Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/47/22. The contractual start date was in March 2016. The final report began editorial review in October 2018 and was accepted for publication in April 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
David Fitzpatrick is a member of the Health Technology Assessment (HTA) Elective and Emergency Specialist Care Panel (2019 to present) and the HTA Prioritisation Committee (2019 to present). Robert Harris-Mayes reports grants from Swansea University during the conduct of the study. Yvette LaFlamme-Williams was employed by the Welsh Ambulance Service NHS Trust as a paramedic site researcher. Her position (on a fixed-term contract) was funded by Swansea University. Suzanne Mason is a member of the Health Services and Delivery Research (HSDR) Commissioned Panel (2013 to present). Heather Morgan reports that her work was funded by the main grant to Swansea University through a subcontract from the University of Aberdeen during the conduct of the study. Katherine McNee reports personal fees from South Western Ambulance Service NHS Foundation Trust during the conduct of the study. Nigel Rees reports grants from Health and Care Research Wales during the conduct of the study. Helen Snooks is a member of the HTA and Efficacy and Mechanism Evaluation Editorial Board (2012 to present) and is a HSDR Senior Scientific Advisor (2016 to present).
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Porter et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Context and background
Introduction
Ambulance services have a vital role in the shift towards the delivery of health care outside hospitals, when this is better for patients, by offering alternatives to transfer to the emergency department (ED). For this to happen safely and effectively, ambulance clinicians must be able to decide which patients will benefit from being treated at the scene or left at home, and ensure that patient information, including details of 999 assessment and care, is passed to community-based care providers. The introduction of information technology (IT) in ambulance services to electronically capture and store patient data in the form of electronic health records (EHRs) has been encouraged by national policy across the UK and is seen as having potential to support a shift towards out-of-hospital care, as well as being part of the wider modernisation agenda within the health service. Additional benefits include the potential to more readily pass on clinical information to both in-hospital and out-of-hospital providers, storage of records that may be used in investigations of adverse events or inquests, and research and clinical audit aimed at improving services.
In this study, we used a multiple-methods approach to examine how emergency ambulance services across the UK are responding to the challenge of digitisation. We were interested in the opportunities and challenges of implementing EHRs and associated technology in emergency ambulances, in how EHRs might support the shift to providing more care out of hospital and in the workforce implications of the digitisation of patient records in a pre-hospital context. Our study assessed the state of progress with the digitisation agenda across the whole of the UK, and focused on four case study areas to examine in more detail what was going on.
The role and organisation of emergency ambulance services in the UK
Across the UK, 14 NHS ambulance services provide emergency medical services (EMSs). All but one are managed as free-standing NHS organisations, the majority as trusts or foundation trusts (the exception being the Isle of Wight NHS Trust, which integrates all health care for the island). Although many UK ambulance services continue to provide non-emergency patient transport services for those travelling to outpatient appointments, our interest in this study is only in emergency ambulance services provided by NHS providers, generally in response to 999 calls.
Ambulance call centres are staffed primarily by non-clinical staff, who answer 999 calls and gather initial key information on the patient and their presenting need, using computer software based on structured algorithms to assign a priority of response (including time target) to the caller. Front-line care is delivered by a range of staff who we refer to collectively as ambulance clinicians. Paramedics are recognised as allied health professionals, regulated by the Health and Care Professions Council, and, increasingly, enter the profession at graduate level. Emergency medical technicians (EMTs) also deliver immediate patient care, but carry out a slightly narrower range of clinical tasks, reflecting their level of training. Finally, a small proportion of paramedics are trained to a higher level, operating in specialist roles, such as advanced paramedic practitioner. All front-line ambulance clinicians in the UK work to guidelines from the Joint Royal Colleges Ambulance Liaison Committee (JRCALC) and the National Institute for Health and Care Excellence (NICE).
In England, each service is jointly commissioned by Clinical Commissioning Groups (CCGs) in their area. In Wales, Scotland and Northern Ireland, ambulance services are part of the respective devolved health service structures and respond to their respective policy priorities. All ambulance services cover the footprints of many acute providers and make their own purchasing and procurement decisions.
Ambulance services in the UK face a variety of challenges. 1 Staff turnover represents a major operational challenge for emergency ambulance services across the UK, with many consistently operating with vacant posts. 2 Services in the UK are faced with rising numbers of 999 emergency calls, presenting major operational challenges in a time of constrained spending on health care. 3 From 2011/12 to 2015/16, ambulance activity rose 30%, yet funding increased by only 16%. 1 In 2016/17, services in England alone received 11.2 million 999 calls, an increase of 2 million over the figure 3 years earlier. 4 Pressures are felt across the whole system, most visibly in the form of ambulances queuing outside EDs waiting to hand over patients.
Roughly 10% of calls are for life-threatening emergencies, whereas 90% are classed as ‘urgent care’. Many of these ‘urgent care’ patients attended by 999 ambulances are not clinically in need of conveyance to an ED, and could be better cared for at home or by an alternative community-based care provider.
Ambulance services in England are performance managed by NHS England through Ambulance Quality Indicators, reported monthly. Traditionally, the emphasis has been on the speed of response to the most serious calls. The devolved nations have their own performance management regimes. In 2017, the Ambulance Response Programme introduced new measures to English ambulance services, similar to those pioneered in Wales in 2015, which brought a more clinical focus to performance management in an attempt to improve clinical outcomes and reduce some of the operational inefficiencies engendered by time-based targets. 1
The emergency and urgent care system has in recent years been the subject of major national policy reviews in England5 and in the devolved administrations of the UK. 6,7 These reviews reinforce the policy objective set out by the Department of Health and Social Care in its 2005 strategy Taking Healthcare to the Patient8 and more recently in NHS England’s Five Year Forward View,9 encouraging more decision-making by ambulance clinicians about the care of 999 ambulance patients and the establishment of safe alternatives to transport to hospital (non-conveyance). The two main models of care for non-conveyed patients are known as (1) ‘hear and treat’, in which needs are resolved through telephone advice, sometimes through the use of clinical hubs, and (2) ‘see and treat’, in which ambulance clinicians attend and clinically assess a patient, provide care and advice where required, and in some cases provide onward referral. However, questions still remain about the effectiveness and safety of alternatives to conveyance, and how they can best be integrated into routine practice.
Rates of non-conveyance in the UK are around 30%, but vary considerably between ambulance services. 10 To enable non-conveyance to happen safely, ambulance clinicians need to be able to decide which patients will benefit from being left at home, to be able to access appropriate referral pathways to alternative care providers and to ensure that appropriate and accurate patient information is passed on to community-based providers.
This increases the demands placed on ambulance clinicians as clinical practitioners, with implications for staffing, professional roles and responsibilities. 11 To date, the workforce implications of changing models of pre-hospital care have received little attention, although there has been a small amount of research focusing on how ambulance personnel carry out their role. This includes studies of the way in which ambulance clinicians make decisions12,13 and of the unresolved tensions around the increasing professionalisation of the role. 14
Ambulance services and patient records
The modern ambulance is a busy care environment generating large numbers of data that may be critical to ongoing care. 15 Ambulance clinicians make ever more complex clinical decisions, which need to be well informed (supported by all relevant information), and for which they are accountable (the decision and the reasons for it need to be recorded). Patient data that are difficult to retrieve during emergency care within the ambulance present the risk of a poor handover of information on arrival at hospital. 16 For patients who are not conveyed to hospital, good communication to the patient, the general practitioner (GP) and others present challenges that require efficient and accurate information storage and retrieval. Poor-quality data hamper audit and medicolegal use,17 and represent a significant organisational burden and financial risk for NHS trusts and health boards.
Electronic health records are becoming the norm throughout the health service and present an array of benefits,18 although their introduction has often been difficult. 19,20 The introduction of IT to capture patient data electronically in the ambulance context has the potential to support the shift to safe out-of-hospital care in a number of ways:
-
As a base onto which other electronic resources and tools to support safe clinical care [e.g. decision-support software, service directories, referral tools and apps (applications)] are built.
-
To allow easy and direct transfer of patient information to other care providers (including GPs), avoiding the risks of error associated with reading and copying data or with verbal handover.
-
To support real-time remote sharing of diagnostic information (including imaging) so that, for example, an ED consultant can advise about the appropriate conveyance and care decisions while the patient is still at home.
-
To facilitate transfer of patient information to ambulance clinicians at the scene or before arrival, in order to support patient care and appropriate decision-making [e.g. by sharing information on past contacts with GPs or if they are on a do not attempt cardiopulmonary resuscitation (DNACPR) directive].
-
To support identifying those who might benefit from a community-based intervention, such as referral to a falls service.
-
To make data more readily available for audit, research and evaluation. 21 EHRs can feed automatically into anonymised warehouses of linked data from other services, which provide vast potential for future research to inform service improvements,22 as well as providing ambulance services with a valuable store of information to run automated clinical and management reports, removing the need to store large quantities of paper records and freeing up valuable space in NHS premises.
The major move towards EHRs seen internationally has, up until now, been focused on records used in acute hospitals and primary care. 23,24 So far, the progress of transition to EHRs in emergency ambulance services in the UK has been uneven and incomplete. This reflects the experience of other Western countries: for example, a 2016 survey of 2453 US paramedics and EMS managers found that, although 73% reported collecting data on clinical processes electronically, other categories of data were far less likely to be recorded electronically, and forms might be completed retrospectively and sketchily, despite a recognition of the potential value of electronic data developments in mobile integrated health care and community paramedicine. 25
Shifting to electronic health records: strategic drivers
In the UK, by the early part of this century, EHRs had become universal in primary care, usually running on one of three main commercial systems. 26 The shift to EHRs in secondary care has been much slower, with a greater diversity of systems, and with EDs often using a separate system from the rest of a hospital.
Acknowledging the potential value of EHRs to both patients and all health-care providers, the government launched the National Programme for Information Technology (NPfIT) in 2002, and the NHS agency Connecting for Health was set up to deliver it. 27 The NPfIT was a highly ambitious 10-year strategic programme aimed at creating one standard IT system for patient records in England, which would readily allow the exchange of patient information between providers. Planned total investment was more than £11B. The NPfIT established the NHS Care Records Service, consisting of the Personal Demographics Service (PDS) and Summary Care Record (SCR) (both shared via NHS Spine), and the Detailed Care Record for patients seen in secondary care; this function has since been taken over by NHS Digital. Contracts for the delivery of detailed care records were awarded to four commercial suppliers, each covering one or more areas of the country. However, the NPfIT was subject to significant delays,28 some contracts were ended early, and, according to the National Audit Office, delivery fell ‘well below expectations’ (p. 8) (© National Audit Office, The National Programme for IT in the NHS: An Update on the Delivery of Detailed Care Records Systems27). By 2011, the NPfIT was abandoned,18 and the Department of Health and Social Care’s approach shifted from a major national programme to building up local systems under the guidance of a newly created National Information Board, providing, as The King’s Fund described it, the ‘electronic glue’ to make sure that different parts of the system work together. 29
A faith in the value and importance of digitisation was embedded in the NHS England strategy document Five Year Forward View,9 which set a target of paperless records everywhere by 2018, and interoperability by 2020. More detailed guidance30 promoted linked hospital and primary care data sets for secondary uses, that is, uses other than providing direct care, such as research, quality improvement and risk stratification. Because anxieties about data-sharing and data security can inhibit data-sharing for secondary uses, the Caldicott review of data security31 proposed new data security standards plus a new consent/opt-out model for secondary uses.
The Treasury announced a £4.2B investment in technology in the NHS in 2016, although it is not clear how much of this was new money. 29 Area-based sustainability and transformation partnerships across England were tasked in 2016 with producing local ‘digital roadmaps’ to help navigate the path to integrated digitisation on their patch, although the level of involvement of ambulance services in sustainability and transformation partnerships has generally been low. 1
A new approach to tackling the challenges of achieving digital modernisation and interoperability, without tying local providers into a cumbersome national programme, came in 2016 with the influential report published by the National Advisory Group on Health Information Technology in England, chaired by Robert Wachter. 18 The Wachter report examined what lessons can be learnt from the USA and from the primary care sector in the UK to guide the secondary care sector in England in harnessing the power of health information technology. Although ambulance services are notably absent from the report, it provides useful guidance for the sector. The Wachter report’s recommendations take a ‘Goldilocks’ approach to implementing digitisation: not too centralised, not too localised, but somewhere in the middle. The authors note the distinction articulated by Heifetz and Laurie32 between ‘technical’ change (know-how applied from the top down) and ‘adaptive’ change (new ways of working learned on the front line) and argue that digitisation in health care ‘is adaptive change of the highest order’, requiring sufficient time, engagement and skills if failure is to be avoided. The measured approach recommended by the report puts the emphasis on developing skills within trusts, working in regional networks, evaluating progress, looking for safety and quality benefits in addition to financial savings, and adaptation as systems mature. Most importantly, it proposed a rewriting of time scales, giving a new target date of 2023, by which trusts would be expected to have achieved a high degree of digital maturity, and beyond which no further central funding for IT developments should be available.
The Wachter report18 was realistic about the variation among secondary care trusts in how far they have progressed down the path to digitisation, proposing a classification based on progress so far, and readiness to advance into the future, with proposals for investment needed, as shown in Table 1.
| State of digitisation | Readiness | |
|---|---|---|
| Ready to advance | Not ready to advance | |
| Digital now | Early adopter (group A): provide moderate funding to achieve even higher state, serve as role model and teach others. Consider creation of a consortium of members of this group to promote shared learning | Stable (group D): provide no or minimal funding to help advance to next stage. Expect higher level of digital maturity over next 3–6 years |
| Not yet digital | Ready to launch (group B): provide substantial funding to buy system, train, Go-Live and support early enhancement. Expect reasonable digital maturity by 2020 | Not ready (group C): provide modest funding to improve readiness, with hope of digital launch (with additional funding) around 2020; expect high level of digital maturity by 2023 |
To enable those ‘early adopter’ health-care providers in group A to develop further and to share their learning with others, NHS England launched the Global Digital Exemplars programme. In 2018, three ambulance services (South Central Ambulance Service NHS Foundation Trust, West Midlands Ambulance Service NHS Foundation Trust and North East Ambulance Service NHS Foundation Trust) were selected to be Global Digital Exemplars 2018, and were given funding of £5M over 30 months ‘to further their digitisation and support others to do the same’ (contains public sector information licensed under the Open Government Licence v3.0). 33
Technical requirements: standard data sets and interoperability
The strategic approach outlined in the Wachter report18 recognises that, for EHRs to achieve their potential, there need to be a level of standardisation in terms of data collected, and efforts made to ensure that providers achieve interoperability29 (the ability of two or more IT systems or components to share information and use that information34).
On behalf of the National Information Board, NHS Digital [formerly known as Health and Social Care Information Centre (HSCIC)] prepared a handbook on interoperability,34 designed as a tool to help local providers put the national strategy into action. It addresses the two problems of interoperability:
-
technical interoperability – the ‘how’
-
semantic interoperability – the ‘what’ (organising data in a common way, using specific coding and messaging schemes).
The handbook did not mandate any particular model for the technical aspects, acknowledging the different functions and advantages of point-to-point models, hub-and-spoke models and hybrid models, and suggesting a range of approaches to document exchange. It did, however, set out a list of ‘key building blocks’ that it suggested providers should adopt as part of a programme of work with built in evaluation in terms of terms of the impact of data exchange on patient satisfaction, efficiency and quality of care. The key building blocks were:
-
adoption of NHS number as primary identifier
-
establishing regional interoperability communities, with clinical leadership at the local level
-
establishing open application programming interfaces within and between integrated digital care records
-
prioritise the uptake of fundamental digital standards as ratified by the NHS England Board
-
for key transfers of care, specifying, introducing and adopting tight and consistent digital standards
-
creating a national patient record locator service
-
extending the use of SCRs.
The other key part of what NHS England has called the Interoperability Architecture Framework34 is a set of common standards for records, the framework for which has been set out by the National Information Board. 30 A set of standards for clinical records in secondary care were first produced by the Academy of Medical Royal Colleges in 2013,35 which were revised and reissued by the Professional Records Standards Body in 2018. 36 Building on these standards, the Royal College of Physicians’ Health Informatics Unit developed a set of standards specifically for emergency ambulance services, published on behalf of NHS England and NHS Digital37 in 2016. 37 The aim of the standards is to support improvements to patient care, to performance management, audit and research, and, as Sir Bruce Keogh wrote in the foreword to the standards:
. . . to create true digital integration from primary care, into the ambulance services and onto acute, community, mental health and other health and care provider organisations. This guidance will allow greater measurement and understanding of clinical care provided by the nation’s ambulance services.
The guidance provides a standard structure for data categories for the ambulance record that are meaningful to clinicians and patients, and each of which has a clinical description. There are 171 subheadings in total, grouped under 31 top-level headings, from the details taken at the time of the initial call to patient disposition. The guidance proposes that ambulance EHR systems should include all of the headings, although not all headings would need to be used in all circumstances, and should be used only when appropriate. Some headings might be pre-coded, whereas others would support the entry of free text; some information could be drawn from other sources, such as call centre data. The guidance recommended that all electronic systems should ensure that the system automatically records the date, time and the identity of the person making each entry. Guidance does not specify which information should be coded and which should be entered as free text.
Understanding the challenges of introducing technology in health care
Although EHRs and other IT applications have potential value in the ambulance context, we note that they have repeatedly been introduced in health care on the assumption that they will bring quality improvements and cost savings, but the reality has often been disappointing compared with the rhetoric. 19 There have been many challenges to implementing informatics systems in the NHS, as seen with the NPfIT and, more recently, the care.data programme, which aimed to enable sharing of primary care patient records. Some systems have been abandoned (e.g. HealthSpace). 38 Indeed, one notable early example of a system failing and being abandoned concerned ambulance control rooms. 39 The introduction of IT into direct care may have unanticipated consequences, and these are likely to differ across care settings and system architectures (see, for example, Ash et al. 40 and Cresswell et al. 41).
The challenges of health IT projects have been explored through several theoretical lenses, as outlined in a 2009 National Institute for Health Research (NIHR) review of electronic patient records. 19 This review suggested the potential for further developing the use of recursive theories to examine the use of technology in health care, looking at the two-way relationship between people and technology, in which technology changes individuals’ practice, but can also be modified, resisted or bypassed, and how practice feeds back into technological developments.
The definition of success in such projects is itself fluid and contested. 19 Success criteria cannot necessarily be predefined or even always predicted, but emerge and are interpreted by stakeholders.
Past research has stressed the interlinked nature of EHR use, workflows and service redesign. 18–20 EHRs will have an effect on processes and capability of staff to manage patients (e.g. decision-support software for treatment or referral). In turn, workforce development will have an effect on the pace and nature of implementation of EHRs. Early adopters of EHRs were limited to devices with a single function: that of presenting and storing the record. Since that time, and with the introduction of smart devices, these systems have become multifunctional. This means that adopting EHRs opens numerous possibilities to provide greater support to ambulance clinicians and patients: telehealth consultations from a patient’s home, access to medicines data, internet/intranet access, record linkage with GPs and hospitals, access to emergency care summaries, embedded patient assessment algorithms and calculators. For the staff specifically, these can include incident reporting, rostering management, leave requests, embedded learning modules and defect reporting. All of these will combine to determine the shape and processes of our workforce into the future, as technology and working practices co-evolve.
Prior research, including by members of the team, has described how EHRs and related technology are used by health-care staff in other contexts, what the challenges to adoption are, and how, why, by whom and at what rate innovations are taken up. It is possible that unintended consequences may arise, including potentially unintended benefits, so we have looked for this happening and not presumed that the only benefits to be measured are those predefined in business cases or that the only dangers are those predefined in risk assessments.
Aims and objectives of the Electronic Records in Ambulances study
Research aim
To understand how EHRs can be most effectively implemented in a pre-hospital context in order to support a safe and effective shift from acute care to community-based care, and how their potential benefits can be maximised.
Objectives
-
To describe the current usage of EHRs and associated IT in ambulance services in the UK:
-
– To describe processes of implementation, uptake and usage.
-
– To investigate what use is currently being made of EHRs in terms of identifying and managing repeat callers, information transfer to other providers, linking with other electronic resources (e.g. for decision support and referral), and research and audit.
-
– To investigate the use and development in ambulance services of other handheld technologies (including apps) to support decision-making and referral to community-based care.
-
-
To understand how the ambulance workforce responds to the introduction of EHRs and associated infrastructure, and what impact they are perceived to have on the role of ambulance clinicians.
-
To investigate risks, benefits and unintended consequences of implementation of EHRs in terms of changes to patient care, working practice of ambulance clinicians, management and organisational practice within ambulance services, and planning and commissioning processes in the wider health economy.
-
To understand the factors that lead to successful implementation of EHRs and adoption by the workforce, and how risks can be minimised and benefits can be maximised.
-
To assess the potential to further develop and implement EHRs, computerised clinical decision-support and referral tools to support the shift to out-of-hospital care.
Outline of the report
Chapter 2 outlines our methods for gathering and analysing original empirical data on the use of EHRs in UK ambulance services. Chapter 3 presents the methods and findings of a rapid review [work package (WP) 1] of the peer-reviewed literature on EHRs in pre-hospital emergency care. We aimed to review the scope of the literature, and to identify any key messages that would inform subsequent phases of the study. Chapter 4 presents findings from WP2: a telephone survey of the state of implementation of EHRs in ambulance services across the UK. Findings from WP3, our case studies on four selected sites, are presented in Chapters 5–7: first describing the situation in each of our case study sites based on our qualitative data collection and examination of documentation; then presenting our analyses of a 2-month snapshot of routine data; and finally looking across the four sites to draw out cross-cutting themes, considering what variation and consistency there is across sites and why this might be. In Chapter 8, we report on WP4, the knowledge-sharing workshop. We discuss our findings, relating them back to previous literature, and present conclusions in Chapter 9.
Chapter 2 Methods
Overall study design
The study had four WPs:
-
a rapid review of published research literature on EHRs and other IT relevant to the ambulance context – details of the methods for this are presented in Chapter 3
-
a telephone survey of NHS trusts providing 999 emergency ambulance services in the UK
-
case studies in four ambulance services, along with their associated health economies, selected to represent services at a range of stages of implementation of EHRs
-
a knowledge exchange and future development workshop.
Theoretical framework
Our study was informed by two large, interdisciplinary reviews funded by NIHR. The first was the 2005 Greenhalgh et al. 42 review and model of diffusion of innovation in health care, which considers the innovation itself, the outer context, the inner context and the processes linking them. The second was the 2009 review by Greenhalgh et al. 19 of research on EHRs that highlighted the value of recursive theories of technology in use, drawing on human–computer interaction research, actor–network theory and others.
We used strong structuration theory (SST) as the theoretical underpinning for this study, following Greenhalgh and Stones20 in incorporating a focus on the implementation of technology. SST with a technological dimension proposes that the outcomes and impact associated with introducing a new technology into use in an organisation are shaped by the interplay between the external structure (in this case of the NHS as a whole and of each ambulance service); the internal structure, in this case both of ambulance clinicians (their knowledge and attitude) and of the technology (its material properties and functionality); and of the actions that the clinicians as human agents take; and that in turn outcomes can reproduce or change structures. SST with a technological dimension recognises the recursive relationship between these elements in order to understand how new processes are, or are not, adopted in practice. 20,43,44 Theory also highlights the agency of technology: that the technology comes with affordances that support certain activities, but also represents ‘frozen fragments’ of social relations, so we have considered how the technology influences work and potential mismatches between those who designed the technology and those using it.
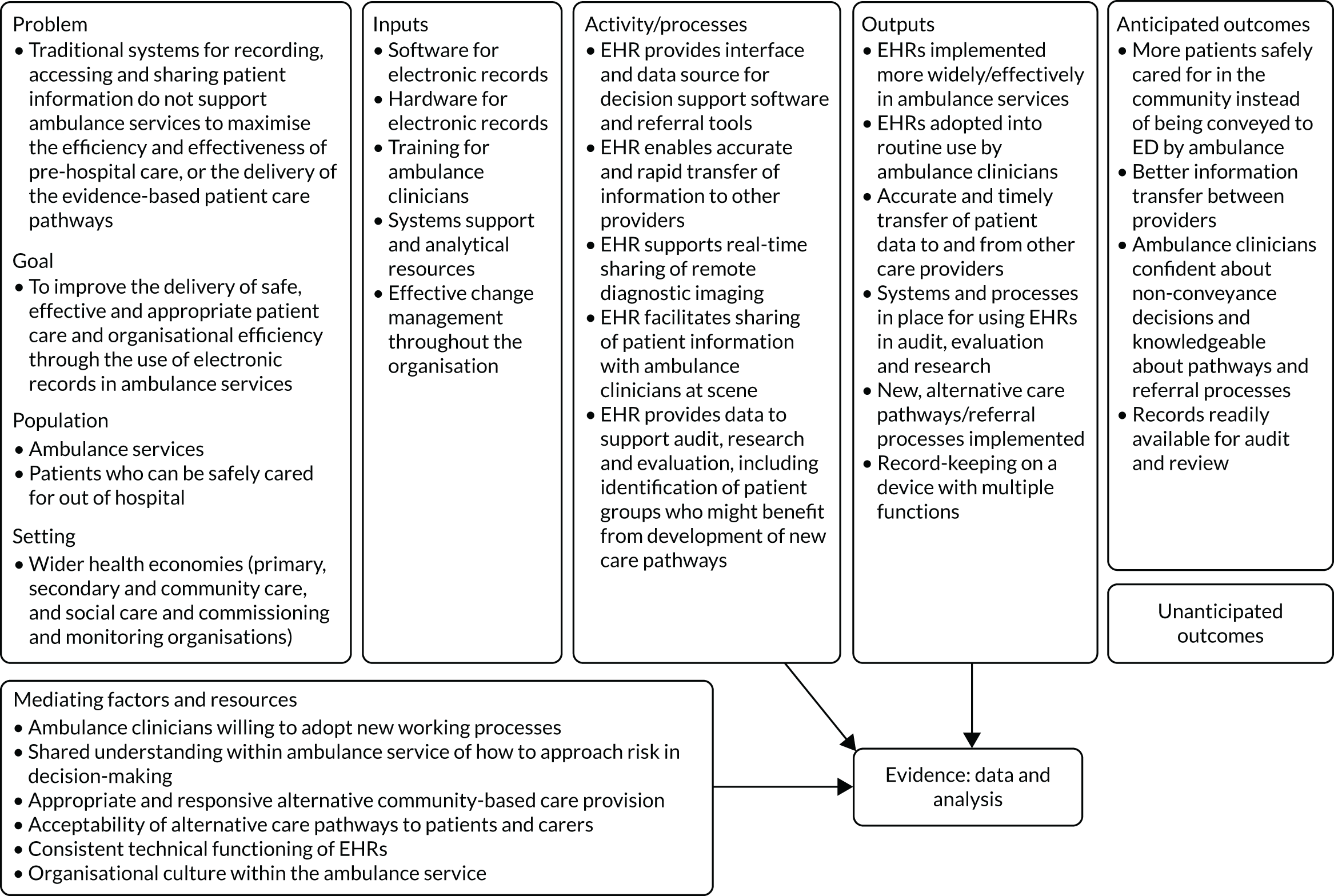
In terms of understanding how EHRs might make a difference to the delivery of patient care, we developed an initial logic model (Figure 1) at the start of our study. The logic model sets out our belief that the adoption and implementation of EHRs in ambulance services might support improvements to the delivery of safe, effective and appropriate patient care and organisational efficiency. We used this logic model to inform our data collection and analysis, and the presentation of our findings is in Chapter 7.
FIGURE 1.
Initial logic model of the proposed impact of EHRs in emergency ambulance services.
Setting and sampling
Work package 2
All free-standing UK ambulance services (n = 13) were used: the three national services for Wales, Scotland and Northern Ireland, and the 10 independent ambulance service trusts in England. The only service not included was the small integrated health-care trust that provides an emergency ambulance service on the Isle of Wight. In each site, we invited, by e-mail, up to two senior or middle managers with knowledge of EHRs to take part in an interview. Potential participants were identified through our professional networks.
Work package 3
Four selected ambulance services, along with their associated health economies, were used. We selected the ambulance services to give a range of experiences. At the time of selection (2015), one service was an established user of EHRs, one had partially adopted EHRs, one was anticipated to be in the early stages of implementation during the time of the fieldwork and one was still discussing introduction of EHRs. Representatives of each ambulance service were co-applicants on this proposal.
Data collection
Work package 2: survey
We conducted semistructured telephone interviews with senior and middle managers in each service to gather descriptive date regarding the implementation, usage and development of IT in pre-hospital care settings in the UK. Building on the rapid review, we developed an interview schedule that covered the current stage of implementation of EHRs in the service, reasons for introduction or non-introduction of EHRs perceived benefits and uses of EHRs, impediments or barriers to their use and other electronic tools used by ambulance clinicians and how they interface with EHRs. If EHRs had not yet been introduced in the ambulance service, we asked about future plans, perceived benefits of EHRs and perceived impediments to their introduction. Verbal consent to participate was taken at the beginning of the telephone call and participants could decline to answer questions or cease to participate simply by indicating that they wished to do so. Interviews were recorded and transcribed in full; respondent identifiers were removed from the transcripts. Interviews were conducted by Victoria Williams during the period February to August 2017.
Work package 3a: case studies
We undertook case studies in four ambulance services and their associated health economies to address objectives 2, 3 and 4. Each case study examined the story of the implementation and use of EHRs in the site, incorporating descriptive analysis of any available routine data on uptake, use and impact of EHRs. We adapted some principles of ethnographic research to incorporate observation of practice on ambulances. To facilitate comparison across sites, we included a particular focus on three tracer conditions known to have potential for increased non-conveyance rates: falls in older people, diabetic hypoglycaemia and mental health crises. We examined how, in each study site, out-of-hospital care pathways are being provided for these patient groups, and how ambulance service data are (or could be) informing both care provision and planning/commissioning decisions.
In each site, we had a part-time site researcher; the role was split between two members of staff in site 2, although only one of them carried out observations. Two researchers (in sites 1 and 4) were registered paramedics. In three sites, the site researchers were employed by the ambulance trust; in the fourth (site 3), the researcher was employed by one of the collaborating universities but maintained close links with the trust. The site researchers’ reflections on their role are summarised in Reflexivity and the site researchers. Fieldwork took place during the period April to October 2017, and involved collecting the following data (also summarised in Table 2):
-
Documentation (business case, minutes, etc.) to track the story and timeline of implementation, including costs (planned and actual) and collection of descriptive data on the EHR systems themselves in terms of hardware, software, data categories and flexibility.
-
Interviews with relevant senior and middle managers and training staff (identified by the local ambulance service lead) within ambulance services to gather their views on the rationale for introducing EHRs in their ambulance service, the way in which the records were introduced, the challenges to introduction and the opportunities presented by EHRs. Interviews were carried out face to face and recorded and transcribed in full. We asked about reasons for non-introduction or delay in introduction, and the choices that may have been made, including decisions relating to the opportunity costs associated with introduction of records. We also asked about care pathways (actual or in development) for the three tracer conditions, and the perceived relevance of EHRs to these.
-
Focus groups with paramedics and ambulance technicians – recorded and transcribed in full, involving participants from a range of ambulance stations within the service. In collaboration with each ambulance service, the site researchers selected a random sample of ambulance clinicians to invite to the focus groups, and thus aimed to ensure that we talked to people with a range of levels of enthusiasm for EHRs. Site researchers had aimed to carry out a focus group in each of the stations from which they carried out their observation, giving a target of three focus groups per case study area. However, it proved difficult to recruit sufficient numbers of staff in several of the areas, largely due to shift patterns that made it difficult to get enough people to attend at any one time. Site researchers tackled this in several ways. In one case study area, the site researcher held a large focus group with clinicians attending a training session, thus capturing views from practitioners from a range of localities in the service. Another researcher held several smaller groups to try to gather a range of views.
Focus groups were conducted within ambulance stations, and we paid participants an honorarium for taking part. The discussion covered participants’ views on the rationale for the introduction of EHRs in their ambulance service, the way in which the records were introduced, the challenges to the introduction, their experience of using EHRs in practice (where relevant) and the opportunities presented by EHRs. We also asked about care pathways (actual or in development) for the three tracer conditions, and the perceived relevance of EHRs to these.
-
Observation of EHRs in use. Site researchers carried out a total of 12 full-shift observations with different crews from different ambulance stations. Although our original plan had been to carry out three observations in each site, owing to local issues in site 3 the site researcher was able to carry out only two observations. In site 2, where a new system was being rolled out, the site researcher decided to observe a fourth shift in an attempt to capture some of the changes to the way patient data were gathered and transferred.
Observations were carried out by the site researcher over the course of a full shift and covered both day and night shifts, modelled on an approach previously used in a study by O’Hara et al. 12 of decision-making in pre-hospital care. The site researcher made recorded observations and reflections using a pre-formatted site researcher notebook (the edited version is in Appendix 3; the full version is available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/144722#/) and a digital recorder, and discussed the use of records with the crews between episodes of patient contact. Shifts were selected to ensure that different clinicians were shadowed, and that observations took place at different times and in different localities. The site researchers were trained in participant observation. They observed the use of electronic and other records (when completed, by whom, processes undertaken) and the use of other data sources to support decision-making. At times when there was no patient in the ambulance, the researchers asked ambulance clinicians for clarification or explanation of processes and decision-making, and then recorded this information.
-
Interviews with other stakeholders, including representatives of the commissioning or funding organisation(s), EDs and community health-care providers. Interviews covered participants’ views on the rationale for the introduction of EHRs in the ambulance service, and their perception of the opportunities and challenges presented by EHRs. We also asked about care pathways (actual or in development) for the three tracer conditions, and the perceived relevance of EHRs to these.
| Site | Collection process | ||||
|---|---|---|---|---|---|
| Observations (n) | Documents (n) | Interviews (n) | Focus groups (n) | ||
| Sessions | Hours | ||||
| 1 | 3 | 36 | 59 | 8 | 2 |
| 2 | 4 | 48 | 50 | 8 | 5 |
| 3 | 2 | 24 | 20 | 6 | 1 |
| 4 | 3 | 36 | 29 | 8 | 3 |
| Total | 12 | 144 | 158 | 30 | 11 |
Work package 3b: routine data
-
Extraction and collation of a sample of routine data to explore the use of electronic patient records. Following the signing of data-sharing agreements with each case study ambulance service, we collected computer-aided dispatch (CAD) data relating to incidents (calls) and resources (vehicles and crews) alongside EHR data for a 2-month ‘snapshot’ period of January and February 2017 from all four ambulance services. Table 3 indicates the variables requested from each service, and the data source from which they were obtained. Patient identifiers were removed before data transfer. We also requested from each service a cover sheet describing the parameters of the data (i.e. date extracted, data sources, data coverage and contact details of those extracting data) and a data dictionary describing and defining the variables (e.g. data source – CAD, EHRs, other; and date ranges).
Following data cleaning, we analysed and profiled the data to show, at each site, the total number of calls attended with an EHR, and identified associations between completion of an EHR and the patient demographic (age and sex), clinical factors (condition type and severity from triage category) and operational factors [crew member identifier (ID), ambulance station, time of day, disposition of patient, hospital to which a patient was conveyed], as recorded in the call centre.
-
We investigated what routinely available data there were (time period, nature of data source) on ambulance attendances and consequent care for the three tracer conditions, in order to understand patterns of disposition and care pathways. This work was primarily exploratory. We sought to establish a minimum data set across all sites based on dispatch codes in order to describe patterns of activity, and looked at how any additional data were collected and used to inform decision-making.
| Variable | Source |
|---|---|
| Incident number | CAD |
| Incident postcode (first four digits) | CAD |
| Call number | CAD |
| Locality | CAD |
| Responding station(s) | CAD |
| Dispatch code | CAD |
| Priority classification | CAD |
| Clinical impression (dispatch) | CAD |
| Disposition (transferred to hospital, treated on scene, referred to other service, etc.) | CAD |
| Time of call – date and time | CAD |
| Responding vehicles | CAD |
| Vehicle type | CAD |
| Double or single crew | CAD |
| Did vehicle arrive on scene? | CAD |
| Time mobile – date and time | CAD |
| Time at scene – date and time | CAD |
| Time left scene – date and time | CAD |
| Time arrived at hospital – date and time | CAD |
| Time of handover – date and time | CAD |
| Hospital | CAD |
| Crew ID | CAD |
| Crew grade (paramedic, technician, emergency care assistant, etc.) | CAD |
| Patient ID | EHRs |
| Response number | ECS |
| Date of birth (if age missing) | ECS |
| Ethnicity | ECS |
| Clinical impression (clinician) | ECS |
| Location | ECS |
| Crew position | ECS |
| Crew level | ECS |
Work package 4: knowledge exchange workshop
We presented our initial findings at a knowledge exchange workshop on 3 July 2018 in central London. The workshop functioned both as a validity check of the findings and as a source of new data. We supplemented the workshop with online and telephone contact with stakeholders both before the workshop (to help to inform the plan for the workshop and to gain initial responses to study findings) and after it (to seek endorsement/comment in relation to conclusions and recommendations). This contact allowed us to obtain input from people who were not able to attend the workshop in person, to gather reflections formed over time rather than immediate responses and to obtain comments in confidence that people might be reluctant to express in a group setting.
The workshop was audio-recorded and notes were made from the recording. WP4 brought together UK ambulance services, secondary care clinicians, patient and public involvement (PPI) representatives, relevant IT suppliers and other relevant policy-makers. We shared learning on successful implementation and discussed potential for, and possible challenges to, future development of EHRs in relation to identifying and managing repeat callers, information transfer, linking with other electronic resources, and research and analysis.
Data analysis
Framework approach
Analysis of the qualitative data drew on the framework approach to analysis for applied policy research. 45 Framework provides a method for researchers to systematically sort and analyse data in relation to key issues and themes within a finite time frame. Framework involves five stages of analysis. The first is familiarisation, whereby a researcher reads the data and begins to form ideas about emerging issues and themes. Next is identifying a thematic framework, based on these issues, and informed by the original research aims and questions; this framework may be revised as analysis progresses. In the indexing stage, the framework is applied to the data, and the data are linked to the themes. Charting the data then entails the researcher reviewing the data theme by theme, and relating text to themes and subthemes. Finally, the mapping stage involves the researcher synthesising and interpreting the data in order to define concepts, map the range and nature of phenomena and provide explanations in relation to the research questions and objectives.
Work package 2: survey
Analysis of the transcripts of the survey interviews was carried out by two members of the research team (VW and AP).
Work package 3: case studies
Analysis of the large number of data (transcripts, observation notes and documentation) generated by the case studies was supported by the use of NVivo 11 software (QSR International, Warrington, UK). As above, our analysis followed the framework approach. The analysis was carried out on a team basis by up to nine members of the research group with experience in qualitative analysis (AP, VW, ZM, HP, KM, DS, RS, HM, YL-W). Analysis began with a workshop event bringing together members of the research team and PPI representatives. Prior to the event, each participant read a sample of texts (observations, interview transcripts and focus groups transcripts). Each text was analysed by a minimum of two researchers for validation.
Routine data about the uptake and use of EHRs were analysed descriptively, and multivariate analysis was used to identify associations and predictors of use.
Analysis of all case study data was first carried out within sites, and was followed by cross-case analysis across sites. 46 Our analysis drew on SST with a technological dimension in order to understand how new processes are, or are not, adopted in practice. 20,44 In each site, we examined the role and practice of the key agent (in this case, the ambulance clinician) using data from observation and focus groups; the political and organisational context, using interview data and documentation; the technology itself, drawing on documentation and observation; and the recursive relationship between these elements, using routine data on usage, interview and focus group information relating to feedback and performance management, and data on response to and provision for the three tracer conditions. We then compared across sites in order to understand consistency or variation in experience, the significance of time in the implementation process and the role of local context.
Work package 4: knowledge exchange workshop and online forum
Consensus methods were used during the workshop to develop shared understanding of future opportunities around use of EHRs in ambulance services. 47
Synthesis
Table 4 summarises how each WP addressed the study’s objectives. The research team members were in regular contact with each other, allowing the different WPs to inform each other’s development. A final overarching synthesis is presented in the discussion and conclusions chapter (see Chapter 9), bringing together the findings of each WP, presenting a summary, interpreting findings, drawing out common themes and presenting any tensions and conflicts between the WPs’ conclusions as higher-order data.
| Objective | WPs |
|---|---|
| 1. To describe the current usage of EHRs and associated IT in ambulance services in the UK: | |
| a. To describe processes of implementation, uptake and usage | WP2, WP3a and WP3b |
| b. To investigate what use is currently being made of EHRs in terms of identifying and managing repeat callers, information transfer to other providers, linking with other electronic resources (e.g. for decision support and referral), and research and audit | WP3a |
| c. To investigate the use and development in ambulance services of other handheld technologies (including apps) to support decision-making and referral to community-based care | WP2 and WP3a |
| 2. To understand how the ambulance workforce responds to the introduction of EHRs and associated infrastructure, and what impact they are perceived to have on the role of ambulance clinicians | WP2 and WP3a |
| 3. To investigate the risks, benefits and unintended consequences of the implementation of EHRs | WP2 and WP3a |
| 4. To understand the factors that lead to the successful implementation of EHRs and adoption by the workforce, and how the risks can be minimised and benefits maximised | WP3a and WP3b |
| 5. By focusing on the three tracer conditions, to carry out a cross-case comparison of how EHRs can support the development and delivery of out-of-hospital care in the four sites as an alternative to conveyance to the ED | WP3a and WP3b |
| 6. To assess the potential to further develop and implement EHRs, computerised clinical decision-support and referral tools to support the shift to out-of-hospital care | Synthesis of WP1–4 |
Ethics
We were advised by Wales Research Ethics Committee 6 (in June 2016) that the project did not require ethics review by an NHS Research Ethics Committee. In September 2016, we received approval for the study from the College of Human and Health Sciences/College of Medicine Research Ethics Committee of Swansea University. All research participants (i.e. interviewees, focus group participants and staff being observed in observation sessions) were given written information sheets and provided written consent to take part in the study. In the observation sessions, we did not gather any data from patients or carers or record any information that might identify them. Patients/carers were asked to verbally consent to the observer being present.
Project management
The core research team members (AP, VW, ZM and HP) kept in regular contact through teleconferences to discuss the day-to-day management of the project and research activities. They were joined in their discussions by the five site researchers during the period they were employed on the study.
The Research Management Group (RMG) was responsible for overseeing the delivery of the project, and brought together co-applicants with members of the core research team and PPI representatives. The RMG met 10 times during the course of the project, with some members joining in by teleconference.
We also convened a Research Advisory Group, bringing together people with expertise in the planning and delivery of emergency care services and in relevant academic research, alongside PPI representation. Membership of the Research Advisory Group is shown in Appendix 10. The Research Advisory Group also fulfilled the role of a Data Monitoring and Ethics Committee. The group met three times during the course of the project, at a venue in central London, with some members joining by teleconference.
Patient and public involvement
Patient and public involvement was considered from the proposal stage of the project onwards, with one PPI member based in Wales being included in the first ever meeting to discuss the proposal. This PPI member (RM-H) then became a co-applicant for the project bid.
Once the project started, the PPI member became part of the RMG, attending meetings as a full member of the team. A second PPI member (PM) was recruited to the RMG. This second member was based in England and was identified as having a different background, thus promoting PPI diversity.
We also recruited a PPI member (AB) to sit on the Research Advisory Group.
During the project, the PPI members in the RMG contributed fully to the meetings, giving descriptions of personal experiences of being treated by ambulance crews and recounting their use of recording systems. They both made relevant comments in the various discussions throughout the project.
Their individual PPI backgrounds, in research activities within the wider health and social care community nationally, regionally and locally, enhanced many of the discussions to shape the overall benefits of the Electronic Records in Ambulances (ERA) project. The involvement of the PPI members contributed to the discussions at the meetings. In fact, no adverse effects at all were felt from their presence.
The activities of the PPI representatives included attending meetings and associated discussions, and participating in the initial analysis workshop and the knowledge exchange workshop. They did not take part in any of the data gathering or literature research.
The meetings were held at appropriate times and locations to allow easy access for the PPI members to attend as required, with full and timely remuneration. There was always the opportunity to dial in and PPI members were reassured that any areas of need, had they arisen, would have been addressed to accommodate the PPI members.
The PPI representatives were involved in reviewing the final report and wrote the Plain English summary.
Reflexivity and the site researchers
The embedded site researchers set up and conducted meetings and focus groups, gathered documentation, carried out observation (in site 2, observation was carried out by only one of the two researchers who were sharing the role) and contributed to analysis of the data.
The degree to which they were ‘insiders’ within the respective ambulance services varied in terms of employment, experience and clinical qualification, as shown in Box 1.
The researcher was a registered paramedic, already employed by AS1 and seconded to the project in a research role. In her usual role, she would work with or alongside the colleagues she was observing, interviewing and conducting focus groups with:
As a paramedic, it was difficult not to put my opinion in on the completion of the EHR or suggestions on what may be wrong with the patient.
Site 2
The two researchers were already employed by AS2 within the governance and audit management team; neither had a clinical qualification, although they came to the study with an understanding of the new EHR system and the ongoing project management associated with it. On observation sessions, the researcher was able to share her knowledge:
[ED receptionist] asked about how to filter patients on the web viewer . . . I showed her how to use the date filter together with the patient name filter to ensure she got the correct incident.
Site 3
The researcher had a background in qualitative research, but no previous experience of working in a pre-hospital context. She was employed by a university and carried out her work in AS3 under an honorary contract. Sometimes she felt outside her comfort zone:
. . . I’m OK personally in emergencies, but not when I have time to think. I go from practical to feeling ill and emotional.
Site 4
The researcher was a registered paramedic, who had been working in a research and training role immediately prior to the study. To carry out the researcher role, she returned to her old employer and encountered many colleagues who already knew her as a paramedic or trainer:
With a notebook in my hand and writing as they are working, I wondered if [paramedic’s] comment hinted that he thought I might have been covertly spying on them.
AS, ambulance service.
All of the site researchers reflected, both during and after the fieldwork period, on their experience of these tasks, particularly the observation sessions. They identified a number of issues that highlight the ambiguities inherent in their role, and the challenges of conducting fieldwork in a way that is consistent across sites and maintains an appropriate level of objectivity:
-
They brought preconceptions and different levels of background knowledge, and all but one of the researchers had some existing personal contacts among those they were working with.
-
They experienced ambiguities about presentation. All researchers were required to dress appropriately for observational shifts, including wearing ambulance service-provided garments/badges marked as ‘observer’. However, researchers found that wearing a ‘hi-vis’ jacket led to assumptions of being part of the clinical team.
-
They took an active role in what was going on, not merely observing. All reported talking to patients and family members to fill silences, provide reassurance or otherwise smooth the encounter. All reported carrying out practical tasks such as fetching bags or holding doors, which they felt legitimised their presence. The two paramedic researchers both stepped in to provide clinical support in cases in which they were more highly qualified than those they were observing or in which an additional person was needed.
-
They experienced marginalisation in many of the encounters. In some cases, this was self-marginalisation, standing back out of respect for privacy or for reasons of space. On occasion, the physical location of the researcher (outside the room, or in the cab of the ambulance) prevented observation of practice.
-
Researchers reflected on their embodiment – feeling nausea when travelling backwards in the ambulance, feeling hungry and thirsty as meal breaks were deferred, and needing the toilet. For the researcher who had never previously ridden in an ambulance, there were particular concerns about being out of the local area and fear of being left at a hospital or other site (with no contact numbers) if not always by the clinicians.
Chapter 3 Literature review
Introduction
We reviewed the scope of the research literature on the use of EHRs in emergency ambulance services. We aimed to identify and conduct a narrative review of evidence that might inform us of the challenges, opportunities and workforce implications associated with the implementation, adoption and usage of electronic patient records in emergency ambulances.
Methods
This review followed a protocol that was developed a priori in reference to the Cochrane Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. 48
Eligibility criteria
We included articles that described experimental or observational studies, including case studies, carried out in the pre-hospital setting and that made reference to EHRs. Articles that did not describe any form of investigation – opinion pieces, advertorial articles, editorials and theoretical design articles – were not included.
Information sources and search strategy
We searched the following databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), The Cochrane Library, Health Management Information Consortium, MEDLINE, Scopus® (Elsevier, Amsterdam, the Netherlands) and Web of Science™ (Clarivate Analytics, Philadelphia, PA, USA). We did not limit for date, nor did we use any study design restrictions. Keywords and medical subject heading (MeSH) terms used to conduct the search are presented in Box 2.
electronic record*
electronic medical record*
electronic health record*
electronic patient record*
electronic care record*
electronic patient care record*
EMR
EPR
EHRs
ECR
ePCR
Ambulancesambulance*
emergency service*
emergency response
emergency response team
Emergency Medical Technician*
Paramedic*
EMS
EMT
Medical subject heading termsemergency medical services
emergency medical technicians
emergency treatment
emergency medicine
ambulances
Study selection
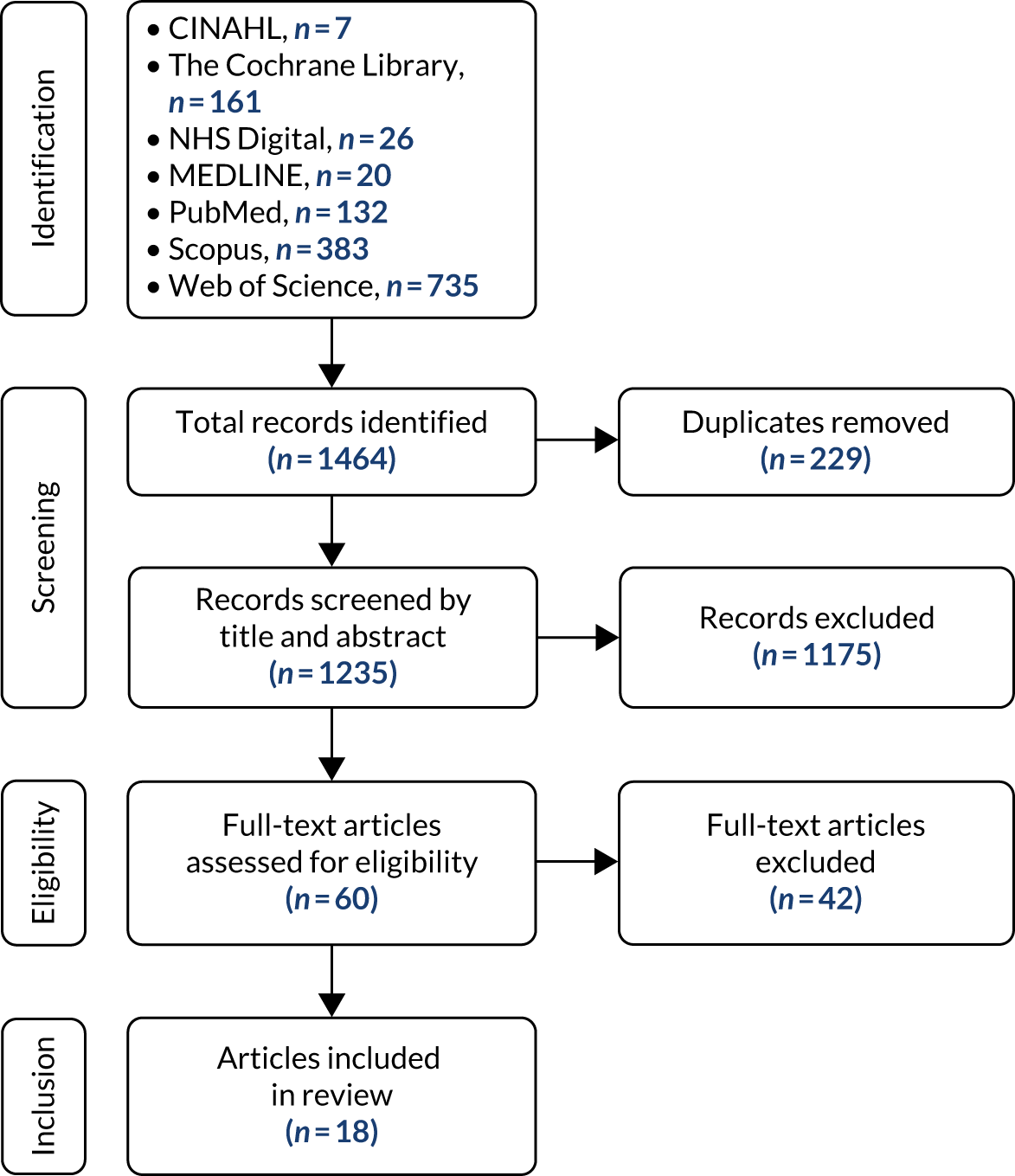
Studies were initially screened by title and abstract content following database searches. Full papers that were deemed suitable based on title and abstract content were then assessed to confirm suitability. The search and selection process is detailed in Figure 2. Our search of the literature in seven databases returned 1464 results. A total of 229 duplicates were removed and 1235 articles were screened. Of the 1235 articles, 1217 articles did not meet the eligibility criteria and were excluded. Data were extracted from the remaining 18 articles, using a standard record sheet, by Matthew Jones and Anisha Badshah.
FIGURE 2.
Study selection flow diagram.
Data reporting
We present findings within seven themes that we developed inductively: (1) implementation and adoption of EHRs, (2) EHRs in use, (3) determining clinical status using EHRs, (4) quality of EHR documentation, (5) EHRs’ impact on call duration, (6) EHRs and real-time data-sharing and (7) EHRs and retrospective data linkage.
Results
Overview
The characteristics of the 18 included studies are summarised in Table 5. All but one study were set in a single country, with one study sampling from the USA and Canada. 49 The majority of the studies (n = 10) were conducted in the USA,50–59 two were conducted in Japan,60,61 two in Australia65,66 and one was conducted in each of Finland,62 Italy63 and the UK. 64 The identified literature is of limited quality. The majority of the empirical research was conducted with small, private emergency services providers with small sample sizes. Three of the studies consider one EHR system within scenario testing over the course of its development. 55,56,58 Publication dates range from 2004 to 2016; the age of the literature is an important consideration as earlier studies illustrate software deficiencies that would not be anticipated today. 59
| Study | Setting | Focus of study | Type of research/study design | Main findings |
|---|---|---|---|---|
| Baird and Boak50 (2016) |
Small, privately owned emergency care provider USA |
Implementation and adoption of EHRs |
Mixed-methods case study, 20 months post system introduction Four semistructured interviews with managers and trainers, 29 surveys with paramedics |
Factors aiding EHR adoption:
|
| Bledsoe et al.52 (2013) |
Emergency physicians USA |
Availability of pre-hospital care records and ED decision-making |
Survey n = 228 |
EHRs were preferred over handwritten records for legibility and accuracy EHRs were mostly unavailable at the time of ED medical decision-making Handwritten records were more readily available |
| Broussard57 (2009) |
Large, privately owned emergency care provider USA |
Implementation and adoption of EHRs | Descriptive case study |
EHRs were used to collect patient data retrospectively (post delivery of care) through direct data entry or dictation EHRs used for reimbursement, clinical audit, workforce training needs analyses and education |
| Burley et al.65 (2008) |
Urban ambulance service Australia |
Implementation and adoption of EHRs |
Qualitative case study, before and after implementation (+ 3 months) 45 semistructured interviews with managers, trainers and paramedics |
EHRs improved legibility, and standardisation of reports and speed of data acquisition/record retrieval, reducing documentation Implementing EHRs led to a loss of narrative in records and increased costs of infrastructure, training and support |
| Buswell et al.64 (2015) |
One emergency ambulance service UK |
Comparison of clinician usage of paper clinical records and EHRs |
Retrospective review of 1 month of paper clinical records data 187 EHRs and 186 paper clinical records |
Clinicians chose record type according to patient disposition Fewer than 1 in 20 patients reported as ‘treated and discharged’ (left at scene) in EHRs group compared with more than one-third in paper clinical records group Almost 85% of patients in EHRs group reported as ‘treated and transported’ compared with 50% in paper clinical records group |
| Chan et al.55 (2011) |
Simulated mass casualty scenario USA |
Multidisciplinary emergency responders Evaluation of quality of patient documentation |
Comparison of paper clinical records and EHRs for simulated patients 50 paper clinical records and 50 EHRs |
Documentation and tracking of victim status (including acuity) significantly improved using the EHR system |
| Chittaro et al.63 (2007) |
Simulation study in an emergency ambulance service Italy |
Evaluation of a PDA-based EHR system |
EHR usability study using survey and informal discussion with paramedics n = 6 |
Overall, a positive user reaction towards most aspects of the PDA-based EHR system except for unsatisfactory handwriting recognition |
| Crilly et al.66 (2011) |
Ambulance, ED and hospital care settings Australia |
Comparison of automated data linkage and manual data linkage |
Data linkage 3469 ambulance records, 10,835 ED records, 3431 hospital admission records |
Automated data linking produced accurate results efficiently, in comparison with manual data linking (even in the absence of a unique identifier) |
| Katzer et al.53 (2012) |
Small, privately owned emergency care provider USA |
Comparison of usage of paper clinical records and EHRs and documentation completion |
Retrospective review of records 77 handwritten records and 77 EHRs |
Completeness of physical examination documentation significantly improved with the use of an EHR system |
| Killeen et al.58 (2006) |
Simulated mass casualty scenario involving multidisciplinary emergency responders USA |
Evaluation of physician- and EHR-determined patient acuity status | Two simulated mass casualty scenarios:
|
During both tests, participants were able to accurately enter most victims into the EHRs Patient triage acuity, which was calculated automatically, did not always correspond with simulated patients’ predetermined acuity |
| Kuisma et al.62 (2009) |
Large, urban dispatch centre Finland |
Impact of EHRs on duration of ambulance calls |
Retrospective cohort study 37,599 ambulance calls (17,950 paper clinical records prior to implementation, 19,649 EHRs 6 months post implementation) |
Documentation method had no significant influence on duration of calls Urgency category and transportation decisions influenced call duration |
| Landman et al.49 (2012) |
EMS providers USA and Canada |
Directors, administrators and paramedics Implementation and adoption of EHRs |
Qualitative study 23 semistructured interviews from 14 provider organisations |
Quality assurance was a main reason for adoption Adoption and implementation of EHRs was found to be challenging Emerging strategies for successful implementation recommended |
| Lenert et al.56 (2011) |
Simulated mass casualty scenario USA |
Multidisciplinary emergency responders |
Randomised trial comparing paper clinical records and EHRs for simulated patients 50 paper clinical records and 50 EHRs |
No significant difference in time requirement of EHRs and handwritten paper clinical records The EHRs reduced the rate of missing and/or duplicated patient identifiers |
| Nakada et al.60 (2016) |
Urban trauma centre Japan |
Evaluation of a pre-hospital vital signs chart sharing system |
Comparison of availability of patient data communicated verbally by telephone (before implementation) or by EHRs (post implementation) 25 pre-system (telephone) records and 25 EHRs |
The number of vital signs shared with the trauma centre increased significantly There was no reduction in the number and duration of telephone calls from the ambulance to the trauma centre |
| Nakae et al.61 (2014) |
Ambulance services Japan |
Comparison of usage of paper records and EHRs on documentation and delivery of care to stroke patients |
Pilot study of smartphone-based EHRs n = 914 |
The EHRs allowed analysis of pre-hospital information of stroke patients to be completed in a short time with little effort Data sent to the server could be used for real-time analysis |
| Newgard et al.54 (2012) |
EMS providers USA |
Comparison of electronic data processing and manual data processing | Retrospective review of patient record data |
n = 418 An electronic data processing strategy led to gains in patient ascertainment, data quality and time efficiency of data processing in comparison with manual data processing |
| Scott et al.51 (2016) |
Two urban EMS providers USA |
Use of EHRs to characterise a patient subpopulation | Retrospective 12-month study of EHRs from a medical priority dispatch system |
n = 19,300 cases (16,736 used in analysis) System codes were found to be feasible for use as criteria to determine patient clinical status Codes were found to be suitable in identifying suitable candidates for secondary nurse triage |
| Tollefsen et al.59 (2004) |
Ambulance service USA |
Ambulance crews Evaluation of an EHR system |
Field trial (semistructured interview and retrospective audit) to evaluate EHR usage compared in parallel with handwritten paper clinical records |
n = 16 medical responses Issues identified with the EHRs included software problems that hindered the flow of data capture (e.g. inability to save, view or edit a record) |
Theme 1: implementation and adoption of electronic health records
Objectives of system implementation
Three studies detailed the objectives of EHR system implementation; all of them were conducted in North America. Baird and Boak50 carried out a case study of one small EMS in the USA 20 months post implementation of an EHR system. They gathered both quantitative and qualitative data from users of the system through interviews with representatives of leadership, mid-management, trainers and junior paramedics, and 29 follow-up surveys completed by paramedics. They found improved billing and quality assurance to be primary motivating factors behind the implementation of an EHR system. Similarly, Landman et al. ,49 through interviews with 23 representatives of 20 EMS agencies in the USA and Canada (medical directors, emergency physicians and EMS agency administrative staff), found improved quality assurance to be a primary objective of the implementation of an EHR system through the increased availability of patient records and improved reporting functionality. Other motivating factors were improved billing, improved legibility of patient records, reduced data loss and state mandates requiring services to adopt EHRs. Similarly, Broussard57 identified quality improvement to be a motivating factor in the development and implementation of an in-house EHR system by a large private ambulance service in the USA. The service was using EHRs for billing purposes, such as generating invoices and for reimbursements, clinical audits, workforce training needs analysis and education.
Barriers to implementation
Three studies identified barriers to the implementation of EHR systems. Landman et al. 49 discussed the challenges posed by high start-up costs, lack of financial resources, lack of leadership, complex organisational structures, poor usability of software, unreliable vendors, concerns about privacy and security, concerns about increased run times and other service disruption, and concerns about difficulty integrating systems within existing ED or hospital systems. In Baird and Boak’s50 study, integration with ED systems was found to be challenging, as 67% of participants reported frustration with a tablet stylus interface. Similarly, Broussard57 found that paramedics faced initial difficulty with the interface for reporting, as long hold times of 15–20 minutes were problematic when EMTs were calling in their reports to live operators who would follow the EHR software template.
Strategies to support implementation
Having identified challenges to implementation, Broussard57 reported on the introduction of two options for alternative interfaces through which information could be recorded onto EHRs: (1) leaving a voicemail that was then transcribed, or (2) entering reports on a laptop or computer during downtime or after shifts and e-mailing them to dispatch centres. The latter was the preferred method, used by 70% of staff; 20% used dictation and 10% called live operators. Baird and Boak50 found that the introduction of optional additional hardware and software tools (e.g. keyboard and private laptop) aided adoption, with the majority of users (86%) finding the system easier to use with the addition of extra hardware tools. All participants in Baird and Boak’s50 research suggested that additional formal training may have aided earlier adoption, and the majority (79%) found informal learning from peers to be very helpful or somewhat helpful. Both Landman et al. ’s49 and Baird and Boak’s50 findings highlight the importance of support and training in aiding adoption.
In Landman et al. ’s49 study, those EMSs that had already adopted EHR systems (14/20) were using strategies to overcome challenges, such as identifying alternative sources of funding (e.g. state road safety officials, billing companies or EHR system vendors) working with regional information organisations to exchange EHR systems data and funding dedicated IT personnel to support the process of implementation and adoption.
Theme 2: electronic health records in use
How electronic health records were used
In Baird and Boak’s50 study, participants were found to have various ways in which they used EHRs: filling in EHRs before arriving at the scene of a call, on the way back to the station, on returning or at the end of their shift after several calls. Buswell et al. 64 found varying preferences of ambulance personnel between the use of paper records and EHRs when attending to older patients. They conducted a retrospective chart review of 373 patients aged > 65 years who were attended by paramedics over a 1-month period. They found that ambulance clinicians were more likely to create a paper record than to use EHRs if discharging patients at their homes, leaving patients and their carers with a copy of the record; only 9 out of 187 (4.85%) patients for whom an EHR was created were left at the scene, whereas 67 out of 186 (36.0%) patients with paper clinical records were left at the scene. Bledsoe et al. 52 surveyed 228 emergency physicians to find out how they used EHRs generated by ambulance clinicians. Handwritten records were found to be more readily available at the time of physician decision-making than EHRs (22.4% vs. 20.4%), and EHRs were not used to support medical decision-making during the provision of care.
Perceived benefits of electronic health records
Five studies examined the perceived benefits of using EHRs, mainly through the comparison of EHRs with paper clinical records. Burley et al. 65 conducted 45 interviews with various stakeholders of an EMS organisation in Australia, including 38 paramedics and seven administrative, IT and management staff, before and after the implementation of an in-house EHR system, which replaced a paper-based system. They found perceived advantages to the new system to include improved legibility, standardisation of reports, reduced documentation, fast data acquisition, speedier record retrieval and scope for easier statistical analysis of patient data. Bledsoe et al. 52 found that the majority (81.6%) of emergency physicians in their survey had encountered EHRs in their practice at least once, and over half (52.2%) preferred EHRs to handwritten records (17.1%); 75% of respondents cited legibility as a benefit of EHRs, whereas only 1% reported legibility as a beneficial aspect of paper reports. Chittaro et al. 63 evaluated the usability of a personal digital assistant (PDA)-based EHR system. Following a short informal training session, six emergency responders in Italy filled in an EHR based on a described scenario of a rescue operation written by an emergency physician. Agreement was registered to a total of 21 statements describing the system using a Likert scale. The highest favourable scores were reported for screen legibility, ease of use, system information, system capabilities and overall reaction. In Baird and Boak’s50 study, the improved quality of charts was mentioned by all interviewees as a benefit to adopting an EHR system. Chittaro et al. 63 found that all six respondents were able to quickly learn how to use a PDA-based system without the need for specific training. Killeen et al. 58 also found this to be the case, with participants of a full-scale disaster drill being able to readily adapt to and use EHR devices (PDAs/tablet computers) with little or no training on the device beforehand. However, Baird and Boak50 found that more training could have aided adoption.
Perceived disbenefits of electronic health records
Four studies identified disbenefits of EHRs. The only disbenefit identified in Chittaro et al. ’s63 study of the PDA-based EHRs was the system’s handwriting recognition aspect, which was perceived as difficult to use, particularly on a moving ambulance and because screen space was insufficient, although two users suggested that this method of input could perform better with practice. Baird and Boak50 also noted the challenges of completing an EHR on a moving ambulance, with interviewees stating that many paramedics felt sick when trying to do so. Burley et al. 65 noted a loss of ‘narrative’ in records, suggesting that EHR systems did not facilitate the recording of qualitative data. Paramedics in Burley et al. ’s65 study also reported that during handover ED staff paid little attention to printed reports from EHRs, speculating that ED staff found it difficult to find what they were looking for. In Bledsoe et al. ’s52 study, 7.5% of respondents stated that there was no advantage to EHRs; however, a greater number (18.9%) believed that there was no advantage of paper records.
Theme 3: determining clinical status using electronic health records
Two studies examined the capability of EHR data in helping to determine clinical status. 51,58 Scott et al. 51 retrospectively used EHR data from a 1-year period from two EMSs in the USA that were using the Medical Priority Dispatch System (MPDS) software package (Priority Dispatch Corp, Salt Lake City, UT, USA), to determine the clinical status of low-acuity patients and to determine the suitability of using EHR data to identify low-acuity patients for emergency nurse triage. EHRs for calls coded as low acuity were extracted from the dispatch database and vital signs for those records were retrieved; 16,736 out of 19,300 records were included in analysis. The researchers were able to retrieve all vital signs from the included records and found that 97.8% of patients had stable vital signs, or low to moderate values, and that only 0.5% of all cases had critical vital signs. They were able to capture data regarding the top 10 ‘chief complaint’ protocols, including the proportion of patients who had at least one high vital sign and/or at least one critical value. Findings showed that system codes were feasible for use as criteria to determine patients’ clinical status and that codes were appropriate for identifying suitable candidates for secondary nurse triage. However, the demographic variable (age) was missing in one of the two systems, leading to an inability to link certain items of the EHRs to dispatch case record; age data had to be aggregately used for the majority of records, suggesting that completeness of record-keeping was an issue.
Killeen et al. 58 used a simulated cohort to evaluate a Wireless Internet Information System for MedicAl Response in Disasters (WIISARD). This was a wireless network made up of several routers at the incident site; sensors to track patient status; PDAs and tablet computers with EHR software; and a command and medical communication system. The system was used to determine acuity of patients in the USA during two simulated terrorist attacks, with 32 patients in the first and 100 patients in the second. The accuracy of acuity level was used as the primary outcome measure (as determined by the level of agreement between acuity that was automatically determined through the EHRs and acuity that was predetermined for the simulated victims by the physicians, based on their own assessment of the scenario). In the first scenario, 25 out of 32 cases were in agreement; for seven cases, WIISARD-recorded acuity was one step higher than the physician estimates for each scenario. In the second scenario, responders triaged and logged 97 out of 100 patients using WIISARD; predesigned scenario estimates stated that 37 out of 100 would be immediate, 39 would be delayed and 25 would be minors. Using WIISARD, responders determined 42 as immediate, 29 delayed and 7 minor, representing differences of 13.5%, –25.6% and –72%, respectively. Findings show that during both tests, participants were able to accurately enter most victims into the EHRs; however, patient triage calculated automatically did not always correspond with simulated patients’ predetermined acuity. Nonetheless, both Scott et al. ’s51 and Killeen et al. ’s58 studies suggest the potential utility of EHRs in determining clinical status and for EHRs to support clinical decision-making.
Theme 4: quality of electronic health record documentation
Improvements in documentation
The WIISARD EHR system was used by Chan et al. 55 and Lenert et al. 56 for evaluating EHR documentation during mass-casualty scenarios. Both studies compared the quality of documentation using EHRs with the quality of documentation using a paper documentation method. Chan et al. 55 compared 50 EHRs with 50 paper records during a simulated mass disaster. Lenert et al. ’s56 study similarly involved a simulated terrorist attack with 100 victims; 50 went through the WIISARD system and 50 through a paper-based system, and 39 EHRs and 32 paper records were included in analysis. Chan et al. 55 found that the greatest improvement in EHR quality of documentation was for perfusion rate (89.7%) and decontamination status (59%), which were not recorded at all in paper records. Lenert et al. 56 found that there were no data integrity problems in EHRs, whereas 47% of patients in the paper records group had some data integrity problems, including lost tags and duplicate identifiers. Field treatments received were recorded in the EHRs in 59% of cases, but not recorded at all in the paper records groups. Improvement of documentation of respiration rate was seen in Chan et al. ’s55 study: 92.3% of EHRs compared with 5.3% of paper records. Lenert et al. 56 found that age was recorded in 95% of cases and gender was recorded in 92% of cases in the EHRs, compared with 26% and 24% on paper, respectively. Chan et al. 55 similarly found that patient age was documented 94.9% of the time in the EHRs, compared with 26.3% in the paper group; gender was documented in 92.3% of cases in EHRs versus 23.7% in paper records, and mental status was documented in 64.1% of EHRs versus 2.6% in paper records. In Lenert et al. ’s56 EHRs, 73% of clinical information fields were completed, compared with 30% using a paper system.
Katzer et al. 53 carried out a retrospective chart review of a larger sample on the quality of documentation, at a small student-run EMS in the USA, comparing quality of physical examination documentation between paper records and EHRs. A total of 154 patient records were analysed (77 paper and 77 electronic). Records were grouped into three complaint categories (respiratory dysfunction, neurological dysfunction and those presenting problems from both). Each record was assessed for documentation completion of vital information depending on the category of complaint. For example, for the respiratory dysfunction category, completion rates for respiratory rate, visual appearance, quality of speech and auscultation were compared. Findings showed a mean increase of 36% in the completion of documentation of physical examination EHRs.
Loss of quality in documentation
Only one study, by Tollefsen et al. ,59 found a loss of quality in documentation using EHRs through the evaluation of an iRevive system, which comprised a PDA running EHR software, with decision-support functionality and wireless sensors that could monitor patients’ vital signs, with data relayed via a central server to receiving EDs. A simulated field trail was carried out alongside existing manual methods over 16 patient transports, involving 12 ambulance clinicians in the USA. The EHRs recorded and documented the same data as the existing manual approach. Problems were experienced by clinicians using the EHRs, including data fields in the ‘wrong’ order for system users (e.g. times and mileage pages placed too early in the process – requiring going back and forth); requirements to record data already recorded by dispatch centre such that EHRs could not be saved unless certain fields were completed; inability to return to previously saved EHRs until synched with the server; lack of appropriate values in some pull-down menus; and insufficient space to record certain clinical data, such as multiple allergies. Although the EHR system complied with local data set requirements, the need for more data-recording capabilities was identified along several different domains. The study did not find the EHRs superior to manual paper-based recording in terms of ease of use, data completion or data content. This may have been due to the technical capabilities of the EHRs given the age of the study, and such functional limitations may be less significant today.
Theme 5: electronic health records’ impact on call duration
Only one study looked at the impact of using EHRs on call duration, defined as the total time from ambulance unit dispatch to when the ambulance was back in service. Kuisma et al. 62 conducted a retrospective observational study examining the impact of a change from paper-based reporting to EHRs on the duration of ambulance calls at a large EMS in Finland. A total of 37,599 calls were analysed, of which 17,950 took place when paper records were in use and 19,649 took place once EHRs had been introduced; 7% of calls were excluded from analysis. The documentation method was not found to be a significant factor determining call duration; however, urgency category, unit level and transportation decision were found to have influenced the call duration. Median call duration was 48 minutes using paper records and 49 minutes using EHRs. Call duration when using EHRs increased from that when using paper records by 2 minutes in urgent calls and by 1 minute in less urgent calls but decreased by 4 minutes for the most urgent category of calls. The call duration was longer during the first 3 months post system implementation for most calls, before returning to baseline. It was concluded by the authors that the temporary increase in call duration reflected adaptation to a new way of working rather than being dependent on transition to EHRs specifically, and that minimal disruption to call duration was attributed to good planning, training and reorganisation of work processes.
Theme 6: electronic health records and real-time data-sharing
Two studies described the use of EHRs for real-time data-sharing. Both were based in Japan and discussed a system that shared vital signs charts through a cloud server. In a study by Nakae et al. ,61 emergency medical staff inputted vital signs data onto a smartphone, along with information related specifically to stroke patients, filled in with the help of the system’s decision-support feature. Once submitted, the data were sent to a cloud server, which sent the data to the receiving hospital. The smartphone-assisted pre-hospital medical information system allowed analysis of pre-hospital information of stroke patients to be completed in a short time with little effort. The data were found to be useable for real-time analysis. Of 914 patients, 874 were analysed; of those analysed, 867 (94.9%) received a pre-hospital diagnosis, 417 of which were for stroke. Of those, 199 (47.7%) were confirmed at radiology (126 infarction and 73 haemorrhagic). For the pre-hospital diagnosis of stroke and transient ischaemic attack, the smartphone-assisted pre-hospital medical information system exhibited a positive predictive value (PPV) of 0.51, with 213 correct positive diagnoses and 214 incorrect positive diagnoses. The system exhibited a negative predictive value (NPV) of 0.95, with 427 correct negative diagnoses and 23 incorrect negative diagnoses. Sensitivity was 0.9 and specificity was 0.68. For subarachnoid haemorrhage, PPV and NPV were similar (0.50 and 0.97, respectively), with a sensitivity of 0.33 and a specificity of 0.99.
A study by Nakada et al. 60 included additional stages: vital signs were collected continuously, directly via patient monitors that were connected to a tablet computer. Vital signs data were stored in the software on the tablet computer as numerical data, then transferred to the cloud server via a cellular telephone communication technology and then to the receiving hospital. Nakada et al. ’s60 study found evidence that significantly more vital signs data could be shared using EHRs than could be shared with the method previously used (EMTs verbally communicating vital signs via telephone). The efficacy of the system in sharing real-time vital signs data for patients with and without severe bleeding was compared; there was no difference in initial blood pressure readings, but a decrease in blood pressure was observable in charts during transfer for those with severe bleeding. In addition, the system recorded and shared significantly increased heart rates for severe bleeding versus non-severe bleeding. Notably, there was no reduction in the number or duration of telephone calls from the ambulance to the trauma centre associated with the introduction of the EHRs.
Theme 7: electronic health records and retrospective data linkage
Two studies looked at the use of EHRs for retrospective data linking. Crilly et al. 66 looked at data linkage and Newgard et al. 54 looked at data processing. Crilly et al. 66 assessed the accuracy of data linkage in emergency care to examine service delivery outcomes in the ED with linked data. A manual approach and an electronic approach to linking data were compared; 3469 EHRs, 10,835 ED records and 3431 hospital admission records from a 2-month period from a teaching hospital in Australia were used. Each data set was cleaned and 423 erroneous records were manually removed prior to linking. Manual data linking was carried out by one of the researchers with previous experience in the process, and electronic data linking utilised health data integration software. Records were linked by age, sex, name, dates/times of arrival at the ED and dates/times of ED discharge and of hospital admission. Automated data linking was found to produce accurate results efficiently in comparison with manual data linking, even in the absence of a unique identifier. Although health data integration linking required 80 hours of initial set-up time, after which data could be quickly linked on an ongoing basis, it took only 5 minutes to link data sets using this method, whereas manual linking took 200 hours. Through a deterministic method, ED records linked with 87.9% of EHRs, compared with 92% using a manual approach. The comparison of electronic linkage of EHRs with ED records with a manual approach demonstrated sensitivity of 95.5%, specificity of 99.6% and a PPV of 87.9%.
Newgard et al. 54 retrospectively looked at data processing and also compared an electronic approach with a manual one. They compared case ascertainment, agreement, validity and missing values for EHR data obtained, processed and linked electronically (using a probabilistic approach) compared with a manual approach, over 21 months, with data from 10 EMS agencies and 16 hospitals in the USA. Their findings showed that an electronic data processing strategy identified gains in patient ascertainment, data quality and time efficiency of data processing in comparison with manual data processing. A total of 629 patients were identified to have met the inclusion criterion of ‘physiological compromise’ from manually processed records, and 3008 were identified through electronic matching. There were 2625 unmatched patients using the electronic approach and 211 unmatched patients using the manual approach. In relation to the 418 patients matched between the two groups, inter-rater agreement was good to excellent (κ = 0.76–0.97). The intraclass correlation coefficient was 0.49–0.97, with exact agreement in 67–99% of cases, and the median difference for all continuous and ordinal variables was 0. Across vital signs, time intervals and field procedures, data loss was broadly similar using both methods. However, electronic matching resulted in a greater loss of hospital outcomes (21%) than manual matching did (3%). The authors highlighted the significance of functional and data format compatibilities to electronic linkage of EHR data for research purposes. Both Crilly et al. ’s66 and Newgard et al. ’s54 findings show that using EHRs can allow data to be linked electronically with time efficiency and accuracy.
Discussion
We were able to identify only a limited literature on EHRs in emergency ambulance services. Studies used a variety of methods, including qualitative, mixed methods, case studies, descriptive case studies, simulated scenarios and observational studies. A significant number of studies were case studies, and findings may not be generalisable. Some studies were conducted retrospectively and many of them used small sample sizes. The majority (10 out of 18) of studies were from the USA, and only one reported on a UK system. The pace of technological development has led to significant differences in systems’ forms and functionalities over the publication period covered by this review, highlighting the relevance of publication date. Findings may also have been skewed by the presence of three studies looking specifically at mass-casualty scenarios and the use of one particular electronic system (i.e. WIISARD).
Studies examining implementation and adoption suggested that EMS agencies are adopting EHRs primarily for quality purposes, including quality assurance and quality improvement, as well as for billing purposes. 49,50,57 Other themes mentioned by one study each were workforce training needs analysis and education,57 and reduced data loss and state mandates requiring services to adopt EHRs. 49
Barriers to EHR adoption included financial, organisational, technical and privacy/security reasons, fears of increasing run times, difficulty integrating EHRs with existing systems and difficultly in complying with legal mandates. Suggested solutions to these challenges included identifying alternative sources of funding, working with regional information organisations to exchange EHR systems data and by funding dedicated IT personnel to support the process. 49 Integrating with ED systems was found to be challenging, but the introduction of flexibility in the choice of interface was found to be helpful in overcoming this challenge. 49,50,57
Perceived benefits of EHRs identified in the literature included better legibility, improved quality of charts, standardisation of reports, and fast data acquisition and speedier record retrieval. The only study to show a loss in quality of documentation was the earliest study identified. 59
Six studies looked at how EHRs were used by clinicians,50,52,58,63–65 finding that clinicians appeared to use discretion in how, and if, they completed an EHR.
We found limited evidence of the use of EHR systems during clinical decision-making, although two studies that looked at the use of EHRs for determining clinical status suggested potential for EHRs to be able to do so. 51,58
Only one study looked at the operational impact of EHRs, and found that they did not have a significant impact on run times of ambulances. 62 Two studies found benefits of EHRs in terms of real-time data-sharing. 60,61 Two studies examined how EHRs could allow for data to be electronically linked accurately, as well as time efficiently. 54,66
Chapter 4 Results: national survey
Participants
We conducted 22 interviews with representatives from all 13 free-standing UK ambulance services that provide emergency responses, giving us almost complete coverage of the UK. The only exception was the Isle of Wight, where a small-scale emergency ambulance service is delivered by the local integrated health-care trust. The services included in our survey varied widely in terms of levels of activity (the largest responding to 1.9 million 999 calls per year, and the smallest responding to 220,000 calls) and in terms of geographical area covered (ranging from 620 to > 30,000 square miles).
We asked to interview people with knowledge of the service’s EHR system or, where EHRs were not in use, people with an understanding of plans for the future. Information on participants is given in Table 6. Interviews were conducted during the period February to August 2017 so responses relate to the situation at that time.
| Ambulance service | Participants | ||||
|---|---|---|---|---|---|
| Information management and technology project manager | Director of operations | Clinical records manager | Clinical effectiveness manager (post held alongside clinical duties) | Medical director/deputy director patient care | |
| AS1 | ✓ | ✓ | |||
| AS2 | ✓ | ✓ | |||
| AS3 | ✓ | ✓ | |||
| AS4 | ✓ | ✓ | |||
| AS5 | ✓ | ||||
| AS6 | ✓ | ✓ | |||
| AS7 | ✓ | ✓ | |||
| AS8 | ✓ | ✓ | |||
| AS9 | ✓ | ✓ | |||
| AS10 | ✓ | ✓ | |||
| AS11 | ✓ | ||||
| AS12 | ✓ | ||||
| AS13 | ✓ | ||||
State of implementation
Systems in use
Use of EHR systems at the time of the interviews (February to August 2017) is summarised in Table 7. Seven services had EHR systems in place. At the time of the interviews (February to August 2017), seven services had EHR systems in place. The length of time that systems had been in place ranged from over a decade to still being in the final stages of roll-out, with most services having had their systems in place for 2–3 years. Three of the services using EHRs were in the process of changing their systems completely, ceasing to use one provider and recommissioning from another. Others had opted for continuous changes and updates to both software and hardware in response to local need.
| Ambulance service | EHR system in place | |
|---|---|---|
| Hardware | Software | |
| AS1 | Panasonic TOUGHBOOK (Panasonic UK Ltd, Bracknell, UK) | Ortivus (Ortivus UK Ltd, Totton, UK) |
| AS2 | Previously used EHRs but reverted to paper records temporarily | |
| AS3 | Terrafix (Terrafix Ltd, Stoke-on-Trent, UK) | Bespoke |
| AS4 | Anoto Digipen (Anoto Group AB, Stockholm, Sweden) | Anoto (Anoto Group AB, Stockholm, Sweden) |
| AS5 | iPad (Apple Inc., Cupertino, CA, USA) | Kainos Evolve (Kainos, Belfast, UK) |
| AS6 | Previously used EHRs but reverted to paper records temporarily | |
| AS7 | Panasonic TOUGHBOOK | Ortivus |
| AS8 | Previously used EHRs but reverted to paper records temporarily | |
| AS9 | Previously used EHRs but reverted to paper records temporarily | |
| AS10 | Panasonic TOUGHBOOK | Bespoke |
| AS11 | Never had an EHR system to date | |
| AS12 | Never had an EHR system to date | |
| AS13 | Getac (Getac Technology Corp., Telford, UK) | Safe Triage Pro (Inmarsat UK, London, UK) |
Six services did not use EHRs, of which two [ambulance service (AS) 11 and AS12] had never had an EHR system in place, although both were planning to introduce one. The other four (AS2, AS6, AS8 and AS9) had temporarily reverted to paper records while they were at various stages of designing, procuring and implementing new systems. These services reported having previously introduced EHRs under the Connecting for Health contract, and using the end of the contract as an opportunity to look for a new system better suited to their needs. Two services (AS4 and AS10) had not fully rolled out the old system to the whole service, largely due to the associated costs. Respondents from two services (AS8 and AS10) commented that they had received negative feedback from staff regarding the old system so were happy to have the opportunity to develop a new system.
AS4 took a different approach from all the other services, choosing, instead of a tablet, a digipen, a device used to write on a paper form that stored information through recording pen strokes.
AS1 and AS7 had installed printers on board ambulances, but most had chosen not to, citing them as unnecessary and a potential source of technical problems.
Time scale of implementation
Respondents described phased roll-out of new systems, generally area by area across a site. For most, this was a process that took around 6 months. As a representative of AS7 reported, this staged approach allowed attention to be given to the support the workforce needed to embed the new system into day-to-day practice:
Individual support through their clinical mentors . . . they’ve had presentations as a group and then we’ve also from the beginning run an [EHR] help desk which is a telephone support line, which we stopped running January of this year but we had the ability 24/7 . . . on the phone to take queries . . . That, I think, was one of the biggest drivers for getting people to use it.
AS7
An exception to this pace was AS13, which transitioned from one EHR system to another, and was keen to limit the return to paper in the interim. A respondent described their approach as:
We went big bang . . . it took about 2 months but we managed to move our full ambulance service across a 2-month period.
AS13
By contrast, AS1 had a much longer roll-out time, of around 19 months. This was determined by the fact that installing the new hardware (and removing the previous generation of EHR software) entailed taking vehicles off the road, so had to be done one at a time to minimise disruption to the service.
Support for the implementation process
Training was regarded as an important part of encouraging adoption. Although respondents did not think that EHR technology was particularly complicated (it was often likened to using a smartphone), they did acknowledge that ambulance clinicians were required to input information in a different way from how they would input information in paper forms, and that it took some time to learn their way around the system. Examples of training and support that were perceived as effective were a package of 1 day of training followed by support provided at each receiving hospital for the first few weeks after the system went live (AS1), and a telephone support line for front-line staff combined with the use of local clinical mentors to encourage a culture change (AS7).
Having a reliable system (devices and the EHR system) was also seen as an important part of staff adoption of EHRs. Battery failures, poor connectivity and an overcomplicated form that led to increased time on the scene all caused front-line staff to lose faith in the EHRs.
Completion rates
We asked respondents to estimate the proportion of patient calls attended that resulted in the creation of an EHR. Most of those currently using EHRs reported that rates of generation of EHRs were ≥ 90%. Services in the process of transition between systems reported that rates were much lower than this when their first generation of EHRs was taken offline, with use ranging from 34% down to 3%, these figures representing a decline in use over time. Some of the reasons presented for non-completion of EHRs are discussed in Problems and challenges associated with electronic health records.
Transferring patient information
Accessing existing patient records
Only a minority of respondents described ambulance clinicians being able to access previous medical records for patients they were attending. AS1, AS3 and AS7 appeared to be at the forefront of enabling this to happen. Although the EHR software did not link directly to previous patient records, ambulance clinicians were able to use the tablet to access the PDS and NHS Spine to look up information about their patients:
They can access the PDS from the tablet and they can do that at any point really. So they can put in a few details about the patient and then they can click the PDS lookup and it actually then connects to the Spine to look up that patient so that they can check things like GP surgery and all that sort of information.
AS7
If ambulance clinicians in AS7 wanted more detailed information, they could insert their NHS smartcard into the hardware to allow them to access the full SCR via NHS Spine. This would allow them to see information such as the reason for the patient’s last contact with their GP, what medication they are currently on and any existing or long-term conditions. For about 85% of patients, the PDS was looked up, either by the ambulance clinician or in the control room. Rates of access for the SCR were slightly lower, but it appeared to be highly valued as a source of information that could potentially support non-conveyance decisions:
The crews absolutely love it because it can give them an indication of, you know, some sort of preterm conditions, long-term conditions, that might be exacerbated in that particular incident and therefore they can look at what the management for that is and then make a decision as to whether they’re going to convey or not convey.
AS7
In AS7, information on previous ambulance service call-outs was available via the PDS. In AS1, as well as having access to information on NHS Spine, ambulance clinicians could use their EHR devices to search for information on previous call-outs if they had the patient’s NHS number. Clinicians in other services were not yet able to access this information.
Transferring patient information to other providers
Of the ambulance services with an EHR system currently in place, only one (AS4) did not support electronic transfer of patient information directly to other health service providers. Five ambulance services (AS1, AS3, AS7, AS10 and AS13) reported that they were able to transfer patient records to both the acute services receiving patients and the patient’s GP. AS9 (in the process of roll-out) and AS5 both supported the transfer of information to acute services but not primary care, whereas AS1, AS3, AS7 and AS13, along with AS2 (in the process of roll-out), supported the transfer of information to primary care, although not to acute services. Table 8 summarises services’ ability to transfer patient records.
| Ambulance service | Not transferred | Health service provider that records can be transferred to | ||
|---|---|---|---|---|
| GP | Hospital | Other | ||
| Ambulance services with EHRs currently in use | ||||
| AS1 | ✓ | ✓ | Yes (e.g. falls service, safeguarding) | |
| AS3 | ✓ | ✓ | ||
| AS4 | ✓ | |||
| AS5 | ✓ | |||
| AS7 | ✓ | ✓ | ||
| AS10 | ✓ | ✓ | ||
| AS13 | ✓ | ✓ (hospital can access record) | ||
| Ambulance services in the process of rolling out a new system | ||||
| AS2 | ✓ | |||
| AS9 | ✓ | |||
Respondents described a range of approaches to facilitating this transfer of information. AS1 and AS10 reported that the record was uploaded to their central database in real time, and could then be accessed by hospital staff via a live portal. In addition, AS1 would, where appropriate, forward the patient’s National Early Warning Score (NEWS) to the receiving hospital so that staff could prepare for the arrival of the patient.
Other services (AS5 and AS3) took the approach of generating a Portable Document Format (PDF) of the patient record, which could then be e-mailed to another health-care provider:
It gets transmitted from the iPads up to a database where the sort of conversion process to generate the PDF happens. It gets saved into the database and the e-mail is generated if that’s what’s requested during the record. So we would request – we would select the hospital we’re going to and that would produce the e-mail and if we don’t select a hospital, i.e. it’s a discharge, then no e-mail is generated.
AS5
AS3 reported sending bulk e-mails overnight of patient record PDFs to patients’ GPs. AS9 had a function on their first-generation system that allowed records to be e-mailed to GPs at the choice of the ambulance clinician, but found that this was not used and this function was not included in the new system.
One service reported encountering challenges with arranging for transfer of patient information to GPs:
Getting GPs across 260 surgeries in [AS1] area to agree on a template on how they should receive information, it is challenging. I think sometimes we need to just, sort of, make decisions nationally and say, ’look, this is the way it should be’.
AS1
Transferring information to patients
Ambulance services’ traditional model of paper patient report forms (PRFs) generally allowed for a paper duplicate that could be left with the patient, particularly if they were not conveyed to hospital. EHR systems did not readily allow for information from the contact with the ambulance service to be transferred to patients. The two ambulance services that had fitted printers to ambulances did not routinely use them to print records for non-conveyed patients. Six ambulance services that either currently had EHRs or had previously used EHRs left leaflets with patients, on which paramedics might write some information about their care if they requested it.
Accessing diagnostic tools and other resources
We asked respondents to describe how EHRs were used to support the use of diagnostic tools or other electronic resources.
Integration of assessment tools and prompts into the electronic health records
The AS7 system had prompts to carry out tests if the paramedic reached the end of the patient record without inputting certain data.
A respondent from AS1 suggested that the level of integration of the EHR system with other data sources meant that it functioned as ‘a clinical decision-support system’, with additional benefits in terms of supporting the ambulance clinician in carrying out their job:
We do an assessment of the patient, we capture other information in terms of social and medical detail, we will perform a series of diagnostics and those diagnostics have been built into the system so there’s not just an electronic patient record system, it’s actually a clinical decision-support system . . . So we have got a whole set of algorithms, things like NEWS score built in, we’ve got pain assessments and other assessments which . . . we find very useful and let’s say a typical paramedic should be performing as a matter of course on all patients but basically we’re guiding them through those things based on the presenting conditions. So fairly intelligent in that respect and . . . it is taking pressure off the paramedic in terms of them needing to remember all of the things that they need to remember when they go down a certain pathway.
AS1
Telemedicine and linking with other apps and devices
AS10 used the hardware to enable telemedicine, which then informed decisions of whether or not to convey the patient:
It then allows us to do a telemetry/telemedicine function live, whilst the crew are with the patient. So I’ll give you a really good example of that from a couple of days ago. I went to a patient that was burnt, took photos of the patient and was able to have a conversation with the burns consultant.
AS10
Respondents gave other examples of integration: AS1 ran its vital signs device through the hardware used for its EHRs and AS13 linked its defibrillator and monitor to the hardware used for the EHRs. AS2 planned to integrate Paramedic Pathfinder into its device.
Accessing information resources
Some devices could be used to access the internet, enabling paramedics to find information about other resources, such as the local directory of services, or drug information.
Others had access to national and local clinical guidelines, which could be used to aid decision-making but should not be considered decision-making tools.
Use of data recorded in electronic health records
Audit, research and analysis
Respondents from all ambulance services with EHRs described how data from the records were used to generate reports for audit, for both external reporting and internal use. Clinical audit teams generally had access to complete records, but, to protect patient confidentiality, other members of staff had only limited access, and queries could be run on specific fields and summaries produced.
The main external reporting function was in relation to the Ambulance Quality Indicators collected by NHS England and equivalent performance measures in the devolved nations. Services also generated audit reports for their own use; for example, AS10 reported running reports to see how many EHRs were being created and completed. There were also limited examples of audit reports triggering an investigation of specific issues: AS7 found that it was dealing with a spate of respiratory issues in one locality, looked at the records and found that they were clustered near a swimming pool where there had been a chlorine leak:
We just seemed to be doing a lot of respiratory jobs in one particular building and it was student accommodation for [name] University, yeah, and it was highlighted there was an issue, we reported it and public health looked into it and that’s what they found.
AS7
There was acknowledgement from most respondents that the scope for analysis and report making was not being fully realised because of capacity issues. Similarly, any engagement in research using the EHRs was inhibited by a lack of capacity within services, although several respondents hoped that this might change in the future:
No immediate plans at the moment – not from not wanting to do it, more from the point of view ‘cause we’re currently working through this process of getting the basic reports we need out we just haven’t really had the time to sort of sit down with anything on a research side.
AS5
Staff feedback and professional development
Three respondents described ways in which EHRs were used to provide feedback to staff and look at the quality of the records to monitor and improve paramedics’ record creation. In AS13, team managers were allowed access to records generated by their own teams, but not by others, to review activity and provide feedback. Ambulance clinicians in AS3 were able to access their own EHRs, giving them the potential to use the records for their own professional development.
Medicolegal uses
Respondents described the ways in which EHRs supported medicolegal requirements, particularly in providing information for the coroner after a patient death or responding to access requests, and were seen as having considerable advantages over paper records because of both the ease with which the record could be retrieved and the quality of information it contained. Respondents stated that there were far fewer missing or incomplete EHRs than missing or incomplete paper records, so providing reports when required was much more straightforward:
From a medicolegal and subject access requests, the problem with paper records historically is even with a really good system it can take up to, you know, it can take 2 weeks to get paper records in. We’ve got these records within minutes of them being completed.
AS13
An additional benefit was reported as the better quality of patient records, which had knock-on effects in terms of demands on clinicians’ time, with EHRs seen as providing:
More accurate and clear information about what’s happened to patients and [they] are calling less of the paramedics to give evidence in coroner’s courts. So it actually releases a significant amount of time back.
AS6
Management of frequent callers
Respondents from two services described ways in which EHRs, in addition to the more generally used CAD data, supported the management of people who make frequent calls to the emergency ambulance services. AS7 had dedicated call demand practitioners, who used records to build a picture of individual behaviour patterns and to see what the ambulance service has done for them:
What they basically do is work on a caseload of the top persistent callers in their area, so they get regular information about that. They can then review all the records that the crews are completing for that particular individual, and they tend to work across services, so they liaise with social services, police or whoever else has got interest in that particular individual. So they use the [EHRs] to really get a true picture of what’s actually been done for that patient when we’ve been there, so that’s quite a big use.
AS7
AS10 took a different approach, reporting that since it began sending EHRs to GPs it had seen a change in the way people were managed, as GPs were becoming aware of those patients who repeatedly called 999.
Perceived benefits of electronic health records
Data quality and completeness
Respondents identified the advantage of EHRs in producing data in a standard format, allowing records to be readily compared and for information transfer to other providers to be more effective. They also noted the value of records that were not handwritten:
It’s actually been very well received by the medical side at the hospitals as well. They love the clarity of the record compared to the carbon copies that ambulance services have always handed over in the past, we’re now handing over a very clear concise record laid out in the same order in every record basically.
AS5
Ease of handling the data
Respondents identified ways in which EHRs streamlined the handling and storing of data, because the data were automatically uploaded to a central hub. This contrasted with the labour involved in dealing with paper records, which had to be physically transported and then scanned. EHRs were seen both as easier to keep track of and as easier to search:
I’ve never ever been not able to find an electronic one, if there’s an electronic one it’s always been found, it’s been the paper ones that have not been there . . . easier to use the data, so what it’s telling you, it should be more easy to mine that data, to get better meaningful intelligence from it.
AS2
Data transfer and referrals
Respondents discussed the value of EHRs in allowing data to be shared with other health-care providers in real time, bringing benefits to patients and to other health-care providers:
And also I think that most of our benefits sit with the hospitals because if they use our system for pre-emptive care, they saw somebody coming in and they got a room ready or a surgeon ready for that patient, you know, they could assist a lot quicker in the pathway. They don’t have to wait for somebody really to make a phone call and turn up, they’ve got a lot more detail behind them.
AS1
Benefits were also identified for the ambulance service in terms of saving time for ambulance clinicians: the respondent from AS5 said that paramedics were able to do things on the road that they previously had to return to the station to do, such as send a report on a vulnerable adult.
Confidentiality and security
Respondents reported that EHRs offered greater security than paper records. As the respondent from AS7 pointed out, once the record was completed and signed off, it was closed and off the device, unlike paper records, which would still be in the ambulance. There was a higher level of confidentiality when records were being searched, as searches could be run without patient identifiers, and only the fields that needed to be accessed were included in the results:
It’s less risky if you’ve got it on a system than a piece of paper. You have the information governance risks, they’re not as high.
AS2
Costs
Respondents mentioned the cost savings associated with EHRs from not having to process, transport and store paper patient records. However, for both AS1 and AS7, EHRs were not primarily about saving money:
The thing about this system, it isn’t a cash-releasing benefit, it’s societal benefit and it’s quality benefit really.
AS1
I think it’s a very difficult one and the business case is based on something which – you know, there’s physical things like printing, running paper records around, scanning them in, you know, there’s all those sorts of cost savings, but how do you actually put a value on the fact that they can access a Summary Care Record for a patient whilst they’re in front of them? These sorts of things you can’t put financial money on, but what you can put is the value to the patient and the patient care.
AS7
Problems and challenges associated with electronic health records
Technical problems
Although EHRs seemed to be associated with fewer missing records than paper systems, some technical glitches were reported. AS3 had lost records from its first-generation devices, for example if the battery had run out before the device could be docked. Other services had taken proactive measures when designing their systems to protect against the loss of information. For example, AS10’s device continuously uploaded data to the server; it had a mobile signal so that even if the device lost power or was damaged, the record would still exist. There were some issues around ‘missing’ records due to lost server connections when making the record, but these had largely been resolved. AS1 had taken similar steps and although the clinician needed to log back in to access the record following a loss of connection, the record still existed on the server.
For some services, poor connectivity and the associated fears that records would be lost were reported as having a negative impact on adoption as crews lacked confidence in the system:
There’s been a big drive on the connectivity behind it, because historically in [county] we’ve got a really poor signal and the crews are finding it – that nothing is uploading, so that was one of the barriers for its use really.
AS2
We had issues with connectivity – serious issues with connectivity. Something to do with the [devices] themselves and the way they’d been installed which took us months and months and months to find out what the issue – and then something else was to do with [mobile network] and a switch that needed switching on and people didn’t recognise this. And it took a lot of fact finding and took a lot out on crews ‘cause they just . . . lost faith in the system so went back to paper very regularly.
AS6
AS4, which used the digipen system, reported that records were not always linked to CAD data as this had to be done manually. Although the EHR was not lost, it was separated from the corresponding dispatch record:
The staff themselves can write the incident number from the original call on the top of the form and then in their vehicles when they’ve finished the job they can put the clinical record number into the field in the job before they shut the job down. That’s how it should happen to make sure that there’s a link to every incident. But unfortunately again they’re forced to put eight characters in and some people don’t put the correct characters in, some of them by accident genuinely, but some it’s deliberate because you get eight zeros and that sort of thing.
AS4
Technical problems were cited by a minority of services as being one of the factors that kept completion rates below 100%. AS2’s first-generation system depended on mobile phone connectivity to work fully, so areas of poor coverage made it challenging. AS9 also reported problems with its first-generation system, which led to a decline in use:
A couple of significant IT, technical and then performance issues. We saw that drop from its high to probably a baseline I reckon of around . . . between probably 50 and 60 per cent for a fair period of time. And then we reached a period about just over a year ago where we had some significant technical issues with the old software it developed all sorts of issues with screens freezing, Wi-Fi links not working da de da de da. That all happened at the same time as the national programme sort of winding up.
AS9
For AS10, technical problems came in the following form:
Occasional failures of the tablet and the very, very occasional failures of our staff, like when they leave them on the roof of the car. So we’ve had a few tablets that have ended up on motorways or being driven over by the ambulance following the car out of the door. But we only see that on our RRVs, on our rapid-response vehicles.
AS10
In AS7, the respondent described difficulties associated with the design of the EHRs, with paramedics reluctant to use the drop-down menus and instead writing the bulk of information into free-text boxes, making it difficult to extract for audit. To try to correct the way clinicians used the records, AS7 had redesigned the EHRs, removing the bulk of the free-text boxes.
Interoperability with acute services
Four ambulance services (AS1, AS2, AS7 and AS10) identified problems with transfer of information to acute services, and suggested this as a reason for ambulance clinicians not completing EHRs. Each ambulance service was conveying patients to a number of different acute services, some of which were able to receive patient records electronically, but some of which were not able to, or perhaps were not willing to:
They like the paper ones at our acute, so the crews find that when they’re going in that the hospitals are saying, ‘oh we prefer the paper ones’ and they’re getting a bit of a hard time and then the administrators at the hospitals are saying, ‘we haven’t got smart cards’, they can’t access them. And then they were having to rewrite the patient information on paper so they just didn’t bother with the electronic one, they did it straight onto paper.
AS2
AS10 reported that there had been some regional variation due to one particular hospital not wanting to receive information on EHRs, so paramedics would use paper records; intervention from AS10’s medical director led to the hospital changing its system to accept EHRs.
Training and compliance issues
Three services (AS8, AS9 and AS2) described challenges with training staff to use the EHR system and then with maintaining compliance, sometimes in the face of technical challenges. AS8, where completion rates were around 3% immediately before it took its first-generation system offline, reported that this represented a substantial drop-off in use from an earlier peak:
In some areas it got to kind of 60–70 per cent but without sort of frequent – because there’s a lot of staff movement across the system, so you know, as soon as we scaled back on the support then it just fell away exponentially, in terms of its use because people were just not – they just weren’t using it. They just, you know, the people would move into an area where [EHRs] was enabled but they didn’t know how to use it. And equally, the people who did know how to use it, you know, would move on to another area . . . No, we never hit a critical mass.
AS8
Although AS8 did put some champions in place once it was clear that there were problems, the respondent felt that they were brought in too late:
They put some people down at ED so if crews would come in they would be there to just help them out and, you know, help them complete the record and things like that. But I think the horse had bolted by that stage and it was too late, there was the reluctance to even start using it . . . you’re in your ambulance for 12 hours with your crew mate and . . . you’ll just follow the path of least resistance and go back to pen and paper. So whilst they did put some champions in, there was nothing really for them to champion.
AS8
Learning from this, AS8 planned to make it compulsory to use the second-generation system once it was implemented:
Respondents from AS2 and AS9 reported problems with delivering training to staff. In AS9 they had found it difficult to find time to release staff for the EHR training. This impacted negatively on adoption as ‘Untrained staff means not using EHRs’.
AS9
Regional variations in completion rates, from 60% to 20%, were also reported by AS9, attributed by the respondent to local champions encouraging take-up in certain localities. They also reported resistance in certain areas, mostly in particularly busy areas where managers were reluctant to release staff for training, describing the reason as:
It’s a cultural thing, if I’m brutally honest. I think we just haven’t managed the usage very well in one area, whereas we will be moving forward. So I think we’ll see that change, so we’ll get all our divisions to a very similar level.
AS2
AS9 kept paper records on board ‘in case’ a backup was required for the EHR system; however, the respondent reported that ambulance clinicians found ‘inventive’ reasons for not using EHRs, so a more arduous system was being introduced to stop this from happening. Similarly, AS2 ascribed some of the challenges to uptake with their first-generation EHR system as being due to clinicians still being allowed the option to use paper – an option that would be removed with the transition to the second-generation system.
Future plans
Plans for introduction in the future
The four services that had previously used EHRs intended to reintroduce them and all except one had clear timelines for doing so. As one respondent remarked:
I think they are completely essential.
AS6
Following the failure to successfully implement EHRs previously, AS6 was working to ensure that its second-generation system was straightforward to use as it anticipated that clinicians’ concerns about time on scene could be a potential reason for non-compliance. AS6 was involving staff in the design and procurement of the new system to encourage better buy-in:
We’ve actually involved a lot more staff in the – in the design of how this would work, we’ve involved a lot more clinical staff in how it looked and how the buttons work and then we’re also involving clinical staff in the actual purchase of the equipment so that hopefully there’s a lot more buy-in from the beginning. And then the other side to this if we add things to it that enable them to have a better experience of say something that they need to get done, something that they need then that will enhance the system for us.
AS6
The two services that had never previously used EHRs were keen to introduce them in the near future. AS12 had recently had its business case approved and was about to go out of procurement. AS11 stated that the introduction of EHRs was a long-term aim, but they had no fixed timeline for doing so owing to the cost of implementation and the difficulties surrounding the logistics of installing devices and training staff.
AS4 planned to continue using its current system but thought that its next steps would be to move to tablet-based EHRs rather than a digipen.
Plans for developing existing electronic health record systems
Respondents discussed their services’ plans for developing the use and value of EHRs in the future, and using them to their full potential. These plans covered a range of themes:
-
improved transfer of patient information to primary care (AS1, AS3, AS5 and AS7) and to secondary providers (AS7)
-
more analysis of patient data to improve service delivery (AS2 and AS5)
-
using NHS numbers to link ambulance service records with other patient information, such as secondary care data, in order to track patient outcomes, described by one respondent as the ‘missing link in the patient care journey – you know, the hospital information’ (AS13)
-
use feedback from patient records to support paramedics’ professional development (AS13).
Summary
Only half of the services had EHRs in use at the time of the interviews. A further two were in the process of implementing new systems and had reverted to paper in the interim. Of those services using EHRs, three were in the process of changing the system they used and one was planning to do so in the near future. These interviews showed the level of change in the ambulance services: implementing EHRs was neither a single event nor a linear process, but instead was an ongoing negotiation between front-line clinicians and managers.
Respondents reported benefits to the accuracy of record-keeping and the ease of extracting data. However, many of the advantages identified were yet to be realised. The potential value of sharing data between ambulances and other parts of the health service was identified but in many cases this was not yet possible, although it was something that services aspired to. They also talked about challenges associated with implementing EHRs, often around technical issues, such as ensuring connectivity in rural areas or making sure that devices had adequate batteries. This often knocked the confidence of the clinicians in the system, potentially prompting them to revert to paper records. Several services planned to combat this by making EHR use mandatory. Despite these challenges, some services reported well-established systems, with almost every patient clinical record (PCR) being created in an electronic format.
Chapter 5 Results: four case studies
Introduction
In this chapter, we present each of our four case study sites in turn. We summarise key facts about the four sites in Table 9. Our case study ambulance services used a range of terminology for describing their electronic records systems, including electronic PRFs, electronic PCRs and electronic patient records. For consistency, we use the expression ‘electronic health records’ (‘EHRs’), regardless of what term was used by the service. Case study sites and their associated ambulance services are identified by number, which corresponds to the numbers used for ambulance services in Chapter 4 (e.g. AS1 in this chapter is the same as AS1 in Chapter 4).
| Characteristic | Site | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| EHR system in use | Panasonic TOUGHBOOK running Ortivus software | Panasonic TOUGHBOOK running Medusa software (Medusa Medical Technologies, Halifax, Nova Scotia, Canada), later transitioned to Getac tablets running Medusa software | Terrafix rugged tablets running bespoke software | Anoto Digipens |
| Date of introduction of system | Roll-out in 2014–2017 | Original EHR system in 2010, new system in 2017 | 2007 | 2015 |
| Population covered | 5.3 million | 4.8 million | 5.4 million | 3.1 million |
| Area covered | Approximately 20,000 square miles | 6425 square miles | Approximately 30,000 square miles | Approximately 8000 square miles |
Verbatim quotations from interviews and focus groups are presented in this chapter and in Chapter 6 in order to illustrate points. Quotations from interviews are identified by site number and interview number for that site; interview numbers were allocated sequentially as they were conducted. Where relevant, we indicate the role of the interviewee in the text introducing the quotation. Quotations from focus group participants are, similarly, identified by site number, focus group number and participant number; all focus group participants were front-line clinicians (paramedics and EMTs). We also present, in a series of boxes, vignettes taken from the observation notes made by the site researchers.
Site 1
Context
Case study site 1 covered a large area of some 20,000 square miles, spanning seven counties; the area is predominantly rural, but also includes some large urban centres as well as island communities. AS1 served a resident population of approximately 5.3 million people, and also responded to calls from the 17.5 million seasonal visitors per year. AS1 had nearly 100 ambulance stations. It was created in 2006, and merged with a neighbouring ambulance service trust in February 2013. AS1 covered 13 CCGs and served 18 acute trusts. It employed over 4000 mainly clinical and operational staff, including paramedics (n = 1788), emergency care practitioners, advanced technicians, ambulance care assistants and nurse practitioners, plus GPs and around 2785 volunteers. In the most recent Care Quality Commission (CQC) inspection, in 2016, AS1 received an overall rating (including its non-emergency services) of ‘Requires improvement’, although in terms of caring it was rated as ‘outstanding.’ The annual budget for AS1 was £240.5M in 2016–17.
Records system
AS1 used a Panasonic TOUGHBOOK running Ortivus software.
Implementation
The timeline of EHR implementation in site 1 is summarised in Table 10.
| Time point | Activity |
|---|---|
| 2011 |
Original business case for ECS incorporating EHRs presented to trust directors Three detailed benefits case studies: for cardiac arrest, interagency working and frequent callers Specification for software requirements drawn up |
| 2012 | Invitation to tender for new ECS issued |
| 2013 |
Ortivus selected as preferred supplier and contract signed Eight-stage implementation plan drawn up |
| 2014 |
Range of SOPs and user guides on use of EHRs developed Hosting service prepared 30-day testing period |
| September 2014 to February 2017 | Roll-out of ECS – installation of device on vehicles, staff training, ‘Go-Live’ in each area beginning with non-conveyed patients, then all patients. Roll-out sequentially across 18 geographical areas |
Design and procurement
AS1 did not identify a suitable ‘off-the-shelf’ EHR system to purchase, so the data management team at AS1 worked closely with the software company in developing the system and identifying changes or improvements that were needed, and its ‘tweaking’ of the system was ongoing (Site 1, Int 1). During the development stage, the team gathered feedback from front-line ambulance staff and ED staff, and had made ‘significant changes’ to the system (Site 1, Int 5). However, there still seemed to be a perception from ED staff that the design of the system and, in particular, its output, was not tailored to the hospital’s needs:
We hadn’t actually seen the system at all, so we were presented with a system which was more or less fully developed and with a start date for implementation.
Site 1, Int 3
Managers reported that the speed and extent of development was limited by the funding available:
The government refused to fund a system that was fully integrated, what they funded was an electronic system that captures data but the output is paper, so it was a bit disappointing really.
Site 1, Int 2
Training and roll-out
The service used ‘cascade training’ to train paramedics in how to use the EHRs. Formal training was carried out in each area and was quite a slow process, partly due to the logistical difficulties in getting clinicians off the road to be trained (Site 1, Int 5) and partly due to the logistics of installing equipment in vehicles. Although the staff member responsible for implementation had found that ‘conquering the workforce’ turned out to be ‘a lot easier’ than expected (Site 1, Int 5), training had ‘cost a huge amount of money’ (Site 1, Int 2), and the slow pace led to some problems for front-line staff:
The way that we delivered training made it very difficult for the user because we delivered training alongside the implementation plan, but unfortunately the devices and the fleet and the logistics weren’t ready . . . so the lag between having their training and then being out and using the device and going live in an area meant that actually it was all of a sudden unfamiliar to people again.
Site 1, Int 9
Implementation officers had been employed during the roll-out of the system to meet with hospital staff and deal with queries they might have, and to make sure that the workstations in the hospitals were installed and able to display the clinical data. There were differences in perspective about how this had gone: a manager from AS1 thought that the training process in hospitals had been ‘easy’ (Site 1, Int 2), but one ED clinician felt that it had been a ‘massive issue’ as staff needed to be trained in how to read the record (Site 1, Int 3).
The roll-out was phased over 2 years, following a trial period in a single area. One respondent described the lengthy roll-out, following a long procurement phase, as causing some problems:
So the tablets that we currently use are now obsolete because you purchase them, you take 2 years to roll out the product, we’re almost a year beyond the final roll-out and the devices become obsolete very quickly.
Site 1, Int 2
Electronic health records in use by ambulance clinicians
On standard ambulances operated by AS1 (converted Mercedes Sprinter, Stuttgart, Germany), the EHR device was stored in the back of the ambulance on the bulkhead adjacent to the patient trolley, as shown in Figure 3. In the single-crewed rapid-response estate cars, the device was stored in the boot of the car.
FIGURE 3.
Plan of typical AS1 ambulance, showing the position of the EHR device when stored. ECS, electronic care system.

The EHR was a complex form with approximately 1400 fields. The person completing the record would be taken to different parts of the form depending on the answers to previous questions. Clinicians entered some data manually, often using free-text boxes to enter supplementary details and negative findings, in addition to using the drop-down menus.
Paramedics could use the tablet to access NHS Spine and view patient demographic information and their SCR, which could provide information on, for example, prescribed medication. Except on rapid-response vehicles (RRVs), data were also entered directly to the device from other pieces of equipment, via a Bluetooth connection, and one senior manager described the benefits of this:
We have the tablet on the vehicle, the tablet is also linked up to the various vital signs equipment, linked up to a piece of equipment that allows a 12-lead ECG [electrocardiogram], blood pressure, SpO2 levels, pulse oximetry all of that feeds into the electronic patient records.
Site 1, Int 11
The tablet had a camera function enabled, which would be used, for example, to photograph a wound before it was dressed. We also observed the camera being used as an ingenious workaround, photographing the electrocardiogram (ECG) display on a RRV not equipped to transfer information directly.
Information was not always entered directly into the tablet, with paramedics also using the traditional method of writing on their glove or in a notebook before transferring the information onto the EHRs:
Everything will be on the back of my glove . . . I don’t have time to be fiddling around with that.
Site 1, FG1, participant 1
In observations, we noted that the tablet was generally taken into the patient’s home (if that was where they were) along with the rest of the kit. If the patient was conveyed to hospital, the EHR might be completed during the journey by the clinician who was sitting in the back of the vehicle with the patient. It might be completed in the patient’s house if they were not being conveyed, or on the way to hospital if they were conveyed. One respondent, an ED consultant, commented that, in some cases, paramedics would complete the record after physically handing the patient over, meaning that hospital staff did not know if the record they could see was the completed EHR or one still in progress, something he felt was a potential patient safety risk (Site 1, Int 3).
In the vignette in Box 3, the site researcher describes how the attending paramedic used a mix of ways to collect and store data when attending a small child: exploiting the connectivity of the system to draw in background information, using paper and pen, and in this case using the researcher as an assistant to process information while she focused on direct patient care.
The attending paramedic asked me to input the patient demographics into the EHR device which I have done and performed a PDS search, bringing up the patient’s details from the NHS Spine. Other assessments [paramedic] is doing include an SpO2 reading where she has had to stick a paediatric probe onto the child’s toe – which she [the child] is not impressed about and starts to pull it off. I suggest putting a sock on the foot to try and keep it on. [Paramedic] makes a note of the reading on her notepad. Then proceeds to start assessing the patient’s chest and tummy all the time asking the patient’s parents questions about coughs, colds, bowel movement and passing urine. All the time [paramedic] is actively listening and making a few notes on her [paper] notepad.
Use of data recorded in electronic health records
Transfer of patient information to support care
The patient record was transferred to a central server remotely, via a subscriber identity module (SIM) card, and hospital staff could then connect to the server via a secure link to download the information. Ambulance clinicians were also able to send the EHRs directly to some receiving hospitals, but this was not possible across the whole of the service area. Staff in some of the hospitals served by AS1 were able to access real-time data, including vital signs information, before the patient arrived in the ED, and so were prepared for the patient when they arrived – something we observed happening and that was seen by a senior ambulance services clinician as a benefit of the system:
The hospital can view the live biometric data, they can look at live ECGs on the clinical workstation, they can almost watch the clinician filling the [EHRs] in . . . one of the benefits we wanted to deliver with that, is that the hospital could better prepare for the patients that are coming in because they know more about them.
Site 1, Int 2
Once the ambulance arrived at the ED, hospital staff either printed the record or saved it on the record system as a PDF or Tagged Image File Format (TIF). In some ways, they were positively received, as one ED doctor reported:
Electronic records are brilliant in the fact that they’re legible, and you can look back at them months and months later.
Site 1, Int 3
In the early stages of implementation, these records could run to 20 A4 pages. The length of the record was commented on by both hospital staff and ambulance clinicians, who were aware that it was likely to be longer than what could reasonably be assimilated by the receiving clinician at the hospital. Two paramedics described how, at handover, hospital staff mainly looked at the presenting complaint box and did not go through the detail of the record:
So when they are looking through the whole record they don’t go through it because, let’s be honest, who has the time for that, so they pick that and go through it so I just try to give as much of a detailed summary in that as I can, and then the rest of it be damned.
Site 1, FG1, participant 2
[The receiving hospital] just want to know what drugs you’ve given, they want to know what your basic observations were and your little write-up of what the chief complaint was and the rest of it is just flummery. They’re not interested. They don’t bother to look at our PCRs, we’re wasting loads of time.
Site 1, FG2, participant 2
The ambulance service could send a record for a non-conveyed patient directly to their GP as long as they were on NHS.net, and this seemed to be viewed favourably by ambulance clinicians:
The single biggest thing that’s happened with the care record that’s been tremendously useful, and I really like it, is the e-mailing the GPs.
Site 1, FG2, participant 2
Ambulance clinicians could also send referral e-mails to their local falls team, depending on what was available in their local area, and make safeguarding referrals.
Decision support and risk prediction
Several managers discussed how they thought that the EHR would support clinician decision-making as it guided paramedics through a set process, prompting them to ask a series of questions, and allowed direct access to clinical guidelines. The EHRs incorporated a calculation of the NEWS, and one respondent reported that the new system had been essential in introducing NEWS to the region (Site 1, Int 6). It also supported the routine calculation of frailty scores.
Secondary uses
Managers in AS1 described as a key benefit of EHRs the ease with which they could access patient data for analysis and development, with large quantities of data being made available promptly for analysis, with potential for supporting change to the service in the future:
Daily we’ve been able to use the data, use the system to develop reports to build, design web-based reports, to use the data to integrate with other data sources . . . it’s almost real-time data so we have access to it within 2 hours.
Site 1, Int 1
The value of the data . . . it’s huge and I think we’ve only just started to mine that data to look at what it’s telling us about what the ambulance service actually does, who we are going to, what’s wrong with them, where they are, how old are they and what are the outcomes that we are generating . . . the data, potentially, the [EHR] has, to redefine the service, to reshape the service, to change it fundamentally in the way that we approach the jobs.
Site 1, Int 2
A stakeholder with a public health perspective also saw the potential value, although the use of words such as ‘probably’ and ‘might’ emphasises that this enthusiasm is for what could be done but is not yet certain:
It’s a fantastic public health resource . . . You’ve now got a very rich database which might show you what the patterns are amongst these patients . . . you might be able to say to the CCG ‘Oh look, it’s looking like this, there’s an opportunity for there to be an intervention in primary care to stop this happening’ . . . You’ve probably got a good picture of the vulnerable cohort, and possibly the vulnerable cohort before they have the fall that breaks their hip.
Site 1, Int 6
Tracer conditions
The EHR had templates for assessing falls and the risk of falls and then offering pathways for the patients. It also incorporated assessment tools for mental health crises (Site 1, Int 5). However, as one manager noted, although moving to EHRs could help facilitate new pathways, ‘having an electronic patient record doesn’t suddenly make a falls pathway appear’ (Site 1, Int 9), and setting up pathways was still a lengthy and potentially complicated process.
In relation to diabetic hypoglycaemia, a data manager identified this as an area where there was potential for future work to support early intervention:
We’re linking in, in a number of areas to try to expand the referral process so that if, for example, if we treat someone with hypoglycaemia and we leave them at home, we can then inform specialist services so they’re more aware of patients, they can intervene earlier and perhaps prevent the deterioration that may occur in that patient’s long-term condition.
Site 1, Int 2
Attitudes to electronic health records
Positive
The EHR was largely seen by ambulance clinicians as a useful tool once they had become familiar with using it. Clinicians valued the fact that the EHR could draw in data directly from other equipment, with the time saving from not having to write down observations described as ‘awesome’ (Site 1, FG1, participant 3). The ability to make referrals to other services had also helped to reduce job time:
There’s no question that it’s improved the speed of referrals as well, of course, because it wasn’t so long ago that we had to return to station to do a referral.
Site 1, FG2, participant 3
A clinician on an observation shift reported that being able to view the patient’s previous EHRs, in particular to compare ECG readouts, helped her to decide whether or not to convey the patient.
A recurrent theme among ambulance clinicians was the importance of having a more accurate, comprehensive patient record from a legal perspective:
I think you can cover your [backside] better now than you could on any paper.
Site 1, FG1, participant 3
You’ll have massively increased quality through that machine. I appreciate there’s a lot of hiccups and annoyances that go alongside it, but when things go wrong and you’re standing in a court of law, and you have to answer for your actions, having a lot more quality paperwork will stand everybody in good stead. And it’s not until things do go wrong that you suddenly realise how much you’re going to rely on what you put into that box [the EHR].
Site 1, FG1, participant 2
Senior managers in the ambulance service were very enthusiastic about the EHR and its potential to link in with other health-care providers. They tended to see the EHRs as potentially transformative to practice and patient care:
Pretty much everyone I’ve spoken to thinks it’s a huge improvement and is of great benefit.
Site 1, Int 1
Hospital clinicians reported finding it very beneficial to have a ‘live’ EHR available to them while the patient was with the ambulance clinicians, before arrival at the ED:
If we had a really sick patient coming in, we could look at it and see all their observations and, you know, bits and pieces that might help us plan what we were going to do for them.
Site 1, Int 3
However, many of the positive comments about EHRs, in particular from ambulance service managers, were considering the future potential of the system rather than current reality.
Negative
Some mixed and downright negative feelings were reported about using the ‘etch-a-sketch’, as one paramedic described the tablet, focusing largely on the materiality of the record. However, as one paramedic noted, this was not to say that it was worse than paper:
I think overall I would not want to go back . . . I did recently have reason, due to a malfunction I think, to actually use the paper form and (a) it was interesting to get back into that but (b) I realised how poor a record the paper form was . . . I think it’s a far superior system to the paper one and I would hate to go back. But I loathe it for other reasons.
Site 1, FG1, participant 2
Negative comments about coming to terms with working with the device included complaints about the time it took to complete a record and irritations about how the device worked. The physical sound of tapping on the screen with a stylus was mentioned as an irritation by a number of ambulance clinicians:
If you need to write a lot you’ve got to get the keyboard out otherwise you’re like a woodpecker on bloody steroids.
Site 1, FG1, participant 1
There was some frustration among clinicians that the EHRs did not always have enough tick boxes or did not allow them to record sufficient detail. The body map was thought to be limited and the form lacked opportunities to negatively assess a patient (to record that something had not been observed), leading to possible overuse of the free-text boxes. One clinician reported that the software felt a bit clumsy:
It doesn’t flow, and it’s not logical.
Site 1, FG1, participant 1
Losing mobile signal had been a problem, particularly given the rural nature of much of the ambulance service area, but the system had been designed to cope with this by synchronising as soon as the device was back in signal.
Several clinicians reported that using the EHRs had a negative impact on their contact with patients, drawing too much of their attention compared with a paper record:
The jobs I really enjoy doing, and 90% of the jobs I see, which are the ones where I’m just going to talk to Mrs Smith for half an hour because no one else is going to give her that much . . . attention . . . that thing [messes] that up royal, ‘cos I’m sat there and I’m doing ‘sorry, I can’t talk, oh yes, he was in the army, yes, just a second’ tap tap tap, [expression of frustration], I pressed the wrong thing.
Site 1, FG1, participant 5
I’ve had patients say, a negative thing about it is they say the clinician is too focused on it. They’ve said they’re constantly looking at that . . . computer screen and tapping and not paying attention to what’s going on in front of them. I’ve heard that said a few times by patients, by patient public involvement groups, and things like that.
Site 1, FG2, participant 2
One ambulance service manager commented that data quality had fallen following the shift to EHRs:
Data quality took a definite hit. I think that’s partly as a result of the flow and the actual device itself, in terms of the software and the configuration of it, but I think it’s in large part due to the time lag between training and actual hands on for people.
Site 1, Int 9
In relation to data received from the system at the ED, one hospital consultant expressed quite negative views on the number of data and how they were formatted. He found that EHRs were much more complicated than the old paper records and that the adjustment to the new system was difficult, particularly when trying to establish what drugs people had been given:
The old report sheets were a single side, more or less, of A3 and everything is in the same place . . . When the new system came in we were being presented with 20 sheets of A4 paper . . . even if there was only 10 pages you still didn’t know where to look to see what drugs had been given, because it might be on a different page. So there was no way of actually quickly finding that information . . . in terms of the clinical usefulness as a document it was a massive step backward.
Site 1, Int 3
In addition, the respondent thought that the EHRs did not give paramedics the opportunity to record some useful information as data entry was mainly through tick boxes:
The richness that you get from a free-text box has masses of important information . . . you don’t get it if you just use tick boxes.
Site 1, Int 3
Site 2
Context
Case study site 2 covered six counties and approximately 6425 square miles. The area contained several large cities, as well as rural areas, and had a population of around 4.8 million people. AS2 employed 3290 staff over 60 locations, and in 2014–15 provided a face-to-face response to 643,115 emergency calls. The service was commissioned by 22 CCGs, with one of these taking the role as co-ordinating commissioner. At its most recent CQC inspection in 2017, AS2 received an overall rating of ‘requires improvement’.
Records system
Site 2 originally introduced EHRs in 2010 in the form of Panasonic TOUGHBOOKs running Siren software from Medusa. During the period in which the site researcher was undertaking the case study interviews, focus groups and observations, the service withdrew its EHR system and rolled out a new one. This new system used GETAC tablets (shown in Figure 4) to run an updated and modified version of the EHR from Medusa. One of the features of the new system was high-specification hardware and software that could be easily updated and adapted.
FIGURE 4.
The EHR device used in AS2. (a) Front view; and (b) rear view.

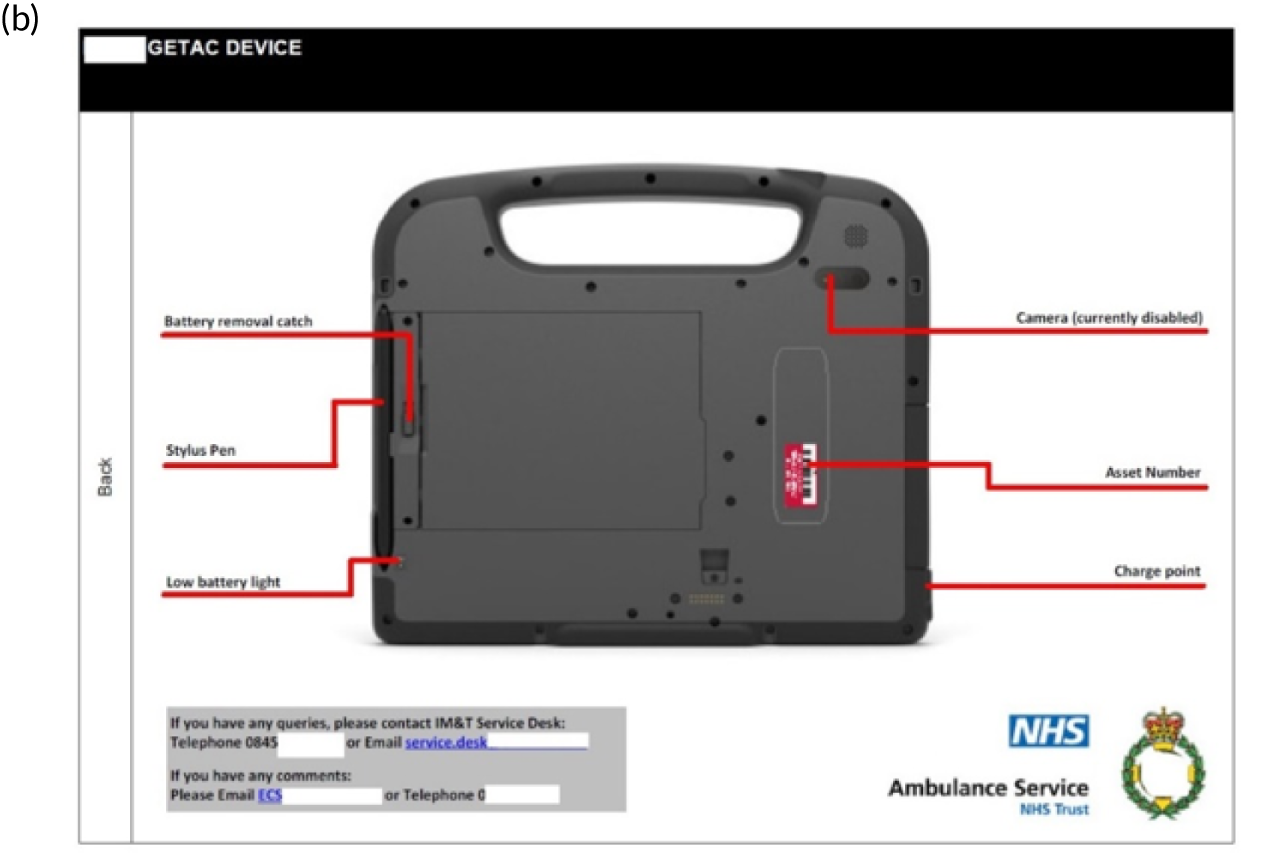
Implementation
Table 11 summarises the timeline of implementation of EHRs in site 2.
| Time point | Activity | |
|---|---|---|
| July 2009 | Presentations to team leaders on planned introduction of first-generation EHRs | |
| May 2010 | Testing of first-generation EHRs – TOUGHBOOKs running Medusa software | |
| September 2010 | Business case submitted for implementation of EHR upgrade | |
| January 2017 | Plans prepared for transition to second-generation EHRs | From January onwards:
|
| February 2017 |
Business case for new EHR system approved by trust board Announcement made to staff and public Hardware orders placed with Getac Software order placed with Medusa |
|
| March 2017 | Hardware (devices and servers) received | |
| April 2017 |
First software received for upload Back-end infrastructure complete CQUIN agreed Devices tested |
|
| May 2017 | Roll-out begins in three stations in county 1a | |
| June 2017 |
Pilot phase commences – non-conveyed patients Roll-out in county 2a |
|
| July 2017 |
Roll-out in counties 2a and 3a Expiry of software contract for first-generation system Recall of TOUGHBOOKs |
|
| September 2017 | Installation 100% complete, training 95% complete | |
| November 2017 |
All hospitals in region ‘live’ for transfer of records to ED Planned upgrade of software – reversion to paper records for 5-hour period |
History
A first-generation EHR system had been installed in 2010, funded by the Department of Health and Social Care through the NPfIT. However, it was never installed in every vehicle. Problems with connectivity (Site 2, Int 7) and faults with some machines affected clinicians’ confidence, and consequently compliance, and there was a tendency to use paper instead:
The biggest problem with the old system was that it didn’t seem to be robust enough and the hardware didn’t seem to be up to the job enough. It was too slow, too cranky and the paramedics seemed to have a general thing they’ll try something twice and if it fails the second time they won’t use it again.
Site 2, Int 2
Design and procurement
When the national contract for EHRs associated with the Department of Health and Social Care funding came to an end, the service took the opportunity to procure its own system:
Now we’re not on a national system and we have the ability to do as we please as opposed to, well it’s the offering, take it or leave it kind of thing.
Site 2, Int 5
Getting funding for the new system has been ‘the biggest challenge’ (Site 2, Int 1). The costs associated with the new device and software had to be balanced against the costs of paper and, although initial costs were high, over time it was expected to be more cost-effective (Site 2, Int 3).
Clinical commissioners had high expectations of the new system and were engaged with its introduction and integration with primary and secondary care. However, they were possibly overambitious in how fast they thought full roll-out could be achieved (Site 2, Int 9).
Training and roll-out
At the time of our fieldwork, AS2 had partially reverted to paper records while rolling out the second-generation EHR system. Although a full, temporary reversion to paper had been discussed, it was decided instead that each area would move to paper and then receive the new EHR system. Most clinicians had had only limited experience of using the new system, and some had not used it. Although we tried to schedule observations to follow roll-out of the new system, on some of the observations the EHRs were not fully operational.
Training was being provided online. Clinicians were asked to do it in their own time and then claim back the time it took, which they felt was a ‘good deal’ (Site 2, FG3, participant 2). However, focus group participants who had experience of the training for the original system did not feel that it compared favourably:
When we did our first TOUGHBOOK training . . . We had 2 days in one of the suites. There was about 10 of us in a room, we’d all got one and we were literally going through page by page by page, stage by stage to log onto it and then to do this and then went through, and you’ve got like, lists of like – there would be about 10/12 patients that you had to work through and you’d be just tapping away doing everything under the guidance of a trainer. So, if you’d got any questions about it, you could ask them. You could ask your mate next to you, say, ‘Oh, where’s that thing? How do you do this?’. You know, this one, it’s assumed that everybody’s completely versed in it, everybody understands IT and can learn off a series of 3-minute videos.
Site 2, FG3, participant 1
Despite this, the focus group participants did not generally feel that they required more training as the system was not very different from the one that they had been using and was thought to be fairly straightforward to use.
Electronic health records in use by ambulance clinicians
Ambulance clinicians described a range of ways in which they used the EHR system, choosing when, how and sometimes whether or not to complete the EHRs. They reported that the position of the tablet in the ambulance meant that they did not automatically pick it up with their other kit, and whether or not they took it in when arriving at the patient would depend on the nature of the call, with providing care taking priority over record-keeping in serious cases:
If I’m going to a life-threatening job, I don’t tend to grab it and take it in with me . . . if it’s a non-life-threatening job, I’ll tend to take it in with me and I open it up straight away . . . I’ll put the observations in it straight away and it’s time stamped straight away.
Site 2, FG4, participant 1
Our observations suggested that use of the EHRs was shaped by the type of call-out, individual practice, and the stage of the roll-out in the area. Clinicians on one shift were observed entering data onto the EHRs once the patient had been transferred to the ambulance, whereas on another shift the tablet was routinely taken into the patient and the record started straightaway. On another shift, clinicians did not routinely take the tablet with them on arrival, instead waiting until they had decided whether or not to convey the patient before fetching the tablet. During the observation, clinicians created EHRs for patients who were not being conveyed, copying the data from the paper form onto the tablet, but took a paper record to hospital with conveyed patients, because hospitals were not yet able to accept EHRs. All EHRs were added to on the ambulance and clinicians often carried on entering information on arrival at the hospital, for example while waiting to hand the patient over.
The EHR system had the potential to allow ambulance clinicians to access GP records and view pertinent patient information, but only where GPs had put the appropriate permissions in place:
At the moment, in theory, we can actually see do not resuscitate decisions, advance care planning, current plans for that patient, e.g. if this patient with chronic airways disease calls you and their saturations are 90 that’s normal, please leave them at home.
Site 2, Int 3
In addition to being entered manually, data were also drawn from the mobile data terminal (MDT), which could autopopulate some parts of the EHR. Information from the LIFEPAK (Physio-Control, Redmond, WA, USA) monitoring equipment was printed and entered retrospectively into the EHRs; the ability to transmit the information via Bluetooth had not yet been activated at the time of the observations (Box 4).
In the patient’s bedroom the paramedic filled out the EHRs balancing the tablet on the end of the bed and using her finger to make entries, whilst the technician carried out basic observations. The technician travelled in the back of the ambulance . . . and continued the EHR, completing the relative’s details and taking further history through conversation with the patient’s wife and reading through the GP’s letter . . . Most of the entries were made using ‘tick’ boxes and dropdown lists with free text used to write in information not captured by the tick boxes/menus. The entries were made using a stylus attached to the tablet. The EHR was transmitted straight through to the hospital where it would be received by equipment based in the A&E department. The final entries to the EHR were added in the ambulance after the patient had been handed over. The EHR was then finalised.
A&E, accident and emergency.
Completion of the EHRs was observed to be something of a ‘team’ approach: one clinician might start the form but have it signed off by their colleague; or one doing observations might tell the colleague what to enter on the record. One clinician commented that the EHRs acted as a prompt to ask or record things that she might not have done if using a paper form, leading to the creation of a more comprehensive record.
Some focus group participants expressed disappointment that they did not have more access to data on previous patient contacts, particularly in relation to people who make frequent use of the service:
It’s a shame that [recent visits] wasn’t included. It doesn’t need to give the information just that you’ve been to this one . . . that’d be useful.
Site 2, FG2, participant 4
Use of data recorded in electronic health records
Transfer of patient information to support care
The intention was that EHRs completed in the newly launched system could be electronically transferred to the receiving hospital, but at the time of the fieldwork, not all of the hospitals were able to receive EHRs and clinicians had to complete a paper record instead. On one shift, clinicians completed paper EHRs when conveying patients to hospital. On another, clinicians were observed sending EHRs ahead to the ED while the patient was being conveyed. It was expected that by the end of the roll-out of the new system, all hospitals would be able to accept EHRs.
The roll-out of the EHRs was reported by ambulance clinicians as having had a negative impact on clinicians’ interactions with ED staff, who wanted to be given paper forms:
Just talk about the hospitals . . . just walk into a reception and be snarled at by a receptionist because you’ve dared to go in with an [EHR] which they’ve got to then click a print button on so, you know, we’re just not working together with it.
Site 2, FG2, participant 2
Records could be shared with GPs, but only if the GPs have given the ambulance service an e-mail address. However, clinicians in the focus groups expressed some scepticism about what happened to the records of non-conveyed patients and what GPs actually did with the information. This had an effect on their confidence in and commitment to the new EHR system:
I see what goes to the doctor . . . but I don’t know whether GPs actually look at them or if they just sit in an inbox or whether they get attached to records. I don’t know where they go.
Site 2, FG1, MS1, participant 1
Clinicians were observed making safeguarding referrals over the radio and liaising with out-of-hours services over the telephone. However, one senior manager anticipated that in the future safeguarding referrals would be sent via e-mail rather than ‘getting hold of one of the safeguarding administrators and speaking to them on the phone for 20 minutes’ (Site 2, Int 6).
Decision support and risk prediction
The new EHR software was designed to provide support with decision-making, and the device could support other software that can help clinicians, such as the tool to calculate the NEWS (a scoring system to detect deterioration of acutely ill patients).
The process of going through the EHR could help with decision-making:
I think even if it’s just used as a reference tool to be able to go through that checklist and tick them off would be a bonus, because then you’ve got the proof that you’ve actually done that . . . and if the clinician then makes a decision at the end of it that, you know, they’re happy, then I think it’s a good thing that you’ve actually recorded it.
Site 2, Int 6
Clinicians echoed this, commenting that it gave them confidence that they had covered all the necessary areas:
It just guides you along and it gives you the confidence to know that you’ve not missed something.
Site 2, FG2, participant 2
Although EHRs can be very helpful in terms of facilitating alternative care pathways (via decision-making support in the record and ease of referral) and non-conveyance to ED, their effectiveness was seen as depending on the working culture of the clinicians.
Secondary uses
For much of the time during which the site researcher was conducting interviews, EHRs were either not in use, or had just been introduced and therefore had not yet generated a bank of data available for secondary uses. However, several managers anticipated that the new EHRs would be used to inform research and audit and help to enable service planning:
There’s the audit facility so, as you know, we can look at various data in there about various aspects, pull it all down.
Site 2, Int 3
I’m sure that clinical audit, etc., will use that information and share that with the wider health economy and us as an organisation, so when we go into meetings about what the pathway is, what time of day is it, where are they coming from, where do we need to put the pathways in, what pathway do we need, what bits of the pathway are missing, I think they will benefit that.
Site 2, Int 2
It was expected that the EHR data would be more comprehensive and easier to interrogate than paper records. This would enable the ambulance service to build a more complete picture of the types of patients attended, and how their needs could best be addressed:
One of the challenges we have as an ambulance service is if you were to do a trawl of code sets of calls into the ambulance service, due to the triage systems that we have, the AMPDS [Advanced Medical Priority Dispatch System] code that we have is quite rudimentary, it’s just based upon that initial telephone, you know, analysis and interpretation. The true clinical representation can be very different . . . And by actually having reliable clinical records we can interrogate that data much better to be able to be in a position where we can help understand what really is the level of activity that we get and what conditions. It then takes it on to that step further about are the pathways in place, so i.e., do we have robust diabetic pathways, do we have true access to falls services as the system may indicate? So I think the platform gives you that real benefit.
Site 2, Int 5
It was also expected that the new EHRs would be useful when compiling reports for the coroner, providing a more complete record, and potentially meaning that paramedics were not required to attend inquests in person:
For clinicians where high usage of electronic records happens, our attendance for coroners’ inquests has dropped by 30%, which is a big improvement for us. Coroners like it because it helps them with their inquest which obviously helps the family in the end anyway.
Site 2, Int 3
So, although the service was not able to make use of the EHR data at the time of the case study, owing to the ongoing implementation process, there were plans to use the information for purposes other than immediate patient care.
Tracer conditions
Both managers and clinicians recognised the potential ways in which EHRs could help refer patients to care pathways. They hoped that the new system would give them opportunities to integrate referrals to care pathways into the form as well as being more time efficient, as the referral could be made electronically rather than over the telephone. This would possibly have a positive impact on paramedic job satisfaction as they are often aware that people are not always getting the right input or support following an emergency visit, but cannot link in with the other care the patient might have received.
Clinicians in one focus group expressed some reticence about doing mental health referrals electronically as they wanted to be confident that the referral had been successfully received and did not trust that this would necessarily happen if carried out via the EHR or e-mail, rather than through a telephone call:
I know someone’s heard it, as opposed to it sitting in an inbox for a week waiting for somebody to pick it up.
Site 2, FG3, participant 3
There were also some problems with implementing a standardised referral system across several CCG areas:
We’re a regional service and the commissioners don’t work regionally.
Site 2, Int 1
This made it difficult to create care pathways for the ambulance service to follow as the services available for clinicians to refer into varied across the region.
Attitudes to electronic health records
Positive
Ambulance clinicians identified a range of benefits to the EHR system: better security for patient data as records could be encrypted and were less likely to be physically misplaced than a paper form; creation of a standardised, legible record; the form acting as a prompt and aid to decision-making; and the potential to transfer information to hospitals, GPs and other health-care providers. At the time of the case study, clinicians had very little experience of the new EHR system and so were either comparing the old system with paper patient report forms or talking in more general terms. Much of the discussion of the benefits of EHRs, particularly among ambulance service managers, was speculative and looking to the future. The vision for the new system was that it would benefit patients, integrate with hospital systems and provide better, more easily accessible data for the ambulance service:
It won’t just be a patient record system which will have integration with the acutes and other aspects of care, so primary care, it will allow us from an audit perspective to be able to interrogate the information in a much more timely manner . . . we will have better-quality data, we will be able to address external enquiries, for example police or coroner processes, to make sure that we can respond in a timely manner.
Site 2, Int 5
Electronic health records were reported to be far less likely to be lost or altered once finalised and it was easier to see when the record had been shared or accessed, helping to make the records more secure. Managers were hopeful that the new EHR system would save time for front-line crews, both by reducing the amount of time spent reporting to the coroner and through streamlining routine processes:
We put time back into the system, we put time back into the lives of the staff and stop them doing things twice.
Site 2, Int 1
Although the immediate benefits concern better data recording and easier access to the data for the ambulance service, the potential to share information across organisations and to be better integrated across the NHS were seen as important wider benefits (Site 2, Int 5), helping patients to access the most appropriate treatment and lead to other pathways being developed (Site 2, Int 7).
Negative
Clinicians participating in the focus groups reported various negative feelings about both the new system and the new device. Perhaps the main issue was a feeling of disappointment that the new system did not give them access to the patient’s existing records or link in easily with other health-care providers:
Do you end up sending someone in that you know would probably have stayed at home if you’d had that background information, because you can’t tell what they’re like normally, to make a decision as to whether the problem they’ve got tonight is new, whether it’s an exacerbation of something, and so you think, at 3 o’clock in the morning when you’re battling to find the information you just think, ‘oh do you know what? I’ll just send them in, somebody will sort them out because they’ll have access to the records when they get to hospital’.
Site 2, FG2, participant 3
There was frustration at the time taken to complete a patient record on the new device, which had an impact on everyone as it meant that fewer crews were available to respond to calls because it took longer to attend to patients.
Front-line clinicians had some complaints that the new on-screen keyboard was ‘awkward’ and that the ergonomics of the new device were ‘poor’. Some paramedics reported difficulties with navigating the screens and writing less free text, which they felt was detrimental to their recording. One was frustrated by the touch screen compared with a keyboard:
There’s no keys on it! It’s quite infuriating to type on.
Site 2, FG2, participant 2
Focus group respondents reported issues with the availability of information on the device. In particular, they felt that the GP database was not as comprehensive as it been on the old system, which made referring patients much harder than it previously had been.
One paramedic commented that the change to EHRs meant that they had lost a potential source of patient information as paper records from previous ambulance call-outs used to be found in patients’ houses.
Site 3
Context
Case study site 3 covered a large geographical area of roughly 30,000 square miles, which included several major cities and urban conurbations, numerous smaller urban areas and some very remote rural areas. AS3 provided emergency care for approximately 5.4 million people. Its operational area included 14 NHS health boards.
Implementation
The timeline of implementation of EHRs in site 3 is summarised in Table 12.
| Time point | Activity |
|---|---|
| 2007 | April–October: first generation of EHRs introduced – Terrafix rugged tablets installed in vehicles, running bespoke software |
| 2011 | Clinical strategy sets out aim to enable transfer of EHRs to GPs |
| 2014 | Piloting of transfer of EHRs to GPs and to receiving EDs |
| 2014 | Ambulance service adopts new ‘Ambulance Telehealth’ programme |
| 2014 | November: outline business case prepared for two-phase upgrade – phase 1 hardware and communication systems, phase 2 software and diagnostic equipment |
| 2015 | AS3 published strategy document looking towards 2020, emphasising the ambition to provide a fully electronic patient record that was integrated into NHS systems |
| 2015–2016 | Roll-out of new hardware |
| 2016 | January: business case prepared for phase 2 of upgrade (software and diagnostic equipment) |
| 2016 | Expiration of contract for first-generation software |
History
AS3 was the first ambulance service in the UK to introduce EHRs, in 2007, and EHRs were firmly embedded in practice. A fully digitised system was envisaged for the service, enabling digital patient records to be shared across the health system – but this had not yet been achieved. The shift to digital records was seen as a way to free up paramedics to deliver more mobile health care in the community; improve the performance of front-line services; improve the integration of national, regional and local health services; provide decision-making support for ambulance clinicians; capture all clinical data in real time; and provide easier analysis to improve clinical performance.
The first-generation EHR system introduced in 2007 used Terrafix rugged tablets and bespoke software, but was not fully integrated with other EHRs within the health service. It was described as:
Basically just a data-gathering tool, so you put your record and all your observations for the patient . . . effectively that was all there was.
Site 3, Int 4
Design and procurement
By 2013, AS3 saw a need to replace the equipment, which had been in continuous use for 6 years, and which was no longer cutting-edge technology and could not support the planned software updates. The expiry of the contract to supply the first-generation EHR system was due in 2016, offering an opportunity to upgrade to a system better able to support data-sharing and new technology, such as video consultation.
AS3’s preferred option was to completely update software and hardware and establish the vehicle as a wireless hub. AS3 planned to continue using EHRs throughout the update process. A business case prepared in 2016 set out plans for the new system with four components: a new EHR system with a user-friendly, intuitive interface; access to a range of back-office systems and internet-based applications and services to support mobile working and improve patient care; a new application to provide key information to service staff about services, pathways and guidelines that will help them to do their job; and infrastructure to enable ambulance telehealth capability.
Training and roll-out
Roll-out of new hardware (tablets, communication hubs and printers) took place during 2015–16. New software was rolled out in the second half of 2017, so was in progress at the time of the interviews. Observations were carried out before the new software was in use. The researcher had originally arranged for some observations to take place once the new technology was in use but delays to the roll-out meant that this was not possible in the fieldwork period. This software roll-out was intended to give paramedics better access to patient data, clinical guidance and electronic access to patient records.
Electronic health records in use by ambulance clinicians
An EHR was generated automatically for every patient for whom an emergency response was sent:
A record is created automatically on allocation of a new incident to the vehicle, so the record is created with some of the detail already pre-populated from our command and control system, so for example the incident number, patient name, patient – any patient demographics that we’ve already picked up from the call-taking is already in there, as well as what we call the dispatch code.
Site 3, Int 1
It was intended that ambulance clinicians would take the device in with them when they saw a patient. In practice though, this did not always happen. During the observations, the site researcher saw notes being written on gloves or other temporary surfaces, and the device then used for the final ‘formal’ version of the patient record, as described in Box 5.
No bag taken in. Patient brought out to ambulance on chair and installed into the bed. Obs performed then [EHR] completed – time to complete as patient stable and ‘sleeping’ . . . Obs recorded. Used back of glove and then typed up. Paramedic standing over attending to patient and cannot handle tablet as well until seated.
Focus group participants told a similar story, reporting that they did not routinely take the device out of the vehicle unless they decided to keep the patient at home. There were concerns that they would not be able to connect to the internet inside the house.
Records for patients who were conveyed to the ED were likely to be completed on the way to the hospital. Focus group respondents thought that this was because they already took ‘probably too much equipment’ (Site 3, FG1, participant 1) in when they first arrived.
The second-generation EHR software was designed to reduce the amount of information recorded as free text by using more drop-down pick lists:
What we’ve tried to do with the new version EHR then is reduce the amount of writing required, so that everything that we would expect to write down, there’s usually a button or something for them to pull down a drop-down list for them to pick from, to choose that information.
Site 3, Int 4
At the time of our fieldwork, ambulance clinicians were not yet able to look at a patient’s previous EHR from earlier call-outs, although there were plans to enable paramedics to access individual patient EHRs for the preceding 3 months. A paramedic would therefore be able to see if a patient had called 999 and been seen in the previous 3 months, and review what had happened. Managers and clinicians reported that patients expected that this already happened:
When we first raised the issue of accessing previous [EHRs] . . . the question is patient confidentiality, etc., etc. And then when we went and assessed it the patients expected that we actually knew that, so the patients do expect our staff to know there was an ambulance there last week or what happened to them . . . people expect us to have that record there and they’re surprised when we don’t have.
Site 3, Int 4
They’ll quite often think you’ve got access to all their records, because they’ll see you ‘Oh, that’ll be on my records’.
Site 3, FG1, participant 2
Use of data recorded in electronic health records
Transfer of patient information to support care
Patient records stayed on the terminal until the end of the shift, and were uploaded to the ambulance service database when the clinician signed off. Printouts of the EHRs were made to hand over at the ED when patients were conveyed, and an abbreviated record was printed and left with the patient for those who stayed at home. There were future plans to upload a copy of the record to a data integration system to be developed to operate across the NHS in site 3.
Although AS3 had a long-term commitment to the integration of their EHRs with other digital systems within the NHS to ensure continuity of care and better case management, this was some way from being fully realised. Although pilots trialling the transfer of records to hospitals had been positive, full roll-out had been delayed by complications arising from the difference between systems in hospitals across the site 3 area.
A specific example of how integration might improve patient care and be of benefit to the ambulance service was the impact of being able to e-mail records to a GP. Previously, with the old system, paramedics would leave a paper summary with patients who were not conveyed because it was felt that they could be treated more appropriately in primary care, with the intention that patients would take this to their GP. However, respondents reported that that patients did not always do this, potentially contributing to the problems associated with frequent callers:
What’s being found is sometimes you go back to regular calls, if you want to call them that, and they can be sitting because they’ve not bothered . . . taking it to the GP. There’s a fault in the line there.
Site 3, Int 4
Under the new system, paramedics could e-mail records directly to the GP, in addition to leaving a paper record with the patient. It was hoped that this would prompt the GP to see the patient and thus reduce the number of repeat ambulance calls.
Decision support and risk prediction
The first-generation system had concentrated on recording patient data and clinical observations. However, the new system, which was being rolled out at the time the case study was done, introduced a range of new tools within the record or loaded onto the device. Checklists for incidents, such as suspected stroke or falls, were built into the record and if certain criteria were met a patient might be eligible for a particular referral pathway and the clinician prompted to look at apps within the device for local information. The purpose of this was to provide some decision-making support and to make them aware of potential alternatives to ED conveyance, rather than replace their clinical judgement.
The new device also had the potential to run other apps and programmes and to have more data transferred to the EHRs electronically. For example, there would be links to the JRCALC guidelines, useful external websites and the NHS service directory.
Secondary uses
Since AS3 introduced EHRs, they had saved patient data in a secure data bank – more than 8 million electronic records at the time of the case study. Managers within the ambulance service were proud of the large number of data they had gathered in their data bank.
One example given by a senior manager of how these data had been put to secondary use concerned the design of a new clinical response model:
The data that we collected from electronic records was fundamental in persuading clinicians and politicians to implement our new clinical response model. We used half a million patient records to show the efficacy of the proposals that we were making . . . it is absolutely fundamental to have been able to show and convince people that the new model is safe and we’ve subsequently updated the model for another half a million records, so that’s 2 years’ worth of data, now that we’re able to show the model as working as intended.
Site 3, Int 6
Tracer conditions
The tracer condition of falls was mentioned as one of the conditions for which decision support leading to a referral pathway was built into the second-generation EHR system:
What we’ve built into the new version is that for certain things, so for stroke, for falls . . . for acute MI patients, we’ve actually built a checklist into the patient report . . . questions will pop up to say: this patient’s suitable for a referral pathway, look at the apps to see local information . . . that’s not to take away their clinical judgement but it’s just to support that judgement for them.
Site 3, Int 4
Attitudes to electronic health records
At the time of case study observations, clinicians were not yet using the new EHR software, so much of the discussion around the impact on practice, patient experience and data collection was speculative. As EHRs had been used in AS3 since 2007, it was difficult for staff to draw comparisons between EHRs and paper records, as a significant number of staff had little or no experience of using paper records. In focus groups, paramedics were generally talking about the first-generation software system on the new device (the interim arrangement), but, in interviews, managers were often talking about the new system on the new device.
Positive
Clinicians valued the EHR’s role as a written record of the encounter with the patient, to show that they had acted appropriately:
It’s about a legal written record of what we’ve done . . . we need a patient record that we can hand over to whoever’s receiving the patient . . . you need to have it legally because we have a responsibility should something happen down the line . . . It’s part of the medical treatment if you like, and it’s part of covering our backs, that we’ve done correct procedures.
Site 3, FG1, participant 3
It’s a safety net for the patient, for ourselves, and for the services.
Site 3, FG1, participant 2
The device was thought to be a useful prompt, reminding clinicians to ask the patient certain questions or take observations. Being able to leave a printout of the record with non-conveyed patients was also thought to be useful, as patients might not be able to take in the information at the time. The EHR was also thought to be useful for clinicians referring people to other services as they were able to pass on a more comprehensive summary of their observations and treatment.
Senior ambulance service managers cited the quality and quantity of data collected and the ease with which EHRs could be accessed for audit and reporting as one of their main benefits. The second-generation system had been designed with this in mind:
A focus of it was to make sure we’re capturing the best data that we can, that allows us to measure new clinical indicators, specially around the response model and things like that.
Site 3, Int 5
Looking ahead, senior managers were very positive about the potential of the new EHR system to support increased sharing of data across NHS organisations and ultimately patients, ‘so that we can provide a more seamless service to patients’ (Site 3, Int 6).
Ambulance clinicians were hoping for future benefits from the system, ranging from being able to use the camera function and being able to transfer photographs to the receiving hospital, to supporting feedback on patient outcomes that could help to improve practice:
Sometimes it’d be useful [to follow up patients], you think I’ll look up and see what they were actually diagnosed with and then for the future if you ever saw something like it . . .
Site 3, paramedic, FG1, participant 5
Negative
Ambulance clinicians had various minor negative views about the functionality of the EHR device, including that the battery did not stay charged for very long so it had to be docked as much as possible, and that the screen was not very sensitive. They also complained that it added to the number of pieces of equipment they were expected to take in when attending a patient.
Negative comments about the EHR software – the first generation of which was still in use at the time of the focus groups and observations – focused on the flow of the EHRs, which could slow down entry:
If you’ve got a time-critical patient or somebody who’s really, really unwell . . . there’s a lot of fields in it . . . and some of it is not quite a logical flow.
Site 3, FG1, participant 4
There were also some criticisms of the available fields, making it tricky to accurately record what the patient reported:
Your chest pain one . . . this whole thing about the time of onset and they’re like ‘oh yeah, I’ve had it for 3 days’ . . . you’ve got to just leave that blank . . . you can only put a time in.
Site 3, FG1, participant 5
Your interpretation of what is actually going on, it could fit into a hundred [codes]!
Site 3, FG1, participant 3
Site 4
Context
Case study site 4 was an area of approximately 8000 square miles, with a population of 3.1 million living in extensive rural areas, busy seaside resorts and large urban conurbations. AS4 attended more than 250,000 emergency calls per year, in addition to providing non-emergency transport and telephone advice. It employed 1310 people on emergency duties working from 90 ambulance stations.
AS4 developed a new clinical model and formally introduced it in 2015, to support innovative ways of responding to and measuring service performance. This model is based on patient clinical outcome rather than the blanket 8-minute response target previously used across the whole of the UK for all high-priority calls.
Records system
Since 2015, AS4 used a hybrid EHR system. Ambulance clinicians wrote on a paper form known as a PCR that was printed with a microdot pattern using a digipen, which is a digitised clinical record pen. As the clinician wrote, making conventional ink marks on the paper, the digital pen took up to 70 images per second, each stroke digitally recorded using a small digital camera. These images were stored as data with the precise position of the pen within the digital pen’s memory and labelled with a time stamp. Each digipen was issued to an individual member of staff and when records were created, the pen’s unique ID was also recorded. At the end of each shift, the digipen was docked and data were uploaded. The digipen and paper form are shown in Figure 5.
FIGURE 5.
Digipen used by AS4, with paper PCR.

Implementation
The timeline of implementation of EHRs in site 3 is summarised in Table 13.
| Time point | Activity |
|---|---|
| 2009 | Initial discussion of EHRs by clinical audit team – but decision not to proceed at this time |
| 2011 | Presentation to board of outline business case for EHRs |
| 2013 |
External review recommended progressing improved data systems as a priority Anoto Digipen introduced on a trial basis in one area – ‘proof of concept’ |
| 2014 | September: business case for digipen presented to board |
| 2015 |
March: trust proposes revised clinical model; ambulance service commissioner advises that digipen should be in place by 1 September 2015 in order to deliver the plan Project group hold meetings twice each month and prepare action plan Funding secured from regional NHS capital programme September: over a 3-week period, roll-out of 1700 digipens across entire trust, alongside introduction of new paper report form, with digital matrix to enable pen to recognise strokes Training delivered on a cascade model Electronic user guide provided for staff October: survey to all staff End of project report |
| 2016 | April: new validation system introduced |
| 2017 | Trust publishes integrated medium-term plan – 3-year strategy, including aim to achieve access to and sharing of electronic patient information |
History
Before the digipen was introduced, AS4 processed approximately 500,000 paper records per year. Paper records were physically transported and then scanned into a system that was able to capture only eight of the available data fields. It could take up to 4 months from the time of the incident to this small proportion of data being available for audit or analysis.
Design and procurement
The digipen was an off-the-shelf product that was used with a revised version of AS4’s existing design of paper form. A transition to EHRs for the service had been under discussion for some time when an external review recommended an upgrade to data systems as a priority. Procurement of the new system then proceeded rapidly, supported by slippage funding secured from an NHS capital programme. The digipen was seen by senior managers as a ‘stepping stone’ to a fully digital electronic PCR, offering a cheaper, simpler alternative to tablet- or laptop-based EHR systems. It also allowed (as the digipen also writes with ink) AS4 to continue to hand over a handwritten paper record at EDs. Stated aims of the 2014 business case included cost savings on the printing and processing of paper forms; improved data quality, security and timeliness; the ability to provide feedback to staff on clinical performance; and the development of algorithms from the clinical data, which would inform the clinical response model.
At the time of the fieldwork, there were plans under discussion to change to a tablet-based system, which would allow the clinicians to make referrals directly to other care providers or safeguarding services, to access an electronic version of the JRCALC guidelines and to use clinical support for decision-making, but there was no agreed plan or time scale for this transition at the time of the fieldwork.
Training and roll-out
Originally, the service had planned to roll the system out gradually. However, the introduction of a new clinical response model, combined with the approval of the cost of the project, put the service under pressure to roll the system out faster than intended – over a 3-week period across the entire service area.
The ease with which the digipen system could be implemented had been part of the reason the ambulance service had chosen this system:
Much easier to teach someone to carry on using a pen and then dock the pen rather than teach them how to use [an EHR with tablet interface] with drop-down menus and so on, if they’re not familiar with computers.
Site 4, Int 1
There was, though, a formal programme of digipen training delivered throughout the implementation period, consisting of a 25-slide PowerPoint® (Microsoft Corporation, Redmond, WA, USA) presentation created by the digipen provider, and a practical demonstration by local digipen champions or clinical team leaders. Training focused largely on the practical features of the pen, such as the battery life and how to dock it. Accompanying the training was information provided on the AS4 intranet: a digital pen PCR user guide and completion instructions, and a clinical memo, in the form of 12 pages of written frequently asked questions and supporting information.
In one area, focus group participants reported that the new system had already been rolled out by the time they received their training. However, the respondents generally thought that training had been sufficient, as the simplicity of the system meant that it was easy to use, and it did not differ much from what they had been doing before:
How much training do you need to write, to use a pen?
Site 4, FG1, participant 2
Electronic health records in use by ambulance clinicians
Clinicians were observed getting patient information from a variety of sources, including information from the ambulance dispatch team, via the MDT, via the Corpuls cardiac monitoring equipment (GS GmbH Kaufering, Germany), from friends and relatives of the patient, and from the patient themselves. They could take the job number from the MDT to record on the PCR and would enter the unique reference on the PCR into the MDT when the job was cleared. This meant that the PCR could be linked to the dispatch data.
Because the PCR was a paper form, clinicians were not able to access information through the PCR and information could not be transferred directly into the form. They decided what data to record and wrote them on the PCR using a digipen as and when they could, as described in Boxes 6 and 7.
At the time of this study, AS4 had recently purchased Corpuls ECG monitors/defibrillators and placed them into ambulances to increase the potential for telemetry. Although the Corpuls equipment had the capacity to share observation data, it could not be linked directly to the patient record, as one clinician reflected:
There’s information being shared but not fully integrated within systems. It’s still very much separate systems talking to each other with a manual input in between. So there is a flow of information but it’s not an integrated flow.
Site 4, Int 4
In two out of the three observations, clinicians did not take the PCR in with them, instead making notes on their gloves or notepads, using this along with data from the Corpuls, and their memory of events, to complete the form once patients were in the ambulance or the decision had been made that the patient would be left at home. The researcher noted that the PCRs were not kept with the equipment that would routinely be taken to a patient for the initial assessment. On the third observation, the crew took the PCR in for the initial patient assessment, and one clinician completed it while with the patient, with the colleague relaying information to them to enter into the form. This was reported by the crew as being a common procedure except in time-critical cases.
[Paramedic] adds more information to the patient record en route. Then his patient suddenly feels sick and he has to stop writing – he stands up to get her a bowl from the cupboard above her head and proceeds to stand alongside her until we stop outside the ED.
On each observation, crews finished filling in the form after handing the patient over to staff in the ED.
As the crew were busy loading the patient into the vehicle and setting her up again on the various observation devices, several pieces of new information came to light via two different sources – a neighbour and the patient’s niece. It seems that the GP had visited the patient twice the day before and someone else stated that the patient had also recently experienced carbon monoxide poisoning but that she had not wanted to go to hospital after it. There were new pieces of information being captured through active and passive listening skills of the crew members. There were distracting ‘planning’ conversations being shared by the niece with me as I tried to observe the crews’ actions around patient records . . . The crew seemed to filter what they needed out of all this noise, responding to some questions and comments, and allowed the other information to fly around them as they cared for the patient in front of them.
Use of data recorded in electronic health records
Transfer of patient information to support care
Clinicians could leave a copy of the PCR with patients who were not conveyed to ED. Clinicians made referrals to other health-care providers over the radio, by telephone or by fax. There was no facility to electronically transfer patient information to other providers.
Ambulance clinicians reported that they would have liked to have been able transfer information to other services more easily:
It’ll take us a good half an hour or hour at the scene sometimes, just trying to arrange all the pathways, if information can be collected straight to them via the digipen that would cut down in time really.
Site 4, FG3, participant 3
There was a lack of interoperability in the hospitals too, and there were no digipen docking cradles in the EDs:
That’s down to issues with our ICT [information and communications technology] department linking in with other ICT departments because each health board runs differently.
Site 4, Int 1
On arrival at an ED, ambulance clinicians would hand over a paper record to the hospital staff. They generally also gave a verbal handover to an ED nurse after booking the patient in with the receptionist, as noted in the observation in Box 8.
The paramedic holds the PCR and speaks to the staff nurse and provides a verbal recollection of History of the Patient’s Presenting Complaint and his assessment of her.
A staff nurse with a fluorescent tabard enters [the ambulance] through the side doors. The paramedic provides her with a brief verbal handover, mainly telling the tale from memory, with the occasional reference to the PCR.
Decision support and risk prediction
Because of the simplicity of the technology used in AS4, it was not able to support any decision-support tools or risk-prediction software.
Secondary uses
Patient records could be retrieved for clinicians if required for a coroner’s inquest. In addition to the clinicians who completed the forms and the hospital staff who received a form when the patient was conveyed, the EHR was used by the clinical audit team for data analysis to inform audit reports. Data from the digipen were also used in conjunction with information from the CAD system for a mortality review system.
The concerns team and patient safety team could also request records for specific purposes. The ease with which records could be retrieved for investigative purposes by the audit team was seen as being a great benefit of the new system, for example if the ambulance service needed to look into a complaint or adverse event and use it for audit purposes. Over 600 fields of information could be collected from a digital record.
Clinical team leaders could use the clinical indicator information, taken from the digital records, to see how their team was performing – not just in terms of compliance around form completion, but also in terms of clinical process and outcomes. They could also use the data to provide feedback to individual members of their team:
They can see graphs and they can see where they are . . . they can measure any variants against other teams. But importantly, all those clinical records that his team have produced for the clinical indicators are accessible to him or her . . . They can have this discussion round outcomes and experience, and review of clinical records, and provide positive feedback.
Site 4, Int 3
Tracer conditions
The ambulance service used the patient records to monitor hypoglycaemia, which was one of its clinical indicators, and had referral pathways for this condition, falls and epilepsy. There were pathways associated with these conditions that attending clinicians could refer patients to, but, as with all pathways, referrals could not be made electronically. Instead, clinicians were required to fill in separate forms and fax them to the relevant people once they returned to the station, or liaise with services over the phone.
Mental health was one area where clinicians felt it would be particularly helpful to have access to a patient’s medical records, either from previous ambulance call-outs or from other medical history.
Staff professional development
AS4 staff were able to access digipen records retrospectively, once data had been checked and cleaned manually by the audit team. Clinical team leaders could request records to assist with their staff’s performance and development reviews. In addition, ambulance clinicians could request access to records themselves for continuous professional development purposes.
Attitudes to electronic health records
Positive
The digipen system was widely seen by clinicians and managers as having had a positive impact on data security, as paper patient records would no longer be stored on vehicles.
The layout of the form helped to prompt the clinician’s memory and helped them to write the ‘story’ of the patient encounter – an important aspect of the record because they were generally writing them while transferring the patient to hospital or once it had been established that the patient would not be conveyed, rather than during the initial encounter.
Clinicians talked about the benefits of paper and digipens compared with other electronic devices. In particular, they thought that some colleagues might find it hard to switch to using a tablet or laptop as they did not have good keyboard skills and, although they might be able to use it at home, using it in the field would be a challenge. In contrast, pen and paper was seen as ‘foolproof’ (Site 4, FG2, participant 1).
Clinicians identified the main benefits as being for ambulance service management. Creating a digitised record alongside the paper form meant that the record could be retrieved more easily, compared with a traditional paper record, which then helped with access to data for research and audit purposes and saved time when reports were needed for coroners’ enquiries. Patient data security was also improved as the information was held in an encrypted form on the digipen. Paper records sometimes went missing, but the digital EHRs were much less likely to get lost as they were held on the pen and then transferred to a data bank when the pen was docked.
For practitioners, the main benefit of the digipen was that it was a simplified way of creating a digital record and required very little change to the way in which they completed a PCR:
We went from pen and paper to fancy pen and paper.
Site 4, FG2, participant 1
Even if the battery ran out, the memory was full or there was a technical error, the clinician could still use the pen to fill in the form.
Clinicians did not discuss potential benefits of the digipen as they did not feel that they did much more with them but they did discuss the possible advantages of having a full tablet-based EHR system. The main perceived benefit was the potential access to a patient’s medical history, from either GP records or previous ambulance attendances. This would provide background knowledge that could help with decision-making.
Respondents saw the possibility of integrated health systems within the NHS as one of the biggest possibilities offered by EHRs:
I think the massive opportunity of an electronic record is the ability to be able to talk to other systems, and as a result then be able to almost have conversations with other health-care providers we’ve never really had before as a result.
Site 4, Int 4
Negative
Negative views on the system included the fact that it was not integrated with other parts of the health service’s electronic systems. This was discussed by front-line clinicians, and, below, by a service manager:
If we took the example of transporting a patient into hospital, we might have the [EHR] electronically or in a data format but currently there’s no actual link, so everything has to be retyped in. The health board don’t even have access to the PDF image of the [EHR] . . . in terms of opportunities I think that’s an area we haven’t really gone anywhere with yet, and I think it’s something we need to do to realise better benefits from an electronic record.
Site 4, Int 6
Although the pens were simple to use, they were still at risk of system failure – early in the implementation, there was a period of some 12 hours when clinicians were not able to download data from their pens.
Managers observed that the system might be straightforward to use, but that it was only as good as those using it:
The downside to it is if staff don’t fill them in properly.
Site 4, Int 2
There were also some issues with the data. First, the number and complexity of the data had been greater than anticipated. Second, validating some records when clinicians had not filled them in entirely accurately proved difficult and slowed down the data processing:
There is a data accuracy issue with a digipen. So obviously the computer tries to pick up what’s written and turn it into usable data. There is an element of error there.
Site 4, Int 4
Although the system’s simplicity was one of its benefits, clinicians still experienced some problems with the pen as batteries went flat without anyone noticing. Pens were also fairly easy to lose or to accidentally put in the washing machine. The pen recorded the time when something was written, which was reported as causing problems if information such as drugs administered was recorded at the time, and then details such as observations were filled in later, as it appeared that the drugs had been given before the proper assessments had been carried out, as reported in Box 9.
There had been concerns that the introduction of the digipen would have a negative impact on time on scene, but because it had not particularly changed clinicians’ way of working, it had not extended the time they spent on scene.
One of the problems with this specific electronic system and due to the nature of this job, it’s not always possible to write patient details and treat at the same time when you work alone. So the second crew in effect ‘started’ writing first (according to the digipen) but this was at a much later time after [paramedic] had already assessed the patient, taken observations and then treated the patient accordingly. Thus making it appear (timewise) as though [paramedic] had not checked the patient’s vital observations in advance of administering the drug.
At an organisational level, we heard of frustration that, for the full benefits of an electronic system to be realised, they would need to link up with other parts of the health service so that data could be transferred electronically. However, senior managers recognised that this would require significant investment in the digital infrastructure of the ambulance service so that their technology could be linked up and then connected to other parts of the NHS, possibly using a patient’s NHS number to access previous medical records:
We know that connectivity is kind of like a foundation that you need to have to be able to reap any benefit from any kind of more electronic record type thing floating around in that vehicle.
Site 4, Int 4
Chapter 6 Results: analysis of routine data from case study sites
Introduction
We requested a 2-month snapshot of data on responses by our case study ambulance services to emergency calls. We had a number of aims: to understand more about the nature of the data sets created by ambulance services and how they compared across services; to profile activity in each case study service to provide context; to assess what proportion of attendances resulted in the generation of an EHR; to see what characteristics might be related to an EHR being produced (assuming that the rate of EHR generation was < 100%); and to see if there was any useful learning from the data in relation to care for the tracer conditions.
We requested a consecutive series of data on calls received, resources allocated and EHRs generated, with patient-identifying information removed, from our four case study areas for January and February 2017. Further details of the data requested are provided in Chapter 3. Box 10 gives definitions relevant to the presentation and analysis of the data.
Call or incident: call to the 999 call centre.
CAD: computer-aided dispatch system (as used in 999 call centre to support call centre staff to process calls). All sites used AMPDS.
Arrived at scene: a resource arrived at the scene of the incident (we only include cases where a date/time was recorded in the appropriate ‘at scene date/time’ data field).
Arrived at patient: resource arrived at scene and patient contact was made.
Resource: vehicle and crew (e.g. ambulance or RRV).
In hours: 08.00 to 18.29, Monday to Friday.
Out of hours: 18.30 to 07.59, Monday to Friday, plus all day Saturday and Sunday and bank holidays.
Weekend: Saturday and Sunday.
Night: 18.30 to 07.59.
Job cycle time: start to finish time for a resource allocated to a call. Measured by the time between resource allocation, and resource cleared or stood down.
Disposition: disposition summary (outcome of call, i.e. what happened to the patient).
AMPDS, Advanced Medical Priority Dispatch System.
Description of the data sets provided in each site
Table 14 summarises the data supplied by each service. Although we made the same request to each site, there were many key points of difference in the data they provided. For example, all four sites at that time used different categories to indicate response priority for calls, as shown in Box 11; AS3 was transitioning between priority systems, which is reflected in the higher number of categories listed. There was also a large range in the number of variables provided. These differences may exist for sound reasons, reflecting different practices and contexts for each site. However, this diversity demonstrates some of the challenges to carrying out comparative analysis using ‘big data’.
| Data set | Ambulance service | |||
|---|---|---|---|---|
| AS1a | AS2b | AS3b | AS4a | |
| CAD (calls/incident) data set (number of calls in period) | 135,941 | 129,233 | 120,042 | 66,217 |
| Telephone advice/hear and treat | NA | 12,390 | 11,991 | NA |
| No resource allocated | NA | 17,381 | 9700 | NA |
| Resources data set (number of resources allocated) | 204,003 | 158,765 | 158,888 | 127,722 |
| Number of calls for which one or more resource was allocated | 135,941 | 111,852 | 110,342 | 66,217 |
| EHR data set (number created) | 125,225 | 33,424 | 225,629 | 60,713 |
-
Purple.
-
Red.
-
Amber.
-
Green.
-
Red 1.
-
Red 2.
-
Green 1.
-
Green 2.
-
Green 3.
-
Green 4.
-
Emergency purple.
-
Emergency red.
-
Emergency yellow.
-
Yellow.
-
Emergency amber.
-
Emergency green.
-
Emergency (no colour).
-
Urgent.
-
Routine.
-
Red.
-
Amber 1.
-
Amber 2.
-
Green 2.
-
Green 3.
AS2 and AS3 supplied data sets that included all calls, including those resolved over the telephone. AS1 and AS4 supplied data for calls where a resource was allocated only; in addition to the calls on which we had data, these services would have received calls that were resolved without an ambulance being sent. The CAD data supplied by AS1 did not include information on the age and gender of patients, although all other data sets did include this information.
Profile of calls
Although each ambulance service used a different set of priority categories, they all followed the same principle of identifying a small group of patients with immediately life-threatening problems who required the fastest response. Figure 6 shows the proportion of calls allocated to each priority category, by service.
FIGURE 6.
Proportion of calls allocated to each priority category, by service. (a) AS1; (b) AS2; (c) AS3; and (d) AS4.
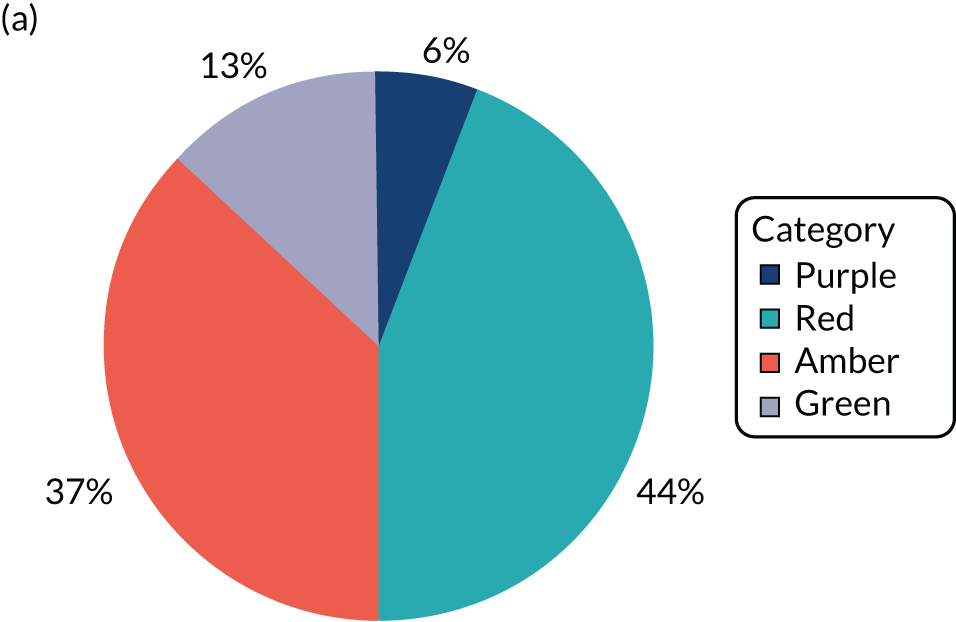
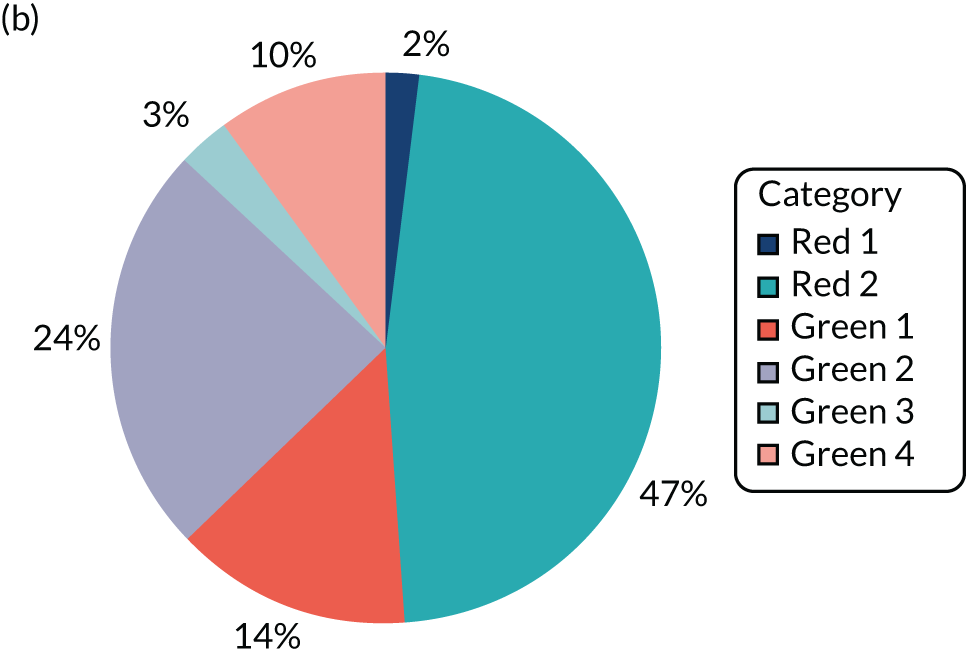
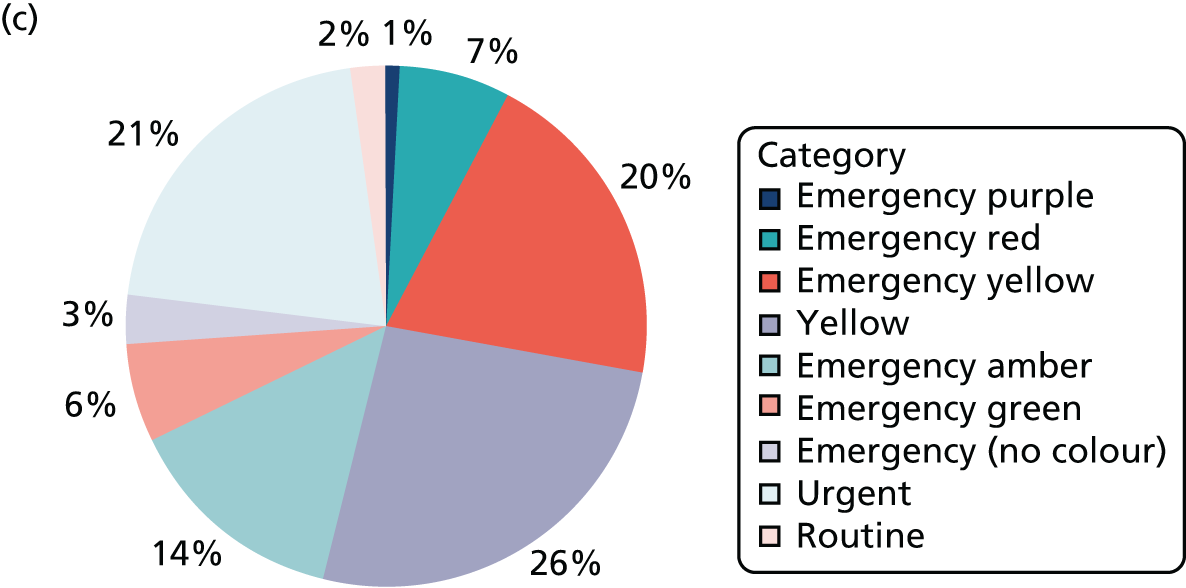

As shown in Table 15, all services showed a slightly uneven spread of demand across the week, with Sundays and Mondays being the busiest days for all services. In the two services for which we were able to obtain these data, a majority of calls were received during the ‘out-of-hours’ period rather than ‘in hours’.
| Call times | Ambulance service, n (%) | |||
|---|---|---|---|---|
| AS1 | AS2 | AS3 | AS4 | |
| Day of week | ||||
| Monday | 20,755 (15.5) | 20,075 (15.5) | 19,320 (16.1) | 10,213 (15.4) |
| Tuesday | 17,821 (13.3) | 19,216 (14.9) | 18,072 (15.1) | 9921 (15.0) |
| Wednesday | 17,913 (13.4) | 17,068 (13.2) | 15,724 (13.1) | 9002 (13.6) |
| Thursday | 17,619 (13.2) | 16,959 (13.1) | 15,542 (12.9) | 8867 (13.4) |
| Friday | 17,756 (13.3) | 17,000 (13.2) | 16,565 (13.8) | 8997 (13.6) |
| Saturday | 19,403 (14.5) | 17,717 (13.7) | 15,919 (13.3) | 8864 (13.4) |
| Sunday | 22,335 (16.7) | 21,198 (16.4) | 18,900 (15.7) | 10,353 (15.6) |
| In/out of hours | ||||
| In hours | Not available | 50,685 (39.2) | 50,677 (42.2) | Not available |
| Out of hours | Not available | 78,548 (60.8) | 69,365 (57.8) | Not available |
Table 16 summarises call disposition, that is, what response was provided to the patient. It indicates that in a proportion of cases (ranging from 4.3% in AS1 to 8.9% in AS4), no ambulance resource arrived at the scene with a patient. Rates of conveyance of patients to hospital or another facility ranged from 64.5% in AS1 to 73.2% in AS3.
| Disposition | Ambulance service, n (%) | |||
|---|---|---|---|---|
| AS1 | AS2 | AS3 | AS4 | |
| (At least one) resource allocated (n) | 135,941 | 111,852 | 110,342 | 66,217 |
| (At least one) resource arrived at scene | 130,155 (95.7) | 103,546 (92.6) | 103,517 (93.8) | 60,356 (91.1) |
| One or more patients treated at scene (and not conveyed) | No data | 25,608 (22.9) | 14,941 (18.1) | 7400 (11.2) |
| Patient conveyed | 87,614 (64.5) | 76,007 (67.9) | 80,856 (73.2) | 43,322 (65.4) |
Table 17 provides a summary of the patient demographics, based on data received through the call centre for AS2, AS3 and AS4, but on EHR data for AS1, as no CAD data were supplied. It shows that in all services but AS4, the biggest patient group by age was those aged ≥ 65 years. There were particularly high levels of missing CAD data for age in AS2 (37.8%). The highest level of missing CAD data for gender was in AS3 (9.2%).
| Patient characteristic | Ambulance service | |||
|---|---|---|---|---|
| AS1 (EHR data) | AS2 (CAD data) | AS3 (CAD data) | AS4 (CAD data) | |
| Age (years) | ||||
| Minimum, maximum | 0, 109a | 0, 109 | 0, 106a | 0, 108 |
| Mean, median | 59.28, 67 | 59.99, 68 | 59.12, 65 | 61.03, 69 |
| Child (0–17), n (%) | 10,615 (7.8) | 5167 (4.9) | 6604 (6.4) | 2288 (3.5) |
| Adult (18–64), n (%) | 45,159 (33.2) | 25,504 (24.0) | 42,801 (41.3) | 37,580 (56.8) |
| Adult (≥ 65), n (%) | 62,386 (45.9) | 35,336 (33.3) | 49,857 (48.2) | 23,137 (34.9) |
| Missing, n (%) | 17,781 (13.1) | 40,139 (37.8) | 4255 (4.1) | 3212 (4.9) |
| Gender, n (%) | ||||
| Female | 63,250 (53.9) | 55,268 (52.1) | 48,061 (46.4) | 33,717 (50.9) |
| Male | 54,346 (46.0) | 49,057 (46.2) | 45,891 (44.3) | 30,336 (45.8) |
| Missing | 564 (0.5) | 1821 (1.7) | 9565 (9.2) | 2164 (3.3) |
| Total (N) | 135,941 | 106,146 | 103,517 | 66,217 |
Generation and completion of electronic health records
Table 18 indicates the number of EHRs generated in each site, and the number of calls attended that resulted in at least one EHR. The lowest rate was in AS2, which had not yet transitioned to the new EHR system at the time of this data sample. Rates of generation of EHRs in AS1 and AS4 were 90.8% and 77.9%, respectively. The rate of 105.8% in AS3 is accounted for by an EHR being automatically started at the time a resource was dispatched, so it still existed on the system even if the resource stood down without attending the patient.
| Item | Ambulance service | |||
|---|---|---|---|---|
| AS1 | AS2 | AS3 | AS4 | |
| Number of calls for which resource arrived at scene | 130,155 | 103,546 | 103,517 | 60,356 |
| Number of paper patient records created | Not supplied | 67,421a | Not recorded | Not supplied |
| Number of EHRs created | 125,225 | 33,424 | 225,629 | 60,712 |
| Number of calls resulting in at least one EHR | 118,160 | 32,981 | 109,502 | 47,033 |
| Proportion of calls attended resulting in generation of EHRs, n/N (%) | 118,160/130,155 (90.8) | 32,981/103,546 (31.8) | 109,502/103,517 (105.8) | 47,033/60,356 (77.9) |
We examined how many key fields were completed on each EHR once it had been generated. As shown in Table 19, it was challenging to compare this across the four services as the only fields that were supplied to us from all four EHR systems were age and gender, both of which, as might be expected, showed higher completion rates from the face-to-face encounter recorded on the EHRs than from the CAD data, which are collected over the phone. For some fields, there was a striking variation between sites: details of the patient’s illness or condition [expressed as clinical impression/final Advanced Medical Priority Dispatch System (AMPDS) code/provisional diagnosis] were recorded on < 50% of EHRs in AS3 and AS4, but twice that rate in AS1 and AS2.
| Data field | Ambulance service, n (%) | |||
|---|---|---|---|---|
| AS1 (N = 125,225) | AS2 (N = 33,424) | AS3 (N = 225,629) | AS4 (N = 60,712) | |
| Patient ID | NA | 33,424 (100) | NA | NA |
| Call number | 125,225, of which 4035 had ‘no’ entered in the field for call number | 33,424 | 225,629 | 3513 records with verified incident numbersa |
| Clinical impression/final AMPDS code/provisional diagnosis | 113,381 (90.5) | 33,424 (100) | 102,805 (45.6) | 26,723 (44.0) |
| Location | 54,609 (43.6) | 25,411 (76.0) | NA | NA |
| Crew position | NA | 33,424 (100) | 224,977 (99.7) | 59,030 (97.2) |
| Time at patient | NA | 9266 (27.7) | 179,131 (79.4) | 51,500 (84.8) |
| Age | 120,736 (96.4) | 33,263 (99.5) | 213,069 (94.4) | 52,636 (86.7) |
| Gender | 121,960 (97.4) | 31,080 (93.0) | 205,036 (90.9) | 55,695 (91.73) |
| Ethnicity | NA | Not supplied (but advised low completion) | 23,377 (10.4) | 21,367 (35.2) |
Characteristics associated with generation of electronic health records, by site
We conducted logistic regressions exploring whether or not certain characteristics were associated with the generation of EHRs. Factors are described in three sections: Electronic health record generation by call characteristics, Electronic health record generation by ambulance service processes and Electronic health record generation by patient characteristics.
Electronic health record generation by call characteristics
Time and day when call was received
In Figure 7, we indicate rates of generation of EHRs by day of the week, which showed little variation across services. We calculated odds ratios for EHR generation by day (presented in Appendix 8), which confirmed that there was no significant variation; that is, an EHR was equally likely to be generated on each day of the week.
FIGURE 7.
Percentage of attended calls resulting in generation of an EHR, by day, for each ambulance service.
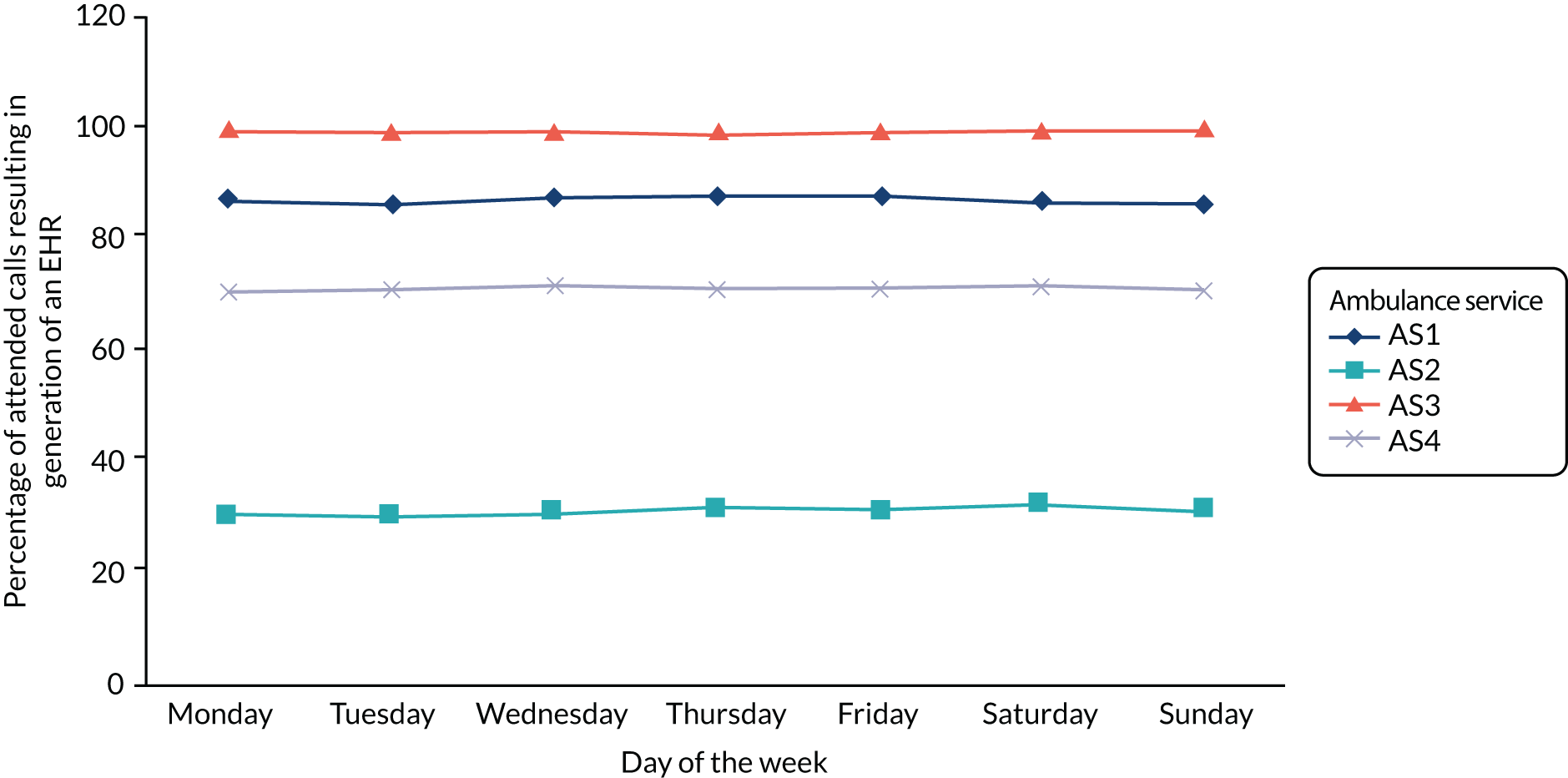
Data were collected over a 9-week period. Because three out of four sites were in a process of transition in terms of record system, we were interested to see whether or not rates of completion changed over that time, as systems became more embedded. In Figure 8, we show rates of generation of EHRs by sample week, over the sample period, by ambulance service. Although we found some variation week to week, there was no clearly discernible or consistent trend across the sites. There was no indication of a consistent relationship across sites between EHR completion and the calendar within our snapshot of the data. Full data, including odds ratios, are presented in Appendix 7.
FIGURE 8.
Percentage of attended calls resulting in generation of an EHR, by sample week, for each ambulance service.

We examined how generation of EHRs varied according to whether the call was received during regular hours or out of hours (AS2 and AS3); for AS1 and AS4, where the data had been coded differently, we compared calls made during the day versus during the night. As shown in Table 20, we found that in AS1, AS2 and AS3, EHRs were more likely to be created during night-time/out-of-hours calls than during daytime/regular hours calls, and the difference was statistically significant. The effect was much more pronounced in AS3. In AS4, EHRs were slightly more likely to be generated in the day, but the effect was not statistically significant.
| Time (Number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS1 | ||||
| Day (74,311) | 64,326 (86.6) | 0.933 | 0.904 to 0.963 | < 0.001 |
| Night (61,630) | 53,834 (87.4) | 1 | – | – |
| AS2 | ||||
| In hours (42,975) | 12,796 (29.8) | 0.910 | 0.886 to 0.935 | < 0.001 |
| Out of hours (63,171) | 20,073 (31.8) | 1 | – | – |
| AS3 | ||||
| In hours (43,823) | 43,393 (99.0) | 0.563 | 0.487 to 0.650 | < 0.001 |
| Out of hours (59,694) | 59,363 (99.4) | 1 | – | – |
| AS4 | ||||
| Day (36,802) | 26,232 (71.3) | 1.028 | 0.994 to 1.063 | 0.113 |
| Night (29,415) | 20,801 (70.7) | 1 | – | – |
Call priority
We examined whether or not there was any difference in likelihood of generating an EHR according to the priority category allocated to the call in the ambulance control centre. In all services, there were significant differences by call priority. As shown in Table 21, the category for which an EHR was least likely to be generated was the lowest-priority category, which would include, for example, transfers to hospital in response to a GP call and taking a patient home from hospital.
| Priority category (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS1 | ||||
| Purple (8633) | 7368 (85.4) | 1 | – | – |
| Red (59,818) | 55,464 (92.7) | 2.187 | 2.045 to 2.339 | < 0.001 |
| Amber (49,265) | 44,063 (89.4) | 1.454 | 1.361 to 1.553 | < 0.001 |
| Green (16,978) | 11,049 (65.1) | 0.320 | 0.299 to 0.342 | < 0.001 |
| AS2 | ||||
| Red 1 (2734) | 860 (31.5) | 1.012 | 0.932 to 1.099 | 0.774 |
| Red 2 (55,659) | 17,363 (31.2) | 1 | – | – |
| Green 1 (16,373) | 5145 (31.4) | 1.011 | 0.973 to 1.049 | 0.579 |
| Green 2 (23,931) | 8290 (34.6) | 1.169 | 1.132 to 1.207 | < 0.001 |
| Green 3 (1087) | 305 (28.1) | 0.860 | 0.753 to 0.983 | 0.027 |
| Green 4 (5559) | 905 (16.3) | 0.429 | 0.399 to 0.462 | < 0.001 |
| AS3 | ||||
| Purple (1282) | 1282 (100.0) | NA | – | 0.989 |
| Red (7890) | 7866 (99.7) | 1.731 | 0.846 to 3.539 | 0.133 |
| Yellow (52,726) | 52,614 (99.8) | 2.481 | 1.333 to 4.615 | 0.004 |
| Amber (16,789) | 16,747 (99.7) | 2.106 | 1.082 to 4.096 | 0.028 |
| Green (2094) | 2083 (99.5) | 1 | – | – |
| AS4 | ||||
| Red (3644) | 2823 (77.5) | 1 | – | – |
| Amber 1 (29,235) | 23,394 (80.0) | 1.165 | 1.072 to 1.265 | < 0.001 |
| Amber 2 (17,412) | 11,948 (68.6) | 0.636 | 0.585 to 0.692 | < 0.001 |
| Green 2 (5451) | 3197 (58.7) | 0.412 | 0.375 to 0.453 | < 0.001 |
| Green 3 (10,475) | 5671 (54.1) | 0.343 | 0.315 to 0.374 | < 0.001 |
For two services (AS1 and AS4), we found that there was a clear and statistically significant pattern. The category for which an EHR was most likely to be generated was the large group (red in the case of AS1, amber 1 for AS4) that fell into the second-most urgent category, requiring an immediate response, and would include patients with conditions such as chest pain, suspected stroke and seizures. The smaller group of immediately life-threatening problems, such as not breathing, cardiac arrest or choking, is allocated the highest-priority response; in AS1 and AS4, they were slightly less likely to have an EHR generated than the next priority group. In both services, the likelihood of an EHR being generated then reduced as the priority of response reduced.
AS2 showed a similar marked drop-off in EHR completion rates for their two lowest-priority categories. Completion rates, however, were similar for red 1, red 2 and green 1 calls, but showed a slight peak for green 2 calls. In AS4, the lowest-priority category showed a slightly, but statistically significant, lower completion rate, but rates were flat in the other categories.
Electronic health record generation by ambulance service processes
Call disposition
We examined whether or not there was an association between an EHR being generated and the patient being conveyed to hospital. As shown in Table 22, in three ambulance services, patients were markedly more likely to have an EHR generated if they were conveyed to hospital. In AS3, the reverse was true: patients were more likely to have an EHR generated if they were not conveyed, although the difference was small. This association was statistically significant in all sites.
| Disposition (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS1 | ||||
| Conveyed to hospital (87,614) | 81,201 (92.7) | 1 | – | – |
| Treated at scene, not conveyed (48,327) | 36,959 (76.5) | 0.257 | 0.248 to 0.265 | < 0.001 |
| AS2 | ||||
| Conveyed to hospital (76,007) | 24,073 (31.7) | 1 | – | – |
| Treated at scene and not conveyed (27,726) | 8381 (30.2) | 0.935 | 0.907 to 0.963 | < 0.001 |
| Treat and refer (1324) | 343 (25.9) | 0.153 | 0.120 to 0.194 | < 0.001 |
| Other (1089) | 72 (6.6) | 0.935 | 0.907 to 0.963 | < 0.001 |
| AS3 | ||||
| Conveyed to hospital (80,856) | 80,196 (99.2) | 1 | – | – |
| Treated at scene and not conveyed (14,941) | 14,898 (99.7) | 2.851 | 2.093 to 3.884 | < 0.001 |
| Other (6552) | 6504 (99.3) | 1.115 | 0.831 to 1.496 | 0.468 |
| AS4 | ||||
| Conveyed to hospital (43,355) | 34,377 (79.3) | 1 | – | – |
| Treated at scene, not conveyed (22,862) | 12,656 (55.4) | 0.324 | 0.313 to 0.335 | < 0.001 |
Job cycle time
For AS2 and AS3, we were able to examine the relationship between job cycle time and likelihood of an EHR being generated, as shown in Table 23. These data were not available for AS1 and AS4. In AS3, there was a statistically significant association between increased job cycle time and decreased likelihood of an EHR being generated, although the absolute differences were small. The situation in AS2 was quite different. Here, the likelihood of an EHR being generated was higher with increased job cycle times, except that the longest job cycle times showed a lower completion rate than for those in the third quartile.
| Job cycle time (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS2 | ||||
| Q1 (≤ 45 minutes) (38,023) | 10,580 (27.8) | 0.843 | 0.817 to 0.869 | < 0.001 |
| Q2 (46–77 minutes) (38,138) | 11,649 (30.5) | 0.961 | 0.932 to 0.991 | 0.012 |
| Q3 (78–104 minutes) (37,988) | 12,985 (34.2) | 1.135 | 1.101 to 1.170 | < 0.001 |
| Q4 (> 104 minutes) (37,444) | 11,755 (31.4) | 1 | – | – |
| Total (151,593) | 46,969 (31.0) | |||
| AS3 | ||||
| Q1 (≤ 19 minutes) (37,020) | 36,962 (99.8) | 1 | – | – |
| Q2 (20–63 minutes) (37,384) | 37,226 (99.6) | 0.370 | 0.274 to 0.500 | < 0.001 |
| Q3 (64–88 minutes) (36,473) | 36,311 (99.6) | 0.352 | 0.260 to 0.475 | < 0.001 |
| Q4 (≥ 89 minutes) (36,278) | 35,842 (98.8) | 0.129 | 0.098 to 0.170 | < 0.001 |
| Total (147,155) | 146,341 (99.4) | |||
Destination hospital
For AS2 and AS3, we were able to examine the relationship between destination hospital to which the patient was conveyed and likelihood of an EHR being generated, as shown in Table 24. These data were not available for AS1 and AS4. We included in our analysis only hospitals to which the service conveyed ≥ 3000 patients in the sample time period. In AS2, there was enormous variation between rates of generation of EHRs by hospital, from 61.3% to 2.6%. There was less variation in AS3 (99.1% to 99.9%), but variation did reach statistical significance.
| Hospital (≥ 3000 conveyances) (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS2 | ||||
| Hospital 1 (4055) | 585 (14.4) | 0.107 | 0.097 to 0.118 | < 0.001 |
| Hospital 2 (4547) | 2181 (48.0) | 0.586 | 0.546 to 0.629 | < 0.001 |
| Hospital 3 (3499) | 481 (13.7) | 0.101 | 0.091 to 0.112 | < 0.001 |
| Hospital 4 (5299) | 140 (2.6) | 0.017 | 0.015 to 0.021 | < 0.001 |
| Hospital 5 (5984) | 2535 (42.4) | 0.467 | 0.438 to 0.498 | < 0.001 |
| Hospital 6 (9330) | 2404 (25.8) | 0.221 | 0.208 to 0.234 | < 0.001 |
| Hospital 7 (4923) | 720 (14.6) | 0.109 | 0.100 to 0.119 | < 0.001 |
| Hospital 8 (5198) | 319 (6.1) | 0.042 | 0.037 to 0.047 | < 0.001 |
| Hospital 9 (10,610) | 6486 (61.1) | 1 | – | – |
| Hospital 10 (8512) | 5220 (61.3) | 1.008 | 0.951 to 1.069 | 0.784 |
| Hospital 11 (3034) | 1236 (40.7) | 0.437 | 0.403 to 0.475 | < 0.001 |
| Total (64,991) | 22,307 (34.3) | |||
| AS3 | ||||
| Hospital 1 (16,110) | 16,086 (99.9) | 1 | – | – |
| Hospital 2 (8755) | 8735 (99.8) | 0.652 | 0.360 to 1.180 | 0.158 |
| Hospital 3 (4284) | 4276 (99.8) | 0.797 | 0.358 to 1.776 | 0.580 |
| Hospital 4 (6456) | 6419 (99.4) | 0.259 | 0.155 to 0.433 | < 0.001 |
| Hospital 5 (3068) | 3062 (99.8) | 0.761 | 0.311 to 1.864 | 0.551 |
| Hospital 6 (7114) | 7090 (99.7) | 0.441 | 0.250 to 0.777 | 0.005 |
| Hospital 7 (11,659) | 11,618 (99.6) | 0.423 | 0.255 to 0.700 | < 0.001 |
| Hospital 8 (5326) | 5317 (99.8) | 0.881 | 0.409 to 1.897 | 0.747 |
| Hospital 9 (8086) | 8052 (99.6) | 0.353 | 0.209 to 0.596 | < 0.001 |
| Hospital 10 (5680) | 5669 (99.8) | 0.769 | 0.376 to 1.571 | 0.471 |
| Hospital 11 (8271) | 8248 (99.7) | 0.535 | 0.302 to 0.948 | 0.032 |
| Hospital 12 (15,781) | 15,692 (99.4) | 0.263 | 0.168 to 0.413 | < 0.001 |
| Hospital 13 (4108) | 4088 (99.5) | 0.305 | 0.168 to 0.553 | < 0.001 |
| Hospital 14 (6446) | 6386 (99.1) | 0.159 | 0.099 to 0.255 | < 0.001 |
| Hospital 15 (4283) | 4274 (99.8) | 0.709 | 0.329 to 1.525 | 0.378 |
| Hospital 16 (5833) | 5789 (99.2) | 0.196 | 0.119 to 0.323 | < 0.001 |
| Total (121,260) | 120,801 (99.6) | |||
By locality
For AS2 and AS3, we examined the relationship between ambulance station locality where the crew were based and likelihood of an EHR being generated, as shown in Table 25. These data were not available for AS1 and AS4. In AS2, there was enormous variation between rates of generation of EHRs by locality, from 58.2% to 1.5%. There was less variation in AS3 (ranging from 98.6% to 100% between localities), but variation did reach statistical significance in relation to seven of the localities.
| Ambulance station locality (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS2 | ||||
| A locality (8344) | 730 (8.7) | 0.075 | 0.069 to 0.081 | < 0.001 |
| B locality (10,674) | 165 (1.5) | 0.012 | 0.010 to 0.014 | < 0.001 |
| C locality (13,913) | 5838 (42.0) | 0.565 | 0.540 to 0.591 | < 0.001 |
| D locality (17,253) | 3529 (20.5) | 0.201 | 0.192 to 0.211 | < 0.001 |
| E locality (10,225) | 2692 (26.3) | 0.279 | 0.265 to 0.294 | < 0.001 |
| F locality (16,618) | 6434 (38.7) | 0.494 | 0.473 to 0.515 | < 0.001 |
| G locality (10,716) | 3575 (33.4) | 0.391 | 0.372 to 0.411 | < 0.001 |
| H locality (16,712) | 9734 (58.2) | 1.090 | 1.045 to 1.137 | < 0.001 |
| I locality (8119) | 2149 (26.5) | 0.281 | 0.266 to 0.298 | < 0.001 |
| J locality (112,10) | 572 (5.1) | 0.042 | 0.038 to 0.046 | < 0.001 |
| K locality (8294) | 954 (11.5) | 0.102 | 0.094 to 0.109 | < 0.001 |
| L locality (18,612) | 10,448 (56.1) | 1 | – | – |
| Total (150,690) | 46,820 (31.1) | |||
| AS3 | ||||
| A locality (11,546) | 11,477 (99.4) | 1 | – | – |
| B locality (5032) | 4979 (98.9) | 0.565 | 0.394 to 0.809 | 0.002 |
| C locality (3369) | 3369 (100.0) | – | – | 0.981 |
| D locality (3355) | 3340 (99.6) | 1.339 | 0.765 to 2.343 | 0.307 |
| E locality (3112) | 3104 (99.7) | 2.333 | 1.121 to 4.855 | 0.024 |
| F locality (3567) | 3556 (99.7) | 1.944 | 1.027 to 3.676 | 0.041 |
| G locality (5247) | 5219 (99.5) | 1.121 | 0.721 to 1.741 | 0.612 |
| H locality (3577) | 3576 (100.0) | – | – | 0.002 |
| I locality (4823) | 4819 (99.9) | 7.243 | 2.642 to 19.858 | < 0.001 |
| J locality (4394) | 4245 (96.6) | 0.171 | 0.128 to 0.228 | < 0.001 |
| K locality (2830) | 2827 (99.9) | 5.665 | 1.782 to 18.012 | 0.003 |
| L locality (3289) | 3267 (99.3) | 0.893 | 0.552 to 1.445 | 0.644 |
| M locality (3579) | 3578 (100.0) | – | – | 0.002 |
| N locality (3942) | 3938 (99.9) | 5.919 | 2.159 to 16.229 | 0.001 |
| O locality (4460) | 4396 (98.6) | 0.413 | 0.293 to 0.581 | < 0.001 |
| Total (N = 66,122) | 65,690 (99.3) | 0.002 | ||
Electronic health record generation by patient characteristics
Age
For AS2, AS3 and AS4, we found that all sites showed broadly similar patterns of EHR generation being more likely with higher age category, as shown in Table 26. Since the only age data for AS1 were from the EHRs, not CAD, we could not study age as a predictor of EHR generation in that site.
| Age in years (CAD data) (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS2 | ||||
| Child (0–17) (5167) | 2361 (45.7) | 0.862 | 0.813 to 0.914 | < 0.001 |
| Adult (18–64) (25,504) | 12,583 (49.3) | 0.997 | 0.966 to 1.030 | 0.862 |
| Adult (≥ 65) (35,336) | 17,459 (49.4) | 1 | – | – |
| Total (66,007) | 32,403 (49.1) | |||
| Missing (40,139) | 466 (1.2) | |||
| AS3 | ||||
| Child (0–17 years) (6604) | 6339 (96.0) | 1 | – | – |
| Adult (18–64 years) (42,801) | 42,631 (99.6) | 10.483 | 8.631 to 12.733 | < 0.001 |
| Adult (≥ 65 years) (49,857) | 49,583 (99.5) | 7.565 | 6.377 to 8.975 | < 0.001 |
| Total (99,262) | 98,553 (99.3) | |||
| Missing (4255) | 4203 (98.8) | |||
| AS4 | ||||
| Child (0–17 years) (2288) | 1613 (70.5) | 1 | – | – |
| Adult (18–64 years) (37,580) | 26,174 (69.7) | 0.960 | 0.875 to 1.053 | 0.391 |
| Adult (≥ 65 years) (23,137) | 17,413 (75.3) | 1.273 | 1.158 to 1.399 | < 0.001 |
| Total (63,005) | 45,200 (71.7) | |||
| Missing (3212) | 1833 (57.1) | |||
Gender
As for AS1, gender data were available only from the EHRs, not CAD, so could not be used in the regression analysis. EHR creation was less common with male patients, but this was only significantly different in AS4, as shown in Table 27.
| Gender (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS2 | ||||
| Male (49,057) | 15,206 (31.0) | 0.981 | 0.956 to 1.007 | 0.157 |
| Female (55,268) | 17,356 (31.4) | 1 | – | – |
| Total (104,325) | 32,562 (31.2) | |||
| Missing (1821) | 307 (16.9) | |||
| AS3 | ||||
| Male (48,061) | 45,655 (99.5) | 0.906 | 0.754 to 1.088 | 0.290 |
| Female (45,891) | 47,837 (99.5) | 1 | – | – |
| Total (93,952) | 93,492 (99.5) | |||
| Missing (9565) | 9264 (96.9) | |||
| AS4 | ||||
| Male (30,336) | 21,488 (70.8) | 0.939 | 0.907 to 0.971 | < 0.001 |
| Female (33,717) | 24,318 (72.1) | 1 | – | – |
| Total (64,053) | 45,806 (71.5) | |||
| Missing (2164) | 1227 (56.7) | |||
Tracer conditions
Tracer conditions were based on the AMPDS codes recorded in the CAD data. The codes used are 13 for diabetes-related incidents, 17 for falls and 25 in relation to mental health (psychiatric/abnormal behaviour/suicide attempt). As shown in Table 28, there were no consistent patterns across the sites. In AS1 and AS4, mental health cases had much lower EHR creation rates. There were no other statistically significant differences in AS4, but AS1 showed higher EHR creation rates for falls and diabetes-related incidents than for non-tracer conditions. AS2 and AS3 showed a different pattern, with falls having a significantly higher rate of generation of EHRs.
| Condition recorded on CAD (N) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| AS1 | ||||
| Non-tracer condition (129,250) | 112,269 (86.9) | 1 | – | – |
| Diabetes related (457) | 415 (90.8) | 1.495 | 1.088 to 2.054 | 0.013 |
| Falls related (5391) | 4865 (90.2) | 1.399 | 1.277 to 1.533 | < 0.001 |
| Mental health related (843) | 611 (72.5) | 0.398 | 0.342 to 0.464 | < 0.001 |
| Total (135,941) | 118,160 (86.9) | |||
| AS2 | ||||
| Non-tracer condition (95,876) | 29,308 (30.6) | 1 | – | |
| Diabetes related (825) | 250 (30.3) | 0.988 | 0.851 to 1.146 | 0.869 |
| Falls related (8269) | 2952 (35.7) | 1.261 | 1.203 to 1.322 | < 0.001 |
| Mental health related (1176) | 359 (30.5) | 0.998 | 0.881 to 1.131 | 0.976 |
| Total (106,146) | 32,869 (31.0) | |||
| AS3 | ||||
| Non-tracer condition (92,505) | 91,766 (99.2) | 1 | – | – |
| Diabetes related (816) | 815 (99.9) | 6.563 | 0.922 to 46.711 | 0.060 |
| Falls related (8442) | 8428 (99.8) | 4.848 | 2.856 to 8.230 | < 0.001 |
| Mental health related (1754) | 1747 (99.6) | 2.010 | 0.953 to 4.237 | 0.067 |
| Total (103,517) | 102,756 (99.3) | |||
| AS4 | ||||
| Non-tracer condition (55,730) | 39,705 (71.3) | 1 | – | – |
| Diabetes related (505) | 373 (73.9) | 1.140 | 0.934 to 1.392 | 0.196 |
| Falls related (8364) | 6016 (71.9) | 1.034 | 0.983 to 1.088 | 0.198 |
| Mental health related (1618) | 939 (58.0) | 0.558 | 0.505 to 0.617 | < 0.001 |
| Total (66,217) | 47,033 (71.0) | |||
Summary and key points
We found that different sites recorded information in different ways, using different fields and different priority categorisation systems; this made it challenging to compare across sites.
All services faced similar challenges in terms of patterns of demand. There were very different levels of EHR creation across the case study sites, from fewer than one-third of calls in AS2 (which had not yet started phasing in its new system at the time of the data sample) to > 99% in AS3, the longest established user of EHRs. Multiple generations of EHRs on dispatch complicate the picture, as each call may result in a number of EHRs being generated. We found that, even when an EHR was generated, not all fields would necessarily be completed.
We analysed rates of EHR creation by a range of variables:
-
Time of completion. In three out of four sites, marginally fewer records were created within routine hours/daytime compared with evenings, nights and weekends, although there was no difference in the fourth site. By day of the week, there were no consistent results.
-
Week of completion. We found no clear pattern. In two sites, record creation was lowest in week 1 (1–7 January 2017) and higher in later weeks. A third site showed lower rates throughout the first half of the period. However, AS1 showed a very different pattern, with the lowest creation rates in February.
-
Call priority. We consistently saw that the lowest creation rates – markedly lower in three out of four sites – were in the least urgent categories.
-
Patient disposition. In three sites, record creation rates were higher when patients were conveyed to hospital, but the opposite was seen in AS3.
-
Patient characteristics. Record creation rates were generally highest for older people and lowest for children. There were no consistent differences in creation rates by gender.
-
Job cycle time. In the two sites for which we had such data, one site saw the fewest records created when the job cycle was shortest, whereas the other found the fewest created when the job cycle was longest.
-
Geography. In the two sites for which we had such data, there was variation by the hospital conveyed to and by ambulance station locality. Both of these variations were very marked in AS2.
-
Tracer conditions. There was no consistent pattern across the four sites. The main result was that, in AS1 and AS4, patients with mental health-related conditions were substantially less likely than those with non-tracer conditions to have an EHR created.
These independent variables are confounded with each other. For example, we would expect age and gender to be related. The biggest effects tended to be by geography and call priority, and these may explain other observed effects.
Chapter 7 Results: comparison and cross-cutting themes
Introduction
In this chapter, we present comparative data and discussion from the case study sites in relation to two broad areas: implementation of the EHRs into practice and the impact that EHRs have had. In relation to implementation, we are informed by SST with a technological dimension, to examine the roles of the various agents and structures involved in implementation and to consider the relationships between them. In relation to impact, we return to the initial logic model that we presented in Chapter 3 and use it to frame our discussion of what change has resulted from the introduction of EHRs, and what might have supported or hindered that change.
Throughout this chapter, we look across all four case study sites and consider the similarities and differences between them, and what might account for the differences.
Implementation of electronic health records
What is the role and practice of the ambulance clinician in bringing electronic health records into use?
Ambulance clinicians are the key agents tasked with bringing EHRs into everyday use. We examined what they had to do to make it work, what motivated them to use the system and how they might resist or modify the intended model of implementation.
At site 4, where the digipen had been introduced, it seemed that the hopes of having a relatively seamless transition to the new system had been realised. Ambulance clinicians reported that it brought no significant change in practice:
No difference to us at all, ‘cause we’ve still got to fill out the [EHR] whether it be digital or biro or pencil or crayons.
Site 4, FG1, participant 2
In the other sites, we found a generally positive attitude towards new systems, a recognition that they did not represent a massive change in practice, and certainly no outright resistance. However, there was some suggestion that the process of bringing them into use was not entirely painless. In site 3, an ambulance clinician anticipated some reluctance from staff to engage with the second-generation system, as they had concerns about its predecessor. In site 1, one ambulance clinician reported what they felt had been the response among peers to the new system:
It’s mixed . . . it doesn’t matter what grade you are or what age you are, some love it and some hate it. Some don’t like it ‘cause it’s different to what they used to do. Some don’t like it ‘cause it’s not one page. Some don’t like it because the battery runs out really quickly.
Site 1, Int 5
As part of the process of the implementation of EHRs, staff in all sites had to undertake formal training. Logistical challenges to this were identified in all sites, for example:
In our busier areas . . . crews are not on stations for any length of time, they are literally on a 12-hour shift and they are out on the road for that whole 12-hour shift, just going from one job to the next, so downtime to complete training is difficult.
Site 3, Int 1
E-learning, sometimes in clinicians’ own time, was one option for training when shift patterns did not allow for formal training sessions. In site 2, clinicians who were asked to complete e-learning from home or an ambulance station reported some resistance to doing it. In another site where e-learning was meant to be taking place, we found that only one of the crews we observed had undertaken the training, and reported that they had not fully engaged with it, choosing instead to run the computer program while washing vehicles and then returning to the computer to answer the questions at the end. The crew members were critical of the new EHR system but admitted that their lack of engagement with training may have made their experience more negative.
Once ambulance clinicians started using a new EHR system, there was (except in site 4) still work involved in adapting to the new system. Whereas a paper form makes it immediately obvious which sections have already been completed, an EHR takes a little more effort to navigate, as one front-line clinician reported:
I do end up repeating things because I’ve forgotten that 20 minutes earlier I ticked that box, it’s taken me that long to go through the drop-down menu, I tend to write my comments bit last, by the time I get to that I’ve forgotten, or it doesn’t flow very well if I miss those bits out.
Site 2, FG5, participant 3
In site 2, a number of front-line clinicians expressed some scepticism about the new EHR system, and there was concern that if it proved slower than paper records, people might want to revert. However, it is important to remember that we were talking to people in the midst of change, and any concerns were likely to have been shaped by the disruption of transition as well as memories of problems with the first-generation system, and were likely to subside over time as people got used to the new system.
In the course of bringing EHRs into use, it seemed that ambulance clinicians developed their own variations in ways of using it, and also learnt from their peers to develop local practice. In site 1, one clinician commented on the way in which colleagues based in different stations would establish their own ways of doing things:
People who all work together very frequently have somewhat attained a kind of a bit of a crossover of how they do things . . . if you went to different stations now I reckon you would see patterns in how data is entered, what is entered, and when it’s entered, and the time it takes to do it . . . I reckon it’s different everywhere.
Site 1, FG1, participant 4
Although all EHR systems were designed to be used live, during patient contact, we found that this was not necessarily the case in practice. We also found that it was not a simple question of EHRs being used or not – instead, they were used in different ways (timing of data entry, order of data entry, use of free-text boxes, sharing of tasks between clinician). EHRs may have all fields completed, or some data missing.
Across all four sites, we observed that data were not always entered directly into the EHR system. Instead, observations would often be written on a glove or notebook, or stored in the paramedic’s memory, before being entered in the EHRs, just as has been traditionally done with paper records:
That’s one of the reasons I wear gloves, it’s just a notepad.
Site 4, observation 3, paramedic
The entry of data onto the EHR sometimes took place much later during the course of the patient contact than the point when the information was obtained. From our observations, it seemed that this should not be read as resistance to using the EHRs, but instead a response to the practical constraints on delivering care in the field.
What is the role of the organisational and political context in bringing electronic health records into use?
In our interviews and focus groups, much of the discussion about the role of the organisation in bringing EHRs into use concentrated on the training of front-line staff. All case study areas had offered training, although the amount varied across the sites. In several areas, there was a time lag between delivering training to clinicians and them being able to use the new device and software, which had an impact on how well clinicians were able to put their skills into practice.
Two services used ‘local champions’ to help support the implementation of EHRs. In site 3, these ‘super users’ were given a full day of training on the tablet being introduced before spending time in the ambulance stations in their local area:
They’d spend the day sitting there ‘right, how are you getting on with your e-learning’ and they would encourage the staff to get the e-learning done. They actually had a tablet with them and they would sit and let them play with it and give them hands-on information.
Site 3, Int 4
Managers in all sites discussed that, to ensure transition to EHRs, staff needed to be given a simple, clear message that they were mandatory. In site 2, this was clearly borne out of experience of implementing the first-generation of EHRs:
I think what we’ve learnt is that we have to make the system mandatory and used, we can’t make it optional.
Site 2, Int 1
For ambulance clinicians, though, it seemed that what was needed was something more than a simple mandate, but an organisational system that was designed to provide feedback to front-line staff and reassure them that the EHR was worth completing:
If we knew that information was going to be used . . . we might all be encouraged to use it . . . if we had the confidence to know that by using this new system, and using it properly, that would possibly sort some of those problems out, it might encourage people to use it.
Site 2, FG2, participant 3
Even before the point when ambulance services were working to encourage change in practice among clinicians, they had tasks to accomplish in terms of designing and specifying the system. Work on these tasks was not limited to only long-serving staff of the ambulance service: external collaborators were involved, as were project staff who may not have had the embedded experience of ambulance service operational requirements to ensure that these were met.
We noticed that there were sometimes differences in perspective between people involved in designing and planning the implementation of EHRs and those tasked with putting it into practice on the ground. For example, in site 2, managers reported that they had engaged widely with internal and external stakeholders in the development of the system, and to plan roll-out. However, a front-line ambulance clinician told a different story:
We’re going at it half-baked, we’re kind of going ‘oh yeah, we need to do this, let’s just run at it headlong’ instead of actually sorting it out and looking at it and getting it all in place and getting everything set up properly and then rolling it out. We’ve jumped straight in.
Site 2, FG1, participant 2
What is the role of the technology itself in bringing electronic health records into use?
For a new technology to become readily embedded into use, it needs to be easy to use, sufficiently similar to previous systems to be easy to learn, and reliable enough that people do not give up on it. We found that, broadly, the EHR systems being introduced were seen as reliable and user friendly. However, even though managers reported that the EHRs had been designed in such a way that they would not change the operational process for completing clinical records (Site 1, Int 2), it seemed that a shift to record-keeping model using drop-down boxes was having an effect on the work practices around data recording for clinicians. One manager from site 1 reported:
I think one of the things that we failed to acknowledge is that we spent the best part of 10 years teaching our staff that in order to make themselves safe and to cover themselves legally, they had to write in what’s known as the medicolegal model . . . so recording all the pertinent negatives as well as all of the things that you do find. And when you then move kind of pretty much wholesale overnight to a system where you have drop-down boxes and some of those things are implied as opposed to explicitly recorded, then people really balked at that.
Site 1, Int 9
These concerns were confirmed by a front-line clinician from the same site:
I’m very much in the school of if I haven’t written it down it hasn’t happened, which I find is a big problem . . . I have to physically write they haven’t got a headache, but what you need is a box saying ‘do they have a headache, yes or no,’ and you say no . . . you’re still having to write things.
Site 1, FG1, participant 4
Also relevant to the implementation process was the way in which the EHRs related to technology being used by other health-care providers. In each case study site, we heard how there were multiple systems in use, making integration difficult:
Every hospital you go to, or every GP surgery you go to, use different systems. If they use different systems they might not be compatible.
Site 1, Int 5
All of our case study services were to a greater or lesser extent transitioning from one system to another and one supplier to another. During our fieldwork period, we observed roll-out of new hardware and software in AS1 and AS2, and new software in AS3. AS4 had started initial discussions about a successor to its system. The progress from one system to another in AS2 had included a partial return to paper records, area by area, as the system was switched over.
Even where there was no major change to new hardware or to a new software supplier, systems were subject to constant minor upgrades. In AS2, for example, managers reported that they had learnt from their previous experience with EHRs and had chosen a records system that would be easier to update than the previous one, and they acknowledged that tweaks would be needed to keep the system up to date (Site 2, Int 6). The device itself had also been selected to be easier to update and adapt(Site 2, Int 3).
Impact of electronic health records
We explored what impact EHRs had had in our four sites. We were interested in what difference EHRs made to interaction with patients, to the workforce and their professional role, to ambulance service organisations themselves, and to care pathways and outcomes, in particular those for our three tracer conditions.
Impact on clinician–patient interaction
We found that the use of EHRs appeared to have only a very limited impact on clinician–patient interaction. Much of the time, the EHR devices did not even feature in the interaction, as they were left in the ambulance while clinicians attended the patient in the home. In only one of the case study ambulance services were clinicians able to access relevant information from past health service encounters in order to inform decision-making: paramedics in this site found this very valuable:
The more access to information that we’ve had the better that we can decide on the best course of treatment for your patient.
Site 1, FG1, participant 3
We also found that the model of information gathering for which the EHR was designed – sequential and complete – did not necessarily tally with the situation of imperfect information that ambulance clinicians were dealing with on the ground. They did not necessarily have access to all of the information they needed to complete the form in full and to inform decision-making; if patients had poor recall, or were unco-operative, there was nothing an EHR system could do to help this. Information does not flow to the clinicians in a pre-set order. Although clinicians could record clinical observations and presenting complaints, there would always be uncertainties and ambiguities in making diagnoses.
Impact on the workforce
We were interested in whether or not the introduction of EHRs had led to any change in ambulance crews’ perceptions of their role, particularly in terms of decision-making about whether or not patients could safely be cared for in the community rather than conveyed to hospital. We found little evidence of this. In site 4, one clinician expressed this very directly. He had had to learn to remember to dock the pen at the end of the shift but:
From the point of view of actually doing the job, it’s made absolutely no difference to us.
Site 4, FG1, participant 1
In site 1, clinicians described using the prompts built into the EHRs, and were seen doing so on shift observations, but emphasised that they were not using them as a diagnostic tool:
You are the clinician diagnosing and this is a clinical record and not a diagnostic tool.
Site 1, FG2, participant 3
Ambulance clinicians talked at length about the role of the EHR in providing a formal record of what they had done, and about how it had the potential to ‘cover their back’ if there was any problem in the future. Clinicians were aware that the EHR was a formal record of what had happened and that it could not be changed, potentially leading them to put extra data into the free-text boxes:
People are inputting so much data into those jobs which are not relevant, and they don’t know when to stop. They’re afraid to stop because they think, alright, when I press the end key here, this is it forever, and I’ve got to have justified this. But for 99% of your jobs it’s irrelevant and the hospital are just not looking at it, they’re not interested.
Site 1, FG2, participant 5
Although ‘covering their back’ is a function also served by paper records, the EHR was slightly different because of some of its technical qualities: it was ‘locked’ on completion, it recorded the time when data were entered (even though this may not have been the time when observations were taken and activities were carried out) and it was seen as leaving some key information implicit, which meant clinicians might enter more free text in order to confirm negative findings.
Impact on the organisation
Ambulance service managers were generally enthusiastic about the benefits of EHRs for their organisations. They reported on efficiency savings from handling data electronically rather than on paper, although none quantified these. AS3, the longest-established user of EHRs, had as long ago as 2008/9 been reporting that EHRs had contributed to improvements in clinical performance and effectiveness, demonstrated by indicators such as an increase in the numbers of patients treated at home and not conveyed to hospital. The exact role played by EHRs in these shifts, among all the complexities of pre-hospital care provision, was hard to identify. In other sites, the impact of EHRs on non-conveyance rates was even harder to assess.
In site 4, a range of potential benefits – including the provision of timely feedback to operational staff on clinical performance to improve delivery of care, and the ability to develop algorithms from the clinical data that inform the management and implementation of the clinical response model – were presented as reasons for implementing the digipen. However, at the time of the fieldwork, these were still no more than possibilities.
Managers from all sites talked very positively about the advantages of sharing EHRs with other health-care providers, and with patients themselves, to improve care. Sharing of data across NHS organisations was seen as one of the biggest potential benefits of EHRs, and one of the biggest challenges:
Absolute top priority for us is to be sharing our [EHR] far and wide and wherever it can go.
Site 3, Int 1
It’s about being able to share our records more easily with the rest of the NHS and ultimately with patients, so that we can provide a more seamless service to patients.
Site 3, Int 6
The true advance in what we need to do . . . that sort of seamless integration between health system and health providers is absolutely key.
Site 2, Int 5
However, these views were generally expressed in terms of the potential of future developments, rather than reporting actual change.
In all sites, respondents reported that a lack of interoperability with hospital systems was a major stumbling block to achieving change through the implementation of EHRs. A clinical commissioner in site 2 commented positively that the involvement of the CCGs was key to the successful integration of a fully electronic system across the NHS because it involved all parts of the health service, not just the ambulance service, across the region. Contact with hospitals was about more than the ED, as a manager from site 1 pointed out:
It’s not just about [site 1] taking patients into the emergency department . . . it’s about taking patients into acute medical wards, into surgical wards, into paediatrics, into maternity. So it wasn’t just about producing kind of workstations in one location, it was about making sure the data was visible across the hospital.
Site 1, Int 2
At a more micro level, however, encouraging GPs to engage with the electronic transfer of EHRs was a particular challenge:
To get GPs to check their e-mail boxes and then disseminate that information as necessary. I think for commissioners, that will be the hardest thing for us to be doing – getting the GP practices to check their secure inboxes regularly enough to pick up an alert, a referral, a letter that crews have been out to see a patient.
Site 2, Int 9
In site 2, we also heard how barriers in hospitals to accessing the ambulance service EHRs delayed the full roll-out of the system and meant that ambulance clinicians were working in an inconsistent environment as some hospitals were able to access the records but others would not receive the new EHRs.
There may be hard-to-resolve differences in what people from different organisations want from an electronic data set. In all sites, there seemed to be challenges in reconciling the interests of clinicians with those of the audit department. This situation was described to us by an ambulance service manager in site 1:
Right from the outset . . . I had the clinical research team in one ear saying ‘I want nothing but structured data’ and I get that completely . . . because structured data enables you to run reports, it enables you to analyse data in a much more timely manner, and then I had ED consultants from the acute trusts who wanted nothing but free text because that’s what they were used to and they didn’t like all the boxes and structure.
Site 1, Int 2
Impact on care pathways and outcomes
Clinicians and managers recognised the potential for developing multiagency working to improve care pathways and outcomes. EHRs could potentially support this in two ways: (1) by providing large data sets, that are relatively easy to analyse, which would help service planners to assess demand and patient flow and to monitor the impact of changes, and (2) by facilitating data transfer to smooth patients’ transitions along care pathways. The first of these functions was highlighted by a manager from AS4, currently as an ambition, but potentially achievable even with the relatively simple technology of the digipen:
Essentially what we want to be able to do is map the patient, be able to link this data to map the patient’s journey from a 999 call, from our arrival right through the system.
Site 4, Int 3
Older people who fall – one of our tracer conditions – were highlighted across all sites as a patient group that could benefit from more information sharing between services to increase the scope for interagency working, but this was made difficult by the need for better technological interoperability.
In terms of transfer of patient information along care pathways, some of the challenges have already been noted. An additional issue was raised by a manager at site 2: although EHRs can be very helpful in terms of facilitating alternative care pathways (via decision-making support and ease of referral), and non-conveyance to ED, their effectiveness depends on the working culture of the clinicians:
If those clinicians are just simply in the traditional mindset of somebody rings 999 for an ambulance, they get an ambulance . . . take them to hospital, even though that facility is available to them on the electronic patient record they simply aren’t going to use it . . . if you don’t address the culture and you just plough on with the strategy, then essentially the culture will win every time.
Site 2, Int 5
To realise all the potential of EHRs requires engagement from other parts of the local health economy and dealing with the variations between systems operated by different providers.
However, integrating systems had proved problematic. Site 3 provides a case study here, but similar issues were experienced in all sites. Different secondary care providers were running different records system, and were not going to be changing them to suit the ambulance service:
The issues we’ve had is with that is the territorial health boards . . . using a mixture of different systems. And we just don’t seem to be able to get onto their priority list to engage with us and our uniform style.
Site 3, Int 1
Negotiating access into secure systems had been a challenge:
What held us back in the initial stages [of developing systems to share electronic records] is because all the different health boards had different firewalls and different systems and in effect networks, that was a huge issue for us. The problems we get now range from questions like, well who do you actually send it to? So does it go to the A&E [Accident & Emergency] receptionist? Does it go to the nurses’ station? Does it go to the doctors’ desk? . . . so there’s some resistance to some of it.
Site 3, Int 4
Although greater interoperability was an aspiration for the new system, it was acknowledged that this was still a significant challenge to achieve owing to the range of systems in use across the NHS and the logistical challenges of implementing a unified system:
It’s frustrating from our point of view because we’ve got it, and we want to share it, but we just can’t quite get the single one size fits all solution for people, which is annoying.
Site 3, Int 1
Summary
We explored the work that was done in bringing EHRs into use in the four sites. Front-line clinicians had to put effort into learning the new systems and adapting their practice. We found that, to a large extent, they maintained some of their old ways of working with the new system; rather than using it as a real-time data source and repository, it was often completed later in the patient encounter, and data were recorded elsewhere before being transferred onto the EHRs. Although the experience of using the technology was not seen as significantly different from paper records, there were some concerns that the design would not allow negative observations to be made, instead leaving them implicit.
To encourage change in practice, ambulance services emphasised the importance of making change mandatory in order to make it embedded. There was some suggestion that feedback to clinicians on the benefits and impact of EHRs would encourage use. There were clear differences in perspective on the smoothness and effectiveness of implementation processes between those in management roles and front-line clinicians. The challenges of achieving interoperability – technically and in terms of information requirements – across a multiorganisation health economy appeared to be one of the factors inhibiting progress.
In terms of impact, we found little evidence of impact of EHRs on patient care or on clinician role. For the ambulance services, there seemed to be benefits in terms of the efficiency of handling data and ease of audit. Other potential benefits were yet to be realised, despite high hopes and expectations for the future expressed by many in senior positions.
Chapter 8 Knowledge exchange workshop
We held a knowledge exchange workshop in July 2018 in a venue in central London, lasting a total of 3.5 hours. We invited representatives from all 13 UK ambulance services, along with members of the research team (including PPI representatives and the Research Advisory Group) and relevant interested parties from other health-care providers, NHS England, other national bodies with an interest in policy, and commercial providers. The invitation list was developed by the research team with input from the Research Advisory Group. Invitations (see Appendix 9) were sent by e-mail.
The event was attended by 23 people. These included representatives of 10 ambulance services, with some ambulance services sending more than one delegate. Two representatives of one ambulance service who were not able to attend in person joined in discussions via a Skype™ (Microsoft Corporation, Redmond, WA, USA) link. Also attending were one ED consultant, one representative of a commercial EHR provider and two participants with a national role in policy. Two PPI representatives were given an honorarium for attending and reimbursed for their travel expenses, but we did not pay other participants for attending.
The event started with a buffet lunch. Participants were given a four-page written summary paper of the project aims and main findings. Members of the research team (AP and MK) then gave a short presentation on the findings of the study, and invited questions and comments.
Participants were then divided into four groups (A–D), as directed by the research team, to ensure that there was a suitable mix of people in each group. Each group was facilitated by one member of the research team (MK, ZM, HP and VW). Participants were asked to discuss the following questions:
-
How could EHRs have an impact on the workforce (e.g. decision-making, role)?
-
What are the limits to the transition to digital?
-
How can services share knowledge/learn from each other?
-
Is it realistic to hope to measure change from EHRs?
-
How can an ambulance service ensure that change happens at all levels to ensure full implementation of EHRs?
Discussion was facilitated by the research team member, who also took notes, and discussions were audio-recorded with permission of the participants. Facilitators then encouraged the group members to develop consensus on three or four key messages from their discussion that they would like to feed into the output from the day. All participants reconvened in a single group, where representatives of the discussion groups fed back their key messages for consideration by their peers. Alison Porter facilitated the discussion and conducted sense checking with the participants when writing up their key messages.
Following the workshop event, we conducted a teleconference with six people we had invited but who were not able to attend on the day. We shared the presentation and the handout with them before the teleconference, and discussed the main findings and implications of the study.
Results
Participants attending the workshop and those in the teleconference confirmed that the main findings of the study seemed to ‘ring true’ and reflect their own experience of working in this field. Participants spoke positively about the value of having a chance to get together, share knowledge and experience with colleagues in other services, and reflect. The key messages that emerged from the workshop are set out in Box 12.
-
Get the software right – and get people to see the value of it.
-
Close the loop on patient contact/feedback.
-
Empowering staff.
-
Feedback.
-
Give them a personal iPad.
-
Gain clinical confidence.
-
Feedback – to support improved practice.
-
Interoperability of kit on ambulance – the vehicle as a communications hub.
-
Scope – what’s the aim? How much risk do you want? Services are different.
-
Devices can be multifunctional and act as a portfolio repository holding, for example, patient records, NICE guidelines, decision-support software, and be used for continuing professional development and e-learning.
-
Data transfer into EDs.
-
Positive as data transferred while the patient is en route gives the receiving ED time to prepare.
-
Work of data collection transferred to paramedics.
-
Time is of the essence, so the EHRs should be kept simple – no Ferraris when a Mini would be enough!
-
Ambulance services should have a single point of ownership for EHRs in the organisation (and not dispersed responsibility) – helps knowledge sharing between organisations. This should be a recognised part of someone’s role so that the development of the records and interaction with other health-care organisations is a priority.
-
Feedback
-
(to paramedics/service clinicians) . . . so that people become confident data are used/useful
-
Feedback on patient outcomes/final diagnoses to crews so that there is a feedback loop
-
Enable crews to have summary information on their performance/experience (e.g. dealt with x cardiac arrests in past year)
-
-
Opportunities of device beyond record, i.e. to bring in JRCALC guideline information, link with directory of services for referrals, etc.
-
Data currency (e.g. of patient data pulled) is it up to date? – if not then can affect confidence, usefulness etc. BUT some data are better than no data.
-
Development of EHRs should be led by clinicians.
Discussion
The single strongest theme among the key messages identified at the workshop, mentioned by three of the four groups, was the potential for EHRs to support the provision of feedback both in order to improve care provision and to encourage thorough and consistent use of EHRs. This was partly an implementation issue, but participants also saw the potential value in EHRs being able to provide ambulance clinicians with information on patient outcomes, and so support improvements to clinical practice and professional development. This is an interesting finding as it is not one of the potential functions or benefits of EHRs that we had identified at the start of the study (see Chapter 1), and there was limited reference to this issue in the four case studies. More generally, discussion around the key messages emphasised the importance of bringing about consistent use of EHRs in order to support further changes in practice.
There was an emphasis on implementation issues, including the importance of having a single point of leadership within ambulance services to drive forward development of EHRs and maximise their benefits. This suggestion is interesting in the light of the dispersal of roles and functions we had identified in WP2 and WP3, in which responsibilities for clinical, business and technological aspects of EHR implementation were often held by different members of staff, with a consequent dispersal of specialist knowledge. There was also acknowledgement of the importance of supporting front-line clinical staff to feel a sense of ‘ownership’ of the technology.
One other key message (groups A and C, see Table 1) was about the importance of making the system simple and easy to use, for both ambulance clinicians and those in partner health providers to whom they might be transferring information. This was seen as a way to support implementation as well as maximise the impact of EHRs.
Although some of the key messages (groups B, C and D, see Table 1) around EHRs as a hub for data exchange and other functions fitted closely with issues we had explored throughout the study, there were two new issues raised that we had not previously examined. The first was that the transfer of data into an EHR system is worthwhile only if those data (whether from primary care, a secondary provider or some other provider) are accurate and up to date, and any anxieties about data quality can reduce confidence in the system itself. The second is that transfer of information gathered on the ambulance to the ED could be seen as a shifting of labour from one service to another and one professional group to another, with implications for workforce and for responsibility for those data.
Chapter 9 Discussion and conclusions
Summary of findings
Work package 1: literature review
The literature review found that, although there is an extensive and theoretically developed literature examining the implementation of technology into health care more generally, there was a very limited range of published literature specifically on EHRs in ambulance services. We identified 18 peer-reviewed papers, mostly not of high quality. They were primarily descriptive and/or concerned with implementation of EHRs rather than their impact.
Work package 2: national survey
The national telephone survey established that only half of the UK emergency ambulance services had a current EHR system in use. There was a range of systems in use. All services seemed, to some extent, to be in a state of flux in relation to EHRs. Some had experience of start–stop implementations, with reversion to paper records not uncommon. External drivers could play a strong and sometimes disruptive role in implementation. Although there were some positive examples of EHR systems acting as hubs for the real-time transfer of data to improve patient care, uses beyond simple data storage were not yet fully developed. The main advantages of EHRs were seen to be around data handling and audit.
Work package 3: case studies
Our case studies identified that all four services were, to a greater or lesser extent, in a state of transition in relation to EHR systems. Although we had planned to observe four services at distinct stages of implementation, we discovered that the situation was more complex and fluid than this.
One service had adopted a technology that was relatively cheap and straightforward, but very limited in its functionality. The others were working with more sophisticated tablet-based systems. Although we saw some indication of data being transferred into and out of systems to support patient care, none of these seemed to yet be being used to their intended potential.
Despite the diversity of systems and contexts, we made some common observations across all sites. Positive aspects of what we observed included:
-
vision and enthusiasm from senior managers
-
front-line staff who were willing and able to readily adapt to new systems
-
benefits being realised in terms of data quality, confidentiality and efficient storage and searching for audit and medicolegal use.
However, we also identified a number of challenges that were being encountered by all services:
-
interoperability in terms of information transfer to and from other parts of the health-care system – the challenges related to information governance and differing information needs of different clinicians, as well as technical aspects
-
technical issues with EHRs – most technical issues were relatively minor or had been resolved, but appeared to have had an influence on clinicians’ response to the EHR system
-
the need to update systems (software and hardware) without undue disruption.
Our analysis of routine data sets found that different sites recorded information in different ways: there was variation in fields and priority categorisation systems. Levels of EHR creation at the time of the data sample (January to February 2017) ranged across sites from fewer than one-third of calls to over 99%. Analysis of factors influencing EHR completion showed broad consistency across sites, although striking variation in relation to some factors. Factors that seemed to be associated with a lower rate of EHR completion included:
-
the call being received within routine working hours (Monday to Friday, 8.00 to 18.30)
-
the call being categorised as low priority
-
the patient not being conveyed (3/4 sites only)
-
the patient being a child
-
a mental health condition as the reason for the call (2/4 sites).
In one site, we found strong associations between completion rates and which hospital the patient was conveyed to, and which locality the crew was based in; it is unclear whether these associations were characteristic only of that time period or if they will have continued with roll-out of the service’s new EHR system.
These independent variables were confounded with each other. The biggest effects tended to be by geography and call priority, and these may explain other observed effects.
Work package 4: knowledge exchange workshop
Ambulance service representatives attending the knowledge exchange workshop felt that the findings resonated with their own experiences. They found it valuable to share knowledge with other ambulance services. Discussion groups identified the following issues:
-
the need to present front-line staff with the optimum software and to ensure that staff see its value
-
the value of empowering staff by providing feedback on patient outcomes
-
the multifunctional potential of EHR devices, for example accessing web resources
-
the need for information handover at the ED to be simple and streamlined
-
the role of a single point of ownership in the organisation (rather than dispersed responsibility) to help knowledge sharing between organisations
-
anxieties about data currency.
Looking across the work packages
Across the WPs, we found remarkable consistency in what we learned.
Key messages
-
Digital diversity. There was no standard hardware or software in use. We found great variety in how (and if) other technology and record systems were linked to the EHRs.
-
Constant change. Services were transitioning from one system to another, and from one supplier to another. Software and hardware underwent routine updates. Progress could be to and fro, including switching back to paper records as a temporary measure.
-
Imperfect information. In real patient encounters, clinicians are likely to be dealing with partial or unclear information, which does not arrive to them in a pre-ordered sequence. It may be challenging to fit this into the structured, sequential format of an EHR.
-
Indirect input. Some patient data can be fed straight into EHRs. However, data entered by clinical staff were still sometimes written on a glove or notebook, or stored in the paramedic’s memory, before being entered into the EHR.
-
Data dump. The primary function of EHRs in all services seemed to be to act as a store for patient data. There was, as yet, limited evidence of EHRs’ full potential being realised to transfer information or support decision-making or changes to patient care.
-
The system is bigger than the service. To realise all the benefits of EHRs requires engagement with other parts of the local health economy. This, in turn, requires dealing with variations between providers and the challenges of interoperability.
-
Different data demands. Clinicians and data managers are likely to want very different things from a data set, and need to be presented with only the information that they need.
-
‘Ford Fiesta, not a Ferrari’. Sometimes simple is best.
Strengths and limitations of the study
Strengths of our study included the combination of breadth (all UK ambulance service trusts included) and depth of exploration in our four selected study sites. Our use of multiple methods allowed us to triangulate findings. In the four study sites, our embedded researchers, working closely with local principal investigators, afforded us an ‘insider’ view to an extent that would not otherwise have been possible. Our study was theoretically informed, and built on previous work on introducing technology into other areas of health care. It took observations of EHRs into a new context, for the first time reporting in detail on EHR use in ambulances. It built on the work of those such as Pinnock et al. ,26 who have examined EHRs in primary care, and expanded their work by considering how EHRs are used in a non-controlled environment without any continuity of care.
In terms of limitations of our study, we acknowledge the small numbers of respondents from each service in WP2, which may have restricted our ability to be informed about the full picture of EHR implementation and use in each service. In WP3, we had difficulties in obtaining sets of matching routine data. We were not able to get a full picture of the data journey as data travelled from the ambulance service to the ED or to other health-care providers. Although our embedded researchers were a strength, they were not able to stay detached from events around them: in particular, the two researchers who were qualified paramedics were on occasion required to take an active role in patient care in response to demands encountered on their shifts. Assessing the impact of EHRs in general, and particularly in relation to the tracer conditions, proved challenging, in part because of the difficulties of attribution in a complex system.
The fact that we were observing systems in flux could be read as both a strength and a weakness. The flux itself was a point of interest, and our work was sensitised to observing it. Although we had planned to include case studies with a clear range of stages of implementation, reality proved more complex. On the other hand, as time has moved on, some of our observations about what systems are in use and levels of completion of EHRs may already be out of date.
Discussion in relation to existing literature
The experience of EHRs in ambulances has many similarities to the story of EHRs in health care more broadly,19 but also reflects the particular context of being on scene and in a vehicle, and the particular roles of paramedics. Greenhalgh and Stones,20 drawing on SST, have described how the successful adoption and use of EHR systems requires a long chain of arrangements at a macro (e.g. national policy), meso (e.g. trust adoptions) and micro (e.g. an electronic device retaining its charge) level to work. 28 Greenhalgh et al. 19 have noted that implementation is often not successful. Likewise, we found that the adoption of EHRs by the ambulance trusts took place within a national policy context (macro level), was affected by the decisions of trusts and other bodies locally (meso level), and depended on the actions of front-line staff (micro level).
The use of the technology is reflected by the context it is in, and, in turn, the technology leads to changed behaviour at an individual level and at a group level. 20 Changes in the behaviour of individual workers may have been planned as part of an implementation, or they may not, as staff devise their own response, perhaps involving workarounds. There can be a mismatch between ideas of how records and associated digital tools are used by paramedics and normal practice. Although future plans and technology could have significant effects on paramedics’ clinical practice, to date there were few examples of this happening at the patient’s side. Observations were often recorded on intermediate media or remembered before later data input on the EHRs. The data in the EHRs were more useful for retrospective purposes than as an immediate tool affecting paramedic practice.
Designing EHRs remains difficult, and the existence of off-the-shelf products suitable for local use may have been overestimated by governments. The mobile context presents some particular challenges: connectivity was often mentioned, but also appears to have been solved up to a point with systems that update automatically when a connection is available. However, intermittent connectivity is a major barrier to using an EHR system for ‘live’ transfer of information in or out of an ambulance.
A particular challenge for the ambulance context is data entry without a desktop computer. In one site, the digipen was readily adopted, but limited the benefits available from a digital system. Tablets are widely used and all future planned adoptions are based on tablet solutions. However, tablets are often not brought to the patient but left in the vehicle and data entry can be experienced by clinicians as slow and fiddly.
The main advantages so far of the systems in use are in later administrative use: in audit and medicolegal contexts, long after the patient was seen. Benefits to immediate clinical care were less common. We did not see much use of decision-support systems, although a checklist effect was noted. That is, the record often acted as a prompt, although this usually meant a prompt to record rather than a prompt to action. Interviewees were sometimes keen to avoid any language of decision-making by software. 67
The optimistic stance of managers – as with the rhetoric of politicians – offers considerable change to come, but timelines for this change are unclear. There was some disconnect between the perspective of managers (often focused on forthcoming functionality) and usual usage on the ground, yet the vision is valuable to drive activity and is an important part of acquiring funding and motivating change.
Ambulance services found EHRs transformative in terms of audit and related processes. However, there is more potential for such data usage. The investigation of trends or data linkage (e.g. to public health) remains rare, and one example reported to us (a cluster of cases pointing to chlorine exposure) was an exception, not the rule. The full potential of big data is not yet being realised.
There can be a mismatch between design assumptions and practice when it comes to how records are used in the field. Systems often appeared to be designed on the presumption that data entry would be done near contemporaneously at the patient’s side during initial assessment and care. This was sometimes the case: often with one paramedic attending to the patient and one taking notes. However, more commonly, paramedics attended to the patient and environment, with any notes written with a pen on the glove or in a notebook. A full record was produced later, when the patient was in the ambulance, often on the move, and sometimes even after handover to a hospital. Sometimes key observations and/or actions (e.g. medication) were recorded contemporaneously, with other details backfilled later. These asynchronies between action and recording raised problems for others’ use of the record.
With EHRs rarely used at the patient’s side during the initial phase of care, there was little possibility to track the impact of EHRs in terms of improvements to clinical care or changes to care pathways. Paramedics valued the ability to find contact details and to send information to other health-care professionals (often the GP), although we do not know how useful or not these other people within the health-care service found the information they received.
Organisational structures remain a challenge for interoperability, as seen in WP2 and WP3. That challenge is around technical aspects of interoperability and also in what information was wanted in what form.
Running through much of the above is a familiar tension between structured and narrative records. As seen in prior health records research outside the ambulance,19 we see the record as a tool to support specific jobs, rather than a context-free record of the patient. Design of records, in terms of the balance between coding and free text, raises implications for data entry, for handover and for ambulance service data retrieval. In some cases, the extensive use of free text was seen as something that could and should be discouraged through design changes. However, free text can also have clinical advantages and was sometimes preferred.
In many cases, we saw high levels of non-use of EHRs. Several adoptions described in WP2 barely warrant that term. In some services, there were lengthy periods of hybrid use: the significant use of EHRs paired with significant continued use of paper. Usage within a service could vary according to geography, which may be about staggered roll-outs across stations, local cultures and difficulties in integrating with local hospital systems. Both contracting a new system and upgrading to a new system, be that installing technology and software updates or re-training, were challenging and could be slow. This appears to be related to a lack of spare capacity, or slack, in services running on tightly constrained budgets. 68 The benefits of digital technologies require investment. 18 To achieve interoperability (at various levels) and the full benefits of digital transformation requires working across organisations, but we found only limited evidence of this. The tension between the local and the national, and the mandatory and the discretionary, remains an issue in relation to the introduction of new systems. 28 The solution needs to be organisational as well as technical, requiring ambulance services to work closely with their partner trusts to achieve it. As ever, though, when one trust is trying to work with many partners, some complicated choreography is needed. Questions remain about whether this can be resolved through direct engagement at a local level or is better addressed through national bodies (e.g. NHS Digital). 69
Ambulance services are keen to share information, but we do not yet know what impact this will have on patient outcomes or service delivery. Ambulance services are trying to achieve a records system that will fit their own organisational and administrative demands, support ambulance clinicians in their work and provide the right information for partner health providers – and it is a struggle to make records systems fit all of these demands. The reality is that different subsets of information are needed for different purposes and different users.
Conclusions
Implications for health care
-
Living with change. Our findings suggest that the implementation of EHRs in emergency ambulance services is not something that can be considered ‘task and finish’ but is a continuous work in progress. This requires a flexible and ongoing approach to managing change.
-
Managing ambitions. Although EHRs are showing benefits, these benefits are not yet as wide as they could be. Realistic planning and an acceptance that change moves slowly will help to sustain what has been achieved so far and reduce the risk of disappointment or cynicism that might inhibit further progress.
-
Flexibility in data collection process. Although EHRs may support standardised processes of clinical observation, data collection and clinical decision-making, there will remain uncertainties, fluidity and ambiguity in the information available to ambulance clinicians. Seeing mismatches between the requirements of the EHRs and the data entered into records as something to be anticipated and planned for is likely to be more helpful than seeing them as failure in compliance.
-
Addressing the interoperability requirement. Ambulance services face challenges in working with their local primary, secondary and acute health-care providers, and with social care, in ensuring that patient data are transferred securely and appropriately to support patient care. This issue is clearly on the policy agenda locally and nationally, but skilled negotiation and priority setting will be required to achieve effective and productive real-time flow of patient information both into and out of emergency ambulance services.
-
Maximising the potential of EHRs as a multifunctional resource. As well as being instruments of data storage, tablet-based EHRs have the potential to act as a portal to the world of information, both on the web and through secure local information databases. Maximising the ability of ambulance clinicians to readily access guidelines, clinical advice or local service directories will ensure that EHR devices get embedded in use and achieve maximum benefit.
-
Maximising use of EHRs to support staff development. Feedback from EHRs has the potential to support staff reflective learning and appraisal, especially if linked to data on patient outcomes following ambulance service contact.
-
Identifying streamlined data sets. Patient records transferred at the time of patient contact are most likely to be used and useful if they are focused and relevant to the receiving clinicians. A streamlined data summary for transfer at the ED, rather than the full EHR, might support this.
-
Coherence of perspective throughout an ambulance service. We identified some differences in perspective between different staff groups within ambulance services about the value and potential of EHRs, with managers typically being more enthusiastic. There may be scope for more mutually beneficial communication to strengthen effective implementation of EHRs.
Recommendations for future research
-
Ambulance services are collecting huge, potentially valuable resources in the form of routine data sets, but have very limited capacity to analyse them beyond routine auditing and reporting. The research community should prioritise finding ways to work with ambulance services to maximise the opportunity these present. Ambulance services are likely to welcome this prospect.
-
There is scope for useful qualitative work on how ambulance service EHRs are used (or not) in the ED and how they could be used better. We identified this opportunity, from the perspective of both ambulance clinicians (who often thought that they were not really being used) and ED staff (who felt that the records were not particularly useful).
-
There is scope to examine patients’ perspectives on records and record-keeping within emergency ambulance services to understand how these views and experiences may affect patient care.
-
Electronic health records provide the potential to offer ambulance clinicians feedback on patient outcomes if records can be linked to other data sets. There is scope to develop this and to evaluate the impact of such initiatives.
Acknowledgements
Contributions of authors
Alison Porter (https://orcid.org/0000-0002-3408-7007) (Associate Professor of Health Services Research) was the chief investigator, led the development of the research question and study design, and was responsible for study delivery and conduct, and the production of the report.
Anisha Badshah (https://orcid.org/0000-0002-4198-1285) (Research Assistant) contributed to the literature review (see Chapter 3).
Sarah Black (https://orcid.org/0000-0001-6678-7502) (Head of Research, Audit and Quality Improvement) was a co-applicant and principal investigator for one study site.
David Fitzpatrick (https://orcid.org/0000-0003-0653-8445) (Clinical Research Paramedic and Senior Lecturer in Health Sciences) was a principal investigator for one study site.
Robert Harris-Mayes (Service User) was a co-applicant and service user advisor.
Saiful Islam (https://orcid.org/0000-0003-3182-8487) (Medical Statistician) undertook the routine data analysis of case study data.
Matthew Jones (https://orcid.org/0000-0002-6974-8725) (Research Officer, Primary and Emergency Care) contributed to the literature review (see Chapter 3).
Mark Kingston (https://orcid.org/0000-0003-2242-4210) (Research Officer, Primary and Emergency Care) was the data manager for the collection and processing of the case study site routine data. He prepared the data tables for Chapter 6.
Yvette LaFlamme-Williams (https://orcid.org/0000-0002-6421-1996) (Site Researcher) gathered qualitative interview and observation data, contributed to the analysis of case study data and helped to prepare the results for publication.
Suzanne Mason (https://orcid.org/0000-0002-1701-0577) (Professor of Emergency Medicine) was a co-applicant and contributed to the study design and conduct.
Katherine McNee (Research Paramedic and Site Researcher) gathered qualitative interview and observation data, contributed to the analysis of case study data and helped to prepare the results for publication.
Heather Morgan (https://orcid.org/0000-0002-6118-8911) (Lecturer in Applied Health Sciences) gathered qualitative interview and observation data, contributed to the analysis of case study data and helped to prepare the results for publication.
Zoe Morrison (https://orcid.org/0000-0003-4655-2268) (Professor) was a co-applicant and contributed to the study delivery and interpretation of findings.
Pauline Mountain (https://orcid.org/0000-0002-6442-0448) (Service User) was a service user advisor.
Henry Potts (https://orcid.org/0000-0002-6200-8804) (Senior Lecturer in Health Informatics) was a co-applicant and contributed to study delivery and interpretation and write-up of findings.
Nigel Rees (https://orcid.org/0000-0001-8799-5335) (Head of Research and Innovation) was a co-applicant and principal investigator for one study site.
Debbie Shaw (https://orcid.org/0000-0003-0532-4007) (Clinical Audit and Research Analyst) gathered qualitative interview and observation data, contributed to the analysis of case study data and helped to prepare the results for publication.
Niro Siriwardena (https://orcid.org/0000-0003-2484-8201) (Academic GP, Professor of Primary and Pre-Hospital Health Care) was a co-applicant and academic advisor for one study site.
Helen Snooks (https://orcid.org/0000-0003-0173-8843) (Professor of Health Services Research) was a co-applicant, contributed to the study design and provided methodological expertise.
Rob Spaight (Clinical Audit and Research Manager) gathered qualitative interview and observation data, contributed to the analysis of case study data and helped to prepare the results for publication.
Victoria Williams (https://orcid.org/0000-0002-4747-9544) (Project Manager) co-ordinated the day-to-day delivery of the study and led the analysis and write-up of qualitative data.
All authors contributed to the writing of the report and approved the final version.
Contributions of others
Thanks to Carys Evans, Neil Jenkinson and Anne Surman for providing administrative support to the study.
Data-sharing statement
All data generated that can be shared are contained within the report. All data queries and requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Wankhade P. The crisis in NHS ambulance services in the UK: let’s deal with the ‘elephants in the room’!!. Ambulance Today 2018;15:13-7. https://research.edgehill.ac.uk/ws/portalfiles/portal/20115801/EHRA+version.pdf (accessed 15 January 2020).
- Association of Ambulance Chief Executives . A Vision for the Ambulance Service: ‘2020 and Beyond’ and the Steps to Its Realisation 2015. http://aace.org.uk/wp-content/uploads/2015/09/Ambulance-2020-and-beyond-the-AACE-vision.pdf (accessed 27 September 2018).
- NHS Confederation . Zero Tolerance – Making Ambulance Handover Delays a Thing of the Past 2012.
- Association of Ambulance Chief Executives . Association of Ambulance Chief Executives (AACE) Annual Report 2016–17 2017. https://aace.org.uk/wp-content/uploads/2017/11/AACE-A4-ANNUAL-REPORT-2016-2017-V8F.pdf (accessed 6 November 2019).
- Keogh B. Transforming Urgent and Emergency Care Services in England. Urgent and Emergency Care Review 2013. www.nhs.uk/NHSEngland/keogh-review/Documents/UECR.Ph1Report.FV.pdf (accessed 20 September 2018).
- Welsh Assembly Government . Delivering Emergency Care Services: An Integrated Approach for Delivering Unscheduled Care in Wales 2008. www.wales.nhs.uk/document/156584 (accessed 20 September 2018).
- McClelland S. Strategic Review of Welsh Ambulance Services. Cardiff: Welsh Government; 2013.
- Department of Health and Social Care . Taking Healthcare to the Patient: Transforming NHS Ambulance Services 2005. http://ircp.info/Portals/11/Future/NHS%20EMS%20Policy%20Recommendation2005.pdf (accessed 20 September 2018).
- Health Education England . The NHS Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 12 September 2018).
- O’Cathain A, Knowles E, Bishop-Edwards L, Coster J, Crum A, Jacques R, et al. Understanding variation in ambulance service non-conveyance rates: a mixed methods study. Health Serv Deliv Res 2018;6. www.journalslibrary.nihr.ac.uk/hsdr/hsdr06190/#/full-report (accessed 25 September 2018).
- Mason S, Snooks H. Alternative services to deliver urgent care in the community. Emerg Med J 2010;27:183-5. https://doi.org/10.1136/emj.2009.073049.
- O’Hara R, Johnson M, Hirst E, Weyman A, Shaw D, Mortimer P, et al. A qualitative study of decision-making and safety in ambulance service transitions. Health Serv Deliv Res 2014;2.
- Porter A, Snooks H, Youren A, Gaze S, Whitfield R, Rapport F, et al. ‘Should I stay or should I go?’ Deciding whether to go to hospital after a 999 call. J Health Serv Res Policy 2007;12:32-8. https://doi.org/10.1258/135581907780318392.
- McCann L, Granter E, Hyde P, Hassard J. Still blue-collar after all these years? An ethnography of the professionalization of emergency ambulance work. Journal of Management Studies 2013;50:750-76. https://doi.org/10.1111/joms.12009.
- Blandford A, Wong BLW, Connell I, Green T, Faulkner X, Finlay J, et al. People and Computers XVI – Memorable Yet Invisible. London: Springer; 2002.
- Talbot R, Bleetman A. Retention of information by emergency department staff at ambulance handover: do standardised approaches work?. Emerg Med J 2007;24:539-42. https://doi.org/10.1136/emj.2006.045906.
- Fitzpatrick G, Ellingsen G. A review of 25 years of CSCW research in healthcare: contributions, challenges and future agendas. Comput Support Coop Work 2013;22:609-65. https://doi.org/10.1007/s10606-012-9168-0.
- National Advisory Group on Health Information Technology in England . Making IT Work: Harnessing the Power of Health Information Technology to Improve Care in England 2016. www.gov.uk/government/publications/using-information-technology-to-improve-the-nhs/making-it-work-harnessing-the-power-of-health-information-technology-to-improve-care-in-england (accessed 12 September 2018).
- Greenhalgh T, Potts HW, Wong G, Bark P, Swinglehurst D. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Q 2009;87:729-88. https://doi.org/10.1111/j.1468-0009.2009.00578.x.
- Greenhalgh T, Stones R. Theorising big IT programmes in healthcare: strong structuration theory meets actor-network theory. Soc Sci Med 2010;70:1285-94. https://doi.org/10.1016/j.socscimed.2009.12.034.
- Morrison Z, Fernando B, Kalra D, Cresswell K, Sheikh A. National evaluation of the benefits and risks of greater structuring and coding of the electronic health record: exploratory qualitative investigation. J Am Med Inform Assoc 2014;21:492-500. https://doi.org/10.1136/amiajnl-2013-001666.
- Dean JM, Vernon DD, Cook L, Nechodom P, Reading J, Suruda A. Probabilistic linkage of computerized ambulance and inpatient hospital discharge records: a potential tool for evaluation of emergency medical services. Ann Emerg Med 2001;37:616-26. https://doi.org/10.1067/mem.2001.115214.
- Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform 2008;77:291-304. https://doi.org/10.1016/j.ijmedinf.2007.09.001.
- Handel DA, Wears RL, Nathanson LA, Pines JM. Using information technology to improve the quality and safety of emergency care. Acad Emerg Med 2011;18:e45-51. https://doi.org/10.1111/j.1553-2712.2011.01070.x.
- National Association of Emergency Medical Technicians (NAEMT) . 2016 National Survey: Data Collection, Use and Exchange in EMS 2016. www.naemt.org/docs/default-source/community-paramedicine/ems-data/naemt_ems_data_report_6_17_2016-5-1.pdf?status=Temp&sfvrsn=0.06606199361250287 (accessed 12 September 2018).
- Pinnock H, Sheikh A, Williams R, Creswell K, Fernando B, Huby G, et al. Evaluation of the Effect of IT on Interactions Between Healthcare Workers and Patients 2011. www.birmingham.ac.uk/research/activity/mds/projects/HaPS/PHEB/CFHEP/reports/projects/010.aspx (accessed 27 September 2018).
- Comptroller and Auditor General . The National Programme for IT in the NHS: An Update on the Delivery of Detailed Care Records Systems 2011. www.nao.org.uk/wp-content/uploads/2011/05/1012888.pdf (accessed 27 September 2018).
- Greenhalgh T, Stramer K, Bratan T, Byrne E, Russell J, Potts HW. Adoption and non-adoption of a shared electronic summary record in England: a mixed-method case study. BMJ 2010;340. https://doi.org/10.1136/bmj.c3111.
- Honeyman M, Dunn P, McKenna H. A Digital NHS? An Introduction to the Digital Agenda and Plans for Implementation. London: The Kings Fund; 2016.
- Department of Health and Social Care . Personalised Health and Care 2020: Using Data and Technology to Transform Outcomes for Patients and Citizens: A Framework for Action 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/384650/NIB_Report.pdf (accessed 12 September 2018).
- Caldicott F. Review of Data Security, Consent and Opt-Outs. Leeds: National Data Guardian; 2016.
- Heifetz RA, Laurie DL. The work of leadership. Harv Bus Rev 1997;75:124-34.
- NHS England . Ambulance Global Digital Exemplars n.d. www.england.nhs.uk/digitaltechnology/connecteddigitalsystems/exemplars/ambulance-global-digital-exemplars/ (accessed 27 September 2018).
- South Central and West Commissioning Support Unit . Interoperability Handbook 2015. www.england.nhs.uk/wp-content/uploads/2017/03/interoperabilty-handbk.pdf (accessed 12 September 2018).
- Academy of Medical Royal Colleges/Royal College of Physicians . Standards for the Clinical Structure and Content of Patient Records 2013.
- Professional Records Standards Body . PRSB Standards for the Structure and Content of Health and Care Records 2018.
- NHS Digital . Professional Guidance on the Structure and Content of Ambulance Records 2014. www.england.nhs.uk/wp-content/uploads/2014/12/amblnce-rec-guid.pdf (accessed 20 September 2018).
- Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ 2010;341. https://doi.org/10.1136/bmj.c5814.
- Finkelstein A, Dowell J. A Comedy of Errors: The London Ambulance Service Case Study (Proceedings of the 8th International Workshop on Software Specification and Design). Institute of Electrical and Electronics Engineers Computer Society; 1996.
- Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc 2004;11:104-12. https://doi.org/10.1197/jamia.M1471.
- Cresswell KM, Bates DW, Williams R, Morrison Z, Slee A, Coleman J, et al. Evaluation of medium-term consequences of implementing commercial computerized physician order entry and clinical decision support prescribing systems in two ‘early adopter’ hospitals. J Am Med Inform Assoc 2014;21:e194-202. https://doi.org/10.1136/amiajnl-2013-002252.
- Greenhalgh T, Robert G, Bate P, Macfarlane F, Kyriakidou O. Diffusion of Innovations in Health Service Organisations: A Systematic Literature Review. Chichester: Blackwell Publishing; 2005.
- Porter A, Dale J, Foster T, Logan P, Wells B, Snooks H. Implementation and use of computerised clinical decision support (CCDS) in emergency pre-hospital care: a qualitative study of paramedic views and experience using strong structuration theory. Implement Sci 2018;13. https://doi.org/10.1186/s13012-018-0786-x.
- Stones R. Structuration Theory. London: Palgrave; 2005.
- Ritchie J, Spencer L, Huberman M, Miles M. The Qualitative Researcher’s Companion. Thousand Oaks, CA: SAGE Publications Ltd; 2002.
- K Yin R. A Review of Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE Publications Ltd; 2003.
- Halcomb E, Davidson P, Hardaker L. Using the consensus development conference method in healthcare research. Nurse Res 2008;16:56-71. https://doi.org/10.7748/nr2008.10.16.1.56.c6753.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. Lancaster: Lancaster University; 2006.
- Landman AB, Lee CH, Sasson C, Van Gelder CM, Curry LA. Prehospital electronic patient care report systems: early experiences from emergency medical services agency leaders. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0032692.
- Baird S, Boak G. Leading change: introducing an electronic medical record system to a paramedic service. Leadersh Health Serv 2016;29:136-50. https://doi.org/10.1108/LHS-04-2015-0012.
- Scott G, Clawson J, Fivaz MC, McQueen J, Gardett MI, Schultz B, et al. Using on-scene EMS responders’ assessment and electronic patient care records to evaluate the suitability of EMD-triaged, low-acuity calls for secondary nurse triage in 911 centers. Prehosp Disaster Med 2016;31:46-57. https://doi.org/10.1017/S1049023X15005567.
- Bledsoe BE, Wasden C, Johnson L. Electronic prehospital records are often unavailable for emergency department medical decision making. West J Emerg Med 2013;14:482-8. https://doi.org/10.5811/westjem.2013.1.12665.
- Katzer R, Barton DJ, Adelman S, Clark S, Seaman EL, Hudson KB. Impact of implementing an EMR on physical exam documentation by ambulance personnel. Appl Clin Inform 2012;3:301-8. https://doi.org/10.4338/ACI-2012-03-RA-0008.
- Newgard CD, Zive D, Jui J, Weathers C, Daya M. Electronic versus manual data processing: evaluating the use of electronic health records in out-of-hospital clinical research. Acad Emerg Med 2012;19:217-27. https://doi.org/10.1111/j.1553-2712.2011.01275.x.
- Chan TC, Griswold WG, Buono C, Kirsh D, Lyon J, Killeen JP, et al. Impact of wireless electronic medical record system on the quality of patient documentation by emergency field responders during a disaster mass-casualty exercise. Prehosp Disaster Med 2011;26:268-75. https://doi.org/10.1017/S1049023X11006480.
- Lenert LA, Kirsh D, Griswold WG, Buono C, Lyon J, Rao R, et al. Design and evaluation of a wireless electronic health records system for field care in mass casualty settings. J Am Med Inform Assoc 2011;18:842-52. https://doi.org/10.1136/amiajnl-2011-000229.
- Broussard LA. My own private ePCR. Acadian ambulance service pioneers its own system. JEMS 2009;34:22-4.
- Killeen JP, Chan TC, Buono C, Griswold WG, Lenert LA. A wireless first responder handheld device for rapid triage, patient assessment and documentation during mass casualty incidents. AMIA Annu Symp Proc 2006:429-33.
- Tollefsen W, Myung D, Moulton S, Gaynor M. iRevive, A Pre-Hospital Mobile Database. New York, NY: Association for Information Systems; 2004.
- Nakada TA, Masunaga N, Nakao S, Narita M, Fuse T, Watanabe H, et al. Development of a prehospital vital signs chart sharing system. Am J Emerg Med 2016;34:88-92. https://doi.org/10.1016/j.ajem.2015.09.048.
- Nakae T, Kataoka H, Kuwata S, Iihara K. Smartphone-assisted prehospital medical information system for analyzing data on prehospital stroke care. Stroke 2014;45:1501-4. https://doi.org/10.1161/STROKEAHA.114.004872.
- Kuisma M, Väyrynen T, Hiltunen T, Porthan K, Aaltonen J. Effect of introduction of electronic patient reporting on the duration of ambulance calls. Am J Emerg Med 2009;27:948-55. https://doi.org/10.1016/j.ajem.2008.07.033.
- Chittaro L, Zuliani F, Carchietti E. Mobile Devices in Emergency Medical Services: User Evaluation of a PDA-Based Interface for Ambulance Run Reporting 2007. https://link.springer.com/chapter/10.1007/978-3-540-75668-2_3 (accessed 1 October 2018).
- Buswell M, Fleming J, Lumbard P, Prothero LS, Amador S, Goodman C. Difference between how ambulance service personnel use paper and electronic patient care records when attending older people at home. Eur J Emerg Med 2015;22:147-8. https://doi.org/10.1097/MEJ.0000000000000237.
- Burley L, Scheepers H, Owen L. The Internal Value of Mobile Computing in Emergency Medical Services: An Australian Case Study. Waikoloa, HI: Institute of Electrical and Electronics Engineers; 2008.
- Crilly JF, Keefe RH, Volpe F. Use of electronic technologies to promote community and personal health for individuals unconnected to health care systems. Am J Public Health 2011;101:1163-7. https://doi.org/10.2105/AJPH.2010.300003.
- Cowburn A. Theresa May says AI revolution will help NHS prevent thousands of cancer-related deaths by 2033. The Independent 2018. www.independent.co.uk/news/uk/politics/nhs-artificial-intelligence-ai-cancer-deaths-2033-technology-promise-a8360451.html (accessed 1 October 2018).
- Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Analysing the role of complexity in explaining the fortunes of technology programmes: empirical application of the NASSS framework. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1050-6.
- Akrich M, Callon M, Latour B. The Key to Success in Innovation Part I: The Art of Interessement – Part II: The Art of Choosing Good Spokespersons 2002;6:207-25.
Appendix 1 Literature search strategy for work package 1
Databases: Web of Science, Scopus, Cumulative Index to Nursing and Allied Health Literature, MEDLINE, Health Management Information Consortium and The Cochrane Library
Date search: 27 July 2017.
Restrictions:
-
date – none
-
design – none.
Search strategy
| Electronic records | Ambulances | MeSH terms |
|---|---|---|
|
electronic record* electronic medical record* electronic health record* electronic patient record electronic care record* electronic patient care record* EMR EPR EHRs ECR ePCR |
Ambulance* Emergency service* Emergency response Emergency response team Emergency Medical Technician* Paramedic* EMS EMT |
emergency medical services emergency medical technicians emergency treatment emergency medicine ambulances |
Appendix 2 Semistructured interview schedule for work package 2
ERA – Electronic Records in Ambulances – work package 2 a telephone survey of all providers of 999 emergency ambulance services in the UK (14 services) (months 4–6)
Interview questions for work package 2
1. Please can you tell me your job title and role within the ambulance service?
2. Does your ambulance service currently use electronic patient records?
-
If yes
-
What system or systems?
-
When were they introduced? Go to question 3.
-
-
If no
-
Are there any plans for introducing electronic patient records?
-
What system(s) and when? Go to question 9.
-
3. What proportion of patient encounters lead to an electronic record being created?
-
Does this vary by area? Over time? By anything else?
-
Why are some records made electronically and some on paper?
4. What was the purpose of introducing electronic patient records into your ambulance service?
-
Stated rationale.
-
Any other purposes?
-
Any value which has come to light subsequently?
5. Please describe the process which the service went through to bring electronic patient records into use.
-
Preparing business case.
-
Identifying funding.
-
Service specification/tendering.
-
Roll-out and training – logistics, time period.
6. How do you think paramedics and EMTs have responded to the introduction of electronic records?
-
Training required.
-
Resistance/reluctance/enthusiasm.
-
Different responses from different staff groups.
-
Changing perception of role.
7. Once an electronic patient record has been created, what then happens to that information?
-
Transferred to another care provider – how, when.
-
Downloaded and stored – how, where.
-
Used for analyses – what.
8. What use does your service make of data from electronic patient records to support performance management or service improvements?
-
Identifying and managing repeat callers.
-
Audit.
-
Research – what?
-
Medicolegal.
9. Do the electronic patient records link with other electronic resources or hand held technologies?
-
For decision support.
-
For referral.
-
Apps.
10. What do you think are the benefits of implementing electronic patient records in the ambulance service?
11. What are the risks of implementing electronic patient records in the ambulance service?
-
Unintended consequences?
12. What do you think will be the next steps for electronic patient records in your ambulance service?
13. How do you think electronic patient records have changed the experience of those using the ambulance service?
14. Are they any reports or documents on the process of adoption (e.g. business cases) or use that you are happy to share?
Appendix 3 Observation handbook for work package 3 (shortened edit)
Appendix 4 Focus group topic guide for work package 3
ERA’s topic guide for focus groups with paramedics/emergency medical technicians in case study sites
Please note this topic guide is indicative. It may be amended following the completion of WP1 and WP2 (rapid review and interviews with representatives from ambulance services across the UK) in line with the project protocol.
1. What do you understand to be the rationale for the introduction of electronic patient records in the ambulance service in this area?
-
Role of national directives.
-
Strategic plans/vision within ambulance service.
-
Potential to support priorities, e.g. increased non-conveyance.
-
Opportunities, e.g. funding made available.
2. What was your experience of the introduction of electronic records in the service?
-
Phased roll-out?
-
Training.
-
Role/responsibility of particular staff members.
3. How do you feel that front-line clinical staff (paramedics and EMTs) have responded to the introduction of electronic patient records?
-
Enthusiasm/resistance.
-
Own opinion/opinions of colleagues.
-
Any change over time?
4. What advantages or opportunities do you think are presented by the use of electronic patient records?
-
Direct impact on patient care.
-
Transfer of information/referrals to/from other providers.
-
Accessing tools to support diagnosis and risk assessment.
-
Audit and record-keeping.
-
Research.
-
Have you seen any evidence of impact on any of these in your service?
5. Are there times or circumstances when you would NOT use an electronic record?
-
Particular patient categories.
-
Technical reasons.
-
Patient disposition.
6. Are you aware of any current or planned new technology (e.g. diagnostic apps, remote consultations) which might link to and enhance electronic patient records?
7. Can you see any negative aspects to the introduction of electronic patient records?
-
Cost.
-
Confidentiality concerns.
-
Opportunity cost/distraction from other priorities.
-
Poorer technical performance/more difficult to use than paper records.
8. We are particularly interested the care pathways for three patient groups: 1. Falls in older people 2. Diabetic hypoglycaemia; 3. Mental health crisis. Do you think there are any particular opportunities for electronic patient records to support improvements to these care pathways?
-
Any evidence of this happening already?
9. Do you have any suggestions for how to get maximum value from the use of electronic patient records in the ambulance service in this area?
-
Impact within wider health economy/other providers.
-
Technical improvements.
-
Improvements in training/support.
-
Additional investment.
-
Senior support/strategy.
Appendix 5 Stakeholder interview schedule for work package 3
ERA’s interviews schedule for key stakeholders in case study sites
Please note this interview schedule is indicative. It may be amended following the completion of WP1 and WP2 (rapid review and interviews with representatives from ambulance services across the UK) in line with the project protocol.
1. What awareness do you have of the implementation of electronic records in the ambulance service in this area?
-
Knowledge of rationale.
-
Knowledge of process.
-
Discussion of potential/opportunities with ambulance service.
2. What opportunities do you think are presented by the use of electronic patient records?
-
Within ambulance service/within other health providers.
-
Direct impact on patient care.
-
Transfer of information/referrals to/from other providers.
-
Accessing tools to support diagnosis and risk assessment.
-
Audit and record-keeping.
-
Research.
-
Have you seen any evidence of impact on any of these in your service?
3. What challenges do you think are presented by the use of electronic patient records?
-
Within ambulance service/within other health providers.
4. Are you aware of any current or planned new technology (e.g. diagnostic apps, remote consultations) which might link to and enhance electronic patient records?
5. We are particularly interested the care pathways for three patient groups: 1. falls in older people; 2. diabetic hypoglycaemia; and 3. Mental health crisis. Do you think there are any particular opportunities for electronic patient records to support improvements to these care pathways?
-
Impact on other providers/care pathway as a whole.
-
Impact of planning/commissioning of care.
-
Any evidence of this happening already?
6. Do you have any suggestions for how to get maximum value from the use of electronic patient records in the ambulance service in this area?
-
Impact within wider health economy/other providers.
-
Technical improvements.
-
Improvements in training/support.
-
Additional investment.
-
Senior support/strategy.
Appendix 6 When should electronic health records be created for each service?
Ambulance service 1
Not supplied.
Ambulance service 2
It was expected but not mandated in policy. EHRs were expected to be created for all of the following:
-
any patient transported to an ED that had the facility to view our EHRs (15 across the region)
-
any patient who was seen but discharged on scene
-
any patient who was seen and made their own way to an ED
-
any incident where the crew arrived on scene but were unable to locate a patient or the patient had absconded prior to the 999 arrival.
Ambulance service 3
Electronic health records are automatically generated on a vehicle when that resource is allocated by the control centre. Limited information will be passed from control to the vehicle at this point, including location of the incident, a brief description of the incident and any information they have about the patient (e.g. name, date of birth).
There are no mandatory fields requiring completion on an EHR.
Ambulance service 4
Not supplied.
Appendix 7 Generation of electronic health records by sample week, for each ambulance service
Ambulance service 1
| Week of call (number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| 1 (1–7 January) (17,198) | 14,661 (85.3) | 1.000 | – | – |
| 2 (8–14 January) (15,847) | 13,743 (86.7) | 1.130 | 1.062 to 1.203 | < 0.001 |
| 3 (15–21 January) (15,678) | 13,686 (87.3) | 1.189 | 1.116 to 1.266 | < 0.001 |
| 4 (22–28 January) (16,369) | 14,244 (87.0) | 1.160 | 1.090 to 1.234 | < 0.001 |
| 5 (29 January–4 February) (16,763) | 14,628 (87.3) | 1.186 | 1.114 to 1.261 | < 0.001 |
| 6 (5–11 February) (15,638) | 13,781 (88.1) | 1.284 | 1.204 to 1.369 | < 0.001 |
| 7 (12–18 February) (15,943) | 13,697 (85.9) | 1.055 | 0.992 to 1.122 | 0.086 |
| 8 (19–25 February) (15,842) | 13,953 (88.1) | 1.278 | 1.199 to 1.363 | < 0.001 |
| 9 (26–28 February) (6663) | 5767 (86.6) | 1.114 | 1.026 to 1.209 | 0.010 |
Ambulance service 2
| Week of call (number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| 1–2 (1–14 January) (25,885) | 8041 (31.1) | 1.000 | – | – |
| 3–4 (15–28 January) (25,337) | 8305 (32.8) | 1.082 | 1.043 to 1.123 | 0.000 |
| 5–6 (29 January–11 February) (24,859) | 7420 (29.8) | 0.944 | 0.909 to 0.981 | 0.003 |
| 7–8 (12–25 February) (24,657) | 7588 (30.8) | 0.987 | 0.950 to 1.024 | 0.481 |
| 9 (26–28 February) (5408) | 1515 (28.0) | 0.864 | 0.809 to 0.922 | 0.000 |
Ambulance service 3
| Week of call (number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| 1–2 (1–14 January) (25,366) | 25,144 (99.1) | 1.000 | – | – |
| 3–4 (15–28 January) (23,971) | 23,754 (99.1) | 0.966 | 0.801 to 1.166 | 0.722 |
| 5–6 (29 January–11 February) (24,490) | 24,350 (99.4) | 1.536 | 1.242 to 1.899 | < 0.001 |
| 7–8 (12–25 February) (24,332) | 24,183 (99.4) | 1.433 | 1.164 to 1.765 | 0.001 |
| 9 (26–28 February) (5358) | 5325 (99.4) | 1.425 | 0.987 to 2.056 | 0.059 |
Ambulance service 4
| Week of call (number of calls) | EHRs, n (%) | 95% CI | p-value |
|---|---|---|---|
| 1 (1–7 January) (8578) | 5762 (67.2) | 1.000 | – |
| 2 (8–14 January) (7750) | 5404 (69.7) | 1.126 | 1.054 |
| 3 (15–21 January) (7653) | 5478 (71.6) | 1.231 | 1.151 |
| 4 (22–28 January) (7596) | 5589 (73.6) | 1.361 | 1.271 |
| 5 (29 January–4 February) (8063) | 5752 (71.3) | 1.216 | 1.139 |
| 6 (5–11 February) (7591) | 5496 (72.4) | 1.282 | 1.198 |
| 7 (12–18 February) (7934) | 5710 (72.0) | 1.255 | 1.174 |
| 8 (19–25 February) (7731) | 5483 (70.9) | 1.192 | 1.115 |
| 9 (26–28 February) (3321) | 2359 (71.0) | 1.198 | 1.098 |
Appendix 8 Electronic health record generation (where a resource was allocated) by day of the week
Ambulance service 1
| Day of week (number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| Monday (20,755) | 20,120 (87.1) | 1.087 | 1.029 to 1.147 | 0.003 |
| Tuesday (17,821) | 15,347 (86.1) | 0.996 | 0.941 to 1.055 | 0.901 |
| Wednesday (17,913) | 15,647 (87.4) | 1.109 | 1.046 to 1.176 | < 0.001 |
| Thursday (17,619) | 15,482 (87.9) | 1.164 | 1.097 to 1.234 | < 0.001 |
| Friday (17,756) | 15,536 (87.5) | 1.124 | 1.060 to 1.192 | < 0.001 |
| Saturday (19,403) | 16,784 (86.5) | 1.029 | 0.973 to 1.089 | 0.311 |
| Sunday (22,335) | 19,244 (86.2) | 1.000 | – | – |
Ambulance service 2
| Day of week (number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| Monday (16,455) | 4965 (30.2) | 0.955 | 0.912 to 1.001 | 0.054 |
| Tuesday (15,888) | 4810 (30.3) | 0.960 | 0.916 to 1.006 | 0.088 |
| Wednesday (14,136) | 4324 (30.6) | 0.974 | 0.928 to 1.023 | 0.290 |
| Thursday (14,022) | 4404 (31.4) | 1.012 | 0.965 to 1.062 | 0.621 |
| Friday (14,212) | 4410 (31.0) | 0.995 | 0.948 to 1.044 | 0.827 |
| Saturday (14,551) | 4698 (32.3) | 1.054 | 1.005 to 1.106 | 0.030 |
| Sunday (16,882) | 5258 (31.1) | 1.000 | – | – |
Ambulance service 3
| Day of week (number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| Monday (16,505) | 16,397 (99.3) | 0.975 | 0.744 to 1.279 | 0.856 |
| Tuesday (15,569) | 15,443 (99.2) | 0.787 | 0.606 to 1.022 | 0.073 |
| Wednesday (13,663) | 13,548 (99.2) | 0.757 | 0.580 to 0.988 | 0.041 |
| Thursday (13,560) | 13,435 (99.1) | 0.690 | 0.531 to 0.897 | 0.006 |
| Friday (14,350) | 14,236 (99.2) | 0.802 | 0.614 to 1.048 | 0.106 |
| Saturday (13,733) | 13,663 (99.5) | 1.254 | 0.925 to 1.700 | 0.145 |
| Sunday (16,137) | 16,034 (99.4) | 1.000 | – | – |
Ambulance service 4
| Day of week (number of calls) | EHRs, n (%) | Odds ratio | 95% CI | p-value |
|---|---|---|---|---|
| Monday (10,213) | 7222 (70.7) | 1.000 | 0.941 to 1.061 | 0.988 |
| Tuesday (9921) | 7035 (70.9) | 1.009 | 0.950 to 1.072 | 0.770 |
| Wednesday (9002) | 6407 (71.2) | 1.022 | 0.960 to 1.088 | 0.792 |
| Thursday (8867) | 6320 (71.2) | 1.027 | 0.965 to 1.093 | 0.401 |
| Friday (8997) | 6416 (71.3) | 1.029 | 0.967 to 1.095 | 0.368 |
| Saturday (8864) | 6311 (71.2) | 1.023 | 0.961 to 1.090 | 0.470 |
| Sunday (10,353) | 7322 (70.7) | 1.000 | – | – |
Appendix 9 Invitation e-mail to potential participants in work package 4 knowledge exchange workshop
Appendix 10 Research Advisory Group terms of reference and membership
Electronic Records in Ambulances to support the shift to out-of-hospital care: challenges, opportunities and workforce implications
Research Advisory Group terms of reference
The role of the group
The Research Advisory Group will provide critical, but friendly, oversight and advice to the researchers across the breadth of the study. It has been established by the RMG to:
-
Offer comment and advice on the overall conduct and progress of the research.
-
Offer comment and advice on the research questions, methods, findings and outputs.
-
Provide oversight of data quality and advice on ethics issues and to act as a Data Monitoring and Ethics Committee for the remainder of the project.
-
Exchanging ideas and information while ensuring the confidentiality of the research and any other information shared within the meetings.
-
The chairperson of the group will report back to the chief investigator.
Membership
Membership will include
-
Members of PPI organisations with an interest in emergency care provision.
-
Members of professional organisations with particular interest in emergency care provision.
-
Academics with research and educational interests in the topics being investigated for the project.
-
It is anticipated that membership of the Research Advisory Group will last for the duration of the research project.
Meetings
-
The group will meet three times over the course of the project for 2 hours per meeting.
-
Meetings will be held in London.
-
Papers will be circulated 1 week prior to the agreed meeting date.
-
Expenses will be met.
Electronic Records in Ambulances Research Advisory Group members
-
Amanda Brewster, PPI representative.
-
Tjeerd Van Staa, Professor in Health e-Research, University of Manchester.
-
Martin McTigue, Ambulance Operations Manager, London Ambulance Service.
-
Alison Clements, Head of Operations, University College London Hospitals NHS Foundation Trust.
-
David Davis, Operational Staff Governor and Deputy Lead Governor, South East Coast Ambulance Service.
-
Janette Turner, Reader in Emergency and Urgent Care Research, University of Sheffield.
-
Catherine Pope, Professor of Medical Sociology in the Faculty of Health Sciences, University of Southampton.
Glossary
- Advanced Medical Priority Dispatch System (Priority Dispatch Corp, Salt Lake City, UT, USA)
- The proprietary brand name for a computer-aided dispatch system used in ambulance call centres to help call handlers select the appropriate response to callers through systematised caller interrogation.
- Ambulance clinician
- A generic term for front-line staff working on emergency ambulances and delivering clinical care, which includes both paramedics and emergency medical technicians.
- Computer-aided dispatch system
- A tool used in ambulance call centres to support staff to select the appropriate response to calls; it also creates a log of all calls received.
- Connecting for Health
- An agency of the Department of Health and Social Care, which existed from 2005 to 2013, and was given responsibility for delivering the National Programme for Information Technology.
- Department of Health and Social Care
- The branch of government responsible for setting health-care policy in England.
- Disposition
- The outcome of a particular contact between patient and health-care provider: what happens next to the patient?
- Electronic health record
- An electronic set of information for a particular patient, likely to include patient details, clinical observations and information on care or treatment delivered.
- Emergency medical service
- A term used to describe care provided by emergency ambulance services, usually delivered by paramedics or emergency medical technicians rather than doctors.
- Emergency medical technician
- A health-care professional generally employed by an ambulance service to deliver pre-hospital care in response to emergency calls, but with a slightly narrower scope of practice than a paramedic and likely to have undergone less extensive training.
- Interoperability
- The ability of two or more information technology systems or components to share information and use that information.
- Job cycle time
- Start to finish time for a resource allocated to a call. Measured by the time between (1) resource allocation and (2) resource cleared or stood down.
- Joint Royal Colleges Ambulance Liaison Committee guidelines
- A set of UK ambulance services clinical practice guidelines produced under the guidance of the Joint Royal Colleges Ambulance Liaison Committee and published by the Association of Ambulance Chief Executives. The guidelines are in a reference book, with an accompanying pocket book and application, to give practical guidance to ambulance clinicians and pre-hospital practitioners on the common conditions and injuries they may encounter, and how best to assess and treat them.
- Mobile data terminal
- A device fitted in the cab of an emergency ambulance that displays details of calls allocated to the crew. The information is transferred from the service call centre.
- National Early Warning Score
- A score based on six patient measures, used to detect clinical deterioration in acutely ill patients. The measures are (1) respiratory rate, (2) oxygen saturations, (3) temperature, (4) systolic blood pressure, (5) pulse and (6) level of consciousness.
- National Programme for Information Technology
- A strategic programme set up in 2002, but since discontinued, which aimed to create one standard information technology system for patient records in England.
- NHS Digital
- An executive non-departmental public body that provides digital services for the NHS and social care in England, including the management of large health informatics programs. It was formerly known as the Health and Social Care Information Centre.
- NHS Spine
- A set of national services managed by NHS Digital, including the Personal Demographics Service, Summary Care Records and Secondary Uses Service.
- Out of hours
- Health care delivered outside the core daytime hours of Monday to Friday. This is defined in our report as 18.30 to 07.59, Monday to Friday, plus all day on Saturdays, Sundays and bank holidays.
- Paramedic
- A clinically trained health-care professional, generally employed by an ambulance service to deliver pre-hospital care in response to emergency calls. In the UK, the title is protected and all paramedics must be registered with the Health and Care Professions Council.
- Patient clinical record
- A term used in some ambulance services for the paper form used to record details of the patient, clinical observations and any immediate care delivered in response to a 999 call. It is the same as a patient report form.
- Patient report form
- A term used in some ambulance services for the paper form used to record details of the patient, clinical observations and any immediate care delivered in response to a 999 call. It is the same as a patient clinical record.
- Personal Demographics Service
- The national electronic database of NHS patient details, such as name, address, date of birth and NHS number (known as demographic information).
- Personal digital assistant
- A small hand-held computer, now largely superseded by smartphones and tablets.
- Rapid-response vehicle
- Used to facilitate the fast arrival of a paramedic, but unable to carry patients.
- Resource
- Vehicle and crew (e.g. ambulance or rapid-response vehicle).
- Summary Care Record
- A summary of a patient’s clinical information, such as allergies and adverse reactions to medicine, accessible via NHS Spine.
- Tablet
- A small portable computer with a touchscreen interface.
List of abbreviations
- AMPDS
- Advanced Medical Priority Dispatch System
- AS
- ambulance service
- CAD
- computer-aided dispatch
- CCG
- Clinical Commissioning Group
- CQC
- Care Quality Commission
- ECG
- electrocardiogram
- ED
- emergency department
- EHR
- electronic health record
- EMS
- emergency medical service
- EMT
- emergency medical technician
- ERA
- Electronic Records in Ambulances
- GP
- general practitioner
- ID
- identifier
- IT
- information technology
- JRCALC
- Joint Royal Colleges Ambulance Liaison Committee
- MDT
- mobile data terminal
- MeSH
- medical subject heading
- NEWS
- National Early Warning Score
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPfIT
- National Programme for Information Technology
- NPV
- negative predictive value
- PCR
- patient clinical record
- PDA
- personal digital assistant
- Portable Document Format
- PDS
- Personal Demographics Service
- PPI
- patient and public involvement
- PPV
- positive predictive value
- PRF
- patient report form
- RMG
- Research Management Group
- RRV
- rapid-response vehicle
- SCR
- Summary Care Records
- SST
- strong structuration theory
- WIISARD
- Wireless Internet Information System for MedicAl Response in Disasters
- WP
- work package
