Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/47/17. The contractual start date was in April 2018. The final report began editorial review in December 2018 and was accepted for publication in June 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Andrew Booth is a member of the National Institute for Health Research Complex Reviews Support Unit Funding Board (2015 to present) and the Health Services and Delivery Research Funding Committee (2019 to present).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Cantrell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background to the topic
In 2015 it was estimated that 2.16% of the adult population living in England had intellectual disabilities (ID). 1 People with ID face considerable, persistent and, to a degree, avoidable health inequalities. 2,3 These arise from disparities in the presence of disease,4 inequalities in access to and use of health-care services,5,6 and increased risk of exposure to common social determinants of ill health,7 for example poverty and social discrimination. 8 The life expectancy of people with ID remains significantly lower than that of the general population. 9 In the past 10 years, several inquiries into the deaths of people with ID have concluded that inadequate health care was a contributory factor and that these deaths were avoidable. 10–12
A number of inquiries into the early deaths of people with ID have reported shortcomings across a range of health services. 12–14 These point to factors, such as poor communication, that may be common across the full range of health services. Although our review covers initial access to primary care services rather than quality of ongoing health care provided, there are important lessons from these inquiries that are relevant to initial access to primary care.
UK government policy is for people with ID to have their health needs met in mainstream services, although there is considerable evidence that some people with ID may not be able to respond to and benefit from uniformly delivered services. 15 The statutory position is that mainstream services have a legal duty to make reasonable adjustments to enable those with protected characteristics to access these services; however, there is little guidance about what constitutes a reasonable adjustment.
People with ID are less likely to be able to access uniformly delivered health interventions. Public bodies have a legal duty to make ‘reasonable adjustments’ to policies and practices to provide fair access and treatment for people with learning disabilities (LDs). 16 However, more needs to be done in primary care, where services are often inaccessible to people with LDs because effective adjustments have not been put in place. 17
Similarly, some of the problems of access to primary health care sit outside health service responsibilities, for example the ability of paid support staff to recognise when an adult with intellectual disabilities might need primary care. Although the focus of this report focuses on access to primary care, the barriers to access and interventions shown by social care providers and disability organisations to be successful in improving access among this population have an important role to play in enabling access to these services.
Evidence suggests that people with ID use primary care services at rates less than or equal to the general population despite having greater health needs18 and their use of primary care is lower than expected in comparison with groups with other long-term conditions. 19 This suggests that people with ID do not access primary care services proportionately to their level of health need. Primary care services are particularly important because they provide an entry point to screening, treatment and secondary care. Difficulty and delay in accessing primary care may lead to serious negative health outcomes and disengagement with future health-care services, with concomitant cost to the individuals and to the UK NHS.
This work complements UK government policy, which emphasises the requirement to support people with ID to lead fully inclusive lives and this means meeting their health needs within mainstream services. 17 Public bodies have a legal duty to make ‘reasonable adjustments’ to policies and practices to provide fair access and treatment for people with LDs16 and health and social care services have a legal duty to reduce health inequalities under the Health and Social Care Act 2012. 20
Definitions
Intellectual disability has been defined as a significantly reduced ability to understand new or complex information and to learn new skills, along with a reduced ability to cope independently where this disability starts before adulthood, with a lasting effect on development. However, in practice, studies may recruit participants on the basis that they are known to statutory service providers. People with severe ID are likely to be known to service providers, however, some people with mild ID may live independently without service intervention, either from choice or because they do not meet eligibility criteria for ID services and, therefore, are not able to access support. This review will use the term ID throughout in recognition of the increasing use of this term in research.
In a review for the NHS Service Delivery and Organisation (SDO) programme, Alborz et al. 21 used Gulliford’s model of access; this distinguishes between having access, where services are notionally available; gaining access, where the user gains entry to and use of an appropriate service; and maintaining access, that is having continued use of a service. 22 We plan to focus on gaining access and use because the review focuses on first contact with services such as primary/community care. In addition, Alborz et al. 21 distinguished between access and effectiveness and focused on the ability to use a service rather than whether or not the service was provided to a high standard. In this review, we focus on access to a service as the primary outcome rather than the quality of the service received. However, we consider that patient engagement is crucial to the success of most health-care interactions; therefore, we will consider the extent to which health-care services are set up or adjusted to facilitate the engagement of people with ID during health appointments. We will also examine evidence for the effectiveness of any measures or interventions designed to improve access to relevant services.
Chapter 2 The mapping review methods
A systematic mapping review was undertaken to map the literature in the topic area and to help decide on the final scope for the targeted systematic review.
The mapping review aimed to examine the volume and characteristics of the available evidence about quality of access to primary health-care services for people with ID. The protocol for the mapping review is provided in Report Supplementary Material 1.
The mapping review includes the following types of health service:
-
NHS primary care
-
first-point community-based services [general practitioners (GPs), pharmacists, dentists and optometrists]
-
sexual health
-
health screening delivered in the context of primary and community care
-
palliative and end-of-life care delivered in the context of primary care.
Research questions
-
What are the gaps in evidence about access to primary and community health care for people with ID?
-
What are the barriers to accessing primary and community health-care services for people with ID and their carers?
-
What actions, interventions or models of service provision improve access to health services for people with ID and their carers?
Methods
The systematic mapping review was conducted in accordance with published methods. 23 The mapping review followed the scope of a previous review,21,24 with the exception that it focused on only primary and community care services.
We chose to build on the existing review for four compelling reasons:
-
We could follow (and hopefully enhance) the methods of the original review.
-
The time that had elapsed since the original work (approximately 15 years) provided a manageable quantity of literature for logistic purposes.
-
The conceptual framework produced by the original team could be used as a template for data extraction if appropriate.
-
Our updated review would follow seamlessly from the original work.
Areas of research activity and research gaps identified in the mapping review helped inform and finalise the scope for the targeted systematic review.
Literature search for the mapping review
The literature search was informed by methods of identifying the literature described by McNally and Alborz. 25
We searched the following databases (seven of the 14 bibliographic databases in the Alborz et al. review21):
-
MEDLINE (via Ovid, 1946 to 2018)
-
Science Citation Index Expanded; Social Sciences Citation Index (via Web of Science, 1900 to 2018)
-
The Cochrane Library
-
Cochrane Database of Systematic Reviews (1996 to 2018)
-
Database of Abstracts of Reviews of Effect (1995 to 2015)
-
Cochrane Central Register of Controlled Trials (1898 to 2018)
-
Health Technology Assessment Database (1995 to 2016)
-
NHS Economic Evaluations Database (1995 to 2015)
-
-
Cumulative Index to Nursing and Allied Health (via EBSCOhost 1974 to 2018)
-
Applied Social Science Index (via ProQuest, 1987 to 2018)
-
PsycINFO (via Ovid, 1806 to 2018)
-
Educational Resources Index (via ProQuest, 1966 to 2018).
The database search strategy was adapted from methods described in the existing review for identifying the literature. 25 The search strategy comprised key terms for ID and access. Additional terminology was added to include the primary care setting (e.g. GPs, dentists, optometrists) and recent or current legislation or guidance terms, such as the Disability Discrimination Act and ‘reasonable adjustments’. The existing review was conducted between 1980 and 2002 so this search was limited from 1 January 2002 onwards, thereby ensuring continuity of the evidence base. The search was also restricted to English-language and human studies. The search strategy is provided in Appendix 1.
Supplementary searching included grey literature searching of the websites of key UK charities and associations to identify reports about initiatives to improve access to services for people with ID. Snowballing by citation searching key studies was also performed in Google Scholar™ (Google Inc., Mountain View, CA, USA) and reference lists of included papers were scrutinised.
Screening
Study screening and selection was undertaken in EPPI-Reviewer 4 (Evidence for Policy and Practice Information and Co-ordinating Centre, University of London, London, UK). A team of three reviewers screened the identified references. An initial 100 references were screened by all three reviewers to check for consistency. Any queries were resolved through discussion with the other two reviewers.
Study selection was undertaken according to the inclusion criteria outlined in Table 1.
| Criterion | Eligibility |
|---|---|
| Population |
|
| Setting |
Evidence from any of the following settings: the UK, Canada, Australia, New Zealand or Europe The above settings have been selected because of their similar health-care systems. Papers from the USA will be excluded because US private service provision is not comparable with the UK primary care setting. However, the mapping review will investigate the impact of including qualitative research papers from the USA depending on their relevance |
| Outcomes |
Access to a service Alborz et al. 21 distinguished between access and effectiveness and focused on the ability to use a service rather than whether or not the service was provided to a high standard. We will also review studies reporting the effectiveness of any measures or interventions designed to improve access to the relevant services |
| Comparator | The general population may offer a comparator in some study types |
| Study design |
|
| Other limitations |
English language only Evidence published since 2002; the Alborz et al. 21 review searched up to 2002 |
Following screening at the title and abstract stage, the references that potentially met the inclusion criteria were considered further, and data were extracted for inclusion in the review. Citations not meeting the inclusion criteria were excluded.
Data extraction
Data extraction based on abstracts was undertaken in EPPI-Reviewer 4 using a template designed for the mapping review (see Appendix 2). Mapping at the abstract level is a typical component of systematic mapping review methodology, given that the primary purpose is to plan a subsequent review. The extraction form comprised the following items: paper identifying code, author, date, study design, setting – country, health-care professional (HCP), specialist topic, study population, sample size, needs assessment, study outcomes, tools used to measure outcomes, study result, and barriers and facilitators. For mapping purposes, references were categorised into sets according to HCP or specialist topic, and ‘needs assessment’ papers were also considered as a separate categorisation. Data extraction was completed using data included in each abstract. If the abstract was unavailable, brief details were extracted from the title for the mapping review on the understanding that the full text would be obtained if included in the targeted systematic review. An example of a completed data extraction table is in Appendix 3.
Patient and public involvement
During the mapping review, we consulted people with ID, family carers and formal paid carers so that the review of access to health care for people with ID could be informed by the views and experiences of stakeholders. The aim of this consultation was to:
-
illuminate the model of access to health care for people with ID
-
inform and refine our search strategies by identifying barriers to accessing health care and any solutions developed
-
identify gaps in the literature.
We contacted the clinical director and senior commissioning manager for services for people with ID in a Clinical Commissioning Group and asked them to identify relevant community groups for people with ID and their carers. We sent information about the review to these groups and asked to visit to discuss their experiences of accessing health care.
We met a group of people with ID (n = 8, plus one personal assistant) and a group of family carers (n = 5). Snowball sampling was used to identify formal carers and we spoke to staff who manage support services (n = 2). These were convenience samples depending on who attended the group or meeting on the day we visited.
Discussions were loosely guided by a topic guide covering how people identify a health need, what actions they take, the issues influencing their decision to take a particular course of action and the barriers to and facilitators of their access and use of the chosen service. 21 Notes were taken during each meeting and these were written up afterwards using bullet points to document the barriers and facilitators. These were organised under the headings ‘identifying and communicating symptoms of ill health’, ‘arranging and attending health appointments’ and ‘continuing access to services’. A brief summary is provided in Table 2.
| Barriers | Facilitators |
|---|---|
| Identifying and communicating symptoms of ill health | |
|
|
| Arranging and attending health appointments | |
|
|
| Continuing access to services | |
|
|
The barriers and facilitators were used to identify relevant search terms and for future comparison with the barriers and facilitators identified in the qualitative literature.
Detailed notes from the patient and public involvement (PPI) meetings are provided in Appendix 4.
We plan to present our findings following completion of the targeted review with the pre-existing groups of people with ID, and their paid and unpaid carers. Comments on the Plain English summary were received from the facilitator of the pre-existing group of people with ID.
We have continued to involve patients and members of the public through the Sheffield Evidence Synthesis Centre PPI group. Members of this group were asked to comment on the scope of the targeted systematic review.
Chapter 3 Mapping review findings
Literature search
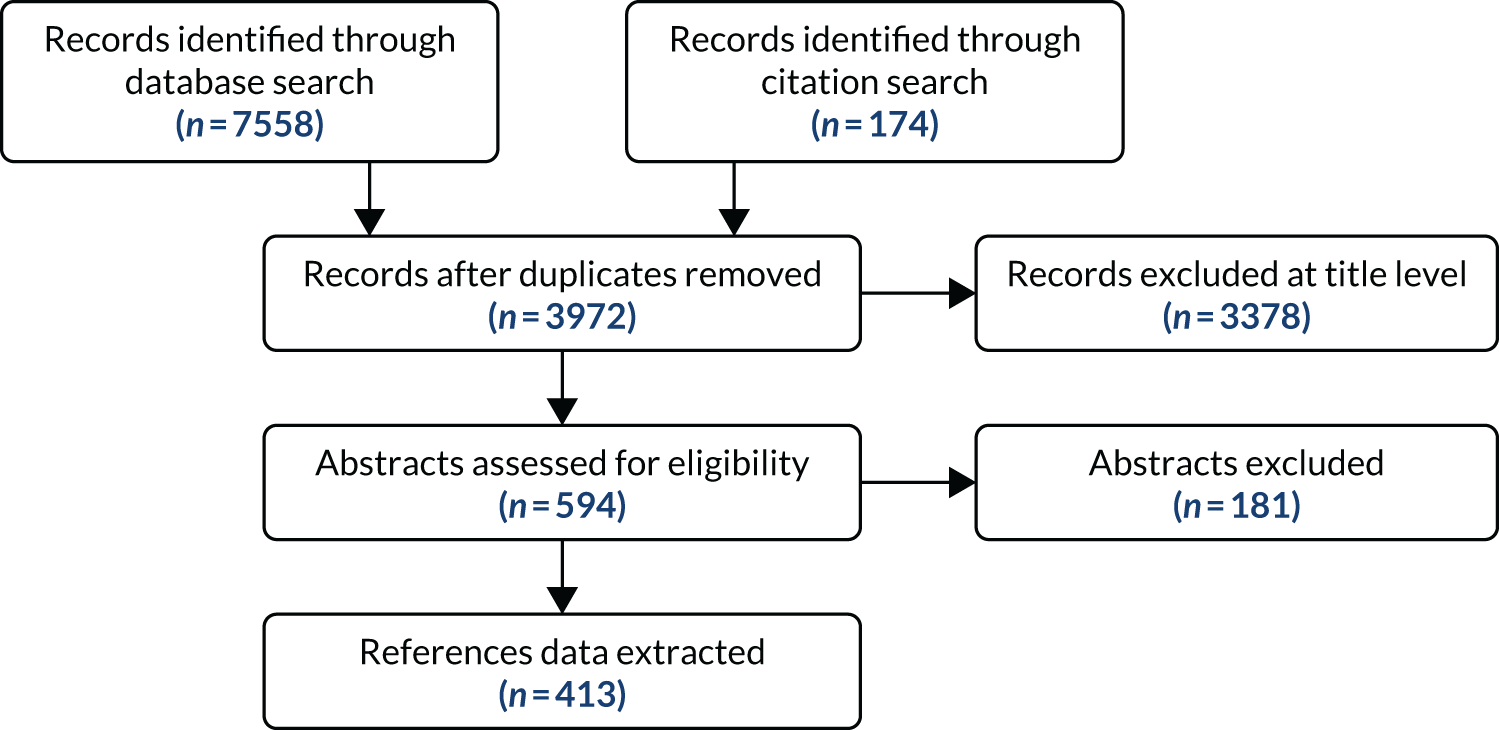
The database search retrieved 7558 records. Following deduplication, a total of 3972 records remained for screening. A total of 594 references were identified as ‘potentially include’. After further scrutiny, 181 of these were excluded. Common reasons for exclusion were that the study setting was secondary rather than primary care, the study was about a different population, the study was not about access to health care and the study was not a research study. A total of 413 papers met the criteria for inclusion in the mapping review (Figure 1).
FIGURE 1.
Modified PRISMA flow diagram for mapping review.
Results
The mapping review comprised 413 studies.
Study design
All included abstracts were coded with one of the following study designs: quantitative, qualitative, mixed methods, review or unclear. Figure 2 shows the number of papers coded with each study design.
FIGURE 2.
Chart detailing study designs.

The chart shows an almost equal distribution of quantitative and qualitative studies. The large number of papers coded as having an unclear study design was a result of the limited information available in abstracts.
Geographical distribution of studies
Table 3 details the country of origin of included studies. The mapping review extracted data from abstracts only, meaning that country information was not available for a large proportion (n = 136) of the studies. The largest proportion of research studies investigated populations in the UK, followed by the USA, Australia and Canada.
| Country | Count |
|---|---|
| UK | 142 |
| USA | 33 |
| Australia | 27 |
| Canada | 20 |
| Ireland | 12 |
| The Netherlands | 11 |
| France | 3 |
| Norway | 2 |
| Spain | 2 |
| China | 1 |
| Germany | 1 |
| Greece | 1 |
| Hong Kong | 1 |
| India | 1 |
| Malaysia | 1 |
| Poland, Romania, Slovenia | 1 |
| Saudi Arabia | 1 |
| Taiwan | 1 |
| International (i.e. multiple countries) | 16 |
| Not stated | 136 |
Health-care professional
Table 4 shows the number of studies in the mapping review in which the role of a specific HCP was researched. A number of the studies were undertaken with multiple HCP participants.
| Code: HCP | Count |
|---|---|
| GP | 127 |
| Dentist | 41 |
| Optometrist | 11 |
| Pharmacist | 7 |
| Other community staff | 101 |
| Total | 287 |
General practitioner
One hundred and twenty-seven of the studies specifically investigated the GP role. The papers investigated a broad range of topics, including quality of primary health care, health checks, education or training for GPs, communication skills of GPs, out-of-hours primary care services and how to identify patients with an intellectual disability.
Dentist
Forty-one papers researched the role of dentists in treating people with ID. These studies investigated a variety of topics, including factors affecting access to dental service, oral care needs of people with ID, experiences of dental services from the viewpoint of people with ID and their carers, training of dentists and ethical issues to consider when treating patients with ID.
Optometrist
The role of the optometrist was researched in 11 of the included studies. These studies investigated the visual health needs of adults and children with ID, diabetic eye screening, inequalities in access to eye care and screening and how optometrists can provide eye care services to this population.
Pharmacist
Seven of the included studies related to the role of pharmacists. Topics researched included knowledge that people with ID have about their medicine, information that they want about their medications, medication-related interventions from pharmacists and whether or not pharmacists could play a role in blood pressure screening for hypertension in this population.
Other community staff
The ‘other community staff’ category covered a diverse range of staff, including practice nurses, health visitors, occupational therapists, community nurses and intellectual disability care staff. Within this large category, issues investigated included the needs of the population, the experiences of professionals and people with ID, health information exchange, the attitudes of professionals towards this population, training of staff, rural health care and the needs of specific groups within this population, including women and children.
Specialist topic
Table 5 shows the number of studies in the mapping review that related to services for specific conditions.
| Code: specialist topic | Count |
|---|---|
| Mental health | 30 |
| Palliative care | 25 |
| Sexual health | 21 |
| Other | 105 |
| Total | 176 |
Sexual health
The delivery of sexual health services was researched in 21 of the included studies. The populations investigated in these studies can be subdivided into people receiving services (14 studies), professionals delivering services (five studies) and carers of people receiving services (one study). In addition, there was one study researching family carers, support workers and professional staff, as shown in Figure 3.
FIGURE 3.
Pie chart of broad populations researched in sexual health studies.
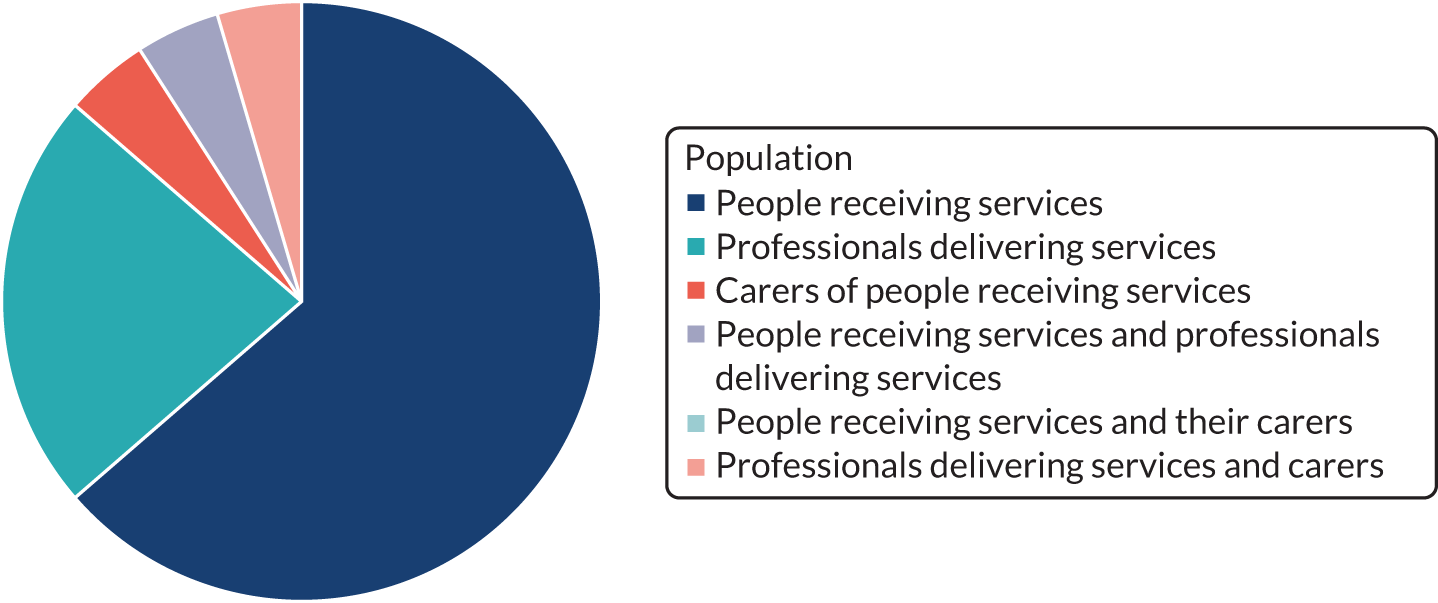
The studies investigated sexual health services for people with ID. Topics of research included services available, self-advocacy, experiences, barriers, contraception, cervical smear testing, capacity to consent to sexual relations, service provision for gay men, and breast screening.
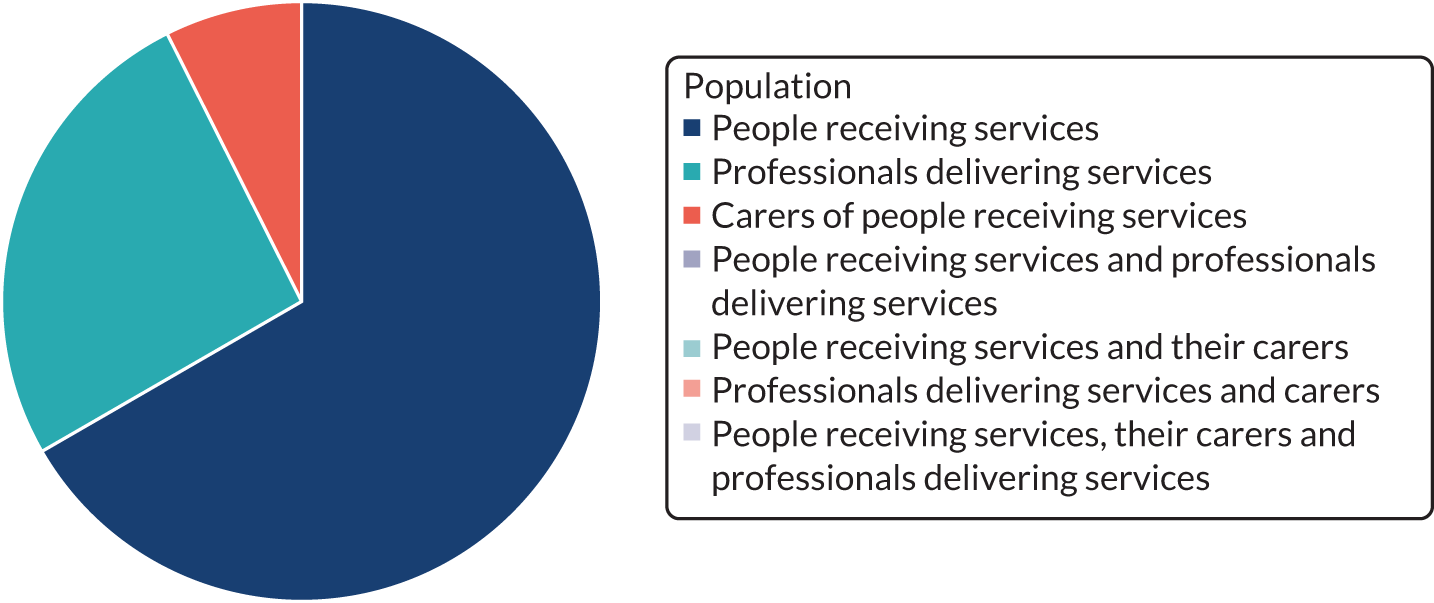
Palliative care
The delivery of palliative care services to people with ID was researched in 25 of the studies. The populations investigated in these studies can be subdivided into people receiving services (11 studies) and professionals delivering services (12 studies); one study researched a person with ID and the professionals involved in his care, and another study considered people with ID and their carers (Figure 4).
FIGURE 4.
Pie chart of broad populations researched in palliative care studies.

The included studies researched challenges in providing palliative care to this population, identification of needs by HCPs, communication about illness, death and dying, and the role of carers in end-of-life care.
Mental health
Thirty of the studies in the mapping review researched the delivery of mental health services to people with ID. The populations investigated in these studies can be subdivided into people receiving services (18 studies) and professionals delivering services (seven studies); three studies researched people receiving the service, their carers and the professionals delivering the service, and two studies considered people with ID and their carers. The breakdown is shown in Figure 5. These studies investigated services available for people with ID and mental health problems, access to these services, experiences of these services and the needs of people with ID who develop dementia.
FIGURE 5.
Pie chart of broad populations researched in mental health studies.
Other
The ‘other’ category covered a broad range of specialist topics; more detail of the different areas of service provision is provided in Table 6.
| Specialist topic | Count |
|---|---|
| Access to health care | 3 |
| Accessible information | 1 |
| Autism | 1 |
| Blood test | 3 |
| Cancer care, not necessarily palliative | 2 |
| Cancer information | 1 |
| Cancer screening (includes breast and cervical) | 17 |
| Children and young people | 4 |
| Communication skills | 3 |
| Dementia | 4 |
| Diabetes services | 4 |
| Epilepsy | 1 |
| General practice | 1 |
| Gynaecological/reproductive health | 1 |
| Health checks/assessments | 13 |
| Health inequalities | 1 |
| Health information exchange | 1 |
| Health promotion | 5 |
| Health status, care utilisation and medical outcomes (review) | 1 |
| Health visiting | 1 |
| Hearing | 2 |
| Mainstream health services | 1 |
| Maternity services | 3 |
| Older people | 4 |
| Oral health care | 3 |
| Out-of-hours care | 2 |
| Pain | 2 |
| Polypharmacy and medication review | 1 |
| Primary care | 3 |
| Range of needs | 1 |
| Research | 1 |
| Satisfaction with care | 1 |
| Social prescribing | 1 |
| Substance use | 1 |
| Preventative health care | 3 |
| Rural health | 1 |
| Training | 1 |
| Transition paediatric to adult health care | 1 |
| Unmet need | 1 |
The ‘other’ category covers a variety of topics. Papers about cancer screening were the most common, followed by papers about health checks/assessments.
Needs assessment
Twenty of the 413 included references were coded as relating to needs assessment. Table 7 provides details of the different populations investigated.
| Population | Number of references |
|---|---|
| Older people | 5 |
| Children and young people | 4 |
| Staff working with people with ID | 2 |
| Palliative care needs of people with ID | 2 |
| Adults with ID | 1 |
| Mental health needs of people with ID | 1 |
| Adults with cerebral palsy and ID | 1 |
| Men with HIV with or without ID | 1 |
| People with ID and dementia | 1 |
| Evaluation of a needs assessment tool | 1 |
| Not given | 1 |
Reasonable adjustments
Several articles specifically considered changes or reasonable adjustments introduced to make services more accessible; examples are a specialist multiprofessional visual assessment clinic at a day centre to provide appropriate eye care to people with ID, techniques to engage people with ID in physical health assessment measures and the implementation of health checks.
Grey literature
A total of 16 UK-based sources (mainly comprising charitable associations) were searched for relevant grey literature (see Appendix 1). Of these, seven provided no further information relevant to the review. The remaining nine sources linked to between one and six documents that appeared relevant from the title, with a total of 28 documents potentially meeting our inclusion criteria.
Twenty-three of the documents were excluded on the grounds that they included no data (these were mainly guidance documents). Of the remaining five reports, one was a short review of the literature, thus providing a source for further identification of includable studies, three contained practice examples and case studies (without reporting outcome data) and one was a qualitative research study (Table 8).
| Author(s) and date | Title | Relevant data | Section(s) and page(s) |
|---|---|---|---|
| Faculty of Dental Surgery 201226 | Clinical Guidelines and Integrated Care Pathways for the Oral Health Care of People with Learning Disabilities | Guidelines with a short review of barriers to oral health care | Barriers to oral health care, pp. 7–10 |
| Public Health England 201527 | Health Checks for People with Learning Disabilities: Including Young People Aged 14 and Over, and Producing Health Action Plans | Suggestions for improving uptake of health checks (no outcome data) | Practice examples and case studies, pp. 11–14 |
| Public Health England 201628 | Making Reasonable Adjustments to Cancer Screening | Background: screening programmes, short review of research, short case studies of reasonable adjustments (no outcome data) | Resources and case studies, pp. 14–44 |
| Public Health England 201629 | People with Learning Disabilities in England: Main Report 2015 | Initiation and uptake of health check for people with ID | Health services, pp. 22–23 |
| The Disability Partnership 201630 | Evaluation Report of the 2015–16 Mencap-led Pharmacy Project | Results from surveys, interviews and focus groups about access to pharmacy services | All (methods and results are included) |
Two reports considered the implementation and uptake of health checks; one focused on reasonable adjustments to encourage uptake of screening for cervical, breast and bowel cancer; one identified barriers to accessing oral health care; and a final, Mencap-led, research study explored access to pharmacy services.
Data in the mapping review related to barriers and facilitators
Data relating to potential barriers to and facilitators of access for people with ID were extracted from results sections, where available. Of the included citations, 87 abstracts mentioned barriers to and 47 mentioned facilitators of access to primary health care. From the information available in the abstracts, we categorised the barriers and facilitators (some abstracts included more than one) in Tables 9 (barriers) and 10 (facilitators).
| Barrier | Number of citations |
|---|---|
| Wider determinants | |
| Independent living | 1 |
| Undefined roles for carers | 1 |
| Lack of knowledge of services | 1 |
| People with ID having difficulties attending (e.g. distance, finances, physical difficulties) | 3 |
| People with ID not understanding information/health literacy | 2 |
| ID factors (general) | 1 |
| People with ID communication skills | 1 |
| Identification of need | |
| Lack of perceived need/lack of willingness/fear of intervention | 4 |
| Organisation of health care | |
| Organisational/primary care characteristics | 5 |
| Facilities | 1 |
| Partnership working | 1 |
| Lack of services (including out of hours) and funding | 2 |
| Waiting times | 1 |
| Time/length of appointment times | 2 |
| Late referrals | 1 |
| HCPs | |
| Lack of guidelines/support for staff | 2 |
| Staff training/education | 3 |
| Staff knowledge/skill/confidence level | 6 |
| Staff awareness | 2 |
| Staff experience with people with ID | 2 |
| Identification of people with ID | 1 |
| Access to first-contact health care | |
| Interpersonal skills/welcoming | 2 |
| Staff communication skills | 11 |
| Staff attitudes and behaviour/lack of understanding/not supporting autonomy/lack of cultural sensitivity | 7 |
| Opportunities to engage in discussion about care | 1 |
| Consent | 2 |
| Comorbidities | 1 |
| Continuing health care | |
| Continuity of care | 1 |
| Monitoring health problems | 1 |
| Facilitator | Number of citations |
|---|---|
| Wider determinants | |
| Social cohesion/community connectedness | 2 |
| Residence (in relation to services) | 2 |
| Family characteristics/support/advocacy for people with ID | 3 |
| Liaison between family and carers | 1 |
| Education (HCP/peers) | 1 |
| Caregiver support/interventions | 3 |
| Identification of need | |
| Health check programmes/regular health checks | 2 |
| Organisation of health care | |
| Financial incentive for health checks (practice) | 1 |
| Walk-in clinics | 1 |
| Co-ordinated care | 1 |
| Adapted resources/methods | 4 |
| Lead practitioner or GP with a special interest | 1 |
| Data-sharing resources | 1 |
| Telephone accessibility | 1 |
| HCPs | |
| Teamwork/interprofessional working | 5 |
| Joined-up approach across agencies | 2 |
| Adopting and encouraging best practice | 2 |
| Staff training/shared learning | 6 |
| Staff skills/competence | 2 |
| Access to first-contact health care | |
| Timeliness and frequency of appointments | 1 |
| Familiar environment | 1 |
| Personal greeting in waiting room | 1 |
| Begin consultation at once | 1 |
| Communication aid | 1 |
| Advance planning/preparation before consultation | 6 |
| Written care plans | 1 |
| Knowledge of the person and their routines | 3 |
| Respectful HCP–service user relationship/personal connection/patience/taking time/patient centred/empowering | 8 |
| Helping people with ID understand/learn skills/recognising and minimising treatment effects | 3 |
| Counselling (screening) | 1 |
| Education/information | 5 |
| Reassure/evaluate anxiety/pain | 1 |
| Continuing health care | |
| Signposting and appropriate referral | 1 |
| Continuity/communicate with people with ID/carer outside consultation | 3 |
Identified barriers were often accompanied by facilitators that were suggested or implemented to minimise the impact of the barriers; for example, an identified lack of communication skills in HCPs could be modified by training staff or by people with ID using communication aids.
Professional communication, knowledge, skills and attitudes appeared to be commonly reported barriers to people with ID seeking primary health care. This is mirrored by facilitators relating to the professional, including service user relationship, staff training, and planning before a consultation. Our adding up of the numbers of citations within these categories needs to be considered with caution; potentially it might not reflect the literature as a whole, as abstracts provide only partial information. It was intended that the information derived from characterising the literature in this way during the mapping review would assist us in prioritising the focus of the systematic review and considering where and how the research in this area had developed since the original review by Alborz et al. 21
Chapter 4 Mapping review discussion
The mapping review identified a large number of studies on access to health-care services for people with ID. The evidence available for barriers to identification of need and continuing care appeared, from this review, to be less than for other domains of the Alborz et al. 21 model. Many barriers and facilitators identified in abstracts resonated with themes generated from the PPI discussions, particularly in arranging and attending health appointments, although less so at this point in identifying and communicating symptoms of ill health, and continuing access to services was also reported less often.
The Alborz et al. 21 review found that the evidence base on general practice was larger than those on many other areas of interest, and this mapping review found that studies specifying a role for the GP constituted the most common single HCP category. The 2003 review21 found only one study on access to optometry services, and we similarly found only a small number considering the specific role of optometrists in screening and eye care, and some on the unmet eye care need of this population. A small number of studies were found on the organisation of dental services in the Alborz et al. 21 review, but no studies were found about entry point access. By contrast, we found a reasonably sized body of literature related to dentists, dental services and oral care.
Limitations of mapping review
Although mapping reviews use systematic methods to identify, screen and code studies, a mapping review is not a systematic review. Mapping reviews generally omit some standard features of systematic reviews, for example study quality assessment, and do not attempt to assess the effects of interventions. The role of mapping reviews is to provide a descriptive account of the published literature and this should be taken into account when assessing the findings of this part of the overall evidence synthesis. The strength of the mapping review is in identifying areas where opportunities for further research or review are either present or not present and not to support actionable practice. For this reason, quality assessment is usually reserved for detailed follow-up analysis using the full text of included studies.
Mapping reviews can be based either on the full text of a limited number of identified studies or, more typically, on the abstracts of a wider literature base. In this specific case, informed by the previous Alborz et al. 21 review and preliminary scoping, we decided that mapping on the basis of abstracts only was the preferred option for logistical reasons. This was particularly appropriate given that revisiting key studies would be necessary for the subsequent systematic review. We recognised that abstracts are of variable quality and may be either informative (e.g. containing a list of key barriers and facilitators) or indicative (e.g. stating that a list of barriers and facilitators is present in the full text of the study). In addition, there is some evidence that the contents of abstracts may not fully reflect the detail of the papers, as authors may omit to revise abstracts when the main body of the text undergoes manuscript revision.
Chapter 5 Targeted systematic review methods
Aims and research questions
This targeted systematic review focused on evidence from the UK, building on the findings of the mapping review. The revised protocol for the targeted systematic review is provided in Report Supplementary Material 2.
The key elements of the targeted systematic review were:
-
development of the research questions based on the findings of the mapping review and information from PPI meetings
-
a focused systematic database search following inspection of the mapping review findings
-
a full data extraction of relevant studies
-
a quality assessment of included full peer-reviewed papers, and no formal quality assessment of conference abstracts or grey literature.
Research questions
-
What are the gaps in evidence about direct access to primary and community health-care services for people with ID?
-
What are the barriers to directly accessing primary and community health-care services for people with ID and their carers?
-
What actions, interventions or models of service provision improve access to primary and community health-care services for people with ID and their carers?
Search strategy
The findings from the mapping review helped develop the search strategy for the targeted systematic review. Searches covered the period 2002–18. We searched MEDLINE, The Cochrane Library, Web of Science, CINAHL (Cumulative Index of Nursing and Allied Health Literature), ASSIA (Applied Social Science Index), PsycINFO and ERIC (Educational Resources Index) for studies published from 1 January 2002 (the end date of the previous SDO review) to September 2018. A validated filter31 was used to identify UK studies. Further details of the database search, including a sample search strategy, can be found in Appendix 5. Further evidence was sought by contacting topic experts, people with ID and their carers. Broad searches for grey literature on ID (irrespective of setting) that were conducted during the mapping review provided the grey literature for the targeted review.
Selection of articles
Search results were uploaded to EPPI-Reviewer 4 for title and abstract screening. Screening was performed by a team of three reviewers, with a random sample of 10% of records from each reviewer double screened by one of the reviewers. Full papers were obtained for records that appeared potentially to meet the inclusion criteria (Table 11) and these were also uploaded to EPPI-Reviewer 4. Screening on full text followed a similar process to title and abstract screening. Any queries were resolved by discussion. The list of papers excluded at full-text review is available in Appendix 6.
| Criteria | Eligibility |
|---|---|
| Population |
|
| Setting |
|
| Outcomes |
Access to a service We will also review studies reporting the effectiveness of any measures or interventions designed to improve access to the relevant services |
| Comparator | The general population may offer a comparator in some study types |
| Study design |
|
| Other limitations |
English language only Evidence published since 2002. The Alborz et al. 21 review searched up to 2002 |
Data extraction
Data extraction was completed in EPPI-Reviewer 4 using a mix of tick-box and open questions (see Appendix 7). We focused on extracting data relating to the barriers to and facilitators of service access, service acceptability and effectiveness of the implementation of reasonable adjustments to primary care services for people with ID. An example data extraction for one of the included studies is in Appendix 8 and the data extraction table for the grey literature is in Appendix 9.
Quality assessment
Risk of bias was assessed using validated checklists published by the US National Heart, Lung and Blood Institute [URL: www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed 19 November 2018)] for quantitative study designs [controlled (randomised and non-randomised) intervention studies, observational cohort and cross-sectional studies, case–control studies and before-and-after studies with no control group]. Qualitative studies were assessed with the Critical Appraisal Skills Programme (CASP) checklist for qualitative studies [URL: https://casp-uk.net/casp-tools-checklists/ (accessed 19 November 2018)]. Mixed-method studies were assessed using the appropriate checklist for the predominant methodology of the study.
Analysing and synthesising data
We performed a narrative synthesis of the evidence. The structure of the synthesis was determined by the themes that emerged from the included studies. We drew on a pathway of care model to explore evidence relating to the patient journey of care, including examination of the barriers and facilitators or influencing factors at each point in the pathway.
Patient and public involvement
Patient and public involvement in the development and conduct of the review is reported in Chapter 2. Further to this, we discussed the findings and recommendations from the review with a family carer representing the group of family carers (n = 1) and with a group of people with LDs (n = 10) plus a member of staff supporting the group (n = 1). These discussions covered the main findings and recommendations from the review. Prompts were used when needed to ensure that the discussions covered whether or not these findings were an accurate reflection of their experiences, whether or not there was anything missing and whether or not there was anything they would like to add to the findings or recommendations.
Chapter 6 Targeted systematic review results
Results of literature search
The 413 potentially relevant references from the mapping review were rescreened against the new inclusion criteria while the additional literature searches for the targeted review were being completed. The database search for the targeted review retrieved 9067 references. After de-duplication of the search results, 5957 additional unique records were available for screening (Figure 6), giving a total of 6370 to be screened.
FIGURE 6.
The PRISMA flow diagram for the targeted systematic review.
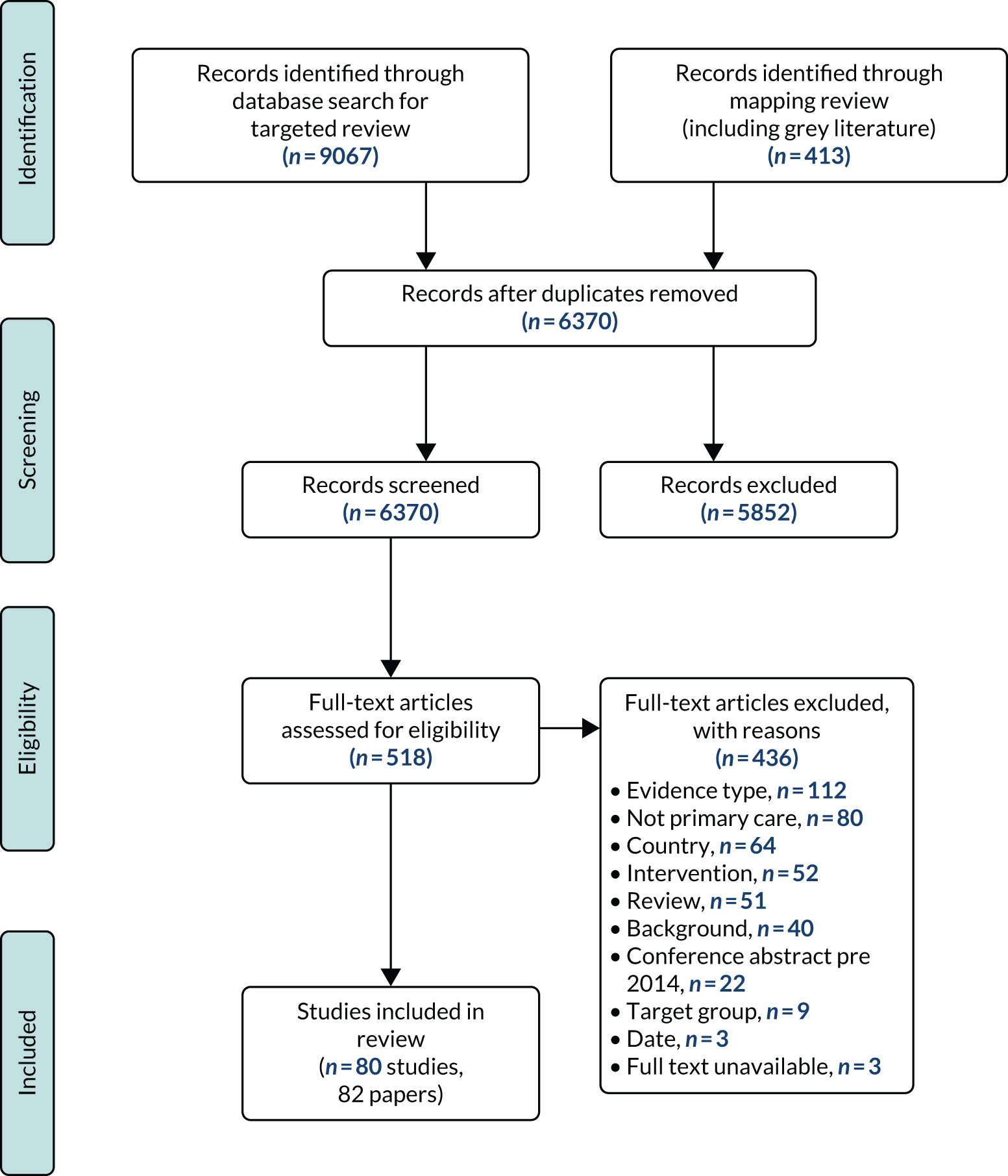
Screening
The screening process was divided between three reviewers. A calculation of inter-rater agreement was made. A kappa coefficient was calculated that demonstrated excellent agreement between the reviewers (κ = 0.933, 95% CI 0.904 to 0.962). A total of 518 references were screened as ‘include’ based on a preliminary title and abstract screen. On further scrutiny of the full text, 436 of these were excluded. Common reasons for exclusion were that the study’s setting was secondary not primary care, the study was about a different population, the study was not about access to health care and the study was not a research study. Eighty-two publications reporting 80 studies were included in the targeted systematic review.
Study characteristics
The review synthesised the evidence from 80 studies reported in 82 publications; an alphabetical list of the included studies is in Appendix 10. All of the included studies were conducted in the UK and investigated adults with ID and their carers (paid or family carers or primary care health professionals working with individuals with ID).
The synthesis was based around a pathway of care encompassing identifying need, accessing services and interaction during a consultation. The pathway model (Figure 7) was not prespecified but emerged from the examination of included study characteristics and was agreed by consensus among the review team. Included studies were grouped into the three clusters corresponding to the stages of the patient pathway. In addition, some studies evaluated innovations/interventions that aimed to improve access, which had an impact at different steps in the pathway model, and these formed a fourth cluster.
FIGURE 7.
Pathway model.
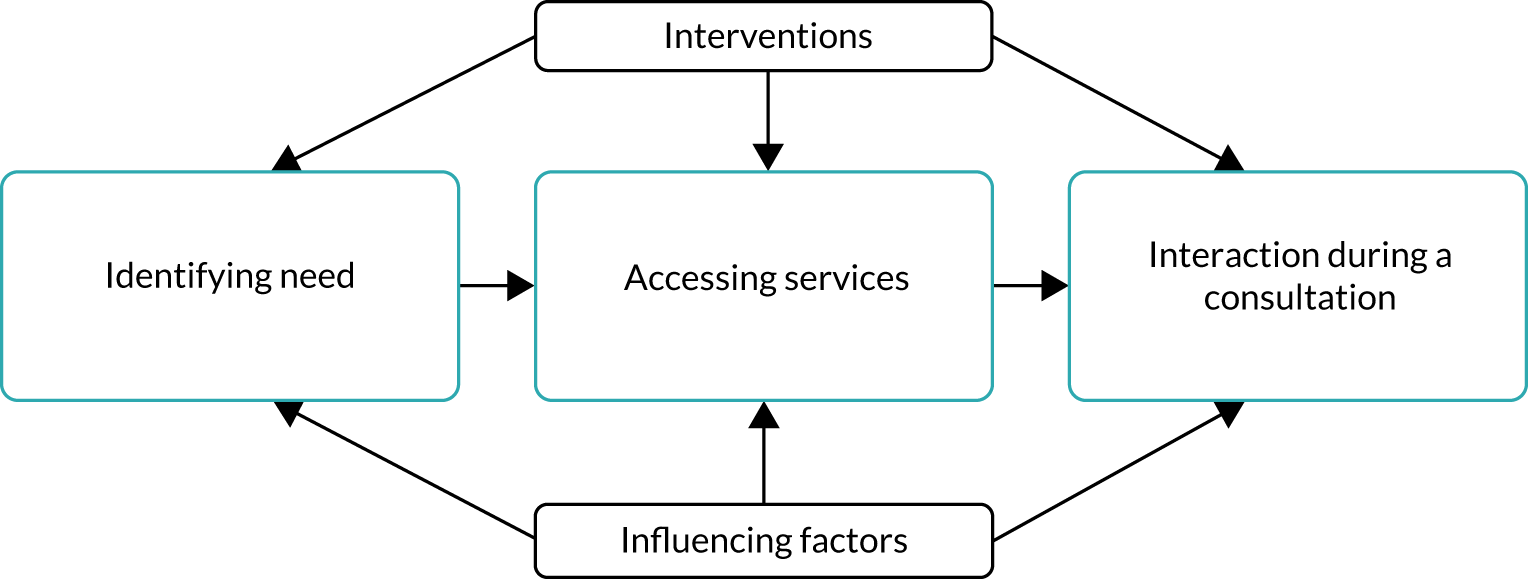
Influencing factors (barriers and facilitators) of access at each stage were also identified within the data. A common group of influencing factors that appeared to act at all stages was used to structure the narrative synthesis for each cluster of studies.
The evidence will thus be outlined within the following four clusters: identifying needs (14 studies), accessing services (24 studies), interaction during a consultation (19 studies) and interventions to improve access (23 studies).
Identifying need
Fourteen studies reported in 16 publications, published from 2003 to 2017, were included in this group (Table 12). Of these, three dealt with general practice,44,45,48 three dealt with a range of primary care services,36,37,49 three dealt with carers working at residential or supported living homes33–35,43 and two dealt with formal and informal carers of people with ID in residential or family homes. 38,39 The other three studies dealt with audiology services,42 cervical and cancer screening40 and sexual health. 41 The majority of the studies included in this cluster had a qualitative design.
| First author and year of study | Type of service | Type of study |
|---|---|---|
| Beacroft 2010/1133,34 | Residential and supported living homes in Surrey |
Cross-sectional33 Qualitative34 |
| Bland 200335 | Nursing homes | Cross-sectional |
| Bollard 201736 | All services | Qualitative |
| Donovan 200237 | All services | Qualitative |
| Findlay 2014/15 (same study)38,39 | Formal and informal carers | Qualitative |
| Hanna 201140 | Cervical screening and other cancer screening | Cross-sectional |
| McCarthy 200941 | Sexual health | Qualitative |
| McShea 201642 | Audiology | Qualitative |
| Northway 201743 | Supported living accommodation for people with ID in Wales | Qualitative |
| Turk 201244 | GP | Cross-sectional |
| Walker 201645 | GP | Very few data; mix of literature review; many relevant data linked to hospitals |
| Willis 201546 | Carers | Qualitative |
| Wilson 201047 | All services | Qualitative |
| Young 201248 | GP | Qualitative |
Accessing services
Twenty-four studies, published between 2003 and 2017, were included in this group (Table 13). Of these, six dealt with a range of primary care services,50,55,58,62,66,67 six dealt with with general practice,51–53,57,60,70 five dealt with cancer screening,59,63,68,69,72 two dealt with dental services,56,64 two dealt with mental health services,54,61 one dealt with diabetic retinopathy screening65 and one dealt with sexual health. 71 The majority of included studies used a cross-sectional (e.g. survey or audit) or qualitative (e.g. interviews or focus groups using qualitative methods for data analysis) design. Only two studies used a cohort or case–control design63,69 and two were classed as mixed methods. 54,71
| First author and year of study | Type of service | Type of study |
|---|---|---|
| Ali 201350 | All services | Qualitative |
| Allgar 200851 | GP | Cross-sectional |
| Black 200452 | GP | Qualitative |
| Carey 201653 | GP | Cross-sectional |
| Chinn 201654 | IAPT | Mixed methods |
| Cooper 201155 | All services | Cross-sectional |
| Doshi 200956 | Dentist | Cross-sectional |
| Jones 200857 | GP | Qualitative |
| Lennox 200358 | All services | Cross-sectional |
| Lloyd 201459 | Cervical screening | Qualitative |
| Lodge 201160 | GP | Cross-sectional |
| McNally 201561 | Community mental health | Qualitative |
| Nicholson 201162 | All services | Cross-sectional |
| Osborn 201263 | Cancer screening | Cohort |
| Owens 201164 | Dentist | Qualitative |
| Pilling 201565 | Diabetic retinopathy screening | Cross-sectional |
| Raghavan 200766 | All services | Cross-sectional |
| Redley 201267 | All services | Qualitative |
| Rees 201168 | Cancer screening | Cross-sectional |
| Reynolds 200869 | Cervical screening | Case–control |
| Russell 201770 | GP | Cross-sectional |
| Starling 20066 | Eye care | Cross-sectional |
| Williams 201471 | Sexual health | Mixed methods |
| Wood 200772 | Cervical screening | Qualitative |
Interaction during a consultation
Nineteen articles, published between 2004 and 2017, were included in this group (Table 14). Six of these studies dealt with GP services,75,79,82,83,91 four dealt with a range of primary services,74,77,78,84 three dealt with palliative or end-of-life care service,86,88,90 two dealt with sexual health services,81,85 two dealt with diabetes services,73,89 one dealt with dental services80 and one study dealt with non-specific cancers in this population. 87 The majority of these studies had a qualitative design,73–77,80,82,83,85,87,89,90 a few had a cross-sectional study design78,79,81,84,85,88,91 and one was a case study. 86
| First author and year of study | Type of service | Type of study |
|---|---|---|
| Brown 201773 | Diabetes | Qualitative |
| Gates 201174 | All services | Qualitative |
| Goldsmith 201375 | GP | Qualitative |
| Hames 200676 | GP | Qualitative |
| Hebblethwaite 200777 | All services | Qualitative |
| Heyman 200478 | All services | Cross-sectional |
| Jones 200779 | GP | Cross-sectional |
| Lees 201780 | Dental | Qualitative |
| McCarthy 201181 | Sexual health | Cross-sectional |
| Murphy 200682 | GP | Qualitative |
| Perry 201483 | GP | Qualitative |
| Powrie 200384 | All services | Cross-sectional |
| Thompson 200885 | Sexual health | Cross-sectional and qualitative |
| Tuffrey-Wijne 200286 | Palliative and end-of-life care | Case study |
| Tuffrey-Wijne 200987 | Cancer | Qualitative |
| Tuffrey-Wijne 200588 | Palliative and end-of-life care | Cross-sectional |
| Turner 201489 | Diabetes | Qualitative |
| Watchman 200590 | Palliative and end-of-life care | Qualitative |
| Williamson 200491 | GP | Cross-sectional |
Innovations to improve access (including health checks)
Twenty-three studies evaluated innovations to improve access (Table 15). The majority of the studies investigated innovations within GP services. 19,93–101,103–105,107–109,111–113 The remaining studies reported innovations in eye health,92 in Improving Access to Psychological Therapies (IAPT), in cardiovascular disease106 and for staff in care homes. 110 One of the included studies was a cluster randomised controlled trial,100 but most had a cross-sectional design.
| First author and year of study | Type of service | Type of study |
|---|---|---|
| Adler 200592 | Eye health | Cross-sectional |
| Baxter 200693 | GP | Cross-sectional |
| Biswas 200594 | GP | Cross-sectional |
| Buszewicz 201495 | GP | Cohort |
| Cassidy 200296 | GP | Case control and qualitative |
| Chauhan 201097 | GP | Cohort |
| Chauhan 201298 | GP | Cohort and qualitative |
| Codling 200799 | GP | Cross-sectional |
| Cooper 2014100 | GP | Cluster randomised controlled trial |
| Cooper 2006101 | GP | Case–control |
| Dagnan 2018102 | IAPT | Before and after |
| Felce 200819 | GP | Retrospective cohort (medical records scrutiny) |
| Ford 2015103 | GP | Cross-sectional |
| Glover 2013104 | GP | Retrospective cohort (routine data trends) |
| Harrison 2005105 | GP | Before–after |
| Holly 2014106 | Cardiovascular | Cross-sectional |
| Martin 2004107 | GP | Cross-sectional |
| McConkey 2015108 | GP | Cross-sectional |
| Romeo 2009109 | GP | Case–control |
| Taylor 2014110 | Care homes | Cross-sectional |
| Walmsley 2011111 | GP | Qualitative |
| Webb 2009112 | GP | Mixed methods |
| Webb 2009113 | GP | Mixed methods |
Study quality
The results of the quality assessment for all included studies, classified by study design, are presented in Appendix 11, Tables 27–32. One case study86 was included in the review but not assessed for quality. The methodological limitations of the included studies are discussed in this section. Overall, the studies in the review were rated as being at relatively high risk of bias. Only two were controlled intervention studies92,100 and only one of these was randomised (by clusters). 100 The randomised trial appeared to be rated as being at low risk of bias, although blinding of outcome assessment was incomplete and the study did not meet the criteria for high adherence to the intervention (see Appendix 11, Table 27). The non-randomised study92 had a number of weaknesses, including differences between groups at baseline, differences in background treatments (other than the intervention being evaluated) and lack of a sample size/power calculation (see Appendix 11, Table 28).
For quantitative (cohort and cross-sectional) observational studies, the main limitations identified were lack of a power calculation or justification of sample size, absence of blinded outcome assessment and not considering possible confounding factors in the analysis (see Appendix 11, Table 29). In the accessing services cluster, only two studies compared a sample of people with ID with a general population control group. 63,69 Studies involving people with ID and carers often had small samples recruited from specialist settings and hence were not necessarily representative. Other studies provided the perspectives of health professionals only, with little or no representation of people with ID. Only a few included studies were classed as case–control or uncontrolled before-and-after studies (see Appendix 11, Tables 30 and 31).
The included qualitative studies met most of the criteria on the CASP checklist for qualitative studies (see Appendix 11, Table 32). Some studies did not consider the relationship between researchers and participants, which is a major limitation in studies involving people with ID. Other studies reported few details of data analysis, so it was unclear whether or not the analysis was sufficiently rigorous.
Identifying need
There were 16 papers reporting 14 different studies in this cluster. Among these studies, health needs were identified by the person with ID,34,36,38,41,44 family carers,49,114 paid carers33,35,39,40,42,48,73,114,115 and health professionals. 37,45,48
Identifying health need depends on some knowledge of potential risks to health. Ten papers reporting eight studies looked at carers’ awareness and knowledge of risks and potential health needs relating to cardiovascular disease,48 hearing,42 cancer,40 men’s health,36 older people35 and pain. 33,34,37–39 Table 16 provides the key findings of the studies in the identifying needs cluster.
| First author and year of study | Type of service | Key findings |
|---|---|---|
| Beacroft 2010/201133,34 | Residential and supported living homes in Surrey | Poor recognition and management of pain |
| Bland 200335 | Nursing homes | Screening rare; generally good access to GPs |
| Bollard 201736 | All services | Useful for GPs and other HCPs to actively promote the health of men with ID, who, with minimal nudging, are prepared to take on health promotion advice |
| Donovan 200237 | All services | Nurses find it hard to explore pain symptoms with people with ID. Ability to interpret non-verbal pain signals was crucial |
| Findlay 2014/2015 (same study)38,39 | Formal and informal carers | Under-reporting of pain by people with ID |
| Hanna 201140 | Cervical screening and other cancer screening | Lack of professional carer knowledge about cancer and screening |
| McCarthy 200941 | Sexual health | Women’s limited knowledge of contraception |
| McShea 201642 | Audiology | Lack of knowledge among support workers about hearing loss |
| Northway 201743 | Supported living accommodation for people with ID in Wales | Role of residential care staff in supporting older people with ID |
| Turk 201244 | GP | People with ID and carers under-report pain/problems |
| Walker 201645 | GP | Mostly descriptive, mentions QOF116 coding |
| Willis 201546 | Carers | Carer role undefined in terms of health care |
| Wilson 201047 | All services | Majority of carers report good access to GPs and dentists but difficulties accessing allied health professionals |
| Young 201248 | GP | Move to engaging with services; suggests ways to improve self-management |
Influencing factors
Influencing factors in the framework were identified in the included studies as summarised in Table 17. The most commonly reported factors were uptake and relationships with staff. Individual factors are briefly discussed in the following sections.
| First author and year of study | Staff knowledge/skills | Joint working with LD services | Service delivery model | Uptake | Appointment making | Carer/support role | Relationships with staff | Time | Accessible information | Communication |
|---|---|---|---|---|---|---|---|---|---|---|
| Beacroft 2010/201133,34 | ✓ | ✓ | ||||||||
| Bland 200335 | ✓ | ✓ | ✓ | |||||||
| Bollard 201736 | ✓ | ✓ | ||||||||
| Donovan 200237 | ✓ | ✓ | ||||||||
| Findlay 2014/2015 (same study)38,39 | ✓ | ✓ | ||||||||
| Hanna 201140 | ✓ | ✓ | ||||||||
| McCarthy 200941 | ✓ | ✓ | ||||||||
| McShea 201642 | ✓ | ✓ | ||||||||
| Northway 201743 | ✓ | ✓ | ||||||||
| Turk 201244 | ✓ | ✓ | ||||||||
| Walker 201645 | ✓ | |||||||||
| Willis 201546 | ✓ | |||||||||
| Wilson 201047 | ✓ | |||||||||
| Young 201248 | ✓ |
Carer knowledge/skills
Many people with ID rely on those supporting them to recognise that they have a health need and that services are available to meet that need. Recognising unmet health need is an important step towards accessing appropriate care. Carers needed an in-depth knowledge of the client to be able to recognise and interpret health-related changes in behaviour, whether acute or long term; recognising when someone is unwell or in pain is an important first step towards accessing primary care services. Five papers33,34,37–39 reporting three studies explored pain recognition and management. One study was an audit exploring residential staff members’ beliefs about pain, strategies for recognising and managing pain33 and experiences of when people with ID had experienced pain. 34 Two qualitative studies explored the experience of pain for people with ID from the perspectives of people with ID and caregivers38,39 and ID nurses. 37 They found that people with ID did not necessarily tell someone when they were in pain, although they relied on others to deal with their pain. 34,38 People with ID demonstrated pain through changes in verbal and non-verbal behaviour;33,37 however, caregivers and residential staff did not always recognise that these were signs of pain. 33,39 Worryingly, some staff still believed that people with ID have a higher pain threshold than the general population, and those with more experience and qualifications were more likely to think that was the case, suggesting that training does not address pain recognition and management. 33 Pain recognition and communication tools were not widely used. 33,34,38 A further study carried out a secondary analysis of health information provided by people with mild to moderate ID and their carers to see how well the two sources corresponded. This study found some evidence that carers did not always recognise all health problems that were significant to the client, and clients reported a high frequency of unreported and untreated pain. Worryingly, some people with ID said that they did not have anyone to talk to about their health. 44
Companion/carer/support worker role
Three studies43,48,114 reported that tensions between services and uncertainty about roles and boundaries affected identification of and response to health needs.
One study used semistructured interviews with managers of supported living accommodation to explore how residential social care staff support older people with ID to meet their health needs. 43 This study found that residential social care staff often felt that their role in recognising, monitoring and meeting clients’ health needs was not always understood by health professionals and that this had an impact on their ability to meet these needs.
One study carried out interviews with paid carers and unpaid family carers to explore views about their role in monitoring the health of people with ID. 114 This study found that there was uncertainty about who among residential care staff, day care services staff, welfare guardians and family members was responsible for recognising and managing health concerns. Relationships, and particularly communication between the different personnel and organisations, could be poor, and this lack of joined-up working contributed to delays and difficulties in identifying and addressing health needs.
These findings were echoed in the third study48 that used qualitative interviews with people with ID, carers and health professionals to look at perceptions of self-management of cardiovascular disease. This study found that paid carers played a pivotal role in supporting health management because they were present regularly in the home and likely to have a trusting relationship with the person with ID. However, the authors raised concerns about poor knowledge about healthy lifestyle choices among social care staff, which could have an impact on their ability to recognise a health need.
Service delivery model
Access to services depends on someone identifying a need and being aware that services are available to address that need. A number of studies35,40–42,117 explored knowledge of health risk and awareness of services to mitigate the risk.
A survey of residential staff carers found gaps in the knowledge of carers about the signs and symptoms of and risks and protective factors for cancer and, therefore, carers did not promote cervical screening or weight management services for cancer prevention. 40 This study also found that staff did not know about risk factors specific to the individual, for example their family history of diseases such as cancer or any previous screening or testing.
A health needs assessment undertaken by the Lincolnshire Learning disabilities Health Needs Assessment steering group also found that the uptake of cervical screening was low among women with ID (28%) compared with women in the general population (71%). It also found that 48% of women with ID declined cervical screening or were ‘exemption reported’, compared with 12% of other women. Women who were exemption reported did not routinely receive future invitations for screening. This highlights the importance of care staff educating and supporting women to undergo screening. The authors speculate that as the Quality and Outcomes Framework (QOF) allows practices to omit exemption reported patients from the data on which their achievement scores are based, there might be a financial incentive to exemption report women who are more difficult to treat, such as women with ID. 45
A survey of care staff working in accommodation for people with ID about health problems in those aged > 65 years and their perceptions about access to support found that many were unaware of the screening tests available and whether or not clients had undergone screening. The authors highlighted the need for staff training to raise awareness of health screening and the age at which screening is appropriate. This includes screening for hearing loss; the patient may be symptom free and it is therefore easy to miss. 35
One study interviewed 20 residential and day care workers, focusing on their knowledge of hearing loss and use of hearing aids. 42 Care workers were aware that it was their responsibility to detect health problems in those unable to do so, but they lacked the skills to detect hearing problems and had reservations about the extent to which audiology services could verify and treat hearing loss in someone with ID. Carers also had negative perceptions about the use of hearing aids, the most common management option for hearing loss, and lacked the necessary skills to support their use in someone with ID.
One study interviewed 23 women with mild to moderate ID living in community-based settings about contraception use. 41 The study found that only 5 of the 23 women used family planning services, with the others preferring to consult their family doctor. Reasons for this may include lack of knowledge about family planning services among women and their carers and a preference for consulting someone familiar and trusted. The study concluded that family planning staff may have more time for consultations but may lack experience of working with women with ID.
Communication
One study49 used semistructured questionnaires and two focus groups with informal family carers of children and adults with ID ranging from mild to severe to explore their perceptions of access to health and social care services. It found that family carers felt that they had to fight to get services and perceived that those that shouted loudest and fought most had better access to services.
Similarly, a study that interviewed men who had mild to moderate ID to explore the factors affecting their health and their capacity to act on health promotion messages found that a good relationship with a GP was important to ensure ongoing access to GP services and that people particularly valued the GP talking to them directly and then talking to the carer if there was a need to clarify information. 36
Monitoring and record-keeping
It is important to record information to maintain an accurate medical history when clients are unable to do this for themselves. Bollard118 found that men with ID in their study used health passports but not all health professionals filled them in on each visit. Residential care managers interviewed by Northway43 raised concerns that some carers may not have the literacy and numeracy skills to maintain health records accurately.
Summary
All of the factors included in the framework were identified as having some influence on identifying need. The studies were mostly weak in design and some of the older studies are unlikely to represent current practice. The most commonly reported factors were uptake and relationships with staff.
Access to services
The access to services cluster comprised 24 studies; the types of services researched and the key findings of each study are provided in Table 18.
| First author and year of study | Type of service | Key findings |
|---|---|---|
| Ali 201350 | All services | Further improvement required in reasonable adjustments |
| Allgar 200851 | GP | Template useful for identifying people with ID in general practice |
| Black 200452 | GP | Many internal and external barriers to equal access |
| Carey 201653 | GP | Continuity of care and longer appointments are key improvements |
| Chinn 201654 | IAPT | Access involves negotiation between patients/carers and service, barriers and facilitators at many levels |
| Cooper 201155 | All services | Deprivation is not associated with worse access to services |
| Doshi 200956 | Dentist | Young Bangladeshi adults with ID have complex and unmet oral health needs |
| Jones 200857 | GP | Access issues identified by patients, social care staff or both |
| Lennox 200358 | All services | Many patients not accessing more specialised primary care (e.g. optician) |
| Lloyd 201459 | Cervical screening | Attendance at cervical screening facilitated by joint working between LD nurses and primary care |
| Lodge 201160 | GP | Relying on Read code searches to identify patients with ID may lead to underdetection |
| McNally 201561 | Community mental health | Mental health and LD specialists identified barriers to people with ID accessing mainstream mental health services |
| Nicholson 201162 | All services | Adults with ID living in rural areas were not disadvantaged compared with those in urban areas |
| Osborn 201263 | Cancer screening | People with ID less likely to be screened for cancer and situation not improving |
| Owens 201164 | Dentist | Improved model of access to dental care needed |
| Pilling 201565 | Diabetic retinopathy screening | National standards for access to screening are not currently being met. Reasonable adjustments (e.g. alternative screening method) could improve matters |
| Raghavan 200766 | All services | Participants accessed primary care services through their GPs. Barriers included lack of awareness, language difficulties and lack of culturally sensitive services |
| Redley 201267 | All services | Access depends on support from family and health professionals |
| Rees 201168 | Cancer screening | Limited awareness among health professionals of some screening programmes and recommended age limits for screening |
| Reynolds 200869 | Cervical screening | Need to improve training for staff taking smears and to improve communication between LD teams and GPs so that patients and carers can receive better support |
| Russell 201770 | GP | Advanced Read code search did not identify large numbers of new patients for register, suggesting other methods needed |
| Starling 20066 | Eye care | Need to monitor people with ID to ensure access to appropriate eye care |
| Williams 201471 | Sexual health | Most younger adults with ID wanted to attend mainstream sexual health services |
| Wood 200772 | Cervical screening | Many practices lacked robust methods to identify women with ID; most felt that there was a need for training and support to deliver cervical screening for women with ID |
Influencing factors
Influencing factors in the framework were identified in the included studies as summarised in Table 19. The most commonly reported factors were uptake and relationships with staff. Individual factors are briefly discussed in the following sections.
| First author and year of study | Staff knowledge/skills | Joint working with LD services | Service delivery model | Uptake | Appointment making | Carer/support role | Relationships with staff | Time | Accessible information | Communication |
|---|---|---|---|---|---|---|---|---|---|---|
| Ali 201350 | ✓ | ✓ | ✓ | ✓ | ||||||
| Allgar 200851 | ✓ | |||||||||
| Black 200452 | ✓ | ✓ | ✓ | |||||||
| Carey 201653 | ✓ | ✓ | ✓ | |||||||
| Chinn 201654 | ✓ | ✓ | ✓ | |||||||
| Cooper 201155 | ✓ | |||||||||
| Doshi 200956 | ✓ | ✓ | ||||||||
| Jones 200857 | ✓ | ✓ | ✓ | |||||||
| Lennox 200358 | ✓ | ✓ | ||||||||
| Lloyd 201459 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Lodge 201160 | ✓ | |||||||||
| McNally 201561 | ✓ | ✓ | ||||||||
| Nicholson 201162 | ✓ | |||||||||
| Osborn 201263 | ✓ | |||||||||
| Owens 201164 | ✓ | ✓ | ✓ | |||||||
| Pilling 201565 | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Raghavan 200766 | ✓ | ✓ | ✓ | |||||||
| Redley 201267 | ✓ | ✓ | ||||||||
| Rees 201168 | ✓ | |||||||||
| Reynolds 200869 | ✓ | ✓ | ||||||||
| Russell 201770 | ✓ | |||||||||
| Starling 20066 | ✓ | |||||||||
| Williams 201471 | ✓ | |||||||||
| Wood 200772 | ✓ | ✓ |
Staff knowledge/skills
The importance of health professionals’ knowledge and skills in relation to access was highlighted in several studies. In most cases, staff in mainstream services lacked confidence in their skills to deliver services to people with ID or at least expressed a need for further training. This was true for cervical screening72 and mental health services. 61 In a study of sexual health services, young adults with ID in Scotland expressed a preference for accessing mainstream services and felt that staff in these services should be able to meet their needs. 71 In relation to cancer screening generally, Rees et al. 68 reported that community staff working with people with ID had low awareness of some national screening programmes and were unsure of age limits and recommended intervals for screening. Lloyd et al. 59 emphasised the importance of primary care staff skills and knowledge for conducting cervical screening, including investment of time in preparing women to be screened.
Joint working with learning disability services
Community learning disability (LD) teams offer specialist support and services to people with ID. Access to services is facilitated when community teams co-operate effectively with general practice, but the included studies revealed a mixed picture. In an early study,52 many GP staff were unaware of the community team and what it could offer their patients. However, when there is awareness, there may still be confusion over the roles of different services and how they can best work together. Chinn et al. 54 identified this as a problem in the context of mental health and the respective roles of IAPT and specialist LD services.
Included studies identified a particular role for joint working between general practice and community services in promoting screening (e.g. for diabetic retinopathy in people with ID and diabetes65 and supporting women with ID to attend cervical screening59).
Service delivery model
This topic overlaps Joint working with learning disability services and should be read in conjunction with it. The included studies identified a number of barriers to access associated with service delivery models. McNally et al. 61 reported that lack of resources limits access by people with ID to mainstream mental health services and it is important that services do not offer ‘false hopes’ about what they can provide. In another study, dental services were reported to not be available at suitable times, again limiting access. 64
Service delivery by general practice is supported by practice registers of patients with ID; however, inaccuracies in registration constitute a barrier to accessing some services (e.g. screening). Three studies examined aspects of searching practice records using Read codes to identify people with ID. The findings were mixed; one study found a simple template useful51 but two others suggested that searches based on Read codes may not identify all patients with ID and need to be supplemented with other methods. 60,70
Pilling65 found that ID was not always recorded for people with diabetes who were eligible for retinopathy screening, while cervical screening history was inadequately documented in another study. 69 Wood and Douglas72 also reported that many general practices lacked robust methods to identify women with ID, which would have a bearing on service provision for cervical screening for this group. These cervical screening studies are more than 10 years old so it may be that they do not reflect current practice. As noted previously, a more recent study59 highlighted the role of joint working across services in promoting cervical screening.
Uptake
This section covers studies reporting on use of services by people with ID (quantitative) and their attitudes to using services (qualitative or mixed methods). People with ID have a higher rate of GP consultations than the general population. 53 Uptake of services may vary across the UK but a study in Scotland found that people in rural areas had more primary care contacts than those living in urban areas, suggesting that living in a rural area is not a barrier to service uptake. 62 Another study55 found no clear connection between the level of neighbourhood deprivation and the uptake of services by people with ID. However, people from minority ethnic communities with ID were reported to lack awareness of services and who was eligible for them. 50,66 In terms of specialist services, many people with ID were found to be receiving eye care below the recommended levels;6 again, this is a relatively old study and may not represent the current situation.
Included studies identified patients’ attitudes and perceptions as important factors influencing service uptake. Chinn and Abraham54 reported an unwillingness to admit to mental health difficulties, while Lloyd and Coulson59 found negative attitudes or apathy towards cervical screening among women with ID. Young Bangladeshi people with ID in Tower Hamlets, London, visited the dentist only when they experienced symptoms rather than regularly, suggesting that they and/or their carers might have had a negative attitude to screening. 56 However, another study64 of dental services identified lack of availability of preferred provider as a barrier to uptake.
Only one study63 compared people with ID with the general population and looked at changes in screening uptake over time. The authors found that differences in uptake between people with ID and control participants have reduced over time for cervical screening but not for breast screening.
In summary, uptake of services among people with ID is often lower than that among the general population and it is unclear whether or not the situation is improving. Initiatives to improve uptake are discussed in Interaction during a consultation, Influencing factors, Uptake.
Appointment making
Only three studies in this group dealt with the mechanics of making an appointment with a health professional. Black52 identified that difficulties using the telephone was a barrier to access experienced by people with ID. Although the study was published in 2004, it is unlikely that the situation has improved as general practice and urgent care increasingly rely on the telephone for access and sometimes as an alternative to face-to-face appointments.
Offering pre-appointment visits to prepare people with ID for tests and other procedures has been recommended as a way of promoting access to cervical59 and eye65 screening but this depends on having the resources available and also on identifying patients with ID. This type of measure could be considered a ‘reasonable adjustment’ for the benefit of people with ID.
Companion/carer/support worker role
Two studies provided limited insight into the role of companions in helping people with ID to access services. Redley et al. 67 reported that GPs preferred people with ID to be accompanied as they felt that this helped to overcome communication problems; however, Ali et al. 50 noted a lack of support for and involvement of carers, although the study was small. Support for carers is closely linked to other issues (e.g. relationships with staff and communication), as discussed in the next section.
Relationships with staff
Evidence about relationships between people with ID and primary care professionals was mixed. Jones et al. 57 found that the attitudes and behaviour of general practice staff were generally positive, although there were some exceptions. By contrast, participants in Ali et al. ’s50 study reported some negative attitudes and behaviour from primary care staff, as did Owens et al. 64 from dental professionals.
Positive relationships between patients and staff are supported by continuity of care, which is not always easy to achieve for people with ID, as Owens et al. 64 reported for dental care. Better continuity of care was identified as a key area for improvement in a recent study of GP services,53 while Lloyd and Coulson59 noted that attendance at cervical screening was facilitated by long-term relationships between patients and LD specialist nurses. Patient preference was identified as a factor in a study of dental health in a Bangladeshi population in Tower Hamlets; for example, women preferred to see a female dentist from a similar background. 56
Finally, a study of IAPT services used the concept of ‘candidacy’ to explore how people with ID and their supporters negotiate access to services. 54 This study used data from health and care professionals and concluded that there are barriers to access at many levels. As well as relationships between individual patients and staff, access to services was influenced by the culture of IAPT teams, specialist LDs mental health teams, managers and service commissioners.
The evidence on relationships with staff and its influence on access to services presents an unclear picture, with most studies being small and involving people from specific geographical areas or cultural groups. National, theory-based studies such as that of Chinn and Abraham54 may offer a route towards better understanding this complex area.
Time
A number of studies highlighted that people with ID need longer appointments both with GPs53 and for procedures such as diabetic retinopathy screening65 or cervical screening. 59 Time pressure was identified as a particular barrier to cervical screening. 59 Longer appointments could be considered a ‘reasonable adjustment’ to facilitate access to primary care services.
Jones et al. 57 identified a different time-related issue, namely that excessive time waiting for appointments can be difficult for some people with ID. The authors recommended not to arrive too early for appointments to minimise this risk.
Accessible information
Accessible information is an additional reasonable adjustment for people with ID. More general communication issues are considered in the next section. Language barriers affect access to services by people with IDs, particularly those whose first language is not English. 50,66 Black et al. 52 noted in 2004 that practice information leaflets were too detailed for people with ID. Easy-read leaflets have been used to promote diabetic retinopathy screening52 and as part of an intervention to improve general practice access for people with ID [see Innovations to improve access (including health checks)].
Communication
In addition to language barriers as mentioned above, included studies identified communication problems arising because people with ID were unable to express their problems clearly. 52 However, another study57 of access to GP services found that communication was not a major problem. This issue is discussed in more detail in Identifying need.
Redley et al. 67 reported that GPs saw communication with people with ID as a problem, but most did not make special arrangements other than allowing extra time for appointments. From the point of view of patients and carers, professionals speaking to the carer rather than directly to the person with ID was highlighted as a problem. 58
In general, health and care services aim to be ‘colour-blind’ rather than adapt to the needs of particular ethnic or religious groups. However, one included study highlighted that this may result in services lacking cultural knowledge or sensitivity. 66
One included study found that communication problems can also arise when people with ID are invited to access services, in this case cervical screening, rather than seeking access themselves. A relatively robust case–control study69 found that women with ID were less likely to respond to invitations and to be screened than those without ID. The authors’ suggestions for improved communication include tailoring invitation letters and informing community LD teams when an invitation letter has been sent.
The included studies have thus identified communication problems as an influencing factor in access to services at different levels before and after an appointment.
Summary
All of the factors included in the framework were identified as having some influence on access to primary care services in UK studies. The studies were mostly weak in design and some date back to the early 2000s and are unlikely to represent current practice. Topics highlighted in recent studies include the need for longer appointments and continuity of care,53 the roles of mainstream versus specialist services54,61 and the continuing need for ‘reasonable adjustments’. 65
Interaction during a consultation
Interaction during a consultation depends on the extent to which an individual can engage and interact with the health care provided. Nineteen papers were considered in this cluster and the majority focused on interactions with GPs and practice nurses, although one paper focused on dental services. 80 Among the papers focusing on general practice, studies considered the provision of palliative and end-of-life care,86–88,90 sexual health and contraception81,85 and diabetes management. 73,89 One study focused on the needs of people with ID who were homeless77 and one focused on the needs of people with Down syndrome and dementia. 90 Details of the type of service investigated and the key study findings are provided in Table 20.
| First author and year of study | Type of service | Key findings |
|---|---|---|
| Brown 201773 | Diabetes | Limitations to providing diabetes services |
| Gates 201174 | All services | Importance of communication and interaction |
| Goldsmith 201375 | GP | Variable amounts of information and explanation given during blood tests. Variable attempts to elicit consent for blood tests. Consent process was rarely followed |
| Hames 200676 | GP | Limited knowledge of LD teams |
| Hebblethwaite 200777 | All services | Homeless people with ID require support in arranging appointments and additional provision |
| Heyman 200478 | All services | Concept of organisational simplification as a restriction to service access |
| Jones 200779 | GP | Appointments differ for people with Down syndrome; GP lack of confidence |
| Lees 201780 | Dental | General satisfaction with dentistry, problems with transition and communication |
| McCarthy 201181 | Sexual health | Challenges in providing contraception |
| Murphy 200682 | GP | Limitations of consultation experiences |
| Perry 201483 | GP | Contact with primary care: the experience of people with ID |
| Powrie 200384 | All services | Nurses require greater co-ordination with LD services |
| Thompson 200885 | Sexual health | Staff tend not to discuss sexual health. Study not specific to ID |
| Tuffrey-Wijne 200286 | Palliative and end-of-life care | Considerations for end-of-life care including consent and communication |
| Tuffrey-Wijne 200987 | Cancer | Challenges in cancer care including reliance on others to negotiate with services |
| Tuffrey-Wijne 200588 | Palliative and end-of-life care | Challenges in communication |
| Turner 201489 | Diabetes | Very limited data; makes suggestions for ways to improve access |
| Watchman 200590 | Palliative and end-of-life care | End-of-life care limitations |
| Williamson 200491 | GP | Provides useful list of recommendations to improve GP services |
Influencing factors
Influencing factors identified in the innovations to improve access cluster are discussed below and shown in Table 21.
| First author and year of study | Staff knowledge/skills | Joint working with LD services | Service delivery model | Uptake | Appointment making | Carer/support role | Relationships with staff | Time | Accessible information | Communication |
|---|---|---|---|---|---|---|---|---|---|---|
| Brown 201773 | ✓ | ✓ | ✓ | |||||||
| Gates 201174 | ✓ | ✓ | ✓ | ✓ | ||||||
| Goldsmith 201375 | ✓ | ✓ | ✓ | |||||||
| Hames 200676 | ✓ | |||||||||
| Hebblethwaite 200777 | ✓ | |||||||||
| Heyman 200478 | ✓ | ✓ | ✓ | ✓ | ||||||
| Jones 200779 | ✓ | ✓ | ||||||||
| Lees 201780 | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| McCarthy 201181 | ✓ | ✓ | ||||||||
| Murphy 200682 | ✓ | ✓ | ✓ | |||||||
| Perry 201483 | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Powrie 200384 | ✓ | ✓ | ||||||||
| Thompson 200885 | ✓ | ✓ | ||||||||
| Tuffrey-Wijne 200286 | ✓ | |||||||||
| Tuffrey-Wijne 200588 | ✓ | |||||||||
| Tuffrey-Wijne 200987 | ✓ | ✓ | ||||||||
| Turner 201489 | ✓ | |||||||||
| Watchman 200590 | ✓ | |||||||||
| Williamson 200491 | ✓ | ✓ | ✓ | ✓ |
Making the appointment
A paper combining the findings of two studies that used focus groups of people with ID found that some patients found the telephone menu system used by general practices confusing and were frustrated by the time taken to get through to the surgery at busy times. Some people preferred to go to the practice to make their appointment. Triage systems were particularly problematic because people found it difficult to wait for a call back. Many of these problems are also experienced by people without ID; however, people with ID are unlikely to have the confidence or persistence of other patients and so are disproportionately affected by these issues and more likely to be disadvantaged by them. 83 A qualitative study77 of people with ID who had experience of being homeless found that support to register at a practice close to any temporary accommodation was important because the distance to appointments was a factor that affected whether or not people attended.
Time needed
Seven studies73,78–80,82,83 raised the issue of extra time to consult with people with ID. This caused problems for some during busy clinics,73 whereas others routinely offered double appointments for people with ID. 79,82 Lees et al. 80 highlighted the importance of not rushing people with ID and Perry et al. 83 found that long waiting times increased anxiety for some people, which had an impact on the consultation. Williamson et al. 91 suggested that people with ID could be offered the first appointment of the clinic if waiting was difficult for them, whereas Perry et al. 83 highlighted the importance of offering flexible appointment times so that people did not miss day services that they might be paying to attend.
Consultation skills
Seven papers74,75,78–81,83 discussed the interpersonal skills that were needed during a consultation with someone with ID. People with ID wanted to be treated with dignity and respect74,78,80 and they wanted to feel that they could trust the person they were talking to. In a study of communication between general practice staff and patients with communication disabilities, including two focus groups comprising people with ID, Murphy82 found that continuity and the opportunity to build a relationship with GP staff over time was important to the development of trust and rapport during consultations. Similarly, a qualitative interview study comprising people with ID and their carers about their experiences of using community dental services found that anxiety increased when people felt that they were not being listened to and that building long-term relationships with members of staff reduced this anxiety. 119 In a study using focus groups with people with ID and their parents and relatives, Gates74 found that people with ID wanted all staff to have some training in working with people with ID so that everyone the patient came into contact with, including receptionists, porters and auxiliary staff, would treat them with respect. Three qualitative studies74,78,83 using interviews with people with ID, family carers, and health and social care professionals all found that, when a carer accompanied a person with ID to a consultation, it was important that the health professional talked to the person with ID directly rather than to the carer. People with ID valued clear, verbal information tailored to their cognitive abilities, which included breaking explanations down into simple elements and using short sentences and simple, jargon-free vocabulary to explain concrete terms. 75,78
Accessible information
Eight papers73–75,80,81,83,89,91 discussed the provision and use of accessible information, tailored to individual abilities, to support verbal communication. In their study of practitioners supporting people with ID who had diabetes, Brown et al. 73 found that some practitioners made information about diabetes accessible by using ‘Talking Mats’ (Talking Mats Ltd, Stirling, UK), easy-read materials, and pictures and symbols, whereas others were not aware that these resources were available. Lees et al. 80 reported service user and carer perspectives on dental services and found that accessible information was important to support self-care and knowledge of what to do in a dental emergency. Perry et al. 83 found that the information sent with an invitation to a health check was confusing, particularly for people with mild ID who did not have access to support. They also found that information in the surgery was difficult for patients to understand; for example, some patients could not read signs and, therefore, were unable to find their way around the building. Two papers discussed the need to maintain accurate patient-held health records with accessible information tailored to the needs of the individuals. 89
Using accessible information to support verbal communication, including pictures and symbols for those who could not read, was particularly important when information was needed to make a decision about whether or not to give consent, for example for a blood test. 75
Support capacity to give consent
Ten papers discussed issues around capacity for people with ID to give consent or make other decisions about their health care,75,84,89 cervical screening,78,84 sexual health,85 contraception81 and end-of-life care. 86–88,90
An ethnographic study75 in which six people with ID were observed having a routine blood test in general practice found that information was not provided in an accessible format to support decision-making and that inconsistent levels of explanation were given for the procedure without checking for understanding. Instead, as patients were known to trust the nurse, their acquiescence was interpreted as consent. Similarly, in an ethnographic study of people with ID who had cancer, Tuffrey-Wijne et al. 87 identified that some health professionals did not seem to be aware that people with ID may have a tendency towards acquiescence and, therefore, the assumptions made about someone without ID may not apply to someone with ID. For example, when someone without ID offers an arm for a blood test it could reasonably be assumed that they are giving consent; however, they may be going along with this action because they are not confident or lack capacity to refuse the test. Turner89 highlighted the importance of providing accessible information to support consent to blood tests and listening and responding to any fears in advance of any procedure. A survey of practice nurses84 found that nurses were concerned about medical decision-making and consent in relation to invasive procedures such as cervical screening. A study78 using focus groups with adults with ID to explore issues of autonomy and consent identified that adults with ID who are capable of giving informed consent are legally entitled to make their own decisions; however, they may not have the same agency and ability to choose as someone without ID because they may be unduly influenced by the views and preferences of carers or family members. The study reported that some health professionals felt that consent was obtained through negotiation with the individual and their relatives and social care staff. 78 A survey81 of GP practice for women with ID attending for contraception found that GPs relied on discussions with carers when women could not consent to treatment. Most GPs felt that carers could facilitate communication between them and the woman with ID to maximise her capacity to consent; however, some respondents indicated that the purpose of this discussion was to gain the carer’s consent, which has no legal basis in the UK. GPs said that they prescribed contraception on the basis of ‘best interests’ when women did not have the capacity to consent; however, the study’s authors noted that it is sometimes difficult to separate the best interests of women with ID from the interests of their relatives and carers. The authors noted that relatively few GPs expressed concerns about whether or not a woman who could not consent to treatment could consent to sex, and it was not clear what those doctors did with their concerns or whether or not they reported them and, if so, to whom.
Four qualitative studies considered decision-making in relation to cancer,87 dementia90 and end-of-life care. 86,88 These studies found that relatives, carers and GPs were unsure about how to communicate with people with ID about terminal diagnoses, prognosis and death, and wanted to protect people with ID from distressing news. However, this led to people with ID feeling scared because they did not know what was happening to them. Doctors did not always give patients clear information about treatment decisions in a format they could understand, sometimes because carers asked them not to. 87 Emotional issues surrounding end-of-life and palliative care affected family and other carers’ decisions, and situations arose where those close to the person with ID had conflicting views about the best course of action. This meant that people with ID were given conflicting information that caused anxiety and, in some cases, prevented them from making decisions about their care. 88
Role of carers
Family carers and paid social care staff clearly played an important role in facilitating communication and interaction during health consultations. However, a survey90 of practitioners working in residential and palliative care settings with people with Down syndrome who had dementia raised the issue of a ‘care culture clash’. This clash occurred when social care staff were employed to provide social care, which emphasised the rights of individuals to autonomy and an independent lifestyle, but their role subsequently changed to include monitoring deteriorating health and diminishing skills, which required more directive and structured services as well as medical and nursing care. 90 An ethnographic study of the experiences of people with ID who had cancer found that carers were committed to their patients but they found it hard to manage the practical and emotional demands of caring for someone with cancer without information and support from health professionals. In some cases, this support was not available because GPs did not explain the reason for a particular course of treatment action (or inaction), so carers did not understand some of the decisions that were made. 87 Similarly, Williamson et al. ’s survey91 of GPs about their interface with people with ID and their supports found that there was poor communication between GPs and social support providers.
Joint working
It was important for mainstream services to have good working relationships with specialist LD services so that they could access support and advice about how to interact with people with ID to meet their health needs.
In a qualitative study85 using interviews with GPs and practice nurses, participants reported that they did not feel adequately trained to support people with ID to address their sexual health needs. A survey of general practice staff, including GPs, found varying levels of awareness of the role that community LD teams have in supporting people with ID to access mainstream health services. The study highlighted the role that these teams could have, particularly relating to screening and health checks, because of their knowledge of the patient’s health needs and condition-specific risk factors. 76 A survey of practice nurses by Powrie84 also suggested that primary care providers would benefit from closer working relationships with community LD teams to support them with dilemmas around autonomy and freedom of choice when discussing lifestyle issues such as overeating and alcohol abuse.
A qualitative study exploring perceptions of diabetes service provision among practitioners, including those delivering diabetes care in primary and secondary care, in ID services and in community care services found that positive working relationships between care providers in different settings were crucial to ensure person-centred care and effective diabetes management. Relatives and carers provided support to enact diabetes management plans but needed training in diabetes care. The study found that the high turnover of support staff meant that delivering this training was time and resource intensive. Diabetes practitioners noted that inconsistency of care by relatives and carers resulted in inaccurate communication with people with ID, leading to confusion and poor management, which highlighted the need for joined-up care between primary health care, specialist ID services, diabetes services and social care support services. 120
Two further studies identified the problems caused by the high turnover of staff. Powrie84 found that the high turnover of social care staff contributed to poor communication between primary and social care services and Tuffrey-Wijne86 found that a reliance on agency staff put more pressure on permanent staff to provide consistency of care and meant that training for care staff was of limited value because of the constant turnover of staff.
Three studies focusing on cancer or end-of-life and palliative care found that mainstream service providers benefited from close working with staff from community LD teams. 86,87,90
Staff uncertainty
Jones and Kemp79 found that only 40% of GPs were confident about taking histories and gathering information from people with Down syndrome and that they valued working in close partnership with LD teams. Thompson et al. 85 found that GPs and practice nurses did not discuss sexual health with people with ID unless this was specifically requested, and they did not feel that they were adequately trained to support clients with ID to address their sexual health needs. Tuffrey-Wijne et al. 88 found that palliative care staff were unsure about how to communicate with and care for people with ID. Tuffrey-Wijne et al. 87 found that GPs and carers lacked confidence in breaking bad news to someone with ID and that sometimes they avoided doing so, which left patients feeling anxious and scared because they did not know what was happening to them. Similarly, Watchman90 explored the experiences of practitioners working with people with Down syndrome and dementia and found that care staff as well as health professionals did not discuss end-of-life care or funeral arrangements with patients because they were unsure how to do so. Powrie84 found that practice nurses were uncertain about how to manage consent or lack of consent for procedures such as blood tests, cervical screening and breast examinations with women with ID.
Summary
All of the factors included in the framework were identified as having some influence on interaction during a consultation. The studies were mostly weak in design and some of the early research is unlikely to reflect current practice. The most common factors were staff knowledge/skills, time, accessible information and communication.
Innovations to improve access (including health checks)
Twenty-three studies evaluated innovations developed to improve access. Fifteen of these studies19,93,95–101,104,105,107–109,111 investigated health checks. Training for staff was investigated in five of the included studies. 92,102,106,110,112 A counselling intervention was evaluated in one study;94 one cross-sectional study researched weekend opening and whom it would benefit103 and one study investigated a training intervention for people with ID. 113 Table 22 provides details of the key findings from studies in this cluster.
| First author and year of study | Type of service | Key findings |
|---|---|---|
| Adler 200592 | Eye health | Training that incorporates clinical experience, and using real patients, is particularly effective, although there is still benefit in providing lecture-type courses. Whenever possible, courses provided should offer hands-on experience with real patients |
| Baxter 200693 | GP | Health checks help to identify health needs |
| Biswas 200594 | GP | Uptake of cervical screening in women with ID was found to be very low, but largely for appropriate reasons. Counselling made a small difference to uptake |
| Buszewicz 201495 | GP | Incentivisation schemes increase testing and checks |
| Cassidy 200296 | GP | Health checks reduce long-term need for onward referral and interventions |
| Chauhan 201097 | GP | Incentivisation increases recording of health data. Need for specific ID targeting of checks |
| Chauhan 201298 | GP | Incentivisation schemes increase checks and identification of disease. Fewer than half received the checks and a number of barriers were identified |
| Codling 200799 | GP | Evaluation of ‘My Health’ booklet – not always completed and information could be poor |
| Cooper 2014100 | GP | Practice nurse health checks. No significant difference in health needs identified or SF-36 but better monitoring of long-term conditions, improved health (EQ-5D), quality-adjusted life-years and costs |
| Cooper 2006101 | GP | Practice nurse health screening increased routine screening and immunisations, more health needs identified |
| Dagnan 2018102 | IAPT | IAPT staff need specialist knowledge and confidence in dealing with people with ID. Outcome measures used by IAPT services are not standardised for people with ID |
| Felce 200819 | GP | Evaluation of health checks. No increase in consultations, but frequency of health promotion activities increased |
| Ford 2015103 | GP | Weekend opening unlikely to benefit people with ID |
| Glover 2013104 | GP | Number of adults receiving checks has increased (to around half). Obstacles remain |
| Harrison 2005105 | GP | Targeted initiative improved uptake of health checks and health action plans |
| Holly 2014106 | Cardiovascular | Evaluation of a training resource for coronary heart disease, initially promising but requires further evaluation |
| Martin 2004107 | GP | Health check uptake 91%. Checks identified unmet need |
| McConkey 2015108 | GP | In Northern Ireland, 64% received a check; variation in uptake; suggestions of barriers |
| Romeo 2009109 | GP | Health check intervention is cost-effective |
| Taylor 2014110 | Care homes | Evaluation of tool and training staff for pain reporting |
| Walmsley 2011111 | GP | Describes reasons for slow implementation of health checks |
| Webb 2009112 | GP | Training for GPs and practice staff can improve access for people with ID but releasing staff to attend training was a barrier |
| Webb 2009113 | GP | 12-week training programme improved knowledge and self-efficacy for accessing primary health care among people with ID, but implementing such programmes in practice would be difficult without additional funding |
Health checks
Health checks were evaluated in 15 studies. These were found to help identify health needs,93,101,107 improve the monitoring of people with long-term conditions,121 reduce the long-term need for referral and interventions96 and increase health promotion activities aimed at people with IDs. 19 Three studies95,97,98 found that incentivisation schemes increased tests and checks and one study found health checks to be cost-effective. 109 A number of studies investigated the uptake of health checks and factors that could influence this. 104,107,108,111 One study99 investigated the use of the ‘My Health’ booklet as part of health checks. Each of the studies will now be discussed in greater depth.
One of the included studies researched health checks carried out by practice nurses using a cluster RCT121 to attempt to determine their clinical effectiveness and cost-effectiveness compared with standard care. The study investigated adults aged > 18 years with ID who were registered at one of the participating practices in Scotland. The practices were randomly assigned either to health checks in addition to standard care or to standard care, and participants were followed up for 9 months. The study found that more newly detected health needs were identified and met in the intervention group than in the control group, although the difference was not significant. The study was well conducted methodologically but was potentially underpowered to detect a significant difference for the outcome of health needs identified and met. Some of the participants disclosed their group to the outcome assessors. In many cases carers completed the measures with or for the individuals with ID and, because of staff turnover, different carers may have completed the measures and interpreted them differently.
Forty GP practices in Wales93 identified adults with ID and then invited them for a structured health check. The practices identified 318 adults eligible for a health check; 190 health checks were conducted and data were available for 181 of these. An audit was undertaken 3 months after checks to determine any health needs identified and actions that had been taken. New health needs were identified in 51% of patients; 63% had one new health need recognised, 25% had two health needs and more than two new health needs were recognised in 12% of patients. New morbidity was discovered in 16 patients. At the 3-month audit, management had been initiated for 90% and treatment for 61% of the new health needs identified. For the 10% of new health needs for which management had not been started, the patient or carer had refused or there had been treatment delays. The study demonstrated that health checks can be an important tool for identifying health needs. The researchers felt that it was important to ensure that common hearing and visual conditions are identified, as they can have an impact on communication. The characteristics of the initially identified 318 people with ID and the final 190 that actually received a health check were similar for age, sex, abilities/disabilities, challenging behaviour and threshold indicators of mental illness. However, the final sample had more patients from staffed accommodations, meaning that the sample was not representative of the whole population of people with ID and potentially any findings might not be applicable. Furthermore, the paper was published in 2006 and, thus, might not be representative of current opinion.
A large cohort study95 used data from The Health Improvement Network primary care database to investigate whether or not the NHS England opt-in incentive scheme to encourage practices to perform health checks for people with ID had improved care after 3 years. Complete data were available for 5256 people with ID; 4645 were registered with an incentivised practice and had received health checks during the study period. Blood tests to measure total cholesterol, health checks specifically for hearing and vision, medication reviews, action plans and referrals to secondary care were more likely to be offered at incentivised practices. Newly identified gastrointestinal, thyroid disorders, constipation rates and weight problems were higher at incentivised practices. People who chose not to attend health checks were younger and lived in more deprived areas. This evidence is important for demonstrating that health checks aimed at people with ID can have positive effects on health service provision, which potentially could contribute to a reduction in avoidable deaths. However, the study authors noted that it was difficult to ascertain which practices had opted into the learning disability direct enhanced service (LD-DES), which provided practices with a financial incentive, as the information was not available. In addition, the quality of the health checks was not assessed.
An analysis of QOF data97 investigated the additional value of a health check for people with ID compared with that for a standard care control group. The study findings suggest that there is a high level of recording for processes that are directly incentivised through the QOF and further significant increases in the recording of information about people with ID. The study authors reported that focusing on health issues common to people with ID could potentially improve care more than the extensive health checks being performed. The study had only a small sample and was for a short time period (6 months). In addition, it was not possible to identify how many people with ID invited for a health check did not attend. Data that had been extracted for the LD-specific process might not be as reliable as QOF data, which are directly linked to GP payment.
A qualitative study98 evaluated the impact of health checks on health professionals, patients and health services through interviews and analysing clinical data from GP clinical systems. Recording of health checks increased during the 2-year study period and the number of people with ID identified by practices increased. Health checks were associated with increased identification of QOF-incentivised conditions. Screening and health promotion activities that were associated with QOF-incentivised processes increased following health checks. There was still considerable variability between recording of data, and additional barriers to the introduction of health checks were identified in the recording of data by practices. The resources available to practices influenced how they introduced them. A facilitator for practices signing up to the LD-DES was the financial incentive and if this was removed then practices are potentially less likely to continue health checks. Reasonable adjustments introduced during the study, for example how appointments are booked, could potentially remain and become part of routine care. The study was potentially not representative of the whole population of people with ID, only one person cared for by their families who had refused a health check was recruited and no-one younger than 24 years was recruited.
A controlled study in GP practices in Scotland examined the service use and cost implications of health checks. 109 Costs considered were the costs of health checks, services, aids and adaptations, and carer costs. The study found that the mean cost of delivering a health check was £82. The 12-month costs of carers and services were lower in the group receiving health checks than in the control group (bootstrapped mean cost difference £22,272, 95% CI £37,657 to £6400); lower costs were mainly attributed to unpaid informal care. It is possible that health check interventions could offer value for money compared with standard care and hopefully benefit people with ID by reducing health inequalities. The study groups were not randomised and there was no information about previous health-care use. No data were provided to inform a sample size calculation, so the study could be underpowered. The study measured only costs; other possible benefits were inferred from the literature.
One study researched trends in health check provision from 2008–9 to 2011–12 using data collected by the Health and Social Care Information Centre from primary care trusts in England. 104 During the study period, uptake of health checks rose 5% from 48% to 53%. This increase in health checks is positive but the study found that a number of strategic health authority and primary care trust areas needed to improve to ensure that minimum standards are being met.
Another study researched the uptake of health checks across general practices in Northern Ireland over 3 years. 108 The study found that practices were identifying increasing numbers of people with ID but that the proportion who had received a check had fallen. There was also wide variation between practices in the number of people with ID receiving a check (6–100%); no differences were found between small and large practices in the number of patients being checked. The majority of identified people with ID (87%) were registered at a practice that performed annual health checks. Of those eligible, < 50% received the annual checks. The study did find that it was more likely that people living in nursing or residential homes and people living in more affluent areas would have had a check. The main reasons GPs gave for not doing health checks were a lack of demand, a desire to avoid extra paperwork and scepticism of their value. Trusts that employed more health facilitators for longer had greater numbers of practices that performed health checks. The total study sample size in this study was unclear and the data provided by GPs did not identify the people receiving the health check, so it was not possible to determine if people had had just one check or regular checks. This study did not evaluate the quality of health checks or their ability to detect health problems.
Trends in implementation of annual health checks in Oxfordshire were investigated in a qualitative study conducted during 2010. 111 The study considered GPs’ experiences of conducting the health checks and any associated problems . The study also obtained perspectives on the checks from people with ID. The study found that the implementation of health checks was still in its infancy in Oxfordshire in 2010. Practices had different lists of people who might be eligible, making it difficult to determine whom to target for health checks. Six practices participated in the study but only two recorded any outcomes. Serious health conditions were identified through the checks, including heart disease and diabetes, and many less serious conditions were also identified and treated. One practice identified 90 health conditions from 65 checks. The practices found the following challenges to implementing health checks: difficult to define eligibility, costs, lack of training in working with people with ID and lack of awareness of ‘reasonable adjustments’. There was limited access to or awareness about support from community LD teams, which could have provided much needed specialist support. The participating practices might not be representative of the whole country. The attitudes of GPs towards checks could have changed since 2010 and also the organisation of services could be different meaning that the findings from this study might not be reflective of the current situation.
A small study19 in Wales investigated the impact of health checks on increased consultations with GPs or another member of the primary care team, increased health promotion activities and increased contact with specialists. Study participants had 5.4 primary care and 1.8 specialist consultations in 1 year. The rates before and after the study were not statistically different. The frequency of health promotion actions outside the health check increased significantly following the introduction of health checks. There was significant sample attrition during this study, one-third of practices declined to participate in the second stage of the study and a further one-fifth of participants chose not to continue in the study. The study authors acknowledge that the final sample did not represent an epidemiological cross-section, meaning that any findings need to be treated cautiously. In addition, the study was published in 2008 and therefore might not be reflective of current practice.
An audit study published in 200799 researched whether or not the ‘My Health’ booklet was being used effectively in practice and whether or not the format met the specific health needs of people with ID. The ‘My Health’ booklet was being used in practice but it was not always fully completed and some of the information recorded was inaccurate. The study was published in 2007 and is potentially not reflective of current practice. The study participants were from a residential home, mostly aged 51–60 years and over, with 60% being male, so any findings are potentially not reflective of the whole population of people with ID.
The introduction of a health screening programme for people with ID was implemented and health gains were investigated 1 year later. 101 The study demonstrated that the benefits of a screening programme were sustained for 1 year, when compared with standard treatment alone, and its routine implementation could potentially reduce health inequalities for people with ID. The study had a control and considered the longer-term impact of a health screening programme. However, the study was conducted prior to 2006 and might not reflect the current situation. The health screening intervention was introduced in isolation without any other changes to services.
A small uncontrolled service evaluation described a project designed to facilitate access to mainstream primary care services by people with ID in Warrington and the surrounding areas. 105 The project introduced a joined-up approach to working involving primary care and community staff and the project outcomes were uptake of health checks by people with ID and production of health action plans. When the study started, 14 of the 62 patients had accessed a health check in the previous year. At the end of the project, 60 had received a health check, with 46 being provided with a health action plan. This small uncontrolled study had promising findings but was conducted only in a single area and would need to be repeated with a larger sample in a range of areas to determine whether or not findings can be replicated.
A small survey conducted in 2002 evaluated a nurse-led health review for people with ID. 107 Fifty-three patients and carers attended health checks; 34 of these already had concerns and the checks identified an average of 1.49 required interventions per patient. In addition, the checks identified unmet health needs. However, the study found that it could be difficult to get patients to return for follow-up tests or interventions. The use of double appointments, a structured questionnaire and input from carers facilitated the health checks. The study used a small sample from one GP practice; a larger more robust study conducted in a number of GP practices would be needed to determine the true impact of the health checks. In addition, the research was conducted in 2002 and is potentially not reflective of current practice.
A small controlled study96 investigated health checks for people with ID to detect, quantify and treat physical and mental health conditions in one Midlands market town. The health checks were performed by a consultant psychiatrist in LDs, a GP and a community LD nurse at the GP’s surgery, and detected and treated a range of health conditions. The checks were performed twice, 1 year apart. At the second check, there were a reduced number of referrals and other interventions, but it was thought that it would still be useful to continue with annual checks. Generally, people with ID and carers were positive about the checks and how the consultations were conducted. A wider range of outcome measures would have helped to produce a fuller understanding of the quality of the consultations. The research was published in 2002 and is potentially not reflective of current practice.
Health checks were found to help identify health needs,93,101,107 improve the monitoring of people with long-term conditions,121 reduce long-term need for referral and interventions,96 and increase health promotion activities aimed at people with ID. 19 Three studies95,97,98 found that incentivisation schemes increased tests and checks and one study found health checks to be cost-effective. 109 A number of studies investigated uptake of health checks and factors that could influence this. 104,107,108,111 These studies found challenges to the introduction and uptake of health checks, including defining eligibility. 111 The included studies did not investigate the quality of the health checks.
Staff training
Five of the innovation studies investigated training of staff. Individual studies investigated training for staff in the following services or areas: eye health,92 IAPT, general practice,112 cardiovascular106 and pain reporting. 110
One controlled study investigated training for optometrists and student optometrists,92 which included a series of lectures and then supervised practice at vision screening for at least 2 days. The results were compared with those of a control group who had received similar lectures but no practical experience. Both groups improved their self-reported knowledge of eye health for people with ID and their confidence in working with them. However, the study found that training that incorporated clinical experience and using real patients was particularly effective, although lectures can still be useful. Courses that provide practical experience should be offered where possible. The study findings were based on self-report data and the questionnaire used for attitude assessment had not been validated. Participants’ actual knowledge would have been better assessed by a formal examination than by self-report data. In addition, the study participants had all volunteered to work at the Special Olympics so this is an area of possible bias as they potentially had a more positive attitude to people with ID than other optometrists.
Another study112 evaluated a project that aimed to raise staff awareness, improve their training and adapt their working practices to improve the accessibility of their services to people with ID. The project was undertaken in three primary care practices in north Essex. The study found that GPs and practice staff were aware of their need for training in providing services to people with ID and training workshops were offered but only one of the three practices was prepared to release all of their reception and administrative staff to attend the training. Practice development plans were produced by all of the practices, which aimed to improve the accessibility of their services to people with ID. In addition, communication was improved between the practices and the community LD team. The study had only limited involvement of people with ID, it had a small sample size and its evaluation was only short term (3 months), so it is not possible to determine if the changes would be sustained.
One study investigated training for IAPT practitioners designed to prepare them for working with people with ID. The study participants, who were therapists working in an English IAPT service, completed measures of confidence, attitudes to people with ID using mainstream health services and their self-efficacy before and immediately after the training, and 3 months after the training. Following the training, there were positive changes in measures of confidence, attitudes to people with ID using mainstream IAPT services and their general therapeutic self-efficacy, which were maintained 3 months after the training. In addition, 12 of the practitioners were interviewed about how the training had affected their practice. The interviews highlighted that the referral and access process for IAPT can act as barriers to people with ID. The skill levels of practitioners can also be a barrier and specialist knowledge is needed to enable them to work effectively with people with ID. Furthermore, scales used at IAPT sessions have not been standardised for people with ID and this is a potential area for further research. The study was small and the training would need to be further evaluated in a larger study with a more robust study design.
A training package for professional carers, to train them to report and manage the pain of people with ID, was evaluated in a cross-sectional study. 110 The staff were from care homes in Kent. Out of 203 people who completed the training, 116 completed evaluations. The majority of staff (82.8%) who completed the evaluations found the training useful and 71.1% believed that they had gained new insights into pain assessment and management. The study authors reported that there was better reporting of pain following the training. However, the study provided data only on the training, not on the reported improvements in recording. The study was based on self-report data, which are open to bias.
One small pilot study106 investigated a training resource for coronary heart disease. The programme trained 17 staff from community support organisations in Scotland about heart disease. Following the training, staff had increased their knowledge of heart disease and felt more confident about improving the health of people with ID. This was an initial study to test the training package and would need to be evaluated with a larger number of staff using a stronger study design to conclusively determine its impact.
Other innovations
A small cross-sectional study94 investigated whether one-to-one counselling improved uptake of cervical screening in eligible women with ID in one primary care trust area in Lancashire. At the start of the study only 16% were having regular screening compared with the national target of 80%. The counselling was time-consuming and uptake was low for mainly appropriate reasons. Following counselling, an extra nine women had cervical screening for the first time, which was a small increase in uptake to 22% and the counselling revealed that the remaining 96 women (60%) had appropriate reasons (e.g. medical reasons, not sexually active, etc.) for not having cervical screening. Counselling provided an opportunity for women with ID to discuss their reasons for not attending cervical screening, which is potentially a discussion that could take place with a patient’s GP or practice nurse. Women included in the study had mild ID and, therefore, were not representative of the whole ID spectrum, meaning that the findings were not applicable to the whole ID population.
A small mixed-methods study developed, implemented and evaluated a teaching programme to empower people with ID to better access health care. 113 The study assessed participants’ knowledge, skills and self-efficacy related to accessing health care and improvements were seen compared with scores before the training. Data from the qualitative interviews suggested that the programme has improved decision-making, symptom awareness, understanding of medical procedures, knowledge of how to access primary care, self-efficacy, ability to plan health care and how to formulate health goals. The project was funded by a research grant and it would be difficult to find the money to implement the programme in normal practice. The findings from this pilot project were promising but the sample size was small and there was no follow-up done. Further larger studies would be necessary to determine if the findings were as a result of the project.
An analysis of the general practice patient survey103 investigated which patient groups were more likely to benefit from weekend opening. Patients with ID were found to be less likely to utilise or want weekend opening, so this innovation would be unlikely to improve GP access for this population. The survey had a low response rate of 33%, meaning that it is not reflective of the whole population and potentially has a degree of participation bias; people who felt strongly that they wanted weekend opening hours could potentially have been more likely to reply. The survey was based on self-report data meaning that potentially the population of people with ID could have been higher but individuals might not have reported that they have ID. In addition, the survey included only patients registered with a GP so that patients who did not have a GP or had recently moved practices would not have been invited to participate, meaning that the views of certain populations (e.g. immigrants, people without a permanent home) might not have been considered. Furthermore, the survey was based on self-report data about people’s perceptions of the usefulness of weekend opening not their actual use.
Influencing factors
Influencing factors identified in the innovations to improve access cluster are discussed below and shown in Table 23.
| First author and year of study | Factor | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Staff knowledge/skills | Joint working with LD services | Service delivery model | Uptake | Appointment making | Carer/support role | Relationships with staff | Time | Accessible information | Communication | |
| Adler 200592 | ✓ | |||||||||
| Baxter 200693 | ✓ | ✓ | ||||||||
| Biswas 200594 | ✓ | |||||||||
| Buszewicz 201495 | ✓ | ✓ | ||||||||
| Cassidy 200296 | ✓ | ✓ | ||||||||
| Chauhan 201097 | ✓ | |||||||||
| Chauhan 201298 | ✓ | ✓ | ✓ | ✓ | ||||||
| Codling 200799 | ||||||||||
| Cooper 2006101 | ||||||||||
| Cooper 2014100 | ||||||||||
| Dagnan 2018102 | ✓ | ✓ | ||||||||
| Felce 200819 | ||||||||||
| Ford 2015103 | ✓ | |||||||||
| Glover 2013104 | ||||||||||
| Harrison 2005105 | ✓ | ✓ | ||||||||
| Holly 2014106 | ✓ | |||||||||
| Martin 2004107 | ✓ | ✓ | ||||||||
| McConkey 2015108 | ✓ | |||||||||
| Romeo 2009109 | ||||||||||
| Taylor 2014110 | ✓ | |||||||||
| Walmsley 2011111 | ✓ | ✓ | ✓ | |||||||
| Webb 2009112 | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Webb 2009113 | ✓ | |||||||||
Staff knowledge/skills
The importance of health professionals’ knowledge and skills in working with people with ID was apparent in several studies. Staff involved in mainstream services lacked confidence in their skills to effectively deliver services to patients with ID or were aware of the need for further training. This was the case for staff in mainstream IAPT services, general practice staff106,111,112 and optometrists. 92 Training to develop the knowledge and skills of health professionals working with people with ID was found to be more effective when it incorporated clinical practice. 92
Joint working with learning disability services
Joint working with LD services was highlighted in three studies. A project to improve access involved practices producing a practice development plan that included reasonable adjustments for people with ID, which was developed by the practices working with the community LD team. 112 One study investigated a joined-up approach involving primary care and community and specialist LD team staff, which improved access to mainstream health care for people with ID. 105 An older study introduced health checks performed by a consultant psychiatrist in ID, a GP and a community intellectual disability nurse at the GP’s surgery. They detected health conditions and were favourably received by people with ID and their carers. 96
Service delivery model
One influencing factor highlighted in this topic was the challenge of identifying who was actually eligible for health checks. 111 A project to improve service access for people with ID introduced a LD register as part of a practice development plan. 112 Read codes were used for specific conditions to help identify patients. 95 However, another study found that there could be variation in coding and coding could be based on social assessment not medical need with no clarity about purpose or value. 98
Another important influencing factor for practices in introducing health checks was financial incentivisation. 95,97,98
Uptake
The uptake of health checks was affected by uncertainty about who was actually eligible. 111 Read codes in GP records for specific conditions could help to identify patients eligible for checks. 95 Two studies93,108 considering uptake found that people in nursing or residential homes were more likely to have health checks, which could be because their eligibility for checks was easier to determine than that for people living in family homes.
Poor uptake could also be associated with problems making an appointment; potential issues were the way patients were invited, poor interagency communication and patients’ individual communication difficulties. 98 The study attempted to make reasonable adjustments for people with ID, including telephoning to arrange an appointment, offering health check appointments at home and telephoning to remind patients of their appointment. 98
One training programme improved the knowledge and confidence of people with ID to access primary care, which could potentially lead to increased uptake of services. 113
Appointment making
As discussed in Uptake, a telephone call to arrange an appointment, the option of an appointment at home and a telephone call reminder about the appointment can help make the appointment process easier. 98
Making appointments to attend other services could also be problematic; the referral and access process for IAPT could be challenging for people with ID.
Companion/carer/support worker role
Input from carers to health review was important. 107
Staff working in care homes need knowledge about pain assessment and management. 110
Relationships with staff
For people with ID, continuity of health professionals was important. 98
Time
Flexible GP appointments could also be introduced as a reasonable adjustment; in one study flexible appointments included offering the first appointment of the clinic to reduce waiting time and offering double-length appointments. 112 Booking double appointments for health reviews ensured that people with ID were not rushed. 107 Providing a quiet waiting area could help people with ID and stop them from getting anxious. 112
One-to-one counselling provides time for discussion and helps identify reasons for low uptake of cervical screening and improved actual uptake by a small percentage. 94
Accessible information
Accessible information is important to people with ID. Reasonable adjustments introduced in one study included a board with staff photographs, visual aids in consultation rooms and an easy-to-read practice leaflet. 112
Communication
Communication can be difficult for people with ID; therefore, if health checks can identify common hearing and visual problems that can affect communication, and if these are treated, this could help people with ID to communicate with primary care health professionals. 93
Grey literature
The mapping review grey literature searches identified 28 reports; following full-text inspection, three reports were included. Of these, only one report comprised a research study,30 using mixed qualitative methods. The remaining two reports, published by Public Health England and using quantitative methods29 and case studies,122 provide only short sections that are relevant to this review.
The Mencap-led Pharmacy Project123 aimed to identify issues reported by pharmacists, people with disabilities and their professional and family carers in accessing pharmacy services. A significant limitation of this study for our review is that the scope was broader than ID, including any disability. This suggests that caution should be used in interpreting the findings as some reported barriers to access, for example, physical barriers, may not be specific to people with ID. Issues that were identified within pharmacies included unclear signage in the pharmacy and lack of a quiet room. One-third of respondents stated that pharmacists could be more patient, and that some attitudes about disabled people were negative. There were reported limitations in pharmacists’ knowledge about disabled people. Health information was reported as too complex or difficult to read. Disabled people may also be unable to adequately describe their symptoms. Pharmacists reported that health review medication may not be checked by a GP and therefore may go unchanged for a considerable time. There was a reported lack of communication between GPs and pharmacists, which leads to communication gaps between the pharmacist and families and/or other service providers. Pharmacists reported that they need to build up trust, assist families’ understanding of the situation and provide information.
Making reasonable adjustments to encourage the uptake of screening for cervical, breast and bowel cancer122 provides a number of innovative case studies. As cervical cancer screening is the only screening programme relevant to this review (being carried out in primary care), the data we have included from the report are limited. One intervention provides resources to help women with ID make informed choices about cervical screening, including a 20-page, easy-to-read guide and a ‘smear test’ film. Another innovation is the introduction of a screening liaison nurse to work with GPs to identify eligible women with ID and also to ensure that they receive the appropriate information. This role is not confined to cervical screening and as yet there are no reported outcomes relating to changes in cervical screening uptake. The role does, however, appear to have made a positive impact on the uptake of breast screening. A Quality Innovation Productivity and Prevention Plan has resulted in statistically significant (no figures supplied) increases in the use and recording of mental capacity and best interest assessments across a range of GP practices; however, there are currently no data on the effects on screening rates. Similarly, implementation of the ‘screening uptake for vulnerable groups’ cluster of the Accelerate, Coordinate, Evaluate (ACE) programme (60 projects, eight clusters) as yet has no reported outcomes.
Initiation and uptake of health checks29 is discussed briefly using quantitative data. The report highlights the increase in registration of people with ID in GP practices from 2008 to 2015, when 252,446 people of all ages were on LD registers. A total of 197,451 of those registered were eligible for an intellectual disability health check and 124,785 were reported to have been carried out (63%) compared with 25,000 in 2008.
Summary
A very small body of data has been identified from grey literature that provides evidence relevant to this review. Only one report comprises a research study and it is limited by its broader disability scope. However, it does provide some insight into the views and experiences of people with disabilities accessing pharmacies as well as pharmacists’ views of their own potential to make adjustments. Further adjustments are being made across a range of conditions and screening programmes, although outcomes are generally not yet reported. One exception is for cervical screening, in which there is limited evidence for initiatives that specifically aim to identify women with ID and ensure that they are made aware of the programme and its implications in an appropriate format. Finally, there is evidence that GP registration for people with ID and uptake of annual health checks, initiated in 2007, are both increasing each year.
Chapter 7 Discussion
Main findings
The literature search identified 82 publications describing 80 studies that met the reviews inclusion criteria. The included studies were published between 2002 and 2018. Three items of grey literature were included. 29,30,122
The overall strength of the evidence base is weak. The methodological quality of the included studies was generally poor, which limits the strength of any findings from the review. The studies generally had small sample sizes and reported short-term outcomes.
The majority of studies focused on studies about access to services provided in or by general practices, a small number of studies referred to IAPT services, optical services, and those provided by sexual health clinics71 and dental clinics. No studies explored access to pharmacy services, NHS 111, and out-of-hours or walk-in general practice centres. Individual studies explored particular settings, including rural health, deprived communities and temporary accommodation for the homeless.
Given the variation and changes in service provision over the time period covered by this review and across different geographical areas, it is difficult to get a clear picture about service provision nationally.
The review found very little new high-quality evidence to add to the review by Alborz et al. in 2003. 21 Some innovations, such as annual health checks, have increased access to and uptake of some health services but not all of those who are eligible for the checks receive them and there is some evidence that actions taken are preferentially directed towards those services that bring financial benefit to the service provider. Some high-profile innovations that have taken place across primary care, since the review by Alborz et al. ,21 have been widely publicised, such as extended opening hours; however, these have not benefited people with ID. 103
The review conceptualised access in three stages: (1) identifying need, (2) accessing services and (3) interacting during a consultation. These three stages reflect a simple pathway to access; however, factors identified from the literature that influenced these stages were common to more than one stage and, in most cases, relevant to all three stages. Influencing factors are considered below.
The review identified the following key factors that influenced access and were cross-cutting across the stages of access reported in the literature:
-
availability of support – from social service providers, relatives and other paid and unpaid supporters
-
consistent person or people providing care or support – enabled a long-term relationship between the person with ID and their supporters, and communication between social service providers, relatives, other supporters and health professionals
-
adequate training for supporters – training for social service providers and all paid supporters to identify health needs
-
effective communication within services – close teamworking, sharing knowledge of the client, and consistency of staff team
-
effective communication between services – mainstream health services, specialist ID services, day services and residential services, family carers, and other formal carers and supporters (e.g. personal assistants, advocates)
-
accurate record keeping
-
communication skills of all who come into contact with people with ID – value, respect, ability to tailor information to the abilities of the individual with ID
-
appropriate use of accessible resources – including use of pain recognition and communication tools
-
time – to communicate and work effectively with people with ID.
Availability of support from a consistent person or people with adequate training in monitoring and addressing the health needs of people with intellectual disabilities
The role of carers and supporters is pivotal and studies reported the importance of long-term relationships to enable staff and supporters to recognise and monitor health-related changes in verbal and non-verbal behaviours. Supporters needed an awareness of health needs relevant to the general population regardless of intellectual disability, as well as those related to any underlying cause of ID, associated comorbidity or polypharmacy. In addition, they needed knowledge of the health needs of a particular individual, for example related to family history of disease, living environment and lifestyle. Several authors reported that high turnover of staff meant that training was time-consuming and of limited value. 86,120 Lack of knowledge about potential health risks and services available leads to unmet health needs and untreated ill health. Powrie84 found that the high turnover of social care staff contributed to poor communication between primary and social care and Tuffrey-Wijne86 found that reliance on agency staff put more pressure on permanent staff who were able to provide consistency of care.
The evidence base demonstrated that people with ID and their carers also valued being able to see the same health professional, and this led to trusting relationships that built up over time. However, health professionals needed greater awareness of the needs of someone with ID and of communication strategies and aids to facilitate good communication during consultations. 110 The opportunity to see the same health professional over time can help reduce anxiety for the person with ID and help the health professional to develop knowledge of an individual, their living circumstances and health needs and the communication skills to work with them effectively. Training can develop health professionals’ specialist knowledge of ID and potentially improve their skills in working with people with ID. Training that includes clinical practices may be more beneficial. 92
Studies found that carers and supporters experienced tension between their role in promoting the autonomy of an individual with ID and promoting good health or, in some cases, safeguarding when a decision had the potential to be harmful to health. 84,90 In some cases, the decision was referred to as a ‘best interest’ decision but there was little clarity about how these decisions were made and some concern that decisions were influenced by the interests of carers or relatives as well as the interests of the individual. This was of particular concern in relation to contraception and to end-of-life care when there are significant emotional and practical consequences for carers and relatives. Clarity about the process and monitoring of best interest decisions is needed.
People are long-term users of services and their past experience has an impact on access. The PPI showed that adults and, particularly, their carers feel that they have to fight for the services that they are accessing. In addition, there is a fear of health professionals making blood tests or dental procedures difficult.
Effective communication within and between services
Communication within services was particularly important to monitor and identify health-related changes in verbal and non-verbal behaviour when people with ID were unable to communicate their health needs verbally. There was evidence that people who use verbal communication did not necessarily disclose health needs and so monitoring is important. There was some uncertainty about whose role it is to monitor health between day and residential care services as both clearly have a role in monitoring and communicating any health concerns when an individual is unable or unlikely to do so for themselves.
Communication between mainstream health services and specialist ID services is important to enable mainstream services to meet the needs of people with ID. The evidence base contained limited evidence of joint working between health professionals and specialist ID staff, and health professionals were not always aware that there was support available from the community LD teams. Similarly, it was important to have good communication between social care and health services and to include informal carers and relatives in this. There was evidence that in some cases families and carers felt that their knowledge of the individual with ID was undervalued or disregarded by health professionals. There was also evidence that cultural differences between organisations had an impact on communication and care for people with ID and that families had to negotiate these differences to access health care.
Accurate record-keeping
Studies highlighted the importance of maintaining accurate health records43,89,99,118 to facilitate communication within and between services when appropriate. One study43 highlighted that some care staff may lack the literacy and numeracy skills to maintain accurate health records. A small number of studies discussed patient-held records such as health passports but there were concerns about how these are used and that they are not completed accurately by all health professionals.
Communication skills including use of accessible information
There was some evidence that communication was important to enable people to make appointments. 52,69,83,98 Sometimes information provided in letters inviting patients to attend for health checks or screening appointments was not understood by the recipient. Some people did not communicate over the telephone and so visited the service to make an appointment instead. Telephone triage appointments were difficult for some patients.
There was considerable evidence highlighting that people with ID want to be treated with dignity and respect by everyone they come into contact with at a service, and that this is not always the treatment they receive. 73,79,80,82,83,91,107,112 The literature suggests that this means talking to the individual first rather than anyone accompanying them to the appointment, although clearly the accompanying person may facilitate this communication. People want clear verbal information tailored to their abilities and supported by information in a format that is accessible to them. There was evidence that some service providers were not confident to communicate with people with ID and joint working with community ID teams could facilitate this. Being able to see the same person at repeat appointments was important to practitioners to develop person-specific knowledge of communication abilities and preferences, and to patients and carers because it reduced anxiety and fostered relationship building and the development of trust. The literature found that to help people with ID interact during a consultation, health professionals needed to give the patient adequate time. Some clinics offered double appointments for people with ID.
Many of the studies discussed the importance of accessible information for people with ID and highlighted that some service providers were not aware of accessible resources that are widely available. 50,52,66,73–75,80,81,83,89,91,112 Provision of accessible information tailored to the abilities of the individual was particularly important to support decision-making, including consent to procedures such as blood tests and cervical screening. There was evidence that consent is a particularly contentious issue and that there is a lack of clarity about actions to support capacity, the process of assessing capacity and the correct action to take when an individual is deemed to lack capacity. 75,78,81,84–90 The evidence suggests that there is a tension between promoting individual autonomy and the right to make decisions, and safeguarding, when people may make choices that are detrimental to their health possibly because they lack accessible information and/or capacity to weigh the future implications of their choices, and that staff were uncertain about how to manage this tension. There was some evidence to suggest that health professionals were basing best interest decisions on the interests of relatives and carers when they should be based on the best interests of the individual alone.
Patient and public involvement contribution to the review
The PPI consultation raised some issues that were not covered in the literature. Formal support staff spoke about the difficulties of supporting people with milder ID who lived independently and had limited support. They spoke about the difficulty in supporting access to services, for example when screening invitations or text appointment reminders were sent to the client who ignored them and did not inform the support staff. They spoke about the difficulties clients had in responding to automated text appointment reminders and said that these created anxiety because clients did not know if they had responded correctly and so were not sure whether an appointment was confirmed or not. The literature did not refer to text reminders, but our PPI work suggests that these have created a further barrier to access for people with ID. They also discussed pharmacy services. None of the included studies referred to pharmacy services but formal carers talked about the difficulties and the danger posed when clients had the ability to go to a pharmacy themselves to request a prescription but did not explain about other medications they were taking or could not understand the instructions they were given about the new medication. This is clearly an area that warrants further exploration. PPI consultations on the findings and recommendations from the review are included in Chapter 8.
Considering these results in relation to the recommendations made in the Learning Disabilities Mortality Review Programme Second Annual Report and the UK government response to this review
Since the Alborz et al. review,21 there has been increasing attention to the preventable deaths of people with ID. The scale of these deaths led to a confidential inquiry into premature deaths of people with LDs [Confidential Inquiry into premature deaths of people with learning disabilities (CIPOLD)], which reported that deaths from causes amenable to good-quality health care were significantly more common for people with ID than for those in a comparator group. 13 The inquiry was across all health services and did not specifically focus on direct access; however, the findings have implications for all those who have a role in ensuring that people with ID can access high-quality health care. The confidential inquiry led to an annual Learning Disabilities Mortality Review (LeDeR). The Learning Disabilities Mortality Review (LeDeR) Programme Annual Report December 2017124 (the second annual LeDeR report) listed nine recommendations, which resonate closely with the influencing factors identified from the literature. The influencing factors identified in this review of the literature have been mapped to the recommendations from the second annual LeDeR report124 and the actions proposed in the UK government’s response to the recommendations in the LeDeR report125 (Table 24).
| Influencing factors | LeDeR recommendation | Action proposed in UK government’s response to LeDeR |
|---|---|---|
|
1. Strengthen collaboration and information sharing, and effective communication, between different care providers or agencies |
|
|
2. Push forward the electronic integration (with appropriate security controls) of health and social care records to ensure that agencies can communicate effectively, and share relevant information in a timely way |
|
|
3. Health action plans developed as part of the LDs annual health check should be shared with relevant health and social care agencies involved in supporting the person (either with consent or following the appropriate MCA decision-making process) |
|
|
4. All people with LDs with two or more long-term conditions (related to either physical or mental health) should have a local, named health-care co-ordinator |
|
|
5. Providers should clearly identify people requiring the provision of reasonable adjustments, record the adjustments that are required and regularly audit their provision |
|
|
6. Mandatory LD awareness training should be provided to all staff, delivered in conjunction with people with LDs and their families |
|
|
7. There should be a national focus on pneumonia and sepsis in people with LDs, to raise awareness about their prevention, identification and early treatment |
|
|
8. Local services strengthen their governance in relation to adherence to the MCA, and provide training and audit of compliance ‘on the ground’ so that professionals fully appreciate the requirements of the Act in relation to their own role |
|
| Not applicable | 9. A strategic approach is required nationally for the training of those conducting mortality reviews or investigations, with a core module about the principles of undertaking reviews or investigations, and additional tailored modules for the different mortality review or investigation methodologies |
Strengths and limitations
The review process
We conducted two large searches for the mapping and targeted review and extensive grey literature searching. However, time constraints meant that it was not possible to do all of the reference checking of reviews described in the protocol (see Report Supplementary Material 2). However, a recent Health Services and Delivery Research review129 found that searching reviews for UK studies was time-consuming because of poor reporting and tended to find only older relevant studies.
There was no agreed pre-existing framework for analysis of the studies and the clusters developed from the literature. The clusters were reflective of the patient pathway and enabled us to focus on the different steps in the pathway. In addition, the clusters being reflective of the patient pathway would make them familiar to the readers. A disadvantage of the clusters is that it imposed a structure that was arbitrary and could mean that issues across the different clusters were not considered.
The evidence base
The methodological quality of the included studies was generally poor, which limits the strength of any findings from the review. The studies generally had small sample sizes and short-term outcomes.
The body of literature included in the review was heterogeneous in nature. Studies researched adults across the whole spectrum of ID, adults living in their own home cared for by formal or informal carers or in residential homes. The differences in study populations made comparing results from different studies difficult and findings from individual studies are therefore potentially not applicable to all adults with ID.
Chapter 8 Conclusions
Implications for health care
The review has identified a number of potential implications for health care or service delivery. The methodological quality of the included studies was generally poor, which limits the strength of any findings from the review.
Consistency of care is important and staff retention is a key aspect of this. Adults with ID are looked after by family or paid carers in their homes or in residential homes. There is a high turnover of paid carers, meaning that it can be difficult for carers to develop a relationship with adults with ID that can enable them to realise when adults with ID are ill or in pain and when they need to access services. Carers who know the adult with ID well can help them in consultations with their GP or other HCPs by providing background health information and helping the adult explain themselves. Improving the retention of paid carers working with people with ID, for example, by fostering a culture that values the quality rather than the speed of care, has the potential to improve access to primary and community health care.
Training of health professionals is important to improve their knowledge of the needs of people with ID and their skills in working effectively with this population. This training could usefully include an awareness of the availability and role of specialist LD services and of the need to make reasonable adjustments to ensure that people with ID receive equitable care. Health professionals need to be able to fulfil the requirements of the Mental Capacity Act 2005 (MCA)128 in relation to consent.
Employers have a responsibility to promote and prioritise staff training to ensure that social care staff and other paid carers have an up-to-date knowledge of health needs and services available to address those needs.
Action is needed to improve collaboration and joint working across funding and organisational boundaries. The failure of services to work together has been a factor contributing to the preventable deaths of people with ID.
Communication with someone with ID needs to be appropriate to their abilities. This may mean using accessible materials and resources to augment verbal communication and allowing extra time to communicate and to assess whether or not information has been understood. Appointments with the same health professional can facilitate communication over time and the opportunity to develop trusting relationships with health professionals may facilitate discussions about health needs and possible actions to take to maintain or improve health. Improved communication also includes ensuring that all information, including signs and notices, is clear and that any materials are available in an accessible format. Written communication, for example invitations to attend for screening, is particularly important and where possible information sent by post will include some mechanism to check that it has been received and understood to the extent of an individual’s capabilities, while ensuring patient confidentiality.
Action is needed to improve compliance with the MCA. 128 This includes practice guidance about how to adhere to the MCA in situations where capacity to consent is lacking, and monitoring to ensure that practices adhere to this guidance. Similarly, guidance about the process of determining best interest and monitoring of this process is needed.
Accurate record keeping at many different levels is important to ensure that information is available within services and between services. Comprehensive and up-to-date practice registers of people with ID facilitate access to annual health checks and enable recording of any reasonable adjustments needed to access care. Accurate health records held by residential care staff facilitate identification of health need and access to services, for example routine dental health screening. Action to improve recording and use of this information in practice is needed.
Patient and public involvement feedback on the implications for health care
Discussions about the implications for health care raised in the report were wide-ranging and energetic. The findings and suggested implications resonated with participants who agreed that they were relevant and important. A summary of key points from the discussions is given below.
-
Improving retention of carers in order to provide consistency of care is important. There should be a career structure for carers. This should recognise when carers have undergone training and are experienced. These carers should be able to earn more money because they have been trained and are more experienced than other carers. Caring should be valued more highly, which means paying carers more for the work they do.
-
People with LDs should be involved in delivering training to HCPs. When this happens the training is stronger and more effective.
-
When talking to someone with LDs, check that the person has understood the information. For example someone with LDs may not understand how often to take their medication if they are told to take it daily. It is important to check that the person understands that this means they should take it once a day.
-
Communication within and between services is important because some people with LDs have multiple health problems and they should be treated holistically taking into account all their health problems and their living arrangements. There has to be someone who knows them well who can communicate between services and organisations, and co-ordinate all their care.
-
Families feel they have to fight for services when services should be proactive in offering services to people who need them.
Recommendations for research
The UK government’s response to the LeDeR Programme Second Annual Report, published in September 2018, details actions to address recommendations from the LeDeR report, and these actions also resonate with the recommendations for practice from this literature review (see Table 24). However, research is needed to evaluate whether these actions are effective at improving access to health care for people, to understand the barriers that prevent actions from being implemented and used in practice and to develop effective interventions to improve staff training and retention, communication skills, collaboration and joined-up working and record-keeping. Recommendations for research are based on the evidence reviewed and are therefore limited by the availability of research. Given the paucity and the poor quality of research available, these recommendations are prioritised pragmatically according to their potential impact on the future health of people with ID rather than by the strength of the evidence supporting them. Fifteen years after the original review by Alborz et al. ,21 the evidence remains patchy and of poor quality because of the complexity of the population, the settings and the interventions under scrutiny and the ethical, logistical and financial challenges these present for randomised controlled designs, seen as the ‘gold standard’ for evaluating health care. 130
-
Creative study designs that are feasible and ethical to implement and that meaningfully include people with ID are needed to address the complex issues highlighted in this review. The value of these designs should be recognised rather than seen as diminishing the quality of the study.
-
Given the range of abilities, living circumstances, support and other resources available within the population of people with ID, future studies should provide greater clarity about participants, including their abilities and circumstances relevant to the subject of the research. Further research is needed to identify how to support access for people in different circumstances with different abilities and with different levels of support and other resources, and across the population. For example, people with mild ID who live independently with little or no support are likely to have different abilities and, therefore, require different support to those people with moderate or severe ID living with higher levels of support. All studies should describe participants, perhaps in terms of living circumstances and relevant support needs, to enable practitioners to determine the extent to which findings are likely to be transferable to another population and for researchers to make meaningful comparisons across different studies.
-
Studies are needed to develop and evaluate solutions aiming to improve communication within services and across funding and organisational boundaries.
-
Studies are needed to explore how training can involve people with ID and improve the knowledge, attitudes and skills of those who work with and for people with ID, and to evaluate this training in terms of the difference it makes to the health of people with ID.
-
Research is needed to analyse the barriers to effectively implementing the MCA and to identify potential solutions to overcome these in order to improve compliance with it.
-
Research is needed to develop and evaluate interventions to improve the retention of care staff in order to provide consistency of care.
-
Interventions are needed to support carers to negotiate the tension between promoting autonomy and safeguarding against risk of harm when supporting individuals who have some capacity to make autonomous decisions. This might include frameworks to support decision-making or theoretical work. People with LDs should be involved in developing these interventions.
-
The majority of included studies addressed GPs’ services; therefore, we recommend that research studies investigate access to other primary care services, for example nurses, pharmacists, opticians, NHS 111 and IAPT, with the aim of developing reasonable adjustments, interventions and service innovations to improve access.
-
Limited research was identified around other axes of difference [lesbian, gay, bisexual, transgender, and queer (or questioning) (LGBTQ), Black, Asian and minority ethnic (BAME), homelessness, etc.], further research is needed into access to health care for people with ID from communities that are already marginalised.
This review focused on access to mainstream primary and community care services and, therefore, did not include specialist community health-care teams for people with learning disabilities (CTALDs) and similar services for young people (aged 16–25 years). These specialist services accept referrals directly from people with ID and their carers and, therefore, a future systematic review of access to these services is needed to provide a full picture of access to community services for people with ID.
Patient and public involvement feedback on the recommendations for research
Discussions about the recommendations for future research centred on the importance of involving people with LDs in all training about working with people with LDs. This may reflect the fact that the PPI group included self-advocates who regularly contributed to training for people working with people with LDs. They also expressed frustration at the lack of progress made despite the research that has been undertaken since the Alborz et al. 21 review in 2003. The recommendations have been changed to reflect this feedback.
Acknowledgements
We are grateful to the Families Lobbying and Advising (FLASh) carers group, Royal Mencap’s ‘Treat Me Well’ group, staff employed by Mencap support unit, SpeakUp Self Advocacy and members of the Sheffield Health Services and Delivery Research Evidence Synthesis Centre PPI Group for their contributions. We thank Veronica Fibisan for help with referencing on EndNote version X8 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA]. We also thank Louise Preston for commenting on the initial draft.
Contributions of authors
Anna Cantrell (https://orcid.org/0000-0003-0040-9853) (Research Associate in Health Economics and Decision Science) was responsible for project co-ordination, protocol development for the mapping and targeted systematic review, study selection for the mapping and targeted systematic review, data extraction for the mapping and targeted systematic review, quality assessment for the targeted systematic review and report writing for the mapping and targeted systematic review.
Elizabeth Croot (https://orcid.org/0000-0002-3666-6264) (Senior Research Fellow in Health Services Research) was responsible for protocol development for the mapping and targeted systematic review, study selection for the mapping and targeted systematic review, data extraction for the mapping and targeted systematic review, quality assessment of the targeted systematic review, report writing for the mapping and targeted systematic review and subject expertise.
Maxine Johnson (https://orcid.org/0000-0003-0850-234X) (Research Fellow in Public Health) was responsible for the protocol development for the mapping and targeted systematic review, study selection for the mapping and targeted systematic review, data extraction for the mapping and targeted systematic review and report writing for the mapping review.
Ruth Wong (https://orcid.org/0000-0002-4536-4794) (Information Specialist in Health Economics and Decision Science) was responsible for information retrieval for the mapping and targeted review.
Duncan Chambers (https://orcid.org/0000-0002-0154-0469) (Research Fellow in Public Health) was responsible for data extraction for the targeted systematic review, quality assessment for the targeted systematic review and report writing for the targeted systematic review.
Susan K Baxter (https://orcid.org/0000-0002-6034-5495) (Senior Research Fellow in Public Health) was responsible for data extraction and quality assessment for the targeted systematic review and co-ordinated the PPI meetings.
Andrew Booth (https://orcid.org/0000-0003-4808-3880) (Reader in Evidence-based Information Practice) was responsible for protocol development for the mapping and targeted systematic review, report writing for the mapping review and methodological expertise.
All authors commented on drafts of the report.
Data-sharing statement
No new data have been created in the preparation of this report and, therefore, there is nothing available for access and further sharing. All queries should be submitted to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Hatton C, Glover G, Emerson E, Brown I. Learning Disabilities Observatory. People With Learning Disabilities in England 2015: Main Report 2016.
- Brown M, MacArthur J, McKechanie A, Hayes M, Fletcher J. Equality and access to general health care for people with learning disabilities: Reality or rhetoric?. J Res Nurs 2010;15:351-61. https://doi.org/https://doi.org/10.1177/1744987110370019.
- Emerson E, Baines S, Allerton L, Welch V. Health Inequalities and People with Learning Disabilities in the UK: 2010. Durham: Improving Health and Lives Learning Disabilities Observatory; 2010.
- Straetmans JM, van Schrojenstein Lantman-de Valk HM, Schellevis FG, Dinant GJ. Health problems of people with intellectual disabilities: the impact for general practice. Br J Gen Pract 2007;57:64-6.
- Michael J, Richardson A. Healthcare for all: the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. Tizard Learn Disabil Rev 2008;13:28-34. https://doi.org/10.1108/13595474200800036.
- Starling S, Willis A, Dracup M, Burton M, Pratt C. Right to sight: accessing eye care for adults who are learning disabled. J Intellect Disabil 2006;10:337-55. https://doi.org/10.1177/1744629506070057.
- Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M. Fair Society, Healthy Lives. The Marmot Review. London: The Marmot Review; 2010.
- Emerson E, Hatton C, Baines S, Robertson J. The physical health of British adults with intellectual disability: cross sectional study. Int J Equity Health 2016;15. https://doi.org/10.1186/s12939-016-0296-x.
- Tyrer F, McGrother C. Cause-specific mortality and death certificate reporting in adults with moderate to profound intellectual disability. J Intellect Disabil Res 2009;53:898-904. https://doi.org/10.1111/j.1365-2788.2009.01201.x.
- Mencap . Death By Indifference 2007.
- Mencap . Death By Indifference: 74 Deaths and Counting. A Progress Report 5 Years On 2012.
- Mazars LLP . Independent Review of Deaths of People With a Learning Disability or Mental Health Problem in Contact With Southern Health NHS Foundation Trust April 2011 to March 2015 2015. www.england.nhs.uk/south/wp-content/uploads/sites/6/2015/12/mazars-rep.pdf (accessed 27 November 2018).
- Heslop P, Blair P, Fleming P, Hoghton M, Marriott A, Russ L. Confidential Inquiry Into Premature Deaths of People With Learning Disabilities (CIPOLD). Bristol Norah Fry n.d. https://rcpsych.ac.uk/pdf/ConfidentialInquiryintoprematuredeathsfullreport.pdf (accessed 27 November 2018).
- Heslop P, Hoghton M. The learning disabilities mortality review (LeDeR) programme. Br J Gen Pract 2018;68. https://doi.org/10.3399/bjgp18X697313.
- Allerton L, Emerson E. British adults with chronic health conditions or impairments face significant barriers to accessing health services. Public Health 2012;126:920-7. https://doi.org/10.1016/j.puhe.2012.08.003.
- Great Britain . Equality Act 2010 2010.
- Department of Health and Social Care . Valuing People Now: A New Three-Year Strategy for People With Learning Disabilities 2009.
- Turk V, Kerry S, Corney R, Rowlands G, Khattran S. Why some adults with intellectual disability consult their general practitioner more than others. J Intellect Disabil Res 2010;54:833-42. https://doi.org/10.1111/j.1365-2788.2010.01312.x.
- Felce D, Baxter H, Lowe K, Dunstan F, Houston H, Jones G, et al. The impact of checking the health of adults with intellectual disabilities on primary care consultation rates, health promotion and contact with specialists. J Appl Res Intellect Disabil 2008;21:597-602. https://doi.org/10.1111/j.1468-3148.2008.00432.x.
- Great Britain . Health and Social Care Act 2012 2012. https://doi.org/10.12968/eqhe.2012.1.7.5.
- Alborz A, McNally R, Swallow A, Glendinning C. From the Cradle to the Grave: A Literature Review of Access to Healthcare for People with Learning Disabilities Across the Lifespan. London: National Coordinating Centre for the Service Delivery and Organisation; 2003.
- Gulliford M, Morgan M, Hughes D, Beech R, Hughes D, Figeroa-Munoz J, et al. Access to Health Care: Report of a Scoping Exercise for the National Co-Ordinating Centre for NHS Service Delivery and Organisation R and D (NCCSDO) 2001.
- James KL, Randall NP, Haddaway NR. A methodology for systematic mapping in environmental sciences. Environ Evid 2016;5. https://doi.org/10.1186/s13750-016-0059-6.
- Alborz A, McNally R, Glendinning C. Access to health care for people with learning disabilities in the UK: mapping the issues and reviewing the evidence. J Health Serv Res Policy 2005;10:173-82. https://doi.org/10.1258/1355819054338997.
- McNally R, Alborz A. Developing methods for systematic reviewing in health services delivery and organization: an example from a review of access to health care for people with learning disabilities. Part 1. Identifying the literature. Health Info Libr J 2004;21:182-92. https://doi.org/10.1111/j.1471-1842.2004.00512.x.
- Faculty of Dental Surgery . Clinical Guidelines and Integrated Care Pathways for the Oral Health Care of People With Learning Disabilities 2012.
- Public Health England (PHE) . Health Checks for People With Learning Disabilities: Including Young People Aged 14 and Over, and Producing Health Action Plans 2015.
- Public Health England (PHE) . Making Reasonable Adjustments to Cancer Screening 2016.
- Public Health England (PHE) . People With Learning Disabilities in England 2015: Main Report 2016.
- Hatton C, Glover G, Emerson E, Brown I. the Disability Partnership . Evaluation Report of the 2015–16 Mencap-Led Pharmacy Project 2016.
- Ayiku L, Levay P, Hudson T, Craven J, Barrett E, Finnegan A, et al. The MEDLINE UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID MEDLINE. Health Info Libr J 2017;34:200-16. https://doi.org/10.1111/hir.12187.
- Ptomey LT, Gibson CA, Lee J, Sullivan DK, Washburn RA, Gorczyca AM, et al. Caregivers’ effect on weight management in adults with intellectual and developmental disabilities. Disabil Health J 2017;10:542-7. https://doi.org/10.1016/j.dhjo.2017.02.001.
- Beacroft M, Dodd K. Pain in people with learning disabilities in residential settings – the need for change. Br J Learn Disabil 2010;38:201-9. https://doi.org/10.1111/j.1468-3156.2009.00593.x.
- Beacroft M, Dodd K. ‘I Feel Pain’– audit of communication skills and understanding of pain and health needs with people with learning disabilities. Br 2011;39:139-47. https://doi.org/10.1111/j.1468-3156.2010.00640.x.
- Bland R, Hutchinson N, Oakes P, Yates C. Double jeopardy? Needs and services for older people who have learning disabilities. J Learn Disabil 2003;7:317-38. https://doi.org/10.1177/1469004703074002.
- Bollard M. Health promotion and intellectual disability: listening to men. Health Soc Care Community 2017;25:185-93. https://doi.org/10.1111/hsc.12291.
- Donovan J. Learning disability nurses’ experiences of being with clients who may be in pain. J Adv Nurs 2002;38:458-66. https://doi.org/10.1046/j.1365-2648.2002.02207.x.
- Findlay L, Williams AC, Scior K. Exploring experiences and understandings of pain in adults with intellectual disabilities. J Intellect Disabil Res 2014;58:358-67. https://doi.org/10.1111/jir.12020.
- Findlay L, Williams AC, Baum S, Scior K. Caregiver experiences of supporting adults with intellectual disabilities in pain. J Appl Res Intellect Disabil 2015;28:111-20. https://doi.org/10.1111/jar.12109.
- Hanna LM, Taggart L, Cousins W. Cancer prevention and health promotion for people with intellectual disabilities: an exploratory study of staff knowledge. J Intellect Disabil Res 2011;55:281-91. https://doi.org/10.1111/j.1365-2788.2010.01357.x.
- McCarthy M. Contraception and women with intellectual disabilities. J Appl Res Intellect Disabil 2009;22:363-9. https://doi.org/10.1111/j.1468-3148.2008.00464.x.
- McShea L, Fulton J, Hayes C. Paid support workers for adults with intellectual disabilities; their current knowledge of hearing loss and future training needs. J Appl Res Intellect Disabil 2016;29:422-32. https://doi.org/10.1111/jar.12201.
- Northway R, Holland-Hart D, Jenkins R. Meeting the health needs of older people with intellectual disabilities: exploring the experiences of residential social care staff. Health Soc Care Community 2017;25:923-31. https://doi.org/10.1111/hsc.12380.
- Turk V, Khattran S, Kerry S, Corney R, Painter K. Reporting of health problems and pain by adults with an intellectual disability and by their carers. J Appl Res Intellect Disabil 2012;25:155-65. https://doi.org/10.1111/j.1468-3148.2011.00642.x.
- Walker C, Beck CR, Eccles R, Weston C. Health inequalities and access to health care for adults with learning disabilities in Lincolnshire. Br J Learn Disabil 2016;44:16-23. https://doi.org/10.1111/bld.12104.
- Willis DS. Inconsistencies in the roles of family-and paid-carers in monitoring health issues in people with learning disabilities: some implications for the integration of health and social care. Br J Learning Disabil 2015;43:24-31. https://doi.org/10.1111/bld.12082.
- Wilson C, Mansell I. Access to health and social care services and information. Learn Disabil Pract 2010;13:32-8.
- Young AF, Naji S, Kroll T. Support for self-management of cardiovascular disease by people with learning disabilities. Fam Pract 2012;29:467-75. https://doi.org/10.1093/fampra/cmr106.
- Devik SA, Hellzen O, Enmarker I. ‘Picking up the pieces’ – Meanings of receiving home nursing care when being old and living with advanced cancer in a rural area. Int J Qual Stud Health Well-Being 2015;10. https://doi.org/10.3402/qhw.v10.28382.
- Ali A, Scior K, Ratti V, Strydom A, King M, Hassiotis A. Discrimination and other barriers to accessing health care: perspectives of patients with mild and moderate intellectual disability and their carers. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070855.
- Allgar V, Mir G, Evans J, Marshall J, Cottrell D, Heywood P, et al. Estimated prevalence of people with learning disabilities: template for general practice. Br J Gen Pract 2008;58:423-8. https://doi.org/10.3399/bjgp08X299272.
- Black D. Improving access to care for the learning disabled. Pract Nurs 2004;15:38-40. https://doi.org/10.12968/pnur.2004.15.1.11956.
- Carey IM, Shah SM, Hosking FJ, DeWilde S, Harris T, Beighton C, et al. Health characteristics and consultation patterns of people with intellectual disability: a cross-sectional database study in English general practice. Br J Gen Pract 2016;66:e264-70. https://doi.org/10.3399/bjgp16X684301.
- Chinn D, Abraham E. Using ‘candidacy’ as a framework for understanding access to mainstream psychological treatment for people with intellectual disabilities and common mental health problems within the English Improving Access to Psychological Therapies service. J Intellect Disabil Res 2016;60:571-82. https://doi.org/10.1111/jir.12274.
- Cooper SA, McConnachie A, Allan LM, Melville C, Smiley E, Morrison J. Neighbourhood deprivation, health inequalities and service access by adults with intellectual disabilities: a cross-sectional study. J Intellect Disabil Res 2011;55:313-23. https://doi.org/10.1111/j.1365-2788.2010.01361.x.
- Doshi M, Burke M, Fiske J. A preliminary investigation into aspects of oral health of Bangladeshi young adults with learning disability in Tower Hamlets. J Disabil Oral Health 2009;10:25-3.
- Jones MC, McLafferty E, Walley R, Toland J, Melson N. Inclusion in primary care for people with intellectual disabilities. J Intellect Disabil 2008;12:93-109. https://doi.org/10.1177/1744629508090982.
- Lennox TN, Nadkarni J, Moffat P, Robertson C. Access to services and meeting the needs of people with learning disabilities. J Learn Disabil 2003;7:34-50. https://doi.org/10.1177/1469004703007001604.
- Lloyd JL, Coulson NS. The role of learning disability nurses in promoting cervical screening uptake in women with intellectual disabilities: A qualitative study. J Intellect Disabil 2014;18:129-45. https://doi.org/10.1177/1744629514528829.
- Lodge KM, Milnes D, Gilbody SM. Compiling a register of patients with moderate or severe learning disabilities: experience at one United Kingdom general practice. Ment Health Fam Med 2011;8:29-37.
- McNally P, McMurray K. Exploration of the dynamic barriers to adults with intellectual disabilities accessing mainstream mental health services. Adv Ment Health Intellect Disabil 2015;9:352-62. https://doi.org/10.1108/AMHID-01-2015-0001.
- Nicholson L, Cooper SA. Access to healthcare services by people with intellectual disabilities: a rural-urban comparison. J Intellect Disabil 2011;15:115-30. https://doi.org/10.1177/1744629511412659.
- Osborn DP, Horsfall L, Hassiotis A, Petersen I, Walters K, Nazareth I. Access to cancer screening in people with learning disabilities in the UK: cohort study in the health improvement network, a primary care research database. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0043841.
- Owens J, Mistry K, Dyer TA. Access to dental services for people with learning disabilities: quality care?. J Disabil Oral Health 2011;12:17-2.
- Pilling RF. Screening for diabetic retinopathy in adults with learning disability: current uptake and adjustments to facilitate equality of access. Br J Learn Disabil 2015;43:62-5. https://doi.org/10.1111/bld.12088.
- Raghavan R, Waseem F. Services for young people with learning disabilities and mental health needs from South Asian communities. Adv Ment Health Learn Disabil 2007;1:27-31. https://doi.org/https://doi.org/10.1108/17530180200700028.
- Redley M, Banks C, Foody K, Holland A. Healthcare for men and women with learning disabilities: understanding inequalities in access. Disabil Soc 2012;27:747-59. https://doi.org/10.1080/09687599.2012.673080.
- Rees G. Increasing access to cancer screening programmes. Learn Disabil Pract 2011;14:14-9. https://doi.org/10.7748/ldp2011.09.14.7.14.c8697.
- Reynolds F, Stanistreet D, Elton P. Women with learning disabilities and access to cervical screening: retrospective cohort study using case control methods. BMC Public Health 2008;8. https://doi.org/10.1186/1471-2458-8-30.
- Russell AM, Bryant L, House A. Identifying people with a learning disability: an advanced search for general practice. Br J Gen Pract 2017;67:e842-e850. https://doi.org/10.3399/bjgp17X693461.
- Williams F, Scott G, McKechanie A. Sexual health services and support: the views of younger adults with intellectual disability. J Intellect Dev Disabil 2014;39:147-56. https://doi.org/10.3109/13668250.2014.899326.
- Wood R, Douglas M. Cervical screening for women with learning disability: current practice and attitudes within primary care in Edinburgh. Br J Learni Disabil 2007;35:84-92. https://doi.org/10.1111/j.1468-3156.2007.00440.x.
- Brown M, Taggart L, Karatzias T, Truesdale M, Walley R, Northway R, et al. Improving diabetes care for people with intellectual disabilities: a qualitative study exploring the perceptions and experiences of professionals in diabetes and intellectual disability services. J Intellect Disabil Res 2017;61:435-49. https://doi.org/10.1111/jir.12369.
- Gates B. The Valued People Project: users’ views on learning disability nursing. Br J Nurs 2011;20:15-21. https://doi.org/10.12968/bjon.2011.20.1.15.
- Goldsmith L, Woodward V, Jackson L, Skirton H. Informed consent for blood tests in people with a learning disability. J Adv Nurs 2013;69:1966-76. https://doi.org/10.1111/jan.12057.
- Hames A, Carlson T. Are primary health care staff aware of the role of community learning disability teams in relation to health promotion and health facilitation?. Br J Learn Disabil 2006;34:6-10. https://doi.org/10.1111/j.1468-3156.2005.00332.x.
- Hebblethwaite A, Hames A, Donkin M, Colman M, Forsyth A. Investigating the experiences of people who have been homeless and are in contact with learning disability services. Learn Disabil Rev 2007;12:25-34. https://doi.org/10.1108/13595474200700020.
- Heyman B, Swain J, Gillman M. Organisational simplification and secondary complexity in health services for adults with learning disabilities. Soc Sci Med 2004;58:357-67. https://doi.org/10.1016/S0277-9536(03)00210-7.
- Jones J, Kemp K. Down syndrome: exploring the knowledge, attitudes and practice of GPs. Learn Disabil Pract 2007;10:18-21. https://doi.org/10.7748/ldp2007.10.10.8.18.c4280.
- Lees C, Poole H, Brennan M, Irvine F. Adults with learning disabilities experiences of using community dental services: service user and carer perspectives. Br J Learn Disabil 2017;45:114-20. https://doi.org/10.1111/bld.12181.
- McCarthy M. Prescribing contraception to women with intellectual disabilities: general practitioners’ attitudes and practices. Sex Disabil 2011;29:339-49. https://doi.org/10.1007/s11195-011-9216-6.
- Murphy J. Perceptions of communication between people with communication disability and general practice staff. Health Expect 2006;9:49-5. https://doi.org/10.1111/j.1369-7625.2006.00366.x.
- Perry J, Felce D, Kerr M, Bartley S, Tomlinson J, Felce J. Contact with primary care: the experience of people with intellectual disabilities. J Appl Res Intellect Disabil 2014;27:200-11. https://doi.org/10.1111/jar.12072.
- Powrie E. Primary health care provision for adults with a learning disability. J Adv Nurs 2003;42:413-23. https://doi.org/10.1046/j.1365-2648.2003.02633.x.
- Thompson K, Casson K, Fleming P, Dobbs F, Parahoo K, Armstrong J. Sexual health promotion in primary care – Activities and views of general practitioners and practice nurses. Prim Health Care Res Dev 2008;9:319-30. https://doi.org/10.1017/S1463423608000881.
- Tuffrey-Wijne I. The palliative care needs of people with intellectual disabilities: a case study. Int J Palliat Nurs 2002;8:222-32. https://doi.org/10.12968/ijpn.2002.8.5.10369.
- Tuffrey-Wijne I, Bernal J, Hubert J, Butler G, Hollins S. People with learning disabilities who have cancer: an ethnographic study. Br J Gen Pract 2009;59:503-9. https://doi.org/10.3399/bjgp09X453413.
- Tuffrey-Wijne I, Hollins S, Curfs L. Supporting patients who have intellectual disabilities: a survey investigating staff training needs. Int J Palliat Nurs 2005;11:182-8. https://doi.org/10.12968/ijpn.2005.11.4.18039.
- Turner S. Making reasonable adjustments to diabetes services for people with learning disabilities: what nurses can do. J Diabetes Nurs 2014;18:189-92.
- Watchman K. Practitioner-raised issues and end-of-life care for adults with Down syndrome and dementia. J Policy Pract Intellect Disabil 2005;2:156-62. https://doi.org/10.1111/j.1741-1130.2005.00026.x.
- Williamson A, Allan L, Cooper SA, Morrison J, Curtice L. The general practitioner interface with people with intellectual disabilities and their supports. Eur J Gen Pract 2004;10:66-7. https://doi.org/10.3109/13814780409094236.
- Adler P, Cregg M, Duignan A, Ilett G, Woodhouse JM. Effect of training on attitudes and expertise of optometrists towards people with intellectual disabilities. Ophthalmic Physiol Opt 2005;25:105-18. https://doi.org/10.1111/j.1475-1313.2004.00253.x.
- Baxter H, Lowe K, Houston H, Jones G, Felce D, Kerr M. Previously unidentified morbidity in patients with intellectual disability. Br J Gen Pract 2006;56:93-8.
- Biswas M, Whalley H, Foster J, Friedman E, Deacon R. Women with learning disability and uptake of screening: audit of screening uptake before and after one to one counselling. J Public Health 2005;27:344-7. https://doi.org/10.1093/pubmed/fdi055.
- Buszewicz M, Welch C, Horsfall L, Nazareth I, Osborn D, Hassiotis A, et al. Assessment of an incentivised scheme to provide annual health checks in primary care for adults with intellectual disability: a longitudinal cohort study. Lancet Psychiatry 2014;1:522-30. https://doi.org/10.1016/S2215-0366(14)00079-0.
- Cassidy G, Martin DM, Martin GH, Roy A. Health checks for people with learning disabilities: community learning disability teams working with general practitioners and primary health care teams. J Learn Disabil 2002;6:123-36. https://doi.org/10.1177/146900470200600202.
- Chauhan U, Kontopantelis E, Campbell S, Jarrett H, Lester H. Health checks in primary care for adults with intellectual disabilities: how extensive should they be?. J Intellect Disabil Res 2010;54:479-86. https://doi.org/10.1111/j.1365-2788.2010.01263.x.
- Chauhan U, Reeve J, Kontopantelis E, Hinder S. Impact of the English Directly Enhanced Service (DES) for Learning Disability 2012. www.choiceforum.org/docs/desmf.pdf (accessed 27 November 2018).
- Codling M, Solomon J. Evaluating health checks. Learn Disabil Pract 2007;10:32-8. https://doi.org/10.7748/ldp2007.05.10.4.32.c4268.
- Cooper SA, Morrison J, Allan LM, McConnachie A, Greenlaw N, Melville CA, et al. Practice nurse health checks for adults with intellectual disabilities: a cluster-design, randomised controlled trial. Lancet Psychiatry 2014;1:511-21. https://doi.org/10.1016/S2215-0366(14)00078-9.
- Cooper SA, Morrison J, Melville C, Finlayson J, Allan L, Martin G, et al. Improving the health of people with intellectual disabilities: outcomes of a health screening programme after 1 year. J Intellect Disabil Res 2006;50:667-77. https://doi.org/10.1111/j.1365-2788.2006.00824.x.
- Dagnan D, Masson J, Thwaites R, James A, Hatton C. Training therapists to work with people with intellectual disability in Improving Access to Psychological Therapies (IAPT) services. J Appl Res Intellect Disabil 2018;31:760-7. https://doi.org/10.1111/jar.12427.
- Ford JA, Jones AP, Wong G, Steel N. Weekend opening in primary care: analysis of the General Practice Patient Survey. Br J Gen Pract 2015;65:e792-8. https://doi.org/10.3399/bjgp15X687673.
- Glover G, Emerson E, Evison F. The uptake of health checks for adults with learning disabilities in England: 2008/9–2011/12. Tizard Learn Disabil Rev 2013;18:45-9. https://doi.org/10.1108/13595471311296012.
- Harrison S, Berry L. Improving primary care services for people with learning disability. Nurs Times 2005;101:38-40.
- Holly D, Sharp J. Addressing health inequities: coronary heart disease training within learning disabilities services. Br J Learn Disabil 2014;42:110-16. https://doi.org/10.1111/bld.12014.
- Martin G, Philip L, Bates L, Warwick J. Evaluation of a nurse led annual review of patients with severe intellectual disabilities, needs identified and needs met, in a large group practice. J Learn Disabil 2004;8:235-46. https://doi.org/https://doi.org/10.1177/1469004704044965.
- McConkey R, Taggart L, Kane M. Optimizing the uptake of health checks for people with intellectual disabilities. J Intellect Disabil 2015;19:205-14. https://doi.org/10.1177/1744629514568437.
- Romeo R, Knapp M, Morrison J, Melville C, Allan L, Finlayson J, et al. Cost estimation of a health-check intervention for adults with intellectual disabilities in the UK. J Intellect Disabil Res 2009;53:426-39. https://doi.org/10.1111/j.1365-2788.2009.01159.x.
- Taylor IR, Conway V, Knight AE. Measuring and addressing pain in people with limited communication skills: The ‘I Hurt Help Me’ pain management project. J Pain Manage 2014;7:129-36.
- Walmsley J. An investigation into the implementation of annual health checks for people with intellectual disabilities. J Intellect Disabil 2011;15:157-66. https://doi.org/10.1177/1744629511423722.
- Webb J, Stanton M. Working with primary care practices to improve service delivery for people with learning disabilities – a pilot study. Br J Learn Disabil 2009;37:221-7. https://doi.org/10.1111/j.1468-3156.2009.00555.x.
- Webb J, Stanton M. Better access to primary healthcare for adults with learning disabilities: evaluation of a group programme to improve knowledge and skills. Br J Learn Disabil 2009;37:116-22. https://doi.org/10.1111/j.1468-3156.2008.00527.x.
- Dafoulas GE, Toulis KA, Mccorry D, Kumarendran B, Thomas GN, Willis BH, et al. Type 1 diabetes mellitus and risk of incident epilepsy: a population-based, open-cohort study. Diabetologia 2017;60:258-61. https://doi.org/10.1007/s00125-016-4142-x.
- Håman L, Barker-Ruchti N, Patriksson G, Lindgren E-C. Orthorexia nervosa: an integrative literature review of a lifestyle syndrome. Int J Qual Stud Health Well-Being 2015;10. https://doi.org/10.3402/qhw.v10.26799.
- NHS Digital . Quality and Outcomes Framework (QOF), Enhanced Services and Core Contract Extraction Specifications (Business Rules) n.d. https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/quality-and-outcomes-framework-qof#targetText=The%20QOF%20is%20a%20voluntary,the%20delivery%20of%20primary%20care (accessed 27 November 2018).
- Unite-CPHVA (Community Practitioners and Health Visitors Association) . Annual Professional Conference: Programme 2016. Community Pract 2016;89:18-9.
- Hussaindeen JR, Shah P, Ramani KK, Ramanujan L. Efficacy of vision therapy in children with learning disability and associated binocular vision anomalies. J Optom 2018;11:40-8. https://doi.org/10.1016/j.optom.2017.02.002.
- Bengani H, Handley M, Alvi M, Ibitoye R, Lees M, Lynch SA, et al. Clinical and molecular consequences of disease-associated de novo mutations in SATB2. Genet Med 2017;19:900-8. https://doi.org/10.1038/gim.2016.211.
- Braga LH, Rickard M, Farrokhyar F, Jegatheeswaran K, Brownrigg N, Li C, et al. Bladder training video versus standard urotherapy for bladder and bowel dysfunction: a noninferiority randomized, controlled trial. J Urol 2017;197:877-84. https://doi.org/10.1016/j.juro.2016.08.089.
- Abbott L, Austin R, Mulkeen A, Metcalfe N. The global classroom: advancing cultural awareness in special schools through collaborative work using ICT. Eur J Special Needs Educ 2004;19:225-40. https://doi.org/10.1080/08856250410001678504.
- Marriott A, Turner S. Making Reasonable Adjustments to Cancer Screening. London: Public Health England; 2016.
- Beadle-Brown J, Mansell J, Whelton B, Hutchinson A. People with learning disabilities in ‘out-of-area’ residential placements: views of families, managers and specialists. Br J Dev Disabil 2009;55:15-31. https://doi.org/10.1179/096979509799103133.
- University of Bristol and NHS England . Learning Disabilities Mortality Review (LeDeR) Programme. Annual Report December 2017 n.d. www.bristol.ac.uk/media-library/sites/sps/leder/leder_annual_report_2016-2017.pdf (accessed 27 November 2018).
- Department of Health and Social Care and NHS England . The Government Response to the Learning Disabilities Mortality Review (LeDeR) Programme Second Annual Report. 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/739560/government-response-to-leder-programme-2nd-annual-report.pdf (accessed 27 November 2018).
- Skills for Health, Skills for Care and Health Education England . Learning Disabilities Core Skills Education and Training Framework 2016. www.skillsforhealth.org.uk/images/resource-section/projects/learning-disabilities/Learning-Disabilities-CSTF.pdf (accessed 27 November 2018).
- NHS England . NHS RightCare Pathways 2019. www.england.nhs.uk/rightcare/products/pathways/ (accessed 27 November 2018).
- Great Britain . Mental Capacity Act 2005 2005.
- Chambers D, Cantrell A, Booth A. Factors that facilitate the implementation of interventions to reduce preventable hospital admissions for cardiovascular or respiratory conditions: an evidence map and realist synthesis. Health Serv Deliv Res 2020.
- Tones K. Evaluating health promotion: a tale of three errors. Patient Educ Couns 2000;39:227-36. https://doi.org/10.1016/S0738-3991(99)00035-X.
- Burton H, Walters L. Access to Medicare-funded annual comprehensive health assessments for rural people with intellectual disability. Rural Remote Health 2013;13.
- Great Britain . Care Act 2014 2014.
- Melville CA, Finlayson J, Cooper SA, Allan L, Robinson N, Burns E, et al. Enhancing primary health care services for adults with intellectual disabilities. J Intellect Disabil Res 2005;49:190-8. https://doi.org/10.1111/j.1365-2788.2005.00640.x.
Appendix 1 Search strategy for mapping review
Epub Ahead of Print, In-Process & Other Non-Indexed Citations, MEDLINE® Daily and MEDLINE®
Date searched: 4 May 2018.
Date range: 2002–18.
Records retrieved: 1090.
| # | Searches |
|---|---|
| 1 | (learning adj (disab* or disorder* or difficult*)).tw. |
| 2 | ((developmental* or intellectual*) adj disab*).ti. |
| 3 | (mental* adj (retard* or handicap* or subnormal* or deficien*)).ti. |
| 4 | intellectual* impair*.ti. |
| 5 | or/1-4 |
| 6 | (access* or advoca* or barrier* or communication* or information or uptake or utili*ation or need* or provision or consent* or help seeking or help-seeking or utili*e or inaccessib* or availab* or prohibit* or affordab* or applicab* or refer*).ti. |
| 7 | (primary care or nhs or general practi* or gp or family practi* or family doctor* or doctor* surgery* or dentist* or dental or optician* or optical or optometrist* or eye or pharmacy* or pharmacist* or clinic or clinics or community service* or community based).ti. |
| 8 | (reasonable adjustment* or equality act or disability discrimination act or mental capacity act or care act).tw. |
| 9 | or/6-8 |
| 10 | 5 and 9 |
| 11 | exp Animals/ |
| 12 | Humans/ |
| 13 | 11 not (11 and 12) |
| 14 | 10 not 13 |
| 15 | limit 14 to english language |
| 16 | limit 15 to yr = ‘2002 -Current’ |
Web of Science
Date searched: 4 May 2018.
Date range: 2002–18.
Records retrieved: 2023.
| # | Searches |
|---|---|
| #1 | TS = ((learning NEAR/1 (disab* or disorder* or difficult*))) |
| #2 | TI = (((developmental* or intellectual*) NEAR/1 disab*)) |
| #3 | TI = ((mental* NEAR/1 (retard* or handicap* or subnormal* or deficien*))) |
| #4 | TITLE: (intellectual* impair*) |
| #5 | #4 OR #3 OR #2 OR #1 |
| #6 | TI = ((access* or advoca* or barrier* or communication* or information or uptake or utili*ation or need* or provision or consent* or help seeking or help-seeking or utili*e or inaccessib* or availab* or prohibit* or affordab* or applicab* or refer*)) |
| #7 | TI = ((primary care or nhs or general practi* or gp or family practi* or family doctor* or doctor* surgery* or dentist* or dental or optician* or optical or optometrist* or eye or pharmacy* or pharmacist* or clinic or clinics or ‘community service*’ or ‘community based’)) |
| #8 | TS = ((‘reasonable adjustment*’ or ‘equality act’ or ‘disability discrimination act’ or ‘mental capacity act’ or ‘care act’)) |
| #9 | #8 OR #7 OR #6 |
| #10 | (#9 AND #5) AND LANGUAGE: (English) Timespan = 2002-2018 |
The Cochrane Library
Date searched: 4 May 2018.
Date range: 2002–18.
Records retrieved: 666.
| # | Searches |
|---|---|
| #1 | (learning near/1 (disab* or disorder* or difficult*)):ti,ab |
| #2 | ((developmental* or intellectual*) near/1 disab*):ti |
| #3 | (mental* near/1 (retard* or handicap* or subnormal* or deficien*)):ti |
| #4 | intellectual* impair*:ti |
| #5 | #1 OR #2 OR #3 OR #5 |
| #6 | (access* or advoca* or barrier* or communication* or information or uptake or utili*ation or need* or provision or consent* or help seeking or help-seeking or utili*e or inaccessib* or availab* or prohibit* or affordab* or applicab* or refer*):ti |
| #7 | (primary care or nhs or general practi* or gp or family practi* or family doctor* or doctor* surgery* or dentist* or dental or optician* or optical or optometrist* or eye or pharmacy* or pharmacist* or clinic or clinics or community service* or community based):ti |
| #8 | (reasonable adjustment* or equality act or disability discrimination act or mental capacity act or care act):ti,ab |
| #9 | #6 OR #7 OR #8 |
| #10 | #5 and #9 Publication Year from 2002 to 2018 |
Cumulative Index of Nursing and Allied Health Literature
Date searched: 4 May 2018.
Records retrieved: 1117.
| # | Searches |
|---|---|
| S1 | TI ((learning N1 (disab* or disorder* or difficult*))) OR AB ((learning N1 (disab* or disorder* or difficult*))) |
| S2 | TI ((developmental* or intellectual*) N1 disab*) |
| S3 | TI (mental* N1 (retard* or handicap* or subnormal* or deficien*)) |
| S4 | TI ‘intellectual* impair*’ |
| S5 | S1 OR S2 OR S3 OR S4 |
| S6 | TI (access* or advoca* or barrier* or communication* or information or uptake or utili*ation or need* or provision or consent* or help seeking or help-seeking or utili*e or inaccessib* or availab* or prohibit* or affordab* or applicab* or refer*) |
| S7 | TI (primary care or nhs or general practi* or gp or family practi* or family doctor* or doctor* surgery* or dentist* or dental or optician* or optical or optometrist* or eye or pharmacy* or pharmacist* or clinic or clinics or community service* or community based) |
| S8 | TI (‘reasonable adjustment*’ or ‘equality act’ or ‘disability discrimination act’ or ‘mental capacity act’ or ‘care act’) |
| S9 | S6 OR S7 OR S8 |
| S10 | S5 AND S9 Limiters - Published Date: 20020101-20181231; English Language |
PsycINFO
Date searched: 4 May 2018.
Date range: 2002–18.
Records retrieved: 1646.
| # | Searches |
|---|---|
| 1 | (learning adj (disab* or disorder* or difficult*)).tw. |
| 2 | ((developmental* or intellectual*) adj disab*).ti. |
| 3 | (mental* adj (retard* or handicap* or subnormal* or deficien*)).ti. |
| 4 | intellectual* impair*.ti. |
| 5 | or/1-4 |
| 6 | (access* or advoca* or barrier* or communication* or information or uptake or utili*ation or need* or provision or consent* or help seeking or help-seeking or utili*e or inaccessib* or availab* or prohibit* or affordab* or applicab* or refer*).ti. |
| 7 | (primary care or nhs or general practi* or gp or family practi* or family doctor* or doctor* surgery* or dentist* or dental or optician* or optical or optometrist* or eye or pharmacy* or pharmacist* or clinic or clinics or community service* or community based).ti. |
| 8 | (reasonable adjustment* or equality act or disability discrimination act or mental capacity act or care act).tw. |
| 9 | or/6-8 |
| 10 | 5 and 9 |
| 11 | exp Animals/ |
| 12 | Humans/ |
| 13 | 11 not (11 and 12) |
| 14 | 10 not 13 |
| 15 | limit 14 to english language |
| 16 | limit 15 to yr = ‘2002 -Current’ |
Applied Social Sciences Index and Abstracts
Date searched: 4 May 2018.
Date range: 2002–18.
Records retrieved: 596.
| # | Searches |
|---|---|
| S1 | (((ti((learning disab* OR learning disorder* OR learning difficult*)) OR ab((learning disab* OR learning disorder* OR learning difficult*))) OR ti((developmental* disab* OR intellectual* disab*)) OR ti((mental* retard* OR mental* handicap* OR mental* subnormal* OR mental* deficien*)) OR ti(intellectual* impair*)) AND (ti((access* OR advoca* OR barrier* OR communication* OR information OR uptake OR utili?ation OR need* OR provision OR consent* OR help seeking OR help-seeking OR utili?e OR inaccessib* OR availab* OR prohibit* OR affordab* OR applicab* OR refer*)) OR ti((primary care OR nhs OR general practi* OR gp OR family practi* OR family doctor* OR doctor* surgery* OR dentist* OR dental OR optician* OR optical OR optometrist* OR eye OR pharmacy* OR pharmacist* OR clinic OR clinics OR community service* OR community based)) OR ti((‘reasonable adjustment*’ OR ‘equality act’ OR ‘disability discrimination act’ OR ‘mental capacity act’ OR ‘care act’)))) AND (la.exact(‘ENG’) AND pd(20020101-20181231)) |
Education Resources Information Center
Date searched: 4 May 2018.
Date range: 2002–18.
Records retrieved: 920.
| # | Searches |
|---|---|
| S1 | TI ((learning N1 (disab* or disorder* or difficult*))) OR AB ((learning N1 (disab* or disorder* or difficult*))) |
| S2 | TI ((developmental* or intellectual*) N1 disab*) |
| S3 | TI (mental* N1 (retard* or handicap* or subnormal* or deficien*)) |
| S4 | TI ‘intellectual* impair*’ |
| S5 | S1 OR S2 OR S3 OR S4 |
| S6 | TI (access* or advoca* or barrier* or communication* or information or uptake or utili*ation or need* or provision or consent* or help seeking or help-seeking or utili*e or inaccessib* or availab* or prohibit* or affordab* or applicab* or refer*) |
| S7 | TI (primary care or nhs or general practi* or gp or family practi* or family doctor* or doctor* surgery* or dentist* or dental or optician* or optical or optometrist* or eye or pharmacy* or pharmacist* or clinic or clinics or community service* or community based) |
| S8 | TI (‘reasonable adjustment*’ or ‘equality act’ or ‘disability discrimination act’ or ‘mental capacity act’ or ‘care act’) |
| S9 | S6 OR S7 OR S8 |
| S10 | S5 AND S9 Limiters - Date Published: 20020101-20181231; Language: English |
Grey literature search
Terms used in the grey literature search in include ‘learning disab*’, ‘learning disorder*’, ‘learning difficult*’, ‘access*’, ‘primary care’ and ‘community’.
-
Association of Chartered Physiotherapists for People with Learning Disabilities – http://acppld.csp.org.uk/ (accessed 10 May 2018).
-
British Institute of Learning Disabilities (BILD) – www.bild.org.uk (accessed 10 May 2018).
-
Dimensions – www.dimensions-uk.org/ (accessed 10 May 2018).
-
Disability Rights UK – www.disabilityrightsuk.org/ (accessed 10 May 2018).
-
Foundation for People with Learning Disabilities – www.mentalhealth.org.uk/learning-disabilities (accessed 10 May 2018).
-
IHaL - The Learning Disabilities Public Health Observatory – www.ndti.org.uk/our-work/our-projects/peoples-health/improving-health-and-lives-ihal (accessed 10 May 2018).
-
Learning Disability Wales – www.ldw.org.uk/ (accessed 10 May 2018).
-
Mencap – www.mencap.org.uk/ (accessed 10 May 2018).
-
Mind – www.mind.org.uk/ (accessed 17 May 2018).
-
Scope – www.scope.org.uk/ (accessed 17 May 2018).
-
The Hearing and Learning Disabilities Group – www.hald.org.uk/ (accessed 17 May 2018).
-
British Academy of Childhood Disability (BACD) – www.bacdis.org.uk/ (accessed 17 May 2018).
-
British Society for Disability and Oral Health (BSDH) – www.bsdh.org/ (accessed 17 May 2018).
-
Focus on Disability – www.focusondisability.org.uk/ (accessed 17 May 2018).
-
Sexual Health and Disability Alliance (SHADA) – http://shada.org.uk/wp2/ (accessed 17 May 2018).
-
Voluntary Organisations Disability Group (VODG) – www.vodg.org.uk/ (accessed 17 May 2018).
Citation search
Citation searches were carried out in Google Scholar on 21 June 2018 on three key publications:
-
Alborz A, McNally R, Swallow A, Glendinning C. From the Cradle to the Grave: A Literature Review of Access to Healthcare for People with Learning Disabilities Across the Lifespan. London: National Coordinating Centre for the Service Delivery and Organisation; 2003. (44 citations.)
-
Alborz A, McNally R, Glendinning C. Access to health care for people with learning disabilities in the UK: mapping the issues and reviewing the evidence. J Health Serv Res Policy 2005;10:173–82. https://doi.org/10.1258/1355819054338997. (111 citations.)
-
McNally R, Alborz A. Developing methods for systematic reviewing in health services delivery and organization: an example from a review of access to health care for people with learning disabilities. Part 1. Identifying the literature. Health Info Libr J 2004; 21:182–92. (19 citations.)
Appendix 2 Data extraction components for mapping review
Study identification number.
Study design:
-
quantitative
-
qualitative
-
mixed methods
-
review
-
unclear.
Setting: country
HCP:
-
GP
-
dentist
-
optometrist
-
pharmacist
-
other community staff.
Specialist topic:
-
sexual health
-
palliative care
-
mental health
-
other.
Study population.
Sample size.
Needs assessment.
Study outcomes.
Tools used to measure outcomes.
Study results.
Barriers.
Facilitators.
Appendix 3 Data extraction mapping review example
| Study identification number | Study design | Setting: country | HCP | Specialist topic | Study population | Sample size | Needs assessment | Study outcomes | Tools | Study results | Barriers | Facilitators |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Burton (2013)131 | Qualitative | Australia |
GP Other community staff: practice nurse |
In-depth interviews were conducted with 18 participants including people with ID, carers/support workers and rural doctors | 18 | Seven themes were identified: (1) health-care barriers in rural areas, (2) cohesion of rural communities, (3) the way rural doctors practice, (4) lack of knowledge/understanding, (5) venturing into new territory, (6) the role of the practice nurse and (7) the health communication triangle | Lack of services in rural areas. Distance to specialists in rural Australia | Increased social cohesion. Community connectedness |
Appendix 4 Information from the patient and public involvement meetings
Consultation meeting at Mencap Sheffield, Norfolk Lodge with group of members who had been working on Royal Mencap’s ‘Treat Me Well’ campaign on 6 June 2018 (EC/AC)
Themes arising from discussion:
-
someone else decided when an appointment was necessary
-
someone to take them to appointments
-
someone to go into appointments with them
-
not having to wait too long (people laughing at me in the waiting area)
-
staff using correct name (not shortening names without asking first)
-
seeing same doctor each time who knows them
-
one member took photos of pills taken so Mum can check correct
-
parents receive any appointment letters or text reminders
-
letters are confusing and use long words
-
knowing where to go – related more to hospital care.
Question – eye tests for people with intellectual disabilities. (URL: www.seeability.org/eye-tests-explained; accessed 30 November 2018).
Showed video they had done about visit hospital – letters confusing, big words, cannot read it, how to get to hospital, where to go, signs confusing, worry late, so many different big words, open wide fear not explained.
Letters – Dad read.
Dad talks to doctor.
Tell parents ears sore, they phone and make appointment wait too long. Happened before so point to ear, know need to go to doctors, Mum or Dad takes, not comfortable asking questions.
Dentist – parents make appointment and take them, parents ring dentist, take them, go in on own.
Opticians – new glasses, need someone to go with. Regular check-ups told need new glasses, do not know what letters are? Parents help choose glasses.
Pain.
Check-ups letters arrive not strange.
Like dentist, nice lady, injections ‘no pain, no gain’ easy to understand.
Optician sends letter, Mum reads, makes appointment, had eye test chose new glasses.
Mum decides need go to doctors, asks if ill, rings doctors to make appointment.
Doctors – do not want to wait too long, get agitated think people laughing. Want staff at doctors to use correct name not shorten.
Seeing same doctor helpful as understanding, knows patient, Mum goes too, Mum talks first then doctor to patient. Does not get upset if sees same doctor.
Important someone to take and go in with, see same Dr.
Takes medicine himself, if Mum not there take photo of medicine taken so she can check correct. Explains medicines when take, colours, size tablets. Pill organiser so in days.
One group member uses diary and Mum writes appointments in.
One group member had ears syringed to clear wax before so was confident to go to hospital himself. Mum decides when need ears syringed.
Consultation meeting with two formal carers employed by national organisation. 18 July 2018 (MJ/EC)
Barriers may be structural – cost and organisation of services, or they may relate to a person’s preferences and priorities, their knowledge, cultural beliefs and attitudes.
General practitioner
Barriers
-
Appointment systems.
-
Receptionists.
-
Confidentiality when someone has reduced capacity but practice are not aware that they have not understood the consultation.
-
Poor communication: not at the level the person can understand.
-
People may not want to talk about their problems or may over/under emphasise relevant symptoms.
-
Patients may make a nuisance of themselves by visiting often for no reason.
-
If patients refuse to go no one can make them attend.
-
Variation in the extent to which GPs will share patient information with carers (fluctuating mental capacity of patient).
Enablers
-
Good provider–patient communication: understanding that it takes time to listen, talking to the person and ensuring that they have understood, making sure the proposed treatment is understood and is acceptable to the person.
-
Seeing the same doctor/nurse so that they build a relationship and get to know the person.
-
Health checks done in the home by a nurse from the practice.
Pharmacy
Barrier/enabler
-
Knowledge of the individual’s capacity.
Optician
Barriers
-
Can be frightening to go to a strange place and do something you do not normally do.
Enablers
-
Able to do home visits if necessary.
-
Suitable methods for testing eyes when someone cannot read.
Dentist
Enabler
-
Formal carers keeping records to track check-ups and ensure that they are not missed.
General
Barriers
-
Person’s understanding and willingness to attend an appointment somewhere unfamiliar.
-
Person’s willingness to attend for unpleasant treatment: cervical screening, vaccination.
-
Negative past experiences.
-
Seeing a different, unfamiliar or unexpected doctor without advanced explanation that this would happen.
-
Person’s inability to flag up a health problem at an early stage (e.g. blister that became badly infected without staff knowing about it).
-
Person who goes to the GP regularly although there is nothing wrong.
-
Person might not attend appointment because they are worried about the outcome (e.g. fear of diabetes diagnosis).
-
Person might appear as though they have capacity to understand but actually not be able to understand or pass on the information they are given.
-
People might not know what information is relevant to tell the doctor.
-
Difficult to identify some health problems that arise over several days or that might not be obvious to a support worker who is only there for short periods at a time (e.g. constipation).
-
Support workers often having to ‘fight’ (advocate) for several people at any one time.
-
Letters/texts appointment reminders go to person and may be ignored.
-
Voicemail messages can cause alarm: from surgical team when no surgery planned.
-
Fragmented service where individual services pass the person between them with no one taking ownership to follow through until the problem is resolved.
-
Lack of understanding of life world of person with disability (support worker) ‘they do not see it from our side’.
-
Different agencies attending patient (risk of missing appointments if patient not ready in time).
Enablers
-
Having support staff who can attend with the person.
-
Having consistent support staff who know the person so can recognise when something is not right.
-
Good lines of communication between support staff and health service providers.
-
Time.
-
Listening to what is needed.
-
Getting to know the person (e.g. their preferences).
-
Talking to the person with ID but then also to the carers to ensure that the information will be acted on.
-
Sending appointment letters and reminders to support workers as well as patients.
-
Someone willing to coordinate care between different services to ensure that the health need is met.
-
Recognising where system/approach requires adjustment to accommodate patient needs.
Patient and public involvement meeting 5 July 2018
Present at the meeting were five members (two male and three female) of the FLASh carers group (all parents of adults with ID).
Introductions were made and discussion followed the guide adapted from the Alborz et al. review. 21
The notes of the discussion points follow.
Identifying/communicating symptoms of ill health
-
Difficulty communicating (e.g. pain; parents used to call for help at every suspicion of pain or other symptom, but then no signs when they see HCP).
-
Can sometimes read facial expressions; have to ask what it means.
-
Not sure if person with ID is giving ‘correct’ response to HCP’s questions.
-
Cannot leave signs/symptoms in case it becomes serious.
-
Example of paramedics saying observations were fine but could not read person with ID’s expression of pain.
-
Communicate in the way people with ID is used to or through stories (example of using ‘Mr Diabetes’).
-
Patient’s views may differ from parent’s views; HCP has to listen to patient.
-
Patient may not understand reason for symptoms (e.g. ‘ageing’ the reason for aches and pains).
-
Pain may be recognised suddenly rather than gradually.
-
People with autism do not like to talk about personal things so may make, for example, depression worse if they are encouraged to do so.
-
People with ID may expect others to be able to ‘know’ what is wrong (‘be psychic’).
-
People with ID not the same all the time.
-
People with ID may get ideas stuck in their heads about certain things (e.g. antidepressants are for bad people).
-
Difficulty understanding that ‘silent symptoms’ (e.g. high blood sugar) are serious whereas obvious symptoms (e.g. painful foot) may be less serious – link between severity of symptom and severity of problem not always helpful.
Arranging and attending health consultations
Barriers
-
Appointments difficult to obtain (discussion of different systems at GP practices including morning triage, afternoon drop in).
-
Cannot always get transport to other services such as walk-in centre (need to book transport in advance).
-
People with ID cannot explain their symptoms to the doctor, they need an advocate.
-
Waiting in the waiting room can raise anxiety for people with ID.
-
A 10-minute consultation time is not enough – need 15 minutes.
-
Some people with ID (e.g. with autism) express more concern about small things than larger ones, so time needed to explore.
-
HCPs not always aware of how ID affects family members.
-
GP practices (and secondary care) do not always share the same computer system, so not easy to share information.
-
Not all practices are linked to out-of-hours service.
-
Late diagnosis of ID.
-
Dentist – paperwork not always clear (ticking wrong boxes could affect funding).
-
Cutting pharmacy support – having to wait for medication – not dealing with patients as too many prescriptions.
Facilitators
-
GP listens to the patient.
-
Quiet area away from waiting room to sit until can see GP.
-
Able to ask for a double appointment.
-
Suggestion – add red flag to patient notes so that the HCP is aware that this is a person with ID.
-
Doctors discussing/sharing best practice, not doing things a certain way because that is how it has always been done.
-
Important role of support worker (triangle: patient–support worker–HCP).
-
Practice receptionists get to know patient and situation after a while.
-
Home visits (GP, dentist, optician).
-
Hospital passport (personal to people with ID, lets staff know needs and requirements), good idea but HCPs do not always read it.
-
Parents involved in HCP training sessions.
Continuing access
-
Take on board patient feelings/fears (e.g. patient with autism may panic over seemingly small things).
-
Patient feeling safe.
-
Knowing patient (e.g. carrying backpack around all the time can lead to chest pains).
-
Continuity – patients like familiarity.
-
Patient story does not always follow patient around from one service/HCP to another.
Other
-
Parents need respite as care is 24/7 and do not get privacy if care is at home.
-
Budget cuts have affected ability to employ support workers (increase in hourly rate/use of agency staff).
-
What will happen when parents no longer there – concern.
-
LD Care Act 2014132 not implemented – clinical commissioning group not bound by it.
-
No support worker cover for holidays – could ask trainees/volunteers to cover?
Appendix 5 Search strategy for targeted systematic review
Adapted from the searches conducted for previous SDO review (i.e. McNally and Alborz25).
-
Strategy informed by the findings from the mapping review.
-
Multiple limits applied: humans, English language, date limits (2002–18), UK filter (Ayiku et al. 31).
-
Seven databases to search.
-
MEDLINE
-
The Cochrane Library (Cochrane Database of Systematic Reviews; Database of Abstracts of Reviews of Effect; Cochrane Central Register of Controlled Trials; Health Technology Assessment Database; NHS Economic Evaluations Database)
-
Web of Science (Science Citation Index Expanded; Social Sciences Citation Index)
-
CINAHL (Cumulative Index to Nursing and Allied Health)
-
ASSIA (Applied Social Science Index)
-
PsycINFO
-
ERIC (Educational Resources Index).
-
MEDLINE
Date of search: 7 September 2018.
Date range searched: 2002–18.
Search strategy
-
(learning adj (disab* or disorder* or difficult*)).tw.
-
((developmental* or intellectual*) adj disab*).tw.
-
(mental* adj (retard* or handicap* or subnormal* or deficien*)).tw.
-
intellectual* impair*.tw.
-
or/1-4
-
(access* or advoca* or barrier* or communication* or information or uptake or utili*ation or need* or provision or consent* or help seeking or help-seeking or utili*e or inaccessib* or availab* or prohibit* or affordab* or applicab* or refer*).tw.
-
(primary care or nhs or general practi* or gp or family practi* or family doctor* or doctor* surgery* or dentist* or dental or optician* or optical or optometrist* or opthalmolog* or eye or eyes or ear or ears or hear or hearing or audiolog* or pharmacy* or pharmacist* or chemist* or clinic or clinics or community service* or community based or community care).tw.
-
(reasonable adjustment* or equality act or disability discrimination act or mental capacity act or care act).tw.
-
or/6-8
-
5 and 9
-
exp Animals/
-
Humans/
-
11 not (11 and 12)
-
10 not 13
-
exp Great Britain/
-
(national health service* or nhs*).ti,ab,in.
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab.
-
(gb or ‘g.b.’ or britain*).ti,ab,jw,in.
-
(british* not ‘british columbia’).ti,ab,jw,in.
-
(uk or ‘u.k.’ or united kingdom*).ti,ab,jw,in.
-
(england* not ‘new england’).ti,ab,jw,in.
-
(‘northern ireland*’ or ‘northern irish*’ or scotland* or scottish* or welsh*).ti,ab,jw,in.
-
((wales or south wales) not ‘new south wales’).ti,ab,jw,in.
-
or/15-23
-
(exp africa/or exp americas/or exp antarctic regions/or exp arctic regions/or exp asia/or exp oceania/) not (exp great britain/or europe/)
-
24 not 25
-
exp Primary Health Care/
-
Community Health Services/
-
Community Mental Health Services/
-
exp Physicians, Family/
-
Pharmacies/
-
Dentists/
-
Optometry/
-
Audiology/
-
exp After-Hours Care/
-
(out of hours or ooh or after hours or walk in centre* or national health service* 111 or nhs* 111 or iapt or improving access to psychological therapies or health check* or screen* or assessment or health service* or care service*).tw.
-
or/27-36
-
5 and 37
-
38 not 13
-
(14 or 39) and 26
-
limit 40 to english language
-
limit 41 to yr = ‘2002 -Current’
Appendix 6 List of excluded studies
Ahmad F, Roy A, Brady S, Belgeonne S, Dunn L, Pitts J. Care pathway initiative for people with intellectual disabilities: impact evaluation. J Nurs Manag 2007;15:700–2.
Albanese A, Hopper NW. Suppression of menstruation in adolescents with severe learning disabilities. Arch Dis Child 2007;92:629–32.
Alborz A, McNally R. Developing methods for systematic reviewing in health services delivery and organization: an example from a review of access to health care for people with learning disabilities. Part 2. Evaluation of the literature – a practical guide. Health Info Libr J 2004;21:227–36.
Alborz A, McNally R, Glendinning C. Access to health care for people with learning disabilities in the UK: mapping the issues and reviewing the evidence. J Health Serv Res Policy 2005;10:173–82. https://doi.org/10.1258/1355819054338997
Alcedo MÁ, Fontanil Y, Solís P, Pedrosa I, Aguado AL. People with intellectual disability who are ageing: perceived needs assessment. Int J Clin Health Psychol 2017;17:38–45. https://doi.org/10.1016/j.ijchp.2016.07.002
Allan L, Morrison J, Cooper SA, Smiley E, Williamson A. Uptake of cervical screening among women with intellectual disabilities. J Appl Res Intellect Disabil 2006;19:250.
Allerton L, Emerson E. British adults with chronic health conditions or impairments face significant barriers to accessing health services. Public Health 2012;126:920–7. https://doi.org/10.1016/j.puhe.2012.08.003
Anderson ES, Smith R, Thorpe LN. Learning from lives together: medical and social work students’ experiences of learning from people with disabilities in the community. Health Soc Care Community 2010;18:229–40. https://doi.org/10.1111/j.1365-2524.2010.00921.x
Anonymous. GP registration moving too slowly. Community Care 2004:7.
Anonymous. HSJ awards 2005. Primary care innovation. Winner: PCT and council set up integrated commissioning for mental health, substance misuse and learning disability. Health Serv J 2005;115(Suppl.):42–3.
Anonymous. Open forum. Community Care 2007:19.
Anonymous. Threat to learning disability nursing. Nurs Times 2007;103:3.
Anonymous. Second equality report slams DH. Nurs Times 2007;103:3.
Anonymous. Chance to improve learning disability care must be taken. Nurs Times 2008;104:1.
Anonymous. Step change Ian McMillan Step change is a Freelance journalist. Nurs Stand 2012;26:18–20.
Anonymous. NHS strategy for learning disability. Nurs Stand 2015;29:10.
Anonymous. Appropriate care for people with learning disabilities. Nurs Stand 2016;30:66.
Antaki C, Young N, Finlay M. Shaping clients’ answers: departures from neutrality in care-staff interviews with people with a learning disability. Disabil Soc 2002;17:435–55.
Antaki C, Finlay WML, Walton C, Sempik J. Communicative Practices In Staff Support of Adults with Intellectual Disabilities. In O'Reilly M, Lester JN, editors. The Palgrave Handbook Of Adult Mental Health: Discourse and Conversation Studies. New York, NY: Palgrave Macmillan; 2016. pp. 613–32.
Atkinson D. Editorial. Br J Learn Disabil 2006;34:1–2.
Atkinson D, Walmsley J. Editorial. Br J Learn Disabil 2003;31:61–2.
Auty E, Scior K. Psychologists’ clinical practices in assessing dementia in individuals with down syndrome. J Policy Pract Intellect Disabil 2008;5:259–68.
Ayre K, Khalifeh H. Immigrant women and women with learning disabilities have complex mental health needs and service use in the perinatal period. Evid Based Ment Health 2017;20:55–7. https://doi.org/10.1136/eb-2017-102607
Azam K, Serfaty M, King M, Martin S, Strydom A, Parkes C, Hassiotis A. The development of manualised cognitive behaviour treatment for adults with mild intellectual disability and common mental disorders. Psychiatriki 2012;23:109–16.
Bailey M, Doody O, Lyons R. Surveying community nursing support for persons with an intellectual disability and palliative care needs. Br J Learn Disabil 2016;44:24–34.
Baines S, Emerson E, Robertson J, Hatton C. Sexual activity and sexual health among young adults with and without mild/moderate intellectual disability. BMC Public Health 2018;18:667. https://doi.org/10.1186/s12889-018-5572-9
Bains H, Bonell E, Speight P. Carer satisfaction with telephone consultations in a community intellectual disability unit. J Intellect Disabil 2010;14:259–65. https://doi.org/10.1177/1744629510390450
Bakker-van Gijssel EJ, Olde Hartman TC, Lucassen PL, van den Driessen Mareeuw F, Dees MK, Assendelft WJ, van Schrojenstein Lantman-de Valk HM. GPs’ opinions of health assessment instruments for people with intellectual disabilities: a qualitative study. Br J Gen Pract 2017;67:e41–e48. https://doi.org/10.3399/bjgp16X688585
Balogh R, McGarry C, McMorris C, Lake J, Dobranowski K, Wilton A et al. Chronic diseases and healthcare utilization in persons with cerebral palsy and intellectual disabilities. J Intellect Disabil Res 2016;60:633.
Balogh R, McMorris CA, Lunsky Y, Ouellette-Kuntz H, Bourne L, Colantonio A, Gonçalves-Bradley DC. Organising healthcare services for persons with an intellectual disability. Cochrane Database Syst Rev 2016;4:CD007492. https://doi.org/10.1002/14651858.CD007492.pub2
Barcham L. Carrots and sticks: incentives and barriers to having a fully qualified workforce in intellectual disability (ID) services in England. J Intellect Disabil Res 2004;48:501.
Barr O, Sowney M. Inclusive nursing care for people with intellectual disabilities using urology services. Int J Urol Nurs 2007;1:138–45.
Barr O. Better services . . . are we there yet? J Intellect Disabil 2012;16:243–5. https://doi.org/10.1177/1744629512467137
Barrett N, Paschos D. Alcohol-related problems in adolescents and adults with intellectual disabilities. Curr Opin Psychiatry 2006;19:481–5. https://doi.org/10.1097/01.yco.0000238474.07078.41
Barriball L. Learning disabilities health check project. Br J Community Nurs 2005;10:81.
Barron DA, Molosankwe I, Romeo R, Hassiotis A. Urban adolescents with intellectual disability and challenging behaviour: costs and characteristics during transition to adult services. Health Soc Care Community 2013;21:283–92. https://doi.org/10.1111/hsc.12015
Barron DA, Hassiotis A. Good practice in transition services for young people with learning disabilities: a review. Adv Mental Health Learn Disabil 2008;2:18–24.
Barron DA, Robotham D, Hassiotis A. A life like no other. A national audit of specialist inpatient healthcare services for people with learning difficulties in England (December 2007). Adv Mental Health Learn Disabil 2008;2:58–62.
Bauer A, Taggart L, Rasmussen J, Hatton C, Owen L, Knapp M. Economic and ethical implications of improving access to health care for older people with intellectual disabilities in England: a cost-effectiveness modelling study of health checks. Lancet 2017;390:S4.
Baumbusch J, Phinney A, Baumbusch S. Practising family medicine for adults with intellectual disabilities. Can Fam Phys 2014;60:E356–E361.
Baxter P. Service provision for people with learning disability. Dev Med Child Neurol 2013;55:972. https://doi.org/10.1111/dmcn.12279
Beadle M, Needham Y, Dearing M. Collaboration with service users to develop reusable learning objects: the ROOT to success. Nurse Educ Pract 2012;12:352–5. https://doi.org/10.1016/j.nepr.2012.04.005
Beake S, Clark LL, Turner T, Bick D. A mixed methods study to develop and pilot a competency assessment tool to support midwifery care of women with intellectual disabilities. Nurse Educ Today 2013;33:901–6. https://doi.org/10.1016/j.nedt.2012.08.007
Beck A, Sanchez-Walker E, Evans LJ, Harris V, Pegler R, Cross S. Characteristics of people who rapidly and frequently reattend the emergency department for mental health needs. Eur J Emerg Med 2016;23:351–5. https://doi.org/10.1097/MEJ.0000000000000349
Beighton C, Victor C, Carey IM, Hosking F, DeWilde S, Cook DG, Manners P, Harris T. ‘I’m sure we made it a better study . . . ’: experiences of adults with intellectual disabilities and parent carers of patient and public involvement in a health research study. J Intellect Disabil 2019;23:78–96.
Bell DM. Over the sea and far away: ways of overcoming some of the difficulties arising in work with adults with learning disabilities living in geographical isolation in the United Kingdom. Br J Learn Disabil 2005;33:180–7.
Belling R, McLaren S, Paul M, Ford T, Kramer T, Weaver T, et al. The effect of organisational resources and eligibility issues on transition from child and adolescent to adult mental health services. J Health Serv Res Policy 2014;19:169–76.
Bergstrom H, Elinder LS, Hagstromer M, Wihlman U. Barriers and facilitators in health education for people with intellectual disabilities: a qualitative study. J Intellect Disabil Res 2012;704.
Bhaumik S, Watson JM, Thorp CF, Tyrer F, McGrother CW. Body mass index in adults with intellectual disability: distribution, associations and service implications: a population-based prevalence study. J Intellect Disabil Res 2008;52(Pt 4);287–98.
Black LA, McConkey R, Roberts P, Ferguson P. Developing a person-centred support service for families caring for children with severe learning disabilities in rural and urban areas. J Intellect Disabil 2010;14:111–31. https://doi.org/10.1177/1744629510381941
Black P, Hyde C. Caring for people with a learning disability, colorectal cancer and stoma. Br J Nurs 2004;13:970–5. https://doi.org/10.12968/bjon.2004.13.16.15973
Blair J. Care adjustments for people with learning disabilities in hospitals. Nurs Manag 2011;18:21–4. https://doi.org/10.7748/nm2011.12.18.8.21.c8841
Blakemore S. NHS England to transform care for people with learning disabilities. Nurs Stand 2015;30:8. https://doi.org/10.7748/ns.30.6.8.s4
Bone A, McGrath-Lone L, Day S, Ward H. Inequalities in the care experiences of patients with cancer: analysis of data from the National Cancer Patient Experience Survey 2011–2012. BMJ Open 2014;4:e004567. https://doi.org/10.1136/bmjopen-2013-004567
Bonell S, Underwood L, Radhakrishnan V, McCarthy J. Experiences of mental health services by people with intellectual disabilities from different ethnic groups: a Delphi consultation. J Intellect Disabil Res 2012;56:902–9. https://doi.org/10.1111/j.1365-2788.2011.01494.x
Boot F H, Voorbrood V, Faber A, Evenhuis H. Systematic multidisciplinary medication reviews for older people with intellectual disabilities and polypharmacy in primary care. J Intellect Disabil Res 2016;60:640.
Bowler M, Nash P. Learning disabilities: improved bowel screening. Nurs Times 2015;111:14–16.
Braynion P. ‘Person-centred care is led by learning disability nurses’. Nurs Times 2011;107:11.
Bright L. File on 4. Community Care 2007;36.
Brodrick D, Lewis D, Worth A. One-page patient passport for people with learning disabilities. Nurs Stand 2011;25:35–40. https://doi.org/10.7748/ns.25.47.35.s49
Broughton S. A review of the literature: interventions to maximize capacity to consent and reduce anxiety of women with learning disabilities preparing for a cervical smear test. Health Serv Manage Res 2002;15:173–85. https://doi.org/10.1258/095148402320176756
Brown H, Flynn M. Supporting people with intellectual disabilities who are dying: What care staff need to know. J Intellect Disabil Res 2008;653.
Brown M, McCann E. Sexuality issues and the voices of adults with intellectual disabilities: A systematic review of the literature. Res Dev Disabil 2018;74:124–38.
Brown M, Sierka A, Karatzias T. Local Area Coordination as a model of social prescribing for adults with intellectual disabilities in primary care in Scotland. J Intellect Disabil Res 2016;772.
Brown M, Taggart L, Karatzias T, Truesdale M, Walley R, Northway R, et al. Improving diabetes care for people with intellectual disabilities: a qualitative study exploring the perceptions and experiences of professionals in diabetes and intellectual disability services. J Intellect Disabil Res 2017;61:435–49. https://doi.org/10.1111/jir.12369
Bunning K, Horton S. ‘Border crossing’ as a route to inclusion: a shared cause with people with a learning disability? Aphasiology 2007;21:9–22.
Burke E, McCallion P, Walsh J, McCarron M. One size does not fit all: making reasonable adjustment to facilitate people with intellectual disabilities to engage in objective health assessments. J Intellect Disabil Res 2016;773.
Buszewicz M, Welch C, Horsfall L, Nazareth I, Osborn D, Hassiotis A, et al. Assessment of an incentivised scheme to provide annual health checks in primary care for adults with intellectual disability: a longitudinal cohort study. Lancet Psychiatry 2014;1:522–30. https://doi.org/10.1016/S2215-0366(14)00079-0
Byrne JH, Ware RS, Lennox NG. Health actions prompted by health assessments for people with intellectual disability exceed actions recorded in general practitioners’ records. Aust J Prim Health 2015;21:317–20.
Cambridge P. The sexual health needs of people with learning disabilities. Nurs Times 2003;99:48–9.
Campbell M. Integrated inspection of services for people with learning disabilities in Scotland: the way forward? Int J Integr Care 2007;7:e40.
Campbell M. Commissioning services for people with learning disabilities in Scotland: linking evidence and practice. Br J Learn Disabil 2009;37:28–33.
Campbell M, and Martin M. Reducing health inequalities in Scotland: the involvement of people with learning disabilities as national health service reviewers. Br J Learn Disabil 2010;38:49–58.
Campbell M, Whoriskey M, Lyall R, Davidson A, McCue M. A national review of health services for people with intellectual disabilities in Scotland. Br J Dev Disabil 2007;53:25–36.
Cannistraci P. Health and wellness: What Adults with Intellectual and Developmental Disabilities Perceive as Facilitators and Barriers. Troy, NY: Sage Graduate Schools; 2011.
Carey IM, Hosking FJ, DeWilde S, Harris T, Beighton C, Cook DG. Learning disability registers in primary care. Br J Gen Prac 2016;66:351–2.
Carter P. ‘Be proud of the UK’s advances in learning disability care’. Nurs Times 2016;112:7.
Castell E, Stenfert Kroese B. Midwives’ experiences of caring for women with learning disabilities – A qualitative study. Midwifery 2016;36:35–42. https://doi.org/10.1016/j.midw.2016.02.001
Caton S, Starling S, Burton M, Azmi S, Chapman M. Responsive services for people with learning disabilities from minority ethnic communities. Br J Learn Disabil 2007;35:229–35.
Chadwick D, Chapman M, Davies G. Factors affecting access to daily oral and dental care among adults with intellectual disabilities. J Appl Res Intellect Disabil 2018;31:379–94. https://doi.org/10.1111/jar.12415
Chadwick D, Davies G, Cunningham D, Starling S. Access to dental care for adults with intellectual disabilities. J Appl Res in Intellect Disabil 2006;251.
Chambers S. Use of non-verbal communication skills to improve nursing care. Br J Nurs 2003;12:874–8. https://doi.org/10.12968/bjon.2003.12.14.11412
Chaplin E, Halls S, Carlile G, Hardy S, Joyce T. Barriers to user involvement in mental health services for people with learning disability. Adv Ment Health Learn Disabil 2009;3:28–33.
Chaplin E, O’Hara J. Policy implementation in England: developments to meet the mental health needs of people with learning disabilities. Adv Ment Health Learn Disabil 2007;1:7–12.
Chaplin E, Taggart L. England and Northern Ireland policy and law update relating to mental health and intellectual disability. Adv Ment Health Intellect Disabil 2012;6:144–50.
Chapman HM. The Health Consultation Experience for People with Learning Disabilities: a Constructivist Grounded Theory Study Based on Symbolic Interactionism. 2014.
Chapman HR, Kirby-Turner N. Visual/verbal analogue scales: examples of brief assessment methods to aid management of child and adult patients in clinical practice. Br Dent J 2002;193:447–50.
Cheak-Zamora NC, Yang X, Farmer JE, Clark M. Disparities in transition planning for youth with autism spectrum disorder. Pediatrics 2013;131:447–54. https://doi.org/10.1542/peds.2012-1572
Chew KL, Iacono T, Tracy J. Overcoming communication barriers - working with patients with intellectual disabilities. Aust Fam Phys 2009;38:10–14.
Chinn D. Review of interventions to enhance the health communication of people with intellectual disabilities: a communicative health literacy perspective. J Appl Res Intellect Disabil 2017;30:345–59. https://doi.org/10.1111/jar.12246
Clapham A. People with learning disabilities in rural Scotland: review of policy. Nurs Stand 2015;30:38–43. https://doi.org/10.7748/ns.30.7.38.s46
Clare IC, Madden EM, Holland AJ, Farrington CJ, Whitson S, Broughton S, et al. ‘What vision?’: experiences of Team members in a community service for adults with intellectual disabilities. J Intellect Disabil Res 2017;61:197–209. https://doi.org/10.1111/jir.12312
Clark LI, O’toole MS. Intellectual impairment and sexual health: information needs. Br J Nurs 2007;16:154–6. https://doi.org/10.12968/bjon.2007.16.3.22968
Clark LL, While A. Meeting the needs of people with intellectual impairment in primary care. Br J Community Nurs 2008;13:550–5. https://doi.org/10.12968/bjcn.2008.13.12.31824
Clegg J. Holding services to account. J Intellect Disabil Res 2008;52:581–7.
Codling M. ‘Eye Know’: translating needs from annual health checks for people with learning disabilities to demand. Br J Learn Disabili 2013;41:45–50.
Codling M, Macdonald N. User-friendly information: does it convey what it intends?. Learn Disabil Prac 2008;11:12–17.
Codling M, Solomon J. Evaluating health checks. Learn Disabil Prac 2007;10:32–8.
Coiffait FM, Marshall K. How to recognise and respond to mental health needs. Learn Disabil Prac 2011;14:23–8.
Cole A. Disabled people face difficulties in accessing primary care. BMJ 2006;333:565.
Collins K, Gratton C, Heneage C, Dagnan D. Employed carers‘ empathy towards people with intellectual disabilities: the development of a new measure and some initial theory. J Appl Res Intellect Disabil 2017;30:133–46.
Connolly J. Barriers to access to cancer screening for people with learning disabilities: a review. Lancet 2013;382:29.
Conyers C, Miltenberger RG, Peterson B, Gubin A, Jurgens M, Selders A, et al. An evaluation of in vivo desensitization and video modeling to increase compliance with dental procedures in persons with mental retardation. J Appl Behav Anal 2004;37:233–8. https://doi.org/10.1901/jaba.2004.37-233
Cooper SA, Hughes-McCormack L, Greenlaw N, McConnachie A, Allan L, Baltzer M, et al. Management and prevalence of long-term conditions in primary health care for adults with intellectual disabilities compared with the general population: a population-based cohort study. J Appl Res Intellect Disabil 2018;31(Suppl. 1):68–81. https://doi.org/10.1111/jar.12386
Corbett J, Thomas C, Prior M, Robson R. Health facilitation for people with learning disabilities. Br J Community Nurs 2003;8:404–10. https://doi.org/10.12968/bjcn.2003.8.9.11573
Corbett J. Health Care Provision and People with Learning Disabilities: a Guide for Health Professionals. New York, NY: John Wiley & Sons Ltd; 2007.
Costello H, Bouras N. Assessment of mental health problems in people with intellectual disabilities. Isr J Psychiatry Relat Sci 2006;43:241–51.
Costello H, Hardy S, Tsakanikos E, McCarthy J. Training Professionals, Family Carers and Support Staff to Work Effectively with People with Intellectual Disability and Mental Health Problems. In Bouras N, Holt G, editors. Mental Health Services For Adults With Intellectual Disability: Strategies And Solutions. New York, NY: Psychology Press; 2010. pp.117–36.
Cowley G. Poor understanding of learning disability careers. Nurs Stand 2012;26:33. https://doi.org/10.7748/ns.26.38.33.s47
Cross H, Cameron M, Marsh S, Tuffrey-Wijne I. Practical approaches toward improving end-of-life care for people with intellectual disabilities: effectiveness and sustainability. J Palliat Med 2012;15:322–6. https://doi.org/10.1089/jpm.2011.0132
Cumella S. Mental health services for people with a learning disability. Adv Ment Health Learn Disabil 2009;3:8–14.
Daaleman TP. Primary Care of Adults with Intellectual and Developmental Disabilities. South Med J 2016;109:12–16. https://doi.org/10.14423/SMJ.0000000000000392
D’Antonio Minh-Lieu V. Evaluating the Effectiveness of Specialist Multi-disciplinary Community Teams for People with Intellectual Disabilities in the United Kingdom. Dissertation Abstracts International: Section B: The Sciences and Engineering 2006;66(12-B):6917.
Davies J, Burke C. Strategic thinking. Ment Health Today 2012;12–14.
Davis C. Everyone welcome. Opening Trusts to patients with learning disabilities. Nurs Stand 2005;19:26–8.
Dawkins B. Getting it right for people with a learning disability. Br J Nurs 2010;19:808. https://doi.org/10.12968/bjon.2010.19.13.48854
Dearden-Phillips C, Fountain R. Real power? An examination of the involvement of people with learning difficulties in strategic service development in Cambridgeshire. Br J Learn Disabil 2005;33:200–4.
Dee B. Registered nurses supporting people with intellectual disabilities: an exploratory survey examining their role in meeting health needs. J Intellect Disabil Res 2016;778.
Devine M, Taggart L. Addressing the mental health needs of people with learning disabilities. Nurs Stand 2008;22:40–8. https://doi.org/10.7748/ns2008.07.22.45.40.c6591
Dodd K, Joyce T, Nixon J, Jennison J, Heneage C. Improving access to psychological therapies (IAPT): are they applicable to people with intellectual disabilities? Adv Ment Health Intellect Disabil 2011;5:29–34.
Doody C, Markey K, Doody O. Health of ageing people with intellectual disability and the role of the nurse in Ireland. J Intellect Disabil 2012;16:275–86. https://doi.org/10.1177/1744629512462181
Doody CM, Markey K, Doody O. Future need of ageing people with an intellectual disability in the Republic of Ireland: lessons learned from the literature. Br J Learn Disabil 2013;41:13–21.
Doody O, Slevin E, Taggart L. Intellectual disability nursing in Ireland: identifying its development and future. J Intellect Disabil 2012;16:7–16. https://doi.org/10.1177/1744629512437091
Douma JC, Dekker MC, De Ruiter KP, Verhulst FC, Koot HM. Help-seeking process of parents for psychopathology in youth with moderate to borderline intellectual disabilities. J Am Acad Child Adolesc Psychiatry 2006;45:1232–42. https://doi.org/10.1097/01.chi.0000230167.31246.db
Doyle C, Byrne K, Fleming S, Griffiths C, Horan P, Keenan PM. Enhancing the experience of people with intellectual disabilities who access health care. Learn Disabil Prac 2016;19:33–8.
Doyle J. Sexual health education for young people with special needs and learning difficulties. Paediatr Nurs 2006;18:12.
Dressler PB, Nguyen TK, Moody EJ, Friedman SL, Pickler L. Use of transition resources by primary care providers for youth with intellectual and developmental disabilities. Intellect Dev Disabil 2018;56:56–68. https://doi.org/10.1352/1934-9556-56.1.56
Dunkley AJ, Tyrer F, Gray LJ, Bhaumik S, Spong R, Chudasama Y, et al. Type 2 diabetes and glucose intolerance in a population with intellectual disabilities: the STOP diabetes cross-sectional screening study. J Intellect Disabil Res 2017;61:668–81. https://doi.org/10.1111/jir.12380
Dunkley S, Sales R. The challenges of providing palliative care for people with intellectual disabilities: a literature review. Int J Palliat Nurs 2014;20:279–84. https://doi.org/10.12968/ijpn.2014.20.6.279
Dunn K, Hughes-McCormack L, Cooper SA. Hospital admissions for physical health conditions for people with intellectual disabilities: systematic review. J Appl Res Intellect Disabil 2018;31(Suppl. 1):1–10. https://doi.org/10.1111/jar.12360
Durà-Vilà G, Hodes M. Ethnic factors in mental health service utilisation among people with intellectual disability in high-income countries: systematic review. J Intellect Disabil Res 2012;56:827–42. https://doi.org/10.1111/j.1365-2788.2011.01466.x
Edge N. My practice. Community Care 2005;39.
Edwards J, Northway R. Helping a person with autism to overcome her fear of needles. Primary Health Care 2011;21:26–29.
Emerson E. Inequalities in access to health screening among adults with intellectual disabilities. J Policy Pract Intellect Disabil 2013;119.
Emerson E, Hatton C, Robertson J, Baines S. Perceptions of neighbourhood quality, social and civic participation and the self rated health of British adults with intellectual disability: cross sectional study. BMC Public Health 2014;14:1252. https://doi.org/10.1186/1471-2458-14-1252
Emmett C. The Mental Capacity Act 2005 and its impact on dental practice. Br Dent J 2007;203:515–21.
Enow H, Nagalingam P, Singh R, Thalitaya MD. Need for a comprehensive sex and relationship education programme for adults with learning disability. Psychiatr Danub 2015;27(Suppl. 1):465–7.
Erickson SR, Kornexl K. Blood pressure screening, control, and treatment for patients with developmental disabilities in general medicine practices. J Pharm Technol 2016;32:234–9.
Evans J, Mir G, Atkin K, Marshall J, Allgar V. Identifying people with learning disabilities in general practice. Living Well 2005;5:18–22.
Evans T. A critical discourse analysis of community access service policy and practice informed by people with intellectual and developmental disabilities in the United Kingdom and Australia. J Intellect Disabil Res 2016;60:664.
Felce D, Allen D. The All Wales Learning Disability Strategy: current status and implications for people with mental health needs or severe challenging behaviour. Adv Ment Health Learn Disabil 2007;1:33–6.
Feldman MA, Owen F, Andrews A, Hamelin J, Barber R, Griffiths D. Health self-advocacy training for persons with intellectual disabilities. J Intellect Disabil Res 2012;56:1110–21. https://doi.org/10.1111/j.1365-2788.2012.01626.x
Ferguson M, Jarrett D, Terras M. Inclusion and healthcare choices: the experiences of adults with learning disabilities. Br J Learn Disabil 2011;39:73–83.
Finlay WM, Rohleder P, Taylor N, Culfear H. ‘Understanding’ as a practical issue in sexual health education for people with intellectual disabilities: a study using two qualitative methods. Health Psychol 2015;34:328–38. https://doi.org/10.1037/hea0000128
Finlayson J, De Amicis L, Gallacher S, Munro R, Crockett J, Godwin J, et al. Reasonable adjustments to provide equitable and inclusive assessment, screening and treatment of osteoporosis for adults with intellectual disabilities: a feasibility study. J Appl Res in Intellect Disabil 2018;2:2.
Fitzgerald C, Withers P. ‘I don’t know what a proper woman means’: what women with intellectual disabilities think about sex, sexuality and themselves. Br J Learn Disabil 2013;41:5–12.
Flatt JF, Guizouarn H, Burton NM, Borgese F, Tomlinson RJ, Forsyth RJ, et al. Stomatin-deficient cryohydrocytosis results from mutations in SLC2A1: a novel form of GLUT1 deficiency syndrome. Blood 2011;118:5267–77. https://doi.org/10.1182/blood-2010-12-326645
Flinton L, Pashley S, Lewington E. Keep your eyes open! Untreated co-morbidities in adults with epilepsy and learning disability. Epilepsia 2013;54:39.
Flood B, Henman MC. Case study: hidden complexity of medicines use: information provided by a person with intellectual disability and diabetes to a pharmacist. Br J Learn Disabil 2015;43:234–42.
Flynn M. Joint investigation into the provision of services for people with learning disabilities at Cornwall Partnership NHS Trust. J Adult Protect 2006;8:28–32.
Flynn M. Unlearned lessons from the Healthcare Commission’s investigation into the service for people with learning disabilities provided by Sutton and Merton Primary Care Trust. J Adult Protect 2007;9:21–26.
Flynn S, Hulbert-Williams L, Bramwell R, Stevens-Gill D, Hulbert-Williams N. Caring for cancer patients with an intellectual disability: attitudes and care perceptions of UK oncology nurses. Eur J Oncol Nurs 2015;19:568–74. https://doi.org/10.1016/j.ejon.2015.03.002
Flynn S, Hulbert-Williams NJ, Hulbert-Williams L, Bramwell R. ‘You don’t know what’s wrong with you’: an exploration of cancer-related experiences in people with an intellectual disability. Psycho-Oncology 2016;25:1198–1205.
Forbat L, Wilkinson H, Kerr D. Intellectual disability and dementia: subjective reflections on experiences and models of care provision. Gerontologist 2004;110.
Fordham M. The lived experience of homeless women: insights gained as a specialist practitioner. Community Pract 2015;88:32–4, 36–7.
Forrester-Jones R, Beecham JK, Barnoux M, Oliver D, Couch E, Bates C. People with intellectual disabilities at the end of their lives: The case for specialist care? J Appl Res Intellect Disabil 2017;30:1138–50. https://doi.org/10.1111/jar.12412
Forsyth B, Winterbottom P. Economic implications of current and future provision of English learning disability health services. Expert Rev Pharmacoecon Outcomes Res 2004;4:457–68. https://doi.org/10.1586/14737167.4.4.457
Forsyth R, Colver A, Alvanides S, Woolley M, Lowe M. Participation of young severely disabled children is influenced by their intrinsic impairments and environment. Dev Med Child Neurol 2007;49:345–9.
Fredheim T, Lien L, Danbolt LJ, Kjønsberg K, Haavet OR. Experiences with general practitioners described by families of children with intellectual disabilities and challenging behaviour: a qualitative study. BMJ Open 2011;1:e000304. https://doi.org/10.1136/bmjopen-2011-000304
Freeman T, Walshe K. Achieving progress through clinical governance? A national study of health care managers’ perceptions in the NHS in England. Qual Saf Health Care 2004;13:335–43.
Friedman C, Arnold CK, Owen AL, Sandman L. ‘Remember Our Voices are Our Tools’: sexual self-advocacy as defined by people with intellectual and developmental disabilities. Sex Disabil 2014;32:515–32.
Friedman SL, Helm DT, Woodman AC. Unique and universal barriers: hospice care for aging adults with intellectual disability. Am J Intellect Dev Disabil 2012;117:509–32. https://doi.org/10.1352/1944-7558-117.6.509
Fyson R, Fox L. Inclusion or outcomes? Tensions in the involvement of people with learning disabilities in strategic planning. Disabil Soc 2014;29:239–54.
Gallagher JE, Fiske J. Special Care Dentistry: a professional challenge. Br Dent J 2007;202:619–29.
Gardiner C, Brown N. Is there a role for occupational therapy within a specialist child and adolescent mental health eating disorder service? Br J Occup Ther 2010;73:38–43.
Gates B. Plus ca change, plus c’est la meme chose: reflection on access to health care in mainstream services by people with intellectual disabilities in England. J Intellect Disabil 2012;16:3–6.
Gates Bob. Planning for health: a contrary reflection on health action plans and health facilitators. J Learn Disabil 2003;7:5–7.
Gates B. ‘Develop learning disability nursing to stop more scandals’. Nurs Times 2011;107:7.
Genders N, Brown B. Shaping policy and provision for people with intellectual disabilities in England: change from within. J Intellect Disabil Res 2012;56:773.
George AP, Pope D, Watkins F, O’Brien SJ. How does front-line staff feel about the quality and accessibility of mental health services for adults with learning disabilities? J Eval Clin Pract 2011;17:196–8. https://doi.org/10.1111/j.1365-2753.2009.01343.x
Gilbert T, Wilkinson T, Crudgington S. Supporting people with intellectual disability in the cancer journey: the ‘Living with cancer’ communication pack. Eur J Oncol Nurs 2007;11:357–61.
Gilbert T, Wilkinson T, Crudgington S. People with intellectual disability and cancer: Issues of communication, access, and comfort. Int J Disabil Hum Dev 2008;7:371–77.
Gill F, Stenfert Kroese B, Rose J. General practitioners’ attitudes to patients who have learning disabilities. Psychol Med 2002;32:1445–55.
Gill F, Stenfert Kroese B, Rose J. General practitioners’ attitudes to patients who have learning disabilities. Psychol Med 2002;32:1445–55.
Gillen S. Learning disability care services ‘are heading towards a timebomb’. Nurs Stand 2012;26:9. https://doi.org/10.7748/ns2012.05.26.35.9.p8231
Glasper A. Every nurse needs to know about learning disabilities. Br J Nurs 2011;20:514–15. https://doi.org/10.12968/bjon.2011.20.8.514
Glidewell L, West R, Hackett JE, Carder P, Doran T, Foy R. Does a local financial incentive scheme reduce inequalities in the delivery of clinical care in a socially deprived community? A longitudinal data analysis. BMC Fam Pract 2015;16:61. https://doi.org/10.1186/s12875-015-0279-9
Glover G, Emerson E. A big data view of the health and healthcare of people with intellectual and developmental disabilities from primary care in England. J Intellect Disabil Res 2016;60:671.
Glover G, Williams R, Heslop P, Oyinlola J, Grey J. Mortality in people with intellectual disabilities in England. J Intellect Disabil Res 2017;61:62–74. https://doi.org/10.1111/jir.12314
Glover G, Christie A, Hatton C. Access to cancer screening by people with learning disabilities in England 2012/13: information from the Joint Health and Social Care Assessment Framework. Tizard Learn Disabil Rev 2014;19:194–8. https://doi.org/10.1108/TLDR-07-2014-0024
Glover G, Emerson E. Patterns of decline in numbers of learning disability nurses employed by the English National Health Service. Tizard Learn Disabil Rev 2012;17:194–8.
Goldring M. End healthcare’s disability apartheid. Community Care 2009;26.
Goodare L. A new strategy for learning disability care. Nurs Times 2003;99:42–3.
Greenwood N W, Ferrari B, Bhakta S, Ostrach B, Wilkinson J. Experiences, beliefs and needs of women with intellectual disabilities in accessing their reproductive rights. Contraception 2014;90:348–9.
Greig R. The policy construct behind community care. Int J Dev Disabil 2015;61:61–7.
Guthrie KS, Beadle-Brown J. Defining and measuring rapport: implications for supporting people with complex needs. Learn Disabil Rev 2006;11:21–30.
Haines D, Brown A. Health professionals working effectively with support workers to enhance the quality of support for adults with intellectual disabilities: A meta-ethnography. J Appl Res Intellect Disabil 2018;31:200–12. https://doi.org/10.1111/jar.12343
Hall E, McGarrol S. Progressive localism for an ethics of care: Local Area Co-ordination with people with learning disabilities. Soc Cult Geogr 2013;14:689–709.
Hall M. Health screening for patients with learning difficulties – a model for GP practices. Living Well 2005;5:21–6.
Hammond J. Signpost – a model of self-directed support and a framework for brokerage. Ment Health Soc Incl 2012;16:48–55.
Harrison R, Williamson J. Promoters of equal access. Nurs Stand 2010;25:20–1.
Harrison S, Berry L. Reports from winners of Foundation of Nursing Studies Awards 2004: access all areas: improving primary care services for patients with learning disabilities. Foundation of Nursing Studies: Developing Practice Improving Care Dissemination Series 2005 pp. 1–2.
Harwood I, Hassiotis A. A re-design of undergraduate medical training in intellectual disability: building psychological capital and imparting knowledge to redress health inequalities. Adv Ment Health Intellect Disabil 2014;8:354–361.
Hassiotis A, Buszewicz M, Welch C, Horsfall L, Nazareth I, Osborn D, et al. Effectiveness of annual health checks for patients with intellectual disability in primary care. J Appl Res Intellect Disabil 2014;27:318.
Hassiotis A, Osborn D, Horsfall L, Petersen I, Walters K, Nazareth I. Access to cancer screening in people with learning disabilities in the UK using a primary care database. J Intellect Disabil Res 2012;56:763.
Haymes LK, Storey K, Maldonado A, Post M, Montgomery J. Using applied behavior analysis and smart technology for meeting the health needs of individuals with intellectual disabilities. Dev Neurorehabil 2015;18:407–19. https://doi.org/10.3109/17518423.2013.850750
Heer K, Rose J, Larkin M. The challenges of providing culturally competent care within a disability focused team: a phenomenological exploration of staff experiences. J Transcult Nurs 2016;27:109–16. https://doi.org/10.1177/1043659614526454
Hemmings C, Bouras N Craig T. How should community mental health of intellectual disability services evolve? Int J Environ Res Public Health 2014;11:8624–31.
Hemmings CP. Community services for people with intellectual disabilities and mental health problems. Curr Opin Psychiatry 2008;21:459–62. https://doi.org/10.1097/YCO.0b013e3283060a6a
Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889–95. https://doi.org/10.1016/S0140-6736(13)62026-7
Heslop P, Hoghton M, Blair P, Fleming P, Marriott A, Russ L. The need for FASTER CARE in the diagnosis of illness in people with intellectual disabilities. Br J Gen Pract 2013;63:661–2. https://doi.org/10.3399/bjgp13X675593
Heslop P, Marriott A. Making a difference – the impact of the Confidential Inquiry into premature deaths of people with learning disabilities. Br J Learn Disabil 2015;43:142–9.
Heslop P, Hoghton M, Marriott A. ‘Reasonable adjustments’ for vulnerable patients. Br J Psychiatry 2014;205:411–12. https://doi.org/10.1192/bjp.205.5.411b
Hill R. Integrated care – foundation trust or social enterprise? Journal of Integrated Care 2007;15:20–3.
Hoghton M, Martin G, Chauhan U. Annual health checks for people with intellectual disabilities. BMJ 2012;345:e7589. https://doi.org/10.1136/bmj.e7589
Hollingsworth L, Kalambouka A. Giving a Voice to the Person in My Dental Chair: Communication with People with Learning Disabilities. Prim Dent J 2015;4:70–6.
Holman Andrew. Will the new system mean more or less equality of access to health care? Community Living 2010;24:8–10.
Holt G, Bouras N. Training residential and day care staff on the mental health needs of people with intellectual disability (ID). J Intellect Disabil Res 2004;495.
Homeyard C, Gaudion A. Aiming for equal access to maternity care for all. Pract Midwife 2014;17:13–16.
Homeyard C, Montgomery E, Chinn D, Patelarou E. Current evidence on antenatal care provision for women with intellectual disabilities: A systematic review. Midwifery 2016;32:45–57. https://doi.org/10.1016/j.midw.2015.10.002
Hoole L, Morgan S. ‘It’s only right that we get involved’: service-user perspectives on involvement in learning disability services. Br J Learn Disabil 2011;39:5–10.
Hosking FJ, Carey IM, Shah SM, Harris T, DeWilde S, Beighton C, Cook DG. Mortality among adults with intellectual disability in England: comparisons with the general population. Am J Public Health 2016;106:1483–90. https://doi.org/10.2105/AJPH.2016.303240
House A, Bryant L, Russell AM, Wright-Hughes A, Graham L, Walwyn R, et al. Randomized controlled feasibility trial of supported self-management in adults with type 2 diabetes mellitus and an intellectual disability: OK Diabetes. Diabet Med 2018;35:776–88. https://doi.org/10.1111/dme.13626
House A, Latchford G, Russell AM, Bryant L, Wright J, Graham E, et al. Development of a supported self-management intervention for adults with type 2 diabetes and a learning disability. Pilot Feasibil Stud 2018;4:106. https://doi.org/10.1186/s40814-018-0291-7
Hovey T, Cheswick C. Copying letters to service users with learning disabilities: opinions of service users, carers and professionals working within learning disability services. Br J Lear Disabil 2009;37:50–5.
Howieson J, Clarke K. Ensuring service users can access crucial information. Learn Disabil Pract 2013;16:22–5.
Hsieh K, Yamaki K. Health status and health care access among adults with intellectual and developmental disabilities living at home. Gerontologist 2009;49:186–7.
Hubert J. Family carers’ views of services for people with learning disabilities from black and minority ethnic groups: a qualitative study of 30 families in a south London borough. Disabil Soc 2006;21:259–72.
Hudson B. Making and missing connections: learning disability services and the transition from adolescence to adulthood. Disabil Soc 2006;21:47–60.
Hughes-McCormack L, Cooper SA, Greenlaw N, McConnachie A, Allan L, Baltzer M, et al. Quality of primary health care of 5,000 people with intellectual disabilities in Scotland. J Intellect Disabil Res 2016;685.
Huneke NT, Gupta R, Halder N, Chaudhry N. Difficult decisions: are intellectually disabled patients given enough information to consent to medical treatment? J Intellect Disabil 2012;16:265–74. https://doi.org/10.1177/1744629512462179
Hurtado B, Jones L, Burniston F. Is easy read information really easier to read? J Intellect Dis Res 2014;58:822–9.
Innes A, McCabe L, Watchman K. Caring for older people with an intellectual disability: a systematic review. Maturitas 2012;72:286–95. https://doi.org/10.1016/j.maturitas.2012.05.008
Jelley D, Walker C. Patient perspective. Copying clinical letters: access issues for specific patient groups. Qual Prim Care 2003;11:215–19.
Jenkins R. Nurses’ views about services for older people with learning disabilities. Nurs Older People 2009;21:23–7. https://doi.org/10.7748/nop2009.04.21.3.23.c7013
Jokinen N. The content of available practice literature in dementia and intellectual disability. Dementia 2005;4:327–39.
Jones A, Tuffrey-Wijne I, Bernal J, Butler G, Hollins S. Meeting the cancer information needs of people with learning disabilities: experiences of paid carers. Br J Learn Disabil 2007;35:12–18.
Kaler M. Special dentistry. Part three: learning disability. Dent Nurs 2011;7:324–27.
Kancherla V, Van Naarden Braun K, Yeargin-Allsopp M. Dental care among young adults with intellectual disability. Res Dev Disabil 2013;34:1630–41. https://doi.org/10.1016/j.ridd.2013.02.006
Kelly M. The implementation of the Care Programme Approach for service users with a learning disability. Building Bridges to the same Old Horizons? J Psychiatr Ment Health Nurs 2017;24:396–402. https://doi.org/10.1111/jpm.12398
Kerr S, Lawrence M, Middleton AR, Fitzsimmons L, Darbyshire C. Tobacco and alcohol use in people with mild/moderate intellectual disabilities: giving voice to their health promotion needs. J Appl Res Intellect Disabil 2017;30:612–26. https://doi.org/10.1111/jar.12255
Kerrigan JC, Hopper C. Implementing policy and good practice in services for people with learning disabilities: factors influencing commissioning and service provision. Tizard Learn Disabil Rev 2017;22:28–37.
Khanlou N, Mustafa N, Vazquez LM, Haque N, Yoshida K. Stressors and barriers to services for immigrant fathers raising children with developmental disabilities. Int J Ment Health Addict 2015;13:659–74. https://doi.org/10.1007/s11469-015-9584-8
Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev 2006;12:70–82. https://doi.org/10.1002/mrdd.20098
Kroese BS, Rose J, Heer K, O’Brien A. Mental health services for adults with intellectual disabilities – what do service users and staff think of them? J Appl Res Intellect Disabil 2013;26:3–13. https://doi.org/10.1111/jar.12007
Lafferty A, McConkey R, Simpson A. Reducing the barriers to relationships and sexuality education for persons with intellectual disabilities. J Intellect Disabil 2012;16:29–43. https://doi.org/10.1177/1744629512438034
Lane M, Taylor M, Ewin M, Schafer J, Mitchell G, Lennox N. Increasing medical students’ awareness of barriers to comprehensive healthcare in adults with intellectual disability. J Intellect Disabil Res 2012;56:761.
Lantman-de Valk, HMJV, Naaldenberg J. Towards tailored primary health care for persons with intellectual disabilities. J Appl Res Intellect Disabil 2014;27:305.
Larkin M, Unwin G, Iyer M, Tsimopoulou I, Zahid S, Malik K, et al. Cultural affordance, social relationships, and narratives of independence: understanding the meaning of social care for adults with intellectual disabilities from minority ethnic groups in the UK. Int J Dev Disabil 2018;64:195–203.
Lennox N, McPherson L, Bain C, O’Callaghan M, Carrington S, Ware RS. A health advocacy intervention for adolescents with intellectual disability: a cluster randomized controlled trial. Dev Med Child Neurol 2016;58:1265–72. https://doi.org/10.1111/dmcn.13174
Lennox N, Taylor M, Rey-Conde T, Bain C, Boyle FM, Purdie DM. Ask for it: development of a health advocacy intervention for adults with intellectual disability and their general practitioners. Health Promot Int 2004;19:167–75. https://doi.org/10.1093/heapro/dah204
Lennox N, Van Driel ML, van Dooren K. Supporting primary healthcare professionals to care for people with intellectual disability: a research agenda. J Appl Res Intellect Disabil 2015;28:33–42. https://doi.org/10.1111/jar.12132
Lennox N, Ware R, Bain C, Taylor Gomez M, Cooper SA. Effects of health screening for adults with intellectual disability: a pooled analysis. Br J Gen Pract 2011;61:193–6. https://doi.org/10.3399/bjgp11X561186
Leyshon S, Clark LL, Epstein L, Higgins S. Caring for people with learning disability using care management. Br J Nurs 2004;13:845–7. https://doi.org/10.12968/bjon.2004.13.14.14311
Li CW, Wong YC, Lo YM, Sham MK, Cheng HW, Lai T, et al. Embracing the setting sun: provision of palliative care via a collaborative model between hospital and community for patients with intellectual disabilities. Ann Palliat Med 2018;7:365–7. https://doi.org/10.21037/apm.2017.08.03
Li JCh, Wong K, Park AS, Fricke TR, Jackson AJ. The challenges of providing eye care for adults with intellectual disabilities. Clin Exp Optom 2015;98:420–9. https://doi.org/10.1111/cxo.12304
Li S, Ng J. End-of-life care: nurses’ experiences in caring for dying patients with profound learning disabilities – a descriptive case study. Palliat Med 2008;22:949–55. https://doi.org/10.1177/0269216308096905
Lindsay P, Burgess D. Care of patients with intellectual or learning disability in primary care: no more funding so will there be any change? Br J Gen Pract 2006;56:84–6.
Ling P, MacPherson J, Craig J. Service review of the joint epilepsy and learning disability clinic in the South Eastern Health and Social Care Trust, Northern Ireland. Epilepsia 2013;54:107.
Mac Giolla Phadraig C, Burke E, McCallion P, McGlinchey E, Nunn J, McCarron M. Dental attendance among older adults with intellectual disabilities in Ireland. Spec Care Dentist 2014;34:265–72. https://doi.org/10.1111/scd.12067
MacArthur J, Brown M, McKechanie A, Mack S, Hayes M, Fletcher J. Making reasonable and achievable adjustments: the contributions of learning disability liaison nurses in ‘Getting it right’ for people with learning disabilities receiving general hospitals care. J Adv Nurs 2015;71:1552–63. https://doi.org/10.1111/jan.12629
Macdonald S, Morrison J, Melville CA, Baltzer M, MacArthur L, Cooper SA. Embedding routine health checks for adults with intellectual disabilities in primary care: practice nurse perceptions. J Intellect Disabil Res 2018;62:349–57. https://doi.org/10.1111/jir.12475
Mafuba K, Gates B. An investigation into the public health roles of community learning disability nurses. Br J Learn Disabil 2015;43:1–7.
Magana S, Seltzer MM, Krauss MW.. Service utilization patterns of adults with intellectual disabilities: a comparison of Puerto Rican and non-Latino white families. J Gerontol Soc Work 2002;37:65–86.
Malouf R, Henderson J, Redshaw M. Access and quality of maternity care for disabled women during pregnancy, birth and the postnatal period in England: data from a national survey. BMJ Open 2017;7:e016757. https://doi.org/10.1136/bmjopen-2017-016757
Malouf R, McLeish J, Ryan S, Gray R, Redshaw M. ‘We both just wanted to be normal parents’: a qualitative study of the experience of maternity care for women with learning disability. BMJ Open 2017;7:e015526. https://doi.org/10.1136/bmjopen-2016-015526
Mander C. An investigation of the delivery of health-related accessible information for adults with learning disabilities. Tizard Learn Disabil Rev 2016:21:15–23.
Markar TN. Communications between psychiatrists and general practitioners in learning disability a clinical audit. Br J Dev Disabil 2002;48:107–12.
Marks B, Sisirak J, Chang YC. Efficacy of the HealthMatters program train-the-trainer model. J Appl Res Intellect Disabil 2013;26:319–34. https://doi.org/10.1111/jar.12045
Marriott A, Turner S, Giraud-Saunders A. Improving access to screening for people with learning disabilities. Nurs Stand 2014;29:37–42. https://doi.org/10.7748/ns.29.9.37.e9123
Marsden D, Giles R. The 4C framework for making reasonable adjustments for people with learning disabilities. Nurs Stand 2017;31:45–53. https://doi.org/10.7748/ns.2017.e10152
Martin G, Gadsby R. Annual health checks for adults with severe learning disabilities in primary care. Br J Gen Pract 2002;52:675–6.
Martin G, Lindsay P. Dying and living with learning disability: will health checks for adults improve their quality of life? Br J Gen Pract 2009;59:480–1. https://doi.org/10.3399/bjgp09X453503
Martin G. Annual health reviews for patients with severe learning disabilities: five years of a combined GP/CLDN clinic. J Learn Disabil 2003;7:9–21.
Mastebroek M, Naaldenberg J, Lagro-Janssen AL, van Schrojenstein Lantman de Valk H. Health information exchange in general practice care for people with intellectual disabilities – a qualitative review of the literature. Res Dev Disabil 2014;35:1978–87. https://doi.org/10.1016/j.ridd.2014.04.029
Mastebroek M, Naaldenberg J, van den Driessen Mareeuw FA, Lagro-Janssen AL, van Schrojenstein Lantman-de Valk HM. Experiences of patients with intellectual disabilities and carers in GP health information exchanges: a qualitative study. Fam Pract 2016;33:543–50. https://doi.org/10.1093/fampra/cmw057
McCann E, Lee R, Brown M. The experiences and support needs of people with intellectual disabilities who identify as LGBT: a review of the literature. Res Dev Disabil 2016;57:39–53. https://doi.org/10.1016/j.ridd.2016.06.013
McCarthy G, Norbrook M. Establishing an integrated level 2 sexual health service for people with learning difficuties. Sexually transmitted infections. British Association for Sexual Health and HIV (BASHH) Annual Conference, Oxford, UK, July 2016.
McCarthy M. Women with intellectual disability: their sexual lives in the 21st century. J Intellect Dev Disabil 2014;39:124–131.
McClimens A, Brewster J, Lewis R. Treatment of people with intellectual disability in the NHS: a report from England. J Appl Res Intellect Disabil 2014;315.
McCray J. Interprofessional practice and learning disability nursing. Br J Nurs 2003;12:1335–44. https://doi.org/10.12968/bjon.2003.12.22.11897
McGlade A, Bickerstaff D, Lindsay J, McConkey R, Jackson J. Making a difference. Visual health needs of people with a learning disability. Br J Learn Disabil 2010;38:187–193.
McGrother C W, Bhaumik S, Thorp C F, Watson J M, Taub N A. Prevalence, morbidity and service need among South Asian and white adults with intellectual disability in Leicestershire, UK. J Intellect Disabil Res 2002;46:299–309.
McIlfatrick S, Taggart L, Truesdale-Kennedy M. Supporting women with intellectual disabilities to access breast cancer screening: a healthcare professional perspective. Eur J Cancer Care 2011;20:412–20. https://doi.org/10.1111/j.1365-2354.2010.01221.x
McInnis EE, Hills A, Chapman MJ. Eligibility for statutory learning disability services in the north-west of England. Right or luxury? Findings from a pilot study. Br J Learn Disabil 2012;40:177–86.
McKenzie K, Metcalfe D, Michie A, Murray G. Service provision in Scotland for people with an intellectual disability who have, or are at risk of developing, dementia. Dementia 2018. https://doi.org/10.1177/1471301218785795
McKenzie K, Smith M, Purcell AM. The reported expression of pain and distress by people with an intellectual disability. J Clin Nurs 2013;22:1833–42. https://doi.org/10.1111/j.1365-2702.2012.04269.x
McLaughlin D. Formal carers providing end-of-life care and bereavement support to people with intellectual disabilities have unmet learning needs. Evid Based Nurs 2018;21:19. https://doi.org/10.1136/eb-2017-102799
McLaughlin D, Barr O, McIlfatrick S, McConkey R. Developing a best practice model for partnership practice between specialist palliative care and intellectual disability services: a mixed methods study. Palliat Med 2014;28:1213–21. https://doi.org/10.1177/0269216314550373
McLaughlin D, Barr O, McIlfatrick S, McConkey R. Service user perspectives on palliative care education for health and social care professionals supporting people with learning disabilities. BMJ Support Palliat Care 2015;5:531–7. https://doi.org/10.1136/bmjspcare-2013-000615
McLaughlin D, Taggart L, Quinn B, Milligan V. The experiences of professionals who care for people with intellectual disability who have substance-related problems. J Subst Use 2007;12:133–43.
McShea L, Corkish C, McAnelly S. Audiology services: access, assessment and aftercare. Learn Disabil Pract 2014;17:20–5.
Melville CA, Cooper SA, Morrison J, Finlayson J, Allan L, Robinson N, et al. The outcomes of an intervention study to reduce the barriers experienced by people with intellectual disabilities accessing primary health care services. J Intellect Disabil Res 2006;50:11–17.
Melville CA, Finlayson J, Cooper SA, Allan L, Robinson N, Burns E, et al. Enhancing primary health care services for adults with intellectual disabilities. J Intellect Disabil Res 2005;49:190–8.
Messent PR. An evaluation of community learning disability nurse teams in two London boroughs. Br J Community Nurs 2003;8:411–13, 416–20. https://doi.org/10.12968/bjcn.2003.8.9.11574
Morton-Nance S, Schafer T. End of life care for people with a learning disability. Nurs Stand 2012;27:40–7. https://doi.org/10.7748/ns2012.09.27.1.40.c9270
Moyle J, James N. Role of reasonable adjustments in improving care: a case study. Learn Disabil Pract 2015;18:32–7.
Murphy GH. Capacity to consent to sexual relationships in adults with learning disabilities. J Fam Plann Reprod Health Care 2003;29:148–9.
Murphy GH, O’Callaghan A. Capacity of adults with intellectual disabilities to consent to sexual relationships. Psychol Med 2004;34:1347–57.
Naaldenberg J, Lantman-de Valk, HMJV, Mastebroek M. Health promotion for people with intellectual disabilities: a systematic review of available literature. J Intellect Disabil Res 2012;56:758.
Naseem M, Shah AH, Khiyani MF, Khurshid Z, Zafar MS, Gulzar S, et al. Access to oral health care services among adults with learning disabilities: a scoping review. Ann Stomatol 2016;7:52–9. https://doi.org/10.11138/ads/2016.7.3.052
Neve J, Briers G. Reducing inequalities in health and life expectancy. Nurs Times 2016;112:12–14.
Nind M, Seale J. Concepts of access for people with learning difficulties: towards a shared understanding. Disabil Soc 2009;24:273–87.
Nocon A, Sayce L. Primary healthcare for people with mental health problems or learning disabilities. Health Policy 2008;86:325–34. https://doi.org/10.1016/j.healthpol.2007.11.009
Nocon A, Sayce L, Nadirshaw Z. Health inequalities experienced by people with learning disabilities: problems and possibilities in primary care. Learn Disabil Rev 2008;13:28–36.
Northfield J. Visual Impairment and People with Learning Disabilities. NLH Learning Disabilities Specialist Library; 2008.
O’Dwyer M, Meštrović A, Henman M. Pharmacists’ medicines-related interventions for people with intellectual disabilities: a narrative review. Int J Clin Pharm 2015;37:566–78. https://doi.org/10.1007/s11096-015-0113-4
Oliver MN, Miller TT, Skillman GD. Factors influencing direct-care paraprofessionals’ decisions to initiate mental health referrals for adults with mental retardation. Ment Retard 2005;43:83–91. https://doi.org/10.1352/0047-6765(2005)43<83:FIDPTI>2.0.CO;2
Ong N, McCleod E, Nicholls L, Fairbairn N, Tomsic G, Lord B, and Eapen V. Paving the way for paeds with needs: attitudes of healthcare staff in the treatment of children and adolescents with intellectual disabilities. J Intellect Disabil Res 2016;804.
O’Regan P, Drummond E. Cancer information needs of people with intellectual disability: a review of the literature. Eur J Oncol Nurs 2008;12:142–7. https://doi.org/10.1016/j.ejon.2007.12.001
Owen S, Khalil E. Addressing diversity in mental health care: a review of guidance documents. Int J Nurs Stud 2007;44:467–78.
Owens J, Dyer TA, Mistry K. People with learning disabilities and specialist services. Br Dent J 2010;208:203–5. https://doi.org/10.1038/sj.bdj.2010.204
Owens PL, Kerker BD, Zigler E, Horwitz SM. Vision and oral health needs of individuals with intellectual disability. Dev Disabil Res Rev 2006;12:28–40.
Parish C. Identifying challenges linked to healthcare provision for people with learning disabilities. Learn Disabil Pract 2013;16:6–7.
Parker M. Caring for vulnerable ostomists: learning disabilities and stoma care. Br J Nurs 2012;21:S4, S6, S8 passim. https://doi.org/10.12968/bjon.2012.21.Sup16.S4
Parrott R, Tilley N, Wolstenholme J. Changes in demography and demand for services from people with complex needs and profound and multiple learning disabilities. Tizard Learn Disabil Rev 2008;13:26–34.
Peate I, Maloret P. Testicular self-examination: the person with learning difficulties. Br J Nurs 2007;16:931–5. https://doi.org/10.12968/bjon.2007.16.15.24517
Pelleboer-Gunnink HA, Van Oorsouw WMWJ, Van Weeghel J, Embregts PJCM. Mainstream health professionals’ stigmatising attitudes towards people with intellectual disabilities: a systematic review. J Intellect Disabil Res 2017;61:411–34. https://doi.org/10.1111/jir.12353
Penfold J. Better primary care for special needs patients. Prim Health Care 2016;26:11.
Perry DW, Shervington T, Mungur N, Marston G, Martin D, Brown G. Why are people with intellectual disability moved ‘out-of-area’? J Policy Pract Intellect Disabil 2007;4:203–9.
Petrovic B, Markovic D, Peric T. Evaluating the population with intellectual disability unable to comply with routine dental treatment using the International Classification of Functioning, Disability and Health. Disabil Rehabil 2011;33:1746–54. https://doi.org/10.3109/09638288.2010.546934
Pilling R. Diabetic eye screening in people with learning disabilities: improving access. J Diabetes Nurs 2014;18:199–202.
Pownall JD, Jahoda A, Hastings RP. Sexuality and sex education of adolescents with intellectual disability: mothers’ attitudes, experiences, and support needs. Intellect Dev Disabil 2012;50:140–54. https://doi.org/10.1352/1934-9556-50.2.140
Pradhan A, Slade GD, Spencer AJ. Access to dental care among adults with physical and intellectual disabilities: residence factors. Aust Dent J 2009;54:204–11. https://doi.org/10.1111/j.1834-7819.2009.01120.x
Proulx R, Mercier C, Lemetayer F, Jutras S, Major D. Challenges in access to breast cancer screening for women with intellectual disability. J Intellect Disabil Res 2008;52:745.
Read S. Toolkits for better health: supporting the health needs of people with intellectual disabilities. J Intellect Disabil Res 2012;56:659.
Read S, Cartlidge D. Critical reflections on end-of-life care for people with intellectual disabilities: a single case study approach. Int J Palliat Nurs 2012;18:23–7. https://doi.org/10.12968/ijpn.2012.18.1.23
Read S, Jackson S, Cartlidge D. Palliative care and intellectual disabilities: individual roles, collective responsibilities. Int J Palliat Nurs 2007;13:430–5. https://doi.org/10.12968/ijpn.2007.13.9.27391
Read S, Thompson-Hill J. Palliative care nursing in relation to people with intellectual disabilities. Int J Palliat Nurs 2009;15:226–32. https://doi.org/10.12968/ijpn.2009.15.5.42348
Redshaw M, Malouf R, Gao H, Gray R. Women with disability: the experience of maternity care during pregnancy, labour and birth and the postnatal period. BMC Pregnancy Childbirth 2013;13:174. https://doi.org/10.1186/1471-2393-13-174
Roberts H, Ingold A, Liabo K, Manzotti G, Reeves D, Bradby H. Moving on: transitions out of care for young people with learning disabilities in England and Sweden. Br J Learning Disabil 2018;46:54–63.
Robertson J, Baines S, Emerson E, Hatton C. Service responses to people with intellectual disabilities and epilepsy: a systematic review. J Appl Res Intellect Disabil 2017;30:1–32. https://doi.org/10.1111/jar.12228
Robertson J, Emerson E, Hatton C, Elliott J, McIntosh B. The Impact of Person Centred Planning. Lancaster: Institute for Health Research, Lancaster University; 2005. URL: www.choiceforum.org/docs/pcpimpact.pdf (accessed 30 November 2018).
Robertson J, Hatton C, Baines S, Emerson E. Systematic reviews of the health or health care of people with intellectual disabilities: a systematic review to identify gaps in the evidence base. J Appl Res Intellect Disabil 2015;28:455–523. https://doi.org/10.1111/jar.12149
Robertson J, Hatton C, Emerson E, Baines S. The impact of health checks for people with intellectual disabilities: an updated systematic review of evidence. Res Dev Disabil 2014;35:2450–62. https://doi.org/10.1016/j.ridd.2014.06.007
Robertson J, Roberts H, Emerson E. Health Checks for People with Learning Disabilities: a Systematic Review of Evidence. Stockton-on-Tees: Improving Health and Lives: Learning Disabilities Observatory; 2010.
Robertson J, Roberts H, Emerson E, Turner S, Greig R. The impact of health checks for people with intellectual disabilities: a systematic review of evidence. J Intellect Disabil Res 2011;55:1009–19. https://doi.org/10.1111/j.1365-2788.2011.01436.x
Rose N, Kent S, Rose J. Health professionals’ attitudes and emotions towards working with adults with intellectual disability (ID) and mental ill health. J Intellect Disabil Res 2012;56:854–64. https://doi.org/10.1111/j.1365-2788.2011.01476.x
Rowe M. Will general practitioners be adequately prepared to meet the complexities of enhanced dementia screening for people with learning disabilities and Down syndrome: key considerations. Br J Learn Disabil 2016;44:43–8.
Rozas NS, Sadowsky JM, Jeter CB. Strategies to improve dental health in elderly patients with cognitive impairment: a systematic review. J Am Dent Assoc 2017;148:236–45.e3.
Ruddick L. Health of people with intellectual disabilities: a review of factors influencing access to health care. Br J Health Psychol 2005;10:559–70.
Russ L. WA10 Working in partnership with people with learning disabilities: academics and people with learning disabilities working together to disseminate the findings of a confidential inquiry into deaths of people with learning disabilities through film. BMJ Support Palliat Care 2015;5(Suppl. 1):A3–4. https://doi.org/10.1136/bmjspcare-2015-000906.10
Sallah D, Kozlowska O. Is information enough? Increasing effectiveness of engagement and signposting for people with intellectual disabilities from migrant communities living in England, UK. J Appl Res Intellect Dis 2014;345.
Sallah D, Kozlowska O. People with learning disabilities from migrant communities, living in England: improving access, experience and outcomes. J Intellect Disabil Res 2015;67.
Saunders J, McEnhill LS. Education for workers caring for people with intellectual disabilities (ID) who are in need of palliative care services: a comprehensive approach. J Intellect Disabil Res 2004;435.
Sawhney I, Tajer A, Morgan J. Copying clinical letters to patients: views of people with learning disability and their carers. Br J Dev Disabil 2007;53:17–23.
Schulte AG, Freyer K, Bissar A. Caries experience and treatment need in adults with intellectual disabilities in two German regions. Community Dent Health 2013;30:39–44.
Scior K, Grierson K. Service provision for young people with intellectual disabilities and additional mental health needs: service-providers’ perspectives. J Appl Res Intellect Disabil 2004;17:173–79.
Shankar R, Bradley-Smith G, Brigham P, Devapriam J, Osborne A, Axby S. Patient- and carer-held health records: can they improve annual health checks for patients with learning disability? Br J Gen Pract 2016;66:210–12. https://doi.org/10.3399/bjgp16X684697
Shankar R, Bradley M, Jory C, Olotu V. Consent to contraceptive treatment among clients with epilepsy. Learn Disabil Pract 2013;16:27–30.
Shooshtari S, Naghipur S, Zhang J. Unmet healthcare and social services needs of older canadian adults with developmental disabilities. J Policy Pract Intellect Disabil 2012;9:81–91.
Skorpen S. Information-tools and cancer for people with intellectual disability. J Intellect Disabil Res 2008;52:649.
Slevin E, Sines D. The role of community nurses for people with learning disabilities: working with people who challenge. Int J Nurs Stud 2005;42:415–27.
Slevin E, Truesdale-Kennedy M, McConkey R, Barr O, Taggart L. Community learning disability teams: developments, composition and good practice: a review of the literature. J Intellect Disabil 2008;12:59–79. https://doi.org/10.1177/1744629507083583
Slowie D, Martin G. Narrowing the health inequality gap by annual health checks for patients with intellectual disability. Br J Gen Pract 2014;64:101–2. https://doi.org/10.3399/bjgp14X677293
Smallman S, Engel B, Nelson J. Obesity services for adults with learning disabilities. J Hum Nutr Diet 2011;24:304–5.
Smiley E, Cooper SA, Miller SM, Robertson P, Simpson N. Specialist health services for people with intellectual disability in Scotland. J Intellect Disabil Res 2002;46:585–93.
Sosnowy C, Silverman C, Shattuck P. Parents’ and young adults’ perspectives on transition outcomes for young adults with autism. Autism 2018;22:29–39. https://doi.org/10.1177/1362361317699585
Southby K. Barriers to non-residential respite care for adults with moderate to complex needs: a UK perspective. J Intellect Disabil 2017;21:366–86. https://doi.org/10.1177/1744629516658577
Sowney M, Barr O. Equity of access to health care for people with learning disabilities: a concept analysis. J Learn Disabil 2004;8:247–65.
Staff writer. Helping people assert their rights. Nurs Times 2005;101:47.
Starr JM, Marsden L. Characterisation of user-defined health status in older adults with intellectual disabilities. J Intellect Disabil Res 2008;52:483–9.
Stauffer-Kruse S. Gay men with learning disabilities: UK service provision. J Gay Lesbian Psychother 2007;11:145–52.
Stein W. Modified Sainsbury tool: an initial risk assessment tool for primary care mental health and learning disability services. J Psychiatr Ment Health Nurs 2005;12:620–33.
Straetmans J, Lantman-de Valk, HMJV, Dinant GJ. Health problems of people with intellectual disabilities (ID): the implications for general practice? J Appl Res Intellect Disabil 2006;19:249.
Stringer K, Terry AL, Ryan BL, Pike A. Patient-centred primary care of adults with severe and profound intellectual and developmental disabilities: patient-caregiver-physician relationship. Can Fam Phys 2008;64:S63–69.
Sullivan WF, Heng J, Cameron D, Lunsky Y, Cheetham T, Hennen B, et al. Consensus guidelines for primary health care of adults with developmental disabilities. Can Fam Phys 2006;52:1410–18.
Swaine JG, Dababnah S, Parish SL, Luken K. Family caregivers’ perspectives on barriers and facilitators of cervical and breast cancer screening for women with intellectual disability. Intellect Dev Disabil 2013;51:62–73. https://doi.org/10.1352/1934-9556-51.01.062
Swaine JG, Parish SL, Luken K, Son E, Dickens P. Test of an intervention to improve knowledge of women with intellectual disabilities about cervical and breast cancer screening. J Intellect Disabil Res 2014;58:651–63. https://doi.org/10.1111/jir.12062
Taggart L, Coates V, Clarke M, Bunting B, Davies M, Carey M, et al. A study protocol for a pilot randomised trial of a structured education programme for the self-management of type 2 diabetes for adults with intellectual disabilities. Trials 2015;16:148. https://doi.org/10.1186/s13063-015-0644-y
Taggart L, McLaughlin D, Quinn B, Milligan V. An exploration of substance misuse in people with intellectual disabilities. J Intellect Disabil Res 2006;50:588–97.
Taggart L, Truesdale M, Dunkley A, House A, Russell AM. Health Promotion and Wellness Initiatives Targeting Chronic Disease Prevention and Management for Adults with Intellectual and Developmental Disabilities: Recent Advancements in Type 2 Diabetes. Curr Dev Disord Rep 2018;5:132–42. https://doi.org/10.1007/s40474-018-0142-5
Tarleton B, Ward L. Changes and choices: finding out what information young people with learning disabilities, their parents and supporters need at transition. Br J Learn Disabil 2005;33:70–6.
Taylor Ian R, Conway Val, and Knight Anneyce E. Measuring and addressing pain in people with limited communication skills: The ‘I hurt help me’ pain management project. J Pain Manage 2014;9:129–36
Taylor NS, Standen PJ, Cutajar P, Fox D, Wilson DN. Smoking prevalence and knowledge of associated risks in adult attenders at day centres for people with learning disabilities. J Intellect Disabil Res 2004;48:239–44.
Taylor S, Markar T. Audit of the quality of general practitioner referral letters to a learning disability service. Br J Dev Disabil 2002;48:101–6.
Thomas B, Atkinson D. Improving health outcomes for people with learning disabilities. Nurs Stand 2011;26:33–6. https://doi.org/10.7748/ns2011.10.26.6.33.c8757
Thomson K, Gripton J, Lutchmiah J, Caan W. Health facilitation in primary care seen from practice and education. Br J Nurs 2007;16:1156–60. https://doi.org/10.12968/bjon.2007.16.18.27514
Timehin C, Timehin E. Prevalence of hearing impairment in a community population of adults with learning disability: access to audiology and impact on behaviour. Br J Learn Disabil 2004;32:128–32.
Tingle J. Tragic failures in learning disability healthcare provision. Br J Nurs 2018;27:648–9. https://doi.org/10.12968/bjon.2018.27.11.648
Trueland J. Show of support. Nurs Stand 2014;28:20–1. https://doi.org/10.7748/ns2014.01.28.20.20.s26
Truesdale-Kennedy M, Taggart L, McIlfatrick S. Breast cancer knowledge among women with intellectual disabilities and their experiences of receiving breast mammography. J Adv Nurs 2011;67:1294–304. https://doi.org/10.1111/j.1365-2648.2010.05595.x
Tuffrey-Wijne I. The palliative care needs of people with intellectual disabilities: a literature review. Palliat Med 2003;17:55–62. https://doi.org/10.1191/0269216303pm668oa
Tuffrey-Wijne I. People with intellectual disabilities and their need for cancer information. EJC Suppl 2007;5:426.
Tuffrey-Wijne I, Bernal J, Butler G, Hollins S, Curfs L. Using Nominal Group Technique to investigate the views of people with intellectual disabilities on end-of-life care provision. J Adv Nurs 2007;58:80–9.
Tuffrey-Wijne I, Bernal J, Hollins S. Assessing the needs of people with intellectual disabilities (ID) who are terminally ill. J Intellect Disabil Res 2008;52:653.
Tuffrey-Wijne I, Bernal J, Jones A, Butler G, Hollins S. People with intellectual disabilities and their need for cancer information. Eur J Oncol Nurs 2006;10:106–16.
Tuffrey-Wijne I, Giatras N, Butler G, Cresswell A, Manners P, Bernal J. Developing guidelines for disclosure or non-disclosure of bad news around life-limiting illness and death to people with intellectual disabilities. J Appl Res Intellect Disabil 2013;26:231–42. https://doi.org/10.1111/jar.12026
Tuffrey-Wijne I, Hogg J, Curfs L. End-of-life and palliative care for people with intellectual disabilities who have cancer or other life-limiting illness: a review of the literature and available resources. J Appl Res Intellect Disabil 2007;20:331–44.
Tuffrey-Wijne I, Hollins S. Preventing ‘deaths by indifference’: identification of reasonable adjustments is key. Br J Psychiatry 2014;205:86–7. https://doi.org/10.1192/bjp.bp.113.142299
Tuffrey-Wijne I, Jones A, Bernal J, Butler G. A video by actors with intellectual disabilities (ID) to improve understanding and access to cancer services. J Intellect Disabil Res 2004;367.
Tuffrey-Wijne I, McEnhill L. Communication difficulties and intellectual disability in end-of-life care. Int J Palliat Nurs 2008;14:189–94. https://doi.org/10.12968/ijpn.2008.14.4.29133
Tuffrey-Wijne I, McEnhill L, Bernal J, Adeline P. End-of-life and palliative care for people with intellectual disabilities who have cancer or other life-limiting illness: a review of the literature and available resources. J Appl Res Intellect Disabil 2006;19:253.
Tuffrey-Wijne I, McEnhill L, Curfs L, Hollins S. Palliative care provision for people with intellectual disabilities: interviews with specialist palliative care professionals in London. Palliat Med 2007;21:493–9.
Tuffrey-Wijne I, Curfs L, Hollins S. Access to palliative care services by people with learning disabilities: Is there equity? Adv Ment Health Learn Disabil 2008;2:42–8.
Turk V, Ashworth M, Burchell S, Burrha S, Corney RH. Factors affecting consultation rates of adults with intellectual disabilities to general practitioners. J Intellect Disabil Res 2008;52:743.
Turnbull J, Chapman S. Supporting choice in health care for people with learning disabilities. Nurs Stand 2010;24:50–5. https://doi.org/10.7748/ns2010.02.24.22.50.c7519
Turner S. Increasing health checks for people with learning disabilities. Nurs Stand 2011;26:35–8. https://doi.org/10.7748/ns2011.10.26.7.35.c8758
Turner S. Improving care for people with learning disabilities. Nurs Stand 2014;29:53–9. https://doi.org/10.7748/ns.29.12.53.e9306
Vrijmoeth C, Christians M, Echteld M, Groot M. Perceptions of healthcare professionals on identification of the need for palliative care in people with intellectual disabilities: an interview-based study. J Intellect Disabil Res 2016;60:819.
Waldman HB, Perlman SP. Dentists must overcome barriers to caring for the developmentally disabled. Dent Abstr 2003;48:22–3.
Ware RS, Lennox NG. Characteristics influencing attendance at a primary care health check for people with intellectual disability: An individual participant data meta-analysis. Res Dev Disabil 2016;55:235–41. https://doi.org/10.1016/j.ridd.2016.04.012
Wark S, Hussain R, Edwards H. Rural and remote area service provision for people aging with intellectual disability. J Policy Pract Intellect Disabil 2013;10:62–70.
Wark S, Hussain R, Edwards H. Impediments to community-based care for people ageing with intellectual disability in rural New South Wales. Health Soc Care Community 2014;22:623–33. https://doi.org/10.1111/hsc.12130
Wark S, Hussain R, Müller A, Ryan P, Parmenter T. Challenges in providing end-of-life care for people with intellectual disability: Health services access. J Appl Res Intellect Disabil 2017;30:1151–9. https://doi.org/10.1111/jar.12408
Watson JM, McDonnell V, Bhaumik S. Valuing people: evaluating referral systems. A study of a multidisciplinary single point of referral system to dedicated adult learning disability health services in Leicester. Br J Dev Disabil 2005;51:155–70.
Watts S. Access to cervical screening for women with learning disabilities. Br J Nurs 2008;17:518–25. https://doi.org/10.12968/bjon.2008.17.8.29205
Webb OJ. Health needs of people with intellectual disabilities: understood but unchanging. J Policy Pract Intellect Disabil 2009;6:156.
Weise J, Pollack A, Britt H, Trollor JN. Primary health care for people with an intellectual disability: an exploration of demographic characteristics and reasons for encounters from the BEACH programme. J Intellect Disabil Res 2016;60:1119–27. https://doi.org/10.1111/jir.12301
Werner S, Yalon-Chamovitz S, Tenne Rinde M, Heymann AD. Principles of effective communication with patients who have intellectual disability among primary care physicians. Patient Educ Couns 2017;100:1314–21.
West SL, Graham CW, Cifu DX. Rates and correlates of alcohol/other drug treatment denials for people with disabilities in the United Kingdom. Alcohol Treat Q 2009;27:317–28.
Whitington J, Ma P. A fast track path improves access to palliative care for people with learning disabilities. Nurs Times 2010;106:13–14.
Whittle EL, Fisher KR, Reppermund S, Lenroot R, Trollor J. Barriers and enablers to accessing mental health services for people with intellectual disability: a scoping review. J Ment Health Res Intellect Disabil 2018;11:69–102.
Wiese MY, Balandin S, Stancliffe RJ. End-of-life care and dying: choices and needs of people with intellectual disability and their carers. J Intellect Disabil Res 2008;52:653.
Wilkinson VJ, Theodore K, Raczka R. ‘As Normal as Possible’: sexual identity development in people with intellectual disabilities transitioning to adulthood. Sex Disabil 2015;33:93–105.
Williams RW, Roberts GW, Irvine FE, Hastings RP. Exploring decision making in intellectual disability nursing practice: a qualitative study. J Intellect Disabil 2010;14:197–220. https://doi.org/10.1177/1744629510386289
Williamson A, Johnson J. Improving services for people with learning disabilities. Nurs Stand 2004;18:43–51. https://doi.org/10.7748/ns2004.02.18.24.43.c3555
Williamson HJ, Contreras GM, Rodriguez ES, Smith JM, Perkins EA. Health care access for adults with intellectual and developmental disabilities: a scoping review. OTJR 2017;37:227–36. https://doi.org/10.1177/1539449217714148
Willis D, Samalin E, Satgé D. Colorectal Cancer in People with Intellectual Disabilities. Oncology 2018;95:323–36. https://doi.org/10.1159/000492077
Willis DS, Kilbride L, Horsburgh D, Kennedy CM. Paid- and family-carers’ views on supporting women with intellectual disability through breast screening. Eur J Cancer Care 2015;24:473–82. https://doi.org/10.1111/ecc.12245
Willis DS, Kilbride L, Horsburgh D, Kennedy CM. Paid- and family-carers’ views on supporting women with intellectual disability through breast screening. Eur J Cancer Care 2015;24:473–82. https://doi.org/10.1111/ecc.12245
Wilson NJ, Cumella S, Parmenter TR, Stancliffe RJ, Shuttleworth RP. Penile hygiene: puberty, paraphimosis and personal care for men and boys with an intellectual disability. J Intellect Disabil Res 2009;53:106–14. https://doi.org/10.1111/j.1365-2788.2008.01133.x
Wilson S, McKenzie K, Quayle E, Murray GC. The postnatal support needs of mothers with an intellectual disability. Midwifery 2013;29:592–8. https://doi.org/10.1016/j.midw.2012.05.002
Wullink M, Lantman-de Valk, HMJV, Dinant GJ. Transfer of care to the general practitioner for people with intellectual disability (ID) who live in the community. J Intellect Disabil Res 2004;48:343.
Wullink M, Lantman-de Valk, HMJV , Metsemakers JFM, Dinant GJ. Education for general practitioners by changing care for people with intellectual disability (ID). J Appl Res Intellect Disabil 2006;19:249.
Yalon-Chamovitz S. Invisible access needs of people with intellectual disabilities: a conceptual model of practice. Intellect Dev Disabil 2009;47:395–400. https://doi.org/10.1352/1934-9556-47.5.395
Yen CF, Hsu SW, Loh CH, Fang WH, Wu CL, Chu CM, Lin JD. Analysis of seasonal influenza vaccine uptake among children and adolescents with an intellectual disability. Res Dev Disabil 2012;33:704–10. https://doi.org/10.1016/j.ridd.2011.11.011
Young-Southward G, Cooper SA, Philo C. Health and wellbeing during transition to adulthood for young people with intellectual disabilities: a qualitative study. Res Dev Disabil 2017;70:94–103.
Young-Southward G, Philo C, Cooper SA. What effect does transition have on health and well-being in young people with intellectual disabilities? A systematic review. J Appl Res Intellect Disabil 2017;30:805–23. https://doi.org/10.1111/jar.12286
Appendix 7 Data extraction components for targeted systematic review
Study details.
Study design:
-
quantitative
-
qualitative
-
mixed methods
-
conference abstract 2015 onwards.
Study population.
Sample size.
Setting.
Study aim.
Reasonable adjustment.
HCP:
-
GP
-
dentist
-
optometrist
-
pharmacist
-
IAPT service staff
-
audiologist
-
disability liaison nurse
-
practice nurse
-
other GP staff
-
other community staff.
Specialist topic:
-
audiology
-
cardiovascular
-
cervical screening
-
dental health
-
diabetes
-
eye health
-
gastrointestinal
-
health checks
-
IAPT
-
mental health
-
palliative and end-of-life care
-
respiratory
-
sexual health
-
transition
-
other.
Study outcomes.
Study results.
Study conclusions.
Barriers.
Facilitators.
Limitations.
Appendix 8 Data extraction targeted systematic review example
Findlay L, Williams AC, Scior K. ‘Exploring experiences and understandings of pain in adults with intellectual disabilities’. J Intellect Disabil Res 2014;58:358–67. Study details:
-
Study design: qualitative (semistructured interviews).
-
Study population: adults with ID – 15 participants (eight men and seven women) with mild to moderate LD took part in the study.
-
Sample size: 15 adults with ID.
-
Setting: participants were invited to participate by professionals working in a community service for people with ID in the London area.
-
Study aim: to explore the experiences that adults with ID have had of being in pain, and what meaning they attribute to both acute and chronic pain.
-
Specialist topic.
-
Other pain.
-
Barriers: people may hide pain or fail to tell people they are in pain because they do not think they will be believed or they will be ignored, or because they think they might be stopped from doing something they enjoy. Someone who can communicate verbally will not necessarily communicate pain.
-
Facilitators: development of a widely accessible checklist of questions to ask could help with the task of assessing pain and its potential causes.
-
Limitations: the recruitment method may have introduced unknown biases, for example two participants did not speak English as their first language and may not have properly understood the question or answered fully. The study relied on service providers to approach potential participants; this poses the risk that not everyone meeting the inclusion criteria had the same chance of being invited to participate. The interviews used pictures and this might have limited the different pains discussed.
Appendix 9 Grey literature data extraction
| Data topic | Details |
|---|---|
| Hatton et al. 201630 | |
| Study design | Qualitative |
| Setting | Pharmacist |
| Specialist topic | General |
| Study population |
PwLD Professional support staff Family carers Pharmacists |
| Sample size | 597 |
| Study results |
57% thought that signage was not clear in the pharmacy < 10% used a quiet room to communicate to staff and 48% did not think that their pharmacy had a quiet room at all 30% wanted their pharmacist to be more patient The average frequency for visits to pharmacists was monthly 15% stated that they did not know why they took their medication Survey work shows that negative experiences of pharmacy services are not the norm but some barriers exist |
| Barriers |
For people with disabilities: Access to information – information presented in ways that were too small, too wordy, too complex, or not suitable Physical barriers – poor accessibility to health-care facilities Administrative barriers – short appointments and long waiting times Communication barriers – inability to describe symptoms, with differential diagnosis difficult and diagnostic overshadowing possible Attitudinal barriers – negative assumptions and attitudes about disabled people Knowledge barriers – limited theory and practice experience of the health needs of disabled people For pharmacists: Health reviews often completed by practice nurses so medication not being checked by a GP and, therefore, can go years without being changed Lack of communication between GP and pharmacy, and then to service providers or families Fear among families of reducing medication, especially if bad experiences in the past and have finally got the situation to a manageable point, they can be scared to alter it Community pharmacists do not have the skills or confidence to support better communications between HCPs Families do not want to have to deal with too many professionals, so there needs to be decision-making and co-ordination at a local level |
| Facilitators | Pharmacists feel they need to build up trust, help the families’ understanding of the situation and give them information |
| Limitations | Not restricted to learning disabilities |
| Public Health England 201629 | |
| Study design | Quantitative |
| Setting | GP (section of report) |
| Specialist topic | Health checks (section of report) |
| Study population | People with LD |
| Sample size | N/A |
| Study results |
At the end of March 2015, there were 252,446 people of all ages on LD registers In 2014 to 2015, GP practices reported that there were 197,451 patients eligible for a LD health check (registered with their GP as having a LD and aged ≥ 14 years). There were 124,785 checks reported, giving an overall apparent coverage of 63.2%. The number of people with LD registered at a GP, eligible for a health check and having a health check has risen each year from 2008/9 when around 25,000 checks were carried out (no data for eligibility in 2013/14) |
| Barriers | Not reported |
| Facilitators | Not reported |
| Limitations | Not reported |
| Marriott and Turner 2016122 | |
| Study design | Case studies
|
| Setting | GP/community |
| Specialist topic | Cervical screening (2 and 3 also include breast and bowel screening) |
| Study population | Women with LD |
| Sample size | Not reported |
| Study results |
|
| Barriers | Not reported |
| Facilitators | Not reported |
| Limitations | Not reported |
Appendix 10 Alphabetical list of included studies
Adler P, Cregg M, Duignan A, Ilett G, Woodhouse JM. Effect of training on attitudes and expertise of optometrists towards people with intellectual disabilities. Ophthalmic Physiol Opt 2005;25:105–18.
Ali A, Scior K, Ratti V, Strydom A, King M, Hassiotis A. Discrimination and other barriers to accessing health care: perspectives of patients with mild and moderate intellectual disability and their carers. PLOS ONE 2013;8:e70855. https://doi.org/10.1371/journal.pone.0070855
Allgar V, Mir G, Evans J, Marshall J, Cottrell D, Heywood P, Emerson E. Estimated prevalence of people with learning disabilities: template for general practice. Br J Gen Pract 2008;58:423–8. https://doi.org/10.3399/bjgp08X299272
Baxter H, Lowe K, Houston H, Jones G, Felce D, Kerr M. Previously unidentified morbidity in patients with intellectual disability. Br J Gen Pract 2006;56:93–8.
Beacroft M, Dodd K. Pain in people with learning disabilities in residential settings – the need for change. Br J Learn Disabil 2010;38:201–9. https://doi.org/10.1111/j.1468-3156.2009.00593.x
Beacroft M, Dodd K. ‘I Feel Pain’ – audit of communication skills and understanding of pain and health needs with people with learning disabilities. Br J Learn Disabil 2011;39:139–47. https://doi.org/10.1111/j.1468-3156.2010.00640.x
Biswas M, Whalley H, Foster J, Friedman E, Deacon R. Women with learning disability and uptake of screening: audit of screening uptake before and after one to one counselling. J Public Health 2005;27:344–7.
Black D. Improving access to care for the learning disabled. Pract Nurs 2004;15:38–40.
Bland R, Hutchinson N, Oakes P, Yates C. Double jeopardy? Needs and services for older people who have learning disabilities. J Learn Disabil 2003;7:317–38.
Bollard M. Health promotion and intellectual disability: listening to men. Health Soc Care Community 2017;25:185–93. https://doi.org/10.1111/hsc.12291
Brown M, Taggart L, Karatzias T, Truesdale M, Walley R, Northway R, et al. Improving diabetes care for people with intellectual disabilities: a qualitative study exploring the perceptions and experiences of professionals in diabetes and intellectual disability services. J Intellect Disabil Res 2017;61:435–49. https://doi.org/10.1111/jir.12369
Buszewicz M, Welch C, Horsfall L, Nazareth I, Osborn D, Hassiotis A, et al. Assessment of an incentivised scheme to provide annual health checks in primary care for adults with intellectual disability: a longitudinal cohort study. Lancet Psychiatry 2014;1:522–30. https://doi.org/10.1016/S2215-0366(14)00079-0
Carey IM, Shah SM, Hosking FJ, DeWilde S, Harris T, Beighton C, Cook DG. Health characteristics and consultation patterns of people with intellectual disability: a cross-sectional database study in English general practice. Br J Gen Pract 2016;66:e264–70. https://doi.org/10.3399/bjgp16X684301
Cassidy G, Martin DM, Martin GH, Roy A. Health checks for people with learning disabilities: Community learning disability teams working with general practitioners and primary health care teams. J Learn Disabil 2002;6:123–36.
Chauhan U, Kontopantelis E, Campbell S, Jarrett H, Lester H. Health checks in primary care for adults with intellectual disabilities: how extensive should they be? J Intellect Disabil Res 2010;54:479–86. https://doi.org/10.1111/j.1365-2788.2010.01263.x
Chauhan U, Reeve J, Kontopantelis E, Hinder S. Impact of the English Directly Enhanced Service (DES) for Learning Disability. 2012. URL: www.choiceforum.org/docs/desmf.pdf (accessed 27 November 2018).
Chinn D, Abraham E. Using ‘candidacy’ as a framework for understanding access to mainstream psychological treatment for people with intellectual disabilities and common mental health problems within the English Improving Access to Psychological Therapies service. J Intellect Disabil Res 2016;60:571–82. https://doi.org/10.1111/jir.12274
Cooper SA, McConnachie A, Allan LM, Melville C, Smiley E, Morrison J. Neighbourhood deprivation, health inequalities and service access by adults with intellectual disabilities: a cross-sectional study. J Intellect Disabil Res 2011;55:313–23. https://doi.org/10.1111/j.1365-2788.2010.01361.x
Cooper SA, Morrison J, Allan LM, McConnachie A, Greenlaw N, Melville CA, et al. Practice nurse health checks for adults with intellectual disabilities: a cluster-design, randomised controlled trial. Lancet Psychiatry 2014;1:511–21. https://doi.org/10.1016/S2215-0366(14)00078-9
Cooper SA, Morrison J, Melville C, Finlayson J, Allan L, Martin G, et al. Improving the health of people with intellectual disabilities: outcomes of a health screening programme after 1 year. J Intellect Disabil Res 2006;50:667–77.
Dagnan D, Masson J, Thwaites R, James A, Hatton C. Training therapists to work with people with intellectual disability in Improving Access to Psychological Therapies (IAPT) services. J Appl Res Intellect Disabil 2018;31:760–7. https://doi.org/10.1111/jar.12427
Donovan J. Learning disability nurses’ experiences of being with clients who may be in pain. J Adv Nurs 2002;38:458–66.
Doshi M, Burke M, Fiske J. A preliminary investigation into aspects of oral health of Bangladeshi young adults with learning disability in Tower Hamlets. J Disabil Oral Health 2009;10:25–35.
Felce D, Baxter H, Lowe K, Dunstan F, Houston H, Jones G, et al. The impact of checking the health of adults with intellectual disabilities on primary care consultation rates, health promotion and contact with specialists. J Appl Res Intellect Disabil 2008;21:597–602. https://doi.org/10.1111/j.1468-3148.2008.00432.x
Findlay L, Williams AC, Baum S, Scior K. Caregiver experiences of supporting adults with intellectual disabilities in pain. J Appl Res Intellect Disabil 2015;28:111–20. https://doi.org/10.1111/jar.12109
Findlay L, Williams AC, Scior K. Exploring experiences and understandings of pain in adults with intellectual disabilities. J Intellect Disabil Res 2014;58:358–67. https://doi.org/10.1111/jir.12020
Ford JA, Jones AP, Wong G, Steel N. Weekend opening in primary care: analysis of the General Practice Patient Survey. Br J Gen Pract 2015;65:e792–8. https://doi.org/10.3399/bjgp15X687673
Gates B. The Valued People Project: users’ views on learning disability nursing. Br J Nurs 2011;20:15–21. https://doi.org/10.12968/bjon.2011.20.1.15
Glover G, Emerson E, Evison F. The uptake of health checks for adults with learning disabilities in England: 2008/9 – 2011/12. Tizard Learn Disabil Rev 2013;18:45–9. https://doi.org/10.1108/13595471311296012
Goldsmith L, Woodward V, Jackson L, Skirton H. Informed consent for blood tests in people with a learning disability. J Adv Nurs 2013;69:1966–76. https://doi.org/10.1111/jan.12057
Hames A, Carlson T. Are primary health care staff aware of the role of community learning disability teams in relation to health promotion and health facilitation? Br J Learn Disabil 2006;34:6–10.
Hanna LM, Taggart L, Cousins W. Cancer prevention and health promotion for people with intellectual disabilities: an exploratory study of staff knowledge. J Intellect Disabil Res 2011;55:281–91. https://doi.org/10.1111/j.1365-2788.2010.01357.x
Harrison S, Berry L. Improving primary care services for people with learning disability. Nurs Times 2005;101:38–40.
Hebblethwaite A, Hames A, Donkin M, Colman M, Forsyth A. Investigating the experiences of people who have been homeless and are in contact with learning disability services. Learn Disabil Rev 2007;12:25–34.
Heyman B, Swain J, Gillman M. Organisational simplification and secondary complexity in health services for adults with learning disabilities. Soc Sci Med 2004;58:357–67.
Holly D, Sharp J. Addressing health inequities: coronary heart disease training within learning disabilities services. Br J Learn Disabil 2014;42:110–16. https://doi.org/10.1111/bld.12014
Jones J, Kemp K. Down syndrome: exploring the knowledge, attitudes and practice of GPs. Learn Disabil Pract 2007;10:18–21.
Jones MC, McLafferty E, Walley R, Toland J, Melson N. Inclusion in primary care for people with intellectual disabilities. J Intellect Disabil 2008;12:93–109. https://doi.org/https://doi.org/10.1177/1744629508090982
Lees C, Poole H, Brennan M, Irvine F. Adults with learning disabilities experiences of using community dental services: Service user and carer perspectives. Br J Learn Disabil 2017;45:114–20. https://doi.org/10.1111/bld.12181
Lennox TN, Nadkarni J, Moffat P, Robertson C. Access to services and meeting the needs of people with learning disabilities. J Learn Disabil 2003;7:34–50. https://doi.org/https://doi.org/10.1177/1469004703007001604
Lloyd JL, Coulson NS. The role of learning disability nurses in promoting cervical screening uptake in women with intellectual disabilities: A qualitative study. J Intellect Disabil 2014;18:129–45.
Lodge KM, Milnes D, Gilbody SM. Compiling a register of patients with moderate or severe learning disabilities: experience at one United Kingdom general practice. Ment Health Fam Med 2011;8:29–37.
Martin G, Philip L, Bates L, Warwick J. Evaluation of a nurse led annual review of patients with severe intellectual disabilities, needs identified and needs met, in a large group practice. J Learn Disabil 2004;8:235–46. https://doi.org/https://doi.org/10.1177/1469004704044965
McCarthy M. Contraception and women with intellectual disabilities. J Appl Res Intellect Disabil 2009;22:363-9. https://doi.org/10.1111/j.1468-3148.2008.00464.x
McCarthy M. Prescribing contraception to women with intellectual disabilities: general practitioners’ attitudes and practices. Sex Disabil 2011;29:339–49. https://doi.org/10.1007/s11195-011-9216-6
McConkey R, Taggart L, Kane M. Optimizing the uptake of health checks for people with intellectual disabilities. J Intellect Disabil 2015;19:205–14. https://doi.org/10.1177/1744629514568437
McNally P, McMurray K. Exploration of the dynamic barriers to adults with intellectual disabilities accessing mainstream mental health services. Adv Ment Health Intellect Disabil 2015;9:352–62. https://doi.org/https://doi.org/10.1108/AMHID-01-2015-0001
McShea L, Fulton J, Hayes C. Paid Support Workers for Adults with Intellectual Disabilities; Their Current Knowledge of Hearing Loss and Future Training Needs. J Appl Res Intellect Disabil 2016;29:422–32. https://doi.org/10.1111/jar.12201
Murphy J. Perceptions of communication between people with communication disability and general practice staff. Health Expect 2006;9:49–59.
Nicholson L, Cooper SA. Access to healthcare services by people with intellectual disabilities: a rural-urban comparison. J Intellect Disabil 2011;15:115–30. https://doi.org/10.1177/1744629511412659
Northway R, Holland-Hart D, Jenkins R. Meeting the health needs of older people with intellectual disabilities: exploring the experiences of residential social care staff. Health Soc Care Community 2017;25:923–31. https://doi.org/10.1111/hsc.12380
Osborn DP, Horsfall L, Hassiotis A, Petersen I, Walters K, Nazareth I. Access to cancer screening in people with learning disabilities in the UK: cohort study in the health improvement network, a primary care research database. PLOS ONE 2012;7:e43841. https://doi.org/10.1371/journal.pone.0043841
Owens J, Mistry K, Dyer TA. Access to dental services for people with learning disabilities: quality care? J Disabil Oral Health 2011;12:17–27.
Perry J, Felce D, Kerr M, Bartley S, Tomlinson J, Felce J. Contact with primary care: the experience of people with intellectual disabilities. J Appl Res Intellect Disabil 2014;27:200–11. https://doi.org/10.1111/jar.12072
Pilling RF. Screening for diabetic retinopathy in adults with learning disability: current uptake and adjustments to facilitate equality of access. Br J Learn Disabil 2015;43:62–5. https://doi.org/10.1111/bld.12088
Powrie E. Primary health care provision for adults with a learning disability. J Adv Nurs 2003;42:413–23.
Raghavan R, Waseem F. Services for young people with learning disabilities and mental health needs from South Asian communities. Adv Ment Health Learn Disabil 2007;1:27–31. https://doi.org/10.1108/17530180200700028
Redley M, Banks C, Foody K, Holland A. Healthcare for men and women with learning disabilities: understanding inequalities in access. Disabil Soc 2012;27:747–59. https://doi.org/10.1080/09687599.2012.673080
Rees G. Increasing access to cancer screening programmes. Learn Disabil Pract 2011;14:14–9.
Reynolds F, Stanistreet D, Elton P. Women with learning disabilities and access to cervical screening: retrospective cohort study using case control methods. BMC Public Health 2008;8:30. https://doi.org/10.1186/1471-2458-8-30
Romeo R, Knapp M, Morrison J, Melville C, Allan L, Finlayson J, Cooper SA. Cost estimation of a health-check intervention for adults with intellectual disabilities in the UK. J Intellect Disabil Res 2009;53:426–39. https://doi.org/10.1111/j.1365-2788.2009.01159.x
Russell AM, Bryant L, House A. Identifying people with a learning disability: an advanced search for general practice. Br J Gen Pract 2017;67:e842–e850. https://doi.org/10.3399/bjgp17X693461
Starling S, Willis A, Dracup M, Burton M, Pratt C. Right to sight: accessing eye care for adults who are learning disabled. J Intellect Disabil 2006;10:337–55.
Taylor IR, Conway V, Knight AE. Measuring and addressing pain in people with limited communication skills: The ‘I Hurt Help Me’ pain management project. J Pain Manage 2014;7:129–36.
Thompson K, Casson K, Fleming P, Dobbs F, Parahoo K, Armstrong J. Sexual health promotion in primary care – Activities and views of general practitioners and practice nurses. Prim Health Care Res Dev 2008;9:319–30. https://doi.org/https://doi.org/10.1017/S1463423608000881
Tuffrey-Wijne I. The palliative care needs of people with intellectual disabilities: a case study. Int J Palliat Nurs 2002;8:222–32. https://doi.org/10.12968/ijpn.2002.8.5.10369
Tuffrey-Wijne I, Bernal J, Hubert J, Butler G, Hollins S. People with learning disabilities who have cancer: an ethnographic study. Br J Gen Pract 2009;59:503–9. https://doi.org/10.3399/bjgp09X453413
Tuffrey-Wijne I, Hollins S, Curfs L. Supporting patients who have intellectual disabilities: a survey investigating staff training needs. Int J Palliat Nurs 2005;11:182–8. https://doi.org/10.12968/ijpn.2005.11.4.18039
Turk V, Khattran S, Kerry S, Corney R, Painter K. Reporting of health problems and pain by adults with an intellectual disability and by their carers. J Appl Res Intellect Disabil 2012;25:155–65. https://doi.org/10.1111/j.1468-3148.2011.00642.x
Turner S. Making reasonable adjustments to diabetes services for people with learning disabilities: what nurses can do. J Diabetes Nurs 2014;18:189–92.
Walker C, Beck CR, Eccles R, Weston C. Health inequalities and access to health care for adults with learning disabilities in Lincolnshire. Br J Learn Disabil 2016;44:16-23. https://doi.org/10.1111/bld.12104
Walmsley J. An investigation into the implementation of annual health checks for people with intellectual disabilities. J Intellect Disabil 2011;15:157–66. https://doi.org/10.1177/1744629511423722
Watchman K. Practitioner-raised issues and end-of-life care for adults with Down syndrome and dementia. J Policy Pract Intellect Disabil 2005;2:156–62. https://doi.org/10.1111/j.1741-1130.2005.00026.x
Webb J, Stanton M. Better access to primary healthcare for adults with learning disabilities: evaluation of a group programme to improve knowledge and skills. Br J Learn Disabil 2009;37:116–22. https://doi.org/10.1111/j.1468-3156.2008.00527.x
Webb J, Stanton M. Better access to primary healthcare for adults with learning disabilities: evaluation of a group programme to improve knowledge and skills. Br J Learn Disabil 2009;37:116–22. https://doi.org/10.1111/j.1468-3156.2008.00527.x
Williams F, Scott G, McKechanie A. Sexual health services and support: the views of younger adults with intellectual disability. J Intellect Dev Disabil 2014;39:147–56. https://doi.org/10.3109/13668250.2014.899326
Williamson A, Allan L, Cooper SA, Morrison J, Curtice L. The general practitioner interface with people with intellectual disabilities and their supports. Eur J Gen Pract 2004;10:66–7, 70. https://doi.org/10.3109/13814780409094236
Willis DS. Inconsistencies in the roles of family-and paid-carers in monitoring health issues in people with learning disabilities: some implications for the integration of health and social care. Br J Learn Disabil 2015;42:24–31.
Wilson C, Mansell I. Access to health and social care services and information. Learn Disabil Pract 2010;13:32–8.
Wood R, Douglas M. Cervical screening for women with learning disability: current practice and attitudes within primary care in Edinburgh. Br J Learn Disabil 2007;35:84–92.
Young AF, Naji S, Kroll T. Support for self-management of cardiovascular disease by people with learning disabilities. Fam Pract 2012;29:467–75. https://doi.org/10.1093/fampra/cmr106
Appendix 11 Quality appraisal of included studies
For the one randomised study the risk of bias was assessed using the checklist produced by the US National Heart Lung and Blood Institute for controlled intervention studies. The checklist can be accessed at URL: www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Table 27).
| Criteria | Cooper et al. 2014100 | ||
|---|---|---|---|
| Yes | No | Other | |
| 1 | Y | ||
| 2 | Y | ||
| 3 | Y, statisticians blinded to group | ||
| 4 | Not possible | ||
| 5 | Partial, some compromise | ||
| 6 | Y | ||
| 7 | Y | ||
| 8 | |||
| 9 | N, 76% received | ||
| 10 | Y | ||
| 11 | Y | ||
| 12 | Y | ||
| 13 | Unclear | ||
| 14 | Y | ||
For the one non-randomised study the risk of bias was assessed using the checklist produced by the US National Heart Lung and Blood Institute for controlled intervention studies. The checklist can be accessed at URL: www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Table 28).
| Criteria | Adler et al. 200592 | ||
|---|---|---|---|
| Yes | No | Other | |
| 1 | N | ||
| 2 | NA | ||
| 3 | Not possible | ||
| 4 | Not possible | ||
| 5 | Unclear | ||
| 6 | N | ||
| 7 | Y | ||
| 8 | Y | ||
| 9 | Y | ||
| 10 | N | ||
| 11 | N | ||
| 12 | N | ||
| 13 | Unclear | ||
| 14 | NA | ||
For the observational, cohort and cross-sectional studies, risk of bias was assessed using the checklist published by the US National Heart, Lung and Blood Institute for observational cohort and cross-sectional studies. The checklist can be accessed at URL: www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Table 29).
| Reference (first author and year of study) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Allgar 200851 | Y | Y | U | Y | N | N | NA | NA | NA | N | Y | U | NA | N |
| Baxter 200693 | Y | Y | U | N | N | Y | Y | NA | Y | N | Y | U | Y | N |
| Bland 200335 | Y | Y | Y | Y | N | NA | Y | NA | NA | N | Y | N | NA | NA |
| Buszewicz 201495 | Y | Y, existing database | Y | U | N | N | NA | NA | Y | N | Y | U | NA | N |
| Carey 201653 | Y | Y | NA | Y | Y | Y | Y | Y | Y | N | Y | N | NA | N |
| Chauhan 201097 | Y | Y | U | Y | N | N | Y | N | Y | N | Y | U | U | N |
| Chauhan 201298 | Y | Y | U | Y | N | N | Y | NA | Y | N | Y | U | U | N |
| Codling 200799 | Y | Y | Y | Y | N | N | Y | NA | Y | N | Y | N | Y | N |
| Cooper 2006101 | Y | Y | Y | Y | N | N | Y | NA | Y | N | Y | U | N | N |
| Cooper 201155 | Y | Y | U | Y | N | N | NA | Y | Y | N | Y | U | NA | Y |
| Doshi 200956 | Y | Y | Y | Y | N | Y | Y | N | Y | N | Y | N | NA | N |
| Felce 200819 | Y | Y | U | U | N | N | Y | NA | Y | N | Y | U | Y | N |
| Ford 2015103 | Y | N | U | N | Y | Y | Y | U | Y | Y | Y | U | Y | Y |
| Glover 2013104 | Y | Y | Y | Y | N | N | Y | NA | Y | N | Y | U | Y | N |
| Hanna 201140 | Y | Y | N | Y | N | NA | Y | NA | NA | N | Y | N | NA | NA |
| Hames 200676 | Y | Y | N | Y | N | N | NA | NA | NA | N | N | U | NA | N |
| Heyman 200478 | Y | Y | N | Y | N | N | NA | N | Y | N | Y | U | NA | N |
| Holly 2014106 | Y | Y | U | Y | N | N | Y | Y | Y | Y | Y | N | Y | N |
| Jones 200779 | Y | Y | N | Y | N | N | NA | N | N | N | Y | U | NA | N |
| Lennox 200358 | Y | Y | Y | Y | N | Y | Y | Y | Y | N | Y | N | NA | Y |
| Lodge 201160 | Y | Y | NA | Y | N | N | NA | NA | N | N | Y | N | NA | NA |
| Martin 2004107 | Y | Y | Y | Y | N | N | NA | NA | Y | N | Y | U | Y | N |
| McCarthy 201181 | Y | Y | N | U | N | N | NA | NA | N | N | N | N | NA | N |
| McConkey 2015108 | Y | Y | Y | Y | N | N | NA | NA | Y | N | Y | U | Y | N |
| Melville 2005133 | Y | Y | Y | Y | N | N | NA | NA | N | N | Y | N | NA | N |
| Nicholson 201162 | Y | Y | N | Y | Y | Y | Y | Y | Y | N | Y | N | NA | Y |
| Osborn 201263 | Y | Y | NA | Y | Y | Y | Y | N | Y | N | Y | N | U | Y |
| Pilling 201565 | Y | Y | Y | Y | N | Y | Y | N | Y | N | Y | N | NA | N |
| Powrie 200384 | Y | Y | Y | Y | N | N | NA | NA | Y | N | Y | N | NA | N |
| Raghavan 200766 | Y | Y | NR | Y | N | Y | Y | N | Y | N | Y | N | NA | N |
| Rees 201168 | Y | Y | Y | Y | N | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Reynolds 200869 | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | N | NA | N |
| Russell 201770 | Y | Y | NA | Y | N | N | NA | NA | NA | NA | N | N | NA | N |
| Starling 20066 | Y | Y | Y | Y | N | Y | Y | Y | U | N | Y | N | NA | Y |
| Taylor 2014110 | Y | Y | U | Y | N | N | Y | N | N | N | N | N | NA | N |
| Tuffrey-Wijne 200588 | Y | Y | N | U | N | N | NA | NA | N | N | NA | N | NA | N |
| Turk 201244 | Y | Y | N | Y | Y | NA | Y | NA | NA | N | Y | N | NA | NA |
| Walker 201645 | Y | Y | NA | Y | N | NA | Y | NA | NA | N | Y | N | NA | NA |
| Williams 201471 | Y | Y | N | Y | N | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Williamson 200491 | Y | Y | Y | Y | N | N | NA | NA | N | N | N | N | NA | N |
For the case–control studies risk of bias was assessed using the checklist published by the US National Heart, Lung and Blood Institute for case–control studies. The checklist can be accessed at URL: www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Table 30).
| Reference (first author and year of study) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cassidy 200296 | Y | Y | N | Y | Y | Y | N | N | Y | Y | U | N |
| Romeo 2009109 | Y | Y | N | Y | Y | Y | NA | Y | Y | Y | U | N |
For the before-and-after studies, risk of bias was assessed using the checklist published by the US National Heart, Lung and Blood Institute for before-and-after studies with no control group. The checklist can be accessed at URL: www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Table 31).
| Reference (first author and year of study) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dagnan 2018102 | Y | Y | Y | U | Y | Y | N | U | Y | Y | N | NA |
| Webb 2009112 | Y | NA | Y | Y | N | N | Y | N | NA | N | N | NA |
| Webb 2009113 | Y | Y | Y | U | N | Y | N | U | Y | Y | N | NA |
| Biswas 200594 | Y | Y | Y | U | Y | Y | N | U | Y | N | N | NA |
Qualitative studies were assessed with the CASP checklist for qualitative studies, which can be accessed at https://casp-uk.net/casp-tools-checklists/ (Table 32).
| Reference (first author and year of study) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Ali 201350 | Y | Y | Y | Y | Y | U | Y | Y | Y | Y |
| Beacroft 2010/201133,34 | Y | Y | Y | Y | Y | N | Y | U | Y | Y |
| Bollard 201736 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Black 200452 | Y | Y | Y | Y | Y | N | U | U | Y | Y |
| Brown 201773 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Chinn 201654 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Donovan 200237 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Findlay 2014/201538,39 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Gates 201174 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Goldsmith 201375 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Hebblethwaite 200777 | Y | Y | Y | Y | Y | U | U | U | Y | Y |
| Jones 200857 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Lees 201780 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Lloyd 201459 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| McCarthy 200941 | Y | Y | Y | Y | Y | N | Y | U | Y | Y |
| McNally 201561 | Y | Y | Y | Y | Y | Y | U | Y | Y | Y |
| McShea 201642 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Murphy 200682 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Northway 201743 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Owens 201164 | Y | Y | Y | U | Y | Y | Y | U | Y | Y |
| Perry 201483 | Y | Y | Y | Y | Y | N | N | Y | Y | Y |
| Redley 201267 | Y | Y | Y | U | U | N | Y | U | Y | Y |
| Thompson 200885 (mixed methods) | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Tuffrey-Wijne 200987 | Y | Y | Y | Y | Y | N | Y | y | y | y |
| Turner 201489 | Y | Y | Y | U | U | N | U | U | Y | Y |
| Walmsley et al. 2011111 | Y | Y | Y | Y | Y | N | N | N | Y | Y |
| Watchman 200590 | Y | Y | Y | U | U | N | U | U | Y | Y |
| Willis 201546 | Y | Y | Y | U | Y | N | Y | Y | Y | Y |
| Wilson 201047 | Y | Y | Y | Y | Y | N | Y | U | Y | Y |
| Wood 200772 | Y | Y | Y | Y | Y | N | U | U | Y | Y |
| Young 201248 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
List of abbreviations
- CASP
- Critical Appraisal Skills Programme
- GP
- general practitioner
- HCP
- health-care professional
- IAPT
- Improving Access to Psychological Therapies
- ID
- intellectual disabilities
- LD
- learning disability
- LD-DES
- learning disability direct enhanced service
- LeDeR
- Learning Disabilities Mortality Review
- MCA
- Mental Capacity Act 2005
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- SDO
- Service Delivery and Organisation
Notes
-
Intellectual disabilities mapping review protocol
-
Intellectual disabilities targeted systematic review protocol
Supplementary material can be found on the NIHR Journals Library report project page under the ‘Download report documents’ section on the Toolkit (https://doi.org/10.3310/hsdr08050).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
