Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/19/16. The contractual start date was in October 2015. The final report began editorial review in February 2018 and was accepted for publication in July 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Catherine Pope reports personal fees from UK higher education institutions, personal fees from the Norwegian Centre for E-health Research, personal fees from Macmillan, McGraw-Hill Education, John Wiley & Sons and the Authors’ Licensing and Collecting Society, grants from Health Education England Wessex and Health Foundation, other from University Hospital Southampton NHS Foundation Trust and other from the National Institute for Health Research (NIHR) Clinical Research Network, outside the submitted work. She is a member and Deputy Director of NIHR Collaboration for Leadership in Applied Health Research and Care Wessex, and a member of the Health Services and Delivery Research (HSDR) Researcher-led Panel. Joanne Turnbull is a current co-collaborator on another HSDR programme project (15/136/12).
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Turnbull et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Rationale
In England, recent policy has called for a focus on providing urgent care services that ‘minimise disruption and inconvenience’ for patients. 1 Local and national policy has centred on guiding patients to ‘get the right advice in the right place, first time,’2 reducing unnecessary emergency department (ED) attendances by providing more responsive urgent care services and providing better support for people to self-care. 1–3 However, the proliferation of different services has created an evolving, complex urgent care landscape for people to access and navigate and this has implications for the decisions and choices that are made. Effective service provision requires a deeper understanding of the factors influencing people’s help-seeking and their choices about accessing care.
The aim of our study was to identify sense-making strategies and help-seeking behaviours that can help to explain the utilisation of urgent care services. We set out to develop a conceptual framework of sense-making and help-seeking that NHS managers and commissioners could use as a foundation for health care planning. This report presents our study of how the public, health-care providers, policy-makers and decision-makers define and make sense of the urgent care landscape. It explores how service users understand and seek help, looking in detail at their choices, how they access urgent (and emergency) care services and the ‘work’ that this may involve for patients and their carers. We focus on three groups:
-
health service policy-makers – for example health-care commissioners, civil servants, and politicians in local and national government
-
health-care providers and health professionals – the organisations that provide and deliver health services and the staff employed by those services
-
health service users – patients and the general public who access and use services.
The remainder of Chapter 1 explores the urgent care context and outlines the aims and conceptual framework for the study.
Urgent care context
In most developed countries, including the UK, the USA, Canada and Australia, urgent care services are often positioned in an ill-defined space somewhere between general practice and emergency care. 1,4–7 Urgent care services are designed to assess and manage unscheduled or unforeseen conditions that arise in the out-of-hours period (typically 18:30 to 08:00 on weekdays, and all day at weekends and on public holidays). 8 The UK Keogh review, for example, describes urgent care as ‘for those people with urgent but non-life threatening needs’ with the goal of delivering:
. . . care in or as close to people’s home as possible, minimising disruption and inconvenience for patients and their families
These services have evolved slightly differently across health systems and have different names, but the services offered reflect wider shifts in care provision, notably their enrolment of new technologies to support access and care delivery,9 increasing fragmentation and differentiation of services, and a consumerist approach10,11 characterised by an emphasis on patient choice. 12,13
In the UK, a range of urgent and emergency care service developments and policy initiatives have taken place since the 1980s14 (Figure 1). These have included changes to existing services (e.g. the growth of general practice out-of-hours co-operatives and the use of telephone triage in the 1990s) and the launch of new services such as the nurse-led telephone service NHS Direct (replaced by NHS 111), NHS walk-in centres (WICs), and minor injuries units (MIUs).
FIGURE 1.
Selected key developments and policy initiatives for the delivery of emergency and urgent care. Reproduced from Turner et al. 14 Contains information licensed under the Non-Commercial Government Licence v2.0.

A key intention of urgent care services is to act as a lever for managing demand, seeking to divert people away from overburdened and overcrowded emergency services. 1–3,15 Research suggests that between 12%16 and 40% of ED attendances can be described as ‘inappropriate’,17 and some 40% of patients are discharged from the ED without treatment. 1 This finding is used to highlight a potential mismatch between the purposes for which services are provided and how they are used. Much of the existing research exploring patient help-seeking predates the expansion in the range of urgent care services offered and the introduction of the NHS 111 telephone triage service, making our investigation into sense-making and help-seeking a timely addition to the evidence base.
How this study builds on our previous work and other work
The study reported here extends our previous research, Health Services and Delivery Research (HSDR) 08/1819/217, completed in 2010,18 and HSDR 10/1008/10, completed in 2012. 19 The first of these examined the use of a single clinical decision support system called NHS Pathways used in three urgent and emergency care settings, focusing on how call handlers triaged and managed patients seeking 999 ambulance services and/or out-of-hours urgent care. The second expanded on this to examine the work and workforce implications of NHS 111 and was able to look at the telephone service itself, the technologies used and the wider network of urgent care provided in primary care. Both of these studies provided a deep and detailed understanding of the new NHS 111 services and delivered insights into the provision of urgent and emergency care in the English NHS. The questions to be addressed by the study move beyond our earlier organisational focus to explain how patients seek help and make choices in the increasingly complex landscape of service provision. Our analyses of call-handling services suggested that patients and the public were confused and that there was considerable variation in their experiences and knowledge of these services. Although the NHS 111 telephone service was conceived to direct patients to the most appropriate service, there is limited evidence that this has been achieved,20 and we wanted to understand this from the perspective of patients and the public, as well as of health-care professionals and policy.
By analysing patients’ experiences of urgent care, we seek to understand both the work required by patients to make sense of and navigate health care (i.e. the work or effort required) and the ways in which changes in provision (including the use of new technologies such as NHS Pathways) have become routine and embedded (i.e. normalised) as strategies for managing health-care needs.
Research aims and objectives
The overarching aim of the study was to identify sense-making strategies and help-seeking behaviours that explain the utilisation of urgent care services. We set ourselves the following objectives:
-
to describe how patients, the public, providers (professionals and managers) and shapers (commissioners and policy-makers) define and make sense of the urgent care landscape
-
to explain how sense-making influences help-seeking strategies and patients’ choices in accessing and navigating available urgent (and emergency) care services
-
to analyse the ‘work’ (the activities and tasks) for patients involved in understanding, navigating and choosing to utilise urgent care
-
to explain urgent care utilisation and identify modifiable factors in urgent care patient decision-making.
Theoretical background to the study
The underlying conceptualisation informing the study is that service users, professionals and providers are working within a system of emergency and urgent care. Urgent care services are part of a complex landscape that includes general practice out of hours, WICs and NHS 111, and have considerable overlap with EDs and 999 services (as well as wider links with other services such as general practice, pharmacies, social care and self-care). Given the well-recognised overlap between urgent and emergency care help-seeking, it is relevant to consider urgent care in a wider context that includes ambulance services, hospital EDs and a range of designated urgent care services.
For the current study we drew on sense-making perspectives21 to help understand contested meanings surrounding urgent care and to see how this might influence people’s attitudes and behaviours around service use (objectives 1 and 2). Sense-making can be understood as individuals’ attempts to structure the unknown by putting things into ‘frameworks, comprehending, redressing surprise, constructing meaning, interacting in pursuit of mutual understanding, and patterning’. 21,22 These perspectives about sense-making have encouraged us to consider patient decision-making, help-seeking behaviour and choices in ways that avoid the simple binaries of ‘appropriate’ or ‘inappropriate’ service use.
The study was informed by the notion of the ‘work’ that people do in understanding, navigating and choosing to use urgent care (objective 3). There are many theories that have conceptualised patient work, such as that of Corbin and Strauss23 and, more recently, burden of treatment theory. 24 Previous theorising around patient work has tended to focus on chronic illness, but it is a useful means of understanding patient decision-making and behaviours concerning urgent care. Existing help-seeking models are explored further in Chapter 6.
Outline of the report
The remainder of this report is structured as follows. Chapter 2 details our methodological approach. Chapter 3 presents the findings from the literature and policy review. Chapters 4 and 5 present the findings from the empirical work. Specifically, Chapter 4 examines how different groups make sense of urgent and emergency care (objective 1), and Chapter 5 examines the help-seeking behaviour, choices and work that services users in accessing, navigating and using urgent care services (objectives 2 and 3). Chapter 6 describes the development of a conceptual model of urgent care help-seeking. Chapter 7 presents the discussion, conclusions, and implications of this work (objective 4).
Chapter 2 Methods
This chapter describes the research design, data collection and analysis used in this study.
Research design
The study used a mixed-methods sequential design consisting of three integrated work packages (WPs) (Figure 2). The first WP (WP1) comprised a literature review and four citizens’ panels with service users and health-care professionals. It aimed to describe and explain how patients and the public, providers (professionals and managers), and shapers (commissioners and policy-makers) define and make sense of the urgent care landscape (objective 1). The second WP (WP2) used serial qualitative interviews to examine the role of sense-making in patient help-seeking strategies accessing and navigating available urgent (and emergency) care services (objectives 1 and 2) and to identify and describe the ‘work’ for people of navigating and using urgent care (objective 3). In WP3 we integrated our analyses of these data to construct a conceptual model of urgent care help-seeking behaviour that explains urgent care utilisation and identifies modifiable factors that affect urgent care patient decision-making (objective 4).
FIGURE 2.
Diagram of the research objectives and study design.
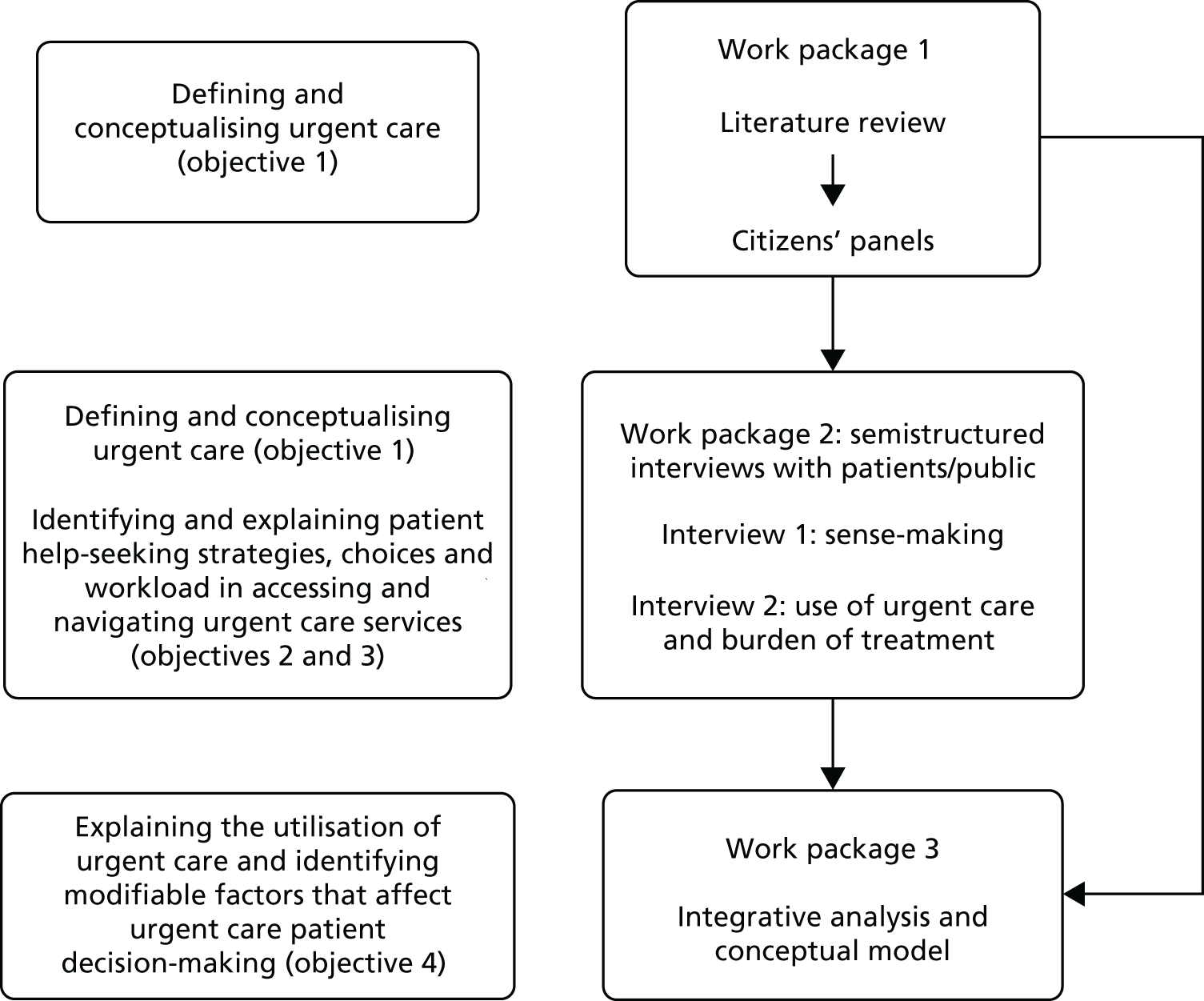
Methods were integrated in two ways. The first was developmentally, such that the findings from one WP informed the design and analysis of subsequent components. The literature review complemented and shaped the focus of the study, as well informing the conduct of the subsequent data collection. The meanings and definitions of urgent care identified in the review were explored in the empirical data collection with service users (interviews in WP2) and with health-care professionals (the citizens’ panels in WP1). The literature review also informed the conceptual model (WP3). Second, the results were integrated by exploring convergence and contradiction in the findings derived from different methods, using this process of ‘crystallisation’ to provide a more comprehensive account than that offered by a single method. 25
Work package 1: literature review and citizens’ panels
Literature review
A structured review of the published literature from 1990 onwards was undertaken with the primary aim of generating meanings and definitions of urgent care from the multiple perspectives of policy-makers, service providers and patients/the public. This was informed by Weick’s sense-making perspective21,26 alerting us to the possibility of contested definitions and meanings of urgent care, which in turn can have implications for people’s attitudes and behaviours associated with the use of urgent care services.
The review included policy documents (and related grey literature) as well as empirical research literature published since 1990 relating to urgent and emergency care. Although not an exhaustive systematic review, it sought to examine the evidence in relation to the following questions:
-
How do service users (patients and the public), providers (professionals and managers) and shapers (commissioners and policy-makers) define and understand urgent care differently?
-
Does the way in which patients and professionals perceive urgency influence the way in which patients seek help for urgent care problems?
Conducting the review
A review team was established to develop and manage the review (JT, GM and JP). We employed the expertise of an information specialist (Karen Welch) to undertake literature searching, and, with input from the team, Karen Welch developed the search strategy [using both free-text and database Medical Subject Headings (MeSH) terms where appropriate]. Joanne Turnbull, Gemma McKenna and Jane Prichard identified, screened and critically appraised the literature identified. Critical appraisal was guided by the Critical Appraisal Skills Programme (CASP) tools appropriate to different types of research designs. 27
Identification and review of key policy documents and grey literature
Our review focused on policy documents and other grey literature since 1990 because many of the developments in urgent care services occurred from the 1990s onwards (see Figure 1) and we focused on the literature that could shed light on policy for urgent or unscheduled care in the UK that also included relevant references to emergency care policy. The search of the SIGLE (System for Information of Grey Literature in Europe) database focused on formal, government-level policy and local-/practice-level policies and guidelines. Specific governmental and health websites were also searched. Key sources are shown in Table 1. Reports from individual urgent care centres (UCCs) and wider policy documents dealing with health-care delivery were included when relevant (e.g. NHS Plan in England, White Papers). In total, 60 documents and information sources were reviewed (last searched November 2017). The 44 sustainability and transformation partnerships proposals were not examined in detail but were briefly examined to confirm that they did not contain important information about urgent care that was not represented in the other documents obtained.
| Type of organisation or body | Key sources |
|---|---|
| NHS organisations, Department of Health and Social Care and government sources | Department of Health and Social Care, NHS England, NHS Wales, NHS Scotland, Scottish Government Health and Social Care, House of Commons Committees reports, NHS Evidence, NHS Choices website |
| Royal colleges and professional associations | Royal College of Emergency Medicine, Royal College of General Practitioners, Royal College of Nursing, British Medical Association |
| Charities and independent bodies | The King’s Fund, The Patient Association, The Nuffield Trust, National Audit Office, Healthwatch England, Urgent Health UK |
Primary documentary research methods were used28 to identify and compare policy and service provider meanings of urgent and unscheduled care. Members of the research team read the documents to identify definitions, and a spreadsheet containing research questions about the policy context and definitions of urgent care was used to extract, examine, summarise and synthesise key information and concepts (Table 2).
| Theme | Questions asked in the data extraction |
|---|---|
| Policy context |
|
| Defining urgent care and examining meaning |
|
Identification and review of the research literature
Structured searches of the research literature were conducted in two stages. First, a detailed search on MEDLINE used a wide range of search terms and a combination of free-text and MeSH terms as well as appropriate subheadings (see Appendix 1). This initial search retrieved a large number of results and was refined to reduce the number of results. One early modification was to include the term ‘ambulatory care’ only if it was linked to urgent or unscheduled care as the term retrieved a large number of results related to hospital outpatient care rather than urgent care. The strategy combined terms relating to urgent care and non-urgent use of emergency care services (‘Set 1’) with terms that focused on patient experiences, for example patient help-seeking and decision-making (‘Set 2’), to produce a final search.
Targeted searches were then undertaken of MEDLINE In Process & Other Non-Indexed Citations, EMBASE, Web of Science, Cumulative Index to Nursing and Allied Health Literature (CINAHL), ProQuest Sociological Search and PsycINFO around urgent and emergency care use and help-seeking (see Appendix 1). Searching was undertaken in November 2015, and updated in September 2017 to identify additional relevant literature. Studies were included if they met the criteria outlined in Table 3. International evidence was included to consider alternative models of urgent care in comparable health-care systems.
| Criteria | Included | Excluded |
|---|---|---|
| Focus of study |
Patient, health-care professional and provider perceptions of urgent and emergency care Patient decision-making, knowledge, beliefs, attitudes, expectations and experiences related to conceptualisations of urgent and emergency care |
Evidence related to specific clinical interventions for specific conditions |
| Health service |
Urgent care (e.g. general practice out of hours; NHS Direct; WICs; MIUs, NHS 111) Emergency care where focus is about the use of ED or ambulance service for ‘non-urgent’ or ‘primary care’ reasons |
General practice Hospital care not related to the ED (e.g. elective admissions; outpatients clinics) |
| Type of study/publication |
Qualitative and mixed-methods studies Quantitative studies of ED use that focused on non-urgent, ‘inappropriate’ use or on help-seeking behaviour High-quality literature reviews |
Editorials; opinion pieces; letters Conference abstracts Low-quality/unstructured reviews Quantitative or statistical reports of rates of service utilisation, satisfaction or referral |
| Study setting | UK, Europe, USA, Canada, Australia, New Zealand | All others |
| Dates of publication | 1990–2017 | Prior to 1990 |
| Language | English | Non-English |
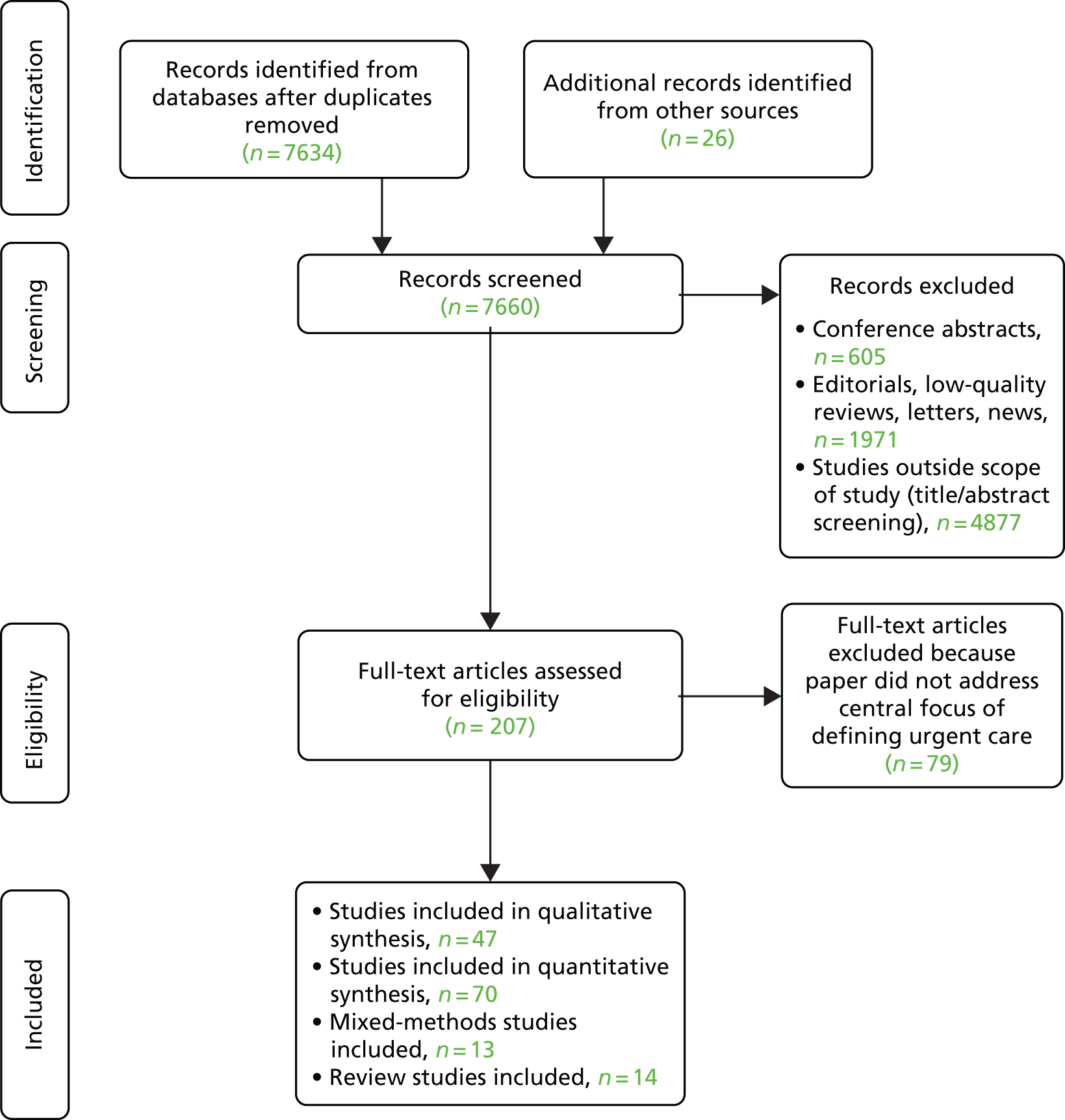
The final search retrieved 7634 results after deduplication. Twenty-six additional papers were identified through other sources (e.g. reference lists, general searching) (Figure 3). In total, 144 papers were included in the final review. Key information about the content of the papers was summarised in tables as part of the critical appraisal process against the questions in the CASP checklists, augmented with additional questions from Table 2. This aided the synthesis and identification of main themes.
FIGURE 3.
Flow diagram of search process using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009.
Citizens’ panels
A number of approaches to seeking public views is identified in the literature, including citizens’ juries and citizens’ panels. We drew on a modified citizens’ panel approach. One of the defining features of a citizens’ panel is to:
bring together a small group of people . . . and present them with a policy question. The panel listen to expert witnesses, examine the evidence, deliberate on the issues and arrive at a policy decision or set of recommendations.
p. 78829
The aim of this type of panel is to ensure deliberative and inclusive involvement directed at executing high-quality citizen contributions that can inform the policy-making process. 30 Citizens’ panels permit participants to ‘engage with evidence, deliberate and deliver recommendations on a range of complex and demanding topics’ (p. 6). 31 They provide an opportunity for citizens to challenge managerial and professional viewpoints and offer a chance for alternative perspectives to be explored. 32 We used citizens’ panels to examine urgent and emergency care policy and to deliberate on the provision of urgent and emergency care, and we asked the participants to help develop agreed definitions of urgent care.
Participants and recruitment
Guided by discussions within the research team and with our advisory board, we agreed that our main criteria for the selection of participants should maximise variation in the people and professions involved, drawn from the urgent and emergency care network of actors. Four separate panels were convened to debate and offer direction about how to define and conceptualise urgent health care. Our ‘citizens’ were drawn from (1) the Polish community, (2) a wider general population, (3) health professionals and (4) members of Clinical Commissioning Groups (CCGs). We purposively sampled to represent a range of perspectives and to include public, provider and policy-maker perspectives.
In our original research proposal, three panels (general public, health-care professionals and NHS commissioners) were envisaged. However, following a review of the literature, and discussion within the advisory group and research team, another panel was included comprising Polish participants. This offered an opportunity to include a group who could be characterised as more ‘marginalised’,29 and whom few previous studies had consulted on the topic of urgent care. It was also a chance to explore the views of recent migrants who have the unique experiences of two very different health-care systems. Our public panels (general population and the Polish community) reflected the populations also chosen for the more detailed qualitative interviews in WP2 (see Work package 2: the qualitative interviews).
Participants in the public panels were recruited via local community groups and networks (e.g. through community centres, local groups and organisations) and reflected the diversity of study setting (Table 4). They were recruited to act as citizens rather than as expert patients or patient representatives, and so they had varying experiences of health-care need and service use. Health-care professional and provider participants were recruited primarily from a single local NHS trust, along with some who were recruited from health-care education programmes at the university (see Table 4). The participants in the panel that was designed to elicit the views of those engaged in local policy-making and shaping were approached via CCG contacts and were representatives of local commissioning bodies (see Report Supplementary Material 1 and 2).
| Panel group | Number of participants | Characteristics of participants | Venue of panel |
|---|---|---|---|
| Mixed general public | 12 | 6 female and 6 male | Community centre |
| Polish community | 12 | 11 female and 1 male | University premises |
| Health-care professionals | 14 | 10 paramedics, student paramedics and paramedic managers; 3 student nurses; 1 student mental health nurse | NHS organisation meeting room |
| NHS shapers and commissioners | 3 | 1 commissioner and 2 representatives of local CCGs | University premises |
In total, 41 participants took part in the panels. The shapers and commissioners’ panel had three participants because of some late decisions not to attend, but the three other panels had between 12 and 14 participants. Public panel members ranged in age from 18 years to ≥ 75 years. The panel format was face-to-face deliberation over 6 hours in a single day, except for the shapers and commissioners’ panel, which took 4 hours, reflecting the smaller number of members (see Table 4). Public panel participants were offered £120 to take part [calculated in line with National Institute for Health Research (NIHR) INVOLVE rates]33 as recompense for the significant time commitment required to participate.
Conducting the citizens’ panels
Each panel took place over one day and was designed to explore a set of questions informed by the literature review, which included:
-
How would you like to see urgent care described and defined?
-
Are there circumstances in which urgent care services are particularly appropriate (or inappropriate)?
-
What benefits and risks do you think that urgent care services have for (1) patients and (2) health-care providers?
-
What principles would you wish to see underpinning developments in the provision of urgent care services?
-
What do you think are the key differences between urgent and emergency care?
-
What range of services do you think come under the heading of ‘urgent care’?
-
Do you think urgent care services – and perceptions of urgent care – have changed over time?
-
As a group how would you describe and define ‘urgent care’?
The research team prepared a set of resources (drawing on web links, videos and other visual resources) and prepared activities designed to facilitate discussion (Figure 4). Prior to the panels taking place, four individuals (drawn from the public panels) acted as a panel advisory group. These individuals were asked for their feedback about some aspects of the panel (e.g. the use of some resources in some of the activities, and the format of some activities, such as whether or not to use small discussion groups). We sought their views (through a series of telephone and e-mail discussions) on the best ways to support and facilitate citizens’ discussions during the panel to ensure that panel members would be comfortable with particular activities and tasks.
FIGURE 4.
Urgent care citizens’ panels: process model.

All participants were sent introductory material including policy statements and findings generated from the literature review. Activities on the day included:
-
brainstorming words associated with urgent care
-
discussion of hypothetical scenarios or case studies derived from the literature review
-
discussions about perceptions of different services prompted by pictures of urgent care and emergency services
-
discussion and debate centred on the diagram of urgent care presented in the Keogh review. 1
Two members of the research team attended each panel to facilitate group discussion. One of the team (GM) led the facilitation and one of the team (JT) supported the day’s events. Members of the research team adopted a neutral role, facilitating participation to ensure that the discussion stayed on topic, and to derive recommendations and reach a consensus. Each panel commenced with an introduction to the study, and then introducing panel members to each other. Some activities took place in small groups, facilitated by Joanne Turnbull and Gemma McKenna. The panel were encouraged to question the researchers about the evidence. Activities also included a large group discussion and agreement on definitions of and terms for urgent care by the end of the day, facilitated by Gemma McKenna and Joanne Turnbull. Data generated from the panel were recorded in contemporaneous notes taken by team members and by audio-recordings, as well as some written data (flip chart summaries, diagrams, and sticky notes used in the discussions). Notes and transcripts of discussions were anonymised.
Work package 2: the qualitative interviews
Qualitative interviews were used to examine, in depth, the role of sense-making in help-seeking strategies and how the respondents accessed and navigated services, and to identify and describe the ‘work’ entailed in navigating and using urgent care (objectives 1–3). To obtain a rich description, qualitative semistructured interviews were undertaken with three carefully selected groups of service users who reflected a diverse range of experiences of urgent care need (see Selection and recruitment of interview participants). A second interview was conducted with a sample of participants to explore the items raised in more detail and to overcome some of the weaknesses associated with ‘one-shot’ interview studies. This use of serial qualitative interviews proved to be effective in building rapport and relationships between interviewee and interviewer, and to generate the kinds of private accounts that may not have been revealed in a single interview. 34 This design added a prospective dimension to the study, offering the respondents and researcher time and space to reflect on and revisit topics from the initial interview, and capture changes between the two time points. The first interview probed how interviewees distinguished between routine, urgent and emergency care needs, and understandings of service availability, and examined attitudes and beliefs about urgent care services. The second interview (conducted between 6 and 12 months after the first) examined, in more detail, interviewees’ experiences of using urgent care services in the intervening months (if at all) and explored the ‘work’ entailed when navigating and accessing care.
Selection and recruitment of interview participants
Participants were sampled from the large geographical area served by a single NHS 111 provider (South Central) which covers four counties (Oxfordshire, Berkshire, Hampshire and Buckinghamshire) that are diverse in their geographic and demographic characteristics. By selecting an area covered by a single NHS 111 provider, we were attempting to recognise geographical boundaries that also ‘made sense’ within the structure of the NHS service provision. Although this setting is not the most socioeconomically deprived compared with other parts of the UK, it includes pockets of deprivation, and some lower layer super output areas are in the most deprived quintile nationally (e.g. parts of Portsmouth, Southampton, Reading and Milton Keynes). It also contains areas that are in the most affluent categories (e.g. Wokingham, New Forest and Aylesbury), as well as major cities (e.g. Portsmouth, Southampton and Oxford), and a mix of urban and accessible, and more remote rural areas.
We purposively sampled from three populations that represented particular facets of urgent care need and a range of participants in terms of socioeconomic and demographic characteristics. Two groups were chosen to reflect populations with known high use of emergency care (people aged ≥ 75 years and those aged 18–26 years), and a third group, people from the East and Central European community, was chosen to represent a population known to be increasing locally as a result of recent migration, and who may, therefore, be vulnerable because they are less familiar with NHS services. 35
Older people (aged ≥ 75 years)
This group represents a key demographic change experienced in the UK whereby the ageing population has led to a significant increase in the population aged > 80 years. 36,37 The research literature suggested that this group had higher rates of attendance at EDs and made greater use of urgent care38 than other age groups. However, this is a group for whom we lack evidence about help-seeking and decision-making around health service use. 39
Younger people (aged 18–26 years)
This group was selected because research evidence suggests that younger adults have the highest rates of ED attendance. 37 Adolescents (aged 15–19 years) are also more likely to attend UCCs than general practice40 and younger adults (aged 20–29 years) tend to access UCCs because they offer convenience and ease of access. 41
East European communities
People from the Accession 8 (A8) countries (Poland, Slovakia, Czechia, Slovenia, Hungary, Latvia, Lithuania and Estonia) were granted rights of free movement across European Union Member States in 2004, and there have been relatively high rates of A8 migration, particularly people from Poland, into the major towns and cities in our chosen setting. Some of the rural areas in our setting have also experienced their first international migration of people from these countries. 42 This is a new and possibly growing population, but we have little research evidence about their health needs, or their knowledge of, and use of, urgent and emergency care. 43,44 There is some evidence that some ethnic and migrant groups are less likely to use urgent care and more likely to use emergency care,45 although this is contested. 46 We refer to this group as East European people, recognising that not all the participants in this group were from the A8 countries (and that the designation of Eastern Europe is contested).
As with all qualitative research, the goal of sampling is not to enable statistical representativeness but to provide a detailed and nuanced understanding. From past experience we are aware that purposive samples allow us to access a range of experiences and to capture rich data about beliefs, attitudes and experiences, and reported behaviours. To achieve an adequate final number of completed serial qualitative interviews, we aimed to conduct 105 first interviews (± 10%), recruiting approximately 35 people from each of the three population groups, and then conduct a second interview with 50% of these (± 10%). In total, we conducted 93 first interviews with 100 people (some in pairs) and 41 second interviews (Table 5).
| Interview | Population group | Number of participants |
|---|---|---|
| Interview 1 | East European people | 18 |
| Older people (aged ≥ 75 years) | 36 | |
| Younger people (aged 18–26 years) | 39 | |
| Total | 100 | |
| Interview 2 | East European people | 12 |
| Older people (aged ≥ 75 years) | 19 | |
| Younger people (aged 18–26 years) | 10 | |
| Total | 41 |
We adopted three recruitment strategies to ensure maximum variation: (1) recruitment from nine NHS urgent and emergency care services, (2) recruitment from the general population via community networks and local advertising and (3) snowball sampling via participant networks following interviews (Table 6). In our original proposal, we had expected most of our participants to be recruited via NHS services. Although we recruited nine NHS organisations to act as participant identification centres (one NHS 111 service, five EDs and three UCCs/WICs), it proved very difficult to identify and recruit participants from these sources, and only 13 participants were found via NHS sites. Poor recruitment via NHS sites may have been due to challenges in identifying individuals that matched our three population groups (there were particular sensitivities about identifying and approaching East European people). In addition, potential participants were sometimes reluctant to engage in conversations about research when attending, or calling, for an urgent care problem. We were largely reliant on staff at sites to approach people about the research on our behalf, which took place in often busy and pressured environments.
| Recruitment means | Site or source of recruitment |
|---|---|
| NHS sites |
NHS 111 service Five EDs across Hampshire and Berkshire Three MIUs/UCCs across Hampshire and Berkshire |
| Advertising across community networks and localities |
Four universities across the south 15 support and carer groups across four counties Seven local community centres and one library Five local community groups One parish council Free advertising (Gumtree website; www.gumtree.co.uk) and three local newspapers Local businesses (e.g. website/posters at a football club and in coffee shops) All-Party Parliamentary Health Group website |
Guided by discussions with our advisory group, we widened our strategy and recruited another 87 participants using a combination of community-based advertising and local media advertising to meet sample targets. To encourage greater uptake of interviews, we successfully applied to the Health Research Authority (HRA) for amended ethics approval to offer £15 in gift vouchers (per interview) to participants as an incentive to take part. (To ensure equity, we contacted those who had already taken part and also offered them this reward.)
Conduct of the interviews
The topic guide for the first interviews was informed by the literature review and the citizens’ panels, and the topic guide for the second follow-up interview drew particularly on notions of patient ‘work’ and the analyses of interview 1 (see Report Supplementary Material 3). Service users were encouraged during interview 2 to explore the networks and resources that support them in their help-seeking or illness tasks. This was aided by using a simple diagram of concentric circles on which participants captured and mapped their social networks (family, friends, groups, professionals, services and third-sector organisations) in order of importance. The location of the interview was determined by interviewee preference, and most were conducted in people’s homes, with a minority taking place at participants’ places of work or study. All interviews were digitally recorded (after consent was obtained) and transcribed, and they typically lasted between 35 minutes and 1.5 hours. The majority of interviews were conducted by the same researcher (GM) supplemented by one other (JT). Participant information sheets and consent forms can be found in Report Supplementary Material 4 and 5.
Work package 3: integrating the analysis to build a conceptual model
Data analysis began alongside data collection, initially focused on the data generated during the citizens’ panels. We undertook a thematic analysis of these data, broadly following the stages described by Braun and Clarke,47 familiarising ourselves with the data, generating initial codes and categories and then identifying themes. To facilitate analysis and discussion among the team, grids and matrices were used to chart and compare the data, and this involved the wider research team, comprising fieldworkers, researchers and clinicians.
Qualitative interview data were analysed using a data clinic approach to share and interpret data collectively, building emergent themes and developing narrative and interpretive summaries. Core team members (GM, CP, JP, AR and JT) initially read and open coded a sample of transcripts independently, and these early codes were discussed and refined to form the basis for a coding scheme that was refined and developed and applied to all transcripts. We drew on a framework analysis approach,48 looking across cases and exploring similarities and differences (paying attention to contradictory cases). These analyses were informed by conceptual ideas drawn from previous research and theorising, including work on sense-making and patient work. As the analysis developed, the themes were refined using matrix techniques to facilitate further comparisons and interpretations. Emerging themes and interpretations were shared with patient and public involvement (PPI) and advisory group members to check the credibility of these and further refine our analyses.
To build a conceptual model to explain urgent care utilisation, we drew together the findings from the literature review, citizens’ panels (WP1) and qualitative interviews (WP2) by examining codes that:
-
described and explained different conceptualisations/definitions of urgent care
-
identified, characterised and explained sense-making strategies that influenced help-seeking choices and behaviours
-
identified and characterised the ‘work’ involved in understanding, navigating and choosing to utilise urgent care.
We created lists, and taxonomies, of influences that shaped choices and reported behaviours. We recognised that interaction with urgent care services was not simply produced by individual help-seeking behaviour but was also a collective phenomenon (such that narratives and processes are shaped by the views and behaviours of multiple participants), and we used this understanding to underpin our analysis. We then explored the identified factors, exploring how they were formed related to each other and to the contexts in which they operate. We continued to use comparative analysis to identify factors that appeared common across different data sources and different care contexts. As the analysis progressed we began to use mind maps, decision trees and logic models to map our interpretations. Our data clinics allowed us to revisit the data from WPs 1 and 2 to test emerging hypotheses concerned with how sense-making and help-seeking related to each other and to identify factors that might be modifiable, which provided the basic material for a framework from which a conceptual model of relational choices about engagement with urgent care was developed.
Ethics approval
The citizens’ panels comprised members of the public (recruited from community groups and local public networks) and health-care staff. This component of the study did not require NHS ethics approval, and was approved by the University of Southampton (Ethics and Research Governance Online, number 20217). NHS/HRA ethics review was required for the qualitative interviews (WP 2) as some participants were recruited via NHS organisations (REC reference number 16/EM/0329).
Chapter 3 Results from the literature review: how do policy-makers, professionals and service users define and make sense of urgent care?
Although policy ‘frames’ urgent and emergency care, it is also shaped by those organisations that provide care and is defined by how service users access, navigate and use services. Four broad definitions of urgent care were identified from the policy and from the literature: (1) physiological symptoms, (2) relational language used to differentiate ‘urgent’ and ‘emergency’, (3) types of services and treatment they offer and (4) patients’ perceived need and legitimacy of service use (Table 7). We examine each of these in relation to policy, provider and service user perspectives and then draw together cross-cutting themes.
| Constructs in conceptualising urgent care | Description of construct |
|---|---|
| Physiological |
Nature of symptoms (e.g. seriousness; suddenness) How quickly symptoms need medical attention |
| Relational | ‘Urgent’ defined in relation to definitions of ‘emergency’ (e.g. ‘less serious’, ‘minor’) |
| Service organisation |
The type of service (e.g. MIU, WIC, UCC, NHS 111) What the service is designed to offer (e.g. convenience; care close to home; signposting; treatment; advice) Service availability (geographic location; opening times) How care is provided (e.g. telephone; UCC) |
| Perceived need and legitimacy |
Patients’ perceived need/urgency and their use of services Notions of appropriateness and legitimacy of health service use |
Policy definitions of urgent care
The current UK policy pertaining to the urgent and emergency care services landscape can be identified from the Urgent and Emergency Care Review. 1,3,49 This paints a picture of urgent and emergency care as a hierarchy of services that are distinct from one another. For those unable to self-care, the urgent care system is identified as providing services for serious health needs requiring quick attention, while the emergency care services are for those with the highest level of need who have more serious and potentially life-threatening conditions. This suggests a landscape of provision in which there is clarity around how the terms ‘urgent’ and ‘emergency’ are understood. However, closer scrutiny reveals that these concepts are ill-defined and inconsistently used. Few policy documents provide a specific working definition of what is meant by either an urgent or an emergency health-care ‘need’. 50–52 Instead, documents touch on these terms briefly when describing which services should be responsible for different needs,1,3 or, more often, there is simply an absence of a definition. 3,53–56
Physiological factors in defining urgent care
Physiological need is the definition most frequently used in policy documents to describe urgent or emergency care. This relates to the seriousness of symptoms and/or whether the need is life-threatening. 1,3,8 Examples are offered of particular conditions or symptoms as being suitable for particular services57,58 (e.g. the speed with which a person needs to be seen,56,59 the onset of illness and the time frame in which a condition or symptom requires treatment) (Table 8).
| Physiological aspects | Urgent definition | Emergency definition |
|---|---|---|
| Severity of illness or injury | Urgent but not life-threatening; not serious; ‘minor’ illness or injury; ‘short-term’ illness1,49,57,60,61 | Life-threatening; serious1,49,58,60 |
| Symptoms appropriate for different types of service | Sprains and strains; broken bones; wound infections; minor burns and scalds; minor head injuries; insect and animal bites; minor eye injuries; injuries to back, shoulder and chest57 | Loss of consciousness; an acute confused state; fits that are not stopping; persistent, severe chest pain; breathing difficulties; severe bleeding that cannot be stopped; severe allergic reactions; severe burns or scalds; heart attack; stroke; major trauma (e.g. serious road traffic accident, serious head injury)58 |
| Onset of illness | Unforeseen; acute; sudden onset or worsening of symptoms50,59 | Unforeseen; acute; sudden onset or worsening of symptoms50,59 |
| Time frame | Does not need immediate medical attention. Cannot wait until the next day. For ‘less serious yet immediate illness or injury’. Needs to be addressed quickly1 | Requires immediate attention1 |
‘Urgent’ may be described as serious but not life-threatening. 57,60 The National Audit Office describes urgent care services as being for ‘people who feel urgently ill’ (p. 37),59 while NHS Choices sets out that ‘If your injury is not serious, you can get help from a MIU or UCC rather than going to an ED’. 57
Some definitions are circular: the word ‘urgency’ is used to define the ‘urgent care’, providing little insight into what is really intended or how one might decide whether or not something is urgent. By contrast, emergency care is defined as those illnesses or injuries that are life-threatening. Broadly, descriptions that relate to emergency services include the words ‘major’ or ‘severe’, in contrast to urgent care, which can include ‘minor’ or ‘problems usually dealt with by a GP [general practitioner]’. 58 Definitions of both urgent and emergency include ‘unforeseen’ need and refer to people requiring care that is ‘unscheduled’ or ‘unplanned’. 2,50 Unscheduled care is defined as:
services that are available for the public to access without prior arrangement where there is an urgent, actual, or perceived need for intervention by a health or social care professional.
Some policies include reference to specific time frames in which particular symptoms should receive treatment; for example, a medical problem needs ‘immediate attention’. 1,57 Although physiological definitions of urgent (and emergency) need appear clear or more objective, this assumes that users are able to accurately interpret the likely seriousness of their symptoms and judge what constitutes ‘less’ or ‘more serious’ illness and/or injury in order to utilise the ‘appropriate’ service.
Relational language
A second theme in policy adds a relational dimension, contrasting emergency with urgent care. Urgent is compared with emergency as ‘not life threatening’ versus ‘life threatening’, or as ‘serious’ versus ‘more serious’. 8,49,60,62 A key example of this relational definition is the strapline for NHS 111, which is ‘when it is less serious than 999’ (the UK national emergency number). 59,62 Indeed, much of the NHS 111 advertising is presented in this way:
When you need medical help fast – but it’s not an emergency.
Policy documents sometimes group urgent and emergency care needs as a single category, labelled as unplanned or unscheduled care,8,64 and so the boundary between urgent and emergency is avoided. 52,62 It is sometimes argued that it is too difficult for patients to distinguish between services because the terms mean different things to different people. 62,65 Elsewhere it is suggested that these services need to be fully integrated and possibly co-located. 66 However, when service users self-refer to services (e.g. the ED, WICs, MIUs) they require an understanding of what different services offer,67 so it continues to be important that service users are able to disentangle these terms and these services.
The language used to conceptualise urgent care has changed over time. In policy documents from the 1990s, general practice out-of-hours services were the main source of ‘urgent care’ and urgent care was closely linked to primary care. From 2010 onwards, the term ‘out of hours’ was replaced by the term ‘urgent care’ and this began to be discussed in relation to emergency care rather than general practice. 1,3,49,61
Health service organisation and provision definitions of urgent care
Currently there are a range of emergency, urgent and routine care services. In addition to established emergency services, there has been an increase in urgent care services, for example NHS WICs, MIUs and UCCs, and other facilities. These are often overlapping and inconsistent in the services or facilities they offer and the time of day they are open (Table 9). Some policy documents define urgent and emergency care by the types of services (or the range of responses) that are available to users, but it has been recognised that efforts to increase access to urgent care by creating service choices have created a fragmented, complex service, creating further confusion. 1,65
| Urgent care services | Emergency services | |
|---|---|---|
| Type of service |
UCC (sometimes called treatment, primary care or out-of-hours centre) WIC (terms can overlap with UCC) MIU NHS 111 telephone service |
999 ambulance service ED (also still referred to as A&E) Major trauma centre |
| What the service offers | MIUs and WICs are either nurse or GP led; UCCs are usually staffed by both GPs and nurses. UCC facilities vary by location | High level of clinical service, expertise and resources to manages a full range of life-threatening illness and injury |
| Availability of services | Varies by location: some open 24/7, some have opening hours (e.g. 08:00–22:00) | 24/7 |
Urgent care has been defined by the services offered to users, including the skill level of providers and the facilities provided. Emergency care is presented as highly specialised in terms of staff and equipment:
For those people with more serious or life threatening emergency care needs we should ensure they [users] are treated in centres with the very best expertise and facilities in order to maximise the chances of survival and a good recovery.
p. 22. 1
Urgent care, on the other hand, is conceptualised as a less specialised service for everything that is not an emergency:
walk-in service developed to have a ‘see and treat’ approach to less serious yet immediate illness or injury
p. 42. 1
Elsewhere, urgent care services are defined by opening times (i.e. operating in the evenings, at night and at weekends)68 but, more recently, policy emphasis has shifted towards describing the range of ‘urgent care’ services that users might access over 24 hours (e.g. some MIUs, NHS 111).
Notions of ‘urgency’ may be defined by where a particular health problem is treated, which might be determined by what services are available in any given location at any given time of day. For example, a broken bone is classed as urgent rather than emergency (see Table 8) and therefore suitable for treatment at an UCC, but when this service is not available the patient would need to attend an ED. Thus, the definition of urgency is fluid depending on service availability:
MIUs and UCCs can treat: sprains and strains; broken bones; wound infections; minor burns and scalds; minor head injuries; insect and animal bites; minor eye injuries; injuries to the back, shoulder and chest. If no minor injuries unit in your area, these services will also be provided by an A&E department.
Patients’ perceived need
There is a recognition on the part of policy-makers and professionals that the responsibility for judging both the seriousness and the suitability of a particular service often lies with the patient. Policy documents from the UK make some reference to this:
Urgent care is the range of responses that health and care services provide to people who require – or who perceive the need for – urgent advice, care, treatment or diagnosis.
p. 12. 50
More recently, policy-makers have sought to reframe urgent care, taking into account a wider range of influences that are involved in the decision-making (e.g. perceived severity of symptoms as well as social factors such as caring commitments).
The importance of patients’ perception of their condition has led to the development of the ‘prudent layperson standard’ in the USA, which promotes a symptom-based determination of urgency. This standard was developed by listing common symptoms and conducting a large-scale survey to determine if a ‘prudent layperson’ would reasonably interpret them as an emergency. 69 What is interesting here is the recognition on the part of policy-makers and professionals that the responsibility for judging both the seriousness and the suitability of a particular service often lies with the patient, yet the decision to intervene is a professional one:
[It is the] responsibility to consider other care options prior to visiting the emergency department.
Guttman et al. 70
Language around what is ‘appropriate’ for particular services or what is a ‘genuine’ medical complaint appears in descriptions of emergency care in the research literature. However, such terms are largely absent from policy, with the exception of a sentence on NHS Choices about what is legitimate for emergency care use:
An A&E department . . . deals with genuine life-threatening emergencies, such as: loss of consciousness; acute confused state and fits that are not stopping; persistent, severe chest pain; breathing difficulties; severe bleeding that cannot be stopped [ ] Less severe injuries can be treated in urgent care centres or minor injuries units.
Provider and professional definitions of urgent care
Conceptualisations of urgent care from the provider and professional perspective place heavy emphasis on physiological definitions of urgent care and the extent to which these legitimise the use of services. Much of the research evidence is based on quantitative surveys of ED use rather than urgent care service use, and ‘urgency’ is discussed in narratives about the ‘inappropriate’ use of EDs and ambulance services. 71–77
Clinical ‘appropriateness’
Unsurprisingly, like the policy definitions discussed, the seriousness of the illness or injury appears to be evident in health-care provider conceptualisations. ‘Inappropriate’ ED use is synonymous, and interchangeable, with service use that is ‘less urgent’, ‘non-urgent’78 or ‘low acuity’79 or for ‘minor illness or injury’,16,17,80 ‘non-life-threatening health problems or injuries’81 or primary care reasons.
Physiological definitions of urgency include assessment of the severity of symptoms and how quickly symptoms need assessing or treating74,75,82–90 and/or whether the condition(s) could be assessed only in the ED or could be addressed elsewhere. 41,87,89,91–98 Many studies of inappropriate ED use do not explicitly specify how attenders were classified as ‘inappropriate’ or ‘non-urgent’. 76,99–103 However, some research has developed explicit criteria for assessing appropriate use,74,75,85,104–106 which include items that assess the severity of illness; the urgency of treatment or intervention needed; referral or transfer from other medical source; and confirmation by diagnostic testing. In such definitions, markers of appropriateness can include both presenting symptoms (prospectively defined) and diagnosis (retrospectively defined).
Koziol-McLain et al. 83 suggest that the term ‘severity’ is embedded in the ‘medical framework of physiologic dysfunction or disease’ so that emergency care is defined as ‘those health services provided to evaluate and treat medical conditions of recent onset and severity’. The term non-urgent is often used in the context of emergency care services and may describe a minor medical problem that is non-acute and non-life-threatening, and does not require immediate attention78,82,107 (i.e. it can be left for several hours or days78 and/or it is short in duration, e.g. it lasts less than 24 hours). 93 This might include symptoms such as coughs, sneezing, weakness or tiredness,72 those that are musculoskeletal,108 or cases that are deemed to require only ‘prescription, bandage, sling, dressing, and steristrips’. 109 Minor illness or injury/’non-urgent problems’ were characterised are those that could be managed by a GP (see next section). 73,78,85,104,109
Health professionals (and researchers) have defined non-urgent ED use by making reference to treating a health problem that could wait until the next day (> 12 hours) for treatment. 110 This is illustrated by a study designed to assess agreement between health-care professionals about ED attenders’ need for urgent care in an urban hospital in the USA, which used a quantitative chart review of 266 patients111 and defined urgency using terms such as ‘major’ illness or injury, whereby a possible danger exists to the patient if the condition is not medically treated within 20 minutes to 2 hours. A non-urgent or ‘minor’ injury or illness, when the patient is usually ambulatory, can be seen between 4 and 6 hours. Another US survey study measuring perceptions of urgency asked ED nurses and physicians to define urgent and non-urgent care. 112 Physicians defined ‘non-urgent’ as something that could be addressed after ≥ 1 hour without the patient’s health being affected, while nurses gave times that ranged from > 30 minutes to up to 4–6 hours.
Assessment of patient urgency differs among types of health professional irrespective of patient condition, even when the same criteria of urgency and appropriateness are applied. 99,107,111 In New Zealand, Richardson et al. 107 found that there was no clear consensus between ambulance staff, ED surgeons, registrars and consultants, ED nurses, GPs and hospital managers about a definition of ‘inappropriate’ attendance. Different groups of professionals used different factors to assess appropriateness; for example, ambulance staff were more likely to see patient admission as an indicator of appropriateness, whereas ED doctors and nurses were more likely to see patient perception of urgency or seriousness as a reliable indicator. In the USA, O’Brien et al. 71 assessed levels of agreement between internists and emergency physicians reviewing the ED nurses’ triage notes of 892 adult patients and reported only moderate agreement (κ = 0.47) between these groups. Emergency physicians were 10.3 times more likely than internists to classify those with minor discharge diagnoses as appropriate for ED care. Health professionals and patients also differ in their assessment of how quickly patients need to be seen. Poor agreement among health professionals raises questions as to how objectively ‘appropriateness’ can be measured and, in turn, how urgency can be defined.
Demarcation of definitions according to place
In defining urgency in the context of the ED, professionals and providers distinguish between condition(s) that could be assessed only in the ED and those that could be addressed elsewhere. 41,87,89,91–98 These definitions echo the ‘right place’, at the ‘right time’, treated by the ‘right professional’ phrasing found in some policy documents. However, in a study of health-care professionals’ perceptions of the effectiveness of a UK GP-led WIC, professionals were more likely to deem service use as appropriate if the user was referred from the ED. 113 A recent qualitative interview study of staff at a GP-led UCC in the UK suggested that health-care professionals believed that patients were ‘unaware of what the GP-led Urgent Care Centre is. They simply want someone to see them’. 114 They also reported that staff believed that patients used the UCC because it was convenient or because they had difficulties accessing other services (e.g. GP appointments).
There is also a strong tendency for health-care providers to define urgency in relation to the lack of emergency. The academic literature about ED use frequently uses relational terms to define degree of urgency, for example describing service use that is ‘less urgent’ (compared with something that is considered an emergency),81,99,115 although concepts of ‘less urgent’ vary. Backman et al. 99 suggest that:
Less urgent users were assessed as being more suitable for primary care and judged to be able to wait for more than 24 h for a medical examination without risk of medical harm.
Backman et al. 99 (emphasis added by authors)
Pileggi et al. 115 define urgent as ‘conditions that could possibly progress to a serious status requiring emergency intervention, perhaps those associated with significant discomfort or dysfunction at work or activities of daily living’ and less urgent as ‘conditions relating to age, distress, or potential for deterioration or complications that would benefit from interventions or reassurance within 1–2 hours’. These are different from ‘non-urgent’:
conditions that are acute and non-urgent as well as conditions which may be part of a chronic problem with or without evidence of deterioration.
Pileggi et al. 115
What these studies highlight is that urgency is often positioned in relation to emergency care, and it is less clear from these studies how urgent care problems are understood.
Value judgements about patient perceived need
Health providers and professionals sometimes recognise that patient perceived need and the subjective nature of lay assessment of symptoms are legitimate components of making sense of urgent care. However, health-care professionals also make value judgements about patient use of services and this shapes how they make sense of urgent care.
There is some evidence that health professionals recognise that service users draw on ‘rational reasons to initiate care’. This can include consideration of access to primary care and the context of how the medical problem developed. In a Canadian study, a survey of patients and physicians examined the appropriateness of WIC visits. 7. Of 142 attendances, physicians judged more than half of the visits as appropriate, compared with most patients, who scored their visits’ urgency as low or medium. The authors concluded that doctors appeared to judge patient factors such as anxiety and access to services as legitimate reasons for attending these services. Similar findings have been reported elsewhere; health-care professionals often approve of patients’ decisions and believe that they act appropriately. 116,117 A qualitative study of 87 patients and 34 health-care professionals, using interviews and direct observation, examined the decision-making patterns of families using EDs, as well as paediatric staff responses. Staff ‘incorporated the realities of daily living under trying circumstances, such as difficulty in contacting primary care for appointments, problems with transportation, financial barriers, and other practical issues’. 117
It appears that the more vulnerable the patient, the more likely the health-care provider is to take societal context into consideration when a ‘non-urgent’ visit is made or being reconsidered. Recognition of the social contexts in which people use emergency services for low-acuity problems has been acknowledged in other studies. 75,117,118 In the ED context, health professionals were more sympathetic to those perceived as ‘inappropriate’; for example, in a study of the use of unscheduled services by people with long-term conditions, health-care professionals felt that use of unscheduled care was a necessary component of care because exacerbations were inevitable in long-term conditions. 118
An American study of non-urgent ED use developed a typology of how providers conceptualised appropriateness of service use including restrictive, pragmatic and all-inclusive provider ideologies. 119 Some professionals held a pragmatic viewpoint: ED use was legitimate if other service options were limited or unavailable, including at times the need for medically non-urgent care. Conversely, other professionals believed that the ED is appropriate for only the most urgent care, that it should not, for example, be used for ‘trivial reasons’ that could be treated in primary care. What this study highlights is that, even within a single setting, health-care professionals hold a range of views about what is ‘appropriate’. This lack of consistency at the supply end raises questions about how service users can be expected to make decisions on the basis of lay knowledge alone if those with medical training have different positions on where people should go to seek care under different circumstances.
The extent to which professionals judge patients as ‘deserving’ of care is relevant to conceptualising ‘appropriateness’. Discussion about the ‘abuse’ and ‘misuse’ of services is particularly apparent in relation to emergency ambulance services. 101 In one study of ED use of ambulance services in the USA, emergency medical services (EMS) providers and patients were asked, ‘Do you think this patient’s medical problem represented a true emergency requiring EMS transport?’ (emphasis added by authors). 103 However, what constitutes a ‘true emergency’ is not defined or described. Muller et al. 102 described how [high demand] ‘inevitably make it more difficult to provide genuine emergencies with rapid treatment, leading to deterioration in the quality of emergency services’ (emphasis added by authors).
Similarly, in telephone-based UCCs, call advisors tended to construct shared understandings about the ‘inappropriate use of services’ and the extent to which patient concerns were ‘genuine’ or not. 18 This is echoed elsewhere in the out-of-hours literature that makes reference to ‘trivial and self-limiting conditions’. 120 Such findings reflect those of Jeffrey’s121 seminal paper of ED staff perceptions of appropriateness. Notions of ‘genuineness’ also featured in a survey study of GPs who were asked about the appropriateness of UK out-of-hours care use. 122 The study found that there was broad consensus about what constituted an appropriate call:
Genuineness was a key concept and the word ‘genuine’ occurred frequently, as in ‘genuine unwellness’ and ‘genuine anxiety’. Calls about potentially serious symptoms, severe symptoms or life-threatening conditions were regarded as appropriate.
Smith et al. 122
There is some evidence that health-care professionals judge some age groups as more vulnerable and that they may deem them as ‘special cases’ who either are more deserving of care or have more reason to make ‘inappropriate’ use of services, for example the elderly,78,122,123 children78,117,124 or patients who are ‘genuinely’ frightened or anxious about the threat of serious illness. 124 In an ethnographic study of ED use in the UK, professionals were more likely to perceive elderly patients and patients who articulated that they did not want to ‘bother’ services as legitimate attenders. 123 Users were also considered more favourably if they had an understanding of the other services available to them, when to approach them, and by which professional they should be seen. In the UK, a study of UCC staff identified a set of motives perceived as ‘more legitimate’ for making contact. 114 These included having acute health needs, access problems (those who ‘honestly’ cannot get an appointment with their GP) and anxiety, and also people not registered in the system (e.g. tourists, students). Conversely, less legitimate motives included convenience (‘claiming’ they cannot get an appointment) and those seen to be ‘playing’ the system.
Service user definitions of urgent care
Some research has examined service users’ help-seeking and decision-making in relation to both urgent and emergency care. From this we can extract some of the ways in which service users define and make sense of urgent care. Although perceived physical symptoms are important, other social and emotional cues, as well as service users’ beliefs and knowledge about health services, also influence the way in which service users define what is ‘urgent’.
Symptoms
Studies about symptom interpretation in relation to out-of-hours or urgent care services have highlighted that symptoms that are perceived to be prolonged, severe,41,67,79,125–128 unusual, worsening or causing pain trigger the help-seeking process. 7,120,129–135 Users’ perceptions of urgency were associated with an awareness of potentially fatal illnesses or conditions (such as meningitis and appendicitis) that were likely to compel contact with emergency or urgent care. 129,131,136 People may also call urgent care services when they are unsure about the severity of their condition67,133 and/or to rule out or prevent serious disease. 137 This suggests that urgent care services provide a preventative/risk management function. There are similar reasons for using the ED for non-urgent illness, whereby attenders typically perceive their problem as urgent or severe,138–150 recent and sudden in onset,151 and/or requiring emergency treatment or ‘immediate’ or ‘rapid’ attention. 102,110,140,152 One study found that half of all parents were unsure about the seriousness of their child’s symptoms98 and this prompted ED attendance. Pain is also a common key driver of ED attendance. 70,140,141,146,151 In a study of ED attendances for people with asthma, Becker et al. 153 sum up the dilemma that a patient faces when having to navigate definitions of urgency:
Individuals with asthma are caught in a bind by extremely narrow definitions of appropriate symptoms in the delivery of health care in the emergency department: they must not delay too long or seek help too soon.
Becker et al. 153
Studies that have compared health professionals’ perceptions of urgency of illness with those of patients attending an ED154–156 suggest that there are substantial differences. Kalidindi et al. 155 reported that most parents believed that their child’s illness required urgent care (defined as care needed within 24 hours), whereas physicians considered 30% of the ED visits as non-urgent (care that could safely wait until the next day). A New Zealand study has attempted to define a ‘health emergency’, a definition based on physiological factors. 154 This study used patient and ED ratings of urgency, and compared these with published literature and policy guidelines. The study reported congruence between the patients’ and health professionals’ perceptions of what constitutes a health emergency and suggested that a combined definition of these two perspectives would be reflected as:
A health emergency is a sudden or unexpected threat to physical health or wellbeing which requires an urgent assessment and alleviation of symptoms.
Morgans and Burgess154
However, Morgans and Burgess154 acknowledged that such physiological assessment is difficult because a health emergency is complex, changeable and not dichotomous.
One UK qualitative study that attempted to define urgent care from the user perspective67 found that participants were unable to identify a lay definition for ‘urgent care’, suggesting that ‘urgent’ could indicate the need for emergency services only or the need to be seen quickly by ‘non-emergency services’. Participants were more consistent in defining the term ‘emergency’ as an illness and/or injury requiring ‘blue flashing lights’ and an ‘ambulance’.
The literature about service users highlights the role of anxiety, feeling helpless or being unsure of what to do in relation to assessing the seriousness of symptoms when contacting urgent care41,67,120,129,132,135,157 or emergency care. 78,150,158,159 Users make contact with services for medical care, but also to seek reassurance from a health service to alleviate anxiety about symptoms. 78,135,146,151,158,160 Anxiety and reassurance appear to be viewed as a legitimate use of services from the patient perspective70,135,161 and sometimes from the professional perspective. 7,116,117,122 There is commonly a positive correlation between anxiety and level of pain151 or between anxiety and participants’ perceptions of the seriousness of the problem. 41
Ambiguous organisational arrangements
Whereas Dale et al. 162 reported that patients choosing between attendance at a MIU or an ED made an appropriate choice, other studies of urgent care have found that people often do not know where to go or who to contact, particularly at night,67,127,162 or when it is appropriate to contact a particular service. 133 A UK study of out-of-hours services found that some service users were unsure if their condition was ‘serious enough’ to warrant contact and some believed that the service was ‘only for seriously ill people’. 133
A study of an English NHS WIC reported that participants were uncertain of the centre’s purpose and its role within the health-care system. 163 A further study based on a survey suggested that most people did not make an ‘active choice’ to attend a WIC. More than half of attenders were unaware of the type of facility that they were attending, and believed that they had been treated in an ED. 164 Cook et al. 165 reported similar confusion about NHS Direct, with some participants believing that it was a WIC or that it provided an out-of-hours service.
Furthermore, service users do not always know what to expect on attending urgent care facilities. Chapple et al. 166 found that half of all interviewees expected to find a doctor at the WIC, with some suggesting that ‘nurses only deal with minor problems’. NHS staff beliefs about service users’ perceptions is that they do not distinguish between the ED, WIC or UCC, and were unaware of the UCC service and what it provides. 114 This confusion suggests that service users may not have a clear conceptualisation about what urgent care services are and what they can offer. Conceptualisations of urgent care are likely to be influenced by familiarity with, or previous experiences of, using these services. 127,128,167
User conceptualisations of urgent care also consider which service is available and able to carry out the care they deemed to be appropriate. 127,163 A qualitative study of NHS WIC attenders found that service users often had some idea or certainty that they knew what was wrong with them and what treatment they required and, as such, they were seeking support to carry out a predetermined treatment plan. 163 In the UK, Shipman et al. 168 reported that if parents had sought GP advice prior to self-referral and if the GP was not able to come out for several hours, then they went to the ED. Over half of participants suggested that they would have contacted their GP had the practice been open. Similarly, service users often report using the ED because other care – either general practice or urgent care – is not available. 83,95,156,169–173 A study from the USA reported that participants initially tended to tolerate symptoms until pain increased to a level at which self-care was no longer possible – and when non-emergency care settings were full. 83 A lack of availability of urgent care may result in ‘urgent cases’ becoming emergency ones. The notion of ED care being used as a GP substitute is not new. Calnan150 reported that patients sometimes made contact with the ED when they believed that the circumstances were inappropriate to contact a GP, for example during the night or at weekends.
There is a tendency for people to use emergency and urgent care services interchangeably depending on perceptions of the availability of services and what they can offer. These might include the perceived unavailability of timely appointments in primary care settings; preference about facilities and staff expertise;174 perceived shorter waiting time; ease of access; and wanting a second opinion when not content with primary care in-hours treatment. 78,120,146,158,168,170 People sometimes use hospitals because they believe that these will provide better care,144 for example that they can offer specialist expertise and facilities that community care cannot. 126,128,143,153,175,176 The focus on expertise and equipment is particularly notable in ED settings. 147,173,177
Choices about access include consideration about personal convenience and the shortest delay. 127,164,165 Chalder et al. 164 found that people initially chose to attend services with a co-located ED and WIC (rather than a ‘traditional’ ED service) because they expected a shorter wait for treatment or that it would be quicker than getting a GP appointment’. NHS Direct ‘users’ identified awareness, ease of use and convenience as facilitators that influenced their decision. 165 Studies of ED use suggest that convenience of location included offering a timely source of care83,145,147,149,156,173,177–179 and proximity. 170,173 A Swedish study of ED use found that it takes less time to go the ED and obtain help than to go to a GP, who may refer the patient to the ED anyway. 156,171 What is convenient in terms of being seen quickly has most salience for those who are working and those with caring responsibilities. 83,127
Perceived need and legitimacy
Like health-care providers and professionals, seekers of urgent care services use notions of what is ‘appropriate’ or ‘inappropriate’ based on perceptions of severity of illness, the time frame in which a problem needs to be addressed, and service availability.
Unsurprisingly, most service users perceive their own attendance or need for contact as legitimate, appropriate or deserving67,133,180 but may judge others’ attendance as ‘inappropriate’. Services users may judge others as ‘time wasters’ who are less rational or cannot justify their help-seeking behaviour. 67
A mixed-methods study of UK service users of primary and emergency care180 using vignettes about the ‘appropriateness’ of using NHS urgent care reported that 65.6% believed that others had used GP or ED services inappropriately. Similar findings were reported in a UK study133 based on focus groups and telephone interviews in which some participants expressed concern about other people who misused services for minor complaints, while emphasising that their own reasons for calling were serious and appropriate. However, unlike in Adamson et al. ,180 some participants also expressed concern for other users around inequality of care. Participants were concerned that the onus was on the patient to convey the urgency of their situation to health-care professionals and that people less articulate and less able to communicate might not get the care they need.
Users of urgent care often express the wish of not wanting to be seen as a ‘burden’ on the service, to place themselves before other NHS users deemed to be in more need, or to place excessive demands on an overstretched health service. 157,181 Service users are aware of potential ‘inappropriate’ use of publicly funded health services that provide universal access. 163,182 Richards et al. 133 reported that users of out-of-hours care said that they worried about calling the service. They also feared wasting the doctor’s time or ‘abusing the system’. Similar findings are reported in attenders of EDs unwilling to go to an ED without medical sanction. 182 This reluctance to use services is particularly observable in older age groups181,182 and among palliative care patients who were found to be reluctant to contact out-of-hours services to seek help. 183 Like health-care professionals, some service users judge some age groups as more vulnerable, and therefore as ‘special cases’ who are more deserving of care. 157,184
Summary
Points of consensus around physiological symptoms as determining urgent and emergency need
Our literature review suggests that there is some consensus between policy and provider perspectives regarding the physiological factors that feature in conceptualisations of urgent care, particularly around severity of symptoms and time frame. Much of the evidence from the provider perspective is drawn from the ED setting rather than from urgent care. A key distinction is made between emergency presentations and less urgent, non-life-threatening physiological presentations as the main determinant of appropriate service use, whereas users’ understanding of the seriousness of physiological symptoms draw on wider social and emotional factors that feed into their perceptions of urgency and time frame for accessing care.
Confusion about what constitutes urgent care
The terms urgent and emergency as categories of care are far from clear in the policy literature. The terms lack specificity, and it is difficult to discriminate between something ‘serious’, and appropriate for an UCC, WIC or minor injuries clinic, and something ‘more serious’ that requires the attention of an ED. There is a lack of consistency in meaning and messages across documents that note that people are confused about which services to use. 1–3,51,185 The health provider perspective examined in the research literature highlighted the variation in definition of ‘urgency’ or appropriateness and, at least in the context of the ED, an absence of consensus about ‘appropriateness’, the constitution of a ‘health emergency’ and what is ‘non-urgent’. From a service user perspective, conceptualisations of different services are shaped by perceptions of availability, accessibility and acceptability,186 which, in turn, may influence whether something is categorised as ‘urgent’ rather than ‘routine’ or ‘emergency’. [For example, if a particular facility is not available in a particular area then an urgent problem may be effectively upgraded to an emergency. In the case of a broken bone, in physiological terms this may not be an emergency (serious, life-threatening) but if a local urgent care facility is not available or does not have radiography facilities, the injury will be treated in the ED and becomes conceptualised as ‘an emergency’ rather than urgent.]
Questions around terminology
Both the policy and the research literature use a wide range of terms to describe both emergency and urgent care. Urgency is often defined (particularly in the policy literature) in relation to emergency (e.g. less urgent, non-emergency). The public are expected to be able to make ‘appropriate’ choices about health services, but it is unclear how these terms are understood by service users.
Defining emergency and urgent is difficult because they are context-specific, dynamic concepts reflected in service users’ wide-ranging and fluid conceptualisations of urgent care. Although there is some recognition from policy and providers that service users’ evaluation of symptoms may vary from those made by clinicians, there is still an expectation that service users can and should make ‘appropriate choices’.
A significant proportion of studies included in the literature review are over 20 years old71,76,77,80,84,85,91,109–111,187,188 and so these earlier definitions of ‘emergency’ and ‘urgent’ may not reflect current service provision. Most of the evidence base that underpins conceptualisations of what counts as urgent or emergency is drawn from studies of ED use (particularly ‘non-urgent’ or inappropriate use). The extent to which these definitions transfer to urgent care settings is unclear. The generalisability of the findings from one location to a wider geographical area or population is limited. This literature is also drawn from a range of countries and there are difficulties in drawing international comparisons about conceptualisations of urgent care because of variations in definitions and differences in the organisation and delivery of health-care systems. For example, unlike some other countries where such research has taken place, the UK offers universal access to primary care services at no cost to patients.
Points of learning for the citizens’ panels and the interviews
Many of the papers in the review focus on particular groups of people (parents, older people, and people with asthma or chronic conditions) and other groups in the population may have different views about urgent care. The policy literature and studies of health providers suggest some narrow ways of thinking about urgent care, notably in relation to acuity of physiological symptoms, but service users also consider various emotional and social factors when deciding whether or not to use urgent care services. These findings prompted us to think about previously neglected population groups to include in the empirical work and to explore these broad conceptualisations of urgent care.
The literature review also highlighted that the language used by policy and professionals about urgent care is unclear. Urgent care is poorly defined, and often only in relational terms (i.e. contrasting with emergency need/care). This language may not be meaningful to or shared by service users. Urgent care policy definitions make a number of assumptions about what patients want, including care close to home, telephone access and self-care advice, and these needed to be tested in our empirical work. To this end we used the citizens’ panels and qualitative interviews to explore understandings of urgent (and emergency care) and people’s experiences of help-seeking, to fill some of the gaps in the literature.
Chapter 4 Making sense of urgent care: findings from the citizens’ panels and qualitative interviews
In this chapter we explore how people define and make sense of urgent care, presenting the findings from the citizens’ panels and qualitative interviews (objective 1). The citizens’ panels examined people’s understandings of the health-care system and specific services, and also considered what ‘urgent care’ meant to them, as service users, providers, and commissioners. In the panels we were able to explore the real and imagined boundaries of urgent and emergency care and the tensions and challenges these provoked. Emergent themes generated in these panels were explored in more detail in the semi-structured interviews with service users. We present the findings in this chapter under three thematic headings, which explore the sense-making in relation to the confusing boundaries of urgent care, the role of moral positioning in making sense of urgent care, and how boundaries of urgent care are reimagined by service users, professionals and providers. ‘CP’ denotes citizens’ panel participants; ‘P’ denotes interview participants.
‘Urgent’ or ‘emergency’? Confusing boundaries of care
We have combined the data from the panels and both interviews here to reflect participants’ initial understandings of urgent care. Before they took part in the panels or the interviews, most participants said that they had not explicitly thought about the concepts of emergency and urgent care. However, it is important to note that the research process itself challenged them to construct meanings as part of the data collection process. P9, for example, illustrates how the interview process prompted them to differentiate between urgent and emergency after initially they had viewed these terms as interchangeable:
If I mention urgent care to you, what would you think of?
I’d think of 999, or A&E, predominantly, I think, sort of, life-threatening is what I would think of.
And if I said to you emergency care, what would you think of?
I think of A&E again, but probably less 999. I don’t know why, I just think urgent is, sort of, then and there . . .
So, what do you think are the similarities and the differences between emergency and urgent care?
I don’t . . . Maybe they both involve, life-threatening as, sort of, an overview . . . I don’t know, thinking about it more, urgent sounds less like an emergency than emergency care.
Younger
The literature review of policy and research identified a clear hierarchy that placed emergency (broadly, life-threatening or serious events that need immediate attention) above urgent care (less serious conditions that require a less immediate response). Service users’ accounts were reasonably consistent with this policy view in defining ‘emergency’ and they talked about the seriousness of the symptom (life-threatening or very serious), how quickly help is required (immediately) and the response or service required (999 or ED response):
I hadn’t really thought about that before . . . well emergency I think it’s just the time scale. If it’s an emergency . . . it would needed to be dealt with now . . . but if it’s urgent it’s still, you still need it to be dealt with soon but you may live with it for a couple of hours . . . So for me emergency is the highest level of urgency and if it’s any lower level then I can either still go to A&E but wait to be treated or I could see an even lower urgency level then I can go to . . . the minor injuries unit or the GP at the lowest level.
P71, East European
Emergency is where life is threatened or health to a large degree is threatened and it has to be dealt with quickly and by highly qualified personnel I would say. Whereas urgent care there are things that still need to be attended to quickly but they wouldn’t be life-threatening.
P4, East European
For a minority of service users, the term ‘emergency’ was not necessarily associated with ED care:
Emergency care, probably something a bit less severe than A&E, but a lot of them . . . Again, there’s no real fine line, is there?
P28, older
However, defining ‘urgent’ was more challenging; there was less consensus and more uncertainty about the term. Although service users understood ‘emergency’ as a term applied to more serious, or life-threatening conditions, they also used the word ‘urgent’ to describe these health-care needs. Terms were often used interchangeably (by participants from all population groups):
Urgent care, I would think of, probably, well, an ambulance, A&E, you know, if it was urgent, yes. Otherwise it would be just a trip up the doctors to see what the problem is, you know.
Yes. OK. And if I mention emergency care, what do you think of?
Emergency care is, well, the same thing, really. Yes. I mean, if I could see there was a major problem with anything . . . well, if it really looked bad, you’d have to ring the 999, I think.
Younger
Reflecting our review of the policy literature, service users often described urgent care in relation to emergency care, using language such as ‘less urgent’ or ‘not an emergency’ to define urgent care:
Well I know that urgent care is not emergency. Emergency is life-threatening, yes? Or at least you think it’s life-threatening. I mean if somebody was in pain I definitely would think that it was emergency and they needed somebody now and then, now. But if it’s something that you thought could be not dashed off straight away I would think it was less urgent.
P29, older
A variety of different terms were used to describe urgent care. Descriptions of health conditions suitable for urgent care services ranged from ‘less serious health problems’ (e.g. ‘not critical’ or ‘minor’) to descriptions that indicated high acuity (e.g. ‘serious’, ‘life-threatening’ or ‘severe’). Similarly, when using a time frame to define urgency, the term ‘urgent’ elicited a broad range of responses ranging from ‘immediate’ to ‘be seen within a day’ (or ‘can’t wait until morning’). The public panels, particularly, suggested that ‘urgent’ need required ‘being seen there and then’, ‘immediately’, ‘instantly’ or ‘quickly’. However, when asked to suggest their own definitions of urgent care, the general public panel struggled to articulate how time factored into the need for health care:
I think I say ‘no time limit’ because once you’ve got time you get . . . if there’s a certain target once you put a time limit on it, that’s then a target . . . I mean that would have to make that a time period. Time in there, and we’ve got 24-hour care. So you’re all saying to me is around timing. That’s what we want to, to imply isn’t it? You know, it’s something that’s as soon as possible. Requiring urgent care.
CP5, general public panel
Several East European participants suggested that there was little distinction between the words ‘urgent’ and ‘emergency’ and that the terms did not directly apply to their experiences of other health-care systems. Participants from Poland and Hungary reported that both ‘urgent’ and ‘emergency’ would apply to emergency services:
Yes, [urgent might be] something that can’t wait for very long or maybe can wait longer than emergency [. . .] But maybe it’s because in . . . Polish I think we don’t have separate words for these two. Maybe that’s why . . . It’s language problem as well, but in Polish, emergency and urgent . . . urgent sounds pretty serious. So maybe that’s why we struggle to distinguish. I don’t know . . . linguistic problem.
P3, East European
We don’t use two different words, emergency and urgent. This is why for me it’s the same. Yes, not in health-care terms.
Yes, not in health-care terms. So for me it’s no different.
There’s no difference. And do you just have the term emergency in Hungarian? What would you call it . . . that would be perhaps a translation here?
So, emergency is more connected with danger, and urgent is something you have to hasten rapidly. Emergency is something that, emergencies, critical, like fire.
But not the hospital?
Yes, probably there is just one service in the hospital, like the ambulance maybe. Yes, but it’s all linked, so you don’t think the ambulance is separate. It’s just the thing that takes you from A to B and tries to preserve your life.
East European
Additional confusion was created through the use of the words ‘urgent’ and ‘emergency’ in different health-care services. For example, the words ‘urgent’ and ‘emergency’ are used in the context of same-day general practice appointments but were understood as different from ‘urgent’ or ‘emergency’ in the context of the ED. For some, daytime general practice was viewed as an urgent care service:
You’ve talked a little bit about [urgency] in terms of offering same-day appointments. Do you think that is urgent care, or do you think that’s something slightly different?
I would think that is urgent care, because . . . it is quick. It’s the same . . . it could be within a couple of hours . . . or even sooner. They sometimes say, ‘oh we can see you in half an hour’. Can you make it? . . . You can get that initial assessment really, really quickly.
East European
Right, I think if I need urgent care, I can phone up the surgery and get an answer and possibly get an appointment that day. If it is out of hours, then you dial 111 and you speak to a colleague on the end.
P7, older
The boundaries between types of health-care services were described as muddled and opaque. The range of services that the general public and health-care professional panels identified as potentially available for urgent and emergency care needs included expected answers such as 999 and the ED, NHS WICs, pharmacies, NHS 111 and general practice. However, panel members also talked about an extended network of specialist services such as mental health, end-of-life and hospice care, geriatric medicine, physiotherapy and dental services, as well as information and advice services, and non-health services including social services, the police, and patient transport. Services were often perceived as equivalent rather than hierarchical, and the boundaries between them were often viewed as flexible at best, or ambiguous. The general public panel struggled to define the boundaries of services.
There was confusion among public panels and from interview participants about what UCCs and MIUs were. Some regarded these as ‘another name for A&E’; although the commissioners’ panel suggested that the boundaries between urgent and emergency care were demarcated by the NHS 111 (urgent) and 999 (emergency) distinction, they also listed same-day GP appointments, MIUs, WICs and the ED as part of the urgent care system. The general public panel thought that pharmacies offered advice for ‘little ailments’ and were a place to ‘seek second opinion’ rather than occupying a clear position within the remit of urgent care services:
So ultimately it’s about providing services that are easier to access, that the public understand. We had a conversation here, didn’t we, about the confusion, and how do you know what to do. And actually, you know, if you’ve used services a lot you know what to do. But if you’ve had an urgent care incident, and you’ve only had one in the last 20 years, how do you know what to do? So it’s . . . For me it’s about getting policy and providers to do a bit more than stick an advert on the back of the bus.
CP6, general public, urgent care ideas exercise
Participants could articulate what particular services might be used for (e.g. NHS 111 for ‘non-emergency’ cases) but typically did not recognise ‘urgent care’ as an umbrella term for a range of services:
So 111 would be more toothache and a nosebleed and mum’s slight bleeding from her rectum . . . But an emergency is an emergency . . . yes, phoning the ambulance if there was somebody not breathing or passing out or . . .
Yes, so there’s urgent care centre, minor injuries, which you talked about with the sprains, and 111. So . . .
Urgent care - is that like an A&E or not? Is that . . . urgent care? I suppose that would be an A&E, wouldn’t it? I don’t know, I really don’t know . . . what the difference would be . . . is it a walk-in centre?
Older
Variation in what different UCCs, MIUs and WICs offer can create confusion for service users and the public. Health-care professionals acknowledged this confusion; indeed, often health professionals were equally confused:
I just think it’s so vague as well. I think that, you know, we have a problem with the definition of emergency, which people don’t tend to . . . [ ] The view of an emergency is so drastically different to a vast proportion of the public . . . And if there’s a vagueness around that, like, an urgent care centre, I mean, is even vaguer. And I don’t even think it’s just patients who don’t really appreciate what it is. I think, actually, the reality is most health-care professionals don’t really understand what an urgent care centre does [ ].
CP1, professionals’ panel
Now, if I struggle to know what unit will accept what, you know . . . They’re forever ringing up and saying ‘Will you see this?’ Because we don’t know what their agreement is, you know? Some will do X-ray, some can’t do X-ray. Some will, you know, be nurse-led, the other will be GP-led. So, I don’t know what hope we have.
CP2, professionals’ panel, urgent care services exercise
The East European panel offered a more restricted list of services under the umbrella of urgent and emergency care, but noted that access to an on-call doctor was important (direct access to doctors was something that recent migrants from Poland said that they had experience of). East European panel members were surprised to learn that policy-makers considered community pharmacies to be part of the urgent care network of services. In addition, interview participants from East European communities suggested that the ways in which services are named pose particular challenges for people whose first language is not English:
For people who come over here from a different country, they take names literally. They don’t see it as an umbrella of things, different services are available to them. They look at the name, and they see the name and they just associate the help with . . . Accident and emergency . . . Emergency, I need to be seen quickly, it’s critical, I need help . . . And then you’ve got out of hours. In the name, itself, it doesn’t have anything to convince you . . . that you would be seen quickly. Emergency, right I can be, sort of, fast-forwarded and be seen quickly. Out of hours, fine, they will see me, but God knows how long the wait will be because there’s no sense of urgency in the name, it’s just out of hours. Minor injury unit, again, injury, it sounds as if someone will take it more seriously than out of hours. So just the way you name things . . . To someone who doesn’t use them regularly, who has no experience of using them, they sort of put them in an order just depending on what they are called.
P2, East European
Both members of the public and health professionals felt that the term ‘urgent care centre’ was problematic: for many it was viewed as suitable for health problems that were ‘more urgent’ than those dealt with by NHS 111 or NHS WICs. Many believed that ‘urgent care centre’ was the name for an ED:
Urgent care centre, I think the word urgent you straightaway think that something is really wrong and you need to be seen straightaway. You think of all possibly the worst outcomes. Minor injuries I just associate with really long waiting queues, a lot of people in casts, a lot of broken arms, broken fingers – that’s what it says on the tin really, minor injuries.
P37, younger
Minor injuries? I don’t think I’ve . . . Oh no, I have been . . . Have I been to minor injuries? Urgent care? You mean accidents and emergencies?
P61, older
Minor injuries units seemed to be less well known, possibly because coverage of these across the country is patchy. The name ‘walk-in centre’ seemed to blur the boundaries of what is viewed as urgent because it conveyed notions of convenient access and not needing an appointment. For some service users, NHS WICs were a convenient alternative service to general practice:
The walk-in centre, to me, never seemed to be urgent care [ ] You’ve got your emergency service and then urgent care confuses me. Because those things aren’t urgent. They’re just us wanting to be seen quicker. You see, urgent, to me, if it was urgent . . . do we have urgent care clinics . . . do we have them? Have we got them in [name of city]? Have we? Where’s our urgent? [ ] Because I’ve never thought of [the walk-in centre] as an urgent care centre because . . . well, I suppose it is, isn’t it? Yes, but because it’s just a walk-in centre . . . I think that because it’s used by people who can’t get appointments at the GP.
P16, older
Walk-in seems so casual. Pop in and out if you want. But urgent, urgent care centre makes it seem . . . If I were to see those two things and you would say to me do you think these two are, you know synonymous or do you think they are, you know two totally opposite things I would probably say a walk-in centre and an urgent care centre seems two different . . . just by the words that are in the names . . . And then what was the third one?
A minor injuries unit?
No clue. I have no clue. Can you tell me?
Younger
NHS 111 was widely recognised by both citizens’ panel and interview participants, and most conceptualised it as a service for information and advice, or for signposting to other services. NHS 111 was not strongly identified as an urgent care service, and it appeared that the advertising of NHS 111 as a ‘non-emergency’ service contributed to this conceptualisation. Younger people in particular viewed NHS 111 as a service for ‘inquiries’ and ‘general health information’:
OK, great and what about the telephone service?
The telephone service 111 is more for inquiry type stuff than it is for emergencies.
Younger
If I was to say to you urgent care centre, a minor injuries unit or the 111 telephone service, what do you think the differences are between those three?
I think 111 is non-emergency I think isn’t it. And then you’ve got minor injuries which I guess is probably something you’d go for . . . I’m guessing it’s an A&E service which goes for minor, or possibly not A&E. Possibly not A&E. No, I don’t think it’s A&E.
Younger
Only a minority thought that NHS 111 was for more urgent or serious cases:
So 111 telephone service I think it would be very serious like maybe someone’s fallen unconscious or they’re unable to get out that sort of thing or, you know, if they’d had a fall or, yes . . . they can’t get to where they need to go or they’re not able to move them I think 111 is definitely the [service].
P46, younger
Moral positioning in making sense of urgent care
In making sense of the boundaries between ‘urgent’ and ‘emergency’ and between different services, people judged and positioned themselves relative to other people and behaviours. Service users often recognised or judged that other people misused services but then rationalised their own behaviour as legitimate, calling on notions of exceptionalism. ‘Others’ included both people known to them (often close family members) and people unknown to them (the general public). The latter were especially prominent in people’s sense-making narratives. Overall, while service users often described their own health service use and that of close family members and friends as legitimate, ‘others’ (i.e. the ‘general public’) were often characterised as ‘time wasters’, seeking help for ‘trivia’. The moral work entailed in making decisions about urgent care and its impact on help-seeking behaviour is explored further in Chapter 5.
Here we focus on how perceptions of legitimacy factor into sense-making. In the panel and interview data collection, we sometimes prompted participants for their views about other people’s use of urgent and emergency care services (we did this as neutrally as possible, avoiding value-laden language such as ‘inappropriate’).
‘Time wasters’ and undeserving cases constituted the construction of moral categories that framed people’s sense-making around what services were for. Medical trivia is a common theme in the wider literature and is often discussed in relation to ‘inappropriate’ service use. Trivia was characterised as illness that could be self-managed, could wait or could be seen somewhere else (e.g. coughs, colds, headaches), or conditions seen as self-inflicted or resulting from behaviour, rather than for reasons of medical seriousness (e.g. resulting from the use of alcohol or drugs). Disapproval was predominantly reserved for those who use the ED unnecessarily:
There was a girl when I was waiting who had cut her finger on Christmas Day, that’s why she was there. But they would be able to dress it and clean it. I mean, those sort of small traumas are not what I think A&E should have to deal with. Yes, I mean, I think it should be sort of really serious things, you know, people who’ve had a stroke or you know, somebody who’s had a coronary . . . that sort of thing . . . I mean, I certainly do not think that it should have to deal with people who have had too much to drink.
P20, older
In hearsay, in stories you sometimes hear about people who have got something absolutely piffling and yet they have gone to A&E or even called an ambulance.
And what would piffling be for you?
You’re coughing a lot or you have cut your finger on the tin opener or you have burnt your wrist on the oven shelf, you know really minor things, or you have got a temperature . . . a lot of people now apparently go to A&E because their child has croup and that I assume is because they have no idea what it is, and it is terrifying when you see it.
Younger
Behaviours such as alcohol and drug use that resulted in health service contact were often viewed as less deserving and irresponsible; however, occasionally service use was considered justified. Several younger service users had made contact with urgent or emergency services, often for a friend who was drunk, but these accounts often provided legitimisations, for example saying that this was a rare event, or, in the quotation below, suggesting that the presence of an underlying health condition might make attendance acceptable even when drunk:
What other things do you think people go to A&E for?
Being too drunk. That’s, being too drunk, OK yes I can imagine if you’ve already got a health condition that’s worsened by being too drunk then you might need to go to A&E but, you know if you’re paralytic go home and sleep it off. Go home and be sick, eat something, drink plenty of water and go to sleep. Don’t go to A&E.
Younger
Some interviewees also highlighted that ‘undeserving’ people make health services more unpleasant for others and may deprive others of the care that they need or are entitled to:
That has happened recently to a friend of mine, whose dad died . . . It’s very easy to call up a 999 in that situation . . . They shouldn’t have done, but they did. But then he ended up dying sort of on the other side of curtain, with somebody who’s . . . Some sort of drug-related problem. The nurse sort of grabbed . . . Have you, you know . . . ‘Have you got any drugs up your arse? We need to . . . Concentrate. Can you concentrate? I need to know if you’ve got any more drugs up your arse?’ And it was all awful while they were saying goodbye to their dad.
P18, older
He said they had been to a party and had some drinks so they wouldn’t be able to come down straight away. Don’t worry I said, I will look after her, we have called the ambulance; and the ambulance couldn’t come because they were dealing with drunks and drug addicts and they were full.
P24, older
This was also linked to beliefs that ‘others’ should take responsibility for their own health more generally:
Because the resources . . . so, how many people we know have been treated by NHS and people are getting older . . . but also I think people are not taking care of themselves from what I can see. And maybe it’s an exaggeration, but sometimes walking through [name of city] . . . I think that people are just not taking care of themselves. I don’t know whether the statistics can show that, but they just don’t look healthy and that is a difference I can see with going back to Poland. I think people look healthier there than here, and there is some responsibility on people themselves to actually look out for being hugely overweight, diabetes, and it’s just like some kind of responsibility is not there.
P54, East European
There was also some disapproval of people using urgent care services for minor ailments such as coughs and colds:
This is an education problem. I think this is most important. Because otherwise maybe lastly we go to the [urgent care] centre for ridiculous problems, like coughing or I don’t know what it is. Don’t call. If they know what they have to do, they stay at home.
P33, East European
I’d like to know what priorities each service treats. I mean, some people must ring up 111 for a headache or something stupid like that. Well that should be made quite clear, that you go to your doctor if you’ve got a headache or any minor cut or anything like that. You don’t ring them and waste their time because you get people who have had too much to drink and they’ve fallen over and they think, ‘oh well I’ll ring the hospital or ring the walk-in centre or whatever is available’. Whereas they could just as well wait until the next day. I feel very sorry for these people [health services] because they’re overstretched all the time by a lot of idiots.
P36, older
There was a perception among the older participants interviewed that other people may lack the necessary knowledge or skills to understand, articulate and interpret health problems, which leads them to make unnecessary contact with health services. Older interviewees used this kind of account as a prelude to a presentation of him- or herself as someone who understood how to use services responsibly (a theme to which we return in Chapter 5):
I think other people get worried . . . Basically, they don’t have the same type of knowledge in their heads that I have, so therefore I think their worry and anxiety is more profound . . . I think it’s worry and anxiety possibly to do with their condition and possibly lack of . . . lack of knowledge . . .
P7, older
I think I have used the 111 on one occasion . . . I would like to think that my husband and I are relatively articulate people, so that we can say what they would need in order to give us information back, but a lot of people couldn’t describe things or would be too stressed, in too much of a panic you know, to handle that.
P20, older
Some were more sympathetic:
You know, we’re not simple people but there are a lot of simple people in the . . . in the world that are even worse off than we are who can’t navigate anything, or maybe they find it easier because they just go and camp outside until somebody looks after them.
P5a, older
However, younger service users were singled out as lacking the education or knowledge to make the right decision, and were considered ‘hypochondriacs’ or ‘attention seekers’. Interestingly, this characterisation of younger service users was often made by those in the younger group:
I think people need reminding of that because I think this generation is full of hypochondriacs. I think they just need to chill out a little bit and educate themselves instead of thinking that, you know minor flu is going to kill them and they need to go sit at A&E. I think it’s a shame that people do that because, like my mum for example has got so many health problems and she’s had to wait because of time wasters, I shouldn’t really say time wasters, but people who are not educated enough for, people that just go there for the attention. Sometimes I’ve found . . . I have personally known people that have gone and there’s not actually been anything wrong with them. They’ve just wanted some attention.
P45, younger
One of things that drives me mad is when you’ve got people there with viral infections that go to A&E . . . You do see it when you go into the waiting room, people taking up time they don’t necessarily need to be there [ ] Usually panicked mothers, to be honest. Yes, mums that are very scared about their children. And also probably young teenagers. And I think a lot of it as well is teenagers who just need a bit of attention, maybe not necessarily for health conditions . . . I’ve seen a lot of people that definitely don’t need to be there and a lot of minor cuts that could probably be done at [MIU].
P49, younger
There was also a belief that others had unreasonable expectations or used services because they were lazy:
For some people it’s just easier, it’s a, kind of, laziness, they think I’d rather go there and wait than go through the palaver of having to make an appointment in the surgery.
P4, East European
Inappropriate service use was linked to perceptions of the consumer society: the idea that people ‘expected’ services to be available 24/7 (i.e. 24 hours a day, 7 days a week) in the same way that many shops and services are:
I think people want things to happen straight away. I think everything’s instant, so if I want something, like, from Amazon I’ll get it straight away; so in the same way people want the doctor to be available 24 hours a day. And I think they abuse . . . I do think they abuse the out-of-hours service. And listening to people talking about the surgery, I think their expectation of what they can get from the NHS and social services isn’t there. I think there’s an expectation but you can’t bridge that gap so everybody’s going to be disappointed; so they go in disappointed, they go in angry.
P16, older
I get really mad when people, like, slate the NHS and A&E because they think they’re the only person with something wrong with them when there’s so many more people who are way more serious [ ] So, because actually there was a time my nan had cancer and she was, like, dying. And she couldn’t breathe and I phoned . . . 999 and they got us in and we went straight in and someone [another patient] was so mad that we’d gone in but she was, like, dying, like. But they were just sat in A&E and they were really mad. And I was just, like, ‘how can you even do it, like, it’s just non-urgent selfishness’ [ ] I think they’re quite selfish in the way that they want to be seen, they want to be seen first. And that’s why you get, like, the arguments in A&E . . . because people think that they’re so much poorlier than someone else. It’s more do with, like, the lack of knowledge and understanding and not knowing that other things are available.
P43, younger
Media representations: ‘those programmes on television’
The portrayal of inappropriate service use in the media – particularly the use of emergency services – had a strong influence on the beliefs of service users and fed into moral positioning. This included both news reports of services under pressure and reality television programmes about emergency care:
Well, you always hear . . . see in media, that people use it too much. I think I’d . . . I would agree with that statement, but at the same time, I’ve never . . . I don’t have any reason to agree with that statement, other than just . . . what I’d read in the BBC News and that kind of thing.
P9, younger
I was scared about my breathing and the pain because I’d never experienced anything like that. And, I wouldn’t do it, you know, lightly. I mean, when you hear these horrendous stories about people going in. I heard it on the radio last week, on Radio 4. People going in to A&E for dandruff, for God’s sake, you know. What is the matter with people?
P12, older
News stories and reality programmes often highlighted extreme cases (such as attending the ED ‘for dandruff’ as in the quotation above), and added to the sense of outrage and talk about the unfairness of paying for other people’s irresponsible behaviour:
After watching those programmes recently on television, I think it’s a little bit irresponsible how they use it sometimes. You know, calling for silly things, or calling, really, just to have a chat. Or if the people are saying to them, you know, don’t call us, it’s not an emergency, you know, call 111, or go to the GP in the morning, they keep calling them again and again. So, this is very upsetting, really, that they are abusing, actually, in the system. In the end of the day, I’m also paying tax here. So, somehow, I’m also paying for their stupid calls.
P6, East European
However, some service users were sceptical about media reports, as in the quotation below:
I’ve never actually used it [NHS 111] personally and you tend to be . . . not guided, but what you read in the newspapers tends to give you a sort of a . . . sometimes a false impression of what’s happening. And you hear a lot of derogatory reports about the 111 and A&E and all this sort of thing and you read about people phoning up because they need a lift home because they’re drunk and all this sort of thing, you know, and it sort of does influence the way you think about it. But from my own experience I couldn’t complain to be quite honest.
P19, older
Moral tensions: contingencies and special cases
While the people we interviewed and talked to in the panels could be judgemental about other people’s help-seeking behaviour, they also acknowledged the moral tensions in these arguments:
To make a moral judgement, as in, does a single mum deserve more care than a 65-year-old pensioner who worked really hard all his life, and it’s really difficult to . . . Like immediately there’s a moral judgement straight away.
CP7, general public panel, vignettes exercise
Moral positioning called on the kinds of contingencies (explored further in the next chapter in relation to people’s own help-seeking behaviour) that appeared to legitimise other people’s use of services, and these blurred the boundaries of urgent and emergency care. Thus, members of the public panel and interviewees noted moral exceptions for ‘special cases’ such as the elderly, children, and those who lacked support. Health-care professionals and commissioner panel members also drew on moral discourses, but also tried to understand the reasons for service use; in the following example, a discussion about an ‘inappropriate’ attender drew on non-health-related drivers of behaviour:
The sentence before last really worries me, because that’s the inappropriate A&E . . . She suspects he might have flu, but she is anxious and has to be at work the next day. You’re kind of like, ‘I can’t afford to take the time off to go see the GP in the morning, so I’m going to go down A&E now’, and that’s exactly the target group’.
CP1, commissioner panel, vignettes exercise
Use of ‘the wrong’ service might be legitimate if people lacked sufficient knowledge to make the right decision, or perceived that they had nowhere else to go. P35, for example, drew a distinction between the undeserving (‘the drunks’) and these more legitimate service users:
If you come from abroad, you have that experience or memory of another system and you try to find commonalities, because you want to orient here in the new system, but there is not much there. People don’t seem to know, even if you talk to people born and bred in this country and brought up in this country, they don’t necessarily know all the intricacies of the system. So it must be a very complex system.
P34, East European
Having been in the waiting rooms up there [the ED] on a Saturday evening with all the drunks and things like that, I think, yes, I think they are definitely misused. But equally, you can understand why some people use it when they may not necessarily need it . . . But people might use it because they feel they need something and they can’t get it elsewhere, you know. If they can’t access a doctor anywhere else at the time, it depends on how they’re feeling as to whether they go there or not. If they’re sufficiently in pain or sufficiently distressed, then they need that reassurance even if it’s only from a triage nurse [ ] I mean it maybe that people don’t always feel confident in phoning 111 because it is a voice on the end of a phone.
P35, older
Similarly, lack of knowledge might lead to panic, and in this case service use might be seen as more reasonable, as P22 suggested:
For instance, if you ever got chest pains and you’ve got no breathing problems then it’s fairly unlikely it’s going to be fatal, on the day at any rate. So you’ve got to consider whether you really need A&E or an ambulance . . . But it’s not easy to say, everyone’s different. It depends on a lot of people’s temperament, you know. Some people are cool and calm and accept things, others go into a blind panic.
Yes, and you think that makes a difference?
I think it does, because no matter what advice or information is available, the one who panics is going to do what they want to do and that’s all there is to it.
Older
In one other example, a panel member suggested that going to the ED might also be a way to signal the severity of an illness:
If she calls her employer and says, well I had to take my child to A&E, we were in hospital all night, I can’t come to work, whereas if she goes like, yes, he was a bit poorly, he still has a temperature, I need to stay at home, she won’t get the same, just, reaction from her employer . . . There’s a status thing about going to the A&E and . . . And needing that care. Sort of having all that, sort of forces people to go to . . . To sort of get validation or . . . You know? She can call her mum or her boyfriend and say, oh, you know what happened? I had to go to A&E, and look at me.
CP8, general public panel, vignettes exercise
Contingent boundaries of need were also influenced by exceptionalism. In common with previous sociological work,189,190 children and babies were considered special cases. Children were seen as legitimate users of health care, and service users often explained the differences between actions they would take for themselves and what they would do for a child. Some suggested that a lack of support elsewhere in the NHS could prompt people to make contact with emergency care:
I’m pretty sure there’s quite a lot of people I know with a kid might be like my kid is sick, I can’t wait to book this appointment so I am going to take them to A&E because they will be looked at . . .
OK, and have they been seen?
Yeah.
And what do you think about that?
Obviously they wouldn’t have to do that if they had the right sort of support type system. It is a very good support system the NHS but it needs improving.
Younger
We’re a bit more worried about the toddler than anyone else.
CP9, general public panel, vignettes exercise
And there’s something about compassion as well. Sort of how a condition like [inaudible] infection wouldn’t be urgent care matter for a very healthy 30-year-old, but it would be very important for baby whose teething or sort of there’s something . . . It needs to be tailored to the person and what their needs are and their mental health state and there’s loads of things that need to be understood before you rate something as urgent or emergency or regular care.
CP10, general public panel, urgent care ideas exercise
Other service users regarded the elderly as special cases who were more deserving of care, or were justified in using services such as ED:
I’m a young person, but maybe if you’re older, a situation that’s not maybe me walking on my foot, with my torn ligament, for me it wasn’t that much of an issue, but for someone who’s older, they might need to go to A&E for that because they might be more, less, I don’t know what the right word is, able to get around and things, they might need to go for that.
P42, younger
Reimagined boundaries of urgent care
The two themes presented above have demonstrated the confusion and moral positioning at play in people’s sense-making about urgent and emergency care. Sense-making is rendered problematic because of a lack of clarity about the definitions and boundaries between urgent and emergency health needs and care services. This is complicated further by the moral positioning that features in sense-making, which serves to reinforce understandings and legitimise one’s own help-seeking while marking out others as inappropriate services users.
The final theme from our data about sense-making is drawn from the exercise in the citizens’ panels where we asked participants to look at the ‘Keogh triangle’,1 a diagram used to depict the urgent and emergency care service landscape (Figure 5). We asked them to consider the range of services that should be included and the routes to accessing these services, as well as the visual representation.
FIGURE 5.
The ‘Keogh triangle’: proposed look and design of the new system. Figure reproduced with permission from NHS England (2013). 1
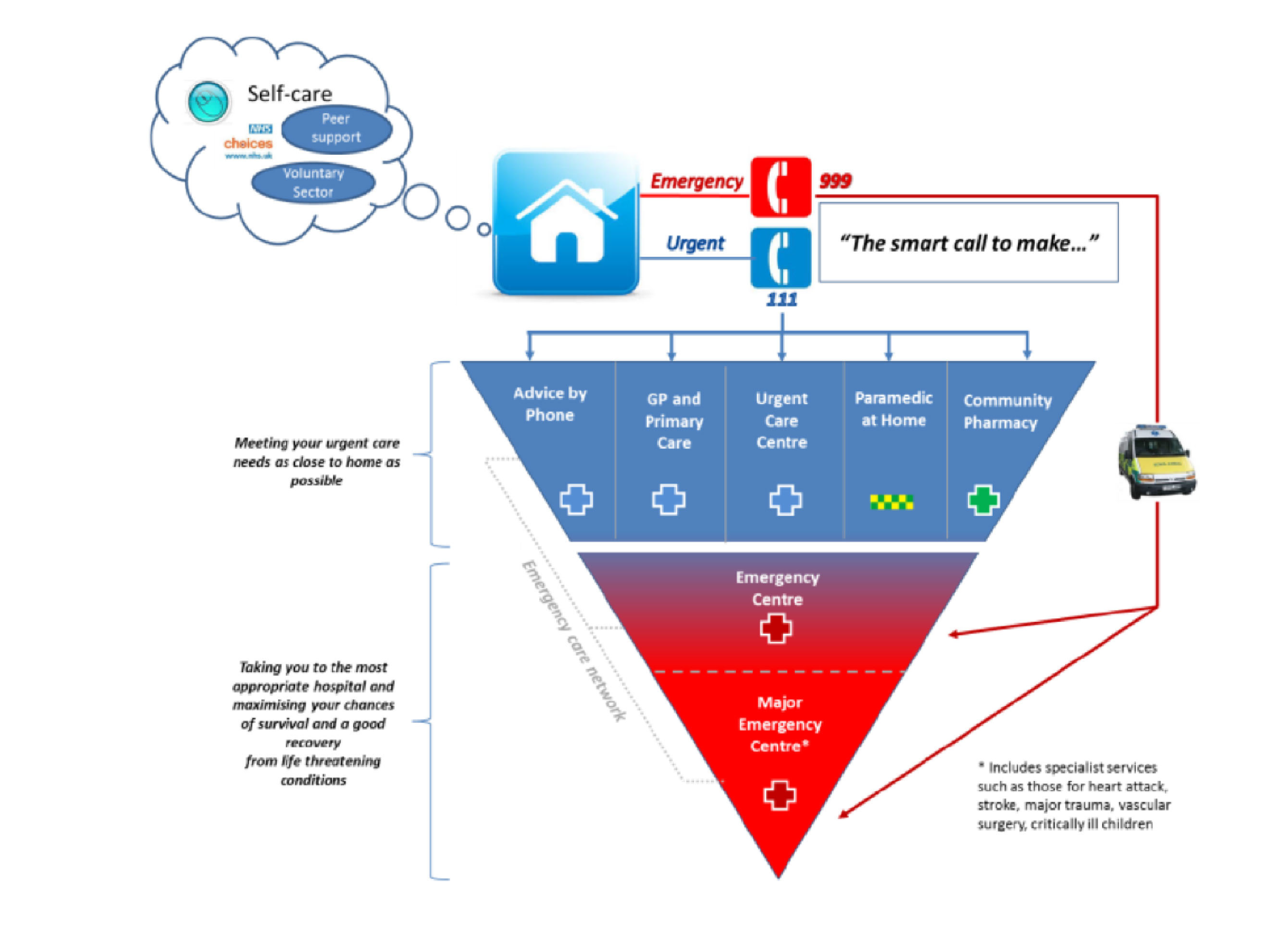
When asked to redraw or adapt the diagram to match their sense-making about urgent and emergency care, the panels’ pictures looked very different (Figure 6). Some groups, such as the commissioners, clearly ‘knew’ this visual representation, but we asked the panels to discuss this representation and reimagine it.
FIGURE 6.
Panels’ representations of the urgent and emergency care system. (a) Commissioners; and (b) general public 1.
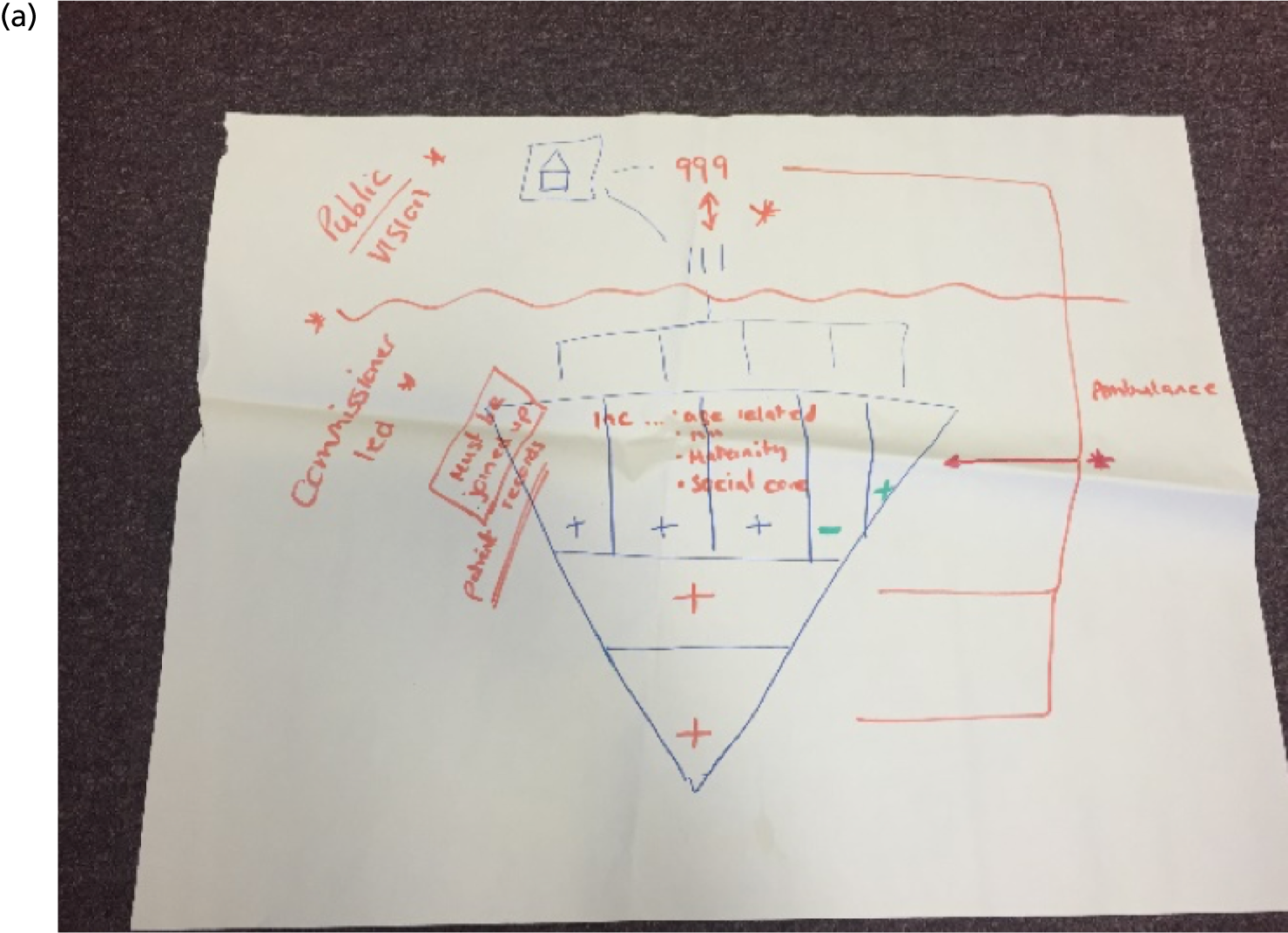
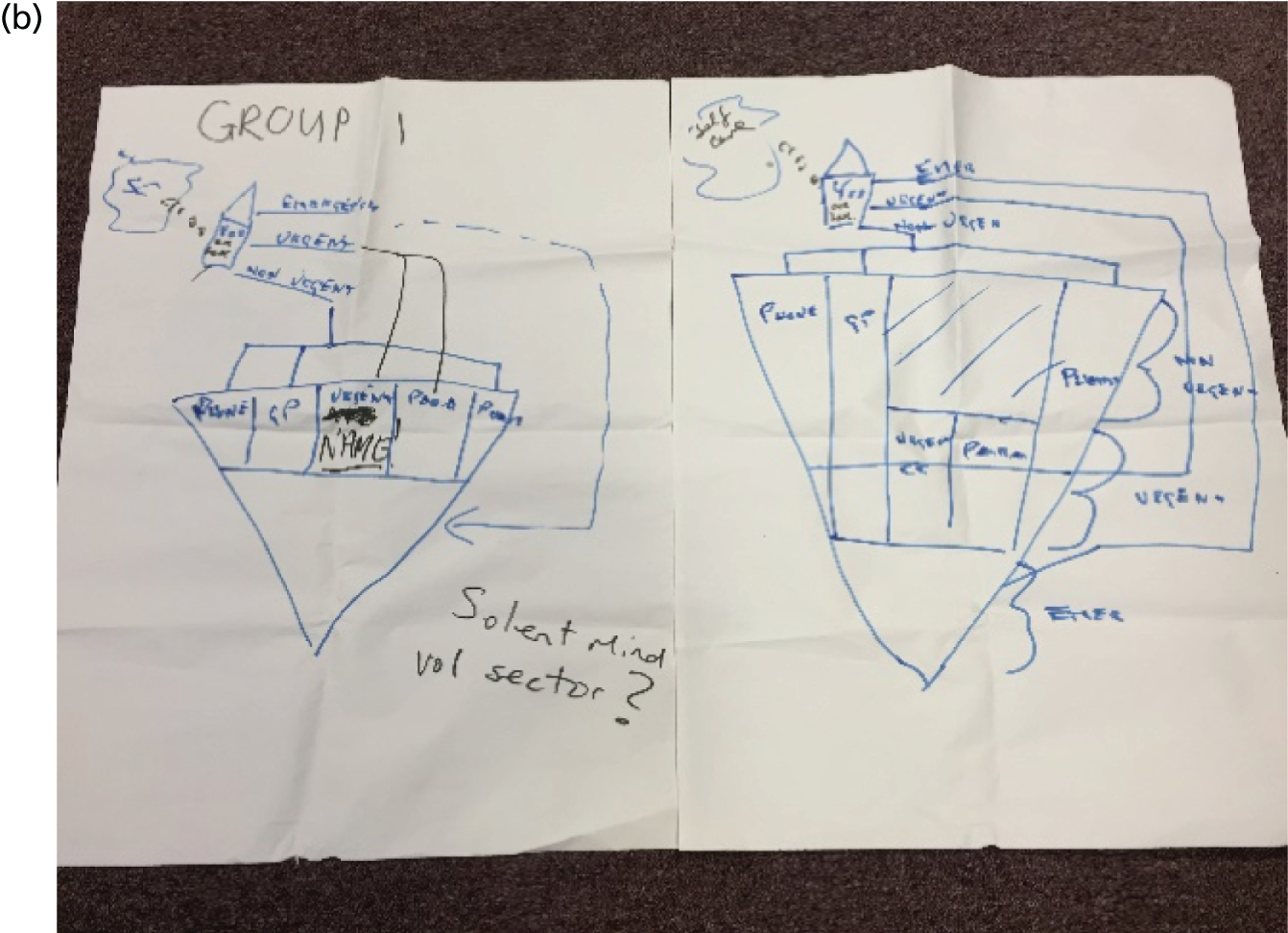
One general public group reproduced the inverted triangle used in the Keogh visualisation, but, like the commissioners’ panel, they began to edit this during the discussion as they considered which services should be identified as urgent care. Both these groups were keen to explore a range of ways to access services:
I think it’s more important to have the definitions of urgent and emergency rather than the outcomes. So that people understand when they should be calling and which service to be calling. We sort of did it . . . And obviously panic is quite subjective, but green being sort of like, oh I’ve got a cough not . . . Like I’m OK, I can make it through. Amber being a bit like, OK, I’m a bit panicked by this, I’m worried, and you know, to being like I’m really, really panicked, whether it’s . . . Which is obviously pretty subjective, but as a general rule.
CP1, general public panel, discussion on Keogh diagram exercise
The discussion around this panel task confirmed that people wanted much clearer information about what different services did to inform their sense-making. Rather than using relational language, they favoured specific examples of the kinds of illness and injury that would be treated at each service. Several public panel members were confused about the placement of the ED at the base of the diagram and felt that this, and the bold red used, drew attention to this service and perhaps encouraged people to attend. This was particularly confusing in the light of the fact that the lines at the top of the diagram (denoting 111 and 999) placed 999 above 111 (the reverse of the diagram):
In the diagram but not with the fonts and I didn’t like the lines at the top. That’s forcing you to use 999 first.
OK, it sends the wrong message?
Yes.
Would you all agree with that?
Yes [it would be better] on the side.
Or even underneath it.
Underneath, yes.
East European panel, discussion on Keogh diagram
In their reimagined drawings, some groups drew traffic lights and other representations that attempted to help make better sense of where to go (Figure 7):
So we thought we’d have a traffic light system which was red, amber and green. With special leaflets for people who’re colour blind. And so the green will be the GP and the internet where you have time to think, you just go, have a little think about it, I’m not too . . . Or perhaps I . . . Perhaps I better see the GP on Monday or whatever. Or the internet reassures you, whatever it might be. So less important, but in green, we’re not sure where to put it.
CP4, general public panel, discussion on Keogh diagram
FIGURE 7.
Panels’ reimagined representations of the urgent and emergency care system. (a) Professionals 1; (b) general public 2; and (c) general public 3.
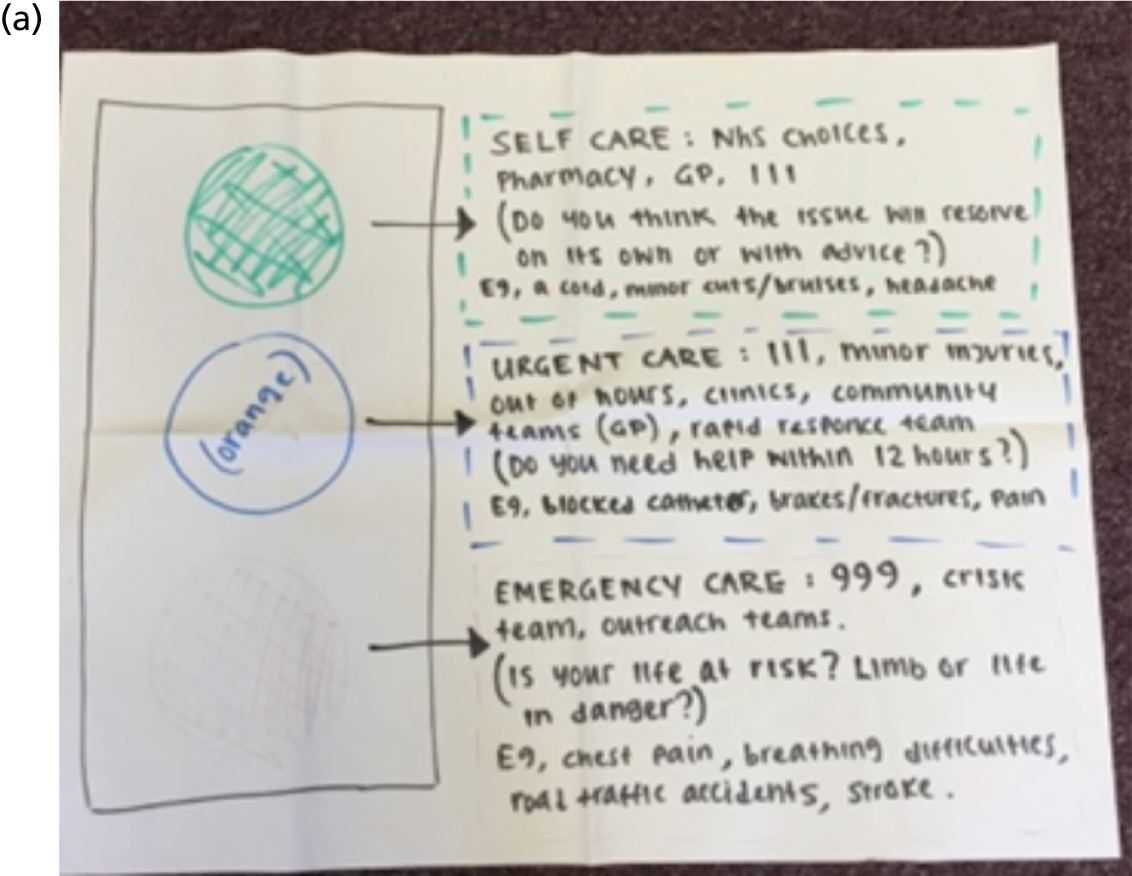
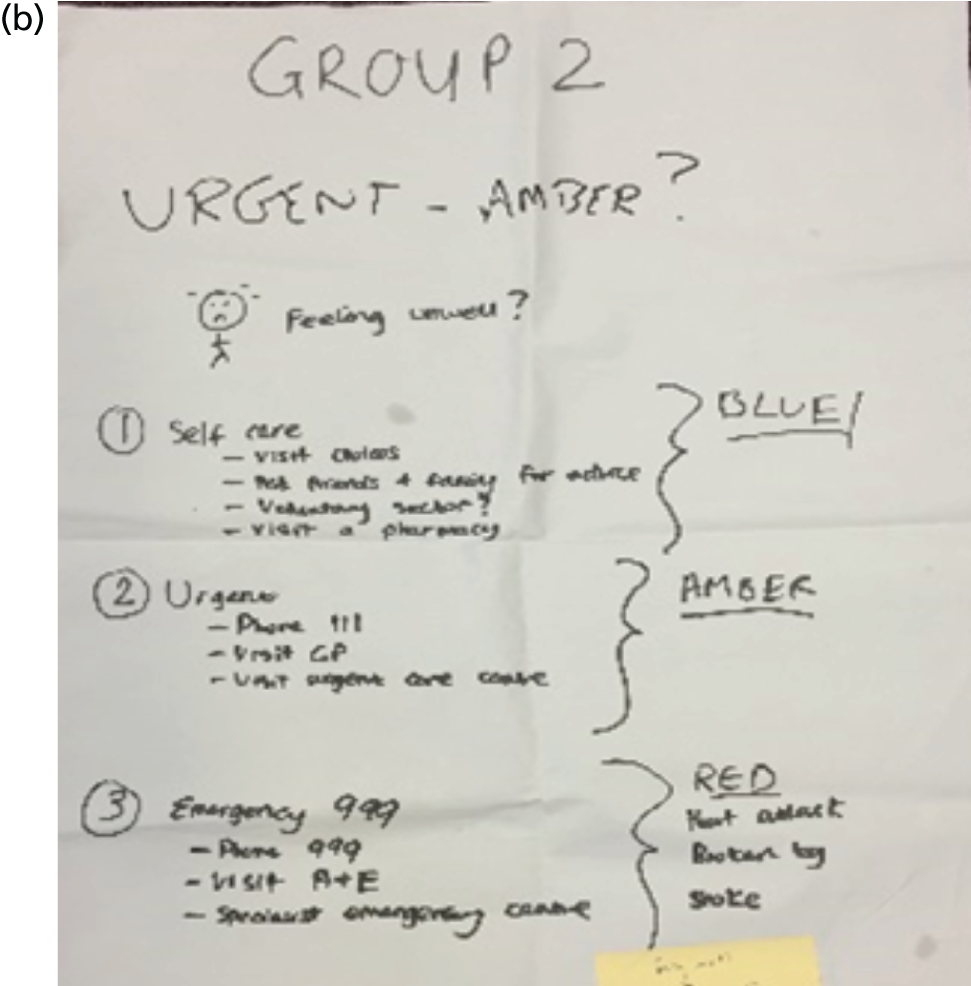
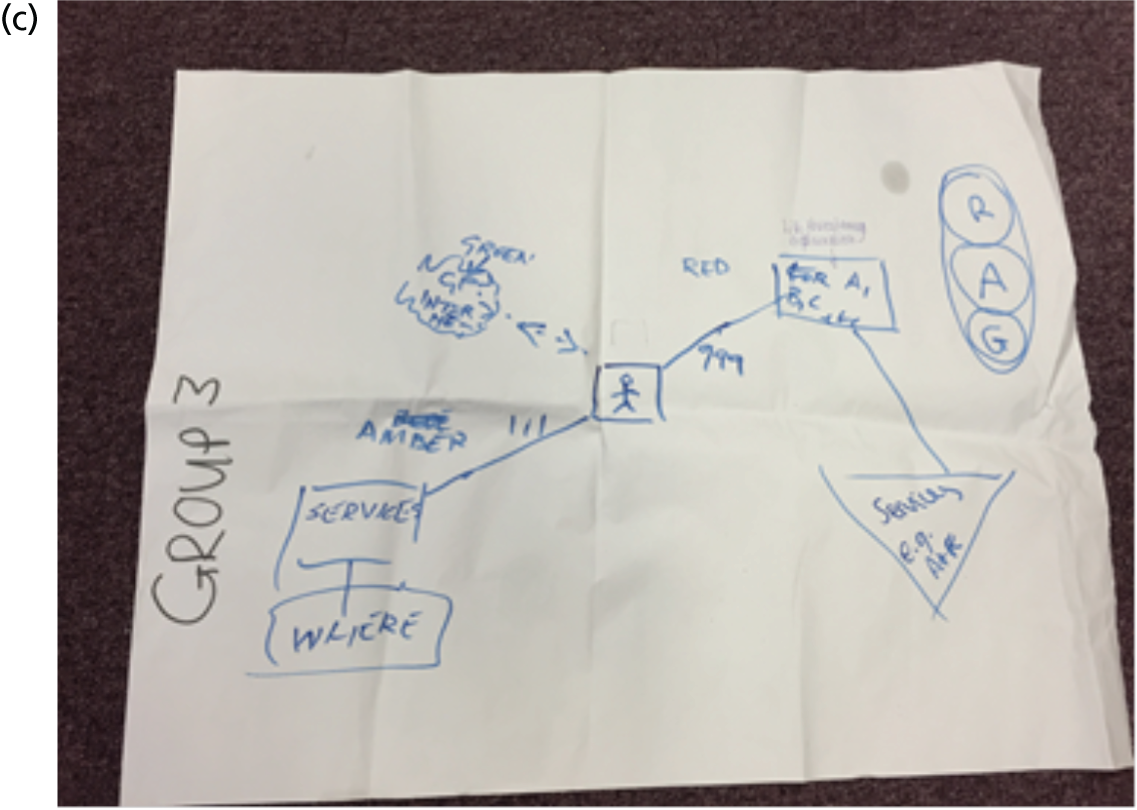
Two groups also specified a role and place for self-care and wanted this to feature prominently in the diagram to support people’s decision-making:
We felt definitely there needed to be more emphasis on this [self-care is in a separate bubble]. In fact, at first [panel member name] didn’t even notice that it was there. So we were saying if that was going to be the flow chart, you should have to go through self-care before you even get the option to go to emergency or urgent.
CP2, professionals panel, discussion about Keogh diagram
The East European panel provided insights into their understandings of different services. Some members suggested that they did not trust telephone services (such as NHS 111) and wanted to see a doctor face to face, which prompted them to seek help at A&E:
We don’t trust phone calls. We don’t use them. Quite often, we don’t communicate well enough to explain what’s happening and take the message from the doctors on the phone. They don’t have Polish speakers or any other languages, you know, on the 111. So that’s why they don’t call and they would like to see a doctor, because the doctor will explain. If they cannot explain, they draw it or they show it on a picture. So then she knows.
CP3, East European panel, discussion about services map
However, in the interviews several East European participants reported that they understood that NHS 111 provided help and advice about urgent health conditions and said that they would use the service. Some of these panel participants also mentioned that language barriers, as well as more direct experiences of racism, influenced their choices about accessing care. These experiences, combined with experiences of the health-care system (e.g. in Poland) and less knowledge of the NHS, led them to read the triangle map of service provision in very different ways. This was an unexpected finding that alerted us to cross-cultural differences in sense-making about urgent care.
Summary
Our exploration of sense-making about urgent and emergency care confirmed that the boundaries between urgent and emergency care are ill-defined and that there is considerable confusion about the appropriate use of the many services on offer. The general public, health-care professionals and service commissioners share this confusion, and this may explain why they find it difficult to navigate this service landscape. Given that the policy review revealed a lack of specificity in defining ‘urgent’, it is perhaps not surprising that the public struggled to articulate what urgent means and to make sense of the care options available. It was interesting that professionals and commissioners also shared this confusion at times. Our panels and interviews suggest that, unlike emergency, the term ‘urgent’ is particularly problematic: it holds little meaning for most people. The term ‘urgent care’ is often used interchangeably with ‘emergency care’. Although much of the policy surrounding urgent and emergency care is predicated on the notion that ‘urgent’ sits neatly between emergency and routine and is clearly distinct from these, the public, in particular, struggle to distinguish it from emergency or routine care in this way.
Although the public in our panels and interviews often found it difficult to articulate the differences between urgent and emergency care, they had strong moral views on the kinds of illness and injury, and the kind of person, deserving of ‘emergency’ care. Although the public recognised a range of contingent factors and special cases that influence people’s help-seeking, their sense-making with regard to emergency care tended to be judgemental and polarised. Fewer moral judgements were made about the ‘misuse’ of urgent care services, perhaps reflecting the lack of clarity about these. This moral positioning is further explored in Chapter 5, when we examine the moral work that service users do when choosing urgent or emergency care.
The panels demonstrated that the public sought a clearer sense of service priorities. Their redrawings of the Keogh diagram attempted to capture a triage system that might help navigate a confusing landscape and aid sense-making about urgent care. Although the Keogh diagram reflects the policy rhetoric that expects people to use NHS 111 as a gateway to urgent care, the public members of our panels and our interviewees were still less familiar with this model. Sense-making about urgent care is varied and complex, and our findings suggest that we cannot simply assume that providing a signpost in the form of NHS 111 will direct patients to the right service at the right time. Chapter 5 of our report examines the data about how sense-making influences people’s choices about which service to use, and probes more deeply into their experiences of help-seeking and the work involved in accessing, navigating and using urgent and emergency health services.
Chapter 5 Help-seeking behaviour, choices, experiences and ‘work’: findings from the qualitative interviews
Introduction
This chapter examines the choices that service users make and the work that they do when seeking help for an urgent health problem (objectives 2 and 3). We also develop a typology of types of work involved in help-seeking: ‘illness work’, ‘moral work’ and ‘navigation work’. This work informs individual sense-making (how people think and feel) and help-seeking behaviour (actions). We also show how help-seeking is influenced by a wider set of psychosocial and contextual factors.
Illness work
Illness behaviour – how people monitor their health, and define and interpret their symptoms – is well documented in the literature191–194 (see also Chapter 6) and has been explored in relation to urgent care129,135,137,195 and emergency care. 150,153,196 The concept of ‘illness work’ has primarily been used in the context of chronic conditions research to refer to ‘diagnostic-related work, regimen work, crisis prevention and management, and symptom management’. 23 We suggest that it also occurs in relation to urgent care needs. People need to interpret and make decisions about the meaning and the severity of symptoms; manage physical symptoms, psychological states and possible risks; decide if access to medical care is needed, and if so, how soon; and decide which service is required. Illness work takes place at the individual level and within a social network that may include family, friends and neighbours.
Individual-level illness work
Our analysis of the interview data helped us to identify a core set of symptoms that were particularly important in prompting contact with urgent care. Such symptoms are sudden in onset, unusual and perceived to be life-threatening or very serious, and typically interfere with daily life (e.g. by impairing mobility in some way). These findings broadly reflect the extensive literature on illness behaviour more generally and it is not our intention to rehearse this in detail. Instead, we focus on responses to symptoms that seem most distinctive as prompts to urgent care help-seeking. We summarised these as ‘pain’ and ‘anxiety’. We contend that subjective interpretations of pain are inextricably linked with emotional responses to illness, characterised as anxiety, and that together these drive decisions about help-seeking.
Interpreting and managing pain
Previous work on urgent care has considered pain in a limited sense as a physiological correlate of a serious specific illness, such as a heart attack or major trauma (see Chapter 3), largely ignoring its psychosocial aspects, and pain has been examined little in relation to urgent care help-seeking more generally. We were surprised at how talk about pain dominated people’s accounts of their help-seeking behaviour. The role of pain in our participants’ decision-making processes was especially interesting given the almost complete absence of reference to pain in definitions of urgent and emergency care services (see Chapter 3).
Service users described how they evaluated the level of pain that they experienced, trying to decide if it indicated serious illness and could be used to identify a cause. They compared it with previous experience and assessed whether or not it was intolerable and if it was impairing their ability to perform everyday activities. They made contact with urgent or emergency health services when they experienced a high level of pain, particularly in conjunction with other symptoms they were worried about, such as shortness of breath or chest pains. High levels of pain were associated with high perceived risk; chest pain, for example, caused particular concern, first because the pain was very acute, and, second, because service users were worried about the possibility of a heart attack:
I woke up again at 03:15 and I could barely breathe and I had the most horrendous pains in my chest. And, I thought, ‘Oh God’. I mean, it really was not funny. It took me ages to get out of bed, stagger out of bed . . . I thought, ‘this is ridiculous’. But, the pain. And, it was so bad I was crying, you know, and I don’t do that normally.
P12, older
High levels of pain that impaired physical functioning, as in this example, affected breathing and movement, that caused crying signalled severity. Other physical responses to pain included ‘curling up in pain’. An important trigger for people making contact with health services was their perception that the pain was exceptional or different from what they had experienced before:
[In] putting more pressure on my left leg, I got a trapped nerve, which was terrible . . . You live and hope that it will improve each day and that, and nearer it got to Christmas it was obvious it wasn’t going to clear up. [I was in a] huge amount of pain! Shooting pain, shooting right down my leg. I couldn’t stand. It was unbearable. It was the worst sort of 6 or 7 days of pain that I’ve had for a long time. I mean nothing that I did seemed to you know, help it. It was excruciating sharp pain [ ].
So you also mentioned that your husband was quite concerned in the period leading up to you going to [name of UCC]?
Well yes he was, because you know, I couldn’t do normal things . . . I mean on Christmas Day . . . we had to find something I could sit on the right level in order to do the cooking on the stove, because I just could not bear any weight on that leg.
Older
Awful pain . . . I was laying back on the sofa . . . and I couldn’t move, I couldn’t move an inch. I couldn’t have even grabbed a phone at that stage. It’s a pain that you can’t describe. I’ve never had a pain like it and I never want it again, but I did have it again.
P36, older
Some described how they usually managed painful symptoms using a ‘wait-and-see’ approach, but help was sought if symptoms persisted when services were available and accessible:
I was trying to manage it myself . . . so I think it’s not an immediate, sort of, first resort, it’s after you’ve tried things yourself and then you go to urgent care.
P88, younger
I think I just knew it was a chest infection because I’m usually, I don’t get ill that much and usually I’m like, ‘I’ll be fine, I’ll be fine’. But then when it got to a point I was, like, ‘no this is definitely, definitely too much’, so I went in.
P90, younger
Help-seeking for a recurrent health problem was precipitated by a change in pain level. P50, for example, had a history of cystitis but attended an ED because her pain seemed different from what she had previously experienced:
It was lower abdomen and it was causing me discomfort so I felt like I needed to urinate and I couldn’t. And I was having a lot of shakes and cold sweats. And, yes, really struggling with the pain and it didn’t feel normal. I’d had, you know, cystitis and things like that in the past. I get it quite often, actually . . . but it was unlike anything I’d had before, which I was worried about.
P50, younger
Pain described as ‘internal’, or that occurred in the absence of an obvious, visible injury or cause, provoked particular anxiety:
I think it’s a lot worse when you can’t see the pain. With a broken arm or a sprained thumb you can see swelling, you can see something is out of place. But when you feel something like a long, sharp, constant pain inside, you can’t see, you’re not used to it so it’s quite a scary thought because it’s just the unknown and it starts the whole, sort of, fear process and just spiralling of your thoughts of what it could be so you want to get that sorted.
P37, younger
Both urgent and emergency care services were considered appropriate help-seeking choices for severe pain. When asked to describe ‘an urgent care problem’, service users, across all population groups, named pain as significant. Urgent care services were viewed as being able to provide pain management or pain relief:
I think emergency would be life and death, like, compared to urgent [which] could be someone who’s in a lot of pain who needs pain relief . . .
If I said to you, what’s urgent, you would say . . .
Pain relief, doctors, things that don’t . . . need to go to A&E. But things that could be dealt with at home, maybe.
Younger
What would you describe as an urgent care problem?
Yes, so for example, if you have a massive toothache, and you don’t know obviously you can’t function because that’s very painful, so you would go. If it’s a night, night time, then you go and seek urgent health care just for strong pain relief or whatever they can do in there, I think.
East European
Advice from NHS 111 was useful for some who experienced unexplained pain, while others sought face-to-face help:
Like the kidney stones, or the strong abdominal pain, really excruciating pain . . . I thought ‘no, rather than rushing, or calling an ambulance and going up there, let’s phone this 111 number and see what they say first’.
P2, East European
If you’ve got something that you couldn’t stop bleeding or you’ve got a terrific earache or something that was so painful, like poor little [name of grandchild] gets, you know, you’ve got to do something, haven’t you, if there’s no doctors available anywhere or you can’t . . .
So you would go to a minor injuries unit for that?
Definitely, yes, because . . . you never know with children, do you?
Older
People described how they made judgements about the likely cause of their pain, and whether or not it could be managed in the short term. This might mean waiting some time for the general practice surgery to open, and using GP appointments in cases of high levels of pain appeared to be more common in the older and the East European groups:
I had tonsillitis, and the pain was really bad and I phoned the doctors. Because it was my throat, so I knew it wasn’t something that I need to be . . . I knew it wasn’t the case of an urgent emergency case. Routine can also be quick; you can still be seen.
P2, East European
I couldn’t get up in the morning, my back was killing me . . . I said [to a friend], ‘No . . . the breathing is agony and I’ve got a pain in my back around the side’ . . . but I had to drive home. There was no other way of getting back [ ] So, it was a 2-hour drive back here and I was fine driving, but, going around roundabouts . . . Nearly died every time because the pain was excruciating. Got home. Rang the surgery first thing the next morning, which was the Monday.
P12, older
Things described as ‘emergency problems’ were strongly associated with severe pain with an unknown cause. A decision to call an ambulance was made when pain was accompanied by other symptoms such as being unable to move:
Well, he was static on the sofa, couldn’t move . . . He’d been like that for three quarters of an hour because I was out, and I came home and found him in a state of . . .
Pain.
Shock and pain and, well, I mean the shopping got left out there, everything was left, and I just phoned 999 straightaway.
Older
Younger interviewees were more inclined to choose to attend the ED to manage pain, and often felt that there were no alternatives to the ED (sometimes because of the time of day, and sometimes because they did not know where else to go):
It just went so bad [hip pain/hypermobility] that there wasn’t any option other than to get the pain sorted at A&E. Which didn’t happen anyway, so I wouldn’t go back to A&E . . . I honestly don’t know what I’d do next time . . . I’ve pretty much said the next time that happens I would phone an ambulance because I’m just not getting the attention and the care I need at the moment.
P49, younger
Interpreting and managing anxiety
High levels of pain, and accompanying uncertainty about symptoms and what to do, often provoked anxiety or panic. Across all three groups, responses to symptoms were frequently described in terms of fear or anxiety, and interviewees articulated this using a range of words such as ‘panic’, ‘scary’ and ‘frightening’. When interviewees talked about panic in relation to the help-seeking behaviour of others this was often used to imply over-reaction, and irrational and/or selfish actions. By contrast, managing their own anxiety was presented as a legitimate reason for making contact with urgent care.
While anxiety was used to legitimise personal decisions to seek help from urgent care services, some service users reflected that their interpretation of urgency might differ from that of a health-care professional and they recognised that anxiety fuelled decisions about what to do ‘in the moment’. This recognition of the subjective nature of illness and the role that anxiety plays in rationalising health service use was more common in the older age group:
It might not be in their definition of a doctor’s emergency, whether they can do something about it or not, if they’re doing from a doctor point of view. But from our point of view, it’s a panic [ ] When calling 999 for my mum . . . just being too floppy to get up . . . It’s not a sort of medical emergency, in their book, in their definition. But it is something that . . . needs to be dealt with . . . And it is something that is pretty concerning . . . It’s just that there’s a sort of boundary thing, the definition. When we were living it, it’s just being in a, sort of, very frightening situation.
P18, older
A minority of service users, particularly in the younger age group, identified themselves as having an anxious personality type and being prone to worrying about their health, and they used this to legitimise their use of urgent or emergency care services:
Blurriness, particularly in my left bottom corner in the left eye, real irritation under my eyelids, a kind of scratchy feeling under my eyelids and just real discomfort. It wasn’t pain, just real discomfort, very dry . . . very dry.
And how did it make you feel?
I think I have a tendency to worry a lot anyway, but when it’s your eyes, they’re a certain thing you can’t help but think about because you see out of them, so I was so aware of it all the time, and I felt a bit . . . I felt quite worried, definitely.
Younger
Older service users described ways in which they tried to manage anxiety, including self-talk (telling themselves that they would be OK) and behaviours (e.g. deep breathing):
‘I’ll get better, I’ll be all right. I’ll be all right, I’ll get better.’ But as time goes on, you realise your chest is getting tighter, OK, your breathing isn’t what it should be, and you’re sweating a bit through anxiety.
P7, older
They [999 ambulance] came almost immediately, then rushed me into hospital because my oxygen were right down low I didn’t hardly have any oxygen and they couldn’t control my heart and so they said you will have to go in. That happened about two or three times . . . and then it settles down when they give me the tablets and if I had it before that I could sit up and tell myself not to panic and do some deep yoga breathing to slow it down.
P24, older
Those reporting less anxiety tended to seek reassurance from urgent care services including NHS 111, but those experiencing more anxiety and high levels of concern about their health problem were prompted to seek help from emergency care. Contacting emergency services was a last resort chosen when they were highly anxious and did not know what else to do. However, for many older people, calling 999 or attending the ED was a first response to a problem when they were anxious and worried:
If you’re worried silly, it’s going to be A&E.
P28, older
Well I didn’t know what else to do at the time because I was in a state. Well not panic, but I was highly stressed and I thought I don’t know what to do so I just dialled 999 and they asked me what was wrong.
P19, older
Across all groups, service users gave examples of how anxiety could influence their judgement about a health problem. They described ‘freezing’ with panic and not being able to undertake basic self-care tasks, and not being able to remember or understand information that may have been given to them by a health service such as NHS 111:
Because your mind runs away with you when you’ve got something wrong, and you could think you got all sorts of things, and it might not be any of that.
P23, older
I’m 25, it’s pathetic. Usually I need someone to come with me . . . because sometimes you don’t listen. So, if you’re panicking or if you’re in pain I just don’t take in information so it’s nice to have someone there with you to be there.
P43, younger
People also talked about how they revaluated their experiences once they had received diagnostic information and they were able to acknowledge that their behaviour was partly driven by anxiety. They described their responses as an ‘over-reaction’, noting that they contacted emergency care when they might have more appropriately made contact with an urgent care service. Such ‘over-reaction’ was also linked to the social context, for example if someone lived alone or if the problem occurred at night. Younger service users were perhaps more likely to describe their help-seeking behaviour in these terms. In some cases, self-reflection prompted changes to help-seeking behaviour, such as seeking out information to manage their anxiety:
In my mind, the worst that could happen was losing my sight, which obviously now it seems like a big over-reaction, but at the time . . . I wasn’t aware of blepharitis and what it was . . . [Now] I think I always try and look up symptoms beforehand just to check if it’s something I can self-diagnose easily, and if not, then I’d be more open to going into urgent care.
P32, younger
Managing risk
Illness work requires service users to assess the risks of action and inaction (e.g. seeking help vs. delaying or not making contact). Managing uncertainty and risk was a key aspect of most accounts in the interviews. For many participants, deciding what to do was not straightforward. Many reported debating – either with themselves or with family members – the best course of action to take. This illness work entails balancing anxiety with action. Fear of serious harm or death was often balanced with ‘bothering services unnecessarily’, and this illness work is undertaken in the context of moral decision-making and judgements about the availability and accessibility of services:
Yes, again reassurance. So . . . because you thought you won’t bother your doctor. Because I thought, ‘well, I won’t get an appointment with the doctor’.
P16, older
Seeking reassurance by consulting health professionals or talking to members of lay networks is also a way of managing risk and can be described as ‘safety netting’. Reassurance was sought to ‘make sure there’s nothing wrong’ or ‘being on the safe side’. NHS 111 was often the first port of call, particularly for the younger and East European interviewees. For some service users, this tactic was used in anticipation, as a pre-emptive action to ease anxiety and worry:
Well, I didn’t want another weekend of worrying about, you know, ‘what shall I do now’, because those nights when I couldn’t sleep, I just sat up in bed, in fact when I can’t breathe, I sit up in bed, and I was just sitting up in bed with the radio on, and sort of drifting in and out of sleep, on and off all night.
P26, older
For many service users, there was a moral tension between wanting to represent themselves as responsible citizens, who were confident in their ability to self-care and make rational judgements, and the desire to delegate illness work to health-care professionals. NHS 111 was valued by some as a service that could provide reassurance and advice, and it was used to check if they were ‘over-reacting’:
It’s 111, because they asked me about symptoms and then they can sense if I’m overdoing it [over-reacting] [ ] But if I can see that something is wrong and I don’t know . . . That’s why it’s easier to phone 111, because they know the symptoms. They know that if I’m overthinking, or if I’m worried too much.
P1, East European
Using an ED for reassurance was less common. For P16, there was a recognition that using the ED to obtain reassurance for less urgent problems may be construed as ‘abusing’ the service, but the immediacy of this service was attractive:
It feels reassuring, and if you’re stuck and you’ve sprained your ankle after a few drinks you go to A&E, don’t you? It’s part of our comfort blanket maybe, A&E. Yes, that’s why we use it . . . and it’s not that we’re abusing it, maybe we just feel safe. You feel safe at A&E because you know even though you wait . . .
That you will be seen.
You will be seen.
Get the reassurance you need, and you feel safe . . .
Yes, whereas maybe we should get the reassurance from the chemist, which is cheaper. Because it costs so much money, doesn’t it? To go to A&E.
Older
I would have gone to A&E directly.
Why would you have done that?
I was not feeling well, so I just wanted to make sure there’s nothing wrong, so I would have gone straight to A&E.
What was at A&E for you that you didn’t think you’d get at another service?
Just the immediate check-up.
East European
P76 suggested that she chose to attend the ED ‘to be on the safe side’. Her previous positive experience, the fact that the ED staff did not pass judgement (‘they were fine about it’), encouraged her to consider it again as an option (see Navigation work):
I have been to A&E before I kind of figured, if it is not life threatening then they probably won’t, like, do any more than go to your doctor’s appointment . . . The problem is because I don’t know, from my perspective, I don’t have any medical knowledge or anything. So I think if something is kind of wrong you should just follow up on it regardless of what you think because sometimes it can be serious and within 24 hours. So that I just wanted to be on the safe side basically. But then it is good to hear from them because they are, like medical professionals, they were fine about it.
Younger
Help-seeking in illness work in social networks
Most service users do not make decisions about seeking help alone; they assess and interpret symptoms with other people,197,198 and these others play a role in sanctioning help-seeking. 199 In this way, social networks influence how illness work ‘gets done’. To examine this, in this section we distinguish ‘strong ties’, such as partners, parents, children and friends, from weaker ties, such as neighbours, community groups and acquaintances. 200
Strong ties
Much illness work involved strong network ties. When a service user had direct responsibility for the health of others (e.g. caring for children or a partner) and when the frequency of interaction between people was high (e.g. living in the same household), these network ties exerted a strong influence on help-seeking. Many service users described a hierarchy of support for their decision-making when experiencing episodes of ill health:
Well it’d be you, wouldn’t it [husband’s name]? Then [our] daughter and then the GP.
P52, older
Illness work may be shared or done on behalf of others, and the responsibility of managing health risks was seen as greater when undertaking illness work on behalf of other family members:
Do you generally go for your health appointments together; do you make appointments together?
I always make them together with [husband’s name].
Otherwise I have to start remembering what has been said . . .
[Interrupting] and he can’t. I always take him. He comes with me, with mine but he doesn’t come in with me because you get a bit confused.
Older
What’s the difficulty? It’s because they’re [parents] bloody wired in a different generation [They say] ‘Don’t need to go, I’m not calling the doctor, I’ll be all right’. And all that sort of stuff. And it’s just like, ‘basically, sorry, Dad, but you’ve banged your head, don’t know what’s happened, I’ve got to take you to hospital, as your son’. That’s it. Imagine if we leave it be to the morning, something happens in the night. I couldn’t face my sisters.
P11, son on behalf of father
Among the older age group, there were differences between married participants and single or widowed service users. For married participants, most illness work was done in consultation with their spouse and they tended not to seek advice or support from others:
Do you look to your neighbours, or your daughter, or anyone else, for your care decisions or information and advice?
Not really, do we? [Name], my daughter, tends to ring us if she’s got a problem.
Yes, she does . . . It’s almost like confirmation of what she’s thinking.
She just likes that reassurance.
It’s a lack of confidence, really.
But we’ve not really got anybody else that we would ring, have we? Not friends or family that . . .
No, well nobody you can trust. That’s horrible for me to say, we know loads of people, but, you know . . .
None of them are that close enough to . . .
Older
And do you generally make your decisions about health care on your own or do you involve your husband, family, anyone else?
No, we usually talk about it, you know, between us.
Yes? And what about neighbours? Do you involve anybody in . . .?
No!
Like taking you places or anything like that?
No.
Older
Older participants without a partner often involved their adult children in illness work:
About 2 weeks ago, for some unknown reason, I had a nosebleed. I managed to stop it the usual way, pinch your nose and this sort of thing. Took about 10 or 15 minutes, maybe longer, to stop completely. Then it happened again for no apparent reason and we stopped that one. Then it was on a Friday morning . . . it started again and it wouldn’t stop. Fortunately my two sons were here because they live with me and the elder of the two phoned up 111 and they said go directly to A&E. So they took me.
P19, older
I would normally call my daughter if I had a [health] problem, because she’s a lot more reliable and a lot more . . . you know, takes control of things. But she sort of more or less runs the local old people’s home, doesn’t she? And so she, you know, she knows she’s up with all the doctors, sort of thing. She’s got no qualifications or anything . . .
P14, older
Younger participants also relied on close family ties (predominantly a parent, a partner or, sometimes, a sibling). Advice from others played a role in how pain was interpreted and helped to sanction decisions – in the case of P32 and P66 – to attend the ED:
I went to urgent care, A&E, about 3 weeks ago. I had a hip operation last year and the pain came back, and I was in quite a lot of pain [ ] I spoke to my sister on the phone quite a lot, and she said to me ‘if you can’t think because of the pain, [you’re] in a lot of pain, you should go to hospital’. I was sat with my boyfriend at the time and he helped me come to the decision. He said, ‘if you want to go, we can go; if not, we don’t have to’ . . . I think they could see how much pain I was in so they told me to go.
P32, younger
I actually called my dad for that one . . . I was like, ‘Dad, I’ll call you, and can you bring a first aid kit and just give me an opinion on whether you think this is a bad enough cut?’ Because I just . . . I didn’t know . . .
P66, younger
Younger participants were often reluctant to involve friends and weaker ties such as neighbours and community organisations when experiencing an illness. Although younger service users discussed illness with their friends, it seemed that they did not place much trust in their friends’ opinions, and instead parents were viewed as a more credible source of help:
My mum was really supportive, friends . . . a little less so, because I think it’s . . . you know, it’s just, especially at that age [18], and I don’t think anybody really, like, had much of a clue. Couldn’t really empathise properly with what I was going through, and you know. He’s just complaining all the time, ‘oh, he’s always ill. It’s probably just you know, just complaining about stuff. Attention and whatever’.
P65, younger
I think I would discuss it with friends. I’d be like, ‘oh, this is really annoying, this is’. But I wouldn’t look to friends with solutions. Like, I’ve been saying to people on my course at the moment, like, ‘the rash is really annoying’. And they say a million and one things, and then they become more annoying than the rash, because they’re like, ‘oh, it might be this’.
P9, younger
P76 was an exception; she described talking with a friend to assess symptoms and decide on the best course of action:
Like with [name of friend] who broke her arm. I sat down with her before we looked to call an ambulance and said ‘look how serious is it’, you know, pain scales, levels, where are you, kind of thing. And when she said she was in a lot of pain I just kind of thought ‘well, probably it is best to just call 111 and find out what we can do’.
P76, younger
East European participants relied heavily on strong ties (family and friends), and reported less wide-ranging social networks, in part because of their migrant status. Lacking geographical proximity to close ties, they connected with family and close friends by telephone:
OK, so I think the most important one would be my mum, as well as my closest friends. The least, would be work. Yes, [and] the internet.
P53, East European
In the case of P63, an extended family of parents, grandparents and aunts interacted and shared information about ill health, partly encouraged by shared experiences of illness in the family:
Yeah, well we all live close by so.
Do you generally call on each other for health-care decision-making and stuff like that?
Yeah, we have had a bit of a year of it really. My aunty had . . . cancer in her kidney and then my dad last year, it turned out to be pericarditis . . . but obviously that [was] quite scary, crying because his chest was hurting very much because he couldn’t breathe. And I wasn’t around for that, I just got a phone call saying we were at A&E, Dad’s gone in [ ] This was during the period of time my grandmother had just come out of hospital as well and she knew because she knew . . . something wasn’t right because my dad was ringing her every day to see how she was, as well as popping round to see her in the morning . . . Like in times of need, I think everyone is there for each other pretty well, so that is good.
Younger
Close family ties with clinical expertise were particularly valued by all groups. When social networks included health professionals, these people were informally consulted to inform decisions about help-seeking:
I can definitely put my husband and mother [as sources of support], I would say. She’s a doctor . . . she’s not a GP, she’s a paediatrician.
P54, East European
My husband jumped out of bed, he’s actually a nurse; he picked him up [son], put him on the bed, raised his legs, but he wasn’t comfortable because his chest was hurting. If he sat up, he was dizzy, so we waited for about 20 minutes. It was quite a difficult situation because my husband, having some knowledge, was wondering what it could be.
P73, older
Some service users sought to avoid involving close ties in illness work. Interrogating the data, it became clear that this was common in parent–child relationships, either because younger people did not want their parents to worry, or, sometimes, because older service users did not want to worry their children. In these circumstances interviewees reported trying to cope on their own, using online resources or drawing on weaker ties:
It was bad, I could hardly breathe . . . I could see I was going blue and I thought I did not want to panic [my husband] so I was trying to cope with it. So in the end I did wake him up and I said I did not feel very well and I thought we ought to call the paramedics.
P24, older
I may use my mum sometimes but I just don’t really want to bother her because she’s just going to be so worried. So I would probably prefer to do this kind of online symptom checks. If there was something that I was really, really worried about and then the next thing would be if it was an emergency I would contact the GP.
P54, East European
Weak ties
Weaker ties, such as acquaintances and neighbours, played a part in older people’s accounts of help-seeking. Those who cared for a partner, were single or widowed, or were more socially isolated categorised weak ties as important. These personal networks included neighbours, pharmacists, tradespeople already providing services, local transport and amenities:
I’m very happy here, I wish I’d moved here before. Because we’ve got a very close-knit community . . . I can always ask people for help . . . I don’t feel awkward asking neighbours to do things because I do things back . . . I’ve got three paramedics living next door to me as well.
P55, older, widower
The neighbours are brilliant. They are so important as they are invariably there . . . or I could phone our really good friends who are a 10-minute drive away . . . then the GP. If I needed my son or daughter for anything that I, well, yes, if I needed them to come, I know they would come.
P93, older, married carer with children far away
In the case of P55 below, older participants were often involved in the care of their elderly neighbours, and sometimes referred to these ties when making help-seeking decisions:
I went to a neighbour, and the neighbour did it for me. I knew she was a first aider. What I’d done, I’d run a knife into my hand and it was bleeding everywhere. I couldn’t stop the bleeding so I went to the lady next door but one and she sorted it all out for me.
P55, older
The younger group talked more about using social media and the NHS Choices website in help-seeking. They were often aware of the pitfalls of using the internet in terms of possibly exacerbating anxiety and providing unreliable information, and so tended to seek advice from the internet in combination with talking to other people:
I’d probably Google search or try the NHS one, and then if I couldn’t find anything that seemed reliable, or . . . even if I found anything I’d probably then call 111.
P65, younger
Run it by, I think, talking to other people. So if I was at my partner’s at the time, or at home with parents, talk to them about it. Probably, I don’t know if I should admit, but probably have a quick look on the internet. See what that says.
P63, younger
Moral work
We use the term ‘moral work’ to capture ideas in the data about ‘being a credible patient’201 and what constitutes an appropriate or legitimate user of health care180 and being a responsible citizen in medical encounters. 10,202 This moral work is closely linked to illness work and navigation work in help-seeking, and, like illness work, it operates at an individual and social network level.
Individual-level moral work
There is a clear moral tension for service users in help-seeking for urgent care needs. There is an expectation that health services should be used ‘appropriately’ and that users should be responsible service users (thus avoiding being labelled as a ‘time waster’ or as overly anxious) but also that users should make decisions that effectively manage health risks.
There was wide recognition across all three groups that urgent and emergency health services experience high demand. Service users were aware that accessing services ‘unnecessarily’ might waste scarce resources, place an unnecessary burden on services and deprive care from those ‘who really need it’. This awareness fed into decision-making. Concern about unnecessary service use was most marked in relation to emergency services (999, ambulance and ED), and was present, but less so, for general practice. Using urgent care services did not appear to create the same level of moral dilemma as the decision to use emergency or GP services:
I think that’s what came to our minds [using an UCC] because she [daughter] wasn’t in critical state, condition. So we thought there is no point to bother hospital . . . if maybe we can see the [out-of-hours] GP and it will be enough. It was night-time, so it’s more convenient for the child as well [ ].
And how easy have you found it to make the decision to use urgent care?
It’s not easy. Well, I don’t like to bother people when it’s not necessary, so you have to really wait.
East European
I don’t know whether that’s just because I’m interested in health and health care, so I don’t want to waste resources, on an individual level.
P9, younger
Across all three groups, participants were keen to demonstrate that their actions were responsible or credible. They provided accounts of when they had not sought help for a health problem and had sought to manage it themselves, giving examples of symptoms they considered to be too trivial to make contact for. Older service users were quick to describe themselves as ‘copers’ and said that they tolerated symptoms, undertook self-care and took actions to reduce unnecessary health service use. Not accessing services was viewed as a sign of stoicism, or resilience, of which many people were proud. Many accounts used ideas of coping to contrast with others who might ‘rush off to the doctors’ (see next section):
I think we were brought up in that generation, like, at the beginning of the war, and you had to get on with life. I always remember . . . I fell out of a tree, broke my arm in three places, and my parents were stood in our lounge, discussing whether they could afford to get a doctor, because National Health hadn’t come in yet . . . I was 10 then . . . My mum was quite strong, and my dad was a strong character, and I think I got it all from them. But you just try not to bother people. I never go to the doctors, if I can help it [ ] But then, you know, they’re [the ambulance service] up to their eyes, aren’t they? And I think this is a lot of problems with older people. It’s so put into their brain that all this is going on, soldier through this and soldier through that, that they don’t want to bother people.
P23, older
Implicit in the accounts of older people was the expectation that over time they had gained the knowledge and experience to make the ‘right decision’. Contact with services for less serious symptoms was morally rationalised by reference to unusual or excessive symptoms, and help-seeking decisions in these cases often were attributed to the insistence of someone else:
I do tend to put up with a lot. When I had that stomach problem, and he [husband] called 999, I mean I wasn’t sure whether it was food poisoning . . . Well, I just started getting these horrendous griping pains. If you’ve got a bout of wind or something, it can be painful. This was just beyond that, and I was sort of shouting out with it . . . And he said ‘oh, I’ll dial 999’. ‘No, no’, I kept saying ‘no’, because I don’t like to be a nuisance. But eventually, he called them. And to be honest, I think at the end of the day it was some sort of wind trapped.
P82, older
Service users did not want to be labelled as ‘time wasters’ by health professionals, and fear of a negative reaction from the emergency services could push them to use urgent care instead. This view was reinforced by media portrayals of NHS service users (see Chapter 4):
I’m conscious of not wanting to get there [ED] and people be like: ‘why are you here?’ Which, I guess, if I was in need of help, they wouldn’t, but it’s also that . . . in the news, people going to A&E that don’t need to be there . . . It almost makes you nervous about using it, because you don’t want to be using it with the wrong, sort of, reasons.
P9, younger
These beliefs also prevented people from making contact with their general practice surgery, as they were afraid of annoying their GP and sought to avoid ‘bothering the doctor’. Some younger people said that they preferred to contact NHS 111 but older people tended to use the pharmacy in preference to going to the general practice surgery:
I think there would be an instinct in me [to use NHS 111], because there always is when I go to the GP if, I don’t want to make a fuss out of something that might not be a fuss or I don’t want to annoy the doctor.
P57, younger
It was pretty easy to make the decision to go to the pharmacy, so I wouldn’t have bothered the doctor or even the nurse, so that was no problem.
P5, older
One interviewee placed the moral work in historical context, and suggested that the wide range of services now available was a change for the better in as much as it removed or reduced the moral burden of calling your own doctor:
I think . . . it’s better now than it ever was because my mother’s generation, they were always very worried about phoning up doctors or bringing anybody out. But that has gone . . . because that’s what they’re there for, doctors, aren’t they? . . . I remember a couple of times when my mum said, ‘Oh, no, no, don’t call the doctors. They don’t want to be woken up in the night’. It would be all this sort of rubbish, you know? . . . And so I think that’s better.
P56a, older
Moral work in a social network
Moral work includes efforts to legitimate help-seeking choices by comparing, referencing or evaluating against those of ‘others’. We identified three subthemes in relation to this aspect of moral work, comparison, sanctioning and entitlement, which are discussed in turn below.
Comparison with others
Interview accounts compared people’s own use with that of ‘others’. As we noted in Chapter 4, other people may often be judged as time wasters, but individuals, as one might expect, justify their own use of services as rational, appropriate and responsible, even for apparently ‘less urgent’ symptoms. P13, for example, was extremely disapproving of others but admitted using the ED for a more minor issue. She legitimised this help-seeking behaviour by referring to the level of panic she experienced, but she was also one of the few interviewees to point out the contradictions in her stance:
I think people panic so much, they can have a little thing like ‘all right you’ve broken your arm, it’s going to hurt like hell, but it’s not a big deal, you’re not dying. It’s not major, so take yourself to the hospital, not A&E, because it’s not an emergency’ . . . You need to go to A&E when you are bleeding like severely, or there is a chance that something . . . could be fatal. You know, that’s what A&E’s for. Unfortunately we were there for something that really was not quite [an emergency] . . . I’m being really, really bad right now, but I panicked about it.
P13, younger
Responsibly using services, especially the GP service (‘not rushing off to the doctors’), was important to many interviewees:
Personally I’m one of these people, I won’t go to the GP unless I really have to and unless I’m near death I just don’t do it. So I think an emergency is literally if you’re really deteriorating quite fast or you’re put in a situation where you’re potentially putting yourself at risk, I think then you need to go to A&E.
P40, younger
I go to the GP quite a lot for valid reasons. I’m not one of those people that go there for no reason. But, like, I do go there quite a lot. I trust my doctor a lot I think he’s really good but if I needed medical help I’d probably go to him first unless obviously I’d like broken my leg or something then I would go to A&E.
P43, younger
P22 criticised others for using the ED for minor illnesses, but acknowledges that ‘others’ may make the same criticism of his actions. He provided an example of calling 999 for a non-life-threatening problem, all the while emphasising his attempts to be a responsible citizen (e.g. going to a WIC first) and indicating later in the interview that his son telephoned for an ambulance:
I take the local paper and the headlines on there is, they found out that [name of] accident and emergency, one in seven [people] shouldn’t be up there. Well I would say that is a very modest estimate, I’d have said one in three from my experience . . . I mean people go up there for the slightest things. Things they used to treat at home, they now go to A&E for [ ] I’d seen a chap who’d . . . He’d burnt his hand with a bit of drain cleaner. Well you know, it was only a little bit, it’s the sort of thing you’d put under the tap and, you know, see what develops as it were [ ] But I mean, they may look at me and say, ‘well, what’s he doing here?’ So it’s swings and roundabouts . . . My foot was hurting . . . then my son turned up. And I said, ‘well you know, you get us down to a walk-in centre’. But I couldn’t walk. And they couldn’t get me down the stairs you see. So my son phoned for an ambulance, 999 ambulance . . . then asked me what it was for and I explained I’d had a fall, and my foot . . . I couldn’t walk because of my foot and all that. He was ‘are you having breathing difficulties or chest pains?’ ‘No.’ ‘Oh right, so it’s not a dire emergency, let’s put it that way.’ I said, ‘No no, not at all, no, not at all. No, I can wait a bit’ . . . They eventually turned up. I had my accident about half past 10, we phoned about 11 o’clock and they came at half past 2.
P22, older
The notion that unnecessarily using care could deprive or delay care for others was perhaps more common among younger people. Sometimes interviewees said that they did not use services because ‘other people need care more than me’:
. . . the pain just shot up my back, so I presumed, ‘OK, I’ve done something to my back here’. And I ended up stuck on the floor. My mum phoned my doctor . . . she wasn’t at home . . . and the doctor prescribed me some painkillers over the phone. I didn’t get to see anyone at that point . . . Looking back now, I probably should have phoned an ambulance because I was unable to move but, again, my attitude is there’s people worse off than me, those people that need the ambulance for.
P49, younger
Sanctioning choices
Members of our participants’ social network helped to sanction or legitimise decision-making, and could alleviate the moral responsibility of decision-making for individuals. Participants gave examples of times when they had been reluctant to contact health services, but were persuaded to do so by others:
Perhaps what other people around you think, because I think sometimes I’m the kind of person that I know I tend to play down a lot of how I’m feeling, because I don’t like going to the doctor and I don’t want to go to hospital, but you know, in that moment my boss said ‘no, I think you need to call 111, you’re clearly not right’.
P68, younger
Younger service users were more likely to cite others (usually parents, but sometimes managers at work) as instrumental in making the decision to seek urgent or emergency care. P9 suggested that her parent had a tendency to over-react, and other younger people indicated that family members (usually parents) experienced high levels of anxiety about their child’s health problems:
I complain a lot [when unwell], but I generally, like, I just, sort of, get over it, and then don’t really . . . I’ve got quite a high pain threshold, I think . . . They [parents] were both quite shocked that something serious was actually happening [ ].
And had you lost consciousness, or . . .?
. . . Yes. I think my mum was quite scared. She was probably more scared than I was.
Younger
In the following account, P51 describes her mother as a someone who has a tendency to ‘panic’ but then justifies her tendency to call on the emergency services as a sign of caring:
So you’d have some people who break their legs and then they’d be like, I might as well get myself there then. And some people, the first thing they’d do is call 999. So yes, I guess it’s just down to how much the person chills and stuff and how unchilled they are I guess [ ] I know like my mum would probably panic immediately kind of thing. She’d like . . . She’s very caring and stuff so if something’s wrong, BAM, kind of thing.
P51, younger
This indicates some of the complex reasoning behind decisions to seek help. In addition, interviewees provided accounts of occasions when help-seeking for an apparently trivial matter had been vindicated when their symptoms had been found to indicate something serious:
[My] mum used emergency services because when mum was pregnant with her, she felt something was wrong. She used the emergency. She called someone and they come up, and told her she had to have an emergency caesarean. Even though we take the mick out of her for being a hypochondriac . . . It turned out to be right that time, and we felt a bit, like, ‘no, Mum, there’s nothing wrong’. OK, there actually was something wrong. We felt quite bad about that.
P38, younger
Entitlement
Some service users felt entitled to use health services. Older and East European interviewees in particular sought to justify their entitlement; they suggested that they were not sick very often, did not use services unnecessarily, and contributed to the health service via taxation. Older people were the most likely to articulate the view that they felt they had a right to use the NHS because they had ‘paid into it all our lives’. This sense of entitlement was particularly strong when a service user perceived that they had been treated as a time waster or that they had not received the care that they had wanted:
I thought, ‘hang on a minute, you know, he might be older, but we paid all our life into this’, you know, and we’ve never asked for anything very much from the National Health, and you’re made to feel as though you’re not wanted, you know.
P23, older
I don’t think, at 82, I should have to wait seven and a quarter hours to see a doctor when I’m in pain. And, it’s obvious one was in pain, because you can cry with pain, and I certainly was crying with pain. I mean, I really didn’t know what to do with myself, other than sit.
P12, older
I am not really a sickly person so I don’t get sick at all. The only time I go to doctors is for smear tests or travel, to have vaccinations. So I don’t go to doctors at all. So I think they knew it must be something I’m really worried about to arrange for an emergency.
P54, East European
The sense of entitlement from paying in via taxation, or, as in the case below, from working in the NHS, extended beyond the discussion of urgent and emergency care help-seeking. For example, this East European interviewee explained why she felt that she should be able to access NHS care:
We tried to get to do regular checks because in Hungary, we used to go, yearly check-ups [for skin cancer] to see what has to be checked because he is, you know, he has loads of spots . . . So we said it’s bonkers to go back. We are paying national insurance. I am working in the NHS, both of my daughters work in the NHS. It’s bonkers that we can’t have this care here. We got a referral after a long while from GP to see a skin specialist in community care, and he was really rude. He said, you know, ‘you don’t have anything major to worry about; you shouldn’t be wasting NHS time’.
P33b, East European
These ideas about entitlement also linked to those concerning fairness – and service users were especially upset when being responsible was not rewarded. The sense of injustice was acute following a negative experience with urgent or emergency care (e.g. when they had been made to feel like time wasters). P55, for example, felt that she had been treated as a nuisance because she was elderly. She perceived that others were able to gain access to care by being more demanding (or more charming):
I’ve been to the walk-in centre . . . Well, I’m not very impressed. You have to wait a long time . . . if you’re an old biddy, they don’t want to know [ ] I went up there one Sunday morning because I knocked a pan of water over my hand and it was all wrapped in a towel and everything. I walked in and I was shaking. I was upset, I was crying. [The nurse said] ‘what’s the matter with you then?’ So I said, ‘well, I’ve scalded myself, I think’ . . . She said hour and a half [waiting time]. So I said, ‘OK, thank you’ . . . Then this young man came in and she said ‘what are we going to do with you here?’ And this happened three times. ‘And, oh, I’ve got a cough. I’ve had it for 3 days.’ ‘Oh, well, we’ll see if we can get a nurse’ . . . Maybe it’s just me but . . . three young men all got charm and I got, ‘well, you’re just a bloody old nuisance’ [ ] It’s my generation. You don’t make a fuss . . . You assume that the system works and that you will eventually be seen. But it strikes me that the louder you shout, the quicker you get heard nowadays [ ] It seemed to me that they’d come for rubbish [to the UCC]. You know, one had got a cough and the other one had not been feeling very well. Probably got a hangover, you know? It seemed quite trivial for me sitting there with a scalded hand. I would have thought that was more of a priority than somebody with a cough.
P55, older
Similarly, P24 was upset and defensive about his experience with the ambulance service and his perceived wider portrayal of the elderly in society as being demanding and high consumers of health care. Again this interviewee drew on the idea of entitlement and having paid for services:
I was completely confused in the end the way they spoke to me [paramedics] . . . he was quite bolshie and I thought ‘well, we started with the NHS in 1948 and we have gone through our lives, we have paid for it and we have not bothered them as much as some people do, we have been pretty healthy’, haven’t we darling?
P24, older
Although not a commonly expressed view, a small minority of elderly service users held the belief that others (notably students and migrants) placed additional demands on pressurised services, thereby depriving them of the health care that they felt entitled to:
I’ve got nothing against students but they are clogging up the system . . . Is it a walk-in place down at the [name of area]? [ ] Why can’t they make that into a student surgery? [ ] Loads of them live around there . . . But it would be a point where they would go, rather than clog the surgeries and [name of ED], of their own.
P23, older
The younger group were much less likely to express individual entitlement although a few suggested that young people were marginalised by health services:
I should think that health-care systems around the world differ quite a lot, like Canada is a lot more efficient than in the UK, even in Australia they seemed a lot quicker in getting you seen. The UK is a bit slow, they just seem to ignore young people. They always put other people first, so they do not give us the services that we need.
P62, younger
Navigation work
To help us think about what is involved in navigation work – that is, the processes of choosing and accessing particular care services – we drew on Penchansky and Thomas’s dimensions of access. 186 In particular, we focused on availability and accessibility, as these themes stood out in the data in relation to urgent and emergency care. We sought to explain how service users made choices between what is available (the type of services and the resources, e.g. staffing and technology), what is accessible (how easily the service user can physically reach a health service) and how they are ‘accommodated’ (how services are organised and configured, e.g. opening hours). We also recognise that navigating health care is informed by previous experiences, knowledge and perceptions about illness and about services and the acceptability of these. We therefore also draw on the concept of ‘recursivity’, which describes a service user’s experiences of health services and their future help-seeking. 128,203 Navigation work thus combines sense-making (based on experience, knowledge and perceptions of risk) and help-seeking behaviours (following a pathway through a care landscape). As with illness work, this takes place at an individual level (service users draw on their personal knowledge, experiences and perceptions) and within a social network that supports action directed towards seeking help.
Individual-level navigation work
To navigate urgent care services, users need to know what is available and when it is available. The literature review (see Chapter 3) and the sense-making findings (see Chapter 4) confirmed that service users are unclear about the different services on offer. Urgent care is provided by a range of services (see Chapter 3), which are available at different times of day and may have different facilities (in terms of advice, diagnosis and treatment). Even services with the same name and branding can vary, as there is a lack of standardisation of what, for example, UCCs, WICs or MIUs actually offer.
Availability
Service availability is contingent on time (i.e. the time of day that the symptom occurs in relation to the time that particular services are available). Service users need to know opening hours, as well as what is offered at each service, in order to navigate the system:
I’m not sure if minor injury unit is open 24 hours, but for me that would be strictly what is the issue. So let’s say he [son] had a fall from stairs and you could see a fracture or whatever, it depends what time. I guess . . . Minor injury is not open during the night so I would probably call first A&E, ask them first.
P67, East European
There was considerable confusion among interviewees, as there had been in the citizens’ panels (see Chapter 4), about what sorts of illnesses and injuries could be dealt with in urgent care. There appeared to be more confidence among interviewees about what services an ED would provide. This was often seen as a ‘one-stop shop’ where a range of specialist facilities could also be accessed. Choosing to attend an ED was a way to maximise the chances that the facilities needed would be available, thereby avoiding the risk of a potentially wasted journey:
If you’ve broken a leg, say, you need it to be not made worse. It needs to be positioned and put in plaster, so your average GP surgery’s not going to be able to do all that . . . If it requires an X-ray, then you clearly . . . I believe the minor injuries [unit] have X-ray facilities . . . but is that known? I think a lot of people go to A&E because they assume or know that they’re going to need an X-ray, but X-ray facilities are available [elsewhere].
P21, older
It’s a nuisance to get to the hospital because it is an hour away but once you are there . . .
It’s all there.
At the hospital [laughs].
So here in, like, town, there are different services taking place at different places and . . .
Yes and that’s a bit of a pain.
Older
However, the ED might also be avoided by those who perceived it as a busy or an unpleasant environment. Urgent care was sometimes described as a more comfortable, less crowded environment (even if its waiting times were similar to those of the ED):
I think I prefer to go to one of the drop-in centres, rather than up to [ED] because that’s . . . it’s usually overflowing, isn’t it, with people waiting to be seen . . . It’s a pleasanter experience, anyway, I have to say, certainly at [WIC]. The [name of WIC] is a bit dire, I suppose . . . it’s rather cramped, and you probably . . . sometimes you can’t get a seat, so . . . it’s just it’s usually crowded, people coughing and spluttering all over the place, kids screaming. I shouldn’t complain about that. It’s just, you know, not a very pleasant environment.
Yes, and what’s your understanding of the difference of the care that you might receive at A&E as opposed to the walk-in centre?
. . . I’ve not experienced any difference in the standard of care, so whenever I’ve had to access these places, it’s always been OK; apart from waiting, car parking at [WIC] is a pain. The . . . car parking at [ED] is not very good now, either.
Older
Some accounts highlighted a lack of confidence in the health-care professionals at particular services, opinions formed from experience and knowledge shared in people’s social networks. When service users felt that they had not been listened to or not taken seriously, this did not deter them from seeking help, but it might change which service they chose:
When you came in the reception and you start speaking with foreign accent, these old ladies are a bit like this to you and they’re, OK, OK. And they talk to you like you are an idiot, if you know what I mean.
P3, East European
I think the difference with the 111 service is you’re talking to somebody on the end of a phone. And sometimes, they’re so harassed that they don’t really . . . I won’t say they don’t listen properly, but they never seem to come over quite right. Whereas, if you go to the walk-in centre . . .
P23, Older
One of the strongest drivers of service choice was the perception of the time it would take to be seen (waiting time). Routine primary care was seen as the least accessible form of care compared with urgent care and the ED. What was really prominent from the accounts was that many service users did not simply choose a service that they knew; rather, they considered several services and chose the one likely to offer the shortest waiting time (often based on previous experience). Service users who had experienced lengthy waiting times in the ED were more likely to use urgent care in the future. What is interesting here is that these accounts of future use were based on an assessment of waiting time rather than on an assessment of severity. Thus, for some the ED was not seen as an ‘inappropriate’ choice, but it would be rejected as less efficient:
They were really good there, as in minor injury unit, or out of hours. So next time, and the queue was shorter, so next time, maybe rather than going straight up to the A&E, I will consider using the minor injury unit.
P2, East European
I still don’t know that I would go to A&E because I know the waiting times are horrendous so I am not sure if I wouldn’t try somewhere else first like a walk-in centre because maybe they would be able to help him there.
P31, East European
However, for others, particularly younger participants, the ED was regarded as the most convenient choice and appeared to offer a prompt service. Choosing to use the ED was about convenience rather than clinical need, with some service users reporting choosing to attend the ED when it was likely to be less busy. The model of the patient as consumer was apparent in such accounts; indeed, one used the consumer term ‘served us’:
The A&E was very calm, they served us pretty quickly in like half an hour or so.
P46, younger
As for things like A&E, for minor injuries, that’s just, sort of, a gamble really. If you think something is not all that wrong but you still need to go to A&E, having the luxury of picking and choosing the time, like go in the early hours of the morning because that might be a bit emptier, you’ll be seen quicker. But for something serious you don’t really have that luxury, so you could be going in whenever and it could be really busy or you could get lucky and there will be no one. Generally there’s usually some sort of wait just to get through admin work.
P37, younger
Anyway, sounds a bit like the emergency clinic, well it is emergency clinic isn’t it, and they asked him all sorts of questions, fill in all sorts of forms and then said go to the accident and emergency clinic. Well he didn’t because he said ‘I’m not going up there this time of night’, it was sort of 10:00 [pm], so he says ‘I’m going in the morning’.
P29, older
To help them assess the availability of timely care, some participants sought out information about waiting times. They looked up information on the internet [some urgent care services use Twitter (www.twitter.com; Twitter Inc., San Francisco, CA, USA) to inform people of their waiting times] or telephoned the ED to enquire about the waiting time before travelling. When P67 did this, she was advised to attend later when it might have been less busy, which can be seen as reinforcing the use of the ED for something that ‘wasn’t that serious’:
I remember with the knee, that was I think Friday or Saturday night, so we actually didn’t want to go to A&E because you obviously spend like, sometimes a few hours and it wasn’t that serious, but you never know if you can just do something, you know by just walking if that will get worse, so we like just rang them up and said what is the approximate waiting time and they tell us.
So you called the A&E ahead?
Yes. And we just asked them and they say . . . I think we asked them in the afternoon and they say it is busy but you can try later on and then we just asked them again and we said that it’s OK or something like this.
East European
I’ve obviously looked at the minor injuries unit when I hurt my ankle, but chose not to use that because of the delays. But, apart from that, I’m not really aware of anything else that’s, sort of, out there.
P9l, younger
Some decisions were made to optimise service users’ own time; for example, urgent care attendance was sometimes co-ordinated with other activities:
Well, I didn’t feel resentful because it was better to have that service even though you had to queue up . . . But if I was there with my son, I would go and do some shopping and he would keep the place. It’s, like, you had to think creatively but it was doable.
P4, East European
In all three groups, urgent care was viewed as an available and more convenient alternative to visiting the general practice. Urgent care services facilitated access and, unlike GPs, did not require an appointment. P1 disliked the lengthy waiting times at the WIC, but she used it when she was unable to obtain a GP appointment:
It’s more difficult to go to walking in centre because most of times you wait, because most of times you’ve got some procedure where you need to go. You fill in loads of forms and definitely it will take you at least 2, 3 hours. So if that would be something that you don’t have an option to go to your GP [ ] I think the walking-in centre is good if you can’t get your appointment at GP.
P1, East European
Other service users arranged care around working patterns. A small number of service users said that they used NHS 111 to bypass the GP. P13 justified working around the system in this way by suggesting that this was also better for the GP by ‘saving the doctor’s time’. This was a particularly common feature of accounts by East European and younger participants, who were more likely to be negotiating health care in the context of paid employment, studying and family commitments:
When I used them for the first time, walk-in centre. I don’t remember how I found out that I can use it for like, yes, the urgent problems, but without going through the process of making an appointment with the GP, because it’s easier, accessible than the GP.
P3, East European
I’ve started taking them [children to the UCC] which is so much easier than going to the doctor . . . I could start work at 14:00 like today, and if it happened today I’d get on the phone now . . . It’s fantastic. Because of work I wouldn’t have time to wait for a doctor’s appointment. You don’t have time to phone your doctors because you can’t ever get through . . . I don’t want to sit in discomfort, so for me that is the easiest way to go about it. And they are so helpful . . . If phone the doctors up I have to wait for an appointment, probably 2 weeks, then you have to go and do a sample, then they have to test it and . . . It’s too much. Why would I go and do that when I have this option which is fantastic? It’s brilliant [ ] Like UTIs [urinary tract infections] and stuff you need antibiotics so it’s the longest thing to attempt to phone up the doctors and wait 2 weeks for a doctor’s appointment. I can’t do that because it hurts so bad, so I phone up 111. They are so good . . . I say ‘I phoned you not long ago, and I complained of this and now I’ve got it again, can you please get a prescription sent to my pharmacy so I can have antibiotics because I just can’t work, you know, it’s really hard’. And they are fine about it . . . And he does literally within the hour . . . ‘fine, yes, we’ll get a prescription faxed over’ . . . Which is the best way ever . . .
So you’re not needing to use primary care. So you’re not going to your GP?
No, why would I want to waste their time when I can do it this way?
Younger
Always . . . 2 hours waiting in the walk-in centre that’s why . . .
That’s why you don’t go back?
Yes we don’t go back . . . If we need to see a doctor we just call 111. Wait 2 hours at home because then we can sort of he can play and get busy around here instead of get bored at the walk-in centre . . . So it’s better to sit here wait for the call and then go to the [UCC] spend half an hour, 40 minutes and that’s it.
East European
Accessibility
Urgent care centres and WICs are typically located where they are accessible and convenient (e.g. in town centres). Participants rarely commented on the ease of access to these (P20 below is one of the few exceptions):
Well until quite recently we did use occasionally the [name] walk-in centre. I mean, we were obviously very against that closing . . . Obviously it was very handy for us because it’s walkable.
P20, older
For many service users, proximity drives their choice of where to go. Help-seeking decisions are primarily driven not by seriousness but by how accessible services are. Younger participants particularly chose services that were closest and offered the shortest wait:
Even if it is something quite severe like a possible broken arm I would call that a minor injury and I might go to, I would go to that drop-in centre if it was out of hours. But I might equally go to A&E if it wasn’t out of hours. I don’t know, it depends on which was the nearest I suppose.
P75, younger
Younger participants also suggested that they felt reassured by living close to an ED:
It’s really positive because you’ve got it right round the corner. So, it’s a bit more reassurance that if I am ill I’m literally 5 minutes away from the hospital and I can get there . . . Air ambulance goes over so you’ve got that big kind of centre near you and it’s kind of a regional, you know, trauma unit. So, you know you’re in safe hands and it’s right round the corner.
P59, younger
Do you think about the time of the day, access . . . transport . . .
Definitely, I think about geography and how close I am to certain services, so if the hospital is closer than others [services] or a doctor’s surgery . . .
It is the convenience isn’t it.
Yes, the convenience and I think, I personally think with A&E, Monday is quite a busy day because everyone waits the weekend . . . Mondays are really very busy. I work 9 to 5 so I would probably try to do it out of hours if possible or over my lunch break.
Younger
Some recognised that using the ED for more minor medical problems was not the most appropriate choice, but said that the difficulties of travelling justified their decision:
But I knew it wasn’t really the correct place, I wanted a walk-in centre but there isn’t a convenient one for here. I mean, there’s the one in Gosport but trying to get into [name of MIU] is murder, and the other one is [a different MIU]. It’s so far away you could die on the way.
P22, older
NHS 111 was popular with younger participants. Telephone access overcame difficult or inconvenient journeys and offered the additional benefit of avoiding unnecessary and unpleasant waiting:
I guess 111 . . . you ring them up and they kind of assess you on the phone. So, it is almost like you do not have to go all the way to them in hospital or anywhere like that you can just ring them up and then they could tell you on the phone what to do. And I think that is quite good because sometimes you don’t really need to go all the way in. Also for me when I went to A&E myself, maybe like talking on the phone beforehand would have been a better option because when you are in A&E you are around so many people who have different problems and a lot of it is people on drugs, or drunk or they have injured themselves doing that and it is just a bit, like, it is a bit overwhelming for the A&E, especially if you have got something fairly minor.
P76, younger
However, others – notably this East European interviewee – preferred a face-to-face rather than a lengthy telephone assessment:
I know when you are not too bad, it doesn’t matter that you wait 2, 3 hours. But if you are really in a critical condition and you still have to go through this telephone interview, very detailed one, you know, someone can die at this, in the meantime [ ] It was fairly easy to access walk-in centre, for example. You just need to walk there if you are able to walk, yes. But I found it a bit more difficult to access GP out of hours.
OK, what was difficult about that?
The telephone interview they take you through.
East European
Social networks and navigation work
Although many of our data suggested that navigation work was performed individually, service users also made health-care choices in consultation with relatives, friends and neighbours. They also drew on a wider network of weaker social ties and made use of the internet. Younger service users accessed the internet to seek out information about service availability, and they used advice gleaned from networks available online as well as from family members to help them navigate services:
I tend to make my own decisions but sometimes I’ll ask my mum. But I know a lot of people, I see it a lot on Facebook [www.facebook.com; Facebook, Inc., Menlo Park, CA, USA], where can I go for, people ask like Facebook sort of thing. Maybe a lot of people that are younger might ask Facebook.
P40, younger
People’s social networks influenced decision-making in different ways. P28, for example, described how she had been persuaded by a friend to use the ED, making a choice that she suggested was different from the one she might have made otherwise:
You know, if you’re on your own, it’s different. I mean, if I hadn’t had [name of friend] to talk to, I wouldn’t have gone to A&E at that stage. Not then. I might have left it a bit later.
OK. So you’d have watched and waited, and . . .
Hm. I would have been trying to think, what shall I do? But then again, I’ve got the experience.
Older
As might be expected, parents usually made the decision about which service to use on behalf of their children. Less commonly, adult children made decisions on behalf of elderly parents:
So you’d had several episodes of a nosebleed and on this particular occasion it was worse, it wasn’t stopping . . .
It wasn’t stopping, no.
And so what happened at that point . . .? Where you thought ‘this isn’t stopping’?
Well my son said ‘I’m going to phone’. He just decided to phone 111.
Older
People’s social networks played a role in informing each other about particular services and making recommendations and could therefore be important influencers on decision-making:
So who are those people who you might find information out from?
Yes, so that would be the close community. People you work with. People you socialise with. You would . . . Sort of, yes, ask them for help. Or they would be, when they talk about their own experiences, when you learn from people’s experiences. And that . . . This is where the negative side of certain services. That sort of comes up to the service where people say, oh, I needed help. But my GP was closed.
East European
I’ve never used the 111 telephone service. Somebody told me the other day that I should use the 111 service . . . 111 service because they’ve got a . . . if you can get to talk to the doctor, they’ve got a secret area at [the ED] that not . . . that nobody knows about that you could get referred to, but I don’t know whether there’s any truth in that.
P5a, older
In general, older participants drew on a mix of strong and weak ties to help with their health-care needs, such as third-sector organisations and patient transport, as well as neighbours, family and friends. These ties were based on geographical proximity and supported daily living as well as help-seeking:
I suppose I’m lucky, because I have backup around me, or even the neighbours. You know, I mean, even for my eyes. I talked to several people within the Close . . . then there’s U3A [University of the Third Age], Fox Choir and the Masons.
P7, older
While close interpersonal ties were highly important for East Europeans in their illness work, navigation work was much more dependent on having local knowledge of health services. This put recent migrants at a disadvantage, especially as their social network was often in another country and so unable to help them. Some East European participants had strong networks of friends to draw on in their local area; however, as P2 explained, fragmented networks could make it difficult to navigate UK health services:
Ages ago, before, if you asked your neighbour, where can I go? They would give you a definite answer [ ] Those families over here are quite . . . Well, the Polish community families, the new families, are quite fragmented. So it’s people who have got to know each other over here, and then they had a child. So, normally, back in Poland, the community is very close . . . Ten years ago, you tended to be born somewhere, find work around that area, study around that area, and have a family not far. So it was a very close community where help was available . . . Someone would be there to advise you. Whereas here, I think people tend to panic a little bit. And they just go to A&E, just to see someone, basically. Because it’s a young family, isolated from everybody. They don’t know who to go to, so go to the A&E, and that puts pressure.
P2, East European
There is quite a lot of Polish people who come in here and they don’t have much family here. And as long as you don’t have any problems you don’t think about it, but when you’re starting to have problems you actually do need to take your kids into car and you need to go.
P1, East European
Was it easy to navigate the services when you first arrived here? Was it obvious?
I don’t think I struggled. Well, it’s not that it wasn’t easy to navigate; there were just things I never knew about. And I only found out years later that I could have used this service [urgent care] rather than struggle. It’s not something that, you know, when you move countries somebody gives you a lovely leaflet and tells you that, that, that, that. You need to find out yourself, so, I went as far as finding out where my GP, which surgery I’d like and what GP. And other things came much later and I didn’t have a family or very good friends initially to point me in the right direction either, so.
East European
Wider social contexts
We have shown that urgent care help-seeking, as described by our interviewees, entails three different kinds of work: illness, moral and navigation work. Although much of the work is performed by individuals themselves, choices are influenced by members of social networks: both strong and weak ties. These influencers can facilitate help-seeking work and shape patterns of service use. Alongside these network effects, we also identified a range of contextual factors that shaped help-seeking. The next section explores some of these features of people’s social contexts that were most prominent in the interview accounts and that appeared to influence help-seeking. These included living arrangements, work commitments, mobility and access to transport, and language. In the discussion that follows, we highlight how these factors influence help-seeking and note too how they can be mediated by the time of day in which help is needed.
Living arrangements
Those who were married or living with partners or other family members had access to support and advice in decision-making about help-seeking, but also for accessing services. For those who lived alone this was more problematic. Social support was more readily available during the day for most people:
Did you feel having your daughter there impacted your decision in any way?
Well actually I’m not quite sure what I would have done if she hadn’t have been there actually because the two other people I would have called on were totally unavailable on that Saturday afternoon. So I was glad that she was there I have to say.
Older
I knew [name of a friend] would take me. But she had to come over from [different area] . . . You’re aware of all the other things going on, then. You know, if somebody’s taking me . . . She’s got to get here, she’s got to get back afterwards. Is it going to be a long time?
P28, older
The time of day and the source of support could influence decisions about when to seek help and which services to attend. Some called on support more quickly for fear of being left without help during the night or to avoid having to bother others at night:
My neighbour on the end of this block, I’ve only got to ring her, and she was around, you know . . . I think it was the 111 she called because it was a Friday night. And she was always there for me, you know, and help me. But it got to the stage where I thought, this is like 7 o’clock at night, 7:30 at night, I’m not going to be able to cope with him on my own, in the night, if something goes on like this. OK, I know [neighbour] . . . if I’d have rung, she can come around. But there’s something different about bothering them in the middle of the night to it is in the daytime. So, she said, come on, [name], we’ve got to get some help.
P23, older
Although most people said that they had someone they could call in an emergency, many were reluctant to bother others late at night, and this was especially true of those who lived alone:
Say if you had a health-care problem that couldn’t wait until the morning, how would you decide what to do? . . .
Is it 111. Ring them, but then again would you get anywhere with them? You read such things in the paper about [them] . . . So I suppose I’d ring that as a first port of call, if I got nowhere then I think I’d do a 999 if I thought it was really . . . if it was pains in my chest or my arm or anything and I thought it was a possible heart attack I would. But other than that, I mean I could try ringing [son], but their phone’s downstairs, would they hear it, and I couldn’t ring my other daughter-in-law because she’s deaf. She wouldn’t have her hearing aids in or anything at night [ ].
So in the end you decided to do nothing [about a recent episode of illness]?
I carried on being sick on in the sink . . . Yes, just work your way through it . . . Well I’ll probably be one of those bodies they find in the hall 4 days later, you know, crawling with maggots.
Older
This kind of anxiety was felt more acutely at night, particularly by those living alone, and the quotation above illustrates the other social factors that are considered, ranging from knowledge of services to illness work and consideration of the social situation of different social network members. Those living alone often recognised that fear and anxiety was worse at night, and interestingly this could encourage them to avoid seeking help:
[There is] the likelihood of me doing it wrong and either overstating it [the health problem] . . . you know, exaggerating. Because it’s me, and I’m on my own. It’s me, me, me. Yes, especially at night things may seem, sort of, a lot more drastic than they really are.
P2, East European
I had this most terrible pain in my thigh that came on in the afternoon, and I went to bed but I couldn’t stay there and at about 1 o’clockish I had to get up and sit in a chair. And I was getting in a bit of a flap because I was wondering if it was a thrombosis, you know. Because, you know, you just don’t know. Anyway, the dark hours and especially the wee small hours are always the worst if you’re ill. If you’ve never been ill you wouldn’t know that but the wee small hours is when you feel at your worst, your lowest.
P22, older
Younger service users reported that changes in their living arrangements (e.g. moving out of the family home) meant that they were required to manage illness and seek help with less family support than they were used to. This too was frightening:
Very scared because I come from a house where there’s always someone around. It’s a very busy house. Someone’s always there. Someone’s always around . . . So coming home to . . . a situation where everyone was not always there it was kind of . . . probably, you know should take this matter seriously because if someone isn’t here to help me or, you know to help me make the call, you know it probably would be a bit more daunting for me.
P30, younger
The other living arrangement that had an impact on help-seeking involved care relationships. Caring for others appeared to amplify illness, moral and navigation work. In addition, the responsibility for others had to be co-ordinated and factored into help-seeking choices; this might include identifying someone to look after children as well as deciding which service to attend. In the case of P1, there was no one easily identifiable if her sister was not available, and so this was factored into her decision-making:
When you’ve got children and I’m with him [husband], you can’t, should I take them with me? I don’t know. And when it’s something serious and you’ve got this option, it’s easier because . . . I don’t know. Probably we would wait until morning, maybe, and you never know what would happen [ ] I don’t know if even I could ask neighbours to come too much. I don’t know because I never actually had to try that. But you can phone for example, my sister, that she could come in. But it’s taking time and if you know that it’s not an emergency then you . . . I think it depends on situation.
P1, East European
Work commitments
Work commitments also influenced help-seeking. For some, it meant accessing care that best fitted around working hours, and this meant attending a walk-in UCC rather than making a GP appointment. For others, it meant avoiding care:
I was really worried about him, he kept dozing off and he looked very white. And I said ‘I think there’s something wrong with you, there’s something more’. And I said ‘I’m going to phone the ambulance’. ‘Don’t you dare phone the ambulance! I’m fine! You know, I’m fit, I’ve got to go into work tomorrow’.
P56a, older
A few people spoke of pressure from work to not take time off sick, or to seek medical care. In the case of P89, this influenced whether or not they would choose to seek help:
It was my boss. I didn’t want to go. But I’m conscious that I’ve been coughing and I’ve been a bit of a nuisance to people in the office. And I didn’t call in sick. I went home a couple of times, like, earlier. But my manager said that you need to get it checked out, because we can’t have you call in sick when we’ve got events happening. And because the week was quite quiet, I made an appointment . . . I called in on Monday. The only available appointment was on Friday. So obviously I got better in that time, but I’m still not fully well. But I guess, if there’s nothing they can do, there’s nothing they can do. But I think, next time, I’m going to tell my manager I’ve been, and I’m not going to go.
P89, East European
Mobility and access to transport
The interviews suggested that for most of our participants access to transport was not a common constraint to help-seeking. Most either had their own transport or could call on others from their social network. Older service users and/or those with mobility difficulties, including people who were frail or recovering from illness or injury, were more likely to enrol others in providing transport:
Well, [name of husband] was in pain and he obviously needed urgent looking at so I phoned for 111 and they said go to emergency. Well at that time my son was living near [name of village] so he was able to take his father to the hospital.
P29, older
Or, it’s urgent, it’s not an emergency, I can get myself to that place, for example, or I can ask a neighbour or someone to give me a lift. The . . . minor injury unit, or the walk-in centre, or out of hours.
P2, East European
The availability of such support and time of day would influence the choice of service attended.
Navigation work was thus more complex for those who relied on others for transport.
Well, if I had an accident or anything like that and they were around, I would . . . you know, if it’s the weekend then I would contact them normally. But they’re not always around, you see? They’re all at work and everything. You can’t rely on your family.
P55, older
I think because obviously I was aware that if I had to see somebody that day I’d have to go to the walk-in clinic and if I had to do that then I was going to have to get somebody to come with me either to drive me or just to accompany me. And I have a boyfriend, you know who lives with me, but he had to help me get back from work and then he didn’t know if he needed to go into work straight away because you can wait around [ ] it wasn’t the end of the world, my boyfriend could have come back from work and if I did need to see somebody that day, but in a perfect world it would have been sooner.
P68, younger
Older service users, although less likely to have access to transport, often described themselves as self-reliant, and they were keen to avoid burdening people they knew:
So [did you] take yourself to A&E?
Yes, that’s why my car sits outside. You know, it’s rather than me bother the family, if I think I’m fit enough to drive, I will get myself wherever I’ve got to go, within a small radius; because I don’t drive too far these days, I have a boundary.
Older
You got on the bus to the walk-in?
Yes. Because it stops at the bottom of the road . . . And then it stops outside the hospital. And it’s free for me because I’ve got a bus pass. Because that’s another thing, you keep taking taxis everywhere, and it eats into your pension, you know. So, if I can, I get there under my own steam. And my neighbour really gets angry with me because I don’t ask for a lift in their car. You are so stubborn. I said, all the time I can do it, I will do it. When I can’t, then I have to ask.
Older
Again, these behaviours can be seen as contributing to the choices they made about service use.
Language
The potential difficulties of English as a second language was not a common theme in our data, and this may well be linked to our data collection method (interviews required some proficiency in English). However, the East European participants did refer to the ways in which language could hinder navigation work:
And sometimes there might be language barrier. And sometimes you might not understand the difference between these numbers. And then it’s good to have someone who can at least calm you down. That’s what my mum was doing. And then you can have step back and think again if it’s really, like, something wrong.
P1, East European
So when you first moved here, was the range of services available to you clear, easy to navigate?
No. Of course, not. No.
Tell me a little bit more about that?
Oh . . . Yes, there was no information whatsoever, and my English wasn’t that bad, so I could find some information on my own. But I didn’t know where to look for. We didn’t have internet at home at that time, so I could only use it at the library, and I didn’t know that I can ask a librarian about things because, you know, in Poland it’s not that obvious that you can . . . People are more left on their own to do things in Poland, so you have to be very resourceful and find your ways. Whereas here you got all these services provided. You just need to know how to use them.
East European
Services accessed by telephone presented more difficulties for some whose second language was English:
I don’t know because this 111 service this need to go through the 20,000 questions but obviously is there like option B? I know what I need can I just tell you I need to see a doctor because I need this antibiotic or double check instead of going through is he breathing? So far yes but . . .
So you’d like to let me know that it would be helpful if there’s another option.
Yes is there like option or is the study going to go somewhere with it? OK this 111 service could go two ways or something you know. To avoid all the questions. Because . . . some sort of . . . obviously people with less understanding English they get confused as well.
East European
Summary
This chapter has presented data about the three related, but distinct, types of work that appear to shape what people think and do when they experience an urgent health-care need. We have suggested that these types of work operate at an individual level and within social networks, but how this work gets done is highly dependent on people’s social context (notably living arrangements, work commitments, mobility and access to transport, and language) and on time (the time of day when help is needed).
Illness work involved interpretation of and decision-making about the meaning and the severity of symptoms, the management of physical symptoms and psychological states and the assessment and management of possible risks. This is used to decide if access to medical care is needed, and, if so, how soon, and which service is required. In our analysis we focused on responses to symptoms that seemed most distinctive as prompts to urgent care help-seeking. We summarised these as ‘pain’ and ‘anxiety’. We contend that subjective interpretations of pain are inextricably linked with emotional responses to illness, characterised as anxiety, and together these drive decisions about help-seeking. When anxiety was high, people reported bypassing more considered decision-making processes, frequently heading to the ED. Service users accessed both urgent care and emergency care to access pain relief or management. Younger service users particularly were equivocal in their service choices to manage pain, considering both urgent and emergency care. The dominant role that service users give to pain and anxiety in urgent care help-seeking is in stark contrast to the absence of these in policy definitions of urgent and emergency care.
Key to illness work is the interpretation and management of risks to health, and, in response, reassurance (rather than diagnosis or treatment), or ‘making sure nothing is wrong’, was a main reason for urgent care help-seeking to manage their anxiety. This was particularly prominent in choosing NHS 111. Illness work was often carried out across social networks to help make sense of symptoms and determine whether or not people should seek help. When people were making decisions on behalf of others, the risk threshold for seeking help was lowered. We also found that there were some differences between groups in relation to how they used their social networks. Older service users and East European service users who were married involved their spouse in illness work. Older people living alone tended to draw on a wider range of family, friends and neighbours than East Europeans, who tended to draw on closer family ties (parents or siblings). Younger participants tended to include their parents in illness work, but were less likely to involve friends.
Help-seeking was guided by moral work: the moral positioning, legitimation and sanctioning work done by service users. There are obvious tensions for services users in receiving the clinical reassurance, advice and treatment they desire to manage their anxiety but ensuring that their use is ‘legitimate’. Service users were keen to portray themselves as responsible users of services (someone who did not waste scarce resources, overburden already busy services or deprive others of care who might really need it). Not accessing services unnecessarily or at all, self-care, and tolerating symptoms were used to construct identifiers of being a ‘coper’, that is, someone who is self-reliant. Service users feared negative reactions from others, particularly from health professionals (although few reported being ‘told off’ when they acknowledged that their use might not have been appropriate). In addition, narratives of seeking to avoid ‘bothering the doctor’ were common. Social networks played a key role in sanctioning decision-making, and comparison with ‘others’ was a key part of moral work. There was often an emphasis on how others were instrumental in persuading them to use health services (against their own judgement). For younger people in particular, other people played an important role in sanctioning their choices. Older people were more likely to feel a sense of entitlement or a sense of unfairness when they had not been rewarded for being a ‘good patient’ (e.g. using services responsibly, paying taxes, not getting sick very often).
Navigation work – the choosing and accessing of services – relates to what is available and accessible. This very much depends on the knowledge and experience of an individual and on the knowledge and experience shared across service users’ social networks. What is available, accessible and acceptable is contingent on time. One of the strongest drives of patient help-seeking was weighing up waiting time and the convenience that different services offered, particularly for younger and East European groups. What was apparent was that people commonly chose the ED because it was convenient (e.g. it offered a shorter waiting time). For many, urgent and emergency care services were equivocal; decisions about where to go were frequently not based on perception of clinical need alone but, rather, were strongly influenced by convenience.
The illness, moral and navigation work evidenced by our participants is not done in a vacuum; rather, it is embedded in social contexts. There are myriad factors at play here, but family arrangements (e.g. living alone, caring responsibilities), work commitments, mobility and access to transport, and language were key. In turn, all of these factors are mediated by both time of day when help is needed and people’s access to social support.
In this chapter we have highlighted some features of the three population groups around their illness work, moral work and navigation work. Much of the work involved in help-seeking was similar across different user groups. For example, pain and anxiety were common reasons for help-seeking and all service users made similar moral distinctions between their own service use and that of others. However, there were also differences across groups, such as how social networks were used. In Table 10 we summarise the main group differences and similarities.
| Population group | Summary for population group |
|---|---|
| East European |
Illness work: this group was similar to other groups Moral work: compared with the younger group, they were more likely to seek to justify their use of services. They suggested they were not sick very often, did not use services unnecessarily, and contributed to the health service via taxation Navigation work: this was most different for this group, often relying heavily on strong ties (family and friends). They reported less wide-ranging social networks. As navigation work is more dependent on having local knowledge of health services, it puts recent migrants at a disadvantage, especially as their social network is often in another country and so unable to help them. Several East European participants suggested that there was little distinction between the words ‘urgent’ and ‘emergency’ and that the terms did not directly apply to their experiences of other health-care systems Wider social context: the potential difficulties of English as a second language was not a common theme in our data, although this may be linked to our data collection method (interviews required some proficiency in English). However, participants did refer to the ways that language could hinder navigation work. Some suggested that they did not trust telephone services (such as NHS 111) and wanted to see a doctor face to face, and this prompted them to seek help at the ED. Urgent care was sometimes used in preference to general practice because it fitted around paid employment, studying and/or family commitments more easily |
| Older |
Illness work: this group gave more recognition to the subjective nature of illness and the role that anxiety plays in rationalising health service use Moral work: they were more likely to describe themselves as ‘copers’ and described how they tolerated symptoms, undertook self-care, and took actions to reduce unnecessary health service use. Not accessing services was viewed as a sign of stoicism, or resilience, of which many people were proud. There was a perception among the older participants that other people may lack the necessary knowledge or skills to understand, articulate and interpret health problems, which leads to unnecessary contact with health services. This group were most likely to articulate the view that they felt they had a right to use the NHS because they had ‘paid into it all our lives’ Navigation work: weaker ties such as acquaintances and neighbours played a part in older people’s accounts of help-seeking. Those who cared for a partner, were single or widowed, or were more socially isolated categorised weak ties as important Wider social context: this group were more likely to have difficulties getting to services because of mobility issues or not being able to drive. This made them more dependent on others for transport. This was further affected by time of day when public transport or friends/family were available, which could delay or bring forward the decision to seek help |
| Younger |
Illness work: younger participants were more likely to go to the ED to manage pain than other groups. They were also more likely to reflect that they may have over-reacted to health concerns. Like other groups, they relied on close family ties to interpret symptoms (predominantly a parent, a partner or sometimes a sibling rather than friends). This group talked more about using social media and the NHS Choices website in help-seeking. They were often aware of the pitfalls of using the internet as possibly exacerbating anxiety and providing unreliable information, and so tended to seek advice from the internet in combination with talking to other people Moral work: young people were more likely to use anxiety about health to legitimise their use of urgent or emergency care services. They were more likely to cite others (usually parents, but sometimes managers at work) as instrumental in making the decision to seek urgent or emergency care. They were less likely than the other two groups to express feelings of entitlement to service use Navigation work: this group were more equivocal in their service choices and were most likely to use both urgent and emergency care for reasons of convenience (closest and shortest wait). This group were more likely to use NHS 111 as a first port of call again for convenience. Like the European group, the younger group were more likely to use urgent care in preference to general practice Wide social context: changes in living arrangements such as moving away from home – a common feature in this group – resulted in them having less support than they were used to |
Chapter 6 describes how we synthesised the analyses to develop a conceptual model of urgent care help-seeking (WP3).
Chapter 6 Model of urgent care help-seeking
We have described how different people – different publics, health professionals and commissioners – make sense of urgent and emergency care needs and the services provided to meet these needs. Chapter 4 showed how confusion about the definitions of ‘urgent’ and the different services offered made it difficult for people to make sense of the urgent care landscape. We also examined how moral positioning influenced sense-making, creating strong legitimation frameworks for personal views and behaviours with regard to help-seeking, and contributed to discourses about the appropriate and inappropriate use of services by others. This moral positioning was influenced by experience, beliefs and stereotypes, some of which were informed by media representations and advertising about services. It was also deeply contingent and nuanced; what people regarded as the legitimate use of services by themselves or others depended on a range of social, psychological and contextual variables, such as family support, access to transport, anxiety, time of day and service opening times.
Chapter 5 looked in more detail at help-seeking behaviours, and at the choices people make when they identify urgent health-care needs. Here we delineated three types of work that underpin help-seeking: illness work related to responding to and managing symptoms, moral work drawing on the legitimation and positioning identified in Chapter 4, and navigation work of finding ways through the landscape of services. This work took place at an individual level but was also heavily influenced by service users’ social networks, which were drawn on to seek information, reassurance or validation of decision-making or, at times, to hand over decision-making. We argued that this work was further highly dependent on context; the effort required was conditional on variables such as family circumstances, mobility and transport, and language.
In this chapter we describe how we synthesised the analyses presented in Chapters 4 and 5 to develop a conceptual model of urgent care help-seeking.
Help-seeking models in the literature
Numerous theories and models from a range of disciplines have been developed to conceptualise illness behaviour, decisions to seek help from health professionals and access to health care. 192 These include microsociological conceptualisations of illness behaviour,204,205 through meso-level psychosocial models to macro-level cultural, demographic, geographic, economic, structural, and service organisation and accessibility factors. These conceptualisations provide frameworks to help us understand how people interact with others and within social contexts to obtain assistance with their health-care needs in terms of understanding, advice, information, treatment and general support.
Social psychology approaches, underpinned by theories of cognition, decision-making and learning, have described cues or triggers for help-seeking. The health belief model, for example, describes psychological and motivational determinants of health service use. These include internal and external cues to action (e.g. pain; interference with everyday life); the readiness to take a particular course of action and the perceived risks and benefits from health-care use. These may be modified by demographic and individual factors such as gender, personality and social class. 206 One of the most extensively referenced sociobehavioural frameworks for studying access to health services is that of Andersen and colleagues. 207–210 Andersen and Newman in 1973 described the inter-relationship of the need for health services with individual-level determinants of utilisation and the organisation of health services and social norms in health-seeking behaviour. 207 These ideas were developed into a behavioural model of access to care208 and adapted in subsequent papers. 210,211 The framework takes health policy as the starting point for determining access, which directly influences the supply of health care. Within the framework, individual determinants of access are grouped into predisposing characteristics (e.g. age, sex and education); enabling determinants – the means by which people use health services (e.g. income, place of residence or supply of service); and need (current health status). The key limitation of these models is that they downplay the importance of social context, wider social influences, networks and processes. Andersen’s behavioural model focuses on outcomes rather than help-seeking as a (social) process. 203 Our findings in Chapter 5 reflect some of the determinants in Andersen’s model, particularly in what we have characterised as illness work, and we extend some of these ideas, particularly around risk work as part of illness work. However, we found that people’s social networks also played a key role in illness, moral and navigation work.
Medical sociology presents help-seeking as a social process,191,198,199,212 explaining how social and contextual influences may prompt or delay help-seeking. Early work by Freidson emphasises how interactions with others in lay referral networks shape help-seeking behaviour. 213 In an influential article, Pescosolido devised a framework termed the social organisation strategy focusing on socially constructed patterns of decisions. 198 It derives from four basic assumptions: the actor is social and pragmatic rather than isolated and consciously rational; the focus is individuals’ patterns of interaction with others; the unit of analysis is the network; and the context includes time and place, representing substantive and structural networks. In this way, it acts as a ‘middle tier between micro and macro-systems’. 192 One of its key strengths is that it recognises a wide range of options for health care, advice and resources. Although in the present study we have, to some extent, attended to micropsychosocial processes of individual sense-making and decision-making, what is important in our model is how individual actions combine with social networks, process and structures to create distinct types of health-seeking work in the context of urgent care.
The process of developing the model
A conceptual model can help us to organise our thoughts and identify a common set of influences that are strongly associated with choosing and using urgent care. Conceptual models are commonly informed by theory but based on empirical evidence so that they are directly applicable to the context and setting being studied. Here, the phenomenon under study is the way in which people make sense of, and seek help from, urgent care services.
The analysis of qualitative data that formed the basis of building a conceptual model was outlined in Chapter 3 (WP3). Using data from the full set of qualitative interviews, the core team (GM, CP, JP, AR and JT) held regular data clinics to examine the transcripts, codes and themes that captured people’s individual choices and reported behaviours, as well as the social processes and networks at play. We used spreadsheets containing the preliminary coding frame, mind maps, decision trees and logic models to map our interpretations. The data were grouped, regrouped and revised into inter-related themes and subthemes to form a final coding framework and a draft of the conceptual model. The core team discussed and worked through how sense-making and help-seeking related to each other and to identify factors and choices that might be modifiable.
We have characterised the underlying and mediating mechanisms through which these factors shape sense-making (thinking, feeling) and help-seeking (action) at the individual and social network level, and explained their operation. We have considered influences that are common across different service user groups, and have identified contingent factors that are specific to each of the service user groups. These are expressed as a set of theoretical constructs mapped onto a conceptual model. Once finalised, associations between components of the model were explored and a visual representation of the conceptual model was developed to show the relationships between them.
The model of urgent care sense-making and help-seeking
From our empirical data we have developed an integrative model of urgent care sense-making and help-seeking behaviour to help us understand variations in health-care utilisation in the context of urgent care. This builds on extant concepts of help-seeking and patient work. The overall structure of the model emphasises that work informs the interaction between what we think and feel about illness and the need to seek care (sense-making), and action, the decisions we take and how we use urgent care (help-seeking). The way in which sense-making leads to help-seeking is influenced by a set of social contextual factors and time.
From our analysis (see Chapters 3–5) we have built a typology of the work that people do in thinking about illness in relation to urgent care. We have conceptualised three related, but distinct, types of work that take place at both the individual level and the social network level in relation to urgent care sense-making and help-seeking (Table 11).
| Concept of work | Individual level | Social network level | Nature of the work |
|---|---|---|---|
| Illness work | Assessing and managing symptoms, regimens and risk, and actions associated with these | Assessing and managing symptoms, regimens and risk, and actions associated with these across social networks |
|
| Moral work | Thinking about appropriate service choices by self and others | Thinking about appropriate service choices in comparison with others and influenced by others |
|
| Navigation work | Thinking about services available (choosing) and deciding which to access (using) | Thinking about services available (choosing) and deciding which to access (using) informed by social network |
|
Having delineated the typology, the next stage in the development of the model focused on describing the way in which these three types of work interact to determine how people make sense of urgent care (Figure 8). Sense-making is what the individual thinks and feels about a set of symptoms (e.g. their cognition, affect, motivation to act). This is informed by their past experiences and knowledge of symptoms and services but also by their social networks. Individuals draw on their social networks to engage in different types of urgent care work, but these also shape how people make sense of urgent care. Social networks conduct and spread information, social norms, attitudes and beliefs to influence urgent care sense-making in a myriad of ways such as helping in risk assessment, providing reassurance and guidance, and sanctioning views, and, in so doing, influence help-seeking behaviours. This complex interplay between individuals and their social networks makes individual differences in sense-making inevitable but also reveals how group-level differences may emerge as factors such as experience, social norms, language and access to knowledgeable networks come into play.
FIGURE 8.
Model of urgent care help-seeking.
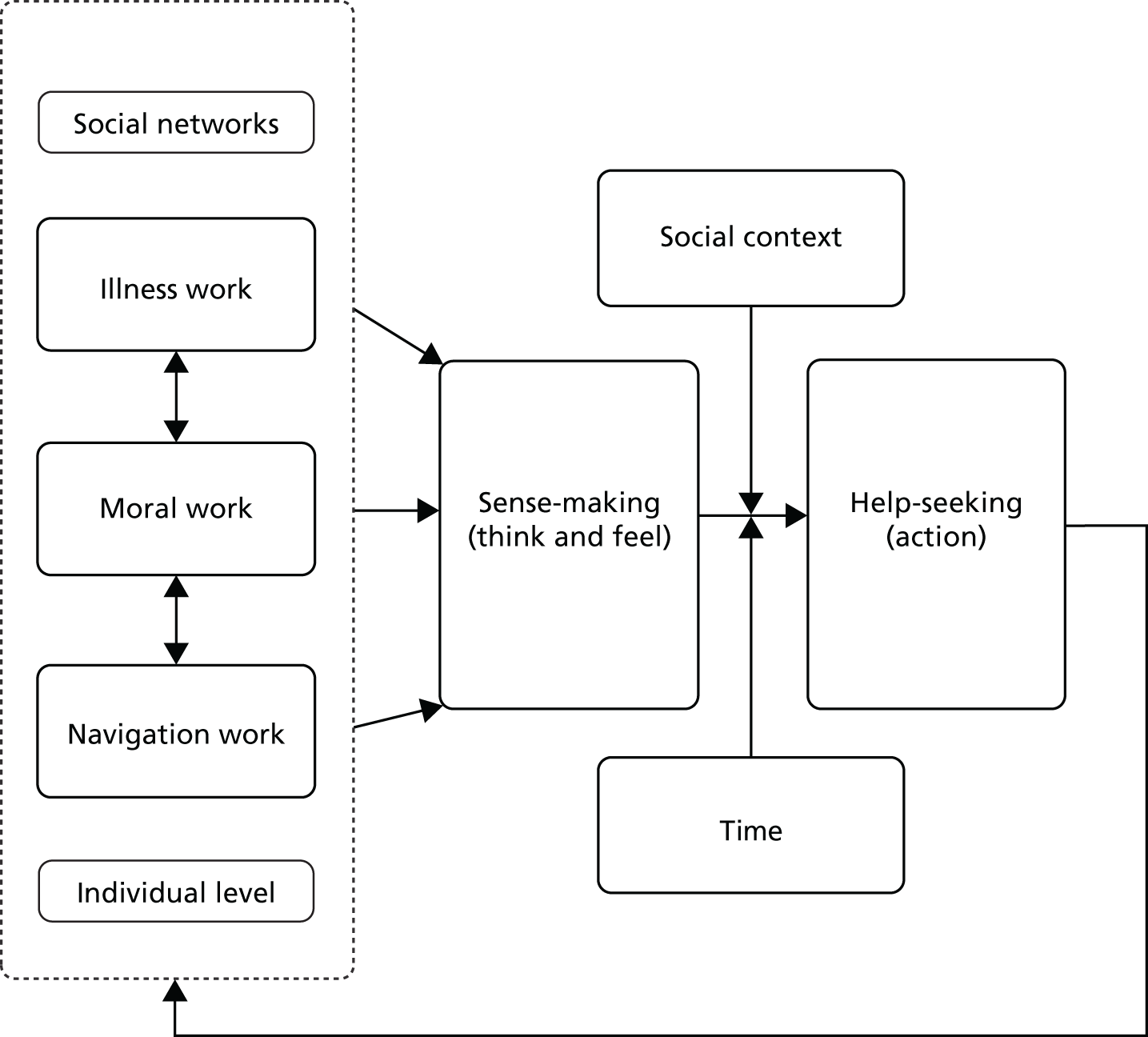
What is particularly interesting about urgent care is that there is no universally agreed, precise definition of ‘urgency’. It is often described in generic or relational terms (see Chapters 3 and 4) and, in everyday talk, ‘urgent’ lacks consistent and clear meaning. The sense-making that people undertake is therefore both based on lay knowledge/interpretation of illness and of health services, and (mis)informed by imprecise definitions of ‘urgent’. It is in this context that an individual has to recognise illness and interpret the meaning of symptoms, how they feel and what to do about it, if health care is needed and what level of urgency or service is required.
Our concept of illness work builds on that of Corbin and Strauss,23 which we have extended to include assessment of risk, decisions about what is being sought (e.g. reassurance, treatment) and what level of care is needed. Alongside this, our interpretations of illness are considered in the light of an individual’s moral position on the use of health services. People made sense of urgent care in assessing their illness in relation to thinking, and making judgements about when urgent care is ‘appropriate’. This is related to decisions about the severity or concern about illness (illness work) balanced against a need to legitimate their use. Assessing legitimacy of service use shapes people’s views about what urgent care ‘is’ and what ‘it is for’. This work also involves assessing a range of urgent and emergency services. Moral work involved situating or legitimating urgent care use in preference to emergency care use. Calnan150 highlights a useful distinction in lay evaluation: specific experiences and reasons, and more general lay images of health and health care, which is useful for thinking about moral work. People’s thinking and moral evaluations come from both individual moral evaluations of specific symptoms in relation to specific experiences of services and evaluations that are constructed by comparison with ‘others’, for example not wasting the doctor’s time as other people might (see Chapter 5).
The final aspect of work is navigation work. People make sense of urgent care by understanding the range of possible services and understanding what is available, accessible and acceptable from different services. As we have highlighted above, urgent care in the UK does not have a clear meaning or definition. Furthermore, urgent care is not a single service with a single identity. It is a collection of different services, offering slightly different things for different purposes. People’s knowledge and experience of this landscape shapes their understanding of what urgent care ‘is’ and what it can provide. We used some aspects of Penchansky and Thomas’s dimensions of access186 on availability and accessibility of urgent care and extended these to acknowledge how sense-making is informed by previous experiences, knowledge and perceptions about illness and about services and the acceptability of these. We also draw on the concept of ‘recursivity’ to emphasise how a service user’s experiences of health services shapes and informs their future help-seeking. 128,203 People make sense of what is ‘urgent’ by recursively drawing on their own experience and knowledge (or sometimes that of others). Navigation work takes place alongside illness and moral work to shape people’s understanding of urgent care, and this in turn shapes help-seeking.
The second stage of the model captures how help-seeking (i.e. the actions that people take in terms of their behaviours, decisions and choices) is influenced by how they make sense of urgent care, and by social context and time. Deciding to act (seeking help) is informed by making sense of illness, and of one’s moral position, and by personal and networked understandings of the urgent care landscape. Help-seeking involves comparing the options, assessing, and synthesising information to evaluate the direct or indirect benefits and costs of alternative choices. Deciding to act involves balancing these (sometimes competing) types of work against each other. For example, a choice of service may involve balancing what is being sought (e.g. reassurance) against moral positioning (views about what is appropriate for a particular service). Thus, help-seeking involves weighing up the risks and seeking reassurance to manage those risks, but also a desire to act as a responsible service user. Although there may be strong motivation to be a ‘legitimate’ user of a particular service, this can be ‘traded off’ against what is most accessible or convenient at a particular time or in a specific context.
The third stage of the model shows how, between sense-making and help-seeking, choices and action, the individual is influenced by social context and by time. Help-seeking is the result of individual, social and structural/organisation practices,214 and the conceptual model we propose emphasises the individual (micro) aspects of sense-making and help-seeking while also accounting for the wider social network and social structure influences. We have demonstrated how sense-making and help-seeking are influenced by social networks and that these networks play a role in illness work (e.g. helping decide how to manage risk), in moral work (e.g. how others can trigger help-seeking by sanctioning health service use)199 and in navigation work (e.g. supporting action directed towards seeking help). Action to seek help is also contingent on the social context, at a given time of day, and together influencers may facilitate or inhibit support-giving and help-seeking. Social context influences the individual’s access to information and social support, including practical support (e.g. transport to services),200 and again this varies with time of day. For example, help-seeking may be facilitated (or, at least, there may be more choices available) for those who live with a partner, own a car or have more flexibility in their working hours. Those who live alone, or who rely on public transport or on other people for a lift, may make different choices. Time of day influences the social context in terms of what help is available and how people feel about asking for help (e.g. at night people worry about burdening others).
Although the model is necessarily presented as linear, there is a feedback loop from help-seeking (action) back into sense-making to illustrate how experiences of help-seeking consolidate or reframe sense-making in a reciprocal relationship. For example, an individual who experiences care positively when using a particular service is likely to use that service again.
In summary, our model suggests that sense-making (thinking, feeling) and help-seeking (action) is a function of illness work, moral work and navigation work (at the individual and social level) but is influenced by social structure and time.
Chapter 7 Discussion and conclusions
In this chapter, we draw together our conclusions, structured around our original research objectives, and discuss the implications of our findings. We outline our strengths and weaknesses and dissemination work, before concluding with what this study adds to the evidence base about urgent and emergency care.
How patients, the public, providers and policy makers define and make sense of the urgent care landscape (objective 1)
We showed that the terms ‘urgent’ and ‘emergency’ as categories of care are not clear in the policy literature, although there was some consensus across policy and provider perspectives regarding the physiological factors that feature in conceptualisations of urgent care. Definitions of urgent were ‘relational’ and focused on comparing urgent care with emergency care. For service users, their construct of ‘urgent’ was more complex, ambiguous and subjective, and was shaped by the help-seeking work that they do [see The ‘work’ of urgent care and the way in which sense-making influences service users understanding, navigating, and use of services (help-seeking strategies) (objectives 2 and 3)]. Initially, most interview participants did not see a distinction between the terms ‘urgent’ and ‘emergency’. Only when asked if there was a difference were interviewees likely to define ‘emergency’ as ‘more serious’ than ‘urgent’.
Policy1–3,51,185,215 and existing research67 has previously identified that people are confused about which services to use, but we found that there is a clear mismatch between how policy and the public conceptualise ‘urgent’. O’Cathain et al. 67 found that people can describe emergency care more easily than urgent care, but there is little in the literature that explains how people think about urgent care. We argue that, although ‘urgent’ care is a term that is used widely, and may have particular meaning for providers and policy-makers, this is not the case for service users. Our citizens’ panels and interviews suggest that, unlike emergency, the term ‘urgent’ is particularly problematic: it holds little meaning for most people. Although many service users understand that services such as NHS 111 or WICs are for less serious symptoms than the ED, they may not assign the label ‘urgent’ to these sorts of services.
In policy, it is often implied that urgent care has a single identity, but this term covers a range of services, which appears to contribute to why service users do not have a clear understanding of it. This raises the question of whether the range of services (e.g. WICs, MIUs, NHS 111) are too broad and too disparate, in terms of when they are available and what they are able to assess and treat, to be meaningfully grouped together under the banner of ‘urgent’ care services.
For service users, there is a lack of urgent care identity and a lack of clarity about what urgent ‘is’ and what it is intended to provide. Historically, service provider definitions of ‘urgent’ reflected those of out-hours services, for example medical problems that ‘cannot wait until morning’. 68 More recently, definitions of ‘urgent’ have focused on descriptions that include ‘not serious’, ‘minor’ illness or injury or ‘urgent but not life-threatening’. These definitions potentially broaden notions of urgency to include more minor – and possibly more routine – health concerns. Our findings have drawn attention to the ways language is used to describe urgent care and how it is presented by health services providers and policy-makers. Lack of clarity may lead to ‘overuse’ of some services41,79,97,147,175,216,217 as people conflate urgent with emergency services and then make decisions about where to seek help in idiosyncratic ways. For example, in our study we report that some used the ED because it was convenient, and this perception is likely to be further exacerbated when primary care services are hard to access in a timely way. Lack of clarity around what ‘urgent’ means to service users may also lead to delays in help-seeking218 and we suggest that some groups (e.g. older people) may wait longer to access care.
Using urgent and emergency care services when seeking reassurance about symptoms was very common in the accounts we obtained from the panels and interviews. This encouraged us to extend our concept of illness work to include how people manage risk when making sense of and using services. Our findings suggest that urgent care services are often seen as offering reassurance and ‘peace of mind’, which may contribute to high levels of satisfaction, but this may not always be the purpose they were intended to serve. The notion of risk in acute help-seeking has not been particularly prominent,137,219 although previous research has considered urgent and emergency service use is seen as a way to manage anxiety. 157,219,220 NHS 111 explicitly offers reassurance, advice and information, and survey research suggests that the majority of those who use this service (86%) fully complied with advice and that nearly three-quarters were satisfied with the service. 221 The position of NHS 111 is somewhat contradictory: on the one hand, it is branded as an ‘urgent care service’, but on the other, it plays this wider role, offering ‘non-urgent’ reassurance, and more general health advice and information. This extended remit may contribute to ambiguity about the term ‘urgent’.
NHS 111 has been presented as a service that can signpost people to other services and provide support for people to self-care. Our findings suggest that service users make contact to sanction, signpost and seek confirmation about what to do next, but many go on to use another urgent or emergency service. The ability of NHS 111 to substitute for other services may be compromised by this help-seeking behaviour. Indeed, using NHS 111 before attending another service may be reinforced by adverts and health education; for example, the NHS self-care week in 2017 promoted NHS Choices as a website that offered information about losing weight, stopping smoking and eating more healthily but also suggested that:222
If you’re worried about an urgent medical concern, call 111 and speak to a fully trained adviser.
This advertising provides normative messages that the remit of NHS 111 includes non-urgent and general health information and advice, rather than urgent care specifically, and further blurs the boundaries between urgent and emergency care. It also signals that NHS 111 is positioned as a gateway to other services (such as ED), which patients and the public may understand more clearly.
Our findings suggest that service users wanted a clearer sense of service priorities. In the panels, redrawings of the Keogh diagram attempted to capture a triage system that might help navigate a confusing landscape and aid sense-making about urgent care. Although the Keogh diagram reflects the policy rhetoric that expects people to use NHS 111 as a gateway to urgent care, the public members of our panels and our interviewees remain less familiar with this model. NHS 111 has the potential to prevent patients using other services unnecessarily (i.e. it could ‘shut the gate’) but this would require people to both understand and accept NHS 111 as the starting point for seeking urgent support. However, in a context in which people do not understand the term ‘urgent’, where their sense-making does not match policy-makers’ vision of service use and where people are free to access other health-care services directly, this ambition will be hard to realise. Sense-making about urgent care is varied and complex, and our findings confirm that we cannot simply assume that providing a signpost in the form of NHS 111 will direct patients to the ‘right service at the right time’.
Judgements of ‘appropriateness’ of service use have tended to reflect policy positioning of services and professional attitudes (see Chapter 3), particularly in relation to ED use. 121 This has tended to focus on ‘blaming the user’ for poor choices, but our findings raise questions for the health-care system that has repeatedly failed to guide people to the ‘right place’. Our work shows that service users were aware of strong messages about choosing between available services and using them ‘appropriately’, particularly for ED. This finding has been noted elsewhere. 223 However, service users frequently rationalise their own use of services, a finding that is consistent with that of Adamson et al. 180 Interestingly, we observed that fewer moral judgements were made about the ‘misuse’ of urgent care services than of that of ED. This may reflect a lack of clarity, as described above, or the perception that services such as NHS 111 provide a much wider remit than urgent care alone. We discuss this further in the context of moral and navigation work in the next section.
The ‘work’ of urgent care and the way in which sense-making influences service users’ understanding, navigating and use of services (help-seeking strategies) (objectives 2 and 3)
We identified three distinct types of work (illness, moral and navigation work) that influence how people make sense of urgent care, and in turn, how and where they seek help.
The way in which service users involved in our study interpret symptoms largely concurs with existing literature. 129,135,137,157 However, a dominant theme in our analysis of illness work was the way in which the interpretation and management of pain was a key reason for seeking help from both emergency and urgent care. While there is relatively little attention given to pain in the policy literature, research has noted that pain is an important reason for attending the ED. 224,225 In addition, a recent study has suggested that those who attend ED because of pain tend to be ‘vulnerable, complex and report significant worry and anxiety’. 224 Although not all of our participants could be described as vulnerable or complex, we have also drawn attention to the role that anxiety plays in help-seeking.
Another key theme in our analysis was the role that services play in reassurance and managing risk. We extended the concept of illness work to include the management of risk.
The role of risk in help-seeking for acute illness has not been particularly prominent in the literature but seeking reassurance from health services has previously been identified,137,219,226 particularly in the context of parents’ help-seeking about their child’s illness137,227 but also more recently in the context of NHS 24 service use. 219 Some studies have identified a risk-averse culture in some urgent and emergency care services, for example in ED clinical decision-making (‘better safe than sorry’224) or in the algorithms underpinning NHS 111. 228 The ways in which services are organised may share risk with service users229 and influence help-seeking behaviours. Our findings concur with those of Doyle,219 who suggests that ruling out risks is a significant feature of urgent care help-seeking: checking that they were ‘doing the right thing’ was a main reason for people making contact. Seeking reassurance is an important part of urgent care help-seeking but this raises questions about the role of urgent care. Is it to assess and treat ‘urgent’ symptoms or is it to provide a wider range of advice and information?
Our findings suggest that people engage in complex moral reasoning when making sense of and using services, and we have extended some of what is already known about moral reasoning to highlight this as a key aspect of help-seeking work. Service users had strong moral views on what kinds of illness and injury and what kind of person deserves ‘emergency’ care and were highly sensitive to ‘inappropriate’ help-seeking. They wished to present as responsible citizens, and feared ‘bothering the doctor’ and criticism from health professionals. This moral work influenced their choices when seeking help. Many people articulated the moral aspects of their help-seeking; they considered the likely impact on staff workload and the opportunity costs of using resources in place of those more deserving, in ways that reflect findings elsewhere in relation to urgent, emergency and GP care. 10,157,163,202,223,230 However, consideration of appropriateness is often externalised so that the moral rules are applied to others (often characterising others as ‘time wasters’, seeking help for ‘trivia’) and not to oneself. Some groups, for example the older age group, rehearsed notions of stoicism or of being ‘someone who copes’180,231 to identify appropriate service use, in comparison with ‘others’ who were less resilient, less knowledgeable or more selfish. While these sentiments were offered in the context of discussions about emergency care, we observed that fewer moral judgements were made about the ‘misuse’ of urgent care services. We conclude from this that moral work may be less influential when considering urgent care help-seeking.
Service users make decisions in the light of the choices that are (or are perceived to be) available and accessible at any given time of day186,203,223 and on how they feel about these (acceptability). Available urgent care services are highly variable; for example, there is inconsistency in what is open, and at what times, in different areas of the country. This is complicated further as services that people have previously relied on are shut down or reconfigured. Road and transport links may influence accessibility, and can mean that a hospital with an ED is nearer or more accessible than a ‘local’ UCC. Previous research supports that those who live closer to services have higher rates of use127,232,233 but our work suggests that proximity may be temporal as well as geographical (e.g. the hospital may be ‘nearer’ at night because of car and motorway access). These features of access are socially patterned: older people, for example, relied on others for support (e.g. transport) more than other groups. We also showed that the lack of a consistent landscape of care makes understanding, and using, services difficult, especially for some groups; for example, East European groups have a different set of experiences in their home country (e.g. no urgent care services) so their sense-making may not transfer to the UK system.
One of the strongest drivers of service choice was the perception of the amount of time it would take to be seen (waiting time). Routine primary care was described as the least accessible form of care in this respect when compared with urgent care and the ED. Here, we can see how navigation work extends beyond choices between urgent and emergency services: many people report using urgent care (and sometimes the ED) because they cannot access a GP appointment. This finding is supported by research that has demonstrated that patients registered with practices that are open fewer than 45 hours per week attend the ED more often. 234 Furthermore, what is apparent from our data is the extent to which convenience drives people’s choices. For many, urgent and emergency care services were equivalent, not distinct, services, and people’s decisions about which to use were not based on perception of clinical need alone but rather were influenced by accessibility and waiting time considerations. Service users, particularly younger ones, sought to maximise the use of their own time (e.g. by choosing services with the shortest expected waiting time, choosing what time was best to access them and/or by choosing services that were more conveniently located). This navigation work involves both finding one’s way and trading off choices about the availability, accessibility and acceptability of services. Although many do not take the decision to consult health services lightly, they also want to use the most convenient service. Convenience is thus a legitimate reason, and important determinant, for using a service.
Our model proposes that sense-making work takes place at both the individual level and the social network level, and that context and time shapes people’s help-seeking. We have shown that individuals often drew on social networks to support illness, moral and navigation work. The use of lay networks in illness work and sanctioning choices are well documented in the help-seeking literature. 197,213 There is a suggestion that weaker social networks may encourage service use; indeed, NHS 111 and its predecessor NHS Direct may substitute for stronger lay networks. 235 We observed that service users often draw on weak and strong ties in social networks for illness advice, but do so in conjunction with making contact with health services. Services such as NHS 111 have not replaced the social network, but have instead become part of a wider network of complementary support to draw on. In addition, social context influenced the way in which help was sought, so that family arrangements (e.g. living alone, caring responsibilities), work commitments, mobility and access to transport, and language also facilitate (or hinder) choices about and access to care.
Modifiable factors in urgent care patient decision-making: implications for urgent care (objective 4)
The proposed conceptual model helps us identify, explain and describe potentially modifiable components of help-seeking (see Chapter 6). Our research suggests that there may be implications for urgent care provision and utilisation. These are summarised below.
Illness work
-
Pain is one of the most common reasons for seeking urgent (and emergency) care: better recognition of this and information about pain symptoms and management of pain would aid service users in deciding when and where to seek help.
-
Clarifying what urgent care services can offer would support service users in sense-making and help-seeking. Is this ‘care that cannot wait until morning’, or is this the wider remit of reassurance and advice offered by services such as NHS 111? Clear information about what different services ‘are for’ would help service users decide which services to use.
Moral work
-
There are numerous examples of the NHS sending out strong normative messages in advertising and health education to prompt people to consider if their use of a service is ‘appropriate’, but service users have a wider moral repertoire. They legitimise their own use by citing a broad range of justifications (e.g. perceived severity, anxiety, uncertainty, lack of access, availability or convenience) and apply different moral standards to other people’s choices. These beliefs are deep-seated, and influencing moral reasoning through the use of advertising alone, without recognising the complex and nuanced moral work people undertake, is unlikely to modify behaviour.
Navigation work
-
There is a need to consider if the range of services currently available are too disparate to be grouped under a single heading of ‘urgent care’. As a minimum, there is a need for clearer information for service users. There is a need for clarity around the language of urgent care and of the nature of different services, for example what they are, what they do, when they are open and what they offer, rather than simply in relational terms (as what they are not). ED is more clearly identified and better understood and could be considered a ‘brand’ (notwithstanding the public’s continued use of A&E terminology). There may be an opportunity to more clearly ‘brand’ urgent care, again in terms of what it is and does rather than in contrast to the ED.
-
There are additional considerations for migrant groups. Many will have no experience of a wide range of different free-at-the-point-of-access services until they come to the UK. Wider access to health-care information could help facilitate sense-making and help-seeking. Other services, and local authority provision, might consider making such information available in relevant languages.
-
The relationship between urgent and emergency services needs to be better specified. Although in policy they are broadly presented as hierarchical, our findings suggest that many perceive these services as equivalent. Until they are regarded as distinct, it seems unlikely that patterns of help-seeking will change.
-
Further standardisation of what services are offered by MIUs, UCCs or WICs would provide consistency and help service users more easily ‘know’ what is available and make choices about where to go.
-
A modified patient-facing model of urgent care, ideally developed using patient centred co-design methods, would better demarcate the routes from self-care and general practice/primary care on to urgent care in ways that patients and the public can understand. Such a model would aid sense-making and support navigation work by patients and the public. This would, for example, give service users a clearer picture of where routine general practice fits into the landscape of urgent and emergency care.
Social context and time
-
Time of day should be more central when discussing urgent care help-seeking and service provision. It has an impact on sense-making (e.g. how people think and feel may be different at night) and on service availability and accessibility (the WIC may be closed or difficult to travel to at night). Better communication of and possibly standardisation of opening hours may aid sense-making and help-seeking decisions. We acknowledge that standardising services is complex – there are a range of political, historical and cultural factors that make wide-scale change difficult – but this should not prevent it being an ambition.
-
Locally there may need to be greater attention to the different needs of different population groups. For example, the work for recent migrants (particularly navigation work) may be greater because of their reduced local social networks and knowledge of services. Older people may be reliant on particular networks for transport and this may shape service use.
-
Attempts to modify sense-making and help-seeking must be aware of the wider social network and contextual influences on behaviour and thinking. Health service advertising and education campaigns could better reflect the social networks and ties that influence decisions and in particular recognise the local factors that might push people towards ED and urgent care (e.g. perceived lack of access to GP services). Policy-makers and providers could make use of our analyses of social networks and contexts to inform educational interventions. Many of our participants felt that lack of knowledge hindered sense-making and help-seeking. The British Medical Association has proposed that schools introduce curricula about appropriate, safe and effective use of health services, and of self-management of health when required,236 and this seems a potentially useful way of modifying behaviour.
Strengths and weaknesses of the study
Like our study, previous research in the UK and elsewhere has identified difficulties people face in accessing urgent and emergency care. 127,133,145,237–239 However, much of this work has been limited in its ability to inform the bigger picture about how and why people use the urgent care system in the ways they do. Study limitations of previous research have included small sample sizes, a focus on a narrow set of help-seeking and sense-making determinants, and/or a focus on particular patient groups such as those with a specific long-term condition. Our study is the first in-depth look at how a large and diverse sample of service users are making sense (or not) of the urgent care system, and how this is informing their decision-making.
The interview component of our work offers particular insight to people’s understanding and use of the urgent care system. With 93 interviews with 100 people, we were able to elicit a diverse range of accounts, including those from people who had used services a lot and those with much less experience. Furthermore, with the focus firmly on service users, we have been able to identify what was important from their perspective rather than those of service providers and the policy-makers who shape service and system design. This has enabled us to develop a more holistic understanding of why and how people access different services at micro, meso and macro levels of analysis by probing them about the foundations of their sense-making and the moderators of their decision-making processes.
In addition, the present study has examined three specific population groups, determined not by the nature of their illness but rather by their demographic features. This has enabled us to consider the impact that age (old and young) and migrant status have on service use and the range of reasons people report seeking urgent care. Although the elderly have been the focus of other studies,36,181,240–244 the young and the migrant populations have received much less attention. Out study has identified the importance of group differences. For example, the findings from our study reveal the challenges for recent migrant populations due to language, lack of cultural understanding of the system and fragmented social networks and how this influences their decision-making about service use.
We cannot be sure that the sample population of our three groups reflected the full range of diverse views and experiences. For example, in the East European group, we found that, in general, those agreeing to participate had very good levels of spoken English and were well educated and articulate. Whether we would have observed similar sense-making and help-seeking choices in a more diverse group is debatable but it seems likely that in the absence of good English, service users would find navigating the urgent care landscape even more problematic than our participants did. Similarly, our younger group were largely recruited through educational establishments and may thus have had a higher level of education than the wider population. Nonetheless, this group revealed a wide range of health encounters and perceptions that can help us to understand their use of urgent and emergency care. Overall, greater understanding of these different groups, made possible by the design of this study, enabled us to consider varied and nuanced approaches to sense-making and decision-making pertinent to each group, with the potential that policy and interventions might be more specifically targeted to support their understanding and appropriate use of services.
Another feature of the research design was the use of second interviews for a subsection of our participants. Although second interviews meant additional time and financial costs for the research, they allowed us to follow up on themes emerging from the first interviews and probe issues in greater depth than would have been possible in a one-shot interview. We also noted that the time between interviews had resulted in participants reflecting on the issues raised by the research. During second interviews, participants often discussed how they had used services differently in the intervening period and how participating in the research had led to a more considered and appropriate response. This finding hints at the possible benefits of informing the public better about the distinctions between urgent and emergency care services and how to use them responsibly.
The design of the study enabled us to capture only the narratives around people’s self-reported service use rather than their actual behaviour. However, the second interviews provided an opportunity to explore encounters with health services that had taken place between the interviews and appeared to result in a more insightful consideration of sense-making and decision-making in the context of a trusting and supportive interviewer–interviewee encounter. Future studies might seek to adapt the design still further to talk to patients while they are waiting at different urgent care facilities to make a clearer link with actual behaviour. However, such designs are limited by patients’ willingness to engage in health-care research while unwell and anxious and would also fail to capture the many episodes of self-care or use of social networks to manage health.
A further strength of our study was the use of citizens’ panels to explore people’s understanding of the definitions of urgent and emergency care and how these might be better defined and communicated. With some exceptions,29,31,245,246 citizens’ panels have been rarely used in health-care research. Some critics suggest that, historically, this methodology has been used to appear democratic and inclusive, but that participant control and engagement is illusory. 247 In our study we tried to minimise bias by having two citizen advocates in each group who assisted the researcher in co-constructing the important themes and helped us to develop the materials used to structure the panel discussions. We note, however, that in a single-day session it is difficult to break established power relations between the researcher and the researched.
User involvement, dissemination and impact
User involvement
In preparing the application
We sought the advice and assistance of the South Central Research Design Service. Conversations with patient and public individuals suggested that the subject area is one of importance to the public. It also evidenced their confusion about the concepts the NHS uses around urgent and emergency care and where to go for different care needs. It also revealed a lack of understanding about newer urgent care services such as NHS 111. As a result we adapted the original protocol to strengthen the quality of the research and ensure that the methods were acceptable to the participants.
During the project
A small group of PPI participants was convened (n = 6) after a local community centre was used to identify members. The group informed the development of participant information sheets and consideration of ethical issues. PPI members also had the opportunity to consider the findings and help interpret these, as well as to be involved in planning dissemination. Two members of the PPI group were also part of the advisory board panel.
Dissemination during the project
The dissemination of early findings followed the completion of each citizens’ panel. All participants received a short report outlining the key data and the findings, and their agreed definition of ‘urgent’ care. Participants were invited to read, comment on, and make suggestions for amendment of the report. This was in line with the collaborative approach embedded in the citizens’ panel methodology. It also acted as a way to keep an open dialogue with participants, which later encouraged them to feed into the process of organising how and where public engagement events would take place to disseminate the findings not only to participants, but also to the wider public. The citizens’ panel data were also presented at the Health Services Research UK annual symposium in Nottingham in July 2017. This paper and the accompanying poster presented an opportunity to share early indications of the complex landscape of urgent care and the conflicting conceptualisations held about what it is, and does, between the public, providers and shapers of services.
Planned dissemination
With guidance from members of our four citizens’ panels, we plan to hold further public engagement events, inviting those who have taken part in the study as well as the wider public. The key objective of these events will be to take our findings and share them in a space that enables the public to explore the complex system of urgent and emergency care in an accessible and engaging way, without the boundaries that academic presentations can create.
A paper reporting findings from the citizens’ panels was presented for the OBHC (Organisational Behaviour in Healthcare) conference, in Montreal, QC, Canada, in May 2018. 248 The theme of the conference was ‘Coordinating care across boundaries and borders’. Our paper highlighted the use of citizens’ panels as a way to arrive at shared understandings of health-care boundaries and barriers to service use. This paper, along with others that focus on sense-making, urgent care work and the conceptual model, will be submitted to relevant health services research and sociology journals.
Further to our engagement with CCGs, Southampton CCG have expressed interest in our participation at local community events. These will share the findings and recommendations of our work and, in particular, feed back on the utility of the Keogh diagram for urgent and emergency care. To conclude our dissemination and outreach activities, we will work with Public Policy|Southampton (www.southampton.ac.uk/publicpolicy/index.page) to produce a policy briefing detailing our recommendations from the study. This will be shared with representatives from NHS England, the All-Party Parliamentary Health Group, the Health Select Committee, local authorities, the NHS and MPs representing the constituencies where research work was undertaken.
Recommendations for future research
Our study has added significantly to the knowledge base by exploring the perspectives of policy, providers and the public in conceptualising urgent care, and by explaining how understanding, navigating and using urgent care requires significant ‘work’ for service users. As such, our research recommendations are as follows.
Defining and establishing an identity for urgent care
-
First, our analysis suggests that the term ‘urgent’ care is not meaningful for service users. Further work is needed to test out definitions and the language that surrounds urgent care so that we can identify and design interventions that would help position urgent care more clearly for service users.
-
There is a need for engagement with stakeholders, including NHS England and commissioners, with a view to agreeing a standardised way of describing and identifying key service characteristics to explain urgent care to service users.
Managing demand
-
Our results suggest that there is a lack of integration between urgent and emergency care and routine general practice that warrants further investigation. A whole-systems approach to considering integration across a wider network of partners is key to understanding the complex relationships between demand, access and the provision of urgent health care.
-
More research is needed to identify better ways of delivering care across service boundaries, particularly for service users for whom access (and care) may be more complex (e.g. those with mental health issues, older patients, those for whom English is not a first language).
-
In addition, recognising that local populations will vary, research is needed to understand the local patterns of need, historical patterns of service provision and changes in what is available, and how this influences help-seeking and produces variation in service use and outcomes.
-
Our results highlight the role that service users play in interpreting and managing risks in illness work. There is a need to further understand how newer urgent care initiatives (such as the NHS 111 service) manage risk. There is some suggestion that NHS 111 may be risk averse and could potentially lead to higher contact rates with services.
Current provision
-
Our research findings suggest that seeking reassurance from both urgent and emergency care is a common reason for making contact with services. Research should address the role of urgent care in managing patient anxiety and providing reassurance.
-
There is also a need to better understand how social networks could be used to support individuals in making health service choices.
-
This study has focused on the ‘work done’ by service users. More research is needed to examine the ‘work done’ by service providers and professionals and how this interacts with the ‘work done’ by service users, for example the ‘work’ involved in ensuring accessibility and in providing appointments, the ‘work’ of triage and prioritisation, the ‘work’ of pathway navigation, or signposting, or the ‘work’ involved in redirecting an issue that has entered the ‘wrong’ pathway. This research would lay the groundwork to help contextualise research needed to identify and predict causal relationships.
-
While we have outlined a detailed understanding of service users’ sense-making and help-seeking in the form of a conceptual model, this model is not predictive. Further work is needed to quantify relationships between sense-making and help-seeking and to identify and predict causal relationships.
Interventions and future provision
Some of the potentially modifiable factors that have been identified (e.g. how pain is conceptualised and managed to shape urgent care help-seeking) need further investigation to determine if, and how, these might be truly ‘modifiable’. This might lead to the development of behaviour change interventions that aim to:
-
help service users assess and mange pain
-
empower service users by improving their skills and knowledge to directly access the services that best meet their needs by presenting clearer public information (both national and local interventions) and examine if interventions could be designed to help the public to do this (e.g. a map of the urgent care system)
-
provide feedback to service users when using a service to help inform them about the nature and role of particular services as a basis for future decision-making (e.g. services could routinely explain to service users what their role is).
Conclusions
The literature about illness behaviour and help-seeking is sizable and raises the question of why we might need more. 249 However, there are still some gaps in our understanding. First, policy and research has highlighted the complexity of urgent care and how provision has changed significantly over the last 20 years. There has been less focus on complex systems that include a range of service choices and newer forms of provision, such as NHS 111. This study was a timely opportunity to empirically investigate how people make sense of care, the work involved in understanding, navigating and choosing, and their use of it. Second, much of the previous research evidence has had a stronger focus on experiences of help-seeking for chronic rather than acute illness and on the management of minor illness and injuries with self-care. 249,250 Third, as Adamson et al. 180 point out, there is little research that examines how service users view ‘appropriate’ service use and the impact that this may have on help-seeking behaviour.
We have drawn quite heavily on older concepts of illness work that have previously been applied to people with chronic illness rather than those with acute health-care needs. We conclude that help-seeking is complex and is influenced by individual and social factors. Re-examining what these older studies can tell us about the nature of patient work in the context of urgent and emergency care has informed our model of urgent care sense-making and help-seeking. This study has been the first to examine in detail how service users are making sense (or not) of the urgent care system across a large data sample and how this is informing their decision-making around their urgent care needs. It has also included a group (East Europeans) about whom there has been little research to date. Recognising that there may be different or additional work for some groups may help design services (and guidance to using services) better in the future.
As expected, we identified a mismatch between policy providers’ and public understanding. Much of the policy surrounding urgent and emergency care is predicated on the notion that ‘urgent’ sits neatly between emergency and routine; however, service users in particular struggle to distinguish it from emergency or routine care in this way. We have drawn attention to the role of risk management in illness work, and developed a concept of ‘navigation work’, alongside moral work. From our empirical data, we have developed a new model of urgent care sense-making and help-seeking behaviour, which places greater focus on work at both the individual and the social levels, encouraging us to think about patient work more broadly. We emphasised that individual work takes place in a social and structural context where there is a range of influencing variables that shape both sense-making and help-seeking. The model aims to frame the interaction between thinking (sense-making) and action (help-seeking) and the work that may be involved (for individuals and their social networks) in accessing urgent care health-care systems. Crucially, as proposed by the model, this individual phenomenological approach is situated within the wider context. This pushes us from examining individual phenomenological study of everyday experiences to understanding the complex network of interactions that drive behaviour. The model helps us understand variations in health-care utilisation in the context of urgent care and has implications for policy and practice as it stresses the importance of the individual and their social networks in their roles as interpreters of illness, moral decision-makers and service navigators.
Acknowledgements
We thank everyone who took part in the interviews and in citizens’ panels. In particular, we are grateful to our patient and public advisors, particularly Mike and Lin Holder, for their help with assembling a PPI group, taking part in it, and securing support from the Lordshill Community Association.
We thank and acknowledge Karen Welch, Information Specialist, for developing the literature review search strategy and running the searches for the literature review.
We would also like to thank members of our advisory board: Mike Holder, Lin Holder and Agnieszka Fularska (PPI representatives); Ed England (South Central Ambulance Service); Professor Louise Locock (University of Oxford); Simon Brook (University of Southampton and NHS); Suzannah Rosenberg (Portsmouth CCG); and Iain Ward (GP and Southampton City CCG).
We would like to thank the anonymous reviewers of the draft report for their helpful comments.
Professor Carl May was initially a co-investigator on the study but was unable to contribute due to pressures of other commitments. We acknowledge his early contributions to our thinking about explanatory theory.
Contributions of authors
Joanne Turnbull (Lecturer, Health Services Research) led the research and the preparation of the report and was involved in the conceptualisation and design of the study, data collection and analysis and data interpretation.
Gemma McKenna (Research Fellow, Health Services Research) was involved in recruitment, data collection, analysis and interpretation of the data and assisted with drafting and revising of the report.
Jane Prichard (Senior Lecturer) was involved in the conception and design of the study, and the analysis and interpretation of data, provided psychological perspectives and assisted with drafting the report.
Anne Rogers (Professor of Health Systems Implementation) supported the design of the study and contributed to the analysis and interpretation of the data. She commented on drafts of the final report.
Robert Crouch (Consultant Nurse) supported the delivery of the study by liaising with NHS services, supporting access to acute trust and pre-hospital services for sampling, and advising on clinical and service provider aspects of the analysis. He commented on drafts of the final report.
Andrew Lennon contributed a perspective as urgent care service provider, liaising with other providers and supporting sample recruitment. He advised on primary and urgent care service and organisation delivery.
Catherine Pope (Professor of Medical Sociology) was centrally involved in the conception and design of the study and the analysis and interpretation of the data. She played a key role in the development of the typology and conceptual model and was also involved in the drafting and revising of the report.
Publications
Pope C, McKenna G, Tunbull J, Prichard J, Rogers A. Navigating and making sense of urgent and emergency care processes and provision [Published online ahead of print January 10 2019]. Health Expectations 2019.
Turnbull J, Pope C, Prichard J, McKenna G, Rogers A. A conceptual model of urgent care sense-making and help-seeking: a qualitative interview study of urgent care users in England. BMC Health Serv Res 2019;19:481.
Data-sharing statement
All qualitative data generated that can be shared are contained within the report. All data queries and requests should be submitted to the corresponding author for consideration.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- NHS England . High Quality Care for All, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England – Urgent and Emergency Care Review. End of Phase 1 Report 2013. www.england.nhs.uk/wp-content/uploads/2013/06/urg-emerg-care-ev-bse.pdf (accessed 16 May 2018).
- Department of Health and Social Care . NHS Next Stage Review. Our Vision for Primary and Community Care. 2008.
- NHS England Urgent and Emergency Care Review Team and Emergency Care Intensive Support Team . Transforming Urgent and Emergency Care Services in England – Update on the Urgent and Emergency Care Review 2014.
- Huibers L, Giesen P, Wensing M, Grol R. Out-of-hours care in western countries: assessment of different organizational models. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-105.
- Weick RM, Bristol SJ, DesRoches CM. Urgent care centers in the US: findings from a national survey. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-79.
- Harris P, Whitty JA, Kendall E, Ratcliffe J, Wilson A, Littlejohns P, et al. The Australian public’s preferences for emergency care alternatives and the influence of the presenting context: a discrete choice experiment. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006820.
- Broekhuis SM, van Dijk WD, Giesen P, Pavilanis A. Walk-in clinics in Quebec, Canada: patients and doctors do not agree on appropriateness of visits. Fam Pract 2014;31:92-101. https://doi.org/10.1093/fampra/cmt069.
- NHS England . Commissioning Standards: Integrated Urgent Care 2015.
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742-52. https://doi.org/10.7326/0003-4819-144-10-200605160-00125.
- Goode J, Hanlon G, Luff D, O’Cathain A, Strangleman T, Greatbatch D. Male callers to NHS Direct: the assertive carer, the new dad and the reluctant patient. Health 2004;8:311-28. https://doi.org/10.1177/1363459304043468.
- Sandman L, Munthe C. Shared decision-making and patient autonomy. Theor Med Bioeth 2009;30:289-310. https://doi.org/10.1007/s11017-009-9114-4.
- Greener I. Patient choice in the NHS: the view from economic sociology. Soc Theory Health 2003;1:72-89. https://doi.org/10.1057/palgrave.sth.8700002.
- Newman J, Vidler E. Discriminating customers, responsible patients, empowered users: consumerism and the modernisation of health care. J Soc Pol 2006;35. https://doi.org/10.1017/S0047279405009487.
- Turner J, Coster J, Chambers D, Cantrell A, Phung V, Knowles E, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015;3.
- Royal College of Emergency Medicine . Tackling Emergency Department Crowding 2015. www.rcem.ac.uk/docs/College%20Guidelines/5z23.%20ED%20crowding%20overview%20and%20toolkit%20(Dec%202015).pdf (accessed 16 May 2018).
- McHale P, Wood S, Hughes K, Bellis MA, Demnitz U, Wyke S. Who uses emergency departments inappropriately and when – a national cross-sectional study using a monitoring data system. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-258.
- Ismail SA, Gibbons DC, Gnani S. Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions. Br J Gen Pract 2013;63:e813-20. https://doi.org/10.3399/bjgp13X675395.
- Turnbull J, Pope C, Rowsell A, Prichard J, Halford S, Jones J, et al. The work, workforce, technology and organisational implications of the ‘111’ single point of access telephone number for urgent (non-emergency) care: a mixed-methods case study. Health Serv Deliv Res 2014;2.
- Pope C, Turnbull J, Halford S, Prichard J, Calestani M, Salisbury C, et al. Ethnography and Survey Analysis of a Computer Decision Support System in Urgent Out-of-Hours, Single Point of Access and Emergency (999) Care. 2010. www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1819-217_V01.pdf (accessed 14 December 2018).
- Turner J, O’Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003451.
- Weick KE. Sensemaking in Organizations. London: Sage; 1995.
- Waterman RH. Adhocracy: The Power to Change. Memphis, TN: Whittle Direct Books; 1990.
- Corbin J, Strauss A. Managing chronic illness at home: three lines of work. Qual Sociol 1985;8:224-47. https://doi.org/10.1007/BF00989485.
- Eton DT, Ramalho de Oliveira D, Egginton JS, Ridgeway JL, Odell L, May CR, et al. Building a measurement framework of burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Relat Outcome Meas 2012;3:39-4. https://doi.org/10.2147/PROM.S34681.
- O’Cathain A, Thomas K, Pope C, Mays N. Qualitative Research in Health Care. Oxford: Blackwell Publishing/BMJ Books; 2006.
- Weick KE, Sutcliffe KM, Obstfeld D. Organizing and the process of sensemaking. Organ Sci 2005;16:409-21. https://doi.org/10.1287/orsc.1050.0133.
- Critical Appraisal Skills Programme . CASP Qualitative Checklist 2018. www.casp-uk.net/checklists (accessed 16 May 2018).
- Rapley T. Doing Conversation, Discourse and Document Analysis. London: Sage; 2007.
- Iredale R, Longley M. From passive subject to active agent: the potential of citizens’ juries for nursing research. Nurse Educ Today 2007;27:788-95. https://doi.org/10.1016/j.nedt.2006.10.012.
- Wakeford T. Teach Yourself Citizens’ Juries Handbook. Newcastle upon Tyne: Policy Ethics and Life Sciences (PEALS); 2013.
- Crosby N, Renn O, Webler T, Wiedel-Mann P. Fairness and Competence in Citizen Participation: Evaluating Models for Environmental Discourse. Boston, MA: Kluwer Academic Press; 1995.
- Pickard S. Citizenship and consumerism in health care: a critique of citizens’ juries. Soc Policy Adm 1998;32:226-44. https://doi.org/10.1111/1467-9515.00100.
- National Institute for Health Research INVOLVE . Payment and Recognition for Public Involvement 2018. www.invo.org.uk/resource-centre/payment-and-recognition-for-public-involvement (accessed 16 May 2018).
- Cornwell J. Hard-Earned Lives: Accounts of Health and Illness from East London. London: Tavistock Publications; 1984.
- Raphaely N. Understanding the Health Needs of Migrants in the South East Region. Oxford: Health Protection Agency; 2010.
- Downing A, Wilson R. Older people’s use of accident and emergency services. Age Ageing 2005;34:24-30. https://doi.org/10.1093/ageing/afh214.
- Baker C. Accident and Emergency Statistics: Demand, Performance and Pressure, Briefing Paper Number 6964. London: House of Commons Library; 2017.
- Lowthian JA, Smith C, Stoelwinder JU, Smit DV, McNeil JJ, Cameron PA. Why older patients of lower clinical urgency choose to attend the emergency department. Intern Med J 2013;43:59-65. https://doi.org/10.1111/j.1445-5994.2012.02842.x.
- Age UK . Improving Later Life. Understanding the Oldest Old 2012. www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/health--wellbeing/rb_feb13_understanding_the_oldest_old_improving_later_life.pdf (accessed 16 May 2018).
- Gnani S, McDonald H, Islam S, Ramzan F, Davison M, Ladbrooke T, et al. Patterns of healthcare use among adolescents attending an urban general practitioner-led urgent care centre. Emerg Med J 2014;31:630-6. https://doi.org/10.1136/emermed-2012-202017.
- Amiel C, Williams B, Ramzan F, Islam S, Ladbrooke T, Majeed A, et al. Reasons for attending an urban urgent care centre with minor illness: a questionnaire study. Emerg Med J 2014;31:e71-5. https://doi.org/10.1136/emermed-2012-202016.
- Hampshire County Council . Hampshire International Migration Data Analysis 2012. www3.hants.gov.uk/migration_data_analysis_-_final_-_april_2012.pdf (accessed accessed 16 May 2018).
- Jayaweera H. Health of Migrants in the UK: What Do We Know?. Oxford, University of Oxford: The Migration Observatory; 2011.
- Institute for Health and Human Development . Health and Social Care Needs Assessment of Eastern European (Including Roma) Individuals Living in Barking and Dagenham 2010.
- Hargreaves S, Friedland JS, Gothard P, Saxena S, Millington H, Eliahoo J, et al. Impact on and use of health services by international migrants: questionnaire survey of inner city London A&E attenders. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-153.
- Petersen J, Longley P, Gibin M, Mateos P, Atkinson P. Names-based classification of accident and emergency department users. Health Place 2011;17:1162-9. https://doi.org/10.1016/j.healthplace.2010.09.010.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- NHS England and the UEC Review Team . Transforming Urgent and Emergency Care Services in England. Safer, Faster, Better: Good Practice in Delivering Urgent and Emergency Care. A Guide for Local Health and Social Care Communities 2015.
- Department of Health and Social Care . Direction of Travel for Urgent Care: A Discussion Document 2006.
- Royal College of General Practitioners . The Future of GP Out of Hours Care. Part One an RGCP Position Statement 2014.
- Primary Care Foundation and NHS Alliance . Breaking the Mould Without Breaking the System. New Ideas and Resources for Clinical Commissioners On the Journey Towards Integrated 24 7 Urgent Care 2011. www.primarycarefoundation.co.uk/images/PrimaryCareFoundation/Downloading_Reports/Reports_and_Articles/Urgent_Care_Commissioning/Breaking_the_Mould_RELEASE.pdf (accessed 16 May 2018).
- The King’s Fund . Transforming Our Healthcare System. Ten Priorities for Commissioners 2011. www.kingsfund.org.uk/sites/default/files/field/field_publication_file/10PrioritiesFinal2.pdf (accessed 16 May 2018).
- The King’s Fund . Urgent and Emergency Care. A Review for NHS South of England 2013.
- Welsh Government . Written Statement – Unscheduled Care Winter Pressures 2015. http://gov.wales/about/cabinet/cabinetstatements/previous-administration/2015/winterpressure/?lang=en (accessed 16 May 2018).
- Scottish Government . Pulling Together: Transforming Urgent Care for the People of Scotland the Report of the Independent Review of Primary Care Out of Hours Services 2015. www.gov.scot/Publications/2015/11/9014/downloads (accessed 16 May 2018).
- NHS . NHS Home Page 2017. www.nhs.uk/using-the-nhs/nhs-services/urgent-and-emergency-care/when-to-visit-an-urgent-care-centre/.
- NHS . NHS Home Page 2017. www.nhs.uk/using-the-nhs/nhs-services/urgent-and-emergency-care/when-to-go-to-ae/ (accessed 16 May 2018).
- National Audit Office . Out of Hours GP Services in England 2014. www.nao.org.uk/wp-content/uploads/2014/09/Out-of-hours-GP-services-in-England1.pdf (accessed 16 May 2018).
- NHS England . Transforming Urgent and Emergency Care Services in England. Urgent and Emergency Care Financial Modelling Methodology 2015. www.nhs.uk/NHSEngland/keogh-review/Documents/UEC-financial-modelling-methodology-FINAL.PDF (accessed 16 May 2018).
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/publication/nhs-five-year-forward-view/ (accessed 16 May 2018).
- Royal College of General Practitioners . Guidance for Commissioning Integrated Urgent and Emergency Care. A ‘Whole System’ Approach 2011. www.rcgp.org.uk/policy/rcgp-policy-areas/urgent-and-emergency-care.aspx (accessed 16 May 2018).
- NHS England . 111 – The New NHS Number 2012. www.nhs.uk/NHSEngland/AboutNHSservices/Emergencyandurgentcareservices/Documents/2012/NHS%20111%20Easy%20Read%20leaflet.pdf (accessed 16 May 2018).
- Department of Health and Social Care . NHS 111 Public Sector Equality Duty (PSED) Analysis of Impact on Equality (AIE) 2012. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213148/NHS111AnalysisOfImpactOnEquality20121.pdf (accessed 16 May 2018).
- Welsh Assembly Government . Delivering Emergency Healthcare Services. An Integrated Approach for Delivering Unscheduled Care in Wales 2008. www.wales.nhs.uk/documents/decsstrategye.pdf (accessed 16 May 2018).
- The Patients Association . Why Our NHS Should Listen and Be Human 2015.
- O’Cathain A, Coleman P, Nicholl J. Characteristics of the emergency and urgent care system important to patients: a qualitative study. J Health Serv Res Policy 2008;13:19-25. https://doi.org/10.1258/jhsrp.2007.007097.
- Department of Health and Social Care . Raising Standards for Patients New Partnerships in Out-of-Hours Care an Independent Review of GP Out-Of-Hours Services in England 2000.
- Morgans A, Burgess S. Judging a patient’s decision to seek emergency healthcare: clues for managing increasing patient demand. Aust Health Rev 2012;36:110-14. https://doi.org/10.1071/AH10921.
- Guttman N, Zimmerman DR, Nelson MS. The many faces of access: reasons for medically nonurgent emergency department visits. J Health Polit Policy Law 2003;28:1089-120. https://doi.org/10.1215/03616878-28-6-1089.
- O’Brien GM, Shapiro MJ, Fagan MJ, Woolard RW, O’Sullivan PS, Stein MD. Do internists and emergency physicians agree on the appropriateness of emergency department visits?. J Gen Intern Med 1997;12:188-91. https://doi.org/10.1007/s11606-006-5028-2.
- Bardelli P, Kaplan V. Non-urgent encounters in a Swiss medical emergency unit. Swiss Med Wkly 2013;143. https://doi.org/10.4414/smw.2013.13760.
- Breen BM, McCann M. Healthcare providers attitudes and perceptions of ‘inappropriate attendance’ in the emergency department. Int Emerg Nurs 2013;21:180-5. https://doi.org/10.1016/j.ienj.2012.08.006.
- Pereira S, Oliveira e Silva A, Quintas M, Almeida J, Marujo C, Pizarro M, et al. Appropriateness of emergency department visits in a Portuguese university hospital. Ann Emerg Med 2001;37:580-6. https://doi.org/10.1067/mem.2001.114306.
- Sempere-Selva T, Peiró S, Sendra-Pina P, Martínez-Espín C, López-Aguilera I. Inappropriate use of an accident and emergency department: magnitude, associated factors, and reasons – an approach with explicit criteria. Ann Emerg Med 2001;37:568-79. https://doi.org/10.1067/mem.2001.113464.
- Thomson H, Kohli HS, Brookes M. Non-emergency attenders at a district general hospital accident and emergency department. J Accid Emerg Med 1995;12:279-81. https://doi.org/10.1136/emj.12.4.279.
- O’Brien GM, Shapiro MJ, Woolard RW, O’Sullivan PS, Stein MD. ‘Inappropriate’ emergency department use: a comparison of three methodologies for identification. Acad Emerg Med 1996;3:252-7. https://doi.org/10.1111/j.1553-2712.1996.tb03429.x.
- Durand AC, Palazzolo S, Tanti-Hardouin N, Gerbeaux P, Sambuc R, Gentile S. Nonurgent patients in emergency departments: rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res Notes 2012;5. https://doi.org/10.1186/1756-0500-5-525.
- Redstone P, Vancura JL, Barry D, Kutner JS. Nonurgent use of the emergency department. J Ambul Care Manage 2008;31:370-6. https://doi.org/10.1097/01.JAC.0000336555.54460.fe.
- Liggins K. Inappropriate attendance at accident and emergency departments: a literature review. J Adv Nurs 1993;18:1141-5. https://doi.org/10.1046/j.1365-2648.1993.18071141.x.
- Hodgins MJ, Wuest J. Uncovering factors affecting use of the emergency department for less urgent health problems in urban and rural areas. Can J Nurs Res 2007;39:78-102.
- Durand AC, Gentile S, Devictor B, Palazzolo S, Vignally P, Gerbeaux P, et al. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med 2011;29:333-45. https://doi.org/10.1016/j.ajem.2010.01.003.
- Koziol-McLain J, Price DW, Weiss B, Quinn AA, Honigman B. Seeking care for nonurgent medical conditions in the emergency department: through the eyes of the patient. J Emerg Nurs 2000;26:554-63. https://doi.org/10.1067/men.2000.110904.
- Lang T, Davido A, Diakite B, Agay E, Viel JF, Flicoteaux B. Non-urgent care in the hospital medical emergency department in France: how much and which health needs does it reflect?. J Epidemiol Community Health 1996;50:456-62. https://doi.org/10.1136/jech.50.4.456.
- Lowe RA, Bindman AB. Judging who needs emergency department care: a prerequisite for policy-making. Am J Emerg Med 1997;15:133-6. https://doi.org/10.1016/S0735-6757(97)90083-8.
- Petersen LA, Burstin HR, O’Neil AC, Orav EJ, Brennan TA. Nonurgent emergency department visits: the effect of having a regular doctor. Med Care 1998;36:1249-55. https://doi.org/10.1097/00005650-199808000-00012.
- Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad Saude Publica 2009;25:7-28. https://doi.org/10.1590/S0102-311X2009000100002.
- Gill JM. Nonurgent use of the emergency department: appropriate or not?. Ann Emerg Med 1994;24:953-7. https://doi.org/10.1016/S0196-0644(94)70213-6.
- Sanders J. A review of health professional attitudes and patient perceptions on ‘inappropriate’ accident and emergency attendances. The implications for current minor injury service provision in England and Wales. J Adv Nurs 2000;31:1097-105. https://doi.org/10.1046/j.1365-2648.2000.01379.x.
- Goeman DP, Aroni RA, Sawyer SM, Stewart K, Thien FC, Abramson MJ, et al. Back for more: a qualitative study of emergency department reattendance for asthma. Med J Aust 2004;180:113-17.
- Afilalo M, Guttman A, Colacone A, Dankoff J, Tselios C, Beaudet M, et al. Emergency department use and misuse. J Emerg Med 1995;13:259-64. https://doi.org/10.1016/0736-4679(94)00157-X.
- Coleman P, Irons R, Nicholl J. Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency?. Emerg Med J 2001;18:482-7. https://doi.org/10.1136/emj.18.6.482.
- Gentile S, Vignally P, Durand AC, Gainotti S, Sambuc R, Gerbeaux P. Nonurgent patients in the emergency department? A French formula to prevent misuse. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-66.
- Hauswald M. Can paramedics safely decide which patients do not need ambulance transport or emergency department care?. Prehosp Emerg Care 2002;6:383-6. https://doi.org/10.1080/10903120290937978.
- Lo S, McKechnie S. Perceptions of service quality and sacrifice in patients with minor medical conditions using emergency care. Int J Clin Pract 2007;61:596-602. https://doi.org/10.1111/j.1742-1241.2006.00974.x.
- Murphy AW. ‘Inappropriate’ attenders at accident and emergency departments I: definition, incidence and reasons for attendance. Fam Pract 1998;15:23-32. https://doi.org/10.1093/fampra/15.1.23.
- Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department?. Emerg Med J 2012;29:487-91. https://doi.org/10.1136/emj.2010.107276.
- Truman CD, Reutter L. Care-giving and care-seeking behaviours of parents who take their children to an emergency department for non-urgent care. Can J Public Health 2002;93:41-6.
- Backman AS, Blomqvist P, Svensson T, Adami J. Health care utilization following a non-urgent visit in emergency department and primary care. Intern Emerg Med 2010;5:539-46. https://doi.org/10.1007/s11739-010-0439-9.
- Dunne MO, Martin AJ. The appropriateness of A&E attendances: a prospective study. Ir Med J 1997;90:268-9.
- Kirkby HM, Roberts LM. Inappropriate 999 calls: an online pilot survey. Emerg Med J 2012;29:141-6. https://doi.org/10.1136/emj.2010.092346.
- Müller U, Winterhalder R, Businger A, Zimmermann H, Exadaktylos AK. Why do walk-in patients prefer a busy urban emergency department during office hours? A pilot survey of 200 consecutive patients from Switzerland. Swiss Med Wkly 2012;142. https://doi.org/10.4414/smw.2012.13565.
- Richards JR, Ferrall SJ. Inappropriate use of emergency medical services transport: comparison of provider and patient perspectives. Acad Emerg Med 1999;6:14-20. https://doi.org/10.1111/j.1553-2712.1999.tb00088.x.
- Benahmed N, Laokri S, Zhang WH, Verhaeghe N, Trybou J, Cohen L, et al. Determinants of nonurgent use of the emergency department for pediatric patients in 12 hospitals in Belgium. Eur J Pediatr 2012;171:1829-37. https://doi.org/10.1007/s00431-012-1853-y.
- Bezzina AJ, Smith PB, Cromwell D, Eagar K. Primary care patients in the emergency department: who are they? A review of the definition of the ‘primary care patient’ in the emergency department. Emerg Med Australas 2005;17:472-9. https://doi.org/10.1111/j.1742-6723.2005.00779.x.
- Prince M, Worth C. A study of ‘inappropriate’ attendances to a paediatric accident and emergency department. J Public Health Med 1992;14:177-82.
- Richardson S, Ardagh M, Hider P. New Zealand health professionals do not agree about what defines appropriate attendance at an emergency department. N Z Med J 2006;119.
- Backman AS, Blomqvist P, Lagerlund M, Adami J. Physician assessment of appropriate healthcare level among nonurgent patients. Am J Manag Care 2010;16:361-8.
- Lowy A, Kohler B, Nicholl J. Attendance at accident and emergency departments: unnecessary or inappropriate?. J Public Health Med 1994;16:134-40. https://doi.org/10.1093/oxfordjournals.pubmed.a042947.
- Young GP, Wagner MB, Kellermann AL, Ellis J, Bouley D. Ambulatory visits to hospital emergency departments. Patterns and reasons for use. 24 Hours in the ED Study Group. JAMA 1996;276:460-5. https://doi.org/10.1001/jama.1996.03540060036032.
- Gill JM, Reese CL, Diamond JJ. Disagreement among health care professionals about the urgent care needs of emergency department patients. Ann Emerg Med 1996;28:474-9. https://doi.org/10.1016/S0196-0644(96)70108-7.
- Quan SD, Morra D, Lau FY, Coke W, Wong BM, Wu RC, et al. Perceptions of urgency: defining the gap between what physicians and nurses perceive to be an urgent issue. Int J Med Inform 2013;82:378-86. https://doi.org/10.1016/j.ijmedinf.2012.11.010.
- Arain M, Baxter S, Nicholl JP. Perceptions of healthcare professionals and managers regarding the effectiveness of GP-led walk-in centres in the UK. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008286.
- Greenfield G, Ignatowicz A, Gnani S, Bucktowonsing M, Ladbrooke T, Millington H, et al. Staff perceptions on patient motives for attending GP-led urgent care centres in London: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-007683.
- Pileggi C, Raffaele G, Angelillo IF. Paediatric utilization of an emergency department in Italy. Eur J Public Health 2006;16:565-9. https://doi.org/10.1093/eurpub/ckl019.
- Brousseau DC, Nimmer MR, Yunk NL, Nattinger AB, Greer A. Nonurgent emergency-department care: analysis of parent and primary physician perspectives. Pediatrics 2011;127:e375-81. https://doi.org/10.1542/peds.2010-1723.
- Chin NP, Goepp JG, Malia T, Harris L, Poordabbagh A. Nonurgent use of a pediatric emergency department: a preliminary qualitative study. Pediatr Emerg Care 2006;22:22-7. https://doi.org/10.1097/01.pec.0000195756.74328.21.
- Drinkwater J, Salmon P, Langer S, Hunter C, Stenhoff A, Guthrie E, et al. Operationalising unscheduled care policy: a qualitative study of healthcare professionals’ perspectives. Br J Gen Pract 2013;63:e192-9. https://doi.org/10.3399/bjgp13X664243.
- Guttman N, Nelson MS, Zimmerman DR. When the visit to the emergency department is medically nonurgent: provider ideologies and patient advice. Qual Health Res 2001;11:161-78. https://doi.org/10.1177/104973201129119028.
- Campbell NC, Iversen L, Farmer J, Guest C, MacDonald J. A qualitative study in rural and urban areas on whether – and how – to consult during routine and out of hours. BMC Fam Pract 2006;7. https://doi.org/10.1186/1471-2296-7-26.
- Jeffery R. Normal rubbish: deviant patients in casualty departments. Sociol Health Illn 1979;1:90-107. https://doi.org/10.1111/1467-9566.ep11006793.
- Smith H, Lattimer V, George S. General practitioners’ perceptions of the appropriateness and inappropriateness of out-of-hours calls. Br J Gen Pract 2001;51:270-5.
- Hillman A. ‘Why must I wait?’ The performance of legitimacy in a hospital emergency department. Sociol Health Illn 2014;36:485-99. https://doi.org/10.1111/1467-9566.12072.
- Smith S, Lynch J, O’Doherty K, Bury G. Patients’ views on out-of-hours care in general practice in Dublin. Ir J Med Sci 2001;170:192-4. https://doi.org/10.1007/BF03173889.
- Lowe R, Porter A, Snooks H, Button L, Evans BA. The association between illness representation profiles and use of unscheduled urgent and emergency health care services. Br J Health Psychol 2011;16:862-79. https://doi.org/10.1111/j.2044-8287.2011.02023.x.
- Langer S, Chew-Graham C, Hunter C, Guthrie EA, Salmon P. Why do patients with long-term conditions use unscheduled care? A qualitative literature review. Health Soc Care Community 2013;21:339-51. https://doi.org/10.1111/j.1365-2524.2012.01093.x.
- Turnbull J, Pope C, Martin D, Lattimer V. Do telephones overcome geographical barriers to general practice out-of-hours services? Mixed-methods study of parents with young children. J Health Serv Res Policy 2010;15:21-7. https://doi.org/10.1258/jhsrp.2009.009023.
- Hunter C, Chew-Graham C, Langer S, Stenhoff A, Drinkwater J, Guthrie E, et al. A qualitative study of patient choices in using emergency health care for long-term conditions: the importance of candidacy and recursivity. Patient Educ Couns 2013;93:335-41. https://doi.org/10.1016/j.pec.2013.06.001.
- Hopton J, Hogg R, McKee I. Patients’ accounts of calling the doctor out of hours: qualitative study in one general practice. BMJ 1996;313:991-4. https://doi.org/10.1136/bmj.313.7063.991.
- Shipman C, Dale J. Using and providing out-of-hours services: can patients and GPs agree?. Health Soc Care Community 1999;7:266-75. https://doi.org/10.1046/j.1365-2524.1999.00187.x.
- Kallestrup P, Bro F. Parents’ beliefs and expectations when presenting with a febrile child at an out-of-hours general practice clinic. Br J Gen Pract 2003;53:43-4.
- Drummond N, McConnachie A, O’Donnell CA, Moffat KJ, Wilson P, Ross S. Social variation in reasons for contacting general practice out-of-hours: implications for daytime service provision?. Br J Gen Pract 2000;50:460-4.
- Richards SH, Pound P, Dickens A, Greco M, Campbell JL. Exploring users’ experiences of accessing out-of-hours primary medical care services. Qual Saf Health Care 2007;16:469-77. https://doi.org/10.1136/qshc.2006.021501.
- Stafford V, Greenhalgh S, Davidson I. Why do patients with simple mechanical back pain seek urgent care?. Physiotherapy 2014;100:66-72. https://doi.org/10.1016/j.physio.2013.08.001.
- de Bont EG, Loonen N, Hendrix DA, Lepot JM, Dinant GJ, Cals JW. Childhood fever: a qualitative study on parents’ expectations and experiences during general practice out-of-hours care consultations. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0348-0.
- Veitch C, Crossland L, Hays R. Consumers’ after hours health care decisions. Comparison between those who did and those who did not seek care in an Australian provincial city. Aust Fam Physician 1999;28:1078-83.
- Hugenholtz M, Bröer C, van Daalen R. Apprehensive parents: a qualitative study of parents seeking immediate primary care for their children. Br J Gen Pract 2009;59:173-9. https://doi.org/10.3399/bjgp09X394996.
- Benger JR, Jones V. Why are we here? A study of patient actions prior to emergency hospital admission. Emerg Med J 2008;25:424-7. https://doi.org/10.1136/emj.2007.050856.
- Williams A, O’Rourke P, Keogh S. Making choices: why parents present to the emergency department for non-urgent care. Arch Dis Child 2009;94:817-20. https://doi.org/10.1136/adc.2008.149823.
- Land L, Meredith N. An evaluation of the reasons why patients attend a hospital Emergency Department. Int Emerg Nurs 2013;21:35-41. https://doi.org/10.1016/j.ienj.2011.12.001.
- Nelson J. Why patients visit emergency units rather than use primary care services. Emerg Nurse 2011;19:32-6. https://doi.org/10.7748/en2011.04.19.1.32.c8448.
- Thornton V, Fogarty A, Jones P, Ragaban N, Simpson C. Why do patients self-present to Middlemore Hospital Emergency Department?. N Z Med J 2014;127:19-30.
- Siminski P, Cragg S, Middleton R, Masso M, Lago L, Green J, et al. Primary care patients’ views on why they present to emergency departments: inappropriate attendances or inappropriate policy?. Aust J Prim Health 2005;11:87-95. https://doi.org/10.1071/PY05026.
- Northington WE, Brice JH, Zou B. Use of an emergency department by nonurgent patients. Am J Emerg Med 2005;23:131-7. https://doi.org/10.1016/j.ajem.2004.05.006.
- Gill JM, Riley AW. Nonurgent use of hospital emergency departments: urgency from the patient’s perspective. J Fam Pract 1996;42:491-6.
- Olsson M, Hansagi H. Repeated use of the emergency department: qualitative study of the patient’s perspective. Emerg Med J 2001;18:430-4. https://doi.org/10.1136/emj.18.6.430.
- Fieldston ES, Alpern ER, Nadel FM, Shea JA, Alessandrini EA. A qualitative assessment of reasons for nonurgent visits to the emergency department: parent and health professional opinions. Pediatr Emerg Care 2012;28:220-5. https://doi.org/10.1097/PEC.0b013e318248b431.
- Uscatescu V, Turner A, Ezer H. Return visits to the emergency department: what can we learn from older adults’ experiences?. J Gerontol Nurs 2014;40:32-40. https://doi.org/10.3928/00989134-20140421-02.
- Lawson CC, Carroll K, Gonzalez R, Priolo C, Apter AJ, Rhodes KV. ‘No other choice’: reasons for emergency department utilization among urban adults with acute asthma. Acad Emerg Med 2014;21:1-8. https://doi.org/10.1111/acem.12285.
- Calnan M. Managing ‘minor’ disorders: pathways to a hospital accident and emergency department. Sociol Health Illn 1983;5:149-67. https://doi.org/10.1111/1467-9566.ep10491503.
- Palmer CD, Jones KH, Jones PA, Polacarz SV, Evans GW. Urban legend versus rural reality: patients’ experience of attendance at accident and emergency departments in west Wales. Emerg Med J 2005;22:165-70. https://doi.org/10.1136/emj.2003.007674.
- Lobachova L, Brown DF, Sinclair J, Chang Y, Thielker KZ, Nagurney JT. Patient and provider perceptions of why patients seek care in emergency departments. J Emerg Med 2014;46:104-12. https://doi.org/10.1016/j.jemermed.2013.04.063.
- Becker G, Janson-Bjerklie S, Benner P, Slobin K, Ferketich S. The dilemma of seeking urgent care: asthma episodes and emergency service use. Soc Sci Med 1993;37:305-13. https://doi.org/10.1016/0277-9536(93)90262-3.
- Morgans A, Burgess SJ. What is a health emergency? The difference in definition and understanding between patients and health professionals. Aust Health Rev 2011;35:284-9. https://doi.org/10.1071/AH10922.
- Kalidindi S, Mahajan P, Thomas R, Sethuraman U. Parental perception of urgency of illness. Pediatr Emerg Care 2010;26:549-53. https://doi.org/10.1097/PEC.0b013e3181ea71b3.
- Ekwall A. Acuity and anxiety from the patient’s perspective in the emergency department. J Emerg Nurs 2013;39:534-8. https://doi.org/10.1016/j.jen.2010.10.003.
- Houston AM, Pickering AJ. ‘Do I don’t I call the doctor’: a qualitative study of parental perceptions of calling the GP out-of-hours. Health Expect 2000;3:234-42. https://doi.org/10.1046/j.1369-6513.2000.00109.x.
- Agarwal S, Banerjee J, Baker R, Conroy S, Hsu R, Rashid A, et al. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emerg Med J 2012;29. https://doi.org/10.1136/emermed-2011-200585.
- Booker MJ, Simmonds RL, Purdy S. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emerg Med J 2014;31:448-52. https://doi.org/10.1136/emermed-2012-202124.
- Rubin GJ, Amlôt R, Carter H, Large S, Wessely S, Page L. Reassuring and managing patients with concerns about swine flu: qualitative interviews with callers to NHS Direct. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-451.
- Stanley R, Zimmerman J, Hashikawa C, Clark SJ. Appropriateness of children’s nonurgent visits to selected Michigan emergency departments. Pediatr Emerg Care 2007;23:532-6. https://doi.org/10.1097/PEC.0b013e318128f84a.
- Dale J, Dolan B. Do patients use minor injury units appropriately?. J Public Health Med 1996;18:152-6. https://doi.org/10.1093/oxfordjournals.pubmed.a024474.
- Jackson CJ, Dixon-Woods M, Hsu R, Kurinczuk JJ. A qualitative study of choosing and using an NHS walk-in centre. Fam Pract 2005;22:269-74. https://doi.org/10.1093/fampra/cmi018.
- Chalder M, Montgomery A, Hollinghurst S, Cooke M, Munro J, Lattimer V, et al. Comparing care at walk-in centres and at accident and emergency departments: an exploration of patient choice, preference and satisfaction. Emerg Med J 2007;24:260-4. https://doi.org/10.1136/emj.2006.042499.
- Cook EJ, Randhawa G, Large S, Guppy A, Chater AM, Ali N. Barriers and facilitators to using NHS Direct: a qualitative study of ‘users’ and ‘non-users’. BMC Health Serv Res 2014;14. https://doi.org/10.1186/s12913-014-0487-3.
- Chapple A, Sibbald B, Rogers A, Roland M. Citizens’ expectations and likely use of a NHS walk-in centre: results of a survey and qualitative methods of research. Health Expect 2001;4:38-47. https://doi.org/10.1046/j.1369-6513.2001.00112.x.
- Claver ML. Deciding to use the emergency room: a qualitative survey of older veterans. J Gerontol Soc Work 2011;54:292-308. https://doi.org/10.1080/01634372.2011.552938.
- Shipman C, Longhurst S, Hollenbach F, Dale J. Using out-of-hours services: general practice or A&E?. Fam Pract 1997;14:503-9. https://doi.org/10.1093/fampra/14.6.503.
- Padgett DK, Brodsky B. Psychosocial factors influencing non-urgent use of the emergency room: a review of the literature and recommendations for research and improved service delivery. Soc Sci Med 1992;35:1189-97. https://doi.org/10.1016/0277-9536(92)90231-E.
- Soliday E, Hoeksel R. Factors related to paediatric patients’ emergency department utilization. Psychol Health Med 2001;6:5-12. https://doi.org/10.1080/713690225.
- Howard MS, Davis BA, Anderson C, Cherry D, Koller P, Shelton D. Patients’ perspective on choosing the emergency department for nonurgent medical care: a qualitative study exploring one reason for overcrowding. J Emerg Nurs 2005;31:429-35. https://doi.org/10.1016/j.jen.2005.06.023.
- Callen JL, Blundell L, Prgomet M. Emergency department use in a rural Australian setting: are the factors prompting attendance appropriate?. Aust Health Rev 2008;32:710-2. https://doi.org/10.1071/AH080710.
- Cooper C, Simpson JM, Hanson R. The district hospital emergency department: why do parents present?. Emerg Med (Fremantle) 2003;15:68-76. https://doi.org/10.1046/j.1442-2026.2003.00411.x.
- Moll van Charante EP, ter Riet G, Bindels P. Self-referrals to the A&E department during out-of-hours: patients’ motives and characteristics. Patient Educ Couns 2008;70:256-65. https://doi.org/10.1016/j.pec.2007.10.012.
- Rieffe C, Oosterveld P, Wijkel D, Wiefferink C. Reasons why patients bypass their GP to visit a hospital emergency department. Accid Emerg Nurs 1999;7:217-25. https://doi.org/10.1016/S0965-2302(99)80054-X.
- Woolfenden S, Ritchie J, Hanson R, Nossar V. Parental use of a paediatric emergency department as an ambulatory care service. Aust N Z J Public Health 2000;24:204-6. https://doi.org/10.1111/j.1467-842X.2000.tb00144.x.
- Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study. Ambul Pediatr 2008;8:360-7. https://doi.org/10.1016/j.ambp.2008.07.001.
- Brown I, Warner A, Mounstephen W, Shaw B. Parents’ reasons for bringing young children to hospital emergency for non-urgent reasons. Early Child Dev Care 2001;167:1-12. https://doi.org/10.1080/0300443011670101.
- Watson MC, Ferguson J, Barton GR, Maskrey V, Blyth A, Paudyal V, et al. A cohort study of influences, health outcomes and costs of patients’ health-seeking behaviour for minor ailments from primary and emergency care settings. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006261.
- Adamson J, Ben-Shlomo Y, Chaturvedi N, Donovan J. Exploring the impact of patient views on ‘appropriate’ use of services and help seeking: a mixed method study. Br J Gen Pract 2009;59:e226-33. https://doi.org/10.3399/bjgp09X453530.
- Foster J, Dale J, Jessopp L. A qualitative study of older people’s views of out-of-hours services. Br J Gen Pract 2001;51:719-23.
- Eastwood A, Jaye C. After hours healthcare for older patients in New Zealand – barriers to accessing care. N Z Med J 2006;119.
- Richards SH, Winder R, Seamark C, Seamark D, Avery S, Gilbert J, et al. The experiences and needs of people seeking palliative health care out-of-hours: a qualitative study. Prim Health Care Res Dev 2011;12:165-78. https://doi.org/10.1017/S1463423610000459.
- Maguire S, Ranmal R, Komulainen S, Pearse S, Maconochie I, Lakhanpaul M, et al. Which urgent care services do febrile children use and why?. Arch Dis Child 2011;96:810-16. https://doi.org/10.1136/adc.2010.210096.
- Nuffield Trust . What’s Behind the A&Amp;E ‘Crisis’? 2015. www.nuffieldtrust.org.uk/resource/what-s-behind-the-a-e-crisis (accessed 16 May 2018).
- Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care 1981;19:127-40. https://doi.org/10.1097/00005650-198102000-00001.
- Kelly LJ, Birtwhistle R. Is this problem urgent? Attitudes in a community hospital emergency room. Can Fam Physician 1993;39:1345-52.
- Frey L, Schmidt J, Derksen DJ, Skipper B. A rural emergency department. West J Med 1994;160:38-42.
- Dingwall R, Murray T. Categorization in accident departments: ‘good’ patients, ‘bad’ patients and ‘children’. Sociol Health Illn 1983;5:127-48. https://doi.org/10.1111/1467-9566.ep10491496.
- Davies A, Strong P. ‘Aren’t Children Wonderful?’: A Study of the Allocation of Identity in Developmental Assessment. Sociol Rev 1976;22:156-75.
- Mechanic D. The concept of illness behavior. J Chronic Dis 1962;15:189-94. https://doi.org/10.1016/0021-9681(62)90068-1.
- Young JT. Illness behaviour: a selective review and synthesis. Sociol Health Illn 2004;26:1-31. https://doi.org/10.1111/j.1467-9566.2004.00376.x.
- Zola IK. Culture and symptoms – an analysis of patients’ presenting complaints. Am Sociol Rev 1966;31:615-30. https://doi.org/10.2307/2091854.
- Wyke S, Adamson J, Dixon D, Hunt K. Consultation and illness behaviour in response to symptoms: a comparison of models from different disciplinary frameworks and suggestions for future research directions. Soc Sci Med 2013;86:79-87. https://doi.org/10.1016/j.socscimed.2013.03.007.
- Shipman C, Dale J. Responding to out-of-hours demand: the extent and nature of urgent need. Fam Pract 1999;16:23-7. https://doi.org/10.1093/fampra/16.1.23.
- Becker J, Dell A, Jenkins L, Sayed R. Reasons why patients with primary health care problems access a secondary hospital emergency centre. S Afr Med J 2012;102:800-1. https://doi.org/10.7196/SAMJ.6059.
- McKinlay J. Social networks, lay consultation and help-seeking behavior. Soc Forces 1973;51:275-92. https://doi.org/10.1093/sf/51.3.275.
- Pescosolido B. Beyond rational choice: the social dynamics of how people seek help. Am J Sociol 1992;97:1096-138. https://doi.org/10.1086/229863.
- Zola IK. Pathways to the doctor-from person to patient. Soc Sci Med 1973;7:677-89. https://doi.org/10.1016/0037-7856(73)90002-4.
- Granovetter M. The strength of weak ties. Am J Sociol 1973;78:1360-80. https://doi.org/10.1086/225469.
- Werner A, Malterud K. It is hard work behaving as a credible patient: encounters between women with chronic pain and their doctors. Soc Sci Med 2003;57:1409-19. https://doi.org/10.1016/S0277-9536(02)00520-8.
- O’Cathain A, Goode J, Luff D, Strangleman T, Hanlon G, Greatbatch D. Does NHS Direct empower patients?. Soc Sci Med 2005;61:1761-71. https://doi.org/10.1016/j.socscimed.2005.03.028.
- Rogers A, Hassell K, Nicolaas G. Demanding Patients. Analysing the Use of Primary Care. Buckingham: Open University; 1999.
- Parsons T. The Social System. London: Routledge & Kegan Paul; 1951.
- Suchman EA. Social patterns of illness and medical care. J Health Hum Behav 1965;6:2-16. https://doi.org/10.2307/2948614.
- Rosenstock IM. Why people use health services. Milbank Mem Fund Q 1966;44:94-127. https://doi.org/10.2307/3348967.
- Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc 1973;51:95-124. https://doi.org/10.2307/3349613.
- Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res 1974;9:208-20.
- Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res 1983;18:49-74.
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter?. J Health Soc Behav 1995;36:1-10. https://doi.org/10.2307/2137284.
- Aday LA, Andersen RM. Equity of access to medical care: a conceptual and empirical overview. Med Care 1981;19:4-27. https://doi.org/10.1097/00005650-198112001-00004.
- Freidson E. Profession of Medicine: a Study in the Sociology of Applied Knowledge. New York, NY: Dodd Mead; 1970.
- Freidson E. Patients’ Views of Medical Practice. New York, NY: Russell Sage; 1961.
- May C. The clinical encounter and the problem of context. Sociology 2007;41:29-45. https://doi.org/10.1177/0038038507072282.
- Healthy London Partnership . Coordinated Consistent and Clear Urgent and Emergency Care: Implementing the Urgent and Emergency Care Vision in London 2015.
- MacKichan F, Brangan E, Wye L, Checkland K, Lasserson D, Huntley A, et al. Why do patients seek primary medical care in emergency departments? An ethnographic exploration of access to general practice. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013816.
- Rati RM, Goulart LM, Alvim CG, Mota JA. ‘Children cannot wait’: why mothers seek urgency and emergency care services for their children in non-urgent situations. Cien Saude Colet 2013;18:3663-72. https://doi.org/10.1590/S1413-81232013001200022.
- Coventry LL, van Schalkwyk JW, Thompson PL, Hawkins SA, Hegney DG. Myocardial infarction, patient decision delay and help-seeking behaviour: a thematic analysis. J Clin Nurs 2017;26:1993-2005. https://doi.org/10.1111/jocn.13607.
- Doyle E. Calling NHS 24: Exploring Caller Decision Making and Help-Seeking Behaviour Within the Context of Out-of-Hours Health Care Provision. Edinburgh: University of Edinburgh; 2015.
- Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med 2017;24:1137-49. https://doi.org/10.1111/acem.13220.
- O’Cathain A, Knowles E, Turner J, Nicholl J. Acceptability of NHS 111 the telephone service for urgent health care: cross sectional postal survey of users’ views. Fam Pract 2014;31:193-200. https://doi.org/10.1093/fampra/cmt078.
- NHS Choices . Self Care Week 2017. www.england.nhs.uk/urgent-emergency-care/nhs-111/ (accessed 18 May 2018).
- Dixon-Woods M, Kirk D, Agarwal S, Annandale E, Arthur T, Harvey J, et al. Vulnerable Groups and Access to Health Care: A Critical Interpretive Review. London: NIHR Service Delivery and Organisation R&D Programme; 2005.
- Daniels J, Osborn M, Davis C. Better safe than sorry? Frequent attendance in a hospital emergency department: an exploratory study. Br J Pain 2018;12:10-9. https://doi.org/10.1177/2049463717720635.
- Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, et al. PEMI Study Group . Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain 2007;8:460-6. https://doi.org/10.1016/j.jpain.2006.12.005.
- Cunningham-Burley S, Maclean U, Wyke S, Hewison J. Child Health Matters: Caring for Children in the Community. Milton Keynes: Open University Press; 1991.
- Cunningham PJ, Clancy CM, Cohen JW, Wilets M. The use of hospital emergency departments for nonurgent health problems: a national perspective. Med Care Res Rev 1995;52:453-74. https://doi.org/10.1177/107755879505200402.
- Turnbull J, Prichard J, Pope C, Brook S, Rowsell A. Risk work in NHS 111: the everyday work of managing risk in telephone assessment using a computer decision support system. Health Risk Soc 2017;19:189-208. https://doi.org/10.1080/13698575.2017.1324946.
- Goode J, Greatbatch D, O’Cathain A, Luff D, Hanlon G, Strangleman T. Risk and the responsible health consumer: the problematics of entitlement among callers to NHS Direct. Crit Soc Policy 2004;24:210-32. https://doi.org/10.1177/0261018304041951.
- Kai J. What worries parents when their preschool children are acutely ill, and why: a qualitative study. BMJ 1996;313:983-6. https://doi.org/10.1136/bmj.313.7063.983.
- Calnan M, Wainwright D, O’Neill C, Winterbottom A, Watkins C. Illness action rediscovered: a case study of upper limb pain. Sociol Health Illn 2007;29:321-46. https://doi.org/10.1111/j.1467-9566.2007.00543.x.
- Turnbull J, Martin D, Lattimer V, Pope C, Culliford D. Does distance matter? Geographical variation in GP out-of-hours service use: an observational study. Br J Gen Pract 2008;58:471-7. https://doi.org/10.3399/bjgp08X319431.
- O’Reilly D, Stevenson M, McCay C, Jamison J. General practice out-of-hours service, variations in use and equality in access to a doctor: a cross-sectional study. Br J Gen Pract 2001;51:625-9.
- National Audit Office . Improving Patient Access to General Practice 2017.
- Nettleton S, Hanlon G, Webster A. New Technologies in Health Care. Health, Technology and Society. London: Palgrave Macmillan; 2006.
- British Medical Association (BMA) . Developing General Practice Today. Providing Healthcare Solutions for the Future 2013.
- Shipman C, Payne F, Dale J, Jessopp L. Patient-perceived benefits of and barriers to using out-of-hours primary care centres. Fam Pract 2001;18:149-55. https://doi.org/10.1093/fampra/18.2.149.
- Kellermann AL. Nonurgent emergency department visits. Meeting an unmet need. JAMA 1994;271:1953-4. https://doi.org/10.1001/jama.1994.03510480077038.
- Farmer J, Iversen L, Campbell NC, Guest C, Chesson R, Deans G, et al. Rural/urban differences in accounts of patients’ initial decisions to consult primary care. Health Place 2006;12:210-21. https://doi.org/10.1016/j.healthplace.2004.11.007.
- Howard R. Reasons for older people attending A&E. Nurs Times 1995;91:40-3.
- Spilsbury K, Meyer J, Bridges J, Holman C. Older adults’ experiences of A&E care. Emerg Nurse 1999;7:24-31. https://doi.org/10.7748/en1999.10.7.6.24.c1296.
- Kihlgren AL, Nilsson M, Skovdahl K, Palmblad B, Wimo A. Older patients awaiting emergency department treatment. Scand J Caring Sci 2004;18:169-76. https://doi.org/10.1111/j.1471-6712.2004.00266.x.
- McMillan RE, Stokes-Lampard H, Large R. What influences recurrent presentations of older people to the emergency department?. N Z Med J 2011;124:93-8.
- Kennelly SP, Drumm B, Coughlan T, Collins R, O’Neill D, Romero-Ortuno R. Characteristics and outcomes of older persons attending the emergency department: a retrospective cohort study. QJM 2014;107:977-87. https://doi.org/10.1093/qjmed/hcu111.
- Mort M, Finch T. Principles for telemedicine and telecare: the perspective of a citizens’ panel. J Telemed Telecare 2005;11:66-8. https://doi.org/10.1258/1357633054461877.
- Iredale R, Longley M, Thomas C, Shaw A. What choices should we be able to make about designer babies? A citizens’ jury of young people in South Wales. Health Expect 2006;9:207-17. https://doi.org/10.1111/j.1369-7625.2006.00387.x.
- Kashefi E, Mort M. Grounded citizens’ juries: a tool for health activism?. Health Expect 2004;7:290-302. https://doi.org/10.1111/j.1369-7625.2004.00295.x.
- Pope C, McKenna G, Tunbull J, Prichard J, Rogers A. Navigating and making sense of urgent and emergency care processes and provision [Published online ahead of print January 10 2019]. Health Expectations 2019.
- Wyke S. Why people use primary care health services? Do we really need more research?. J Health Serv Res Policy 2003;8:55-7. https://doi.org/10.1177/135581960300800111.
- Lawton J. Lay experiences of health and illness: past research and future agendas. Sociol Health Illn 2003;25:23-40. https://doi.org/10.1111/1467-9566.00338.
Appendix 1 Search strategy and key search terms for the literature review
| Health service: urgent care use | Ambulatory care (linked to urgent or unscheduled care); GP out-of-hours; unplanned care; unscheduled care; minor injuries unit; walk-in centre; NHS 111; NHS Direct; NHS 24; after hours care; mobile health units | Set 1 |
| Health service: (non-urgent) emergency care use | Emergency service, hospital; emergency medical services; emergency nursing; critical care; paramedic (linked to emergency or urgent); ambulances; ambulance service; emergency care teams | Set 1 |
| Patient experiences: help-seeking, decision-making, and use of services |
Patient help-seeking; sense-making; decision making patient decision, experience, perception, feedback, attitude, empower, satisfaction, expectation, participation, choice, motivation, behaviour, acceptance; satisfaction; understanding, comprehension, navigation, involvement, use; communication; health education; health knowledge, practice, behaviour; health literacy; public opinion; health services misuse; socioeconomic factors; anthropology, cultural; educational status; service user; access inappropriate use; correct advice; right advice; best advice; burden of treatment; opinion of stakeholder, professional, manager, policy, service provider, public Attitude of Health Personnel; delivery of health care; health services accessibility; health services needs and demand; health policy; marketing of Health Services; patient-centered care; personnel staffing and scheduling; organizational innovation; clinical governance; decision Support Systems, Clinical; Decision Support Systems, Management; Practice Management, Medical; Professional Practice Location/Health Facilities – Utilization and Planning; Hotlines; needs assessment; referral and consultation; patient care planning; Patient Compliance; Patient Care Management; Professional role/practice; Professional-Patient Relations; Interprofessional Relations; Quality Assurance/Improvement; Health Planning; Process Assessment (Health Care); Utilization Review; Models, Organizational; Linear Models; Systems Analysis; Outcome Assessment (Health Care; Organizational Case Studies; Seasons) |
Set 2 |
| Database, host, years searched, keywords added | Search strategy | Results |
|---|---|---|
|
Ovid MEDLINE(R) 1946 to November Week 1 2017 Restricted 1990–2017 Searched 17 November 2017 Keywords added: URGENT CARE SEARCH KW MEDLINE |
|
5387 |
|
Ovid MEDLINE In Process & Other Indexed Citations Searched 18 November 2017 Restricted 1990–2017 Keywords added MEIP URGENT CARE SEARCH KW |
As per MEDLINE | 66 |
|
Ovid EMBASE 1980 to 2017 Week 46 Restricted 1990–2017 Searched 18 November 2017 Keywords added MEIP URGENT CARE SEARCH KW |
|
2547 |
|
Web Of Science Indexes=SCI-EXPANDED, SSCI, CPCI-S Timespan=1990-2017 Searched 18 November 2017 Keywords Added: URGENT CARE SEARCH KW (WOS identified in web url, so keyword not added) |
# 1 761(TS=((‘urgent care’) and (service* or provider* or provision or policy or policies or centre* or center* or commission* or department* or clinic* or setting*))) # 2 38 (TS=(‘GP out of hours’)) # 3 192(TS=(‘out of hours service*’)) # 4 63 (TS=(‘minor injury unit*’ or ‘minor injuries unit*’)) # 5 91(TS=(‘walk in center*’ or ‘walk in centre*’)) # 6 29(TS=(‘walk in service*’)) # 7 13(TS=(‘NHS 111’)) # 8 32 (TS=(‘mobile health unit*’)) # 9 13 (TS=(‘NHS 24’)) # 10 258(TS=(‘NHS Direct’)) # 11 1,403 #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 # 12 466,350 (TS=((patient*) NEAR (educat* or decision* or experience* or perception* or perceiv* or feedback or attitude* or empower* or satisfaction or satisfied or expectation or participat* or choice* or motivat* or behaviour* or behaviour* or understand* or comprehen* or navigat* or involvement or perspective*))) # 13 189,253(TS=(‘sense-making’ or ‘health seeking’ or ‘decision making’)) # 14 1,079,170 (TS=(expectation or experience*)) # 15 232,796(TS=(utilization or utilisation)) # 16 722(TS=(‘consumer panel*’ or ‘patient panel*’ or ‘customer panel*’ or ‘citizen panel*’)) # 17 944,480(TS=(questionnaire* or survey*)) # 18 41,640 (TS=(opinion* AND (patient* or consumer* or stakeholder* or professional* or manager* or policy or service provider or public))) # 19 77,249 (TS=(attitude* AND (patient* or consumer* or stakeholder* or professional* or manager* or policy or service provider or public))) # 20 24,283 (TS=(misuse or misusing or misunderstanding)) # 21 791,786(TS=(opinion* or attitude* or behaviour* or behaviour*)) # 22 3,096,869#21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 # 23 747#22 AND #11 # 24 221(TI=‘urgent care’) # 25 895#24 OR #23 |
895 |
|
CINAHL EBSCOhost Searched 24 November 2017 Restricted 1990–2017 Keywords added: URGENT CARE SEARCH KW |
S1TI ‘urgent care’(253) S2‘urgent care’ N5 (clinic* or setting* or center* or centre* or practice* or nurs* or patient* or facilit* or practitioner* or system* or service* or provider* or commission* or policy or policies)) (588) S3(MH ‘Ambulatory Care Facilities’) OR (MH ‘Ambulatory Care Information Systems’) OR (MH ‘Ambulatory Care Nursing’) OR (MH ‘Ambulatory Care’) (13,453) S4TX ‘urgent care’ (4142) S5S3 AND S4 (225) S6(MH ‘Emergency Nurse Practitioners’) OR (MH ‘Emergency Service’) OR (MH ‘Emergency Service Information Systems’) OR (MH ‘Emergency Patients’) OR (MH ‘Emergency Nurses Association’) (37,608) S7S4 AND S6 (477) S8TX ‘GP out of hours’ (185) S9TX ‘General Practice out of hours’ (34) S10TX ‘out of hours service*’ (741) S11TX (‘minor injury unit*’ or ‘minor injuries unit*’) (623) S12TX (‘walk in center*’ or ‘walk in centre*’) (1154) S13TX ‘walk in service’ (65) S14TX ‘NHS 111’ (231) S15TX (‘NHS 24’ or ‘NHS Direct’) (2078) S16S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 (4143) S17S4 AND S16 (271) S18S1 OR S2 OR S5 OR S7 OR S17 (1319) S19(appropriate* or inappropriate* or misuse or misusing or misunderstand* or ‘unnecessary attendance’) (91,036) S20(‘sense-making’ or ‘health seeking’ or ‘decision making’) (86,138) S21(expectation* or experience*) (230,918) S22(opinion* or attitude* or behaviour* or behaviour*) (259,386) S23(‘consumer panel*’ or ‘patient panel*’ or ‘customer panel*’ or ‘citizen panel’) (104) S24(questionnaire* or survey*) (413,699) S25(MH ‘Decision Making’) OR (MH ‘Decision Making, Organizational’) OR (MH ‘Decision Making, Computer Assisted’) OR (MH ‘Decision Making, Patient’) (46,472) S26(MH ‘Questionnaires+’) (269,196) S27(MH ‘Qualitative Studies’) (67,006) S28(MH ‘Focus Groups’) OR (MH ‘Pilot Studies’) (77,545) S29S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 (892,832) S30S4 AND S29 (1072) S31S18 AND S29 (435) S32S30 OR S31 (1169) S33S1 OR S32 (1398) |
1398 |
|
ProQuest Sociology search Searched 25 November 2017 Restricted 1990–2017 Keywords added: URGENT CARE SEARCH KW |
(‘urgent care’ or ‘GP out of hours’ or ‘NHS Direct’ or ‘NHS 111’)18 (‘Ambulatory care’£ and urgent)1 record already in database so not downloaded ‘emergency care’ 22 records2 downloaded ‘out of hours service’ 3 records 1 downloaded ‘out of hours’ – 14 results – nothing downloaded relevant items in database already |
21 |
|
EBSCOhost PsycInfo Searched 25 November 2017 Keywords added: URGENT CARE SEARCH KW |
S1TI ‘urgent care’ OR KW ‘urgent care’(42) S2‘NHS 111’ (1) S3‘NHS Direct’ (36) S4GP out of hours’ (8) S5‘general practice out of hours’ (2) S6‘NHS 24’ (6) S7‘walk in centre*’ OR ‘walk in center*’ OR ‘walk in service’ (53) S8‘walk in clinic*’ OR TX ‘walk in medical clinic*’ (197) S9‘after hours’ (165) S10‘minor injuries unit*’ OR ‘minor injury unit’ (1) S11S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 (448) S12TX urgent (6133) S13‘sense-making’ OR ‘help-seeking’ (8674) S14DE ‘Help-seeking Behavior’ OR DE ‘Health Care Seeking Behavior’ OR DE ‘Health Care Utilization’ (19,817) S15DE ‘Decision Making’ OR DE ‘Group Decision Making’ OR DE ‘Management Decision Making’ OR DE ‘Decision Support Systems’ OR DE ‘Decision Theory’ OR DE ‘Health Literacy’ (66,222) S16DE ‘Questionnaires’ (15,430) S17DE ‘Qualitative Research’ (6318) S18‘consumer panel*’ OR ‘citizen panel*’ OR ‘patient panel*’ (204) S19S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 (116,448) S20S11 AND S19 (69) S21TX ‘urgent care’ (202) S22S13 OR S14 OR S15 OR S16 OR S17 OR S18 (110,621) S23S21 AND S22 (53) S24S1 OR S20 OR S23 (135) |
135 |
|
Delphis (university cross database search resource) Searched 1 December 2017 Restricted 1990–2017 Keywords added: URGENT CARE SEARCH KW DELPHIS |
Various quick title searches as a double check for formal search strategy | 1 |
List of abbreviations
- A&E
- accident and emergency
- CASP
- Critical Appraisal Skills Programme
- CCG
- Clinical Commissioning Group
- ED
- emergency department
- EMS
- emergency medical services
- GP
- general practitioner
- HRA
- Health Research Authority
- HSDR
- Health Services and Delivery Research
- MeSH
- Medical Subject Headings
- MIU
- minor injuries unit
- NIHR
- National Institute for Health Research
- PPI
- patient and public involvement
- UCC
- urgent care centre
- WIC
- walk-in centre
- WP
- work package
