Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/154/07. The contractual start date was in November 2015. The final report began editorial review in November 2017 and was accepted for publication in March 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
This report contains transcripts of interviews conducted in the course of research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Gridley et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Carers are the mainstay of the support system for disabled and frail children and adults. The UK 2011 Census1 identified almost 6 million people who defined themselves as carers, over half of whom cared for > 50 hours per week. In total, UK carers provide the equivalent of 17 million working hours of care per week. Furthermore, both the population of carers overall and the proportion who provide the longest hours of care have increased since the 2001 Census.
Carers are most likely to be over the age of 50 years, and are more likely than others of the same age to report poor or indifferent health, and, although people who become carers are more likely than others to be in poor health before they become carers,2 caring (further) affects both physical and mental health. 3
Evidence of the effectiveness of specific ‘carer interventions’ is poor (see below), but we do know that mainstream services for the people who carers support also help carers themselves. 4,5 However, the most recent nationally representative survey of carers showed that only 11% of the people being supported by carers had a visit from a paid home help or care worker at least once per month. Although in most cases carers said that visits from home carers were ‘not needed’, 25% of those not in contact did express some type of need. The proportions of people receiving visits from all other types of health or social care staff at least once per month were even smaller, and with similar levels of expressed need for most. 6 Further analysis of these data has compared them with those from a similar 1985 survey. This has shown that, despite an intensification in caring activity and impact over the past 30 years, and policy preoccupations with supporting carers, smaller proportions of the people who carers help now receive health and social care support and smaller proportions of carers experience respite. 7
Carers of people with dementia are potentially an even more disadvantaged group than the generality of carers. They experience repeated transitions in their personal, social, economic and psychological lives as the dementia journey progresses, and a substantial body of literature has documented the impact of becoming and being a carer for a person with dementia. 8 They are more likely to report negative physical and psychological outcomes than otherwise similar carers who support people without dementia. 9–11 Spouses who care for partners with dementia are themselves often elderly and frail, although some of those who care for parents may also still have responsibility for their own children.
Without carers, the health and social care system would be hard pressed to provide alternative care for people with dementia. 12,13 However, despite considerable policy interest in dementia over recent years,13–15 and a (largely separate) policy stream designed to ensure that carers are supported,16–19 evidence about how best to support carers through the dementia ‘journey’ remains elusive. This is largely because of the relative paucity and poor quality of existing evaluative research. 20–22 A particular weakness in the evidence base is the lack of studies that can throw any light on the cost-effectiveness of interventions to support carers. When there is evidence of effectiveness, there is rarely evidence of costs, whether to health and social care services or to carers and families themselves.
There is one dementia-specific, specialist nursing service in the UK that targets support at the carers of people with dementia – Admiral Nursing (AN) – and it is this that we have evaluated here.
What is Admiral Nursing and what do we know about its impact?
Admiral Nursing, based within the charity Dementia UK, is the only UK-based, dementia-specific, specialist nursing service that targets carers of people with dementia. The service was first piloted in Westminster in 1990 and as of June 2018 provides support via 85 teams (staffed by 221 nurses) around the country.
Admiral Nursing services vary in their composition, remit, funding models, case mix and other key characteristics, although they all work to a core set of values to support carers and family members of people with dementia. Some are commissioned and/or hosted by the NHS, whereas others are commissioned and/or hosted by local authorities or third-sector organisations. AN services are currently found in memory assessment services, community AN teams, care homes, hospitals, palliative and end-of-life care settings and third-sector settings. The service also runs a national helpline (Admiral Nursing DIRECT), which was established in 2008 and was staffed by an additional 31 nurses at the time the research was carried out.
Dementia UK describes the AN service thus:
Admiral Nurses are specialist dementia nurses who work closely with families living with the effects of dementia. They provide psychological support, expert advice and information to help families understand and deal with their thoughts, feelings and behaviour and to adapt to the changing situation. Admiral Nurses seek to improve the quality of life for people living with dementia and their families by using a range of interventions to help people live positively with the condition and to develop skills to improve communication and maintain relationships. Admiral Nurses also uniquely join up different parts of the health and social care system and enable the needs of family carers and people with dementia to be addressed in a coordinated way. They provide consultancy and education to professionals to model best practice and improve dementia care in a variety of care settings.
All Admiral Nurses are mental health nurses who have specialised in the care of people with dementia. However, although they do increasingly work with people with dementia, their main objective is to support carers and family members of the person with dementia.
A recent systematic evidence synthesis by Bunn et al. 24 scoped the existing literature about AN to determine, among other things, the scope, nature and key attributes of the AN role. This work identified two main themes that underpinned Admiral Nurses’ work with carers:
-
relational support (including taking a carer-centred approach, providing individually tailored support and being a ‘friend’)
-
co-ordination and personalisation of support (including facilitating access to other services and support, collaborating with other service providers and advocating on the carer’s behalf).
A third theme related to organisational and delivery issues, including the management of caseload, providing care across the dementia journey, the definition of the role and the dynamics of relationships with other parts of the health and social care system for people with dementia.
As these descriptions suggest, AN has all of the key characteristics of a complex intervention, as defined in the Medical Research Council guidance on the evaluation of such interventions. 25 It can involve large numbers of (and interactions between its) components, significant numbers and difficulty of behaviours for those who deliver and receive the intervention, targets for change at more than one organisational level, numerous and variable outcomes, and flexible and tailored delivery of the intervention.
The Bunn et al. 24 synthesis suggested that carers value the emotional support and education that Admiral Nurses provide and that their expectations of what Admiral Nurses might provide and what they actually do provide largely match. However, it also pointed out that, although there has been some qualitative research and one quantitative evaluation of AN outcomes in the past,26 the evidence base on their effectiveness, costs, cost-effectiveness and relationships to other health and social care services was still very limited.
The need for the research
The evidence synthesis from Bunn et al. ,24 commissioned by Dementia UK itself, showed that few studies provided evidence about outcomes for carers or evaluated the specific inputs of AN services. However, the synthesis also found little clear evidence about the cost-effectiveness of any other model of community-based support for people with dementia and their carers.
More recently, an updated metareview of evidence on support for carers suggested that contact between the carers of people with dementia and other people who know about dementia may improve some aspects of carers’ mental health and their perceptions of burden and stress. 21 However, very different types of intervention seemed to produce this effect, and it was often not clear what control groups were experiencing as ‘usual care’, making it difficult to come to robust conclusions about how best to provide support.
In 2009, the Department of Health and Social Care announced a new role, the dementia adviser, which was intended to enable ‘easy access to care, support and advice following diagnosis’ (© Crown copyright 2009. Contains public sector information licensed under the Open Government Licence v3.0). 13 This model appears to have been widely adopted,27 but navigating the complex health and social care system after diagnosis remains an obstacle to effective care and support,5,12 and people with dementia have recently been shown to receive less primary preventative health care than people without dementia. 28 In fact, dementia advisers were never intended to provide intensive support at the level offered by specialist services, such as Admiral Nurses,13 and qualitative evidence suggests that there continues to be a demand for a more intensive approach. 24
Indeed, a systematic review of case-management programmes for people with dementia29 concluded that the intensity of case management interventions was one of two factors determining the magnitude of their effects, the other being the integration level of the system in which the case managers worked.
Most recently, and since our research was completed, the review to update the National Institute for Health and Care Excellence (NICE) guideline on dementia30 identified only one cost–utility analysis on the subject of care planning, review and co-ordination for people with dementia or their carers. This analysis did suggest that intensive case management could result in cost savings, but the impact on quality of life was equivocal. 31
The review also identified moderate-quality evidence for a reduction in ‘carer burden’, along with improvements in quality of life for people with dementia and reduced rates of entry into residential care for those offered case management versus usual care. Across the studies, larger gains were seen in interventions with more frequent follow-up in which the case manager was a nurse and contact was made face to face in the person’s home.
Previous research has suggested that specialist nurses could be particularly effective in enhancing the continuity of care for people with complex conditions32 and that the disease-specific knowledge of specialist nurses in particular is highly valued by recipients. 33 Specht et al. 34 compared the outcomes of an existing dementia case management service with those of a new nurse care management model and found benefits to carer stress, well-being and endurance potential in the nurse care management group. From anecdotal evidence accompanying their study, the authors suggested that it could have been that having a nurse, in particular, leading the care management of the person with dementia and their carer led to these differences, as the nurse was able to pick up and help to manage associated health concerns, but they did not demonstrate this robustly. 34 A more recent systematic review of the evidence for ‘key worker type support roles’ for people with dementia and their carers concluded that one of the key ingredients of success was the support worker having a skilled background (i.e. they were a nurse, an occupational therapist or a social worker trained in dementia). 35
The detailed implications for research outlined in the Bunn et al. 24 synthesis included the need to:
-
evaluate the specific input of AN practitioners, set alongside outcomes for carers
-
explore the in-reach and training role of AN in acute hospitals, care homes and other practice settings and practitioners
-
investigate the contribution of AN services from the perspectives of other health and social care stakeholders
-
understand the profile of carers whom AN services support.
In the work we report here, we hoped to throw light on these types of issues by building on the earlier evidence and our existing partnership with Dementia UK to develop a rigorous quantitative and qualitative approach to address our main research question:
What are the costs and benefits for carers, families and people with dementia of providing specialist nursing support?
However, in addressing this question, we also wanted to explore the wider effects on health and social care of specialist support services for carers of people with dementia and the impact that receiving services has on carers’ navigation of other parts of the health and social care system.
As Bunn et al. 24 point out, as others have experienced,36 and as we know from our recent research on an intervention in dementia care,37 there are substantial challenges in setting up and carrying out an evaluation of complex interventions, and particularly in the area of dementia care.
Reflecting both the lack of current evidence and the difficulty of generating new evidence, our proposed project therefore had a dual purpose. The first aim was to make the best use of the existing data to examine outcomes for carers alongside inputs from AN, while also exploring the perceived systemic impact of specialist nursing support for carers. The second purpose was to test the feasibility of collecting outcomes and costs data and then to undertake exploratory research comparing the outcomes and costs of specialist nursing to support the carers of people with dementia against ‘usual care’, which might include other forms of carer support services.
Exploring how specialist community nursing services can support carers has the potential to reduce financial costs for health and social care services and, more importantly, social, health and financial costs for carers themselves. It also fits closely with current policy preoccupations, not only in relation to dementia and carers per se, but also in relation to the role of specialist community-based nurses in supporting the health and well-being of adult carers. 38 Among other issues, Compassion in Practice39 outlines clearly the need for carers and those they support to receive help from community-based practitioners who are experienced and knowledgeable, for the improved use of specialist roles and for greater harnessing of expertise to provide good-quality support. All of these and many other issues outlined in this policy document have clear relevance to the provision of specialist dementia nursing.
Without carers, the UK health and social care system would be unable to cope with the additional demands placed on it; finding effective and efficient ways of supporting carers to continue caring, if this is what they and the person they care for want, is thus of key importance in a country dealing with an ageing population. However, despite carers’ potential vulnerability and the repeated policy focus on the need to support them, we seem to be little nearer to delivering adequate support than we were when the first national survey of carers was carried out in 1985. 40
We currently know very little about the services available to carers of people with dementia across England, how carers engage with them and whether or not they answer carers’ needs. This study is a first step in understanding the national picture and preparing for a future full-scale evaluation.
Chapter 2 Study design and methods
In this chapter, we describe the detailed aims and objectives of the study, its design and the methods used to carry out the six work packages (WPs) that made up the project.
Design
In the absence of a secure evidence base for cost-effective interventions to provide support for carers of people with dementia, any high-quality evaluation will provide value. However, as the Medical Research Council guidance on the evaluation of complex interventions advises, it is important not to rush to a full-scale summative evaluation, such as a randomised controlled trial, before developing an understanding of the context within which interventions are delivered, their potential effects and the feasibility of a full-scale formal evaluation. 25 Developing such an understanding is what we aimed to do by adopting a mixed-methods approach, using secondary analysis of an existing administrative data set, along with primary quantitative and qualitative data collection.
We hoped that this approach would allow us to make the best use of existing and newly collected data to explore the potential effects and costs of specialist support for carers of people with dementia, while at the same time exploring the feasibility of formal evaluation in subsequent research. The work was thus intended to address two major uncertainties identified in the Bunn et al. 24 review:
-
limited quantitative evidence on the effectiveness, costs and cost-effectiveness of AN services, addressed by:
-
secondary analysis of the AN administrative database to identify preliminary evidence on the effectiveness (outcomes) of AN services
-
a survey of carers using AN services and carers in similar areas without AN services to generate preliminary evidence on the effectiveness and costs of AN services
-
-
an understanding of the relationship of AN with other health and social care services, addressed by:
-
an analysis of the AN administrative database to describe any (other) service support begun or discontinued after input from AN services
-
an analysis of all service receipt by carers using AN services and by carers in similar areas without AN services, using statistical methods to control for possible confounding variables
-
an in-depth exploration, in four case study areas, with health and social care commissioners and service providers of the impact of specialist dementia services, including AN, on the perceived impact on other health and social care services.
-
Patient and public involvement
This project was made possible by a partnership between the research team and Dementia UK, a third-sector organisation that campaigns for and supports people with dementia and their carers. AN is a Dementia UK service, and the charity had, for some time, sought support to explore its outcomes. Discussions between the research team and Dementia UK thus formed the basis of the original proposal.
In designing the study, we also consulted extensively with carers and people with dementia through the White Rose (University of York, University of Sheffield and University of Leeds) collaboration on dementia, cognition and care. Specialist nursing support for carers (or, more accurately, its lack) was one of the main priorities for future research identified through consultation. When the current project commenced, we continued to work with two of the carers on the White Rose consultation group, both of whom joined the project steering group and contributed throughout.
We also worked with Together in Dementia Everyday (TiDE), a national network of carers hosted by the Life Story Network community interest company, to establish a virtual advisory group of seven carers of people with dementia who were consulted throughout the project to advise on study design, project documentation and question wording for the survey. The group facilitator, a former carer herself, linked this group with the project steering group, attending meetings of the latter to present the views of the carers’ group. A further three carers regularly attended the steering group. This arrangement allowed carers to express their views in a facilitated and supportive environment. We found this approach to be of great value: carers were empowered to be both critical and supportive of the research, and their accounts of the lived experience of caring undoubtedly improved the project.
Towards the end of the project, we held a stakeholder workshop to discuss the study findings and their implications. Members of the virtual advisory group and other carers linked to the project were invited and supported to attend, and one-third of those who booked to attend the day said that they were current or former family carers. This workshop was extremely helpful to the research team in testing out the findings (see Appendix 1), and the presence of so many carers ensured that the implications and the next steps were grounded in the real-world experiences of those caring for people with dementia.
Aims and objectives
The aims of the project were to:
-
explore the processes, the individual and system-wide impacts and the effect on outcomes and costs of specialist support for carers of people with dementia (using the largest such service – AN – as an exemplar)
-
produce guidance to inform service delivery, organisation, practice and commissioning of specialist support for such carers.
Using a mixed-methods approach, the objectives were:
-
to carry out secondary analysis of an existing administrative database maintained by AN to explore the relationships between the characteristics of carers and people with dementia, AN service type and input and outcomes
-
using qualitative methods (interviews, focus groups and cognitive interviewing) with carers, to develop and test data collection methods to inform a subsequent cost-effectiveness evaluation
-
to conduct a survey of carers of people with dementia with and without access to AN services, in order to explore the effect on outcomes and costs of AN services, compared with usual care, and to determine the feasibility of a large-scale evaluation
-
using qualitative methods (face-to-face interviews with health and social care stakeholders in four case sites – two with and two without AN services), to explore the perceived system-wide impact of providing specialist support services for carers of people with dementia, compared with usual care
-
to implement new data collection methods to facilitate future evaluative research in AN, which could be used by other dementia service providers
-
to build on the findings of all elements of the project and work with key stakeholders to devise best-evidence guidelines for service organisation and commissioning.
Methods
The project had six interlinked WPs. In this section, we outline the main methods of each, as originally planned. Because of the mixed-methods design we adopted, further details of the methods that we actually used are provided in the individual chapters below.
Work package 1: secondary analysis of the Admiral Nursing administrative data set
Work package 1 prepared the administrative data maintained by AN for research purposes and then analysed the data to explore the links between carer characteristics, the characteristics of the person with dementia, AN input and outcomes over time (objective 1).
The data set
Admiral Nursing has maintained a database of its activities with individual carers since 2005. Data on carers’ personal characteristics, support needs, burden and physical and mental health, and some details of the person being cared for and on services provided, are collected by AN when it carries out its first assessment of carers’ needs, and these are entered into the data record. Data on variables, such as needs, burden and health, as well as AN input, are also collected at follow-up, allowing the exploration of outcomes over time. Needs assessment is carried out using AN’s own tool, with standard coding.
On the day when the anonymised data were securely transferred to the research team (11 March 2016), these included 24,825 records in a Microsoft Excel® 2013 (Microsoft Corporation, Redmond, WA, USA) data set and were made up of both ‘primary’ carers and other family members defined as secondary carers, as well as cases that were now closed. It also included records that log follow-up data for primary carers. Owing to the size of the database, the data were split into several data sets (see Table 8) to ease transfer and data manipulation. Dementia UK transformed the data into a format that was compatible with the data analysis software package that was being used for analysis [IBM Statistical Product and Service Solutions (SPSS) Statistics version 24 (IBM Corporation, Armonk, NY, USA)], while ensuring that the baseline and follow-up data on individuals remained linked across the data sets.
Based on a preliminary discussion with AN, we expected to find data for 1360 carers whose needs were assessed at both baseline and at least one follow-up point. For a small number of carers, the data set also included standardised outcome measures, of which the Zarit Burden Inventory41 is the one most often completed. In September 2014, around 3% of open cases of carers had a completed Zarit Burden Inventory in their record.
Preparation of data for analysis
Admiral Nursing provided a cleaned and anonymised data set containing the records of carers who had used the service since 2005. However, as would be the case with any administrative data set, the following issues had to be addressed before we could export the data and start the analysis for research purposes:
-
Creating flat structures for all of the data, to allow linking across individual records.
-
As maintained by AN, each question in the needs assessment tool and the standardised outcome measures is entered on a separate row in the Excel spreadsheet. For example, the answers to questions 1–22 for the first carer who completed the Zarit Burden Inventory appear in the first 22 rows of the relevant sheet in the Excel spreadsheet. These data had to be converted into a flat structure (with all 22 answers in a single row) to allow us to easily and securely link the answers to the rest of the record for that carer. AN carried out this work, but it created substantial challenges, which are described in Chapter 3.
-
-
Linking baseline and follow-up (outcome) records for individual carers.
-
Each carer in the database had a unique identifier, but follow-up data were recorded in a separate file. We therefore needed to use the identifier to create single records for those carers for whom follow-up data were available. Although it had originally been planned that AN would carry out this work, it was eventually done at the University of York.
-
-
Devising a coding framework for data currently entered as text.
-
The research team reviewed all of the data and liaised with Dementia UK to ensure that they understood the concepts and questions behind the data, the mode of data entry – that is, entered by staff or system-generated – and the data codes that existed in the data sets received. For example, data related to needs assessments were already coded from 0 to 3. We accessed the relevant assessment documents and, when appropriate, spoke with members of the Dementia UK data team to clarify coding systems, so that we were able to determine the meaning of each code (for the example given above, this was 0 = no need, 1 = need currently met, 2 = unmet need, 3 = not known).
-
Some data, such as the carer relationship to the person with dementia, country of birth and risk screening, were in text form. These forms of data had to be transformed into numerical codes to enable analysis. Two members of the research team (GP and FA) reviewed the text and identified summary categories for these data using filtering commands in Excel, and the data were recoded accordingly.
-
In two of the data sets – daily activity log and risk screening – the data were qualitative and extensive. To carry out the planned analysis, we needed to create numerical (categorical) data from the text. We started to develop a coding framework by taking a systematic sample of records and examining the text for commonalities and differences in the text for each ‘question’, and then devised and piloted the coding framework. Once the coding framework was finalised, we aimed to apply it to all textual material, thereby creating categorical variables. However, after reading the data and identifying the initial codes, we felt that these data required more in-depth qualitative analysis to maintain data integrity and to illustrate the complexity of cases that Admiral Nurses were dealing with and that clients were experiencing. A summary of these qualitative data is provided in Chapter 3.
-
-
Creating variables to summarise the type of AN service received.
-
We had planned to create descriptive variables for the current AN services, using another AN data set that logged service details, including team composition and size, geographical area covered, referral processes, funding source and staff complement. This would have allowed us to explore relationships between service characteristics and outcomes. We encountered considerable challenges in this part of the planned work, mainly because of difficulties in accessing information about teams that were in existence when we did the work and the impossibility of obtaining data for teams that no longer existed. We therefore did not, in the end, conduct these analyses.
-
Analysis
We first used analysis of this unique data set to provide a detailed picture of the carers who have used AN services. We then attempted to use records when needs assessment had been carried out at more than one point to explore how AN input affected outcomes. We had hoped to carry out a range of univariate, bivariate and multivariate (regression) analyses and to establish the links between type and intensity of AN input, service user characteristics and needs and outcomes. The initial univariate and bivariate analyses were intended to explore patterns of change in the outcomes, create change variables and identify service types. The generalised regression and multilevel approaches would then explore the unique and inter-related contributions of carer characteristics, service input and team types to outcomes. For reasons explained in Chapter 3, we were unable to progress beyond the univariate and bivariate analyses. However, the large amount of work that has gone into turning an administrative data set into something that can be used for research lays the base for multivariate exploration in the future.
Individual AN services have changed over time in their characteristics and functions, and, since 2005, some have ceased to operate, whereas others have started up. We could not, therefore, use the data simply to ‘describe’ AN services. However, we did use the data to analyse what type of work was done, and used this to develop a picture of the AN service ‘offer’.
All analyses were carried out by the University of York team.
Work package 2: develop and test data collection methods for the survey and the new data set
Work package 2 was designed to establish a data collection framework and processes for the survey in WP 3 (objective 2).
There were two elements to the package. First, we wanted to establish what outcomes are important to carers in terms of their actual or anticipated use of specialist nursing support. Second, we needed to identify robust ways of measuring those outcomes, that were acceptable to and feasible for carers, both for our survey in WP 3 and for use in service settings (WP 5). The in-depth exploration of the acceptability and the feasibility of the framework and processes was an essential element, given the acknowledged challenges of evaluative research in dementia care.
Sample
We identified two areas with an AN service and two areas without and recruited carers in each, aiming for a total sample of around 30 carers, with a wide range of characteristics and circumstances. The details of the recruitment processes and outcomes are provided in Chapter 4.
Although we had initially planned to hold focus groups on the University of York campus, we soon realised that it would be more convenient for carers to hold these groups in meeting places (churches, community centres, etc.) that were local to the carers’ own homes. We also offered carers the option of an individual interview by telephone or in their home, or somewhere else to suit them. We offered to pay for the costs of substitute support for the person with dementia when this would help the carer to participate.
Methods
Developing the survey
We talked to carers twice, using focus groups or, when requested, individual interviews.
At the first contact, we used in-depth qualitative methods to explore with carers the outcomes that they would like to experience if receiving support from specialist dementia services that were focused on carers. For those who lived in areas without AN services, we first described the support that they might get from such a service, so that they could focus their responses on this type of service.
At the end of each group session or interview, we fed back the learning from the discussion and worked with the carers to finalise the outcomes they wanted us to take forward to the next stage of work. We recorded the groups and interviews (with carers’ permission), but did not fully transcribe all of them. After the interviews, we reviewed the recordings, first to ensure that we did not miss any outcomes in the summing up and, second, to carry out a brief analysis of the material, under each of the outcomes identified. We used the framework principles of case- and theme-based analysis and data reduction through summarisation and synthesis42 to do this.
We then identified robust, standardised measures that are available to assess the main outcomes that carers had identified. In doing this, we were guided by the work that Early detection and timely INTERvention in DEMentia (INTERDEM) has done to identify good-quality outcome measures in dementia care. 43 This work and the measures that we selected – the EuroQol-5 Dimensions (EQ-5D),44 Adult Social Care Outcomes Toolkit (ASCOT) for Carers (ASCOT-Carer) (the ASCOT-Carer measure was used in the study with permission from the University of Kent on an all rights reserved basis. The measure should not be used for any purposes without the appropriate permissions from the University of Kent. Please visit www.pssru.ac.uk/ascot or email ascot@kent.ac.uk to enquire about permissions)45 and the Family Caregivers’ Self-Efficacy for Managing Dementia (SEMD) scale46 – are described in detail in Chapter 4.
The questionnaire had a dual purpose within our proposed work. First, it was to collect data on the carers of people with dementia in areas with and areas without AN for WP 3 (see Work package 3: survey and analysis of outcomes and analysis of outcomes and costs) and, second, it was to provide the basis for a draft data collection framework for AN to use routinely (see Work Package 5: implement a new data collection system for Admiral Nursing and promote it to other dementia service providers). The questionnaire included:
-
Questions on the demographic and socioeconomic characteristics of the carer and of the person with dementia (e.g. age, sex, ethnicity, education and household resource level).
-
Instruments that measured the outcomes that were important to carers (see above and Chapter 4).
-
Questions on the time and resource use associated with caring. These included unpaid (informal) care time, out-of-pocket costs for care services, health [e.g. hospital appointments, general practitioner (GP) appointments], social care (e.g. home care) and non-statutory sector resources. These also included questions on specialist dementia services accessed by the carer (both AN and other services).
We then carried out cognitive interviews with carers. These explored the carers’ understanding of the questionnaire and its acceptability to them. We also talked to them about the feasibility of carers completing a questionnaire of this type online and in hard copy, and the pros and cons of self-completion versus face-to-face or telephone interviews.
We tested the administration of the survey, both electronically and in hard copy, with a small number of carers (n = 9) who had been involved with the earlier work and with members of our carers’ virtual advisory group and our steering group.
The survey was developed within, and administered using, Qualtrics [February 2017; www.qualtrics.com (Provo, UT, USA and Seattle, WA, USA)]. This is sophisticated, internet-based survey software that allowed us to produce and distribute high-quality online questionnaires. We also produced a paper version of the questionnaire, which is reproduced in Appendix 2.
Work package 3: survey and analysis of outcomes and costs
The key aims of WP 3 were to address objective 3 by:
-
understanding the characteristics of carers, the people with dementia whom they support and their outcomes and costs with and without AN services
-
exploring the effect on outcomes and costs of AN by comparing relevant carer outcomes and costs in areas with and areas without AN services
-
evaluating the feasibility of recruiting carers and collecting their outcomes via online and postal questionnaires in future research.
Rationale for our chosen survey design
Our aim in this section of the proposed work was to compare the carers of people with dementia who used AN services with those who did not (who received ‘usual care’), both to judge the likely effect of AN services on carers’ outcomes and to assess the costs of AN services against any benefits that might be identified.
Admiral Nursing is the only specialist nursing service for the carers of people with dementia, so we felt relatively sure that carers in non-AN areas would not be receiving any carer-focused, dementia-specific services. Other services that both AN and non-AN carers might use include visits from community-based mental health nurses, home care services and social work input. However, we expected to see substantial heterogeneity, given the diversity of support services for people with dementia and their carers and the diversity of provision across the country. It is possible that AN services substitute for other forms of services that carers might otherwise have received. However, at the outset, we thought that it was more likely, given the objectives of AN services, that they would enhance carers’ access to other services, via signposting and direct liaison.
We had hoped to strengthen our analysis by also surveying a small number of carers who lived in AN areas but did not use AN services. The substantial challenges of identifying those not using AN services, described in more detail in Chapter 5, meant that we did not achieve this secondary aim.
Choice of design
Our chosen design was a cross-sectional survey. We chose this approach because the carers of people with dementia are a precious research resource, and longitudinal data collection would impose additional burdens on them and, in all likelihood, reduce response rates over time. However, we intended that the design of the sampling and analysis strategies would allow us to carry out a robust cross-sectional comparison between those who did and those who did not use AN services.
First, the sample selection processes aimed to reduce heterogeneity, both within the AN services being evaluated and between carers in areas with and without AN services.
Choice of sampling frame
We generated simple, two-stage cluster samples of local authority (LA) areas that had ‘standard’ AN services (see below for a definition) and broadly similar (matched) LA areas without AN services. We then intended to carry out proportionate random sampling of current users of AN services in the former areas and of carers in contact with TiDE in the latter areas to generate the respondents for the survey. For the reasons described in detail in Chapter 5, identifying carers in non-AN areas was extremely challenging and we were not able to carry out this element of the design. We did, however, carry out proportionate sampling of carers in our selected AN services.
‘Standard’ model of Admiral Nursing services
As outlined in Chapter 1, AN services vary in their composition, remit, funding models, case mix and other key characteristics. For the purposes of this WP, however, we needed to compare the outcomes from services that were typical of the majority. We therefore selected areas with AN services that delivered a ‘standard’ model, which, after discussion with AN, we defined as services that:
-
were based in the community (rather than in a long-term care setting)
-
provided support mainly to carers when supporting a person still living in a private household
-
were funded to provide support to any carer (thus excluding third-sector-funded services that provided support only to a subgroup of carers).
Matched areas
We defined ‘broadly similar’ areas in terms of statistical neighbourhood, as defined by the Chartered Institute of Public Finance and Accountancy (CIPFA)’s statistical model (www.cipfastats.net/default_view.asp?content_ref=18003; accessed 16 October 2018). Statistical neighbourhood is used by local authorities themselves, and across government, to allow comparisons between authorities that are similar in terms of population size and characteristics, such as age distribution, deprivation and ethnicity. For example, the Department of Health and Social Care has developed an interactive adult social care efficiency tool (www.gov.uk/government/publications/adult-social-care-efficiency-tool; accessed 16 October 2018), which compares local authorities’ performance on service provision to, and expenditure on, older people and people with a learning disability. It was this latter tool that we eventually used to match areas.
Sample size
Sample size calculation for cross-sectional surveys of populations is simple when the sole aim of the survey is to describe the population within given statistical tolerances. Similarly, sample size calculation is relatively simple when the sole aim is to compare outcomes between equivalent groups that vary only in their receipt or not of an intervention. However, this calculation does also require prior knowledge about, or an indication of, what size of effect one might be expecting, or what average level of a chosen outcome one might expect to see in the selected population prior to intervention.
In our survey, we wished both to describe and to draw inferences about what effect using AN services might have on carers of people with dementia. Although our sampling strategy (see above) was intended to reduce some of the likely variation between users and non-users of AN services, we also needed to control for any other differences between them that would become evident after collecting data. This was so that we could feel confident that we were seeing the effect (if any) of AN services on measured outcomes, and not the effect of some other differences between carers.
It was challenging to find any up-to-date population-based evidence about the average levels of (for example) the quality of life of carers of people with dementia, or any UK-based comparative studies that might hint at possible effect sizes from similar types of intervention.
Given these challenges, we took a pragmatic approach to sample size calculation using three different approaches. The first was a simple population survey sample calculation. The second was a sample calculation for comparative research, using the effect sizes found in a randomised controlled trial of community occupational therapy in the Netherlands47 that aimed to help carers to use ‘effective supervision, problem solving, and coping strategies’ with a view to sustaining both their own and the person with dementia’s ‘autonomy and social participation’. This intervention also included similar input for the person with dementia and found very substantial differences on a range of outcomes at the 3-month follow-up point. We then assessed how many independent variables could be included in a multivariate analysis, based on the sample sizes generated by these two approaches. The results of these calculations are in Table 9 in Appendix 3.
A pragmatic decision about an achievable sample size, within reasonable resource use, took us to a decision about original sample size somewhere between the two figures of 26 and 640 generated by this process. Assuming that we would need to control for up to 20 independent variables in a regression analysis, we calculated that an achieved sample of 320 participants would be needed to detect differences of the size observed in the Graff et al. 47 study.
We assumed that the response rate in non-AN areas might be lower than that for AN users [e.g. 50%, rather than the 60% we had achieved in a recent survey of carers in another National Institute for Health Research (NIHR)-funded project]. 37 Subsequent discussion with AN prompted us to reduce the anticipated response rate further to 30%. Taken together, to achieve 160 participants in each group, we needed to sample around 480 carers from AN services and 480 carers in non-AN areas: a total of 960 carers.
While preparing the original proposal, the team had discussions with staff at Dementia UK about the likely caseloads that might be found in individual AN services. Although services varied in size, the general view was that an average of 35 active cases per site was likely. We therefore needed to sample at least 16 teams to achieve our required sample size (again assuming a 30% response rate for this group). This also gave us the recommended minimum number of 30 clusters (15 AN areas and 15 matched non-AN areas) for this type of survey design.
Admiral Nursing teams identified carers who were currently using the service in the selected AN areas. A range of approaches was used to identify carers in the non-AN areas (see Chapter 5).
When the number of cases per AN team was greater than needed for sampling, we used proportionate random sampling to generate the required numbers.
Methods
Survey
In our 16 AN areas, we asked the AN services to identify carers of people on their current caseload and to facilitate distribution of the questionnaire developed in WP 2. We also worked with a range of statutory and non-statutory organisations to identify carers of people with dementia in the 16 matched, non-AN areas. In both cases, we offered the option of electronic and paper-based delivery, depending on individual preferences. Our earlier discussions with AN had suggested that electronic distribution would be the preferred option for AN carers but, in reality, this was not the case, as many selected services did not have e-mail addresses for the carers. We therefore ended up with a majority of AN returns on paper and, because of the way in which we sampled them, a majority of electronic returns from carers in non-AN areas. Further details of this are in Chapter 5 and a copy of the paper questionnaire is in Appendix 2.
For paper-based questionnaires, we included a leaflet explaining our study and its objectives, the questionnaire and a prepaid envelope for returning directly to the research team. For questionnaires delivered electronically, we attached the same leaflet to an e-mail, which also provided a unique electronic link to the survey.
We offered carers a £10 voucher on receipt of their completed questionnaire to thank them for taking the time and the effort to answer the questions and contribute to our research.
Further details of the sample identification and selection and the questionnaire administration are in Chapter 5.
Data entry
Data gathered via Qualtrics were initially exported as an Excel spreadsheet, which, after some editing, was exported to statistical software (SPSS and Stata®, StataCorp LP, College Station, TX, USA) for analysis. Data returned via paper-based questionnaires were checked for quality and then entered into Qualtrics manually.
Analysis
We carried out a number of descriptive and econometric analyses that enabled us to understand the characteristics of carers and the person they support and how these related to their outcomes and costs, with and without AN services. We also used data on responses to the survey to assess the feasibility of future research to collect data on carers and the people with dementia they care for via online and postal questionnaires.
The analysis plan was designed to include the exploration and analysis of outcomes and costs, and also methodological learning.
Describing outcomes
The first stage described the characteristics of carers and explored their relationship with outcomes. The univariate and bivariate analyses explored carers’ demographic and socioeconomic characteristics; the characteristics of the person with dementia; carer-specific variables, such as type and hours of care provided; scores on our selected outcome measures; and resource use and costs.
This preliminary work also allowed us to compare the overall characteristics of the AN carers and people with dementia with the characteristics of carers and people with dementia in the non-AN areas. This enabled us to specify potential confounding variables for the subsequent analysis of outcomes and costs, as well as to establish the representativeness of carers who had completed the survey.
In the second stage of the analysis, we costed the health and social care services used by carers using national unit costs when available, or using the local unit costs of services otherwise. A descriptive analysis of the resources used by carers, and the costs of those resources, was carried out, and the relationship between the carers’ characteristics, the characteristics of the person with dementia, outcomes and costs was evaluated. The relationship between costs to the health and social care sector by type of area (with and without AN), controlling for the characteristics of the carer and the person with dementia, was of particular interest, as it might indicate whether or not AN services can generate savings in the health and social care sector by providing support to carers.
Analysis of outcomes and costs
Building on stages 1 and 2, we then carried out an analysis of outcomes and costs using regression analysis, propensity score matching (PSM) and an instrumental variables (IVs) approach to establish the associations between the carers’ characteristics, costs and outcomes.
The analysis aimed to evaluate the costs and effects associated with AN compared with usual care for carers. Our focus was on carers, given that AN was primarily designed to support the carer rather than the person with dementia. A broad perspective was taken to account for the costs falling on the NHS, social services and voluntary-sector services.
The aim was that the primary analysis would involve an analysis of outcomes and costs using the NICE reference case for health-care interventions taking the NHS and Personal Social Services (PSS) perspective. 48 This includes the costs falling on the NHS and PSS budgets and the outcomes that were relevant to carers. The costs falling on the NHS and PSS budgets included hospital appointments, primary care appointments (GP, nurse and so on), home care funded by the LA and the AN service itself. Resource use was costed using published, national average unit costs49,50 and NHS reference costs51,52 when available, so that the cost analysis was as generalisable across England as possible.
In addition, we ran a descriptive analysis to compare out-of-pocket costs and other informal (unpaid) care costs across AN and non-AN carers.
Dealing with comparability and unknown confounders
Given the non-randomised, cross-sectional nature of the data collection process, quantifying an association between outcomes and the availability of AN services requires us to be sure that carers responding to the survey in areas with and in areas without AN services are comparable in observed and unobserved factors that might affect outcomes.
For this reason, the analysis was in five stages, described in detail in Chapter 6: descriptive analysis, linear regression analysis, PSM, IV analysis and sensitivity analysis. We conducted the descriptive analysis to understand the characteristics of the sample and to select the variables to use in the subsequent analyses. With the linear regression analysis, we analysed the associations between having AN services and outcomes and costs, controlling for the observed differences between carers with and without AN services. We used PSM to generate comparable groups of carers with and without AN services. 53
Linear regression and PSM can deal only with observed differences in the two groups of carers. We had some concerns that there might be unobserved differences (i.e. differences in characteristics on which we could not collect data). The implication was that carers in non-AN areas would not represent carers in AN areas in the absence of AN services, even after controlling for observed characteristics. This is known as selection bias (also known as confounding or endogeneity).
The IV approach may reduce the risk of selection bias in the presence of good instruments. The instrument was the travel time between the carer and the AN provider. Carers living far from the AN provider may not be eligible, because the service is limited to a specific geographical area. Moreover, carers living at long travel distances from the AN provider may be less likely to be informed about AN than carers living in proximity to AN teams; thus, carers living near AN providers may be more likely to be eligible for or to access the service. Similar to Forder et al. ,54 we used the type of LA as an instrument. The type of LA may indeed determine the LA’s culture and, in turn, the LA’s propensity to invest in services for carers; the culture, however, will not have a direct effect on the carer’s outcomes.
Work package 4: understand the wider impact of specialist support for carers of people with dementia
The effects of specialist dementia services may extend beyond individual outcomes and resource use, having effects also at a system level. For example, if services enable carers to care for longer or help them to remain healthy, they may reduce costs to both health and social care systems. WP 4 explored with health and social care stakeholders what they perceived to be the system-wide effects of supporting carers of people with dementia, with a specific emphasis on specialist nursing support of the type AN provides.
Sample
We selected two areas with AN services that delivered a ‘standard’ model, defined in the same way as for WP 3 (see ‘Standard’ model of Admiral Nursing services in Work package 3: survey and analysis of outcomes and analysis of outcomes and costs).
We then selected two areas that did not have AN services but that were broadly similar areas to those with AN services. We selected areas that were also selected for WP 3 in the hope that we could triangulate our qualitative and quantitative findings in these areas (thus treating them as case studies). For reasons explained in Chapter 7, it was not possible to triangulate the findings as originally envisaged.
Within each area, we identified the key health and social care stakeholders in dementia care and support for carers. This included both statutory and third-sector (e.g. senior managers of local Age UK or Carers UK) stakeholders. We started with the main health service or social care commissioner for dementia services in each area and then used snowballing techniques to identify other stakeholders.
We intended to grow the sample until we were learning nothing new (i.e. we achieved saturation of the data) and expected to identify between 12 and 15 key stakeholders in each area to achieve saturation. Chapter 7 describes the outcomes of this approach.
Methods
We carried out in-depth, semistructured interviews with stakeholders that explored the perceived system-wide impact of carer services, such as AN, compared with ‘usual care’ (objective 4).
The interview aide-memoire covered the following topics:
-
the current provision and cost of support for carers of people with dementia
-
the perceived impact of support for carers of people with dementia (or its lack) on other health and social care services
-
the balance between the costs and benefits of supporting carers
-
future plans for (further) developing support for carers of people with dementia.
In the AN areas, we also covered topics specific to AN, such as commissioning arrangements and intentions.
We also used this stage to explore the feasibility of implementing routine collection of outcome and resource use data.
Work package 5: implement a new data collection system for Admiral Nursing and promote it to other dementia service providers
Using the learning from WP 2, we worked with AN services to develop a new data collection framework to provide the data required for future evaluative research, while also meeting their administrative needs. This built on the work in prior stages to understand the feasibility for dementia service providers, and acceptability to carers, of using a range of validated outcome measures as part of routine data collection.
Following the general shape of the survey questionnaire, we expected the framework broadly to include socioeconomic data, quality-of-life measures (both generic and carer-specific), informal carer time and health and social care resource use, as well as administrative data that describe AN activity and input for individual carers. We aimed to pilot the new framework with one AN team to test its feasibility in the field and to work with Dementia UK to inform its approach to routine data collection across all services going forward.
Further details about the ways in which this WP was carried out are in Appendix 1.
Work package 6: develop best-evidence guidance for service commissioning and the delivery of support for carers of people with dementia
The final stage of our project was a stakeholder workshop that presented the findings of all elements of our research. We worked with stakeholders during a full-day event to begin drafting a statement about the current evidence for specialist support for carers of people with dementia, how different models of support might influence outcomes and how to collect data at a local level so that they inform both service development and evaluation.
We invited a range of stakeholders, including carers, decision-makers from health and social care commissioning and provider organisations (including those in the third sector) and local and regional policy-makers. Key points from this workshop are presented in Appendix 1. These fed into a summary of the project findings, which was circulated to participants and other stakeholders and is now available as a project output. 55
Chapter 3 Analysis of the Admiral Nursing administrative data set
Work package 1 of the project focused on preparing Dementia UK’s AN administrative data set for analysis of its routinely collected data for research purposes. The aim of this analysis was to help to understand the characteristics of carers who use AN services and the characteristics of the person they care for, the type and level of input carers receive from AN services and the outcomes carers experience when using AN services. As outlined in Chapter 2, because of the size of the database, the data were split into several data sets to ease transfer and data manipulation. Table 8 (see Appendix 3) provides an overview of the data sets received.
Analysis
Each data set was initially analysed separately and, when appropriate and practical, then joined and analysed alongside other data sets.
Some data held within the database were collected at a single point in time and some were longitudinal. Data collected at a single time point – usually at entry to the service – included information about the sociodemographic characteristics of carers, agencies involved in the case at admission to AN and other family members involved. We analysed these data descriptively.
The Likert scale-derived data about the needs of the dyad of the carer and the person with dementia were longitudinal. There were two main data sets with such repeated measures, both related to needs assessment. One data set held data from an older version of the AN service’s own needs assessment form and the other held data from a new version of the form. The current needs assessment contained 18 questions and the legacy assessment contained 19 questions. Most of these were about comparable topics, but the response options were different. On the legacy needs assessment, the five-point Likert scale responses were about whether or not there was a need that required intervention and the severity/urgency of that need/intervention (i.e. none, minimal, some, considerable, urgent). The current needs assessment tool used a four-point Likert scale to ascertain whether or not there was a need that might require intervention, but did not refer to the severity or urgency of that need/intervention (i.e. no need, needs currently met, unmet need, not known). The legacy assessment asked a specific question about information in relation to understanding dementia symptoms, but this was not included in the current tool. The current tool included a question about risk that was not on the legacy tool (see Appendix 3, Table 10). Because of these differences, the two data sets were analysed separately.
The data sets held legacy needs assessments for 2074 carers and current needs assessments for 2541 carers. Some carers were assessed up to eight times using the legacy needs assessment and up to nine times using the current needs assessment; however, the majority of carers had only one assessment recorded (see Appendix 3, Table 11). To ensure that we would be able to detect any changes in needs assessment over time while retaining an adequate sample size, we limited the analysis of assessments to carers’ first three assessments. To be able to do this, we undertook additional restructuring of the data sets.
First, we conducted a match-text analysis on unique identification numbers to identify carers who had been assessed using both assessment formats. This showed that 51 carers were assessed using both the legacy and the current assessments forms. The analysis of these 51 cases across the two data sets confirmed that the legacy needs assessments were completed before the current needs assessments. Thus, we were able to remove the 51 duplicate cases from the current needs assessment data set.
Second, when we received the data, they were not in any particular date order. On speaking with the administrator of the database, it became clear that, when the data were converted from their original structure to the required ‘flat’ structure (as outlined in Chapter 2), they had been ordered by the date on which they were entered onto the system rather than the date on which assessments were undertaken. To correct this problem, we had to convert the data set back to its original structure and then restructure it again into a flat format in order of the dates of the assessments. Assessments without dates were removed from the data set being analysed.
Finally, we removed all cases in which there were fewer than three assessments on each of the forms. This left us with active data sets of 157 cases for the legacy needs assessment and 201 cases for the current assessment (see Appendix 3, Table 12).
These longitudinal data were then subject to descriptive analyses and Friedman’s tests to analyse the variance in responses to the needs assessment questions over three consecutive time points. The Friedman test is appropriate for examining differences in ordinal values over time when the samples are related (as they are here) and produces a chi-squared statistic. When the results of the Friedman test were significant, we then carried out Wilcoxon signed-rank post hoc tests with Bonferroni adjustment, resulting in a significance level set at a p-value of < 0.017, to establish which pairs of needs assessment data accounted for the differences.
The cases data set
Of all of the data sets, the ‘cases’ data provided the most complete and up-to-date overview of clients of AN services, with information about all 24,825 current and previous clients. Of these client cases, 85% were closed (see Appendix 3, Table 13). When relevant, the findings are presented to enable a comparison of closed (previous), open (current; 14%) and waiting-list (future; 1%) client cases.
Demographics of carers and people with dementia
Almost three-quarters of carers (71%), whether previous or current clients, were the main carer for the person with dementia. Information about living situation was recorded for only one-quarter of the people with dementia. Most lived with their main carer (57%) or alone (14%). Most carers were female (70%), whereas the people with dementia were split almost equally in terms of sex (53% female, 47% male). Over three-quarters of carers (77%) were > 55 years of age, as, unsurprisingly, were most people with dementia (98%). Almost two-thirds of the primary carers were retired, but an important minority (15%) were in full-time employment. Ninety-one per cent of both the carers and the people with dementia were described as being of white ethnicity (see Appendix 3, Tables 14–19).
Table 20 in Appendix 3 shows the relationship between the age of carers and the age of people with dementia. Almost one in three carers (32%) were in the oldest age group (aged ≥ 75 years) and were caring for someone in the oldest age group. The similarity in age is not surprising, given that the majority of carers (88%) receiving support from the AN service were married and were most likely supporting their spouse or partner (see Appendix 3, Tables 21 and 22).
Diagnoses
Seventy per cent of the cases in the cases data set reported whether or not the person with dementia had been diagnosed when they were referred to the AN service; almost half of these people had been formally diagnosed. When a diagnosis was recorded, the most common were Alzheimer’s disease (39%) and vascular dementia (30%). Table 23 in Appendix 3 shows that there was little variation in diagnoses among closed, open or waiting-list client cases, although open cases were somewhat less likely yet to have received a diagnosis, as might be expected.
Service provision
The intensity of input that carers received from Admiral Nurses was recorded for current clients. In almost half of the cases, when the data were entered into the data set, Admiral Nurses were still working with carers to determine their longer-term input requirements (45%). Almost one-third of carers (31%) were recorded as receiving a medium level of intervention, which could include, for example, monthly one-to-one meetings and planned telephone, e-mail or group contacts between meetings (see Appendix 3, Table 24). Carers classified as being in the ‘holding pool’ (13%) had the lowest level of intervention: 3- to 6-monthly telephone or face-to-face contacts, and contact at other times if initiated by the carer. Eleven per cent of carers were in the intensive category: the highest level of intervention that Admiral Nurses provide. Intensive support could be monthly or more frequent visits in combination with support group attendance and could include both planned and unplanned contacts and multiagency working.
This analysis suggests that Admiral Nurses are accessible through different routes and at times when carers need them and thus are able to provide a responsive and flexible service, responding to carers’ requirements at different times. By enabling those carers who need the least amount of support to request additional contacts if necessary, Admiral Nurses empower carers to take the helm as they travel through their caring journey.
Daily activity log data set
Support given by Admiral Nurses
As outlined in Chapter 2, we undertook a thematic analysis of a sample of the textual data that Admiral Nurses recorded about their daily work and that was entered in the daily activity log data set. This illustrated the wide variety of tasks that Admiral Nurses undertook to support carers. We categorised these as:
-
assessment and monitoring
-
discussion, information provision and advice
-
care co-ordination
-
emotional support/counselling
-
practical support.
Admiral Nurses also provided education to other service providers and professionals involved in their clients’ and the wider community’s care, and organised and ran carers’ groups. These last two roles are not discussed here because no detail was provided in the data set about what these roles entailed.
Assessment and monitoring
As the range of data listed in Appendix 3, Table 8 shows, Admiral Nurses formally assessed carers, their needs for support and the risks that they might be experiencing. The textual data from the daily activity log showed that, as appropriate, they also undertook assessments of the person with dementia, such as the Mini Mental State Examination, to help in planning and providing support to the carer. In addition to these more formal assessments, Admiral Nurses monitored carers’ mood and mental health during contacts, so that input could be adapted to respond to carers’ changing needs. One of the key assessments that Admiral Nurses undertook was risk assessment, which we analyse later in the chapter.
Discussion, information provision and advice
One of the central roles that Admiral Nurses played was spending time with carers, giving them the opportunity to discuss their practical concerns and fears and gain confidence. The data indicated that, drawing on their expertise about dementia to provide relevant and timely information and advice, Admiral Nurses talked with carers about managing the person with dementia’s behaviour, including safety and changing needs, addressed fears about the future, provided advice about coping strategies and identified services that might help in caring for the person with dementia and/or supporting the carer.
Care co-ordination
Admiral Nurses made and ‘chased up’ referrals to other services on carers’ behalf and also facilitated carers’ ability to lead referrals themselves by providing relevant forms. This helped to provide carers and people with dementia with timely access to services. The data indicated that they provided a conduit for communication between the carer/person with dementia and services, providing both sides with updates on progress with referrals and care management decisions, including transitions between different care settings. Admiral Nurses also took a lead role in co-ordinating care, liaising with, for example, health, social care and benefit services, the LA and community police services. An interesting part of their role was liaising with community policing to implement strategies to minimise risks that people with dementia might face, for example opening the door to untrustworthy people. The work of the police service in relation to dementia is not well explored in the existing literature on dementia care,56 but could serve to reduce both the risk to the person with dementia and the carer’s levels of anxiety.
Emotional support and counselling
The main way that Admiral Nurses supported carers emotionally was spending time listening to them. Their emotional support focused on helping carers to see that it was beneficial to care for themselves as well as the person with dementia, encouraging them to have confidence in their ability as a carer and being there when carers needed reassurance or guidance about how to deal with a new situation. Their expertise about dementia and the symptoms that might occur meant that Admiral Nurses were able to reassure carers about behaviour that the person with dementia was displaying and about the future and the services that would be able to support them. They could also help carers to appreciate that respite care for the person with dementia could be beneficial for both of them.
Practical support
Admiral Nurses also provided practical support to make caring more manageable. Alongside helping carers to understand and complete benefit forms, apply for voucher schemes, and register with their GP as a carer, Admiral Nurses also helped by visiting the person with dementia while he or she was in respite care, so that carers could have a proper break and be reassured that the person would be visited. Some Admiral Nurses also helped by collecting and delivering medications and continence aids and taking medical equipment to respite facilities.
These data showed the variety of roles that Admiral Nurses adopted, including providing support for people with dementia themselves, to help support their client in their caring role.
Risk screening data set
The sample of data reviewed in the risk assessment data set showed that up to 40% of dyads were judged to be at some form of risk. Risks could be related to:
-
Health conditions – such as mobility, sensory impairments and medical conditions – that could increase the risk of falling, infection, constipation and pressure ulcers.
-
Abuse of the person with dementia, including physical, psychological, financial, sexual, social and verbal abuse.
-
Intentional or accidental self-harm in terms of dietary intake, alcohol use, wandering, suicidal ideation and refusing care.
-
The person with dementia harming others physically, verbally or psychologically. Some carers also expressed concern to Admiral Nurses about the person with dementia’s sexualised behaviour to strangers and about their reluctance to give up driving, thus putting other people at risk.
Admiral Nursing records indicated that Admiral Nurses advised carers about minimising both the risk of these problems occurring and the impact of the risks on themselves and the person with dementia. Admiral Nurses also worked with other agencies when appropriate, such as social service safeguarding teams, the police and other health care-providers, to minimise risks.
Referral data set
Referral data described which services referred the carer to AN services and to what services carers and/or people with dementia were referred. A wide variety of professionals and services, as well as family members, referred carers to AN services. Over one-third of referrals came from mental health services, including psychiatrists, community psychiatric nurses (CPNs) and memory clinics (see Appendix 3, Table 25). However, almost one-fifth of clients self-referred to the service.
Admiral Nurses referred clients onto other services for particular support, including to social services, occupational therapy and day care services. In their efforts to support the carer, Admiral Nurses also sometimes referred the person with dementia to other services, including to other health-care professionals, such as physiotherapists, district nurses and social services, and specialist psychiatric support, including consultant psychiatrists and CPNs. It is not possible to be sure from the administrative data whether or not this referral represented the first contact that carers and the person with dementia had with these services or if they were ongoing/previous clients of the service and the Admiral Nurse was making a referral for review or a rereferral. As the next section shows, very few dyads were not using any services.
‘Agencies involved in the case’ data set
Admiral Nurses recorded the type of services that were involved with the carer and the person with dementia at the point that they were referred to the AN service. As Table 26 in Appendix 3 shows, most dyads received support from at least one service (98%). However, the majority of these dyads (64%) received support from just one service, and very few were receiving input from five or more services (1%). The range of services that dyads were using when they were referred into the AN service is shown in Table 27 in Appendix 3. Overall, dyads were most likely to use social services, mental health services for older people and community mental health teams. Those dyads who reported using only one service were most likely to be receiving support from social services (43%), mental health services for older people (15%) and community mental health teams [12% (see Appendix 3, Table 28)].
‘Other people involved’ data set
On admission to the AN service, Admiral Nurses recorded any family members, friends or neighbours who were ‘involved’ in the case but who were not clients of the AN service in their own right. Most carers (98.9%) reported having some support from at least one other family member or friend (see Appendix 3, Table 29).
From the analysis of the ‘cases’ data set, we know that the majority of primary carers were spouses (44%) or adult children (33%). Given this, it is unsurprising that a large majority of the other people reported as being ‘involved’ were adult children [84% (see Appendix 3, Table 30)]. As Table 31 in Appendix 3 shows, this pattern was similar when there was only one other person involved.
Needs assessment data set
Descriptive data from the needs assessment are given in Tables 32 and 33 of Appendix 3, and the results of the analysis of variance between the three time points per question are shown in Tables 34 and 35 of Appendix 3. Only significant results of the analysis of variance, after Bonferroni adjustment, are reported in this section. The analysis showed that responses to 11 questions in the legacy needs assessment and 12 questions in the current needs assessment changed significantly at some point across the first three assessments.
For the first occurrence of this – the second question on the legacy assessment – a fully worked example reporting all of the relevant statistics is presented. However, to avoid repeating data that can be found in Tables 34 and 35 (see Appendix 3), the remainder are simply summarised in Tables 1 and 2.
| Outcome domain | Significant difference between time points (yes/no) | ||
|---|---|---|---|
| Time point 1 and time point 2 | Time point 2 and time point 3 | Time point 1 and time point 3 | |
|
1. Physical health: person with dementia |
No | No | No |
|
2. Mental health: person with dementia |
Yes | No | Yes |
|
3. Physical health: carer |
No | No | No |
|
4. Mental health: carer |
No | No | No |
|
5. Medication management |
No | Yes | Yes |
|
6. Insight into dementia |
Yes | Yes | Yes |
|
7. Dementia symptoms |
Yes | Yes | Yes |
|
8. Coping with behaviour/symptoms |
Yes | Yes | Yes |
|
9. Communication: professionals and carer |
No | No | No |
|
10. Environment/accommodation |
No | No | No |
|
11. Financial issues |
Yes | Yes | Yes |
|
12. Practical aids |
No | No | No |
|
13. Practical support |
Yes | No | No |
|
14. Informal support |
Yes | No | Yes |
|
15. Adjustment to loss |
No | No | No |
|
16. Balancing needs |
No | No | No |
|
17. Time for self |
No | No | Yes |
|
18. Time for self: longer respite |
Yes | Yes | Yes |
|
19. Looking to the future |
Yes | No | Yes |
| Outcome domain | Significant difference between time points (yes/no) | ||
|---|---|---|---|
| Time point 1 and time point 2 | Time point 2 and time point 3 | Time point 1 and time point 3 | |
|
1. Physical health: person with dementia |
No | No | Yes |
|
2. Mental health: person with dementia |
No | No | Yes |
|
3. Physical health: carer |
Yes | No | Yes |
|
4. Mental health: carer |
Yes | No | Yes |
|
5. Medication management |
No | No | Yes |
|
6. Insight into dementia |
Yes | Yes | Yes |
|
7. Coping with behaviour/symptoms |
Yes | Yes | Yes |
|
8. Communication: professionals and carer |
– | – | – |
|
9. Environment/accommodation |
No | No | Yes |
|
10. Financial issues |
– | – | – |
|
11. Practical aids |
– | – | – |
|
12. Practical support |
No | No | Yes |
|
13. Informal support |
Yes | No | Yes |
|
14. Adjustment to loss |
No | No | No |
|
15. Balancing needs |
Yes | Yes | Yes |
|
16. Time for self |
No | No | Yes |
|
17. Looking to the future |
– | – | – |
|
18. Risk |
– | – | – |
The Friedman test showed that there was a significant difference between responses to the question about the mental health of the person with dementia across the three time points in the legacy needs assessment [χ2 = 28.828, degrees of freedom (df) = 2; p < 0.001]. The post hoc tests (Wilcoxon signed-rank tests) showed that there was no significant difference between the second and third assessments [z = –0.093; p = 0.926 (significance was set at the higher Bonferroni-adjusted level of < 0.017)], but there was a significant difference between the first and second assessments (z = –4.354; p < 0.001) and between the first and third assessments (z = –4.725; p < 0.001). This reflects a reduction in reported need in relation to the mental health of people with dementia at the second and third assessments undertaken by Admiral Nurses (see Appendix 3, Table 34). The same topic on the current needs assessment also showed a significant difference in the reported level of need (p = 0.016) between assessment 1 and assessment 3 (see Appendix 3, Table 35).
The key change of interest is, of course, that between time point 1 and time point 3, indicating that change has occurred and has been sustained. Such change was reported in the legacy needs assessment in relation to the mental health of the person with dementia, medication management, carers’ insight into dementia, dementia symptoms, carers’ ability to cope with dementia behaviour and symptoms, financial issues, informal support, carers’ time for themselves both in the short term and the longer term, and looking to the future (see Appendix 3, Table 8). In almost all cases, positive progress was evident through all three time points.
The results of the comparison across the three time points in the current needs assessment data were similar, but with less consistent patterns of change over time. A significant change was observed between the first and third assessments in both the physical and mental health of the person with dementia, the physical and mental health of the carer, medication management, insight into dementia, coping with behaviour and dementia symptoms, communication between the carer and professionals, environment and accommodation, practical support, informal support, balancing needs and time for the carer.
All but one of these significant differences reflect a reduction in the level of reported need in the topic that was asked about. The only difference that appears to indicate that the level of need increased over the three assessments was related to carers relinquishing their role as primary carers (question 19 in the legacy needs assessment). The question on a similar topic in the current needs assessment did not show any significant difference. The apparent increase in the level of need to support carers to relinquish their caring role is, perhaps, unsurprising if it relates to people’s situation becoming more complex and having to consider alternative care arrangements over time.
Comparison of the Admiral Nursing administrative cases with the Admiral Nursing carer survey
Having the AN administrative data allowed us to see how successful our survey of carers (see Chapter 5) had been in sampling carers who were similar to all AN carers. We therefore compared the sample of AN carers who completed the survey with carers who were included in the AN database. The carers who responded to the survey were similar to the carers included in Dementia UK’s AN administrative database in relation to several key demographic characteristics. However, carers responding to the survey were more likely to be caring for a spouse/partner and less likely to be caring for a parent than carers included in the Dementia UK database. Related to these differences, the survey carers were supporting people who were older and more likely to be living at home with their main carer than those supported by all AN carers (Figures 1 and 2).
FIGURE 1.
Comparison of carers’ demographic data in the Dementia UK AN data set and those of AN carers in our survey.

FIGURE 2.
Comparison of demographic data of the person with dementia between the Dementia UK data and the survey data.
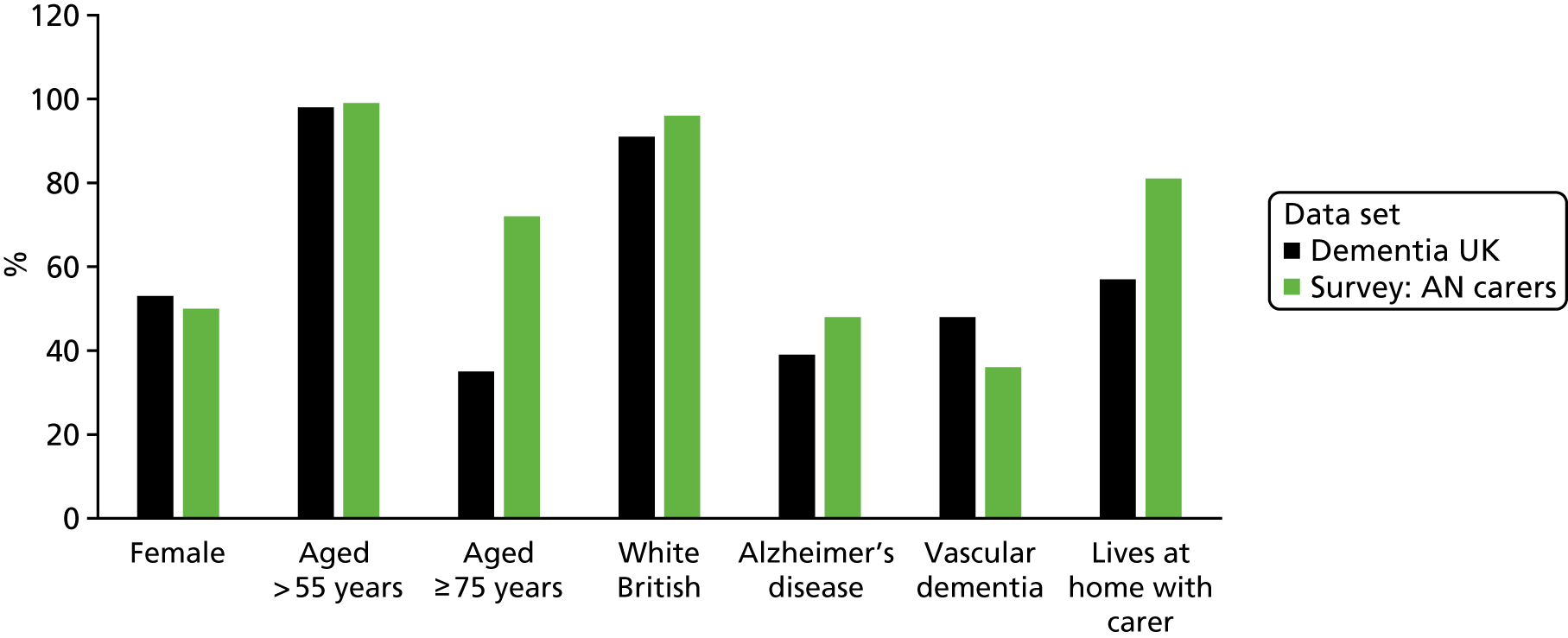
Several factors might explain these differences, for example the fact that carers self-selected into the survey, whereas Dementia UK’s database held administrative information about all of their clients. Differences in service organisation and delivery in the localities in which carers were recruited might also contribute to these differences. For example, if carers lived in a locality with poor access to residential/care homes or, indeed, greater access to support for caring at home, this could account for more people with dementia being cared for at home well into older age.
Conclusions
The analysis of the Dementia UK database showed that, although wider family members and friends and neighbours helped, the person who was most often the main carer to people with dementia on the AN caseload was their spouse or partner. This explains why almost one-third of carers included on the database were aged > 75 years and were caring for someone aged > 75 years. The findings suggest that Admiral Nurses are successfully targeting the potentially most vulnerable cases. This should be of interest to service commissioners, as carers of this age are more likely to have age-related conditions that could be affected by the demands of caring and that could in themselves make their role as a carer fragile.
The needs assessment data indicated that, on average, the needs of carers being supported by Admiral Nurses reduced over time. We are not able definitively to link reduction in need over time to the input of the Admiral Nurses, because we do not have direct information about AN input in response to the needs identified and/or the impact of AN input on carers’ continued level of need. However, as we know from the analysis of textual data, Admiral Nurses do provide the types of support that would be likely to help to reduce carers’ levels of need over time, or at least to maintain these levels of need when situations become more complex. Despite this, given that we do not know what else might have changed in carers’ circumstances, it may be just as feasible to argue that a reduction in need is related to other changes. A multivariate analysis of the data that are now fully prepared for this type of analysis may allow us to explore this further in the future.
Cases are triaged to help Admiral Nurses to manage their caseloads, and their tiered approach to service provision, whereby those with the most need receive greater levels of input, reflects this. This approach enables Admiral Nurses to be flexible in terms of the types of support they provide and to be responsive in terms of method and regularity of access. We argue that this empowers carers by enabling them to decide when and how to contact Admiral Nurses and to be involved in decisions about the type of support they, and the person they care for, receive as their needs change throughout their caring journey.
Challenges of using administrative data
The four main problems associated with using these types of data – determining availability, receiving the data, merging multiple data sets and understanding what the data really mean57 – were, for the most part, overcome by us working in partnership with Dementia UK as part of this research project. Nonetheless, we still experienced several challenges in working with these data.
First, when the project was developed, both Dementia UK and the research team were under the impression that all AN services entered data into the central database. However, once Dementia UK started to prepare the database for research purposes (as outlined in Chapter 2), it became apparent that some services had stopped entering information into it. Rather, these AN services were storing information locally on the paper or electronic systems in the organisation in which they were based/commissioned. We are not aware of any systematic bias between services that are using this database and those that are not, but it is something to be aware of in interpreting our results.
Understanding and transforming the administrative data into a format that was appropriate for research was extremely time-consuming and required several face-to-face and telephone meetings in addition to many e-mail communications. Understanding the focus and meaning of all of the variables, questions, response options and precoded data was essential and could require several e-mail/telephone communications each day until a thorough understanding was gained. Some of the data sets and/or variables were particularly troublesome; examples of this are the date variables, as outlined earlier, which were in several formats within the data sets we received. Indeed, in data sets with more than one date field, formats could differ within the data set. This made transferring data to SPSS for analysis challenging, and required many attempts before the formats were consistent.
There was no information about the factors that triggered a reassessment of needs. As Admiral Nurses provide support tailored to individuals’ needs, it was perhaps unsurprising that times between needs assessments were not consistent between carers. Did Admiral Nurses complete needs assessments only when they thought that carers’ needs had changed? Although this approach would clearly be right for clinical and service management, it can be problematic for research that seeks to understand how people’s needs change over time.
Furthermore, as the needs assessment tools used by Admiral Nurses are not standardised measures that have undergone cognitive and/or reliability testing, we do not know whether or not Admiral Nurses are interpreting questions and response options similarly over time or between themselves and we also do not know about the mode of completion. Do Admiral Nurses complete the assessment with carers or complete it on return to the office? By their nature, these types of service administrative data reflect how a service works and so can limit the analysis we can undertake. Despite this, we have been able to provide a summary of the type of clients that Dementia UK’s AN service supported, an overview of the interventions that Admiral Nurses offer and an estimate of the changes in dyads’ needs over time.
Chapter 4 The outcomes of carer support and development of the carer questionnaire (work package 2)
Introduction
The aims of WP 2 were to establish a data collection framework to be used in the survey of carers reported in Chapter 5 (objective 2). There were two elements to the package:
-
to establish what outcomes are important to carers in terms of their actual or anticipated use of specialist nursing support
-
to identify robust ways of measuring these outcomes that would be acceptable to and feasible for carers, for both our survey in WP 3 and for use in service settings (WP 5).
We began with qualitative research with carers to learn about the outcomes that they felt were influenced by the quality and level of support they received, either from AN (in areas with this service) or from the alternative support available (in areas without AN). This included investigating the outcomes of not receiving support or of receiving poor support. From our analysis, the outcome areas were identified and mapped onto pre-existing standardised outcome measures and the selected measures were incorporated into a data collection framework. The in-depth exploration of the acceptability and feasibility of the framework was an essential element of this WP, given the acknowledged challenges of evaluative research in dementia care.
Sample
We were aiming for a total sample of around 30 carers recruited from a wide range of characteristics and circumstances. We identified two areas with an AN service (AN areas) and two areas without (non-AN areas). The intention was to recruit seven or eight carers from each area through AN (in the AN areas) and TiDE, a national network of carers of people with dementia (in the non-AN areas). These carers would be invited to take part in a focus group or individual interview either by telephone or face to face in their home or another place of their choosing. We offered to pay travel expenses and the costs of substitute support for the person with dementia when this would help the carer to participate. All documents and processes were reviewed and approved by the Health Research Authority (HRA) London – Chelsea Research Ethics Committee [Integrated Research Application System (IRAS) identification number 195413; see the documentation at www.journalslibrary.nihr.ac.uk/programmes/hsdr/1415407/#/].
Methods
We talked to all carers once, and we talked to a subsample of carers twice. At the initial interviews and focus groups, we used in-depth, qualitative methods to explore with carers the outcomes they had or would like to experience from specialist dementia services focused on carers, as well as the outcomes of not receiving this or other support. The sessions were structured around established types of carer support,58 such as emotional and financial, as potential ‘inputs’ (see the topic guides in the documentation at www.journalslibrary.nihr.ac.uk/programmes/hsdr/1415407/#/). Carers were asked to think about the outcomes of receiving this support, and what happened when they did not get these types of support or when the support they received was of poor quality. At the end of each focus group or interview, we fed back the learning from the discussion and worked with participants to agree the outcomes they wanted us to take forward to the next stage of work.
Focus groups and interviews were audio-recorded (with participants’ permission) and these recordings were reviewed and analysed to finalise the key outcomes. As the data provided by carers were very rich, a portion of the recordings were fully transcribed to allow a more in-depth analysis. We used the Framework principles of case- and theme-based analysis, data reduction through summarisation and synthesis to do this. 42 We then identified robust, standardised measures of relevant carer outcomes and mapped these onto the main outcomes that carers had identified to see which were the best fit.
The second time we spoke to carers was to explore their understanding of the draft questionnaire and its acceptability to them. We carried out in-depth cognitive interviews with a subsample of carers and also collected feedback from our virtual carer advisers and steering group. Carers were asked about the feasibility of completing a questionnaire of this type electronically and in hard copy. We also discussed with them the pros and cons of self-completion versus face-to-face or telephone interviews.
The questionnaire had a dual purpose: first, to collect data from carers of people with dementia in areas with and without AN for WP 3 and, second, to provide the basis for a draft data collection framework for AN to use routinely (see WP 5, reported in Appendix 1). The survey was developed within, and administered using, Qualtrics. This is sophisticated, internet-based survey software that enables the user to produce and distribute high-quality online questionnaires. In addition to outcome measures (the identification of which is set out in detail in Findings), the survey questionnaire included questions on the demographic and socioeconomic characteristics of the carer and the person with dementia, as well as resource and time use questions associated with caring.
Recruitment
Carers were recruited through AN services in the two AN areas and through alternative routes in the two non-AN areas. Our original intention had been to recruit carers in the non-AN sites through TiDE alone, but this proved to be challenging. In addition to TiDE, we attempted to recruit in these areas through:
-
carers’ centres, forums and trusts
-
Dementia Action Alliances
-
dementia-specific and older people’s voluntary-sector organisations
-
local carer-led peer support groups (most successful)
-
local papers (unsuccessful)
-
Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) (unsuccessful)
-
Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) (unsuccessful).
Focus groups were smaller than planned (mainly because of carers’ availability) and a larger than expected number of carers opted to be interviewed individually. Across the four sites, we carried out:
-
six small focus groups (each had two to five participants)
-
13 individual interviews.
All of the interviews were conducted by the same researcher, but other members of the team were present at the larger focus groups. In total, we spoke to 35 carers (18 from AN areas and 17 from non-AN areas) as follows:
-
18 carers from AN sites:
-
female-to-male ratio = 10 : 8
-
spouses-to-adult children ratio = 12 : 6
-
current-to-former carers ratio = 16 : 2
-
-
six carers from AN site 1:
-
one focus group with three participants
-
three individual interviews
-
-
12 carers from AN site 2:
-
one focus group with four participants
-
one focus group with two participants
-
six individual interviews (two together)
-
-
17 carers from areas without AN:
-
female-to-male ratio = 9 : 8
-
spouses-to-adult children ratio = 10 : 7
-
current-to-former carers ratio = 11 : 6
-
-
10 carers from non-AN site 1:
-
one focus group with five participants
-
one focus group three participants
-
two individual interviews
-
-
seven carers from non-AN site 2:
-
one focus group with five participants
-
two individual interviews.
-
Findings
The outcomes of support identified by carers could be grouped into three broad areas as follows:
-
confidence in caring (carer self-efficacy)
-
carer quality of life
-
carer health (mental and physical).
Once the analysis to identify the outcomes was complete, we undertook a mapping exercise to ascertain which tools could most accurately measure these outcomes when self-completed by the carers of people with dementia. As is set out below, a shortlist of quality-of-life measures was mapped onto the findings, leading us to select ASCOT-Carer as the most appropriate tool to measure this outcome. For mental and physical health, we chose the EQ-5D, five-level version (EQ-5D-5L), as a measure that would give us data that could be compared with other studies and used in the health economic analysis. Confidence in caring is a less commonly measured outcome, but after some searching we identified the SEMD scale,46 which mapped well onto our analysis.
The remainder of this chapter sets out the key themes from the qualitative data and explains in more detail how these led us to choose the three outcome measures used in our survey.
1. The impact of carer support on confidence in caregiving (or carer self-efficacy)
Participants were asked what they thought the outcomes of good support were for them and, conversely, what happened when support was poor or not available. Carers in both the AN and the non-AN areas talked about the difficulties they faced in caring and how hard it could be to ‘cope’, access support and plan for the future. Those who had experienced good support described how this could give them the confidence to continue caring in spite of the difficulties they faced. Notably, when participants with an Admiral Nurse were asked to sum up the impact of having this service, confidence was a consistent theme:
What ultimately . . . is the result or outcome of you having this Admiral Nurse?
Um, I think confidence is a lot of it, confidence that I can get help, confidence that I’m not alone, there’s someone out there to help, who fully understands and who is trained in the specific illness.
From interview in AN area 2
In addition, a participant from focus group 1 in AN area 1 stated that:
I think [wife] and I would have been where we are now [with wife going into a care home] 2 or 3 years ago, had it not been for [local charity] and the Admiral Nurse . . . I wouldn’t have felt I had the support to do it [carry on caring for wife at home], I wouldn’t feel I had the confidence to do it . . .
Responses relating to carer confidence mapped well onto the two domains of carer self-efficacy used by Fortinsky et al. 46 in their SEMD scale. This is a 10-item scale, which loads onto two separate domains: one domain in the SEMD relating to efficacy in managing dementia (SXEFF) and the other relating to efficacy in accessing and using services (SERVEFF).
Carer self-efficacy domain 1: self-efficacy for symptom management
Handling the symptoms of dementia, especially distressing behaviour and, to a lesser extent, memory loss and ‘wandering’, was a common theme that appeared to influence carers’ confidence in their ability to ‘cope’ and continue caregiving (item 1). The confidence to handle these symptoms appeared to be related to the support the carer had access to. For example, a participant who felt that she received little support said:
I just think I feel lost, because we’ve got a situation and I think I don’t know how to handle this . . . At times I just feel I just don’t know where to turn and what to do . . . At times I feel as if I’m sinking . . .
NAN2C6, non-AN area 2
This carer’s mother had regular (6-monthly) appointments with the memory service, which both mother and daughter attended, and she also had contact with social services and her GP, but still felt that she could not get satisfactory answers to her questions about how to handle her mother’s worsening symptoms. Primarily, she felt that this was because of a lack of continuity in the professionals she came into contact with, which meant that no one with expertise in dementia had got to know her family or understood their needs:
. . . it’d be nice for [there to be] somebody that, once you are diagnosed, they know you, [and] the person with it, and come and see you . . . and as the illness progresses and deteriorates, you have this support that ‘Have you tried this?’ or ‘Have you tried that?’
NAN2C6
This was exactly the sort of ongoing, personalised support that carers who did sound confident in their ability to handle situations said that they received. Primarily, it was carers in the AN group who said that they received this sort of support and, indeed, some described a difference between the time before they had had an Admiral Nurse, when they had been struggling, and the time afterwards, when they felt better equipped to cope:
I was off work with stress because I just really did not know what to do . . . I contacted them [Admiral Nurses] and I have to say that my life changed the minute I spoke to them, and the minute they came through the door. They basically took me by the hand and said ‘Look, we need to do this, we need to do this . . .’
Focus group 1, AN area 2
November and December were horrendous . . . I don’t think I could have done another 6 months of that without any help and support . . . Now, I do feel he’s getting worse, but I do feel I can cope, and I now have a vision for the future that I know how it will go.
Focus group 2, AN area 2
Facing the future was a particularly important issue for the current carers of people with dementia in our sample, caring as they were for people with a deteriorating condition. Again, the division between those with Admiral Nurses, who could answer carers’ questions about how the illness might progress and, crucially, what was happening to their loved ones at the moment, and those without Admiral Nurses was noticeable. Those with an Admiral Nurse had someone who could answer their questions (item 5), whereas it was common for those without an Admiral Nurse to feel ‘at sea’:
. . . once the illness takes over . . . the support isn’t always there, I’ve been trying for long enough to have the psychiatrist check my wife’s illness and tell me, because I, I actually don’t really know what stage she’s in and I seem to be having quite a bit of problem of getting the doctor to look at my wife, to be honest.
NAN1C1, non-AN area 1
Some of the carers in the non-AN groups had accessed training and advice through third-sector agencies, such as the Alzheimer’s Society, which runs a caring and coping course, which can help to prepare carers for the things to come. Some read books or used ‘Talking Point’, the Alzheimer’s Society’s online forum, to get advice from other carers. Indeed, peer support, whether elicited online or face to face, was a valued source of information that carers in both groups felt that they could trust. However, there was agreement from those in the AN groups that the Admiral Nurse was their first port of call when a new situation arose or when they were concerned about how things would progress (item 2):
The thing about the Admiral Nurses is . . . my mum would do something really random and I’d think ‘Is this part of it? Is this part of the disease, is this how it works?’ They always, always had time to speak to me.
They always know what to say.
They just calm you down, and explain in a fashion that you understand.
Focus group 1 in AN area 2
Item 3 in domain 1 of the SEMD asks carers about their confidence in their ability to deal with ‘the frustrations of caring’ that they experience in caring for the person with dementia. This is an especially relevant outcome in areas such as dementia care, in which some situations may not be resolvable (given current medical knowledge) but their impact on the carer could be altered. The outcome is therefore derived not by changing a situation, but by learning to deal with its frustrations. Much of the training run by Admiral Nurses focuses on supporting carers to find ways to deal with the frustrations in their lives, which could involve reframing situations (helping carers to view the same situation differently) or making practical suggestions about how to handle or respond to situations. An example given was of a carer facing a ‘battle’ every night with her mother over getting ready for bed. The Admiral Nurse reframed the situation, asking if it mattered whether her mum changed her clothes at night, as long as she was happy and healthy. As the carer explained, the Admiral Nurses taught her to ‘. . . manage the things that you can, but if you can’t, leave it’. Another carer agreed:
. . . it is acceptance, that what you’re doing is OK.
Focus group 1, AN area 2
The final item to mention under domain 1 is item 4, which relates to carers’ confidence in their ability to do something to keep their relative as independent as possible. This was less of a prominent theme in our interviews and focus groups, possibly because our topic guides were designed to orientate participants to tell us about their needs and the outcomes for them, as carers, of receiving or not receiving support. As a result, we cannot speculate on the role or otherwise of Admiral Nurses or other support providers in influencing carers’ confidence in their ability to keep their relative independent.
Carer self-efficacy domain 2: self-efficacy for community support service use
The first item under this second domain, item 6, relates to carers’ confidence in their ability to care for their relative without help from organisations or agencies that provide services. This item sits awkwardly with our aim of understanding the impact of carer support services on carer outcomes, as a low score on this item would imply a greater need for support in situations in which none was available and a high score would indicate that support was possibly not needed, but neither of these would tell us how well a service is meeting carers’ needs currently. Carers with an Admiral Nurse, for example, told us that without their Admiral Nurse they would be ‘struggling’, and some went as far as to say that they did not think they would have been able to carry on caring without his or her support:
. . . I honestly don’t believe that we would be able to manage them [both parents need care] in their own homes without that support. They would have definitely been in a nursing home by now, and neither of them want that . . .
Focus group 2, AN area 2
This participant was making a positive point here, saying that, because she received such good support, she was able to support her parents to stay at home, which was their wish. However, as item 6 asks how certain she is that she could care for them without help, presumably she would enter a low score (indicating a poor outcome) here. Item 9 similarly asks about carers’ confidence in their ability to arrange for services themselves, implying that they would be doing this without support, which does not fit neatly with a questionnaire evaluating support.
At first glance, item 7 also seems a little circular, as it asks how confident carers are in their ability to access support. Participants in a study evaluating a service would, by virtue of their being in either the intervention group or the control group, already have access or otherwise to the service in question. However, if we take this question to refer to carers’ ability to access other or additional services, then it may indeed be relevant. One of the stated aims of AN is to ‘join up different parts of the health and social care system’,23 and other professionals, such as dementia advisers and social workers, also aim to link carers up with the services they need. Participants felt that a good service would help them to access further support as and when they needed it and to take the pressure off them to organise those services themselves. Certainly this was not always forthcoming, and simply being in contact with a professional in the system did not guarantee easy access to other services:
. . . I’ve had 4 and a half years of looking after [wife] without one single day off not having to think about it . . . so I talked to [CPN] about doing this . . . a sanity break . . . she said ‘oh, I don’t know much about that, it’s social services’.
Focus group 1, non-AN area 2
This participant was eventually given the name of a respite provider and advised to look this up himself on the internet. His experience contrasted starkly with the intense support provided by an Admiral Nurse and social worker described below, whereby the carer needed support not only to access help, but also to accept it:
. . . [the AN] was suggesting . . . a home visit so that I could get out of the house . . . not pushing but, you know, sort of encouraging me in the right direction and, . . . if only I’d taken that on board a little bit sooner, but again, he suggested day centres as well, and alongside the social worker; he knew [my husband’s] interests . . . and together they found this fantastic day centre for [husband] to attend . . . Again, I didn’t, I didn’t give in soon enough [laughs] not realising that it was not just for me . . . but also for [husband].
AN2C1, AN area 2
There was general agreement from the carers we spoke to that signposting alone was often not enough to help them to access the help that they needed. Indeed, knowing that there were more agencies to contact, more numbers to look up and more forms to fill in could add to the stresses that they were experiencing. Not knowing the quality or track record of a service provider could similarly be a source of anxiety for carers, and carers highly valued Admiral Nurses who were able to vouch for the quality of a service or look into it for them. This ties in with item 8, which asks how confident the carer is that they will get answers to all of their questions about the services they require. In the example given above, the Admiral Nurse actually visited the day centre when the carer’s husband was there and fed back to her on his progress, reassuring her that he was happy there, enabling her to relax.
The final item under domain 2 of the SEMD scale relates to carers’ confidence in their ability to find ways to pay for services. In the UK, health care is delivered free at the point of use through the NHS. However, the majority of services required by carers of people with dementia are in fact classed as social care, the funding for which is subject to stringent means-testing. Many people with dementia and/or their carers contribute financially towards the services they receive, and carers’ confidence in their ability to find ways to pay for services may well be linked to the quality of the support they receive from those who are tasked with helping them. A number of participants reported receiving useful information about finances and support to access benefits from voluntary-sector organisations, such as Age UK. The most significant role for Admiral Nurses in this respect appeared to be advocacy, particularly when carers were attempting to access continuing care funding. As this carer explained, in these negotiations, Admiral Nurses are able to speak on behalf of families with some authority (which the families themselves felt that they lacked) and without a vested interest in gatekeeping funds:
. . . because social services and the CCG [Clinical Commissioning Group – health service commissioners] are trying to downplay it [the person’s needs], whereas if they actually do it properly they’re going to end up paying, so they’re trying to avoid that, whereas the Admiral Nurses have got the authority to say ‘No, I have seen this, I know that this is happening’, and they can support you.
Focus group 1, AN area 2
Table 3 shows the degree of fit between the outcomes identified through our focus groups and interviews with carers and the items on the SEMD scale. 46
| Item number | Question: how certain are you right now that you can: | Degree of fit |
|---|---|---|
| Domain 1: self-efficacy for symptom management | ||
| 1 | Handle any problems your relative has, like memory loss, wandering, or behaviour problems? | Good |
| 2 | Handle any problems that might come up in the future with your relative’s care? | Good |
| 3 | Deal with the frustrations of caring for your relative? | Good |
| 4 | Do something to keep your relative as independent as possible? | Unclear |
| 5 | Get answers to all of your questions about your relative’s problems? | Good |
| Domain 2: self-efficacy for community support service use | ||
| 6 | Care for your relative without help from organisations or agencies that provide services? | Poor |
| 7 | Find organisations or agencies in the community that provide services to help you care for your relative? | Good |
| 8 | Get answers to all of your questions about these services? | Good |
| 9 | Arrange for these services yourself? | Poor |
| 10 | Find ways to pay for these services? | Good |
Although the SEMD scale was a good fit for many of the data on carer outcomes affected by support, it by no means covered all of the identified themes. A considerable chunk of these fitted more squarely with quality of life, and it is this area of outcomes that we address next.
2. The impact of carer support on quality of life
The outcomes identified by carers were mapped against a shortlist of six validated measures of quality of life:
-
ASCOT-Carer45
-
Carer Experience Scale (CES)59
-
Care-related Quality of Life instrument, seven demensions (CarerQol-7D)60
-
ICEpop CAPability measure for Older people (ICECAP-O)61
-
ICEpop CAPability measure for Adults (ICECAP-A)62
-
ASCOT quality of life. 63
Table 4 shows how well the items in each of the shortlisted measures fit with the outcomes that carers told us were influenced by support (or the absence of support).
| Quality-of-life measure | |||||
|---|---|---|---|---|---|
| ASCOT-Carer | CES | CarerQol-7D | ICECAP-O | ICECAP-A | ASCOT quality of life |
| Q1: occupation (spending time as you want) – good fit | Q1: activities outside caring – good fit | Q1: fulfilment from caregiving – not a prominent theme | Q1: love and friendship – good fit | Q1: feeling settled and secure – not a prominent theme | Q1: control over daily life – partial fit |
| Q2: control over daily life – partial fit | Q2: support from family and friends – partial fit | Q2: relational problems with the person cared for – not a prominent theme | Q2: thinking about the future – partial fit | Q2: love, friendship and support – good fit | Q2: personal cleanliness and comfort – not a prominent theme |
| Q3: self-care (looking after yourself) – partial fit | Q3: assistance from organisations and the government – partial fit | Q3: mental health problems – good fit | Q3: doing things that make you feel valued (Q3) – not a prominent theme | Q3: being independent – not a prominent theme | Q3: food and drink – partial fit |
| Q4: safety (how safe do you feel) – partial fit | Q4: fulfilment from caring – not a prominent theme | Q4: problems combining daily activities with care – good fit | Q4: enjoyment and pleasure – good fit | Q4: achievement and progress – partial fit | Q4: personal safety – partial fit |
| Q5: social participation (contact with people you like) – good fit | Q5: control over the caring – not a prominent theme | Q5: financial problems – partial fit |
Q5: independence – not a prominent theme No more questions |
Q5: enjoyment and pleasure – good fit No more questions |
Q5: social participation – good fit |
| Q6: space and time (to be yourself) – good fit |
Q6: getting on with the person you care for – not a prominent theme No more questions |
Q6: support with lending care (from family and friends) – partial fit | Q6: occupation (spending time as you want) – good fit | ||
|
Q7: encouragement and support – good fit No more questions |
Q7: physical health problems – good fit No more questions |
Q7: accommodation cleanliness and comfort – not a prominent theme | |||
| Q8: support (how getting support makes you feel about yourself) – not a prominent theme | |||||
| Q9: dignity (how the way you are treated makes you feel about yourself) – not a prominent theme | |||||
|
ASCOT-Carer All seven Qs were relevant (four were fully relevant, three were partially relevant) |
CES 3/6 Qs were relevant (one was fully relevant, two were partially relevant) |
CarerQol-7D 5/7 Qs were relevant (three were fully relevant, two were partially relevant) |
ICECAP-O 3/5 Qs were relevant (two were fully relevant, one was partially relevant) |
ICECAP-A 3/5 Qs were relevant (two were fully relevant, one was partially relevant) |
ASCOT quality of life 5/9 Qs were relevant (two were fully relevant, three were partially relevant) |
On the basis of this mapping, ASCOT-Carer was selected as the quality-of-life measure for use in the survey of carers. A more detailed analysis is given below of the relevance of this measure to the outcomes of support that were identified by carers.
Adult Social Care Outcomes Tool for Carers to measure the impact of the carer on quality of life
The first question in ASCOT-Carer asks to what degree carers are able to spend time doing things that they value or enjoy (including leisure activities, formal employment, voluntary or unpaid work and caring for others). Question 6 follows this up, asking carers to think about the amount of space and time that they have in their daily life ‘to be yourself’. These were key themes in our data, with most carers reporting that time for themselves was highly restricted. As one carer noted, when he was interrupted by his wife during our interview:
. . . that’s what it’s like being a carer . . . you know, it’s very difficult to get on with it, any, anything I want to do . . .
AN2C2, AN area 2
As dementia progresses, the demands on carers’ time could become all-consuming. Carers talked about their loved ones ‘following me round the house’ or not being able to leave their side for a minute for safety reasons:
. . . for example, she’d take a boiling kettle and pour it over the cooker . . .
AN1C5
Under The Care Act 2014,19 social services departments have a responsibility to assess carers’ needs. Resultant care plans may, among other things, recommend that carers obtain some respite from caregiving. Options include a paid carer or ‘sitter’ coming into the home to look after the person, or the person with dementia attending a day centre or staying overnight (usually for 1 week) at a residential care home. However, a number of the carers we spoke to did not feel that the latter options, which required the person with dementia to go somewhere, offered a satisfactory solution, either because the person with dementia would be unsettled in another place or because the carer did not trust that they would be well cared for there. Although carers in both the AN and the non-AN groups expressed these concerns, we heard instances of Admiral Nurses helping to overcome these barriers, either by acclimatising people with dementia to settings and alternative care workers or by checking in on people while they were at day centres or in care homes, enabling their family carers to relax and engage in some of the activities necessary to maintain their quality of life. These activities can be split into two broad categories, one being social and leisure activities, such as seeing friends or engaging in hobbies, and the other being time to undertake ‘jobs’, such as shopping, cleaning and gardening, or even to continue in paid employment. Such time was highly valued. One participant, for example, was helped by two voluntary-sector organisations, Age Concern and Crossroads Care, to have a few hours off per week and remarked that:
It was only 2 hours, but it’s 2 hours that I had all to myself – yippee! I could go and get my hair cut, I could do anything I liked. It sounds small, but by God I looked forward to that . . . You could just kick your heels! . . . and it was very relieving.
Focus group 2 in non-AN area 1
As dementia symptoms progressed, carers’ time for themselves tended to be more and more limited. Some carers from both AN and non-AN areas paid an individual to come into the home regularly (or even to live in the home) to provide some of the hands-on care that they would otherwise be providing themselves, and this made a considerable difference to their quality of life. Access to funding to pay for replacement care may therefore be a key facilitator in the quality of life of carers:
. . . none of these things are free . . . If you’ve got the money you’ve got far more choices and you can go ‘yeah well actually it is costing quite a bit having someone coming in so I can go and do that, but it means I can go and do something normal’, or I know that she’s OK on a Tuesday afternoon because I know the befriender’s coming round that day. So it’s peace of mind. It all costs [a lot of money].
Focus group 1, non-AN area 1
Arguably, carers’ time to themselves and the ability to spend time as they want could be influenced more by their personal means, or those of the person they care for, than by the quality of support they receive from services. However, some carers did receive benefits or funds through social services to help to pay for replacement care, and support to access these funds varied greatly. Moreover, the ability to pay for respite or a ‘sitter’ was not the only factor influencing whether or not a carer accessed replacement care; some described the practical help and encouragement that had helped them to find the right person or provider to deliver this. A service’s awareness of, and emphasis on, the needs of the carer appeared to be particularly important here. As the carers in one of our focus groups explained, the Admiral Nurse ‘gives you permission’ to do something for yourself and to enjoy it. Guilt was a common emotion experienced by many of the carers trying to balance their needs with those of the person they cared for and, without a service that saw them as the client, some felt unable to take advantage of the limited replacement care, day care and respite available to them. Indeed, some former carers talked of still experiencing guilt long after their loved ones had passed away. Conversely, other carers described a process whereby, with the right support, they had been able to ‘step back’ and allow others to take on some of their caring responsibilities, for example allowing them to go on holiday.
Two further items in ASCOT-Carer are linked to the amount of time carers have for themselves: how much contact they have with people they like (question 5) and how well they are able to look after themselves (question 3). Unfortunately, instances in which carers felt socially isolated were abundant in our data:
. . . it’s like you’re in this little bubble that he doesn’t want anybody [else] to be in . . . [and] I cannot make a choice to go out anywhere because I’ve got always [husband] to consider . . .
NAN2C7, non-AN area 2
. . . you become isolated with that person you’re looking after, being completely isolated . . .
For me, that’s the biggest thing . . .
. . . that can lead to carer breakdown so quickly . . .
Focus group 1 in non-AN area 2
Some carers recounted experiences of friends, and even family members, dropping away as the person’s symptoms grew more pronounced. Others said that friends and family members still called, but carers did not want to burden them with the realities of their situation so had little to talk about. Still others said that the person with dementia found it hard to accept carers seeing friends, or that they behaved in other ways that made socialising difficult. Carers’ social groups and dementia-specific activities, such as ‘Singing for the Brain’ (a service provided by the Alzheimer’s Society), were therefore highly valued as opportunities for social contact and peer support.
Similarly, a number of carers felt that their caregiving had affected their ability to look after themselves, either because they did not have the time (e.g. to exercise or cook healthy meals) or because the necessities of caregiving more directly affected their ability to sleep or protect their health:
. . . I became a diabetic. And they said ‘you’d have always become one, but you’re doing it 7 years earlier because you’re neglecting yourself’ . . .
Focus group 2, non-AN area 1
Some carers said that they had been subject to violence, as the person they cared for could be aggressive, and others were concerned that they might be injured in the course of caring, for example when lifting the person with dementia in and out of the bath. Both of these concerns could be captured by question 4, which asks carers how safe they feel, and both could arguably be influenced by the support that carers receive. A carer from focus group 1 in AN area 2, for example, talked about her husband being violent towards her and the Admiral Nurse supporting her through the process of realising that, for her safety, the situation could not go on as it had:
. . . she was there with me every step of the way, which nobody else would be.
Question 2 in ASCOT-Carer asks how much control carers feel they have over their daily lives. In the main, the carers we spoke to felt that they had very little control, in terms of either how they spent their time now or how things might develop in the future. To some extent, this may be the nature of caring for someone with a degenerative disease that can be unpredictable, but services did have a role in giving caregivers more or less control over their situations. For example, some of the participants with Admiral Nurses talked about being supported to take back some control, whether that was through helping them to challenge the person’s medication regime or looking into options for replacement care. By contrast, one participant without an Admiral Nurse felt that social services were actively stopping her from taking control of her life:
. . . when I was thinking about care, long-term care, I was probably thinking there’s a light at end of this tunnel for me, for my life . . . But then when they were telling me all this [that he wasn’t ready to go into a care home] and I, I just wanted to be able to put his name down because I liked the place and I thought he would be happy . . . I am a person that needs to plan . . . But I seem to be blocked that way . . .
NAN2C7, non-AN area 2
Despite disclosing to social services that she sometimes felt suicidal, this carer did not feel that her husband’s social worker or any other professional was particularly interested in her needs as a carer. By contrast, one of the recurring themes from our interviews and focus groups with people with an Admiral Nurse was the feeling that they, as carers, had support from a professional whose job it was to focus on their needs. In part, this was an advocacy role (e.g. supporting carers in meetings with hospital or care home staff and adding weight to their arguments), but often it was about helping them to recognise and meet their own needs.
. . . you know you’re not on your own then . . . and she was one of the ones that said, ‘you know, you’ve really got to think of yourself too’ . . .
AN1C5, AN area 1
An important point made by carers was that Admiral Nurses are specialists in dementia care, with clinical expertise, and yet they make home visits and get to know the family, which other clinicians generally do not have the time to do. Indeed, some carers felt that their Admiral Nurse was the only professional who had truly got to know them and their situation, as was demonstrated by this example:
. . . we both commented . . . you could see the difference between [the AN’s] report and the others; theirs is just sort of academic, but [the AN’s] report, you could see it was actually somebody who’s been in contact with us and there was exactly what’s going on . . . you could see it the way she’d written it.
Joint interview with AN2C9 and AN2C10, AN area 2
A key difference between ASCOT-Carer and the other quality-of-life measures in our shortlist is that ASCOT-Carer has an item that specifically asks carers to what degree they feel supported and encouraged in their present situation. It was clear from our data that feeling supported was an important outcome for carers in and of itself. Although this question could pick up encouragement from family and friends, those well supported by a professional or service would presumably score higher than those who felt abandoned by the system or taken for granted. Carers in both AN and non-AN areas received emotional support informally through carers’ groups, and some had accessed more formal counselling, either while still caring or after the person with dementia had passed away. Those with an Admiral Nurse consistently reported feeling relieved that they had someone to turn to who knew them and who could respond quickly, and who would also check in on them proactively. In part, the reassurance came from someone taking the time to listen and provide emotional support as and when it was needed, but it was also important to carers that that person was a professional who was knowledgeable about dementia:
[The AN] . . . takes a bit of the pressure away, you know. It’s having somebody who’s, who’s knowledgeable in that field who can [say] ‘Oh right, OK, you’re going to need this, you’re going to need that, and how’s about the other’ . . .
AN1C1, AN area 1
. . . the emotional help is very valuable, but more than that she was able to, oh, comfort me, if you want, . . . for example [wife] was having a problem with her bowels, so we were able to talk about that, and the way things were going. Sleeping, we were able to talk about that . . .
AN1C5, AN area 1
Anyone who’s dealt with dementia can give you practical tips, but the Admiral Nurses properly get to know you, care for you, and provide the essential emotional support . . . somebody understands, and that, I think, is more important than anything, somebody actually understands what you’re going through.
Focus group 1, AN area 2
3. Carer health (mental and physical)
A final theme from our interviews and focus groups with carers was the impact that caregiving could have on the mental and physical health of the caregiver and how support could alleviate this. It is well documented that caregiving is associated with poor health (particularly mental health) outcomes and that carers of people with dementia may have poorer health not only compared with the general population, but also with carers of people with other diseases or impairments. 3,8,9,11,64 Our data from both carers with and those without Admiral Nurses underline the detrimental impact that caring can have on the caregiver’s mental health:
. . . let down, frustrated, annoyed, upset, suicidal. [laughs] . . . I’m quite strong, but even I’ve thought about stepping off and going back to heaven . . .
NAN1C2, non-AN area 2
I don’t like using the word depression, but that’s how you feel.
Focus group 1, AN area 1
The impact mentally . . . I was just all over the place for huge amounts of time, mentally . . .
Focus group 1, non-AN area 2
The impact of caring and support (or its absence) on physical health was less pronounced in our data, but its influence was there in examples of when stress and sleep deprivation had manifested themselves as physical illness (headaches, shingles) or a risk of injury.
The emotional support described above could arguably influence carers’ mental health, as could space and time ‘to be yourself’ and indeed any other of the quality-of-life themes covered by ASCOT-Carer, and these may in turn influence physical health. However, ASCOT-Carer does not ask directly about mental or physical health. For this, we selected the health-related quality-of-life measure known as the EQ-5D. 65 This is the standard measure, preferred by NICE, that is used to calculate quality-adjusted life-years (QALYs) in health economics. The version we selected has five items, covering mobility, self-care, usual activities, pain and discomfort and anxiety and depression. We would expect the final item, anxiety and depression, to be most relevant to carers of people with dementia.
Conclusion
The aim of this WP was to establish a data collection framework for the survey in the final stages of our proposed work (objective 2). Through interviews and focus groups with 35 carers of people with dementia, we identified three key outcome areas that are important to carers and that appear to be influenced by carer support (and AN in particular) and three standardised instruments with which to measure these:
-
carer confidence, as measured by the SEMD scale46
-
carer quality of life, as measured by ASCOT-Carer45
-
carer mental and physical health, as measured by the EQ-5D-5L. 65
Design of the final survey questionnaire
The final paper version of the survey questionnaire is shown in full in Appendix 2. This included:
-
questions on the demographic and socioeconomic characteristics of the carer and of the person with dementia (i.e. age, sex, ethnicity, education and household resource level)
-
the following instruments to measure the outcomes that were important to carers:
-
questions on the time and resource use associated with caring, including unpaid (informal) care time, out-of-pocket costs, health (hospital appointments, GP appointments) and social care (e.g. home care) and non-statutory sector resources (e.g. volunteer befriending service).
Exploration of acceptability and feasibility
We carried out in-depth cognitive interviews with nine of the initial carer participants, using a ‘think-aloud’ methodology66 to explore the carers’ interpretations of each question in turn. This was conducted for the electronic version of the questionnaire only, but demonstrated that the electronic version was easy to use and not off-putting to the carers in our sample. The data collected about the content and wording of the questions were very valuable, but we reached saturation more quickly than expected; rather than conduct 20 full cognitive interviews, we decided to stop at nine and further ‘check’ the comprehensibility and feasibility of the questionnaire by sending it to our carer ‘virtual’ advisory group and our steering group. Comments from these groups were fed into the questionnaire design at our second steering group meeting.
The final documents and processes for the survey were reviewed and approved by the HRA London – Chelsea Research Ethics Committee as a substantial amendment to our original application (IRAS identification number 195413).
The following chapter sets out in detail our approach to administering the questionnaire, including the challenges we faced in recruiting to the non-AN comparison group, and it also sets out the survey findings.
Chapter 5 Analysis of the survey of carers of people with dementia
Constructing the sampling framework
Sample selection for the survey of Admiral Nursing services
Dementia UK provided us with a list of current AN services in the spring of 2016, from which we selected those that were providing the ‘standard model’ (see Chapter 2 for the definition of this term). We then matched the sites to LA areas in order to facilitate matching of the non-AN areas, usually by contacting the services to establish which postcode areas they covered. We also examined current caseload sizes to ensure that with 16 sites we would be able to achieve our required sample size, and excluded those with fewer than 35 service users. Some services that we subsequently contacted for inclusion did not feel able to participate at that point. By the end of this process, we had 17 eligible services, one of which did not respond to our contacts.
The 16 services selected had, between them, around 3230 clients on their active caseloads and we calculated that we needed to generate a sample size of around 480 clients to achieve the desired number of returned surveys of around 160 (assuming a 30% response rate). However, there was wide variation in the numbers of clients between the services: from 40 clients in the smallest service to 974 clients in the largest service. To create a representative sample of individuals from the totality of AN services selected, we therefore identified individuals using a sampling fraction of 1 in 6 (or around 17%).
A random number between 1 and 6 was generated for each site using Stat Trek (https://stattrek.com). Sites ordered their current caseload either by date of most recent contact or alphabetically by surname, depending on their current practice. We then instructed them to select the nth case (where n was the randomly generated number for that site) and every following sixth case, to the end of the caseload. Based on the caseload numbers the sites had given us, we expected this to generate a sample of around 484 carers. Because of some increase in caseloads between issuing the sampling fractions and the services selecting carers, 497 carers were eventually identified and sent a paper questionnaire.
Comparison group sample
We identified 16 ‘broadly similar’ areas in terms of statistical neighbourhood, as defined by CIPFA’s statistical model. Statistical neighbourhood is used by LAs themselves and across government to allow comparisons between authorities that are similar in terms of population size and characteristics, such as age distribution, deprivation and ethnicity. The tool eventually used was the Department of Health and Social Care’s social care efficiency tool (www.gov.uk/government/publications/adult-social-care-efficiency-tool), which is based on the CIPFA model.
Learning from the challenges we had faced recruiting carers to WP 2 (for the qualitative interviews and focus groups with carers, see Chapter 4), we worked with Join Dementia Research (JDR) and a number of local voluntary-sector organisations in the matched neighbourhoods, as well as TiDE, to identify and recruit current carers. Despite us taking this multipronged approach, recruitment in these matched areas was labour intensive and very time-consuming.
Over 500 paper questionnaire packs were posted out and over 400 e-mails with the link to the e-survey were distributed to non-AN areas. The link was also advertised online on multiple websites. Details of where and to whom the questionnaire packs and e-mails were sent are given below:
-
Through JDR, 103 carers were e-mailed the questionnaire and a further nine people received a hard copy through the post.
-
Together in Dementia Everyday contacted 31 carers directly (28 by e-mail and three by post), as well as publicising the survey more generally through e-mail and social media.
-
Fifteen local voluntary-sector organisations (mainly local carers’ groups) were sent a total of 427 hard-copy packs, and six of these organisations also advertised the survey online or by e-mail. One of these organisations e-mailed the link to 300 carers of people with dementia in their locality.
-
Three local NHS partners were sent a total of 72 hard-copy packs (but we know that at least 10 of these were never distributed).
-
Seven further organisations (local and national) advertised the survey online or by e-mail.
Responses
Calculating an overall response rate for our survey is impossible, because we can be sure about the number of questionnaires or links distributed for the AN and the JDR groups only. Although we know how many paper questionnaires we sent to control-area third-sector organisations, we do not know how many they actually handed on. Furthermore, although we know to which organisations we sent the electronic survey, we do not know how many people received the link but chose not to open it.
After the survey was distributed, we had 10 responses from carers who told us that the person they had been caring for had died. We contacted this group to thank them for letting us know and to pass on our sympathies. A further six questionnaires were returned as undeliverable and two people contacted us to tell us that the person they had cared for was now in long-term care. Six paper questionnaires were returned blank, which we classed as refusals.
In total, we received 430 responses to the survey, either by post or electronically; however, not all were usable or within our scope. First, 22 electronic surveys, all from those contacted via the third sector, had been opened, but no data had ever been entered. We classed these as refusals. Second, 37 carers told us that the person they cared for was living in long-term care and 25 carers told us that they were no longer caring for a person with dementia. Both of these groups were outside the scope of our survey, which focused exclusively on those currently caring for a person with dementia who was still living in the community.
Table 36 in Appendix 3 summarises what we know about how many paper questionnaires or links to the electronic survey were distributed and the numbers of refusals or out-of-scope responses we had from each source. Twenty-six per cent of the paper questionnaires we distributed to the AN services and third-sector organisations were returned to us and were within the scope of our survey, but without knowing the total number actually passed on to carers we cannot calculate an overall response rate. For the two organisations for which we knew how many links were sent to carers, 25% and 43% of carers provided in-scope responses.
In total, we received 346 completed questionnaires that were within the scope of our survey, 158 (46%) of which were from AN service users in our selected areas and 188 (54%) of which were from carers in non-AN areas.
Description of the whole sample
In describing the whole sample of carers we surveyed, we compared them with carers of people with dementia identified in the most recent nationally representative, detailed survey of carers: the Survey of Carers in Households – England, 2009–10 (SCH). 67 This comparison helps us to understand whether or not the group as a whole could be considered to be representative of all carers of people with dementia (see Appendix 3, Table 37, for a full comparison).
Figure 3 shows that our survey sample as a whole was broadly similar in respect of the sex of the carer, although a higher proportion of our survey carers were in the older age groups. Our survey carers were more likely to be caring for a man with dementia and somewhat less likely to be caring for someone over the age of 75 years than the SCH carers (Figure 4).
FIGURE 3.
The sex and age of the carer: SCH carers and carers from our survey.
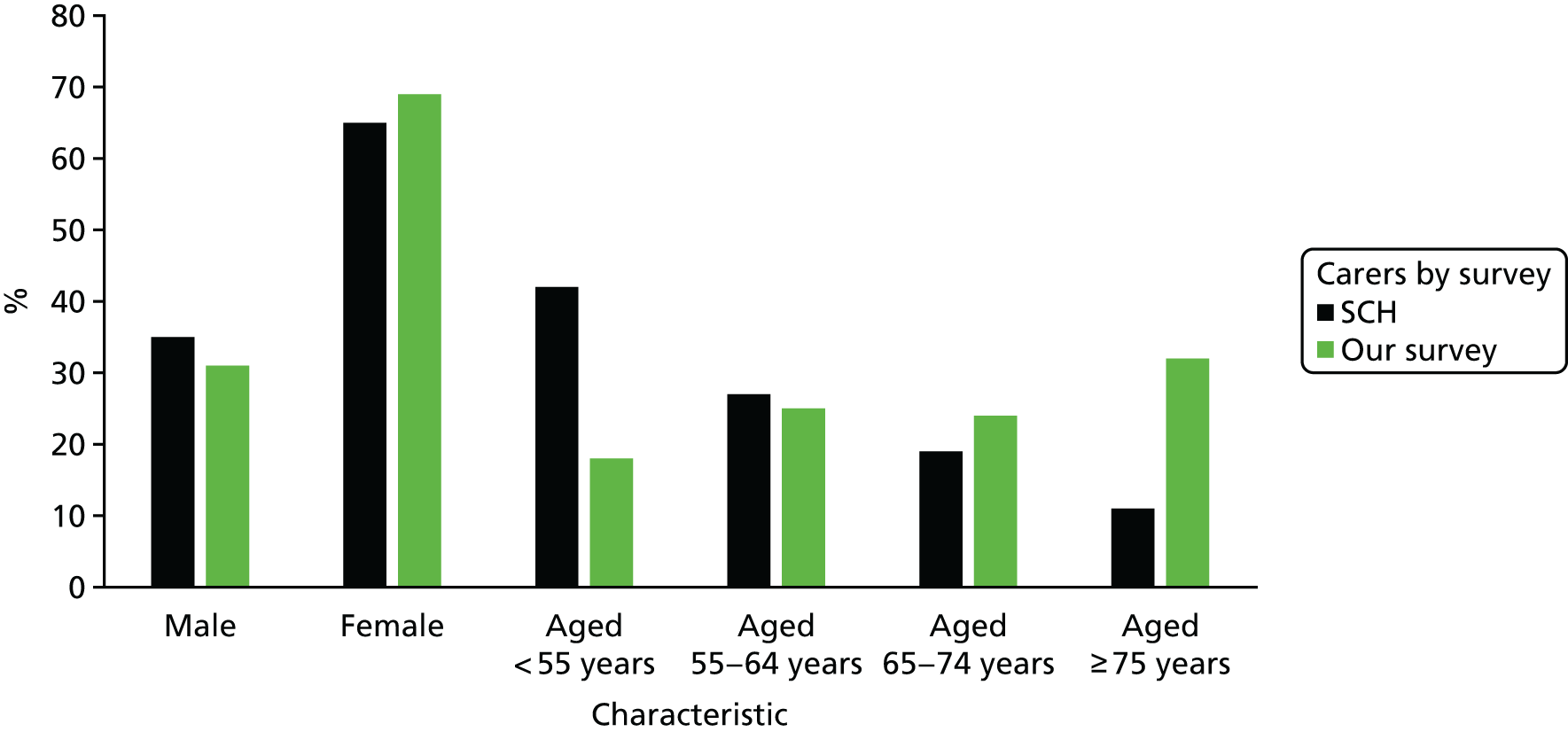
FIGURE 4.
The sex and age of the person with dementia: SCH carers and carers from our survey.
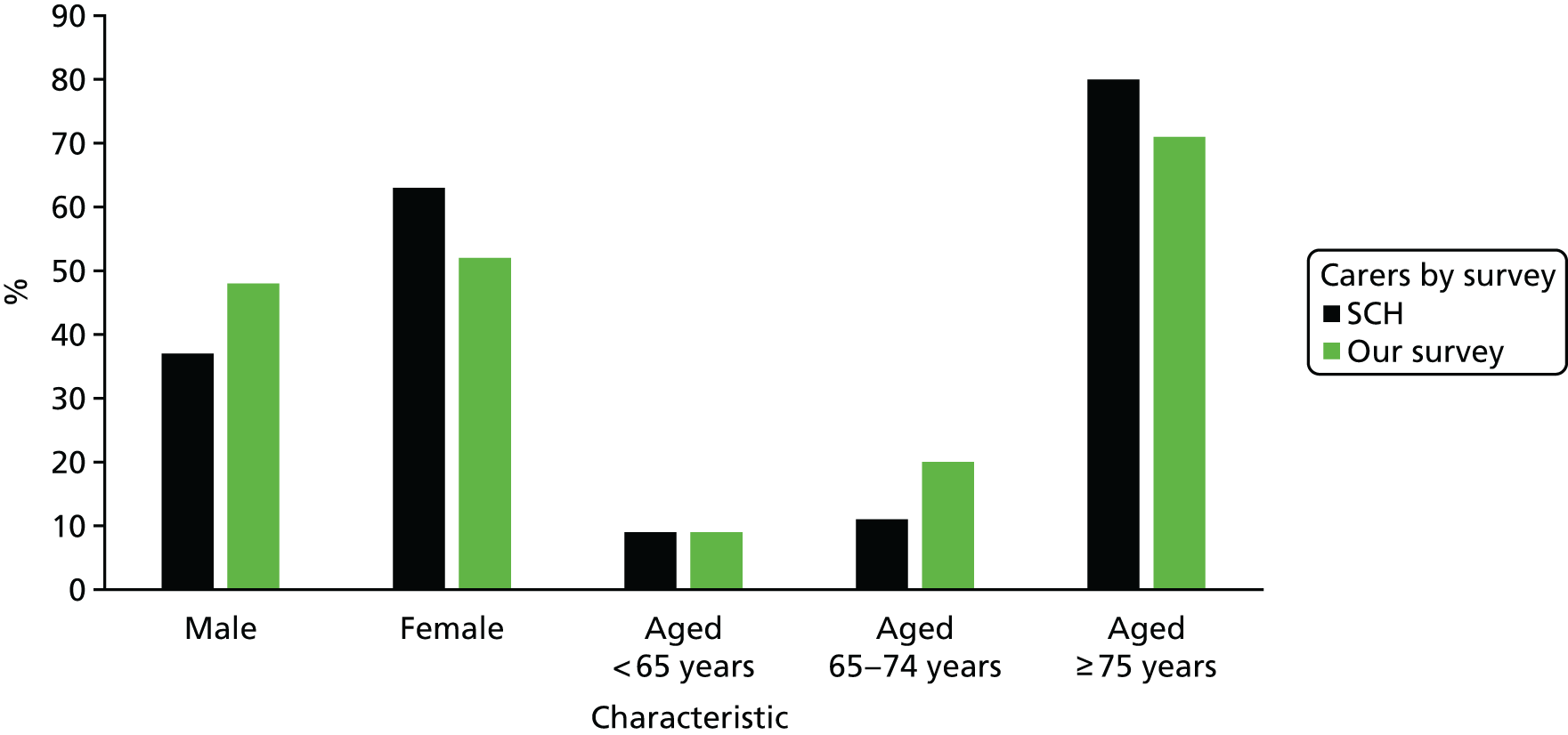
Beyond this, however, our survey carers were very different from the SCH carers, in that they were much more likely to be supporting a spouse or partner, much more likely to be heavily involved in caring (providing both personal and physical care) and much less likely to be in paid employment (Figure 5).
FIGURE 5.
Relationship of the person with dementia to the carer, the type of care provided and paid employment: SCH carers and carers from our survey.

Our survey sample was thus different in several important respects from the carers of people with dementia included in the nationally representative sample of carers.
However, the SCH was a large survey of over 2000 adult carers of people with any condition, and only a single question differentiated between those caring for someone with dementia and other carers. Furthermore, the SCH was carried out before the recent policy emphasis on the importance of the diagnosis of dementia and the consequent increase in the numbers of people who know what their condition is. It is possible that a repeat of the SCH now would reveal both a higher proportion of carers reporting that they supported someone with dementia (11% of the total in 2009–10) and, therefore, a different pattern of socioeconomic characteristics. However, the differences between the carers in our survey and the SCH carers are so large that it seems unlikely that even this change would increase their comparability. The ways in which we recruited our carers – through service providers and third-sector organisations – perhaps inevitably led us to the most heavily involved and vulnerable (by virtue of their age) carers who needed support and had started to access it.
Comparison of Admiral Nursing and non-Admiral Nursing area carers
Demographic and socioeconomic status
By matching the AN and non-AN areas using a statistical neighbourhood approach, we hoped to minimise the differences between possible service outcomes for the two groups based on local characteristics, such as expenditure on older people’s services and the proportion of older people living in the area. However, given that all AN carers were, by definition, using at least one service, we expected that our matching approach would not necessarily produce matching groups of carers in terms of their demographic and socioeconomic status. Our analysis (see Appendix 3, Table 38) shows that the main differences between the two groups were in the age of the carer and in the variables related to that age difference.
Respondents receiving AN support were more likely than those not receiving such support to be over the age of 75 years, caring for a spouse/partner, the main or sole carer, caring for someone with vascular dementia, without formal educational qualifications and retired from paid work. By contrast, respondents not supported by an Admiral Nurse were more likely to be caring for a parent/in-law, caring for someone with Alzheimer’s disease, aged between 45 and 54 years, educated to master’s degree level or above and in full-time work.
The differences in the carers’ ages are obviously related to the differences in relationship (older carers are more likely to be spouses/partners and younger carers are more likely to be children or children-in-law of the person with dementia) and to the differences in educational and economic status. The differences in the type of dementia are more difficult to explain, given that there was little difference in the ages or sex of the people with dementia in the two groups. The differences in main/sole carer status is perhaps explained by the natural history of caring in dementia; that is, when people with dementia are married or in a partnership, the spouse takes on the main caring role until the point when she or he has become too old and frail to continue alone. At this point, the help of a daughter or son may enable the person with dementia to remain at home and the spouse/partner is thus no longer the sole or main carer.
Caring activity
The information that carers provided about the caring tasks they carried out was summarised using the typology developed by Parker and Lawton68 and used subsequently to analyse large national surveys of carers. 7,68,69
The typology categorises six types of caring activity: personal and physical care; personal but not physical care; physical but not personal care; practical care without personal or physical care; practical help only; and other combinations not including personal, physical or practical care. These categories have been shown to distinguish between more heavily involved and less heavily involved carers in terms of total hours of care, carer status, impact on employment and other carer characteristics. 68
Admiral Nursing carers were more likely than carers in non-AN areas to be involved in the heaviest type of care (personal and physical care: χ2 = 5.57, df = 1; p = 0.018).
The distribution of total hours for which carers said they provided care to the person with dementia was highly skewed, with 18% of all respondents reporting that they had spent the maximum possible number of hours (24) caring the previous day. We therefore used non-parametric statistics to explore the differences between carers in AN and non-AN areas. This showed that AN carers reported caring for significantly more hours than did carers in non-AN areas (Wilcoxon test, z = –2.599; p = 0.009). Almost one-third of AN carers (31%) reported caring for 18 hours or more the day before the survey, compared with 19% of carers in non-AN areas. Table 39 in Appendix 3 shows the data recoded into quartiles. The largest difference lies in the ≥ 18 hours category.
Income
Given the differences between the two groups’ economic status, household incomes were more similar than expected at the lower end. Similar proportions (28% and 27%) had gross incomes of £15,000 or less per year. At the higher end, however, 16% of AN carers had gross household incomes of £35,000 and above, compared with 28% of carers from non-AN areas. The number of carers who chose to answer this question (243/346) was lower than for any other question, so these data need to be interpreted with care. The related question about how people felt that they were managing financially, however, was answered by more people (310/346), and this showed a significant difference; in total, 72% of AN carers said that they had ‘some’ or ‘severe’ financial difficulties, compared with 50% of non-AN area carers (χ2 = 13.62, df = 5; p = 0.018).
Outcome measures
Before we could examine the relationship between AN and non-AN area carers in terms of our chosen outcome measures (see Chapter 6), we needed to explore whether or not any of the variables on which the two groups varied significantly also varied significantly with these outcome measures, across the whole group. This analysis is reported in Appendix 4 (see also Appendix 3, Tables 40–46).
The overall conclusion from this analysis was that the age of the carer was a major driver of the other socioeconomic differences we saw between AN carers and those from non-AN areas. However, the type of dementia that the person being supported had and, for ASCOT-Carer only, the carer’s status and activity (sole/main carer or not, type of care provided and hours of care) may also be crucial areas to be controlled for when comparing the outcome measures.
Overall, we gained the sense that the EQ-5D-5L worked as it should: reflecting carers’ underlying state of health, with some dimensions (mobility, usual activities and pain) being affected by age but not, by and large, by caring status or activity.
The ASCOT-Carer also seemed to work as it should: reflecting caring status and activity but not, by and large, the carer’s age. However, the ASCOT-Carer did seem to be sensitive to the nature of the relationship between the carer and the person being supported, with spouses/partners having poorer scores. There was also a relationship between type of dementia and ASCOT-Carer scores (with those caring for people with Alzheimer’s disease seeming to fare better than those caring for people with vascular and ‘other’ dementias), which deserves future investigation.
The SEMD measure showed relatively few differences related to carer characteristics, caring status and activity or type of dementia. However, we found higher levels of confidence about finding and arranging services among those caring for people with Alzheimer’s disease, and a non-linear relationship with hours of care, which could suggest that the SEMD measure is sensitive to service support.
The outcome measures for AN and non-AN area carers are compared in Chapter 6.
Carers’ use of services
We asked a range of questions about the health and social care services that carers and the person with dementia had ever used and were currently using.
Admiral Nursing service use
We started with a section about the use of AN services and guided respondents either to an explanatory leaflet that came with the paper questionnaire or to a link to the AN website that was included in the electronic questionnaire. However, despite this and the fact that we had selected half of our sample via AN services and half via organisations in areas in which there were no AN services, some people in the former half of the sample said that they had never used AN services and some in the latter half said that they had. In both cases, evidence from answers to other questions suggested misunderstanding in both halves of the sample. AN service users who said that they had never used an AN service were mostly people who later reported that they attended carers’ groups; it might have been that they did not know that the group they attended was run by an Admiral Nurse. Among non-AN area respondents, there was again some misunderstanding, with some claiming to have used ‘other’ types of AN services, such as sitting services, where no such services exist in reality. It is also possible that some carers in non-AN areas had used AN services that had subsequently closed, or had previously lived somewhere that did have AN services.
Because of this issue, the analysis in this subsection, in which we explored carers’ experiences of using AN services, is based on the 140 carers who were identified via AN services and who were aware that they had used an AN service.
More than half of the AN service users were recent: 54% had first used an AN service in the previous 12 months and only 6% had been in contact for 5 years or more. The majority (90%) had been in contact most recently in the previous 6 months. Face-to-face visits from Admiral Nurses were the most frequent type of contact reported (94%), followed by telephone contact (54%), AN group meetings (20%) and e-mail contact (10%). As these figures suggest, most people had more than one type of contact with the service.
The two-thirds (n = 89; 65%) of carers who had been in any AN contact in the previous 4 weeks were then asked how many of what type of contact there had been (see Appendix 3, Table 47).
In total, 89 carers had had at least 193 contacts, of different types, with an AN service in the previous 4 weeks (an average of 2.2 each). Of these, face-to-face visits and telephone calls were the most frequent.
Those who had been in contact with an AN service in the previous 4 weeks were asked about a range of types of support they might have received. Providing emotional and social support to the carer (mentioned by 90%) and providing information, advice and knowledge (92%) were the most frequently reported types of support, followed by practical help, including liaison with other services (75%) and assessing the carer’s needs (72%). Less often mentioned were attending support groups and carer training (26%), and recommendations about medication for the person with dementia (21%). Educating and supporting other professionals in touch with the carer (12%) and clinical examination of the person with dementia (7%) were reported less frequently. Two carers mentioned other types of support: one mentioned that the Admiral Nurse had facilitated a meeting with another carer and one mentioned that the Admiral Nurse spent time with the carer.
Other services intended for carers
There are other services specifically intended to support carers, although they may also help the person with dementia. All carers were asked if they had ever used short breaks/respite, when the person with dementia is looked after away from home; services when someone sits with the person with dementia or takes them out during the day to give the carer time for themselves; night-time sitting services to enable the carer to get a full night’s sleep; carers’ advice services; and support groups for carers.
It was clear from subsequent answers given about day care services (the main purpose of which is to provide activity for the person with dementia during the day) that some carers had misinterpreted the short breaks/respite category (which we had intended to be understood as care away from home for more than 1 day to provide the carer with an extended break) as day care. This confusion had not been evident during the cognitive interviewing (see Chapter 4). When it was clear that this misunderstanding had occurred, we recoded the data appropriately. When it was not clear, we left the answers as originally given. It is therefore possible that this category of carer support service may be slightly over-represented and that day care may be slightly under-represented. The totality of support to carers and the person with dementia, of course, remains the same.
Given the age and level of involvement of the carers in our survey, the proportions receiving any kind of support services that gave them some space for themselves was low: 15% had ever used respite care, 26% had ever used a sitting or ‘taking out’ service and 4% had ever used a night-sitting service. Rather more had used a carers’ advice service (45%) or had attended a carers’ support group (41%), which is not surprising, given the way in which we identified carers.
There were some differences between AN carers and non-AN area carers: AN carers were significantly more likely than non-AN area carers ever to have used a respite service (20% and 11%, respectively; χ2 = 4.32, df = 1; p = 0.038) and less likely to have used a carers’ advice service (39% and 55%, respectively; χ2 = 8.49, df = 1; p = 0.004). Again, this last finding is not surprising, given that we found many of our non-AN area carers via third-sector organisations that run advice services. There were no other differences between AN carers and non-AN area carers in relation to ever having used services for carers.
We asked those who had ever used these services what type of support they felt that they had received from them. As Table 48 in Appendix 3 shows, this question distinguished well between the types of support that different services provided to carers. Thus, time for themselves or to allow them to do other things was mentioned by almost 8 in 10 of those who had used respite and day-sitting/taking out services, whereas half of the small numbers who had used a night-sitting service reported this as an outcome. By contrast, half of those who used carers’ support groups reported receiving emotional or social support from these groups, whereas the most frequently mentioned type of support gained from carers’ advice services was information, advice and knowledge (mentioned by 76% of those who had used this service). Overall, these figures suggest that our sample found carers’ support groups less helpful than carers’ advice services.
A small number of carers who had used each of the services had found them to be of no support at all.
Carers were much less likely to report recent use of all of these services (see Appendix 3, Table 49), suggesting very low levels of ongoing support. For example, only 17% of all carers reported having attended a carers’ support group in the previous 4 weeks. Recent use was different for carers in AN carers and non-AN area carers only in relation to this type of support; as might be expected, given how we recruited carers in the non-AN areas, AN carers were less likely to have attended a support group recently (32% and 48%, respectively, χ2 = 3.84, df = 1; p = 0.05).
In terms of the perceived usefulness of the services used recently (see Appendix 3, Table 49), we found lower levels of reporting of emotional and social support and receipt of information, advice and knowledge than we found among recent AN service users.
A small number of carers had used services frequently in the previous 4 weeks: 5 out of the 21 carers who reported using respite had done so eight times, 12 out of the 64 carers who had used day-sitting/taking out services had used them 10 times or more and two out of the seven carers who had used night-sitting services had done so 10 times or more. By contrast, most of those using advice services (33 out of 50) reported only a single use, as did 35 out of the 57 carers who had been to a carers’ support group. Only one carer reported using a carers’ advice service and one reported using a carers’ support group 10 times or more in the previous 4 weeks.
In total, 60% of all carers reported no use of a service for carers in the previous 4 weeks, 25% of carers had used one service, 11% of carers had used two services and one person had used four services. There was no difference between carers in AN carers and non-AN areas in whether or not they had used a carer service recently. Nor was there any difference between older and younger carers or between those who were more or less involved, whether this was defined by hours of care, number of care tasks undertaken, main carer responsibility or type of care provided.
On the face of it, this might suggest poor targeting of services for carers, that the services on offer are not reaching those in most need or that the services on offer are not what carers want or need. We therefore looked at current carer service use by our outcome measures. This showed no relationship between any of the ASCOT-Carer domains or the total ASCOT-Carer score and carer service use. One EQ-5D-5L domain – anxiety and depression – was significantly related to current carer service use, with service users being more likely to report problems in this domain than those who were not using services (84% and 74%, respectively; χ2 = 4.64, df = 1; p = 0.031). Those currently using carer services had significantly poorer total SEMD scores on symptom management efficacy than those who were not using carer services (mean ranks 143.36 and 164.74, respectively; Wilcoxon W, z = –2.081; p = 0.037).
Looking at each type of service by each type of outcome measure showed few relationships. However, there are one or two that are worth mentioning. First, carers using day-sitting/taking out services were more likely than those who were not using these services to report problems in the EQ-5D-5L anxiety and depression domain (80% and 58% respectively; χ2 = 4.57, df = 1; p = 0.032). This was also the case with those who were using night-sitting services compared with those who were not (86% and 63%, respectively), but the numbers involved were small and the difference did not reach statistical significance. Those using carers’ advice services were also more likely to report problems in this domain (92% and 77%, respectively; χ2 = 4.95, df = 1; p = 0.026).
All of those using respite services reported problems in the ASCOT-Carer domain related to how they spent their time (100% compared with 79% of those not using respite; χ2 = 4.95, df = 1; p = 0.026). Carers using respite were also more likely to report problems in feeling that they had control over their lives (95% and 74%, respectively; χ2 = 4.11, df = 1; p = 0.043). There was no other relationship between any ASCOT-Carer domain and use of any carer service in the previous 4 weeks.
None of the SEMD individual questions, or the SXEFF and SERVEFF scores (see Chapter 4), showed any relationship to recent use of any carers’ service.
Of course, different types of services may be related to different types of outcome measures in different ways. For example, one would hope that those using respite or sitting services would feel that they had more time to be themselves, whereas those using advice services would feel more confident about their knowledge about dementia and about services. However, given that it is not possible to distinguish cause from effect in this cross-sectional survey, it may be found that carers using such services report more problems in these areas because services have been targeted at their specific concerns.
Future multivariate analysis is clearly necessary to explore the relative contributions of carer characteristics, carer involvement and carer services to outcome assessment.
Health service use by carers
In the 4 weeks before completing the questionnaire, 45% of carers had seen their GP and 16% had seen a practice or district nurse (see Appendix 3, Table 50). In terms of hospital-based services, 23% had had at least one outpatient appointment. Table 50 also reports the average number of contacts per carer and the average number of contacts per carer using the service.
There was only one difference between AN carers and non-AN area carers in terms of hospital or primary care use: AN carers were significantly more likely to report having seen a nurse specialist of some type in the previous 4 weeks than were non-AN area carers (11% and 4%, respectively, χ2 = 4.59, df = 2; p = 0.032). This question did make it clear that we did not want carers to include in their response any contact with an Admiral Nurse, so this may suggest that AN carers were more likely to be seeing other nurse specialists in addition to using the AN service.
The lack of other differences in health service use is slightly surprising given that the AN carers were significantly older than those in non-AN areas and that older people are usually seen as more frequent users of health-care services.
Further analysis of health service use by age and level of involvement of the carer (main carer status, hours of care provided in the previous 24 hours and type of care provided) showed only one relationship: those caring for a relatively small number of hours (0–5 hours) were more likely to report having seen a therapy health professional (21%, compared with 12% of all carers; χ2 = 8.52, df = 3; p = 0.036).
Examining our outcome variables and health service use throws up some interesting and, in the case of ASCOT-Carer, some potentially disturbing results (see Table 5).
First, as one might expect, as a health status measure, problems in some domains of the EQ-5D-5L – mobility, ability to carry out usual activities and pain – were related to health service use in the previous 4 weeks and, in particular, to seeing a GP.
Analysis of the ASCOT-Carer data showed some relationships between needs and health service use, despite the fact that the ASCOT measures are not designed to be sensitive to health service use. In particular, having needs in the ‘feeling safe’ domain was related to more use by carers of outpatient and other hospital appointments, seeing the GP and seeing a practice or district nurse. Although our data are cross-sectional, these relationships give pause for thought: are carers using more health services because not feeling safe affects their health indirectly or, more worryingly, because it affects their health directly through physical injury?
Some of these outcome domains were also related to overall health service use. So, with the EQ-5D-5L, 60% of those who had used health services three or more times in the previous 4 weeks reported mobility problems, whereas only 31% of those who had not used health services had mobility problems (χ2 = 12.89, df = 3; p = 0.005). Similarly, 74% of those using three or more services reported problems in carrying out their usual activities, compared with 46% of those who used no health services. With ASCOT-Carer, 23% of those who reported three or more uses of health services had needs in relation to feeling safe, compared with 6% of those who reported no use of health services (χ2 = 14.06, df = 3; p = 0.003).
As there was little relationship between carer age and the use of individual or total health services, the EQ-5D-5L results shown in Table 5 presumably reflect differences in health unrelated to age. It is also possible that the ASCOT-Carer relationships reflect physical injury sustained as a carer, but this remains to be explored in future research.
| Outcome measure domain | Health service used | % of carers not using service who reported needs | % of carers using service who reported needs | χ2; df | p-value | n |
|---|---|---|---|---|---|---|
| EQ-5D | ||||||
| Mobility | Outpatient appointment | 37 | 58 | 9.45; 1 | 0.002** | 317 |
| GP | 34 | 49 | 8.11; 1 | 0.004** | 317 | |
| Usual activities | Outpatient appointment | 53 | 71 | 7.41; 1 | 0.006** | 317 |
| GP | 51 | 64 | 4.97; 1 | 0.026* | 317 | |
| Therapy professional | 56 | 74 | 4.74; 1 | 0.030* | 314 | |
| Pain | GP | 62 | 78 | 9.34; 1 | 0.002** | 317 |
| ASCOT-Carer | ||||||
| How the carer spends time | Practice or district nurse | 85 | 71 | 5.54; 1 | 0.019* | 314 |
| Looking after self | GP | 42 | 55 | 5.05; 1 | 0.025* | 317 |
| Feeling safe | Outpatient appointment | 6 | 15 | 5.83; 1 | 0.016* | 315 |
| Other hospital appointment | 7 | 23 | 6.42; 1 | 0.011* | 312 | |
| GP | 5 | 12 | 4.64; 1 | 0.031* | 312 | |
| Nurse specialist | 7 | 22 | 5.76; 1 | 0.016* | 310 | |
| Feeling supported | Nurse specialist | 57 | 78 | 4.00; 1 | 0.045* | 306 |
Use of services by the person with dementia
Health services
We also asked carers who were completing the questionnaire how many times the person they supported had used health services in the previous 4 weeks. Responses highlighted the importance of primary care – both GPs and practice and district nurses – in the lives of people with dementia (see Appendix 3, Table 51). Over half had seen a GP in the previous 4 weeks and just under one-third had seen a nurse. However, there was also a relatively high use of outpatient appointments, with almost one-third of respondents reporting this. For those who had used a service recently, the average number of contacts was highest for practice or district nurses, therapy professionals and nurse specialists.
There were no significant differences in the use of individual health services or the total number of services used in the previous 4 weeks by the person with dementia between AN carers and non-AN area carers.
There were no obvious relationships between the use of services and the age of the person with dementia. The only statistically significant result here was non-linear; people aged 75–84 years were less likely (23%) and those aged 85–94 years were more likely (44%) to have seen a practice or district nurse in the previous 4 weeks than all people with dementia (30%) (χ2 = 12.04, df = 5; p = 0.034), but there was nothing that suggested a clear relationship with increased age. These are surprising findings, given the relationship between age and health service use in the general population.
Carers who reported that the person they cared for had a type of dementia other than Alzheimer’s disease or vascular dementia were more likely to report that the person had had an outpatient appointment in the previous 4 weeks [25% of people with Alzheimer’s disease, 27% of people with vascular dementia and 46% of people with another type of dementia (χ2 = 7.11, df = 2; p = 0.029)]. There was also a tendency for men to be more likely to have had an outpatient appointment (34% of men and 24% of women), but this difference did not reach statistical significance. These differences are not explained by the recency of symptoms (when one might expect more contact with health services). Indeed, there was no relationship between any type of health service used in the previous 4 weeks and how long carers reported being aware of the person’s symptoms. However, men were significantly more likely to have ‘other’ types of dementia, so there is clearly some clustering of difference here. Looking behind the ‘other’ classification, men in the survey were more likely than women to have Parkinson’s disease-related dementia, Korsakoff syndrome/alcohol-related dementia or corticobasal dementia. It may be that services for these conditions are more developed than those for other types of dementia, or perhaps that services stay in contact with these patients for longer after diagnosis.
People with vascular dementia were more likely than others to have had a planned overnight admission to hospital [0% of people with Alzheimer’s disease, 5% of people with vascular dementia and 2% of people with another type of dementia (χ2 = 9.33, df = 2; p = 0.003)], but numbers, and thereby cell sizes, were small here, so this difference needs to be interpreted with care. Men were also more likely to have used this type of service [3% of men and 0% of women (χ2 = 4.77, df = 1; p = 0.029)], but there is the same proviso about small cell sizes.
There were no relationships between whether or not the person with dementia had a formal diagnosis of their condition and the use of any health service.
Finally, we looked at health service use and the level of severity of dementia, as reported by the carer. There was a single statistically significant relationship here: those reported as having ‘mild’ dementia were more likely (25%), and those reported as having ‘moderate’ dementia were less likely (10%), to have seen a therapy professional in the previous 4 weeks than those with ‘severe’ dementia (17%) (χ2 = 6.35, df = 2; p = 0.042).
Social care services
We asked carers whether the person with dementia had made any use of day care, home care, meals services and memory cafés, or if they had had an appointment with staff from social services in the previous 4 weeks.
Carers reported that the majority of people with dementia had not recently used any of the individual services we asked about (Table 6). However, counting up use across all of these services, 59% of all carers reported some use in the previous weeks, with an average of at least nine contacts during that time. As this contrast suggests, some individuals had used multiple social care services recently and, among those who had, some had had many contacts. For example, those using home care had at least an average of 8.39 contacts in the previous 4 weeks.
| Type of social care service | Use (% of people with dementia) | Minimum total number of uses in the previous 4 weeks | n (100%) | Minimum average number of contacts per person with dementia (all people with dementia) | Minimum average number of contacts per person with dementia using services | |
|---|---|---|---|---|---|---|
| Not used | Used | |||||
| Day care centre | 72 | 27 | 494a | 335 | 1.47 | 5.74 |
| Other type of day care provision | 89 | 10 | 105b | 335 | 0.31 | 3.39 |
| Home care | 72 | 27 | 705c | 335 | 2.10 | 8.39 |
| Meals service (at home or elsewhere) | 91 | 8 | 157d | 335 | 0.47 | 6.54 |
| Memory café | 85 | 14 | 142 | 335 | 0.42 | 2.25 |
| Appointment with social services | 80 | 19 | 73 | 335 | 0.22 | 1.66 |
| Any social care service | 41 | 59 | 1711 | 336 | 5.09 | 8.77 |
In a few cases, the carer did not know whether or not the person with dementia had used the service; this is why the row percentages in Table 6 do not always sum to 100%.
There were differences between the AN carers and the others in terms of use of two individual services. Non-AN area carers were more likely than AN carers to report the use of ‘other’ types of day service (i.e. not day care centres): 14% versus 6%, respectively (χ2 = 5.54, df = 1; p = 0.019). Non-AN area carers were also more likely than AN carers to report the use of memory cafés (27% vs. 11%, respectively) (χ2 = 13.69, df = 1; p < 0.001).
We also examined whether or not any characteristics of the person with dementia or the carer were related to individual service use. We examined the sex and the age of both the person with dementia and the carer, how long symptoms had been present, whether or not a formal diagnosis had been received, reported severity, the relationship between the person with dementia and the carer, main carer status and the type and hours of care provided. Relatively few of these characteristics were statistically significantly related to service use (see Appendix 3, Table 52).
Five services did show some relationship to the characteristics of the person with dementia or the carer: day centres, other types of day care, home care, meals and attendance at a memory café.
Women with dementia were more likely to have used other types of day care and home-care services in the previous 4 weeks, whereas men were more likely to have attended a memory café. Although people with Alzheimer’s disease were somewhat more likely to have used a memory café than people with other forms of dementia (although this difference did not reach statistical significance), men were less likely than women to have Alzheimer’s disease, as we saw earlier. However, men with dementia in our survey were significantly less likely to be over the age of 85 years, so this may explain the difference.
Home care was more likely when the person with dementia was aged 85 years or over, but both day centre and memory café use were less likely for this age group. Those aged 65–74 years were more likely than other people with dementia to have used a day centre. Day centre use and other day care services were also related to the reported severity of dementia, with those in the ‘severe’ category being more likely than others to have used these services recently. When the carer reported having been aware of the symptoms of dementia for under a year, meals provision was more likely.
There were only two areas in which the nature of the caring relationship was related to service use. Those caring for a parent/in-law were much more likely, and those caring for a spouse/partner were much less likely, to report the use of home care, whereas those caring for 6–11 hours were more likely to report meals provision.
Some of these differences make sense in terms of the progression of dementia (day care being more evident when dementia is severe, but with extreme age likely to depress its use) or what we know from other work on the services that are in place when a carer is also present (home care use is more often in place when the person with dementia is female and/or very old, but it is less often in place when the carer is supporting a spouse or partner). One can also understand why very old people with dementia might not be using memory cafés, which in turn may explain the sex difference in the use of this service.
Non-AN area carers were more likely to report the use of any kind of social care service (63%, compared with 55% of AN area carers), but this difference was not large enough to reach statistical significance (χ2 = 2.11, df = 1; p = 0.146). Nor was there any difference between the groups in the reported total number of contacts with social care services over the previous 4 weeks (Wilcoxon W test, z = –1.029; p = 0.304).
We also explored any social care service use alongside the characteristics of the person with dementia and the carer. Neither the sex of the person with dementia nor their age was related to total social care service use.
People with a formal diagnosis were more likely to be using any social care service [62%, compared with 46% of those without a formal diagnosis and 0% of those for whom the carer did not know if a diagnosis had been given (χ2 = 8.88, df = 2; p = 0.012)]. However, neither the type of dementia nor the length of time for which the carer reported that symptoms had been evident was related to social care service use. By contrast, reported severity did play a part: 72% of people whose carer reported that the dementia was ‘severe’ had used some form of social care service in the previous 4 weeks, compared with 58% of those with ‘moderate’ dementia and 46% of those with ‘mild’ dementia (χ2 = 8.15, df = 2; p = 0.017).
The sex and age of the carer were not significantly related to the use of any social care service, and nor was the relationship of the carer to the person with dementia. However, there was a relationship with whether or not the carer had the main, or the sole, responsibility for caring. Those defined as a ‘joint main carer’ were less likely to report any use of social care services (29%) than those who were the main/sole carers (61%) or who did not have the main responsibility as a carer (67%), and this difference was statistically significant (χ2 = 6.32, df = 2; p = 0.043). Despite this, there was no relationship between the intensity of the carers’ involvement, as defined by the type of care being provided or the total number of hours of care provided, and the use of any social care service.
Unlike health services, social care services are not necessarily free at the point of use, as they are subject not only to assessment of need, but also to means testing, if the LA social services department becomes involved. Furthermore, as there is an active private market in social care, individuals with adequate resources can bypass the assessment of need and pay directly for services themselves. These issues make it difficult to determine here the extent to which services are responding to need or if individuals are making their own judgements about what they require to help the person with dementia to continue to live in the community. We move on to these issues in the next section, in which we examine which services carers and the person with dementia paid for.
Paying for services
In terms of services intended for carers, four out of five of the carers who had used respite in the previous 4 weeks said that they or the person with dementia, or both, had paid for the service. Half of those who reported using a day-sitting service, two out of the seven who had used a night-sitting service and 1 in 10 of those attending a carers’ group also reported payment for the services. No one reported paying anything for using a carers’ advice service.
Payment was also common in relation to most social care services for the person with dementia: 78% of those using the service paid for day centre care, 63% paid for other types of day care, 74% paid for home care and 92% paid something for meals provision. Payment was less common for memory cafés, but even here 46% reported paying something for attendance.
We asked those who reported paying something for the service both how many times they had used the service in the previous week and what they had paid each time they had used it. This information is analysed fully in Chapter 6, in which we explore the health economics aspects of our study. Here we simply report totals, when it is possible to calculate them, and analyse these alongside data on carers’ household financial situation.
Table 7 indicates the substantial financial burden that some carers and people with dementia were bearing to buy, or contribute towards the cost of, services to support them. The wide range of costs per use – particularly in relation to respite, day and home care – is likely to reflect the fact that some people were paying the full cost of these services, whereas others were making means-tested contributions.
| Type of service | Cost (£) | Number of carers reporting cost per use/total number paying | ||
|---|---|---|---|---|
| Range of cost per use | Range of total cost in previous4 weeks | Median cost in previous 4 weeks | ||
| Respite | 8–850 | 18–850 | 252.00 | 14/15 |
| Day sitting/taking outa | 6–100 | 26–1000 | 120.00 | 28/30 |
| Night sitting | 100–140 | 1000–1400 | 1200.00 | 2/2 |
| Carers’ groupa | 3–8 | 3–24 | 8.00 | 5/5 |
| Day carea | 5–130 | 5–950 | 156.00 | 65/66 |
| Other day carea | 3–55 | 5–250 | 25.50 | 18/19 |
| Home carea | 1–213 | 2–1917 | 150.00 | 56/57 |
| Mealsa | 3–40 | 5–400 | 49.50 | 20/23 |
| Memory café | 2–40 | 2–160 | 8.00 | 24/24 |
| All carers’ services | – | 3–2000 | 190.00 | 42 |
| All services for the person with dementia | – | 2–1925 | 120.00 | 147 |
| Total social care service costs | – | 2–3008 | 120.00 | 164 |
As indicated earlier, we asked whether it was the carer or the person with dementia, or both, who paid for the service. In this next section of analysis, in which we look at costs alongside household finances, we confine the analysis to the 256 respondents who lived in the same household as the person with dementia. First, we look at estimated gross annual income, for which 177 of these ‘same-household’ respondents provided information, and then at how people felt that they were ‘getting on’ financially, for which we had information from 232 respondents.
Over half (57%) of the carers who provided information reported an annual household income of ≤ £25,000; 23% had an annual household income of ≤ £15,000. At the other end of the income range, 14% of carers reported a household income of ≥ £40,000 per year. Over two-thirds of carers reported that they had some (34%) or severe (35%) financial difficulties.
It is not surprising, perhaps, to find that those with the lowest incomes were most likely to report severe financial difficulties; 75% of those with incomes of ≤ £15,000 reported severe problems, as did 56% of those with incomes between £15,001 and £19,999. At the other end of the income scale, 46% of those with incomes between £35,000 and £39,999 and 41% of those with incomes of ≥ £40,000 reported that they managed very or quite well. These differences were statistically significant (χ2 = 41.457, df = 12; p < 0.001).
One might have expected that household income and the costs of services would vary in a linear fashion, with those with the lowest incomes having the lowest costs (because they were accessing means-tested services and paying little) and those with the highest incomes having the highest costs (because they were paying the maximum towards means-tested services or choosing to buy in the private market). There was, in fact, little evidence of this relationship in those households in which the carer and the person with dementia lived together. Non-parametric testing of the costs of carers’ services, services for the person with dementia and all social care services showed little relationship to household income.
There was also no significant relationship between the costs of services and how carers reported that they were getting on financially. However, the median cost of both carers’ services and the total cost of social care services was higher for those reporting severe difficulties than for others (£3302 and £1742 per annum, respectively, compared with £988 and £1560 per annum for those reporting that they were managing quite or very well, and £2652 and £1248 per annum for those reporting that they were getting by or had some difficulties). These figures suggest that the high costs of respite, day-sitting and night-sitting services could be driving some of these differences.
Future testing of the relationships between the costs of services and the characteristics of the person with dementia and the carer is needed.
Conclusions
Overall, the total sample of carers was older and more heavily involved in caring activities than all carers of people with dementia. Furthermore, the AN carers were older and more heavily involved than carers in non-AN areas. Both the general and the specific differences are likely to reflect the routes through which respondents were recruited. Carers who have started attending carers’ groups and who are known to statutory and third-sector organisations are likely to be some way into the dementia caring journey, rather than at its beginning. Those known to AN services are likely to be even further into this journey and/or, as we see in Chapter 7, struggling with their caring responsibilities.
The other differences between the AN carers and non-AN area carers perhaps show something of the ‘natural history’ of caring for someone with dementia and the role that AN support might play in maintaining people in their own homes. Thus, the first port of call for support, when people are married or in long-term relationships, is the partner, who acts as the main carer. If younger family members or friends are available, they may act as joint or non-main carers. If the main carer becomes frail or ill themselves or dies, or for other reasons the person with dementia needs more support than the main carer can provide alone, the younger generation takes over as the main carer, and the partner moves into the joint or non-main carer role. Alternatively, AN services may step in to support older or more heavily involved carers to continue.
Carers who had used AN services recently were more likely to report receiving emotional and social support and receipt of information, advice and knowledge from that source than were carers who had recently accessed other types of services for carers. This may reflect the personal and targeted nature of the relationship that Admiral Nurses are able to develop with carers compared with that which is possible in, say, carers’ groups or advice services.
Given the heavy involvement of all our carers, in terms of their caring status and activity, their overall levels of use of, and practical support from, other health and social care services were surprisingly low. Moreover, those carers who were accessing services related to their caring activities were often paying large amounts of money to do so and, for some perhaps, with consequent financial difficulties.
As other work shows,20,21 and as participants in the stakeholder workshop pointed out (see Appendix 1), there is no single ‘silver bullet’ model of service that could possibly provide support for carers of people with dementia all the way from initial symptoms becoming evident, through the worsening of behaviour and physical health, to death. Carers’ needs across the dementia journey will vary substantially, both as symptoms and circumstances change and in relation to individual characteristics and the support networks they do or do not have around them. Our survey results show that AN services are supporting the very oldest and most burdened carers, many of whom may be very close to the end of that journey.
Chapter 6 Exploratory analysis of the outcomes and the costs of Admiral Nursing compared with those of usual care
This chapter reports WP 3, the health economics component of the project. The overall aim of WP 3 was to undertake an exploratory analysis of the outcomes and the costs of AN compared with those of usual care.
Background
Carers of people with dementia provide an essential resource in supporting people with dementia to remain living in the community. Their support has implications for service use across the economy, including health and care services. In supporting carers of people with dementia, therefore, Admiral Nurses may also affect service use across the economy. It is important to quantify the impact of AN in terms of the cost of AN and the services used alongside AN, but also the cost of alternative provision, namely usual care. If AN is not available, what other services are available and what are the associated costs? In embarking on this study, usual care was defined as outlined in Chapter 2, but this work also allowed the project team to identify in more detail, and quantify, what this involved.
Admiral Nursing and usual care might also have an impact in terms of benefits, so these should also be considered. In offering any kind of support to carers, funders in health and social care services require information about the available options, what works (which service has a beneficial impact), what works best (of the alternative services compared, which one has the most beneficial impact), at what cost and for whom. This information can be used to inform decisions about which services it is most worthwhile to invest in. The key question then becomes ‘Is AN associated with better outcomes and lower costs compared with usual care?’ This chapter explores this question.
Methods
As noted in Chapter 2, this WP explored the feasibility of undertaking a full economic evaluation of specialist nursing support for carers versus usual care, based on a cross-sectional survey of carers of people with dementia. To do this, we examined the outcomes, resource use and costs associated with AN and non-AN, including informal (unpaid) care time, out-of-pocket costs for carers, health (e.g. hospital appointments, GP appointments), social care (e.g. home care) and non-statutory sector resources, as described next.
Carer outcomes
At the project inception stage, we hypothesised that the AN service could have an impact on health-related quality of life (HRQoL), carer-related quality of life (CQoL) and general well-being, in addition to specific outcomes that are valuable to carers.
Health-related quality of life
To measure HRQoL, the EQ-5D-5L was selected, given its common use in economic evaluation and NICE’s recommendation of its use to evaluate health and social care interventions. 70 As the analysis progressed, however, it became increasingly clear that AN was unlikely to have an impact on overall HRQoL. AN support is meant to help carers cope, rather than improve their health or HRQoL. For this reason, HRQoL was excluded from the analysis of carers’ outcomes and instead was used as a covariate in the econometric analyses to capture carers’ health. In the sensitivity analysis checks, however, the analysis of the EQ-5D-5L and EQ-5D, three-level version (EQ-5D-3L), scores, when used as dependent variables, was included.
The EQ-5D-5L was selected as a generic measure of HRQoL. 65 The measure consists of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. 71 Each dimension is described on five levels: no problems, slight problems, moderate problems, severe problems and unable to/extreme problems. The EQ-5D-5L thus describes 3125 potential health states, including worst health to full health. These health states can be converted into a preference-based score, anchored at 0 for death to 1 for full health, using a national tariff. The preference-based score reflects the preference for one health state over another. The national tariff reflects the preferences of 996 adults who were selected as a representative sample of the general public in England. 71 The preference-based scores range from –0.281 (for extreme problems on all dimensions) to 1 (for no problems on any dimensions).
The National Institute for Health and Care Excellence recently issued a position statement,44 in which it recommended using the van Hout et al. 72 cross-walk tariff from the EQ-5D-5L to the EQ-5D-3L to ensure consistency between appraisals (NICE), rather than using the Devlin et al. 73 values. We used the Devlin et al. 73 approach initially, as the base case, and tested the impact of using the van Hout et al. 72 approach in the sensitivity analysis.
Care-related quality of life
There is currently no consensus on the use of a CQoL measure in health economic evaluation. As described in Chapter 4, we carried out in-depth qualitative work with the carers of people with dementia to inform the selection of outcomes that might be influenced by supporting carers and tools to measure these outcomes. The selection was made from a shortlist of validated quality-of-life measures that have (or will have in the near future) a preference-based scoring system. This means that the scoring of the measure reflects people’s preferences for one dimension over another. We selected the ASCOT-Carer45 from this shortlist, as it was the measure that covered the most dimensions of CQoL that carers identified as being important in the interviews and focus groups.
The ASCOT-Carer measures social care-related quality of life in carers who care for adults with a variety of long-term conditions, impairments or problems related to old age. It includes seven questions/dimensions, with four levels each. The dimensions measure quality of life related to spending time on valued or enjoyable activities, having control over daily life, looking after oneself, feeling safe, having social contact, having space and time to be oneself and feeling encouraged and supported in the caring role. Preference weights for this instrument are currently in development and should be available soon. 74 In the meantime, the ASCOT-Carer can be presented as a summed score, ranging from 0 (lowest CQoL) to 21 (highest CQoL). 45
Carer self-efficacy
The qualitative work with carers also found that self-efficacy (or confidence in caring) was an important outcome to carers that was not captured in the ASCOT-Carer. There are very few tools that measure this outcome, and only one that is both validated and developed specifically for the carers of people with dementia. This is the Fortinsky et al. 46 SEMD scale. This is a 10-item scale with two domains: domain 1 is about self-efficacy in relation to the management of dementia (SXEFF) and domain 2 is about self-efficacy in relation to service use (SERVEFF).
The dementia management domain (SXEFF) comprises five questions with answers on a 10-point scale on how certain carers are that they can manage problems related to dementia presentation. The items are handling any problems the person with dementia currently has, handling any problems that might come up, dealing with the frustrations of caring for the person with dementia, doing something to keep the person with dementia as independent as possible and getting answers to all their questions about the person with dementia’s problems. The scale runs from 1, representing ‘not at all certain’, to 10, representing ‘very certain’. A summed score can be derived by adding the question scores, with a possible range of 5 (least self-efficacy) to 50 (greatest self-efficacy). 46
The items in the SXEFF domain cover finding care for the person with dementia without help from organisations or agencies that provide services, finding organisations or agencies that provide services to help care for the person with dementia, getting answers to all questions about the services and arranging for the services. A further question, about finding ways to pay for the services, does not load on to either domain. Thus, although the scaling of responses is the same as for domain 1, the summary scoring for domain 2 has a possible range of 0–40.
Overall life satisfaction and happiness
To obtain a sense of carer well-being overall, carers were also asked how satisfied they were with their life nowadays and to rate this on a scale of 0–10, with 0 meaning ‘not at all satisfied’ and 10 meaning ‘completely satisfied’. This question is used in the Office for National Statistics (ONS)’s annual population survey75 and has previously been used to value informal care. 76,77
Carers were also asked how happy they felt yesterday using the same scaling. This question is also used in the ONS’s annual population survey. 75
Resource use and costs
One of the objectives of the survey was to understand the use of services by and costs for carers with and without AN services. The questionnaire included sections about service use by carers and the person with dementia, which covered specialist support services for carers (including AN), health care, social care and voluntary-sector services, as well as any out-of-pocket costs incurred in accessing or using associated services. This part of the questionnaire was developed by the whole research team, tested through cognitive interviewing and then changed in response to this and to preliminary piloting.
We costed resource use using nationally available unit costs49,78,79 to aid the transferability of results (see Appendix 3, Table 53). Costs relate to the financial year 2015–16.
Measuring and costing informal care
We included questions about the time carers spent caring for the person with dementia in the 24 hours prior to answering the questionnaire.
First, we used the questions included in the most recent survey of carers in private households about the things that carers usually did for the person they cared for. 6 These questions have been used in every official representative survey of carers since the 1985 General Household Survey. 40 We followed this with a question about how much time carers had spent on these tasks in the previous 24 hours. When people had indicated that they were involved in three or more tasks, we asked them to provide the information about hours of care only for the three tasks that had taken up the most time. Finally, we asked carers to record how much time they had spent caring, in total, in the previous 24 hours.
We costed informal care time using two alternative methods: the opportunity cost method and the proxy good method. 80 The opportunity cost method values informal care time as the income that would have been forgone by the carer as a result of the time spent caring had the carer been in active employment. We used the average gross hourly pay in the UK in 2016, of £15.72 per hour. 81 The proxy good method values informal care time with the market price of a close substitute, which may be activity specific.
Cost of the Admiral Nursing service
In the survey, we asked carers if they had been in contact with the AN service in the previous 4 weeks and, if so, what type of contact they had had (face-to-face visits, telephone contact, e-mail contact, support group meetings or other types of contacts specified by the carer) and how often. In our qualitative work, we understood that AN nurses can be employed at band 5, 6 or 7; hence, we assumed for the costing that, on average, an Admiral Nurse is employed at band 6 (£44 per working hour). 49 We also assumed that the duration of face-to-face visits was 2 hours, including travel time, and that telephone contacts lasted 1 hour on average. We had no information on the resources involved in organising and facilitating support group meetings, and assumed that group meetings required 1 hour of AN time. We assumed that e-mail contacts took 15 minutes. We have assumed that the cost of AN falls on the health and social care budget through commissioning, although this might not always be the case and varies across localities.
We have also calculated the cost of the AN service using information from Dementia UK. Dementia UK provided programme budgeting information on six AN services funded by charitable organisations. This was the only information available at the time of this research and may not be generalisable to all AN services. Dementia UK also provided the average number of carers served by one full-time equivalent Admiral Nurse. We averaged the costs of setting up and running a new AN service staffed with one nurse and divided this by the average number of carers supported by a full-time equivalent nurse over 1 year. This assumes that the Admiral Nurse dedicates all of her or his time to supporting carers directly, although in practice some time is also spent supporting commissioners and health-care professionals in their services for people with dementia and their carers.
Exploratory analysis of outcomes and costs
To explore the effect on outcomes and costs of AN services compared with usual care, we compared the differences in outcomes and costs for carers we recruited via AN with those for carers recruited in areas without AN (for simplicity, respectively, AN and non-AN carers from now on). We used an economic evaluation framework to draw learnings to inform future economic evaluations of interventions of specialist support services for carers. Economic evaluation is a systematic approach used to inform decision-makers about the costs and effects of a range of mutually exclusive courses of action. 82 In the UK health-care setting, this has typically focused on analysing which option will maximise health outcomes subject to the health-sector budget constraint. In the case of specialist support services for the carers of people with dementia, such as AN services, a broader perspective may be appropriate, and NICE guidance on the economic evaluation of interventions with a social care focus is likely to be more appropriate. 48 For this reason, we considered health and social care outcomes and included costs falling on a broad perspective, including resource and service use associated with AN in the NHS, social care sector, voluntary sector and services paid for out of pocket. We also costed informal care using the opportunity cost and the proxy good method. Table 54 in Appendix 3 summarises the unit costs for the proxy good method.
The survey design was cross-sectional and went to a varied population of carers of people with dementia. Although the sampling strategy was designed to minimise differences between AN carers and those from non-AN areas, there were important differences between the respondents in the two groups (see Chapter 5). Differences in the people with dementia whom they cared for were much less marked.
Although drawing inferences on the effect of receiving AN services on outcomes or costs was conditional on the carers recruited and the data collected, the latter did provide an opportunity to explore whether or not using econometric methods could account for differences in the carers and still estimate the impact of AN services on outcomes and costs. We thus undertook an exploratory analysis, owing to both the scope of the project and the limitations of the data.
In undertaking this evaluation, the aim was to compare the impact of the intervention on carer outcomes. To do this in a scientifically robust way, the two interventions (AN and usual care) should be given to two groups of carers that do not differ systematically, as such systematic differences between the two groups can bias the results. Random allocation is used to avoid bias, but this was not possible in this study. We hypothesised that non-AN carers were similar to AN carers once we had controlled for the observed carer characteristics that differed across the two groups. Under this assumption, we estimated the effect of AN services on the carers who used AN services using linear regression analysis and PSM.
The qualitative work suggested that AN services tend to target the carers with the greatest need for support and, therefore, that AN carers would have greater needs than non-AN carers. Although the survey included several questions that indicate proxy need (e.g. severity of dementia, informal care time, informal care activities), some dimensions of the carers’ needs are, in all likelihood, still unobserved. To address this issue, an IVs approach was used.
A complete-case analysis was employed in all of the approaches. Cases that are missing variables in any proposed analysis are dropped from the analysis, leaving only complete cases. The analysis was in five stages, summarised below. Appendix 5 details our approach in econometric terms.
Description of Admiral Nursing and non-Admiral Nursing carers
We described the outcomes, resource use and costs of AN and non-AN carers and assessed how comparable AN and non-AN carers were based on their observed characteristics. A detailed comparison of AN and non-AN carer characteristics is provided in Chapter 5 and Appendix 4.
Regression analysis
We used linear regression analysis to control for the observed differences between AN and non-AN carers, as differences between groups may bias the estimate of the average effect of the AN service on AN carers. There may be carer characteristics that have an influence on their costs and outcomes, which vary depending on whether or not the carer has used the AN service. For example, AN carers may be older, and older people tend to have a lower quality of life. 83 Therefore, in this example, a naive comparison between the outcomes of AN and non-AN carers could underestimate the effect of the AN service on quality of life.
Regression analysis allows us to control for the effect of carer characteristics on the outcomes, such as CQoL, when those characteristics are not equally distributed between groups. Regression analysis provides unbiased estimates of the effect of the AN service on outcomes or costs under two key conditions. First, the regression needs to include all characteristics that affect outcomes and costs and can be confounded with the effect of AN. Second, the effect of AN and all characteristics on outcomes and costs is linear; that is, the effect of a variable on the outcome or cost is constant for any value of the variable.
Propensity score matching
We used PSM as an alternative to linear regression. PSM compares the average outcomes and costs between AN and non-AN carers after matching observations in the two groups of carers that are similar in their probability of having the AN service, given their observed characteristics (i.e. their propensity score). Unlike regression analysis, PSM does not require linearity, but it requires the matched AN and non-AN carers to have a similar propensity score distribution, that is, a similar probability of being in the AN group, conditional on observed characteristics.
Instrumental variable analysis
Regression analysis and matching analysis using PSM control for observed differences, but there may be unobserved factors that determine whether or not carers receive AN and that affect carers’ outcomes, such as their resilience and ability to care. IV analysis can deal with these unobserved factors through a variable, the instrument, that is correlated with having AN, but has no direct effect on outcomes and costs and is not correlated with unobserved factors that affect costs and outcomes. Instead of computing the effect of AN on AN carers’ outcomes (as with regression analysis and PSM), IV estimates the effect of AN on those carers who are estimated to use AN because of the variable contained within the instrument. We decided that the travel time between the carer and the AN provider is a good instrument in the analysis of outcomes and costs. Carers living far from the AN provider may not be eligible because the service is limited to a specific geographical area. Moreover, carers living long travel distances from the AN provider may be less likely to be informed about AN than carers living close to AN teams. This implies that carers living near AN providers are more likely to be eligible for, or to access, the service. This condition does not exclude the possibility that carers living close to the AN provider are ineligible because of low needs. Similarly, it does not exclude the existence of carers who access the AN service even if they live far from the provider.
The travel time to the closest AN provider is unlikely to be related to carers’ outcomes, costs and needs because carers may live either close to or far from the AN provider regardless of their levels of needs or CQoL. Following Forder et al. ,54 we argue that the type of LA is also a good instrument in the analysis of outcomes because it determines the LA’s culture and, in turn, the LA’s propensity to invest in services for carers. Some LAs will therefore be more willing than others to fund AN, but the culture will not have a direct effect on carers’ outcomes. We tested the relevance of the instruments (i.e. the strength of the relationship between the instrument and the AN dummy) through the Cragg–Donald F-statistic. 84 Using additional instruments, we also tested if travel time was unrelated to outcomes.
Sensitivity analysis
We ran seven sensitivity analyses to test the robustness of our results. The findings from these analyses are provided in Appendix 5.
Results
Outcomes of Admiral Nursing and non-Admiral Nursing carers
Table 55 in Appendix 3 reports the descriptive statistics for the outcome data. CQoL using the ASCOT-Carer was 10.1 on average (minimum 0, maximum 21) and was statistically significantly lower (worse) for AN carers than for non-AN carers (9.6 vs. 10.6) at the 5% level. Similarly, HRQoL using the EQ-5D-5L was on average significantly lower for AN carers (0.744 vs. 0.802). AN carers also reported significantly lower life satisfaction (4.3 vs. 5). Self-efficacy on symptom management was on average 27.4 and self-efficacy on service use was 22.3 (minima and maxima of 5–50 and 4–40, respectively). AN and non-AN carers were statistically similar on both measures of self-efficacy. AN carers were also typically as happy as non-AN carers. Thus, on a straight comparison and without controlling for differences between them, AN carers had lower CQoL and HRQoL, but showed similar levels of self-efficacy and happiness.
Resource use and costs of Admiral Nursing and non-Admiral Nursing carers
Table 56 in Appendix 3 summarises the use of services in the previous 4 weeks. Typically, there was sporadic use of hospital services among both carers and people with dementia, but, on average, the number of visits by carers to a GP in the previous 4 weeks was just under 1. However, the use of resources among carers varied, as the standard deviation was always greater than the mean. There were no substantial statistical differences in the amount of support, hospital and community services used by AN and non-AN carers.
Costs to the public sector
Table 57 in Appendix 3 reports descriptive statistics on health and social care costs in the previous 4 weeks. These do not discount out-of-pocket costs, which in most cases were copayments for social care services and, as we saw in Chapter 5, were substantial for some carers.
On average, the cost of using the AN service was £86 over the previous 4 weeks. As noted earlier, we have assumed that the AN services are funded from health and social care budgets.
Across all carers, the overall cost of health and social service use in the previous 4 weeks, including AN for those who used it, was around £1000. Carers cost the NHS around £239 for their use of health-care services, being costlier in terms of hospital costs (£309) than in terms of community services (£28). Such costs varied considerably across carers, as the standard deviation was sometimes five times the mean (e.g. for hospital costs). AN carers were less costly than non-AN carers for hospital services (£221 vs. £391), but more costly for community health-care services (£30 vs. £26), although the differences were not statistically significant.
Overall, the costs of the health-care services used by people with dementia followed a similar pattern, with the total costs being £324 and with higher hospital costs than community costs (£383 vs. £40, respectively). Social care services costs were, on average, £627. People with dementia cared for by AN carers had lower hospital costs (£372 vs. £393), but higher costs for community health-care services (£42 vs. £37) and social care (£663 vs. £594). The differences were not statistically significant.
Out-of-pocket costs
Table 58 in Appendix 3 summarises the out-of-pocket costs for a single use of carer support services other than AN in the previous 4 weeks (the total out-of-pocket costs of carer support services are described in Chapter 5). These out-of-pocket costs largely refer to payments for social care, as LA social services are means tested, or payment for services is arranged privately. The out-of-pocket costs were asked about in relation to the carer, the person with dementia or both and hence these related to the carer–person with dementia dyad. Fourteen out of the 21 carers using short respite/break services reported paying, on average, £240 per use, 27 out of the 64 carers using day-sitting services paid £37 per use, and two out of the seven carers using night-sitting services paid £120 per use. No carers paid for advice services, whereas carers using support group services (5 out of 57) paid, on average, £6 per use.
Table 59 in Appendix 3 summarises the out-of-pocket costs for a single use of social care services for the person with dementia in the previous 4 weeks (the total out-of-pocket costs of social care services are described in Chapter 5). Out of the 86 carers who said that the person with dementia used a day care centre, 65 carers paid for the service and reported an average payment of £40 per use, with AN carers reporting a payment of £13 less than non-AN carers. Nineteen out of the 27 carers who said that the person with dementia used other day care services paid an average of £15 per use. Of the 84 carers who reported the use of home care, 55 paid £29 per use, with AN carers paying £25 less than non-AN carers. Most (23/24) of those who said that they used meal services paid for them out of pocket, with an average payment of £10 per use; 2 out of the 44 carers reporting a visit from someone from social services paid £30 per use. Finally, 24 out of the 63 carers who said that the person with dementia had visited a memory café paid £7 per use.
Informal care time and costs
Table 60 in Appendix 3 shows the time spent and the value of the top three informal care tasks that carers carried out in the previous 24 hours, using the opportunity cost method and the proxy good method.
The informal care task that in our sample took the most time was keeping an eye on the person with dementia, with, on average, carers spending 11 hours in the previous day on this. AN carers spent 2 hours per day more than non-AN carers on this task and the difference was statistically significant. Given that AN carers were more likely than non-AN carers to live in the same household as the person with dementia, this difference is not surprising.
The second most important task in terms of hours spent caring in the previous 24 hours was keeping company with the person with dementia. AN carers spent 2 hours per day more on this task than non-AN carers, and this result is also statistically significant. Again, the reasons for this are probably to do with household composition.
The care task among the ‘top three’ that took up the least time was help with dealing with care services and benefits (e.g. making appointments and calls, filling forms). On this task, AN and non-AN carers spent around 2 hours on the day before completing the questionnaire.
The total value of the top three informal care tasks in the previous day was £293 using the opportunity cost method, on average, and £459 using the proxy good method. There was no statistically significant difference in these costs between AN and non-AN carers.
Use and costs of the Admiral Nursing service
Table 61 in Appendix 3 shows the use of the AN service. In the previous 4 weeks, among all AN carers receiving an AN service, carers received an average of 0.7 face-to-face visits, 0.3 telephone contacts and 0.2 e-mails and attended 0.2 support group meetings. Under the assumptions in Cost of the Admiral Nursing Service, AN services over the previous 4 weeks cost an average of £136 per AN carer.
Table 62 in Appendix 3 summarises the information on the cost of AN services based on programme budget information from Dementia UK. The six AN services we received information on were each staffed by one full-time equivalent AN nurse. In addition to the employment costs, the host organisation bears the cost of recruitment, employment, training, travel, subscription and insurance, equipment, indirect costs and overheads. This amounts to £52,350 in year 1 and £50,034 in year 2. An ongoing study between Dementia UK and the Personal Social Services Research Unit (PSSRU)/the London School of Economics and Political Science shared some preliminary results regarding the caseload per full-time equivalent AN at 70.6 carers per year. Using this information, we calculated the cost of AN to be £709–742 per carer per year. This is, however, likely to be an overestimate of the true cost of AN per carer per year, because the nurses carry out other activities in addition to carer support (e.g. training health-care professionals, advocacy), which we were unable to disentangle.
Regression analysis
We showed that AN and non-AN carers are different in their outcomes but similar in their costs. Such differences may be explained by differences in the characteristics of the carers, the people with dementia and the caring experience reported in Chapter 5. Hence, in our exploratory analysis, we constructed a set of explanatory variables on the basis of the carer and care recipient characteristics described in Appendix 3, Table 63. The objective was to use these explanatory variables to control for the differences between AN and non-AN carers and to estimate the effect of AN on outcomes and costs.
Table 64 in Appendix 3 reports the regression results for the outcome analysis. Being an AN carer is always associated with better outcomes, although the differences are not statistically significant (except for the self-efficacy measure on service use, which is weakly significant at the 10% level). This suggests that AN carers have similar levels of CQoL, self-efficacy and happiness to those of non-AN carers.
Table 64 in Appendix 3 also shows the effect of the covariates on the outcomes. In general, better outcomes were associated with higher HRQoL, whereas worse outcomes were associated with female sex, financial difficulties, the lack of a replacement for a break, and more severe dementia.
Having a job or being retired had a non-significant or weakly significant positive effect on the outcomes. Being the joint main carer or not the main carer (compared with being the main carer) had no significant effect on any outcome. Caring for a parent or parent-in-law or any other relative/friend (as opposed to caring for a spouse or partner) had no significant effect on outcomes.
The type and total hours of care had varying effects on outcomes. For example, an additional hour of care had a negative impact on the ASCOT-Carer, but a positive impact on self-efficacy in relation to symptom management. This suggests that the more intense caring role may have a negative impact on the ASCOT-Carer, but a positive impact on how confident carers feel in their caring role. Having been a carer for longer was significantly associated with greater self-efficacy in service use. Not having anyone to rely on to look after the person with dementia for a couple of days was negatively associated with all outcomes. There was no substantial effect of the age of the person with dementia on carer outcomes and no evidence of effect of the reported duration of the symptoms of dementia.
Table 65 in Appendix 3 includes the regression results on health and social care costs. There was no statistically significant association between being an AN carer or not and costs. The covariates were statistically insignificant, with a few exceptions. For example, care recipients with vascular dementia were associated with greater health-care costs.
Propensity score matching
After assessing the validity of PSM in a number of ways, we argued that there was a satisfactory balance of the observed characteristics between AN and non-AN carers (Appendix 3, including Table 66 and Figures 6 and 7, provides more details on the statistical tests carried out). Table 67 in Appendix 3 shows that the results of the PSM analysis on the outcome are mostly in line with the regression analysis, except for the effect of AN on the self-efficacy measure related to service use, which becomes statistically significant at the 5% level. AN carers showed greater self-efficacy on service use of almost 3 points than non-AN carers. Table 68 in Appendix 3 shows that PSM produces a statistically insignificant estimate of the effect of AN on costs, similar to the regression analysis.
These tables illustrate the estimated coefficients of the logit regression on the AN dummy used to calculate the propensity score. Carers taking care of a person with vascular dementia have twice the odds of being in the AN group than carers of people with Alzheimer’s disease. By contrast, carers with master’s or higher degrees had between 15% and 23% lower odds of being in the AN group than carers with no university education. The longer the time since the dementia diagnosis, the less likely carers were to be in the AN group.
Instrumental variable analysis results
As explained earlier, we considered travel time and type of LA as instruments for this analysis. Table 69 in Appendix 3 shows descriptive statistics for the instruments. Non-AN carers were, on average, 17 minutes (0.286 hours) away from AN services, whereas AN carers were 9 minutes (0.151 hours) away, as would be expected, given the way in which we identified carers. This difference is statistically significant at the 1% level. There was also a significant difference in the distribution of carers by type of LA: AN carers were most likely to reside in county LA areas, whereas non-AN carers were most likely to reside in unitary LA areas.
Tables 70 and 71 in Appendix 3 show the results of the IV approach for outcomes and costs, respectively, when travel time is used as an instrument. IV results are in line with those from the regression and PSM analysis. The coefficient on the AN dummy is not statistically significant for any outcome or cost measure except ASCOT, which is weakly significant (at the 10% level). The effect of the covariates on outcomes is similar to what we observed in the regression analysis results.
Travel time is a strong instrument, as the Cragg–Donald F-statistic is between 41 and 56 (well above 10). As shown in Table 72 in Appendix 3, we cannot reject the hypothesis of no effect of travel time on outcomes when additional instruments are employed. In other words, this suggests that travel time has no relationship with the outcomes.
Discussion
In general, better outcomes were consistently associated with lower health needs, as captured by higher HRQoL through the EQ-5D-5L score, whereas worse outcomes were consistently associated with financial difficulties, the lack of a replacement for a break, and more severe dementia. Similarly, financial difficulties may substantially decrease the carer’s self-efficacy and may preclude the purchasing of support services to complement statutory services. Moreover, AN carers were less likely to have a master’s degree or higher education and report that the symptoms of dementia had been in existence for > 1 year. A higher level of education might imply better caring skills (even when age is controlled for; for example, see Appendix 3, Table 67). AN carers are more likely to be caring for a person with vascular dementia, which might be associated with more severe cases.
There were differences between AN and non-AN carers, as highlighted in Chapter 5 and in Tables 63–65 in Appendix 3. AN carers were older, had lower education, were more likely to be retired and had more financial difficulties. AN carers were also more likely to care for their spouse/partner, to be the main carer, to carry out the heaviest tasks (e.g. personal or physical care) and to look after a person with Alzheimer’s disease or vascular dementia, but less likely to have someone who could replace them if they were in need of a break. This suggests that carers may be in receipt of AN support on the basis that their needs are greater than those of carers with no AN support. A naive comparison indicated that AN carers had worse outcomes than non-AN carers. Once we controlled for the different characteristics, however, AN carers were found to have better outcomes, although these results were mostly not statistically significant. Similarly, we found little difference in costs between AN carers and non-AN carers or in the costs of the people with dementia they care for.
Strengths and limitations
To our knowledge, this is the first time that costs and outcomes have been compared between users of AN and non-AN carers.
Typically, within a standard economic evaluation framework, it is useful to collect data over multiple points in time. Although a cross-sectional study may provide a useful insight, it increases the uncertainty about the results because of a higher risk of selection bias (e.g. because of unobserved needs). Even if the IV helps to address the selection bias, its estimate of the effect of AN refers to a subgroup of AN carers (i.e. those carers who are estimated to use AN because of the variable contained within the instrument).
Other limitations are strictly related to the nature of AN. For instance, the effect on carers who received AN support in the past may be difficult to disentangle from other support services that may also have been utilised. Diversity in the referral process (in some cases, carers are referred to AN after a triage assessment; in other cases, they can self-refer) across AN providers may generate high heterogeneity within the group of AN carers, which may hamper us from identifying an effect. Finally, we are unable to estimate a summary indicator, such as an incremental cost-effectiveness ratio (ICER), to inform decision-making. Our CQoL measure, although generic to carers, is not generic to all members of the community. In addition, at the time of reporting, no preference weights for the ASCOT-Carer are available. We were unable to calculate a measure akin to a QALY, given that currently we do not have information on time in state or a CQoL preference weight. In addition, based on this, there is no decision rule available to interpret an ICER and no empirical estimate of the cost-effectiveness threshold for decision-making in social care to assist decision-makers.
Chapter 7 Understanding the wider impact of specialist support for carers of people with dementia
Introduction
The effects of specialist dementia services may extend beyond individual outcomes and resource use, having an impact also at a system level. In theory, for example, if services enable carers to care for longer or help them to remain healthy, they may reduce costs to both health and social care systems. In WP 4, we explored with health and social care stakeholders what they perceived to be the system-wide effects of the services in their areas that were designed to support the carers of people with dementia, with a specific emphasis on specialist nursing support of the type AN provides.
Methods
We selected two areas with AN services and two areas that did not have AN but were broadly similar (in terms of ethnic diversity and urban/rural mix) to the AN areas. All four were areas that had also been selected for WP 3 (the survey). However, it was not possible to triangulate the findings from the two WPs, as we did not receive any eligible survey responses from two of the four case study areas. The case study findings set out below are, therefore, informed by qualitative interviews alone.
Within each area, we identified the key health and social care stakeholders in relation to dementia care and support for carers from both the statutory care sector and the third sector. We began by inviting commissioners through the NHS research offices and then used snowballing techniques to identify other stakeholders. We expected to identify between 12 and 15 key stakeholders in each area whom we could invite to take part.
Stakeholders were invited to take part in an in-depth, semistructured telephone interview to explore the perceived system-wide impact of carer services, such as AN, compared with ‘usual care’ (objective 4). The interview aide-memoire covered:
-
current provision for the carers of people with dementia
-
commissioning arrangements and intentions
-
the impact (if any) of AN and other relevant services on health and social care
-
how services interact
-
views on the costs and benefits of AN and other relevant services
-
future plans for (further) developing support for carers of people with dementia.
We also asked stakeholders how they measured the impact of their services in order to explore the feasibility of implementing routine collection of outcome and resource use data in the future.
All interviews were digitally recorded and transcribed. Data from the transcripts were then ‘charted’ (summarised and organised in spreadsheets using the Framework approach)42 and analysed thematically. All documents and processes were reviewed and approved by the HRA London – Chelsea Research Ethics Committee (IRAS ID 195413; see the documentation at www.journalslibrary.nihr.ac.uk/programmes/hsdr/1415407/#/).
Case study sites and participants
The four case study sites selected were:
-
a mixed rural/urban area with an AN service hosted by a dementia charity
-
a large, ethnically diverse city with an AN service hosted by the mental health trust
-
a mixed rural/urban county without an AN service
-
an ethnically diverse city without an AN service.
Across the four case study areas, 58 professional stakeholders in key positions were identified and invited to take part in a telephone interview. Of these, 20 eventually took part, with the remaining 38 either actively declining to be interviewed or failing to respond after a reminder. Recruitment was very challenging in all areas, but particularly so in the areas without AN, where perhaps there was less motivation to learn about the impact of this model.
We were most successful in recruiting professionals in case study site 1, with seven agreeing to be interviewed (out of a total of 14 invited). Recruitment in case study site 2 was more difficult, with only 5 out of the 16 invited professionals agreeing to take part (less than one-third). Recruitment in case study site 3 started well, with two commissioners and two front-line nurses agreeing to be interviewed. However, it was not possible to interview anyone from the voluntary sector, and senior (strategic) staff from the mental health trust were also unavailable. We eventually spoke to just 4 out of the 10 professionals identified in this area. Two further stakeholders had initially agreed to take part, but when we contacted them to arrange the interview they did not respond, perhaps reflecting the time pressures facing professionals who in principle would like to contribute to research, but in practice do not have the time.
Recruitment to case study site 4 was particularly challenging, and, given what we now know about the potential decommissioning of key services and resultant instability in that area, this is perhaps not surprising. Recruitment was initially led by the local research office, which contacted commissioners, but with no success. The University of York research team then began contacting potential participants at all levels directly (via e-mail). Of the 18 professionals contacted, only four agreed to be interviewed. The reasons for refusal ranged from not having the ‘level of detail’ the stakeholder thought would be useful to the research to being in the process of being made redundant. This was clearly a difficult time for service providers, as is explained further in Results.
Table 73 in Appendix 3 shows the areas of responsibility of all professionals who took part in the case studies, as well as of those who were invited but did not participate. Box 1 lists those who did take part.
WP4W1: dementia charity.
WP4W2: commissioning.
WP4W3: AN.
WP4W4: community organisation.
WP4W5: palliative care.
WP4W6: dementia charity.
WP4W7: commissioning.
Professionals interviewed from site 2 City with Admiral NursingWP4X1: AN.
WP4X2: occupational therapy.
WP4X3: carers’ charity.
WP4X4: commissioner.
WP4X5: dementia charity.
Professionals interviewed from site 3 Mixed rural/urban area without Admiral NursingWP4Y1: commissioner.
WP4Y2: commissioner.
WP4Y3: nurse.
WP4Y4: nurse.
Professionals interviewed from site 4 City without Admiral NursingWP4Z1: commissioner.
WP4Z2: nurse.
WP4Z3: carers’ charity.
WP4Z4: dementia charity.
Results
Case study 1: a mixed rural/urban area with an Admiral Nursing service hosted by a dementia charity
In this site, the Admiral Nurses were hosted by a voluntary-sector organisation jointly commissioned by three CCGs and a LA. The service provided a tiered dementia support service with a number of elements. It had two Admiral Nurses, each of whom worked with a team of dementia support advisors, enabling them to reach greater numbers of families than they could do alone, yet still provide continuity as people’s needs changed over time. A representative of the provider organisation explained:
. . . the Admiral Nurse sits above a team of dementia support advisors . . . almost like a triaging system; so referrals come in, we support people from early diagnosis, or even pre-diagnosis, through to end of life, and at any given time if the support advisor sees fit, they can escalate it up to an Admiral Nurse. She does intensive input on what that particular problem is, with the family, the carers, and then when she feels things are stabilised, if they have, she will pass it back to the support advisors.
WP4W1
The service also ran two helplines and various group activities and had been recently commissioned to pilot a practice-based dementia navigator, which was a non-clinical role that would be attached to a GP practice and mentored by an Admiral Nurse. The nurses also provided regular dementia training to palliative care staff, as well as to home-care and voluntary-sector organisations. From the perspective of the service, a core part of the AN role was to work alongside the memory clinic, adult social care and GPs. However, the Admiral Nurses themselves were not commissioned by the CCGs or the LA, did not feature in the contract for the wider service that hosted them and, indeed, were funded entirely through voluntary donations. As one commissioner explained:
. . . from [my] perspective having an Admiral Nurse that’s funded by [the charity] is really good because we couldn’t afford to employ her, I don’t think. So obviously we’re very grateful for, about that . . . we’ve got a several million pound deficit and we can’t invest in anything . . . that won’t produce at least equivalent savings.
WP4W2
This commissioner had heard good things about Admiral Nurses, but had no actual evidence about their impact or the potential cost savings they could deliver. We do know that the Admiral Nurse took referrals from across the health, social care and voluntary sectors, particularly when other services were struggling with a complex situation or were unable to provide further help to a person or their family. They were thought by some to be used as an ‘overflow’ for NHS services. However, the cases they took on tended to be very complex and there did not appear to be any other professionals in the service system with the skills, capacity and remit to take those cases. A (real) example was given of a person with dementia with multiple problems whose family was struggling to cope, but who had been told by the community mental health team that there was nothing they could do (no medication, no specific intervention), so the person and their family had been discharged. The LA adult social care services then picked up the case, but called in the Admiral Nurse, who explained how she became involved:
. . . because they [adult social care] also couldn’t do anything, because although . . . [there was a] high state of self-neglect, some risky behaviours, family just on their knees, there’s nothing they can do yet.
Right. So what can you do?
Just help reduce family stress and look at strategies to help to get through the, you know, the tricky times. So some of it is emotional, so listening to them and supporting them . . . and some of it is to try and find ways of problem-solving and, you know, dealing with some of the risky behaviours . . . I rang them up and then went to the house and did a visit, and then actually there was some safeguarding stuff, so I ended up liaising with their care manager at adult community services, I’ve spoken to the GP; everybody’s floundering and not knowing what to do . . . I’ve also maintained regular phone contact with the stressed [family member so] she feels like she’s supported . . . and every time a little blip happens, something happens, I sort of steer her through that about what’s appropriate to do . . .
This was not an isolated case. Nevertheless, the view of another commissioner was that, although the Admiral Nurse was doing a valuable job, this might not be necessary if the statutory service system worked more effectively. The Admiral Nurse was, in effect, plugging the gaps in a system that, with the right developments, should be able to meet the needs of its population without this expensive service:
I think it [the Admiral Nurse] is having a value at this point in time. I do think though that Health could and should be better providing the dementia awareness support and education for their staff; I think that if that was in place . . . you can almost perceive that there would not need to be an Admiral Nurse.
WP4W7
This commissioner argued that the key priorities for improvement locally were professional education, information and signposting. However, the carers interviewed for WP 2 (see Chapter 4) made a clear distinction between signposting and the intensive support they received from Admiral Nurses to help them access services, and to encourage them and the people they cared for to accept help. A professional working in palliative care confirmed that such support could be very valuable for people with complex needs:
. . . [the Admiral Nurse would] refer on to Adult Social Care but what they would do is they would support them in the meanwhile, and they would co-ordinate the referrals and liaise with them in terms of getting the support available. And also the person themselves, in accepting that help, can be very difficult; so they can be that person that helps them to come to terms with the fact that they need a referral. Because otherwise . . . say the GP saw them and just said, ‘oh can I refer you to social services’, and the person said ‘no’, pretty much that’d be it, whereas the Admiral Nurse would go in on a regular basis and . . . be a little bit more persuasive over a period of time, but they’re, they’re able to do that because of the pre-existing relationship they’ve got . . .
WP4W5
This professional saw continuity as the key factor distinguishing the Admiral Nurses from other services: other professionals could (and should) be better trained and dementia aware, but she was doubtful that they would have the capacity to work with families affected by dementia in the intense, continuous way that the Admiral Nurse could. Crucially, the ongoing relationship afforded by the tiered approach (whereby support advisers engaged with people early on in their journey and retained contact) meant that, if and when the Admiral Nurse became involved, the family and their situation were already known. A representative from another community organisation working with older people similarly commented that it was the dementia charity as a whole, with its support advisers supervised by the Admiral Nurses, that was the valuable resource:
. . . it’s not just the Admiral Nurse that we liaise with really, but, you know, in terms of the expertise of her training, that was really helpful, and also knowing that within [the charity] they do have that nursing expertise for people who really need it . . .
WP4W4
This account contrasted with that of another dementia charity, which provided a number of services locally (information and advice, social groups and training for carers) but had very little to do with AN or the organisation that hosted it. Unlike the other organisations we spoke to, this charity did not often refer to the Admiral Nurses or access staff training from them. As a representative of the organisation explained:
. . . we generally are quite skilled at supporting people ourselves, we know who to refer to, you know, for financial advice and support like Age UK and other things, and also we know the need to refer back to the GPs occasionally or the mental health team, [and] we do do a lot of in-house training in our teams . . .
WP4W6
This organisation did not provide ongoing case management, except for a ‘very small minority’ (WP4W6), and did not have in-house clinical expertise, but would refer on to other services if it felt that this was required.
A final relevant service in the area was a dedicated carers’ service mentioned by several interviewees, but which did not respond to our invitations to be interviewed. We know that the support advisers liaised closely with this service and did joint home visits, but we do not know what the carers’ service thought about its impact or that of the Admiral Nurses.
It is clear that, in this case study site, not everyone had an Admiral Nurse, and, indeed, one commissioner pointed out that there appeared to be very little awareness of the service among the general public. However, having this specialist resource locally and being able to draw on it was highly valued by services on the ground that came into contact with people with dementia and their carers but were not specialist dementia organisations themselves. The view from commissioners was ambivalent, recognising that having Admiral Nurses might add value to the system but not being convinced that this would justify investment, particularly as there did not seem to be demand for AN from the general public. There was, however, strong demand for improved, more consistent services, rather than the fragmented ‘postcode lottery’ currently experienced by many.
Case study 2: a large, ethnically diverse city with an Admiral Nursing service hosted by the mental health trust
This site was a large city with a small AN service based in community mental health services. The service was a small part of a large block contract, but was one of a handful of dementia services within that contract that came under a Section 75 pooled budget within the Better Care Fund. 85 The aim of the service was to provide specialist support to carers with complex needs or comorbidities, and referrals came primarily from the mental health trust itself. Interviewees explained that the service had to be quite selective and take on carers with the highest needs only, because ‘if everybody was referred, we wouldn’t be able to cope with the demand . . .’ (WP4X1). When fully staffed, the service should have had three full-time and two part-time nurses, all at band 6, but at the time of the interviews it was two nurses short. The service had responded to this restricted capacity by using its time more efficiently through running clinics and groups, being ‘economical with home visits’ and staff taking laptops when they did go out so that they could work anywhere, rather than having to return to their office. Nevertheless, reduced capacity and tight referral criteria meant that their impact on, and integration with, the wider service system seemed limited. The service was not contracted to take referrals from primary care or social services, although if referrals came who met the criteria they would not be turned away. The local carers’ service was aware of the Admiral Nurses, but did not work closely with them. The memory service, although based in the same building, rarely referred to the AN service, as they tended to see people with dementia at the start of the journey (i.e. assessment and diagnosis), when carers’ needs were not generally so pronounced. Joint working was more likely between the Admiral Nurses and other elements of the community mental health team:
. . . we’ll liaise with the community mental health teams and we work with them, such as reporting any concerns to psychiatrists, especially if someone’s suicidal or if they come out with any ideas, and also if we have any concerns such as if there’s changes in the caring role that’s going to impact on their mental health we’ll liaise with the mental health team as well. So that’s a good form of communication, we’re on the system, we can e-mail, we can inform, we can find out what’s happening, we can enter things on their notes so that whoever comes in can see exactly what we’ve done.
WP4X1
Our interviewee from AN did think that the work done by Admiral Nurses reduced pressure on primary and secondary care. Carers on the AN caseload could go to them rather than to a GP for advice, and those who attended their training would be able to spot signs of infection in the person with dementia and access treatment early, before a hospital admission was required. However, they knew of no way of measuring this impact.
The commissioner leading on dementia and carers agreed that demonstrating the impact of dementia services was very difficult for two reasons: (1) if you prevent an admission, it does not take place, so it cannot be observed or measured; and (2) any impact may take years to take effect. She also pointed out that the AN service was only a small part of the dementia service system and worked with only a few hundred carers per year. She argued that the model had strength as part of a tiered pathway:
. . . it’s about having a menu of options.
WP4X4
She explained that some people do not need much support (some people just want a few appointments with a dementia adviser, or to be signposted to dementia cafés or other services), whereas other people want longer-term support, and some people will have very complex needs that can be met only by the Admiral Nurses:
. . . That’s what we’re paying them for, mental health expertise. So I would expect them to still link people in with dementia advisers as a long-term thing, because they cannot case manage eight and a half thousand people with a diagnosis. . . . my expectation as a commissioner would be that they would hold onto the most complex ones, because we’re paying them for clinical expertise, they’re a much more expensive service in that way than if you go to the third sector. . . . if I found out that they were working with the same people, you know, they were doing a dementia adviser type role, I wouldn’t be very happy because you pay [for a] nurse . . .
WP4X4
The dementia advisers this interviewee referred to are part of a commissioned service provided locally by a dementia charity. The usual pathway for newly diagnosed people with dementia was to be referred from the memory service to a dementia adviser, who would work with the person for up to 6 months. If a person needed support more than 6 months after diagnosis, they would be referred to a dementia support worker (or, in some areas, a dementia navigator) and these workers would also support carers (something that was not an official part of the dementia adviser role). Although a little disjointed, this model had far greater coverage than the AN service, reaching 700 or 800 people per year. However, the service did not have the capacity to provide active case management to that many people in the long term; rather, people were expected to move in and out of the service:
We’re not about creating a dependency, you know, we’re about empowering people to . . .
So you do [between] one and three visits and then, what . . . do you close the case . . . ?
It, yeah, yeah, the aim is, when we meet somebody, that we say we’re here to help and support you, once we’ve met your needs we’ll back off when, about you living your life and getting on with life, we’ll back off and if you need us in the future you come back to us, we don’t close people . . . until we’ve met the outcomes . . .
. . . and if they need support again, can they access the same adviser or worker?
We, we try as much as possible to, to keep that continuity, you know, it isn’t always possible, but in the main we will try to keep that continuity going.
The view of this interviewee, as well as of the commissioner we spoke to, was that most people do not want a service involved all the time; the important thing is that they can access support when they need it. This contrasts somewhat with the findings of our interviews and focus groups with carers (see Chapter 4), who said that ongoing support from someone who knew them and their situation well was important and meant that, when crises did arise, a professional was already involved and so was better positioned to help them.
The tiered approach seen here has some similarities to the model described in case study site 1, and also some differences. Although the Admiral Nurses in site 1 were employed by the same organisation as the support advisers and worked very closely with them (passing on expertise and escalating or de-escalating cases, but not closing them), the relationship between the Admiral Nurses and the dementia advisers and support workers in site 2 was less developed. Each service would refer to the other, but there did not appear to be much joint working or formal professional education. Although the Admiral Nurses did provide dementia training to local hospices, the dementia advisers and support workers accessed their own training in-house and from elsewhere. Nevertheless, they recognised the Admiral Nurses as a ‘resource to tap into, in what feels, sometimes, like an ever-decreasing resource pool’ (WP4X5) and said ‘the gift’ of the Admiral Nurses was their clinical expertise and dementia specialism.
One other significant resource for the carers of people with dementia in this area was a consortium of 15 carers’ organisations commissioned by the LA. The service was described as ‘diagnosis neutral’, but all carers were welcomed and 18,000 people in total were registered with the service. The overall aim of the consortium was to help carers navigate an otherwise complicated service system but, rather than simply signpost, they assessed needs centrally and retained overall responsibility for the carer so that multiple and future needs could be met in a co-ordinated manner:
. . . we will tap people into those services, as well as provide any additional wrap around services that we feel the carer might need around their own well-being . . . They stay on our books, so it’s not, ‘OK, we signpost you and we close the case’, carers can come back whenever they want for that information [and] support . . . So we’ve got lots of carers that at any point in time are accessing services from more than one provider. That’s great . . .
WP4X3
Although this consortium appeared to have overcome the challenge of co-ordinating support from a number of specialist services and maintaining continuity, it should be noted that none of the services signed up to the consortium was for carers of people with dementia in particular. Interviewees did tell us about one final service that had been commissioned specifically to provide information to the carers of people with dementia. However, no one from this service was available to be interviewed, so our knowledge of it is limited.
On paper, the availability of the information service for the carers of people with dementia, together with the larger consortium for carers, the routine care co-ordination for people with dementia and their carers available through the dementia advisers and support workers services and the more specialist support for carers with complex needs through AN, presents a picture of a well-designed tiered service system meeting the needs of carers and people with dementia across the city. However, the commissioner we interviewed explained that in practice there was not enough capacity in dementia services to reach the 11,500 people with dementia who were expected to reside in the city (8500 currently diagnosed) and all of their carers:
I mean for [the dementia carers’ information service] there’s something like, I think it’s less than 10 workers. So for a city the size of [site 2], eight and half thousand people with dementia, that’s not a huge service. . . . we’ve got dementia cafés and memory cafés as well, we’ve got probably 13 of those, and then the dementia café only usually operates once a month sort of for half a day. So what I say to the GPs is, ‘well if all eight and a half thousand people with a diagnosis turn up to a dementia café on the same day it’s going be really, really difficult’ . . .
WP4X4
Moreover, site 2 was a very diverse city, with large numbers of people from different ethnic backgrounds, but it had very few dementia services or services for carers designed specifically to meet the needs of these different groups. As the commissioner explained:
. . . the services that we’ve got are expected to cope with that, because there’s, whilst there’s no money to commission generic services, there’s no, there’s totally no money to commission specialist ones . . .
WP4X4
When asked specifically about the AN service, the commissioner again felt that this small service, although highly targeted, did not have the capacity to adequately serve the city, citing the low prioritisation of dementia services and the problems in demonstrating impact as the reasons for this:
[It’s the] tip of the iceberg . . . I mean what you’d ideally have is a bigger service that would offer more of what they’ve got, because I’m sure there’s lots of people that could benefit from the [AN] service but can’t actually access it. But it’s just about finding the funding, you know, funding for dementia services is usually the bottom of the pile and it’s just really difficult because there’s no evidence that the, these services make a difference to persuade the people that hold the money that they should invest.
WP4X4
Case study site 3: a mixed rural/urban county without an Admiral Nursing service
This site was a large county with both rural and urban parts. The dementia strategy was compiled jointly by the CCG and LA and was jointly funded, partly through the Better Care Fund. The site did not have an AN service, but did have a voluntary-sector dementia support worker service and a generic carers’ service, as well as acute care-based assistant practitioners and support workers assisting the memory service and home treatment teams. The latter received clinical supervision and dementia training via an innovative nurse practitioner position within the memory service, which appeared to fulfil a role that in other areas might have been undertaken by an Admiral Nurse:
. . . this is clinical supervision, clinical education, doing it ‘on the job’ . . . and doing it through experiences and reflection. But I’ve also just started . . . my medical educator master’s degree as well so I’m bringing that education into the workplace.
WP4Y3
The home treatment team also delivered professional education, helping staff in care homes, for example, to recognise the underlying factors that might be causing distress to people with dementia, and diffusing situations before they became acute. Although this team also provided some follow-up to dementia patients in the community and during inpatient stays, there was a view from some professionals that this was not enough. An interviewee working with patients with early-onset dementia, for example, said that he would keep patients with vascular dementia and frontotemporal lobe dementia on his caseload rather than transferring them to mainstream mental health services, because he was concerned about the lack of follow-up:
. . . if I transferred them over to the memory service, because they don’t need any medication reviewing they therefore aren’t eligible to any reviews so they’d be discharged. If they needed home treatment, of course the teams would get involved, but, you know, I feel that they deserve more than that . . .
WP4Y1
This was also the view of one of the commissioners we interviewed, who was proposing to commission a new dementia companions service to ‘beef up’ the existing dementia support worker service. The dementia companions would be non-clinical workers supported by practice-based dementia specialist nurses, who themselves would primarily be focused on diagnosis, but with the availability to provide advice and support should that be required. Again, this proposed model does not sound dissimilar to the model described in case site 1, where teams of support workers worked under Admiral Nurses, although the proposed model here would be primary care, rather than voluntary sector-based care.
Interestingly, in a neighbouring district, there was an AN service that at least one of our interviewees could refer to for carers living within that boundary. This enabled a direct comparison of current support between the areas with and without AN, and this interviewee felt that support for carers in the area without this service was lacking:
And what if someone has that kind of need that you’ve recognised, particularly the carer is not coping, needs help, but they’re not in the area where they’ve got the Admiral Nurses?
Well it’s really difficult. So we refer most people to [charity that provides dementia support workers] . . . but again [they’re] quite limited, they’re unqualified staff; so, you know, although they’re very good it’s not quite to the level that the Admiral Nurses can give. So we just have to manage but it’s not ideal; and I do struggle more with people in [the area without the AN service] than I do in [the area with the AN service] . . .
No one from the existing voluntary-sector dementia support worker service in this area was available to be interviewed, but the commissioner explained that this service did not currently provide continuous support to families affected by dementia and had only limited capacity. By contrast, the aim of the proposed service was to make available a ‘go-to person’ to people with dementia and their families, with whom they could develop an ongoing relationship. As the dementia progressed, the home treatment team might also become involved, but this would not replace the dementia companion:
They’ll be with the person, very similar to how the Admiral Nurse works, throughout the entirety of the dementia journey . . . the dementia companion remains in contact, you know, they have a go-to person, if you like, for the person with dementia and their carer. Then as the journey progresses it may well be that the home treatment team is required in future. Now this home treatment team will be a team that responds to people with, with fairly moderate-stage dementia, moderate to end stage where the, the symptoms and behaviours become quite pronounced . . .
WP4Y2
The home treatment team did currently exist, but the commissioner said that its role would be developed and standardised. In terms of services having an impact on acute admissions and reducing the need for residential care, the general view was that this was the role of the home treatment team. The commissioner explained that, at present, there is no way of measuring this impact, but that this is one of the developments being proposed. No one from the home treatment team was available to be interviewed.
The service was envisaged to be for carers as well as for people with dementia, and this would complement the existing generic carers’ service. It should be noted, however, that the dementia companion model, with its aspirations for continuity and joint working with primary and secondary care, had not yet been commissioned, and it is impossible to say how it might work in practice.
Case study site 4: an ethnically diverse city without an Admiral Nursing service
This site was a diverse city without an AN service. At the time of the interviews, both the city and the county council, together with the three CCGs covering the area, were jointly undertaking ‘a live procurement exercise around dementia support services’ (WP4Z1), which made the recruitment of interview participants very challenging. A number of provider services faced uncertain futures and some of those in commissioning seemed reluctant to talk about current and future provision. The LA dementia support service was one of the services currently out to tender and, as a result, no one from this service was available to speak to us.
An interview was conducted with a lead commissioner for the city who set out the vision for support services for people with dementia and their carers going forward. The aim was to commission a service that would provide advice and information, one-to-one (short-term) support, training for carers, group support and advocacy. The commissioner explained:
. . . the service will provide that consistent first point of contact for people, which is, I know that’s something that the Admiral Nurses do . . .
WP4Z1
However, the service would most likely be staffed by non-clinical support workers and provide time-limited support:
. . . what we don’t want to do is, is obviously there’s the finite volume to this service, we don’t want it to get silted-up with people who require ongoing support necessarily; the idea being that the service will be a point of contact, a consistent point of contact for the person and their carer, and that they can zip in and out of the service as they require.
WP4Z1
It is impossible to know the potential impact of this service, as it had not yet been commissioned, but interviewees were asked about their hopes for the service and how any impact would be measured. The commissioner explained that there would be a greater focus on measuring outcomes for service users than there had been in previous contracts. In terms of the wider impact, although it was envisaged that the service could reduce pressure on health services, this was not a primary aim and there were no plans to measure this:
We do not expect the provider to answer for the NHS and for their targets. We do think there will be an impact, hopefully, if we get it right, because what the service will be doing when it links with people who are in hospital, they’ll be linking with the discharge teams as well. So there’ll be that sort of facilitating role between the discharge teams back into the community and, and maybe into adult social care too. So I do think that we will, well I’m hoping that we will see improvements but we’re not expecting this service to be accountable for that . . .
WP4Z1
The existing LA support service was felt, at least by some stakeholders, already to provide continuity of care and to dovetail well with clinical services. When we asked a participant from memory services what she hoped the new service would achieve, she said that she was mainly hoping that there would be no deterioration in the high quality of care that people with dementia and their carers currently received from the existing LA service. She considered this service to be ‘invaluable’, because it was staffed by very experienced workers and provided continuity, which was something the memory service, with its focus on assessment and diagnosis, could not do:
. . . one of the hardest things that I do and my colleagues do is actually say to someone ‘We’ve given you a diagnosis and treated your dementia, it’s stable at the moment but that won’t be that way forever, but we’re going to have, we’re going to discharge you’. What it can be reassuring is knowing, and saying to them, here is a contact number, here is someone that, who will actually help you; and if you’ve got confidence in that level of support that’s great.
WP4Z2
Moreover, in her view, the involvement of these support workers did save the health service time and resources, as they would pick up problems in the community (such as urine infections or constipation that could be affecting a person’s well-being and behaviour and, in turn, the carer’s ability to manage) and act on these to prevent crisis. Unfortunately, she knew of no way to quantify this impact.
This nurse trusted the judgement of the support workers, despite their not having a clinical background, valuing their experience and commitment above qualifications. However, she was aware that these qualities were attributes of the individual workers and not necessarily of the support worker model in general, and she was concerned that a newly commissioned service, which on paper looked similar, might in practice not operate so effectively:
I could put them alongside a new member of nursing staff and I, I think they’d give them a run for their money really. . . . but that’s what’s hard to replicate, experience and dedication, and that is a problem . . . you can have a model that works or you can have staff who are absolutely great. You could say, oh this works because that person’s done it for years and they know what they’re doing; but that’s not, that’s not replicable . . .
WP4Z2
No other health or social care services were identified that focused primarily on support for the carers of people with dementia in this case study site. CPNs and the unscheduled care service might get involved at crisis points, but they came under the umbrella of general mental health services, rather than targeting dementia in particular. We invited numerous managers covering these community mental health services to take part in an interview, as well as a senior mental health nurse, but all declined or did not respond.
Professionals working in the voluntary sector were more forthcoming. We identified two main voluntary-sector services providing support to the carers of people with dementia: one a dementia charity that provided some services for carers and the other a generic carers’ service that worked with some carers of people with dementia. As such, neither service specialised in supporting the carers of people with dementia and, as they were both non-clinical services, neither directly replicated AN. However, there were elements of both services that might be delivered by Admiral Nurses in other areas. The dementia charity, for example, ran an advocacy service for people with dementia and their carers, as well as peer support groups and carers’ information and support programmes. Our interviewee from the memory service said that she might refer someone with low-level needs to these services rather than to the LA support workers, because the latter’s caseloads were often very high, but her service did not do this routinely. The interviewee from the dementia charity agreed that their services reduced the pressure on statutory services, in particular by taking on non-clinical support issues and advocacy so that GPs and CPNs could focus on medical issues. This impact was captured, to some extent, in case studies, but it was not recorded systematically and these case studies could be used selectively:
. . . we’ve got into the habit of writing case studies and keeping them on file . . . we send those with the monitoring, and I think they’re often really good because, you know, they can actually see outcomes from that basically . . .
And so do you do that systematically, that for every case that comes through, or just for certain ones?
Not for every case because otherwise we’d, well there’d be hundreds of case studies . . . we choose, actually, when the monitoring’s due . . . which one is best to, you know, to fit with outcomes . . .
The carers’ charity was a generic carers’ organisation working with all adult carers, including carers of people with dementia, but without any services or projects targeting specific conditions. Staff from the charity saw it as a prevention service, providing practical training and stress management for carers, as well as advocacy. This service argued that helping somebody to deal with stress might prevent illness, helping them to continue caring for longer and reducing pressure on other services. However, the staff we interviewed did not feel that they were in a position to measure or demonstrate their impact on the statutory sector and felt that this made services like theirs vulnerable to cuts:
. . . is there any way that the impact of that is measured . . . whether or not you’re able to actually prevent admissions or prevent use of care home or home care?
This is the big problem, because generally you don’t really see it [sighs], I don’t know how they would measure it, we certainly are not in a position to measure it, and this is one of the problems with preventative approaches . . . it’s one of the reasons why social care service [commissioners], when they’re looking to make cuts, will not cut the emergency stuff, the crisis management stuff, they’ll cut the prevention . . .
There were contrasting views on the value of AN from the different professionals we interviewed. The commissioner felt that there were advantages to the model, but had always thought of AN as ‘quite an expensive resource’ (WP4Z1). The interviewee from memory services described AN as ‘unmatched’ in the level of support and continuity they could provide. However, she too felt that it was unrealistic to expect this service to be commissioned in this area:
And what are you hoping for? What would be a good outcome from this [re-tendering process]?
What would be a good outcome? Admiral Nursing across, across the city [laughs] but that’s never going to happen, is it? No, no.
Right, OK. So, and why do you say that?
Um, because I, as much as I think it’s a wondrous, wonderful model, it’s an expensive model.
Staff from both voluntary-sector organisations were asked if they felt that the services their charity provided replicated AN services or negated the need for AN in their area, and both said ‘no’. The representatives from the dementia charity pointed out that the charity’s staff were non-clinical and their role was primarily to provide a voice for people with dementia and their carers while navigating the health and social care system. Similarly, the representives from the carers’ charity felt that its staff did not have the expertise in dementia and could not offer the intensive case management that Admiral Nurses provide:
. . . an Admiral Nurse can help the person to deal with the situation they’re dealing with at home, and to understand what’s going on with the person that they’re looking after, which is a completely different thing. We can only do that up to a point, but we don’t know the individual case, we don’t know the specific diagnosis, bearing in mind how many different types of dementia there are and we do not know enough about it to go any further than the basics . . .
WP4Z3
Discussion
A key aim of this WP was to better understand the perceived system-wide impact of services such as AN. What is immediately clear is that this impact is not well understood. Although, in the main, AN and other dementia care co-ordination services, notably dementia advisers and support workers, undertake activity that in theory could reduce the impact on acute health services (such as emergency admissions and hospital bed-days) and adult social care (in particular the need for long-term care), this was rarely measured. Indeed, there was a suggestion that such effects were particularly difficult to capture, as prevented crises could not be observed. Nevertheless, the consensus was that these preventative services were valuable and did reduce pressure on statutory services.
In all four of the case study sites, the LAs and CCGs jointly commissioned the dementia services and so, in theory at least, the cost savings from both sectors would be reaped jointly and could be ploughed back into integrated preventative services. In practice, we heard that a large proportion of the funding for preventative services (including the Admiral Nurses themselves in case study site 1) came from donations or other charitable sources and that statutory funding for prevention and continuity appeared to be reducing. A common theme across all sites was the significant financial pressure that commissioners and providers were under, exacerbated not only by funding cuts, but by growing demand as the diagnoses of dementia increased. Admiral Nurses were valued, but seen as an expensive resource, a luxury that those with were grateful for and those without thought that they could not afford.
In both of the case study sites that had AN, the nurses were called on to work only with carers with the most complex needs. Often this was when other services were struggling. Indeed, they appeared in these areas to be the only professionals with the skills, capacity and remit to take on some of these cases. In the areas without AN, it was difficult to establish who was fulfilling this role. Although there were non-clinical care co-ordination services (and plans for these to be developed further in some areas), the staff were not qualified to work with the most complex cases, and the more specialised NHS services did not have the capacity to provide continuity under current working conditions. Although commissioners stressed the importance of linking up services, carers told us that information and signposting was not always sufficient (see Chapter 4); they wanted a relationship with a named professional whom they could turn to as things progressed.
Given the challenge of reaching, and providing continuity to, the growing numbers of people with a diagnosis of dementia and their carers across any given area, one solution does appear to be the tiered approach through which specialist nurses, such as Admiral Nurses, work with and mentor less-qualified support workers and escalate/de-escalate cases as and when necessary, without discharging them. However, it remains to be seen if the wider impact of such an approach can be demonstrated.
Chapter 8 Discussion and conclusions
Policy interest in dementia has continued since our project was funded,86 and with particular injunctions to the NHS to improve the quality of post-diagnostic support for people with dementia and their carers. 87 A 2016 report, Making a Difference in Dementia: Nursing Vision and Strategy,88 set out how nurses can provide high-quality compassionate care and support for people with dementia and their carers. The report set out how nurses can care for the carers of people with dementia to meet the aspirations of the Prime Minister’s Challenge,86 including offering the opportunity for respite, education, training, emotional and psychological support, so that carers feel able to cope with their caring responsibilities and to have a life alongside caring.
However, as a recent House of Commons Library briefing demonstrates,89 most progress in England seems to have been in relation to diagnosis, with little evidence about actual improved support for the specific needs of carers of people with dementia. This seems particularly the case in relation to support towards the end, rather than at the beginning, of the dementia journey.
Our report thus comes at an opportune moment to explore how some of these policy aspirations are evidenced in the real lives of the carers of people with dementia.
In this final chapter we first discuss the strengths and limitations of our complex, multimethod study. This provides the context within which the subsequent discussion of the results and our conclusions can be understood.
Strengths and limitations
Working with Dementia UK
We were lucky to work in partnership with Dementia UK, both in planning the project and throughout all of its elements. Dementia UK wanted to evaluate the AN service, which is a large part of what it does, and to have this evaluation carried out by independent researchers. In this, it demonstrated a wish to learn from impartial evaluators about what Admiral Nurses currently do and to use this learning to improve what they do in the future. This openness to outside scrutiny is, perhaps, not as common among health and social care providers as it might be.
Officers at Dementia UK enabled access to their administrative database and answered very many questions from the research team to make it possible for the team to carry out the analyses on it. They also provided a vital link between the research team and the AN services selected for the survey, ensuring that paper questionnaires and electronic links to the questionnaire were distributed in accordance with the research team’s sampling strategy. A senior member of the Dementia UK management team was an ex officio member of our project advisory group in order to facilitate all of our links with the organisation, but did not have an advisory role in relation to the conduct of the research.
Despite all of these facilitative links, for which the research team was very grateful, this was an independent evaluation, with the York researchers being responsible for all aspects of the design and conduct of all of the WPs, and analysis and interpretation of all of the results.
Analysis of the administrative data set (work package 1)
We experienced four main problems associated with using administrative data for research purposes: determining availability, receiving the data, merging multiple data sets and understanding what the data really meant. Although these were largely overcome because we could work in partnership with Dementia UK, several challenges remained. These included only partial coverage of all AN services in the central database, the time-consuming nature of fully understanding and transforming those data into a format suitable for research purposes, and the lack of clarity about what triggered the reassessment of carers’ needs.
We worked to address these challenges, but some remained unresolvable, either completely or in part. So, for example, we could not detect any obvious differences in the types of services that did or did not use the central database, but without data from these services we could not formally test this. Although we worked hard with Dementia UK to ensure that the data we received were as usable as possible, resolving issues around date fields and differing data formats took a long time and reduced the amount of analysis we could then carry out. Similarly, although we also worked hard to understand AN practice in relation to needs assessment, there were no data that explained why needs were reassessed (or not). Finally, the needs assessments did not use standardised tools, so they relied on the nurses’ (inevitably subjective) appraisal of the position of both the carer and the person with dementia.
By their nature, these types of administrative data reflect how a service works and so can limit the analysis that can be undertaken in a research project. Despite this, we were able to provide a summary of the type of clients that the AN service supported, an overview of the interventions that the nurses offered and an estimate of the changes in dyads’ needs over time. Furthermore, we now have a prepared data set that offers opportunities for future multivariate analysis that we had hoped to carry out as part of the project, but which was constrained by the amount of time it took just to get the data into a usable form.
Qualitative work (work packages 2 and 4)
We experienced challenges in recruiting the carers of people with dementia for WP 2. Initially, we had intended to recruit 30 carers through TiDE and to conduct focus groups in York, but we did not recruit the number of carers we needed via this route. In response, we engaged with local community organisations and we were able to identify several peer support groups for the carers of people with dementia, from which we recruited participants. We had originally intended to conduct the bulk of our data collection for this WP through focus groups but, in response to carers’ preferences, we adopted a more flexible approach to data collection depending on individual preferences. Although this responsive and flexible approach meant that recruiting carers for WP 2 took more time than had been anticipated, we recruited more carers than originally planned (n = 35).
A strength of this study was that the survey design was informed by the priorities of carers and their views about which outcomes were likely to be influenced by the services they received. The analysis of the interviews and focus group data from carers fed directly into our choice of outcome measures. Moreover, we were able to test the full questionnaire with a subgroup of these carers, ensuring that the final design was acceptable to them and that carers and researchers had a shared understanding of the meanings of all questions.
We were unable to triangulate findings from the survey and the qualitative interviews with professional stakeholders in WP 4 because there were insufficient survey responses from the case study areas. The number of stakeholders who agreed to participate was also smaller than we had hoped. The pressures of reorganisation, responsibilities for areas other than dementia care and time constraints all seemed to contribute to reluctance among some stakeholders to share their views with us. Despite this, however, we did feel that our material reached saturation in most areas.
The survey and health economics analysis (work package 3)
The main challenge of this part of our work was identifying carers from non-AN areas. We had originally hoped to recruit people from our matched LA areas, using the third-sector organisation TiDE. However, TiDE was, at that point, a relatively new organisation and had not yet been able to rebuild the cohort of carers that its predecessor organisation had access to. We then tried to find carers in our chosen areas via JDR; although this gave us a potentially larger number of carers, using the JDR system was time-consuming. It also identified a fair proportion of carers who were no longer caring at home, because the person they cared for had entered long-term care or had died; in most cases, this was not evident until carers returned the questionnaire.
We therefore spent much time contacting local organisations in our selected non-AN areas to identify carers’ groups and similar. We also put a link to the electronic questionnaire on some national organisations’ websites, including the Alzheimer’s Society’s Talking Point, and recruited some carers via statutory organisations that had approached us directly. Because of the complexity of the recruitment strategy and our lack of control over how many carers actually received the paper questionnaire or the link to the electronic questionnaire, we cannot calculate an overall response rate. A ‘guesstimate’ of between 25% and 45% is all that we can hazard.
The team did finally manage to identify enough carers to have similar numbers of AN and non-AN carers, but the latter were different from the former in a number of important respects, which are discussed in Chapter 5. The variety of sources through which we recruited also made administration of the survey more complicated than we had originally planned.
The survey itself worked well; most carers who responded answered most questions, demonstrating that our chosen outcome measures were, indeed, feasible to use in future evaluation and that carers were willing and able to provide useful information about services that they and the person with dementia used and how much they paid for them.
We think the survey may be the largest, independent, detailed, national survey of carers of people with dementia yet carried out in England. In purely descriptive terms, then, it has value that goes beyond its specific role in this project. The carers we surveyed were, on average, older and more heavily involved in care than those identified in the most recent national survey of carers,6 thus giving a unique insight into a potentially vulnerable group.
In terms of the health economics analysis, and as far as we are aware, this is also the first time that costs and outcomes have been compared between users of specialist nursing services for carers and those receiving usual care.
Typically, within a standard economic evaluation framework, it is useful to collect data over multiple points in time. Although a cross-sectional study may provide a useful insight, it increases the uncertainty about the results because of a higher risk of selection bias (e.g. due to unobserved needs). Even if the IV approach that was used helps to address the selection bias, its estimate of the effect of AN refers to a subgroup of AN carers (i.e. those carers who are estimated to use AN because of the variable contained within the instrument).
Other limitations are strictly related to the nature of AN. For instance, the effect on carers who received AN support in the past may be difficult to disentangle from other support services that may also have been used. Diversity in the referral process (in some cases, carers are referred to AN after a triage assessment; in other cases, they can self-refer) across AN providers may generate high heterogeneity within the group of AN carers, which may hamper us in identifying an effect. Finally, we are unable to estimate a summary indicator, such as an ICER, to inform decision-making. Our CQoL measure, although generic to carers, is not generic to all members of the community. In addition, at the time of reporting, no preference weights for the ASCOT-Carer were available. We were unable to calculate a measure akin to a QALY, given that currently we do not have information on time in state or a CQoL preference weight. In addition, based on this, there is no decision rule available to interpret an ICER and no empirical estimate of the cost-effectiveness threshold for decision-making in social care to assist decision-makers.
Informing future practice and evaluation (work package 5)
The AN service we trained to use the chosen carer measures had not had time to implement these into their routine data collection systems before the project came to a close. However, Dementia UK as a whole is keen to integrate these measures into the data collection systems used by all services and we will continue to work with the charity to support this.
Integrating the views of stakeholders to strengthen our findings (work package 6)
Work package 6 involved a workshop attended by 36 stakeholders, including carers, practitioners and commissioners. Participants discussed the research findings and fed back key messages and implications. These included overall messages from the research, messages relating to AN in particular and messages relating to the future evaluation of services for carers of people with dementia. We also discussed the ways in which data are collected and used locally to inform and improve services. A full account of the messages from this workshop is given in Appendix 1.
The workshop gave us a valuable opportunity to discuss our initial interpretations of the study findings with professionals and carers with direct experience of the issues under consideration. An example would be the issue of balancing the intensive, specialist nature of AN support (which not everyone requires at all times) with the desire for continuity and full coverage for all carers and people with dementia. There were stakeholders at the workshop who represented organisations that could provide greater coverage than most AN services, but not the intensive specialist support that AN offers, and there was a consensus in the room that these services should work together via a tiered model to ensure continuity and access to specialist support for all. This discussion added weight to our conclusion that, if embedded well into dementia services across a locality, AN could enable the system as a whole to offer appropriate ‘end-to-end’ care and support for all carers and people with dementia.
However, although the feedback from this workshop was useful, we did not feel that it provided a secure base for the production of best-evidence guidelines. Instead, we have produced a short summary of findings, which is now being widely disseminated and is available to download from the project webpage (www.york.ac.uk/spru/projects/admiral-nursing/).
Discussion of results
The analysis of the Dementia UK database (WP 1) showed that, on average, the needs of carers being supported by Admiral Nurses reduced over time. However, as we were unable to link changes in carers’ needs to the input of the Admiral Nurses, we cannot say what caused this reduction. The Admiral Nurses do provide the types of support that are likely to help reduce carers’ level of need over time, or at least maintain these when situations become more complex, but to show a link between input and outcomes, additional information would be needed that the Admiral Nurses do not currently collect.
The database confirmed that Admiral Nurses are successfully targeting older carers, who are more likely to be affected by the demands of caring. The model employed typically involves triage, whereby those in most need receive greater levels of input, but those with lower levels of need can be escalated if/when their needs change.
The qualitative research with carers for WP 2 emphasised the value that carers place on continuity and ‘feeling supported’ as things progress. We identified three key outcome areas through this WP that are important to carers and appear to be influenced by carer support (and AN in particular). The first was confidence in caring, which carers said that they gained when they were supported by a specialist in dementia who knew them and their situation well. Having an ongoing relationship with such a professional, to whom they could turn to as things progressed, could give them the confidence to continue caring in spite of the difficulties and uncertainty they faced. We chose to measure carer confidence using the SEMD scale. 46
The second outcome area identified by carers was their own quality of life, which we chose to measure using the ASCOT-Carer,45 as this mapped most accurately onto the analysis of the qualitative data. In particular, the ASCOT-Carer was the only tool in our shortlist of validated quality-of-life measures with a specific question on ‘feeling supported and encouraged’.
Finally, and not surprisingly, carers told us that the level and quality of support they received could affect their physical and mental health. We chose to measure this using the EQ-5D-5L65 because of its common use in economic evaluation and its relevance for NICE. However, subsequent health economic understanding the AN service convinced us that AN services are unlikely to have an effect on EQ-5D-5L scores, and therefore we used this variable in the economic analysis as an explanatory variable in our main analysis.
Feedback from testing suggested that our questionnaire was acceptable and comprehensible to carers. The acceptability of our chosen outcome measures was later confirmed by the high rates of completion of the outcome questions by survey participants. We thus feel that the questionnaire provides a useful evaluation framework for other dementia care services that might be expected to have an impact on carers.
Through the survey we identified a group of carers who were, as a group, older and more heavily involved in caring activity than found in nationally representative data about the carers of people with dementia. However, within this, the AN carers were even older and more heavily involved in caring, echoing what was observed in the administrative data. These differences probably reflect the study recruitment; carers who attend carers’ groups and who are known to statutory care and third-sector organisations are likely to be some way into the dementia caring journey, rather than at its beginning. Those known to AN services are likely to be even further into this journey and/or, as we saw in Chapter 4, struggling with caring.
Admiral Nursing carers were more likely to report receiving emotional and social support and information, advice and knowledge from Admiral Nurses than carers using other types of carer support services, perhaps reflecting the personal and targeted nature of the relationship that Admiral Nurses are able to develop with carers.
We suspect that some differences between our AN and non-AN carers reflect the ‘natural history’ of caring for someone with dementia and the role that specialist support might play in maintaining people in the community. Spouses and partners were the largest group of main carers, both in the administrative data and among all carers in our survey. If the main carer is no longer able to provide the care that the person with dementia needs, younger family members may take over as the main carer, while the partner moves into a less involved role. The administrative data showed that increasing the amount of informal support that carers could access was a key part of what the Admiral Nurses were doing. Alternatively, AN services may step in to support older or more heavily involved carers who have no other source of informal support to continue, by improving their coping strategies and enabling them to take time for themselves. This, we conjecture, may thus prevent or delay admission to long-term care.
Given the heavy involvement of all of the carers, in terms of their caring status and activity, their overall levels of use of and practical support from other health and social care services were surprisingly low. Moreover, those carers who were accessing services related to their caring activities were often paying large amounts of money to do so and, for some perhaps, with consequent financial difficulties.
The health economics work, based on data collected through the survey, explored outcomes in the group of carers as a whole and compared AN and non-AN carers, in both cases controlling for other variables that might affect these outcomes.
Better health was associated with better carer outcomes, whereas worse carer outcomes were consistently associated with financial difficulties, the lack of anyone to stand in for the carer if they needed a short break, and reported severity of dementia.
The older age and heavier involvement of carers using AN services suggests that they may be receiving appropriately targeted support through AN on the basis that their needs are greater than those of carers with no AN support. Although initial analysis showed that AN carers had worse outcomes than non-AN carers, once the differences between the two groups were controlled for in the analysis, this difference disappeared. Indeed, AN carers had better outcomes, although these results were mostly not statistically significant. Similarly, there was little difference in health and social care costs between AN and non-AN carers or in the costs of the people with dementia they cared for.
A key aim of WP 4 was to understand stakeholders’ views on the system-wide impact of services, such as AN, but it was clear that this impact was not well understood. Although support for carers might be able to reduce the impact on acute health and adult social care (in particular the need for long-term care), this was rarely measured. Nevertheless, participants in this part of the study did feel that preventative services were valuable and likely to reduce pressure on statutory services.
With an increasing use of joint commissioning for dementia services, cost savings from services that had a preventative role could accrue to both health and social care services. In fact, a large proportion of preventative services funding (including the Admiral Nurses themselves in one site) came from donations or other charitable sources, and as statutory funding grew scarcer, prevention and continuity seemed to be suffering.
Admiral Nurses were seen as a valuable, but expensive, resource. This was despite the fact that, in both of the sites that had AN, the nurses worked only with carers with the most complex needs, and often when other services were struggling. The difficulty of the cases they worked with was such that Admiral Nurses seemed to be the only professionals with the skills, capacity and remit to take them on. In the areas without AN, it was difficult to know who would deal with similar complexity. Other staff in dedicated dementia services were generally not qualified to work with the most complex cases, and the more specialised NHS services did not have the capacity to provide continuity. Although commissioners stress the importance of linking up services, information and signposting are not always sufficient for carers; they want and need a relationship with a named professional whom they can turn to as dementia progresses and its demands increase.
Given the challenge of reaching, and providing continuity to, growing numbers of people with dementia and their carers, the tiered approach through which specialist nurses work with and mentor less qualified support workers and escalate/de-escalate cases as and when necessary, without discharging them, seems promising.
The routine evaluation of services to support the carers of people with dementia (or, indeed, any carers) is still not in place. Our outcome measurement tools and data collection system were acceptable to carers and seen as relevant and useful to the Admiral Nurses we trained to use them. However, when it came to incorporating them into the routine data collection systems of one service for our pilot, the service could not find the capacity to try them out. In a climate of increased demand and reduced resources, improving data collection and evaluation systems is rarely prioritised. However, it is just such evaluative data that can prove the value of services to commissioners.
Dementia UK has agreed to incorporate the selected outcome measures into its new AN national data collection system, as hoped for as an outcome of this work. However, services and professionals need protected time to apply these and use the data collected to evaluate their services and demonstrate impact.
As other work shows,20,21 and as participants in our stakeholder workshop pointed out (see Appendix 1), there is no single model of service that could possibly provide support for carers of people with dementia all the way from initial symptoms becoming evident, through the worsening of behaviour and physical health, to death. Carers’ needs across the dementia journey will vary substantially, both as symptoms and circumstances change and in relation to their characteristics and the support networks they do or do not have around them. Overall, the results of this study show that specialist nursing services can support the very oldest and most burdened carers, many of whom may be very close to the end of that journey. They can also act as resources for non-clinical dementia support workers and, indeed, other clinicians, and, if embedded well into dementia services across a locality, enable the system as a whole to offer appropriate ‘end-to-end’ care and support.
Areas for future research
-
Findings from across our WPs underline the role of specialist nursing support with carers who are under considerable stress, whether by virtue of their age, their caring activity or their coping skills. This raises the inevitable research question of whether support of this type, for carers at this stage, delays or prevents admission of the person with dementia to long-term care.
-
Analysis of the textual data in the administrative data set showed that carers and people with dementia could be at risk of problems related to their health (e.g. falls), as well as physical and verbal assault and other forms of abuse. These data would benefit from further analysis, alongside professional and carer accounts, to explore this issue in greater detail. This material also highlighted the role of the police service in dealing with risk in dementia. We feel that this would benefit from further exploration in research specifically designed to focus on this under-researched (in relation to dementia care) service.
-
Our work has demonstrated the use of econometric analysis for economic evaluation in analysing observational, cross-sectional data. This is particularly relevant in the context of social care, in which it is not always possible to implement randomised controlled trials and the use of quasi-experimental data sets is more common. The high response rates in the survey suggest that routine collection of these data is possible and can be used to examine the impact of the service on individuals over time. Future research may use routinely collected data in the same individuals over time to explore whether or not econometric methods that take time into account (e.g. difference in differences) may help to reduce uncertainty in the results and further address potential selection bias.
-
An in-depth, qualitative analysis of the remainder of the daily activity data in the AN administrative data set, in addition to the 200 cases we thematically reviewed for this study, might shed more light on the day-to-day work of Admiral Nurses and how this affects carers’ lives and their capacity to continue to support people with dementia.
-
The AN administrative data sets are now fully prepared for multivariate analysis that would allow us to understand other factors that might affect changes in carers’ needs over time.
Acknowledgements
First, our thanks must go to the carers of people with dementia who took part in this project, both as participants and as advisers, when they had many other demands on their time and energy. Thanks also go to the professional stakeholders who took time out of their busy schedules to take part in the study.
We would not have been able to undertake this research without the support of our partners Dementia UK, who ensured that we had access to all of the necessary information and services. Particular thanks are due to Laura Maio, who provided invaluable information about AN services across England and about the administrative data, to Pete Henshall for preparing the administrative data for our use and to Karen Harrison-Dening who facilitated our work with AN. We would like to thank them for their enthusiasm throughout the project.
Similarly vital were our links to carers through TiDE and the Life Story Network community interest company. Thanks go especially to Louise Langham and Anna Gaughan for working tirelessly to reach carers for our survey and qualitative work, and to Jean Tottie, who organised and liaised with our virtual advisory group.
We would like to thank all members of the project advisory group, including those on the ‘virtual’ advisory group. A special thank you goes to our carer members – Ray Carver, Frances Garside and Frank Arrojo – who provided invaluable comments and guidance throughout the study.
We are grateful to all of the Admiral Nurses who helped us to reach carers with our survey and to the many voluntary-sector workers and organisations, from the Alzheimer’s Society to small, independent groups, that helped us to reach carers in the comparison areas.
We are indebted to the authors of the outcome measures we selected for allowing us to use these in our research: Stacey Rand, Juliette Malley, Ann Netten and Julien Forder for the ASCOT-Carer; Richard H Fortinsky, K Kercher and C Burant for the SEMD scale; and the EuroQol Group for the EQ-5D-5L.
Finally, our thanks go to Dawn Rowley-White, who provided invaluable administrative support throughout the project and in the production of this report, to Sarah Boatman, for assisting with the questionnaire mailouts, and to Michelle Stewart, for many hours of data entry.
Contributions of authors
Ms Kate Gridley [Research Fellow, Social Policy Research Unit (SPRU)] was the project manager. She led WPs 2, 4, 5 and 6 (the qualitative research and implementation work) and wrote Chapters 4 and 7, and elements of Chapter 8, of the final report. She also contributed to WPs 1 and 3, including recruitment for the survey.
Dr Fiona Aspinal (Research Fellow, SPRU) led the analysis of the administrative data set for WP 1, wrote Chapter 3 of the final report and contributed to Chapter 8. She also contributed to WPs 2, 3 and 6.
Professor Gillian Parker (Professor of Social Policy Research, SPRU) was the principal investigator. She designed the study, led the design of the survey, analysed and wrote up all of the material included in Chapter 5, contributed to the writing of Chapters 1, 2, 3 and 8, and was responsible for editing the final report. She also contributed to WPs 1, 2, 4, 5 and 6.
Dr Helen Weatherly [Senior Research Fellow, Centre for Health Economics (CHE)] led on the health economic design for WP 3. She worked with Rita Faria and jointly supervised Francesco Longo, and co-wrote Chapter 6 (the economic evaluation). She also contributed to WP 6.
Dr Rita Faria (Research Fellow, CHE) developed the health economic design, and worked alongside Kate Gridley, Gillian Parker and Fiona Aspinal on WP 2 in developing the data collection processes for WP 3 and selecting the study sites. She jointly supervised Francesco Longo with Helen Weatherly and co-wrote Chapter 6 (the economic evaluation). She also contributed to WP 6.
Dr Francesco Longo (Research Fellow, CHE) was the lead quantitative analyst for the economic evaluation and co-wrote Chapter 6 (WP 3). He also contributed to WP 6.
Professor Bernard van den Berg (Professor of Health Economics, CHE) provided high-level advice to support the health economic design, regression analysis and write-up for WP 3 (see Chapter 6).
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- White C. 2011 Census Analysis: Unpaid Care in England and Wales, 2011 and Comparison with 2001. London: Office for National Statistics; 2013.
- Hutton S. Poverty Over Time for those Recorded as Carers in the British Household Panel Survey. York: University of York, Social Policy Research Unit; 1998.
- Hirst M. Carer distress: a prospective, population-based study. Soc Sci Med 2005;61:697-708. https://doi.org/10.1016/j.socscimed.2005.01.001.
- Arksey H, Jackson K, Croucher K, Weatherly H, Golder S, Hare P, et al. Review of Respite Services and Short-Term Breaks for Carers of People with Dementia. London: NHS Service Delivery Organisation R&D Programme; 2004.
- Newbronner L, Chamberlain R, Borthwick R, Baxter M, Glendinning C. A Road Less Rocky: Supporting Carers Of People With Dementia. London: Carers Trust; 2013.
- Survey of Carers in Households – England, 2009–10. Leeds: NHS Digital; 2010.
- Parker G, Kampanellou E, Beresford B, Hirst M. The Changing Face of Caring: Secondary Analysis of the 1985 General Household Survey and the 2009/10 Survey of Carers in Households. York: University of York, Social Policy Research Unit; 2017.
- Ory MG, Hoffman RR, Yee JL, Tennstedt S, Schulz R. Prevalence and impact of caregiving: a detailed comparison between dementia and nondementia caregivers. Gerontologist 1999;39:177-85. https://doi.org/10.1093/geront/39.2.177.
- Schoenmakers B, Buntinx F, Delepeleire J. Factors determining the impact of care-giving on caregivers of elderly patients with dementia. A systematic literature review. Maturitas 2010;66:191-200. https://doi.org/10.1016/j.maturitas.2010.02.009.
- Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging 2003;18:250-67. https://doi.org/10.1037/0882-7974.18.2.250.
- Goren A, Montgomery W, Kahle-Wrobleski K, Nakamura T, Ueda K. Impact of caring for persons with Alzheimer’s disease or dementia on caregivers’ health outcomes: findings from a community based survey in Japan. BMC Geriatr 2016;16. https://doi.org/10.1186/s12877-016-0298-y.
- Prince M, Knapp M, Guerchet M, McCrone P, Prina M, Comas-Herrera A, et al. Dementia UK: Update. London: Dementia UK; 2014.
- Living Well with Dementia: A National Dementia Strategy. London: Department of Health and Social Care; 2009.
- Prime Minister’s Challenge on Dementia: Delivering Major Improvements in Dementia Care and Research by 2015. London: Department of Health and Social Care; 2012.
- Dementia: Post-Diagnostic Care and Support. London: Department of Health and Social Care; 2016.
- Carers (Recognition and Services) Act 1995. London: The Stationery Office; 1995.
- Caring about Carers: The National Strategy for Carers. London: The Stationery Office; 1999.
- Recognised, Valued and Supported: Next Steps for the Carers Strategy. London: Department of Health and Social Care; 2010.
- The Care Act 2014. London: The Stationery Office; 2014.
- Parker G, Arksey H, Harden M. Meta-Review of International Evidence on Interventions to Support Carers. York: University of York, Social Policy Research Unit; 2010.
- Thomas S, Dalton J, Harden M, Eastwood A, Parker G. Updated meta-review of evidence on support for carers. Health Serv Deliv Res 2017;5.
- Prince M, Comas-Herrera A, Guerchet M, Karagiannidou M, Knapp M. World Alzheimer Report 2016. Improving Healthcare for People Living with Dementia: Coverage, Quality and Costs Now and in the Future. London: Alzheimer’s Disease International; 2016.
- Dementia UK . Dementia UK Strategic Plan 2014–2017 n.d. www.dementiauk.org/wp-content/uploads/2015/11/Strategic-plan-new-branded.pdf (accessed 25 September 2018).
- Bunn F, Pinkney E, Drennan V, Goodman C. An Evaluation of the Role of the Admiral Nurse: A Systematic Evidence Synthesis to Inform Service Delivery and Research. London: Dementia UK; 2013.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Woods RT, Wills W, Higginson IJ, Hobbins J, Whitby M. Support in the community for people with dementia and their carers: a comparative outcome study of specialist mental health service interventions. Int J Geriatr Psychiatry 2003;18:298-307. https://doi.org/10.1002/gps.822.
- Dementia Advisers Survey. London: Ipsos MORI; 2016.
- Cooper C, Lodwick R, Walters K, Raine R, Manthorpe J, Iliffe S, et al. Inequalities in receipt of mental and physical healthcare in people with dementia in the UK. Age Ageing 2017;46:393-400. https://doi.org/10.1093/ageing/afw208.
- Somme D, Trouve H, Dramé M, Gagnon D, Couturier Y, Saint-Jean O. Analysis of case management programs for patients with dementia: a systematic review. Alzheimers Dement 2012;8:426-36. https://doi.org/10.1016/j.jalz.2011.06.004.
- Dementia – Assessment, Management and Support for People Living with Dementia and their Carers: Draft Guidance Consultation. London: NICE; 2018.
- MacNeil Vroomen J, Bosmans JE, Eekhout I, Joling KJ, van Mierlo LD, Meiland FJ, et al. The cost-effectiveness of two forms of case management compared to a control group for persons with dementia and their informal caregivers from a societal perspective. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0160908.
- Aspinal F, Gridley K, Bernard S, Parker G. Promoting continuity of care for people with long-term neurological conditions: the role of the neurology nurse specialist. J Adv Nurs 2012;68:2309-19. https://doi.org/10.1111/j.1365-2648.2011.05928.x.
- Wilson E, Aubeeluck A. Knowledge in practice: the specialist nurse role in Huntington’s disease. BJNN 2016;12:185-9. https://doi.org/10.12968/bjnn.2016.12.4.185.
- Specht J, Bossen A, Hall GR, Zimmerman B, Russell J. The effects of a dementia nurse care manager on improving caregiver outcomes outcomes. Am J Alzheimers Dis Other Demen 2009;24:193-207. https://doi.org/10.1177/1533317508330466.
- Goeman D, Renehan E, Koch S. What is the effectiveness of the support worker role for people with dementia and their carers? A systematic review. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1531-2.
- Iliffe S, Waugh A, Poole M, Bamford C, Brittain K, Chew-Graham C, et al. The effectiveness of collaborative care for people with memory problems in primary care: results of the CAREDEM case management modelling and feasibility study. Health Technol Assess 2014;18.
- Gridley K, Brooks J, Birks Y, Baxter K, Parker G. Improving care for people with dementia: development and initial feasibility study for evaluation of life story work in dementia care. Health Serv Deliv Res 2016;4.
- Community Nursing Programme: Professional Pathway for Community Nurses: Supporting the Health and Wellbeing of Adult Carers. London: Department of Health and Social Care; 2013.
- Compassion in Practice: Nursing, Midwifery and Care Staff – Our Vision and Strategy. Leeds: Department of Health and Social Care/NHS Commissioning Board; 2012.
- Green H. Informal Carers. A Study Carried Out on Behalf of the Department of Health and Social Security as Part of the 1985 General Household Survey. London: The Stationery Office; 1988.
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 1980;20:649-55. https://doi.org/10.1093/geront/20.6.649.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Moniz-Cook E, Vernooij-Dassen M, Woods R, Verhey F, Chattat R, Vugt MD, et al. A European consensus on outcome measures for psychosocial intervention research in dementia care. Ageing Ment Health 2008;12:14-29. https://doi.org/10.1080/13607860801919850.
- Position Statement on Use of the EQ-5D-5L Valuation Set. London: NICE; 2017.
- Rand SE, Malley JN, Netten AP, Forder JE. Factor structure and construct validity of the Adult Social Care Outcomes Toolkit for Carers (ASCOT-Carer). Qual Life Res 2015;24:2601-14. https://doi.org/10.1007/s11136-015-1011-x.
- Fortinsky RH, Kercher K, Burant CJ. Measurement and correlates of family caregiver self-efficacy for managing dementia. Aging Ment Health 2002;6:153-60. https://doi.org/10.1080/13607860220126763.
- Graff M, Vernooij-Dassen M, Thijssen M, Dekker J, Hoefnagels W, OldeRikkert M. Effects of community occupational therapy on quality of life, mood and health status in dementia patients and their caregivers: a randomized controlled trial. J Gerontol A Biol Sci Med Sci 2007;62:1002-9. https://doi.org/10.1093/gerona/62.9.1002.
- The Social Care Guidance Manual. London: NICE; 2013.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: University of Kent, Personal Social Services Research Unit; 2016.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: University of Kent, Personal Social Services Research Unit; 2014.
- Reference Cost Collection: National Schedule of Reference Costs – Year 2015–2016 – NHS Trust and NHS Foundation Trusts. London: Department of Health and Social Care; 2016.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Rosenbaum PR, Rubin DB. The central role of the Propensity Score in observational studies for causal effects. Biometrika 1983;70:41-55. https://doi.org/10.1093/biomet/70.1.41.
- Forder J, Malley J, Towers A-M, Netten A. Using cost-effectiveness estimates from survey data to guide commissioning: an application to home care. Health Econ 2014;23:979-92. https://doi.org/10.1002/hec.2973.
- Gridley K, Aspinal FJ, Parker GM, Weatherly HLA, Neves De Faria RI, Longo F, et al. Supporting Carers of People with Dementia: A Mixed Methods Evaluation and Feasibility Study. York: University of York, Social Policy Research Unit; 2018.
- Bantry White E, Montgomery P. Dementia, walking outdoors and getting lost: incidence, risk factors and consequences from dementia-related police missing-person reports. Aging Ment Health 2015;19:224-30. https://doi.org/10.1080/13607863.2014.924091.
- Maxwell K. Issues in Accessing and Using Administrative Data, OPRE Report #2017–24. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families; 2017.
- Action for Carers: A Guide to Multi-Disciplinary Support at Local Level. London: The King’s Fund; 1988.
- Al-Janabi H, Flynn T, Coast J. Estimation of a preference-based Carer Experience Scale. Med Decis Making 2011;31:458-68. https://doi.org/10.1177/0272989X10381280.
- Hoefman RJ, van Exel NJ, Looren de Jong S, Redekop WK, Brouwer WB. A new test of the construct validity of the CarerQol instrument: measuring the impact of informal care giving. Qual Life Res 2011;20:875-87. https://doi.org/10.1007/s11136-010-9829-8.
- Flynn TN, Chan P, Coast J, Peters TJ. Assessing quality of life among British older people using the ICEPOP CAPability (ICECAP-O) measure. Appl Health Econ Health Policy 2011;9:317-29. https://doi.org/10.2165/11594150-000000000-00000.
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res 2012;21:167-76. https://doi.org/10.1007/s11136-011-9927-2.
- Netten A, Burge P, Malley J, Potoglou D, Towers AM, Brazier J, et al. Outcomes of social care for adults: developing a preference-weighted measure. Health Technol Assess 2012;16. https://doi.org/10.3310/hta16160.
- Dassel KB, Carr DC. Does dementia caregiving accelerate frailty? Findings from the health and retirement study. Gerontologist 2016;56:444-50. https://doi.org/10.1093/geront/gnu078.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Beatty P, Willis G. Research synthesis: the practice of cognitive interviewing. Public Opin Q 2007;71:287-311. https://doi.org/10.1093/poq/nfm006.
- Survey of Carers in Households – England, 2009–10. Leeds: NHS Digital; 2010.
- Parker G, Lawton D. Different Types of Care, Different Types of Carer: Evidence from the General Household Survey. London: The Stationery Office; 1994.
- Rowlands O, Parker G. Informal Carers. An Independent Study Carried Out by the Office for National Statistics on Behalf of the Department of Health as Part of the 1995 General Household Survey. London: The Stationery Office; 1998.
- Developing NICE Guidelines: The Manual. London: NICE; 2014.
- Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337-43. https://doi.org/10.3109/07853890109002087.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Devlin N, Shah K, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L set for England. Health Econ 2018;27:7-22. https://doi.org/10.1002/hec.3564.
- Batchelder L, Saloniki E-C, Malley J, Burge P, Lu H, Forder J. Carer Social Care-Related Quality of Life Outcomes: Establishing Preference Weights for the Adult Social Care Outcomes Toolkit for Carers n.d.
- Harmonised Concepts and Questions for Social Data Sources. Interim Harmonised Principle. Personal Well-being. Version 1.1. Newport: ONS; 2015.
- van den Berg B, Ferrer-i-Carbonell A. Monetary valuation of informal care: the well-being valuation method. Health Econ 2007;16:1227-44. https://doi.org/10.1002/hec.1224.
- van den Berg B, Fiebig DG, Hall J. Well-being losses due to care-giving. J Health Econ 2014;35:123-31. https://doi.org/10.1016/j.jhealeco.2014.01.008.
- Glendinning C, Jones K, Baxter K, Rabiee P, Curtis L, Wilde A, et al. Home Care Re-ablement Services: Investigating the Longer-Term Impacts (Prospective Longitudinal Study). York: University of York, Social Policy Research Unit; 2010.
- NHS Reference Costs 2015 to 2016. London: Department of Health and Social Care; 2016.
- Weatherly H, Faria R, Berg BVD, Culyer A. Encyclopedia of Health Economics. San Diego, CA: Elsevier; 2014.
- All Data Related to Annual Survey of Hours and Earnings: 2016 Provisional Results. Newport: ONS; 2017.
- Drummond M, Sculpher M, Claxton K, Stoddart G, Torrance G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: University of York; 1999.
- Cragg JG, Donald SG. Testing identifiability and specification in instrumental variables models. Econ Theory 1993;9:222-40. https://doi.org/10.1017/S0266466600007519.
- Better Care Fund: Policy Framework. London: Department of Health and Social Care; 2014.
- Prime Minister’s Challenge on Dementia 2020. London: Department of Health and Social Care; 2015.
- The Government’s Mandate to NHS England for 2016–17. London: Department of Health and Social Care; 2017.
- Making a Difference in Dementia: Nursing Vision and Strategy. London: Department of Health and Social Care; 2016.
- Dementia: Policy, Services and Statistics. London: House of Commons Library; 2016.
- McKee K, Spazzafumo L, Nolan M, Wojszel B, Lamura G, Bien B. Components of the difficulties, satisfactions and management strategies of carers of older people: a principal component analysis of CADI-CASI-CAMI. Aging Ment Health 2009;13:255-64. https://doi.org/10.1080/13607860802342219.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- Homes J. UKHCA Summary. An Overview of the Domiciliary Care Market in the United Kingdom. Wallignton: United Kingdom Home Care Association Limited; 2016.
- Light D, Delves J. A Guide to Setting Up a Memory Café 2015. https://dementiapartnerships.com/a-guide-to-setting-up-a-memory-cafe (accessed 21 September 2018).
- Knapp M, Bauer A, Perkins M, Snell T. Building community capital in social care: is there an economic case. Community Dev J 2012;48:313-31. https://doi.org/10.1093/cdj/bss021.
- NHS Employers . Agenda for Change. NHS Terms and Conditions of Service Handbook 2017 n.d. www.nhsemployers.org/media/Employers/Documents/Pay-and-reward/AfC-pay-bands-from-1-April-2017---FINAL.pdf (accessed 17 October 2018).
- Reenen Mv, Oppe M. EQ-5D-5L User Guide. Basic Information on How to Use the EQ-5D-5L Instrument. EuroQol Research Foundation; 2015.
- Jones A, Rice N, Glied S, Smith PC. The Oxford Handbook of Health Economics. Oxford: Oxford University Press; 2011.
- Woolridge J. Introductory Econometrics: A Modern Approach. Boston, MA: Cengage Learning; 2015.
- White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica 1980;48:817-38. https://doi.org/10.2307/1912934.
- Heckman J, Ichimura H, Todd P. Matching as an econometric evaluation estimator: evidence from evaluating a job training programme. Rev Econ Stud 1997;64:605-54. https://doi.org/10.2307/2971733.
- Horvitz DG, Thompson DJ. A generalization of sampling without replacement from a finite universe. J Am Stat Assoc 1952;47:663-85. https://doi.org/10.1080/01621459.1952.10483446.
- Angrist J, Hahn J. When to control for covariates? Panel asymptotics for estimates of treatment effects. Rev Econ Stat 2004;86:58-72. https://doi.org/10.1162/003465304323023679.
- Staiger D, Stock J. Instrumental variables regression with weak instruments. Econometrica 1997;65:557-86. https://doi.org/10.2307/2171753.
- Cameron AC, Trivedi PK. Microeconometrics: Methods and Applications. Cambridge: Cambridge University Press; 2005.
Appendix 1 Work packages 5 and 6: ensuring that the study findings inform future research and practice
Work package 5
Work package 5 was designed to ensure that the learning from this research informs practice and supports future service evaluation. We proposed to work with Dementia UK to inform its data collection processes, using the data collection framework established in WP 2 as a starting point. The aim was to improve systems to collect data required for future evaluative research while also meeting the organisation’s administrative needs. This built on the work in prior stages to understand the feasibility for dementia service providers, and acceptability to carers, of using a range of validated outcome measures as part of routine data collection. We planned to pilot the new framework with one AN team to test its feasibility in the field.
Work package 5 began with a meeting between the University of York research team and the Dementia UK research team, as well the Dementia UK director of clinical services, the information technology development leads and the professional and practice development lead. It was agreed to concentrate on encouraging and supporting a local AN team to use the three standardised measures of carer outcome selected for the national survey (ASCOT-Carer, the EQ-5D and the SEMD) in their routine work.
An AN service was invited and agreed to take part. The researchers provided training to staff from this service, along with other interested Admiral Nurses, at a practice development day in June 2017. The training covered:
-
findings of the development work leading to the selection of the three outcome measures (WP 2)
-
what these measures can be used for
-
how to use the measures (including how to attribute scores and measure change over time).
Participants tried using the three measures during the session through role play and fed back to colleagues and the research team about their experiences. The ASCOT-Carer and the SEMD were felt to be very relevant to the work of the Admiral Nurses. It was noted that all three measures were straightforward to use, especially as self-completed questionnaires. In interview form, however, the questions could sound cumbersome, and it was noted that being asked to respond verbally to the nurse who delivered their care might encourage carers to respond in ways that they perceived to be desirable.
Participants considered the possibility of posting out the ASCOT-Carer to carers before their first appointment. As ASCOT-Carer is a short and user-friendly tool, it was generally felt that this could be successful. The selected service settled on this as its approach to pilot in WP 5.
The SEMD was felt to be particularly suited to measuring the outcomes of the training that the Admiral Nurses provide. Again, the selected service agreed to pilot the use of this tool, encouraging carers to complete it before they began training, at the end of training and at a follow-up point.
The research team kept in contact with the service over the following months. However, the service manager reported experiencing staffing shortages over this time, and towards the end of the pilot period she reported that there had not yet been any opportunity to build the new measures into their working practices. She was hopeful that over time they would be able to use the measures, but this would not be within the lifetime of the current NIHR Health Services and Delivery Research project.
Towards the end of the project, a representative from our research team joined a Dementia UK meeting to discuss and agree the outcome measures to be integrated into a new national AN data collection system. In the light of the findings from this research, and other feedback from key stakeholders, the tools chosen to measure outcomes for carers were the ASCOT-Carer and the SEMD.
Work package 6
The final stage of our project, WP 6, centred on a stakeholder workshop. Here we presented the findings of all elements of the research and worked with stakeholders to:
-
identify key messages arising from the research
-
discuss the collection of data at a local level to inform both service development and evaluation.
We invited a range of stakeholders to the workshop, including people with dementia and their carers, decision-makers from health and social care commissioning and provider organisations (including the third sector) and local and national policy-makers.
Key messages arising from the research
The workshop was attended by 36 stakeholders, including carers, practitioners, commissioners and six members of the research team. Participants discussed the research findings and fed back key messages and implications. These have been grouped below under three headings: (1) overall messages from the research, (2) messages relating to AN in particular and (3) messages relating to the future evaluation of services for carers of people with dementia.
1. Overall messages from the research
-
Participants noted the inconsistency of carer support across the country.
-
Continuity of support for the carers of people with dementia is very important: people do not stop having dementia, so carers’ needs are ongoing.
-
Participants were struck by the financial pressures carers are under (as evidenced by the survey findings). Statutory services do not always understand the financial impact of caring.
-
Sleep deprivation seems to have a huge impact on carers’ lives. Night-sitting services are therefore very important, but they are also very costly.
2. Messages relating to Admiral Nursing in particular
-
The specialist knowledge that Admiral Nurses have (their unique insight into dementia and the service landscape, as well as their clinical background) is key.
-
AN support and education is an important way to create, maintain and improve carer confidence (e.g. a positive steps programme). It is likely to enable the carers to carry on caring at home for longer.
-
Admiral Nurses also work across service and professional boundaries to ensure access to other services.
-
Admiral Nurses are a valuable resource, but they cannot be the answer for everything. In particular, they are involved in only the more complex cases; carers want the practitioners they deal with to have the type of expertise that Admiral Nurses have.
-
There are not enough Admiral Nurses to help all carers, and not all carers have complex needs. However, preventing carers’ needs from escalating is also important. Admiral Nurses need to work collaboratively with other support workers to have the greatest reach, facilitating continuity and access to specialist knowledge more widely.
3. Messages relating to the future evaluation of services for carers of people with dementia
-
This research seems to have looked at two different populations [one of carers with particularly complex needs (recruited through AN) and a ‘comparison’ group of carers with lower needs (recruited through voluntary-sector organisations and carers’ groups)]. What population of carers would be comparable with the carers who receive AN services?
-
Part of the problem of identifying carers for research is that there is nowhere that carers are routinely and formally identified. People do not always self-identify as carers and so it can be difficult to know how many carers of people with dementia there are.
-
As well as hidden carers, there are carers whose full caring roles are hidden (such as those caring for more than one person) and carers with comorbidities.
-
It is important to collect evidence of things that are harder to quantify, such as the impact of Admiral Nurses and other support services for carers.
Collecting data at a local level to inform both service development and evaluation
In the second group work session of the day, participants were asked about the information that services currently collect from dementia carers and what other information might be useful for service evaluation. The key points have been grouped under three headings: (1) problems/challenges with evaluating carers’ services, (2) missed opportunities/things that could be done better and (3) ways forward.
1. Problems/challenges with evaluating carers’ services
-
Carers are asked the same questions repeatedly. This is probably because services and assessments are fragmented.
-
Voluntary-sector organisations might not have the infrastructure to collect all of the information that commissioners are asking for.
-
There is variability in the quality of commissioning of services for the carers of people with dementia.
-
There are many things that could be measured and a multiplicity of commissioners and funders who may want different data about different outcomes. This can be a burden on services and on carers.
-
When assessing services and aiming to improve them, it is important to consider context. We are currently in a service and policy context of austerity (cost savings) and this will influence what information can/should be collected.
-
What do you do with the data when you have them?
2. Missed opportunities/things that could be done better
-
Different measures are used by different services (so the evidence is not comparable).
-
Some services use outcome measures at the initial assessment (baseline), but these are not followed up later on.
-
Not all carers are getting carers’ assessments, and, if they are, these are not often reviewed. The carers who do get a carers’ assessment are asked important questions, but often nothing is done with the information collected. Carers’ assessments and reviews need to be turned into action.
-
Outcome measures are used in other services: why not dementia/carers’ services? Some collect a lot of statistics about service user characteristics but nothing about outcomes. We need a change in culture.
3. Ways forward
-
It would help to have a steer from commissioners about what outcomes they want to see.
-
In some localities, qualitative key performance indicators were used to shape the outcomes that commissioners want.
-
Case studies can be used to demonstrate an impact in business cases.
-
It is important to have a baseline for measurement. Carers’ assessments could be used to create a real foundation for carer-related baseline information.
-
Goal-setting with individuals and monitoring progress could be another solution. This can be embedded into everyday practice with the carer, but it is important that workers are committed to the measure.
-
Sensitivity and good communication skills are needed to enable staff to ask baseline questions early in the service provision relationship.
-
It is easier to do before-and-after assessments when it comes to evaluating training. (Perhaps this is why there is more evidence on the impact of carer training than on other forms of intervention?)
-
In other areas of health and social care, the expectation is often that a person will get better; this is not the case for people with dementia, and so services (and carers) need to manage their deterioration. This requires access to information through learning, education and support. Good questions to assess whether or not a service is supporting a carer well are:
-
How confident do carers feel in making decisions about the person they care for?
-
How much confidence do carers have in the professionals they come into contact with?
-
These key points were circulated to workshop participants for final comments and then used alongside the project findings to inform a four-page project summary, which was distributed widely as one of our project outputs.
Flyer from the workshop
Appendix 2 Support for the carers of people with dementia survey
© ASCOT Carer SCT4 v1.1 (with IP): © PSSRU at the University of Kent. This questionnaire has been developed by members of the Personal Social Services Research Unit (PSSRU) at the University of Kent at Canterbury, United Kingdom (UK). The work has been substantially funded by the Quality and Outcomes of Person-Centred Care Research Unit (QORU) under the Policy Research Programme in the UK Department of Health and Social Care. The views expressed are not necessarily those of the Department. The University of Kent is the sole owner of the copyright in these materials. The University of Kent authorises non-commercial use of this questionnaire on the condition that anyone who uses it contacts the ASCOT team (ascot@kent.ac.uk) to discuss this use and enable the PSSRU at University of Kent to track authorised non-commercial use. The University of Kent does not authorise commercial use of this questionnaire. Anyone wishing to obtain a licence for commercial use of any of the ASCOT materials should contact the ASCOT team, who will put them in touch with Kent Innovation & Enterprise. The ASCOT measure is disclosed in full herein with permission from the University of Kent on an all rights reserved basis. The measure should not be used for any purposes without the appropriate permissions from the University of Kent. Please visit www.pssru.ac.uk/ascot or e-mail ascot@kent.ac.uk to enquire about permissions.
Survey of Carers in Households 2009/10: copyright © 2010, The Health and Social Care Information Centre. All rights reserved.
Please note that this page has been amended from the questionnaire used in the trial because of copyright restrictions.
This section has been redacted owing to copyright restrictions. Please refer to Fortinsky et al. 46 Please contact the corresponding author for a copy of the full questionnaire.
Appendix 3 Tables and figures
| Data set | Number of | Information held | Data analysed | |
|---|---|---|---|---|
| Cases | Variables | |||
| CADIa | 57 | 38 | Needs assessments (based on published assessment tools) for carers, focusing on stress, coping and rewards. Only one time point and too few cases to analyse | No |
| CASIa | 51 | 36 | ||
| CAMIa | 45 | 44 | ||
| Agency | 3543 | 24 | Agencies ‘involved’ in the case | Yes |
| Other family members | 2342 | 12 | Other family members are involved in the case, but they are not clients of the AN service in their own right | Yes |
| Work | 24,825 | 5 | Client’s status – also reported in the cases data set, so no additional relevant data | No |
| Cases | 24,825 | 51 | The latest core descriptive information held on each current or previous client | Yes |
| Current needs assessment | 2541 | 24 (covering 18 areas of need) | Needs assessment, using the latest version of the in-house needs assessment tool | Yes |
| Daily activity log | 17,362 | 1 | Details of the actual input Admiral Nurses have provided to clients over time. Sample of 200 cases analysed | Yes – qualitatively |
| Legacy needs assessment | 2074 | 25 (19 needs) | Needs assessment using the previous version of the in-house needs assessment tool | Yes |
| Person with dementia status | 6609 | 3 | Living circumstances of the person with dementia. Information already available in the cases data set | No |
| Referral | 24,088 | 4 | Services and professionals who referred the carer to the AN service and services referred to | Yes |
| Review pro forma | 2276 | 4 | Discretionary field that Admiral Nurses can use to make additional notes. No data | No |
| Risk screening tool | 1091 | 24 | Risk assessment based on in-house screening tool. Summarised a 5% sample of data | Yes – qualitatively |
| Triage assessment | 2517 | 4 | System-generated output. Does not link to other data | No useful data |
| Type of calculation | Assumptions | Assumed response rate | Total achieved sample size required (original sample size to ensure this) | Number of independent variables in regression using more and less conservative inflators (10 observations or 5 observations per variable) |
|---|---|---|---|---|
| Population survey sample calculation |
66% of people with dementia live in the community with the support of a carer (population size circa 528,000) 30 clusters Design effect of 1 (random sampling) |
60% | 384 (640) | Achieved sample size would allow for 38 independent variables using a conservative ratio, 76 using a less conservative ratio |
| Comparative research sample calculation | Mean difference of –5.0 points on the GHQ, with 5% confidence level and 80% power | 60% | 16 (26) | Achieved sample size would allow one independent variable using a conservative ratio and three using a less conservative ratio |
| Question topics | Needs assessment | |
|---|---|---|
| Legacy | Current | |
| Physical health: person with dementia | Q1 | Q1 |
| Mental health: person with dementia | Q2 | Q2 |
| Physical health: carer | Q3 | Q3 |
| Mental health: carer | Q4 | Q4 |
| Medication management | Q5 | Q5 |
| Insight into dementia | Q6 | Q6 |
| Dementia symptom | Q7 | – |
| Coping with behaviour/symptoms | Q8 | Q7 |
| Communication: professionals and carer | Q9 | Q8 |
| Environment/accommodation | Q10 | Q9 |
| Financial issues | Q11 | Q10 |
| Practical aids | Q12 | Q11 |
| Practical support | Q13 | Q12 |
| Informal support | Q17 | Q13 |
| Adjustment to loss | Q16 | Q14 |
| Balancing needs | Q18 | Q15 |
| Time for self | Q14 | Q16 |
| Time for self: longer respite | Q15 | – |
| Looking to the future | Q19 | Q17 |
| Risk | – | Q18 |
| Number of assessments completed | Needs assessment (number of carers) | |
|---|---|---|
| Legacy | Current | |
| 1 | 1628 | 1987 |
| 2 | 281 | 343 |
| 3 | 105 | 134 |
| 4 | 33 | 40 |
| 5 | 20 | 23 |
| 6 | 5 | 6 |
| 7 | 1 | 6 |
| 8 | 1 | – |
| 9 | – | 2 |
| Total | 2074 | 2541 |
| Eligible cases for analysis | 165 | 554 |
| Eligibility for analysis | Needs assessment (n) | |
|---|---|---|
| Legacy | Current | |
| Eligible cases (more than three assessments) | 165 | 211 |
| Excluded: no dates | 8 | 1 |
| Excluded: duplicate from legacy needs assessment | – | 9 |
| Total | 157 | 201 |
| Case status in data set | n (%) |
|---|---|
| Closed case (previous) | 21,073 (85) |
| Open case (current) | 3510 (14) |
| Waiting (future) | 242 (1) |
| Total | 24,825 (100) |
| Type of carer | n (%) |
|---|---|
| Main | 17,557 (71) |
| Secondary | 1641 (7) |
| Not yet set | 5604 (23) |
| Total | 24,802 (100) |
| Missing cases | 23 |
| Living circumstances of the person with dementia | n (%) |
|---|---|
| Living with AN carer | 3704 (57) |
| Living with another carer | 453 (7) |
| Living alone | 916 (14) |
| Residential care/nursing home | 425 (7) |
| Deceased | 660 (10) |
| In hospital | 243 (4) |
| Supported living | 62 (1) |
| Other | 37 (1) |
| Total | 6500 (100) |
| Missing | 18,325 |
| Sex | Carer, n (%) | Person with dementia, n (%) |
|---|---|---|
| Female | 14,647 (70) | 10,774 (53) |
| Male | 6258 (30) | 9452 (47) |
| Total | 20,905 (100) | 20,226 (100) |
| Missing | 3920 | 4599 |
| Employment status | Carer, n (%) | Person with dementia, n (%) |
|---|---|---|
| Employed full-time | 2114 (15.3) | 20 (0.3) |
| Employed part-time | 1240 (9.0) | 11 (0.1) |
| Self-employed | 331 (2.4) | 15 (0.2) |
| Retired | 8682 (62.7) | 7238 (98.1) |
| Unemployed | 783 (5.7) | 84 (1.1) |
| Left work to become a carer | 695 (5.0) | 9 (0.1) |
| Total | 13,845 (100.0) | 7377 (100) |
| Missing | 10,980 | 17,448 |
| Ethnic group | Carer, n (%) | Person with dementia, n (%) |
|---|---|---|
| White | 13,899 (90.8) | 12,668 (90.7) |
| Mixed | 63 (0.4) | 40 (0.3) |
| Asian/Asian British | 517 (3.4) | 498 (3.6) |
| Black African/Caribbean/British | 580 (3.8) | 549 (3.9) |
| Other | 253 (1.7) | 218 (1.6) |
| Total | 15,312 (100.0) | 13,973 (100.0) |
| Missing | 9513 | 10,852 |
| Age group (years) | Carer, n (%) | Person with dementia, n (%) |
|---|---|---|
| < 16a | 99 (0.8) | 169 (0.9) |
| 16–24 | 43 (0.4) | 3 (0.02) |
| 25–34 | 143 (1.2) | 6 (0.03) |
| 35–44 | 595 (4.9) | 14 (0.08) |
| 45–54 | 1860 (15.3) | 113 (0.63) |
| 55–64 | 2425 (20.0) | 696 (3.9) |
| 65–69 | 1265 (10.4) | 1068 (5.9) |
| 70–74 | 1430 (11.8) | 2107 (11.7) |
| ≥ 75 | 4261 (35.2) | 13,855 (76.8) |
| Total | 12,121 (100.0) | 18,031 (100.0) |
| Missing | 12,704 | 6794 |
| Carer age group (years) | Person with dementia age group (years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| < 16 | 16–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–69 | 70–74 | ≥ 75 | Total | |
| < 16a | 16 | 0 | 1 | 0 | 0 | 2 | 1 | 8 | 52 | 80 |
| 16–24 | 1 | 0 | 0 | 1 | 3 | 5 | 5 | 5 | 18 | 38 |
| 25–34 | 1 | 0 | 1 | 1 | 5 | 24 | 17 | 17 | 64 | 130 |
| 35–44 | 5 | 0 | 0 | 2 | 5 | 32 | 47 | 95 | 316 | 502 |
| 45–54 | 12 | 0 | 0 | 1 | 26 | 65 | 43 | 147 | 1303 | 1597 |
| 55–64 | 15 | 0 | 0 | 2 | 12 | 215 | 172 | 129 | 1596 | 2141 |
| 65–69 | 7 | 0 | 0 | 0 | 3 | 56 | 230 | 266 | 578 | 1140 |
| 70–74 | 7 | 0 | 0 | 1 | 1 | 19 | 89 | 387 | 782 | 1286 |
| ≥ 75 | 24 | 1 | 0 | 1 | 8 | 6 | 29 | 192 | 3505 | 3766 |
| Total | 88 | 1 | 2 | 9 | 63 | 424 | 633 | 1246 | 8214 | 10,680 |
| Marital status | Carer, n (%) | Person with dementia, n (%) |
|---|---|---|
| Married | 14,429 (84.5) | 10,481 (69.5) |
| Widowed | 315 (1.8) | 3648 (24.2) |
| Divorced | 387 (2.3) | 265 (1.8) |
| Separated | 107 (0.6) | 87 (0.6) |
| Single | 1242 (7.3) | 316 (2.1) |
| Living in a partnership | 604 (3.5) | 287 (1.9) |
| Total | 17,084 (100.0) | 15,084 (100.0) |
| Missing | 7741 | 9741 |
| Carer’s marital status | Carer’s relationship to the person with dementia, n (%) | ||||||
|---|---|---|---|---|---|---|---|
| Spousea | Child (adult) | Sibling | Neighbour/friend | Grandchild (adult) | Other | Total | |
| Married | 10,327 (72.8) | 3562 (25.1) | 118 (0.8) | 24 (0.2) | 33 (0.2) | 129 (0.9) | 14,193 (100.0) |
| Widowed | 87 (29.4) | 134 (45.3) | 40 (13.5) | 20 (6.8) | 0 (0.0) | 15 (5.1) | 296 (100.0) |
| Divorced | 35 (9.4) | 305 (81.6) | 10 (2.7) | 16 (4.3) | 0 (0.0) | 8 (2.1) | 374 (100.0) |
| Separated | 20 (19.8) | 72 (71.3) | 0 (0.0) | 5 (5.0) | 0 (0.0) | 4 (4.0) | 101 (100.0) |
| Single | 13 (1.1) | 1025 (84.9) | 49 (4.1) | 48 (4.0) | 43 (3.6) | 29 (2.4) | 1207 (100.0) |
| Living in a partnership | 287 (49.3) | 253 (43.5) | 5 (0.9) | 9 (1.5) | 18 (3.1) | 10 (1.7) | 582 (100.0) |
| Not entered | 80 (8.0) | 806 (80.7) | 37 (3.7) | 25 (2.5) | 20 (2.0) | 31 (3.1) | 999 (100.0) |
| Total | 10,849 (61.1) | 6157 (34.7) | 259 (1.5) | 147 (0.8) | 114 (0.6) | 226 (1.3) | 17,752 (100.0) |
| Dementia type | Current case status, n (%) | |||
|---|---|---|---|---|
| Closed | Open | Waiting list | Total | |
| Alzheimer’s disease | 4124 (19.6) | 642 (18.3) | 48 (19.8) | 4814 (19.4) |
| Vascular dementia | 3194 (15.2) | 434 (12.4) | 41 (16.9) | 3669 (14.8) |
| Dementia (non-specific) | 574 (2.7) | 105 (3.0) | 25 (10.3) | 704 (2.8) |
| Mixed vascular and Alzheimer’s disease | 1441 (6.8) | 219 (6.2) | 16 (6.6) | 1676 (6.8) |
| Lewy body disease | 329 (1.6) | 44 (1.3) | 5 (2.1) | 378 (1.5) |
| Other forms of dementia | 255 (1.2) | 46 (1.3) | 8 (3.3) | 309 (1.2) |
| Frontotemporal lobe dementia | 268 (1.3) | 45 (1.3) | 2 (0.8) | 315 (1.3) |
| Parkinson’s disease | 260 (1.2) | 34 (1.0) | 3 (1.2) | 297 (1.2) |
| Alcohol-related dementia | 60 (0.3) | 7 (0.2) | 1 (0.4) | 68 (0.3) |
| Not entered | 3032 (14.4) | 144 (4.1) | 22 (9.1) | 3198 (12.9) |
| No diagnosis | 7539 (35.8) | 1790 (51) | 71 (29.3) | 9397 (37.9) |
| Total | 21,073 (100) | 3510 (100) | 242 (100) | 24,825 (100) |
| Intensity of input | n (%) |
|---|---|
| Maintaining | 1093 (31) |
| Holding pool | 434 (13) |
| Not yet set | 1591 (45) |
| Intensive | 392 (11) |
| Total | 3510 (100) |
| Service referring carers to AN | n (%) |
|---|---|
| Mental health professional/service | 5925 (24.9) |
| Psychiatrist (including consultant) | 3275 (13.6) |
| Self | 4362 (18.3) |
| Other health-care professional | 2719 (11.4) |
| Social services (including day care) | 2081 (8.7) |
| Other | 1869 (7.9) |
| GP | 1355 (5.7) |
| Relative | 613 (2.6) |
| Voluntary agency/third sector | 539 (2.3) |
| Carer support worker | 470 (2.0) |
| Community health | 465 (2.0) |
| Other carer | 89 (0.4) |
| Friend/neighbour | 57 (0.2) |
| Not clear | 3 (0.0) |
| Total | 23,822 (100.0) |
| Missing | 1003 |
| Number of services involved | Number of dyads (%) |
|---|---|
| 0 | 77 (2) |
| 1 | 2268 (64) |
| 2 | 777 (22) |
| 3 | 281 (8) |
| 4 | 93 (3) |
| ≥ 5 | 47 (1) |
| Total | 3543 (100) |
| Type of service | Number of dyads receiving the service |
|---|---|
| Adult mental health services | 218 |
| Alzheimer’s Society | 98 |
| Carer dementia support service | 3 |
| Carer’s group | 43 |
| Community mental health team | 503 |
| Day care | 329 |
| Day centre | 18 |
| District nursing | 8 |
| Elderly mental health services | 652 |
| General Medical Services | 222 |
| Home care | 15 |
| Independent sector | 331 |
| Hospital-based multidisciplinary team | 1 |
| National hospital | 2 |
| Primary care | 355 |
| Social services | 1818 |
| Voluntary organisation | 217 |
| Type of service | Number of dyads using only this one service (%) |
|---|---|
| Adult mental health services | 110 (5) |
| Alzheimer’s Society | 44 (2) |
| Carer’s group | 20 (1) |
| Community mental health team | 262 (12) |
| Day care | 87 (4) |
| Day centre | 5 (0) |
| District nursing | 2 (0) |
| Elderly mental health services | 349 (15) |
| General Medical Services | 93 (4) |
| Independent sector | 117 (5) |
| Primary care | 124 (5) |
| Social services | 977 (43) |
| Voluntary organisation | 78 (3) |
| Total | 2268 (100) |
| Number of other people | Number of dyads reporting this number of other people (%) |
|---|---|
| 0 | 25 (1.1) |
| 1 | 1926 (82.2) |
| 2 | 303 (12.9) |
| 3 | 72 (3.1) |
| 4 | 11 (0.5) |
| 5 | 3 (0.1) |
| 6 | 2 (0.1) |
| Total | 2342 (100) |
| Relationship of the family member to the person with dementia (all other family members) | Number of dyads reporting this relationship (%) |
|---|---|
| Spouse/partner | 120 (5) |
| Adult child/child-in-law | 2012 (84) |
| Sibling | 60 (3) |
| Grandchild | 81 (3) |
| Neighbour/friend | 38 (2) |
| Other | 81 (3) |
| Total | 2392 (100) |
| Relationship of the family member to the person with dementia (cases when only one other person was involved) | Number of dyads reporting this relationship (%) |
|---|---|
| Spouse | 101 (5) |
| Adult child | 1646 (85) |
| Sibling | 44 (2) |
| Grandchild | 54 (3) |
| Neighbour/friend | 25 (1) |
| Other | 56 (3) |
| Total | 1926 (100) |
| Question number_time | n | Responses – level of intervention needed (%) | Total (%) | Median | ||||
|---|---|---|---|---|---|---|---|---|
| None (0) | Minimal (1) | Some (2) | Considerable (3) | Urgent (4) | ||||
| 1_1 | 154 | 63 | 31 | 5 | 0 | 1 | 100 | 0 |
| 1_2 | 154 | 75 | 20 | 3 | 1 | 1 | 100 | 0 |
| 1_3 | 147 | 73 | 22 | 3 | 1 | 1 | 100 | 0 |
| 2_1 | 155 | 43 | 31 | 17 | 7 | 2 | 100 | 1 |
| 2_2 | 154 | 69 | 21 | 7 | 2 | 1 | 100 | 0 |
| 2_3 | 147 | 71 | 19 | 8 | 2 | 0 | 100 | 0 |
| 3_1 | 155 | 67 | 22 | 8 | 3 | 0 | 100 | 0 |
| 3_2 | 157 | 67 | 27 | 4 | 2 | 0 | 100 | 0 |
| 3_3 | 157 | 64 | 27 | 7 | 1 | 1 | 100 | 0 |
| 4_1 | 154 | 39 | 32 | 24 | 5 | 0 | 100 | 1 |
| 4_2 | 157 | 41 | 34 | 24 | 1 | 0 | 100 | 1 |
| 4_3 | 157 | 40 | 42 | 15 | 3 | 0 | 100 | 1 |
| 5_1 | 152 | 78 | 10 | 8 | 3 | 1 | 100 | 0 |
| 5_2 | 154 | 78 | 17 | 3 | 1 | 1 | 100 | 0 |
| 5_3 | 145 | 89 | 9 | 1 | 1 | 0 | 100 | 0 |
| 6_1 | 154 | 25 | 27 | 24 | 16 | 8 | 100 | 1 |
| 6_2 | 155 | 54 | 32 | 13 | 0 | 1 | 100 | 0 |
| 6_3 | 147 | 78 | 15 | 5 | 1 | 1 | 100 | 0 |
| 7_1 | 156 | 22 | 29 | 29 | 16 | 4 | 100 | 1 |
| 7_2 | 155 | 46 | 36 | 16 | 1 | 1 | 100 | 1 |
| 7_3 | 147 | 66 | 26 | 5 | 1 | 2 | 100 | 0 |
| 8_1 | 153 | 21 | 33 | 30 | 13 | 3 | 100 | 1 |
| 8_2 | 155 | 35 | 43 | 18 | 4 | 0 | 100 | 1 |
| 8_3 | 148 | 53 | 37 | 6 | 2 | 2 | 100 | 0 |
| 9_1 | 156 | 69 | 18 | 8 | 4 | 1 | 100 | 0 |
| 9_2 | 156 | 74 | 17 | 8 | 1 | 0 | 100 | 0 |
| 9_3 | 151 | 71 | 20 | 6 | 3 | 0 | 100 | 0 |
| 10_1 | 154 | 88 | 6 | 2 | 3 | 1 | 100 | 0 |
| 10_2 | 154 | 88 | 10 | 1 | 1 | 0 | 100 | 0 |
| 10_3 | 149 | 90 | 8 | 1 | 1 | 0 | 100 | 0 |
| 11_1 | 154 | 54 | 30 | 12 | 4 | 0 | 100 | 0 |
| 11_2 | 156 | 73 | 24 | 3 | 0 | 0 | 100 | 0 |
| 11_3 | 153 | 87 | 10 | 2 | 1 | 0 | 100 | 0 |
| 12_1 | 146 | 86 | 10 | 3 | 1 | 0 | 100 | 0 |
| 12_2 | 151 | 93 | 4 | 3 | 0 | 0 | 100 | 0 |
| 12_3 | 143 | 91 | 6 | 2 | 1 | 0 | 100 | 0 |
| 13_1 | 155 | 70 | 21 | 8 | 1 | 0 | 100 | 0 |
| 13_2 | 153 | 83 | 14 | 2 | 1 | 0 | 100 | 0 |
| 13_3 | 145 | 85 | 10 | 3 | 1 | 1 | 100 | 0 |
| 14_1 | 155 | 45 | 28 | 17 | 8 | 2 | 100 | 1 |
| 14_2 | 151 | 60 | 26 | 11 | 1 | 2 | 100 | 0 |
| 14_3 | 143 | 69 | 24 | 5 | 1 | 1 | 100 | 0 |
| 15_1 | 140 | 70 | 17 | 8 | 4 | 1 | 100 | 0 |
| 15_2 | 143 | 70 | 18 | 8 | 3 | 1 | 100 | 0 |
| 15_3 | 139 | 73 | 17 | 7 | 2 | 1 | 100 | 0 |
| 16_1 | 141 | 48 | 25 | 16 | 10 | 1 | 100 | 1 |
| 16_2 | 151 | 44 | 30 | 18 | 7 | 1 | 100 | 1 |
| 16_3 | 155 | 53 | 27 | 12 | 8 | 0 | 100 | 0 |
| 17_1 | 157 | 81 | 13 | 4 | 1 | 1 | 100 | 0 |
| 17_2 | 155 | 83 | 14 | 1 | 1 | 1 | 100 | 0 |
| 17_3 | 151 | 90 | 7 | 2 | 0 | 1 | 100 | 0 |
| 18_1 | 155 | 50 | 29 | 13 | 8 | 0 | 100 | 1 |
| 18_2 | 154 | 60 | 26 | 11 | 3 | 0 | 100 | 0 |
| 18_3 | 149 | 69 | 22 | 7 | 2 | 0 | 100 | 0 |
| 19_1 | 137 | 73 | 20 | 6 | 1 | 0 | 100 | 0 |
| 19_2 | 142 | 66 | 20 | 8 | 6 | 0 | 100 | 0 |
| 19_3 | 138 | 59 | 25 | 9 | 5 | 2 | 100 | 0 |
| Question_time | n | Responses – level of intervention needed (%)a | Total (%) | Median | ||
|---|---|---|---|---|---|---|
| No need (0) | Needs currently met (1) | Unmet need (2) | ||||
| 1_1 | 188 | 26 | 62 | 12 | 100 | 1 |
| 1_2 | 172 | 29 | 66 | 5 | 100 | 1 |
| 1_3 | 175 | 29 | 68 | 3 | 100 | 1 |
| 2_1 | 189 | 16 | 65 | 19 | 100 | 1 |
| 2_2 | 175 | 22 | 65 | 13 | 100 | 1 |
| 2_3 | 175 | 22 | 67 | 11 | 100 | 1 |
| 3_1 | 186 | 35 | 51 | 14 | 100 | 1 |
| 3_2 | 177 | 41 | 52 | 7 | 100 | 1 |
| 3_3 | 179 | 40 | 53 | 7 | 100 | 1 |
| 4_1 | 190 | 26 | 24 | 50 | 100 | 1.5 |
| 4_2 | 178 | 33 | 37 | 30 | 100 | 1 |
| 4_3 | 176 | 35 | 35 | 30 | 100 | 1 |
| 5_1 | 187 | 47 | 44 | 9 | 100 | 1 |
| 5_2 | 171 | 47 | 48 | 5 | 100 | 1 |
| 5_3 | 171 | 52 | 46 | 2 | 100 | 0 |
| 6_1 | 187 | 17 | 22 | 61 | 100 | 2 |
| 6_2 | 177 | 22 | 29 | 49 | 100 | 1 |
| 6_3 | 175 | 29 | 34 | 37 | 100 | 1 |
| 7_1 | 186 | 16 | 19 | 65 | 100 | 2 |
| 7_2 | 180 | 22 | 24 | 54 | 100 | 2 |
| 7_3 | 178 | 30 | 25 | 45 | 100 | 1 |
| 8_1 | 185 | 64 | 24 | 12 | 100 | 0 |
| 8_2 | 168 | 66 | 25 | 9 | 100 | 0 |
| 8_3 | 169 | 70 | 21 | 9 | 100 | 0 |
| 9_1 | 173 | 62 | 32 | 6 | 100 | 0 |
| 9_2 | 159 | 65 | 32 | 3 | 100 | 0 |
| 9_3 | 163 | 70 | 29 | 1 | 100 | 0 |
| 10_1 | 180 | 36 | 48 | 16 | 100 | 1 |
| 10_2 | 167 | 42 | 52 | 6 | 100 | 1 |
| 10_3 | 168 | 45 | 50 | 5 | 100 | 1 |
| 11_1 | 176 | 61 | 34 | 5 | 100 | 0 |
| 11_2 | 167 | 62 | 33 | 5 | 100 | 0 |
| 11_3 | 168 | 68 | 29 | 3 | 100 | 0 |
| 12_1 | 180 | 40 | 42 | 18 | 100 | 1 |
| 12_2 | 173 | 43 | 46 | 11 | 100 | 1 |
| 12_3 | 169 | 48 | 44 | 8 | 100 | 1 |
| 13_1 | 181 | 35 | 47 | 18 | 100 | 1 |
| 13_2 | 172 | 39 | 53 | 8 | 100 | 1 |
| 13_3 | 170 | 42 | 53 | 5 | 100 | 1 |
| 14_1 | 171 | 30 | 24 | 46 | 100 | 1 |
| 14_2 | 169 | 36 | 24 | 40 | 100 | 1 |
| 14_3 | 171 | 39 | 30 | 31 | 100 | 1 |
| 15_1 | 178 | 22 | 30 | 48 | 100 | 1 |
| 15_2 | 175 | 31 | 35 | 34 | 100 | 1 |
| 15_3 | 172 | 36 | 44 | 20 | 100 | 1 |
| 16_1 | 183 | 25 | 38 | 37 | 100 | 1 |
| 16_2 | 181 | 31 | 37 | 32 | 100 | 1 |
| 16_3 | 176 | 35 | 41 | 24 | 100 | 1 |
| 17_1 | 159 | 28 | 27 | 45 | 100 | 1 |
| 17_2 | 163 | 29 | 29 | 42 | 100 | 1 |
| 17_3 | 174 | 31 | 31 | 38 | 100 | 1 |
| 18_1 | 24 | 71 | 25 | 4 | 100 | 0 |
| 18_2 | 63 | 56 | 30 | 14 | 100 | 0 |
| 18_3 | 86 | 62 | 22 | 16 | 100 | 0 |
| Question_time | n | Mean rank | χ2 (df = 2) | p-value (Friedman) | Pairs being tested | z | p-value (Wilcoxon) |
|---|---|---|---|---|---|---|---|
| 1_1 | 144 | 2.1 | 4.895 | 0.087 | |||
| 1_2 | 1.93 | ||||||
| 1_3 | 1.97 | ||||||
| 2_1 | 145 | 2.28 | 28.848 | 0.000 | 1 to 2 | –4.354 | 0.000 |
| 2_2 | 1.85 | 1 to 3 | –4.725 | 0.000 | |||
| 2_3 | 1.87 | 2 to 3 | –0.093 | 0.926 | |||
| 3_1 | 155 | 2.02 | 0.589 | 0.745 | |||
| 3_2 | 1.97 | ||||||
| 3_3 | 2.01 | ||||||
| 4_1 | 154 | 2.04 | 1.574 | 0.455 | |||
| 4_2 | 2.02 | ||||||
| 4_3 | 1.94 | ||||||
| 5_1 | 141 | 2.09 | 11.253 | 0.004 | 1 to 2 | –1.609 | 0.108 |
| 5_2 | 2.03 | 1 to 3 | –3.478 | 0.001 | |||
| 5_3 | 1.88 | 2 to 3 | –2.399 | 0.016 | |||
| 6_1 | 143 | 2.58 | 132.991 | 0.000 | 1 to 2 | –7.928 | 0.000 |
| 6_2 | 1.88 | 1 to 3 | –8.271 | 0.000 | |||
| 6_3 | 1.55 | 2 to 3 | –4.314 | 0.000 | |||
| 7_1 | 145 | 2.51 | 104.739 | 0.000 | 1 to 2 | –7.418 | 0.000 |
| 7_2 | 1.9 | 1 to 3 | –7.917 | 0.000 | |||
| 7_3 | 1.59 | 2 to 3 | –4.002 | 0.000 | |||
| 8_1 | 143 | 2.4 | 65.49 | 0.000 | 1 to 2 | –5.833 | 0.000 |
| 8_2 | 1.94 | 1 to 3 | –6.756 | 0.000 | |||
| 8_3 | 1.66 | 2 to 3 | –3.442 | 0.001 | |||
| 9_1 | 150 | 2.06 | 3.619 | 0.164 | |||
| 9_2 | 1.93 | ||||||
| 9_3 | 2.01 | ||||||
| 10_1 | 147 | 2.02 | 1.326 | 0.515 | |||
| 10_2 | 2.01 | ||||||
| 10_3 | 1.97 | ||||||
| 11_1 | 150 | 2.29 | 49.805 | 0.000 | 1 to 2 | –4.719 | 0.000 |
| 11_2 | 1.95 | 1 to 3 | –5.752 | 0.000 | |||
| 11_3 | 1.76 | 2 to 3 | –3.244 | 0.001 | |||
| 12_1 | 133 | 2.07 | 5.396 | 0.067 | |||
| 12_2 | 1.95 | ||||||
| 12_3 | 1.98 | ||||||
| 13_1 | 141 | 2.13 | 12.339 | 0.002 | 1 to 2 | –2.906 | 0.004 |
| 13_2 | 1.94 | 1 to 3 | –2.221 | 0.026 | |||
| 13_3 | 1.92 | 2 to 3 | –0.328 | 0.743 | |||
| 14_1 | 138 | 2.22 | 22.302 | 0.000 | 1 to 2 | –3.281 | 0.001 |
| 14_2 | 1.96 | 1 to 3 | –4.385 | 0.000 | |||
| 14_3 | 1.82 | 2 to 3 | –2.076 | 0.038 | |||
| 15_1 | 122 | 2.07 | 2.197 | 0.333 | |||
| 15_2 | 1.95 | ||||||
| 15_3 | 1.98 | ||||||
| 16_1 | 140 | 2.06 | 4.502 | 0.105 | |||
| 16_2 | 2.04 | ||||||
| 16_3 | 1.9 | ||||||
| 17_1 | 151 | 2.07 | 8.845 | 0.012 | 1 to 2 | –1.333 | 0.182 |
| 17_2 | 2.01 | 1 to 3 | –2.921 | 0.003 | |||
| 17_3 | 1.92 | 2 to 3 | –2.065 | 0.039 | |||
| 18_1 | 145 | 2.21 | 27.992 | 0.000 | 1 to 2 | –2.563 | 0.010 |
| 18_2 | 1.99 | 1 to 3 | –3.907 | 0.000 | |||
| 18_3 | 1.8 | 2 to 3 | –2.434 | 0.015 | |||
| 19_1 | 118 | 1.87 | 9.869 | 0.007 | 1 to 2 | –2.761 | 0.006 |
| 19_2 | 2.01 | 1 to 3 | –3.456 | 0.001 | |||
| 19_3 | 2.12 | 2 to 3 | –1.500 | 0.134 |
| Question_time | n | Mean rank | χ2 (df = 2) | p-value (Friedman) | Pairs being tested | z | p-value (Wilcoxon) |
|---|---|---|---|---|---|---|---|
| 1_1 | 158 | 2.08 | 6.721 | 0.035 | 1 to 2 | –2.351 | 0.019 |
| 1_2 | 1.98 | 1 to 3 | –2.592 | 0.010 | |||
| 1_3 | 1.95 | 2 to 3 | –0.192 | 0.847 | |||
| 2_1 | 158 | 2.11 | 10.685 | 0.005 | 1 to 2 | –2.370 | 0.018 |
| 2_2 | 1.98 | 1 to 3 | –2.408 | 0.016 | |||
| 2_3 | 1.91 | 2 to 3 | –1.766 | 0.077 | |||
| 3_1 | 160 | 2.09 | 7.597 | 0.022 | 1 to 2 | –2.448 | 0.014 |
| 3_2 | 1.97 | 1 to 3 | –2.498 | 0.012 | |||
| 3_3 | 1.94 | 2 to 3 | –0.010 | 0.992 | |||
| 4_1 | 161 | 2.21 | 29.779 | 0.000 | 1 to 2 | –4.380 | 0.000 |
| 4_2 | 1.93 | 1 to 3 | –3.719 | 0.000 | |||
| 4_3 | 1.86 | 2 to 3 | –0.592 | 0.554 | |||
| 5_1 | 155 | 2.08 | 11.176 | 0.004 | 1 to 2 | –1.422 | 0.155 |
| 5_2 | 2.01 | 1 to 3 | –3.064 | 0.002 | |||
| 5_3 | 1.91 | 2 to 3 | –2.353 | 0.019 | |||
| 6_1 | 160 | 2.23 | 47.722 | 0.000 | 1 to 2 | –3.505 | 0.000 |
| 6_2 | 2.01 | 1 to 3 | –5.497 | 0.000 | |||
| 6_3 | 1.76 | 2 to 3 | –3.959 | 0.000 | |||
| 7_1 | 158 | 2.19 | 38.273 | 0.000 | 1 to 2 | –3.250 | 0.001 |
| 7_2 | 2.01 | 1 to 3 | –4.995 | 0.000 | |||
| 7_3 | 1.8 | 2 to 3 | –3.737 | 0.000 | |||
| 8_1 | 152 | 2.07 | 4.762 | 0.092 | |||
| 8_2 | 2.00 | ||||||
| 8_3 | 1.93 | ||||||
| 9_1 | 139 | 2.10 | 13.850 | 0.001 | 1 to 2 | –2.172 | 0.030 |
| 9_2 | 1.99 | 1 to 3 | –3.535 | 0.000 | |||
| 9_3 | 1.91 | 2 to 3 | –1.831 | 0.067 | |||
| 10_1 | 147 | 2.08 | 4.908 | 0.086 | |||
| 10_2 | 1.98 | ||||||
| 10_3 | 1.94 | ||||||
| 11_1 | 147 | 2.02 | 5.150 | 0.076 | |||
| 11_2 | 2.04 | ||||||
| 11_3 | 1.93 | ||||||
| 12_1 | 150 | 2.11 | 10.953 | 0.004 | 1 to 2 | –1.933 | 0.053 |
| 12_2 | 2 | 1 to 3 | –2.465 | 0.014 | |||
| 12_3 | 1.89 | 2 to 3 | –1.559 | 0.119 | |||
| 13_1 | 148 | 2.12 | 12.457 | 0.002 | 1 to 2 | –2.687 | 0.007 |
| 13_2 | 1.97 | 1 to 3 | –3.073 | 0.002 | |||
| 13_3 | 1.91 | 2 to 3 | –0.878 | 0.380 | |||
| 14_1 | 145 | 2.09 | 10.307 | 0.006 | 1 to 2 | –0.473 | 0.636 |
| 14_2 | 2.02 | 1 to 3 | –2.359 | 0.018 | |||
| 14_3 | 1.89 | 2 to 3 | –1.835 | 0.066 | |||
| 15_1 | 151 | 2.24 | 42.306 | 0.000 | 1 to 2 | –3.144 | 0.002 |
| 15_2 | 2 | 1 to 3 | –5.377 | 0.000 | |||
| 15_3 | 1.77 | 2 to 3 | –3.173 | 0.002 | |||
| 16_1 | 155 | 2.10 | 14.304 | 0.001 | 1 to 2 | –1.525 | 0.127 |
| 16_2 | 2.04 | 1 to 3 | –3.162 | 0.002 | |||
| 16_3 | 1.86 | 2 to 3 | –1.726 | 0.084 | |||
| 17_1 | 129 | 2.05 | 2.651 | 0.266 | |||
| 17_2 | 2.01 | ||||||
| 17_3 | 1.94 | ||||||
| 18_1 | 22 | 2.05 | 0.667 | 0.717 | |||
| 18_2 | 1.98 | ||||||
| 18_3 | 1.98 |
| Approach | Source of carers identified for the survey | Totals | |||
|---|---|---|---|---|---|
| AN services | JDR | Third-sector organisations | TiDE | ||
| Number of paper questionnaires distributed (excluding reminder packs) | 497 | 9 | 501 | 3 | 1010 |
| Paper questionnaires returned | 194 | 4 | 108 | 0 | 304 |
| Paper questionnaire refusals | 1 | 2 | 3 | – | 6 |
| Paper questionnaires attempted and in scope | 158 | 2 | 98 | 0 | 258 |
| Response rate (% returned and in scope) | 32 | 22 | 20 | 0 | 26 |
| Number of organisations sent an anonymous electronic link for distribution | N/A | N/A | 6 | N/A | N/A |
| Number of individual links sent via organisations | N/A | 103 | At least 300 | 28 | N/A |
| Electronic survey returns | 0 | 35 | 76 | 15 | 126 |
| Refusals via electronic survey | 0 | 2 | 20 | 2 | 24 |
| Electronic surveys in scope | 0 | 26 | 50 | 12 | 88 |
| % response rate | N/A | 25 | N/A | 43 | N/A |
| Total returned and in scope | 158 | 28 | 148 | 12 | 346 |
| Characteristic | Type of carer (%) | |||
|---|---|---|---|---|
| AN carers | Non-AN area carers | All survey carers | SCH carers of people with dementia | |
| Sex of the carer | ||||
| Male | 36 | 26 | 31 | 35 |
| Female | 64 | 74 | 69 | 65 |
| Age (years) of the carer | ||||
| < 55 | 10 | 25 | 18 | 42 |
| 55–64 | 20 | 29 | 25 | 27 |
| 65–74 | 30 | 19 | 24 | 19 |
| ≥ 75 | 40 | 26 | 32 | 11 |
| Sex of the person with dementia | ||||
| Male | 51 | 45 | 48 | 37 |
| Female | 49 | 55 | 52 | 63 |
| Age (years) of the person with dementia | ||||
| < 65 | 7 | 12 | 9 | 9 |
| 65–74 | 21 | 18 | 20 | 11 |
| ≥ 75 | 72 | 69 | 71 | 80 |
| Relationship of the person with dementia to the carer | ||||
| Spouse or partner | 76 | 58 | 66 | 22 |
| Parent/in-law | 22 | 37 | 30 | 57 |
| Other | 3 | 5 | 4 | 21 |
| Type of care provided | ||||
| Personal and physical | 49 | 36 | 42 | 22 |
| Other | 51 | 64 | 58 | 78 |
| Economic activity | ||||
| In paid employment | 15 | 29 | 23 | 49 |
| Not in paid employment | 85 | 77 | 77 | 51 |
| Maximum number | 158 | 188 | 346 | 249 |
| Characteristic | Key categories | % of AN carers | % of non-AN area carers | χ2 value and dfa | Statistical significance (two-sided) p-value | n |
|---|---|---|---|---|---|---|
| Person with dementia | ||||||
| Where the person with dementia lives | Living at home with carer | 81 | 68 | 9.404, df = 4 | 0.052 | 346 |
| Relationship of the person with dementia to the carer | Spouse/partner | 76 | 58 | 332 | ||
| Parent/in-law | 22 | 37 | 11.095, df = 2 | 0.004** | 332 | |
| Sex of the person with dementia | Male | 51 | 45 | 1.058, df = 1 | 0.304 | 332 |
| Age (years) of the person with dementia | 75–84 | 43 | 39 | 3.758, df = 5 | 0.585 | 331 |
| Self-reported ethnicity of the person with dementia | ‘White’ | 96 | 95 | 5.47, df = 4 | 0.140 | 338 |
| How long the dementia symptoms had been present | 1–5 years | 60 | 59 | 1.119, df = 3 | 0.773 | 339 |
| Whether the person has a formal diagnosis of dementia | Yes | 95 | 96 | 0.391, df = 2 | 0.822 | 340 |
| Diagnosis | Alzheimer’s disease | 52 | 66 | 7.043, df = 1 | 0.008** | 346 |
| Vascular dementia | 39 | 27 | 5.727, df = 1 | 0.017* | 346 | |
| Carer-reported severity of dementia | Moderate | 65 | 62 | 3.412, df = 2 | 0.182 | 339 |
| Carer | ||||||
| Sex of the carer | Female | 64 | 74 | 3.546, df = 1 | 0.060 | 340 |
| Age (years) of the carer | 45–54 | 9 | 18 | |||
| ≥ 75 | 40 | 26 | 23.202, df = 7 | 0.002** | 340 | |
| Self-reported ethnicity of the carer | ‘White’ | 96 | 97 | 6.444, df = 5 | 0.265 | 340 |
| Highest level of qualification of the carer | Master’s level or above | 3 | 14 | |||
| None | 24 | 13 | 23.902, df = 6 | 0.001*** | 339 | |
| Economic status of the carer | In full-time work | 2 | 12 | 13.195, df = 1 | < 0.001*** | 346 |
| Retired from paid work | 63 | 50 | 5.577, df = 1 | 0.018* | 346 | |
| Carer status | Is the sole or main carer | 97 | 84 | 15.662, df = 2 | < 0.001*** | 336 |
| How long the carer has been caring for the person with dementia | 1–3 years | 35 | 30 | 4.854, df = 6 | 0.563 | 339 |
| Hours of care provided on the previous day | Type of carer (%) | ||
|---|---|---|---|
| AN carers | Non-AN area carers | All | |
| 0–5 | 19 | 26 | 23 |
| 6–11 | 22 | 27 | 25 |
| 12–17 | 28 | 27 | 27 |
| ≥ 18 | 31 | 19 | 25 |
| N (100%) | 153 | 175 | 328 |
| EQ-5D dimension | % of carers in each age group (years) (all carers) | χ2 value and df | Statistical significance (two-sided) p-value | N | ||||
|---|---|---|---|---|---|---|---|---|
| < 55 | 55–64 | 65–74 | ≥ 75 | Total | ||||
| Mobility | ||||||||
| No problems | 76 | 71 | 67 | 32 | 59 | |||
| Problems | 24 | 29 | 33 | 63 | 41 | 45.53, df = 3 | < .001** | 330 |
| Self-care | ||||||||
| No problems | 95 | 96 | 93 | 87 | 92 | |||
| Problems | 5 | 4 | 7 | 13 | 8 | 7.03, df = 3 | 0.071 | 329 |
| Usual activity | ||||||||
| No problems | 53 | 51 | 45 | 30 | 43 | |||
| Problems | 48 | 49 | 55 | 71 | 57 | 12.42, df = 3 | 0.006** | 330 |
| Pain/discomfort | ||||||||
| No problems | 48 | 33 | 32 | 20 | 31 | |||
| Problems | 53 | 67 | 68 | 80 | 69 | 13.59, df = 3 | 0.004** | 330 |
| Anxiety and depression | ||||||||
| No problems | 27 | 14 | 20 | 28 | 22 | |||
| Problems | 73 | 86 | 81 | 72 | 78 | 6.02, df = 3 | 0.111 | 330 |
| ASCOT-Carer domain | % of carers in each age group (years) (all carers) | χ2 value and df | Statistical significance (two-sided) p-value | N | ||||
|---|---|---|---|---|---|---|---|---|
| < 55 | 55–64 | 65–74 | ≥ 75 | Total | ||||
| How the carer spends time | ||||||||
| No needs | 24 | 19 | 13 | 16 | 18 | |||
| Needs | 76 | 81 | 87 | 84 | 82 | 2.79, df = 3 | 0.426 | 330 |
| Control over daily life | ||||||||
| No needs | 46 | 29 | 22 | 23 | 28 | |||
| Needs | 54 | 71 | 78 | 77 | 72 | 12.22, df = 3 | 0.007** | 331 |
| Looking after self | ||||||||
| No needs | 58 | 46 | 50 | 57 | 53 | |||
| Needs | 42 | 54 | 50 | 43 | 47 | 2.82, df = 3 | 0.421 | 329 |
| Feeling safe | ||||||||
| No needs | 93 | 94 | 88 | 91 | 91 | |||
| Needs | 7 | 6 | 12 | 9 | 9 | 2.27, df = 3 | 0.518 | 327 |
| Social contact | ||||||||
| No needs | 48 | 36 | 29 | 32 | 35 | |||
| Needs | 52 | 64 | 71 | 68 | 65 | 5.72, df = 3 | 0.126 | 329 |
| Space and time to be oneself | ||||||||
| No needs | 32 | 27 | 24 | 21 | 25 | |||
| Needs | 68 | 73 | 76 | 79 | 75 | 2.43, df = 3 | 0.489 | 327 |
| Feeling supported and encouraged | ||||||||
| No needs | 38 | 31 | 48 | 49 | 42 | |||
| Needs | 62 | 69 | 52 | 51 | 58 | 7.915, df = 3 | 0.048* | 322 |
| ASCOT-Carer score | % of carers in each age group (years) (all carers) | ||||
|---|---|---|---|---|---|
| < 55 | 55–64 | 65–74 | ≥ 75 | Total | |
| 0–7 | 19 | 29 | 30 | 24 | 26 |
| 8–9 | 14 | 23 | 20 | 24 | 21 |
| 10–12 | 37 | 25 | 28 | 28 | 29 |
| ≥ 13 | 30 | 24 | 23 | 23 | 24 |
| N (100%) | 57 | 80 | 80 | 99 | 316 |
| ASCOT-Carer domain | % of carers in each relationship to the person with dementia (all carers) | χ2 value and df | Statistical significance (two-sided) p-value | N | |||
|---|---|---|---|---|---|---|---|
| Spouse or partner | Parent or parent-in-law | Other | Total | ||||
| How the carer spends time | |||||||
| No needs | 15 | 27 | 8 | 18 | |||
| Needs | 86 | 73 | 92 | 82 | 7.66, df = 2 | 0.022* | 323 |
| Control over daily life | |||||||
| No needs | 24 | 39 | 17 | 28 | |||
| Needs | 76 | 61 | 83 | 72 | 8.71, df = 2 | 0.013* | 324 |
| Looking after self | |||||||
| No needs | 51 | 57 | 50 | 53 | |||
| Needs | 49 | 43 | 50 | 47 | 0.925, df = 2 | 0.630 | 323 |
| Feeling safe | |||||||
| No needs | 91 | 94 | 92 | 92 | |||
| Needs | 9 | 6 | 8 | 8 | 0.635, df = 2 | 0.728 | 321 |
| Social contact | |||||||
| No needs | 31 | 43 | 33 | 35 | |||
| Needs | 69 | 57 | 67 | 65 | 4.47, df = 2 | 0.107 | 322 |
| Space and time to be oneself | |||||||
| No needs | 21 | 35 | 17 | 25 | |||
| Needs | 79 | 65 | 83 | 75 | 7.53, df = 2 | 0.023* | 320 |
| Feeling supported and encouraged | |||||||
| No needs | 44 | 39 | 25 | 42 | |||
| Needs | 56 | 61 | 75 | 58 | 2.10, df = 2 | 0.349 | 315 |
| ASCOT-Carer domain | % of carers in each carer category (all carers) | χ2 value and df | Statistical significance (two-sided) p-value | N | |||
|---|---|---|---|---|---|---|---|
| Sole/main carer | Joint main carer | Not main carer | Total | ||||
| How the carer spends time | |||||||
| No needs | 15 | 15 | 53 | 17 | |||
| Needs | 85 | 85 | 47 | 83 | 17.46, df = 2 | < 0.001*** | 328 |
| Control over daily life | |||||||
| No needs | 25 | 54 | 58 | 28 | |||
| Needs | 75 | 46 | 42 | 72 | 14.44, df = 2 | 0.001*** | 328 |
| Looking after self | |||||||
| No needs | 50 | 85 | 58 | 52 | |||
| Needs | 50 | 15 | 42 | 48 | 6.27, df = 2 | 0.043* | 326 |
| Feeling safe | |||||||
| No needs | 91 | 92 | 100 | 91 | |||
| Needs | 9 | 8 | 0 | 9 | 1.95, df = 2 | 0.378 | 324 |
| Social contact | |||||||
| No needs | 31 | 62 | 68 | 34 | |||
| Needs | 69 | 38 | 32 | 66 | 15.55, df = 2 | < 0.001*** | 326 |
| Space and time to be oneself | |||||||
| No needs | 23 | 31 | 56 | 25 | |||
| Needs | 77 | 69 | 44 | 75 | 10.22, df = 2 | 0.006** | 324 |
| Feeling supported and encouraged | |||||||
| No needs | 41 | 33 | 59 | 41 | |||
| Needs | 59 | 67 | 41 | 59 | 2.55, df = 2 | 0.280 | 318 |
| ASCOT-Carer domain | % of carers in each category of hours of care provided in the previous 24 hours (all carers) | χ2 value and df | Statistical significance (two-sided) p-value | N | ||||
|---|---|---|---|---|---|---|---|---|
| 0–5 hours | 6–11 hours | 12–17 hours | ≥ 18 hours | Total | ||||
| How the carer spends time | ||||||||
| No needs | 31 | 20 | 7 | 13 | 17 | |||
| Needs | 69 | 80 | 93 | 87 | 83 | 17.87, df = 3 | < 0.001*** | 324 |
| Control over daily life | ||||||||
| No needs | 43 | 31 | 22 | 17 | 28 | |||
| Needs | 57 | 69 | 78 | 83 | 72 | 14.82, df = 3 | 0.002** | 325 |
| Looking after self | ||||||||
| No needs | 71 | 57 | 43 | 42 | 53 | |||
| Needs | 29 | 43 | 57 | 58 | 47 | 17.19, df = 3 | 0.001*** | 325 |
| Feeling safe | ||||||||
| No needs | 96 | 93 | 93 | 85 | 92 | |||
| Needs | 4 | 7 | 7 | 15 | 8 | 6.50, df = 3 | 0.090 | 322 |
| Social contact | ||||||||
| No needs | 55 | 34 | 26 | 27 | 35 | |||
| Needs | 45 | 66 | 74 | 73 | 65 | 18.06, df = 3 | < 0.001*** | 324 |
| Space and time to be oneself | ||||||||
| No needs | 42 | 28 | 13 | 19 | 25 | |||
| Needs | 58 | 72 | 87 | 82 | 75 | 20.93, df = 3 | < 0.001*** | 323 |
| Feeling supported and encouraged | ||||||||
| No needs | 53 | 46 | 35 | 32 | 41 | |||
| Needs | 47 | 54 | 65 | 68 | 59 | 9.73, df = 3 | 0.021* | 318 |
| ASCOT-Carer domain | % of carers supporting someone with this type of dementia (all carers) | χ2 and df | Statistical significance (two-sided) p-value | N | |||
|---|---|---|---|---|---|---|---|
| Alzheimer’s disease | Vascular dementia | Other type of dementia | Total | ||||
| How the carer spends time | |||||||
| No needs | 21 | 14 | 4 | 17 | |||
| Needs | 79 | 86 | 96 | 83 | 7.65, df = 2 | 0.022* | 303 |
| Control over daily life | |||||||
| No needs | 32 | 21 | 17 | 28 | |||
| Needs | 68 | 79 | 83 | 72 | 6.04, df = 2 | 0.049* | 305 |
| Looking after self | |||||||
| No needs | 57 | 48 | 31 | 52 | |||
| Needs | 43 | 52 | 69 | 48 | 10.79, df = 2 | 0.005** | 303 |
| Feeling safe | |||||||
| No needs | 92 | 89 | 89 | 91 | |||
| Needs | 8 | 11 | 11 | 9 | 0.624, df = 2 | 0.732 | 301 |
| Social contact | |||||||
| No needs | 40 | 27 | 23 | 35 | |||
| Needs | 60 | 73 | 77 | 65 | 6.23, df = 2 | 0.044* | 303 |
| Space and time to be oneself | |||||||
| No needs | 28 | 16 | 17 | 24 | |||
| Needs | 72 | 84 | 83 | 76 | 4.47, df = 2 | 0.107 | 301 |
| Feeling supported and encouraged | |||||||
| No needs | 49 | 37 | 28 | 43 | |||
| Needs | 51 | 63 | 72 | 57 | 7.88, df = 2 | 0.019* | 296 |
| Type of contact | Number of carers reporting specified frequency of contact | Number not reported | Minimum number of individual contacts | ||||||
|---|---|---|---|---|---|---|---|---|---|
| None | 1 | 2 | 3 | 4 | 5 | 6 | |||
| Face-to-face visit | 3 | 56 | 15 | 3 | 0 | 0 | 0 | 2 | 97 |
| Telephone contact | 12 | 20 | 7 | 1 | 2 | 0 | 0 | 1 | 46 |
| AN group meeting | 3 | 12 | 1 | 1 | 1 | 0 | 0 | – | 21 |
| 1 | 5 | 0 | 1 | 2 | 1 | 1 | – | 27 | |
| Other | 1 | 2 | 0 | 0 | 0 | 0 | 0 | – | 2 |
| Total number of contacts | – | 95 | 46 | 18 | 20 | 5 | 6 | 3 | 193 |
| Type of support received | Carer support services ever used: carers reporting the type of support received from the service | ||||
|---|---|---|---|---|---|
| Respite (n) | Day-sitting/taking out (%) | Night-sitting (n) | Carers’ advice service (%) | Carers’ support group (%) | |
| Emotional and social support | 7 | 16 | 2 | 39 | 50 |
| Information, advice or knowledge | 7 | 12 | 1 | 76 | 17 |
| Practical help | 12 | 10 | 1 | 40 | 26 |
| Time for self | 40 | 75 | 6 | 6 | 11 |
| Assessment of carer’s needs | 5 | 4 | 2 | 27 | 9 |
| Other type of support | 2 | 3 | 2 | 7 | 9 |
| No support | 5 | 8 | 1 | 3 | 4 |
| Number of carers who ever used this service | 53 | 91 | 13 | 157 | 138 |
| Type of support received | Carer support services used in the previous 4 weeks: carers reporting the type of support received from the service | ||||
|---|---|---|---|---|---|
| Respite (n) | Day-sitting/taking out (%) | Night-sitting (n) | Carers’ advice service (%) | Carers’ support group (%) | |
| Emotional and social support | 2 | 13 | 2 | 26 | 37 |
| Information, advice or knowledge | 3 | 10 | 1 | 42 | 41 |
| Practical help | 4 | 7 | 1 | 25 | 20 |
| Time for self | 18 | 52 | 4 | 4 | 9 |
| Assessment of carer’s needs | 2 | 3 | 2 | 19 | 7 |
| Other type of support | 1 | 1 | 1 | 3 | 5 |
| No support | 1 | 3 | 0 | 1 | 0 |
| Number (%) of all carers who had used this service in the previous 4 weeks | 21 (6) | 65 (19) | 7 (2) | 51 (15) | 58 (17) |
| Type of health service use | Not used: % of carers | Used: % (n) of carers | Total number of events | N (100%) | Average contacts per | |
|---|---|---|---|---|---|---|
| Carer (all carers) | Carer using services | |||||
| Elective overnight admission | 99 | 1 (2) | 4 | 318 | 0.012 | 2.000 |
| Elective day admission | 96 | 4 (14) | 23 | 318 | 0.072 | 1.643 |
| Outpatient appointment | 77 | 23 (74) | 113 | 320 | 0.353 | 1.486 |
| Emergency admission | 99 | 1 (4) | 4 | 318 | 0.012 | 1.000 |
| Other hospital appointment | 93 | 7 (23) | 30 | 318 | 0.094 | 1.304 |
| GP contact | 55 | 45 (145) | 211 | 320 | 0.659 | 1.455 |
| Practice or district nurse | 84 | 16 (52) | 76 | 317 | 0.240 | 1.461 |
| Nurse specialist | 93 | 7 (23) | 26 | 314 | 0.082 | 1.130 |
| Therapy professional (including occupational therapist, physiotherapist, speech therapist) | 88 | 12 (39) | 80 | 317 | 0.252 | 2.051 |
| Type of health service use | Not used: % of people with dementia | Used: % (n) of people with dementia | Total number of events | N (100%) | Average contacts per person with dementia (all people with dementia) | Average contact per person with dementia using services |
|---|---|---|---|---|---|---|
| Elective overnight admission | 98 | 2 (4) | 4 | 313 | 0.013 | 1.00 |
| Elective day admission | 96 | 4 (12) | 13 | 313 | 0.041 | 1.083 |
| Outpatient appointment | 71 | 29 (92) | 152 | 320 | 0.474 | 1.652 |
| Emergency admission | 90 | 10 (31) | 47 | 315 | 0.149 | 1.516 |
| Other hospital appointment | 88 | 12 (36) | 43 | 315 | 0.137 | 1.194 |
| GP contact | 47 | 53 (168) | 275 | 322 | 0.854 | 1.637 |
| Practice or district nurse | 69 | 31 (95) | 204 | 314 | 0.650 | 2.147 |
| Nurse specialista | 86 | 14 (40) | 73 | 311 | 0.235 | 1.825 |
| Therapy professional (including occupational therapist, physiotherapist, speech therapist)a | 87 | 12 (39) | 82 | 313 | 0.262 | 2.103 |
| Type of service | Characteristic (% who used the service) | |||||
|---|---|---|---|---|---|---|
| Sex of person with dementia | Age (years) of the person with dementia | Severity of dementia | How long they had been aware of symptoms | Relationship of the person with dementia to the carer | Hours of care provided | |
| Day centre use |
65–74: 37% 85+: 18% χ2 = 7.99, df = 2; p = 0.046 |
Severe: 43% χ2 = 15.74, df = 2; p < 0.001 |
||||
| Other day care |
Female: 14% χ2 = 5.86, df = 1; p = 0.015 |
Severe: 19% χ2 = 10.129, df = 2; p = 0.006 |
||||
| Home care |
Female: 36% χ2 = 11.97, df = 1; p = 0.001 |
85+: 39% χ2 = 9.17, df = 3; p = 0.027 |
Parent/in-law: 40% Spouse/partner: 21% χ2 = 13.35, df = 2; p = 0.001 |
|||
| Meals |
Under 1 year: 31% χ2 = 15.59, df = 3; p = 0.001 |
6–11 hours: 16% χ2 = 9.61, df = 3; p = 0.022 |
||||
| Memory café |
Male: 25% χ2 = 4.73, df = 1; p = 0.030 |
85+: 10% χ2 = 10.04, df = 3; p = 0.018 |
||||
| Item | Unit cost (£) | Source | Notes |
|---|---|---|---|
| Hospital services | |||
| Hospital outpatient appointment | 120 | NHS Reference Costs 2015 to 2016 79 | Average consultant led, non-consultant led and outpatient procedures |
| Planned hospital admission without staying overnight | 733 | NHS Reference Costs 2015 to 2016 79 | Average day case |
| Planned hospital admission with an overnight stay | 3750 | NHS Reference Costs 2015 to 2016 79 | Average elective inpatient |
| Unplanned hospital admission | 1609 | NHS Reference Costs 2015 to 2016 79 | Trim point = average non-elective inpatient, including short stay |
| Other hospital admissions | 389 | NHS Reference Costs 2015 to 2016 79 | Regular day or night admissions |
| Other health-care services | |||
| GP appointment | 36 | PSSRU 2016,49 p. 154 | Per-surgery consultation of 9.22 minutes, including direct care staff costs and qualification costs |
| Nurse appointment | 11 |
PSSRU 2016,49 p. 152 PSSRU 2015,91 p. 183 |
Nurse based at a general practice, including qualification costs: £44 per hour Average contact duration is 15.5 minutes (PSSRU 2015) |
| Nurse specialist appointment | 13 | PSSRU 2016,49 p. 151, PSSRU 2015,91 p. 184 |
Nurse band 7, including qualification costs: £52 per hour Assumes that the average contact duration is 15.5 minutes (PSSRU 2015), as per a nurse based at a general practice |
| Therapist appointment: occupational therapist, physiotherapist, speech therapist, chiropodist, podiatrist | 9 | PSSRU 2016,49 p. 194 |
Allied health professionals band 5: £34 per hour Assumes that the average contact duration is 15.5 minutes (PSSRU 2015), as per a nurse based at a general practice |
| Social care services | |||
| Home care, per appointment | 12 | PSSRU 2016,49 p. 169 |
Face-to-face weekday: £24 per hour Assumes 30 minutes per session (UKHCA 2016 report92) |
| Day care, per hour | 61 | PSSRU 2016,49 p. 37 | £61 per client attendance |
| Meals, per meal | 4 | Glendenning et al.78 p. 201; inflated to 2015–16 | |
| Social service appointment: social worker | 20 | PSSRU 2016,49 p. 165 |
Per hour of client-related work including qualifications = £79 Assumes that the average contact duration is 15.5 minutes (PSSRU 2015), as per a nurse based at a general practice |
| Memory café, per session | 14 | Rotary club 201593 | Based on example of a memory café, at £138.33 per monthly session. Assumes 10 carer–dementia pairs per session |
| Item | Unit cost (£) | Source | Notes | Informal care activity |
|---|---|---|---|---|
| Paid carer, per hour | 24.60 | PSSRU 2016,49 p. 169 | Weighted average of weekday, night and weekend hours | Personal care, physical help, keeping company, transport, keeping an eye |
| Citizens Advice Bureau adviser, per hour | 52.00 | PSSRU 2016,49 p. 171 | Knapp et al. 201394 used the cost of a family support worker to reflect the cost of an adviser | Dealing with care services and benefits |
| Finance administrator, per hour | 25.00 | PSSRU 2016,49 p. 146; NHS Agenda for Change95 | Finance officer is at Agenda for Change band 395 | Dealing with other paperwork and financial matters |
| Cleaner/handy person, per hour | 21.00 | PSSRU 2016,49 p. 146 | Housekeeping assistant is at Agenda for Change band 1. Mid-point band 1 is £15,500 per year.95 Calculated from the ratio wages/hourly cost band 2 | Practical help |
| Outcome measure | All carers | AN | Non-AN | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Mean | SD | Min. | Max. | Obs. | Mean | Obs. | Mean | ||
| ASCOT score | 317 | 10.1 | 4.0 | 0 | 21 | 147 | 9.6 | 170 | 10.6 | 0.019 |
| Self-efficacy on symptoms management | 310 | 27.4 | 10.5 | 5 | 50 | 142 | 26.6 | 168 | 28.0 | 0.238 |
| Self-efficacy on service use | 302 | 22.3 | 9.3 | 4 | 40 | 137 | 22.5 | 165 | 22.0 | 0.654 |
| Overall life satisfaction | 330 | 4.7 | 2.3 | 0 | 10 | 153 | 4.3 | 177 | 5.0 | 0.008 |
| Happiness yesterday | 328 | 5.0 | 2.5 | 0 | 10 | 154 | 4.8 | 174 | 5.1 | 0.278 |
| EQ-5D-5L score | 330 | 0.775 | 0.181 | 0 | 1 | 153 | 0.744 | 177 | 0.802 | 0.004 |
| Variable | All carers | AN | Non-AN | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Mean | SD | Min. | Max. | Obs. | Mean | Obs. | Mean | ||
| Carer | ||||||||||
| Number of hospital services used in the previous 4 weeks | ||||||||||
| Elective overnight | 318 | 0.013 | 0.158 | 0 | 2 | 153 | 0.000 | 165 | 0.024 | 0.172 |
| Elective day | 318 | 0.072 | 0.425 | 0 | 5 | 153 | 0.065 | 165 | 0.079 | 0.778 |
| Outpatient | 320 | 0.366 | 0.784 | 0 | 4 | 153 | 0.399 | 167 | 0.335 | 0.477 |
| Emergency | 318 | 0.013 | 0.112 | 0 | 1 | 153 | 0.013 | 165 | 0.012 | 0.941 |
| Other | 318 | 0.126 | 0.518 | 0 | 4 | 153 | 0.144 | 165 | 0.109 | 0.554 |
| Number of community services used in the previous 4 weeks | ||||||||||
| GP | 320 | 0.659 | 0.937 | 0 | 6 | 153 | 0.686 | 167 | 0.635 | 0.628 |
| Practice nurse | 317 | 0.240 | 0.724 | 0 | 8 | 152 | 0.276 | 165 | 0.206 | 0.390 |
| Nurse specialist | 314 | 0.083 | 0.309 | 0 | 2 | 151 | 0.113 | 163 | 0.055 | 0.097 |
| Other therapist | 317 | 0.252 | 0.783 | 0 | 5 | 152 | 0.276 | 165 | 0.230 | 0.609 |
| Care recipient | ||||||||||
| Number of hospital services used in the previous 4 weeks | ||||||||||
| Elective overnight | 313 | 0.013 | 0.113 | 0 | 1 | 152 | 0.020 | 161 | 0.006 | 0.300 |
| Elective day | 313 | 0.042 | 0.230 | 0 | 2 | 152 | 0.053 | 161 | 0.031 | 0.403 |
| Outpatient | 320 | 0.475 | 0.892 | 0 | 6 | 154 | 0.461 | 166 | 0.488 | 0.788 |
| Emergency | 315 | 0.149 | 0.633 | 0 | 8 | 151 | 0.073 | 164 | 0.220 | 0.033 |
| Other | 315 | 0.137 | 0.404 | 0 | 2 | 153 | 0.098 | 162 | 0.173 | 0.099 |
| Number of community services used in the previous 4 weeks | ||||||||||
| GP | 322 | 0.854 | 1.065 | 0 | 6 | 153 | 0.824 | 169 | 0.882 | 0.619 |
| District nurse | 314 | 0.650 | 1.434 | 0 | 8 | 152 | 0.763 | 162 | 0.543 | 0.167 |
| Nurse specialist | 311 | 0.235 | 0.947 | 0 | 10 | 152 | 0.276 | 159 | 0.195 | 0.451 |
| Therapist | 313 | 0.262 | 1.048 | 0 | 10 | 152 | 0.296 | 161 | 0.230 | 0.579 |
| Number of social care services used in the previous 4 weeks | ||||||||||
| Day care centre | 327 | 1.830 | 4.141 | 0 | 28 | 152 | 2.277 | 175 | 1.442 | 0.077 |
| Other day care service | 324 | 0.262 | 0.996 | 0 | 8 | 152 | 0.118 | 172 | 0.390 | 0.008 |
| Home care | 325 | 8.657 | 20.2 | 0 | 112 | 151 | 7.278 | 174 | 9.853 | 0.253 |
| Meals | 329 | 0.829 | 3.887 | 0 | 28 | 154 | 1.160 | 175 | 0.538 | 0.152 |
| Social services | 327 | 0.223 | 0.745 | 0 | 9 | 154 | 0.182 | 173 | 0.260 | 0.335 |
| Memory café | 330 | 0.430 | 1.062 | 0 | 6 | 153 | 0.242 | 177 | 0.593 | 0.002 |
| Variable | All carers | AN | Non-AN | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Mean | SD | Min. | Max. | Obs. | Mean | Obs. | Mean | ||
| Overall costs | 260 | 999 | 1327 | 0 | 7000 | 121 | 1047 | 139 | 958 | 0.567 |
| Carera | ||||||||||
| Cost of AN | 323 | 36 | 72 | 0 | 440 | 135 | 86 | 188 | 0 | 0.000 |
| Total health-care costs | 306 | 239 | 841 | 0 | 9110 | 150 | 198 | 156 | 277 | 0.393 |
| Hospital costs | 317 | 309 | 1506 | 0 | 17,932 | 153 | 221 | 164 | 391 | 0.304 |
| Community costs | 310 | 28 | 37 | 0 | 238 | 151 | 30 | 159 | 26 | 0.338 |
| Care recipienta | ||||||||||
| Total health-care costs | 297 | 324 | 837 | 0 | 6940 | 148 | 290 | 149 | 358 | 0.483 |
| Hospital costs | 308 | 383 | 1071 | 0 | 9206 | 151 | 372 | 157 | 393 | 0.857 |
| Community costs | 305 | 40 | 47 | 0 | 273 | 150 | 42 | 155 | 37 | 0.419 |
| Total social care costs | 307 | 627 | 1096 | 0 | 6928 | 144 | 663 | 163 | 594 | 0.588 |
| Variable | All carers | AN | Non-AN | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Mean | SD | Min. | Max. | Obs. | Mean | Obs. | Mean | ||
| Short respite/break | ||||||||||
| Ever used (p) | 334 | 0.159 | 0.366 | 0 | 1 | 158 | 0.203 | 176 | 0.119 | 0.051 |
| Used in the previous 4 weeks (p) | 53 | 0.396 | 0.494 | 0 | 1 | 32 | 0.406 | 21 | 0.381 | 1.000 |
| Used in the previous 4 weeks (n) | 21 | 3.048 | 3.057 | 1 | 8 | 13 | 2.308 | 8 | 4.250 | 0.154 |
| Who pays | ||||||||||
| Carer (p) | 19 | 0.421 | 0.507 | 0 | 1 | 11 | 0.455 | 8 | 0.375 | 0.036 |
| Care recipient (p) | 19 | 0.211 | 0.419 | 0 | 1 | 11 | 0.364 | 8 | 0.000 | |
| Both (p) | 19 | 0.158 | 0.375 | 0 | 1 | 11 | 0.182 | 8 | 0.125 | |
| Neither (p) | 19 | 0.211 | 0.419 | 0 | 1 | 11 | 0.000 | 8 | 0.500 | |
| Cost per single use (£) | 14 | 240 | 305 | 8 | 850 | 10 | 297 | 4 | 97 | 0.101 |
| Day-sitting | ||||||||||
| Ever used (p) | 334 | 0.272 | 0.446 | 0 | 1 | 158 | 0.291 | 176 | 0.256 | 0.538 |
| Used in the previous 4 weeks (p) | 91 | 0.714 | 0.454 | 0 | 1 | 46 | 0.674 | 45 | 0.756 | 0.488 |
| Used in the previous 4 weeks (n) | 64 | 6.522 | 7.144 | 1 | 28 | 30 | 5.510 | 34 | 7.416 | 0.266 |
| Who pays | ||||||||||
| Carer (p) | 61 | 0.213 | 0.413 | 0 | 1 | 27 | 0.222 | 34 | 0.206 | 0.556 |
| Care recipient (p) | 61 | 0.230 | 0.424 | 0 | 1 | 27 | 0.222 | 34 | 0.235 | |
| Both (p) | 61 | 0.049 | 0.218 | 0 | 1 | 27 | 0.000 | 34 | 0.088 | |
| Neither (p) | 61 | 0.508 | 0.504 | 0 | 1 | 27 | 0.556 | 34 | 0.471 | |
| Cost per single use (£) | 27 | 37 | 21 | 6 | 100 | 12 | 31 | 15 | 41 | 0.222 |
| Night-sitting | ||||||||||
| Ever used (p) | 334 | 0.039 | 0.194 | 0 | 1 | 158 | 0.032 | 176 | 0.046 | 0.581 |
| Used in the previous 4 weeks (p) | 13 | 0.538 | 0.519 | 0 | 1 | 5 | 0.600 | 8 | 0.500 | 1.000 |
| Used in the previous 4 weeks (n) | 7 | 4.714 | 4.386 | 1 | 10 | 3 | 1.333 | 4 | 7.250 | 0.003 |
| Who pays | ||||||||||
| Care recipient (p) | 7 | 0.286 | 0.488 | 0 | 1 | 3 | 0.000 | 4 | 0.500 | 0.286 |
| Neither (p) | 7 | 0.714 | 0.488 | 0 | 1 | 3 | 1.000 | 4 | 0.500 | |
| Cost per single use (£) | 2 | 120 | 28 | 100 | 140 | 0 | 0 | 2 | 120 | – |
| Advice | ||||||||||
| Ever used (p) | 334 | 0.470 | 0.500 | 0 | 1 | 158 | 0.386 | 176 | 0.545 | 0.004 |
| Used in the previous 4 weeks (p) | 156 | 0.327 | 0.471 | 0 | 1 | 61 | 0.295 | 95 | 0.347 | 0.600 |
| Used in the previous 4 weeks (n) | 50 | 2.120 | 4.148 | 0 | 30 | 16 | 3.313 | 34 | 1.559 | 0.335 |
| Who pays | ||||||||||
| Neither (p) | 47 | 1.000 | 0.000 | 1 | 1 | 14 | 1.000 | 33 | 1.000 | – |
| Cost per single use (£) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | – |
| Support group | ||||||||||
| Ever used (p) | 334 | 0.413 | 0.493 | 0 | 1 | 158 | 0.361 | 176 | 0.460 | 0.075 |
| Used in the previous 4 weeks (p) | 138 | 0.420 | 0.495 | 0 | 1 | 57 | 0.316 | 81 | 0.494 | 0.054 |
| Used in the previous 4 weeks (n) | 57 | 1.860 | 1.663 | 1 | 10 | 17 | 2.176 | 40 | 1.725 | 0.433 |
| Who pays | ||||||||||
| Carer (p) | 56 | 0.107 | 0.312 | 0 | 1 | 17 | 0.118 | 39 | 0.103 | 1.000 |
| Neither (p) | 56 | 0.893 | 0.312 | 0 | 1 | 17 | 0.882 | 39 | 0.897 | |
| Cost per single use (£) | 5 | 6 | 2 | 3 | 8 | 2 | 7 | 3 | 6 | 0.914 |
| Variable | All carers | AN | Non-AN | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Mean | SD | Min. | Max. | Obs. | Mean | Obs. | Mean | ||
| Day care centre | ||||||||||
| Used in the previous 4 weeks (p) | 335 | 0.269 | 0.444 | 0 | 1 | 158 | 0.285 | 177 | 0.254 | 0.076 |
| Used in the previous 4 weeks (n) | 86 | 6.958 | 5.447 | 1 | 28 | 43 | 8.050 | 43 | 5.867 | 0.051 |
| Who pays | ||||||||||
| Carer (p) | 87 | 0.218 | 0.416 | 0 | 1 | 44 | 0.159 | 43 | 0.279 | 0.587 |
| Care recipient (p) | 87 | 0.149 | 0.359 | 0 | 1 | 44 | 0.159 | 43 | 0.140 | |
| Both (p) | 87 | 0.253 | 0.437 | 0 | 1 | 44 | 0.295 | 43 | 0.209 | |
| Neither (p) | 87 | 0.379 | 0.488 | 0 | 1 | 44 | 0.386 | 43 | 0.372 | |
| Cost per single use (£) | 65 | 40 | 27 | 5 | 130 | 35 | 34 | 30 | 47 | 0.029 |
| Other day care service | ||||||||||
| Used in the previous 4 weeks (p) | 335 | 0.099 | 0.298 | 0 | 1 | 158 | 0.057 | 177 | 0.136 | 0.016 |
| Used in the previous 4 weeks (n) | 27 | 3.148 | 1.703 | 1 | 8 | 7 | 2.571 | 20 | 3.350 | 0.254 |
| Who pays | ||||||||||
| Carer (p) | 30 | 0.233 | 0.430 | 0 | 1 | 8 | 0.375 | 22 | 0.182 | 0.565 |
| Care recipient (p) | 30 | 0.300 | 0.466 | 0 | 1 | 8 | 0.375 | 22 | 0.273 | |
| Both (p) | 30 | 0.100 | 0.305 | 0 | 1 | 8 | 0.000 | 22 | 0.136 | |
| Neither (p) | 30 | 0.367 | 0.490 | 0 | 1 | 8 | 0.250 | 22 | 0.409 | |
| Cost per single use (£) | 19 | 15 | 15 | 3 | 55 | 6 | 13 | 13 | 16 | 0.585 |
| Home care | ||||||||||
| Used in the previous 4 weeks (p) | 335 | 0.266 | 0.442 | 0 | 1 | 158 | 0.228 | 177 | 0.299 | 0.144 |
| Used in the previous 4 weeks (n) | 84 | 33.49 | 27.42 | 1 | 112 | 33 | 33.30 | 51 | 33.62 | 0.961 |
| Who pays | ||||||||||
| Carer (p) | 85 | 0.212 | 0.411 | 0 | 1 | 33 | 0.212 | 52 | 0.212 | 0.869 |
| Care recipient (p) | 85 | 0.447 | 0.500 | 0 | 1 | 33 | 0.424 | 52 | 0.462 | |
| Both (p) | 85 | 0.082 | 0.277 | 0 | 1 | 33 | 0.061 | 52 | 0.096 | |
| Neither (p) | 85 | 0.259 | 0.441 | 0 | 1 | 33 | 0.303 | 52 | 0.231 | |
| Cost per single use (£) | 55 | 29 | 36 | 1 | 213 | 20 | 13 | 35 | 38 | 0.002 |
| Meals | ||||||||||
| Used in the previous 4 weeks (p) | 335 | 0.081 | 0.273 | 0 | 1 | 158 | 0.095 | 177 | 0.068 | 0.120 |
| Used in the previous 4 weeks (n) | 24 | 11.36 | 9.517 | 1 | 28 | 14 | 12.76 | 10 | 9.41 | 0.376 |
| Who pays | ||||||||||
| Carer (p) | 26 | 0.192 | 0.402 | 0 | 1 | 15 | 0.333 | 11 | 0.000 | 0.131 |
| Care recipient (p) | 26 | 0.385 | 0.496 | 0 | 1 | 15 | 0.267 | 11 | 0.545 | |
| Both (p) | 26 | 0.346 | 0.485 | 0 | 1 | 15 | 0.333 | 11 | 0.364 | |
| Neither (p) | 26 | 0.077 | 0.272 | 0 | 1 | 15 | 0.067 | 11 | 0.091 | |
| Cost per single use (£) | 23 | 10 | 9 | 3 | 40 | 14 | 11 | 9 | 8 | 0.320 |
| Social services | ||||||||||
| Used in the previous 4 weeks (p) | 335 | 0.137 | 0.345 | 0 | 1 | 158 | 0.120 | 177 | 0.153 | 0.698 |
| Used in the previous 4 weeks (n) | 44 | 1.659 | 1.328 | 1 | 9 | 18 | 1.556 | 26 | 1.731 | 0.610 |
| Who pays | ||||||||||
| Care recipient (p) | 39 | 0.051 | 0.223 | 0 | 1 | 17 | 0.000 | 22 | 0.091 | 0.495 |
| Neither (p) | 39 | 0.949 | 0.223 | 0 | 1 | 17 | 1.000 | 22 | 0.909 | |
| Cost per single use(£) | 2 | 30 | 14 | 20 | 40 | 0 | 0 | 2 | 30 | - |
| Memory café | ||||||||||
| Used in the previous 4 weeks (p) | 335 | 0.194 | 0.396 | 0 | 1 | 158 | 0.108 | 177 | 0.271 | 0.000 |
| Used in the previous 4 weeks (n) | 63 | 2.254 | 1.344 | 1 | 6 | 15 | 2.467 | 48 | 2.188 | 0.509 |
| Who pays | ||||||||||
| Carer (p) | 63 | 0.143 | 0.353 | 0 | 1 | 17 | 0.118 | 46 | 0.152 | 0.708 |
| Care recipient (p) | 63 | 0.064 | 0.246 | 0 | 1 | 17 | 0.000 | 46 | 0.087 | |
| Both (p) | 63 | 0.254 | 0.439 | 0 | 1 | 17 | 0.235 | 46 | 0.261 | |
| Neither (p) | 63 | 0.540 | 0.502 | 0 | 1 | 17 | 0.647 | 46 | 0.500 | |
| Cost per single use (£) | 24 | 7 | 8 | 2 | 40 | 1 | 6 | 23 | 7 | 0.712 |
| Variable | All carers | AN | Non-AN | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Mean | SD | Min. | Max. | Obs. | Mean | Obs. | Mean | ||
| Informal care tasks | ||||||||||
| Personal care | 137 | 2.547 | 2.584 | 1 | 24 | 60 | 2.533 | 77 | 2.558 | 0.951 |
| Physical help | 66 | 3.152 | 4.203 | 1 | 24 | 27 | 2.481 | 39 | 3.615 | 0.209 |
| Help with care services | 62 | 1.984 | 1.895 | 1 | 11 | 12 | 1.583 | 50 | 2.080 | 0.166 |
| Help with paperwork | 68 | 2.147 | 2.377 | 1 | 15 | 12 | 1.667 | 56 | 2.250 | 0.176 |
| Other practical help | 243 | 3.650 | 3.030 | 1 | 24 | 105 | 3.686 | 138 | 3.623 | 0.874 |
| Keeping company | 183 | 7.120 | 6.115 | 1 | 24 | 80 | 8.188 | 103 | 6.291 | 0.035 |
| Taking out | 85 | 3.694 | 2.980 | 1 | 14 | 22 | 3.545 | 63 | 3.746 | 0.773 |
| Giving medicines | 67 | 2.448 | 4.190 | 1 | 24 | 16 | 2.688 | 51 | 2.373 | 0.788 |
| Keeping an eye | 216 | 11.25 | 7.861 | 1 | 24 | 97 | 12.63 | 119 | 10.12 | 0.017 |
| Any other help | 13 | 6.846 | 7.163 | 1 | 24 | 5 | 7.600 | 8 | 6.375 | 0.790 |
| Informal care costs (£): opportunity cost method | ||||||||||
| Personal care | 137 | 40 | 41 | 16 | 377 | 60 | 40 | 77 | 40 | 0.951 |
| Physical help | 66 | 50 | 66 | 16 | 377 | 27 | 39 | 39 | 57 | 0.209 |
| Help with care services | 62 | 31 | 30 | 16 | 173 | 12 | 25 | 50 | 33 | 0.166 |
| Help with paperwork | 68 | 34 | 37 | 16 | 236 | 12 | 26 | 56 | 35 | 0.176 |
| Other practical help | 243 | 57 | 48 | 16 | 377 | 105 | 58 | 138 | 57 | 0.874 |
| Keeping company | 183 | 112 | 96 | 16 | 377 | 80 | 129 | 103 | 99 | 0.035 |
| Taking out | 85 | 58 | 47 | 16 | 220 | 22 | 56 | 63 | 59 | 0.773 |
| Giving medicines | 67 | 38 | 66 | 16 | 377 | 16 | 42 | 51 | 37 | 0.788 |
| Keeping an eye | 216 | 177 | 124 | 16 | 377 | 97 | 199 | 119 | 159 | 0.017 |
| Any other help | 13 | 108 | 113 | 16 | 377 | 5 | 120 | 8 | 100 | 0.790 |
| Total costs | 323 | 293 | 267 | 16 | 1902 | 149 | 283 | 174 | 301 | 0.547 |
| Informal care costs (£): proxy good method | ||||||||||
| Personal care | 137 | 63 | 64 | 25 | 590 | 60 | 62 | 77 | 63 | 0.951 |
| Physical help | 66 | 78 | 103 | 25 | 590 | 27 | 61 | 39 | 89 | 0.209 |
| Help with care services | 62 | 103 | 99 | 52 | 572 | 12 | 82 | 50 | 108 | 0.166 |
| Help with paperwork | 68 | 54 | 59 | 25 | 375 | 12 | 42 | 56 | 56 | 0.176 |
| Other practical help | 243 | 77 | 64 | 21 | 504 | 105 | 77 | 138 | 76 | 0.874 |
| Keeping company | 183 | 175 | 150 | 25 | 590 | 80 | 201 | 103 | 155 | 0.035 |
| Taking out | 85 | 91 | 73 | 25 | 344 | 22 | 87 | 63 | 92 | 0.773 |
| Giving medicines | 67 | 60 | 103 | 25 | 590 | 16 | 66 | 51 | 58 | 0.788 |
| Keeping an eye | 216 | 277 | 193 | 25 | 590 | 97 | 311 | 119 | 249 | 0.017 |
| Any other help | 13 | 168 | 176 | 25 | 590 | 5 | 187 | 8 | 157 | 0.790 |
| Total costs | 323 | 459 | 427 | 25 | 3181 | 149 | 437 | 174 | 477 | 0.393 |
| Variable | Obs. | Mean | SD | Min. | Max. |
|---|---|---|---|---|---|
| Use of AN | |||||
| Yes | 158 | 0.886 | 0.319 | 0 | 1 |
| No | 158 | 0.101 | 0.303 | 0 | 1 |
| Do not know | 158 | 0.013 | 0.112 | 0 | 1 |
| First use | |||||
| < 1 month ago | 158 | 0.076 | 0.266 | 0 | 1 |
| 1–2 months ago | 158 | 0.076 | 0.266 | 0 | 1 |
| 3–6 months ago | 158 | 0.165 | 0.372 | 0 | 1 |
| 7–12 months ago | 158 | 0.139 | 0.347 | 0 | 1 |
| 1–2 years ago | 158 | 0.177 | 0.383 | 0 | 1 |
| 2–5 years ago | 158 | 0.139 | 0.347 | 0 | 1 |
| > 5 years ago | 158 | 0.051 | 0.220 | 0 | 1 |
| Do not know | 158 | 0.025 | 0.158 | 0 | 1 |
| Did not answer | 158 | 0.152 | 0.360 | 0 | 1 |
| Last use | |||||
| Up to 6 months ago | 158 | 0.772 | 0.421 | 0 | 1 |
| 7–12 months ago | 158 | 0.032 | 0.176 | 0 | 1 |
| 1–2 years ago | 158 | 0.032 | 0.176 | 0 | 1 |
| Do not know | 158 | 0.025 | 0.158 | 0 | 1 |
| Did not answer | 158 | 0.139 | 0.347 | 0 | 1 |
| Kind of contact | |||||
| Face-to-face visit | 158 | 0.835 | 0.372 | 0 | 1 |
| Telephone contact | 158 | 0.481 | 0.501 | 0 | 1 |
| E-mail contact | 158 | 0.089 | 0.285 | 0 | 1 |
| Support group meeting | 158 | 0.177 | 0.383 | 0 | 1 |
| Other contact | 158 | 0.038 | 0.192 | 0 | 1 |
| Use of AN in the previous 4 weeks | |||||
| Yes | 158 | 0.563 | 0.498 | 0 | 1 |
| No | 158 | 0.310 | 0.464 | 0 | 1 |
| Did not answer | 158 | 0.127 | 0.334 | 0 | 1 |
| Contacts in the previous 4 weeks | |||||
| Face-to-face visit | 135 | 0.704 | 0.754 | 0 | 3 |
| Telephone contact | 135 | 0.333 | 0.743 | 0 | 4 |
| E-mail contact | 135 | 0.200 | 0.871 | 0 | 6 |
| Support group meeting | 135 | 0.156 | 0.531 | 0 | 4 |
| Other contact | 135 | 0.015 | 0.121 | 0 | 1 |
| Cost of AN in the previous 4 weeks (£) | 86 | 136 | 78 | 11 | 440 |
| Type of cost | Project | General template | Average | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| Recruitment, year 1 | 4103 | NR | 3000 | 3000 | NR | NR | 4265 | 3592 |
| Employment | ||||||||
| Year 1 | 39,582 | 33,630 | 45,346 | 45,346 | 41,678 | 38,281 | 41,145 | 40,715 |
| Year 2 | 41,459 | 37,873 | 41,557 | 40,296 | ||||
| Training | 3% of salary | |||||||
| Year 1 | 1026 | 1200 | 1800 | 1077 | 1276 | |||
| Year 2 | 1056 | 135 | 1077 | 756 | ||||
| Travel | ||||||||
| Year 1 | 4500 | 1814 | 3421 | 3421 | 1149 | 8969 | 4500 | 3968 |
| Year 2 | 4500 | 4227 | 4500 | 4409 | ||||
| Subscription and insurance per year | 70 | 100 | 704 | 704 | 100 | 395 | ||
| Equipment | ||||||||
| Year 1 | 1618 | 8411 | 850 | 850 | 4101 | 1000 | 1618 | 2635 |
| Year 2 | 550 | 322 | 450 | 441 | ||||
| Indirect costs (HR, finance) per year | 987 | NR | NR | NR | = service 1 | 987 | ||
| Overheads per year | 3000 | 3000 | 3000 | 2000 | NR | NR | 2750 | |
| Dementia UK costs | ||||||||
| Database licence per year | 600 | 600 | 600 | 600 | 600 | 875 | 600 | |
| Academy support per year | 3500 | 3000 | 3000 | 3000 | 3000 | 1750 | 2000 | |
| Dementia UK pioneer time | NR | 4000 | 2000 | 2000 | 3000 | 600 | 4900 | |
| Dementia UK overheads | NR | NR | NR | NR | 4000 | NR | 5964 | |
| Management recharge cost | 9156 | 9473 | ||||||
| Covariates | All carers | AN (mean) | Non-AN (mean) | |||
|---|---|---|---|---|---|---|
| Mean | SD | Min. | Max. | |||
| Carer’s characteristics | ||||||
| Male (ref.) | 0.309 | 0.463 | 0 | 1 | 0.341 | 0.280 |
| Female | 0.691 | 0.463 | 0 | 1 | 0.659 | 0.720 |
| Aged 16–54 years (ref.) | 0.177 | 0.383 | 0 | 1 | 0.121 | 0.227 |
| Aged 55–64 years | 0.252 | 0.435 | 0 | 1 | 0.220 | 0.280 |
| Aged 65–69 years | 0.110 | 0.313 | 0 | 1 | 0.129 | 0.093 |
| Aged 70–74 years | 0.149 | 0.357 | 0 | 1 | 0.167 | 0.133 |
| Aged ≥ 75 years | 0.312 | 0.464 | 0 | 1 | 0.364 | 0.267 |
| Below university-level education (ref.) | 0.720 | 0.450 | 0 | 1 | 0.773 | 0.673 |
| Bachelor’s degree | 0.195 | 0.397 | 0 | 1 | 0.197 | 0.193 |
| Master’s degree or above | 0.085 | 0.280 | 0 | 1 | 0.030 | 0.133 |
| Full- or part-time job | 0.209 | 0.407 | 0 | 1 | 0.159 | 0.253 |
| Looking after person with dementia full-time | 0.248 | 0.433 | 0 | 1 | 0.295 | 0.207 |
| Retired | 0.582 | 0.494 | 0 | 1 | 0.614 | 0.553 |
| No difficulties (ref.) | 0.234 | 0.424 | 0 | 1 | 0.197 | 0.267 |
| Some difficulties | 0.326 | 0.470 | 0 | 1 | 0.311 | 0.340 |
| Severe difficulties | 0.316 | 0.466 | 0 | 1 | 0.379 | 0.260 |
| Do not know/prefer not to say | 0.124 | 0.330 | 0 | 1 | 0.114 | 0.133 |
| EQ-5D score | 0.774 | 0.182 | 0 | 1 | 0.752 | 0.793 |
| Caring role | ||||||
| Main carer (ref.) | 0.926 | 0.263 | 0 | 1 | 0.977 | 0.880 |
| Joint or not main carer | 0.075 | 0.263 | 0 | 1 | 0.023 | 0.120 |
| Spouse/partner (ref.) | 0.674 | 0.470 | 0 | 1 | 0.742 | 0.613 |
| Parent/parent-in-law | 0.287 | 0.453 | 0 | 1 | 0.227 | 0.340 |
| Other relationship | 0.039 | 0.194 | 0 | 1 | 0.030 | 0.047 |
| Personal care | 0.702 | 0.458 | 0 | 1 | 0.750 | 0.660 |
| Physical care | 0.482 | 0.501 | 0 | 1 | 0.538 | 0.433 |
| Total hours | 12 | 7 | 0 | 24 | 13 | 11 |
| Duration of < 1 year (ref.) | 0.064 | 0.245 | 0 | 1 | 0.046 | 0.080 |
| Duration of 1–3 years | 0.323 | 0.468 | 0 | 1 | 0.364 | 0.287 |
| Duration of 3–5 years | 0.277 | 0.448 | 0 | 1 | 0.235 | 0.313 |
| Duration of 5–10 years | 0.234 | 0.424 | 0 | 1 | 0.250 | 0.220 |
| Duration of ≥ 10 years | 0.103 | 0.304 | 0 | 1 | 0.106 | 0.100 |
| Replacement for a break (ref.) | 0.411 | 0.493 | 0 | 1 | 0.326 | 0.487 |
| No replacement for a break | 0.589 | 0.493 | 0 | 1 | 0.674 | 0.513 |
| AN | 0.468 | 0.500 | 0 | 1 | 1.000 | 0.000 |
| Care recipient’s characteristics | ||||||
| Aged 45–64 years (ref.) | 0.099 | 0.300 | 0 | 1 | 0.076 | 0.120 |
| Aged 65–74 years | 0.202 | 0.402 | 0 | 1 | 0.212 | 0.193 |
| Aged ≥ 75 years | 0.699 | 0.460 | 0 | 1 | 0.712 | 0.687 |
| Symptoms for < 1 year (ref.) | 0.046 | 0.210 | 0 | 1 | 0.061 | 0.033 |
| Symptoms for 1–5 years | 0.589 | 0.493 | 0 | 1 | 0.598 | 0.580 |
| Symptoms for 6–10 years | 0.280 | 0.450 | 0 | 1 | 0.265 | 0.293 |
| Symptoms for ≥ 11 years | 0.085 | 0.280 | 0 | 1 | 0.076 | 0.093 |
| Formal diagnosis (ref.) | 0.965 | 0.185 | 0 | 1 | 0.970 | 0.960 |
| No diagnosis/do not know | 0.036 | 0.185 | 0 | 1 | 0.030 | 0.040 |
| Alzheimer’s disease | 0.606 | 0.489 | 0 | 1 | 0.515 | 0.687 |
| Vascular dementia | 0.333 | 0.472 | 0 | 1 | 0.439 | 0.240 |
| Other dementia | 0.270 | 0.444 | 0 | 1 | 0.258 | 0.280 |
| Mild (ref.) | 0.103 | 0.304 | 0 | 1 | 0.068 | 0.133 |
| Moderate | 0.631 | 0.483 | 0 | 1 | 0.644 | 0.620 |
| Severe | 0.266 | 0.443 | 0 | 1 | 0.288 | 0.247 |
| Variable | ASCOT score | Self-efficacy on | Overall life satisfaction | Happiness yesterday | |
|---|---|---|---|---|---|
| Symptom management | Service use | ||||
| AN | 0.382 | 1.243 | 1.990* | 0.087 | 0.433 |
| (0.397) | (1.317) | (1.060) | (0.266) | (0.279) | |
| Carer’s characteristics | |||||
| Female | –0.539 | –2.384 | –3.842*** | –0.166 | 0.001 |
| Aged 55–64 years | –0.134 | –2.399 | –1.712 | –0.387 | –0.618 |
| Aged 65–69 years | 0.127 | –2.214 | 0.596 | –0.181 | –0.300 |
| Aged 70–74 years | 0.202 | –1.761 | 1.448 | –0.015 | 0.227 |
| Aged ≥ 75 years | 0.833 | –3.149 | –5.370* | 0.629 | 0.545 |
| Bachelor’s degree | –0.483 | –2.408* | –2.403* | –0.456 | –0.467 |
| Master’s degree or above | –0.871 | –3.096 | –1.205 | –0.083 | 0.157 |
| Full- or part-time job | 1.212* | 2.045 | 1.227 | 0.069 | –0.042 |
| Looking after person with dementia full-time | 0.273 | 0.264 | 0.743 | 0.050 | 0.055 |
| Retired | 1.159** | 2.216 | 2.152 | 0.289 | 0.499 |
| Some financial difficulties | –1.531*** | –1.384 | –3.928*** | –0.830** | –1.075*** |
| Severe financial difficulties | –2.281*** | –2.936 | –3.926*** | –1.308*** | –1.382*** |
| Do not know/prefer not to say | –2.636*** | –1.904 | –4.371** | –0.740 | –1.136** |
| EQ-5D score | 7.131*** | 13.295*** | 8.581*** | 4.129*** | 4.160*** |
| Caring role | |||||
| Joint or not main carer | 0.543 | 2.790 | 3.307 | 0.823* | 0.535 |
| Parent/parent-in-law | 0.889 | 0.375 | –2.327 | 0.336 | 0.407 |
| Other relationship | 0.063 | –4.703 | –5.352* | –0.200 | –0.206 |
| Personal care | –0.495 | –1.076 | –0.896 | –0.214 | –0.031 |
| Physical care | –0.578 | 2.578* | 0.964 | 0.108 | 0.003 |
| Total hours | –0.084*** | 0.213** | 0.042 | –0.023 | –0.029 |
| Duration of 1–3 years | –0.142 | 2.512 | 6.458*** | 0.274 | 0.765 |
| Duration of 3–5 years | –0.195 | 1.496 | 4.667** | 0.331 | 0.895 |
| Duration of 5–10 years | –0.108 | 2.149 | 5.895** | –0.141 | 0.453 |
| Duration of ≥ 10 years | –0.658 | 0.493 | 4.568 | –0.021 | 0.360 |
| No replacement for a break | –1.192*** | –3.433** | –2.829*** | –0.746*** | –0.772*** |
| Care recipient’s characteristics | |||||
| Aged 65–74 years | 0.782 | 0.187 | 1.552 | 0.529 | 0.640 |
| Aged ≥ 75 years | 0.665 | 2.396 | 4.932** | 0.290 | 0.367 |
| Symptoms for 1–5 years | 0.107 | 1.565 | 0.402 | 0.961 | –0.185 |
| Symptoms for 6–10 years | –0.247 | 2.725 | 0.117 | 1.260 | 0.429 |
| Symptoms for ≥ 11 years | 0.993 | 6.705 | 1.174 | 1.567* | 0.985 |
| No diagnosis/do not know | –1.424 | –6.734*** | –4.891* | –0.208 | –0.329 |
| Vascular dementia | –0.722 | –1.211 | –1.682 | –0.096 | 0.159 |
| Other dementia | –0.561 | –0.827 | –4.162*** | –0.062 | 0.218 |
| Moderate severity | –0.585 | –2.828 | –3.692** | –0.827* | –1.012* |
| Severe severity | –1.722** | –5.450** | –4.208** | –1.574*** | –1.795*** |
| Constant | 7.928*** | 17.986*** | 18.970*** | 2.271 | 2.782* |
| Observations | 282 | 274 | 268 | 287 | 285 |
| R 2 | 0.459 | 0.260 | 0.350 | 0.340 | 0.335 |
| Variables | Costs | |||
|---|---|---|---|---|
| Overall | Health care | Care recipient’s total social care | ||
| Carer’s total | Care recipient’s total | |||
| Carer’s characteristics | ||||
| AN | 26.575 | –170.163 | –96.722 | 58.072 |
| (202.900) | (145.300) | (132.800) | (146.100) | |
| Female | –39.048 | 249.835 | 20.416 | 11.324 |
| Aged 55–64 years | –467.576 | 128.496 | –141.026 | –335.640 |
| Aged 65–69 years | –334.156 | 291.419 | –73.958 | –339.032 |
| Aged 70–74 years | –123.763 | 195.256 | 300.093 | –556.264* |
| Aged ≥ 75 years | –251.914 | 477.933 | –23.456 | –270.283 |
| Bachelor’s degree | 366.745 | –132.246* | –121.511 | 347.939** |
| Master’s degree or above | 356.185 | –24.123 | –148.834 | 288.675 |
| Full- or part-time job | 106.192 | –161.379 | 200.487 | –159.649 |
| Looking after person with dementia full-time | –207.212 | –130.192 | –64.121 | –68.701 |
| Retired | 273.644 | 62.005 | 23.403 | 324.513* |
| Some financial difficulties | 70.590 | –5.400 | 36.713 | –38.273 |
| Severe financial difficulties | 32.179 | 148.637 | –86.977 | 222.563 |
| Do not know/prefer not to say | 714.671 | 339.305 | 457.131 | 104.296 |
| EQ-5D score | 287.667 | –480.094 | –39.793 | 272.184 |
| Caring role | ||||
| Joint or not main carer | 52.862 | –175.647 | 83.663 | 12.641 |
| Parent/parent-in-law | 12.912 | 133.233 | –100.213 | 101.146 |
| Other relationship | 195.767 | 131.535 | –79.843 | 115.261 |
| Personal care | 191.701 | 77.500 | –79.857 | 129.525 |
| Physical care | 193.175 | 33.166 | 206.183 | 17.289 |
| Total hours | 3.924 | –10.643 | 10.046 | –13.727 |
| Duration of 1–3 years | 398.569 | 110.028 | 160.741 | 141.011 |
| Duration of 3–5 years | 440.687 | –148.956 | 257.482 | 138.329 |
| Duration of 5–10 years | 208.638 | –146.994 | –145.185 | 397.548 |
| Duration of ≥ 10 years | 213.159 | –403.659* | –441.864 | 699.565* |
| No replacement for a break | –6.526 | –246.425* | –124.837 | 40.765 |
| Care recipient’s characteristics | ||||
| Aged 65–74 years | –179.399 | –89.527 | –149.343 | 101.373 |
| Aged ≥ 75 years | –9.698 | –58.444 | 123.903 | –75.069 |
| Symptoms for 1–5 years | –333.064 | 300.841* | –1.208 | –65.940 |
| Symptoms for 6–10 years | –280.120 | 224.415 | 46.416 | –117.714 |
| Symptoms for ≥ 11 years | 29.423 | 317.816 | 562.790 | –404.817 |
| No diagnosis/do not know | 173.043 | –193.276 | 89.217 | –227.561 |
| Vascular dementia | 2.554 | –20.470 | 274.529** | –199.234 |
| Other dementia | 26.060 | 133.562 | 239.774 | –76.373 |
| Moderate severity | –182.493 | 71.698 | –189.708 | 29.877 |
| Severe severity | 480.491 | 480.773 | –2.824 | 561.472** |
| Constant | 407.519 | 113.887 | 112.560 | 179.663 |
| Observations | 227 | 269 | 259 | 266 |
| R 2 | 0.173 | 0.174 | 0.170 | 0.164 |
| Technique | Sample | Mean bias | Median bias |
|---|---|---|---|
| Kernel | Unmatched | 14.4 | 11.4 |
| Matched | 3.4 | 3.1 | |
| Nearest neighbour | Unmatched | 14.4 | 11.4 |
| Matched | 8.4 | 7.6 | |
| Calliper (0.2) | Unmatched | 14.4 | 11.4 |
| Matched | 8.4 | 7.6 |
| Variables | ASCOT score | Self-efficacy on | Overall life satisfaction | Happiness yesterday | |
|---|---|---|---|---|---|
| Symptoms management | Service use | ||||
| AN | 0.648 | 1.618 | 2.634 | 0.171 | 0.575 |
| (0.562) | (1.505) | (1.328)** | (0.333) | (0.346)* | |
| Coefficient on covariates from logit regression when the AN dummy is the dependent variable | |||||
| Carer’s characteristics | |||||
| Female | 0.816 | 0.972 | 0.901 | 0.897 | 0.914 |
| Aged 55–64 years | 1.905 | 1.698 | 1.590 | 1.933 | 1.674 |
| Aged 65–69 years | 3.129 | 3.204 | 2.943 | 3.588* | 3.075 |
| Aged 70–74 years | 2.036 | 1.943 | 2.195 | 2.356 | 1.861 |
| Aged ≥ 75 years | 1.935 | 2.206 | 2.048 | 2.587 | 1.948 |
| Bachelor’s degree | 1.015 | 1.124 | 1.003 | 1.055 | 1.027 |
| Master’s degree or above | 0.222** | 0.165** | 0.153*** | 0.233** | 0.233** |
| Full- or part-time job | 1.115 | 0.946 | 0.895 | 1.245 | 1.083 |
| Looking after person with dementia full-time | 1.241 | 1.261 | 1.043 | 1.285 | 1.289 |
| Retired | 0.832 | 0.763 | 0.729 | 0.837 | 0.793 |
| Some financial difficulties | 1.088 | 1.153 | 1.152 | 1.062 | 1.044 |
| Severe financial difficulties | 1.697 | 1.852 | 1.822 | 1.604 | 1.645 |
| Do not know/prefer not to say | 1.258 | 1.225 | 1.243 | 1.202 | 1.145 |
| EQ-5D score | 0.483 | 0.429 | 0.586 | 0.483 | 0.475 |
| Caring role | |||||
| Joint or not main carer | 0.398 | 0.283* | 0.267* | 0.289* | 0.328 |
| Parent/parent-in-law | 0.829 | 0.784 | 0.776 | 0.873 | 0.726 |
| Other relationship | 1.154 | 1.201 | 1.197 | 1.368 | 1.122 |
| Personal care | 1.300 | 1.587 | 1.437 | 1.347 | 1.284 |
| Physical care | 1.117 | 0.979 | 1.061 | 1.074 | 1.135 |
| Total hours | 1.009 | 1.000 | 1.000 | 1.007 | 1.006 |
| Duration of 1–3 years | 3.834* | 3.673 | 3.845* | 3.814* | 3.965* |
| Duration of 3–5 years | 2.327 | 2.378 | 2.592 | 2.502 | 2.677 |
| Duration of 5–10 years | 3.860 | 3.725 | 3.954 | 4.692* | 4.598* |
| Duration of ≥ 10 years | 3.871 | 3.814 | 4.408 | 4.509 | 4.366 |
| No replacement for a break | 1.512 | 1.634 | 1.505 | 1.613 | 1.560 |
| Care recipient’s characteristics | |||||
| Aged 65–74 years | 0.986 | 1.028 | 0.980 | 0.944 | 0.999 |
| Aged ≥ 75 years | 1.132 | 1.024 | 1.096 | 0.978 | 1.152 |
| Symptoms for 1–5 years | 0.135** | 0.141** | 0.140** | 0.122** | 0.136** |
| Symptoms for 6–10 years | 0.084** | 0.082** | 0.085** | 0.068*** | 0.078** |
| Symptoms for ≥ 11 years | 0.067** | 0.075** | 0.090** | 0.057** | 0.065** |
| No diagnosis/do not know | 0.668 | 0.545 | 0.484 | 0.539 | 0.540 |
| Vascular dementia | 2.456*** | 2.479*** | 2.359** | 2.329*** | 2.263** |
| Other dementia | 1.055 | 0.988 | 1.090 | 1.045 | 1.035 |
| Moderate severity | 2.367 | 2.367 | 2.278 | 2.346 | 2.291 |
| Severe severity | 2.444 | 2.380 | 2.091 | 2.347 | 2.241 |
| Constant | 0.440 | 0.475 | 0.466 | 0.417 | 0.479 |
| Observations | 282 | 274 | 268 | 287 | 285 |
| Variable | Overall costs | Carer’s total health-care costs | Care recipient’s total health-care costs | Care recipient’s total social care costs |
|---|---|---|---|---|
| AN | –113.215 | –207.220 | –186.252 | 10.682 |
| (215.731) | (145.259) | (142.972) | (144.031) | |
| Coefficient on covariates from logit regression where the AN dummy is the dependent variable | ||||
| Carer’s characteristics | ||||
| Female | 0.799 | 0.881 | 0.976 | 0.801 |
| Aged 55–64 years | 1.287 | 1.825 | 1.831 | 1.490 |
| Aged 65–69 years | 2.562 | 2.750 | 3.088 | 3.270 |
| Aged 70–74 years | 1.811 | 2.238 | 2.115 | 1.786 |
| Aged ≥ 75 years | 1.055 | 1.655 | 1.815 | 1.632 |
| Bachelor’s degree | 1.386 | 0.965 | 1.179 | 1.045 |
| Master’s degree or above | 0.155** | 0.268** | 0.261** | 0.164** |
| Full- or part-time job | 0.882 | 1.068 | 0.864 | 0.939 |
| Looking after person with dementia full-time | 1.172 | 1.094 | 1.121 | 1.231 |
| Retired | 0.641 | 0.858 | 0.619 | 0.713 |
| Some financial difficulties | 1.536 | 1.000 | 1.097 | 1.346 |
| Severe financial difficulties | 2.705** | 1.430 | 1.723 | 2.215* |
| Do not know/prefer not to say | 1.667 | 1.064 | 1.370 | 1.232 |
| EQ-5D score | 0.775 | 0.329 | 0.680 | 0.400 |
| Caring role | ||||
| Joint or not main carer | 0.441 | 0.268* | 0.284* | 0.367 |
| Parent/parent-in-law | 0.527 | 0.777 | 0.593 | 0.710 |
| Other relationship | 0.432 | 1.027 | 0.596 | 1.125 |
| Personal care | 1.493 | 1.188 | 1.389 | 1.347 |
| Physical care | 1.412 | 1.383 | 1.263 | 0.987 |
| Total hours | 1.015 | 1.004 | 1.007 | 1.016 |
| Duration of 1–3 years | 3.830 | 4.196* | 4.467* | 3.810 |
| Duration of 3–5 years | 2.364 | 2.585 | 2.712 | 2.950 |
| Duration of 5–10 years | 3.737 | 4.696* | 5.076* | 4.249 |
| Duration of ≥ 10 years | 2.286 | 3.665 | 3.707 | 4.370 |
| No replacement for a break | 1.653 | 1.583 | 1.487 | 1.519 |
| Care recipient’s characteristics | ||||
| Aged 65–74 years | 1.123 | 0.999 | 0.854 | 1.156 |
| Aged ≥ 75 years | 1.966 | 1.033 | 1.301 | 1.398 |
| Symptoms for 1–5 years | 0.238 | 0.125** | 0.151* | 0.153** |
| Symptoms for 6–10 years | 0.198 | 0.089** | 0.098** | 0.084** |
| Symptoms for ≥ 11 years | 0.217 | 0.070** | 0.085** | 0.071** |
| No diagnosis/do not know | 0.359 | 0.398 | 0.325 | 0.606 |
| Vascular dementia | 2.334** | 1.922** | 2.065** | 2.270** |
| Other dementia | 0.817 | 0.932 | 0.903 | 0.872 |
| Moderate severity | 1.660 | 2.293 | 2.221 | 2.009 |
| Severe severity | 1.233 | 2.213 | 1.892 | 2.256 |
| Constant | 0.170 | 0.875 | 0.388 | 0.478 |
| Observations | 227 | 269 | 259 | 266 |
| Variable | All carers | AN | Non-AN | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Mean | SD | Min. | Max. | Obs. | Mean | Obs. | Mean | ||
| Travel time (hours) | 327 | 0.222 | 0.151 | 0 | 1 | 155 | 0.151 | 172 | 0.286 | 0.000 |
| Type of LA | ||||||||||
| County | 327 | 0.287 | 0.453 | 0 | 1 | 155 | 0.484 | 172 | 0.110 | 0.000 |
| London | 0.131 | 0.338 | 0 | 1 | 0.116 | 0.145 | ||||
| Metropolitan | 0.217 | 0.413 | 0 | 1 | 0.194 | 0.238 | ||||
| Unitary | 0.364 | 0.482 | 0 | 1 | 0.206 | 0.506 | ||||
| Variable | ASCOT score | Self-efficacy on | Overall life satisfaction | Happiness yesterday | |
|---|---|---|---|---|---|
| Symptoms management | Service use | ||||
| AN | 1.462* | 2.871 | 3.276 | 0.249 | 0.989 |
| (0.854) | (3.130) | (2.633) | (0.658) | (0.636) | |
| Carer’s characteristics | |||||
| Female | –0.494 | –2.532* | –3.951*** | –0.173 | –0.019 |
| Aged 55–64 years | –0.266 | –2.572 | –1.835 | –0.407 | –0.670 |
| Aged 65–69 years | –0.122 | –2.542 | 0.345 | –0.217 | –0.413 |
| Aged 70–74 years | 0.060 | –1.903 | 1.291 | –0.037 | 0.175 |
| Aged ≥ 75 years | 0.704 | –3.031 | –5.289** | 0.623 | 0.539 |
| Bachelor’s degree | –0.490 | –2.513* | –2.458** | –0.461 | –0.480 |
| Master’s degree or above | –0.606 | –2.924 | –1.027 | –0.061 | 0.246 |
| Full- or part-time job | 1.191* | 1.989 | 1.213 | 0.059 | –0.060 |
| Looking after person with dementia full-time | 0.213 | 0.015 | 0.619 | 0.033 | –0.001 |
| Retired | 1.189** | 2.299 | 2.233 | 0.293 | 0.518 |
| Some difficulties | –1.543*** | –1.395 | –3.937*** | –0.829** | –1.072*** |
| Severe difficulties | –2.407*** | –2.917* | –3.933*** | –1.311*** | –1.404*** |
| Do not know/prefer not to say | –2.684*** | –1.986 | –4.443** | –0.746* | –1.153** |
| EQ-5D score | 7.298*** | 13.911*** | 8.962*** | 4.176*** | 4.306*** |
| Caring role | |||||
| Joint or not main carer | 0.654 | 3.149* | 3.596* | 0.855* | 0.632 |
| Parent/parent-in-law | 0.932 | 0.669 | –2.088 | 0.354 | 0.483 |
| Other relationship | 0.042 | –4.439 | –5.139* | –0.189 | –0.156 |
| Personal care | –0.552 | –1.060 | –0.868 | –0.213 | –0.029 |
| Physical care | –0.593 | 2.230* | 0.707 | 0.084 | –0.071 |
| Total hours | –0.087*** | 0.226*** | 0.052 | –0.022 | –0.027 |
| Duration of 1–3 years | –0.389 | 2.215 | 6.206*** | 0.241 | 0.642 |
| Duration of 3–5 years | –0.327 | 1.635 | 4.723** | 0.331 | 0.870 |
| Duration of 5–10 years | –0.350 | 1.876 | 5.646** | –0.176 | 0.328 |
| Duration of ≥ 10 years | –0.901 | 0.339 | 4.382 | –0.048 | 0.261 |
| No replacement for a break | –1.279*** | –3.537*** | –2.895*** | –0.758*** | –0.809*** |
| Care recipient’s characteristics | |||||
| Aged 65–74 years | 0.774 | 0.062 | 1.469 | 0.523 | 0.619 |
| Aged ≥ 75 years | 0.613 | 2.399 | 4.906** | 0.290 | 0.346 |
| Symptoms for 1–5 years | 0.497 | 2.048 | 0.800 | 1.016 | –0.002 |
| Symptoms for 6–10 years | 0.249 | 3.239 | 0.562 | 1.325 | 0.647 |
| Symptoms for ≥ 11 years | 1.547 | 7.128 | 1.520 | 1.631* | 1.209 |
| No diagnosis/do not know | –1.336 | –6.644*** | –4.785** | –0.196 | –0.280 |
| Vascular dementia | –0.919** | –1.533 | –1.936* | –0.125 | 0.064 |
| Other dementia | –0.578 | –0.536 | –3.979*** | –0.045 | 0.264 |
| Moderate | –0.782 | –3.192 | –3.986** | –0.860* | –1.120** |
| Severe | –1.932** | –5.480** | –4.241** | –1.587*** | –1.846*** |
| Constant | 7.594*** | 16.919*** | 18.190*** | 2.186 | 2.503* |
| Observations | 281 | 273 | 267 | 286 | 284 |
| R 2 | 0.442 | 0.254 | 0.343 | 0.337 | 0.320 |
| First-stage estimated coefficient of the instrument and F-statistic | |||||
| Travel time | –1.314*** | –1.242*** | –1.303*** | –1.267*** | –1.284*** |
| (0.140) | (0.142) | (0.153) | (0.141) | (0.143) | |
| Cragg–Donald F-statistic | 48.153 | 41.741 | 41.138 | 45.057 | 45.341 |
| Variables | Costs | |||
|---|---|---|---|---|
| Overall | Health care | Care recipient’s total social care | ||
| Carer’s total | Care recipient’s total | |||
| AN | –84.789 | –26.945 | 183.325 | –485.907 |
| (424.300) | (220.400) | (235.300) | (325.800) | |
| Carer’s characteristics | ||||
| Female | –43.503 | 247.528 | 15.399 | –10.760 |
| Aged 55–64 years | –460.986 | 111.659 | –172.661 | –290.753 |
| Aged 65–69 years | –311.635 | 264.837 | –136.340 | –206.945 |
| Aged 70–74 years | –111.880 | 174.031 | 263.621 | –497.466* |
| Aged ≥ 75 years | –250.737 | 478.223* | –43.945 | –226.171 |
| Bachelor’s degree | 374.071* | –132.752* | –133.293 | 354.348** |
| Master’s degree or above | 325.279 | –4.059 | –97.005 | 132.848 |
| Full- or part-time job | 101.672 | –164.674 | 208.777 | –167.638 |
| Looking after person with dementia full-time | –203.433 | –138.609 | –77.242 | –40.900 |
| Retired | 262.168 | 64.582 | 47.587 | 287.262 |
| Some difficulties | 79.236 | –2.703 | 33.939 | –9.724 |
| Severe difficulties | 54.450 | 146.511 | –112.209 | 312.202* |
| Do not know/prefer not to say | 726.467* | 337.062 | 439.764 | 130.765 |
| EQ-5D score | 282.471 | –432.785 | –6.379 | 171.143 |
| Caring role | ||||
| Joint or not main carer | 39.986 | –144.610 | 133.295 | –56.076 |
| Parent/parent-in-law | –2.780 | 147.888 | –63.445 | 54.819 |
| Other relationship | 172.630 | 143.890 | –38.175 | 93.189 |
| Personal care | 199.606 | 80.022 | –94.520 | 156.414 |
| Physical care | 201.990 | 8.679 | 183.537 | 22.129 |
| Total hours | 4.180 | –10.290 | 9.859 | –12.197 |
| Duration of 1–3 years | 424.923 | 78.139 | 92.416 | 270.099 |
| Duration of 3–5 years | 456.227 | –154.424 | 229.955 | 235.502 |
| Duration of 5–10 years | 234.233 | –178.270 | –216.822 | 535.651 |
| Duration of ≥ 10 years | 228.892 | –423.710* | –492.216 | 838.114** |
| No replacement for a break | 4.059 | –257.263* | –144.867 | 82.728 |
| Care recipient’s characteristics | ||||
| Aged 65–74 years | –174.957 | –94.208 | –143.724 | 123.119 |
| Aged ≥ 75 years | 7.603 | –59.864 | 106.349 | –25.234 |
| Symptoms for 1–5 years | –360.584 | 348.865** | 86.623 | –248.950 |
| Symptoms for 6–10 years | –311.801 | 275.298 | 155.216 | –363.265 |
| Symptoms for ≥ 11 years | –2.090 | 374.579 | 677.913 | –673.275 |
| No diagnosis/do not know | 151.458 | –170.216 | 147.718 | –279.431 |
| Vascular dementia | 20.869 | –38.935 | 234.759** | –112.184 |
| Other dementia | 21.787 | 146.556 | 255.082 | –91.738 |
| Moderate | –170.357 | 43.524 | –238.101 | 111.622 |
| Severe | 486.253 | 465.856 | –32.586 | 654.281** |
| Constant | 422.567 | 26.884 | 14.125 | 362.846 |
| Observations | 227 | 268 | 258 | 266 |
| R 2 | 0.171 | 0.170 | 0.150 | 0.105 |
| First-stage estimated coefficient of the instrument and F-statistic | ||||
| Travel time | –1.376*** | –1.354*** | –1.444*** | –1.277*** |
| (0.141) | (0.141) | (0.136) | (0.142) | |
| Cragg–Donald F-statistic | 47.155 | 49.597 | 56.661 | 43.216 |
| Variable | ASCOT score | Self-efficacy on | Overall life satisfaction | Happiness yesterday | |
|---|---|---|---|---|---|
| Symptoms management | Service use | ||||
| AN | 0.910 | 2.514 | 3.149* | 0.005 | 0.609 |
| (0.642) | (2.367) | (1.811) | (0.468) | (0.458) | |
| Observations | 281 | 273 | 267 | 286 | 284 |
| R 2 | 0.454 | 0.256 | 0.344 | 0.338 | 0.331 |
| First-stage estimated coefficient of the instrument and F-statistic | |||||
| Travel time | –1.119*** | –1.088*** | –1.145*** | –1.127*** | –1.123*** |
| County LA | 0.418*** | 0.395*** | 0.428*** | 0.386*** | 0.399*** |
| London LA | 0.052 | –0.003 | –0.015 | –0.004 | 0.015 |
| Metropolitan LA | 0.090 | 0.086 | 0.080 | 0.068 | 0.071 |
| Cragg–Donald F-statistic | 25.267 | 0.630 | 24.255 | 22.990 | 23.712 |
| Sargan–Hansen test (p-value) | 0.187 | 0.889 | 0.112 | 0.783 | 0.441 |
| Case study site | Number of professionals | Areas of responsibility of professionals interviewed | |
|---|---|---|---|
| Invited to take part | Agreed to be interviewed | ||
| Site 1 | 14 | 7 | Commissioning (health), commissioning (social care), AN, palliative care, dementia charity (×2) and one ‘other’ community organisation |
| Site 2 | 16 | 5 | Commissioning (joint health and social care), AN, occupational therapy, carers’ charity, dementia charity |
| Site 3 | 10 | 4 | Commissioning (health), commissioning (social care), memory services (×2) |
| Site 4 | 18 | 4 | Commissioning (social care), memory services, carers’ charity, dementia charity |
| Overall | 58 | 20 | Commissioning (health and social care), dementia charities, carers’ charities, AN, palliative care, occupational therapy, memory services and one ‘other’ community organisation |
FIGURE 6.
Adult Social Care Outcomes Toolkit score: bias reduction for each covariate after matching.
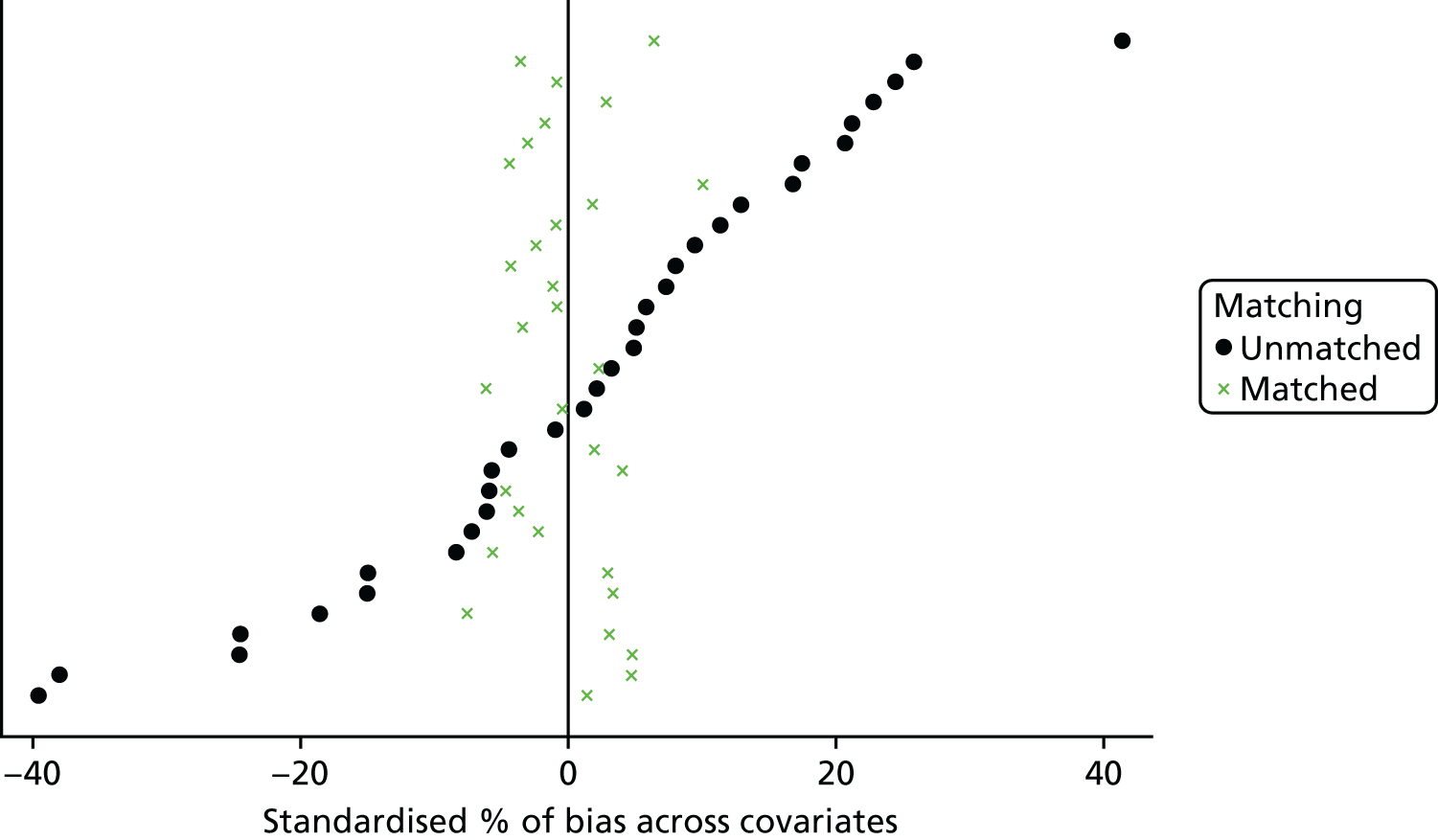
FIGURE 7.
Adult Social Care Outcomes Toolkit score: propensity score distributions. (a) Before matching; and (b) after matching.
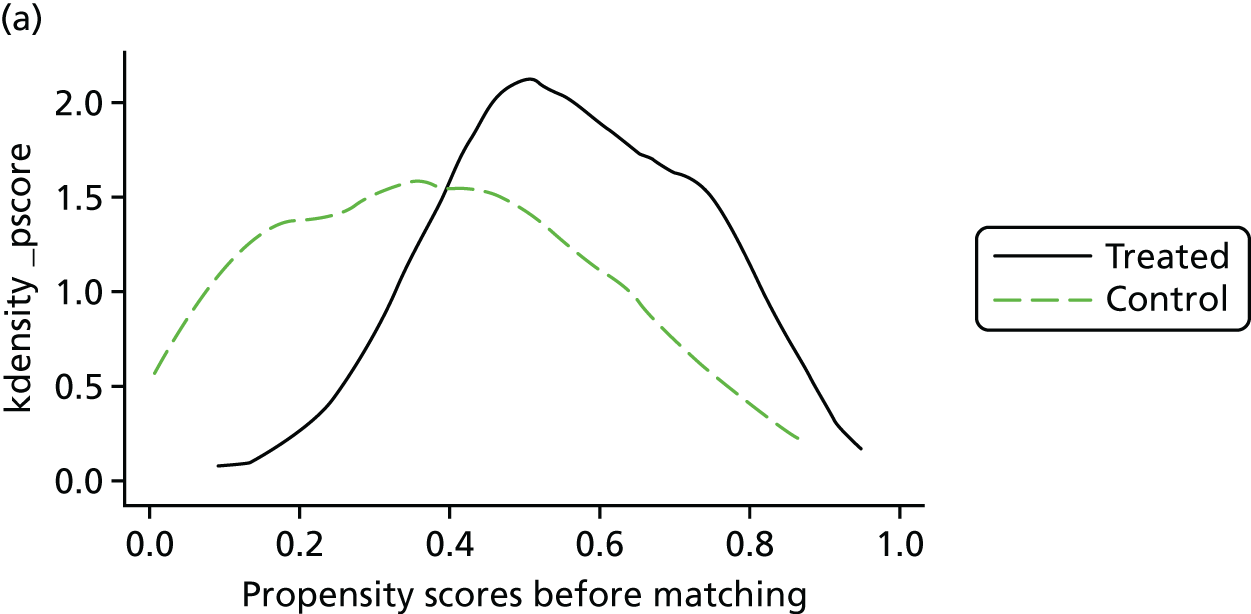
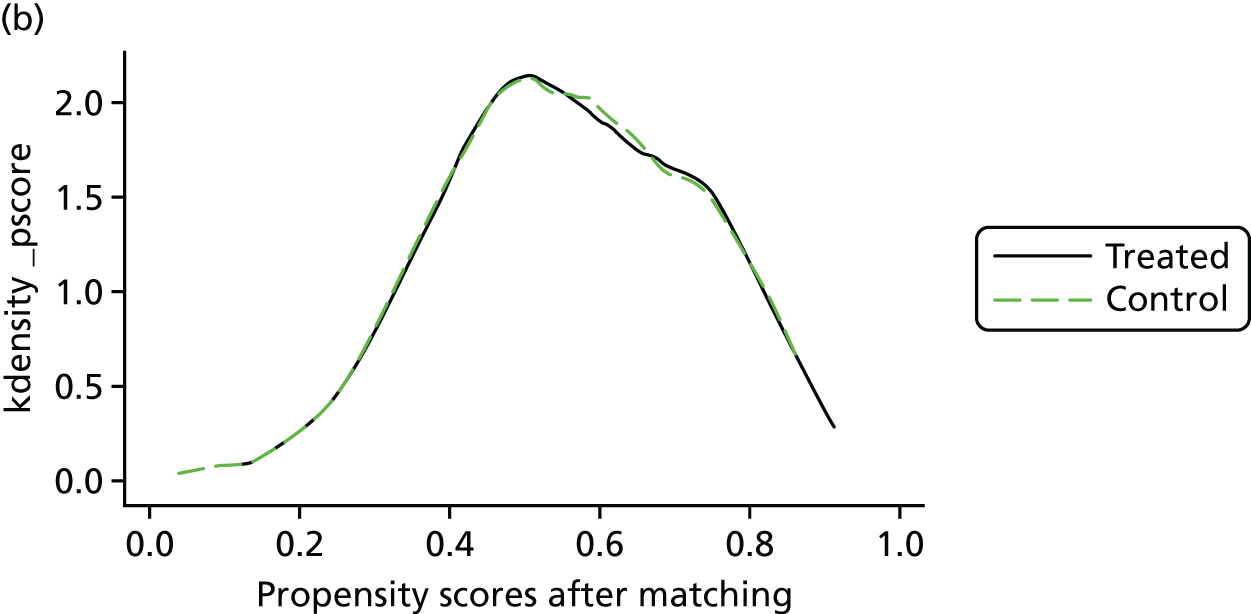
Appendix 4 Analysis from Chapter 5
Exploration of outcome measures by the characteristics in which Admiral Nursing and non-Admiral Nursing carers differed
Carer age and EuroQol-5 Dimensions results
Following guidance on the presentation of the EQ-5D results in survey research,96 for this part of our analysis we dichotomised the EQ-5D levels into ‘no problems’ and ‘problems’ and presented the results as frequencies (see Table 40).
There were strong linear and significant relationships between carer age and the reporting of problems in three dimensions: mobility, usual activity and pain/discomfort. Although older people were also more likely than younger people to report problems in relation to self-care, the difference did not reach statistical significance. The relationship with age and anxiety/depression appeared to be more complex, with those aged 55–64 years being more likely and the oldest (aged ≥ 75 years) being less likely than would be expected to report problems in this area; again, however, the difference did not reach statistical significance.
In sum, then, it is clear that age is related to problems in most EQ-5D dimensions. Whether the restrictions in usual activities are related to mobility issues or to the restrictions that caring for a person with dementia can create is not immediately clear.
Carer age and the Adult Social Care Outcomes Toolkit for Carers
We took the same approach to exploring the relationship between carer age and the ASCOT-Carer score, converting the data into ‘needs’ and ‘no needs’ and reporting frequencies in each of the seven domains (see Table 41). We also explored the total ASCOT-Carer score, as recommended by its developers. 45
Unlike the EQ-5D, there was only one domain in the ASCOT-Carer with a strong linear relationship to age – control over daily life – in which younger carers (aged < 55 years) were much less likely to report feeling that they had only some or no control over their daily life. There was also a significant, but weaker, relationship between age and feeling supported or encouraged, but this was not easy to interpret, as it was the 55- to 64-year-olds who were most likely to report needs in this area. As we mentioned above, this was also the age group most likely to report problems in the anxiety/depression domain of the EQ-5D.
The ASCOT-Carer scores can be simply summed to give a total score that ranges from 0 (lowest social care-related quality of life) to 21 (highest social care-related quality of life). First, we explored the distribution of this total score across the group as a whole, using the Kolmogorov–Smirnov test. This showed that the distribution of the ASCOT-Carer total score was not normal (Kolmogorov–Smirnov statistic = 0.092, df = 317; p < 0.001). Given this, we used non-parametric tests to explore total score by age of carer. This showed that there was no difference in the total score by carer age (Kruskal–Wallis χ2 = 3.45, df = 3; p = 0.328). For presentation here we also divided the scores roughly into quartiles. The frequencies of the ASCOT-Carer total scores by age of carer are provided in Table 42.
Carer age and self-efficacy
Our chosen outcome measure in this area was the SEMD scale. 46 This was the only one of our measures that had been developed specifically with and for the carers of people with dementia. The measure has 10 domains, nine of which load onto two factors: carers’ self-efficacy in relation to dementia symptom management (SXEFF) and carers’ self-efficacy in relation to community support service use (SERVEFF). We analysed the results for all 10 domains and the summary scores on the two main factors.
None of the distributions for the individual domains, or those for the two summary scores, was normally distributed, tested by the Kolmogorov–Smirnov test. As with the ASCOT-Carer, we therefore used non-parametric tests to explore the relationship between SEMD scores and carers’ age. Two of the individual domains were significantly related to the age of the carer (tested using the Kruskal–Wallis test): how certain carers felt about being able to get answers about the problems experienced by the person with dementia (Kruskal–Wallis test χ2 = 8.22, df = 3; p = 0.042, n = 314) and their certainty about getting answers to their questions about support services (Kruskal–Wallis test χ2 = 12.67, df = 3; p = 0.005, n = 308). Both of these questions contribute to the SERVEFF measure, so it was not surprising to find that this also varied by age (Kruskal–Wallis test χ2 = 9.36, df = 3; p = 0.025, n = 302). However, the direction of the relationship was not linear – those aged 65–74 years were the most confident (mean rank = 174.74), followed by those aged ≥ 75 years (150.60), then those aged < 55 years (149.17) and, finally, those aged 55–64 years (141.84).
The symptom management summary score did not vary with age.
There were more missing cases for this measure than for the others we used. This perhaps reflects the length of the scale. However, we are also aware that in the paper version of the questionnaire, some respondents turned over two pages at once, thus, for this measure, missing out questions 5–10. It is not possible to calculate the summary scores without answers to these questions; as a result, there were 37 missing cases for SXEFF and 44 for SERVEFF.
Relationship to the person with dementia and the EuroQol-5 Dimensions, five-level version
None of the EQ-5D-5L domains showed any difference in the reporting of problems versus reporting no problems when examined alongside the type of relationship between the carer and the person with dementia.
Relationship to person with dementia and Adult Social Care Outcomes Toolkit for Carers
Three ASCOT-Carer domains showed a statistically significant relationship with the relationship of the carer to the person with dementia (see Table 43). In all three domains – how carers spent their time, how much control they felt they had over their daily lives and whether they had space and time to be themselves – spouses/partners were more likely than expected to report needs than the other two groups.
These findings may reflect whether or not the carer and the person with dementia were living in the same household, which we explore below.
The total ASCOT-Carer score also varied with relationship to the person with dementia, with those caring for spouses/partners being more likely (51%) and those caring for parents/parents-in-law being less likely (36%) to score below 9 (the lower the score, the more problems were reported) when the score was analysed in quartiles. However, this difference did not reach statistical significance (χ2 = 10.02, df = 6; p = 0.124).
Relationship to the person with dementia and Family Caregivers’ Self-Efficacy for Managing Dementia
Two of the individual dimensions of the SEMD were significantly related to relationship: how certain the carer felt about being able to handle any problems the person with dementia might have and being able to deal with any frustrations of caring. In both cases, however, the mean rank scores suggested that it was those caring for ‘other’ relatives/friends/neighbours who were least likely to feel confident about handling these issues. There were only 12 such people in the sample, so this result needs to be treated carefully.
There were no differences in the SXEFF or SERVEFF summary scores.
Carer educational level and outcome measures
Only two domains of the EQ-5D showed any relationship with the carers’ educational level: those who had no qualifications were significantly more likely to report mobility problems (χ2 = 16.89, df = 6; p = 0.01), whereas those who preferred not to say what qualifications they had were more likely to report problems with self-care.
None of the ASCOT-Carer domains or the total ASCOT-Carer score showed any relationship with carer qualifications.
There was only one significant relationship between individual SEMD questions and carers’ qualification level: those with no qualifications or qualifications at a secondary level only were more likely to feel confident about caring without help than those with higher-level qualifications (Kruskal–Wallis test, χ2 = 16.49, df = 5; p = 0.006; n = 308). Indeed, the relationship here was completely linear (mean ranks: no qualifications = 177.86, secondary-level education = 171.04, 16+ qualifications = 161.30, college-level qualifications = 146.68, bachelor’s degree level = 137.79, master’s degree level and above = 108.76).
There were no differences in SXEFF or SERVEFF summary scores.
Carer economic activity and outcome measures
Two EQ-5D domains displayed a relationship with carers’ economic activity. Those in full-time work were less likely to report problems in relation both to mobility (χ2 = 8.03, df = 1; p = 0.005) and to usual activity (χ2 = 7.17, df = 1; p = 0.007), whereas those who were retired were more likely to report problems with mobility (χ2 = 10.19, df = 1; p = 0.001). Both of these sets of relationships seem highly likely to be related to age.
There was only one significant relationship between any ASCOT-Carer domain and carers’ economic activity: those who were in full-time work were less likely to report having problems with control over their daily life (χ2 = 4.81, df = 1; p = 0.028).
There was no relationship between any of the individual SEMD questions or the SXEFF and SERVEFF summary scores and whether or not carers were in full-time work. By contrast, being retired was associated with being more confident about finding support services (Wilcoxon test, z = –2.548; p = 0.011) and getting answers about such services (z = –2.937; p = 0.005). As a consequence, those who were retired also had higher overall SERVEFF summary scores (Wilcoxon test, z = –2.749; p = 0.006).
Carer status and outcome measures
We saw earlier that AN carers were much more likely to be the sole or main carer (spending the most time caring) than those in non-AN areas.
The only difference in EQ-5D domains related to sole/main carer status was usual activity, in which sole/main carers were much more likely to report problems in doing their usual activities (χ2 = 8.69, df = 2; p = 0.013). This is an interesting finding, suggesting that, despite the wording of the EQ-5D, which focuses on health, carers may have been interpreting the question in terms of restrictions on their lives that arose from being a carer.
Table 44 shows that four domains of the ASCOT-Carer were highly sensitive to carer status. Sole/main carers were much more likely than would be expected to report needs in relation to how they spent their time, control over their daily life, social contact and the space and time to be themselves. By contrast, there were no obvious differences in relation to looking after themselves, feeling safe and feeling supported and encouraged.
Although the total ASCOT-Carer scores, when analysed by quartiles, did not show an overall significant difference by carer status, the adjusted standardised residuals showed that those who were sole/main carers were much less likely (22%) to have a total score of ≥ 13 (a score that indicates a higher quality of life) than joint main carers (33%) and people who were not main carers at all (53%).
Only one individual question in the SEMD showed any relationship with carer status: those who were not main carers were more likely to feel confident with getting answers about support services (Kruskal–Wallis test χ2 = 6.06, df = 2; p = 0.048). Overall, this subgroup also scored the highest on the SERVEFF summary (Kruskal–Wallis test χ2 = 6.27, df = 2; p = 0.044).
Although there was a very strong relationship between age and main carer status (35% of main carers were aged ≥ 75 years, compared with none of the joint main carers and 10% of those who were not main carers, χ2 = 61.76, df = 6; p < 0.001) the analysis in this section, and the contrast with the section that explored carers’ age, suggests that the two variables may be operating differently in relation to our outcome measures.
There were very strong relationships between the ASCOT-Carer scores and whether or not carers were providing the most intense type of care, as defined by our typology (see Chapter 5). Those providing both personal and physical care were more likely to report problems in how they spent their time (χ2 = 4.89, df = 1; p = 0.027), how much control they had over their daily lives (χ2 = 20.37, df = 1; p < 0.001), their ability to look after themselves (χ2 = 8.78, df = 1; p = 0.003), whether or not they felt safe (χ2 = 4.19, df = 1; p = 0.041) and the space to be themselves (χ2 = 8.28, df = 1; p = 0.004). There were no differences in relation to social contact or feeling supported or encouraged. As would be expected given these differences on individual dimensions, carers providing both personal and physical care were much more likely than other carers to have total ASCOT-Carer scores in the lowest quartile (χ2 = 11.86, df = 3; p = 0.008).
None of the EQ-5D dimensions showed any differences between those providing both personal and physical care and other carers. This was also the case with the SEMD individual questions and the SEXEFF and SERVEFF summary scores.
Finally, in this section, we explore whether or not the total hours of care in the previous 24 hours was related to any of our outcome measures.
In terms of the EQ-5D, carers who reported caring for ≥ 18 hours the previous day were more likely than others to report mobility problems (χ2 = 8.56, df = 3; p = 0.039) and restricted activity (χ2 = 11.36, df = 3; p = 0.010). No other dimensions showed any significant relationship with hours of care.
By contrast, with the exception of feeling safe, ASCOT-Carer scores were highly sensitive to hours of care (see Table 45).
As would be expected, total ASCOT-Carer score, recoded into quartiles, also showed that those caring for ≥ 18 hours in the previous day were most likely to have scores indicating the poorest quality of life (χ2 = 33.16, df = 9; p < 0.001). In all, 39% of those caring for this number of hours were in the lowest quartile, compared with 32% of those caring for 12–17 hours, 22% of those caring for 6–11 hours and 11% of those caring for ≤ 5 hours.
Some questions in the SEMD varied with hours of care: confidence about keeping the person with dementia independent (Kruskal–Wallis test χ2 = 8.43, df = 3; p = 0.038), getting answers about dementia (Kruskal–Wallis test χ2 = 11.49, df = 3; p = 0.009), finding services (Kruskal–Wallis test χ2 = 9.17, df = 3; p = 0.027), getting answers about services (Kruskal–Wallis test χ2 = 8.13, df = 3; p = 0.043) and arranging services (Kruskal–Wallis test χ2 = 12.65, df = 3; p = 0.005). Both the SXEFF (Kruskal–Wallis test χ2 = 9.55, df = 3; p = 0.023) and the SERVEFF (Kruskal–Wallis test χ2 = 13.61, df = 3; p = 0.003) also varied with hours of care.
As with age of the carer, examining the mean ranks showed that the relationships between hours of care and carer self-efficacy were not linear. Those who were least confident about managing dementia were those caring for between 6 and 11 hours, whereas those who were most confident were those caring for ≥ 18 hours. In relation to confidence about services, those who were least confident were caring for 6–11 hours and those who were most confident were caring for ≤ 5 hours. The relationships with SXEFF and SERVEFF were also non-linear.
Overall, this could suggest that the SEMD is sensitive to contact with services; younger and less heavily involved carers may be less likely to be in contact with services and therefore less confident about their ability to care and to find and engage with services. This will be explored later.
Type of dementia and the outcome measures
We saw earlier that the two groups (AN and non-AN area) differed in the reported type of dementia of the person the carer supported, with AN carers being less likely than non-AN area carers to be supporting someone with Alzheimer’s disease and more likely to be supporting someone with vascular dementia.
An analysis of the five EQ-5D-5L dimensions by type of dementia showed no significant differences in reporting of problems in any dimension.
By contrast, there were significant differences in five of the ASCOT-Carer dimensions. People supporting someone with Alzheimer’s disease were less likely than expected to report problems in relation to how they spent their time, control over their daily lives, being able to look after themselves, social contact and feeling supported and encouraged (see Table 46). In three domains – how the carers spent their time, being able to look after themselves, and feeling supported and encouraged – the main contrast was between those caring for people with Alzheimer’s disease and those caring for people with ‘other’ types of dementia.
As would be expected given the individual domain scores, the total ASCOT-Carer score also varied for those caring for someone with Alzheimer’s disease, who were least likely to have scores between 0 and 7 and most likely to have scores of ≥ 13, when analysed in quartiles (χ2 = 16.32, df = 6; p = 0.012). Again, the contrast here was with those caring for people with ‘other’ types of dementia, who were most likely to have scores between 0 and 7, and least likely to have scores of ≥ 13 (χ2 = 16.32, df = 6; p = 0.012).
There were also differences in the SEMD between those caring for someone with Alzheimer’s disease and other carers. In two SEMD areas, the carers of people with Alzheimer’s disease were, on average, more confident than other carers; these areas were getting answers about support services (Kruskal–Wallis test χ2 = 7.84, df = 2; p = 0.020) and arranging for such services (Kruskal–Wallis test χ2 = 13.59, df = 2; p = 0.01). In relation to paying for services, those caring for people with ‘other’ types of dementia were less likely to feel confident than those caring for someone with Alzheimer’s disease or vascular dementia (Kruskal–Wallis test χ2 = 8.65, df = 2; p = 0.013).
As would be expected, given the differences in the individual elements of the SEMD, the carers of people with Alzheimer’s disease had higher (better) overall SERVEFF scores, followed by those caring for people with vascular dementia and then, with the lowest level of overall confidence, those caring for people with ‘other’ types of dementia (Kruskal–Wallis test χ2 = 6.98, df = 2; p = 0.03). There was no difference in the SXEFF scores.
There were no significant differences in the reported severity of dementia symptoms by type of dementia. Indeed, those caring for people with Alzheimer’s disease were slightly more likely than others to report that the dementia was ‘severe’ (29% for Alzheimer’s disease, 24% for vascular dementia and 23% for ‘other’ types of dementia), whereas those caring for people with ‘other’ types of dementia were slightly more likely to report that the dementia was ‘mild’ (9% for Alzheimer’s disease, 3% for vascular dementia and 17% for ‘other’ types of dementia). Perceived severity of the condition is not, therefore, a likely explanation for these differences in the ASCOT-Carer and SEMD scores.
Appendix 5 Analysis from Chapter 6
Summary of analytical methods in econometric terms
Regression analysis
Regression analysis estimates the average treatment effect on the treated (ATET)97 as follows:
where yi is the outcome or cost of the carer i = 1, . . ., N, di is a dummy variable indicating whether or not the carer receives AN services, Xi is a vector of covariates that control for differences across carers (e.g. age, relationship with the care recipient) and εi is the error term capturing all unobserved factors that influence yi.
Our key coefficient of interest was β, which estimates the ATET. It captures whether or not AN carers have, on average, different levels of outcomes or costs from non-AN carers. For example, β > 0 indicates that AN carers had greater levels of outcomes or costs than non-AN carers.
The regression model in the equation is estimated by the ordinary least squares (OLS) estimator. A crucial assumption for the unbiasedness of the OLS is exogeneity, that is, no correlation between independent variables and the error term. In this context, unbiasedness relies on a weaker condition, called the ignorability assumption, which implies that the intervention assignment is independent of (i.e. ‘ignores’) the outcome of the untreated individuals, conditional on Xi. This implies that Xi should include all potential factors correlated with both yi and di. As carers are not randomly assigned to the AN service but are generally admitted after a triage process that assesses their needs, those with high needs are more likely to access AN and also to have a low quality of life. Instead, carers who are not referred to AN are more likely to have low needs and a higher quality of life. If Xi does not allow for such a difference in the carers’ needs, the regression will underestimate the true ATET on outcomes.
The OLS estimator is the best linear unbiased estimator (BLUE) under the standard Gauss–Markov assumptions98 (p. 52): (i) there exists a linear relationship between dependent and independent variables, which implies that the model in (1) is linear in its parameters, whereas non-linearity may occur in the variables (e.g. a squared or log-transformed covariate); (ii) observations in the sample are randomly drawn; (iii) there is no perfect collinearity between independent variables; (iv) the independent variables are exogenous, that is, there is no correlation between the independent variables and the error term; and (v) the variance of εi is homoscedastic, that is, it is constant conditional on the independent variables. If assumption (v) is violated, OLS is no longer BLUE, but it is still an attractive estimator because it is unbiased and consistent.
We relax the homoscedasticity assumption and estimate standard errors that are robust to heteroscedasticity,99 because the variance of the error term may vary systematically across observations. For example, suppose that there is a positive relationship between using AN services and outcomes (i.e. suppose that β > 0). The variability of such a relationship may increase with the carer’s age, because older carers may have greater needs and their outcome may therefore be more uncertain. If we do not account for this, standard errors and, in turn, inference will be invalid.
Propensity score matching
The PSM is implemented in three steps. First, we regress the treatment variable di on the covariates Xi using a logit. Under the assumption that this model is well specified, the propensity scores, p(Xi), are computed as the predicted values of the dependent variable (di), which capture the carers’ conditional probability of receiving AN, given the observed characteristics Xi. Second, we match carers in the treatment and control group with similar propensity scores through the kernel matching. The kernel matching compares each treated individual with a counterfactual constructed as the kernel weighted average of multiple individuals in the control group. The counterfactual will depend on the distance between propensity scores of the treated and untreated individual within a specific bandwidth. We set the bandwidth to 0.06 to optimise the trade-off between variance and bias of the matching estimator. 100 Finally, we estimate the ATET by comparing the average outcome or cost of the treated and untreated carer in the matched sample.
As well as regression analysis, PSM requires the ignorability assumption for the estimation of the ATET, but now conditional on p(Xi) instead of Xi. In addition, we assume weak overlap (or common support), which implies that the sample includes treated and untreated individuals with the same propensity score. We test this assumption through visual inspection of the propensity score’s distribution between AN and non-AN carers.
Unlike regression analysis, PSM is non-parametric and it therefore avoids the linearity assumption by dropping all observations with no common support. Instead, regression analysis preserves portions of the sample with no overlap between treated and untreated individuals by replacing the missing observations through extrapolation. Jones and Rice97 suggest that good estimates of the ATET in regression analysis depend on the balancing of the means of the covariates between the treatment and control groups. If common support is small and linearity does not hold true, extrapolation may perform poorly and, in turn, the means of the covariates may not be balanced.
Overall, as Horvitz and Thompson101 show, PSM and linear regression are similar. Angrist and Hahn,102 however, argue that PSM may produce more precise estimates of the ATET (i.e. estimates with smaller standard errors) in finite samples than regression analysis. Such an instance may occur in the presence of omitted covariates that do not predict the intervention, but do have a statistically small impact on the outcome. More specifically, omitting some covariates from a regression that help to predict the outcome (although only to a lesser extent) but not the treatment will decrease precision. Moreover, with small samples, the inclusion of such covariates in the regression may not necessarily increase precision, because it may reduce statistical power owing to fewer degrees of freedom. Omitting the same covariates from the PSM, however, will not affect precision. This may well be our case because of the limited sample size and availability of covariates. For example, having polite neighbours might reduce stress and marginally improve the outcome of the carer, but polite neighbours are unlikely to directly influence the use of AN. As we did not observe the politeness of neighbours, PSM might be preferable to regression analysis.
Validity of propensity score matching
We assessed the validity of the PSM analysis in a number of ways. First, we tested the balancing property to check the balance of the covariates within a specific number of blocks of the propensity score distribution. This is always satisfied with five blocks, with the exception of the self-efficacy measure on symptoms management for which the balancing property is satisfied under less desirable conditions, that is, 11 blocks. Then, we checked whether the standardised difference for each covariate between AN and non-AN carers was reduced because of the matching. For ASCOT, for example, Figure 6 shows that the standardised difference is reduced below 10 for most of the covariates (a similar result is observed for all other outcome and cost measures). Moreover, we test the presence of common support through visual inspection of the propensity score distribution in the two groups of carers before and after the matching. Again for ASCOT, for example, Figure 7 shows that there was a good overlap between propensity score distributions before the matching, and that such an overlap becomes almost perfect after the matching (a similar result is observed for all other outcome and cost measures). Finally, we choose the kernel PSM technique because it minimises the average standardised difference of the covariates. Table 66 shows that kernel PSM has a smaller average standardised difference of the covariates than the nearest neighbour and the calliper technique.
Instrumental variable analysis
We implemented an IV approach, using the distance between the carer and the AN provider as an instrument (zi). The IV approach relaxes the ignorability assumption and assumes that the instrument is relevant, that is, correlated to the treatment variable, and exogenous, that is, not correlated to the outcome and to unobserved factors having an effect on the outcome. The distance between carer and AN provider is likely to be relevant because carers living far from the AN provider may not be eligible, as the service is delimited to a specific geographical area. Moreover, carers living long travel distances from the AN provider may have lower chances of being informed about AN than carers living in proximity to AN teams. Carers living in rural areas, for example, may have fewer peers and lower chances of being informed about AN than carers living in urban areas, where AN teams are usually based. This implies that carers living near AN providers are more likely to be eligible for, or to access, the service. We tested relevance through the Cragg–Donald F-statistic. As a rule of thumb, instruments are relevant if the F-statistic is > 10. 103 zi is also likely to be exogenous, because the distance is predetermined with respect to the location of the AN provider; carers are likely to live either close to or far from the AN provider, regardless of their levels of needs or care-related quality of life.
We use the types of LA as an additional set of instruments in the regression of the outcomes. Following Forder et al. ,54 we argue that the types of LA determine different cultures and, in turn, different propensity to invest in support services for carers. Some LAs will therefore be more willing to fund AN services than others, but the culture will not have a direct effect on outcomes. We use these additional instruments to implement the Sargan–Hansen overidentification test of exogeneity.
We estimated the IV regression using the two-stage least squares estimator and, similarly to regression analysis, we computed robust standard errors. The two-stage least squares estimates the local average treatment effect (LATE) rather than the ATET. The LATE measures the treatment effect on the ‘compliers’, that is, the individuals who are induced to participate in the treatment because of the change in zi. Intuitively, in our study, compliers are carers who live closer to the AN provider. In practice, the use of a continuous instrument, such as travel time, makes the interpretation of the LATE more complex, because the resulting estimate is a weighted average across groups of compliers. The identification of the LATE also requires the monotonicity assumption, which implies that the closer carers are to the AN services, the higher the probability of using AN. 104
Sensitivity analysis
Methods
We ran seven types of sensitivity check to test the robustness of our results.
First, we implemented the regression and PSM analysis by focusing on carers who looked after a spouse/partner because we believed, based on Chapter 5, that these carers were more likely to share similar needs.
Second, we carried out a regression analysis for all outcome and cost measures, after accounting for whether the carer completed an electronic or paper questionnaire (see Chapter 5 for further details).
Third, we tested any effect of AN on the EQ-5D-5L score and on the EQ-5D-3L. 72
Fourth, we checked the effect of AN on all outcome and cost measures by regression and PSM analysis after classifying carers as AN or non-AN according to their responses in the survey rather than by the way they received the questionnaire (via an AN service or via other organisations in areas without AN services). Although all AN carers were on the caseload of an AN service, some indicated that they had not received AN services; conversely, some non-AN carers had indicated that they had received an AN service (see Chapter 5). These answers may reflect confusion about the AN service or they may reflect the services that these carers actually received. If this is the case, there may be some non-AN carers in the AN carer group and vice versa, which would dilute our measures of association. For this reason, we tested whether or not the results changed if we classified carers according to their answers rather than their route of recruitment to the survey.
Fifth, we carried out regression and PSM analysis on a subsample in which all carers completed questions for all variables in the analysis (complete-case analysis).
Sixth, we estimated the effect of AN on health care and AN costs (excluding social care costs) through regressions and PSM.
Finally, in regression analysis, we undertook a subgroup analysis exploring the impact of sex, severity of dementia, and relationship with the care recipient on the outcome in the two groups, through interacting the AN dummy with the female dummy, the severity of dementia dummies and the relationship with the care recipient dummies, respectively.
Results
All tables including the results of the sensitivity analysis are available in Report Supplementary Material 1 (see www.journalslibrary.nihr.ac.uk/programmes/hsdr/1415407/#/). The regression (Table S1 and S2) and PSM results (Tables S3 and S4), after focusing on a more homogeneous group of carers who look after their spouse/partner, also suggested no effect of AN on outcomes, except for self-efficacy in service use (at the 10% significance level in regression analysis and at the 5% level in PSM) and costs.
The regression results, after controlling for whether the carer completed an electronic or a paper questionnaire, are in line with the key results presented so far, showing no or weak statistical significance for the outcome and cost measures (Tables S5 and S6). As expected, AN has no effect on HRQoL, as measured by the EQ-5D-5L and the EQ-5D-3L, as the estimated coefficient on the AN dummy in both the regression analysis and the PSM analysis, although negative, is small and non-significant (Table S7). The results are also similar to those of the main analysis, when we reanalysed all outcome and cost measures by regression and PSM analysis after classifying carers as AN or non-AN according to their responses in the survey, rather than by the way they received the questionnaire (Tables S8–S11), and when running the complete-case analysis (Tables S12–S15). The effect of AN on health care and AN costs (excluding social care costs), estimated through regression and PSM, is also statistically insignificant (Table S16).
Finally, the analysis of interactions between the AN dummy and some variables suggested that AN has a significantly positive effect on women compared with men and that self-efficacy on service use significantly increases more for carers looking after someone with any relationship other than a spouse/partner or parent/parent-in-law [although this group includes only 14 carers (Table S17)]. The results are similar to the base case in the regression analysis on costs (Table S18).
List of abbreviations
- AN
- Admiral Nursing
- ASCOT
- Adult Social Care Outcomes Toolkit
- ASCOT-Carer
- Adult Social Care Outcomes Toolkit for Carers
- ATET
- average treatment effect on the treated
- BLUE
- best linear unbiased estimator
- CarerQol-7D
- Care-related Quality of Life instrument, seven demensions
- CCG
- Clinical Commissioning Group
- CES
- Carer Experience Scale
- CHE
- Centre for Health Economics
- CIPFA
- Chartered Institute of Public Finance and Accountancy
- CPN
- community psychiatric nurse
- CQoL
- carer-related quality of life
- df
- degrees of freedom
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GP
- general practitioner
- HRA
- Health Research Authority
- HRQoL
- health-related quality of life
- ICECAP-A
- ICEpop CAPability measure for Adults
- ICECAP-O
- ICEpop CAPability measure for Older people
- ICER
- incremental cost-effectiveness ratio
- IRAS
- Integrated Research Application System
- IV
- instrumental variable
- JDR
- Join Dementia Research
- LA
- local authority
- LATE
- local average treatment effect
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OLS
- ordinary least squares
- ONS
- Office for National Statistics
- PSM
- propensity score matching
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- SCH
- Survey of Carers in Households
- SEMD
- Family Caregivers’ Self-Efficacy for Managing Dementia
- SERVEFF
- domain in the Family Caregivers’ Self-Efficacy for Managing Dementia scale relating to efficacy in accessing and using services
- SPRU
- Social Policy Research Unit
- SPSS
- Statistical Product and Service Solutions
- SXEFF
- domain in the Family Caregivers’ Self-Efficacy for Managing Dementia scale relating to efficacy in managing dementia
- TiDE
- Together in Dementia Everyday
- WP
- work package
