Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/04/28. The contractual start date was in December 2015. The final report began editorial review in May 2018 and was accepted for publication in April 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Miranda Scanlon reports grants from the National Institute for Health Research (NIHR) during the conduct of the study. Outside the submitted work, Miranda Scanlon reports personal fees from Which? (London, UK), the National Perinatal Epidemiology Unit (University of Oxford, Oxford, UK), Rod Gibson Associates Ltd (Wotton-under-Edge, UK) and the Midwifery Unit Network, and grants from NIHR. Jim Thornton is a member of the NIHR Health Technology and Assessment and Efficacy and Mechanism Evaluation Editorial Board (from 2012 to present).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Walsh et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Parts of this report are reproduced from Walsh et al. 1 © Author(s) (or their employer(s)) 2020. Re-use permitted under CC BY. Published by BMJ. https://creativecommons.org/licenses/by/4.0/ This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/.
Introduction
Since 1993, maternity care policy in England has promoted women’s choice of place of birth. This became the national choice guarantee in Maternity Matters in 2007,2 with three options: (1) birth in a maternity hospital [obstetric-led unit (OU)]; (2) birth in two types of midwifery-led units (MUs), either alongside midwifery unit (AMU) or free-standing midwifery unit (FMU); or (3) birth at home. Department of Health and Social Care-commissioned research into the outcomes of childbirth in different settings3 reported that outcomes for low-risk pregnant women and their babies were better and costs reduced if birth occurred in MUs, both AMUs or FMUs, rather than OUs. Planning to have a baby in a MU reduced caesarean rates by two-thirds.
The most recent National Institute for Health and Care Excellence (NICE) guidelines on intrapartum care therefore recommend MUs for low-risk women (i.e. women without significant health risk factors who would be predicted to have a normal labour and birth). 4 Sandall et al. ’s5 research suggests that this could be around 45% of all birthing women. However, despite the advantages of MUs, a recent survey found that only 11% of women gave birth in MUs, with the vast majority continuing to give birth in OUs. 6 If 20% of births occurred in MUs, savings to the NHS maternity budget could be around £85M. This represents a 3% saving on the current budget of £2.6B for maternity care. 7
In addition, our survey showed that MUs were not equally distributed across the country. One-third of local maternity services had no MUs, whereas others achieved 20% of all births in these facilities (designated ‘high performing’), and the remainder had MUs but they were frequently underutilised, with < 10% of all births in MUs (designated ‘low performing’).
The explanation for the survey results is unclear. There may be a range of context-specific or more general barriers to establishing and operating MUs. Little is currently known about such barriers or what facilitates MU provision. However, the unequal provision may result in many women being unnecessarily exposed to the risk of caesarean and to a birth experience that is less satisfying, although this may also be explained by the selection of women likely to achieve better outcomes. In addition, local maternity services may not be realising the cost savings of MUs.
Rationale for the research
This study explored the reasons for organisational anomalies in the provision of maternity services by undertaking comparative case studies of NHS trusts with contrasting MU configurations in England. Specifically, we investigated higher-performing trusts (those with > 20% of their total births in MUs) and lower-performing trusts (those with < 10% of their total births in MUs). In addition, we undertook case studies in trusts without MUs. The study also sought to identify interventions to address barriers to and facilitators of the provision of MUs and developed service guidance to inform future maternity service commissioning and provision.
Home birth was excluded from our study because our focus was only on MUs.
Aims and objectives
The study set out to:
-
describe the configuration, organisation and operation of MUs, both AMUs and FMUs, in England
-
build an understanding of key issues and barriers to uptake by women that MUs face (including why some maternity units have closed MUs)
-
explore why some maternity services in England have no MUs
-
identify why some maternity services in England have ≥ 20% of all births in MUs
-
identify why some maternity services in England have MUs, but are running at substantial undercapacity (≤ 10% of all births)
-
convene a national maternity care stakeholders’ workshop to discuss appropriate interventions and service guidance to inform future maternity service commissioning and provision regarding improving the availability and utilisation of MUs.
Structure of the report
Chapter 1 describes the background and rationale for the study. Chapter 2 describes the research approach and methods, with details of the design and analysis. Chapter 3 reports the findings of the national mapping survey of MUs in England. Chapter 4 describes the findings from the case study sites. Chapter 5 describes the stakeholder workshop, which included individuals from a range of constituencies, designed to generate guidance for maternity care providers and commissioners. Chapter 6 discusses in more depth the integrated findings from stages 1–3. Chapter 7 is the conclusion, summing up the key findings, their implications for maternity services and recommendations for further research.
Updated literature review
The literature review, updated from the original research submission, identifies the existing, contemporary (from 2000 to 2017), English-language research of MUs (AMU and/or FMU). The search terms ‘birth cent*’, ‘midwife led unit’, ‘birthplace and midwife’, ‘place of birth’ and ‘midwife’ as title or keyword were used to search four databases: MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE and PubMed. A manual search of key journals and article references was also undertaken.
There was a range of study designs utilised in research evaluating MU clinical outcomes, including randomised controlled trials (RCTs) or quasi-RCTs, prospective cohort studies, retrospective cohort studies and mixed-methods case studies. Although one RCT8 and one cohort study9 have been undertaken in the context of the opening of a MU, with access to it being dependent on agreement to participate in the study, the RCT was confounded by the two arms receiving different models of care. 8,9 RCTs may not be appropriate or possible (acceptable to women) in a context in which women already have ready access to either birthplace type. 10 Although observational studies are subject to selection bias, which weakens the ability to draw causal inferences,11,12 this design can accommodate several outcomes within the same study. 13 Arguably, they are the best design for answering research questions regarding the identification of differences in clinical outcomes between the different birthplace types, given the complexity of both childbirth and birthplace. 14–16
The Cochrane review into alternative (MUs) compared with conventional settings (OUs) for birth included 10 trials, including a total of 11,795 women, relating to AMUs only, with six of them undertaken over 25 years ago. 3,17–21 There are also several observational studies into AMUs, with comparison OU outcomes. 19,22,23 The limited contemporary research into the comparative clinical outcomes for FMUs and OUs includes prospective studies,24–26 a retrospective study27 and population-based cohort studies. 19,28 There are also studies reporting only MU clinical outcomes, with no OU comparison outcomes from the same context. 29–32 All but a few of these studies report similar or improved neonatal outcomes for women planning a MU birth compared with women of similar risk planning an OU birth. The few discrepant studies reporting worse neonatal outcomes for FMU babies than those born in an OU are from the USA. 33–35 The lack of integration of MUs in the US maternity system arguably limits the applicability of this, and other research from the USA, in the UK context. Studies that are not relevant to the context or focus of the MU study are not for inclusion here, for example those combining all out-of-hospital births for comparison with OU births,36 those evaluating a model of care rather than birthplace type37 or those from remote rural38 or developing country contexts (e.g. Nepal).
The Birthplace in England study3 is the largest and most comprehensive comparative birthplace research to date. It included 64,538 women defined as ‘low risk’ (19,706 women planning a OU birth, 16,710 women planning an AMU birth, 11,282 women planning a FMU birth and 16,840 women planning a home birth). This study is relatively recent and set in the local context, making it the dominant reference in the birthplace literature and in the latest NICE intrapartum and birthplace guidelines. 39
Specifically, the caesarean rate varied from 11% (OUs) to 4% (MUs), the assisted vaginal birth rate (forceps and vacuum assisted) varied from 15% (OUs) to 7% (MUs) and the rate of normal birth varied from 73% (OUs) to 90% (MUs). In addition, in OUs and MUs the epidural rate was 30% and 12.5%, the intravenous oxytocin rate was 23% and 8.5% and the episiotomy rate was 19% and 10%, respectively. 3 These differences are critically important. Operative births and labour interventions put the mother at greater risk both physically and psychologically. The major complications of caesareans are severe haemorrhage, thromboembolism, infection and risks for subsequent pregnancies. 40 Emergency caesareans are also linked to post-traumatic stress. 41 Assisted vaginal birth is associated with perineal trauma, anal sphincter tear and urinary stress incontinence. 42 Epidurals increase the risk of assisted vaginal birth43 and intravenous oxytocin is more likely to be associated with fetal compromise. 44 Higher rates of episiotomy are linked with additional perineal trauma. 45
The reduction in all of these labour interventions and operative birth outcomes could be achieved if low-risk women birth in MUs. Critically, outcomes for babies when women birth in MUs are no different from those born in OUs. 3 The Birthplace in England study also found that having a baby in a MU was cheaper. The unadjusted mean costs were £1435, £1461 and £1631 for births in FMUs, AMUs and OUs, respectively. 46 MUs also improve continuity of care and one-to-one care in labour47 and increase women’s sense of control and their satisfaction with care,17 areas in which the Care Quality Commission say current maternity services need to improve. 48
In 2014, McCourt et al. 49 reported follow-up research to the Birthplace in England study3 on AMUs’ organisation, staffing and provision. They called for further research into the facilitators of and barriers to expansion of MU capacity.
In the past 2 years, research from New Zealand,50,51 Australia52 and the Netherlands53 on MU outcomes continues to show the consistent trend to fewer birth interventions. In addition, an English study found that FMUs were cost-effective. 54
This updated literature review provides additional background evidence and context for the rationale for this study, outlined at the beginning of this chapter (see Rationale for the research).
The next chapter details the research approach and methods.
Chapter 2 Research approach and methods
This chapter details the research design and rationale for the methods of the three stages of the research. It describes the individual components of each stage, including a discussion of the theoretical underpinning for the analyses of the case studies.
It also provides a brief overview of how the study was organised and managed, and the public involvement throughout all stages.
Study organisation and management
The study was overseen by the co-investigators, a Project Management Team (made up of the researchers and a subset of the research team, which met monthly) and an advisory group (which met twice a year). The overall role of the advisory group was to ensure that the study was conducted in line with the protocol, and that the design, execution and findings were valid and appropriate for all stakeholders in maternity care. The role was also to ensure linkages with any emerging intelligence related to the topic.
Public involvement in the research
Public involvement was integrated into the study throughout all phases, including project design, implementation, management and dissemination. Four service users were recruited through an established local service user maternity network [URL: www.nottsmaternity.ac.uk (accessed 8 July 2019)] that worked with the university maternity research group. Black, Asian and minority ethnic representatives were part of this group, but none volunteered for our project. This service user reference group reviewed the study design, all study documents and the research process, including data collection and feedback on emergent findings presented at the stakeholder workshop, and have continued with dissemination activities with their networks over the past 12 months.
User involvement in the study design
One of the co-investigators (MD) has had a long history with maternity care research in the UK as a service user representative. She contributed to the original idea for the research and to the subsequent protocol.
User involvement in the study implementation
A service user reference group was established once the funding had been secured and met twice per year over the lifetime of the project. Group members advised on approaches to achieve recruitment of women into focus groups. All members participated in data collection, specifically in facilitating women’s focus groups at the six case study sites across England. In preparation for this, they, together with other members of the research team, participated in a bespoke training workshop on focus group facilitation. At the stakeholder workshop, one member of the service user reference group co-presented the preliminary findings to stakeholders and two other members co-facilitated two of the small group discussions held throughout the day.
Research design and methods
The design was in three stages, utilising mixed methods. The mixed-methods approach is most aptly described as explanatory sequential. 55 Within this typology, quantitative data collection and analysis (stage 1) inform later stages of qualitative data collection and analysis (stages 2 and 3). This is then followed by a final interpretation phase (Figure 1).
FIGURE 1.
Stages of the mixed-methods research.

The six objectives of the project overall are mapped as follows (and outlined in Chapter 1) to these three stages, commencing with stage 1.
Stage 1 (objectives 1 and 2)
Objective 1
To describe the configuration, organisation and operation of MUs (both AMUs and FMUs) in England.
Method
Telephone survey of all NHS trusts in England with maternity services.
Data collection
Our data collection was aided by information provided by BirthChoiceUK and the consumer organisation Which? Both of these companies provide web-based information about maternity service provision across the UK. BirthChoiceUK holds a database containing details of maternity unit configurations, which was supplied to Which? for the development of the Which? Birth Choice website. 56 Which? also audits MU provision and utilisation across the UK. We entered into a data agreement with Which? for it to share the details of maternity units and configurations along with information it had collected about birth numbers in MUs in England. We developed our own data collection pro forma after consulting both the Birthplace in England mapping data collection tool57 and pages on the Which? Birth Choice website relating to maternity units, and populated it from the Which? Birth Choice data. Heads of midwifery (HoMs) in the 134 trusts across England were then sent the survey. We then telephoned the HoMs, who confirmed, clarified or completed missing entries in the survey for their current maternity services. These telephone interviews, which lasted up to 30 minutes, took place over a 3-month period between March and May of 2016. Actual annual number of births was completed using the Which? Birth Choice data and updated in the telephone interviews, as required.
Ethics
This first stage of the research was classed as service evaluation and thus did not require Research Ethics Committee (REC) approval.
Sample
One hundred and thirty-four HoMs, representing all NHS trusts providing all publicly funded maternity care in England, were contacted by the research staff. Home birth was excluded from our data.
Analysis
Descriptive summary statistics and narrative description of configuration, organisation and operation of AMUs and FMUs was undertaken.
Objective 2
To build an understanding of key issues and barriers to uptake facing MUs (including why some maternity services have closed FMUs).
In trusts in which a FMU had been closed within the previous 8 years, the HoM was interviewed to gain their perceptions of the reasons for closure. An analysis of media (newspaper, radio, television) coverage of the closure of the relevant units was also undertaken.
Method
A systematic search of media reports, content and discourse analysis was carried out guided by framing theory. 58
Data collection
The LexisNexis database was searched systematically to identify all media reports directly relating to the 14 FMUs in England that had closed between 2008 and 2015. Multiple FMUs from the same NHS trust were considered as one site, as were two units from different but nearby trusts that had closed after recommendations from the same service review. After screening, two services (Mid Yorkshire Hospitals NHS Trust, Wakefield Birth Centre; and Wiltshire Primary Care Trust, St Peter’s Maternity Unit, Shepton Mallet) were found to have no relevant articles, leaving a remaining eight services. The number of articles about each site ranged from 2 to 65. A total of 190 articles were included in the analysis. These included local newspaper articles (n = 175), transcripts of local television news items (n = 5) (all from one site) and articles from national publications (industry publications and national newspapers) (n = 11).
Analysis
Data were extracted onto a bespoke template in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), which provided a framework for analysis, working on two levels, to (1) identify and analyse the relevant content using a structured approach and (2) identify and analyse the discourse present in the media reporting in each case. The approach enabled us to capture the range of voices and to compare perspectives, identifying who the authors and speakers were in each report and relating this to extracted content and discourse. The aim of this was not to triangulate in terms of validation but to recognise that media analysis captures events not as ‘facts’ but as representations of them. The template was drafted in relation to the study objectives and discussed and revised within the research team. It was intended to be used flexibly, allowing for the amendment of categories when needed, and some categories on the template were combined in the light of the initial data extraction work. Two team members extracted data for each site independently of each other, using a separate sheet for each media report, and any areas of difference were discussed to reach consensus. Using a purpose-built macro, the data were then collated into a single spreadsheet for each site and a thematic approach was used to synthesise the findings within and then across all services.
Once the emergent themes had been identified, framing theory58,59 was used to guide the synthesis of themes in relation to discourse.
Stage 2 (objectives 3–5)
Objectives
To explore why some maternity services in England achieve ≥ 20% of all births in MUs.
To explore why some maternity services in England have opened MUs but are running under capacity (≤ 10%).
To explore why some maternity services in England have no MUs.
Method and justification
Case study methodology was the most appropriate approach for these aims, as it facilitates the exploration of large, complex organisations, such as maternity services. It does this by combining a range of data collection methods, including interviews and focus groups, with a variety of sampling techniques, to achieve data saturation and thus gain an in-depth understanding of the social processes and organisational culture within each study site. 60 Specifically, this project explored why organisational change, premised on a relatively strong evidence base, had not been achieved across England in relation to the provision and utilisation of MUs. Within each site, both individual interviews and focus groups were used to produce a detailed and rounded analysis of the case. A comparative case study approach enabled the identification of common and differentiating determinants of the successful implementation of MUs. 61 In-depth exploration of each study site was necessary to gain an understanding of the complex set of inter-related factors that played a role in the local uptake and implementation of MUs. The case studies provided sufficiently detailed descriptions of the local social processes and contextual factors to develop an understanding of the potential for individual findings to be sensitively generalised to other sites. 62
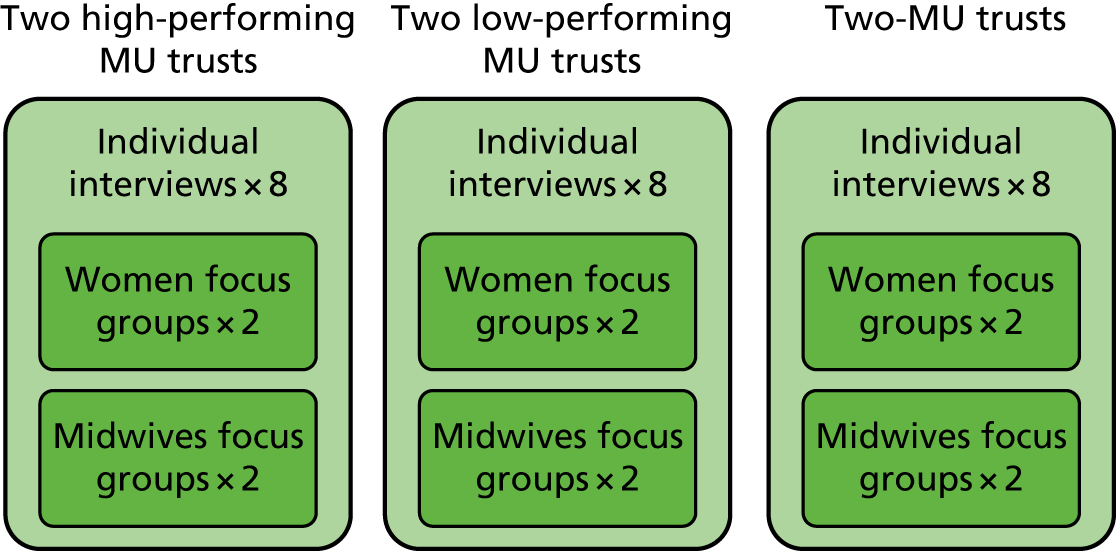
Using the data from stage 1, six case study sites were purposively sampled to identify:
-
two high-performing services with both an AMU and a FMU, achieving ≥ 20% of total births
-
two low-performing services with one or more MUs (AMU or FMU), achieving ≤ 10% of total births
-
two services with no MUs.
Within each of the three categories, study sites were chosen to represent both rural and urban settings to enhance diversity. Six sites (two from each category above) were chosen to obtain a cross-section of local maternity care services that might approximate typical adoption, integration and utilisation of MU services.
Theoretical/conceptual framework
The theoretical and conceptual frameworks underpinning the case study methodology are described below.
This research sought to identify and analyse factors that help to explain variations in MU provision, with a view to identifying routes to overcoming barriers to change. Findings of the potential economic efficiency of MUs over OUs46 suggest that financial drivers alone do not explain the inequitable provision of MUs across the country. In recent years, there has been a widespread focus on the gap between research evidence and practice. 63,64 Prior research supported by the National Institute for Health Research describes multifaceted barriers to and drivers of change in the NHS, including contextual conditions, the nature of innovations and the processes of implementation. 65,66 Considering this work, a wide range of factors may be thought to facilitate or create barriers to the establishment and utilisation of MUs. Previous research has identified a number of important institutional factors shaping maternity services and potentially hindering innovation, including issues of professional power and the midwifery–obstetrics relationship,67,68 resource constraints and workforce issues,69 the environment of litigation and risk management,70,71 as well as inaccurate media portrayals of birth. 72 Currently, however, the prevalence and impact of potential barriers to the creation and utilisation of MUs remains unclear. In addition, a large body of research on innovation diffusion and implementation has demonstrated that innovations, particularly those that involve complex organisational change, do not move directly from evidence into practice, but are adapted, and in some cases transformed, through the process of implementation. 67,73 To explicate this process, our study utilised Damschroder et al. ’s74 Consolidated Framework for Implementation Research (CFIR), supplemented by theory that considers the wider institutional forces shaping health-care organisations and organisational change. 75,76
The CFIR provides useful insights for investigating why implementations fail, or are only partially successful, to guide future implementation efforts. 77 This was selected to provide a conceptual framework to analyse the contexts of MU implementation and systematically identify the factors influencing the extent to which MUs are adopted into practice and utilised. The CFIR was developed through meta-review of previous implementation literature and theories, and identifies 39 underlying constructs previously found to have an impact on the course and extent of implementation. The CFIR has now been used by a number of studies to identify factors affecting implementation, including the implementation of complex service initiatives,78–80 and has been found to be an effective tool to identify barriers to and facilitators of implementation. 81 Within the CFIR, constructs are divided between five major domains:
-
characteristics of the intervention itself, including the essential ‘core’ and adaptable ‘periphery’ elements, its design, complexity, cost and degree of flexibility
-
outer context of change, including pressure from patients, partners and other stakeholders
-
inner context of change, including the features of the local organisation, its culture, structure, practices and resources
-
individuals involved in change, their preferences, beliefs and identities
-
process of change itself, including details of planning, engaging and executing.
This framework is not intended to be applied wholesale, but rather offers a long list of constructs to consider for inclusion when investigating particular instances of implementation. We drew on CFIR to identify relevant constructs in early stages of the study to inform data collection and subsequent approaches to analysis, as outlined in the sections below. The current research sought to explore both the variation in initial engagement with MUs as well as subsequent implementation in sites that do engage. Therefore, the CFIR, geared towards understanding specific instances of implementation, was supplemented by theory geared towards consideration of the factors affecting MU adoption at a more general level. A large volume of recent work on health-care organisations has identified regulative, normative and cultural features of the health-care institutional environment75 that shape the potential for innovation and change. 76 Waring et al. 82 suggested the guiding categories of power, organisation, culture and knowledge, which have previously been adopted to make sense of the complex set of inter-related social factors known to affect processes and outcomes of health-care organisations. These categories guided the analysis of the more macro elements of the ‘outer context’ of change.
Data collection
Data collection consisted of in-depth telephone interviews and focus groups of midwives and service users, held locally (Figure 2).
FIGURE 2.
Case studies.
The interview schedule was developed by the research team, drawing on the findings from the first stage of the study, existing literature regarding the organisation of maternity services and literature on implementation and organisational change, and was reviewed by the service user reference group and the advisory group. Questions were focused on discussing the evolution of services in each of the sites.
Interviews
At each site, digitally recorded semistructured telephone interviews were undertaken with the chief executive of the NHS trust, HoM, senior obstetrician, community midwifery lead, business manager for maternity service, neonatologist, GP commissioner of local maternity services, Maternity Services Liaison Committee service user or user group representative and local maternity support/campaigning groups. These interviews lasted between 30 and 60 minutes and a minimum of eight interviews were carried out at each site. They were professionally transcribed verbatim.
Focus groups
Focus groups with service users and with clinical midwives were conducted at each site. The focus group guides were developed by the research team in collaboration with service users.
In each site, two focus groups were held with six to eight women who had given birth in the previous 12 months. These groups were held at venues in the local community of case study sites. The groups were co-facilitated by a service user from the Nottingham Maternity Research Network (service user reference group) and a member of the research team. They lasted on average 45 minutes and were digitally recorded and transcribed. Topics explored included interviewees’ perception of local service options around place of birth and the functioning of MUs. Within each site, we attempted to recruit as diverse a sample of participants as possible (e.g. different ethnic groups, different socioeconomic classes, different parity and age), but this was hampered by having to rely on local informants. In the end, we recruited women whom informants knew through Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) contacts mainly. We achieved diversity in relation to age, parity and minority ethic Asian representation, but not very well in relation to social class.
In addition, we undertook two focus groups with six to eight midwives in each site, exploring how choice of place of birth was presented, how MUs were functioning where they existed and midwives’ perceptions of why they had not been developed in sites without them.
Ethics approval
The stage 2 case study was reviewed and given a favourable opinion by the West Midlands – Solihull REC on 1 April 2016 (REC reference number 16/WM/0136).
Analysis plan and revisions
The process for analysis of qualitative case study data was as follows.
Both DW and CG attempted to each code a women’s focus group discussion according to the CFIR, but it became clear from early on in this exercise that the transcript codes did not map across to the CFIR domains and constructs, except in very selected areas. This was because the women’s transcripts reflected their personal experience of care and not the broad sweep of a major service implementation project. Following a team discussion, it was decided that the women’s focus group discussion would be open-coded and analysed thematically, utilising the principles of thematic analysis as outlined by Braun and Clarke,83 supported by NVivo software (QSR International, Warrington, UK). This approach follows six distinct stages: (1) familiarisation with data, (2) generating initial codes, (3) searching for them, (4) reviewing themes, (5) defining and naming themes and (6) writing up findings.
All other interviews and the midwives focus groups (MFGs) were analysed using the CFIR. First, in the pilot analysis, five members of the research team (DW, DC, HS, CG and SB) coded the same three interviews to the constructs in the CFIR, which are grouped into six domains, mentioned above. This coding was placed within NVivo, with nodes and subnodes created to match the domains and constructs of the CFIR. These team members then met to compare coding and discuss how data related to each of the constructs. A second pilot round was then undertaken with the same team members coding an additional two transcripts. Once it had been agreed that a shared understanding of CFIR constructs had been achieved, case study sites were then divided between the project members involved in coding (DC two sites, DW two sites, SB one site and HS one site). The remaining interviews and MFGs were then coded according to the constructs within the CFIR. It was considered appropriate for an individual coder to complete analysis of a whole site in order to develop an in-depth understanding of the case. During this stage, ‘open’ codes were also added within CFIR constructs to further identify how the data related to the broader construct. For example, data relating to the construct ‘patient needs and resources’ were also coded by the nature of specific patient needs and resources referred to, such as ‘patient need for choice’ or ‘patient need for convenient locale’.
At this stage, a number of issues with coding data to the constructs in the CFIR were encountered. One issue that arose was that there were differences in the number of open codes created by each coder, with some coders adding a larger number of codes with greater specificity in relation to the data. In addition, data from the MFGs and the individual interviews often related to multiple constructs, and were therefore coded in several places, under the framework. One of the consequences of this was the production of many additional nodes within NVivo, which made handling the full data set cumbersome; it also meant that it was difficult to test inter-rater reliability following this coding stage.
To address this, following this coding, a wider team of co-investigators (DW, HS, SB, CMc and LC) who had previously undertaken case study analysis met to start the process of collapsing codes into themes. In addition, the research fellow who had not participated in the coding, but was very familiar with the data scrutinised, reorganised and reduced the codes within each construct to reflect the important themes of the data and relate this to the logic of the CFIR construct in which it was located, in a process akin to axial coding.
This process of reduction revealed six cross-cutting themes that were relevant under multiple CFIR constructs (see Table 22). We then had to make a decision on how to report the findings: whether to give priority to the cross-cutting themes or to the CFIR domains as the organising headings. If we chose the former, it rendered the theoretical underpinning of the CFIR redundant, superseded by these six primary themes. However, the CFIR, as well as being empirically validated in multiple organisational research projects,74 had provided us with a heuristic template via its five headline domains of (1) intervention characteristics, (2) outer setting, (3) inner setting, (4) individual characteristics and (5) process. We therefore decided to locate the cross-cutting themes within these domains.
In addition, narrative summaries and within-site comparisons of each case study site were produced to tell the ‘story’ from each site and to tease out areas of unanimity and dissonance between the respondents. These sections utilised and synthesised elements of the broad domains of the CFIR (inner setting, outer setting, characteristics of individuals, intervention characteristics and process) to shape each story. This facilitated more congruence in the reporting of the data collected in each site, which lost some of its distinctiveness and rootedness when coded as one data set into NVivo.
A ‘within-case’ analysis proceeded to ‘cross-case’ comparisons. Waring’s84 categories of power, organisation, culture and knowledge assisted in providing a macro-lens to inform this level of analysis. In this way, a comprehensive picture of both the ‘inner’ and ‘outer’ context for change assisted in distilling the key barriers to and facilitators of MUs developed (see Chapter 6).
The CFIR assisted analysis of interviews and MFGs were juxtaposed with the thematically analysed women’s focus group at the level of the cross-case analysis.
Stage 3 (objective 6)
Objective
Convene a national maternity care stakeholders’ workshop to discuss appropriate interventions and service guidance to inform future maternity service commissioning and provision, regarding improving the availability and utilisation of MUs.
The workshop aimed to engage participants in a dialogue to enhance the ontological, educative and catalytic authenticity of the research. 85 The team presented their findings from stages 1 and 2. Workshop participants collaborated in mixed interdisciplinary small groups, led by two facilitators from the project team, service user network and advisory group, in examining and suggesting potential interventions. This was done in the following way. The participants were asked first to discuss appropriate interventions in response to the findings, and then to categorise these as immediate/short term (up to 3 months), medium term (6–12 months) or long term (> 12 months). Underpinning this process, we impressed on delegates the importance of remaining cognisant of the feasibility and utility of each of the proposed interventions in relation to their own organisations or areas of work. Finally, we asked the groups to target their interventions according to different stakeholder groups: providers (managers, different professional groups), commissioners and service users. The workshop thus linked research knowledge with decision-making processes and potential interventions. 86
Data collection
Data were captured by field notes and on flip charts throughout the day, which were then transcribed. Through this process of debate and discussion, further service guidance was co-developed by stakeholders and the research team.
Sample
The workshop was attended by 56 people. Our objective was to include all groups representing those involved in the maternity services, including service users, maternity care professionals, NHS trust managers, maternity policy representatives, service providers, service commissioners and politicians, and academics with an interest in maternity care.
Stakeholder workshop attendees were:
-
four members of the service user reference panel
-
head of policy of the National Childbirth Trust
-
representative of the chief executive of the Royal College of Midwives (RCM)
-
midwifery representative from the Department of Health and Social Care
-
three co-investigators on the Birthplace in England study3
-
national clinical director for Maternity and Women’s Health in NHS England
-
director of nursing, Commissioning and Health Improvement
-
chairperson of NICE Intrapartum Guideline Group
-
knowledge mobilisation research fellow (maternity services)
-
two representatives of former local supervising authority midwifery officers
-
two consultant midwives
-
neonatologist
-
consultant obstetrician
-
three representatives of Maternity Transformation, NHS England
-
chief executive officer (CEO) of Birthrights
-
two doulas
-
midwifery clinical leads from an AMU and a FMU
-
two representatives of the Midwifery Unit Network
-
two representatives from two maternity and neonatal networks in England.
Ethics
This third stage of the research was classed as service evaluation and thus did not require REC approval.
Analysis
The workshop data were synthesised by HS and reviewed by DW and LC.
Changes to the protocol
The original protocol had included local media analysis regarding changes in MU provision at the case study sites. However, as a result of extensive delays with clinical governance approvals at most of the sites, there was insufficient time to undertake the local media analysis and undertake all of the focus group and individual interviews. Only site 1 had undergone recent, significant maternity service reconfiguration and this process was covered quite comprehensively in individual interviews. In addition, our media analysis of closed FMUs from stage 1 became more extensive than originally intended. We were confident that this aspect of the project illustrated the impact of local media commentary on service reconfigurations and therefore adequately compensated for the loss of media analysis from the case study sites.
Documentary analysis was also in our protocol and was to include minutes of strategic meetings about MU service changes and local policy and guidance about MU access, organisation and operation. However, when we asked case study sites for these records, they were either unable or unwilling to produce them, despite repeated requests. We made the pragmatic decision to not pursue this.
The next chapter details the results for stage 1 of the project: the mapping, organisation and operation of MUs and the findings about the closure of FMUs, both from the media analysis and the interviews with HoMs of MUs where FMUs had closed.
Chapter 3 Findings phase 1: mapping, organisation and operation of midwifery-led units
The aim of the initial phase was to report on the types, numbers and utilisation of MUs in England, 6 years on from the Birthplace in England study,3 and present the results from the first part of a larger funded study of the facilitators of and barriers to optimal use of MUs. It compares the results with the Birthplace Mapping Survey57 and comments on the changes that have occurred over that time. In addition, it discusses in more depth the potential utility of MUs to birth a greater proportion of low-risk women. This has already been published and is referenced in the Acknowledgements.
Definition of alongside midwifery units
To enable accurate mapping of service configuration it was first necessary to review how terms are operationalised. MUs are defined as a clinical location offering care to women with straightforward pregnancies during labour and birth, in which midwives take primary professional responsibility for care. Although the definition of a FMU is clear (MU that is a geographical distance from a host OU and therefore requires a vehicle transfer if complications occur in labour), an AMU is less clearly defined. The Birthplace in England study3 defined it as a MU in which diagnostic and therapeutic medical services, including obstetric, neonatal and anaesthetic care, are available, should they be needed, in the same building, or in a separate building on the same site. 57 Transfer will normally be by trolley, bed or wheelchair. Follow-on research projects from the Birthplace in England study3 add that AMUs should be able to accurately identify their admissions and births in their record systems. 87 However, these criteria allow for a number of hybrid arrangements, for example:
-
midwifery-led rooms within the physical space of a traditional labour ward
-
a midwifery-led area adjacent to a labour ward, but with no separate staffing or management
-
a midwifery-led area that allows for labour interventions, such as continuous fetal monitoring
-
a midwifery-led area that is regularly used for labour ward overflow
-
no separate data collections of processes or outcomes within the MU.
Within our team, we had extensive discussions before agreeing the following criteria for defining AMUs for the mapping stage of our study:
-
midwifery-led care setting
-
‘low-risk’ women, with case-by-case exceptions only
-
separate physical space from OU, with minimum demarcation being a line on the floor that excludes (e.g. having a AMU-style room within an obstetric labour ward)
-
only emergency secondary/tertiary-level care is permissible within the space; epidurals, continuous electronic fetal monitoring and medical induction/augmentation require transfer to the adjacent OU
-
does not provide care for labouring high-risk women when the OU is short of rooms (unless exceptional circumstances)
-
ability to measure number of births per year.
These criteria are slightly more restrictive than the Birthplace in England study3 and we estimate that they resulted in the exclusion of a very small number (possibly two or three) AMUs included in the previous research. Our data set therefore reflects this number.
Results
All 134 trusts participated in the survey (response rate 100%).
The results will be presented in four ways: (1) number and type of MUs as an indicator of place of birth choice, (2) changes since the Birthplace in England study,3 (3) the number of births per year in AMUs compared with FMUs and (4) MU births as a percentage of all births within each individual trust, excluding home birth. The last gives some indication of the utilisation of MUs as defined by percentage of women on a midwifery-led pathway that birth in them.
Number and type of midwifery-led units
The local configuration of maternity services (trusts) in England is constantly evolving. There has been a tendency for trusts to expand and merge so that there are now fewer trusts in England providing maternity services than at the time of the Birthplace Mapping Survey57 in 2010, reduced from 148 to 134. There has been a similar reduction in the overall number of OUs, from 177 to 159. Many of the existing small OUs operate in areas that are more rural. Most trusts have just one OU (n = 106), but 25 trusts now have two OUs and one trust has three.
One hundred and thirty-two trusts have at least one OU and, of these, 65% have at least one AMU. The majority of trusts (52.2%) have one OU and one AMU. Almost 27% of trusts have one OU and no AMU. Ten trusts with two OUs have no AMUs. The trust with three OUs has two OUs with an attached AMU and one OU without an AMU. This accounts for all 97 AMUs (Table 1).
| Number of OUs in the trust | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||||||
| n | % | n | % | n | % | n | % | n | % | |
| Number of AMUs in the trust | ||||||||||
| 0 | 2a | 1.5 | 36 | 26.9 | 10 | 7.5 | 0 | 0.0 | 48 | 35.8 |
| 1 | 0 | 0.0 | 70 | 52.2 | 5 | 3.7 | 0 | 0.0 | 75 | 56.0 |
| 2 | 0 | 0.0 | 0 | 0.0 | 10 | 7.5 | 1 | 0.7 | 11 | 8.2 |
| Total n/% of trusts | 2 | 1.5 | 106 | 79.1 | 25 | 18.7 | 1 | 0.7 | 134 | 100.0 |
Twenty-nine per cent of all trusts (39 out of 134) have a FMU. Of these, six trusts have two FMUs, five trusts have three FMUs and two trusts have four FMUs, with the majority of trusts with FMUs having only one. Of these, there are two FMUs that are not part of a trust with an OU. Multiple FMUs were found to exist exclusively in rural areas. In total, there are 61 FMUs (Table 2).
| Number of OUs in the trust | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||||||
| n | % | n | % | n | % | n | % | n | % | |
| Number of FMUs in the trust | ||||||||||
| 0 | 0 | 0.0 | 79 | 59.0 | 16 | 11.9 | 0 | 0.0 | 95 | 70.9 |
| 1 | 2 | 1.5 | 16 | 11.9 | 8 | 6.0 | 0 | 0.0 | 26 | 19.4 |
| 2 | 0 | 0.0 | 5 | 3.7 | 0 | 0.0 | 1 | 0.7 | 6 | 4.5 |
| 3 | 0 | 0.0 | 4 | 3.0 | 1 | 0.7 | 0 | 0.0 | 5 | 3.7 |
| 4 | 0 | 0.0 | 2 | 1.5 | 0 | 0.0 | 0 | 0.0 | 2 | 1.5 |
| Total n/% of trusts | 2 | 1.5 | 106 | 79.1 | 25 | 18.7 | 1 | 0.7 | 134 | 100.0 |
In summary, there are 23 trusts with an AMU attached to an OU and at least one FMU.
Within these 23 trusts there are:
-
three trusts with two AMUs and one FMU
-
eight trusts one AMU and two FMUs
-
three trusts with one AMU and three FMUs
-
one trust with one AMU and four FMUs.
The clusters of FMUs (e.g. three or more) attached to trusts (hub and spoke arrangement) tend to exist in counties that are more rural.
Figure 3 represents the current configuration.
FIGURE 3.
Flow chart of trusts, AMUs, FMUs and OUs.

Changes since the Birthplace in England study
Over a 6-year period, there has been an increase of 44 AMUs and three FMUs since the Birthplace Mapping Survey was undertaken in 2010. 57 The number of trusts without a MU has fallen from 75 (50%) to 32 (24%), and, of these 32 trusts, 27 have one OU and five have two OUs (Figure 4).
FIGURE 4.
Numbers of AMUs, FMUs and trusts without MUs in England: change since Birthplace in England study. 3
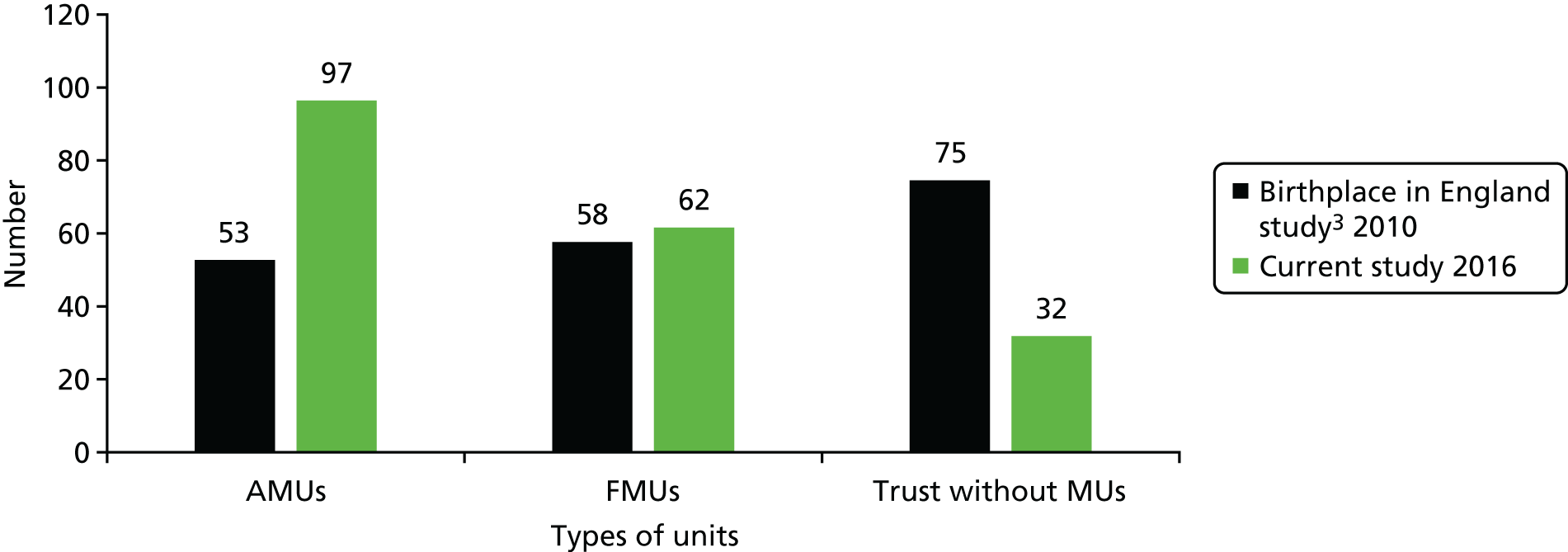
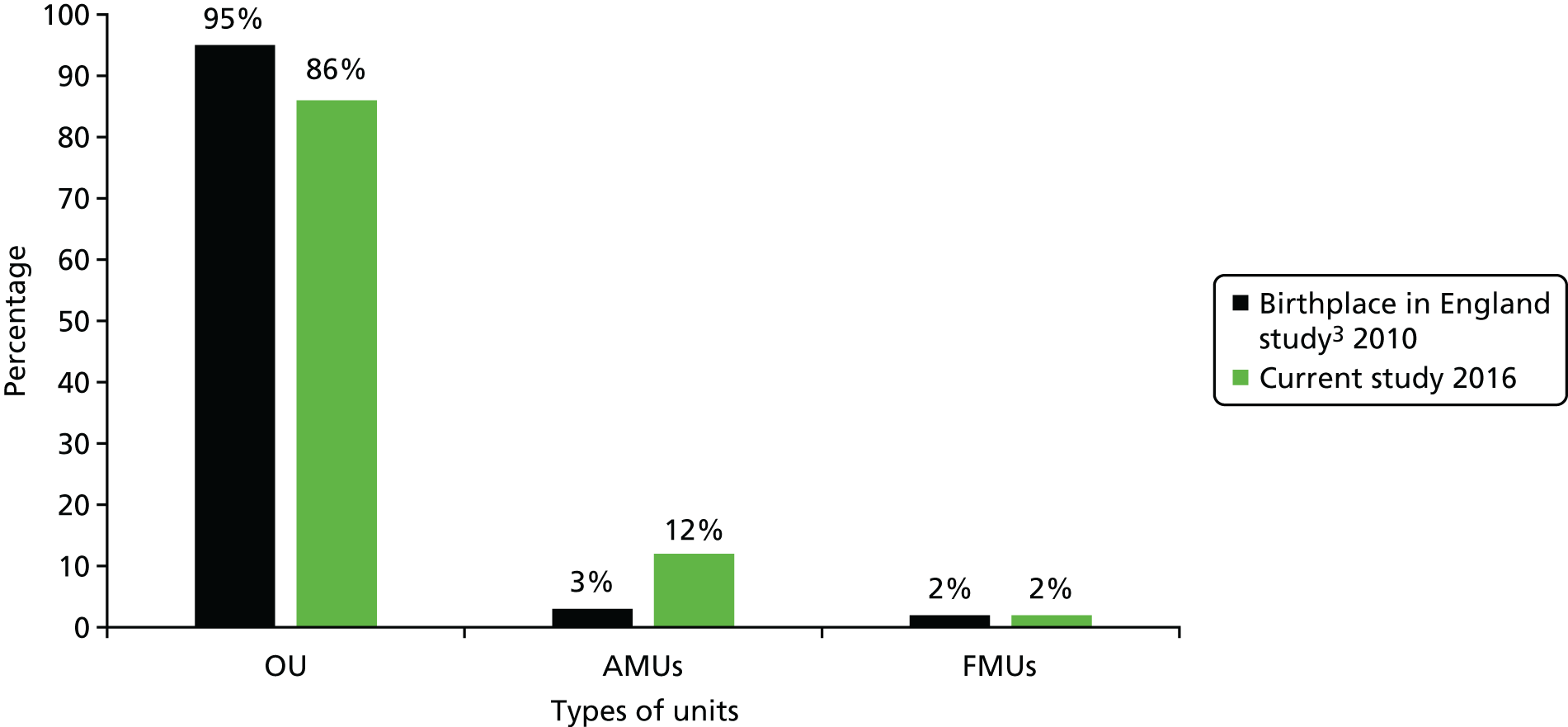
The increase in the number of MUs is reflected in a higher national percentage of all births occurring in such units. In comparison with findings from the Birthplace Mapping Survey,57 MU births across England increased from 5% to 14% of all births over the 6-year period, almost entirely related to the increase in AMU provision (Figure 5).
Number of births per year in midwifery-led units
The number of births in each AMU varies considerably, from 100 to 2000 births per year, but most range between 500 and 1000 births per year. Below we have categorised AMUs into bands based on their number of births per year (Figure 6).
FIGURE 6.
Size of AMUs: numbers of births per year.
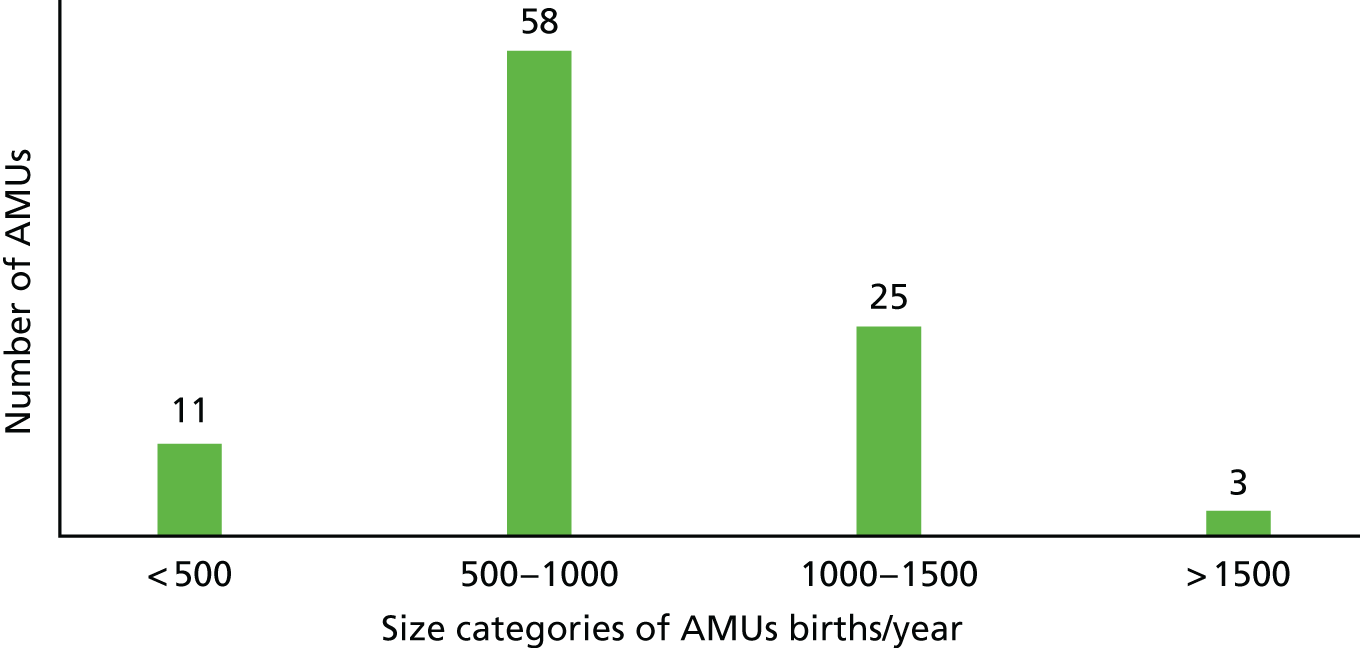
Size categories of alongside midwifery units birth per year
The differences in the number of births per year between AMUs is partly related to the number of births in their linked OU. For example, three of the five largest AMUs in England are linked to the three largest OUs. However, number of births is also dependent on the ability of each local maternity service to optimise access to its AMUs. A later section of the findings highlights this (see Chapter 4, Information and knowledge about midwifery-led units).
The number of births in FMUs is much smaller than in AMUs because they generally serve smaller population areas, typically more rural communities. 57 They appear to have more restrictive access criteria. 89 For example, women planning a vaginal birth after a previous caesarean are not encouraged to birth in FMUs, but it became clear in our survey that some local services allow this in AMUs, as we asked a question about access criteria for the two types of MU. The range was between 10 births per year to 650 births per year, with the majority between 10 and 200 births per year. As above, we categorised FMUs into bands based on their number of births per year (Figure 7).
FIGURE 7.
Size of FMUs: number of births per year.
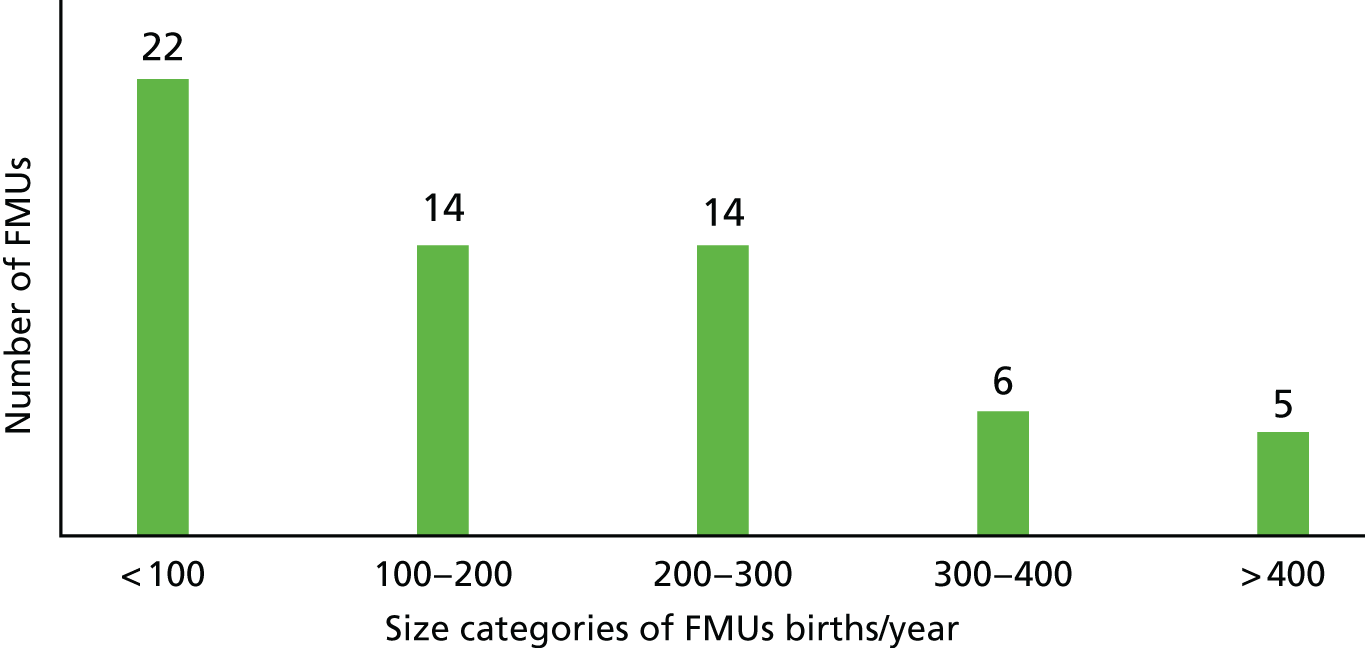
Thirty-six of the 61 FMUs (59%) are supporting < 200 births per year. There has been a small but steady trend towards metropolitan FMUs opening in a town or city where an OU has closed in the past 15 years. 90 The three FMUs with the highest number of births in England were established in the last 5 years because of this change. Two other FMUs, supporting in excess of 400 births, opened in large cities where existing OUs were situated.
Midwifery-led unit percentage of all births per linked trust
After excluding home birth, the number of MU births as a percentage of all births per linked trust gives some indication of their optimum utilisation. This is based on the assumption that the best care for women on a midwifery-led pathway includes access to MUs for labour and birth. For the purpose of this study, we calculated the number of MU births as a percentage of all trust births, excluding home births (in trusts with both AMUs and FMUs, trusts with just AMUs and trusts with just FMUs), to reflect utilisation. We then counted the number of trusts that had MUs birthing women according to different percentage bands (0–5%, 5–10%, 10–15%, 15–20%, 20–15%, 25–30%, > 30%). This revealed wide variations (Figure 8).
FIGURE 8.
Utilisation of MUs: numbers of trusts by percentage bands of MU births/all trust births.
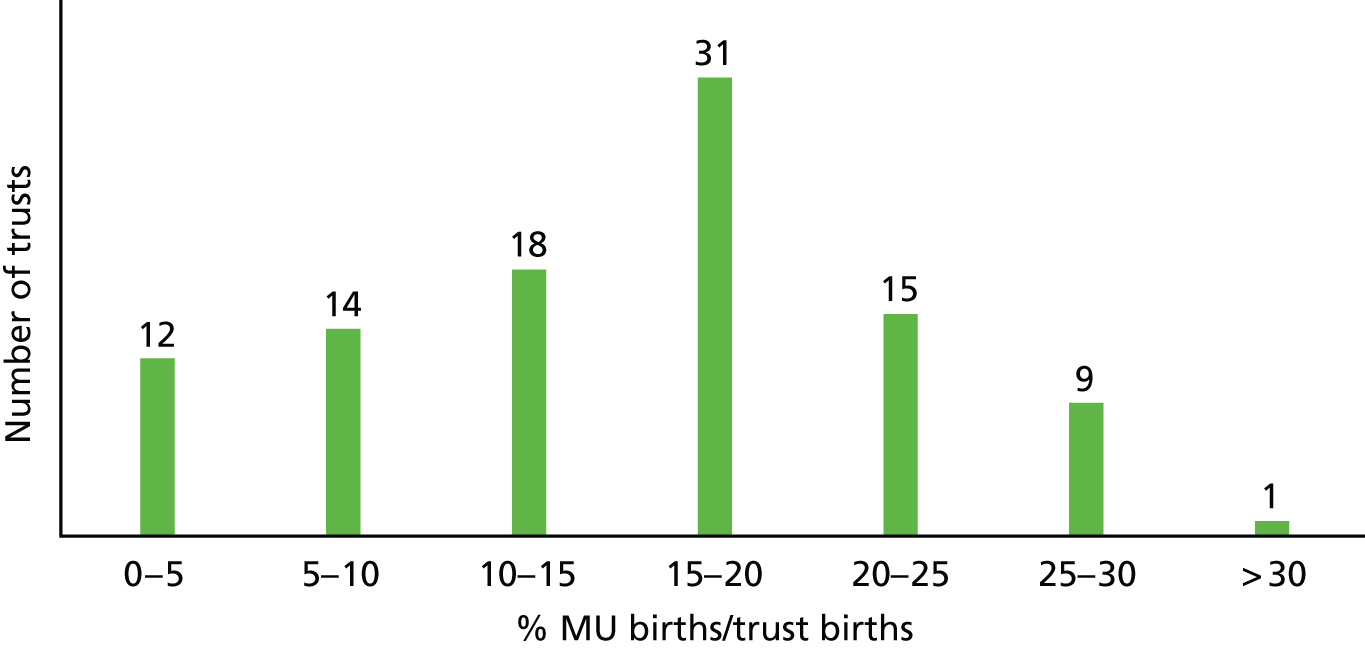
In the trust with the lowest percentage of all births in its MU(s) the figure was 4% and in the trust with the highest it was 31%. Seventy-two per cent (72%) of MUs were birthing < 20% of their total trust births, excluding home births, with only 11% achieving > 25%. AMU utilisation (number of AMU births as a percentage of all attached unit births) was similar (Figure 9).
FIGURE 9.
Utilisation of AMUs numbers of OUs by percentage bands of AMU births/all units births.

Trusts without any midwifery-led units
Of the 32 trusts without MUs, five have two OUs. Of these five trusts, four have their OUs in different towns or cities covered by the trust and the other has two OUs in one large city. The size of these OUs varies from 1300 births per year to 5700 births per year (Figure 10).
FIGURE 10.
Size of OUs without MUs: number of births per year.
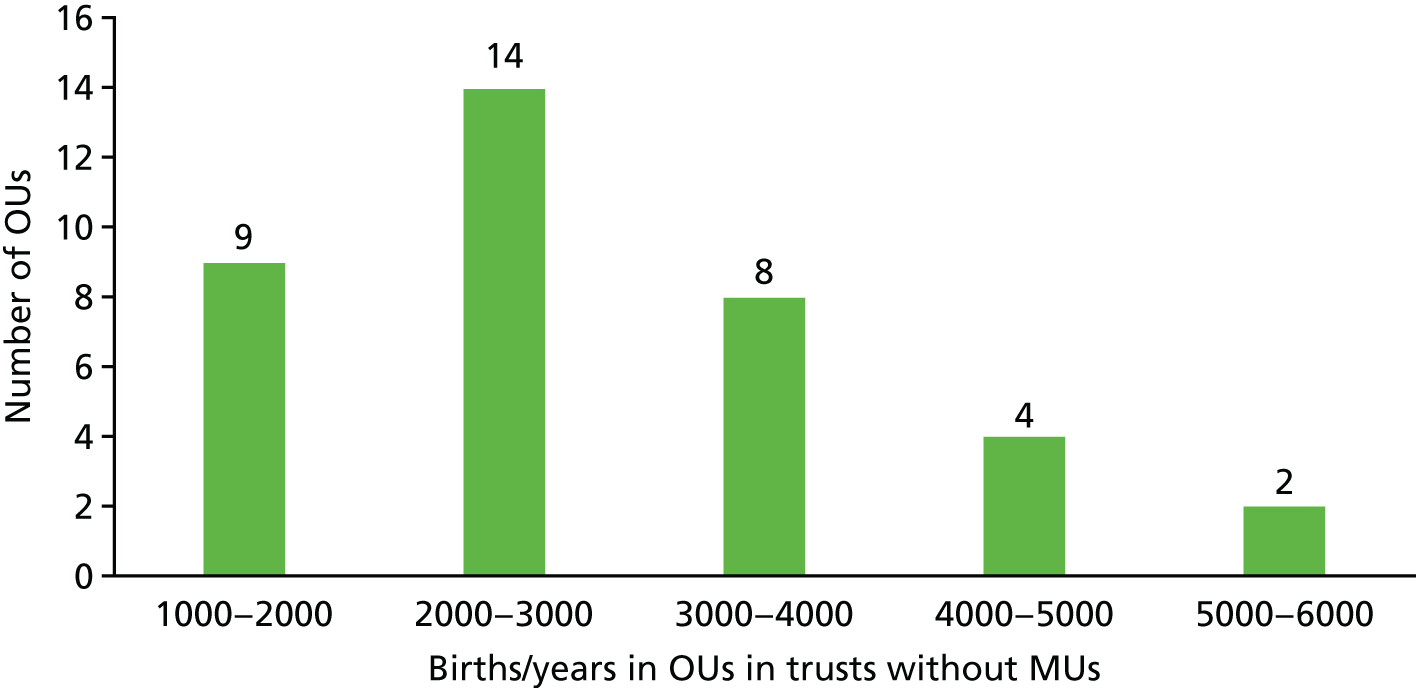
Size of OUs does not appear to affect whether or not an AMU is established. Variations in choice of MUs are particularly striking in large metropolitan areas, where we found examples of a city having two AMUs for a population of 10,000 births, whereas a city in the same region with a similar number of births had no MUs.
Results of the organisation and operation of midwifery-led units
This second section reports the results from both AMUs and FMUs of how they are organised and operated.
Alongside midwifery units
Staffing
We recorded whether or not AMUs had core staff (i.e. designated midwives assigned to permanently staff the AMU, rather than midwives allocated from the OU for each shift or some other variant). We then compared trusts achieving > 20% of all trust births in their AMUs with those trusts achieving 10% to 20% and those under 10% (Table 3).
| AMUs | AMU core staff, n (%) | ||
|---|---|---|---|
| Yes | No | Missing | |
| Trusts with AMUs (N = 97) | 87 (89.7) | 10 (10.3) | 0 |
| Trusts > 20% (N = 26) | 23 (88.5) | 3 (11.5) | 0 |
| Trusts 10–20% (N = 53) | 47 (88.7) | 6 (11.3) | 0 |
| Trusts < 10% (N = 7) | 6 (85.7) | 1 (14.3) | 0 |
Eighty-six AMUs had core staff and there was no difference between higher-performing and lower-performing trusts.
The vast majority of AMUs have a designated midwife clinical lead, but lower-performing AMUs are less likely to (Table 4).
| AMUs | Midwife clinical lead for AMU(s), n (%) | ||
|---|---|---|---|
| Yes | No | Missing | |
| Trusts with AMUs (N = 97) | 90 (92.8) | 6 (6.2) | 1 (1) |
| Trusts > 20% (N = 26) | 24 (92.3) | 1 (3.8) | 1 (3.8) |
| Trusts 10–20% (N = 53) | 50 (94.3) | 3 (5.7) | 0 |
| Trusts < 10% (N = 7) | 6 (85.7) | 1 (14.3) | 0 |
Community midwives staff approximately 60% of AMUs on a shift system (Table 5).
| AMUs | Community midwife scheduled shifts in AMU, n (%) | ||
|---|---|---|---|
| Yes | No | Missing | |
| Trusts with a community midwife in AMU (N = 58) | 34 (58.6) | 24 (41.4) | |
| Trusts > 20% (N = 17) | 10 (58.8) | 7 (41.2) | 0 |
| Trusts 10–20% (N = 36) | 21 (58.3) | 15 (41.7) | 0 |
| Trusts < 10% (N = 5) | 3 (60) | 1 (20) | 1 (20) |
Staff movement to obstetric-led unit
Nearly all (97%) AMU midwives are moved into OUs to work for part or all shifts regularly. This means that they may often be caring for low-risk women on OUs who are suitable for MUs (Table 6).
| AMUs | Staff moved from/to AMU(s) during shift, n (%) | ||
|---|---|---|---|
| Yes | No | Missing | |
| Trusts with AMU(s) (N = 86) | 83 (96.5) | 2 (2.3) | 1 (1.2) |
Closures
Related to the movement of staff out of AMUs was the finding that one-third of AMUs experience closures, with one-fifth closing frequently (more than once per month) (Tables 7 and 8). The closure lasts for the duration of a shift in most cases. Lower-performing AMUs close three times more often than higher-performing AMUs. Movement of staff out of AMUs to OUs and closure of AMUs were expedient and a response to shortage of midwives on OUs and/or workload on OUs. Movement was almost always asymmetrical, in the direction of OU.
| AMUs | AMU(s) closed at any time, n (%) | ||
|---|---|---|---|
| Yes | No | Missing | |
| Trusts with AMUs (N = 86) | 24 (27.9) | 59 (68.6) | 3 (3.5) |
| Trusts > 20% (N = 26) | 5 (19.2) | 21 (80.8) | 0 |
| Trusts 10–20% (N = 53) | 15 (28.3) | 35 (66) | 3 (5.7) |
| Trusts < 10% (N = 7) | 4 (57.1) | 3 (42.9) | 0 |
| AMUs | AMU closure frequency, n (%) | |||||
|---|---|---|---|---|---|---|
| Frequently (≥ 1/month) | Infrequently (every 6 weeks) | Rarely (every 6 months) | Very rarely | Other | Missing | |
| Trusts in which AMU closed (N = 24) | 5 (20.8) | 3 (12.5) | 8 (33.3) | 4 (16.7) | 3 (12.5) | 1 (4.2) |
Capacity
Higher-performing AMUs had more birth rooms (five to eight), whereas lower-performing AMUs had fewer birth rooms (two to four). The latter had fewer births per room (< 200/year), although even the larger AMUs underutilised their room capacity. Thus, all AMUs could absorb more births per year.
Access and physical location
Data were collected on whether trusts had an opt-out or opt-in model for women accessing their AMU (Table 9). Opt-out implies that low-risk women wanting a hospital birth were sent to the AMU unless they specifically requested to labour in the OU (i.e. a standard midwife-led or low-risk pathway). Opt-in means that women are sent to the OU unless they ask for the AMU. In addition, a small number of services operate a hybrid model that, for example, leaves the decision to the admitting midwife.
| AMUs | AMU(s) opt-out or opt-in policy, n (%) | |||
|---|---|---|---|---|
| Opt out | Opt in | No/other | Missing | |
| Trusts with AMUs (N = 86) | 49 (56.9) | 22 (25.6) | 14 (16.3) | 1 (1.2) |
| Trusts > 20% (N = 26) | 19 (73.1) | 2 (7.7) | 4 (15.4) | 1 (3.8) |
| Trusts 10–20% (N = 53) | 29 (54.7) | 15 (28.3) | 9 (17) | 0 |
| Trusts < 10% (N = 7) | 1 (14.3) | 5 (71.4) | 1 (14.3) | 0 |
Fifty-seven per cent of AMUs had an opt-out policy and this appeared to be associated with higher utilisation. Of the higher-performing AMUs, 73% had an opt-out policy, whereas only 14% of the lower-performing AMUs had an opt-out policy.
Eighty-one per cent of trusts used NICE recommendations91 to ascertain women’s eligibility for AMU care, though > 50% of trusts adapted or broadened these recommendations to allow other women access to their AMU (Table 10).
| AMUs | AMU eligibility criteria guidelines source, n (%) | |||
|---|---|---|---|---|
| NICE | NICE and adapteda | Other/own | Missing | |
| Trusts with AMUs (N = 86) | 30 (34.9) | 40 (46.5) | 9 (10.5) | 7 (8.1) |
| Trusts > 20% (N = 26) | 10 (38.5) | 12 (46.2) | 2 (7.7) | 2 (7.7) |
| Trusts 10–20% (N = 53) | 18 (33.9) | 24 (45.3) | 6 (11.3) | 5 (9.4) |
| Trusts < 10% (N = 7) | 2 (28.6) | 4 (57.1) | 1 (14.3) | 0 |
| All trusts with MU (N = 102) | 40 (39.2) | 45 (44.1) | 9 (8.8) | 8 (7.8) |
We also asked if women who did not meet the local eligibility criteria were sometimes allowed access to AMU (Table 11).
| AMUs | AMU access for ineligible women, n (%) | |||
|---|---|---|---|---|
| Yes | No | Other | Missing | |
| Trusts with AMUs (N = 86) | 72 (83.7) | 9 (10.5) | 4 (4.6) | 1 (1.2) |
| Trusts > 20% (N = 26) | 25 (96.2) | 1 (3.8) | 0 | 0 |
| Trusts 10–20% (N = 53) | 41 (77.4) | 7 (13.2) | 4 (7.5) | 1 (1.9) |
| Trusts < 10% (N = 7) | 6 (85.7) | 1 (17.3) | 0 | 0 |
High-performing trusts were more likely to allow this eligibility.
Alongside midwifery units were co-located in three ways: (1) 63% were on the same floor as the main labour ward, (2) 36% were on a different floor and (3) 1% were in a different building (Table 12).
| AMUs | AMU location, n (%) | ||
|---|---|---|---|
| Same floor | Different floor | Different building | |
| Trusts with AMUs (N = 97) | 61 (61.9) | 35 (36.1) | 1 (1) |
| Trusts > 20% (N = 27) | 15 (55.6) | 11 (40.7) | 1 (3.7) |
| Trusts 10–20% (N = 63) | 40 (63.5) | 23 (36.5) | 0 |
| Trusts < 10% (N = 7) | 6 (85.7) | 1 (14.3) | 0 |
There may be an association between smaller MU birth numbers and the location of the AMU on the same floor, but the numbers were too small to be conclusive.
Facilities
Number of rooms
The majority of AMUs had two to four rooms and very few had more than eight rooms.
Trusts with a small proportion of births in MUs were very likely to have small numbers of rooms in their AMU, and more than twice as likely to do so as trusts with > 20% of MU births. Nearly half of trusts with > 20% MU births had five to eight rooms in their AMUs (Table 13).
| AMUs | Number of rooms, n (%) | ||
|---|---|---|---|
| 2–4 | 5–8 | 9–12 | |
| Trusts with AMUs (N = 97) | 52 (53.6) | 39 (40.2) | 6 (6.2) |
| > 20% MU births AMUs (N = 27) | 10 (37.0) | 13 (48.1) | 4 (14.8) |
| 10–20% MU births AMUs (N = 63) | 36 (57.1) | 25 (39.7) | 2 (3.2) |
| < 10% MU births AMUs (N = 7) | 6 (85.7) | 1 (14.3) | 0 |
Birthing pools
Nearly all AMUs had at least one birthing pool (98%), but trusts with higher proportions of births in MUs did not appear to have a greater proportion of rooms with pools than trusts with lower proportions of births in MUs (Table 14).
| AMUs | Proportion of rooms with birth pools, n (%) | ||
|---|---|---|---|
| < 25% | 25–75% | > 75% | |
| Trusts with AMUs with pools (N = 84) | 5 (6.0) | 60 (71.4) | 19 (22.6) |
| Trusts > 20% (N = 26) | 3 (11.5) | 18 (69.2) | 5 (19.2) |
| Trusts 10–20% (N = 51) | 2 (3.9) | 35 (68.6) | 14 (27.5) |
| Trusts < 10% (N = 7) | 0 | 7 (100) | 0 |
Free-standing midwifery units
Staffing
Approximately half of the trusts with FMUs had core midwifery staff in their FMUs (Table 15). The differences between the three groups (< 10%, 10–20% and > 20%) must be interpreted with caution, as the FMUs did not figure strongly in overall birth proportions, particularly in trusts with both AMUs and FMUs.
| FMUs | FMU core staff, n (%) | |||
|---|---|---|---|---|
| Yes | No | Other | Missing | |
| Trusts with FMUs (N = 39) | 21 (53.8) | 12 (30.8) | 5 (12.8) | 1 (2.6) |
| Trusts > 20% (N = 15) | 10 (48) | 3 (25) | 1 (6.7) | 1 (6.7) |
| Trusts 10–20% (N = 13) | 6 (29) | 5 (42) | 2 (15.4) | |
| Trusts < 10% (N = 11) | 5 (24) | 4 (33) | 2 (18.2) | |
For FMUs with no core staff, community midwives must staff them when they accompany women for birth.
Just over 50% of FMUs were staffed 24 hours per day, whereas the remainder were either open during daytime hours only (e.g. for clinics) or open when women booked there went into labour. Nearly all FMUs had a midwife clinical lead. Community midwives played a major role in staffing, mostly as the second midwife for births. Twelve trusts ran their FMU by a fully integrated model of core staff and community midwives.
Staff movement
Over half of FMU staff were moved within or between shifts, most often to the host OU (Table 16).
| FMUs | FMU staff moved (N = 22) (trusts with FMU N = 39), n (%) | ||||
|---|---|---|---|---|---|
| FMU to OU | FMU to AMU | Community to FMU | Unspecified or anywhere | Missing | |
| Trusts with FMU staff moved | 8 (36.4a) | 5 (22.7a) | 4 (18.2a) | 3 (13.6a) | 3 (13.6a) |
Closures
Nearly 40% of FMUs were closed more than once every 6 months (Table 17).
| FMUs | FMU(s) closed at any time, n (%) | ||||
|---|---|---|---|---|---|
| Yes | No | Open for births only | Other | Missing | |
| Trusts with FMUs (N = 39) | 15 (38.5) | 15 (38.5) | 12 (30.8) | 6 (15.4) | 1 (2.6) |
Access
Unlike AMUs, only 5% of FMUs had an opt-out policy, whereas nearly 50% operated an opt-in policy (Table 18).
| FMUs | FMU policy, n (%) | ||||
|---|---|---|---|---|---|
| Opt out | Opt in | Unclear | No | Missing | |
| Trusts with FMUs (N = 39) | 2 (5.1) | 18 (46.2) | 16 (41) | 1 (2.6) | 2 (5.1) |
Just over one-third of trusts had stricter eligibility criteria for their FMU than for their AMUs (Table 19).
| FMUs | FMU eligibility criteria guidelines stricter than AMU, n (%) | ||||
|---|---|---|---|---|---|
| N/A, no AMU | Yes | No | Other | Missing | |
| Trusts with FMUs (N = 39) | 16 (41) | 14 (35.9) | 6 (15.4) | 2 (5.1) | 1 (2.6) |
Facilities (birthing pools)
Almost all FMUs (98%) had rooms with birthing pool facilities and most had more than one (Table 20).
| FMUs | FMU proportion of rooms with birth pools, n (%) | ||
|---|---|---|---|
| < 25% | 25–75% | > 75% | |
| Trusts with FMUs with pools (N = 39) | 3 (7.7) | 20 (51.3) | 16 (41.0) |
Consultant midwives attached to midwifery-led units
Only 40% of trusts had a dedicated consultant midwife and these tended to be in higher-performing sites (43% vs. 29%) (Table 21).
| MUs | Consultant midwives attached to MU, n (%) | ||
|---|---|---|---|
| Yes | No | Missing | |
| Trusts with MU(s) (N = 102) | 38 (37.3) | 61 (59.8) | 3 (2.9) |
| Trusts > 20% (N = 28) | 12 (42.9) | 15 (53.6) | 1 (3.6) |
| Trusts 10–20% (N = 57) | 21 (36.8) | 35 (61.4) | 1 (1.8) |
| Trusts < 10% (N = 17) | 5 (29.4) | 11 (64.7) | 1 (5.9) |
Case-loading and midwifery-led units
Although 20% of trusts say they had some form of case-load model (care from a midwife or small group of midwives throughout all phases of care), the percentage of women who could avail themselves of it was only 1–2%. In fact, only two AMUs and two FMUs had case-load models for some of their women. Women planning a home birth are the most common group to have access to case load care, although one trust had case-load midwifery implemented for > 50% of its population.
Closure of free-standing midwifery units in England
As part of the mapping phase of this study, we identified 10 FMU services in England closed permanently in the 10 years prior to the analysis. This first section (see Media analysis) explores the representation of the closure of these units in print and television media to better understand the public rationale for closure decisions and the climate or public atmosphere in which such decisions take place.
A second section reports on the findings from interviews of HoMs where FMUs closed (see Head of midwifery interviews).
Media analysis
Despite persuasive evidence in favour of FMUs, maternity policies along with professional organisations such as the Royal College of Obstetricians and Gynaecologists (RCOG) have supported AMUs over FMUs. 92 The opening and closing of FMUs has been tracked for a report to the RCM,90 which identified that in England in February 2013 there were 59 FMUs (compared with 53 in April 2001). During these 12 years, 30 new units opened and 21 units were permanently closed. A further three were temporarily closed, with the possibility that they will not reopen. Previous studies have documented the cyclical struggle for survival of FMUs in England, their small size and invisibility having rendered them vulnerable to closure by their larger host organisations. 93,94 This is of interest, given evidence from the Birthplace in England study3 that FMUs outperform AMUs regarding reductions in labour and birth interventions. 25 They are also more cost-effective than AMUs in relation to the primary outcome of neonatal adverse outcome and the secondary outcome of maternal morbidity, although this is reduced if only low-risk women without complications at the onset of labour are compared. 46 In addition, organisational research has found that midwifery satisfaction is very high in these settings95 and they are much less prone to problems of staff recruitment and retention, which are a contemporary challenge to the sustainability of the maternity workforce. 96
The aim of this part of the project was to explore what an analysis of media coverage of the closure of FMUs might tell us about the reasons given for the closures, how are these closures presented publicly and by whom, and whether media representations support or disrupt pervading cultural norms around place of birth in England.
The methods we utilised are described in Chapter 2.
Content analysis
The articles reported on planned or proposed changes to the existing maternity services in their areas. These plans all involved the closure of a local FMU, with some including the opening of a new AMU on a hospital site in a nearby town or city. A simple count showed that service users were quoted almost twice as often (46 times) as the next most frequently quoted stakeholders [local council politicians and commissioners (24 times)]. These were followed by senior trust staff (mostly directors of nursing and a few HoMs), at 22 times, health campaigners (18 times), CEOs (16 times) and members of parliament (14 times).
A preliminary analysis of the basic content of the articles revealed a number of trends. The newspaper coverage appeared to present a binary relationship between a medical model of care (in which birth close to medical back-up, such as in or close to an OU, was regarded as safer and more desirable) and a contrasting social model of care (in which birth was kept locally within the community).
A straightforward count of the reasons given for the closures revealed two predominant reasons: the perceived underuse of the units and the assumed high cost of running them.
Those in favour of closing units often argued that women were not choosing to use them, resulting in underuse of the facilities, which were then presented as unaffordable.
Commissioners and trust senior managers used the press releases on which many of the newspaper articles were based to justify their decisions to close units. Thus, closures were constructed as inevitable or unavoidable and largely outside their control. Often the underlying assumptions behind this discourse were not challenged within the articles.
When opposing voices were represented, those in favour of keeping the units open were more likely to be of the opinion that the units were desirable from the point of view of a social model of care, keeping birth within the local community, avoiding long journeys in labour, and that underuse was caused by lack of eligibility or provision of relevant information. Opposing voices were mainly those of service users, local politicians and community campaigners.
Voices supporting closures
Our content analysis revealed that very little of the media reporting focused on safety per se and made very little reference at all to clinical evidence. However, the assumption that being closer to obstetric care was safer, despite this being contrary to the evidence, was implicit in the arguments in support of the closure of FMUs in favour of AMUs:
We feel that a midwife-led unit close to the maternity department would provide the best of both worlds – the possibility of a natural birth without medical intervention, but the security of knowing an obstetrician is close by in case of emergencies.
Trust chief executive, Scarborough Evening News97
Free-standing midwifery units were often portrayed as undesirable or inferior places to give birth:
The vast majority [of women in Grantham] opt to give birth at other hospitals where they can get:
None of which they can currently get at the Midwifery Led Birthing Unit at Grantham Hospital.
Journalist, Grantham Journal. 98
Trust CEOs, commissioners and some journalists asserted that the problem was that there was a lack of demand for FMUs from women. Women were assumed to have a free and informed choice about where they plan their births and they were not choosing FMU care:
The midwives do a great job but women are clearly choosing to go elsewhere for their care.
Clinical Commissioning Group accountable officer, Grantham Journal. 98
Chief executive officers and commissioners also used the articles to explain how much money their FMU was costing their service, quoting the specific amount of money that they perceived was ‘lost’ each year. In some cases, the financial losses were attributed directly to women’s decisions on place of birth:
Only 274 out of 5440 new mothers from Brent gave birth there in 2006, along with 18 from Harrow, leading to a deficit of £300,000 a year.
First-time mother, Kentish Gazette99
In Brent, where the FMU had been opened on the site of a closed OU, the CEO presented his decision to close the unit as a moral one:
I have a responsibility to make the best use of taxpayers’ money and the Brent Birthing Centre is losing £300,000 a year. As an accountable officer, that is not something I can sustain.
CEO, Harrow Times100
Articles deployed a combination of managerialist and consumerist discourses whereby managers were depicted as sharing out limited resources for the greater good, whereas women exercised a ‘free, consumer choice’ not to birth in FMUs:
It’s important we provide the best care possible for every pound spent, for everyone in Derbyshire.
Medical director, Derby Evening Telegraph101
It’s about how you provide the best model of maternity service for the area. We can’t continue to run the whole service in this way and something has to change.
Hospital trust CEO, Hull Daily Mail102
Often the proposed changes involved the closure of the FMU and the opening of an AMU in another of the trust’s hospitals. This was at times framed as a ‘relocation’ of the FMU, rather than a closure, and in the case of the Brent Birth Centre the new AMU was given the same name as the closed FMU.
Closures were frequently framed as ‘gains’, for example the opening of a new MU or more money to invest in other services:
What do the proposals mean for women living in North Tyneside? When a woman becomes pregnant, no matter whether she is considered to be low or high risk she will be able to choose to deliver her baby at either Northumbria Specialist Emergency Care Hospital or Royal Victoria Infirmary, Newcastle.
Commissioner, Chronicle Live103
I hope that most of the journal’s readers will be reassured to know that the changes that have been announced this week will bring about an expansion in the services on offer at Grantham Hospital and an improvement in the treatment and care given to local people.
Nick Boles, MP, Grantham Journal104
Voices opposing closure
Service users and campaigners privileged women’s right to birth locally, expecting that trusts had a duty to provide and support women’s opportunities to choose these places of birth.
In Kent, campaign messages emphasised the importance of women being able to birth locally to avoid long journeys in labour and to retain birth within the local community. Changes were questioned by service users using highly emotive language that drew on images of family, home and community:
The move would force Canterbury mothers-to-be into long journeys to hospital and mean Kent’s only city would disappear from birth certificates [our emphasis].
Kentish Gazette 105
Both of my children were born there as were their mother and me. I was therefore hoping to see a third generation eventually come into the world at Buckland.
Philip Moore, East Kent Mercury106
Service users and campaigners argued that the FMUs remained desirable places to give birth, but that many women were prevented from using FMUs through eligibility guidelines or a lack of information:
I think one of the fundamental issues is the lack of publicity the centre gets from GPs and midwives at booking in appointments. Two friends of the family who are expecting didn’t know the Jubilee Birth Centre existed until I told them!
Half the pregnant ladies were not given the chance to use it. They were told, you have to go to Lincoln.
Campaigner, Yorkshire and Lincolnshire Regional News and Weather107
For those opposing the closures, the arguments were more likely to be framed in terms of a ‘loss’. The loss of the unit or of local services and possible implications for the economic well-being of a local community, and other local services:
So North Tyneside General . . . will soon have no A&E [accident and emergency] and likely no maternity at all after already being degraded. What is to become of it? A cottage hospital where people go to die in old age? The demise of hospital services for residents . . . is disgraceful.
Claire Louise Keys, service user, Evening Chronicle108
However, campaigners supporting the Jubilee Birth Centre in Hull were reported as satisfied with the trust’s proposal to ‘relocate’ the FMU to the main hospital to become an AMU:
Jubilee Supporters' Group campaigner Sian Alexander, said: ‘While I am sad to see the Jubilee close permanently, I'm glad the trust at least acknowledges the importance of midwifery-led care and I hope the spirit of the Jubilee will be able to live on, albeit in another place’.
Hull Daily Mail 109
Head of midwifery interviews
Thematic analysis of the HoM interviews relating to 8 of the 10 FMU closures from the media analysis revealed common threads across most sites. These were:
-
underutilisation issues in relation to falling numbers of annual FMU births, which subsequently increased the costs of keeping the MUs open
-
distance of FMUs from their host OUs, exacerbated by traffic congestion and/or poor weather, especially in rural FMUs, which could theoretically impact on safety
-
relative popularity of AMUs and rationalisation of OUs led to the opening of more AMUs which were seen as a replacement for the closed FMUs.
Underutilisation
Seven were said to be ‘undercapacity’, although no justification exists in the literature of a threshold for utilisation that equates to viability. Some FMUs open only for intrapartum care, remaining closed the rest of the time, but the argument is made that utilities, such as heating, lighting and water, are required continuously. However, there still exists a significant number (53) of FMUs with 50–250 births per year, mostly in rural areas. Some units provide antenatal and postnatal care and other community-based services for a rural area.
Distance from host obstetric-led unit
This rationale for closure applies exclusively to rural units, where it was judged that journeys of > 15 miles, or time taken to transfer of > 30 minutes, may impact on safety. It was interesting that none of the closures had been precipitated by clinical incidents, at least according to the HoMs interviews, and this was also reflected in our analysis of media content and discourses, which focused on economic and staffing issues, with little reference to clinical safety concerns.
Popularity of alongside midwifery units and rationalisation of obstetric-led units
A number of the interviewees mentioned that AMUs were opened in virtually all trusts where FMUs were closed. They were seen as a more popular alternative to FMUs, but this appears to be a professional view, rather than a service user view. Certainly, their capacity is greater, sometimes by as much as 10 times. However, this greater volume of births is primarily derived from women who would have previously accessed the main OU. Interestingly, at two of the closed FMU sites, home birth rates went up, suggesting that some local women chose to birth at home over attending the neighbouring OU/AMU.
There were some interesting examples of closures that did not fit the above categories. One FMU closed despite having > 300 births per year, although the rationale given was underutilisation. A metropolitan FMU closed because its local population of mainly immigrant women perceived it as a second-class service, because there were no doctors on staff. The FMU was built in an industrial estate that meant low visibility in the local community. More than one comment was made that small FMUs represented a ‘Rolls Royce’ service that few women could benefit from.
The next chapter describes in detail the findings from the six case study sites.
Chapter 4 Findings phase 2: case studies
The findings from the six case study sites are derived from MFGs, women’s focus groups and all individual interviews. These present a picture of the local maternity cultures, organisational processes regarding the functioning of MUs, relationships between stakeholders and key actors who shape the MU service.
In the first section, each site is described in a narrative summary, outlining why it was selected, its configuration, its throughput of births, relevant historical backdrop to the current configuration and any current contextual issues impinging on its MU provision.
This is followed by a within-case analysis. The within-case analysis distilled themes that emerged from the particularities of each case. These have been mapped to the CFIR (see Cross-case analysis), but to highlight individual differences between cases they are reported here as ‘stand-alone’ themes. These stand-alone themes are individual constructs, extracted from the CFIR five domains (see Table 22) that matched most closely to the data.
The themes for this section are leadership, culture and beliefs about the intervention MUs, resources and priorities, organisation, staffing and change. Not all themes apply in each site.
Each site has been given a pseudonym, the first letter of which is used to identify where the respondents are from in all excerpts from MFGs (e.g. ‘AMFG1’), women’s focus groups (e.g. ‘BWFG2’) and interviews (e.g. ‘Clnt3’).
After this section, the analysis of the women’s focus groups is detailed and the chapter concludes with a substantive section on the cross-case analysis. The structure of the findings is given in Box 1.
Within-case analysis based on their primary themes: leadership, culture and beliefs about the intervention MUs, resources and priorities, organisation, staffing, change.
Women’s focus groups based on primary themes: information and knowledge about MUs, influences on birthplace decision-making, administrative and logistical issues.
Cross-case analysis based on the most important constructs from each of the CFIR five domains: intervention characteristics, outer setting, inner setting, characteristics of individuals, process.
Narrative summaries and within-case analysis
Armidale narrative summary
Armidale was one of the ‘high-performing’ sites (see Chapter 2 for definitions) and consisted of one OU, one AMU and two FMUs (Figure 11).
FIGURE 11.
Site 1: Armidale.
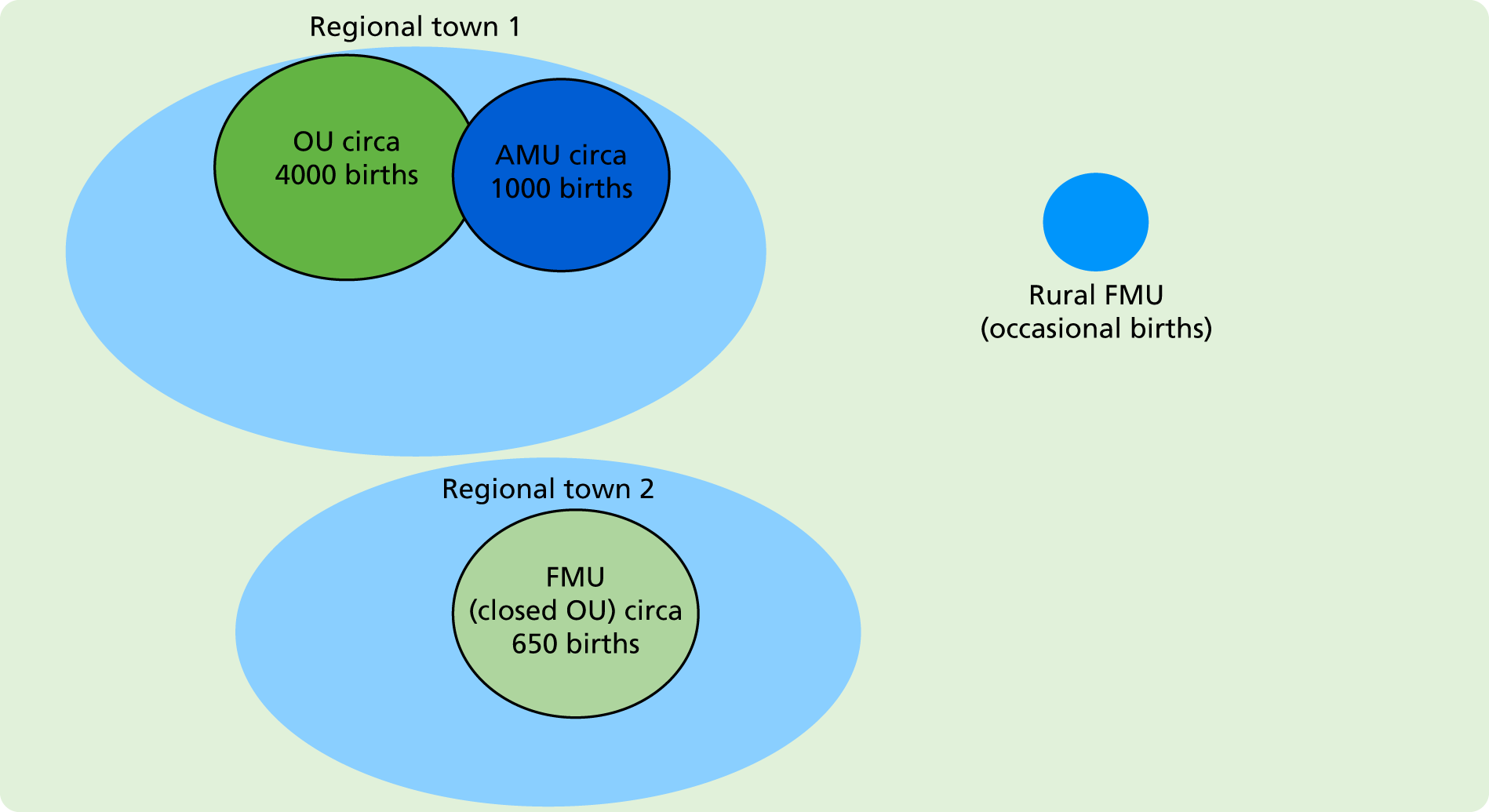
Within Armidale, one of the FMUs was in a town where an OU previously existed, and it was one of the best-utilised FMUs in the country, with > 600 births per year. The OU, which was in a nearby town, had around 4000 births per year and had an AMU with about 1000 births per year. Apart from the two towns, the trust also covered a sizable rural area. The long-standing smaller and rurally located FMU hosted only occasional births and was described as being at risk of closure during interviews.
The AMU and larger FMU were developed following a trust-wide reconfiguration of the maternity services. This involved the reorganisation of obstetric and neonatal facilities and services across two towns at some geographical distance, and this reorganisation enabled the scene to be set for maternity systems change. Of the two recently developed MUs, the new FMU (in a town where the OU was closing) and the development of the new OU in the other town were prioritised. Having the new FMU opened and running prior to the closure of the OU in the same town was seen as an important part of embedding it into the maternity service. The AMU in the new OU was developed to provide women with a ‘low-risk’ birthplace option in the town with a large OU.
The staffing model for both the FMU and AMU was integrated hospital and community midwives, which is a relatively unusual staffing configuration in England. The midwives worked both in the community and on shifts in their particular MU, providing antenatal, labour/birth and postnatal care. The AMU-based team also operated the small FMU, which was opened only for births, and were sometimes moved within shifts from the AMU to the OU, depending on service demand. Sometimes the midwives on shift in the larger FMU were moved to the OU/AMU to cover staff shortages. The MUs had no core staff, apart from the clinical lead.
Leadership
Interviews and focus group data revealed a commonly held view that the reconfiguration developed from extremely strong midwifery leadership and widespread, multilayered and multidisciplinary consultation and engagement with both internal and external stakeholders:
. . . it’s crucial to have an inspirational leader. If you don’t have somebody at the very top who is passionate about it happening, it won’t happen. And they must cascade, get everybody onboard.
AMFG2
One of the important characteristics of a leader that midwives and service user representatives identified was charisma:
. . . a charismatic leader to kind of bring it together . . . unless you’ve got that then I think it’s quite hard to bring it to fruition.
AInt9
The longstanding, active and ongoing support of the trust’s MUs by key senior obstetricians was also viewed as very important. A senior obstetrician who was interviewed was a very strong advocate of MUs and normal birth. She described an enduring commitment to collaboration with midwives and to challenging the medicalised practice of service:
. . . ultimately I suppose it’s with them [women] having that better experience and it’s reducing C-section [caesarean] rates and the medicalisation of birth and bringing it back to something a bit more of the emotional, social, psychological side of birth.
AInt5
The importance of continuity of vision when new service leaders came into post was referred to by the senior obstetrician, the midwives and the service users. They suggested that recent changes in midwifery leadership had resulted in a reduction in staffing on the MUs and less service user engagement. This was perceived to contribute to falling numbers of births in both the large FMU and the AMU:
I think the birth centres are being used less at the moment, and that does seem to coincide with a change of leadership.
AInt9
Culture and beliefs about midwifery-led units
The midwives from each of the MUs identified strongly with their work context and organisation. They saw themselves as normality advocates, grounded in a social/midwifery model of childbirth:
I think that the birth centre philosophy is a social model of care . . . This is where we wanted to work with the community midwives who wanted the normality as well.
AMFG1
The midwives talked of the importance of a strong team culture in the MUs, with the need to trust your colleagues, especially in an emergency. This was facilitated by frequent, random unannounced skills drills, which the senior midwives set up.
In both the FMU and the AMU, there was a potent sense of ownership and a commitment to promoting their units and a strong commitment to the integrated MU community model:
. . . the midwives very much take ownership of the [AMU], and you don’t see a lot of higher management on the unit here, where you might do in some of the other areas.
AMFG1
The FMU midwives engaged in considerable promotional activity within the local community (e.g. providing information stands at local shops) and at the unit itself (e.g. Christmas parties for the local community to join):
So you have to do a lot of positive promotion, you have to get out there. And you’re almost selling a product. And that’s how we saw it. So we did lots of promotional events, and got lots in the press, about the positive things that we were doing . . .
AMFG1
The AMU staff had also held fundraising events to purchase equipment/’extras’, which had helped build the staff culture as well as increase the unit’s visibility:
. . . it’s like the fundraising [name] just mentioned, we did use to do that quite often, to promote, to raise money for us to use on the birth centre [AMU]. To decorate our rooms.
AMFG2
Change
The reconfiguration was not without resistance from staff, with two main contributors to this: first, a loss of workplace identity and culture for the staff (obstetric, neonatal and midwifery) from the OU which closed; second, the adjustment to a new model of practice for midwives:
[Staff] will tell you themselves that it wasn’t without challenge, etc. . . . the way they had to totally change the culture and the way they worked, even down to the language that was used rather than . . . they don’t use language around ‘delivery’ now, it’s about ‘birth’, and yeah, I think it was met with some resistance from staff initially . . .
AInt1
The development of the MUs met more resistance from the neonatologists, who were not supportive of a FMU initially:
As a team of neonatologists we clearly always see the extreme end of the spectrum in terms of, you know, babies who get into difficulties because those are the ones who we come in contact with, so obviously there were anxieties.
AInt9
The neonatologists’ engagement with the process was through the development of protocols. They strongly argued for the presence of a neonatal life support (NLS)-trained midwife on every shift at the FMU and this was implemented.
Organisation and staffing
From the outset, community midwives and a small team of core midwives staffed the MUs. This integrated staffing model was described very positively by those working in it, with there being a strong recommendation that the integrated model is desirable for an effectively functioning MU:
If you have an integrated model you develop a really highly skilled, flexible workforce, which can move to where the activity is.
AMFG2
The midwives valued the relational continuity of care, however limited, that the integrated model provided. They experienced this if they cared for women in labour whom they had previously met during the antenatal period.
This site demonstrated that strategic planning, visionary leadership and widespread sign-up from stakeholders set the conditions for successful MU development. In addition, developing a sense of identity and ownership in the MU staff facilitated MU promotion and optimum utilisation.
Borodale narrative summary
Borodale was one of the ‘low-performing’ sites and consists of two OUs, one AMU and one FMU (Figure 12).
FIGURE 12.
Site 2: Borodale.
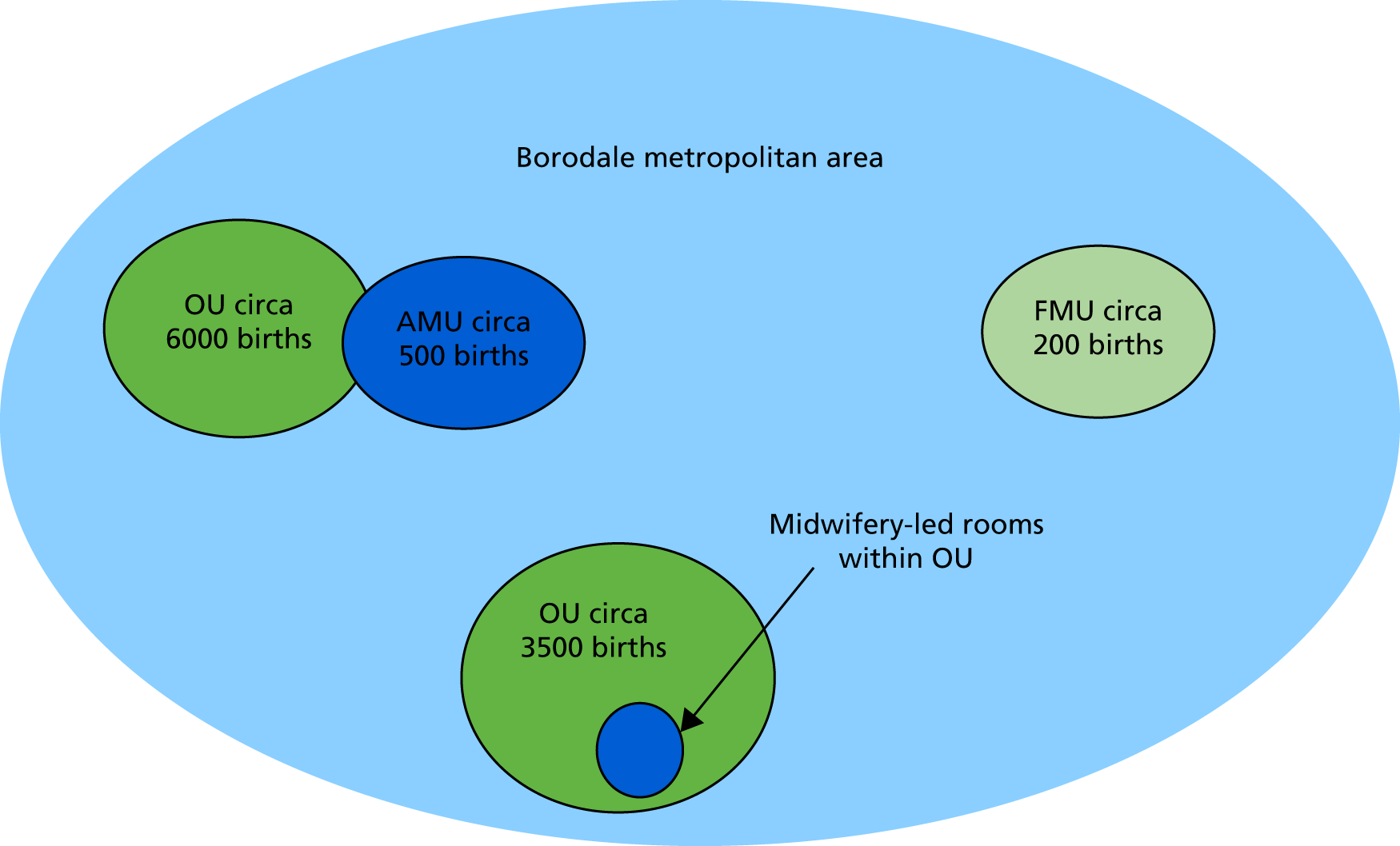
Within Borodale, the tertiary-level OU was in a large metropolitan area and had > 6000 births per year, with an attached small, three-room AMU that had 500–600 births per year.
The smaller secondary-level OU was in an adjacent urban centre and had between 3500 and 4000 births per year. The FMU was located in a smaller community at one end of the trust area and had < 200 births per year. A number of the respondents described it as being at risk of closure. The AMU and FMU had core staff with a clinical lead.
The trust had experienced several boundary and service reconfigurations during the preceding 10 years; these uncertainties were continuing at the time of data collection. The trust acquired the second OU following a relatively recent amalgamation of trusts. Prior to that, a small OU within a larger community hospital had been closed after losing its neonatal services. The FMU was opened within that previous OU facility several years ago. The reconfiguration of OU to FMU met with great resistance from both midwives and obstetricians who worked there prior to its closure.
Leadership
In contrast to Armidale, there was an apparent lack of maternity service leadership during the reconfigurations at Borodale. A maternity service manager at the time of data collection commented that she was distracted from promoting the FMU as she was addressing other priorities in the trust:
And sometimes you have to go all through that before you get the thinking time to think actually, are we doing it the right way? Do you know what I mean? But when you’re in the middle of it, this is what you’ve got to do . . .
You’re firefighting almost?
Yeah.
Other staff interviews expressed uncertainty about whether or not the problems with leadership existed at trust or maternity unit level:
We are constrained by the trust and so you know, if people did say, hang on this isn’t working, we’ve got to get everything on one site, the trust won’t countenance that. So it’s difficult for me to know whether it’s maternity leadership or whether it’s them [the trust].
BMFG1
Culture and beliefs about the intervention
Across the trust and midwifery management of Borodale, there were a number of conflicting views regarding the value of MUs. Illustrative of those with negative views was one trust manager who suggested that the midwives:
. . . believe that you have to have padlocks, bolted door with machine guns and guard dogs between a unit that’s midwife run and a unit that has obstetricians.
BInt5
However, other trust managers were supportive of AMUs:
They are recommended by national guidelines – I don’t see an issue . . .
BInt4
There had been poor service user engagement in the trust. One of the commissioners was very positive about MUs and referred to a recently developed place of birth tool for midwives to use when discussing birthplace options with women. She was open to innovation in both organisation and provision of MUs, if they met the needs of women, and was keen to engage service users who reflected the trust’s population of childbearing women in this process:
We need to really reconsider how we’re doing engagement with women. The maternity service liaison committee is not representative of our service users. And they’re not current service users, but white middle class woman who gave birth years ago.
BInt6
The midwifery and obstetric management at the OU without an AMU wanted to open one and optimise its utilisation. They were keen for the MU to be opt-out and for the OU to be only for women receiving obstetric care:
. . . it should be an opt-out, which was something we’ve sort of been driving for over the past year . . .
BInt7
They also wanted a new AMU to be on a different floor, to properly distinguish the MU from the OU. This was in contrast to the lead obstetrician at the OU that already had an AMU, who, while believing AMUs were safe, insisted they needed to be on the same floor and as close as possible to the OU:
. . . an alongside midwifery-led unit needs to be on the same floor because the lift is, you know, takes too long if you have a cord prolapse.
Bint9
A senior manager spoke about outright hostility from midwives working in the OU that was closed and replaced with a FMU:
. . . they were completely horrified at the idea of having a standalone midwifery-led unit.
BInt3
She went on to say that most of them were redeployed to work in the new FMU, despite their resistance. This had contributed to a gradual fall in numbers of women birthing there and, at the time of our data collection, there was discussion about it being no longer viable.
Relationships and communication between midwifery staff working in the FMU and those working in the local community were reportedly poor, even though the community midwives were based in the same building as the FMU. For example, when the prospect was raised that community midwives might be required to do shifts in the FMU, it appeared that they were then even less likely to promote the FMU to women, because this increased the chances of being called in to work there:
. . . there have been situations where the community midwives don’t promote a unit because it increases their workload.
BMFG2
Poor relationships between AMU and OU midwives were also described:
. . . really sad I think, because obviously you acknowledge the [OU] midwives and the high-risk care they give, but equally you have to acknowledge the low-risk care that low-risk midwives are giving, they’re all important but there is a sort of ‘them and us’.
BMFG1
Overall, it was apparent that Borodale lacked a consistent strategy for MU development. There were a number of points of fragmentation in the organisational structure with contradictory and conflicting views about MUs’ value and how they should be operationalised. This was contributing to poor interunit relationships and underutilisation of the FMU in particular.
Cliffdale narrative summary
Cliffdale was one of the sites with no MU (Figure 13).
FIGURE 13.
Site 3: Cliffdale.
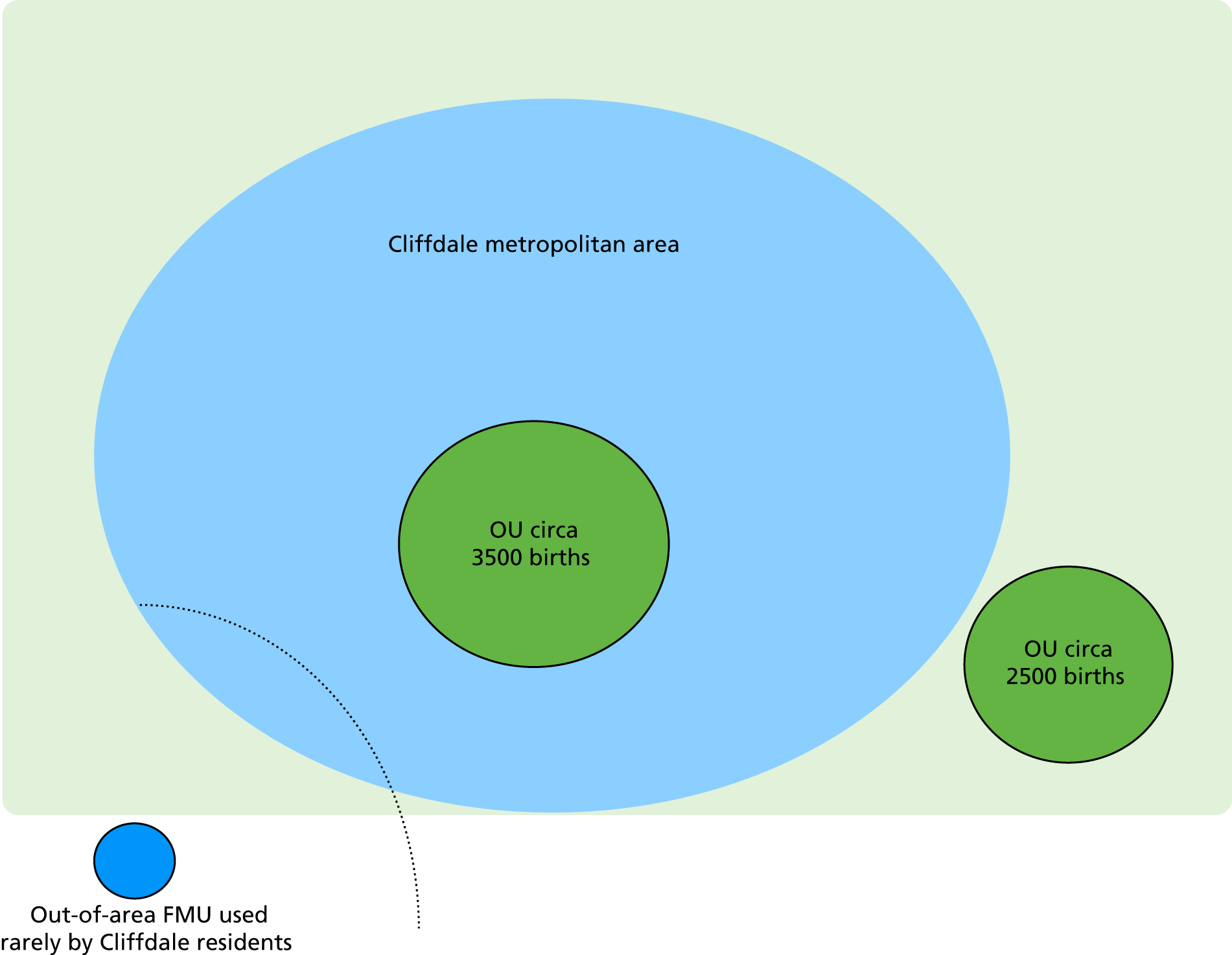
Cliffdale had two OUs, the larger of which was a tertiary-level centre based in a city with approximately 3500 births per year. The other OU was a secondary-level centre in a town, with approximately 2500 births per year. There was a rurally located FMU in a nearby trust, which was accessed by a small number of women from the trust.
The site had been trying to get an AMU on the larger OU hospital site for many years and had sign-up from a wide range of stakeholders. However, for a range of reasons (elaborated on below), this had never come to fruition.
Cliffdale also had one of the highest home birth rates in England, at 5% (national average 2%).
Resources and priorities
Financial constraints were cited as playing a major part in the delays in developing MUs, with the trust currently in ‘financial special measures’. In this context, plans that did not involve generating income were low priority. Attracting women across borders from other trusts was unlikely to work because neighbouring trusts were already well served with MUs.
One difficulty was quantifying the financial benefit of MUs according to a midwifery manager:
Reducing the caesarean section rate for example, yes that’s great, but actually it doesn’t really make that much difference because we’re paid for maternity with a tariff, so in terms of actually getting more money for doing less caesarean sections it just doesn’t happen. So from a financial perspective it’s a difficult business case to write.
CInt6
(It should be noted that the tariff system has been updated recently to eliminate this perverse incentive.)
The maternity management team had successfully put the case to the trust board on the basis of ‘patient satisfaction’ and instituting a midwife-led pathway of care, with the focus on women and responding to national guidelines, rather than money. The proposal was accepted by the trust on that basis, but then floundered later and was never implemented. Cliffdale was very proud of as its high home birth rate and this was mentioned many times in staff interviews:
We’ve also got a really, really good home birth service with a high birth rate, so we try and encourage, try and give women that choice, and facilitate that choice.
CInt6
One manager expressed uncertainty about how opening a MU would affect this:
So I’ve often thought, if we did have the midwifery-led unit would our home birth rate go down and then once that goes down it gets less easy to support and promote.
CInt8
The women’s focus groups also suggested there might be a trade-off between home and MUs:
I think we’ve got the highest number of kind of home births in the country. I think a lot of those women, if they had a choice, might consider going to MUs.
CWFG1
Leadership
An additional barrier to the development of MUs had been the high turnover of both trust and maternity service leadership. The trust had had six CEOs in the last 10 years. This had contributed to the proposal for a MU being revised at least three times.
Leadership changes in midwifery also during this period had also brought ‘rethinks’ of proposals, slowing momentum, and resulted in the postponement of MU development. The current midwife manager, who was about to leave to work in another trust, was keen on developing an AMU on the site of the smaller OU. She had been influential in the previously approved AMU not proceeding:
The problem with the current hospital at [OU 2] is that, you know, it’s an old build, creaking at the seams, you know, so there was never the ideal place to create the right sort of environment. That fell through because a new midwifery manager turned up at the last minute and said, actually this space isn’t big enough.
CInt8
The midwifery manager had been very active in shaping the development of a proposal for an AMU on the site of the smaller OU:
I have been part of the initial discussions and been asked, ‘could we just make this room the MLU’? And I’ve said, ‘No, we cannot put a sticking plaster over it. If we want to do this we’ve got to do it properly’. It’s got to be co-located, so I think we all agree that that’s what we want . . . we want the midwifery and obstetric team to embrace it for it to work.
CInt2
However, as the CEO left during the development of the proposal and, as reported in interviews, the trust experienced financial difficulties, the MU proposal was shelved. One of the midwifery managers was also opposed to developing a FMU outside the city, which had been suggested by some service users. She was strongly committed to an AMU as the best form of MU. Her rationale for this included the likelihood that an AMU would be more popular with service users, the fact that FMUs were situated in nearby trusts and that it might ‘improve obstetric and midwifery relationships’ as a result of medical students and junior doctors observing normal births.
Women in the focus group felt that the neighbouring FMU was inaccessible, which was compounded by the fact that transfers from the FMU go to an OU even further away. It was not seen as a reasonable option for most women in the trust:
. . . the FMU outside of trust is a long way away and you end up at another trust if something happens. So it isn’t really viable for many women, and then the only other option is home birth which obviously won’t suit everyone.
CWFG2
This site demonstrated how perceptions about finances in the wider trust, tariffs and cross-boundary complexity can impinge on MU plans. When combined with frequent turnover of senior management posts, these factors can frustrate the realisation of a cohesive, longstanding plan for establishing MUs.
Dewsdale narrative summary
Dewsdale was one of the high-performing sites and consisted of two OUs, each with an attached AMU, and one FMU (Figure 14).
FIGURE 14.
Site 4: Dewsdale.
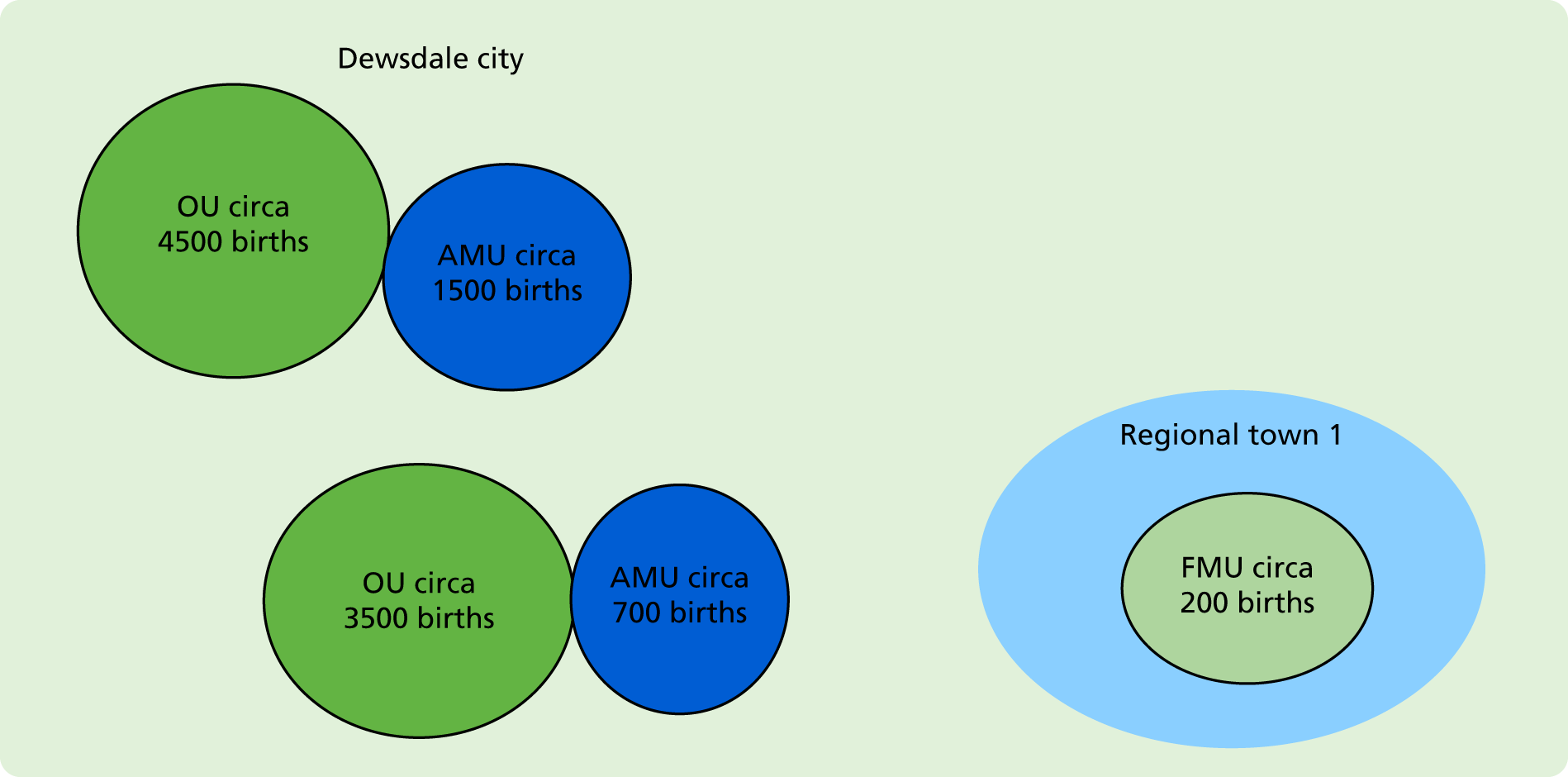
Both hospitals were in the same city. One OU was tertiary level with > 4500 births per year and its AMU had > 1500 births per year. The smaller OU was secondary level with > 3500 births per year and its AMU had > 700 births per year. The FMU was located in a smaller town, in a rural area, at some distance from the city. It had < 200 births per year and at the time of the study the trust was considering closing it as part of a major reconfiguration of maternity facilities. Other elements of the reconfiguration included the proposed closure or conversion of the smaller OU/AMU to a FMU, and the rebuild and expansion of the larger OU/AMU (with the AMU in a separate building on the site, rather than its current location beside the OU). At the time of data collection, the trust was consulting the public regarding reconfiguration proposals.
The trust had a long history of both an AMU and a FMU, despite several proposals for closure of the latter over the years. Both AMUs and the FMU had core staff, with one clinical lead for the two AMUs and one in the FMU. The staffing model was ‘traditional’. The AMUs were staffed by hospital midwives and the FMU by a combination of core staff and local community midwives.
Culture and beliefs about the intervention
Although this site had the longest history of MUs of all the sites, staff working in the MUs generally felt unsupported, particularly at the FMU, which was under threat of closure during the data collection period. The FMU midwives reported poor levels of consultation by the host unit’s midwifery managers regarding policy changes related to the FMU and said that the trust obstructed their FMU promotional activities:
Well they [trust management] always pay me lip service . . . the staff said when they met with the managers, ‘but you don’t promote us’. And they said, ‘well we do’ but we’ve been fighting for a year to get a video on the trust website, of a tour of our birth centre – there’s promotion and there’s promotion!
DMFG3
They reported experiencing hostility when transferring women to the linked OU and believed that neighbouring area community midwives were advising women against booking at the FMU because of the likelihood of transfer. They summed up their feelings by commenting:
You do feel like the poor relation. And it seems so bizarre, because the women love it, but they [management] don’t seem to care what the women want. They just seem to care what works for them.
DMFG3
Not surprisingly, a fairly strong oppositional culture between midwives in the different work contexts (MUs and OUs) was expressed in each of the three MFGs:
It’s a very ‘them and us’ sort of culture. And it’s not fair, it’s not nice, because we’re all in the same profession.
MFG. 4.1
The two city-based women’s focus groups, which were mainly composed of women of Asian ethnicity, both stated that there was a lack of information about the AMUs:
To be fair, I didn’t even know there were other choices. And I thought the one in [FMU], for some reason, was privatised. So I thought it was something that you’d go to and pay for if you wanted it.
DWFG1
They believed that the trust had a responsibility to inform women about MUs.
In contrast, a senior midwifery manager reported that community midwives do inform women about the range of birthplace options and also:
Do an assessment at 36 weeks . . . and review the notes again, we’ve got a chance to offer home birth and renew the AMU information as well.
DInt2
However, she did not mention whether or not this included the FMU option.
The MFGs revealed that the trust had recently updated the maternity care notes to include the choice of AMUs but not the FMU, which had to be selected under the category of ‘other’ and requested specifically.
Organisation and staffing
The larger and longer-established AMU functioned more effectively than the smaller AMU. There have been ongoing problems, according to the MFGs, in establishing the AMU’s autonomy at the smaller AMU, which is located more centrally in the OU. The dividing doors were rarely closed, and the obstetric staff enter it and monitor activity:
The other birth centre, just feels like an alcove of the main delivery suite, and it doesn’t have much of a sitting area. The rooms are lovely, but it just doesn’t feel as separate when you walk in.
DMFG2
It had only recently established core staff and still did not have its own clinical lead. Staff from the smaller AMU are also moved to the OU more frequently than those based in the larger AMU, disrupting the functioning of the unit and the sense of identity of the midwives with the AMU:
. . . they’ll ring from delivery suite and say we need a midwife. And because I’m rotational, it’s me that has to go. And then you’re like, all huffy about it, and I don’t even know why because I work on delivery suite a lot, so I know delivery suite. But it’s that mentality. I’m on the birth centre so I can get pulled off there . . .
DMFG1
The midwives also reported that the AMUs were used as overflow rooms for the OU, with high-risk women receiving care there:
The other day we came in, and we might as well have been an OU. We’d got 23 weekers, and 30. There wasn’t one lady in there who was low risk.
DMFG2
Leadership
Dewsdale, although categorised as a high-performing MU site in terms of percentage of women birthing in a MU, was hindered by poor support and communication mechanisms between the MUs and the rest of maternity services. In contrast to the other high-performing sites, no mention was made of there being strong or effective midwifery leadership. Staff in the MUs felt marginalised and ignored, especially in the FMU. There was also dissonance between management perceptions of MU choice and women’s experience of it.
The relatively recent opening of a second AMU sits uneasily alongside a provisional plan at the trust to close the OU where it is based, possibly replacing it with a FMU, and situating a very large AMU at the other OU with combined births at that hospital of > 10,000. This plan also includes the closure of the existing rural FMU. The new AMU may have a capacity of > 2000 births per year, making it the largest AMU in England.
Eisedale narrative summary
Eisedale was one of the ‘low-performing’ sites and consisted of one OU and one AMU (and a case-loading home-birth team, with a home birth rate above the national average), located in a large city (Figure 15).
FIGURE 15.
Site 5: Eisedale.
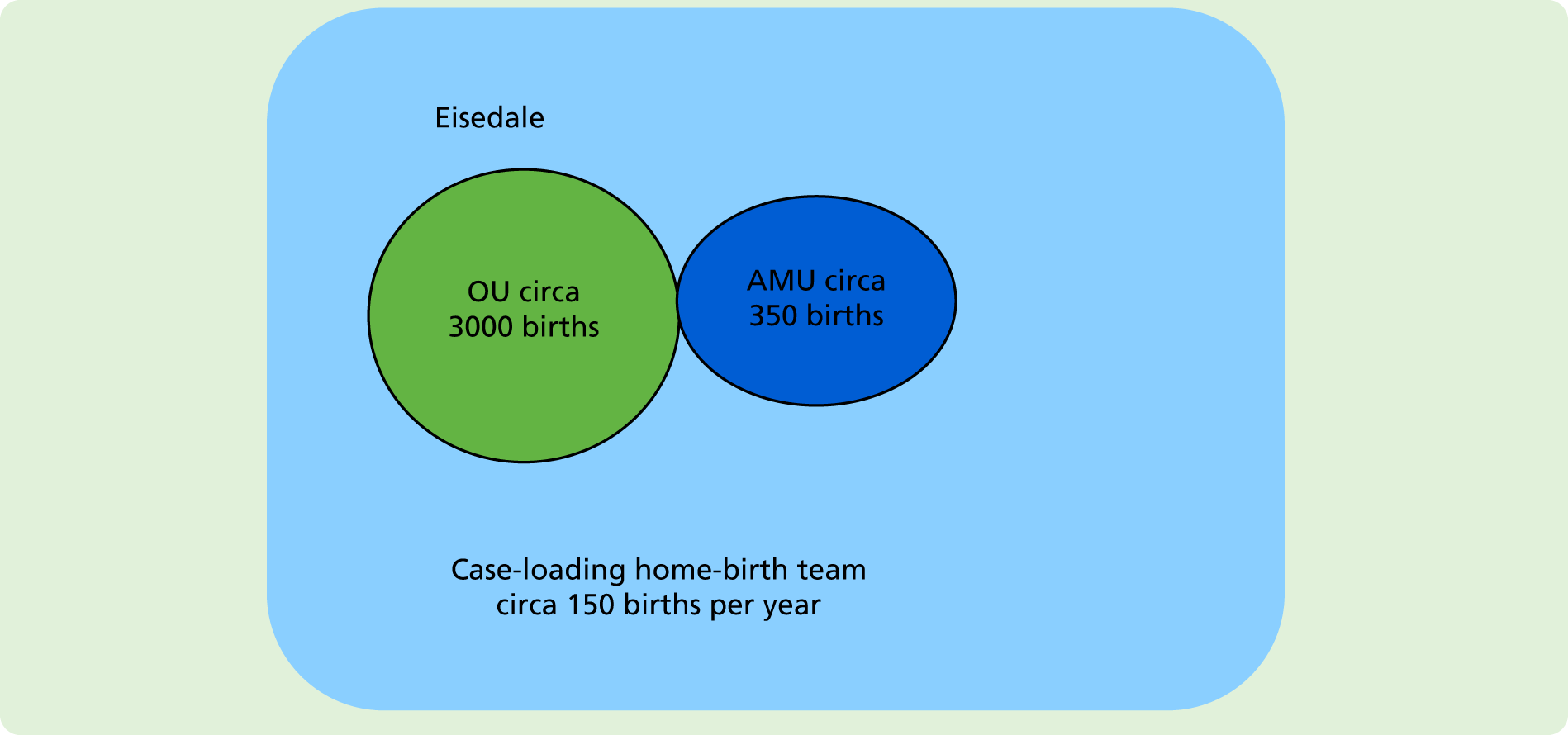
This site had an OU with > 3000 births per year and an AMU with ≈350 births per year. The AMU had core staff.
According to several respondents, the trust had a relatively longstanding history of a poor reputation, including related to its maternity services. The trust had made several changes to address this, but some problems remained and some GPs still recommend women go elsewhere to give birth. The trust used to have about 15% of women giving birth in its AMU and the reduction to just under 10% was reported to have resulted from a leadership change. A new senior midwifery leadership had recently been appointed and had begun work to improve the performance of the AMU. The AMU had a reputation for closing frequently, with staff transferred to work on the OU.
Culture and beliefs about the intervention
There was an overarching shared vision at strategy level from both the trust and maternity managers for improving the utilisation of the MU:
The vision is to increase the numbers, so we have the quality boards, and we have the numbers, and we are aiming to increase the deliveries in the midwifery-led unit, and home deliveries . . . we are continuously striving to increase it.
EInt4
Actually, a home birth service was well established and thriving, with its own case load team. It had a very good reputation beyond the boundaries of the trust, as described by a woman in a focus group:
And the trust home birth service has got a really good reputation, so I’d heard on social media how good the service was. And you get to have a midwife that comes to your house, so you see the same midwife. And she was the one that actually delivered.
EWFG1
The home birth service was the only example in the case study sites of a functioning case load model. It had also established a popular and well-used Facebook page.
Managers did not perceive that there would be any trade-off between the MU and home birth, unlike Cliffdale:
. . . for a lot of women it’s [AMU] that halfway house, you know, home birth feels a little bit too out there, but they don’t want to be on an obstetric-led ward.
EInt5
Although the staff believed that there was a commitment to developing MU services, women in the focus groups experienced a different agenda. There was still an impression of dominance by medical staff:
However, there is still this perceived hierarchy of doctors. Doctors know best, got to do as they say, and sometimes the language that’s used and the way things are presented, women feel . . . what I hear at reunions and when I speak to the women who have babies there, they feel that there wasn’t much choice. We had to do what the doctor said, or, we had to have this intervention because . . .
EInt3
Organisation and staffing
The workload on the OU took priority over the MU, resulting in MU midwives frequently being transferred there. From time to time, this meant that the AMU had to be closed:
When delivery is busy the first port of call is let’s grab a birth centre midwife. So of course you’re already then depleting your two midwives leaving potentially one on, or zero if they’re that busy, and so that service is then shut, it’s closed, you know, you can’t then offer that for the women.
EMFG2
The closure of the AMU filtered back to women, who became wary of booking there. They interpreted this to mean that the AMU was an optional extra to the main service provision on the OU:
Basically if you had a baby there you were lucky . . . it got round to women and every now and then I still meet a woman that says oh, but is it open?
EWFG1
When I did visit the trust hospital, they [the midwives] said that the midwife-led unit can shut if the labour ward is busy, they have to pull the midwives out of there. So the labour ward will always take precedent over it.
EWFG2
Resources and priorities
The trust undertook a number of promotional activities for the AMU, including the 36-week antenatal appointment in the AMU to encourage women to choose the AMU for birth. However, midwives commented that 36 weeks seemed a little late for planning place of birth, because many women will have made a decision before then:
. . . it’s difficult because that choice isn’t made until 36 weeks and I understand why, let’s wait until 36-week appointment and then assess the suitability for birth centre. But I think by then women have already sort of got their head around where they’re going to have their baby. It’s too late.
EMFG2
Some midwives described having very little time to discuss birthplace options with women. They believed that low-risk women should be encouraged to express their preference in a care plan:
I just think we don’t give women enough time and education to make proper informed choices . . . they get told where to go and what to do, and that’s it. But it’s never mentioned to them along the way, if you would like to have a more low-risk environment.
EMFG1
The trust also had monthly ‘early pregnancy evening’ promotional events in the maternity unit which included tours of the AMU.
EMFG1
Eisedale was struggling to overturn a poor reputation within the wider trust, but had a vision for MUs alongside its existing and popular case-loading home-birth team. However, an obstetric focus undermined its ability to operationalise MU care because the OU demands always took precedence over those of the AMU. It also operated an opt-in policy for accessing the AMU. Together, these factors resulted in the frequent transfer of AMU midwives and closures of the service.
Ferndale narrative summary
This was the second trust without any MU and consisted of two large OUs in a major city (Figure 16).
FIGURE 16.
Site 6: Ferndale.

Both OUs were described as being very busy, with > 10,000 births between them per year. Surrounding trusts had MUs that women can access, but it seemed that these other locations were not promoted by midwives. There appeared to be very little drive to have a MU, with the vast majority of midwives having only ever worked in an OU environment since qualifying. Many believed that they were already providing good low-risk care in their OUs, reporting that the OUs had low caesarean rates.
A strategy document had been put forward, suggesting the development of a FMU as part of a wider reconfiguration of services. The plan suggested merging all children’s and women’s services onto one site and then having a FMU at the other site. This was in the very early stages of discussion, but there appeared to be very few supporters for any kind of MU, apart from one of the senior midwifery team.
Culture and beliefs about the intervention
Within Ferndale, the culture and beliefs were particularly focused on reducing risk. It was also evident that the culture was loaded towards a preference for obstetric-led care. One corollary of this was a pervasive paternalism according to many respondents:
It’s very, very medicalised. But I think a lot of it is obviously within the hearts and minds of the midwives . . . what I know from other things that I’ve been involved in is that as midwives we don’t realise we use a lot of closed questioning of women. So we talk about choice, but we don’t actually mean choice, we mean choice for ourselves and what’s, you know . . . what choice suits us.
FInt6
Normal labour and birth was perceived to be the exception and was therefore commented on when it occurred:
I was walking out of the delivery suite and an obstetrician was walking next to me and there was a mum and new baby just leaving to go to a postnatal ward. And he said, ‘oh isn’t it lovely to see a nice normal birth’? And it was like, oh goodness me, you know, we don’t need to be hearing and saying those sorts of thing . . . said in complete innocence, but actually when you think about what they were saying in a way it’s like what we aren’t able to offer women.
FInt4
Some staff took the view that there was no need for a MU because low-risk care was already provided on the OUs:
But what’s quite interesting is that the current obstetric service can accommodate low-risk deliveries. So I mean if you look at both sides of the city there’s about 30% of all the women come through never see a doctor, so they could deliver anywhere really, the place of delivery is actually a lot less critical.
Int3
However, others felt that the strong team ethos between obstetricians and midwives was on the obstetrician’s terms:
I’m really impressed by how supportive the obstetricians are of the midwives; they are incredibly supportive, you know. It’s really fantastic team working. But I just feel it’s all meeting the obstetric point of view and we are midwives.
FInt7
Newly qualified midwives who trained locally were able to handle complications with confidence because that was what they were regularly exposed to, but they felt deskilled about normal birth:
I think, that because everyone has worked in such a high-risk environment, you become deskilled to an extent, and feel a bit apprehensive about trusting that women can have babies who are low risk.
FMFG1
Leadership
Once again, leadership came up as key reason why MUs had not been developed:
I think it’s lack of leadership and influence that’s probably blocking change because you need that leadership and vision. And as I keep telling people, the modern NHS doesn’t appoint leaders it appoints managers . . .
FInt2
. . . if we had that leadership and we had that real definite, yeah we’re going to do this, we’re going to . . . you know, walls could be knocked down and things could be done.
FMFG1
One of the new senior midwifery managers wanted to develop MUs, but felt that midwives would resist it because they would not have the confidence to work in them. She did not believe it would be possible to open an AMU owing to the obstetric dominance there, and favoured recruiting an entirely new team of midwives with a commitment to FMUs:
. . . the midwives would find it very difficult to sort of just be left alone because they quite like the way that they work at the moment. And I think that we need different talent group of midwives going into a standalone with a different philosophy of care.
FInt3
Resources and priorities
Some staff believed that maternity services reconfiguration depended, first of all, on how neonatal services would be rationalised. Until final decisions were made about this, no decision could be made about obstetric services and staff lamented the loss of maternity independence over recent years:
And if you look back in history it was obstetricians that developed neonatal services but now paediatricians have taken over neonatal services so they control them and we have to follow them.
FInt8
There were also concerns about the cost of furnishing a new FMU, as the trust had significant financial challenges:
I think the resistance comes from, how can we financially afford this? The trust is hugely in debt.
FInt7
Ferndale demonstrated how an embedded culture can frustrate change profoundly, using a range of strategies, including believing that the desired outcome (midwife-led care) is already being achieved, or by rationalising why the change will not work in this unique setting, or by projecting the rationale for no change onto another cause.
Summary
A primary theme to emerge from the within-case analysis was the importance of leadership for the development of MUs. Leaders need a strategic plan and to be able to achieve sign-up from as many stakeholders as possible. Strategic plans benefit from continuity of management personnel or at least a consistency with existing plans when new managers come into post.
Beliefs in the value of MUs cannot be assumed, even when a strong evidence base exists and national guidelines support their introduction. Strong but different preferences on the relative merits of FMUs and AMUs, and how each should be operationalised, were evident within and between different stakeholders. The challenge for services is how to reconcile these, without compromising the availability and effectiveness of both types of units.
The culture of settings can facilitate or create barriers to the success of MUs. Organisational processes that optimise MU utilisation need embedding. These include the ongoing promotion of MUs, streamlining care pathways for access to them, staffing models that facilitate ownership and the respectful mutually supportive intersection with OUs.
Women’s focus groups
Women in the six case study sites were invited to participate in a focus group to discuss MUs. Eligible women had given birth in the trust in the last 12 months, were well women (midwife-led pathway) and aged 18–40 years. Thirteen focus groups and three interviews were undertaken, with a total of 76 women (7% white European, 30% Asian and 63% white British).
As stated in Chapter 2, these data were thematically analysed outside the CFIR. The main issues that women spoke about are summarised here, with illustrative quotations used, under the three themes:
-
information and knowledge about MUs
-
influences on birthplace decision-making
-
administrative and logistical issues.
Information and knowledge about midwifery-led units
There was a wide variation in the information women had, or were given, about MUs, within and between trusts. Twice as many women mentioned not receiving information as those who received information. There appeared to be differences between ethnicities, with those who were not white British less well informed by midwives (see Individual characteristics). This was especially apparent in one of the focus groups that comprised mainly Asian women. They knew less about the option of a MU than women in other focus groups. Participants from five of the six case study trusts mentioned not being given information about the local MUs (including the two that had > 20% of women giving birth in a MU):
Well it’s just that nobody gave us the information about it [MUs]. That’s the main thing. I didn’t know nothing about it. I didn’t even know it even existed.
DWFG1
The four case study trusts that had MUs also had women mention receiving information on MUs, mostly from midwives:
I was given like an information pack on each one. And my midwife encouraged me to try and book an appointment, or to turn up to see which one I wanted to go to, which one I felt more comfortable with. And she ran through the different options with me as well.
EWFG2
Many participants spoke of seeking information from the internet [using Google (Google Inc., Mountain View, CA, USA), Which? or NHS], either to augment or in lieu of information from midwives:
I highly relied on the internet [for information]. I wasn’t aware of things like [MUs], at the midwife appointment we went in, they did the checks on me, we went out. There was no sort of consultation, or discussion, or otherwise with me.
BWFG2
Women’s knowledge of MUs varied widely also, with four times as many mentioning not knowing about MUs at all, or just some of the details of the kind of care provided or available in them. This was not confined to the two case study trusts with no MUs, but included those with MUs, where all, some or none of the trust’s MUs were known about:
. . . because I didn’t know about [FMU] anyway.
AWFG1
Women were asked what sort of information they would find helpful for their own decision, and also if they had a friend having a baby, what would they recommend that they access to inform their decision. They had numerous suggestions for things that would help, including the better use of trust websites, the addition of a social media platform to enable more active engagement and provision of information in (trust-provided) antenatal classes, which may or may not be in the MU.
The option most wanted by women was visiting the MU, as part of antenatal care or classes, or a formal or informal tour, with a virtual tour raised as a much less desirable substitute. Apart from seeing the unit, the possibility of meeting the midwives who work there was valued:
I actually went to the actual live [tour], like they show you around [AMU], just so that we kind of knew where everything was, so that we’d know where to go . . . it was good to look around first, and it actually gave me a lot of peace of mind because the lady showing us around was really nice, and everything looked really good.
AWFG2
I did the online tour for [nearby trust], and I went in person for [trust]. And I think, speaking for me, having done both, I think going in person was probably much more powerful.
EWFG2
The next most frequently requested option was for written information, which could be given to women for them to take away and consider the options before having to make their birthplace decision. Some women acknowledged the possibility of getting too much, with others adding the qualification of wanting the written information to be used to help inform a later discussion with a midwife. Women suggested that the leaflet include a range of information, such as the MU facilities and scope of care, transfer rates, pools and pictures of the rooms:
I think it’s important for them to talk through the options with you, but I also think it’s good to have it written down somewhere, that you can go away with.
DWFG3
I think it’s just more facts. People want facts, the likelihood of anything going wrong, although you can’t know that, if you were told it’s this likelihood of going in an ambulance.
BWFG1
Influences on birthplace decision-making
Environment of midwifery-led unit
The environment is a very important aspect of women’s decision to go to a MU.
The look and feel of the unit was the most significant feature for participants. This included it feeling homely, comfortable and private and facilitating a sense of relaxation or calm:
I remember picturing me and my partner in that really nice room, and it made the whole prospect of giving birth, which is scary when it’s your first, a lot easier to deal with.
EWFG2
. . . it’s like being home but with midwives, so they’ve got like, lovely flowery duvet covers or whatever, like it feels homely and cosy and that was really appealing.
CWFG2
Birth pools were the most frequently wanted facility, with lighting, kitchenette, music playing and balls less frequently mentioned.
Familiarity with the midwifery-led unit
When women were familiar with the MU – its environment, staff, location and accessibility – it assisted them to plan to give birth there.
When a MU (particularly a FMU) offered more than a birthplace (e.g. antenatal classes, postnatal checks or breastfeeding support), it was valued by women and often contributed to them planning to use the facility:
. . . so for us it was kind of ‘oh yeah, we’ve already been a few times’ [for antenatal care], you know where you’re going, it’s easier to drive there [FMU], because you’re already there, you know about the parking . . . you know your facilities and stuff like that, so you’re a bit more familiar with it. So it’s not as scary.
AInt1
After going to our antenatal classes at [FMU] I actually changed my mind and decided that I loved it there and wanted to go there.
AInt1
Continuity of midwifery care
Women expressed their desire for continuity of care, experience or lack of continuity. They indicated that continuity of midwifery care is important to, and wanted by, women. It was only experienced by women planning home birth in one site, or informally due to integrated FMU/community care in two sites, where women may see a midwife they know from antenatal care if she is rostered in FMU when they labour. Women in a site without a MU thought that continuity would be part of the package. If MUs offered continuity of care they would attract more women:
Because my midwife was my community midwife who also worked at [FMU], so for me I wanted that.
BWFG1
. . . And if I could have been at least partially guaranteed that I could have had the same midwife at [FMU] that I was seeing, and I would see the same person through the pregnancy, that would really encourage me to go to the MU rather than the [OU/AMU] hospital, because I would have felt like I had that advocate.
AWFG2
Influential people in birthplace decision-making
Women mentioned midwives as positively influential in their MU birthplace decision-making, more often than others, most often as a result of their practice and/or their promotion of the MU. Some women experienced midwives as not providing any information, making assumptions or not promoting MUs:
I think because the staff have been there [FMU] so long, they’re so positive about what they have. And the minute you speak to them about it then it just reassures you. But their experience and their passion for the place just sort of encourages you to stay there really.
DWFG3
I think the problem with it is, they make you aware that it’s there, but they tell you about the negatives, not the positives of it . . .
BWFG2
Other influences on the women (not always for a MU birth) were antenatal classes, family and community, and then, much less frequently, friends, their partner and a doctor:
I had already made up my mind, but then NCT [National Childbirth Trust antenatal class] definitely, like yeah I’ve made the right decision, I definitely need to go to the [MU], it’s the best, it’s amazing, and all of that.
AWFG2
And there was just a lot of fear amongst everyone [in antenatal class] about how to cope with giving birth. And I think that sort of reinforced my feeling that I would need a medicalised birth.
CWFG1
And then my mum and stepdad are paramedics, and so they convinced me, I suppose, in a way, to pick [OU/AMU]. So, because they know, they blue light people over there.
AWFG2
Role of facilities and services in decision
Many women planned to give birth in an OU, or in an AMU adjacent to one, because there are specialist facilities and services available there:
Just the idea of being in a hospital room and the doctor just being outside the door. Even though they could be busy, and there might be delays that way, I think just the safety of knowing that they’re there.
FWFG2
The belief that birth is inherently risky and unpredictable was widespread for women who planned an OU or AMU birth, where they believed that they and their baby would be ‘safe’:
. . . [regarding AMU] they’ve got a delivery suite [OU] underneath, because to me that would take away everything for me. If the risk was my only panic, that’s me, it’s mitigated, it’s gone.
BWFG1
A much smaller proportion of women had confidence in the birth process and the safety of a FMU. Some women mentioned their desire to avoid the risk of (unnecessary) intervention in the OU as part of their decision to plan to give birth in a MU:
I thought it’s very, very unlikely that something’s going to happen where literally I need medical intervention like this within the next 10 minutes, so to speak. And so because of that I thought I’m prepared to take that risk that if I need to be transferred, that transfer will be safe.
BWFG1
Location of midwifery-led unit
The location of a birthplace was an important factor in many women’s decision-making. For some, it was related to how close it was to their home, for access in labour. For others, the unit’s location relative to the referral OU, for access on transfer, took priority. The close location of AMUs to an OU was frequently mentioned as optimal:
. . . so even that, even if it’s a 5-minute drive, to me, [OU/AMU] like less than 5 minutes. But it just felt like hours just getting there, because you’re in so much pain. So to me, [FMU town] just like way far.
DWFG2
So you’re half an hour down the motorway then, haven’t you, and if you have a poorly baby you don’t – you want to be 30 seconds in next door, not 30 minutes down the motorway.
AWFG1
In contrast, the distant location of FMUs from the OU was an issue for some women, although not mentioned as frequently as the distance the FMU was from their home for access during labour (particularly when the FMU is rurally located and the women live in a city with an OU ± AMU):
I wanted to go to [FMU] because it was literally 2 minutes from my house. And I really didn’t . . . because trying to get to [OU/AMU] from my house, if you got stuck in traffic, it would just be . . . and I had my second one on the toilet at home.
BWFG1
Because my anxiety is that if anything goes wrong it’s a long way to hospital, which if you’re at [FMU], for me, that’s how I felt about it.
DWFG3
Cross-trust boundary issues were a factor for some women, with some being discouraged from booking to give birth in another trust and others denied the option:
I got told ‘no’ to [nearby trust town].
BWFG2
I think it depends on your postcode actually, so possibly someone that lived more in central [trust area] might not be able to go to [nearby trust].
EWFG1
Administrative and logistical issues
Booking process and timing
Women expressed uncertainty about the booking process, such as whether or not it is necessary, how it is done, if it is possible to change your mind and if it is for births or scans (where notes are to be held).
Most sites complete the booking early in pregnancy, at the booking visit, with those appearing to have less discussion and flexibility. Others have some flexibility, although women reported experience of different processes within the same trust.
Some of those sites that formalise the booking later postpone the decision for MU birth until ‘low-risk’ status is confirmed in the third trimester. Some of these are well women who cannot plan a MU birth ‘just in case’ they develop a risk factor that will make them ineligible, whereas others are women who have a risk factor, such as a low-lying placenta, which requires review in the third trimester to see if it has resolved:
I wasn’t aware that you had to decide before you went in for your booking appointment, so I was asked on the spot and I didn’t know. But the midwife said that you have to choose now because they have to book the hospital in advance.
BWFG2
Yeah, because maybe sometimes you feel like well I’ve made my decision now, so that’s what I need to do. As opposed to knowing that it is actually changeable.
DWFG2
Eligibility criteria
Some women had poor knowledge of eligibility criteria, whereas others challenged them or were frustrated by them and others accepted them. There was a sense that the criteria were very risk averse and overly restrictive. Women also found variation in the way they were interpreted or implemented. The ability to have a review with a senior midwife or obstetrician was valued by some, but felt unnecessarily bureaucratic by others. There was a sense that a ‘fight’ was necessary to get a reasonable compromise:
At first they said with her she was going to be too big. Then they scanned me and said she was too small. So yeah, it was literally on border whether I could go or not.
BWFG1
[Regarding FMU] it’s so low risk though, if you’ve got any slight thing and it’s just took off you.
BWFG1
Capacity
Midwifery-led unit capacity is an issue for women, either the whole unit being full or closed, or an unstaffed FMU not able to be opened for a birth owing to no staff being available. Women had also experienced OUs being full. They found it problematic to plan to give birth somewhere when there was uncertainty about its availability when they were in labour and tried to book somewhere where this was least likely to happen, which sometimes meant changing the location or type of maternity unit they booked. Some women commented on the stress that those working in the NHS are under, with particular focus on midwives, who were seen as having high work pressures, limited time and providing reduced or minimal care:
What is scary is the number of rooms, you think if you get there and it’s full . . . and you’ve planned that for 9 months in your head . . . Like the day we went in there [AMU] for the tour, all the rooms were full . . . because they’d have to overflow into the labour one, I think god, that would have been really upsetting.
EWFG2
So I was thinking of going to, to the [nearby trust], purely because there’s a Which? Birth Choices thing [website], which said that the [AMU] had been closed so and so many times in the previous year due to understaffing. And I thought I’m not going to risk getting there on the day and ending up in labour ward [OU].
EWFG1
And I don’t think that’s the fault of the midwives concerned at all, I just think there aren’t enough of them. But that’s the thing, there aren’t enough of them.
DWFG3
Summary
There were some similarities and some differences in the experiences and views of participants, both within and between trusts. The theme of ‘information and knowledge about MUs’ had the greatest range of responses, with women in some trusts receiving quite different information about the MUs available either within their trust or in neighbouring trusts, in trusts without a MU. The second theme with divergent responses was ‘administrative and logistical issues’, with women both within and between trusts experiencing these processes differently. The theme with the most consistency in responses was ‘influences on birthplace decision-making’, which women reported more consistently within and across sites, although they were still dependent on the information shared and processes undertaken by midwives providing antenatal care and information.
Cross-case analysis
These findings are reported using the CFIR with its constituent five domains.
Although we had anticipated a clear difference in the experiences of midwifery-led services in the high- and low-performing sites, overall, our findings suggest that across all sites the delivery of midwifery-led services was considered challenging and was perceived as a struggle. The cross-case analysis is structured around the most salient constructs within each of the domains of the CFIR. Although the data gathered covered many of the CFIR constructs, here we focus on issues that were seen as most strongly having an impact on the uptake and development of midwifery-led services from each of the CFIR domains. Namely, this covers factors from the ‘outer context’ of public policy and the broader health system; distinguishing features of midwifery-led services themselves as an ‘intervention’ for health service improvement; the ‘characteristics of the individuals’ from stakeholder groups involved in leading and running maternity services; factors within the ‘inner context’ of the midwifery service systems; and features of the ‘process of change’. Each of the CFIR domains contributes to a holistic overview of change within complex organisations. These are described with their relevant attendant constructs where they linked to the cross-cutting themes.
The CFIR constructs are mapped to the cross-cutting themes in Table 22. See Chapter 2, Theoretical/conceptual framework for more detail on the constituents in this table.
| CFIR domains and linked constructs | Cross-cutting themes | ||||||
|---|---|---|---|---|---|---|---|
| Culture and beliefs about the intervention | Resources and priorities | Organisation | Staffing | Leadership | Change | ||
| I. Intervention characteristics | |||||||
| A | Intervention source | ||||||
| B | Evidence strength and quality | ||||||
| C | Relative advantage | ||||||
| D | Adaptability | ||||||
| E | Trialability | ||||||
| F | Complexity | ||||||
| G | Design quality and packaging | ||||||
| H | Cost | ||||||
| II. Outer setting | |||||||
| A | Patient needs and resources | ||||||
| B | Cosmopolitanism | ||||||
| C | Peer pressure | ||||||
| D | External policy and incentives | ||||||
| III. Inner setting | |||||||
| A | Structural characteristics | ||||||
| B | Networks and communications | ||||||
| C | Culture | ||||||
| D | Implementation climate | ||||||
| 1 | Tension for change | ||||||
| 2 | Compatibility | ||||||
| 3 | Relative priority | ||||||
| 4 | Organisational incentives and rewards | ||||||
| 5 | Goals and feedback | ||||||
| 6 | Learning climate | ||||||
| E | Readiness for implementation | ||||||
| 1 | Leadership engagement | ||||||
| 2 | Available resources | ||||||
| 3 | Access to knowledge and information | ||||||
| IV. Characteristics of individuals | |||||||
| A | Knowledge and beliefs about the intervention | ||||||
| B | Self-efficacy | ||||||
| C | Individual stage of change | ||||||
| D | Individual identification with organisation | ||||||
| E | Other personal attributes | ||||||
| V. Process | |||||||
| A | Planning | ||||||
| B | Engaging | ||||||
| 1 | Opinion leaders | ||||||
| 2 | Formally appointed internal implementation leaders | ||||||
| 3 | Champions | ||||||
| 4 | External change agents | ||||||
| C | Executing | ||||||
| D | Reflecting and evaluating | ||||||
In the following section, we have chosen to describe and evidence only the most pertinent construct under each domain.
We commence with the ‘outer context’ construct because it provides the backdrop and rationale for the development of MUs.
Outer context
External policy and incentives
The macro context of national maternity policy in England has a number of intersecting priorities that frustrate commissioner and provider strategic planning for MUs in local settings, and examples of this are given in this section.
Although the evidence base of MUs is quite well disseminated and national guidelines recommend them for every trust, a number of other macro factors impinge on developing them. These include the medicalisation of birth, contributing to greater obstetric surveillance that has overseen a shift to birthing on busy obstetric-led labour wards, the increased complexity of risks in the childbearing population, such that fewer women are eligible for MUs, and a risk-averse culture that militates against the use of MUs.
The provision of choice around place of birth has been policy in maternity services for > 20 years, but local services are not audited on how they operationalise this regarding MUs, and hence our data show considerable inconsistency.
Finally, financial constraints on the NHS were spoken about ubiquitously. As one respondent expressed it, ‘we’re in a period of austerity now’ (AInt4).
The medicalisation of birth, so that the wider population views giving birth as safe only on a labour ward, was highlighted in a number of interviews and focus groups:
I think also as we’ve been culturally accustomed to birth taking place in hospital since the 1970s, and to step outside of that model you’ve got to face your family and your peers and actually have a good reason why you want to birth outside that accepted model . . . you’re battling a mindset. Hospital is perceived as safety, the ‘just in case’ option. They’ve lost the ability to believe in their own bodies haven’t they, this sort of generation coming through don’t actually think even that it’s a natural thing for a woman’s body to do, they just see it as a medicalised model of giving birth.
BMFG2
Changing this perception was seen to require a major cultural shift:
We need to change some of the culture I think. The low-risk women would automatically go there, so it would be seen as part of the norm. But that’s a massive culture shift isn’t it, probably which would take almost a generation, wouldn’t it? So actually a generation of teenagers out there now who are going to have babies in the next 10 years, the message would be, actually if everything is low risk this is the place of birth, this is where you would go and have your baby.
CInt4
The changing perceptions of risk among health professionals was having an impact on access to MUs:
We’ve seen a bit of a reduction [in FMU births], because of the impact of Saving Babies’ Lives [NHS England. Saving Babies’ Lives. A Care Bundle for Reducing Stillbirth. London: NHS England; 2016].
Right, yeah. The policy framework . . .
So we’re seeing more women being scanned for growth, and being induced. More inductions because of the query that the growth’s falling off, or static, or reduced movement. So we are losing births to that.
Services therefore tended to attribute low provision, or take-up, of MUs to what they perceived to be increasing levels of obstetric risk:
Because we have many ladies who are desperate to use the birth centre, but they just don’t fit the criteria. We’re a high-risk population in other words.
DInt5
I think it’s difficult as well, because a lot of our ladies are high risk. We do get the low-risk ladies, but the majority are inductions, we induce a lot of people. It is generally a high-risk population we’re dealing with.
FMFG1
Two of these sites were high performing, indicating that, despite apparently having a higher-risk population, their MUs were still well used. This challenges the view that a changing risk profile in local women is a justification for not having a MU or a rationale for a reduced throughput in an existing MU.
A risk and litigation agenda was clearly evident in all sites but was predominantly constructed around the risks of birthing in MUs:
There’s also the potential clinical risks of people giving birth in those areas [AMUs]. And we had an unfortunate death about 3 years ago, someone who didn’t want a vaginal examination and ended up fully dilated pushing for a considerable period of time and in the end the decision was made, we’ve just got to transfer, and unfortunately the baby died in transfer.
BInt4
There might be a degree of fear that if people started saying that, you can go in there [to the MU], you are constantly like . . . women have to be told the risks . . . because of the litigation now.
FMFG1
We’ve got ladies going through solicitors, it’s going very, very high up within the trust to make sure that these MU women are safe, and make sure the midwives are covered and safe with these ladies. Because they [midwives] are scared.
BMFG2
These litigation concerns expose a paradoxical element because the evidence shows that healthy women who plan birth in OUs are subjecting themselves to greater risk.
Patient needs and resources
The second salient construct of the outer setting was that of patient needs and resources.
Respondents’ awareness about resource scarcity within the NHS was widespread across the case study sites:
You know, the limiting factors are the fact that the country’s in a financial crisis and health care is crippled in terms of finance. So it comes down to the money. I think, you know, there’s a will, there’s an understanding but actually being able to finance these things [MUs] means that you need money from the treasury to do so.
CInt3
I think the whole financial situation within the trust at the moment is a driver . . . Unfortunately all our finance team will only see is the figure at the bottom of the page . . . it is a sort of finance-driven organisation and you’re forever trying to find ways of saving money, cutting costs, etc.
BInt5
I think the finances is something that we all skim around but I guess that’s the crux of what’s gone on, it is the money . . .
DInt1
I just have this undertone that decisions, some of the decisions are being made not for the women, but for money. Not to gain money, but to save money.
EMFG1
This discourse of scarcity was not questioned by anyone we interviewed and there was a sense of resignation to having to compete with other trust services for a limited and apparently diminishing reservoir of money.
These factors emanating from the national context are having real effects on the implementation of MU services locally.
All sites were aware of the imperative to provide the choice of MU provision for service users of a MU, but its application was generally suboptimal, both in the availability of MUs and in the mechanism of how choice was presented. Two case study sites had no AMU and three had no FMU. In sites with MUs, women reported that they either did not know about them or did not know they could choose to birth there:
But I mean, I’ll be honest, MUs, are they a relatively new concept? I didn’t know they existed.
EWFG2
Well it’s just that nobody gave us the information about it. That’s the main thing. I didn’t know nothing about it . . .
DWFG1
I even didn’t know I’d got a choice [where to birth], but then friends said go to the birth centre. I said am I allowed? So then I did my own search.
AWFG1
These women’s experiences raise important questions about how embedded MUs are as a mainstream place of birth option alongside OUs within local maternity services, and to what extent trusts headline their value and purpose.
Under the CFIR, the domain of intervention characteristics and its constructs of ‘cost’ and ‘adaptability’ will be explored next.
Intervention characteristics
Cost
One of the respondents’ key concerns about the introduction of MUs, especially FMUs, was their perceived cost. Economic evaluations of both AMUs and FMUs have been favourable, as discussed in Chapter 1. However, there is a paucity of information about the set-up costs of developing them. All but two of our sites already had MUs, either an AMU or a FMU, and three sites had both. Start-up costs were therefore relevant in only two sites. Virtually all of our findings around cost pertained to FMUs.
Within an environment of financial constraint, the perception that a service is underused quickly translates into it being viewed as inefficient and poor value for money. This especially affected low-volume FMUs, for which, across three case study sites, there were plans to close them:
If you spoke to any of the consultants I am sure they would say it [FMU] should be closed because it’s a waste of money. And it’s an unfair allocation of resources, in a relatively resource-poor environment.
BInt3
Well it [FMU] is small and we do have to understand how viable it [FMU] is because you can’t spread yourself so thin. And I mean, to be fair, we can only provide so much, you can’t spread yourself too thinly and become unsafe. So it [FMU] is difficult to manage because we’re covering so many other areas, and the birth rates numbers are very low.
AInt3
. . . That’s essentially where we’re coming from there, and also our plans look to shut the very small unit that we have . . . because that’s just not viable, the numbers are falling.
DInt5
In addition, the start-up costs for staffing a new FMU were judged to be prohibitive at Ferndale, which had no MUs:
You couldn’t possibly do a standalone unit without having more staff, so it’s a cost thing. It’s staffing levels. And unless the trust are willing to put the money into it, you wouldn’t be able to do it, it wouldn’t be feasible.
FInt2
Adaptability
A second feature of the introduction of MUs was their perceived adaptability and compatibility with existing services. For example, finding an appropriate space was paramount. One approach has been to recommission space within an existing footprint, a less challenging and less costly option than commissioning a new build. This is how AMUs have been principally developed in the case study sites. However, that has also been problematic because of the increased birth rate nationally, so many existing OUs already had capacity issues:
But the problem with [OU/AMU], it was designed for 4500 deliveries and they’re now delivering 6700 through [OU/AMU].
BInt7
Only one site commissioned a new build for a MU. More commonly, consideration of this option did not result in a new MU but years of plans, revisions and more plans:
We had three kind of projects to rebuild in the last 12 years because we are underspaced, undercapacity, each of which have kind of got so far, got the architects plans and then the trust have said, actually we need an A&E [accident and emergency], or we need money for this . . .
BInt1
One potential solution to unequal provision of MUs would be for adjoining local maternity services to share MU facilities (e.g. one service that does not have a FMU could share with a neighbouring service that does have one). Our data showed that this rarely happened and, if it did, it created organisational and logistic problems, as well as access problems for women and their families. This was because of the tariff system of payment, premised on a competitive model:
. . . at the moment the tariff does provide a complete barrier because if we were expecting our two trusts to work together then each trust is going to want to retain all the tariff for the women. So there isn’t an incentive for the women living in the [trust] catchment area to be cared for by the [other trust] because they lost the tariff.
BInt6
Two trusts operated other services from their FMUs, including antenatal clinics, antenatal education and scanning, as a way of attaching women to the service and optimising alternative uses for the building. Respondents believed that this helped justify continued investment in the FMU.
Individual characteristics
Beliefs about the intervention
Convictions about the benefits of an intervention are known to strongly influence its successful introduction. 110,111 Despite the evidence base of MUs being well known locally, interviews and focus groups revealed substantial ambivalence about value of MUs, especially among clinicians. It was clear that having an AMU or a FMU and working in them positively influenced perceptions, especially among midwives:
. . . it is great and it’s, you know, less medical intervention, it’s cheaper and it’s better for the women. It’s just better all round . . .
AInt6
I think the beauty of midwifery-led units is that it helps midwives to be autonomous practitioners. It allows for choice for the women.
CInt2
Similar comments were made by obstetricians and neonatologists:
I have mainly had positive experiences with midwifery-led units. I worked as a registrar in [place] and there was a co-located one there and from a neonatal point of view I wouldn’t say there are any more troublesome deliveries there than there are elsewhere.
BInt5
Some of the trust staff expressed a preference for an AMU over a FMU:
I think majority of women and all my friends will opt for alongside, because most women do want the option of midwifery led but if anything goes wrong they just want to go down that corridor, through that door.
DInt4
It was notable that, despite the national evidence indicating difference in rates of intervention according to setting, some midwives in strategic posts expressed the view that midwifery care for low-risk women could occur effectively within an OU, with or without dedicated low-risk rooms:
Well there is what we call a midwifery-led unit which is incorporated within the delivery suite in the [OU2] which was set up by [name] which must be about 25 years ago . . . two or three rooms where the midwife-led care was given.
FInt1
. . . it’s about ensuring that you have quite a high percentage of vaginal delivery, and again midwifery-led care being delivered in labour ward and . . . and the protection of it, that’s the important thing . . .
EInt1
. . . you can deliver a woman on midwife-led care wherever you are. We don’t need to have these alongside units. A midwife is a midwife is a midwife.
BInt2
The midwife manager cited above went on to criticise the OU staff for not utilising the three low-risk rooms within the OU:
There are three beautiful, low-risk, midwife-led rooms on the end of the [OU] delivery suite. But for some reason the staff on that site cannot see them in that way, and instead want an AMU.
BInt2
The view that FMUs were unsafe was held by some midwives according to the MFGs:
We’ve had students come back to us and say that the [midwife] mentors have said they’re [FMUs] not safe to birth with in, especially primips, because . . . and they’ve said to the women, you have a greater risk of dying.
DMFG2
Finally, some staff believed that women from particular ethnic groups preferred OUs to MUs. Those expressing this view presented it as something that could not be addressed or changed:
. . . We have women from ethnic minorities that back home, for them, they want the continuous monitoring, they want the doctors to deliver them. So they have that mentality. Yeah, we’ve got couches in our birth centre and they’re like, where’s the bed. On the birth centre, they won’t stay here, there’s no bed.
EMFG2
. . . women coming through of a different culture, and they particularly want it obstetric led.
BInt4
However, two sites with significant populations of women with Asian ethnic backgrounds had AMUs and FMUs that were popular and heavily used by these women. The staff discussed the strategies they used to engage with these communities and change inaccurate perceptions regarding MUs:
We have had others suggest that Asian women are not going to buy into midwifery-led units. I used to speak the husbands, get them to come and visit and talk to them because they’re, oh my husband doesn’t want me . . . now he wants me to go to . . . one lady that came to my clinic and all her family had been to the OU so she was going there . . . I said, just come to the [FMU] and have a look round. And she came and had a fantastic birth. So it’s word of mouth. The Asian girls love it, they absolutely love it.
AMFG1
Although across all case study sites, the provision of MUs was generally viewed favourably, for some maternity stakeholders personal opinions or beliefs about them appeared to trump evidence and this is likely to have affected MU provision and utilisation in some of the case study sites.
Inner setting
Access to knowledge and information
The provision of evidence-based sources and appropriate skills training by local health services is known to facilitate the introduction of optimum care models. 112,113 Working in MUs, although it should be the basic default skill set for every midwife, may require considerable adjustment for midwives more used to working in OUs. Many interviewees suggested that midwives were losing the skills for caring for normal labour and birth:
Because everyone has worked in such a high-risk environment, you become deskilled to an extent, and feel a bit apprehensive about, I don’t know, caring for . . . you know, trusting that women can have babies low risk.
FMFG2
One of the effects that that has had, is that is has decreased a lot of the midwives’ confidence in this unit, of providing low-risk care, because they don’t have the environment, a consistent one, in which to do it properly . . . when you’re on labour ward you become over-reliant on the doctors . . .
EMFG2
Respondents felt that midwives need particular sensory skills and a holistic outlook to work effectively in MUs:
You’re using your eyes and your ear and your hands and you’re more tuned into that woman . . . which is what you need if you go midwifery led.
DInt4
The ability to work autonomously was also seen as important:
It’s for us to show them [students] what working autonomously as a midwife looks like, and how these . . . you know, truly let our women labour uninterrupted under her own steam in a calm and peaceful environment, what it actually looks like. And that’s a precious thing, it really is, and we need to spread the word.
AMFG1
Midwives in the focus groups said there was a need for training in normal birth skills for qualified midwives:
I’d like to make physiological birth and normal birth more accessible to them . . . our sort of mandatory week of training that we do is very obstetric led. So what I would love to do is a session, a day, on physiological birth, and normal birth, and making midwives more confident in doing it.
EMFG1
Others suggested that the default training for student midwives should be in low-risk care. From there, midwives can then learn to recognise risk, rather than the other way around:
I trained at the satellite birth centre and then went on to go to our birth centre. But not every student has the opportunity to actually train on the birth centre, so you are trained in that thought process. You are trained in completely low risk, and then you spot the high risk. Whereas there are a lot of new midwives who are trained solely on high risk because there aren’t enough places on birth centres to send these students.
One case study site had introduced NLS training, especially for midwives working in FMUs:
. . . a few of the midwives in the birth centres are NLS instructors, so they have helped raise the profile of that even higher, so even more than what we thought was the basic requirement, they’ve actually taken it, you know, one step further . . . on every shift there was an NLS-trained midwife. So we’ve actually made that, mandatory really . . .
AInt7
Readiness for implementation
Consulting widely and inclusively, with a particular focus on meaningful and ongoing dialogue with local service users when developing MUs, was highlighted in many interviews:
. . . it’s that desire for genuine and well-informed public consultation so that they know really what is being proposed and what the implications are for it.
EInt4
Armidale was especially effective in this area, particularly during the major reconfiguration, but many participants recognised the need to this to be ongoing:
. . . there was a big consultation with service users, and that was called the Meeting Patient Needs programme . . . I think that was the big driver. It meant massive change for the service in [FMU place] having standalone unit.
AInt2
So I think having service users in at the ground level . . . Having genuine engagement with them rather than tick box; and I suppose also building a network of people that are interested in birth centres to work alongside the midwives, people from the community. But then they’ll be back in their own communities talking to women and that helps filter out information.
AMFG1
Some services struggled to engage with a truly representative sample of service users:
We need to really reconsider how we’re doing engagement with women. We’ve got a couple maternity service liaison committees, but they’re not representative of our service users. So it might be a white middle-class woman who gave birth 8 years ago chairing them, and they’ve got chips on their shoulders about certain aspects of care.
BInt6
I’ve been what’s known as a patient partner, and I think this might be unique, certainly in terminology. And it just means that I go give a patient’s point of view at various board meetings. I’m not . . . I mean I’m not elected, I’m not a representative patient or anything like that, simply a patient.
DInt2
Therefore, multidisciplinary collaboration within the trust, with sign-up across the organisation, was also identified:
In order to get a birth centre off the ground, there has to be the political will and you need all the obstetricians on board.
CInt7
So you know, just good communication as well between the birth centre and labour ward that everybody is singing from the same hymn, and that includes, you know, the multidisciplinary, the obstetricians as well.
EInt9
Culture, networks, communication
Many of the MUs described a poor interface with their linked OUs:
There will always be a ‘them and us’. And I think, because of the medical model of obstetrics, I think there’s always been higher importance put on obstetric care.
AInt7
It seemed that a ‘them and us’ dynamic was exacerbated by individuals:
I think unfortunately the issue was the previous lead. She managed to create that ‘us and them’.
EMFG1
I think, we have certain sort of delivery suite co-ordinators who have no time for the birth centres at all . . . there is a bit of ‘them and us’.
EMFG2
One manifestation of this was the negative reception some FMU midwives received on the OU when transferring a woman:
I went on a transfer, and the reception I got was non-existent.
What do you mean?
There was nobody waiting. They weren’t waiting for me when we go there, there wasn’t a cot in the room, no midwife came, I had to find somebody.
But they were told, they’re always told ahead that you’re coming?
Oh yeah, they know you’re coming. I’ve been greeted with oh, here comes another failure from [FMU].
The MU midwives felt that some OU staff had a perception that workload on MUs was less intense:
I think there is this myth that we low-risk midwives perhaps sit around twiddling our thumbs quite often and we don’t. I think that’s something that’s sort of spread around, the rumour. It’s really sad, it is a very ‘them and us’ situation.
BInt4
It was noticeable that staff in FMUs in two of the three sites had felt detached from and unsupported by their host trusts. In one site, the staff’s attempts at promoting the FMU have been frustrated by lack of engagement from the trust:
And they [trust management] kept putting us back, putting us back . . . If you look at all the leaflets that they do send out from the trust, [FMU]’s this little add-on at the end, in the fine print at the bottom. It’s not promoted, you know.
CMFG3
The staff at another FMU said that the two linked OUs, which seemed ambivalent regarding encouraging women to birth in the FMU, were nevertheless happy to use them for postnatal transfers when they got busy:
And they’re quick to send women back to us with their feeding concerns, because obviously bed shortages over at their units.
Oh I see, you still take postnatal inpatients?
Yeah. From everywhere, yeah. Regularly. And that’s what’s promoted. If they’re busy at their ward, which they always are because they’re rammed, we get phone calls. Can you take them? . . . We’re kind of like a half-way house sometimes, it feels like. But that’s because that suits them. When we talk about being here [for births], they’re – but you’re too far out, nobody can come.
Process
Planning
When establishing a new MU, promotional events and materials, especially regarding FMUs, was crucial. In one site, where a FMU was thriving, promotion initiatives and positive messages from the midwives were fundamental to its success:
I think if you’ve got that promotion, and we’ve got films on our website where we are promoting the birth centre and so I think it’s about promotional material to make sure women know.
AInt5
I think there needs to be a very good website – because I know women shop around and look at websites and we’ve got films on our website where we are promoting the birth centre.
EInt1
Promotional activities need to be ongoing, as another site with an established FMU stopped tours of the facility for women and this appeared to diminish bookings:
One of the things I’ve heard, certainly around the standalone is that they used to have regular tours as part of the introduction for the women, but that was pulled. And I think women will hear about it and they can go and have a look, but it’s that automatic tour that was part of the introduction that they felt affected the numbers.
BInt3
One site actually performance managed their staff on recruiting women to their new FMU:
I guess one of the thoughts was has integration of your community with your birth centre, has that influenced the promotion of birth centres by the community midwives?
Yeah, greatly. When we were really, really trying to embed the unit and promote it, we really needed the midwives to embrace it. So we set targets . . . we had to audit everybody’s referrals. To see how many mums they did, and if they didn’t do any we wanted to know why. We said if you don’t start referring women, we’ll pull you off your clinic.
Finally, writing a strong business case is especially important to help win the financial argument:
It’s a difficult business case to write and in the end the trust accepted that there would never be a financial motivation for this, that it would always be about patient satisfaction, pathway of patient care and it would be all about the patient, so it was not going really going to be about making more money.
CInt6
It really needs the trust, the managers of maternity services, to write a business case, and to get that signed off by their board.
FInt1
Engaging: champions
The second aspect in the process of developing a MU was harnessing the persuasive power of champions to engage and influence other key stakeholders, especially those who remain ambivalent about the change:
If you can get a good obstetrician to support you, in terms of that, I think you need that one person to champion your corner from that clinical leadership side that would be key.
AInt1
Champions are often individuals who have worked within the model previously as they are more likely to be familiar with the arguments against the change:
I think they need a champion. There needs to be someone in the system that drives it who has worked in a midwifery-led unit in the past, they obviously have a very strong view and a very strong voice.
EInt4
Having that presence at a strategic level is also important:
I still think we have a long way to go at getting maternity services discussed at board level, and having an identified board-level champion within the CCG [Clinical Commissioning Group], as well as within the provider, and making sure that that role is more than just a name.
EInt6
Executing
One of the findings from the mapping survey in the first stage of the project was that a key to high utilisation of MUs was the streamlining of the care pathway to access them when women go into labour.
This did not happen in the majority of sites and was especially commented on by the WFGs.
Many women were not aware that they were birthing in a MU, or that they existed within their local maternity service. The actualising of choice was compromised by poor organisational processes that sometimes required a choice of place of birth at the beginning of pregnancy:
I wasn’t aware that you had to decide [where to birth] before you went in for your booking appointment, so I was asked on the spot and I didn’t know. But the midwife said that you have to choose now because they have to book the hospital in advance. Then I called up my mum and she suggested [OU/AMU].
BWFG1
Yeah, because maybe sometimes you feel like well I’ve made my decision [about place of birth] now, so that’s what I need to do. As opposed to knowing that it is actually changeable.
DWFG2
However, on other occasions women were discouraged from booking in a FMU because they might develop complications:
They said ‘don’t make the decision now . . . wait until towards the end and see if you are still OK’ . . .
BInt4
This had a negative effect because the woman wanted the reassurance of having a plan.
Instead, a graduated discussion commencing at the booking appointment and then revisiting it on a later occasion and especially at 36 weeks was recommended:
So I think that orientation into the community needs to include that birthplace discussion and promote birth centres . . . to make sure they offer low-risk women the birth centre.
EInt7
I think when they have their birth plans done at around 36 weeks it’s worth mentioning it [MU] then, because at booking when you get bombarded with so much information, so many leaflets and often they’ll say to us, oh I haven’t read it, or I haven’t had a chance to read it. So giving that a bit later on when they’ve had chance to digest all of that information, might be more beneficial.
DMFG1
Having an opt-out policy was commonly viewed as the best way to maximise access to MUs:
The AMU has a very well-established co-located MU and it works really well and it continues to. So the MU is the default place to go for everybody and that’s where they go when they come in the door and then they’re only sent to the higher-risk unit if there’s a reason, so everybody is in the MU.
DInt9
I think whether you set it up as opt in or opt out makes a big difference. So if you’re low risk you are automatically booked at the birth centre, unless you explicitly opt out. That probably encourages more people to use it because if you present to them this is the appropriate normal place for you to go for your birth because you are low risk, it’s more likely that they’ll agree with it, rather than saying which would you rather have?
FInt2
An opt-out policy would help with solving another recurrent issue, especially for AMUs in the case study sites: the frequency of MU midwives being moved regularly during shifts to OUs to care for women there. Midwives complained about this a lot:
I think it’s dangerous once we start seeing staffing pull from the birth centres to deal with problems in the obstetric unit . . . can be unsettling for the junior midwives coming in to [FMU] work and then being asked to go. And it limits their experience here, so they’ve not got the exposure to the lovely normal births, so they just see the birth centre and somewhere where they get moved from to go and cover the shifts at the OU.
AInt2
There’s been a lot of staffing issues with [AMU], so they were constantly pulling off midwives and shutting it.
BInt12
They don’t like coming out to help on delivery suite, and they probably feel like if they need help they don’t get it as easily as they’re dragged out to help on delivery suite. So that can cause a bit of friction.
DInt2
Only a few sites saw addressing this as a priority for optimising the use of MUs:
I think now it’s been recognised that we’ve worked the wrong way round actually. You need to staff your alongside units, keep the capacity off the labour ward, and let midwives deal with the normal stuff.
BInt4
Having core staff who could not be moved was one way of keeping MUs open:
I would like birth centre to have a proper core of midwives. The staffing are separate from the labour ward, postnatal, so they, obviously they’re still there, but they’re not counted in the numbers. Because birth centre has its own numbers. So midwives can go there to work and not have this fear of being pulled.
EMFG2
Only one site had an integrated staffing pattern with community midwives working shifts in both the FMU and the AMU. This clearly contributed a sense of ownership and pride in the facility and solidarity with the women:
Because midwives like to see the women, you know, not just when they’re coming in in labour, and it helps to give that approach. Although, you know, we can’t do a named midwife as such, but then that helps us so that women fundamentally will only have like the maternity services, a group of four to six women that they know. So in the main the women at the [FMU] birth centre will have met the woman.
AInt5
Reflecting and evaluating
Respondents from one site in particular spoke about the need to audit and reflect on how their MUs were working:
The important thing is to keep auditing their activity making sure that you know, lessons are learnt and people can sort of, you know help their practice get better . . . you know, get improved for the better really.
AInt7
And I think in establishing it I think that’s important, but then also maintaining that. There’s always a risk that things start dwindling if you don’t constantly review and constantly make sure that those underpinning values are still there.
AInt3
This site had the largest FMU in England and one of the highest utilisation rate regarding their MUs.
Summary
The case study analysis has distilled key themes that need addressing if the English maternity services want to maximise the dividend of MUs. The domains of the CFIR (outer setting, intervention characteristics, individual characteristics, inner setting and process) enable the complexity of change to be broken down into overlapping and interwoven processes that maintains a holistic perspective while identifying component parts that either facilitate or confound the introduction of MUs.
A number of broader societal discourses and factors in the national political landscape, such as the medicalisation of birth and NHS budgetary constraints, impinged on MU’s development in all the case study sites. The latter linked directly to the perceived cost of the intervention itself and its propensity for adaptability into the existing service.
Despite MUs having a strong evidence base, personal beliefs about their efficacy and legitimacy, especially among individuals in strategic posts, had a considerable impact locally. In the case study sites, the readiness for implementation of MUs was dependant on midwives having the appropriate knowledge and skills, and on an inclusive, thorough engagement with maternity care stakeholders.
The process of implementing MUs required services to transit through the classic stages of change management: planning, in which robust promotional activities were especially important; executing, in which the more successful sites devised a streamlined pathway that maximised access and utilisation; and finally reflecting and evaluating, in which processes were tweaked to increase effectiveness.
The women’s focus groups were a litmus test of how effective trusts had been with all of these stages of change, with many women being unaware that they had a choice of a MU and some even birthing in them without realising it.
One site had implemented a comprehensive MU service in recent years and provided an instructive template for others. Some of our sites had a long history of MUs, but their place within local maternity care provision had been progressively eroded by a number of the factors mentioned above. Other sites had resisted external pressure to open MUs or failed to follow through on existing strategic plans, whereas two other services had MUs but they were underperforming for mostly local contextual reasons.
High-performing sites shared similar tensions, challenges and uncertainties surrounding the utilisation of MUs as low-performing sites. We had anticipated, probably naively in retrospect, that high-performing sites would demonstrate the main facilitators that enhance MU utilisation and operation, and that low-performing sites would be illustrative of the barriers to this. However, the picture was more mixed, with high-performing sites exemplifying some of the barriers (poor leadership) and low-performing sites the facilitators (clear vision for MUs).
The central challenge in all sites was that of embedding an alternative configuration into an existing mainstream, ‘taken for granted’ model.
Fundamental to addressing these complexities is effective leadership, especially at the top of organisations, and investment from a broad constituency of maternity care stakeholders, especially service users whose voices were marginalised in most case study settings. This has to be sustained and maintained by streamlined care pathways and organisational processes.
The next chapter details the third stage of the project: a stakeholder workshop that aimed to arrive at a consensus of how to address the barriers to and facilitators of establishing MUs that had been identified in the findings.
Chapter 5 Findings phase 3: stakeholder workshop
The programme for the stakeholder event followed the structure below. A social media embargo was requested to avoid publication of preliminary findings. Attendees were provided with copies of presentations on arrival and seated in mixed constituency groups, with roundtable discussions jointly facilitated by a member of the project’s advisory group/research team and a member of the service user panel.
Programme
-
A presentation by a member of the research team (CG) of the findings on utilisation and organisation of MUs in England.
-
This was followed by a general discussion to achieve early participation of all attendees.
-
-
A presentation delivered jointly by a member of the research team (CG) and a service user collaborator (LS), reporting the findings of women’s views and perceptions of MUs.
-
A presentation by the chief investigator (DW) and a member of the research team (CG) on barriers to and facilitators of MUs in England.
-
This was followed by group discussions and generation of suggestions to consider barriers to and facilitators of increased access to and utilisation of MUs.
-
-
The suggestions were generated and collated under themes and a further group activity required attendees working in groups to suggest interventions that might improve the uptake of AMUs and FMUs over the short term (up to 6 months), medium term (6–18 months) and longer term (18 months to 3 years).
-
The final activity required attendees to suggest priorities for interventions that could be carried forward by different constituencies:
-
service providers, including leaders and managers, clinical midwives, obstetricians and neonatologists
-
commissioners
-
service user groups
-
professional bodies.
-
The sections below provide a summary of the responses to the presentations and questions posed, the range of interventions identified, by time periods, and responsible group.
Response of stakeholders to barriers and facilitators
Keeping midwifery-led units
The importance of keeping MUs open, especially FMUs, by using them for a range of activities and recognising them as community/family resource/early year’s assets was considered helpful. Some of the suggested activities that could be provided in FMUs include antenatal clinics, childbirth education classes, outreach high-risk antenatal clinics, complementary therapies and smoking cessation support.
Frame midwifery-led units as a real option
It was considered important to frame MUs as a real option. Encouraging women to identify and retain MUs as an option in their birth planning, rather than the majority contemporary approach of requiring that women make binding decisions about birthplace early in pregnancy. There was support for presenting MUs as the default option for healthy women without pregnancy complications and for whom a straightforward labour and birth can be anticipated. This was suggested as an approach that would engender confidence in MUs as a place of birth. This would also require that women are provided with information about different options to counter fears about out-of-hospital birth that are prevalent.
Influential individuals
The importance of influential individuals believing in MUs who should be active in their support was identified. Such individuals included obstetricians and senior midwifery managers; the latter should be in positions in which they influence service provision and commissioning decisions (e.g. trust and commissioning boards).
Risk culture
The prevalent risk culture that dominates NHS maternity services was considered a significant negative factor for MUs.
Use of financial information
There were particular concerns around the understanding and use of financial information related to MUs, with perceptions that finance directors required access to better data and improved understanding of the evidence base.
Continuity of midwifery carer
The relative dearth of NHS trusts where care in a MU could be accompanied by access to continuity of a midwifery carer was of particular concern. Other aspects of the organisation of midwifery staffing also perceived as threats related to the default option of supporting OUs by drawing on midwives from AMUs and FMUs.
General comments
General comments included the need for ways to change the discussion around MUs. This encompassed moving from discussion of MUs as a ‘nice opportunity’ to a conversation related to safety.
The provision of information both in a range of ways and at different times in women’s pregnancies was considered important to meet the needs of different families. The need to broaden conversations to consider care provided prior to transfer, rather than simply the birth and increased use of the internet for local maternity systems to demonstrate what their ‘offer’ is to women, were all ideas that should also be considered. The imperative to provide accurate information was considered the responsibility of a wide range of health-care staff, including GPs, receptionists and community midwives. Increased use of MUs again featured, ensuring appropriate senior trust staff, rather than OU labour wards midwives, made decisions on closing units on a short-term basis.
Midwifery leaders were charged with the importance of collecting robust data and utilising it appropriately, including publishing annual reports for their MUs.
Boundary issues featured as current obstacles to women’s ability to access a MU. Ways of sharing access to notes through common care portals and enabling women to access options across trust boundaries were suggested.
Key themes and how to address them
Key themes were beliefs, change, leadership, organisation and management, resources, staffing and training. For each theme, methods of addressing these barriers were sought. Some of the issues and actions overlap those identified above.
Interventions to address beliefs
Reliance on the evidence base was considered insufficient to address some individual’s beliefs. It was acknowledged that using established, theoretically based approaches, such as implementation science or MU champions, was required. The goal should be to ensure equity of access through avoiding stereotypical assumptions about the preferences of women from different ethnic groups. The influence of individual practitioner’s beliefs or views of evidence could be reduced by engaging in a more public campaign, including a range of media (local and social) to raise the local profile of MUs. Additionally, involving those who have recently used a service and community groups (e.g. the Women’s Institute) would enable a range of contributions. Language should move from the terminology of risk assessment to that of birth planning. Learning from and sharing positive experiences, and increasing the collection and use of good-quality data, were all considered approaches that might address concerns and to modify beliefs about MUs.
Interventions to support change
Some of the interventions identified above (see Interventions to address beliefs) also featured here, including involving women and the wider community; using media; increasing use of MUs for activity, in addition to intrapartum care (e.g. antenatal education); changing from a predominantly opt-in to an opt-out model; and utilising appropriate language. Additional potential interventions related to reviewing culture and interdisciplinary relationships within trusts, increasing normalisation of birth in OUs and training for health-care professionals in the provision of information about birthplace.
Interventions to address leadership
Identifying what has worked elsewhere, including internationally, and supporting midwifery leaders, including consultant midwives, heads and directors of midwifery, were considered important, although specific approaches were not identified. It was suggested that midwifery leaders for MUs and OUs should have similar levels of responsibility. Relationships also required enhancing across organisations, for example between midwifery leaders and commissioners; local maternity systems could support cross-trust collaborations and alignment of policies.
Interventions to address organisational and managerial issues
Several aspects related to business and performance were identified as having negative impacts on use of MUs. Tariffs were considered a particularly urgent problem requiring review; these encompassed systems of financial coding that supported a ‘forcing’ of women’s birthing choices in early pregnancy and lack of subsequent opportunity to flex these. Reducing the impacts of cross-boundary restrictions and increasing the use of FMUs for a broader range of activity were identified as important organisational interventions that would require the development of new business cases. There was also a view that current key performance indicators are obstetrically defined and may not reflect important aspects of MU activity.
Effort should be engaged in moving away from an ‘us and them’ culture within trusts and enhancing cohesion across community and hospital midwifery and between MU and OU midwives.
Interventions to address resource issues
The challenges of communicating resource issues was identified. It was noted that cost-effectiveness can be misrepresented as rationing. The local maternity systems were considered to have a role in these communications and there was a need to try to equalise perceived power imbalances within trusts, between OUs and MUs. Again, several suggestions were made to achieve a multipurpose use of MUs to encompass, for example, antenatal education and breastfeeding support. Women should have access to information about all of the options available to them for planned place of birth, including achieving equal information provision for all women. Clearer communication is required about the importance of investment in maternity services and the resulting benefits accrued across other NHS services, beyond maternity. Key features of AMUs were considered to be an assessment room, its own entrance, location on a separate floor to the OU, its own triage area and separate telephone line. As stated above, models that are based around the needs of women, rather than the organisation/trust configuration, were seen as key. The support of NHS England and the transformation team in publicising a small number of easily identifiable messages was recommended.
Interventions to address staffing and training
Supporting midwives to work in continuity models and in how to present information to women were recurrent themes. Re-evaluating the midwifery and related team as a whole, including the contribution of support workers to postnatal care, was considered to offer a potential means to help midwives in achieving continuity models.
Training that supports normality, rather than a focus on risk and frameworks that give due acknowledgement to competencies in normal labour and birthing, was considered important in redressing the current weighting towards higher-risk skill development. Identifying midwives to provide that training and to act as role models was challenging. Maintaining ‘high-risk skills’ for midwives working in MUs was essential and multidisciplinary training comprising midwives, doctors and paramedics was considered important.
For this and interventions to tackle some of the other barriers, the importance of starting during midwifery training was identified. Current challenges for student midwives in achieving an optimal amount of experience in MUs were acknowledged.
Short-, medium- and long-term actions
The next part of the programme required attendees to identify interventions that could be actioned in the short, medium and long term. Owing to the nature of group work, some interventions appeared more than once, as different groups envisaged them as action at different time points. Some contributions comprised comment rather than intervention.
Interventions that could be actioned in the short term
An intervention to ensure that women have access to high-quality, evidence-based information to inform their decision-making about place of birth, which may require support by existing or new tools that should be available in different languages or with the provision of language support. Information and discussion of place of birth should not be a single event, but something that is revisited several times during pregnancy. Women should not be required to make binding decisions on place of birth in early pregnancy.
Use of an ‘opt-out’ model for MU use should be considered, when this is not already in place.
Midwifery-led units need leadership and management by midwives, without competing responsibilities. Consultant midwives appear ideally placed to lead and champion MUs, but may need support in achieving this.
Linkage with the Midwifery Unit Network (established in 2016, but probably underutilised) may be helpful for individual organisations to benefit from shared good practice and support with developing their business case.
Midwifery-led units require a marketing campaign, including local and social media, with endorsement of their value by national NHS leaders/local members of parliament/similar.
Maintaining a MU requires collection of robust data, including outcomes relevant to MU care and approaches. Consideration could be given to developing a MU ‘kite mark’ award and for AMU and FMU data to be included in dashboards.
Midwives working in, or rotating to, MUs require access to a continuing education programme that both supports the maintenance of skills related to the care of women with straightforward maternities, but also in maintaining skills if emergencies occur.
Consideration should be given to how continuity of midwifery care can be provided.
Language and terminology should reflect a focus on normality and positive choices and outcomes.
Free-standing midwifery units should be used for a wider range of activity in addition to intrapartum care. This may include consideration of use by other agencies in order that they are identified as a community resource, open continuously or for longer periods of time, and thus perceived as less costly to maintain.
Interventions that could be actioned in the medium term
Several of the interventions suggested for the medium-term action echoed those identified for short-term action. This may have been an artefact caused by the nature of parallel group work or because they were seen as requiring continuing effort. Publicity about MUs is one example and developing educational provision for both qualified midwives and those in training another. Leadership and management, data collection, staffing (continuity and rotational) models and ensuring FMUs were seen as a community hub were all identified as interventions to be applied in the medium term.
Interventions that first appeared in the medium-term grouping comprised those with a wider political perspective and achieving influence (e.g. engaging politicians as allies through the secretary of state/prime minister’s office or engaging influential women’s groups). Engaging local maternity systems as influencers, ensuring senior midwives were appropriately positioned on boards, and involving service users on appointment panels for midwives and obstetricians were all identified. An additional medium-term intervention concerned offering place of birth discussions for groups rather than individual women.
Mentioned for the first time was the need to consider the 32 units where there was currently no MU available to women, although this lacked specific actions.
Interventions that could be actioned in the long term
Similar themes emerged to those reported previously, but with an emphasis on actions that could be embedded to achieve sustained change. It was acknowledged that this would not be without challenge. Here, interventions were linked with the contemporary maternity policy priorities of embedding personalised care planning and integrating MUs fully into maternity transformation plans. Models of midwifery working were again considered important through scaling up continuity approaches and there was emphasis on preparing student midwives during training for work in those models on registration. Cultural and systems issues, again, featured with changes to the risk and blame culture in maternity, advocated together with financial and contracting changes required, including tariff.
Interventions for midwives, obstetricians and neonatologists
These included promotion and awareness-raising related to MUs as a means of increasing perception of MUs as a choice. Avoiding divisions and enabling positive and respectful cultures within organisations, and working across boundaries and with service users in a co-production approach, were all seen as interventions for this group. Preparing future midwives to have the appropriate skills to work confidently in low-risk settings and moving beyond safety as the only outcome to celebrate excellence, innovation and improved experience through collaboration at all levels of the system were also ascribed to this group.
Interventions for commissioners
During the stakeholder meeting, it became evident that some commissioners were perceived as lacking a detailed knowledge of the evidence base supporting use of MUs. Their future role was seen as supporting continuity models and of utilising existing NHS performance measures, such as CQUIN (Commissioning for Quality and Innovation), to ensure targets exist and are reached for the use of MUs. The commissioners’ role encompassed supporting personalised care and influencing local maternity system redesign. Commissioners’ perceived remit, to support collaborative activity, was seen as key to including work with providers and local maternity systems and in promoting information about all options for labour and birthing. Their role in ensuring quality and safety encompassed influencing training provision to achieve appropriately skilled practitioners across all settings.
Interventions for professional bodies
There was some uncertainty about how professional bodies were currently influencing policy and transformation of services at the level of local maternity systems. Influencing local maternity systems now was seen as imperative.
Professional bodies should promote use of evidence, support shared educational provision and the development of jointly agreed standards. Development of leadership focusing on normality and within professional groups required action.
Interventions for service user groups
A number of ways were envisaged to involve service user groups, both maternity-specific users of individual services and members of the wider community in intervening on behalf of MUs.
A number of approaches used to gain service user perspectives and feedback were shared. These included the Maternity Voices project. Local service users could contribute to professional training, involvement in guideline development, as ‘Friends of the Birth Centre’ or in providing a ‘meet and greet’ service for potential MU users. It was considered that evidence of service user impact was required to draw down resources that would increase service user involvement. The latter was valued as a means of making experiential knowledge visible and as a means of influencing a broader range of markers of experience than those currently used; the example of dignity was provided.
Summary
The extent to which similar comments were made, and the interventions suggested for different barriers, offers encouragement that some interventions may reach a range of targets. This encouragement may be needed in the context that some of the challenges are complex, longstanding and require considerable change for systems and, in some cases, for individual practitioners.
The ideas below are derived from the research findings, discussion and contributions at the stakeholder event, and further input from the research team.
Ideas for increasing the utilisation of midwifery-led units
Local
-
Ensure leadership within trusts, named champions and designated time for those managing MUs. Consideration should be given to the involvement of consultant midwives in leadership of MUs where this system does not currently exist.
-
Heads and directors of midwifery should be enabled to operate at a strategic level in which they can inform and champion MUs. Such locations include trust boards, local maternity system boards and commissioning groups.
-
Midwifery managers responsible for MUs should be at an equivalent level in their organisation to those responsible for OU birth facilities and free of competing work.
-
In each trust, an obstetrician should act as champion for MU.
-
MUs require fresh campaigns to raise awareness among various groups: commissioners, health professionals and the local community. This may include a range of local and social media. Campaigns to promote use may benefit from involving those who have used and wish to be ambassadors for these services. Consideration should be given to the involvement of key women’s groups in the local community and in engaging national maternity policy-makers or politicians.
-
To enable women to have a realistic choice of accessing MUs, barriers that need to be removed include the absence of information about MUs as an option. This information should be available to all women and include existing and, if required, new tools to present women with information about all of the options for birthplace in language that moves beyond the current emphasis on risk.
-
Discussions about birthplace should not be available ‘once only’ in early pregnancy and subsequently binding. They should be revisited throughout pregnancy, especially at 36 weeks, as part of a birth options discussion and again at onset of labour. 114 Encouraging women to retain a number of options should be encouraged, and discussions and language should follow an approach in which normality is the default expectation for the majority of childbearing women.
-
Getting potential service users across the threshold was perceived as key in enabling women to start to consider MUs as an option. All of the above should be embedded in a midwife-led care pathway that is standardised across the entire service and addresses criteria for referral from midwifery to obstetric services and the process of referral.
-
The current predominant model is that birthing in MUs is available as an opt in rather than opt out. This should be changed so that offering AMUs, where available, should become the default for women with straightforward maternity and should be explored by trusts as the default in settings with FMUs; impacts on utilisation should subsequently be evaluated.
-
The ongoing collection of robust data related to MU use, women’s experiences, as well as outcomes, is a priority, as is the regular publication of these. Consideration should be given to framing outcomes in the context of supporting women’s perinatal mental health.
-
In the context of MU utilisation, reconsideration of models of midwifery working. There are two main components to this. First, the need to reduce diminishing MU midwifery resources by moving midwives from MUs to OUs in times of high workload, as this may be followed by closure and threaten unit viability. A key to addressing this is the embedding of the MU as equal and necessary as the OU so that women are cared for in the appropriate setting. One suggestion was that in OUs, once per shift, a review is done of the risk status of women to see if any can be transferred to the AMU. Second, the need for women accessing MUs also to benefit from continuity models.
-
Reconsideration is required for developing and maintaining skill sets. This includes increasing attention to the skills required to support normality in birthing, including consideration of an advanced competency set that focuses on supporting normal childbirth and thereby increasing midwives’ confidence for normality-focused practice settings. However, maintaining skills for practice when complications develop or when, for example, babies require more assistance at birth is also essential and it may be beneficial to increase multidisciplinary education to support this. Random emergency skill drills in FMUs was highly valued by staff in one case study site and is worthy of consideration by other FMUs.
-
Finance managers should be provided with detailed information about the evidence base and wider health economic implications related to utilisation of MU.
-
Women’s choice should not be constrained by geographical or organisational boundaries. Systems that support appropriate access to maternity records across geographical areas require exploration. The development of digital records as recommended in Implementing Better Births: A Resource Pack for Local Maternity Systems115 is a priority.
-
Within organisations, attention must be given to avoiding divisions between staff groups and encouraging respect for different roles. Maintaining the sense of coherence of a wider service is essential, together with the acknowledgement made by each part of a service. The provision of multidisciplinary education and training may facilitate this.
-
Increasing the use of FMUs to include activities beyond intrapartum care has potential to result in FMUs being open for longer periods or all of the time. This may counter both perceptions that FMUs are closed most of the time and some women’s concerns about whether or not the unit will be available to them when their labour starts. Utilisation of FMUs for other activities and as the community hubs, envisaged in Implementing Better Births: A Resource Pack for Local Maternity Systems115 may counter perceptions of elite and limited services and, depending on services using them, has potential to increase income into the maternity directorate.
Commissioning
-
Commissioners may benefit from a clear and detailed briefing on the evidence base to MUs and how these can support their efforts to ensure high-quality, accessible services for all women. All Clinical Commissioning Groups (CCGs) should appoint a clinical lead for maternity and, as a minimum, ensure that the focus is specifically detailed in the job description of a CCG clinical lead.
-
The option to co-commission services such as FMUs should be explored across geographical and commissioning boundaries, with the development of clear referral pathways. This would facilitate collaboration and provide potential efficiencies.
-
The potential for local maternity systems to provide leadership and support for development and utilisation of MUs should be explored.
Midwifery education
-
The importance of continuing education for the qualified midwifery workforce was addressed above.
-
Preparation of future practitioners needs to include work in continuity models, with consideration of the numbers of births that should be achieve in MU, or similar, settings. Preceptorship following qualification may need review to incorporate support in developing confidence in birth in MU settings.
General
-
The Midwifery Unit Network is a useful resource and source of support for individuals and organisations, enabling sharing of good practice and preparation of business cases.
-
The use of social marketing campaigns to increase awareness of MUs should be considered.
The subsequent chapter considers all findings in the context of contemporary policy and extant evidence.
Chapter 6 Discussion
This chapter examines the findings from all phases of the project to better understand substantive mechanisms that may explain and underpin them. It commences with a summary of the findings from stage 1 and the picture that the findings paint of current MU provision in England as marginalised and undervalued. We then discuss possible explanations for this, based on the case study findings, highlighting the role of medicalisation, risk, financial constraints, managerialism and the interplay between beliefs and evidence. The status of FMUs is explored in some detail.
The second half of the chapter discusses possible strategies to address these issues.
Availability of midwifery-led units
According to NICE intrapartum guidance,39 optimum provision of MUs consists of having an AMU attached to each trust and the option of a FMU in ‘the local area or in a neighbouring area’. The mapping exercise revealed that, although significant increases have occurred in both the availability and utilisation of MUs across England, just under one-quarter of all local maternity services do not have any MUs and nearly all those that do are significantly underutilised. Only 17% of trusts in England have both an AMU and a FMU. Furthermore, our mapping revealed that the 10% growth in all births in MUs since 2011 has occurred almost exclusively in AMUs where numbers have nearly doubled, whereas FMUs have remained broadly the same. These results remain broadly consistent with those of the recent national audit of maternity services, which confirmed the trend of a steady increase in numbers of AMUs, but stagnation in FMUs. 116 Women’s access to FMUs is poor in some major population centres. This is especially concerning given the recent publication of a subanalysis of the Birthplace in England study,3 which showed that FMUs are associated with a lower rate of instrumental delivery and a higher rate of vaginal birth than AMUs25 and a lower rate of serious maternal morbidity (third- or fourth-degree perineal trauma or maternal admission to higher-level care) among multiparous women than in AMUs. 25
For the project we calculated that the optimum use of MUs approximated to ≥ 30% of all births,88 but our mapping survey found only one trust achieved this, with a relatively small number achieving between 20% and 30%. Over 70% of trusts had < 20% of births in the MU.
The results from the survey of the organisational and operational features of MU, in combination with the findings from the in-depth case studies across six sites, provided persuasive rationales for why MU provision is so unequal and so underutilised across England. A picture emerged of an alternative model of provision (MUs) struggling to embed itself alongside the existing, historical, ‘taken for granted’, default model (OUs), which is supported by powerful interest groups and dominant societal norms.
Evidence of the undervaluing of midwifery-led units
A number of findings from our study pointed towards a picture of MUs being a marginalised, optional service that always gave way to the demands of the OU service, as McCourt et al. 49 also suggested in their case studies of AMUs.
Ninety-seven per cent of AMU midwives and 50% of FMU midwives were moved regularly during shifts, usually to the OU, with the resultant effect of one-third of AMUs and half of FMUs being closed more than once every 3 months for short periods of time. The net result was that often MU midwives were looking after low-risk women in OUs while the AMUs or FMUs stood vacant. Midwives in all the case study sites complained about this scenario. AMUs that were underutilised (i.e. birthing < 20% of all women) were closed three times as frequently as units birthing > 20% women. Miah and Adamson117 comment on the implications of regularly moving midwives back to the OU in their case study of the establishment of a new AMU. It undermined the ability of staff to build a ‘safe normality’ culture in the AMU because they were not only regularly removed from their preferred setting but had to adjust their philosophy to practice in the high-risk environment of the OU. Blaaka and Schauer Eri118 describe this experience of ambivalence as a consequence of trying to straddle two belief systems and link it to occupational stress. Russell119 also alludes to this in her review of factors that facilitate the embedding of midwifery-led care in hospital settings, suggesting that organisational and bureaucratic obstacles can ‘make it impossible for workers to achieve a way of working true to their value and beliefs’. 119 The only exception to this would be the movement of midwives from MUs to OUs when women are transferred as it enables continuity of carer to be maintained,120 though this was uncommon in the case study sites.
Women’s focus groups revealed that the choice of a MU, though supported by all the provider interviewees in the case study sites that had MUs, did not translate into the experience of choice for service users. Some did not know that MUs were a birthplace option, some gave birth in MUs without knowing it and some did not even know a MU existed. At the same time, providers suggested that particular groups of women, sometimes based on ethnicity, did not like MUs, although this was not borne out by the women’s responses. This echoes the findings of McCourt et al. ’s study49 of AMU provision, which was published prior to the updating of NICE intrapartum guidelines. 91 There was also considerable variation across the case study sites regarding the process for accessing MUs and this could vary not just by organisational idiosyncrasies but also by how local policies and processes were interpreted and enacted by individual midwives. Thus, a picture emerged across many sites of a haphazard, muddled pathway for gaining access to MUs, which defaulted to the dominant OU model frequently. A number of authors have critiqued the framing of birthplace choice, with evidence strongly suggesting that health-care professionals may guide women’s choices by offering little information about alternatives to OU birth,121 resulting in what has been variously called ‘protecting steering’122 or ‘informed compliance’. 123,124 This was also found in our media analysis.
Factors that have an impact on midwifery-led units
Economic
The case study findings helped illuminate potential underlying mechanisms that begin to explain the low status of MU in contemporary maternity services. The first of these is the NHS climate of financial constraints.
Financial probity within trusts was mentioned across all sites as frustrating the development of MUs, thus illustrating the impact of the economic policy of austerity. 125 All respondents appeared to accept the need for trusts to save money as a ‘fait accompli’ and positioned maternity as competing with other trust services for a share of a limited budget. Within this competition for limited resources, management decisions from within the trusts were criticised for diverting resources to other specialisms away from maternity and MUs.
McCourt et al. 49 reported that MUs were often perceived by maternity care managers as a drain on the human and economic resources of OUs, with more limited awareness in evidence of the ways in which they provide cost-effective care through reducing the throughput of women in busy OUs and rates of unnecessary intervention.
We also found evidence that the understanding of tariffs and contracting in maternity services was poorly understood by clinicians within trusts. Cross-border collaboration, especially in regard to accessing neighbouring FMUs, was frowned on by some providers because they lost income to the FMU’s host trust and were disliked by some women because, if they needed an intrapartum transfer, they could be moved to another hospital much further from home. Thus, the competitive nature of an internal market in health generated perverse incentives126 and mitigated against choice.
Risk and safety
The second factor gleaned from the case study sites with deleterious impacts on MUs was how culture and beliefs affected the respondents’ interpretation of the evidence base of MUs. Risk127 and safety128 concerns were major contributors to these beliefs, with an acceptance that the medicalisation of birth was inevitable. These beliefs were shared across professional groups and have undermined efforts to develop MUs; they have effectively countered the evidential claims of the benefits of MUs. 39 Clinicians’ concerns about risk in MU services are especially anomalous because the MUs-intended client group is, by definition, low risk, and one of the primary advantages of the model is lowering the risk of caesarean in this group. 3 Thus, the strapline for MUs should be that they improve the safety of low-risk women. However, respondents seemed unable or unwilling to make this distinction. Recent policy papers from the NHS England129 and the RCOG130 on safety in relation to reducing stillbirth omit mention of the contribution of midwifery-led care and continuity of carer to the broader context of safety, even though systematic reviews on both of these aspects of midwifery care show lower preterm birth rates and lower overall fetal and neonatal death rates. 131
Medicalisation and a preoccupation with risk reduction may well have influenced the disproportionate increase in the numbers of AMUs in comparison with FMUs, reflecting a bias towards the hospitalisation of birth as AMUs are co-located with OUs by definition. Some of our case study data indicate provider preference for AMUs, with respondents assuming an equivalence in regard to the evidence base of AMUs and FMUs. However, the Birthplace in England study3 unequivocally showed the superior performance of FMUs over AMUs, in both clinical outcomes and cost of each,46,132 and subsequent analysis has strengthened this difference. 25 Our findings on institutional marginalisation and neglect of FMUs may also illustrate ambivalence in providers about the primary or secondary care status of low-risk maternity care. Policy documents already endorse community hubs and the choice of home birth. The vast majority of antenatal and postnatal services are situated in a community context, albeit provided by a mix of primary and secondary services, and keeping patients out of secondary care is a central driver for broader health-care policy. 133 Already a FMU has opened in a community hub,134 so conceptualising low-risk maternity care as an explicitly primary care domain could assist in protecting women’s option of a FMU birth.
Another aspect of the risk and safety discourse that became evident in the HoM interviews was closures of FMUs. This concerned the safety implications of a transfer time from FMU to OU. A transfer time in excess of 30 minutes was given as another rationale for closure, despite the fact that audits of transfers from FMUs suggest that more than half are non-urgent. 87 In addition, there was no evidence from the Birthplace in England study3 of poorer neonatal or maternal outcomes from FMUs132 that are rurally located, and birth outcomes in countries with very rural populations, including Scotland,135 New Zealand,51 Canada38 and Australia,24 indicate that careful risk assessment and judicious decision-making that anticipates complications can ameliorate this. 136 In fact, none of the FMU closures from the media analysis or the HoM interviews had been precipitated by clinical incidents.
Our data highlight a further unintended consequence of medicalisation: the deskilling of midwives in supporting normal labour and birth. This has been a consistent concern of authors ever since the almost universal hospitalisation of birth in the UK from the early 1970s. 42,137,138 At one level, this is a disturbing finding, as the World Health Organization, Nursing and Midwifery Council, which regulates midwifery practice in the UK, and university undergraduate midwifery programmes all define the role of the midwife in relation to normal birth skills. 139,140 Respondents in our study recommended mandatory training in normal birth skills to address this concern. Linked to a perceived deficit in skills, and arguably more influential, was a lack of confidence to make decisions in MU settings where midwives are more autonomous. The research on MUs shows that they provide exactly the environment to facilitate and develop this ability. 47,96
Inadequate leadership
One of the curious findings from the case study sites was the ambivalence expressed by midwifery leaders and clinical midwives about the value of MUs given their well disseminated evidence base and the opportunity they present as a discrete, autonomous sphere of practice to bolster the professional status, work satisfaction, retention and well-being of midwives. We have already suggested that this may be partly explained by the internalisation by midwives of risk and medicalisation discourses that they are constantly exposed to and the lack of support for midwives from their managers when adverse events occur. 141 Organisational theory proffers another explanation: system justification theory. 142 This states that individuals hold system-justifying beliefs, even when it works against their interests, because it serves a palliative psychological function, protecting them from unknowns while perpetuating a sense of dependence. System-justifying theory applies in the context of individuals or groups with a relative sense of powerlessness143 and a body of research has illuminated this phenomenon in NHS midwives. 68,144,145 This resonates with Roberts’ analysis146 of the behaviours of oppressed groups, using nursing as a focus, and may explain why some midwifery managers express ambivalence about MUs. Roberts146 suggests that in order to gain promotion, managers learn to acquiesce to the values of the dominant group, in this case obstetricians, who are more likely to be opposed to MUs. 147
Gender
Finally, in seeking to make explicit how Waring’s84 typology of power, organisation, culture and knowledge intersect to undermine the embedding of MUs into maternity services, an examination of gender is apposite, as MUs serve women and are staffed almost exclusively by women. Like wider society, the NHS reflects patriarchal values and practices regarding the gender pay gap,148 gendered effects on health inequality,149 fewer promotional opportunities for women in the medical specialties,150 under-researching of women’s health151 and the subordination of the predominantly female nursing and midwifery professions. 152,153 Midwifery and maternity care has a well-documented history of gender discrimination,68,154 a legacy of which persists through to the present. 155 In addition, some feminists have criticised managerialism as toxic to innovation and self-governing small teams,156 both of which are characteristic of FMUs, in particular. 93,157 Though no specific references were made by respondents to the impact of gender on the development and sustainability of MUs, the nature of the broader contextual factors support this view.
The plight of free-standing midwifery units
Rationale for closures
The stagnation in the growth of FMUs since the Birthplace in England study3 (while AMUs have nearly doubled in numbers), was a surprising finding and is further evidence that FMUs are viewed as an optional and marginal element in service provision. The findings from the media analysis and HoM interviews of closed FMUs demonstrate that FMUs function within the influence of strong cultural norms around place of birth, and that awareness and understanding of the evidence is low not only among media reporters but also among health service decision-makers.
The two dominant problems posited as reasons for closure – that FMUs were underused and too expensive – were used to frame the media coverage. These were underpinned by a number of strong cultural assumptions around provision of a FMU service:
-
the superior safety of the medical model
-
that FMUs are costly and not sustainable
-
that FMUs and AMUs offer essentially an identical service
-
that women have a free choice about where to give birth and do not choose this care.
Despite evidence to the contrary about each of these assumptions, media reporting presented proposed closures of FMUs and the justifications for them in the above terms, using women, their families and campaigners against closures to offer an ‘alternative perspective’, with the harder task of refuting the dominant narrative and countering these assumptions.
These rationales for closure were common, despite the extant scientific evidence that FMUs are as safe as hospital for babies and safer for mothers,3 and that FMUs are the most cost-effective birthplace for low-risk women, even when occupancy is at an average rate of 30%. 46,54 They also failed to acknowledge the evidence that women are offered limited information138 and that the choice to plan birth out of hospital is highly constrained by social norms. 158
One way of understanding the rationale for closures is that decision-making often takes place within managerial utilitarian frameworks,156 which consider the directly observable local costs of buildings and staffing of FMUs, without including reference to corresponding savings in the acute service of, for example, theatre time or medical staffing. Nor do the economic implications for the whole maternity service or the negative impact on rural communities appear to figure in these judgements. It also reflects a widespread belief that consumer choices of women are primary and that women have the means to exercise free informed choice in relation to place of birth. Positioning the service user as a ‘consumer’ therefore favours existing models that are already known to women and accepted and preferred by many health professionals. A managerialist framework also suggests that maternity services should operate on a market model and that such a model produces efficiency and effectiveness;159 this sets up an expectation that the service should sustain itself through its own generated income and mitigates against the more comprehensive analysis provided by health economic evaluation, which takes into account the consequences of decisions and actions by the individual woman and other parts of the system (e.g. the costs of higher intervention rates in OUs).
In contrast to the managerial view described above, service users and politicians campaigning against closure of FMUs privileged women’s rights to birth locally. They believed that trusts had a duty to provide FMUs and support women’s opportunities to choose them. This ‘rights’ model implies that a hospital trust would have responsibility to provide a clinically effective service, regardless of whether or not it was financially self-sustaining. The arguments for or against closure in the media analysed were rarely supported by evidence on the cost or clinical outcomes of FMUs themselves, possibly as commentators’ lack access to such knowledge.
Thematic analysis of the HoM interviews where FMUs had closed demonstrated an acceptance of the underutilisation and cost rationales that dominated the media coverage. In regard to underutilisation, no justification exists in the literature of a threshold of viability for FMUs. Our mapping survey revealed that some FMUs only open for intrapartum care, whereas others run other maternity-related services (e.g. antenatal and postnatal clinics, antenatal education classes and ultrasound scanning) out of these facilities. This helps justify the ongoing utility costs. We found only one trust that kept their rural FMUs open to honour local women’s choice of birthing there, rather than close them as a perception of saving money, in an echo of the ‘rights’ model mentioned above. The rarity of this illustrates how much financial arguments dominate trusts’ decision-making.
Institutional control
Although findings from the media analysis help to explain the stagnation in numbers of FMUs, the case study data suggest another dynamic at work. FMUs are by definition detached and separate from their trust host sites and their scale is dwarfed by comparison. We found evidence that they can be subjected to a mixture of managerial neglect and authoritarian control from their host trusts. This manifests in using FMUs to solve capacity crises in the host trust, while threatening them with closure at other times, restricting opportunities for FMU staff to promote their services, low FMU visibility in maternity notes that record place of birth choice, FMU midwives experiencing a negative reception in OUs when transferring women in labour and FMU staff not being consulted on strategic changes that affect them. These behaviours are suggestive of a form of institutional or organisational bullying/discrimination in which a dominant model takes precedence over a subordinate model.
We did an extensive search of the literature to help explain the treatment of smaller organisational units within a larger umbrella institution. We are capturing another dynamic of ‘organisational/institutional bullying’ that operates at the organisational/institutional level and should not be explained away by blaming rogue individual managers. 160,161 This does not wholly capture the dynamic we observed. Part of the explanation may reside with the advent of new managerialism exercised within the NHS,162 which emphasises organisational control, a centralised hierarchy and performance. This provides a strong rationale for penalising underperformance (e.g. low birth numbers in a FMU) without examining how this could be addressed collaboratively. Douglas’s theory163 of grids and groups in organisation refers to enclaves: autonomous, non-hierarchical small spaces, which McCourt et al. 95 liken to MUs. Though enclaves can create a therapeutic space in which both staff and clients can flourish, they tend to have an uneasy relationship with their host organisations, which operate hierarchically. Over a decade ago, the contrast between host trust and FMU management styles were juxtaposed as typical of modern compared with postmodern organisations,93 with the former characterised by ‘command and control’ and the latter by a decentralised and autonomous ethos. 164 The current NHS England strategic initiative of sustainability and transformation plans (STPs)165 appears to exhibit some features of the modern organisation. Walshe166 has criticised STPs for not consulting local stakeholders and being driven by an imperative to rationalise services, a claim supported by findings from two case study sites in which midwives advised that STPs are recommending the closure of their respective FMUs.
There also appears to be an element of horizontal bullying among midwives, particularly from OU midwives of FMU midwives at the point of transfer from FMU to OU, a phenomena that McCourt et al. 49 found at the AMU/OU interface and also Curtis et al. 145 in the broader maternity services.
Unpopular with women?
One key finding from across the study was that there is a widely held belief that women are unlikely to willingly choose FMUs, and this was frequently cited within our case studies and in our media analysis as a reason for either closing or failing to establish a FMU. However, previous research has suggested this notion requires further critical engagement. van Teijlingen et al. ’s167 reflections challenge this idea. They expounded on the limitations of satisfaction surveys in maternity care by coining the phrase ‘what is, must still be best’. This phrase captures the idea that people default to what they have experienced when asked to appraise one type of care in comparison to an alternative not currently available. In addition, previous studies examining information provision for services users have found that women are frequently either not provided with information or provided with information that is not neutral and evidence based. 49,168 An instructive example of its application occurred in the 1990s post the Changing Childbirth Report,169 which recommended that women be cared for by a known midwife in labour. This required major change to midwives’ work pattern and was resisted by many local maternity services that argued that women were happy with the status quo of being cared for in labour by a competent, kind but unknown midwife. 170 However, as the evaluations of continuity of carer schemes, such as case load midwifery, were published, it became clear that having a known carer in labour was highly valued by women who experienced it171,172 and has subsequently become a central feature of current maternity care policy. 173 Thus, provider beliefs that service users would not choose FMUs may spring from a spurious rationale.
Increasing the utilisation of midwifery-led units
Leadership and champions
We have identified a number of the underlying factors that deter the development of MUs in England. We now turn to ways of addressing these by examining evidence-based strategies shown to assist large organisational change and exemplars of good practice from our case study sites.
A body of organisational research has systematically reviewed the research on change of this magnitude in health-care systems. Best et al. ’s174 realist review found five factors that facilitated large-scale system change. They were:
-
blending designated leadership (someone in charge of the programme) with distributed leadership (professionals/partner organizations sharing responsibility for delivering the programme)
-
establishing a feedback loop (measures of effectiveness)
-
attending to history (local timeline, events and circumstances)
-
engaging physicians
-
including patients and families.
The importance of leadership was a key finding from our case studies. For the successful development and operationalisation of MUs, leadership needs to be exercised vertically, via the layers of organisational hierarchy, and horizontally, across different professional groups, and at each of these levels designated leadership and distributive leadership should be combined.
Armidale best illustrated this approach. There was a strategic vision for MUs that was shared across the senior managers from the trust, the maternity unit and the commissioners. A well-networked and respected leader led the project (first factor). There was sign-up by middle and clinical managers and their teams in the maternity unit hierarchy, including obstetricians and paediatricians (fourth factor), one of whom acted as an additional champion. This was followed by an extensive engagement exercise with service users (fifth factor). Apart from achieving a consensus from maternity unit stakeholders, this strategic approach acted as a catalyst for devising organisational models and processes that facilitated the realisation of the vision in practice. Reflection and evaluation were part of the process (third factor). Other case study sites lacked this planned approach or the ability to sustain a plan over time and were characterised by procrastination, frequent revision of existing plans and poor organisational processes when plans were implemented. Leaders’ ambivalence regarding the vision for MUs, contradictory views about the appropriate model of MUs among clinicians and the absence of serious engagement with a representative sample of service users were also evident in some of the case study sites.
An important component of leadership was the identification and subsequent impact of having ‘champions’. Champions of MUs were clinicians, managers or service users who were highly influential in promoting the service and recruiting support for it. The marketing research literature is instructive in evidencing the value of brand champions175 and how leaders can facilitate the identification and empowering of brand champions. 176 Morhart et al. 176 demonstrated that a combination of both transactional (quid pro quo) leadership and transformational (inspiring and modelling) leadership contribute to producing brand champions. This was reflected in our data, in which services employed an element of performance management targets to increase MU usage and high-visibility, passionate advocates to lead MU initiatives.
More often in the case study sites, individuals lamented the lack of leadership and the absence of champions, which they believed was a central contributor to the under performance of their MUs.
Core staff and consultant midwives
Having core staff, especially in AMUs, may contribute to better utilisation and although this is an established principle in recent Australian maternity care reform,177 there is very little mention of it in the UK maternity care literature. McCourt et al. 95 commented on the presence of core staff in MUs in their case studies of AMUs, reporting that managers saw an appropriate level of core staffing as vital to maintain skills and continuity of care in the unit. Our mapping revealed almost universal presence of core staff in AMUs, perhaps reflecting the wisdom of promoting ownership of AMUs by their presence. Having a clinical lead midwife in an AMU was less common; however, those trusts with a clinical lead midwife also had a higher percentage of overall births in their AMU. However, it is the role of a consultant midwife that may be the most effective way of both developing and supporting MUs. The RCM and the RCOG92 recommend the employment of one consultant midwife per 900 low-risk births and Guest et al. ’s178 review of the role found that it increased midwifery-led care births. The opening of some MUs has been led by consultant midwives179 and our data suggest that their presence in MUs increases their utilisation. However, only 40% of MUs in our mapping survey had a consultant midwife. When consultant posts in nursing and midwifery were introduced in 2000, the policy rhetoric was that they were a nursing/midwifery equivalent to consultants in the medical specialities. However, 20 years on, consultant midwife numbers in maternity units are nowhere near approaching those of obstetricians, whose absence from OUs would be unthinkable. The original intention of this role was to provide better outcomes for patients by improving the quality of services, strengthen clinical leadership and to assist in retaining experienced nurses and midwives by increasing the range of career options. 178 We are therefore encouraging every trust with MUs birthing > 900 women per year to consider appointing a consultant midwife.
Operational models
Our evidence suggests that having a policy whereby low-risk women are routinely allocated to the AMU (opt out) contributed significantly to higher usage. McCourt et al. 49 stressed that this organisational arrangement optimised AMU use in their ethnographic studies related to the Birthplace in England study. 3 It could be argued that an opt-out policy compromises women’s choice of an OU if they are low risk. However, it is how the choice is framed that is the key. It was clear from our study (see Chapter 4) that inequality of access to information is primarily a matter of women not being given information about the option of MU care. Similarly, McCourt et al. ,49 in their study of AMUs, found that women’s key concern in relation to informed choice was that of not having information that MUs were an option for them. The opt-out policy reflects the research evidence concerning the benefits of AMUs for low-risk women and therefore should be understood as the appropriate care setting in the same way that an OU is the appropriate setting for a woman with pregnancy or labour complications. As AMUs are adjacent to OUs, transfer if requested by women can be seamless. Having an opt-out policy for FMUs could also be explored. FMUs have the additional advantage of being a local provision and therefore meeting the wider health service principle of moving care closer to home. 180 If particular ethnic groups have reservations about an opt-out policy, this can be addressed by how staff approach engaging with them as demonstrated in case study site 1 (see Chapter 4, Individual characteristics).
Another interesting finding from our survey was the frequency of access criteria being changed to allow medium-risk women into AMUs. This may have inflated the utilisation of higher-performing AMUs and resulted in more obstetric involvement in them, presumably because complications occurred more often. This appears inconsistent with clinical governance policy, especially when some suitable low-risk women are being cared for on OUs. However, Gillen and Healy181 make the argument for more flexible criteria for access to AMUs on the basis that immediate back-up is available, and they have produced new guidance for Northern Ireland in this regard. McCourt et al. 49 reported that obstetric consultants often expressed a preference for higher-risk women to be admitted to an AMU outside usual guidelines, in preference to a choice to birth at home, although some clinical midwives expressed concerns about the possible implications for practice in MUs. This perhaps reflects the documented view in obstetrics that AMUs offer a kind of halfway option owing to their proximity to the OU. 182 McCourt et al. 49 also found in their AMU study that consultant midwives played a key role in some sites in facilitating higher-risk women birthing in AMUs where they ran special clinics in close liaison with obstetricians. Nonetheless, an analysis of the clinical outcomes of higher-risk women in the Birthplace in England study3 found that higher-risk women who planned birth at home had comparable outcomes to those who planned birth in an OU. 183 Rates of adverse outcome overall were greater than for lower-risk women, but no difference was found between OUs and out-of-hospital settings. The women who opted for home birth ‘out of guidelines’ tended to have more moderate risk levels, such as one prior caesarean section. Their profile is perhaps similar to that of women who are in some cases able to plan care in AMUs. The issue requires investigation in further studies.
Increasing the availability of free-standing midwifery units
Addressing the plight of FMUs is urgent in the current climate. The most successful FMU in our case study (Armidale) was introduced following an extensive engagement process with multiple maternity care stakeholders, particularly service representative groups. Armidale’s experience challenged the notion that some ethnic groups resist FMUs because a minority community that the FMU serves accepted and embraced the idea after the engagement period. After the opening of the FMU, trust maternity staff prioritised promoting the service to the local population and continue to do so. As it is a new service and therefore unfamiliar to childbearing women, this promotion was essential in their view. The midwives actively recruit women into the FMU and this recruitment was regularly reviewed. The integrated staffing model promoted a sense of ownership and attachment to the FMU among the midwives, and increased the likelihood of them caring for women in labour from their case load, which further incentivised them to attract women to the unit.
Most importantly, trusts need to view their FMU(s) as central to the broader maternity service provision and a necessary choice for low-risk women. In particular, the common perception that FMUs are a financial burden unless operating at maximum capacity is challenged by the available evidence stating that they are cheaper than birthing the same women in an OU, even when they are being used around 30% of the time. This is because health economists factored in the savings they generate in less maternal morbidity. 46,54 FMU facilities could also be used for other outpatient services and could arguably operate as part of a community hub as envisaged by the Better Births115,173 policy document. Wirral University Teaching Hospital NHS Foundation Trust has opened a ‘pop-up’ FMU within Seacombe Children’s Centre in an innovative response to the government’s call for more women to birth in MUs. 134 They view it as a transition phase towards a permanent FMU for women in that area.
Addressing professional territorialism
An ‘us and them’ culture between MUs and OUs found in the case study sites reprises an existing theme in the midwifery literature, highlighted in research into both midwifery-led care47 and birth centres. 184 Research and policy have previously asserted the importance of team work for ensuring a safe maternity service,128,185 but this has sometimes been invoked to resist separate midwifery-led spaces in maternity hospitals21 and to install obstetricians as heads of teams. 186 Walsh and Devane47 have written about the need for mutual respect, trust and collaboration at the interface of midwifery-led care and obstetric-led care, a relationship that mirrors the interface between primary and secondary care. 187 Role modelling from midwifery and obstetric leaders,188 regular audit meetings based on equality and reciprocity22 and a shared vision for quality in service delivery189 can ameliorate any conflict at this interface.
Continuity models
Finally, our findings regarding case-loading services available across MUs in England have implications for the implementation plan following on from Better Births,115,173,190 which has the objective of embedding continuity of carer models (e.g. case load) through all phases of childbirth care. Case loading was extremely uncommon in our study, with only 1–2% of women having access to it. However, service users expressed a strong desire for continuity of carer models, including during the intrapartum phase, and some expected it to be integral to MU care. We believe that the development of MUs provides an ideal opportunity for trusts to explore continuity of carer models. In addition, a case-loading model, building on the integration of community midwifery teams with some MUs, may help to address some of the staffing challenges reported by maternity services managers, including the ‘pulling’ of midwives identified in our mapping survey.
The next chapter details the overall conclusions from the study, the study’s strengths and weaknesses and the implications for policy, education, practice and research.
Chapter 7 Conclusions
Maternity care policy has remained consistent on the need for women to be offered choice regarding place of birth in England, to specifically include MUs, both alongside and freestanding, as well as provision for home birth care, since 2007. 2,173 Since 2014, the NICE intrapartum guidelines have recommended MUs for low-risk women because they reduce labour and birth interventions, notably caesarean rates. 39 Our mapping showed that there are now more MUs than ever before and that the growth has been in AMUs. 88 There has been an associated increase in the percentage of births in MUs in England by 9% over a 6-year period. However, the growth in MUs is unequally distributed across the country, there remains a minority of trusts without any MUs and the provision of FMUs is limited compared with AMUs. In addition, the utilisation of MUs is extremely variable, with the majority providing birthing services for < 20% of their total population. Best available evidence suggests that this figure could be as high as 36%,5 but only one trust in our survey exceeded 30%.
The stagnation in the numbers of FMUs is concerning, given their marginally better evidence base, both in clinical effectiveness and in cost-effectiveness, compared with AMUs. 25,46,54
One can extrapolate from these results that many low-risk women continue to birth in OUs where the risk of caesarean and other birth interventions is increased, maternal satisfaction is decreased and care is more expensive. Potentially, this could represent around 45,000 low-risk women per year in England who could birth in a MU but currently have no access to one or are not using existing ones. 7
The mapping exercise also described suboptimal organisational processes within MUs, with the frequent movement of staff out of them to work on OUs and the regular closure of MUs as a consequence. Access to MUs was frustrated by the absence of a streamlined care pathway during pregnancy and inadequate mechanisms for service users to obtain information and exercise choice about and for them.
Local media analysis of a recognised cycle of opening and closing of FMUs revealed how dominant discourses of safety191 and austerity192 resist the competing discourse of women’s choice regarding place of birth. 173 In fact, it co-opts the choice discourse by repositioning it as evidence that women do not want FMUs. Interviews with senior midwifery managers in sites where a FMU had closed revealed that these safety and austerity discourses were broadly endorsed by them.
The case study analysis helped illuminate why MUs are still not available in some trusts and underused in many. The OU model has had decades to establish itself as the default, overwhelmingly dominant place of birth in England. Home birth and FMU have existed alongside it over those decades, but in a marginal way, consistently accounting for < 3% of all birth. 193 AMUs are a relatively new phenomenon, yet they have seen an exponential increase in use over the past 6 years, which, in itself, could reflects a bias to an OU model, as AMUs are co-located. Our analysis revealed the potent influence of a number of discourses favouring the status quo, including risk127 and medicalisation. 194 Managerialism in large host trusts, emphasising organisational control, a centralised hierarchy and performance,162 can result in the marginalisation of smaller, detached organisational units, like FMUs, which become a soft target for closure.
Based on the findings from all three phases of the study, we have suggested a range of potential strategies in Chapter 6 to increase the access and utilisation of MUs within current English maternity services. These are directed at providers, commissioners, educational institutions and service users. This ‘whole systems’195 approach may be required to address the powerful underlying mechanisms shaping current service provision.
The next section summarises these implications.
Implications
For maternity services to maximise women’s choice and to develop and fully utilise FMUs and AMUs, commissioners need a thorough knowledge of the evidence base of both FMUs and AMUs, both their clinical and their financial benefits. They also need to understand the clinical and organisational differences between these two forms of MU and their respective merits for service users and midwives. CCGs could consider appointing a clinical lead for maternity. Joint commissioning of FMUs could be explored across geographical and commissioning boundaries so that FMUs are an option for women wherever they live. Issues around tariffs, sharing maternal records and maintaining clinical continuity would need to be resolved to make this seamless.
Our research suggests that local maternity systems115 could provide leadership and support for development and utilisation of both AMUs and FMUs and their interface with STPs needs to be addressed.
The following suggestions, aimed at providers, are offered to address the current low status and priority that MUs occupy compared with OUs; addressing these has potential to achieve a more integrated and balanced approach to maternity service provision.
Our research suggests that heads and directors of midwifery could operate at a strategic level to include trust boards, local maternity system boards and commissioning groups, where they can inform and champion MUs. Trusts with > 1000 birth per year in their MUs could consider appointing a consultant midwife to oversee that provision. In addition, MUs could explore having a designated midwifery and obstetric champion and MU managers being at an equivalent level in their organisation to those responsible for OUs.
There is a need to raise the profile of MUs among commissioners, primary care health professionals and the local community, and this could include social media platforms and local media outlets. One approach to extending choice is making sure all women are provided with information about MUs as a place of birth option in accessible language that communicates their evidence base. Discussion about birthplace could be raised by community midwives in early pregnancy and revisited throughout the pregnancy, especially at 36 weeks as part of a birth options discussion, and again at onset of labour. 114 Given the prior evidence and the findings from case studies within this research, one approach that could be considered for more general adoption is allocating women to AMUs and FMUs as an ‘opt out’ rather than a secondary option. Visiting an AMU or FMU, hosting antenatal clinics and holding antenatal education in them is to be encouraged for all women considering them as a place of birth. Audit data related to MU use, women’s experiences and outcomes is important. All of the above could be embedded in a midwife-led care pathway that is standardised across the entire service and addresses criteria for referral from midwifery to obstetric services and the process of referral.
The study found frequent movement of staff out of MUs to OUs and altering these staffing arrangements would appear to be important in maximising MU availability and utilisation. This could be addressed by robust triaging at the point of labour admission so that women labour in the appropriate setting for their risk status. Transfer of midwives from AMU to OU is sensible in the context of accompanying a woman who has developed complications to ensure continuity of carer, though this was uncommon in our case study sites. Arguably, implementing case load models would be the most rational way of ending frequent staff movement, as then a midwife would follow the woman she is caring for according to the woman’s clinical need.
The stakeholder discussion proposed that the nurturing of skills for working in MUs be addressed through incorporating a range of normal birth skills as part of mandatory training requirements. These could include examining decision-making processes, using actual case scenarios, especially when there is clinical uncertainty. The maintenance of emergency skills drills, already mandatory, could be augmented by random emergency skill drills in FMUs, which were highly valued by midwives in one of the case study sites.
The discussion also highlighted that to help avoid divisions between staff groups and location settings (OUs and MUs), multidisciplinary education and review meetings could be considered.
Finally, the stakeholders emphasised that trust finance managers may benefit by being provided with detailed but accessible information about the evidence base and wider health economic implications related to utilisation of MUs.
Free-standing midwifery units in some of the case study sites were used for a variety of day and evening clinics and/or education purposes for local childbearing women. This served the dual role of maximising the usefulness of the space and countering negative perceptions held by some women that FMUs were closed if they were not being used for births. Another potential use is as a community hub envisaged in Implementing Better Births: A Resource Pack for Local Maternity Systems115 and, depending on services using them, this has potential to increase income for the maternity service.
Recommendations for future research
Our recommendations for future research comprise questions to further evaluate and explicate MU provision and the appropriate combination of mixed methods for examining major organisational change:
-
examine optimum staffing models for MUs, including case load, integrated community and hospital midwives’ models and the core staff model
-
undertake a comparison of adjacent AMUs and different floor locations of AMUs to ascertain optimum functioning
-
more detailed mapping of MU organisational processes to identify best practice, to include developing a more streamlined MU pathway that tracks referrals back from obstetric-led care if complications resolve
-
action research to examine best practice at the MU/OU interface
-
examine how best to integrate, value and sustain FMU provision within the envelope of other maternity service provision
-
explore rural settings where multiple small FMUs exist, to investigate how appropriate models can be developed and sustained.
Strengths and limitations
Securing a 100% response rate was important in undertaking a service mapping of all provision of MUs in England. However, service configurations are constantly changing, in terms of trusts merging, the opening of AMUs and FMUs and the closing of FMUs in particular, so our results will need updating within 5 years. Data on the number of births in MUs were revised sometimes by HoMs when their initial figures were at variance with Which? data that we already had. The robustness of data systems varies across trusts so we cannot be sure of the accuracy of exact birth figures, but we are confident that they are accurate ± 100 births per year.
We were able to identify organisational characteristics of MUs not previously recorded in the literature that either facilitated or created barriers to MU use (e.g. movement of MU staff, process for accessing MUs). These were subsequently fed back to the stakeholder workshop and stimulated attendees to devise possible strategies to address them. However, the examination of organisational processes within MUs was hampered by missing data in a few of the categories (e.g. frequency and time length of closures of FMUs). In addition, the structured questionnaire did not capture enough detail in some of the categories to adequately understand some processes. Though we had piloted the questionnaire, there are so many organisational variations between MUs that our questions could not cover all variants. Thus, our ability to delineate processes was hampered. However, the strength of a comparative case study methodology is the richness and breadth of data that can be captured across multiple sites with contrasting organisational characteristics. In addition, focus groups generated discussion and insight that is unlikely to be obtained by individual interviews. They were particularly effective in comparing service user perspectives with provider perspectives from within the same case. We were unable to get access to trust documentation regarding MU policies and organisation, which may have helped triangulate data from the interviews and focus groups. However, we did interview a wide spectrum of stakeholders across all case study sites and the focus groups were well attended. Inevitably, we were not able to include all representative groups of service users in the focus groups (e.g. we did not have translation services), so all respondents needed to speak English. In addition, as previously mentioned, we were reliant on local informants to assist us with recruitment to service user focus groups. This resulted in a spread of women of different parity, age, ethnicity and from rural and metropolitan areas, but was not as successful in relation to social class. Another limitation was that we did not consider factors, apart from geography, that could impact equity of access as a criterion for service user recruitment. Despite considerable efforts, we were only able to recruit one finance director and this may have reduced the comprehensiveness of our finance-related data. Having only six case study sites out of a possible 134 may compromise the transferability of our implications, although we developed careful criteria for selecting the sites to make them as representative as possible.
The CFIR utilised for analysing the case study data was helpful in making explicit generic categories that had an impact on implementation. However, it was less useful when complex interventions had been introduced over varying time frames, across a range of sites, because some of the domains of the framework (e.g. process) assume a comparable timeline.
The strength of the stakeholder workshop was in bringing together and achieving multiconstituency discussion of barriers to and facilitators of the utilisation of MUs in England. It is by no means easy to engage some of these constituencies because of the varied demands on them. A further strength was in the continued active contribution of members of the service user group for this research through presentation and co-facilitation of group discussions.
Perhaps unsurprisingly, the focus of discussions prioritised barriers and interventions to address these. In hindsight, although some very innovative examples of good practice were shared, greater emphasis on identifying supportive factors and how those could be further enabled may have generated additional actionable strategies.
Acknowledgements
We are extremely grateful to all who contributed to the study, including HoMs for their support to the stage 1 mapping phase, all who contributed in interviews or focus groups in the stage 2 case study phase and participants at the stage 3 stakeholder event.
We would also like to thank the members of the service user reference panel for their invaluable contributions: Melissa Thomas, Leanne Stamp, Samantha Foulke and Joanne Wyler.
We would like to thank Dr Juliet Rayment for her contribution to the media analysis of FMUs that had closed and Which? Birth Choice for allowing us access to their data.
We would also like to acknowledge and thank Sheila Adamson at the University of Nottingham for all her work as the research secretary over 24 months.
Contributions of authors
Denis Walsh (Chief Investigator, Associate Professor in Midwifery) was the principal author, was responsible for drafting and revising content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published, and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Helen Spiby (Co-investigator, Professor in Midwifery) authored Chapter 5, drafted and revised content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Christine McCourt (Co-investigator, Professor in Maternal Health) was the author of Chapter 3, drafted and revised content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dawn Coleby (Senior Research Fellow) was responsible for drafting and revising content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Celia Grigg (Research Fellow) was the author of the updated literature review and women’s focus group findings (see Chapters 1 and 4), drafted and revised content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Simon Bishop (Co-investigator, Senior Lecturer in Business School) was responsible for drafting and revising content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Miranda Scanlon (Co-investigator, Service User) drafted and revised content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Lorraine Culley (Co-investigator, Emeritus Professor of Social Science and Health) drafted and revised content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jane Wilkinson (GP Commissioner) drafted and revised content critically for important intellectual content, provided final approval of the version to be published, provided substantial contribution to the interpretation of data and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Lynne Pacanowski (HoM) drafted and revised content critically for important intellectual content, provided final approval of the version to be published, provided substantial contribution to the interpretation of data and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jim Thornton (Professor of Obstetrics) drafted and revised content critically for important intellectual content, provided substantial contribution to the interpretation of data, provided final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Publications
Walsh D, Spiby H, Grigg CP, Dodwell M, McCourt C, Culley L, et al. Mapping midwifery and obstetric units in England. Midwifery 2018;56:9–16.
Walsh D, Spiby H, McCourt C, Grigg C, Coleby D, Bishop S, et al. Factors influencing the utilisation of free-standing and alongside midwifery units in England: a qualitative research study. BMJ Open 2020;10:e033895.
Data-sharing statement
All available data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Walsh D, Spiby H, McCourt C, Grigg C, Coleby D, Bishop S, et al. Factors influencing the utilisation of free-standing and alongside midwifery units in England: a qualitative research study. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-033895.
- Department of Health and Social Care . Maternity Matters: Choice, Access and Continuity of Care in a Safe Service 2007.
- Brocklehurst P, Hardy P, Hollowell J, Linsell L, Macfarlane A, McCourt C, et al. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ 2011;343. https://doi.org/10.1136/bmj.d7400.
- National Institute for Health and Care Excellence (NICE) . Intrapartum Care Quality Standard 2015.
- Sandall J, Murrells T, Dodwell M, . The efficient use of the maternity workforce and the implications for safety and quality in maternity care: a population-based, cross-sectional study. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02380.
- National Audit Office (NAO) . Maternity Services in England 2013.
- Walsh D, Spiby H, McCourt C, Bishop S, Dodwell M, Culley L, et al. Factors Influencing the Utilisation of Free-Standing and Alongside Midwifery Units in England: A Mixed Methods Research Study n.d. www.journalslibrary.nihr.ac.uk/programmes/hsdr/140428/#/ (accessed 10 September 2019).
- Bernitz S, Rolland R, Blix E, Jacobsen M, Sjøborg K, Øian P. Is the operative delivery rate in low-risk women dependent on the level of birth care? A randomised controlled trial. BJOG 2011;118:1357-64. https://doi.org/10.1111/j.1471-0528.2011.03043.x.
- Cheung NF, Mander R, Wang X, Fu W, Zhou H, Zhang L. Clinical outcomes of the first midwife-led normal birth unit in China: a retrospective cohort study. Midwifery 2011;27:582-7. https://doi.org/10.1016/j.midw.2010.05.012.
- Hendrix M, Van Horck M, Moreta D, Nieman F, Nieuwenhuijze M, Severens J, et al. Why women do not accept randomisation for place of birth: feasibility of a RCT in the Netherlands. BJOG 2009;116:537-42. https://doi.org/10.1111/j.1471-0528.2008.02103.x.
- Berger ML, Dreyer N, Anderson F, Towse A, Sedrakyan A, Normand SL. Prospective observational studies to assess comparative effectiveness: the ISPOR good research practices task force report. Value Health 2012;15:217-30. https://doi.org/10.1016/j.jval.2011.12.010.
- Yang W, Zilov A, Soewondo P, Bech OM, Sekkal F, Home PD. Observational studies: going beyond the boundaries of randomized controlled trials. Diabetes Res Clin Pract 2010;88:3-9. https://doi.org/10.1016/S0168-8227(10)70002-4.
- Jepsen P, Johnsen SP, Gillman MW, Sørensen HT. Interpretation of observational studies. Heart 2004;90:956-60. https://doi.org/10.1136/hrt.2003.017269.
- Downe S. Beyond evidence-based medicine: complexity and stories of maternity care. J Eval Clin Pract 2010;16:232-7. https://doi.org/10.1111/j.1365-2753.2009.01357.x.
- Sackett D, Straus S, Richardson W, Rosenberg W, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. London: Churchill Livingstone; 2000.
- Keirse MJ. Evidence-based medicine and perinatal care: from dawn to dusk. Birth 2012;39:296-300. https://doi.org/10.1111/birt.12004.
- Hodnett ED, Downe S, Walsh D. Alternative versus conventional institutional settings for birth. Cochrane Database Syst Rev 2012;8. https://doi.org/10.1002/14651858.CD000012.pub4.
- Laws PJ, Xu F, Welsh A, Tracy SK, Sullivan EA. Maternal morbidity of women receiving birth center care in New South Wales: a matched-pair analysis using linked health data. Birth 2014;41:268-75. https://doi.org/10.1111/birt.12114.
- Gaudineau A, Sauleau EA, Nisand I, Langer B. Obstetric and neonatal outcomes in a home-like birth centre: a case-control study. Arch Gynecol Obstet 2013;287:211-16. https://doi.org/10.1007/s00404-012-2553-6.
- Eide BI, Nilsen AB, Rasmussen S. Births in two different delivery units in the same clinic – a prospective study of healthy primiparous women. BMC Pregnancy Childbirth 2009;9. https://doi.org/10.1186/1471-2393-9-25.
- Gottvall K, Winbladh B, Cnattingius S, Waldenström U. Birth centre care over a 10-year period: infant morbidity during the first month after birth. Acta Paediatr 2005;94:1253-60. https://doi.org/10.1111/j.1651-2227.2005.tb02085.x.
- Hofmeyr GJ, Mancotywa T, Silwana-Kwadjo N, Mgudlwa B, Lawrie TA, Gülmezoglu AM. Audit of a new model of birth care for women with low risk pregnancies in South Africa: the primary care onsite midwife-led birth unit (OMBU). BMC Pregnancy Childbirth 2014;14. https://doi.org/10.1186/s12884-014-0417-8.
- Dencker A, Smith V, McCann C, Begley C. Midwife-led maternity care in Ireland – a retrospective cohort study. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1285-9.
- Monk A, Tracy M, Foureur M, Grigg C, Tracy S. Evaluating Midwifery Units (EMU): a prospective cohort study of freestanding midwifery units in New South Wales, Australia. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006252.
- Hollowell J, Li Y, Bunch K, Brocklehurst P. A comparison of intrapartum interventions and adverse outcomes by parity in planned freestanding midwifery unit and alongside midwifery unit births: secondary analysis of ‘low risk’ births in the birthplace in England cohort. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1271-2.
- Overgaard C, Møller AM, Fenger-Grøn M, Knudsen LB, Sandall J. Freestanding midwifery unit versus obstetric unit: a matched cohort study of outcomes in low-risk women. BMJ Open 2011;1. https://doi.org/10.1136/bmjopen-2011-000262.
- Davis D, Baddock S, Pairman S, Hunter M, Benn C, Wilson D, et al. Planned place of birth in New Zealand: does it affect mode of birth and intervention rates among low-risk women?. Birth 2011;38:111-19. https://doi.org/10.1111/j.1523-536X.2010.00458.x.
- Homer CS, Thornton C, Scarf VL, Ellwood DA, Oats JJ, Foureur MJ, et al. Birthplace in New South Wales, Australia: an analysis of perinatal outcomes using routinely collected data. BMC Pregnancy Childbirth 2014;14. https://doi.org/10.1186/1471-2393-14-206.
- Kataoka Y, Eto H, Iida M. Outcomes of independent midwifery attended births in birth centres and home births: a retrospective cohort study in Japan. Midwifery 2013;29:965-72. https://doi.org/10.1016/j.midw.2012.12.020.
- Stapleton SR, Osborne C, Illuzzi J. Outcomes of care in birth centers: demonstration of a durable model. J Midwifery Womens Health 2013;58:3-14. https://doi.org/10.1111/jmwh.12003.
- Morano S, Cerutti F, Mistrangelo E, Pastorino D, Benussi M, Costantini S, et al. Outcomes of the first midwife-led birth centre in Italy: 5 years’ experience. Arch Gynecol Obstet 2007;276:333-7. https://doi.org/10.1007/s00404-007-0358-9.
- Jackson DJ, Lang JM, Swartz WH, Ganiats TG, Fullerton J, Ecker J, et al. Outcomes, safety, and resource utilization in a collaborative care birth center program compared with traditional physician-based perinatal care. Am J Public Health 2003;93:999-1006. https://doi.org/10.2105/AJPH.93.6.999.
- Wax JR, Pinette MG, Cartin A, Blackstone J. Maternal and newborn morbidity by birth facility among selected United States 2006 low-risk births. Am J Obstet Gynecol 2010;202:152.e1-5. https://doi.org/10.1016/j.ajog.2009.09.037.
- Grünebaum A, McCullough LB, Sapra KJ, Brent RL, Levene MI, Arabin B, et al. Apgar score of 0 at 5 minutes and neonatal seizures or serious neurologic dysfunction in relation to birth setting. Am J Obstet Gynecol 2013;209:323.e1-6. https://doi.org/10.1016/j.ajog.2013.06.025.
- Grünebaum A, McCullough LB, Sapra KJ, Brent RL, Levene MI, Arabin B, et al. Early and total neonatal mortality in relation to birth setting in the United States, 2006–2009. Am J Obstet Gynecol 2014;211:390.e1-7. https://doi.org/10.1016/j.ajog.2014.03.047.
- Snowden JM, Tilden EL, Snyder J, Quigley B, Caughey AB, Cheng YW. Planned out-of-hospital birth and birth outcomes. N Engl J Med 2015;373:2642-53. https://doi.org/10.1056/NEJMsa1501738.
- Benatar S, Garrett AB, Howell E, Palmer A. Midwifery care at a freestanding birth center: a safe and effective alternative to conventional maternity care. Health Serv Res 2013;48:1750-68. https://doi.org/10.1111/1475-6773.12061.
- Van Wagner V, Osepchook C, Harney E, Crosbie C, Tulugak M. Remote midwifery in Nunavik, Québec, Canada: outcomes of perinatal care for the Inuulitsivik health centre, 2000–2007. Birth 2012;39:230-7. https://doi.org/10.1111/j.1523-536X.2012.00552.x.
- National Institute for Health and Care Excellence (NICE) . Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. Clinical Guideline 190 2014.
- Goer H, Romano A, Sakala C. Vaginal or Cesarean BIRTH: What is at Stake for Women and Babies? A Best Evidence Review. New York, NY: Children Connection; 2012.
- Olde E, van der Hart O, Kleber R, van Son M. Posttraumatic stress following childbirth: a review. Clin Psychol Rev 2006;26:1-16. https://doi.org/10.1016/j.cpr.2005.07.002.
- Walsh D. Evidence and Skills for Normal Labour and Birth: A Guide for Midwives. Abingdon: Routledge; 2011.
- Anim-Somuah M, Smyth RM, Jones L. Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev 2011;12. https://doi.org/10.1002/14651858.CD000331.pub3.
- Oscarsson ME, Amer-Wåhlin I, Rydhstroem H, Källén K. Outcome in obstetric care related to oxytocin use. A population-based study. Acta Obstet Gynecol Scand 2006;85:1094-8. https://doi.org/10.1080/00016340600804530.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev 2009;1. https://doi.org/10.1002/14651858.CD000081.pub2.
- Schroeder E, Petrou S, Patel N, Hollowell J, Puddicombe D, Redshaw M, et al. Birthplace in England Collaborative Group . Cost effectiveness of alternative planned places of birth in woman at low risk of complications: evidence from the Birthplace in England national prospective cohort study. BMJ 2012;344. https://doi.org/10.1136/bmj.e2292.
- Walsh D, Devane D. A metasynthesis of midwife-led care. Qual Health Res 2012;22:897-910. https://doi.org/10.1177/1049732312440330.
- Care Quality Commission . National Findings From the 2013 Survey of Women’s Experiences of Maternity Care 2013.
- McCourt C, Rayment J, Rance S, Sandall J. An ethnographic organisational study of alongside midwifery units: a follow-on study from the Birthplace in England programme. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02070.
- Bailey DJ. Birth outcomes for women using free-standing birth centers in South Auckland, New Zealand. Birth 2017;44:246-51. https://doi.org/10.1111/birt.12287.
- Grigg CP, Tracy SK, Tracy M, Daellenbach R, Kensington M, Monk A, et al. Evaluating Maternity Units: a prospective cohort study of freestanding midwife-led primary maternity units in New Zealand-clinical outcomes. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016288.
- Monk AR, Grigg CP, Foureur M, Tracy M, Tracy SK. Freestanding midwifery units: maternal and neonatal outcomes following transfer. Midwifery 2017;46:24-8. https://doi.org/10.1016/j.midw.2017.01.006.
- de Jonge A, Peters L, Geerts CC, van Roosmalen JJM, Twisk JWR, Brocklehurst P, et al. Mode of birth and medical interventions among women at low risk of complications: a cross-national comparison of birth settings in England and the Netherlands. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0180846.
- Schroeder L, Patel N, Keeler M, Rocca-Ihenacho L, Macfarlane AJ. The economic costs of intrapartum care in Tower Hamlets: a comparison between the cost of birth in a freestanding midwifery unit and hospital for women at low risk of obstetric complications. Midwifery 2017;45:28-35. https://doi.org/10.1016/j.midw.2016.11.006.
- Cresswell J, Klassen AC, Clark VLP, Smith KC. Best Practices for Mixed Methods Research in the Health Sciences. Bethesda, MD: Office of Behavioral and Social Sciences Research; 2013.
- Which? Birth Choice n.d. www.which.co.uk/birth-choice (accessed 10 August 2016).
- Redshaw M, Rowe R, Schroeder L, Puddicombe D, Macfarlane A, Newburn M, et al. Mapping Maternity Care: The Configuration of Maternity Care in England. Birthplace in England Research Programme. Final Report Part 3 2011.
- McCombs M. Setting the Agenda: Mass Media and Public Opinion. Chichester: John Wiley & Sons; 2014.
- Bacchi C. Analysing Policy. Australia: Pearson Higher Education; 2009.
- Anderson RA, Crabtree BF, Steele DJ, McDaniel RR. Case study research: the view from complexity science. Qual Health Res 2005;15:669-85. https://doi.org/10.1177/1049732305275208.
- Yin RK. Case Study Research: Design and Methods. UK: Sage; 2013.
- Payne G, Williams M. Generalization in qualitative research. Sociology 2005;39:295-314. https://doi.org/10.1177/0038038505050540.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003;362:1225-30. https://doi.org/10.1016/S0140-6736(03)14546-1.
- Cooksey D. A Review of UK Health Research Funding. London: The Stationery Office; 2006.
- Iles V, Sutherland K. Change: A Review for Health Care Managers, Professionals and Researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2002.
- Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F, Peacock R. How to Spread Good Ideas: A Systematic Review of the Literature on Diffusion, Spread and Sustainability of Innovations in Health Service Delivery and Organisation. Southampton: IHR Service Delivery and Organisation Programme; 2004.
- Ferlie E, Fitzgerald L, Wood M, Hawkins C. The nonspread of innovations: the mediating role of professionals. Acad Manag J 2005;48:117-34. https://doi.org/10.5465/amj.2005.15993150.
- Donnison J. Midwives and Medical Men: A History of Inter-Professional Rivalry and Women’s Rights. London: Heinemann Educational Books; 1977.
- Smith AH, Dixon AL, Page LA. Health-care professionals’ views about safety in maternity services: a qualitative study. Midwifery 2009;25:21-3. https://doi.org/10.1016/j.midw.2008.11.004.
- Wise J. Litigation in maternity care is rising, says National Audit Office. BMJ 2013;347. https://doi.org/10.1136/bmj.f6737.
- Hankins GD, MacLennan AH, Speer ME, Strunk A, Nelson K. Obstetric litigation is asphyxiating our maternity services. Obstet Gynecol 2006;107:1382-5. https://doi.org/10.1097/01.AOG.0000220531.25707.27.
- Morris T, McInerney K. Media representations of pregnancy and childbirth: an analysis of reality television programs in the United States. Birth 2010;37:134-40. https://doi.org/10.1111/j.1523-536X.2010.00393.x.
- Pope C, Robert G, Bate P, Le May A, Gabbay J. Lost in translation: a multi-level case study of the metamorphosis of meanings and action in public sector organizational innovation. Public Adm 2006;84:59-7. https://doi.org/10.1111/j.0033-3298.2006.00493.x.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Scott WR. Institutional Change and Healthcare Organizations: From Professional Dominance to Managed Care. Chicago, IL: University of Chicago Press; 2000.
- Reay T, Goodrick E, Casebeer A, Hinings CR. Legitimizing new practices in primary health care. Health Care Manage Rev 2013;38:9-19. https://doi.org/10.1097/HMR.0b013e31824501b6.
- Sorensen JL, Kosten T. Developing the tools of implementation science in substance use disorders treatment: applications of the consolidated framework for implementation research. Psychol Addict Behav 2011;25:262-8. https://doi.org/10.1037/a0022765.
- Damschroder LJ, Lowery JC. Evaluation of a large-scale weight management program using the consolidated framework for implementation research (CFIR). Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-51.
- Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the Consolidated Framework for Implementation Research. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0437-z.
- Lash SJ, Timko C, Curran GM, McKay JR, Burden JL. Implementation of evidence-based substance use disorder continuing care interventions. Psychol Addict Behav 2011;25:238-51. https://doi.org/10.1037/a0022608.
- Breimaier HE, Heckemann B, Halfens RJ, Lohrmann C. The Consolidated Framework for Implementation Research (CFIR): a useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital-based nursing practice. BMC Nurs 2015;14. https://doi.org/10.1186/s12912-015-0088-4.
- Waring J, Allen D, Braithwaite J, Sandall J. Healthcare quality and safety: a review of policy, practice and research. Sociol Health Illn 2016;38:198-215. https://doi.org/10.1111/1467-9566.12391.
- Braun V, Clarke V. Using thematic analysis in psychology. Quali Res in Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Waring J, Hollnagel E, Braithwaite J. Resilient Health Care. Farnham: Ashgate Publishing; 2013.
- Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handb Qual Res 1994;2.
- Smith A, Dixon A. The Safety of Maternity Services in England. London: The King’s Fund; 2007.
- Walsh D, Spiby H, Grigg CP, Dodwell M, McCourt C, Culley L, et al. Mapping midwifery and obstetric units in England. Midwifery 2018;56:9-16. https://doi.org/10.1016/j.midw.2017.09.009.
- Rowe RE, Townend J, Brocklehurst P, Knight M, Macfarlane A, McCourt C, et al. Duration and urgency of transfer in births planned at home and in freestanding midwifery units in England: secondary analysis of the birthplace national prospective cohort study. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-224.
- Rowe RE, Fitzpatrick R, Hollowell J, Kurinczuk JJ. Transfers of women planning birth in midwifery units: data from the birthplace prospective cohort study. BJOG 2012;119:1081-90. https://doi.org/10.1111/j.1471-0528.2012.03414.x.
- Dodwell M. Trends in Freestanding Midwife-led Units in England and Wales 2001–13. Edinburgh: Royal College of Midwives; 2013.
- National Institute for Health and Care Excellence (NICE) . Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth (CG190) 2014.
- Royal College of Obstetricians and Gynaecologists (RCOG) . Safer Childbirth: Minimum Standards for the Organisation and Delivery of Care in Labour 2007.
- Walsh D. Improving Maternity Services: Small is Beautiful – Lessons From a Birth Centre. Abingdon: Radcliffe Publishing; 2006.
- Deery R, Hughes D, Kirkham M. Tensions and Barriers in Improving Maternity Care: The Story of a Birth Centre. Abingdon: Radcliffe Publishing; 2010.
- McCourt C, Rayment J, Sandall J, Rance S. Place of birth and concepts of wellbeing: an analysis from two ethnographic studies of midwifery units in England. Anthropol Action 2016;23:17-29. https://doi.org/10.3167/aia.2016.230303.
- Kirkham M, Morgan R, Davies C. Why Do Midwives Stay. UK: Bedfordshire & Hertfordshire Workforce Development Confederation, Department of Health and Social Care; 2006.
- Editor . Maternity decision based on safety – comment on this story. Scarborough Evening News 2008.
- Graham N. Breaking news: Grantham Hospital to lose maternity unit in health shake-up. Grantham Journal 2012.
- Royston J. First mother – I was happy with it. Kentish Gazette 2008.
- Kirk T. Birthing centre closure supported. Harrow Times 2007.
- Mallett C. ‘Overwhelming’ support to save birth centre. Derby Evening Telegraph 2011.
- Health chief has ‘nothing to hide’ over birth centre . Hull Daily Mail 2011.
- Commissioner in ‘Call for North Tyneside mothers to have their say on maternity services’. Chronicle Live 2014.
- Boles N. Nick Boles: I support decision to close midwifery unit. Grantham Journal 2013.
- Williams A. Health bosses receive our 450 named petitions. Kentish Gazette 2011. https://doi.org/10.1177/1536504211399047.
- Chance to have say on future of birthing centre . East Kent Mercury 2011.
- BBC1 . Yorkshire and Lincolnshire Regional News and Weather 2013.
- Davies K. Mums lead calls to save at-risk maternity unit. Evening Chronicle 2013.
- Wood K. Birthing centre will shut doors for good. Hull Daily Mail 2012.
- Kulier R, Gee H, Khan KS. Five steps from evidence to effect: exercising clinical freedom to implement research findings. BJOG 2008;115:1197-202. https://doi.org/10.1111/j.1471-0528.2008.01821.x.
- Downe S. Beliefs and values moderate evidence in guideline development. BJOG 2016;123. https://doi.org/10.1111/1471-0528.13634.
- Straus SE, Ball C, Balcombe N, Sheldon J, McAlister FA. Teaching evidence-based medicine skills can change practice in a community hospital. J Gen Intern Med 2005;20:340-3. https://doi.org/10.1111/j.1525-1497.2005.04045.x.
- O’Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2007;4. https://doi.org/10.1002/14651858.CD000409.pub2.
- Hinton L, Dumelow C, Rowe R, Hollowell J. Birthplace choices: what are the information needs of women when choosing where to give birth in England? A qualitative study using online and face to face focus groups. BMC Pregnancy Childbirth 2018;18. https://doi.org/10.1186/s12884-017-1601-4.
- NHS England . Implementing Better Births: A Resource Pack for Local Maternity Systems 2017.
- Blotkamp A, Cromwell D, Dumbrill B, Gurol-Urganci I, Harris T, Hawdon J, et al. National Maternity and Perinatal Audit: Organisational Report 2017 2017.
- Miah R. Adamson. Creating a culture of ‘safe normality’: developing a new inner city alongside midwifery unit. Br J Midwifery 2015;23:498-50. https://doi.org/10.12968/bjom.2015.23.7.498.
- Blaaka G, Schauer Eri T. Doing midwifery between different belief systems. Midwifery 2008;24:344-52. https://doi.org/10.1016/j.midw.2006.10.005.
- Russell K. Factors that support change in the delivery of midwifery led care in hospital settings. A review of current literature. Women Birth 2018;31:e134-e141. https://doi.org/10.1016/j.wombi.2017.08.129.
- Rowe R, Kurinczuk J, Locock L, Fitzpatrick R. Women’s experience of transfer from midwifery unit to hospital obstetric unit during labour: a qualitative interview study. BMC Pregnancy Chilbirth 2012;12. https://doi.org/10.1186/1471-2393-12-129.
- Coxon K, Chisholm A, Malouf R, Rowe R, Hollowell J. What influences birth place preferences, choices and decision-making amongst healthy women with straightforward pregnancies in the UK? A qualitative evidence synthesis using a ‘best fit’ framework approach. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1279-7.
- Levy V. Protective steering: a grounded theory study of the processes by which midwives facilitate informed choices during pregnancy. J Adv Nurs 2006;53:114-22. https://doi.org/10.1111/j.1365-2648.2006.03688.x.
- Stapleton H, Kirkham M, Thomas G. Qualitative study of evidence based leaflets in maternity care. BMJ 2002;324. https://doi.org/10.1136/bmj.324.7338.639.
- McCourt C. Supporting choice and control? Communication and interaction between midwives and women at the antenatal booking visit. Soc Sci Med 2006;62:1307-18. https://doi.org/10.1016/j.socscimed.2005.07.031.
- Jordà Ò, Taylor AM . The time for austerity: estimating the average treatment effect of fiscal policy. Economic J 2016;126:219-55. https://doi.org/10.1111/ecoj.12332.
- Marshall L, Charlesworth A, Hurst J. The NHS Payment System: Evolving Policy and Emerging Evidence. London: The Nuffield Trust; 2014.
- Scamell M. Childbirth within the risk society. Sociol Compass 2014;8:917-28. https://doi.org/10.1111/soc4.12077.
- Department of Health and Social Care . Safer Maternity Care: The National Maternity Safety Strategy – Progress and Next Steps 2017.
- NHS England . Saving Babies’ Lives. A Care Bundle for Reducing Stillbirth 2016.
- Robertson L, Knight H, Snelling EP, Petch E, Knight M, Cameron A, et al. Each Baby Counts: National Quality Improvement Programme to Reduce Intrapartum-Related Deaths and Brain Injuries in Term Babies. Seminars in Fetal and Neonatal Medicine. London: Elsevier; 2017.
- Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2015;9. https://doi.org/10.1002/14651858.CD004667.pub4.
- Hollowell J, Puddicombe D, Rowe R, Linsell L, Hardy P, Stewart M, et al. The Birthplace National Prospective Cohort Study: Perinatal and Maternal Outcomes by Planned Place of Birth Birthplace in England Research Programme. Oxford: National Perinatal Epidemiology Unit; 2011.
- Purdy S. Avoiding Hospital Admissions. What Does the Research Evidence Say?. London: The King’s Fund; 2010.
- Pop up’ birthing centre offers new choice to pregnant women . Wirral View 2018.
- Harris FM, van Teijlingen E, Hundley V, Farmer J, Bryers H, Caldow J, et al. The buck stops here: midwives and maternity care in rural Scotland. Midwifery 2011;27:301-7. https://doi.org/10.1016/j.midw.2010.10.007.
- Denham S, Humphrey T, Taylor R. Quality of care provided in two Scottish rural community maternity units: a retrospective case review. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1374-9.
- Robinson S, Golden J, Bradley S. A Study of the Role and Responsibilities of the Midwife. London: Chelsea College, University of London; 1983.
- McCourt C, Rayment J, Rance S, Sandall J. Organisational strategies and midwives’ readiness to provide care for out of hospital births: an analysis from the birthplace organisational case studies. Midwifery 2012;28:636-45. https://doi.org/10.1016/j.midw.2012.07.004.
- Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014;384:1129-45. https://doi.org/10.1016/S0140-6736(14)60789-3.
- Hands C, Reid E, Meredith P, Smith GB, Prytherch DR, Schmidt PE, et al. Patterns in the recording of vital signs and early warning scores: compliance with a clinical escalation protocol. BMJ Qual Saf 2013;22:719-26. https://doi.org/10.1136/bmjqs-2013-001954.
- Stapleton H, Kirkham M, Thomas G, Curtis P. Midwives in the middle: balance and vulnerability. BR J Midwifery 2002;10:607-11. https://doi.org/10.12968/bjom.2002.10.10.10621.
- Jost JT, Banaji MR, Nosek BA. A decade of system justification theory: accumulated evidence of conscious and unconscious bolstering of the status quo. Polit Psychol 2004;25:881-919. https://doi.org/10.1111/j.1467-9221.2004.00402.x.
- van der Toorn J, Feinberg M, Jost JT, Kay AC, Tyler TR, Willer R, et al. A sense of powerlessness fosters system justification: Implications for the legitimation of authority, hierarchy, and government. Polit Psychol 2015;36:93-110. https://doi.org/10.1111/pops.12183.
- Kirkham M. The culture of midwifery in the National Health Service in England. J Adv Nurs 1999;30:732-9. https://doi.org/10.1046/j.1365-2648.1999.01139.x.
- Curtis P, Ball L, Kirkham M. Why do midwives leave? (Not) being the kind of midwife you want to be. Br J Midwifery 2006;14:27-31. https://doi.org/10.12968/bjom.2006.14.1.20257.
- Roberts SJ. Development of a positive professional identity: liberating oneself from the oppressor within. ANS Adv Nurs Sci 2000;22:71-82. https://doi.org/10.1097/00012272-200006000-00007.
- Behruzi R, Klam S, Dehertog M, Jimenez V, Hatem M. Understanding factors affecting collaboration between midwives and other health care professionals in a birth center and its affiliated Quebec hospital: a case study. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1381-x.
- Smith J, Gosling J. Moving on up: women in healthcare leadership. Pract Manag 2017;27:24-7. https://doi.org/10.12968/prma.2017.27.2.24.
- Scott-Samuel A, Crawshaw P, Oakley A. ‘Men behaving badly’: patriarchy, public policy and health inequalities. Int J Mens 2015;14.
- Crompton R, Lyonette C. Women’s career success and work–life adaptations in the accountancy and medical professions in Britain. Gend Work Organ 2011;18:231-54. https://doi.org/10.1111/j.1468-0432.2009.00511.x.
- Payne S, Doyal L, Detels R, Gulliford M, Karim QA, Tan CC. Oxford Textbook of Public Health. Oxford: Oxford University Press; 2009.
- Kouta C, Kaite CP. Gender discrimination and nursing: a literature review. J Prof Nurs 2011;27:59-63. https://doi.org/10.1016/j.profnurs.2010.10.006.
- Witz A. Professions and Patriarchy. UK: Routledge; 2013.
- Stewart M. Pregnancy, Birth and Maternity Care: Feminist Perspectives. London: Books for Midwives Press; 2003.
- Walsh D. Gender inequality in maternity services. Int J Childbirth 2015;5:178-9. https://doi.org/10.1891/2156-5287.5.4.178.
- Davies B. Death to critique and dissent? The policies and practices of new managerialism and of ‘evidence-based practice’. Gend Educ 2003;15:91-103. https://doi.org/10.1080/0954025032000042167.
- Kirkham M. Birth Centres: A Social Model for Maternity Care. UK: Elsevier Health Sciences; 2003.
- Coxon K, Sandall J, Fulop NJ. To what extent are women free to choose where to give birth? How discourses of risk, blame and responsibility influence birth place decisions. Health Risk Soc 2013:51-67. https://doi.org/10.1080/13698575.2013.859231.
- Pollock AM, Price D, Viebrock E, Miller E, Watt G. The market in primary care. BMJ 2007;335:475-7. https://doi.org/10.1136/bmj.39303.425359.AD.
- Cilliers F. A systems psychodynamic description of organisational bullying experiences. SA J Ind Psychol 2012;38:44-55. https://doi.org/10.4102/sajip.v38i2.994.
- Pope R. A model of organisational dysfunction in the NHS. J Health Organ Manag 2013;27:676-97. https://doi.org/10.1108/JHOM-10-2012-0207.
- O’Reilly D, Reed M. The grit in the oyster: professionalism, managerialism and leaderism as discourses of UK public services modernization. Organ Stud 2011;32:1079-101. https://doi.org/10.1177/0170840611416742.
- Douglas M. Natural Symbols: Explorations in Cosmology. London: Routledge; 1970.
- Iles V, Sutherland K. Organisational Change: A Review for Health Care Managers, Professionals and Researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organisation Research and Development; 2001.
- Ham C. Sustainability and Transformation Plans (STPs) Explained. London: The King’s Fund; 2017.
- Walshe K. Sustainability and transformation plans for the NHS in England: radical or wishful thinking?. BMJ 2017;356. https://doi.org/10.1136/bmj.j1043.
- van Teijlingen ER, Hundley V, Rennie AM, Graham W, Fitzmaurice A. Maternity satisfaction studies and their limitations: ‘what is, must still be best’. Birth 2003;30:75-82. https://doi.org/10.1046/j.1523-536X.2003.00224.x.
- Henshall C, Taylor B, Kenyon S. A systematic review to examine the evidence regarding discussions by midwives, with women, around their options for where to give birth. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0832-0.
- Expert Maternity Group . Changing Childbirth: Report of the Expert Maternity Group; Part 2: Survey of Good Communications Practice in Maternity Services 1993.
- Green JM, Renfrew MJ, Curtis PA. Continuity of carer: what matters to women? A review of the evidence. Midwifery 2000;16:186-96. https://doi.org/10.1054/midw.1999.0208.
- Forster DA, McLachlan HL, Davey MA, Biro MA, Farrell T, Gold L, et al. Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomised controlled trial. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0798-y.
- McCourt C, Stevens T. Continuity of carer: what does it mean and does it matter to midwives and birthing women. Can J Midwifery Res Pract 2005;4:10-2.
- NHS England . National Maternity Review. Better Births; Improving Outcomes of Maternity Services in England 2016.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. https://doi.org/10.1111/j.1468-0009.2012.00670.x.
- Löhndorf B, Diamantopoulos A. Internal branding: social identity and social exchange perspectives on turning employees into brand champions. J Serv Res 2014;17:310-25. https://doi.org/10.1177/1094670514522098.
- Morhart FM, Herzog W, Tomczak T. Brand-specific leadership: turning employees into brand champions. J Mark 2009;73:122-42. https://doi.org/10.1509/jmkg.73.5.122.
- Hartz DL, White J, Lainchbury KA, Gunn H, Jarman H, Welsh AW, et al. Australian maternity reform through clinical redesign. Aust Health Rev 2012;36:169-75. https://doi.org/10.1071/AH11012.
- Guest D, Peccei R, Rosenthal P, Redfern S, Wilson-Barnett J, Dewe P, et al. An Evaluation of the Impact of Nurse, Midwife and Health Visitor Consultants. London: King’s College London; 2014.
- Richardson J. Are you normal? Implementing normality in the maternity unit. RCM Midwives 2005;8:462-3.
- Monitor . Moving Healthcare Closer to Home: Literature Review of Clinical Impacts 2015.
- Gillen P, Healy M. Planning Birth in a Midwife-Led Unit: GAIN Guideline for the Admission to Midwife-led Units in Northern Ireland. London: Royal College of Midwives; 2016.
- Royal College of Obstetricians and Gynaecologists . RCOG Statement on the Results of the NPEU Birthplace Study 2011. www.rcog.org.uk/what-we-do/campaigning-and-opinions/statement/rcog-statement-results-npeu-birthplace-study (accessed 15 July 2019).
- Li Y, Townend J, Rowe R, Brocklehurst P, Knight M, Linsell L, et al. Perinatal and maternal outcomes in planned home and obstetric unit births in women at ‘higher risk’ of complications: secondary analysis of the Birthplace national prospective cohort study. BJOG 2015;122:741-53. https://doi.org/10.1111/1471-0528.13283.
- Walsh DJ. A birth centre’s encounters with discourses of childbirth: how resistance led to innovation. Sociol Health Illn 2007;29:216-32. https://doi.org/10.1111/j.1467-9566.2007.00545.x.
- Day-Stirk F, McConville F, Campbell J, Laski L, Guerra-Arias M, Hoope-Bender PT, et al. Delivering the evidence to improve the health of women and newborns: State of the World’s Midwifery, report 2014. Reprod Health 2014;11. https://doi.org/10.1186/1742-4755-11-89.
- Walsh D. Euphemisms for an Obstetric-Led Agenda. London: MA Healthcare; 1999.
- Hibberd PA. The primary/secondary interface. Cross-boundary teamwork – missing link for seamless care?. J Clin Nurs 1998;7:274-82. https://doi.org/10.1046/j.1365-2702.1998.00233.x.
- Byrom S, Downe S. ‘She sort of shines’: midwives’ accounts of ‘good’ midwifery and ‘good’ leadership. Midwifery 2010;26:126-37. https://doi.org/10.1016/j.midw.2008.01.011.
- Reiger K, Morton C. Standardizing or individualizing? A critical analysis of the ‘discursive imaginaries’ shaping maternity care reform. Int J Childbirth 2012;2:173-86. https://doi.org/10.1891/2156-5287.2.3.173.
- NHS England . Implementing Better Births: Continuity of Carer 2017.
- Walker KF, Cohen AL, Walker SH, Allen KM, Baines DL, Thornton JG. The dangers of the day of birth. BJOG 2014;121:714-18. https://doi.org/10.1111/1471-0528.12544.
- Braedley S, Luxton M. Neoliberalism and Everyday Life. Montreal, QC: McGill–Queen’s University Press; 2010.
- National Audit Office . Maternity Services in England 2013.
- Johanson R, Newburn M, Macfarlane A. Has the medicalisation of childbirth gone too far?. BMJ 2002;324:892-5. https://doi.org/10.1136/bmj.324.7342.892.
- Davies J. Off centre. Whole systems approach is a driver of change in prompting a new direction of travel in impenetrable NHS jargon. Health Serv J 2004;114:14-5.
Glossary
- Alongside midwifery unit
- Midwifery-led care setting for ‘low-risk’ women, with case-by-case exceptions only. Separate physical space from obstetric-led unit with minimum demarcation being a line on the floor. Only emergency secondary/tertiary level care is permissible within the space. Does not provide care for labouring ‘high-risk’ women when the obstetric-led unit if short of rooms (unless exceptional circumstances). Number of births per year can be measured.
- Free-standing midwifery unit
- An NHS clinical location offering care to low-risk women during labour and birth in which midwives take primary professional responsibility for care. During labour and birth, diagnostic and treatment medical services (including obstetric, neonatal and anaesthetic care) are not immediately available but are located on a separate site should they be needed. Transfer will normally involve car or ambulance.
- High-performing trust
- An NHS local maternity service with an alongside midwifery unit and/or free-standing midwifery unit where > 20% of all women give birth in its midwifery-led unit(s).
- Low-performing trust
- A NHS local maternity service with an alongside midwifery unit and/or free-standing midwifery unit where < 10% of all women give birth in its midwifery-led unit(s).
- Obstetric-led unit
- An NHS clinical location in which care is provided by a team, with obstetricians taking primary professional responsibility for women at high risk of complications during labour and birth. Midwives offer care to all women in an obstetric-led unit, whether they are considered at high or low risk, and take primary responsibility for women with straightforward pregnancies during labour and birth. Diagnostic and treatment medical services (including obstetric, neonatal and anaesthetic care) are available on site, 24 hours per day.
List of abbreviations
- AMU
- alongside midwifery unit
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- CFIR
- Consolidated Framework for Implementation Research
- FMU
- free-standing midwifery unit
- HoM
- Head of midwifery
- MFG
- midwives focus group
- MU
- midwifery-led unit
- NICE
- National Institute for Health and Care Excellence
- NLS
- neonatal life support
- OU
- obstetric-led unit
- RCM
- Royal College of Midwives
- RCOG
- Royal College of Obstetricians and Gynaecologists
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- STP
- sustainability and transformation plan