Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/77/05. The contractual start date was in August 2016. The final report began editorial review in September 2017 and was accepted for publication in January 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Karen Spilsbury is a member of the National Institute for Health Research Health Services and Delivery Research board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Hanratty et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
NHS England’s ‘vanguard programme’ has been leading on innovating and integrating services to meet the changing needs of local populations. Four categories of vanguard site were defined: integrated primary and acute care systems, multispecialty community providers, urgent and emergency care systems, and care for older people living in care homes. This evidence synthesis aims to provide empirical underpinning for the innovation that is already under way in the six vanguard care home sites. It will also contribute to the evolution and refinement of new care models as they are developed, evaluated and disseminated across the NHS and social care.
The mixed economy in the care home sector poses unique challenges to the integration of services. The funding of care homes, resident care and in-reach services is a mix of public and private. The majority of care homes are commercial bodies that must work across organisational and disciplinary boundaries, and liaise with state-funded health and social care services, independent professionals, social enterprises and charities. 1 Residents of care homes have increasingly complex health-care needs. Levels of multimorbidity, frailty and disability are rising as the care home population ages. 2 Across the care home sector, recruiting and retaining the nursing and support workforce and high staff turnover are ongoing challenges. Technology offers many potential benefits to care and communication, but the availability and uptake of this are variable. Over recent years, a consensus has emerged that services for care home residents need to improve in a range of ways. These include better access to co-ordinated and multidisciplinary care, partnership working,3 enhanced dignity and privacy, and staffing levels matched to the needs of residents. 3,4 The vanguard programme is part of the policy response to these identified needs. It aims to develop and evaluate new models of care, with a renewed emphasis on prevention, active rehabilitation and health promotion in care homes. This is expected to enhance well-being while also reducing resource use. 5
This report presents the findings from a rapid synthesis of the evidence on enhancing health in care homes through the organisation, delivery and quality of services to care home residents. The six vanguard care home sites are, and have been, developing locally appropriate services that have potential for national replicability, adaption and spread. To maximise the benefit to the wider NHS from the investment in this programme, it is important that innovation is followed by dissemination, and underpinned, when possible, by existing evidence. A review now is timely to ensure that any changes that are spread across the NHS are grounded in evidence-based good practice. Gaps in our knowledge also need to be identified for ongoing evaluation and research. Vanguard sites are being encouraged to learn from international experience. Our review will provide an objective, critical synthesis of relevant findings from other countries that aims to help vanguard sites and others to consider novel ways of working and radical change to enhance care.
Our work is focused around four inter-related issues: technology, communication and engagement, workforce and evaluation. These are key enablers of care home vanguard success, as identified in early guidance for vanguard sites. 6 They are also expected to be enduring issues with relevance to other settings. By considering some of the issues pertinent to developing and evaluating new models of care in and with the care home sector, this work aims to inform the ongoing work of the vanguard programme to meet the challenges of commissioning and delivering care across a range of providers.
The term ‘care home’ is used in this report to describe residential care for older adults in facilities with registered nurses (RNs) on site (nursing homes) and those without (residential care). Under this umbrella term, we have considered research on similar settings in high-income countries.
Chapter 2 Aims and objectives
The aim of this review was to identify and synthesise evidence underpinning new models of care to enhance health in care homes. The focus was in four key areas: technology, communication and engagement, workforce and evaluation.
Objectives
Our objectives were to:
-
identify the potential uses, benefits and challenges of technology in care homes and for enhancing communication between care homes and partner organisations (what is the impact of technology, who benefits and how?)
-
identify flexible uses of the nursing and support workforce, and innovative ways of working and retaining staff to benefit resident care
-
identify and critically describe the key characteristics and benefits of effective communication and engagement between care homes, communities and other health-related organisations, including barriers to and facilitators of the initiation and maintenance of successful relationships
-
summarise existing evidence on approaches to the evaluation of new models of care in care homes, including an assessment of the quality of care received by residents.
Specification of questions for rapid systematic reviews
We worked with the vanguard sites to ensure that we specified questions for review that were relevant to commissioners, providers and front-line staff. After completing the mapping reviews, we identified a range of potential questions for each of the four themes (technology, communication and engagement, workforce and evaluation) that could be answered by a focused evidence synthesis. An interactive workshop with representatives of the vanguard sites and NHS England was held to prioritise single questions for each theme. The potential questions are shown in Appendix 1. The selected questions are as follows:
-
Technology – which technologies have a positive impact on resident health and well-being?
-
Communication and engagement – how should care homes and the NHS communicate to enhance resident, family and staff outcomes and experiences?
-
Evaluation – which measurement tools have been validated for use in UK care homes?
-
Workforce – what is the evidence that staffing levels (i.e. ratio of RNs and support staff to residents or different levels of support staff) influence resident outcomes?
Chapter 3 Methods: overview
For each of the four themes, the evidence synthesis comprised two stages: (1) a broad mapping review of published material within the theme and (2) a systematic review that addressed a specific question. The general methods for each are described in this chapter, including details of the how the methods were tailored to each specific theme.
Literature searches
Two information scientists developed the search strategies. They combined relevant search terms with indexed keywords [such as medical subject headings (MeSH)] and text terms that appeared in the titles and/or abstracts of database records. The searches were applied to selected, specific databases for each topic, in addition to a common set of databases that included MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Science Citation Index, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects (DARE) and the Index to Theses. Searches were restricted to studies published in English between 2000 and 2016 in high-income countries (see Appendix 2). Grey literature and unpublished studies were sought via GoogleTM (Mountain View, CA. USA) and websites of organisations relevant to each search.
Technology searches also included PsycINFO, the Association of Computing Machinery’s Digital Library and IEEE Xplore® Digital Library, alongside the following grey literature resources: ProQuest Dissertations & Theses, NHS Evidence, Health Management Information Consortium, The King’s Fund, Nuffield Trust, Health Foundation, Social Care Institute for Excellence, National Institute for Health and Care Excellence, and Archiv.org.
Communication and engagement searches included PsycINFO, Cochrane Central Register of Controlled Trials (CENTRAL), Health Technology Assessment, NHS Economic Evaluation Database (NHS EED) and Applied Social Sciences Index and Abstracts (ASSIA). Grey literature searches were not undertaken.
Workforce searches included Arts and Humanities Citation Index and ASSIA. In addition, grey literature sources included Google, GreyLit.org, Theses Canada, Open Grey, ProQuest Dissertations & Theses, Care Quality Commission, Age UK, Alzheimer’s Society, Nuffield Trust, Carers UK, Abbeyfield, The King’s Fund, National Institute for Health Research School for Social Care, Personal Social Services Research Unit, Royal College of Nursing, Vanguards and the Joseph Rowntree Foundation.
Evaluation searches included Cochrane Database of Methods Studies, CENTRAL, Health Technology Assessment, NHS EED and PsycINFO. Grey literature sources included Google, Joseph Rowntree Foundation, Kellogg, The King’s Fund, Nuffield Trust, ProQuest, RAND Corporation, Robert Wood Johnson Foundation and Social Care Online.
References and abstracts of journal articles and grey literature were downloaded into an EndNote X7 (Thomson Reuters, CA, USA) library and deduplication was undertaken. Two researchers screened titles and abstracts for initial inclusion. Initial screening was undertaken in EndNote or Rayyan (Mourad Ouzzani, Hossam Hammady, Zbys Fedorowicz, and Ahmed Elmagarmid. Rayyan – a web and mobile app for systematic reviews. Systematic Reviews 2016;5:210); the latter is a web application for title and abstract screening for systematic reviews. 7 The criteria used across all four mapping reviews were inclusive. By allowing any study design or outcome, the review team were able to fully scope the available evidence base. Full papers were retrieved for all studies that met the broad criteria and were of potential relevance to the mapping review. All papers retrieved were further scrutinised to obtain a final set of papers for inclusion in the mapping review.
Mapping review: broad inclusion criteria
Technology
Any study concerning the use of novel digital technology to enhance health and well-being in care homes, encompassing novel technologies as well as established technologies that are new to the care home setting, which reported staff, resident or service outcomes and/or barriers and facilitators.
Communication and engagement
The focus of eligible studies was communication or engagement between more than one care home, or between care homes and communities or health-related organisations. Studies also needed to report one of the following outcomes:
-
a measure of communication or engagement external to the care home (i.e. studies of communication between patients and/or staff only within a care home were not included)
-
resident outcomes (e.g. quality of care, health and safety, clinical outcomes)
-
staff outcomes (e.g. well-being, safety, satisfaction).
Workforce
Studies that report on new staff roles (e.g. a NHS ‘in-reach’ role in a care home or an enhanced role for support workers in the home) or report on staffing levels in care homes. Studies were also required to report one or more of the following outcomes:
-
resident outcomes – health status, improvement or maintenance of functional ability, activities of daily living (ADL), falls, mortality, quality of life or well-being measures
-
staff outcomes – well-being, satisfaction or recruitment and retention
-
service use outcomes – on use of external NHS and social care, or other, services and care home organisation or profits/commercial success
-
impacts on relationships or integration between care homes and partner organisations.
Evaluation
Studies including tools for measuring quality of care, or aspects of patient health or quality of life, validated in a UK care home, that reported any of the following outcomes: (1) resident outcomes (health status, improvement or maintenance of functional ability, ADL, falls, mortality, quality of life or well-being measures) and (2) methods of care quality assessment.
Mapping review: data extraction
Information was extracted from each study into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet. The data included citation, location (country) of study, study design, target population, name and brief details of the intervention. Mapping data extraction was conducted by one reviewer and checked by a second reviewer.
Data extraction: technology mapping
Data were also extracted on the presence of an assessment of the costs of, barriers to, and facilitators of, the implementation and acceptability of the technologies. For each of the mapped studies, the interventions were listed, and descriptive categories were developed from this list: digital records, telehealth, surveillance and monitoring, robots, communication (excluding telemedicine or telehealth interventions), education and gaming. An eighth category (technologies) was used for the heterogeneous mix of studies that did not fall into any of the preceding seven categories.
Data extraction: communication and engagement mapping
Data were also extracted on target population (whether in the care home or communication partner) and setting of communication partner (e.g. another care home or a hospital emergency department), and outcomes were separated according to whether they related to communication or engagement, care home residents, staff or organisation.
Data extraction: workforce mapping
Outcomes were classified as relating to staff, residents or services.
Data extraction: evaluation mapping
Additional data extracted included sample size, sample characteristics, description of the intervention and control comparator conditions, outcomes and outcome measures used, and results.
Mapping review: synthesis
Mapping findings were tabulated in tables and narratively. These results were presented to the vanguard group and used to help formulate potential review questions for each theme. A range of potential questions for each of the four themes (technology, communication and engagement, workforce and evaluation) were derived that could be answered with a focused evidence synthesis. An interactive workshop with representatives of the vanguard sites and NHS England was held to prioritise single questions for each theme.
Systematic review questions
-
Technology: which technologies have a positive impact on resident health and well-being?
-
Communication and engagement: how should care homes and the NHS communicate to enhance resident, family and staff outcomes and experiences?
-
Evaluation: which measurement tools have been validated for use in UK care homes?
-
Workforce: what is the evidence that staffing levels (i.e. ratio of RNs and support staff to residents or different levels of support staff) influence resident outcomes?
The systematic reviews were conducted according to the principles outlined in Centre for Reviews and Dissemination’s guidance on the conduct of systematic reviews8 and reported following the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 9 The protocols were written in accordance with the new PRISMA-P initiative10 and registered on PROSPERO, the international database of prospectively registered systematic reviews in health and social care (www.crd.york.ac.uk/prospero/).
Inclusion and exclusion criteria
After being mapped, papers were screened once more (independently by two reviewers) to identify those that met the criteria for inclusion for each systematic review. For three of the themes (communication and engagement, evaluation and workforce), additional focused searches were conducted to ensure that the material included in the review was comprehensive.
The inclusion criteria for each systematic review are now outlined.
Technology review
Types of participants
Studies had to be focused on care homes, nursing homes or residential aged care facilities.
Intervention
The intervention of interest was equipment or methods that incorporate digital technology (any electrical device that can store, generate and transfer data) to enhance health and well-being in care homes, encompassing novel technologies as well as established technologies that are new to the care home setting.
Outcomes
The relevant outcome was care home residents’ health, functional ability or well-being.
Study design
Relevant study designs included randomised controlled trials (RCTs) (including parallel-group trials, cluster randomised trials and crossover trials) and non-randomised controlled studies.
Communication and engagement review
Types of participants
Studies had to be focused on care homes, nursing homes or residential aged care facilities; the communication partner could be a hospital, another health-related organisation or a community health partner.
Intervention
The intervention of interest was some form of tool that improved communication or an explicit statement that that the study was focusing on communication between care homes and other health-related organisations. Studies were excluded if the focus of communication was not relevant to the UK (e.g. US Medicaid or Medicare processes).
Outcomes
Communication or engagement outcomes, for example staff views on communication, resident outcomes (health/well-being, safety and quality of care) and/or staff outcomes (well-being, safety and satisfaction).
Study design
Randomised controlled trials, cluster RCTs, quasi-experimental studies, interrupted time series and pre- and post-intervention studies.
Workforce review
Types of participants
The populations of interest were staff and residents from a care home setting. The term ‘staff’ included people paid a salary or wage (not volunteers) within any of the following categories: (1) people employed directly by care homes, (2) staff employed by the NHS, excluding pharmacist interventions, (3) staff of local authority social services and (4) staff of private providers. Relevant staff employed by care homes included (1) registered or licensed nurses; (2) personnel providing personal care and support with ADL and instrumental ADL who are not registered or licensed nurses – job titles may include care assistant, nursing assistant (NA), auxiliary and social care worker; (3) care home managers; and (4) personnel who provide and/or direct activities in the home.
Intervention
The intervention of interest was staffing levels, which was defined as the ratio of RNs and support staff to residents or different levels of support staff, and the role mix of staff within nursing homes.
Outcomes
Relevant resident outcomes were one or more of the following: health status, quality of life or well-being measures, improvement or maintenance of functional ability (e.g. ADL), adverse events (e.g. falls), health service utilisation and mortality. Relevant staff outcomes were measures of health, well-being, satisfaction or recruitment/retention/turnover.
Study design
Relevant study designs were systematic reviews, RCTs, non-randomised trials, primary and secondary cohort/panel studies and cross-sectional studies.
Evaluation review
Types of participants
The population of interest was residents, families, carers or staff from a care home setting.
Intervention
The intervention of interest included approaches to the evaluation of new models of care in care homes, and approaches to the assessment of the quality of care received by care home residents.
Outcomes
Relevant outcomes were (1) resident outcomes (health status, improvement or maintenance of functional ability, ADL, falls, mortality, quality of life or well-being measures) and (2) methods of care quality assessment.
Study design
All comparative studies were considered eligible.
Data extraction and quality assessment
For all reviews, data extraction was conducted by one researcher and checked by a second researcher for accuracy, with any discrepancies resolved by discussion or consultation with a third researcher when necessary. A standardised data extraction form for each review was developed, piloted on an initial sample of papers and refined as necessary. Data extracted included study citation, country of origin, design, sample size, sample characteristics, description of the intervention and control comparator conditions, outcomes and outcome measures used, and findings. All data extraction was undertaken in Microsoft Excel.
Quality assessment was undertaken alongside the data extraction. The quality of RCTs was assessed using the Cochrane Risk of Bias tool, which focuses on the domains shown to have an impact on the trial results in particular (selection, performance and detection biases and attrition). 11 All and non-RCTs (observational studies) were assessed using the ROBINS-I (Risk of Bias In Non-Randomised Studies – of Interventions) tool, which also focuses on the bias domains likely to have an impact on results (selection, measurement, performance, attrition, detection and outcome). 12 Both tools focus on the internal validity of a study. Discrepancies between reviewers’ ratings were resolved through discussion. For some interventions considered, the blinding of participants would have been impractical and the blinding of assessors would have been challenging. For this reason, ratings of the measurement of outcome data were considered to be less important. Most of the studies were given a low quality score in this domain. To summarise the ratings from the ROBINS-I, each domain was judged to exhibit low, moderate, serious or critical risk of bias. Low risk of bias indicates that the study is comparable with a well-performed randomised trial in the domain being evaluated. Moderate risk of bias indicates that the study is sound for a non-randomised study but not comparable with a rigorous randomised trial. Serious risk of bias indicates the presence of important problems, and critical risk of bias indicates that the study is too problematic to provide any useful evidence on the effects of intervention. If insufficient information is provided to determine the risk of bias of a certain domain, the domain is marked as having no information.
Data synthesis
Data from the individual studies were tabulated and discussed in a narrative overview. Owing to the nature of the available evidence, a quantitative analysis of the results, including a meta-analysis, was not appropriate. There was extensive heterogeneity in study design, settings and outcome measures across the included studies.
Chapter 4 Mapping and rapid evidence syntheses
In the following sections, the findings are presented from four mapping reviews and four rapid, systematic evidence syntheses. The mapping reviews are broad-ranging and intended to provide a flexible and interactive resource. In this report, the data are tabulated for information. For dissemination purposes, they will be made available in a colourful, diagrammatic and interactive format.
Section 1: digital technology interventions and care home residents’ health, well-being and functional status
Background
Digital technology is expected to play an increasingly important role in enhancing the health, well-being and safety of care home residents. The list of potential applications of technology in this setting is long, and includes remote monitoring, communication between care homes and external agencies and families, medicines optimisation, assistive technologies and the promotion of physical and social activity. 13 Recent developments have focused in particular on the introduction of platforms that link electronic health and care data records,14,15 tools for remote consultation and diagnosis, sensor-based technologies that monitor movement and physical activity16,17 and social robots that act as companions or serve to support ADL. 18
Research in this field has accumulated rapidly over the last 10 years, but a clear message on the most acceptable, effective and cost-effective choices for care home residents, providers and commissioners has yet to emerge. Previous evidence syntheses have examined the effectiveness of individual technologies (e.g. robotic pets, sensors and telehealth), specific outcomes (e.g. wandering, falls)19–22 and the implementation of complex infrastructure information technology (IT) systems. Telemedicine in long-term care has been used to enable a range of medical specialists to provide advice in care homes. 21,23 Existing reviews of the evidence suggest that this is a feasible approach, but this work is dominated by qualitative and descriptive studies of service utilisation and staff satisfaction. Similarly, a review of the use of gaming technologies in long-term care settings points to positive effects on physical and social activity and a potential role in rehabilitation, but the six included studies were mainly descriptive or small. 24 Wearable or environmental sensors have multiple potential uses in residential care: they detect movement by pressure, position and infrared light, and can alert staff that a resident has risen from a chair or got out of bed and may be at risk of falling. A recent systematic review of the effectiveness of sensors in geriatric institutions described a high rate of false alarms and inconsistent findings, and only 1 of the 12 included studies was conducted in a care home. 20 Robots in older adult care have also attracted a great deal of attention from researchers and practitioners. They can be divided into two groups: rehabilitative robots that are designed to support physical assistive technology and are not interactive (e.g. smart wheelchairs and artificial limbs) and assistive robots that either support ADL or have a companion function. Research generally reports positive findings for the impact of robots on older people’s well-being. Kachouie’s review of social assistive robots25 also suggested that these may have potential to reduce nurses’ workload. However, this work identified limitations common to many existing studies, including a failure to consider cultural and linguistic sensitivities or to elicit participants’ expectations or perceptions, a gender bias among research participants (the majority are older women), little work with residents’ families, and methodological concerns about study design, conduct and reporting. 25
Previous research has provided useful insights, but important gaps remain in our understanding of the value, impact and best use of digital technology in care homes. Care home organisations are interested in the potential of technology to enhance quality of life, boost social interaction and enhance resident safety. Policy-makers and commissioners may also wish to advocate for the use of technology to increase efficiency and reduce demands on health services. All are faced with a disparate body of evidence from a wide range of sources, some of which is relevant to long-term care. Previous reviews of the evidence have synthesised research from across different care settings and have included qualitative, non-experimental and small-scale studies that provide useful information on the acceptability of and satisfaction with technological interventions, but are an uncertain basis for resource allocation decisions. Care homes and their residents are unique in many ways, and it cannot be assumed that an intervention that is suitable for the community can be readily transferred to a care home. To our knowledge, no review has focused exclusively on technological interventions in care homes.
The aim of this work was to (1) map the existing evidence on the use and outcomes of digital technology interventions in care homes, describe the body of work, and identify gaps in our understanding and areas where evidence is strong; and (2) conduct a focused systematic review on the impact of digital technology interventions on the health, well-being and functional status of care home residents.
Methods
See Chapter 3 for details of methods.
Findings of mapping review
Which technologies have a positive impact on resident health and well-being?
Number and characteristics of studies
After deduplication, 6240 studies were identified for title and abstract screening, and 338 were identified for full-text screening. In total, 281 articles were included in the mapping review, listed in Table 1. Basic data on all of the studies in this mapping review are presented in Report Supplementary Material 1,Table 1.
| First author | Year of publication | Review |
|---|---|---|
| Abdelrahman26 | 2015 | Technology |
| Age UK27 | 2013 | Technology |
| Age UK28 | 2010 | Technology |
| Age UK29 | 2012 | Technology |
| Alexander30 | 2009 | Technology |
| Alexander31 | 2015 | Technology |
| Alexander32 | 2016 | Technology |
| Aloulou33 | 2013 | Technology |
| Alzheimer’s Society34 | 2011 | Technology |
| Alzheimer’s Society35 | 2015 | Technology |
| Anonymous36 | 2009 | Technology |
| Anonymous37 | 2011 | Technology |
| Anonymous38 | 2010 | Technology |
| Anonymous39 | 2008 | Technology |
| Anonymous40 | 2009 | Technology |
| Anonymous41 | 2013 | Technology |
| Babalola42 | 2014 | Technology |
| Bäck43 | 2013 | Technology |
| Bäck44 | 2012 | Technology |
| Baker45 | 2015 | Technology |
| Bakerjian46 | 2009 | Technology |
| Banks47 | 2008 | Technology |
| Banks48 | 2013 | Technology |
| Barbour49 | 2016 | Technology |
| Baril50 | 2014 | Technology |
| Baril51 | 2014 | Technology |
| Barrett52 | 2009 | Technology |
| Bartle53 | 2017 | Technology |
| Beeckman54 | 2013 | Technology |
| Beedholm55 | 2016 | Technology |
| Bemelmans19 | 2012 | Technology |
| Bemelmans56 | 2015 | Technology |
| Bemelmans57 | 2016 | Technology |
| Bennett58 | 2015 | Technology |
| Bennett59 | 2016 | Technology |
| Bereznicki60 | 2014 | Technology |
| Bezboruah61 | 2014 | Technology |
| Biglan62 | 2011 | Technology |
| Biglan63 | 2009 | Technology |
| Blair Irvine64 | 2012 | Technology |
| Bobillier Chaumon65 | 2014 | Technology |
| Bollen66 | 2005 | Technology |
| Bond67 | 2000 | Technology |
| Bowen68 | 2013 | Technology |
| Brandt69 | 2011 | Technology |
| Brankline70 | 2009 | Technology |
| Bratan71 | 2004 | Technology |
| Braun72 | 2014 | Technology |
| Broadbent73 | 2016 | Technology |
| Broder74 | 2015 | Technology |
| Brown75 | 2000 | Technology |
| Bruun-Pedersen76 | 2015 | Technology |
| Burdea77 | 2015 | Technology |
| Burns78 | 2007 | Technology |
| Bygholm79 | 2014 | Technology |
| Campbell80 | 2011 | Technology |
| Campbell81 | 2017 | Technology |
| Castle82 | 2009 | Technology |
| Centre for Workforce Intelligence83 | 2013 | Technology |
| Chae84 | 2001 | Technology |
| Chan85 | 2000 | Technology |
| Chan86 | 2001 | Technology |
| Chang87 | 2013 | Technology |
| Chang88 | 2014 | Technology |
| Chang89 | 2015 | Technology |
| Chen90 | 2012 | Technology |
| Cherry91 | 2011 | Technology |
| Chesler92 | 2015 | Technology |
| Clark93 | 2009 | Technology |
| Cobb94 | 2007 | Technology |
| Courtney95 | 2006 | Technology |
| Centre for Policy on Ageing96 | 2014 | Technology |
| Curyto97 | 2002 | Technology |
| Daly98 | 2005 | Technology |
| Damant99 | 2015 | Technology |
| De Luca100 | 2016 | Technology |
| De Luca101 | 2016 | Technology |
| de Veer102 | 2011 | Technology |
| Degenholtz103 | 2008 | Technology |
| Degenholtz104 | 2010 | Technology |
| Degenholtz105 | 2011 | Technology |
| Degenholtz106 | 2016 | Technology |
| Demiris107 | 2008 | Technology |
| Demiris108 | 2013 | Technology |
| Dewsbury109 | 2012 | Technology |
| Dorsten110 | 2009 | Technology |
| Doshi-Velez111 | 2012 | Technology |
| Driessen112 | 2016 | Technology |
| Eccles113 | 2012 | Technology |
| Edirippulige23 | 2013 | Technology |
| Elliott114 | 2016 | Technology |
| Eyers115 | 2013 | Technology |
| Field116 | 2008 | Technology |
| Filipova117 | 2015 | Technology |
| Fossum118 | 2011 | Technology |
| Fossum119 | 2012 | Technology |
| Fournier120 | 2004 | Technology |
| Freedman121 | 2005 | Technology |
| Fu122 | 2015 | Technology |
| Gaver123 | 2011 | Technology |
| Gerling124 | 2012 | Technology |
| Gerling125 | 2015 | Technology |
| Ghorbel126 | 2013 | Technology |
| Gietzelt127 | 2014 | Technology |
| Grabowski128 | 2014 | Technology |
| Grant129 | 2014 | Technology |
| Guilfoyle130 | 2003 | Technology |
| Guilfoyle131 | 2002 | Technology |
| Hamada132 | 2008 | Technology |
| Handler133 | 2013 | Technology |
| Hardy134 | 2016 | Technology |
| Harrington135 | 2003 | Technology |
| Hensel136 | 2006 | Technology |
| Hensel137 | 2007 | Technology |
| Hensel138 | 2009 | Technology |
| Hex139 | 2015 | Technology |
| Hitt140 | 2016 | Technology |
| Hobday141 | 2010 | Technology |
| Hoey142 | 2010 | Technology |
| Hofmeyer143 | 2016 | Technology |
| Hori144 | 2004 | Technology |
| Hori145 | 2006 | Technology |
| Hoti146 | 2012 | Technology |
| Hsu147 | 2011 | Technology |
| Hui148 | 2001 | Technology |
| Hui149 | 2002 | Technology |
| Hung150 | 2007 | Technology |
| Hustey151 | 2009 | Technology |
| Hustey152 | 2010 | Technology |
| Hustey153 | 2012 | Technology |
| Iio154 | 2014 | Technology |
| Irvine155 | 2012 | Technology |
| Irvine156 | 2012 | Technology |
| Jiang157 | 2014 | Technology |
| Johansson-Pajala158 | 2016 | Technology |
| Johnston159 | 2001 | Technology |
| Jøranson160 | 2015 | Technology |
| Jøranson161 | 2015 | Technology |
| Jøranson162 | 2016 | Technology |
| Jung163 | 2009 | Technology |
| Kachouie25 | 2014 | Technology |
| Kanstrup164 | 2015 | Technology |
| Kapadia165 | 2015 | Technology |
| Keogh166 | 2014 | Technology |
| Khosla167 | 2012 | Technology |
| Khosla168 | 2013 | Technology |
| Kidd169 | 2006 | Technology |
| Kidd21 | 2010 | Technology |
| Knapp170 | 2015 | Technology |
| Kong171 | 2012 | Technology |
| Kosse20 | 2013 | Technology |
| Lai172 | 2015 | Technology |
| Lattanzio173 | 2014 | Technology |
| Lawrence174 | 2010 | Technology |
| Lesnoff-Caravaglia175 | 2005 | Technology |
| Libin176 | 2004 | Technology |
| Lin177 | 2014 | Technology |
| Little178 | 2016 | Technology |
| Loh179 | 2009 | Technology |
| Loveday16 | 2016 | Technology |
| Low180 | 2013 | Technology |
| Lyketsos181 | 2001 | Technology |
| MacDonald182 | 2005 | Technology |
| Maiden183 | 2013 | Technology |
| Mansdorf184 | 2009 | Technology |
| Mariño185 | 2016 | Technology |
| Marston24 | 2013 | Technology |
| Martin-Khan186 | 2012 | Technology |
| McDonald187 | 2012 | Technology |
| McGibbon188 | 2013 | Technology |
| McNeil189 | 2013 | Technology |
| Meador190 | 2009 | Technology |
| Meißner191 | 2014 | Technology |
| Michel-Verkerke192 | 2012 | Technology |
| Mickus193 | 2002 | Technology |
| Millington194 | 2015 | Technology |
| Miskelly195 | 2004 | Technology |
| Mitzner196 | 2014 | Technology |
| Morley197 | 2012 | Technology |
| Morley198 | 2016 | Technology |
| Morrissey199 | 2015 | Technology |
| Moyle200 | 2013 | Technology |
| Moyle201 | 2013 | Technology |
| Moyle202 | 2015 | Technology |
| Moyle203 | 2017 | Technology |
| Munyisia204 | 2012 | Technology |
| Munyisia205 | 2011 | Technology |
| Munyisia206 | 2013 | Technology |
| Murphy207 | 2005 | Technology |
| My Home Life208 | 2012 | Technology |
| Naganuma209 | 2015 | Technology |
| Nagayama210 | 2016 | Technology |
| Nakai211 | 2000 | Technology |
| Namazi212 | 2003 | Technology |
| Niemeijer213 | 2011 | Technology |
| Niemeijer214 | 2014 | Technology |
| Niemeijer215 | 2015 | Technology |
| Novek216 | 2000 | Technology |
| Oliver217 | 2006 | Technology |
| Oliver218 | 2010 | Technology |
| Pallawala219 | 2001 | Technology |
| Park220 | 2012 | Technology |
| Pillemer221 | 2009 | Technology |
| Pillemer222 | 2012 | Technology |
| Potts223 | 2011 | Technology |
| Qadri224 | 2009 | Technology |
| Qian225 | 2015 | Technology |
| Rabinowitz226 | 2010 | Technology |
| Rantz227 | 2010 | Technology |
| Rantz228 | 2013 | Technology |
| Rantz229 | 2015 | Technology |
| Rantz230 | 2017 | Technology |
| Ratliff231 | 2005 | Technology |
| Remington232 | 2015 | Technology |
| Richardson233 | 2014 | Technology |
| Robinson22 | 2006 | Technology |
| Robinson234 | 2007 | Technology |
| Robinson235 | 2013 | Technology |
| Robinson236 | 2013 | Technology |
| Robinson237 | 2015 | Technology |
| Robinson238 | 2016 | Technology |
| Rochon239 | 2006 | Technology |
| Rosen240 | 2002 | Technology |
| Rosen241 | 2003 | Technology |
| Rudston242 | 2013 | Technology |
| Russell243 | 2015 | Technology |
| Šabanović244 | 2013 | Technology |
| Sabelli245 | 2011 | Technology |
| Sanctuary Care246 | 2016 | Technology |
| Sävenstedt247 | 2003 | Technology |
| Sävenstedt248 | 2004 | Technology |
| Schneider249 | 2016 | Technology |
| Shibata250 | 2004 | Technology |
| Sicurella251 | 2016 | Technology |
| Silverman252 | 2006 | Technology |
| Smith253 | 2014 | Technology |
| South East Health Technologies Alliance254 | 2016 | Technology |
| Specht255 | 2001 | Technology |
| Spiro256 | 2005 | Technology |
| Stephens257 | 2015 | Technology |
| Sugihara258 | 2015 | Technology |
| Sung259 | 2015 | Technology |
| Tabar260 | 2015 | Technology |
| Tak261 | 2007 | Technology |
| Tak262 | 2008 | Technology |
| Tak263 | 2012 | Technology |
| Tak264 | 2013 | Technology |
| Tang265 | 2001 | Technology |
| Thorpe-Jamison266 | 2013 | Technology |
| Tinder Foundation267 | 2016 | Technology |
| Tiwari268 | 2011 | Technology |
| Toh269 | 2015 | Technology |
| Toh270 | 2015 | Technology |
| Torres-Padrosa271 | 2011 | Technology |
| Trinkle272 | 2003 | Technology |
| Tseng273 | 2013 | Technology |
| Van der Ploeg274 | 2016 | Technology |
| Vandenberg275 | 2015 | Technology |
| Vogelsmeier276 | 2007 | Technology |
| Vowden277 | 2013 | Technology |
| Wagner278 | 2004 | Technology |
| Wagner279 | 2001 | Technology |
| Wakefield280 | 2004 | Technology |
| Walker281 | 2006 | Technology |
| Walker282 | 2008 | Technology |
| Wang283 | 2011 | Technology |
| Webster284 | 2014 | Technology |
| Weiner285 | 2002 | Technology |
| Weiner286 | 2004 | Technology |
| Welsh287 | 2010 | Technology |
| Wigg288 | 2010 | Technology |
| Yu289 | 2006 | Technology |
| Yu290 | 2007 | Technology |
| Yu291 | 2013 | Technology |
| Zelickson292 | 2003 | Technology |
| Zhang293 | 2012 | Technology |
| Zhang294 | 2016 | Technology |
| Zhuang295 | 2013 | Technology |
| Zwijsen296 | 2010 | Technology |
| Zwijsen297 | 2012 | Technology |
Countries
The USA was the setting for around two-fifths of the work (114 studies). 26,30–32,36,42,46–49,64,67–70,74,75,77,82,87–89,91,93–95,97,98,103–108,110–112,117,120,121,128,129,133,134,136–138,140,141,143,151–153,155,156,159,172,175,176,178,181,184,189,190,192,196–198,212,217,218,221,222,224,226–233,239–241,243,244,250,252,255,257,260–264,266,272,276,278–282,285,286 A further 94 (33%) studies were from high-income countries outside the USA and Europe. 19,23–25,33,37–41,50–52,61,62,66,73,78,81,84–86,90,92,101,114,116,122,125,130–132,142,144–150,154,157,164–168,171,174,177,179,180,182,185–187,201–205,209–211,216,219,220,225,235–238,245,249,251,253,256,258,259,265,268–270,273–275,283,289–291,293,295 A minority of studies were conducted in Europe (n = 78, 28%), half of these in the UK. 16,20–22,27–29,34,35,43–45,53–60,63,65,71,72,76,79,80,83,96,99,100,102,109,113,115,118,119,123,124,126,127,134,139,158,160–162,164,170,173,183,188,191,192,194,195,199,200,206–208,213–215,223,234,242,246–248,254,267,271,277,284,296,297 Most of the work was recent, with a rapid increase in the annual publication rate post 2009: approximately three-quarters of the articles were published after that date.
All of the 38 UK studies were published after 2010. They comprised 14 reviews or reports relating to technology and care homes,21,22,27–29,35,83,96,99,170,208,234,254,267 three case studies,80,134,246 three qualitative studies,115,124,194 two observational studies,16,139 one pilot RCT,277 one protocol,45 12 descriptive studies58,59,71,109,113,123,188,195,207,223,242,284 and two opinion pieces. 34,53 Telehealth and surveillance technologies were both the subject of six articles,16,71,113,115,195,234 and single articles were identified on gaming,125 robots,80 digital records134 and communication technologies. 246 The remaining 21 studies comprised a mix of topics, including general overviews of technology in long-term care, digital exclusion and assistive technologies.
Methodologies
A range of research methods had been employed, but most studies fell into the lower categories of the established hierarchies of evidence. 298 The biggest single group of studies (n = 78, 28%) comprised those that were descriptive or non-experimental, including case studies and small feasibility studies. 36,38,40,42,44,48,50–52,58–61,63,68,71,74–77,79,80,88–90,93–95,97,98,109,111,113,114,120,123,126,134,137,142,144,145,150,167,169,173,174,178,180,182,183,185,188,190,193,195–197,200,207,209,211,218–220,223,226,228,242,243,246,249,250,255,258,265,267,271,284,285,288,290,294 A further 16 (6%) were opinion pieces34,46,53,189,198,217,232,239,251,256,260,278,279,286,287,292 and a small number were of narrative, non-systematic overviews of the current state of research. Qualitative methods have been extensively used to explore various aspects of technology in care homes; these were the main focus of 59 (21%) studies. 30,31,33,55,57,65,66,69,78,103,107,108,110,115,118,119,121,124,129,130,136–138,140,146,158,159,164,168,171,176,179,192,194,199,212–216,224,225,233,237,241,245,247,248,257,268,270,273,275,276,283,291,293,296,297
Table 2 shows the breakdown of research methods by intervention topic. Qualitative and descriptive studies form the largest groups for all topics. However, for robots, gaming and education, more than one-third of the studies are experimental or quasi-experimental.
| Study design | Topic, n (%) | Total, n | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Digital records | Telehealth | Communications | Robots | Surveillance | Gaming | Education | Technologies | ||
| Systematic review | 2 (5) | 2 (3) | 0 | 2 (5) | 2 (6) | 1 (7) | 0 | 2 (3) | 11 |
| Experimental and quasi-experimental | 5 (12) | 11 (18) | 3 (27) | 12 (31) | 2 (6) | 5 (36) | 8 (57) | 9 (16) | 55 |
| Observational | 3 (7) | 11 (18) | 0 | 5 (13) | 4 (13) | 2 (14) | 1 (7) | 3 (20) | 29 |
| Cross-sectional | 7 (16) | 2 (3) | 2 (18) | 1 (3) | 1 (3) | 0 | 0 | 3 (20) | 16 |
| Qualitative | 12 (28) | 9 (15) | 5 (45) | 7 (18) | 9 (42) | 2 (14) | 2 (14) | 13 (19) | 59 |
| Descriptive | 10 (23) | 19 (32) | 1 (9) | 11 (28) | 13 (33) | 4 (28) | 2 (14) | 23 (52) | 83 |
| Overview and reports | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 (16) | 11 |
| Other | 4 (9) | 6 (10) | 0 | 1 (3) | 0 | 0 | 1 (7) | 6 (25) | 18 |
| Total | 43 (100) | 60 (100) | 11 (100) | 39 (100) | 31 (100) | 14 (100) | 14 (100) | 70 (100) | 282 |
Qualitative research can provide invaluable insights into resident and staff experiences and perceptions of new uses of technology. Fifty-nine of the included articles described studies that used qualitative methods to investigate interventions in all categories. 30,31,33,55,57,65,66,69,78,103,107,108,110,115,118,119,121,124,129,130,136–138,140,146,158,159,164,168,171,176,179,192,194,199,212–216,224,225,233,237,241,245,247,248,257,268,270,273,275,276,283,291,293,296,297 Twelve explored technologies related to digital records, nine related to telehealth and surveillance technologies, seven related to robots, two related to communication technologies and two related to gaming. The remaining 18 studies covered a mix of topics.
One in 10 articles (n = 29, 10%) reported on observational (case control and cohort) studies, and just under one in five (n = 53, 19%) was an experimental or a quasi-experimental design, including before-and-after studies. Many of these were pilot studies and did not appear to be powered to detect significant differences between any intervention and control groups. Eleven systematic reviews of previous evidence were identified. Only two of these followed established guidance for producing systematic reviews. 19,22
Interventions or topics
The mapped studies described technologies directed at care processes, resident and staff experiences and outcomes of care. More than half of all articles (n = 145, 51%) related to the use of technologies that were likely to directly influence experiences and processes of care (communication, telehealth, digital health records, surveillance and monitoring). Thirty-nine articles (14%) related to the use of robots that may have companion or rehabilitative functions. 19,25,39,43,47,48,55–57,73,80,87–89,132,160–162,167–169,176,196,200–203,209,220,235–238,244,245,250,251,259,268 The use of technology for education or training with staff or residents’ families (e.g. online training in dementia care or injury prevention) was the subject of 14 (5%) articles. 45,64,134,141,155,156,171,182,184,240,241,243,281,282
Studies were concerned with the impact of technology on residents (n = 106, 38%), staff (n = 78, 28%) or a mix of residents and staff (n = 95, 34%). Only a small minority were concerned exclusively with residents’ families (n = 3, 1%).
When outcomes were measured or discussed, these related to residents in 107 (38%) articles and to staff in 70 (25%) articles. Thirty-three (12%) articles considered the impact of technology on the use of other services, and 30 (11%) presented or discussed costs or any form of economic assessment.
Barriers to, and facilitators of, technology use in care homes
Barriers to, and facilitators of, technology use were considered in just under half (n = 123, 43%) of the articles. One hundred and thirteen of these described interventions in telehealth, digital records or communication, topics of particular importance and current relevance to health care in care homes. The barriers and facilitators listed in these articles were examined more closely and grouped into 10 categories. Table 3 shows the number of articles mentioning barriers or facilitators, by category. Many of the identified barriers were also potential facilitators of the uptake and use of technology. The most frequently occurring issues were ease of use, staff attitudes and structural concerns. Cost and ease of use were most often discussed as barriers, whereas staff attitudes and work demands were more likely to be facilitators.
| Factor | Articles, n (%) | ||
|---|---|---|---|
| Communication technologies (N = 11) | Digital records (N = 43) | Telehealth (N = 60) | |
| Cost | |||
| Barrier | 2 (18) | 3 (7) | 10 (17) |
| Facilitator | 1 (9) | 2 (5) | 3 (5) |
| Structural issues | |||
| Barrier | 4 (36) | 10 (23) | 11 (18) |
| Facilitator | 0 | 0 | 0 |
| Ease of use | |||
| Barrier | 4 (36) | 8 (19) | 4 (7) |
| Facilitator | 1 (9) | 10 (23) | 4 (7) |
| Staff attitudes/motivation | |||
| Barrier | 3 (27) | 8 (19) | 4 (7) |
| Facilitator | 2 (18) | 12 (28) | 8 (13) |
| Integration with existing systems | |||
| Barrier | 3 (27) | 2 (5) | 2 (3) |
| Facilitator | 0 | 0 | 0 |
| Access to training | |||
| Barrier | 4 (36) | 2 (5) | 3 (5) |
| Facilitator | 1 (9) | 4 (10) | 2 (3) |
| Reliability of technology | |||
| Barrier | 1 (9) | 3 (7) | 5 (8) |
| Facilitator | 0 | 1 (2) | 0 |
| Legal/regulatory issues | |||
| Barrier | 1 (9) | 1 (2) | 1 (2) |
| Facilitator | 0 | 1 (2) | 0 |
| Incentives | |||
| Barrier | 0 | 1 (2) | 0 |
| Facilitator | 0 | 1 (2) | 1 (2) |
| Work demands | |||
| Barrier | 0 | 5 (12) | 6 (10) |
| Facilitator | 1 (9) | 11 (26) | 4 (7) |
Table 3 shows the number of articles on communication technologies, digital records and telehealth that discuss barriers to, and facilitators of, the implementation or use of technology.
Findings of systematic evidence synthesis
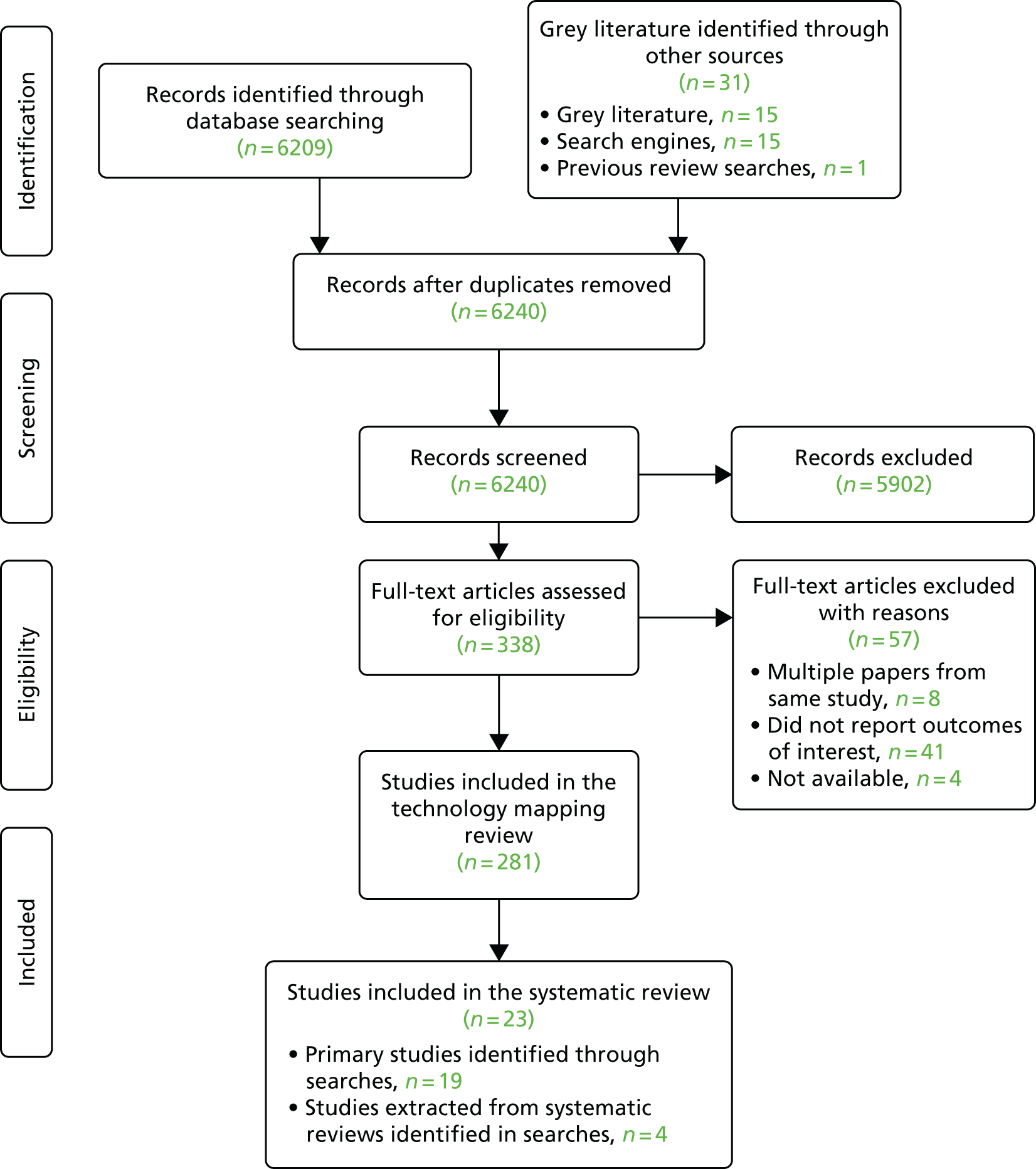
Twenty-three studies met the inclusion criteria for the systematic review. The PRISMA diagram for this study is shown in Figure 1. Ten studies were conducted in the USA,47,169,176,210,222,227,230,299–301 two in Australia,203,274 two in New Zealand166,236 and one in each of Belgium,54 Canada,147 Italy,101 Japan,250 Singapore,163 Norway,160 Taiwan,177 the Netherlands56 and the UK. 277 Thirteen randomised studies were included (six individually randomised parallel group trials, two individually randomised crossover trials and five cluster randomised trials),47,54,101,147,160,177,203,210,230,236,274,277,299 as were 11 non-randomised studies of interventions. 56,161,163,166,168,169,176,222,227,250,300,301 Details of the studies included in this systematic review are shown in Tables 4–7.
FIGURE 1.
Technology PRISMA flow diagram.
| Authors, year of publication, location | Design | Sample size (care home residents) | Sample characteristics | Interventions and comparators | Outcomes and measures | Overall risk of bias rating | Results |
|---|---|---|---|---|---|---|---|
| Beeckman, 2013, Belgium54 | Cluster RCT | 11 wards in four nursing homes (464 residents and 118 professionals) | Mean resident age 84.5 years, 76% female, (intervention group); mean age 84.9 years, 82.8% female (control group) |
|
Prevalence of pressure ulcers, prevention measures, knowledge and attitudes among staff | High | Residents in the intervention group were significantly more likely to receive adequate pressure ulcer prevention, but there were no differences in pressure ulcer prevalence between the groups. Professionals’ knowledge was unchanged |
| Hsu et al., 2011, Canada147 | Crossover RCT | 34 residents | Mean age 80 years; 71% female (whole sample); participants were cognitively intact, with upper extremity dysfunction |
|
Scores on the following measures: a numeric rating scale of pain intensity, Physical Activity Enjoyment Scale and a six-item measure of functional capacity | High | Enjoyment of activity was significantly greater in the intervention group (p = 0.014); for all other outcomes similar improvements were shown in both groups |
| Jung et al., 2009, Singapore163 | Quasi-experimental study | 45 residents | Age range 56–92 years (whole sample) (gender balance not stated) |
|
Scores on the UCLA Loneliness and Rosenberg Self-Esteem scales; Bradburn Affect Balance Scale; Physical Activity Questionnaire for Elderly Japanese | Critical | Intervention group participants scored significantly higher on affect (p < 0.05), self-esteem and physical activity and significantly lower on loneliness (p < 0.01) than those in the control group |
| Keogh et al., 2014, New Zealand302 | Quasi-experimental study | 34 residents | Mean age 83 years; 88% female |
|
Functional ability (bicep curl and Four Square Step Test), physical activity (Rapid Assessment of Physical Activity) and quality of life World Health Organization Quality of Life Questionnaire – Brief Australian version) | Critical | Significantly greater increases in functional ability, physical activity and quality of life in the intervention group (p < 0.05) |
| Lin et al., 2014, Taiwan177 | Randomised study, parallel groups | 24 residents | Residents in long-term care facilities with chronic stroke. Mean age 74.6 years, 16.6% female (intervention group); mean age 75.6 years, 41.6% female (control group) |
|
Balance and satisfaction, measured using scores from the Berg Balance Scale and Barthel Index. Technology satisfaction was based on the technology acceptance model | Some concerns | Significant effect on Berg Balance Scale scores, total and self-care score of Barthel Index and basic daily activity were observed in both groups (p < 0.05). No significant changes in mobility were observed (p = 0.088), and measures of perceived usefulness and satisfaction were similar in both groups |
| Nagayama, 2016, USA210 | Pilot cluster RCT | 12 facilities (44 residents) | Mean age 82.1 years; 85.2% female (whole sample) |
|
Health status, measured using the Short Form questionnaire-36 items (SF-36) and the Short Form Questionnaire-6 Dimensions (SF-6D) utility score; quality-adjusted life-years; scores on the Barthel Index of Daily functioning and total care cost | High | The intervention group had a significantly greater improvement in Barthel scores (p = 0.027). No other outcome was significantly different between groups. The incremental cost-effectiveness ratio, calculated using the change in BI score, was US$63.10 |
| Authors, year of publication, location | Design | Sample size (care home residents) | Sample characteristics | Interventions and comparators | Outcomes and measures | Overall risk of bias rating | Results |
|---|---|---|---|---|---|---|---|
| Bemelmans et al., 2015, the Netherlands56 | Quasi-experimental time series study (ABAB) within-subject comparison | 91 residents | Female 80.3%; residents with dementia and (1) undesirable psychological/psychosocial unrest or mood, and (2) care providers experienced difficulties in providing ADL-related care |
|
IPPA scores | Serious | IPPA scores and mood improved significantly following the therapeutic PARO intervention (p < 0.01). No effects were seen with the care support application |
| De Luca et al., 2016, Italy101 | Randomised study | 59 residents | Mean age 79 years; 67.8% female |
|
Measures of neurobehavioral symptoms and quality of life; blood pressure and heart rate; admissions to health-care services | High | Significant reductions in Geriatric Depression Scale (p < 0.01), Brief Psychiatric Rating Scale (p < 0.05) scores, mean blood pressure, heart rate and admission to health-care services (p < 0.05) and improved quality of life (p < 0.05) between groups favouring the intervention |
| Jøranson et al., 2015, Norway160 | Cluster RCT | 10 care homes; 60 residents | Age range 62–95 years; 67% women; diagnosed with dementia or cognitive impairment (MMSE score of < 25/30) |
|
Regular medication prescribed, assessed using the Anatomical Therapeutic Chemical Classification System; scores on the Brief Agitation Rating Scale and Norwegian versions of the Cornell Scale for Symptoms of Depression in Dementia and MMSE | High | The intervention group experienced significant reductions in agitation and depression at 3 months. Symptoms increased in the control group |
| Libin and Cohen-Mansfield, 2004, USA176 | Quasi-experimental | Nine nursing home residents | Mean age 90 years, all female; residents with dementia |
|
Agitated behaviour, measured using the Mapping Instrument (ABMI); affect, measured using Lawton’s Modified Behaviour Stream; residents’ engagement with the stimuli, assessed using various measures but not validated tools | Serious | The intervention group experienced significant increases in pleasure (p = 0.007) and interest (p = 0.028). Non-significant effects in relation to anger, anxiety and engagement were reported in both groups |
| Moyle et al., 2017, Australia203 | Parallel, three-group cluster RCT | 28 long-term care facilities (415 residents) | Mean age 84 years, 73% female (main intervention group); mean age 86 years, 81% female (second intervention group); mean age 85 years, 72% female (control group), documented diagnosis of dementia |
|
Changes in participants’ levels of engagement, mood states, and agitation, using the video coding protocol – incorporating observed emotion Scheme, and the CMAI-SF. Measurements were taken at baseline and at 1, 5, 10 and 15 weeks | Some concerns | Participants in the PARO group were more engaged verbally (3.61 points) and visually (13.06 points) than participants with the plush toy. Both PARO (3.09 points) and the plush toy (3.58 points) had significantly greater reductions in neutral affect than usual care. PARO was more effective than usual care in improving pleasure (1.12 points) and agitation (3.33 points). When measured using the CMAI-SF, there was no difference between the groups |
| Robinson et al., 2013, New Zealand236 | RCT with parallel groups | 40 residents in a residential care facility | Age range 55–100 years, 67.5% female |
|
Loneliness (UCLA loneliness scale), depression (Geriatric Depression Scale), and quality of life (Quality of Life for Alzheimer’s Disease scale) | High | Compared with the control group, residents who interacted with the robot had significant decreases in loneliness during the study period. Residents talked to and touched the robot significantly more than the real resident dog (p < 0.05). There were no other significant differences in change scores from baseline to follow-up between groups |
| Shibata et al., 2004, Japan250 | Quasi-experimental | 23 residents/attendees at health service facility that provides nursing home stays, rehabilitation and day care | Mean age 84.6 years, 66.6% female (intervention group); mean age 85.5 years, 81.8% female (control group) |
|
Participant mood, assessed using a face scale, Profile of Mood States and comments from the nursing staff | Moderate | Average face scale scores improved by an average of 2 points for the intervention group and by 0.7 in the control group; decreases in Profile of Mood States ‘depression-dejection’ ratings were by an average of 14 points in the intervention group and 7 points in the control group |
| Van der Ploeg et al., 2016, Australia274 | Pilot randomised, crossover, repeated measures study | Nine residents from five nursing homes in Melbourne | Mean age 86.7 years (range 83–93 years); 66% female |
|
Changes in Cohen-Mansfield Agitation scores | High | Skype conversations lasted longer than telephone calls (12 vs. 10.3 minutes). Mean agitation counts fell by 24.1 points during Skype calls and 12.9 points during landline calls. These differences were not statistically significant |
| Authors, year of publication, location | Design | Sample size (care home residents) | Sample characteristics | Interventions and comparators | Outcomes and measures | Overall risk of bias rating | Results |
|---|---|---|---|---|---|---|---|
| Banks et al., 2008, USA47 | Cluster RCT | 38 residents in three long-term care facilities | Age and gender profile of the sample not stated |
|
Resident loneliness (UCLA scale) and attachment to pets (MLAPS) | Some concerns | Residents receiving a dog intervention (robotic or living) were significantly less lonely than those in the control group (p < 0.05), regardless of their attachment to pet score. There were no differences between the robotic or living dog group in reducing loneliness |
| Jung et al., 2009, Singapore163 | Quasi-experimental study | 45 residents | Age range 56–92 years (whole sample) (gender balance not stated) |
|
Scores on the UCLA Loneliness and Rosenberg Self-Esteem scales; Bradburn Affect Balance Scale; Physical Activity Questionnaire for Elderly Japanese | Critical | Intervention group participants scored significantly higher on affect (p < 0.05), self-esteem and physical activity and significantly lower on loneliness (p < 0.01) than the control group |
| Kidd et al., 2006, USA169 | Quasi-experimental | 23 residents | No data on age and gender of the participants |
|
Questions relating to social interaction and play with the robot designed specifically for this study | Critical | Participant responses to questions indicated higher levels of social interaction and play in the intervention condition |
| Robinson et al., 2013, New Zealand236 | RCT with parallel groups | 40 residents in a residential care facility | Age range 55–100 years; 67.5% female |
|
Loneliness (UCLA Loneliness Scale), depression (Geriatric Depression Scale), and Quality of Life (Quality of Life for Alzheimer’s Disease scale) | High | Compared with the control group, residents who interacted with the robot had significant decreases in loneliness over the study period. Residents talked to and touched the robot significantly more than the real dog (p < 0.05). There were no other significant differences in change scores from baseline to follow-up between the groups |
| Vowden and Vowden, 2013, UK277 | Cluster RCT (pilot study) | 16 nursing homes (39 patients) | Mean age 79.47 years, 58.8% female (intervention); mean age 82.67 years, 55.6% female (control) |
|
Cost savings and usefulness of the system, assessed using opinions and quotations provided by experts and care home staff | High | No statistical analysis because of small sample size; the study authors reported that the case studies included in their article illustrate the potential benefits of the system |
| Authors, year of publication, location | Design | Sample size (care home residents) | Sample characteristics | Interventions and comparators | Outcomes and measures | Overall risk of bias rating | Results |
|---|---|---|---|---|---|---|---|
| Holmes et al., 2007, USA300 | Quasi-experimental design | Two units; 118 residents | Average age on both units was 87 years (±7.5 years); 78 residents (38 on the intervention unit and 40 on the comparison unit) |
|
Reduction of falls, accidents and injuries for residents; decrease in staff time spent on direct care and staff burden | Critical | No significant reduction in falls and injuries, but there was a significant improvement in affective disorder in the intervention group, relative to the comparison group |
| Kelly et al., 2002, USA301 | Crossover design | 47 patients | 66% (n = 31) were female; no data on age |
|
Fall rate per 100 patient-days | Critical | Significant reduction in fall rate of 91% (p = 0.02). Patients had 11 falls in the pre period (4.0 falls per 100 days), 1 fall in the during period (0.3 falls per 100 days) and 17 falls in the post period (3.4 falls per 100 days) |
| Lapane et al., 2011, USA299 | Cluster RCT (to determine the extent to which the use of a clinical informatics tool for monitoring plans reduces adverse outcomes) | 25 homes comprising 3480 residents | 50% aged ≥ 85 years, 33% aged 75–84 years, 18% aged 65–74 years; 73% female (intervention recipients) |
|
Incidence of delirium, falls, hospitalisations and mortality | High | Significant difference in the rate of potential delirium onset between groups (adjusted hazard ratio 0.42, 95% confidence interval 0.35 to 0.52) favouring the intervention. No other significant effects were observed |
| Pillemer et al., 2012, USA222 | Quasi-experimental study to investigate the impact of introducing a HIT system on resident outcomes | 761 residents | Mean age, 79.6 years, female 68.17% (intervention group); mean age 79.2 years, 63.55% female (control group) |
|
Resident satisfaction with care; average number of falls; ADL (Performance Activities of Daily Living scale); mood (Feeling Tone Questionnaire); Observed behaviour frequency of behavioural states based on rater observations | Critical | No statistically significant impact of the introduction of HIT system on residents for any outcomes, except a negative effect on behavioural symptoms |
| Rantz et al., 2010, USA227 | Quasi-experimental study to investigate the contribution of bedside EMRs and on-site clinical consultation by gerontological expert nurses on cost, staffing and quality of care in nursing homes | 18 facilities; 8166 residents | No data were provided on age or gender. Facilities were split into four groups, all willing to implement bedside EMR systems |
|
Cost reports (total costs per resident and nursing staff), staffing and retention, various quality indicators and measures for resident outcomes including ADL, motion, behavioural/depressive symptoms, pressure sores, urinary tract infection, delirium, physically restrained | Serious | Total costs increased in the intervention groups that implemented technology. Staffing and retention remained constant. Improvement trends were detected in resident outcomes for ADLs, range of motion, and pressure sores in intervention groups |
| Rantz et al., 2017, USA230 | Prospective, randomised controlled study to assess the effectiveness and cost-effectiveness of using data from an environmentally embedded sensor system for early recognition of illness | 171 residents in 13 assisted living communities | Mean age 83.6 years, 74.4% female (intervention group); mean age 86 years, 72.9% female (control group) |
|
SF-12, GDS, MMSE, activities/instrumental ADL and IADL, gait speed and profile (GAITRite), hand grip, falls, emergency room visits, hospitalisations, nursing home stays, physician visits | Some concerns | Functional decline was significantly more rapid in the comparison group, suggesting that alerts from sensor data promote early detection and intervention. No differences were identified in SF-12, GDS, MMSE, ADL or IADL scales, or grip strength measures between groups. There were no difference in health-care costs between groups |
Study quality
Thirteen of the included studies were RCTs; the remaining 11 were non-randomised, observational studies. Full details of the validity assessment are presented in Appendix 3, Table 18. The quality of reporting was variable between studies and across criteria. Of the 13 RCTs, nine were considered overall at a high risk of bias, whereas the other four were rated overall as having some concern of bias. Risk of bias across the domains for each RCT was variable, but in general RCTs were either rated as being at high risk of bias because of the measurement of outcomes or flagged as having some concerns because of deviations from intended interventions. Although the lack of blinding of participants and/or assessors may be justifiable given the nature of the interventions, the deviations from the intended interventions support the overall risk-of-bias assessment of high or some concern. None of the RCTs was rating as being at a low overall risk of bias.
Of the 11 non-randomised studies, 10 were considered to be at serious or critical risk of bias, with one considered to be at moderate risk. The majority (n = 10) were considered as having serious or critical risk of bias owing to confounding and measurement outcomes. Confounding relates to when one or more prognostic factor that predicts the outcome also influences or predicts who receives the intervention. Although the lack of blinding may be justifiable given the nature of the interventions, because of issues with confounding all 10 studies remained at serious or critical risk of bias.
The quality of the studies for each of the individual interventions is summarised alongside the results. With only one non-randomised study rated as being at moderate risk of bias and four RCTs rated as having some concern of bias, the overall evidence base to support the effectiveness of individual technologies is weak.
Quality assessments are shown in Appendix 3, Tables 18 and 19.
Results of evidence synthesis
The findings from the 24 studies investigating associations between digital technology interventions and care home residents’ health, functional ability and well-being are synthesised in the following section, grouped by outcome.
Studies investigating the effects of interventions on physical health, physical activity and functional status
Six studies assessing the effects of interventions on physical health, physical activity and functional status were included. They were conducted in Singapore, Taiwan, New Zealand, Belgium, Canada and the USA. 54,147,163,177,210,302 The Belgian study involved 144 participants; the sample size of the other five studies ranged from 34 to 45 residents. 54 Two were quasi-experimental studies, two were randomised studies (one with parallel groups and one crossover) and two were cluster randomised studies. All except one were rated as being at high or critical risk of bias.
Research teams from three countries have evaluated the potential of Nintendo® (Windsor, UK) Wii technology to enhance physical functioning, in addition to reporting on outcomes such as health and quality of life. Playing specific Wii games appeared to have a greater impact on physical and psychological health than playing traditional board games when implemented over a 6-week period with 45 residents of a Singapore care home. 163 This quasi-experimental study was successful in its aim to increase physical activity; participants also reported increases in positive affect and self-esteem, and lower levels of loneliness, than those in the control group, suggesting that the intervention has the potential to have a broad impact on well-being. 163 A quasi-experimental mixed-methods study166 from New Zealand evaluated the impact of an 8-week programme of Nintendo Wii sports games. Significantly greater increases in functional ability, self-reported physical activity levels and quality of life were reported among the 13 members of an intervention group than among 13 residents who continued with their normal ADL. However, the Wii was less successful when used with residents in Canada who had existing impairments. A Nintendo Wii bowling game was added to standard care for 34 residents with upper limb dysfunction from two long-term care facilities. Wii bowling participants reported greater enjoyment of physical activity than residents receiving standard care, but changes in functional status, pain intensity and the extent to which pain disturbed the resident were similar in both groups after the intervention. 147
Other studies of digital technology interventions failed to demonstrate any improvement in functional status over and above usual care. In a pilot trial in Taiwan,177 the effectiveness of balance training via a telerehabilitation system was compared with conventional therapy for 24 care home residents with chronic stroke. During a 4-week period, balance and functional status improved, but there were no significant differences between the intervention and control groups. Mobility, including 50-yard walking and going up and down stairs, was unaffected. Another pilot cluster RCT,210 this time from the USA, evaluated an iPad (Apple Inc., Cupertino, CA, USA) application [the Aid for Decision-making in Occupation Choice (ADOC)]. This application was developed for use with occupational therapists, and displayed images of daily activities that could be selected by the clients in an attempt to promote shared decision-making and occupation-based goal-setting. The ADOC was found to be acceptable to therapists and clients, and able to maintain or improve ADL, compared with an impairment-based approach. The authors report that it also appeared to be a cost-effective intervention. No significant differences in health status or quality of life were detected between the intervention and control groups.
This combination of studies does not present strong evidence for a positive impact of technological interventions on the physical health and functional status of care home residents. However, the Nintendo Wii appears to be a promising intervention for increasing physical activity and enhancing mood and social functioning.
Studies investigating the effectiveness of interventions for improving mental health and well-being
Ten studies described digital interventions aimed at influencing mental health and well-being in care home residents. 56,101,132,160,163,169,176,236,250,274 A majority measured symptoms of depression and dementia. They also report on agitation, a set of behaviours associated with emotional distress that impair social functioning and ADL. Examples of agitation include excessive motor activity, such as pacing and/or verbal and physical aggression. Agitation is common in dementia and cognitive impairment, but it is important to note that it can have other causes. 303
Mood and agitation
The influence of robotic animals on mood and agitation among care home residents has been investigated in studies from five countries: the Netherlands,56 Norway,160 New Zealand,236 Japan250 and the USA. 176 In all but one of these studies,176 the intervention was with PARO, a robotic seal (www.PAROrobots.com). A sixth study, from Korea, discussed the need to explain and promote the PARO intervention with care home staff, but it presented no data on outcomes and is not included in this review. 132
PARO is the most commonly available robotic pet developed for use by people living with dementia. PARO is built to resemble a baby seal, and moves its head and legs and makes sounds when interacting with people. PARO contains sensors that detect touch, light, sound, temperature and position. This allows the PARO device to respond when it is being held or stroked, and move in the direction of sounds. PARO can be programmed to respond in a certain way to stimuli, and remember the users’ previous actions and behaviour patterns.
Two studies rated as being at high/serious risk of bias described the positive impact of PARO on mood and agitation. The short-term effects of intervening with PARO robotic seal were assessed in a quasi-experimental time series study (with within subject comparisons) in the Netherlands.
The effects of PARO on the psychological well-being and psychosocial functioning of residents with dementia were measured, along with its ability to facilitate daily care activities. Ninety-one residents completed this study. The authors described a strong positive effect of PARO on mood and on an individual goal attainment scale (Inventory of Positive Psychological Attitudes) when used in a therapeutic intervention. The potential of PARO to support delivery of care by enhancing resident co-operation was unproven. 56 PARO has also been used successfully in Norway in group interventions to tackle symptoms of agitation and depression among care home residents with dementia or cognitive impairment. A cluster RCT160 involving 60 residents described significant improvements in the intervention group, 3 months after the end of a 12-week intervention. Medication usage was unchanged. In a smaller study in Japan,250 PARO also appeared to have a positive impact on mood when deployed with 11 older people living in a long-stay facility. Twelve people in a second facility were given a less interactive version of PARO as a placebo, but the results between the groups were similar, which implies that PARO’s ability to move and interact may not be an essential component of the intervention.
Only one published study,236 a RCT from New Zealand rated as being at moderate risk of bias, failed to detect any positive effects on quality of life for PARO. The intervention was compared with a real dog who lived with residents in a care home. No differences were detected between the groups in quality of life or depression. 236 This study is discussed further in Social relationships (loneliness and isolation): the influence of robotic animals.
A robotic cat was the subject of a pilot study in the USA. 176 It had many similarities to PARO: inbuilt sensors and basic artificial intelligence allowed a range of sounds (purring, meowing and hissing) and non-verbal (stretching, wagging tail, lying down) responses to stimuli. Researchers compared the impacts of the robotic and toy cats on mood and engagement with the stimulus (attention, attitude and intensity measured on a five-point scale) of nine people living with dementia in one nursing home. The residents gained pleasure from interacting with the robotic cat, but both cats held participants’ interest and appeared to reduce agitation.
In summary, robot interventions reported in published literature appear likely to have a positive effect on resident mood, agitation and interaction, but it is not clear that they offer greater benefits than real pet animals, other than in ease of access and availability. Evaluations of the costs and benefits of robotic interventions, and comparisons with existing practice, would all be helpful.
Other interventions to influence mood and reduce agitation
The impacts of telemonitoring were investigated in a study of 59 residents of a single Italian care home, allocated randomly into two groups in sequential order of recruitment. The intervention included transfer of patient data by text, monitoring of clinical signs (heart rate and blood pressure) and specialist neurological/psychological counselling. Quality of life had improved for all participants at 6 months. The intervention group also experienced reductions in depression scores and mean blood pressure. However, some caution is needed in extrapolating from this study, as it had a number of methodological limitations, including small sample size, baseline differences between the groups and method of allocation. 101
The impact on agitation of video calls with relatives was compared with that of standard telephone calls for people with dementia. Nine residents in five Australian care homes took part in a pilot randomised crossover study. Reductions in agitation during the calls was greater for video calls, suggesting that this might be worthy of further scrutiny in a larger study. 274
Social relationships (loneliness and isolation): the influence of robotic animals
Nintendo Wii and PARO have both been shown to have some influence on loneliness among care home residents. The study in Singapore care homes comparing the Nintendo Wii with traditional board games reported lower levels of loneliness in the intervention group. 163 In New Zealand, PARO was deployed in a RCT involving 40 older people in one retirement home facility (17 were in the rest home area and 13 were in the hospital area). Twice-weekly sessions with PARO were more effective than interactions with a real dog in reducing loneliness. The authors observed that residents spoke to and touched PARO more often than residents in the control group interacted with the real dog. 236 PARO has also been reported to support social interaction in a small study in two US nursing homes. The researchers worked with 23 residents, visiting every 2 weeks over 4 months. Although they reported positive outcomes, they also noted that some residents were reluctant to interact with PARO because they perceived a seal to be a wild, aquatic animal. In particular, some residents were concerned that it may be stranded on land. 169
In summary, interventions that bring people together and prompt them to interact with a digital intervention, such as a robotic pet, or other residents appear to have a positive effect on loneliness and social isolation. However, there is no evidence of the superiority of technological interventions over non-digital alternatives on these outcomes.
Complex information technology systems and a range of resident outcomes
This section considers the remaining studies that did not fit into the preceding section. They describe the impact of complex interventions on multiple resident outcomes.
Seven articles were identified that evaluated the impact of complex IT systems or telemonitoring on resident outcomes. In most of these, technology is a vehicle for delivering complex care, and it is difficult to isolate the contribution of the technology. This is particularly pertinent to studies in telehealth, when the expert advice delivered into the care home is likely to be the active ingredient.
Impact of information technology systems in care homes on mood, functional status and mortality
A non-randomised study from the USA examined the effects on nursing home residents of introducing a broad-ranging IT system. 222 Patient records were converted from paper to electronic. The IT system enabled scheduling, mobile capture of assessments and treatments, online entry of notes, and real-time reporting of sentinel events, quality indicators and quality measures. Mobile electronic devices for certified nursing assistants (CNAs) and nurses allowed them to access to resident records at the bedside or anywhere within the facility. Desktop personal computers were configured on every nursing station and within every department for clinical management. Physicians were also able to access records and approve prescriptions remotely. Residents reported being satisfied with the changes. No statistically significant changes were detected in mood, functional status or mortality, but there was an increase in the observation of disruptive behaviours. The researchers hypothesised that the IT system would have an impact on resident outcomes via quality of care and anticipated that greater use of IT might be associated with adverse outcomes by promoting less personalised care and reducing time spent with residents. When outcomes were measured 9 months after implementation, this did not appear to be the case. 222
Clinical decision support systems and pressure ulcer incidence
In a large randomised study,54 researchers in Belgium evaluated the use of an electronic clinical decision support system (computer program) to increase adherence to guidelines in care homes. Individually tailored pressure ulcer prevention protocols were developed for care home residents and compared with paper- and classroom-based introduction of the guidelines. The intervention was associated with a significantly greater reduction in grade I–IV pressure ulcers than that in the control group (intermediate outcome). However, this was a multifaceted intervention, including education, reminders, monitoring and the introduction of new nurse roles. The role of digital technology is difficult to disentangle, and it is not clear that it was an essential component of this intervention. 54
In a similar study in the USA,299 bespoke software was used with pharmacists and nurses to identify care home residents at risk of falls and delirium, and to implement monitoring plans and medication reviews. The aim was to reduce adverse events associated with medication use. This intervention was evaluated in a RCT in 25 care homes served by two long-term care pharmacies. Plans were triggered for 461 (14%) out of the 3480 residents in the intervention homes. Newly admitted residents who received the intervention had lower rates of delirium, hospitalisation and mortality than residents in usual care. Among longer-stay residents, there were no significant differences between the intervention and control groups. 299
Impact of telemonitoring on clinical outcomes, including mood
The impacts of telemonitoring were investigated in a study of 59 residents of a single Italian care home,101 allocated randomly into two groups in order of recruitment. The intervention comprised transferring patient data by text, video and audio, regularly monitoring vital clinical signs (heart rate and blood pressure), and intermittent specialist neurological and psychological teleconsulting. Quality of life had improved for all participants at 6 months. The intervention group also experienced non-significant reductions in depression scores and mean blood pressure. However, it is difficult to draw firm conclusions, as this study had a number of methodological limitations, including small sample size, baseline differences between the groups and method of allocation. 101 A pilot cluster RCT in a northern English city investigated the impact of remote expert advice on wound care for staff in nursing homes. Patient information and images were uploaded and transferred via smartphone for the 17 patients in the intervention group, whereas the nine control patients received usual care. The authors concluded, from an analysis of patient pathways, that the intervention had potential benefits for patients and staff. 277
Technology for surveillance is in use in care homes in the USA and Europe. This may be why few evaluative studies were identified that were published after the year 2000. Holmes and colleagues300 assessed the impact of bed, bedroom and bathroom exit monitors in a quasi-experimental study with 118 residents. They did not report any reduction in falls or injuries, but they did note improvement in mood for residents subject to the intervention. The mechanism for this is unclear.
Discussion
Summary of findings
There are multiple applications for technology in care homes. Much of the research effort has been directed at telehealth, digital records, social robots, surveillance or monitoring, gaming, education and communication. We identified 22 topic overviews or systematic reviews published since the year 2000 in high-income countries. We also identified a paucity of research that met the quality standards for robust evidence used in health-related research. 304 Descriptive and qualitative studies form the main body of work. They are essential to inform the implementation of technologies, with insights into, for example, acceptability and barriers to utilisation. In some areas – notably robots and telehealth – there are several experimental and quasi-experimental studies that aim to evaluate effectiveness.
Digital technology has the potential to enhance the health and well-being of care home residents. The most promising interventions appear to be those that promote physical activity or enhance mental health and well-being. Robotic pets and games that stimulate group activity are the most common interventions that have been subject to experimental evaluation. Other interventions that may have greater practical application to care – for example monitoring and digital records– are less likely to have been studied in this way. There is a paucity of comparative studies within the body of empirical evidence in this review. This means that it is impossible to conclude that the digital interventions are of greater benefit to residents’ health and well-being than less costly alternatives. There is an urgent need for properly conducted experimental research in this field.
The introduction of technologies into care homes raises a range of moral and ethical concerns, a discussion of which was outside the remit of this rapid evidence synthesis. However, it is important to acknowledge that issues of consent, dignity, privacy and care that prioritises the best interests of the resident should be central considerations when technological innovations are being considered in this setting.
Strengths and limitations
We applied systematic methods to synthesise existing evidence on technology to enhance the health and well-being of care home residents. A focus on resident outcomes enabled us to draw conclusions from a disparate body of work on diverse technologies. Our searches were designed to be comprehensive and identify work beyond traditional academic outputs, which we expected to be less relevant to this subject. There are two potential areas of weakness in our work. Hierarchies of research design that are used to judge the quality of health-related research place a high value on randomised controlled studies that are able to prove causation. Until recent years, the number of RCTs conducted with care home residents has been small. This may be because of the ethical, methodological and practical challenges of working in care homes. Participants are aged and living with multiple conditions, including cognitive and physical frailty. They may stay in a home for a relatively short time, and experience rapid deterioration in their health. Long-term care is also a setting that has not always attracted significant research funding, and RCTs may be costly. However, it is also possible that new technologies do not lend themselves to evaluation in a RCT. Interventions are often complex, with multiple effects and outcomes for a range of participants (staff, residents, families). Systems need updating and tweaking as the technology is implemented, which may result in the intervention being modified after the study has started. A qualitative evaluation of the process of implementation often yields the most useful information in the early stages of implementation, and when the technology is established, motivation to evaluate its impact in a RCT may be low. Whatever the underlying reasons, the paucity of experimental research will make it difficult for any review to draw conclusions that are based on traditional concepts of strong evidence. We have taken this into account in our narrative. It is also important to acknowledge that the USA and East Asia are the two main geographical foci of development in technology for care homes. Without translation from languages other than English, it is possible that we have omitted some relevant work.
Gaps in research knowledge
UK-relevant research
This review points to an overall paucity of research on technology and UK care homes, and a notable lack of experimental and observational studies. Only one pilot RCT from the UK was identified in our mapping review. Telehealth and technology for surveillance and monitoring have attracted some attention from UK researchers. Other applications of technology, including digital records and companion or rehabilitative robots, have yet to be formally evaluated and results published from UK settings.
Robust experimental studies
In recent years, an increasing number of RCTs have been conducted in care homes. In this review, a minority were powered to be able to detect statistically significant differences between groups. Such studies have generated useful findings on the acceptability and feasibility of novel interventions, but cannot provide evidence of a firm link between an intervention and observed outcome. There are many practical applications of technology. Experimental research to date has focused on robotics and games, to the detriment of other interventions.
Economic evaluation
Our work identified few studies that considered costs and no formal economic evaluations of introducing novel technologies into long-term care. Training staff to operate and maintain any technologies that are introduced is also important and should be considered as an ongoing cost. This is an omission, as cost is likely to be a particularly important consideration in a sector characterised by financial insecurity and narrow profit margins.
Impact on all stakeholders
Caring for older adults requires time, and staff workload is a key issue for care homes. Any technology that places demands on staff would need to offset this with significant benefits to residents, staff or the organisation. Our review identified a large number of studies that considered barriers to and facilitators of the use and implementation of technology. However, few considered the consequences for staff and organisations.
Implications for the UK care home sector
Digital technology pervades all aspects of care services, and there is no reason to expect care homes to be immune from new developments. But without formal, independent assessment of the positive and negative consequences of new technologies or new use of existing technology, it will be impossible to make rational choices about the allocation of future resources. The care home sector requires support to evaluate new interventions, and service commissioners have an important contribution to make with expertise and funds. The technology industry could also play a key role. With shared protocols for implementation of new interventions and collection of information on outcomes, it may be possible to pool data from multiple locations and generate a more robust evaluation. The robot PARO provides an example of where such an approach could have been beneficial. It has been the subject of many small studies that provide a poor basis for decision-making. If these studies had been more homogeneous in approach, data on PARO could have been available from a significant number of care home residents.
Evaluating new technologies requires resources, time and commitment across the long-term care economy. Funding studies of sufficient size and duration in this setting will require considerable resources, and funders may have been reluctant to support the evaluation of commercially marketed interventions. Consideration should be given to joint working and sponsorship of independent research. Credible evidence for impact of a new intervention if of benefit to all concerned, including manufacturing companies, commissioners and residents.
Section 2: communication and engagement
Background
In England, most care homes sit outside the NHS and statutory services, but work alongside a wide range of public and private service providers. This is a unique context and poses particular challenges to communication between professional carers working for different organisations. Good communication is essential to the successful integration of services, and is particularly important when care is delivered by many different providers. Collaboration with health and social care professionals is believed to benefit care quality and promote person-centred care for care home residents. 305,306 In addition, good communication between care homes, hospices and acute services is known to improve quality and resource use. 307,308 Care homes have long seen the benefits of collaboration with their local communities to enhance residents’ quality of life and break down some of the misconceptions and stigma surrounding care homes. Initiatives such as community tea parties, adopt-a-resident and communal gardening initiatives are perceived to be of benefit to quality of life and boost a home’s commercial success. 309,310
Communication and engagement are cross-cutting issues, relevant to a care homes’ relationships with health services, social care, commercial companies and community groups. To date, no review has brought together current understanding of which approaches to communication and engagement are most likely to enhance resident health and well-being. This work intends to fill this gap, and be of value to decision-makers in care homes and commissioning organisations with limited time and resources.
In this review, communication was defined as the transfer or sharing of information by speaking, writing or other media. Engagement was understood to refer to meaningful contact or connection and/or involvement (or the feeling of being connected or involved).
Methods
See Chapter 3 for details of methods.
Findings of mapping review
Number and characteristics of studies
After deduplication, 3607 references were available for title and abstract screening (see Figure 2). Of these, the full texts of 250 references were retrieved for further assessment of eligibility, and the details of 94 studies were mapped (Table 8 and Report Supplementary Material 1, Table 2). Of those that were not reviews, 61 (64%) took place in the USA, 11 (12%) took place in the UK, five took place in the rest of Europe, six (9%) took place in Australia, four took place in Canada and one took place in each of New Zealand, Singapore and Sweden. There were 16 (17%) experimental studies: seven RCTs, two quasi-experimental studies, five pre–post and two interrupted time series studies. There were also five (5%) relevant published protocols: three for RCTs and two for quasi-experimental studies. Nine (9%) studies reported surveys, two (2%) reported retrospective reviews of data, 13 (14%) reported qualitative research (interviews or focus groups) and five (5%) described case studies. Eighteen (19%) studies utilised mixed methods, including a mix of surveys, qualitative, action research and process evaluations. Fifteen (16%) studies provided descriptions of interventions or methods of communication and three were discussion papers. Finally, eight (8%) systematic reviews were found.
| First author | Year of publication | Review |
|---|---|---|
| Agar311 | 2015 | Communication and engagement |
| Alexander312 | 2014 | Communication and engagement |
| Alexander31 | 2015 | Communication and engagement |
| Amador313 | 2016 | Communication and engagement |
| AMDA314 | 2011 | Communication and engagement |
| Anderson315 | 2010 | Communication and engagement |
| Anonymous316 | 2011 | Communication and engagement |
| Anonymous317 | 2013 | Communication and engagement |
| Anonymous318 | 2014 | Communication and engagement |
| Anonymous319 | 2015 | Communication and engagement |
| Anrys320 | 2016 | Communication and engagement |
| Arendts321 | 2014 | Communication and engagement |
| Arling322 | 2014 | Communication and engagement |
| Badger323 | 2012 | Communication and engagement |
| Banda324 | 2015 | Communication and engagement |
| Baur325 | 2010 | Communication and engagement |
| Beck305 | 2014 | Communication and engagement |
| Bensadon326 | 2014 | Communication and engagement |
| Bokhour327 | 2006 | Communication and engagement |
| Boockvar328 | 2007 | Communication and engagement |
| Anonymous329 | 2016 | Communication and engagement |
| Cadogan330 | 1999 | Communication and engagement |
| Cassidy331 | 2005 | Communication and engagement |
| Catic332 | 2014 | Communication and engagement |
| Colon-Emeric333 | 2013 | Communication and engagement |
| Conway334 | 2015 | Communication and engagement |
| Cortes335 | 2004 | Communication and engagement |
| Cowley336 | 2012 | Communication and engagement |
| Crotty337 | 2004 | Communication and engagement |
| Crotty338 | 2004 | Communication and engagement |
| Cwinn339 | 2009 | Communication and engagement |
| Dalawari340 | 2011 | Communication and engagement |
| Davis341 | 2005 | Communication and engagement |
| Davies342 | 2011 | Communication and engagement |
| Dearing343 | 2017 | Communication and engagement |
| Ellis344 | 2006 | Communication and engagement |
| Field345 | 2011 | Communication and engagement |
| Fisch346 | 2014 | Communication and engagement |
| Furman347 | 2006 | Communication and engagement |
| Ghorbel126 | 2013 | Communication and engagement |
| Gillespie348 | 2010 | Communication and engagement |
| Gillespie349 | 2010 | Communication and engagement |
| Gilmore-Bykovskyi350 | 2013 | Communication and engagement |
| Goodman351 | 2005 | Communication and engagement |
| Goodman352 | 2009 | Communication and engagement |
| Goodman353 | 2013 | Communication and engagement |
| Griffiths354 | 2014 | Communication and engagement |
| Hasson355 | 2008 | Communication and engagement |
| Hearn356 | 2015 | Communication and engagement |
| Heckman357 | 2016 | Communication and engagement |
| Hewison358 | 2009 | Communication and engagement |
| Hustey359 | 2010 | Communication and engagement |
| Hustey152 | 2010 | Communication and engagement |
| Hustey153 | 2012 | Communication and engagement |
| Huynh360 | 2013 | Communication and engagement |
| Jarboe361 | 2015 | Communication and engagement |
| Jones362 | 2010 | Communication and engagement |
| King363 | 2013 | Communication and engagement |
| Kirsebom364 | 2013 | Communication and engagement |
| Krol365 | 2017 | Communication and engagement |
| LaMantia366 | 2010 | Communication and engagement |
| Lea367 | 2016 | Communication and engagement |
| Longo368 | 2002 | Communication and engagement |
| Martz369 | 2011 | Communication and engagement |
| McGilton370 | 2009 | Communication and engagement |
| Ouslander371 | 2009 | Communication and engagement |
| Ouslander372 | 2011 | Communication and engagement |
| Ouslander373 | 2014 | Communication and engagement |
| Ouslander374 | 2016 | Communication and engagement |
| Reed375 | 2003 | Communication and engagement |
| Renz376 | 2013 | Communication and engagement |
| Renz377 | 2015 | Communication and engagement |
| Renz378 | 2016 | Communication and engagement |
| Richardson233 | 2014 | Communication and engagement |
| Romøren379 | 2017 | Communication and engagement |
| Sankaran380 | 2010 | Communication and engagement |
| Sutton381 | 2016 | Communication and engagement |
| Tabar382 | 2013 | Communication and engagement |
| Tena-Nelson383 | 2012 | Communication and engagement |
| Terrell384 | 2005 | Communication and engagement |
| Tjia385 | 2009 | Communication and engagement |
| Toh269 | 2015 | Communication and engagement |
| Tsakitzidis386 | 2016 | Communication and engagement |
| van Dongen387 | 2016 | Communication and engagement |
| Vogelsmeier388 | 2011 | Communication and engagement |
| Weiner389 | 2001 | Communication and engagement |
| White390 | 2015 | Communication and engagement |
| Whitson391 | 2008 | Communication and engagement |
| Wroth392 | 2011 | Communication and engagement |
| Yang393 | 2009 | Communication and engagement |
| Young394 | 2010 | Communication and engagement |
| Zafirau395 | 2012 | Communication and engagement |
Features of communication under investigation in the studies
Interpersonal communication within care homes was the focus of 18 (19%) studies. These discussed existing systems or proposed new methods for improving staff communication. Some described the use of formalised meetings or networks. Others focused more on one-to-one communication between staff members, and discussed barriers to successful communication or suggested strategies to improve it. A number of articles related to educational interventions to help staff focus on and improve communication.
One-quarter of studies (n = 22, 24%) had an explicit focus on the process of transferring patients between care home and hospital or communication between care home and hospital staff. The documentation used during this process was a topic of interest, and studies were concerned with the introduction of an improved and/or standardised form, or a different way of transferring the information (e.g. electronic transfer). Some articles looked more broadly at how information is communicated between staff members in the care home and hospital. Two studies examined communication between different care homes, and three investigated features of communication with multiple stakeholders (e.g. staff, hospital, academics and community representatives).
Named quality improvement tools were the focus of 27 (29%) of the studies. The most common (n = 8, 8%) was INTERACT (Interventions to Reduce Acute Care Transfers), which was originally conceived and tested in the USA as a tool to reduce hospitalisations from care homes. 372,383 It was improved through two rounds of expert consultation and focus groups and evolved into INTERACT 3. 373 This is a quality improvement programme that focuses on managing acute changes in the condition of residents in care homes, with the aim of reducing admissions to hospital. The focus of INTERACT 3 is the management of an acute change in condition, and it incorporates several fundamental strategies. First, it explicitly uses principles of quality improvement: it demands a designated champion and strong leadership support, provides the means to measure, track and benchmark defined outcomes, and generates root-cause analyses of hospitalisations. Staff receive feedback and guidance about translating these outcomes into improvements in the process of care and educational interventions. INTERACT 3 aims to promote early identification and evaluation of changes in a resident’s condition, using specific tools, STOP and WATCH and the Situation, Background, Assessment and Recommendation (SBAR) tool. Appropriate management in the care home should then prevent some residents from becoming so unwell that they require hospital transfer. INTERACT 3 also enables advance care planning and use of palliative or hospice care, when appropriate and chosen by the resident as an alternative to hospitalisation. Finally, it enables improved communication and documentation within the nursing home, between the nursing home staff and families, and between the nursing home and the hospital. INTERACT tools for improving communication with acute hospitals include a checklist of key transfer documents, lists of critical data to be communicated during transfer, examples of forms to document these data and a tool to assist with medication reconciliation at the time of transfer to the nursing home. The keys to the success of the programme are described as executive leadership support, a culture dedicated to quality improvement and engagement of staff by an INTERACT champion; choosing the right person for this last role is described as one of the most important decisions. 372
Selected examples of other quality improvement projects follow.
The Empira Fall Prevention Program322 is a quality improvement collaborative of older adult service providers in the USA. It includes nursing and other leaders from participating care homes. The aim is to get every employee involved in determining the root causes of a resident’s fall. The programme provided guidance for ‘first responders’ – those who found a fallen resident – along with attending nurses. The concept of a ‘fall huddle’ was introduced: the charge nurse and all staff members who had been working in the area of the fall would gather as soon as the resident was stabilised. The aim was to enhance understanding of the circumstances that led to the fall by recreating the scenario (with the resident if possible) and generating a list of questions to answer.
Connections, Communication, and Problem solving (CONNECT)333 is a multicomponent intervention designed in the USA to promote the systematic use of management practices. Staff are provided with training and tools to improve day-to-day interactions, encouraged to establish social networks for creative problem-solving, and work with mentors to help them to maintain the newly acquired behaviours. 333 This approach aims to strengthen interdependencies among staff and address common barriers to interdisciplinary problem-solving, such as passing responsibility to people further up the hierarchy. CONNECT intends to be widely generalisable to care home settings, because it enhances the capacity of existing staff to learn and improve.
Essence of Care353 is a benchmarking tool designed in the UK to improve the quality of resident or patient care. It helps practitioners to take a patient-focused and structured approach to sharing and comparing practice across health and social care settings. Nine ‘fundamental aspects of care’ are identified, each with its own set of benchmarks, including one that focuses on communication between patients and/or carers and health-care personnel. The toolkit contains an overall patient outcome for each of these aspects of care and a number of factors that need to be considered to improve the outcome. Each factor consists of a benchmark of best practice, indicators to monitor progress, guidance, and forms to document and chart activity.
Nurses Improving Care for Health system Elders (NICHE) provides geriatric education for all levels of staff in the acute and long-term care areas. It also promotes collaboration across the continuum through NICHE organisational strategies, clinical improvement models and other resources. 396 It was devised in the USA and is now also used in Canada, Bermuda and Australia.
Communication outcomes
Process measures were commonly reported in studies that evaluated communication tools. For example, an evaluation of the introduction of a transfer form would record the number of completed forms. In other studies, the number of meetings or interactions would be recorded. Authors have also described gaps in information that arose, and made comparisons with a defined gold standard. Most commonly, qualitative methods were used to understand perceptions of the levels or value of communication, or satisfaction with interactions.
Other outcomes
Around one-fifth of the articles (n = 19; 20%) reported clinical outcomes. Some studies were set up to look at communication with the idea of improving a particular clinical outcome; for example, two of the studies aimed to reduce fall rates in the care homes, and another aimed to improve bowel health. Other studies were targeted at improving the administration of medication or reducing medication errors. A small number reported quality-of-life outcomes.
Staff outcomes were a focus of interest in around 26 (28%) of studies. A majority reported on changes in staff satisfaction, knowledge or attitudes, or adherence to a communication tool. Few studies reported organisational-level outcomes; the most commonly reported were related to patient transfer or readmission to hospital.
UK studies
Twelve of the mapped studies (13%) were published from the UK, including one systematic review and one discussion paper. Eight (8%) used qualitative methods, two of these were action research projects and two were mixed methods. Seven (7%) were concerned with quality improvement tools or frameworks, including Essence of Care353 and the Gold Standards Framework. 358 All the UK studies were focused on care home staff communication with external health professionals, either community based (e.g. district nurses) or hospital.
Summary
This mapping review has identified 94 articles on communication and engagement in care homes, three-quarters of which were published in 2010 or later. Two-thirds of the research originated from the USA, with only 12 studies from the UK. The three major topics of interest to researchers have been quality improvement tools or frameworks, resident transfer to and from hospital, and interpersonal communication within care homes. Little published research was found on care homes’ communication and engagement with their local communities. No comparative studies of quality improvement frameworks were identified.
Findings of systematic evidence synthesis
How should care homes and the NHS communicate to enhance resident, family and staff outcomes and experiences?
Communication and engagement methods: systematic evidence synthesis
This review followed the methods previously described (see Methods). The PRISMA flow diagram is shown in Figure 2.
FIGURE 2.
Communication and engagement PRISMA flow diagram.
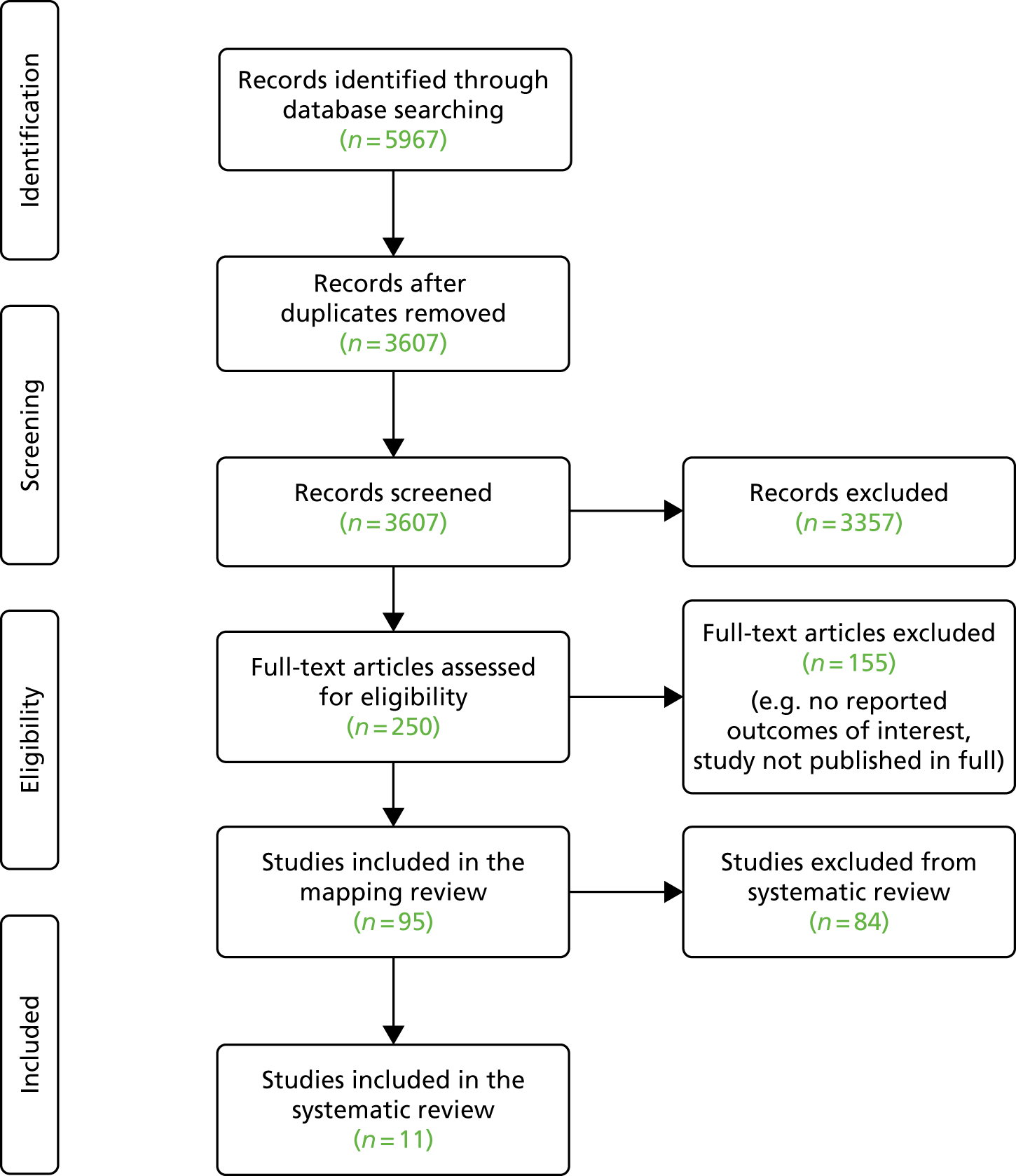
Results of evidence synthesis
A total of 5967 references were identified in the online search. After screening the titles and abstracts, 95 references were identified as potentially suitable for inclusion and retrieved for full-text assessment. In total, 13 references (11 studies) were included in the final review (Table 9).
| Authors, year of publication | Aims/purpose | Design | Participants | Settings | Type of intervention | Key findings |
|---|---|---|---|---|---|---|
| Arling et al., 2014322 | To explore the association between participation in a nursing home quality improvement collaborative and resident outcomes (changes in fall rates) |
Mixed-methods approach (quantitative surveys and qualitative interviews) Interrupted time series design |
RNs, n = 12; recreational therapist, n = 3; others including administrator, activity director and social worker, n = 14 |
Nursing facilities Empira project (n = 15) and other nursing facilities (n = 357) |
Empira quality improvement falls reduction collaborative |
Reductions in fall rates were highest in facilities where respondents experienced the highest levels of communication with collaborative members outside scheduled meetings, and where respondents perceived that the collaborative kept them informed and provided new ideas Clinicians felt that participation in a quality-improvement collaborative positively influenced their ability to share innovative ideas and expand the quality improvement programme within their nursing home |
| Bensadon et al., 2014;326 Musante, 2014397 | Evaluation of INTERACT. This is a comprehensive quality improvement programme designed to promote prompt, local management of residents by promoting early identification, assessment and communication of changes in resident status | RCT | 203 long-term care staff | 72 nursing homes | INTERACT | Preliminary data suggest that implementing INTERACT can promote positive cultural change in long-term care and reduce preventable (re)hospitalisations. Aggregated interview data showed measurable improvement in six outcomes: communication (86%; 174/203), nursing assessment (83%; 168/203), documentation (73%; 149/203), quality improvement procedures (75%; 153/203), hospital relations (66%; 133/203) and reduced hospitalisation rates (58%; 118/203) |
| Colon-Emeric et al., 2013333 | To determine whether or not an intervention that improves nursing home staff connections, communication and problem-solving (CONNECT) would improve implementation of a falls reduction education programme (FALLS) | Cluster RCT | Staff in any role with resident contact (n = 497) | Four community nursing homes and four Veterans Affairs community living centres | CONNECT tool and FALLS intervention | CONNECT was associated with significant improvements in staff perceptions of communication quality, participation in decision-making, safety climate, caregiving quality and use of local interaction strategies in intervention community nursing homes (treatment-by-time effect p = 0.01) but not in Veteran Affairs nursing homes. Fall risk reduction documentation did not change significantly, and the direction of change in individual facilities did not relate to observed direction of change in fall rates. Fall rates did not change in control facilities (falls/bed per year: baseline, 2.61; after intervention, 2.64) but decreased by 12% in intervention facilities (falls/bed per year: baseline, 2.34; after intervention, 2.06); the effect of treatment on rate of change was 0.81 (95% CI 0.55 to 1.20) |
| Conway et al., 2015334 | To evaluate the impact of a nurse-led telephone support service to RACFs on a range of measures relating to the transfer of acutely unwell residents to the ED of a large tertiary referral hospital in New South Wales, Australia, over a 9-month period | Pre- and post- evaluative intervention design | 50 staff from ED and 26 staff from RACFs participated | 12 RACFs (4 intervention vs. 8 control) | A nurse-led telephone support service provided by an APN | Reduced presentations of older people to the ED from the four pilot RACFs occurred. High levels of satisfaction among staff in RACFs were reported |
| Cwinn et al., 2009339 | To measure the prevalence of information gaps that occurred when patients were transferred to an ED from a nursing home or seniors residence, and to assess effectiveness of a regionally standardised transfer form on reducing information gaps in the region | Retrospective study of care reporting database: standardised vs. institutional form | Transfer forms for consecutive patients aged ≥ 60 years who were transferred by ambulance from a nursing home or seniors residence within a 6-month period in 2004 | Nursing homes or senior residence | Record review of transfer documents | A standardised transfer form was used in 42.7% of transfers. When the form was used, information gaps were present in 74.9% of transfers compared with 93.5% of the transfers when the form was not used (p < 0.001) |
| Dalawari et al., 2011340 | To assess the extent to which transfer forms facilitate communication between nursing home and ED staff based on proposed criteria | Retrospective review: pre and post quality improvement | Transfer documents for patients aged ≥ 65 years transferred by emergency medical services from nursing homes to St Louis University ED between January and June 2009 | Nursing home including extended care facilities | Transfer forms | Information deemed valuable in caring for a patient in the ED has an increased chance of transmission when transfer forms are used. The transfer form group had available, on average, 71% of the essential items, compared with 28% for cases without a transfer form (p < 0.001). However, the availability of this information did not translate into observable differences in case resolution time (p = 0.94) and disposition status (p = 0.12) |
| Field et al., 2011345 | To improve the quality and safety of anticoagulation management in the nursing home | RCT | A representative of each nursing homeIntervention homes, n = 13; control homes, n = 13 | Nursing homes | SBAR tool | Facilitated telephone communication between nurses and physicians using the SBAR approach modestly improves the quality of warfarin management for nursing home residents. In intervention homes, residents’ international normalised ratio values were in the therapeutic range a statistically significant 4.50% more often than in control homes (95% CI 0.31% to 8.69%) |
| Hustey and Palmer, 2010152 | To determine whether or not the implementation of an internet-based communication system improves the amount of essential information conveyed between a SNF and the ED during patient care transitions | Before-and-after intervention | Transfer documents of patients transferred from a SNF to the ED over 16 months | A 55-bed subacute SNF | SNF–ED transfer form | The use of an internet-based system increased the amount of information communicated during SNF–ED care transitions and significantly reduced the number of pages in which this information was contained. There was more critical patient information (1.85 vs. 4.29 of nine elements; p < 0.001) contained within fewer pages of transfer documents (24.47 vs. 5.15; p < 0.001) after the intervention |
| Renz et al., 2013;376 Renz, 2015377 | To evaluate the influence of SBAR protocol and training on nurse communication with medical providers, as perceived by nurses and physicians, using a pre–post questionnaire | Single-site repeated measures design (pre–post intervention) | 40 nurses (21 RNs and 19 LPNs) and 7 physicians | 137-bed skilled nursing home, part of a continuing care retirement community | INTERACT 2 SBAR communication tool | Implementation of the INTERACT 2 SBAR tool suggests improvement in nurse satisfaction with communication, although not statistically significant. Twenty-eight nurses (87.5%) found the tool useful, one nurse did not find it useful and three did not comment. Twenty-two nurses (69%) reported no limitations with the SBAR tool, although nine (28%) found the tool time-consuming |
| Tena-Nelson et al., 2012383 | To describe a replication of the INTERACT programme among member facilities of a New York City area nursing home provider association (INTERACT NY) and estimate its effect on hospital transfers | Pre- and post-intervention design | Nurse administrators, unit-based nurses, medical directors and attending physicians, nursing home administrators, CNAs, case managers and social workers | 30 nursing homes | INTERACT NY | Overall, there was a non-significant 10.6% reduction in hospital admissions from 4.07 to 3.64 per 1000 resident-days from pre to post INTERACT NY (p = 0.332). Among nursing homes with high engagement, there was a non-significant 14.3% reduction in hospital admissions from 4.19 to 3.59 per 1000 resident-days (p = 0.213). Among nursing homes in the highest tertile of baseline (pre-INTERACT NY) hospital admission rates, there was a non-significant 27.2% reduction in hospital admissions from 7.32 to 5.33 per 1000 resident-days (p = 0.102) |
| Terrell et al., 2005384 | To improve communication between ECFs and the ED. This study tested the hypothesis that a one-page, standard ECF to ED transfer form with essential data elements would change the rate of successful documentation of ECF patient information | Pre- and post-intervention investigation | Transfer documents for patients transferred by ambulance from ECF to the ED | ECFs defined as either a skilled nursing care facility or an intermediate care facility | Transfer forms | Use of a one-page, standard ECF to ED transfer form increased the number of essential data provided to the ED. Post intervention, the proportion of transfers with successful documentation was 77.8% (56/72), an increase of 19.3% (95% CI 4.0% to 34.7%) during the pre-intervention period. In 31.9% (23/72) of post-intervention ED transfers, the transfer form was transported with the patient. Successful documentation was achieved in 22 (95.6%) of these 23 transfers |
Included studies
Four references326,333,345,397 reported randomised controlled studies evaluating the effectiveness of a communication tool, one322 had a mixed-methods approach including a pre and post segment, seven references152,334,340,376,377,383,384 described pre- and post-intervention investigations on a single site and one339 was a retrospective comparative study of patient transfer records.
Country
One study took place in Canada,339 another took place in Australia334 and the remainder took place in the USA. 152,322,326,333,340,345,376,383,384 All studies were conducted in nursing homes or residential aged care facilities.
Types of interventions
The included studies assessed a variety of interventions to improve the quality of communication between nursing homes and other health-care organisations. Four studies analysed the effect of standard communication tools, such as INTERACT,326,383 SBAR345 and a combined INTERACT II SBAR tool. 376 Two studies evaluated the effect of a quality improvement initiative to enhance clinical care outcomes for the residents, the Empira Quality Improvement falls reduction collaborative,322 and CONNECT333 in combination with a falls reduction education (FALLS) programme. 311 Four studies152,339,340,384 evaluated the effectiveness of standardised transfer forms as a communication platform between nursing homes and hospital emergency departments. One study334 used a pre–post design to evaluate the effect of a telephone-led support system by an aged care emergency advanced practice nurse for residential aged care facility (RACF) staff during transfer of residents to an emergency department. The outcome measures were heterogeneous, with studies reporting measures of staff communication with other organisations, effects of communication tools on the quality of communication and effects on resident outcomes such as bowel-related care, falls risk and quality and safety of anticoagulation management.
Participants
These interventions were targeted at providers and staff of the care or nursing homes (including administrators, directors of nursing, RNs and NAs) and other health service providers (including general practitioners, social workers, medical staff and pharmacy staff).
Excluded studies
Thirteen studies were excluded from this focused review: five311,320,321,389,398 because they were protocols, six269,337,338,353,361,390 because they did not explicitly state that they were focusing on communication outcomes in the study aims, one323 because it evaluated the impact of a standard framework, and one349 because it has not been published in full.
Risk of bias in included studies
Of the 11 included studies, 10 were rated as being at high to moderate risk of bias and one was rated as being at low risk. Full details of the validity assessment are presented in Appendix 3, Table 20. The quality of reporting was variable between studies and across the criteria. However, many of the RCTs suffered from high levels of bias because of data collection issues and bias in the measurement of outcomes. The lack of blinding was not considered to be critical for this assessment; however, the overall level of bias for three of RCTs remained moderate to high, with only one being considered as being at low risk of bias.
With only one RCT rated as being at low risk of bias, the overall evidence base to support the effectiveness of individual communication and engagement interventions is weak.
Effects of interventions
Staff reports of communication outcomes
Two RCTs and a mixed-methods study322,326,333 from the USA investigated the impacts of complex quality improvement interventions in care homes. They report the views of staff on some measure of communication quality alongside resident outcomes. All three studies reported improvements in this domain after intervention, although the measured outcomes were different and none of the evidence was strong. One of the trials received a moderate quality rating333 and the other two studies were rated as weak. 322,326
A cluster randomised pilot trial333 with 497 nursing home staff investigated whether or not an intervention to improve nursing home staff connections, communication and problem-solving could improve implementation of a falls reduction programme. The authors reported a significant improvement in staff perceptions of communication quality and safety culture over 6 months, measured using standard scales (openness mean score: baseline, 3.51; after intervention, 3.64; 3.7%, p = 0.02; safety culture: baseline, 4.45; after intervention, 4.69; 3.6%, p = 0.004). The second trial in this section assessed the implementation of a programme to promote early detection of deterioration in residents’ condition (the INTERACT tool). 322,326 Involving over 200 care home staff in 72 nursing homes, this study also investigated the ability of the programme to facilitate cultural change in an organisation. Positive improvements in communication were reported. However, the brevity of reporting and complexity of the intervention make it difficult to interpret the significance of the changes.
The mixed-methods study included in this section looked at the impact that staff communication outside arranged group meetings had on residents’ fall rates. 322 The 29 participants in the qualitative interviews highlighted the importance of sharing ideas with other colleagues, and the link between frequent communication and the staff feeling informed. In turn, they felt that this helped them to improve resident outcomes.
In summary, these three studies provide weak evidence that complex, quality improvement interventions may positively influence communication from the perspective of staff.
Clinical outcomes
Three studies322,333,345 reported positive effects on a range of clinical outcomes from interventions to improve communication. Two were included in the previous section on staff outcomes, the mixed-methods study and the pilot RCT. 322,333
Participating in a quality improvement programme was reported to be associated with a reduction in fall rates in care homes, in Arling’s mixed-methods study. 322 Of particular importance were communication with other colleagues outside scheduled meetings, a perception that the collaborative kept staff informed and that it was effective in fostering new ideas. An intervention to improve nursing home staff connections, communication and problem-solving was tested on its ability to enhance the implementation of a falls reduction programme in a pilot cluster RCT. 333 Over a 6-month period, there was a 12% reduction in the falls rate in the intervention facilities pre and post intervention, but no statistically significant differences in control facilities. In this case, the communication intervention may have been successful in enhancing the implementation of the falls reduction programme.
Structured communication was the subject of a RCT in 26 US nursing homes. 345 This study evaluated the effect of introducing structured telephone communication between nurses and physicians about warfarin management for 453 residents. A template was used based on the SBAR approach, which focuses communication about patients under four headings: situation, background, assessment and recommendations. In the intervention homes, residents were significantly more likely to have optimal anticoagulation management, measured by an international normalised ratio value blood test within the target therapeutic range. There were no differences in the correct ordering of follow-up blood tests between intervention and control homes.
In summary, tools to structure communication, such as SBAR, have the potential to enhance clinical outcomes for care home residents. Complex interventions to improve communication may also improve resident clinical outcomes, but the evidence is limited.
Health service outcomes
Four studies326,334,377,383 reported the impact of interventions on hospitalisation from care homes. Three articles326,377,383 described outcomes from the Interventions to Reduce Acute Care Transfers programme in the USA, one of which implemented the SBAR tool. 377 Two of these studies were rated as moderate quality,377,383 and one was rated as weak. 326
The largest326 of the three studies of INTERACT implementation reported reduced hospitalisation rates of 58% (118/203) post intervention across 72 nursing homes. The study set in 30 nursing homes383 found no significant difference in the rate of hospital transfers, and a non-significant reduction in hospital admissions from 4.07 to 3.64 per 1000 resident-days, pre and post intervention. A single-site study377 reported that the number of hospital transfers decreased after implementation of the SBAR tool; however, there were no differences in the number of avoidable transfers during intervention (1.75 transfers per month).
In the fourth study in this set,334 a nurse-led telephone support service provided by an advance practice nurse was evaluated in a controlled pre and post intervention study in Australia. This study involved 50 staff from emergency departments and 26 from RACFs. In the 9 months after the implementation of the intervention, there were reductions in emergency department presentations (16%), admissions (19%) and total inpatient days (35%) from the 26 RACFs. The outcome of telephone calls to the service were examined for a 6-month period post intervention. Almost two-thirds (57/97, 60%) of the calls made to the telephone support service resulted in transfers being made to the emergency department, and half (29, 51%) of those residents transferred were admitted to hospital.
Overall, these studies reported small reductions in the rate of hospitalisation after intervention of complex interventions to enhance communication and reduce hospital transfers. Tools to structure communication between nursing homes and health services and telephone support services also appear to have potential to reduce transfers of care home residents to hospital. However, all of the evidence is graded as moderate or weak quality. It is also important to acknowledge that transfer to hospital is sometimes associated with the best outcome for the resident.
Transfer forms
Four studies evaluated the effectiveness of transfer forms to promote communication between nursing homes and hospital emergency departments. 152,339,340,384 Two studies, one from Canada339 and one from the USA,340 used a retrospective study design. The other two US studies were pre- and post-interventional studies. 152,340,384 All four studies were rated as being of moderate quality. The number of transfers reviewed in the studies ranged from 60339 to 513. 152 All studies reported that the number of items of vital data transferred between nursing homes and hospitals increased following implementation of a transfer form. In Canada, a care-reporting database was used to evaluate the impact of standardised transfer forms on information provided to the hospital. Information gaps were observed in three-quarters (75%) of the transfers when the forms were used, compared with 94% when they were not used (p < 0.001). 339 A similar retrospective study of transfers between nursing homes and emergency departments in St Louis found that essential information was transferred in 71% of cases when a form was used, compared with 28% when a form was not used (p < 0.0001). 340 Documentation of transfers also increased by around 20% to 78% (56/72) after the introduction of a standard transfer form between extended care facilities and emergency departments. 384
A study on a single site in the USA152 evaluated the impact of an internet-based system on the information transferred with residents moving between skilled nursing facilities and emergency departments. The new system was used in 40% of care transitions and nine elements of patient information were assessed with a point being awarded for each element included in the transfer. Communication of vital information increased, whereas the total amount of information transferred reduced. 152
In summary, the use of standardised data collection forms appears to promote the transfer of vital information with residents who are referred to hospital. The studies reviewed provided no data on the impact of transfer forms on patient outcomes.
Discussion
Summary of findings
Around two-thirds of the research on communication and engagement originated from the USA, with only 1 in 10 studies conducted in the UK. Communication about resident transfers to hospital was a major focus of attention. A number of ways of structuring communication have been evaluated, and this appears to offer potential benefits to care home residents and staff. Tools such as SBAR and structured transfer forms have enhanced communication and may have influenced resident outcomes in US studies. A number of the complex interventions aimed at reducing resident transfers to hospital have included a component directed at modifying communication between care home staff and health service personnel.
Strengths and weaknesses
There is extensive literature that may offer insights into communication in and with care homes, and our searches were designed to be comprehensive. However, to manage the volume of material identified, we focused our attention on studies that had an explicit aim or interest in influencing resident-related communication. We also omitted any research that was concerned with communication that was entirely internal to the care home. Nevertheless, we have included studies in our review that describe broad-ranging quality improvement programmes. Most of these programmes aimed to reduce the number of residents transferred to hospital, and modifying communication was one of the strategies employed to meet this aim. The data generated by these studies on staff perception of communication quality are valuable and can be used to judge the relevance of interventions in other settings. The findings that relate to the achievement of programmatic outcomes – notably reductions in hospital transfers – are less useful, as it is often not clear how enhanced communication has influenced outcomes.
The USA has produced a high proportion of the worldwide research into long-term care, and most of the larger studies. However, there are many differences in the organisation and practice of health and social services between the USA and the UK. Any generalisation of the findings of US research to the UK requires careful consideration of the context in which the study was conducted. Communication practices are likely to be very sensitive to cultural contexts, which emphasises the importance of locally appropriate research.
Gaps in research
Care homes in the UK are increasingly active in engaging with their local communities. Many homes host tea parties, bring-and-buy sales and dances. Some have hosted polling stations at election time. These activities are believed to encourage social interaction between residents and local communities, and aim to break down barriers and preconceptions about life in a care home. There is little research in this area to guide care homes and other organisations. This review identified a gap in our understanding of which activities offer the most benefit to residents, and which are acceptable and cost-effective. Future research could usefully further our understanding of the value of the care home as a community resource, and the role of volunteers in promoting engagement between communities and care homes. There is increasing interest in intergenerational initiatives with care home residents, and a need for well-designed evaluative research. A longitudinal perspective on the most effective ways of engaging with local populations and the long-term benefits to residents of greater community engagement would be particularly helpful.
Complex interventions to reduce the number of residents transferred to hospital have been implemented and evaluated in the USA. There is some evidence that these broad-ranging quality improvement programmes have a positive impact on communication and some resident outcomes. However, questions remain about the transferability of these interventions to the UK. The effectiveness and cost of different aspects of different component parts of the interventions may also vary. Research is needed to identify the active ingredients in broad-ranging and complex programmes. It is likely that some aspects of these programmatic interventions are likely to be more applicable to the UK context than others.
Structured communication between care homes and hospitals has been introduced via transfer forms to record information and tools to guide communication by care home staff. These approaches have been shown to enhance information transfer in studies from the USA. The impact on resident outcomes is unknown, but is assumed to be positive.
Telephone support lines for care homes, staffed by advanced nurse practitioners, appear to be effective in reducing transfers of residents to hospital in Australia. These models are in use in the UK but have not been evaluated.
Implications for the UK care home sector
Existing research offers little guidance for UK care homes on how best to promote engagement from local communities or specific groups. This is an area where the care home sector is active, and collaboration with researchers would help to develop the evidence base.
Structured communication tools are available to support care home staff to liaise with the NHS. Although they appear to be effective, they have not been the subject of formal evaluation in the UK, and there is no off-the-shelf solution available for the sector. Evaluation of such tools is essential to ensure that they are modified to be appropriate for the UK situation. Telephone support lines provided by the NHS for care homes are in place in the UK, but no evaluative evidence was found. Formal study of these interventions would be helpful to extend the evidence base.
Section 3: approaches to evaluation in care homes
Background
Evaluating novel interventions or ways of working is essential to ensuring that we understand and can quantify the impact on care home residents, staff and systems. This is particularly important when changes are being proposed to established practice, with implications for the quality and efficiency of care delivery. NHS England’s care home vanguard programme aimed to identify interventions that could be rolled out across the NHS. Without effective evaluation, it will be impossible to identify effective interventions, or to understand which are the active ingredients of new models of care or the influential contextual factors for promoting enhanced care.
Evaluation in long-term care may be particularly challenging. Multiple organisations contribute to the care received, and there are few routine data on health-care experiences or health outcomes for residents. The USA has a national minimum data set on residents of Medicare- or Medicaid-certified care homes. 399,400 In England, there are no similar accessible, aggregated outcome data to monitor residents’ health and care, and a high proportion of residents are removed from monitoring data produced by general practice for financial payments. 401 Residents are often excluded from a majority of population surveys. 402 This places an emphasis on data collection, which is both costly and a potential burden on busy care homes.
A number of reviews have been published on specific topics relevant to care home evaluation, but there is no overarching synthesis of the current evidence to guide commissioners towards an appropriate evaluation framework. Authors have looked at the ways in which care is organised and how these affect residents, including interdisciplinary interventions in care homes,403 the impact of case management404 or optimal organisation of homes for dementia care. 405 Much previous work investigated specific aspects of care, such as medication management and prescribing in care homes, with a particular focus on reducing polypharmacy and minimising the use of psychotropic drugs,406–408 prevention of falls and exercise promotion/rehabilitation409,410 or infection control and oral care. 411,412 Process and outcome measures in these areas have been taken as indicators of care quality in care homes, although it is noteworthy that more attention has been given to objective measures of physical status and functioning, rather than to quality of life or resident-identified priorities. The aim of this work is to produce a synthesis of the current evidence that will be useful to guide commissioners to an appropriate evaluation framework. The mapping review will collate information on approaches to evaluation in care homes and tools used, whereas the systematic rapid evidence synthesis will identify tools validated for use in UK care homes.
Methods
The methods are described in a previous section of this report.
Findings of mapping review
This mapping review had two component parts. In the first, articles were sought that described general evaluations of care, to produce an overview of approaches to evaluation in this setting. In the second, measurement tools used to evaluate different aspects of care in this setting were identified.
Approaches to evaluation
Number and characteristics of studies
The database search returned 3799 records. After deduplication and application of the inclusion criteria, 266 articles were selected for screening based on their titles and abstracts by two independent reviewers. Disagreements were resolved through discussion. Of these, 64 articles were judged to have met the inclusion criteria and included in the mapping review (Table 10).
| First author | Year of publication | Review |
|---|---|---|
| Axelsson413 | 2000 | Evaluation |
| Bartoszek414 | 2016 | Evaluation |
| Bettger415 | 2012 | Evaluation |
| Bowers416 | 2008 | Evaluation |
| Bravo417 | 2005 | Evaluation |
| Brownie418 | 2013 | Evaluation |
| Castle419 | 2005 | Evaluation |
| Chenoweth420 | 2007 | Evaluation |
| Chin421 | 2011 | Evaluation |
| Chiu422 | 2005 | Evaluation |
| Corradi423 | 2016 | Evaluation |
| Corazzini424 | 2003 | Evaluation |
| Crogan425 | 2006 | Evaluation |
| Crogan426 | 2006 | Evaluation |
| Cutler427 | 2006 | Evaluation |
| Davis428 | 2016 | Evaluation |
| Drouin429 | 2015 | Evaluation |
| Edvardsson430 | 2008 | Evaluation |
| Fisher431 | 2006 | Evaluation |
| Flores432 | 2009 | Evaluation |
| Forsyth433 | 2000 | Evaluation |
| French434 | 2007 | Evaluation |
| Froggatt435 | 2011 | Evaluation |
| Graney436 | 2000 | Evaluation |
| Halfens437 | 2013 | Evaluation |
| Harrington438 | 2003 | Evaluation |
| Jones 439 | 2015 | Evaluation |
| Kapoor440 | 2008 | Evaluation |
| Kehinde441 | 2011 | Evaluation |
| Kovach442 | 2008 | Evaluation |
| Lepore443 | 2012 | Evaluation |
| Levenson444 | 2010 | Evaluation |
| Merilahti445 | 2016 | Evaluation |
| Mor446 | 2011 | Evaluation |
| Mukamel447 | 2007 | Evaluation |
| O’Reilly448 | 2007 | Evaluation |
| Peak449 | 2002 | Evaluation |
| Port450 | 2003 | Evaluation |
| Reijula451 | 2009 | Evaluation |
| Rosen452 | 2006 | Evaluation |
| Ryan453 | 2004 | Evaluation |
| Saivar454 | 2004 | Evaluation |
| Sales455 | 2015 | Evaluation |
| Sangl456 | 2005 | Evaluation |
| Schnelle457 | 2004 | Evaluation |
| Schnelle458 | 2005 | Evaluation |
| Shier459 | 2014 | Evaluation |
| Simmons460 | 2000 | Evaluation |
| Stevenson461 | 2009 | Evaluation |
| Swafford462 | 2009 | Evaluation |
| Thompson463 | 2006 | Evaluation |
| Tolson464 | 2013 | Evaluation |
| Van Camp465 | 2005 | Evaluation |
| Wagner466 | 2008 | Evaluation |
| Wan467 | 2003 | Evaluation |
| Werner468 | 2009 | Evaluation |
| Winters469 | 2014 | Evaluation |
| Woitha470 | 2015 | Evaluation |
| Worden471 | 2006 | Evaluation |
| Wu472 | 2009 | Evaluation |
| Xholi473 | 2004 | Evaluation |
| Yeager474 | 2014 | Evaluation |
| Yeh475 | 2003 | Evaluation |
| Zhang476 | 2009 | Evaluation |
Countries
Excluding the five studies that were reviews,414,418,429,462,463 38 studies were carried out in the USA,415,419,423–427,431–434,436,438,440–444,446,447,449,450,452–454,456–461,465–468,472,474,476 six in Australia,420,421,428,430,439,448 three in multiple sites (one in 30 countries,464 one in 25 European countries470 and one in Australia, the Netherlands and Switzerland437), two each from Canada417,455 and Finland445,451 and one each from China,422 the Netherlands,469 Sweden413 Taiwan475 and the UK. 435 Three of the studies416,471,473 did not mention the country where study took place in the title or the abstract.
Methodologies
Of the 64 studies included, eight were experimental studies: five non-randomised trials,425,426,430,455,466 two RCTs417,420 and one before-and-after study. 452 There were also 19 cross-sectional studies415,416,419,422,427,431,437,440,445,447,451,454,457,461,464,467,469,470,472 and one study employed the Delphi methods process. 428 Three of the studies provided descriptions of the methods of evaluations439,453,458 and two were discussion papers. 444,456 The rest of the studies used observational methods, including surveys, cohort studies, longitudinal, retrospective data analyses and a case study.
Clinical care outcomes
Most of the studies (80%, 51/64) described ways to improve the clinical care outcomes of residents in nursing or residential homes. 413,414,417,419–426,428–434,437,439–441,444,445,447–449,452–473,475,476 Thirty of these studies (60%) assessed approaches to measuring the well-being and quality of care of residents. 417,419–421,424,428,429,432,437,438,444,447–450,453–459,461,463,466–469,471,472,475 For example, one study469 assessed measures for monitoring change in client-reported and professional indicators over a period of time, and another451 assessed perceived well-being among elderly people. Six of the studies (12%) focused on measures to promote or maintain the mental health of residents, in particular cognitive ability, delirium status and dementia. 413,420,423,430,439,442 Some of the studies reported on measures to improve mobility (n = 5, 10%), nutrition (n = 3, 6%), pain (n = 3, 6%) and skin care (n = 2, 4%), and only one study assessed the measures to improve clinical assessment.
Influencing the culture of nursing homes
Four of the studies (6%) in the mapping assessed approaches to improving the culture of care home facilities. One427 provided insights into the use of checklists to assess room, bathing, unit and facility environments, whereas another416 assessed measures of improving provider performance. Another study421 reported on the effects of observing and interviewing residents to identify elements of the built and social environments that may influence their well-being. The other study474 was a systematic review that sought to examine and summarise ways in which using the resource dependency theory perspective has an impact on how to operationalise the market environment in health-care settings.
Palliative care
Three (5%) studies also reported on approaches to improve palliative care. One435 examined the use of a framework that aimed to develop staff knowledge about palliative care by implementing informal, reflective debriefing sessions and using a model (the ÄldreVäst Sjuhärad) to make judgements about the quality of partnership working with older people. A systematic review463 focused on describing the various methods of measuring the quality of end-of-life care, including measures of satisfaction and perception, quality of life/dying, and structures and processes of care. The reliability and feasibility of a set of quality indicators of palliative care across 25 European countries were presented in a study that argued for their use as a starting point for quality improvement activities. 470
Staff and staff–resident interactions
Six (9%) studies focused on measures to improve staff practice and staff–resident relationships to long-term care outcomes. Three studies assessed methods to improve change in staff behaviour by monitoring their adherence to protocols and procedures418,452 and their responses to provider feedback. 455 Two420,465 focused on improvement measures to staff and resident interactions and the impact that this would have on the quality of care. Only one study438 focused on measures that examine the impact of quality improvement on indirect staff outcomes such as retention rates, financial indicators (e.g. wages), complaints and deficiencies.
Summary: approaches to evaluation
Over half of the mapped studies were concerned with general aspects of evaluation in care homes, with measurements of quality of care, quality of life or well-being. A majority employed descriptive methods. Experimental approaches were most often applied to specific interventions, rather than general approaches to care.
Methods: evaluation – measurement tools validated in UK care homes
Scrutiny of the mapped literature and specific, focused searches were used to identify articles that described measurement tools used in care homes. Further database searching and an examination of the reference lists of articles using the identified tools served to locate papers describing the validation process. The following section describes tools that have been validated in the UK for use in care homes.
For methods, see Chapter 3. The PRISMA flow diagram is shown in Figure 3.
FIGURE 3.
Evaluation PRISMA flow diagram.

Findings of systematic evidence synthesis
The complete list of tools used in care homes is presented in Appendix 4. Further details of the retrieved articles are presented in Report Supplementary 1, Table 4. In total, we identified 65 tools.
In this section, data are presented on six tools that were identified as having been validated in a UK care home setting (Table 11).
| Validation study (authors, year of publication) | Measurement tool | Description | Patient/participant characteristics | Population size | Assessor |
|---|---|---|---|---|---|
| Dutta et al., 2015477 | MMRI-R | Measures a resident’s risk of dying within the next 6 months |
Nursing home residents Median age 87 years; 55.7% female |
183 | Researchers |
| Faulkner et al., 2006478 | CARE profiles | Identifies the frequency of positive events over a specified time based on the perceptions of residents, relatives and staff in care home settings |
Care home residents (n = 23), relatives (n = 53) and staff (n = 55) Mean ages: relatives (60.85 years), staff (36.5 years), residents (78.95 years) |
131 | Researchers (RNs) |
| Fossey et al., 2002479 | DCM | Observational tool that looks at the care of people with dementia from the viewpoint of the person with dementia |
Nursing and residential home residents Cohort A (mean age 82.3 SD 7.4 years) Cohort B (mean age 78.2 SD 9.1 years) |
Cohort A (n = 123) Cohort B (n = 54) |
Researchers |
| Moniz-Cook et al., 2001480 | CBS | A behavioural rating scale for older adults living in care with behaviour that staff find difficult to manage |
Nursing and residential home residents Mean age 82.7 years (SD 8.14 years) |
382 | Nursing home staff |
| Sutcliffe et al., 2000481 | GDS-12R | A short version of the 30-item GDS, which is a measure for depression among older adults |
Nursing and residential home residents Mean age 83 years (SD 7.6 years); 69% female |
308 | Researchers |
| Towers et al., 2015482 | ASCOT | Measures the outcomes of social care for individuals living in a variety of care settings | 28 professional and 17 lay stakeholders for care homes | 45 | Researchers |
Measurement tools and evidence of reliability and validity
All of the included studies report on measurement of various aspects of health and well-being in care homes, including dementia, challenging behaviour, depression and general social care. Internal consistency was evaluated in four of the studies,478–481 followed by criterion validity (measured in three studies)479–481 and then reliability in two studies479,480 and content validity482 and hypothesis testing477 in one study each. None of the studies evaluated measurement error, structural validity, or cross-cultural validity and responsiveness for their corresponding tools, and none of the studies applied any item response theory models to their tests, and therefore the results of these properties were not presented. All studies that evaluated the methodological quality for internal consistency were scored as poor because they did not provide information on whether or not factor analysis was performed, nor did they refer to any similar study where it could be performed. For criterion validity, all three studies were scored as poor because the criterion used to judge the measurement could not be considered an adequate reflection of a gold standard. 483 Table 12 provides a summary of the methodological qualities of these measures and Description of measurement tools presents a narrative summary of these measures.
| Authors, year of publication | Tool | Internal consistency | Reliability | Content validity | Hypothesis testing | Criterion validity |
|---|---|---|---|---|---|---|
| Dutta et al., 2015477 | MMRI-R | N/A | N/A | N/A | Good | N/A |
| Faulkner et al., 2006478 | CARE profiles | Poor | N/A | N/A | N/A | N/A |
| Fossey et al., 2002479 | DCM | Poor | Fair | N/A | N/A | Poor |
| Moniz-Cook et al., 2001480 | CBS | Poor | Good | N/A | N/A | Poor |
| Sutcliffe et al., 2000481 | GDS-12R | Poor | N/A | N/A | N/A | Poor |
| Towers et al., 2015482 | ASCOT | N/A | N/A | Good | N/A | N/A |
Description of measurement tools
The MMRI-R tool is a 10-item score sheet simplified from the original Minimum Data Set Mortality Risk Index designed to monitor quality of care in nursing homes. It uses selected Minimum Data Set (MDS) items to determine a resident’s risk of dying within the next 6 months. 484 The quality of hypotheses testing for the tool was rated as good after the study theorised that the MMRI-R score could predict 6-month mortality. In this case, hypotheses testing refers to the degree to which the scores of the MMRI-R tool derived from the theory are supported. The evidence, presented as area under the curve of 0.723 for death at 6 months, was consistent with the value of 0.76 in the original MMRI-R validation study based in the USA. 477
The Combined Assessment of Residential Environments (CARE) profiles were developed to identify the frequency of positive events over a specified time based on the perceptions of residents, relatives and staff in care home settings. 478 They were derived from the Events Frequency Approach,485 which encourages the involvement of representative members of a target group, including residents and staff. The process takes place in two phases. Phase 1 involves asking target members to nominate events that they believe are important and enjoyable in a care home. Phase 2 involves judging the nominated events using a 5-point rating scale. Based on limited evidence, Cronbach’s alpha, a statistic used to measure the degree of internal consistency between items in a questionnaire,486 showed acceptable scores (≥ 0.7) ranging from 0.7 to 0.89 for residents, 0.91 to 0.94 for relatives and 0.78 to 0.92 for staff. 478 However, owing to poor methodological quality (factor analysis not being performed), the quality of internal consistency of the tool was rated as poor.
Dementia care mapping (DCM) is an approach used to improve the quality of care for people with dementia living in various care settings. 487 It was developed in the UK by the Bradford Dementia Group from the psychosocial theories of dementia. 488 DCM involves recording observations every 5 minutes for up to 6 hours on a patient’s behaviour and assigning a behaviour category code and perceived quality of life, and assigning a well-being and ill-being score. To assign a behaviour category code, the observer selects from a list of 24 codes, the one that best describes the behaviour of the resident during the 5-minute observation period, whereas well-being and ill-being values are judged on a six-point scale from very negative (–5) to very positive (+5). 479 Internal consistency, test–retest reliability and concurrent validity were evaluated by investigating the correlations between key DCM indices, the hour before lunch and the total observation period, respectively, using Spearman’s rank correlation. 489 Although the study showed that there was excellent agreement between the different DCM indices, internal consistency of the study was rated as poor because of factor analysis not being performed on the tool. The study showed good levels of agreement for well-being (r = 0.58; p < 0.0001) and well-being and ill-being score (r = 0.55; p < 0.0001) and more moderate scores for activities (r = 0.4; p = 0.003) and social withdrawal (r = 0.33; p = 0.007); however, the test–retest reliability of the tool was rated as fair because the study did not report on whether there were any missing items or participants and this affected the rating. 483 The quality of criterion validity was also rated as poor because the measurement tool that DCM was evaluated against, the Blau Scale,490 could not be considered as gold standard483 even though there was evidence of strong correlation between the well-being and ill-being score (DCM) and quality of life score (Blau Scale) (r = 0.73; p < 0.0001).
The CBS is a 25-item rating scale that records staff reports of the incidence, frequency and management difficulty of residents’ behaviour, and it can also identify challenging residents through a computed score. The frequency of a behaviour is rated from 1 (occasionally present or less than once per month) to 4 (present daily) and severity of the behaviour is rated from 1 (minimal management difficulty) to 4 (extreme management difficulty). Scores are then calculated as totals of incidence (0–25), frequency (0–100) and difficulty (0–100). The fourth measure, a computed score, is calculated as the sum of the products of frequency and difficulty ratings for each behavioural item on the scale (0–400). 480 Internal consistency of the scale was rated as poor because of factor analyses not being performed;483 however, based on the limited evidence presented in the study, Cronbach’s alpha486 for the four subscales showed acceptable scores: 0.85 (incidence), 0.82 (frequency), 0.87 (difficulty) and 0.85 (challenge). 480 Criterion validity of the tool was also rated as poor because the analysis was explored by correlating the total scores for each of the four CBS measures: incidence (r = 0.45; p = 0.01), frequency (r = 0.46; p = 0.001), difficulty (r = 0.36; p0.001) and challenge (r = 0.35; p = 0.001). It was difficult to ascertain if this criterion method could be considered as gold standard. 483 Reliability of the scale was rated as good based on the presented evidence, and test–retest and inter-rater reliability were shown to be good. 480
The Geriatric Depression Scale – Residential (GDS-12R) scale is a screening measure for depression appropriate for use with older people in nursing and residential care. It is a short form of the 30-item Geriatric Depression Scale (GDS), shown to be effective in distinguishing between depressed and non-depressed older adults. The GDS-12R is based on the 15 item Geriatric Depression Scale (GDS-15) and reflects the differences between living in the community and living in institutions such as nursing homes. The scale consists of 12 questions, with responses awarded points for either positive statements [yes (0) and no (1)] or negative statements [yes (1) and no (0)]. The total score is calculated as the sum of points for all 12 questions with a minimum score (0) and maximum score (12). 481 Based on the evidence presented in the study, internal reliability scores were all high (> 0.8) for each of the three data collection points: at admission (alpha = 0.85), at 5 months (alpha = 0.848) and at 9 months (alpha = 0.812). The quality of assessing internal consistency was rated as poor, however, as factor analyses were not performed in the study. 483 Based on limited evidence, using another indicator of depressed mood from another tool, the Affect Balance Scale491 as a comparator showed that the GDS-12R gives higher levels of specificity and sensitivity than the original GDS-15. However, criterion validity was rated as poor because no current measurement tools are considered to be an adequate gold standards for comparison. 483
The Adult Social Care Outcomes Toolkit (ASCOT) was developed as a multiattribute preference-weighted measure of social care-related quality of life. It has eight conceptually distinct attributes: personal cleanliness and comfort, food and nutrition, control over daily life, personal safety, accommodation cleanliness and comfort, social participation and involvement, occupation, and dignity. The toolkit can be administered as self-completion questionnaires, face-to-face interviews or observations depending on the needs of an individual, and service users applying the relative importance or preference weights to obtain an overall social care-related quality of life score, which is rated between zero and one and quantifies the a service user’s well-being based on personal experiences. 492 Face validity of the study was rated as good because experts within the field were asked to reflect on whether or not the toolkit actually measured the construct it was supposed to measure, based on their experiences in social care. 482
Discussion
This review identified six measurement tools that have undergone some validation for use in UK care homes. These included measures of depression, behaviours that staff find difficult to manage, a resident’s risk of dying within 6 months and dementia care from the resident’s perspective. Only two measures of more general outcomes of care were included: ASCOT and CARE. None of the included tools scored highly in our assessment of measurement properties.
A broad range of measurement tools have been described in the English-language care home literature. From 65 articles in our mapping that described use of a tool or measure published since the year 2000, we were able to identify only six tools with associated, published validation work from the UK. Validation of one of the general measures, the care home version of ASCOT, involved 29 professional and 17 lay stakeholders, However, this supplements development work for the original, earlier versions of this measure. Validation of the remaining five tools involved study populations of between 131 and 308. In all but one study, researchers performed the assessments.
Many care home residents living with cognitive impairment or dementia may be unable to respond to surveys or interview questions. Proxy respondents in the form of staff or relatives are often used to provide a resident’s perspective. Some measures, such as the CARE profiles, deliberately seek responses from all parties to generate a rounded picture. Others may need specific tailoring to application by a proxy. Both approaches have strengths and weaknesses, and the important point is that they should be explicitly addressed in tool development and administration. In this study, we made no comment on the length of the tools, although this is relevant to all residents and likely to influence completion rates.
The search for appropriate performance measures in long-term care has been the subject of an extensive literature. 493,494 A manual of 94 institutional-level indicators for use in long-term care has been produced by a European consortium that included the My Home Life Project authors. 494 Starting from a conceptual analysis of quality of care and quality of life in this setting, the indicators were derived from a range of sources, including regulatory frameworks. Although a majority of these indicators do not require a specific measurement tool, the extent of this project serves to illustrate the complexity of evaluating the outcomes of care in this setting. 494 A number of the indicators related directly to the domains of the CARE framework.
Strengths and limitations
To be comprehensive, this review accepted a broad definition of measure or tool, but this has generated a heterogeneous group of studies. Restricting this work to research published after the year 2000 gave a focus on measures likely to be in current usage. The search for validation papers was not restricted by year so that it would reflect the times involved in the development and adoption of new measures. Many measurement tools used in care homes will be dementia specific, and it is possible that our focus on the care home setting led us to overlook some of these. Similarly, by focusing on UK-validated measures, we will have omitted tools that may work well in the UK. (The Oral Health Assessment Tool, for example, features in National Institute for Health and Care Excellence guidance, but was developed for use in Western Australia. 495) It is also plausible that measures used in hospitals or during primary care consultations could be transferable to the care home setting. However, the unique context provided by care homes, which are home to residents living with multiple conditions and frailty, and have staff who may not be familiar with the application of measurement tools, suggests that tools should be tested in that environment.
Implications
This review did not identify a well-validated general outcome measure for use in UK care homes. Our assessment of the methodological quality of ASCOT and CARE identified strengths, weaknesses and possible areas for future work. A broad range of measures has been used in care homes worldwide. Some of these measures merit assessment of their suitability for use in a UK setting to avoid the need to develop completely new tools.
Close scrutiny of the measures in this review provides some guidance as to the sources and types of data that may be helpful to evaluate the quality and impact of health and other service inputs to care homes. There is no comprehensive, easily accessible source of information on health, well-being or quality of life in care homes across England and Wales. However, this information could inform the future development of any care home minimum data set.
Section 4: care home workforce
Background
A care home’s workforce is its life blood, and is central to the provision of high-quality care. Yet, for a range of reasons, recruitment and retention in this sector are ongoing challenges. The low-wage economy is an important factor in the employment of care assistants. In a recent review of the literature on training and ongoing professional development for the RN workforce, the absence of a career path for care home nurses, low levels of confidence in their own skills and poor access to training were particular areas of concern. 496 High staffing levels and job satisfaction are believed to be associated with better-quality care, whereas high staff turnover is linked with poor outcomes for residents. 497–500 The drive to enhance care has led to calls for innovative thinking around the care home workforce, the skills and expertise required of staff and the roles adopted.
This section of the report presents a mapping review of literature on the care home workforce. It aims to inform flexible and innovative uses of the nursing and support workforce to benefit resident care. The linked rapid review examines the relationship between staffing levels (the ratio of RNs and support staff to residents or different levels of support staff) and resident outcomes.
Methods
See Chapter 3 for overview section.
Findings of mapping review
Number and characteristics of studies
After deduplication, 5383 studies were identified for title and abstract screening, and 535 identified for full-text screening. Three hundred and sixteen articles met the broad inclusion criteria for the mapping review (Table 13).
| First author | Year of publication | Review |
|---|---|---|
| Abraham501 | 2008 | Workforce |
| Abrahamson502 | 2013 | Workforce |
| Adams-Wendling503 | 2005 | Workforce |
| Akinci504 | 2005 | Workforce |
| Alexander505 | 2008 | Workforce |
| Alzheimer’s Society506 | 2007 | Workforce |
| Anderson507 | 2004 | Workforce |
| André508 | 2014 | Workforce |
| Anonymous511 | 2001 | Workforce |
| Anonymous509 | 2005 | Workforce |
| Anonymous510 | 2009 | Workforce |
| Anonymous512 | 2009 | Workforce |
| Anonymous316 | 2011 | Workforce |
| Arling513 | 2007 | Workforce |
| Atkins514 | 2010 | Workforce |
| Backhaus516 | 2014 | Workforce |
| Backhaus515 | 2015 | Workforce |
| Banaszak-Holl517 | 2015 | Workforce |
| Bates-Jensen518 | 2004 | Workforce |
| Berta519 | 2013 | Workforce |
| Blekken520 | 2015 | Workforce |
| Blinkhorn521 | 2012 | Workforce |
| Boorsma522 | 2011 | Workforce |
| Bostick524 | 2002 | Workforce |
| Bostick523 | 2004 | Workforce |
| Bostick525 | 2006 | Workforce |
| Boumans526 | 2008 | Workforce |
| Bowblis527 | 2011 | Workforce |
| Bowers528 | 2000 | Workforce |
| Brown529 | 2007 | Workforce |
| Brown530 | 2016 | Workforce |
| Brulhart531 | 2011 | Workforce |
| Buettner532 | 2009 | Workforce |
| Bunn533 | 2015 | Workforce |
| Burgio534 | 2004 | Workforce |
| California Health Care Foundation536 | 2006 | Workforce |
| California Health Care Foundation535 | 2008 | Workforce |
| Care Quality Commission573 | 2013 | Workforce |
| Carrier537 | 2009 | Workforce |
| Carter538 | 2003 | Workforce |
| Cassidy331 | 2005 | Workforce |
| Cassie539 | 2012 | Workforce |
| Castle540 | 2000 | Workforce |
| Castle541 | 2001 | Workforce |
| Castle542 | 2005 | Workforce |
| Castle543 | 2006 | Workforce |
| Castle544 | 2006 | Workforce |
| Castle545 | 2007 | Workforce |
| Castle546 | 2007 | Workforce |
| Castle547 | 2008 | Workforce |
| Castle548 | 2008 | Workforce |
| Castle549 | 2008 | Workforce |
| Castle550 | 2008 | Workforce |
| Castle551 | 2010 | Workforce |
| Castle552 | 2011 | Workforce |
| Castle553 | 2011 | Workforce |
| Castle554 | 2011 | Workforce |
| Castle555 | 2012 | Workforce |
| Castle556 | 2014 | Workforce |
| Castle557 | 2015 | Workforce |
| Chang559 | 2005 | Workforce |
| Chang558 | 2006 | Workforce |
| Chapman560 | 2007 | Workforce |
| Chen561 | 2015 | Workforce |
| Cherubini562 | 2012 | Workforce |
| Chipantiza563 | 2014 | Workforce |
| Choi564 | 2012 | Workforce |
| Chou566 | 2002 | Workforce |
| Chou565 | 2003 | Workforce |
| Chu567 | 2014 | Workforce |
| Clare568 | 2013 | Workforce |
| Collier569 | 2008 | Workforce |
| Collier570 | 2008 | Workforce |
| Comondore571 | 2009 | Workforce |
| Corazzini572 | 2013 | Workforce |
| Crickard574 | 2005 | Workforce |
| de Jonge575 | 2014 | Workforce |
| Decker576 | 2008 | Workforce |
| Dellefield577 | 2000 | Workforce |
| Dhaini578 | 2016 | Workforce |
| Dill579 | 2013 | Workforce |
| Dixon580 | 2010 | Workforce |
| Donoghue581 | 2007 | Workforce |
| Donoghue582 | 2010 | Workforce |
| Dwyer583 | 2011 | Workforce |
| Dwyer584 | 2015 | Workforce |
| Dyck586 | 2004 | Workforce |
| Dyck585 | 2007 | Workforce |
| Eckstrom587 | 2016 | Workforce |
| Ersek588 | 2014 | Workforce |
| Eyers589 | 2003 | Workforce |
| Figueirido590 | 2013 | Workforce |
| Finnema591 | 2005 | Workforce |
| Fitzler592 | 2016 | Workforce |
| Freeman593 | 2003 | Workforce |
| Gao594 | 2014 | Workforce |
| Sandoval Garrido595 | 2014 | Workforce |
| Gloth596 | 2011 | Workforce |
| Goldberg597 | 2000 | Workforce |
| Gorski598 | 2004 | Workforce |
| Goyder599 | 2012 | Workforce |
| Grabowski600 | 2008 | Workforce |
| Gray-Siracusa601 | 2005 | Workforce |
| Halcomb602 | 2009 | Workforce |
| Harahan603 | 2011 | Workforce |
| Harden604 | 2015 | Workforce |
| Harrington608 | 2000 | Workforce |
| Harrington606 | 2003 | Workforce |
| Harrington607 | 2012 | Workforce |
| Harrington605 | 2016 | Workforce |
| Harvath609 | 2008 | Workforce |
| Hasson355 | 2008 | Workforce |
| Havig610 | 2011 | Workforce |
| Havig611 | 2014 | Workforce |
| Heath612 | 2012 | Workforce |
| Hedrick613 | 2009 | Workforce |
| Heeren614 | 2014 | Workforce |
| Hegeman615 | 2005 | Workforce |
| Help the Aged616 | 2007 | Workforce |
| Hendrix618 | 2000 | Workforce |
| Hendrix617 | 2001 | Workforce |
| Heponiemi619 | 2011 | Workforce |
| Hewison358 | 2009 | Workforce |
| Hickey620 | 2005 | Workforce |
| Hodgkinson621 | 2011 | Workforce |
| Hofmann622 | 2003 | Workforce |
| Hollingsworth623 | 2016 | Workforce |
| Horn624 | 2005 | Workforce |
| Horn625 | 2010 | Workforce |
| Hovey626 | 2015 | Workforce |
| Hunt627 | 2014 | Workforce |
| Hutt629 | 2003 | Workforce |
| Hutt628 | 2008 | Workforce |
| Hyde630 | 2014 | Workforce |
| Hyer631 | 2011 | Workforce |
| Ikegami632 | 2013 | Workforce |
| Intrator633 | 2011 | Workforce |
| Irvine634 | 2013 | Workforce |
| Jette635 | 2004 | Workforce |
| Jogerst636 | 2008 | Workforce |
| Johnson637 | 2005 | Workforce |
| Jordan638 | 2009 | Workforce |
| Kajonius639 | 2016 | Workforce |
| Kang640 | 2008 | Workforce |
| Karsh641 | 2005 | Workforce |
| Kash643 | 2006 | Workforce |
| Kash642 | 2010 | Workforce |
| Katz645 | 2009 | Workforce |
| Katz644 | 2011 | Workforce |
| Kayser-Jones646 | 2003 | Workforce |
| Kayser-Jones647 | 2008 | Workforce |
| Kayyali648 | 2014 | Workforce |
| Keogh302 | 2014 | Workforce |
| Kerr649 | 2008 | Workforce |
| Killett650 | 2013 | Workforce |
| Kim651 | 2006 | Workforce |
| Kim652 | 2009 | Workforce |
| Kim653 | 2009 | Workforce |
| King654 | 2001 | Workforce |
| Kinjerski655 | 2008 | Workforce |
| Kirkevold658 | 2004 | Workforce |
| Kirkevold657 | 2006 | Workforce |
| Kirkevold656 | 2008 | Workforce |
| Klay659 | 2005 | Workforce |
| Klitch660 | 2000 | Workforce |
| Konetzka662 | 2005 | Workforce |
| Konetzka661 | 2008 | Workforce |
| Kovner663 | 2000 | Workforce |
| Kovner665 | 2000 | Workforce |
| Kovner664 | 2001 | Workforce |
| Kramer666 | 2002 | Workforce |
| Krichbaum667 | 2000 | Workforce |
| Kris669 | 2004 | Workforce |
| Kris668 | 2009 | Workforce |
| Krueger670 | 2002 | Workforce |
| Kuo671 | 2008 | Workforce |
| Laakso672 | 2001 | Workforce |
| Laging673 | 2015 | Workforce |
| Landreville674 | 2005 | Workforce |
| Lange675 | 2011 | Workforce |
| Lapane677 | 2004 | Workforce |
| Lapane676 | 2007 | Workforce |
| Lapane678 | 2011 | Workforce |
| LaPorte679 | 2007 | Workforce |
| Lee682 | 2002 | Workforce |
| Lee681 | 2009 | Workforce |
| Lee680 | 2014 | Workforce |
| Leland683 | 2012 | Workforce |
| Lerner684 | 2013 | Workforce |
| Lerner498 | 2014 | Workforce |
| Lewis685 | 2004 | Workforce |
| Li686 | 2015 | Workforce |
| Lin687 | 2014 | Workforce |
| Lisk688 | 2012 | Workforce |
| Liu689 | 2011 | Workforce |
| Lucas691 | 2007 | Workforce |
| Lucas690 | 2009 | Workforce |
| Maas692 | 2008 | Workforce |
| MacEntee693 | 2007 | Workforce |
| Manitoba Nurses’ Union694 | 2006 | Workforce |
| Marcotte695 | 2009 | Workforce |
| Masterson696 | 2004 | Workforce |
| Matsudaira697 | 2012 | Workforce |
| Mattingly698 | 2015 | Workforce |
| Mayrhofer699 | 2016 | Workforce |
| McAiney700 | 2008 | Workforce |
| McGilton701 | 2007 | Workforce |
| McGilton702 | 2014 | Workforce |
| McGregor704 | 2005 | Workforce |
| McGregor705 | 2011 | Workforce |
| McGregor703 | 2014 | Workforce |
| McKinney706 | 2016 | Workforce |
| McNulty707 | 2006 | Workforce |
| Meade708 | 2016 | Workforce |
| Meehan709 | 2015 | Workforce |
| Miller710 | 2016 | Workforce |
| Mitchell711 | 2003 | Workforce |
| Molinari712 | 2008 | Workforce |
| Monarch713 | 2005 | Workforce |
| Monkhouse714 | 2003 | Workforce |
| Morgan715 | 2008 | Workforce |
| Moxon716 | 2001 | Workforce |
| Moxon717 | 2003 | Workforce |
| Moyle718 | 2003 | Workforce |
| Mueller719 | 2006 | Workforce |
| Mueller720 | 2012 | Workforce |
| Muirhead721 | 2004 | Workforce |
| National Center for Health Workforce Analyses722 | 2004 | Workforce |
| Nazir403 | 2013 | Workforce |
| Neuman723 | 2014 | Workforce |
| Noel724 | 2000 | Workforce |
| Older People’s Commissioner for Wales725 | 2014 | Workforce |
| Orellana726 | 2014 | Workforce |
| Ottem727 | 2004 | Workforce |
| Painter728 | 2000 | Workforce |
| Painter729 | 2000 | Workforce |
| Park730 | 2009 | Workforce |
| Parsons731 | 2003 | Workforce |
| Paulsen732 | 2005 | Workforce |
| Personal Social Services Research Unit733 | 2011 | Workforce |
| Phillips734 | 2000 | Workforce |
| Pillemer735 | 2008 | Workforce |
| Pittman736 | 2015 | Workforce |
| Rahnfeld737 | 2016 | Workforce |
| Rai738 | 2012 | Workforce |
| Rantz739 | 2014 | Workforce |
| RCN740 | 2004 | Workforce |
| RCN742 | 2010 | Workforce |
| RCN743 | 2010 | Workforce |
| RCN741 | 2012 | Workforce |
| Redfern744 | 2002 | Workforce |
| Rico745 | 2013 | Workforce |
| Riggs746 | 2001 | Workforce |
| Rondeau747 | 2009 | Workforce |
| Rosen748 | 2011 | Workforce |
| Ryden749 | 2000 | Workforce |
| Sawan750 | 2016 | Workforce |
| Schnelle751 | 2004 | Workforce |
| Schwendimann752 | 2016 | Workforce |
| Scott-Cawiezell753 | 2007 | Workforce |
| Scottish Care754 | 2015 | Workforce |
| Scottish Care755 | 2015 | Workforce |
| Scottish Care756 | 2016 | Workforce |
| Scottish Care757 | 2016 | Workforce |
| Shin758 | 2008 | Workforce |
| Shin759 | 2008 | Workforce |
| Shin760 | 2012 | Workforce |
| Shin761 | 2013 | Workforce |
| Shin762 | 2014 | Workforce |
| Shin763 | 2015 | Workforce |
| Shipman764 | 2007 | Workforce |
| Shippee765 | 2015 | Workforce |
| Simmons767 | 2001 | Workforce |
| Simmons766 | 2004 | Workforce |
| Spector768 | 2013 | Workforce |
| Spilsbury499 | 2011 | Workforce |
| Spilsbury496 | 2015 | Workforce |
| Spilsbury769 | 2015 | Workforce |
| Stearns770 | 2007 | Workforce |
| Stolee771 | 2006 | Workforce |
| Suen772 | 2006 | Workforce |
| Tamura773 | 2013 | Workforce |
| Temple774 | 2011 | Workforce |
| Thomas777 | 2009 | Workforce |
| Thomas776 | 2010 | Workforce |
| Thomas775 | 2014 | Workforce |
| Thompson778 | 2002 | Workforce |
| Tong779 | 2011 | Workforce |
| Trinkoff780 | 2005 | Workforce |
| Trinkoff500 | 2013 | Workforce |
| Unruh781 | 2005 | Workforce |
| Wagner782 | 2008 | Workforce |
| Walker783 | 2008 | Workforce |
| Wan784 | 2006 | Workforce |
| Way785 | 2008 | Workforce |
| Weech-Maldonado786 | 2004 | Workforce |
| Wild787 | 2010 | Workforce |
| Woo788 | 2005 | Workforce |
| Xing789 | 2013 | Workforce |
| Xu790 | 2013 | Workforce |
| Yamaguchi791 | 2016 | Workforce |
| Yassi792 | 2004 | Workforce |
| Yeatts793 | 2000 | Workforce |
| Yeh794 | 2002 | Workforce |
| Zhang795 | 2004 | Workforce |
| Zhang796 | 2005 | Workforce |
| Zhang797 | 2008 | Workforce |
| Zhang798 | 2009 | Workforce |
| Zhang799 | 2013 | Workforce |
| Zimmerman800 | 2002 | Workforce |
| Zúñiga802 | 2014 | Workforce |
| Zúñiga801 | 2015 | Workforce |
Countries
The USA was the setting for two-thirds of the work (n = 201, 64% studies). A further 48 (15%) were from high-income countries other than the USA and Europe. Forty-one studies (13%) were conducted in the UK, and the remaining 26 (8%) studies were conducted in the rest of Europe (for study details see Report Supplementary Material 1).
Study design
Twenty-nine (9%) of the included studies presented a review of existing research evidence, of which 14 (4%) used a systematic approach. Thirty-one (10%) were experimental and quasi-experimental studies. Observational studies were the biggest single group by design (n = 159, 50%); the majority of these were cross-sectional (n = 127, 40%). Fifteen (5%) were purely qualitative studies, and a further 21 (7%) used mixed methods. The remaining studies were reports (n = 18, 6%), descriptive or case studies (n = 26, 8%), or opinion pieces (n = 17, 5%) (for study details see Report Supplementary Material 1).
Staff groups of interest
All of the included articles were concerned in some way with care home staffing, but the main focus varied. In Report Supplementary Material 1, Table 5, all articles are labelled with the aspect of staffing that they cover. One-third of the articles (109, 34%) were focused on topics that were the most likely to inform new or flexible ways of working; staff roles (n = 35, 11%), mix of staff (n = 35,11%), training (n = 27, 9%), teamworking (n = 7, 2%) and leadership (n = 5, 2%) (for study details see Report Supplementary Material 1).
When studies covered more than one aspect of staffing, the most prominent or important was selected for the mapping. In most cases, this was staff numbers. One hundred and forty of the mapped studies (44%) dealt with staff numbers or staff hours. Smaller numbers of studies were included on job satisfaction (n = 16, 5%), turnover (n = 42, 13%), regulations for minimum staff numbers (n = 5, 2%) and staff absenteeism (n = 2, 1%) (for study details see Report Supplementary Material I).
Target population
The population of interest was recorded for each mapped study. (Many studies included more than one staff group, so percentages total more than 100.) Two hundred and thirteen articles (67%) were concerned with nurses; in 160 (51%) of these the nurses were registered or licensed. NAs or aids were the subject of 100 (32%) studies, and 49 (16%) studies were concerned with management or administrative staff. Physicians were the subject of 11 (3%) studies. Sixty-six (21%) studies dealt with residents and a further 16 (5%) dealt with families.
Outcomes
A majority of studies (n = 228, 72%) measured or discussed resident outcomes. Among these, clinical outcomes were the most commonly reported (n = 136, 43%). A smaller number of studies reported on resident functional status (n = 47, 15%) and satisfaction, well-being or quality of life (n = 45, 14%). Almost half of the mapped studies discussed staff outcomes (n = 142, 45%). Process measures of care, and system outcomes, such as service utilisation, were considered in 55 (17%) and 86 (27%) studies respectively (for study details see Report Supplementary Material 1).
UK studies
Forty-one (13%) of the mapped studies were published from the UK between 2000 and 2016. The majority (n = 28) were published from 2010 onwards. One-third of UK studies (n = 15) were reports, primarily from care home organisations and non-governmental organisations, such as Skills for Care and the Royal College of Nursing. Seven publications presented syntheses of existing evidence, three of which were systematic reviews. Five were mixed-method studies, six were cross-sectional studies, two were RCTs, two were quasi-experimental studies, two were descriptive studies, two were qualitative studies, one was a case study and one was an opinion piece (for study details see Report Supplementary Material 1).
Novel staff roles or ways of working for care home staff
To describe the evidence base for novel staff roles and new or flexible ways of working in more detail, two researchers screened the titles of the mapped literature for publications that provided empirical data on these topics. The full texts of 36 titles were examined and 20 of these were selected for closer scrutiny. Table 14 provides information on the selected studies, including aim, design, outcomes and findings. Seven US studies were included, as were three each from the UK and Australia, two each from Canada and the Netherlands and one from Finland (for study details see Report Supplementary Material 1). A majority reported data from single or very small sites, including a single general practice708 and one,521,532,672,793 two,526,560,602,716 or three749,771,787 care homes. Studies were not subject to quality appraisal, but they varied widely in study design, size and setting. All of the published studies reported positive findings.
| Authors, year of publication, country | Aim of study | Design | Sample size | Sample characteristics | New staff role or way of working | Outcomes and measures | Findings | Positive outcome? |
|---|---|---|---|---|---|---|---|---|
| Blinkhorn et al., 2012, Australia521 | To improve the oral health of residents in an aged care mental health unit through the introduction of an innovative nursing intervention | Mixed methods | 28 residents; nursing staff from nine hospital wards NP | Residents of a aged care mental health unit; qualified nurses | Enhanced role for staff in oral hygiene |
Resident: plaque and gingival index, pocket depth, views of new protocol Staff: interviews |
Staff training and implementation of protocols resulted in improved oral care for residents. Reductions were seen in plaque scores, gingivitis and pocket depths. The oral hygiene protocol was positively accepted into a daily routine and the knowledge of staff in matters relating to oral health increased | Yes |
| Boumans et al., 2008, Netherlands526 | To examine the implementation of integrated care in nursing homes and its effects on the quality of caregivers’ work | Quasi-experimental (pre and post) | Two nursing homes | Intervention nursing home (three physical disability wards and two psychogeriatric wards). Control nursing home (two physical and two psychogeriatric wards) | Integrated care model with three components: home-like environment, care in line with resident demands and co-ordinated care provision |
Demographic and ward characteristics, care load (SIVIS-Help Index), bespoke scale measuring three characteristics of integrated care Quality of work measures. Staff satisfaction |
Integrated care intervention was only successful on the wards caring for people with physical disabilities, where it was easier to implement Increases were reported in collaboration and support from supervisors and a decrease in job demands. There were no changes in workers’ outcomes, such as job satisfaction |
Yes |
| Brownie and Nancarrow, 2013, Australia418 | Effects of person-centred care on residents and staff in aged care facilities: a systematic review | Systematic review | Nine studies | One cluster RCT, eight controlled quasi-experimental or pre–post design | Interventions to deliver person-centred care. These were multifaceted, and included leadership and management changes, staffing models to empower staff, and allocating staff to individual residents, as well as modifications to the environment | A broad range of outcome measures, including resident, family and staff satisfaction, resident quality of life, functional status, psychological well-being and infection rates | Some of the included studies describe interventions that are likely to require new ways of working by care home staff. The authors concluded that some person-centred interventions were associated with improved outcomes for residents. However, the quality of the included studies in this review was low, making it difficult to draw robust conclusions. Specific interventions, such as the Eden alternative (a framework for introducing person-centred care), were highlighted as being associated with improvements in residents’ psychological well-being, including reduction in boredom and loneliness | Some |
| Buettner, 2009, USA532 | To evaluate a training programme to improve staff knowledge and skills in engaging residents in meaningful activity | Descriptive | 29 staff staff members of one care home | New role for recreational therapist as trainer for care home staff | Twenty-item multiple-choice questionnaire on dementia, skills in engaging residents observed and rated on a 5-point scale, measure of perceived stress | A recreational therapist delivering 10 training sessions to care home staff was able to increase staff knowledge and reduce their stress levels | Yes | |
| Burgio et al., 2004, USA534 | To compare resident and staff outcomes across two types of staffing patterns, permanent and rotating assignment (or primary and team nursing), and work shift | Between-groups comparison | 91 CNAs delivering primary nursing, 87 team nursing | CNAs from four nursing homes (two using primary care nursing/permanent assignment staffing and two using team nursing/rotating assignment staffing) | Primary care nursing model vs. team nursing | CNAs’ job satisfaction, burnout, absenteeism and turnover rates | In homes using primary care/permanent assignment staffing, personnel were assigned to specific residents. With this model, absenteeism was higher, but CNAs had greater job satisfaction. Evening shifts had higher turnover rates in all homes | Yes |
| Chapman and Toseland, 2007, USA560 | To evaluate the effectiveness of an AICT in two nursing homes | RCT (partial crossover design) | 118 residents in two nursing homes | Residents with a diagnosis of dementia, scoring ≤ 23 on the MMSE and ≥ on the GDS, plus requiring assistance on ≥ 4 ADLs | Formation of AICTs from care home staff, with external input from clinical social workers |
Resident clinical outcomes: Cohen-Mansfield Agitation Inventory; Face, Legs, Activity, Cry, Consolability Behavioral Pain Scale; Cornell Scale for Depression in Dementia; Pain in Advanced Dementia |
Working in multidisciplinary advanced illness care teams made up of care home and external staff led to reduced pain and agitation among residents | Yes |
| Finnema et al., 2005, Netherlands591 | To evaluate the effect of emotion-orientated care on care home residents with dementia and NAs | RCT | 146 residents and 99 staff | Residents with dementia in 14 care homes; 99 NAs | NAs trained to provide emotion-orientated care | Measures of resident mood and behaviour. NA stress and general health |
NAs were trained to deliver care aimed at improving emotional and social functioning and quality of life was integrated with usual care Positive effects were reported on anxiety and dissatisfaction for residents with mild or moderate dementia. Staff who felt that they had acquired skills reported fewer stress reactions |
Yes |
| Halcomb, 2009, Australia803 | To examine the feasibility, acceptability and sustainability of multidisciplinary case conferencing in residential care | Mixed methods | 31 case conferences | Staff in two aged care facilities in Australia | Care staff taking a leading role in multidisciplinary case conferencing | Interviews with 11 residential care staff; questionnaires with all participating staff | Multidisciplinary case conferencing in residential care appears to be feasible, with care staff playing a role. Finding time to complete resident assessments before case conferences was challenging, but staff found the meetings valuable for learning more about residents’ health and care | Yes |
| Hollingsworth et al., 2016, USA623 | To compare the quality of feeding assistance provided by trained non-nursing staff with care provided by CNAs | Mixed methods | 126 residents and 113 staff |
Residents: 61 in intervention group, 65 in usual care control group Staff: 50 in intervention group plus 39 trained staff and 73 CNAs (for interview) |
Non-nursing staff trained in feeding assistance | Care processes including standardised observations of feeding assistance care processes, calories per meal, in-depth interviews with staff | Staff who received feeding assistance training performed significantly better than CNAs for 12 of 13 care process measures. Residents also consumed significantly more calories per snack offer from trained staff. The majority of staff reported a positive impact of the training programme | Yes |
| Laakso and Routasalo, 2001, Finland672 | To explore how nursing home residents, families and nurses experienced a change to primary nursing in a nursing home | Qualitative interviews | 30 interviewees (10 care home residents, 10 family members, 10 nursing staff) | Ten residents, 10 family members and 10 nursing staff | Primary nursing/patient-centred working | Qualitative exploration of experiences of the change in care | Primary nursing provided continuity of care staff for individual residents. Residents reported no change in care. Family members noticed a change in nurse behaviour. Nurses felt that their job was more challenging and rewarding, but some felt that the new model was a threat | Yes; mixed views |
| Lisk et al., 2012, UK688 | To explore the impact of four strategies to reduce hospital admissions for nursing home residents | Quasi-experimental | 1954 residents | Hospital admissions from nursing homes over a 3-year period in one NHS trust | Change in ways of working with NHS services, involving regular in-person and telephone meetings | Reduction of emergency admissions, length of stay in hospital, cost analysis | Geriatrician input into nursing homes had a significant impact on admissions from nursing homes and length of stay. Costs (service and medication use) were reduced | Yes |
| Low et al., 2013, Singapore180 | A systematic review of interventions to change staff care practices to improve resident outcomes in nursing homes | Systematic review | 63 studies | RCTs and quasi-experimental studies | Interventions to change staff practice to improve resident outcomes (educational materials, training, audit and feedback, monitoring, champions, team meetings, policy or procedures and organisational restructure) | Staff behaviour, other staff outcomes, resident clinical outcomes, but not satisfaction | No single intervention component; combination of components or increased number of components was associated with greater likelihood of enhanced outcomes. Studies targeting care tasks (e.g. oral care) were more likely to produce positive outcomes than those addressing more global changes. This review did not explicitly identify new staff roles, and many included studies describe improved delivery of existing roles | Yes |
| McAiney et al., 2008, Canada700 | To examine the impact of a practice model for NPs in long-term care homes on staff confidence, hospital admission and early discharge | Descriptive/cross-sectional survey | 21 staff members, 2135 clinical NP contacts over 12 months | Three NPs and 18 directors of care | Integration of NPs into long-term care homes | Nurse practitioner clinical activities over a 1-year period: number of referrals, contacts, contact location, referral source and person. Promotion and impact of early hospital discharge (back to long term care). Impact on staff confidence | The majority of contacts were for uncomplicated medical problems or more complex but straightforward medical issues, and had positive outcomes. NPs judged that their intervention prevented hospital admission in 43% of cases. NPs had a positive impact on improving staff confidence, but did not promote early discharge from hospital | Yes |
| Meade et al., 2016, Australia708 | To describe and examine the effect on service provision and GPs of a new nurse-led model of team care for rural aged care facilities in a rural general practice | Mixed-methods case study | Six staff from one general practice |
Four GPs, one practice nurse and one practice manager Analysis of claims data on RACF service provision in 2005–6 and 2009–10 |
A new team model of nurse-led primary care for residents. The GP practice nurse was the lead |
Number of standard and after-hours consultations, before and after implementing new model Payment claims for comprehensive medical assessments, medication reviews and GP contribution to care plans. Qualitative data on perceptions and experiences of the new model |
Residents in RACF access to GP consultations almost doubled, (from 6.69 to 14.09 per resident per year). After-hours consultations were reduced. The provision of quality improvement services increased. GPs reported decreases in workload and stress, and increase in professional satisfaction | Yes |
| Moxon et al., 2001, UK716 | (1) To determine if training will increase the ability of residential care home staff to recognise depression, and (2) to implement a care planning intervention to help residents to manage their depression | Before-and-after study; no comparison group | 22 care staff in two residential care homes | Care staff with no previous training in depression | Enhanced role for care staff in detecting depression | Detection of depression using Brief Assessment Scale and Judgements of Residential Health Status scale | Training for residential care staff by community mental health team (four x 3 hours), was associated with increased ability to detect depression over time. A care planning intervention was successfully implemented with eight residents | Yes |
| Nazir et al., 2013, USA403 | To study the impact of interdisciplinary interventions on resident health outcomes, and document features of successful interventions, in the nursing home setting | Systematic review | 27 studies | All RCTs of interdisciplinary interventions from 1990 to August 2011. Ten trials in the USA, four in Australia, three in the UK, three in Netherlands and the remainder in other countries | Shift to integrated working with health-care professionals. Provision of education for staff | Various resident clinical/functional outcomes, including reduction in antipsychotic use, falls, depression, pain, incontinence, restraint use, and increase in appropriate medication use and positive nutritional status | This review was concerned with interdisciplinary working. A change in staff role is implied by this, but is not explicit in all included studies. All interventions that included residents’ primary care providers and/or a pharmacist had positive outcomes. In trials that used formal team-based care, communication, co-ordination and leadership were consistent features of successful interventions | Yes, n = 18 studies. Without benefit, n = 7 studies; no, n = 2 studies |
| Ryden et al., 2000, USA749 | To determine the effect on clinical outcomes when APNs worked with care home staff | Quasi-experimental (controlled pre and post) | 319 residents in three nursing homes | Newly admitted residents | Introduction of APNs into care homes | Four clinical outcomes: incontinence (Modification of Incontinence Monitoring Schedule), pressure ulcers (Braden Scale for Pressure Sore Risk; Staging of Pressure Ulcers), depression (Geriatric Depression Scale, Philadelphia Geriatric Center Morale Scale, Apparent Emotion Scale), and aggressive behaviour (Ryden Aggression Scale), plus the MMSE |
Residents with APN input experienced significantly greater improvement or less decline in incontinence, pressure ulcers and aggressive behaviour, and they had higher mean composite trajectory scores compared with residents receiving usual care Residents in the treatment group experienced significantly less deterioration in mood |
Yes |
| Stolee et al., 2006, Canada771 | To identify factors that facilitate or impede implementation of the NP role in three long-term care facilities | Mixed methods | 110 staff | 109 long-term care facility staff and 1 NP | Assignment of NP to three long-term care facilities |
Views of long-term care staff on the impact of the NP on various practice activities, including preadmission assessments, timely access to care, availability of geriatric assessment, continuity of care, comprehensive documentation, effectiveness and satisfaction with the NP role The NP’s views of their involvement in the long term care |
The NP was introduced to conduct pre-admission assessments and medication reviews, but high caseload and rapid admissions meant this was not achieved. Staff perceived the NP to be greatest benefit in wound management, and appreciation of the NP increased, with greater contact | Yes |
| Wild et al., 2010, UK787 | To provide an in-depth evaluation of approaches to enhancing care in residential homes (through education and training for staff to take on extended care or new roles) | Qualitative/multimethod | 141 staff in three residential care homes | Staff with NVQs. RNs from two homes, number not stated | Staff trained for extended care and/or new roles | Bespoke questionnaires, interviews, focus groups, documentary analysis | The three participating care homes adopted different approaches:
|
Yes |
| Yeatts and Seward, 2000, USA793 | To define and provide the rationale for SMWTs and examine factors influencing performance | Qualitative (observation, interviews) | 31 staff in one care home | CNAs, RNs, supervisors, managers | Autonomous working teams in nursing homes | Staff turnover, job satisfaction | Higher job satisfaction for SMWTs. The facility employing SMWTs had a lower staff turnover than average | Yes |
In the following section, the mapped literature that was pertinent to new care home staff roles or new ways of working is described.
Working together in care homes
The need for different health and social care disciplines to work together was a common theme in the literature on new ways of working in care homes. Nazir and colleagues403 conducted a systematic review of RCTs of interdisciplinary interventions in care homes, and examined their impact on resident outcomes. A change in staff roles is implied, but this was not always explicit in the included studies. In formal team-based care, communication, co-ordination and leadership were consistent features of success. Involving the residents’ primary care provider was also associated with positive outcomes.
A systematic review and individual studies in this mapping review also described complex models of care, with implied changes in working practice for care home staff. For example, introducing person-centred care would require the adoption of new or different ways of working by many staff. The review by Brownie and Nancarrow418 investigated the impact of person-centred care in care homes, but drew limited conclusions because of the quality of the included studies. In a study in the Netherlands,526 care described as integrated was introduced into two nursing homes. The provision of a home-like environment, care in line with resident demands and co-ordination of care produced positive outcomes for staff and for residents with physical disabilities.
Teams in care homes
The formation of teams to deliver care is a common approach in long-term care. However, in this set of studies, some potentially novel initiatives were described. Chapman and colleagues560 described a multidisciplinary advanced illness care team that drew in external professionals to work in a team with existing care home staff. In a RCT with 118 residents, this approach was successful in reducing pain and agitation among residents with dementia. Staff from residential facilities often have limited involvement in case conferences dominated by health-care providers. In an Australian study,602 residential care staff were given a leading role in multidisciplinary case conferences. An analysis of 31 case conferences suggested that staff found this greater involvement beneficial for learning more about their residents’ health and care, but finding the time to prepare for the case conferences was a challenge. 602 In 2000, Yeatts and Seward793 gave a qualitative account of the development of a self-managed team within a US care home, where a group of staff worked with a high level of autonomy, organising their own schedules and making decisions. This was the only publication identified on this topic, which suggests that it may not have been widely adopted.
In nursing, different approaches to team working have been in place for a number of decades. A Cochrane review621 compared established primary and team nursing models. Primary nursing describes the situation where nurses are consistently allocated to care for the same resident, providing continuity and enhanced understanding of each resident’s needs. Team nursing is a model in which staff are rotated and responsibilities shared. Two additional studies in this mapping review also addressed this question. Hodgkinson’s 2012 review621 (discussed in the systematic evidence synthesis shortly) reported some evidence for improved resident outcomes with primary nursing. In the two additional studies from different countries, primary nursing was also perceived to be more rewarding for staff, but also more challenging. 534,672
Enhanced roles for care home staff
Studies that described novel roles for care home staff fell into two categories. In the first, the staff took on tasks or responsibilities that would not normally be allocated to someone in their discipline. For example, in a novel UK study,787 care home staff were trained to take on tasks that are generally the responsibility of RNs. This was a genuinely new role for staff without nursing training, which appeared to offer potential benefits to residents, staff and care home organisations. Other studies described an enhanced role for staff in tasks that are already part of the daily routine in a care home. In one study, staff were given training in helping residents at meal times, which led to the adoption of a more standardised approach to support eating and an increase in residents’ calorie intake. 623 Similar programmes have been described to enhance staff roles in oral hygiene and emotion-orientated care (reminiscence). 521,591 Some initiatives formalised an aspect of care that is likely to be happening already but on an ad hoc basis. An example of this is provided by Moxon and colleagues,716 who described a training programme to extend the role of care staff to detect depression and implement appropriate care planning.
Low and colleagues804 conducted a systematic review of interventions to change staff practice to improve resident outcomes. The interventions included training, audit and feedback, monitoring, champions, team meetings and new procedures. These are likely to have encompassed both new and enhanced roles for staff, although not described in these terms. Interventions that were compliant with intervention theory and those directed at specific care tasks were more likely to be associated with improved resident outcomes.
Specialist nurses in new roles in care homes
Specialist nurses have been introduced into care homes in a number of countries. Their remit has included a focus on newly admitted residents749,771 and acceptance of referrals for specialist advice. 700 Generally, they worked with care home staff to provide clinical input and pass on their knowledge and expertise. There is also one report included of a nurse from a single general practice who was tasked with leading on care home resident care, which appeared to reduce some of the perceived burden on doctors. 708 The long-term implications of this model for staff relationships and resident outcomes are unknown.
Summary
This mapping of literature relevant to the care home workforce, published since the year 2000, has identified an extensive body of work. It is dominated by work from the USA and of cross-sectional design. Identifying literature on new ways of working is challenging, as novelty is context specific. In general, initiatives that promote joint working within and beyond the care home appear to be associated with enhanced outcomes for residents. Promising interventions include multidisciplinary teams, primary nursing and a focus on specific care tasks. Only one study from the UK787 described personnel taking on traditional nursing tasks without the qualifications, but this was perceived to show promise.
Findings of systematic evidence synthesis
What are the effects of care home staffing levels on staff and resident outcomes?
For methods, see Chapter 3.
Figure 4 shows the flow of studies through the mapping and review process. The literature searches identified 5741 abstracts, with an additional 35 identified from grey literature sources. After deduplication, 5383 were screened for eligibility and 340 were included in the mapping. Of those, 13 were deemed eligible for inclusion in the systematic review.
FIGURE 4.
Workforce PRISMA flow diagram.
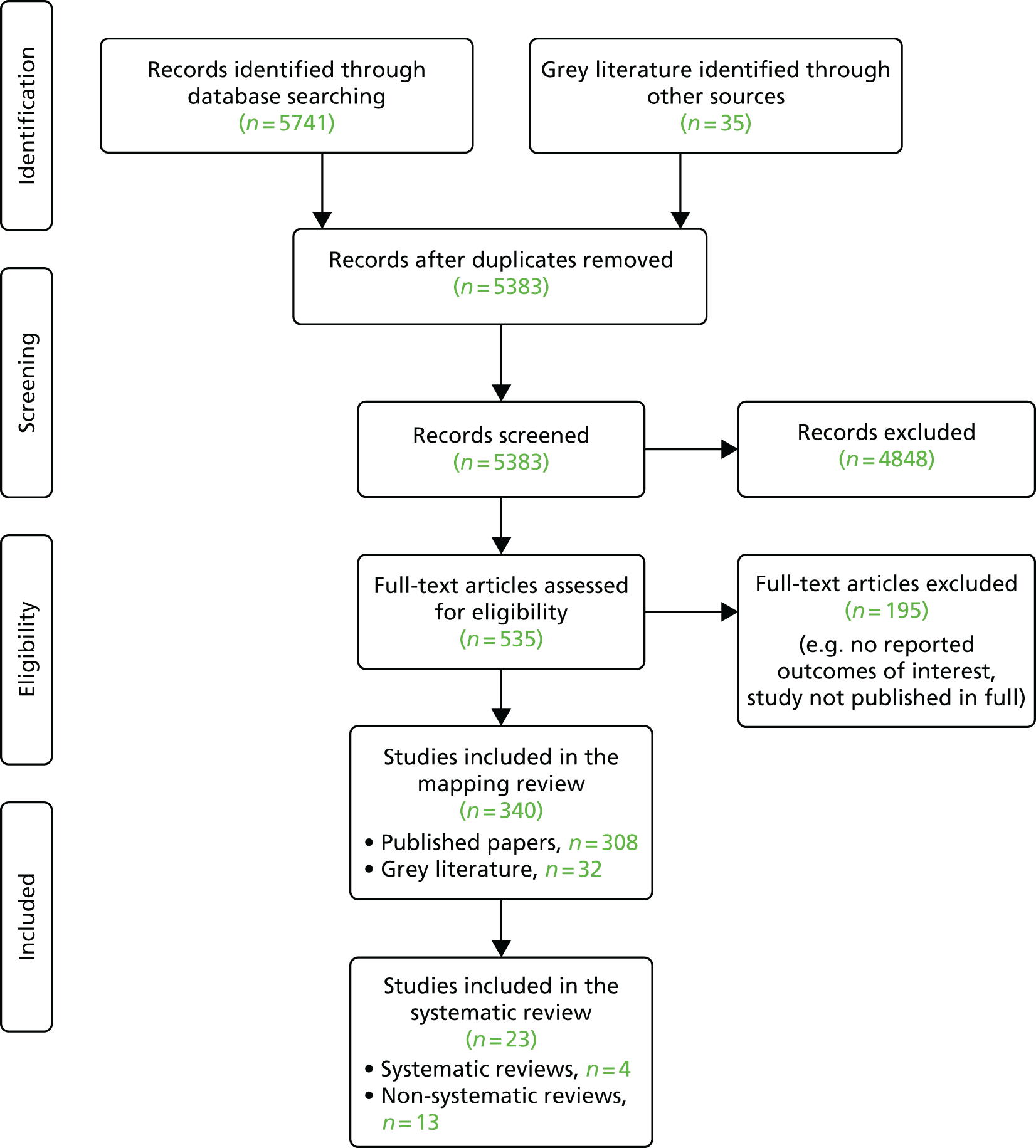
Study populations
Study populations were reported as the number of residents or the number of wards/units in nursing homes/facilities, or a standardised measure of person-year observations. When the number of residents was reported, this ranged from 380794 to 365,895. 585
Nurse staffing measures
The main measures of staffing in this review are (1) numbers of staff in different grades/roles of nurse staffing [i.e. RN, licensed practical nurse (LPN), CNA/NA], (2) the ratio of staff members to residents, (3) employment of agency staff and (4) imposition of staffing standards.
Data sources from the USA
A small number of key sources provided many of the US data. In the USA, certified providers of long-term care are required to submit a MDS based on a standardised assessment system. To receive funding from Medicaid and Medicare a provider must meet certain quality conditions. Annual inspections are carried out by state surveyors, and any shortfall in care quality is noted as a ‘deficiency’ in a range of domains, including food sanitation, accident environment, unnecessary medications and dignity. Staffing is one of the assessed quality domains that may result in a deficiency.
Nursing Home Compare is a national online nursing home report card that provides information on Medicare- and Medicaid-certified nursing homes in each US state. It provides information by provider and facility on (1) the results of state inspections from a database containing survey information [Online Survey, Certification and Reporting (OSCAR)], (2) the results of fire and safety inspections and (3) the history of penalties or complaints over the last 3 years.
Nineteen quality measures are used for public reporting on long-term care facilities in the USA. They are generated out of the MDS and highlight issues of clinical importance, such as pain, pressure ulcers, changes in ADL and use of long-term urinary catheters. Each nursing home also receives a rating on a scale of one to five stars based on health inspection results, quality measures and staffing levels.
Results of evidence synthesis
Thirteen reviews of the literature published since the year 2000 were identified as potentially relevant to this review. They are listed in Tables 15 and 16. Nine reviews explored the relationship between staffing and quality of care (broadly defined); four reviews208,692,763,790 considered resident quality of life as an outcome. One review584 considered staffing among a number of influences on emergency transfers to hospital for care home residents.
| Authors, year of publication | Date of searches | Question or aim | QoL | QoC | Study designs and numbers | Finding | Comment |
|---|---|---|---|---|---|---|---|
| Castle, 2008549 | 2006 | To review the evidence on staffing levels and quality in nursing homes | Y | Cross-sectional and longitudinal studies (n = 59) | Higher staffing levels appear to be associated with better quality indicators. The methodological limitations of research in this area are emphasised | ||
| Collier and Harrington, 2008570 | 2007 | To synthesise the literature on staffing levels, turnover and QoC in nursing homes (literature from 2002 to 2007) | Y | Expert opinion, reports, published studies, qualitative and quantitative (n = 71) | The author concludes that RN staffing levels should be increased and action taken to reduce turnover to enhance quality | ||
| Dellefield, 2000577 | Not stated | To review literature that has addressed the relationship between traditional nurse staffing in nursing homes and various types of quality indicator | Y | Not stated | Higher total staffing levels are associated with some quality indicators. The relationship between staff skill mix and outcomes are unclear, making conclusions about staff skill mix premature | ||
| Maas et al., 2008692 | Not stated | To summarise research on the relationship between staffing levels and QoC and QoL of care home residents | Y | Y | Not stated | The author concludes that RN staffing is related to quality and minimum staffing standards are needed | |
| Masterson, 2004696 | Not stated | Review of some of the literature that care home managers and commissioners might find useful in planning staff skill mix of services | Y | Not stated | The relationship between staffing and outcomes is complex. Attention is required to the attitudes, values and training of staff. High levels of educated and senior RN involvement are needed | Overview, informed by literature | |
| Mattingly, 2015698 | Not stated | Not stated. Review of staffing and appropriate antipsychotic use in care homes | Y | Not stated (n = 11) | Inverse relationship between staffing levels and antipsychotic use; no link between staffing hours and antipsychotic use | Clinician overview; no methods presented | |
| My Home Life, 2007208 | 2005 | To adopt an appreciative inquiry approach to synthesising the literature on experiences of residents, family caregivers and staff to identify strategies to enhance the QoL of residents and support caregivers | Y | Y | A broad range of study designs was included | This is a broad-ranging review, with multiple narrative findings across a range of domains | |
| Shin and Bae, 2012763 | 2011 | To produce an integrated literature review of the relationship between staffing and QoL and QoL outcomes in US nursing homes | Y | Y | Cross-sectional or longitudinal (n = 17), experimental/quasi-experimental (n = 4), not stated (n = 7) | Higher staffing levels are associated with better outcomes, but the methodological quality of the evidence is low | |
| Spilsbury et al., 2011499 | February 2008 | To review the evidence for the relationship between nursing home nurse staffing (proportion of RNs and support workers) and how this affects QoC for nursing home residents, and to explore methodological lessons for future international studies | Y | Cohort and cross-sectional studies (n = 50) | There is tentative evidence that total nurse, RN and NA numbers have a positive influence on resident care. The existing evidence base has multiple limitations | Systematic mapping review |
| Authors, year of publication | Date of searches | Question or aim | QoL | QoC | Study designs and numbers | Finding | Quality assessment |
|---|---|---|---|---|---|---|---|
| Backhaus et al., 2014516 | April 2013 | To summarise the findings from longitudinal studies on the relationship between nurse staffing and QoC in nursing homes | Y | Longitudinal studies (n = 20 studies) | No consistent evidence was found for a positive relationship between staffing and QoC. Major methodological and theoretical weaknesses limit interpretation of results | High quality (++) | |
| Dwyer et al., 2015584 | August 2014 | To synthesise evidence on clinical and organisational determinants of emergency transfer to hospital for acute illness or injury among frail, elderly people living in residential aged care facilities | Y | Observational studies (n = 78) | Facilities with poorer staff-to-patient ratios have higher transfer rates than those with higher RN and medical practitioner staffing | Acceptable (+) | |
| Hodgkinson et al., 2011621 | August 2007 | To identify which staffing models are associated with the best patient and staff outcomes in long-term aged care | Y | Interrupted time series (n = 1); controlled before-and-after study (n = 1) | A primary care model of nursing produces slightly better resident outcomes than the comparator (team nursing or usual care). Overall little firm evidence | High quality (++) | |
| Xu et al., 2013790 | March 2012 | To synthesise evidence on the association between nursing home ownership, affiliation, location, chain membership, percentage of private rooms, facility size, staffing and residents’ QoL | Y | Cross-sectional studies (n = 10); longitudinal, quasi-experimental (n = 1) | Studies rated as having low or medium risk of bias found that RN, LPN/LVN and total nursing staff had no significant relationship with QoL | High quality (++) |
Four of these516,584,621,790 reviews used systematic methods, and met the criteria for inclusion for our review. To decide if a review could be considered as a systematic review, criteria used by the University of York Centre for Reviews and Dissemination DARE (www.crd.york.ac.uk/CRDWeb/) were used:
-
Were inclusion/exclusion criteria reported?
-
Was the search adequate?
-
Were the included studies synthesised?
-
Was the quality of the included studies assessed?
-
Are sufficient details about the individual included studies presented?
To be included, reviews had to meet at least four out of the five criteria.
Quality assessment
The methodological quality of each study was assessed using the ROBINS-I tool. This tool provides a detailed framework for assessing and judging the of risk of bias that may arise from confounding, selection of participants into the study, measurement of interventions, departures from intended interventions, missing data, measurement of outcomes and selection of reported results.
Based on a review of the literature concerning confounders, age, ethnicity or race, physical activity and education were identified as critical confounders that required suitable adjustment for study results to be rated as having a low risk of bias.
Each domain is determined to exhibit low, moderate, serious or critical risk of bias. Low risk indicates that the study is comparable with a well-performed randomised trial in the domain being evaluated. Moderate risk indicates that the study is sound for a non-randomised study but not comparable with a rigorous randomised trial. Serious risk indicates that the presence of important problems, whereas critical risk of bias indicates that the study is too problematic to provide any useful evidence on the effects of intervention. If insufficient information is provided to determine the risk of bias of a certain domain, the domain is marked as having no information.
It is worth noting that the domains for classification of interventions and deviations from interventions were omitted as they did not apply to this review. All of the studies were cross-sectional (secondary data from surveys), and, therefore, no interventions were administered. The ROBINS-I tool is equally appropriate for cross-sectional studies as quality assessments are independent of study design.
Table 16 lists the systematic reviews that were included in our review.
Summary of previous systematic reviews
Evidence from reviews
Four relevant systematic reviews were identified, three of high quality516,621,722 and one that was assessed as of acceptable quality584 (see Table 16). A systematic scoping review499 has also been included in this synthesis. Spilsbury and colleagues’ review499 was not classified as systematic because it contained no explicit assessment of the quality of individual studies. However, study quality and its implications are discussed at length, and (with the exception of quality assessment) systematic review methods were adopted. In addition, this work formed the starting point for one of our included reviews, which searched for literature published after Spilsbury and colleagues’ review.
Two reviews restricted their work by study design. Hodgkinson’s Cochrane review621 was limited to quasi-experimental studies and Backhaus and colleagues restricted their review,516 published in 2013, to longitudinal studies. The remaining reviews included observational studies.
Risk of bias in individual studies
Of the 18 observational studies included, eight were rated as being at serious risk of bias, two were rated as being at critical risk and eight were rated as being at moderate risk. Whereas those at serious and critical risk of bias do not offer robust evidence, those with a moderate rating offer some evidence to support interventions; although they cannot be considered as robust as evidence derived from a good-quality RCT. Full details of the validity assessment are presented in the Appendix 3, Table 21. The quality of reporting was variable between studies and across the criteria. The majority of the studies had moderate issues with missing data and selection of the reported results, two important areas of bias. However, those rated as being at serious or critical risk of bias generally also had issues of bias in terms of confounding. Issues with bias across several of the domains greatly reduces the reliability of the findings. The quality of the studies for each of the individual interventions is summarised alongside the results (Table 17).
| Authors, year of publication, country | Study design | Sample size | Data sources | Outcomes and measures | Overall risk of bias | Results |
|---|---|---|---|---|---|---|
| Abrahamson et al., 2013,502 USA | Secondary data analysis of cross-sectional survey data | n = 14,381 (13,983 residents) | The 2007 Minnesota Nursing Home Resident Quality of Life and Consumer Satisfaction Survey | Influence of nursing facility characteristics (staffing levels) on resident quality of life using the Minnesota Nursing Home Resident Quality of Life and Consumer Satisfaction Survey | Serious | Activity and certified nursing aide staff significantly associated with higher QoL (p < 0.001; p = 0.012); no statistically significant association between RN and LPN staff hours per resident day and QoL (p > 0.05) |
| Alexander, 2008,505 USA | Cross-sectional study: retrospective | n = 510 nursing homes |
Nursing home Compare site in February 2004 database |
Eleven long-stay quality measures; five short-stay quality measures | Serious | Significant differences in outcomes associated with CNA/LPN/RN staffing-level mix, with two measures (loss of bowel and bladder control, and assistance with ADL) and two short-stay measures (moderate to severe pain and presence of pressure ulcers) |
| Backhaus et al., 2015;515 Backhaus et al., 2017,805 the Netherlands | Cross-sectional study | N = 282 wards [n = 117 somatic wards (n = 2604 residents); n = 165 psychogeriatric wards (n = 3541 residents)] and N = 6145 residents | Questionnaire data on 95 Dutch long-term care facilities | Relationship between staffing levels and clinical, process-related and administrative outcomes | No consistent relationship was found between nurse staffing and QoC; higher staffing levels were associated with better as well as lower QoC indicators | |
| Bowblis, 2011,527 USA | Cohort study (panel data) | n = 94,371 survey observations | The OSCAR surveys from 1999 to 2004 merged with Minimum Direct Care Staffing requirements | Outcome quality measures in the following: pressure ulcers; facility-acquired pressure ulcers; incontinent (bladder); incontinent (bowel); significant weight change; rash; and total number of deficiencies | Moderate | Higher MDCS requirements increase the total number of staff in a nursing home. Skill mix moved slightly towards using more CNAs, whereas among licensed staff, LPNs are substituted for RNs |
| Carrier et al., 2009,537 Canada | Cross-sectional study | 395 residents in 38 public nursing homes | Interviews with cognitively intact residents; primary institutional caregivers completed a questionnaire for cognitively impaired residents | Resident quality of life measures using the Quality of Life in Dementia instrument; and measures of activity and positive and negative affect | Moderate | Ratio of residents per RA significantly associated with Quality of Life in Dementia in cognitively intact (β = 0.458; p = 0.016) and cognitively impaired residents (β = 0.454; p = 0.023) |
| Castle and Engberg, 2008,545 USA | Secondary analysis of cross-sectional survey data | n = 6005 nursing homes | Survey of nursing home administrators conducted March–June 2005 and January–March 2006; 2004 Nursing Home Compare; 2005 OSCAR; and 2006 Area Resource File | Eleven long-stay quality measures; three quality measures for short-stay residents | Serious | Dependent variables (Nursing Home Compare). Variables not statistically significantly different (p > 0.05) from national averages reported in Nursing Home Compare for 2004 |
| Castle et al., 2008,546 USA | Secondary analysis of survey data | n = 2946 surveys returned in 2005 | National Nursing Home Staffing Study; OSCAR database; Nursing Home Compare web-based report card; and Area Resource File data | Eleven long-stay quality measures; three quality measures for short-stay residents are percentage of residents | Moderate | Use of nurse aide agency staff of < 14 full-time equivalents per 100 beds has little influence on quality; nurse aide agency staff of > 25 full-time equivalents per 100 beds has a substantial influence on quality |
| Chen and Grabowski, 2015,561 USA | Secondary analysis of panel survey data | n = 45,738 nursing home-year observations | The OSCAR database, with the state regulation data (Survey of the Nursing Home Staffing Standards, and a Department of Health and Human Services 2003 report) | Five facility-level quality measures to examine the effects of minimum nursing hours per resident day regulations on nursing home staffing levels and care quality (deficiencies, use of physical restraints, catheters, psychoactive medications and pressure ulcer incidence) | Moderate | The percentage of nursing homes with a severe deficiency decreased by 60%; high prevalence of psychoactive drug usage (50%) was present in nursing homes; nearly one-third of the residents had contractures; and about 7% of the residents had pressure ulcers |
| Gray-Siracusa, 2005,601 USA | Cross-sectional survey | n = 81,023 residents | Ohio nursing home data from Centers for Medicare and Medicaid Services OSCAR; MDS in 2000 |
Prevalence of range of no motion, the use of antipsychotics and pressure ulcers Outcomes in nutrition or physical functioning; adverse outcomes, including skin care, maintenance of catheters and prevention from infection or accidents; adverse outcomes with behavioural or emotional patterns and the use of antipsychotropic drugs |
Serious | As the RN staffing difference increased by 1.0 HPRD (less staffing) the prevalence of residents with weight loss decreased by 2.2%, with tube feedings increased by 3.2% and remaining bedfast increased by 1.9% |
| Havig et al., 2011,610 Norway | Cross-sectional study | n = 40 wards (one–four wards in 21 nursing homes) | Self-report questionnaires; interviews/questionnaires; telephone interviews; field observations | Satisfaction of care, social activities and social interactions appraised by staff, relatives and field workers using self-report questionnaires | Moderate | Non-significant associations in ratio of RNs to outcomes (p > 0.05); ratio of unlicensed staff showed a significant relationship with quality as assessed by relatives (p < 0.05) and field observations (p < 0.01), but not with quality as assessed by staff (p > 0.05) |
| Heeren et al., 2014,614 Belgium | Survey | n = 570 older adults, 23 wards within seven nursing homes from the Flemish Navigator Network | Data collected from 1 November to 31 December 2011 | Relationship between staffing levels and use of physical restraints | Critical | Compared with non-restrained residents, restrained residents were cared for by a caregiver with significantly fewer NAs and fewer LPNs and more RNs (p < 0.05) |
| Kajonius and Kazemi, 2016,639 Sweden | Cross-sectional survey | n = 95,000 elderly people | National survey, including a wide range of quality indicators for elderly care services, conducted in 2012 at the request of the Swedish National Board of Health and Welfare | Elderly persons’ perceived satisfaction with quality of care and nursing home staffing | Moderate | Non-significant association between nursing home staffing and satisfaction with care (0.09; p > 0.05) |
| Leland et al., 2012,683 USA | Cross-sectional survey | n = 230,730 individuals | MDS | Relationship between nursing home staffing levels and residents’ falls | Moderate | Nursing homes with more CNAs had lower rates of falls (adjusted odds ratio 0.97, 95% confidence interval 0.95 to 0.99; p < 0.05); RN and LPN hours per resident per day was not significant in predicting falls (p > 0.05) |
| Lerner, 2013,684 USA | Secondary data analysis of cross-sectional data | n = 225 nursing homes | Nursing Home Compare website | The association between nurse staffing levels, and skill mix and number and severity of nursing home deficiencies | Serious | Severity of deficiencies influenced by number of beds (b = 0.29) location of the home (b = –0.138) and NA hours per patient day (b = –0.206) |
| Lin, 2014,687 USA | Secondary data analysis of panel data | N = 3275 nursing homes | OSCAR (1999–2003); Area Resource File; Centres for Medicare & Medicaid Services; and most recent population census | Relationship between nursing home staffing levels and reported deficiencies using OSCAR | Moderate | Both RN and NA staffing have a non-significant impact on quality of care (p > 0.05); increasing RN staffing by 0.3 hours per resident day (one standard deviation in the data) would increase quality by > 16%, which is equivalent to lowering the number of deficiencies from the average of 7.4 to 6.2; NA staffing does not have a statistically significant impact on quality of care |
| Park and Stearns, 2009,730 USA | Secondary data analysis of panel data | n = 55,248 facility-year observations |
OSCAR (1998–2001); state minimum staffing standards from Harrington 2002806 and U.S. Department of Health and Human Services 2003;807 state Medicaid per-diem rates from Brown University Survey of State Policies and State Data Book on Long-Term Care Programme and Market Characteristics808 Market-level variables from the Area Resource File, a publicly available data set containing economic and demographic variables for each county (U.S. Department of Health and Human Services 2006) Population data from the US Census Bureau |
Impact of state minimum staffing standards on the level of staffing and quality of care (restraint use and deficiencies) | Serious | Minimum standards were associated with reductions in restraint use (p < 0.01) and the number of total deficiencies (p < 0.01) at all types of facilities except for-profit facilities |
| Zhang et al., 2008,799 USA | Cross-sectional study | n = 14,184 Medicare- and Medicaid-certified facilities | 2003 OSCAR data; Area Resource File data from 2000 from the Health Resources and Services Administration | Relationship between facility service environments and psychosocial care quality using 2003 OSCAR data | Critical | Qualified social service and mental health staffing is significantly negatively associated with psychosocial care deficiencies (p < 0.05); qualified social service staff (OR 0.132, 95% CI 0.050 to 0.349); mental health services staff (OR 0.024, 95% CI 0.001 to 0.571) |
| Zhang et al., 2013,797 USA | Secondary data analysis of panel survey data | n = not reported | OSCAR (1997–2009) | Relationship between nursing home nurse staffing and resident needs (medications, pressure ulcers, catheter use and ADL) based on data from OSCAR | Serious | Private-concentrated nursing homes: mismatch between changes in RN hours per resident day and the percentage of Medicare residents; Medicare-concentrated nursing homes: mismatch between changes in LPN hours per resident day and the number of medications per resident |
| Zúñiga et al., 2015,801 Zúñiga et al., 2014,802 Switzerland | Cross-sectional study |
n = 400 units In Zúñiga et al. 802 (2015), 4311 care workers from 402 units and 77 additional care team were not assigned to a specific unit (e.g. night shift team) |
Swiss Nursing Home Human Resources Project; survey administered between May 2012 and April 2013 | Relationship between nursing home staff turnover and long-term absence with quality of care (pressure ulcers, fall-related injuries and weight loss) using survey data | Serious | Work environment factors, work stressors and rationing of nursing care were significantly related to quality of care, whereas staffing level, staff mix and turnover were not |
With no RCTs included, there is a lack of high-quality, robust evidence; however, the eight observational studies rated as being at moderate risk of bias provide some support for the potential effectiveness of the workforce interventions.
Care home staffing and resident quality of life
Evidence of the association between staffing and resident quality of life is presented in the following section, separate from other resident outcomes. Quality of life and resident well-being are being highlighted here as they are important direct or indirect outcomes of care that have been relatively neglected in studies of care home staffing. 499
Evidence on staffing and quality of life, from previous reviews
Four reviews621,692,763,790 were identified that investigated the relationship between staffing and care home resident quality of life. Two met the quality threshold and were included in our study. Xu and colleagues790 synthesised data from US studies790 and found no clear evidence of an association between nurse staffing and quality of life. The four studies in Xu and colleagues’790 review were assessed as being at low or medium risk of bias, and found no relationship between RN, LPN/licensed vocational nurse (LVN), and total nurse staffing and residents’ quality of life. Other findings were inconsistent, with the majority suggesting either no association or a tendency for higher staffing levels to be beneficial for residents.
Hodgkinson621 conducted a Cochrane review to identify and assess the quality of all experimental research designed to evaluate the effectiveness of specific nursing models in improving resident quality of life and health outcomes. Two studies were included in their review, one interrupted time series and one controlled before-and-after study. Both studies compared a primary nursing model with either team-based nursing or usual care. (The primary care nursing model consisted of 24-hour accountability and decision-making by one nurse for several patients, direct communication between caregivers and a change in the head nurse’s role to more of a facilitator. By contrast, team nursing is a hierarchical system in which patient care is supervised by a RN, and the provision of care is assigned to personnel of different skill levels, according to the complexity of the patients’ needs.) The primary care model performed slightly better on some resident outcomes but had no impact on resident well-being. 621
Evidence from additional individual studies
Two additional studies502,537 were identified that were not part of the reviews discussed above. One was a more recent publication502 and the other was conducted in Canada. 537 Both were assessed as being at moderate risk of bias and would not have met the threshold for inclusion in Hodgkinson’s Cochrane review. 621 Both studies suggest that care assistants may be important to residents’ quality of life. An analysis502 of cross-sectional data from almost 14,000 participants of the Minnesota Nursing Home Residents Quality of Life and consumer satisfaction survey found no relationship between resident quality of life and the number of registered or licensed nurses and nursing administrators. However, CNA staff hours per resident day were associated with higher quality of life. These data are drawn from a probability sample of residents from all 388 nursing homes in the state. A much smaller Canadian study reported similar findings. A cross-sectional study537 with 395 residents of 38 Canadian nursing homes investigated the association between quality of life and staffing as part of a study of dining experiences and food services. The ratio of residents per resident assistant was positively associated with quality of life for both cognitively intact and cognitively impaired residents.
Summary: staffing and quality of life
A single high-quality systematic review of US literature and two additional cross-sectional studies all failed to identify any relationship between the numbers of RNs or LPNs/LVNs and quality of life. A review of a primary care nursing model also found no evidence of any impact on resident well-being. There is mixed evidence that the numbers or hours of care provided by staff without nursing qualifications may be an important influence on residents’ quality of life. However, it is important to acknowledge the limitations of the measures for both staffing and quality of life. This is discussed later.
Care home staffing and health-related resident outcomes
Two high-quality systematic reviews499,516 and one systematic scoping review621 have synthesised evidence on care home staffing and health-related outcomes.
Evidence from existing systematic reviews
Backhaus and colleagues516 conducted a systematic review of longitudinal studies that examined nurse staffing and quality of care outcomes in nursing homes. Their intention, in focusing on longitudinal studies, was to avoid the methodological weaknesses inherent in reviews of cross-sectional studies. Searches retrieved articles published between 2007 and 2013; older longitudinal studies were extracted from Spilsbury and colleagues’ review. 499 In total, 20 studies were included, one from Italy and the rest from the USA. The authors distinguished between clinical (e.g. pressure ulcers), process (e.g. restraints) and administrative (e.g. deficiencies) outcomes of care. Measures of staffing were carefully identified and documented, along with the source of outcome variables. This review found no consistent evidence of a relationship between staffing and quality of care. For pressure ulcers, there was a consensus across the studies that more staff of any grade were associated with better outcomes. For other outcomes, such as catheterisation, a greater number of staff could be associated with better or worse outcomes, depending on the study.
Evidence from additional individual studies
Seven studies that were not included in preceding reviews investigated the relationship between staffing numbers and resident outcomes. They were conducted in Norway, Sweden, Belgium, Switzerland and the USA. A majority of publications from the USA have analysed information from the nursing home MDSs, generating a body of work that uses common, mainly clinical, outcome measures. Elsewhere, researchers have collected data on outcomes, such as pressure ulcers, but greater attention has been paid to staff and resident perceptions of care outcomes.
In Norway, a cross-sectional study610 in 21 nursing homes investigated the association between staffing and relatives’ perceptions of a range of process measures of care quality. Interviews and questionnaire responses were obtained from 444 staff and 378 relatives, and supplemented with field observations. Care quality was assessed through scores for satisfaction and general ratings of care processes, including treating residents with dignity and taking the time to talk. Staffing levels and the ratio of RNs to the total number of care staff were not found to be statistically significantly related to any of the composite indices of care quality. However, the ratio of unlicensed staff to total care staff numbers was inversely related to quality as assessed by relatives and researchers’ field observations, but not to quality assessed by staff. This study focused on relative- and staff-perceived satisfaction with care, social activities and social interactions, and did not include any of the commonly reported clinical outcome measures. Similar findings emerged from Sweden,639 where a cross-sectional survey of 31,073 care home residents found no association between staffing and overall satisfaction with care. In this case, the staffing ratio was calculated as the number of trained staff relative to the total older population in each municipality.
A cross-sectional survey802 of a nationally representative sample of 163 Swiss nursing homes found no association between staffing, turnover or long-term absences and any measured quality indicators (pressure ulcers, falls and weight loss). When 4311 Swiss care workers were surveyed,801 care worker-perceived quality of care was also unrelated to staffing level, although an association was noted with work environment, work stressors and the implicit rationing of nursing care. In Belgium, a survey614 of seven nursing homes (570 residents) in a Flemish network found no associations between staffing intensity and the use of restraints. Restrained residents were cared for by a team with fewer LPNs and NAs.
In the USA, OSCAR data have been used extensively in analyses of care home staffing. A comparison of trends in nursing home nurse staffing and resident nursing care needs between 1997 and 2009 revealed a complex picture. 797 Taking the data from all US care homes, the number of RNs decreased slightly, whereas the number of LPNs and NAs rose, suggesting that some substitution took place. Medications, pressure ulcers, catheter use and ADL were used as proxies for nursing needs. Levels and trends in measures of staffing and resident needs all varied depending on the proportion of Medicare, Medicaid or private residents in the homes. The authors concluded that there is a mismatch between the trends in staffing and pressure ulcers, catheters, ADLs and medications, with staffing failing to keep up with needs. In the cross-sectional analysis of OSCAR data discussed earlier,799 the same research group investigated the relationship between nursing home service environments, which included staffing levels, and care deficiencies. Qualified social service and mental health staffing was inversely related to the recording of psychosocial care deficiencies. The greater the number of qualified social services and mental health services staff, the higher the likelihood of good-quality psychosocial care.
Summary: staffing numbers or ratios, and resident outcomes
Outside the USA, staffing numbers or staffing resident ratios appear to have no association with resident and staff perceptions of care quality or clinical outcome measures. US data suggest that there may be a positive relationship between numbers of some staff groups and resident outcomes. However, interpreting analyses of the US MDS is complicated by the influence of funding sources and the use of regulatory judgements (deficiencies) as proxies for resident outcomes.
Staff skill mix and resident outcomes
Many of the studies in the preceding section investigated the relationship between numbers of nurses within different groups (e.g. RNs, licensed nurses, NAs) and resident outcomes. This section collates studies that had a specific focus on the comparative impact of nurses with different levels of training. One study is from the Netherlands805 and five are from the USA505,601,683,684,687, all of which make use of the US MDS. Three out of the five US studies make use of reported care home deficiencies as a proxy for resident outcomes.
Evidence from the Netherlands suggests that employment of nurses with higher academic qualifications may be associated with better resident outcomes in certain situations. A cross-sectional study in Dutch care homes analysed data on 6145 residents from the 2016 LPZ (Landelijke Prevalentiemeting Zorgkwaliteit or the International Prevalence Measurement of Care Problems in Care Homes). 805 The authors looked at the relationship between the employment of baccalaureate-educated RNs and a range of resident outcome measures across 282 wards in 95 care homes. They found no consistent association between the employment of baccalaureate-educated RNs and resident outcomes. On wards that looked after residents with physical disabilities, the presence of baccalaureate-educated RNs was linked to reduced numbers of medication incidents, adjusting for background characteristics. Residents in wards that provided psychogeriatric care were slightly more likely to fall and receive antipsychotic medication and less likely to have an indwelling catheter when baccalaureate-educated RNs were employed. The probability of developing pressure ulcers was not associated with the employment of baccalaureate-educated RNs in either setting. 515,805
Five studies analysed information from the US MDSs on staff mix and resident outcomes. Data on the 230,730 people admitted to US nursing homes in 2006 were analysed in a cross-sectional study. 683 Nursing homes with higher NA staffing were noted to have lower rates of falls, but RN and LPN hours per resident per day were not predictive of falls. Routine data from 225 Maryland nursing homes684 found that the NA hours per day influenced the number of deficiencies reported, while RN hours were associated with the severity of the deficiencies. In another study with OSCAR data (from 1999 to 2004), Lin and colleagues687 reported that both RN and NA staffing had a small but non-statistically significant impact on quality of care, measured by reported deficiencies. Using an instrumental variables approach, they estimated that increasing RN staffing by 0.3 hours per resident day (one standard deviation in the data) would increase quality by more than 16%.
A smaller study on 510 Missouri nursing homes505 (data from 2004) explored the relationship between staffing level mix and quality indicators in a cross-sectional study. Positive associations between staffing level mix and quality measures were reported. Two measures (the percentage of residents who become incontinent and the percentage who need help with ADL) appeared to be sensitive to change in staffing level mix. 505
In most of the included studies in this review, staffing levels were measured without any reference to resident needs or acuity. Gray-Siracusa601 used an established classification to calculate staffing levels based on resident case mix, and compared them with reported staffing levels. Shortfalls between reported and required staffing adversely influenced some measures of care quality (use of antipsychotic medications, pressure ulcers) and the number of reported deficiencies recorded by the US nursing home certification authorities. This doctoral thesis was based on data from Ohio nursing homes, available from OSCAR and MDS.
Summary: staff skill mix and resident outcomes
It is difficult to extract a clear message from research on the relationship between skill or role mix and resident outcomes. The data suggest that there may be a relationship between the number of different staff available in a care home and resident outcomes. NAs and RNs both appear to influence different aspects of care. A focus on numbers of staff, and not on the role and tasks performed, limits the value of this body of work.
Minimum staffing requirements and resident outcomes
Four studies from the USA examined the relationship between regulations on minimum staffing levels and resident outcomes. All were observational studies that analysed the same data set (OSCAR) from similar time periods, and shared some common outcome measures. They differed in the geographical level under scrutiny. The four studies were rated as being at high risk of bias. The most recent study527 examined the impact of minimum direct care staffing (MDCS) requirements on care quality outcomes (antipsychotic and psychotropic medications, use of restraints and catheters, pressure ulcer incidence) as part of a study into the impact of MDCS on nurse staffing levels and nurse skill mix. Using national data (94,371 observations) from the OSCAR surveys (1999–2004), the authors found that minimum requirements were associated with improved patient outcomes. They noted that organisations’ responses to MDCS differed depending how reliant they were on Medicaid. A similar study730 using data from 1998 to 2001 examined the impact of introducing or increasing minimum standards for staffing in nursing homes within 16 US states. Regulations varied from state to state but included numbers of total, registered and licensed staff, staff ratios and care standards. Restraint use and the total number of deficiencies fell. The imposition of minimum standards had the greatest impact on the not-for-profit homes that were at, or below, the imposed level. Facilities with higher staffing levels to start with were relatively unaffected. 730 A similar picture emerged from analyses of 45,738 observations from Californian and Ohio OSCAR data between 1996 and 2006. Increasing minimum staffing standards was associated with a decrease in the total number of deficiencies and a reduction in the rate of contractures, but no changes in any of the other four measures (use of physical restraints, catheters, psychoactive medications and pressure ulcer incidence). 561 In a related analysis of cross-sectional OSCAR data from 2003, Zhang and colleagues799 found higher levels of reported care home deficiencies when requirements for qualified social services staffing exceeded minimum federal regulations. 799
Summary: minimum staffing requirements and resident outcomes
Observational studies of routine US data suggest that the imposition of minimum standards for staffing in care homes has a positive impact on some resident outcomes. This is of uncertain relevance to other countries.
Discussion
Summary of findings
This systematic, rapid evidence synthesis examined the relationship between care home staffing and resident outcomes. It serves to update and extend previous reviews, the majority of which have focused on quality of care. No strong evidence was identified of a relationship between the numbers of staff, staff-to-resident ratios, staff skill mix or nursing care models and any resident outcomes. There is limited evidence to suggest that the number of staff without nursing qualifications may influence residents’ quality of life. There is a paucity of research on resident outcomes from outside the USA. Studies that consider the duties and activities of different groups of staff may be more useful in defining a care home workforce that will promote health and well-being of residents. It is noteworthy that the extensive published literature on care home staffing and resident outcomes is predominantly from the USA and concerned with quality of care, defined in many different ways.
Previous reviews have identified and discussed at length the methodological limitations that are common in works on care home staffing. 499,516,692,790 Extensive use has been made of cross-sectional studies that are liable to a range of biases. Systematic reviews that have attempted to overcome this problem by focusing on longitudinal or experimental work have also reported negative findings. 516,621 This may point to a true absence of any association between staffing and outcomes, but it could also be secondary to other study limitations. Measuring resident outcomes is dominated in this work by the US MDSs. Much of the information is collected to monitor quality of care in nursing homes and determine payments. Such measures provide uncertain proxies for resident outcomes, and are unlikely to reflect resident and family priorities. Deficiencies, for example, are a measure of how well a care home meets various process and outcome measures in their annual state inspection. This variable has been used extensively in research, but it is clear that some (e.g. prescribing) may be a better measure of the outcomes of resident care than others (e.g. administration). In many instances, components of MDS information analysed in US studies have been collected at different points in time. This is problematic when measuring staffing levels, which may vary appropriately over time and with the changing needs of residents. The dearth of longitudinal studies limits our understanding of the direction of the relationship between staffing and outcomes.
Strengths and limitations
In our systematic review, we made best use of previous, high-quality evidence syntheses to avoid duplication of effort. When we looked at material that postdated the reviews, we attempted to fill in the gaps between the previous work. Spilsbury and colleagues’ review499 was wide ranging, but those that followed were limited by study design516 or outcome measures. 790 We did not impose strict study design inclusion criteria and, as a result, have included some studies that would not have met the criteria for the previous systematic reviews. Although this has drawbacks, it served to generate a comprehensive overview of the current state of the evidence base.
The topic of new or flexible ways of working was a challenging one for a review. The subject did not lend itself to focused database searches and we were obliged to conduct a very broad mapping review. If the cataloguing and keywords did not alert us to relevant content, we were reliant on the title and abstract screening. With a large review completed in a short time, it is impossible to eliminate errors, and it is almost inevitable that we will have overlooked some relevant material. In addition, publication bias is a particular concern in this area. Roles that are perceived to be novel in one setting may be well established in another, and not worthy of publication. Similarly, facilities that trial new initiatives may seek to publish only their success stories, or find that journals have little interest in certain aspects of their work, such as flexible working.
Gaps in research knowledge
There is a paucity of UK-specific research on the care home workforce. A majority of the included studies were from the USA, where both health and long-term care are distinct from the UK context.
The majority of research in this field is observational. Studies of this type cannot answer questions about the personal qualities, values, skills and experience needed to provide care in care homes. The US data sets have generated an extensive body of observational studies, and encouraged a focus on numbers of staff and a narrow range of resident and staff outcomes.
Future research needs to appreciate the complexity of care delivery, with measurement of outcomes that are important to residents, and more nuanced insights into the nature of care delivered. This suggests a move away from numbers of staff and greater focus on resident experiences and staff roles and tasks.
Implications
There is an extensive literature on care home staffing, and it has been extensively reviewed. However, it provides few insights for UK providers and commissioners of care, as the majority originates from the USA, and analyses data sets specific to their setting. Multiple reviews have failed to identify a robust evidence base to link staffing levels to resident outcomes. In the future, a greater focus on the fate of staff may, however, be useful, and provide insights into how to promote recruitment and retention.
Studies of staff taking on new roles or working flexibly were difficult to identify, and our mapping is unlikely to be comprehensive. Research described staff taking on genuinely new tasks, and others that involved adoption an enhanced role in an established task. Joint working within and beyond the care home, multidisciplinary teams, primary nursing and a focus on specific care tasks all appear to have potential to enhance outcomes.
Chapter 5 Discussion
This report covers four distinct topic areas. A mapping review and systematic evidence synthesis have been presented for each, with individual discussions. In the following section, some of the strengths and weaknesses of our overall approach are discussed, followed by a brief consideration of the possible implications of the work for the NHS, and recommendations for research.
Strengths and weaknesses of our approach
Our focus on care homes as a distinct setting has allowed us to collate a disparate literature and produce findings that are relevant to resident care, irrespective of diagnosis. However, a high proportion of care home residents are living with dementia, and this report should be interpreted alongside the growing body of work on that subject. The four topic areas – technology, communication and engagement, workforce and evaluation – were identified by NHS England in their strategy documents. We worked with the care home vanguard teams to define questions for systematic evidence syntheses to ensure that our work would be of use. In three of the four areas, this produced a novel and potentially useful review. In the workforce review, the question of staffing levels and resident outcomes has been addressed many times, and a number of reviews were available. Our conclusions echo those of previous authors, but the need for both a different lens on workforce issues and more robust research methods is an important point to reiterate. In retrospect, the inclusion of staffing levels in the options considered by the stakeholders should have been accompanied by clear explanations of the limitations of any future review. Following the production of this report, further work is planned to examine the relationship between staffing levels and staff outcomes, as the impact on staff health, in particular, appears to be a relatively neglected area.
The mapping reviews did not examine outcomes in any detail, with the exception of the section on new ways of working. We did investigate the nature of the outcomes, and which group of stakeholders – residents, staff, families or organisations – were involved. This has generated a resource that should be useful to people looking for information on a particular topic, but it does not substitute for a robust systematic or scoping review. In the 12 months allocated to this project, it was not possible, or our intention, to go beyond this.
Similarly, resources did not allow us to update our database searches before submitting this report. In some cases, this means that the searches are 10 months old.
Our methodological approach had a standard hierarchy of evidence at its centre. Quality appraisal of studies was completed with a tool from The Cochrane Library. This choice is justified by the identification of a number of experimental studies, particularly in the section on technology. The challenges of conducting trials in long-term care may be an argument against judging the quality of research with a framework that would be appropriate in a hospital setting. However, this implies that a lower quality of evidence may be acceptable in care home research. The potential vulnerabilities and multiple conditions among residents suggest that robust evidence for the effectiveness of interventions is essential.
Public and patient involvement
This study benefited from input from the Newcastle University Care Home Interest Group. This is an open forum of people with an interest in care home research, drawn from the general public and social and health care professionals. Members were recruited under the auspices of Voice North, a Newcastle University-led organisation to promote involvement of the public in research. All have an interest in care homes, but a number of members are current or former social care workers. They include a former Care Quality Commission inspector, current and former care home managers, specialist nurses and many people who have cared for relatives who moved into care homes. The proposal and research questions were discussed with the wider group, and, after funding was secured, a subgroup volunteered to take a particular interest in this study. They have been involved in prioritising questions and interpreting results, and are having a major role in the development of dissemination materials.
Chapter 6 Conclusions
Implications for health care
Digital technology
Digital technology has multiple potential applications in care homes, and researchers have investigated a range of interventions using experimental study designs. However, a majority of studies are pilot or feasibility trials of insufficient size to detect clinically significant outcomes. Cost, ease of use and staff demands are frequently identified as both barriers to and facilitators of the implementation and use of technology. There is limited evidence that games that promote activity and robotic interventions may have some benefits for residents’ mental well-being. However, these interventions are more likely to have been evaluated, and it is not clear that they are superior to non-technological solutions. Digital records, monitoring technologies and telehealth may also have positive impacts, but the evidence base does not allow firm conclusions to be drawn.
Communication and engagement
The evidence base for communication interventions was weak. However, the use of standardised data collection forms appears to promote the transfer of vital information with residents who are referred to hospital. The studies reviewed provided no data on the impact of transfer forms on patient outcomes. Tools to structure communication, such as SBAR, have been evaluated outside the UK and appear to have the potential to enhance clinical outcomes for care home residents. Complex interventions to improve communication may also improve resident clinical outcomes, and reduce hospital transfers, but the evidence is limited. There was, as anticipated, a paucity of research into how care homes engage with their local communities.
Evaluation
There are many measurement tools that have been used in care homes and described in the English-language literature. Only six of the recently used tools had undergone any validation in a UK setting. This does not mean that other tools are not useful, but, if they are to be introduced into routine use, some work is needed to explore their measurement properties and to ensure that they are appropriate for this context. The two general measures of care outcomes that had undergone some validation for use in UK care homes have different origins. We found no data to enable us to recommend one over the other. None of the included tools scored highly in our assessment of methodological quality.
Workforce
The literature relevant to care home staffing is extensive, but much of it has limited relevance to the UK context. Initiatives in flexible deployment of staff or in new roles were difficult to identify in the published literature. However, interventions that promote joint working within and beyond the care home, multidisciplinary teams, primary nursing and a focus on specific care tasks all appear to have merit. There is no strong evidence of a relationship between the numbers of staff, staff-to-resident ratios, staff skill mix or nursing care models and any resident outcomes. There is limited evidence to suggest that the number of staff without nursing qualifications may influence residents’ quality of life.
Recommendations for research
Technology
There is a general need for appropriately powered experimental studies in this area, and to address the paucity of economic evaluations. Greater focus on interventions with practical applications to health care, such as the use of digital records and telehealth interventions, is needed. Their use and benefits could be addressed with mixed-methods and quasi-experimental designs. The burden of new interventions on care home staff is another important topic for future research. In addition, the impact of technology on families appears to have been neglected in this research area, and this should be rectified in future studies. Joint working between care homes, researchers and the manufacturers of new technologies may be helpful to generate robust evidence of effectiveness from multiple sites.
Communication and engagement
Formal evaluation in a UK setting of the use of transfer forms and tools such as SBAR would be valuable, before, or as, they are introduced across the NHS. If the complex, multifaceted interventions that have been used in US settings are introduced to the UK, they require multimethod, long-term evaluation to produce evidence that would support wider implementation.
Investigation is needed into the most effective and appropriate ways for care homes to engage with local communities, and the long-term impact on residents and the public perception of care homes. This is an area that would benefit from ethnographic and other qualitative approaches.
Evaluation
Care home commissioners and providers would benefit from an easy to administer, robust measure of care outcomes. The two general measures of care outcomes discussed, CARE profiles and ASCOT, have had some validation for UK use; however, the assessment of methodological quality suggests that publication of further validation work would help to promote this. The burden on residents, staff and care homes, the training needed, and the costs involved in administering and analysing data from both CARE and ASCOT all merit closer scrutiny before these measures are implemented across the NHS. There are many measurement tools developed elsewhere, and our mapping review provides some evaluative work to select candidate tools for testing in the UK.
Workforce
The evidence base on the care home workforce needs to be supplemented with research that is specific to the UK. Future work could usefully consider the experiences and perceptions of staff and residents, and the qualities and values that would promote high-quality care. Further measurement or analysis of the number of staff and a search for associations with resident outcomes cannot be justified. The impact of staffing practices on staff outcomes, particularly health, may be informative.
Acknowledgements
We are grateful to the ongoing contribution of the Newcastle University Care Home Interest Group/Voice North participants for their critical and supportive input into our work.
Contributions of authors
Barbara Hanratty (Professor of Primary Care and Public Health, Institute for Health and Society, Newcastle University) led the project and contributed to all reviews.
Dawn Craig (Director of the Evidence Synthesis Team, Institute for Health and Society, Newcastle University) led the design and provided expert methodological advice throughout the project.
Katie Brittain (Associate Professor of Ageing and Health, Northumbria University) and John Vines (Professor of Design, Northumbria University) led the technology review.
Karen Spilsbury (Professor of Nursing Research, University of Leeds) contributed to the design and all reviews.
Paul Wilson (Senior Research Fellow at the Alliance Manchester Business School and National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care Greater Manchester) provided expert methodological advice throughout the project.
Data-sharing statement
Owing to the nature of this study and the type of data collected, there are a limited number of data that can be shared further. All queries should be submitted to the corresponding author in the first instance.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Laing W. Care of Older People: UK Market Report. London: LaingBuisson; 2014.
- Office for National Statistics (ONS) . Changes in the Older Resident Care Home Population Between 2001 and 2011 2014. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/changesintheolderresidentcarehomepopulationbetween2001and2011/2014-08-01 (accessed August 2018).
- British Geriatrics Society . Quest for Quality. British Geriatrics Society Joint Working Party Inquiry into the Quality of Healthcare Support for Older People in Care Homes: A Call for Leadership, Partnership and Quality Improvement 2011.
- Care Quality Commission . The State of Health Care and Adult Social Care in England in 2011 12 2012.
- NHS England . Five Year Forward View 2014.
- NHS England . The Forward View Into Action: Planning for 2015 16 2014.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan – a web and mobile app for systematic reviews. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0384-4.
- Centre for Reviews and Dissemination (CRD) . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2009.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4. https://doi.org/10.1186/2046-4053-4-1.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- International Federation on Ageing . Long Term Care and Technology: Senior Government Officials Meeting, Final Report 2012. www.ifa-fiv.org/wp-content/uploads/2012/11/som-2012-ltc-and-technology-final-report.pdf (accessed August 2018).
- Jiang T, Yu P, Hailey D, Ma J, Yang J. The impact of electronic health records on risk management of information systems in Australian residential aged care homes. J Med Syst 2016;40. https://doi.org/10.1007/s10916-016-0553-y.
- Richardson S, Mishuris R, O’Connell A, Feldstein D, Hess R, Smith P, et al. ‘Think aloud’ and ‘near live’ usability testing of two complex clinical decision support tools. Int J Med Inform 2017;106:1-8. https://doi.org/10.1016/j.ijmedinf.2017.06.003.
- Loveday A, Sherar LB, Sanders JP, Sanderson PW, Esliger DW. Novel technology to help understand the context of physical activity and sedentary behaviour. Physiol Meas 2016;37:1834-51. https://doi.org/10.1088/0967-3334/37/10/1834.
- Chernbumroong S, Cang S, Atkins A, Yu H. Elderly activities recognition and classification for applications in assisted living. Expert Syst Appl 2013;40:1662-74. https://doi.org/10.1016/j.eswa.2012.09.004.
- Broekens J, Heerink M, Rosendal H. Assistive social robots in elderly care: a review. Gerontechnology 2009;8:94-103. https://doi.org/10.4017/gt.2009.08.02.002.00.
- Bemelmans R, Gelderblom GJ, Jonker P, de Witte L. Socially assistive robots in elderly care: a systematic review into effects and effectiveness. J Am Med Dir Assoc 2012;13:114-20.e1. https://doi.org/10.1016/j.jamda.2010.10.002.
- Kosse NM, Brands K, Bauer JM, Hortobagyi T, Lamoth CJ. Sensor technologies aiming at fall prevention in institutionalized old adults: a synthesis of current knowledge. Int J Med Inform 2013;82:743-52. https://doi.org/10.1016/j.ijmedinf.2013.06.001.
- Kidd L, Cayless S, Johnston B, Wengstrom Y. Telehealth in palliative care in the UK: a review of the evidence. J Telemed Telecare 2010;16:394-402. https://doi.org/10.1258/jtt.2010.091108.
- Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al. A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use. Health Technol Assess 2006;10. https://doi.org/10.3310/hta10260.
- Edirippulige S, Martin-Khan M, Beattie E, Smith AC, Gray LC. A systematic review of telemedicine services for residents in long term care facilities. J Telemed Telecare 2013;19:127-32. https://doi.org/10.1177/1357633X13483256.
- Marston HR, Greenlay S, van Hoof J. Understanding the Nintendo Wii and Microsoft Kinect consoles in long-term care facilities. Technol Disabil 2013;25:77-85. https://doi.org/10.3233/TAD-130369.
- Kachouie R, Sedighadeli S, Khosla R, Chu MT. Socially assistive robots in elderly care: a mixed-method systematic literature review. Int J Hum Comput Interact 2014;30:369-93. https://doi.org/10.1080/10447318.2013.873278.
- Abdelrahman N, Abdelrahman A, Elfadil M. Utilization of a mobile videoconferencing tool (FaceTime) for real-time evaluation of critically ill residents in skilled nursing facilities. J Am Med Dir Assoc 2015;16.
- Age UK . Digital Inclusion Evidence Review 2013. www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/active-communities/rb_sept13_age_uk_digital_inclusion_evidence_review.pdf (accessed August 2018).
- Age UK . Technology and Older People Evidence Review 2010. www.ageuk.org.uk/Documents/EN-GB/For-professionals/Research/Evidence_Review_Technology.pdf?dtrk=true.
- Age UK . The Digital Inclusion of Older People in Care Homes 2012. www.ageuk.org.uk/Documents/EN-GB/For-professionals/Services%20for%20Later%20Life/ID200921%20Digital%20Inclusion%20In%20Care%20Homes%2024ppA4.pdf?dtrk=true (accessed 30 August 2017).
- Alexander GL, Madsen R. IT sophistication and quality measures in nursing homes. J Gerontol Nurs 2009;35:22-7. https://doi.org/10.3928/00989134-20090527-05.
- Alexander GL, Rantz M, Galambos C, Vogelsmeier A, Flesner M, Popejoy L, et al. Preparing nursing homes for the future of health information exchange. Appl Clin Inform 2015;6:248-66. https://doi.org/10.4338/ACI-2014-12-RA-0113.
- Alexander GL, Madsen RW, Miller EL, Wakefield DS, Wise KK, Alexander RL. The state of nursing home information technology sophistication in rural and nonrural US markets. J Rural Health 2016;22.
- Aloulou H, Mokhtari M, Tiberghien T, Biswas J, Phua C, Kenneth Lin JH, et al. Deployment of assistive living technology in a nursing home environment: methods and lessons learned. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-42.
- Alzheimer’s Society . Assistive Technology. Position Paper 2011. www.alzheimers.org.uk/download/downloads/id/1098/alzheimers_society_position_paper_on_assistive_technology.pdf (accessed 30 August 2017).
- Alzheimer’s Society . Assistive Technology – Devices to Help With Everyday Living 2015. www.alzheimers.org.uk/download/downloads/id/1779/factsheet_assistive_technology_%E2%80%93_devices_to_help_with_everyday_living.pdf (accessed 30 August 2017).
- Anonymous . Electronic Medication Administration Records Improve Communication and Decisionmaking in Nursing Homes 2009. https://archive.ahrq.gov/news/newsletters/research-activities/jul09/0709RA29.html (accessed 30 August 2017).
- Anonymous . Using health information technology to reduce adverse drug events in long-term care facilities. Ann LongTerm Care 2011;19.
- Anonymous . Nursing Home Users of Information Technology Start to See Its Benefits 2010. https://archive.ahrq.gov/news/newsletters/research-activities/apr10/0410RA34.html (accessed 30 August 2017).
- Anonymous . Real or robotic dogs wag away loneliness. J Gerontol Nurs 2008;34.
- Anonymous . Residential facility adopts environmentally friendly pharmacy. J Gerontol Nurs 2009;34.
- Anonymous . Computerized Clinical Decision Support Produces Only Modest Savings for Nursing Home Residents With Impaired Kidney Function 2013. https://archive.ahrq.gov/news/newsletters/research-activities/13jan/0113RA22.html (accessed 30 August 2017).
- Babalola EO, Baier RR, Gravenstein S, Capizzo L, Zimmerman A, Gardner R. Building a health information technology infrastructure in long-term care. Ann LongTerm Care 2014;22:43-7.
- Bäck I, Makela K, Kallio J. Robot-guided exercise program for the rehabilitation of older nursing home residents. Ann LongTerm Care 2013;21:38-41.
- Bäck I, Kallio J, Perälä S, Mäkelä K. Remote monitoring of nursing home residents using a humanoid robot. J Telemed Telecare 2012;18:357-61. https://doi.org/10.1258/jtt.2012.120305.
- Baker C, Huxley P, Dennis M, Islam S, Russell I. Alleviating staff stress in care homes for people with dementia: protocol for stepped-wedge cluster randomised trial to evaluate a web-based mindfulness-stress reduction course. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0703-7.
- Bakerjian D, Scherger JE. Are you on the health information technology bandwagon?. J Am Med Dir Assoc 2009;10:368-9. https://doi.org/10.1016/j.jamda.2009.03.002.
- Banks MR, Willoughby LM, Banks WA. Animal-assisted therapy and loneliness in nursing homes: use of robotic versus living dogs. J Am Med Dir Assoc 2008;9:173-7. https://doi.org/10.1016/j.jamda.2007.11.007.
- Banks WA. Artificial emotions: robots caring for the elderly. J Am Med Dir Assoc 2013;14:635-6. https://doi.org/10.1016/j.jamda.2013.04.011.
- Barbour PJ, Arroyo J, High S, Fichera LB, Staska-Pier MM, McMahon MK. Telehealth for patients with Parkinson’s disease: delivering efficient and sustainable long-term care. Hosp Pract 2016;44:92-7. https://doi.org/10.1080/21548331.2016.1166922.
- Baril C, Gascon V, Brouillette C. Impact of technological innovation on a nursing home performance and on the medication-use process safety. J Med Syst 2014;38. https://doi.org/10.1007/s10916-014-0022-4.
- Baril C, Gascon V, St-Pierre L, Lagacé D. Technology and medication errors: impact in nursing homes. Int J Health Care Qual Assur 2014;27:244-58. https://doi.org/10.1108/IJHCQA-03-2013-0029.
- Barrett M, Larson A, Carville K, Ellis I. Challenges faced in implementation of a telehealth enabled chronic wound care system. Rural Remote Health 2009;9.
- Bartle C. The Role of Technology in Care Homes 2017. www.linkedin.com/pulse/role-technology-care-homes-caroline-bartle (accessed 30 August 2017).
- Beeckman D, Clays E, Van Hecke A, Vanderwee K, Schoonhoven L, Verhaeghe S. A multi-faceted tailored strategy to implement an electronic clinical decision support system for pressure ulcer prevention in nursing homes: a two-armed randomized controlled trial. Int J Nurs Stud 2013;50:475-86. https://doi.org/10.1016/j.ijnurstu.2012.09.007.
- Beedholm K, Frederiksen K, Lomborg K. What was (also) at stake when a robot bathtub was implemented in a Danish elder center: a constructivist secondary qualitative analysis. Qual Health Res 2016;26:1424-33. https://doi.org/10.1177/1049732315586550.
- Bemelmans R, Gelderblom GJ, Jonker P, de Witte L. Effectiveness of robot PARO in intramural psychogeriatric care: a multicenter quasi-experimental study. J Am Med Dir Assoc 2015;16:946-50. https://doi.org/10.1016/j.jamda.2015.05.007.
- Bemelmans R, Gelderblom GJ, Jonker P, de Witte L. How to use robot interventions in intramural psychogeriatric care: a feasibility study. Appl Nurs Res 2016;30:154-7. https://doi.org/10.1016/j.apnr.2015.07.003.
- Bennett P, Hinder H, Kozar S, Bowdler C, Massung E, Cole T, et al. TopoTiles: Storytelling in Care Homes With Topographic Tangibles n.d. https://doi.org/10.1145/2702613.2732918.
- Bennett P, Hinder H, Cater K. Rekindling Imagination in Dementia Care With the Resonant Interface Rocking Chair n.d.:2020-6. https://doi.org/10.1145/2851581.2892505.
- Bereznicki LR, Jackson SL, Kromdijk W, Gee P, Fitzmaurice K, Bereznicki BJ, et al. Improving the management of warfarin in aged-care facilities utilising innovative technology: a proof-of-concept study. Int J Pharm Pract 2014;22:84-91. https://doi.org/10.1111/ijpp.12035.
- Bezboruah KC, Paulson D, Smith J. Management attitudes and technology adoption in long-term care facilities. J Health Organ Manag 2014;28:344-65. https://doi.org/10.1108/JHOM-11-2011-0118.
- Biglan KM, Killoran A, Scoglio N, Cayea-Delker S, Friedman V, Hadfield T, et al. The generalizability of telemedicine for providing care to individuals with chronic neurological conditions residing in nursing homes. Mov Disord 2011;26:S350-1.
- Biglan KM, Voss TS, Deuel LM, Miller D, Eason S, Fagnano M, et al. Telemedicine for the care of nursing home residents with Parkinson’s disease. Mov Disord 2009;24:1073-6. https://doi.org/10.1002/mds.22498.
- Blair Irvine A, Billow MB, Eberhage MG, Seeley JR, McMahon E, Bourgeois M. Mental illness training for licensed staff in long-term care. Issues Ment Health Nurs 2012;33:181-94. https://doi.org/10.3109/01612840.2011.639482.
- Bobillier Chaumon M-E, Michel C, Tarpin Bernard F, Croisile B. Can ICT improve the quality of life of elderly adults living in residential home care units? From actual impacts to hidden artefacts. Behav Inf Technol 2014;33:574-90. https://doi.org/10.1080/0144929X.2013.832382.
- Bollen C, Warren J, Whenan G. Introduction of electronic prescribing in an aged care facility. Aust Fam Physician 2005;34:283-7.
- Bond GE, Wolf-Wilets V, Fiedler FE, Burr RL. Computer-aided cognitive training of the aged: a pilot study. Clin Gerontologist 2000;22:19-42. https://doi.org/10.1300/J018v22n02_03.
- Bowen ME, Wingrave CA, Klanchar A, Craighead J. Tracking technology: lessons learned in two health care sites. Technol Health Care 2013;21:191-7. https://doi.org/10.3233/THC-130738.
- Brandt K, Paniagua MA. The use of Nintendo Wii with long-term care residents. J Am Geriatr Soc 2011;59:2393-5. https://doi.org/10.1111/j.1532-5415.2011.03692.x.
- Brankline AL, Coyle CM, Jencks KA, Mullegama A, O’Brien MW. Practical innovations: technology-assisted referrals. Soc Work Health Care 2009;48:768-76. https://doi.org/10.1080/00981380902958213.
- Bratan T, Jones R, Clarke M. A new monitoring service for long term residential care. Stud Health Technol Inform 2004;103:374-80.
- Braun SM, Kleynen M, Bleijlevens MH, Moser A, Beurskens AJ, Lexis MA. ‘Interactive surfaces’ technology as a potential tool to stimulate physical activity in psychogeriatric nursing home residents. Disabil Rehabil Assist Technol 2014;28.
- Broadbent E, Kerse N, Peri K, Robinson H, Jayawardena C, Kuo T, et al. Benefits and problems of health-care robots in aged care settings: a comparison trial. Australas J Ageing 2016;35:23-9. https://doi.org/10.1111/ajag.12190.
- Broder K, Chau D, Bodor R, Yourman L. Skilled nursing facility/plastic surgery interdisciplinary team approach: utilizing inter-professional collaboration and innovative telemedicine technologies to provide comprehensive wound care across the healthcare continuum. J Am Med Dir Assoc 2015;16.
- Brown AC, Garrison C. The emerging role of telemedicine in extended-care risk management. Manag Care Interface 2000;13:66-8.
- Bruun-Pedersen JR, Serafin S, Kofoed LB. Simulating Nature for Elderly Users – A Design Approach for Recreational Virtual Environments n.d.:1566-71.
- Burdea G, Polistico K, Krishnamoorthy A, House G, Rethage D, Hundal J, et al. Feasibility study of the BrightBrainerTM integrative cognitive rehabilitation system for elderly with dementia. Disabil Rehabil Assist Technol 2015;10:421-32. https://doi.org/10.3109/17483107.2014.900575.
- Burns P, Perkins DA, Larsen K, Dalley A. The introduction of electronic medication charts and prescribing in aged care facilities: an evaluation. Australas J Ageing 2007;26:131-4. https://doi.org/10.1111/j.1741-6612.2007.00237.x.
- Bygholm A, Kanstrup AM. Learning from an ambient assisted living lab: the case of the intelligent bed. Stud Health Technol Inform 2014;205:318-22.
- Campbell A. Dementia care: could animal robots benefit residents?. Nurs Resident Care 2011;13:602-4. https://doi.org/10.12968/nrec.2011.13.12.602.
- Campbell B, Stirling C, Cummings E. Continuity matters: examining the ‘information gap’ in transfer from residential aged care, ambulance to emergency triage in southern Tasmania. Int Emerg Nurs 2017;32:9-14. https://doi.org/10.1016/j.ienj.2016.05.001.
- Castle N, Liu D. Information technology and quality of nursing home care. Gerontologist 2009;49.
- Centre for Workforce Intelligence . The Technology Horizon: Preliminary Review on Technologies Impacting the Future Health &Amp; Social Care Workforce 2013. www.escholar.manchester.ac.uk/uk-ac-man-scw:211237 (accessed 30 August 2017).
- Chae YM, Heon Lee J, Hee Ho S, Ja Kim H, Hong Jun K, Uk Won J. Patient satisfaction with telemedicine in home health services for the elderly. Int J Med Inform 2001;61:167-73. https://doi.org/10.1016/S1386-5056(01)00139-3.
- Chan HH, Woo J, Chan WM, Hjelm M. Teledermatology in Hong Kong: a cost-effective method to provide service to the elderly patients living in institutions. Int J Dermatol 2000;39:774-8. https://doi.org/10.1046/j.1365-4362.2000.00034.x.
- Chan WM, Woo J, Hui E, Hjelm NM. The role of telenursing in the provision of geriatric outreach services to residential homes in Hong Kong. J Telemed Telecare 2001;7:38-46. https://doi.org/10.1258/1357633011936129.
- Chang W-L, Sabanovic S, Huber L. Use of Seal-Like Robot PARO in Sensory Group Therapy for Older Adults With Dementia n.d. https://doi.org/10.1109/HRI.2013.6483521.
- Chang WL, Sabanovic S, Huber L. Observational Study of Naturalistic Interactions With the Socially Assistive Robot PARO in a Nursing Home n.d.:294-9. https://doi.org/10.1109/ROMAN.2014.6926268.
- Chang W-L, Sabanovic S. Studying Socially Assistive Robots in Their Organizational Context: Studies With PARO in a Nursing Home n.d. https://doi.org/10.1145/2701973.2702722.
- Chen ST, Huang YGL, Chiang IT. Using Somatosensory Video Games to Promote Quality of Life for the Elderly With Disabilities n.d.:258-62. https://doi.org/10.1109/DIGITEL.2012.68.
- Cherry B, Carpenter K. Evaluating the effectiveness of electronic medical records in a long term care facility using process analysis. J Healthc Eng 2011;2:75-86. https://doi.org/10.1260/2040-2295.2.1.75.
- Chesler J, McLaren S, Klein B, Watson S. The effects of playing Nintendo Wii on depression, sense of belonging and social support in Australian aged care residents: a protocol study of a mixed methods intervention trial. BMC Geriatr 2015;15. https://doi.org/10.1186/s12877-015-0107-z.
- Clark R, Kraemer T. Clinical use of Nintendo Wii bowling simulation to decrease fall risk in an elderly resident of a nursing home: a case report. J Geriatr Phys Ther 2009;32:174-80. https://doi.org/10.1519/00139143-200932040-00006.
- Cobb D. The case for IT investment: while daunting upfront costs prevent many providers from embracing information technology, IT systems can prove well worth the investment. Provider 2007;33:41-3.
- Courtney KL. Privacy And Senior Adoption of Assistive Technology in Residential Care 2006.
- Centre for Policy on Ageing . The Potential Impact of New Technologies 2014.
- Curyto K, Roos B, Sanford J, Calkins M. Bringing technology into the nursing home: barriers and opportunities. Gerontologist 2002;42:83-4. https://doi.org/10.4017/gt.2002.02.01.110.00.
- Daly JM, Jogerst G, Park JY, Kang YD, Bae T. A nursing home telehealth system: keeping residents connected. J Gerontol Nurs 2005;31:46-51. https://doi.org/10.3928/0098-9134-20050801-14.
- Damant J, Knapp M. What are the Likely Changes in Society and Technology Which Will Impact Upon the Ability of Older Adults to Maintain Social (Extra-Familial) Networks of Support Now, in 2025 and in 2040?. London: Government Office for Science; 2015.
- De Luca R, Bramanti A, De Cola MC, Leonardi S, Torrisi M, Aragona B, et al. Cognitive training for patients with dementia living in a Sicilian nursing home: a novel web-based approach. Neurol Sci 2016;37:1685-91. https://doi.org/10.1007/s10072-016-2659-x.
- De Luca R, Bramanti A, De Cola MC, Trifiletti A, Tomasello P, Torrisi M, et al. Tele-health-care in the elderly living in nursing home: the first Sicilian multimodal approach. Aging Clin Exp Res 2016;28:753-9. https://doi.org/10.1007/s40520-015-0463-8.
- de Veer AJ, Fleuren MA, Bekkema N, Francke AL. Successful implementation of new technologies in nursing care: a questionnaire survey of nurse-users. BMC Med Inform Decis Mak 2011;11. https://doi.org/10.1186/1472-6947-11-67.
- Degenholtz H, Handler S, Lin M, Kobelak C, Zaharoff J. Health information technology in nursing homes: clinical care processes that can benefit from automation. Gerontologist 2008;48.
- Degenholtz HB, Lin MK, Handler SM, Resnick AL. Implementing health information technology in US nursing homes: a report on adoption and use. Gerontologist 2010;50.
- Degenholtz HB, Handler SM, Lin MK, Resnick AL. Health information technology in US nursing homes: availability and use. Gerontologist 2011;51.
- Degenholtz HB, Resnick A, Lin M, Handler S. Development of an applied framework for understanding health information technology in nursing homes. J Am Med Dir Assoc 2016;17:434-40. https://doi.org/10.1016/j.jamda.2016.02.002.
- Demiris G, Oliver DR, Hensel B, Dickey G, Rantz M, Skubic M. Use of videophones for distant caregiving: an enriching experience for families and residents in long-term care. J Gerontol Nurs 2008;34:50-5. https://doi.org/10.3928/00989134-20080701-02.
- Demiris G, Thompson H, Boquet J, Le T, Chaudhuri S, Chung J. Older adults’ acceptance of a community-based telehealth wellness system. Inform Health Soc Care 2013;38:27-36. https://doi.org/10.3109/17538157.2011.647938.
- Dewsbury G, Ballard D. Is your home telecare aware?. Nursing &Amp; Residential Care 2012;14:422-4. https://doi.org/10.12968/nrec.2012.14.8.422.
- Dorsten AM, Sifford KS, Bharucha A, Mecca LP, Wactlar H. Ethical perspectives on emerging assistive technologies: insights from focus groups with stakeholders in long-term care facilities. J Empir Res Hum Res Ethics 2009;4:25-36. https://doi.org/10.1525/jer.2009.4.1.25.
- Doshi-Velez F, Li W, Battat Y, Charrow B, Curtis D, Curthis D, et al. Improving safety and operational efficiency in residential care settings with WiFi-based localization. J Am Med Dir Assoc 2012;13:558-63. https://doi.org/10.1016/j.jamda.2012.04.010.
- Driessen J, Castle NG, Handler SM. Perceived benefits, barriers, and drivers of telemedicine from the perspective of skilled nursing facility administrative staff stakeholders. J Appl Gerontol 2016;5.
- Eccles R, Anderson A. Telehealthcare in care homes: the use of falls detectors and bed/chair sensors to enhance the safety and experience of care home residents. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.905.
- Elliott RA, Lee CY, Hussainy SY. Evaluation of a hybrid paper-electronic medication management system at a residential aged care facility. Aust Health Rev 2016;40:244-50. https://doi.org/10.1071/AH14206.
- Eyers I, Carey-Smith B, Evans N, Orpwood R. Safe and sound? Night-time checking in care homes. Br J Nurs 2013;22:827-30. https://doi.org/10.12968/bjon.2013.22.14.827.
- Field TS, Rochon P, Lee M, Gavendo L, Subramanian S, Hoover S, et al. Costs associated with developing and implementing a computerized clinical decision support system for medication dosing for patients with renal insufficiency in the long-term care setting. J Am Med Inform Assoc 2008;15:466-72. https://doi.org/10.1197/jamia.M2589.
- Filipova AA. Health information exchange capabilities in skilled nursing facilities. Comput Inform Nurs 2015;33:346-58. https://doi.org/10.1097/CIN.0000000000000169.
- Fossum M, Ehnfors M, Fruhling A, Ehrenberg A. An evaluation of the usability of a computerized decision support system for nursing homes. Appl Clin Inform 2011;2:420-36. https://doi.org/10.4338/ACI-2011-07-RA-0043.
- Fossum M, Ehnfors M, Fruhling A, Ehrenberg A. The experiences of using a computerized decision support system. NI 2012 2012;2012:113-5.
- Fournier D, Gosselin D, Rioux N. Implementing an EHR system. Provider 2004;30:37-8.
- Freedman VA, Calkins M, Van Haitsma K. An exploratory study of barriers to implementing technology in U.S. residential long-term care settings. Gerontechnology 2005;4:86-100. https://doi.org/10.4017/gt.2005.04.02.004.00.
- Fu AS, Gao KL, Tung AK, Tsang WW, Kwan MM. Effectiveness of exergaming training in reducing risk and incidence of falls in frail older adults with a history of falls. Arch Phys Med Rehabil 2015;96:2096-102. https://doi.org/10.1016/j.apmr.2015.08.427.
- Gaver W, Boucher A, Bowers J, Blythe M, Jarvis N, Cameron D, et al. The Photostroller: Supporting Diverse Care Home Residents in Engaging With the World n.d. https://doi.org/10.1145/1978942.1979198.
- Gerling K, Livingston I, Nacke L, Mandryk R. Full-Body Motion-Based Game Interaction for Older Adults n.d. https://doi.org/10.1145/2207676.2208324.
- Gerling KM, Mandryk RL, Linehan C. Long-Term Use of Motion-Based Video Games in Care Home Settings n.d. https://doi.org/10.1145/2702123.2702125.
- Ghorbel M, Betge-Brezetz S, Dupont MP, Kamga GB, Piekarec S, Reerink J, et al. Multimodal notification framework for elderly and professional in a smart nursing home. J Multimodal User Interfaces 2013;7:281-97. https://doi.org/10.1007/s12193-012-0116-6.
- Gietzelt M, Feldwieser F, Gövercin M, Steinhagen-Thiessen E, Marschollek M. A prospective field study for sensor-based identification of fall risk in older people with dementia. Inform Health Soc Care 2014;39:249-61. https://doi.org/10.3109/17538157.2014.931851.
- Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Aff 2014;33:244-50. https://doi.org/10.1377/hlthaff.2013.0922.
- Grant LA, Rockwood T, Stennes L. Testing telehealth using technology-enhanced nurse monitoring. J Gerontol Nurs 2014;40:15-23. https://doi.org/10.3928/00989134-20140808-01.
- Guilfoyle C, Wootton R, Hassall S, Offer J, Warren M, Smith D, et al. User satisfaction with allied health services delivered to residential facilities via videoconferencing. J Telemed Telecare 2003;9:52-4. https://doi.org/10.1258/135763303322196349.
- Guilfoyle C, Wootton R, Hassall S, Offer J, Warren M, Smith D, et al. Videoconferencing in facilities providing care for elderly people. J Telemed Telecare 2002;8:22-4.
- Hamada T, Okubo H, Inoue K, Maruyama J, Onari H, Kagawa Y, et al. Robot Therapy As for Recreation for Elderly People With Dementia – Game Recreation Using a Pet-Type Robot n.d.:174-9.
- Handler SM, Boyce RD, Ligons FM, Perera S, Nace DA, Hochheiser H. Use and perceived benefits of mobile devices by physicians in preventing adverse drug events in the nursing home. J Am Med Dir Assoc 2013;14:906-10. https://doi.org/10.1016/j.jamda.2013.08.014.
- Hardy R. ‘It was so simple and easy’: the nursing home improving care with tech. The Guardian 2016. www.theguardian.com/social-care-network/2016/jul/26/nursing-home-technology-improve-care (accessed 30 August 2017).
- Harrington SS, Walker BL. Is computer-based instruction an effective way to present fire safety training to long-term care staff?. J Nurses Staff Dev 2003;19:147-54. https://doi.org/10.1097/00124645-200305000-00007.
- Hensel BK, Oliver DP, Demiris G, Willis L. A telehealth case study of videophone use between family members. AMIA Annu Symp Proc 2006;948.
- Hensel BK, Parker-Oliver D, Demiris G. Videophone communication between residents and family: a case study. J Am Med Dir Assoc 2007;8:123-7. https://doi.org/10.1016/j.jamda.2006.09.012.
- Hensel BK, Parker-Oliver D, Demiris G, Rantz M. A comparison of video-based resident-family communication in a nursing home and a congregate living facility. J Am Med Dir Assoc 2009;10:342-7. https://doi.org/10.1016/j.jamda.2009.02.006.
- Hex N, Tuggey J, Wright D, Malin R. Telemedicine in care homes in Airedale, Wharfedale and Craven. Clin Gov 2015;20:146-54. https://doi.org/10.1108/CGIJ-07-2015-0022.
- Hitt LM, Tambe P. Health care information technology, work organization, and nursing home performance. ILR Review 2016;69:834-59. https://doi.org/10.1177/0019793916640493.
- Hobday JV, Savik K, Smith S, Gaugler JE. Feasibility of internet training for care staff of residents with dementia: the CARES program. J Gerontol Nurs 2010;36:13-21. https://doi.org/10.3928/00989134-20100302-01.
- Hoey J, Poupart P, von Bertoldi A, Craig T, Boutilier C, Mihailidis A. Automated handwashing assistance for persons with dementia using video and a partially observable Markov decision process. Comp Vision Image Understanding 2010;114:503-19. https://doi.org/10.1016/j.cviu.2009.06.008.
- Hofmeyer J, Leider JP, Satorius J, Tanenbaum E, Basel D, Knudson A. Implementation of telemedicine consultation to assess unplanned transfers in rural long-term care facilities, 2012–2015: a pilot study. J Am Med Dir Assoc 2016;17:1006-10. https://doi.org/10.1016/j.jamda.2016.06.014.
- Hori T, Nishida Y, Aizawa H, Murakami S, Mizoguchi H. Sensor Network for Supporting Elderly Care Home n.d.;2:575-8. https://doi.org/10.1109/ICSENS.2004.1426230.
- Hori T, Nishida Y, Murakami S. Evidence-Based Nursing Care Support Enhanced by Minimally Privacy Invasive and Pervasive Sensing Technology n.d.;51:537-42. https://doi.org/10.1109/percomw.2006.51.
- Hoti K, Hughes J, Sunderland B. Medication supply to residential aged care facilities in Western Australia using a centralized medication chart to replace prescriptions. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-25.
- Hsu JK, Thibodeau R, Wong SJ, Zukiwsky D, Cecile S, Walton DM. A ‘Wii’ bit of fun: the effects of adding Nintendo Wii(®) Bowling to a standard exercise regimen for residents of long-term care with upper extremity dysfunction. Physiother Theory Pract 2011;27:185-93. https://doi.org/10.3109/09593985.2010.483267.
- Hui E, Woo J, Hjelm M, Zhang YT, Tsui HT. Telemedicine: a pilot study in nursing home residents. Gerontology 2001;47:82-7. https://doi.org/10.1159/000052778.
- Hui E, Woo J. Telehealth for older patients: the Hong Kong experience. J Telemed Telecare 2002;8:39-41.
- Hung LH, Zhang HW, Lin YJ, Chang IW, Chen HS. A Study of the Electronic Healthy Diet and Nutrition Assessment System Applied in a Nursing Home n.d.:64-7. https://doi.org/10.1109/HEALTH.2007.381604.
- Hustey F, Palmer RM. The use of a computerized system to improve information transfer during patient transition from a skilled nursing facility to the emergency department. J Am Geriatr Soc 2009;57.
- Hustey FM, Palmer RM. An internet-based communication network for information transfer during patient transitions from skilled nursing facility to the emergency department. J Am Geriatr Soc 2010;58:1148-52. https://doi.org/10.1111/j.1532-5415.2010.02864.x.
- Hustey FM, Palmer RM. Implementing an internet-based communication network for use during skilled nursing facility to emergency department care transitions: challenges and opportunities for improvement. J Am Med Dir Assoc 2012;13:249-53. https://doi.org/10.1016/j.jamda.2010.07.003.
- Iio T, Shiomi M, Kamei K, Sharma C, Hagita N. Social Acceptance by Elderly People of a Fall-Detection System With Range Sensors in a Nursing Home n.d. https://doi.org/10.1145/2658861.2658910.
- Irvine B, Billow MB, Gates DM, Fitzwater EL, Seeley JR, Bourgeois M. An internet training to reduce assaults in long-term care. Geriatr Nurs 2012;33:28-40. https://doi.org/10.1016/j.gerinurse.2011.10.004.
- Irvine AB, Billow MB, Gates DM, Fitzwater EL, Seeley JR, Bourgeois M. Internet training to respond to aggressive resident behaviors. Gerontologist 2012;52:13-2. https://doi.org/10.1093/geront/gnr069.
- Jiang T, Yu P. The impact of electronic health records on client safety in aged care homes. Stud Health Technol Inform 2014;201:116-23.
- Johansson-Pajala RM, Gustafsson LK, Jorsater Blomgren K, Fastbom J, Martin L. Nurses’ use of computerised decision support systems affects drug monitoring in nursing homes. J Nurs Manag 2016;13.
- Johnston D, Jones BN. Telepsychiatry consultations to a rural nursing facility: a 2-year experience. J Geriatr Psychiatry Neurol 2001;14:72-5. https://doi.org/10.1177/089198870101400205.
- Jøranson N, Pedersen I, Mork AM, Ihlebaek C. Effects of participation in robot-assisted activity groups for nursing home patients with dementia on symptoms of agitation and depression – a cluster-randomized controlled trial. Int Psychogeriatr 2015;27:S48-9.
- Jøranson N, Pedersen I, Rokstad AM, Ihlebæk C. Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: a cluster-randomized controlled trial. J Am Med Dir Assoc 2015;16:867-73. https://doi.org/10.1016/j.jamda.2015.05.002.
- Jøranson N, Pedersen I, Rokstad AM, Aamodt G, Olsen C, Ihlebæk C. Group activity with Paro in nursing homes: systematic investigation of behaviors in participants. Int Psychogeriatr 2016;28:1345-54. https://doi.org/10.1017/S1041610216000120.
- Jung Y, Li KJ, Janissa NS, Gladys WLC, Lee KM. Games for a Better Life: Effects of Playing Wii Games on the Well-Being of Seniors in a Long-Term Care Facility n.d. https://doi.org/10.1145/1746050.1746055.
- Kanstrup AM, Bygholm A. Monitoring technology meets care work: challenges of monitoring wet-beds in a nursing home. Stud Health Technol Inform 2015;215:157-67.
- Kapadia V, Ariani A, Li J, Ray PK. Emerging ICT implementation issues in aged care. Int J Med Inform 2015;84:892-900. https://doi.org/10.1016/j.ijmedinf.2015.07.002.
- Keogh JW, Power N, Wooller L, Lucas P, Whatman C. Physical and psychosocial function in residential aged-care elders: effect of Nintendo Wii Sports games. J Aging Phys Act 2014;22:235-44. https://doi.org/10.1123/japa.2012-0272.
- Khosla R, Chu M-T, Kachouie R, Yamada K, Yoshihiro F, Yamaguchi T. Interactive Multimodal Social Robot for Improving Quality of Care of Elderly in Australian Nursing Homes n.d. https://doi.org/10.1145/2393347.2396411.
- Khosla R, Chu MT, Nguyen K. Affective Robot Enabled Capacity and Quality Improvement of Nursing Home Aged Care Services in Australia n.d.:409-14. https://doi.org/10.1109/COMPSACW.2013.89.
- Kidd CD, Taggart W, Turkle S. A Sociable Robot to Encourage Social Interaction Among the Elderly n.d.:3972-6. https://doi.org/10.1109/ROBOT.2006.1642311.
- Knapp M, Barlow J, Comas-Herrera A, Damant J, Freddolino PP, Hamblin K, et al. The Case for Investment in Technology to Manage the Global Costs of Dementia 2015. www.piru.ac.uk/assets/files/Dementia_IT_PIRU_publ_18.pdf (accessed 30 August 2017).
- Kong E, Evans LK. Development of an educational app and website on restraint-free care for Korean nursing homes. Gerontologist 2012;52.
- Lai YL, Chen CL, Chang CH, Hsu CY, Lai YK, Tseng KK, et al. An intelligent health monitoring system using radio-frequency identification technology. Technol Health Care 2015;24:421-31. https://doi.org/10.3233/THC-151109.
- Lattanzio F, Abbatecola AM, Bevilacqua R, Chiatti C, Corsonello A, Rossi L, et al. Advanced technology care innovation for older people in Italy: necessity and opportunity to promote health and wellbeing. J Am Med Dir Assoc 2014;15:457-66. https://doi.org/10.1016/j.jamda.2014.04.003.
- Lawrence E, Sax C, Navarro KF, Qiao M. Interactive Games to Improve Quality of Life for the Elderly: Towards Integration into a WSN Monitoring System n.d.:106-12.
- Lesnoff-Caravaglia G. Gerontechnology in healthcare settings: myth or reality. Gerontechnology 2005;4:46-51. https://doi.org/10.4017/gt.2005.04.01.006.00.
- Libin A, Cohen-Mansfield J. Therapeutic robocat for nursing home residents with dementia: preliminary inquiry. Am J Alzheimers Dis Other Demen 2004;19:111-16. https://doi.org/10.1177/153331750401900209.
- Lin KH, Chen CH, Chen YY, Huang WT, Lai JS, Yu SM, et al. Bidirectional and multi-user telerehabilitation system: clinical effect on balance, functional activity, and satisfaction in patients with chronic stroke living in long-term care facilities. Sensors 2014;14:12451-66. https://doi.org/10.3390/s140712451.
- Little MO, Rantz M, Lynn GA. Health information technology in long-term care: potential for the future. J Am Med Dir Assoc 2016;17:379-80. https://doi.org/10.1016/j.jamda.2016.02.029.
- Loh PK, Flicker L, Horner B. Attitudes toward information and communication technology (ICT) in residential aged care in Western Australia. J Am Med Dir Assoc 2009;10:408-13. https://doi.org/10.1016/j.jamda.2009.02.012.
- Low JA, Beins G, Lee KK, Koh E. Last moments of life: can telemedicine play a role?. Palliat Support Care 2013;11:353-5. https://doi.org/10.1017/S1478951512000995.
- Lyketsos CG, Roques C, Hovanec L, Jones BN. Telemedicine use and the reduction of psychiatric admissions from a long-term care facility. J Geriatr Psychiatry Neurol 2001;14:76-9. https://doi.org/10.1177/089198870101400206.
- MacDonald C, Stodel EJ, Casimiro L. Online training for healthcare workers: improving the quality of life for dementia patients in long-term care facilities. ELearn 2005;9. https://doi.org/10.1145/1104985.1104991.
- Maiden N, D’Souza S, Jones S, Muller L, Pannese L, Pitts K, et al. Computing technologies for reflective, creative care of people with dementia. Communications of the ACM 2013;56:60-7. https://doi.org/10.1145/2500495.
- Mansdorf IJ, Sharma R, Perez M, Lepore AM. Falls reduction in long-term care facilities: a preliminary report of a new internet-based behavioral technique. J Am Med Dir Assoc 2009;10:630-3. https://doi.org/10.1016/j.jamda.2009.06.005.
- Mariño R, Tonmukayakul U, Manton D, Stranieri A, Clarke K. Cost-analysis of teledentistry in residential aged care facilities. J Telemed Telecare 2016;22:326-32. https://doi.org/10.1177/1357633X15608991.
- Martin-Khan M, Beattie E, Edirippulige S, Gray LC, Russell T, Smith AC, et al. Telehealth for nursing homes: utilisation of specialists services. Australas J Ageing 2012;31.
- McDonald T, Russell F. Impact of technology-based care and management systems on aged care outcomes in Australia. Nurs Health Sci 2012;14:87-94. https://doi.org/10.1111/j.1442-2018.2011.00668.x.
- McGibbon F, Dorrian C, O’Keeffe R. Lochaber telemedicine clinic – a new approach managing dementia in care homes. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.1412.
- McNeil R. Technology enhances employee learning, resident care. Long Term Living Contin Care Prof 2013;62:28-9.
- Meador R. Linking technology implementation to resident centered care in nursing homes. Gerontologist 2009;49:130-1.
- Meißner A, Schnepp W. Staff experiences within the implementation of computer-based nursing records in residential aged care facilities: a systematic review and synthesis of qualitative research. BMC Med Inform Decis Mak 2014;14. https://doi.org/10.1186/1472-6947-14-54.
- Michel-Verkerke MB, Hoogeboom AMGM. Evaluation of an Electronic Patient Record in a Nursing Home: One Size Fits All? n.d.:2850-9. https://doi.org/10.1109/HICSS.2012.258.
- Mickus MA, Luz CC. Televisits: sustaining long distance family relationships among institutionalized elders through technology. Aging Ment Health 2002;6:387-96. https://doi.org/10.1080/1360786021000007009.
- Millington B. Exergaming in retirement centres and the integration of media and physical literacies. J Aging Stud 2015;35:160-8. https://doi.org/10.1016/j.jaging.2015.08.005.
- Miskelly F. A novel system of electronic tagging in patients with dementia and wandering. Age Ageing 2004;33:304-6. https://doi.org/10.1093/ageing/afh084.
- Mitzner TL, Chen TL, Kemp CC, Rogers WA. Identifying the potential for robotics to assist older adults in different living environments. Int J Soc Robot 2014;6:213-27. https://doi.org/10.1007/s12369-013-0218-7.
- Morley JE. High technology coming to a nursing home near you. J Am Med Dir Assoc 2012;13:409-12. https://doi.org/10.1016/j.jamda.2012.04.002.
- Morley JE. Telemedicine: coming to nursing homes in the near future. J Am Med Dir Assoc 2016;17:1-3. https://doi.org/10.1016/j.jamda.2015.10.012.
- Morrissey K, McCarthy J. Creative and Opportunistic Use of Everyday Music Technologies in a Dementia Care Unit n.d. https://doi.org/10.1145/2757226.2757228.
- Moyle W, Jones C, Cooke M, O’Dwyer S, Sung B, Drummond S. Social Robots Helping People With Dementia: Assessing Efficacy of Social Robots in the Nursing Home Environment n.d.:608-13. https://doi.org/10.1109/HSI.2013.6577887.
- Moyle W, Cooke M, Beattie E, Jones C, Klein B, Cook G, et al. Exploring the effect of companion robots on emotional expression in older adults with dementia: a pilot randomized controlled trial. J Gerontol Nurs 2013;39:46-53. https://doi.org/10.3928/00989134-20130313-03.
- Moyle W, Beattie E, Draper B, Shum D, Thalib L, Jones C, et al. Effect of an interactive therapeutic robotic animal on engagement, mood states, agitation and psychotropic drug use in people with dementia: a cluster-randomised controlled trial protocol. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009097.
- Moyle W, Jones CJ, Murfield JE, Thalib L, Beattie ERA, Shum DKH, et al. Use of a robotic seal as a therapeutic tool to improve dementia symptoms: a cluster-randomized controlled trial. J Am Med Dir Assoc 2017;18:766-73. https://doi.org/10.1016/j.jamda.2017.03.018.
- Munyisia EN, Yu P, Hailey D. The impact of an electronic nursing documentation system on efficiency of documentation by caregivers in a residential aged care facility. J Clin Nurs 2012;21:2940-8. https://doi.org/10.1111/j.1365-2702.2012.04157.x.
- Munyisia EN, Yu P, Hailey D. Does the introduction of an electronic nursing documentation system in a nursing home reduce time on documentation for the nursing staff?. Int J Med Inform 2011;80:782-92. https://doi.org/10.1016/j.ijmedinf.2011.08.009.
- Munyisia EN, Yu P, Hailey D. Caregivers’ time utilization before and after the introduction of an electronic nursing documentation system in a residential aged care facility. Methods Inf Med 2013;52:403-10. https://doi.org/10.3414/ME12-01-0024.
- Murphy J, Tester S, Hubbard G, Downs M, MacDonald C. Enabling frail older people with a communication difficulty to express their views: the use of Talking Mats as an interview tool. Health Soc Care Community 2005;13:95-107. https://doi.org/10.1111/j.1365-2524.2005.00528.x.
- My Home Life . My Home Life: Digital Technology 2012. http://myhomelife.org.uk/wp-content/uploads/2014/11/mhl_bulletin_14.pdf (accessed 30 August 2017).
- Naganuma M, Ohkubo E, Kato N. Use of robotic pets in providing stimulation for nursing home residents with dementia. Stud Health Technol Inform 2015;217:1009-12.
- Nagayama H, Tomori K, Ohno K, Takahashi K, Ogahara K, Sawada T, et al. Effectiveness and cost-effectiveness of occupation-based occupational therapy using the Aid for Decision Making in Occupation Choice (ADOC) for older residents: pilot cluster randomized controlled trial. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0150374.
- Nakai H, Ishihara K, Miyake Y, Watanabe M. Non-Restrictive Visual Respiration Monitoring n.d.;4:647-51. https://doi.org/10.1109/ICPR.2000.903001.
- Namazi KH, McClintic M. Computer use among elderly persons in long-term care facilities. Educ Gerontol 2003;29:535-50. https://doi.org/10.1080/713844391.
- Niemeijer AR, Frederiks BJ, Depla MF, Legemaate J, Eefsting JA, Hertogh CM. The ideal application of surveillance technology in residential care for people with dementia. J Med Ethics 2011;37:303-10. https://doi.org/10.1136/jme.2010.040774.
- Niemeijer AR, Depla M, Frederiks B, Francke AL, Hertogh C. CE: Original research: the use of surveillance technology in residential facilities for people with dementia or intellectual disabilities: a study among nurses and support staff. Am J Nurs 2014;114:28-37. https://doi.org/10.1097/01.NAJ.0000457408.38222.d0.
- Niemeijer AR, Depla MF, Frederiks BJ, Hertogh CM. The experiences of people with dementia and intellectual disabilities with surveillance technologies in residential care. Nurs Ethics 2015;22:307-20. https://doi.org/10.1177/0969733014533237.
- Novek J, Bettess S, Burke K, Johnston P. Nurses’ perceptions of the reliability of an automated medication dispensing system. J Nurs Care Qual 2000;14:1-13. https://doi.org/10.1097/00001786-200001000-00003.
- Oliver DP, Demiris G, Hensel B. A promising technology to reduce social isolation of nursing home residents. J Nurs Care Qual 2006;21:302-5. https://doi.org/10.1097/00001786-200610000-00005.
- Oliver DP, Wittenberg-Lyles E, Demiris G, Oliver D. Giving long-term care residents a passport to the world with the internet. J Nurs Care Qual 2010;25:193-7. https://doi.org/10.1097/NCQ.0b013e3181d7964a.
- Pallawala PM, Lun KC. EMR-based TeleGeriatric system. Stud Health Technol Inform 2001;84:849-53. https://doi.org/10.1016/S1386-5056(01)00144-7.
- Park C, Kang S, Kim J, Oh J. A Study on Service Robot System for Elder Care n.d.:546-7. https://doi.org/10.1109/URAI.2012.6463070.
- Pillemer K, Meador R, Teresi JA, Henderson C. Health information technology evaluation in nursing homes: resident outcomes. Gerontologist 2009;49.
- Pillemer K, Meador RH, Teresi JA, Chen EK, Henderson CR, Lachs MS, et al. Effects of electronic health information technology implementation on nursing home resident outcomes. J Aging Health 2012;24:92-112. https://doi.org/10.1177/0898264311408899.
- Potts V, Earwicker T. Telehealth: monitoring residents in care homes. Practice Nursing 2011;22:602-6. https://doi.org/10.12968/pnur.2011.22.11.602.
- Qadri SS, Wang J, Ruiz JG, Roos BA. Personal digital assistants as point-of-care tools in long-term care facilities: a pilot study. Educ Gerontol 2009;35:294-305. https://doi.org/10.1080/03601270802467049.
- Qian S, Yu P, Hailey DM. The impact of electronic medication administration records in a residential aged care home. Int J Med Inform 2015;84:966-73. https://doi.org/10.1016/j.ijmedinf.2015.08.002.
- Rabinowitz T, Murphy KM, Amour JL, Ricci MA, Caputo MP, Newhouse PA. Benefits of a telepsychiatry consultation service for rural nursing home residents. Telemed J E Health 2010;16:34-40. https://doi.org/10.1089/tmj.2009.0088.
- Rantz MJ, Hicks L, Petroski GF, Madsen RW, Alexander G, Galambos C, et al. Cost, staffing and quality impact of bedside electronic medical record (EMR) in nursing homes. J Am Med Dir Assoc 2010;11:485-93. https://doi.org/10.1016/j.jamda.2009.11.010.
- Rantz MJ, Skubic M, Miller SJ, Galambos C, Alexander G, Keller J, et al. Sensor technology to support aging in place. J Am Med Dir Assoc 2013;14:386-91. https://doi.org/10.1016/j.jamda.2013.02.018.
- Rantz M, Lane K, Phillips LJ, Despins LA, Galambos C, Alexander GL, et al. Enhanced registered nurse care coordination with sensor technology: Impact on length of stay and cost in aging in place housing. Nurs Outlook 2015;63:650-5. https://doi.org/10.1016/j.outlook.2015.08.004.
- Rantz M, Phillips LJ, Galambos C, Lane K, Alexander GL, Despins L, et al. Randomized trial of intelligent sensor system for early illness alerts in senior housing. J Am Med Dir Assoc 2017;18:860-70. https://doi.org/10.1016/j.jamda.2017.05.012.
- Ratliff CR, Forch W. Telehealth for wound management in long-term care. Ostomy Wound Manage 2005;51:40-5.
- Remington L. Long-term and post-acute electronic health records (EHR) initiatives. Remington Report 2015;23:12-4.
- Richardson JE, Malhotra S, Kaushal R. HITEC Investigators . A case report in health information exchange for inter-organizational patient transfers. Appl Clin Inform 2014;5:642-50. https://doi.org/10.4338/ACI-2014-02-CR-0016.
- Robinson L, Hutchings D, Corner L, Finch T, Hughes J, Brittain K, et al. Balancing rights and risks: conflicting perspectives in the management of wandering in dementia. Health Risk Soc 2007;9:389-406. https://doi.org/10.1080/13698570701612774.
- Robinson H, MacDonald BA, Kerse N, Broadbent E. Suitability of healthcare robots for a dementia unit and suggested improvements. J Am Med Dir Assoc 2013;14:34-40. https://doi.org/10.1016/j.jamda.2012.09.006.
- Robinson H, Macdonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc 2013;14:661-7. https://doi.org/10.1016/j.jamda.2013.02.007.
- Robinson H, MacDonald B, Broadbent E. Physiological effects of a companion robot on blood pressure of older people in residential care facility: a pilot study. Australas J Ageing 2015;34:27-32. https://doi.org/10.1111/ajag.12099.
- Robinson H, Broadbent E, MacDonald B. Group sessions with PARO in a nursing home: structure, observations and interviews. Australas J Ageing 2016;35:106-12. https://doi.org/10.1111/ajag.12199.
- Rochon PA, Field TS, Bates DW, Lee M, Gavendo L, Erramuspe-Mainard J, et al. Clinical application of a computerized system for physician order entry with clinical decision support to prevent adverse drug events in long-term care. CMAJ 2006;174:52-4. https://doi.org/10.1503/cmaj.050099.
- Rosen J, Mulsant BH, Kollar M, Kastango KB, Mazumdar S, Fox D. Mental health training for nursing home staff using computer-based interactive video: a 6-month randomized trial. J Am Med Dir Assoc 2002;3:291-6. https://doi.org/10.1097/01.JAM.0000027201.90817.21.
- Rosen J, Mittal V, Mulsant BH, Degenholtz H, Castle N, Fox D. Educating the families of nursing home residents: a pilot study using a computer-based system. J Am Med Dir Assoc 2003;4:128-34. https://doi.org/10.1097/01.JAM.0000062035.91165.A0.
- Rudston S. Facing the future: touchscreen technology for residents. Nurs Resident Care 2013;15:555-7. https://doi.org/10.12968/nrec.2013.15.8.555.
- Russell K, Uddin Z, Maennle D. Telemedicine: one way to reduce Clostridium difficile infection in hospitals and long-term care facilities. Am J Clin Pathol 2015;144. https://doi.org/10.1093/ajcp/144.suppl2.183.
- Šabanović S, Bennett CC, Chang WL, Huber L. PARO robot affects diverse interaction modalities in group sensory therapy for older adults with dementia. IEEE Int Conf Rehabil Robot 2013;2013. https://doi.org/10.1109/ICORR.2013.6650427.
- Sabelli AM, Kanda T, Hagita N. A Conversational Robot in an Elderly Care Center: An Ethnographic Study n.d. https://doi.org/10.1145/1957656.1957669.
- Sanctuary Care . Harry’s Story: Using Technology to Keep in Touch 2016. www.sanctuary-care.co.uk/about-us/case-studies/residents-stories/harrys-story-using-technology-keep-touch.
- Sävenstedt S, Zingmark K, Sandman PO. Video-phone communication with cognitively impaired elderly patients. J Telemed Telecare 2003;9:52-4. https://doi.org/10.1258/135763303322596264.
- Sävenstedt S, Zingmark K, Sandman PO. Being present in a distant room: aspects of teleconsultations with older people in a nursing home. Qual Health Res 2004;14:1046-57. https://doi.org/10.1177/1049732304267754.
- Schneider R, Dorsey ER, Biglan K. Telemedicine care for nursing home residents with Parkinsonism. Mov Disord 2015;30.
- Shibata T, Wada K, Saito T, Tanie K, Wiederhold BK, Riva G. Annual Review of CyberTherapy and Telemedicine: Interactive Media in Training and Therapeutic Interventions. San Diego, CA: Interactive Media Institute; 2004.
- Sicurella T, Fitzsimmons V. Robotic pet therapy in long-term care. Nursing 2016;46:55-7. https://doi.org/10.1097/01.NURSE.0000482265.32133.f6.
- Silverman M, Lettier R, Moffitt L, Blondet R, Wiley V, Roos BA. A pilot study of the use of high technology sensors and nursing education to reduce falls in a large nursing home. J Am Geriatr Soc 2006;54.
- Smith AC, Caffery LJ, Saunders R, Bradford NK, Gray LC. Generating new telehealth services using a whole of community approach: experience in regional Queensland. J Telemed Telecare 2014;20:365-9. https://doi.org/10.1177/1357633X14552371.
- South East Health Technologies Alliance (SEHTA) . Technology and Innovation in Care Homes: The SEHTA Review 2016. https://sehta.co.uk/cms-data/depot/sehta/Technology-Innovation-in-Care-Homes-The-SEHTA-Review.pdf (accessed 30 August 2017).
- Specht JK, Wakefield B, Flanagan J. Evaluating the cost of one telehealth application connecting an acute and long-term care setting. J Gerontol Nurs 2001;27:34-9. https://doi.org/10.3928/0098-9134-20010101-11.
- Spiro RF, Saxton C. Electronic-prescribing: will long-term care be ready?. Consult Pharm 2005;20:651-4. https://doi.org/10.4140/TCP.n.2005.651.
- Stephens C, Halifax E, Bui N, Harrington C, Lee SJ, Ritchie C, et al. Stakeholder perspectives on the use of emerging health technologies to reduce nursing home resident ER transfers. J Am Geriatr Soc 2015;63:S178-S9.
- Sugihara T, Fujinami T, Jones R, Kadowaki K, Ando M. Enhancing care homes with assistive video technology for distributed caregiving. AI Soc 2015;30:509-18. https://doi.org/10.1007/s00146-014-0560-9.
- Sung HC, Chang SM, Chin MY, Lee WL. Robot-assisted therapy for improving social interactions and activity participation among institutionalized older adults: a pilot study. Asia Pac Psychiatry 2015;7:1-6. https://doi.org/10.1111/appy.12131.
- Tabar P. EHRs: progress or pileup. Long Term Living Contin Care Prof 2015;64:12-8.
- Tak SH, Beck C, McMahon E. Computer and internet access for long-term care residents: perceived benefits and barriers. J Gerontol Nurs 2007;33:32-40.
- Tak S. Cognitive exercise with computer games and activities among nursing home residents with dementia. Gerontologist 2008;48.
- Tak SH, Hong S. Therapeutic computer activity intervention for nursing home residents with dementia. Gerontologist 2012;52.
- Tak SH, Beck C, Hong SH. Feasibility of providing computer activities for nursing home residents with dementia. Nonpharmacol Ther Dement 2013;3:1-10.
- Tang WK, Chiu H, Woo J, Hjelm M, Hui E. Telepsychiatry in psychogeriatric service: a pilot study. Int J Geriatr Psychiatry 2001;16:88-93. https://doi.org/10.1002/1099-1166(200101)16:1<88::AID-GPS282>3.0.CO;2-W.
- Thorpe-Jamison PT, Culley CM, Perera S, Handler SM. Evaluating the impact of computer-generated rounding reports on physician workflow in the nursing home: a feasibility time-motion study. J Am Med Dir Assoc 2013;14:358-62. https://doi.org/10.1016/j.jamda.2012.11.008.
- Tinder Foundation . Health and Digital: Reducing Inequalities, Improving Society. An Evaluation of the Widening Digital Participation Programme 2016.
- Tiwari P, Warren J, Day K, MacDonald B, Jayawardena C, Kuo IH, et al. Feasibility Study of a Robotic Medication Assistant for the Elderly n.d.;117:57-66.
- Toh HJ, Chia J, Koh E, Lam K, Magpantay GC, De Leon CM, et al. Increased Engagement in Telegeriatrics Reduces Unnecessary Hospital Admissions of Nursing Home Residents n.d.;578:81-90. https://doi.org/10.1007/978-3-319-27695-3_5.
- Toh HJ, Chia J, Koh E, Lam K, Magpantay GC, De Leon CM, et al. Virtual Geriatric Care: User Perception of Telegeriatrics in Nursing Homes of Singapore n.d.;578:91-105. https://doi.org/10.1007/978-3-319-27695-3_6.
- Torres-Padrosa V, Calle E, Marzo JL, Rovira M. A Medicosocial Videoconferencing Tool for the Elderly, Impaired and Long-Term Care Patients n.d.;221:11-20. https://doi.org/10.1007/978-3-642-24352-3_2.
- Trinkle D. Geriatric psychiatry telemedicine consultation project to rural nursing homes in Virginia. Int Psychogeriatr 2003;15.
- Tseng KC, Hsu CL, Chuang YH. Designing an intelligent health monitoring system and exploring user acceptance for the elderly. J Med Syst 2013;37. https://doi.org/10.1007/s10916-013-9967-y.
- Van der Ploeg ES, Eppingstall B, O’Connor DW. Internet video chat (Skype) family conversations as a treatment of agitation in nursing home residents with dementia. Int Psychogeriatr 2016;28:697-8. https://doi.org/10.1017/S1041610215001854.
- Vandenberg AE, van Beijnum B, Capezuti EE, Overdevest VG, Johnson TM. Technology as a contributor to nursing home falls: findings from a cross-national site comparison. Gerontologist 2015;55. https://doi.org/10.1093/geront/gnv240.02.
- Vogelsmeier A, Scott-Cawiezell J, Zellmer D. Barriers to safe medication administration in the nursing home – exploring staff perceptions and concerns about the medication use process. J Gerontol Nurs 2007;33:5-12.
- Vowden K, Vowden P. A pilot study on the potential of remote support to enhance wound care for nursing-home patients. J Wound Care 2013;22:481-8. https://doi.org/10.12968/jowc.2013.22.9.481.
- Wagner L. New technologies enhance patient safety. Provider 2004;30.
- Wagner L. Telemedicine offers promise to long-term care. Provider 2001;27:28-9.
- Wakefield BJ, Buresh KA, Flanagan JR, Kienzle MG. Interactive video specialty consultations in long-term care. J Am Geriatr Soc 2004;52:789-93. https://doi.org/10.1111/j.1532-5415.2004.52220.x.
- Walker BL, Harrington SS, Cole CS. The usefulness of computer-based instruction in providing educational opportunities for nursing staff. J Nurses Staff Dev 2006;22:144-9. https://doi.org/10.1097/00124645-200605000-00009.
- Walker BL, Harrington SS. Computer-based instruction and the web for delivering injury prevention training. Educ Gerontol 2008;34:691-708. https://doi.org/10.1080/03601270802055778.
- Wang RH, Kontos PC, Holliday PJ, Fernie GR. The experiences of using an anti-collision power wheelchair for three long-term care home residents with mild cognitive impairment. Disabil Rehabil Assist Technol 2011;6:347-63. https://doi.org/10.3109/17483107.2010.519096.
- Webster G, Hanson VL. Technology for supporting care staff in residential homes. ACM Trans Access Comput 2014;5:1-23. https://doi.org/10.1145/2543577.
- Weiner M, Schadow G, Lindbergh D, Warvel J, Abernathy G, Perkins SM, et al. Conducting a study of internet-based video conferencing for assessing acute medical problems in a nursing facility. Proc AMIA Symp 2002:874-8.
- Weiner M, Schadow G, McDonald C. Camera on call: videoconferencing between nursing home residents and off-site clinicians. Am J Nurs 2004;104:44-5.
- Welsh PG, Durham C, Richards M. Innovations in North Carolina skilled nursing care: new uses of technology and approaches to the routines of care. N C Med J 2010;71:168-9.
- Wigg JM. Liberating the wanderers: using technology to unlock doors for those living with dementia. Sociol Health Illn 2010;32:288-303. https://doi.org/10.1111/j.1467-9566.2009.01221.x.
- Yu P, Qiu Y, Crookes P. Computer-based nursing documentation in nursing homes: a feasibility study. Stud Health Technol Inform 2006;122:570-4.
- Yu P, Yu H, Mu Y. The Acceptance of a Clinical IT Innovation by the Care Givers in Residential Aged Care 11-Weeks After the Software Implementation in Australia n.d.;115:6549-52. https://doi.org/10.1109/WICOM.2007.1607.
- Yu P, Zhang Y, Gong Y, Zhang J. Unintended adverse consequences of introducing electronic health records in residential aged care homes. Int J Med Inform 2013;82:772-88. https://doi.org/10.1016/j.ijmedinf.2013.05.008.
- Zelickson BD. Teledermatology in the nursing home. Curr Probl Dermatol 2003;32:167-71. https://doi.org/10.1159/000067357.
- Zhang Y, Yu P, Shen J. The benefits of introducing electronic health records in residential aged care facilities: a multiple case study. Int J Med Inform 2012;81:690-704. https://doi.org/10.1016/j.ijmedinf.2012.05.013.
- Zhang N, Lu SF, Xu B, Wu B, Rodriguez-Monguio R, Gurwitz J. Health information technologies: which nursing homes adopted them?. J Am Med Dir Assoc 2016;17:441-7. https://doi.org/10.1016/j.jamda.2016.02.028.
- Zhuang JP, Fang R, Feng X, Xu XH, Liu LH, Bai QK, et al. The impact of human-computer interaction-based comprehensive training on the cognitive functions of cognitive impairment elderly individuals in a nursing home. J Alzheimers Dis 2013;36:245-51. https://doi.org/10.3233/JAD-130158.
- Zwijsen S, te Boekhorst S, Hertogh C, Francke A. Assistive technology as an alternative to physical restraints in psychogeriatric nursing homes. J Clin Nurs 2010;19.
- Zwijsen SA, Depla MF, Niemeijer AR, Francke AL, Hertogh CM. Surveillance technology: an alternative to physical restraints? A qualitative study among professionals working in nursing homes for people with dementia. Int J Nurs Stud 2012;49:212-19. https://doi.org/10.1016/j.ijnurstu.2011.09.002.
- Petticrew M, Roberts H. Evidence, hierarchies, and typologies: horses for courses. J Epidemiol Community Health 2003;57:527-9. https://doi.org/10.1136/jech.57.7.527.
- Lapane KL, Hughes CM, Daiello LA, Cameron KA, Feinberg J. Effect of a pharmacist-led multicomponent intervention focusing on the medication monitoring phase to prevent potential adverse drug events in nursing homes. J Am Geriatr Soc 2011;59:1238-45. https://doi.org/10.1111/j.1532-5415.2011.03418.x.
- Holmes D, Teresi JA, Ramirez M, Ellis J, Eimicke J, Kong J, et al. An evaluation of a monitoring system intervention: falls, injuries, and affect in nursing homes. Clin Nurs Res 2007;16:317-35. https://doi.org/10.1177/1054773807307870.
- Kelly KE, Phillips CL, Cain KC, Polissar NL, Kelly PB. Evaluation of a nonintrusive monitor to reduce falls in nursing home patients. J Am Med Dir Assoc 2002;3:377-82. https://doi.org/10.1097/01.JAM.0000036702.12824.82.
- Keogh K. CQC says greater effort is needed to boost care sector’s workforce. Nurs Stand 2014;29. https://doi.org/10.7748/ns.29.8.9.s7.
- Cummings J, Mintzer J, Brodaty H, Sano M, Banerjee S, Devanand DP, et al. Agitation in cognitive disorders: International Psychogeriatric Association provisional consensus clinical and research definition. Int Psychogeriatr 2015;27:7-17. https://doi.org/10.1017/S1041610214001963.
- Greenhalgh T. How to Read a Paper: The Basics of Evidence-based Medicine. London: Wiley-Blackwell; 2014.
- Beck C, Gately KJ, Lubin S, Moody P, Beverly C. Building a state coalition for nursing home excellence. Gerontologist 2014;54:87-9. https://doi.org/10.1093/geront/gnt110.
- LaPorte M. Providers, surveyors join forces to achieve mutual goals. A look at some innovative approaches to boosting person-centered care. Provider 2014;40:20-6.
- Miller SC, Mor V. The opportunity for collaborative care provision: the presence of nursing home/hospice collaborations in the U.S. states. J Pain Symptom Manage 2004;28:537-47. https://doi.org/10.1016/j.jpainsymman.2004.10.007.
- Mort JR, Sailor R, Hintz L. Partnership to decrease antipsychotic medication use in nursing homes: impact at the state level. S D Med 2014;67:67-9.
- Cox R. Alverno Green Thumb Club grows strong community ties. Provider 1986;12.
- Troyer DR. Hillhaven’s Adopt-A-Resident program a sharing of hearts. J Am Health Care Assoc 1985;11.
- Agar M, Beattie E, Luckett T, Phillips J, Luscombe G, Goodall S, et al. Pragmatic cluster randomised controlled trial of facilitated family case conferencing compared with usual care for improving end of life care and outcomes in nursing home residents with advanced dementia and their families: the IDEAL study protocol. BMC Palliat Care 2015;14. https://doi.org/10.1186/s12904-015-0061-8.
- Alexander GL, Pasupathy KS, Steege LM, Strecker EB, Carley KM. Multi-disciplinary communication networks for skin risk assessment in nursing homes with high IT sophistication. Int J Med Inform 2014;83:581-91. https://doi.org/10.1016/j.ijmedinf.2014.05.001.
- Amador S, Goodman C, Mathie E, Nicholson C. Evaluation of an organisational intervention to promote integrated working between health services and care homes in the delivery of end-of-life care for people with dementia: understanding the change process using a social identity approach. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2426.
- American Medical Directors Association ad hoc Work Group on Role of the Attending Physician and Advanced Practice Nurse . Collaborative and supervisory relationships between attending physicians and advanced practice nurses in long-term care facilities. J Am Med Dir Assoc 2011;12:12-8. https://doi.org/10.1016/j.jamda.2010.08.003.
- Anderson KA, Dabelko-Schoeny HI. Civic engagement for nursing home residents: a call for social work action. J Gerontol Soc Work 2010;53:270-82. https://doi.org/10.1080/01634371003648323.
- Anonymous . Hospitals, SNFs Team Up to Improve Transitions 2011. www.ahcmedia.com/articles/132187-hospitals-snfs-team-up-to-improve-transitions (accessed 30 August 2017).
- Anonymous . Transition CMs Reduce Readmissions from SNFs 2013. www.ahcmedia.com/articles/64648-transition-cms-reduce-readmissions-from-snfs (accessed 30 August 2017).
- Anonymous . Hospitals, SNFs Team to Prevent Readmissions 2014. www.ahcmedia.com/articles/31331-hospitals-snfs-team-to-prevent-readmissions (accessed 30 August 2017).
- Anonymous . Tools Improve Communication With SNFs, Reduce Readmissions 2015. www.ahcmedia.com/articles/134863-tools?v=preview (accessed 30 August 2017).
- Anrys P, Strauven G, Boland B, Dalleur O, Declercq A, Degryse JM, et al. Collaborative approach to Optimise MEdication use for Older people in Nursing homes (COME-ON): study protocol of a cluster controlled trial. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0394-6.
- Arendts G, Etherton-Beer C, Howard K, Lewin G, Sim M, Pickstock S, et al. Nurse led care coordination: trial protocol and development of a best practice resource guide for a cluster controlled clinical trial in Australian aged care facilities. Arch Gerontol Geriatr 2014;58:15-9. https://doi.org/10.1016/j.archger.2013.07.004.
- Arling PA, Abrahamson K, Miech EJ, Inui TS, Arling G. Communication and effectiveness in a US nursing home quality-improvement collaborative. Nurs Health Sci 2014;16:291-7. https://doi.org/10.1111/nhs.12098.
- Badger F, Plumridge G, Hewison A, Shaw KL, Thomas K, Clifford C. An evaluation of the impact of the Gold Standards Framework on collaboration in end-of-life care in nursing homes. A qualitative and quantitative evaluation. Int J Nurs Stud 2012;49:586-95. https://doi.org/10.1016/j.ijnurstu.2011.10.021.
- Banda V, Guidry T, Beal L, Lacour M. Improving care transitions: standardizing discharge care plans from hospital to nursing home. J Am Med Dir Assoc 2015;16. https://doi.org/10.1016/j.jamda.2015.01.036.
- Baur VE, Abma TA, Widdershoven GA. Participation of marginalized groups in evaluation: mission impossible?. Eval Program Plann 2010;33:238-45. https://doi.org/10.1016/j.evalprogplan.2009.09.002.
- Bensadon BA, Rojido MC, Wolf D, Shutes J, Tappen RM, Ouslander JG. Barriers & approaches to implementing the interact quality improvement program. J Am Geriatr Soc 2014;62.
- Bokhour BG. Communication in interdisciplinary team meetings: what are we talking about?. J Interprof Care 2006;20:349-63. https://doi.org/10.1080/13561820600727205.
- Boockvar KS, Burack OR. Organizational relationships between nursing homes and hospitals and quality of care during hospital–nursing home patient transfers. J Am Geriatr Soc 2007;55:1078-84. https://doi.org/10.1111/j.1532-5415.2007.01235.x.
- Anonymous . Hospitals, SNFs team up to improve transitions. Hosp Case Manage 2011;19:157-8.
- Cadogan MP, Franzi C, Osterweil D, Hill T. Barriers to effective communication in skilled nursing facilities: differences in perception between nurses and physicians. J Am Geriatr Soc 1999;47:71-5. https://doi.org/10.1111/j.1532-5415.1999.tb01903.x.
- Cassidy EL, Rosen C, Cook J, Greenbaum MA, Chow H, Solano N, et al. Assessment to intervention: utilizing a staff needs assessment to improve care for behaviorally challenging residents in long term care (part I). Clin Gerontol 2005;28:29-42. https://doi.org/10.1300/J018v28n04_03.
- Catic AG, Mattison ML, Bakaev I, Morgan M, Monti SM, Lipsitz L. ECHO-AGE: an innovative model of geriatric care for long-term care residents with dementia and behavioral issues. J Am Med Dir Assoc 2014;15:938-42. https://doi.org/10.1016/j.jamda.2014.08.014.
- Colon-Emeric CS, McConnell E, Pinheiro SO, Corazzini K, Porter K, Earp KM, et al. CONNECT for better fall prevention in nursing homes: results from a pilot intervention study. J Am Geriatr Soc 2013;61:2150-9. https://doi.org/10.1111/jgs.12550.
- Conway J, Higgins I, Hullick C, Hewitt J, Dilworth S. Nurse-led ED support for residential aged care facility staff: an evaluation study. Int Emerg Nurs 2015;23:190-6. https://doi.org/10.1016/j.ienj.2014.11.005.
- Cortes TA, Wexler S, Fitzpatrick JJ. The transition of elderly patients between hospitals and nursing homes. Improving nurse-to-nurse communication. J Gerontol Nurs 2004;30:10-5. https://doi.org/10.3928/0098-9134-20040601-05.
- Cowley S, Ward L. Better communication within care home services. Nurs Times 2012;108.
- Crotty M, Halbert J, Rowett D, Giles L, Birks R, Williams H, et al. An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing 2004;33:612-17. https://doi.org/10.1093/ageing/afh213.
- Crotty M, Rowett D, Spurling L, Giles LC, Phillips PA. Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized, controlled trial. Am J Geriatr Pharmacother 2004;2:257-64. https://doi.org/10.1016/j.amjopharm.2005.01.001.
- Cwinn MA, Forster AJ, Cwinn AA, Hebert G, Calder L, Stiell IG. Prevalence of information gaps for seniors transferred from nursing homes to the emergency department. CJEM 2009;11:462-71. https://doi.org/10.1017/S1481803500011660.
- Dalawari P, Duggan J, Vangimalla V, Paniagua M, Armbrecht ES. Patient transfer forms enhance key information between nursing homes and emergency department. Geriatr Nurs 2011;32:270-5. https://doi.org/10.1016/j.gerinurse.2011.05.001.
- Davis MN, Brumfield VC, Smith ST, Tyler S, Nitschman J. A one-page nursing home to emergency room transfer form: what a difference it can make during an emergency!. Ann LongTerm Care 2005;13.
- Davies SL, Goodman C, Bunn F, Victor C, Dickinson A, Iliffe S, et al. A systematic review of integrated working between care homes and health care services. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-320.
- Dearing JW, Beacom AM, Chamberlain SA, Meng J, Berta WB, Keefe JM, et al. Pathways for best practice diffusion: the structure of informal relationships in Canada’s long-term care sector. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0542-7.
- Ellis J, Zorowitz R, Novotny J, Cheng H, Teresi J, Maurer MS. Communication between long term care facilities and an acute care hospital: the impact on transitional care. J Am Geriatr Soc 2006;54.
- Field TS, Tjia J, Mazor KM, Donovan JL, Kanaan AO, Harrold LR, et al. Randomized trial of a warfarin communication protocol for nursing homes: an SBAR-based approach. Am J Med 2011;124:179.e1-7. https://doi.org/10.1016/j.amjmed.2010.09.017.
- Fisch J, McNamara SE, Lansing BJ, Mody L. The 24-hour report as an effective monitoring and communication tool in infection prevention and control in nursing homes. Am J Infect Control 2014;42:1112-14. https://doi.org/10.1016/j.ajic.2014.07.001.
- Furman CD, Pirkle R, O’Brien JG, Miles T. Barriers to the implementation of palliative care in the nursing home. J Am Med Dir Assoc 2006;7:506-9. https://doi.org/10.1016/j.jamda.2006.07.008.
- Gillespie SM, Gleason LJ, Karuza J, Shah MN. Health care providers’ opinions on communication between nursing homes and emergency departments. J Am Med Dir Assoc 2010;11:204-10. https://doi.org/10.1016/j.jamda.2009.09.002.
- Gillespie SM, Panzer RJ, Shah MN, Katz PR. An interdisciplinary multi-site program to improve transitions of care between hospitals and nursing homes. J Am Geriatr Soc 2010;58.
- Gilmore-Bykovskyi AL, King BJ, Roil R, Bowers B, Roberts TJ, . Factors that impact the quality of hospital-to-skilled nursing facility transitions for persons with dementia: a qualitative study. Gerontologist 2013;53.
- Goodman C, Robb N, Drennan V, Woolley R. Partnership working by default: district nurses and care home staff providing care for older people. Health Soc Care Community 2005;13:553-62. https://doi.org/10.1111/j.1365-2524.2005.00587.x.
- Goodman C, Davies S, Leyshon S, Fader M, Norton C, Morris J, et al. Understanding Care Homes: A Research and Development Perspective. London: Jessica Kingsley Publishers; 2009.
- Goodman C, Davies SL, Norton C, Fader M, Morris J, Wells M, et al. Can district nurses and care home staff improve bowel care for older people using a clinical benchmarking tool?. Br J Community Nurs 2013;18:580-7. https://doi.org/10.12968/bjcn.2013.18.12.580.
- Griffiths D, Morphet J, Innes K, Crawford K, Williams A. Communication between residential aged care facilities and the emergency department: a review of the literature. Int J Nurs Stud 2014;51:1517-23. https://doi.org/10.1016/j.ijnurstu.2014.06.002.
- Hasson F, Kernohan WG, Waldron M, Whittaker E, McLaughlin D. The palliative care link nurse role in nursing homes: barriers and facilitators. J Adv Nurs 2008;64:233-42. https://doi.org/10.1111/j.1365-2648.2008.04803.x.
- Hearn L, Slack-Smith L. Oral health care in residential aged care services: barriers to engaging health-care providers. Aust J Prim Health 2015;21:148-56. https://doi.org/10.1071/PY14029.
- Heckman GA, Boscart VM, D’Elia T, Kelley ML, Kaasalainen S, McAiney CA, et al. Managing heart failure in long-term care: recommendations from an interprofessional stakeholder consultation. Can J Aging 2016;35:447-64. https://doi.org/10.1017/S071498081600043X.
- Hewison A, Badger F, Clifford C, Thomas K. Delivering ‘gold standards’ in end-of-life care in care homes: a question of teamwork?. J Clin Nurs 2009;18:1756-65. https://doi.org/10.1111/j.1365-2702.2008.02613.x.
- Hustey FM. Care transitions between nursing homes and emergency departments: a failure to communicate. Ann LongTerm Care 2010;18:17-9.
- Huynh S, Culler F, Gustafson D, Murray S. At the table: a communication network model for local public health, acute care, long-term care, and community partners. Am J Infect Control 2013;41:165-6. https://doi.org/10.1016/j.ajic.2012.02.019.
- Jarboe DE. The effect of evaluating a quality improvement initiative on reducing hospital transfers of nursing home residents. Dissert Doct Stud Coll 2015. https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=1282&context=dissertations (accessed 1 August 2018).
- Jones SA, Jarvis J, Powell P, Deaville J. Improving diabetes care for residents in care homes in a rural setting. FoNS: Devel Pract Improv Care Dissem Ser 2010;5:1-4.
- King BJ, Gilmore-Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJ. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc 2013;61:1095-102. https://doi.org/10.1111/jgs.12328.
- Kirsebom M, Wadensten B, Hedström M. Communication and coordination during transition of older persons between nursing homes and hospital still in need of improvement. J Adv Nurs 2013;69:886-95. https://doi.org/10.1111/j.1365-2648.2012.06077.x.
- Krol M, Allen C, Setji N, Shepherd T, English W, White H. Improving transitions for elders from the hospital to skilled nursing facilities through HOPE (Health Optimization Program for Elders). J Am Med Dir Assoc 2017;18. https://doi.org/10.1016/j.jamda.2016.12.042.
- LaMantia MA, Scheunemann LP, Viera AJ, Busby-Whitehead J, Hanson LC. Interventions to improve transitional care between nursing homes and hospitals: a systematic review. J Am Geriatr Soc 2010;58:777-82. https://doi.org/10.1111/j.1532-5415.2010.02776.x.
- Lea E, Andrews S, Haines T, Nitz J, Haralambous B, Moore K, et al. Developing networks between residential aged care facilities as a result of engagement in a falls prevention project: an action research study. Contemp Nurse 2016;52:163-75. https://doi.org/10.1080/10376178.2015.1129911.
- Longo DR, Young J, Mehr D, Lindbloom E, Salerno LD. Barriers to timely care of acute infections in nursing homes: a preliminary qualitative study. J Am Med Dir Assoc 2004;5:4-10. https://doi.org/10.1097/01.JAM.0000027250.76379.B2.
- Martz K, Gerding A. Perceptions of coordination of care between hospice and skilled nursing facility care providers. J Hosp Palliat Nurs 2011;13:210-21. https://doi.org/10.1097/NJH.0b013e3182135ddd.
- McGilton KS, Boscart V, Fox M, Sidani S, Rochon E, Sorin-Peters R. A systematic review of the effectiveness of communication interventions for health care providers caring for patients in residential care settings. Worldviews Evid Based Nurs 2009;6:149-59. https://doi.org/10.1111/j.1741-6787.2009.00155.x.
- Ouslander JG, Perloe M, Givens JH, Kluge L, Rutland T, Lamb G. Reducing potentially avoidable hospitalizations of nursing home residents: results of a pilot quality improvement project. J Am Med Dir Assoc 2009;10:644-52. https://doi.org/10.1016/j.jamda.2009.07.001.
- Ouslander JG, Lamb G, Tappen R, Herndon L, Diaz S, Roos BA, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc 2011;59:745-53. https://doi.org/10.1111/j.1532-5415.2011.03333.x.
- Ouslander JG, Bonner A, Herndon L, Shutes J. The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. J Am Med Dir Assoc 2014;15:162-70. https://doi.org/10.1016/j.jamda.2013.12.005.
- Ouslander JG, Naharci I, Engstrom G, Shutes J, Wolf DG, Alpert G, et al. Lessons learned from root cause analyses of transfers of skilled nursing facility (SNF) patients to acute hospitals: transfers rated as preventable versus nonpreventable by SNF staff. J Am Med Dir Assoc 2016;17:596-601. https://doi.org/10.1016/j.jamda.2016.02.014.
- Reed J, Stanley D. Improving communication between hospitals and care homes: the development of a daily living plan for older people. Health Soc Care Community 2003;11:356-63. https://doi.org/10.1046/j.1365-2524.2003.00436.x.
- Renz SM, Boltz MP, Wagner LM, Capezuti EA, Lawrence TE. Examining the feasibility and utility of an SBAR protocol in long-term care. Geriatr Nurs 2013;34:295-301. https://doi.org/10.1016/j.gerinurse.2013.04.010.
- Renz SM. Implementing an SBAR Communication Protocol: A Quality Improvement Project n.d.
- Renz SM, Carrington JM. Nurse–physician communication in long-term care literature review. J Gerontol Nurs 2016;42:30-7. https://doi.org/10.3928/00989134-20160615-04.
- Romøren M, Pedersen R, Førde R. One patient, two worlds – coordination between nursing home and hospital doctors. Tidsskr Nor Laegeforen 2017;137:193-7. https://doi.org/10.4045/tidsskr.16.0099.
- Sankaran S, Kenealy T, Adair A, Adair V, Coster H, Whitehead N, et al. A complex intervention to support ‘rest home’ care: a pilot study. N Z Med J 2010;123:41-53.
- Sutton E, Dixon-Woods M, Tarrant C. Ethnographic process evaluation of a quality improvement project to improve transitions of care for older people. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010988.
- Tabar P. The power of partnerships. Long Term Living Contin Care Prof 2013;62:10-3.
- Tena-Nelson R, Santos K, Weingast E, Amrhein S, Ouslander J, Boockvar K. Reducing potentially preventable hospital transfers: results from a thirty nursing home collaborative. J Am Med Dir Assoc 2012;13:651-6. https://doi.org/10.1016/j.jamda.2012.06.011.
- Terrell KM, Brizendine EJ, Bean WF, Giles BK, Davidson JR, Evers S, et al. An extended care facility-to-emergency department transfer form improves communication. Acad Emerg Med 2005;12:114-18. https://doi.org/10.1197/j.aem.2004.10.013.
- Tjia J, Mazor KM, Field T, Meterko V, Spenard A, Gurwitz JH. Nurse-physician communication in the long-term care setting: perceived barriers and impact on patient safety. J Patient Saf 2009;5:145-52. https://doi.org/10.1097/PTS.0b013e3181b53f9b.
- Tsakitzidis G, Timmermans O, Callewaert N, Verhoeven V, Lopez-Hartmann M, Truijen S, et al. Outcome indicators on interprofessional collaboration interventions for elderly. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2017.
- van Dongen JJ, van Bokhoven MA, Daniëls R, van der Weijden T, Emonts WW, Beurskens A. Developing interprofessional care plans in chronic care: a scoping review. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0535-7.
- Vogelsmeier A, Scott-Cawiezell J. Achieving quality improvement in the nursing home: influence of nursing leadership on communication and teamwork. J Nurs Care Qual 2011;26:236-42. https://doi.org/10.1097/NCQ.0b013e31820e15c0.
- Weiner M, Schadow G, Lindbergh D, Warvel J, Abernathy G, Dexter P, et al. Secure Internet video conferencing for assessing acute medical problems in a nursing facility. Proc AMIA Symp 2001:751-5.
- White H, Pavon J, Setji N, Shepherd T, Stilwagon M, O’Brien M, et al. Optimizing hospital to skilled nursing facility transitions. J Am Geriatr Soc 2015;63.
- Whitson HE, Hastings SN, Lekan DA, Sloane R, White HK, McConnell ES. A quality improvement program to enhance after-hours telephone communication between nurses and physicians in a long-term care facility. J Am Geriatr Soc 2008;56:1080-6. https://doi.org/10.1111/j.1532-5415.2008.01714.x.
- Wroth T. Linking primary care with adult care homes. N C Med J 2011;72:207-8.
- Yang C, Campbell J. Change management and partnership: achieving a solution to provide peritoneal dialysis in a long-term care setting. CANNT J 2009;19:29-33.
- Young Y, Barhydt NR, Broderick S, Colello AD, Hannan EL. Factors associated with potentially preventable hospitalization in nursing home residents in New York State: a survey of directors of nursing. J Am Geriatr Soc 2010;58:901-7. https://doi.org/10.1111/j.1532-5415.2010.02804.x.
- Zafirau WJ, Snyder SS, Hazelett SE, Bansal A, McMahon S. Improving transitions: efficacy of a transfer form to communicate patients’ wishes. Am J Med Qual 2012;27:291-6. https://doi.org/10.1177/1062860611427413.
- Brown HL, Bub L. Care transitions across the continuum: improving geriatric competence. Geriatr Nurs 2016;37:68-70. https://doi.org/10.1016/j.gerinurse.2015.12.005.
- Musante A. Two studies examine the triumphs and struggles of INTERACT for quality improvement. Ann LongTerm Care 2014;22:16-8.
- Field TS, Tjia J, Mazor KM, Donovan JL, Kanaan AO, Harrold LR, et al. A randomized trial of a warfarin management protocol to enhance communication between nursing home staff and physicians: the SBAR approach. Pharmacoepidemiol Drug Saf 2010;19:S132-3.
- Shin JH, Scherer Y. Advantages and disadvantages of using MDS data in nursing research. J Gerontol Nurs 2009;35:7-17. https://doi.org/10.3928/00989134-20090101-09.
- Poss JW, Jutan NM, Hirdes JP, Fries BE, Morris JN, Teare GF, et al. A review of evidence on the reliability and validity of minimum data set data. Healthc Manage Forum 2008;21:33-9. https://doi.org/10.1016/S0840-4704(10)60127-5.
- Shah SM, Carey IM, Harris T, Dewilde S, Cook DG. Quality of chronic disease care for older people in care homes and the community in a primary care pay for performance system: retrospective study. BMJ 2011;342. https://doi.org/10.1136/bmj.d912.
- Hanratty B, Stow D, Collingridge Moor D, Valtorta NK, Matthews FS. Loneliness as a risk factor for care home admission in the English Longitudinal Study of Ageing. Age and Ageing 2018;47:896-900.
- Nazir A, Unroe K, Tegeler M, Khan B, Azar J, Boustani M. Systematic review of interdisciplinary interventions in nursing homes. J Am Med Dir Assoc 2013;14:471-8. https://doi.org/10.1016/j.jamda.2013.02.005.
- You EC, Dunt DR, Doyle C. Case managed community aged care: what is the evidence for effects on service use and costs?. J Aging Health 2013;25:1204-42. https://doi.org/10.1177/0898264313499931.
- Zimmerman S, Anderson WL, Brode S, Jonas D, Lux L, Beeber AS, et al. Systematic review: Effective characteristics of nursing homes and other residential long-term care settings for people with dementia. J Am Geriatr Soc 2013;61:1399-409. https://doi.org/10.1111/jgs.12372.
- Alldred DP, Raynor DK, Hughes C, Barber N, Chen T, Spoor P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev 2013;2. https://doi.org/10.1002/14651858.CD009095.pub2.
- Plakiotis C, Bell JS, Jeon YH, Pond D, O’Connor DW. Deprescribing psychotropic medications in aged care facilities: the potential role of family members. Adv Exp Med Biol 2015;821:29-43. https://doi.org/10.1007/978-3-319-08939-3_8.
- Tjia J, Velten SJ, Parsons C, Valluri S, Briesacher BA. Studies to reduce unnecessary medication use in frail older adults: a systematic review. Drugs Aging 2013;30:285-307. https://doi.org/10.1007/s40266-013-0064-1.
- Weening-Dijksterhuis E, de Greef MH, Scherder EJ, Slaets JP, van der Schans CP. Frail institutionalized older persons: a comprehensive review on physical exercise, physical fitness, activities of daily living, and quality-of-life. Am J Phys Med Rehabil 2011;90:156-68. https://doi.org/10.1097/PHM.0b013e3181f703ef.
- Vlaeyen E, Coussement J, Leysens G, Van der Elst E, Delbaere K, Cambier D, et al. Characteristics and effectiveness of fall prevention programs in nursing homes: a systematic review and meta-analysis of randomized controlled trials. J Am Geriatr Soc 2015;63:211-21. https://doi.org/10.1111/jgs.13254.
- Hughes C, Smith M, Tunney M, Bradley MC. Infection control strategies for preventing the transmission of methicillin-resistant Staphylococcus aureus (MRSA) in nursing homes for older people. Cochrane Database Syst Rev 2011;12.
- Sjögren P, Nilsson E, Forsell M, Johansson O, Hoogstraate J. A systematic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc 2008;56:2124-30. https://doi.org/10.1111/j.1532-5415.2008.01926.x.
- Axelsson K, Ahrel K, Friström A, Hallgren L, Nydevik I. Pain among persons living at a nursing home. Nordic J Nurs Res 2000;20:20-3. https://doi.org/10.1177/010740830002000205.
- Bartoszek G, Fischer U, Müller M, Strobl R, Grill E, Nadolny S, et al. Outcome measures in older persons with acquired joint contractures: a systematic review and content analysis using the ICF (International Classification of Functioning, Disability and Health) as a reference. BMC Geriatr 2016;16. https://doi.org/10.1186/s12877-016-0213-6.
- Bettger JP, Sochalski JA, Foust JB, Zubritsky CD, Hirschman KB, Abbott KM, et al. Measuring nursing care time and tasks in long-term services and supports: one size does not fit all. J Nurs Res 2012;20:159-68. https://doi.org/10.1097/jnr.0b013e318263d977.
- Bowers B, Reinhard S. A standardized approach to identifying and measuring consumer determined quality outcomes in community based long term care. Gerontologist 2008;48:649-50.
- Bravo G, Dubois MF, Roy PM. Using goal attainment scaling to improve the quality of long-term care: a group-randomized trial. Int J Qual Health Care 2005;17:511-19. https://doi.org/10.1093/intqhc/mzi064.
- Brownie S, Nancarrow S. Effects of person-centered care on residents and staff in aged-care facilities: a systematic review. Clin Interv Aging 2013;8:1-10. https://doi.org/10.2147/CIA.S38589.
- Castle NG, Degenholtz H, Engberg J. State variability in indicators of quality of care in nursing facilities. J Gerontol A Biol Sci Med Sci 2005;60:1173-9. https://doi.org/10.1093/gerona/60.9.1173.
- Chenoweth L, Jeon YH. Determining the efficacy of dementia care mapping as an outcome measure and a process for change: a pilot study. Aging Ment Health 2007;11:237-45. https://doi.org/10.1080/13607860600844226.
- Chin L. An approach to improving the quality of life of residents living in aged care facilities: from the perspectives of the residents. Aust Occup Ther J 2011;58.
- Chiu Y, Lin W, Hsieh P, Li C, Chiou C. A survey to identify effective nutritional assessment indicators in long-term care facilities. J Evidence-Based Nurs 2005;1:112-22.
- Corradi JP, Chhabra J, Mather JF, Waszynski CM, Dicks RS. Analysis of multi-dimensional contemporaneous EHR data to refine delirium assessments. Comput Biol Med 2016;75:267-74. https://doi.org/10.1016/j.compbiomed.2016.06.013.
- Corazzini K, Jones K. Improving nursing home care: using case study methods for interdisciplinary research to improve quality. Gerontologist 2003;43.
- Crogan NL, Alvine C. Testing of the Individual Nutrition Rx assessment process among nursing home residents. Appl Nurs Res 2006;19:102-4. https://doi.org/10.1016/j.apnr.2005.10.003.
- Crogan NL, Alvine C, Pasvogel A. Improving nutrition care for nursing home residents using the INRx process. J Nutr Elder 2006;25:89-103. https://doi.org/10.1300/J052v25n03_07.
- Cutler LJ, Kane RA, Degenholtz HB, Miller MJ, Grant L. Assessing and comparing physical environments for nursing home residents: using new tools for greater research specificity. Gerontologist 2006;46:42-51. https://doi.org/10.1093/geront/46.1.42.
- Davis J, Morgans A, Burgess S. Information management for aged care provision in Australia: development of an aged care minimum dataset and strategies to improve quality and continuity of care. Health Inf Manag 2016;45:27-35. https://doi.org/10.1177/1833358316639453.
- Drouin H, Walker J, McNeil H, Elliott J, Stolee P. Measured outcomes of chronic care programs for older adults: a systematic review. BMC Geriatr 2015;15. https://doi.org/10.1186/s12877-015-0136-7.
- Edvardsson D, Katz B, Nay R. The aged care pain chart: an innovative approach to assessing, managing and documenting pain in older people. Australas J Ageing 2008;27:93-6. https://doi.org/10.1111/j.1741-6612.2008.00283.x.
- Fisher SE, Burgio LD, Thorn BE, Hardin JM. Obtaining self-report data from cognitively impaired elders: methodological issues and clinical implications for nursing home pain assessment. Gerontologist 2006;46:81-8. https://doi.org/10.1093/geront/46.1.81.
- Flores C, Newcomer R. Monitoring quality of care in residential care for the elderly: the information challenge. J Aging Soc Policy 2009;21:225-42. https://doi.org/10.1080/08959420902955735.
- Forsyth KA. Using the Minimum Data Set to Measure Change in Functional Status of Nursing Home Residents 2000.
- French DD, Werner DC, Campbell RR, Powell-Cope GM, Nelson AL, Rubenstein LZ, et al. A multivariate fall risk assessment model for VHA nursing homes using the minimum data set. J Am Med Dir Assoc 2007;8:115-22. https://doi.org/10.1016/j.jamda.2006.08.005.
- Froggatt K, Hockley J. Action research in palliative care: defining an evaluation methodology. Palliat Med 2011;25:782-7. https://doi.org/10.1177/0269216311420483.
- Graney MJ, Engle VF. Stability of performance of activities of daily living using the MDS. Gerontologist 2000;40:582-6. https://doi.org/10.1093/geront/40.5.582.
- Halfens RJ, Meesterberends E, van Nie-Visser NC, Lohrmann C, Schönherr S, Meijers JM, et al. International prevalence measurement of care problems: results. J Adv Nurs 2013;69:e5-17. https://doi.org/10.1111/jan.12189.
- Harrington C, O’Meara J, Collier E, Schnelle JF. Nursing indicators of quality in nursing homes. A web-based approach. J Gerontol Nurs 2003;29:5-11. https://doi.org/10.3928/0098-9134-20031001-04.
- Jones C, Sung B, Moyle W. Assessing engagement in people with dementia: a new approach to assessment using video analysis. Arch Psychiatr Nurs 2015;29:377-82. https://doi.org/10.1016/j.apnu.2015.06.019.
- Kapoor A, Kader B, Cabral H, Ash AS, Berlowitz D. Using the case mix of pressure ulcer healing to evaluate nursing home performance. Am J Med Qual 2008;23:342-9. https://doi.org/10.1177/1062860608316109.
- Kehinde JO, Pope C, Amella EJ. Methodological issues in fall prevention research involving older adults in long-term care facilities. Res Gerontol Nurs 2011;4:294-30. https://doi.org/10.3928/19404921-20110503-02.
- Kovach CR, Morgan S, Noonan PE, Brondino M. Using principles of diffusion of innovation to improve nursing home care. J Nurs Care Qual 2008;23:132-9. https://doi.org/10.1097/01.NCQ.0000313762.79396.ec.
- Lepore M. Multi-method assessment of person-centered care outcomes across long-term care settings. Gerontologist 2012;52.
- Levenson SA. The basis for improving and reforming long-term care. Part 4: identifying meaningful improvement approaches (segment 1). J Am Med Dir Assoc 2010;11:84-91. https://doi.org/10.1016/j.jamda.2009.11.009.
- Merilahti J, Viramo P, Korhonen I. Wearable monitoring of physical functioning and disability changes, circadian rhythms and sleep patterns in nursing home residents. IEEE J Biomed Health Inform 2016;20:856-64. https://doi.org/10.1109/JBHI.2015.2420680.
- Mor V, Intrator O, Unruh MA, Cai S. Temporal and geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-78.
- Mukamel DB, Spector WD, Zinn JS, Huang L, Weimer DL, Dozier A. Nursing homes’ response to the nursing home compare report card. J Gerontol B Psychol Sci Soc Sci 2007;62:S218-25. https://doi.org/10.1093/geronb/62.4.S218.
- O’Reilly M, Courtney M, Edwards H. How is quality being monitored in Australian residential aged care facilities? A narrative review. Int J Qual Health Care 2007;19:177-82. https://doi.org/10.1093/intqhc/mzm002.
- Peak T, Sinclair SV. Using customer satisfaction surveys to improve quality of care in nursing homes. Health Soc Work 2002;27:75-9. https://doi.org/10.1093/hsw/27.1.75.
- Port CL, Hebel JR, Gruber-Baldini AL, Baumgarten M, Burton L, Zimmerman S, et al. Measuring the frequency of contact between nursing home residents and their family and friends. Nurs Res 2003;52:52-6. https://doi.org/10.1097/00006199-200301000-00008.
- Reijula J, Rosendahl T, Reijula K, Roilas P, Roilas H, Sepponen R. A new method to assess perceived well-being among elderly people – a feasibility study. BMC Geriatr 2009;9. https://doi.org/10.1186/1471-2318-9-55.
- Rosen J, Mittal V, Degenholtz H, Castle N, Mulsant BH, Hulland S, et al. Ability, incentives, and management feedback: organizational change to reduce pressure ulcers in a nursing home. J Am Med Dir Assoc 2006;7:141-6. https://doi.org/10.1016/j.jamda.2005.08.003.
- Ryan J, Stone RI, Raynor CR. Using large data sets in long-term care to measure and improve quality. Nurs Outlook 2004;52:38-44. https://doi.org/10.1016/j.outlook.2003.11.001.
- Saivar SR. Veterans’ and Family Members’ Perceptions of Quality of Care in VA-Placed Community Nursing Homes 2004.
- Sales AE, Fraser K, Baylon MA, O’Rourke HM, Gao G, Bucknall T, et al. Understanding feedback report uptake: process evaluation findings from a 13-month feedback intervention in long-term care settings. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0208-2.
- Sangl J, Saliba D, Gifford DR, Hittle DF. Challenges in measuring nursing home and home health quality: lessons from the First National Healthcare Quality Report. Med Care 2005;43:I24-32. https://doi.org/10.1097/00005650-200503001-00005.
- Schnelle JF, Bates-Jensen BM, Levy-Storms L, Grbic V, Yoshii J, Cadogan M, et al. The minimum data set prevalence of restraint quality indicator: does it reflect differences in care?. Gerontologist 2004;44:245-55. https://doi.org/10.1093/geront/44.2.245.
- Schnelle JF, Osterweil D, Simmons SF. Improving the quality of nursing home care and medical-record accuracy with direct observational technologies. Gerontologist 2005;45:576-82. https://doi.org/10.1093/geront/45.5.576.
- Shier V, Khodyakov D, Cohen LW, Zimmerman S, Saliba D. What does the evidence really say about culture change in nursing homes?. Gerontologist 2014;54:6-16. https://doi.org/10.1093/geront/gnt147.
- Simmons SF, Reuben D. Nutritional intake monitoring for nursing home residents: a comparison of staff documentation, direct observation, and photography methods. J Am Geriatr Soc 2000;48:209-13. https://doi.org/10.1111/j.1532-5415.2000.tb03914.x.
- Stevenson DG, Mor V. Targeting nursing homes under the Quality Improvement Organization program’s 9th statement of work. J Am Geriatr Soc 2009;57:1678-84. https://doi.org/10.1111/j.1532-5415.2009.02401.x.
- Swafford KL, Miller LL, Tsai PF, Herr KA, Ersek M. Improving the process of pain care in nursing homes: a literature synthesis. J Am Geriatr Soc 2009;57:1080-7. https://doi.org/10.1111/j.1532-5415.2009.02274.x.
- Thompson GN, Chochinov HM. Methodological challenges in measuring quality care at the end of life in the long-term care environment. J Pain Symptom Manage 2006;32:378-91. https://doi.org/10.1016/j.jpainsymman.2006.05.014.
- Tolson D, Rolland Y, Katz PR, Woo J, Morley JE, Vellas B. An international survey of nursing homes. J Am Med Dir Assoc 2013;14:459-62. https://doi.org/10.1016/j.jamda.2013.04.005.
- Van Camp CM, Lerman DC, Cherry KE, Bielecki J. A methodology for evaluating the relationship between staff attention and disruptive behavior displayed by nursing home residents with dementia. Clin Gerontol 2005;29:11-25. https://doi.org/10.1300/J018v29n01_02.
- Wagner LM, Capezuti E, Clark PC, Parmelee PA, Ouslander JG. Use of a falls incident reporting system to improve care process documentation in nursing homes. Qual Saf Health Care 2008;17:104-8. https://doi.org/10.1136/qshc.2007.022947.
- Wan TT. Nursing care quality in nursing homes: cross-sectional versus longitudinal analysis. J Med Syst 2003;27:283-95. https://doi.org/10.1023/A:1022579512926.
- Werner RM, Konetzka RT, Stuart EA, Norton EC, Polsky D, Park J. Impact of public reporting on quality of postacute care. Health Serv Res 2009;44:1169-87. https://doi.org/10.1111/j.1475-6773.2009.00967.x.
- Winters S, Kool RB, Klazinga NS, Huijsman R. The influence of corporate structure and quality improvement activities on outcome improvement in residential care homes. Int J Qual Health Care 2014;26:378-87. https://doi.org/10.1093/intqhc/mzu057.
- Woitha K, Hasselaar J, van Beek K, Ahmed N, Jaspers B, Hendriks JC, et al. Testing feasibility and reliability of a set of quality indicators to evaluate the organization of palliative care across Europe: a pilot study in 25 countries. Palliat Med 2015;29:157-63. https://doi.org/10.1177/0269216314562100.
- Worden A, Challis D. Assessing care home quality using routine regulatory information. Qual Ageing 2006;7:33-44. https://doi.org/10.1108/14717794200600018.
- Wu N, Mor V, Roy J. Resident, nursing home, and state factors affecting the reliability of minimum data set quality measures. Am J Med Qual 2009;24:229-40. https://doi.org/10.1177/1062860609332510.
- Xholi C, O’Toole R, Nicholas C. An interdisciplinary approach to improved outcomes for an aged care unit. Australas J Ageing 2004;23.
- Yeager VA, Menachemi N, Savage GT, Ginter PM, Sen BP, Beitsch LM. Using resource dependency theory to measure the environment in health care organizational studies: a systematic review of the literature. Health Care Manage Rev 2014;39:50-65. https://doi.org/10.1097/HMR.0b013e3182826624.
- Yeh SH, Lin LW, Lo SK. A longitudinal evaluation of nursing home care quality in Taiwan. J Nurs Care Qual 2003;18:209-16. https://doi.org/10.1097/00001786-200307000-00007.
- Zhang NJ, Paek SC, Wan TT. Reliability estimates of clinical measures between minimum data set and online survey certification and reporting data of US nursing homes. Med Care 2009;47:492-5. https://doi.org/10.1097/MLR.0b013e31818c014b.
- Dutta R, Hooper J, Dutta D. Use of the MMRI-R prognostic tool for older patients discharged to nursing homes from hospital: a prospective cohort study. Age Ageing 2015;44:673-6. https://doi.org/10.1093/ageing/afv012.
- Faulkner M, Davies S, Nolan M, Brown-Wilson C. Development of the combined assessment of residential environments (CARE) profiles. J Adv Nurs 2006;55:664-77. https://doi.org/10.1111/j.1365-2648.2006.03967.x.
- Fossey J, Lee L, Ballard C. Dementia care mapping as a research tool for measuring quality of life in care settings: psychometric properties. Int J Geriatr Psychiatry 2002;17:1064-70. https://doi.org/10.1002/gps.708.
- Moniz-Cook E, Woods R, Gardiner E, Silver M, Agar S. The Challenging Behaviour Scale (CBS): development of a scale for staff caring for older people in residential and nursing homes. Br J Clin Psychol 2001;40:309-22. https://doi.org/10.1348/014466501163715.
- Sutcliffe C, Cordingley L, Burns A, Mozley CG, Bagley H, Huxley P, et al. A new version of the geriatric depression scale for nursing and residential home populations: the geriatric depression scale (residential) (GDS-12R). Int Psychogeriatr 2000;12:173-81. https://doi.org/10.1017/S104161020000630X.
- Towers AM, Holder J, Smith N, Crowther T, Netten A, Welch E, et al. Adapting the adult social care outcomes toolkit (ASCOT) for use in care home quality monitoring: conceptual development and testing. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0942-9.
- Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol 2010;10. https://doi.org/10.1186/1471-2288-10-22.
- Porock D, Parker-Oliver D, Petroski GF, Rantz M. The MDS Mortality Risk Index: The evolution of a method for predicting 6-month mortality in nursing home residents. BMC Res Notes 2010;3. https://doi.org/10.1186/1756-0500-3-200.
- Faulkner M. A measure of patient empowerment in hospital environments catering for older people. J Adv Nurs 2001;34:676-86. https://doi.org/10.1046/j.1365-2648.2001.01797.x.
- Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess 2003;80:99-103. https://doi.org/10.1207/S15327752JPA8001_18.
- Brooker D, Abou-Saleh MT, Katona C, Kumar A. Principles and Practice of Geriatric Psychiatry. Oxford: Wiley-Blackwell; 2011.
- Kitwood T. Brain, mind and dementia: with particular reference to Alzheimer’s disease. Ageing Soc 1989;9:1-15. https://doi.org/10.1017/S0144686X00013337.
- Bland M. An Introduction to Medical Statistics. Oxford: Oxford University Press; 2015.
- Blau TH. Quality of life, social indicators, and criteria of change. Prof Psychol 1977;8. https://doi.org/10.1037/0735-7028.8.4.464.
- Harding SD. Psychological well-being in Great Britain: an evaluation of the Bradburn affect balance scale. Pers Individ Dif 1982;3:167-75. https://doi.org/10.1016/0191-8869(82)90031-9.
- Smith N, Towers A, Razik K. Adult Social Care Outcomes Toolkit (ASCOT) SCT4 Guidance. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- Challis D, Clarkson P. Performance Indicators in Social Care for Older People. Abingdon: Routledge; 2006.
- Hoffman F, Maas F, Rodrigues R, Bruckmüller A, Gross S, Kattnigg A, et al. Measuring Progress, Indicators for Care Homes 2013. http://myhomelife.org.uk/wp-content/uploads/2015/02/EU-Report-on-Quality-Indicators-in-Care-Homes.pdf (accessed 30 August 2017).
- National Institute for Health and Care Excellence (NICE) . Oral Health for Adults in Care Homes 2016. www.nice.org.uk/guidance/ng48 (accessed 30 August 2017).
- Spilsbury K, Hanratty B, McCaughan D. Supporting Nursing in Care Homes: Project Report for the RCN Foundation 2015. www.rcnfoundation.org.uk/?a=620718&now=1429088648 (accessed 30 August 2017).
- Dellefield ME, Castle NG, McGilton KS, Spilsbury K. The relationship between registered nurses and nursing home quality: an integrative review (2008–2014). Nurs Econ 2015;33:95-108.
- Lerner NB, Johantgen M, Trinkoff AM, Storr CL, Han K. Are nursing home survey deficiencies higher in facilities with greater staff turnover. J Am Med Dir Assoc 2014;15:102-7. https://doi.org/10.1016/j.jamda.2013.09.003.
- Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. Int J Nurs Stud 2011;48:732-50. https://doi.org/10.1016/j.ijnurstu.2011.02.014.
- Trinkoff AM, Han K, Storr CL, Lerner N, Johantgen M, Gartrell K. Turnover, staffing, skill mix, and resident outcomes in a national sample of US nursing homes. J Nurs Adm 2013;43:630-6. https://doi.org/10.1097/NNA.0000000000000004.
- Abraham J, Grant LA. Leadership competencies and employee satisfaction in nursing homes. Seniors Hous Care J 2008;16:11-23.
- Abrahamson K, Lewis T, Perkins A, Clark D, Nazir A, Arling G. The influence of cognitive impairment, special care unit placement, and nursing facility characteristics on resident quality of life. J Aging Health 2013;25:574-88. https://doi.org/10.1177/0898264313480240.
- Adams-Wendling L. The Relationship Between Nurse Staffing and Quality in Nursing Facilities 2005.
- Akinci F, Krolikowski D. Nurse staffing levels and quality of care in Northeastern Pennsylvania nursing homes. Appl Nurs Res 2005;18:130-7. https://doi.org/10.1016/j.apnr.2004.08.004.
- Alexander GL. An analysis of nursing home quality measures and staffing. Qual Manag Health Care 2008;17:242-51. https://doi.org/10.1097/01.QMH.0000326729.78331.c5.
- Alzheimer’s Society . Home from Home: A Report Highlighting Opportunities for Improving Standards of Dementia Care in Care Homes 2007.
- Anderson RA, Corazzini KN, McDaniel RR. Complexity science and the dynamics of climate and communication: reducing nursing home turnover. Gerontologist 2004;44:378-88. https://doi.org/10.1093/geront/44.3.378.
- André B, Sjøvold E, Rannestad T, Ringdal GI. The impact of work culture on quality of care in nursing homes – a review study. Scand J Caring Sci 2014;28:449-57. https://doi.org/10.1111/scs.12086.
- Anonymous . Staffing Levels in Aged Care Below Ministry Guidelines 2005. www.highbeam.com/doc/1G1-138396446.html (accessed 30 August 2017).
- Anonymous . Staffing Level Mix Affects Quality of Care in Nursing Homes 2009. https://archive.ahrq.gov/news/newsletters/research-activities/mar09/0309RA8.html (accessed 30 August 2017).
- Anonymous . Case managers emerge as focal point of unique team. Hosp Case Manag 2001;9:173-6.
- Anonymous . Adequate Staffing Helps Ensure Patients in Nursing Homes Receive Proper Treatment for Pneumonia: Research Activities, April 2009 2009. https://archive.ahrq.gov/news/newsletters/research-activities/apr09/0409RA15.html (accessed 30 August 2017).
- Arling G, Kane RL, Mueller C, Bershadsky J, Degenholtz HB. Nursing effort and quality of care for nursing home residents. Gerontologist 2007;47:672-82. https://doi.org/10.1093/geront/47.5.672.
- Atkins MA. Staff Turnover in Long-Term Care: An Intervention Study in a Group of Care Homes 2010.
- Backhaus R, van Rossum E, Verbeek H, Halfens RJ, Tan F, Capezuti EE, et al. Relationship between RN staffing and quality of care in Dutch long-term care facilities. Gerontologist 2015;55.
- Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JP. Nurse staffing impact on quality of care in nursing homes: a systematic review of longitudinal studies. J Am Med Dir Assoc 2014;15:383-93. https://doi.org/10.1016/j.jamda.2013.12.080.
- Banaszak-Holl J, Castle NG, Lin MK, Shrivastwa N, Spreitzer G. The role of organizational culture in retaining nursing workforce. Gerontologist 2015;55:462-71. https://doi.org/10.1093/geront/gnt129.
- Bates-Jensen BM, Schnelle JF, Alessi CA, Al-Samarrai NR, Levy-Storms L. The effects of staffing on in-bed times of nursing home residents. J Am Geriatr Soc 2004;52:931-8. https://doi.org/10.1111/j.1532-5415.2004.52260.x.
- Berta W, Laporte A, Deber R, Baumann A, Gamble B. The evolving role of health care aides in the long-term care and home and community care sectors in Canada. Hum Resour Health 2013;11. https://doi.org/10.1186/1478-4491-11-25.
- Blekken LE, Vinsnes AG, Gjeilo KH, Mørkved S, Salvesen Ø, Norton C, et al. Effect of a multifaceted educational program for care staff concerning fecal incontinence in nursing home patients: study protocol of a cluster randomized controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0595-3.
- Blinkhorn F, Weingarten L, Boivin L, Plain J, Kay M. An intervention to improve the oral health of residents in an aged care facility led by nurses. Health Educ J 2012;71:527-35. https://doi.org/10.1177/0017896911412127.
- Boorsma M, Frijters DH, Knol DL, Ribbe ME, Nijpels G, van Hout HP. Effects of multidisciplinary integrated care on quality of care in residential care facilities for elderly people: a cluster randomized trial. CMAJ 2011;183:E724-32. https://doi.org/10.1503/cmaj.101498.
- Bostick JE. Relationship of nursing personnel and nursing home care quality. J Nurs Care Qual 2004;19:130-6. https://doi.org/10.1097/00001786-200404000-00010.
- Bostick JE. The Relationship of Nursing Personnel and Nursing Home Care Quality 2002.
- Bostick JE, Rantz MJ, Flesner MK, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. J Am Med Dir Assoc 2006;7:366-76. https://doi.org/10.1016/j.jamda.2006.01.024.
- Boumans NP, Berkhout AJ, Vijgen SM, Nijhuis FJ, Vasse RM. The effects of integrated care on quality of work in nursing homes: a quasi-experiment. Int J Nurs Stud 2008;45:1122-36. https://doi.org/10.1016/j.ijnurstu.2007.09.001.
- Bowblis JR. Staffing ratios and quality: an analysis of minimum direct care staffing requirements for nursing homes. Health Serv Res 2011;46:1495-516. https://doi.org/10.1111/j.1475-6773.2011.01274.x.
- Bowers BJ, Esmond S, Jacobson N. The relationship between staffing and quality in long-term care facilities: exploring the views of nurse aides. J Nurs Care Qual 2000;14:55-64. https://doi.org/10.1097/00001786-200007000-00009.
- Brown Wilson CR. Exploring Relationships in Care Homes: A Constructivist Inquiry 2007.
- Brown PB, Hudak SL, Horn SD, Cohen LW, Reed DA, Zimmerman S. THRIVE Research Collaborative . Workforce characteristics, perceptions, stress, and satisfaction among staff in Green House and other nursing homes. Health Serv Res 2016;51:418-32. https://doi.org/10.1111/1475-6773.12431.
- Brulhart MI, Wermeille JP. Multidisciplinary medication review: evaluation of a pharmaceutical care model for nursing homes. Int J Clin Pharm 2011;33:549-57. https://doi.org/10.1007/s11096-011-9506-1.
- Buettner LL. Evidence to support an advanced role for recreational therapists: staff trainer in long term care. Am J Recreat Ther 2009;8:29-34.
- Bunn D, Jimoh F, Wilsher SH, Hooper L. Increasing fluid intake and reducing dehydration risk in older people living in long-term care: a systematic review. J Am Med Dir Assoc 2015;16:101-13. https://doi.org/10.1016/j.jamda.2014.10.016.
- Burgio LD, Fisher SE, Fairchild JK, Scilley K, Hardin JM. Quality of care in the nursing home: effects of staff assignment and work shift. Gerontologist 2004;44:368-77. https://doi.org/10.1093/geront/44.3.368.
- The Health Services Marketing Group Ltd . Improving End-Of-Life Care in California’s Nursing Homes 2008. https://chcf.org/wp-content/uploads/2017/12/PDF-EOLCareNursingHomes.pdf (accessed 1 August 2018).
- Harrington C, O’Meara J, Kang T. Snapshot: Staffing and Quality in California’s Nursing Homes. Oakland, CA: California Healthcare Foundation; 2006.
- Carrier N, West GE, Ouellet D. Dining experience, foodservices and staffing are associated with quality of life in elderly nursing home residents. J Nutr Health Aging 2009;13:565-70. https://doi.org/10.1007/s12603-009-0108-8.
- Carter MW, Porell FW. Variations in hospitalization rates among nursing home residents: the role of facility and market attributes. Gerontologist 2003;43:175-91. https://doi.org/10.1093/geront/43.2.175.
- Cassie KM, Cassie WE. Organizational and individual conditions associated with depressive symptoms among nursing home residents over time. Gerontologist 2012;52:812-21. https://doi.org/10.1093/geront/gns059.
- Castle NG, Ferguson-Rome JC. Influence of nurse aide absenteeism on nursing home quality. Gerontologist 2015;55:605-15. https://doi.org/10.1093/geront/gnt167.
- Castle N. Changes in staff-mix and quality in nursing homes. Gerontologist 2014;54.
- Castle NG, Anderson RA. Caregiver staffing in nursing homes and their influence on quality of care: using dynamic panel estimation methods. Med Care 2011;49:545-52. https://doi.org/10.1097/MLR.0b013e31820fbca9.
- Castle N. Nursing home deficiency citations for abuse. J Appl Gerontol 2011;30:719-43. https://doi.org/10.1177/0733464810378262.
- Castle NG. Differences in nursing homes with increasing and decreasing use of physical restraints. Med Care 2000;38:1154-63. https://doi.org/10.1097/00005650-200012000-00002.
- Castle NG, Engberg J. Further examination of the influence of caregiver staffing levels on nursing home quality. Gerontologist 2008;48:464-76. https://doi.org/10.1093/geront/48.4.464.
- Castle NG, Engberg J, Aiju M. Nurse aide agency staffing and quality of care in nursing homes. Med Care Res Rev 2008;65:232-52. https://doi.org/10.1177/1077558707312494.
- Castle NG, Engberg J. The influence of staffing characteristics on quality of care in nursing homes. Health Serv Res 2007;42:1822-47. https://doi.org/10.1111/j.1475-6773.2007.00704.x.
- Castle NG. Reviewing the evidence base for nurse staffing and quality of care in nursing homes. Evid Based Nurs 2012;15:23-4. https://doi.org/10.1136/ebn.2011.100186.
- Castle NG. Nursing home caregiver staffing levels and quality of care – a literature review. J Appl Gerontol 2008;27:375-40. https://doi.org/10.1177/0733464808321596.
- Castle NG. The influence of consistent assignment on nursing home deficiency citations. Gerontologist 2011;51:750-60. https://doi.org/10.1093/geront/gnr068.
- Castle NG, Lin M. Top management turnover and quality in nursing homes. Health Care Manage Rev 2010;35:161-74. https://doi.org/10.1097/HMR.0b013e3181c22bcb.
- Castle NG. State differences and facility differences in nursing home staff turnover. J Appl Gerontol 2008;27:609-30. https://doi.org/10.1177/0733464808319711.
- Castle NG, Engberg J, Men A. Nursing home staff turnover: impact on nursing home compare quality measures. Gerontologist 2007;47:650-61. https://doi.org/10.1093/geront/47.5.650.
- Castle NG. Measuring staff turnover in nursing homes. Gerontologist 2006;46:210-19. https://doi.org/10.1093/geront/46.2.210.
- Castle NG. Administrator turnover and quality of care in nursing homes. Gerontologist 2001;41:757-67. https://doi.org/10.1093/geront/41.6.757.
- Castle NG, Engberg J. Organizational characteristics associated with staff turnover in nursing homes. Gerontologist 2006;46:62-73. https://doi.org/10.1093/geront/46.1.62.
- Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Med Care 2005;43:616-26. https://doi.org/10.1097/01.mlr.0000163661.67170.b9.
- Chang CC, Wykle ML, Madigan EA. The effect of a feeding skills training program for nursing assistants who feed dementia patients in Taiwanese nursing homes. Geriatr Nurs 2006;27:229-37. https://doi.org/10.1016/j.gerinurse.2006.03.007.
- Chang CC, Lin LC. Effects of a feeding skills training programme on nursing assistants and dementia patients. J Clin Nurs 2005;14:1185-92. https://doi.org/10.1111/j.1365-2702.2005.01240.x.
- Chapman DG, Toseland RW. Effectiveness of advanced illness care teams for nursing home residents with dementia. Soc Work 2007;52:321-9. https://doi.org/10.1093/sw/52.4.321.
- Chen MM, Grabowski DC. Intended and unintended consequences of minimum staffing standards for nursing homes. Health Econ 2015;24:822-39. https://doi.org/10.1002/hec.3063.
- Cherubini A, Eusebi P, Dell’Aquila G, Landi F, Gasperini B, Bacuccoli R, et al. Predictors of hospitalization in Italian nursing home residents: the U.L.I.S.S.E. project. J Am Med Dir Assoc 2012;13:84.e5-10. https://doi.org/10.1016/j.jamda.2011.04.001.
- Chipantiza NI. A Quantitative Analysis of Nurse Staffing Skill Mix to Quality of Care in Nursing Homes 2014.
- Choi J, Flynn L, Aiken LH. Nursing practice environment and registered nurses’ job satisfaction in nursing homes. Gerontologist 2012;52:484-92. https://doi.org/10.1093/geront/gnr101.
- Chou SC, Boldy DP, Lee AH. Factors influencing residents’ satisfaction in residential aged care. Gerontologist 2003;43:459-72. https://doi.org/10.1093/geront/43.4.459.
- Chou SC, Boldy DP, Lee AH. Staff satisfaction and its components in residential aged care. Int J Qual Health Care 2002;14:207-17. https://doi.org/10.1093/oxfordjournals.intqhc.a002612.
- Chu CH, Wodchis WP, McGilton KS. Turnover of regulated nurses in long-term care facilities. J Nurs Manag 2014;22:553-62. https://doi.org/10.1111/jonm.12031.
- Clare L, Whitaker R, Woods RT, Quinn C, Jelley H, Hoare Z, et al. AwareCare: a pilot randomized controlled trial of an awareness-based staff training intervention to improve quality of life for residents with severe dementia in long-term care settings. Int Psychogeriatr 2013;25:128-39. https://doi.org/10.1017/S1041610212001226.
- Collier EJ. Quality of Care &Amp; California Nursing Homes: The Effects of Staffing, Organizational, Resident and Market Characteristics 2008.
- Collier E, Harrington C. Staffing characteristics, turnover rates, and quality of resident care in nursing facilities. Res Gerontol Nurs 2008;1:157-70. https://doi.org/10.3928/00220124-20091301-03.
- Comondore VR, Devereaux PJ, Zhou Q, Stone SB, Busse JW, Ravindran NC, et al. Quality of care in for-profit and not-for-profit nursing homes: systematic review and meta-analysis. BMJ 2009;339. https://doi.org/10.1136/bmj.b2732.
- Corazzini KN, Anderson RA, Mueller C, Thorpe JM, McConnell ES. Licensed practical nurse scope of practice and quality of nursing home care. Nurs Res 2013;62:315-24. https://doi.org/10.1097/NNR.0b013e31829eba00.
- Care Quality Commission (CQC) . Time to Listen in Care Homes: Dignity and Nutrition Inspection Programme 2012 2013. www.cqc.org.uk/sites/default/files/documents/time_to_listen_-_care_homes_main_report_tag.pdf (accessed 30 August 2017).
- Crickard KB. A West Virginia Nursing Facility Structure and Its Effects on Quality Outcomes 2005.
- de Jonge J, Gevers J, Dollard M. Managing employee creativity and health in nursing homes: the moderating role of matching job resources and matching occupational rewards. Int J Stress Manag 2014;21:361-83. https://doi.org/10.1037/a0038149.
- Decker FH. The relationship of nursing staff to the hospitalization of nursing home residents. Res Nurs Health 2008;31:238-51. https://doi.org/10.1002/nur.20249.
- Dellefield ME. The relationship between nurse staffing in nursing homes and quality indicators. J Gerontol Nurs 2000;26:14-28. https://doi.org/10.3928/0098-9134-20000601-05.
- Dhaini S, Zúñiga F, Ausserhofer D, Simon M, Kunz R, De Geest S, et al. Absenteeism and presenteeism among care workers in Swiss nursing homes and their association with psychosocial work environment: a multi-site cross-sectional study. Gerontology 2016;62:386-95. https://doi.org/10.1159/000442088.
- Dill JS, Morgan JC, Marshall VW, Pruchno R. Contingency, employment intentions, and retention of vulnerable low-wage workers: an examination of nursing assistants in nursing homes. Gerontologist 2013;53:222-34. https://doi.org/10.1093/geront/gns085.
- Dixon S, Kaambwa B, Nancarrow S, Martin GP, Bryan S. The relationship between staff skill mix, costs and outcomes in intermediate care services. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-221.
- Donoghue C, Castle NG. Organizational and environmental effects on voluntary and involuntary turnover. Health Care Manage Rev 2007;32:360-9. https://doi.org/10.1097/01.HMR.0000296791.16257.44.
- Donoghue C. Nursing home staff turnover and retention: an analysis of national level data. J Appl Gerontol 2010;29:89-106. https://doi.org/10.1177/0733464809334899.
- Dwyer D. Experiences of registered nurses as managers and leaders in residential aged care facilities: a systematic review. Int J Evid Based Healthc 2011;9:388-402. https://doi.org/10.1111/j.1744-1609.2011.00239.x.
- Dwyer R, Stoelwinder J, Gabbe B, Lowthian J. Unplanned transfer to emergency departments for frail elderly residents of aged care facilities: a review of patient and organizational factors. J Am Med Dir Assoc 2015;16:551-62. https://doi.org/10.1016/j.jamda.2015.03.007.
- Dyck MJ. Nursing staffing and resident outcomes in nursing homes: weight loss and dehydration. J Nurs Care Qual 2007;22:59-65. https://doi.org/10.1097/00001786-200701000-00012.
- Dyck MJ. Nursing Staffing and Resident Outcomes in Nursing Homes 2004.
- Eckstrom E, Neal MB, Cotrell V, Casey CM, McKenzie G, Morgove MW, et al. An interprofessional approach to reducing the risk of falls through enhanced collaborative practice. J Am Geriatr Soc 2016;64:1701-7. https://doi.org/10.1111/jgs.14178.
- Ersek M, Sefcik JS, Lin FC, Lee TJ, Gilliam R, Hanson LC. Provider staffing effect on a decision aid intervention. Clin Nurs Res 2014;23:36-53. https://doi.org/10.1177/1054773812470840.
- Eyers IA. Meeting the Needs of Older People? A Comparative Study of Care Home Staff in England and Germany 2003.
- Figueiredo D, Barbosa A, Cruz J, Marques A, Sousa L. Empowering staff in dementia long-term care: towards a more supportive approach to interventions. Educ Gerontol 2013;39:413-27. https://doi.org/10.1080/03601277.2012.701105.
- Finnema E, Dröes RM, Ettema T, Ooms M, Adèr H, Ribbe M, et al. The effect of integrated emotion-oriented care versus usual care on elderly persons with dementia in the nursing home and on nursing assistants: a randomized clinical trial. Int J Geriatr Psychiatry 2005;20:330-43. https://doi.org/10.1002/gps.1286.
- Fitzler S, Raia P, Buckley FO, Wang M. Does nursing facility use of habilitation therapy improve performance on quality measures?. Am J Alzheimers Dis Other Demen 2016;20. https://doi.org/10.1177/1533317516662335.
- Freeman IC. Assuring safety for people with dementia in long-term care facilities: a focus on staffing. J Ethics Law Aging 2003;9:107-24.
- Gao F, Newcombe P, Tilse C, Wilson J, Tuckett A. Models for predicting turnover of residential aged care nurses: a structural equation modelling analysis of secondary data. Int J Nurs Stud 2014;51:1258-70. https://doi.org/10.1016/j.ijnurstu.2014.01.011.
- Sandoval Garrido FA, Tamiya N, Kashiwagi M, Miyata S, Okochi J, Moriyama Y, et al. Relationship between structural characteristics and outcome quality indicators at health care facilities for the elderly requiring long-term care in Japan from a nationwide survey. Geriatr Gerontol Int 2014;14:301-8. https://doi.org/10.1111/ggi.12098.
- Gloth FM, Gloth MJ. A comparative effectiveness trial between a post-acute care hospitalist model and a community-based physician model of nursing home care. J Am Med Dir Assoc 2011;12:384-6. https://doi.org/10.1016/j.jamda.2010.11.010.
- Goldberg SL. Keys to retaining staff: the Jewish home & hospital experience. Nursing Homes: Long Term Care Management 2000;49:24-68.
- Gorski MS. Quality of Care in Nursing Homes: The Relationship Between State Level Health Care Policy and Selected Quality Measures 2004.
- Goyder J, Orrell M, Wenborn J, Spector A. Staff training using STAR: a pilot study in UK care homes. Int Psychogeriatr 2012;24:911-20. https://doi.org/10.1017/S1041610211002559.
- Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev 2008;65:3-39. https://doi.org/10.1177/1077558707308754.
- Gray-Siracusa K. Acuity-Based Staffing in Long Term Care: Does It Influence Quality? 2005.
- Halcomb EJ. Feasibility and sustainability of a model of multidisciplinary case conferencing in residential aged care. Aust J Prim Health 2009;15:238-43. https://doi.org/10.1071/PY08073.
- Harahan MF, Sanders A, Stone RI, Bowers BJ, Nolet KA, Krause MR, et al. Implementation and evaluation of LVN LEAD. A leadership and supervisory training program for nursing home charge nurses. J Gerontol Nurs 2011;37:26-33. https://doi.org/10.3928/00989134-20110302-01.
- Harden JT, Burger SG. They are called nursing homes for a reason: RN staffing in long-term care facilities. J Gerontol Nurs 2015;41:15-20. https://doi.org/10.3928/00989134-20151116-01.
- Harrington C, Schnelle JF, McGregor M, Simmons SF. The need for higher minimum staffing standards in U.S. nursing homes. Health Serv Insights 2016;9:13-9. https://doi.org/10.4137/HSI.S38994.
- Harrington C, Swan JH. Nursing home staffing, turnover, and case mix. Med Care Res Rev 2003;60:366-92. https://doi.org/10.1177/1077558703254692.
- Harrington C, Olney B, Carrillo H, Kang T. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Serv Res 2012;47:106-28. https://doi.org/10.1111/j.1475-6773.2011.01311.x.
- Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing home staffing and its relationship to deficiencies. J Gerontol B Psychol Sci Soc Sci 2000;55:S278-87. https://doi.org/10.1093/geronb/55.5.S278.
- Harvath TA, Swafford K, Smith K, Miller LL, Volpin M, Sexson K, et al. Enhancing nursing leadership in long-term care. A review of the literature. Res Gerontol Nurs 2008;1:187-96. https://doi.org/10.3928/00220124-20091301-06.
- Havig AK, Skogstad A, Kjekshus LE, Romøren TI. Leadership, staffing and quality of care in nursing homes. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-327.
- Havig AK, Skogstad A, Romoren T, Kjekshus L. Staffing and quality of care in Norwegian nursing homes. Gerontologist 2014;54.
- Heath H. How to optimise the registered nurse contribution in care homes. Nurs Older People 2012;24:23-8. https://doi.org/10.7748/nop2012.03.24.2.23.c8954.
- Hedrick SC, Guihan M, Chapko MK, Sullivan J, Zhou XH, Manheim LM, et al. Assisted living pilot program: health outcomes. J Aging Health 2009;21:190-207. https://doi.org/10.1177/0898264308328929.
- Heeren P, Van de Water G, De Paepe L, Boonen S, Vleugels A, Milisen K. Staffing levels and the use of physical restraints in nursing homes: a multicenter study. J Gerontol Nurs 2014;40:48-54. https://doi.org/10.3928/00989134-20140407-03.
- Hegeman CR. Turnover turnaround. Health Prog 2005;86:25-30.
- Help the Aged . My Home Life: Quality of Life in Care Homes. A Review of the Literature 2007. www.scie.org.uk/publications/guides/guide15/files/myhomelife.pdf (accessed 30 August 2017).
- Hendrix TJ, Foreman SE. Optimal long-term care nurse-staffing levels. Nurs Econ 2001;19:164-75.
- Hendrix TJ. Optimal Nursing Home Staffing 2000.
- Heponiemi T, Elovainio M, Kouvonen A, Kuusio H, Noro A, Finne-Soveri H, et al. The effects of ownership, staffing level and organisational justice on nurse commitment, involvement, and satisfaction: a questionnaire study. Int J Nurs Stud 2011;48:1551-61. https://doi.org/10.1016/j.ijnurstu.2011.05.015.
- Hickey EC, Young GJ, Parker VA, Czarnowski EJ, Saliba D, Berlowitz DR. The effects of changes in nursing home staffing on pressure ulcer rates. J Am Med Dir Assoc 2005;6:50-3. https://doi.org/10.1016/j.jamda.2004.12.003.
- Hodgkinson B, Haesler EJ, Nay R, O’Donnell MH, McAuliffe LP. Effectiveness of staffing models in residential, subacute, extended aged care settings on patient and staff outcomes. Cochrane Database Syst Rev 2011;6. https://doi.org/10.1002/14651858.CD006563.pub2.
- Hofmann MT, Bankes PF, Javed A, Selhat M. Decreasing the incidence of falls in the nursing home in a cost-conscious environment: a pilot study. J Am Med Dir Assoc 2003;4:95-7. https://doi.org/10.1097/01.JAM.0000052517.44062.8A.
- Hollingsworth EK, Long EA, Simmons SF. Comparison between quality of care provided by trained feeding assistants and certified nursing assistants during between-meal supplementation in long-term care settings. J Appl Gerontol 2016;22. https://doi.org/10.1177/0733464816669806.
- Horn SD, Buerhaus P, Bergstrom N, Smout RJ. RN staffing time and outcomes of long-stay nursing home residents: pressure ulcers and other adverse outcomes are less likely as RNs spend more time on direct patient care. Am J Nurs 2005;105:58-70. https://doi.org/10.1097/00000446-200511000-00028.
- Horn SD, Sharkey SS, Hudak S, Smout RJ, Quinn CC, Yody B, et al. Beyond CMS quality measure adjustments: identifying key resident and nursing home facility factors associated with quality measures. J Am Med Dir Assoc 2010;11:500-5. https://doi.org/10.1016/j.jamda.2009.10.008.
- Hovey SL, Kim M, Dyck MJ. Hospital Readmission rates following skills training for nurses employed in long-term care facilities. J Nurs Care Qual 2015;30:380-4. https://doi.org/10.1097/NCQ.0000000000000117.
- Hunt SR, Corazzini K, Anderson RA. Top nurse-management staffing collapse and care quality in nursing homes. J Appl Gerontol 2014;33:51-74. https://doi.org/10.1177/0733464812455096.
- Hutt E, Radcliff TA, Liebrecht D, Fish R, McNulty M, Kramer AM. Associations among nurse and certified nursing assistant hours per resident per day and adherence to guidelines for treating nursing home-acquired pneumonia. J Gerontol A Biol Sci Med Sci 2008;63:1105-11. https://doi.org/10.1093/gerona/63.10.1105.
- Hutt E, Frederickson E, Ecord M, Kramer AM. Associations among processes and outcomes of care for Medicare nursing home residents with acute heart failure. J Am Med Dir Assoc 2003;4:195-9. https://doi.org/10.1097/01.JAM.0000073964.19754.C0.
- Hyde P, Burns D, Killett A, Kenkmann A, Poland F, Gray R. Organisational aspects of elder mistreatment in long term care. Qual Ageing Older Adults 2014;15:197-209. https://doi.org/10.1108/QAOA-06-2014-0010.
- Hyer K, Thomas KS, Johnson CE, Harman JS, Weech-Maldonado R. Do Medicaid incentive payments boost quality? Florida’s direct care staffing adjustment program. J Aging Soc Policy 2013;25:65-82. https://doi.org/10.1080/08959420.2012.705629.
- Ikegami N, Ikezaki S. Nursing homes and end-of-life care in Japan. J Am Med Dir Assoc 2013;14:718-23. https://doi.org/10.1016/j.jamda.2013.02.008.
- Intrator O, Minca E, Lima JC, Wetle T. Medical staff organization and rehospitalizations: hospital-based versus free-standing nursing homes. Gerontologist 2011;51.
- Irvine AB, Beaty JA, Seeley JR, Bourgeois M. Use of a dementia training designed for nurse aides to train other staff. J Appl Gerontol 2013;32:936-51. https://doi.org/10.1177/0733464812446021.
- Jette DU, Warren RL, Wirtalla C. Rehabilitation in skilled nursing facilities: effect of nursing staff level and therapy intensity on outcomes. Am J Phys Med Rehabil 2004;83:704-12. https://doi.org/10.1097/01.PHM.0000137312.06545.D0.
- Jogerst GJ, Daly JM, Hartz AJ. State policies and nursing home characteristics associated with rates of resident mistreatment. J Am Med Dir Assoc 2008;9:648-56. https://doi.org/10.1016/j.jamda.2008.05.005.
- Shanti C, Johnson J, Meyers AM, Jones GR, Fitzgerald C, Lazowski DA, et al. Evaluation of the restorative care education and training program for nursing homes. Can J Aging 2005;24:115-26. https://doi.org/10.1353/cja.2005.0065.
- Jordan F, Byrne G, Bushell A. Improving mental health in residential aged care facilities through staff training and resident’s interventions. Australas J Ageing 2009;28.
- Kajonius PJ, Kazemi A. Structure and process quality as predictors of satisfaction with elderly care. Health Soc Care Community 2016;24:699-707. https://doi.org/10.1111/hsc.12230.
- Kang D. The Effects of Resident Ethnic Mix, Staffing Patterns, and Medicaid Census on Quality of Care and Quality of Life in New York State Nursing Homes 2008.
- Karsh B, Booske BC, Sainfort F. Job and organizational determinants of nursing home employee commitment, job satisfaction and intent to turnover. Ergonomics 2005;48:1260-81. https://doi.org/10.1080/00140130500197195.
- Kash BA, Naufal GS, Cortes L, Johnson CE. Exploring factors associated with turnover among registered nurse (RN) supervisors in nursing homes. J Appl Gerontol 2010;29:107-27. https://doi.org/10.1177/0733464809335243.
- Kash BA, Castle NG, Naufal GS, Hawes C. Effect of staff turnover on staffing: a closer look at registered nurses, licensed vocational nurses, and certified nursing assistants. Gerontologist 2006;46:609-19. https://doi.org/10.1093/geront/46.5.609.
- Katz PR, Karuza J, Lima J, Intrator O. Nursing home medical staff organization: correlates with quality indicators. J Am Med Dir Assoc 2011;12:655-9. https://doi.org/10.1016/j.jamda.2010.06.004.
- Katz PR, Karuza J, Intrator O, Mor V. Nursing home physician specialists: a response to the workforce crisis in long-term care. Ann Intern Med 2009;150:411-13. https://doi.org/10.7326/0003-4819-150-6-200903170-00010.
- Kayser-Jones J, Schell E, Lyons W, Kris AE, Chan J, Beard RL. Factors that influence end-of-life care in nursing homes: the physical environment, inadequate staffing, and lack of supervision. Gerontologist 2003;43:76-84. https://doi.org/10.1093/geront/43.suppl_2.76.
- Kayser-Jones J, Kris AE, Lim KC, Walent RJ, Halifax E, Paul SM. Pressure ulcers among terminally ill nursing home residents. Res Gerontol Nurs 2008;1:14-2. https://doi.org/10.3928/19404921-20080101-06.
- Kayyali A. The impact of turnover in nursing homes. Am J Nurs 2014;114:69-70. https://doi.org/10.1097/01.NAJ.0000453762.61882.82.
- Kerr D, Cunningham C, Wilkinson H. Supporting Older People in Care Homes at Night. York: Joseph Rowntree Foundation; 2008.
- Killett A, Hyde P, Burns D, Gray R, Poland F. How organizational factors interact to influence the quality of care of older people in the care home sector. J Health Serv Res Policy 2013;18:14-22. https://doi.org/10.1177/1355819613476016.
- Kim H. A Longitudinal Study of the Relationship Between Nurse Staffing and Quality of Care in Nursing Homes 2006.
- Kim H, Harrington C, Greene WH. Registered nurse staffing mix and quality of care in nursing homes: a longitudinal analysis. Gerontologist 2009;49:81-90. https://doi.org/10.1093/geront/gnp014.
- Kim H, Kovner C, Harrington C, Greene W, Mezey M. A panel data analysis of the relationships of nursing home staffing levels and standards to regulatory deficiencies. J Gerontol B Psychol Sci Soc Sci 2009;64:269-78. https://doi.org/10.1093/geronb/gbn019.
- King MA, Roberts MS. Multidisciplinary case conference reviews: improving outcomes for nursing home residents, carers and health professionals. Pharm World Sci 2001;23:41-5. https://doi.org/10.1023/A:1011215008000.
- Kinjerski V, Skrypnek BJ. The promise of spirit at work: increasing job satisfaction and organizational commitment and reducing turnover and absenteeism in long-term care. J Gerontol Nurs 2008;34:17-25. https://doi.org/10.3928/00989134-20081001-03.
- Kirkevold Ø, Engedal K. Quality of care in Norwegian nursing homes – deficiencies and their correlates. Scand J Caring Sci 2008;22:560-7. https://doi.org/10.1111/j.1471-6712.2007.00575.x.
- Kirkevold O, Engedal K. The quality of care in Norwegian nursing homes. Scand J Caring Sci 2006;20:177-83. https://doi.org/10.1111/j.1471-6712.2006.00396.x.
- Kirkevold O, Sandvik L, Engedal K. Use of constraints and their correlates in Norwegian nursing homes. Int J Geriatr Psychiatry 2004;19:980-8. https://doi.org/10.1002/gps.1197.
- Klay M, Marfyak K. Use of a continence nurse specialist in an extended care facility. Urol Nurs 2005;25:101-2.
- Klitch BA. Survey survival. Staffing to avoid deficiencies. Nurs Homes Long Term Care Manage 2000;49:14-114.
- Konetzka RT, Stearns SC, Park J. The staffing-outcomes relationship in nursing homes. Health Serv Res 2008;43:1025-42. https://doi.org/10.1111/j.1475-6773.2007.00803.x.
- Konetzka RT, Stearns SC, Konrad TR, Magaziner J, Zimmerman S. Personal care aide turnover in residential care settings: an assessment of ownership, economic, and environmental factors. J Appl Gerontol 2005;24:87-107. https://doi.org/10.1177/0733464804270854.
- Kovner C, Mezey M, Harrington C. Research priorities for staffing, case mix, and quality of care in U.S. nursing homes. J Nurs Scholarsh 2000;32:77-80. https://doi.org/10.1111/j.1547-5069.2000.00077.x.
- Kovner C. The impact of staffing and the organization of work on patient outcomes and health care workers in health care organizations. Jt Comm J Qual Improv 2001;27:458-68. https://doi.org/10.1016/S1070-3241(01)27040-0.
- Kovner CT, Harrington C. Nursing counts. Quality of care linked to nurse staffing levels. Am J Nurs 2000;100. https://doi.org/10.1097/00000446-200009000-00041.
- Kramer RG. Of costs and caregivers. Analyzing the impact of staffing recommendations. Contemp Longterm Care 2002;25.
- Krichbaum KE, Pearson V, Hanscom J. Better care in nursing homes: advanced practice nurses’ strategies for improving staff use of protocols. Clin Nurse Spec 2000;14:40-6. https://doi.org/10.1097/00002800-200001000-00014.
- Kris A. Influence of staffing levels on pressure ulcer management in nursing homes. Gerontologist 2009;49.
- Kris A, Kayser-Jones J. Staffing and symptom management in nursing homes. Gerontologist 2004;44.
- Krueger P, Brazil K, Lohfeld L, Edward HG, Lewis D, Tjam E. Organization specific predictors of job satisfaction: findings from a Canadian multi-site quality of work life cross-sectional survey. BMC Health Serv Res 2002;2. https://doi.org/10.1186/1472-6963-2-6.
- Kuo HT, Yin TJ, Li IC. Relationship between organizational empowerment and job satisfaction perceived by nursing assistants at long-term care facilities. J Clin Nurs 2008;17:3059-66. https://doi.org/10.1111/j.1365-2702.2007.02072.x.
- Laakso S, Routasalo P. Changing to primary nursing in a nursing home in Finland: experiences of residents, their family members and nurses. J Adv Nurs 2001;33:475-83. https://doi.org/10.1046/j.1365-2648.2001.01687.x.
- Laging B, Ford R, Bauer M, Nay R. A meta-synthesis of factors influencing nursing home staff decisions to transfer residents to hospital. J Adv Nurs 2015;71:2224-36. https://doi.org/10.1111/jan.12652.
- Landreville P, Dicaire L, Verreault R, Lévesque L. A training program for managing agitation of residents in long-term care facilities: description and preliminary findings. J Gerontol Nurs 2005;31:34-42. https://doi.org/10.3928/0098-9134-20050301-08.
- Lange JW, Mager D, Greiner PA, Saracino K. The ELDER Project: educational model and three-year outcomes of a community-based geriatric education initiative. Gerontol Geriatr Educ 2011;32:164-81. https://doi.org/10.1080/02701960.2011.572056.
- Lapane KL, Hughes CM. Considering the employee point of view: perceptions of job satisfaction and stress among nursing staff in nursing homes. J Am Med Dir Assoc 2007;8:8-13. https://doi.org/10.1016/j.jamda.2006.05.010.
- Lapane KL, Hughes CM. Which organizational characteristics are associated with increased management of depression using antidepressants in US nursing homes?. Med Care 2004;42:992-1000. https://doi.org/10.1097/00005650-200410000-00008.
- Lapane KL, Hughes CM, Christian JB, Daiello LA, Cameron KA, Feinberg J. Evaluation of the fleetwood model of long-term care pharmacy. J Am Med Dir Assoc 2011;12:355-63. https://doi.org/10.1016/j.jamda.2010.03.003.
- LaPorte M. Nurse practitioners given hands-on role. Provider 2007;33:24-5.
- Lee HY, Blegen MA, Harrington C. The effects of RN staffing hours on nursing home quality: a two-stage model. Int J Nurs Stud 2014;51:409-17. https://doi.org/10.1016/j.ijnurstu.2013.10.007.
- Lee HY. Quality of Care: Impact of Nursing Home Characteristics 2009.
- Lee CL, Liu TL, Wu LJ, Chung UL, Lee LC. Cost and care quality between licensed nursing homes under different types of ownership. J Nurs Res 2002;10:151-60. https://doi.org/10.1097/01.JNR.0000347594.28520.61.
- Leland NE, Gozalo P, Teno J, Mor V. Falls in newly admitted nursing home residents: a national study. J Am Geriatr Soc 2012;60:939-45. https://doi.org/10.1111/j.1532-5415.2012.03931.x.
- Lerner NB. The relationship between nursing staff levels, skill mix, and deficiencies in Maryland nursing homes. Health Care Manag 2013;32:123-8. https://doi.org/10.1097/HCM.0b013e31828ef5f9.
- Lewis T, Arling G, Mueller C. Staff perceptions of involvement and self-value in nursing homes: does position matter?. Gerontologist 2004;44.
- Li Y, Harrington C, Mukamel DB, Cen X, Cai X, Temkin-Greener H. Nurse staffing hours at nursing homes with high concentrations of minority residents, 2001–11. Health Aff 2015;34:2129-37. https://doi.org/10.1377/hlthaff.2015.0422.
- Lin H. Revisiting the relationship between nurse staffing and quality of care in nursing homes: an instrumental variables approach. J Health Econ 2014;37:13-24. https://doi.org/10.1016/j.jhealeco.2014.04.007.
- Lisk R, Yeong K, Nasim A, Baxter M, Mandal B, Nari R, et al. Geriatrician input into nursing homes reduces emergency hospital admissions. Arch Gerontol Geriatr 2012;55:331-7. https://doi.org/10.1016/j.archger.2011.10.014.
- Liu LF, Liu WP, Wang JY. Work autonomy of certified nursing assistants in long-term care facilities: discrepant perceptions between nursing supervisors and certified nursing assistants. J Am Med Dir Assoc 2011;12:524-34. https://doi.org/10.1016/j.jamda.2010.05.006.
- Lucas R, Atkinson C, Godden J. Nursing Homes, Residential Homes and Domicilliary Care Establishments. A Research Project Conducted for Skills For Care 2009. www.skillsforcare.org.uk/Document-library/NMDS-SC,-workforce-intelligence-and-innovation/Research/Research-Reports/Rewards-and-incentives/Rewards-and-Incentives-Phase-2-CaseStudies.pdf (accessed 30 August 2017).
- Lucas JA, Levin CA, Lowe TJ, Robertson B, Akincigil A, Sambamoorthi U, et al. The relationship between organizational factors and resident satisfaction with nursing home care and life. J Aging Soc Policy 2007;19:125-51. https://doi.org/10.1300/J031v19n02_07.
- Maas ML, Specht JP, Buckwalter KC, Gittler J, Bechen K. Nursing home staffing and training recommendations for promoting older adults’ quality of care and life: part 1. Deficits in the quality of care due to understaffing and undertraining. Res Gerontol Nurs 2008;1:123-33. https://doi.org/10.3928/19404921-20080401-03.
- MacEntee MI, Wyatt CC, Beattie BL, Paterson B, Levy-Milne R, McCandless L, et al. Provision of mouth-care in long-term care facilities: an educational trial. Community Dent Oral Epidemiol 2007;35:25-34. https://doi.org/10.1111/j.1600-0528.2007.00318.x.
- Manitoba Nurses’ Union . Long Term Care in Manitoba 2006. www.cbc.ca/manitoba/features/nursinghomes/union_report.pdf (accessed 30 August 2017).
- Marcotte A. Resident-Centered Care and Work Satisfaction of Health Care Aides Working With Personal Care Home Residents Living With Dementia 2009.
- Masterson A. Towards an ideal skill mix in nursing homes. Nurs Older People 2004;16:14-6. https://doi.org/10.7748/nop2004.06.16.4.14.c2313.
- Matsudaira JD. Government regulation and the quality of healthcare evidence from minimum staffing legislation for nursing homes. J Hum Resour 2014;49:32-7. https://doi.org/10.1353/jhr.2014.0003.
- Mattingly TJ. A review exploring the relationship between nursing home staffing and antipsychotic medication use. Neurol Ther 2015;4:169-75. https://doi.org/10.1007/s40120-015-0032-2.
- Mayrhofer A, Goodman C, Smeeton N, Handley M, Amador S, Davies S. The feasibility of a train-the-trainer approach to end of life care training in care homes: an evaluation. BMC Palliat Care 2016;15. https://doi.org/10.1186/s12904-016-0081-z.
- McAiney CA, Haughton D, Jennings J, Farr D, Hillier L, Morden P. A unique practice model for nurse practitioners in long-term care homes. J Adv Nurs 2008;62:562-71. https://doi.org/10.1111/j.1365-2648.2008.04628.x.
- McGilton KS, McGillis Hall L, Boscart V, Brown M. Effects of director of care support on job stress and job satisfaction among long-term care nurse supervisors. Nurs Leadersh 2007;20:52-66. https://doi.org/10.12927/cjnl.2007.19288.
- McGilton KS, Boscart VM, Brown M, Bowers B. Making tradeoffs between the reasons to leave and reasons to stay employed in long-term care homes: perspectives of licensed nursing staff. Int J Nurs Stud 2014;51:917-26. https://doi.org/10.1016/j.ijnurstu.2013.10.015.
- McGregor MJ, Abu-Laban RB, Ronald LA, McGrail KM, Andrusiek D, Baumbusch J, et al. Nursing home characteristics associated with resident transfers to emergency departments. Can J Aging 2014;33:38-4. https://doi.org/10.1017/S0714980813000615.
- McGregor MJ, Cohen M, McGrail K, Broemeling AM, Adler RN, Schulzer M, et al. Staffing levels in not-for-profit and for-profit long-term care facilities: does type of ownership matter?. CMAJ 2005;172:645-9. https://doi.org/10.1503/cmaj.1040131.
- McGregor MJ, Baumbusch J, Abu-Laban RB, McGrail KM, Andrusiek D, Globerman J, et al. A survey of nursing home organizational characteristics associated with potentially avoidable hospital transfers and care quality in one large British Columbia health region. Can J Aging 2011;30:551-61. https://doi.org/10.1017/S071498081100047X.
- McKinney SH, Corazzini K, Anderson RA, Sloane R, Castle NG. Nursing home director of nursing leadership style and director of nursing-sensitive survey deficiencies. Health Care Manage Rev 2016;41:224-32. https://doi.org/10.1097/HMR.0000000000000072.
- McNulty CAM, Bowen J, Foy C, Gunn K, Freeman E, Tompkins D, et al. Is there an opportunity to reduce urinary catheter-related infections? Exploring variation in catheterisation rates in care homes. Br J Infect Contr 2006;7:22-8. https://doi.org/10.1177/14690446060070010701.
- Meade C, Ward B, Cronin H. Implementation of a team model for RACF care by a general practice. Aust Fam Physician 2016;45:218-22.
- Meehan TP, Qazi DJ, Van Hoof TJ, Ho SY, Eckenrode S, Spenard A, et al. Process evaluation of a quality improvement project to decrease hospital readmissions from skilled nursing facilities. J Am Med Dir Assoc 2015;16:648-53. https://doi.org/10.1016/j.jamda.2015.02.015.
- Miller EL, Alexander GL, Madsen RW. Effects of staffing and regional location on influenza and pneumococcal vaccination rates in nursing home residents. J Gerontol Nurs 2016;42:38-44. https://doi.org/10.3928/00989134-20151124-05.
- Mitchell SL, Kiely DK, Gillick MR. Nursing home characteristics associated with tube feeding in advanced cognitive impairment. J Am Geriatr Soc 2003;51:75-9. https://doi.org/10.1034/j.1601-5215.2002.51021.x.
- Molinari V. Development of a model for staff training to address serious mental illness in nursing homes. Gerontologist 2008;48.
- Monarch K. The quality of care provided in nursing homes: nurses can help facilities do the right things. Am J Nurs 2005;105:70-2. https://doi.org/10.1097/00000446-200505000-00032.
- Monkhouse C. Beyond the medical model – the Eden Alternative® in practice: a Swiss experience. J Soc Work Long Term Care 2003;2:339-53. https://doi.org/10.1300/J181v02n03_11.
- Morgan JC, Konrad TR. A mixed-method evaluation of a workforce development intervention for nursing assistants in nursing homes: the case of WIN A STEP UP. Gerontologist 2008;48:71-9. https://doi.org/10.1093/geront/48.Supplement_1.71.
- Moxon S, Lyne K, Sinclair I, Young P, Kirk C. Mental health in residential homes: a role for care staff. Ageing Soc 2001;21:71-93. https://doi.org/10.1017/S0144686X01008054.
- Moxon S. The Role of Care Staff in Identifying and Managing Depression in Residential Homes 2003.
- Moyle W, Skinner J, Rowe G, Gork C. Views of job satisfaction and dissatisfaction in Australian long-term care. J Clin Nurs 2003;12:168-76. https://doi.org/10.1046/j.1365-2702.2003.00732.x.
- Mueller CA. Staffing standards for long-term care facilities: where is the evidence?. J Nurs Adm 2006;36. https://doi.org/10.1097/00005110-200605000-00009.
- Mueller C, Corazzini K, Anderson RA. Nurse staffing and practice patterns in nursing homes. Gerontologist 2012;52.
- Muirhead G, Sachs C. A multidisciplinary approach to LTC patients with behavioral problems. Psychiatric Times 2004;21:76-9.
- US Department of Health and Human Services . Nursing Aides, Home Health Aides, and Related Health Care Occupations–National and Local Workforce Shortages and Associated Data Needs 2004. https://bhw.hrsa.gov/sites/default/files/bhw/RNandHomeAides.pdf (accessed 30 August 2017).
- Neuman MD, Wirtalla C, Werner RM. Association between skilled nursing facility quality indicators and hospital readmissions. JAMA 2014;312:1542-51. https://doi.org/10.1001/jama.2014.13513.
- Noel MA, Pearce GL, Metcalf R. Front line workers in long-term care: the effect of educational interventions and stabilization of staffing ratios on turnover and absenteeism. J Am Med Dir Assoc 2000;1:241-7.
- Older People’s Commissioner for Wales . ‘A Place to Call Home?’ – A Review into the Quality of Life and Care of Older People Living in Care Homes in Wales 2014. www.olderpeoplewales.com/Libraries/Uploads/A_Place_to_Call_Home_-_A_Review_into_the_Quality_of_Life_and_Care_of_Older_People_living_in_Care_Homes_in_Wales.sflb.ashx (accessed 30 August 2017).
- Orellana K. Care Home Managers: A Scoping Review of Evidence 2014. www.kcl.ac.uk/sspp/policy-institute/scwru/pubs/2014/reports/Orellana-2014-Scoping-review-care-home-managers.pdf (accessed 30 August 2017).
- Ottem P. Changing staff mix. Nurs BC 2004;36:11-2.
- Painter W, Kennedy B. The evolving role of certified nursing assistants in long-term care facilities. Director 2000;8:105-7.
- Painter W, Kennedy B. The evolving role of certified nursing assistants in long-term care facilities. Part three. Director 2000;8:56-9.
- Park J, Stearns SC. Effects of state minimum staffing standards on nursing home staffing and quality of care. Health Serv Res 2009;44:56-78. https://doi.org/10.1111/j.1475-6773.2008.00906.x.
- Parsons SK, Simmons WP, Penn K, Furlough M. Determinants of satisfaction and turnover among nursing assistants. The results of a statewide survey. J Gerontol Nurs 2003;29:51-8. https://doi.org/10.3928/0098-9134-20030301-11.
- Paulsen B, Halvorsen T, Harsvik T. Staffing, organisation, and quality of care. A multi-level analysis of staff-made quality assessments in nursing homes. Eur J Public Health 2005;15.
- Personal Social Services Research Unit . Measuring the Productivity of Workforce Development in Care Homes 2011. www.pssru.ac.uk/pub/skills-for-care.pdf (accessed 30 August 2017).
- Phillips DM, Wesley RM, Kruse JE, Gail D. Health status, staffing, and Medicaid reimbursement in nursing homes: 1985 to 1995. J Am Med Dir Assoc 2000;1:253-7.
- Pillemer K, Meador R, Henderson C, Robison J, Hegeman C, Graham E, et al. A facility specialist model for improving retention of nursing home staff: results from a randomized, controlled study. Gerontologist 2008;48:80-9. https://doi.org/10.1093/geront/48.Supplement_1.80.
- Pittman P, Forrest E. The changing roles of registered nurses in Pioneer Accountable Care Organizations. Nurs Outlook 2015;63:554-65. https://doi.org/10.1016/j.outlook.2015.05.008.
- Rahnfeld M, Wendsche J, Ihle A, Müller SR, Kliegel M. Uncovering the care setting-turnover intention relationship of geriatric nurses. Eur J Ageing 2016;13:159-69. https://doi.org/10.1007/s10433-016-0362-7.
- Rai GS. Organizational commitment among long-term care staff. Adm Soc Work 2012;36:53-66. https://doi.org/10.1080/03643107.2010.550671.
- Rantz MJ, Alexander G, Galambos C, Vogelsmeier A, Popejoy L, Flesner M, et al. Initiative to test a multidisciplinary model with advanced practice nurses to reduce avoidable hospitalizations among nursing facility residents. J Nurs Care Qual 2014;29:1-8. https://doi.org/10.1097/NCQ.0000000000000033.
- Royal College of Nursing (RCN) . RCN Care Home Survey 2004: Impact of Low Fees for Care Homes in the UK. Policy Report 10 2004 2004.
- Royal College of Nursing (RCN) . Persistent Challenges to Providing Quality Care: An RCN Report on the Views and Experiences of Frontline Nursing Staff in Care Homes in England. Policy Report, 03 2012 2012. www.rcn.org.uk/about-us/policy-briefings/pol-0812 (accessed 30 August 2017).
- Royal College of Nursing (RCN) . Care Homes Under Pressure – An England Report. RCN Policy Report 04 2010 2010. www.rcn.org.uk/about-us/policy-briefings/pol-0410 (accessed 30 August 2017).
- Royal College of Nursing (RCN) . Guidance on Safe Nurse Staffing Levels in the UK. Policy Report 12 2010 2010. www.rcn.org.uk/about-us/policy-briefings/pol-003860 (accessed 30 August 2017).
- Redfern S, Hannan S, Norman I, Martin F. Work satisfaction, stress, quality of care and morale of older people in a nursing home. Health Soc Care Community 2002;10:512-17. https://doi.org/10.1046/j.1365-2524.2002.00396.x.
- Rico JS. Staffing the Nation’s Nursing Homes 2013.
- Riggs CJ, Rantz MJ. A model of staff support to improve retention in long-term care. Nurs Adm Q 2001;25:43-54. https://doi.org/10.1097/00006216-200101000-00009.
- Rondeau KV, Williams ES, Wagar TH. Developing human capital: what is the impact on nurse turnover?. J Nurs Manag 2009;17:739-48. https://doi.org/10.1111/j.1365-2834.2009.00988.x.
- Rosen J, Stiehl EM, Mittal V, Leana CR. Stayers, leavers, and switchers among certified nursing assistants in nursing homes: a longitudinal investigation of turnover intent, staff retention, and turnover. Gerontologist 2011;51:597-609. https://doi.org/10.1093/geront/gnr025.
- Ryden MB, Snyder M, Gross CR, Savik K, Pearson V, Krichbaum K, et al. Value-added outcomes: the use of advanced practice nurses in long-term care facilities. Gerontologist 2000;40:654-62. https://doi.org/10.1093/geront/40.6.654.
- Sawan M, Jeon YH, Fois RA, Chen TF. Exploring the link between organizational climate and the use of psychotropic medicines in nursing homes: a qualitative study. Res Social Adm Pharm 2016;5.
- Schnelle JF, Simmons SF, Harrington C, Cadogan M, Garcia E, Bates-Jensen BM. Relationship of nursing home staffing to quality of care. Health Serv Res 2004;39:225-50. https://doi.org/10.1111/j.1475-6773.2004.00225.x.
- Schwendimann R, Dhaini S, Ausserhofer D, Engberg S, Zúñiga F. Factors associated with high job satisfaction among care workers in Swiss nursing homes – a cross sectional survey study. BMC Nurs 2016;15. https://doi.org/10.1186/s12912-016-0160-8.
- Scott-Cawiezell J, Pepper GA, Madsen RW, Petroski G, Vogelsmeier A, Zellmer D. Nursing home error and level of staff credentials. Clin Nurs Res 2007;16:72-8. https://doi.org/10.1177/1054773806295241.
- Scottish Care . In the Front Line: Supplementary Report on the Use of Agency Staffing 2015. www.scottishcare.org/wp-content/uploads/2016/06/Agency-Report-Final.pdf (accessed 30 August 2017).
- Scottish Care . Independent Sector Nursing Data 2016 2016. www.scottishcare.org/wp-content/uploads/2016/11/SC-Independent-Sector-Nursing-Data-2016.pdf (accessed 30 August 2017).
- Scottish Care . Voices From the Front Line 2016. www.scottishcare.org/wp-content/uploads/2016/06/Voices-from-the-Front-Line.pdf (accessed 30 August 2017).
- Scottish Care . In the Front Line: Social Care Providers Survey Report on Recruitment and Retention 2015. www.scottishcare.org/wp-content/uploads/2016/06/Scottish-Care-In-the-Front-Line-Report.pdf (accessed 30 August 2017).
- Shin JH, Hyun TK. Nurse staffing and quality of care of nursing home residents in Korea. J Nurs Scholarsh 2015;47:555-64. https://doi.org/10.1111/jnu.12166.
- Shin JH, Park T, Huh IS. Nursing staffing and quality of life in western New York nursing homes. West J Nurs Res 2014;36:788-805. https://doi.org/10.1177/0193945913511154.
- Shin JH. Relationship between nursing staffing and quality of life in nursing homes. Contemp Nurse 2013;44:133-43. https://doi.org/10.5172/conu.2013.44.2.133.
- Shin J, Specht J, Dyck M, Bern-Klug M, Reed D, Ansley T, et al. Relationship between nursing staffing and quality of life in Iowa nursing homes. Gerontologist 2008;48.
- Shin JH. Relationship Between Nurse Staffing and Quality of Life in Nursing Homes 2008.
- Shin JH, Bae SH. Nurse staffing, quality of care, and quality of life in US nursing homes, 1996–2011: an integrative review. J Gerontol Nurs 2012;38:46-53. https://doi.org/10.3928/00989134-20121106-04.
- Shipman D, Hooten J. Are nursing homes adequately staffed? The silent epidemic of malnutrition and dehydration in nursing home residents. Until mandatory staffing standards are created and enforced, residents are at risk. J Gerontol Nurs 2007;33:15-8.
- Shippee TP, Hong H, Henning-Smith C, Kane RL. Longitudinal changes in nursing home resident-reported quality of life: the role of facility characteristics. Res Aging 2015;37:555-80. https://doi.org/10.1177/0164027514545975.
- Simmons SF, Schnelle JF. Individualized feeding assistance care for nursing home. J Gerontol A Biol Sci Med Sci 2004;59:M966-73. https://doi.org/10.1093/gerona/59.9.M966.
- Simmons SF, Osterweil D, Schnelle JF. Improving food intake in nursing home residents with feeding assistance: a staffing analysis. J Gerontol A Biol Sci Med Sci 2001;56:M790-4. https://doi.org/10.1093/gerona/56.12.M790.
- Spector WD, Limcangco R, Williams C, Rhodes W, Hurd D. Potentially avoidable hospitalizations for elderly long-stay residents in nursing homes. Med Care 2013;51:673-81. https://doi.org/10.1097/MLR.0b013e3182984bff.
- Spilsbury K, Hanratty B, McCaughan D. Understanding the Registered Nursing Workforce in Care Homes 2015. www.rcn.org.uk/-/media/royal-college-of-nursing/documents/professional-development/research/2016-research-conference/2-6-1.pdf?la=en&hash=7BB8413204FA33D548DD3AB0E455D66F42C4BD3E (accessed 30 August 2017).
- Stearns SC, Park J, Zimmerman S, Gruber-Baldini AL, Konrad TR, Sloane PD. Determinants and effects of nurse staffing intensity and skill mix in residential care/assisted living settings. Gerontologist 2007;47:662-71. https://doi.org/10.1093/geront/47.5.662.
- Stolee P, Hillier LM, Esbaugh J, Griffiths N, Borrie MJ. Examining the nurse practitioner role in long-term care: evaluation of a pilot project in Canada. J Gerontol Nurs 2006;32:28-36.
- Suen W, Hickey E, Berlowitz D. Do staffing levels predict quality improvement implementation in nursing homes?. J Am Geriatr Soc 2006;54.
- Tamura BK, Bell CL, Masaki KH, Amella EJ. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: a systematic review of the literature. J Am Med Dir Assoc 2013;14:649-55. https://doi.org/10.1016/j.jamda.2013.02.022.
- Temple A, Dobbs D, Andel R. Exploring correlates of turnover among nursing assistants in the National Nursing Home Survey. J Nurs Adm 2011;41:34-42. https://doi.org/10.1097/NNA.0b013e318221c34b.
- Thomas KS, Rahman M, Mor V, Intrator O. Influence of hospital and nursing home quality on hospital readmissions. Am J Manag Care 2014;20:e523-31.
- Thomas KS, Hyer K, Branch L. Do Florida nursing homes improve quality as nurse staffing levels increase?. Gerontologist 2010;50.
- Thomas KS, Hyer K, Mehra S. Outcomes of increased nurse staffing policies in Florida nursing homes: staffing levels, quality, and costs. Gerontologist 2009;49:20-1.
- Thompson TP, Brown HN. Turnover of licensed nurses in skilled nursing facilities. Nurs Econ 2002;20:66-9.
- Tong PK. The effects of California minimum nurse staffing laws on nurse labor and patient mortality in skilled nursing facilities. Health Econ 2011;20:802-16. https://doi.org/10.1002/hec.1638.
- Trinkoff AM, Johantgen M, Muntaner C, Le R. Staffing and worker injury in nursing homes. Am J Public Health 2005;95:1220-5. https://doi.org/10.2105/AJPH.2004.045070.
- Unruh L, Zhang N. Impact of Medicare reimbursement changes on staffing and the quality of care in nursing homes. Gerontologist 2005;45.
- Wagner K. Nursing Homes’ Organizational Factors and Resident Mistreatment 2008.
- Walker MJ. Effects of the medication nursing assistant role on nurse job satisfaction and stress in long-term care. Nurs Adm Q 2008;32:296-300. https://doi.org/10.1097/01.NAQ.0000336726.03065.9f.
- Wan TT, Zhang NJ, Unruh L. Predictors of resident outcome improvement in nursing homes. West J Nurs Res 2006;28:974-93. https://doi.org/10.1177/0193945906289331.
- Way M. Job Demand, Job Control, and Support: A Comparison of Three Nursing Work Environments 2008.
- Weech-Maldonado R, Meret-Hanke L, Neff MC, Mor V. Nurse staffing patterns and quality of care in nursing homes. Health Care Manage Rev 2004;29:107-16. https://doi.org/10.1097/00004010-200404000-00004.
- Wild D, Szczepura A, Nelson S. Residential Care Home Workforce Development 2010. www.jrf.org.uk/report/residential-care-home-workforce-development-rhetoric-and-reality-meeting-older-residents%E2%80% (accessed 30 August 2017).
- Woo J, Chi I, Hui E, Chan F, Sham A. Low staffing level is associated with malnutrition in long-term residential care homes. Eur J Clin Nutr 2005;59:474-9. https://doi.org/10.1038/sj.ejcn.1602096.
- Xing J, Mukamel DB, Temkin-Greener H. Hospitalizations of nursing home residents in the last year of life: nursing home characteristics and variation in potentially avoidable hospitalizations. J Am Geriatr Soc 2013;61:1900-8. https://doi.org/10.1111/jgs.12517.
- Xu D, Kane RL, Shamliyan TA. Effect of nursing home characteristics on residents’ quality of life: a systematic review. Arch Gerontol Geriatr 2013;57:127-42. https://doi.org/10.1016/j.archger.2013.03.015.
- Yamaguchi Y, Inoue T, Harada H, Oike M. Job control, work-family balance and nurses’ intention to leave their profession and organization: a comparative cross-sectional survey. Int J Nurs Stud 2016;64:52-6. https://doi.org/10.1016/j.ijnurstu.2016.09.003.
- Yassi A, Cohen M, Cvitkovich Y, Park IH, Ratner PA, Ostry AS, et al. Factors associated with staff injuries in intermediate care facilities in British Columbia, Canada. Nurs Res 2004;53:87-98. https://doi.org/10.1097/00006199-200403000-00004.
- Yeatts DE, Seward RR. Reducing turnover and improving health care in nursing homes: the potential effects of self-managed work teams. Gerontologist 2000;40:358-63. https://doi.org/10.1093/geront/40.3.358.
- Yeh SH, Sehy YA, Lin LW. The quality of nursing home care in Taiwan. J Gerontol Nurs 2002;28:13-21. https://doi.org/10.3928/0098-9134-20020801-06.
- Zhang N, Unruh L, Wan T, Marathe S. Quality adjusted minimum nurse staffing ratios for nursing homes. Gerontologist 2005;45.
- Zhang X, Grabowski DC. Nursing home staffing and quality under the nursing home reform act. Gerontologist 2004;44:13-2. https://doi.org/10.1093/geront/44.1.13.
- Zhang NJ, Unruh L, Wan TT. Gaps in nurse staffing and nursing home resident needs. Nurs Econ 2013;31:289-97.
- Zhang NJ, Unruh L, Ni L, Hong Y, Wan T. State nurse staffing policy and quality of care in nursing homes. Gerontologist 2009;49.
- Zhang NJ, Gammonley D, Paek SC, Frahm K. Facility service environments, staffing, and psychosocial care in nursing homes. Health Care Financ Rev 2008;30:5-17.
- Zimmerman S, Gruber-Baldini AL, Hebel JR, Sloane PD, Magaziner J. Nursing home facility risk factors for infection and hospitalization: importance of registered nurse turnover, administration, and social factors. J Am Geriatr Soc 2002;50:1987-95. https://doi.org/10.1046/j.1532-5415.2002.50610.x.
- Zúñiga F, Ausserhofer D, Hamers JP, Engberg S, Simon M, Schwendimann R. The relationship of staffing and work environment with implicit rationing of nursing care in Swiss nursing homes – a cross-sectional study. Int J Nurs Stud 2015;52:1463-74. https://doi.org/10.1016/j.ijnurstu.2015.05.005.
- Zúñiga F, Ausserhofer D, De Geest S, Schwendimann R. Staffing, turnover, and long-term absences do not relate with quality of care in Swiss nursing homes. Gerontologist 2014;54:152-3.
- Halcomb EJ. Feasibility and sustainability of a model of multidisciplinary case conferencing in residential aged care. Aust J Prim Health 2009;15:238-43. https://doi.org/10.1071/PY08073.
- Low LF, Fletcher J, Goodenough B, Jeon YH, Etherton-Beer C, MacAndrew M, et al. A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0140711.
- Backhaus R, van Rossum E, Verbeek H, Halfens RJ, Tan FE, Capezuti E, et al. Relationship between the presence of baccalaureate-educated RNs and quality of care: a cross-sectional study in Dutch long-term care facilities. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-016-1947-8.
- Harrington C. Nursing Home Staffing Standards. The Kaiser Commission on Medicaid and the Uninsured; 2002.
- US Department of Health and Human Services (DHHS) Assistant Secretary for Planning and Evaluation Office of Disability . State Experiences With Minimum Nursing Staff Ratio for Nursing Facilities: Finding from Case Studies of Eight States 2003.
- Harrington C, Swan JH, Griffin C. 1998 State Data Book on Long-Term Care Program and Market Characteristics. Baltimore, MD: US Department of Health and Human Services; 1999.
- World Bank Group . World Bank Country and Lending Groups 2016. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed August 2018).
Appendix 1 Candidate questions for systematic evidence synthesis
Technology
-
Which technologies have a positive impact on resident health and well-being?
-
What is the impact of technologies on resident health and well-being?
-
What are the barriers to and facilitators of the use of technology in care homes?
-
How can technology improve resident engagement/social interactions?
-
What are staff and resident experiences of using technology to improve communication (and the barriers to and facilitators of this use)?
Communication and engagement
-
How can care homes engage with their local communities to promote resident well-being/quality of life?
-
What are the benefits for care homes of engaging with their local communities?
-
How should care homes and the NHS communicate to enhance resident, family and staff outcomes and experiences?
Evaluation
-
Which measurement tools have been validated for use in UK care homes?
-
Is there any evidence that any of the tools are superior to others, (reliability, validity, replicability, acceptability, cost-effectiveness)?
-
What are the common problems that evaluators encounter in this setting and how may these be overcome?
Workforce
-
What is the evidence that staffing levels (i.e. ratio of RNs and support staff to residents or different levels of support staff) influence resident outcomes?
-
What are the effects of staffing levels on staff outcomes?
-
What are the effects of introducing a new role on resident care outcomes and care home team working?
Appendix 2 List of high-income economies
Andorra, Antigua and Barbuda, Aruba, Australia, Austria, The Bahamas, Bahrain, Barbados, Belgium, Bermuda, British Virgin Islands, Brunei Darussalam, Canada, Cayman Islands, Channel Islands, Chile, Croatia, Curaçao, Cyprus, Czech Republic, Denmark, Estonia, Faroe Islands, Finland, France, French Polynesia, Germany, Gibraltar, Greece, Greenland, Guam, Hong Kong, China, Hungary, Iceland, Ireland, Isle of Man, Israel, Italy, Japan, Korea, Kuwait, Latvia, Liechtenstein, Lithuania, Luxembourg, Macao, Malta, Monaco, Nauru, the Netherlands, New Caledonia, New Zealand, Northern Mariana Islands, Norway, Oman, Poland, Portugal, Puerto Rico, Qatar, Saint-Martin, San Marino, Saudi Arabia, Seychelles, Singapore, Sint Maarten, Slovak Republic, Slovenia, Spain, St Kitts and Nevis, Sweden, Switzerland, Taiwan, Trinidad and Tobago, Turks and Caicos Islands, United Arab Emirates, UK, USA, Uruguay and Virgin Islands.
Source: World Bank Country and Lending Groups, 2016. 809
Appendix 3 Quality appraisal tables
| Authors, year of publication | Randomisation process | Timing of randomisation (cluster RCTs only) | Deviations from intended interventions | Missing outcome data | Measurement of outcome data | Selection of the reported result | Overall rating |
|---|---|---|---|---|---|---|---|
| Banks et al., 200847 | Low | Low | Some concerns | Some concerns | Low | Some concerns | Some concerns |
| Beeckman et al., 201354 | Low | Low | Low | Low | High | Low | High |
| De Luca et al., 2016101 | Some concerns | No information | High | High | High | Low | High |
| Hsu et al., 2011147 | Low | No information | High | Some concerns | Low | Low | High |
| Jøranson et al., 2015161 | Low | Some concerns | Some concerns | Low | High | Low | High |
| Lapane et al., 2011299 | Some concerns | Some concerns | Some concerns | Low | Some concerns | Some concerns | High |
| Lin et al., 2014177 | Low | No information | Some concerns | Low | Low | Low | Some concerns |
| Moyle et al., 2017203 | Low | Some concerns | Some concerns | Low | Low | Some concerns | Some concerns |
| Nagayama et al., 2016210 | Low | Low | Some concerns | Low | Low | Some concerns | High |
| Rantz et al., 2017230 | Some concerns | No information | Some concerns | Some concerns | Low | Low | Some concerns |
| Robinson et al., 2013236 | Low | No information | Some concerns | Low | High | Low | High |
| Van der Ploeg et al., 2016274 | High | Some concerns | Some concerns | High | Low | Some concerns | High |
| Vowden and Vowden, 2013277 | Some concerns | Low | Some concerns | Low | High | Critical | High |
| Authors, year of publication | Confounding | Selection | Classification of interventions | Deviations from interventions | Missing data | Measurement of outcomes | Selection in the reported results | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|
| Bemelmans et al., 201556 | Serious | Serious | Low | Serious | Moderate | Serious | Moderate | Serious |
| Holmes et al., 2007300 | Critical | Serious | Low | No information | Serious | Serious | Low | Critical |
| Jung et al., 2009163 | Critical | No information | Low | No information | No information | Serious | Low | Critical |
| Kelly et al., 2002301 | Critical | Low | Critical | Low | Moderate | Serious | Moderate | Critical |
| Keogh et al., 2014166 | Serious | No information | Moderate | Low | Moderate | Critical | Low | Critical |
| Kidd et al., 2006169 | Critical | Critical | Serious | Critical | Critical | Serious | No information | Critical |
| Libin and Cohen-Mansfield, 2004176 | Serious | Low | Low | Low | Low | Serious | Low | Serious |
| Pillemer et al., 2012222 | Critical | Serious | Low | No information | Moderate | Serious | No information | Critical |
| Rantz et al., 2010227 | Serious | Low | Low | Low | Low | Serious | Low | Serious |
| Shibata et al., 2004250 | Low | Moderate | Low | Low | No information | Moderate | Low | Moderate |
| Authors, year of publication | Selection bias | Study design | Confounders | Blinding | Data collection methods | Withdrawals and dropouts | Global rating |
|---|---|---|---|---|---|---|---|
| Arling et al., 2014322 | Moderate | Moderate | Weak | Moderate | Moderate | Weak | Weak |
| Bensandon et al., 2014326 | Moderate | Strong | Weak | Moderate | Moderate | Weak | Weak |
| Colon-Emeric et al., 2013333 | Weak | Strong | Moderate | Moderate | Moderate | Moderate | Moderate |
| Conway et al., 2015334 | Moderate | Weak | Weak | Moderate | Moderate | Strong | Weak |
| Cwinn et al., 2009339 | Strong | Weak | N/A | Moderate | Moderate | Strong | Moderate/weak? |
| Dalawari et al., 2011340 | Strong | Weak | N/A | ? | Moderate | ? | Moderate/weak? |
| Field et al., 2011345 | Strong | Strong | Moderate | Moderate | Strong | Strong | Strong |
| Hustey and Palmer, 2010152 | Strong | Moderate | N/A | Moderate | ? | Strong | Moderate |
| Renz et al., 2013376 | Moderate | Weak | N/A | Moderate | Moderate | Strong | Moderate |
| Tena-Nelson et al., 2012383 | Strong | Moderate | Strong | Moderate | Moderate | Strong | Moderate |
| Terrell et al., 2005384 | Strong | Moderate | N/A | Moderate | Moderate | Weak | Moderate/weak? |
| Authors, year of publication | Confounding | Selection | Missing data | Measurement of outcomes | Selection in the reported results | Overall risk of bias |
|---|---|---|---|---|---|---|
| Abrahamson et al., 2013502 | Serious | Low | Moderate | Low | Serious | Serious |
| Alexander, 2008505 | Serious | Low | Moderate | Low | Moderate | Serious |
| Backhaus, et al., 2017805 | Low | Low | Moderate | Low | Moderate | Moderate |
| Bowblis, 2011527 | Low | Low | Moderate | Low | Moderate | Moderate |
| Carrier et al., 2009537 | Low | Low | Moderate | Low | Moderate | Moderate |
| Castle et al., 2008546 | Moderate | Low | Moderate | Low | Moderate | Moderate |
| Castle and Engberg, 2008545 | Moderate | Low | Moderate | Low | Serious | Serious |
| Chen and Grabowski, 2015561 | Low | Low | Moderate | Low | Moderate | Moderate |
| Gray-Siracusa, 2005601 | Low | Low | Moderate | Low | Serious | Serious |
| Havig et al., 2011610 | Moderate | Low | Moderate | Low | Moderate | Moderate |
| Hereen et al., 2014614 | Low | Low | Critical | Low | Moderate | Critical |
| Kajonius and Kazemi, 2016639 | Moderate | Low | No information | Low | Moderate | Moderate |
| Leland et al., 2012683 | Low | Low | Moderate | Low | Moderate | Moderate |
| Lerner, 2013684 | Low | Low | Serious | Low | Moderate | Serious |
| Lin, 2014687 | Moderate | Low | Moderate | Low | Moderate | Moderate |
| Park and Stearns, 2009730 | Serious | Low | Moderate | Low | Serious | Serious |
| Zhang et al., 2008799 | Critical | Low | Low | Low | Moderate | Critical |
| Zhang et al., 2013797 | Moderate | Low | Moderate | No information | Serious | Serious |
| Zúñiga et al., 2015;801 Zúñiga et al., 2014802 | Serious | Low | Low | Low | Moderate | Serious |
| Authors, year | Tool | Internal consistency | Reliability | Content validity | Hypothesis testing | Criterion validity |
|---|---|---|---|---|---|---|
| Dutta et al., 2015477 | MMRI-R | N/A | N/A | N/A | Good | N/A |
| Faulkner et al., 2006478 | CARE profiles | Poor | N/A | N/A | N/A | N/A |
| Fossey et al., 2002479 | DCM | Poor | Fair | N/A | N/A | Poor |
| Moniz-Cook et al., 2001480 | CBS | Poor | Good | N/A | N/A | Poor |
| Sutcliffe et al., 2000481 | GDS-12R | Poor | N/A | N/A | N/A | Poor |
| Towers et al., 2015482 | ASCOT | N/A | N/A | Good | N/A | N/A |
Appendix 4 Evaluation tools identified by use in care homes
-
Agitated Behavior Mapping Instrument.
-
Ambiance Scale.
-
Antipsychotic Use in Dementia Assessment.
-
Apparent Emotion Rating Scale.
-
ASCOT.
-
Attitudes About Families Checklist.
-
Beck’s PAINCQ-33.
-
Brief Interview for Mental Status.
-
Care Dependency Scale.
-
Caregiver Stress Inventory.
-
Cohen-Mansfield Agitation Inventory.
-
Composite Above Average Quality Score.
-
Consumer Quality Index Long-term Care.
-
Continuous (or Continuity) Assessment Record and Evaluation.
-
Core Nurse Resource Scale.
-
Cornell Scale for Depression in Dementia.
-
Discomfort Scale – Dementia of Alzheimer Type.
-
End of Life in Dementia – Satisfaction With Care.
-
End of Life in Dementia – Symptom Management.
-
End of Life in Dementia – Comfort Assessment in Dying.
-
Falls Prevention and Management Audit Tool.
-
Family Distress in Advanced Dementia Scale.
-
Family Perceptions of Caregiving Role.
-
Family Perceptions of Physician–Family Caregiver Communication.
-
Functional Abilities Checklist.
-
Geriatric Depression Scale.
-
Huber Badrak Borders Scales.
-
Incontinence-Associated Dermatitis Intervention Tool.
-
Intellectual Disability Supplement to The Irish Longitudinal Study on Ageing.
-
International Classification of Functioning, Disability and Health – Usability Scale.
-
Malnutrition Universal Screening Tool.
-
Minimum Data Set 2.0.
-
Minimum Data Set 3.0: Brief Interview for Mental Status.
-
Minimum Data Set bedfast quality indicator.
-
Minimum Data Set versions 1 and 2: mood assessment.
-
Minimum Data Set: depression prevalence.
-
Minimum Data Set: prevalence of restraint.
-
Mini-Suffering State Examination.
-
Models of Care Instrument.
-
Neuropsychiatric Inventory.
-
Neuropsychiatric Inventory – Clinician Rating.
-
Neuropsychiatric Inventory – Nursing Home Version.
-
Neuropsychiatric Inventory – Nursing Home Version – Occupational Disruptiveness Scale.
-
Nursing Home Composite Measure Score.
-
Nursing Home Confusion Assessment Method.
-
Nursing Home Survey on Patient Safety Culture.
-
Nursing Minimum Data Set.
-
Nursing Older People – Competence Evaluation Tool.
-
Observable Indicators of Nursing Home Care Quality.
-
Older Patient Assessment of Chronic Illness Care.
-
Pain Assessment in Advanced Dementia.
-
Pain Assessment Checklist for Seniors with Limited Ability to Communicate.
-
Pain Assessment in the Communicatively Impaired.
-
Palliative Care Outcome Scale.
-
Palliative Care Survey.
-
Patient Assessment of Chronic Illness Care.
-
Patient Health Questionnaire-9.
-
Patient Health Questionnaire Observational Version.
-
Person-Centered Care Assessment Tool.
-
Pleasant Events Schedule: Alzheimer Disease.
-
Professional Care Team Burden.
-
Program of All-Inclusive Care for the Elderly.
-
Purpose-in-Life Test.
-
QUALIDEM.
-
Quality of Dying in Long-Term Care.
-
Relational Care Scale.
-
Satisfaction with Life Scale.
-
Quality of Life Scale.
-
Schedule for the Evaluation of Individual Quality of Life: Direct Weighting.
-
Scope and Severity Index.
-
Seated Posture Scale.
-
Sheffield Care Environment Assessment Matrix.
-
Special Care Unit Environmental Quality Scale.
-
Staff Perceptions of Caregiving Role.
-
Therapeutic Environment Screening Scale-2+.
-
Thriving of Older People Assessment Scale.
Appendix 5 MEDLINE search strategies
Technology review
Database(s): Ovid MEDLINE(R) 1946 to week 4 September 2016.
Search date: 11 October 2016.
Search strategy
-
Respite Care/
-
Long-Term Care/
-
exp Nursing Homes/
-
Homes for the Aged/
-
“Home? for the Aged”.mp.
-
“Old Age Home?”.mp.
-
“Skilled Nursing Facilit*”.mp.
-
“Intermediate Care Facilit*”.mp.
-
“Nursing Home?”.mp.
-
“Respite Care?”.mp.
-
“care home?”.mp.
-
“residential home?”.mp.
-
(“long-term care facilit*” or “long term care facilit*”).mp.
-
(“aged care facilit*” or “aged-care facilit*”).mp.
-
or/1-14
-
exp “Diffusion of Innovation”/
-
Safety Management/
-
Cloud Computing/
-
Digital Divide/
-
Electronic Health Records/
-
Electronic Prescribing/
-
Health Information Exchange/
-
Health Smart Cards/
-
Medical Records Systems, Computerized/
-
Internet/
-
exp Microcomputers/
-
Mobile Applications/
-
Video Games/
-
Radio Frequency Identification Device/
-
exp Telemedicine/
-
Remote Sensing Technology/
-
Smartphone/
-
Social Media/
-
exp Telemedicine/
-
Wireless Technology/
-
Clinical Alarms/
-
exp telemetry/
-
Point-of-Care Systems/
-
exp Technology/
-
“Meaningful Use”/
-
self-help devices/ or communication aids for disabled/
-
(technolog* or digital* or computer* or internet* or wireless).ti,ab,kf,kw.
-
(mobile device* or mobile phone* or cellphone or cell phone or smartphone* or smart phone* or ipad* or iphone* or software or app or apps or augmented realit* or virtual realit* or robot*).ti,ab,kf,kw.
-
((tangible or user) adj2 interface*).ti,ab,kf,kw.
-
(telecare or telemedic* or telehealth).ti,ab,kf,kw.
-
(remote adj2 (care or medic* or health*)).ti,ab,kf,kw.
-
(smarthome* or smart home* or smart environment* or smartcard* or smart card*).ti,ab,kf,kw.
-
or/16-47
-
15 and 48
-
adolescent/ or exp child/ or exp infant/
-
(adolescen* or paediatric* or pediatric*).mp.
-
(animals not (humans and animals)).sh.
-
or/50-52
-
49 not 53
-
limit 54 to (english language and yr=“2000 -Current”)
Workforce review
Staff levels
Database(s): Ovid MEDLINE(R) 1946 to week 4 September 2016.
Search date: 10 October 2016.
Search strategy
-
“Personnel Staffing and Scheduling”/
-
((staff* or nurse?) adj2 (schedul* or roster* or rota? or rotation or level? or balanc*)).ti,ab,hw.
-
staffing.ti,ab.
-
manpower.fs,ti,hw.
-
((day* or night* or work* or job? or rotat* or team* or interval? or “long-hour?” or alternat* or enhanc* or shared or group? or overtime) adj shift?).ti,ab.
-
(skill? adj2 mix*).ti,ab.
-
personnel management/ or personnel downsizing/ or personnel selection/ or “personnel staffing and scheduling”/ or personnel turnover/
-
“Personnel Staffing and Scheduling Information Systems”/
-
or/1-8
-
Homes for the Aged/
-
Skilled Nursing Facilities/
-
Intermediate Care Facilities/
-
Nursing Homes/
-
Respite Care/
-
“Home? for the Aged”.mp.
-
“Old Age Home?”.mp.
-
“Skilled Nursing Facilit*”.mp.
-
“Intermediate Care Facilit*”.mp.
-
“Nursing Home?”.mp.
-
“Respite Care?”.mp.
-
“care home?”.mp.
-
“residential home?”.mp.
-
(“long-term care facilit*” or “long term care facilit*”).mp.
-
(“aged care facilit*” or “aged-care facilit*”).mp.
-
or/10-24
-
9 and 25
-
limit 26 to (english language and yr=“2000 -Current”)
Staff roles
Database(s): Ovid MEDLINE(R) 1946 to week 4 September 2016.
Search date: 6 October 2016.
Search strategy
-
exp professional role/
-
Patient Care Team/
-
staff development/
-
delegation, professional/
-
(extend* adj3 (role? or skill? or scope?)).ti,ab,kw.
-
(role? adj7 (development? or develop or developing or developed)).ti,ab,kw.
-
(role? adj7 impact?).ti,ab,kw.
-
(expand* adj3 (role? or skill? or scope? or responsibilit* or practice?)).ti,ab,kw.
-
((extra or added or additional) adj4 responsibilit*).ti,ab,kw.
-
(emerging adj3 (role? or skill? or scope? or responsibilit* or practice?)).ti,ab,kw.
-
(advanced adj2 (role? or skill? or scope? or practice?)).ti,ab,kw.
-
(blur* adj4 (boundar* or role?)).ti,ab,kw.
-
(develop* adj4 responsibilit*).ti,ab,kw.
-
((evolution or evolv*) adj3 (practice? or role?)).ti,ab,kw.
-
non-medical.ti,ab,kw.
-
((inter?disciplin* or inter?professional or multi?disciplin* or multi?faceted) adj5 (work or working or role? or team? or staff or practice?)).ti,ab,kw.
-
(substitut* adj2 role?).ti,ab,kw.
-
(medical adj2 substitut*).ti,ab,kw.
-
(new adj3 role?).ti,ab,kw.
-
(scope adj3 practice?).ti,ab,kw.
-
(greater adj2 role?).ti,ab,kw.
-
((nurse or nursing) adj3 (skill? or role? or impact? or scope? or practice?)).ti,ab,kw.
-
(trends adj7 (nurse or nursing or role? or skill? or scope?)).ti,ab,kw.
-
(impact? adj9 (nurse or nursing or role? or skill? or scope?)).ti,ab,kw.
-
(integrat* adj5 (nurse or nursing or role? or skill? or scope?)).ti,ab,kw.
-
(innovati* adj5 (nurse or nursing or role? or skill? or scope? or practice?)).ti,ab,kw.
-
(co?operati* adj5 (work or working or role? or team? or practice? or nurse or nursing)).ti,ab,kw.
-
or/1-27
Communication and engagement review
Database(s): Ovid MEDLINE(R) 1946 to week 4 March 2016.
Search date: 31 March 2017.
Search strategy
-
Respite Care/
-
Long-Term Care/
-
exp Nursing Homes/
-
Homes for the Aged/
-
“Home? for the Aged”.mp.
-
“Old Age Home?”.mp.
-
“Skilled Nursing Facilit*”.mp.
-
“Intermediate Care Facilit*”.mp.
-
“Nursing Home?”.mp.
-
“Respite Care?”.mp.
-
“care home?”.mp.
-
“residential home?”.mp.
-
(“long-term care facilit*” or “long term care facilit*”).mp.
-
(“aged care facilit*” or “aged-care facilit*”).mp.
-
or/1-14
-
Communication/
-
Persuasive Communication/
-
Interdisciplinary Communication/
-
exp Communication Barriers/
-
Health Communication/
-
Hospital Communication Systems/ or Emergency Medical Service Communication Systems/
-
exp Computer Communication Networks/
-
exp Communications Media/
-
Information Dissemination/
-
((share or shared or sharing or disseminat*) adj5 information).ti,ab,kf.
-
Cooperative Behavior/
-
Community-Based Participatory Research/
-
or/16-27
-
Health Facilities/
-
exp Ambulatory Care Facilities/
-
exp Hospital Units/
-
exp Hospitals/
-
Community Health Services/
-
Adult Day Care Centers/
-
Community Health Nursing/
-
Hospices/
-
Senior Centers/
-
Health Services/
-
exp Emergency Medical Services/
-
Health Services for the Aged/
-
exp Nursing Services/
-
exp Nursing Care/
-
Palliative Care/
-
exp Terminal Care/
-
Community Networks/
-
Community Participation/
-
exp Organizational Innovation/
-
or/29-47
-
15 and 28 and 48
-
Community-Institutional Relations/ or Interinstitutional Relations/ or Intersectoral Collaboration/
-
Public-Private Sector Partnerships/
-
((community or communities or primary care or general practice* or family practice* or hospital* or health service* or clinic* or hospice* or institution* or department* or provider* or stakeholder*) adj5 (communicat* or collaborat* or cooperat* or co-operat* or coordinat* or co-ordinat* or engag* or network* or integrat* or share* or sharing or link* or partner* or coalition* or volunteer* or relationship* or transition* or transfer* or innovat*)).ti,ab,kf.
-
or/50-52
-
15 and 53
-
49 or 54
-
adolescent/ or exp child/ or exp infant/
-
(adolescen* or paediatric* or pediatric*).mp.
-
(animals not (humans and animals)).sh.
-
or/56-58
-
55 not 59
-
limit 60 to (english language and yr=“2000 -Current”)
Evaluation review
Initial search
Database(s): Ovid MEDLINE(R) 1946 to week 1 December 2016.
Search date: 19 December 2016.
Search strategy
-
Respite Care/
-
Long-Term Care/
-
exp Nursing Homes/
-
Homes for the Aged/
-
“Home? for the Aged”.mp.
-
“Old Age Home?”.mp.
-
“Skilled Nursing Facilit*”.mp.
-
“Intermediate Care Facilit*”.mp.
-
“Nursing Home?”.mp.
-
“Respite Care?”.mp.
-
“care home?”.mp.
-
“residential home?”.mp.
-
(“long-term care facilit*” or “long term care facilit*”).mp.
-
(“aged care facilit*” or “aged-care facilit*”).mp.
-
or/1-14
-
“outcome and process assessment (health care)”/ or “outcome assessment (health care)”/ or “process assessment (health care)”/
-
Program Evaluation/
-
Quality Assurance, Health Care/
-
Quality Improvement/
-
or/16-19
-
mt.fs.
-
exp “Evaluation Studies as Topic”/
-
exp “Epidemiologic Study Characteristics as Topic”/
-
or/21-23
-
20 and 24
-
((evaluat* or assess* or measur* or apprais* or monitor* or improv* or assur*) adj5 (methodolog* or framework* or theory or theories or approach*)).tw,kw.
-
((evaluat* or assess* or measur* or apprais* or monitor* or improv* or assur*) adj5 (method* or model*)).ti.
-
or/26-27
-
or/25,28
-
15 and 29
-
adolescent/ or exp child/ or exp infant/
-
(adolescen* or paediatric* or pediatric*).mp.
-
(animals not (humans and animals)).sh.
-
or/31-33
-
30 not 34
-
limit 35 to yr=“2000 –Current”
Focused searching for tools (lines 1–34 same as initial search)
Database(s): Ovid MEDLINE(R) 1946 to week 4 July 2016.
Search date: August 2016.
Search strategy
-
Respite Care/
-
Long-Term Care/
-
exp Nursing Homes/
-
Homes for the Aged/
-
“Home? for the Aged”.mp.
-
“Old Age Home?”.mp.
-
“Skilled Nursing Facilit*”.mp.
-
“Intermediate Care Facilit*”.mp.
-
“Nursing Home?”.mp.
-
“Respite Care?”.mp.
-
“care home?”.mp.
-
“residential home?”.mp.
-
(“long-term care facilit*” or “long term care facilit*”).mp.
-
(“aged care facilit*” or “aged-care facilit*”).mp.
-
or/1-14
-
“outcome and process assessment (health care)”/ or “outcome assessment (health care)”/ or “process assessment (health care)”/
-
Program Evaluation/
-
Quality Assurance, Health Care/
-
Quality Improvement/
-
or/16-19
-
mt.fs.
-
exp “Evaluation Studies as Topic”/
-
exp “Epidemiologic Study Characteristics as Topic”/
-
or/21-23
-
20 and 24
-
((evaluat* or assess* or measur* or apprais* or monitor* or improv* or assur*) adj5 (methodolog* or framework* or theory or theories or approach*)).tw,kw.
-
((evaluat* or assess* or measur* or apprais* or monitor* or improv* or assur*) adj5 (method* or model*)).ti.
-
or/26-27
-
or/25,28
-
15 and 29
-
adolescent/ or exp child/ or exp infant/
-
(adolescen* or paediatric* or pediatric*).mp.
-
(animals not (humans and animals)).sh.
-
or/31-33
-
30 not 34
-
limit 35 to yr=“2000 –Current”
-
ASCOT.ti. and (valid* or reliab*).ti,ab.
-
(score* or status* or scale* or survey* or indicator* or tool* or framework* or diagnos* or instrument* or assess* or inventor* or questionnaire* or index or indices or measure*).ti.
-
15 and 38
-
*Nursing Homes/
-
(nursing home* or care home*).ti.
-
40 or 41
-
38 and 42
-
(valid* or reliab*).ti,ab.
-
43 and 44
-
(valid* or reliab*).ti.
-
43 and 46
-
45 not 36
-
47 not 36
-
limit 48 to english language
Glossary
- Medicaid
- A social insurance programme in the USA that covers institutional nursing services on a means-tested basis.
- Medicare
- A federally funded programme of health care in the USA for people aged > 65 years.
- OSCAR
- Online Survey, Certification and Reporting (United States database containing survey information on state inspections of nursing homes).
- PsycINFO
- Psychological Abstracts database.
- Telehealth
- The provision of health care remotely by means of telecommunications technology.
- Telemedicine
- The remote diagnosis and treatment of patients by means of telecommunications technology.
List of abbreviations
- ADL
- activities of daily living
- APN
- advanced practice nurse
- ASCOT
- Adult Social Care Outcomes Toolkit
- ASSIA
- Applied Social Sciences Index and Abstracts
- CARE
- Combined Assessment of Residential Environments
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CNA
- certified nursing assistant
- DARE
- Database of Abstracts of Reviews of Effects
- DCM
- dementia care mapping
- GDS-12R
- Geriatric Depression Scale – Residential
- INTERACT
- Interventions to Reduce Acute Care Transfers
- IT
- information technology
- LPN
- licensed practical nurse
- LVN
- licensed vocational nurse
- MDCS
- minimum direct care staffing
- MDS
- minimum data set
- MeSH
- medical subject heading
- MMRI-R
- Minimum Dataset Mortality Risk Index – Revised
- NA
- nursing assistant
- NHS EED
- NHS Economic Evaluation Database
- NIHR
- National Institute for Health Research
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RACF
- residential aged care facility
- RCT
- randomised controlled trial
- RN
- registered nurse
- ROBINS-I
- Risk of Bias In Non-Randomised Studies of Interventions
- SBAR
- situation, background, assessment and recommendation
