rapid response scheme PRISMA-style diagram.

Early Warning Scores
FIGURE 18.
Early Warning Score PRISMA-style diagram.
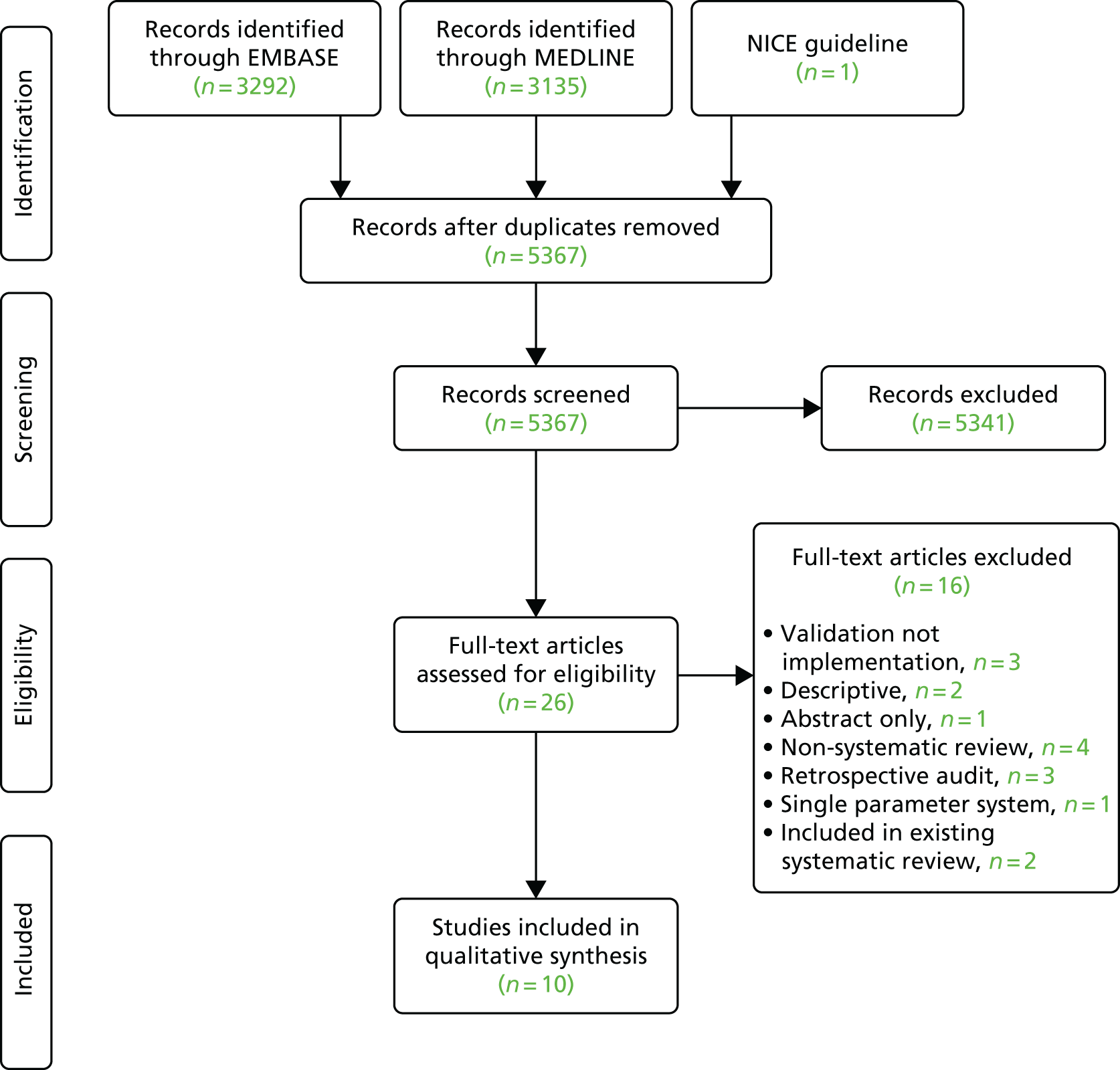
Standardised handover tools
FIGURE 19.
Standardised handover tools PRISMA-style diagram.
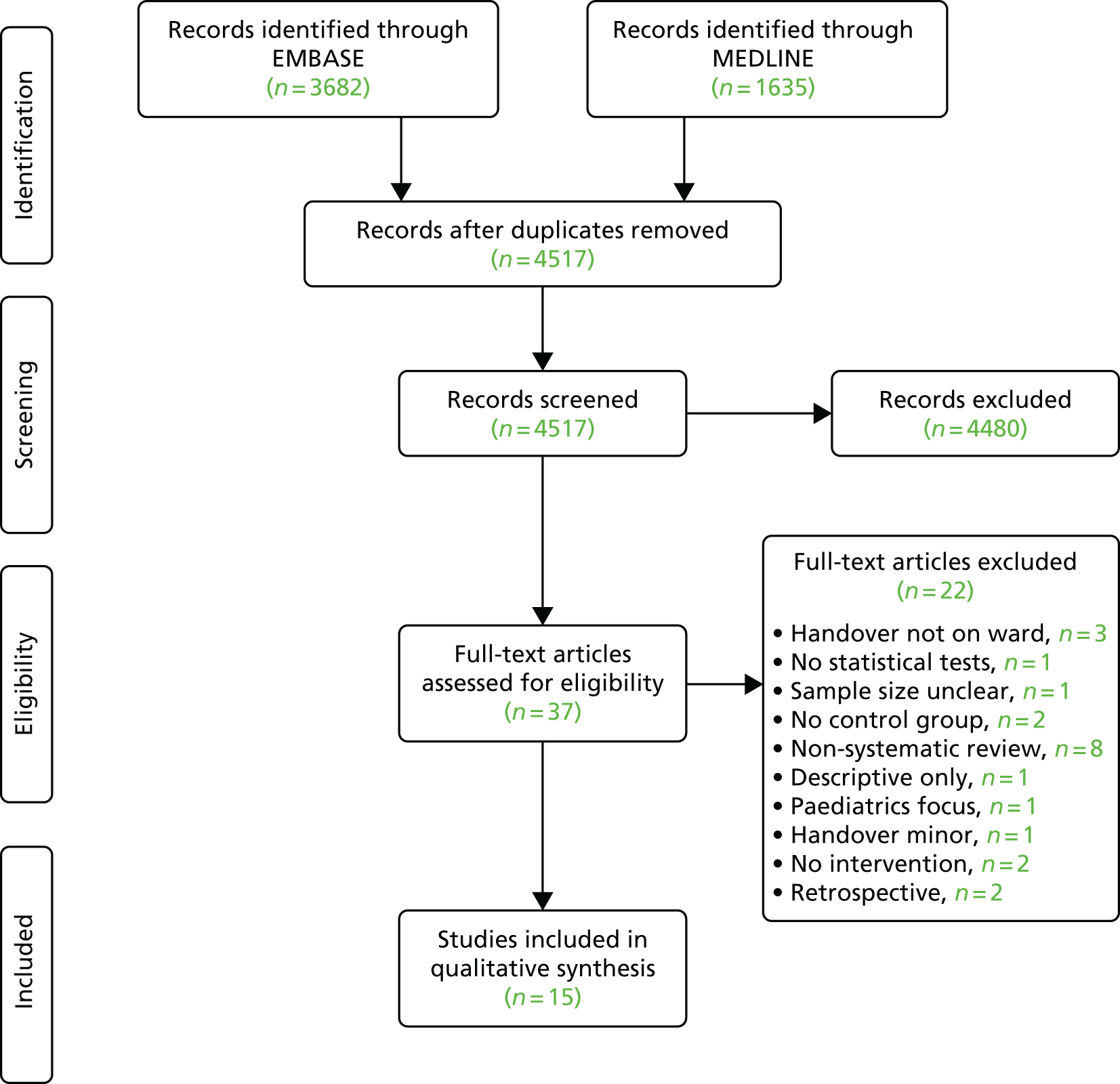
Continuing education
FIGURE 20.
Continuing education PRISMA-style diagram.
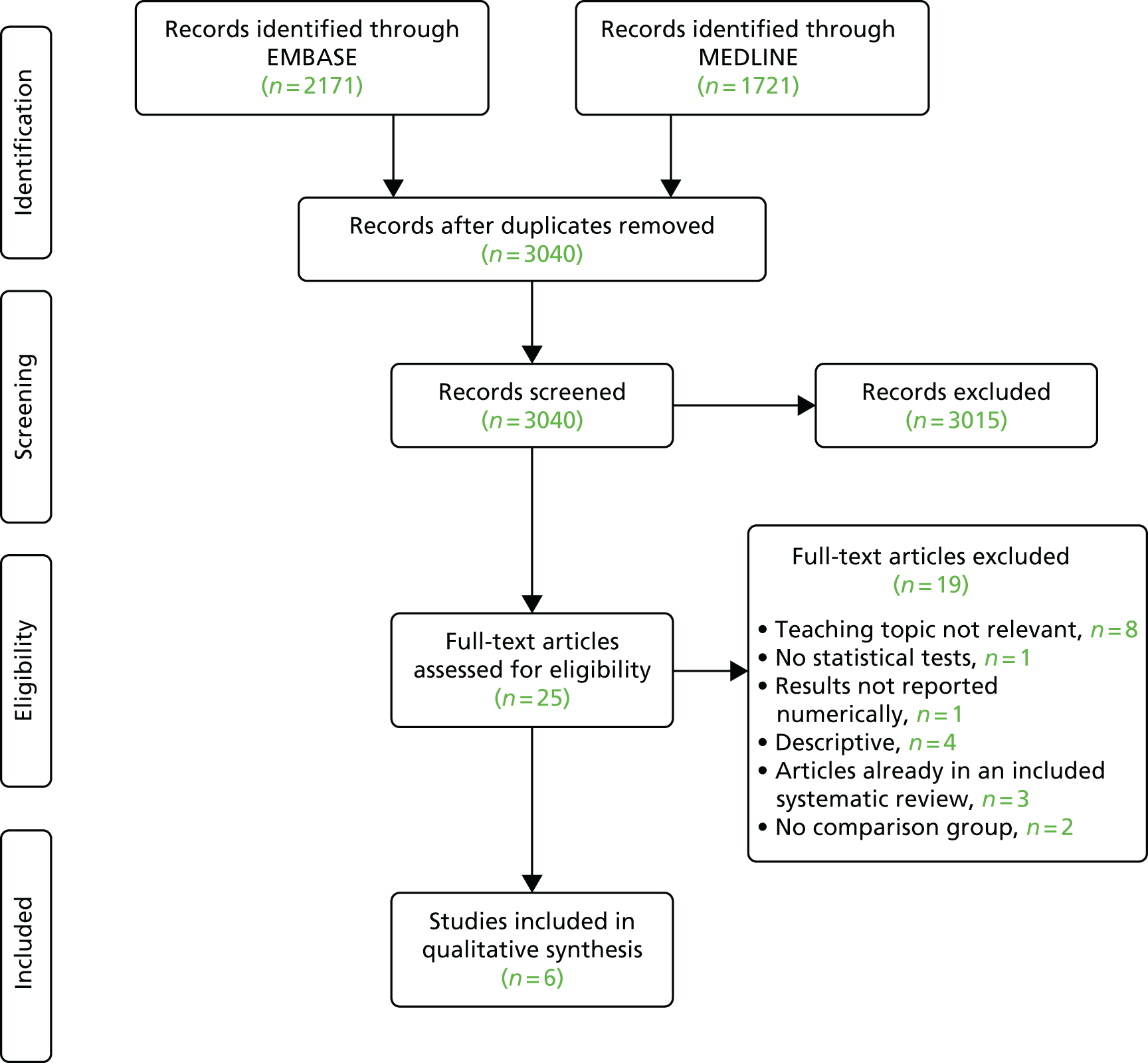
Appendix 4 Data items extracted from papers
Systematic review
-
Quality assessment:
-
focus
-
relevant studies
-
rigorous literature search
-
critical appraisal of studies
-
description of methodology
-
overall quality rating.
-
-
Method:
-
author’s objective and rationale
-
participants
-
interventions
-
comparisons
-
outcomes
-
study design
-
eligibility criteria
-
search method
-
screening method
-
assessment of quality method
-
data extraction method
-
summary measures
-
synthesis method.
-
-
Results:
-
study selection
-
summary – strength of evidence for each main finding
-
synthesis of results
-
additional analysis.
-
-
Limitations.
-
Conclusions.
Primary study
-
Study type:
-
study design
-
data collection method
-
study duration (observation, intervention and follow-up).
-
-
Population:
-
number of participants
-
setting
-
age
-
gender
-
inclusion and exclusion criteria.
-
-
Risk of bias:
-
selection bias (systematic baseline differences between the comparison groups)
-
performance bias (systematic differences between groups in the care provided, apart from the intervention under investigation)
-
attrition bias (systematic differences between the comparison groups with respect to loss of participants)
-
detection bias (bias in how outcomes are ascertained, diagnosed or verified)
-
other concerns about bias
-
overall quality rating.
-
-
Intervention type:
-
aim, intervention and control details: what was delivered, by whom, to whom, how, when, where, how often, how long
-
Implementation adherence:
-
content – the treatment, skills or knowledge that the intervention seeks to deliver to its recipients
-
dose (frequency, duration, or coverage)
-
intervention complexity
-
intervention moderators (e.g. the provision of manuals, guidelines, training, and monitoring and feedback for those delivering the intervention)
-
intervention moderators – quality of delivery
-
intervention moderator – participant responsiveness.
-
-
-
Outcomes.
-
Funding source.
-
Limitations.
Glossary
- Commissioning for Quality and Innovation
- An incentivised payment framework that encourages NHS providers to undertake quality improvement activities related to a particular service.
- Critical illness
- A life-threatening medical condition.
- ‘Do not attempt cardiopulmonary resuscitation’ decisions
- A decision framework that informs the medical team about the views of the patient with respect to cardiopulmonary resuscitation. The decision is normally documented after a discussion between the patient and/or relatives and the consultant directing the patient’s care. The decision does not affect other medical treatments.
- Health-care assistants
- Individuals who work under the supervision of qualified, registered nurses who undertake routine tasks on the ward, such as assisting with patient meals and mobility, as well as undertaking monitoring of physiological measures, such as temperature or blood pressure.
- In-hospital cardiac arrest
- A cardiorespiratory arrest occurring within hospital as opposed to one that occurs prior to admission.
- Intensive care unit
- A hospital unit that provides care for patients with acute, life-threatening illness usually affecting more than one major organ system (e.g. heart and kidneys). They are staffed by doctors and nurses with specialist training and have a high staff-to-patient ratio.
- Outreach team
- Nurse-led rapid response team with responsibility for developing critical care skills amongst ward staff, providing clinical support to ward staff in managing patient deterioration, monitoring intensive care unit discharges and promoting the uptake of track-and-trigger systems to track patient observations and trigger appropriate responses.
- Physiological/vital signs
- Measurements that provide an indication of how well the body’s life-sustaining functions are doing. Routinely measured by clinicians to monitor a patient’s well-being and the progress of an illness. They generally include measurements of respiratory rate, blood oxygen levels, temperature, blood pressure and heart rate.
- Rapid response system
- A system for identifying and responding to deteriorating patients on the ward consisting of an ‘afferent arm’ (a scoring system based on physiological signs and graded criteria for calling) and ‘efferent arm’ (responsive) arm that brings the appropriate clinical response to the bedside (e.g. a rapid response team visit).
- Rapid response team
- A hospital-wide team designated to respond to patients who are deteriorating on the ward before that patient reaches the point of cardiac arrest. The team may be nurse led (e.g. critical care outreach team) or doctor led (e.g. medical emergency team) and may include personnel who make up the resuscitation team, but are usually not synonymous with this team. Hospitals may have both types of teams and differentiation may be based on the stage or rapidity of deterioration at which the team intervenes and additional roles; for instance, critical care outreach teams are more likely to follow up patients discharged from the intensive care unit to the ward.
- Resuscitation team
- Also commonly called the cardiac arrest team. This is a medically led multidisciplinary team with advanced life-support skills that is called (via the emergency number 2222) when an individual has a cardiac or respiratory arrest or is just about to do so. The team is responsible for implementing cardiopulmonary resuscitation.
- Situation, background, assessment, recommendation
- A structured method for communicating vital clinical information between clinical staff that requires immediate attention and action. It includes four steps: (1) caller identification and current location, (2) patient’s medical background, (3) patient’s current clinical condition and (4) caller’s requested action.
- Track-and-trigger system
- A guide used by clinicians to determine the degree of illness of a patient and the appropriate response. Physiological signs are entered into a paper or electronic scoring system. Scores are then related to specific actions that need to be taken, including a change in frequency of monitoring or a request for further support depending on the severity of the patient’s clinical condition.
- Treatment escalation plans
- A tool to deliver the appropriate level of clinical care given a patient’s clinical condition and wishes. The plan is usually drawn up after a discussion between the patient and/or relatives and the consultant directing the patient’s care. It informs other clinical staff about key treatment decisions such as whether or not the patient is to have mechanical ventilation in the case of respiratory failure.
List of abbreviations
- ALERT™
- Acute Life-Threatening Events Recognition and Treatment
- CCOT
- critical care outreach team
- CCU
- coronary care unit
- CG50
- Clinical Guideline 50
- CI
- confidence interval
- CPR
- cardiopulmonary resuscitation
- CQUIN
- Commissioning for Quality and Innovation
- DHSC
- Department of Health and Social Care
- DNACPR
- do not attempt cardiopulmonary resuscitation
- EWS
- Early Warning Score
- HCA
- health-care assistant
- HDU
- high-dependency unit
- HES
- Hospital Episode Statistics
- ICNARC
- Intensive Care National Audit & Research Centre
- ICU
- intensive care unit
- IHCA
- in-hospital cardiac arrest
- IRR
- incidence rate ratio
- LOS
- length of stay
- MERIT
- Medical Early Response, Intervention and Therapy
- MET
- medical emergency team
- MEWS
- Modified Early Warning Score
- NCAA
- National Cardiac Arrest Audit
- NCEPOD
- National Confidential Enquiry into Patient Outcome and Death
- NEWS
- National Early Warning Score
- NICE
- National Institute for Health and Care Excellence
- ONS
- Office for National Statistics
- OR
- odds ratio
- PMG
- Project Management Group
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCP
- Royal College of Physicians
- RCT
- randomised controlled trial
- R&D
- research and development
- RRT
- rapid response team
- SBAR
- situation, background, assessment, recommendation
- SG
- Steering Group
- TEP
- treatment escalation plan
- TTS
- track-and-trigger system
