Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/54/34. The contractual start date was in September 2015. The final report began editorial review in January 2018 and was accepted for publication in November 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Peter Bullock is Chief Executive of Age UK North Staffordshire and reports that a contract between Keele University and Age UK was set up to enable Age UK support workers to deliver the intervention during the study. Carolyn A Chew-Graham, Simon Gilbody and Peter Bower are and have been in receipt of funding from the National Institute for Health Research outside the submitted work. Simon Gilbody is a member of the Health Technology Assessment (HTA) Commissioning Board, HTA Efficient Study Designs, HTA End of Life Care and Add-on Studies and HTA Funding Boards Policy Group.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Burroughs et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Context and background
Definitions and epidemiology
Depression is a major global public health burden, and by 2030 depressive disorders are predicted to be the second leading cause of disease burden and disability worldwide. 1 Anxiety and depression often coexist and are prevalent among older people, with up to 20% of older people reporting symptoms of depression. 2,3
Should the prevalence rates for these mental health problems remain stable in the future, we are still likely to witness an increase in the total number of older people with mental health problems owing to demographic changes (i.e. an ageing population). This will lead to an increased demand for treatment and an increased burden on health and social care. 4 Untreated anxiety and depression present a particular challenge and lead to increased health and social care utilisation and mortality. 5
Living with comorbidities (the presence of one or more additional conditions) is a common occurrence in later life: 36% of people aged 65–74 years and 47% of people aged ≥ 75 years experience a limiting chronic condition, and comorbidities present a significant risk to mental health. 6 The presence of long-term physical conditions increases the prevalence of depression and anxiety; for example, up to 30% of people with diabetes experience depression and up to 25% of people with chronic obstructive pulmonary disease (COPD) experience anxiety. 7 The presence of two or more long-term physical conditions increases the likelihood of depression by as much as seven times. 8
For older people with undetected depression, longer-term prognosis is poorer than for those whose depression is known by their general practitioner (GP). 9
Older adults face adversity in the areas of health, bereavement and loss, which is associated with depression. Isolation, loneliness and loss may be important contributors to anxiety and depression. This has clinical relevance for psychological interventions for older adults to consider social context and social support. 10
Depression and anxiety in older people are poorly detected and can be poorly managed in primary care,11 particularly in people with chronic physical ill health. 12 One impediment to detection is that older people may not present to their GP with depression because of the stigma they perceive about mental health problems. 13 Older people with chronic physical illness may normalise their depression, or view it as a ‘justifiable’ cause of low mood. 12–14 As a result, older people may hold negative views about help seeking. 15 Diagnosis and treatment led by a narrow biomedical model may overlook important social and contextual factors of mental health that can inform management. 16 One way around this is to treat people with mild to moderate depression and anxiety in a way that underserved individuals, such as older people, find non-stigmatising.
Management of anxiety and depression in older adults
The National Service Framework for Older People17 made specific references for the improvement of health-care services in England. The framework suggested that older adults who have mental health problems should have access to specialist older people’s mental health services with integrated social service elements, provided by the NHS and local councils, to ensure effective diagnosis, treatment and support. This framework was followed by a new older people’s mental health service development guide from the Department of Health and Social Care, Everybody’s Business,18 which made it clear that older people’s mental health spans health and social care, physical and mental health and mainstream and specialist services. The strategy document No Health Without Mental Health19 emphasises the importance of improving outcomes for people with mental health problems through high-quality services, for people of all ages, that are accessible to all.
A total of 90% of people with mental health problems are managed in primary care, and the population of older adults is no exception, with most older people with GP-recognised anxiety and/or depression being managed solely in primary care. In addition, older adults are under-represented in referrals to Improving Access to Psychological Therapies (IAPT). 20–22
The National Institute for Health and Care Excellence (NICE)’s guidelines for depression23 and anxiety24 advocate a stepped care approach in the management of depression and anxiety, as outlined in Figures 1 and 2.
FIGURE 1.
The NICE stepped care model for depression. 23 © NICE 2009 Depression: Treatment and Management of Depression in Adults. Clinical Guideline 90. Available from www.nice.org.uk/guidance/cg90 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this publication.
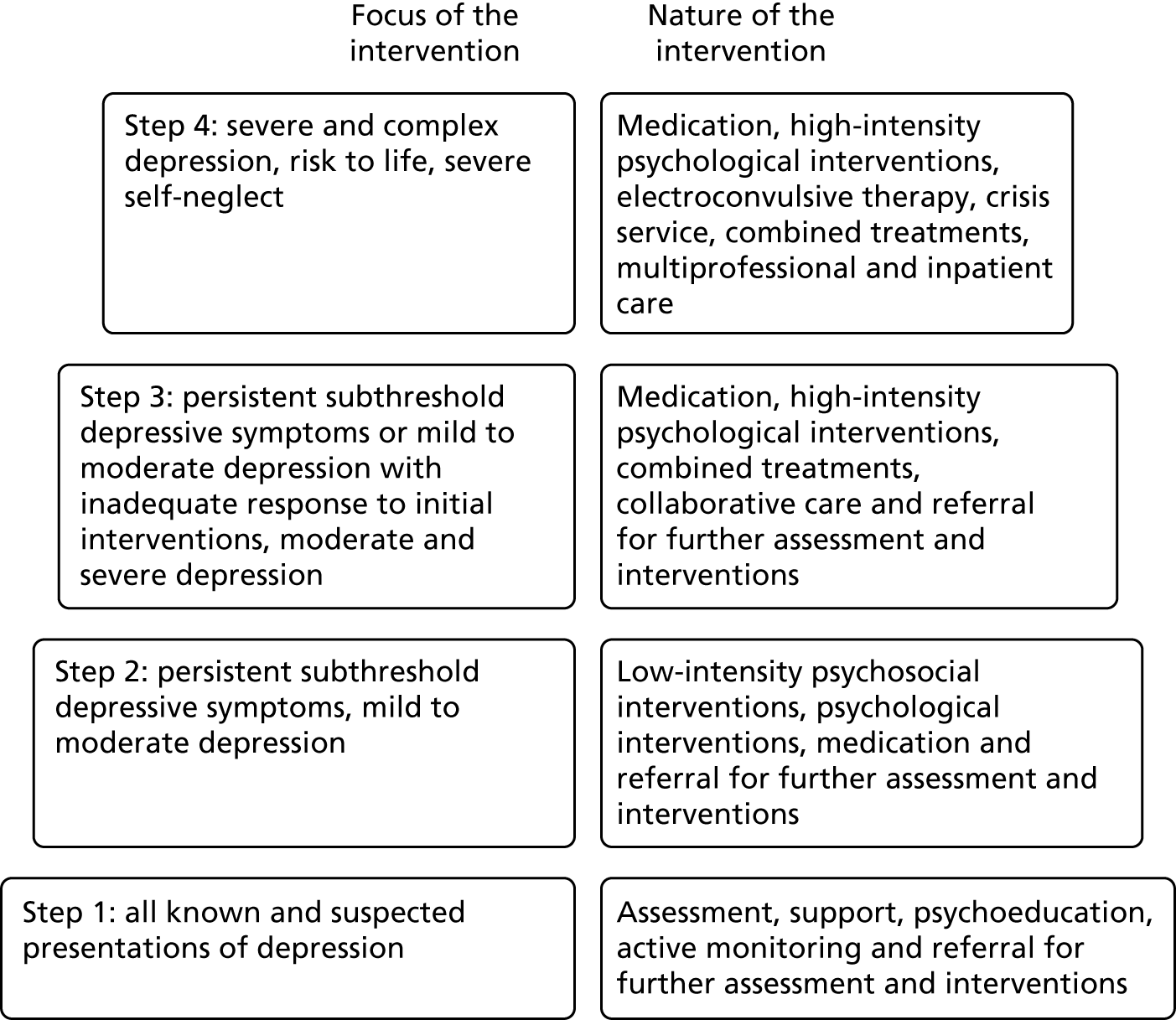
FIGURE 2.
The NICE stepped care model for anxiety. 24 CBT, cognitive–behavioural therapy; GAD, generalised anxiety disorder. © NICE 2011 Generalised Anxiety Disorder and Panic Disorder in Adults: Management. Clinical Guideline 113. Available from www.nice.org.uk/guidance/cg113 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this publication.
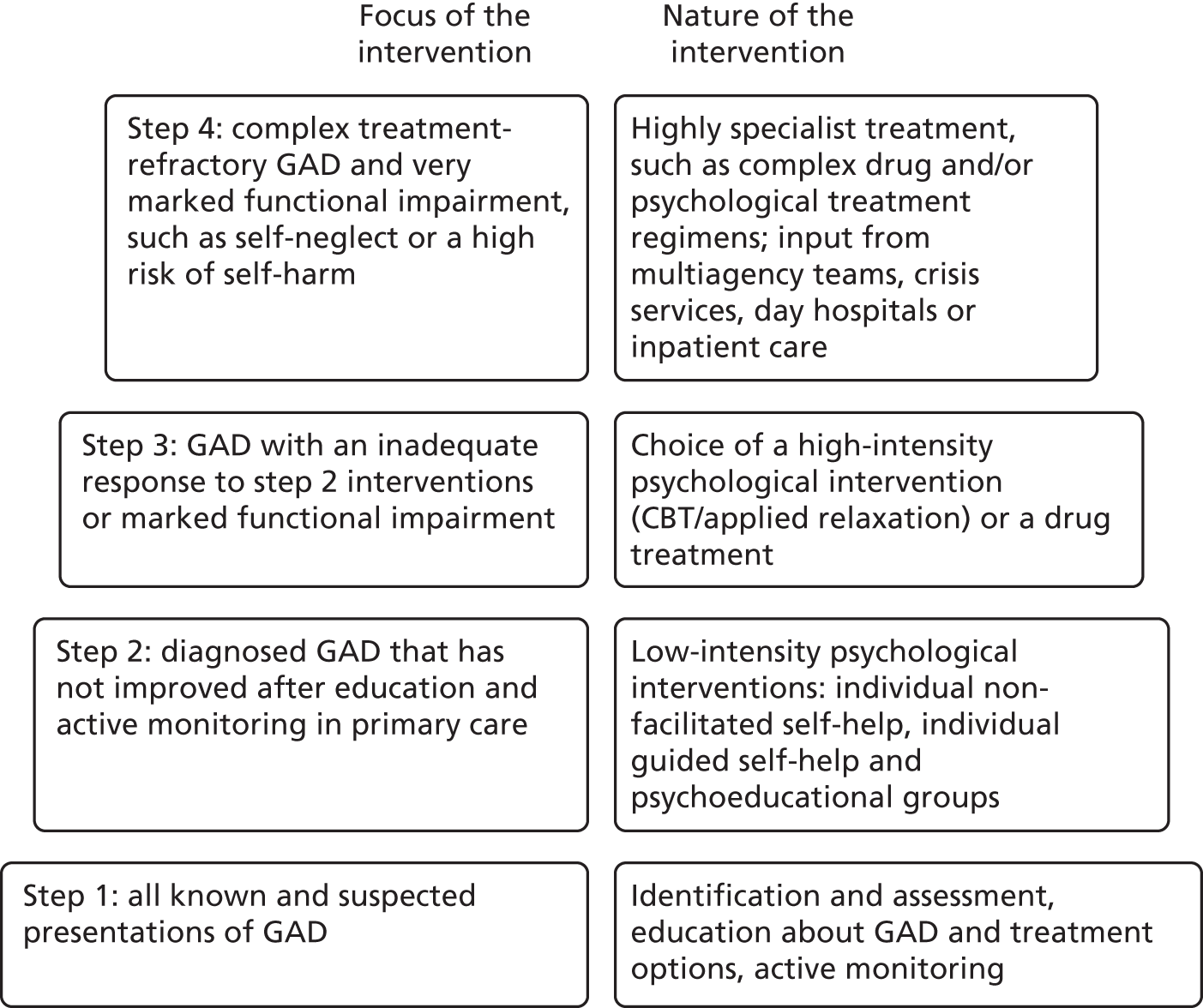
The NICE guidelines advocate that mild to moderate ‘cases’ of anxiety and depression are offered, at steps 1 and 2, advice about lifestyle by GPs and low-intensity interventions, respectively, which may include provision by non-statutory or third-sector bodies. There is limited evidence of the effectiveness of such providers in improving patient outcomes.
The NICE guidelines for common mental disorders25 emphasises the need to promote access to services for people with common mental health disorders from a range of socially excluded groups including older people, with suggestions, such as using different explanatory models of common mental health disorders, interventions in the person’s home or other residential settings or assistance with travel, and signposting to self-help and support groups.
Evidence base for the management of depression in older adults
A range of individual treatments has been shown to be effective in older people, including antidepressants and psychosocial interventions. 26 Antidepressants may not be an acceptable option for older people and, therefore, concordance is likely to be poor. 15 In addition, evidence repeatedly suggests that older people are not referred for ‘talking treatments’. 22 There is evidence that befriending (a one-to-one intervention) is effective in reducing depression in older people. 27 Befriending has been defined as ‘a relationship between two or more individuals which is initiated and supported and monitored by an agency that has defined one or more parties as likely to benefit. Ideally the relationship is non-judgemental, mutual, and purposeful, and there is a commitment over time’. 28
Lester et al. 29 suggest that befriending provides older people with desired opportunities to develop social ties that they perceive as reciprocal, to share intimacies and establish trust. Moriarty and Manthorpe30 emphasise the need for further research to evaluate the effectiveness of befriending-type interventions.
Other literature, however, suggests that a one-to-one intervention for older people with depression is insufficient: according to a systematic review of interventions for isolated and depressed older people,31 9 out of the 10 effective interventions included were group activities with an educational or support input, whereas six of the eight ineffective interventions provided one-to-one social support, advice and information or health-needs assessment. Therefore, befriending alone is unlikely to achieve a lasting effect, and the practitioner delivering the intervention needs to encourage change in behaviour and activity in the older person.
We attempted to conduct a systematic review32 into the effectiveness of psychosocial interventions for treating depression and anxiety in older people to evaluate which interventions are effective. The aim was to identify which components of psychosocial interventions are most effective in reducing the symptoms of depression and anxiety in older people, which was to inform the NOTEPAD (NOn-Traditional providers to support the management of Elderly People with Anxiety and Depression) intervention. However, the studies identified in the search were too heterogeneous for a metasynthesis, with divergent statistical tests and reporting, follow-up periods, depression scales and control conditions (see Appendix 1). Nine of the interventions were group-based activities and a major difficulty is disentangling the effectiveness of the activity from the effectiveness of being part of a group regardless of the activity that is taking place. Collaborative care as a framework for delivery or complex multicomponent interventions seem to be the most effective. Individual components such as cognitive–behavioural therapy (CBT) and group reminiscence are also promising. However, the study reporting the effectiveness of group reminiscence did not differentiate the reminiscence therapy from socialising as part of a group.
Loneliness and isolation are risk factors for developing depression and anxiety10 and, because increasing age is associated with loneliness and isolation, new methods of treatment of depression and anxiety among older people should focus on addressing loneliness. Kharicha et al. 33 suggested that older people experiencing, or at risk of, loneliness may not consider that primary care has a role in alleviating this. In addition, they reported that older people with characteristics of loneliness generally know about local resources but do not consider services advertised as being for ‘lonely older people’ to be desirable or helpful. Participants in their qualitative study reported that group-based activities with a shared interest are preferred to one-to-one support or social groups.
Behavioural activation (BA) is a short-term CBT-based intervention known to be effective in the management of depression, which can be delivered by practitioners who do not have specialist mental health training. 34 BA focuses on activity scheduling to encourage participants to approach activities that they may have previously enjoyed but are currently avoiding owing to increasing life changes (e.g. loss of spouse), or to develop new activities, and on analysing the function of cognitive processes (e.g. rumination) that serve as a form of avoidance. Participants are thus refocused on their goals and valued directions in life. The main advantage of BA-oriented interventions over traditional CBT for depression is that it may be easier to train non-clinical staff to deliver the intervention. 34 BA within a collaborative care model forms the cornerstone of trials35–39 in which the intervention is delivered by psychological well-being practitioners. 30,35–37 In addition, behavioural therapies have been shown to be effective in older people. 40,41 BA is therefore likely to be effective in older adults with anxiety and depression.
In the CASPER plus (CollAborative care for Screen-Positive EldeRs with major depression) trial,42–44 the BA intervention was acceptable for many of the older adults with depression and could readily be delivered over the telephone, following a face-to-face meeting. This approach may be able to reduce the stigma of the label of mental illness and resolve misconceptions around antidepressant medication prescribed by GPs. 29,30 However, some participants reported that the intervention was intrusive, and felt that talking and thinking about their symptoms made them feel uncomfortable.
An observation among all trials of people with depression has been the failure to integrate these effective elements of care into routine primary care services. 31,44
Collaboration with the third sector
The argument for working with the third sector, specifically Age UK, is based on previous collaborations with Age UK, and that older adults may find third-sector services less stigmatising.
Age UK has funded previous evaluations such as ‘Fit as a fiddle’45 and ‘Call me’. 46 Fit as a fiddle was a £15.1M portfolio of activities funded by the Big Lottery Fund and delivered across the nine English regions between 2007 and 2009. The aim was to increase the opportunities for older people to undertake physical activities and improve their eating habits, contributing to an overall improvement in mental health. The evaluation demonstrated a significant improvement in physical and mental well-being and an increase in volunteering capacity. The model has been accepted by Age Action Alliance as the preferred model for delivering healthy ageing services. Findings from the Call me project demonstrated that tailoring activities to a participant’s interests increases engagement in social activities and participant satisfaction and encourages sustainability.
Rationale for the NOTEPAD study
There is a need to improve the quality of care for older people with anxiety and depression. Improving quality of care means addressing not only the effectiveness of interventions but also the issue of limited access to acceptable care.
Older adults are a vulnerable and underserved group, often experiencing difficulty in accessing mental health care. 47 This is compounded by social isolation, loneliness and economic deprivation. 36,48 Given the ageing population and the public health implications of depression in older people, it is clear that acceptable community interventions focused on older people with anxiety and depression are needed. 49
Previous studies, such as Dowrick et al. ,50 explored ways to improve access for particular patient groups with limited access to care (e.g. older people). In the AMP (Access to Mental Health in Primary Care) study,50 psychological well-being practitioners (seconded from local IAPT services) delivered a brief psychosocial intervention to older people, which participants found to be acceptable. 51 In the same programme,50 third-sector workers were trained to deliver a similar intervention to South Asian women. Delivery by therapists or mental health practitioners is costly, which makes an intervention less likely to be commissioned in the NHS. Whether or not third-sector workers can deliver such an intervention to older people, and whether or not it is acceptable to patients and effective in improving outcomes, is unknown.
A further argument for increasing social participation is that loneliness and depression are strongly associated in older people52 and loneliness is an independent risk factor for depression. 48 Evidence from the USA53 suggests that for lonely older people there is a potential benefit from a social group or educational activities. Thus, it is reasonable to postulate that group activity might be a useful adjunct to treatment for mild to moderate depression.
Further evidence from a systematic review of social interventions targeting loneliness in older people54 suggests that the most successful interventions for loneliness, measured by improvement in the domains of physical, mental and social health, tend to be group based and participatory and offer some activity. 55–58 Such community-based interventions have been shown to have additional benefits in terms of social inclusion and social cohesion. 59–61
It has been argued that creativity plays an important role in later life and has positive implications for health and well-being and the maintenance of social networks by older people. 62–65 Creative activity has also been shown to provide therapeutic benefits,66 further evidenced by the rise in community-based ‘art for health’ across the UK. 67
A report from the Baring Foundation68 argues that the arts are an effective way to tackle loneliness, offering opportunities to connect and contribute, and to develop friendships and a sense of being valued, so that resilience is enhanced. It also notes that they are often overlooked by older people’s services. Despite the growing call for a diverse range of support for older people, there remains a paucity of evidence on what works best and Dickens et al. 54 suggest that there is a need for more studies to add to the evidence base.
From the literature, it is likely that the ideal intervention would be a tailor-made, flexible combination of elements, with some individual psychological therapy if necessary, followed by a group-based social activity that the participant might find enjoyable and/or meaningful.
In this older population, however, there are likely to be barriers to recipients of BA resuming previously enjoyed activities, such as difficulties with transport or lack of confidence. One solution would be for support workers (SWs) to initially accompany participants to activities to support their attendance.
The proposed intervention was supported by a wide theoretical basis, including social identity theory69 and self-concept theory,70 which examine how a person’s self-concept is affected by membership of social groups, and self-efficacy theory,65 which is highly relevant to health behaviours and posits that self-efficacy can be directly influenced by modelling or social persuasion within groups. These theories indicate how group interventions might help to foster good mental health framed within a critical gerontology approach. Critical gerontology challenges traditional notions of ageing as problematic and burdensome, and argues for older people to be seen as assets and contributors to the societies in which they live. This approach emphasises diversity and the need to take account of the wide range of issues that profoundly structure the experience of ageing, including life-course, sex, health and disability, socioeconomic status, ethnicity, sexual orientation and the physical environment. 71
Whether or not third-sector workers can deliver such an intervention to older people, and whether or not it is acceptable to patients and effective in improving outcomes, is unknown.
Summary
The overall aim of the NOTEPAD study was to explore whether SWs from the third-sector organisation Age UK North Staffordshire can deliver a non-stigmatising psychosocial intervention to support and manage older people with anxiety and depression recruited from primary care.
Research aims and objectives
This was a study composed of three phases, each informed by a patient and public involvement and engagement (PPIE) group:
-
phase 1 – qualitative work with older people and third-sector providers, plus a consensus group to refine the intervention, training, SW manuals and patient participant materials
-
phase 2 – recruitment and training of SWs
-
phase 3 – feasibility study to test recruitment procedures and assess fidelity of delivery of the intervention; interviews with study participants, SWs and GPs to assess acceptability of the intervention and impact on routine care.
Aims
Phase 1: to refine a community-based psychosocial intervention for older people with anxiety and/or depression, to be delivered by non-traditional providers (NTPs)/SWs in the third sector.
Phase 2: to determine whether or not NTPs/SWs can be trained to deliver this intervention to older people with anxiety and/or depression.
Phase 3: to determine if it is feasible to recruit and randomise patients, to pilot procedures and to conduct a process evaluation to provide essential information and data to inform an application for a full randomised trial.
Objectives
Phase 1: to refine a psychosocial intervention to be delivered by third-sector NTPs/SWs to older people with anxiety and/or depression.
Phase 2: to assess feasibility of recruiting and training NTPs/SWs to participate in the study and to assess fidelity of delivery of the psychosocial intervention to older people with anxiety and/or depression.
Phase 3: to answer the questions below.
-
Feasibility:
-
Can we recruit general practices to participate in a study to evaluate the feasibility of this approach?
-
Can we recruit and retain older adult participants in a randomised study, including the completion of follow-up questionnaires?
-
Can the NTPs/SWs deliver a psychosocial intervention to older people with anxiety and/or depression?
-
Can this intervention be implemented in routine NHS service delivery?
-
-
Process evaluation:
-
Do older people find working with an Age UK SW, and joining groups, acceptable?
-
What are the perspectives of the SWs about training, support to deliver the intervention, and how did they find working with older people in a more structured way?
-
Were the manuals developed to support training and delivery of the psychosocial intervention acceptable and useful to SWs?
-
What did participating primary care clinicians understand by the study and how did it impact on their work?
-
Figure 3 illustrates how the three phases link together.
FIGURE 3.
Model of the NOTEPAD study phases. TAU, treatment as usual.

Chapter 2 Qualitative study to inform the NOTEPAD intervention
The following description of the qualitative study is informed by our research output, Kingstone et al. 49 Content from this publication has been reproduced and/or adapted for the purposes of this report under the creative commons licence. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Aims and objectives
The objective of phase 1 of the NOTEPAD study was to inform the refinement of the psychosocial intervention to be delivered by SWs recruited from the third sector to older people with anxiety and/or depression. Based on the previous work of the research team, and on the existing literature, it was anticipated that the intervention would comprise a two-stage process of one-to-one contact, utilising BA, based on the principles of CBT, and including the option of signposting to a group activity.
In addition, an objective of phase 1 was to contribute to the development of training for the SWs, including the development of manuals for the SWs and for patient participants.
Design and setting
Ethics approval was obtained from the Keele University Ethical Review Panel on 23 September 2015.
Patient and public involvement and engagement
A PPIE group was established to support the development of the whole NOTEPAD study. The group helped to create the NOTEPAD logo and strapline ‘Supporting Mental Strength’.
The PPIE group suggested that the term ‘non-traditional providers’ used in the application for funding was unlikely to be acceptable to older people, and suggested that the term ‘support workers’ would be more appropriate.
The PPIE group suggested that the terms ‘depression’ and ‘anxiety’ may not be acceptable to older adults owing to stigma and could limit engagement with the study. Alternative terms ‘low mood’ and ‘stress’ were suggested by the PPIE group members and used thereafter. The term ‘stress’ is not clinically equivalent to anxiety; however, the research team accepted that there is sufficient overlap between these terms to support exploration in the qualitative interviews.
The PPIE group provided advice on the design of participant-facing documents (e.g. participant information sheet, consent forms), on the language and terminology used and on the layout of documents.
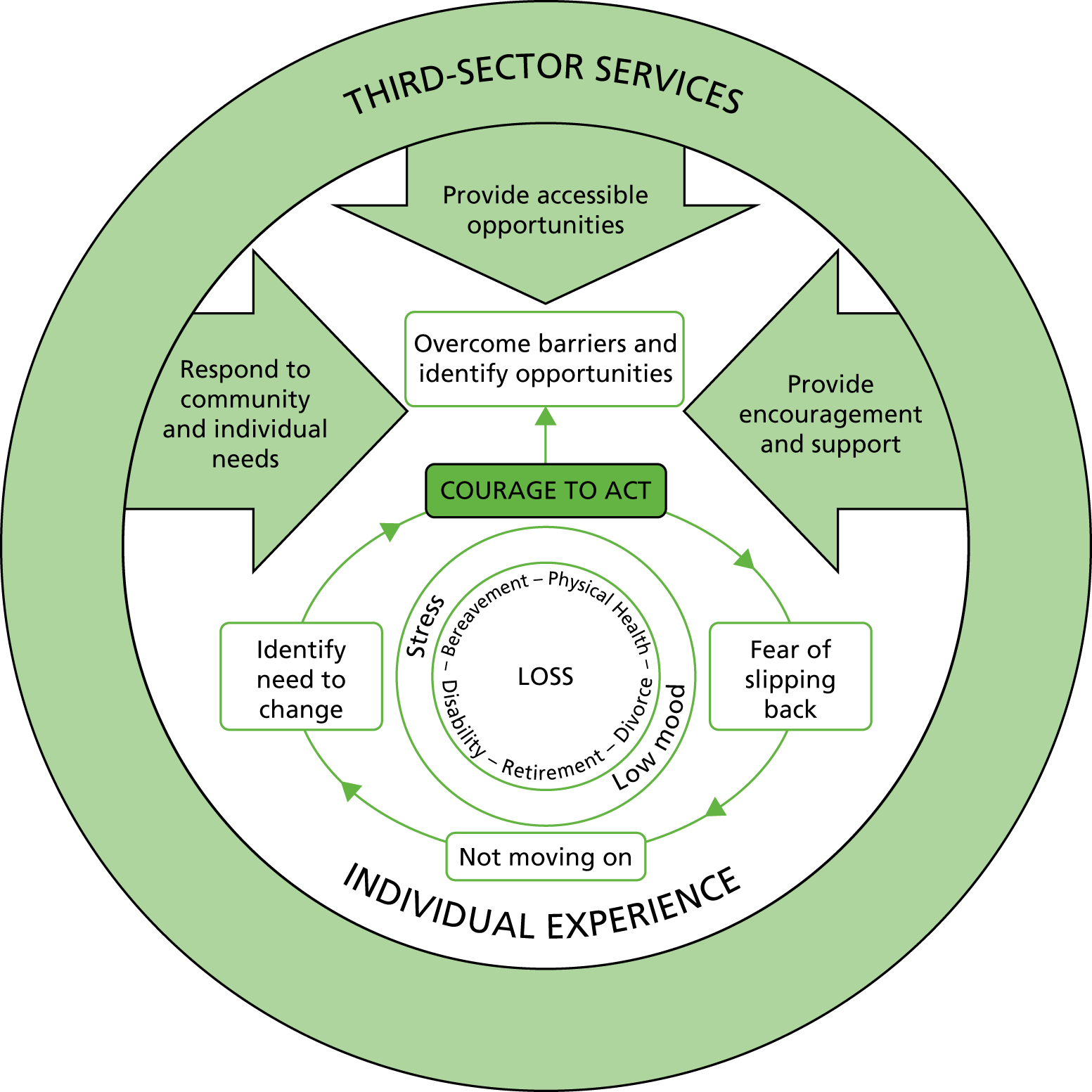
Towards the end of the qualitative study, the results of the emerging analysis were presented to the PPIE group, and they contributed to the development of a model that mapped the perspectives of older adults and third-sector workers on older adult responses to loss, which informed the intervention (Figure 4).
FIGURE 4.
Older people’s and third-sector service responses to distress and loss in later life. Reproduced from Kingstone et al. 49 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Methods
Qualitative methods were used to explore older people’s experiences of, and perspectives on, low mood and stress, and third-sector workers’ perspectives on working with people suffering from mental health problems. In addition, the views of participants on how to manage low mood and stress were sought, along with what an intervention delivered by third-sector workers to older people might look like.
Semistructured interviews were used to generate data.
The approach to sampling was purposive. We sought to recruit older adults (aged ≥ 65 years) living in the community and interested in sharing their views about experiencing low mood and/or stress in old age. We also sought to recruit individuals who were either in paid employment or volunteering with third-sector organisations and involved in the provision of community-based support for older people who may or may not experience low mood and stress.
Recruitment
Researchers (TK and HB) attended group activities (e.g. keep fit classes, line dancing classes, knitting groups and luncheon clubs) hosted in North Staffordshire by third-sector organisations with which the research team had established links [for example, Age UK North Staffordshire, Royal Voluntary Service (www.royalvoluntaryservice.org.uk), Beth Johnson Foundation (www.bjf.org.uk)]. With the assistance of activity group leaders, the researchers explained the study and distributed participant information packs comprising an invitation letter, a participant information sheet, a consent to further contact slip and a prepaid envelope. Snowball sampling72 was used to reach older people who did not attend groups and participant information packs were provided to group attendees to share with friends. Packs were also provided to non-statutory workers to distribute to service users outside these groups (e.g. befriending, signposting services). On return of consent to further contact slips, prospective participants were contacted to confirm willingness to participate and to arrange a convenient time and place for the interview, typically a private room at the community-based venue where group activities were held. Written consent was recorded immediately before the interview. Interviews lasted between 30 and 60 minutes.
Third-sector workers were identified through third-sector organisations (e.g. Age UK North Staffordshire, Royal Voluntary Service and Beth Johnson Foundation). Worker information packs were distributed via team managers within these organisations and contained equivalent information to the participant information packs for older people (as described). On return of consent to further contact slips, prospective participants were contacted to confirm willingness to participate and to arrange a convenient time and place for the interview.
Informed consent
The study was verbally explained to prospective participants and information packs were distributed. On return of consent to further contact slips, prospective participants were contacted to confirm willingness to participate and to arrange a convenient time and place for the interview, usually a private room at the community-based venue where group activities were held. Written consent was recorded immediately before the interview: two consent forms were signed, with the participant given a copy to keep.
Topic guides
Two topic guides were used: one for older people and one for third-sector workers. The topic guide for older people contained a series of open questions (see Appendix 2) to act as a basis for the discussion and explore their views on mood problems/depression and anxiety, seeking help and from where, and acceptable management approaches. Older people’s views on (and any experiences of) third-sector workers delivering one-to-one interventions were explored.
The topic guide for third-sector workers (see Appendix 3) also contained a series of open questions. They were used as a basis for the discussion and to explore perspectives on, and experiences of, working with older people, recognising depression or anxiety, concerns over working with people with anxiety and/or depression, and how receptive workers would be to receiving training to deliver a psychosocial intervention to older people.
Data coding and analysis
All interviews were digitally recorded with consent and transcribed by an external company. The transcripts were checked against the digital recording by HB or TK. The study was exploratory in nature; thus, thematic analysis was used to analyse the data. 73 Coding of the transcripts was undertaken by five members of the research team from different professional backgrounds to increase the trustworthiness of the analysis. 74 All transcripts were coded inductively by the first and second authors; the third, fourth and last authors independently coded five transcripts each. Each data set (older people, third-sector workers) was coded separately, and then comparisons across the two data sets were made. Data were stored and managed in NVivo 10 (QSR International, Warrington, UK).
Themes and subthemes emerging from the coding were discussed in team meetings and modified to account for alternative interpretations. The key themes and a model of the analysis were agreed.
Results
Participants
Interviews were completed with 19 older people and 9 third-sector workers (demographic information is provided in Tables 1 and 2).
| ID | Sex | Age (years) |
|---|---|---|
| Older adult 1 | Female | 72 |
| Older adult 2 | Female | 76 |
| Older adult 3 | Male | 65 |
| Older adult 4 | Female | 70 |
| Older adult 5 | Female | 76 |
| Older adult 6 | Female | 66 |
| Older adult 7 | Female | 78 |
| Older adult 8 | Female | 67 |
| Older adult 9 | Female | 86 |
| Older adult 10 | Female | 76 |
| Older adult 11 | Female | 77 |
| Older adult 12 | Female | 85 |
| Older adult 13 | Female | 83 |
| Older adult 14 | Female | 76 |
| Older adult 15 | Female | 70 |
| Older adult 16 | Female | 80 |
| Older adult 17 | Female | 67 |
| Older adult 18 | Female | 69 |
| Older adult 19 | Female | 74 |
| ID | Sex | Role |
|---|---|---|
| Worker 1 | Female | Volunteer (unpaid) |
| Worker 2 | Female | Worker (paid) |
| Worker 3 | Female | Worker |
| Worker 4 | Male | Volunteer |
| Worker 5 | Female | Worker |
| Worker 6 | Female | Worker |
| Worker 7 | Female | Worker |
| Worker 8 | Female | Volunteer |
| Worker 9 | Female | Volunteer |
Findings
Analysis of the interview data revealed the following themes: experiencing multiple forms of loss; distress as a personal burden to bear; having courage and providing/receiving encouragement; opportunities to increase self-worth; and barriers, tensions and gaps in service provision. Each theme is described below; data are given to support the analysis and each data extract labelled with a participant identifier (ID).
A conceptual model was developed to map older adult and third-sector worker perspectives on older adult responses to loss (a key contributing factor to low mood and stress). The contribution of this analysis to refinement of the intervention and the NOTEPAD feasibility study is described.
Experiencing multiple forms of loss
The older people we interviewed described multiple forms of loss in later life, which contributed to feelings of low mood and stress. The forms of loss described included loss of significant relationships (i.e. with spouses, friends, confidantes), changes to physical health and mobility (e.g. osteoarthritis, joint replacement operations), changes in capabilities and established activities (e.g. driving, employment roles) and loss of control of daily life (e.g. burden of providing caregiving).
Typically, older people experienced combinations of these losses. For example, one older person described a sequence of losses, which affected how she dealt with her own low mood:
My husband died and I had a hip replacement and then, 3 months after, I fell and broke the other [hip] . . . I’m trying to get over that now but, of course, I’ve had to give my work up, which doesn’t help because you’re more or less stuck in the house 24 hours.
Older adult 14
The experience of successive losses contributed to a sense of decline – of being on a ‘downward slope’ (older adult 6) or in a ‘downward trend’ (older adult 17).
This experience of loss was typically experienced as a crossroads when older adults found themselves thrown back onto their own resources. They described coming to the realisation that they would have to choose whether to make a conscious effort to get out of the house and forge new social links or to avoid participation and stay indoors. Several interviewees reflected that they feared that the latter choice could result in ‘giving up’ and becoming isolated.
Workers recognised the habitual nature of staying indoors:
A lot of people I see are in their late 80s, early 90s; they have become used to staying at home. I wouldn’t say they’re housebound; they’ve got out of the habit of going out.
Worker 4
The worker implies an important distinction between older people who are housebound (i.e. owing to physical health impairment) and those who are ‘out of the habit’ of getting out from their home environment. Thus, not going out has become a habitual behaviour for some older people and is not a result of physical impairment, centralising the importance of behaviour to overcome social isolation and losses attributable to this.
Distress as a personal burden to bear
One older adult described the way in which her friend coped with low mood as follows: ‘it was her cross and she would carry it’ (older adult 12). This metaphor captures common experiences of older people with low mood or stress: it is a personal burden for older people to bear. One older adult described:
I had six major operations within about 3 years. So that really knocked me off my pedestal and nobody really knows . . . That’s the thing. Depression. Nobody knows what you’re going through . . . you put on a smile and everybody thinks you’re fine, you’re doing alright, aren’t you? But they don’t realise inside that you’ve been through a hell and back and you’re suffering.
Older adult 10
The invisibility of such distress, as described, implies an opportunity to control the perceptions of others. A reluctance to share mental health experiences with others was apparent:
You don’t really want to pick up the phone and talk to friends because if you’re miserable I’m not going to make her miserable, you know. You’ve got to do something for yourself.
Older adult 5
The reluctance stems from not wanting to burden other people; to share their misery. Some older people did describe sharing these apparent burdens with their GP, seeking to obtain support, but people reported disappointment that they were prescribed antidepressants. Some older people reported taking antidepressants whereas others reported that this was not an acceptable course of action and that their problems remained unresolved.
Workers acknowledged that some older people may not want to talk about mental health problems, such as anxiety, with them:
Somehow anxiety has got a capital A; they might talk about feeling a bit low or something, so I think people don’t always find it easy to identify.
Worker 5
Older men were particularly identified as a group reluctant to discuss mental health. However, workers described being able to overcome reluctance to talk and perceived stigma around mental health by providing time and developing trust:
[P]eople do, once they trust you, feel that they can confide, and so people have talked about issues around mental health and you listen . . . Quite often it has been enough just to listen but sometimes we would encourage people to have a chat with the GP or maybe direct them towards some counselling.
Worker 5
The opportunity to establish meaningful, quality relationships and develop listening skills was felt to be important to facilitate disclosure of mood problems to others.
Having courage and receiving/providing encouragement
Older people described themselves as having to build up courage and determination to participate in group activities, despite suggesting that this may help to alleviate their feelings of low mood and/or stress. One participant described actualising their sense of courage, referring to the time that they discovered an advert for a group activity:
I thought, ‘that sounds good’, but, of course, I hadn’t got the courage because, as I said, [my husband had] only been gone 3 or 4 months. ‘Well’, I thought, ‘I’ll cut the thing off the [newspaper]’, which I did, and I popped it into this thing in the kitchen. I had to take it out from time to time and look at it. It took me 6 months to find the courage to, to phone up.
Older adult 1
Courage was an important part of accepting the need to reach out and make social contact. One participant described requiring ‘grim determination’ (older adult 5), perhaps indicating how difficult it was to find the necessary courage to engage in a new social activity.
Older people indicated a fear of slipping backwards with regard to sustaining a change in behaviour and continuing to attend and participate in group activities. Sustaining courage and motivation can be challenging, as one participant describes:
[O]nce you drop something it’s so difficult to pick up again afterwards. You think ‘oh, I haven’t been for a long while; what will they think of me if I turn up now?’ you know. But it takes a lot of willpower and not everybody’s got that willpower.
Older adult 10
In counterpoint to the courage that older people described, workers identified the importance of providing encouragement. Workers expressed empathy towards older people, seeking to initiate new social activities and practical help, as the following worker describes:
They need that encouragement to go to the befriending group. I do make contact with everybody a week before to remind them, to say ‘do you need a taxi?’, ‘do you need a lift?’
Worker 4
Attention and encouragement may act to support an older person’s own sense of courage to overcome challenges of low confidence. Encouragement was reported to be essential to support joining in any new activity.
Opportunities to increase self-worth
Older adults described how both one-to-one support and participation in group activities were valuable in improving mood and reducing the distress associated with loss. One older adult participant described attending an exercise class as an opportunity for respite from being a caregiver for her husband:
I don’t work, but this is my ‘day off’ where I come and enjoy the exercising. I enjoy being with the people . . . I love my husband, don’t get me wrong, but it’s just nice. He’s in, I can have the car, I can come down here, and it’s just a release sometimes, just to switch off and everything.
Older adult 16
Participation in group activities was valued for several reasons: the provision of opportunities to develop social relationships and participate in activities and roles, to redevelop or maintain a routine and to experience a change of environment.
Participation in group activities also supported a sense of self-worth within the group, as one participant described: ‘I really enjoy it and I’m the tea lady’ (older adult 15). It was clear that participation could also include assuming specific roles within these groups; others described providing supportive roles for newcomers to the groups.
Workers acknowledged the importance and range of benefits and opportunities that participating in group activities had for older people. One worker described an exercise group in the following way:
It isn’t just about sticking the music on and moving your arms and legs, it’s about the interaction with you and the folks in the group and the interaction between each [participant] . . . just going once a week, say to an exercise group, when they have maybe suffered from depression for 2 years and have never been out of the house maybe following a bereavement, it’s more than a lifeline.
Worker 5
Acknowledging the significance of the social element of group activities (i.e. that these are not solo activities but performed in groups) is important because it has implications for older people in terms of maintaining participation, self-confidence and social relationships.
However, workers recognised that group settings were not appropriate for everyone:
Even though some of them are still fairly mobile, that lack of confidence, I think, of being in a group situation has put them off trying.
Worker 4
When addressing inertia, it is important to provide support and encouragement to overcome apprehension and lack of confidence regarding group activities.
Barriers to, tensions and gaps in service provision
Internal (intrapersonal) and external (interpersonal and systemic) barriers were identified from the experiences of older people. Lack of acceptance and difficulties in acknowledging need (i.e. poor mental health arising from social isolation or loss of meaningful activities) among older people presented a barrier to engagement with the third-sector services; this was evidenced in the continuation of avoidance-style behaviours and social withdrawal. One older adult described how she coped with her low mood: ‘if I feel a bit low, I put the television on’ (older adult 12). Another shared her views about her friend whom she describes as experiencing low mood:
She has no hobbies, no interests at all . . . But she still gets very low and, to my mind, almost enjoys it. That sounds odd, I suppose, but it’s become a way of life and she doesn’t mind saying so.
Older adult 17
A lack of opportunities to engage in activities may perpetuate this cycle of social withdrawal. For some of the older adult participants, suitable opportunities were considered to be lacking, providing a further disincentive to increase social contact.
Transport was identified as a barrier to participation in group activities. Some older people in the study were still able to drive and used their own transport to access these groups, whereas others could no longer drive and described public transport as either unsuitable or non-existent: ‘There is no community transport here at all’ (older adult 9). Workers acknowledged transport as an issue in the provision of services:
This is a problem that we have. We know that there are people that are stuck at home . . . but it’s just getting them out and transport is always an issue.
Worker 3
Although some workers reported that they provided transport to older people, using their own vehicle, the capacity to maintain this raised concerns about sustainability:
In the past I might have taken people – picked people up a bit more – but we just haven’t got the capacity to do that.
Worker 6
Financial cuts to services were described by older people and third-sector workers, which were typically attributed to current policies of fiscal austerity and remained an ongoing concern. Workers would often talk to service users during group activities about financial cuts and service losses, as one older adult describes:
[She’s] always saying they’re cutting back on the company where she works for, Age UK, you know. It’s such a shame because a lot of people need these groups.
Older adult 16
When services had been cut, gaps in provision had not been filled and so the needs of those older people who had utilised these services went unmet.
Workers described tensions around the boundaries of their roles as facilitators of group activities (in a paid or voluntary capacity) and responsibility for older people experiencing mental health problems. Workers identified a lack of mental health training:
We kind of work, maybe, try and instinctively to chat to people and reassure them. We don’t really know if that’s making much of a difference.
Worker 6
Workers had concerns about managing boundaries with older people who presented severe mental health needs:
You would need to have . . . good boundaries, I think, when you’re working with people . . . so you don’t get drawn in to all sorts of things that are going on with that person’s life.
Worker 6
This concern was shared by others and reflected a lack of sufficient, tailored training. Workers also identified a tension in the lack of collaboration between third-sector and primary care services, important in the context of clients with apparent mental health needs (e.g. older people with dementia or clients who self-harm).
Conceptual model
The conceptual model illustrated in Figure 4 is derived from the thematic analysis of the interview data. The experience of loss, as a contributing factor to the mental health needs of older people, is central to the model. How older people respond to this loss varies and is individualised, with courage required to accept that a problem exists and to do something about it. Not moving on, and not acknowledging a need arising from social isolation or the loss of meaningful activities, may then lead to inactivity and increasing social withdrawal. The identification of opportunities to support self-worth is important, as is the capacity to overcome barriers (e.g. access, transport, low confidence). Third-sector organisations provide a crucial support role (e.g. through provision of group activities). It is this population of increasingly socially withdrawn older people who are at risk of being overlooked by the services offering support.
Views about the proposed NOTEPAD intervention
Overall, older people and third-sector workers in this study were positive about the potential for an intervention to be delivered by third-sector workers as part of the NOTEPAD study. However, participants felt that it might take some skilled intervention to persuade older people with low mood or stress to take part in the study, specifically group activities:
If you’ve got a person who wants to sit in the house and not do anything and is not willing to do anything, nothing on this earth will get you out of it.
Older adult 3
Older people in the study did not typically associate Age UK North Staffordshire with providing mental health services. Workers confirmed during interview that mental health services were not typically provided by the Age UK North Staffordshire. Workers identified training needs, the need for supervision and the opportunity to debrief as important in the development of the intervention for the NOTEPAD study:
You need access to a supervisor and I think depending on when you were having contact with the individuals concerned you would need to be able to debrief. If you had an urgent concern, you would need to be able to debrief straight after . . . you probably also need to be writing something down.
Worker 5
Documenting interventions and actions seemed important. Regarding the design of the intervention, the inclusion of one-to-one and group activities was identified as important:
You’ve got to try and get them out. You can’t just listen to what they say and don’t do anything. Get them to join things like – to join things like this and keep going, you know? Keep going for them and it’ll do them good because then they – like they’ll be talking to ordinary people [older people] but ordinary people know just as much as some psychiatrists.
Older adult 2
Group activities were not seen as suitable for everybody, and one-to-one interventions were considered essential to provide the opportunity to develop trusting relationships:
Depression. Nobody knows what you’re going through. And my relatives and friends, you know, you put on a smile and everybody thinks you’re fine, you’re doing alright, aren’t you? But they don’t realise inside that you’ve been through a hell and back and you’re suffering, and nobody knows . . . I, I got no sympathy from anybody from what I’d been through . . . You know, it is very very difficult and, and if, it’s partly that no sympathy that makes you depressed. If you’ve got somebody there helping you, you don’t get depressed, if you’ve got somebody there with you, you know. [. . .] You need, you need somebody there.
Older adult 1
Furthermore, having a worker accompany an older adult to new group settings was considered crucial to providing support and much needed encouragement:
I wouldn’t mind at all if somebody came, picked me up, took me out and brought me back again, that would be lovely! Yeah! [Laughter] Yes, [when I was depressed] it took a lot of will to go and do them [group activities], but I knew myself that I had to do them because if I didn’t it wouldn’t do me any good at all.
Older adult 1
Table 3 summarises the contribution of the qualitative study to the design of the intervention.
| Aspect of study | How intervention has been adapted |
|---|---|
| Facilitating relationships and trust |
|
| Facilitating self-management (and ongoing data gathering) |
|
| Maintaining participant engagement |
|
| Supporting third-sector workers |
|
Patient and public involvement and engagement
During the analysis of the interview data, a meeting was held with our PPIE group during which the findings were discussed. Members of the group suggested that the analysis resonated with their experiences (and experiences of older people they are in contact with) and that the model made sense to them. The group discussed how the analysis could inform the design of the intervention and contributed to Table 3.
Discussion
Summary of results
The themes presented map out how experiences of loss contributed to the mental health of older people in a community sample, their engagement with third-sector services, and the provision of these services by those involved in delivery. The process is depicted in the conceptual model (see Figure 4).
The experience of loss was described in multiple forms and was a central theme from the interviews. Loss and its ramifications for older people is a complex and individualised experience; responses to loss, although supported by third-sector services, are influenced by biographical factors (e.g. existing support networks, a sense of one’s own courage, and personal agency). Older people described a reluctance to talk about mental health problems with friends, for fear of burdening them, and described difficulty in acknowledging the need to do so. Those participants who self-identified as experiencing low mood or stress said that they would talk to third-sector workers once a trusting relationship had been developed. Older people in this study were already actively participating in group activities in an effort to maintain social networks and roles, reporting that this did support good mental health; older people valued being members of these groups because of the opportunity for social interaction and to support self-confidence. The role of courage and to receive (or provide) encouragement was highlighted as important in supporting this participation, highlighting a key function of third-sector workers. Older people revealed an ongoing concern of slipping back to avoidance behaviours; this suggests that maintaining positive behaviours requires ongoing support and encouragement. The findings highlighted and informed important areas for development of the intervention for the NOTEPAD feasibility study: facilitating relationships and trust, the importance of self-management as an integral part of the intervention, maintaining participant engagement and supporting third-sector workers.
Comparison with previous literature
The analysis supports other research that identifies the need to take a broader perspective on mental health and its management than a biomedical model permits. For instance, Burroughs et al. 13 described how GPs normalised and justified depression among older people as a social problem, reinforced by GPs’ sense of powerlessness to respond; they perceived that there were very limited options available to them. In the present study, older people identified feelings of distress as a personal burden. Many disclosed antidepressant usage but that their problems remained unresolved, and older people in this study took it on themselves to identify opportunities to attend group activities, which supported their social mental health. Maintaining participation in activities and social interaction seemed important for older people in this study to support their quality of life and mental health, as identified in other research,75,76 but also to support coping with, and moving on from, the experience of loss. The process of ‘moving on’ has been identified previously in relation to depression;14 the role of others (the case managers in the trial) was seen as important in providing encouragement to increase activity and social participation. Chew-Graham et al. 15 described perceived stigma as preventing older people from sharing mental health problems with their GP, which may relate to the fear of burdening others that has been described. In the present qualitative study, a link between loss (in multiple forms) and anxiety and depression was identified; thus, third-sector workers may be well placed, with greater contact time, to develop relationships, support disclosure and respond to mental health risk factors. Targeting loss, supporting responses of older people to loss, and overcoming avoidance-type behaviours that may lead to rumination may be a useful point of entry for third-sector services.
Strengths and limitations
Strengths
This study explored multiple perspectives on anxiety and depression among older people in the community and identified the central role of loss as a potential contributing factor in such mental health problems. Recruiting older people from community groups means that we accessed the views of people not necessarily accessing primary care. This is the first study to our knowledge to report the views of third-sector workers on supporting older people with anxiety/depression (stress and low mood) and the potential role they might play. The analysis contributed to the refinement of the NOTEPAD intervention.
Interviews were conducted with older people who were already accessing group activities and services in their local community; thus, the perspectives of older people who do not attend community groups are not reported. We did not specifically recruit participants who were experiencing or had experienced low mood or stress.
The views of housebound individuals were limited to those shared by other participants; that is, some participants shared the views of others whom they knew to be potentially housebound. These views may have been shared as a means of supporting social comparisons. This limitation occurred despite efforts from the researchers to recruit more broadly. A male perspective was lacking. This may have been a result of the recruitment strategy, which focused on local groups (which were mostly attended by women). A ‘Men in Sheds’ group was attended by the researchers, but no-one agreed to participate in an interview. More broadly, this also reflects a lack of male-oriented activity groups available in the community.
Summary
This phase of the study identified the central role of loss in later life as a potential contributing factor in mental health problems; the findings have important implications for the proposed feasibility study, training of third-sector workers delivering the intervention and clinical practice. Third-sector workers reported regular contact with older people presenting apparent mental health problems and needs related to the community; typically, such contact occurred at group activities and services not designed to respond to mental health needs nor with staff or volunteers appropriately trained. Phase 1 affirmed that, with appropriate training, third-sector workers could be well placed to deliver a low-intensity psychosocial intervention to older people, as recommended in the stepped care approach in NICE guidelines for anxiety and depression, and would provide both older people and primary care professionals with choice for management. The analysis contributed to the refinement of the NOTEPAD intervention and the development of the SW training, SW manual, and the resources intended for study participants. This will be discussed in Chapter 3.
Chapter 3 Phase 2: refining and delivering the NOTEPAD intervention
Aims
The aims of phase 2 of the NOTEPAD study were to:
-
identify the effective components of an intervention that aims to improve the management of depression and anxiety, reduce social isolation, increase participation and promote good mental health in older people
-
develop, refine and integrate interventions that respond to patients’ self-reported difficulties and may include lifestyle and activity advice, psychoeducation, BA techniques (a simple CBT-based intervention) and referral to existing third-sector resources (which might include referral to a befriending service, patient or carers group, Age UK or other local groups) to reduce social isolation
-
develop training for SWs from the third sector (Age UK) to enable them to conduct the assessment and deliver the psychosocial intervention
-
develop a manual for the SWs to structure the intervention and support and supervise their work with study participants
-
develop resources for study participants to use with a SWs’ support.
Refining the intervention
The intervention was built on the literature, the research team’s previous experience39,42,76 and consensus achieved in an expert group.
The evidence base underpinning the NOTEPAD study is outlined in Chapter 1. The systematic review (see Appendix 1) confirmed the premise of the application; that the ideal intervention would be a tailor made combination of individual psychological support and subsequent group-based social activity that the participant might find enjoyable and/or meaningful. Our review suggested that reminiscence therapy might be useful but that the effects were not well differentiated from the effects of merely socialising as part of a group.
The research team drew on previous interventions that incorporated BA that they had been responsible for developing and delivering within trials. 39,42,76 BA is a structured programme of reducing the frequency of negatively reinforced avoidant behaviours in parallel with increasing the frequency of positively reinforcing behaviours to improve functioning and mood. The intervention for this study was to include signposting to local agencies and activities, when acceptable to the study participants, and the SWs were encouraged to accompany the study participants to a first visit to a group. The intervention was designed to be delivered by SWs recruited from Age UK North Staffordshire.
The research team considered that adaptations would need to be made to the information gathered at the initial session by the SW. Older adults are more likely to experience long-term health problems and a reduced level of functioning, with their psychological status often closely linked to their physical functioning. 77 Additional questions regarding health conditions and their impact were therefore thought to be needed as part of the initial assessment by the SW. The team considered that the SWs should adopt a person-centred approach. Depression in older adults is associated with impaired social support;78 therefore, additional questions regarding social contacts and family were felt to be important, especially as we anticipated that signposting to local groups to reduce social isolation should be an integral part of the intervention. The team felt that the risk assessment in the intervention and the suicide ideation protocol in the feasibility study – available on the project webpage [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)] – should be adapted to enquire about past passive and past active suicide ideation as well as current plans and preparations, as past suicidality is a risk factor for current suicidal behaviour. 79
The qualitative study conducted in phase 1 (see Chapter 2) highlighted important areas for inclusion in the intervention for the NOTEPAD feasibility study: the need for an empathic relationship and the development of trust, acknowledgement of loss, the importance of self-management as an integral part of the intervention, maintenance of participant engagement, and the need for adequate support for the SWs delivering the intervention.
At the PPIE meetings in January and September 2016, participants were presented with results of the qualitative study and an outline of the proposed intervention. Comments from the group were also sought on examples of patient manuals used in previous trials39,42,76 and views taken to present and discuss further at the consensus group. Members of the PPIE group particularly commented on the size (A4) of the example materials, which they felt were not convenient for carrying or storing. In addition, the group felt that the manuals used in the previous trials39,42,76 contained too much jargon and that the text needed breaking up with more illustrations and pictures. The PPIE group also strongly felt that the term ‘non-traditional provider’ would not be appealing or understandable to older adults and suggested that the term ‘support workers’ should be used.
The consensus expert group was held in January 2016 to draw together the evidence base, views from the PPIE group and findings from the qualitative study. The group comprised clinicians (GPs, psychiatrists, IAPT practitioners), academics and researchers with knowledge and expertise about the management of older people’s mental health. During development of the funding application, it had been agreed that the intervention would use the principles of BA plus signposting to existing third-sector resources. The group members were tasked with responding to outstanding questions posed by the research team and achieving consensus by the end of the day in the following areas:
-
What intervention for anxiety?
-
How many sessions in the intervention?
-
Should we use a measure/assessment of mood within the NTP/SW–study participant consultations?
-
How should the participant manual look?
-
What are the implications of phase 1 for the SW training?
The group discussion resulted in a consensus as presented in Table 4 and Box 1.
| Intervention component | Consensus |
|---|---|
| Intervention for anxiety |
‘Keep it simple’; focus on BA rather than a separate intervention labelled ‘for anxiety’ to avoid ‘complicating things’ for SWs. Activity scheduling should also help anxiety symptoms The key is to the ensure that SWs can recognise where anxiety is a problem:May include active relaxation (e.g. scheduling deep-breathing exercises) |
| Psychosocial intervention |
Four to six sessions: mixed face-to-face and telephone sessions; face-to-face session initially to establish a relationship (unless an older person expressed preference for all telephone contacts) Venue (if face-to-face session) following patient preference: home, GP practice (if negotiated with GP) or Age UK venue The SW accompanying the person to a group will be considered equivalent to one session Delivered over 8 weeks (maximum 12 weeks). Perhaps weekly for three or four weeks, then spread out; final ‘booster’ session where ‘ending’ is dealt with, and ‘staying well’ strategies put in place Duration: face-to-face session up to 1 hour; telephone session up to 30 minutes ‘Reminder’ phone call the day before a session, if possible (in addition to six sessions) The role of family/carers to be recognised; may try to engage in facilitating increased activity, but the SW should try to achieve privacy in interactions/consultations Only one session will be considered to be a ‘drop-out’ |
| Use of measure to assess change |
Whichever scale is used, Clinical Global Impression or Patient Global Impression, it has to be person-centred, simple and meaningful The mood thermometer might be a more acceptable (to SWs and study participants) instrument to use |
| Patient manual |
The intervention is not guided self-help; thus, the patient ‘manual’ should be simple, clear and short. An existing Age UK leaflet is a good example Content could be built up over time and thus more tailored to the individual Key information to be included:Title should be something like: ‘Follow your plan, not your mood’ Format: colourful and bright; clear language; include photographs of local area Include a pen Mixed views on format: organiser, folder or leaflet(s) |
| Directory of resources |
Use the term ‘list’ rather than ‘directory’ so that details of specific activities/services can be given to the older person once their interests have been explored – will feel tailored to the individual Details can be kept by older person in the patient manual (particularly if in organiser format) |
Deliver training over 2 to 3 days.
Include information on anxiety and depression.
Ensure that risk assessment and managing risk is covered.
Explain and provide the rationale for BA.
Instruct SW to:
-
establish and maintain a relationship with the older person
-
pick up cues
-
identify/clarify the problem
-
deliver the BA intervention face to face and/or by telephone
-
safeguard
-
plan to end contact
-
work with families/carers (and ensure time/privacy with the older person)
-
make telephone contact
-
explain how to use patient resources/manual
-
document contact (noting duration and activity within the session)
-
provide digital recordings of some SW–patient sessions.
Explain what to take to supervisions.
Explain when to contact the GP.
Explain working within a research study (while remaining person-centred).
Ensure inclusion of role play (with simulated patient) to emphasise concept of ‘person-centredness’.
The SW manual needs to fit with the patient manual; the SWs should feel comfortable working with the study participants and in supporting them to use the participant manual.
The NOTEPAD materials can be found on the project web page [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)].
The final NOTEPAD intervention
At a PPIE meeting in February 2016 the NOTEPAD intervention, as agreed at the consensus meeting, was presented to the group and supported by members.
The final intervention is outlined against the Template for Intervention Description and Replication (TIDieR) checklist80 in Table 5.
| Item number | Item | Description |
|---|---|---|
| 1 | Brief name | NOTEPAD intervention |
| 2 | Why |
Anxiety and depression are underdiagnosed and undermanaged in older adults. Current interventions may not be not acceptable to older people. Loneliness and depression are strongly associated. There is limited evidence for the effectiveness of one-to-one interventions, such as befriending, for depressive symptoms. There is evidence that the most successful interventions for anxiety and depression in older people, measured by improvement in the domains of physical, mental and social health, tend to be group based and participatory and offer some activity (social or educational). BA has a good evidence base for older adults with depression Third-sector services are increasingly commissioned to provide these services but the effectiveness of non-traditional or third-sector providers delivering a psychosocial intervention has not been tested |
| 3 | What: materials |
Resources for study participants Set of training slides SW manual [All available on the project webpage – see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)] |
| 4 | What: procedures | The SW intervention is described in Table 4 (see ‘Psychosocial intervention’ row) and here [and on the project webpage – see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)] |
| 5 | Who provided |
SWs recruited from Age UK employees Recruited using advertisement and interview Training given as described in Box 1 and Delivering the support worker training [and on the project webpage – see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)] |
| 6 | How | One-to-one face-to-face and/or telephone session with or without the SW accompanying the study participant to a local group |
| 7 | Where |
One-to-one face-to-face session in the patient’s home, or a local third-sector provider (depending on study participant’s preference) and/or telephone sessions. The SW may also accompany the study participant to a local group The SW can claim for intervention contact time and travel costs. See Appendix 4 for breakdown of costs |
| 8 | When and how much | Up to six sessions (up to 1 hour face-to-face contact and up to 30 minutes telephone contact) with reminder phone calls prior to sessions |
| 9 | Tailoring | Intervention was refined as described in Table 4 (see ‘Psychosocial intervention’ row) and here, and training will emphasise that the intervention needs to be flexible to accommodate the needs of the study participant |
| 10 | Modifications | No modifications planned during the feasibility study |
| 11 | How well: planned | Fidelity to be assessed via digital recordings of the SWs’ first two contact sessions |
| 12 | How well: actual | See Chapter 5 |
The NOTEPAD participant resources
Format and content
As described in Tables 4 and 5, the format of the patient manual was discussed at PPIE meetings and with consensus groups, building on existing manuals developed by the research team for previous studies. It was agreed (see Table 4) that we would need to make adaptations to the language and content and that information in the manual would need to tailored to meet the needs of older adults. 81 In addition, we noted the suggestion from the PPIE group that the manual should take the form of an organiser to which additional, relevant information could be added. In addition, as suggested by the PPIE group, we acknowledged the need to use a larger font and simple language. We also included photographs of the local area to break up the text.
We intended to include, in the manual, examples of older people or case studies with which study participants could identify, and these needed to be age and context appropriate, including bereavement and loss of role, to facilitate engagement and make the information easier to relate to.
Functional equivalence and keeping well
The importance of staying well was thought to be an integral part of the intervention and the participant manual. To this end, the manual had sections added on the importance of helping patients to identify functionally equivalent activities, and a ‘Keeping Well Plan’ to prompt participants to continue to identify functionally equivalent activities which might replace previously enjoyed activities that they were no longer able to undertake.
At a PPIE meeting in February 2015, a draft A5 patient material file was presented to the group. This was well received, with particularly positive feedback on the personalisation of the file via the addition of a photograph of the patient’s allocated SW and on the ability of the SW to offer relevant information for the participant to add to their file.
Materials developed for NOTEPAD participants can be found on the project web page [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)].
Support worker manual
The SW manual was developed by members of the training team (CC-G, HB, KL, DB and LG), with input from co-investigator Peter Bullock from Age UK North Staffordshire. The manual supported the SW training and complemented the participant resources. The manual included suggestions to the SWs about how to introduce aspects of the NOTEPAD intervention, for example establishing the problem, and included a section on risk assessment, which was covered in the SW training.
The SW manual can be found on the project web page [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)].
Recruitment of support workers
Support workers were recruited from Age UK North Staffordshire via a job advertisement giving extensive information about the NOTEPAD study. This was devised by Peter Bullock (Chief Executive, Age UK North Staffordshire) and Heather Burroughs. Peter Bullock personally drew the attention of suitable workers to the advertisement, answered any questions that they had and encouraged them to apply by submitting a written application. The applicants were then shortlisted and selected for interview. Peter Bullock and Heather Burroughs interviewed the applicants, and six of the eight applicants were appointed. At the suggestion of the NOTEPAD study steering committee (SSC), a seventh, substitute worker was also recruited to ensure that we had enough SWs should any of them drop out.
Characteristics of recruited support workers
The previous experience, expertise and training of the SWs, as described by the SWs, in the area of mental health are outlined in Table 6.
| SW | Characteristic | ||
|---|---|---|---|
| Highest educational qualification | Training in field of mental health | Work in the field of mental health | |
| 1 | Masters | Training (2 days) about anxiety and depression in a community group setting | Better able to identify people with anxiety and depression in own groups following training |
| 2 | University degree | Counselling certificate | No |
| 3 | University degree |
Psychology as part of degree Counselling diploma |
Yes, as Samaritans (www.samaritans.org) volunteer and for victim support |
| 4 | GCSE | Dementia awareness training | Some clients have dementia |
| 5 | University degree |
Counselling training Drugs and alcohol |
Alcohol and drug addiction service |
| 6 | A level | Certificate in counselling | No |
Delivering the support worker training
The NOTEPAD training was developed from training used in previous trials,37,39,42,76 modified in line with suggestions made at the consensus group meeting (see Table 4 and Box 1).
The training was delivered over 3 days at Keele University in May 2016 by the training team (CC-G, HB, KL, DB and LG). The training was supported by a set of slides and the SW manual. Skills practice was facilitated by the use of simulated patients (SPs) recruited from the pool used for educational events at Keele University School of Medicine.
The training included a description of the role of the SW in the NOTEPAD study, discussion and revision of the risk assessment and safeguarding policies for Age UK, advice regarding note keeping about study participants and details required for the feasibility study. In addition, the requirement for recording the first two sessions with each study participant was reinforced, with training on how to use the recorder and transfer recordings to the study team. Arrangements for supervision were given during the training.
A ‘refresher’ training event, again with skills practice using SPs, was held in August 2016 owing to a delay in recruitment to the feasibility study.
All training materials can be found on the project web page [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)].
Evaluation of the training
Questionnaires were completed by the SWs before the first session and following the third session of training to assess usefulness of the training. The results are shown in Tables 7 and 8. The shift in scores to the right suggest that the training achieved what was intended. One SW indicated that they were still ‘not sure’ about how to use BA as a technique and were ‘not sure’ about how to manage people with anxiety symptoms. A different SW was ‘not sure’ about how to work with the study participants using the NOTEPAD file (patient participant resources). These items were covered in the refresher training.
| Statement number | Statement | Number of responses | ||||
|---|---|---|---|---|---|---|
| Strongly disagree | Disagree | Not sure | Agree | Strongly agree | ||
| 1 | I understand the aims of the NOTEPAD study | 3 | 3 | |||
| 2 | I understand the role of the SW in the NOTEPAD study | 4 | 2 | |||
| 3 | I have reasonable knowledge and understanding of anxiety and depression in older people | 2 | 4 | |||
| 4 | I understand how the SW will be working with the NOTEPAD study participants | 2 | 3 | 1 | ||
| 5 | I understand what the NOTEPAD ‘intervention’ is | 1 | 1 | 1 | 3 | |
| 6 | I understand why it is important to encourage older people to increase their activity | 3 | 3 | |||
| 7 | I feel confident that I can conduct a ‘person-centred’ assessment | 2 | 2 | 2 | ||
| 8 | I understand the ‘ABC’ model of emotion | 1 | 2 | 3 | ||
| 9 | I feel confident that I can help a NOTEPAD study participant understand and define their mental health | 1 | 2 | 3 | ||
| 10 | I understand the importance of assessment of risk | 1 | 3 | 2 | ||
| 11 | I feel confident that I can manage risk in older people | 2 | 3 | 1 | ||
| 12 | I understand the principles of ‘safeguarding’ | 2 | 3 | 1 | ||
| 13 | I know when to contact the GP of a study participant | 1 | 2 | 3 | ||
| 14 | I feel confident that I can structure a NOTEPAD session | 1 | 3 | 1 | ||
| 15 | I understand what BA is | 1 | 3 | 2 | ||
| 16 | I feel confident that I can use BA techniques with the NOTEPAD study participants | 3 | 1 | 1 | 1 | |
| 17 | I feel confident that I can use a diary with study participants to plan activities | 1 | 2 | 3 | ||
| 18 | I feel confident that I can work with the NOTEPAD study participants to develop their goals | 2 | 2 | 2 | ||
| 19 | I feel confident in supporting people to manage anxiety symptoms | 1 | 2 | 3 | ||
| 20 | I understand the principles of staying well | 1 | 2 | 3 | ||
| 21 | I understand how to communicate with a person face to face and over the telephone | 5 | 1 | |||
| 22 | I know how to use the SW manual | 3 | 2 | 1 | ||
| 23 | I know how to use the NOTEPAD contact sheet | 3 | 2 | 1 | ||
| 24 | I know how to work with the NOTEPAD study participant using the NOTEPAD file | 3 | 2 | 1 | ||
| 25 | I know how to contact members of the NOTEPAD team | 1 | 3 | 2 | ||
| 26 | I understand the value of supervision in the NOTEPAD study | 1 | 2 | 2 | 1 | |
| 27 | I know how to prepare for supervision in the NOTEPAD study | 2 | 1 | 1 | ||
| 28 | I understand what constitutes an adverse event in the NOTEPAD study | 3 | 3 | |||
| 29 | I know how to report an adverse event | 3 | 2 | 1 | ||
| 30 | I have a good knowledge of the local groups available that I might encourage the NOTEPAD study participants to join | 6 | ||||
| Statement number | Statement | Number of responses | ||||
|---|---|---|---|---|---|---|
| Strongly disagree | Disagree | Not sure | Agree | Strongly agree | ||
| 1 | I understand the aims of the NOTEPAD study | 1 | 5 | |||
| 2 | I understand the role of the SW in the NOTEPAD study | 2 | 4 | |||
| 3 | I have reasonable knowledge and understanding of anxiety and depression in older people | 4 | 2 | |||
| 4 | I understand how the SW will be working with the NOTEPAD study participants | 3 | 3 | |||
| 5 | I understand what the NOTEPAD ‘intervention’ is | 3 | 3 | |||
| 6 | I understand why it is important to encourage older people to increase their activity | 2 | 4 | |||
| 7 | I feel confident that I can conduct a ‘person-centred’ assessment | 4 | 2 | |||
| 8 | I understand the ‘ABC’ model of emotion | 4 | 2 | |||
| 9 | I feel confident that I can help a NOTEPAD study participant understand and define their mental health | 6 | ||||
| 10 | I understand the importance of assessment of risk | 4 | 2 | |||
| 11 | I feel confident that I can manage risk in older people | 6 | ||||
| 12 | I understand the principles of ‘safeguarding’ | 3 | 3 | |||
| 13 | I know when to contact the GP of a study participant | 6 | ||||
| 14 | I feel confident that I can structure a NOTEPAD session | 3 | 3 | |||
| 15 | I understand what BA is | 3 | 3 | |||
| 16 | I feel confident that I can use BA techniques with the NOTEPAD study participants | 1 | 2 | 3 | ||
| 17 | I feel confident that I can use a diary with study participants to plan activities | 4 | 2 | |||
| 18 | I feel confident that I can work with the NOTEPAD study participants to develop their goals | 2 | 4 | |||
| 19 | I feel confident in supporting people to manage anxiety symptoms | 1 | 2 | 3 | ||
| 20 | I understand the principles of staying well | 4 | 2 | |||
| 21 | I understand how to communicate with a person face to face and over the telephone | 1 | 5 | |||
| 22 | I know how to use the SW manual | 5 | 1 | |||
| 23 | I know how to use the NOTEPAD contact sheet | 1 | 5 | |||
| 24 | I know how to work with the NOTEPAD study participant using the NOTEPAD file | 1 | 5 | |||
| 25 | I know how to contact members of the NOTEPAD team | 4 | 2 | |||
| 26 | I understand the value of supervision in the NOTEPAD study | 3 | 3 | |||
| 27 | I know how to prepare for supervision in the NOTEPAD study | 4 | 2 | |||
| 28 | I understand what constitutes an adverse event in the NOTEPAD study | 3 | 3 | |||
| 29 | I know how to report an adverse event | 4 | 2 | |||
| 30 | I have a good knowledge of the local groups available that I might encourage the NOTEPAD study participants to join | 5 | 1 | |||
Feedback from the SPs was encouraging: it suggested that the SWs had understood the training; the SPs felt more comfortable with each of the SWs during role play on the third day of training and seemed very confident in the refresher training.
Support worker supervision
Supervision for the SWs was offered in two ways:
-
Group meetings (with refreshments) at Keele University with Carolyn A Chew-Graham and Heather Burroughs to discuss practicalities of the NOTEPAD feasibility study (including the documentation and how to use the digital recorder) and to share experiences and accumulated knowledge of local resources.
-
One-to-one supervision, either face to face or by telephone, between Carolyn A Chew-Graham and the individual SWs, at intervals to suit the SWs. The SWs were asked to complete a form to prepare for supervision. Carolyn A Chew-Graham documented each supervision session. SWs also received usual and on-going support for their work with Age UK North Staffordshire from their nominated manager at Age UK.
SWs were encouraged to claim the costs of their time and travel to attend both group meetings and individual supervision sessions.
Summary
This section has outlined phase 2 of the NOTEPAD study: refining the psychosocial intervention, developing and delivering the training for SWs and finalising the manual for use by NOTEPAD study participants. Chapter 4 describes the methods for the feasibility study within which this intervention was tested.
Chapter 4 Feasibility study methods
Aim
The aim of phase 3 of the NOTEPAD study was to determine whether or not it is feasible to recruit and randomise participants to the study, to test procedures and to conduct a process evaluation to provide essential information and data to inform a future application for a full randomised trial. The objectives were to assess feasibility in terms of recruitment of general practices and patient participants, retention, delivery of intervention, acceptability of intervention to participants, SWs and GPs, and questionnaire completion rates in both intervention and usual-care arms.
To determine feasibility, findings will be assessed against the following criteria:
-
Engage GP practices – at least six practices to participate.
-
Recruit, train and retain SWs – at least six SWs to be retained.
-
High response rates to the screening questionnaire – receive useable responses from at least 40% of those mailed.
-
Recruitment – at least two out of five individuals eligible from the screening questionnaire randomised to the trial at a rate of at least one individual per practice per week.
-
High response rates to a follow-up questionnaire – at least 75% for the primary outcome.
-
Adherence to intervention – data to be drawn from SW notes and recordings of sessions. A participant will have at least one contact with a SW. This will be investigated in more detail with the in-depth qualitative interviews with the participants, SWs and GPs to determine the barriers to, and facilitators of, intervention delivery/reception.
-
Acceptability of the intervention – to be explored using qualitative interviews.
-
Fidelity checking.
Study methods and design
Study design
The NOTEPAD study was organised into three phases as presented in Figure 3. Phases 1 and 2 are described in Chapters 5 and 6, respectively. The protocol described here relates to phase 3, the feasibility study.
The feasibility study aimed to assess whether or not it is possible to recruit and randomise patients, deliver a psychosocial intervention to older people and conduct a process evaluation. We conducted a process evaluation to explore whether or not this intervention was acceptable to participants and SWs, and to GPs. The study was conducted within primary and community care in Stoke and North Staffordshire Clinical Commissioning Groups (CCGs). This included a range of geographical areas (inner city, urban and rural) so the patient populations had a range of characteristics.
The process of phase 3 is presented in Figure 5; each stage is described in the sections that follow.
FIGURE 5.
Diagram of the NOTEPAD phase 3 processes. CASP-12, Control, Autonomy, Self-realisation and Pleasure-12 items; CIS-R, Clinical Interview Schedule-Revised; EQ-5D-5L, EuroQol-5 Dimensions, five-level version; GAD-7, Generalised Anxiety Disorder-7 items; PHQ-9, Patient Health Questionnaire-9 items; RN, research nurse.
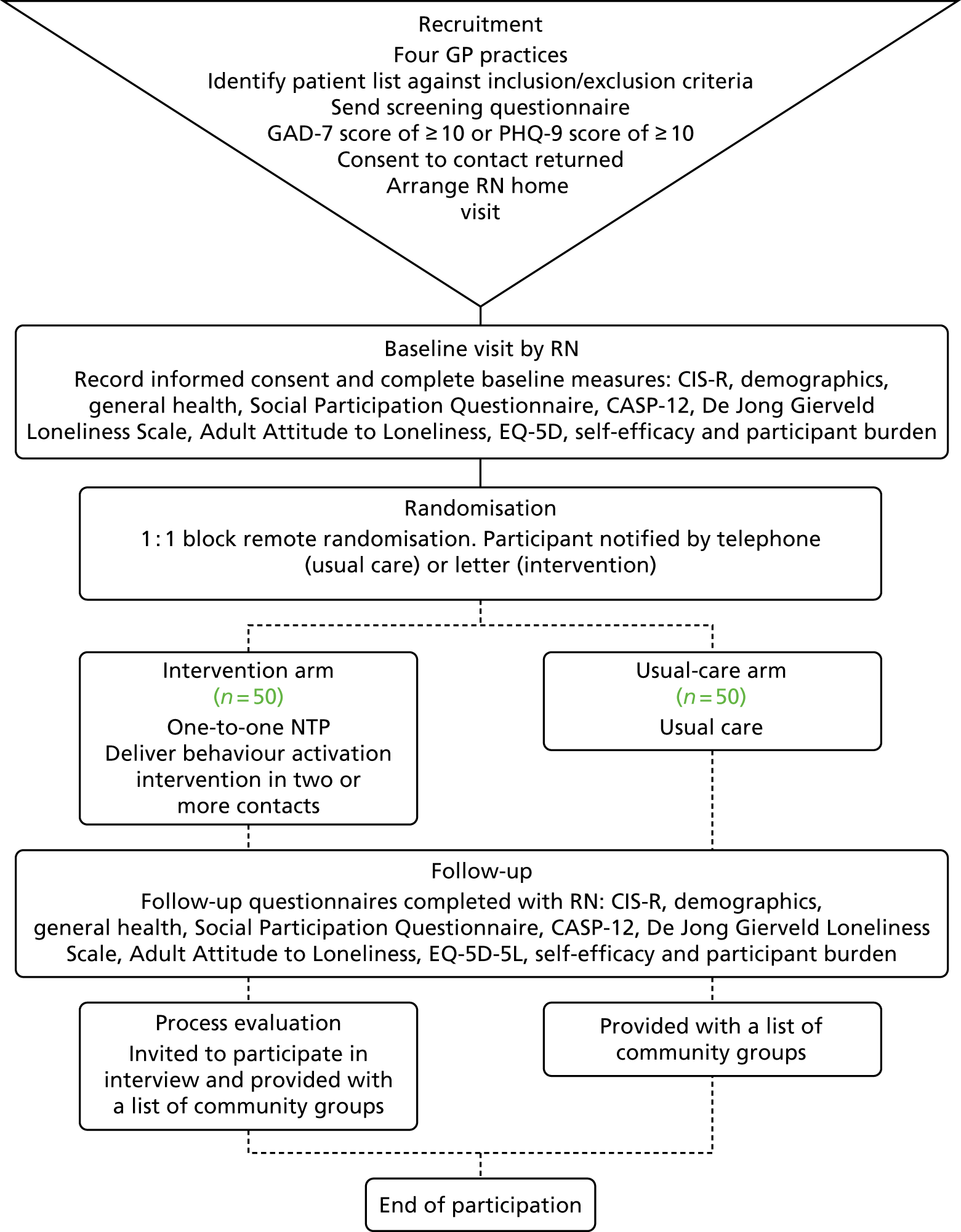
Ethics approvals and research governance
The study population comprised older adults who have depression and/or anxiety.
This study was conducted in accordance with the principles of Good Clinical Practice. 82
Research ethics approval was obtained from the National Research Ethics Committee North West – GM West on 16 August 2016 [Research Ethics Committee (REC) reference number 16/NW/0552].
Appropriate NHS Health Research Authority (HRA) approvals were obtained prior to study commencement. Amendments to study protocols and documentation were reviewed and approved by the NHS REC and HRA. A log of amendments is available on the project web page [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)].
Patient participants had full access to NHS services throughout their study participation.
Trial registration
The study is registered with the International Standard Randomised Controlled Trial Number (ISRCTN) registry as ISRCTN16318986. Registered 10 November 2016.
Study oversight
The study was hosted and sponsored by Keele University. The NOTEPAD feasibility study was managed by the trial management group consisting of the chief investigator (CC-G), principal investigator (HB), Keele co-applicants, including Peter Bullock (Chief Executive, Age UK North Staffordshire), and the study co-ordinator from Keele Clinical Trials Unit (CTU). Monthly meetings ensured that study progress, targets and any problems were monitored and reviewed.
Additional governance oversight was provided by an independent SSC. Details of the SSC members are provided in Appendix 5, Table 34.
Recruitment setting and sample size
Recruitment of general practices
Six general practices in North Staffordshire and Stoke-on-Trent were recruited to identify eligible participants. The practices were recruited through the NIHR Clinical Research Network West Midlands (CRN WM). Practice recruitment was staggered, beginning with searches and a mail-out to potential participants from two practices before increasing the number of practices as needed.
Recruitment of participants
Practice lists from the participating general practices were searched (by CRN WM clinical studies officers) for people aged ≥ 65 years. We asked GPs to screen the resulting lists and remove people who met the exclusion criteria: at risk of self-harm/suicide, under secondary/specialist care mental health services, alcohol/substance abuse, in the palliative phase of an illness, lacking capacity to consent, inability to understand or read English or living in a care home.
People on the resulting list of potential participants were sent an invitation pack consisting of an invitation letter, a participant information sheet, a postal screening questionnaire with a consent-to-contact form and a stamped addressed envelope, all of which are available on the project web page [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)].
The postal screening questionnaire consisted of the Patient Health Questionnaire-9 items (PHQ-9),83 Generalised Anxiety Disorder-7 items (GAD-7)84 and a section seeking consent to further contact (see Appendix 6). Individuals returning a completed questionnaire with a score of ≥ 10 on the PHQ-9 and/or the GAD-7 and who consented to further contact formed the sample for invitation to the feasibility study. A research nurse (RN) contacted these individuals and recompleted the PHQ-9 and/or GAD-7 over the telephone to ensure that depression and anxiety symptoms had not been transient. For those who scored ≥ 10 on the PHQ-9 and/or the GAD-7, the RN arranged a home visit with the potential study participant to complete the baseline assessment. Those who scored ≤ 9 on both the PHQ-9 and the GAD-7 conducted over the telephone were thanked by the RN for their time, informed that they were not eligible for the study and were offered a copy of the resource directory if they would like it.
If no response to the postal screening questionnaire was received after 14 days, a reminder postcard was sent to potential participants on the practice list. Where an illegible, missing or erroneous contact number was received, a letter requesting clarification of the contact number was sent.
Sample size
Because this was not a hypothesis-testing trial, a formal power calculation was not required. Nonetheless, as this is a feasibility study, we aimed for each arm to consist of 30–40 participants to reliably estimate process outcomes relating to recruitment, retention and attrition rates, which would inform a fully powered randomised controlled trial (RCT). 85 We anticipated that the total combined loss to follow-up would not exceed 20% at 4 months and, therefore, aimed to recruit 50 participants to each study arm.
We anticipated that six practices would enable us to recruit the required number of participants. Approximately 1000 people aged > 65 years are expected to be registered in an average-sized general practice of 5000 patients. On the assumption that 50% of people would respond to the postal screening questionnaire, of whom we expected 20% to have anxiety and/or depression, we anticipated a potential sample size of 100 per practice. We expected that 30% of these might give consent to take part, resulting in an anticipated recruitment of approximately 30 participants per practice over a 9-month period. Confirming these screening and enrolment rates was part of the reason for performing the feasibility study.
Baseline visit
The baseline visit was conducted by a clinical research network (CRN) RN who had previously received training (from the research team) about the study and how to conduct assessments. At the baseline visit, the RN discussed the study further with the potential participant, responding to any questions that the person had. Although patients were screened against the exclusion criteria by their GP prior to the initial mail-out, the RN was asked to again check the potential participants against the inclusion/exclusion criteria (exclusion criteria: at risk of self-harm/suicide, under secondary/specialist care mental health services, alcohol/substance abuse, in the palliative phase of an illness, lacking capacity to consent, inability to understand or read English or living in a care home). The RN was also asked to administer an assessment of cognitive capacity using a cognitive capacity proforma. If a participant scored > 0 they were deemed unsuitable for recruitment to the study.
The RN explained to those potentially eligible for the NOTEPAD study what participating in the study would involve – the completion of baseline and follow-up questionnaires and, if randomised to the intervention arm, participation in up to six meetings with the Age UK SW, a qualitative interview (subsample only) and an audio-recording of up to two of the consultations with the Age UK SW – and sought written consent before inviting the participant to complete the baseline questionnaires.
Outcome measures
The computerised Clinical Interview Schedule-Revised (CIS-R)85 total score was our primary outcome, but its performance was examined in the feasibility study in terms of its precision [based on the 95% confidence interval (CI)], completion rate at the item and scale level and any evidence of floor or ceiling effects. The CIS-R was administered by the RN via laptop.
Secondary outcome measures included:
-
PHQ-9 score83
-
GAD-7 score84
-
self-efficacy score86 (for those who disclosed a long-term condition)
-
quality of life score [Control, Autonomy, Self-realisation and Pleasure-12 items (CASP-12)]87
-
health-related quality of life score [EuroQol-5 Dimensions, five-level version (EQ-5D-5L)]88
-
De Jong Gierveld Loneliness Scale score89
-
Adult Attitude to Loneliness score90
-
Social Participation Questionnaire score. 91
Demographic questions covering age, sex, ethnic background, marital status, general health and household economic status were included in the baseline questionnaire.
The level of respondent burden (for completion of the questionnaires) was monitored by free text that was intended to be analysed as part of the process evaluation. We asked the RN to offer breaks between completion of scales; the optimum method of administration will be determined to help inform the methods of a full trial application.
Randomisation
Once written informed consent and the baseline measures were collected, participants were randomised by the study administrator to either the intervention arm or the usual GP care arm. After the baseline visit, the RN contacted the study administrator, who randomised the participant using the study-specific database. A researcher (HB) informed those allocated to the usual-care arm of the outcome by telephone. Where a participant was randomised to the intervention arm, they received a letter informing them that an Age UK SW would make contact with them in the next week. The participant’s contact details were sent to Age UK by Safe Haven fax. Peter Bullock then allocated the study participant to a SW. It was intended that allocation would enable an equitable distribution of participants to each SW. We had hoped that SWs would align themselves to one or two practices, but the staggered recruitment from one practice at a time did not allow this.
Randomisation was in a 1 : 1 ratio, using randomly permuted blocks of sizes 4, 6 and 8 to ensure that there was a balanced allocation to each arm of the trial. The study statisticians (RO and EN) and the study team members involved in the collection of follow-up data were blinded. Each participant’s GPs was sent a letter informing them of their patient’s participation and randomisation allocation.
Usual-care arm
Participants randomised to the usual-care arm received whatever care is judged to be suitable by the primary care practitioners in contact with them. No constraints were placed on what constituted as ‘usual care’. We intended to use the feasibility study to describe care for participants in the usual-care arm of the study: data on self-reported health and social care utilisation were collected at follow-up at 4 months. At follow-up, participants in the usual-care arm were offered a list of local community groups that they could choose to access.
Intervention arm
Participants randomised to the intervention arm were offered an individual appointment with the Age UK SW in the participant’s home or at a local third-sector service (depending on the participants’ preference). The SW was to work with the study participant and deliver the intervention as described in Chapter 3.
We anticipated that there would be 4–6 contacts between the participant and the SW, utilising a combination of face-to-face and telephone contact. The intervention was intended to be tailored to patient preference, so there was flexibility regarding the precise number of sessions, interval, mode of delivery and format. Participant preference for the type of session was intended to be explored in the process evaluation interviews. The content of the intervention was monitored for fidelity by digitally recording the first two sessions the SW had with each participant. These digital recordings were checked against a fidelity checklist (by CC-G and HB) as part of the process evaluation.
Intervention group participants also received treatment as usual from their general practice.
The SWs were asked to record basic information about participation activities, including referrals, signposting or accompanying participants to third-sector services. Each SW was asked to complete a brief summary of the content of each participant contact.
We asked the participants to record a one-line summary of their sessions with the SW and activities that they attended (or had been signposted to but had not attended). Our PPIE group helped us to develop the optimum method of collecting such data, which was incorporated into the organiser-style participant resource.
Follow-up
Follow-up data collection was intended to be completed for all participants 4 months after baseline. All randomised participants were contacted and a home visit with a RN arranged. A follow-up questionnaire consisting of the following scales was used:
-
CIS-R administered by laptop
-
PHQ-9
-
GAD-7
-
health-related quality of life (EQ-5D-5L)
-
quality of life (CASP-12)
-
De Jong Gierveld Loneliness Scale
-
Adult Attitude to Loneliness
-
self-efficacy score
-
Social Participation Questionnaire.
Process evaluation
The aim of the process evaluation was to determine whether or not Age UK SWs can deliver the NOTEPAD psychosocial intervention to older people with sufficient fidelity to the training. The process evaluation explored whether or not the one-to-one intervention, delivered by SWs, is acceptable to older adult participants and whether or not the intervention affected GPs in participating practices. Interviews were used to explore whether or not the intervention made sense to the study SWs and whether or not the training, support materials and supervision were acceptable.
Analysis of responses about completion of questionnaires
To explore the acceptability of the baseline and follow-up questionnaires in terms of participant burden, the text in the free-text boxes at the end of the questionnaires was collated and thematically analysed.
Fidelity checking
It was intended that the first two consultations between the SWs and patient participants would be digitally recorded with both parties’ consent. Researchers from the qualitative team examined the recordings from the SW sessions with the NOTEPAD participants and used a fidelity checklist specifically developed for the study (see Appendix 7) to assess whether or not components of the SW sessions that were intended to be included, and focused on during training, were demonstrated by the SW in the recorded session. A descriptive analysis was produced. Data collected from the digital recordings will be available for future thematic analysis.
Interviews with key informants
Patient participants
To assess the acceptability of the intervention to participants, we aimed to conduct up to 20 semistructured interviews with participants in the intervention group shortly after the follow-up visit by the RN at 4 months. We also aimed to conduct interviews with any older person who dropped out of the intervention.
A letter was sent to participants after their follow-up appointment to let them know that a researcher would contact them by telephone and arrange a time and date for interview. Consent for this contact was obtained at entry into the study. We aimed to sample on baseline characteristics to ensure views from a diverse sample were sought. The participants who took part in the process evaluation interviews were offered a £20 shopping voucher as a ‘thank you’ for participating.
Telephone interviews with people who declined to participate in the study
As the study progressed, the research team were concerned about the large number of people declining to participate at the telephone call with the RN. At the suggestion of the SSC (March 2017), an amendment to the ethics approval was applied for and obtained to enable members of the research team to contact people who were eligible for the study but declined, and explore their reasons for declining. These data were collated by the research team.
General practitioners
Letters were sent to GPs in participating practices, inviting them to participate in a semistructured interview. We aimed to interview up to 12 GPs from the participating practices.
Support workers
Letters were sent to the SWs, followed up by an e-mail and telephone call, to arrange a time for an interview. The SWs agreed to participate in the interview as part of their appointment to the SW role. They were invited for interview within 4 weeks of the last appointment with their last participant.
Data generation
Interviews were conducted by Bernadette Bartlam or Heather Burroughs at a time and place convenient to the participants. GPs were offered the option of a telephone interview or joint interviews with colleagues in the practice.
The topic guide for patient participants (in the intervention arm) explored:
-
their overall perspectives on the intervention
-
whether or not the questionnaires were acceptable
-
participant equipoise and propensity to undergo randomisation in a pilot RCT
-
how acceptable and useful they found the one-to-one sessions with the SW
-
preference for face-to-face or telephone intervention sessions
-
what they recalled doing with the SW
-
whether or not they attended any groups and whether or not (and how) this was facilitated by the SW
-
how closely the group interventions matched the interests of the participants
-
how acceptable and useful they found the group sessions
-
satisfaction with the group intervention
-
whether or not the intervention was flexible enough to meet their needs
-
whether or not they had previous contact with services and reasons why they did or did not
-
barriers to and facilitators of their (non-)engagement with the SW or with groups
-
use of the participant manual (notepad file) and diaries
-
whether or not their engagement in a group has continued.
The topic guide for people who had ‘dropped out’ explored:
-
reasons for interest in the study
-
whether or not the questionnaires were acceptable
-
participant equipoise and propensity to undergo randomisation in a pilot RCT
-
reasons for discontinuing
-
overall perspectives on the intervention
-
preference for face-to-face or telephone intervention sessions
-
how acceptable and useful they found the one-to-one sessions with the SW
-
what they recalled doing with the SW.
The topic guide for people who declined to participate explored their understanding of the study and reasons for declining.
The topic guide for GPs explored:
-
their perspectives on managing older people with anxiety and depression
-
experiences of barriers to and facilitators of working with the third sector
-
clinician’s position of equipoise regarding the treatment arms
-
any feedback that they have received from older patients involved in the NOTEPAD study
-
any contact with the SWs or study team and the impact on themselves and the practice
-
whether or not (and how) their management of older people with anxiety and/or depression has changed.
The topic guide for SWs explored:
-
their reflections on the NOTEPAD intervention and working with the research team
-
their experiences of training
-
their experiences of delivering the NOTEPAD intervention to older people, attitudes to outcome assessment, experiences of assessing and dealing with risk and experiences of signposting to groups
-
views on the SW manual and client resources, the NOTEPAD file, use of diaries and use of mood thermometers
-
their experiences of support and supervision
-
their views on liaison with primary care (if this took place) and other statutory agencies (e.g. IAPT)
-
barriers to and facilitators of implementation of such an intervention.
Data management
All information and documentation relating to this study is stored securely on password-protected computers or filed in locked cabinets in Keele CTU. In accordance with Keele CTU standardised operating procedures (SOPs), data have been anonymised, are held securely (in locked cabinets and/or on secure servers) and will be archived for at least 5 years after the grant has ended. Keele CTU is legally obliged to store research data securely and this has been done by removing all personally identifiable information from all sources at an appropriate stage of the study. Paper-based consent records that are personally identifiable are stored separately from research data. The processing of data (in line with the Data Protection Act 1998)92 will occur within Keele CTU. Once personal data have been processed and are not required for contact with the participant, they are destroyed and research databases are anonymised using a unique code ID allocated to each participant. All questionnaires completed by/with participants are identified by the participant’s unique code and are therefore anonymised.
The computerised CIS-R data were kept on an encrypted Universal Serial Bus (USB) stick and this was used to move the data from the laptop. The RN then uploaded the data directly from the USB stick into the CTU secure server using a CTU file transfer protocol.
All sensitive data sets are retained on a secure server and access is restricted dependent on study team role at Keele CTU. Access to all research data sets is controlled by password protection and additional permissions to access folders pertaining to the data.
Study and participant information from the qualitative interviews as part of the process evaluation is stored and processed securely (as above). Any identifying information provided to the study team has been dealt with in the strictest confidence under the terms of the Keele University Code of Research Conduct.
Data analysis
The data collected in this study include sequential quantitative and qualitative types owing to the mixed methods being applied.
Quantitative data
Statistical analysis followed a detailed statistical analysis plan (SAP) formally agreed with the SSC prior to data analysis. The analysis has focused on (1) describing the key process measures to decide if a main trial would be feasible, (2) baseline description of the study sample, (3) exploratory analysis of clinical outcomes, (4) reports of adverse events in any of the treatment arms, (5) descriptive summaries of the contacts made with the SW (in relation to adherence with randomised intervention) and satisfaction with care and (6) extent of missing data and data accuracy. There was no emphasis on hypothesis testing, which is reserved for a future main trial. Feasibility outcomes were estimated using descriptive statistics (with 95% CI). The assessment of key process measures will include determining the engagement of GP practices, recruitment, training and retention of SWs, response rate to the screening questionnaire, participant’s recruitment uptake and response to follow-up.
At follow-up at 4 months we intended to compare the key patient characteristics of those followed up and those lost to follow-up and to investigate how similar these are across the treatment arms to assess possible attrition bias in data collection.
The extent of protocol adherence will be reported within the intervention group in terms of participants who adhere to the intervention that they were allocated to receive or comply with the scheduled visits.
A baseline table will compare important demographic and clinical characteristics between the two trial arms. The primary clinical outcome measure at 4 months will be analysed on an intention-to-treat basis (participants analysed according to the arm to which they were randomised, irrespective of whether or not they actually received the intervention as intended) using a linear regression model adjusted for baseline outcome scores, age and sex to estimate the probable range of intervention effects, that is, to determine if the mean total CIS-R score differs between the intervention and the usual-care arms after controlling for the differences at baseline. The emphasis is on CIs of effect-size estimations rather than hypothesis testing to explore the imprecision around effect sizes. The SAP outlined the intention to conduct mixed-effect ordered logistic regression models adjusted for age and sex to be used to compare the individual symptoms of the CIS-R between the trial arms. Scores on each of the 14 symptom groups on the CIS-R will be entered into the models as ordinal dependent variables. We intended to analyse between-group differences in secondary outcomes at 4 months and provide point and 95% CI estimates from linear or logistic regression models as appropriate to the outcome data being analysed (linear for numerical measures and logistic for categorical measures).
Qualitative data
Analysis of narrative in response to question about participant burden
Participants were asked by the RN about their views on the length of, and questions in, the baseline and follow-up questionnaires to assess participant burden. Comments were collated by the research team.
Analysis of digitally recorded consultations (fidelity checking)
The SWs were asked to record their first two meetings with a NOTEPAD participant (with study participant’s consent). Researchers (HB and CCG) listened to the audio recordings from the SW sessions with the NOTEPAD participants and used a fidelity checklist specifically developed for the study (see Appendix 7) to assess whether or not components of the SW sessions intended to be included, and focused on during training, were demonstrated by the SW in the recorded session. A descriptive analysis was produced. Data collected from the audio recordings will be available for future thematic analysis.
The recordings and paper copies of the sessions will be kept securely for a minimum of 5 years after funding has ended and after this time they will be destroyed. If any of the recordings contain comments or information that might identify a third party (e.g. a GP) or an institution (e.g. health centre/general practice), we will amend them to ensure that the person or institution cannot be identified in any account or published report of this study.
Analysis of interview data
The interviews were transcribed verbatim, the transcripts forming the data for analysis. Data were stored, managed and analysed using NVivo 10. Initially the data were analysed using the constant comparison method93 within each data set (patient participants, SWs and GPs). Analysis was then conducted across the three data sets presented using the principles of framework analysis,93 a method appropriate for applied policy research that allows the development of an understanding of how the intervention was implemented (or not) and operationalised by respondents. A team of researchers (CCG, BB and HB) conducted analysis individually and then agreed themes through discussion; conducting analysis with researchers of different professional backgrounds increases the trustworthiness of the analysis. 74
Ethics considerations
Confidentiality
The standard data protection procedures operating in the Keele CTU have been employed to protect confidentiality and anonymity. Only on receipt of a consent-to-contact form did the study team have access to personal details of participants. Personal identifiable data were used only for the purpose of mailing out study-related documentation and conducting study-related telephone calls.
A subsample of study participants were mailed an invitation to participate in a semistructured interview. Mailing data were held in a separate database to research data. At the end of the study the mailing database was stripped of all identifiable information and an anonymised version retained so that the study team has a record of numbers mailed, numbers responded, exclusion reasons, etc.
The Keele CTU has robust data security systems and procedures in place, which are regularly reviewed and which achieve the legal obligations set by the Data Protection Act 199892 and follow General Medical Council (GMC), Caldicott Guardian and British Computer Society standards and guidelines. Any personal identifiable data will only be held for as long as they are needed (e.g. to undertake mailing) and identifiable data are removed from research databases as soon as possible. Each person was allocated a unique study number so that only anonymised data are used for analysis. All electronic data are held on a dedicated, password-protected, firewalled university server. All recorded content was anonymised and coded for analysis and writing up of the research. Only members of the study team and the SWs delivering the intervention had access to participants’ personal data during the study.
Confidentiality and anonymity has been maintained for all participants. Full information about the purpose and uses of participants’ contributions was given. Participants were free to withdraw from the study at any time; however, any information provided up until the point of withdrawal was kept as agreed via the consent process.
Participant burden
The burden of taking part in this study included the completion of questionnaires delivered by the RN, and participants randomised to the intervention arm were asked to participate in up to six consultations with the SW, a qualitative interview (subsample only) and audio recording of up to two of their consultations with the SW.
The baseline visit was anticipated to take approximately 90 minutes to complete, and the follow-up interview up to 45 minutes to complete.
Study management and safety reporting procedures are reported in Appendix 5.
Patient and public involvement and engagement
Because a key study objective was to develop an intervention that was person-centred, it was particularly important to incorporate a large PPIE component within the study.
As described in Chapter 2, our PPIE group played an integral part in the development of the NOTEPAD study. The group’s input to the feasibility study included advising that the term ‘non-traditional provider’ would not be acceptable to older people and that we should use the term ‘support worker’. The PPIE group contributed to the logo used for the study and the strapline ‘Supporting Mental Strength’ (Figure 6).
FIGURE 6.
The NOTEPAD logo.
The PPIE group contributed to the refinement of the NOTEPAD intervention and patient materials, which was fed into the consensus group meeting (see Chapter 3), and advised on patient-facing documents for participant recruitment as part of the ethics approval.
The group met in May 2017 to discuss recruitment and contributed to discussion of findings towards the end of the study.
The PPIE members were reimbursed for their time (£12 per hour, paid in vouchers), with an average meeting length of 2–3 hours plus preparation time, and travel expenses and had refreshments provided. Two members of the PPIE group were also members of the SSC (see Table 10).
Summary
This section has outlined the methods for the NOTEPAD feasibility study. The results are presented in Chapter 5.
Chapter 5 Results of NOTEPAD feasibility study
Quantitative results
Practice recruitment
Six practices were identified by the CRN but, owing to delays in the process of ethical review and HRA approvals, recruitment was limited to a 5-month recruitment period in four practices. Characteristics of the four practices which recruited patients are included in Table 9.
| General practice ID | Number of GP partners | Size of list | Geographical area |
|---|---|---|---|
| Practice 1 | 2 | 4648 | Inner city |
| Practice 2 | 4 | 7028 | Rural |
| Practice 3 | 4 | 7255 | Urban |
| Practice 4 | 6 | 10,978 | Urban |
Patient recruitment
The searches of practice records identified 3822 people aged ≥ 65 years. Of these, 60 met the study exclusion criteria so were excluded by GPs.
Information packs and screening questionnaires were mailed to 3762 people. The flow of participants in the feasibility study is shown as a Consolidated Standards of Reporting Trials (CONSORT) flow diagram in Figure 7.
FIGURE 7.
The CONSORT recruitment flow diagram for NOTEPAD phase 3.
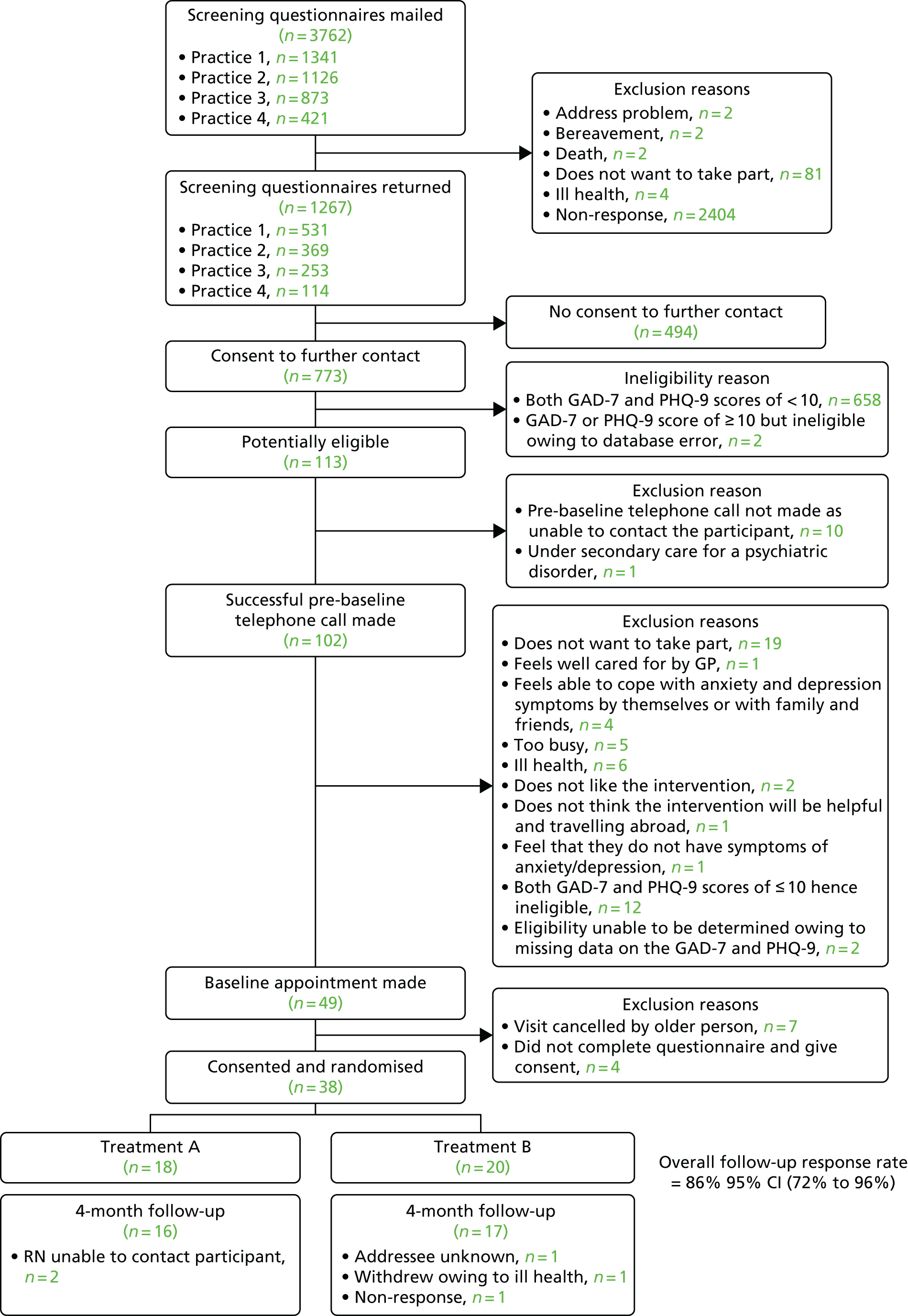
Notably, out of 113 potentially eligible people identified, 38 were randomised. Ten people were not contactable by the RN and 54 declined to participate in the study. The RN documented reasons for declining and these included ‘not wanting to take part’ (19 people). One person directly said that anxiety or depression was not a problem, and five people described having mood problems but felt that they were sufficiently supported by family, friends or their GP.
As outlined in Chapter 4, an ethics amendment was obtained to enable the research team to contact people declining to participate at this stage, to explore reasons for declining. Analysis of data generated by these telephone calls is given in Process evaluation results, Analysis of qualitiative data, Findings, and Decliners.
Participant characteristics
The descriptive characteristics of the 38 study participants are given in Table 10.
| Characteristic | Arm | Total (N = 38) | |
|---|---|---|---|
| Intervention (N = 18) | Usual care (N = 20) | ||
| Female sex, n (%) | 10 (56) | 12 (60) | 22 (58) |
| Age, median (IQR) | 73 (69–78) | 70 (67–72) | 71 (68–76) |
| Ethnic group, n (%) | |||
| English/Welsh/Scottish/Northern Irish/British | 18 (100) | 20 (100) | 38 (100) |
| Employment status, n (%) | |||
| In full-time paid work | 0 (0) | 1 (6) | 1 (3) |
| Looking after home/dependants | 1 (7) | 1 (6) | 2 (6) |
| Retired | 14 (93) | 14 (88) | 28 (90) |
| Marital status, n (%) | |||
| Married | 10 (56) | 12 (60) | 22 (58) |
| Cohabiting (living as married) | 1 (6) | 1 (5) | 2 (5) |
| Widowed | 5 (28) | 7 (35) | 12 (32) |
| Divorced or separated | 2 (11) | 0 (0) | 2 (5) |
| Never married | 0 (0) | 0 (0) | 0 (0) |
| Social class, n (%) | |||
| Large employers and higher managerial and administrative occupations | 1 (6) | 1 (5) | 2 (5) |
| Higher professional occupations | 0 (0) | 2 (10) | 2 (5) |
| Lower managerial, administrative and professional occupations | 7 (39) | 3 (15) | 10 (26) |
| Intermediate occupations | 3 (17) | 4 (20) | 7 (18) |
| Small employers and own account workers | 1 (6) | 2 (10) | 3 (8) |
| Lower supervisory and technical occupations | 3 (17) | 2 (10) | 5 (13) |
| Semi-routine occupations | 0 (0) | 5 (25) | 5 (13) |
| Routine occupations | 3 (17) | 1 (5) | 4 (11) |
| Living situation, n (%)a | |||
| Live alone | 5 (28) | 7 (35) | 12 (32) |
| Live with one other person | 10 (56) | 11 (55) | 21 (55) |
| Live with more than one other person | 3 (17) | 2 (10) | 5 (13) |
| General health, n (%) | |||
| Excellent | 2 (11) | 0 (0) | 2 (5) |
| Very good | 3 (17) | 4 (20) | 7 (18) |
| Good | 2 (11) | 4 (20) | 6 (16) |
| Fair | 3 (17) | 6 (30) | 9 (24) |
| Poor | 8 (44) | 6 (30) | 14 (37) |
| Taking medication for low mood or stress, n (%) | 8 (44) | 10 (50) | 18 (47) |
| Has a long-standing illness, disability or infirmity, n (%) | 16 (89) | 20 (100) | 36 (95) |
| Number of long-standing illnesses, mean (SD) | 4.2 (2.3) | 3.1 (1.4) | 3.6 (1.9) |
| CIS-R score (0–57), mean (SD) | 21.7 (10.1) | 23.2 (7.3) | 22.5 (8.7) |
| PHQ-9 score (0–27), mean (SD) | 15.5 (4.9) | 15.8 (4.5) | 15.6 (4.7) |
| GAD-7 score (0–21), mean (SD) | 12.5 (4.7) | 14.3 (5.4) | 13.4 (5.1) |
| Self-efficacy score (1–10), mean (SD) | 4.7 (2.6) | 5.1 (1.6) | 4.9 (2.1) |
| EQ-5D-5L score [–0.281 (extreme problems on all dimensions) to 1 (no problems on any dimension)], mean (SD) | 0.51 (0.36) | 0.50 (0.24) | 0.51 (0.30) |
| CASP-12b score (0–33), median (IQR) | 18 (15–24) | 19.5 (18–23) | 18.5 (16–23) |
| De Jong Gierveld Loneliness Scale score (0–6), mean (SD) | 2.4 (1.5) | 3.9 (1.9) | 3.2 (1.9) |
| Adult Attitude to Loneliness scale score (0–36), mean (SD) | 18.6 (3.8) | 20.6 (4.8) | 19.6 (4.4) |
| Social Participation Scale score (0–94), mean (SD) | 25.3 (10.0) | 21.9 (11.9) | 23.4 (11.0) |
We managed to recruit both men and women to participate in the study. All participants were white, reflecting the ethnic mix of the recruiting practices in North Staffordshire. A total of 32% participants lived alone. A total of 38% participants rated their health as ‘fair’ or ‘poor’ and participants reported a mean of 3.6 long-term health conditions, including arthritis, pain, ‘heart problems’ and diabetes.
The mean CIS-R score of 22.5 indicated high psychological morbidity; a CIS-R score of ≥ 18 denotes more severe or pervasive symptoms ‘of a level very likely to warrant intervention such as medication or psychological therapy’. 85
Table 11 compares the PHQ-983 and GAQ-784 scores of potentially eligible participants with those who were subsequently randomised to the study. The PHQ-9 and/or GAD-7 scores were slightly higher in the randomised participants.
| Instrument | Participants, mean (SD) | |
|---|---|---|
| Potentially eligible on the screening questionnaire (n = 113) | Randomised (n = 38) | |
| PHQ-9 score | 13.7 (5.3) | 15.6 (4.7) |
| GAD-7 score | 11.8 (5.3) | 14.3 (5.4) |
The mean PHQ-9 scores indicated that participants had major depression (moderate severity) and the mean GAD-7 scores indicated that participants had moderate anxiety. Almost half the participants reported that they were taking tablets for low mood or stress, suggesting that they are consulting primary care but that their mood problems are not being adequately managed. Thus, the participants recruited to the study had high levels of psychological and physical morbidity.
The results of the primary outcome (CIS-R) score are shown in Table 12. Scores were reduced in both intervention and usual-care arms at the follow-up at 4 months; the reduction was greater in the usual-care arm.
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| CIS-R score, mean (SD) | 21.7 (10.1) | 23.2 (7.3) | 22.5 (8.7) |
| CIS-R score, mean (95% CI) | 21.7 (16.7 to 26.8) | 23.2 (19.8 to 26.6) | 22.5 (19.7 to 25.3) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| CIS-R score, mean (SD) | 17.7 (10.0) | 15.5 (9.2) | 16.5 (9.5) |
| CIS-R score, mean (95% CI) | 17.7 (12.4 to 23.0) | 15.5 (10.8 to 20.2) | 16.5 (13.2 to 19.9) |
| Treatment effect, mean (95% CI) | –2.2 (–9.0 to 4.6) | ||
| Adjusted treatment effect, mean (95% CI) | –2.9 (–9.1 to 3.3) | ||
Outcomes
There were insufficient numbers of participants to analyse between-group differences in secondary outcomes at 4 months.
Similar reductions were seen in PHQ-9 and/or GAD-7 scores at 4 months in both intervention and usual-care arms (Tables 13 and 14).
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| PHQ-9 score, mean (SD) | 15.5 (4.9) | 15.8 (4.5) | 15.6 (4.7) |
| PHQ-9 score, mean (95% CI) | 15.5 (13.1 to 17.9) | 15.8 (13.4 to 18.2) | 15.6 (14.0 to 17.3) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| PHQ-9 score, mean (SD) | 12.9 (7.3) | 8.8 (5.5) | 10.7 (6.7) |
| PHQ-9 score, mean (95% CI) | 12.9 (8.8 to 16.9) | 8.8 (5.8 to 11.7) | 10.7 (8.3 to 13.2) |
| Treatment effect, mean (95% CI) | –4.1 (–8.8 to 0.61) | ||
| Adjusted treatment effect, mean (95% CI) | –3.6 (–8.3 to 1.1) | ||
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| GAD-7 score, mean (SD) | 12.5 (4.7) | 14.3 (5.4) | 13.4 (5.1) |
| GAD-7 score, mean (95% CI) | 12.5 (10.1 to 14.9) | 14.3 (11.6 to 16.9) | 13.4 (11.7 to 15.2) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| GAD-7 score, mean (SD) | 10.0 (5.7) | 9.4 (5.7) | 9.7 (5.6) |
| GAD-7 score, mean (95% CI) | 10.0 (7.0) | 9.4 (6.5 to 12.4) | 9.7 (7.7 to 11.7) |
| Treatment effect, mean (95% CI) | –0.6 (–4.6 to 3.5) | ||
| Adjusted treatment effect, mean (95% CI) | –2.0 (–5.8 to 1.8) | ||
Table 15 illustrates that self-efficacy was essentially unchanged at 4 months.
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| Self-efficacy score, mean (SD) | 4.7 (2.6) | 5.1 (1.6) | 4.9 (2.1) |
| Self-efficacy score, mean (95% CI) | 4.7 (3.3 to 6.0) | 5.1 (4.3 to 5.9) | 4.9 (4.2 to 5.6) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| Self-efficacy score, mean (SD) | 4.5 (2.3) | 5.6 (1.8) | 5.1 (2.1) |
| Self-efficacy score, mean (95% CI) | 4.5 (3.2 to 5.9) | 5.6 (4.5 to 6.6) | 5.1 (4.2 to 5.9) |
| Treatment effect, mean (95% CI) | 1.04 (–0.5 to 2.6) | ||
| Adjusted treatment effect, mean (95% CI) | 0.79 (–0.78 to 2.3) | ||
EQ-5D-5L scores were similar in both intervention and usual-care arms, although scores seemed to increase at follow-up at 4 months in the usual-care arm (Table 16).
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| EQ-5D-5L score, mean (SD) | 0.51 (0.36) | 0.50 (0.24) | 0.51 (0.30) |
| EQ-5D-5L score, mean (95% CI) | 0.51 (0.33 to 0.69) | 0.50 (0.39 to 0.62) | 0.51 (0.41 to 0.61) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| EQ-5D-5L score, mean (SD) | 0.55 (0.36) | 0.64 (0.24) | 0.60 (0.30) |
| EQ-5D-5L score, mean (95% CI) | 0.55 (0.36 to 0.74) | 0.64 (0.52 to 0.77) | 0.60 (0.49 to 0.70) |
| Treatment effect, mean (95% CI) | 0.09 (–0.12 to 0.31) | ||
| Adjusted treatment effect, mean (95% CI) | 0.14 (–0.03 to 0.31) | ||
Table 17 illustrates that the quality-of-life measure, CASP-12, scores were similar in both intervention and usual-care arms at baseline, but were slightly lower in the usual-care arm at follow-up at 4 months.
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| CASP12µ score, mean (SD) | 19.7 (7.2) | 20.3 (5.1) | 20.0 (6.1) |
| CASP12µ score, mean (95% CI) | 19.7 (16.1 to 23.2) | 20.3 (17.9 to 22.7) | 20.0 (18.0 to 22.0) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| CASP12µ score, mean (SD) | 20.3 (7.1) | 17.9 (6.6) | 19.0 (6.8) |
| CASP12µ score, mean (95% CI) | 20.3 (16.3 to 24.2) | 17.9 (14.5 to 21.3) | 19.0 (16.6 to 21.5) |
| Treatment effect, mean (95% CI) | –2.3 (–7.3 to 2.6) | ||
| Adjusted treatment effect, mean (95% CI) | –2.3 (–6.5 to 1.9) | ||
Table 18 illustrates that scores on the De Jong Gierveld Loneliness Scale were similar in both arms at baseline and 4-month follow-up.
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| De Jong Gierveld Loneliness Scale score, mean (SD) | 2.4 (1.5) | 3.9 (1.9) | 3.2 (1.9) |
| De Jong Gierveld Loneliness Scale score, mean (95% CI) | 2.4 (1.6 to 3.1) | 3.9 (2.9 to 4.8) | 3.2 (2.5 to 3.8) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| De Jong Gierveld Loneliness Scale score, mean (SD) | 2.9 (1.8) | 3.4 (2.2) | 3.2 (2.0) |
| De Jong Gierveld Loneliness Scale score, mean (95% CI) | 2.9 (1.9 to 3.9) | 3.4 (2.2 to 4.5) | 3.2 (2.4 to 3.9) |
| Treatment effect, mean (95% CI) | 0.42 (–1.06 to 1.90) | ||
| Adjusted treatment effect, mean (95% CI) | –0.76 (–2.15 to 0.64) | ||
Table 19 illustrated that there was no treatment effect on the Adult Attitude to Loneliness scale.
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| Adult Attitude to Loneliness score, mean (SD) | 18.6 (3.8) | 20.6 (4.8) | 19.6 (4.4) |
| Adult Attitude to Loneliness score, mean (95% CI) | 18.6 (16.7 to 20.5) | 20.6 (18.3 to 22.8) | 19.6 (18.2 to 21.1) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| Adult Attitude to Loneliness score, mean (SD) | 20.3 (3.1) | 20.6 (4.7) | 20.5 (4.0) |
| Adult Attitude to Loneliness score, mean (95% CI) | 20.3 (18.6 to 22.1) | 20.6 (18.2 to 23.0) | 20.5 (19.0 to 21.9) |
| Treatment effect, mean (95% CI) | 0.25 (–2.67 to 3.18) | ||
| Adjusted treatment effect, mean (95% CI) | –0.00 (–2.62 to 2.61) | ||
Scores for social participation were slightly higher in the intervention arm at baseline and increased at follow-up; however, a similar increase in score was seen in the usual-care arm (Table 20).
| Outcome | Arm | Total | |
|---|---|---|---|
| Intervention | Usual care | ||
| Baseline, n | 18 | 20 | 38 |
| Social participation score, mean (SD) | 25.3 (10.0) | 21.9 (11.9) | 23.4 (11.0) |
| Social participation score, mean (95% CI) | 25.3 (19.7 to 30.8) | 21.9 (16.0 to 27.8) | 23.4 (19.5 to 27.3) |
| Follow-up at 4 months, n | 16 | 17 | 33 |
| Social participation score, mean (SD) | 26.3 (10.3) | 23.8 (12.7) | 25.0 (11.5) |
| Social participation score, mean (95% CI) | 26.3 (20.4 to 32.2) | 23.8 (17.1 to 30.6) | 25.0 (20.7 to 29.3) |
| Treatment effect, mean (95% CI) | –2.47 (–11.19 to 6.24) | ||
| Adjusted treatment effect, mean (95% CI) | –4.09 (–13.05 to 4.87) | ||
Completion rates of the baseline and follow-up questionnaires
The overall follow-up response rate was 86% (95% CI 72% to 96%), with a follow-up rate for the intervention arm of 89% (16/18) (95% CI 65% to 99%) and for the usual-care arm of 85% (17/20) (95% CI 62% to 97%).
Overall, the completion rate of items on the questionnaires was very good. All questions had missing data rates of < 10%, with the exception of:
-
question A4 at baseline (current employment status – missing data rate, 16%)
-
question B7 at baseline (the way in which each illness limits activity – missing data rate, 11%).
Adverse events and breaches
There were no adverse events.
There was one serious breach that was reported to the sponsor and ethics committee. This breach occurred at the follow-up RN visit at 4 months, when a participant had answered positively on question 9 (question on suicidality) of the PHQ-9. This should have triggered the RN to act according to the suicide ideation protocol. This did not happen and the error was detected when data were entered onto the database. The participant was immediately contacted by Heather Burroughs; the participant stated that he had sought help from his GP and felt that he was improving. Heather Burroughs obtained consent from the participant to contact their GP and spoke to the GP, who advised that the practice were aware of this participant’s mental health needs and that the participant had consulted and had been prescribed suitable medication within the time period of the suicidal ideation being identified. The chief investigator was notified.
The sponsor and ethics committee were satisfied that this breach had been dealt with appropriately.
Summary
Six general practices were recruited, agreeing to recruit older people to the study. Recruitment of participants had been planned to take place over a 9-month period but, owing to delays in ethics and HRA approvals, this was reduced to a 5-month recruitment period between February and June 2017. Owing to limited capacity in the CRN and CTU, mailings were restricted to four practices. There were 3762 initial mailings, with 1267 returned questionnaires. There was a response rate of 33% (against a predicted response rate of 40%).
The participants recruited to the study had high levels of psychological and physical morbidity. Almost half the participants reported that they were taking tablets for low mood or stress, suggesting that they are consulting primary care but that their mood problems are not being adequately managed.
The overall follow-up response rate was 86% (95% CI 72% to 96%), with a high completion rate of questionnaires. The study was not powered to demonstrate differences in outcomes. There was no signal that the intervention might be more effective than usual care.
Process evaluation results
This section outlines the findings of the process evaluation. We begin with feedback from study participants on the burden of completing the questionnaires; comments from RNs on completion of assessment are also included.
Contact times between SWs and study participants are tabulated in this section; details of supervision times and a description of topics covered in supervision are provided.
The bulk of this section focuses on the analysis of the qualitative interviews, conducted with study participants, SWs and GPs.
Participant burden
The respondents’ comments about completion of baseline questionnaires with the RN were organised into four main themes, shown in Table 21.
| Theme | Data |
|---|---|
| The questionnaires | Length of questionnaire quite long to concentrate onThe questions are ambiguous and difficult to answer fullyQuestions could be clearerQuestions obscure, not able to pinpoint the right picture of how feeling generally |
| Needed help from RN to complete questions | I would have found the questions difficult to answer on my own |
| Experience of RN visit | I enjoyed the nurse’s company and felt cheered upA very nice person came to see me, which made a great difference to how I feltQuite happy to answer questions on my own; I found [name of RN] very easy to talk to and appreciated her understanding and gave me ample time to answer the questions’ |
| Impact of visit | I didn’t like the experience as it brought everything to the front of my mindIt made my stomach drop and I felt myself slump. It brought me downI’ve enjoyed the experience and found the questions enlighteningI felt the questions were relevant and I could easily answer them |
Several participants reported that they found the questionnaire long, ‘repetitive’, ‘tortuous’ and ‘convoluted’ and that they found it difficult to maintain concentration for the necessary length of time. Some participants felt that some of the questions were confusing. They reported that often the nature of the questions did not fit their situation and were ‘ambiguous’, ‘obscure’ or ‘nonsensical’. This group of participants needed the RN’s help to complete the questionnaire. Because they found the questionnaire long and confusing, they reported that they would have found it difficult to answer the questions on their own and that the support of the RN was appreciated.
Some people reported that they found the RN’s visit positive, commented that the RN was helpful and polite and that they enjoyed her company. Other people reported finding the experience of answering the questionnaire distressing and ‘a little depressing’. They reported that they felt the assessment brought up painful emotions, which made them feel worse. Other participants reported that they found the experience ‘thought-provoking’ and enlightening in that it made them reflect on what was happening to them at the time.
The RNs were asked to record their impressions of participant burden on completion of baseline and follow-up questionnaires. On one occasion, the RN reflected her concern that she ‘came away feeling that I had brought a lot of painful emotions to the forefront of his mind and that I was leaving him feeling worse than when I arrived’. Although the possibility that the potential study participants may become distressed during the baseline interview had been discussed with the RNs during training, this highlights the need to ensure that adequate support is given to the RNs.
Support worker–study participant contact
Intervention contact times
Five of the six SWs who had participated in training were allocated study participants. One withdrew owing to moving home to care for a family member and reduced hours at Age UK. One SW withdrew at the time that a study participant was allocated; this study participant proved hard to contact, and family illness meant that the SW had limited time to work on the study.
Four SWs were allocated 18 participants. One SW was unable to contact a person allocated to her.
Contact sheets from three SWs were returned, which detailed the durations of 52 sessions with 13 study participants. The sessions ranged from 15 minutes to 4 hours (in the 4-hour session the SW took the patient to a shop to buy disability equipment for the participant’s wife, the main worry for the client when first visited by the SW). Table 22 summarises the contact times for 13 participants in the intervention arm.
| Participant ID | Session number | Duration (minutes) |
|---|---|---|
| P3009 | 1 | 60 |
| 2 | 60 | |
| 3 | 45 | |
| 4 | 45 | |
| 5 | 90 | |
| 6 | 60 | |
| P3512 | 1 | 60 |
| 2 | 60 | |
| P2777 | 1 | 85 |
| 2 | 60 | |
| 3 | 45 | |
| 4 | 60 | |
| P2662 | 1 | 75 |
| 2 | 80 | |
| 3 | 45 | |
| 4 | 45 | |
| 5 | 60 | |
| 6 | 60 | |
| P1061 (dropout) | 1 | 90 |
| P145 | 1 | 60 |
| 2 | 60 | |
| 3 (telephone) | 25 | |
| 4 | 30 | |
| 5 | 75 | |
| P3560 | 1 | 60 |
| 2 | 50 | |
| 3 | 20 | |
| P2977 | 1 | 60 |
| 2 | 45 | |
| 3 (telephone) | 15 | |
| 4 | 75 | |
| 6 | 70 | |
| P3060 (dropout) | 1 | 60 |
| P11 | 2 (telephone) | 20 |
| 3 | 90 | |
| 4 | 20 | |
| 5 | 60 | |
| P441 | 1 | 80 |
| 2 | 90 | |
| 3 | 240 | |
| 4 | 90 | |
| 5 | 90 | |
| P2427 | 1 | 60 |
| 2 | 150 | |
| 3 | 30 | |
| 4 | 150 | |
| P2589 | 1 | 210 |
| 2 | 120 | |
| 3 | 60 | |
| 4 | 150 |
The mean session length was 69 minutes and the median was 60 minutes. This does not include brief telephone calls of < 10 minutes’ duration that were made between the SWs and the study participants to confirm or reschedule an appointment or to give information to the participants.
Content of support worker–study participant sessions
Three SWs returned their contact sheets. Activities recorded on the contact sheets were counted and are outlined in Table 23. Each item was counted once per study participant.
| Activity | n |
|---|---|
| Listening | 13 |
| Risk assessment | 13 |
| Education/information about mood | 12 |
| Discussion of physical health problems | 11 |
| Discussion of responsibilities as a carer | 7 |
| Explanation of BA | 13 |
| Problem-solving | 10 |
| Relaxation techniques | 3 |
| Use of patient diary | 12 |
| Use of mood thermometer | 4 |
| Giving written information (often posted out after initial visit) | 13 |
| Signposting to groups (e.g. computer classes, art groups, ‘Men in Sheds’, walking groups) | 13 |
| Signposting to other activities (e.g. swimming, walking, bowls) | 7 |
| Accompanying to groups | 4 |
| Accompanying to other services (e.g. mobility and equipment shop) | 2 |
| Other support (e.g. help completing forms, advice about benefits) | 6 |
| Discussion with family | 5 |
| Staying well discussion | 13 |
Supervision of support workers
A summary of the one-to-one supervision time between Carolyn A Chew-Graham and the four SWs who delivered the intervention is outlined in Table 24.
| SW | Number of study participants | Number of telephone supervision sessions | Total (minutes) |
|---|---|---|---|
| A | 5 (including one dropout) | 3 | 60 |
| B | 3 | 3 | 75 |
| C | 3 | 4 | 280 |
| D | 6 | 6 | 85 |
| E | One dropout | 0 | 0 |
In addition to one-to-one individual supervision, two face-to-face group meetings (90 minutes each) with Heather Burroughs and Carolyn A Chew-Graham were held. When the study was delayed owing to delays in HRA approvals, Heather Burroughs hosted a ‘coffee morning’ to update the SWs. A final meeting to review the study and present initial results was held, with Heather Burroughs and Carolyn A Chew-Graham, which lasted 90 minutes. SWs were encouraged to claim for the time to attend meetings as well as travel expenses.
The above does not include the time that SWs talked with each other, and with Peter Bullock at Age UK, particularly exploring what could be done to support the study participants and what signposting opportunities there might be; this time was not documented by the SWs.
At the final group meeting, the SWs emphasised how important it was for them to have the supervision time to reflect on their sessions with study participants, which they suggested enabled them to work out what could be done to support their ‘clients’. Discussion of risk assessment was also said to be important to the SWs.
The different times required by the SWs illustrates the need to offer flexible supervision, as each SW had different needs for support and monitoring, with some SWs seeking supervision after each study participant contact.
Discussion during supervision sessions
The one-to-one supervision sessions were structured around the supervision and participant contact sheets that were included in the SW manual (and given to SWs as A4 sheets for use by the SWs with each study participant). The discussion included the SW talking through their recent contact(s) with each study participant, identification of problems, assessment of risk, goal-setting, resources/groups suggested to the study participant and arrangements for follow-up or planning to end contact. The sessions were focused on the needs of the individual SWs and the concerns that they raised for discussion. Two examples of supervision are given in Box 2 using pseudonyms.
Admits to long-standing depression and pain in addition to arthritis.
Lives alone, has transport (car).
In the past, has enjoyed painting.
The SW visited on a Saturday to suit Paul.
No risk identified.
The SW was aware of a local art class and men’s group. The SW felt that the client might be interested in the art class but had seemed dismissive of the men’s group.
Paul engaged in the art class (attended alone) but did not enjoy the men’s group even though initially accompanied by the SW.
Supervision focused on identifying Paul’s problems, considering possible goals, identifying local groups and working through the participant manual. The SW reported that Paul had articulated that he wanted to do something useful and that the men’s group did not provide this.
The SW expressed no concerns about Paul, reporting confidence in conducting the risk assessment, and did not feel that mood thermometers were useful for Paul. The SW delivered four sessions and had introduced the concept of ‘staying well’ to Paul.
MaryLives with husband.
Multiple medical problems (including shortness of breath owing to bronchitis, which restricts ability to walk). Has stopped going out.
Husband drives. Family close by.
The SW identified social withdrawal as a problem, and recognised the resources that Mary has (e.g. daughter and husband).
The SW reported using the diary in the participant manual to help Mary realise how inactive she had become, and identified a number of activities that Mary might resume. The SW accompanied Mary to a local craft group, which seemed to be acceptable as there were only three other participants and Mary felt she could deal with this. The SW encouraged Mary’s daughter to take her swimming, and this happened twice during the time the SW visited.
The SW reported confidence in assessing risk and using the mood thermometer with Mary at each session. The SW introduced breathing exercises to help Mary deal with anxiety and help with her feelings of breathlessness. The SW suggested that Mary might find yoga helpful but could not identify a beginner’s group to suit Mary.
The SW introduced the idea of ‘staying well’ and encouraged Mary to continue to use the diary when the intervention finished. Five sessions completed.
Fidelity checking
Tables 25–27 show the results of fidelity checking the recorded sessions. Overall, 22 sessions were recorded by four SWs. Fourteen of the sessions recorded were first sessions, six were second sessions and two were subsequent sessions (recorded by the SW when the client gave permission for recording later in the intervention).
| Aspect of consultation | Yes | Partially | No |
|---|---|---|---|
| Verbal explanation given of the NOTEPAD study | 13 | 1 | |
| Explanation of the evidence for the beneficial effects of social participation for depression | 9 | 3 | 2 |
| Evidence of exploring the older person’s problems | 13 | 1 | |
| Assessment of risk | 8 | 3 | 3 |
| Activities/social participation goals discussed | 14 | ||
| Activity/social participation goals set | 12 | 1 | 1 |
| The NOTEPAD personal file given along with a verbal explanation of how to use it | 10 | 4 | |
| Signposting (e.g. to exercise groups, craft classes) | 9 | 4 | 1 |
| Participant understanding of what has been discussed and agreed is checked | 11 | 2 | 1 |
| Barriers/motivators to increasing activity discussed and/or addressed | 11 | 2 | 1 |
| Next session discussed and arranged (face to face or telephone) | 13 | 1 |
| Action | Yes | Partially | No |
|---|---|---|---|
| Review mood – mood thermometers | 3 | 1 | 2 |
| Review progress – diary | 4 | 1 | 1 |
| Feedback given regarding any progress made | 6 | ||
| Barriers/motivators to increased activity/participation discussed and/or addressed | 4 | 2 | |
| Activity/social participation goals discussed | 3 | 1 | 2 |
| Activity/social participation goals set | 2 | 2 | 1 |
| Signposting (e.g. to craft groups, adult learner classes) | 2 | 1 | 3 |
| Remind about use of the NOTEPAD personal file | 2 | 1 | 3 |
| Relapse prevention/’staying well’ strategies discussed (e.g. support and guidance) | 2 | 3 | 1 |
| Possible personal issues/difficulties encountered while increasing activity/social participation | 3 | 3 | |
| Relevant contact details are given in case of any problems, issues or further advice required | 4 | 2 |
| Action | Yes | Partially | No |
|---|---|---|---|
| Review mood – mood thermometers | 1 | 1 | |
| Review progress – diary | 2 | ||
| Feedback given regarding any progress made | 2 | ||
| Barriers/motivators to increased activity/participation discussed and/or addressed | 2 | ||
| Activity/social participation goals discussed | 2 | ||
| Activity/social participation goals set | 2 | ||
| Signposting (e.g. to craft groups, adult learner classes) | 1 | ||
| Remind about use of the NOTEPAD personal file | 1 | 1 | |
| Relapse prevention/’staying well’ strategies discussed (e.g. support and guidance) | 2 | ||
| Possible personal issues/difficulties encountered while increasing activity/social participation | 2 | ||
| Relevant contact details are given in case of any problems, issues or further advice required | 2 |
Reasonable delivery of the intervention was achieved, particularly in the first session. Use of the mood thermometers was not felt to be helpful; the SWs admitted in the supervision session that they found this to be the most challenging part of the discussion with their clients.
Analysis of qualitative data
Analysis of the data was conducted both independently and subsequently collectively by three members of the qualitative research team (HB, BB and CCG). Transcripts were read and re-read, themes arising during analysis and data collection were discussed within the team and the topic guides were modified as data collection and analysis progressed. The qualitative research team met regularly to discuss and agree coding, revisiting the data from each dataset in an iterative manner to verify coding and themes generated from these codes. This process was repeated until it was agreed that each dataset had reached saturation. Analysis was initially conducted within each data set, then comparison carried out across the data sets. NVivo 10 was used to store and manage data and aid analysis.
Study participants
In this section, we outline the key findings from the interviews with patient participants. Of the 18 people who were allocated to the intervention group, two people did not complete the intervention. These are denoted as ‘dropouts’. We also interviewed SWs (n = 6) and GPs (n = 12). A total of 17 older people in the intervention arm were interviewed.
The mean duration of interviews was 23 minutes for patients (range 12–68 minutes), 37 minutes for SWs (range 30–51 minutes) and 23 minutes for the GPs (range 11–28 minutes).
Tables 28–30 provide details of the participants.
| Participant ID | Characteristic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Sex | Ethnic group | Employment status | Marital status | Living situation | General health | Taking medication for low mood or stress | Long-standing illness/disability | Completer/dropout | |
| P11 | 76 | Male | White British | Retired | Married | Lives with more than one other person | Poor | No | Yes | Completer |
| P145 | 67 | Male | White British | Retired | Divorced or separated | Lives with another person | Poor | Yes | Yes | Completer |
| P441 | 84 | Male | White British | Carer | Married | Lives with another person | Fair | No | Yes | Completer |
| P467 | 80 | Male | White British | Missing | Married | Lives with another person | Fair | No | Yes | Completer |
| P589 | 67 | Female | White British | Retired | Divorced or separated | Lives alone | Poor | No | Yes | Completer |
| P1061 | 76 | Female | White British | Retired | Widowed | Lives alone | Poor | No | Yes | Dropout |
| P1093 | 74 | Female | White British | Retired | Married | Lives with more than one other person | Poor | Yes | Yes | Completer |
| P2427 | 79 | Female | White British | Retired | Widowed | Lives alone | Very good | Yes | Yes | Completer |
| P2589 | 73 | Female | White British | Retired | Widowed | Lives alone | Fair | No | Yes | Completer |
| P2662 | 85 | Female | White British | Missing | Widowed | Lives with another person | Poor | No | Yes | Completer |
| P2777 | 78 | Male | White British | Retired | Married | Lives with another person | Poor | Yes | Yes | Completer |
| P2945 | 72 | Female | White British | Retired | Married | Lives with another person | Excellent | Yes | No | Completer |
| P2977 | 66 | Male | White British | Retired | Married | Lives with another person | Good | Yes | Yes | Completer |
| P3009 | 73 | Female | White British | Retired | Co-habiting (living as married) | Lives with another person | Poor | Yes | Yes | Completer |
| P3060 | 71 | Male | White British | Missing | Married | Lives with another person | Very good | No | Yes | Dropout |
| P3512 | 70 | Male | White British | Retired | Married | Lives with more than one other person | Very good | No | No | Completer |
| P3560 | 69 | Female | White British | Retired | Widowed | Lives alone | Good | Yes | Yes | Completer |
| General practice | List size | Number of interviewees | Sex |
|---|---|---|---|
| Practice 1 | 4648 | 2 | 2M |
| Practice 2 | 7028 | 3 | 2M, 1F |
| Practice 3 | 7255 | 1 | M |
| Practice 4 | 10,978 | 4 | 2M, 2F |
| Practice 5 | 5545 | 2 | 2M |
| Characteristic | n |
|---|---|
| Female | 5 |
| Male | 1 |
| Age (years) | |
| 45–50 | 2 |
| 55–60 | 2 |
| 60–65 | 1 |
| 65–70 | 1 |
General practitioners at practice 4 had agreed to participate in the study, recruiting older people, but, owing to lack of capacity in CTU and CRN, the final two practices identified were not used for recruitment. Four GPs did agree to be interviewed at the end of a practice meeting to discuss the management of depression in older people and their reasons for agreeing to participate in the NOTEPAD study.
Limited data are given about the SWs to ensure anonymity is preserved.
Findings
Perspectives of patient participants
A number of key, interlinked themes emerged from the patient interview data: recognising depression and the long-standing nature of mental health problems, comorbid physical and mental health problems, loneliness, support received and views and reflections on the NOTEPAD intervention. Data will be provided to support each of the themes presented, with participant IDs (which include ‘dropout’ for the two participants who did not complete the intervention but agreed to be interviewed).
Participants recognised that they were suffering from depression, and that it was currently, and had previously, caused difficulties in their lives:
I’ve been up and down, I mean I’ve had it 50 years to tell you the truth so I had it in my 20s yeah. . . . the first time I was depressed in [my] early 20s.
P3512
I’ve had this depression and anxiety for about 7 years now, but my last 4 years has been horrendous.
P145
Linked to the long-standing nature of their problems, people reported diverse experiences of treatments ranging from interventions by GPs and counselling services to psychologists and psychiatrists. These included both psychological and pharmaceutical approaches:
I’ve been treated for depression since – when was it – 1998. I’m still on tablets now for depression. I’ve been to see, talk to somebody, like a psychiatrist . . . It weren’t a psychiatrist, it was . . . [trails off].
A psychologist?
Something like that.
Reflecting on answering the postal questionnaires and completing the questionnaires with the RNs, the older people interviewed reported multiple illnesses:
Yes, yes, I’ve got it all. You name it, if it’s free I have it. Now I’ve got, what is it? Cholesterol, COPD, diabetes two, blood pressure. I’ve just been up and had blood taken this morning. Mmm, I’ve got ‘em all.
P11
So, as well as the cancer, you mentioned you’ve got arthritis as well?
Yeah . . . you know, I can’t run, I can’t kneel, I can’t stoop, I have to do anything like tying shoelaces I have to sit on the floor, things like that . . . well, it affects everything in every way.
Right OK, and do you – does it affect your sleep?
Yes.
And do you have a lot of pain with it?
Oh yes, yeah . . . I’m on morphine patches at the moment. I’ve got a heart condition as well.
In addition to physical health problems, some participants’ experiences were compounded by difficulties with their families:
I’ve had depression in the past, severe depression and there’s a family history of depression and I’ve had episodes of depression. So the depression comes and goes a bit. You know, there some times when I’m feeling really low, and other times when I’m not too bad mood-wise . . . but it’s all what’s happening within the family and what’s happening within my physical health is all, is all sort of jumbled up together. So if I’m having a good day one day, there’s quite a few things that can make it not so good the next day.
P589
There are currently, and there has been for about 18 years, quite severe family problems and they’re getting worse as well with certain, certain parts of the family. And that’s causing a lot of stress and distress.
P589
Other participants were busy with caring responsibilities:
I was at a stage where I was running backwards and forwards to my mother and then when my mother died I suppose it made it easier because then it was only my husband but I mean he got, I had to take him [to] the toilet, in other words it was full on. I had to wash him, dress him, everything.
P3650
Some participants reported financial difficulties thay they felt affected their health:
The disability living allowance, it’s, it’s gone to PIP [Personal Independence Payment] now and I had my assessment . . . but I’m just waiting to hear from that now, to, you know, know whether I’m going to keep me car and that. It’s just – because I’d be lost without the car because . . . I can’t walk and get buses now, I can’t even sit on a bus, so I’m worried sick about that because I don’t know what I’d do if I – do you know what I mean?
P145
Some study participants expressed feelings of loneliness and isolation, acknowledging that loneliness exacerbated their feelings of anxiety and depression:
I do suffer from anxiety and depression and I worry a lot. I worry tremendously. I never used to worry this much but I do now and I think it’s because . . . I think it’s because I’m on my own . . . every little thing . . . and when I draw the curtains at night I’m thinking, ‘oh gosh what’s that’ and it’s probably absolutely nothing. Just a car passing.
P2427
Respondents who were lonely described their families as living far away or busy with work or their own family commitments:
I’ve got two sons who try very hard to be supportive but are quite some distance away, work 7 days a week, have family of their own, so are not as available.
P589
Other respondents reported that they were not lonely or isolated, but despite this, still suffered from depression:
You know people with [. . .] anxiety and depression and, that’s one thing I’ve suffered for a lot of, great many years, off and on like . . . I mean I’m not lonely because I’m very busy, I’ve got three daughters so I’m not lonely.
P3512
The GPs were seen as an important source of support for the variety and complexity of described problems, particularly physical. However, a number of patients reported that the treatment offered by their GP for low mood had been ineffective in the past, particularly where a pharmaceutical approach was taken, as P1093 describes:
OK, have you spoken to your GP about it or . . . ?
I have done, yeah, but they just give you tablets.
Right, so have you taken tablets?
Yeah, I do, yeah.
You do? For your mood?
Yeah, yeah.
Yeah, and do you find that helps or not?
Not really, no.
Moreover, patients had little expectation that their GP could offer any alternative owing to time constraints on the length of consultations:
I know, having worked with GPs, you know, their time is so short it’s very difficult to deal with any problems but particularly mood and depression. It’s very hard for them to deal in the surgery with how people are feeling because, you know, it’s not a 5- or 10-minute thing, is it?
P2977
All of the patients who completed the intervention suggested that it was acceptable, even though some were initially uncertain about what it might involve:
At first I wasn’t quite sure what it was about, I couldn’t quite grasp what it was about . . . and then as time went on a bit I started to realise you were really trying to find out what elderly people want and what their needs are really. And then it sort of got a bit more interesting to me and I thought, ‘oh, somebody actually asking me [what you want]’ . . . I just felt that my answers mattered because I feel as if I’m just one in millions as just feel the same.
P2427
The patients reported that the empathic approach of the SWs and the time available to be listened to by the SWs were valuable experiences, regardless of whether or not they considered themselves lonely. The personal qualities of the SWs were particularly commented upon:
She actually listened, which a lot of people don’t do . . . she very quickly seemed to grasp the struggle I was having.
P2589
I thought she was quite professional; she was empathetic and I felt she was listening to me.
P3009
Patients also reported that the practical support offered by the SWs was helpful and reported receiving help with claiming benefits and filling in forms, in addition to signposting to local groups and activities:
She gave me a lot of contact information about organisations that could help with bereavement, for instance, and benefits, finance things, and she also found me a support group called [name of local group].
P589
And he found out other interests or other things I could do in [the] area . . . he found indoor bowling as well, down the leisure centre. Then I go swimming occasionally as well. It’s different groups I didn’t know about in [the area], community groups where you can go. Just like to play dominoes or a book club or things like that.
P2977
In helping older people identify their goals, respondents suggested that the SWs also went beyond simply mentioning possible activities:
And she said, ‘Do you want me to come with you?’ And I said, ‘Yes, that would be nice’. So she came with me the first time. She didn’t stay for the whole session but she said, before we went in, she said, ‘Let me know if you feel at any time that you’re OK and that you don’t need me there,’ sort of thing. And so she went halfway through. She went by our agreement.
P589
Some patients reported attending groups to be helpful:
It’s quite a positive thing. Everybody sits around and talks about what sort of day or week they’ve had and things come out, you know? Like I was struggling about my dad, and about some other family issues, and the rest of the group all sort of say, you know, they sort of give you encouragement. Like saying, you know, ‘Well, you’ve done really well to do this and do that’. So it was good and I think I will go again.
P3009
Other people reported that they did not want to attend social or activity groups, even when they acknowledged that the SWs seemed to have tried hard to find a group to match their interests and help to overcome psychological and/or practical barriers to attending. Those people who did not find attending social or activity groups appealing did not feel themselves to be lonely or in need of company or activity. They lived with spouses or other family members or were busy with caring responsibilities:
She [the SW] desperately wanted me to go to, erm, places that I haven’t been to before like there’s a leisure place in [local town] where they do various clubs. I didn’t want to go. I really didn’t want to meet people I didn’t know.
P1061 [dropout]
But the more I thought of it, I didn’t really want that ‘cause I aren’t on me own, I’ve got me family and me wife here. I thought it was more for people on their own sort of thing, you know, no company or anything like that. So I was quite happy myself.
P3060 [dropout]
Participants reported that they valued activity that they felt to be personally meaningful and were not interested in groups that did not contribute in that way:
Yes, well, it didn’t help but he [the SW] was helpful. Helpful in the list of things. He did try to get me to go to Men in Sheds and all that. I just didn’t fancy driving all that way to sit and drink tea. But I don’t drink tea and so I just couldn’t see a future for me there of any kind.
P11
However, those who engaged with the intervention but did not want to attend groups still reported that the time spent with the SW, being listened to, was beneficial to them:
You see, I don’t want to go out to these groups as I’ve explained cos I can’t . . . but having somebody coming to talk to you relaxes you and all that, it’s great.
P1093
Most participants reported that they felt better having met with the SW, such as P441, who was the main carer for his wife and attributed this change to the SW visiting:
We’re working better now than it has done in the past. She [the SW] has done wonders. I’ve got [my wife] used to the routine and I’m on a routine which we can cope with, I can cope with well. And I think if anything [my wife’s] better than she has been, she’s yeah, she is, she’s better.
P441
The SW intervention prompted P3009 to visit their GP for a change in medication:
I mean, one thing because of talking to [name of SW] is I finally did go to the GP and I’m on a different antidepressant.
P3009
The following model (Figure 8) illustrates how the distinction between loneliness and depression is an important one. Those who were lonely needed supportive listening as well as help to access meaningful group activity. The group who would characterise themselves as ‘not lonely’ because they have supportive family nearby did not want to attend groups but still wanted and valued being listened to. This model was checked out with the study PPIE group. We debated the idea that the ‘GP is not helpful’, and considered alternative ways of expressing this, but the group felt that this phrase represented the data from both study participant and GP data sets.
FIGURE 8.
Conceptual model.
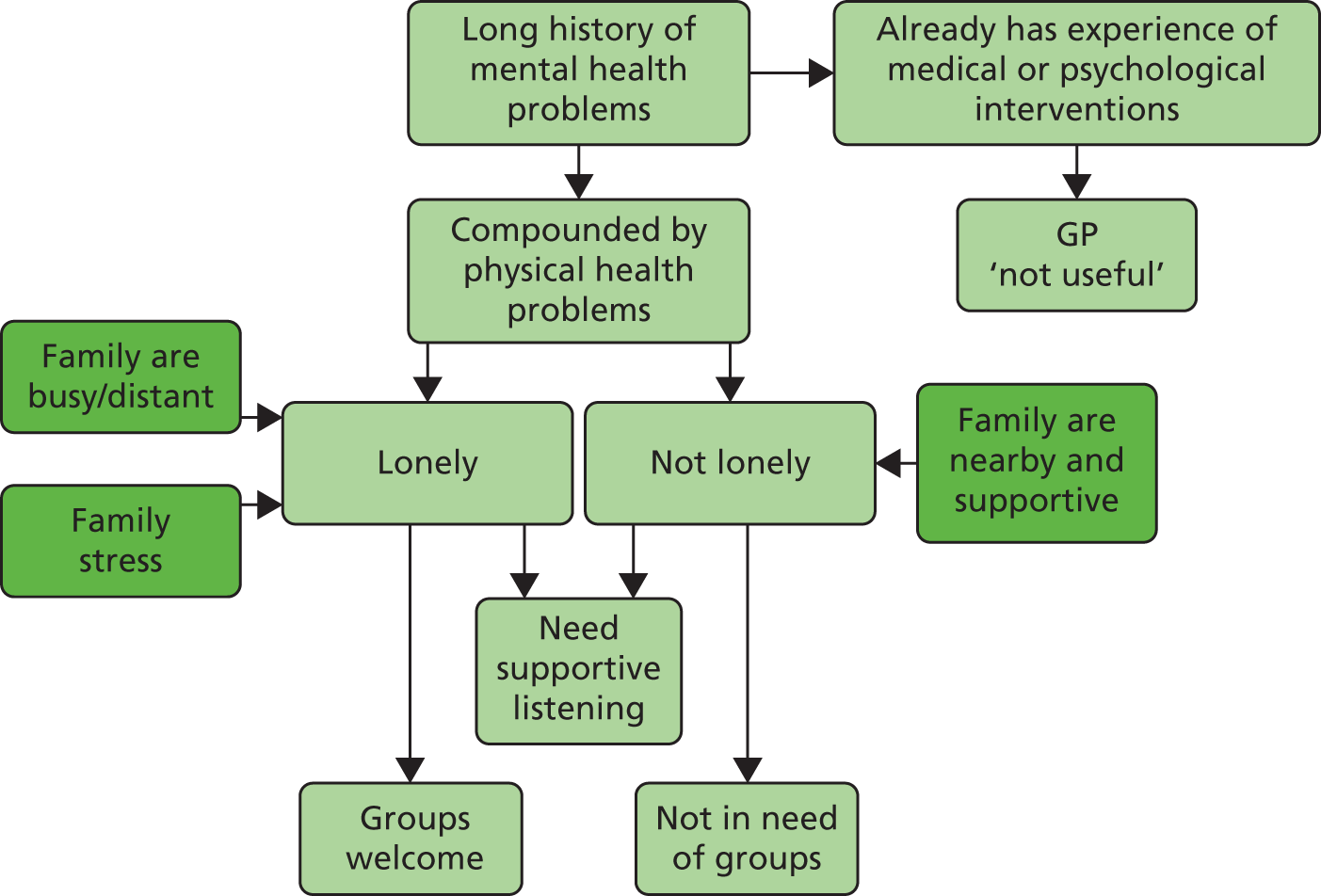
Decliners
Potential participants who were eligible to participate in the NOTEPAD study but had declined to take part at the point of the RN telephone call without making an appointment for a visit by the RN were considered to be ‘decliners’. Thirty-seven people were telephoned by Heather Burroughs or Bernadette Bartlam to attempt to explore their reasons in more detail. These telephone calls were very brief, with older people apparently not wishing to discuss this, or justify their decision, further. Where people did give a reason for declining to participate, this was noted and Table 31 lists the reasons given for declining to take part (some people gave more than one reason).
| Reason for declining | n |
|---|---|
| Could not be contacted | 5 |
| Declined to discuss | 4 |
| Ill health | 8 |
| Carer | 5 |
| Too busy | 7 |
| Does not do surveys | 5 |
| Does not want anyone to visit | 4 |
| Does not want to take part/study is not for me | 7 |
| Does not feel depressed | 6 |
Perspectives of support workers
The interviews with the SWs focused on the training, supervision, delivery of the intervention, and suggestions for refining the intervention. Data will be provided, with participant IDs, to support each of the themes presented.
The SWs all reported that they found the idea of the study novel and interesting:
I was looking for, you know, a bit of a new challenge really. Because my son’s gone off to university and, and I just thought, ‘Oh, do something a bit different’, that I’m interested in, you know? Because I’m quite interested in helping people, really. I’ve always been in the caring profession really, so. It just sounded interesting, really.
SW1
I mean, overall, I think it was – it’s been really good to be involved. I thought kind of the initial information we got about what and why, you know, I thought was really well sort of researched and it seemed like it was a really good idea.
SW3
The above data reflect the detailed information given about the study by Peter Bullock and the research team during the recruitment process.
The SWs described a wealth of prior professional experience and some had done courses in counselling:
I’d been a teacher in a former life and then became a trainer in the voluntary sector . . . I did some study, it was just a year’s psychology for everyday life and I’d done psychology for my degree years ago anyway.
SW 6
My first degree is sociology so my interest is across the board . . . I’ve managed community centres . . . I’ve also managed a drugs and alcohol rehab and I’ve written alcohol counselling training nationally . . . I’ve lectured in universities and college.
SW2
I did counselling courses when I was young, maybe about 10 years ago now, so I have a bit of a basic foundation of one-to-one interaction with people.
SW4
Thus, the SWs recruited from Age UK had broad knowledge and skills on which the NOTEPAD training could build on.
The SWs all spoke of experiencing anxiety prior to and during the training:
We were all scared, we were all really scared. I mean, we were very well supported on the training and, to be kind of, doing the skills practice and have people sitting there observing, was initially very scary.
SW6
I mean overall, I think it was – it’s been really good to be involved. I thought kind of the initial information we got about what and why, you know, I thought was really well sort of researched and it seemed like it was a really good idea right. I think – yeah, the training was really good.
SW3
One SW, however, suggested that the theory included in the training was excessive:
[It needed to be] more experiential, more practical . . . That’s a big block to learning, that there’s too much here, once one of them [the SWs] said, ‘if I’d have known it was going to be like this’ . . . I just thought I was going to visit people and find out what they wanted to do . . . and I’m just wondering if you needed all that other stuff. You didn’t need a lecture in psychiatry.
SW1
All of the SWs reported that the training manual was essential:
In terms of the training manual, how useful did you find that?
Oh, very, very good actually, very good. Because it’s something to keep going back to if you’re not sure of things . . . Everything is in there that we could possibly need, you know. And I just sort of had started to sort of do a little check list for myself, you know, when I went out. Just a little card, just to remind me of, so I didn’t sort of forget anything.
SW1
It, it was very helpful. You know, it rejogs your memory, builds on the foundations that you had in, yeah. It refreshes you, and I found that I was reading, the session one, every time I was going into the person, and reading session two every time I was going in to see them, see them the second time and the third time and the familiarising myself with the mood thermometers, and explaining that to them.
SW4
Some of the SWs described how they had made their own summaries of the key messages in the manual, which were vital in the first couple of encounters, but eventually needed them less as they became more confident working with their clients:
I made my own prompt sheet because you feel a bit, like everything’s entering your head at once sort of thing. So, it was just sort of all the things. That was one of the most difficult things. There were all sorts of aspects that you had to include but, one of the tricky things was, how do I order this? Should I say, should I broach that part before that? Do I make the list before we go into this part? So, the prompt sheet was really useful for that.
SW5
As the SWs became more experienced, the manual was used less:
I did read, more or less read through that each time, you know, well I wouldn’t say before every contact, because the further I went on with contact and settled into it and could actually see, you know, see BA in practice and how actually, you were able to engage with somebody and it did, it did make sense, that gave me a bit more confidence and I felt I was internalising it, I wasn’t so focused on, oh you know, I’ve got all these things written down, how am I going to remember it all, because it was, it was making sense.
SW6
Most of the SWs reported experiencing anxiety following the training and prior to visiting their first client and carrying out the intervention:
I felt completely overwhelmed by what I was hearing, I think it was far, far more [complex] than I had ever anticipated . . . because I was so nervous, throughout the first 10 minutes, my heart, you know, I could feel my heart was going like this, I could barely speak, because I was stuttering and I thought for goodnees sake, get a grip, get a grip of yourself . . . I felt this pressure . . . I felt quite a responsibility that, you know, we’d had this time invested, this knowledge given to us and I didn’t want to let anybody down.
SW6
The SWs reported that there were particular areas that they initially found difficult, such as doing the risk assessment, but which they became more confident in as they saw more clients:
I think you said it was the first client that you saw who had attempted suicide previously. More generally in terms of assessing risk, how comfortable or not where you in doing that?
I’m a lot more comfortable now after seeing six people than when I started. It’s just a shame he was the very first one, you see? It was like [a] baptism of fire really. But I managed to, broach the subject with everybody, and I was getting a lot better at it . . . So, yeah, I’m much more comfortable than I was at the start. But I found the training very useful.
SW5
Because they were already employed by Age UK and were running activity groups, SWs felt they had a comprehensive knowledge about benefits and resources, services and support groups available in the local area:
Obviously I know about the Age UK and benefit type things and I use the internet a lot to find social groups and things that were available. And perhaps my local knowledge, because a lot of the, clients I got, because I think they were from [health centre], the last group. Because I run my befriending scheme in [town] I knew what was available there so that was useful.
SW5
Recruiting SWs with this local knowledge was key.
The SWs found dealing with the complex needs of some clients challenging and requiring careful thought beyond simply delivering an intervention:
I’m thinking, ‘how am I going to help this man, how am I going to help him?’ But if I’d said, ‘oh well, you know, why don’t you ring [a group]’, that would have been completely inappropriate . . . And just thinking, you know, what, how, you know? I can’t wave a magic wand and make this go away, but it wasn’t about that, and then, you know, you come away and you make your notes and you reflect.
SW6
The SWs sometimes found that organised groups, of which they had prior knowledge, may not be appropriate for their clients, and finding alternatives required careful investigation, with often a number of suggestions offered to clients:
I’d kind of gently kept coming back to these groups and I thought, ‘Maybe this isn’t kind of what they want’. So I asked them, ‘Well,’ you know, ‘kind of what, what – where do you go? What, what do you do? What, what do you like doing?’ And they said, ‘Going to garden centres. He loves B&Q [B&Q plc, Eastleigh, UK]. Doing things around the house’. And I said, ‘Right, OK. It doesn’t have to be a bladder cancer support group,’ you know. ‘If, if that’s what you would like to go to,’ you know, ‘what about planning it?’
SW3
Reflecting on the challenges in working with clients with complex needs, SWs reported a sense of satisfaction when goals were achieved:
She did [go to the group], she did! Oh, it was, I kind of ran round the office going, ‘yes, yes’. It was great. I was just in the office with my colleague who runs these groups, and my colleague took a phone call and then my colleague said to me the lady’s name and she said, ‘well, she’s just phoned up to enquire about the computer groups and she’s going to come along on Thursday’. So that was thrilling. That was really, really thrilling.
SW6
We discussed different types of respite and after a while, he, this is another visit, he told me that he had decided that he and his wife were going to go together and have respite in this lovely residential facility. He said ‘it’s so posh’, and he told me all about it. It was marvellous [to hear] and they were booking in for 2 weeks and very, very excited about it. And they’d never done that before, so I’m hoping that just by, you know, prompting him to think about his own needs and maybe, you know, were there things they could do together that would give him respite? So that was a good thing.
SW6
The SWs also reported that they thought some clients had carried on attending groups after they had ended contact, which they felt indicated that they had made an impact:
I went up there and physically supported them by standing next to them, and I also passed on the information on paper, and as far as I know they went on and carried it forward themselves.
SW4
Sometimes improvements were reported by SWs to be more subtle, reflecting patients’ accounts of the importance of feeling heard:
You know, I was just going along and sitting down and saying, ‘tell me, tell me, you know, I’ve got time and I want to listen and you can be as honest with me as you want, just tell me because I care about what you’re going to say’. And I think that is such a simple thing, but it is absolutely key, because just the fact that somebody would want to do that and be genuinely interested, even if you can’t help them resolve it or maybe only a bit, because with that participant we did make some progress.
SW4
The SWs suggested that one of the main factors contributing to helping clients was the time they invested in people:
I think a lot of what was positive about this was, I think, the person visiting, just keeps showing that person that they are important and you do care about them and I think that was quite a motivating factor.
SW3
The SWs reported that the one-to-one supervision offered was helpful in dealing with their anxieties, particularly after the first visit to the first client:
The first supervision that I did on the phone was very, reassuring . . . just to, just to know that there was somebody else there who I could offload to myself, and that was welcomed.
SW4
[Supervision was] quite good really. They were all over the phone. I did think, I don’t know whether it was, we were supposed to some have supervision meetings. I initially thought that it would be a supervision session [right] somewhere. I didn’t think it would just be on the phone. But it was ok, you know, it was fine. But because I didn’t have any really major problems, it was just really talking about each case so, that was very useful I think.
SW5
Face-to-face meetings were held between the SWs and Carolyn A Chew-Graham and Heather Burroughs, but these were seen by the SWs more as group support meetings than as formal ‘supervision’ sessions.
Some SWs felt that the intervention could be improved by building in a follow-up session with clients a few months after the six sessions:
Hopefully that there would be an opportunity to engage over a longer time. I think also, some kind of follow-up could be built in, say at possibly a 3-month or 6-month point, perhaps a year or something like that.
SW6
Other SWs felt that the limited time of the intervention helped to motivate patients to make the most of the sessions:
More than one person said to me, ‘well, I’ve only got you for a short time, so I better make good use of you’, sort of thing, so, it spurred them in a way, really, they’re all, oh, I’ve only got like four or five sessions, or six sessions so, if I’m going to do something, I’ve got to do it now type of thing, without making them feel rushed in anyway, but, it took, sometimes took a few weeks to get to that stage but, no, I thought it was really good.
SW5
Thus, SWs recognised that people in the study had complex problems, and to meet this challenge required the support of their peers on the study, colleagues at Age UK and the opportunity to discuss at supervision. The knowledge and expertise that the SWs already had through previous training, and concurrent experience working with Age UK, were perceived as vital in suggesting local groups to study participants, being able to contact the group leaders and feeling comfortable accompanying people to groups.
Perspectives of general practitioners
Recruiting GPs to participate in interviews was challenging. GPs seemed reluctant to spare the time to be interviewed and those who were spoken to commented that they had not been affected by the NOTEPAD study. The researchers needed to be very flexible in organising interview times.
The interviews with GPs identified themes around working with patients with complex needs and GPs’ views on the study.
GPs recognised that there is a group of older adults who may be depressed, or lonely or socially isolated (GPs used these terms interchangeably), and who may benefit from simply having a conversation with someone:
We used to have a receptionist here who was very astute, who would say, ‘do you realise, if I had a kettle, teapot and a packet of biscuits, half these people coming in to see you wouldn’t need to come in and see you?’
GP practice 3
Initially, I think more face-to-face chat and probably seeing them every week and just giving them a bit of support and listening to them and acknowledging what’s happening.
GP practice1
They reported, however, that they were personally unable to provide time to listen owing to a lack of capacity within the practice and the constraints of time-limited consultations:
I think all she came to do was talk to me and that’s fine, and might have been fine in general practice 20 years ago, 25 years ago. It ain’t any more. It’s too task orientated, it’s too problem orientated and there’s too much pressure as the hospital dump more and more long-term conditions on us to look after. We’ve just not got that . . . We’ve not got that capacity, we’ve not got that sort of pastoral effect we used to have. We’ve just not got time.
GP practice 2
The GPs reported that they often had difficulty in making a diagnosis of mental health problems in this group of patients with already complex needs, with mental health not being a priorty for the GP or the older adult. GPs also identified differences between consultations with older adults and younger populations:
We don’t diagnose that well because they have other conditions, like dementia . . . so we tend to forget about and it’s not probably screened. And also they don’t ask for support as much as the younger people do, and because older people actually they say, ‘it’s just anxiety, I’ll get over it’. Whereas younger people, they work, and their work stress and everything, they want to take some time off or they want a sick note, that sort of thing.
GP practice 4
The GPs all reflected on the poor provision of services for older adults, who they felt would benefit from further input, whether this was a result of loneliness, being isolated or having a depressive illness. Even if services were reported to be available, GPs noted that patients could not access them in a timely manner:
There’s huge delays for older people. It has improved a lot but it’s still not great.
GP practice 2
Some GPs reported knowledge of accessible and acceptable NHS-commissioned well-being services, and mentioned an awareness of third-sector organisations, such as Age UK, providing support. However, GPs were reluctant make a diagnosis of anxiety or depression without being certain that there were services available to support older adults:
I think the other thing we must consider is to find underlying depression and anxiety in elderly patients without making sure we’ve got adequate resources to cope with this. It will be a shame to diagnose depression in an elderly patient and then it would be a further shame that then there’s nothing to help them and possibly that will make them worse really.
GP practice 5
Thus, although GPs recognised that older people were a vulnerable group, they suggested that they had little time to personally offer pastoral support to older people, and that there were limited resources to which to refer people to.
Some GPs had difficulty recalling that their practice was taking part in the study:
I wasn’t aware about it [the NOTEPAD study] but I may have been told but I didn’t know about it.
GP practice 2
Some GPs were generally supportive of the concept behind the NOTEPAD study, recognising a need for such an intervention for older people, and recognising that primary care could not fulfil this role. Other GPs were vocal in their criticism of recent cuts in mental health services and suggested that using non-medical personnel to work patients with mental health problems was not appropriate, especially when the responsibility to assess suicide risk remained with the GP. This was felt particularly strongly in the context of cuts to secondary care psychiatric services in the local area (this was documented in field notes, summarising conversations recorded prior to an interview and a focus group).
Some GPs reported feeling annoyed by the NOTEPAD risk protocol, which required a member of the research team to notify them if one of their patients expressed suicidal ideation. Some GPs felt that risk was being raised unnecessarily, generating additional work:
I had contact with the [researcher] who was worried that the patient had suicidal thoughts. I think I’ve had two or three of those and the patient had to speak to me but that was just depressing thoughts they were having. The [researcher] was very worried but the patient wasn’t.
Did that annoy you at all?
Yeah, a bit . . . a lot, actually.
GP practice 2
Other than being contacted by researchers as part of the risk protocol, GPs did not feel that participating in the NOTEPAD study had affected their routine practice. They could not recall any contact with the SWs, and did not recollect any patients discussing participation in the NOTEPAD study with them in consultations. GPs were not able to suggest if or how the NOTEPAD intervention might be implemented in practice.
Summary
Potentially eligible people who declined to be further assessed by the RN, or consented to randomisation, suggested, when contacted by members of the research team to explore reasons for declining further, that they did not have anxiety or depression, or did not feel that the study was appealing to them. These people had scored ≥ 10 on the PHQ-9 and/or GAD-7 but did not recognise depression or anxiety as labels that might apply to them, or did not feel that the study had any relevance for them.
Analysis of the digital recordings of SW–study participant sessions suggested that the SWs could be trained to deliver the intervention as intended, and analysis of contact sheets completed by the SWs suggested adherence to most of the components of the intervention.
Older people recruited to the study disclosed long-standing mental health problems together with physical health problems. This complexity was echoed by the SWs and GPs interviewed. The SWs described additional challenges posed by social situations that could include caring responsibilities, family stresses and financial worries. Despite this complexity, older people reported that the SW intervention was useful in a variety of ways, emphasising the value of being listened to and having someone interested in them and spending time with them.
That the SW visited the older person at home was felt to be valuable by both older people and SWs. The older people also valued information provided by the SWs and in the manual that was developed as part of the intervention. Some older people found signposting to groups, with the offer of accompanying to a group, acceptable, particularly when this group was felt to be personally meaningful. Other study participants did not feel that a group was suitable or appropriate for them, either because they were not interested in groups where they felt they were ‘passive recipients’ of a service or because they did not feel that loneliness or social isolation were problems for them. The flexibility of the SW intervention allowed negotiation between the SWs with their clients about attending groups. This person-centredness was valued by the older people interviewed and the SWs.
The GPs interviewed reported that they had little understanding of the NOTEPAD study and were not aware of what the intervention entailed or the content of the interaction between SWs and their patients. Participation in the NOTEPAD study had not affected their routine work.
Chapter 6 Discussion and conclusions
Introduction
The NOTEPAD study is the first study, to our knowledge, that attempted to train SWs from the third sector to deliver a psychosocial intervention to older people with anxiety and/or depression recruited from primary care. The study was conducted in collaboration with Age UK North Staffordshire.
As outlined in Chapter 1, the research aims and objectives of the NOTEPAD study were as follows.
Aims
Phase 1: to refine a community-based psychosocial intervention for older people with anxiety and/or depression, to be delivered by NTPs/SWs in the third sector.
Phase 2: to determine whether or not NTPs/SWs can be trained to deliver this intervention to older people with anxiety and/or depression.
Phase 3: to determine if it is feasible to recruit and randomise patients, to pilot procedures and to conduct a process evaluation to provide essential information and data to inform an application for a full randomised trial.
Objectives
Phase 1: to refine a psychosocial intervention to be delivered by third-sector NTPs/SWs to older people with anxiety and/or depression.
Phase 2: to assess feasibility of recruiting and training NTPs/SWs to participate in the study and to assess fidelity of delivery of the psychosocial intervention to older people with anxiety and/or depression.
Phase 3: to answer the questions below.
-
Feasibility:
-
Can we recruit general practices to participate in a study to evaluate the feasibility of this approach?
-
Can we recruit and retain older adult participants in a randomised study, including the completion of follow-up questionnaires?
-
Can the NTPs/SWs deliver a psychosocial intervention to older people with anxiety and/or depression?
-
Can this intervention be implemented in routine NHS service delivery?
-
-
Process evaluation:
-
Do older people find working with an Age UK SW, and joining groups, acceptable?
-
What are the perspectives of the SWs about training, support to deliver the intervention, and how did they find working with older people in a more structured way?
-
Were the manuals developed to support training and delivery of the psychosocial intervention acceptable and useful to SWs?
-
What did participating primary care clinicians understand by the study and how did it impact on their work?
-
Summary of main findings
In this study, we developed and evaluated a psychosocial intervention for delivery by Age UK SWs to older people with anxiety and/or depression recruited from primary care.
Development of the intervention
The NICE guidelines for common mental disorders25 emphasise the need to promote access to services for people with common mental health disorders from a range of socially excluded groups, including older people, with suggestions, such as using different explanatory models of common mental health disorders, interventions in the person’s home or other residential settings or assistance with travel, and signposting to self-help and support groups. The NOTEPAD intervention was based on the research team’s previous research, refined in the light of phase 1 qualitative data analysis (see Chapter 2) and input from our PPIE group and an expert consensus group (see Chapter 3) comprising clinicians (GPs, psychiatrists and IAPT practitioners), academics and researchers with an interest and expertise in the management of mental health problems in primary care.
The psychosocial intervention comprised one-to-one contact between older people with anxiety and/or depression with encouragement to attend and participate in a group activity. The intervention was a person-centred, one-to-one psychosocial intervention based on the principles of BA, which is a structured programme of reducing the frequency of negatively reinforced avoidant behaviours in parallel with increasing the frequency of positively reinforcing behaviours to improve functioning and improve mood. The intervention was to be delivered by SWs recruited from Age UK North Staffordshire. The intervention also included signposting to local agencies and activities, where acceptable to the study participants, with the possibility of the SW accompanying the older person to a group. We developed training materials, a SW manual and a patient participant manual to support the intervention.
The objective of phase 1 of the NOTEPAD study was therefore met.
Recruitment of support workers
We recruited six SWs currently employed by Age UK North Staffordshire. We delivered 3 full days of training to these six SWs, and to a manager from Age UK who had agreed to act as a ‘backup SW’, to enable them to deliver the intervention to study participants. We delivered a refresher training session because of a delay in starting recruitment to the study. The digital recordings of a sample of SW–study participant sessions allowed fidelity checking of intervention delivery.
The objective of phase 2 of the NOTEPAD study was therefore met.
Results of feasibility study
Quantitative results
Six general practices were recruited, agreeing to recruit older people to the study. Recruitment of participants during a 9-month period had been planned, but, owing to delays in ethics and HRA approvals, this was reduced to a 5-month recruitment period, February to June 2017. As previously described, mailings were restricted to four practices owing to limited capacity in the West Midlands CRN and Keele CTU.
There were 3762 initial mailings, with 1267 returned questionnaires. This was a response rate of 33%, against a predicted response rate of 40%.
A total of 775 people consented to further contact. Out of these, 113 people were potentially eligible for the study (scoring ≥ 10 on PHQ-9 and/or GAD-7). A total of 49 baseline visits were conducted by CRN RNs, with 38 participants randomised.
The consent rate among potentially eligible people was slightly higher than anticipated [38 out of 113 (34%) against 30% estimated in the protocol].
Overall follow-up response rate was 86% (95% CI 72% to 96%) against an anticipated follow-up response rate of 75% at 4 months.
The completion rate of items on the questionnaires was very good. All questions had missing data rates of < 10% with the exception of:
-
question A4 at baseline (current employment status – missing data rate 16%)
-
question B7 at baseline (the way in each illness limits activity – missing data rate 11%).
Five of the six SWs who were trained to deliver the intervention were allocated study participants and four SWs worked with participants in the intervention arm. Two of the SWs withdrew from the study owing to changes in their personal circumstances and employment status with Age UK.
Baseline participant characteristics
All participants were white British, with a median age of 71 years. Most were retired, over half were married and one-third lived alone. Nearly half reported taking medication for low mood or stress and nearly all disclosed long-standing illness or disability, with a mean number of comorbidities of 3.6 [standard deviation (SD) 1.9].
The PHQ-9 and/or GAD-7 scores of randomised participants were higher than potentially eligible participants.
Outcomes
Overall follow-up response rate was 86% (95% CI 72–96%).
The primary outcome measure was CIS-R; secondary outcomes included PHQ-9, GAD-7, self-efficacy, EQ-5D-5L, CASP-12, De Jong Gierveld Loneliness Scale, Social Participation Scale and Adult Attitude to Loneliness scale scores. The study was not powered to demonstrate differences in outcomes. There was no indication that the intervention might be more effective than usual care.
To assess feasibility, we assessed our findings against criteria as outlined in Table 32.
| Criterion | Intended | Actual |
|---|---|---|
| Engagement of general practices | Six practices to participate | Six practices recruited, but reduced time for participant recruitment and limitations in capacity of CRN and CTU meant that participant recruitment was from four practices |
| Recruit, train and retain SWs | At least four SWs to be retained | Four SWs delivered intervention within the NOTEPAD study |
| Useable response rate to screening questionnaire (%) | 40 | 33 |
| Consent rate among potentially eligible people (%) | 30 | 33 |
Thus, the objective of phase 3 regarding feasibility was partially met. We have data that will inform a future RCT, although we recognise that we did not recruit to target. This was partly because of delays in obtaining ethics and HRA approvals and a lack of capacity in the RN team in the CRN WM and Keele CTU. In this study we invited all older adults aged ≥ 65 years, aiming to identify people with ‘hidden’ depression14 and recruit people who did not ordinarily attend their GP. In fact, many participants disclosed long-standing mental health problems and 18 out of the 38 participants were on medication for low mood or stress.
A suggested recruitment strategy for future studies would be to send invitations to people aged > 65 years with two or more long-term physical conditions rather than to all registered patients aged > 65 years, as in the CASPER plus trial. 42–44 An alternative approach in future studies would be to recruit people already on antidepressants, as nearly half of participants in the NOTEPAD study were taking medication. Aiming to recruit people who live alone is difficult as ‘living alone’ is unlikely to be Read coded on GP computer systems.
Process evaluation
Potentially eligible people who declined to be further assessed by the RN, or consented to randomisation, suggested, when contacted by members of the research team to explore reasons for declining further, that they did not have anxiety or depression, or did not feel that the study was appealing to them. These people had scored ≥ 10 on the PHQ-9 and/or GAD-7 but did not recognise depression or anxiety as labels that might apply to them, or did not feel that the study had any relevance for them. Some people stated that they were ‘too busy’, describing caring responsibilities or the burden of managing physical health problems.
The RNs asked potential study participants at baseline visits for their views on the baseline questionnaires. Some people suggested that the questionnaires were too long but that the RN support was helpful in enabling them to complete the questionnaires. There were positive comments about the personal qualities and supportive nature of the RNs. Views expressed about the content of the questions were variable, with some potential participants reflecting on negative emotions evoked by some of the questions.
We assessed adherence and acceptability of the intervention in the process evaluation. Sixteen out of the 18 people randomised received the intervention, one person who had been randomised and allocated was not contactable by the SW and one person dropped out.
The number of sessions and contact times between SWs and study participants varied between 3 and 6 sessions, each lasting from 15 minutes to 4 hours. Requirements for the supervision for each SW varied, with one-to-one supervision time varying between 60 and 280 minutes per SW.
Analysis of the digital recordings of SW–study participant sessions (fidelity checking) suggested that the SWs could be trained to deliver the intervention as intended.
Analysis of contact sheets completed by the SWs suggested adherence to most of the components of the intervention. SWs reported, during supervision, that using the mood thermometers was challenging and they admitted that they did not do this with all clients. This was confirmed in analysis of contact sheets and fidelity checking of recorded sessions.
Analysis of the data generated from interviews with SWs suggested that the training was acceptable to the SWs, who also valued the SW manual. The SWs reported that the intervention offered older people the opportunity to talk, and that this could be seen to legitimise their problems and concerns. Giving time and showing empathy was thought to ensure that older people developed trust with the SW.
The opportunity to visit people in their own home was thought to make the intervention more accessible to older people as well as giving the SW the opportunity to appraise the social contact of the study participant. SWs also valued the flexibility of the intervention, working with the individual to determine time to be spent at each session.
The SWs reflected on the complexity of the problems disclosed by study participants; such complexity was challenging, requiring the support of their peers in the NOTEPAD study, colleagues at Age UK and the opportunity to discuss at supervision. The knowledge and expertise that the SWs already had through previous training, and concurrent experience working within Age UK, were perceived as vital in suggesting local groups to study participants, being able to contact the group leaders and feeling comfortable accompanying people to groups. The SWs described the positive feelings they themselves experienced when they felt that they had made a difference to the study participants.
Although the SWs reported that the prospect of assessing risk of self-harm and suicide had made them feel uncomfortable during the training, they reported that they had developed confidence when doing this in practice.
A number of the SWs suggested that the training could have included more about dealing with families (in addition to safeguarding, which was included), as they reported that they had worked with family carers to support the study participant.
All SWs who had delivered the intervention to the NOTEPAD study participants and received supervision reflected on the value of the face-to-face group meetings and the one-to-one telephone supervision sessions. The amount of one-to-one supervision time required varied between each of the SWs (see Table 24); the supervision was led by the SW requirements and not limited by the supervisor. If the level of supervision required by SW C (see Table 24) in the NOTEPAD study was the level required for all SWs from Age UK, this would have resource implications, making the intervention costly.
All SWs made suggestions about how the intervention might be improved: the need for at least two sessions before problems could be fully defined and solutions (including signposting to groups) suggested; the need for a follow-up session (at 3 and 6 months were suggested) after the more intensive intervention had ended.
Older people recruited to the study disclosed long-standing mental health problems; some older people reported loneliness, which was not always linked with being socially isolated or a lack of close relationships.
All participants described positive experiences of meeting with the SWs; they described and valued the positive personal qualities of their individual SW and appreciated the opportunity to talk to, and be listened to by, the SW. Such support was not seen to be available either within their family or from statutory services. The GP was not seen as a potential source of support.
Participants who completed the intervention valued the home visits made by the SW, being seen as less stigmatising than attending a building associated with a mental health service, of which many of them had previous experience, and also fitting in with competing commitments and caring responsibilities of some of the study participants.
Some older people reported that the opportunity to be introduced and accompanied to local groups was a positive feature of the NOTEPAD intervention. Some participants reported valuing activities that they felt to be personally meaningful; they were not interested in groups where they felt they were ‘passive recipients’ of a service and expressed the necessity of a reciprocal relationship.
The NOTEPAD resources were valued by older adults, particularly the diary, information about local groups and information about staying well.
Analysis of data enabled the development of a model for further refinement of the intervention, focusing on developing the relationship, and more emphasis on determining who might wish to attend, and benefit from attending, groups.
Although GPs recognised that older people were a vulnerable group, they suggested that they had little time to offer pastoral support to older people, and that there were limited resources to which to refer people. GPs admitted that they had little understanding of the NOTEPAD study, which had not affected their routine work, and were not aware of the work done by SWs with their patients. Some GPs expressed irritation about instances when the suicide ideation protocol resulted in a telephone call to the practice. Although discussion of communication with the study participant’s GP was discussed within the SW training, it was mainly around risk. Encouraging liaison between SWs and GPs, perhaps with co-location of the SW within the general practice, might encourage engagement by GPs.
Thus, the process evaluation suggests that we were successful in recruiting and retaining SWs from Age UK. The SWs delivered the NOTEPAD intervention to fidelity; the SW manual and training improved SW confidence, were acceptable and supported delivery of the intervention. One-to-one and group supervision sessions were valued. The one-to-one sessions with SWs were acceptable to, and valued by, older people who participated in the study, but not all participants took up the option of joining a local group.
Comparison with previous studies
Pettit et al. 21 report that older adults are still under-represented in IAPT services, and the NICE guidelines on common mental disorders25 suggests the need to modify interventions to improve access. It is important to establish whether or not changes to service configuration, treatment options, and GP behaviour can increase referrals for middle-aged and older adults. In response to the knowledge that older people are one of the vulnerable groups for whom access to mental health services needs to improve, the AMP research programme50 developed a model to improve access and develop acceptable interventions. In the AMP study,94 one of the vulnerable groups in which a new model of care was evaluated was older people with depression, but the intervention was delivered by IAPT practitioners who worked closely with local groups offered by Age Concern (the group in Manchester preferred to be known as ‘Age Concern’ rather than ‘Age UK’). The NOTEPAD study was an attempt to increase access to care for people with anxiety and depression by developing and testing the acceptability of a less stigmatising intervention delivered by SWs from the third sector.
In the CASPER plus trial,43 older people reported the value of receiving the screening questionnaires and being invited to participate in a trial about depression. The study team suggested that this might facilitate an older person to disclose their feelings, name the problem and seek help. The NOTEPAD process evaluation suggests that some, although not all, older people found the screening questionnaires disconcerting and uncomfortable. The study participants in the CASPER plus trial43 were thought to be from areas of higher socioeconomic status, in contrast to the participants in the NOTEPAD study, who were recruited from deprived areas in Stoke-on-Trent.
In the CASPER plus trial,43 it was reported that offering older people an opportunity to talk outside the primary care consultation was valued by patients and GPs and that psychosocial intervention in the primary care setting may fill the gap in the care of older people with depression. Our findings confirm this.
In a service development evaluation in which practice nurses (PNs) delivered a psychosocial intervention to patients with long-term conditions,95 the patients valued the availability of PNs to listen to their concerns.
In the process evaluation in the COINCIDE trial (a trial of a psychological intervention for the management of depression in adults with diabetes and/or heart disease),37 it was reported that patients with long-term conditions and comorbid depression preferred a protected space to discuss mental health issues, and study participants in the NOTEPAD study alluded to their beliefs that they did not feel it was appropriate to discuss low mood or stress and distress with their GPs. The PNs and IAPT practitioners in the COINCIDE trial expressed a wish to maintain barriers around physical and mental health expertise. In our study, GPs suggested that they could not offer support to older people with anxiety and depression and lacked services to refer them to. The SW role might meet this need.
The GPs interviewed as part of the process evaluation suggested that the NOTEPAD study had only affected the practice when a call was received in relation to the risk protocol. The SWs had no contact with the practices from which study participants were recruited. Although a safe space perceived to be outside the primary care consultation was valued, it might have been better if we had achieved closer liaison between the SWs and practices, perhaps linking one SW with one practice. This was achieved in the DeepEnd initiative in Glasgow,96 where ‘community links practitioners’ (CLPs) were embedded in practices in Glasgow; these CLPs carried out one-to-one working with patients to support patients’ use of community services.
This study has improved our understanding of the link between depression and loneliness48 (see Chapter 2), people’s response to it and the potential role of the third sector in delivering a one-to-one intervention and signposting group activities. The qualitative study by Kharicha et al. 33 suggested that older people with characteristics of loneliness generally know about local resources but may not consider services that they perceive as being for ‘lonely older people’ as desirable, helpful or relevant to them. Our study suggests that groups can be acceptable to some people who perceive themselves to be lonely; group-based activities with a shared interest are preferred to social groups. Our study resonates with Kharicha’s findings that older people experiencing loneliness may not consider that primary care has a role in alleviating this.
Patient and public involvement and engagement
This study’s design and processes were informed by PPIE in accordance with INVOLVE’s recommendations [URL: www.invo.org.uk/resource-centre/resource-for-researchers/ (accessed on 10 October 2018)]. Participants at the meetings prior to submission of the funding application endorsed the concept of a ‘non-medicalised’ approach to the management of depression and anxiety in older people, and welcomed partnering with third-sector groups such as Age UK. PPIE members also supported the idea of a one-to-one intervention delivered by a worker from Age UK. Members of the group felt that most older people would be happy to talk to the SW and strongly supported the idea of tailoring activities to the older person’s interests. Many felt that older people might need some encouragement and reassurance to take part. They also felt strongly that barriers to participation, such as transport and lack of confidence, would need to be addressed. These factors were at the heart of the intervention.
In subsequent meetings, the PPIE group provided input on the patient information sheets, letters and participant resources for phases 1 and 3. The group contributed to the NOTEPAD logo and suggested the strapline ‘Supporting Mental Strength’, which was adopted by the research team.
The group met during the feasibility study and reflected on the slow recruitment. In particular, group members commented on the formality of the language used in public-facing documents (which had been modified with the group’s input) and how the stringent requirements of the regulatory procedures might negatively affect recruitment.
The group reflected on the results of the process evaluation, supporting the development of the model (see Figure 8).
Strengths and limitations of the methods
Strengths
A strength of the study is the development of a complex psychosocial intervention for older adults with anxiety and/or depression, built on the literature, knowledge and expertise of the research team, initial qualitative work, PPIE and agreement of components in an expert consensus group. The components of the resources for study participants, SW manual and SW training were similarly developed. These materials are available on the project webpage [see www.journalslibrary.nihr.ac.uk/programmes/hsdr/135434/#/ (accessed 20 March 2019)].
We recruited six SWs from staff employed by Age UK North Staffordshire, and trained these six, plus a manager to act as a backup SW.
A strength of this study is the PPIE input throughout the study, with PPIE input into the original funding application; comments on the proposed intervention, SW training and manual, and patient resources; advice on documents for ethics applications; reflections on analysis; and advice on dissemination.
Table 33 summarises the reporting of the PPIE contribution following the Guidance for Reporting Involvement of Patients and the Public-updated version (GRIPP2) framework. 97
| Number | Topic | Item | Reported |
|---|---|---|---|
| 1 | Aim | Report the aim of PPIE in the study | Aims of PPIE involvement reported in Chapters 2, 3 and 4 |
| 2 | Methods | Provide a clear description of the methods used for PPIE in the study |
Group meetings Study design and processes were informed by PPIE Reported in Chapters 2, 3 and 4 |
| 3 | Study results | Report the results of PPIE in the study, including both positive and negative outcomes | Reported in Chapters 2, 3, 4 and 6 |
| 4 | Discussion and conclusions | Comment on the extent to which PPIE influenced the study overall. Describe positive and negative effects of PPIE | Reported in Chapter 2, Results, PPIE and Chapter 6, NOTEPAD participant resources |
| 5 | Reflections/critical perspective | Comment critically on the study, reflecting on the things that went well and those that did not, so others can learn from this experience |
Group reflected on phases 1 and 3 of the study Reported in Chapter 2, Results, PPIE and Chapter 6, NOTEPAD participant resources |
Limitations
Target recruitment was not achieved; this was partly owing to delays in ethics and HRA approvals, leading to a reduction in the recruitment period from 9 to 5 months. In addition, recruitment was affected by a limited capacity of the RNs in the CRN and administrative support from Keele CTU to increase the number of mail-outs when this was advised by the SSC. The SSC suggested that recruitment might have been more successful if members of the research team were directly responsible for recruitment.
The study was conducted in one geographical site and with one third-sector provider (Age UK North Staffordshire), which limits the generalisability of the study. Age UK North Staffordshire, at the time of the study, working with primary care was enthusiastic about; other third-sector services may not share this enthusiasm. It should be noted, however, that such services were commissioned on short-term contracts and the decommissioning of a number of services (by the CCG) occurred during the course of the NOTEPAD study.
Two of the six SWs were unable to continue working on the study (although they had participated in training and were interviewed as part of the process evaluation) owing to family circumstances (they both had increased caring responsibilities and needed to reduce the number of hours they worked). Four SWs delivered the intervention, which reduces the generalisability of the study.
The study was not powered to provide evidence of cost-effectiveness.
Conclusions
Although recruitment was lower than anticipated, it was feasible to recruit and randomise patients, to test procedures and to conduct a process evaluation to provide essential information and data to inform a future randomised trial. Workers in third-sector services have the potential to deliver non-stigmatising interventions to support and manage older people with anxiety and depression, which is potentially useful within a resource-poor NHS.
Implications for health and social care
We have demonstrated that SWs, recruited from staff employed by Age UK North Staffordshire, were capable of working with older adults with anxiety and depression and delivering the psychosocial intervention as intended. The NOTEPAD intervention was acceptable to older adults, the personal qualities of the SWs were valued and the intervention was perceived to be less stigmatising than statutory services. Signposting to group activities was not acceptable to all older adults; older males, particularly, did not want to be passive recipients of services and suggested a preference for more reciprocal relationships in any new activities they embarked on. This emphasises the need to be person-centred, assessing the likelihood of a patient accepting this approach prior to a referral for such an intervention.
The SWs recruited for the study reported broad experience and expertise of working with older adults. This expertise is currently under-recognised and underutilised and is a source of expertise that could be of benefit to primary care, particularly given that our qualitative study suggests that GPs have little time for, and do not prioritise, supporting older adults.
Supervision was perceived by the SWs to be necessary, with supervision duration varying between the four SWs in the study. If this intervention was commissioned as a service, supervision costed in would be limited, which may reduce the confidence of SWs from the third sector to deliver the intervention.
Depression in older adults is a common condition, with a prevalence of depressive symptoms of up to 20%. 2,3 At policy level, there is a need to increase access to psychological services98 for older adults with anxiety and depression to reduce disease burden and costs for the individual and the NHS. There is evidence that older people still do not access IAPT services. 21 An intervention, such as the NOTEPAD intervention, delivered by SWs from the third sector, might be less stigmatising and more acceptable to older adults. Assessment of cost-effectiveness of commissioning third-sector services, rather than facilitating recruitment of older people to existing IAPT services, is necessary.
We demonstrated a lack of engagement by GPs participating in the NOTEPAD study. GPs disclosed that they have little time to support vulnerable older adults. One option would be to locate the SWs in the practice, which would support liaison between the SW and the GP.
Research recommendations
-
Before a fully powered RCT to evaluate the clinical effectiveness and cost-effectiveness of a psychosocial intervention delivered by third-sector workers can be considered, further work is needed to refine procedures and intervention, focusing on older adults with physical long-term conditions already on antidepressants and people living alone. Assessment of cost-effectiveness would be required in a RCT.
-
The intervention might be improved by the inclusion of a structured liaison with primary care/co-location of SWs within practices.
-
Future work should explore partnership with a range of third-sector providers, across more geographical sites, to see if the SW intervention can be delivered at scale.
-
Future research using other existing primary care professionals to deliver the intervention, for example health care assistants and PNs, would be useful to explore integration in routine primary care.
-
A longitudinal implementation study using ethnographic methods would be useful to assess the contribution and long-term sustainability of third-sector organisations in the management of older people with anxiety and depression.
Acknowledgements
We would like to thank the following people and groups for their invaluable contributions as part of the NOTEPAD study:
-
participants and their carers
-
SWs at Age UK North Staffordshire
-
participants in the consensus group held in January 2016
-
GP practices, GPs and practice staff who participated in the study
-
collaborators Professor Linda Gask (Emeritus Professor of Primary Care Mental Health, University of Manchester) and Della Bailey (Research Fellow, University of York) who contributed to delivering the training to Age UK SWs
-
SSC members Professor Christopher Dowrick (Chair), Professor Margaret Maxwell, Dr Peter Kimani, Mrs Carol Williams and Mr John Pemberton
-
Research User Group, Research Institute, Primary Care and Health Sciences, Keele University, particularly Carol Rhodes and Adele Higginbotham
-
the NOTEPAD PPIE group
-
Janine Proctor for contribution to the development of the patient participant resources and the process evaluation protocol
-
database managers Jo Smith and Zoe Mayson, Keele CTU
-
study co-ordinators Tom Shepherd, Stephanie Butler-Whalley and Stephanie Griffiths, Keele CTU
-
research administrator Jane Mason, Keele CTU
-
NHS North Staffordshire and Stoke CCGs
-
CRN WM.
This study was designed and conducted in collaboration with the Keele CTU, a registered UK Clinical Research Collaboration (UKCRC) CTU in receipt of National Institute for Health Research CTU support funding.
Contributions of authors
Heather Burroughs (Research Fellow, Keele University) was principal investigator. She contributed to the grant application and the training of SWs and was trial manager of the feasibility study. She made a major contribution to the final report.
Bernadette Bartlam (Senior Lecturer, Keele University) contributed to the grant application, qualitative work in phase 1 and the process evaluation in phase 3.
Peter Bullock (Chief Executive of Age UK North Staffordshire) contributed to the grant application and supported recruitment and retention of the SWs.
Karina Lovell (Professor of Mental Health, University of Manchester) contributed to the grant application and development of the intervention and training and delivered the training to the SWs.
Reuben Ogollah (Associate Professor of Medical Statistics, University of Nottingham) contributed to the grant application and developed the SAP.
Mo Ray (Professor of Health and Social Care Integration, University of Lincoln) contributed to the grant application and phase 1 of the study.
Peter Bower (Professor Health Sciences, University of Manchester) contributed to the grant application and development of the intervention and feasibility study.
Waquas Waheed (Professor of Primary Care Psychiatry, University of Manchester) contributed to the grant application and development of the intervention.
Simon Gilbody (Professor and Director of the Mental Health and Addictions Research Group, University of York) contributed to the grant application and development of the intervention and feasibility study.
Tom Kingstone (Research Associate, Mental Health, Keele University) contributed to the qualitative work in phase 1, the NOTEPAD protocol and the process evaluation papers.
Elaine Nicholls (Research Fellow, Biostatistics, Keele University) led the quantitative analysis in phase 3.
Carolyn A Chew-Graham (Professor of General Practice Research, Keele University) was chief investigator in this study, led the grant application, co-conceived and designed the study, led the research team, provided clinical input and was lead author on the following sections of the final report: Abstract, Plain English summary, Scientific summary, Chapter 1 and Chapters 3–6. She is the guarantor.
All authors contributed to the final report.
Publications
Kingstone T, Burroughs H, Bartlam B, Ray M, Proctor J, Shepherd T, et al. Developing a community-based psycho-social intervention with older people and third sector workers for anxiety and depression: a qualitative study. BMC Fam Pract 2017;18:77.
Burroughs H, Bartlam B, Ray M, Kingstone T, Shepherd T, Ogollah R, et al. The feasibility and acceptability of an intervention for older people with depression and anxiety delivered by third sector workers: the NOTEPAD feasibility study protocol. BMC Trials 2018;19:172.
Presentations
Bartlam B, Burroughs H, Kingstone T, Bullock P, Ray M, Chew-Graham CA. Lay Perspectives on Supporting Older People with Anxiety and Depression: A Qualitative Study to Develop a Community-Based Psychosocial Intervention Working with Non-Traditional Providers. Paper presented at the British Society of Gerontology, Stirling, July 2016.
Kingstone T, Bartlam B, Burroughs H, Bullock P, Ray M, Chew-Graham CA. Refining a Psychosocial Intervention for Older People with Anxiety and/or Depression to be Delivered by Third Sector Providers: a Qualitative Study. Paper presented at the Society for Academic Primary Care, Dublin, July 2016.
Burroughs H, Kingstone T, Bartlam B, Bullock P, Ray M, Chew-Graham CA. Development of a Psychosocial Intervention for Older People with Anxiety and Depression to be Delivered by Third Sector Practitioners: a Qualitative Study. Poster presented at the Royal College of General Practitioners’ annual conference, Glasgow, October 2016.
Burroughs H, Kingstone T, Bartlam B, Bullock P, Ray M, Chew-Graham CA. Refining a Community-Based Psychosocial Intervention, Delivered by Third Sector Practitioners, for Older People with Depression and Anxiety: Focus on Role of PPIE in Shaping a Feasibility Study. Poster presented at the Keele University ten-year anniversary PPIE event, Keele, Staffs, October 2016.
Kingstone T, Bartlam B, Burroughs H, Bullock P, Ray M, Chew-Graham CA. Exploring Views about Anxiety and Depression Among Older People in the Community in Order to Refine a Psychosocial Intervention Delivered by Third Sector Workers: A UK Qualitative Study. Paper presented at the North American Primary Care Research Group, Colorado Springs, CO, November 2016.
Burroughs H, Kingstone T, Bartlam B, Bullock P, Ray M, Chew-Graham CA. Developing a Community-Based Psychosocial Intervention for Anxiety and Depression: The Views of Older People and Third Sector Workers. Poster presented at the Health Service Research UK symposium, Nottingham, July 2017.
Burroughs H, Bartlam B, Kingstone T, Bullock P, Ray M, Lovell K, et al. The Acceptability of a Psychosocial Intervention Delivered by Age UK Support Workers to Older Adults with Anxiety and Depression: A Qualitative Analysis. Paper presented at Primary Care Mental Health Conference, Southampton, April 2018.
Chew-Graham CA, Kingstone T, Burroughs H, Bullock P, Gilbody S, Bower P, et al. Development and Evaluation of a Brief Psycho-Social Intervention for Delivery by Support Workers from Age UK North Staffordshire, to Support Older People with Anxiety and Depression: A Feasibility Study. Poster presented at the SAPC, London, July 2018.
Chew-Graham CA, Kingstone T, Burroughs H, Bullock P, Gilbody S, Bower P, et al. Development and Evaluation of a Psycho-Social Intervention for Delivery by Support Workers from Age UK North Staffordshire, to Support Older People with Anxiety and Depression: A Feasibility Study. Poster presented at Public Health England, Warwick, September 2018.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLOS Med 2006;3. https://doi.org/10.1371/journal.pmed.0030442.
- Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand 2006;113:372-87. https://doi.org/10.1111/j.1600-0447.2006.00770.x.
- Steffens DC, Fisher GG, Langa KM, Potter GG, Plassman BL. Prevalence of depression among older Americans: the aging, demographics and memory study. Int Psychogeriatr 2009;21:879-88. https://doi.org/10.1017/S1041610209990044.
- Laidlaw K, Pachana NA. Aging, mental health, and demographic change: challenges for psychotherapists. Prof Psych Res Pract 2006;40. https://doi.org/10.1037/a0017215.
- Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci 2003;58:M249-M265. https://doi.org/10.1093/gerona/58.3.M249.
- Age UK . Later Life in the United Kingdom 2018. www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/later_life_uk_factsheet.pdf (accessed 7 January 2018).
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370:851-8. https://doi.org/10.1016/S0140-6736(07)61415-9.
- Katon W, Ciechanowski P. Impact of major depression on chronic medical illness. J Psychosom Res 2002;53:859-63. https://doi.org/10.1016/S0022-3999(02)00313-6.
- Licht-Strunk E, Beekman AT, de Haan M, van Marwijk HW. The prognosis of undetected depression in older general practice patients. A one year follow-up study. J Affect Disord 2009;114:310-15. https://doi.org/10.1016/j.jad.2008.06.006.
- Donoghue HM, Traviss-Turner GD, House AO, Lewis H, Gilbody S. Life adversity in depressed and non-depressed older adults: a cross-sectional comparison of the brief LTE-Q questionnaire and life events and difficulties interview as part of the CASPER study. J Affect Disord 2016;193:31-8. https://doi.org/10.1016/j.jad.2015.12.070.
- Chew-Graham CA, Baldwin R, Burns A. Treating depression in later life: we need to implement the evidence that exists. BMJ 2004;329. https://doi.org/10.1136/bmj.329.7459.181.
- Coventry PA, Hays R, Dickens C, Bundy C, Garrett C, Cherrington A, et al. Talking about depression: a qualitative study of barriers to managing depression in people with long term conditions in primary care. BMC Fam Pract 2011;12. https://doi.org/10.1186/1471-2296-12-10.
- Burroughs H, Lovell K, Morley M, Baldwin R, Burns A, Chew-Graham C. ‘Justifiable depression’: how primary care professionals and patients view late-life depression? A qualitative study. Fam Pract 2006;23:369-77. https://doi.org/10.1093/fampra/cmi115.
- Overend K, Bosanquet K, Bailey D, Foster D, Gascoyne S, Lewis H, et al. Revealing hidden depression in older people: a qualitative study within a randomised controlled trial. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0362-2.
- Chew-Graham C, Kovandžić M, Gask L, Burroughs H, Clarke P, Sanderson H, et al. Why may older people with depression not present to primary care? Messages from secondary analysis of qualitative data. Health Soc Care Community 2012;20:52-60. https://doi.org/10.1111/j.1365-2524.2011.01015.x.
- Scholz B, Crabb S, Wittert GA. ‘Males don’t wanna bring anything up to their doctor’: men’s discourses of depression. Qual Health Res 2017;27:727-37. https://doi.org/10.1177/1049732316640294.
- Department of Health and Social Care . National Service Framework for Older People n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/198033/National_Service_Framework_for_Older_People.pdf (accessed 7 January 2018).
- Department of Health and Social Care . Everybody’s Business n.d. www.scie-socialcareonline.org.uk/everybodys-business-integrated-mental-health-services-for-older-adults-a-service-development-guide/r/a11G00000017vMyIAI (accessed 7 January 2018).
- Department of Health and Social Care . No Health Without Mental Health n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/138253/dh_124058.pdf (accessed 22 December 2017).
- NHS England . Adult Improving Access to Psychological Therapies Programme n.d. www.england.nhs.uk/mental-health/adults/iapt/ (accessed 7 January 2018).
- Pettit S, Qureshi A, Lee W, Stirzaker A, Gibson A, Henley W, et al. Variation in referral and access to new psychological therapy services by age: an empirical quantitative study. Br J Gen Pract 2017;67:e453-e459. https://doi.org/10.3399/bjgp17X691361.
- Prina AM, Marioni RE, Hammond GC, Jones PB, Brayne C, Dening T. Improving access to psychological therapies and older people: findings from the Eastern Region. Behav Res Ther 2014;56:75-81. https://doi.org/10.1016/j.brat.2014.03.008.
- National Institute for Health and Care Excellence (NICE) . Depression: Treatment and Management of Depression in Adults n.d. www.nice.org.uk/guidance/cg90 (accessed 7 January 2018).
- National Institute for Health and Care Excellence (NICE) . Generalised Anxiety Disorder and Panic Disorder in Adults: Management n.d. www.nice.org.uk/guidance/cg113 (accessed 7 January 2018).
- National Institute for Health and Care Excellence (NICE) . Common Mental Disorders: Identification and Pathways to Care n.d. www.nice.org.uk/cg123 (accessed 7 January 2018).
- Baldwin RC, Anderson D, Black S, Evans S, Jones R, Wilson K, et al. Faculty of Old Age Psychiatry Working Group, Royal College of Psychiatrists: guideline for the management of late-life depression in primary care. Int J Geriatr Psychiatry 2003;18:829-38. https://doi.org/10.1002/gps.940.
- Mead N, Lester HE, Gask L, Chew-Graham C, Bower P. A meta analysis of befriending in the treatment of depression. Brit J Psychiatry 2010;196:96-101. https://doi.org/10.1192/bjp.bp.109.064089.
- Dean J, Goodlad R. Supporting Community Participation: The Role and Impact of Befriending. York: Joseph Rowntree Foundation; 1998.
- Lester H, Mead N, Graham-Chew CA, Gask L, Reilly S. An exploration of the value and mechanisms of befriending for older adults in England. Ageing Soc 2012;32:307-28. https://doi.org/10.1017/S0144686X11000353.
- Moriarty J, Manthorpe J. Diversity in Older People and Access to Services: An Evidence Review. London: Age UK; 2012.
- Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc 2005;25:41-67. https://doi.org/10.1017/S0144686X04002594.
- Burroughs H, Chew-Graham C, Seal B, Hanjari M. Systematic Review of Community Based Psychosocial Interventions for Older People With Depression and Anxiety. PROSPERO 2016: CRD42016029502 n.d. www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=29502&VersionID=53837 (accessed 22 December 2017).
- Kharicha K, Iliffe S, Manthorpe J, Chew-Graham CA, Cattan M, Goodman C, et al. What do older people experiencing loneliness think about primary care or community based interventions to reduce loneliness? A qualitative study in England. Health Soc Care Community 2017;25:1733-42. https://doi.org/10.1111/hsc.12438.
- Ekers D, Richards D, Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychol Med 2008;38:611-23. https://doi.org/10.1017/S0033291707001614.
- Veale D. Behavioural activation for depression. Adv Psychiatr Treat 2008;14:29-36. https://doi.org/10.1192/apt.bp.107.004051.
- Bristow K, Edwards S, Funnel E, Fisher L, Gask L, Dowrick C, et al. Help seeking and access to primary care for people from ‘hard-to-reach’ groups with common mental health problems. Int J Family Med 2011;2011. https://doi.org/10.1155/2011/490634.
- Coventry P, Lovell K, Dickens C, Bower P, Chew-Graham C, McElvenny D, et al. Integrated primary care for patients with mental and physical multimorbidity: cluster randomised controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. BMJ 2015;350. https://doi.org/10.1136/bmj.h638.
- Mitchell N, Hewitt C, Adamson J, Parrott S, Torgerson D, Ekers D, et al. A randomised evaluation of CollAborative care and active surveillance for Screen-Positive EldeRs with sub-threshold depression (CASPER): study protocol for a randomized controlled trial. Trials 2011;12. https://doi.org/10.1186/1745-6215-12-225.
- Richards DA, Hill JJ, Gask L, Lovell K, Chew-Graham C, Bower P, et al. Clinical effectiveness of collaborative care for depression in UK primary care (CADET): cluster randomised controlled trial. BMJ 2013;347. https://doi.org/10.1136/bmj.f4913.
- Samad Z, Brealey S, Gilbody S. The effectiveness of behavioural therapy for the treatment of depression in older adults: a meta-analysis. Int J Geriatr Psychiatry 2011;26:1211-20. https://doi.org/10.1002/gps.2680.
- Wilson KC, Mottram PG, Vassilas CA. Psychotherapeutic treatments for older depressed people. Cochrane Database Syst Rev 2008;1. https://doi.org/10.1002/14651858.CD004853.pub2.
- Overend K, Lewis H, Bailey D, Bosanquet K, Chew-Graham C, Ekers D, et al. CASPER plus (CollAborative care in Screen-Positive EldeRs with major depressive disorder): study protocol for a randomised controlled trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-451.
- Bosanquet K, Adamson J, Atherton K, Bailey D, Baxter C, Beresford-Dent J, et al. CollAborative care for Screen-Positive EldeRs with major depression (CASPER plus): a multicentred randomised controlled trial of clinical effectiveness and cost-effectiveness. Health Technol Assess 2017;21. https://doi.org/10.3310/hta21670.
- Taylor AK, Gilbody S, Bosanquet K, Overend K, Bailey D, Foster D, et al. How should we implement collaborative care for older people with depression? A qualitative study using normalisation process theory within the CASPER plus trial. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0813-7.
- Bartlam B, Sim J, Ray MG, Smith N. Fit as a fiddle: the impact of Age UK’s wellbeing programme on the health and wellbeing of participants: preliminary findings. J Aging Phys Act 2012;20.
- Beech R, Murray M. Social engagement and healthy ageing in disadvantaged communities. Qual Ageing Older Adults 2013;14:12-24. https://doi.org/10.1108/14717791311311076.
- Dowrick C, Gask L, Edwards S, Aseem S, Bower P, Burroughs H, et al. Researching the mental health needs of hard-to-reach groups: managing multiple sources of evidence. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-226.
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging 2006;21:140-51. https://doi.org/10.1037/0882-7974.21.1.140.
- Kingstone T, Burroughs H, Bartlam B, Ray M, Proctor J, Shepherd T, et al. Developing a community-based psycho-social intervention with older people and third sector workers for anxiety and depression: a qualitative study. BMC Fam Pract 2017;18. https://doi.org/10.1186/s12875-017-0648-7.
- Dowrick C, Chew-Graham C, Lovell K, Lamb J, Aseem S, Beatty S, et al. Increasing equity of access to high-quality mental health services in primary care: a mixed-methods study. Programme Grants Appl Res 2013;1.
- Lovell K, Lamb J, Gask L, Bower P, Waheed W, Chew-Graham C, et al. Development and evaluation of culturally sensitive psychosocial interventions for under-served people in primary care. BMC Psychiatry 2014;14. https://doi.org/10.1186/s12888-014-0217-8.
- Heikkinen RL, Kauppinen M. Depressive symptoms in late life: a 10-year follow-up. Arch Gerontol Geriatr 2004;38:239-50. https://doi.org/10.1016/j.archger.2003.10.004.
- Frost H, Haw S, Frank J. Promoting Health and Wellbeing in Later Life: Interventions in Primary Care and Community Settings. Edinburgh: Medical Research Council Scottish Collaboration for Public Health Research and Policy; 2010.
- Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-647.
- Andersson L. Intervention against loneliness in a group of elderly women: an impact evaluation. Soc Sci Med 1985;20:355-64. https://doi.org/10.1016/0277-9536(85)90010-3.
- Tennstedt S, Howland J, Lachman M, Peterson E, Kasten L, Jette A. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci Soc Sci 1998;53:P384-92. https://doi.org/10.1093/geronb/53B.6.P384.
- Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, Diehr P, et al. Community-integrated home-based depression treatment in older adults: a randomized controlled trial. JAMA 2004;291:1569-77. https://doi.org/10.1001/jama.291.13.1569.
- McAuley E, Blissmer B, Marquez DX, Jerome GJ, Kramer AF, Katula J. Social relations, physical activity, and well-being in older adults. Prev Med 2000;31:608-17. https://doi.org/10.1006/pmed.2000.0740.
- Greaves CJ, Farbus L. Effects of creative and social activity on the health and well-being of socially isolated older people: outcomes from a multi-method observational study. J R Soc Promot Health 2006;126:134-42. https://doi.org/10.1177/1466424006064303.
- Staricoff RL. Arts in health: the value of evaluation. J R Soc Promot Health 2006;126:116-20. https://doi.org/10.1177/1466424006064300.
- Johnson V, Stanley J. Capturing the contribution of community arts to health and well-being. Int J Ment Health Promotion 2007;9:28-35. https://doi.org/10.1080/14623730.2007.9721836.
- Burroughs H, Wilkie R, Chew-Graham CA, Ray M. Mental Health and Older People: A Guide for Primary Care Practitioners. New York, NY: Springer International Publishing; 2016.
- Ray M, Chew-Graham CA, Ray M. Mental Health and Older People: A Guide for Primary Care Practitioners. New York, NY: Springer International Publishing; 2016.
- Flood M, Scharer K. Creativity enhancement: possibilities for successful aging. Issues Ment Health Nurs 2006;27:939-59. https://doi.org/10.1080/01612840600899832.
- Bandura A. Self Efficacy: The Exercise of Control. New York, NY: W.H. Freeman; 1997.
- Wikström BM. Social interaction associated with visual art discussions: a controlled intervention study. Aging Ment Health 2002;6:82-7. https://doi.org/10.1080/13607860120101068.
- Everitt A, Hamilton R. Art, Health and Community: A Study of Five Community Arts in Health Projects. Durham: Centre for Arts and Humanities in Health and Medicine; 2003.
- Cutler D. Tackling Loneliness in Older Age: The Role of the Arts. London: The Baring Foundation; 2012.
- Hogg MA, Abrams D. Social Identifications: A Social Psychology of Intergroup Relations and Group Processes. London: Routledge; 1998.
- Harter S. The Construction of the Self. New York, NY: Guildford; 1999.
- Roberts D, Scharf T, Bernard M, Crome P. SCIE Research Briefing 21: Identification of Deafblind Dual Sensory Impairment in Older People. London: Social Care Institute for Excellence (SCIE); 2007.
- Morgan D. The SAGE Encyclopaedia of Qualitative Research Methods. Newbury Park, CA: Sage Publications Ltd; 2008.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psych 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Henwood KL, Pidgeon NF. Qualitative research and psychological theorizing. Br J Psychol 1992;83:97-111. https://doi.org/10.1111/j.2044-8295.1992.tb02426.x.
- Age Concern . Promoting Mental Health and Well-Being in Later Life 2006. www.mentalhealth.org.uk/sites/default/files/promoting_mh_wb_later_life.pdf (accessed 7 January 2018).
- Chew-Graham CA, Lovell K, Roberts C, Baldwin R, Morley M, Burns A, et al. A randomised controlled trial to test the feasibility of a collaborative care model for the management of depression in older people. Br J Gen Pract 2007;57:364-70.
- Zeiss AM, Lewinsohn PM, Rohde P, Kato P, Mann T. Handbook of Diversity Issues in Health Psychology. New York, NY: Plenum Press; 1996.
- Blazer DG. Depression in late life: review and commentary. Focus 2009;7:118-36. https://doi.org/10.1176/foc.7.1.foc118.
- Joiner TE, Conwell Y, Fitzpatrick KK, Witte TK, Schmidt NB, Berlim MT, et al. Four studies on how past and current suicidality relate even when ‘everything but the kitchen sink’ is covaried. J Abnorm Psychol 2005;114:291-303. https://doi.org/10.1037/0021-843X.114.2.291.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Pasterfield M, Bailey D, Hems D, McMillan D, Richards D, Gilbody S. Adapting manualized behavioural activation treatment for older adults with depression. Cognitive Behaviour Therapist 2014;7. https://doi.org/10.1017/S1754470X14000038.
- National Institute for Health Research . Good Clinical Practice (GCP) n.d. www.nihr.ac.uk/our-research-community/clinical-research-staff/learning-and-development/national-directory/good-clinical-practice/ (accessed 30 April 2019).
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care 2008;46:266-74. https://doi.org/10.1097/MLR.0b013e318160d093.
- Lewis G, Pelosi AJ, Araya R, . Measuring psychiatric disorders in the community: a standardised assessment for use by lay interviewers. Psychol Med 1992;22:465-86. https://doi.org/10.1017/S0033291700030415.
- Lorig K, Stewart A, Ritter P, González V, Laurent D, Lynch J. Outcome Measures for Health Education and Other Health Care Interventions. Thousand Oaks, CA: Sage Publications Ltd; 1996.
- Wiggins RD, Netuveli G, Hyde M, Higgs P, Blane D. The evaluation of a self-enumerated scale of quality of life (CASP-19) in the context of research on ageing: a combination of exploratory and confirmatory approaches. Soc Indic Res 2008;89:61-77. https://doi.org/10.1007/s11205-007-9220-5.
- Brooks R, Rabin R, de Charro F. The Measurement and Valuation of Health Status Using EQ-5D: A European Perspective. Berlin: Springen; 2003.
- de Jong Gierveld J, van Tilburg T. 6-item scale for overall, emotional, and social loneliness: confirmatory tests on survey data. Res Ageing 2006;28:582-98. https://doi.org/10.1177/0164027506289723.
- Sim J, Machin L, Bartlam B. Identifying vulnerability in grief: psychometric properties of the Adult Attitude to Grief Scale. Qual Life Res 2014;23:1211-20. https://doi.org/10.1007/s11136-013-0551-1.
- Densley K, Davidson S, Gunn JM. Evaluation of the Social Participation Questionnaire in adult patients with depressive symptoms using Rasch analysis. Qual Life Res 2013;22:1987-97. https://doi.org/10.1007/s11136-013-0354-4.
- Great Britain . Data Protection Act 1998 2005.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Gask L, Bower P, Lamb J, Burroughs H, Chew-Graham C, Edwards S, et al. Improving access to psychosocial interventions for common mental health problems in the United Kingdom: narrative review and development of a conceptual model for complex interventions. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-249.
- Webster LA, Ekers D, Chew-Graham CA. Feasibility of training practice nurses to deliver a psychosocial intervention within a collaborative care framework for people with depression and long-term conditions. BMC Nurs 2016;15. https://doi.org/10.1186/s12912-016-0190-2.
- Mercer SW, Fitzpatrick B, Grant L, Chng NR, O’Donnell CA, Mackenzie M, et al. The Glasgow ‘Deep End’ Links Worker Study Protocol: a quasi-experimental evaluation of a social prescribing intervention for patients with complex needs in areas of high socioeconomic deprivation. J Comorb 2017;7:1-10. https://doi.org/10.15256/joc.2017.7.102.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Department of Health and Social Care . How to Make IAPT More Accessible to Older People: A Compendium 2013.
- Unützer J, Katon W, Callahan CM, Williams JW, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002;288:2836-45. https://doi.org/10.1001/jama.288.22.2836.
- Mather AS, Rodriguez C, Guthrie MF, McHarg AM, Reid IC, McMurdo ME. Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder: randomised controlled trial. Br J Psychiatry 2002;180:411-15. https://doi.org/10.1192/bjp.180.5.411.
- McNeil JK, LeBlanc EM, Joyner M. The effect of exercise on depressive symptoms in the moderately depressed elderly. Psychol Aging 1991;6:487-8. https://doi.org/10.1037/0882-7974.6.3.487.
- Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of progressive resistance training in depressed elders. J Gerontol A Biol Sci Med Sci 1997;52:M27-35. https://doi.org/10.1093/gerona/52A.1.M27.
- Tsang HW, Fung KM, Chan AS, Lee G, Chan F. Effect of a qigong exercise programme on elderly with depression. Int J Geriatr Psychiatry 2006;21:890-7. https://doi.org/10.1002/gps.1582.
- Tsang HW, Tsang WW, Jones AY, Fung KM, Chan AH, Chan EP, et al. Psycho-physical and neurophysiological effects of qigong on depressed elders with chronic illness. Aging Ment Health 2013;17:336-48. https://doi.org/10.1080/13607863.2012.732035.
- Ko HJ, Youn CH. Effects of laughter therapy on depression, cognition and sleep among the community-dwelling elderly. Geriatr Gerontol Int 2011;11:267-74. https://doi.org/10.1111/j.1447-0594.2010.00680.x.
- Korte J, Bohlmeijer ET, Cappeliez P, Smit F, Westerhof GJ. Life review therapy for older adults with moderate depressive symptomatology: a pragmatic randomized controlled trial. Psychol Med 2012;42:1163-73. https://doi.org/10.1017/S0033291711002042.
- Mastel-Smith BA, McFarlane J, Sierpina M, Malecha A, Haile B. Improving depressive symptoms in community-dwelling older adults: a psychosocial intervention using life review and writing. J Gerontol Nurs 2007;33:13-9.
- Pot AM, Bohlmeijer ET, Onrust S, Melenhorst AS, Veerbeek M, De Vries W. The impact of life review on depression in older adults: a randomized controlled trial. Int Psychogeriatr 2010;22:572-81. https://doi.org/10.1017/S104161020999175X.
- Preschl B, Maercker A, Wagner B, Forstmeier S, Baños RM, Alcañiz M, et al. Life-review therapy with computer supplements for depression in the elderly: a randomized controlled trial. Aging Ment Health 2012;16:964-74. https://doi.org/10.1080/13607863.2012.702726.
- Shellman JM, Mokel M, Hewitt N. The effects of integrative reminiscence on depressive symptoms in older African Americans. West J Nurs Res 2009;31:772-86. https://doi.org/10.1177/0193945909335863.
- Zhou W, He G, Gao J, Yuan Q, Feng H, Zhang CK. The effects of group reminiscence therapy on depression, self-esteem, and affect balance of Chinese community-dwelling elderly. Arch Gerontol Geriatr 2012;54:e440-7. https://doi.org/10.1016/j.archger.2011.12.003.
- Banerjee S, Shamash K, Macdonald AJ, Mann AH. Randomised controlled trial of effect of intervention by psychogeriatric team on depression in frail elderly people at home. BMJ 1996;313:1058-61. https://doi.org/10.1136/bmj.313.7064.1058.
- Gitlin LN, Harris LF, McCoy MC, Chernett NL, Pizzi LT, Jutkowitz E, et al. A home-based intervention to reduce depressive symptoms and improve quality of life in older African Americans: a randomized trial. Ann Intern Med 2013;159:243-52. https://doi.org/10.7326/0003-4819-159-4-201308200-00005.
- Klug G, Hermann G, Fuchs-Nieder B, Panzer M, Haider-Stipacek A, Zapotoczky HG, et al. Effectiveness of home treatment for elderly people with depression: randomised controlled trial. Br J Psychiatry 2010;197:463-7. https://doi.org/10.1192/bjp.bp.110.083121.
- Chan MF, Chan EA, Mok E, Kwan Tse FY. Effect of music on depression levels and physiological responses in community-based older adults. Int J Ment Health Nurs 2009;18:285-94. https://doi.org/10.1111/j.1447-0349.2009.00614.x.
- Brenes GA, Miller ME, Williamson JD, McCall WV, Knudson M, Stanley MA. A randomized controlled trial of telephone-delivered cognitive–behavioural therapy for late-life anxiety disorders. Am J Geriatr Psychiatry 2012;20:707-16. https://doi.org/10.1097/JGP.0b013e31822ccd3e.
- Moss K, Scogin F, Di Napoli E, Presnell A. A self-help behavioral activation treatment for geriatric depressive symptoms. Aging Ment Health 2012;16:625-35. https://doi.org/10.1080/13607863.2011.651435.
Appendix 1 Systematic review table
| Trial | Author | Date | Intervention | Number of participants in trial | Measurement of depression | Control | Group or individual | Result (p-value) |
|---|---|---|---|---|---|---|---|---|
| A randomised controlled trial to test the feasibility of a collaborative care model for the management of depression in older people | Chew-Graham et al.76 | June 2006 | Collaborative care with a care manager |
Intervention, 53 Normal treatment, 52 |
GDS | Usual care | Individual | 0.036 |
| Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial | Unützer et al.99 | December 2002 | IMPACT collaborative care management programme |
Intervention, 906 Usual care, 895 |
2-item depression screener adapted from the PRIME-MD study | Usual care | Individual | < 0.01 |
| Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder | Mather et al.100 | 2002 | Exercise classes |
Exercise, 43 Control, 43 |
GDS and Hamilton Rating Scale for Depression | Twice weekly educational talks | Group | 0.05 |
| The effect of exercise on depressive symptoms in the moderately depressed elderly | McNeil et al.101 | July 1989 | Exercise therapy with social interaction | 30 | Beck Depression Inventory | Waiting list | Individual | < 0.001 |
| A randomized controlled trial of progressive resistance training in depressed elders | Singh et al.102 | 1997 | Progressive resistance training |
Exercise, 17 Control, 15 |
Beck Depression Inventory | Interactive health education programme of lectures and videos followed by discussion | Group | 0.067 |
| Effect of a qigong exercise programme on elderly with depression | Tsang et al.103 | 2006 | Qigong, which involves meditation, breathing exercise and body movement |
Intervention, 48 Control, 34 |
GDS (Chinese version) | No treatment | Group | 0.041 |
| Psycho-physical and neurophysiological effects of qigong on depressed elders with chronic illness | Tsang et al.104 | 2013 | Qigong, which involves meditation, breathing exercise and body movement |
Intervention, 21 Control, 17 |
DSM-IV, GDS and Hamilton Rating Scale for Depression | No treatment | Group | 0.007 |
| Effects of laughter therapy on depression, cognition and sleep among the community-dwelling elderly | Ko and Youn105 | 2011 | Laughter therapy |
Intervention, 48 Control, 61 |
GDS | No treatment | Group | 0.027 |
| Life review therapy for older adults with moderate depressive symptomatology: a pragmatic randomized controlled trial | Korte et al.106 | March 2011 | Life review therapy |
Intervention, 100 Control, 102 |
CES-D | Usual care | Group | < 0.001 |
| Improving depressive symptoms in community-dwelling older adults a psychosocial intervention using life review and writing workshop | Mastel-Smith et al.107 | May 2007 | Life story workshop |
Intervention, 16 Waiting list, 17 |
Brief Symptom Inventory–18 | Waiting list | Individual | 0.03 |
| The impact of life review on depression in older adults: a randomized controlled trial | Pot et al.108 | December 2009 | Preventative life-review course, ‘Looking for Meaning’ |
Intervention, 83 Movie watching, 88 |
CES-D | Watched a movie | Group | 0.01 |
| Life-review therapy with computer supplements for depression in the elderly: a randomized controlled trial | Preschl et al.109 | December 2011 | Life review therapy with depression programmes on the computer |
Intervention, 19 Control, 21 |
Beck Depression Inventory | Waiting list | Individual | < 0.01 |
| The effects of integrative reminiscence on depressive symptoms in older African Americans | Shellman et al.110 | October 2009 | Integrative reminiscence |
Reminiscence intervention group, 19 Attention control group – health education, 19 Control group, 18 |
CES-D | No intervention | Group | 0.001 |
| The effects of group reminiscence therapy on depression, self-esteem, and affect balance of Chinese community-dwelling elderly | Zhou et al.111 | May 2012 | Group reminiscence |
Intervention, 62 Control, 67 |
GDS | Health education | Group | 0.001 |
| Randomised controlled trial of effect of intervention by psychogeriatric team on depression in frail elderly people at home | Banerjee et al.112 | 1996 | Individual package of care that was formulated by the community psychogeriatric team |
Intervention, 33 Control, 36 |
Self-care questionnaire and AGECATa | Usual GP care | Individual | 0.005 |
| Community-integrated home-based depression treatment in older adults: a randomized controlled trial | Ciechanowski et al.57 | 2004 | Home-based programme of detecting and managing minor depression or dysthymia: PEARLS |
PEARLS, 72 Usual care, 66 |
DSM-IV and PRIME-MD | Usual care | Individual | 0.02 |
| A home-based intervention to reduce depressive symptoms and improve quality of life in older African Americans | Gitlin et al.113 | August 2013 | Home-based intervention delivered by social workers: ‘Beat the Blues’ |
Intervention, 106 Waiting list, 102 |
PHQ-9 | Waiting list | Individual | 0.001 |
| Effectiveness of home treatment for elderly people with depression: randomised controlled trial | Klug et al.114 | November 2010 | Home treatment |
Intervention, 30 Control, 30 |
ICD-10 and GDS | Usual care | Individual | < 0.001 |
| Effect of music on depression levels and physiological responses in community-based older adults | Chan et al.115 | July 2009 | Music therapy |
Intervention, 23 Control, 24 |
GDS | No treatment | Individual | < 0.001 |
| A randomized controlled trial of telephone-delivered cognitive-behavioral therapy for late-life anxiety disorders | Brenes et al.116 | August 2012 | Telephone CBT |
CBT, 30 Information only, 30 |
Penn State Worry Questionnaire and State Trait Anxiety Index | Given information and a list of referral options | Individual | 0.03 |
| A self-help behavioral activation treatment for geriatric depressive symptoms | Moss et al.117 | August 2011 | Bibliotherapy: requires an individual to read a self-help book to alleviate a particular psychological problem |
Intervention, 30 Control, 30 |
GDS and Hamilton Rating Scale for Depression | Waiting list | Individual | 0.004 |
Appendix 2 Topic guide for older adults
Appendix 3 Topic guide for third-sector workers
Appendix 4 Breakdown of costs
Keele University Research Project – AUNS Costings 2014 for 6 NTPs (Version 3)
NTP engagement with patients – agreed assumptions:
-
Patient group = 50
-
Each NTP – average caseload of 8.33 patients (= 6 NTPs)
-
Each patient will require ‘at least 4 contacts’ > ’5 to be budgeted’
-
NTP contact visit with a patient – each requires ‘3 hours’ including face-to-face visit, travel time, visit record keeping
—————————————————————————————————————————————
TRAVEL COSTS (paid at 45p/mile)
-
At an average of 8 miles/contact visit – 8.33 patients × 5 contact/visits × 8 miles each visit × 45p/mile = £150 per NTP
-
+ £14.40 (i.e. 4 training/reflection days at 8 miles each day)
-
= £164.40 per NTP;
-
× 6 NTPs = £986.40
TIME/NTP (assuming 6 NTPs) – 155 hours per NTP
-
8.33 patients × 5 contacts/patient × 3 hours/contact visit = 125 hours
-
+ 28 hours training/reflection time (4 days × 7 hours)
-
+ 2 hours Age UK 1 : 1 supervision (3 sessions during the project: 1 hour + 30 minutes + 30 minutes)
TOTAL COST of 6 NTPs
-
930 hours in total
-
= £11,625 (@ £12.50/hour inclusive of management/supervision/organisational costs)
+ £250 – recruitment costs
+ £200 – DBS processing
Total: £13,061.40 for 6 NTPs (= £261/patient)
Appendix 5 Study management information
Safety reporting
This feasibility study did not involve any investigational medicinal products and was therefore a non-CTIMP (Clinical Trial of an Investigational Medicinal Product) trial. The following describes the safety reporting procedures for this study.
Adverse event reporting
Box 3 outlines the study procedure for severe adverse event recording.
The NHS HRA defines a serious adverse event (SAE) as an untoward occurrence during the conduct of the study that:
-
results in death
-
is life-threatening
-
requires hospitalisation or prolongation of existing hospitalisation
-
results in persistent or significant disability or incapacity
-
is otherwise considered medically significant by the investigator(s).
A SAE occurring to a study participant must be reported to the REC if, in the opinion of the principal investigator (PI), the event resulted from administration of the intervention (it was ‘related’ to the study) and it was ‘unexpected’.
All participants remained under the care of their GP throughout the study. We asked all participating GPs to report SAEs within 24 hours of becoming aware of these. Reporting procedures were made clear during general practice initiation sessions and were built into site service level agreements, copies of which were available within a local site file held at every participating practice. All participants were provided with the contact details of the study co-ordinator and asked to self-report any such events to the NOTEPAD team as soon as possible. Participants randomised to the NOTEPAD intervention interacted with the SW during the intervention; therefore, we also asked the SWs to ask about, record and report any potential participant SAEs that they become aware of to the team.
When a potential SAE was reported to a member of the NOTEPAD research team, this information was passed to the study co-ordinator at Keele CTU, who ensured that a SAE reporting form was completed and informed the Keele PI and appointed study GP (or designated cover) immediately. The appointed study GP (or designated cover) then assessed whether or not any reported SAE was related to the study intervention, according to the process laid out in Keele CTU’s SOP (SOP 20: Safety Reporting and Pharmacovigilance). Any unexpected SAE considered to be related to the study procedures was reported to the REC by the PI within 15 days of becoming aware of the event. In addition, all related unexpected SAEs were reported to the study sponsor and SSC.
Risk
A risk protocol was created for this study should participants express thoughts of suicide or self-harm. Researchers and SWs were instructed to initiate the suicide ideation protocol if a study participant expressed thoughts of suicide or self-harm. This could have been as a result of responses to questionnaire items (including the postal screening questionnaire) or during an interview or any contact that leads the researcher or SW to believe that there was a suicide risk. In both instances, the researcher or SW, with the study participant’s permission, was asked to inform the study participant’s GP and notify the clinical investigator (or nominated deputy).
If the study participant refused permission for the researcher to inform the GP then the researcher was asked (in the risk protocol) to immediately consult the clinical investigator or nominated deputy, who would then examine the study participant’s data and, if necessary, assess the study participant by telephone in the first instance. If it was concluded that there is a significant risk, the study participant’s GP would be notified with or without the study participant’s consent. However, the clinical investigator or deputy would contact the GP without first assessing the study participant herself/himself if the situation was urgent, again with or without the study participant’s consent. In these cases, the decision would be explained to the study participant as soon as possible.
We used the Keele CTU standard risk protocol to deal with distress in participants, along with debriefing, support and regular supervision of researchers.
Insurance and indemnity
Keele University carries professional liability and medical malpractice insurance to indemnify it, subject to the terms and conditions of the policy, for its legal liability for claims or damages arising out of any bodily injury, mental injury, illness, disease or death of any participant caused by negligent act, error or omission committed by the university in the course of its business.
Age UK has full insurance cover for all those acting on their behalf (staff and volunteers) as well as public liability insurance to the value of £10M.
Feasibility study management
Study steering committee
The research team has been guided by research governance guidelines provided by the NIHR. A SSC was convened and comprised the members outlined in Table 34.
| Title and name | Position |
|---|---|
| Independent members | |
| Professor Christopher Dowrick | Professor of Primary Medical Care, University of Liverpool |
| Professor Margaret Maxwell | Deputy Director and Professor of Health Services and Mental Health Research, University of Stirling |
| Dr Peter Kimani | Assistant Professor, Statistics and Epidemiology, University of Warwick |
| Ms Carol Williams | Research User Group member, Keele University |
| Mr John Pemberton | Research User Group member, Keele University |
| Internal member | |
| Professor Carolyn A Chew-Graham | Chief investigator |
| Dr Heather Burroughs | Principal investigator and trial manager |
| Miss Stephanie Butler | Study co-ordinator |
| Dr Reuben Ogollah | Study statistician |
| Dr Bernadette Bartlam | Co-investigator |
The SSC met on four occasions (in February 2016, October 2016, March 2017 and October 2017) with e-mail communication between formal meetings. The aim was to monitor and supervise overall progress and adherence to protocol, patient safety and consideration of new information of relevance to the research question. Terms of reference were agreed and signed off by Professor Dowrick at the first meeting.
Management meetings and risk register
The NOTEPAD study team (chief investigator, principal investigator, study co-ordinator, statistician, administration lead, CRN research facilitator and co-investigators) held monthly meetings to discuss study progress. Identified risks were documented on the NOTEPAD ‘risk register’ and each item on the risk register was discussed in every study management meeting, relating to level of risk (low, medium or high) and the impact on the study (low, medium or high).
Monitoring and audit
The NOTEPAD study was monitored in line with the protocol and Keele CTU SOPs. The independent members of the SSC also monitored the progress of the study. Monitoring was also undertaken by the approving REC and HSDR in the format of progress reports.
Data preservation
All research staff involved in this study adhered to robust data security procedures and have explicit duties of confidentiality. All confidentiality arrangements adhered to relevant regulations and guidelines (Data Protection Act 1998,92 Caldicott, GMC, Medical Research Council, Research Governance Framework).
The transfer of audio files from the recording device to computer for transcription was carried out by the researcher conducting the interviews. Any transfer of personal information between the CRN staff/GP practice staff and the study team was via the NHSmail service (Accenture plc, Dublin, Ireland) and between NHSmail endpoints (from one NHS e-mail to another NHS e-mail address). The transfer of the CIS-R output file was carried out by the RN who used an encrypted USB drive to store the file on the CTU secure network.
The identification of, and invitation to, potentially eligible participants from general practice was supported by CRN staff. Patients’ identification details (e.g. names and addresses) were made available to the research team only once the patient had provided consent to take part in the study.
Specific consent was taken prior to the start of each qualitative interview to enable the research team to use anonymised direct quotes in future publications.
Anonymised paper copies of transcripts and questionnaires are stored in a locked filling cabinet at the Research Institute for Primary care and Health Sciences, Keele University. Consent forms are stored in a separate cabinet to the anonymised data.
All study and participant information is housed in the Keele CTU secure network, which is a secure virtual network, requiring two-factor authentication to access it. Roles and permissions are applied to users to restrict what data a user can access. The CTU secure network has been independently audited and achieved level one of the government-backed Cyber Essentials scheme.
The study data have been anonymised for analysis. All identifiable information was removed once the data collection was complete.
All research staff involved in this study work to robust data security procedures and have explicit duties of confidentiality, equivalent to the duty placed on NHS staff, written into their employment contracts. Access to patient identifiable data are highly restricted, using predefined roles and privileges, and views of the data are restricted so that authorised study team members see only the data that are required to carry out their role. Data access is fully auditable in this system.
Hardcopy data held by Keele CTU have been archived in the designated Keele CTU archive facility and site data and documents have been archived at the participating sites. Keele CTU will proceed to confidential destruction of the data 20 years after the grant expires. Electronic data from the study have had any identifiable information removed, and on this basis will be kept indefinitely, and may be used for future research (where the participant has given consent).
Dr Reuben Ogollah was the data custodian of the quantitative research data; this role has now been taken up by Dr Elaine Nicholls. Professor Carolyn A Chew-Graham is the data custodian of the process evaluation data.
Changes to study design
Amendments to the study design after the protocol were recorded and approved.
One important amendment was approved in May 2017, which we submitted for ethics approval on the advice of the SSC, following a meeting at which recruitment was discussed. It was noted that the conversion of ‘potentially eligible participants’ to people who agreed to be randomised was lower than expected (about 50%). Although the RNs had been asked to keep verbatim notes on reasons for people declining, the research team suggested it would be useful to try to interview people who declined to participate. The SSC supported this, so ethics approval was obtained to contact people who were were potentially eligible to participate in the NOTEPAD study but who had declined at the stage of the RN telephone call. Ethics approval was obtained for these people to be contacted by telephone and brief questions asked about reasons for declining.
Appendix 6 The postal screening questionnaire consisting of the PHQ-9 and the GAD-7 and a section seeking consent to further contact
Appendix 7 Fidelity checklists
First intervention
| Activity | Yes | Partially | No | N/A |
|---|---|---|---|---|
| Verbal explanation given of the NOTEPAD study | ||||
| Explanation of the evidence for the beneficial effects of social participation and depression | ||||
| Evidence of exploring the older person’s problems | ||||
| Assessment of risk | ||||
| Activities/social participation goals discussed | ||||
| Activity/social participation goals set | ||||
| The NOTEPAD personal file given along with a verbal explanation of how to use it | ||||
| Signposting (e.g. exercise groups, craft classes) | ||||
| The participant understanding of what has been discussed and agreed is checked | ||||
| Barriers/motivators to increasing activity discussed and/or addressed | ||||
| Next session discussed and arranged (face to face or telephone) |
Second intervention
| Activity | Yes | Partially | No |
|---|---|---|---|
| Review mood – mood thermometers | |||
| Review progress (diary) | |||
| Feedback given regarding any progress made | |||
| Barriers/motivators to increased activity/participation discussed and/or addressed | |||
| Activity/social participation goals discussed | |||
| Activity/social participation goals set | |||
| Signposting (e.g. craft groups, adult learner classes) | |||
| Remind about use of the NOTEPAD personal file | |||
| Relapse prevention/staying well strategies discussed (e.g. support and guidance) | |||
| Possible personal issues/difficulties encountered while increasing activity/social participation | |||
| Relevant contact details are given in case of any problems, issues or further advice required |
Glossary
- Age UK
- The UK’s largest charity working with older people.
List of abbreviations
- AMP
- Access to Mental Health in Primary Care
- BA
- behavioural activation
- CASP-12
- Control, Autonomy, Self-realisation and Pleasure-12 items
- CASPER plus
- collaborative care for screen-positive elders with major depression
- CBT
- cognitive–behavioural therapy
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CIS-R
- Clinical Interview Schedule-Revised
- CLP
- community links practitioner
- CONSORT
- Consolidated Standards of Reporting Trials
- COPD
- chronic obstructive pulmonary disease
- CRN
- clinical research network
- CRN WM
- Clinical Research Network West Midlands
- CTU
- Clinical Trials Unit
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GAD-7
- Generalised Anxiety Disorder-7 items
- GMC
- General Medical Council
- GP
- general practitioner
- GRIPP2
- Guidance for Reporting Involvement of Patients and the Public-updated version
- HRA
- Health Research Authority
- IAPT
- Improving Access to Psychological Therapies
- ID
- identifier
- NICE
- National Institute for Health and Care Excellence
- NOTEPAD
- NOn-Traditional providers to support the management of Elderly People with Anxiety and Depression
- NTP
- non-traditional provider
- PHQ-9
- Patient Health Questionnaire-9 items
- PI
- principal investigator
- PN
- practice nurse
- PPIE
- patient and public involvement and engagement
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RN
- research nurse
- SAP
- statistical analysis plan
- SD
- standard deviation
- SOP
- standardised operating procedure
- SP
- simulated patient
- SSC
- study steering committee
- SW
- support worker
- TIDieR
- Template for Intervention Description and Replication
- USB
- Universal Serial Bus
