Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1023/17. The contractual start date was in June 2013. The final report began editorial review in February 2018 and was accepted for publication in August 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Tamsin Ford is chairperson of the Child and Adolescent Psychiatry Surveillance Service that was used to run part of the study, which is an unpaid position (other than travel expenses). Kandarp Joshi reports grants from Sunovion Pharmaceuticals, Inc., outside the submitted work. He was principal investigator for the Aberdeen site for a Sunovion-sponsored multisite trial on the efficacy and safety of lurasidone in paediatric schizophrenia. Jonathan Kelly reports that Beat has contracts with some NHS trusts and clinical commissioning groups that provide and commission, respectively, community eating disorders services for children and young people. In these contracts, Beat works with the local services to deliver awareness-raising training for professionals and, in some cases, to offer peer coaching for carers. The funding Beat receives in return for its role in this project is not ‘on my behalf’. Beat is a co-applicant on another research project called ‘TRIANGLE’ (short title), which is also funded by the National Institute for Health Research. The funding Beat receives in return for its role in this project is not ‘on my behalf’. Beat is a co-applicant on another research project called ‘Mind the Gap’ (short title), which is funded by the Welsh Assembly Government and is investigating referral pathways from identification to specialist treatment for people with eating disorders (of all ages) in Wales.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Byford et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
Anorexia nervosa is a serious and enduring eating disorder and mental health problem, with high morbidity and the highest mortality among psychiatric disorders. 1,2 The annual incidence in the most vulnerable group (adolescent girls aged 15–19 years) is between 110 and 135 per 100,000. 3,4 Anorexia nervosa is commonly associated with severe physical, psychological and social impairments, and a significant cost burden. 5,6 Although the majority of adolescents with anorexia nervosa eventually recover, the illness is often protracted, with a mean duration of 5–6 years. 7 Because of the life-threatening nature of this condition, a significant proportion of young people with anorexia nervosa are treated as inpatients in hospital. In England, the number of hospital admissions for anorexia nervosa rose consistently by 37% between 2011–12 and 2015–16. 8,9 Although some admissions (mainly on paediatric wards) are brief, many are as long as 6–12 months, and some are even longer. Hospital stay is disruptive to school, family and social life, and relapse rates for inpatient treatment are high (25–30% after first admission and 50–75% after subsequent admission),7,10 with evidence that clinical outcomes may be worse even when severity is accounted for. 11 By contrast, among those who respond well to outpatient family therapy, relapse rates are as low as 5–10%. 12–14
In the UK, at the time the Cost-effectiveness of models of care for young people with Eating Disorders (CostED) study began, there were several possible referral routes for young people with anorexia nervosa. One was from primary care to a generic child and adolescent mental health service (CAMHS) with varying levels of expertise in eating disorders and a variable mix of individual or family-based treatments. In some cases, this may include a specific eating disorders ‘mini team’. Another referral route was from primary care directly to a specialist community eating disorders service for children and young people. These are dedicated tertiary-level multidisciplinary services that cover a larger geographical area than single CAMHS and have been reported to reduce rates of admission to hospital by as much as 60–80%. 15 Other routes into specialist community care include referrals from accident and emergency, social care and education. Finally, patients may be so unwell that they are admitted immediately to paediatric care or to an inpatient facility, thus bypassing community services.
To date, few studies have compared the relative benefits of different care pathways for young people with anorexia nervosa. The available evidence, although limited, supports a case for specialist outpatient treatment having a higher probability than CAMHS and inpatient treatment of being the most effective strategy. 16,17 Other indicators found to favour a community eating disorders service for children and young people over a generic CAMHS include case identification, rates of hospital admission and continuity of care. Evidence suggests that case identification of adolescent anorexia nervosa in specialist areas is 50% higher than in non-specialist areas; hospital admission rates are significantly lower among patients whose treatment started in a specialist service (16%) than among those whose treatment started in a generic CAMHS (40%), and continuity of care is notably better for young people whose treatment began in a specialist outpatient service than for those whose initial assessment took place in generic CAMHS. 17
Economic evidence also supports the case for specialist outpatient treatment for young people with anorexia nervosa, suggesting that specialist outpatient treatment is cost-effective compared with both inpatient treatment and generic outpatient treatment. 18 However, the data for this study were collected between 2000 and 2003, so service configurations may now be very different. A recent systematic review19 of economic evaluations of prevention and treatment for eating disorders identified only 13 such studies in total; only three of these focused on anorexia nervosa, and only one focused specifically on young people, which was the study already identified. 18
Despite these findings, many parts of the UK and the Republic of Ireland (RoI) had little or no specialist eating disorders provision for young people, although this has started to change in England following the publication of guidance for commissioning standards and requirements for the provision of community-based eating disorders services for children and young people in June 2015. 20 The available evidence suggests that, if the above findings are generalised, investing in the development of such services could have significant implications for the NHS, with the potential to improve health outcomes through reductions in relapse rates, to reduce costs through reductions in hospital admissions and to improve the quality of life of young people and their families. The CostED study aimed to provide evidence of the potential savings to be made from investment in specialist eating disorders services, alongside evidence that patient and family outcomes will be enhanced or at least be no worse than the situation at the time that the CostED study was undertaken.
Aims and objectives
The primary aims of the CostED study were to evaluate the cost and cost-effectiveness of alternative community-based models of service provision for child and adolescent anorexia nervosa and to model the impact of potential changes to the provision of specialist NHS services using decision-analytic modelling techniques. The data collected for this purpose were also used to generate up-to-date estimates of the incidence of anorexia nervosa in secondary care services for young people in the UK and the RoI, and to map specialist and generic services for eating disorders across the UK and the RoI.
The specific objectives of the study were to:
-
identify all new community-based incident cases of anorexia nervosa in young people aged between 8 years and 17 years and 11 months in the UK and the RoI over an 8-month period using a psychiatric surveillance system
-
classify the model of community-based care provided for each case identified at baseline as either specialist or generic, using information from reporting clinicians on service characteristics and applying consensus criteria obtained using a Delphi survey
-
calculate the relative cost of all notified incident cases of child and adolescent anorexia nervosa in the UK and the RoI and determine the cost-effectiveness of different models of care provision at 6- and 12-month follow-ups through questionnaires to reporting clinicians
-
model the impact on cost and cost-effectiveness of potential changes to the provision of specialist services in the UK and the RoI using decision-analytic modelling techniques.
The hypotheses of the study were that:
-
assessment and treatment by highly specialist or tertiary specialist community-based eating disorders services for child and adolescent anorexia nervosa in the UK and the RoI would be less costly to health services over a period of 12 months than assessment and treatment by, or referral via, generic (non-specialist) CAMHS
-
assessment and treatment by highly specialist or tertiary specialist community-based eating disorders services for child and adolescent anorexia nervosa in the UK and the RoI would be more cost-effective from the health service perspective over a period of 12 months than assessment and treatment by, or referral via, generic (non-specialist) CAMHS
-
increasing the availability of highly specialist or tertiary specialist community-based eating disorders services for child and adolescent anorexia nervosa in the UK and the RoI would be cost saving to health services over the medium to long term.
Chapter 2 Methods
Parts of this chapter have been reproduced from Petkova et al. 21 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Study design
An observational surveillance study was undertaken using the Child and Adolescent Psychiatry Surveillance System (CAPSS), a system designed to ascertain cases of rare childhood mental health conditions in the UK and the RoI through monthly reporting by clinicians. 22
This method of case identification aimed to identify all new community-based incident cases of anorexia nervosa in young people aged between 8 years and 17 years and 11 months in the UK and the RoI over an 8-month period (objective 1). Data were collected directly from clinicians who notified cases to CAPSS and included information on service characteristics to enable each notifying service to be classified as either specialist or generic (objective 2), use of health services to support the calculation of the cost of all notified cases (objective 3), and clinical characteristics and outcome measures, which were used alongside the cost data to assess the cost-effectiveness of different models of care provision (objective 3) and to model the impact on cost and cost-effectiveness of potential changes to the provision of specialist services in the UK and the RoI using decision-analytic modelling techniques (objective 4).
Objective 2, to classify the model of community-based care provided for each case identified as either specialist or generic, additionally required information on criteria considered to be important to support the classification of a service as a specialist eating disorder service. These criteria were identified using a Delphi survey to achieve consensus.
Sampling
The study comprised young people aged between 8 years and 17 years and 11 months in contact with child and adolescent mental health services for a first episode of anorexia nervosa in accordance with Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), diagnostic criteria. 23 New cases of anorexia nervosa were notified by clinicians via CAPSS on a monthly basis for a period of 8 months, from 1 February 2015 to 30 September 2015. The CAPSS methodology, which, in order to maximise the accuracy of incident data, does not require patient consent, has been operating successfully since 2009 and is based on the well-established British Paediatric Surveillance Unit system (www.rcpch.ac.uk/work-we-do/bpsu; accessed 8 February 2019). CAPSS aims to facilitate epidemiological surveillance and research into uncommon child and adolescent mental health conditions, to increase awareness within the medical profession and public alike and to allow psychiatrists to participate in surveillance of uncommon child and adolescent mental health conditions. 22
At the time of the CostED study, CAPSS used a report card, known as the yellow card, which contains a list of the conditions currently being surveyed at any one point in time. More recently, CAPSS introduced an e-mail system, but that was not available at the time of the CostED study. The yellow cards (or e-mail notifications), along with reporting instructions and protocols for new studies, are sent every month to all hospital, university and community child and adolescent consultant psychiatrists across the UK and the RoI. The reporting clinicians are sent the yellow cards (or e-mail notifications) from the CAPSS office and asked to tick boxes against any of the reportable conditions they have seen in the preceding month, or to tick a ‘nil return’ box if none has been seen, and return the card to the CAPSS office. A tear-off slip is provided with the card to enable psychiatrists to keep a record of patients reported. ‘Positive’ returns are identified by the CAPSS administrator, allocated a unique CAPSS ID (identifier) number and notified to the appropriate research investigator, who then contacts the reporting clinician directly to request completion of a brief data collection form using the CAPSS ID.
For the CostED study, the report card contained a tick box for anorexia nervosa and was sent to reporting clinicians along with a study-specific protocol card detailing the case notification definition for anorexia nervosa (Box 1). Yellow cards or e-mails were sent monthly for the 8-month period of surveillance. The case notification definition, which was approved by the CAPSS Executive Committee, was based on DSM-5 diagnostic criteria for anorexia nervosa and was intended to aid clinicians in their decision of whether to tick ‘yes’ or ‘no’ on the yellow card, and therefore notify a case. It was not intended to identify whether or not a case met study inclusion criteria, which was determined by the CostED research group after receipt of all relevant data.
Please report any child/young person aged 8 to 17 years and 11 months inclusive, who meets the case notification definition criteria below for the first time in the last month. One bullet point criterion from each group below should be fulfilled.
Group A-
Restriction of food, low body weight, or
-
Weight less than expected for age.
-
Fear of gaining weight, or
-
Fear of becoming fat, or
-
Behaviour that interferes with weight gain, for example excessive exercising, self-induced vomiting, use of laxatives and diuretics.
-
Body image disturbance, or
-
Persistent lack of recognition of the seriousness of the current low body weight.
-
Patients who are not underweight.
-
Patients with bulimia nervosa, binge eating disorder, avoidant restrictive food intake disorder or other failure to thrive presentations.
Setting
Cases were notified by clinicians in community-based or hospital-based secondary or tertiary NHS CAMHS in the UK or the RoI.
Procedures
On receipt by the CAPSS system of a new notification of a case of child and adolescent anorexia nervosa, reporting clinicians were sent a baseline questionnaire for each case that they reported (identified via the unique CAPSS ID number). The questionnaire covered characteristics of the notifying service (to enable classification of services as specialist or generic), clinical characteristics of the notified case (to assess case eligibility for follow-up and for inclusion in the incidence study and to provide baseline assessments of outcome) and referral pathway information for the notified case (to ensure that assessment and diagnosis had not happened prior to the study surveillance period). Data collected via the baseline questionnaires are detailed in full below (see Data).
In line with CAPSS procedures and ethics requirements, the baseline questionnaire also contained a limited set of standard patient identifiers. The patient identifiers included a NHS or a Community Health Index number (unique patient identifiers used in the regions of interest), a hospital number, the first half of the postcode or the town of residence for the RoI, sex, date of birth and ethnicity (white, mixed, Asian, black, Chinese, other or unknown). In Northern Ireland, identifiers were further limited to age in years and months (instead of date of birth) and hospital identifier (instead of hospital number) to further reduce the risk of patient identification, given the relatively small geographical area. In keeping with the requirements of the Northern Ireland Privacy Advisory Committee, all patient-identifiable data from Northern Ireland were retained by the local research team, deduplicated, anonymised and subsequently sent for analysis to the central research team at King’s College London.
Inclusion and exclusion criteria
For the incidence study (objective 1), cases were assessed as eligible for inclusion if the young person (1) was between 8 years and 17 years and 11 months of age, (2) had no previous episode of anorexia nervosa that came to the attention of services, (3) had received a clinical assessment in the reporting service during the study surveillance period (1 February 2015 to 30 September 2015), (4) had not been referred from another secondary health service (to ensure that assessment and diagnosis had not happened prior to the study surveillance period) and (5) had the following clinical symptoms: ‘restriction of energy intake relative to requirements’ and ‘persistent behaviour that interferes with weight gain, despite low weight’. For all other study objectives (objectives 2–4), cases additionally had to be notified by a community-based service, thus excluding notifications from inpatient services. However, cases excluded because they were notified by an inpatient service were eligible for inclusion if they were subsequently notified by a community-based service after discharge from the inpatient service.
The two symptoms noted above were initially used to assess eligibility, but these were later checked using a tighter analytical definition based on the DSM-5 criteria. The purpose of this two-stage approach was to be overinclusive and maximise the likelihood of the sample reflecting the actual population of young people accepted for treatment by CAMHS. The tighter analytical definition included the following symptoms:
-
‘restriction of energy intake relative to requirements’
-
‘intense fear of gaining weight or of becoming fat’ or ‘persistent behaviour that interferes with weight gain, despite low weight’
-
‘perception that body shape/size is larger than it is’ or ‘preoccupation with body weight and shape’ or ‘lack of recognition of the seriousness of the current low body weight’.
Only one case that met the broad criteria failed to meet the tighter criteria, thus confirming the validity of the broad criteria applied.
Cases were excluded if the clinician-reported data were insufficient to assess eligibility. Duplicates were identified by comparing NHS/Community Health Index numbers, hospital numbers/hospital identifiers and date of birth/age in years and months, as appropriate. The management of duplicates was dependent on the outcome for the original notification for which a duplicate had been identified. Four scenarios were considered, and each was assessed in different ways, as follows:
-
If the first notification met the study inclusion criteria, the duplicate notification was excluded and the original notification retained.
-
If the first notification resulted in exclusion on grounds of age (patient too young) or clinical ineligibility, the duplicate notification was assessed as a new case to determine if the case now met eligibility criteria.
-
If the first notification had been excluded because of a previous episode of anorexia nervosa, an assessment and diagnosis date prior to the study recruitment period, or referral from another secondary care service, the duplicate notification was also excluded.
-
If the first notification contained insufficient information to judge eligibility for study inclusion (e.g. missing date of birth), the duplicate notification was checked to see if it contained the missing information and, if it did, the first notification was reassessed for eligibility and the duplicate was excluded.
Data
On notification from CAPSS, clinicians reporting cases of anorexia nervosa were sent a baseline questionnaire, and, if the case was found to be eligible for study inclusion, follow-up questionnaires were sent 6 months and 12 months after the date of initial assessment and diagnosis (as reported by clinicians in the baseline questionnaires). Clinicians completed questionnaires from clinical records. Although 12 months is a relatively short period in the treatment of anorexia nervosa, this had to be balanced against the burden on clinicians, NHS interest in the results and the impact on the total duration of the study.
Items missing from baseline or follow-up questionnaires were pursued directly with reporting clinicians by e-mail and telephone. Unreturned or incomplete forms were also chased by e-mail and post. If any of the symptoms required for case definition was absent despite chasing, cases were individually assessed for eligibility by a consultant child and adolescent psychiatrist co-investigator (MS). If there were too many missing data to assess the case, the case was excluded.
In addition to the patient identifiers described in Procedures, the baseline questionnaires contained sections on characteristics of the service, clinical characteristics, outcomes and care pathway of the case notified. In addition, the baseline questionnaire asked whether or not the patient had experienced a previous episode of anorexia nervosa for which they received treatment and whether or not the service was an inpatient service, as the study inclusion criteria focus on community-based new, incident cases of anorexia nervosa. The 6- and 12-month follow-up questionnaires contained identical sections but excluded the question on previous episodes of anorexia nervosa, and in addition included a section on health service use to provide data for costing purposes.
Service characteristics
Service characteristics included in the baseline and both follow-up questionnaires were initially identified using UK definitions of specialist eating disorders services that were available at the time the CostED study started (2013). 24 The criteria were then refined through discussions with clinical members of the CostED study research group to minimise the burden on reporting clinicians while retaining the criteria considered most critical to the classification of services in the CostED study as specialist or generic. The following questions were included:
-
How many cases of eating disorders does the service see per year?
-
Does the service offer specialist outpatient treatment for eating disorders?
-
Does the service hold weekly multidisciplinary meetings dedicated to eating disorders?
-
Does the service provide multidisciplinary specialist outpatient clinics dedicated to eating disorders?
-
How long has the service existed: < 1 year, between 1 and 2 years, between 3 and 5 years or > 6 years?
Clinical characteristics
Clinical characteristics for each notified young person were included in the baseline and follow-up questionnaires to enable assessment of case eligibility by the CostED research team at baseline and to assess outcomes for the young people at follow-up. Clinical characteristics included weight and height and the following clinical features, which required a response of yes, no, not known or not applicable: restriction of energy intake relative to requirements, intense fear of gaining weight or of becoming fat, persistent behaviour that interferes with weight gain despite low weight, perception that body shape/size is larger than it is, preoccupation with body weight and shape, lack of recognition of the seriousness of the current low body weight, excessive exercise, self-induced vomiting (plus estimate of frequency if yes), laxative or diuretic abuse and binge eating (plus estimate of frequency if yes). In addition, clinicians were asked if females had reached menarche and, if they had, whether or not they exhibited secondary amenorrhoea. Note that although amenorrhoea is no longer included in the diagnostic criteria, it is an indicator of significant weight loss and would support the diagnosis of anorexia nervosa.
Weight and height were used to calculate percentage of median expected body mass index (BMI) for age and sex (%mBMI), which involves dividing the young person’s BMI by the median (i.e. 50th centile) BMI for the same height, age and sex taken from appropriate growth charts such as those of the Child Growth Foundation. 25,26
Outcomes
Clinicians were asked to report scores for two generic outcome measures at baseline and both follow-ups: the Children’s Global Assessment Scale (CGAS)27 and the Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). 28 The CGAS is completed by clinicians and is used to rate the emotional and behavioural functioning of children and adolescents in the family, school and social context. Clinicians score the young person on a scale from 1 to 100 using a classification that includes 10 categories ranging from ‘extremely impaired’ (score 1–10) to ‘doing very well’ (score 91–100). The questionnaires contained a copy of the CGAS classification system, describing each of the 10 categories, to support scoring by clinicians. 27 The HoNOSCA is a routine outcome measurement tool rating 13 clinical features on a 5-point severity scale. It assesses behaviours, impairments, symptoms and social functioning of children and adolescents with mental health problems, producing a total score on a scale from 0 to 52, with a higher score indicating a poorer outcome. More specific emotional and behavioural routinely used outcome measures, such as the Strengths and Difficulties Questionnaire,29 are poor at capturing eating disorders, and, although there are eating disorders-specific outcome measures in use, such as the Eating Disorders Examination Questionnaire,30 these are less likely to be used in non-specialist services.
In addition, all cases were classified as ‘no remission’, ‘partial remission’ or ‘full remission’ at the 6-month follow-up and as ‘no remission’, ‘partial remission’, ‘full remission’ or ‘relapse’ at 12 months. These categories were defined by clinical members of the research group as follows.
Full remission at 6 months
Menstruating at 6 months if amenorrhoea at baseline and above minimally healthy weight (%mBMI of > 85%) and no compensatory behaviours or bingeing (i.e. ‘no’ to all of the following five symptoms: restricted eating, excessive exercise, self-induced vomiting, laxative abuse and binge eating) and minimal impact on function (CGAS score of > 70).
Partial remission at 6 months
Do not meet criteria for full remission and above minimally healthy weight (%mBMI > 85%) and limited impact on function (CGAS score of > 60).
No remission at 6 months
Do not meet criteria for full remission or partial remission.
Relapse criteria at 12 months (if in partial or full remission at 6 months)
Admission to hospital between 6 and 12 months or ‘yes’ to symptoms of vomiting and/or binge eating or weight loss of > 5% of %mBMI combined with ‘yes’ to any one of the following symptoms: restricted eating, excessive exercise, self-induced vomiting, laxative abuse or binge eating.
Full remission at 12 months (if no remission or partial remission at 6 months)
Menstruating at 12 months if amenorrhoea at 6 months and above minimally healthy weight (%mBMI > 85%) and no compensatory behaviours or bingeing (‘no’ to all of the following five symptoms: restricted eating, excessive exercise, self-induced vomiting, laxative abuse and binge eating) and minimal impact on function (CGAS score of > 70).
Partial remission at 12 months (if no remission at 6 months)
Do not meet criteria for full remission and above minimally healthy weight (%mBMI > 85%) and limited impact on function (CGAS score of > 60).
No change at 12 months (if no remission, partial remission or full remission at 6 months)
If a participant is in no remission at 6 months and does not meet the criteria for either partial remission or full remission at 12 months, then the participant remains in no remission. If a participant is in partial remission at 6 months and does not meet criteria for relapse or full remission at 12 months, then the participant remains in partial remission. If a participant is in full remission at 6 months and does not meet criteria for relapse at 12 months, then the participant remains in full remission.
Referral pathway
Referral pathway information was included in the baseline questionnaire to ensure that assessment and diagnosis had not happened prior to the study surveillance period and clinicians were asked to report whether or not the case had been referred from another secondary health service. If yes, the clinician was asked to report the type of service (inpatient psychiatry, paediatrics, specialist CAMHS, specialist eating disorders service or other – please specify). To enable us to follow up those who had moved to another CAMHS, clinicians were asked in the baseline and follow-up questionnaires if the patient had been referred to another service and, if so, to which service.
Health service use
As data were to be collected from clinical records, the perspective of the economic evaluation was limited to secondary/tertiary health services for which data were likely to be available to all reporting clinicians. The 6- and 12-month follow-up questionnaires contained a section on the use of these health services, which included hospital inpatient admissions (including the following ward types: paediatric, general child/adolescent psychiatry, general adult psychiatry, child/adolescent eating disorders unit, adult eating disorders unit or other), outpatient attendances [including paediatrics, specialist eating disorders service (CAMHS or adult) and other psychiatric service (CAMHS or adult)] and day-patient attendances [including paediatrics, specialist eating disorders service (CAMHS or adult) and other psychiatric service (CAMHS or adult)]. For inpatient admissions, respondents were additionally asked to report whether or not the facility was in the independent sector.
In a previous study [the Treatment Outcome for Child and Adolescent Anorexia Nervosa (TOuCAN) study], which took a societal perspective, 2-year total costs were found to be heavily dominated by hospital costs and CAMHS community outpatient costs. 18 Together, these accounted for > 90% of the total 2-year costs. 31 Similarly, a more recent study found that service costs in a population of adolescents with eating disorders were driven by hospital admissions. 32 Thus, although our approach was narrower than that usually adopted for an economic evaluation (i.e. excluding broader health and social care services), it was considered appropriate to minimise respondent burden while still providing evidence of the key costs in this population.
Sample size
The calculation of a sample size (which allows inferences to be made about the population as a whole) was not appropriate for the CostED study, because the aim of the study was to collect population-level data. However, some estimate of expected numbers was considered beneficial to support the estimation of study resources. The following provides estimates for expected baseline and follow-up rates, based on evidence available for the UK.
Primary care incidence of anorexia nervosa estimates
Based on data from primary care in the UK, between 1994 and 2000, the incidence rate of anorexia nervosa among children and adolescents (aged between 10 and 19 years) was 34.6 per 100,000 for females and 2.3 per 100,000 for males. 33 Among children aged 0–9 years, the incidence rate was zero. More recent UK estimates using data from 2000 to 2009 for young people aged 10–19 years indicate a small increase in incidence rates to 37.1 per 100,000 for females and 3.2 per 100,000 for males. 34 We applied these more recent estimates, broken down by age and sex when possible, to population data for the UK and the RoI35,36 for young people aged between 10 and 18 years. Estimates for younger children were available only from the earlier study. 33 The results are reported in Table 1. These incidence rates suggested an estimated number of new cases of anorexia nervosa in those < 18 years old in primary care in the UK and the RoI over an 8-month period of 886 (approximately 810 females and 76 males).
| Age (years) and sex | Incidence | Population by age | Number of cases | Source | |||
|---|---|---|---|---|---|---|---|
| UK | RoI | UK | RoI | Total | |||
| 8–9 | |||||||
| Both | 0.00 | 1,333,900 | 126,416 | 0 | 0 | 0 | Currin et al.33 |
| 10–14 | |||||||
| Female | 24.00 | 1,741,600 | 147,415 | 418 | 35 | 453 | Micali et al.34 |
| Male | 2.50 | 1,825,400 | 155,076 | 46 | 4 | 50 | Micali et al.34 |
| 15–18 | |||||||
| Female | 47.50 | 1,494,000 | 110,237 | 710 | 52 | 762 | Micali et al.34 |
| Male | 3.80 | 1,581,800 | 115,700 | 60 | 4 | 65a | Micali et al.34 |
| Total 12 months | 1329 | ||||||
| Total 8 months | 886 | ||||||
Secondary care incidence of anorexia nervosa estimates
Data from secondary care studies were more limited. Data from a London care pathways study17 suggested an incidence rate of 54.6 per 100,000 for young women aged between 13 and 18 years, including anorexia nervosa and eating disorders not otherwise specified – anorexia nervosa sub-type (EDNOS-AN), a proportion of whom would now be diagnosed with anorexia nervosa using DSM-5 criteria. Data for young men were not reported as the numbers were so small. For the younger ages, data were available from a British national surveillance study carried out in 2005/6 using the CAPSS system. 37 Application of these rates to UK and the RoI population data35,36 is reported in Table 2, broken down by age and sex when data allowed. For males aged 13–18 years, primary care rates were used because of the lack of secondary care data for this group. 34 These incidence rates suggested an estimated number of new cases of anorexia nervosa in the UK and the RoI of 957 over an 8-month period, which is slightly higher than the primary care estimate above. However, given that the majority of these cases were estimated using London data (females aged 13–18 years),17 we adjusted the London data downwards to take into account the fact that incidence rates in London may be higher than the UK and the RoI more broadly as a result of higher incidence of eating disorders in urban versus rural areas,38 as well as a higher concentration of specialist eating disorders services. We reduced London incidence rates by 10% and by 20%, as shown in Table 2.
| Age (years) | Sex | Incidence | Population by age | Number of cases | Source | |||
|---|---|---|---|---|---|---|---|---|
| UK | RoI | UK | RoI | Total | ||||
| 8 | Total | 0.00 | 666,300 | 63,581 | 0 | 0 | 0 | Nicholls et al.37 |
| 9 | Total | 0.72 | 667,600 | 62,386 | 5 | 0 | 5 | Nicholls et al.37 |
| 10 | Total | 1.42 | 683,300 | 61,181 | 10 | 1 | 11 | Nicholls et al.37 |
| 11 | Total | 1.69 | 703,100 | 60,587 | 12 | 1 | 13 | Nicholls et al.37 |
| 12 | Total | 3.63 | 715,500 | 60,926 | 26 | 2 | 28 | Nicholls et al.37 |
| 13–18 | Female | 54.60 | 2,208,700 | 168,213 | 1206 | 92 | 1298 | House et al.17 |
| 13–14 | Male | 2.50 | 750,300 | 61,018 | 19 | 2 | 20a | Currin et al.33 |
| 15–18 | Male | 3.80 | 1,581,800 | 115,700 | 60 | 4 | 65a | Currin et al.33 |
| Total 12 months | 1440 | |||||||
| Total 8 months | 960 | |||||||
| London incidence rate at 8 months, reduced by 10% | 864 | |||||||
| London incidence rate at 8 months, reduced by 20% | 768 | |||||||
Estimated incidence of anorexia nervosa
The estimates presented in Primary care incidence of anorexia nervosa estimates and Secondary care incidence of anorexia nervosa rates suggest a total population of new cases of anorexia nervosa of between 800 and 900 over the 8-month surveillance period. Using data from the previous British national surveillance study,37 Table 3 reports expected rates of case notification at baseline and response rates at 6- and 12-month follow-up, dependent on whether the number of new cases is the higher (n = 900) or the lower (n = 800) of these estimates. The estimates in Table 3 suggest that approximately 590–660 notifications should be received at baseline and follow-up data should be available for between 300 and 330 cases at 6 months and between 220 and 250 cases at 12 months.
| Expected rates of notification and follow-up | Lower estimate | Higher estimate |
|---|---|---|
| Baseline notifications | ||
| Expected new cases in UK and the RoI | 800 | 900 |
| 75% referred by psychiatrists (excludes paediatricians) | 600 | 675 |
| 85% of all psychiatrists expected to report | 510 | 574 |
| Plus 15% expected duplicatesa = total baseline notifications | 587 | 660 |
| Follow-up rates | ||
| Expected new cases excluding duplicates | 510 | 574 |
| 85% with sufficient data to assess eligibilityb | 434 | 488 |
| 80% with no reporting errorsc | 347 | 390 |
| 85% response rate at first follow-up = 6-month estimate | 295 | 332 |
| 75% response rate at second follow-up = 12-month estimate | 221 | 249 |
Incidence of child and adolescent anorexia nervosa
Accurate epidemiological estimates of the number of new cases of anorexia nervosa per year are helpful for service planning. In the UK, the most recent incidence data available are from 2000 to 2009. 34 To date, the majority of incidence estimates have come from primary care records,33,34 which may fail to accurately record all cases of eating disorders. 39,40 This may be particularly true in the UK context, given guidelines41 requiring assessment and diagnosis of anorexia nervosa to be carried out by child and adolescent psychiatrists in secondary or tertiary care settings. As a result, secondary care records are a more reliable source of data on anorexia nervosa incidence than are primary care records.
Aim
The incidence component of the CostED study (objective 1) aimed to estimate the incidence of anorexia nervosa in secondary care services among all young people, male and female, between the age of 8 years and 17 years and 11 months in the UK and the RoI, using cases notified to the CostED study.
Analysis: incidence study
All data analyses were carried out in the software packages Stata® IC version 14.2 (StataCorp LP, College Station, TX, USA) and Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA).
Observed incidence rates (IRs) (IR0), defined as the number of new cases occurring during a specified period of time in a population at risk of developing the disease, were calculated as follows: the number of confirmed new cases of anorexia nervosa in the study’s 8-month surveillance period converted to 12 months [(number of cases over 8 months/8) × 12], then divided by the population at risk and multiplied by 100,000 to give the observed incidence rate per 100,000 young people:
The population at risk, used as the denominator, was calculated as the total number of children of each sex and each year of age between 8 and 17 in the UK and the RoI, minus the number of prevalent cases of patients who, once diagnosed, are no longer part of the ‘at-risk’ population. Population data for young women and young men aged 8 to 17 years in 2015 were obtained from the Office for National Statistics for the UK35 and from the Central Statistics Office for the RoI. 42 To estimate the number of prevalent cases each year, incident cases in the previous age band were used as a proxy. For example, incident cases of patients aged 8 years were used as a proxy for prevalent cases in the estimation of the ‘at-risk’ population aged 9 years, and so on.
To consider incidence among unobserved missing cases, adjustments were needed to take into account unreturned notification cards to CAPSS and unreturned questionnaires for positive case notifications.
Just over half of all CAPSS notification cards sent out were returned (50.16%). To account for incidence among the 49.84% of unreturned cards, two assumptions were made about the unreturned cards, and a correction applied to the observed incidence rate as appropriate.
-
Assumption 1: to take into consideration the possibility that unreturned cards are more likely to be negative (i.e. ‘nil’ returns), it was assumed that half of the unreturned cards (24.92%) were ‘negative’ and the other half followed the same proportion of ‘negative’ and ‘positive’ as the returned cards. This assumption translates to a correction coefficient of 1.50, derived from (24.92 + 50.16)/50.16.
-
Assumption 2: assuming no bias in the likelihood of unreturned cards being either negative or positive returns, it was assumed that all unreturned notification cards followed the same proportion of ‘negative’ and ‘positive’ as the returned cards. This assumption translates to a correction coefficient of 1.99 derived from (49.84 + 50.16)/50.16.
These assumptions provide a range of incidence rates from a minimum (observed incidence rates) to a maximum (assumption 2), within which the actual rate is likely to fall. It is hypothesised that assumption 1 provides the most realistic estimate because it assumes that there is a bias in the response rates with greater likelihood that unreturned cards are negative (i.e. clinicians are less likely to return ‘nil’ returns than ‘positive’ returns) but does not assume that all unreturned cards are ‘nil’ returns.
Approximately two-thirds of the questionnaires that were sent to clinicians reporting positive cases of anorexia nervosa were returned (63%), leaving one-third (37%) unreturned. As all these questionnaires relate to a ‘positive’ notification, we applied a correction coefficient of 1.59, derived from (37 + 63)/63, which assumes that the incidence rate for the unreturned questionnaires is the same as the incidence rate identified in the returned questionnaires for each year of age.
As well as reporting the observed incidence rates (IR0), we combined the correction coefficients described above to generate two adjusted incidence rates.
Adjusted incidence rate 1
Confirmed new cases of anorexia nervosa converted to 12 months, multiplied by the correction for unreturned CAPSS notification cards under assumption 1, multiplied by the correction for unreturned questionnaires, then divided by the population at risk and multiplied by 100,000. This estimate applies the proportion of observed positive and negative cases to half of the cases unobserved as a result of unreturned CAPSS notification cards (the other half assumed ‘nil’ returns) and to all data unobserved because of unreturned questionnaires:
Adjusted incidence rate 2
Confirmed new cases of anorexia nervosa over 12 months, multiplied by the correction for unreturned CAPSS notification cards under assumption 2, multiplied by the correction for unreturned questionnaires and then divided by the population at risk and multiplied by 100,000. This estimate applies the proportion of observed positive and negative cases to all data unobserved as a result of unreturned CAPSS notification cards and to all data unobserved as a result of unreturned questionnaires:(3)IR2=(confirmed new cases of anorexia nervosa converted to 12 months×1. 99×1. 59)/the population at risk×100,000
For each incidence rate, IR0, IR1 and IR2, total, age-specific and sex-specific annual incidence rates for anorexia nervosa for the year 2015 and 95% confidence intervals (CIs) were calculated based on the Poisson distribution43 using the Stata version 14.2 command ‘ci means [N new anorexia nervosa cases 12m], Poisson [exposure(total population)]’ for positive integers/whole incidence numbers (Stata interprets any non-integer decimal point number between 0 and 1 as the fraction of events and converts it to an integer number) and an online CI calculator for rational/fraction numbers (www.openepi.com/PersonTime1/PersonTime1.htm; accessed 13 February 2017). Annual incidence rates were stratified by discrete age (8–17 years) and sex.
Classification of child and adolescent mental health services as specialist or generic
Specialist eating disorders services are not clearly defined, with definitions changing over time20,24 and little indication of how these criteria have been determined. The absence of a clear consensus on what constitutes a specialist eating disorders service hampers attempts to evaluate the clinical effectiveness and cost-effectiveness of such services, and thus to assess the value of future investment to expand provision to a greater proportion of the population.
Aim
The aim of the service classification component of the CostED study was to obtain consensus on the key features of a specialist child and adolescent eating disorders service from a range of stakeholders in order to support the classification of notifying services as either specialist or generic (objective 2).
Study design
The Delphi survey method was used to collect opinions from a wide range of stakeholders in eating disorders, and to reach consensus on the key criteria for a community-based CAMHS to be classified as a specialist eating disorders service. The Delphi approach is a technique designed to combine individual opinions into group consensus, iteratively, through a series of rounds of structured questionnaires. Responses from each round are analysed, summarised and fed back to the participants, who are given an opportunity to respond again to the emerging data. 44–50 The availability of online survey platforms enabled this study to use the Delphi technique to involve geographically distant respondents in larger numbers than are traditionally used in studies employing face-to-face discussion.
Respondents
A range of stakeholders, including service users and their families, child and adolescent psychiatrists, paediatricians, other eating disorders professionals and service commissioners, were invited to take part in the Delphi survey using two different methods: direct e-mail contact and an open web link invitation. Direct e-mails were sent to 687 named child and adolescent psychiatrists using the CAPSS database and to five service commissioners known by the research group to be working in child and adolescent mental health. The open web link invitation was circulated by a range of networks including the eating disorders faculty of the Royal College of Psychiatrists, a group of approximately 1500 child and adolescent and adult psychiatrists, and the Child and Adolescent Feeding and Eating Disorders Network (Café-Net). Café-Net is a multidisciplinary network of approximately 300 child and adolescent feeding and eating disorders professionals working in eating disorders services, whose members include child and adolescent psychiatrists, paediatricians, psychologists, psychotherapists, family therapists, dietitians and nurses. Service users and their families were invited to take part via a survey web link advertised by Beat, the UK national eating disorders charity, via its e-newsletter (approximately 21,500 e-mail addresses) and its research e-newsletter (approximately 456 e-mail addresses of people who signed up to receive updates about opportunities to take part in research).
Criteria for specialist eating disorders services
Criteria relevant to the classification of specialist eating disorders were identified as described in Service characteristics. The included criteria are summarised in Table 4, alongside the UK guideline criteria available at the time24 and, for comparison, guideline criteria for England that became available after the CostED study began. 20
| Criterion | Guidelines available at the start of the CostED study24 | Associated questions included in questionnaire to clinicians | Comment | Guidelines that became available after the CostED study began20 |
|---|---|---|---|---|
| Interventions | Patients are offered individual interventions, including CBT and family-based interventions | ‘Does the service offer specialist outpatient treatment for eating disorders?’ | The clinical group advised that a wide range of interventions are available and that focusing only on CBT and family-based interventions would be too narrow | Use up-to-date evidence-based interventions to treat the most common types of coexisting mental health problems (e.g. depression and anxiety disorders) alongside the eating disorder |
| Staff | The service will have a multidisciplinary staff team, including at least one consultant psychiatrist, one nurse and one therapist | ‘Does the service hold weekly multidisciplinary meetings dedicated to eating disorders?’ and ‘Does the service provide multidisciplinary specialist outpatient clinics dedicated to eating disorders?’ | Given the CAPSS requirement to keep the CostED questionnaire brief to minimise reporting burden, it was not possible to request data on all staff in reporting services so the focus was placed on the multidisciplinary nature of the eating disorders provision | Include medical and non-medical staff with significant eating disorders experience |
| Activity | There will be ≥ 25 new referrals per annum | ‘How many cases of eating disorders does the service see per year?’ | Included | The service should receive ≥ 50 new eating disorders referrals per year, which are likely to include anorexia nervosa, bulimia nervosa, binge eating disorder and related diagnoses |
| Population | Not stated | ‘Approximate population of catchment area covered by the service?’ | Included on the advice of clinical research team members on the assumption that specialist services are more likely to be made available to a wider catchment area | Cover a minimum general population of 500,000 (all ages) |
| Age of service | Criteria not included | ‘How long has the service existed for?’ | Included on the advice of clinical research team members on the assumption that more established services will have had longer to become ‘specialist’ | Criteria not included |
| Intensity | Outpatient and inpatient treatment are provided | Criteria not included | Excluded as the focus of the CostED study was on community-based services | Criteria not included |
| Referral pathway | Criteria not included | Criteria not included | Criteria outlined as part of guidelines published after the CostED study began | Enable direct access to community eating disorders treatment through self-referral and from primary care services (e.g. GPs, schools, colleges and voluntary sector services) |
These criteria were included in the Delphi survey and respondents were asked to rate the importance of each criterion in considering whether or not a community-based eating disorders service can be classified as a specialist service. Responses were rated on a 5-point Likert scale from 1 = not important to 5 = extremely important. Full details of the criteria, associated questions and responses are contained in Table 5. Some questions were associated with follow-up subquestions that were asked only of those who rated the main criterion as important (2 = slightly important, 3 = moderately important, 4 = very important or 5 = extremely important).
| Question | Criterion | Question | Response |
|---|---|---|---|
| 1 | Offering specialist (evidence-based) outpatient treatment for eating disorders | How important is this in considering whether or not a community-based eating disorders service can be classified as a specialist service? | 1 = not important, 2 = slightly important, 3 = moderately important, 4 = very important, 5 = extremely important |
| 2 | Holding weekly multidisciplinary meetings dedicated to eating disorders | How important is this in considering whether or not a community-based eating disorders service can be classified as a specialist service? | 1 = not important, 2 = slightly important, 3 = moderately important, 4 = very important, 5 = extremely important |
| 3 | Providing multidisciplinary specialist outpatient clinics dedicated to eating disorders | How important is this in considering whether or not a community-based eating disorders service can be classified as a specialist service? | 1 = not important, 2 = slightly important, 3 = moderately important, 4 = very important, 5 = extremely important |
| 4 | Number of cases of eating disorders a service sees per year | How important is this in considering whether or not a community-based eating disorders service can be classified as a specialist service? | 1 = not important, 2 = slightly important, 3 = moderately important, 4 = very important, 5 = extremely important |
| Sub 5 | Number of cases of eating disorders a service sees per year | If important, what is the minimum number of cases of eating disorders that a community-based eating disorders service should see per year before it can be classified as a specialist service? | 1 = ≥ 10, 2 = ≥ 25, 3 = ≥ 50, 4 = ≥ 75, 5 = ≥ 100 |
| 6 | Population size of the catchment area covered by the service | How important is this in considering whether or not a community-based eating disorders service can be classified as a specialist service? | 1 = not important, 2 = slightly important, 3 = moderately important, 4 = very important, 5 = extremely important |
| Sub 7 | Population size of the catchment area covered by the service | If important, what is the minimum approximate population of the catchment area that a community-based eating disorders service should cover before it can be classified as a specialist service? | 1 = ≥ 25,000, 2 = ≥ 50,000, 3 = ≥ 100,000, 4 = ≥ 250,000, 5 = ≥ 500,000, 6 = ≥ 750,000, 7 = ≥ 1,000,000, 8 = national coverage |
| 8 | Length of time a service has existed | How important is this in considering whether or not a community-based eating disorders service can be classified as a specialist service? | 1 = not important, 2 = slightly important, 3 = moderately important, 4 = very important, 5 = extremely important |
| Sub 9 | Length of time a service has existed | How long should a community-based eating disorders service have existed for before it can be classified as a specialist service? | 1 = < 1 year, 2 = 1–2 years, 3 = 3–5 years, 4 = ≥ 6 years |
Procedure
The Delphi survey involved two rounds. Round 1 took place between 29 January 2016 and 6 May 2016 and included all six main questions and three subquestions listed in Table 5. Round 2 took place between 20 July 2016 and 20 September 2016 and included only the main questions (and their associated subquestions, if relevant) when consensus had not been reached in round 1. For each question and subquestion included in round 2, data from round 1 were reported to allow respondents to consider their response in relation to the group average from round 1. If consensus was not reached in round 2, the item was excluded from the final criteria checklist for analysis purposes but included in a sensitivity analysis. For brevity and to encourage maximum participation, no other information was collected as part of the survey, apart from e-mail addresses, which were included in round 1 in order to be able to recontact round 1 participants to complete the round 2 survey.
Consensus
Consensus decision rules for the main criteria in this study were finalised prior to data analysis and focused on the percentage of respondents rating each criterion as either 4 (very important) or 5 (extremely important). The literature to date does not provide a clear definition of what percentage agreement is required before consensus is reached in Delphi panels. Values vary from 51% to 100%,44–50 with 75% being the median threshold to define consensus. 44 We conservatively chose 80% as our threshold to conclude that consensus had been reached that a criterion was essential when categorising a service as a specialist eating disorders service. The threshold below which we considered consensus to have been reached to exclude a criterion was set at < 50%, again relatively conservatively compared with previous literature. 49 Percentage responses between 50% and 79% were considered ‘consensus not reached’, and criteria falling into this range in round 1 were included in round 2 of the Delphi survey. The decision rules are summarised in Table 6.
| Percentage of respondents rating criterion as 4 or 5 (%) | Decision rule |
|---|---|
| 80–100 | Consensus reached and item included in checklist |
| 50–79 | Consensus not reached |
| 0–49 | Consensus reached and item excluded from checklist |
Analysis: classification study
Responses to the Delphi survey were collected using the online survey platform SurveyMonkey® (Palo Alto, CA, USA). Following survey completion, responses were imported in Microsoft Excel 2010 and converted to a Stata IC version 14.2 data set when analysis was conducted. Responses were summarised using descriptive statistics, including the number and percentage of responses in each category and the median and mode measures of central tendencies for ordinal data. The predetermined consensus decision rules described above were applied to all responses.
Using data from the CostED study, consensus criteria were applied at both the service level and the patient level to provide estimates of the proportion of notifying services classified as specialist or generic, and the proportion of CostED participants being assessed in specialist versus generic community-based services. In the main analysis, services were classified using only those criteria for which consensus had been reached in the Delphi survey. Classification was repeated in a sensitivity analysis that additionally included criteria that remained uncertain after both Delphi survey rounds. Data from subquestions are reported only when associated with a main question for which consensus was reached to include the criterion or when consensus was uncertain and thus the criterion was included in the sensitivity analysis.
Cost, effectiveness and cost-effectiveness analysis
Cost of health service contacts
Data on inpatient, outpatient and day-patient health service contacts, described in Health service use, were used to calculate the 6- and 12-month costs of all cases eligible for follow-up and to assess the relative cost of alternative community-based models of service provision (objective 3). All resource use data related to the period February 2015 to September 2016 (8 months of surveillance and 12-month follow-up) and costs, in Great British pounds, were for the 2015/16 financial year. Discounting was not necessary as the follow-up length was not more than 12 months. Costs for NHS hospital admissions and outpatient and day-patient contacts, which included CAMHS contacts, were taken from NHS Reference Costs 2014–15. 51 The cost of independent sector hospital admissions and contacts were provided by a range of independent sector organisations and NHS trusts via personal communications and the average cost used when more than one figure was provided. Unit costs are summarised in Table 7.
| Service | Unit cost (£) | Source |
|---|---|---|
| NHS inpatient cost per night | ||
| Eating disorders unit: child/adolescent | 510.14 | NHS Reference Costs 2014–15 51 |
| Eating disorders unit: adult | 455.02 | NHS Reference Costs 2014–15 51 |
| General psychiatry: child/adolescent | 633.07 | NHS Reference Costs 2014–15 51 |
| General psychiatry: adult | 197.29 | NHS Reference Costs 2014–15 51 |
| Paediatric if stay is 1 night | 426.99 | NHS Reference Costs 2014–15 51 |
| Paediatric if stay is > 1 night | 592.27 | NHS Reference Costs 2014–15 51 |
| Other NHS | 389.10 | NHS Reference Costs 2014–15 51 |
| Independent sector inpatient cost per night | ||
| Eating disorders unit: child/adolescent | 695.00 | Personal communication |
| General psychiatry: child/adolescent | 668.00 | Personal communication |
| Outpatient cost per contact | ||
| Eating disorders service | 262.12 | NHS Reference Costs 2014–15 51 |
| Other psychiatry | 298.57 | NHS Reference Costs 2014–15 51 |
| Paediatric | 194.36 | NHS Reference Costs 2014–15 51 |
| Day-patient cost per contact | ||
| Eating disorders service | 274.21 | NHS Reference Costs 2014–15 51 |
| Other psychiatry | 326.16 | NHS Reference Costs 2014–15 51 |
| Paediatric | 446.60 | NHS Reference Costs 2014–15 51 |
Analysis: costs and outcomes
All analyses compared participants initially assessed and diagnosed in specialist eating disorders services with those initially assessed and diagnosed in generic CAMHS, with services classified using the results of the Delphi analysis already described (see Classification of children and adolescent mental health services as specialist or generic). All analyses were adjusted for prespecified baseline covariates including baseline CGAS score, baseline %mBMI, age, sex and region (England, Wales, Scotland, Northern Ireland or the RoI).
Total costs per participant in each group over the 6- and 12-month follow-up periods were compared using standard parametric t-tests. Although cost data are commonly skewed, the advantage of this approach, as opposed to logarithmic transformation or non-parametric tests, is the ability to make inferences about the arithmetic mean, which is more meaningful from a budgetary perspective. 52 The robustness of this approach was confirmed using bootstrapping. 53 Outcomes tested for differences at the 6- and 12-month follow-up points included the CGAS score, HoNOSCA and %mBMI. All were tested using standard t-tests.
We had originally proposed additionally exploring differences between children (between 8 and 12 years old) and adolescents (between 13 and 17 years old) and between young people living in rural or urban areas. However, neither proved possible. For the comparison of children and adolescents, the sample of children proved too small, with only 35 (12%) of the follow-up sample being between 8 and 12 years of age. Furthermore, full 12-month cost data were available for only 18 cases and outcome data were available for a maximum of 23 cases (%mBMI) and a minimum of three cases (HoNOSCA) at 6-month follow-up and for a maximum of 13 cases (%mBMI) and a minimum of three cases (HoNOSCA) at 12-month follow-up. For the purpose of comparing rural and urban areas, the first half of a postcode proved inadequate to enable locations to be accurately classified, with a large proportion of the first halves of postcodes covering a mixture of rural and urban areas. Without full postcodes, this analysis could not be undertaken.
All analyses used complete-case data. Missing items in questionnaires were chased up directly with reporting clinicians via both e-mail and telephone. Missing follow-up questionnaires (or cases that could not be included as a result of key missing items) were assumed to be missing at random, and sensitivity analysis examined the effect of these missing cases on total costs (over the periods 0–6 months, 6–12 months and 0–12 months) and outcomes (%mBMI, CGAS score and HoNOSCA at 6 and 12 months) using multiple imputations to test the robustness of the complete-case analyses. 54
Analysis: cost-effectiveness analysis
Individual-level cost and outcome data were used to calculate the relative cost-effectiveness of initial assessment and diagnosis of anorexia nervosa in a community-based specialist eating disorders service compared with initial assessment and diagnosis in a community-based generic CAMHS at the 6- and 12-month follow-up points. Although the 12-month follow-up point was considered the primary end point given the chronic and long-term nature of anorexia nervosa, missing data were expected to be higher at the 12-month point, so assessment of cost-effectiveness at the 6-month follow-up point was also considered important.
The prespecified primary measure of effectiveness for the cost-effectiveness analysis, as outlined in the proposal and the original protocol, was the HoNOSCA. The %mBMI was specified as a secondary cost-effectiveness analysis because, although more narrowly focused on weight, data on weight and height were expected to be available for a greater proportion of the population than data on clinical outcomes. The preference in economic evaluation is to measure outcomes using broad, preference-based, generic measures of quality of life capable of generating quality-adjusted life-years (QALYs). 55 However, the CostED study was limited to measures of outcome likely to be available from clinical records and, although weight-related outcomes are key to anorexia measures, the HoNOSCA was chosen as the primary measure because it is a broader measure of outcome than %mBMI.
It became clear from the baseline questionnaires, however, that the number of missing HoNOSCA data was substantial (79% missing at baseline), suggesting that this measure was not being routinely used in many outpatient services. For this reason, the protocol was amended, replacing the HoNOSCA with the CGAS, for which a greater proportion of data were available (8% missing at baseline). As expected, the number of missing data was smallest for %mBMI (1% missing at baseline), and, therefore, %mBMI was retained as the measure of effectiveness in a secondary cost-effectiveness analysis.
The cost-effectiveness of specialist versus generic services was explored in a decision-making context, with a focus on the probability of one service model being cost-effective compared with the other given the data available, rather than a focus on statistical significance. This is the recommended approach for economic evaluation in the UK context. 56 Cost-effectiveness analysis is concerned with the combined difference in costs and effects between interventions and was assessed by taking the recommended net benefit approach. 57 One treatment can be defined as cost-effective relative to a comparator if (1) it is less costly and more effective and is thus dominant; (2) it is more costly and more effective, but the additional cost per extra unit of effectiveness is considered worth paying by decision-makers; or (3) it is less costly and less effective and the additional cost per extra unit of effectiveness generated by the alternative is not considered worth paying. In scenario (1), in which one intervention is dominant, cost-effectiveness is confirmed. In scenarios involving a trade-off, such as (2) and (3), incremental cost-effectiveness ratios are calculated as the difference in mean costs between one intervention and another (in this case specialist minus generic services) divided by the difference in mean effect between the two groups.
A joint distribution of incremental mean costs and effects for the two groups was generated using non-parametric bootstrapping53 to explore the probability that each treatment is the optimal choice, subject to a range of possible maximum values (ceiling ratio) that a decision-maker might be willing to pay for an additional unit of outcome gained. Willingness to pay was varied from £0 to £30,000. Cost-effectiveness acceptability curves were then generated by plotting these probabilities for a range of possible values of the ceiling ratio. 58,59 These curves are the recommended decision-making approach to dealing with the uncertainty that exists around the estimates of mean costs and effects as a result of sampling variation and uncertainty regarding the maximum cost-effectiveness ratio that a decision-maker would consider acceptable. 56,59
Cost-effectiveness planes are also presented to illustrate the spread of scatter points across the four quadrants of the plane, whose four quadrants can be described as follows:
-
North-west quadrant – the costs of the intervention group are higher than the costs of the control group (above the x-axis) and the outcomes are worse (to the left of the y-axis); thus, the control dominates.
-
North-east quadrant – the costs of the intervention group are higher than the costs of the control group (above the x-axis) and the outcomes are better (to the right of the y-axis); thus, there is a trade-off between the two groups.
-
South-west quadrant – the costs of the intervention group are lower than the costs of the control group (below the x-axis) and the outcomes are worse (to the left of the y-axis); thus, there is a trade-off between the two groups.
-
South-east quadrant – the costs of the intervention group are lower than the costs of the control group (below the x-axis) and outcomes are better (to the right of the y-axis); thus, the intervention dominates.
Decision-analytic modelling
Aim
The aim of the decision modelling component of the CostED study was to explore the economic impact of changes to the configuration of specialist eating disorders services for children and adolescents, specifically the impact of increasing the availability of specialist services. The decision model was therefore designed to enable us to vary the proportion of a hypothetical cohort of young people who received specialist eating disorders services or generic CAMHS. As a result, model results are presented for the full hypothetical cohort, rather than separately for specialist eating disorders services versus generic CAMHS. Thus, these results are not attempting to explore the relative cost-effectiveness of specialist versus generic services but are instead focused on the overall impact for the cohort, as the proportion of young people being assessed by specialist or generic services is varied.
Design
Decision analysis is a structured way of thinking about the likely impact of a decision or policy change. It involves the construction of a logical model to represent the relationship between inputs (costs) and outputs (outcomes) in order to inform resource allocation decisions under conditions of uncertainty. 60 Decision models use mathematical relationships to define possible consequences that flow from a set of alternative options being evaluated. 61 Each pathway in a decision model is associated with a probability, an outcome and a cost, with the cost being the sum of the costs of each of the events an individual experiences in that pathway. Decision modelling commonly uses existing data on costs, outcomes and probabilities from a range of possible sources including from completed studies, from the literature or from expert opinion.
Once constructed, the assumptions and the data used in a model can be varied, for example as new data become available. In addition, models can be used to explore ‘what if?’ scenarios to provide decision-makers with information on the likely impact of changes to services, such as changes in treatment length, personnel or capacity. This is the approach taken in the CostED study, with data being taken from the CostED surveillance study but alternative scenarios being explored.
Model structure
The structure of the model was based on knowledge and understanding of the course of anorexia nervosa over time and was developed in close collaboration with the clinicians and service managers in the research group. The model was developed to determine the economic impact of changes to the configuration of specialist eating disorders services for children and adolescents, specifically the impact of increasing the availability of specialist services. To do this, the model needed to summarise the possible pathways that a young person could take following a diagnosis of anorexia nervosa in a generic CAMHS or in a specialist eating disorders service, and the relative treatment effect afforded by each treatment option, in order to then be able to alter the mix or number of patients taking each pathway. Changes to the data passing through the pathways would then support the exploration of changes to the provision of specialist services in the UK and the RoI.
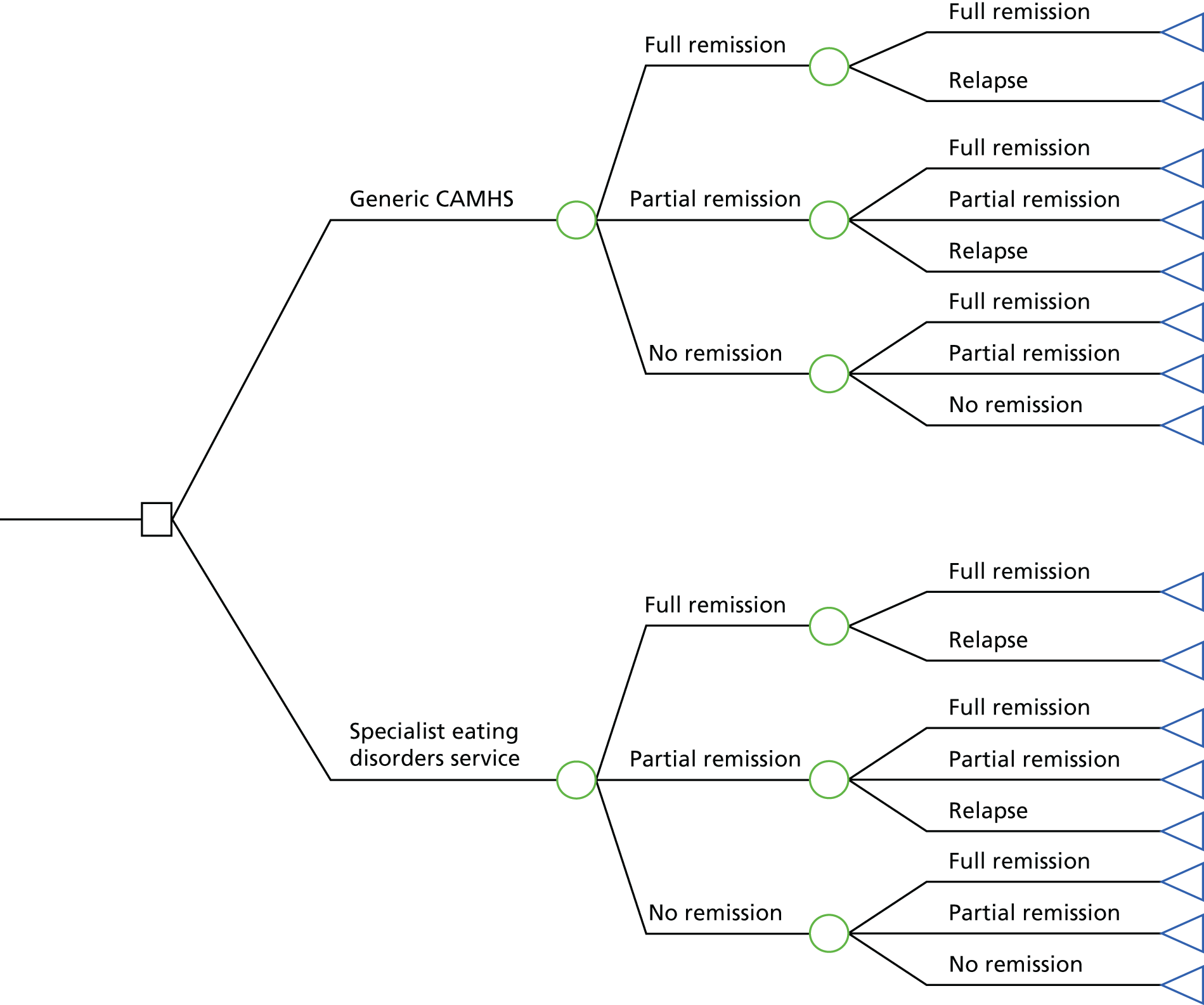
The basic decision model structure is shown in Figure 1. The pathway starts on the far left, where a young person is assessed and diagnosed with anorexia nervosa in either a generic CAMHS or a specialist eating disorders service. As outlined earlier (see Outcomes), young people are then assessed at 6 months and at 12 months for their remission or relapse status. At 6 months, the young person is in full remission, partial remission or no remission. At 12 months, young people who had been in full remission at 6 months can either remain in full remission or relapse at 12 months, young people who had been in partial remission at 6 months can relapse, remain in partial remission or enter full remission at 12 months, and young people who had been in no remission at 6 months can remain in no remission or enter partial or full remission at 12 months.
FIGURE 1.
Decision-analytic model.
A second model, to be run over 5 years, was originally planned using data from the TOuCAN study (see Health service use), which included a 5-year follow-up in addition to the original 2-year follow-up. 62 The TOuCAN study included both cost and HoNOSCA data over the full 5-year period, and thus would have been of value had the HoNOSCA remained the primary outcome measure of the CostED study. However, the substantial number of missing HoNOSCA data meant that it was not possible to use the HoNOSCA in the CostED study in any meaningful way and the primary outcome measure had to be changed to the CGAS (see Analysis: cost-effectiveness analysis), which was not included as an outcome measure in the TOuCAN study. No other sources of long-term cost and CGAS data for young people with anorexia nervosa were identified.
Model inputs
The model used data collected in the CostED study and followed the same timeline (12 months). Each remission and relapse state has cost, effect and outcome variables associated with it, as well as a probability of being in each state.
Model probabilities
Probabilities were calculated based on the number of people in each remission or relapse state in each arm (generic CAMHS or specialist eating disorders service) at the two time points (i.e. the 6- and 12-month follow-ups). All participants start with diagnosed anorexia nervosa and baseline CGAS scores equal to the mean CGAS score among all young people in the relevant study arm (generic CAMHS or specialist eating disorders service). No historical treatment data are factored into their treatment as all are incident (new) cases of anorexia nervosa.
Model costs
Costs were estimated directly from the study data as the total cost of all participants in the relevant remission or relapse state, in each arm and for each time period (baseline to 6 months and 6 months to 12 months), divided by the number of people in that state, to get the average cost per person in each state.
Model effects
The size of the treatment effect of an intervention is the power of that intervention to achieve a chosen outcome. To build a flexible model that can be used to test scenarios, a relative treatment effect needs to be developed. In this case, change in CGAS score was chosen as the treatment effect, with the change score selected on the basis that this study is not a randomised controlled trial (RCT) and thus there is no reason to assume that CGAS scores will be similar at baseline. This was calculated by combining two variables: the number of people in each remission or relapse state at each time period, and the average change in CGAS scores in each state. A weighted average of CGAS scores by each remission and relapse state in each arm was estimated to give the total treatment effect of each group.
The calculation of the treatment effect can be illustrated using the data contained in Table 8. The calculation for the treatment effect for generic CAMHS is (20% × 90%) + (25% × 75%) + (55% × –5%) = 34%. For specialist services, the treatment effect would be (25% × 85%) + (25% × 80%) + (50% × 5%) = 44%. Although generic CAMHS have a higher change in CGAS score for those in full remission, because specialist eating disorders services have more people in both types of remission (full and partial), when weighted, specialist services generate a 10-percentage-point increase in CGAS scores compared with generic CAMHS.
| Arm | Percentage | ||||||
|---|---|---|---|---|---|---|---|
| Patients in full remission | Patients in partial remission | Patients not in remission | Change in CGAS scores if in full remission | Change in CGAS scores if in partial remission | Change in CGAS scores if no remission | Treatment effect | |
| Generic | 20 | 25 | 55 | 90 | 75 | –5 | 34 |
| Specialist | 25 | 25 | 50 | 85 | 80 | 5 | 44 |
Model outcomes
The final outcome for this evaluation is change in CGAS scores. In the example in Table 8, we know from the treatment effect calculation that each arm has a relative increase in points, which we refer to as the treatment effect. As these are relative (percentage change from baseline) rather than absolute increases, they rely on the baseline CGAS scores, and if both arms start at the same baseline CGAS measurement, as would be the case in a RCT, then this would be straightforward. However, in a naturalistic surveillance study, such as the CostED study, there is no guarantee that baseline CGAS scores will be similar in both groups, so the final CGAS gain is calculated as baseline CGAS score × percentage increase in CGAS score. As an example, let the generic CAMHS baseline score be 48 points, and the specialist eating disorders services baseline score be 44 points. Using the data in Table 8, the outcome for generic services = 48 × 34% = 16.32 and for specialist eating disorders services = 44 × 44% = 19.36, which is equivalent to a 3-point difference between the two arms.
Analysis: decision model
The cost-effectiveness of alternative patient flow scenarios was explored using total cost per CGAS point gained for the full sample of young people. Incremental analysis is not appropriate for the economic modelling because there is no comparison between two groups; instead, the model explores the total cost per gain in outcome for the full population of young people, dependent on the proportion of those young people who are initially assessed in specialist eating disorders services or generic CAMHS.
To provide more clinically meaningful results, cost per CGAS point gained was converted to a cost per 10 points gained, because CGAS scores are used to classify patients into one of 10 categories of outcome, with each range covering 10 points on the scale (e.g. ‘extremely impaired’ is associated with a score between 1 and 10 points; ‘doing very well’ is associated with a score between 91 and 100 points). 27 In this way, cost per 10-point improvement on the CGAS score provides information on the additional cost needed to generate an improvement in functioning from one CGAS category to the next category, which is more clinically meaningful than a 1-point improvement.
The cost per 1-point gain in CGAS score is calculated as (total cost of young people initially assessed in specialist services + total cost of young people initially assessed in generic CAMHS)/[(total CGAS points gained by young people initially assessed in specialist services + total CGAS points gained by young people initially assessed in generic CAMHS)/10]. The results provide information on the cost needed to generate an average improvement in CGAS score from one category to the next category for each young person in a hypothetical cohort, dependent on where the cohort of patients is treated. The proportion of young people in the cohort initially assessed in either specialist or generic services is then varied from 100% specialist eating disorders services to 100% generic CAMHS, to see if there is an optimal structure that minimises the costs for the benefits gained.
In the base-case scenario, all cost and outcome data and the proportion of young people following the specialist eating disorders services pathway and the generic CAMHS pathways were taken from the results of the CostED study. Alternative scenarios were then evaluated to explore the implications of changes to the proportion of young people following each pathway, including:
-
0% specialist, 100% generic
-
50% specialist, 50% generic
-
100% specialist, 0% generic.
Two-way sensitivity analyses were carried out for each scenario using different assumptions about baseline CGAS scores and the treatment effect, in order to explore uncertainty in the model structure and the implications of any differences in baseline CGAS scores and to assess whether differential treatment effect was determined by baseline differences or reflected real treatment effects. The sensitivity analyses were as follows:
-
Sensitivity analysis 1a. Baseline mean CGAS scores for both specialist and generic groups are set equal to the baseline value for the generic group (12-month treatment effect as per the base case).
-
Sensitivity analysis 1b. Baseline mean CGAS scores for both specialist and generic groups are set equal to the baseline value for the specialist group (12-month treatment effect as per the base case).
-
Sensitivity analysis 2a. The size of the treatment effect at 12 months for both specialist and generic groups is set equal to the generic group value (baseline CGAS score as per the base case).
-
Sensitivity analysis 2b. The size of treatment effect at 12 months for both specialist and generic groups is set equal to the specialist group value (baseline CGAS score as per the base case).
In addition, a one-way sensitivity analysis was used to explore the sensitivity of the model to the cost and CGAS inputs (parameter, or second-order, uncertainty). 63 In a one-way sensitivity analysis, only one variable was changed at a time (either cost or CGAS scores) and these were varied using the 95% CIs for the relevant variable and expressed as the incremental cost per 10-point CGAS score gain.
Finally, a probabilistic sensitivity analysis was carried out to test the overall robustness of the model. Probabilistic sensitivity analysis is an approach to the uncertainty associated with inputs in an economic model that involves assigning distributions to all input parameters and running simulations to test the strength and suitability of the model and thus the level of confidence we can have in the results of a model. 61 Probabilistic sensitivity analysis allows all parameters to be varied simultaneously, rather than one or two at a time, as with the sensitivity analyses described above. In line with previous research by Jones et al. 64–66 log-normal distributions were assigned to the probabilities and a normal distribution was assigned to the change in CGAS scores and the change in costs, and 10,000 patients were simulated. In other words, the model was run 10,000 times, each time with a new set of parameters.
Ethics approvals and study registration
The study was approved by the CAPSS Committee, King’s College London Research Ethics Committee [PNM/13/14-105], and by the Health Research Authority Confidentiality Advisory Group [CAG 4-03(PR1)/2014]. Health Research Authority Confidentiality Advisory Group approval was for exemption from obtaining participant consent, under Section 251 of the National Health Service Act 2006,67 which enables disclosure of confidential patient information when it is not possible to use anonymised information and seeking consent is not practical. The study is registered with the International Standard Randomised Controlled Trial Number (ISRCTN) Register [ISRCTN12676087].
Public and patient involvement
The CostED study included a patient and a parent representative on the study steering committee, and actively encouraged public and patient participation in the Delphi study for the classification of services as specialist eating disorders services. We used Beat Young Ambassadors to comment on CostED outputs and will use them to support the development of plain English summaries of the study results for wide dissemination to patients, parents and the general public. Beat Young Ambassadors are volunteers aged between 18 and 25 years who have recovered from an eating disorder and have been out of inpatient treatment for at least 1 year. Young Ambassadors are recruited to share their experiences, campaign for better treatment and help more people get the support and understanding that they need.
Chapter 3 Results
Parts of this chapter have been reproduced from Petkova et al. 21 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Study sample
Case ascertainment is illustrated in Figure 2. Over the 8-month surveillance period, 6401 yellow cards were sent to reporting clinicians, of which 3211 were returned (50.16%). Of the 3211 yellow cards received, 997 positive cases of anorexia nervosa were reported and 2214 were nil returns. Of the 997 positve returns, 48 (5%) were immediately excluded because of reporting errors or because clinicans stated that they did not wish to be included in the study or to complete any questionnaires (because of retirement, shortage of capacity, etc.).
FIGURE 2.
Flow diagram of case ascertainment.
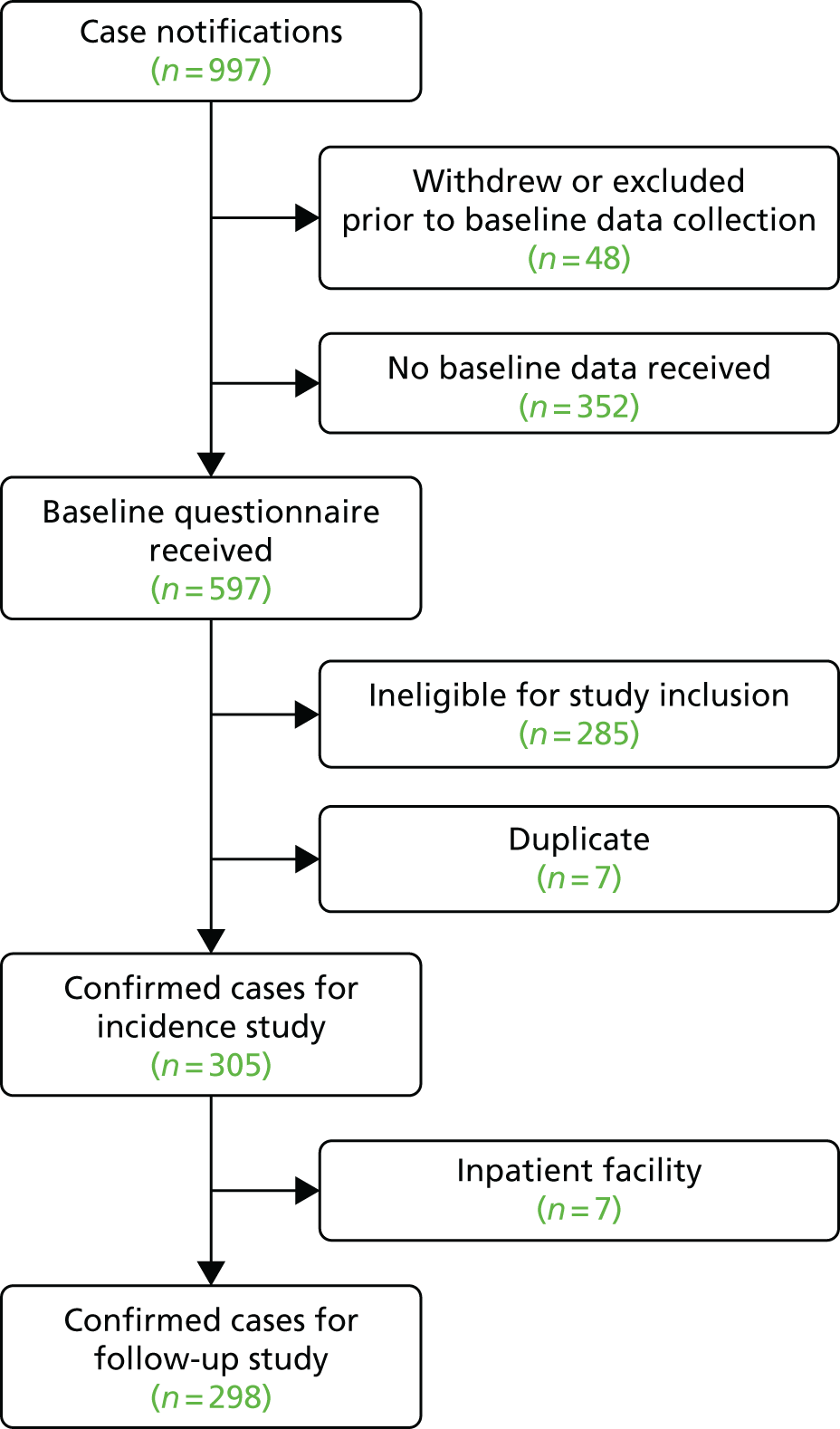
Baseline questionnaires were sent to clinicians who reported the remaining 949 positive returns, and 352 of these positive returns (37%) were subsequently excluded when clinicians failed to return the questionnaires, as no data were available to assess case eligibility. Questionnaires were completed and returned for 597 notified cases, of which 285 (48%) were ineligible for a number of reasons related to age, previous episode of anorexia nervosa, date of assessment being outside the study’s surveillance period, referral from another secondary care service or insufficient information to assess diagnosis. Of 312 notifications that met inclusion criteria, seven (2.2%) were duplicate notifications, leaving 305 incident cases of anorexia nervosa. Seven individuals were reported as being currently in an inpatient facility and thus were excluded from the follow-up study, which focused on young people assessed and diagnosed in a community-based service. Thus, 305 cases were included in the incidence study and 298 cases were included in the follow-up study of cost and cost-effectiveness.
Of the 298 cases included in the follow-up study, clinicians completed and returned a 6-month follow-up questionnaire for 220 cases (74%) and a 12-month follow-up questionnaire for 187 cases (63%).
Demographics and clinical features
As the sample included in the incidence component of the study was only very slightly larger (n = 305) than the sample included in the cost and cost-effectiveness analysis (n = 298) and the demographic and clinical features of the two different samples are almost identical, we report the demographic and clinical features of the larger incidence sample only (Table 9).
| Characteristic | n | Mean (SD) or percentage |
|---|---|---|
| Age (years), mean (SD) | 305 | 14.56 (1.66) |
| Age, category (%) | ||
| Children (8–12 years) | 36 | 11.80 |
| Adolescents (13–17 years) | 269 | 88.20 |
| Sex (%) | ||
| Female | 279 | 91.48 |
| Male | 26 | 8.52 |
| Ethnicity (%) | ||
| Any white | 274 | 91.64 |
| White and Asian | 6 | 2.01 |
| White and black Caribbean | 2 | 0.67 |
| White and black African | 1 | 0.33 |
| Other mixed | 1 | 0.33 |
| Indian | 3 | 1.00 |
| Pakistani | 2 | 0.67 |
| Bangladeshi | 1 | 0.33 |
| Other Asian | 4 | 1.34 |
| Black Caribbean | 2 | 0.67 |
| Chinese | 1 | 0.33 |
| Ethnicity not known | 2 | 0.67 |
| Baseline clinical status, mean (SD) | ||
| %mBMI | 303 | 83.23 (10.99) |
| CGAS score | 280 | 44.61 (14.08) |
| HoNOSCA | 63 | 19.40 (8.17) |
Of the 305 incident cases of DSM-5 anorexia nervosa, the vast majority were girls (91%), from England (70%) and were coded as white (92%; any white background), with a mean age of 14.6 years (±1.66 years). These findings are in line with published literature regarding the demographic at risk for anorexia nervosa and peak age at onset. 68 Although the majority were classified as coming from ‘any white background’, it is worth noting the wide range of ethnic groups represented in the sample. Twelve per cent of the sample were children (aged between 8 and 12 years) whereas the remaining 88% were adolescents (aged between 13 and 17 years).
Baseline clinical variables suggest that these young people were significantly impaired. Mean %mBMI (the deviation from expected body weight) was 83.23% (±10.99%), falling within the range expected for a diagnosis of anorexia nervosa (< 85%). The mean CGAS score for the sample was 44.61 (±14.08), which falls within the range for ‘obvious problems – moderate impairment in most areas or severe in one area’ (41–50) on a scale from 1 to 100 (1 being the worst and 100 the best emotional and behavioural functioning). The mean total HoNOSCA was 19.40 (± 8.17) on a scale from 0 to 52, indicative of a severity similar to that at inpatient admission. 16,69
The proportion of the included sample notified from each region within the UK and the RoI is reported in Table 10, alongside the population of young people aged 8–17 years in each region. England has the largest population of all regions (78%) and notified 70% of cases included in the study. Scotland, despite containing only 7% of the total population of young people aged 8–17 years in the UK and the RoI, notified 14% of the sample. Similarly, Northern Ireland, containing only 3% of the total population, notified 13% of the sample. By contrast, the RoI notified only 2% of cases, despite containing 8% of the total population of young people, and Wales notified no eligible cases (some cases were notified but did not meet inclusion criteria), despite containing 4% of the total population of young people.
| Region | Sample size | Percentage of samplea | Population size | Percentage of population |
|---|---|---|---|---|
| England | 213 | 69.84 | 6,194,444 | 77.83 |
| Scotland | 44 | 14.43 | 561,490 | 7.06 |
| Northern Ireland | 41 | 13.44 | 231,822 | 2.91 |
| RoI | 7 | 2.30 | 628,251 | 7.89 |
| Wales | 0 | 0.00 | 342,627 | 4.31 |
| Total | 305 | 7,958,634 |
Incidence of anorexia nervosa in the UK and the Republic of Ireland
Table 11 details observed incidence rates (IR0) by age and incidence rates after adjustment for missing data using the two approaches outlined in Chapter 2, Incidence of child and adolescent anorexia nervosa: IR1 and IR2. Incidence rates ranged from a minimum of 5.75 per 100,000 young people (95% CI 5.23 to 6.30; IR0) to a maximum of 18.22 per 100,000 young people (95% CI 17.29 to 19.18; IR2), with IR1, the rate hypothesised to be the most accurate, falling between these two values at 13.68 per 100,000 young people (95% CI 12.88 to 14.52). Focusing on IR1 incidence rates, total incidence increased steadily with age, peaking at the age of 16 (30.37, 95% CI 26.70 to 34.41), with a substantial drop at the age of 17 (14.35, 95% CI 11.88 to 17.19).
| Age (years) | Incidence | |||||
|---|---|---|---|---|---|---|
| Observed (IR0) | Adjusted (IR1) | Adjusted (IR2) | ||||
| IR | 95% CI | IR | 95% CI | IR | 95% CI | |
| 8 | 0.18 | 0.01 to 0.76 | 0.43 | 0.10 to 1.14 | 0.57 | 0.18 to 1.35 |
| 9 | 0.18 | 0.01 to 0.77 | 0.44 | 0.11 to 1.17 | 0.58 | 0.18 to 1.38 |
| 10 | 0.19 | 0.01 to 0.80 | 0.45 | 0.11 to 1.21 | 0.60 | 0.19 to 1.43 |
| 11 | 1.53 | 0.79 to 2.67 | 3.65 | 2.43 to 5.25 | 4.85 | 3.43 to 6.65 |
| 12 | 4.91 | 3.47 to 6.76 | 11.69 | 9.39 to 14.38 | 15.56 | 12.89 to 18.63 |
| 13 | 8.39 | 6.44 to 10.73 | 19.95 | 16.89 to 23.42 | 26.58 | 23.02 to 30.54 |
| 14 | 11.71 | 9.41 to 14.39 | 27.85 | 24.25 to 31.84 | 37.10 | 32.92 to 41.66 |
| 15 | 12.39 | 10.05 to 15.10 | 29.47 | 25.80 to 33.52 | 39.25 | 35.50 to 43.88 |
| 16 | 12.76 | 10.42 to 15.47 | 30.37 | 26.70 to 34.41 | 40.45 | 36.19 to 45.07 |
| 17 | 6.03 | 4.47 to 7.96 | 14.35 | 11.88 to 17.19 | 19.12 | 16.24 to 22.35 |
| Total | 5.75 | 5.23 to 6.30 | 13.68 | 12.88 to 14.52 | 18.22 | 17.29 to 19.18 |
Table 12 reports the same incidence rates by age and by sex. Incidence among young men followed a similar pattern to overall incidence rates reported in Table 11, being highest at the age of 16 (5.14 per 100,000) and half that at age 17 (2.54 per 100,000). Among young women, incidence peaked at 1 year younger than in young men, at the age of 15 years (57.77 per 100,000); at age 16 years the rate remained much the same (56.95 per 100,000), before dropping by more than half at age 17 years (26.82 per 100,000).
| Age (years) | Incidence | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Observed (IR0) | Adjusted (IR1) | Adjusted (IR2) | ||||||||||
| Female | Male | Female | Male | Female | Male | |||||||
| IR | 95% CI | IR | 95% CI | IR | 95% CI | IR | 95% CI | IR | 95% CI | IR | 95% CI | |
| 8 | 0.36 | 0.02 to 1.55 | 0.00 | 0.00 to 0.00 | 0.87 | 0.21 to 2.34 | 0.00 | 0.00 to 0.00 | 1.16 | 0.36 to 2.76 | 0.00 | 0.00 to 0.00 |
| 9 | 0.00 | 0.00 to 0.00 | 0.35 | 0.02 to 1.52 | 0.00 | 0.00 to 0.00 | 0.85 | 0.21 to 2.28 | 0.00 | 0.00 to 0.00 | 1.13 | 0.35 to 2.69 |
| 10 | 0.39 | 0.02 to 1.65 | 0.00 | 0.00 to 0.00 | 0.93 | 0.23 to 2.48 | 0.00 | 0.00 to 0.00 | 1.23 | 0.39 to 2.93 | 0.00 | 0.00 to 0.00 |
| 11 | 2.35 | 1.07 to 4.46 | 0.75 | 0.15 to 2.18 | 5.59 | 3.47 to 8.51 | 1.77 | 0.71 to 3.63 | 7.44 | 4.96 to 10.72 | 2.37 | 1.11 to 4.42 |
| 12 | 8.05 | 5.43 to 11.50 | 1.92 | 0.80 to 3.86 | 19.17 | 14.98 to 24.16 | 4.56 | 2.69 to 7.22 | 25.53 | 20.66 to 31.21 | 6.09 | 3.89 to 9.08 |
| 13 | 16.36 | 12.48 to 21.06 | 0.78 | 0.16 to 2.28 | 38.93 | 32.81 to 45.86 | 1.85 | 0.75 to 3.79 | 51.83 | 44.72 to 59.74 | 2.47 | 1.16 to 4.62 |
| 14 | 22.35 | 17.83 to 27.67 | 1.53 | 0.56 to 3.32 | 53.19 | 46.08 to 61.10 | 3.64 | 2.00 to 6.07 | 70.84 | 62.58 to 79.88 | 4.84 | 2.91 to 7.55 |
| 15 | 24.28 | 19.59 to 29.74 | 1.11 | 0.33 to 2.71 | 57.77 | 50.41 to 65.90 | 2.65 | 1.31 to 4.78 | 76.93 | 68.39 to 86.23 | 3.54 | 1.95 to 5.91 |
| 16 | 23.94 | 19.36 to 29.28 | 2.16 | 0.99 to 4.11 | 56.95 | 49.75 to 64.90 | 5.14 | 3.20 to 7.83 | 75.87 | 67.52 to 84.97 | 6.85 | 4.57 to 9.87 |
| 17 | 11.27 | 8.22 to 15.08 | 1.07 | 0.32 to 2.60 | 26.82 | 21.98 to 32.40 | 2.54 | 1.25 to 4.58 | 35.71 | 30.09 to 42.07 | 3.39 | 1.87 to 5.67 |
| Total | 10.78 | 9.77 to 11.87 | 0.96 | 0.68 to 1.30 | 25.66 | 24.09 to 27.30 | 2.28 | 1.84 to 2.79 | 34.17 | 32.36 to 36.06 | 3.03 | 2.52 to 3.62 |
There was a noticeable difference in the pattern of age at onset between girls and boys (Figure 3). Among girls, the incidence of anorexia nervosa followed a bell-shaped curve, starting from its lowest rates at the ages of 8 and 9 years, gradually increasing with each consecutive year of age, peaking at 15 years and decreasing thereafter. Boys exhibited a more irregular pattern of anorexia nervosa incidence, which is likely to be caused by the small number of males in the sample, so caution is required in the interpretation of these results.
FIGURE 3.
Annual incidence of anorexia nervosa for young men and women per 100,000 population; adjusted IR1.

Delphi classification of services
Delphi round 1
A total of 474 responses were received in round 1 of the Delphi survey and responses relating to the criteria being assessed by respondents (questions 1–4, 6 and 8 from Table 5) are summarised in Table 13. Two criteria were rated as either 4 = very important or 5 = extremely important by ≥ 80% of respondents in round 1 (offering specialist, evidence-based outpatient treatment for eating disorders, 91%; providing multidisciplinary specialist outpatient clinics dedicated to eating disorders, 87%). Both of these criteria met the predefined threshold for consensus to be included in the checklist of criteria for a specialist eating disorders service.
| Criteriona | Response, n (%) | Median | Mode | Consensus | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 = not important | 2 = slightly important | 3 = moderately important | 4 = very important | 5 = extremely important | 4 or 5 | ||||
| Round 1 | |||||||||
| Q1. Offering specialist (evidence-based) outpatient treatment for eating disorders | 3 (0.6) | 9 (1.9) | 32 (6.75) | 150 (31.7) | 280 (59.1) | 430 (90.7) | 5 | 5 | Include |
| Q2. Holding weekly multidisciplinary meetings dedicated to eating disorders | 7 (1.5) | 13 (2.7) | 85 (17.9) | 182 (38.4) | 187 (39.5) | 369 (77.9) | 4 | 5 | Uncertain |
| Q3. Providing multidisciplinary specialist outpatient clinics dedicated to eating disorders | 5 (1.1) | 8 (1.7) | 50 (10.6) | 176 (37.1) | 235 (49.6) | 411 (86.7) | 4 | 5 | Include |
| Q4. Number of cases of eating disorders a service sees per year | 27 (5.7) | 44 (9.3) | 157 (33.1) | 157 (33.1) | 89 (18.8) | 246 (51.9) | 4 | 3–4 | Uncertain |
| Q6. Population size of the catchment area covered by the service | 85 (18.5) | 80 (17.4) | 163 (35.4) | 88 (19.1) | 44 (9.6) | 132 (28.7) | 3 | 3 | Exclude |
| Q8. Length of time a service has existed | 179 (40.1) | 117 (26.2) | 111 (24.9) | 28 (6.3) | 11 (2.5) | 39 (8.7) | 2 | 1 | Exclude |
| Round 2 | |||||||||
| Q2. Holding weekly multidisciplinary meetings dedicated to eating disorders | 8 (3.3) | 5 (2.0) | 25 (10.2) | 94 (38.4) | 113 (46.1) | 207 (84.5) | 4 | 5 | Include |
| Q4. Number of cases of eating disorders a service sees per year | 6 (2.5) | 17 (6.9) | 86 (35.1) | 100 (40.8) | 36 (14.7) | 136 (55.5) | 4 | 4 | Uncertain |
Two criteria were rated as either 4 = very important or 5 = extremely important by < 50% of respondents (population size of the catchment area covered by the service, 29%; length of time a service has existed, 9%) and thus met the predefined threshold for consensus to be excluded from the checklist.
The final two criteria were rated as either 4 = very important or 5 = extremely important by between 50% and 79% of respondents (holding weekly multidisciplinary meetings dedicated to eating disorders, 78%; number of cases of eating disorders a service sees per year, 52%) and thus consensus was not achieved. Both of these criteria were therefore included in round 2 of the Delphi survey.
Delphi round 2
Of the 474 respondents in round 1, 245 (52%) responded in round 2, which included only the two criteria that failed to achieve consensus in round 1. One of these items (holding weekly multidisciplinary meetings dedicated to eating disorders) was rated as either 4 = very important or 5 = extremely important by 85% of respondents in round 2, increasing from 78% in round 1, and thus met the threshold for consensus to be included in the checklist.
The second item included in round 2 (number of cases of eating disorders a service sees per year) remained uncertain, with 56% of respondents rating it as either 4 = very important or 5 = extremely important, compared with 52% in round 1. Consensus was therefore not reached in either round 1 or round 2 and the item was excluded from the checklist and from the main analyses presented in the report, which compared services classified as either specialist eating disorders services or generic CAMHS using the three criteria on which consensus as to their inclusion had been achieved.
However, given that the criterion of a minimum number of cases of eating disorders seen per year is now included in the most recent guidelines describing the characteristics of specialist eating disorders services,20 and was the only criterion that failed to achieve consensus for either inclusion or exclusion, the decision was made to include this criterion in sensitivity analyses (denoted Delphi sensitivity analyses throughout the report to distinguish from other sensitivity analyses). So, the main analyses included three criteria for the classification of services as specialist eating disorders services (offering specialist, evidence-based outpatient treatment for eating disorders; providing multidisciplinary specialist outpatient clinics dedicated to eating disorders; and holding weekly multidisciplinary meetings dedicated to eating disorders) and the Delphi sensitivity analyses included four criteria – all the criteria from the main analysis plus an additional criterion relating to a minimum number of cases of eating disorders seen per year.
To do this, it was necessary to refer to the associated subquestion regarding the minimum number of eating disorders cases a service should see per annum in order to be classified as a specialist eating disorders service. Of all respondents who considered this an important criterion, 55% (n = 75) indicated that a service should see a ‘minimum of 50’ cases per year to be classified as a specialist eating disorders service. As this value represents the majority of responses, and is in line with the most recent guidelines,20 this threshold was selected for the Delphi sensitivity analyses.
Service-level classification of services
Classification of the services that assessed and diagnosed the 298 young people meeting eligibility criteria for the CostED follow-up study is reported in Table 14. Case notifications for the included cases were received from a total of 99 separate services across the UK and the RoI over the 8-month surveillance period and, of these, 79 services notified cases that were found to be eligible for study inclusion. Of the 79 services, 37% (n = 29) met the three criteria for classification as a specialist eating disorders service in the main analysis (see Delphi round 2). This fell to 19% (n = 15) in the Delphi sensitivity analysis that additionally included the criterion to see a minimum of 50 cases per annum.
| Classification of services | Analysis, n (%) | |
|---|---|---|
| Main | Delphi sensitivity | |
| Services (N = 79) | ||
| Specialist | 29 (36.71) | 15 (18.99) |
| Generic | 50 (63.29) | 64 (81.01) |
| Young people (N = 298) | ||
| Specialist | 192 (64.43) | 138 (46.31) |
| Generic | 106 (35.57) | 160 (53.69) |
Although the exact number of CAMHS in the UK and the RoI is unknown to the authors, we were able to identify data to suggest that there are 122 CAMHS in England and 45 CAMHS in Scotland, which between them notified approximately 85% of all eligible cases in the CostED study and cover approximately 85% of the population of young people aged 8–17 years. Thus, the minimum number of CAMHS in the UK and the RoI is 167. Given notifications from a total of 99 different services, this suggests that a maximum of 59% of CAMHS notified at least one case to the CostED study.
Patient-level classification of services
In the main analysis, 64% (n = 192) of the 298 notified cases meeting inclusion criteria for the follow-up study were assessed in a service classified using the results of the Delphi survey as a specialist eating disorders service (see Table 14). This number fell to 46% (n = 138) in the Delphi sensitivity analysis.
Table 15 reports the demographic and baseline clinical characteristics of young people classified as being assessed and diagnosed in a specialist service compared with a generic service, both for the main analysis and for the Delphi sensitivity analysis. In both analyses, mean age was similar in both groups (approximately 15 years of age), although specialist services had higher proportions of adolescents than generic services (91% vs. 84% in the main analysis) and lower proportions of children (9% vs. 16% in the main analysis). The proportion of participants who were female was identical in the specialist and generic groups for the main analysis (92%), but slightly higher in the specialist group for the Delphi sensitivity analysis (96% vs. 88%). Ethnicity was similar across groups for both analyses (92–94% coded as any white background).
| Characteristics | Main analysis | Delphi sensitivity analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| Specialist | Generic | Specialist | Generic | |||||
| n | Mean (SD) or % | n | Mean (SD) or % | n | Mean (SD) or % | n | Mean (SD) or % | |
| Age (years), mean (SD) | 192 | 15.09 (1.60) | 106 | 14.84 (1.66) | 138 | 15.13 (1.53) | 160 | 14.89 (1.71) |
| Age category (years) (%) | ||||||||
| Children (8–12) | 18 | 9.38 | 17 | 16.04 | 11 | 7.97 | 24 | 15.00 |
| Adolescents (13–17) | 174 | 90.63 | 89 | 83.96 | 127 | 92.03 | 136 | 85.00 |
| Sex (%) | ||||||||
| Female | 176 | 91.67 | 97 | 91.51 | 132 | 95.65 | 141 | 88.13 |
| Male | 16 | 8.33 | 9 | 8.49 | 6 | 4.35 | 19 | 11.88 |
| Ethnicity (%) | ||||||||
| Any white | 174 | 91.58 | 95 | 94.06 | 126 | 92.65 | 143 | 92.26 |
| Other | 16 | 8.42 | 6 | 5.94 | 10 | 7.36 | 12 | 7.77 |
| Clinical status, mean (SD) | ||||||||
| %mBMI | 191 | 82.70 (11.11) | 105 | 83.60 (9.90) | 137 | 81.42 (11.20) | 159 | 84.40 (10.05) |
| CGAS score | 174 | 43.22 (14.40) | 99 | 47.86 (13.29) | 125 | 41.51 (13.18) | 148 | 47.76 (14.36) |
| HoNOSCA | 45 | 21.04 (8.43) | 16 | 14.88 (5.77) | 34 | 21.74 (8.36) | 27 | 16.52 (7.25) |
In terms of clinical status, all indicators suggest that those assessed in a specialist service had poorer clinical status at baseline than those assessed in a generic service, for both the main and the Delphi sensitivity analyses. Rates of %mBMI, for which higher scores reflect better outcomes, were only very slightly lower for the specialist groups than for the generic groups (82.7% vs. 83.6% in the main analysis; 81.4% vs. 84.4% in the Delphi sensitivity analysis). In the case of the CGAS scores (higher values of which reflect better outcomes) differences were more marked (mean score 43 points specialist vs. 48 points generic in the main analysis; mean score 42 points specialist vs. 48 points generic in the Delphi sensitivity analysis). The same pattern was seen for the HoNOSCA, with high scores reflecting poorer outcomes (mean score 21 points specialist vs. 15 points generic in the main analysis; mean score 22 points specialist vs. 17 points generic in the Delphi sensitivity analysis).
Geographical location of services
To map services across the UK and the RoI, all community-based services notifying a positive case of anorexia nervosa and returning a baseline questionnaire containing service characteristics necessary for service classification were included, not just those services notifying a case found to be eligible for inclusion in the incidence or follow-up studies. This was to maximise the number of services available for the mapping and thus the accuracy of the mapping. In particular, this ensured that tertiary specialist eating disorders services were included – services that see a large number of eating disorders cases, but that were excluded from the CostED study because young people in these services had all been referred from another secondary health service (referral from another secondary service was an exclusion criterion because the focus of the CostED study was on the service where the initial assessment and diagnosis took place, rather than services to which young people may be subsequently referred). In addition, with referred cases it was not possible to confirm whether or not the original assessment and diagnosis took place during the study surveillance period.
The total number of community-based services notifying a positive case of anorexia nervosa and returning a baseline questionnaire containing service characteristics necessary for service classification was 99, adding an additional 20 services to the services notifying at least one case meeting eligibility for inclusion in the CostED follow-up study.
Two maps are presented: services classified in Figure 4 used only the criteria for which consensus was achieved in the Delphi survey (the main analysis) and services classified in Figure 5 additionally used the criterion requiring services to see a minimum of 50 cases per year that remained uncertain in the Delphi survey (the Delphi sensitivity analysis). Services classified as specialist eating disorders services are marked with orange pins and services classified as generic CAMHS are marked with pink pins. In the main analysis (Figure 4), specialist services appear relatively well spread out in England, Northern Ireland and Scotland (the number of notifying services in Wales and the RoI was too small to come to any conclusions) but this is not the case in the Delphi sensitivity analysis (Figure 5), with far fewer services being classified as specialist once the number of cases seen per year was taken into consideration.
FIGURE 4.
Location of specialist (orange) and generic (pink) services: main analysis. Map data © 2017 GeoBasis-DE/BKG (© 2009), Google Inst. Geogr. Nacional. Created using www.doogal.co.uk/BatchGeocoding.php.
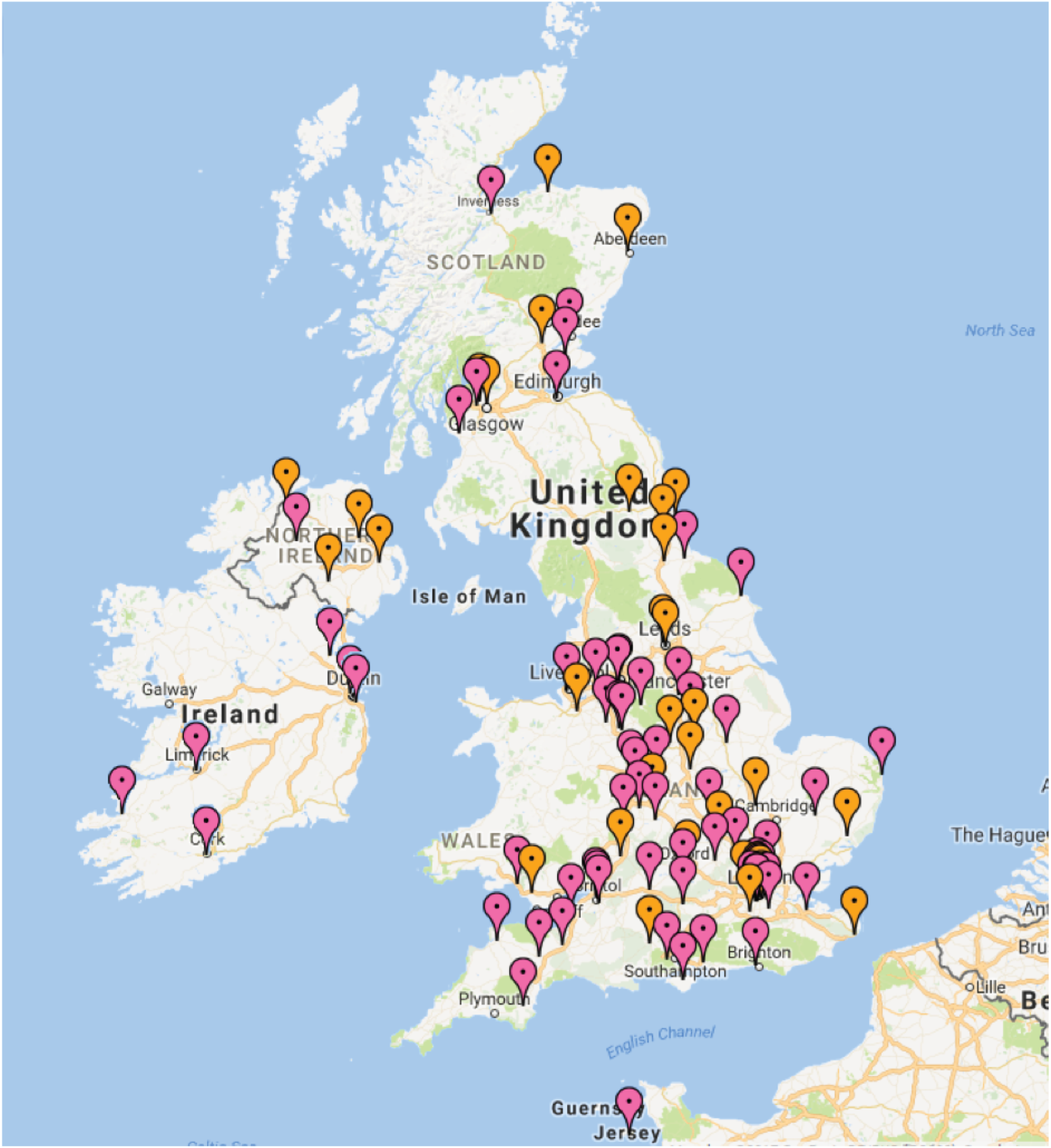
FIGURE 5.
Location of specialist (orange) and generic (pink) services: Delphi sensitivity analysis. Map data © 2017 GeoBasis-DE/BKG (© 2009), Google Inst. Geogr. Nacional. Created using www.doogal.co.uk/BatchGeocoding.php.

Cost, effectiveness and cost-effectiveness
Service use
Mean use of inpatient, outpatient and day-patient health services over the 12-month follow-up period, with services classified using the three criteria for which consensus had been achieved (the main analysis), is reported in Table 16. We received only one report of a young person having an admission to an adult eating disorders unit and one report of an admission to an adult general psychiatry ward, so eating disorders and general psychiatry admissions in child and adolescent facilities and adult facilities are not reported separately. Mean use of health services over the periods from baseline to 6-month follow-up and from 6-month to 12-month follow-up can be found in Appendix 1.
| Service | Group | |||
|---|---|---|---|---|
| Specialist (n = 137) | Generic (n = 50) | |||
| Mean (SD) | Percentage using | Mean (SD) | Percentage using | |
| Inpatient admissions | 0.54 (1.06) | 28.47 | 0.60 (1.20) | 30.00 |
| Inpatient nights | 31.75 (80.03) | 28.47 | 30.78 (68.65) | 30.00 |
| Paediatric: NHS | 2.18 (9.28) | 15.33 | 4.72 (12.96) | 20.00 |
| Eating disorders: NHS | 5.56 (37.72) | 2.92 | 0.28 (1.98) | 2.00 |
| Eating disorders: independent | 14.28 (57.93) | 8.76 | 12.84 (49.89) | 8.00 |
| Psychiatry: NHS | 5.38 (24.47) | 6.57 | 11.58 (39.42) | 12.00 |
| Psychiatry: independent | 1.39 (12.43) | 2.19 | 1.36 (9.62) | 2.00 |
| Other: NHS | 0.53 (6.15) | 1.46 | 0.00 (0.00) | 0.00 |
| Outpatient attendances | 29.98 (17.70) | 98.54 | 27.14 (32.62) | 96.00 |
| Paediatric | 0.07 (0.34) | 5.11 | 0.98 (2.46) | 28.00 |
| Eating disorders | 27.11 (18.11) | 92.70 | 14.58 (32.07) | 56.00 |
| Psychiatry | 2.80 (8.94) | 17.52 | 11.58 (13.55) | 68.00 |
| Day-patient attendances | 4.61 (16.60) | 10.95 | 0.86 (5.66) | 4.00 |
| Paediatric | 0.00 (0.00) | 0.00 | 0.06 (0.42) | 2.00 |
| Eating disorders | 4.25 (16.13) | 10.22 | 0.80 (5.66) | 2.00 |
| Psychiatry | 0.37 (4.27) | 0.73 | 0.00 (0.00) | 0.00 |
Mean number of inpatient admissions (0.54 specialist, 0.60 generic) and mean number of inpatient nights per participant (32 specialist, 31 generic) were similar between the two groups in total. However, young people initially assessed in specialist services spent longer, on average, in an eating disorders facility (20 vs. 13 nights, respectively) and less time on a general psychiatry ward (7 vs. 13 nights). The majority of nights spent in an eating disorder unit were accounted for by NHS-funded patients admitted to units in the independent sector and the majority of nights in a general psychiatry ward were NHS based. This reflects the distribution of eating disorders beds in the country.
The pattern for outpatient attendances, used by over 96% of the sample, was similar to the pattern for inpatient stays, with young people initially assessed in a specialist service having more contacts in eating disorders facilities on average (27 vs. 15 attendances) but fewer general psychiatry contacts (3 vs. 12 attendances) than those initially assessed in a generic service, and a similar number of contacts in total (30 vs. 27 attendances).
Day-patient services were accessed by 11% of the specialist group but only 4% of the generic group, with the average number of attendances also being higher for the specialist group (five attendances vs. one attendance). The vast majority of these contacts took place in eating disorders services.
Mean use of health services over the 12-month follow-up period, with services classified additionally using the fourth criterion of a minimum of 50 cases seen per year (the Delphi sensitivity analysis), is reported in Table 17. Again, separate results for the period from baseline to 6-month follow-up and the period from 6-month to 12-month follow-up can be found in Appendix 1.
| Service | Group | |||
|---|---|---|---|---|
| Specialist (n = 104) | Generic (n = 83) | |||
| Mean (SD) | Percentage using | Mean (SD) | Percentage using | |
| Inpatient admissions | 0.60 (1.15) | 28.91 | 0.51 (1.02) | 28.85 |
| Inpatient nights | 35.91 (87.50) | 28.91 | 25.95 (61.38) | 28.85 |
| Paediatric: NHS | 2.56 (10.41) | 17.31 | 3.23 (10.48) | 15.66 |
| Eating disorders: NHS | 7.33 (43.19) | 3.85 | 0.17 (1.54) | 1.20 |
| Eating disorders: independent | 16.88 (64.51) | 8.65 | 10.16 (42.44) | 8.43 |
| Psychiatry: NHS | 5.46 (26.65) | 4.81 | 9.01 (32.24) | 12.05 |
| Psychiatry: independent | 0.47 (3.63) | 1.92 | 2.52 (17.10) | 2.40 |
| Other: NHS | 0.01 (0.10) | 0.96 | 0.87 (7.90) | 1.20 |
| Outpatient attendances | 31.41 (17.98) | 98.08 | 26.47 (27.19) | 97.59 |
| Paediatric | 0.04 (0.24) | 2.88 | 0.66 (1.97) | 21.69 |
| Eating disorders | 29.15 (18.55) | 92.31 | 17.00 (26.70) | 71.08 |
| Psychiatry | 2.22 (7.47) | 17.31 | 8.81 (13.50) | 48.19 |
| Day-patient attendances | 5.46 (18.32) | 12.50 | 1.29 (7.13) | 4.82 |
| Paediatric | 0.00 (0.00) | 0.00 | 0.07 (0.33) | 1.20 |
| Eating disorders | 5.46 (18.32) | 12.50 | 0.65 (4.63) | 2.41 |
| Psychiatry | 0.00 (0.00) | 0.00 | 0.60 (5.49) | 1.20 |
The patterns of service use in the Delphi sensitivity analysis were very similar to those in the main analysis, with young people initially assessed in a specialist service making greater use of eating disorders services and less use of general psychiatry-based services in all service categories. However, total numbers of inpatient nights were higher for the specialist group, on average (36 vs. 26 nights), as were outpatient contacts (31 vs. 27 attendances). Results for day-patient contacts in the Delphi sensitivity analysis differed little to those in the main analysis, remaining higher and being used more by the specialist group (six attendances vs. one attendance).
Cost of health services used
Total costs per participant over the baseline to 6-month, 6-month to 12-month and baseline to 12-month follow-up periods for young people initially assessed in specialist and those initially assessed in generic services, where services were classified using the three criteria for which consensus had been achieved (the main analysis), are reported in Table 18. In terms of unadjusted analyses, there were no significant differences between the specialist and generic groups, with only small observed differences in total costs over all time periods. Adjustment for prespecified baseline variables made a substantial difference as a result of the baseline differences in CGAS score and %mBMI (see Outcomes). Adjusted analyses suggest larger differences in favour of participants in specialist services (costs lower on average), although again these differences are not significant.
| Service | Group, cost (£), mean (SD) | Unadjusteda mean difference (£) (95% CI) | p-value | Adjusteda,b mean difference (£) (95% CI) | p-value | |
|---|---|---|---|---|---|---|
| Specialist | Generic | |||||
| Baseline to 6 months | n = 147 | n = 73 | ||||
| Inpatient | 11,105 (28,877) | 11,179 (29,050) | ||||
| Outpatient | 4764 (2866) | 4310 (3975) | ||||
| Day patient | 947 (3468) | 299 (1708) | ||||
| Total | 16,817 (28,469) | 15,789 (28,184) | 1028 (–6979 to 9036) | 0.801 | –3586 (–11,999 to 4827) | 0.402 |
| 6 to 12 months | n = 137 | n = 50 | ||||
| Inpatient | 8153 (24,763) | 8224 (20,894) | ||||
| Outpatient | 3103 (3058) | 3279 (5775) | ||||
| Day patient | 306 (1703) | 44 (310) | ||||
| Total | 11,562 (24,905) | 11,547 (22,133) | 14 (–7875 to 7903) | 0.997 | –2785 (–11,241 to 5670) | 0.516 |
| Baseline to 12 months | n = 137 | n = 50 | ||||
| Inpatient | 19,462 (49,946) | 19,755 (44,677) | ||||
| Outpatient | 7955 (4722) | 7470 (8499) | ||||
| Day patient | 1284 (4608) | 246 (1559) | ||||
| Total | 28,700 (49,716) | 27,471 (44,317) | 1230 (–14,529 to 16,988) | 0.878 | –7106 (–23,590 to 9379) | 0.396 |
Mean costs per participant over the baseline to 6-month, 6-month to 12-month and baseline to 12-month follow-up periods, with services classified by additionally including the fourth criterion of a minimum of 50 cases seen per year for which consensus had not been achieved (the Delphi sensitivity analysis), are reported in Table 19. Observed differences are larger than in the main analysis, with costs per young person in the specialist group being higher, on average, than in the generic group, but these differences remained statistically non-significant. Adjustment for prespecified baseline factors had a similar impact in the Delphi sensitivity analysis to that found in the main analysis, with the results becoming more favourable for the specialist group, but non-significant. Over the 6- to 12-month period, costs in the specialist group were higher, on average, than those in the generic group, but the difference between the two groups reduced in adjusted analyses. Between baseline and 6 months and for the full period between baseline and 12 months, adjustment reversed the findings of the unadjusted analysis, with observed cost differences being higher, on average, for participants in specialist services but adjusted cost differences being higher, on average, for participants in generic services.
| Service | Group, cost (£), mean (SD) | Unadjusteda mean difference (£) (95% CI) | p-value | Adjusteda,b mean difference (£) (95% CI) | p-value | |
|---|---|---|---|---|---|---|
| Specialist | Generic | |||||
| Baseline to 6 months | n = 112 | n = 108 | ||||
| Inpatient | 12,052 (29,992) | 10,174 (27,762) | ||||
| Outpatient | 4897 (2744) | 4319 (3735) | ||||
| Day patient | 1098 (3660) | 353 (2094) | ||||
| Total | 18,047 (29,321) | 14,847 (27,272) | 3200 (–4331 to 10,731) | 0.4033 | –3362 (–11,718 to 4994) | 0.428 |
| 6 to 12 months | n = 104 | n = 83 | ||||
| Inpatient | 10,071 (27,905) | 5792 (17,014) | ||||
| Outpatient | 3281 (3207) | 2987 (4742) | ||||
| Day patient | 367 (1917) | 73 (483) | ||||
| Total | 13,718 (27,898) | 8851 (18,180) | 4868 (–2124 to 11,860) | 0.1713 | 1893 (–6156 to 9942) | 0.643 |
| Baseline to 12 months | n = 104 | n = 83 | ||||
| Inpatient | 22,251 (54,762) | 16,144 (39,273) | ||||
| Outpatient | 8313 (4757) | 7214 (7152) | ||||
| Day patient | 1498 (5024) | 391 (2181) | ||||
| Total | 32,061 (54,191) | 23,749 (39,318) | 8311 (–5676 to 22,299) | 0.2426 | –3309 (–19,018 to 12,401) | 0.678 |
A further sensitivity analysis explored the impact of missing data. Table 20 reports the results of the main analysis with imputation of missing total cost data. Imputation made very little difference to the results of the main analysis, with costs remaining very similar in both groups. Unadjusted differences remained small and non-significant; adjusted differences remained larger in favour of specialist services (costs lower) but still non-significant.
| Service | Group, cost (£), mean (SD) | Unadjusteda mean difference (£) (95% CI) | p-value | Adjusteda,b mean difference (£) (95% CI) | p-value | |
|---|---|---|---|---|---|---|
| Specialist (n = 192) | Generic (n = 106) | |||||
| Baseline to 6 months | ||||||
| Total | 16,076 (25,326) | 16,036 (23,946) | 40 (–5877 to 5957) | 0.989 | –2491 (–8511 to 3528) | 0.416 |
| 6 to 12 months | ||||||
| Total | 11,254 (21,196) | 11,904 (15,533) | –650 (–5265 to 3964) | 0.782 | –1184 (–5934 to 3565) | 0.516 |
| Baseline to 12 months | ||||||
| Total | 27,596 (42,640) | 28,617 (31,868) | –1021 (–10,346 to 8305) | 0.830 | –3439 (–12,699 to 5822) | 0.465 |
Outcomes
Mean outcomes at baseline and at the 6- and 12-month follow-ups are reported in Table 21 for young people initially assessed in specialist versus generic services, where services were classified using the three criteria for which consensus had been achieved (the main analysis). At baseline, %mBMI was slightly lower (poorer), on average, in the specialist group than in the generic group, but the difference was not significant. However, both CGAS score and HoNOSCA were significantly worse in the specialist group. At the 6-month follow-up, in adjusted analyses, %mBMI was significantly higher (better) in the specialist group than in the generic group. Although %mBMI remained higher in the specialist group at the 12-month follow-up, the difference between the groups was no longer significant. No significant differences between groups in CGAS score or HoNOSCA were identified at either the 6- or the 12-month follow-up, in unadjusted or adjusted analyses.
| Outcome measure | Group | Unadjusteda mean difference (95% CI) | p-value | Adjusteda,b mean difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|---|---|
| Specialist | Generic | |||||||
| n | Mean (SD) | n | Mean (SD) | |||||
| Baseline | ||||||||
| %mBMI | 191 | 82.70 (11.10) | 105 | 83.60 (9.90) | –0.90 (–3.46 to 1.66) | 0.489 | ||
| CGAS score | 174 | 43.22 (14.40) | 99 | 47.86 (13.29) | –4.64 (–8.11 to –1.17) | 0.009c | ||
| HoNOSCA | 45 | 21.04 (8.43) | 16 | 14.88 (5.77) | 6.17 (1.60 to 10.74) | 0.009c | ||
| 6 months | ||||||||
| %mBMI | 143 | 91.98 (8.51) | 67 | 89.62 (12.89) | 2.37 (–0.59 to 5.31) | 0.116 | 2.58 (0.16 to 5.01) | 0.037c |
| CGAS score | 115 | 58.94 (17.17) | 55 | 63.27 (17.05) | –4.33 (–9.88 to 1.21) | 0.125 | 0.49 (–5.14 to 6.12) | 0.864 |
| HoNOSCA | 17 | 9.47 (7.43) | 16 | 11.88 (10.31) | –2.40 (–8.76 to 3.95) | 0.446 | –6.61 (–15.54 to 2.31) | 0.140 |
| 12 months | ||||||||
| %mBMI | 106 | 94.70 (10.61) | 39 | 93.36 (9.46) | 1.34 (–2.48 to 5.16) | 0.489 | 0.09 (–3.54 to 3.73) | 0.960 |
| CGAS score | 97 | 68.39 (17.95) | 38 | 71.58 (21.41) | –3.19 (–10.37 to 4.00) | 0.382 | –0.65 (–8.26 to 6.96) | 0.866 |
| HoNOSCA | 12 | 7.42 (4.48) | 7 | 13.57 (16.94) | –6.15 (–16.88 to 4.57) | 0.243 | –12.42 (–31.07 to 6.23) | 0.171 |
Mean outcomes at baseline and at the 6- and 12-month follow-ups among young people initially assessed in specialist or generic services, where services were classified additionally including the fourth criterion of a minimum of 50 cases seen per year for which consensus had not been achieved (the Delphi sensitivity analysis), are reported in Table 22. At baseline, the specialist group had significantly poorer scores than the generic group on all three measures. At the 6-month follow-up, CGAS scores remained significantly poorer in the specialist group in unadjusted analysis but not in adjusted analysis, and no significant differences were seen for %BMI or HoNOSCA. No significant differences were evident on any of the three measures at the 12-month follow-up.
| Outcome measure | Group | Unadjusteda mean difference (95% CI) | p-value | Adjusteda,b mean difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|---|---|
| Specialist | Generic | |||||||
| n | Mean (SD) | n | Mean (SD) | |||||
| Baseline | ||||||||
| %mBMI | 137 | 81.42 (11.20) | 159 | 84.40 (10.05) | –2.98 (–5.41 to –0.55) | 0.016c | ||
| CGAS score | 125 | 41.51 (13.18) | 148 | 47.76 (14.36) | –6.25 (–9.56 to –2.94) | 0.0002c | ||
| HoNOSCA | 34 | 21.74 (8.36) | 27 | 16.52 (7.25) | 5.22 (1.15 to 9.28) | 0.013c | ||
| 6 months | ||||||||
| %mBMI | 109 | 91.69 (8.39) | 101 | 90.73 (11.77) | 0.95 (–1.81 to 3.72) | 0.498 | 1.66 (–0.73 to 4.04) | 0.172 |
| CGAS score | 88 | 57.11 (16.95) | 82 | 63.80 (16.89) | –6.69 (–11.82 to –1.56) | 0.011c | –0.94 (–6.52 to 4.64) | 0.740 |
| HoNOSCA | 13 | 9.08 (7.83) | 20 | 11.65 (9.57) | –2.57 (–9.06 to 3.92) | 0.425 | –5.40 (–13.56 to 2.77) | 0.186 |
| 12 months | ||||||||
| %mBMI | 80 | 95.00 (10.61) | 65 | 93.53 (9.91) | 1.47 (–1.94 to 4.87) | 0.396 | 1.37 (–2.03 to 4.78) | 0.426 |
| CGAS score | 74 | 67.29 (18.96) | 61 | 71.26 (19.48) | –3.60 (–10.08 to 2.88) | 0.274 | –3.43 (–10.64 to 3.77) | 0.347 |
| HoNOSCA | 9 | 7.89 (4.34) | 10 | 11.30 (14.55) | –3.41 (–14.07 to 7.25) | 0.509 | –7.21 (–23.79 to 9.36) | 0.359 |
Table 23 reports the results for the main analysis with imputation of missing outcome data. As was found for total cost data, imputation made very little difference to the results of the main analysis, with imputed results being very similar to complete-case results and all differences between groups being non-significant, with the exception of %BMI at 6-month follow-up, which was significantly higher (better outcome) in the specialist group.
| Outcome measure | Group | Unadjusteda mean difference (95% CI) | p-value | Adjusteda,b mean difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|---|---|
| Specialist | Generic | |||||||
| n | Mean (SD) | n | Mean (SD) | |||||
| 6 months | ||||||||
| %mBMI | 192 | 91.60 (7.70) | 106 | 90.39 (10.82) | 1.21 (–0.92 to 3.33) | 0.265 | 1.64 (0.00 to 3.29) | 0.050c |
| CGAS score | 192 | 59.71 (14.17) | 106 | 62.74 (13.07) | –3.03 (–6.31 to 0.25) | 0.071 | 0.24 (–2.88 to 3.38) | 0.877 |
| HoNOSCA | 192 | 13.56 (6.08) | 106 | 12.07 (5.87) | 1.50 (–0.07 to 2.92) | 0.040 | –0.48 (–1.24 to 0.28) | 0.213 |
| 12 months | ||||||||
| %mBMI | 192 | 94.09 (8.56) | 106 | 94.68 (7.12) | –0.59 (–2.51 to 1.34) | 0.547 | –0.11 (–1.72 to 1.51) | 0.896 |
| CGAS score | 192 | 68.56 (13.51) | 106 | 70.31 (13.57) | –1.75 (–4.97 to 1.47) | 0.285 | –0.59 (–3.78 to 2.60) | 0.714 |
| HoNOSCA | 192 | 4.97 (9.43) | 106 | 7.41 (8.21) | –2.43 (–4.58 to –0.29) | 0.027 | –0.43 (–1.12 to 0.27) | 0.227 |
Given the differences in clinical measures between the groups at baseline, observed changes in clinical measures over time are reported in Tables 24 (main analysis) and 25 (Delphi sensitivity analysis). In the main analysis, both groups showed improvements over time and these improvements were greater in the specialist group than in the generic group for %mBMI at 6 months (9% vs. 6% improvement) and 12 months (12% vs. 11% improvement), for CGAS score at 6 months (17-point vs. 13-point improvement) and 12 months (27-point vs. 21-point improvement) and for HoNOSCA at 6 months (12-point vs. 1-point improvement) and 12 months (16-point vs. 2-point improvement).
| Outcome measure | Group | |||
|---|---|---|---|---|
| Specialist | Generic | |||
| n | Change from baseline | n | Change from baseline | |
| %mBMI | ||||
| Baseline to 6 months | 142 | 9.16 | 67 | 6.29 |
| Baseline to 12 months | 105 | 11.70 | 39 | 10.76 |
| CGAS score | ||||
| Baseline to 6 months | 113 | 17.17 | 52 | 12.83 |
| Baseline to 12 months | 93 | 27.43 | 37 | 20.92 |
| HoNOSCA | ||||
| Baseline to 6 months | 16 | –12.25 | 7 | –1.00 |
| Baseline to 12 months | 11 | –16.09 | 7 | –1.50 |
| Outcome measure | Group | |||
|---|---|---|---|---|
| Specialist | Generic | |||
| n | Change from baseline | n | Change from baseline | |
| %mBMI | ||||
| Baseline to 6 months | 108 | 9.87 | 101 | 6.50 |
| Baseline to 12 months | 79 | 13.01 | 65 | 9.54 |
| CGAS score | ||||
| Baseline to 6 months | 87 | 17.81 | 78 | 13.55 |
| Baseline to 12 months | 72 | 28.79 | 58 | 21.56 |
| HoNOSCA | ||||
| Baseline to 6 months | 12 | –13.25 | 11 | –4.00 |
| Baseline to 12 months | 8 | –16.75 | 9 | –3.78 |
Similar to the main analysis, both groups showed improvements over time in the Delphi sensitivity analysis, and these improvements were greater in the specialist group than in the generic group for %mBMI at 6 months (10% vs. 7% improvement) and at 12 months (13% vs. 10% improvement), for CGAS score at 6 months (18-point vs. 14-point improvement) and at 12 months (29-point vs. 22-point improvement) and for HoNOSCA at 6 months (13-point vs. 4-point improvement) and at 12 months (17-point vs. 4-point improvement).
Remission and relapse rates for the main and Delphi sensitivity analyses are reported in Table 26. In the main analysis at 6 months, the proportion of patients who were in partial remission was higher in the specialist eating disorders group (25%) than in the generic CAMHS group (22%), but the proportion who had achieved full remission was lower in the specialist group (6%) than in the generic group (14%). At 12 months, the proportion who were in partial remission was similar in both groups (27%) and a smaller proportion of the specialist group were in full remission (21% vs. 27%), although it was also the case that a smaller proportion of the specialist group had relapsed (5% vs. 6%). In total, 31% of the specialist eating disorders group were in partial or full remission at 6 months and 48% were so at 12 months, compared with 36% of the generic CAMHS group at 6 months and 53% at 12 months. Relapse at the 12-month follow-up was low in both groups. The majority of young people remained in no remission in both groups at both time points (69% in specialist services and 64% in generic CAMHS at 6 months; 47% in specialist services and 41% in generic CAMHS at 12 months).
| Remission and relapse | Analysis, n (%) | |||
|---|---|---|---|---|
| Main | Delphi sensitivity | |||
| Specialist | Generic | Specialist | Generic | |
| 6 months (n = 220) | ||||
| No remission | 102 (69.39) | 47 (64.38) | 83 (74.11) | 66 (61.11) |
| Partial remission | 36 (24.49) | 16 (21.92) | 25 (22.32) | 27 (25.00) |
| Full remission | 9 (6.12) | 10 (13.70) | 4 (3.57) | 15 (13.89) |
| 12 months (n = 180) | ||||
| No remission | 62 (47.33) | 20 (40.82) | 48 (48.98) | 34 (41.46) |
| Partial remission | 35 (26.72) | 13 (26.53) | 30 (30.61) | 18 (21.95) |
| Full remission | 28 (21.37) | 13 (26.53) | 18 (18.37) | 23 (28.05) |
| Relapse | 6 (4.58) | 3 (6.12) | 2 (2.04) | 7 (8.54) |
In the Delphi sensitivity analysis, a smaller proportion of the specialist group than of the generic group achieved partial remission (22% vs. 25%) or full remission (4% vs. 14%) at 6 months. At 12 months, a greater proportion of participants in the specialist group were in partial remission (31% vs. 22%) but a smaller proportion of the specialist group were in full remission (18% vs. 28%). In total, 26% of the specialist eating disorders group were in partial or full remission at 6 months, compared with 39% of the generic CAMHS group. However, rates of partial or full remission at 12 months were similar in both groups (49% specialist services, 50% generic CAMHS). Relapse rates were lower in the specialist group than in the generic group (2% vs. 9%). As with the main analysis, the majority of young people remained in no remission in both groups at both time points (74% in specialist services and 61% in generic CAMHS at 6 months; 49% in specialist services and 42% in generic CAMHS at 12 months).
Cost-effectiveness of specialist versus generic services: main analysis
In the main analysis using the CGAS score (the primary measure of effect in the cost-effectiveness analysis) at the 12 month follow-up (the primary end point), adjusted total costs per participant were lower and adjusted CGAS scores were slightly lower (poorer outcome) in the specialist group than in the generic group, generating an incremental cost-effectiveness ratio (the additional cost of one intervention compared with another divided by the additional effects) of £10,932 (–£7106/–0.65). This suggests that being initially assessed in a generic service generates a 1-point improvement in CGAS scores for an additional cost of approximately £11,000 compared with a specialist eating disorders service. The cost-effectiveness plane in Figure 6 illustrates the scatterplots of the bootstrapped cost and effectiveness pairs for specialist versus generic services at 12 months using the CGAS score. The points in the scatterplot fall in all four quadrants of the cost-effectiveness plane, but the majority fall below the x-axis, indicating that the specialist group is less costly than the generic CAMHS group, and a slightly larger proportion fall to the left of the y-axis, indicating that the specialist group demonstrated poorer outcomes than the generic CAMHS group. In terms of the four quadrants, the largest proportion is in the south-west quadrant, where specialist services are cheaper (below the x-axis) and less effective (to the left of the y-axis), and so there is a trade-off between the two interventions and a decision must be made as to whether or not the additional effects of generic services are worth the additional costs.
FIGURE 6.
Cost-effectiveness plane for CGAS scores at 12 months showing specialist minus generic cost and effectiveness pairs: main analysis.
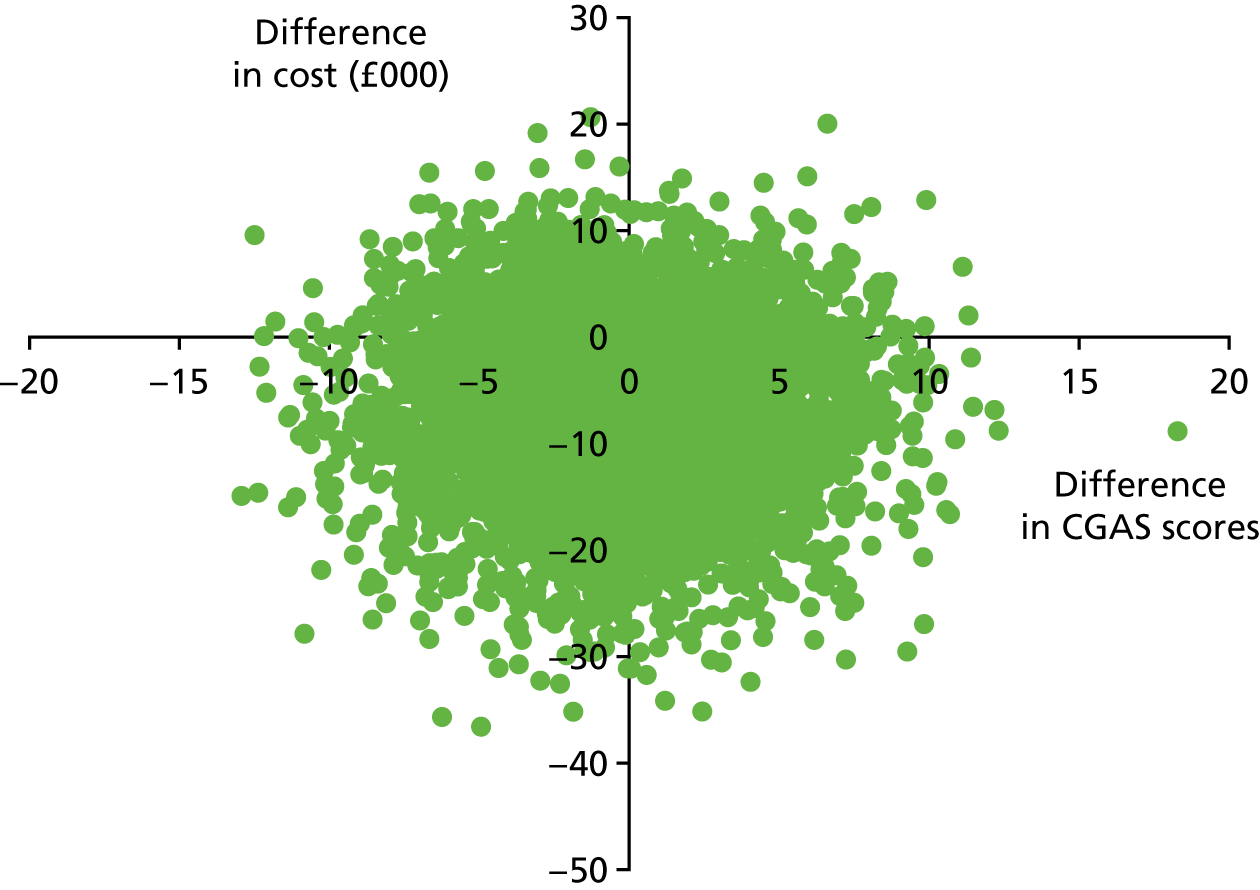
At the 6-month follow-up, adjusted total costs per participant were lower in the specialist group and adjusted CGAS scores were slightly higher (better outcomes), so initial assessment in a specialist service dominates initial assessment in a generic service. In the cost-effectiveness plane for CGAS score at 6 months (Figure 7), the largest proportion of replications is in the south-east quadrant, where specialist services are cheaper (below the x-axis) and more effective (to the right of the y-axis), and thus dominate generic services.
FIGURE 7.
Cost-effectiveness plane for CGAS scores at 6 months showing specialist minus generic cost and effectiveness pairs: main analysis.
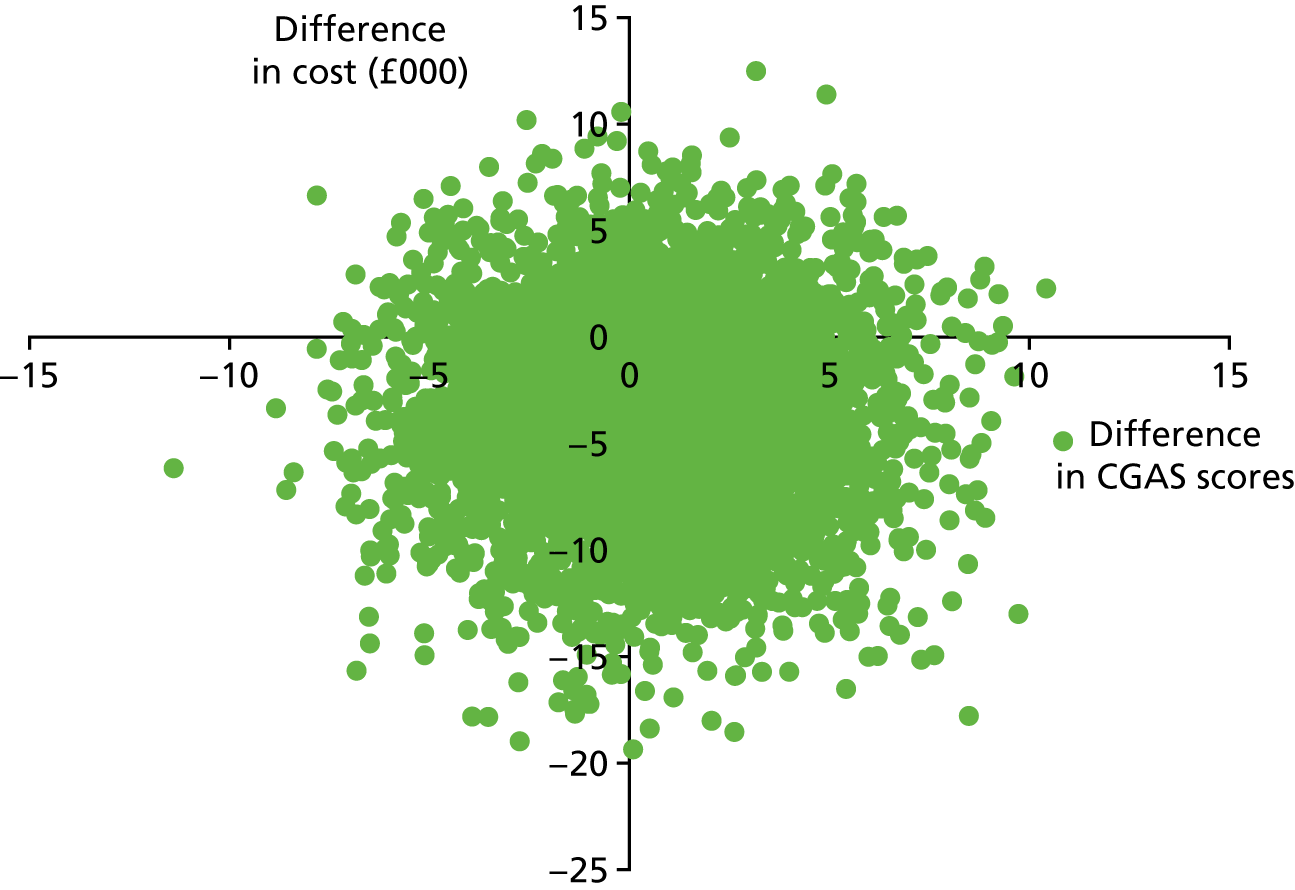
Statistical uncertainty around the incremental cost-effectiveness ratios was explored through the calculation of cost-effectiveness acceptability curves, shown in Figure 8 for CGAS scores at 12 months and at 6 months. Both cost-effectiveness acceptability curves suggest that there is > 50% probability of initial assessment in a specialist service being cost-effective compared with a generic service, with probabilities ranging from approximately 90% at zero willingness to pay for improvements in effectiveness to approximately 50% at a willingness-to-pay value of £30,000.
FIGURE 8.
Cost-effectiveness acceptability curves for CGAS scores at 6 and 12 months: main analysis.
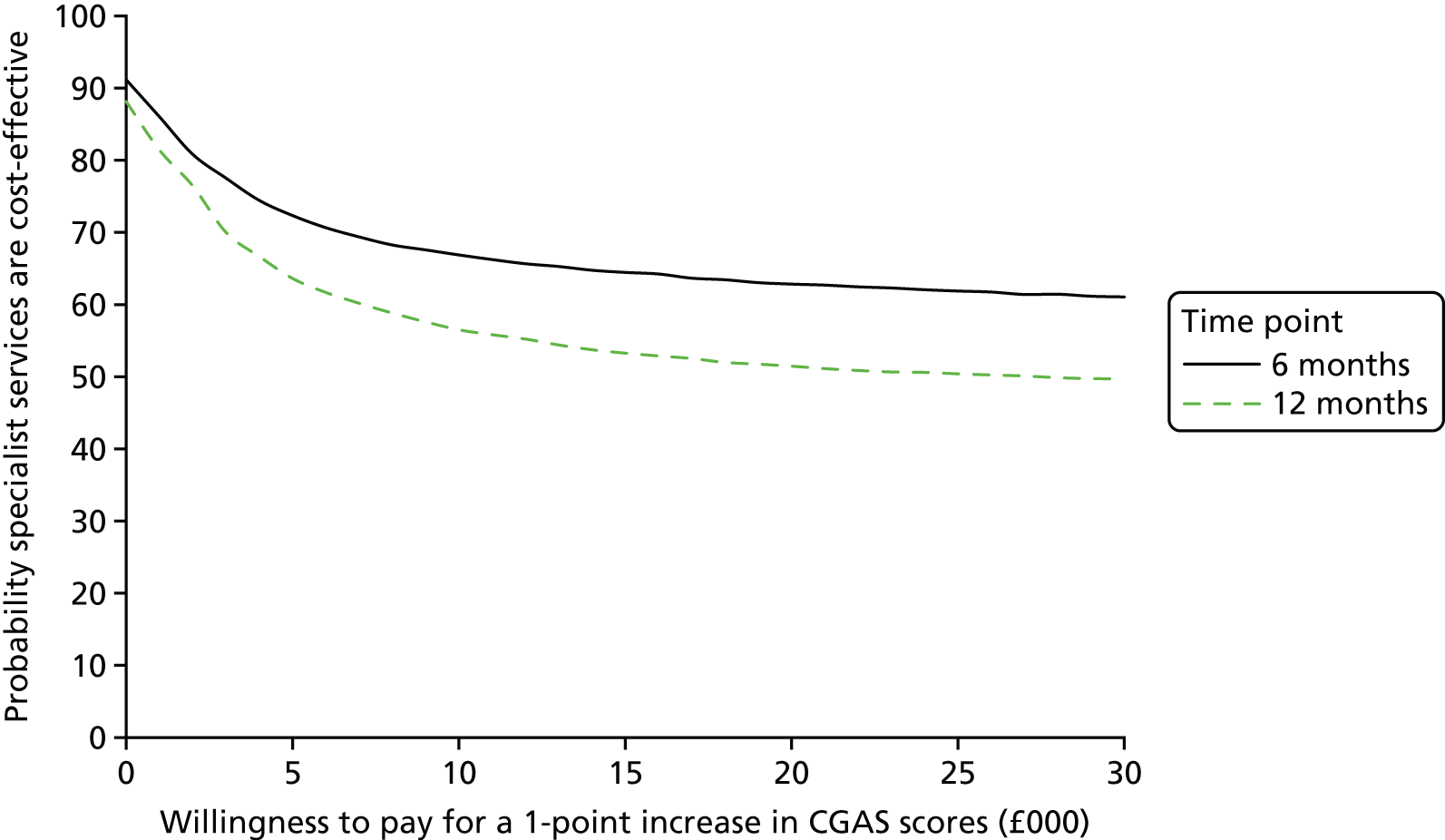
In terms of %mBMI for age and sex (the secondary measure of effect in the cost-effectiveness analysis) at the 12-month follow-up (the primary end point) in the main analysis, adjusted total costs per participant were lower and %mBMI scores were very slightly higher (better outcome) in the specialist group than in the generic group, so initial assessment in a specialist service dominates initial assessment in a generic service. The cost-effectiveness plane in Figure 9 illustrates the scatterplots of the bootstrapped cost and effectiveness pairs for specialist versus generic services at 12 months using %mBMI. The vast majority of the points in the scatterplot fall in the south quadrants below the x-axis, where specialist services are cheaper than generic services, and effectiveness is similar (equally distributed to the left and the right of the y-axis).
FIGURE 9.
Cost-effectiveness plane for %mBMI at 12 months showing specialist minus generic cost and effectiveness pairs: main analysis.
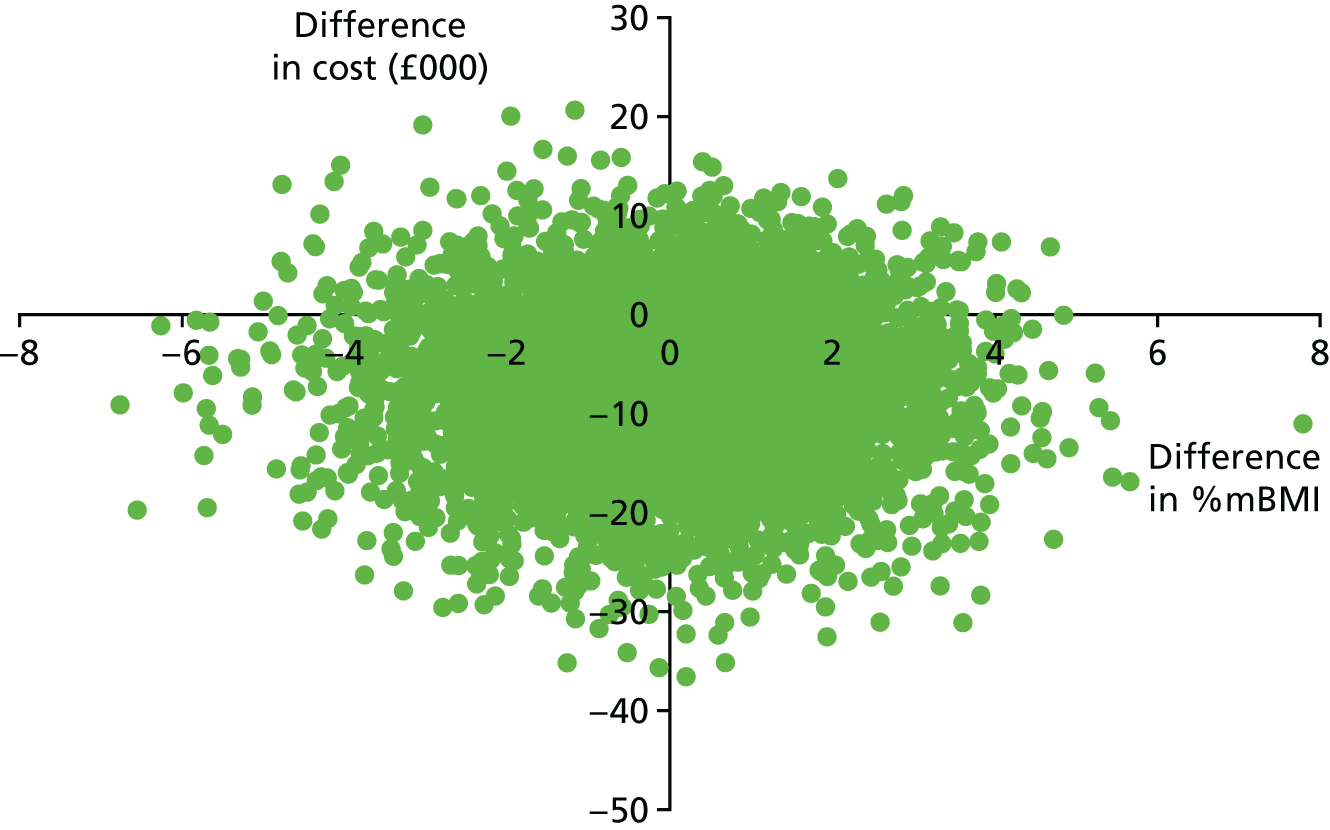
At the 6-month follow-up, results were similar, with adjusted total costs per participant being lower in the specialist group and %mBMI being higher (better outcomes), so initial assessment in a specialist service dominates initial assessment in a generic service. The cost-effectiveness plane in Figure 10 illustrates the scatterplots of the bootstrapped cost and effectiveness pairs for specialist versus generic services at 12 months using %mBMI. The vast majority of the points in the scatterplot fall in the south-east quadrant, where specialist services are cheaper (below the x-axis) and more effective (to the right of the y-axis) than generic services, illustrating that specialist services dominate generic CAMHS.
FIGURE 10.
Cost-effectiveness plane for %mBMI at 6 months showing specialist minus generic cost and effectiveness pairs: main analysis.
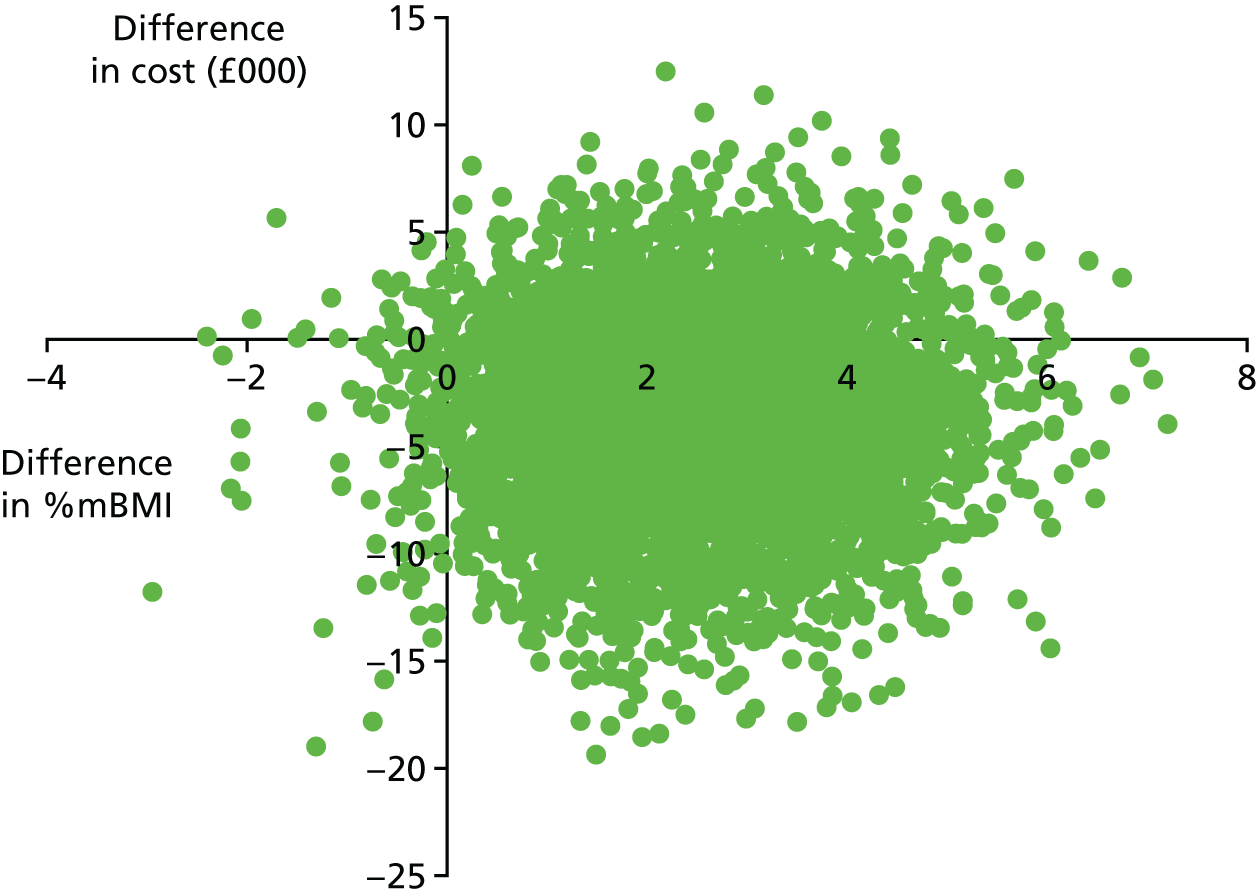
The cost-effectiveness acceptability curves for %mBMI at 12 months and 6 months are shown in Figure 11. Both cost-effectiveness acceptability curves suggest that there is a > 50% probability of initial assessment in a specialist service being cost-effective compared with a generic service, with probabilities ranging from 76% at zero willingness to pay to 56% at a willingness-to-pay value of £30,000 in the 12-month analysis and from approximately 69% at zero willingness to pay for improvements in effectiveness to > 98% at a willingness-to-pay value of £30,000 in the 6-month analysis.
FIGURE 11.
Cost-effectiveness acceptability curve for %mBMI at 6 and 12 months: main analysis.
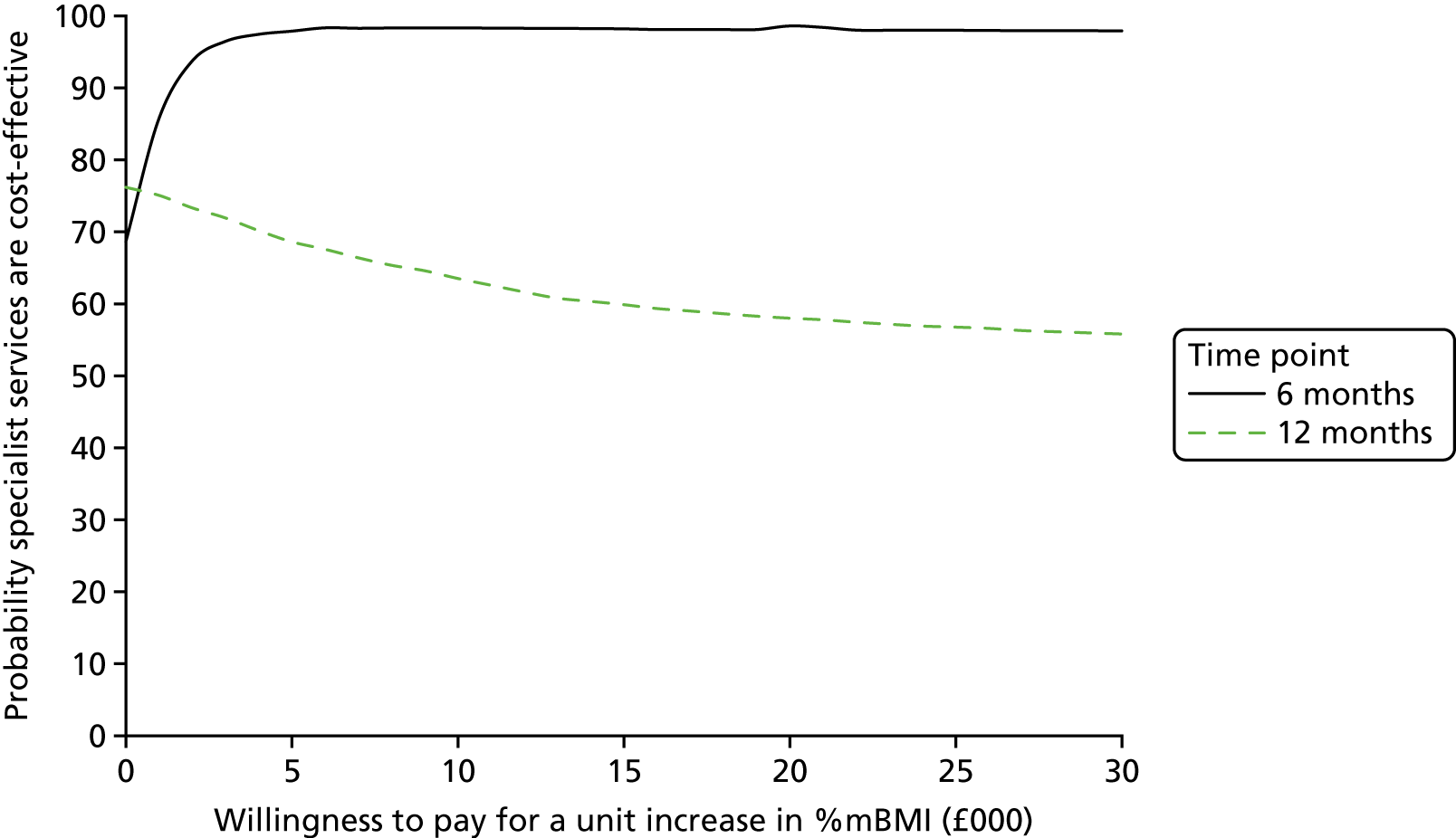
Cost-effectiveness of specialist versus generic services: Delphi sensitivity analysis
In the Delphi sensitivity analysis using the CGAS score, adjusted total costs per participant were lower and adjusted CGAS scores were lower (poorer outcome) in the specialist group than in the generic group, generating an incremental cost-effectiveness ratio of £965 (–£3309/–3.43) at 12 months and £3577 (–£3362/–0.94) at 6 months. The cost-effectiveness planes are presented in Appendix 2.
The cost-effectiveness acceptability curves for CGAS scores at 12 months and 6 months are shown in Figure 12. At 6 months, the cost-effectiveness acceptability curve suggests that there is a > 50% probability of initial assessment in a specialist service being cost-effective compared with a generic service for willingness-to-pay values between £0 and £8000, but the probability falls to < 50% for higher values of willingness to pay, with probabilities falling to 42% at a willingness-to-pay value of £30,000 for unit improvements in CGAS scores. At 12 months, the results are similar, with the probability of initial assessment in specialist services being cost-effective compared with generic services ranging from 93% at zero willingness to pay to 55% at a willingness-to-pay value of £3000, but falling to 22% at a willingness-to-pay value of £30,000.
FIGURE 12.
Cost-effectiveness acceptability curves for CGAS scores at 6 and 12 months: Delphi sensitivity analysis.
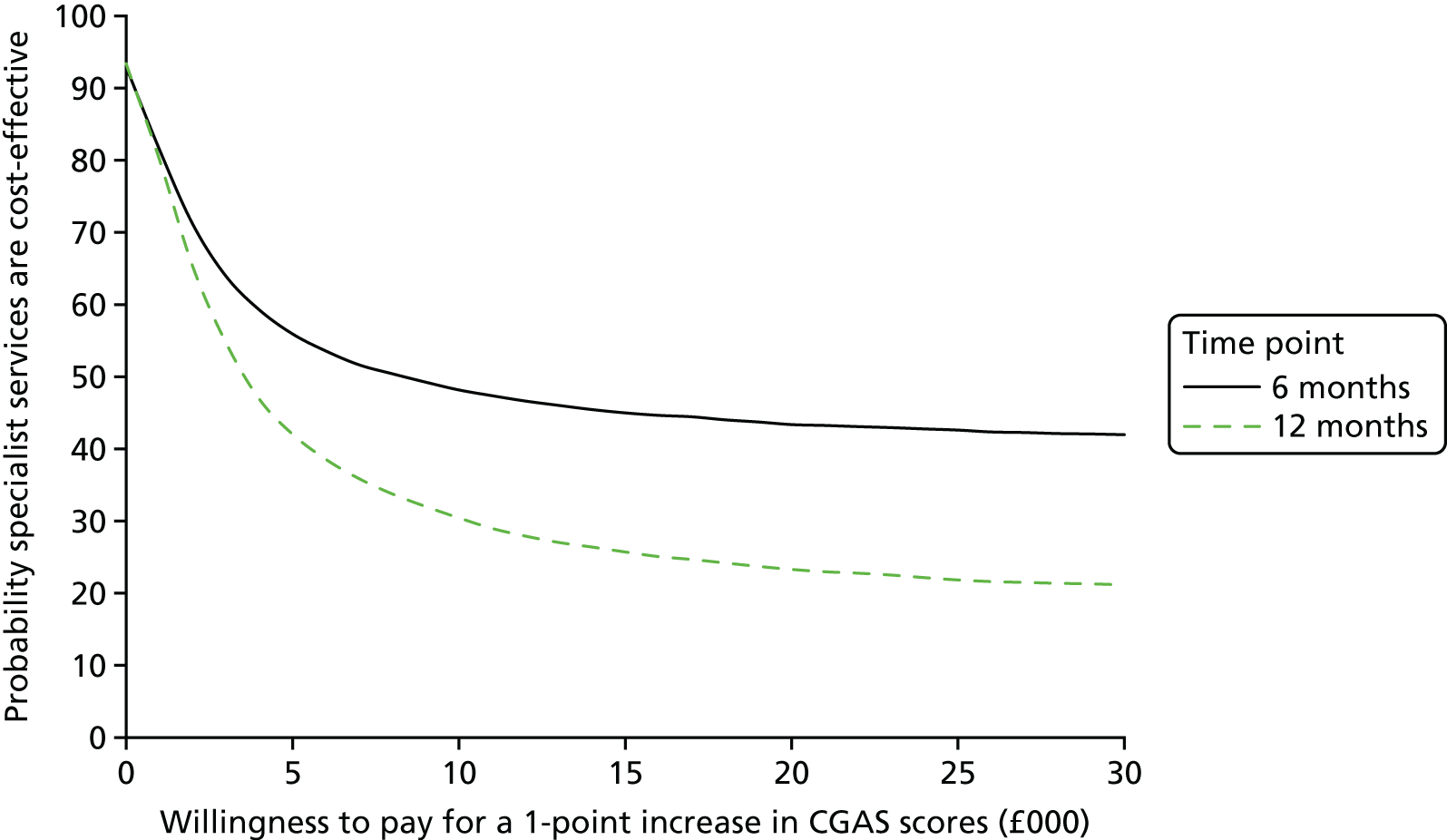
In terms of %mBMI for age and sex, adjusted total costs per participant were lower and %mBMI scores were higher (better outcome) in the specialist group than in the generic group at both the 12-month and the 6-month follow-ups, so initial assessment in a specialist service dominates. The cost-effectiveness planes are presented in Appendix 2.
The cost-effectiveness acceptability curves for %mBMI at 12 months and 6 months are shown in Figure 13. Both cost-effectiveness acceptability curves suggest that there is a > 50% probability of initial assessment in a specialist service being cost-effective compared with a generic service, with a minimum probability of specialist services being cost-effective of 80% in the 12-month analysis and 71% at 6 months.
FIGURE 13.
Cost-effectiveness acceptability curves for %mBMI at 6 and 12 months: Delphi sensitivity analysis.
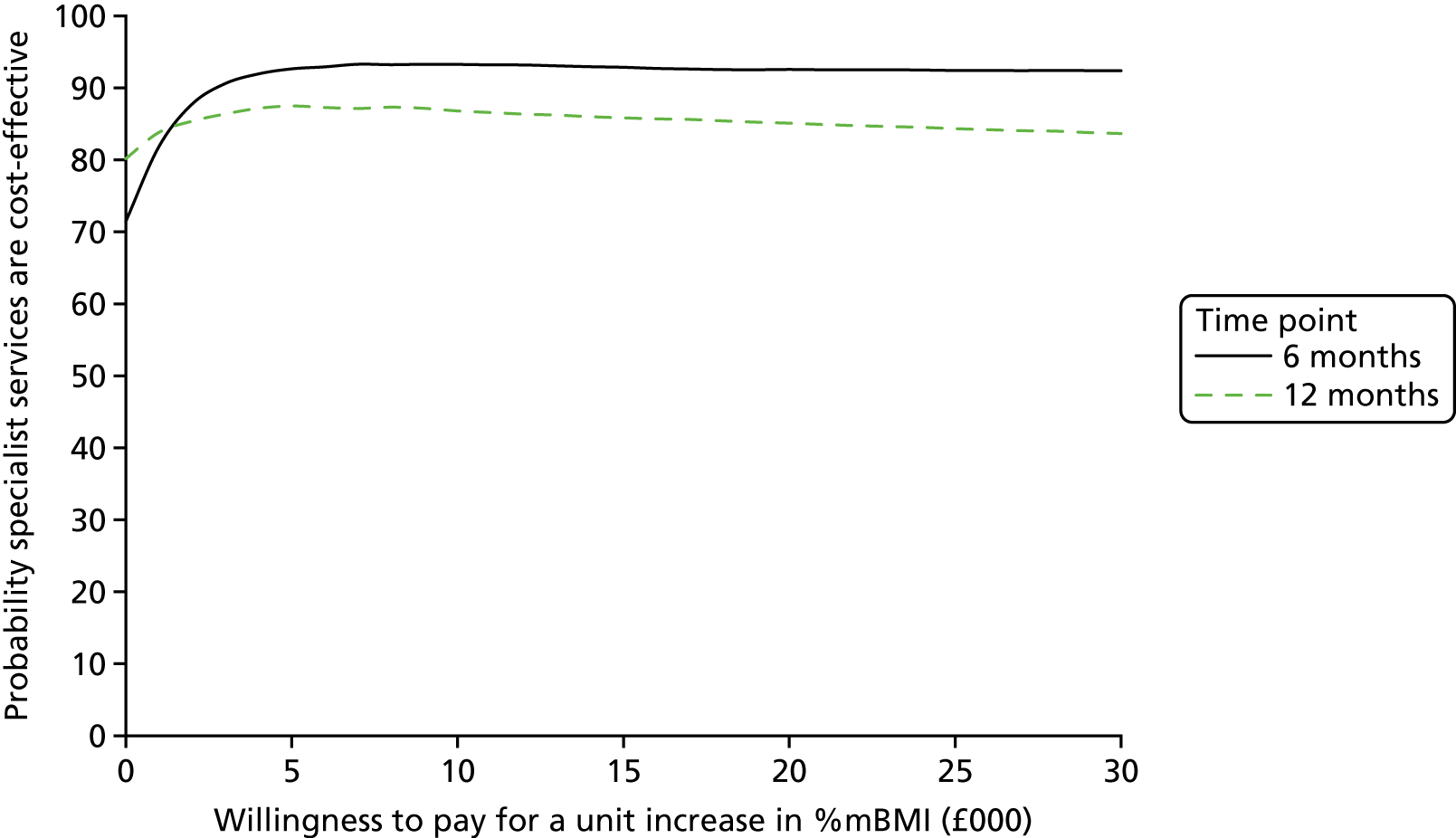
Decision modelling
Model inputs
Model inputs are summarised in Table 27. Costs, which are reported for the periods baseline to 6 months and 6 months to 12 months, were, on average, substantially higher in both groups for participants who had not achieved remission than for those who had (approximately £20,000 vs. £8000 at 6 months and £18,000 vs. £6000 at 12 months, respectively), and higher for participants who achieved only partial remission than for those in full remission (approximately £9000 vs. £4000 at 6 months and £7000 vs. £4000 at 12 months, respectively). Participants who were classified as relapsed at the 12-month follow-up were, on average, substantially less costly in the specialist eating disorders group (£8531) than in the generic CAMHS group (£29,236); however, numbers were small so firm conclusions cannot be reached.
| Inputs | Group | |||
|---|---|---|---|---|
| Specialist | Generic | |||
| Mean | n (%) | Mean | n (%) | |
| Cost (£) | ||||
| 6 months | n = 147 | n = 73 | ||
| No remission | 20,904 | 102 (69.4) | 19,680 | 47 (64.4) |
| Partial remission | 8327 | 36 (24.5) | 11,893 | 16 (21.9) |
| Full remission | 4451 | 9 (6.1) | 3735 | 10 (13.7) |
| 12 months | n = 131 | n = 49 | ||
| No remission | 18,640 | 62 (47.3) | 17,431 | 20 (40.8) |
| Partial remission | 6809 | 35 (26.7) | 8678 | 13 (26.5) |
| Full remission | 4956 | 28 (21.4) | 2171 | 13 (26.5) |
| Relapse | 8531 | 6 (4.6) | 29,236 | 3 (6.1) |
| CGAS score | ||||
| Baseline | 43.22 | 174 | 47.86 | 99 |
| 6 months | n = 115 | n = 55 | ||
| No remission | 48.97 | 70 (60.9) | 51.69 | 29 (52.7) |
| Partial remission | 72.53 | 36 (31.3) | 71.50 | 16 (29.1) |
| Full remission | 82.11 | 9 (7.8) | 83.70 | 10 (18.2) |
| 12 months | n = 97 | n = 38 | ||
| No remission | 51.09 | 33 (34.0) | 47.11 | 9 (23.7) |
| Partial remission | 73.81 | 32 (33.0) | 72.30 | 13 (34.2) |
| Full remission | 85.50 | 26 (26.8) | 90.00 | 13 (34.2) |
| Relapse | 60.50 | 6 (6.2) | 62.00 | 3 (7.9) |
A similar pattern was seen for CGAS outcomes, with mean CGAS scores being, on average, substantially lower (poorer outcome) in both groups for participants who had not achieved remission than for those who had (approximately 50 vs. 75 points at 6 months and 50 vs. 80 points at 12 months), and lower for participants who achieved only partial remission than for those in full remission (approximately 72 vs. 83 points at 6 months and 74 vs. 87 points at 12 months). Participants who were classified as relapsed at the 12-month follow-up had a mean score of approximately 60 points on the CGAS, which was higher than that for those who had not achieved remission (50 points) but lower than for those in partial or full remission (75 points).
At baseline, as noted previously (see Outcomes), participants in the specialist eating disorders service group had, on average, poorer baseline CGAS scores than those in the generic CAMHS group (43 vs. 48); however, in terms of CGAS health states, mean scores in both groups lie within the ‘obvious problems – moderate impairment in most areas or severe in one area’ health state on the CGAS. 27 At both the 6- and 12-month follow-ups, the average score of those who had not achieved remission remained in the ‘obvious problems – moderate impairment in most areas or severe in one area’ category (scores between 41 and 50) or improved slightly to fall into the next category of ‘some noticeable problems – in more than one area’ (scores between 51 and 60). The average score of those in partial remission fell into the ‘doing all right – minor impairment’ category (scores between 71 and 80) and the average score of those in full remission was in the ‘doing well’ category (scores between 81 and 90).
Comparing the two groups, costs and outcomes for participants who had not achieved remission at 6 months were very similar. In the case of those in partial remission, costs were lower and CGAS scores were slightly higher for those in the specialist eating disorders group than in the generic CAMHS group, but for those in full remission, costs were slightly higher and outcomes were slightly lower for the specialist eating disorders group. At 12 months, among those failing to achieve remission, costs were higher and outcomes were better in the specialist eating disorders group than in the generic CAMHS group. Among those in remission, the pattern was the same as at 6 months, with specialist services being associated with lower costs and better outcomes for those in partial remission but with higher costs and poorer outcomes for those in full remission.
Model effects
Calculation of the weighted average overall gain in outcome at 12 months, taking into consideration both the proportion of patients who go into remission and the CGAS score gain, found that young people initially assessed in specialist eating disorders services had improved, on average, by 46.97%, compared with only 41.87% for young people initially assessed in generic CAMHS.
To explore whether the results were driven by the disparity in baseline CGAS scores or by the treatment effect in each arm, two-way sensitivity analyses were carried out to examine the relationship between the baseline CGAS score and the treatment effect. Four scenarios were considered for the economic modelling, which are outlined in Chapter 2, Model analysis, and the calculations to derive the model inputs for these sensitivity analyses, expressed as CGAS score gain from baseline, are reported in Table 28.
| Scenario | Baseline CGAS score (points) | Treatment effect (%) | CGAS score gain (points) |
|---|---|---|---|
| Base case | |||
| Specialist | 43.22 | 47 | 20.31104 |
| Generic | 47.86 | 42 | 20.04116 |
| Sensitivity analysis 1a: generic baseline CGAS | |||
| Specialist | 47.86 | 47 | 22.49158 |
| Generic | 47.86 | 42 | 20.04116 |
| Sensitivity analysis 1b: specialist baseline CGAS | |||
| Specialist | 43.22 | 47 | 20.31104 |
| Generic | 43.22 | 42 | 18.09818 |
| Sensitivity analysis 2a: generic treatment effect | |||
| Specialist | 43.22 | 42 | 18.09818 |
| Generic | 47.86 | 42 | 20.04116 |
| Sensitivity analysis 2b: specialist treatment effect | |||
| Specialist | 43.22 | 47 | 20.31104 |
| Generic | 47.86 | 47 | 22.49158 |
Model results
Model results are presented as the average cost per 10-point gain in CGAS score per young person in the full hypothetical cohort and are not presented separately for specialist eating disorders services versus generic CAMHS. Thus, these results are not attempting to explore the relative cost-effectiveness of specialist versus generic services but are instead focused on the overall impact on the cohort as the proportion of young people being assessed by specialist or generic services is varied.
The cost per 10-point gain in CGAS score per young person generated for the base-case scenario, the three alternative scenarios varying the percentage of young people initially assessed in specialist eating disorders services and generic CAMHS and the two-way sensitivity analyses varying baseline CGAS scores and the 12-month treatment effect is reported in Table 29.
| Scenario | Cost per 10-point improvement in CGAS score (£) |
|---|---|
| Base case | |
| 0% specialist, 100% generic | 13,757.47 |
| 50% specialist, 50% generic | 13,996.64 |
| 73% specialist, 27% generic (as per CostED sample) | 14,105.59 |
| 100% specialist, 0% generic | 14,232.64 |
| Sensitivity analysis 1a: baseline CGAS as per generic CAMHS | |
| 0% specialist, 100% generic | 13,757.47 |
| 50% specialist, 50% generic | 13,279.07 |
| 73% specialist, 27% generic (as per CostED sample) | 13,077.04 |
| 100% specialist, 0% generic | 12,852.79 |
| Sensitivity analysis 1b: baseline CGAS as per specialist group | |
| 0% specialist, 100% generic | 15,234.44 |
| 50% specialist, 50% generic | 14,704.68 |
| 73% specialist, 27% generic (as per CostED sample) | 14,480.96 |
| 100% specialist, 0% generic | 14,232.64 |
| Sensitivity analysis 2a: treatment effect as per generic CAMHS | |
| 0% specialist, 100% generic | 13,757.47 |
| 50% specialist, 50% generic | 14,808.73 |
| 73% specialist, 27% generic (as per CostED sample) | 15,329.15 |
| 100% specialist, 0% generic | 15,972.86 |
| Sensitivity analysis 2b: treatment effect as per specialist group | |
| 0% specialist, 100% generic | 12,258.62 |
| 50% specialist, 50% generic | 13,195.34 |
| 73% specialist, 27% generic (as per CostED sample) | 13,659.06 |
| 100% specialist, 0% generic | 14,232.64 |
In the base-case scenario, the cost per 10-point gain in CGAS score per young person was slightly higher if all young people were initially assessed and diagnosed in a specialist eating disorders service (£14,233) than if they were assessed and diagnosed in a generic service (£13,758). The results were similar in sensitivity analyses 2a and 2b, but the opposite was the case in sensitivity analyses 1a and 1b, with the cost per 10-point gain in CGAS per young person being slightly lower in specialist services than in generic CAMHS. Across all scenarios, there was little variation in the cost per 10-point gain in CGAS score.
The variation is shown more clearly in Figure 14, which depicts the results of the base-case scenario and the four sensitivity analyses, varying the proportion of young people in the specialist eating disorders group from 100% to 0% (and thus the proportion of young people in the generic group from 0% to 100%), a total of 500 scenarios. The base-case results are almost horizontal, suggesting little difference in the cost per 10-point gain in CGAS score as the proportion in each group is varied. The slopes on all sensitivity analyses are greater than in the base-case scenario, suggesting greater variation as the proportion in each group changes, with sensitivity analyses 1a and 1b favouring specialist eating disorders services and sensitivity analyses 2a and 2b favouring generic CAMHS.
FIGURE 14.
Economic model base-case scenario and two-way sensitivity analysis results. SA, sensitivity analysis.

One-way sensitivity analysis was used to explore the sensitivity of the model to the cost and CGAS inputs into the model by varying each of the inputs using the relevant 95% CIs. The results indicated that the model was not particularly sensitive to a 95% CI change in CGAS scores (cost per 10-point gain in CGAS score ranged from £12,900, the lower end of the 95% CI, to £13,913, the upper end of the 95% CI) or in cost (cost per 10-point gain in CGAS score ranged from £12,122, the lower end of the 95% CI, to £15,151, the upper end of the 95% CI).
Probabilistic sensitivity analysis was used to explore the uncertainty in the cost-effectiveness results, in relation to the cost per 10-point gain in CGAS score. The results of this analysis are shown in the cost-effectiveness plane in Figure 15. The distribution of the results (the scatter points) indicate that there is substantial variation in both the CGAS scores and the costs, but the mean of these simulations remains similar to the main results, with little difference in costs (points equally spread above and below the x-axis) and little difference in outcomes (points equally spread to the left and the right of the y-axis).
FIGURE 15.
Probabilistic sensitivity analysis exploring cost-effectiveness of specialist vs. generic services in terms of cost per 10-point gain in CGAS score.

As there is no cost-effectiveness threshold for CGAS score (no point below/above which society is willing/unwilling to pay for a unit improvement in outcome), we also used probabilistic sensitivity analysis to explore the incremental cost per 10-point gain in the CGAS score in terms of the percentage of simulations that fell below various hypothetical willingness-to-pay thresholds for a 10-point gain in CGAS score. This threshold analysis found that 76% of simulations fell below £10,000 per 10-point CGAS score gain, 86% fell below £20,000 per 10-point CGAS score gain, 90% fell below £30,000 per 10-point CGAS score gain and 94% fell below £50,000 per 10-point CGAS score gain.
As noted in Chapter 2, Model structure, a lack of suitable data made a longer-term model impossible, but given consistent similarities in both cost and outcome between the two groups, and the initial differences in baseline, it is hypothesised that modelling further into the future would continue to suggest limited variation between the two groups.
Chapter 4 Discussion
Parts of this chapter have been reproduced from Petkova et al. 21 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Overview of the main results
The primary aims of the CostED study were to evaluate the cost and cost-effectiveness of existing community-based models of service provision for children and adolescents aged between 8 and 17 years with anorexia nervosa in the UK and the RoI and to use economic decision analysis to model the impact on cost and cost-effectiveness of potential changes to the provision of specialist eating disorders services in these regions.
The results of the cost-effectiveness analyses suggest that initial assessment in a specialist eating disorders service has a higher probability of being cost-effective than initial assessment in a generic CAMHS, for willingness-to-pay thresholds for improvements in outcome ranging from £0 to £30,000. This was true for both the CGAS score (primary analysis) and %mBMI for age and height (secondary analysis) and at both the 6- and 12-month follow-ups. However, without knowledge of the exact value society is willing to pay for improvements in either CGAS score or %mBMI, no firm conclusions can be reached.
From the decision modelling, there was no evidence to suggest that changes to the provision of specialist eating disorders services would generate savings for the NHS, with results from the economic model suggesting that the cost per 10-point improvement in CGAS score (i.e. an improvement from one CGAS category to the next) varies very little as the percentage of participants taking the specialist or the generic pathway is varied. These results were not found to be sensitive to variation in parameters or in probabilistic sensitivity analysis.
Cost-effectiveness of specialist versus generic services
The cost-effectiveness findings in favour of specialist eating disorders services were the result of very similar costs and outcomes in the two groups over the 12-month follow-up period, alongside poorer baseline clinical status in the specialist eating disorders group. Thus, despite the fact that young people in specialist eating disorders services were more severely ill at the point of assessment and diagnosis than those in generic CAMHS, specialist eating disorders services were achieving clinical outcomes 12 months after baseline similar to generic CAMHS, using a similar level of NHS secondary and tertiary services, and therefore a similar cost.
A sensitivity analysis (the Delphi sensitivity analysis) was carried out with services classified as either specialist or generic on the basis of criteria that had achieved consensus in the Delphi survey plus an additional criterion on which consensus had not been achieved, and for which there was evidence of a clear split in respondents’ beliefs about its importance (see Criteria for the classification of services as specialist). This analysis reduced the proportion of the sample classified as being assessed in a specialist service and results were less favourable for the specialist group than in the main analysis, with similar outcomes generated in the two groups, but higher costs in the specialist group. Although the specialist eating disorders group retained the higher probability of cost-effectiveness for the analysis using %mBMI, the results were less clear for CGAS scores, with the probability of specialist services being cost-effective falling below 50% at willingness-to-pay levels exceeding £3000 in the 12-month analysis and £8000 in the 6-month analysis. The results of the CGAS score analysis were therefore sensitive to the criteria used for classification of services.
These results are in line with previous evidence to support the cost-effectiveness of specialist eating disorders services for the treatment of young people with anorexia nervosa. 18 The TOuCAN trial,16 a multicentre RCT comparing inpatient psychiatric treatment, specialist outpatient treatment and general outpatient treatment for young people with anorexia nervosa, was carried out in the UK approximately 12 years prior to the collection of the CostED data (TOuCAN data were collected between 2000 and 2003; CostED data were collected in 2015). Outcomes among the specialist outpatient group in the TOuCAN trial were found to be similar to those observed in the inpatient and general outpatient groups, but specialist outpatient treatment was less costly over the 2-year follow-up period, with cost-effectiveness analysis suggesting that specialist outpatient treatment had the highest probability of being cost-effective. 18
A second study compared specialist eating disorders services with general CAMHS in terms of service use, evaluating referrals over a 2-year period with a 1-year follow-up. Data were collected from clinical notes for adolescents aged 13–17 years with an eating disorder in all services beyond primary care across London. 32 Admission rates in the London study, which excluded admissions for medical stabilisation, were significantly different between groups, being 15% among those assessed and treated in a specialist service, 19% among those receiving a non-specialist assessment but treated in a specialist service and 40% among those assessed and treated in a non-specialist service. Those referred to non-specialist outpatient services were also found to have incurred approximately twice the costs of those referred to specialist services, with no statistically significant differences in outcome. In the CostED study, the proportion of young people experiencing an admission was similar in the specialist and generic groups (approximately 30% in both groups), and, after removing paediatric admissions to enable comparison with the London study, admission rates remained similar (20% specialist, 18% generic). Although the rate of admissions of those assessed in specialist services was similar in the CostED study (20%) to that in the London study (15%), the admission rate among those assessed in a generic service (irrespective of where they were treated) was much lower in the CostED study (18%) than in the London study (approximately 30%).
The two studies are not directly comparable as a result of differences in the data collection methods, the sample size and the socioeconomic and demographic characteristics of the samples and possible changes in health-care commissioning of inpatient services since the London study was completed. Nevertheless, it seems unlikely that these factors alone could fully explain the considerable difference in the findings of the two studies. There are several other possible explanations for these differences. First, they could be attributable, at least in part, to differences in accessibility of inpatient services in London and in the broader geographical area covered in the CostED study. However, given evidence to suggest an overall increasing rate of hospital admissions for eating disorders in recent years,70 it seems unlikely that this would account for the lower rates of admissions reported for generic services in the CostED study than for those in the London study. Second, the sample sizes in the London study were relatively small, with follow-up data being based on a total of 84 participants, including only 31 participants referred to a non-specialist service. 32 It is possible that the small numbers of participants resulted in biased findings. However, the admission rates from specialist services are comparable with the 10–15% rates reported from treatment studies conducted in specialist services,71,72 and the findings are also consistent with clinical and audit reports of 50–80% reductions in hospital admissions when specialist eating disorders services that are accessible directly from primary care are introduced. 73
Third, it is possible that the CostED study underestimated the number of admissions from generic services. The CostED study recruited during a period when thresholds for referrals to generic CAMHS had been raised and significant numbers of patients remained on waiting lists until they had to be admitted to hospital. 74 These often quite severely ill patients may not have been included in the CostED study, thus making the results from the generic services group appear more favourable. A further potential bias might arise from the fact that, when patients with eating disorders are admitted to hospital from a generic CAMHS, they are not always discharged back to their local service and may therefore not have been included in the follow-up data. In terms of the CostED methodology, it is possible that generic CAMHS that felt that they were doing well at supporting young people with eating disorders were more likely to refer cases to the study. In addition, CostED was not set up to consider transfers between service types, which may have contributed to bias in the results given findings in the London study to suggest that admissions rates were lower among young people who were assessed in generic CAMHS and then transferred to a specialist community service for treatment. As CostED focused on the service in which young people were assessed, rather than treated, cases of this type would have remained classified as generic in the CostED study; thus, any reductions in admissions as a result of subsequent referral to specialist services would have been attributed to generic services, where the young person was initially assessed, and not to specialist services, where the young person was treated.
Economic evaluations of services for eating disorders are rare. A systematic review of existing cost-effectiveness analyses in eating disorders carried out in 201175 identified only two such studies: the TOuCAN study discussed previously18 and a study focused on guided self-help treatment for recurrent binge eating in adults. 76 This review covered all eating disorders and included adults as well as young people, and thus was broad in scope. 77 A more recent review of economic evidence, carried out in 2017,19 which also covered all eating disorders in people of all ages, identified 13 studies, three of which focused on anorexia nervosa, with the remainder focusing on bulimia nervosa or prevention of eating disorders. Among the anorexia nervosa studies, the review identified, in addition to the TOuCAN study,18 one study that was carried out alongside a RCT and explored the cost-effectiveness of focal psychodynamic therapy and enhanced cognitive–behavioural therapy in adults with anorexia nervosa78 and an economic modelling study comparing ‘adequate care’ with usual care for people of unspecified age. 79 Neither was of relevance to the current study and, given this lack of economic evidence, further comparisons with existing literature proved impossible.
Impact of changes to the provision of specialist services
Despite these cost-effectiveness findings in favour of specialist eating disorders services, economic decision modelling, which varied the proportion of young people initially assessed in specialist eating disorders services compared with generic CAMHS, did not suggest that changes to the provision of specialist eating disorders services would generate savings for the NHS. In fact, the results of the economic modelling show only limited variation between specialist eating disorder services and generic CAMHS, with similar cost per 10-point gain in CGAS score per young person, irrespective of whether the young person is initially assessed in a specialist or a generic service. Thus, the results of the modelling suggest that the two groups are relatively similar in terms of providing improvements in functioning.
In the economic model, costs and outcomes were explored by remission and relapse status and, as in the cost-effectiveness analysis, these costs and outcomes were very similar in both groups. However, the baseline differences observed between the two groups, discussed further (see Outcomes), were dealt with using change scores for the primary outcome measure (the CGAS score) rather than through statistical adjustment by prespecified baseline characteristics. These findings suggest that the economic results presented are sensitive to the baseline characteristics of the young people in the study and the method selected for adjusting for these differences.
Health service use and costs
Exploring the service use and cost components of the cost-effectiveness analysis in more detail, the results of the CostED study demonstrate that, although the number and length of hospital admissions and the number of outpatient contacts, including CAMHS contacts, were similar in the specialist and generic CAMHS groups, young people initially assessed in specialist services were more likely to receive care in an eating disorders facility, whereas young people initially assessed in generic CAMHS were more likely to receive care in general psychiatry facilities, which may simply reflect geography and the location of services. Day-patient contacts, which primarily took place in eating disorders facilities, were accessed more by the specialist group than by the generic group, again supporting the findings that the specialist group were more likely to receive care in an eating disorders service than in general psychiatry services.
In the Delphi sensitivity analysis, with services classified as either specialist or generic on the basis of criteria that had achieved consensus in the Delphi survey plus the additional criterion when consensus had not been achieved, numbers of inpatient nights and outpatient contacts were higher in the specialist group but the specialist group remained more likely than the generic CAMHS group to receive care in eating disorders facilities than in general psychiatry facilities.
It is also interesting to note that inpatient stays were longer in eating disorders facilities, particularly eating disorders facilities in the independent sector, than in general psychiatry and because young people initially assessed in specialist eating disorders services were more likely to receive services in eating disorders facilities, this difference is more marked in the specialist group, and contributes substantially to the cost differences between the two groups in the Delphi sensitivity analysis. If young people who were admitted from specialist services had not been admitted to eating disorder units or independent sector units, but instead had been admitted to general psychiatry facilities, the results in favour of specialist eating disorder services may have been stronger.
Although there were no significant differences in total costs between the specialist and generic groups in either unadjusted or adjusted analyses, adjustment for baseline variables resulted in observed differences favouring participants in specialist services (costs lower on average), in both the main analysis and the Delphi sensitivity analysis. This was because of the baseline differences identified, with those initially assessed in a specialist service having poorer CGAS scores and %mBMI, both of which were prespecified covariates.
Outcomes
In terms of the outcome side of the cost-effectiveness equation, at baseline both CGAS score and HoNOSCA were significantly poorer, on average, in the specialist group than in the generic group in both the main analysis and the Delphi sensitivity analysis, and %mBMI for age and sex was significantly lower in the Delphi sensitivity analysis. This suggests that specialist services are more likely to assess and diagnose more severely ill young people or those with more complex needs than generic services.
The fact that more unwell patients present to specialist services may not be a coincidence. There may be two factors at play. First, in areas where both specialist and generic services are accessible, patients who are more unwell are perhaps more likely to be referred to specialist services than to generic services. Second, and perhaps more importantly for the interpretation of the CostED study results, in areas where specialist services are not accessible, there may be an increased likelihood of the most unwell young people being admitted to paediatrics and then to inpatient treatment, thus bypassing community non-specialist treatment. The CostED study tracked young people only from the point of access to community-based mental health services, and thus would have excluded any young people admitted straight to hospital without any contact with CAMHS. This is a limitation of sampling at the community-based, secondary care level, and potentially introduces a bias in favour of generic CAMHS because caring for these ‘hidden’ young people as inpatients will be considerably more expensive than treating them in the community, and this additional cost would not have been captured in the CostED analyses.
By the 6-month follow-up, %mBMI was significantly higher in the specialist group than the generic group, and it remained higher at the 12-month follow-up, although the difference was no longer significant. No significant differences in CGAS score or HoNOSCA between the specialist and generic groups were identified at either the 6- or the 12-month follow-up, despite the significantly lower scores in the specialist group at baseline, with young people initially assessed in specialist services demonstrating greater improvements in outcome over the 12-month follow-up period than those in generic services.
In terms of remission and relapse rates in the main analysis, the results were not as clearly in favour of specialist services. Although partial remission was evident in a greater proportion of young people assessed in specialist services at 6 months, rates were similar in the two groups by 12 months. Full remission was evident for only a small proportion of the total sample (approximately 10% at 6 months and 24% at 12 months) and the full remission rate was lower in the specialist group than in the generic group at both time points. Relapse rates at 12 months were small and differed little between groups (approximately 5% of the total sample). In the Delphi sensitivity analysis, the proportion in full remission by 12 months was lower in the specialist group than in the generic group, which may be expected given the significantly poorer clinical status at baseline. However, a greater proportion of the specialist group were in partial remission and a smaller proportion had relapsed.
Incidence of anorexia nervosa in young people aged 8–17 years
In addition to the assessment of the cost and cost-effectiveness of alternative models of care for young people with anorexia nervosa and exploration of the impact on cost and cost-effectiveness of potential changes to the provision of specialist eating disorders services in the UK and the RoI, the CostED study aimed to identify incident cases of anorexia nervosa in young people aged between 8 and 17 years in the UK and the RoI and to classify the model of care provided to each young person as either a specialist eating disorders service or a generic CAMHS.
The first of these objectives, the identification of incident cases of anorexia nervosa in the UK and the RoI, provided an opportunity to calculate new estimates of the incidence of anorexia nervosa in the population sampled. These analyses suggest that, for the population as a whole, incidence rates have remained steady over the last few years, but there is evidence to suggest that rates for children have increased.
The missing data-adjusted estimate of the incidence of anorexia nervosa among young people aged 8–17 years, which we hypothesised to be the most accurate of the three estimates presented (IR1), was 14 per 100,000. This is lower than previous estimates from primary care-based data of 18–20 per 100,000 young people aged between 10 and 19 years. 33,34 However, these studies are difficult to compare as a result of the difference in the age range, with the CostED study including children aged 8 and 9 years, among which group the incidence was relatively low, and excluding older young people aged 18 and 19 years, among whom the incidence is relatively high. This age difference is likely to have had the impact of making the CostED estimates lower than those of these previous studies.
It was possible, however, to compare the incidence rates for those age groups covered by both the CostED study and a previous primary care study34 that collected data from the General Practice Research Database (GPRD) between 2000 and 2009. These data suggest that, among young people aged between 10 and 14 years, incidence rates have in fact remained steady over the last decade or so, with incidence rates of 12.6 per 100,000 reported in the CostED study, compared with 13.1 per 100,000 reported in the GPRD study. 34 For young females, the incidence rates were 23.3 per 100,000 in the CostED study and 24.0 per 100,000 in the GPRD study, and, for males, the rates were 2.4 and 2.5 per 100,000, respectively. 34
Only one secondary care study that included estimates of the incidence of anorexia nervosa among children in the UK or the RoI was identified. 37 This study estimated that, between 2005 and 2006, the overall incidence rate of anorexia nervosa, bulimia nervosa and eating disorders that were not otherwise specified among children aged between 6 and 12 years was 3.01 per 100,000. 37 The rates by disorder were 1.09 for anorexia nervosa and 1.35 for other eating disorders (i.e. bulimia nervosa, eating disorders that were not otherwise specified and binge eating disorder). Using the data available in the publication of the previous study,37 the incidence rate of anorexia nervosa among children aged between 8 and 12 years (thus excluding those aged 6 and 7 years for comparability with the CostED study) was approximately 1.5 per 100,000. Although the incidence rate may in fact have been higher had the study used DSM-5 diagnostic criteria rather than Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (because a proportion of those with eating disorders that were not otherwise specified would be diagnosed with anorexia nervosa using DSM-5), combining the anorexia nervosa category with those in the ’other eating disorders’ category meeting CostED criteria for DSM-5 anorexia nervosa (estimated from the original data by DN) gives an approximation of the DSM-5 incidence for children aged 8–12 years of approximately 2.1 per 100,000. This compares with a rate of 3.2 per 100,000 in the CostED study for children in the same age range of 8–12 years. Thus, the CostED DSM-5 incidence rate was higher than the estimated DSM-5 rate for 2006, suggesting that incidence rates for children aged 8–12 years may have increased in the last decade, whereas the overall rates, including adolescents aged 14–17 years, have remained steady. Although rates in children remain lower than rates in adolescents, this finding suggests that the onset of anorexia nervosa may be earlier for some young people than suggested by previous research.
Criteria for the classification of services as specialist
To classify services notifying incident cases of young people with anorexia nervosa in the CostED assessment of cost-effectiveness, a Delphi survey design was used to determine consensus for a number of possible classification criteria, which were identified primarily via review of existing guidelines for specialist eating disorder services. The two-stage Delphi survey was carried out online, rather than taking the more traditional face-to-face approach, to maximise the number of key stakeholder respondents and thus increase the validity of the results.
Two criteria achieved clear consensus for inclusion in round 1 (offering specialist outpatient treatment for eating disorders and providing multidisciplinary specialist outpatient clinics dedicated to eating disorders) and a third (holding weekly multidisciplinary meetings dedicated to eating disorders), which almost achieved consensus in round 1, achieved consensus in round 2. These criteria suggest that, to be classified as a specialist eating disorders service for young people, a service must provide evidence-based services for the treatment of eating disorders, must be multidisciplinary and must have a clear focus on, and expertise in, eating disorders.
A fourth criterion remained uncertain after both rounds of the Delphi survey (the number of cases of eating disorders seen per year), with approximately half the respondents rating it as either very important or extremely important. Previous evidence supports the inclusion of case size in terms of the effectiveness of services, particularly in surgery. For example, a study80 of the frequency and outcome of biliary atresia in infancy, which collected data from paediatricians via the British Paediatric Surveillance Unit in a similar way as data were collected in the CostED study from psychiatrists via CAPSS, found better outcomes and survival rates for children who received surgery in surgical centres with higher caseloads. It concluded that children with biliary atresia should be managed in surgical centres with experience in managing the condition. 80 There is thus evidence to support the concentration of treatment for rarer conditions within a small number of services that can develop expertise in that area. The empirical evidence showing that the same principles may be applicable to mental health problems such as eating disorders is less clear. Surgery is very different from the types of treatments commonly provided to young people with anorexia nervosa, which tend to be psychological and family based, albeit alongside management of physical complications. In addition, the chronic nature of eating disorders means that treatment takes place over months and years and increasingly on a day-care or outpatient basis. Although receipt of a surgical procedure some distance from home may be realistic, long-term day-care or outpatient treatment needs to be geographically located within reach of the young person’s home. The current guideline20 for the treatment of child and adolescent eating disorders in England, which recommended early intervention by specialist, community-based services, included the number of cases as a criterion (as well as a recommendation for a minimum catchment area population of 500,000) on largely pragmatic grounds. This is because of the experience that smaller specialist eating disorders teams tend to be less resilient to staff turnover, rather than on the grounds of evidence indicating that smaller specialist teams are less skilled and less able to deliver good health and social outcomes. 20
The lack of consensus regarding the number of cases of patients with eating disorders seen by a service per year in the CostED study is likely to be a reflection of the differences in the configuration of services across geographical regions at the time the Delphi survey was undertaken, with more heavily populated areas being more likely to receive a larger number of eating disorders referrals than rural areas and thus rural areas being less likely to rate this as important because any minimum number may not be achievable within the population they serve. The development of a large number of new dedicated eating disorders services across England, which vary in size and service organisation, will provide an opportunity to determine empirically what level of referrals is needed to make a specialist service viable. It will ensure that good outcomes are achieved, and at the same time ensure that unnecessary and costly inpatient admissions are avoided and therefore justify the investment in such services.
Although it is possible to argue that having a regular throughput of cases is needed for a team to achieve specialist expertise, specifying an actual minimum number of cases is always going to be somewhat arbitrary. There may be an argument, therefore, for including this criterion only descriptively to differentiate smaller and larger services but not including it in the main definition of a specialist service to avoid penalising services that may be ‘specialist’ in accordance with all other criteria but that may find it difficult to achieve a minimum of 50 cases per year because of the size the population they serve.
n the CostED analyses, this fourth criterion was excluded from the main analyses but included in sensitivity analyses (the Delphi sensitivity analyses), to explore the implication of its inclusion or exclusion. Its inclusion resulted in a decrease in the proportion of cases judged to have been initially assessed in specialist services and an increase in the proportion judged to have been assessed in generic CAMHS. Although follow-up outcomes remained similar between the two groups, differences in baseline clinical scores were more pronounced, with those patients classified as having been assessed in a specialist service being more severely ill at the point of assessment, and differences in cost were more pronounced and higher in specialist services than in generic services. These Delphi sensitivity analyses suggest that, in common with the results of the main analysis, more severely ill young people are more likely to be referred to specialist services and, despite this baseline disparity, specialist eating disorders services are able to achieve similar outcomes to generic CAMHS, although at greater cost. In terms of cost-effectiveness, results were less favourable for specialist services as a result of the greater cost differences, but specialist services remained more likely to be cost-effective than generic CAMHS over a range of willingness-to-pay thresholds for improvements in outcome. Thus, the results of the CostED study were not found to be sensitive to the inclusion of this criterion.
Two remaining criteria reached consensus for exclusion in round 1 of the Delphi survey (the size of the population of the catchment area and the age of the service). The population of the catchment area was not included in the original guidelines that were used to support the development of the CostED study service characteristics, which were included in the questionnaires to clinicians and the Delphi survey questions,24 but it was included on the advice of clinical research group members and was included in more recent guidance published in 2015. 20 This criterion was not considered important by ≥ 70% of the Delphi survey respondents, suggesting that it could be removed from future guidelines. Again, the failure of this criterion to achieve consensus for inclusion could reflect differences in services across geographical regions and the small population covered by services in more rural areas, which would otherwise meet criteria for specialist eating disorders services.
Age of a service was not included as a criterion in either the original guidelines used to support the CostED study methodology24 or the more recent guidelines published in 2015,20 but again was included on the advice of CostED clinical research group members. Only 9% of respondents rated this as very or extremely important, suggesting clear consensus that it should be excluded from the definition of specialist eating disorders services for young people.
One criterion that was not included in the CostED study, but is now included in more recent guidelines, is the availability of evidence-based interventions to treat comorbidities alongside the eating disorder. 20 Further research may be needed to explore the value of this criterion.
Application of the criteria identified through the Delphi survey to CostED cases and services suggests that between 46% and 65% of the young people meeting eligibility for inclusion in the CostED follow-up study were assessed in a specialist eating disorders service and that between 20% and 37% of the services that notified these cases were specialist eating disorders services, dependent on whether services were classified using three or four criteria (the main or the Delphi sensitivity analysis). Although these data may imply that a relatively small number of specialist eating disorders services are working with a much larger proportion of the total population of young people with anorexia nervosa than generic services, this may also indicate bias in the reporting of cases, discussed further below (see Timing of the CostED study). Although it should also be noted that the majority (≥ 60%) of notifying services were generic CAMHS, previous research suggests that up to 50% of individuals with anorexia nervosa never present to clinical services,81 but that they are more likely to present for help where specialist services exist,17 which may account for this finding.
Timing of the CostED study
As noted in the introduction (see Chapter 1, Background), the provision of community-based eating disorders services for children and young people in England has started to change following the publication of guidance for commissioning standards and requirements for the provision of community-based eating disorders services for children and young people in June 2015 and the announcement of £30M of recurrent funding to support the transformation of these services in England. 20 Although the funding announcement was made in the autumn of 2014, the first allocation of funding to services was not made until April 2016, after the commissioning standards guidance was developed and published in 2015. 20
The CostED sample was identified during the period February 2015 to September 2015 and subsequently followed up for 12 months to the end of September 2016. Although there is some overlap with the beginning of the funding allocation period, the entire CostED study surveillance period, all the 6-month follow-up data and approximately half of all the 12-month follow-up data were collected prior to any funding being allocated to services. It is, therefore, possible that some generic services had received funding that was available for the last few months of the CostED data collection period (around May to September 2016) and were beginning to develop their services into specialist eating disorders services. Such developments, which may include staff recruitment and training, take time, however, so the overall impact on the CostED data is likely to be minimal and would have enhanced the generic pathway, thus reducing the likelihood of finding differences between the two groups. Any bias would therefore be in favour of generic services rather than specialist services, so the results presented are conservative.
Strengths and limitations
Anorexia nervosa is a relatively rare disorder, making it difficult to recruit adequately powered samples for clinical trials. This surveillance study was able to gather case notifications from almost 100 services across the UK and the RoI, 79 of which reported at least one case that met the CostED study eligibility criteria. Recruitment of this number of services in a clinical trial would be prohibitively expensive; thus, surveillance studies are an important means to evaluate services for rarer conditions. Using CAPSS methodology has the important advantage of providing national data, and minimising loss of data owing to lack of patient consent. The CostED study included young people with anorexia nervosa, diagnosed using stringent DSM-5 criteria, from across the UK and the RoI, and thus it avoided the biases inherent in studying clinical samples via a small number of specialist centres in a narrow range of geographical locations.
During the 8-month surveillance period, 997 case notifications were received, which was substantially higher than the number estimated prior to the study start (between 590 and 660). After accounting for duplicates and withdrawals, 305 cases were eligible for inclusion in the incidence study and 298 cases were eligible for inclusion in the cost-effectiveness study, which, applying the incidence estimates calculated in the study (see Chapter 3, Incidence of anorexia nervosa in the UK and Republic of Ireland) to recent population data (see Chapter 3, Demographics and clinical features), was approximately 40% of all incident cases of anorexia nervosa in the UK and the RoI over an 8-month period. Although follow-up rates were lower than expected at both 6 months (n = 220, compared with estimates of between n = 300 and n = 330) and 12 months (n = 187, compared with estimates of between n = 220 and n = 250), this sample is still larger than RCTs carried out in this population of young people have been able to achieve to date. 16,82,83
The CAPSS notification cards were returned by approximately 50% of all clinicians included on the CAPSS system; however, 35% of those who provided a positive notification failed to return the baseline questionnaires, so the absence of some data was a constraint. There are many reasons why clinicians may fail to return notification cards or questionnaires. For example, clinicians may have retired or resigned, left the country, moved to work in different services and not received the CAPSS yellow cards or CostED questionnaires, assumed that a case had been reported by a colleague, failed to return yellow cards if there were nil returns, or simply had competing priorities that left them with no time to respond. 84
In addition, anorexia nervosa is a more common disorder than those usually supported by the CAPSS system, which may have depressed response rates. Recent studies include one focusing on gender identity disorders, which, in the first 9 months of surveillance (compared with the 8-month surveillance period in the CostED study), identified 80 cases notified from both the CAPSS (psychiatry) and the British Paediatric Surveillance Unit (paediatric) surveillance systems;85 and a study of childhood non-affective psychoses, which received only 15 notifications over a 12-month period via the CAPSS system. 86 We attempted to offset this through engagement activities, and to minimise the impact on clinicians by reducing the time period for reporting from the typical 12 months to 8 months. Nonetheless, the system relies on data from busy clinicians, which may not be readily available if the patient has moved between services.
In the analyses of costs, outcomes and cost-effectiveness, missing items in returned questionnaires were few and we contacted clinicians directly about missing data to minimise data loss. The one variable that differed was the HoNOSCA, for which a substantial proportion of responses were missing (approximately 80% at baseline, rising to almost 90% at the 6-month follow-up and 94% at the 12-month follow-up). This result strongly suggests that community-based clinical services are not using the HoNOSCA in routine practice and that the HoNOSCA had to be removed as the prespecified primary outcome measure and replaced with the CGAS score, for which response rates were substantially higher. To explore the impact of these missing data resulting from missing follow-up questionnaires for eligible cases, analyses of both costs and outcomes were repeated using multiple imputation. The results were very similar to the findings in complete-case analyses, thus giving greater confidence in the results presented.
In the incidence study, both missing notifications (from the 50% of clinicians who failed to return CAPSS yellow cards) and missing cases that could not be assessed for eligibility owing to missing baseline questionnaires were addressed using a novel approach for adjusting the observed incidence rates under different assumptions about the likely incidence rate among each of the two types of missing cases, which provided incidence rates hypothesised to be the most accurate, but also a range within which the true rates are likely to fall.
The CostED study sample collected via the CAPSS methodology was also limited to young people seen by consultant child and adolescent psychiatrists. Cases that would not be identified by this methodology include those managed by GPs in primary care and those in the care of mental health services with little or no psychiatric input, such as nurse-led facilities. We attempted to mitigate this by contacting those specialist services known to have little or no psychiatry input, in order to identify an alternative clinical lead respondent. For example, this was a particular issue in Northern Ireland, where, because of initial low numbers of notifications, investigation identified a number of nurse-led facilities that were invited to contribute, and subsequently reported just over half of all cases in Northern Ireland.
For the Delphi study, the issues were less about missing data, as the online nature of the survey allowed a much larger sample to be included than would be the case for a face-to-face panel, and more about the limited information available on the respondents. In order to minimise respondent burden and encourage participation, the survey did not ask for any identifying personal information, apart from the respondent’s e-mail address for the purpose of contacting them for round 2 of the Delphi survey. It is therefore not possible to know exactly which stakeholders responded and, thus, whether or not there were any particular biases in terms of the representation of different groups. However, the invited sample was broad, and the sample size achieved was substantially larger than would be expected from any face-to-face Delphi panel. In addition, a clear increase in responses was observed after advertising the Delphi survey on the Beat website, suggesting representation from patients and the public, and similar increases were seen after reminders were sent to professional groups. We are, therefore, confident that responses represent a wide range of expert opinions.
Other known limitations of Delphi surveys that are carried out online – known as e-Delphi studies – focus on internet access and research control. 87 In terms of access, concerns have been raised about the availability and reliability of internet access, particularly in remote, rural and developing areas, which may limit the representativeness of respondents. Although such concerns cannot be dismissed, this is unlikely to be a major concern in the current study, which primarily targeted stakeholders based in the UK and the RoI in order to gain consensus about the classification of UK- and RoI-based services. Individuals invited to take part by personal e-mail with an individual link to the survey included 687 named child and adolescent psychiatrists identified via the CAPSS database, which records contact details for psychiatrists within the UK and the RoI only. Although some respondents from outside the UK and the RoI may have responded via the open weblink advertised on the Beat website (www.beateatingdisorders.org.uk; accessed February 2019), these are likely to be in the minority. Research control may be more of an issue for the CostED Delphi study, with concerns being raised regarding false representation, lack of verbal interaction and participant distractions. 87 One of the main suggestions to limit research control issues is to provide a secure hyperlink to expert participants, which the CostED study was able to do for a proportion of the respondents, as already noted, but it is not possible to assess false representation or errors resulting from lack of verbal interaction, so this must be considered when drawing conclusions from the CostED Delphi study.
In addition, the Delphi survey did not include all aspects of a specialist child and adolescent eating disorders service that may be considered important and, in particular, did not include all criteria outlined in more recent guidance, as this was not available when the CostED study began. 20 The choice of questions on service characteristics was finalised with consideration of the burden on reporting clinicians and the requirement from CAPSS to keep questionnaires as brief as possible. However, there was substantial overlap between the CostED study criteria and the recent guidelines, outlined in Table 4 (see Chapter 2, Criteria for specialist eating disorders services), including the size of the catchment area, the number of cases seen per year, the existence of multidisciplinary teams with eating disorders experience and the provision of evidence-based services, although not for coexisting mental health problems as required by the current guideline. The current study additionally included the age of the service but did not include questions relating to referral pathways, included in the recent guidelines20 but not in earlier guidelines. 24 In addition, we were not able to collect data on staff composition and skill mix because of the substantial reporting burden this would have added, and more nuanced aspects of the quality of service delivery, such as team coherence and philosophy or treatment approach, could not be captured meaningfully by this methodology.
The absence of clear thresholds for Delphi consensus was a limitation, and so a decision was made to conservatively set a relatively high percentage for inclusion of 80%, which was 5% above the median used in similar studies. 44 However, a lower threshold for inclusion would have made no difference to the final results of the current study, although a threshold for inclusion of 75% would have meant that holding weekly multidisciplinary meetings dedicated to eating disorders, which met criteria for inclusion in round 2, would have met criteria for inclusion in round 1. No excluded criteria would have met criteria for inclusion, even with a threshold as low as 60%.
Bias in reporting and questionnaire completion is likely to be a problem in the CostED study. Specialist eating disorders services will tend to see more eating disorders cases than generic CAMHS, placing a much greater questionnaire completion burden on individual clinicians. In the CostED study, some clinicians provided > 20 case notifications, each of which required a baseline questionnaire and potentially also 6- and 12-month follow-up questionnaires. This burden may reduce clinicians’ willingness or ability to respond to notifications and questionnaires. However, those in specialist eating disorders services are also more likely to have a vested interest in the results of the study, which may make them more willing to take part. Overall, it is difficult to assess the extent or the direction of bias in the CostED data. A much larger proportion of CAMHS provided at least one notification (> 60%), but those specialist services that responded provided a much higher proportion of eligible notifications (approximately 65%).
The CostED study was also open to bias in terms of loss to follow-up owing to discharge, because follow-up data were less likely to be available for those young people who were doing well and had been discharged by services prior to the 6- or 12-month follow-up point. Again, it is difficult to hypothesise the differential impact of this problem between the two different service types. Those initially assessed in specialist eating disorders services showed greater improvements in functioning over the follow-up period, whereas those in generic services were more likely to be in remission by the 12-month follow-up point. Overall, there were only small differences in outcomes between the two groups at 12 months, suggesting that loss to follow-up owing to discharge is very likely to be similar in both service types. However, the loss of data on young people doing relatively well at follow-up will have an additional impact on the overall outcome and cost results presented for the two groups. Had full data been available, it is likely that the 12-month outcome scores per young person would be more improved and the total cost per young person over the 12-month period would be lower, on average, than the results presented here.
A further bias, discussed previously (see Outcomes), was the exclusion of young people admitted directly to inpatient facilities without any contact with CAMHS, which may have been more likely in areas where no specialist eating disorders services are available. This potentially introduces a bias in favour of generic CAMHS because the care that these young people receive as inpatients will be considerably more expensive than the costs of treating them in the community as might be the case had they instead been treated by generic CAMHS. The emphasis in the recent investment in specialist services is on ease of access to specialist eating disorders services (direct referral) and early intervention, in the hope that young people are accessing care before they become sick enough to require hospitalisation.
A crucial characteristic of the CostED study to note as a limitation is the fact that all the analyses focused on the service in which the young person was initially assessed and diagnosed, and not necessarily the service in which all treatment was received. In other words, the CostED study did not aim to track the movements of young people between service types. Thus, a young person initially assessed in a specialist eating disorders service may have recovered after an initial period of treatment and subsequently been referred to generic CAMHS for monitoring and treatment. Alternatively, a young person initially assessed in generic CAMHS may have been referred for treatment in a specialist service if, for example, he or she was particularly ill. In addition, a young person may have refused treatment in one service and requested treatment elsewhere, perhaps in a service closer to home. The CostED study, having data at only three time points (0, 6 and 12 months), cannot accurately track all shifts between service types, but a broader assessment of changes at 6 and 12 months is possible, and this work, which does not form part of the original proposal, will be undertaken and published separately.
It is worth noting, however, that previous evidence from the London care pathways study does not suggest substantial movement between specialist and generic services. 32 In a sample of 84 young people in London with a diagnosis of either anorexia nervosa or EDNOS-AN and who were assessed and treated in NHS services (rather than private services), 81% were treated in the same type of service that they were assessed in (63% assessed in a specialist service and received treatment in a specialist service and 18% assessed in a non-specialist service and received treatment in a non-specialist service). Only 19% were assessed in a non-specialist service and subsequently received treatment in a specialist service.
The results presented in the CostED study were clearly affected by the baseline differences in the young people initially assessed in specialist eating disorders services and those initially assessed in generic CAMHS. This will always be a limitation of evaluations that do not randomly allocate participants to one or another group. However, as noted earlier in this section, anorexia nervosa is a relatively rare disorder, making it difficult and prohibitively expensive to recruit adequately powered samples for clinical trials, with the CostED study recruiting a much larger sample (n = 298) than RCTs carried out in this population of young people have been able to achieve to date. 16,82,83 However, although surveillance studies are an important approach to the evaluation of services for rarer conditions, the results must be considered alongside the limitations. Baseline differences in the CostED study were found to influence the results presented, with cost-effectiveness results in favour of specialist eating disorders services, but economic modelling results showing little difference between the two groups.
Current UK clinical guidelines developed by the National Institute for Health and Care Excellence require economic evidence with effectiveness assessed in terms of quality-adjusted life-years (QALYs) to allow comparison across a diverse range of disorders and to support decision-making with reference to a specified threshold for incremental cost per QALY. 88 As the CostED study relied on data from clinical records, no measure capable of generating QALYs was available, so it is not possible to confirm the cost-effectiveness of specialist eating disorders services using standard thresholds. Future research should consider approaches to the collection of outcome data suitable for economic decision-making, such as the EuroQol measure of health-related quality of life,89 currently recommended by the National Institute for Health and Care Excellence,88 or the Child Health Utility instrument, which may be more suitable for young people. 90
Finally, it was not possible to explore our proposed subgroups (children vs. adolescents and rural vs. urban locations) or to model cost-effectiveness over the longer term. In terms of the subgroups, the number of children in the sample (those aged ≤ 12 years) was too small to undertake any meaningful statistical analyses (n = 35 at baseline; 12% of the total sample) and the classification of locations as rural or urban proved impossible with only the first half of the postcode. Although some half-postcodes were clearly rural or clearly urban (all postcodes starting with that first half of the postcode had the same classification), many were a mix of both urban and rural. Future research must balance the need to explore rural versus urban differences against the need to minimise the risk of patient identification through the use of limited identifiers such as the first half of a postcode. In terms of the longer-term modelling, data to support this were not available, highlighting a serious lack of cost and outcome data for young people with anorexia nervosa, which is likely to be an important feature in many rarer disorders.
Future research
Future research should carefully consider all the limitations of the CostED study outlined in the previous section. In terms of service evaluation, future research should focus on assessment of eating disorders services as they evolve following the publication of commissioning standards for the provision of community-based eating disorders services for young people in England in July 2015 and the announcement of £30M of recurrent funding to support the transformation of these services. 20 This investment, which had an explicit aim of overall cost reduction, will allow the impact not only of specialist provision but also of early intervention and staff training in evidence-based care to be evaluated.
Given that anorexia nervosa can take a chronic or relapsing course, future research should also consider the need for longitudinal follow-up to provide data to support assessment of the longer-term costs and benefits of CAMHS for young people as they transition into adulthood, and whether or not lifespan services provide a cost-effective alternative to age-specific care.
The CostED study, which focused on community-based services, also raises questions about the contribution of inpatient facilities and the differential use and impact of specialist eating disorders versus generic facilities. Future research should consider exploration of the full range of hospital and community-based services to get a broader picture of the relative effectiveness and cost-effectiveness of specialist services compared with generic CAMHS.
In terms of the classification of service types, further research is needed to consider the importance of certain criteria that were excluded from the CostED study primarily in order to minimise the reporting burden on clinicians. This includes the availability of evidence-based services for coexisting mental health disorders and the skill mix and composition of staff. It might be possible to better identify the location, number and characteristics of services via a multistakeholder mapping study of the kind in progress, as has been used in the National Institute for Health Research-funded study of transition in young adults with attention deficit hyperactivity disorder (the CATChuS study: https://medicine.exeter.ac.uk/catchus/mapping/adhdservices/; accessed February 2019). Seeking one informant per area to report on services is likely to fail, as no stakeholder group has perfect knowledge, and CostED has demonstrated differences in opinion over what constitutes a specialist service. A multistakeholder, multi-informant study that involved direct contact with relevant practitioners and was promoted via multiple pathways, including social media, may provide data to support a definitive map, which could be maintained over time so that practitioners and patients can continue to access it. More complex, but also of value, would be studies considering the quality of the mental health services provided to young people with anorexia nervosa, not just the characteristics.
From a methodological point of view, future research should consider approaches for the collection of outcome data suitable for economic decision-making, such as generic, preference-based measures capable of generating QALYs, currently recommended by the National Institute for Health and Care Excellence and similar health technology assessment bodies in a number of countries around the world. In addition, future studies should consider approaches to minimise missing data, balancing the need for larger samples and adequate levels of follow-up data against the cost of collecting data from young people themselves or the bureaucracy involved in gaining permission to collect data from the clinical records of a very large number of clinics, rather than relying on clinicians to provide the data. Future studies should also consider novel designs, possibly utilising routine data sources and the use of existing data sets, such as inpatient Hospital Episode Statistics data sets from NHS Digital, given the prohibitively high cost of carrying out RCTs in rare disorders such as anorexia nervosa in young people.
Conclusion
The CostED study suggests that, for young people aged 8–17 years with anorexia nervosa assessed in a community-based mental health service, initial assessment in a specialist eating disorders service may have a higher probability of being cost-effective than initial assessment in a generic CAMHS, but we were unable to reach a firm conclusion as a result of the methodological limitations of the study, in particular the lack of clear willingness-to-pay thresholds for the outcomes measured in the study.
Although the data presented suggest that costs and outcomes at the 12-month follow-up were similar in both groups, specialist services were achieving these equivalent outcomes for a similar cost while supporting young people who were more severely ill. In other words, young people initially assessed in specialist services showed a larger improvement in outcomes over the 12 months, without the need for additional expenditure.
From a pragmatic, decision-making point of view, when this evidence is combined with previous evidence to support the cost-effectiveness of specialist community-based services18 and to suggest that specialist services reduce admissions and reduce costs, with no difference in outcome,32 the body of evidence as a whole supports the provision of specialist eating disorders services, rather than generic services. The present uneven geographical spread of specialist eating disorder services is a concern given the need for young people who are more severly ill to be able to access local services without undue disruption to education, family or social life. In addition, the equivocal CostED results should be considered alongside other factors of relevance to any decision to invest in specialist eating disorders services,32,91,92 in particular the preferences of patients and carers, with much evidence suggesting a preference for specialist services.
Acknowledgements
We would like to thank all the clinicians who were kind enough to give up their time to provide the CostED study with CAPSS notifications and to complete questionnaires. We know your time is precious and in short supply and we are truly grateful. We would also like to thank the team at the Child and Adolescent Psychiatry Surveillance System, based at the Royal College of Psychiatrists’ Centre for Care Quality and Improvement, for its support with the design and running of the surveillance aspect of this study, and our study steering committee for their invaluable advice.
Contributions of authors
Sarah Byford (Professor of Health Economics) led the study, managed the King’s College London research staff, contributed to the design of the study and the data analysis, and drafted the report.
Hristina Petkova (Postdoctoral Researcher and CostED Trial Manager) contributed to data collection, data entry, data cleaning, data analysis, economic model development and drafting of the final report.
Ruth Stuart (Research Assistant) contributed to data collection, data entry, data cleaning and data analysis, and commented on and approved the final report.
Dasha Nicholls (Consultant Child and Adolescent Psychiatrist and Honorary Senior Lecturer) contributed to the design of the study, provided expertise on CAPSS methodology and clinical expertise, and commented on and approved the final report.
Mima Simic (Consultant Child and Adolescent Psychiatrist) contributed to the design of the study, provided clinical expertise and commented on and approved the final report.
Tamsin Ford (Professor of Child and Adolescent Psychiatry) contributed to the design of the study, provided clinical expertise and commented on and approved the final report.
Geraldine Macdonald (Professor of Social Work) contributed to the design of the study, managed the Northern Ireland research staff and commented on and approved the final report.
Simon Gowers (Professor of Adolescent Psychiatry) contributed to the design of the study, provided clinical expertise and commented on and approved the final report.
Sarah Roberts (Research Associate in Health Economics) contributed to the development of the economic model and the drafting of the economic model sections of the final report, and commented on and approved the final report.
Barbara Barrett (Senior Lecturer in Health Economics) contributed to data analysis and economic model development, and commented on and approved the final report.
Jonathan Kelly (Policy Officer, Beat) contributed to the design of the study, led the involvement of the Beat Young Ambassadors and commented on and approved the final report.
Grace Kelly (Research Fellow) contributed to data collection, data entry and data management in Northern Ireland, and commented on and approved the final report.
Nuala Livingstone (Research Fellow) contributed to data collection, data entry and data management in Northern Ireland, and commented on and approved the final report.
Kandarp Joshi (Consultant Child and Adolescent Psychiatrist and Honorary Senior Lecturer) provided clinical expertise and commented on and approved the final report.
Helen Smith (Consultant Child and Adolescent Psychiatrist) provided clinical expertise and commented on and approved the final report.
Ivan Eisler (Emeritus Professor of Family Psychology and Family Therapy) contributed to the design of the study, provided clinical support to the research team and commented on and approved the final report.
Publication
Petkova H, Simic M, Nicholls D, Ford T, Prina AM, Stuart R, et al. Incidence of anorexia nervosa in young people in the United Kingdom and the Republic of Ireland: a national surveillance study. BMJ Open 2019;9:e027339.
Data-sharing statement
Owing to the nature of the data collected and conditions attached to ethical/Health Reseach Authority approval, there are limitations on making data available for wider use. All queries should be submitted to the corresponding author in the first instance. Access to available anonymised data may be granted following review and if appropriate agreements are in place.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry 2011;68:724-31. https://doi.org/10.1001/archgenpsychiatry.2011.74.
- Hoang U, Goldacre M, James A. Mortality following hospital discharge with a diagnosis of eating disorder: national record linkage study, England, 2001–2009. Int J Eat Disord 2014;47:507-15. https://doi.org/10.1002/eat.22249.
- Lucas AR, Crowson CS, O’Fallon WM, Melton LJ. The ups and downs of anorexia nervosa. Int J Eat Disord 1999;26:397-405. https://doi.org/10.1002/(SICI)1098-108X(199912)26:4<397::AID-EAT5>3.0.CO;2-0.
- van Son GE, van Hoeken D, Bartelds AI, van Furth EF, Hoek HW. Time trends in the incidence of eating disorders: a primary care study in the Netherlands. Int J Eat Disord 2006;39:565-9. https://doi.org/10.1002/eat.20316.
- Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, Rosenheck RA. One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: evidence from a national database of health insurance claims. Int J Eat Disord 2000;27:381-9. https://doi.org/10.1002/(SICI)1098-108X(200005)27:4<381::AID-EAT2>3.0.CO;2-U.
- Simon J, Schmidt U, Pilling S. The health service use and cost of eating disorders. Psychol Med 2005;35:1543-51. https://doi.org/10.1017/S0033291705004708.
- Strober M, Freeman R, Morrell W. The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int J Eat Disord 1997;22:339-60. https://doi.org/10.1002/(SICI)1098-108X(199712)22:4<339::AID-EAT1>3.0.CO;2-N.
- NHS Digital . Hospital Episode Statistics, Admitted Patient Care – England, 2011–12 [NS], Primary Diagnosis 4 Characters n.d. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/hospital-episode-statistics-admitted-patient-care-england-2011-12 (accessed February 2019).
- NHS Digital . Hospital Admitted Patient Care Activity, 2015–16 [NS]. Primary Diagnosis 4 Characters n.d. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2015-16 (accessed February 2019).
- Lay B, Jennen-Steinmetz C, Reinhard I, Schmidt MH. Characteristics of inpatient weight gain in adolescent anorexia nervosa: relation to speed of relapse and re-admission. Eur Eat Disord Rev 2002;10:22-40. https://doi.org/10.1002/erv.432.
- Gowers SG, Weetman J, Shore A, Hossain F, Elvins R. Impact of hospitalisation on the outcome of adolescent anorexia nervosa. Br J Psychiatry 2000;176:138-41. https://doi.org/10.1192/bjp.176.2.138.
- Eisler I, Simic M, Russell GF, Dare C. A randomised controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa: a five-year follow-up. J Child Psychol Psychiatry 2007;48:552-60. https://doi.org/10.1111/j.1469-7610.2007.01726.x.
- Eisler I, Dare C, Russell GF, Szmukler G, le Grange D, Dodge E. Family and individual therapy in anorexia nervosa. A 5-year follow-up. Arch Gen Psychiatry 1997;54:1025-30. https://doi.org/10.1001/archpsyc.1997.01830230063008.
- Lock J, Couturier J, Agras WS. Comparison of long-term outcomes in adolescents with anorexia nervosa treated with family therapy. J Am Acad Child Adolesc Psychiatry 2006;45:666-72. https://doi.org/10.1097/01.chi.0000215152.61400.ca.
- Berelowitz M. Management of anorexia nervosa revisited: emphasis needs to continue to shift to outpatient care. BMJ 2004;328. https://doi.org/10.1136/bmj.328.7447.1075-b.
- Gowers SG, Clark A, Roberts C, Griffiths A, Edwards V, Bryan C, et al. Clinical effectiveness of treatments for anorexia nervosa in adolescents: randomised controlled trial. Br J Psychiatry 2007;191:427-35. https://doi.org/10.1192/bjp.bp.107.036764.
- House J, Schmidt U, Craig M, Landau S, Simic M, Nicholls D, et al. Comparison of specialist and nonspecialist care pathways for adolescents with anorexia nervosa and related eating disorders. Int J Eat Disord 2012;45:949-56. https://doi.org/10.1002/eat.22065.
- Byford S, Barrett B, Roberts C, Clark A, Edwards V, Smethurst N, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. Br J Psychiatry 2007;191:436-40. https://doi.org/10.1192/bjp.bp.107.036806.
- Le LK, Hay P, Mihalopoulos C. A systematic review of cost-effectiveness studies of prevention and treatment for eating disorders. Aust N Z J Psychiatry 2018;52:328-38. https://doi.org/10.1177/0004867417739690.
- NHS England . Access and Waiting Time Standard for Children and Young People With an Eating Disorder: Commissioning Guide 2015.
- Petkova H, Simic M, Nicholls D, Ford T, Prina AM, Stuart R, et al. Incidence of anorexia nervosa in young people in the UK and Ireland: a national surveillance study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027339.
- Lynn RM, Viner RM, Nicholls DE. Ascertainment of early onset eating disorders: a pilot for developing a national child psychiatric surveillance system. Child Adol Ment Health 2012;17:109-12. https://doi.org/10.1111/j.1475-3588.2011.00613.x.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders 2013.
- Royal College of Psychiatrists . Eating Disorders in the UK: Service Distribution, Service Development and Training. College Report CR170 March 2012 (CR 87) 2012.
- Le Grange D, Doyle PM, Swanson SA, Ludwig K, Glunz C, Kreipe RE. Calculation of expected body weight in adolescents with eating disorders. Pediatrics 2012;129:e438-46. https://doi.org/10.1542/peds.2011-1676.
- Child Growth Foundation . UK Cross-Sectional Reference Data: 1990 91 1990.
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children’s global assessment scale (CGAS). Arch Gen Psychiatry 1983;40:1228-31. https://doi.org/10.1001/archpsyc.1983.01790100074010.
- Gowers SG, Harrington RC, Whitton A, Lelliott P, Beevor A, Wing J, et al. Brief scale for measuring the outcomes of emotional and behavioural disorders in children. Health of the Nation Outcome Scales for children and Adolescents (HoNOSCA). Br J Psychiatry 1999;174:413-16. https://doi.org/10.1192/bjp.174.5.413.
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. https://doi.org/10.1097/00004583-200111000-00015.
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire?. Int J Eat Disord 1994;16:363-70.
- Byford S. The Design of Clinical and Economic Evaluations of Child and Adolescent Mental Health Services in the UK: Policy and Practice 2009.
- Schmidt U, Sharpe H, Bartholdy S, Bonin EM, Davies H, Easter A, et al. Treatment of anorexia nervosa: a multimethod investigation into translating experimental neuroscience into clinical practice. Programme Grants Appl Res 2017;5.
- Currin L, Schmidt U, Treasure J, Jick H. Time trends in eating disorder incidence. Br J Psychiatry 2005;186:132-5. https://doi.org/10.1192/bjp.186.2.132.
- Micali N, Hagberg KW, Petersen I, Treasure JL. The incidence of eating disorders in the UK in 2000–2009: findings from the General Practice Research Database. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-002646.
- Office for National Statistics (ONS) . Population Estimates for UK, England and Wales, Scotland and Northern Ireland 2015.
- Central Statistics Office . Population by Age Last Birthday, at Each Year of Age, Sex and Census Year, 2011 2011.
- Nicholls DE, Lynn R, Viner RM. Childhood eating disorders: British national surveillance study. Br J Psychiatry 2011;198:295-301. https://doi.org/10.1192/bjp.bp.110.081356.
- van Son GE, van Hoeken D, Bartelds AI, van Furth EF, Hoek HW. Urbanisation and the incidence of eating disorders. Br J Psychiatry 2006;189:562-3. https://doi.org/10.1192/bjp.bp.106.021378.
- Lask B, Bryant-Waugh R, Wright F, Campbell M, Willoughby K, Waller G. Family physician consultation patterns indicate high risk for early-onset anorexia nervosa. Int J Eat Disord 2005;38:269-72. https://doi.org/10.1002/eat.20163.
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample (reprinted from Br J Psychiatry 2000;177:534–9). Int Rev Psychiatr 2003;15:166-72. https://doi.org/10.1080/0954026021000046128.
- National Institute for Health and Care Excellence (NICE) . Eating Disorders: Recognition and Treatment 2017.
- Central Statistics Office . PEA11: Population Estimates from 1926 by Single Year of Age, Sex and Year 2015.
- Hakulinen T, Dyba T. Precision of incidence predictions based on Poisson distributed observations. Stat Med 1994;13:1513-23. https://doi.org/10.1002/sim.4780131503.
- Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 2014;67:401-9. https://doi.org/10.1016/j.jclinepi.2013.12.002.
- Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0020476.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs 2006;53:205-12. https://doi.org/10.1111/j.1365-2648.2006.03716.x.
- Jorm AF. Using the Delphi expert consensus method in mental health research. Aust N Z J Psychiatry 2015;49:887-97. https://doi.org/10.1177/0004867415600891.
- Morrison AP, Barratt S. What are the components of CBT for psychosis? A Delphi study. Schizophr Bull 2010;36:136-42. https://doi.org/10.1093/schbul/sbp118.
- Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLOS Med 2011;8. https://doi.org/10.1371/journal.pmed.1000393.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2014–15 2015.
- Barber JA, Thompson SG. Analysis of cost data in randomized trials: an application of the non-parametric bootstrap. Stat Med 2000;19:3219-36. https://doi.org/10.1002/1097-0258(20001215)19:23<3219::AID-SIM623>3.0.CO;2-P.
- Efron B, Tibshirani RJ. An Introduction to the Bootstrap. New York, NY: Chapman & Hall; 1993.
- Schafer JL. Multiple imputation: a primer. Stat Methods Med Res 1999;8:3-15. https://doi.org/10.1177/096228029900800102.
- Drummond Michael F SM, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluations of Health Programmes. Oxford: Oxford University Press; 2015.
- Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ 1999;18:341-64. https://doi.org/10.1016/S0167-6296(98)00039-3.
- Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 1998;18:68-80. https://doi.org/10.1177/0272989X98018002S09.
- van Hout BA, Al MJ, Gordon GS, Rutten FF. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 1994;3:309-19. https://doi.org/10.1002/hec.4730030505.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8. https://doi.org/10.1192/bjp.187.2.106.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8. https://doi.org/10.3310/hta8360.
- Briggs A, SM, Claxton K. Decision Analytic Modelling for Health Economic Evaluation. Oxford: Oxford University Press; 2006.
- Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al. A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14150.
- Briggs AH, Weinstein MC, Fenwick EA, . Model parameter estimation and uncertainty: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force – 6. Value Health 2012;15:835-42. https://doi.org/10.1016/j.jval.2012.04.014.
- Jones AM, Lomas J, Rice N. Healthcare cost regressions: going beyond the mean to estimate the full distribution. Health Econ 2015;24:1192-212. https://doi.org/10.1002/hec.3178.
- Jones AM, Lomas J, Rice N. Applying beta-type size distributions to healthcare cost regressions. J Appl Economet 2014;29:649-70. https://doi.org/10.1002/jae.2334.
- Jones AM, Lomas J, Moore P, Rice N. A Quasi-Monte Carlo Comparison of Developments in Parametric and Semi-Parametric Regression Methods for Heavy Tailed and Non-Normal Data: With an Application to Healthcare Costs. York: Health Econometrics and Data Group, University of York; 2013.
- Great Britain . National Health Service Act 2006 2006.
- Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 2012;14:406-14. https://doi.org/10.1007/s11920-012-0282-y.
- Gowers S, Levine W, Bailey-Rogers S, Shore A, Burhouse E. Use of a routine, self-report outcome measure (HoNOSCA-SR) in two adolescent mental health services. Health of the Nation Outcome Scale for Children and Adolescents. Br J Psychiatry 2002;180:266-9. https://doi.org/10.1192/bjp.180.3.266.
- CAMHS Tier 4 Report Steering Group . Child and Adolescent Mental Health Services Tier 4 Report 2014.
- Eisler I, Dare C, Hodes M, Russell G, Dodge E, Le Grange D. Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions. J Child Psychol Psychiatry 2000;41:727-36. https://doi.org/10.1111/1469-7610.00660.
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry 2010;67:1025-32. https://doi.org/10.1001/archgenpsychiatry.2010.128.
- Research Excellence Framework . Impact Case Studies: Maudsley Family Therapy For Anorexia Nervosa n.d. http://impact.ref.ac.uk/CaseStudies/CaseStudy.aspx?Id=41186 (accessed February 2019).
- Faculty of Child and Adolescent Psychiatry . Survey of In-Patient Admissions for Children and Young People With Mental Health Problems 2015.
- Stuhldreher N, Konnopka A, Wild B, Herzog W, Zipfel S, Löwe B, et al. Cost-of-illness studies and cost-effectiveness analyses in eating disorders: a systematic review. Int J Eat Disord 2012;45:476-91. https://doi.org/10.1002/eat.20977.
- Lynch FL, Striegel-Moore RH, Dickerson JF, Perrin N, Debar L, Wilson GT, et al. Cost-effectiveness of guided self-help treatment for recurrent binge eating. J Consult Clin Psychol 2010;78:322-33. https://doi.org/10.1037/a0018982.
- Le LK, Barendregt JJ, Hay P, Sawyer SM, Paxton SJ, Mihalopoulos C. The modelled cost-effectiveness of cognitive dissonance for the prevention of anorexia nervosa and bulimia nervosa in adolescent girls in Australia. Int J Eat Disord 2017;50:834-41. https://doi.org/10.1002/eat.22703.
- Egger N, Wild B, Zipfel S, Junne F, Konnopka A, Schmidt U, et al. Cost-effectiveness of focal psychodynamic therapy and enhanced cognitive-behavioural therapy in out-patients with anorexia nervosa. Psychol Med 2016;46:3291-301. https://doi.org/10.1017/S0033291716002002.
- Crow SJ, Nyman JA. The cost-effectiveness of anorexia nervosa treatment. Int J Eat Disord 2004;35:155-60.
- McKiernan PJ, Baker AJ, Kelly DA. The frequency and outcome of biliary atresia in the UK and Ireland. Lancet 2000;355:25-9. https://doi.org/10.1016/S0140-6736(99)03492-3.
- Keski-Rahkonen A, Hoek HW, Susser ES, Linna MS, Sihvola E, Raevuori A, et al. Epidemiology and course of anorexia nervosa in the community. Am J Psychiatry 2007;164:1259-65. https://doi.org/10.1176/appi.ajp.2007.06081388.
- Herpertz-Dahlmann B, Schwarte R, Krei M, Egberts K, Warnke A, Wewetzer C, et al. Day-patient treatment after short inpatient care versus continued inpatient treatment in adolescents with anorexia nervosa (ANDI): a multicentre, randomised, open-label, non-inferiority trial. Lancet 2014;383:1222-9. https://doi.org/10.1016/S0140-6736(13)62411-3.
- Eisler I, Simic M, Hodsoll J, Asen E, Berelowitz M, Connan F, et al. A pragmatic randomised multi-centre trial of multifamily and single family therapy for adolescent anorexia nervosa. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1129-6.
- Knowles RL, Friend H, Lynn R, Mitchell S, Michie C, Ihekweazu C. British Paediatric Surveillance Unit (BPSU). Surveillance of rare diseases: a public health evaluation of the British Paediatric Surveillance Unit. J Public Health 2012;34:279-86. https://doi.org/10.1093/pubmed/fdr058.
- Khadr SN, Carmichael P, Holt V, Roche E, Viner R. Surveillance study of gender identity disorder in children and adolescents. Arch Dis Child 2013;98. https://doi.org/10.1136/archdischild-2013-304107.002.
- Tiffin PA, Kitchen CE. Incidence and 12-month outcome of childhood non-affective psychoses: British national surveillance study. Br J Psychiatry 2015;206:517-18. https://doi.org/10.1192/bjp.bp.114.158493.
- Donohoe H, Stellefson M, Tennant B. Advantages and limitations of the e-Delphi technique. American J Health Ed 2012;43:38-46. https://doi.org/10.1080/19325037.2012.10599216.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal. Process and Methods [PMG9] 2013.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2011;9:157-69. https://doi.org/10.2165/11587350-000000000-00000.
- Mitrofan O, Petkova H, Janssens A, Kelly J, Edwards E, Nicholls D, et al. Care experiences of young people with eating disorders and their parents: a qualitative study. BJPsych Open 2019;5.
- Escobar-Koch T, Banker JD, Crow S, Cullis J, Ringwood S, Smith G, et al. Service users’ views of eating disorder services: an international comparison. Int J Eat Disord 2010;43:549-59. https://doi.org/10.1002/eat.20741.
Appendix 1 Service use
| Service use | Group, mean (SD); % using | |
|---|---|---|
| Specialist (n = 147) | Generic (n = 73) | |
| Inpatient days | 17.57 (44.95); 24.49 | 17.40 (44.52); 19.18 |
| Paediatric | 1.86 (8.70); 14.29 | 2.58 (10.18); 10.96 |
| Eating disorders | 10.03 (34.76); 9.52 | 8.59 (36.08); 6.85 |
| Psychiatry | 5.67 (25.73); 6.80 | 6.23 (25.25); 8.22 |
| Other | 0.01 (0.08); 0.68 | 0.00 (0.00); 0.00 |
| Outpatient attendances | 17.95 (10.64); 94.56 | 15.64 (14.66); 91.78 |
| Paediatric | 0.05 (0.26); 4.76 | 0.52 (1.67); 19.18 |
| Eating disorders | 16.14 (10.53); 89.12 | 8.41 (11.56); 60.27 |
| Psychiatry | 1.76 (6.08); 14.29 | 6.71 (9.17); 52.06 |
| Day-patient attendances | 3.39 (12.38); 9.52 | 0.97 (5.60); 4.11 |
| Paediatric | 0.00 (0.00); 0.00 | 0.04 (0.35); 1.37 |
| Eating disorders | 3.03 (11.77); 8.16 | 0.44 (3.75); 1.37 |
| Psychiatry | 0.35 (4.13); 1.36 | 0.49 (4.21); 1.37 |
| Service use | Group, mean (SD); % using | |
|---|---|---|
| Specialist (n = 137) | Generic (n = 50) | |
| Inpatient days | 13.90 (41.16); 13.87 | 12.66 (31.87); 20.00 |
| Paediatric | 0.26 (2.18); 1.46 | 0.96 (4.55); 8.00 |
| Eating disorders | 9.80 (36.35); 9.49 | 5.80 (23.74); 6.00 |
| Psychiatry | 3.31 (18.40); 4.38 | 5.90 (19.56); 12.00 |
| Other | 0.53 (6.15); 0.73 | 0.00 (0.00); 0.00 |
| Outpatient attendances | 11.72 (11.56); 77.37 | 11.96 (21.97); 76.00 |
| Paediatric | 0.02 (0.15); 2.19 | 0.26 (0.90); 10.00 |
| Eating disorders | 10.77 (11.42); 70.80 | 7.26 (22.27); 36.00 |
| Psychiatry | 0.92 (3.62); 11.68 | 4.44 (6.50); 54.00 |
| Day-patient attendances | 1.12 (6.21); 4.38 | 0.16 (1.13); 2.00 |
| Paediatric | 0.00 (0.00); 0.00 | 0.00 (0.00); 0.00 |
| Eating disorders | 1.12 (6.21); 4.38 | 0.16 (1.13); 2.00 |
| Psychiatry | 0.00 (0.00); 0.00 | 0.00 (0.00); 0.00 |
| Service use | Group, mean (SD); % using | |
|---|---|---|
| Specialist (n = 112) | Generic (n = 108) | |
| Inpatient days | 19.21 (46.96); 25.89 | 15.74 (42.40); 19.44 |
| Paediatric | 2.16 (9.73); 16.07 | 2.04 (8.65); 10.19 |
| Eating disorder | 11.37 (36.85); 9.82 | 7.67 (33.32); 7.41 |
| Psychiatry | 5.68 (26.07); 6.25 | 6.04 (25.05); 8.33 |
| Other | 0.01 (0.10); 0.89 | 0.00 (0.00); 0.00 |
| Outpatient attendances | 18.51 (10.37); 93.75 | 15.81 (13.65); 93.52 |
| Paediatric | 0.02 (0.13); 1.79 | 0.41 (1.40); 17.59 |
| Eating disorders | 17.21 (10.84); 88.39 | 9.81 (10.88); 70.37 |
| Psychiatry | 1.29 (4.66); 12.50 | 5.59 (9.29); 41.67 |
| Day-patient attendances | 4.00 (13.35); 11.61 | 1.12 (6.62); 3.70 |
| Paediatric | 0.00 (0.00); 0.00 | 0.03 (0.29); 0.93 |
| Eating disorders | 3.98 (13.35); 10.71 | 0.30 (3.08); 0.93 |
| Psychiatry | 0.02 (0.19); 0.89 | 0.80 (5.90); 1.85 |
| Service use | Group, mean (SD); % using | |
|---|---|---|
| Specialist (n = 104) | Generic (n = 83) | |
| Inpatient days | 16.53 (45.85); 15.39 | 9.86 (27.41); 15.66 |
| Paediatric | 0.35 (2.50); 1.92 | 0.58 (3.55); 4.82 |
| Eating disorders | 12.91 (41.29); 12.50 | 3.49 (18.57); 3.62 |
| Psychiatry | 3.27 (19.64); 3.85 | 4.92 (17.52); 9.64 |
| Other | 0.00 (0.00); 0.00 | 0.87 (7.90); 1.21 |
| Outpatient attendances | 12.40 (12.13); 78.85 | 11.00 (18.00); 74.70 |
| Paediatric | 0.02 (0.14); 1.92 | 0.17 (0.71); 7.23 |
| Eating disorders | 11.55 (11.93); 73.08 | 7.69 (18.19); 46.99 |
| Psychiatry | 0.84 (3.55); 12.50 | 3.15 (5.81); 36.15 |
| Day-patient attendances | 1.34 (6.99); 4.81 | 0.27 (1.76); 2.41 |
| Paediatric | 0.00 (0.00); 0.00 | 0.00 (0.00); 0.00 |
| Eating disorder | 1.34 (6.99); 4.81 | 0.27 (1.76); 2.41 |
| Psychiatry | 0.00 (0.00); 0.00 | 0.00 (0.00); 0.00 |
Appendix 2 Cost-effectiveness analysis: Delphi sensitivity analysis
FIGURE 16.
Cost-effectiveness plane for CGAS score at 12 months: Delphi sensitivity analysis.

FIGURE 17.
Cost-effectiveness plane for CGAS score at 6 months: Delphi sensitivity analysis.
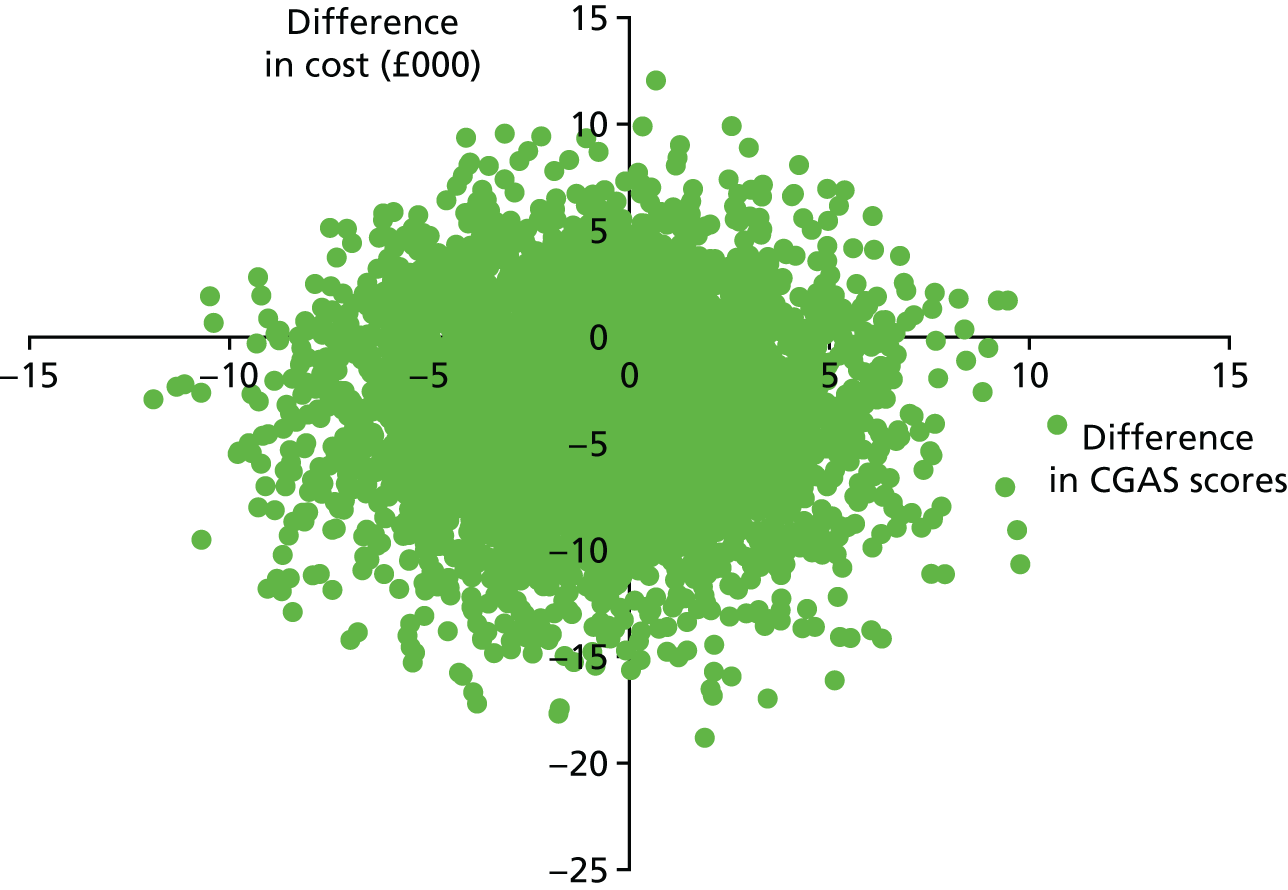
FIGURE 18.
Cost-effectiveness plane for %mBMI at 12 months: Delphi sensitivity analysis.
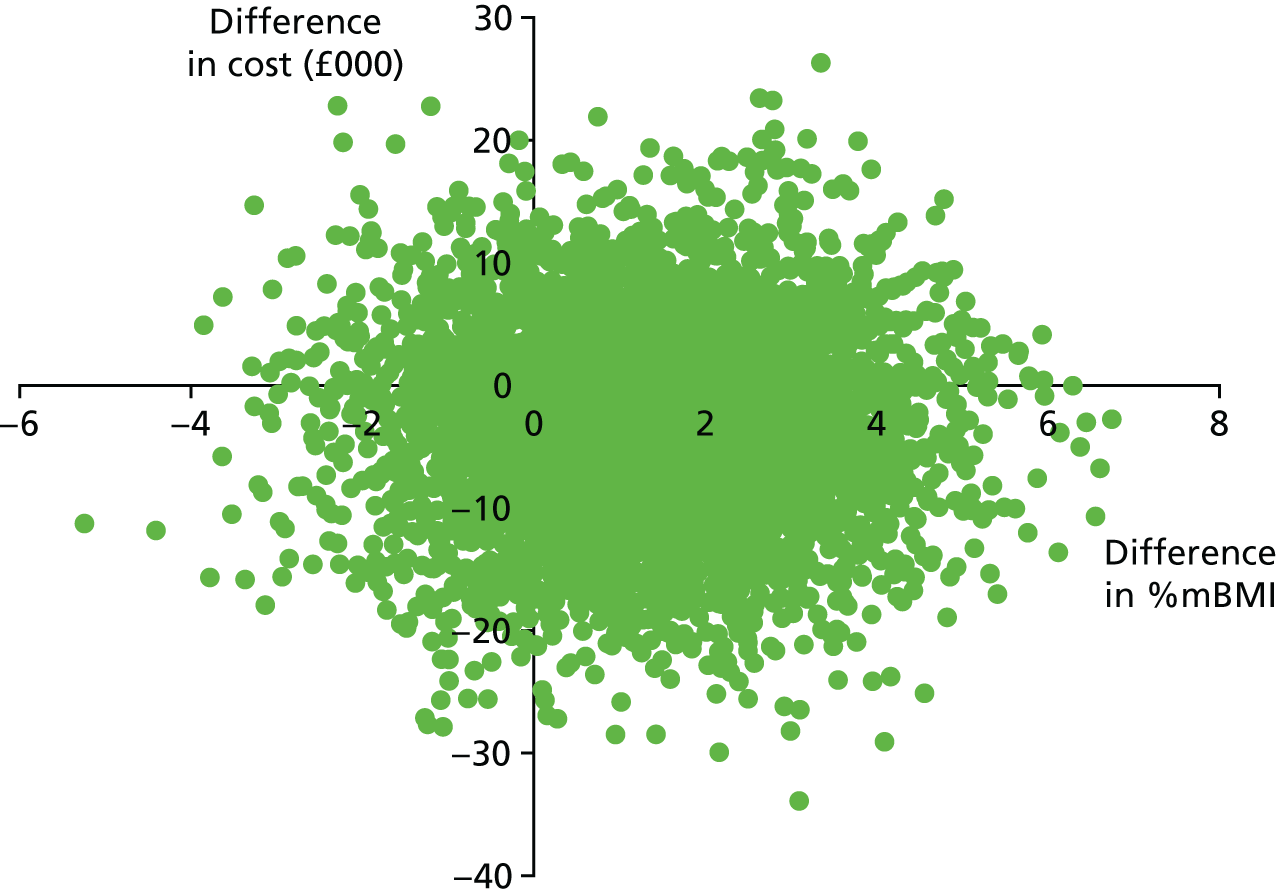
FIGURE 19.
Cost-effectiveness plane for %mBMI at 6 months: Delphi sensitivity analysis.
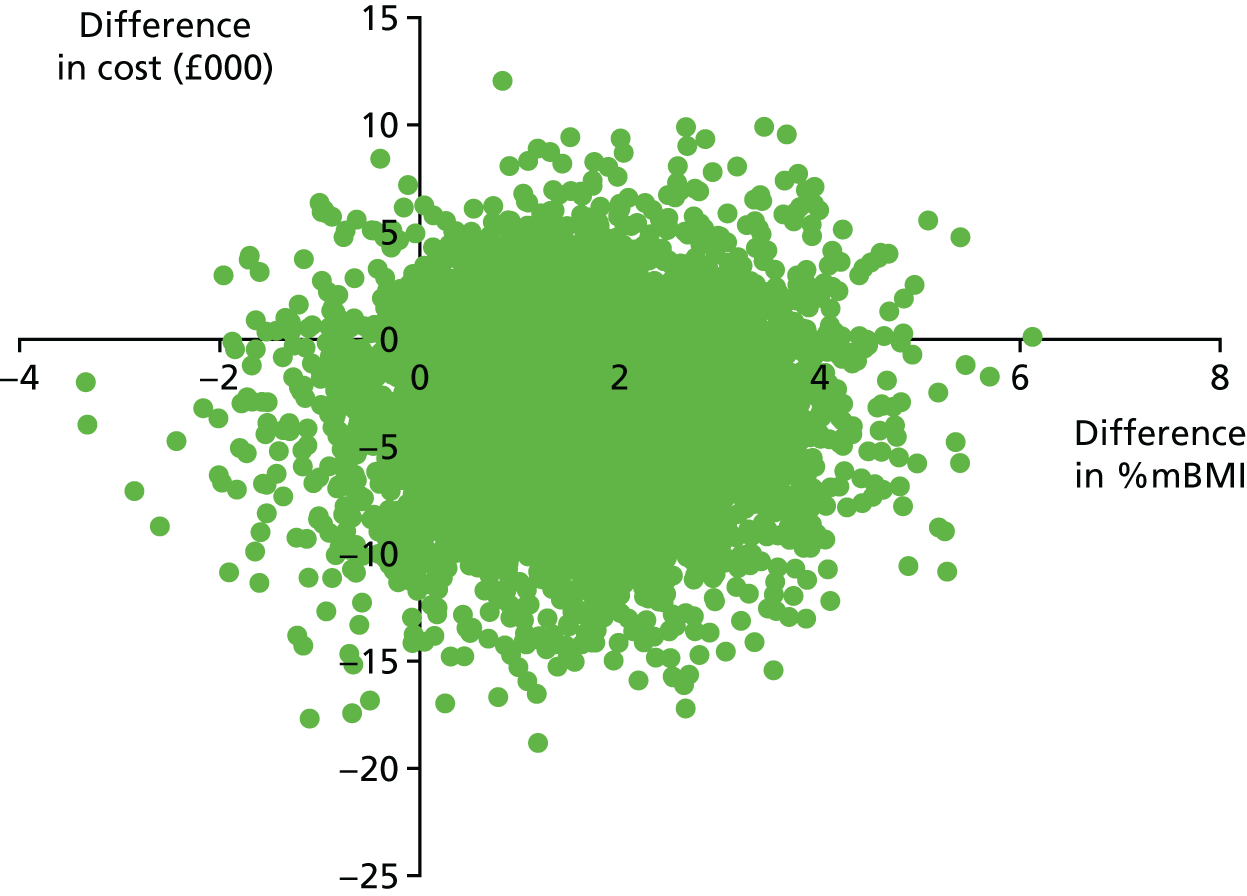
Glossary
- Anorexia nervosa
- An eating disorder and mental health condition in which a person keeps their body weight as low as possible.
- Body mass index
- A measure of body fat based on height and weight that is used to determine if a person is underweight, of normal weight, overweight or obese. The body mass index is calculated by dividing a person’s body mass (weight) by the square of their height. In children and adolescents, the body mass index varies with growth and needs to be adjusted for age and sex. The percentage median BMI is calculated by dividing the young person’s body mass index by the median (i.e. 50th centile) body mass index for young people of the same height, age and sex.
- Cost-effectiveness acceptability curve
- A curve showing the probability that one treatment is cost-effective compared with another treatment, subject to a range of possible maximum values that a decision-maker might be willing to pay for an additional unit of outcome gained.
- Cost-effectiveness analysis
- A method of economic evaluation that compares the relative costs and outcomes (effects) of different courses of action.
- Incidence
- A measure of the probability of a given medical condition occurring in a population within a specified period of time, which is generally reported as the number of new cases occurring per year.
- Incremental cost-effectiveness ratio
- The difference in mean costs between one intervention and another divided by the difference in mean effects between the two groups.
List of abbreviations
- %mBMI
- percentage of median expected body mass index for age and sex
- BMI
- body mass index
- CAMHS
- child and adolescent mental health services
- CAPSS
- Child and Adolescent Psychiatry Surveillance System
- CGAS
- Children’s Global Assessment Scale
- CI
- confidence interval
- CostED
- Cost-effectiveness of models of care for young people with Eating Disorders
- DSM-5
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- EDNOS-AN
- eating disorders not otherwise specified – anorexia nervosa sub-type
- GP
- general practitioner
- GPRD
- General Practice Research Database
- HoNOSCA
- Health of the Nation Outcome Scales for Children and Adolescents
- IR
- incidence rate
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RoI
- Republic of Ireland
- TOuCAN
- Treatment Outcome for Child and Adolescent Anorexia Nervosa study