Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/137/04. The contractual start date was in March 2017. The final report began editorial review in July 2018 and was accepted for publication in January 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Evans et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Female genital mutilation/cutting
Female genital mutilation (or female genital cutting) – henceforth abbreviated to FGM/C (female genital mutilation/cutting) – refers to all procedures that involve the partial or total removal of the external female genitalia or other injury to the female genital organs for non-medical reasons. 1 FGM/C is categorised by the World Health Organization (WHO)1 into four types, with differing degrees of severity, as described in Box 1.
Often referred to as clitoridectomy, this is the partial or total removal of the clitoris (a small, sensitive and erectile part of the female genitals), and in very rare cases, only the prepuce (the fold of skin surrounding the clitoris).
Type 2Often referred to as excision, this is the partial or total removal of the clitoris and the labia minora (the inner folds of the vulva), with or without excision of the labia majora (the outer folds of skin of the vulva).
Type 3Often referred to as infibulation, this is the narrowing of the vaginal opening through the creation of a covering seal. The seal is formed by cutting and repositioning the labia minora, or labia majora, sometimes through stitching, with or without removal of the clitoris (clitoridectomy).
Type 4This includes all other harmful procedures in the female genitalia for non-medical purposes (e.g. pricking, piercing, incising, scraping and cauterising the genital area).
Female genital mutilation/cutting is practised in 30 countries across north and sub-Saharan Africa and in parts of the Middle East and Asia. 2 The UK is in a period of ‘super-diversity’, which is characterised by high rates of migration from countries all over the world (rather than mainly from former colonies as in previous decades). 3–6 As a consequence, the UK’s population is increasingly diverse and includes many groups from countries where FGM/C is practised. 5–7 Hence, the need to address FGM/C within the NHS is already significant and is expected to increase. 6,8–10
Evidence suggests that women and girls who have undergone FGM/C experience many barriers to accessing appropriate care in the UK. 11 Research also suggests that health professionals lack knowledge, experience and confidence in addressing FGM/C-related issues. 12 FGM/C-related services in England and Wales are reported to be fragmented and highly variable, lacking clear referral or care pathways, and difficult for women/girls to access. 13–15 FGM/C therefore presents a growing health issue for the NHS and there is a need to develop more and better services in this area. 13
This project seeks to inform the development of services for FGM/C-related health care through two syntheses of qualitative evidence regarding the views and experiences of service access, service provision and quality of care from the perspectives of (1) women/girls who have undergone FGM/C and (2) health professionals.
Size of the problem
Globally, it is estimated that over 200 million women and girls have experienced FGM/C. 2 In Europe, where many nations are ‘destination’ countries for migrants from FGM/C-practising areas, it is thought that over half a million women and girls are FGM/C survivors. 16 In England and Wales, a comprehensive report published in 2015 estimated FGM/C to be a significant problem, with over 137,000 women/girls directly affected, as follows:9
-
10,000 girls aged < 15 years
-
103,000 women and girls aged 15–49 years
-
24,000 women aged ≥ 50 years.
The same report estimates that women with FGM/C have made up approximately 1.5% (nearly 11,000) of all UK maternity episodes since 2008. 9 In the recording cycle April 2016 to March 2017, there were 9179 attendances reported in NHS trusts and general practices in England where FGM/C was identified or where a procedure for FGM/C was undertaken. Eighty-seven per cent of these attendances were in midwifery or obstetric services. 17 The 2017–18 figures for England show a slight reduction in numbers, to 6195 newly recorded attendances. 18 The figures show that all major urban areas in the UK have significant populations affected by FGM/C, with most areas of the country affected to some extent. 9,17
The current figures from England suggest that FGM/C attendances are primarily by women of childbearing age. For example, out of 6195 recorded attendances in 2017–18, only 2.9% were for women aged ≥ 45 years. 18
With respect to FGM/C-related needs among girls, It has been estimated that approximately 60,000 girls in the UK aged 0–14 years have been born to mothers who have undergone FGM/C and may themselves be at risk of the procedure. 9 However, current figures from England suggest that it is primarily adult women rather than girls/teenagers who are accessing NHS services. For example, in 2017–18, only 1.13% of all recorded attendances were for girls under the age of 18 years. 18
Health consequences of female genital mutilation/cutting
Female genital mutilation/cutting is associated with significant negative physical, psychological and sexual health sequelae. 19–21 In the short term, these include infection, urinary retention or injury to other tissues (e.g. vaginal fistulae). In the longer term, they include psychological problems, post-traumatic stress disorder, painful intercourse and other sexual problems, relationship problems, chronic pain, chronic infections, infertility and complications in childbirth. 22–25 Hence, it is essential that women and girls affected by FGM/C have access to services that can identify and meet these multiple complex health needs and that services include mental health-care as well as physical health-care provision. 13,20,21,26
Health problems may be particularly severe for women with type III FGM/C, also referred to as infibulation. This type of FGM/C is practised predominantly (but not exclusively) in countries in the Horn of Africa, such as Somalia, Sudan, Ethiopia, Eritrea and parts of Kenya. Women with type III FGM/C require a degree of deinfibulation in order to have sexual intercourse and to give birth.
Currently, deinfibulation is recommended for women and girls reporting medical or psychosexual symptoms related to type III FGM/C, or on request (i.e. personal choice). 1 In addition, national and global guidelines specifically recommend that deinfibulation is undertaken to prevent obstetric complications. 14,27–29 However, the optimal timing for deinfibulation is unclear. 30,31 The evidence base regarding outcomes of antepartum deinfibulation compared with intrapartum deinfibulation is weak. 28,32–34 Nonetheless, there are compelling clinical reasons for preferring antepartum deinfibulation. 35 These include the fact that it can be carried out under local anaesthetic in an outpatient setting, thus reducing costs and risks associated with any emergency procedures that may emerge during labour. In addition, given the lack of familiarity with type III FGM/C of many health professionals in destination countries (such as the UK), planned antepartum deinfibulation ensures that it is undertaken by trained and experienced professionals. 32
Costs of female genital mutilation/cutting
There is a lack of data on the economic burden of FGM/C in high-income countries such as the UK. 36 However, recent policy documentation cites a report commissioned by the Department of Health and Social Care estimating the annual cost of FGM/C to the NHS to be £100M if all needs were met/treated in a single year. This estimate comprises £34M associated with physical health needs and £66M associated with mental health needs. 15
Legal and policy context of female genital mutilation/cutting in the UK
Female genital mutilation/cutting has been illegal in the four countries of the UK since 1985 and is considered a form of abuse (FGM/C undertaken outside the UK on UK nationals or residents was criminalised through additional Acts in 2003 for England37 and 2005 for Scotland38). In 2014, the UK Government published a declaration to end FGM/C, and initiated a National FGM/C Prevention Programme. 39 A series of policy changes have been introduced as part of this programme in order to obtain more accurate information on the size and scale of the problem and to enhance safeguarding processes; these are (1) mandatory recording, (2) mandatory reporting and (3) use of a FGM/C Risk Indication System (RIS).
Acute NHS trusts in England have had to record all cases of FGM/C within a FGM/C prevalence database since April 2014. This database has now been re-named the FGM/C Enhanced Dataset (an Information Standard – SCCI2026). The Information Standard requires clinicians across all NHS health-care settings to record in clinical notes when patients with FGM/C are identified and what type of FGM/C has been identified (patient consent is not required). 15 In addition to mandatory recording, from October 2015 a new statutory duty has been introduced through the Serious Crime Act40 requiring all regulated health professionals to report cases of FGM/C in girls under the age of 18 years to the police (known as ‘mandatory reporting’). In addition, a new national health system, the FGM/C RIS, was introduced in 2015, aiming to support safeguarding of girls up to the age of 18 years. The system allows health professionals to add an indicator on a girl’s electronic summary care record to highlight that she may be at risk. This information can then be confidentially shared among health professionals. To set the indicator, professionals are required to seek parental consent.
These measures signal a new policy drive across the NHS to address FGM/C prevention (as well as care) and to significantly improve the identification of women and girls have who undergone FGM/C. 10,13,26 However, all of the above measures place an additional burden of work on health professionals and require additional training and support to understand the legal complexities, the logistics of how to use the systems and the sensitivities of discussing FGM/C with patients/communities and greater awareness of local safeguarding pathways. 15,41 The ways in which these changes will have an impact on the experience of health-care delivery from a patient’s or professional’s perspective are, as yet, unclear. However, systematically examining the existing evidence base on FGM/C may help to identify some of the potential implications of these new policies for practice and future research.
In some communities (particularly in Sudan) in which FGM/C type III is common, reinfibulation is practised after childbirth. However, in the UK and most high-income countries, it is illegal for professionals to undertake reinfibulation. 42,43
Female genital mutilation-/cutting-related service provision and development in the UK
Currently, there is limited evidence regarding the availability and accessibility of FGM/C-related care across the UK. However, there are strong indications that it is it poorly co-ordinated and sub-optimal. 13 To date, FGM/C-related care within the NHS has primarily been provided in the context of maternity services. Specialist clinics run by specialist midwives have been established in a number of maternity services, which provide medical interventions as well as access to counselling and other psychological services. However, the majority of maternity services do not offer this specialist provision, although most now have a designated lead for FGM/C. In these non-specialist settings, care tends to be focused primarily on medical management (e.g. deinfibulation), with limited attention to other health needs or to considering the FGM/C-prevention agenda [Project Advisory Group (PAG) opinion]. 13,44 Accurate information on the accessibility and quality of FGM/C-related care within maternity services is difficult to estimate as there are no up-to-date statistics available.
There is a lack of evidence on FGM/C management in non-maternity settings. However, the view of the expert PAG for this project is that communication about, or management of, FGM/C in non-maternity settings is currently poor, with a lack of clear referral or care pathways, and with health professionals lacking confidence and experience around FGM/C. Access to any non-maternity-focused specialist FGM/C services is, therefore, limited and highly variable across the UK.
As of 2017, there were 16 specialist FGM/C clinics across England (these numbers may now have changed as services are re-commissioned, but are not thought to be greatly increased). 45 Many of these specialist services are actually based within maternity services and referral pathways from other services are not well established. Moreover, the majority of these specialist clinics (n = 11) are located in London, with the remaining five based in other urban areas. 13,45 Therefore, many FGM/C-affected communities currently do not have access to specialist services, and this is an issue particularly for those living in rural areas and other low-prevalence areas. This situation potentially creates inequalities in access to care, as highlighted in recent reports. 8,46,47
In the current policy and legislative climate, health professionals across all sectors, especially primary and maternity care, are required to be knowledgeable about FGM/C and to have the requisite skills to deal with affected women/girls and communities in a sensitive and appropriate manner. 10,13 This is particularly important not only to ensure that health-care encounters are focused on supporting women/girls who are living with the consequences of FGM/C but also to address the sensitive issue of prevention. 13 To achieve this agenda, NHS England has recently published health professional training standards. 41 In addition, several professional and multi-agency guidelines have been published that call for greater levels of specialist and holistic service provision, clearly delineated FGM/C-related care pathways and clear referral pathways, backed up by enhanced training of health professionals. 10,13–15,26,27,29
Why this research is needed and why it is needed now
Currently, there are limited resources to inform FGM/C-related training and service development. Much of the existing body of research relates to understanding the practice of FGM/C,48 the prevention of FGM/C49–51 and the psychosocial and clinical consequences of FGM/C. 19,21,24,52,53 A recent expert commentary on FGM/C identified key gaps in the evidence on clinical management and on models of service delivery. 30 Furthermore, a recent series of systematic reviews undertaken by WHO to inform global guideline development found that evidence on the clinical effectiveness or cost-effectiveness of different models of care for FGM/C is lacking. 54,55
Given the complexity of service development and the sensitivity of FGM/C, it is imperative to take into account the views and experiences of all stakeholders. This project therefore proposed to undertake two systematic reviews focusing specifically on qualitative evidence: one related to women’s/girls’ experiences of health care in relation to their FGM/C and one related to health-care professionals’ views and experiences of service provision. Given the current focus in the UK on the development of care pathways for non-pregnant women as well as pregnant women,15 the reviews sought to understand relevant issues across all health-care settings and across the life course. In addition, in order to ensure that the equity agenda was addressed, the reviews sought to explore issues around access to care as well as experience of care.
A brief look at the existing evidence indicates further why these reviews are important and what kind of issues they will illuminate to be useful for service development.
Perspectives of women/girls who have undergone female genital mutilation/cutting
In the UK context, evidence suggests that several barriers to FGM/C-related care-seeking exist from the perspective of women/girls. Some of these relate to accessibility in terms of not knowing where to go or who to speak to and not being aware of any specialist provision. 11 Other barriers highlighted in existing research relate more directly to quality of care, such as feeling judged or misunderstood or feeling unable to communicate about FGM/C-related problems. 11,56–59
At the time of project development, rigorous searches were undertaken to identify any existing published reviews, protocols, registered reviews and registered review titles [including on PROSPERO, The Cochrane Library and the Joanna Briggs Institute (JBI) Database of Systematic Reviews and Implementation Reports databases]. At that time, there was no registered ongoing work in relation to women’s/girls’ views and experiences of FGM/C-related health care. This was a key gap. Since this project commenced, the above-mentioned WHO systematic review series was published54 and included three qualitative reviews. However, these were focused on evidence related only to specific clinical interventions rather than health-care experiences more generally. Hence, they identified a very limited number of studies. Nonetheless, they highlighted that women’s experiences were often negative and characterised by unmet needs for information and support. 60–62 Two additional reviews, by Hamid et al. 63 and Turkmani et al. ,64 have very recently been published, focusing specifically on the pregnancy and birth experiences of migrant women affected by FGM/C. Their findings are consistent and conclude that pain and anxiety around birth could be exacerbated by traumatic memories of FGM/C and by a perceived lack of provider competence in managing FGM/C. They also found that attitudes to FGM/C changed as women adjusted to life in a new country, but that this process could be difficult as women encountered negative reactions to FGM/C from health-care professionals from the West. 63,64
Health professional perspectives and service delivery issues
There are three existing systematic reviews on health professional perspectives around FGM/C. 12,65,66 These have identified a significant lack of knowledge, confidence and competence around FGM/C and have concluded that more and better training is required. These reviews provide useful evidence but still leave gaps in our understanding. In particular, the reviews have focused primarily on quantitative evidence, which, while highlighting trends, have been unable to provide a more nuanced picture of barriers to and facilitators of service provision. The need to consider wider factors in understanding health professionals’ practice is illustrated by a 2013 study of FGM/C management in a large London maternity unit. 67 This found that, in spite of the existence of protocols, guidelines and training, clinical care for women/girls with FGM/C was suboptimal. The maternity unit had access to a FGM/C specialist service, but 41% of women with FGM/C were not identified until they arrived in the labour ward. Hence, even though a specialist service existed, it was not being optimally used to benefit women with FGM/C, and a significant percentage of opportunities were missed to provide women with specialist care. Similar findings were reported from a study in a maternity unit in Switzerland where, in spite of staff training and the existence of clear guidelines, FGM/C was correctly identified and managed in only 34 (26.4%) of 129 cases reviewed. 68 Likewise, an audit in Lothian in Scotland (between 2010 and 2013) showed that of 487 women from FGM/C-practising countries, only 18% had any documentation relating to FGM/C, suggesting that opportunities for detection may have been missed. 69 The reasons for this lack of adherence to protocols are unclear; hence, we suggest that reviewing the related qualitative evidence may shed greater light on organisational and personal factors that may influence health professionals’ views and behaviour in this area. 70–80
Gaps in existing knowledge: what this project will add
With the exception of the reviews by Hamid et al. 63 and Turkmani et al. ,64 existing reviews on women’s and health professionals’ experiences have all taken a multicontext (or ‘lumping’) approach to the evidence81,82 and have included research from high- and low-income settings across the world. Many key themes from these reviews are therefore drawn from evidence from very different cultural and health system contexts and are not easily transferable to a UK or high-income setting. In order to address this shortcoming, the reviews in this project included evidence from high-income Organisation for Economic Co-operation and Development (OECD) contexts only.
The recent reviews by Hamid et al. 63 and Turkmani et al. 64 are similar to the review that we have undertaken with respect to women’s/girls’ experiences. However, those reviews focused only on English-language papers and looked only at the birth experience, whereas the reviews in this project have looked at all aspects of FGM/C-related health care, including factors influencing care-seeking and service access. In addition, in contrast to Hamid et al. 63 and Turkmani et al,64 the reviews in this project have looked at all clinical settings and at all stages of the life course, not just maternity. This wider perspective is particularly important in terms of illuminating decision-making on topics such as timing of deinfibulation and care for non-pregnant women who may be experiencing symptoms. In addition, in accordance with The Cochrane Library83 and JBI84 methods, our reviews have included grey literature and research published in languages other than English. Hence, our reviews provide a significantly more detailed, holistic and comprehensive picture. This is exemplified by the fact that the review on women’s experiences (review 1, see Chapter 3) identified 57 relevant papers, whereas the reviews by Hamid et al. 63 and Turkmani et al. ,64 identified only 14 and 16 papers, respectively.
Situating female genital mutilation/cutting within a wider migration-related health policy and service context
Although this project is concerned specifically with health care related to FGM/C, it is important to situate this within the wider UK health-care context of service provision for migrant populations in a context of super-diversity. 5–7,85,86 The vast majority of women with FGM/C in the UK are first-generation migrants and evidence shows that this group experiences a wide range of challenges around seeking and receiving health care. 87–89 Likewise, health providers report a range of challenges in delivering care to migrant populations. 90,91 These challenges are particularly acute within maternity settings, where many women with FGM/C are first identified, where migrant women are consistently shown to have poorer outcomes and where improvement of patient safety is a national policy imperative. 92–98 Likewise, the NHS is under pressure to develop service models that can address the needs of a super-diverse population. 3,7,99 In a time of stretched resources, more innovation and better evidence is needed to help guide this endeavour. Therefore, we hope that, although the reviews are specific to FGM/C, the reviews may also serve to illuminate key issues that may help this wider effort.
Research aims and purpose
The aim of this study was to undertake two separate systematic reviews of qualitative evidence to understand the experiences, needs, barriers and facilitators around seeking and providing FGM/C-related care from the perspectives of (1) women and girls who have undergone FGM/C and (2) health professionals. The two separate sets of review results will be integrated into a final synthesis and used to (1) formulate recommendations for NHS training, service development and improvement, (2) pinpoint key dimensions of quality of care that can be operationalised for use in future service improvement evaluations or patient-reported outcome measures and (3) identify areas where further research is required.
Aim and objectives of review 1
Aim
To explore the experiences of FGM/C-related health care across the life course for women and girls who have undergone FGM/C.
Objectives
From the perspective of women and girls who have undergone FGM/C:
-
illuminate factors that influence FGM/C-related health-care-seeking and access to health services across the life course
-
explore how quality of care is perceived and experienced in different health-care settings and with different groups of health-care professionals
-
characterise and explain elements of service provision considered important for the provision of acceptable and appropriate health care
-
describe factors perceived to influence open discussion and communication around FGM/C (including prevention) with health professionals.
Aim and objectives of review 2
Aim
To explore the views and experiences of health professionals of all cadres of providing care for women/girls who have undergone FGM/C.
Objectives
From the perspective of health professionals:
-
explore how quality of care for women/girls who have undergone FGM/C is perceived in different health-care settings and among different professional groups
-
characterise and explain elements of service provision considered important for the provision of high-quality care to women/girls who have undergone FGM/C
-
illuminate factors perceived to facilitate or hinder appropriate provision of care for women and girls who have undergone FGM/C
-
identify processes and practices perceived to influence open discussion and communication around FGM/C (including prevention) with women/girls from affected communities.
Research team and patient/public involvement
This project was conducted by a core research team that was advised by a PAG. The core team comprised (1) academics with expertise in ethnicity and health, gender-based violence, qualitative methodologies and systematic reviewing (CE, RT, GH and JM), (2) an information specialist (JE), (3) a FGM/C specialist midwife who has served as part of NHS England’s National FGM Prevention Programme (JA) and (4) a FGM/C and women’s rights activist who runs a community organisation promoting African women’s rights, runs many anti-FGM/C campaigns nationally and internationally and runs a local FGM/C support group (VN). The PAG also comprised individuals with expertise in a range of areas, including obstetrics, general practice, midwifery, the voluntary sector (focusing on FGM/C issues) and specialist commissioning. In terms of patient and public involvement, we took the approach of ensuring that our community expert was a co-applicant on the project from its inception. Indeed, the project itself was co-constructed out of conversations between Valentine Nkoyo and Catrin Evans. Hence, patient and public involvement has been built into every stage of this project and has been key to its execution.
Structure of the report
Chapter 2 of this report presents the methodology underpinning the two reviews and the methods used. It includes a detailed description of the literature search that was undertaken. The results of the search are also presented in Chapter 2. This is because a single literature search was undertaken for both reviews, hence it needs to be presented in depth only once. Chapters 3 and 4 provide detailed descriptions of the results of reviews 1 and 2, respectively. Chapter 5 presents an integrated synthesis of reviews 1 and 2 that illuminates the health-care challenges around FGM/C in a holistic manner to account for, and explain, both patient and professional viewpoints and experiences. Chapter 6 discusses the review findings in the context of the wider literature and sets out the implications and recommendations of the synthesis. Chapter 7 presents the project conclusions.
Chapter 2 Methodology and methods
Introduction
In this chapter, we describe the methodology and methods used in both reviews. The literature search was conducted for both reviews at the same time (i.e. as one step). However, the other stages were conducted sequentially (i.e. we undertook all of the stages of review 1 first, followed by those of review 2). Given that the methods followed were exactly the same, the methods used in each stage are described in this chapter only once.
The research aims and objectives were constructed to identify insights about lay/health professional experiences of FGM/C-related health care and perceived appropriateness and acceptability of services. These are questions best answered by qualitative research;100,101 indeed, it is increasingly recognised that qualitative evidence syntheses have an essential role to play in understanding barriers to and facilitators of service initiatives. 102,103 The overall design and synthesis methodology for each review was the same. Both have been reported as per Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) guidelines. 104
Methodology
There are many possible approaches to qualitative evidence synthesis, with most discussions in this area characterising the different types along a continuum between aggregation and interpretation. 105 If the purpose of a synthesis is to generate new theoretical insights, a highly interpretive approach such as meta-ethnography may be most suitable, informed by an idealist epistemological stance. However, if the purpose is to inform policy or practice, a more aggregative or thematic approach informed by a realist epistemology is often advocated. 106 The latter is also suggested in cases in which the existing evidence is likely to be descriptive (as in much health services research) rather than highly theoretical or conceptual. 107 An initial scoping of the literature suggested that this was the case for the proposed syntheses. A thematic synthesis approach involves using thematic analysis techniques to identify key themes from primary research studies. 108,109 Synthesis involves an iterative and inductive process of grouping themes into overarching categories and exploring the similarities, differences and relationships between them. Thematic synthesis explicitly aims to move beyond generating a list of descriptive themes (as would be the case in meta-aggregation110) in order to identify new, higher-order, analytical insights that can contribute to new understandings of a phenomenon. Review recommendations, however, are clearly formulated to inform policy and practice. As such, thematic synthesis was considered the most suitable approach for the two systematic reviews. 111 Both reviews were conducted following the guidance set out by the Cochrane Qualitative and Implementation Methods Group. 83,103,110–114
Protocol and PROSPERO registration
Both review proposals were registered separately with the PROSPERO database. 115,116 A combined protocol for both reviews has been published in BMJ Open. 117
Search strategy and study selection
An exhaustive and sensitive search strategy was developed by an experienced information scientist (JE). The search strategy was designed to identify papers for both reviews; thus, it is reported here as one search.
Search inclusion and exclusion criteria
The review inclusion and exclusion criteria are set out in Table 1.
| Criteria | Details |
|---|---|
| Inclusion criteria | |
| Population |
Review 1: women and girls who have undergone any form of FGM/C, as defined by the WHO1 Review 2: any cadre of health-care professionals or health-care students who are involved in the care of women/girls who have undergone FGM/C |
| Phenomenon of interest |
Review 1: experiences of FGM/C-related health care across the life course Review 2: views on, and experiences of, providing care for women/girls who have undergone FGM/C |
| Country/context/setting | The reviews were limited to studies that were undertaken in high-income OECD country settings. The OECD grouping118 includes the majority of countries with similar social and political value systems and levels of economic development, and, therefore, whose research findings could be transferable to the UK (see List of Organisation for Economic Co-operation and Development countries). In addition, in terms of migration, high-income OECD countries tend to be migrant ‘destination’ countries and share a need and a challenge to adapt their health services to the needs of communities that practise FGM/C. ‘High income’ was defined in accordance with the World Bank criteria.119 Both reviews included studies from any health-care setting, health sector or health context within a high-income OECD country |
| Study design | Any type of qualitative study and any type of mixed-methods study that reported qualitative findings |
| Language | Any language |
| Date | No date limit |
| Exclusion criteria | |
| Context | Studies relating to middle- and low-income countries or non-OECD high-income countries |
| Participants |
Review 1: studies not related to women’s or girls’ experiences of health care or health professionals Review 2: studies that did not include the views/experiences of health-care professionals or students |
| Study design | Quantitative study designs and papers that did not report empirical research (e.g. commentaries or opinion pieces) |
List of Organisation for Economic Co-operation and Development countries
-
Australia.
-
Austria.
-
Belgium.
-
Canada.
-
Chile.
-
Czech Republic.
-
Denmark.
-
Estonia.
-
Finland.
-
France.
-
Germany.
-
Greece.
-
Hungary.
-
Iceland.
-
Ireland.
-
Israel.
-
Italy.
-
Japan.
-
Korea.
-
Latvia.
-
Luxembourg.
-
Mexico.
-
The Netherlands.
-
New Zealand.
-
Norway.
-
Poland.
-
Portugal.
-
Slovak Republic.
-
Slovenia.
-
Spain.
-
Sweden.
-
Switzerland.
-
Turkey.
-
UK.
-
USA.
Search strategy
The searching process was conducted in three phases.
The first phase consisted of searching 10 electronic literature resources [both individual databases and hosted multifile collections (see Table 2 for full details)] that covered the relevant disciplinary areas, so that empirical research published in peer-reviewed journals or book chapters could be identified. The searching used a combination of index terms and text-based queries. Several of the resources (e.g. MEDLINE® In-Process & Other Non-Indexed Citations) provide access to literature not yet assigned to a medical subject heading (MeSH) term or other indexing, so it was important to include text-based queries for comprehensive and current retrieval.
Key index terms included:
-
exp Circumcision, Female/ (MeSH and MEDLINE)
-
exp female genital mutilation/ (Emtree and EMBASE)
-
exp circumcision/ (Ovid PsycINFO).
The different terminologies reflect different indexing principles and practices in the individual literature databases, and were incorporated into the overall strategies for completeness. Following the initial searches, the same strategies were set up as monthly alerts for four main literature databases (see Table 3 for details) until 31 December 2017 (i.e. the searching was not completed as a one-off process). Example full strategies for Ovid MEDLINE and CINAHL (Cumulative Index to Nursing and Allied Health Literature) on EBSCOhost are provided in Appendices 1 and 2.
The second phase comprised an extensive search for relevant grey literature, particularly to identify research reports or theses not formally published but still available in the public domain through institutional websites or thesis repositories. 120–122 This part of the searching process included five resources to help identify this type of grey literature (see Table 2). Google (Google Inc., Mountain View, CA, USA) and Google Scholar were also interrogated and key experts in the field were contacted to elicit additional suggestions of relevant documents. 123
The third phase of the search involved hand-searching the reference lists of related systematic reviews and of all the included studies.
Table 2 provides a list of the databases searched and the search dates. Box 2 provides a list of the grey literature sources.
| Electronic databases searched [date range] | Date of search |
|---|---|
| Ovid multifile search (MEDLINE, EMBASE, PsycINFO) [inception to 10 March 2017] | 10 March 2017 |
| POPline (via www.popline.org/) [1970 to present] | 10 March 2017 |
| ProQuest multifile searcha [inception to 10 April 2017] | 10 April 2017 |
| ASSIA on ProQuest [1987 to present] | 26 May 2017 |
| Ovid MEDLINE [1948 to present] and MEDLINE In-Process & Other Non-Indexed Citations [1948 to 26 July 2017] | 26 July 2017 with monthly alert thereafter (cut-off date for included results: 31 December 2017) |
| Ovid EMBASE [1980 to 2017 week 11] | 3 August 2017 with monthly alert thereafter (cut-off date for included results: 31 December 2017) |
| CINAHL Plus with Full Text/EBSCOhost [inception to 2017] | 11 August 2017 with monthly alert thereafter (cut-off date for included results: 31 December 2017) |
| Ovid PsycINFO [1972 to March week 3 2017] | 14 August 2017 with monthly alert thereafter (cut-off date for included results: 31 December 2017) |
| MIDIRS on Ovid [1971 to April 2017] | 18 August 2017 |
| HMIC on Ovid [1979 to present] | 18 August 2017 |
| Clarivate Analytics Web of Scienceb [1900–2017] | 18 August 2017 |
-
The British Library EThOS (ethos.bl.uk).
-
Networked Digital Library of Theses and Dissertations (www.ndltd.org).
-
National Institute for Health and Care Excellence (www.nice.org.uk).
-
Trove – National Library of Australia (trove.nla.gov.au).
-
Open Grey (www.opengrey.eu/).
-
Google (www.google.com).
-
Google Scholar (https://scholar.google.co.uk).
-
Experts in the field.
Balancing sensitivity versus specificity within the search strategy
In developing the original search strategies for the reviews, search terms around FGM/C seemed to generate suspiciously small answer sets in the main literature databases (MEDLINE and EMBASE) despite the use of a large range of synonyms for FGM/C. To address this, the librarian devised additional search statements that brought in terms relating to the possible physical or psychological complications that are identified as health impacts of FGM/C, making use of the descriptors in a UK Department of Health and Social Care FGM/C guidance document. 124 This aimed to retrieve relevant documents, based on symptoms or impacts described, without necessarily mentioning FGM/C or other synonyms. These search statements can then be seen as a proxy for FGM/C in the strategy. In addition, we identified from hand-searching that some relevant studies were not indexed in the databases using FGM/C-related terminology. This appeared to be attributable to the study’s main focus being on a different issue, for example pregnancy experiences or care for a particular migrant group (e.g. Somali). Therefore, the search strategy was broadened by using additional ‘proxies’ for FGM/C (originating countries, e.g. “Somali*”) plus pregnancy terms OR physical/mental complications/disorders associated with FGM/C to draw in such papers, which did not overtly capture FGM/C in the title, abstract or MeSH/Emtree indexing. Because these proxy search statements are necessarily less specific, the high sensitivity was tempered by focusing the strategies to limit retrieval to studies relating to OECD countries and specifically excluding RCTs.
Management of identified records
All retrieved data sets were downloaded into group sets within an EndNote library (Clarivate Analytics, Philadelphia, PA, USA). Using the EndNote grouping functionality, individual group folders were created for each of the database search results sets. Each record was annotated to identify from which database search it had originated. The ‘Find Duplicates’ feature was used to identify duplicate articles from across the different database searches. The duplicates were then moved to a separate ‘Duplicates’ group, leaving one unique representative of each article in the ‘Search Results’ group, usually selecting the MEDLINE representative to be retained, if available.
Screening and selection
Two members of the project team independently screened all potential studies based on a review of titles and abstracts, grouping them into yes, no or unsure using the screening tool in Table 3. Areas of disagreement were resolved through discussion and by consultation with other team members at team meetings.
| Screening criteria | Y | N | U |
|---|---|---|---|
Does the study report findings related to………………
|
|||
| Is the study conducted in an OECD country? | |||
|
Is it a qualitative study? Or Does it report qualitative findings from a mixed-methods study? |
|||
Are the participants………………
|
Full texts of all studies with an initial assessment of yes or unsure were then obtained. These were retrieved via online searches and using the interlibrary loan scheme. If papers and reports could not be retrieved through these channels, authors were contacted by e-mail or via ResearchGate (www.researchgate.net) with full-text requests. All full-text papers were then independently assessed by two team members, alongside discussion with the wider team in cases of uncertainty. Reasons for exclusion were documented (see Appendix 3 for a table of all excluded studies with reasons).
Management of foreign-language papers
Non-English-language papers found to be relevant on the basis of their English-language abstract were sent for complete academic translation. This included a summary of the study purpose or aims and the complete methods and findings sections of the studies. A total of 13 papers were translated by outsourced translators who had experience and training in research. After translation, these texts were then assessed for inclusion and quality appraised and data were extracted if selected for inclusion.
Quality assessment
The role of critical appraisal in qualitative evidence synthesis is contested and there is a lack of agreement on (1) the appropriateness of excluding studies, (2) the potential impact (or not) of excluding eligible papers on review outcomes and (3) the criteria on which quality should be established. 126–129 For these reasons, the team adopted an inclusive approach to critical appraisal, using the appraisal process to enable an in-depth understanding of each paper and to facilitate a critical, questioning approach to the study findings. 130 Studies were not excluded on the basis of quality; rather, the quality assessment was used (1) to judge the relative contribution of each study to the overall synthesis and (2) to assess the methodological rigour of each study as part of a process of assessing confidence in the review findings. 131–135
Following the guidance of the Cochrane Qualitative Methods and Implementation Group136 and the JBI,84 reports and theses from the grey literature were appraised in the same way as papers that were published in peer-reviewed journal articles. 120,122,123
Study quality was assessed by two reviewers (RT and CE) using the Joanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI). 137,138 The domains examined in this tool have been found to be more coherent and more sensitive to assessment of validity than other commonly used tools (see Appendix 4). 128 Team meetings were used to achieve a shared and consistent approach in operationalising the domains in the tool. A third reviewer (GH or JM) was asked to comment on any papers for which there was uncertainty or disagreement and discussions were held until a final consensus on assessment for all the papers was achieved.
The JBI-QARI has 10 questions. These were applied to each individual paper and an aggregate score was calculated (Table 4). In addition, reviewers’ comments were recorded, providing an explanatory rationale for why questions had been answered in a particular way. There is some debate over the use of critical appraisal tools to ‘score’ papers, especially if arbitrary scores are used to exclude papers from a review. 110,135,140 However, as explained above, we did not use the score to exclude papers. Rather, we adopted this approach primarily to enable us to determine an overall, if somewhat crude, picture of the quality of the whole body of evidence within each review, and to assist with the assessment of methodological limitations as a key part of the process of establishing the level of confidence in each of the review findings (see Assessment of confidence in the review findings: CERQual). 112 A criticism of ‘scoring’ qualitative critical appraisals is that it can be hard to distinguish between the poor conduct of a study and poor reporting, especially where journal word limits constrain the level of detail that can be reported. 110 In addition, there is no consensus regarding the relative importance of any one domain within an assessment tool over another, and, hence, whether or not they should all be given an equal weight. In view of these concerns, we chose to adopt a ‘weighting system’ used in previous studies by Higginbottom et al. ,141,142 in which papers were grouped into one of three ‘bands’ (high, medium or low) to enable a broad-brush evaluation to be made of their relative quality, as shown in Table 4.
| Quality evaluation | JBI-QARI aggregate score | Definition |
|---|---|---|
| High | > 7 | A study with a rigorous and robust scientific approach that meets most JBI benchmarks (perhaps 7 or more ‘Yes’) |
| Medium | 5–7 | A study with some flaws but not seriously undermining the quality and scientific value of the research conducted (perhaps 5–7 ‘Yes’) |
| Low | < 5 | A study with flaws and poor scientific value (perhaps below 5 of the benchmarks met) |
As an additional strategy for overcoming the potential limitations of solely relying on a checklist to assess quality, we also chose to assess the ‘richness’ of the studies. This is an approach outlined by Popay et al. ,143 and subsequently operationalised further in Noyes and Popay144 and Higginbottom et al. 141,142 This approach defines study ‘richness’ as ‘the extent to which the study findings provide explanatory insights that are transferable to other settings’. 144 ‘Thick’ papers create or draw on theory to provide in-depth explanatory insights that can potentially be transferable to other contexts. By contrast, ‘thin’ papers provide limited or superficial description and offer little opportunity for generalising. Each paper was assessed by Ritah Tweheyo and Catrin Evans against the criteria, as set out by Higginbottom et al. 141 (Table 5), and categorised as either ‘thick’ or ‘thin’.
| Richness | Operational definition |
|---|---|
| Thick papers |
|
| Thin papers |
|
Extraction of study characteristics
Details of each of the included papers were extracted into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) file using the domains from the JBI data extraction template (see Appendix 5). 137,146 Data extraction of study characteristics was primarily undertaken by one reviewer (RT); however, a second and third reviewer (CE and JM) double-checked the extractions of a subsample of papers for accuracy. In addition, the team had regular meetings to discuss any uncertainties, to ensure consistency of approach and to agree definitions.
Categorisation of study relevance
After data extraction, papers were categorised by Ritah Tweheyo and Catrin Evans in terms of their relevance to the respective review question. This assessment was made in order to gain a better understanding of the nature of the body of evidence, and also to facilitate the coding process, as described further in Thematic analysis and synthesis. Study relevance was defined as high, medium or low, as set out in Table 6.
| Study relevance | Definition |
|---|---|
| High (specific) | FGM/C-specific health care, for example the study is focused on a specific aspect of care related directly to FGM/C (e.g. deinfibulation, childbirth for women who have had FGM/C, psychological care) |
| Medium (direct) | Other health-care context (e.g. where the study focus is on the maternity care experience of a particular group more generally and where some of the findings relate to the experience of FGM/C) |
| Low (indirect) | Where the study focus is on general attitudes towards FGM/C and/or experiences and consequences of FGM/C, and where some FGM/C-related health-care issues are reported, but are not the main focus of the paper |
Extraction of study findings
PDF (Portable Document Format) files of all of the included papers were imported into NVivo 11 (QSR International, Warrington, UK) software and the ‘findings/results’ sections were coded and analysed. If ‘findings’ were located in other parts of the papers (e.g. the discussion sections), these were also coded. 147
Thematic analysis and synthesis
Analysis and synthesis of the study findings followed the principles of inductive thematic analysis,108,109 and comprised four stages, as suggested by Thomas and Harden. 107 This was followed by a final, fifth step in which the findings from both reviews were combined into an integrated synthesis from which implications for policy, practice, education and research were derived.
The first stage involved intensive and repeated reading of all of the included papers to gain an overall in-depth understanding of their context and key findings. This stage was returned to many times during the analysis and synthesis to ensure that emerging interpretations remained deeply contextualised.
The second stage involved line-by-line coding of the findings of the primary studies. We coded only findings that were directly relevant to the review question. Where there were multiple papers from the same study, we ensured that distinct findings were coded from each (i.e. we did not code duplicate findings). Owing to the large number of papers in each review, we decided to start the development of the coding framework by focusing on studies that were likely to yield the richest and most relevant findings. Hence, we started with the studies that had been categorised as both ‘thick’ and highly relevant. These generated a large number of free codes, assigned line by line to the text according to its meaning and content. Subsequent studies were coded using the initial framework of codes and adding to them as new codes were identified. Ritah Tweheyo and Catrin Evans both independently coded the initial set of studies, conferring until the initial coding framework was agreed. Subsequently, Ritah Tweheyo completed the rest of the coding, with Catrin Evans and Gina Higginbottom regularly reviewing and discussing the evolving framework.
The third stage involved analysing the codes to explore areas of similarity or difference, grouping them together based on shared meanings to create new codes, and then organising these into a set of descriptive themes that captured the meaning of their constituent codes. In NVivo, this was represented as a hierarchical tree structure with several layers. Each theme was formulated to describe a key phenomenon in such a way as to capture its core meanings but also to explain and account for possible differences or variations in the phenomenon. To ensure rigour of the analytical process, the team actively sought to identify and understand possible ‘disconfirming’ cases that might challenge emerging interpretations,148 and to explore possible subgroup or contextual differences. These processes were aided by the creation of a theme matrix (see Appendices 8 and 12), in which each theme was mapped to its constituent studies. This helped the team to clearly see how common the theme was among the studies and what kind of study contexts or samples the theme related to, and to explore why it may have been present in some studies but not in others. During the analysis, the team referred to a list of questions to help them to develop the descriptive themes, as set out in Box 3.
-
Define, explain and contextualise the core concept.
-
Explore key groups it may (or may not) apply to.
-
Explore key settings/circumstances it may manifest in or be affected by.
-
Explore causes, manifestations, variations and consequences in terms of perceived quality of care and potential clinical outcomes or clinical trajectories.
-
Identify ‘gaps’ within the theme.
-
Explore any key variations between the studies and the study contexts.
-
Explore implications of the date ranges of the included studies.
-
Explore and understand examples where the theme does not seem to apply.
Descriptive themes are derived from an interpretative process of constructing codes based on underlying meanings and considering how and in what ways these codes are related to each other. Thus, they represent a highly rigorous process that combines the findings of each study into a whole via a listing of themes. Nonetheless, Thomas and Harden107 argue that descriptive themes represent only the first step of synthesis, as, at this point, they generally do not yet ‘go beyond’ the findings of the primary studies to identify new concepts, understandings or hypotheses. This is achieved in the fourth stage, comprising the development of higher-order or ‘analytical’ themes, which constitute the key findings of the reviews.
For the fourth stage of synthesis, analytical themes were evolved through an in-depth process of comparing and contrasting the meanings of the descriptive themes, analysing these in relation to how they were, or were not, able to illuminate the review questions, and inferring broader phenomena, categories of meaning or social processes that they related to. This was a cyclical process that involved re-reading the papers, re-reading the codes and in-depth discussion among team members. Using this analytical process, the descriptive themes were organised into five analytical themes for review 1 and six analytical themes for review 2.
As far as possible, the descriptive and analytical themes were formulated as ‘directive’ findings indicating clear messages and/or suggesting clear lines of action for policy and practice. 137
The fifth and last stage of the synthesis involved bringing the findings from both reviews together to generate an overarching novel synthesis. This was done by creating short statements of findings for all of the themes (descriptive and analytical) in each review, listing them out, juxtaposing review 1 themes against review 2 themes and comparing and contrasting these. This process enabled the team to identify key phenomena that could explain and illuminate aspects of FGM/C-related health care through understanding both women’s and professionals’ views and experiences together. An overarching synthesis comprising four ‘synthesised findings’ was then drafted and extensively consulted and revised by the whole team until a final version was agreed.
Assessment of confidence in the review findings: CERQual
Assessment of confidence in the findings of each review was undertaken using the Confidence in the Evidence from Reviews of Qualitative Research (CERQual) approach. 110,112,131,136,149–153 Ritah Tweheyo and Catrin Evans led this process, working together and discussing the final assessments with the research team. CERQual is a relatively new, transparent method for assessing confidence in the findings in qualitative evidence syntheses; it is akin to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach for establishing confidence in evidence of effectiveness for each outcome in a quantitative review. 154 The assessment of confidence in the evidence is made for each individual review finding and considers four elements: (1) methodological limitations (the extent to which there are problems in the design or conduct of primary studies that contributed to evidence of a review finding),136 (2) relevance (the extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context specified in the review question),149 (3) coherence (whether or not the finding is well grounded in data from the primary studies and can provide a convincing explanation for patterns found in the data)152 and (4) adequacy of data (an overall determination of the degree of richness and number of data supporting a review finding). 151 Based on assessments made of any concerns across these four individual domains, each review finding is assigned one of four levels of confidence: high, moderate, low and very low.
In this project, the CERQual assessment was made for each of the descriptive review findings. Each descriptive review theme was summarised into a succinct ‘summary of a review finding’. These were then presented in a ‘summary of qualitative findings table’ containing several columns, including the summary of the review finding, the studies that contributed to the review finding, the assessments for each of the CERQual domains, the overall CERQual assessment of confidence in the evidence and an explanation of this assessment (see Appendices 9 and 13).
The CERQual assessment was made for each of the descriptive review findings (themes), rather than for the analytical themes or the themes in the overarching integrated synthesis, as the latter comprise an aggregation of descriptive themes as well as descriptions of patterns or explanations that are inferred as part of the interpretative process. There is, as yet, relatively little guidance for, or experience with, applying CERQual to higher-level analytical themes or theories. 150 The process of applying CERQual to our higher-order themes would, therefore, have required an extended period of methodological development and testing, which was beyond the scope of this project, and which is recognised as being part of the ongoing research agenda for CERQual development. 150
As of yet, unlike GRADE assessments, ‘dissemination bias’ within qualitative evidence synthesis is rarely discussed and needs further methodological consideration. 153 However, in this review, we sought to minimise possible dissemination bias by undertaking an exhaustive literature search that (1) was highly sensitive rather than specific, (2) included a range of grey literature (research reports, evaluations and theses) as well as published papers, (3) did not limit the date, (4) did not limit the language and, (5) included the original thesis or report in addition to the published paper when the former contained findings that were not reported in the latter. In addition, as noted above, we maintained an inclusive approach and did not exclude any studies on the basis of quality.
Reflexivity, rigour and quality of the synthesis
As with primary qualitative research, there are a number of strategies that can be adopted to enhance the rigour and trustworthiness of qualitative evidence synthesis. 148,155 We utilised a range of different approaches, as outlined in this section.
First, we were aware that our own theoretical, cultural and political positions might influence the ways in which we engaged with the texts and developed the interpretations. 156,157 The initial analysis and synthesis process was undertaken primarily by two reviewers (RT and CE), aided by the wider project team. Ritah Tweheyo is a black African public health researcher, originally from Uganda, and Catrin Evans is a white nurse and health services researcher from the UK. Neither has direct experience of FGM/C, and neither has worked clinically with women/girls who have experienced FGM/C. Both have had experiences of ‘being migrants’ and having to adjust to foreign health systems, but in different contexts. Both have experienced childbirth. Both consider themselves to be feminists and anti-racist (but again, these standpoints have emerged from different subjectivities). Both are anti-FGM/C but recognise the inherent political and epistemological tensions that exist when individuals located ‘outside’ cultures and communities try to explain a phenomenon that is deeply culturally and socially shaped. During the analysis, we continually challenged ourselves by asking if and how our emerging interpretations were being influenced by our own perspectives and repeatedly returned to the original papers to re-embed coded text within its wider study context and to check our interpretations. As an example, there were many accounts in the papers in review 1 in which women described extremely humiliating, distressing and stigmatising experiences in their health-care encounters, often linked to their race or ethnicity. Although we knew from prior reading that such experiences had previously been reported, reading so many accounts at first hand proved to be a shocking and distressing experience for us as reviewers. We had not expected this to be such a pervasive theme and we felt strongly that we wanted this aspect of women’s experience to be heard in the review. However, we occasionally wondered if we were perhaps giving too much prominence to women’s negative experiences and failing to give sufficient attention to instances where women had reported positive care experiences. This led us back to reading and, in some instances, re-coding the original papers, and this prompted us to develop a more nuanced approach to understanding women’s care experiences.
Second, the analysis process also explicitly drew on the expertise within, and challenge from, the project team. Team members were sent exemplar papers to read before meetings, so that our discussions were grounded in the papers and hence enabled challenge and conceptual development of the initial interpretations of Ritah Tweheyo and Catrin Evans. The same approach was used during consultations with the PAG. However, this consultative process was not always straightforward, as all involved had vast experience and strong views. At times, we had to step back and remind ourselves to base our interpretations on the data from the included papers and not on our own wider experiences.
Third, once the descriptive and analytical themes had been finalised by the project team, we organised a national research stakeholder engagement event in which the draft review findings were presented. Over 65 people attended this event, representing FGM/C survivors, FGM/C activists, community organisations with FGM/C as a remit, academics, researchers, midwives and general practitioners (GPs). Their inputs contributed to the report in four important ways: (1) to explore the credibility of the key findings, (2) to put these into the contemporary UK context, (3) to identify gaps in evidence/understanding and (4) to put forward key implications/recommendations for service development and future research.
The nature of stakeholder validation in the context of a review is controversial and poorly described. 158 Generally, non-author stakeholders have not necessarily read the included papers and thus are not directly familiar with the underlying research findings; they may or may not have direct experience of the issues to which they pertain, hence there is some debate over their ability to ‘validate’ the emergent themes. Therefore, as suggested by Booth et al. ,148 we used our stakeholder event to challenge our interpretations as well as to explore the credibility of our findings. After each of the review presentations, stakeholders were asked to comment on the questions in Box 4.
-
Based on your own experience and perspectives, do the themes seem to capture the main issues?
-
Were any review themes surprising for you? Why?
-
Were there any review themes that you do not agree with? Why?
-
Do you think that there are any issues missing from the review findings that you would have expected to see?
The feedback from the event was reassuring in that there was a very strong sense of validation of the findings. When participants indicated that they had found a theme surprising, we returned to that theme and re-examined it. For example, two of the descriptive themes in review 2 (around professionals’ experiences of deinfibulation and reinfibulation) were rewritten in a more nuanced manner as a result of this process. Participants had felt that further detail and country-specific exploration was required in these themes, as they felt that in the UK context, professionals would know the relevant laws and would not experience the ambivalence described. Likewise, participants noted a number of perceived omissions (e.g. nothing on the impact of mandatory reporting and little on mental health issues), which, again, prompted us to go back and check that these were actual omissions in the evidence and did not reflect errors in the review process. Some comments helped us to analyse the findings in more detail (e.g. one participant asked how the policy and legal context around FGM/C in different countries might have influenced the findings). The event was also used to elicit suggestions for the implications of the review (see Appendix 14 for a full description of the stakeholder event).
Finally, in order to capture feedback from medical practitioners (a group that had been largely absent from the national event), the review findings were then also presented to a group of 30 obstetric and gynaecology registrars during one of their training days. This group included doctors working in cities with a relatively high prevalence of FGM/C as well as some working in settings with a very low prevalence. The subsequent discussions of their own experiences showed a very high level of congruence with the findings of review 2 (at least within the English context), and further helped to shape the implications from a medical perspective (see Appendix 17 for detailed feedback from this group).
Summary of the review process
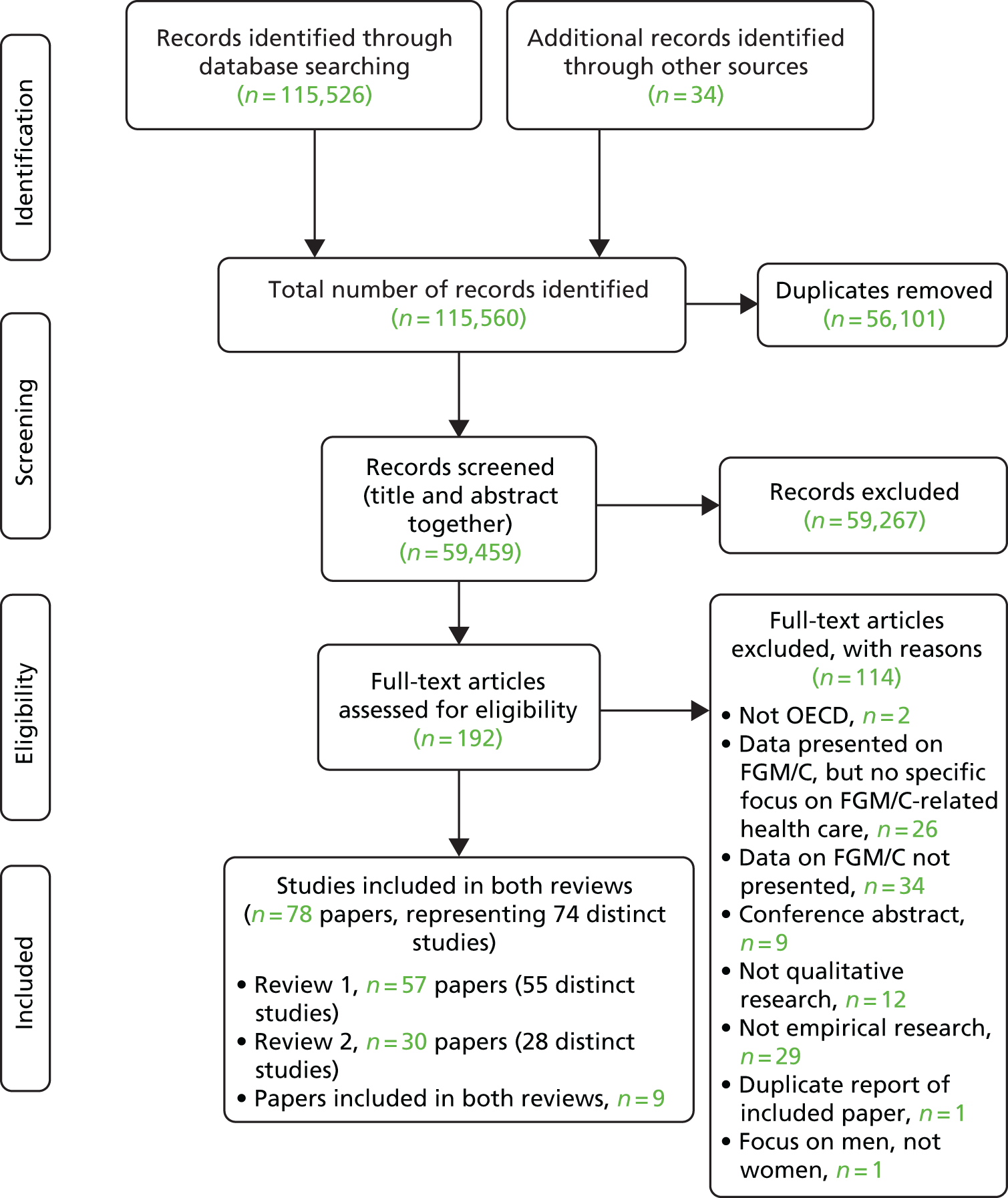
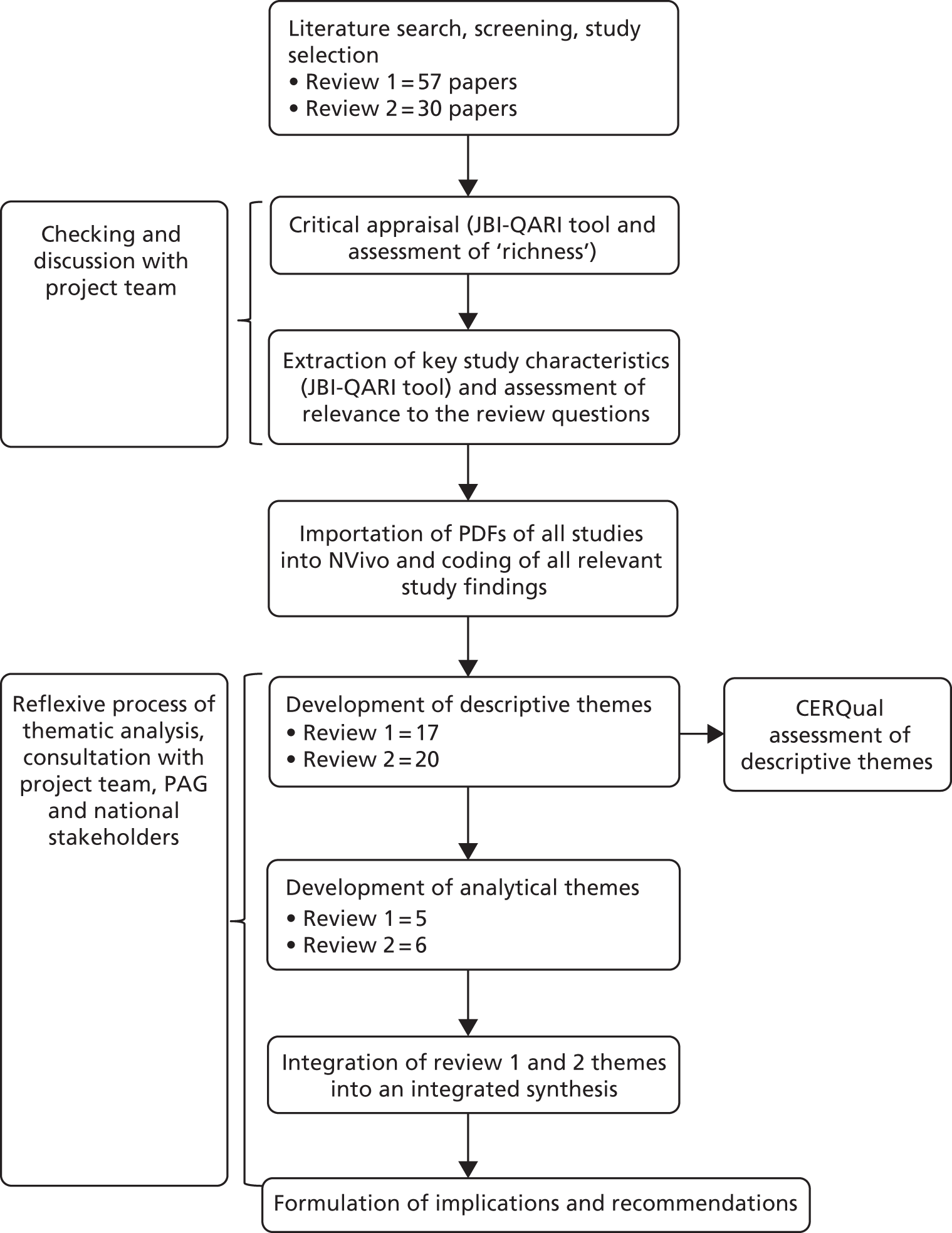
Figure 2 provides a clear depiction of all of the steps in the review process.
FIGURE 2.
Flow chart of the review process.
Chapter 3 Review 1 results
Characteristics of studies in review 1
As described in Chapter 2, 57 papers met the inclusion criteria for review 1. Two studies were reported in multiple publications,159–162 hence review 1 includes 55 distinct studies reported in 57 publications. Regarding these duplicate studies, in both cases these were a doctor of philosophy (PhD) thesis and an associated peer-reviewed journal article. The PhD theses were included in addition to the journal article, as they contained relevant findings that were not reported in the published paper.
Of the 55 distinct studies, 46 were unique to review 1 and nine were also included in review 2 (as their samples included health professionals as well as patients). 56,78,161,163–169 Fifty-three papers were in the English language; two were in German170,171 and two were in Spanish. 172,173
See Appendix 6 for a detailed summary of study characteristics.
Type of publications
Over half of the included papers were peer-reviewed journal articles. In total, the review included 13 master’s and PhD theses,78,159,161,165,170,171,173–179 10 unpublished research reports,47,57,58,164,168,169,180–183 one book chapter184 and 33 peer-reviewed journal articles. 56,59,160,162,163,166,167,172,185–209
Date range of studies
The studies represented a mixture of older and more-recent research, with publication dates ranging from 1985 to 2017. However, 29 papers had been published since 2011, hence half of the papers reflected a more contemporary context.
Geographical setting of studies
The studies represented a wide range of OECD countries, covering 14 different countries in Europe, North America and Australasia. Specifically, review 1 included studies from Australia,168,169,197,203 Austria,171 Canada,159,160,175,177,178,191 Finland,192 France,193 Germany,164,170 the Netherlands,206,208 New Zealand,165,197 Norway,167,199 Spain,172,173 Sweden,186,189,194,200,209 Switzerland,161,162 Scotland (UK),174,181,182 England (UK)47,56–59,163,179,180,183–185,196,202,204,205 and the USA. 78,166,176,187,188,190,195,198,201,207 Research undertaken in the UK (including Scotland and England) provided the most input to the review, contributing over one-third of the papers (n = 18), followed by research undertaken in the USA (n = 10).
Sample/population/type of female genital mutilation/cutting
The studies were primarily of adult women. Only one study included girls under the age of 18 years but did not report health-related experiences of this group. 186 There were no studies that focused specifically on health-care issues related to FGM/C in older (post-childbearing) women. Hence, although the aim of the review was to explore FGM/C across the life course, the studies all focused on generic issues relating to adult women and no further age-specific differentiation could be made.
The vast majority of studies were of women from FGM/C-practising countries in sub-Saharan Africa, and the majority of these included women specifically from countries in the Horn of Africa (Somalia, Sudan and Eritrea), where type III FGM/C is most commonly practised. Hence, the findings included in the review predominantly reflect issues affecting these population groups and issues that may be specific to having experienced type III FGM/C. Only three studies explicitly reported including women from Egypt/the Middle East but did not differentiate these women’s experience from the rest of the sample. 166,176,184 The sample compositions of the included studies were as follows: Somali women,56,59,78,159,160,163,167,175,177,178,184–188,190–192,194,195,198,201,202,206,207,209 Somali and Eritrean women,161,162,168,205 Eritrean women,170,200 Somali and Sudanese women,57,179,199 Senegalese and Nigerian women,172 and mixed samples including women from several different countries. 47,58,164–166,169,171,173,174,176,180–183,189,193,196,197,203,204,208 Almost half of the studies (n = 27) focused exclusively on women from Somalia.
Where there were mixed samples, none of the studies provided an in-depth differentiation of women’s experiences on the basis of the type of FGM/C they had experienced.
Focus, context and relevance of studies
The studies had varied research aims and foci; for example, some studies focused very directly on FGM/C-related health experiences (e.g. Moxey and Jones202), whereas others explored FGM/C as a general issue, not focusing only on health (e.g. O’Brien et al. 181). Other studies explored health issues in a general way (e.g. Abdullahi et al. 185), or focused on sexuality/identity (e.g. Abdi163) or on different aspects of life as a migrant (e.g. Guerin et al. 197), but all included some findings that concerned FGM/C-related health care.
The largest number of studies (n = 18) focused specifically on women’s birth/maternity care experiences. 56,59,78,165,167,174,187–189,191,193,194,198,200,202,203,209 Other study contexts were as follows: general views on health care,57,160,166,168–171,173,184,204,207 general attitudes towards FGM/C,47,58,159,163,164,178,181–183,186,201 experiences of sexual/reproductive health services,161,162,172,176,192,197 cervical screening,185,190,195,206 psychological issues,179,196,208 deinfibulation, 199,205 GP services,180 identity175 and pain/embodiment. 177
Notably, only three studies included psychological health-care needs/experiences as a specific issue. 179,196,208 There were no studies that examined women’s experiences of surgical reconstruction following FGM/C.
As described in Chapter 2, in order to assist development of the initial coding framework, we categorised each of the papers according to their overall relevance to the research aims. Sixteen papers were rated as being of high relevance,59,78,161,167–169,174,175,179,183,189,193,196,200,202,207 19 papers were rated as being of medium relevance56,162,165,172,178,180,185,187,188,190–192,195,199,203,206,208,209 and 22 papers were rated as being of low relevance. 47,57,58,159,160,163,164,170,171,173,176,177,181,182,184,186,194,197,198,201,204,205
Methodological quality of included studies
The papers were each appraised by two reviewers using the JBI-QARI138 (see Appendix 7 for full details of the quality appraisal of each paper).
As described in Chapter 2, a broad scoring range was used to provide a ‘rough’ sense of the overall quality of the body of evidence. In accordance with this categorisation, 30 papers were assessed as being of high quality,59,78,159,161,163,167–169,173,174,177–179,181–183,186,190,192,193,195,196,199–203,205,206,208 21 papers were assessed as being of medium quality47,56–58,162,164,165,170,172,175,176,185,187–189,191,194,198,204,207,209 and six papers were assessed as being of low quality. 160,166,171,180,184,197
A methodological weakness in many studies was a lack of apparent philosophical standpoint (question 1 of the JBI-QARI), making it difficult to assess the congruency of the chosen methodology. Likewise, many studies did not identify any clear methodology (simply stating that they adopted a generic ‘qualitative approach’), making it difficult to judge the congruence of the methodology with the research question and the methods (questions 2 and 3 on the JBI-QARI). Finally, a weakness across many studies was a lack of discussion of reflexivity (questions 6 and 7 on the JBI-QARI). Given the sensitive nature of FGM/C (and sexuality or migrant health care) as a topic, the failure to explore the researcher’s own theoretical position or their role, professional background, ethnicity, experience of FGM/C or relationship to the participants makes it hard to judge the dependability of the findings. 155 A related issue that could affect the transferability of the findings concerns the study samples and the methods of recruitment that were used. 155 The JBI-QARI does not assess in detail how recruitment was conducted; however, many studies had derived their samples from community organisations or used snowball sampling. The majority of studies did not discuss the potential implications of these recruitment strategies for influencing the results towards a particular standpoint (e.g. for or against FGM/C) or towards a particular view of health care or willingness to openly discuss FGM/C.
In addition to the JBI-QARI quality assessment, the papers were also categorised according to their ‘richness’ in terms of being ‘thick’ or ‘thin’ (i.e. their relative ability to provide explanatory insights and plausible interpretations based on a clear account of the research process). 141–143 Thirty-three papers were classified as ‘thin’47,56–58,159,160,162–164,166,170–173,176–178,180–182,184–188,191,192,194,197,201,205,208,209 and 24 papers were classified as ‘thick’. 59,78,161,165,167–169,174,175,179,183,189,190,193,195,196,198–200,202–204,206,207 The ‘thicker’ papers tended to be studies that were informed by an anthropological theoretical approach, that had followed a clear methodological stance or that had moved beyond mere description in their analysis towards a more interpretive and analytical account of the phenomenon of interest.
As noted previously, 23 papers were unpublished research reports or master’s and PhD theses (i.e. grey literature). 47,57,58,78,159,161,164,165,168–171,173–183 The lack of peer review in these included papers could be considered a potential threat to the quality of the review findings; however, our detailed quality appraisal did not indicate any clear correlation between being published and the quality rating. For example, four theses and three unpublished research reports were rated both ‘thick’ and of ‘high quality’ (30% of the grey literature). 78,161,168,169,174,179,183 However, out of 33 peer-reviewed journal articles, only 11 were rated as being both high quality and ‘thick’ (33% of the published journal articles – a very similar percentage). 59,167,190,193,195,196,199,200,202,203,206 Indeed, of the six papers rated as being low quality (all of which were also rated ‘thin’), half (n = 3) were peer-reviewed journal articles160,166,197 and one was a peer-reviewed book chapter. 184 Most of the papers were rated as being somewhere between high quality and low quality.
Review 1 themes
The findings from the 57 studies in review 1 have been synthesised into five analytical themes, which, in turn, represent a synthesis and interpretive analysis of 17 descriptive themes (Table 7). To start the coding process, studies that were both ‘thick’ and ‘highly relevant’ were identified and used to build an initial coding framework. Findings from other studies were then added into this initial coding framework and the framework itself was then further developed as necessary as new codes were identified. In review 1, 16 papers were categorised as ‘thick’ and ‘highly relevant’ and were used for the first stage of coding. 59,78,161,167–169,174,175,179,183,189,193,196,200,202,207
| Analytical theme | Descriptive theme |
|---|---|
| 1. Communication is key |
1.1. Language barriers and interpretation challenge 1.2. ‘Can’t talk, not asked’: double silence and cultural taboo 1.3. Cultural (in)sensitivity |
| 2. Access to care: influenced by an interaction of multilevel community and health service processes |
2.1. Influence of cultural norms 2.2. Influence of the family 2.3. Knowledge and information about FGM/C services 2.4. ‘Hit and miss’ care |
| 3. Cultural and bodily dissonance: striving for cultural and bodily integrity |
3.1. Moving from normal to different 3.2. Threat to the self: reliving FGM/C pain during clinical interventions 3.3. Being opened: complexities around deinfibulation 3.4. Being changed: complexities around reinfibulation |
| 4. Disempowering care encounters |
4.1. Being exposed and humiliated 4.2. Being judged and stereotyped 4.3. Lacking choice, power and control 4.4. Feeling unsafe and vulnerable |
| 5. Positive care encounters |
5.1. Trusting and appreciating providers and the system 5.2. Voicing health-care needs and preferences |
The analytical themes were shaped to directly illuminate the objectives of the review in terms of exploring factors that influence communication, health-care-seeking and access, describing women’s experiences of care in various settings and identifying key elements of service provision that are considered important for good-quality service provision.
In the following sections, we present each analytical theme as a whole, followed by a discussion of each of their constituent descriptive themes. Owing to the large number of studies that contributed findings to each descriptive theme, rather than ‘crowd’ the text with multiple repetitive references to these individual studies, we have created a matrix (see Appendix 8) that shows which studies have contributed findings to each theme. Hence, we reference only individual studies in order to provide particular examples of issues that are identified within the themes or to illustrate a particular nuance within a theme.
Analytical theme 1: communication is key
The review found that communication was a key interpersonal process that underpinned women’s ability to seek care, to obtain care and to have a positive care experience. Conversely, difficulties in communication negatively affected all of these dimensions. Communication about FGM/C was characterised by issues that might be expected within migrant women’s encounters with new destination country health-care systems, such as language barriers in consultations. However, communication about FGM/C presented an additional layer of complexity related to the fact that FGM/C was seen by both women and health-care providers as a deeply personal, private and sensitive issue touching on a range of taboos associated with gender, culture and sexuality – all issues that in many societies are shrouded in secrecy and silence. When women encountered providers who were able to overcome taboos and cultural differences, it forged bonds of trust and facilitated an environment in which women were able to talk about their FGM/C and to explore options for care. However, the majority of studies reported challenges and problems with communication that led to women being unable to talk about their problems or to explore appropriate treatment options, led them to avoid health care in general and generated a sense of mistrust in the system.
Theme 1.1: language barriers and interpretation challenges
The majority of studies (n = 31) reported that communication about FGM/C was severely hindered by language barriers. This was particularly a problem for older migrant women and women who had recently arrived in a destination country. Language barriers meant that women were unable to form a trusting relationship with their provider, adequately express their needs or understand information or advice. This led to frustration and increased anxiety, especially in a context where consultation times were often limited. 56,165 In some cases, women felt that they had had poor clinical experiences as a direct result of their inability to communicate about FGM/C. 165,181,186 In other examples, women avoided mentioning their FGM/C at all because they knew that they would not be able to explain it. 57,162,165
Language barriers were usually addressed through the use of formal or informal interpreters, and studies identified a range of associated challenges. These were partly related to accessibility and partly related to the sensitivities of talking about an issue that was usually regarded as personal, private and taboo and for which specialist terminology may be required. For example, in some cases, there was no formal interpretation available (or it necessitated long waits) and women had to rely on family members, their husbands or other community members. 58 Although this was sometimes a useful strategy, as a sensitive and private issue FGM/C was considered an unsuitable topic to discuss in front of children or informal lay interpreters (such as neighbours). 56 Husbands were sometimes reported not to translate correctly. 207 Where formal interpretation services were used, women reported that interpreters sometimes did not know the correct terminology, did not understand FGM/C or were embarrassed and did not translate fully or correctly. 56,190 Likewise, women reported particularly severe embarrassment if an interpreter was male and hence would be reluctant to discuss FGM/C at all:195
‘It is a really scary experience not to have someone who can explain’ . . . While many participants described as helpful the use of husbands or relatives as interpreters, others were embarrassed to explain aspects of childbirth in front of a relative.
Australia203
This theme mainly related to maternity care interactions, but also to communication about cervical cancer screening. 168,169,206
Theme 1.2: ‘can’t talk, not asked’ – double silence and cultural taboo
The studies suggest that in many cultures, as an issue related to sex and sexuality, FGM/C is shrouded in a culture of silence and is rarely discussed. This theme was reported by 37 studies. Women reported a lack of open discussion about FGM/C and related health matters within their own communities. 57,160,174,179,180,183,204
At the same time, owing to prevailing cultural taboos and uncertainty about how professionals would react, women reported feeling highly embarrassed and hesitant about mentioning FGM/C to their health providers and often would not mention it at all, even when they had questions or anxieties. 47,57,165,179,200 This finding was reported across all country contexts and with all cadres of health-care professionals, including midwives174,189 and medical doctors. 175,187 Some studies reported that, if available, women would seek out providers from their own cultural backgrounds as communication was then easier. 175 Other studies reported that women were particularly hesitant about raising the subject of FGM/C if they thought that the provider was unfamiliar with the issue, for example GPs and providers in lower-prevalence areas where there were no specialist services. 47
Two recent studies from the UK reported that women might be hesitant to mention FGM/C for fear of being reported to the authorities. 47,182
The silence around FGM/C was also attributed to providers failing to raise the topic. Hence, a commonly reported finding was that, even when women appropriately accessed relevant services, for example GPs or antenatal services,47,58,202 and might appreciate the general care offered,173,192 health-care providers often did not ask about FGM/C, even when the consultations were for pregnancy-related check-ups. The consequence was that FGM/C was sometimes not identified or discussed until women presented in the labour room, so opportunities for care planning or birth planning were missed. 174
Interestingly, many studies suggested that women strongly preferred health providers to initiate FGM/C-related conversations and found it acceptable to be asked, as long as it was done in a sensitive manner. In addition, as hinted at by the quotation above, some studies reported that women found communication to be easier when supported by a knowledgeable community advocate or confident peer. 174,175,180,183,190 Other studies emphasised that open communication was predicated on being able to develop a trusting relationship with the health professional, which, in turn, required time and continuity of care. 56,168,169,202
The majority of studies reported this finding in relation to the uptake of maternity care, but several also mentioned women being reluctant to seek out smear tests because they felt unable to discuss their FGM/C. 180,181,206
Theme 1.3: cultural (in)sensitivity
This theme was reported by 34 studies. In many studies, women described experiencing comments and questions from health providers that were perceived as clumsy, insensitive or intrusive. As a result, women reported feeling ashamed, scared or stigmatised. Such encounters inhibited women from talking about their FGM/C and, in some cases, led to them avoiding examinations or health-care services:170,176
The doctor was not comfortable with me. He asked if I enjoy violent sex with my husband. I don’t feel comfortable to talk about sex even with females – yet here is a male doctor examining my genitals and making mean comments.
USA191
By contrast, culturally sensitive communication was greatly appreciated and enabled women to openly discuss their FGM/C and related questions. 182,193,202
Analytical theme 2: access to care – influenced by an interaction of multilevel community and health service processes
The review found that access to care related to FGM/C was influenced by an interaction of factors operating at individual and community levels as well as at health system and service levels. For example, at individual and community levels, studies showed that care-seeking was influenced by cultural norms around health and sexuality, collective approaches to decision-making and the knowledge and information that individuals and communities had about FGM/C and health service availability. These factors influenced whether or not a woman would seek care, at what stage of her life and where. However, the studies also showed that care-seeking choices were shaped by the types of services available and that outcomes were influenced by the extent to which the health system, health services and health practitioners were ready and able to provide the range of support that women may need at different points in their lives. Hence, the review showed that there were challenges within communities in terms of seeking care and finding the right services. However, even when services were appropriately accessed, care was sometimes haphazard and suboptimal owing to variable levels of staff expertise and inconsistent and unclear referral pathways, policies and procedures. This analytical theme was derived from four descriptive themes, which are outlined in turn in the following sections.
Theme 2.1: influence of cultural norms
The studies showed that cultural norms around health and sexuality strongly influenced women’s views towards, and access of, health services. Thirty-five studies contributed to this theme. Particular dimensions of this are directly relevant in relation to FGM/C. For example, many migrant groups represented in the papers came from low-income countries with fragile health systems, where care has to be paid for by individuals. Women noted that, consequently, common ‘Western’ forms of care-seeking, such as preventative care-seeking (e.g. cervical cancer screening) or going for check-ups and tests, were unfamiliar and were sometimes viewed as unnecessary. For such communities, health care was more likely to be sought only when acutely symptomatic or at key life stages such as pregnancy. Likewise, extensive planning, discussions and tests during antenatal care (e.g. for birth planning or to consider options around deinfibulation) were not always expected and were not seen as the norm:
What would my friends in Somalia say if I went a long way to hospital for a check-up, knowing that everything was OK with the pregnancy? – Somalian women do not always want to go to the doctor . . . if something goes wrong we will feel it.
Sweden194
Furthermore, cultural norms around sexuality had a strong influence on the timing of care-seeking. In many studies, women reported that strong cultural imperatives valuing premarital chastity and virginity meant that they would avoid procedures requiring gynaecological examinations [e.g. Pap (Papanicolaou) smear testing58,169,195,206], and, especially for those with type III FGM/C, the general norm was to avoid seeking deinfibulation prior to marriage and pregnancy owing to the cultural pressure to maintain chastity, prove their virginity and to remain ‘closed’ for their husbands. 161,165,166,195,199,202
This norm was so strong that some studies reported younger women wishing that they could undergo deinfibulation, experiencing unpleasant symptoms and being aware of services but feeling unable to resist community pressure. 179,199,205 Some exceptions to this norm were reported, but mainly in the context of needing help for particularly difficult or painful symptoms. 202
Cultural and religious norms also led to a very strong reported preference for female health providers. Many studies reported that women would feel comfortable talking to, or being examined by, only a female health provider and might avoid care altogether if the provider was known to be male. 57,58,161,162,168,175,177,180,185,188,190,195,198,202,206–208
Care-seeking in relation to mental health issues associated with FGM/C was infrequently reported and a few studies suggested that this may also be linked to cultural norms in which mental health is still often viewed as a stigmatised issue and, like FGM/C itself, is seen as hard to talk about. 58,165,178,179,198
Theme 2.2: influence of the family
Nineteen studies reported that access to care in terms of health-care decision-making, especially among Somali women, was strongly influenced by the views and advice of the wider family and peer group. In the maternity context, this had an impact on the decision-making around uptake of antenatal care and caesarean sections. 78,175,179,195,198,202,209 The family also influenced decision-making around FGM/C specifically; for example, as mentioned in Theme 2.1: influence of cultural norms, women considering premarital deinfibulation reported that they might avoid informing their direct family members as they were aware that they would otherwise come under strong pressure to change their mind owing to fears over their future marital prospects. 183,205
For married women with type III FGM/C, studies indicated that the views of husbands were of paramount importance and that women generally felt that they needed their husband’s permission to undergo deinfibulation (outside the context of childbirth):
. . . my friend she wants to do that [deinfibulation] but her husband doesn’t let her . . . I told her, this is good for you – go and do. She said OK but her husband said no . . . Maybe if she did this [deinfibulation], it would have been a big problem in the family.
England205
Theme 2.3: knowledge and information about female genital mutilation/cutting services
Accessing care was also linked to women’s knowledge and information about FGM/C. Thirty-four studies contributed to this theme. Many studies reported that women felt that they lacked knowledge and information about FGM/C itself and about the availability of specialist service provision. In some studies, women expressed a desire to be informed in more depth about what care options might be available and noted that the main emphasis within services appeared to be on pregnancy issues in general rather than management of FGM/C specifically:162,165,196
They need to have someone that talks to you before and while you have a baby. I would have wanted someone to help me and tell me what was going to happen but I never got that . . . You know someone who is specially trained . . . who understands FGM [female genital mutilation].
England196
In some studies, women expressed a desire for more information. Some suggested that leaflets should be available providing this detail,58 but others noted that some groups of women would prefer information to be provided face to face or via community-based education approaches rather than through leaflets, which could be hard to understand, especially if there were language barriers. 59,167,169
Regarding knowledge of services, some women reported being aware of mainstream services such as GPs and maternity services, but were much less aware of specialist services related to FGM/C. 58
In one study from the UK, this seemed to be particularly likely if women lived in low-prevalence areas. 47 Women were also less likely to know about the existence of non-maternity-related FGM/C specialist services (e.g. counselling or group support). 58,179,181
Theme 2.4: ‘hit and miss’ care
This theme, reported in 38 studies, relates to a common finding across countries and time periods that women had problems with receiving appropriate care in relation to management of their FGM/C. As in Theme 2.3: knowledge and information about FGM/C services, in some cases this could be attributed to lack of availability of specialist services but also to providers or the ‘system’ being unprepared. Hence, obtaining the right care appeared to be ‘hit and miss’, dependent (somewhat by chance) on finding a particular service or a particular care provider rather than care provision being offered or available consistently across care contexts. 168
Many studies cited situations in which opportunities to identify FGM/C during a consultation were missed, which was attributed to providers lacking awareness of FGM/C (and associated specialist services) and hence failing to ask the right questions, undertake an examination or make timely referrals. 58
Maternity services were more likely to have knowledgeable providers and responsive systems, but even here women reported situations in which they felt that their FGM/C had been mismanaged owing to a lack of awareness and a lack of appropriate referrals. 58,173,180,183 The most common issue was failure to have been asked about FGM/C, meaning that it was not included in birth planning discussions and was identified only once labour had started:
She said that her friend was FGM and she had heard that she can get it open before delivery, but unfortunately her midwife didn’t know about the clinic . . . My friend stopped searching and . . . the labour was so difficult . . . they didn’t have time to open her first so she [tore] under the delivery.
England196
Two studies58,203 noted how continuity of care was a good way of ensuring that adequate relationships and, hence, care plans could be developed:
Participants experienced frustration over a lack of continuity of care . . . This meant explaining themselves to each new person they encountered, which was described as . . . ‘very hard and challenging.’ Conversely, when participants accessed a service with good continuity of care, they would recommend it to their friends.
Australia203
Women were also more likely to express satisfaction when they had received care from specialist services. 181,202
Analytical theme 3: cultural and bodily dissonance – striving for cultural and bodily integrity
The review found that FGM/C and its clinical management involves experiences of cultural and bodily dissonance and striving for cultural and bodily integrity. This analytical theme refers to changes in and challenges to women’s sense of cultural and bodily identity and integrity as a result of their experiences associated with FGM/C in the destination country, and particularly through their encounters with the health-care system (manifested during experiences of clinical examinations, childbirth, deinfibulation and reinfibulation). The theme also describes women’s responses to experiences of dissonance, in which their decision-making and actions can be understood as a desire to maintain a sense of cultural and bodily integrity. This theme highlights differences in and changes to cultural meanings and values related to FGM/C and how these differences and changes influence the way that women and health professionals define health issues, make decisions around FGM/C care and experience that care. When mutual interpersonal cultural understanding is not achieved, women may experience suboptimal care and may distrust the health system and their health providers. If women feel understood, they feel safe and reassured, resulting in a sense of bodily and emotional integrity. This theme comprises four descriptive themes.
Theme 3.1: moving from normal to different
This theme was reported in many studies (n = 40). Some women described becoming aware of FGM/C as something that is ‘different’ only once they moved to another culture. At this point, some started to become aware of the suffering and symptoms that their FGM/C may have caused them. They started to question and resist aspects of their culture that they had previously taken for granted and to feel uncomfortable with their own bodies and sexual identity. 168
However women also reported feeling shame and anger at being labelled as ‘different’ and ‘mutilated’ by the dominant discourse in the destination country and by health professionals. They felt that their culture was misunderstood. 163,170,183,185,193
This experience of dissonance made some women feel reluctant to mention FGM/C to health providers or caused them to feel extremely uncomfortable during health-care consultations, thereby limiting the opportunity to discuss the issues more openly and to achieve greater mutual understanding. 78,168,189
Theme 3.2: threat to the self – reliving female genital mutilation/cutting pain during clinical interventions
Potential challenges to cultural or bodily integrity were manifested at key points in women’s health-care experiences and were explored in 28 studies. For some women, childbirth, episiotomies, caesarean sections and procedures involving vaginal examinations (such as smear tests) could evoke traumatic flash backs of the original FGM/C:59,208
You always remember it. They decide to cut me, and when she went to do it she didn’t explain to me and I panic. I nearly kick her. Two of the nurses held me down. That was it . . . I was a little girl again being held down.
England196
In addition, some women reported being extremely fearful of undergoing medical procedures (tending to avoid these where possible) and reported these as causing severe pain, bodily reactions (such as shaking) and emotional trauma. 177,184,189,193,196 These reactions were not always consciously linked to FGM/C and in some studies it was clear that neither the women nor the provider understood why the women might be reacting with such fear and apprehension, making it easy for women to be labelled as ‘difficult’, when they actually needed care and support:191,210
I was so scared of childbirth I kept fainting and the doctor got cross with me . . . and said I was doing it on purpose, but that wasn’t true . . . I had to pretend it wasn’t me there as the pain was too bad as they had to cut me up again.
England196
Furthermore, many women came from societies in which childbirth is a dangerous life event, and this social context added to other fears. Linked to this, a key area of dissonance and distress was around caesarean section, with many studies (primarily with Somali women) reporting women expressing particular fears of having to undergo a caesarean section, linked variously to a strong cultural preference for ‘natural’ childbirth as a mark of successful womanhood, a fear of being cut again and a fear of death. 78,194,202,203,211 When put together with communication barriers, childbirth decisions regarding caesarean sections were often mistrusted by women, described as a punishment, or as a Western way of birth control, to get the women to conform to having fewer children. 56,78,187 Many studies reported women feeling that health-care professionals preferred carrying out caesarean sections if their patient had undergone FGM/C because of a lack of medical knowledge of vaginal delivery in circumcised women. 58,162,178 Mistrust ensued when women felt that they were not listened to in their preference for, or given an opportunity to try to have, a vaginal birth and there was a view that health professionals did not treat women fairly in overprescribing of caesarean births when there was often no medical indication for it. In one study, women reported avoiding attending the hospital until the last minute as a way of avoiding medical interventions. 211
Theme 3.3: being opened – complexities of deinfibulation for women with type III female genital mutilation/cutting
The experience of dissonance and quest for integrity was also seen in views and experiences around deinfibulation and was reported on by 28 studies. As noted in Theme 2.1: influence of cultural norms, for cultural reasons, ‘being opened’ medically was seen as necessary primarily after marriage and primarily in the context of pregnancy and childbirth rather than at an earlier stage of a woman’s life. 159,160 There were no studies that explicitly or exclusively focused on the views or experiences of unmarried women, but some studies reported examples of unmarried women for whom the need to maintain cultural and bodily integrity outweighed the experience of physical pain or discomfort, even when women knew about the option to seek surgical deinfibulation. 165,179,199 There were few reported exceptions to this rule, although one study suggested that, for some women, finding out about the option for surgical deinfibulation was empowering and deinfibulation was subsequently seen as a way of asserting control over their bodies and lives. 183
Most studies reported that women preferred to be ‘opened’ during labour to avoid the pain and trauma of being cut twice. 78,161,177,199,202,205 However, some studies suggested that this view could change towards the medically preferred advice of antepartum deinfibulation if there were opportunities for women to have appropriate discussions conducted in a sensitive way in the context of a trusting relationship with a health-care provider. 181,189
However, given that FGM/C is often not discussed during health-care consultations, women’s current reported preferences around deinfibulation timing may also reflect the fact that they may not be receiving the right information at the right time, and thus may not be in a good position to make informed decisions on this matter. 165,170,181,183
Theme 3.4: being changed – complexities around reinfibulation
A consistent finding across the studies within this theme (n = 19) was that ‘being opened’ could involve significant emotional, physical, social and relational adjustments as women’s bodies were changed. For some women, deinfibulation was firmly welcomed, although still required a period of ‘getting used to’ a different way of looking and feeling. 168,205 For other women (especially women from Sudan where it is a cultural norm in some regions to be closed again after childbirth), there was ambivalence about these changes and some women requested to be ‘closed again’ to varying degrees. 165,168,175,183,188,199,200,205
In most OECD countries, reinfibulation is illegal, and some studies reported women feeling very upset when their requests were denied by health professionals, experiencing this as a denial of their agency and integrity:170,197
I became a victim in Sudan already when I was 4 years old; I had no choice. Now I have to become a victim again after delivery, when the midwives refuse to resuture me. I just ask for a few stitches, not to have an open wound.
Sweden189
Consequently, some women reported seeking medical deinfibulation during holidays in their home countries. 181 One study in Australia168 reported that women were sometimes unclear about the meaning of reinfibulation vis a vis suturing following episiotomy, with some women unsure about whether or not surgical repair constituted reinfibulation.
Analytical theme 4: disempowering care encounters
In many situations, the care received by women in relation to their FGM/C was experienced as fundamentally disempowering. Women described experiencing negative attitudes or behaviours from health professionals and poorly managed clinical interventions in which they felt that they were not respected or listened to. Many studies reported examples of care encounters that left women feeling retraumatised, voiceless, without power to question interventions and vulnerable in the hands of an unprepared system. Such experiences caused women to feel unsafe and disempowered. There were many examples where women felt that care had gone wrong or where experiences had been poor, and women felt that these situations could have been avoided with better communication, cross-cultural understanding and sensitivity. Some women actively resisted being stereotyped or controlled and tried to assert their autonomy within a care encounter, strategies that were sometimes perceived by professionals as ‘being difficult’ and that then compounded an already-challenging situation. Some women responded by avoiding health services where possible, and/or lost trust in their providers or sought out ‘known’ providers recommended through peer networks. This analytical theme comprises four descriptive themes that cut across all countries, time periods, population groups and care contexts.
Theme 4.1: feeling exposed and humiliated
Across many studies (n = 40), women reported that the reactions of health-care professionals to their FGM/C had left them feeling ashamed, objectified, humiliated and exposed. This was primarily the case with health-care professionals who were unfamiliar with FGM/C and who were encountering it for the first time. In these situations, women reported that health-care professionals often reacted with extreme shock when they saw that a woman had been cut. Some tried to hide their shock and avoided mentioning anything at all, making the encounter feel uncomfortable. Others openly expressed horror or disgust or reacted insensitively by asking intrusive or inappropriate questions. In many cases, colleagues were called in to be consulted or to ‘have a look’ (sometimes without consent189,191), causing women to feel that their privacy had been violated and that they had been put on display. Such experiences left women feeling angry or very distressed. 78 Indeed, in one study in France, a participant likened her experience to being re-violated:
I was installed with my legs spread apart – they all came to see . . . I didn’t see any reason why they came . . . except for the fact that I was excised. All those people . . . entered into my intimacy without my authorization . . . didn’t ask . . . I felt that it was an aggression.
France193
In some cases, these experiences left women wanting to avoid further contact with services and/or feeling unable to discuss their care any further as it was clear that the provider had limited knowledge about FGM/C. 176 Several studies made the point that negative experiences of a particular service or provider would then be discussed within peer and community networks, and hence could have an impact beyond the individual woman, potentially affecting the way others in the community might engage with care. 78,160,170,174,192,196,208
Theme 4.2: feeling judged and stereotyped
Many studies (n = 36) reported that women often felt judged and discriminated against by care providers. Women reported feeling that health professionals made negative assumptions about them and provided suboptimal care based on racial, religious or other stereotypes and misconceptions about their culture in general as well as about FGM/C specifically. Such experiences caused distress, anger and avoidance of that particular health professional or service.
The studies reported experiences of stereotyping on assumed characteristics related to race, ethnicity, religion or socioeconomic status (i.e. these were experiences that may be common to migrant women in general, not just related to FGM/C). 59,180,183 For example, women reported health professionals making assumptions or disparaging remarks about them having too many babies, lacking language ability, being poor or being uneducated. 168–170,173,174 These encounters left women feeling judged and treated as if they lacked personal agency, sometimes causing them avoid health services:
The women described how the attitudes of the caregivers made them reluctant to return to the regular antenatal controls at the health centers. Women stated that they preferred to stay at home, even if they knew that they had health problems during pregnancy, to avoid alleged insults from the midwives.
Sweden189
With regard to FGM/C, women felt that health professionals often appeared to look down on their culture as ‘barbaric’. 57,58,78,159,197,204 At the same time, they expressed annoyance at being treated over-simplistically as ‘victims’ and, hence, objectified. 164,196,204,208
Theme 4.3: lack of choice, power and control
In this theme, reported by 32 studies, women reported experiences in which they felt that they had lacked choice or control within the health-care encounter, especially in the maternity setting and around key interventions such as caesarean sections or episiotomies. Lack of control was experienced in terms of feeling excluded from health-care decision-making, not being informed, not being listened to, feeling at the mercy of ‘the system’ and feeling unable to express their needs. These experiences were exacerbated when women were treated by inexperienced providers, when there were language barriers and for women still new to a country and unfamiliar with the health system:
Participants experienced an overwhelming sense of fear, loneliness, and ‘not knowing’ during their birth experience, as often they had no prior contact with the Australian health system . . . All participants felt that what was happening in the hospital environment was not adequately explained.
Australia203
Such experiences could be highly traumatising, and women’s attempts to assert control were sometimes construed by health professionals as being ‘difficult’:78,170,187,191,196,198
They decide to cut me, and when she went to do it, she didn’t explain . . . and I panic. I nearly kick her. Two of the nurses held me down. That was it . . . I was a little girl again being held down . . . It was like a bad dream and I couldn’t wake up.
England196
In labour, women described that FGM/C was often not discussed at all or that they were not consulted about interventions such as deinfibulation or caesarean section. This led to suspicion and fear and was particularly reported in studies conducted with the Somali community:
I can’t say that the birth went well. The midwife said that I couldn’t give birth without being cut . . . otherwise the baby won’t come without a caesarean section or I can lose the baby. Nobody asked me what I thought. I was there . . . without pain relief, nothing.
France193
Theme 4.4: feeling unsafe and vulnerable
Many studies (n = 46) reported care encounters where women ended up feeling unsafe and vulnerable, primarily when they were treated by providers who they perceived to be inexperienced in dealing with FGM/C, and, as above, when they faced language barriers or were unable to express their own preferences. Such encounters often led to the perception of poor-quality care or poor clinical outcomes. The following example (from England) describes the experience of a woman in labour (approaching delivery) who was infibulated:
. . . the midwife and junior medical staff . . . appeared confused and undecided as to how to manage her infibulation. The woman tried to communicate that she needed an anterior episiotomy, but was unable to do so, owing to her lack of English and, she felt, their lack of effort . . . in trying to understand her.
England56
This woman was eventually given a mediolateral (downwards) episiotomy, which she felt was not sufficient, and, as the baby emerged, she developed a large perineal tear.
Women expected health providers to be knowledgeable, competent and confident in managing their FGM/C. Many women reported times when this did not seem to be the case. The consequences ranged from providers failing to recognise, identify or discuss FGM/C174 to situations in which they felt that their care had been adversely affected as a direct result of poor provider skills (e.g. having unnecessary caesarean sections or extensive perineal tearing). 58,165,167,170,173,174,186,200,202,204,207 Women endured such situations feeling unsafe and highly vulnerable, often describing painful and traumatic experiences. 168
Feelings of vulnerability were heightened for women who lacked social support. 57,189,193,202 In contrast, women reported feeling safe and highly reassured when they encountered providers who appeared to be knowledgeable or experienced:56,58,168,169,174,182,183,196,200
I was lucky when I met a midwife in Sweden who knew about circumcised women. This was a great help to make me feel secure because it was my first time to be pregnant and to live far from my parents and family.
Sweden200
Analytical theme 5: positive care encounters
As seen in previous sections, the review has revealed many reports of poor care and difficult experiences in relation to FGM/C. However, many studies reported a mixture of experiences, including both good and poor care. High-quality care was conceptualised by women as care that is safe, respectful, culturally sensitive and compassionate. The essential process underpinning the experience of ‘good’ care was having a sense of trust, both in the individual provider and in the ‘system’ as a whole. Trust was essential for, and developed from, positive care experiences. Positive experiences were associated with the development of a good relationship with health professionals who were perceived to be knowledgeable and culturally sensitive, facilitating open communication and a sense of being in safe hands. Trust in the ‘system’ was linked to women’s appreciation of the availability and accessibility of services (compared with those in their home countries) but particularly when services were perceived to be prepared to be responsive to community needs (e.g. provision of appropriate interpretation services) and to manage issues relating to FGM/C (e.g. by having specialist services or specialist providers). This analytical theme has two constitutive descriptive themes. The first describes women’s actual experiences of ‘good’ care. The second sets out women’s views on what good care should look like, and includes their recommendations and suggestions.
Theme 5.1: trusting and appreciating providers and the system
Women’s accounts, reported in 34 studies, identified many instances of good care and of being satisfied with their care, as well as highlighting an appreciation of services that may not have been available in their own countries. With respect to maternity services in particular, there were many narratives of satisfaction with a warm welcoming environment, kind caring staff (especially midwives) and responsiveness to language barriers. 58,165,168,169,181,182,192,194,196,202,209,211
On an interpersonal level, women’s narratives highlighted two key elements that underpinned women’s positive care experiences. The first was feeling that they were in safe hands and in the care of an experienced provider. Trust was greatly enhanced if women felt that providers were knowledgeable about FGM/C:56–58,168–170,172,174,177,182,196,200,202
My first meeting with a midwife was very good because I was lucky to meet a midwife who knew about circumcision from her previous work in Africa. Thanks to God, she had experience so it went well.
Sweden200
The second element was the experience of respectful and sensitive care, which was essential to enable the development of a trusting relationship. Women greatly appreciated being treated with respect and compassion, being given choices and experiencing open and culturally sensitive communication:
The midwives can talk about it during the pregnancy. You need to talk to the woman, ask her opinion, explain the bad parts to her so that she won’t do it to her daughter. During the labour, they spoke to me about my circumcision and I was happy . . .
France193
We have a tendency to hide the situation. But if you talk about it, you need to be gentle: ‘Madam, I see something isn’t normal, have you been circumcised?’ There. And then, you touch on the subject. You can talk about it.
France193
Once women had established a trusting relationship with a health provider, they were more likely to engage in conversations about their care (e.g. birth planning) and, in some cases, were more likely to follow current medical guidelines, for example on issues such as deinfibulation timing. 57 Some studies explicitly linked the ability to form good relationships to services that enabled continuity of care:56,202
The women receiving caseload care and those who received more continuity of care from hospital-based midwives spoke of the effort made by midwives to overcome the language barrier. ‘They listened well and took time in trying to explain things’.
England56
Participants in some studies (in the UK in particular) felt that service provision around FGM/C in general seemed to have improved in recent years, and that new models of care with higher levels of provider training and clear referral pathways were providing better care and achieving greater engagement with the affected communities. 57,58,168,169,202
Theme 5.2: voicing health-care needs and preferences
This theme presents women’s views, reported in 45 studies, on key elements of good-quality care and appropriate service provision. Women’s recommendations fell into two main domains: interpersonal provider characteristics and service organisation issues.
In terms of providers, women identified the following characteristics and behaviours that, from their perspective, would constitute high-quality care:57,165,166,170,174,175,177–179,181–183,187,188,190–193,196–199,203
-
being culturally sensitive
-
being respectful
-
taking the initiative to raise the topic of FGM/C
-
listening and acknowledging women’s needs and preferences
-
providing women with detailed information and knowledge, especially around birth choices and options for deinfibulation timing
-
knowing about available services and signposting women to these
-
encouraging women to ask questions.
In terms of service organisation, women identified the following strategies and approaches that would constitute a high-quality service:47,57,162,165,168,169,175,179,182–184,188–191,196,201,204
-
providing appropriate adequately trained interpreters and/or community-liaison workers or advocates
-
providing specialist services, including services that address mental health and psychosexual issues
-
have staff who are knowledgeable and skilled
-
provide staff with education and training to develop both cultural and clinical competencies around FGM/C
-
ensure that female health workers are available
-
involve communities in awareness raising, service development and delivery
-
provide information and awareness raising through a variety of channels, including leaflets, face-to-face discussions, community activities and community health workers.
Summary, reflections and conceptual model of analytical themes
The overall aim of review 1 was to explore the experiences of FGM/C-related health care across the life course for women and girls who have undergone FGM/C. The review findings provide an important account of these experiences through five analytical constructs.
With respect to factors that influence care-seeking, the review shows that access to care is influenced by multiple interlinked factors operating at different levels. Once a woman accesses care, the findings show that care experiences can be both positive and highly negative. Care experiences are affected by the way in which women are treated by health professionals and the nature of the relationship that is achieved with them, and by whether women feel safe or unsafe/vulnerable in relation to provider competence and preparedness of the system to deal with FGM/C. The review shows that both care-seeking and care experiences are strongly affected by two key phenomena, each of which is, in turn, shaped by cultural norms, processes of cultural change and cultural understanding. The first of these is communication, both within communities and between patients and providers. The reviews show how FGM/C is characterised by silence and secrecy. The second is the experience of cultural and/or bodily dissonance and of seeking cultural and bodily integrity that may arise when women encounter health-care situations in Westernised settings. Here, experiences around FGM/C are characterised by stigma, shame and stereotyping. The inter-relationships between women’s experiences and these explanatory phenomena are depicted in a conceptual model (Figure 3). The conceptual model has grouped the analytical constructs relating to disempowering and positive care experiences together under a single heading: ‘care experiences’. Indeed, in some ways, one analytical construct (positive) is the converse of the other (disempowering). However, in the thematic synthesis (see Review 1 themes), we chose to disaggregate these two constructs and to represent them separately. This was a deliberate decision as we felt it was extremely important for women’s disempowering experiences to be made visible and to be analysed and understood in some detail. Only in this way can appropriate corrective action be taken. Merging negative and positive experiences together would have limited our ability to do this.
FIGURE 3.
Review 1 conceptual model of analytical themes. Reproduced from Evans et al. 139 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.

The CERQual assessment
Appendix 9 provides a detailed summary of findings table, with a CERQual assessment of confidence for each of the above individual descriptive review findings. 131 Ten review findings (descriptive themes) have been graded as ‘high confidence’ and seven review findings (descriptive themes) have been graded as ‘moderate confidence’. The main cause for downgrading a review finding was concerns related to methodological limitations; however, these were often offset by the number of studies contributing to a review finding and the consistency with which a finding was reported across varied contexts, settings and cultural groups.
Discussion of review 1
There has been much research documenting the challenges faced by migrant populations in accessing health care in a new country, especially in a maternity care setting (including language barriers, lack of familiarity with the health system, cultural beliefs and health-seeking strategies that may be very different from Western biomedicine, and challenges in forming good relationships with providers). 89,93–95,142,212 This review has highlighted all of these issues, but has shown that, when obtaining care for FGM/C-related issues, all of these challenges are exacerbated. Silence, secrecy, stigma and lack of familiarity with FGM/C within the system combine and act as obstacles to identifying FGM/C or to providing women with appropriate care. However, the review has also shown that, in some circumstances, women and providers can overcome these obstacles. Key to this are knowledge of services, community engagement, the availability of specialist services, addressing language barriers and providing care that is person centred, culturally sensitive and respectful. 95
The findings from this review are discussed further in Chapter 6, in an integrated discussion section, following a final synthesis in which reviews 1 and 2 are considered together.
Limitations and evidence gaps in review 1
This was an extremely comprehensive review. Nonetheless, there were some limitations. First, the review highlighted several gaps in the evidence base around FGM/C. There were very few studies that focused specifically on mental health needs, hence the findings related to this area lack depth, and the issue would benefit from further research. Decision-making around deinfibulation is another area that would benefit from more specific research [in the UK, a National Institute for Health Research (NIHR) Health Technology Assessment (HTA)-funded study (project number 16/78/04) is currently investigating this issue, and will also explore men’s views and influence on decision-making]. There were no studies that focused specifically on girls and on their experiences. The literature search did not find any in-depth evaluations of interventions or services. This means that development of models of ‘good care’ still needs to be inferred and innovated rather than being based on sound evidence. Second, the review also reflects the methodological limitations of its included studies. Many papers displayed a homogenising tendency in terms of the affected communities as well as FGM/C types. For example, in papers that had mixed community samples, there was little attempt to explore cultural differences in relation to FGM/C. Likewise, it was not always clear which type of FGM/C was being studied. In research with Somali or Sudanese communities, the assumption can reasonably be made that their focus was FGM/C type III. However, in studies with mixed samples, there was very little differentiation on the basis of FGM/C type. As a result, there is limited specific knowledge on the needs or experiences of women with type I, II or IV FGM/C.
Relevance to the UK context
The results of review 1 are derived from studies across many OECD countries. However, of the 57 papers included in review 1, 18 (31.5%) were conducted in the UK. Of these 18, 11 were conducted in the last decade (since 2011) and nine were published within the last 5 years (2013–18). 47,174,180–182,196,202,204,205 Of these nine, one was a MSc (master of science) thesis,174 four were research reports47,180–182 and four were peer-reviewed journal papers. 196,202,204,205 A subgroup analysis exploring their findings and examining the theme matrix was undertaken of UK studies in general, and particularly of the nine published in the last 5 years. This found that the UK-based studies, including the more recent ones, contributed findings across all of the major themes reported in review 1. Hence, we feel that it is reasonable to conclude that the review 1 findings are generally applicable to the UK context.
Chapter 4 Review 2 results
Characteristics of studies in review 2
As described in Chapter 2, 30 papers met the inclusion criteria for review 2. Two studies were reported in multiple publications,56,213–215 hence review 2 includes 28 distinct studies reported in 30 publications. One of the duplicate studies comprised a research report213 and an associated peer-reviewed journal article. 56 The report was included in addition to the journal article, as it contained relevant findings that had not been reported in the published paper. The other duplicate study reported different aspects of study findings in two different journal articles. 214,215
Of the 28 distinct studies, 19 were unique to review 2 and nine were also included in review 1 (as their samples included patients as well as health professionals). 56,78,161,163–165,167–169 Twenty-four of the 30 papers were published in the English language, five were published in Swedish216–220 and one was published in Spanish. 221
See Appendix 10 for a detailed summary of study characteristics.
Type of publications
Half of the included papers were peer-reviewed journal articles (n = 15). 56,76,79,80,163,167,210,214,215,221–226 In addition, the review included 11 master’s and PhD theses78,161,165,216–220,227–229 and four research reports. 164,168,169,213
Date range of studies
The studies represented a mixture of older and more-recent research, with publication dates ranging from 1997 to 2017. However, two-thirds of the papers (n = 20) had been published since 2011, hence the majority of the papers reflected a more contemporary context.
Geographical setting of studies
The studies represented a wide range of OECD countries, covering nine countries in Europe, North America and Australasia. Specifically, review 2 included studies from Australia,76,168,169,214,215 Germany,164 New Zealand,165 Norway,167,210,224 Spain,221 Sweden,79,80,216–220,223,226 Switzerland,161 the UK56,163,213,222,228 and the USA. 78,225,227,229 Sweden contributed the most papers to the review (n = 9), followed by the UK (n = 5) and Australia (n = 5). The other countries contributed between one and three papers each.
Sample
As per the inclusion criteria for review 2, the studies all included health professionals in their samples. Some studies focused on a single cadre of health worker whereas others included multiple cadres. The samples were as follows: midwives (n = 9),76,80,214–216,219,221,223,226,228 health visitors (n = 1),222 district nurses (n = 1),218 a mixed group of nurses (n = 1),217 school nurses (n = 1),220 doctors (n = 1)79 and mixed groups of health professionals (n = 14, including doctors from a variety of specialisms, nurses and midwives). 161,163–165,168,169,224,227,22956,78,167,210,213,225 Within the 14 ‘mixed’ sample papers, in addition to midwives, nurses and doctors, two studies included counsellors163,224 and four studies included community health and social workers. 56,168,169,213,224 There were no studies that included students.
It is notable that only two studies included any kind of mental health professional perspective; however, the findings were not sufficiently differentiated to explore their views as a distinct group. 163,224
Focus, context and relevance of studies
The studies had varied research aims and foci. Some focused directly on professionals’ experiences of supporting/managing women who have undergone FGM/C (e.g. Johansen210), whereas others were more indirect (e.g. Lazar et al. 225). Some studies focused on care of refugee women in general, but included aspects relating to FGM/C (e.g. Burchill and Pevalin222 and Jatau227). Eleven papers specifically focused on professionals’ experiences with women from countries where infibulation is commonly practised (i.e. women who have experienced type III FGM/C). 56,78–80,163,167,210,213,223–225 However, the findings of most of the papers reflected a sense that professionals were often conflating FGM/C in general with type III specifically. Hence, it is our contention that the findings in review 2 are skewed towards health-care professionals’ experiences of, and views on, FGM/C type III.
There were no studies that examined health professionals’ views/experiences of cervical screening for women who have experienced FGM/C. There were also no qualitative studies that explored views on surgical reconstruction following FGM/C. Only one study (of school nurses) focused explicitly on professionals’ views of supporting younger women or girls who had undergone FGM/C. 220
As described in Chapter 2, in order to assist development of the initial coding framework, we categorised each of the individual papers according to how relevant their specific focus was to the review aims. Nineteen papers were rated as being of high relevance,76,78–80,161,165,167–169,210,214–218,225,226,228,229 seven papers were rated as being of medium relevance56,213,220,221,223,224,227 and four papers were rated as being of low relevance. 163,164,219,222
Methodological quality of included studies
The papers were each appraised by two reviewers using the JBI-QARI138 (see Appendix 11 for full details of the quality appraisal of each paper).
As described in Chapter 2, a broad scoring range was used to provide a ‘rough’ sense of the overall quality of the body of evidence. In accordance with this categorisation, 15 papers were assessed as being of high quality,78–80,161,163,167–169,215,218,222,226,227,229 12 papers were assessed as being of medium quality56,76,164,165,210,214,216,219–221,223,225 and three papers were assessed as being of low quality. 213,217,228
A methodological weakness in many studies was a lack of apparent philosophical standpoint (question 1 of the JBI-QARI), making it difficult to assess the congruency of the chosen methodology. Likewise, many studies did not identify any clear methodology (simply stating that they adopted a generic ‘qualitative approach’), making it difficult to judge the congruence of the methodology with the research question and the methods (questions 2 and 3 on the JBI-QARI). Finally, a weakness across many studies was the lack of discussion of reflexivity (questions 6 and 7 on the JBI-QARI). Given the sensitive nature of FGM/C (or sexuality or migrant health care) as a topic, the failure to explore the researcher’s own theoretical standpoint makes it hard to judge the dependability of the findings. 155 Likewise, the researcher’s own professional background may have influenced their viewpoint (e.g. as insiders or outsiders to a profession), their ability to build rapport with their participants or their interpretation of the findings, but this was rarely discussed.
In addition to the JBI-QARI quality assessment, the papers were also categorised according to their ‘richness’ in terms of being ‘thick’ or ‘thin’ (i.e. their relative ability to provide explanatory insights and plausible interpretations based on a clear account of the research process). 141–143 Twelve papers were classified as ‘thin’56,163,164,213–220,228 and 18 papers were classified as ‘thick’. 76,78–80,161,165,167–169,210,221–227,229 The thicker papers tended to be studies that were informed by an anthropological theoretical approach, that had followed a clear methodology or that had moved beyond mere description in their analysis towards a more interpretive and analytical account of the phenomenon of interest.
As noted in Type of publications, half of the papers were unpublished research reports or master’s and PhD theses (n = 15). 78,161,164,165,168,169,213,216–220,227–229 Lack of peer review in these included papers could be considered a potential threat to quality; however, our detailed quality appraisal made it hard to draw any clear conclusions along these lines. For example, 12 out of the 30 papers were ranked as both ‘thick’ and high quality. 78–80,161,167–169,222,224,226,227,229 Out of these 12 papers, six (50%) were PhD theses or research reports. 78,161,168,169,227,229 However, three of the 30 papers were ranked as low quality and ‘thin’ (two master’s dissertations217,228 and one research report213).
Review 2 themes
The findings from the 30 papers in review 2 have been synthesised into six analytical themes, which, in turn, represent a synthesis and interpretive analysis of 20 descriptive themes (Table 8). The analytical themes were shaped to directly illuminate the objectives of the review, which were to explore health professionals’ perspectives on the factors that influence appropriate service provision, communication and quality of care for FGM/C-affected women/girls in different health-care settings.
| Analytical theme | Descriptive theme |
|---|---|
| 1. Knowledge and training |
1.1. Knowledge and awareness 1.2. Education and training |
| 2. Communication is key |
2.1. Language barriers and interpretation challenges 2.2. Talking about a sensitive issue 2.3. Women also find FGM/C hard to talk about |
| 3. Encountering the ‘other’ in clinical practice: negotiating cultural dissonance and achieving cultural understanding within health-care relationships |
3.1. Attitudes towards FGM/C – mixed emotions 3.2. Cultural dissonance – control and resistance in clinical encounters 3.3. Acknowledging the role of the family 3.4. Gender of the provider 3.5. Crossing the cultural divide – strategies and elements of culturally sensitive care |
| 4. Identifying FGM/C |
4.1. Presentation and help seeking 4.2. Practices and processes around identifying FGM/C |
| 5. Clinical management practices: inconsistent and variable |
5.1. Deinfibulation timing 5.2. Deinfibulation practice 5.3. Reinfibulation ambivalence 5.4. Need for guidelines around deinfibulation/reinfibulation 5.5. Psychological issues |
| 6. Optimal service development |
6.1. Provider’s role in prevention 6.2. Community engagement and education 6.3. Specialist services |
In the following sections, we present each analytical theme as a whole, followed by a discussion of each of their constituent descriptive themes. Owing to the large number of studies that contributed findings to each descriptive theme, rather than ‘crowd’ the text with multiple repetitive references to these individual studies, we have created a matrix (see Appendix 12) that shows which studies have contributed findings to each theme. Hence, we will reference only individual studies in order to provide particular examples of issues that are identified within the themes or to illustrate a particular nuance within a theme.
Analytical theme 1: knowledge and training
For health providers, feeling confident and able to deliver appropriate FGM/C-related care is strongly linked to having adequate knowledge and skills. The review found that providers want and need the right knowledge and skills to provide appropriate FGM/C-related care and felt that there was a lack of knowledge (or variable knowledge) around FGM/C. This includes knowledge of sociocultural and legal aspects of the practice as well as clinical knowledge. A lack of knowledge could lead to missed opportunities for discussing FGM/C, poor interpersonal care and poor clinical management, as described in later themes. It also contributed to provider anxiety and stress when having to deal with situations in which they did not feel confident or competent. Many studies reported a desire for more education and training, citing a perception that there is a lack of (or insufficiently in-depth) basic pre-registration training and continuing professional development (CPD).
Theme 1.1: knowledge and awareness
Professionals had variable knowledge around FGM/C, depending on the practitioner’s work setting, role, exposure to FGM/C and exposure to training. This theme was reported in 25 studies. Many studies described a lack of provider awareness around FGM/C or provider reports of having insufficient, inaccurate or partial knowledge and skills (especially around deinfibulation), leading to misconceptions, lack of awareness, fear and uncertainty about how to talk about FGM/C and how best to support women with FGM/C:
. . . midwives also described having ‘mini panic attacks’ when they saw the sticker on the women’s notes indicating that they had FGM/C, as they felt that their practice was inadequate. Midwives also stated that they did not have enough experience to identify FGM/C, saying it was not always ‘clear-cut’ to classify.
Australia76
This finding was reported among medical as well as nursing and midwifery staff. Several studies noted that providers may lack knowledge around differentiating the different types of FGM/C (particularly types I and II). 76,164,217 In addition, providers had many questions (especially around cultural aspects, sex and sexuality) that they were hesitant to ask because of concerns about appearing culturally insensitive. 217
Providers linked being knowledgeable to being aware that FGM/C was a potential issue for a woman, being more confident in discussing FGM/C with women, being able to understand women’s cultures or experiences better, being more confident in providing appropriate care and having greater job satisfaction. Providers also recognised a need for specific knowledge related to clinical management, cultural meanings and the legal context.
Theme 1.2: education and training
Professionals in 21 studies identified a perceived need for greater education and training in all aspects associated with the management of women and girls with FGM/C, and that training would greatly enhance provider confidence. 222 Health providers identified a lack of basic (pre-service) education (or an input that was too brief and superficial)76,78,80,165,167,168,214,216,219,221,225,227,228 and a need for regular CPD around FGM/C that included in-depth information, practical skill development and access to mentorship and clinical supervision where relevant. In the absence of training, health provider perceptions and practices were based on personal experiences, consulting colleagues, self-study or information from the media. Some studies emphasised a view that training must cover all aspects of FGM/C (e.g. communication, sexual and cultural issues), as well as medical aspects so that cultural competence as well as clinical competence was improved; this need was expressed by providers from ‘high-prevalence’ and as well as ‘low-prevalence’ settings. 169
Analytical theme 2: communication is key
Providers reported multiple challenges in talking about FGM/C with women but recognised that good communication was key to providing good-quality care. Language barriers were reported as a significant hindrance to effective communication. Use of interpreters was a common intervention but posed a number of challenges. In addition to the language barrier, the nature of FGM/C as a taboo, sensitive and specialised topic, was seen to add another layer of complexity. Communication problems led both providers and women to avoid the topic of FGM/C, thereby hindering the identification of FGM/C. Communication challenges also led to difficulties in forming quality, trusting relationships with women and providing women with appropriate information and choice about their care. This analytical theme has three constitutive descriptive themes.
Theme 2.1: language barriers and interpretation challenges
This theme, reported in 20 studies, relates to language barriers that affect communication and relationship building between professionals and patients and the challenges that providers experience when addressing this by working through interpreters. The studies showed that language barriers were an issue that could significantly compromise care:
They don’t know that much about their bodies at all. It takes a very long time to explain . . . in an easy way . . . And you have the same amount of time as for any well-informed Swedish patient . . . You have to lower the bar. [Obstetricians]
Sweden79
Language was particularly an issue with women who were still relatively recent migrants. The language barrier affected providers’ ability to elicit in-depth information from women or to provide in-depth explanations and engage in shared decision-making. Moreover, the language barrier deterred providers from asking questions about FGM/C at all, as it was seen to be too difficult to try and address such a sensitive topic requiring specialist vocabulary in a short consultation:
And you see it and, what do you do? Ask them about it? When it’s already too late to do anything about it? ‘You don’t understand, communication is terrible enough without having to talk about FGM/C as well’; ‘It is very difficult to address this matter given the communication issues’ [Midwives].
Switzerland221
Use of interpreters was variable and inconsistent. 56,76,79,80,161,168,169,213,218,220,225,228,229 Some providers preferred to rely on informal interpreters who women would bring with them. However, others expressed concern about maintaining women’s confidentiality given that communities could be tightly knit, and about women’s abilities to open up honestly in front of known family/community members (especially if their husband was acting as an interpreter). 56,168,169,213,220,225,229 Providers also had concerns about the accuracy and quality of interpretation (both with formal and informal interpreters) given the specialist nature of FGM/C, the niche vocabulary and the sensitivity of the topic:56,168,169,213,220,229
I’ve actually had interpreters who don’t exactly say what we say and sort of side with the family . . . because they think we’re trying to do something that’s a problem – you have no idea what they’re saying . . . [Female OB/GYN resident]
USA225
Providers experienced various challenges in using formal interpretation services. First, it could be difficult to predict when women were attending, hence interpreters were not booked in advance, leading to long waits. For these reasons, providers would often fall back on the use of informal interpreters. Pre-booking interpreters was time-consuming or difficult to predict, hence was often not done. Telephone interpretation was seen as particularly challenging owing to the impersonal nature of it when trying to discuss sensitive issues. 56,76,169,213 Providers noted particular difficulties when interpreters were male, as this would make both the interpreter and the woman uncomfortable:
A midwife described feeling uncomfortable and that women were embarrassed when male interpreters were assigned, as female interpreters were often unavailable.
Australia76
Time constraints were also cited as obstacles to using an interpreter, as interpretation inevitably lengthened the consultation time, yet providers were often not given additional time. Finally, using formal interpretation services affected the provider’s ability to establish continuity of care, as a different interpreter might be available each time. Some studies noted that staff had not received adequate training or support in using interpreters:56,76,168,169,213
You don’t have time with all the interpreter situations . . . So the care they receive is definitely not as good, that’s for certain . . . and you can miss an incredible amount because of that, and maybe miss that it’s not a normal pregnancy. [Obstetricians]
Sweden79
Theme 2.2: talking about a sensitive issue
This theme, reported by 24 studies, refers to the sensitive and taboo nature of FGM/C owing to its association with sex, sexuality and ‘private parts’. The nature of the topic compounded potential language barriers and made FGM/C hard to talk about, even when a language barrier was not present.
Some health providers viewed FGM/C as a highly sensitive topic and did not want to offend or stigmatise women or girls. They felt awkward or fearful to broach the issue and felt that women/girls may experience questions as intrusive and that discussing such matters might jeopardise their relationships. 76,80,169,210,217,218,220,221,225 Hence, in order to be culturally sensitive or non-judgemental, some health providers would not ask about FGM/C at all, assuming that women would raise the issue if there was a problem. This hindered communication and could lead to the topic not being discussed at all, hence opportunities for timely interventions could be missed:
There are circumstances where a patient will ask questions and somehow open the door for me and then I feel more comfortable, but I don’t really know how to communicate about that effectively . . . (Nurse-Midwife)
USA225
I guess my biggest fear is coming across really judgmental. I don’t want to hurt a woman’s feelings during an exam . . . So I feel like that’s a real deficit. (Nurse-Midwife)
USA225
Some health providers noted that every woman was different and communication strategies had to be tailored accordingly. 76,216,228 Others emphasised the importance of using and being attentive to non-verbal communication to guide them as to when and how to discuss sensitive issues. 216,228 Some health providers noted that communication was a process (e.g. the topic may need to be addressed several times over different consultations) and relied on being able to develop a trusting relationships with clients – which, in turn, was facilitated by practises such as continuity of care or by having sufficient time in consultations. 56,213,218,220,227 Some health providers felt that it was best to ask openly and directly about FGM/C. 219 Direct communication was considered easier if it was seen to be part of a routine process in a consultation (e.g. a standard question on an assessment form). 169,220,222,223,228 Experience and training were noted to improve health provider’s confidence in addressing FGM/C:219,220,222,223
The female genital mutilation is a very difficult one . . . I have had clients with that and it’s asking the question . . . I found that the few people that I did ask quite often had had it – when asked they were very open about it. [Health Visitor]
England222
Theme 2.3: women also find female genital mutilation/cutting hard to talk about
Thirteen studies reported provider’s views that women rarely proactively mentioned FGM/C in the context of a consultation. 76,78,161,165,167–169,215,217,220,223,225,229 Providers attributed this to cultural taboos within women’s own societies, feeling ashamed and embarrassed or being fearful of being judged. 161
Analytical theme 3: encountering the ‘other’ in clinical practice – negotiating cultural dissonance and achieving cultural understanding
The health-care encounter between professionals and FGM/C-affected women was a site where different cultures and values met and needed to be negotiated. Cross-cultural encounters evoked emotional reactions that affected professional behaviour and interpersonal processes, as well as requiring adjustments to practical aspects of service provision (e.g. responding to women’s preferences for a female provider or interpreter). Achieving cultural understanding and mutual respect led to culturally appropriate care provision. When this was not achieved, quality of care was compromised.
Studies showed that cultural differences were directly related to the practice of FGM/C but also indirectly to more generic issues found when working with patients from different backgrounds and countries. It was evident that many professionals (especially midwives) valued and endeavoured to provide culturally sensitive care, and attempted to deliver this by adopting a non-judgemental and person-centred approach. These professional behaviours were linked to the potential for better-quality care and a greater likelihood of optimal clinical outcomes. However, in other cases, cultural dissonance could cause frustration on both sides and resulted in situations in which professionals and communities struggled to exert control within the health-care encounter and failed to communicate. The consequences could be provider stress, suboptimal clinical outcomes and traumatic experiences for women. Achieving a good relationship between health providers, women and communities affected by FGM/C required cross-cultural understanding, sensitivity to cultural difference and trust. In addition, cultural preferences related to the gender of the provider were important in enabling or hindering the development of a trusting relationship.
Theme 3.1: attitudes towards female genital mutilation/cutting – mixed emotions
This theme was reported by 17 studies, and describes provider views and attitudes around FGM/C. Many providers expressed strong emotions around FGM/C, including shock, disgust and horror. It exemplified a huge cultural difference, with providers describing women’s bodies after FGM/C as different, not ‘normal’ and mutilated. At the same time, providers (especially midwives and nurses) expressed great empathy and sympathy for the women, and tried to be supportive. 76,216,217 Women were often talked about as victims of cultures that were violent, barbaric and patriarchal. Some providers mentioned a struggle to maintain their professionalism around this topic, having to hide their feelings of horror when they first encountered FGM/C. They also expressed anger towards the ‘other’ society and particularly towards the men in that society:
As a woman yourself, you kind of feel . . . a sorrow . . . It is difficult, because you’re so angry. You get so . . . get enraged at the whole situation, at the whole culture . . . how the hell can they subject women to that . . . I become furious at men . . . I try not to show it. [Midwives]
Sweden80
However, some studies reported views of providers who were widely travelled and who, through experience, had developed a more nuanced and culturally relative position, in which FGM/C was seen as a practice that is different, but that needed to be understood in its own context. 78,229
Theme 3.2: cultural dissonance – control and resistance in clinical encounters
This theme, reported in 20 studies, refers to cultural differences between health providers and patients, and to cultural assumptions and stereotypes that may exist and that may affect care by undermining trust and communication. In many of the papers, providers seemed to be referring to their experiences with Somali patients in particular.
In some studies, providers reflected that they, as health professionals, sometimes held stereotyped views, particularly of Somali FGM/C-affected women, which may affect their care (e.g. assumptions that Somali women were ‘tough’ and did not require or want pain relief during labour), hence failing to see women as individuals, especially when there was a language barrier. 56,78–80,219,220,225–227,229
Conversely, there was a widespread sense that Somali patients in particular did not trust the Western health-care system and held fears and assumptions about what may happen to them:
I think they come in with some preconceived notions as well – that we’re forcing health care on them (Female nurse practitioner) . . .
USA225
The bigger problem is the belief in the community that we’re somehow not acting in their best interest . . . it’s mistrust. I think they think we’re trying to hurt them. I don’t know why. I wish it wasn’t there. (Male OB/GYN)
USA225
The studies indicated that key areas of cultural difference manifested in differences in views around pain behaviour, caesarean sections, episiotomies/deinfibulation, vaginal examinations (e.g. pap smears)227 and other clinical interventions. The caesarean section was a particular matter of contestation and resistance, with providers across multiple studies reporting women’s and families’ resistance to this procedure even when medically indicated. 56,78,79,210,219,225–227,229 Providers felt that this was due to religious reasons, ‘ignorance’ or cultural preferences for natural childbirth, but also owing to fears that providers would opt for a caesarean section as a way of managing the FGM/C. Many studies reported examples in which providers became perplexed and frustrated that patients did not follow their advice. Such encounters could become highly charged, with different stakeholders (providers, women and families) all seeking to exert control over the clinical situation. 78
The studies provided several examples of situations that were not well managed, leading to resistance, misunderstandings, miscommunication and poor clinical outcomes (such as women being denied pain relief, enduring traumatic births, refusing to have a caesarean section where it was indicated, or where providers imposed a caesarean section without proper informed consent and explanation). 78,167,210,225,229 One in-depth anthropological study in particular (of Somali women and providers in a maternity setting in Norway) provides many examples of the miscommunication and misunderstandings that can happen as a result of a provider’s lack of cultural understanding and assumptions about the Somali community. 210 However, this and other studies also provide examples showing that, when care was taken to build trust and mutual understanding, clinical situations could become easier to manage. 167,227
Theme 3.3: acknowledging the role of the family
This theme, reported by 15 studies, refers to the significant role of the family in influencing women’s decision-making and actions, in contrast to ‘Western’ patients for whom care decisions are more often made on an individual basis. Providers recognised that women’s health-care decisions and behaviours were strongly influenced by their husbands and wider family. 76,78–80,161,215,218,226 This was, at times, experienced as frustrating, but involvement of the family was seen as important for effective communication and effective care:
. . . it’s the influence the men have over the women [that] is very difficult for us to understand, because again if a Somali woman is there . . . I want her opinion, I don’t want his opinion . . . a lot of times they’ll just look to the side and you have to talk to somebody else. (Female OB/GYN resident)
USA225
However, one study from Sweden reported that providers often held assumptions about gender relations and the role of men in influencing women’s health-care decisions, often assuming men to have a negative influence, and reporting surprise when they encountered husband–wife relationships that appeared supportive and caring, or where the men clearly opposed FGM/C. 226
With respect to FGM/C specifically, family involvement was seen to be particularly crucial in decision-making in relation to deinfibulation timing76,228 and reinfibulation:76,80,161,210
One midwife described the influence of an older woman on the decision to have a de-infibulation prior to birth, citing that ‘their mother or aunty said no’.
Australia76
Theme 3.4: gender of the provider
This theme, reported in eight studies, relates to how the provider’s gender influences the care of women with FGM/C. The studies reported a strong perception that women from FGM/C-affected communities preferred to be seen by a female health professional and that a provider’s ability to form an open and trusting relationship with their patients was more likely if they were female. 78,80,161,169,215,218,221,227 The gender of the provider was said to affect women’s willingness to seek help, to talk openly to the practitioner and, finally, to be examined (so that even if the problem had been disclosed, a patient may refuse further examination if the practitioner was male). 215 Knowing patients’ discomfort with male providers could also make male professionals reluctant to raise the issue of FGM/C at all. 161 Midwives and nurses in particular felt that being female helped them to build rapport with their patients:221
In this matter, female midwives are best because the women completely refuse to be seen by men. There is a complete gender-based affinity between women [Female midwife].
Spain221
Theme 3.5: crossing the cultural divide – strategies and elements of culturally sensitive care
This theme, reported in 23 studies, refers to strategies and outlooks that were adopted by providers in their endeavours to ‘cross cultural divides’. It was evident that many providers tried hard to be culturally sensitive and saw this as an essential aspect of their professional identity and practice. Hence, many papers described strategies and approaches that providers felt were important to build good relationships with FGM/C-affected women and, thus, to provide appropriate care. A good relationship was seen to be founded on trust, and this, in turn, rested on open communication. 228
In addition, study participants noted the importance of understanding FGM/C in the context of women’s wider non-health-care needs and culture (i.e. being person centred as well as ‘culturally’ sensitive), and having time to build rapport. 161,164,168,169,217,219,220,225,229
Additional prerequisites to the development of good patient–provider relationships were having good knowledge about FGM/C,216 sufficient time, continuity of care,169,213,227 managing language barriers, the importance of having a non-judgemental and open attitude, and the involvement of family:76,215
So I’m not treating them as ‘like this is bad’ [focus group discussion (FGD) 4] . . . Once you’ve built up a rapport, the information that you get from these women is amazing and you talk about sex with them and they answer the questions easily (FGD 3).
Australia76
In one hospital ‘very enthusiastic and very client-focused’ medical liaison officers were described as an important part of developing rapport with women (FGD 3).
Australia76
Finally, midwives in several studies noted that providing culturally sensitive care included avoiding making assumptions and stereotyping, and treating each woman as an individual. 76,192,215,219,228 Culturally sensitive care was particularly discussed by midwives and nurses.
Analytical theme 4: identifying female genital mutilation/cutting
A key review finding was that appropriate identification of FGM/C is a ‘hit and miss’ process dependent on individual provider behaviour as well as the existence (or not) of relevant organisational systems and processes. The timely and appropriate identification of FGM/C was dependent on individual providers recognising FGM/C as a potentially relevant health issue regardless of how and when women presented to care, feeling confident to ask women about FGM/C and subsequently having processes and procedures in place to enable women to access appropriate care. The studies suggested that these aspects varied according to a provider’s role and clinical setting. Identification of FGM/C was also related to whether or not there were organisational systems and processes in place to prompt practitioners to ask about FGM/C and to record and act on that information in a systematic way, with considerable variability being reported across settings.
Theme 4.1: presentation and help seeking
In this theme, providers in 15 studies reported a range of experiences in how women presented to services and how they might identify FGM/C. Some, especially in lower-prevalence areas, felt that they had encountered it only rarely,79,80,164,165,168,169,216,218,220,221 whereas others who worked in locations with large migrant populations were more familiar. 169,215,217,219 There was a feeling that women primarily sought medical help only once symptomatic or for pregnancy. Even then, women may not make a connection between their symptoms (e.g. frequent urinary tract infections) and their FGM/C:161,163,164,218,229
I see many women coming to me with infections, obviously I know why it has happened, because they are not allowed to heal before they have sex. However, none of the women will ever believe that that is the reason for it. It’s very frustrating.
England163
As a result, given that many medical procedures and consultations do not require physical examination, providers felt that FGM/C may not be identified at all unless they specifically asked. 161,163,164,169,218,219,229 However, one study with midwives in Spain221 noted that FGM/C could be missed even in an examination unless providers had been specifically trained to look out for it:
’I have never seen a case:’
‘Me neither:’
‘We don’t see that here:’
‘When you examine a women it doesn’t occur to you to look at the clitoris. I have never seen a case, although I have seen women from countries where it is practiced’ [Midwives].
Spain221
Likewise, some studies noted that it could be particularly hard to identify type I or type II FGM/C during examination and that this might account for apparently ‘low’ rates of identification. 76,79,80,161,169
Another study,159 in which a doctor who worked in a refugee health centre in Australia was interviewed, noted that the cervical cancer screening presented a good opportunity to identify FGM/C; however, this practitioner did not appear to routinely address the issue in this context. 169
A few studies mentioned a view that younger women may be becoming more ‘bold’ in seeking out care to alleviate their symptoms. 161,216,220 For example, a Swiss study161 described doctors from family planning centres noticing that young women were increasingly coming to them to request help for problems related to FGM/C. 161
In general, the studies consistently noted that it was the provider who needed to take the initiative to ask about FGM/C and that women may be reluctant to raise the subject of FGM/C themselves. 79,80,163 However, there were exceptions, namely when there were specialist services or experienced providers available, who women might seek out themselves via personal recommendations or on the advice of friends/family:76,164,169,218
I can tell when women turn up at my clinic and I’ve never met them before but they know me, and they know where I’m from and they know it’s because they’ve been recommended by somebody, or we’ve been recommended by somebody. Word of mouth is a really powerful recommendation.
Australia76
The main focus of the papers reporting on this theme was on the maternity context. It is unclear to what extent providers in other settings saw it as their responsibility to consider FGM/C. However, a study of school nurses in Sweden reported that school nursing education sessions proved to be a useful way of encouraging girls to come forward to discuss their FGM/C. 220 Likewise, a study with health visitors in England also showed that they were able to identify and support women with FGM/C through their routine interactions outside the maternity context. 222 In contrast, GPs in an Australian study did not see identification of FGM/C as part of their role or as necessary unless there was a medical problem. 169
Theme 4.2: practices and processes around identifying female genital mutilation/cutting
Twenty studies across many contexts indicated that the presence of organisational and system-related mechanisms to identify FGM/C was variable, and that practices could be inconsistent and unco-ordinated. They argued that a lack of knowledge of the procedures and protocols for the management for obstetric care for women with FGM/C was a substantial challenge to the provision of culturally appropriate care. They described that use of guidelines was ‘ad hoc’. 228
There was a general agreement among providers that, especially for pregnant women, FGM/C should be identified antenatally where possible but this did not always happen. 79,80,169,228 As indicated in Theme 4.1: presentation and help seeking, a key barrier to early and appropriate identification of FGM/C was that providers did not ask about FGM/C. However, several studies identified that organisational systems and processes were often not adequately set up to prompt them to ask or to ensure that follow-up would then take place. Organisational and system-related barriers to FGM/C identification were related to (1) the existence (or not) of clear guidelines, procedures, referral pathways56,76,79,80,167,169,215,216,218,221 and record-keeping processes,56,76,79,167,218,221,228 (2) clarity of roles and responsibilities and (3) the need for communication/co-ordination between organisational units and professional groups. 78,79,161,167,218 For example, some studies reported a confusion between community clinics and hospital inpatient centres over whose responsibility it was to record FGM/C and to provide counselling and care planning. 79,167 As a result, examinations of women and care planning might not happen. One study from Sweden79 described how there was no consensus among doctors regarding how and when women with FGM/C should be informed of deinfibulation options, what information they needed or how best to convey information between antenatal clinics and the hospital:
It was assumed that the ANC-midwives [antenatal care midwives] write necessary information in the notes carried by the patient, although there seemed to be no standard for what information should be included.
Sweden79
Other studies reported a lack of record-keeping,56,76,79,167,218,221,228 so that FGM/C failed to be recorded on the relevant medical notes and then failed to be discussed further during subsequent consultations. 225 For pregnant women, this could lead to situations in which women arrived at the labour ward with no prior counselling regarding their FGM/C:76,225
It is hugely dreadful when you have to do an anterior episiotomy with somebody who’s transitional . . . , who’s just walked in, in that state; there’s no counselling around that. So you are actually doing a procedure that is very uncomfortable because you cannot rationalise with the woman in that state.
Australia76
A unique care plan was seen by several midwives to be a useful way forward (FGD 4). Without this information, they admitted they felt very unprepared.
Australia76
However, even when procedures were in place, one study with midwives in Australia identified several reasons why they might not always be followed. 76 These related to lack of time, a feeling that additional reporting created overly burdensome bureaucracy that was hard to fit into existing work routines and a lack of understanding of how the systems worked:
Time pressures and lack of experience were seen as barriers to data collection . . . In one hospital, labels were placed on women’s files to indicate FGM. This was entered onto the computer under an alert function. However, one midwife admitted that these were not properly assessed by staff.
Australia76
Some midwives were aware of where they could record FGM on the database under ‘other surgeries’ but felt that it was often missed and that FGM needed its own indicator, or a ‘direct question’ for clarity. Participants were not supportive of additional forms, as there were too many already.
Australia76
Analytical theme 5: clinical management practices – inconsistent and variable
The review found that clinical management of FGM/C can be variable and inconsistent dependent on individual provider knowledge and skills, as well as the existence (or not) of relevant clinical guidelines. Although some providers expressed confidence in managing clinical interventions around FGM/C, many of the studies identified uncertainty in terms of good practice and highlighted inconsistencies in clinical practice, including with regard to psychological care. The inconsistency was linked to a perceived lack of clinical guidelines, meaning that the care provided to women could be variable, depending on the experience, confidence and preferences of individual practitioners. Many findings contributing to this theme came from studies looking specifically at obstetric care for women with type III FGM/C and to clinical management practices around deinfibulation and reinfibulation.
Theme 5.1: deinfibulation timing
This theme, reported in eight studies, concerns professionals’ views on the timing of deinfibulation for women with type III FGM/C. The majority of providers felt that women preferred deinfibulation to be carried out in the second stage of labour (rather than antenatally) to avoid having to be cut twice. In contrast, most providers would have preferred to undertake deinfibulation antenatally (although some felt that this might be an unnecessary additional trauma for the woman), but the usual practice seemed to be deinfibulation in the second stage of labour, as the baby’s head is crowning. 76,79,80,161,167,169,215,228
In studies specifically of midwives, it was emphasised that, ideally, decision-making around deinfibulation should be a ‘shared’ process taking place as a result of discussions and counselling between providers and women during the antenatal period;76,215,228 however, this did not always happen. 79,80,167,169,228 A UK study228 noted that discussions with women about defibulation should include asking them when they would like it to be carried out. Participants in the study noted that midwives should discuss the feasibility of women’s requests and should note the woman’s wishes for intervention and pain relief. 228 In some studies, providers noted that women’s decisions around deinfibulation timing were influenced by family members, especially older women. 76,228
Theme 5.2: deinfibulation practice
With regard to deinfibulation, findings reported from 21 studies revealed that providers’ confidence, competence and experience around the procedure varied considerably depending on the professional group, training and setting. Hence, the care that women received could be variable depending on whose care they happened to fall under. Several studies noted that midwives in particular could be anxious and uncertain about deinfibulation:56,76,78,80,168,169,215,217,219
Having done the anterior episiotomy, my biggest fear is having to do a lateral episiotomy as well. We’ve had one occasion where we did have to do that. It felt like we’d mutilated that woman even further (FDG 2).
Australia76
Other participants were worried about undertaking clinical procedures that they were not confident with . . . ’I had to actually do an anterior episiotomy on her. I found that very unnerving to actually have to cut upwards . . . The fear is how far is it going to extend and what it’s going to do’.
Australia76
Two studies, both involving midwives, highlighted uncertainty about how best, and to what extent, to suture and manage the perineum following deinfibulation. 80,210 In another study, a midwife described how, with experience, deinfibulation became a normal routine procedure. 78
Midwives in an Australian study76 described how support from a FGM/C specialist midwife was perceived as extremely helpful in alleviating their anxiety:
In one hospital, midwives said they received referrals from a midwife with specialist training with the women’s history and suggestions for care (FDG 4).
Australia76
Studies that included medical practitioners generally indicated a higher level of professional confidence, even when formal training had not been received:78,79,165,167,225
I think they can muddle through it (circumcision management) . . . I think we do OK with that . . . we do a pretty good job with our education in general . . . and in making those kind of decisions (Male OB/GYN).
USA225
Several studies nonetheless identified inconsistencies in medical practice regarding deinfibulation:76,79,80,161,167
Different suggestions were given for [management of] infibulated women. Most . . . doctors advocated defibulation with care taken to protect underlying anatomical structures, sometimes accompanied with a medio-lateral episiotomy. Others suggested a medio-lateral episiotomy only, thus recommending the same procedure as with non-infibulated women.
Sweden79
Furthermore, three studies reported that doctors were sometimes quick to decide to recommend a caesarean section, owing to uncertainty or lack of experience, and especially when this was compounded by difficulties in being able to undertake routine monitoring in labour:78,79,167
It’s like going back [in time] a bit . . . You’re nervous since you’re not in control and you can’t check . . . that labour progresses as it should . . . there is always the question if you should cut it up [the infibulation] or if you should do a caesarean section straight away without knowing anything . . .
Sweden79
One study highlighted how decision-making around deinfibulation could also be influenced by practitioners’ assumptions about women’s preferences based on cultural stereotypes rather than discussing the issue with them. 210 In a study conducted among midwives in Norway,210 midwives knew that infibulation was of cultural importance to the Somali community. They therefore assumed that Somali women wanted to remain infibulated. Hence, in an attempt to be culturally sensitive, some midwives reported undertaking extensive episiotomies rather than deinfibulation:
‘Therefore, I just made episiotomies, to avoid tears in front.’ . . . When asked whether she had considered that Amina might have wanted defibulation, Katrine replied in surprise: ‘No! Of course she wants to remain the way she is.’
Norway210
Finally, five studies of midwives noted that it was important to provide women with counselling and in-depth information after deinfibulation so that they could adjust to an altered body image and altered physical sensations. 76,167,215,217,228
Theme 5.3: reinfibulation ambivalence
With respect to reinfibulation, findings from 11 studies demonstrated that professionals’ attitudes towards reinfibulation could be ambivalent, and that their practice relating to reinfibulation was variable.
In general, health practitioners were clear that reinfibulation was illegal and should not be carried out. However, in three studies, practitioners reported having undertaken some degree of reinfibulation161,167,210 (but it should be noted that these were all old studies and may no longer reflect current practice).
Although knowing that reinfibulation was illegal, some midwives felt unsure about the detail of FGM/C and the law; therefore, they were unsure about how to best explain the issue in a culturally sensitive way when requested. 214,215 However, where there was clarity on the law, it was perceived to be a helpful way of supporting practitioners in explaining why they were refusing reinfibulation. 80,228
Although reinfibulation was known to be illegal, several studies reported that practitioners sometimes felt ambivalence and a moral dilemma about refusing to reinfibulate a client if she was clearly requesting it, and felt that it should be done. Refusing a patient’s request was seen to contradict the principles of person-centred care. These practitioners worried that refusing reinfibulation may cause harm in terms of causing marital problems for women and their husbands or may cause women distress in terms of adjusting to an altered body image. 76,79,80,161,167,168,210,214,215,219,224
Several studies highlighted the important role of husbands in decision-making around reinfibulation (this varied in terms of requesting it or not wanting it for their wives) and, where appropriate, of the benefit of involving them in women’s care. 76,80,210,226
Theme 5.4: need for guidelines
Fifteen studies reported a lack of (or lack of awareness of) clinical guidelines that would help to establish clarity and consistency of practice around deinfibulation timing, procedure and reinfibulation:
Rather than referring to scientific reasoning and professional guidance, the doctors instead seemed to rely largely on personal knowledge, values and experiences when reasoning about their practice.
Sweden79
None of the clinical sites where study participants worked had formal protocols on the management of circumcised women. One participant mentioned that they had considered adopting a protocol to address requests for reinfibulation . . . however, the protocol was never created.
USA225
Where guidance existed, it was perceived to be highly useful. 169,228
Theme 5.5: psychological issues
Twelve studies reported providers’ experiences that FGM/C could evoke painful and difficult psychological responses in women at any life stage, and some practitioners emphasised the importance of offering counselling and psychological support. 76,215–217 Interestingly, these aspects were mainly mentioned by nurses/midwives, and the studies throughout the review in general gave most prominence to physical rather than psychological aspects of women’s care. Although recognised as a need, in most of the studies reporting this theme the actual availability of counselling or psychological support as a routine part of care was not clear. 168,217
Clinical interventions in particular were recognised as potentially traumatic for women in terms of inducing flashbacks from the original procedure, heightening pain and, in the context of birth, sometimes leading to difficult deliveries. In a maternity context, several studies noted a need to be extra attentive to information giving and counselling in the antenatal period and to pain management during labour and perineal suturing to try and mitigate emotional distress. 56,76,164,167,210,215,217 However, dealing with these situations could also be emotionally challenging for the providers:76,167,210,215
This lady had a small tear . . . and I was actually stitching her up . . . And she was crying and crying, and afterwards I said, ‘Are you OK,’ but she told me it brought back all those memories, you know, being sewn up before. So that was distressing, how she felt. (Midwife 6)
Australia215
Analytical theme 6: optimal service development for female genital mutilation/cutting care
This theme relates to service development and perceived service gaps related to FGM/C prevention and care. The studies identified a perceived need for service development in three interlinked areas: (1) community engagement, (2) prevention and (3) specialist service provision. The studies identified variable engagement of providers in addressing FGM/C prevention on an individual level, but there was strong support for the development of specialist holistically focused services that would cover FGM/C care as well as prevention. Providers saw community engagement as essential for prevention as well as for raising awareness of, and trust in, services.
Theme 6.1: provider’s role in prevention
Apart from school nurses, whose role explicitly encompasses safeguarding and sexual health for children/teenagers,217,220,224 relatively few studies reported practitioners addressing FGM/C prevention (either directly with young people or indirectly via discussions with mothers/families) as part of their practice, although several studies reported that this should be part of any practitioners’ role, including GPs. 76,161,164,167,217,219,220 As a result, prevention discussions appeared to take place in an ad hoc way (dependent on individual providers) rather than as a routinised aspect of care. This theme was reported in 13 studies. 76,80,161,164,167,168,217–220,224,226,228 Ten of these related to prevention discussions with women/families,76,80,161,164,167,168,218,219,226,228 and three (specific to school nurses) included findings regarding FGM/C discussions directly with young people. 217,220,224
Some key barriers to initiating prevention discussions in a clinical setting were identified in six studies (but several of these are now rather old). 76,80,161,167,219,226 These included lack of time, inappropriate timing (referring to the difficulty of having a prevention discussion when a woman was in labour or had just given birth), feeling that the prevention discussion is someone else’s responsibility, not having enough knowledge or confidence, feeling unsure if women’s responses could be trusted, lack of privacy (e.g. if family members were present) and language barriers.
School nurses did report having discussions with young people about prevention, although it was described as a sensitive and difficult topic to address. 217,220,224 Nurses in one study220 reported that discussions were easier if it was possible to speak to the young people alone. One study highlighted that school health practitioners were perhaps overly focused on discussing the clinical or legal aspects of FGM/C and a different approach might be to address sexual/relational concerns and impacts with young people and that this approach might engage them more. 224 For example, in a study from Norway,224 a school nurse described how she ran discussion groups for youth on FGM/C:
When asked whether sexual concerns and the motivation for FGM/C were topics for reflection and discussion in her groups, she was surprised by her own omission. She simply had not considered these topics. Her focus had been on the law and the health risks associated with FGM/C.
Norway224
Theme 6.2: community education and engagement
This theme, reported by 11 studies, refers to provider views on community engagement and education. Practitioners identified a need for greater education and awareness raising among affected communities, both on FGM/C itself and associated services but also on prevention. 76,161,164,165,168,169,217,219,220,224,228 They suggested that this should include men/boys as well as women/girls. Providers also identified a need for better information resources for communities. 76,161,217,220 Practitioners suggested that community engagement needed to be built on relationships of trust and concern for wider community needs (not just FGM/C) and some suggested that community outreach/liaison roles might be beneficial. 76,168,169
Theme 6.3: specialist services
This theme refers to a perceived need for specialist services. Nine studies identified that providers valued and recommended having specialist centres for FGM/C management where women could be referred and where expertise, advice and training could be accessed. 165
Such specialist centres were seen as a particularly important potential link to communities, in terms of building trust and working together with community outreach workers and trained interpreters:76,223
At some units, particularly at family health centers, midwives worked in networks with social workers, health-care professionals, and bi-lingual health advisors of Somali origin. They felt this created a more holistic approach.
Sweden223
In addition, the need for additional counselling services was highlighted by some studies. 76,161,217 Having access to specialist centres was seen as particularly important for practitioners in low-prevalence or rural areas. 165,168,169,228 Finally, four studies stressed the importance of ensuring equity of service provision, especially across lower-prevalence or rural areas. 165,168,169,228
Summary and conceptual model of analytical themes
Review 2 shows that providers’ ability to appropriately identify FGM/C, to provide appropriate clinical and psychological care and to engage in prevention discussions depends on individual provider characteristics, such as knowledge, clinical skills, cultural understanding and communication skills. However, it also requires clear organisational systems, processes and guidelines that support providers to ask the right questions and offer correct care and follow-up, including having systems in place to address language barriers and sufficient time (or continuity of care models) to build relationships with women and their significant others. Particular consideration may be needed for service configuration in low-prevalence settings, where providers appreciate specialist support. These inter-relationships are depicted in Figure 4.
FIGURE 4.
Review 2 conceptual model of analytical themes.

The CERQual assessment
Appendix 13 presents a summary of findings table with a CERQual assessment of confidence for each individual descriptive review finding. 131 Eight review findings (descriptive themes) have been graded as ‘high confidence’, 11 have been graded as ‘moderate confidence’ and one as ‘low confidence’. The main causes of downgrading a review finding were concerns related to methodological limitations and coherence (in some cases, not all studies reported all aspects of a review finding). In addition, several findings had moderate concerns related to ‘adequacy’ in terms of having relatively ‘thin’ data contributing to a finding. However, most findings were relevant across professional group, contexts and countries.
Discussion of review 2
There has been much research documenting the challenges faced by health providers in destination countries in delivering health care to migrant populations in a context of super-diversity (e.g. language barriers, cultural differences and lack of time to manage complex patient needs). 85,86,89–91,230 As with review 1, this review has highlighted all of these issues, and has shown that, when delivering care related to FGM/C, these challenges can all become exacerbated. This is primarily a result of the cultural sensitivities associated with FGM/C, lack of provider knowledge/experience and haphazard organisational processes. Together, these can result in provider stress and suboptimal care. However, the review has also shown that these obstacles can be overcome. Key to this are well-trained, knowledgeable and skilled providers, good communication (especially strategies to address language barriers and to involve families where appropriate) and effective organisational systems and processes.
The findings from this review will be discussed further in Chapter 6, in an integrated discussion section in which reviews 1 and 2 are considered together.
Limitations and evidence gaps in review 2
This was an extremely comprehensive review; however, the key limitations are that there was very limited evidence on providers’ practices around prevention and safeguarding and, as highlighted previously, little explicit research on factors that facilitate or hinder adherence to guidelines around FGM/C identification and record-keeping. In addition, the majority of papers have focused on maternity care settings and maternity care professionals. There is very little evidence to date on the views, experiences and practices of professionals in primary care or other non-obstetric settings (e.g. sexual health, health visiting and school nursing). This is an area for future research.
Relevance to the UK context
The results of review 2 are derived from 30 papers, representing 28 studies across many OECD countries. Five papers, representing four studies, were undertaken in the UK: 14% of all studies in review 2. 56,163,213,222,228 Of these four studies, three were undertaken in the last decade, all of which were conducted between 2012 and 2014. 163,222,228 There are no UK studies from within the last 5 years. A more in-depth analysis of the findings reported by the UK studies showed that two studies (both low quality) contributed findings to analytical themes 1–5. 56,213,228 Only one study contributed findings to theme 6 (optimal service configuration). 228 All studies reported on analytical theme 3 (encountering the ‘other’ in clinical practice) and three of the four studies reported on analytical themes 1–3. In conclusion, although the UK studies do contribute across the themes (particularly themes 1–3), given the relatively small number of UK studies in review 2, their relatively poor quality and the dates when they were conducted, it is hard to judge to what extent review 2 findings are applicable specifically to the current UK context.
Chapter 5 Integrated synthesis
In this chapter, we present an integrated synthesis derived from 78 publications in total for both reviews, representing 74 distinct studies. Fifty-seven papers representing 55 studies were included in review 1. Thirty papers representing 28 studies were included in review 2. Nine studies were common to both reviews.
Integration and synthesis were undertaken by juxtaposing the findings (analytical and descriptive themes) from reviews 1 and 2 and considering whether or not, by taking both women’s and professionals’ perspectives into account, they could be combined to produce integrated and novel insights. Four final syntheses (as illustrated in Figure 5) were formulated, which are able to (1) capture the meaning and complexity of a key FGM/C health-care-related issue or concept, (2) illuminate this and (3) propose its potential antecedents and consequences.
FIGURE 5.
Formulation of integrated synthesis.

The findings within each of the four synthesis domains are depicted in Table 9.
| Synthesis domains | Findings |
|---|---|
| 1. Factors influencing health-care-seeking around FGM/C |
|
| 2. Identifying and talking about FGM/C |
|
| 3. Clinical management and care experiences |
|
| 4. Service configuration and resourcing |
|
Synthesis 1: health-care-seeking around female genital mutilation/cutting
There are multiple interlinked factors that influence whether or not a woman seeks out health care in relation to having experienced FGM/C. These factors, described in the following sections, can operate as barriers or facilitators depending on a women’s life stage and family/community context.
Perceptions about female genital mutilation/cutting
For many women, FGM/C is perceived as ‘normal’ within their cultural context, hence they may not seek out care because they are comfortable in their own body and life situation and see no reason or perceive no need to seek help. This perception may change once they are exposed to anti-FGM/C discourses. Some women may then wish to seek out care (e.g. deinfibulation) because they wish to challenge or resist their own cultural norms and take control over their lives.
Knowledge about services
Women may not be aware of specialist support or services that can address issues related to their FGM/C (even when aware of mainstream services such as maternity services or GPs). This lack of awareness may be related to a lack of information about FGM/C and a lack of service availability but it may also be related to the fact that FGM/C and associated gynaecological, sexual or emotional problems are private, sensitive and taboo issues in many African cultures, and are rarely openly discussed within communities.
Experiencing symptoms
Women will usually seek out care only if they are experiencing acute symptoms or if they are pregnant. However, they may not initially make an explicit connection between their symptoms or medical issues and their FGM/C.
Family and peer influence
Choice of service may be influenced by women’s families, husbands and peer networks. Generally, women will seek help on the advice/recommendation of others and, if it relates to FGM/C, they would aim to seek help from a provider who they (or the community) trust and perceive as competent around FGM/C.
Cultural norms
Care-seeking choices (including around deinfibulation or reinfibulation) are strongly influenced by family members, by husbands and by cultural norms around the body, sexuality and appropriate female behaviour. Women may avoid seeking care owing to embarrassment or shame at having to discuss a private personal issue. They may particularly avoid male health-care providers. Within communities that practise FGM/C type III, there are strong cultural pressures to maintain premarital virginity and chastity, hence most women will avoid undergoing deinfibulation before marriage, even if symptomatic, unless their perceptions around FGM/C change. After marriage, decisions around deinfibulation (and requests for reinfibulation) are particularly influenced by husbands.
Previous health-care experience
Women may avoid seeking care related to FGM/C as a result of having had previous poor health-care experiences causing them to lose trust in the system. Conversely, previous positive experiences would enhance the likelihood of feeling that they can trust the provider/service and this would also enhance the likelihood of women recommending a particular provider or service to their friends/family.
Social circumstances
Some women are facing difficult life circumstances (e.g. in relation to immigration issues or personal histories associated with migration) and may not have the time or capacity to address issues around their FGM/C until/unless their more immediate needs are met.
Synthesis 2: identifying and talking about female genital mutilation/cutting
Once a woman has sought care, the initial identification of, and discussion about, FGM/C is ‘hit and miss’ and is affected by communication challenges and prevailing organisational processes. The challenges and their consequences are described in the following sections.
Communication challenges
Discussion about FGM/C is greatly hindered by language barriers and challenges with accessing appropriate interpretation support. This is further complicated by time pressures within consultations, which may inhibit the ability to talk about complex issues. In addition, as a sensitive and taboo topic, discussion about FGM/C is hindered by embarrassment and uncertainty. Women may feel embarrassed and/or fear being judged, and providers may avoid the subject because of uncertainty over how to talk about it, an assumption that women would mention it themselves if relevant or out of a desire not to offend or intrude. Hence, opportunities to identify and discuss FGM/C may be missed. Providers and women both mentioned that discussion is more likely if the provider takes the initiative to ask/talk about FGM/C rather than waiting for the woman to mention it. Open discussions about FGM/C (including deinfibulation timing) are more likely if the provider is knowledgeable and confident and exhibits cultural sensitivity and respect, and when a good patient–provider relationship has been established (e.g. through continuity-of-care models).
Organisational/system issues
Discussion about FGM/C is hindered if it is not part of routine organisational processes (e.g. providers being prompted to ask about FGM/C for record-keeping requirements or as part of routine questions during assessments). Even in an obstetric context, FGM/C may not be identified during antenatal care unless there are routine processes in place to ask about and record FGM/C status. In addition, it may not always be clear whose role or responsibility it is to undertake identification and management/counselling in relation to FGM/C, and hence it may be missed. Organisational barriers to adhering to existing processes include time and resistance due to the additional administrative burden.
Synthesis 3: clinical management and care experiences
Clinical management of FGM/C can be stressful and difficult for both women and providers owing to challenges in achieving a sense of cultural understanding and safety. The nature and quality of experiences are strongly linked to the level of cultural and clinical competence and professional behaviour of the provider, as indicated in this section.
Seeking respectful care across cultural divides
Women reported experiencing a wide range of negative, discriminatory and insensitive comments and reactions from providers in relation to their FGM/C. These negative experiences caused great distress, with women reporting feeling objectified and humiliated and losing trust in the system/provider. Some women reported subsequently avoiding care (or avoiding mentioning FGM/C) as a result of their negative experiences. Providers, likewise, reported experiencing strong negative reactions to FGM/C. Many providers admitted that they found the issue difficult to deal with emotionally and felt unsure of how to respond to women and their families. Nonetheless, many providers did endeavour to treat women with compassion and empathy, and women were highly appreciative of situations in which they felt that they had been treated with respect, dignity and kindness.
Anxiety, apprehension and professional dominance
Some women were highly anxious and apprehensive about childbirth or vaginal examinations, and the experience of childbirth or vaginal examinations could trigger flashbacks of their original FGM/C and cause extreme emotional or physical reactions. In addition, some women were fearful of clinical interventions, such as caesarean sections, and of how deinfibulation would be managed. Women’s experiences of care in these situations was strongly influenced by the provider’s response. In some cases, providers appeared to feel that women were resisting their advice or ‘being difficult’ and challenging (especially if the family became involved) and confrontational situations could ensue, which were distressing for both providers and women and in which both parties struggled to exert some control. Indeed, women reported many care experiences in which they felt that they had lacked control and that had increased their anxiety. In contrast, in situations in which providers were able to build relationships with women and understand their fears and concerns, they were in a better position to provide appropriate information, support, appropriate family involvement and clinical management. Women expressed great appreciation of such care. Counselling support was recommended by providers for women experiencing psychological difficulties. However, there was a lack of evidence on the ways in which distress was identified by providers and on women’s subsequent experiences of psychological care.
Cultural understanding for shared decision-making
Many providers lacked knowledge of the cultural meanings associated with FGM/C and related bodily procedures (e.g. deinfibulation or reinfibulation), and this, coupled with language barriers, could make it difficult to achieve shared understandings or decision-making in relation to clinical interventions or management of birth. Providers sometimes made assumptions about women’s preferences for deinfibulation (or not) and sometimes found managing requests for reinfibulation challenging. There was a need for women to have more information and support in planning interventions such as deinfibulation and in adjusting to bodily changes following deinfibulation. These issues did not appear to be routinely discussed except in specialist centres or by highly experienced staff.
Being in safe hands
Both women and providers recognised that some providers lacked knowledge and skills around FGM/C, particularly in the management of birth and deinfibulation for women with type III FGM/C. In situations in which providers lacked knowledge, women felt anxious, unsafe and highly vulnerable and providers reported heightened anxiety and stress. Such situations were clearly linked to poorer care experiences, and some women reported avoiding care in the future as a result. In some contexts, there appeared to be a lack of clinical practice guidelines or clear care pathways, and providers reported that these were needed. Both providers and women identified that there was a need for in-depth provider training and skills development around FGM/C. Midwives in particular appeared to be uncertain about their skills in undertaking deinfibulation. Women reported seeking out providers who were known to be experienced in dealing with women with FGM/C, and expressed great relief and satisfaction when they were looked after by providers who appeared knowledgeable and competent.
Synthesis 4: configuration and resourcing of services
Approaches to service provision for FGM/C were not well described but appeared to be highly variable.
Role of specialists and specialist centres
The most positive experiences or recommendations were reported from approaches to care where there were specialist centres or where specialist expertise was available, with clear guidelines and referral pathways between services.
Addressing key barriers
Positive experiences were reported from approaches to care that sought to overcome language barriers, lack of knowledge or lack of trust in communities, including community outreach and engagement strategies, having trained interpreters, community-liaison workers and approaches that encouraged continuity of care.
Filling knowledge and service gaps
There were a number of issues related to service provision that were particularly poorly reported. Current service provision appeared to be strongly focused on clinical (physical) care. There was much less emphasis and evidence on mental health, although some providers clearly recognised it as a need. Likewise, there was relatively little focus on providers’ roles (apart from school nurses) in addressing FGM/C prevention either with young people directly or with mothers or families, although providers recognised that this was an important issue. Women and providers both reported the need for greater community engagement in prevention, information giving, awareness raising and care, but there was relatively little detail available on how this was being operationalised.
Chapter 6 Discussion, implications and recommendations
Introduction
The two reviews show that FGM/C – literally and symbolically – embodies complex processes of cultural change and cultural interaction that are occurring as a result of globalisation, migration and super-diversity. These processes manifest themselves very concretely in health care in terms of influencing how individuals seek care, how care is delivered and experienced by all involved and how services are configured. 3,6,99 Responding and adapting to super-diversity is perhaps one of the major contemporary challenges facing the NHS. This discussion considers these challenges in relation to the review findings on FGM/C-related care and will illuminate these with reference to concepts of ‘cultural competence’ and ‘cultural safety’.
Developing culturally safe care for female genital mutilation/cutting in a context of super-diversity
There is a major body of literature that explores concepts such as cultural awareness and cultural competence. These are often depicted on a continuum whereby practitioners (and also organisations and systems) move from developing an awareness of the needs of clients from other cultures, to being aware of one’s own cultural values and how these shape service provision, to being able to effectively engage across cultures to build relationships and provide culturally responsive and appropriate services. 231 In Canada, Australia and New Zealand, the concept of cultural competence has been extended even further into a commonly used discourse of ‘cultural safety’. Cultural safety derives from critical social theory and argues that traditional approaches to cultural competence fail to adequately take into account power relations within health-care delivery that are historically unequal between migrant or indigenous groups and health-care providers and services. 232 Within a cultural competence discourse, it is argued that the power to define norms of health behaviour and/or to prescribe appropriate courses of action usually lies with health professionals. 233 As such, migrant groups remain represented as the ‘other’ and may be viewed within a deficit model – as a problem that needs to be fixed – rather than as equal partners whose knowledge and values can and should contribute equally to a relationship or to service development initiatives. Culturally safe practice, by contrast, is predicated on relationships of mutual trust and respect. It is a transformative and rights-based approach, seeking to uphold the principles of respect, dignity, empowerment, safety and autonomy. 234 Cultural safety envisages the health-care encounter as a negotiated and equal partnership in which trust plays a central role. The health-care practitioner’s role is to enable patients to say how a service can be adapted and to negotiate an agreed approach – a key aspect of shared decision-making. 235 The converse of cultural safety is ‘cultural risk’236 in that culturally unsafe practices are defined as ‘any actions that diminish, demean or disempower the cultural identity and well being of an individual or group’. 237 However, cultural safety is not just a feature of individual practice. It is argued that culturally safe practice must be institutionalised through organisational policies and structures so that it becomes part of mainstream health-care provision rather than being dependent on individual practitioners who may or may not adopt its values and approach. As with cultural awareness and competence, advocates of cultural safety call for organisations and systems to enshrine its principles through, for example, policy, training, flexible service development or resource allocation. 238–240
Care associated with FGM/C is an exemplar of the challenges of achieving cultural safety in a context of super-diversity. The two reviews have highlighted areas of good practice and positive experiences, but have also highlighted many challenges in care-seeking and care delivery, including poor care experiences. Furthermore, the reviews suggest that the positive experiences are more often associated with individual practitioners’ abilities and values, rather than being part of a systematic mainstreamed approach within a service. As such, the reviews highlight three key areas in which change and development are required. First, there is a need to address and better understand cultural competence and cultural safety in health-care interactions. Second, there is a need for service delivery models and organisational processes to adapt towards culturally safe service provision in a context in which vulnerable migrant women increasingly form a significant percentage of patient groups. Finally, there is a need for professional training and community engagement to be implemented to support appropriate care-seeking and care delivery. These three issues are discussed in the following sections in relation to the findings from both reviews. 241,242
Cultural safety in health-care encounters associated with female genital mutilation/cutting
Culturally safe or culturally competent care is predicated on achieving relationships based on trust and respect. This, in turn, is based on an ability to communicate and to be heard. These issues are considered further in this section.
Respectful care
The majority of the papers in the two reviews focused on the maternity setting. Globally, there is currently enormous emphasis on promoting respectful care during childbirth. 243,244 However, the two reviews (especially review 1) show that for many women affected by FGM/C, the care they receive in OECD countries, including the UK, is perceived as profoundly disrespectful and disempowering. A recent systematic review of disrespect and abuse in childbirth created a typology of six forms of disrespect/abuse:245
-
physical and verbal abuse
-
stigma and discrimination
-
failure to meet professional standards of care
-
poor rapport between women and providers
-
health system conditions and constraints
-
impact on utilisation of maternity services.
Many of the findings of review 1 map very clearly onto the subthemes within these broad categories. As such, it reveals an unacceptable picture of care for FGM/C-affected women during childbirth and highlights an urgent need to take action. Although the aforementioned systematic review245 was developed with specific reference to maternity settings, many of the same typologies of disrespect would also appear to be relevant to the other care settings highlighted in review 1, where women nonetheless needed to discuss an issue that is personal and sensitive and that relates to their sexuality, identity and genital area.
Again, with reference to maternity settings, work is under way to explore how ‘respectful’ care is defined and experienced by women. 246 A recent global review247 identified 12 domains, as follows:
-
being free from harm and mistreatment
-
maintaining privacy and confidentiality
-
preserving women’s dignity
-
prospective provision of information and seeking informed consent
-
ensuring continuous access to family and community support
-
enhancing quality of physical environment and resources
-
providing equitable maternity care
-
engaging with effective communication
-
respecting women’s choices, strengthening their capabilities to give birth
-
availability of competent and motivated human resources
-
provision of efficient and effective care
-
continuity of care.
All of these domains were also highlighted by women in review 1 and some professionals in review 2, as being relevant to, and having an impact on, the care experience. In women’s descriptions of positive care experiences, they particularly emphasised open communication, being treated with dignity, being free from harm/provider competence, being given information and choices, involving the family and continuity of care as a key feature that enabled high-quality relationships to form. Together, these features enable a woman to feel safe and to have trust in the system. 87,248
The same dimensions of respectful care are being promoted as a core work stream of the UK’s Maternity Transformation Programme, linked to ‘Better Births’. 98 It would seem highly important that these packages specifically include the needs of women affected by FGM/C.
Communication, relationships and trust
Both reviews highlighted the critical role of communication both in disclosing or identifying FGM/C and in delivering appropriate care. Discussions about FGM/C could be hindered by language barriers and cultural differences/misunderstandings but also by an apparent lack of trust of women in the provider or in the system generally.
The review findings concur with a large body of literature on language barriers affecting the care of migrant groups and on the importance of configuring services to address these,249 an issue that is discussed in more detail in Service configuration to promote access and equity. The review findings also strongly concur with studies that show that trust is essential for building effective health-care relationships,87,250,251 but the findings also show that this may be particularly challenging because of the sensitivity of FGM/C. The reviews showed that lack of trust was a potential issue with interpreters, health professionals and the ‘system’ as a whole.
With respect to language barriers, the reviews showed that a common strategy used by practitioners was to use interpreters, either formal (professional) or informal (e.g. family members). The reviews are consistent with the existing evidence base in this area, and showed that both of these strategies could be problematic. 252,253 There could be a lack of trust between women and either group of interpreters but also between interpreters and providers who were unsure if the interpreter was translating correctly. Existing evidence supports the lack of confidence in informal interpreters, for example a recent study in Holland showed that informal interpreters translated less than half of what was actually communicated. 254 Problems with informal interpretation can potentially be addressed by increased training and by increased availability of professional interpreters. 255 However, in the context of the reviews, owing to the sensitivity of the topic, it was shown to be imperative that women and providers were able to trust the interpreter. The reviews cited suggestions made by women and professionals of utilising community advocates or liaison workers with an expanded role, to act not just as an interpreter but as a cultural mediator who could raise awareness, befriend women, signpost to services and act as an advocate for their rights. Such approaches have been positively evaluated in other settings,256–260 but need further exploration with reference to FGM/C. Nonetheless, they seem consistent with a cultural safety agenda, in that this model seeks to empower women to interact on an equal footing with providers rather than simply to overcome language differences.
The reviews showed that women’s trust in providers and the ‘system’ was affected when women felt disrespected or disempowered or when they sensed that providers lacked experience and skill. In this latter sense, women felt physically at risk as well as perceiving a potential threat to their identity or culture. However, the findings also suggested that trust could be successfully established, but required contexts where providers were knowledgeable, displayed cultural understanding, sought to understand woman’s own needs and preferences without stereotyping and engaged in dialogue with women to provide them with a sense of control. 261 Thus, the review findings pointed to positive experiences when practitioners utilised a trusting relationship to engage in shared decision-making and to offer person-centred care. Most health-care practitioners are trained in these approaches, but the review supports existing evidence showing how challenging it can be to implement these when there is limited time and poor communication. 262,263 The reviews suggested that continuity of care could be a key strategy for helping to build trusting relationships in order to provide better-quality care. In the UK, these models are particularly being advocated in the maternity care setting, but could also be implemented in primary care. 92,98,264 Furthermore, the Better Births Maternity Transformation Programme has a workstream on developing personalised care plans to help shared decision-making with women throughout pregnancy and birth. 98 This would seem to be a particularly useful mechanism for helping women and maternity professionals to communicate more effectively about approaches to care in relation to FGM/C. 265
A final point relating to trust and respectful care concerns the FGM/C prevention and safeguarding agenda. Although direct or indirect prevention were not prominent themes in either of the reviews, the findings consistently pointed to the fact that women felt able to have open communication with providers if they felt respected and if they trusted the provider and the service. From this, it can be inferred that discussions around prevention and safeguarding are far more likely to happen and to be meaningful if good relationships and respectful care can be ensured.
Culturally safe service delivery and service configuration
Addressing trauma and mental health needs
A clear finding from both reviews was that, for some women affected by FGM/C, childbirth and other clinical interventions could be traumatising, triggering flashbacks of their original cutting, creating profound anxiety and distress and potentially leading to poor care experiences or avoidance of services. 210,266 The reviews were unable to illuminate in any further depth how such women might best be identified or treated, or which women might be most at risk. This is an important agenda for future research. 30,62,267–271 However, maternity care services in the UK all have well-established processes in place for dealing with highly anxious women or women who have experienced trauma. It would seem important for services to ensure that these interventions are also available for women affected by FGM/C. 63,272 A minority of the specialist FGM/C services in the UK do offer psychotherapy or counselling support and the latest commissioning guidelines15 specifically recommend the provision of these services. 273 The findings from these reviews strongly endorse this recommendation. Likewise, the reviews show that, for some women, the move to a Western country can prompt difficult feelings with respect to their culture and their bodies as they started to re-evaluate the practice of FGM/C. 266 Some of these women may likewise benefit from counselling or from support from relevant community organisations. Hence, the reviews also endorse the recent commissioning guidance on promoting community engagement and working in partnership with community organisations. 15
Management of deinfibulation and culturally safe care
The reviews showed that a key area of concern for women and for clinicians related to management of deinfibulation. 27,28,31,32,34 Deinfibulation raises concerns for physical safety but also cultural safety as it reflects an embodied process linked to a sense of cultural and bodily integrity and is a phenomenon that requires negotiation and cross-cultural understanding between practitioners and patients. Hence, it is given specific consideration here.
Globally, the evidence around optimal timing (before pregnancy, antenatally or in labour) is equivocal. 31,34 However, in pregnancy, most medical guidelines recommend antenatal deinfibulation in order to avoid any possible complications during labour, and also because services in Western countries are not always optimally configured to manage a women with type III FGM/C in labour. 27,28 The reviews found that women’s deinfibulation preferences were strongly shaped by cultural norms around maintenance of chastity and virginity, making it difficult for unmarried women to contemplate deinfibulation, even when they may have wanted it. In some cases, they did make this choice, but it was unusual and was associated either with severe symptoms or with a deliberate choice to empower themselves. Once married, some women were supported to seek deinfibulation by their husbands if intercourse was proving difficult. However, this was not a cultural norm, and it was more usual for husbands to deinfibulate over the course of time. Our stakeholder engagement group noted that deinfibulation outside pregnancy was now also increasingly being requested as a way of providing documentation to support asylum claims. Hence, social norms may slowly be changing and community engagement (particularly the involvement of men) around this topic may encourage some women to seek deinfibulation before or just after marriage. 199,274,275 However, this choice depends on women knowing that services are available and how to access them. Our reviews found that service availability and knowledge of these could be patchy at best. Hence, there is a need for more service development in this area. 61 Thus, our review findings endorse the recent commissioning guidance to ensure that care pathways for non-pregnant women are established. 15
Our review findings on this topic are supported by several recent studies and reviews. 61,274 For example, in a specialist London referral clinic for children, four out of 18 girls with confirmed FGM/C (over a 1-year period, 2014–15) had type III FGM/C. All four girls and their parents wanted to wait until planning marriage before considering deinfibulation. 276 Likewise, a study in Norway found that, among 82 female Somalis aged 16–25 years who had had type III FGM/C, 81% were unmarried and only 20.3% had sought health advice. 277
With respect to pregnancy, the two reviews suggest that intrapartum deinfibulation is preferred by most women to avoid being cut twice. However, the findings also show that many women are fearful of how deinfibulation will take place during labour and that being cut or tearing can be a major source of anxiety for them leading up to, and during, the birth. These fears are greatly exacerbated when women encounter or hear about providers who lack confidence or experience in undertaking the procedure. A key finding was that deinfibulation was often not discussed during consultations, and women missed out on opportunities to find out more and to make informed choices. Interestingly, the reviews showed that when women were able to establish good relationships with knowledgeable providers over a period of time, they were able to inform themselves and were more likely to agree to antepartum deinfibulation. 278
Finally, our reviews found that, for some women, deinfibulation could involve significant bodily, emotional and relational changes that required a time of adjustment, and that some women (particularly from Sudan, where it is a cultural norm) desired a degree of reinfibulation. This finding supports WHO recommendations that women could benefit from greater counselling and information about what to expect after the procedure. 61,279,280
A key gap in review 1 was that there were no studies that specifically looked at deinfibulation from the perspective of unmarried or non-pregnant women or girls. Likewise, a key gap in review 2 was a lack of studies that looked specifically at information-giving and communication practices around deinfibulation or at the management of more-complex cases. These are areas that would benefit from future research.
Supporting and routinising culturally safe care with female genital mutilation-/cutting-related guidelines and protocols
Review 2, in particular, has shown that in many cases professionals reported a lack of knowledge of guidelines or protocols, both for identifying FGM/C and for managing FGM/C. These findings are supported by existing evidence. 12,65,281 In relation to identifying FGM/C, both reviews showed that women were often reluctant or embarrassed to discuss FGM/C and preferred providers to raise the issue (as long as it was done in a sensitive manner). However, review 2 showed that providers often missed opportunities to discuss FGM/C, partly owing to lack of knowledge and confidence, but also because it may not have been considered to be a routine part of assessment or history-taking processes. Professionals noted that guidelines would help them to ask the key questions at the right time, and subsequently to be confident about care management, especially deinfibulation and dealing with requests for reinfibulation. Therefore, our reviews have shown that it is imperative for questions about FGM/C to be routinised within certain settings, and for clear guidelines to be developed within different services. 15 Similar approaches have been very successfully utilised to address other health topics that communities and practitioners have traditionally felt uncomfortable with discussing, for example human immunodeficiency virus testing282,283 and domestic violence. 284,285 The review’s PAG suggests that such routinisation may now be happening across the UK within midwifery services (although this needs to be confirmed), but is certainly not the case within other services. Our review suggests that routine questioning and follow-up care pathways should also be implemented within primary care, sexual health, obstetrics/gynaecology and health visiting.
The reviews also aimed to illuminate the question of why guidelines, even when they did exist, may not always be followed. Our reviews were unable to identify a great deal of in-depth information in relation to this question, as we did not find any process evaluations of interventions. However, the evidence was able to offer limited insights of issues that may potentially affect implementation. These include lack of clarity over roles and responsibilities, workload burden of reporting, unclear systems of recording FGM/C and unclear follow-up care pathways.
There is a wide body of evidence exploring barriers to guideline and intervention implementation286–289 that falls broadly within the field of implementation science. 290 For example, the Supporting the Use of Research Evidence (SURE) guidance used by WHO on the implementation of new interventions/protocols/guidelines offers a potentially useful way of categorising barriers and facilitators. 289 It includes several broad analytical domains, within which are subdomains, and associated barriers and facilitators. Some of these map well onto our initial review findings. For example, one of the domains is ‘providers of care’ and includes subdomains of ‘knowledge and skills’, ‘attitudes regarding programme acceptability, appropriateness and credibility’ and ‘motivation to change or adopt new behaviour’. Another domain is ‘health system constraints’, which includes, among others, subdomains of ‘human resources’, ‘clinical supervision’, ‘communication’, ‘patient flow processes’, ‘incentives’ and ‘bureaucracy’. Future research or evaluation on FGM/C-related guideline implementation would benefit from utilising an established framework such as SURE to analyse, understand and address potential barriers further, specifically in a UK context. This is particularly important as the recently introduced policies of mandatory reporting and recording introduce a layer of complexity into an already-sensitive topic area and a layer of bureaucracy into consultation processes that are already stretched for time (especially when there are language barriers to negotiate).
Service configuration to promote access and equity
In terms of configuration of services for FGM/C, the reviews highlighted two issues. The first related to the availability and accessibility of specialist expertise. The second related to the nature of services provided (i.e. the model of care).
The reviews suggested that care experiences were better when care was delivered by specialists. In addition, the reviews highlighted that the availability of this specialist expertise in areas of low prevalence or in rural areas could be challenging. The reviews did not identify any qualitative studies evaluating models of care. However, stakeholders at the national engagement event suggested that a hub and spoke model or mobile clinics might be a way forward in low-prevalence areas.
The review findings also indicate that local commissioning should consider and address particular needs to extend beyond provision of medical care to include counselling/psychotherapy and specialist sexual health services. These findings are supported by the wider evidence. 30,42,291–294 In addition, stakeholders at the national engagement event strongly supported the development of more-holistic models of care. Importantly, as noted previously, this needs to include adequate access to trained and trusted interpretation services. Several such models already exist in England; the majority are based within maternity services but there are also excellent models (e.g. in Oxford and Bristol) based in primary care. 46,57 All include a strong element of community partnership. Further mapping and evaluation of models of care would be beneficial to better understand their differential impact on accessibility, outcomes, cost and patient satisfaction.
Knowledge, training and community engagement for culturally safe care
Both reviews showed that the delivery of culturally safe and effective care requires greater knowledge and training for professionals, and greater awareness among communities regarding care-seeking and engagement with services.
Professionals
The reviews confirm findings from other studies that show an unmet training need for knowledge and skill development in all aspects of FGM/C-related care and in the development of cultural comptence. 12,65,66,281,295–299 This applies to all cadres of health professional. 300–305 In a UK context, there are a range of excellent training resources now available, mostly online; hence, it is important that different NHS services ensure that these are adequately disseminated and utilised. Likewise, UK national standards have recently been developed to guide curriculum development. 41 In addition, WHO has just released a clinical management handbook that provides excellent comprehensive guidance for practitioners. 279 It is unclear to what extent knowledge may have improved as a result of these recent initiatives or to what extent FGM/C is now embedded within pre- or post-registration training curricula in the UK. This is an area in need of future research. Although now somewhat out of date, a UK survey of 1756 midwives conducted in 2012 by the Royal College of Midwives306 suggests that some improvement may still needed. The results showed that the majority of the sample did not know where they should refer a woman with FGM/C and only 15.3% had attended a training session. 306 Likewise, a 2015 survey307 among a mixed sample of 157 doctors and midwives at a district hospital in London with a high prevalence of FGM/C found that 71.4% felt that they would benefit from further training on the subject, and only 21% of respondents stated that they would feel comfortable discussing FGM/C with patients. The majority of health-care professionals (65.3%) had not read any guidelines relating to FGM/C. 307 Another 2015 survey308 conducted among 75 midwives and nurses at a district general hospital in the North East of England found low levels of knowledge and confidence regarding clinical management but higher levels around legal and safeguarding issues (only 16.7% felt confident caring for patients with FGM/C and just 5.6% felt sufficiently trained, but 80.6% were aware that FGM/C was illegal in the UK and 77.8% knew about appropriate safeguarding measures). 308
The review findings suggest that additional training seems to be particularly required in relation to communication around FGM/C, awareness of women’s psychological needs and management of clinical interventions (particularly deinfibulation, where it was clear that competency was highly variable).
Review 2, in particular, showed that professionals can find FGM/C a difficult issue to understand and that some of their clinical experiences can be stressful, especially when they feel that they lack clinical competence and when cross-cultural misunderstandings arise. Similar findings have been reported in other contexts. 298 Hence, staff may also benefit from opportunities to discuss FGM/C-related issues face to face in a supportive environment with experts, including FGM/C survivors. Furthermore, as with any skill, it is important for professionals who may be called on to undertake deinfibulation to have adequate training that extends beyond watching an e-learning video (the current minimum requirement for UK obstetric registrars). This was a point strongly made by a group of 30 obstetric registrars who attended a presentation on the review.
Recent systematic reviews have highlighted that the evidence on the most effective approaches to training around FGM/C is unclear, and that this area would benefit from further research. 301,309 One study by Jacoby and Smith,300 however, showed a clear increase in knowledge, confidence and cultural competence among midwives in the USA following a training programme that included didactic teaching, case studies, a cultural roundtable discussion and a hands-on skills session on deinfibulation and repair.
Women and communities
Review 1 showed that awareness of services and knowledge about possible interventions related to FGM/C (e.g. deinfibulation, counselling, reinfibulation issues) were limited among women, especially in low-prevalence areas. The reviews pointed to a need for more information resources to be available for women on all aspects of care around FGM/C. 60,310,311 There is, as yet, no clear evidence on the most-effective approaches to health education.
Both reviews highlighted the important role that families and husbands had on women’s care-seeking and health decision-making. These findings support existing evidence49,312,313 and NHS commissioning guidance15 on the need for greater information- and awareness-raising approaches within communities, and for these to include husbands and families. 314,315 Both reviews had findings in which women and professionals called for a need for working in partnership with communities – an approach that is strongly endorsed by programmes in the UK316,317 and by findings from a recent research study that interviewed policy-makers and activists across Europe. 318
Implications and recommendations
The implications of the reviews are presented in the following sections. These are integrated implications (i.e. representing implications from both reviews taken together). As with the discussion, the decision was taken to integrate the implications in order to avoid repetition as many of the implications from the reviews address the same underlying issues (e.g. training of health workers or strategies to address language barriers).
UK stakeholder input and UK relevance of implications and recommendations
Although the review evidence reflects a variety of OECD country contexts, the implications/recommendations in this report have been formulated specifically with a UK NHS context in mind.
The implications and recommendations have been shaped by an extensive process of consultation with the whole project team and PAG (see Chapter 2). They have been further refined at a national stakeholder consultation event with 65 participants from a wide range of organisations and professional groups (see Appendices 14–16). In addition, the findings have been discussed at a meeting with 30 obstetric/gynaecology registrars (see the report in Appendix 17). Participants at these events strongly endorsed the findings from both reviews as being largely consistent with their own experiences (see Appendix 14). However, there are certain issues that need more nuanced UK-specific exploration. For example, given the relatively small number of UK-based studies in review 2, the applicability of its findings to UK health professionals remains somewhat unclear. In addition, in the light of recent UK training initiatives, it is unclear whether or not there would be key differences between professional groups.
Implications for practice, service configuration and training
Table 10 presents the implications for practice, service configuration and training.
| Domain | Implications |
|---|---|
| Service delivery and professional practice | |
| Communication |
|
| Respectful, person-centred and culturally appropriate care |
|
| Service development and configuration | |
| Care pathways, protocols and guidelines |
|
| Service gaps |
|
| Training health professionals | |
|
|
| Awareness raising and community engagement | |
Strategies to enhance community engagement may be important for:
|
|
Recommendations for research
The recommendations for research are presented in Box 5. For clarity, recommendations have been grouped into specific topic areas. The whole list has also been numbered to reflect research priorities. Priority areas were discussed during the national stakeholder event and finalised through further discussion among the review team.
1. The review did not include studies that were conducted following the mandatory reporting and mandatory recording policy changes in the UK. However, it is important to evaluate how this new policy context may now be influencing care-seeking and care quality from women’s and providers’ perspectives. In particular, given the review findings that communication around FGM/C is already challenging and yet critical for ‘good’ care, it is particularly important to explore how the new policy context might be affecting communication around FGM/C and provider–patient/community relations in general.
2. There is a need to understand how providers are (or are not) currently engaging in prevention/safeguarding discussions with women/communities, what the barriers and facilitators are for this and which strategies are most appropriate/effective.
Understanding and developing best practice in service delivery models3. In areas where clear guidelines/pathways/protocols already exist, it is important to better understand why professionals may not always be adhering to these or may not know about them, for example by undertaking studies informed by implementation science theories.
4. There is a need to map and to determine effectiveness and patient satisfaction of different models of service delivery for pregnant and non-pregnant women (including girls) in different settings.
Understanding women’s/girls’ needs better5. There is a need to understand women’s information needs better in relation to FGM/C at different life points and for different types of FGM/C. In particular, (1) what women’s information and support needs are in pregnancy, in preparation for birth and during birth, and (2) what women’s information and support needs are in relation to deinfibulation specifically (at different life stages).
6. There is a need to explore what mode of information delivery is most appropriate for different groups of women (e.g. leaflets, face to face, apps).
7. There is a need to understand what women’s mental-health-related needs may be at different time points, to evaluate women’s experiences with mental health services and to evaluate different options for mental-health-care provision, including models of community-based support.
8. There is a need to explore and better understand the potential needs, experiences and care-seeking of non-pregnant or unmarried women/girls.
11. There is a need to develop and evaluate tools to accurately identify women who may need psychological support and to evaluate the most appropriate strategies for dealing with anxiety and trauma during and after birth/clinical procedures.
Community engagement9. There is a need for more research to understand what models of community engagement already exist, what the barriers and facilitators are and how communities and services can best work together around FGM/C health care.
10. There is a need to evaluate the role and cost benefit of using community health advocates/liaison workers to support FGM/C services.
Training12. In the UK context, it would be useful to undertake knowledge/attitude/practice studies with different professional groups to determine current levels of knowledge and practices around FGM/C in order to identify and address topic-specific and cadre-specific knowledge gaps.
13. There is a need to evaluate the most appropriate models of provider training around the different components of FGM/C-related care.
Research methodology14. Future research should adopt a more nuanced anthropological approach in order to explore care issues in terms of difference as well as similarities associated with ethnicity, migration experience, age, FGM/C type or FGM/C experience.
Chapter 7 Conclusions
The reviews presented in this report have focused exclusively on OECD countries, producing findings that are relevant to the UK context. To our knowledge, they are the first to have considered all aspects of FGM/C-related health care at all stages of the life course, in all clinical settings, and to bring together the perspectives of women and health professionals. In addition, in contrast to other systematic reviews in this field, they have, for the first time, included relevant grey literature and papers in languages other than English. As a result, the reviews in this project have been able to present an exceptionally comprehensive and detailed picture of current care experiences. Furthermore, by moving beyond the usual focus on maternity care contexts,63,64 the reviews have been able to advance current knowledge beyond an understanding of experiences (although this is important) to provide a more analytical and holistic interpretation of factors influencing care-seeking, decision-making for deinfibulation surgery, service access and the development of care pathways.
In the last 5 years, the UK has made enormous strides in developing policy, training and commissioning guidance around FGM/C. However, the reviews (which include papers and reports from 22 UK-based studies) suggest that the seeking and providing of FGM/C-related health care is often characterised by processes of silence, secrecy, stigma, shame and stereotyping. Hence, although positive experiences are reported (and greatly appreciated), there still appear to be many challenges. Particularly concerning are the reports of disrespectful care, ad hoc service provision and health professionals who lack clinical and cultural competence.
Many of the challenges relate to FGM/C specifically (e.g. management of deinfibulation or specific mental health needs), but many (e.g. language barriers) also relate to wider challenges in care delivery for migrant populations in a context of super-diversity. Therefore, it is important to consider the findings from these reviews within the wider context of service configuration and resourcing for super-diverse population groups (e.g. provision of accessible and appropriate interpretation services, choice of female health providers, continuity of care models, personalised care models or training of health professionals for culturally safe practice).
Dissemination of the reviews
Activities undertaken to date include:
-
publication of the review protocol117
-
a national stakeholder event
-
presentation to obstetrics and gynaecology registrars across the East Midlands region
-
two oral presentations at an international conference in Montreal, Canada, on 28/29 May 2018 [2nd International Expert Meeting on Female Genital Mutilation/Cutting: Sharing Data and Experiences, Improving Collaboration; www.fourwav.es/view/644/info/ (accessed 12 July 2019)]
-
two publications (one from each review) in international peer-reviewed journals. 139,145
Knowledge translation and impact
-
The review findings have been shared with the Nottingham and Nottinghamshire joint FGM/C steering group. A health task force has now been established, with a first meeting in July 2018 to consider how to implement the review findings.
-
Two members of the review team (CE and JA) have been invited onto the project oversight committee of a recently funded NIHR HTA research project being conducted by a team at the University of Birmingham [HTA 16/78/04; Female Genital Mutilation: a qualitative study exploring survivors’ and health-care professionals’ views on the timing of deinfibulation surgery (FGM/C Sister Study)].
-
The project has led to research capacity development within the team. Valentine Nkoyo has started a PhD at the University of Nottingham focusing on FGM/C prevention as part of its pioneering ‘Rights Lab’. Juliet Albert has received funding from the Health Education England/NIHR Integrated Clinical Academic Pre-doctoral Clinical Academic Fellowship to develop a PhD application on FGM/C.
Acknowledgements
We would like to thank all those who have contributed time and valuable insights to this project. We would particularly like to thank all those who gave up their day to attend the national stakeholder consultation event. Special thanks go to Carol McCormick (FGM/C Specialist Midwife) for her support and input at the start of this project.
Acknowledgement of the Project Advisory Group
We gratefully acknowledge the invaluable contributions of our PAG:
-
Ms Kinsi Clarke, Nottingham and Nottinghamshire Refugee Forum, Co-founder of Nottingham FGM/C survivor’s group
-
Professor Jim Thornton, Consultant Obstetrician, Nottingham University Hospital Trust and University of Nottingham
-
Dr Phoebe Abe, GP, London
-
Ms Amanda Wickham (FGM/C Specialist Midwife), Nottingham University Hospital Trust
-
Ms Helen Denness, Consultant in Public Health, Nottingham City Council
-
Ms Grace Brough, Insight Specialist (public health), Nottingham City Council, Chair of Nottingham and Nottinghamshire FGM/C Steering Group.
Contributions of authors
Dr Catrin Evans (Associate Professor, Health Sciences) was principal investigator, initiated the project and oversaw all stages, led the interpretation/synthesis phases and drafted all chapters of the report.
Dr Ritah Tweheyo (Research Fellow) contributed to all stages of the review and led the data extraction, coding, quality appraisal and CERQual components.
Dr Julie McGarry (Associate Professor, Nursing) acted as a second reviewer for quality appraisal, contributed to the evolving synthesis and assisted with drafting the report tables.
Ms Jeanette Eldridge (Information Specialist) designed the literature search strategy, advised the team on all aspects of information retrieval and undertook the main database searches.
Ms Juliet Albert (FGM/C Specialist Midwife) provided clinical expertise and expertise relating to professional training and the UK policy context, contributed to the evolving interpretation/synthesis and contributed to formulation of the implications and recommendations.
Ms Valentine Nkoyo (Director of Mojatu Foundation, FGM/C, women’s rights activist and Co-founder of Nottingham FGM/C survivor’s group) was involved in the project from its inception, contributed key insights from a community perspective, contributed to the evolving interpretation/synthesis, helped organise the national stakeholder event and contributed to formulation of the implications and recommendations.
Professor Gina Higginbottom (Professor, Ethnicity and Community Health) acted as a second reviewer for quality appraisal, contributed to the evolving synthesis and provided methodological expertise.
Publications
Evans C, Tweheyo R, McGarry J, Eldridge J, McCormick C, Nkoyo V, Higginbottom G. What are the experiences of seeking, receiving and providing FGM-related healthcare? Perspectives of health professionals and women/girls who have undergone FGM: protocol for a systematic review of qualitative evidence. BMJ Open 2017;7:e018170.
Evans C, Tweheyo R, McGarry J, Eldridge J, Albert J, Nkoyo V, Higginbottom G. Crossing cultural divides: a qualitative systematic review of factors influencing the provision of healthcare related to female genital mutilation from the perspective of health professionals. PLOS ONE 2019;14:e0211829. https://doi.org/10.1371/journal.pone.0211829
Evans C, Tweheyo R, McGarry J, Eldridge J, Albert J, Nkoyo V, Higginbottom G. Seeking culturally safe care: a qualitative systematic review of the healthcare experiences of women and girls who have undergone female genital mutilation/cutting. BMJ Open 2019;9:e027452.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- WHO . Female Genital Mutilation: Fact Sheet 2014.
- United Nations Children’s Fund (UNICEF) . Female Genital Mutilation Cutting: A Global Concern 2016.
- Green G, Davison C, Bradby H, Krause K, Mejías FM, Alex G. Pathways to care: how superdiversity shapes the need for navigational assistance. Sociol Health Illn 2014;36:1205-19. https://doi.org/10.1111/1467-9566.12161.
- Newall D, Phillimore J, Sharpe H. Migration and maternity in the age of superdiversity. Pract Midwife 2012;15:20-2.
- Phillimore J. Migrant maternity in an era of superdiversity: new migrants’ access to, and experience of, antenatal care in the West Midlands, UK. Soc Sci Med 2016;148:152-9. https://doi.org/10.1016/j.socscimed.2015.11.030.
- Vertovec S. Super-diversity and its implications. Ethn Rac Stud 2007;30:1024-54. https://doi.org/10.1080/01419870701599465.
- Phillimore J. Approaches to health provision in the age of super-diversity: accessing the NHS in Britain’s most diverse city. Crit Soc Policy 2011;31:5-29. https://doi.org/10.1177/0261018310385437.
- Trust for London . Taking Local Action on FGM: An Essential Guide for Local Authorities 2015.
- Macfarlane A, Dorkenoo E. Prevalence of Female Genital Mutilation in England and Wales: National and Local Estimates. London: City University; 2015.
- Department of Health and Social Care . Commissioning Services to Support Women and Girls With Female Genital Mutilation 2015.
- Brown E. The FGM Initiative: Summary of PEER Research Findings: Endline Phase 1. London: Options Consultancy Services; 2013.
- Dawson A, Turkmani S, Fray S, Nanayakkara S, Varol N, Homer C. Evidence to inform education, training and supportive work environments for midwives involved in the care of women with female genital mutilation: a review of global experience. Midwifery 2015;31:229-38. https://doi.org/10.1016/j.midw.2014.08.012.
- Creighton S, Hodes D. Chapter 3: Female Genital Mutilation. London: Department of Health and Social Care; 2015.
- UNITE . Intercollegiate Guidelines Tackling FGM in the UK: Intercollegiate Recommendations for Identifying, Recording and Reporting 2013.
- Commissioning Services to Meet the Needs of Women and Girls With FGM 2018.
- Van Baelen L, Ortensi L, Leye E. Estimates of first-generation women and girls with female genital mutilation in the European Union, Norway and Switzerland. Eur J Contracept Reprod Health Care 2016;21:474-82. https://doi.org/10.1080/13625187.2016.1234597.
- NHS Digital . Female Genital Mutilation (FGM): Annual Report 2016 7 [PAS] 2017.
- NHS Digital . Female Genital Mutilation (FGM): Annual Report 2017 18 2018. https://doi.org/10.7748/phc.28.1.18.s19.
- WHO . A Systematic Review of the Health Complications of Female Genital Mutilation Including Sequelae in Childbirth 2013.
- Mulongo P, McAndrew S, Hollins Martin C. Crossing borders: discussing the evidence relating to the mental health needs of women exposed to female genital mutilation. Int J Ment Health Nurs 2014;23:296-305. https://doi.org/10.1111/inm.12060.
- Mulongo P, Martin CH, McAndrew S. The psychological impact of female genital mutilation/cutting (FGM/C) on girls/women’s mental health: a narrative literature review. J Reprod Infant Psychol 2014;32:469-85. https://doi.org/10.1080/02646838.2014.949641.
- Berg RC, Denison EAF. Psychological, Social and Sexual Consequences of Female Genital Mutilation/Cutting (FGM/C): A Systematic Review of Quantitative Studies. Oslo: Centre for Reviews and Dissemination, Norwegian Knowledge Centre for the Health Services; 2010.
- Berg RC, Denison E. Does female genital mutilation/cutting (FGM/C) affect women’s sexual functioning? A systematic review of the sexual consequences of FGM/C. Sex Res &Amp; Soc Pol 2012;9:41-56. https://doi.org/10.1007/s13178-011-0048-z.
- Berg RC, Underland V. The obstetric consequences of female genital mutilation/cutting: a systematic review and meta-analysis. Obstet Gynecol Int 2013;2013. https://doi.org/10.1155/2013/496564.
- Berg RC, Underland V, Odgaard-Jensen J, Fretheim A, Vist GE. Effects of female genital cutting on physical health outcomes: a systematic review and meta-analysis. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006316.
- HM Government . Multi-Agency Practice Guidelines: Female Genital Mutilation 2014.
- Royal College of Obstetricians and Gynaecologists . Green-Top Guideline No. 53: Female Genital Mutilation and Its Management 2015.
- WHO . WHO Guidelines on the Management of Health Complications from Female Genital Mutilation 2016.
- Royal College of Nursing . Female Genital Mutilation: An RCN Resource for Nursing and Midwifery Practice (2nd Ed) 2015.
- Abdulcadir J, Rodriguez MI, Say L. Research gaps in the care of women with female genital mutilation: an analysis. BJOG 2015;122:294-303. https://doi.org/10.1111/1471-0528.13217.
- Esu E, Udo A, Okusanya BO, Agamse D, Meremikwu MM. Antepartum or intrapartum deinfibulation for childbirth in women with type III female genital mutilation: a systematic review and meta-analysis. Int J Gynaecol Obstet 2017;136:21-9. https://doi.org/10.1002/ijgo.12055.
- Albert J, Bailey E, Duaso M. Does the timing of deinfibulation for women with type 3 female genital mutilation affect labour outcomes?. Br J Midwifery 2015;23:430-7. https://doi.org/10.12968/bjom.2015.23.6.430.
- Paliwal P, Ali S, Bradshaw S, Hughes A, Jolly K. Management of type III female genital mutilation in Birmingham, UK: a retrospective audit. Midwifery 2014;30:282-8. https://doi.org/10.1016/j.midw.2013.04.008.
- Okusanya BO, Oduwole O, Nwachuku N, Meremikwu MM. Deinfibulation for preventing or treating complications in women living with type III female genital mutilation: a systematic review and meta-analysis. Int J Gynaecol Obstet 2017;136:13-20. https://doi.org/10.1002/ijgo.12056.
- Gayle C, Rymer J. Female genital mutilation and pregnancy: associated risks. Br J Nurs 2016;25:978-83. https://doi.org/10.12968/bjon.2016.25.17.978.
- Bishai D, Bonnenfant YT, Darwish M, Adam T, Bathija H, Johansen E, et al. Estimating the obstetric costs of female genital mutilation in six African countries. Bull World Health Organ 2010;88:281-8. https://doi.org/10.2471/BLT.09.064808.
- Great Britain . UK Female Genital Mutilation Act [2003] 2003. www.legislation.gov.uk/ukpga/2003/31/contents (accessed 28 January 2019).
- Great Britain . Prohibition of Female Genital Mutilation (Scotland) Act 2005 2005. www.legislation.gov.uk/asp/2005/8/contents (accessed 25 June 2019).
- GOV.UK . New Government Measures to End FGM n.d. www.gov.uk/government/news/new-government-measures-to-end-fgm (accessed 25 June 2019).
- Great Britain . Serious Crime Act 2015 2015. www.legislation.gov.uk/ukpga/2015/9/part/5/enacted (accessed 25 June 2019).
- NHS England . Female Genital Mutilation: Standards for Training Professionals 2018.
- Baillot H, Murray N, Connelly E, Howard N. Addressing female genital mutilation in Europe: a scoping review of approaches to participation, prevention, protection, and provision of services. Int J Equity Health 2018;17. https://doi.org/10.1186/s12939-017-0713-9.
- Johansen REB, Ziyada MM, Shell-Duncan B, Kaplan AM, Leye E. Health sector involvement in the management of female genital mutilation/cutting in 30 countries. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3033-x.
- McCormick C, Marshall J, Raynor M. Myles Textbook for Midwives. London: Elsevier Health Sciences; 2014.
- NHS England . NHS Specialist Services for Female Genital Mutilation n.d. www.nhs.uk/NHSEngland/AboutNHSservices/sexual-health-services/Documents/List%20of%20FGM%20Clinics%20Mar%2014%20FINAL.pdf (accessed 28 April 2018).
- Clayton-Hathway K. A Pilot Evaluation of Health Services for Communities Affected by FGM in Oxfordshire: Final Report 2016.
- Norman K, Gegzabher SB, Otoo-Oyortey N. ‘Between Two Cultures’: A Rapid PEER Study Exploring Migrant Communities’ Views on Female Genital Mutilation in Essex and Norfolk, UK. London: FORWARD & National FGM Centre Report; 2016.
- Berg RC, Denison E. A tradition in transition: factors perpetuating and hindering the continuance of female genital mutilation/cutting (FGM/C) summarized in a systematic review. Health Care Women Int 2013;34:837-59. https://doi.org/10.1080/07399332.2012.721417.
- Varol N, Turkmani S, Black K, Hall J, Dawson A. The role of men in abandonment of female genital mutilation: a systematic review. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2373-2.
- Norwegian Knowledge Centre for the Health Services . Effectiveness of Interventions Designed to Reduce the Prevalence of Female Genital Mutilation-Cutting 2009.
- Berg RC, Denison EM. A realist synthesis of controlled studies to determine the effectiveness of interventions to prevent genital cutting of girls. Paediatr Int Child Health 2013;33:322-33. https://doi.org/10.1179/2046905513Y.0000000086.
- Norwegian Knowledge Centre for the Health Services . Psychological, Social and Sexual Consequences of Female Genital Mutilation Cutting: A Systematic Review of Quantitative Studies 2010.
- Berg RC, Taraldsen S, Said MA, Sørbye IK, Vangen S. Reasons for and experiences with surgical interventions for female genital mutilation/cutting (FGM/C): a systematic review. J Sex Med 2017;14:977-90. https://doi.org/10.1016/j.jsxm.2017.05.016.
- Sunday-Adeoye I, Serour G. Management of health outcomes of female genital mutilation: systematic reviews and evidence syntheses. Int J Gynaecol Obstet 2017;136:1-2. https://doi.org/10.1002/ijgo.12041.
- Stein K, Hindin MJ, Chou D, Say L. Prioritizing and synthesizing evidence to improve the health care of girls and women living with female genital mutilation: an overview of the process. Int J Gynaecol Obstet 2017;136:3-12. https://doi.org/10.1002/ijgo.12050.
- Bulman KH, McCourt C. Somali refugee women’s experiences of maternity care in west London: a case study. Crit Public Health 2002;12:365-80. https://doi.org/10.1080/0958159021000029568.
- Hussein E. Women’s Experiences, Perceptions and Attitudes of Female Genital Mutilation: The Bristol PEER Study. London: FORWARD; 2010.
- Norman K, Hemmings J, Hussein E, Otoo-Oyortey N. ‘FGM is Always With Us’: Experiences, Perceptions and Beliefs of Women Affected by Female Genital Mutilation in London: Results from a PEER Study. London: Options Consultancy Services and FORWARD; 2009.
- Straus L, McEwen A, Hussein FM. Somali women’s experience of childbirth in the UK: perspectives from Somali health workers. Midwifery 2009;25:181-6. https://doi.org/10.1016/j.midw.2007.02.002.
- Smith H, Stein K. Health information interventions for female genital mutilation. Int J Gynaecol Obstet 2017;136:79-82. https://doi.org/10.1002/ijgo.12052.
- Smith H, Stein K. Surgical or medical interventions for female genital mutilation. Int J Gynaecol Obstet 2017;136:43-6. https://doi.org/10.1002/ijgo.12053.
- Smith H, Stein K. Psychological and counselling interventions for female genital mutilation. Int J Gynaecol Obstet 2017;136:60-4. https://doi.org/10.1002/ijgo.12051.
- Hamid A, Grace KT, Warren N. A meta-synthesis of the birth experiences of African immigrant women affected by female genital cutting. J Midwifery Womens Health 2018;63:185-95. https://doi.org/10.1111/jmwh.12708.
- Turkmani S, Homer CSE, Dawson A. Maternity care experiences and health needs of migrant women from female genital mutilation-practicing countries in high-income contexts: a systematic review and meta-synthesis [published online ahead of print June 28 2018]. Birth 2018. https://doi.org/10.1111/birt.12367.
- Dawson A, Homer CS, Turkmani S, Black K, Varol N. A systematic review of doctors’ experiences and needs to support the care of women with female genital mutilation. Int J Gynaecol Obstet 2015;131:35-40. https://doi.org/10.1016/j.ijgo.2015.04.033.
- Reig-Alcaraz M, Siles-Gonzalez J, Solano-Ruiz C. A mixed-method synthesis of knowledge, experiences and attitudes of health professionals to female genital mutilation. J Adv Nurs 2015;72:245-60. https://doi.org/10.1111/jan.12823.
- Zenner N, Liao LM, Richens Y, Creighton SM. Quality of obstetric and midwifery care for pregnant women who have undergone female genital mutilation. J Obstet Gynaecol 2013;33:459-62. https://doi.org/10.3109/01443615.2013.767785.
- Abdulcadir J, Dugerdil A, Boulvain M, Yaron M, Margairaz C, Irion O, et al. Missed opportunities for diagnosis of female genital mutilation. Int J Gynaecol Obstet 2014;125:256-60. https://doi.org/10.1016/j.ijgo.2013.11.016.
- Ford CM, Darlow K, Massie A, Gorman DR. Using electronic maternity records to estimate female genital mutilation in Lothian from 2010 to 2013. Eur J Public Health 2018;28:657-61. https://doi.org/10.1093/eurpub/cky045.
- Cappon S, L’Ecluse C, Clays E, Tency I, Leye E. Female genital mutilation: knowledge, attitude and practices of Flemish midwives. Midwifery 2015;31:e29-35. https://doi.org/10.1016/j.midw.2014.11.012.
- Isman E, Mahmoud Warsame A, Johansson A, Fried S, Berggren V. Midwives’ experiences in providing care and counselling to women with female genital mutilation (FGM) related problems. Obstet Gynecol Int 2013;2013. https://doi.org/10.1155/2013/785148.
- Kaplan-Marcusán A, Del Rio NF, Moreno-Navarro J, Castany-Fàbregas MJ, Nogueras MR, Muñoz-Ortiz L, et al. Female genital mutilation: perceptions of healthcare professionals and the perspective of the migrant families. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-193.
- Kaplan-Marcusan A, Torán-Monserrat P, Moreno-Navarro J, Castany Fàbregas MJ, Muñoz-Ortiz L. Perception of primary health professionals about female genital mutilation: from healthcare to intercultural competence. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-11.
- León-Larios F, Casado-Mejía R. Knowledge, attitudes and professional experiences of midwives in primary health care in Seville on female genital mutilation. Matronas Profesion 2014;15:56-61.
- Tamaddon L, Johnsdotter S, Liljestrand J, Essén B. Swedish health care providers’ experience and knowledge of female genital cutting. Health Care Women Int 2006;27:709-22. https://doi.org/10.1080/07399330600817741.
- Dawson AJ, Turkmani S, Varol N, Nanayakkara S, Sullivan E, Homer CS. Midwives’ experiences of caring for women with female genital mutilation: insights and ways forward for practice in Australia. Women Birth 2015;28:207-14. https://doi.org/10.1016/j.wombi.2015.01.007.
- Degni F, Suominen S, Essén B, El Ansari W, Vehviläinen-Julkunen K. Communication and cultural issues in providing reproductive health care to immigrant women: health care providers’ experiences in meeting the needs of [corrected] Somali women living in Finland. J Immigr Minor Health 2012;14:330-43. https://doi.org/10.1007/s10903-011-9465-6.
- Fawcett L. Somali Refugee Women and Their U.S. Healthcare Providers: Knowledge, Perceptions and Experiences of Childbearing 2014. https://pdfs.semanticscholar.org/8676/82b17de150aee7281a365e984214acaa855d.pdf (accessed 12 July 2019).
- Widmark C, Levál A, Tishelman C, Ahlberg BM. Obstetric care at the intersection of science and culture: Swedish doctors’ perspectives on obstetric care of women who have undergone female genital cutting. J Obstet Gynaecol 2010;30:553-8. https://doi.org/10.3109/01443615.2010.484110.
- Widmark C, Tishelman C, Ahlberg BM. A study of Swedish midwives’ encounters with infibulated African women in Sweden. Midwifery 2002;18:113-25. https://doi.org/10.1054/midw.2002.0307.
- Hannes K, Harden A. Multi-context versus context-specific qualitative evidence syntheses: combining the best of both. Res Synth Methods 2011;2:271-8. https://doi.org/10.1002/jrsm.55.
- Weir MC, Grimshaw JM, Mayhew A, Fergusson D. Decisions about lumping vs. splitting of the scope of systematic reviews of complex interventions are not well justified: a case study in systematic reviews of health care professional reminders. J Clin Epidemiol 2012;65:756-63. https://doi.org/10.1016/j.jclinepi.2011.12.012.
- Noyes J, Hannes K, Booth A, Harris J, Harden A, Popay J, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 5/3 (updated October 2015). The Cochrane Collaboration; 2015.
- Joanna Briggs Institute . JBI Reviewer’s Manual n.d. https://wiki.joannabriggs.org/display/MANUAL/JBI+Reviewer%27s+Manual (accessed 12 August 2019).
- Zeeb H, Makarova N, Brand T, Knecht M. Super-diversity: a new concept for migrant health?. Public Health Forum 2015;23:124-5. https://doi.org/10.1515/pubhef-2015-0045.
- Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet 2013;381:1235-45. https://doi.org/10.1016/S0140-6736(12)62086-8.
- O’Donnell CA, Higgins M, Chauhan R, Mullen K. Asylum seekers’ expectations of and trust in general practice: a qualitative study. Br J Gen Pract 2008;58:e1-1. https://doi.org/10.3399/bjgp08X376104.
- Ochieng B. Black African migrants: the barriers with accessing and utilising health promotion services in the UK. Eur J Public Health 2013;23:265-9. https://doi.org/10.1093/eurpub/cks063.
- Agudelo-Suárez AA, Gil-González D, Vives-Cases C, Love JG, Wimpenny P, Ronda-Pérez E. A metasynthesis of qualitative studies regarding opinions and perceptions about barriers and determinants of health services’ accessibility in economic migrants. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-461.
- Suphanchaimat R, Kantamaturapoj K, Putthasri W, Prakongsai P. Challenges in the provision of healthcare services for migrants: a systematic review through providers’ lens. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1065-z.
- Robertshaw L, Dhesi S, Jones LL. Challenges and facilitators for health professionals providing primary healthcare for refugees and asylum seekers in high-income countries: a systematic review and thematic synthesis of qualitative research. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-015981.
- Department of Health and Social Care . Midwifery 2020: Delivering Expectations 2010.
- Balaam M-C, Akerjordet K, Lyberg A, Kaiser B, Schoening E, Fredriksen A-M, et al. A qualitative review of migrant women’s perceptions of their needs and experiences related to pregnancy and childbirth. J Adv Nurs 2013;69:1919-30. https://doi.org/10.1111/jan.12139.
- Benza S, Liamputtong P. Pregnancy, childbirth and motherhood: a meta-synthesis of the lived experiences of immigrant women. Midwifery 2014;30:575-84. https://doi.org/10.1016/j.midw.2014.03.005.
- Wikberg A, Bondas T. A patient perspective in research on intercultural caring in maternity care: a meta-ethnography. Int J Qual Stud Health Well-Being 2010;5. https://doi.org/10.3402/qhw.v5i1.4648.
- National Institute for Health and Care Excellence (NICE) . Pregnancy and Complex Social Factors: A Model for Service Provision for Pregnant Women With Complex Social Factors 2010.
- Gagnon AJ, Zimbeck M, Zeitlin J, Alexander S, Blondel B, Buitendijk S, et al. Migration to western industrialised countries and perinatal health: a systematic review. Soc Sci Med 2009;69:934-46. https://doi.org/10.1016/j.socscimed.2009.06.027.
- NHS England . National Maternity Review. Better Births: Improving Outcomes of Maternity Services in England 2016.
- Phillimore J, Klaas F, Padilla B, Hernandez-Plaza S, Rodrigues V. Adaptation of Health Services to Diversity: An Overview of Approaches, Working Paper No. 15. Birmingham: Institute for Research into Superdiversity, University of Birmingham; 2016.
- Popay J, Williams G. Qualitative research and evidence-based healthcare. J R Soc Med 1998;91:32-7. https://doi.org/10.1177/014107689809135S08.
- Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995;311:42-5. https://doi.org/10.1136/bmj.311.6996.42.
- Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev 2013;10. https://doi.org/10.1002/14651858.CD010414.pub2.
- Hannes K, Booth A, Harris J, Noyes J. Celebrating methodological challenges and changes: reflecting on the emergence and importance of the role of qualitative evidence in Cochrane reviews. Syst Rev 2013;2. https://doi.org/10.1186/2046-4053-2-84.
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12. https://doi.org/10.1186/1471-2288-12-181.
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009;9. https://doi.org/10.1186/1471-2288-9-59.
- Paterson B, Hannes H, Lockwood C. Synthesizing Qualitative Research: Choosing the Right Approach. Oxford: Wiley Blackwell BMJ Books; 2012.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Boyatzis R. Transforming Qualitative Data: Thematic Analysis and Code Development. London: Sage Publications Ltd; 1998.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, et al. Cochrane Qualitative and Implementation Methods Group guidance series-paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol 2018;97:49-58. https://doi.org/10.1016/j.jclinepi.2017.06.020.
- Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, et al. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions, Version 1. Cochrane Collaboration Qualitative Methods Group; 2011.
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0688-3.
- Noyes J, Booth A, Cargo M, Flemming K, Garside R, Hannes K, et al. Cochrane Qualitative and Implementation Methods Group guidance series-paper 1: introduction. J Clin Epidemiol 2018;97:35-8. https://doi.org/10.1016/j.jclinepi.2017.09.025.
- Harris JL, Booth A, Cargo M, Hannes K, Harden A, Flemming K, et al. Cochrane Qualitative and Implementation Methods Group guidance series-paper 2: methods for question formulation, searching, and protocol development for qualitative evidence synthesis. J Clin Epidemiol 2018;97:39-48. https://doi.org/10.1016/j.jclinepi.2017.10.023.
- Evans C, Higginbottom G, McGarry J, McCormick C, Eldridge J, Nkoyo V, et al. The experiences of healthcare across the life course for women and girls who have undergone female genital mutilation: a qualitative systematic review. PROSPERO n.d. www.crd.york.ac.uk/prospero/display_record.php?RecordID=30001 (accessed 12 August 2019).
- Evans C, Higginbottom G, McGarry J, McCormick C, Eldridge J, Nkoyo V, et al. Exploring health professionals’ views on, and experiences of, providing care for women and girls who have undergone female genital mutilation (FGM): a qualitative systematic review. PROSPERO n.d. www.crd.york.ac.uk/prospero/display_record.php?RecordID=30004 (accessed 12 August 2019).
- Evans C, Tweheyo R, McGarry J, Eldridge J, McCormick C, Nkoyo V, et al. What are the experiences of seeking, receiving and providing FGM-related healthcare? Perspectives of health professionals and women/girls who have undergone FGM: protocol for a systematic review of qualitative evidence. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-018170.
- Organisation for Economic Co-operation and Development (OECD) . About n.d. www.oecd.org/about/ (accessed 2 January 2018).
- World Bank . World Bank Country and Lending Groups n.d. http://data.worldbank.org/about/country-and-lending-groups#High_income (accessed 2 January 2018).
- National Information Center on Health Services Research and Healthcare Technology (NICHSR) . Health Services Research and Health Policy Grey Literature Project: Summary Report 2006.
- Adams J, Hillier-Brown FC, Moore HJ, Lake AA, Araujo-Soares V, White M, et al. Searching and synthesising ‘grey literature’ and ‘grey information’ in public health: critical reflections on three case studies. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0337-y.
- Mahood Q, Van Eerd D, Irvin E. Searching for grey literature for systematic reviews: challenges and benefits. Res Synth Methods 2014;5:221-34. https://doi.org/10.1002/jrsm.1106.
- Adams RJ, Smart P, Huff AS. Shades of grey: guidelines for working with the grey literature in systematic reviews for management and organizational studies. Int J Manag Rev 2017;19:432-54. https://doi.org/10.1111/ijmr.12102.
- Department of Health and Social Care . FGM Safeguarding and Risk Assessment: Quick Guide for Professionals 2017.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Carroll C, Booth A, Lloyd-Jones M. Should we exclude inadequately reported studies from qualitative systematic reviews? An evaluation of sensitivity analyses in two case study reviews. Qual Health Res 2012;22:1425-34. https://doi.org/10.1177/1049732312452937.
- Cohen DJ, Crabtree BF. Evaluative criteria for qualitative research in health care: controversies and recommendations. Ann Fam Med 2008;6:331-9. https://doi.org/10.1370/afm.818.
- Hannes K, Lockwood C, Pearson A. A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research. Qual Health Res 2010;20:1736-43. https://doi.org/10.1177/1049732310378656.
- Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J, et al. ‘Trying to pin down jelly’ – exploring intuitive processes in quality assessment for meta-ethnography. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-46.
- Hannes K, Pearson A, Hannes K, Lockwood C. Synthesizing Qualitative Research: Choosing the Right Approach. London: BMJ Books, Wiley Blackwell; 2012.
- Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001895.
- Dixon-Woods M, Sutton A, Shaw R, Miller T, Smith J, Young B, et al. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Policy 2007;12:42-7. https://doi.org/10.1258/135581907779497486.
- Dixon-Woods M, Booth A, Sutton AJ. Synthesizing qualitative research: a review of published reports. Qual Res 2007;7:375-422. https://doi.org/10.1177/1468794107078517.
- Dixon-Woods M, Shaw RL, Agarwal S, Smith JA. The problem of appraising qualitative research. Qual Saf Health Care 2004;13:223-5. https://doi.org/10.1136/qhc.13.3.223.
- Sandelowski M, Barroso J. Reading qualitative studies. Int J Qual Methods 2002;1:74-108. https://doi.org/10.1177/160940690200100107.
- Munthe-Kaas H, Bohren MA, Glenton C, Lewin S, Noyes J, Tunçalp Ö, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 3: how to assess methodological limitations. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0690-9.
- Pearson A, Robertson-Malt S, Rittenmeyer L. Synthesizing Qualitative Evidence. Philadelphia, PA: Lippincott-Joanna Briggs Institute; 2011.
- Joanna Briggs Institute . JBI QARI Critical Appraisal Checklist for Interpretive and Critical Research n.d. https://joannabriggs.org/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Qualitative_Research2017_0.pdf (accessed 12 August 2019).
- Evans C, Tweheyo R, McGarry J, Eldridge J, Albert J, Nkoyo V, et al. Seeking culturally safe care: a qualitative systematic review of the healthcare experiences of women and girls who have undergone female genital mutilation/cutting. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027452.
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-21.
- Higginbottom GM, Morgan M, Alexandre M, Chiu Y, Forgeron J, Kocay D, et al. Immigrant women’s experiences of maternity-care services in Canada: a systematic review using a narrative synthesis. Syst Rev 2015;4. https://doi.org/10.1186/2046-4053-4-13.
- Higginbottom GM, Hadziabdic E, Yohani S, Paton P. Immigrant women’s experience of maternity services in Canada: a meta-ethnography. Midwifery 2014;30:544-59. https://doi.org/10.1016/j.midw.2013.06.004.
- Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qual Health Res 1998;8:341-51. https://doi.org/10.1177/104973239800800305.
- Noyes J, Popay J. Directly observed therapy and tuberculosis: how can a systematic review of qualitative research contribute to improving services? A qualitative meta-synthesis. J Adv Nurs 2007;57:227-43. https://doi.org/10.1111/j.1365-2648.2006.04092.x.
- Evans C, Tweheyo R, McGarry J, Eldridge J, Albert J, Nkoyo V, et al. Crossing cultural divides: a qualitative systematic review of factors influencing the provision of healthcare related to female genital mutilation from the perspective of health professionals. PLOS ONE 2019;14. https://doi.org/10.1371/journal.pone.0211829.
- Joanna Briggs Institute . JBI QARI Data Extraction Form for Interpretive and Critical Research n.d. https://wiki.joannabriggs.org/display/MANUAL/Appendix+2.3%3A+JBI+Qualitative+data+extraction+tool (accessed 12 August 2019).
- Sandelowski M, Barroso J. Finding the findings in qualitative studies. J Nurs Scholarsh 2002;34:213-19. https://doi.org/10.1111/j.1547-5069.2002.00213.x.
- Booth A, Carroll C, Ilott I, Low LL, Cooper K. Desperately seeking dissonance: identifying the disconfirming case in qualitative evidence synthesis. Qual Health Res 2013;23:126-41. https://doi.org/10.1177/1049732312466295.
- Noyes J, Booth A, Lewin S, Carlsen B, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings–paper 6: how to assess relevance of the data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0693-6.
- Lewin S, Bohren M, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 2: how to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0689-2.
- Glenton C, Carlsen B, Lewin S, Munthe-Kaas H, Colvin CJ, Tunçalp Ö, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 5: how to assess adequacy of data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0692-7.
- Colvin CJ, Garside R, Wainwright M, Munthe-Kaas H, Glenton C, Bohren MA, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 4: how to assess coherence. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0691-8.
- Booth A, Lewin S, Glenton C, Munthe-Kaas H, Toews I, Noyes J, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 7: understanding the potential impacts of dissemination bias. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0694-5.
- Guyatt G, Oxman A, Kunz R, Falck-Ytter Y, Vist G, Liberati A, et al. Rating quality of evidence and strength of recommendations: going from evidence to recommendations. BMJ 2008;10:1170-3. https://doi.org/10.1136/bmj.39504.506319.80.
- Lincoln Y, Guba E. Naturalistic Inquiry. California, CA: Sage Publications Ltd; 1985.
- Finlay L, Gough B. Reflexivity: A Practical Guide for Researchers in Health and Social Sciences. Oxford: Blackwell Science Ltd; 2003.
- Newton BJ, Rothlingova Z, Gutteridge R, LeMarchand K, Raphael JH. No room for reflexivity? Critical reflections following a systematic review of qualitative research. J Health Psychol 2012;17:866-85. https://doi.org/10.1177/1359105311427615.
- Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ 2000;320:50-2. https://doi.org/10.1136/bmj.320.7226.50.
- Khaja K. Female Circumcision: Life Histories of Somali Women 2004.
- Khaja K, Lay K, Boys S. Female circumcision: toward an inclusive practice of care. Health Care Women Int 2010;31:686-99. https://doi.org/10.1080/07399332.2010.490313.
- Thierfelder C. Female Genital Mutilation and the Swiss Health Care System 2003. https://edoc.unibas.ch/139/ (accessed 12 July 2019).
- Thierfelder C, Tanner M, Bodiang CM. Female genital mutilation in the context of migration: experience of African women with the Swiss health care system. Eur J Public Health 2005;15:86-90. https://doi.org/10.1093/eurpub/cki120.
- Abdi R. Carving culture: creating identity through female genital cutting. Durham Anthropol J 2012;18:115-53.
- Behrendt A. Listening to African Voices: Female Genital Mutilation/Cutting Among Immigrants in Hamburg: Knowledge, Attitudes and Practice. Hamburg: Plan; 2011.
- Hussen MA. Services for Women With Female Genital Mutilation in Christchurch: Perspectives of Women and Their Health Providers 2014. https://ir.canterbury.ac.nz/handle/10092/10437 (accessed 12 July 2019).
- Shaw E. Female circumcision: perceptions of clients and caregivers. J Am Coll Health 1985;33:193-7. https://doi.org/10.1080/07448481.1985.9939604.
- Vangen S, Johansen RE, Sundby J, Traeen B, Stray-Pedersen B. Qualitative study of perinatal care experiences among Somali women and local health care professionals in Norway. Eur J Obstet Gynecol Reprod Biol 2004;112:29-35. https://doi.org/10.1016/S0301-2115(03)00313-0.
- Vaughan C, White N, Keogh L, Tobin J, Ha B, Ibrahim M, et al. Listening to North Yarra Communities About Female Genital Cutting. Melbourne VIC: The University of Melbourne; 2014.
- Vaughan C, White N, Keogh L, Tobin J, Murdolo A, Quiazon R, et al. Female Genital Mutilation Cutting in Regional Victoria. Research to Practice. Report No. 1470-0328 2014. www.netfa.com.au/downloads/FGMC-in-Regional-Victoria-Report-WEB.pdf (accessed 12 July 2019).
- Asefaw F. Female Genital Mutilation: A Field Study With Special Consideration of the Background As Well As the Health and Psychosexual Consquences for Those Affected and Their Partners in Eritrea and in Germany 2007. https://refubium.fu-berlin.de/handle/fub188/13487?show=full (accessed 12 July 2019).
- Maier C. Echoes of Silence: Voices of Concern for Genital Mutilation in African Immigrant Women in Vienna: An Ethnological Study 2003.
- Ballesteros Meseguer C, Almansa Martinez P, Pastor Bravo MdM, Jimenez Ruiz I. The voice of women subjected to female genital mutilation in the region of Murcia, Spain. Gac Sanit 2014;28:287-91. https://doi.org/10.1016/j.gaceta.2014.02.006.
- Bravo Pastor del Mar M. Women Subjected to Female Genital Mutilation: Knowledge for the Nursing Discipline 2014.
- Baldeh F. Obstetric Care in Scotland: The Experience of Women Who Have Undergone Female Genital Mutilation (FGM) 2013. http://etheses.qmu.ac.uk/1469 (accessed 12 July 2019).
- Betts V. Transnational Gender, Sexuality and Identity Construction: Ambivalent Subjectivities of Somali Refugee Women in the GTA 2011.
- Gali MA. Female Circumcision: A Transcultural Study of Attitudes, Identity and Reproductive Health of East African Immigrants 1997. https://elibrary.ru/item.asp?id=5531937.
- Glazer E. Embodiment, Pain and Circumcision in Somali-Canadian Women 2012.
- Shermarke MAA. Understanding the Canadian Community Context of Female Circumcision 1996.
- Jones A. Working Psychologically with Female Genital Mutilation: An Exploration of the Views and Experiences of Women who have Experienced FGM and of Clinical Psychologists. London: University of East London; 2010.
- Maternity Action . Women’s Voices on Health: Addressing Barriers to Accessing Primary Care 2014.
- O’Brien O, Baldeh F, Hassan J, Baillie M. My Voice: Participatory Action Research Project with Men, Women and Young People on Female Genital Mutilation (FGM) in Scotland: (Phase 2). Edinburgh: Waverly Care, Queen Margaret University; 2017.
- O’Brien O, Baldeh F, Sivapatham S, Brown E, O’May F. Participatory Action Research Project With Men, Women and Young People on Female Genital Mutilation (FGM) in Scotland: (Phase 1) 2016. www.fgmaware.org/uploads/4/6/7/9/46792493/my_voice_report_2016.pdf (accessed 12 July 2019).
- Palfreyman A, Brown E, Nam S. Understanding Female Genital Mutilation in Birmingham: Findings from a PEER Study. Options Consultancy Services and Birmingham & Solihull Women’s Aid; 2011.
- Ahmed M, Momoh C. Female Genital Mutilation. London: Radcliffe; 2005.
- Abdullahi A, Copping J, Kessel A, Luck M, Bonell C. Cervical screening: perceptions and barriers to uptake among Somali women in Camden. Public Health 2009;123:680-5. https://doi.org/10.1016/j.puhe.2009.09.011.
- Ahlberg BM, Krantz I, Lindmark G, Waroame M. ‘It’s only a tradition’: making sense of eradication interventions and the persistence of female ‘circumcision’ within a Swedish context. Crit Soc Policy 2004;24:50-78. https://doi.org/10.1177/0261018304241003.
- Ameresekere M, Borg R, Frederick J, Vragovic O, Saia K, Raj A. Somali immigrant women’s perceptions of cesarean delivery and patient-provider communication surrounding female circumcision and childbirth in the USA. Int J Gynecol Obstet 2011;115:227-30. https://doi.org/10.1016/j.ijgo.2011.07.019.
- Beine K, Fullerton J, Palinkas L, Anders B. Conceptions of prenatal care among Somali women in San Diego. J Nurse Midwifery 1995;40:376-81. https://doi.org/10.1016/0091-2182(95)00024-E.
- Berggren V, Bergström S, Edberg AK. Being different and vulnerable: experiences of immigrant African women who have been circumcised and sought maternity care in Sweden. J Transcult Nurs 2006;17:50-7. https://doi.org/10.1177/1043659605281981.
- Carroll J, Epstein R, Fiscella K, Gipson T, Volpe E, Jean-Pierre P. Caring for Somali women: implications for clinician-patient communication. Patient Educ Couns 2007;66:337-45. https://doi.org/10.1016/j.pec.2007.01.008.
- Chalmers B, Omer-Hashi K. What Somali women say about giving birth in Canada. J Reprod Infant Psychol 2002;20:267-82. https://doi.org/10.1080/0264683021000033183.
- Degni F, Suominen SB, El Ansari W, Vehviläinen-Julkunen K, Essen B. Reproductive and maternity health care services in Finland: perceptions and experiences of Somali-born immigrant women. Ethn Health 2014;19:348-66. https://doi.org/10.1080/13557858.2013.797567.
- d’Entremont M, Smythe L, McAra-Couper J. The sounds of silence – a hermeneutic interpretation of childbirth post excision. Health Care Women Int 2014;35:300-19. https://doi.org/10.1080/07399332.2013.838245.
- Essén B, Johnsdotter S, Hovelius B, Gudmundsson S, Sjöberg NO, Friedman J, et al. Qualitative study of pregnancy and childbirth experiences in Somalian women resident in Sweden. BJOG 2000;107:1507-12. https://doi.org/10.1111/j.1471-0528.2000.tb11676.x.
- Ghebre RG, Sewali B, Osman S, Adawe A, Nguyen HT, Okuyemi KS, et al. Cervical cancer: barriers to screening in the Somali community in Minnesota. J Immigr Minor Health 2015;17:722-8. https://doi.org/10.1007/s10903-014-0080-1.
- Glover J, Liebling H, Barrett H, Goodman S. The psychological and social impact of female genital mutilation: a holistic conceptual framework. J Int Stud 2017;10:219-38. https://doi.org/10.14254/2071-8330.2017/10-2/16.
- Guerin PB, Allotey P, Hussein Elmi F, Baho S. Advocacy as a means to an end: assisting refugee women to take control of their reproductive health needs. Women Health 2006;43:7-25. https://doi.org/10.1300/J013v43n04_02.
- Hill N, Hunt E, Hyrkas K. Somali immigrant women’s health care experiences and beliefs regarding pregnancy and birth in the United States. J Transcult Nurs 2012;23:72-81. https://doi.org/10.1177/1043659611423828.
- Johansen RE. Undoing female genital cutting: perceptions and experiences of infibulation, defibulation and virginity among Somali and Sudanese migrants in Norway. Cult Health Sex 2017;19:528-42. https://doi.org/10.1080/13691058.2016.1239838.
- Lundberg PC, Gerezgiher A. Experiences from pregnancy and childbirth related to female genital mutilation among Eritrean immigrant women in Sweden. Midwifery 2008;24:214-25. https://doi.org/10.1016/j.midw.2006.10.003.
- McNeely S, Christie-de Jong F. Somali refugees’ perspectives regarding FGM/C in the US. Int J Migr Health Soc Care 2016;12:157-69. https://doi.org/10.1108/IJMHSC-09-2015-0033.
- Moxey JM, Jones LL. A qualitative study exploring how Somali women exposed to female genital mutilation experience and perceive antenatal and intrapartum care in England. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009846.
- Murray L, Windsor C, Parker E, Tewfik O. The experiences of African women giving birth in Brisbane, Australia. Health Care Women Int 2010;31:458-72. https://doi.org/10.1080/07399330903548928.
- Recchia N, McGarry J. ‘Don’t judge me’: narratives of living with FGM. Int J Hum Rights Healthc 2017;10:4-13. https://doi.org/10.1108/IJHRH-10-2016-0016.
- Safari F. A qualitative study of women’s lived experience after deinfibulation in the UK. Midwifery 2013;29:154-8. https://doi.org/10.1016/j.midw.2011.12.005.
- Salad J, Verdonk P, de Boer F, Abma TA. ‘A Somali girl is Muslim and does not have premarital sex – is vaccination really necessary?’ A qualitative study into the perceptions of Somali women in the Netherlands about the prevention of cervical cancer. Int J Equity Health 2015;14:1-13. https://doi.org/10.1186/s12939-015-0198-3.
- Upvall MJ, Mohammed K, Dodge PD. Perspectives of Somali Bantu refugee women living with circumcision in the United States: a focus group approach. Int J Nurs Stud 2009;46:360-8. https://doi.org/10.1016/j.ijnurstu.2008.04.009.
- Vloeberghs E, van der Kwaak A, Knipscheer J, van den Muijsenbergh M. Coping and chronic psychosocial consequences of female genital mutilation in the Netherlands. Ethn Health 2012;17:677-95. https://doi.org/10.1080/13557858.2013.771148.
- Wiklund H, Aden AS, Högberg U, Wikman M, Dahlgren L. Somalis giving birth in Sweden: a challenge to culture and gender specific values and behaviours. Midwifery 2000;16:105-15. https://doi.org/10.1054/midw.1999.0197.
- Johansen RE. Care for infibulated women giving birth in Norway: an anthropological analysis of health workers’ management of a medically and culturally unfamiliar issue. Med Anthropol Q 2006;20:516-44. https://doi.org/10.1525/maq.2006.20.4.516.
- Essén B, Binder P, Johnsdotter S. An anthropological analysis of the perspectives of Somali women in the West and their obstetric care providers on caesarean birth. J Psychosom Obstet Gynaecol 2011;32:10-8. https://doi.org/10.3109/0167482X.2010.547966.
- Higginbottom GM, Safipour J, Yohani S, O’Brien B, Mumtaz Z, Paton P. An ethnographic study of communication challenges in maternity care for immigrant women in rural Alberta. Midwifery 2015;31:297-304. https://doi.org/10.1016/j.midw.2014.09.009.
- Bulman K, McCourt C. Report on Somali Womens’ Experiences of Maternity Services 1997.
- Ogunsiji O. Female genital mutilation (FGM): Australian midwives’ knowledge and attitudes. Health Care Women Int 2015;36:1179-93. https://doi.org/10.1080/07399332.2014.992521.
- Ogunsiji O. Australian midwives’ perspectives on managing obstetric care of women living with female genital circumcision/mutilation. Health Care Women Int 2016;37:1156-69. https://doi.org/10.1080/07399332.2016.1215462.
- Bergqvist H, Svensson J. Midwives Experiences of Encounters Wth Young Women Who Come from Areas Where the Practice of Genital Mutilation Is Common. 2016.
- Bibi N, Rahimian N. Nurses’ Experience and Knowledge about Female Genital Mutilation 2013. http://shh.diva-portal.org/smash/record.jsf?pid=diva2%3A693139&dswid=-9636 (accessed 12 July 2019).
- Brodin E, Mårtensson N. [District Nurses’ Knowledge and Experience of Female Genital Mutilation] Distriktssköterskors Kunskap Och Erfarenhet Av Kvinnlig Könsstympning 2016.
- Gertsson M, Serpan H. Meeting With the Unthinkable: Value Conflicts in Meetings With Women Vulnerable to Female Genital Mutilation 2009. www.diva-portal.org/smash/record.jsf?pid=diva2%3A290536&dswid=-170 (accessed 12 July 2019).
- Holm L, Kammensjö H. School Nurses’ Experiences of Female Genital Mutilation Among Girls 2012.
- León-Larios F, Casado-Mejía R. Influence of gender on knowledge, perception and approach to harmful traditional practices: female genital mutilation. Evidentia 2012;9:1-7.
- Burchill J, Pevalin DJ. Demonstrating cultural competence within health-visiting practice: working with refugee and asylum-seeking families. Divers Equal Health Care 2014;11:151-9. https://doi.org/10.21767/2049-5471.100010.
- Byrskog U, Olsson P, Essén B, Allvin MK. Being a bridge: Swedish antenatal care midwives’ encounters with Somali-born women and questions of violence; a qualitative study. BMC Pregnancy Childbirth 2015;15. https://doi.org/10.1186/s12884-015-0429-z.
- Johansen RE. Virility, pleasure and female genital mutilation/cutting. A qualitative study of perceptions and experiences of medicalized defibulation among Somali and Sudanese migrants in Norway. Reprod Health 2017;14. https://doi.org/10.1186/s12978-017-0287-4.
- Lazar JN, Johnson-Agbakwu CE, Davis OI, Shipp MP. Providers’ perceptions of challenges in obstetrical care for somali women. Obstet Gynecol Int 2013;2013. https://doi.org/10.1155/2013/149640.
- Leval A, Widmark C, Tishelman C, Maina Ahlberg B. The encounters that rupture the myth: contradictions in midwives’ descriptions and explanations of circumcised women immigrants’ sexuality. Health Care Women Int 2004;25:743-60. https://doi.org/10.1080/07399330490475593.
- Jatau M. Living Between Two Cultures: A Reproductive Health Journey of African Refugee Women 2011. https://repository.asu.edu/items/14386 (accessed 12 July 2019).
- Moore K. Female Genital Mutilation and Cultural Competency: Moving Towards Improved Management of Obstetric Care 2012. https://eresearch.qmu.ac.uk/handle/20.500.12289/7180 (accessed 12 July 2019).
- Rubin EA. When Cultures Collide: An Exploration of Cultural Competence and Cross-Cultural Communication Between American Medical Providers and Immigrant Women Who Have Been Circumcised 2000.
- Van den Muijsenbergh M, Van Weel-Baumgarten E, Burns N, O’Connell C, Mair F, Spiegel W. Communication in cross-cultural consultations in primary care in Europe: the case for improvement. Prim Health Care Res Dev 2014;15:122-33. https://doi.org/10.1017/S1463423613000157.
- Leininger M, MacFarlane M. Transcultural Nursing: Concepts, Theories, Research and Practice. New York, NY: McGraw-Hill; 2002.
- Browne AJ, Varcoe C, Smye V, Reimer-Kirkham S, Lynam MJ, Wong S. Cultural safety and the challenges of translating critically oriented knowledge in practice. Nurs Philos 2009;10:167-79. https://doi.org/10.1111/j.1466-769X.2009.00406.x.
- Ramsden I. Cultural Safety and Nursing Education in Aotearoa and Te Waipounamu 2002. https://croakey.org/wp-content/uploads/2017/08/RAMSDEN-I-Cultural-Safety_Full.pdf (accessed 12 July 2019).
- Phiri J, Dietsch E, Bonner A. Cultural safety and its importance for Australian midwifery practice. Collegian 2010;17:105-11. https://doi.org/10.1016/j.colegn.2009.11.001.
- Duke J, Connor M, McEldowney R. Becoming a culturally competent health practitioner in the delivery of culturally safe care. J Cult Divers 2009;16:40-9.
- Gerlach AJ. A critical reflection on the concept of cultural safety. Can J Occup Ther 2012;79:151-8. https://doi.org/10.2182/cjot.2012.79.3.4.
- Cooney C. A comparative analysis of transcultural nursing and cultural safety. Nurs Prax N Z 1994;9:6-12.
- Brascoupé S, Waters C. Cultural safety: exploring the applicability of the concept of cultural safety to aboriginal health and community wellness. J Aborig Health 2009;5:6-41.
- Wepa D. Cultural Safety in Aotearoa New Zealand. North Shore City: Pearson Prentice Hall; 2005.
- Johnstone MJ, Kanitsaki O. An exploration of the notion and nature of the construct of cultural safety and its applicability to the Australian health care context. J Transcult Nurs 2007;18:247-56. https://doi.org/10.1177/1043659607301304.
- Vissandjée B, Denetto S, Migliardi P, Proctor J. Female genital cutting (FGC) and the ethics of care: community engagement and cultural sensitivity at the interface of migration experiences. BMC Int Health Hum Rights 2014;14. https://doi.org/10.1186/1472-698X-14-13.
- Narruhn R, Schellenberg IR. Caring ethics and a Somali reproductive dilemma. Nurs Ethics 2013;20:366-81. https://doi.org/10.1177/0969733012453363.
- WHO . WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience 2018.
- White Ribbon Alliance . Respectful Maternity Care Charter: The Universal Rights of Childbearing Women 2011.
- Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001847.
- Denny E. Respectful maternity care needs to be the standard for all women worldwide (mini-commentary). Br J Obstet Gynaecol 2017;125. https://doi.org/10.1111/1471-0528.15055.
- Shakibazadeh E, Namadian M, Bohren MA, Vogel JP, Rashidian A, Nogueira Pileggi V, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. Br J Obstet Gynaecol 2018;125:932-42. https://doi.org/10.1111/1471-0528.15015.
- Sripad P, Ozawa S, Merritt MW, Jennings L, Kerrigan D, Ndwiga C, et al. Exploring meaning and types of trust in maternity care in peri-urban Kenya: a qualitative cross-perspective analysis. Qual Health Res 2018;28:305-20. https://doi.org/10.1177/1049732317723585.
- Bischoff A, Bovier PA, Rrustemi I, Gariazzo F, Eytan A, Loutan L. Language barriers between nurses and asylum seekers: their impact on symptom reporting and referral. Soc Sci Med 2003;57:503-12. https://doi.org/10.1016/S0277-9536(02)00376-3.
- Gilson L. Trust and the development of health care as a social institution. Soc Sci Med 2003;56:1453-68. https://doi.org/10.1016/S0277-9536(02)00142-9.
- Murray B, McCrone S. An integrative review of promoting trust in the patient-primary care provider relationship. J Adv Nurs 2015;71:3-23. https://doi.org/10.1111/jan.12502.
- Greenhalgh T, Voisey C, Robb N. Interpreted consultations as ‘business as usual’? An analysis of organisational routines in general practices. Sociol Health Illn 2007;29:931-54. https://doi.org/10.1111/j.1467-9566.2007.01047.x.
- Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev 2005;62:255-99. https://doi.org/10.1177/1077558705275416.
- Zendedel R, Schouten BC, van Weert JCM, van den Putte B. Informal interpreting in general practice: are interpreters’ roles related to perceived control, trust and satisfaction?. Patient Educ Couns 2018;101:1058-65. https://doi.org/10.1016/j.pec.2018.01.012.
- Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res 2007;42:727-54. https://doi.org/10.1111/j.1475-6773.2006.00629.x.
- Martin M, Phelan M. Interpreters and cultural mediators: different but complementary roles. Migr Health 2010;6:1-8.
- Akhavan S, Edge D. Foreign-born women’s experiences of community-based doulas in Sweden – a qualitative study. Health Care Women Int 2012;33:833-48. https://doi.org/10.1080/07399332.2011.646107.
- Akhavan S, Lundgren I. Midwives’ experiences of doula support for immigrant women in Sweden – a qualitative study. Midwifery 2012;28:80-5. https://doi.org/10.1016/j.midw.2010.11.004.
- Dundek LH. Establishment of a Somali doula program at a large metropolitan hospital. J Perinat Neonatal Nurs 2006;20:128-37. https://doi.org/10.1097/00005237-200604000-00006.
- Shelp A. Women helping women: the Somali doula initiative. Int J Childbirth Educ 2004;19:4-7.
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter?. Milbank Q 2001;79:613-39. https://doi.org/10.1111/1468-0009.00223.
- Moore L, Britten N, Lydahl D, Naldemirci Ö, Elam M, Wolf A. Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scand J Caring Sci 2017;31:662-73. https://doi.org/10.1111/scs.12376.
- Gravel F, Legare F, Graham I. Barriers and facilitators to implementing shared decision making in clincial practice: a systematic review of health professional’s perceptions. Implement Sci 2006;1. https://doi.org/10.1186/1748-5908-1-16.
- Mainous AG, Baker R, Love MM, Gray DP, Gill JM. Continuity of care and trust in one’s physician: evidence from primary care in the United States and the United Kingdom. Fam Med 2001;33:22-7.
- Saha S, Beach MC, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Natl Med Assoc 2008;100:1275-85. https://doi.org/10.1016/S0027-9684(15)31505-4.
- Johansen RE. Pain as a counterpoint to culture: toward an analysis of pain associated with infibulation among Somali immigrants in Norway. Med Anthropol Q 2002;16:312-40. https://doi.org/10.1525/maq.2002.16.3.312.
- James S. Women’s experiences of symptoms of posttraumatic stress disorder (PTSD) after traumatic childbirth: a review and critical appraisal. Arch Womens Ment Health 2015;18:761-71. https://doi.org/10.1007/s00737-015-0560-x.
- Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health 2015;38:216-26. https://doi.org/10.1097/FCH.0000000000000071.
- Abdulcadir J, Bianchi Demicheli F, Willame A, Recordon N, Petignat P. Posttraumatic stress disorder relapse and clitoral reconstruction after female genital mutilation. Obstet Gynecol 2017;129:371-6. https://doi.org/10.1097/AOG.0000000000001835.
- Abayomi O, Chibuzor MT, Okusanya BO, Esu E, Odey E, Meremikwu MM. Supportive psychotherapy or client education alongside surgical procedures to correct complications of female genital mutilation: a systematic review. Int J Gynaecol Obstet 2017;136:51-5. https://doi.org/10.1002/ijgo.12042.
- Adelufosi A, Edet B, Arikpo D, Aquaisua E, Meremikwu MM. Cognitive behavioral therapy for post-traumatic stress disorder, depression, or anxiety disorders in women and girls living with female genital mutilation: a systematic review. Int J Gynaecol Obstet 2017;136:56-9. https://doi.org/10.1002/ijgo.12043.
- Jones A, Byrne A. Working psychologically with female genital mutilation: an exploration of the views and experiences of women who have experienced FGM and of clinical psychologists. Clin Psychol Forum 2013;246:26-30.
- Albert J. Female genital mutilation: the role of the midwife. Midirs 2016;26:159-65.
- Johnsdotter S. The impact of migration on attitudes to female genital cutting and experiences of sexual dysfunction among migrant women with FGC. Curr Sex Health Rep 2018;10:18-24. https://doi.org/10.1007/s11930-018-0139-4.
- O’Neill S, Dubourg D, Florquin S, Bos M, Zewolde S, Richard F. ‘Men Have a Role to Play But They don’t Play it’: A Mixed Methods Study Exploring Men’s Involvement in Female Genital Mutilation in Belgium, the Netherlands and the United Kingdom: Full Report 2017.
- Creighton SM, Dear J, de Campos C, Williams L, Hodes D. Multidisciplinary approach to the management of children with female genital mutilation (FGM) or suspected FGM: service description and case series. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010311.
- Mbanya VN, Gele AA, Diaz E, Kumar B. Health care seeking patterns for female genital mutilation/cutting among young Somalis in Norway. BMC Public Health 2018;18. https://doi.org/10.1186/s12889-018-5440-7.
- Rone M, Carter J, Wright C, Bayly J, Wright A. Female genital mutilation (FGM): a prospective audit of the management of women with FGM in antenatal clinic. Br J Obstet Gynaecol 2015;122.
- WHO . Care of Girls and Women Living With Female Genital Mutilation: A Clinical Handbook 2018.
- Bello S, Ogugbue M, Chibuzor M, Okomo U, Meremikwu MM. Counselling for deinfibulation among women with type III female genital mutilation: a systematic review. Int J Gynaecol Obstet 2017;136:47-50. https://doi.org/10.1002/ijgo.12044.
- Zurynski Y, Sureshkumar P, Phu A, Elliott E. Female genital mutilation and cutting: a systematic literature review of health professionals’ knowledge, attitudes and clinical practice. BMC Int Health Hum Rights 2015;15. https://doi.org/10.1186/s12914-015-0070-y.
- Evans C, Nalubega S, McLuskey J, Darlington N, Croston M, Bath-Hextall F. The views and experiences of nurses and midwives in the provision and management of provider-initiated HIV testing and counseling: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep 2016;13:130-286. https://doi.org/10.11124/jbisrir-2015-2345.
- WHO . Service Delivery Approaches to HIV Testing and Counselling (HTC): A Strategic Programme Framework 2012.
- Hamberger LK, Rhodes K, Brown J. Screening and intervention for intimate partner violence in healthcare settings: creating sustainable system-level programs. J Womens Health 2015;24:86-91. https://doi.org/10.1089/jwh.2014.4861.
- O’Doherty L, Hegarty K, Ramsay J, Davidson LL, Feder G, Taft A. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev 2015;7. https://doi.org/10.1002/14651858.CD007007.pub3.
- Stokes T, Shaw EJ, Camosso-Stefinovic J, Imamura M, Kanguru L, Hussein J. Barriers and enablers to guideline implementation strategies to improve obstetric care practice in low- and middle-income countries: a systematic review of qualitative evidence. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0508-1.
- Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation – a scoping review. Healthcare 2016;4. https://doi.org/10.3390/healthcare4030036.
- Imamura M, Kanguru L, Penfold S, Stokes T, Camosso-Stefinovic J, Shaw B, et al. A systematic review of implementation strategies to deliver guidelines on obstetric care practice in low- and middle-income countries. Int J Gynaecol Obstet 2017;136:19-28. https://doi.org/10.1002/ijgo.12005.
- The Supporting the Use of Research Evidence (SURE) Collaboration . SURE Guides for Preparing and Using Evidence-Based Policy Briefs, No.5: Identifying and Addressing Barriers to Implementing Policy Options n.d. www.who.int/evidence/sure/guides (accessed 3 May 2018).
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0242-0.
- Abdulcadir J, Rodriguez MI, Say L. A systematic review of the evidence on clitoral reconstruction after female genital mutilation/cutting. Int J Gynaecol Obstet 2015;129:93-7. https://doi.org/10.1016/j.ijgo.2014.11.008.
- De Schrijver L, Leye E, Merckx M. A multidisciplinary approach to clitoral reconstruction after female genital mutilation: the crucial role of counselling. Eur J Contracept Reprod Health Care 2016;21:269-75. https://doi.org/10.3109/13625187.2016.1172063.
- Dominguez Garcia L, Dominguez L, Hopkins K, Mutalak O, Harish S, Alcayde D, et al. Meeting the sexual health needs of women with female genital mutilation: an integrated model of care. Int J STD AIDS 2013;24.
- Low-Beer N, Dominguez-Garcia L, Alcayde D, Jones R, Ayida G. Accessible integrated care to meet the complex needs of women with female genital mutilation (FGM). Br J Obstet Gynaecol 2013;120.
- Turkmani S, Homer C, Varol N, Dawson A. A survey of Australian midwives’ knowledge, experience, and training needs in relation to female genital mutilation. Women Birth 2018;31:25-30. https://doi.org/10.1016/j.wombi.2017.06.009.
- Relph S, Inamdar R, Singh H, Yoong W. Female genital mutilation/cutting: knowledge, attitude and training of health professionals in inner city London. Eur J Obstet Gynecol Reprod Biol 2013;168:195-8. https://doi.org/10.1016/j.ejogrb.2013.01.004.
- Leye E, Ysebaert I, Deblonde J, Claeys P, Vermeulen G, Jacquemyn Y, et al. Female genital mutilation: knowledge, attitudes and practices of Flemish gynaecologists. Eur J Contracept Reprod Health Care 2008;13:182-90. https://doi.org/10.1080/13625180701780957.
- Kai J, Beavan J, Faull C, Dodson L, Gill P, Beighton A. Professional uncertainty and disempowerment responding to ethnic diversity in health care: a qualitative study. PLOS Med 2007;4. https://doi.org/10.1371/journal.pmed.0040323.
- Oringanje CM, Okoro A, Nwankwo ON, Meremikwu MM. Providing information about the consequences of female genital mutilation to healthcare providers caring for women and girls living with female genital mutilation: a systematic review. Int J Gynaecol Obstet 2017;136:65-71. https://doi.org/10.1002/ijgo.12057.
- Jacoby SD, Smith A. Increasing certified nurse-midwives’ confidence in managing the obstetric care of women with female genital mutilation/cutting. J Midwifery Womens Health 2013;58:451-6. https://doi.org/10.1111/j.1542-2011.2012.00262.x.
- Balfour J, Abdulcadir J, Say L, Hindin MJ. Interventions for healthcare providers to improve treatment and prevention of female genital mutilation: a systematic review. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1674-1.
- Elliott C, Creighton SM, Barker MJ, Liao LM. A brief interactive training for health care professionals working with people affected by female genital mutilation: initial pilot evaluation with psychosexual therapists. Sex Relation Ther 2016;31:70-82. https://doi.org/10.1080/14681994.2015.1093614.
- Jackson C. Counselling professionals’ awareness and understanding of female genital mutilation/cutting: training needs for working therapeutically with survivors. Couns Psychother Res 2017;17:309-19. https://doi.org/10.1002/capr.12136.
- Leye E. Midwifery training needs identified when caring for women with female genital mutilation. Evid Based Nurs 2016;19. https://doi.org/10.1136/eb-2015-102080.
- Roberts TL, Poblete X. G55(P) Female genital mutilation: a survey of awareness, training and current practice. Arch Dis Child 2015;100. https://doi.org/10.1136/archdischild-2015-308599.54.
- Royal College of Midwives . Female Genital Mutilation: Midwives’ Views and Knowledge 2012.
- Gabrasadig R, Asamoah F, Wilson N. Female genital mutilation: knowledge, training and experience of healthcare professionals at a London Hospital. Arch Dis Child 2015;100:A23-4. https://doi.org/10.1136/archdischild-2015-308599.55.
- Nash E, Ranka P. Female genital mutilation: knowledge, confidence and approach to care in clinical practice of midwives and nurses in the UK. Int J Gynecol Obstet 2015;131.
- Abdulcadir J, Say L, Pallitto C. What do we know about assessing healthcare students and professionals’ knowledge, attitude and practice regarding female genital mutilation? A systematic review. Reprod Health 2017;14. https://doi.org/10.1186/s12978-017-0318-1.
- Esu E, Okoye I, Arikpo I, Ejemot-Nwadiaro R, Meremikwu MM. Providing information to improve body image and care seeking behavior of women and girls living with female genital mutilation: a systematic review and meta-analysis. Int J Gynaecol Obstet 2017;136:72-8. https://doi.org/10.1002/ijgo.12058.
- Waigwa S, Doos L, Bradbury-Jones C, Taylor J. Effectiveness of health education as an intervention designed to prevent female genital mutilation/cutting (FGM/C): a systematic review. Reprod Health 2018;15. https://doi.org/10.1186/s12978-018-0503-x.
- Abdulcadir J, McLaren S, Boulvain M, Irion O. Health education and clinical care of immigrant women with female genital mutilation/cutting who request postpartum reinfibulation. Int J Gynaecol Obstet 2016;135:69-72. https://doi.org/10.1016/j.ijgo.2016.03.027.
- Abdulcadir O, Catania L, Caselli A. Female genital mutilation (FGM): a comparison between the male and the female view. Int J Gynaecol Obstet 2012;119:S262-3. https://doi.org/10.1016/S0020-7292(12)60436-6.
- Local Government Association . Community Engagement on Female Genital Mutilation 2016.
- Finke E. Genital mutilation as an expression of power structures: ending FGM through education, empowerment of women and removal of taboos. Afr J Reprod Health 2006;10:13-7. https://doi.org/10.2307/30032454.
- Khalifa S, Brown E. Communities Tackling FGM in the UK: Best Practice Guide. London: Tackling Female Genital Mutilation Initiative and Options Consultancy Services Limited; 2016.
- Department for Education . National FGM Centre: An Evaluation: Research Report 2017.
- Connelly E, Murray N, Baillot H, Howard N. Missing from the debate? A qualitative study exploring the role of communities within interventions to address female genital mutilation in Europe. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021430.
- Giorgi A. The Descriptive Phenomenological Method in Psychology: A Modified Husserlian Approach. Pittsburg, PA: Duquesne University; 2009.
- Quickfall J. Developing a model for culturally competent primary care nursing for asylum applicants and refugees in Scotland: a review of the literature. Diversity in Health and Social Care 2004;1:53-64.
- Heidegger M. Being and Time (Translated by Macquarrie J and Robinson E). New York, NY: Harper and Row; 1962.
- Guba E, Lincoln Y. Fourth Generation Evaluation. Newbury Park, CA: SAGE Publications Ltd; 1989.
Appendix 1 The MEDLINE search strategy
Reproduced from Evans et al. 145 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. Also reproduced from Evans et al. 139 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Ovid MEDLINE In-Process & Other Non-indexed Citations and Ovid MEDLINE
Date range searched: 1946 to present.
Date searched: 4 August 2017.
| Search statement | Search terms | Number of hits | Notes on strategy |
|---|---|---|---|
| 1 | exp Circumcision, Female/or (exp Genitalia, Female/and exp Medicine, Traditional/) | 1367 | |
| 2 | (“female genital mutilation” or “female circumcision” or “female genital cutting” or “traditional female genital surgery” or infibulat* or reinfibulat* or defibulat* or clitoridect*).mp. | 1509 | |
| 3 | ((((ritual* or traditional* or ceremon* or sociali#ation*) adj3 (practic* or cut or cutting or surg*)) or circumcis* or excis*) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 2924 | |
| 4 | (FGM or FGC or TFGS or FGMC or “FGM/C”).mp. | 1133 | |
| 5 | (thara or tahar or khitan or khifad or khafad or megrez or absum or mekhnishab or kutairi or ibi or ugwu or sunna or bondo or sonde or gudiniin or halalays or qodiin or tahoor or bagne or gadja or ganza or “fanadu di mindjer” or niaka or kuyango or “musolula karoola”).mp. not (thara or tahar or khitan or khifad or khafad or megrez or absum or mekhnishab or kutairi or ibi or ugwu or sunna or bondo or sonde or gudiniin or halalays or qodiin or tahoor or bagne or gadja or ganza or “fanadu di mindjer” or niaka or kuyango or “musolula karoola”).au,in. | 1650 | Expanded terms to include country of origin terminology as described in Department of Health and Social Care guidance124 |
| 6 | 4 or 5 | 2779 | |
| 7 | limit 6 to female | 1200 | In order to exclude irrelevant records from terminology from other disciplines, or male circumcision-related hits |
| 8 | ((FGM or FGC or TFGS or FGMC or “FGM/C” or thara or tahar or khitan or khifad or khafad or megrez or absum or mekhnishab or kutairi or ibi or ugwu or sunna or bondo or sonde or gudiniin or halalays or qodiin or tahoor or bagne or gadja or ganza or “fanadu di mindjer” or niaka or kuyango or “musolula karoola”) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 507 | Adjacency to “female” terms to complement “limit to female” hit set |
| 9 | (egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*).ti,ab. | 151,913 | Country of origin used as proxy for FGM/C terms – as FGM/C is so common, inference is that women from these countries will fit a FGM/C profile even without the term being explicitly mentioned |
| 10 | limit 9 to female | 46,657 | |
| 11 | ((egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 5441 | |
| 12 | 1 or 2 or 3 or 7 or 8 or 10 or 11 | 51,901 | All women with FGM/C |
| 13 | “Emigrants and Immigrants”/or Refugees/or “Transients and Migrants”/or “Emigration and Immigration”/ | 45,756 | |
| 14 | (immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or (ex adj pat*) or transients or newcomer* or (new adj comer*) or alien* or incomer* or (in adj comer*)).mp. | 79,630 | |
| 15 | ((immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or (ex adj pat*) or transients or newcomer* or (new adj comer*) or alien* or incomer* or (in adj comer*)) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 4382 | |
| 16 | (refugee* or (asylum adj seek*) or asylee* or (refused adj3 (asylum* or refugee*)) or (displaced adj person*) or exile* or (new adj arrival) or (country adj2 (birth or origin)) or transnational*).mp. | 17,539 | |
| 17 | ((refugee* or (asylum adj seek*) or asylee* or (refused adj3 (asylum* or refugee*)) or (displaced adj person*) or exile* or (new adj arrival) or (country adj2 (birth or origin)) or transnational*) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 1462 | |
| 18 | (foreigner* or (foreign adj (born or citizen* or national* or origin*)) or (non adj (citizen* or native*)) or ((adoptive or naturali#ed) adj (citizen* or resident*)) or overstay* or trafficked or “spousal migrant*”).mp | 11,442 | |
| 19 | ((foreigner* or (foreign adj (born or citizen* or national* or origin*)) or (non adj (citizen* or native*)) or ((adoptive or naturali#ed) adj (citizen* or resident*)) or overstay* or trafficked or “spousal migrant*”) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 753 | |
| 20 | (((established or long-term or “first generation*” or new* or recent* or current*) adj3 (migrant* or migrat* or immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or (ex adj pat*) or transient* or alien*)) or newcomer* or (new adj comer*) or incomer* or (in adj comer*) or ((international or overseas or foreign) adj2 (student* or employee* or worker*))).mp. | 18,239 | |
| 21 | ((((established or long-term or “first generation*” or new* or recent* or current*) adj3 (migrant* or migrat* or immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or (ex adj pat*) or transient* or alien*)) or newcomer* or (new adj comer*) or incomer* or (in adj comer*) or ((international or overseas or foreign) adj2 (student* or employee* or worker*))) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 559 | |
| 22 | (“non-UK-born” or “born outside the UK” or “length of residence in the UK” or ((“not lawful*” or “not legal*” or unlawful* or illegal* or unauthori#ed* or “not authori#ed” or uncertain or insecure or legal* or legitimate* or permit* or visa* or irregular* or refused or undocumented) adj3 (residen* or student* or worker* or employee* or unemployed or immigrant* or imigrat* or migrant* or migrat*))).mp. | 2887 | |
| 23 | ((“non-UK-born” or “born outside the UK” or “length of residence in the UK” or ((“not lawful*” or “not legal*” or unlawful* or illegal* or unauthori#ed* or “not authori#ed” or uncertain or insecure or legal* or legitimate* or permit* or visa* or irregular* or refused or undocumented) adj3 (residen* or student* or worker* or employee* or unemployed or immigrant* or imigrat* or migrant* or migrat*))) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 136 | |
| 24 | exp Vulnerable Populations/ | 8275 | |
| 25 | ((vulnerab* or disadvantag* or minorit*) adj3 (individ* or person* or people* or population* or communit* or group*)).ti,ab. | 33,112 | |
| 26 | ((vulnerab* or disadvantag* or minorit*) adj3 (individ* or person* or people* or population* or communit* or group*) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 1756 | |
| 27 | exp Ethnic Groups/ | 139,042 | |
| 28 | (ethnic* or ethno* or race or racial*).mp. | 248,038 | |
| 29 | (“Black and Minority Ethnic” or “Black & Minority ethnic” or BME or BAME or black african*).mp. | 3756 | |
| 30 | ((ethnic* or ethno* or race or racial* or “Black and Minority Ethnic” or “Black & Minority ethnic” or BME or BAME or black african*) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 9504 | |
| 31 | exp african continental ancestry group/or exp asian continental ancestry group/ | 136,483 | |
| 32 | (africa* or “middle east*” or asia* or iran* or iraq* or israel* or oman* or “united arab emirat*” or UAE or “saudi arabia*” or palestin* or india* or indonesia* or malaysia* or pakistan*).ti,ab. | 520,081 | |
| 33 | (egypt* or yemen* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or kenya* or uganda* or tanzania* or camero?n* or chad* or niger* or benin* or togo* or ghana* or burkin* or ivory coast* or cote d’ivoire or liberia* or guinea* or sierra leone or leonean* or gambia* or senegal* or mauritan* or mali or malian* or “sara subgroup” or ngama).ti,ab. | 259,558 | |
| 34 | ((africa* or “middle east*” or asia* or iran* or iraq* or israel* or oman* or “united arab emirat*” or UAE or “saudi arabia*” or palestin* or india* or indonesia* or malaysia* or pakistan* or egypt* or yemen* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or kenya* or uganda* or tanzania* or camero?n* or chad* or niger* or benin* or togo* or ghana* or burkin* or ivory coast* or cote d’ivoire or liberia* or guinea* or sierra leone or leonean* or gambia* or senegal* or mauritan* or mali or malian* or “sara subgroup” or ngama) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 58,342 | |
| 35 | 13 or 14 or 16 or 18 or 20 or 22 or 24 or 25 or 27 or 28 or 29 or 31 or 32 or 33 | 1,117,829 | |
| 36 | limit 35 to female | 491,179 | Keywords for immigrant populations limited to female (MEDLINE standard limit feature) |
| 37 | (13 or 24 or 27 or 31) and (female* or wom#n or girl* or child* or adolescen*).mp. | 177,101 | MeSHs for immigrant populations limited by “female” keywords |
| 38 | 15 or 17 or 19 or 21 or 23 or 26 or 30 or 34 or 36 or 37 | 526,145 | Terms for immigrant populations, including specific terms for countries of origin where FGM/C is known to be practised, limited to female |
| 39 | exp Community Health Workers/or exp Volunteers/ | 23,517 | All health and allied workers (who may come into contact with women with FGM/C) |
| 40 | exp Occupational Groups/ | 531,564 | |
| 41 | exp Health Personnel/ | 454,091 | |
| 42 | exp Midwifery/ | 17,848 | |
| 43 | exp General Practitioners/or exp Physicians/ | 117,502 | |
| 44 | exp Nurses/or exp Nurses, Community Health/ | 81,947 | |
| 45 | exp Nurses’ Aides/or exp Nursing Staff, Hospital/or exp Nursing Staff/ | 66,494 | |
| 46 | exp Social Workers/or exp Police/ | 4605 | |
| 47 | 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 | 562,187 | |
| 48 | exp Pregnancy/or (pregnan* or birth* or childbirth* or matern* or gyn#e* or obstetric* or menstru* or labo#r* or vulv* or vagina* or uter*).ti,ab. | 1,391,519 | Physical complications or disorders as identified as health impacts of FGM/C in Department of Health and Social Care guidance,124 already “female” by context of terms – so proxy for FGM/C |
| 49 | exp Pregnancy Complications/or exp Pregnancy High Risk/ | 401,801 | |
| 50 | ((pregnan* or birth* or childbirth* or matern* or gyn#e* or obstetric* or menstru* or labo#r* or vulv* or vagina* or uter*) adj3 (poor* or adverse or complicat* or difficult* or disorder* or dysfunction* or disease* or pain* or risk* or danger* or problem* or issue* or concern* or infect* or inflamm*)).ti,ab. | 137,220 | |
| 51 | exp Obstetric Labor Complications/ | 63,618 | |
| 52 | exp Female Urogenital Diseases/ | 1,161,123 | |
| 53 | exp Menstruation Disturbances/ | 27,153 | |
| 54 | exp Genital Diseases, Female/or exp Vaginal Diseases/or exp Vulvar Diseases/ | 432,325 | |
| 55 | exp Vaginismus/or exp Vulvodynia/or exp Dyspareunia/or exp Vaginitis/or exp Vulvovaginitis/ | 14,171 | |
| 56 | exp Pelvic Inflammatory Disease/ | 10,694 | |
| 57 | exp Vaginal Fistula/or exp Rectovaginal Fistula/ | 4659 | |
| 58 | exp Genital Diseases, Female/ | 432,325 | |
| 59 | exp Infertility, Female/ | 27,170 | |
| 60 | ((pelvic* or back* or urolog* or urogenit* or urinat* or genit* or abdomin*) adj3 (poor* or adverse or complicat* or difficult* or disorder* or dysfunction* or disease* or pain* or risk* or danger* or problem* or issue* or concern* or infect* or inflamm*) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 29,027 | |
| 61 | exp Urologic Diseases/ | 698,515 | Physical complications or disorders as identified as health impacts of FGM/C in Department of Health and Social Care guidance,124 limited to “female” (female genital diseases, etc.) – so proxy for FGM/C |
| 62 | exp Pelvic Pain/ | 8163 | |
| 63 | exp Sexual Dysfunctions, Psychological/ | 24,271 | |
| 64 | exp Pelvic Infection/ | 5409 | |
| 65 | exp Kidney Diseases/ | 474,329 | |
| 66 | exp Urinary Fistula/or exp Rectal Fistula/or exp Urinary Bladder Fistula/ | 11,750 | |
| 67 | 61 or 62 or 63 or 64 or 65 or 66 | 737,520 | |
| 68 | limit 67 to female | 352,622 | |
| 69 | 67 and (female* or wom#n or girl* or child* or adolescen*).mp. | 397,916 | |
| 70 | 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 68 or 69 | 2,386,342 | |
| 71 | exp Mental Disorders/ | 1,122,844 | |
| 72 | exp Depressive Disorder, Major/or exp Suicide/or exp Depression/or exp Suicidal Ideation/or exp Depressive Disorder/or exp Bipolar Disorder/or exp Suicide, Attempted/ | 259,964 | |
| 73 | exp Self-Injurious Behavior/or exp Substance-Related Disorders/or exp Social Isolation/ | 329,005 | |
| 74 | exp Sexually Transmitted Diseases, Viral/or exp Sexually Transmitted Diseases/ | 319,070 | |
| 75 | (anxiet* or anxious* or depress* or self-harm* or self-injur* or suicid*).mp. | 650,968 | |
| 76 | ((anxiet* or anxious* or depress* or self-harm* or self-injur* or suicid*) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 30,927 | |
| 77 | (((sex* or viral* or virus* or bacteria*) adj3 diseas*) or HIV or STD* or AIDS).mp. | 516,543 | |
| 78 | ((((sex* or viral* or virus* or bacteria*) adj3 diseas*) or HIV or STD* or AIDS) adj3 (female* or wom#n or girl* or child* or adolescen*)).mp. | 29,597 | |
| 79 | 71 or 72 or 73 or 74 or 75 or 77 | 2,107,493 | |
| 80 | limit 79 to female | 932,164 | |
| 81 | 79 and (female* or wom#n or girl* or child* or adolescen*).mp. | 1,098,666 | |
| 82 | 76 or 78 or 80 or 81 | 1,098,666 | Psychological or STD-related impacts of FGM |
| 83 | exp United Kingdom/or (“united kingdom” or “great britain” or britain or england or scotland or wales or “northern ireland” or british or english or scottish or welsh or “northern irish” or hebrid* or “isle of man”).ti,ab,gc,ia,pl,in. | 1,167,455 | |
| 84 | (AUSTRALIA* or AUSTRIA* or BELGIUM* or belgian* or CANAD* or CHILE* or CZECH* or DENMARK* or danish* or ESTONIA* or FINLAND or finnish or FRANCE or french).mp. | 641,227 | |
| 85 | (GERMAN* or GREECE or greek* or HUNGAR* or ICELAND* or IRELAND or irish or ISRAEL* or ITALY or italian* or JAPAN* or KOREA* or LATVIA* or LUXEMB* or MEXIC*).mp. | 791,022 | |
| 86 | (NETHERLAND* or holland* or dutch or “low countries” or europe* or “NEW ZEALAND*” or NORWAY or norwegian* or POLAND or polish or PORTUGAL or portuguese).mp. | 597,994 | |
| 87 | (SLOVAK* or SLOVENIA* or SPAIN or spanish or SWED* or SWITZERLAND or swiss or TURK* or “UNITED KINGDOM” or “UK” or britain or british or england or english or scot* or wales or welsh or UNITED STATES or “USA” or america*).mp. | 3,770,430 | |
| 88 | 83 or 84 or 85 or 86 or 87 | 5,147,200 | UK or other OECD countries |
| 89 | randomized controlled trial.pt. | 470,445 | |
| 90 | controlled clinical trial.pt. | 94,472 | |
| 91 | randomized.ab. | 403,685 | |
| 92 | placebo.ab. | 189,129 | |
| 93 | clinical trials as topic.sh. | 187,621 | |
| 94 | randomly.ab. | 280,498 | |
| 95 | trial.ti. | 181,309 | |
| 96 | (animals not (humans and animals)).sh. | 4,412,254 | |
| 97 | 89 or 90 or 91 or 92 or 93 or 94 or 95 | 1,138,847 | |
| 98 | 97 not 96 | 1,049,209 | Standard search hedge for randomised clinical trials in MEDLINE – adapted from SIGN |
| 99 | 38 and 47 and (70 or 82) | 7952 | Female immigrants AND Health Workers AND (physical or mental disorders) |
| 100 | 47 and 12 | 1144 | |
| 101 | 12 or 99 or 100 | 59,304 | Women with FGM or (Female immigrants AND Health Workers AND (physical or mental disorders)) or (Health workers AND FGM) |
| 102 | 101 and 88 | 12,154 | . . . AND OECD countries |
| 103 | 102 not 98 | 11,547 | EXCLUDE RCTs |
| 104 | 103 not 96 | 9261 | EXCLUDE animal studies |
Appendix 2 Cumulative Index to Nursing and Allied Health Literature search strategy
Date range searched: 1937 to 10 August 2017.
Date searched: 10 August 2017.
| Number | Query | Limiters/expanders | Results |
|---|---|---|---|
| S1 | (MH “Circumcision, Female”) OR ((MH “Genitalia, Female+”) AND (MH “Medicine, Traditional+”)) | 1184 | |
| S2 | TX (“female genital mutilation” or “female circumcision” or “female genital cutting” or “traditional female genital surgery” or infibulat* or reinfibulat* or defibulat* or clitoridect*) | 1549 | |
| S3 | TX (((ritual* or traditional* or ceremon* or sociali#ation*) N3 (practic* or cut or cutting or surg*)) or circumcis* or excis*)) N3 (female* or wom#n or girl* or child* or adolescen*) | 2449 | |
| S4 | TX (FGM or FGC or TFGS or FGMC or “FGM/C”) | 1167 | |
| S5 | TX (thara or tahar or khitan or khifad or khafad or megrez or absum or mekhnishab or kutairi or ibi or ugwu or sunna or bondo or sonde or gudiniin or halalays or qodiin or tahoor or bagne or gadja or ganza or “fanadu di mindjer” or niaka or kuyango or “musolula karoola”) | 2518 | |
| S6 | S4 OR S5 | Limiters – sex: female | 1354 |
| S7 | TX ((FGM or FGC or TFGS or FGMC or “FGM/C” or thara or tahar or khitan or khifad or khafad or megrez or absum or mekhnishab or kutairi or ibi or ugwu or sunna or bondo or sonde or gudiniin or halalays or qodiin or tahoor or bagne or gadja or ganza or “fanadu di mindjer” or niaka or kuyango or “musolula karoola”) N3 (female* or wom#n or girl* or child* or adolescen*)) | 736 | |
| S8 | TI (egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*) OR AB (egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*) | 10,311 | |
| S9 | (MH “Immigrants+”) OR (MH “Emigration and Immigration”) OR (MH “Transients and Migrants”) OR (MH “Refugees”) | 21,741 | |
| S10 | TX (immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or ex-pat* or transients or newcomer* or new-comer* or alien* or incomer* or in-comer*) | 96,836 | |
| S11 | TX (immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or ex-pat* or transients or newcomer* or new-comer* or alien* or incomer* or in-comer*) N3 (female* or wom#n or girl* or child* or adolescen*) | 7648 | |
| S12 | TX (refugee* or (asylum N1 seek*) or asylee* or (refused N3 (asylum* or refugee*)) or (displaced N1 person*) or exile* or (new N1 arrival) or (country N2 (birth or origin)) or transnational*) | 21,170 | |
| S13 | TX (refugee* or (asylum N1 seek*) or asylee* or (refused N3 (asylum* or refugee*)) or (displaced N1 person*) or exile* or (new N1 arrival) or (country N2 (birth or origin)) or transnational*) N3 (female* or wom#n or girl* or child* or adolescen*) | 2862 | |
| S14 | TX (foreigner* or (foreign N1 (born or citizen* or national* or origin*)) or (non N1 (citizen* or native*)) or ((adoptive or naturali#ed) N1 (citizen* or resident*)) or overstay* or trafficked or “spousal migrant*”) | 7560 | |
| S15 | TX (foreigner* or (foreign N1 (born or citizen* or national* or origin*)) or (non N1 (citizen* or native*)) or ((adoptive or naturali#ed) N1 (citizen* or resident*)) or overstay* or trafficked or “spousal migrant*”) N3 (female* or wom#n or girl* or child* or adolescen*) | 1165 | |
| S16 | TX (((established or long-term or “first generation*” or new* or recent* or current*) N3 (migrant* or migrat* or immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or ex-pat* or transient* or alien*)) or newcomer* or new-comer* or incomer* or in-comer* or ((international or overseas or foreign) N2 (student* or employee* or worker*))) | 24,924 | |
| S17 | TX (((established or long-term or “first generation*” or new* or recent* or current*) N3 (migrant* or migrat* or immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or ex-pat* or transient* or alien*)) or newcomer* or new-comer* or incomer* or in-comer* or ((international or overseas or foreign) N2 (student* or employee* or worker*))) N3 (female* or wom#n or girl* or child* or adolescen*) | 1448 | |
| S18 | TX (“non-UK-born” or “born outside the UK” or “length of residence in the UK” or ((“not lawful*” or “not legal*” or unlawful* or illegal* or unauthori#ed* or “not authori#ed” or uncertain or insecure or legal* or legitimate* or permit* or visa* or irregular* or refused or undocumented) N3 (residen* or student* or worker* or employee* or unemployed or immigrant* or imigrat* or migrant* or migrat*))) | 8980 | |
| S19 | TX (“non-UK-born” or “born outside the UK” or “length of residence in the UK” or ((“not lawful*” or “not legal*” or unlawful* or illegal* or unauthori#ed* or “not authori#ed” or uncertain or insecure or legal* or legitimate* or permit* or visa* or irregular* or refused or undocumented) N3 (residen* or student* or worker* or employee* or unemployed or immigrant* or imigrat* or migrant* or migrat*))) N3 (female* or wom#n or girl* or child* or adolescen*) | 454 | |
| S20 | TX ((vulnerab* or disadvantag* or minorit*) N3 (individ* or person* or people* or population* or communit* or group*)) | 64,064 | |
| S21 | (MH “Special Populations”) | 4275 | |
| S22 | TX ((vulnerab* or disadvantag* or minorit*) N3 (individ* or person* or people* or population* or communit* or group*)) N3 (female* or wom#n or girl* or child* or adolescen*) | 5658 | |
| S23 | (MH “Ethnic Groups+”) | 111,173 | |
| S24 | TI (ethnic* or ethno* or race or racial*) OR AB (ethnic* or ethno* or race or racial*) | 77,242 | |
| S25 | (TI (ethnic* or ethno* or race or racial*) OR AB (ethnic* or ethno* or race or racial*)) N3 (female* or wom#n or girl* or child* or adolescen*) | 1218 | |
| S26 | TI (“Black and Minority Ethnic” or “Black & Minority ethnic” or BME or BAME or black african*) OR AB (“Black and Minority Ethnic” or “Black & Minority ethnic” or BME or BAME or black african*) | 2147 | |
| S27 | (TI (“Black and Minority Ethnic” or “Black & Minority ethnic” or BME or BAME or black african*) OR AB (“Black and Minority Ethnic” or “Black & Minority ethnic” or BME or BAME or black african*)) N3 (female* or wom#n or girl* or child* or adolescen*) | 125 | |
| S28 | (MH “Blacks”) | 43,581 | |
| S29 | (MH “Asians+”) | 23,913 | |
| S30 | TI (africa* or “middle east*” or asia* or iran* or iraq* or israel* or oman* or “united arab emirat*” or UAE or “saudi arabia*” or palestin* or india* or indonesia* or malaysia* or pakistan*) OR AB (africa* or “middle east*” or asia* or iran* or iraq* or israel* or oman* or “united arab emirat*” or UAE or “saudi arabia*” or palestin* or india* or indonesia* or malaysia* or pakistan*) | 124,141 | |
| S31 | (TI (africa* or “middle east*” or asia* or iran* or iraq* or israel* or oman* or “united arab emirat*” or UAE or “saudi arabia*” or palestin* or india* or indonesia* or malaysia* or pakistan*) OR AB (africa* or “middle east*” or asia* or iran* or iraq* or israel* or oman* or “united arab emirat*” or UAE or “saudi arabia*” or palestin* or india* or indonesia* or malaysia* or pakistan*)) N3 (female* or wom#n or girl* or child* or adolescen*) | 9250 | |
| S32 | TI (egypt* or yemen* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or kenya* or uganda* or tanzania* or camero?n* or chad* or niger* or benin* or togo* or ghana* or burkin* or ivory coast* or cote d’ivoire or liberia* or guinea* or sierra leone or leonean* or gambia* or senegal* or mauritan* or mali or malian* or “sara subgroup” or ngama) OR AB (egypt* or yemen* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or kenya* or uganda* or tanzania* or camero?n* or chad* or niger* or benin* or togo* or ghana* or burkin* or ivory coast* or cote d’ivoire or liberia* or guinea* or sierra leone or leonean* or gambia* or senegal* or mauritan* or mali or malian* or “sara subgroup” or ngama) | 29,763 | |
| S33 | (TI (egypt* or yemen* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or kenya* or uganda* or tanzania* or camero?n* or chad* or niger* or benin* or togo* or ghana* or burkin* or ivory coast* or cote d’ivoire or liberia* or guinea* or sierra leone or leonean* or gambia* or senegal* or mauritan* or mali or malian* or “sara subgroup” or ngama) OR AB (egypt* or yemen* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or kenya* or uganda* or tanzania* or camero?n* or chad* or niger* or benin* or togo* or ghana* or burkin* or ivory coast* or cote d’ivoire or liberia* or guinea* or sierra leone or leonean* or gambia* or senegal* or mauritan* or mali or malian* or “sara subgroup” or ngama)) N3 (female* or wom#n or girl* or child* or adolescen*) | 2660 | |
| S34 | S9 OR S10 OR S12 OR S14 OR S16 OR S18 OR S20 OR S21 OR S23 OR S24 OR S26 OR S28 OR S30 OR S32 | Limiters – sex: female | 179,858 |
| S35 | S11 OR S13 OR S15 OR S17 OR S19 OR S22 OR S25 OR S27 OR S31 OR S33 | 28,486 | |
| S36 | S34 OR S35 | 191,459 | |
| S37 | (MH “Mandatory Reporting”) | 4536 | |
| S38 | TI (prevent* or interven* or safeguard* or “duty of care” or ((report* or indicat* or record*) N3 (mandat* or polic* or authorit* or risk*))) OR AB (prevent* or interven* or safeguard* or “duty of care” or ((report* or indicat* or record*) N3 (mandat* or polic* or authorit* or risk*))) | 487,205 | |
| S39 | TI (prevent* or safeguard* or “duty of care” or ((report* or indicat* or record*) N3 (mandat* or polic* or authorit* or risk*))) OR AB (prevent* or safeguard* or “duty of care” or ((report* or indicat* or record*) N3 (mandat* or polic* or authorit* or risk*))) | 253,530 | |
| S40 | S37 OR S39 | 257,178 | |
| S41 | (MH “Community Health Workers”) OR (MH “Community Health Nursing+”) OR (MH “Health Personnel+”) | 448,692 | |
| S42 | (MH “Volunteer Workers”) OR (MH “Police”) OR (MH “Social Workers”) | 24,006 | |
| S43 | (MH “Nurse Midwives”) OR (MH “Midwives+”) OR (MH “Physicians, Family”) | 24,307 | |
| S44 | (MH “Nurses+”) OR (MH “Community Health Nursing+”) OR (MH “Community Mental Health Nursing”) OR (MH “Nursing Assistants”) | 213,388 | |
| S45 | S41 OR S42 OR S43 OR S44 | 460,602 | |
| S46 | (MH “Female Urogenital Diseases and Pregnancy Complications+”) | 219,968 | |
| S47 | (MH “Urinary Tract Infections+”) OR (MH “Pelvic Pain+”) OR (MH “Kidney Diseases+”) | 70,808 | |
| S48 | (MH “Sexual Dysfunction, Female+”) OR (MH “Female Urogenital Diseases+”) | 163,253 | |
| S49 | (MH “Urinary Fistula+”) OR (MH “Rectal Fistula”) OR (MH “Bladder Fistula+”) | 749 | |
| S50 | (MH “Vaginal Fistula+”) OR (MH “Vesicovaginal Fistula”) | 388 | |
| S51 | TI ((pregnan* or birth* or childbirth* or matern* or gyn#e* or obstetric* or menstru* or labo#r* or vulv* or vagina* or uter*) N3 (poor* or adverse or complicat* or difficult* or disorder* or dysfunction* or disease* or pain* or risk* or danger* or problem* or issue* or concern* or infect* or inflamm*)) | 14,683 | |
| S52 | AB ((pregnan* or birth* or childbirth* or matern* or gyn#e* or obstetric* or menstru* or labo#r* or vulv* or vagina* or uter*) N3 (poor* or adverse or complicat* or difficult* or disorder* or dysfunction* or disease* or pain* or risk* or danger* or problem* or issue* or concern* or infect* or inflamm*)) | 35,023 | |
| S53 | TI ((pelvic* or back* or urolog* or urogenit* or urinat* or genit* or abdomin*) N3 (poor* or adverse or complicat* or difficult* or disorder* or dysfunction* or disease* or pain* or risk* or danger* or problem* or issue* or concern* or infect* or inflamm*)) N3 (female* or wom#n or girl* or child* or adolescen*) | 1416 | |
| S54 | AB ((pelvic* or back* or urolog* or urogenit* or urinat* or genit* or abdomin*) N3 (poor* or adverse or complicat* or difficult* or disorder* or dysfunction* or disease* or pain* or risk* or danger* or problem* or issue* or concern* or infect* or inflamm*)) N3 (female* or wom#n or girl* or child* or adolescen*) | 2425 | |
| S55 | (S46 OR S48 OR S50 OR S51 OR S52 OR S53 OR S54) | 248,635 | |
| S56 | S47 OR S49 | Limiters – sex: female | 31,567 |
| S57 | (S46 OR S48 OR S50 OR S51 OR S52 OR S53 OR S54) | Limiters – sex: female | 159,946 |
| S58 | ((S46 OR S48 OR S50 OR S51 OR S52 OR S53 OR S54)) AND (S56 OR S57) | 159,946 | |
| S59 | TI (egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*) OR AB (egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*) | Limiters – sex: female | 4343 |
| S60 | TI ((egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*) N3 (female* or wom#n or girl* or child* or adolescen*)) OR AB ((egypt* or sudan* or ethiopi* or somali* or djibouti* or eritrea* or burkin* or guinea* or sierra leone or leonean* or mauritan* or mali or malian*) N3 (female* or wom#n or girl* or child* or adolescen*)) | Limiters – sex: female | 825 |
| S61 | S1 OR S2 OR S3 OR S6 OR S7 OR S59 OR S60 | 8475 | |
| S62 | (MH “Pregnancy+”) | 149,766 | |
| S63 | (MH “Pregnancy+”) OR TI ((pregnan* or birth* or childbirth* or matern* or gyn#e* or obstetric* or menstru* or labo#r* or vulv* or vagina* or uter*)) OR AB ((pregnan* or birth* or childbirth* or matern* or gyn#e* or obstetric* or menstru* or labo#r* or vulv* or vagina* or uter*)) | 318,410 | |
| S64 | ((MH “Menstruation Disorders+”) OR (MH “Genital Diseases, Female+”) OR (MH “Female Urogenital Diseases+”)) OR ((MH “Vaginal Diseases+”) OR (MH “Vulvar Diseases+”) OR (MH “Vulvodynia”) OR (MH “Dyspareunia”) OR (MH “Vaginitis+”) OR (MH “Vulvovaginitis+”)) OR AB vaginismus OR TI vaginismus | 163,297 | |
| S65 | (MH “Pelvic Inflammatory Disease+”) OR (MH “Pelvic Floor Disorders”) | 992 | |
| S66 | TX ((pelvic* or back* or urolog* or urogenit* or urinat* or genit* or abdomin*) N3 (poor* or adverse or complicat* or difficult* or disorder* or dysfunction* or disease* or pain* or risk* or danger* or problem* or issue* or concern* or infect* or inflamm*) N3 (female* or wom#n or girl* or child* or adolescen*)) | 9648 | |
| S67 | (MH “Urologic Diseases+”) | 93,197 | |
| S68 | S46 OR S48 OR S50 OR S51 OR S52 OR S53 OR S54 OR S62 OR S63 OR S64 OR S66 | 462,716 | |
| S69 | S47 OR S49 OR S65 OR S67 | Limiters – sex: female | 43,874 |
| S70 | (MH “Behavioral and Mental Disorders+”) | 601,398 | |
| S71 | (MH “Suicidal Ideation”) | 4248 | |
| S72 | (MH “Self-Injurious Behavior”) | 2827 | |
| S73 | (MH “Substance Use Disorders+”) | 120,792 | |
| S74 | (MH “Social Isolation+”) | 8038 | |
| S75 | (MH “Sexually Transmitted Diseases+”) | 84,478 | |
| S76 | (anxiet* or anxious* or depress* or self-harm* or self-injur* or suicid*) | 186,507 | |
| S77 | (((sex* or viral* or virus* or bacteria*) N3 diseas*) or HIV or STD* or AIDS) | 125,927 | |
| S78 | S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 | Limiters – sex: female | 328,002 |
| S79 | TX (“united kingdom” or “great britain” or britain or england or scotland or wales or “northern ireland” or british or english or scottish or welsh or “northern irish” or hebrid* or “isle of man”) | 5,325,378 | |
| S80 | (MH “United Kingdom+”) | 277,182 | |
| S81 | TX (AUSTRALIA* or AUSTRIA* or BELGIUM* or belgian* or CANAD* or CHILE* or CZECH* or DENMARK* or danish* or ESTONIA* or FINLAND or finnish or FRANCE or french) | 821,662 | |
| S82 | TX (GERMAN* or GREECE or greek* or HUNGAR* or ICELAND* or IRELAND or irish or ISRAEL* or ITALY or italian* or JAPAN* or KOREA* or LATVIA* or LUXEMB* or MEXIC*) | 1,770,319 | |
| S83 | TX (NETHERLAND* or holland* or dutch or “low countries” or europe* or “NEW ZEALAND*” or NORWAY or norwegian* or POLAND or polish or PORTUGAL or portuguese) | 2,046,199 | |
| S84 | TX (SLOVAK* or SLOVENIA* or SPAIN or spanish or SWED* or SWITZERLAND or swiss or TURK* or “UNITED KINGDOM” or “UK” or britain or british or england or english or scot* or wales or welsh or UNITED STATES or “USA” or america*) | 5,366,848 | |
| S85 | S79 OR S80 OR S81 OR S82 OR S83 OR S84 | 5,403,319 | |
| S86 | ((MH “Clinical Trials+”) OR (MH “Random Assignment”) OR (MH “Placebos”) OR (MH “Quantitative Studies”)) OR PT Clinical trial OR TX ((clinic* n1 trial*) OR (randomi* control* trial*)) OR TX (((singl* n1 blind*) OR (singl* n1 mask*)) OR ((doubl* n1 blind*) or (doubl* n1 mask*)) OR ((tripl* n1 blind*) or (tripl* n1 mask*)) OR ((trebl* n1 blind*) or (trebl* n1 mask*))) OR (placebo* OR (allocat* random*) OR (random* allocat*)) | 1,209,497 | |
| S87 | (MH “Animal Studies”) | 78,080 | |
| S88 | S68 OR S69 OR S78 | 733,358 | |
| S89 | S36 AND S45 AND S88 | 4365 | |
| S90 | S45 AND S61 | 698 | |
| S91 | S61 OR S89 OR S90 | 12,615 | |
| S92 | S85 AND S91 | 12,609 | |
| S93 | S92 NOT S86 NOT S87 | 8628 |
Appendix 3 Excluded studies (with reasons for exclusion)
| Reference | Reason for exclusion |
|---|---|
| Abdel Halim AM. Honorable Daughters: The Lived Experience of Circumcised Sudanese Women in the United States. PhD thesis. Ann Arbor, OH: Ohio University; 2003 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Abdel Magied A, Shareef S. Knowledge, perception and attitudes of a sector of female health providers towards FGM – case study: female doctors. Ahfad J 2003;20:4–17 | Not OECD |
| Abdulcadir O, Catania L, Caselli A. Female genital mutilation (FGM): a comparison between the male and the female view. Int J Gynaecol Obstet 2012;119:S262–3 | Conference abstract |
| Alizadeh V, Hylander I, Kocturk T, Törnkvist L. Counselling young immigrant women worried about problems related to the protection of ‘family honour’ – from the perspective of midwives and counsellors at youth health clinics. Scand J Caring Sci 2010;24:32–40. https://doi.org/10.1111/j.1471-6712.2009.00681.x | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Alizadeh V, Tornkvist L, Hylander I. Counselling teenage girls on problems related to the ‘protection of family honour’ from the perspective of school nurses and counsellors. Health Soc Care Community 2011;19:476–84 | Data on FGM/C not presented |
| Allag F, Abboud P, Mansour G, Zanardi M, Quereux C. Female genital mutilation. Women’s point of view. Gynecologie Obstetrique Fertilite 2001;29:824–8 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Aquino M, Edge D, Smith DM. Pregnancy as an ideal time for intervention to address the complex needs of black and minority ethnic women: views of British midwives. Midwifery 2015;31:373–9 | Data on FGM/C not presented |
| Ariyo D, Ssali R, King-Webb L, Ikpaahindi S. Voices of the Community: Exploring Female Genital Mutilation in the African Community Across Greater Manchester. London: AFRUCA; 2015 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Beck-Karrer C, Levin T, Levin T. Lion women. Conversations with Somalian women and men about female circumcision. Eur J of Womens Stud 1998;5:533–6 | Not empirical research |
| Brown E, Carroll J, Fogarty C, Holt C. ‘They get a C-section . . . they gonna die’: Somali women’s fears of obstetrical interventions in the United States. J Transcult Nurs 2010;21:220–7 | Data on FGM/C not presented |
| Brown E, Porter C. The Tackling FGM Initiative: Evaluation of the Second Phase (2013–2016). London: Options UK; 2016 | Not empirical research |
| Buckland RL. The Everyday Experience of Somali Women in Canada: Implications for Health. MSc thesis. Ottowa, ON: University of Ottawa; 1997 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Burchill J. Safeguarding vulnerable families: work with refugees and asylum seekers. Community Practitioner 2011;84:23–6 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Carolan M. Antenatal care perceptions of pregnant African women attending maternity services in Melbourne, Australia. Midwifery 2010;26:189–201 | Data on FGM/C not presented |
| Chalmers B, Hashi KO. 432 Somali women’s birth experiences in Canada after earlier female genital mutilation. Birth 2000;27:227–34 | Not qualitative research |
| Christiansen CD. The Lived Experience of Circumcision in Immigrant Somali Women: A Heideggerian Hermeneutic Analysis. MA thesis. Champaign, IL: University of Illinois; 1995 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Clarke ALF. The Process of Changed Meanings: A Study of the Canadian Experience of Somali women in the Kitchener-Waterloo Area in Regard to Female Circumcision. PhD thesis. Ann Arbor, MI: Wilfrid Laurier University; 1995 | Not empirical research |
| Clayton-Hathway K. A Pilot Evaluation of Health Services for Communities Affected by FGM in Oxfordshire: Final Report. Oxford: Healthwatch Oxfordshire; 2016 | Not qualitative research |
| Connor JJ, Hunt S, Finsaas M, Ciesinski A, Ahmed A, Robinson BBE. Sexual health care, sexual behaviors and functioning, and female genital cutting: perspectives from Somali women living in the United States. J Sex Res 2016;53:346–59 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Dahlen UM. Female Genital Cutting: Phenomenological Interviews on the Ethiopian Immigrant Mothers’ Experience. Master’s thesis. London: Regent University; 2011 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Degni F, Suominen S, Essen B, El Ansari W, Vehvilainen-Julkunen K. Communication and cultural issues in providing reproductive health care to immigrant women: health care providers’ experiences in meeting the needs of Somali women living in Finland. J Immigr Minor Health 2012;14:330–43 | Data on FGM/C not presented |
| Essen B, Binder P, Johnsdotter S. An anthropological analysis of the perspectives of Somali women in the West and their obstetric care providers on caesarean birth. J Psychosom Obstet Gynecol 2011;32:10–8 | Data on FGM/C not presented |
| Essen B, Johnsdotter S, Binder P. Not too far to walk but too far for reciprocity: maternal mortality in a migration context using the ‘three delays’ framework. Obstet Gynecol Int J 2012;119:S343 | Conference abstract |
| Feldman R. When maternity doesn’t matter: dispersing pregnant women seeking asylum. Bri J Midwifery 2014;22:23–8 | Data on FGM/C not presented |
| Finnstrom B, Soderhamn O. Conceptions of pain among Somali women. J Adv Nurs 2006;54:418–25 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| García Aguado S, Sánchez López MI. Knowledge of healthcare professionals about female genital mutilation. Metas de Enfermería 2013;16:18–22 | Not qualitative research |
| Gele AA, Kumar B, Hjelde KH, Sundby J. Attitudes toward female circumcision among Somali immigrants in Oslo: a qualitative study. Int J Womens Health 2012;4:7–17 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Gele AA, Sagbakken M, Kumar B. Is female circumcision evolving or dissolving in Norway? A qualitative study on attitudes toward the practice among young Somalis in the Oslo area. Int J Womens Health 2015;7:933–43 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Gerrish K, Naisby A, Ismail M. Experiences of the diagnosis and management of tuberculosis: a focused ethnography of Somali patients and healthcare professionals in the UK. J Adv Nurs 2013;69:2285–94 | Data on FGM/C not presented |
| Glavin K, Sæteren B. Cultural diversity in perinatal care: Somali new mothers’ experiences with health care in Norway. Health Science Journal 2016;10:1–9 | Data on FGM/C not presented |
| Glazer E. Gendering chronic pain: socio-cultural embodiment and circumcision in Somali women in Toronto. Gend Med 2010;7:528 | Conference abstract |
| Goldblatt H. Caring for abused women: impact on nurses’ professional and personal life experiences. J Adv Nurs 2009;65:1645–54 | Data on FGM/C not presented |
| Hai DNT, Ghebre R. Comparison of barriers to cervical cancer screening among Somali and Vietnamese women. J Womens Health 2013;22:36 | Conference abstract |
| Henderson A. Factors influencing nurses’ responses to abused women: what they say they do and why they say they do it. J Interpers Violence 2001;16:1284–306 | Data on FGM/C not presented |
| Herrel N, Olevitch L, DuBois DK, Terry P, Thorp D, Kind E, Said A. Somali refugee women speak out about their needs for care during pregnancy and delivery. J Midwifery Womens Health 2004;49:345–9 | Data on FGM/C not presented |
| Houston AR. (In)visible Embodiment: Somali Perspectives of Diabetes and Mental Health in Diaspora. MSc thesis. Boston, MA: Boston University; 2016 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Hoyt MA. In her own words: an exploration of immigrant women’s experiences of reproductive health care through ethnographic narrative. MA thesis. Fredericton, NB: University of New Brunswick; 2010 | Data on FGM/C not presented |
| Isman E, Ekeus C, Berggren V. Perceptions and experiences of female genital mutilation after immigration to Sweden: an explorative study. Sex Reprod Health 2013;4:93–8 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Jacoby SD, Lucarelli M, Musse F, Krishnamurthy A, Salyers V. A mixed-methods study of immigrant Somali women’s health literacy and perinatal experiences in Maine. J Midwifery Womens Health 2015;60:593–603 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Johansen REB. Experiencing Sex in Exile: Can Genitals Change Their Gender? On Conceptions and Experiences Related to Female Genital Cutting (FGC) Among Somalis in Norway. In Hernlund Y, Shell-Duncan B, editors. Transcultural Bodies: Female Genital Cutting In Global Context. New Brunswick, NJ, Rutgers University Press; 2007. pp. 248–77 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Johnsdotter S, Ingvarsdotter K, Ostman M, Carlbom A. Koran reading and negotiation with jinn: strategies to deal with mental ill health among Swedish Somalis. Mental Health, Religion & Culture 2011;14:741–55 | Data on FGM/C not presented |
| Johnsdotter S, Essén B. It is only a tradition: making sense of Swedish Somalis’ narratives of female circumcision and avoiding submission to hegemonic political discourse. Crit Soc Policy 2005;25:577–89 | Not empirical research |
| Johnsdotter S, Essen B. Cultural change after migration: circumcision of girls in Western migrant communities. Best Pract Res Clin Obstet Gynaecol 2016;32:15–25 | Not empirical research |
| Johnsdotter S, Moussa K, Carlbom A, Aregai R, Essen B. ‘Never my daughters’: a qualitative study regarding attitude change toward female genital cutting among Ethiopian and Eritrean families in Sweden. Health Care Women Int 2009;30:114–33 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Johnson-Agbakwu CE, Helm T, Killawi A, Padela AI. Perceptions of obstetrical interventions and female genital cutting: insights of men in a Somali refugee community. Ethn Health 2014;19:440–5 | Focus on men, not women |
| Kallon I, Dundes L. The cultural context of the Sierra Leonean Mende woman as patient. J Transcult Nurs 2010;21:228–36 | Not empirical research |
| Kaplan-Marcusan A, Del Rio NF, Moreno-Navarro J, Castany-Fabregas MJ, Nogueras MR, Munoz-Ortiz L, et al. Female genital mutilation: perceptions of healthcare professionals and the perspective of the migrant families. BMC Public Health 2010;10:193 | Not qualitative research |
| Kay M, Wijayanayaka S, Cook H, Hollingworth S. Understanding quality use of medicines in refugee communities in Australian primary care: a qualitative study. Br J Gen Pract 2016;66:e397–409 | Data on FGM/C not presented |
| Koukoui S, Hassan G, Guzder J. The mothering experience of women with FGM/C raising ‘uncut’ daughters, in Ivory Coast and in Canada. Reproductive Health 2017;14:1–11 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Lazar J, Shipp M, Johnson C. Provider perceptions of sexual desire and dyspareunia among Somali women with female genital cutting. J Sex Med 2010;7:148 | Conference abstract |
| Lane J, Cole G. Pregnancy, prenatal care and delivery perceptions and beliefs of resettled African refugee women in the western United States. Contraception 2013;88:313 | Conference abstract |
| Leishman J. Perspectives of cultural competence in health care. Nurs Stand 2004;19:33 | Data on FGM/C not presented |
| Lephard E, Haith-Cooper M. Pregnant and seeking asylum: exploring women’s experiences ‘from booking to baby’. Bri J Midwifery 2016;24:130–6 | Data on FGM/C not presented |
| Lewig K, Arney F, Salveron M. Challenges to parenting in a new culture: implications for child and family welfare. Eval Program Plann 2010;33:324–32 | Data on FGM/C not presented |
| Leye E. Midwifery training needs identified when caring for women with female genital mutilation. Evid Based Nurs 2016;19:7 | Not empirical research |
| Liao LM, Elliott C, Ahmed F, Creighton SM. Adult recall of childhood female genital cutting and perceptions of its effects: a pilot study for service improvement and research feasibility. J Obstet Gynaecol 2013;33:292–5 | Not qualitative research |
| Lien IL, Schultz JH. Internalizing knowledge and changing attitudes to female genital cutting/mutilation. Obstet Gynecol Int 2013;2013:467028 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| McCarthy R, Haith-Cooper M. Evaluating the impact of befriending for pregnant asylum-seeking and refugee women. Bri J Midwifery 2013;21:404–9 | Data on FGM/C not presented |
| McLeish J. Maternity experiences of asylum seekers in England. Bri J Midwifery 2005;13:782–5 | Data on FGM/C not presented |
| Mitello L, Proietti A. Feminine genitals modification: survey of a new phenomenon for nurse today. Second Part. Prof Inferm 2006;59:242–5 | Not qualitative research |
| Mitello L, Proietti A. Female genital modification: survey of new phenomenon for nurses today. First Part. Prof Inferm 2006;59:171–81 | Not empirical research |
| Morris MD, Popper ST, Rodwell TC, Brodine SK, Brouwer KC. Healthcare barriers of refugees post-resettlement. J Community Health 2009;34:529–38 | Data on FGM/C not presented |
| Morison LA, Dirir A, Elmi S, Warsame J, Dirir S. How experiences and attitudes relating to female circumcision vary according to age on arrival in Britain: a study among young Somalis in London. Ethnicity & Health 2004;9:75–100 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Mwangi-Powell F. Female Genital Mutilation: a Case Study in Birmingham. FORWARD; 2000 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Nash E, Ranka P. Female genital mutilation: knowledge, confidence, and approach to care in clinical practice of midwives and nurses in the UK. Int J Gynecol Obstet 2015;131:E110 | Not qualitative research |
| Nur Z. Cultural Competence in Health Care: Exploring the Experiences of Muslim Women within the Ontario Healthcare System. MSc thesis. Oshawa, ON: University of Ontario Institute of Technology; 2014 | Data on FGM/C not presented |
| Ogbagzy RA. The Construction of Eritrean Women’s Identity in the Canadian Context. MA thesis. Toronto, ON: University of Toronto; 1999 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Ogunsiji O. Understanding the dilemma of de-infibulation for women living with female genital mutilation. Australian Nursing & Midwifery Journal 2015;22:51 | Not empirical research |
| Ogunsiji O, Wilkes L. Cultural explanations and procedures about female genital mutilation. Aus Nur Midwifery J 2015;22:51 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Ogunsiji O, Wilkes L, Peters K, Jackson D. Knowledge, attitudes and usage of cancer screening among West African migrant women. J Clin Nurs 2013;22:1026–33 | Data on FGM/C not presented |
| Olsson E, Lau M, Lifvergren S, Chakhunashvili A. Community collaboration to increase foreign-born women’s participation in a cervical cancer screening program in Sweden: a quality improvement project. Int J Equity Health 2014;13:62 | Data on FGM/C not presented |
| Pavlish CL, Noor S, Brandt J. Somali immigrant women and the American health care system: discordant beliefs, divergent expectations, and silent worries. Soc Sci Med 2010;71:353–61 | Data on FGM/C not presented |
| Peters K. Reasons why women choose a medical practice or a women’s health centre for routine health screening: worker and client perspectives. J Clin Nurs 2010;19:2557–64 | Data on FGM/C not presented |
| Phillimore J. Migrant maternity in an era of superdiversity: new migrants’ access to, and experience of, antenatal care in the West Midlands, UK. Soc Sci Med 2016;148:152–9 | Data on FGM/C not presented |
| Quilliam S. Female genital mutilation: three questions for us to consider. J Fam Plann Reprod Health Care 2015;41:235–7 | Not empirical research |
| Radford K. ‘Unkind cuts’: health policy and practice versus the health and emotional well-being of asylum-seekers and refugees in Ireland. J Ethn Migr Stud 2010;36:899–915 | Data on FGM/C not presented |
| Razzak M. Sexual medicine: pain and pleasure-reconstruction after female genital mutilation. Nat Rev Urol 2012;9:447 | Not empirical research |
| Reis E. Culture and cutting. The Hastings Center Report 2012;42:3 | Not empirical research |
| Rimmer SN. [Theme: circumcision. Somali women talk about taboo.] Sygeplejersken 1994;94:12–13 | Not empirical research |
| Roberts TL, Poblete X. Female Genital Mutilation: A Survey of Awareness, Training and Current Practice. Archives of Disease in Childhood: Annual Conference of the Royal College of Paediatrics and Child Health, RCPCH 2015. Birmingham: BMJ Publishing Group; 2015 | Conference abstract |
| Rogers C, Earnest J. A cross-generational study of contraception and reproductive health among Sudanese and Eritrean women in Brisbane, Australia. Health Care Women Int 2014;35:334–56 | Data on FGM/C not presented |
| Rosenberg LB, Gibson K, Shulman JF. When cultures collide: female genital cutting and U.S. obstetric practice. Obstet Gynecol 2009;113:931–4 | Not empirical research |
| Rosenberg E, Kirmayer LJ, Xenocostas S, Dao MD, Loignon C. GPs’ strategies in intercultural clinical encounters. Fam Pract 2007;24:145–51 | Data on FGM/C not presented |
| Roth K. Giving refuge: reflections on working with asylum seekers. J Pain Symptom Manage 2010;40:149–54 | Not empirical research |
| Sala R, Manara D. Nurses and requests for female genital mutilation: cultural rights versus human rights. Nurs Ethics 2001;8:247–58 | Not empirical research |
| Schuster S. ‘Gosh’: a cross-cultural encounter with a Somali woman, a male interpreter and a gynecologist on female genital cutting/mutilation. Patient Educ Couns 2015;98:127–8 | Not empirical research |
| Shelp A. Women helping women: the Somali doula initiative. Int J Childbirth Educ 2004;19:4–7 | Not qualitative research |
| Shipp MPL, Francis SA, Fluegge KR, Asfaw SA. Perceived health issues: a perspective from East-African immigrants. Health, Culture and Society 2014;6:13–32 | Data on FGM/C not presented |
| Sigurjonsson H, Jordal M, Lundgren TK. Reconstructive surgery after female genital mutilation. Int J Gynecol Obstet 2015;131:E318–9 | Conference abstract |
| Simpson J, Robinson K, Creighton SM, Hodes D. Female genital mutilation: the role of health professionals in prevention, assessment, and management. Br Med J 2012;344:e1316 | Not empirical research |
| Sokolik L. Somali immigrant and refugee women’s experience of pregnancy and childbirth in the American healthcare system. Commun Nurs Res 2007;40:538 | Conference abstract |
| Sudbury H, Robinson A. Barriers to sexual and reproductive health care for refugee and asylum-seeking women. Bri J Midwifery 2016;24:275–81 | Not empirical research |
| Sundby J. Genital mutilation of women--is it a concern for Gynecologists? Acta Obstet Gynecol Scand 1996;75:513–5 | Not empirical research |
| Talle A. From ‘Complete’ to ‘Impaired’ Body: Female Circumcision in Somalia and London. Disability in Local and Globalworlds. Berkeley, CA: University of California Press; 2007 | Not empirical research |
| Taillens F. [‘I will not circumcise my daughter’.] Krankenpflege - Soins Infirmiers 2012;105:55 | Not empirical research |
| Tait P. Refugee women in Australia and woman-centered midwifery care. Nuritinga 2013:31–9 | Not empirical research |
| Tantet C, Aupiais C, Sorge F, Levy D, Lafon-Desmurs B, Faye A. MIG-01 – Female genital mutilations: evaluation of the knowledge of general practitioners and physicians in travel counseling. Med Mal Infect 2016;46:77 | Not qualitative research |
| Tatah EF. Female Circumcision: A Phenomenological Study of Somalian Immigrants to the United States. PhD thesis. Minneapolis, MN: Walden University; 2016 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Trueland J. School nurses take lead on FGM. Nurs Stand 2014;28:22–3 | Not empirical research |
| Vercoutere A, Temmerman M, Leye E. Female genital mutilation, a story far away from home? Ethical, legal and clinical aspects of mutilated women in western countries. Tijdschrift voor Geneeskunde 2011;67:237–41 | Not empirical research |
| Villani M. From the ‘maturity’ of a woman to surgery: conditions for clitoris repair. Sexologies 2009;18:259–61 | Not qualitative research |
| Villani M. The way of speaking about ‘mutilation’ and performing ‘repairing’. J Sex Med 2011;8:242 | Not qualitative research |
| Villani M. Experiences with clitoris repair with counselling or counselling only in France, for effect on sexual satisfaction for women with FGM. Int J Gynecol Obstet 2012;119:S255 | Conference abstract |
| Villani M, Griffin J, Bodenmann P. In their own words: the health and sexuality of immigrant women with infibulation living in Switzerland. Soc Sci 2016;5:1 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Vissandjee B, Denetto S, Migliardi P, Proctor J. Female genital cutting (FGC) and the ethics of care: community engagement and cultural sensitivity at the interface of migration experiences. BMC Int Health Hum Rights 2014;14:1–18 | Not empirical research |
| Vloeberghs E, Knipscheer J, van der Kwaak A, Naleie Z, van den Muijsenbergh M. Veiled Pain: A Study in the Netherlands on the Psychological, Social and Relational Consequences of Female Genital Mutilation. Pharos–Dutch National Knowledge and Advisory Centre on Refugees and Migrants’ Health; 2010 | Duplicate report of included paper Vloeberghs E, et al.208 |
| Wade L. The politics of acculturation: female genital cutting and the challenge of building multicultural democracies. Soc Probl 2011;58:518–37 | Data presented on FGM/C, but no specific focus on FGM/C-related health care |
| Williams KW. Somali Bantu Health Experience: Refugee Resettlement in South Carolina. PhD thesis. Columbia, SC: University of South Carolina; 2006 | Data on FGM/C not presented |
| Williams N, Offer GJ, Williams S, Everson N. Parental attitude in children referred for circumcision. Br J Surg 1997;84:1722–3 | Data on FGM/C not presented |
| Willis S. The cutting season. J Fam Health 2014;24:9–12 | Not empirical research |
| Wimmer-Puchinger B, Wolf H, Engleder A. [Female migrants in the health care system. Health care utilisation, access barriers and health promotion strategies.] Migrantinnen im Gesundheitssystem Inanspruchnahme, Zugangsbarrieren und Strategien zur Gesundheitsforderung Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2006;49:884–92 | Not empirical research |
| Young H, McGrath K. A Review of Circumcision in New Zealand: ‘I Never Liked Doing Them and I was Pleased to Give Them Up’. Understanding Circumcision: A Multi-Disciplinary Approach to a Multi-Dimensional Problem. Dordrecht, the Netherlands: Kluwer Academic Publishers; 2001 | Data on FGM/C not presented |
| Yusuf L, Negash S. Vaginal calculus following severe form of female genital mutilation: a case report. Ethiop Med J 2008;46:185–8 | Not in an OECD country |
| Zenner N, Liao LM, Richens Y, Creighton SM. Quality of obstetric and midwifery care for pregnant women who have undergone female genital mutilation. J Obstet Gynaecol 2013;33:459–62 | Not qualitative research |
Appendix 4 The JBI-QARI critical appraisal questions
Appendix 5 The JBI data-extraction tool
Appendix 6 Review 1: study characteristics
| Study: authors (year of publication) | Country | Study aims, focus and/or research question | Region and setting (where specified) | Methodology and/or theoretical perspective | Methods and recruitment (where stated) | Data analysis | Whole study sample | Eligible participants and country of origin |
|---|---|---|---|---|---|---|---|---|
| Abdi (2012)163 | UK | To determine the role of FGM/C in creating a social, individual and gendered identity for a Somali woman |
East and north-east regions of London African Well Women’s Service in North London |
Narrative and life history approach |
In-depth interviews. Recruited women who held a strong anti-FGM/C opinion Snowball sampling used |
Analysis using theoretical concept of the ‘three bodies’ |
Two gynaecologists, one counsellor and one midwife 16 Somali women Two men Age range: 20–72 years |
16 Somali women |
| Abdullahi et al. (2009)185 | UK | To explore the barriers to uptake of cervical screening and to identify strategies for overcoming these barriers |
London boroughs, UK, London, Borough of Camden North London Somali community centre |
Qualitative methods |
Focus groups and in-depth interviews Recruitment from a range of settings Included snowball sampling |
Thematic analysis informed by an interpretivist approach |
50 Somali-born women Age range: 25–64 years |
50 Somali-born women |
| Ahlberg et al. (2004)186 | Sweden | Questions why FGM/C persists despite eradication interventions and the migration to non-FGM/C-practising areas | Different forums including a school, youth clinics and a girls’ football team | Emergent research design in the tradition of qualitative research |
Individual and group interviews Snowball sampling used |
Thematic analysis | 30 men, 50 women, 10 girls, five boys and 15 professionals | 50 women of Somali origin |
| Ahmed (2005)184 | UK | To explore the influence of cross-cultural psychology, women’s experience of FGM/C and their attitudes towards it |
West, East and South London and Sheffield Women’s homes, community centre and a mosque |
Qualitative methods | Focus groups recruited via word of mouth, through attending Somali community centres and verbal advertising of the project | Thematic analysis |
56 women Age range: 18–70 years |
56 women. The majority born in Somalia – with some born in UK and the Middle East |
| Ameresekere et al. (2011)187 | USA | To assess the prevalence of FGM/C in the interviewed sample, gain insight into commonly held beliefs about caesarean delivery and understand patient perceptions of communication surrounding caesarean delivery and FGM/C by obstetric providers in the USA | Greater Boston | Exploratory qualitative study |
Semistructured in-depth interviews Snowball sampling and linkage with the Somali Development Centre, a local community-based organisation |
Thematic analysis |
23 Somali immigrant women Age range: 25–52 years |
23 Somali participants |
| Asefaw (2007)170 | Eritrea and Germany | To explore whether or not migration changes the participants’ attitude towards FGC. How do circumcised women deal with it in a society that opposes FGC? Can coherence and reasons be determined for why circumcised women subjectively suffer more in migration compared with when they live in their country of origin? | In the migrant’s homes, in clinics or as part of awareness campaigns of the woman’s organisation FORWARD | Mixed methods. Survey and qualitative methods | Survey and semistructured qualitative interviews | Unclear |
420 women and 50 men Age range: 15–70 years |
31 Eritrean migrants |
| Baldeh (2013)174 | Scotland | To explore the experiences of obstetric care in Scotland among women who have undergone FGM/C. The objectives are to explore how women with FGM experience obstetric care in Scotland; the role of health workers in helping or hindering communication; potential changes and improvements in services |
Glasgow and Edinburgh In participants’ homes |
Qualitative approach, interpretivist paradigm and a feminist perspective |
In-depth interviews Convenience sampling used |
Thematic analysis | Seven women | Seven women in total |
| Ballesteros Meseguer et al. (2014)172 | Spain | To explore the perceptions of a group of women who had experienced FGM/C regarding their sexual and reproductive health, with an aim to consider the impact on their sexual relationships, pregnancy and labour, as well as the social repercussions of this practice |
Region of Murcia, Spain In participants’ homes |
Phenomenological qualitative study |
In-depth interviews using structured open-ended approach Informal conversations with midwives |
Discourse analysis |
Nine sub-Saharan Africa women Mean age: 30 years |
Nine women from Senegal |
| Behrendt (2011)164 | Germany | To listen to the opinions, perceptions and propositions of immigrants from sub-Saharan Africa regarding the practice of FGM/C. To develop an effective and locally adapted approach to promote the abandonment of FGM/C among immigrant groups in Hamburg | Hamburg | Participatory, co-operative approach that engages community members in a joint evaluation research process. Triangulated research design behaviour change model |
Mixed methods Qualitative and quantitative data collection from different target groups:Snowball sampling |
Qualitative data analysed and classified into themes. Quantitative data analysed using IBM SPSS Statistics (IBM Corporation, Armonk, NY, USA) |
Total number of 1767 participants with African migration background were interviewed for the quantitative survey 91 semistructured interviews with African community members 27 interviews with health professionals Age range: 15–83 years |
91 key informant interviews – largely from Ghana, Nigeria and Togo |
| Beine et al. (1995)188 | USA | To understand their cultural beliefs and behaviours better during pregnancy and to determine their attitudes towards their prenatal care experiences in San Diego, in order to inform providers and enhance culturally relevant service programmes | Conducted at International Rescue Committee office or private homes of group participants | Exploratory study |
Focus group interview Recruitment via community social networks |
Content analysis |
14 women Age range: 20–42 years |
14 Somali women |
| Berggren et al. (2006)189 | Sweden | To explore the experience of FGM and the experiences of encounters with Swedish maternal health care among women from Eritrea, Somalia, and Sudan living in Sweden |
Three cities in Sweden Conducted in the women’s homes |
Exploratory qualitative study | 26 interviewees recruited via snowball sampling or network sampling | Latent content analysis |
22 women, six from Eritrea, 11 from Somalia, and five from Sudan (one excluded as no FGM) Age range: 24 to 73 years |
21 women from Eritrea, Somalia or Sudan |
| Betts (2011)175 | Canada | To critically examine popular ideas of Somali women’s identity, gender and sexuality in Canada and to evaluate Somali women’s experiences with Canadian health-care professionals, and how it compares with their experiences with medical professionals in Somalia | Greater Toronto area, Canada. From a community centre in a small office | Anthropological methods | Individual and paired interviews; one discussion group of 14 women | Placed loosely into categories | Thirteen women aged 18–65 years | 13 Somali women |
| Bravo Pastor del Mar (2014)173 | Spain | To identify the knowledge, attitudes and experiences regarding FGM of a group of women from sub-Saharan African countries where FGM/C is a traditional practice |
Region of Murcia, Spain The interviews were held individually at the homes of the participants, at their request, always in the absence of the husband and occasionally in the presence of children |
A qualitative study using the life story method |
Life story interviews held until data saturation was reached. Informal conversations including telephone calls, e-mails, informal chats and informal meetings with key informants. Sociodemographic questionnaire Contact through different associations for African women and snowball sampling |
The analysis was carried out using the categories that emerged from the narratives collected in the interviews |
20 Senegalese women, two Nigerian women and two Gambian women Age range: 23–42 years |
20 Senegalese women, two Nigerian women and two Gambian women |
| Bulman and McCourt (2002)56 | UK | To develop an understanding of the reality faced by Somali women in their contacts with the maternity services in the UK and to explore professionals perceptions of Somali women and their maternity care needs – how they approached providing for these needs and their ideas for improving services |
West London Conducted in participants’ homes or clinics |
Qualitative (ethnographic context narrative approach) |
Six individual interviews and two focus groups with Somali women, recruited via snowball sampling method Two focus groups with midwives, (caseload and hospital midwives) Individual interviews with a Somali health-link worker, a woman on the Health and Race Working Group and an obstetric registrar |
Thematic analysis |
12 Somali women participating in qualitative interviews Health workers (number not specified) were also interviewed |
12 Somali women |
| Carroll et al. (2007)190 | USA | To explore the range of Bantu and other Somali women’s experiences with communication about preventative health services in the USA in order to understand the role communication plays in disparities in this population | Rochester, NY, USA. At a time and place convenient to the participant | Grounded theory | Individual interviews, a Somali women’s focus group was conducted to check thematic validity and clarify questions and concepts. Word of mouth, key informants and primary care provider referrals; and snowballing | Grounded theory, a coding/editing method that extracts emerging themes |
34 women Age range: 18–53 years (median age: 27 years) |
34 Somali refugee women |
| Chalmers et al. (2002)191 | Canada | To explore recent perinatal experiences in Canada | Greater Toronto region, at participants’ homes | Unclear |
Sampling from community sites and snowball sampling Structured questionnaire with four open-ended questions, administered face to face involving reflection and discussion |
Unclear |
432 Somali women Mean age: 34 years |
415 Somali women (who responded to the open-ended questions) |
| Degni et al. (2014)192 | Finland | To explore immigrant Somali women’s experiences of reproductive and maternity health-care services and their perceptions about the service providers |
Helsinki, Vantaa, Espoo and Turku in Finland Conducted at women’s homes and swimming pool hall |
Exploratory, qualitative study | Focus group discussions via purposeful sampling | Guided by concepts of cultural care |
70 women Age range: 18–50 years |
70 Somali women |
| d’Entremont et al. (2014)193 | France | Explored the experiences of childbirth for women who have been excised | At a place of the woman’s choosing | Hermeneutic phenomenology Gadamerian philosophy |
Interviews Purposive sampling methods |
Constant, circular process of thematic, textual interpretations | Four women | Four women from different countries |
| Essén et al. (2000)194 | Sweden | To explore the attitudes, strategies and habits of Somalian immigrant women related to pregnancy and childbirth, in order to gain an understanding as to how cultural factors might affect perinatal outcome | Localities of the different Somalian immigrant associations in their own residential areas | Qualitative | Qualitative in-depth interviews. Recruited from community organisations | Systematic textual analysis |
15 women Age range: 20–55 years |
15 Somali women |
| Fawcett (2014)78 | USA | To identify and measure patterns of cultural knowledge and variations (cross-cultural agreement and disagreement) between Somali resettled refugee women and health-care providers on childbearing models. To investigate and measure intracultural variations in the domain of childbearing knowledge among Somali resettled refugee women. To explore the subjective and intersubjective perceptions of female circumcision | Arizona Metropolitan Phoenix area, in a cafe or participants’ homes |
Quantitative survey and ethnographic methodologies and phenomenological approaches using open-ended semistructured interviews Used theory of Cultural Consensus Model and concepts of embodiment |
Culture consensus questionnaire, participatory observations, in-depth semistructured interviews Used snowball sampling via community organisations |
Phenomenological analysis and inductive explorative approach |
Questionnaires (n = 174) Interviews: Somali resettled refugee women (n = 30) Health-care providers (n = 10) Age range: 18–70 years |
30 Somali resettled refugee women |
| Gali (1997)176 | USA | To explore the relationship between the psychological and the medical concerns circumcised women face and barriers to reproductive health-care delivery in the USA | San Francisco Bay area | Qualitative exploratory research |
Semistructured interviews were conducted in person and by mail Recruitment using community organisations |
Content analysis | 26 women aged 21–45 years | 26 women from Sudan, Eritrea, Ethiopia and Egypt |
| Ghebre et al. (2015)195 | USA | Exploring suitable language, structure and context to describe cervical cancer prevention and screening methods among women in Minnesota’s Somali community |
Minnesota Community locations |
Qualitative study with community engagement socioecological framework | Informant interviews. Used snowball sampling | Themes and subthemes using the socioecological framework |
23 participants Age range: 26–45 years |
23 Somali women |
| Glazer (2012)177 | Canada | Aimed to explore women’s interpretations of FGM and its associated pain | Greater Toronto Area, Canada, at a community health centre | Mixed methods, including a qualitative component drawing on interpretive and embodied phenomenology | Qualitative interview semistructured interviews using a convenience sample | Phenomenological analysis |
14 Somali-Canadian participants Age range: 21–46 years |
14 Somali-Canadian participants |
| Glover et al. (2017)196 | UK | Investigate the experiences of women who had undergone FGM and the psychological effects they had experienced. It also sought to understand the psychological impact of physical health complications, survivor’s resilience and their cultural context | Multiple UK settings |
A qualitative methodology of grounded theory Principles of feminist research were observed |
In-depth interviews from a non-probability convenience sampling frame based on snowballing sampling | Theoretical memos and grounded theory analysis |
20 women survivors of FGM Mean age 38 years (standard deviation 6.5, range 25–51 years) |
20 women from various countries: Somalia (n = 10), Kenya (n = 2), South Africa (n = 6) and The Gambia (n = 2) |
| Guerin et al. (2006)197 | Australia and New Zealand | To enhance the understanding of the immigration experience on the reproductive health of women from Horn of African and Middle Eastern countries resident in Victoria to provide a safe means by which Somali women could express their views about FGM/C |
Melbourne, Australia, and New Zealand In homes of the participants |
Ethnographic cohort design Community-based participatory research |
In-depth, open-ended and unstructured interviews, focus group discussions and participant observation Sampling involved using community networks and snowball approach |
Thematic analysis |
Australia (n = 255) and New Zealand (n = 64) African women in the sample (n = 141) Middle Eastern women (n = 114) 574 women Age range: 19–50 years |
10 women from Somalia, Ethiopia, Eritrea, Sudan and Nigeria |
| Hill et al. (2012)198 | USA | To describe and better understand Somali immigrant women’s health-care experiences and beliefs regarding pregnancy and birth in the USA |
North-eastern USA Setting not given |
Qualitative study | Focus group convenience sampling and women in turn identified friends and family | Thematic content analysis |
18 participants Age range: 27–42 years |
18 Somali women |
| Hussein (2010)57 | UK | To gain an in-depth understanding of some of the experiences and perceptions of women coming from countries with high prevalence rates of FGM/C living in Bristol | Setting not given | PEER and tenets of social construct | Informal in-depth interviews in third-person, loosely structured interviews. Equipping members from the community to become ‘PEER researchers’ | Not stated | Eight adult women | Eight Somali and Sudanese adult women |
| Hussen (2014)165 | New Zealand | To understand the situation of both the Christchurch women with FGM and their health providers in order to increase knowledge of FGM and ensure improved health services for women with this condition | Christchurch, New Zealand, at community gatherings | Qualitative descriptive research methods |
Focus group approach for women from East Africa known to the social worker and researcher Individual interviews with health professionals |
Thematic analysis |
20 focus group participants – mean age 21–65 years Three health providers |
20 women from Eritrea, Ethiopia, Somalia and Sudan |
| Johansen (2017)199 | Norway | Explores experiences and perceptions of premarital deinfibulation. It explores whether Somali and Sudanese men and women understand deinfibulation as a purely medical issue or whether their use of the services is also affected by the cultural meaning of infibulation | Oslo and other villages and towns in Norway. From participants’ homes, workplaces or public spaces, such as a coffee bar or a park | Qualitative study |
In-depth and key informant interviews Participant observation validation seminars. Utilised Snowball sampling |
Themes and patterns |
23 women and 13 men Age range: 18–65 years |
23 Somali and Sudanese women |
| Jones (2010)179 | UK | To understand the experiences and views of women who had undergone FGM/C | South England, UK, in participants’ own homes or the community centre | IPA relativist approach | Semistructured interview. Recruited from FORWARD, community group | IPA |
Six participants Age range: 19–45 years |
Six participants from Sudan and Somalia |
| Khaja (2004)159 | Canada and the USA | To describe their experiences with circumcision and to share the personal and cultural meanings of those experiences | Toronto, Canada, and Salt Lake City, Utah, USA. Setting not stated | Life history methodology/ethnographic | Face-to-face, individual life history interviews. Purposive sampling recruited with the assistance of targeted Somali community members or service providers | Content analysis |
17 women Age range: 20–79 years |
17 Somali women |
| Khaja et al. (2010)160 | Canada and the USA | Examined the lives of Somali Muslim women who were circumcised |
Ontario, Canada, and Salt Lake City, Utah, USA Setting not stated |
Exploratory qualitative | Face-to-face interviews | Not stated |
17 circumcised Somali women Age range: 20–79 years |
17 circumcised Somali women |
| Lundberg and Gerezgiher (2008)200 | Sweden | To explore the experiences from pregnancy and childbirth related to FGM/C among Eritrean immigrant women | At informants’ homes or in a separate room | Ethnographic method |
Semistructured and open-ended in-depth interview Purposive sampling with snowball sampling technique |
Thematic analysis |
15 women Age range: 31–45 years |
15 Eritrean women |
| Maier (2003)171 | Austria | Three questions:
|
Not stated | Qualitative research | Guided interviews with a relatively open design | Not stated | Three women | Three women from different countries |
| Maternity Action (2014)180 | UK | To explore potential barriers to health care, both for women in general and for women who experience comparatively poor health outcomes, in order to contribute to an understanding of how these may be addressed | Leeds, Manchester and London, UK. Community groups were hosted and facilitated organisations | Online survey and a series of focus groups | Focus groups recruited from service user networks | Themes from the literature |
261 in the survey 23 women in focus groups |
23 women from several countries |
| McNeely and Christie-de Jong (2016)201 | USA | To explore perspectives of Somali refugees on FGM/C and potential changes in these after migration to the USA | Denver metropolitan area, USA, in participants’ homes | Descriptive, sociocultural study | Semistructured and open-ended interviews; snowball sampling with two gatekeepers | Thematic content analysis |
13 Somali refugees Age range: 20–70 years |
13 Somali women |
| Moxey and Jones (2016)202 | UK | To explore how Somali women exposed to FGM experience and perceive antenatal and intrapartum care in England |
Birmingham, West Midlands In a private room at a community centre |
Descriptive qualitative methodology | Semistructured face-to-face interviews purposively sampled from community centres and using a snowball approach | Inductive thematic analysis |
10 women Age range: 20–49 years |
10 Somali women |
| Murray et al. (2010)203 | Australia | To uncover first-person descriptions of the birth experiences of African refugee women in Brisbane, Australia, and to explore the common themes that emerged from their experiences | In room at a clinic or in participants’ own homes | Phenomenology Husserlian phenomenological framework | Semistructured interviews; purposeful, snowball strategy | Giorgi’s phenomenological analysis319 |
10 women Age range: 20–40 years |
10 women from Sudan, Liberia, Ethiopia and Somalia |
| Norman et al. (2016)47 | UK | Rapid participatory study among migrant communities in Norfolk and Essex, to help shed more light on this issue and to support their community engagement programme | Norfolk, and Essex, in the community | PEER – a qualitative, participatory research methodology | Interviews using snowball sampling | Participatory thematic analysis | 18 peer researchers and 33 interviewees (each of the peer researchers chose two friends/peers to interview) | 33 women from various countries |
| Norman et al. (2009)58 | UK | To gain in-depth insights from women originally from high-prevalence FGM countries, and currently living in and around Westminster | Borough of Westminster, London, in the community | PEER – a qualitative, participatory research method | In-depth conversational interviews; snowball sampling used | Participatory thematic analysis |
10 peer researchers conducted interviews with three friends each (n = 30). Peer researchers were also interviewed Mean age: ≥ 25 years |
40 women (10 peer researchers who were also interviewed and 30 other women) from Sudan, Eritrea and Somalia |
| O’Brien et al. (2017)181 | Scotland | To facilitate community engagement with FGM-affected populations, to enable their voices to contribute to the development of awareness raising around FGM and to ensure culturally appropriate FGM services for Scotland | Glasgow and Edinburgh, Scotland, in the community | PEER ethnographic research principles | Interviews with contacts in community-based organisations and friends | Participatory analysis | 19 peer researchers (who were also interviewed) who then carried out 29 interviews | 48 women (19 peer researchers who were also interviewed and 29 women) from Sudan, Nigeria and Zimbabwe |
| O’Brien et al. (2016)182 | Scotland | To facilitate community engagement on FGM with women, men, young people and religious leaders to enable their voices to be heard and contribute to the development of awareness raising around FGM as well as ensuring culturally appropriate services for Scotland | Glasgow and Edinburgh, Scotland, in the community | PEER ethnographic research principles | Interviews and focus groups. Convenience and snowball sampling through contacts | Participatory analysis | 28 peer researchers (12 women, 16 men) who carried out 78 interviews | 39 women (nine female peer researchers who were also interviewed and 30 women) from 17 African countries |
| Palfreyman et al. (2011)183 | UK | To explore FGM within the context of Birmingham | Birmingham | PEER | In-depth semistructured interviews with and by peers recruited using community organisations and snowball sampling | Participatory thematic analysis |
15 peer researchers conducted a total of 90 interviews Age range: 17–48 years |
105 women (15 peer researchers who were also interviewed and 90 women) from Somali, Eritrea, Sudan, Sierra Leone and The Gambia |
| Recchia and McGarry (2017)204 | UK | The overall aim of the study was to develop and facilitate a participant-led arts-based workshop with women who were survivors of FGM in order to explore their experiences and the impact of FGM on their health and well-being |
Nottingham At a local FGM specialist support organisation |
Creative narrative approach, which included the sharing of personal stories, the creation of pottery models and the sharing of artefacts – arts-based research approach using a feminist theoretical framework | The composition of the workshop essentially encompassed two main strands: the creation of a persona and sharing artefacts. Recruited through a local FGM specialist support organisation | Narrative approach |
Six women agreed to take part in the project Age range: 25–51 years |
Six women from Kenya, Nigeria and Ethiopia |
| Safari (2013)205 | UK | Explored women’s experience of deinfibulation and its aftermath |
London At an NHS hospital or the participant’s home |
Qualitative approach IPA |
Semistructured interview | IPA |
Nine women Age range: 19–44 years |
Nine women from Somalia and Eritrea |
| Salad et al. (2015)206 | The Netherlands | To explore the perceptions of Somali women living in the Netherlands regarding measures to prevent cervical cancer | In cafes, libraries, schools and community centres |
Qualitative approach |
Semistructured interviews, group discussions, recruited through purposive sampling using snowball sampling | Framework of intersectionality enabled a comprehensive thematic content analysis |
Interviews with 14 young women (aged 17–21 years) and six older women (mothers aged 30–46 years) Group discussions with 26 women (mothers aged 23–66 years) |
46 Somali women |
| Shaw (1985)166 | USA | To (1) provide a summary of basic information about female circumcision, (2) summarise the results of an exploratory study that identified special needs and concerns of circumcised women who have used the Western medical system while living in the USA and (3) identify problems and concerns student health-care providers have encountered while caring for this group of women | Southwestern University town | Exploratory study | Informal interviews | Thematic analysis |
12 circumcised women Six planned parenthood centres and four obstetric gynaecological clinics responded |
12 circumcised women from Sudan, Egypt and Somalia |
| Shermarke (1996)178 | Canada | Explores female circumcision within the Canadian community perspective |
Montreal, Quebec and Ottawa, Ontario In homes of the interviewees or in selected, quiet, public places |
Case study and qualitative methods | Individual interviews selected through personal contacts | Thematic analysis |
Four interviewees from Montreal and four from Ottawa Age range: 16–58 years |
Eight Somali women |
| Straus et al. (2009)59 | UK | To examine cultural and social aspects of childbirth, and to determine how they intersect with the needs and experiences of Somali women in the UK. To explore the experiences and needs of Somali women in the UK during pregnancy and childbirth |
London In the community |
Ethnographic approach Narrative approach |
In-depth narrative interviews Recruitment from two community Somali women’s groups and snowballing |
Thematic analysis |
Eight Somali women Age range: 23–57 years |
Eight Somali women |
| Thierfelder (2003)161 | Switzerland | To analyse the specific situation of genitally mutilated African immigrant women and the health-care providers who encounter them in the Swiss health-care system |
Cantons of Geneva, Vaud and Zürich Setting not stated |
Qualitative research |
Semistructured, in-depth interviews and focus group discussions Utilised purposive sampling and snowball sampling drawing on contacts with migrant-support and community organisations |
Thematic content analysis |
Women (n = 29) and men (n = 8) with Swiss health-care providers (20 physicians and 17 midwives) Age range: 17–64 years |
29 women from Somalia and Eritrea |
| Thierfelder et al. (2005)162 | Switzerland | To analyse how immigrant women with FGM experience gynaecological/obstetrical care in the Swiss health-care system and to investigate if physicians and midwives treat and counsel FGM-related complications adequately | Zürich, Lausanne and Geneva, Switzerland. Setting not stated | Qualitative methods |
Four focus group discussions and interviews Purposive sampling via migrant-support and community organisations |
Unclear | 29 women; 37 health-care professionals | 29 women from Somalia and Eritrea |
| Upvall et al. (2009)207 | USA | To explore the health-care perspectives of Somali Bantu refugees in relation to their status as women who have been circumcised and recently resettled in the USA | South-western Pennsylvania, at a local refugee centre | Qualitative study | Focus groups, purposive sample identified by a local non-profit organisation | Thematic analysis |
23 resettled Somali women, a local female physician Age range: 19–43 years |
23 resettled Somali women |
| Vangen et al. (2004)167 | Norway | To explore how perinatal care practice may influence labour outcomes among circumcised women | At women’s homes or public cafes or hospital | Qualitative method drawing on theories of empowerment | In-depth interviews. Recruited from Somali’s association and in health facilities and through snowball sampling | Thematic analysis |
23 Somali immigrants and 36 Norwegian health-care professionals Age range: 18–55 years |
23 Somali women |
| Vaughan et al. (2014)168 | Australia | To improve understanding of the impacts of FGC and to make suggestions for service development – by engaging with local women, communities and health providers |
North Yarra Carlton, Collingwood and Fitzroy Research conducted in community centre meeting rooms |
Community-based qualitative approach |
Eight focus group discussions, four small group discussions, 10 individual interviews with community members. Recruitment from community consultations, community organisations and networks 11 interviews with service providers |
Thematic analysis |
123 individuals 112 migrant men and women and 11 health providers |
87 migrant women from Eritrea, Ethiopia, Somalia and Sudan |
| Vaughan et al. (2014)169 | Australia | To identify the FGC-related service needs prioritised by affected communities living in Victorian regional centres, and to build evidence as to the training, education and professional development required for service providers working in regional Victoria to be able to meet these needs |
Australia, Regional Victoria Ballarat, Geelong, Latrobe Valley and Shepparton Research conducted in community meeting rooms |
Community-based qualitative approach |
Focus group discussions Recruitment from migrant support agencies and then using snowball sampling |
Thematic analysis |
51 migrant community members 950 women, one man 15 health service providers |
50 women from Togo, Sudan and Kenya |
| Vloeberghs et al. (2012)208 | The Netherlands | Explored psychosocial and relational problems of African immigrant women in the Netherlands who underwent FGM/C, the causes they attribute to these problems and the way they cope with these health complaints | In participants’ homes |
Mixed-methods study using standardised questionnaires as well as in-depth interviews, and qualitative participatory methods Grounded theory |
In-depth interviews using peer researchers. Snowball sampling used | Thematic framework analysis |
66 women Age range: 18–69 years |
66 women from Somalia, Sudan, Eritrea, Ethiopia or Sierra Leone |
| Wiklund et al. (2000)209 | Sweden | To study the childbirth experiences of Somali women and men in Sweden | Umea and nearby municipalities; in women’s homes | Grounded theory | Interviews were semistructured. Recruited from the Swedish Medical Birth Register and ‘patient’ records | Grounded theory analysis | Nine women and four husbands of the women studied, and an additional three men Age range: 21–55 years | Nine Somali women |
Appendix 7 Review 1: quality assessment
| Study: authors (year of publication) | Question | Score | Quality band | Richness: thick or thin | Type of publication | Relevance: high, medium or low | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||||||
| Abdi (2012)163 | Y | Y | Y | N | Y | Y | Y | N | Y | Y | 8 | High | Thin | Journal | Low |
| Abdullahi et al. (2009)185 | N | U | Y | Y | Y | N | N | Y | Y | Y | 6 | Medium | Thin | Journal | Medium |
| Ahlberg et al. (2004)186 | U | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 | High | Thin | Journal | Low |
| Ahmed (2005)184 | N | N | U | U | Y | N | N | P | Y | Y | 3.5 | Low | Thin | Book chapter | Low |
| Ameresekere et al. (2011)187 | U | Y | Y | Y | Y | N | N | P | Y | Y | 6.5 | Medium | Thin | Journal | Medium |
| Asefaw (2007)170 | N | U | U | N | Y | Y | Y | Y | Y | Y | 6 | Medium | Thin | PhD thesis | Low |
| Baldeh (2013)174 | U | Y | Y | Y | Y | Y | P | Y | Y | Y | 8.5 | High | Thick | MSc thesis | High |
| Ballesteros Meseguer et al. (2014)172 | Y | Y | Y | N | Y | N | N | P | Y | Y | 6.5 | Medium | Thin | Journal | Medium |
| Behrendt (2011)164 | U | Y | Y | Y | U | N | N | P | Y | Y | 5.5 | Medium | Thin | Research report | Low |
| Beine et al. (1995)188 | N | U | U | Y | Y | P | N | Y | Y | Y | 5.5 | Medium | Thin | Journal | Medium |
| Berggren et al. (2006)189 | N | U | Y | Y | Y | N | N | Y | Y | Y | 6 | Medium | Thick | Journal | High |
| Betts (2011)175 | U | U | U | N | Y | Y | P | Y | Y | Y | 5.5 | Medium | Thick | MA thesis | High |
| Bravo Pastor del Mar (2014)173 | Y | Y | Y | Y | Y | Y | N | P | Y | U | 7.5 | High | Thin | PhD thesis | Low |
| Bulman and McCourt (2002)56 | N | N | Y | Y | P | P | Y | P | Y | U | 5.5 | Medium | Thin | Journal | Medium |
| Carroll et al. (2007)190 | Y | Y | Y | P | Y | N | P | Y | Y | Y | 8 | High | Thick | Journal | Medium |
| Chalmers et al. (2002)191 | N | U | U | U | Y | P | P | Y | Y | Y | 5 | Medium | Thick | Journal | Medium |
| Degni et al. (2014)192 | U | Y | Y | Y | Y | P | P | Y | Y | Y | 8 | High | Thin | Journal | Medium |
| d’Entremont et al. (2014)193 | Y | Y | Y | Y | Y | U | P | Y | Y | Y | 8.5 | High | Thick | Journal | High |
| Essén et al. (2000)194 | U | U | U | N | Y | Y | P | P | Y | Y | 5 | Medium | Thin | Journal | Low |
| Fawcett (2014)78 | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | 9 | High | Thick | PhD thesis | High |
| Gali (1997)176 | U | U | U | U | Y | Y | N | Y | Y | Y | 5 | Medium | Thin | PhD thesis | Low |
| Ghebre et al. (2015)195 | Y | Y | Y | Y | Y | N | N | P | Y | Y | 7.5 | High | Thick | Journal | Medium |
| Glazer (2012)177 | Y | Y | Y | Y | Y | P | N | Y | Y | Y | 8.5 | High | Thin | MSc thesis | Low |
| Glover et al. (2017)196 | Y | Y | Y | Y | Y | N | N | Y | Y | Y | 8 | High | Thick | Journal | High |
| Guerin et al. (2006)197 | U | U | U | Y | P | N | P | N | Y | Y | 4 | Low | Thin | Journal | Low |
| Hill et al. (2012)198 | N | U | U | Y | Y | Y | N | Y | Y | Y | 6 | Medium | Thick | Journal | Low |
| Hussein (2010)57 | Y | Y | Y | N | Y | N | P | Y | N | Y | 6.5 | Medium | Thin | Research report | Low |
| Hussen (2014)165 | N | U | Y | Y | Y | Y | P | Y | U | Y | 6.5 | Medium | Thick | MSc thesis | Medium |
| Johansen (2017)199 | U | U | Y | Y | Y | Y | P | Y | Y | Y | 7.5 | High | Thick | Journal | Medium |
| Jones (2010)179 | Y | Y | Y | Y | N | P | P | Y | Y | Y | 8 | High | Thick | PhD thesis | High |
| Khaja (2004)159 | U | Y | Y | Y | Y | P | N | Y | Y | Y | 7.5 | High | Thin | PhD thesis | Low |
| Khaja et al. (2010)160 | N | U | Y | N | U | N | N | P | N | Y | 2.5 | Low | Thin | Journal | Low |
| Lundbergand Gerezgiher (2008)200 | U | Y | Y | Y | Y | P | P | Y | Y | Y | 8 | High | Thick | Journal | High |
| Maier (2003)171 | N | N | N | N | Y | Y | N | Y | U | Y | 4 | Low | Thin | PhD thesis | Low |
| Maternity Action (2014)180 | U | U | Y | U | Y | N | P | Y | U | U | 3.5 | Low | Thin | Research report | Medium |
| McNeely and Christie-de Jong (2016)201 | U | Y | Y | Y | Y | Y | P | N | Y | Y | 7.5 | High | Thin | Journal | Low |
| Moxey and Jones (2016)202 | U | Y | Y | Y | Y | Y | P | Y | Y | Y | 8.5 | High | Thick | Journal | High |
| Murray et al. (2010)203 | Y | Y | Y | Y | Y | Y | P | Y | Y | Y | 9.5 | High | Thick | Journal | Medium |
| Norman et al. (2016)47 | Y | Y | Y | U | U | P | P | Y | N | Y | 6 | Medium | Thin | Research report | Low |
| Norman et al. (2009)58 | Y | Y | Y | U | U | P | P | Y | N | Y | 6 | Medium | Thin | Research report | Low |
| O’Brien et al. (2017)181 | Y | Y | Y | U | Y | P | P | Y | Y | Y | 8 | High | Thin | Research report | Low |
| O’Brien et al. (2016)182 | Y | Y | Y | N | Y | P | P | Y | Y | Y | 8 | High | Thin | Research report | Low |
| Palfreyman et al. (2011)183 | N | Y | Y | Y | Y | P | P | Y | Y | Y | 8 | High | Thick | Research report | High |
| Recchia and McGarry (2017)204 | U | Y | Y | U | Y | N | N | Y | U | Y | 5 | Medium | Thick | Journal | Low |
| Safari (2013)205 | Y | Y | Y | Y | Y | N | P | Y | Y | Y | 8.5 | High | Thin | Journal | Low |
| Salad et al. (2015)206 | U | U | Y | Y | Y | Y | P | Y | Y | Y | 7.5 | High | Thick | Journal | Medium |
| Shaw (1985)166 | N | U | U | Y | Y | N | P | Y | U | P | 4 | Low | Thin | Journal | Low |
| Shermarke (1996)178 | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | 9 | High | Thin | MSc thesis | Medium |
| Straus et al. (2009)59 | U | Y | Y | Y | Y | Y | P | Y | Y | Y | 8.5 | High | Thick | Journal | High |
| Thierfelder (2003)161 | N | N | Y | Y | Y | Y | P | Y | Y | Y | 7.5 | High | Thick | PhD thesis | High |
| Thierfelder et al. (2005)162 | N | N | Y | U | Y | P | P | Y | Y | Y | 6 | Medium | Thin | Journal | Medium |
| Upvall et al. (2009)207 | N | N | Y | Y | Y | P | P | Y | Y | Y | 7 | Medium | Thick | Journal | High |
| Vangen et al. (2004)167 | Y | Y | Y | Y | Y | P | N | P | Y | Y | 8 | High | Thick | Journal | High |
| Vaughan et al. (2014)168 | U | Y | Y | Y | Y | Y | P | Y | Y | Y | 8.5 | High | Thick | Research report | High |
| Vaughan et al. (2014)169 | U | Y | Y | Y | Y | Y | P | Y | Y | Y | 8.5 | High | Thick | Research report | High |
| Vloeberghs et al. (2012)208 | Y | Y | Y | Y | Y | P | P | Y | Y | Y | 9 | High | Thin | Journal | Medium |
| Wiklund et al. (2000)209 | Y | Y | U | Y | Y | N | N | Y | Y | Y | 7 | Medium | Thin | Journal | Medium |
Appendix 8 Review 1: theme matrix
| Study: author (year of publication) | Theme | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Communication is key | 2. Access to care: influenced by an interaction of multilevel community and health service processes | 3. Cultural and bodily dissonance: striving for cultural and bodily integrity | 4. Disempowering care encounters | 5. Positive care encounters | |||||||||||||
| 1.1 | 1.2 | 1.3 | 2.1 | 2.2 | 2.3 | 2.4 | 3.1 | 3.2 | 3.3 | 3.4 | 4.1 | 4.2 | 4.3 | 4.4 | 5.1 | 5.2 | |
| Abdi (2012)163 | ✗ | ✗ | ✗ | ✗ | |||||||||||||
| Abdullahi et al. (2009)185 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||
| Ahlberg et al. (2004)186 | ✗ | ✗ | ✗ | ||||||||||||||
| Ahmed (2005)184 | ✗ | ✗ | ✗ | ✗ | |||||||||||||
| Ameresekere et al. (2011)187 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||
| Asefaw (2007)170 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Baldeh (2013)174 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Ballesteros Meseguer et al. (2014)172 | ✗ | ✗ | ✗ | ✗ | |||||||||||||
| Behrendt (2011)164 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Beine et al. (1995)188 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| Berggren et al. (2006)189 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Betts (2011)175 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Bravo Pastor del Mar (2014)173 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Bulman and McCourt (2002)56 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Carroll et al. (2007)190 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||
| Chalmers et al. (2002)191 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Degni et al. (2014)192 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| d’Entremont et al. (2014)193 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| Essén et al. (2000)194 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||
| Fawcett (2014)78 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Gali (1997)176 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Ghebre et al. (2015)195 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||
| Glazer (2012)177 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Glover et al. (2017)196 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Guerin et al. (2006)197 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| Hill et al. (2012)198 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Hussein (2010)57 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Hussen (2014)165 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Johansen (2017)199 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||
| Jones (2010)179 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| Khaja (2004)159 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||
| Khaja et al. (2010)160 | ✗ | ✗ | ✗ | ✗ | |||||||||||||
| Lundbergand Gerezgiher (2008)200 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Maier (2003)171 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Maternity Action (2014)180 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| McNeely and Christie-de Jong (2016)201 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||
| Moxey and Jones (2016)202 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Murray et al. (2010)203 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Norman et al. (2016)47 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||
| Norman et al. (2009)58 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| O’Brien et al. (2017)181 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| O’Brien et al. (2016)182 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| Palfreyman et al. (2011)183 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Recchia and McGarry (2017)204 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||
| Safari (2013)205 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||
| Salad et al. (2015)206 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Shaw (1985)166 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||
| Shermarke (1996)178 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||
| Straus et al. (2009)59 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Thierfelder (2003)161 | ✗ | ✗ | |||||||||||||||
| Thierfelder et al. (2005)162 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Upvall et al. (2009)207 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Vangen et al. (2004)167 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Vaughan et al. (2014)168 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Vaughan et al. (2014)169 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Vloeberghs et al. (2012)208 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Wiklund et al. (2000)209 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Total number of studies per theme | 31 | 37 | 34 | 35 | 19 | 34 | 38 | 40 | 28 | 28 | 19 | 40 | 36 | 32 | 46 | 34 | 45 |
Appendix 9 Review 1: CERQual assessment and summary of findings table
| Summary of review finding | Studies coded to finding | Methodological limitations | Coherence | Adequacy | Relevance | CERQual assessment | Explanation of CERQual score |
|---|---|---|---|---|---|---|---|
| Analytical theme 1: communication is key | |||||||
| 1.1. Language barriers and interpretation challenges | |||||||
| For women who did not speak the destination country language well, communication about FGM/C was hindered by language barriers and problems with accessing interpretation support that was appropriate for discussing highly sensitive and personal issues | n = 3156–59,78,162,165,167–169,175,176,180–183,185,186,189–193,195,198,202,203,206–209 |
Moderate concerns regarding methodological limitations Most studies contributing to this finding are of high quality (16 studies of high quality, one study of low quality, 14 studies of medium quality). However, many studies do not report their theoretical paradigm and present only partial or no reflexivity (n = 17). There are serious concerns with three studies that do not describe ethics processes, one study has an unclear fit of methodology to methods and poor analysis. There are moderate concerns in some studies owing to unclear analysis (n = 3) and participant voices not being well presented (n = 2) |
No concerns regarding coherence |
Minor concerns regarding adequacy 18 of the 31 studies presented data classified as ‘thick’ or ‘rich’. Over half of the papers (31/57) report this theme |
Minor concerns regarding relevance The studies for this finding represented 12 OECD countries. Many studies (n = 12) represented the maternity care contexts, but other contexts were also reflected. Almost half of the studies (n = 15) were exclusively of Somali women, but other nationalities were also represented |
High confidence | There were moderate concerns about methodological limitations, but no (or very minor) concerns about the other domains |
| 1.2. ‘Can’t talk, not asked’: double silence and cultural taboo | |||||||
| As a private, sensitive and taboo issue, communication around FGM/C was hindered by a double silence. Women reported that it was rarely discussed within their own communities and, likewise, they found it hard to discuss with health providers, especially if these (or the interpreters) were male. For this reason, women preferred the topic to be raised by health providers | n = 3747,57,58,78,159,162,164,165,167–170,173–175,177–184,187–189,192,193,200–209 |
Moderate concerns regarding methodological limitations Most studies are of high quality (n = 21); 15 are medium quality and one is low quality. Several studies had unclear, partial or no reflexivity. There were serious concerns for five studies with unclear ethics processes, and seven studies had unclear methodology and data analysis processes |
No concerns regarding coherence Two studies present slightly divergent views but with reasons (based on the relationship established with health-care providers) |
Minor concerns regarding adequacy The majority (n = 23) of studies related to this review finding provide thick (rich) data. Over half of the included review papers report on this theme (37/57) |
No concerns regarding relevance Studies come from a wide range of different countries, with a range of participant groups. They also reflected a range of different health-care contexts |
High confidence | There were moderate concerns about methodological limitations (in particular the predominance of grey literature reports), but there were no (or very minor) concerns about the other domains |
| 1.3. Cultural (in)sensitivity | |||||||
| Clumsy and intrusive questioning and comments made women feel stigmatised and embarrassed and led them to avoid further discussion or health-care interactions. By contrast, women valued culturally sensitive and respectful communication from health providers around FGM/C and this facilitated open discussion | n = 3447,56–59,78,159–161,163–165,167–170,173–177,180,182–184,188–191,196,197,203,204,207–209 |
Moderate concerns regarding methodological limitations Three studies are of low methodological quality, 17 of medium quality and 14 of high quality. Seventeen of the studies gave only partial or no detail on methodological perspective or reflexivity, and six studies had unclear methods and analysis. In three studies, there was inadequate detail about participants’ voices |
Moderate concerns regarding coherence Some findings were ambiguous and overlapping with other themes |
Minor concerns regarding adequacy Twenty-one studies provided rich data and 13 were thin (describing single aspects of this theme or lacking detail in women’s voices). Over half of the studies in the review reported on this theme (34/57) |
No concerns regarding relevance Studies related to this theme represented diverse health-care contexts (10 specific to obstetric care, but other contexts represented), diverse countries (n = 9) and diverse population groups |
Moderate confidence | Two of the four domains have only moderate confidence. Many studies do report on this theme, but there are some concerns regarding their quality and some of the findings are ambiguous |
| Analytical theme 2: access to care – influenced by an interaction of multilevel community and health service processes | |||||||
| 2.1. Influence of cultural norms | |||||||
| Women’s care-seeking in relation to FGM/C was strongly influenced by wider cultural norms around sexuality and health, including cultural norms on the importance of premarital virginity, avoiding male health providers and lack of familiarity with preventative care-seeking. These factors led women to avoid seeking care unless symptomatic or pregnant | n = 3556–59,159,162,165,167–171,175,177,179,180,185,187–192,195,198–200,202,203,205–209 |
Moderate concerns regarding methodological limitations There are six low-quality, 13 medium-quality and 16 high-quality studies. The main methodological limitations relate to unclear fit of methodology, limited ethics descriptions and no reflexivity. Other concerns relate to inadequate representation of participant voices |
Moderate concerns regarding coherence Cultural norms relate to, and influence, a wide range of different health-care phenomena |
Moderate concerns regarding adequacy 35 papers report on this theme. Seventeen studies provide thin data. There are 12 studies with medium richness explaining two or more aspects of this theme and eight studies provide very rich data accounting for all aspects of the theme |
Minor concerns regarding relevance The studies are primarily from UK (n = 10) and US (n = 8) contexts, but with good representation of other contexts. The majority of the studies (n = 19) are exclusively focused on Somali participants, and almost half are focused on maternity care contexts (n = 15). However, other health-care contexts are also included, and several studies with ‘thick’ data reflect a mix of participant groups |
Moderate confidence | Three of the four domains have moderate concerns related primarily to methodological limitations and ‘thin-ness’ of the data, but also to the fact that cultural norms influence health care in many different ways, not all of which were explored in great depth |
| 2.2. Influence of the family | |||||||
| Women’s decision-making in health care related to FGM/C was often a collective rather than individual phenomenon, requiring consultation with husbands and other family members | n = 1959,78,159,163,167,168,171,175,179,189,192,193,195,198,200,205–207,209 |
Moderate concerns regarding methodological limitations Moderate concerns owing to methodology and theoretical framework not stated and/or lack of reflexivity (n = 13) |
Moderate concerns regarding coherence Some findings relate to the importance of social support from the family and provide relatively superficial descriptions about the family’s role specifically related to decision-making |
Minor concerns regarding adequacy Rich data from 13 studies. One-third of studies in the review (19/57) report on this theme |
Moderate concerns regarding relevance Includes studies from 10 countries. The theme is reported on from studies with various foci, although mainly with Somali participants (n = 12), and relating mainly to obstetric care situations |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodological quality, coherence and relevance |
| 2.3. Knowledge and information about FGM/C services | |||||||
| Women’s knowledge of, and familiarity with, health services was variable. In some cases, women lacked familiarity with the destination country health system and this impeded their ability to access care in general. In other cases, women reported being aware of maternity and primary care services. However, there was a particular lack of knowledge and information of FGM/C-related specialist services and where and when it may be appropriate to seek help | n = 3447,56,58,59,159,162,165–169,171–173,175,176,179,181–183,185,187,189,191,194–198,202,203,206,207,209 |
Moderate concerns regarding methodological limitations Two studies had low methodological quality, 18 were designated as medium quality and 14 were high quality. The majority of the studies are journal articles (n = 21). There are serious concerns in two studies where ethics processes are poorly described; there is lack of clarity in the fit of methods to methodology in three studies and 16 studies lack a discussion of reflexivity |
Moderate concerns regarding coherence There was variability in the extent to which studies reported women as being familiar with the general health system in the destination country. However, findings relating to women’s lack of awareness of specialist FGM/C services were coherent across the studies |
Minor concerns regarding adequacy The majority of studies in the review report on this theme (34/57). Over half of the studies provide ‘rich’ (thick) data related to this finding (n = 23); 11 provide thin data |
Minor concerns regarding relevance The contributing studies cover 11 countries. Just under half focus exclusively on Somali women (n = 16); one-third of studies focus on the maternity context (n = 13). However, overall, there is a good mix of focus and participant countries |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodological quality and coherence |
| 2.4. ‘Hit and miss’ care | |||||||
| When accessing health care, women reported that the identification of FGM/C and provision of appropriate treatment or referrals could be a ‘hit and miss’ process, depending on individual provider characteristics and practices rather than being a result of standardised organisational systems and processes. Continuity of care was rare, but when it occurred, women reported that it helped to facilitate communication and access to appropriate care | n = 3847,56–59,78,162,164–171,173–178,180–183,189–192,194,196,198,200–203,208,209 |
Moderate concerns regarding methodological limitations There is variable quality of studies relating to this finding: high quality (n = 20), medium quality (n = 15) and low quality (n = 3). There are serious concerns with six studies that report unclear ethics procedures, and moderate concerns with 11 studies that report no or unclear methodological perspectives. A large number of studies (n = 21) had no or partial reflexivity |
No concerns regarding coherence |
Minor concerns regarding adequacy 38/57 studies report on this theme. Most studies (n = 32) contribute relatively rich data to this review finding |
No concerns regarding relevance Studies represent 13 countries and a mixture of participant backgrounds and settings |
High confidence | Three out of four domains have no or only minor concerns. Lack of reflexivity as a methodological limitation is less of a concern for this finding as it is not such a highly sensitive topic |
| Analytical theme 3: cultural and bodily dissonance – striving for cultural and bodily integrity | |||||||
| 3.1. Moving from normal to different | |||||||
| Women described a shift from feeling ‘normal’ to ‘different’ about FGM/C, their bodies and their culture as part of their transition to living in the destination country. Some women started to become aware of the suffering and symptoms that their FGM/C may have caused them. Some women started to question and/or resist previously taken for granted aspects of their culture and to feel uncomfortable with their own bodies. However, women also reported feeling shame and anger at being labelled as different and mutilated and felt that their culture was misunderstood | n = 4057–59,78,160,162,164–171,173–183,189,191,192,196–201,203,205–209 |
Minor concerns regarding methodological limitations Thirty-five of the studies are rated as high or medium quality. Five are low quality. However, many studies failed to report issues relating to reflexivity |
No concerns regarding coherence |
Minor concerns regarding adequacy The majority of studies in the review present rich data on this theme. Eight studies provide only thin data where detailed information is not given |
No concerns regarding relevance The studies represented mixed contexts, 13 countries and a range of population groups. Eighteen out of 40 studies had an exclusively Somali sample |
High confidence | All domains report no or only minor concerns |
| 3.2. Threat to the self: reliving FGM/C pain during clinical interventions | |||||||
| Many studies reported women’s experiences of gynaecological clinical interventions and childbirth as events that threatened their sense of bodily and cultural integrity. Women reported great pain, suffering, fear and apprehension around clinical interventions – and related this to their previous health-care experiences and, especially, to reliving the original trauma they had experienced during their FGM/C. These emotions were exacerbated in encounters where women felt a loss of control or lack of respect | n = 2857,58,78,162,163,165–172,174,176,177,181,185,189,191,193,195,196,200–202,206,208 |
Moderate concerns regarding methodological limitations Serious concerns for three studies owing to no ethics statements, poor descriptions of methodology and unclear fit of methods There are moderate concerns for nine studies owing to lack of stated methodology, inadequate participant voices and lack of reflexivity. Sixteen studies are rated high quality |
Moderate concerns regarding coherence There was variability in the extent to which studies reported direct experiences of reliving trauma as opposed to avoidance of care or services owing to apprehension of pain, trauma and anxiety |
No concerns regarding adequacy The majority of studies present rich data of women’s voices, with just four studies presenting thin data on this particular finding. Almost half of the papers in the review report on this finding |
Minor concerns regarding relevance Data are spread across several countries and focused on different health-care settings. Eleven studies have an exclusively Somali sample. The focus is specifically on obstetric care in 10 studies. Nine studies are based in the UK |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodological quality and coherence |
| 3.3. Being opened: complexities around deinfibulation | |||||||
| For women with type III FGM/C, decision-making around ‘being opened’ (deinfibulation) was influenced by cultural norms and medical imperatives. Some younger women specifically sought out medical deinfibulation before marriage as a way of asserting control over their bodies and lives, but the majority of women considered medical deinfibulation only in the context of pregnancy, and the majority preferred the procedure to be carried out during labour (rather than antenatally) to avoid additional cutting and pain | n = 2858,59,159,162,165,166,168–171,173–177,179,181,183,188,189,192,196–200,202,205 |
Moderate concerns regarding methodological limitations This finding is primarily derived from high-quality studies (n = 15) even though many are either research reports or theses. Half of the studies are journal articles but these include papers of low and medium methodological quality stemming from poor or no reporting of theoretical perspective and methodology, and poor analysis or presentation of participant voices. There are serious concerns with two papers because of no ethics description (n = 1) and very weak methodology (n = 1) |
Moderate concerns regarding coherence This was because some studies reported specifically on deinfibulation related to obstetric care, whereas others included this topic in discussions on other issues, hence the findings were less specific, but generally still consistent with the theme |
Minor concerns regarding adequacy Twenty-eight studies present this theme. Three of these provide only ‘thin’ data in relation to this finding. Data from the other studies are relatively rich, providing explanatory insights or in-depth descriptions of women’s views |
Moderate concerns regarding relevance Although several of these studies are, as expected, in maternity settings (n = 8), there is a wide diversity of other study foci presenting on this theme and across different nationalities that practise type III FGM/C. However, there is little in-depth exploration of any potential differences between different ethnic groups |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodological quality, coherence and relevance |
| 3.4. Being changed: complexities around reinfibulation | |||||||
| For women with type III FGM/C, ‘being opened’ (deinfibulation) was reported as a process involving significant emotional, physical, social and relational adjustments as their bodies became changed. Some women felt ambivalent about these changes and sometimes wanted to be closed again (reinfibulated) to varying degrees, feeling upset if their requests were denied by health providers | n = 19161,166,168–171,173,175,176,181,183,188,189,192,196,197,199,200,205 |
Moderate concerns regarding methodological limitations Moderate concerns owing to lack of reflexivity in 13 of the papers |
Minor concerns regarding coherence Not all papers reported on the issue of requests for reinfibulation |
Minor concerns regarding adequacy There are 19 papers reporting on this theme, with the majority contributing rich data (n = 16). Three studies present thin data |
Moderate concerns regarding relevance The data are well spread across the included studies, representing 11 countries, involving diverse participant groups with FGM/C type III. However, there is little in-depth exploration of any potential differences between different ethnic groups |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodological quality and relevance |
| Analytical theme 4: disempowering care encounters | |||||||
| 4.1. Being exposed and humiliated | |||||||
| Many studies reported women feeling exposed, objectified and ‘on display’ during health-care encounters owing to the health provider’s reactions to their FGM/C. They reported feeling a lack of concern for their privacy or dignity and felt humiliated and stigmatised. These experiences led them to lose trust in the health provider and ‘the system’ more generally | n = 4047,57–59,78,160,162–165,167–171,173–177,180–185,188,189,191,193,196,197,201–204,206–209 |
Moderate concerns regarding methodological limitations The majority of studies are high quality (n = 28). There are moderate concerns in some studies owing to unclear presentation of the research paradigm (n = 8) and no discussion of reflexivity (n = 8). There are serious concerns regarding the data from six papers owing to lacking ethics descriptions (n = 2), unclear methodological fit with methods (n = 3) and weak analysis/detail of participant voices (n = 1) |
No concerns regarding coherence |
Minor concerns regarding adequacy Most papers (n = 31) provide rich data in relation to this theme. Nine papers provide only thin data Over half of the papers in the review report on this theme (40/57) |
Minor concerns regarding relevance There is good representation of OECD countries, but 14 of the 40 studies are from the UK. A range of population groups are included, but 17 studies focus exclusively on Somali women. A range of health-care contexts are covered (13 out of 40 papers focus specifically on obstetric care situations) |
High confidence | A large of number of papers and highly coherent data are presented in this theme with only a small number of poor-quality studies. Data cover a mixture of contexts and not only on maternity settings |
| 4.2. Being judged and stereotyped | |||||||
| Women reported feeling judged and discriminated against within some of their health-care encounters. They reported feeling that health providers made negative assumptions about them and provided suboptimal care based on racial, religious or other stereotypes and misconceptions about their culture in general as well as about FGM/C. Such experiences caused distress, anger and avoidance of the health provider or service | n = 3647,56–59,78,160,162,164,167–171,173–176,178–180,183,186,187,189–193,196,197,203,204,207–209 |
Moderate concerns regarding methodological quality There are methodological concerns across studies owing to lack of reflexivity, no stated paradigm and serious concerns resulting from no or inadequate ethics statements (n = 4), inadequate participant voices (n = 1) and a mismatch between methodology and methods (n = 1) |
Minor concerns regarding coherence There was minor variability across studies in terms of the ways in which this phenomenon was experienced |
Minor concerns regarding adequacy Thirty-six papers report on this theme. The majority of these papers report relatively rich or in-depth findings, with only two studies providing thin data |
Minor concerns regarding relevance Studies span several contexts and 13 countries, involving mainly Somali participants (n = 15) but with several studies involving more than three participant groups (n = 15) and two other participant groups (n = 4) |
High confidence | Even though there are some studies with serious methodological concerns (n = 6), there are good-quality studies across mixed contexts and participant groups, with very minor concerns on coherence, adequacy and relevance |
| 4.3. Lacking choice, power and control | |||||||
| Women reported experiences when they felt that they lacked control within the health-care encounter, especially in the maternity setting and around key interventions such as caesarean sections or episiotomies. They reported feeling excluded from health-care decision-making, not listened to, at the mercy of the system and unable to express their needs. Such experiences could be highly traumatising. Attempts to assert themselves were sometimes construed as being ‘difficult’ | n = 3256,58,59,78,159,162,164,167–171,174–178,180,181,187–189,191,193,194,196–198,200,202,203,208,209 |
Moderate concerns regarding methodological quality Overall, most studies are high quality. Some studies present moderate concerns (n = 15) owing to lack of reflexivity, and no stated paradigm. Two studies have serious concerns owing to lack of ethics descriptions |
No concerns regarding coherence |
Minor concerns regarding adequacy A large number of studies report this theme. Most of these provide rich data to this theme, with only eight studies providing ‘thin’ accounts |
Minor concerns regarding relevance The studies span 13 OECD countries. The majority of studies involve Somali participants (n = 20), and the majority refer to obstetric care contexts (n = 18) – as stated in the theme |
High confidence | Although there are moderate methodological concerns mainly owing to studies not stating their methodology or theoretical paradigm, the conduct of majority studies was good and there are only minor concerns regarding coherence, adequacy and relevance |
| 4.4. Feeling unsafe and vulnerable | |||||||
| Women expected health providers to be knowledgeable, competent and confident in managing their FGM/C. Some women reported times when this did not seem to be the case and where they felt that their care had been adversely affected as a result of poor provider skills. In such situations, women felt unsafe and highly vulnerable, describing painful and traumatic clinical experiences. Feelings of vulnerability were heightened for women who lacked social support | n = 4656–59,78,159,162,164–183,186–191,193,194,196–198,200–204,206,207,209 |
Moderate concerns regarding methodological quality Half of the papers are high quality with only minor concerns (n = 23). Limitations in studies are mainly owing to partial or lack of reflexivity, which is deemed to be of particular relevance to the reporting of this theme. Five studies have more serious concerns owing to lacking ethics statements, poor methodology and partial participant voices |
No concerns regarding coherence |
No concerns regarding adequacy This theme has a high number of studies contributing to it (n = 46). The majority of these provide rich or in-depth data (n = 42) in relation to this finding |
No concerns regarding relevance Studies involve mixed participant groups, and across a range of health contexts, topics and countries |
High confidence | There are a few studies with serious methodological concerns, and some concern regarding the lack of reflexivity. However the data are very rich and consistent across contexts, hence there are no concerns regarding adequacy, coherence or relevance |
| Analytical theme 5: positive care encounters | |||||||
| 5.1. Trusting and appreciating providers and the system | |||||||
| Women appreciated the good medical services available in the destination country. Women also expressed great appreciation for providers who made them feel safe and respected. Such providers were described as knowledgeable and experienced, who treated women with respect, who understood their individual needs and who involved them in their care. Women described these characteristics as facilitating trust and leading to open communication about FGM/C. This, in turn, enhanced the likelihood of women being involved in, and receiving, appropriate care | n = 3456,58,164,165,167–173,175–179,181–183,187–189,191–194,196,198,200,202,203,207–209 |
Moderate concerns regarding methodological limitations There are three studies with serious concerns for not having clear ethics, no paradigm and poor description of methods. There are moderate concerns in 13 papers owing to no stated paradigm, lack of reflexivity or inadequate participant voices |
No concerns regarding coherence |
No concerns regarding adequacy A large number of papers report this theme (n = 34). The majority of papers (n = 29) provide rich or in-depth data in relation to this finding. Only five papers report thin data |
No concerns regarding relevance Diverse studies across different countries. Fourteen studies are exclusively with Somali women, but other groups (or mixed samples) are also represented. This theme occurs in relation to a range of health-care contexts |
High confidence | There are some concerns owing to methodological limitations. However, the data are rich and consistent across contexts, and there are no concerns regarding adequacy, coherence or relevance |
| 5.2. Voicing health-care needs and preferences | |||||||
| Women’s recommendations for good-quality safe FGM/C-related care and services they could trust included (1) interpersonal provider characteristics and behaviours (such as providers being willing and able to talk about FGM/C, providers being skilled and knowledgeable around FGM/C, providers offering culturally sensitive and respectful care) and (2) service organisation issues (such as having specialist services for FGM/C, being given information and awareness about FGM/C-related services and involving women and affected communities in FGM service development) | n = 4547,56–59,78,160,162,165,166,168–171,173–185,187–193,196–202,204,207–209 |
Moderate concerns regarding methodological limitations The major limitation across studies relates to lack of reflexivity. It is unclear to what extent this may have affected this particular review finding |
Minor concerns regarding coherence Studies report on several aspects of what women would like with regard to health-care services related to FGM/C. Not all studies report on all the different elements of this theme |
Minor concerns regarding adequacy Forty-five studies report this theme. The majority have rich or in-depth data (n = 31), but 14 have relatively thin data owing to limited representation of participant voices or only small aspects of the theme reported on |
No concerns regarding relevance Studies report these recommendations across all care settings for women (including studies that did not specify a care setting). This finding included studies from 13 countries. The studies included a good mix of participants. Nineteen studies were exclusively focused on Somalis (n = 19). A relatively large number of studies were based in the UK (n = 16) |
High confidence | Lack of reflexivity may be an issue; however, the data are highly consistent across contexts, hence there are no or only minor concerns regarding adequacy, coherence or relevance |
Appendix 10 Review 2: study characteristics
| Study: authors (year of publication) | Country | Purpose or aims | Region and setting | Methodology, theory and framework | Methods and recruitment | Data analysis | Whole sample | Relevant number |
|---|---|---|---|---|---|---|---|---|
| Abdi (2012)163 | UK | To establish the way in which Somali women living in London begin to perceive themselves and their identity as they carry out their everyday lives. How do they react to the questioning and probing gaze of others, for example, within a health setting? |
East and north-east regions of London Clinic setting |
Narrative and life history approach | Interviews were mainly flowing narratives. Recruited by snowballing sampling method | Analysis using theoretical concept of the ‘three bodies’ |
16 Somali women and two men Two gynaecologists, one counsellor and one midwife |
Two gynaecologists, one counsellor and one midwife |
| Behrendt (2011)164 | Germany | To gather first-hand information on how the immigrant populations feel about and deal with the practice of FGM/C in the context of migration. Where and under what circumstances do women who have undergone FGM/C seek medical care? What precautions do they take during pregnancy? Do they participate in preventative care programmes? | Hamburg | Participatory, co-operative approach, which engages community members in a joint evaluation research process. A triangulated research design using qualitative and quantitative data from different target groups |
Mixed methods Qualitative and quantitative data collection from different target groups:Contacted gynaecologists working in neighbourhoods with a high proportion of immigrants and health personnel of African origin |
Qualitative data analysed and classified into themes. Quantitative data analysed using SPSS |
Total number of 1767 participants with African migration background were interviewed for the quantitative survey 91 semistructured interviews with African community members 13 interviews with health professionals Age range: 15–83 years |
13 health professionals: six female gynaecologists, other health personnel (midwives, nurses, dermatologist, paediatrician) |
| Bergqvist and Svensson (2016)216 | Sweden | To highlight midwives’ experiences at youth clinics when they met with women who came from areas where FGM/C was common |
Southwestern Sweden At the midwives’ workplace in a separate room. One telephone interview |
Qualitative methods and an inductive approach |
Semistructured interviews The head of department/area manager was asked to select respondents based on the criteria and invite them to participate in the study |
Content analysis |
Eight midwives Age range: 32–59 years |
Eight midwives |
| Bibi and Rahimian (2013)217 | Sweden | To investigate nurses’ knowledge and experience of FGM |
Stockholm In a private room at the department or clinic where the nurse worked and in a cafe |
Qualitative interview study |
Semistructured interviews Participants recruited from selected centres |
Thematic analysis | 11 nurses | 11 nurses (six nurses employed at gynaecological departments, one school nurse, one health centre nurse and three nurses working in a geriatric department) |
| Brodin and Mårtensson (2016)218 | Sweden | To describe the knowledge and experiences of district nurses in caring for women with FGM/C |
A region of central Sweden All nine interviews took place in a private room at the participant’s workplace |
A qualitative interview study – descriptive design with an inductive approach | Unstructured interviews | Content analysis |
Nine participants Age range: 33–64 years, with a median age of 51 years |
Nine female district nurses |
| Bulman and McCourt (2002)56 | UK | To develop an understanding of the reality faced by Somali women in their contacts with the maternity services in the UK and to explore professionals’ perceptions of Somali women and their maternity care needs – how they approached providing for these needs and their ideas for improving services |
West London Conducted in participants’ homes or clinics |
Qualitative (ethnographic context narrative approach) |
Two focus groups with midwives, (caseload and hospital midwives) Individual interviews with a Somali health-link worker, a woman on the health and race working group and an obstetric registrar Six individual interviews and two focus groups with Somali women, recruited via snowball sampling method |
Thematic analysis |
Health workers interviewed (exact number not specified) 12 Somali women interviewed |
Two focus groups with midwives (number not stated) Individual interviews with three others (a Somali health-link worker, a woman on the health and race working group and an obstetric registrar) |
| Bulman and McCourt (1997)213 | UK |
Conducted as part of the evaluation of one-to-one midwifery, which was implemented by Queen Charlotte and Chelsea and Hammersmith maternity services in 1993 To develop an understanding of the reality faced by Somali women in their contacts with the maternity services in the UK and to explore professionals’ perceptions of Somali women and their maternity care needs – how they approached providing for these needs and their ideas for improving services |
West London | Qualitative study | Interview approach was open and semistructured | Not stated | Not stated |
Two focus groups with midwives (number not stated) Individual interviews with three others (a Somali health-link worker, a woman on the health and race working group and an obstetric registrar) |
| Burchill and Pevalin (2014)222 | UK | Explored the experiences of health visitors working with refugee and asylum seeking families in central London, and assessed the dimensions of their cultural competency | A borough of London, at the various health centres in which participants worked | Qualitative study using Quickfall’s five-step model320 | In-depth interviews. The health visitors who worked in the borough were approached at their main professional meeting, where a presentation provided details of the study with a request for participation | An interpretive, thematic-based analytical method using the Framework approach | 14 health visitors | 14 health visitors |
| Byrskog et al. (2015)223 | Sweden | To explore ways in which antenatal care midwives in Sweden work with Somali-born women and the questions of exposure to violence | Middle and north of Sweden; setting not stated | A qualitative approach |
Semistructured interviews A purposive sample of midwives was recruited from 11 antenatal clinics; one to two midwives from each clinic |
Thematic analysis | 17 midwives | 17 midwives |
| Dawson et al. (2015)76 | Australia | To provide an insight into midwives’ views and experiences of working with women affected by FGM | Urban New South Wales – in meeting rooms in the hospitals in which midwives worked during time allocated for professional educational development | A descriptive-interpretive qualitative research method |
Focus group discussions with midwives Clinical nurse midwifery unit manager distributed the invitation to registered midwives working in the hospital with a range of skills and experience. Four antenatal clinics and birthing units in three hospitals were purposively selected |
Thematic analysis | 48 midwives | 48 midwives |
| Fawcett (2014)78 | USA | To identify and measure patterns of cultural knowledge and variations (cross-cultural agreement and disagreement) between Somali resettled refugee women and health-care providers on childbearing models. To investigate and measure intracultural variations in the domain of childbearing knowledge among Somali resettled refugee women. To explore the subjective and intersubjective perceptions of female circumcision |
Arizona Six of the interviews were conducted in the clinical settings, two in a cafe and two in private homes |
Quantitative survey and ethnographic methodologies and phenomenological approaches using open-ended semistructured interviews Used the theory of ‘Cultural Consensus Model’ and concepts of embodiment |
Methods included culture consensus questionnaires, semistructured interviews and participatory observations A group of health-care providers were purposively selected for the in-depth semistructured interviews |
Phenomenological analysis and inductive explorative approach |
Questionnaires (n = 174) Interviews with Somali resettled refugee women (n = 30) and health-care providers (n = 10) All health professional participants were female, with an age range of 18–70 years |
10 health professionals (two medical doctors, one midwife, two nurse practitioners and five labour and delivery nurses) |
| Gertsson and Serpan (2009)219 | Sweden | To explore how professionals meet with women who have been subjected to female genital mutilation – in order to gain a greater understanding of how professionals handle cultural meetings and the conflict of values that may arise when encountering vulnerable women |
A medium-sized Swedish city in an area with a high population of immigrants Conducted at the education centre |
Qualitative method using case study |
Semistructured qualitative interviews with four people using a prepared questionnaire Purposive sampling from centres that come into contact with women who have experienced female genital mutilation |
Comprehensive analysis | Four professional participants: one midwife, one social worker, one teacher and one community support officer | One midwife |
| Holm and Kammensjö (2012)220 | Sweden | To highlight school nurses’ experience of female genital mutilation in schools |
Municipality in southern Sweden Setting was school nurses’ workplaces |
A qualitative approach | Semistructured interviews. School nurses were invited by e-mail | Qualitative content analysis | 11 school nurses | 11 school nurses |
| Hussen (2014)165 | New Zealand | To understand the situation of both women with FGM and their health providers in order to increase knowledge of FGM and ensure improved health services for women |
Christchurch At health providers’ work place |
A narrative approach using qualitative descriptive research methods |
Individual semistructured interviews with service providers Focus groups with women from east Africa |
Thematic analysis |
Three health providers 20 women in focus groups |
Three health providers (GP, nurse and health social worker) |
| Jatau (2011)227 | USA | Explored the reproductive health experiences and perceptions of African refugee women, and the nature of their relationship with health-care providers in order to provide information to enhance the clinical encounters of refugees and health-care providers |
Phoenix Arizona Health-care providers interviewed at the Maricopa Medical Centre |
Qualitative study Postcolonial feminism, intersectionality, and human rights provided the theoretical frameworks |
Demographic questionnaire; in-depth semistructured interviews and observation Purposive sampling |
Thematic analysis | 30 interviews [20 African refugee women (between the ages of 18 and 55 years) and 10 health-care providers] | 10 female health-care providers (one obstetrician/gynaecologist, two health social workers, two certified nurse midwives and five registered nurses) |
| Johansen (2006)210 | Norway | Explored Norwegian health-care workers’ experience and management of birth care of women who have undergone infibulation | Norway – conducted in hospitals and clinics | Interviews and participant observation |
In-depth interviews and case interviews on specific deliveries that were conducted immediately afterwards. Participant observation in a perinatal clinic and in a maternity ward Participants were recruited from three hospitals and three antenatal clinics with a high proportion of immigrant patients |
Not stated | 40 health workers |
40 health workers (25 midwives, nine gynaecologists, three GPs and three nurses) |
| Johansen (2017)224 | Norway | To explore the factors that encourage and hinder women and girls in seeking medicalised deinfibulation | Norway | Qualitative study using interviews | In-depth interviews with women and men of Somali and Sudanese origin and health providers, recruited through formal channels based on their experience and work with FGM/C and/or refugees | Thematic analysis |
30 health service providers 66 women and men of Somali and Sudanese origin |
30 health professionals (included employees from health clinics that conducted deinfibulation, school nurses, sexual counsellors for youth and other refugee and asylum seeker personnel) |
| Lazar et al. (2013)225 | USA | To obtain information about providers’ experiences, training, practices and attitudes surrounding the prenatal care, delivery and management of women with FGM/C |
Columbus, Ohio Setting was in hospitals’ cafeteria, in hospitals’ staff lounge or in physicians’ offices |
Exploratory study |
Semistructured interviews Recruited via the hospital and clinics’ public websites in areas where Somalis are known to access care or/and through referral from interviewed physicians |
Content analysis |
14 obstetricians/gynaecologists and nurse midwives Age range: 30–70 years |
14 health providers (nine obstetricians and one family practice physician who was Somali, three nurse midwives and one nurse practitioner) |
| León-Larios and Casado-Mejía (2012)221 | Spain | To explore the influence of midwives’ gender on knowledge, perception and approach to female genital mutilation | Province of Seville at participants’ work centres | Qualitative study |
Three focus group discussions Purposive sampling |
Discourse analysis |
24 midwives from primary health-care centres Age range: 29–57 years |
24 midwives |
| Leval et al. (2004)226 | Sweden | To investigate midwives’ perceptions and attitudes towards circumcision and circumcised women and their experiences of providing care for them | Sweden | Qualitative – using the anthropological concept of ethnocentrism | Focus group discussions and interviews | Thematic analysis |
26 midwives Age range: 37–53 years (all but one were born in Sweden) |
26 midwives |
| Moore (2012)228 | UK | To investigate how obstetric complications for women with FGM are currently managed in the UK and to elicit the opinions and experiences of midwives with regard to providing culturally competent care for women who have undergone FGM | Across the UK | An exploratory study |
Interviews conducted via Skype™ (Microsoft Corporation, Redmond, WA, USA) and telephone Recruited from websites and contacts |
Principles of ‘Framework Analysis’ | Four midwives (all having experience of caring for women with FGM) | Four midwives |
| Ogunsiji (2015)214 | Australia | Explored the knowledge and attitude of Australian midwives caring for women living with FGM. Part of a larger qualitative study that explored meaning of care and care-giving experiences of Australian midwives who are caring for women with FGM |
Sydney, New South Wales Setting was nearby university classrooms and public libraries |
Interpretive qualitative approach – as suggested by Heidegger321 |
In-depth face-to-face interviews A generic e-mail containing the title and aim of the study was sent to expert midwives in a school of nursing and midwifery at an Australian university |
Constant comparison and identification of emerging themes |
11 midwives All female. Age range: 25–60 years |
11 midwives |
| Ogunsiji (2016)215 | Australia | To report Australian midwives’ stories about how they manage obstetric care of women living with FGM. Part of the study that explored the experiences of Australian midwives caring for women living with FGM | Sydney, New South Wales, Australia | Heideggerian qualitative interpretive approach |
Face-to-face, unstructured, in-depth, audio-taped interview Recruited from staff profile of a university website in Sydney, Australia, and by snowball sampling |
Analysis and identification of emerging themes through selective or highlighting approach | 11 midwives | 11 midwives |
| Rubin (2000)229 | USA | Explored multiple cultural and psychological factors that influence how North American medical providers communicate with immigrant women who have been circumcised | USA | A qualitative-phenomenological research design influenced by psychodynamic and feminist theories of psychotherapy |
Face-to-face interviews using a semistructured interview Purposeful, non-random sampling method |
By clustering the data from each participant into variables identified during the design of the study |
10 semistructured interviews with licensed medical providers. Two participants also worked in private practices Age range: 30–54 years |
10 female health-care providers (five nurse-midwives, three paediatricians, one internist and one nurse practitioner) |
| Thierfelder (2003)161 | Switzerland |
To let circumcised women speak for themselves about the Swiss health-care system To find out what key health-care providers of different professions think about the situation and to compare the two To analyse the attitudes, readiness and information needs of Swiss health-care providers to treat genitally mutilated women |
Cantons of Geneva, Vaud, Zürich and Berne, Basel, Solothurn and Appenzell With the exception of two interviews, all in-depth-interviews with health-care professionals were telephone interviews |
Qualitative design with triangulation of data sources |
Structured, in-depth interviews with different categories of health-care professionals Purposeful sampling (snowball sampling, and sampling according to confirming/disconfirming assumptions) were carried out. Targeted the professions most directly confronted with the phenomenon of FGM in Switzerland |
Content analysis |
In-depth interviews (n = 37) with Swiss health-care providers Sixty-six individual interviews and focus group discussions with women (n = 29) and men (n = 3) of migrant communities from Somalia and Eritrea |
37 health providers (17 midwives, 20 physicians; 17 gynaecologists/obstetricians, three GPs) |
| Vangen et al. (2004)167 | Norway | To explore how perinatal care practice may influence labour outcomes among circumcised (Somali) women |
Oslo Interviewed in the conversation room at their working place |
Qualitative method drawing on empowerment – and disempowerment theories |
Repeated in-depth interviews with the Somali immigrants and health-care professionals Recruited from the obstetric wards, the maternal and child health centres |
Analysed by the main themes and contrasting views on the various issues raised | 59 participants (36 Norwegian health-care professionals and 23 Somali immigrants) | 36 health-care professionals (eight gynaecologists, 22 midwives, three public health doctors and three public health nurses) |
| Vaughan et al. (2014)168 | Australia | To improve understanding of the impacts of FGC and to make suggestions for service development – by engaging with local women, communities and health providers |
North Yarra area (Carlton, Collingwood and Fitzroy) in inner Melbourne, VIC, Australia Interviewed at a time and location of their convenience |
Community-based qualitative study |
Interviews with health-care service providers Focus group discussions, small group discussions and individual interviews with community members Recruitment from community consultations, community organisations and networks |
Thematic analysis |
123 individuals 112 migrant men and women and 11 health providers |
11 health service providers [a senior women’s health clinician, senior clinical midwife, two obstetrician/gynaecologists, a GP, community midwife and four FARREP (community outreach) workers] |
| Vaughan et al. (2014)169 | Australia | To identify the FGC-related service needs prioritised by affected communities living in Victorian regional centres, and to build evidence as to the training, education and professional development required for service providers working in regional Victoria to be able to meet these needs | Australia, regional Victoria, Ballarat, Geelong, Latrobe Valley and Shepparton | Community-based qualitative approach |
Interviews with service providers Focus group discussions with community members Service providers were recruited from networks of the Multicultural Centre for Women’s Health and the Royal Women’s Hospital |
Thematic analysis |
15 health service providers 51 migrant community members (950 women, one man) |
15 health service providers (three medical consultants, four GPs, one senior midwife, one sexual health practitioner, one midwife, three refugee health workers, a community health worker and a community development worker) |
| Widmark et al. (2010)79 | Sweden | To explore obstetricians’ perspectives on caring for women with FGC in Sweden: how do they describe, explain and reason about care and policies? | Sweden | A qualitative study | Open-ended, semistructured interviews from a purposeful sample | Analysis was based on tenets of interpretive description | 20 participants (one interview excluded owing to technical error) | 19 obstetricians (13 senior obstetricians and seven senior house officers) |
| Widmark et al. (2002)80 | Sweden | To investigate Swedish midwives’ experiences of caring for infibulated women, midwives’ perceptions and attitudes towards infibulation and infibulated women, the education and training provided to enable midwives to care for and deliver infibulated women, concerns and problems in providing care and, finally, strategies employed by midwives to deal with dilemmas that may occur | Central Sweden in quiet rooms at the midwives’ workplace, and some at the researchers’ workplace | Qualitative. Drew on principles from Guba and Lincoln’s ‘fourth generation evaluation’322 |
Three focus group discussions and three individual interviews Recruited using a multistage sampling procedure |
Grouping of all meaning bearing units relevant to the research, followed by thematic analysis |
26 midwives Age range: 37–53 years |
26 midwives |
Appendix 11 Review 2: quality assessment
| Study: authors (year of publication) | Question | Score | Quality band | Richness: thick or thin | Type of publication | Relevance: high, medium or low | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||||||
| Abdi (2012)163 | Y | Y | Y | N | Y | Y | Y | N | Y | Y | 8 | High | Thin | Journal | Low |
| Behrendt (2011)164 | U | Y | Y | Y | U | N | N | P | Y | Y | 5.5 | Medium | Thin | Research report | Low |
| Bergqvist and Svensson (2016)216 | N | U | Y | Y | Y | N | N | Y | Y | Y | 6 | Medium | Thin | MSc thesis | High |
| Bibi and Rahimian (2013)217 | N | N | U | Y | Y | N | N | Y | U | Y | 4 | Low | Thin | MSc thesis | High |
| Brodin and Mårtensson (2016)218 | N | Y | Y | Y | Y | P | P | Y | U | Y | 7.5 | High | Thin | MSc thesis | High |
| Bulman and McCourt (2002)56 | N | N | Y | Y | P | P | Y | P | Y | U | 5.5 | Medium | Thin | Journal | Medium |
| Bulman and McCourt (1997)213 | N | N | Y | N | P | P | Y | P | N | U | 3.5 | Low | Thin | Research report | Medium |
| Burchill and Pevalin (2014)222 | Y | Y | Y | Y | Y | N | N | Y | Y | Y | 8 | High | Thick | Journal | Low |
| Byrskog et al. (2015)223 | N | U | Y | Y | Y | N | N | Y | Y | Y | 6 | Medium | Thick | Journal | Medium |
| Dawson et al. (2015)76 | U | Y | Y | Y | Y | N | N | Y | Y | Y | 7 | Medium | Thick | Journal | High |
| Fawcett (2014)78 | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | 9 | High | Thick | PhD thesis | High |
| Gertsson and Serpan (2009)219 | U | Y | Y | Y | Y | N | P | Y | U | U | 5.5 | Medium | Thin | MSc thesis | Low |
| Holm and Kammensjö (2012)220 | N | U | Y | Y | Y | N | N | Y | U | Y | 5 | Medium | Thin | MSc thesis | Medium |
| Hussen (2014)165 | N | U | Y | Y | Y | Y | P | Y | U | Y | 6.5 | Medium | Thick | MSc thesis | High |
| Jatau (2011)227 | Y | Y | Y | Y | Y | Y | P | Y | Y | Y | 9.5 | High | Thick | PhD thesis | Medium |
| Johansen (2006)210 | U | U | Y | Y | Y | P | P | Y | Y | Y | 7 | Medium | Thick | Journal | High |
| Johansen (2017)224 | U | U | Y | Y | Y | Y | P | Y | Y | Y | 7.5 | High | Thick | Journal | Medium |
| Lazar et al. (2013)225 | U | Y | U | Y | Y | N | N | Y | Y | Y | 6 | Medium | Thick | Journal | High |
| León-Larios and Casado-Mejía (2012)221 | U | P | Y | Y | Y | P | P | Y | P | Y | 7 | Medium | Thick | Journal | Medium |
| Leval et al. (2004)226 | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 9 | High | Thick | Journal | High |
| Moore (2012)228 | N | U | N | Y | Y | N | N | P | U | Y | 3.5 | Low | Thin | MSc thesis | High |
| Ogunsiji (2015)214 | U | U | Y | Y | Y | N | N | P | Y | Y | 5.5 | Medium | Thin | Journal | Low |
| Ogunsiji (2016)215 | Y | Y | Y | Y | Y | N | N | Y | Y | Y | 8 | High | Thin | Journal | High |
| Rubin (2000)229 | Y | Y | Y | Y | P | Y | Y | N | Y | Y | 8.5 | High | Thick | PhD thesis | High |
| Thierfelder (2003)161 | N | N | Y | Y | Y | Y | P | Y | Y | Y | 7.5 | High | Thick | PhD thesis | High |
| Vangen et al. (2004)167 | Y | Y | Y | Y | Y | P | N | P | Y | Y | 8 | High | Thick | Journal | High |
| Vaughan et al. (2014)168 | U | Y | Y | Y | Y | Y | P | Y | Y | Y | 8.5 | High | Thick | Research report | High |
| Vaughan et al. (2014)169 | U | Y | Y | Y | Y | Y | P | Y | Y | Y | 8.5 | High | Thick | Research report | High |
| Widmark et al. (2010)79 | U | Y | Y | Y | Y | P | P | Y | Y | Y | 8 | High | Thick | Journal | High |
| Widmark et al. (2002)80 | U | Y | Y | Y | Y | P | N | Y | Y | Y | 7.5 | High | Thick | Journal | High |
Appendix 12 Review 2: theme matrix
| Study: author (year of publication) | Theme | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Knowledge and training | 2. Communication is key | 3. Encountering the ‘other’ in clinical practice: negotiating cultural dissonance and achieving cultural understanding | 4. Identifying FGM/C | 5. Clinical management practices: inconsistent and variable | 6. Optimal service development | |||||||||||||||
| 1.1 | 1.2 | 2.1 | 2.2 | 2.3 | 3.1 | 3.2 | 3.3 | 3.4 | 3.5 | 4.1 | 4.2 | 5.1 | 5.2 | 5.3 | 5.4 | 5.5 | 6.1 | 6.2 | 6.3 | |
| Abdi (2012)163 | ✗ | ✗ | ||||||||||||||||||
| Behrendt (2011)164 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||
| Bergqvist and Svensson (2016)216 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||
| Bibi and Rahimian (2013)217 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Brodin and Mårtensson (2016)218 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| Bulman and McCourt (2002)56 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||
| Bulman and McCourt (1997)213 | ✗ | ✗ | ||||||||||||||||||
| Burchill and Pevalin (2014)222 | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||
| Byrskog et al. (2015)223 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||
| Dawson et al. (2015)76 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Fawcett (2014)78 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Gertsson and Serpan (2009)219 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||
| Holm and Kammensjö (2012)220 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Hussen (2014)165 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||
| Jatau (2011)227 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||
| Johansen (2006)210 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||
| Johansen (2017)224 | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||
| Lazar et al. (2013)225 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| León-Larios and Casado-Mejía (2012)221 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||
| Leval et al. (2004)226 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||
| Moore (2012)228 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Ogunsiji (2015)214 | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||||
| Ogunsiji (2016)215 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| Rubin (2000)229 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||
| Thierfelder (2003)161 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Vangen et al. (2004)167 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Vaughan et al. (2014)168 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Vaughan et al. (2014)169 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Widmark et al. (2010)79 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Widmark et al. (2002)80 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Total number of studies per theme | 25 | 21 | 20 | 24 | 13 | 17 | 20 | 15 | 8 | 23 | 15 | 20 | 8 | 21 | 11 | 15 | 12 | 13 | 11 | 9 |
Appendix 13 Review 2: CERQual assessment and summary of findings table
| Summary of review finding | Studies coded to finding | Methodological limitations | Coherence | Adequacy | Relevance | CERQual assessment | Explanation of CERQual score |
|---|---|---|---|---|---|---|---|
| Analytical theme 1: knowledge and training | |||||||
| 1.1. Knowledge and awareness | |||||||
| Health-care providers had variable knowledge around FGM/C, depending on their work setting, role, exposure to FGM/C and exposure to training. Many studies described a lack of provider awareness around FGM/C or provider reports of having insufficient, inaccurate or partial knowledge and skills, leading to misconceptions, lack of awareness, fear and uncertainty about how to talk about FGM/C and how to support women with FGM/C | n = 2556,76,78–80,161,164,165,167–169,210,214–221,224–228 |
Moderate concerns Some papers (n = 9) have limitations related to no stated paradigm, unclear methodology, and no or partial reflexivity. Two studies have serious concerns from lacking ethics description, no reflexivity and weak methods (n = 2). However, the majority of studies pose minor concerns related to no stated paradigm, and partial reflexivity (n = 14) |
No concerns |
Minor concerns 25 papers report on this theme. The majority of studies contribute rich data to this theme (n = 17) |
Minor concerns A good mix of cadres of staff and contexts. More studies among midwives only (n = 9), with the majority conducted in Sweden (n = 8). Only three studies were conducted in the UK. The majority (n = 19) of the studies were published in the last 10 years |
High confidence | There are moderate methodological concerns, but a large number of studies consistently report this theme. There are rich data from a mixture of contexts and participants |
| 1.2. Education and training | |||||||
| Practitioners expressed a perceived need for greater education and training in all aspects associated with the management of women and girls with FGM/C. Health providers identified a lack of basic (pre-service) education (or an input that was too brief and superficial) and a need for regular in-depth CPD around FGM/C that included all aspects of FGM/C (e.g. communication, sexual and cultural issues, as well as clinical management), practical skill development and access to mentorship and clinical supervision where relevant | n = 2176,79,80,161,164,165,167–169,213,214,217,218,220–222,225,228 |
Moderate concerns Two papers pose serious concerns arising from poor methodology and unclear processes, but the majority are high-quality studies (n = 11). Some pose moderate concerns owing to no stated paradigm, and partial or no reflexivity (n = 8) |
No concerns |
Minor concerns The majority of studies report this theme (n = 21). Of these, 14 present rich data towards this theme |
Minor concerns There is a mix of contexts involving nine countries and seven participant groups (different cadres and roles). Six studies have mixed groups of health professionals. The majority (n = 17) of the studies were published in the last 10 years |
High confidence | There are moderate methodological concerns, but a large number of studies consistently report this theme. There are rich data from a mixture of contexts and participants |
| Analytical theme 2: communication is key | |||||||
| 2.1. Language barriers and interpretation challenges | |||||||
| Language barriers and problems with accessing suitable interpretation significantly compromised health providers’ abilities to provide appropriate FGM/C-related care. It affected health providers’ abilities to ask questions about FGM/C or to provide relevant information. This was particularly an issue with women who were still relatively recent migrants | n = 2056,76,78–80,161,164,168,169,216–218,220,221,223,225,227–229 |
Moderate concerns The majority of studies are of good quality (n = 12), with moderate concerns owing to unclear methods, no paradigm and partial reflexivity (n = 6), and two studies with more serious concerns related to lack of ethics statements and very poor methodology |
No concerns |
No concerns Two-thirds of papers report this theme. The majority of these present rich data to illuminate the theme (n = 15) |
No concerns Well-distributed studies covering several different countries and a range of professional groups |
High confidence | There are moderate methodological concerns. However, two-thirds of studies report this theme. Most of the data are rich, representing a mixture of contexts and participants |
| 2.2. Talking about a sensitive topic | |||||||
| As a sensitive and taboo topic, health providers found it difficult to talk about FGM/C with patients. Sometimes this was a result of trying to show cultural sensitivity and not offend patients, and sometimes it was because the health providers felt awkward and embarrassed. Open communication was seen to require trust, time and experience, and some health providers felt that routinising FGM/C-related questions would be useful | n = 2456,76,78,80,161,165,167–169,210,215–223,225–229 |
Moderate concerns The majority of studies contributing to this theme are high/medium quality (n = 15). There are moderate concerns owing to partial or no reflexivity and no stated paradigm. One paper has more serious concerns owing to very poor methods |
No concerns |
No concerns 24 studies report on this theme, with the majority contributing rich data (n = 15) |
Minor concerns One-third of the studies are from Sweden (n = 8). Nine papers involve midwives only or other obstetric care providers (n = 4). However, there are seven other countries and other cadres also represented |
High confidence | There are moderate methodological concerns, but a large number of studies consistently report this theme. There are rich data from a mixture of contexts and participants |
| 2.3. Women also find FGM/C hard to talk about | |||||||
| Health providers perceived that women rarely proactively mentioned FGM/C in the context of a consultation. Providers attributed this to cultural taboos within women’s own societies, feeling ashamed and embarrassed or being fearful of being judged | n = 1376,78,161,165,167–169,215,217,220,223,225,229 |
Moderate concerns Seven studies are high quality, five are medium quality and one is low quality. There are moderate concerns in the medium- and low-quality groups owing to poor reflexivity and unclear description of methodology and methods |
Moderate concerns The data present providers’ perceptions of this issue, hence the conclusions are largely inferred |
Moderate concerns Thirteen studies report this theme. Only six papers present rich data – the others provide a more superficial description |
Moderate concerns All studies are from non-UK contexts (Sweden, the USA and Australia). Four of the studies focus exclusively on midwives but other groups are also represented |
Moderate confidence | There are moderate concerns in all of the domains |
| Analytical theme 3: encountering the ‘other’ in clinical practice – negotiating cultural dissonance and achieving cultural understanding | |||||||
| 3.1. Attitudes towards FGM/C: mixed emotions | |||||||
| FGM/C elicited strong emotional reactions in providers. Many providers expressed negative reactions to FGM/C, including shock, disgust and horror. FGM/C exemplified a profound cultural difference between host providers and migrant patients, with women’s bodies seen to be ‘different’ and mutilated. At the same time, providers expressed empathy and support for affected women and saw them as victims of a violent or patriarchal culture. Some providers who had travelled or who were more experienced expressed a more nuanced position, where FGM/C was seen as a practice that was different, but that needed to be understood in its own context | n = 1776,78–80,161,163,167,168,210,214,216,217,219,220,225,226,228,229 |
Moderate concerns One paper poses serious concerns owing to poor methods and no reflexivity. There are moderate concerns in five papers owing to lack of discussion of reflexivity, which may be particularly salient for this theme |
No concerns |
Minor concerns 17 studies report on this theme. Data are generally rich/in-depth. Only three papers contribute thin data |
Minor concerns The majority of studies reporting this theme are among midwives (n = 7). However, seven studies with mixed groups also report the theme. Six of the studies are from Sweden, but a range of other countries are also represented. Eleven studies were published in the last 10 years |
High confidence | There are moderate methodological concerns, but a large number of studies consistently report this theme. There are rich data from a mixture of contexts and participants |
| 3.2. Cultural dissonance – control and resistance in clinical encounters | |||||||
| Studies reported cultural stereotyping and misunderstandings between patients and providers to be common. Some health providers held stereotyped views of FGM/C-affected women, leading to a failure to address individual needs. Studies described how health providers become perplexed that clients sometimes did not follow their advice and sought to exert control over the clinical situation. Some patients resisted such medical dominance or challenged stereotypes, leading to misunderstandings and miscommunication (especially around caesarean sections and episiotomies), which, in turn, led to suboptimal care and/or suboptimal clinical outcomes | n = 2056,76,78–80,161,167–169,210,217,219–221,223–227,229 |
Moderate concerns Most studies pose no major methodological concerns. There are moderate concerns in six papers owing to lack of discussion of reflexivity and theoretical stance, which may be particularly salient in this theme |
No concerns |
No concerns Two-thirds of studies report this theme (n = 20). The majority provide relatively rich data, with only two studies providing thin data regarding this finding |
Moderate concerns Almost one-third of studies are from Swedish contexts (n = 7) and the majority are related to pregnancy or childbirth as most papers are on experiences from midwives (n = 6) and obstetricians (n = 6). Other studies also provide data on other countries and contexts and other groups. Two-thirds of the papers (n = 13) were published in the last 10 years |
Moderate confidence | Moderate confidence owing to methodological concerns and concerns about relevance, with the majority of studies related to the maternity care context |
| 3.3. Acknowledging the role of the family | |||||||
| Providers reported that families and husbands played a strong role in health-care decision-making related to FGM/C (especially around caesarean section, timing of deinfibulation and preferences around reinfibulation). The need for family involvement was sometimes perceived as frustrating as it could delay decision-making but was recognised as an essential part of effective care | n = 1576,78–80,161,210,213,215,217,218,221,225,226,228,229 |
Moderate concerns Most papers are high (n = 8) or medium (n = 4) quality. There are moderate concerns about poor reporting of reflexivity in seven studies, which may be particularly salient in this theme. There are serious concerns with three papers that have low quality due to lack of methodological reporting, no reflexivity and poor discussion of ethics |
Minor concerns Some of the data appear to be based on assumptions, whereas other data are based on examples from practice |
No concerns Half of the studies report this theme. The majority (n = 14) present medium/high ‘rich’ data |
Minor concerns One-third of studies (n = 5) are from Sweden, and one-third are with midwives only (n = 5). However, the other studies report a mix of contexts and cadres |
High confidence | There are moderate methodological concerns, but half of the studies report this theme and there are rich data from a mixture of contexts and participants |
| 3.4. Gender of the provider | |||||||
| Health providers reported a strong perception that women from FGM/C-affected communities preferred to be seen by a female health professional and that a provider’s ability to form an open and trusting relationship with their patients was more likely if they were female. The gender of the provider was said to affect women’s willingness to seek help, to talk openly to the practitioner and to be examined | n = 878,80,161,169,215,218,221,227 |
Minor concerns Seven studies are classified as high quality and one is medium quality. Minor concerns due to lack of reflexivity; however, this is considered to be of less significance for this theme |
Moderate concerns Some of the data appear to be based on assumptions and inference rather than from having discussed the issue with women themselves |
Minor concerns Eight studies report on this theme. Six studies contribute rich data |
Moderate concerns Studies from five countries (all non-UK). Three studies specifically relate to the maternity care context. The other studies reflect a range of health-care providers |
Moderate confidence | Moderate confidence due to moderate concerns in two domains (relevance and coherence) |
| 3.5. Crossing the cultural divide – strategies and elements of culturally sensitive care | |||||||
| Many papers described strategies and approaches to build good relationships with FGM/C-affected women and thus to cross cultural divides and provide appropriate care. Key features were an understanding of FGM/C in the context of women’s wider needs and culture (i.e. being person centred as well as ‘culturally’ sensitive), and taking time to build rapport and trust. Prerequisites were knowledge, time, communication, a non-judgemental, open attitude and family involvement. Culturally sensitive care was particularly discussed by midwives and nurses | n = 2356,76,78–80,161,164,165,168,169,214–220,222,223,225,227–229 |
Moderate concerns The majority of studies are high (n = 11) or medium (n = 10) quality. There are moderate concerns in six studies owing to lack of discussion of reflexivity |
No concerns |
Minor concerns This theme is reported across the majority of papers in the review (n = 23) and 14 studies contribute very rich data |
Minor concerns The studies are mainly from Sweden (n = 8) and Australia (n = 5), with minor concerns as they are mostly among midwives (n = 9). However, other cadres are also represented |
High confidence | There are moderate methodological concerns, but over two-thirds of the studies report this theme and there are rich data from a mixture of contexts and participants |
| Analytical theme 4: identifying FGM/C | |||||||
| 4.1. Presentation and help seeking | |||||||
| Providers reported that women primarily seek care related to FGM/C when symptomatic or for pregnancy. Women may not link their attendance reason to FGM/C and may not mention FGM/C unless the provider asks. Given that many medical procedures and consultations do not require physical examination, FGM/C may not be identified at all unless the provider specifically asks. Women were reported to be reluctant to raise the subject themselves. The exception was where specialist services or experienced providers exist in which case women may seek them out via family and social networks. The main focus of providers’ attention was on gynaecological symptoms and the maternity context. They generally did not ask about sexual problems or psychological problems and women rarely raised these issues | n = 1576,80,161,163–165,168,169,215–219,221,229 |
Moderate concerns Out of 15 papers, eight are high quality, six are medium quality and one is low quality. Five papers in particular present moderate concerns owing to lack of reflexivity and partial/unclear reporting of participants’ voices. The other papers present minor or no concerns |
Moderate concerns Not all papers report all aspects of this finding |
Minor concerns Half of the papers in the review report this theme (n = 15). All papers contribute rich or relatively rich data |
Moderate concerns One-third of the studies are from Sweden (n = 5), with only one UK study. Over one-third of papers (n = 6) represent midwives’ views specifically. However, other cadres of health professional are represented in other papers. This finding relates primarily to the maternity care or primary care context. The majority of the papers (n = 12) were published in the last 10 years |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodology, relevance and coherence |
| 4.2. Practices and processes around identifying FGM/C | |||||||
| Organisational and system-level mechanisms to identify FGM/C were reported to be inconsistent and unco-ordinated. A key barrier to early and appropriate identification of FGM/C was that providers did not ask about FGM/C, but also that organisational systems and processes were often not adequately set up to prompt them to ask or to ensure that follow-up would occur. Organisational and system barriers to FGM/C identification were related to the existence (or not) of clear guidelines, procedures and referral pathways, record-keeping processes and to the need for clarity of roles and responsibilities and communication/co-ordination between organisational units and professional groups | n = 2056,76,78–80,161,165,167–169,210,215–218,221,223,225,227,228 |
Moderate concerns There are serious concerns regarding one study related to poor methods, partial ethics and no reflexivity. There are moderate concerns in six studies related to no paradigm, unclear analysis and partial reflexivity. The rest of the studies have minor concerns related to lack of reflexivity |
Moderate concerns Not all papers report all aspects of this finding |
Minor concerns 20 papers describe this theme, with rich data from over half of these (n = 12), and moderately rich data (n = 6), with only two papers having thin findings |
Minor concerns Several studies conducted in Sweden (n = 6) and among midwives (n = 7), but with a good representation among other professionals and seven other countries. Fifteen of the 20 papers were published in the last 10 years |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodology and coherence |
| Analytical theme 5: clinical management practices – inconsistent and variable | |||||||
| 5.1. Deinfibulation timing | |||||||
| The majority of providers reported that women preferred deinfibulation to be done in the second stage of labour (rather than antenatally) and that these decisions were influenced by the wider community. In contrast, most providers preferred deinfibulation to be undertaken antenatally (although some felt that this might be an unnecessary additional trauma for the woman), but in most cases, the usual practice was to undertake intrapartum deinfibulation | n = 876,79,80,161,167,169,215,228 |
Moderate concerns The majority of the papers are high (n = 6) or medium (n = 2) quality, and one was low quality with serious concerns owing to poor reporting of ethics and poor reflexivity |
No concerns |
Minor concerns This theme is reported by relatively few of the review studies (n = 8). However, all present rich data |
Moderate concerns Half of the studies reporting this theme are among midwives (n = 4). Other studies include mixed cadres (n = 2), nurses (n = 1) and doctors (n = 1). The studies represent five countries. All the studies refer to deinfibulation only in the context of maternity care |
Moderate confidence | Moderate confidence owing to moderate concerns regarding relevance as no studies report on this theme outside the maternity context |
| 5.2. Deinfibulation practice | |||||||
| Providers in several studies (especially midwives), expressed uncertainty regarding the best way to manage deinfibulation; there was variability in practice and caesarean sections were sometimes performed too hastily (particularly in the US context) in order to avoid having to undertake a deinfibulation. Uncertainty was compounded by difficulties in being able to undertake examinations or fetal monitoring to determine progress of labour. Midwives in particular expressed fear and stress when dealing with women with type III FGM/C owing to their lack of familiarity with deinfibulation and uncertainty over how best to manage it | n = 2156,76,78–80,161,165,167–169,210,215–221,225,227,228 |
Moderate concerns The studies are a mix of high (n = 10), medium (n = 9) and low (n = 2) quality. There are moderate concerns, particularly in seven studies owing to poor description of methods processes, no paradigm, and no reflexivity |
Moderate concerns Not all papers report all aspects of this finding |
Moderate concerns Many studies report on this theme (n = 21), with rich data from over half of these studies (n = 11), but the data in 10 studies are quite ‘thin’ |
Minor concerns The majority of studies discuss this finding in relation to maternity care contexts. Papers from seven countries report this finding. Eighteen of the 21 papers were published in the last 10 years |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodology, adequacy and coherence |
| 5.3. Reinfibulation ambivalence | |||||||
| Studies reported variable attitudes towards, and practice of, reinfibulation. Practitioners were generally aware that reinfibulation is illegal but reinfibulation was reported in three studies (all over 10 years old). Some practitioners reported moral ambivalence about refusing to reinfibulate a client if she was clearly requesting it, as refusal of a patient’s request was seen to contradict the principles of person-centred care. Practitioners felt that it was important to involve husbands in discussions around reinfibulation | n = 1176,79,80,161,167,210,214,215,219,226,228 |
Moderate concerns Most studies relating to this theme are high (n = 6) or medium (n = 4) quality and one is low quality. However, there are moderate concerns in seven studies relating to no or partial discussion of reflexivity |
Moderate concerns Not all papers report all aspects of this finding |
Minor concerns Nine of the 11 papers provide rich data towards this theme |
Moderate concerns All papers relate to the maternity context. Six studies are exclusively with midwives. The studies represent five countries. However, five of the papers were over 10 years old, therefore it is not clear if their findings are still relevant |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodology, coherence and relevance |
| 5.4. Need for guidelines | |||||||
| Many studies reported a lack of (or lack of awareness of) clinical guidelines to direct practice around deinfibulation timing, procedure and reinfibulation. Providers reported a need for guidelines to establish clarity and consistency in clinical practice | n = 1556,76,79,80,161,167–169,215,216,218,220,221,225,228 |
Moderate concerns There are moderate concerns in five papers owing to unclear methods, partial ethics and no reflexivity, and serious concerns related to one paper owing to weak methodology, unclear processes and partial ethics (n = 1). The rest of the studies are of minor (n = 7) to very minor (n = 2) concern owing to no paradigm and partial reflexivity |
No concerns |
Minor concerns 15 papers report on this theme, with the majority presenting rich data (n = 12) |
Moderate concerns The majority of papers relate to the maternity care context. There are studies from seven different countries. Four of the papers are over 10 years old |
Moderate confidence | There are moderate concerns regarding methodological limitations and relevance |
| 5.5. Psychological issues | |||||||
| Several studies highlighted providers’ experiences that women could experience emotional difficulties in relation to their FGM/C and that clinical interventions in particular could be traumatic for women in terms of inducing flashbacks from the original procedure and heightening pain. Practitioners emphasised the importance of providing counselling and psychological support. These aspects were mainly mentioned by nurses/midwives. Although recognised as a need, in most of the studies reporting this theme, the actual availability of counselling or psychological support as a routine part of care was not clear | n = 1256,76,78,161,164,167,168,210,215–218 |
Moderate concerns Among the studies, six are high quality, five are medium quality and one is low quality. There are moderate concerns related to poor reporting of reflexivity and partial reporting of participants’ voices |
Moderate concerns Not all papers report all aspects of this finding. Some of the findings appear to be inferred rather than based on in-depth descriptions of experiences with women |
Moderate concerns Just over one-third of studies report on this theme. Only six of these provide rich data |
Minor concerns Six countries are represented and the studies reflect a range of health professionals |
Moderate confidence | Moderate confidence owing to moderate concerns regarding methodological limitations, coherence and adequacy |
| Analytical theme 6: optimal service development for FGM/C care | |||||||
| 6.1. Provider’s role in prevention | |||||||
| Apart from school nurses whose role explicitly encompasses safeguarding and sexual health, relatively few studies reported practitioners addressing prevention as part of their FGM/C-related care, although several studies reported that this should be part of any practitioner’s role, including GPs. Prevention discussions appeared to take place in an ad hoc way (dependent on individual providers) rather than as a routinised aspect of care. Barriers to initiating prevention discussions in a clinical setting included lack of time, inappropriate timing, feeling that the prevention discussion is someone else’s role, not having enough knowledge or confidence, feeling unsure if women’s responses could be trusted, lack of privacy and language barriers | n = 1376,80,161,164,167,168,217–220,224,226,228 |
Moderate concerns Studies were a mix of high (n = 7), medium (n = 4) and low (n = 2) quality. Moderate concerns for several studies (n = 6) owing to lack for clarity in methods and lack of reflexivity and serious concerns in two studies owing to lack of ethics reporting |
Moderate concerns Not all papers report all aspects of this finding |
Serious concerns Over one-third of studies contributed to this theme. However, the majority (n = 8) contributed relatively thin data |
Minor concerns Most studies are from Sweden (n = 6) and in maternity settings (n = 7). The other studies were from four other countries and among a mixture of professionals |
Low confidence | Low confidence owing to moderate concerns regarding methodological limitations, coherence and serious concerns regarding adequacy |
| 6.2. Community engagement and education | |||||||
| Practitioners identified a need for greater education and awareness raising among affected communities, both on FGM/C itself and associated services but also on prevention. They suggested that this should include men/boys as well as women/girls and identified a need for better information resources for community engagement. Practitioners also suggested that community engagement needed to be built on relationships of trust and concern for a community’s other needs (not just FGM/C) and some suggested that community outreach/liaison roles might be beneficial | n = 1176,161,164,165,168,169,217,219,220,224,228 |
Moderate concerns Study quality was mixed (high, n = 4; medium, n = 5; low, n = 2). Moderate concerns in four papers owing to partial participant voices, no paradigm and unclear processes, and serious concerns (n = 2) owing to weak methods and unclear ethics processes |
No concerns |
Minor concerns Just over one-third of studies in the review reported this theme. The majority provided relatively rich data. Three contributed only thin data |
Minor concerns Studies were distributed across seven countries, mainly Sweden (n = 3) and Australia (n = 3), and among several different cadres. Nine of the papers were published in the last decade. Nine of the papers focused on the maternity context |
High confidence | High confidence owing to no/minor concerns in three domains (adequacy, relevance, coherence) and only moderate concerns regarding methodological limitations |
| 6.3. Specialist services | |||||||
| In terms of service development, providers (especially in lower-prevalence areas) valued and recommended having specialist centres for holistic FGM/C management, counselling and prevention activities, with links to affected communities. Ensuring equity of access to services was a key concern | n = 976,80,161,165,168,169,217,223,228 |
Moderate concerns Study quality was mixed (high, n = 3; medium, n = 4; low, n = 2). The majority of studies have minor concerns (n = 7) owing to no stated paradigm and partial reflexivity. Moderate concerns (n = 1) and serious concerns (n = 1) owing to partial ethics descriptions, poor methods and no reflexivity |
Moderate concerns Not all papers report all aspects of this finding |
Moderate concerns Owing to relatively few studies reporting on this theme (9/30), and most contribute thin data |
Minor concerns Studies reflect five different countries, mainly Sweden (n = 3) and Australia (n = 3). A good mix of different cadres, with slightly more midwives (n = 4) |
Moderate confidence | Moderate concerns regarding methodological limitations, coherence and adequacy |
Appendix 14 Feedback from the national stakeholder engagement event
Introduction
Stakeholder involvement has been a central consideration throughout this research. Once the key findings from the reviews had been established, the project team organised a stakeholder engagement event, which included a wide range of national stakeholders (including researchers, educators, clinicians, commissioners and community organisations). A list of participants is provided in Appendix 15. The programme for the event, held on 6 March 2018 in Nottingham, is provided in Appendix 16. It included the presentation of the findings from reviews 1 and 2.
Following each presentation, participants were asked to complete a short evaluation form to provide feedback on the findings. The questions were:
-
Based on your own experience and perspectives, do the themes seem to capture the main issues?
-
Were any review themes surprising for you? Why?
-
Were there any review themes that you don’t agree with? And why?
-
Do you think that there are any issues missing from the review findings that you would have expected to see?
-
Any other comments?
After the presentations were complete, there was a roundtable discussion session to explore the key implications of the findings for practice, policy, education and research. Questions for discussion were:
-
What are the implications of the review findings for (1) service delivery, development and commissioning, (2) training and (3) community engagement?
-
What are the key gaps in our current evidence (knowledge) base?
-
What do we still need to know?
The event included specific discussion on the implications of the review findings within the context of recent policy changes around FGM/C in the UK.
Feedback from presentation of findings from review 1 (health-care experiences of women/girls who have undergone female genital mutilation/cutting)
Theme 1: capturing the main issues
Overall, participants in the stakeholder event felt that the themes presented from the review captured the main issues:
I think that this is particularly so in terms of women being treated as a ‘medical dilemma’.
I think the review covered everything well.
The themes relate to feedback that we have had from women we work with in counselling.
Many of the participants commented that the majority of evidence surrounding FGM/C appeared to have a maternal health focus, and, although this may be anticipated given the implications of FGM/C within this particular health-care context, they felt that there were key areas of health care that are not well evidenced within the existing literature. For example, community and primary care did not feature strongly within the review:
Absolutely, [captured the main issues] including the focus on maternal care and the relative lack of information for other service provision across the life course.
All of the participants found resonance with the themes, although one participant felt that women’s feelings with regard to the legal context of FGM/C, although perhaps central to their interactions with health-care professionals, did not feature in the findings:
The only point where I was surprised was the absence of feelings of criminalisation [among the women who presented to health services].
Theme 2: unanticipated findings
Although the themes may have captured the main issues as anticipated by participants, many also reported being surprised or feeling ‘shocked’ at the responses of health-care professionals towards women who they encountered, as presented in the findings:
I was surprised by the [negative] attitude of the midwife and health care professional towards the lady.
Some of the examples of negative health professional’s behaviour were shocking and show how important it is that we professionals think about how we treat people and the impact on them.
Some of the healthcare professional’s attitudes were shocking especially the way women were made to feel as if they had done something wrong or felt judged.
Theme 3: unexpected omissions
For the majority of participants, there were few if any unexpected omissions from the findings as presented. However, several participants expressed surprise at the absence of evidence surrounding the psychological impact of FGM/C or the role of men and/or the wider family:
The focus [literature] seems to have been on maternal health. The psychological presentations have not really been gone into although also important. We struggle to have this recognised properly and commissioned.
Partner’s views or how women feel about their partner’s knowledge and help seeking behaviour.
Feedback from presentation of findings from review 2 (health-care professionals’ experiences of providing care to women/girls who have undergone female genital mutilation/cutting)
Theme 1: capturing the main issues
For the majority of participants, the main themes presented captured the issues that they were aware of or had encountered in practice:
Clearly communication and lack of knowledge.
The difficulties in communication and interpretation resonates as does staff feeling less confident and less supported.
The knowledge gaps are clear.
Especially the ‘hit and miss’ approach and lack of consistency of care provision.
Theme 2: unanticipated findings
For many of the participants, the similarity of reported issues among health-care professionals across disciplines and lack of co-ordination of services was surprising, particularly in the light of perceived service reduction in some areas:
I thought that health-care professionals would be better prepared.
The number of women reporting similar experiences yet we are seeing services supporting women being closed due to lack of funding.
The inconsistency and lack of coordination around FGM/C [is surprising].
Theme 3: unexpected omissions
Participants reported that there were a number of omissions in the evidence, including education and/or training, the impact for health-care professionals in asking about FGM/C and the absence of research beyond maternal health:
How is the capacity of health-care professionals to manage FGM/C cases influenced by the content of current training?
I find it surprising that professionals don’t mention wishing that they had more training as students.
There was an absence of discussion among professionals regarding any existing specialist services.
Mainly focused on obstetrics but may map onto other services.
Given the recent developments concerning mandatory reporting in the UK, a number of participants were surprised about the absence of legal or safeguarding considerations within the findings (this may in part be explained by the relatively recent reporting legislation):
Safeguarding and FGM/C as a safeguarding issue not raised at all by professionals – the law and impact on clinical encounters.
The role of the law is missing.
Feedback from roundtable discussion
The implications and recommendations from the group discussions are described here.
The need for service development across all health-care services with a particular focus towards:
-
Specialist services or centres of excellence with continued support for practitioners from colleagues with experience and expertise.
-
Clear referral pathways and signposting for professionals working in mainstream services and for women who access services.
-
Visual presence and accessibility of services, for example the development of mobile community-based clinics.
-
Development of services that meet the particular needs of women with different life circumstances, for example those seeking asylum.
-
Integrated services including mental health care.
-
Utilising models from other ‘parallel’ areas of health care, for example specialist women’s services.
-
Consistency and ‘gold standard’ of service delivery.
The need for structured education and training for health-care professionals:
-
Development of education and training for those who are already qualified practitioners and the inception of mandatory education and training at pre-qualifying level.
-
Education and training needs to be quality assured – that it is delivered to the right standard and is meeting needs appropriately.
-
Training needs to include communication skills and psychological support as well as more practical application.
The need for community engagement in any service development plans:
-
Community engagement is vital and, as such, needs to be funded appropriately rather than reliance on voluntary support.
-
Services need to be developed in collaboration with local communities and community leaders – creation of community consortium.
-
Need for whole family engagement including men.
The need for more research and in particular research that addresses the following:
-
What are the best and most cost-effective models of care?
-
What are the best and most effective models for interpretation services?
-
What do women want to know about birth preparation and birth options?
-
What is care like for women in midwifery-led settings?
-
How do communities and health-care professionals feel about mandatory reporting (this would include enquiry and affect professional–women relationships)?
-
What are the mental health needs of women who have experienced FGM/C?
-
What is the impact of FGM/C on the health (physical and psychological) needs of women across the life course?
-
What are men’s views on FGM/C?
-
Do experiences of health care affect women’s attitudes towards undertaking FGM/C in the future?
Appendix 15 National stakeholder event participant list
| Prefix | First name | Surname | Company |
|---|---|---|---|
| Dr | Charles | Abe | Yoruba Community Association |
| Mr | Keyrellous | Adib | University of Nottingham |
| Miss | Agatha | Adogho | University of Nottingham |
| Mrs | Sarah | Agnela Simons | World Society of Victomology |
| Mr | Tunde | Akinbowale | GAIN Diapora |
| Ms | Jennifer | Akuamoh-Boateng | University of Nottingham |
| Ms | Juliet | Albert | Imperial College Healthcare NHS Trust and Barnardos National FGM Centre |
| Ms | Obi | Amadi | CPHVA and Unite |
| Mrs | Joanna | Andrews | Sheffield Hallam University |
| Mr | Samwel | Awolola | |
| Dr | Heather | Bird | University of Surrey |
| Mrs | Paula | Booker | NUH |
| Miss | Grace | Brough | Nottingham City Council |
| Mrs | Alison | Byrne | HEFT |
| Mr | Han Yang | Chung | MPH, University of Nottingham |
| Mrs | Kinsi | Clarke | Nottingham & Nottinghamshire Refugee Forum |
| Miss | Deqa | Dirie | NHS |
| Dr | Amanda | DiRosa | Queen Margaret University |
| Dr | Bernie | Divall | University of Nottingham |
| Dr | Sharon | Dixon | Nuffield Department of Primary Care Health Sciences |
| Dr | Sharon | Dixon | Primary Care Department, University of Oxford |
| Miss | Jeanette | Eldridge | University of Nottingham |
| Dr | Catrin | Evans | University of Nottingham |
| Dr | Kerry | Evans | University of Nottingham/NUH |
| Miss | Astrid | Fairclough | NHS England |
| Dr | Meg | Fassam-Wright | National FGM Centre |
| Miss | Velma | Hamilton | Self Help UK |
| Miss | Amira | Haridy | University of Nottingham |
| Professor | Gina | Higginbottom | University of Nottingham |
| Ms | Alya | Howard | LSHTM |
| Dr | Natasha | Howard | LSHTM |
| Dr | Basharat | Hussain | University of Nottingham |
| Ms | Abdoulie | Jah | |
| Dr | Mariam | Johari | University of Nottingham |
| Dr | Laura | Jones | University of Birmingham |
| Mr | Frank | Kamau | Mojatu Foundation |
| Ms | Angela | Karigambe | University of Nottingham |
| Ms | Kekeli | Kpognon | FORWARD |
| Mr | Fadhili | Maghiya | Sub Sahara Advisory Panel |
| Dr | Carol | McCormick | Retired |
| Ms | Joanne | McEwan | Royal College of Nursing |
| Dr | Julie | McGarry | University of Nottingham |
| Mrs | Emma | Mills | Aneurin Bevan University Health Board |
| Ms | Cecily | Mwaniki | Berkshire Health Foundation Trust |
| Miss | Srabani | Nath | University of Nottingham |
| Ms | Valentine | Nkoyo | Mojatu Foundation |
| Ms | Edith | Ogochukwu | Mojatu Foundation |
| Mrs | Rosemary | Omae | Nursing Personnel Agency |
| Dr | Phoebe | Pallotti | University of Nottingham |
| Ms | Veronica | Pickering | Mojatu Foundation |
| Dr | Natasha | Recchia | University of Nottingham |
| Ms | Louise | Robertson | Dahlia Project |
| Mr | Mashair | Saeed | |
| Mr | Alex | Segal | Imperial College Healthcare NHS Trust |
| Mrs | Sarah Agnela | Simons | Member of World Society of Victimology |
| Ms | Bethel | Tadesse | Hidden Scars |
| Dr | Laila | Tata | University of Nottingham |
| Dr | Julie | Taylor | University of Birmingham |
| Professor | Jim | Thornton | University of Nottingham |
| Mr | Morro | Touray | University of Surrey |
| Dr | Ritah | Tweheyo | University of Nottingham |
| Ms | Edith Lucky | Uweh | |
| Dr | Tobe Levin | von Gleichen | Hutchins Centre, Harvard University |
| Mrs | Clare | Watson | NUH |
| Mrs | Amanda | Wickham | NUH |
Appendix 16 National stakeholder engagement event programme
National Stakeholder Engagement Event: FGM/C Systematic Review Project, Clinical Sciences Building, City Hospital, Nottingham, 6 March 2018, 11.00 to 17.00
| Time | Activity | Facilitator/presenter |
|---|---|---|
| 11.00–11.30 | Arrival, registration, coffee/tea | Project team |
| 11.30–12.00 | Introduction to the project and to the day: expected outcomes | Valentine Nkoyo and Dr Catrin Evans |
| 12.00–12.15 | How the systematic reviews were undertaken: brief overview of methods | Dr Ritah Tweheyo |
| 12.15–12.50 | Findings from review 1 (health-care experiences of women/girls who have undergone FGM/C) | Dr Catrin Evans |
| 12.50–13.40 | Lunch | |
| 13.40–14.15 | Findings from review 2 (health-care professionals’ experiences of providing care to women/girls who have undergone FGM/C) | Dr Catrin Evans |
| 14.15–15.00 | Tabletop discussions to identify key implications of the review findings | Project team |
| 15.00–15.45 | Feedback from tabletop discussions | Dr Catrin Evans and Dr Ritah Tweheyo |
| 15.45–16.00 | Break | |
| 16.00–16.15 | Critical reflections on the review findings and future directions for FGM/C services and commissioning in England | Astrid Fairclough |
| 16.15–16.45 | Situating FGM/C care within the wider context of international migration and maternity care in the UK | Professor Gina Higginbottom and Dr Basharat Hussain |
| 16.45–17.00 | Concluding reflections and close | Veronica Pickering |
Appendix 17 Engagement event with obstetricians/gynaecologists
There were relatively few medical doctors present at the national stakeholder engagement, and they were primarily GPs. For this reason, the project findings were presented to a group of 30 trainee obstetrics and gynaecology registrars from across the East Midlands region during a training day. They were asked to provide comments and feedback. Their feedback is presented below.
The group strongly supported the project findings that some medical practitioners are uncertain about deinfibulation and are inexperienced in, and apprehensive of, managing women with FGM/C. They cited several examples in which this had led to difficulties in the management of labour for women with type III FGM/C. The group noted that their current training around FGM/C consists of completing e-learning modules. This was felt to be insufficient. A key recommendation was for more practical skill training.
Feedback included:
-
Insightful project.
-
Helpful findings.
-
Need more training – a physical training day on FGM where we are taught deinfibulation.
-
Perhaps using models so we can better manage these women. Case studies would be useful.
-
It was good to learn about the managerial aspects of FGM. I would like more practical training relating to FGM procedures when encountered in labour.
-
Some more practical clinical teaching would be useful – e.g. what language to use with patients, how to deinfibulate, risk and benefits, how to consent for deinfibulation.
List of abbreviations
- CERQual
- Confidence in the Evidence from Reviews of Qualitative Research
- CPD
- continuing professional development
- FGM/C
- female genital mutilation/cutting
- GP
- general practitioner
- GRADE
- Grading of Recommendations Assessment, Development, and Evaluation
- HTA
- Health Technology Assessment
- JBI
- Joanna Briggs Institute
- JBI-QARI
- Joanna Briggs Institute Qualitative Assessment and Review Instrument
- MeSH
- medical subject heading
- MSc
- master of science
- NIHR
- National Institute for Health Research
- OECD
- Organisation for Economic Co-operation and Development
- PAG
- Project Advisory Group
- PhD
- doctor of philosophy
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RIS
- Risk Indication System
- SURE
- Supporting the Use of Research Evidence
- WHO
- World Health Organization