Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/55/03. The contractual start date was in February 2017. The final report began editorial review in May 2018 and was accepted for publication in March 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Higginbottom et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Equality is a key aim for the NHS in the UK. 1 Over one in four births (28.2%) in the UK is to a foreign-born woman (rising yearly). 2 Fifty-six per cent of births in London in 2013 were to foreign-born women, creating superdiversity among maternity care clients. 3 Of concern is the fact that immigrant women appear disproportionately in confidential inquiries into maternal and perinatal mortality, indicating possible deficits in the care pathways. 4,5 Rapid demographic change and the need to maximise health potential in our diverse, multicultural UK society6 provides an urgent imperative in respect of drawing knowledge together in a systematic fashion. A synthesis of knowledge related to maternity care access and interventions is urgently required to inform policy and practice to appropriately configure interventions as per the NHS Midwifery 2020 vision, to guide the professional development of health-care professionals (HCPs) and to reshape care to ensure culturally congruent maternity care. The UK is in a period of superdiversity, defined as ‘distinguished by a dynamic interplay of variables among an increased number of new, small and scattered, multiple origin, transnationally connected, socio-economically differentiated and legally stratified immigrants7 largely arriving in the UK post 1990’. Consequentially, enhancements to maternity care for immigrant women will not only benefit these women but will also improve the health of future generations in the UK. 5,6,8 Insights into and understanding of the ethnocultural orientation of immigrant women in maternity is critical because it contributes not only to successful integration and social cohesion, but also to social justice in health care. 9–11 Moreover, the socioeconomic marginalisation and vulnerability of immigrant women may be exacerbated by pregnancy, making maternity a critical focus of attention for the health-care system. 10,12,13
Why now?
A knowledge synthesis is required to build a coherent evidence base that elicits an understanding of the factors behind disparities in accessibility, acceptability and outcomes during maternity care that can be used to improve and reconfigure this care. Substantial diversity exists within immigrant women populations; however, examples of commonalities may be found (e.g. late bookings for antenatal care,4,14 higher maternal and perinatal mortality,4,5 poor care and discrimination,9 obesity,15 postpartum depression,10,16 low birth weights and poor birth outcome,17,18 and higher rates of gestational diabetes15). These problems create an economic burden for the NHS. 19
Costs to the NHS
The effective and efficient use of precious NHS resources is vital to the UK, but the higher prevalence of poorer birth outcomes among immigrant populations increases costs for the NHS. Unfortunately, economic modelling of these costs is lacking, so definitive data cannot be provided.
An urgent imperative due to demographic change
This period of superdiversity in the UK means that many new and diverse groups now reside in this country. 20 Historically, the UK has hosted communities within whom a relationship existed via colonisation and the establishment of the commonwealth. However, in particular, increasing migration from Eastern Europe and non-Commonwealth countries is rapidly changing the demography of the UK. If the nation is to realise the full health potential of these future citizens, the NHS urgently needs a synthesis of the knowledge related to immigrant experiences of access and interventions in maternity care. Moreover, addressing health inequalities is a major goal of current NHS directives. The directives entitled Equity and Excellence: Liberating the NHS21 and Midwifery 2020: Delivering Expectations22 demanded enhancements to patient experiences. Developing interventions to militate against inequalities can make major contributions towards redressing inequalities. At present, NHS maternity services are so pressed for resources that they may not be accessible and acceptable to immigrant women. To improve outcomes for these women, effective recommendations for future policies may well sit outside the NHS.
Theoretical framework
A theory of access to services developed by Gulliford et al. 23 maps out four dimensions (Figure 1):
-
service availability
-
utilisation of services and barriers to access (which includes personal, financial and organisational barriers)
-
relevance, effectiveness and access
-
equity and access.
FIGURE 1.
Gulliford theory of access. 23 Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
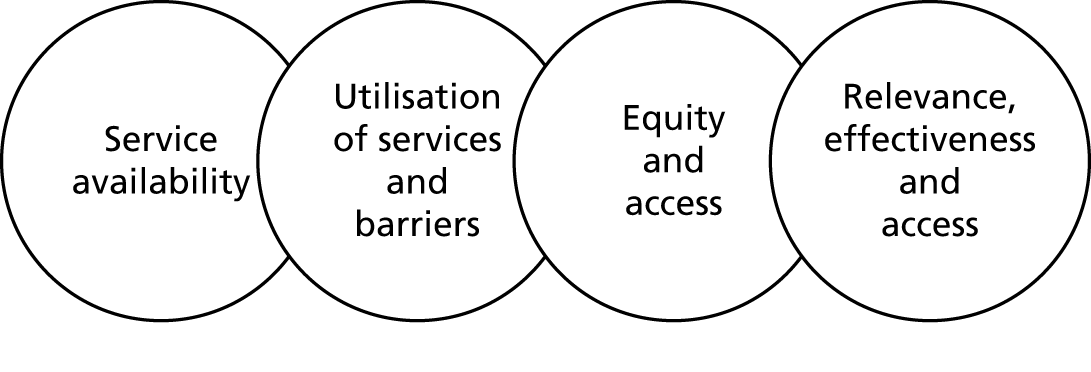
We used this theoretical model in our systematic review, which was based on a synthesis project funded by the National Institute for Health Research (NIHR). Unlike most access models in the USA, this framework reflects the philosophy of the NHS in that its key principles are to provide horizontal access (ensuring equality of access in the population) and vertical access (meeting the needs of particular groups in the population, such as minority ethnic groups). The application of these principles is influenced by availability, accessibility and acceptability. The Gulliford et al. 23 model has been widely used in empirical research, with the main paper having been cited at least 386 times. With its emphasis on accessibility, acceptability, relevance and effectiveness, this model is entirely appropriate for assessing the provision of maternity services to minority ethnic groups. In this study, the theory of access was used in the configuration of the review findings. 23
This approach correlates with the research recommendations of the National Institute for Health and Care Excellence (NICE) on access and models of service provision. 25 Using a comprehensive theoretical framework was crucial, because previous reviews lacked comprehensiveness by addressing only women’s skilled use of maternity services,26 the early initiation of antenatal care by socially disadvantaged women,27 or the early initiation of antenatal care by black and minority ethnic (BME) women. 27 Moreover, in these reviews it was unclear whether or not the women in the studies were immigrants. Our review addresses these deficits.
Policy relevance
Evidence-based health care demands synthesised evidence to ensure that the highest-quality evidence is used to appropriately configure maternity services. 22 Synthesised evidence is also needed to realise the goals of the NHS National Maternity Review,6 which directly informs the NHS Five Year Forward View,1 the professional development of HCPs and organisational change.
Significance and wider context
Some UK locations have historically been destinations of choice for immigrants, but other rural and urban locations are increasing in diversity. These changes are resulting in challenges to the provision of maternity care. Ultimately, enhancements to maternity care for immigrant women benefit not only the women using the service, but also the health of future British generations. Listening and responding to the perspectives of these service users (via the research studies included in our review) will be essential for configuring services in ways that are culturally congruent and culturally safe. 28 Understanding the ethnocultural orientations of immigrant women in maternity is crucial; it contributes to successful integration and social cohesion, and ultimately to social justice in health care. 29,30 Women’s needs and rights are often marginalised within families, communities and legislation. Socioeconomic marginalisation and the subsequent vulnerability of immigrant women can be further exacerbated by pregnancy and childbirth, making these factors an important focus of attention for those concerned with enhancing maternal health. 12,31–34 Critically important is the strategic commitment in the UK to improve maternity services for all service users. 22 In this context, it is imperative to implement service models that are effective for the disadvantaged and to ensure that these services are appropriately personalised.
The UK is in a period of superdiversity,20 with a wide range of populations accessing UK maternity care. Facilitating the provision of appropriate health care for immigrant populations in the UK will be crucial for maximising their well-being and their health potential. Without the delivery of culturally appropriate and culturally safe maternal care, negative event trajectories may occur, ranging from simple miscommunications to life-threatening incidents,35 risking increased maternal and perinatal mortality. Indeed, immigrant women are over-represented in mortality statistics. 11,36,37 Although recent reviews have focused on specific aspects of maternity care,26,27,38 they have not considered a comprehensive conceptualisation of access23 or the current superdiversity. 20 Reconfiguration and redesign of NHS maternal services to meet the needs of immigrant women requires integration of all these aspects.
Globally, a considerable commonality exists among developed nations in the maternity care experiences of immigrant women: studies in the USA,17,39 Canada,13,40–43 Australia,44,45 Sweden46 and Germany10 all provided evidence of this in earlier international reviews led by Higginbottom et al. ,10,12 Small et al. ,8 and Gagnon et al. 41 However, the international comparative reviews by Small et al. 8 and Gagnon et al. 41 focused on South Asian and Somali women in the UK, thereby reflecting more established groups of immigrants and not the more recent superdiversity and current immigration patterns. In addition, two of the national surveys included in the Small et al. 8 and Gagnon et al. 41 reviews did not specify the number of immigrant women, limiting the overall usefulness of those reviews. We have addressed this deficit in our current review.
Our experienced information scientist-assisted search strategy (see Appendix 1) established that a systematic review of immigrant-receiving countries in Europe found substantial disadvantages for immigrant women in all of their maternal outcomes. The risk of low birth weight was 43% higher, the risk of preterm delivery was 24% higher, the risk of perinatal mortality was 50% higher and the risk of congenital malformations was 61% higher. 18 Providing appropriate maternity care successfully to immigrant women requires the legitimisation and incorporation of their pervasive traditional beliefs and practices to which they often adhere despite their new milieu. 47 Their beliefs and practices related to maternity care may differ considerably from Western biomedical perspectives,9,48 and the women may also be affected by migration issues and language barriers. 9,31,33–35,48,49 Maternity care interventions may mitigate many of these issues, thereby enhancing the health of the mothers and their children.
Providing culturally safe and relevant maternity care in an era of superdiversity
The provision of culturally safe50,51 and relevant maternity care is contingent on the recognition and comprehension of key theoretical concepts. In the following paragraphs we explore these key concepts in the context of superdiversity.
Cultural competence
Meeting the maternity care needs of diverse populations demands consideration of the issues of cultural safety and cultural competence. Leininger,52 a seminal theorist, described ‘culturally competent care as care that is sensitive and meaningful to the patients, that intersects well with their cultural beliefs, norms and values’. This type of care may consist of actions that identify, respect and promote the cultural uniqueness of each individual. 53 These important behaviours may be enhanced by continuing education for nurses and other health-care providers. 54 Although Leininger made an important contribution in this field in the last century, her work has been critiqued extensively,55 largely for its assumption that care and services will be improved by knowledge of different cultures without recognition of ‘the very complex ways in which race, socioeconomic status, gender and age may intersect’. 56 The approach tends to promote culture negatively, potentially contributing to stereotypical attitudes and propagating power imbalances. 57 Serrant-Green58 stressed that the diversity within all ethnic communities needs to be addressed.
The term cultural competence means different things to different people; it can be said to represent a diverse set of skills, knowledge, attitudes and behaviours. Cultural competence can operate at the level of the individual practitioner, within a service setting, and at the broader levels of the health-care organisation and in the wider health-care system.
Key dimensions of cultural competence are the following:
-
knowledge about diversity in beliefs, practices, values and world views, both within and between groups and communities, and recognition of similarities and differences across individuals and groups, as well as the dynamic and complex nature of social identities (sometimes called cultural knowledge)
-
acceptance of the legitimacy of cultural, social and religious differences, and valuing and celebrating diversity (sometimes called cultural awareness)
-
awareness of one’s own identity, beliefs, values, social position, life experiences and so on, and their implications for the provision of care (sometimes called cultural awareness or reflexivity)
-
understanding of power differentials and the need to empower service users (sometimes considered part of cultural awareness)
-
the ability to empathise, show respect and engender trust in service users (sometimes called cultural sensitivity)
-
recognition of social, economic and political inequalities and discrimination, and how these shape health-care experiences and outcomes for minority groups; and a commitment to address such inequities
-
effective communication strategies, including resources for cross-lingual and cross-cultural communication
-
resourcefulness and creativity to resolve issues arising during the provision of care across differences. 59
Organisational cultural competence
Organisational cultural competence refers to the structures, processes and strategies that operate within health-care organisations, to ensure the delivery of high-quality care and equitable outcomes to all clients, regardless of their ethnic, cultural or religious identities. This type of competence usually encompasses critical reflection on the inner workings of the organisation, including the underlying ways of operating that serve the interests of the dominant group within society. Cultural competence at an organisational level involves the commitment of adequate resources to support appropriate responses at the service delivery level.
Cultural safety
Culture is one of the most difficult terms or concepts to define, but is usually taken to be the beliefs, values, practices and symbols that are recognised by individuals who belong to a particular ethnic group. Although our focus here is on cultural safety,51 the issue of intersectionality must be acknowledged, because in reality a number of axes of inequality exist. For example, social class, ‘race’, ethnicity and gender intersect with culture and may increase the vulnerability60 of women in accessing maternity care services. Focusing on a narrow definition of culture when providing health care may lead to the stereotyping of clients and potentially to an inability of the practitioner to deal with diversity. Cultural safety aims to address these deficits by considering the historical and social processes that impact power relationships within and beyond health care. 50,51 Cultural safety is achieved when programmes, instruments, procedures, methods and actions are implemented in ways that do not harm any members of the culture or ethnocultural group who are the recipients of care. 61,62 Those within the culture are best placed to know what is or is not safe for their culture, which suggests the need for increased dialogue with immigrant women and a need for collaborative partnership approaches. 63,64
Cultural safety was first conceptualised in New Zealand by Dr Irihapeti Ramsden, a Maori nurse, in response to a need to acknowledge the impact of colonisation on the Maori population and its lasting effects in the provision of health care. 63 Ramsden conceptualised cultural safety as a product of nursing and midwifery education that facilitates culturally safe care as defined by the recipients. 50 Cultural safety has been endorsed by the Nursing Council of New Zealand64 and has been a key component of international nursing and midwifery education since the early 1990s. The concept is less commonly used in the UK context, although it seems to be eminently transferable and has a strong empirical basis which other models do not have. Hence, it has been adopted as the cultural safety model by statutory bodies in both New Zealand and Canada. 62
In the current period of superdiversity3,20 in the UK, responding to diverse needs of immigrant women in maternity care is an urgent imperative. 8,37 It would seem necessary to draw on the concepts of cultural safety51 and cultural competence65 in order to provide optimal care, the fundamental axioms and precepts being that the values and norms of the host community determine the service configuration and in fact NHS employees are the bearers of these cultural norms via professional practice. Other nation states, notably Canada,62 Australia and New Zealand,50,63 have integrated the key dimensions of cultural safety (e.g. into professional education for HCPs). Intersecting the primacy of host community values is the idea within the notion of cultural safety, that power dimensions exist between the dominant cultural groups and new ethnocultural groups, resulting in unequal power dimensions in the health-care interaction. These unequal power dimensions often have historical antecedents; an exemplar of this is the notion that Commonwealth immigrants arriving in the UK, and in sociological terms, may be regarded as ‘the other’. Culturally competent and safe care demands not just a focus on individual professional practice, but an embedding of the principles of culturally safe and competent maternity care at the organisational level via policies, procedures, guidelines, education and training of health professionals.
How is an immigrant defined: international and UK perspectives
Defining the term immigrant is complex and lacks consensus. Internationally, the term ‘immigrant’ is defined in various ways. For example, according to the Canadian Council for Refugees, an immigrant is an individual who relocates to permanently reside in Canada. 66 The Canadian Council for Refugees further explains that a person is a permanent resident if the right to live permanently in Canada is granted by the government to that person. The entry of the person into Canada may be as an immigrant or as a refugee. This definition indicates that in Canada an immigrant is defined on the basis of their legal residence status.
In Australia, the United Nations (UN) definition of international migration67 is used to define an immigrant. Accordingly, a person is an immigrant if they are born outside Australia and have been (or are expected to be) living in Australia for a period of ≥ 12 months. 68
In the USA, the Department of Homeland Security is responsible for collecting data on immigrants. According to the Department of Homeland Security, immigrants are foreign-born individuals and they are required to obtain legal permanent residence in the USA. 69 Here, the foreign-born individuals are the individuals who are not US citizens at the time of their birth. This definition includes naturalised US citizens, legal permanent residents (immigrants), temporary migrants (foreign students), humanitarian migrants (refugees and asylum seekers) and persons residing illegally in the USA. 69 This definition indicates that the USA defines immigrants according to different categories (e.g. permanent and short-term residence).
In the UK, there is inconsistency in defining the term ‘immigrant’ in different data sources and data sets relating to migration. 70 The terms immigrant and migrant are often used interchangeably to confer the same meaning. For example, the Annual Population Survey of Workers and Labour Force Survey71 uses country of birth as a basis for defining a ‘migrant’. According to these data sources, a person born outside the UK is classified as a ‘migrant’. However, many workers born outside the UK may become British citizens over a period of time.
A second source of data on migrants is applications made for obtaining a National Insurance number. This data source defines a migrant on the basis of nationality. Accordingly, applicants that hold nationality other than the UK are migrants. However, similar to the above, the nationality of a person is also subject to change over a period of time and, in some instances, individuals may acquire dual citizenship of a different nation state.
A third and important source of data on migrants is the Office for National Statistics (ONS). The ONS classifies migrants’ data in two data sets (i.e. short-term international migrant and long-term international migrant). Here ‘long term’ means holding the intention of staying > 1 year, whereas ‘short term’ is the intention of staying < 1 year. This suggests that the ONS considers the length of stay of a person in the UK important in determining migrant status. The classification of migrants into short and long term is recommended by the UN. The ONS uses the UN definition of long-term international migrant and estimates migrants both inside and outside the UK. Accordingly, a migrant is a person who relocates and changes his or her country of residence for a minimum of 12 months; therefore, the country of destination in essence becomes the country of usual residence. 72 In long-term international migration data, students and asylum seekers are also included, which is not the case in the USA.
Immigrants and the UK NHS
In service provision, the NHS follows rules set by the central government that determine an immigrant’s entitlement to free NHS care. These rules relate to the kind of services and the immigration status of the user. 73 This approach suggests that an asylum-seeker woman may not be entitled to full maternity care because of immigration status. 74 Furthermore, the collection of data on ‘immigrants’ in the health-care setting is not well established and the NHS usually collects data on ethnicity and nationality and not on the migration-related variables such as length of stay and country of origin.
Researchers in the University of Oxford’s Centre on Migration, Policy and Society have defined immigrants in health-care research based on ‘country of birth’, with recent immigrants being foreign-born individuals who have been living in the UK for ≤ 5 years. 75 Similarly, in another briefing paper on the health of migrants in the UK,74 researchers from the Centre on Migration, Policy and Society defined migrants as all those born outside the UK. The authors acknowledged that currently it is challenging to achieve a comprehensive understanding of migrants’ health due to the lack of evidence on migration-related variables (e.g. country of birth, length of stay in the UK, immigration status).
The statement of NICE, which provides clinical guidelines for health-care practice in the UK, is worth noting here. NICE,25 in its guidelines Pregnancy and Complex Social Factors: A Model for Service Provision for Pregnant Women with Complex Social Factors, identified recent migrant women having complex social needs. NICE defined a recent migrant as a woman who moved to the UK within the previous 12 months. In the guidelines, migrant women are conflated with asylum seekers, refugees and those lacking English-language proficiency. This suggests that there is implicit acceptance of the term migrant women in health care in respect of being born outside the UK, being in the purview of immigration control and having deficits in English-language proficiency.
Defining immigrants in health-care research
There is no consensus on the operational definition of ‘immigrants’ in the health-care research literature. For example, Urquia and Gagnon76 conducted a review of the literature (2000–9) to explore how the term ‘immigrants’ is defined in health-care research. The authors noted heterogeneity and ambiguity in the terminologies used in the field. The authors documented the following definition for international migrants:
A change of residence involving the spatial movement of persons across country borders. The change of residence may result in a new permanent residence (if the person is allowed to reside indefinitely within a country) or a temporary residence, as in . . . of international students and contract labour migrant workers . . .
Urquia and Gagnon76
The above definition is based on ‘length of stay’ and includes asylum seekers and refugees; however, in this definition the terms ‘permanent’ and ‘temporary’ are not further defined and specified. In fact, the authors are based in Canada, and therefore their definition may be mediated by Canadian perspectives on migration, which are somewhat different from those in the UK.
There are studies in which an immigrant is classified on the basis of country of birth. For example, Small et al. 8 published a systematic and comparative review of studies on women’s health in five developed countries, including the UK. For the purposes of their review, the authors defined ‘immigrant women as those women not themselves born in the country in which they are giving birth’. 8 In another study on maternity care,77 the author used similar terms (i.e. Somali-born women in the Finland context). This suggests that being born outside the country in which a women gives birth is the main defining factor. Salt78 has consistently used a definition of immigrant ‘as a person born outside the UK’ in his work. This is similar to a case in the US context, in which a systematic review on the health of immigrant women79 defined immigrant as ‘foreign born’.
In some other studies, the researchers have used broader terms to define immigrants. For example, an integrative review of the literature examining the potential influence of HCPs’ attitudes and behaviours on health-care disparities80 used a ‘broad definition’ and included all groups that, owing to ethnicity, place of birth, citizenship, residence status or the related variables, have minority status in the country in which they reside. The same approach is taken by a meta-synthesis81 undertaken on refugee and immigrant women’s experience of postpartum depression in three major European countries with high levels of immigration (Germany, Italy and the UK). The authors of this aforementioned meta-synthesis noted that there is inconsistency in the use of the term immigrant and thus ‘extended the inclusion criteria to all articles, where research had been undertaken on “ethnic minorities”, “migrants”, “refugees” and “asylum seekers” in the given country‘. 81
It is observed that ‘nationality’ is also used in maternity care-related research to classify immigrant women. For example, acknowledging the challenge of categorising immigrant and ethnic minority women, Jentsch et al. 82 used ‘overseas nationals’ in their study. In another review, Collins et al. 83 excluded papers that looked at second-generation immigrant women and those whose samples were selected only on the basis of ethnicity rather than immigration. In the UK, the terms ‘old’ and ‘new’ migrants are also used when talking about the demographic diversity and challenges of delivering public services, including health care. 7
Immigrant women in our proposal for the National Institute for Health Research
Our proposal submitted to NIHR noted various features of immigrant women in the UK that are related to the aforementioned discussion. The proposal acknowledged heterogeneity and diversity in the immigration pattern of immigrant women in the UK. The proposal highlights a variety of reasons for migration, diversity in country of birth and length of stay in the UK:
Our review is focused on immigrant women. This is heterogeneous group with migratory pattern that might be related to economic migration, the transgression of human rights and war, or have origins in the UK’s colonial history . . . The UK is in a period of superdiversity that is new and more diverse migrant groups (this includes both recent migrants and those who have been settled in the UK for many years) are resident in the UK, creating challenges for the National Health Service [NHS]. Increasing migration from Eastern Europe and non-commonwealth countries means that the synthesis of knowledge related to immigrant experiences of maternity care interventions and access is an urgent imperative because of rapidly changing demography and the potential to realise health potential of future citizens.
Higginbottom et al. 84 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
The operational definition of an immigrant women used in this review
The preceding paragraphs suggests that the term ‘immigrant’ is defined in various ways in different countries and by different authors. However, two features are frequently referred to in these definitions (i.e. country of birth and length of stay). These factors are also noted in NICE guidelines on the provision of maternity care25 and are important in the entitlement, access and ability to use health care in the UK. For example, if you are born outside the UK, it is likely that you are knowledgeable about the UK health-care provision.
We adopted the following definition of an immigrant woman for our review and to inform our inclusion and exclusion criteria. A woman is an immigrant if she:
-
is born outside the UK
-
has lived in the UK for > 12 months or had the intention to live in the UK for ≥ 12 months (or more) when she first entered.
Therefore, we included studies on immigrant women in which the population studied fulfilled these two criteria. According to this definition, studies on population groups of foreign students, asylum seekers, recent legal refugees and immigrants, and illegal immigrants will also be eligible for inclusion. In many cases the study populations/sample may not be accurately and fully described. We therefore used linguistic ability (e.g. the need for an interpreter) as a proxy for immigrant status. Notwithstanding all of these perspectives, we acknowledge that the term ‘immigrant women’ is generic and refers to a highly heterogeneous group of individuals, with a complex and vast array of ethnocultural orientation, linguistic skills abilities, motivations for migration and socioeconomic status. However, there may be a commonality of experience in respect of the use of and familiarity with maternity care services in the UK. What is profoundly critical is the over-representation of immigrant women in maternal and perinatal mortality statistics.
Chapter 2 Aims and objectives
Our aim was to undertake a narrative synthesis (NS) of a wide range of empirical literature, including grey literature, to provide stakeholders with perspectives on maternity care access and interventions (NHS and non-NHS) directed at immigrant women in the UK. The topic is of great significance to the NHS because of the strategic commitment to address inequalities and the changing patterns of migration to the UK. Because established immigrant communities feature disproportionately in maternal and perinatal mortality, and because 26.5% of all UK births in 2013 were to foreign-born women,2 the topic is highly relevant.
We planned to identify the most effective and appropriate methods of services delivery by identifying the acceptability of relevant processes at the individual, community and organisational levels. These factors are recognised to be critical determinants of the effectiveness of services and of patient and client outcomes. We also planned to identify specific critical points in care delivery, which will enable the provision of tailored solutions for policy and practice changes. In addition, we aimed to explore the factors affecting the implementation of particular interventions that are designed to enhance access, equity, and clinical and psychosocial outcomes for immigrant women. To reach this aim, we used a Project Advisory Group (PAG) that included not only patient and public involvement, but also clinicians [an obstetrician, a general practitioner (GP) and midwives], commissioners and a policy-maker. This group was initiated during the establishment of our research questions and our early plans for dissemination, and its involvement continued for the entire duration of the project. We wanted to meet the following objectives:
-
to identify, appraise and synthesise empirical studies on the topic that used qualitative, quantitative or mixed methods of research
-
to identify, appraise and synthesise grey literature and non-empirical reports
-
to identify additional knowledge users and mechanisms of knowledge transfer
-
to share our findings through strategic end-of-grant knowledge transfer (ultimately, we wanted to establish the current knowledge base and generate important recommendations for future policy, practice and programming, thus mapping out pathways to health equity).
Methodology
Protocol and PROSPERO registration
Our study is registered with PROSPERO as CRD42015023605 (URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015023605; accessed 5 June 2019) and the protocol has been published. 84
Narrative synthesis methods
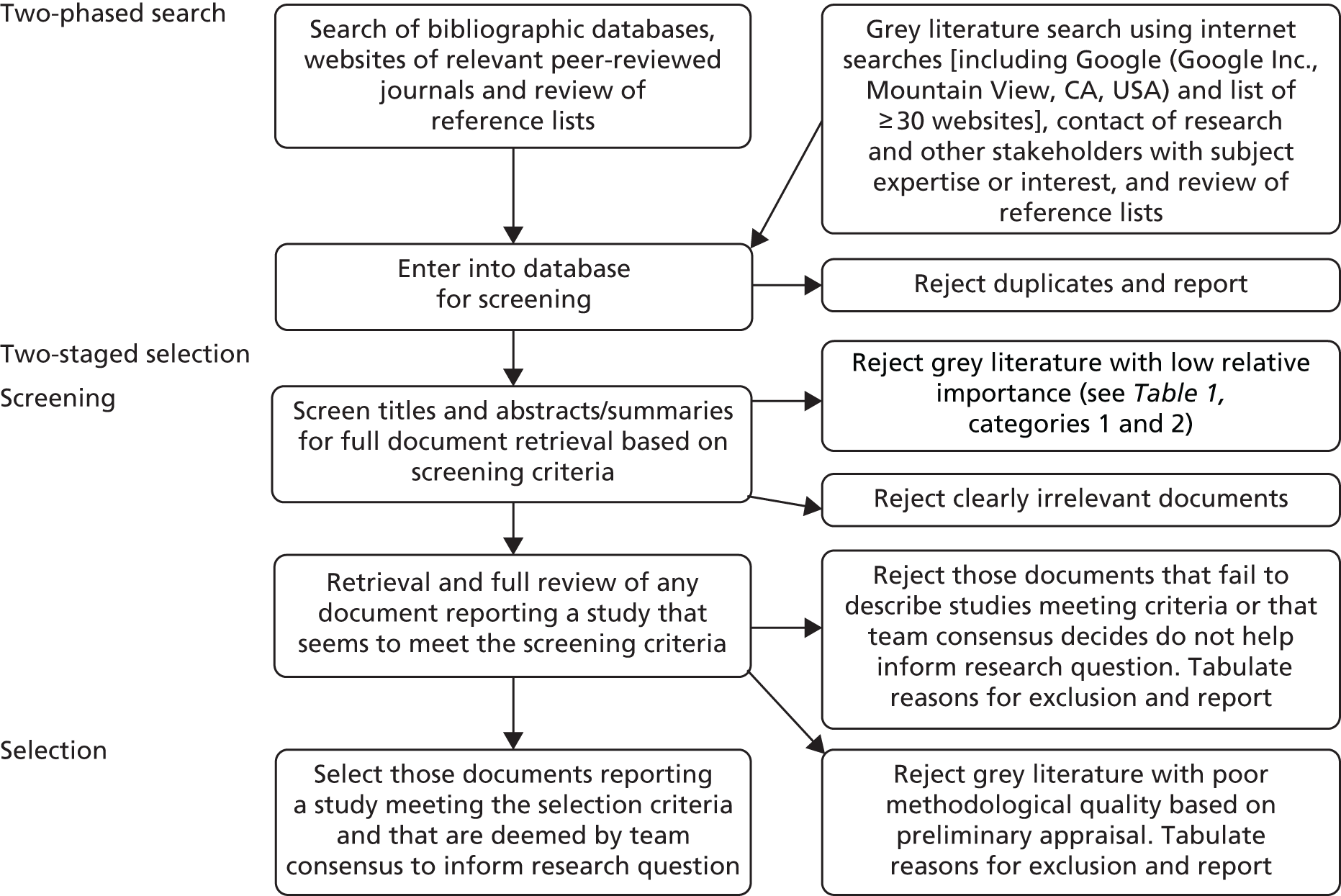
A NS review comprises four main elements (Box 1 and Figure 2).
Element 1: developing a theory of why and for whom.
Element 2: developing a preliminary synthesis of the findings of the included studies, following implementation of the search strategy.
Element 3: exploring relationships in the data.
Element 4: assessing the robustness of the synthesis.
FIGURE 2.
The four elements of a NS review. Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.

Although a wide range of approaches exist on the spectrum of systematic reviews, ranging from aggregative to interpretive approaches,85 the purpose of selecting a NS approach (see Figure 2) was to produce highly relevant policy and practice evidence. Some systematic reviews are highly theoretical in nature; however, in considering our initial scoping review, it was established that much of our evidence was likely to be descriptive in nature and suitable for a thematic analysis which is associated with NS. A focus on narrative findings and the production of a thematic analysis is not merely the collation of key perspectives; importantly, the theming achieves a level of abstraction that produces new and potentially innovative insights. We conducted the review taking account of the original conceptualisation of the NS approach86 and of the new and emerging insights and guidance.
Element 1: developing a theory
This review had no predefined hypotheses. Our review focus on immigrant women’s access to and interventions in maternity care was developed and refined by mapping the available knowledge, and also ensuring the relevance of the knowledge synthesis (to policy-makers, other potential knowledge users and immigrant communities). The literature spanned a range of specific maternity care services, including antenatal, labour and postnatal care; maternal risk factors; health promotion; access to and availability and competency of maternity services; the role of culture and tradition; maternity outcomes in relation to perceived maternal risk factors; and responses to care interventions. We engaged in additional consultation with our PAG to further refine the review questions to increase their relevancy. We utilised Gulliford et al. ’s23 theory of access to inform our thematic outcomes (Box 2 gives an example of the scoping search strategy and Appendix 1 gives an exemplar of a final search strategy).
-
exp Maternal Health Services/or exp Postnatal Care/or exp Preconception Care/or exp Prenatal Care/or exp Perinatal Care/or exp Infant Care/or exp Midwifery/or exp Obstetrics/or exp Obstetric Nursing/
-
exp maternal welfare/or exp maternal care/or exp maternal child health care/or exp newborn care/or exp prepregnancy care/
-
exp General Practitioners/or exp Primary Health Care/or exp Family Health/or exp Community Health Nursing/
-
(((maternal or child* or baby or babies or fetus* or fetal* or embryo* or obstetric*) adj3 (health* or nurs* or care or service*)) or (midwif* or midwiv*)).ti,ab.
-
((birth* or matern* or mother* or pregnan* or childbearing or child-bearing or prenatal or pre-natal or postnatal or post-natal or perinatal or peri-natal or preconception or pre-conception or antenatal or ante-natal or postpartum or puerperium) adj3 (health* or nurs* or care or service*)).ti,ab.
-
exp Health Services Accessibility/or exp Healthcare Disparities/or exp Health Services/
-
(3 or 6) and (matern* or child* or baby or babies or fetus* or fetal* or embryo* or obstetric* or birth* or mother* or pregnan* or childbearing or child-bearing or prenatal or pre-natal or postnatal or post-natal or perinatal or peri-natal or preconception or pre-conception or antenatal or ante-natal or postpartum or puerperium).ti,ab.
-
1 or 2 or 4 or 5 or 7
-
(‘use’ or access* or utili* or consum* or block* or hurdl* or barrier* or hindr* or hinder* or obstacle* or exclu* or discrimin* or disparit* or disproportion* or inequal* or unequal* or inadequat* or insuffic* or stratif* or limit* or lack* or unreliab* or poor* or poverty* or depriv* or disadvantag* or insecur* or insensit* or status* or entitl* or uninform* or ill-inform* or benefit* or interven* or deliver* or effective* or cost effective*).ti,ab.
-
(3 or 6) and 9
-
‘Emigrants and Immigrants’/or Refugees/or ‘Transients and Migrants’/or ‘Emigration and Immigration’/
-
(((established or long-term or ‘first generation*’ or new* or recent* or current*) adj3 (migrant* or migrat* or immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or (ex adj pat*) or transient* or alien*)) or newcomer* or (new adj comer*) or incomer* or (in adj comer*) or ((international or overseas or foreign) adj2 (student* or employee* or worker*))).ti,ab.
-
(refugee* or (asylum adj seek*) or asylee* or (refused adj3 (asylum* or refugee*)) or (displaced adj person*) or exile* or (new adj arrival) or (country adj2 (birth or origin)) or transnational*).ti,ab.
-
(foreigner* or (foreign adj (born or citizen* or national* or origin*)) or (non adj (citizen* or native*)) or ((adoptive or naturali#ed) adj (citizen* or resident*)) or overstay* or trafficked or ‘spousal migrant*’).ti,ab.
-
(‘non-UK-born’ or ‘born outside the UK’ or ‘length of residence in the UK’ or ((‘not lawful*’ or ‘not legal*’ or unlawful* or illegal* or unauthori#ed* or ‘not authori#ed’ or uncertain or insecure or illegal or legal or legitimate* or permit* or visa* or irregular* or refused or undocumented) adj3 (residen* or student* or worker* or employee* or unemployed* or immigrant* or imigrat* or migrant* or migrat*))).ti,ab.
-
exp Ethnic Groups/or (ethnic* or ethno* or race or racial*).ti,ab.
-
exp african continental ancestry group/or exp asian continental ancestry group/
-
exp Vulnerable Populations/or ((vulnerab* or disadvantag* or minorit*) adj3 (individ* or person* or people* or population* or communit* or group*)).ti,ab.
-
(‘Black and Minority Ethnic’ or ‘Black and Minority ethnic’ or BME or BAME or african caribbean* or afro caribbean* or black african* or (west adj (indies or indian*))).ti,ab.
-
(south asia* or afghan* or bangladesh* or bengal* or bhutan
Chapter 3 Search strategy refinement and implementation
The comprehensive search strategy generated high rates of retrieval of records relevant to the research question of this project.
The search strategy used key terms used in consistently formulated text-based queries and search statements. These terms were based on subject headings, thesaurus terms, or related indexing and categorisation terms, appropriate for each literature database. An example of a detailed final search strategy is given in Appendix 1.
The strategies were also adapted to searching other data sources, such as existing systematic reviews, theses and clinical studies, to ensure the maximum possible retrieval of relevant records. Less-structured search queries were used to search various types of grey literature.
Refinements to the search strategy
In developing the search strategy across a number of the different databases, it became evident that terminologies used for maternal health-care services and immigrant status differ significantly, not only across the original journal articles but also in the different literature resources, in their standardisations of terms for subject headings, thesauri and other indexing and categorisation systems.
For example, across three major databases (MEDLINE, EMBASE and PsycINFO), parallel but differing terminologies were found. Moreover, medical subject headings (MeSH) (originally developed for MEDLINE) are searchable across all three databases, but they do not retrieve comparable answer sets and may need to be replaced or enhanced to do so (i.e. by using Emtree in EMBASE and enhanced MeSH terms in PsycINFO) (see Report Supplementary Material 1).
These concerns required iterative modifications to the original search strategies in each database to ensure that the observed variations in terminology were adequately reflected in both the index terms and the text-based queries that were developed for all of the databases.
Search strategy and study selection
We included all empirically based studies that used a variety of methodologies (see Appendix 2) and focused on immigrant women, maternity care experiences, experiences and interventions, published between January 1990 and January 2018. Studies were published in English and included study locations in the UK (Table 1). We found several studies arising from Scotland and one from Wales; the remaining studies were based in England (see Appendix 3 for the table of excluded studies).
| Citation | |||
|---|---|---|---|
| Criteria for selection: | Yes | No | Cannot say |
| 1. Publication date of January 2000 to January 2018 | |||
| 2. English | |||
| 3. Empirical research and findings | |||
| 4. Study participants live in the UK | |||
| 5. Study participants are immigrant women (if the study includes both immigrant and non-immigrant women, it must have findings specific to immigrant women) | |||
| 6. Related to maternity care access, interventions or experiences of maternity | |||
The NS approach relies primarily on the use of words and text to summarise and explain the findings of the synthesis, which are informed by a synthesis of the narrative findings of included papers. 86 Gina Higginbottom and Myfanway Morgan have successfully employed this review genre previously and have vast expertise in its usage. 87 Narrative synthesis is suitable for both quantitative and qualitative studies, as the emphasis is on an interpretive synthesis of the narrative findings of research, rather than on a meta-data analysis. 86 After applying rigorous systematic procedures for searching, screening and selecting literature for inclusion in the review, the articles were appraised for quality and the NS of the findings progressed.
We included studies that focused on immigrant women and adopted the following definition of an immigrant woman for the purposes of our review. A woman is an immigrant if she:
-
is born outside the UK
-
has lived in the UK for > 12 months or had the intention to live in the UK for ≥ 12 months when she first entered the UK.
Therefore, we included studies on immigrant women in which the population studied fulfilled these characteristics. Based on this, studies that focused on the following population groups were also eligible for inclusion: foreign students, asylum seekers, illegal immigrants and recent legal refugees and immigrants. In many cases the study populations/sample was not accurately and fully described. We therefore used linguistic ability (e.g. the need for an interpreter as a proxy for immigrant status). Our focus was on first-generation immigrant women regardless of their phenotype. Meaning that women of all ethnic groups are including women of white ethnicities, although we encountered few studies that focused on the latter and our review was constrained by the lack of various studies in the scientific literature. For example, we did not identify any studies meeting our criteria that focused on solely white immigrant women, such as Eastern European women.
The search and selection strategies drew on established systematic review methods88 and incorporated recent guidelines for the selection and appraisal of grey literature. 89 Two search and selection phases were conducted. The first consisted of searching electronic databases and websites of relevant journals to identify empirical papers published in peer-reviewed journals. We considered empirical papers to be primary research publications that investigated working hypotheses or research questions and tested them by means of observations or experimentation, qualitative investigation or mixed-methods designs. The second phase targeted grey literature and included searches of selected databases, internet-based searches (see Report Supplementary Material 1), reviews of reference lists, and e-mail or telephone contacts with researchers and other stakeholders that had expertise or interest in the target topic. The processes we used to conduct the search and selection process are summarised in Figure 3.
FIGURE 3.
Summary of the search and selection methodology. Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
Our focus was on access and interventions designed to promote or enhance maternity care for immigrant women, as articulated in the original review question. We chose the definition of intervention to be an integration of program facets or strategies designed to create behaviour changes or enhance health status amongst individuals or an entire population’. 90 In fact, in practice we identified few interventions that have been rigorously and scientifically appraised (that is not to suggest that these interventions do not exist, merely that they have not been evaluated).
We adopted the population, intervention, control and outcome of interest (PICO) approach to implement the search strategy as follows:
-
population – immigrant women
-
interest – maternity care
-
control – non-immigrant women (implicit comparator emerging in the results)
-
outcome of interest – experience of care.
Therefore, our search strategy development was based on:
-
search concept 1 – pregnancy, childbirth (implicitly females requiring maternity care), explicit terms covering women/females requiring all types of maternity care (antenatal, perinatal, postnatal, etc.)
-
search concept 2 – immigrant populations (which would not fully distinguish between ‘new’ and ‘second-generation’ immigrants, this would be done at the selection stage)
-
search concept 3 – terms used to identify access to, use of, deficiencies in, etc., service provision (to help identify groups with poorer health outcomes or vulnerabilities)
-
our final answer set of citations included concepts 1, 2 and 3.
Data search strategy and implementation
Development of literature database search strategies and search implementation
Team member Jeanette Eldridge is an experienced information scientist with whom we developed the scoping search strategy (see Box 2). An exemplar of final search strategies (see Appendix 1) incorporated revisions, as per the knowledge base of the academic team members (GH, MM, KB and CE) and included internet and literature database searches. Jeanette Eldridge constructed the detailed search strategies for each literature database and conducted the searches after review of these strategies by the entire team, including the PAG. The search focus was on studies that described access and compared interventions to improve maternity care experiences for immigrant women in the UK (Box 3).
Population: immigrant women from any country other than England, Scotland, Northern Ireland or Wales.
Phenomena of interest: maternity care.
Context setting: UK.
Study designs: qualitative, quantitative and mixed-methods studies.
Language: English.
Date limitations: January 1990 to January 2018.
Exclusion criteriaContext studies: located in any country other than England, Scotland, Northern Ireland or Wales.
Participants: BME women born in the UK.
Study design: non-empirical research, opinion pieces or editorial.
Search implementation included independent double-screening and team review of ambiguous studies. Our search strategy was adapted for each of these databases so that relevant controlled vocabulary, searching techniques and keywords were used consistently. The reference lists of the included studies were reviewed for relevant citations. Additional hand-searches were undertaken of major relevant journals (e.g. Journal of Immigrant and Minority Health, Journal of Health Services Research & Policy and Canadian Journal of Public Health) and in reviews published by topical research groups (e.g. Reproductive Outcomes and Migration, an international research collaboration). 41
We used a screening tool (see Table 1) to select studies congruent with our review questions (Box 4) and to ensure robustness of the NS. 86 A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)91 flow chart illustrates the selection process that we implemented (Figure 4).
What interventions exist that are focused specifically on improving maternity care for immigrant women in the UK?
-
How do these interventions address inequality?
-
How do accessibility and acceptability manifest as important dimensions of access to maternity care services, as perceived and experienced by immigrant women?
FIGURE 4.
The PRISMA flow chart of the final selection process. Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
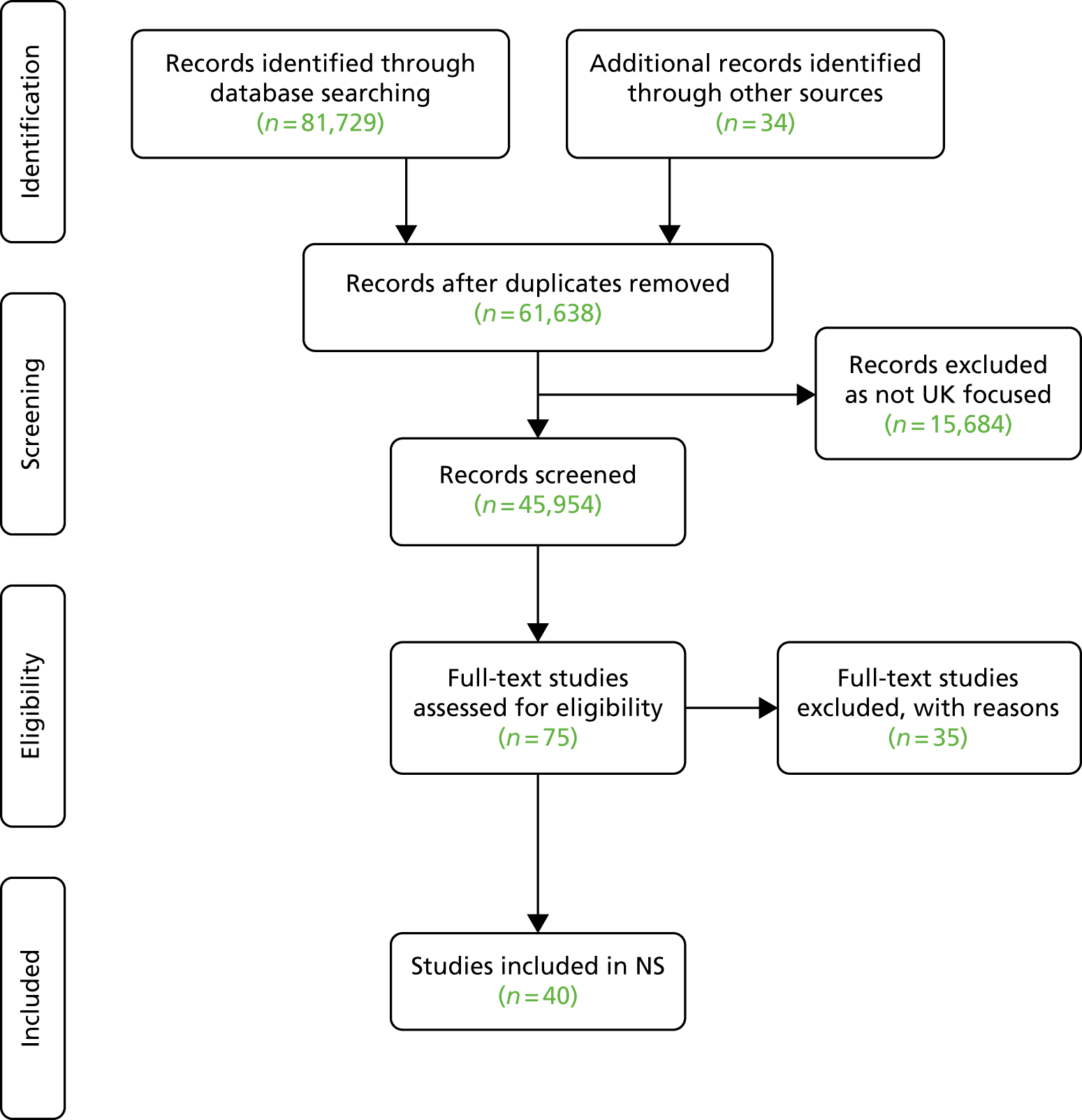
We included studies that focused on immigrant women; therefore, we included studies on immigrant women in which the population studied fulfilled the characteristics previously mentioned (see Search strategy and study selection).
A relevancy appraisal of each record was undertaken by first reviewing the title and abstract (GH, CE, MM, JE, KB and BH). Records were shared with team members via the EndNote, Version 7, collaborative function (Clarivate Analytics, Philadelphia, PA, USA). We retrieved potentially relevant articles for further assessment against our inclusion criteria, with the entire team making the final decision. We used a PRISMA flow chart (see Figure 4) to document the steps used in the search and selection process. 91
Management of non-empirical reports and grey literature
Grey literature is a field in library and information science that deals with the production, distribution and access to multiple document types produced at all levels of government, academia, industry and other organisations. It can be in electronic and print formats, and it may not necessarily be controlled by commercial publishing (i.e. in cases in which publishing is not the primary activity of the producing body). 89,92 It is not published commercially or indexed by major databases, although can have an impact on research, teaching and learning. 89,92 Some examples include theses and dissertations, conference proceedings and abstracts, newsletters, research reports (completed and uncompleted), technical specifications, standards and annual reports.
We utilised the approach of McGrath et al. 93 to systematically review high-quality international grey literature (and non-empirical reports identified in the database searches). We also followed the principles expounded by the US National Library of Medicine. 89 The process consisted of (1) identifying the grey literature (including constructing a list of websites); (2) selecting documents via screening, preliminary selection, final selection and data extraction; (3) organising and tabulating data into categories; and (4) undertaking a narrative review of data. Our previous database searches had identified some grey literature, but further identification of grey literature required searches of the following databases: Web of Knowledge Science Citation Index, Web of Knowledge ISI Proceedings, ProQuest Dissertations & Theses Database and the Cochrane Methodology Register. We also searched using Google and Google Scholar (Google Inc., Mountain View, CA, USA). In addition, we hand-searched the reference lists of all synthesised materials and approached relevant organisations, especially through the contacts of the PAG. We also corresponded with information specialists and other experts within this field. The PAG assisted with the identification and final selection of grey literature and the interpretation of findings.
Outcomes and management of identified records
The retrieved data sets (Box 5) were downloaded into an EndNote library. Duplicate records were identified and retained in a separate group within the EndNote library. The downloaded records normally included the title and abstract. Keyword terms and other bibliographic information were also included when available.
-
Ovid MEDLINE: 1948 to the present.
-
MEDLINE In-Process & Other Non-Indexed Citations: to daily update.
-
Ovid EMBASE: 1980 to Week 11 2017.
-
Ovid PsycINFO: 1972 to March Week 3 2017.
-
CINAHL Plus with full text/EBSCOhost: January 1990 to January 2017.
-
MIDIRS on Ovid: 1971 to April 2017.
-
Thomson Reuters Web of Science:a 1900 to 2017.
-
ASSIA on ProQuest: 1987 to the present.
-
HMIC on Ovid: 1979 to January 2017.
-
POPLINE (via www.popline.org/): 1970 to the present.
ASSIA, Applied Social Sciences Index and Abstracts; CINAHL, Cumulative Index to Nursing and Allied Health Literature; HMIC, Health Management Information Consortium; MIDIRS, Midwives Information & Resource Service.
Thomson Reuters Web of Science includes the following: Science Citation Index Expanded:1900 to 2017; Social Sciences Citation Index: 1956 to 2017; Conference Proceedings Citation Index – Science: 1990 to 2017; Conference Proceedings Citation Index – Social Science and Humanities: 1990 to 2017; Book Citation Index – Science: 2008 to 2017; Book Citation Index – Social Science and Humanities: 2008 to 2017; and Emerging Sources Citation Index: 2015 to 2017.
When individual full-text documents were required, they were obtained through a number of routes, including the EndNote ‘Find Full Text’ option, subscriptions to electronic journals and access to other physical or electronic resources available through the University of Nottingham, interlibrary loans of articles or books and direct contact with the authors or the originating institutions.
When records could not be definitively selected or excluded, they were assigned to a separate group and further reviewed by two members of the team. The full library was then annotated to show the final decision.
The bibliographic databases that were searched are listed in Box 5.
Data extraction
We conducted the following foundational activities in order to extract data:
-
Textual description: a systematic textual narrative was written for each study. We used headings adapted from Popay et al. :86 setting, participants, aim, sampling and recruitment, method, analysis and results (see Appendix 4).
-
Tabulation and summarisation of all studies to be included: these tables described the attributes of the studies and the results. Information was extracted from the textual description using the same headings as above and additional headings as necessary. Papers in the portable document format (PDF) were imported into ATLAS.ti qualitative data analysis software (Scientific Software Development GmbH, Berlin, Germany) using the ‘Attributes’ option to allow the tabulation of relevant data.
Element 2: developing a preliminary synthesis
Our analysis process began with the selection of included papers by the research team, with the final selected papers being reviewed by one researcher and the data of each paper extracted into a one-page textual summary (see Appendix 5). A second team member confirmed the study selection; furthermore, the entire team confirmed the selection at the reflective team meeting. We shared advance information with team members prior to meetings so that views could be elicited in an efficient fashion, with careful recording of views and decision-making processes in meeting minutes. Meetings included incisive debate regarding contentious papers. Team members Myfanwy Morgan, Catrin Evans and Gina Higginbottom are experienced systematic reviewers (evidenced in previous publications94), so we harnessed this expertise for the benefit of this review; pertinent practice perspectives by CM and Janette Eldridge provided technical systematic knowledge.
We engaged in careful reading and re-reading of papers to ensure familiarisation with the content. Once the final selection for inclusion was established, we undertook a tabulation of key variables of all included studies and an exemplar can be found in Appendix 5. Tabulation and extraction of key findings was facilitated by the production of the one-page textual summaries, as this format facilitated comparison and contrast of study findings in a systematic and coherent fashion.
The project principal investigator (GH) also undertook a detailed analysis of the narrative findings of each study using ATLAS.ti computer-assisted qualitative data analysis software, engaging in a line-by-line analysis of the narrative findings of each included study. The analysis created over 250 codes. The two perspectives were then merged to create a cohesive interpretation. The aforementioned processes are human resource intensive, iterative and demanded reconsideration several times. However, differences in interpretation between the researchers may still exist, although these differences are likely to be marginal and will not have an impact on the critical conclusions and implications for practice. Inevitably, the perspectives and foci of the research studies included limit our conclusions.
In element 2 (Table 2), we also applied the critical appraisals tools, made an appraisal and included this in the one-page textual summary we created (see Appendix 5).
| Element | Task | Explanation |
|---|---|---|
| Element 2: developing a preliminary synthesis | Textual description of the studies | A descriptive narrative was produced with the headings of setting, participants, aim, sampling and recruitment, method, analysis and results |
| The data extracted for the textual description allowed papers to be grouped and thus enabled patterns between and within studies to be identified. This grouping was informed by the research questions. Data were grouped by a particular feature; for example, the method, the country of origin of the sample studied, the maternity care setting, or the main findings | ||
| Translating data: thematic analysis | Main or recurrent themes in the findings were identified | |
| Element 3: exploring relationships within and between studies | Moderator variables and subgroup analysis | Study characteristics that vary between studies or sample (subgroup) characteristics that might help explain differences in findings were identified |
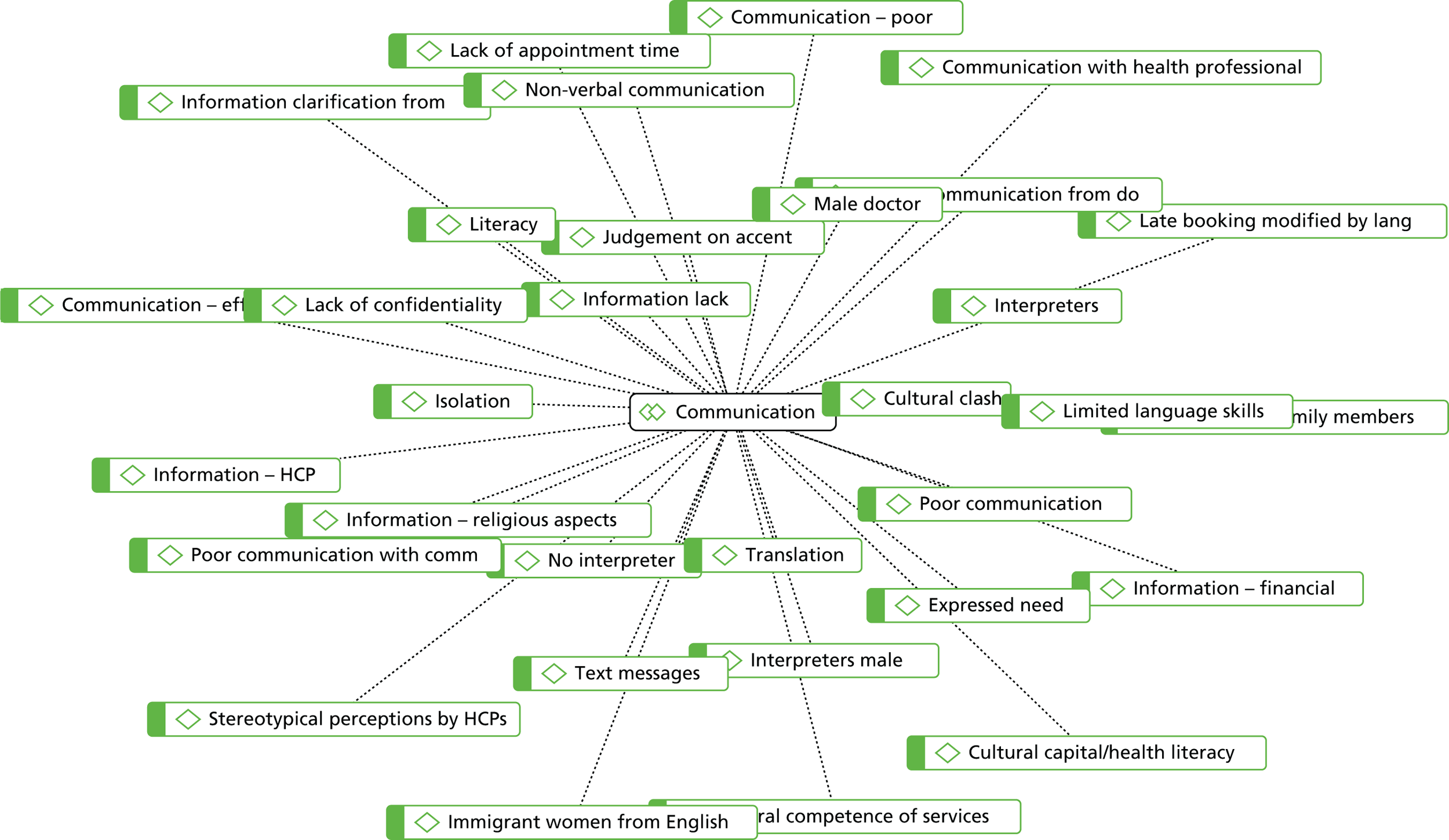
| Ideas webbing and concept mapping | ‘Ideas webbing’ conceptualises and explores connections between the findings reported in the review studies and often takes the form of a spider diagram. ‘Concept mapping’ links multiple pieces of information from individual studies, using diagrams and flow charts to construct a model with relevant key themes | |
| Qualitative case descriptions | Outliers or exemplars of why particular results were found in the outcome studies were described | |
| Element 4: assessing the robustness of the synthesis | Critical reflection | A summary discussion was developed that covered the following: (1) the synthesis methodology used (focusing on the limitations and their possible effects on the results); (2) evidence used (quality, reliability, validity and generalisability); (3) assumptions made; (4) discrepancies and uncertainties identified and how discrepancies were handled; (5) areas in which the evidence was weak or non-existent; (6) possible areas for future research; and (7) a discussion of the evidence, considering the ‘thick’ and ‘thin’ evidence and commenting on similarities and/or differences between the various sources of evidence |
We proceeded to group and cluster the studies in respect of the data extracted for the textual description. This enabled identification of patterns between and within studies. During this grouping process, the research questions remained salient in our cognition. A particular feature grouped data, for example the method, the country of origin of the sample studied, the maternity care setting, or the main findings. We identified major themes in the narrative findings (see tables in Report Supplementary Material 1).
Following construction of the preliminary themes, we produced code/narrative theme tables to demonstrate how the basic meaning units related to the theme, utilising the codes produced in ATLAS.ti and aligning these to the manually extracted key findings. We defined codes individually in ATLAS.ti, enabling the essential meaning of key phenomena to be captured, facilitating cross-comparison and variations in phenomena to be established and observed. Codes are defined by Miles and Huberman95 as:
. . . tags or labels for assigning meaning to the descriptive of inferential information compiled during a study. Codes usually are attached to ‘chunks’ of varying size words, phrases, sentences or who paragraphs, connected or unconnected to a specific setting. They can take the form of a straightforward category label of a more complex one (e.g. a metaphor).
Miles and Huberman, p. 5695
‘Code families’ can be produced in ATLAS.ti and imported into the graphic ‘network builder’ in ATLAS.ti, resulting in topical or hierarchical graphic outputs. We assigned the codes to code families as illustrated in Figure 5, which shows all the codes associated with code family entitled ‘communication’. This code family is a constituent of theme 3 and serves as an exemplar of the extensive analytical work undertaken. ATLAS.ti facilitated a more sophisticated and nuanced analysis than via manual extraction. These data contributed to the production of a descriptive narrative in respect of each theme. Moreover, we created a tabular matrix illustrating how the themes that occurred are distributed over the individual studies (see Appendix 6). This distribution, to some extent, illustrates the weight of evidence in each theme.
FIGURE 5.
Graphic representation of communication theme using ATLAS.ti. HCP, health-care professional. Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
During the analytical processes we interrogated the data identifying using the following concept suggested by Roper and Shapira:96
-
setting – the environment or context
-
activities – patterns of behaviour that occur often
-
events – rare and infrequent activities
-
relationships and social structures – kinship, friendship, bonds, enemies, hierarchical
-
general perspectives – the group’s shared understandings
-
specific perspectives on the research topic(s) – how people understand the phenomena
-
strategies – ways of achieving goals
-
process – flow of events how things change over time
-
meaning – significance and understanding of behaviour
-
repeated phases – depictions of thought processes.
We presented these analytical processes and products at our reflective team meetings to ensure the rigour and robustness of our analytical steps. Through reflection and debate, team members were able to challenge initial interpretations, identify outliers and confirm the coherence of emerging interpretations. Team members independently produced interpretations of the possible meanings of these preliminary themes in order to achieve abstraction, prior to formulation of the higher-level final themes.
Our thematic findings are evolved via a systematic, comprehensive and thorough collaborative team process of comparing and contrasting the emergent themes to establish the ways in which these themes revealed and provided insights into the concepts embedded within the review questions. This iterative process, similar to qualitative research, involved deconstructing the narrative findings into meaning units and social processes as they manifested in the maternity care experiences of immigrant women. As mentioned, individual team members engaged in independent theming of tabular and coded data. We subsequently merged these individual perspectives to form the final harmonised themes, representing a ‘meta-inference’ in respect of the narrative findings of the included studies. Meta-inference is a term used in mixed-methods research to describe the merging of findings from the positivistic and the interpretative paradigms, as is the case in this NS. Tashakorri and Teddlie97 describe meta-inference as ‘an overall conclusion, explanation of understanding developed from the integration of inferences obtained from the qualitative and quantitative strands’.
We have constructed the themes in an indicative fashion (i.e. containing implicit indications) to provide tangible guidance for policy and practice that might be developed into transformational policy- and practice-relevant strategies that will benefit immigrant women and the NHS.
Element 3: exploring relationships within and between studies
Patterns emerging from cross-literary comparisons were subjected to further rigorous evaluation to identify factors that may explain differences, including variance in women’s experiences, in the effects of maternity interventions and in the implementation of maternity services (entire team involvement). This evaluation contributed to our understanding of barriers and enablers that shape maternity services for immigrant women. We also evaluated not only the relationships between the study characteristics and the reported findings, but also the ways in which these relationships may correspond with those reported in other types of literature, including non-empirical and grey literature (which was evaluated separately). Careful attention was paid to the heterogeneity of research methods, methodologies and population characteristics encompassed in the literature through the application of narrative methods. 98 Such methods are particularly suited to synthesising such findings. 86 Narrative methods99 help us to understand and acknowledge the broader influences of theoretical and contextual variables, such as race, gender, socioeconomic status and geographical location. These methods also enable researchers to understand the shaping of differences between reported outcomes for various study designs, in this case those related to childbearing populations, and the development and implementation of maternity services and health interventions across diverse settings.
Data synthesis and establishing relationships
Grouping and clustering
The data extracted in the tabulation allowed papers to be grouped and thus enabled patterns between and within studies to be identified. Groupings were organised by a particular feature (e.g. location, method, ethnic groups, form of analysis, or main findings) (GH, CE, BH and the PAG).
Thematic analysis
Systematically recurrent or salient themes or concepts across studies were identified. ATLAS.ti was used to manage the data and relevant themes were identified on an inductive basis. We generated over 250 codes in ATLAS.ti and these were mapped against the tabular thematic analysis (see Figure 5).
Ideas webbing and concept mapping
‘Ideas webbing’ conceptualises and explores connections among the findings reported in the review studies and it often takes the form of a spider diagram. ‘Concept mapping’ links multiple pieces of information from individual studies using diagrams and flow charts to construct a model with relevant key themes (all team members were involved).
Critical reflection
Popay et al. 86 recommended that a summary discussion of the synthesis should be provided, which includes the following: (1) methodology of the synthesis, focusing on the limitations and their possible impacts on the results; (2) evidence used in terms of quality, reliability, validity and generalisability (for quantitative papers), and possible sources of bias (for qualitative papers); we applied the principles of Lincoln and Guba100 (confirmability, transferability, credibility and dependability); (3) assumptions made; (4) discrepancies and uncertainties identified, and how discrepancies were handled; (5) areas in which evidence is weak or non-existent as possible areas for future research; and (6) whether the evidence is ‘thick’ or ‘thin’ and the similarities and differences in the evidence (entire team).
Methodological quality of included studies and quality appraisal
Key to ensuring the robustness of the synthesis is the methodological quality of key literature, the quality and quantity of the evidence base and the analytical methods used to develop the NS. We critically appraised research studies and weighted each accordingly (GH, MM, CE, and BH). Studies that lacked technical quality or were of questionable methodological integrity101 were critiqued and/or noted for key flaws in the synthesis. Although we identified a number of studies rated as weak, we did not reject any studies on the basis of quality. Despite debates existing regarding the availability of well-established methods for evaluating the reliability and trustworthiness of qualitative and mixed-methods studies, the methodological analysis and synthesis were conducted in a relational and systematic manner.
Appraisal of included studies was assessed using tools from the Center for Evidence-Based Management (CEBMa). 102 We used Good Reporting of A Mixed Methods Study (GRAMMS) for the mixed-methods studies. 103
We used high, medium and low as appraisal categories. 94 This approach is congruent with recent publications from the Cochrane Qualitative Research Group’s Confidence in the Evidence from Reviews of Qualitative Research (CERQual) publications, as they use this type of evaluation104 and it was previously used by Higginbottom et al. in published studies. 87 Studies are classified in three domains, high, medium and low, to enable a ‘macro’ evaluation:
-
High was assigned to studies that used a rigorous and robust scientific approach that largely met all CEBMa benchmarks, perhaps equal to or exceeding 7 out of 10 for qualitative studies, 9 out of 12 for cross-sectional surveys, or 5 out of 6 for mixed-methods research.
-
Medium was assigned if a study had some flaws but these did not seriously undermine the quality and scientific value of the research conducted, perhaps scoring 5 or 6 out of 10 for qualitative studies, 6–8 out of 12 for cross-sectional surveys, or 4 out of 6 for mixed-methods research.
-
Low was assigned to studies that had serious or fatal flaws and poor scientific value, and scored below the numbers of benchmarks listed above for medium-level appraisals in each type of research.
The past decade has witnessed a growth in the development of new approaches to systematic reviews, especially in the domain of qualitative evidence synthesis. Concurrently, innovative approaches to assessing quality have evolved. Popay et al. 86 suggest that we do evaluate the ‘richness’ of studies. Furthermore, this research team have utilised this approach in previous funded studies and publications. 86 Popay et al. 86 defined richness as ‘the extent to which study findings provide in-depth explanatory insights that are transferable to other settings’ (Table 3). We used established criterion in previous studies87 and appraised all the studies in this review using this evaluative tool (Table 4).
| Assessment | Conceptual definition |
|---|---|
| Thick papers |
Studies that offer greater insights into the outcomes of interest Provide a clear account of processes, including sample, its selection, and limitations and biases noted Clear description of analytical processes Present a developed and plausible explanation |
| Thin papers |
Offer only limited insights Lack a clear account of processes by which the findings are produced Present an underdeveloped and weak interpretation of findings produced Present a weak and underdeveloped interpretation of the analysis based on the data presented |
| Manual reference number | Quality as per the CEBMa tool | Relevance | Thick/thin |
|---|---|---|---|
| 1 | Low | High | Thin |
| 2 | Low | High | Thin |
| 3 | Low | High | Thin |
| 4 | Low | High | Thick |
| 5 | High | High | Thick |
| 6 | Medium | High | Thick |
| 7 | Low | High | Thin |
| 8 | Low | High | Thin |
| 9 | Low | High | Thin |
| 10 | Medium | High | Thin |
| 11 | Medium | High | Thin |
| 12 | Medium | High | Thin |
| 13 | Medium | Low | Thin |
| 14 | Medium | Medium | Thin |
| 15 | High | High | Thin |
| 16 | High | High | Thin |
| 17 | Medium | High | Thin |
| 18 | Medium | Medium | Thick |
| 19 | High | High | Thin |
| 20 | Medium | High | Thick |
| 21 | High/medium | High | Thin |
| 22 | High | High | Thick |
| 23 | Medium | Medium | Thin |
| 24 | High | High | Thick |
| 25 | Medium | High | Thin |
| 26 | High | High | Thick |
| 27 | Low | Medium | Thin |
| 28 | Medium | High | Thin |
| 29 | Low | High | Thin |
| 30 | Medium | Medium | Thin |
| 31 | High | High | Thick |
| 32 | Low | High | Thick |
| 33 | High | High | Thick |
| 34 | Low | High | Thin |
| 35 | High | High | Thick |
| 36 | Low | Low | Thin |
| 37 | Medium | Medium | Thin |
| 38 | Medium | High | Thick |
| 39 | High | High | Thin |
| 40 | High | High | Thick |
Element 4: rigour, reflexivity and the quality of the synthesis
Reflexivity in research demands a self-conscious and explicit acknowledgement of the impact of the researcher on the research processes, interpretations and research products. Reflexivity also requires acknowledgement of inherent power dimensions, hierarchies and prevailing ideologies that might influence interpretations and subsequent knowledge production and research products. Our social identities, gender, sexuality, professional socialisation, ethnocultural orientation and political lenses further coalesce to provide a specific perspective on any given phenomenon.
The review team members come from diverse ethnocultural backgrounds and have researched in the fields of ethnicity and health for > 20 years in several global contexts, conducting many externally funded studies. We are imbued with a strong personal and professional commitment to the eradication of inequalities and allegiance to contemporary equality and diversity agendas. From a reflexive perspective, this is important given that immigration is a global phenomena and given the inherent vulnerability of some immigrant women.
Reflexive analysis alerts us as researchers to emergent themes and informs the formal and systematic process of analysis. Murphy et al. 105 define reflexivity as:
. . . we mean sensitivity to the ways in which the researcher’s presence in the research setting has contributed to the data collected and their own a priori assumptions have shaped the data analysis.
Murphy et al. 105
Team members hold a deep knowledge of the semantics associated with describing ethnocultural groups and study populations, which varies between global and sociopolitical contexts. The term immigrant is regarded as pejorative in nature in some contexts. We hold deep understandings of ideologies that manifest in research, publications and, indeed, funding and review processes. Two team members are immigrants to the UK and two team members are UK citizens who have been immigrants to other countries. Of note is that the primary researcher and post-doctoral fellow was a male researcher of Pakistani heritage, which may have created some implicit threats/bias to the interpretation of findings and data. We believe our reflective team meetings, consensus decision-making and incisive debates mitigated these tensions.
Our reflective team meetings enabled and facilitated challenges to primary selection of included papers, emerging interpretations and the extent to which individual subjective lenses had influenced these decisions. The development of themes included an exercise undertaken independently by each team (five team members and one PAG member). Our joint deliberations necessitated the constant review and reading and, in some cases, reviewing the theme allocation and evidence. Therefore, we achieved a refined and nuanced approach, gaining insights into the focus of review.
All decisions and processes were reviewed in reflective team meetings by the research team in order to achieve consensus in decision-making. In our proposal (submitted to the NIHR in 2016) we elected to use the newly conceptualised CERQual, owing to the interpretive nature of our review with a focus on narrative findings. This relatively new tool maps out pertinent dimensions demanding consideration of each individual review finding, considering four dimensions: (1) methodological limitations; (2) relevance, meaning the extent to which the relevant study findings interface with the review question; (3) coherence, that is, the extent to which the finding is grounded in the data from the relevant studies; and (4) adequacy of data, an assessment of the richness of the data informing the finding.
We applied these dimensions to our NS findings that arose from qualitative, quantitative and mixed studies, following personal communication with a CERQual author (Dr Andrew Booth, ScHARR, University of Sheffield 2018),104 regarding the utility of CERQual to our NS. Booth agreed that a modified version may be applicable. We developed and applied this modified version. However, we found the application of CERQual to be problematic because the concepts embedded within it are wholly orientated towards qualitative research. There is little guidance on applying this tool, although team members did engage in an online workshop. In our view, this tool is not wholly orientated towards a NS review. Nevertheless, we did engage in this process and, certainly for the qualitative papers, established a moderate to high level of confidence and relevance in respect of our included studies.
Within the published NS reviews we have seen little evidence of attention to publication bias; however, we sought to eradicate any potential bias by undertaking a comprehensive and exhaustive literature review that included grey literature and follow-up e-mails with authors seeking greater clarity and explanation of opaque issues. A number of the included research studies were identified via ProQuest and e-Theses and do not appear as publications in peer-reviewed scientific journals.
At our national research symposium, we presented our preliminary findings to a wide range of health professions: obstetricians, GPs, midwives, two immigrant women with experience of maternity care services, academics, and voluntary and community workers (see Report Supplementary Material 2). The approach can possibly be considered contentious in respect of systematic review, as participants have no knowledge of the original included papers but do hold deep topic knowledge. However, we found broad support for our findings and facilitated group work activities in order to challenge our initial interpretations. These challenges resulted in the construction of theme 5 (discrimination, racism, stereotyping, cultural sensitivity, inaction and cultural clash in maternity care for immigrant women). These focused activities collectively contribute to the confidence in the review findings, providing verification and validation of the themes.
Individual and group work at the symposium focused on four questions (Box 6). The symposium programme consisted of six sessions and is contained in Report Supplementary Material 2. We shared preliminary findings from the review along with commentary from a GP (CM), on the implications of the findings for practice, and a critical race theorist (KS, Director of Centre for Research on Race and Rights, University of Nottingham). Two recent immigrant women (service users) also shared their experiences of using maternity care services in the UK. The participants were afforded the opportunity to reflect on the implications of the findings for policy and practice both individually and in small groups.
-
Please share your perspectives on implications of the findings for maternity care and service delivery (identifying three key points from each group).
-
From your knowledge and/or professional experience, please identify any intervention(s) that have been or are being implemented to address maternity care needs of immigrant women. Please specify the place, the context and contact details from which we can get further information.
-
How can current policy be used to empower immigrant women to receive good-quality maternity care?
-
In your view, who needs to know the implications of findings from this review?
Our event also included immigrant women with experience of maternity care services who gave presentations regarding their experiences (see Report Supplementary Material 2). We used the event to confirm the credibility of the team’s interpretation and synthesis of the included studies. We gave presentations regarding the theme and then elicited comments. The additional comments elicited at the event were used to inform the discussion; we have not used any of the information elicited in the actual themes, as these are based on the scientific research evidence.
Practical challenges
Use of EndNote for reference management
As the review team was scattered geographically, the sharing features of EndNote proved unhelpful for double-blind screening. References downloaded very slowly from main library.
The EndNote library was set up as a shared library for all of the project team to access. This involved setting up the senior research fellow as the ‘owner’ of the library. The EndNote desktop program installed for each project member could share access to this library and synchronise the content through EndNote online. The library could be backed up regularly using the compressed library feature.
However, issues with synchronisation and with speed of access to the EndNote library prevented full exploitation of the sharing and collaboration features. Although the issues were raised with EndNote support and a number of potential corrections explored, these suggestions did not resolve the problems within a reasonable time, so the project team adopted a different tactic for sharing the EndNote library content for review. The full library content was split into tranches of roughly equal numbers of records and provided to each project member as a separate EndNote library to review individually. The full library content was then annotated to reflect the selections and exclusions from each of the reviewers.
Access to full-text studies
A few small-scale studies that had been conducted back in the 1990s were not available in a digital format. We requested hard copies, but the authors themselves struggled to find them.
Studies published in low-ranked or uncommon journals
The University of Nottingham did not subscribe to some of these journals, so we asked The British Library for access. In some cases, The British Library had to order the articles from another site, which resulted in delayed access.
Lack of full participation from volunteers for patient and public involvement
Some volunteers who signed up initially did not participate later. All were sent invitations to attend the meetings, but a few sent their apologies, others did not respond, and two cited other commitments and resigned.
Conceptual challenges
We observed that authors used a variety of terms to identify participants. Terms used included BME, disadvantaged, immigrants, South Asian origin women, Somali women, Somali refugee women, Palestinian women and Chinese women (including women from Hong Kong, Taiwan and mainland China). However, the term ‘Chinese’ could be used without clearly specifying whether or not the women were born outside the UK. It could refer to immigrants or to UK-born participants who still shared Chinese culture, beliefs and experiences, or to their parents who were born elsewhere. 106 The titles and abstracts alone were often insufficient to make a decision about exclusion, so we read all the papers in detail. When there was a lack of clarity about the study sample, we contacted the authors to ask whether or not the participants were immigrants. Maintaining a contemporary contact list of these authors was challenging, as some of them had retired or held new positions. Our first step was to e-mail the authors to confirm immigrant status. In some cases, however, no valid e-mail address was available.
Challenges were accounted identifying specific findings for immigrant women in mixed population studies.
Search results
Studies included in the review, findings and evidence
Overview of the included studies
Our systematic review using NS86 identified 40 research studies in the scientific and grey literature. A broad range of ethnocultural groups and methodological genres are included in this review (see Appendix 6 and Figure 6 for theme development).
FIGURE 6.
The total numbers of studies involved in each theme. Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
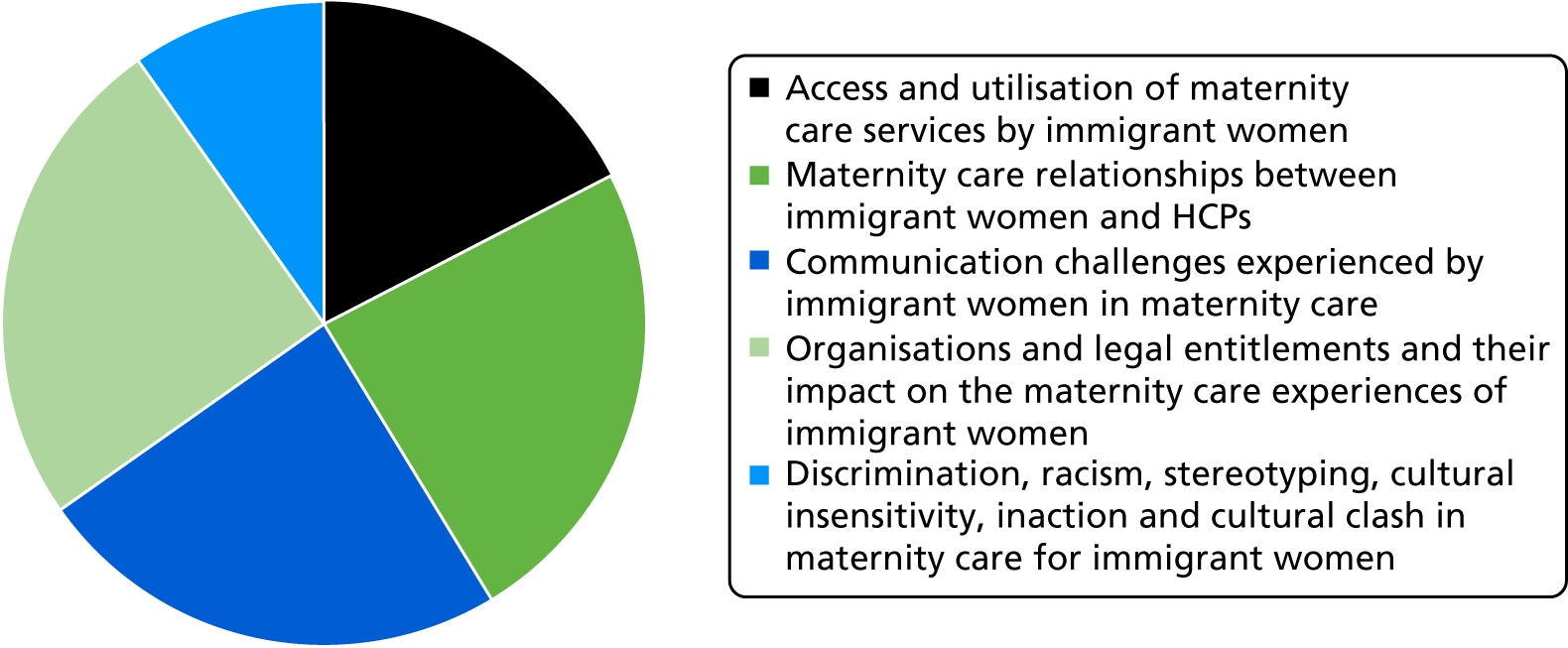
Methodological genres
Qualitative studies
Of the 40 studies included in this review (Figure 7; see Appendix 2), we identified 22 as qualitative research studies, employing a range of qualitative methodologies and approaches. 4,107–127 However, many of these studies did not specify a qualitative methodological genre, but instead employed a more generic qualitative approach and described only the data collection tools used. For example, some presented multiple longitudinal case studies of participants (asylum seekers and refugees), about their maternity care experiences that included photographs taken by the participants, field notes and observations, in addition to researcher interviews. Another example109 was a case study of an ethnocultural group, immigrant women of Somali origin, that used semistructured interviews and focus groups. Some studies used focus groups and interviews conducted in the language of the population group, for example Bengali, Sylheti, Urdu and Arabic. Others used in-depth interviews, open-ended questions, group story-sharing sessions and individual biographical life-narrative interviews. By contrast, a few studies specified a qualitative interpretive approach, which used hermeneutic phenomenology and focused ethnography.
FIGURE 7.
The range of publication dates for the included studies (1990–2016). Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
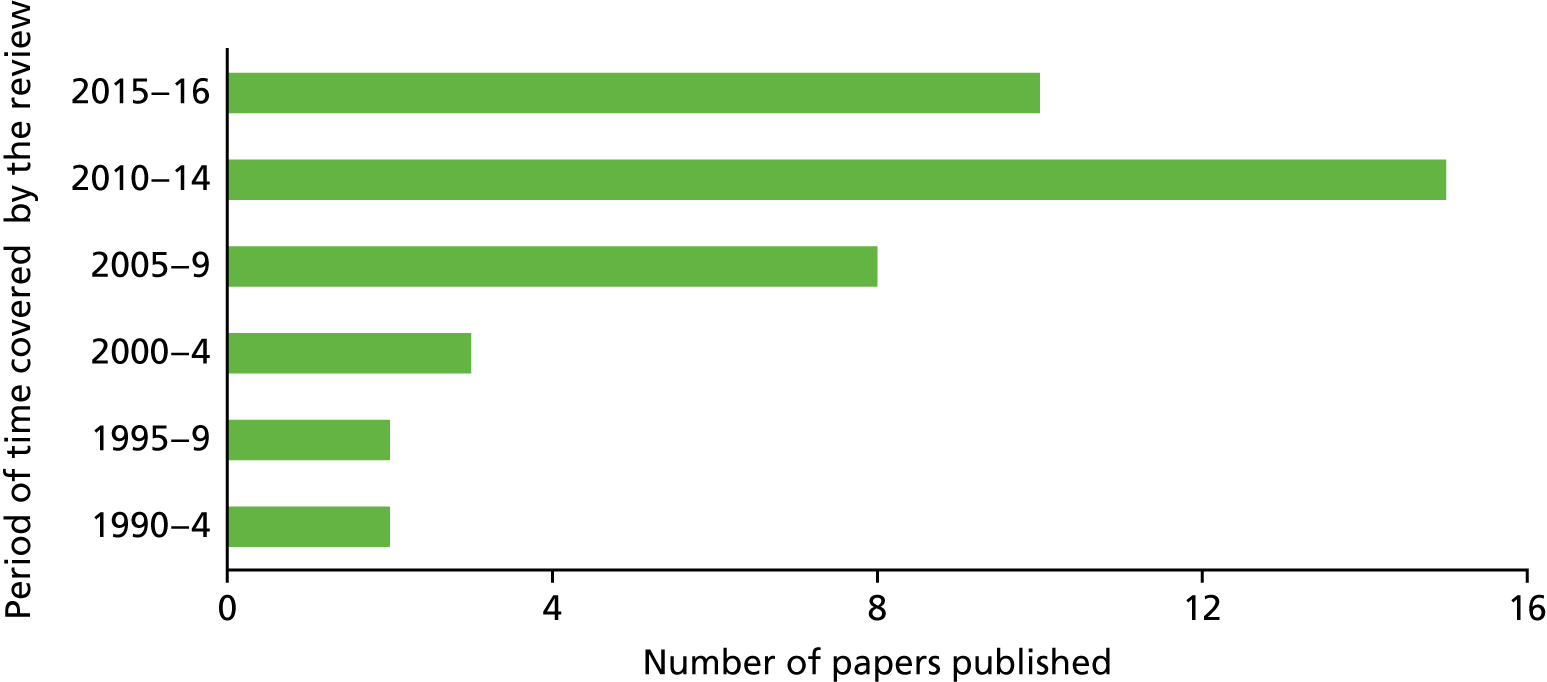
Quantitative studies
We identified eight quantitative studies that used a questionnaire as a tool for data collection. 14,49,128–133 All of these population-based studies and cohort surveys were cross-sectional; none was longitudinal.
Mixed-methods studies
We identified 10 mixed-methods studies using a range of designs (i.e. these studies employed both qualitative and quantitative dimensions). 3,20,47,134–140 For example, Duff et al. 134 reported a two-stage psychometric study in which focus groups and interviews were used in the first stage to develop a questionnaire for an ethnocultural group (Sylheti). In the second stage, quantitative methods were used to test and evaluate the acceptability, reliability and validity of the questionnaire. Other mixed-methods designs included (1) interviewing a small sample of the participants after collecting data from a large-scale survey; (2) conducting semistructured interviews with a small sample of participants based on quantitative data routinely collected from a large group of participants; and (3) using face-to-face, postal and online questionnaires to collect data. One of the studies used Q methodology, which uses questionnaires with structured and unstructured questions.
Studies focusing on specific ethnocultural groups
The chosen studies included participants from a wide range of ethnocultural groups that originated in diverse countries on different continents, including Asia (e.g. Bangladesh and Pakistan), Africa (e.g. Somalia and Ghana) and Europe (e.g. Poland). In some cases, the sample was drawn from a single ethnocultural group, such as Bangladeshi. 136 However, most of the studies were undertaken on mixed samples of immigrant women originating from different countries (e.g. Somalia, Bangladesh and Eastern Europe). Of the studies with mixed populations, we only included those in which the findings where clearly assigned to immigrant women. We encountered a number of relevant studies that did not do so; therefore, we excluded them and entered them in the list of excluded studies (see Appendix 3). Please see Report Supplementary Material 1 for a detailed overview of the characteristics of study participants.
Studies focusing on immigrant women without a clearly specified ethnocultural group
We identified 16 studies that used the term ‘immigrant women’ generically and did not clearly specify an ethnocultural group. In deciding to include these studies, we believed that legitimate proxies for immigrant status could be the specified use of an interpreter or the participants having countries of origin or birth outside the UK. Some studies reported immigrant women arriving from 14 different countries, but did not specify the women’s country of birth; these studies were included.
Studies sorted by immigrant category of the participants
More than half of the included studies (26 in total4,47,49,107,111,112,115,119–121,123–126,128–136,138–140) did not clearly specify the immigrant category of the population they studied (such as economic migrant, asylum seeker or refugee).
Other studies specified the immigrant category as asylum seekers only;109,114,118,122,137 refugees only;108,113,117 or a mix of immigrant categories that included spousal immigrants, economic migrants, asylum seekers and refugees. 3,14,20,116,127 Although a range of identifiers were used, we noted a pattern of reducing immigrant women and their complex cultures, ethnicities and lives to simplified contexts or situations (e.g. ‘asylum seekers’) and of using ‘immigrant’ as a generic label for non-British and potentially for non-white women.
Studies sorted by phase of maternity care
Of the included studies, 17 studies3,20,47,108–110,112,118–121,123–125,133,134,136,140 were undertaken across all phases of maternity care (antenatal, intrapartum and postnatal). Nine studies14,49,111,114–117,128,138 reported on antenatal care alone and six studies116,119,126,131,135,137 focused on postnatal care. Two studies122,129 focused on antenatal and postnatal care, but did not include the intrapartum phase. One study107 focused on the intrapartum and postnatal phases of maternity care and one study4 did not specify the maternity care setting.
Studies sorted by year of publication
The dates of publication for the included studies range from 1990 to 2016 (see Figure 7).
Gaps in the evidence
Few studies focus on (1) recent immigrant and refugees (e.g. from Eastern Europe or Syria) or women of white ethnicities; (2) intrapartum care and immigrant women; (3) quantitative work using sophisticated analyses of relationships, predictability or socioeconomic variables relating to immigrant women and maternity care needs; and (4) economic analyses.
Studies excluded from the review
Some studies of mixed populations gave no clear indication of whether or not the findings were specific to immigrant populations (see Appendix 3).
In the UK context, the term ‘BME’ is usually used in research literature141–143 and policy literature6 to describe population groups that have come to the UK from other countries. However, BME is a very broad term that masks the heterogeneity of this population,144 and individuals in this group would have different expectations of health services and diverse engagement experiences. 144 For example, BME groups would include both first- and second-generation immigrants. However, the two generations of immigrants would have different experiences when engaging with health-care services. Crucially, the first generation often experiences language barriers, but the second generation is born and socialised in the UK and do not usually experience the same linguistic challenges. 145 Nonetheless, both groups are labelled together as BME. Such studies were therefore excluded.
We identified two studies146,147 that reported on mixed samples of non-immigrants and immigrants and provided no separate or clearly identifiable findings for immigrant women. We excluded such studies, as our review focused on only maternity care experiences of immigrant women. Using aggregated findings from mixed samples would have contaminated specific findings for immigrant women in maternity care and would have damaged the integrity of the review.
Chapter 4 Thematic findings
In the following narrative, we present our synthesis of evidence in a thematic form derived from the systematic review process (Figure 8). We define each by scoping out the parameters of the theme. We then examine the context and the mitigating factors, enablers and barriers in the maternity care pathway. Finally, we establish the distribution of themes across the included studies (see Appendix 6 and Figure 7). This contributes towards an evaluation and understanding of the weight of evidence in each theme.
FIGURE 8.
Flow chart of the NS review processes. Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
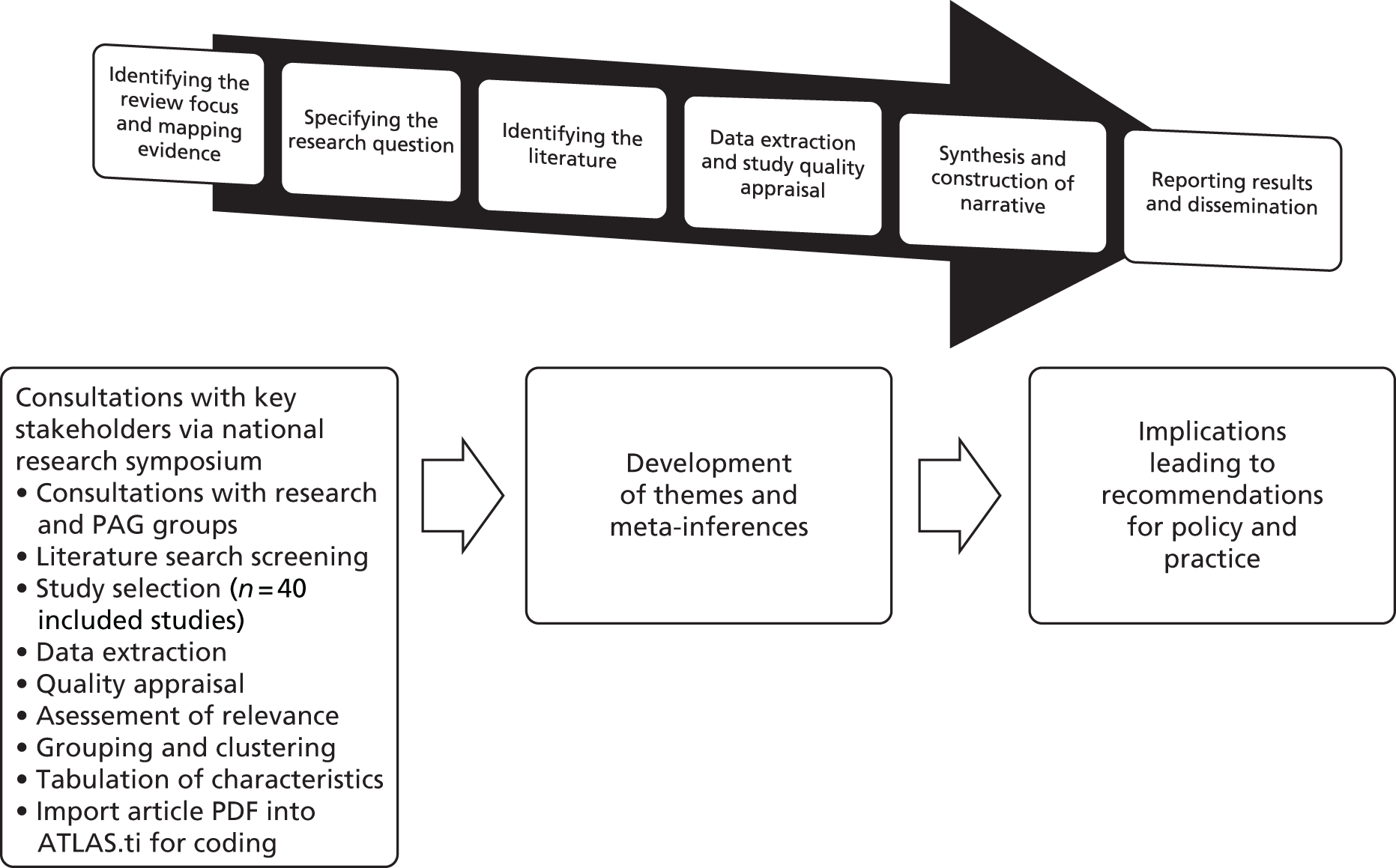
To organise our themes, we used the theoretical framework adopted by Gulliford et al. 23 and the associated four domains of access:
-
service availability
-
personal barriers
-
financial barriers
-
organisational barriers.
In our review, we found research evidence in all four domains that determined access to maternity care. It is worth noting that utilisation of maternity care services is determined not just by adequacy of supply, but also by social or cultural obstacles, financial hurdles and organisational issues, such as the acceptability of services.
These four dimensions proved to be extremely useful for providing a theoretical lens to organise our evidence and investigate the experience of immigrant women. The NHS seeks to provide a universal and egalitarian service; consequently, this might be the most profound and significant dimension of access. Though complex, our review has provided the opportunity for a nuanced and comprehensive exploration of the four facets of access. This stance also interfaces well with NICE research recommendations25 on access and models of service provision.
Theme 1: access and utilisation of maternity care services by immigrant women
Theme 1 maps out and describes the factors that affect immigrant women’s access to and utilisation of formal health-care services relating to their maternity needs, including services delivered through primary care and community settings, in addition to hospital settings. The women received three types of maternity care services: antenatal, intrapartum/delivery and postnatal. Findings in this theme arise from the following ethnocultural groups: women from specific countries in Africa (Somalia, Ghana, Nigeria, Senegal, Eritrea, The Gambia, Ghana and Sudan), Asia (Bangladesh, India, Sri Lanka, Pakistan, Afghanistan and Nepal), Europe (Poland), as well as women from the Middle East and black women from unspecified countries in Africa. The categories of immigrants studied included asylum seekers, refugees, and economic and spousal migrants.
Antenatal services: accessibility and utilisation by immigrant women
Access to antenatal services
The findings identified late antenatal bookings and low rates of attendance for parent education classes among the immigrant women. 121 For example, a study conducted in London found that, out of 29 women, only five (17%) had their first antenatal appointment before the recommended 10 weeks’ gestation. 47 The study noted that 11 out of 29 (38%) women had their first antenatal appointments during their first 12 weeks of pregnancy, whereas 10 (34%) did not visit antenatal services until after 20 weeks’ gestation or even later in their pregnancies. The study noted that 50% of the sample (17/34) attended fewer than the minimum recommended number of antenatal appointments. 47 Late booking among immigrant women was also noted in large studies across England49 and in the West Midlands. 3
Immigrants who had been placed in the category of ‘no recourse to public funds’ (NRPF) (not entitled to welfare benefits), failed asylum seekers, and spousal and economic migrants with short-term employment contacts were less likely to attend antenatal classes or follow-up appointments. 3 Attending follow-up appointments posed a significant challenge for new migrants, who frequently changed address at short notice and then would forget or did not have time to share the new address with maternity services. 3
The legal status of the immigrant women could influence their choice to register with maternity services. For example, women with immigration challenges did not register with maternity services because they feared that immigration authorities would access the data, track them and then remove them from the UK. 3 As a host of systems and services that are geared towards immigration status engage in increasing levels of scrutiny of residency or citizenship documentation, this concern should be seen as emblematic of the health-care system’s role within a wider system of surveillance. Some women were not clear about the purpose of the antenatal appointments121 and reported that the duplication of activities within the antenatal appointments was frustrating. 111
Many immigrant women were not aware of parent education classes, particularly asylum seekers and those with low levels of English. 121 Women with female genital mutilation (FGM) coupled with low levels of English were also identified as more likely to experience difficulties in accessing antenatal services. 117 Some immigrant women also mentioned that they were not aware of the content of parent education classes. 121
A study exploring experiences of maternity care in the UK by women of Muslim faith noted that HCPs tended to assume that immigrant women (in this case of Asian origin) were not interested in attending parent education classes. 121
Other reasons cited for not accessing antenatal services are lack of transport and not being able to afford transport. 3 Some immigrant women did not attend antenatal care because they feared that they would be required to pay. 47
Immigrant women of Somali, non-Somali African and Eastern European origin had much higher rates of late booking than native British women. 47 However, the ability of immigrant women to access antenatal services increased over time. 117 Additional time spent in England improved the English-language skills and social support networks of immigrant women, and both these factors helped to improve their access to antenatal services. A study117 also noted that if these services had a bad reputation in the community, informal communication via social networks can discourage immigrant women from accessing the services. Other factors affecting their access to antenatal services included family size, the number of young children, the financial conditions of the women, the ability to drive or to use public transport, the geographical proximity of the health services and the marital status of the women. 117
Immigrant women in the asylum-seeking category did not receive formal support to understand the configuration and delivery of maternity care, these women only became aware of the availability, processes and practices of maternity services through informal social networks of other asylum seekers. 118 These challenges delayed their initial booking visits for antenatal care. 118 A study3 conducted in the Midlands found that half of the immigrant women in the sample did not have the name of the midwife to contact when they were in need of support or advice.
Legal requirements governing the asylum-seeking process also hampered some women in accessing antenatal care. For example, a study3 reported a case of a human immunodeficiency virus (HIV)-positive asylum-seeking African woman who was detained for 2 months and barred from accessing maternity care:
The Home Office put me in detention centre so I could not attend my appointments. There were no maternity services there for me for the 2 months I was there. I was offered appointments, but they were cancelled at short notice without anyone telling me why.
African, undocumented and at that time an asylum seeker20
Asylum-seeking women were also noted to be heavily engaged with their asylum-seeking cases, the legal process involved and their fundamental needs (e.g. acquiring housing), all of which were more important to them than attending antenatal care and follow-up appointments. 3 Some women in the economic immigrant class feared that their employers would not give them time off to attend follow-up appointments and consequently skipped these appointments. 3 Some new immigrant women did not have access to a telephone and so could not book an antenatal appointment. 3 The new immigrant women also experienced difficulties in locating the hospital and in finding the correct public transport to access antenatal care. 3 The findings noted that, in the UK maternity care system, procedures and processes are based on the assumption that the service users have the cultural health capital required to navigate and access relevant services; however, this may not be true for immigrant women.
The evidence suggests that immigrant women of Somali and Bangladeshi origin perceived antenatal classes as a medicalisation of childbirth, which for them is a natural process. This perception is a barrier to antenatal care uptake. 3 However, a study focusing on preventing adverse obstetric outcomes among Somali women found that the women did have knowledge of emergency health care and the NHS emergency telephone number, which was reassuring. 4
Utilisation of services
Some immigrant women stopped attending antenatal appointments because they perceived that their husbands, who were being used as interpreters, were not communicating their concerns and the care procedures. 3 Many women avoided going to parent education classes because they were offered only in English. 20 The evidence in the studies indicated that Muslim male partners did not find it appropriate to attend antenatal care classes that were composed of Muslim and non-Muslim women. 121 A few women in the study also felt that the male presence in parent education classes was inappropriate and argued that childbirth should be a women-only sphere. 121 Other women in the study wanted their husbands to take part in the classes so that the women could get support from them:121
If they are going be there at the birth, then they need to know.
Participant xyz. 121
I just felt that my husband could have been better prepared if he knew, you know, what area to support me in.
Participant xyz. 121
You know, like you have to tell him everything. It is better that someone tells him before you have the baby that this is the kind of support she will need, because then you feel like a nag.
Participant xyz. 121
In one study, some immigrant women were not clear about the value of routine ultrasound scans; hence, they stopped attending antenatal visits. 111 Other women in the study111 considered seeing an obstetrician even for low-risk pregnancies. Immigrant Somali women with FGM indicated their disapproval for deinfibulation in the antenatal period. 117
The culturally defined health behaviour of immigrant women is an important facet of their access to and navigation of maternity care services. Some studies reported findings related to cultural influences on women’s health behaviour. For example, a qualitative study115 exploring sociocultural influences on the behaviour of South Asian women with diabetes in pregnancy noted an absence of personal coping strategies and a lack of intention to make changes in lifestyle, such as diet and exercise, to reduce the risks.
What would a good antenatal service encompass?
This review evidenced new models for antenatal care for immigrant women in the UK. 121 For example, in a study soliciting views of immigrant women and HCPs, the findings suggested the provision of community-based antenatal services that are culturally and religiously sensitive and that involve local community and volunteer groups along with midwives and other HCPs. 121 Some women were of the view that male-only antenatal care might encourage their Muslim husbands to attend these classes so that they would be better able to help them in their pregnancies. 121 The women in this study121 further suggested that the antenatal care classes for Muslim women should include a Muslim educator who could provide culturally and religiously sensitive explanations on pregnancy and childbirth.
To increase awareness of antenatal services, Somali immigrant women in one study117 suggested that graphic representations in a ‘comic book-style brochure’ on health education could be helpful. Such brochures could present the advantages of prepregnancy deinfibulation. Some immigrant women found that receiving text messages from antenatal clinics on their mobile telephones to remind them of their appointments was also helpful. 111
Intrapartum care services: accessibility and utilisation
Findings from a review by Gorman et al. 131 indicated that Polish immigrant mothers had higher rates of instrumental delivery in Scotland than in their country of origin. Somali immigrant women perceived hospital birth to be safer and they had a strong preference for this over home birth. 117 However, they expressed mixed views on the need for a caesarean compared with normal birth.
Somali immigrant women who anticipated an episiotomy preferred to have deinfibulation in the final stages of labour stage to prevent experiencing surgical interventions twice. 117 Some Somali women delayed accessing intrapartum services because they feared creating trouble in the system, which may not be helpful in preventing adverse obstetric outcomes:4
My husband and I were waiting to see if the pain got worse. We did not want to cause trouble in the system.
Somali woman, aged 24 years, 2 years in UK, three children4
Although we note that such statements could be interpreted to mean that the women did not wish to cause undue fuss and attention by announcing any problems or issues to their practitioners, we also note that women who had already had high levels of stress and agency interaction, such as asylum-seeking pregnant women, may be especially concerned about being ‘in trouble’ within the system.
Pictorial representations in health education brochures were found to be a useful tool for increasing the knowledge of immigrant Somali women regarding emergency caesarean sections. 117
Postnatal services: accessibility and utilisation
Evidence from included studies suggested that participants found that their hospital stays were longer than they expected. For example, one study47 found that 24 out of the 35 immigrant women sampled (68.57%) reported inpatient stays that were 2–11 days longer than they expected. The reasons for longer stays related to both the baby and the mother, such as the baby requiring antibiotics, the mother having high blood pressure, or the mother recovering from a caesarean section and loss of blood.
Lack of money limited the opportunities of many of the participants in our included studies to access and utilise postnatal services. Women from the asylum-seeking and refugee categories were often unable to buy clothes and pushchairs or to attend baby health-check appointments with health visitors. 20 Evidence suggested that immigrant women with no access to welfare benefits found it challenging to manage the expense of feeding their babies with formula milk. 116 Sometimes these mothers prioritised their child’s dietary and health needs over their own:
It is so hard to live on vouchers only. I can’t go for an appointment.
Congolese asylum seeker, Birmingham3
One study demonstrated that participants were not well informed about the amenities available at the hospitals, such as baby changing and feeding facilities. 139 For example, an immigrant woman from the Middle East was not aware of the toilet facilities and she did not ask about it owing to her limited English-language ability. In addition, some women were not aware that a male circumcision facility was available in the hospital.
Acceptability of baby care
A study on the evaluation of postnatal care found that immigrant women of Middle Eastern and European origin received adequate and appropriate information, as well as practical demonstrations from hospital staff, on a wide range of information about caring for their baby,139 for example how to carry the baby, bathe the baby, change nappies, clean the baby’s navel area, settle the baby, massage the baby’s stomach, clean a baby’s sticky eye, maintain safe sleeping positions, control the room temperature, burp the baby, immunise the baby and address the baby’s jaundice. The women from the Middle East rated the baby support that they received in the UK more positively than that in their home country.
A study evaluating bilingual peer support for breastfeeding noted that the support worker did not inform the immigrant women about the breastfeeding classes and none of the women from the study sample attended such classes. 135
Advice on infant nutrition
Evidence regarding advice on infant nutrition was reported by one study. 140 The women reported being confused and disoriented when they were attempting to balance the information received from NHS literature, from health visitors, and from their own social and ethnic network:140
In Africa I was observing what my mothers were doing, what another woman are doing. I introduced solid food to my kids when they were at 4 months. Here information is different. It is confusion because my mother-in-law is telling one thing and a health visitor is telling other.
Maggie, African mother. 140
The evidence from that study also indicates that the midwife can play a very important role in advising women on infant nutrition:140
When I was pregnant, midwife visited me. She left me some leaflets, some of them were in Polish language so it was very helpful. It was very useful . . . It was my first contact with NHS.
Kasia, Polish mother140
Suggestions for improvement in antenatal care included setting up a local community-based ethnicity-specific (e.g. Asian) parent support group, with targeted marketing to increase attendance. 121 These women found their support group helpful in terms of learning how to better care for their children. The women mentioned that they would not have attended if the group had been held in a health-care clinic.
Conclusion
Evidence from our included studies indicated that many participants experienced several accessibility barriers to maternity care. They also faced many challenges in uptake and continuing to utilise these services because of perceived insensitivity to their culture and religious needs. The system was also reported as being designed primarily for the general population and not for immigrant women, highlighting the ways that the health-care system may not currently accommodate diversity.
Gaps in the evidence
More studies are needed relating to interventions and their effectiveness in enhancing accessibility and utilisation of maternity care for immigrant women.
Theme 2: maternity care relationships between immigrant women and health-care professionals
Maternity care relationships in the context of this review mean interpersonal relationships between HCPs and immigrant women during the provision of technical or physical maternity care, and emotional, physical, and psychological support. The relationships between service users and maternity care professionals, such as midwives, GPs and health visitors, are significant in determining the accessibility and quality of maternity care. This theme discusses in more detail the dynamics of building positive relationships between immigrant women and HCPs in maternity care. The findings were mixed, suggesting both positive and negative relationships between maternity care professionals and immigrant women. Positive relationships facilitated a safe environment in which women were able to engage with maternity care professionals in identifying their care and many had a positive experience with maternity services. Positive relationships had good communication, cultural sensitivity and no stereotyping or cultural humility. 148 By contrast, negative relationships are the opposite and may manifest in negative behaviours, such as lack of respect, dismissive communication, failure to respect cultural norms and poor or ineffective communication.
The following subsections give critical accounts of various dimensions of a positive relationship.
Relationships with midwives
From the perspective of immigrant women, a good relationship with the midwife is established when the midwife is caring, kind and helpful in enabling the needs of the immigrant women to be met. 127 However, we identified substantive evidence indicating that the immigrant women born outside the UK continue to be unclear on the role of the midwife in meeting their maternity care needs. 138 This lack of clarity may be due to different perceptions of doctors and midwives in the birth countries of the participants. For example, most of the maternity care needs during the antenatal phase in the UK are provided by midwives, whereas pregnant women with physiologically uncomplicated pregnancies in some other countries (e.g. South Korea and Pakistan) visit gynaecologists and medical doctors for maternal check-ups and medical tests. 127
We identified variability in the quality of, and perceived satisfaction with, the relationships between midwives and immigrant women in different maternity care settings. For example, in a study110 involving asylum-seeking women and maternity care services, high levels of satisfaction with antenatal care were expressed and some of the women had good relationships with their community and specialist midwives:
I received information about depression that women may have after having baby. This gives me some comfort that this may happen to all of us. It was important for me not to feel ashamed that I feel depressed and where I get support. It was very useful for me.
Susanne, Czech mother140
However, relationships during labour and postnatal periods were sometimes reported to be poor, with some, but not all, women experiencing perceived racism, indifference, rudeness and disrespect, as well as feelings of being powerless and coerced. 110 When seen through the lens of the previous considerations of surveillance, racism and causing ‘trouble’ within the system, these issues suggest that more systemic dynamics may be at play, which are less to do with the insensitivities of some, but not all, individual members of staff and more indicative of a system-wide framing of service delivery and care for immigrant women who may disadvantage them because of assumptions about their experiences and capabilities.
The findings suggested that asylum-seeking black women of unspecified African origin perceived that some of the care and health-care practices were coercive. For example, decisions about commencing an induction or a caesarean section appeared to be taken exclusively by the staff. 109 To highlight such coercion, McLeish109 cited a participant quotation:
When they wanted me to stay in hospital because of my high blood pressure I refused . . . I went home . . . They took me by force. They rang the police and told them to bring me back to the hospital.
Participant 5 staff109
When combined with the potential instability and uncertainty in some immigrant women’s lives, especially due to their immigration status and social circumstances, the participation of the health-care system in what appears to be violent and compulsory practices is concerning. Rather than taking sides, however, we see this participant’s perspective as crucial to spurring a reassessment of the practice of service and the challenges of properly communicating procedures and risks, especially within circumstances that may already be fraught with tension and mistrust of authority figures (which would include the NHS from the perspective of some of the mothers).
In cases when women did not have open communication with their midwives (e.g. feeling comfortable in disclosing their FGM), they were unable to share all their concerns and cultural needs. 117 Some immigrant women perceived their midwives to be cruel,108 and a woman in one study124 reported a very bad experience during labour. The midwife asked this woman to walk to the labour ward with her membranes ruptured, shouted at her during labour, refused to hold her hand and argued with the woman’s birthing partner about the practice of FGM.
During the postnatal phase some immigrant women reported that the midwives were angry with them when they approached midwives for help. 108 Midwives were also reported as being unkind, unfriendly and uncaring. 107 For example, an African immigrant woman complained that, after she had undergone a caesarean birth, the midwife did not look after her vomiting baby and left her alone at night. 107
Clearly, some women felt that their interactions with the midwives were devoid of cultural safety. These situations can occur when the demands of the system on the birth practitioners are translated by the women as culturally insensitive care:
I do not think the midwives were friendly with me. When I was delivering him, without my mum . . . I took one of their hands she said to me ‘Don’t touch me!’ I had to say to her ‘Sorry!’ . . . I thought she might hate me she might not help me.
Participant 1109
Although the study107 did not identify the maternity care setting clearly (such as antenatal, postnatal, or labour suites), the event was in a hospital setting. Furthermore, immigrant women feel midwives are too busy in hospitals and they lack support from midwives, particularly if the women had undergone caesarean deliveries. 107
Some women described experiencing more positive birth experiences in their countries of origin than in the UK. 123 This view often developed from poor treatment by midwives. However, this result conflicts with evidence we presented earlier that Middle Eastern women preferred UK birth experiences:
I am so disappointed that I delivered here, in spite of the midwife was nice, but she did not compensate for the general way [I was dealt with]. I maintain that delivery in Jordan is much better – there is no comparison . . . ‘Third World’, they empathise . . . here the indifference is perceptible.
Participant, Rahma. 123
Some women felt that community midwife visits were too short and were not helpful or congruent with the level of support they needed. 139 These women also expressed that the midwives engaged in poor communication, although the study did not explain how this poor communication manifested. 139 By contrast, a few women from the same study thought that their community midwives were most helpful and that the midwives offered them and their babies optimal maternity care and clinical support. 139 Instances of positive relationships with midwives postnatally also included new mothers reporting ‘very good’ support and education on baby care. 139
Immigrant women from the asylum-seeking category felt that midwives did not know their difficulties and never asked them about their immigration status. 118 The midwives also did not take into account their poverty and living conditions when giving maternity advice; therefore, such advice was not helpful for these women because it was not tailored to their specific situation. 118
Factors promoting satisfactory and positive relationships
When the midwives and immigrant women reported an open, comfortable and safe relationship, the women were able to discuss sensitive issues such as FGM,139 asylum-seeking and parenting. 137 Awareness of the immigrant women’s religion and culture played an important role for the midwives in developing positive relationships. 117 It indicated a high level of cultural sensitivity55,65,149 and an appropriate regard for the cultural safety51 of the immigrant women. The analysis identified positive examples of midwives who offered wider treatment options to immigrant women as a matter of course, and showed respect for their cultural and religious needs. In a study108 based in West London, the participating women reported that they had received helpful information on pregnancy and labour from their midwives. In a qualitative study,107 mothers also reported positive and trusting relationships with their midwives during labour and postnatally. Factors that strengthened a trusting relationship with the midwives and increased the quality of communication included maintaining a continuous presence during labour (which was seen as a comfort for the women) and keeping the husband fully informed and aware of the situation.
In some instances, midwives intervened to improve the living circumstances and the access to benefits of asylum-seeking women by referring them to the appropriate services. For example, one study118 reported how a midwife supported an asylum-seeking woman by writing a letter to the Home Office to prevent her dispersal (forced relocation to another area). Another community midwife helped an asylum-seeking woman to get her benefits, and a community midwife visited a woman on the postnatal ward to provide additional support to reduce her isolation and loneliness. In this same study, immigrant women felt that more time and attention, rather than less, was needed from the midwives during the postnatal period, because they lacked sufficient energy and resources to look after their baby properly after giving birth. 139
Rather than receiving ‘orders’ from midwives, the women understandably wanted to be actively involved, have choices and receive explanations of procedures:
She [the midwife] was asking me, ‘Why do you want this medication? You have a sour stomach now?’ . . . the doctor always gives me Zantac with any medication. If you are not convinced, call the doctor. But she would not listen to me.
Participant xyz123
Improved staffing levels on the postnatal ward (a universal theme) were needed to improve the quality and experience of care. 107 Although women preferred early discharge, they expected that the postnatal home midwifery care would replicate the care offered in a hospital setting. 110
Relationships with general practitioners and medical staff
Some findings related to the relationships between immigrant women and GPs and other medical staff. Immigrant women complained that often they were not treated with respect and sometimes misunderstood communications articulated by medical staff. 133 Some immigrant women reported experiencing aggressive behaviour from health professionals (unspecified), and one service user even reported a breach of confidentiality by her GP who was also a family friend. 126 Some immigrant women reported a lack of communication from doctors. 139 Overall, GPs were perceived to have a minimal role to play in antenatal care, which reflects the midwifery-led UK model of maternity care. However, this lack of medical input may contrast with the care women received in their country of origin. 111
Evidence of negative relationships was found when doctors did not explain to the immigrant women why they would not get the medicines they were normally prescribed for minor illnesses. 124 The studies highlighted differences in prescribing practices between the UK and the immigrant women’s countries of origin that led to unmet expectations. This negative perception was attributed to the UK emphasis on ‘self-management’ and ‘over-the-counter’ medicines, rather than prescribed remedies, for treating minor illnesses when compared with countries such as Pakistan127 and South Korea. 124 Consequently, the immigrant women reported feelings of insecurity and perceived that this lack of medical treatment might increase their risk of complications during their pregnancy. 124
Some immigrant women experienced racism or stereotypical comments and attitudes from some medical staff. 107 One study that provided an example of a racist attitude included the use of the term ‘Asian woman syndrome’, suggesting that the professionals perceived that women from an Asian background commonly exaggerated their symptoms and complained too much about minor illnesses. 121 These cultural assumptions were expressed in ways that the mothers felt were not only unprofessional but also may have jeopardised their care. Evidence arising from one study suggests that the negative attitudes and behaviour of some but not all GPs resulted in poorer access to care for the immigrant women and non-adherence to health-care advice. 111 In some cases, women (in this case Muslim women) would compromise on their cultural needs to avoid insensitive treatment from maternity care professionals:121
When I was referred, I was given the choice of a woman consultant, but the woman consultant is a nightmare. She’s really, really insensitive, so I chose to be referred to the man because of the insensitivity of the female.
Participant xyz. 121
Relationships with health-care professionals
Under this subtheme, we present findings from studies that used the terms HCPs or maternity care providers, but did not make clear which professional group they studied. Health visitors are included here because they are registered nurses or midwives who have undergone further training and gained additional qualifications.
The findings highlighted the relationships between immigrant women and health visitors and the ways in which these relationships affected care. Health visitors were reported by some women to be the best professionals they saw in the community setting, these professionals were keen to help the women and provided health-care support, emotional support and childcare needs. However, other immigrant women reported superficial engagement and a lack of thoroughness by health visitors who, for example, failed to explore their postnatal mental health in sufficient depth. 126
The women from the asylum-seeking category perceived feeling ‘labelled’ as asylum seekers and consequently felt that they experienced poorer and different care. In one instance, staff made assumptions about the woman’s health-care needs, such as undertaking a vaginal scan and asking her, unprompted, if she would like to terminate the pregnancy:118
They do me . . . vaginal scan? To check the baby . . . They ask me again if you want to take out the baby?
Participant 5118
The asylum-seeking women were distressed by being treated differently when accessing care. For example, a receptionist in a walk-in clinic shouted at a woman when asking her to provide her passport. Another woman had a negative experience when she encountered a receptionist who made derogatory comments about her non-working status, demonstrating her ignorance of the ineligibility for employment of asylum-seeking women:118
To register in our nearest GP . . . reception ask us . . . You have to bring . . . bills. And I told her, we don’t have bills ‘So you’re not working?’ . . . And I feel like! . . . I’m forbidden to . . . I feel . . . very bad.
Participant 5118
The immigrant women noted both subtle and direct forms of discrimination from the staff. 121 Subtle discrimination was by non-verbal communication and by addressing immigrant women’s requests and questions in angry and inappropriate ways. Direct discrimination included unfair, racist and stereotypical comments and assumptions being made based on a woman’s perceived cultural background:
I saw a consultant . . . She was not nice. She was very abrupt. ‘Did you circumcise?’ . . . I didn’t know women can be circumcised! ‘I’m asking you, are you circumcised?’ I don’t understand.
Participant 3118
No one offered me any antenatal classes . . . Nobody mentioned it to me . . . I really wanted to go but they [health professionals] don’t mention it to you. That’s the thing . . . [They think] Asian people don’t want to come to these antenatal classes.
Participant xyz. 121
Some professionals were found to be stereotyping immigrant African women as having an abnormally high pain threshold. 20 The stereotypes held by professionals on pain negatively affected the care received by the immigrant women, who perceived that they were not offered timely and sufficient pain relief. Some women also complained about a lack of emotional involvement by the HCPs. 123 That lack, together with discrimination, was felt to impair them from providing proper explanations and committing to shared decision-making during the care of immigrant women. 3,110
One study139 noted that a few immigrant European and Middle Eastern women felt that the professionals at the hospitals were easily accessible to them all the time, and they could ask them for prompt explanations and information at ‘the press of a button’:
If I ask them about something, they always told me what to do and they show me how to do this . . . Actually, they were everywhere, so it was easier for me to ask . . . if I press the button. They came to check what is wrong. 139
The women from European and Middle Eastern backgrounds also perceived community HCPs to be accessible, including by telephone. Some women were less satisfied with the telephone contacts because of their limited English-language skills. 139 Even though language was a barrier,108 the immigrant women in the asylum-seeking and refugees categories in many instances felt welcomed by ‘the staff’,110 cared for,122 and offered good service coupled with high attention, consideration123 and equal care. 139
The findings identified a lack of trust between maternity care providers and some immigrant women, especially on the need for caesarean section as a mode of delivery. 107 Mistrust between the maternity care professionals and the immigrant women can negatively affect the ability of the professionals to provide the expected quality in service. 113 If sufficient mistrust exists between the professionals and the immigrant women, some of the women might get their maternity care outside the UK. 4
To improve these relationships, the immigrant women highlighted that empathy and culturally congruent care from the professionals would help them to feel more positive about their experience of maternity care. 111 For some immigrant women, employing maternity care professionals of similar ethnocultural origin was important in building trust and enhancing communication. An alternative view argued that qualities such as being respectful and professional were more important than ethnocultural similarity. 113
Conclusion
This theme identified that positive relationships between immigrant women and maternity HCPs was critical in the access to and uptake of maternity care. Multiple factors influenced these relationships positively or negatively. Being respectful, caring and professional were key dimensions in developing positive relationships with immigrant women and these positive dimensions are reported in a number of studies. Conversely, stereotyping, racism and disrespect from maternity care professionals discouraged immigrant women from obtaining equitable access to the services and impeded adherence to professional advice.
Gaps in the evidence
Studies using social and psychological theories of ‘otherness’ and ‘difference’ are needed to more completely address the factors associated with negative and positive relationships between HCPs and immigrant women. Additional studies are needed, emphasising the structural dynamics within health systems that may encourage negative relationships between service users and health professionals.
Theme 3: communication challenges experienced by immigrant women in maternity care
Communication extends beyond articulated words; therefore, this theme covers both verbal and non-verbal types of communication. It also includes written information on maternity care offered by health-care services in antenatal, intrapartum and postnatal care settings in the UK. Verbal communication occurs through words of a shared language among individuals. English is the language of everyday business for maternity care services in the UK. Therefore, immigrant women with low levels of English-language proficiency find it difficult to communicate with and understand their service providers, particularly if medical or professional language is used,150 and this can result in inability to access maternity care and a lack of interaction within it. This theme is central, as the findings have identified that ‘language is really the key to everything’117 in maternity care.
Non-verbal communication occurs without words and it includes facial expressions, gestures and pictorials. 151 It can be explicit or non-explicit. Importantly, non-verbal communications are culturally defined; for example, a particular gesture can have different meanings for different ethnocultural groups.
Studies included in this theme also report findings on how verbal and non-verbal communication can affect the abilities of immigrant women to access and utilise maternity care services equally. Some studies reported interventions and their effectiveness in improving direct communication between HCPs and immigrant women. This theme also covers interventions to enhance the accessibility and uptake of printed and digital information for immigrant women.
The HCPs with whom immigrant women communicated in these various studies included midwives, GPs, community midwives working in primary and secondary care, obstetricians and sonographers. 111
Findings in this theme relate to the following ethnocultural groups: Indian (Punjabi, Gujarati, Urdu and Tamil speakers), black African and Caribbean women of unspecified origin, African (Somalian, Sudanese, Gambian, Ghanaian and Eritrean), Pakistani, Bangladeshi, Middle Eastern (Arabic and Kurdish speakers) and Eastern European (Polish and Czech). The participants were either asylum seekers, refugees, or spousal or economic migrants.
Impacts of language and communication barriers to access and utilisation of maternity care
The findings indicated that some immigrant women were able to neither speak nor write in English. 132 Women with limited levels of English-language proficiency used gestures to express their needs:110
I waved my hands [to communicate].
Abeba, 2 weeks postnatal110
Lack of proficiency in understanding, speaking and reading English resulted in many challenges for immigrant women in maternity care services, including a limited awareness of available services, an inability to access services, an inability to articulate their health and maternity needs to service providers, and an inability to be understood by HCPs. Importantly, abuse and safeguarding issues may not be noticed without proper language support. These issues can be especially important in countries in which patriarchy is the cultural norm, such as India and Pakistan. One study3 reported the following situation from their sample:
One ‘No Recourse to Public Funds’ South Asian respondent, raped by her husband, told us she had wanted an abortion. However, her husband attended every appointment speaking directly with maternity professionals while clearly excluding her from decisions. She explained that she wanted an interpreter to report the abuse.
Phillimore3
Language fluency and communication play an important role in developing maternity care relationships. Lack of mutual understanding between immigrant women and HCPs led to visible frustration and anger on the part of the HCPs, hindering relationship development:113
The problem we Somalis have here as a refugee or as foreigners or as immigrants is the language . . . Everyone will be fed up with you if you can’t understand what they are saying – if you can’t talk to them . . . sometimes they will just ignore you.
Somali woman, informant 1113
Before they discharge me, the midwife came to me, my husband was there. She tried to explain a few things how to lie down the baby in bed and how to register his birth and how to look after the baby, how to feed him. But he didn’t understand.
Meena, 2 weeks postnatal110
Lack of speaking and understanding the English language often resulted in miscommunication between immigrant women and HCPs. 20 Often the immigrant women did not understand care procedures and their outcomes, discouraging them from fully taking advantage of maternity care services111 and negatively affecting their experience with the health professionals. 126
Language and communication barriers affected almost all phases of maternity care. In terms of antenatal care, language and communication barriers are cited as reasons for immigrant women booking late3 and therefore failing to access the recommended minimum number of antenatal appointments. 47 In a multivariable model of a quantitative study,14 the authors noted that the inability to speak English had an independent effect, increasing the late initiation of antenatal care among immigrant women [do not speak English and not born in the UK: n = 1060, odds ratio = 1.47 (95% confidence interval 1.23 to 1.76)]. 14 In another study, immigrant women wanted to attend parent education classes but did not because they were offered in only English. 20
Immigrant women with limited English-language proficiency felt both frightened107 and ignored by HCPs. 113 Consequently, the women developed the view that they were not being supported properly by HCPs and worried that they would develop complications in their pregnancies. 108 Limited language proficiency in some women hindered their involvement and decision-making regarding their care, specifically during delivery. 121 Often women gave consent for clinical procedures without fully understanding the explanations provided by the HCPs:20
How are they asking people if they do not even understand, you know? It is the matter of understanding . . . Most . . . don’t even understand the questions they are asking, so how do they expect them to, you know, give their consent for whatever is being done to them?
Participant xyz121
I was referred to another hospital, they did not advise why. At my third appointment, I had an interpreter. The whole process was rushed, I did not know what to expect. I did not feel involved in any of the decisions – someone else always made them for me.
Chinese, failed asylum seeker20
Limited English-language proficiency also limited the offers the immigrant women would receive for a wide range of available care options. Such women did not receive proper advice on baby care, including on immunisation139 and feeding their babies. 110 In one case, the communication barriers between HCPs and a service user resulted in the service user misunderstanding that formula milk was a better option for her baby than breastfeeding. 110 Immigrant women who experienced discontinuity in maternity care experienced more difficulties relating to communication. 108 However, some women or their partners were found to initiate communications in organising appointments and clarifying procedures in their care. 123 Poor communication between the women and HCPs sometimes occurred when the professionals noted a possible challenge in the pregnancy but did not share their concerns with the women. 111 Other manifestations of poor communication included the HCPs sometimes being discourteous, compassionless and abrupt. 111
The evidence indicates that the women regarded a reassuring and engaging type of communication as more effective. 111 Furthermore, women with low levels of English proficiency felt that receiving written information, such as a letter for referral, from the HCP was more helpful than receiving verbal information alone. 122 Similarly, careful listening to the concerns of the women and taking time to explain things also improved communication. 108
Interventions to reduce communication barriers that impair access and utilisation
The findings from this review identified three types of interventions to address the language and communication challenges, and to improve communication between HCPs and immigrant women: (1) formal interpreting services; (2) informal interpreting by family or friends; and (3) linkworker and advocate services.
Formal interpreting services
The findings highlight that not all women with low proficiencies in spoken English had interpreting support. The availability of interpreting services within maternity services was variable at best. It was often poor or not available when needed. 113 For example, participants in one study noted that the interpreters were not provided during their postnatal stay at the wards and postnatal visits:
I asked them [the midwife], ‘[Can] we cancel the meeting until we get an interpreter . . . I didn’t understand you and you didn’t understand me.’ She said, ‘No, it’s OK, we can go on – you understand English’.
Participant 3118
In some cases, the women were not aware of the availability of formal interpreting services such as the Commission for Racial Equality service (since replaced by the Equality and Human Rights Commission), or a telephone interpreting service called LanguageLine (LanguageLine Solutions, London, UK). 108 The women found the telephone ‘LanguageLine’ service difficult to use and confusing for effective communication, but they were happy with the Commission for Racial Equality interpreters. 108 The HCPs also noted that this telephone interpreting service was complicated to use. 113
Given the increasing diversity of language needs, it was challenging for the HCPs to organise formal interpreters to facilitate appropriate examinations of the immigrant women. Often the HCPs were not able to identify interpreters for languages not spoken widely or were unable to book interpreters in time. Sometimes interpreters were unable to attend appointments or were not able to understand complex medical terminologies. In some instances, male interpreters were available, but the religious norms for immigrant women of the Muslim faith made male interpreters unacceptable. Often, husbands would interpret for their wives instead. 121
Informal interpreting by family or friends
Informal interpreting is a second type of intervention. Immigrant women often had no option other than to arrange their own interpreters from among their family or friends, including their own children or even male associates. However, these women were unhappy about the quality of the informal interpreting, and women who could not arrange their own interpreters missed appointments in antenatal care111 and hospital settings. 108 The HCPs also viewed informal interpreters as being unable to properly understand and translate complex medical information. 20
Immigrant women in this review noted that getting interpreting support from family members and friends can result in communication challenges for users as well as HCPs. 138 For example, using the husband or partner as an interpreter and not having direct communication with the women can result in a patriarchal and controlling relationship. 20 In cases of domestic violence in which the perpetrator is the husband or partner, the conveyance of correct information between the HCPs and the women is not guaranteed. 121 When using their children as interpreters, the women felt embarrassed sharing their sensitive and private maternity concerns:121
It is awful always having to depend upon someone else, always having to call them up when you know that they are busy, and it makes their lives difficult.
Participant108
He was a man and was not my brother or my husband, and when they were checking me, I asked him to go out, but I really needed to understand.
Participant108
Informal interpreting support was provided not only by family and friends of service users but also by HCPs and other workers, including porters, nurses, midwives and doctors. 128 Owing to language barriers and the challenges involved in organising formal and informal interpreting support, one analysis identified that the time of day was important in determining the quality of maternity care obtained by non-English-speaking immigrant women. 121
Linkworker and advocate services
The recruitment of linkworkers and advocates from the immigrant population was documented as an intervention used to address language-related issues in maternity care. Although noted by only one study,120 this intervention enabled women with low levels of proficiency in English to utilise maternity care services. This study noted that the linkworkers and advocates enabled the immigrant women to communicate better with HCPs and to feel more confident and reassured while accessing maternity care services. The HCPs also appreciated the role of linkworkers in helping them to provide better maternity care to women with limited English.
Despite the benefits of using linkworkers to help immigrant women in maternity care, these linkworkers appeared to be available in antenatal settings only during standard working hours,128 suggesting that their presence overnight and at weekends was not ensured. 120 In addition, the linkworkers were not always properly trained for the role. Many HCPs thought that the linkworkers added their own opinions or comments during interpreting, which could harm the quality of antenatal care. 128 The HCPs also viewed the linkworker position as a low-status role. 128 The linkworker role was criticised by some representatives of immigrant groups because linkworkers are employees of the NHS, therefore may feel conflicted in respect of challenging institutional racism present in the system. 120 To address some of the limitations associated with the linkworker role, the authors128 suggested allocating more resources for training linkworkers and offering linkworker service on a 24-hour shift basis.
According to the immigrant women, constructive communication by HCPs includes having an emphatic and engaging conversational style, being reassuring and enhancing rapport, being open to questions for further clarification, offering time to the women to talk and not giving the impression of being rushed. 111
Impacts of language and communication barriers on the provision of maternity care information
Immigrant women with limited proficiency in English are unable to benefit from written and spoken material on maternity care. 121 Translated content on maternity care is available only in the languages of established immigrant communities and new immigrants usually find such information inaccessible to them. 20 Consequently, many immigrant women with limited English-language proficiency were not knowledgeable about the systems and processes of maternity care services in the UK, the range of treatment options available to them, and their usual rights and entitlements. Therefore, these women were not well prepared for the birth of their babies. 121 Moreover, not all immigrant women receive maternity care information from health-care providers. For example, nearly half of the women sampled in one study20 did not receive dietary information. Consequently, immigrant women with limited proficiency in speaking or reading English have access to only those resources that are provided in their native language. 133 These women therefore depend on their ethnic peers to seek and provide them with information on maternity care, such as infant and maternal nutrition.
Interventions to reduce communication barriers that impair the provision of information
In the review, we found two types of interventions that have been implemented in the past: (1) provision of information in the appropriate ethnocultural languages and (2) provision of bilingual support workers.
Provision of maternity care information in ethnocultural languages
The findings indicated the benefits of providing immigrant women with maternity care information in ethnocultural languages. For example, translating English information into Polish. 140 The immigrant women emphasised that their understanding of maternity care services was highly improved when they were offered information in their first language, resulting in their improved access to and utilisation of maternity services.
Provision of bilingual support workers
Bilingual workers are individuals who can speak English as well as another ethnocultural language. The findings on this intervention were reported by only one small-scale study in which immigrant women favourably commented on offers of breastfeeding advice by a bilingual support worker. 135 Furthermore, compared with paper-based communication materials, the women thought that videos on maternity care and breastfeeding were more helpful because not all women could read their ethnic languages. 116,135
The review135 also noted instances of poor communication among maternity care professionals. During discharge, one participant felt a lack of communication between the maternity care professionals working in the hospital and those working in the community. One of the women in another study111 experienced a so-called ‘silo culture’ between her primary care professionals and the hospital because they failed to share clinical information with one another, resulting in confusion over the first point of contact in need and frustration for that woman.
Conclusion
This theme has identified that immigrant women with limited English-language skills experience communication barriers in accessing and utilising satisfactory maternity care in the UK. These barriers were persistently highlighted in the decades-long time frame covered in this review (1990–2017). However, very few interventions were found that focused on improving verbal and non-verbal communication between HCPs and the immigrant women accessing maternity care; and most were dated. Moreover, evidence on evaluating the effectiveness of these interventions was considered to be methodologically weak and dated, and these interventions may not be relevant for the super-diverse population currently accessing maternity care in the UK.
Gaps in the evidence
The intrapartum phase is a high-risk and critical time, but studies focusing on communication challenges and interventions in this phase are almost absent. Many of the existing studies in respect of communication were conducted several decades ago. In the current period of ethnocultural superdiversity in the UK, with many new and more diverse groups needing maternity care, more contemporary evidence is required. The system lacks comprehensive strategies, at scale, that consider interventions as part of an integrated system of maternal care.
Theme 4: organisation of maternity care, legal entitlements and their impact on the maternity care experiences of immigrant women
This theme provides evidence of how the organisation of maternity care services and legal entitlements impact the experiences of immigrant women in accessing and using these services. This theme also covers findings relating to baby care and breastfeeding.
Organisation of maternity care services and the experiences of immigrant women
The immigrant women in the studies we reviewed had mixed experiences in relation to the maternity care services they received in the UK. 127
Positive experiences
Some immigrant women had the positive experiences of feeling safe in giving birth at a hospital rather than at home,117 being able to register a complaint if poor health care was received,136 reaching a hospital facility in time because of its proximity and not being declined access to a maternity service because of limitations in space or the availability of medical supplies. 4
Some studies also reported that the women had good experiences with postnatal care:123,136,139
The midwife comes to see you, to help with breast feeding . . . and everything before they refer you to the next person, the health visitor. It is really good. I’ve had no problem with them.
Participant 002136
My blood group is B negative. After miscarriage they give me an anti-D injection . . . The positive thing was that the anti-D was sent to my home and the people who brought it to me made an appointment [for me] with the midwife to come and give me the injection.
Participant xyz. 123
No matter whether it was during the day, or at night, they were ready to help . . . Even during Christmas, they like to see a smile on their patients’ faces.
M19, translated from Arabic139
Negative experiences
Other women had negative experiences, resulting from not being able to see the same maternity care providers such as a doctor132 or a midwife3 each time:
Most migrant participants expressed opinions regarding the continuity of carer in the community. Some migrant participants preferred to deal with the same HCP throughout the postnatal period, especially if the baby developed any health problems, as the HCP would be familiar with the case.
Almalik139
I would like to have the same midwife throughout my pregnancy, because she can continue to help me . . . Without, I am starting new every time I see a new midwife.
Spousal migrant, Birmingham3
We identified evidence of limited options of birth place and failure to be offered parent education. 133 Lack of integration of primary and secondary care was evident, and specifically poor communication was seen between GPs and antenatal caregivers. Owing to staff shortages in the hospitals, the caseloads of the HCPs were reportedly not adjusted to provide enough time to meet the multiple and complex needs of immigrant women:20
I wanted an epidural. It was on my birthing plan, but the doctor wasn’t available, so I just had to stick to the gas and air. So, it is whatever is available.
Participant xyz. 121
Sometimes they just don’t give you a choice . . . They took me to theatre, and they gave me epidural . . . had to actually take it, the placenta, out by hand . . . They didn’t ask me for my consent that they are going to put me to sleep.
Participant xyz. 121
The findings identified that there were no policies and procedures in place to address FGM-related care needs during labour and the immigrant women with FGM suffered tears during the perinatal period. 112
Furthermore, it was found that antenatal services were organised on the presumption that the immigrant women would be aware of how these services worked in practice. 20 This assumption was negated by the evidence, which suggested that immigrant women experienced difficulties in understanding most structural aspects of antenatal care. 117 In some cases, the women did not have resources to pay for transport to attend antenatal care. 3 Not only was antenatal care inaccessible to the women, but they were also not aware of all the complexities and internal organisation of the NHS in the UK. 140 Some immigrant women expressed confusion regarding the NHS appointment system and indicated that they were not proficient in using it. 127 All of these challenges created a mismatch between their expectations of care and the maternity care actually received, resulting in consequent disappointment among the service users. 139
Evidence from the included studies suggested that study participants were also unhappy regarding the bureaucracy involved in receiving maternity care. They also found dissonance between the maternity care models in the UK and their home countries (e.g. women of Middle Eastern origin), especially around labour, for which the women expected more proactive medicalised obstetric interventions, rather than the UK ‘normality’ model. 123 The views of immigrant women differed across the trajectory of models of provision of maternity care. Evidence suggests that immigrant women with expectations of frequent access to and preference for more medicalised maternity care were less satisfied with their midwifery-orientated care. 127 Similarly, for the caesarean section births, the biomedical care model of the UK providers was found to be different from emic care models in which the cultural aspects of the women’s care would also be given due consideration:112
They are unemotional and practical here, while we are sentimental by nature. She was telling me that the baby was distress and that we had to deliver it immediately, which was true. I understood what she said, but I could not tell her what I wanted.
Participant xyz. 123
Rights and entitlements for maternity care and the experiences of immigrant women
The rights and entitlements of immigrant women for maternity care in the UK had an important bearing on the experiences of women in accessing and utilising maternity care. The immigrant women without entitlement to free maternity care services in the UK were deterred by the charges and confidentiality of their legal status; hence, they did not access timely antenatal care. 47 Many women in the undocumented and asylum-seeking immigrant category missed their maternity services appointments, as they did not have recourse to public funds. 20
Asylum-seeking women were sometimes dispersed in the final phase of their pregnancy, which resulted in discontinuity in the care process and the loss of their social networks. 20 The dispersed women felt that they did not have any control or power over their lives. 20 The dispersal process, whether in early or late stages of pregnancy, was a main factor in increasing mental stress for pregnant asylum-seeking women.
Pregnant asylum-seeking women reported having to live in accommodation with other unknown asylum-seeking women. Living with other asylum seekers who had their own problems generated more stress and constituted an unsatisfactory environment for the pregnant asylum-seeking women:
If you live with . . . other women [who] are asylum seeker like us, and everyone have problems like stress . . . One is cleaning, one not. One is like, shouting, one is quiet. One is like . . . the TV loud . . . better to stay like, all by your own.
Participant x118
These negative views from asylum-seeking women were also supported by the views of HCPs in one study. 122 Maternity care was delivered to asylum seekers as per their health needs assessments, which gave priority to the views of HCPs rather than being a coproduction with asylum seekers. For example, one of the participants in the study noted the following:
It is not a service that is led by them [asylum seekers] . . . at all, it is a maternity-led service.
Participant M1122
The women in spousal migrant categories were also not entitled to public recourse for the first 24 months of their arrival in the UK and retained no right to live in the UK if their marriage was dissolved. Such women were specifically discouraged from reporting their personal health needs, particularly those arising from domestic violence. 20
Breastfeeding support from maternity services and the experiences of immigrant women
The findings have identified mixed experiences regarding support the women received from HCPs for breastfeeding their babies.
Positive experiences
Findings in our included studies also report that some women are receiving breastfeeding support from their midwives: they provided good information on breastfeeding and its benefits, including a practical demonstration on positioning the baby for breastfeeding. 139 The health visitors also offered practical support on breastfeeding to the women when they were in hospitals and encouraged them to continue breastfeeding after discharge from the hospitals. The HCPs also provided digital versatile discs (DVDs) and booklets on breastfeeding to the immigrant women, which they found helpful.
Evidence suggests that having a named HCP for breastfeeding advice and support, and attending a peer support group, facilitated successful breastfeeding. For women with low levels of English-language fluency, the availability of a bilingual peer support worker was found to be helpful in initiating and maintaining breastfeeding. 139 The findings noted that primiparous women were more influenced by their bilingual support worker to breastfeed than multiparous women, because the peer support worker was the main source of information for them. Other aspects of positive breastfeeding support included the effective communication of the bilingual peer support worker, her significant knowledge of breastfeeding and her good accessibility to the immigrant women. The findings noted that some immigrant women held the influences of their family and the cultural traditions of country of origin for initiating and continuing breastfeeding in high regard. 116
The breastfeeding support offered to the immigrant women included the provision of specific information and support to women with inverted and sore nipples, as well as demonstrations of how to use a breast pump to ensure a supply of milk for breastfeeding. 139
Negative experiences
Immigrant women from European and Middle Eastern countries identified a lack of support from hospital staff as the main reason for not breastfeeding their babies. 139 Another group of women identified lack of support from hospital staff as one of the reasons for having difficulties in exclusive breastfeeding. 135 A third study focusing on the maternity experiences of immigrant women of Muslim faith noted that some women received poor breastfeeding support in hospital, especially from health-care assistants. 121
One study reported that women with low levels of English-language fluency were not satisfied with breastfeeding support both in the hospital and at home. 139 First-time mothers were especially unhappy about the support. Women with low English-language fluency also experienced delays in receiving support for breastfeeding. For example, an immigrant woman from the Middle East who birthed her baby in the evening did not receive any breastfeeding support until the following afternoon, because the practitioners required time to organise an interpreter. In the absence of professional support for breastfeeding, the immigrant women desired social support from family members, such as their mothers. However, some immigrant women reported that they lacked social support and their subsequent isolation hindered their ability to breastfeed their babies appropriately.
National health-care guidelines and hospital procedures negatively affected some women who wanted to breastfeed their babies. For example, some immigrant women of the Muslim faith felt that privacy was lacking in the hospitals, which interfered with their ability to breastfeed their babies. This situation was particularly problematic when the hospital staff would not allow a curtain to be drawn around their bed. 121 Health-care guidelines in the UK suggest that HIV-positive women should avoid breastfeeding their babies to prevent transmission of HIV infection. Some immigrant women were not happy with this restriction, but they nonetheless opted for formula feeding as suggested by the HCPs.
The findings suggested that some immigrant women were not aware of breastfeeding support programmes and organisations such as the ‘Sure Start’ programme. This result is consistent with earlier findings in which some participants reported that they did not attend breastfeeding classes, because their support worker had not informed them about such classes.
Reducing negative impacts
To address organisational and legal entitlement issues in accessing and utilising maternity care, evidence from earlier studies highlighted the need to establish maternity clinics locally, which reduces hospital travel times and minimises waiting times to see HCPs. 132 Evidence from this review suggests that immigrant women want to see their midwives as and when needed, even on the same day, and in some instances they also wished increased frequencies of scans and regular check-ups in the early stages of their pregnancies. 127
Many women in the asylum-seeking and refugee categories felt lonely and isolated, and they expressed a need for HCPs who could offer them the opportunity to talk, listen and understand their ideas and concerns. 110 They also wanted better opportunities to give feedback on the maternity care services they were offered. 136
To address poor care due to staff shortages, the women suggested that the maternity services should have policies and procedures to allow their husbands or partners to stay with them in the hospital so that they could assist with the support of the women after birth. 107 At the hospital, the women who had delivered by caesarean section wanted more help after the birth of their babies and wanted practical demonstrations on positioning the baby onto the breast for feeding. The evidence arising from the review indicated that supporting immigrant women with breastfeeding could be accomplished by integrating their health and social care and by involving experienced refugee mothers in the support of new ones. To offer continuity in maternity care, the evidence from the review highlighted the importance of having a named midwife for each immigrant woman. 121
Conclusion
The evidence from this review suggested that inflexibilities in the organisation of maternity care services in the UK affected its accessibility to and utilisation by immigrant women.
Gaps in the evidence
Most immigrant women come from countries where breastfeeding is a cultural norm, but it is not in the UK. We need more research on how to maintain existing breastfeeding practices, as the health benefits are substantial and they contribute to the health of the nation.
The impact of the limited legal rights on the health of the mother and infant requires further research.
Theme 5: discrimination, racism, stereotyping, cultural sensitivity, inaction and cultural clash in maternity care for immigrant women
This theme addresses all three phases of maternity care (antenatal, intrapartum and postnatal). Reported findings on this theme arise from 12 of the 40 included studies (see Appendix 6). The findings were related to midwives, GPs, gynaecologists and radiologists, and pertained to a range of immigrant categories (asylum seekers, refugees and economic migrants).
Discrimination in maternity care means withholding care or offering poor maternity care to immigrant women because of their perceived ethnocultural backgrounds. 152 Racism ‘in general terms consists of conduct or words or practices which disadvantage or advantage people because of their colour, culture, or ethnic origin’ (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). 153 Stereotyping has been defined as having negative attitudes towards certain social groups, such as immigrants. 154 Cultural sensitivity in maternal care is the practice of recognising and respecting differences in cultural needs and offering maternity care that meets the cultural needs of service users from different cultural backgrounds. 65 Inaction in maternity care is the lack of response to a care need presented by a service user. 155 Cultural clash is the dissonance between conflicting ideas or advice, resulting from the superposition of differing ethnocultural backgrounds. 156
Discrimination and racism
The findings identified that discriminatory treatment and care was received by some immigrant women from HCPs, during various phases of maternity. Discrimination in maternity care services mitigates the delivery of good-quality maternity care. 20 The discrimination was often subtle and difficult to specify, but direct and blatant discrimination was also experienced in some cases. 121 Subtle discrimination included the staff responding to women’s questions or requests in rigid and inappropriate manners. Evidence from one study reports that immigrant women were often not welcomed or greeted in a friendly manner and not made to feel safe. 3 Some women suffered acute negative feelings when they were seen and treated differently by maternity care staff. 118
Direct discrimination included health-care staff uttering stereotypical and racist comments:
I got an infection in my scar . . . I went to the midwife and said I’m feeling cold, and all my body shakes . . . She looked at me like this and said, ‘You are OK’. . . . She said to another midwife, ‘These Africans . . . they come here, they eat nice food, sleep in a nice bed . . . I just cried – she doesn’t know me, who I am in my country. The other midwife said ‘What’s wrong with them’ some of them laughed.
Participant 24109
Somali women are not into preventive medicine at all.
White British doctor 6112
Immigrant women from the Muslim faith criticised the assumption held by HCPs that their partners or husbands should collaborate with the women during labour. Study participants also challenged the assumptions of the HCPs around their food practices. Sometimes other immigrant women are accused of overusing maternity services as a result of exaggerating symptoms, an accusation that is called the ‘Asian woman syndrome’:121
They [health professionals] should not make the assumption that they [Muslim men] are going to be present at the birth. My husband was not there, I didn’t want him there. My mother was there. 121
Why do they assume that all Muslims want to eat curry? You ask for a halal meal, they will send you a curry. Maybe not everybody likes a curry. There are Chinese Muslims, there are Caucasian Muslims, you know? Muslims from all over. 121
Several women talked about staff belittling their worries and concerns, implying they were exaggerating symptoms, wasting time or complaining about ‘minor’ problems in order to get help. The women said staff often referred to this as ‘Asian woman syndrome’. 121
I have had doctors who tell me to have a coil put in after I have had the baby . . . and when I say I want to carry on having babies, he said, ‘You want to receive more benefits. That’s why you are having more babies’. 121
Similarly, women from an African background reported being stereotyped as having high pain thresholds and long labours; hence, they were not given timely or adequate pain relief. 20 Other examples of labelling and assumptions being made based on a woman’s perceived cultural background were also found:
I saw a consultant . . . She was not nice. She was very abrupt. ‘Did you circumcise?’ . . . I didn’t know women can be circumcised! ‘I’m asking you. Are you circumcised?’ I don’t understand.
Participant 3118
They do me . . . vaginal scan? To check the baby . . . They ask me again if you want to take out the baby?
Participant 5118
Some women felt labelled as an asylum seeker, with staff making assumptions about their needs. In one case, this meant a presumed need to terminate the pregnancy. 118
Similarly, a GP is reported in another study to have expressed the view that offering counselling services to asylum-seeking women did not fit with their needs because it was a ‘very Western concept’. 122
Immigrant women from a Muslim faith noted increases in discrimination and were viewed as a different and dangerous people. 121 However, this evidence was from one small study identified in the grey literature. 121
The findings highlighted perceived racism in maternity care when immigrant women from specific countries were advised by HCPs to undertake a specific medical intervention owing to their national origin or race:
They targeted me and my baby as high risk for TB [tuberculosis] and offered the BCG [Bacillus Calmette–Guérin] vaccine . . . a difficult decision to make after giving birth. Singled out because Chinese . . . I am very upset by this and my baby has a huge scar! It was pure racism in my mind.
Chinese woman, non-UK born107
Disrespect, inaction and lack of attention
Findings from one study suggest that participants perceived that the staff did not treat them as human beings with due respect and full attention. 109 Because of this lack of respect from HCPs, the women felt devalued, unsupported and fearful when receiving maternity care. Such findings were reported in antenatal, intrapartum and postnatal care settings:
I feel I am treated like the air.
Participant 13109
I am rubbish. I haven’t got anything left. I have no value. I pretend too much to be happy but inside me I am dead.
Participant 6109
I couldn’t move or breast feed the baby, but they did not help me . . . only if I asked . . . When they sent me to the postnatal . . . my baby choked started frothing at the mouth. I rang the bell more than once until they came. I said, ‘Look at baby! I can’t move’.
Participant Fatima. 123
I went to the hospital they let me wait . . . Then they examined me. I was in pain no one came and talked with us. They only said to wait . . . I told my husband. ‘I can’t stand it anymore. Go and talk with them’ . . . They said, ‘Sorry, we are coming’.
Participant xyz. 123
Some of the midwives spoke to me very arrogantly. Sometimes I got scared as I don’t know the English language very well. It would be very nice if they gave you a smile now and then. Also, it would be nice if they didn’t give orders.
Pakistani woman, non-UK born107
Culturally sensitive maternity care
The evidence in the review noted a prevalence of anxiety about childbirth among the immigrant women in the UK. 123 This was expressed by a participant in the study as follows:
They do not stitch you up after delivery, nor do they perform any cosmetic suturing; I don’t know if this is true or not . . . The second concern is that I heard that they do not give a woman any anaesthetic during delivery, which worries me a lot.
Participant Rahma123
The findings indicate a lack of cultural sensitivity and cultural understanding among HCPs working in maternity care, thus resulting in culturally insensitive care for immigrant women. 121 The findings indicated that immigrant women of the Muslim faith did not optimally benefit from antenatal classes because they were delivered by non-Muslim educators who were not knowledgeable about the Islamic faith related to maternity. In addition, the sessions were with men and women and included other ethnic and religious backgrounds:121
They [women in Muslim-only antenatal classes] would be able to ask and people would understand about religion, like needing a female doctor . . .
Participant xyz. 121
A participant highlighted the lack of cultural knowledge and cultural sensitivity of the staff during the intrapartum phase:
I had a full circumcision, but basically there was no one who had the experience to deliver the baby, so they had to call someone from another hospital. He was a Sudanese man, so I had to have a male doctor to deliver the baby because there was no one else.
Participant xyz. 121
Some immigrant women of Muslim faith felt that the maternity care services were unable to understand and meet their cultural and religious needs on the postnatal wards for breastfeeding:121
I wanted the privacy. The dads are there . . . I just wanted to be able to have privacy to breastfeed without people walking around, because I wear hijab as well. The English women, or the non-Muslim women, are happy to breastfeed openly . . . I didn’t want that.
Participant xyz. 121
Similarly, in another case, an immigrant woman (whose faith was not indicated) complained as follows:
. . . [she had] asked for placenta for religious condition to be buried, but it was taken away.
Indian woman, non-UK born107
Another cultural condition that the immigrant women felt that the staff lacked understanding about and proper responses to FGM. 108
In addition to the staff’s lack of cultural understanding, maternity care services, as a whole, were reported as not meeting the cultural needs of immigrant women:121
I don’t even allow my husband to be in the labour room . . . because I feel uncomfortable with men . . . Even he [my husband] refused to come in. 121
The views held by immigrant women about culturally insensitive maternity care was endorsed by maternity HCPs, as noted by a study in the West Midlands:20
I don’t think the system works well at all. It’s terrible and it’s geared up for white middle-class women.
Midwife, Birmingham20
By contrast, the findings also noted that in a few cases the midwives were happy to meet the cultural and religious needs of the immigrant women in antenatal and postnatal settings. 121 For example, by acting proactively, a midwife was able to discuss the cultural and religious needs of an immigrant woman. When a Muslim woman asked the midwife to sweeten her new baby’s mouth with a date or honey (an Islamic custom), the midwife happily did:121
The midwives were happy to do that, she said, ‘Whatever you have to do’, so they were quite sensitive. They know what we had to do. 121
Cultural clash and conflicting medical advice
The findings identified instances of cultural clash and conflicting advice during pregnancy and maternity care. 123 Cultural clash and conflicting medical advice resulted because cultural practices and the established medical and maternity care systems differ in the UK from those in the home countries of the participants:
I came here in October, and in January I was pregnant. During that time, I spoke to my doctor in my own country. I don’t want to be confused between [the advice I was getting from the] two doctors, so I am not following [the doctor’s advice] here.
Participant xyz. 123
During this pregnancy, my mother was with me and she always reminded me that I was pregnant . . . In my country there is a list of forbidden things.
Zahra. 123
On the first visit, the midwife told me, ‘You are not sick, you are pregnant’. In Egypt, they let you feel that you are sick and that this is abnormal, which is why they pay more attention to it.
Participant xyz. 123
Conclusion
This theme presented evidence that immigrant women were often the subject of discrimination and stereotyping and were offered poor maternity care in the UK. Some maternity care services and staff lacked cultural sensitivity when delivering care to immigrant women. Discrimination and cultural insensitivity in maternity care services contributed to the generation of inequalities in access, utilisation and outcomes for immigrant women in maternity care.
Gaps in the evidence
No intervention was reported that focused on addressing discrimination, stereotyping, racism or cultural insensitivity to improve maternity care for immigrant women.
Chapter 5 Discussion and implications
Introduction
The aim of this study was to map out the experiences of immigrant women accessing maternity care in the UK, and to identify the existence of interventions that were focused on enhancing the accessibility and acceptability of maternity care services for these women. Although there are many pertinent issues that might impact on the experience, the nature of a systematic review means that we can only report on those issues and factors that have been investigated and appear in the scientific journals. For example, we did not encounter studies that featured solely on ‘white ethnicities’. The primary focus was on the perspectives of women. As the UK is in a period of superdiversity (see Chapter 1, Background), the navigation of health services for many is challenging. The level of superdiversity presents challenges for the NHS in the provision of optimal and individualised maternity care. We consider these challenges framed by the theoretical perspectives of cultural safety62 and cultural competence. 51,61,157 Midwives and obstetricians predominantly provide maternity care in the UK; however, virtually none of the studies we identified and included in this review focused on the role of obstetricians and the care they provided. However, we did find evidence of perspectives from women regarding the maternity care provided by GPs, health visitors, community midwives, linkworkers, care assistants and breastfeeding support workers in primary and secondary care.
We reported findings from all three phases of maternity care: antenatal, intrapartum and postnatal. The immigrant population categories studied included asylum seekers, refugees, and spousal and economic immigrants. The ethnocultural groups mentioned include immigrant women of Bangladeshi, Pakistani, European and Middle Eastern origins; black African women from unspecified countries; and women from specific African countries (from Somalia, Ghana, Senegal, Eritrea, Gambia, Sierra Leone, Ivory Coast, Algeria, Congo, Angola and Nigeria).
This NS review identified 61,638 papers (after removal of duplicates), following implementation of our search strategy. We excluded 15,684 papers, meaning that only 0.06% of papers met our inclusion and exclusion criteria. We appraised the quality of each study using the CEBMa tools for the qualitative and quantitative studies and GRAMMS103 for the mixed-methods studies. Following appraisal and organisation into themes as described earlier, we established five significant themes; providing definitions, the scope and parameters of the theme, and exemplars in the form of verbatim comments from included studies and constructing a meta-inference.
Summary of findings
Our themes were as follows:
-
access and utilisation of maternity care services by immigrant women
-
maternity care relationships between immigrant women and health-care professionals
-
communication challenges experienced by immigrant women in maternity care
-
organisation of maternity care, legal entitlements and their impact on the maternity care experiences of immigrant women
-
discrimination, racism, stereotyping, cultural sensitivity, inaction and cultural clash in maternity care for immigrant women.
Our review established strong and robust evidence for three themes presented above (themes 1, 2 and 3).
Although we found evidence to support our theme development for themes 4 and 5, the evidence was less comprehensive. Nevertheless, themes 4 and 5 highlight important critical dimensions of care. Please see Appendix 6 for an overview of the studies supporting each theme.
Theme 1: access and utilisation of maternity care services by immigrant women
Late booking emerged as an important dimension in this theme, that is that immigrant women study participants tended to book and access antenatal care later than the recommended time frame (during the first 10 weeks of pregnancy). This issue was found to be multifactorial in nature, including issues such as limited English-language proficiency, immigration status, lack of awareness of the services, lack of understanding of the purpose of the services, income barriers, the presence of FGM, differences between the maternity care systems of their countries of origin and the UK, arrival in the UK late in the pregnancy, frequent relocations after arrival, the poor reputations of antenatal services in specific communities and perceptions of regarding antenatal care as a facet of medicalisation of childbirth. The factors affecting the access and utilisation of postnatal services were similar to those reported for antenatal services.
Theme 2: maternity care relationships between immigrant women and health-care professionals
Our included studies evidenced the perception of service users in this group and their interactions and therapeutic encounters with HCPs. These interactions were significant in understanding access, utilisation, outcomes and the quality of their maternity care experience.
Included studies in this theme demonstrated that the perceptions of study participants regarding the ways in which HCPs delivered maternity care services were both positive and negative. A number of studies illustrated positive relationships between HCPs and immigrant women. Study participants asserted that the HCPs were caring, respected confidentiality and communicated openly in meeting their medical, as well as emotional, psychological and social, needs. Conversely, studies showed evidence of negative relationships between participants and HCPs. Studies showed HCPs, from the perspective of immigrants, as being rude, discriminatory, or insensitive to the cultural and social needs of the women. Consequently, women tended to avoid accessing/utilising maternity care services consistently.
In our included studies, participants expressed a desire for the HCPs to be empathetic, respectful, culturally congruent and professional when providing maternity care services. Some women also suggested employing HCPs from the immigrant population.
Theme 3: communication challenges experienced by immigrant women in maternity care
It is axiomatic that limited English-language fluency presents verbal communication challenges between the HCPs and their patients, families and carers. Moreover, this is compounded when HCPs use complex medical or professional language that is difficult to comprehend. Non-verbal communication is culturally defined and challenges can occur through misunderstandings of facial expressions, gestures or pictorial representations. Our evidence shows that poor communications result in limited awareness of available services. Communication challenges also create miscommunication with HCPs. Study participants often expressed challenges accessing services; failed to understand procedures and their outcomes; were constrained in their ability to articulate their health or maternity needs to health-care providers; were disempowered in respect of their involvement in decision-making; often gave consent for clinical procedures without fully comprehending the risks and benefits; and did not receive understandable advice on baby care. Studies identified that communication was not reciprocal and HCPs often misunderstood participants. This created feelings of isolation, fear and a perception of being ignored. Interventions to address the language challenges included the provision of formal and informal services, bilingual support workers and written maternity care information in the necessary languages.
Theme 4: organisation of maternity care, legal entitlements and their impact on the maternity care experiences of immigrant women
The legal status of immigrant women in the UK has a profound influence on their access to maternity care. Women without entitlement to free maternity care services in the UK were deterred from accessing timely antenatal care by the costs and by the confidentiality of their legal status. Moreover, some women arrived in the UK during the final phase of their pregnancies, which resulted in fractures in the care process, loss of their social networks, reduced control over their lives, increased mental stress and increased vulnerability to domestic violence.
The study participants in our included studies had mixed experiences with the maternity care services in the UK. Positive and commendable experiences included feeling safe in giving birth at a hospital, rather than at home; being able to register a complaint if poor health care was received; being close to a hospital facility; not being denied access to a maternity service; and having good experiences with postnatal care. Conversely, negative experiences included lack of continuity (e.g. not being able to see the same maternity care providers each time and being unaware of the configuration of maternity services work, limiting navigation). Participants in our included studies found services within the UK maternity care model to be bureaucratic, and perceived a propensity towards medical and obstetric intervention and lower segment caesarean section births.
Positive experiences included receiving information from their midwives on the benefits of breastfeeding, together with demonstrations on how to position the baby. Negative experiences included poor support from hospital staff on how to breastfeed their babies. Consequently, these reported experiences are mixed.
Theme 5: discrimination, racism, stereotyping, cultural sensitivity, inaction and cultural clash in maternity care for immigrant women
Inequalities in access, navigation, utilisation and the subsequent maternity care outcomes are influenced by discrimination and cultural insensitivity in maternity care services, according to the perspectives established in our included studies. Discrimination was often subtle and difficult to identify, but direct and overt discrimination was reported in some studies. The findings informing this theme arise from 12 of the 40 included studies.
Specifically, study participants of Muslim faiths challenged assumptions held by HCPs, including those held regarding Muslim food practices and that their partners or husbands should help the women during labour. In addition, evidence from our included studies suggested that they also felt that they were regarded as different and dangerous people. Moreover, HCPs were reported in some studies to lack cultural sensitivity and cultural understanding. For example, these women did not optimally benefit from antenatal classes facilitated by a non-Muslim educator who had no knowledge of the relationships of Muslim culture to maternity. Furthermore, studies reported participant dissatisfaction of antenatal classes with a gender mix, which contravened religious edicts. Studies illustrated that some women of Muslim faith felt that their cultural and religious needs for breastfeeding were not met on the postnatal wards and they felt that the staff lacked insight, knowledge and understanding of FGM.
Evidence from our included studies suggest that immigrant women perceived that the staff did not treat them with respect or full attention. They felt devalued, unsupported and fearful when receiving maternity care. In a few cases, however, midwives were happy to meet the cultural and religious needs of the study participants in our included studies, in both antenatal and postnatal settings; this is a positive finding.
Our findings also identified instances of cultural clash and conflicting advice during pregnancy and maternity care, mostly resulting from differences between the home countries of the immigrants and the UK in their cultural practices and medical systems.
A theory or model is a postulation of reality and provides a systematic and logical explanation for the meta-inferences and observed phenomena in our included studies. We present a conceptual model of our findings, embedding the key drivers and influences. These key drivers and influences form the critical domains or foci that require interventions and service enhancement to enhance the maternity care experiences of women in the UK maternity care services. Policy and practice development focusing on these domains can therefore bring about benefits and enhancements to maternity care (Figure 9).
FIGURE 9.
Maternity care experiences of immigrant women. Reproduced from Higginbottom et al. 24 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
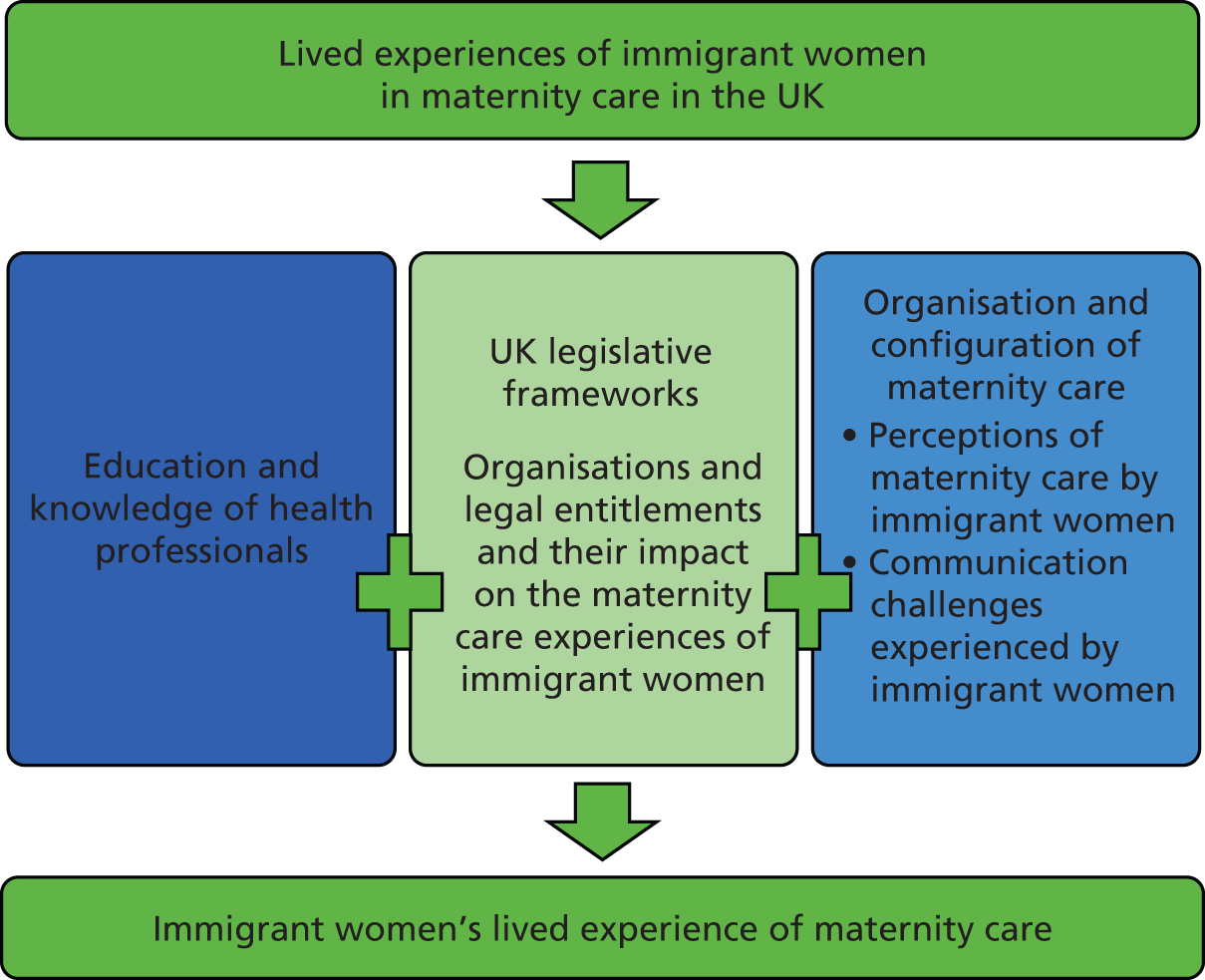
Policy context
Maternity services are essentially public health services that play an important role in improving health and reducing inequalities. Recently policy recommendations that call for modernisation of maternity service, for example National Maternity Review. Better Births; Improving Outcomes of Maternity Services in England,6 A Maternity Strategy for Northern Ireland 2012–2018,158 Refreshed Framework for Maternity Care in Scotland159 and A Strategic Vision for Maternity Services in Wales. 160 The overall vision for the maternity services in the UK is to improve the safety and quality of maternity care. National Maternity Review. Better Births; Improving Outcomes of Maternity Services in England6 set out a 5-year vision for improving the quality of maternity care, providing women and newborn infants with safer, more personalised, kinder, more professional and more-family friendly care, ‘where every woman has access to information to enable her to make decisions about her care; and where she and her baby can access support that is centred around their individual needs and circumstances’ (contains public sector information licensed under the Open Government Licence v3.0). 6 These goals and aspirations match many of the concerns identified by women in our included studies.
The premise behind this vision in the UK is that the services should be flexible and individualised, designed to fit around the needs of the woman and newborn infant, and her family’s journey through pregnancy, childbirth and parenthood. Women and their partners should be supported and encouraged to have as normal a pregnancy and birth as possible. This ambition with regard to the provision of individualised care intersects very well with the findings of this review in respect of immigrant women and maternity care services.
Safety features throughout the Maternity Transformation Programme (this programme is responsible for achieving the vision set out in Better Births) aims to drive improvement in maternity services. Likewise, proposals in the government’s Safer Maternity Care: Next Steps Towards the National Maternity Ambition146 focus on five key drivers for delivering safer maternity care, which are ‘leadership’, ‘learning and best practice’, ‘multi-professional team working’, ‘intelligent use of data’ and ‘innovation’.
Consideration might be given to maternity services improving interagency arrangements (through clinical and local social services networks), including protocols for information sharing and a lead professional, to ensure that women from disadvantaged groups have adequate support and benefit from other agencies (such as housing), referring women, with consent, to local maternity services.
Our findings highlight the criticality that interpreting services are provided for women for whom English is not their first language. Relatives should not act as interpreters. It is paramount in terms of addressing inequalities that funding must be made available for interpreting services in the community, especially in emergency or acute situations.
Successfully providing appropriate maternity care requires the legitimisation and incorporation of the pervasive traditional beliefs and practices of immigrant women, to which these women often adhere despite their new milieu. Their beliefs on maternity care may differ considerably from Western biomedical perspectives. However, a recognition is required that beliefs may change over time due to acculturation. Care provision based on a rigid perception of ethnocultural orientation may lead to stereotyping, and therefore a nuanced strategy of care is required. Overcoming migration issues and language barriers will also be a major factor.
In a diverse pluralistic society, maternity service, care provision and delivery to immigrant women should be everyone’s business. Consideration to addressing the findings from this review might be addressed via the following mechanisms, as articulated in the Transforming Maternity Care programme.
Decision-makers and health-care leaders should address the findings at a strategic level. A focus on diversity, equality and the needs of immigrant women could reasonably be embedded in the role and responsibility of ‘board-level maternity champions’ and of ‘maternity clinical networks’. Maternity service providers could consider the appointment of one obstetrician and one midwife jointly responsible for championing maternity care provision to immigrant women in their organisation, as these dimensions feature in the bespoke maternity safety improvement plan. 161
Key areas of action include:
-
focus on learning and best practice, issues of equality and diversity should be featured in the saving babies’ lives care bundle for use by maternity commissioners and providers
-
focus on multiprofessional team working, continuous personal and professional training
-
focus on data, greater focus on ethnicity and immigration within the maternity services data set and other key data sets
-
focus on innovation, create space for accelerated improvement and innovation at local level.
In Table 5 we provide a summary of the review implications, illustrating their relationship to the review themes and the underpinning evidence from the review.
| Domain | Implication | Theme evidence | Key points derived from review evidence |
|---|---|---|---|
| Service delivery | Focus on strategies to facilitate early booking for immigrants (the evidence in respect of early booking and the potential outcomes is comprehensive and well known) | 1, 2, 3, 5 |
|
| Focus on the development of personalised care, continuity of care and named midwives could help to address inequalities in maternity care services | 1, 2, 3, 5 |
|
|
| Communication | Development of early communication strategies in languages understood by the immigrant women, in geographical locations where cohorts of women are large enough to make this economically viable. Use of a variety of modes of communication: website, videos, text message, social media groups | 2, 3, 5 |
|
| Outreach strategies with immigrant women in their communities and provision of the necessary maternity care education holds the potential to improve access | 4, 5 |
|
|
| Existing networks and mechanisms exist via immigrant support agencies and ethnocultural group community associations. Potential exists to use these avenues as vehicles for outreach to immigrant women |
|
||
| The NHS in the UK has a hugely diverse ethnocultural workforce with a vast untapped linguistic resource. Strategies could be developed to harness this resource in a non-exploitative way for the benefit for patients, families and HCPs, with, of course, due regard for remuneration and non-exploitative strategies | 1, 3 | ||
| Service organisation and reconfiguration | Asylum-seeking women and refugees with wider circumstances and legal position impinging on access and utilisation of maternity care. Specific strategies are required for these groups to use maternity care services effectively | 1, 4, 5 |
|
| Geographically responsive maternity care services are required, as there is a vast difference in demography throughout the UK | All themes |
|
|
| Responding to geographical need the provision of permanent linkworkers and a 24-hour interpretation service | 1, 2, 3 |
|
|
| Generic issues exist that all maternity care users experience; for example, need for greater support, lack of continuity, reducing appointment times, which may reflect both service organisation and scarcity/pressure on services. Therefore, general policies and directives could be utilised to improve the experience of minority immigrant women | All themes |
|
|
| Our findings have indicated a lack of interventions focused on maternity care and immigrant women. Therefore, a policy focus on the development of interventions, implementation and evaluation of such interventions might be considered | All themes |
|
|
| Evidence from the review suggests that the current maternity care service structure is often rigid and repeats what was tried unsuccessfully in the past. Maternity care services need more flexibility to meet the needs of our super-diverse population | 4 |
|
|
| Education and training | Improving relationships of patient–health-care provider, includes addressing discrimination/racism and the provision of culturally appropriate care. Increasing the cultural sensitivity of services and providers emerges from this review as a paramount concern | 1, 2, 5 |
|
| Greater education and training of all maternity care professions, regarding caring for women who have experienced FGM. A focus on all elements of care (e.g. antenatal, intrapartum and postpartum) | All themes |
|
|
| Specifically focusing on immigrant groups sometimes results in stereotyping and further discrimination and a focus of attention might be ‘mainstreaming’ in the context of maternity care | All themes |
|
What is the value of this synthesis for the education and training of health-care professionals?
To improve maternity care experiences for immigrant women, we need to improve these women’s access to the services and increase the acceptability of these services. We suggest that the education and training of HCPs needs to take into account the dimensions shown in Box 7, both in the core education programme and in ongoing professional development.
Cultural humility incorporates a lifelong commitment to self-evaluation and self-critique, to redressing the power imbalances in the patient–physician dynamic, and to developing mutually beneficial and non-paternalistic clinical and advocacy partnerships with communities on behalf of individuals and defined populations. 148
Cultural sensitivity
Cultural sensitivity refers to the acquisition of fundamental knowledge and the possession of specific attitudes towards health-care beliefs and traditions that are culturally defined. 162
Cultural awareness
Cultural awareness includes an awareness of one’s own identity, beliefs, values, social position, life experiences and so on, and their implications for the provision of care. 55
Cultural competence
Cultural competence is a process in which critical thinking and awareness, harmonious behaviours, appropriate attitudes and manageable policies, come together in a system, agency, or among professionals to enable the system or professionals to work effectively in cross-cultural situations. 163
Cultural safety
This concept is based on the theoretical framework frequently referred to as critical social theory, which suggests that nursing is unsafe as defined by clients. In this respect, they mean feel humiliated, disenfranchised, or oppositional care or accessing care. 50
The strength of this concept is that cultural safety is not about cultural practices; rather, it involves the recognition of the social, economic, and political position of certain groups and the historical antecedents that contributed to the power hierarchies that exist in all societies. 61
The reality of the UK context as a super-diverse society demands health-care providers who are culturally competent and culturally safe so that they will be able to communicate effectively with immigrant women and their families. The goal is the delivery of high-quality maternity care for immigrant women who are from diverse sociocultural, economic and environmental backgrounds and provide them with quality health care. 164 A number of different definitions, typologies and models have evolved55 to assist in the identification of the key components of culturally safe and competent care as well as ways in which practitioners and organisations can enhance their performance and delivery of care in this area. Prior to embarking on a learning path to develop skills in culturally safe and competent care provision, a theoretical grounding is imperative. Moreover, cultural safety and competence improves patient satisfaction, as many ethnocultural groups value relational quality (as established in this review) and the resultant individualised care.
We suggest that a focus on cultural safety and competence could provide vehicles and mechanisms for improving maternity care services for immigrant women in the UK.
Limitations of the review
This review was challenging to undertake because of the great variation in language and diversity of terminology used by researchers to describe ethnocultural and immigrant groups in the UK. We worked closely with our information scientist to ensure that we had selected the correct terms and to develop robust inclusion and exclusion criteria. In the UK, researchers most frequently use the terms BME or specify the ethnocultural group without an indication of the immigrant status. As noted in this report, reductionism in the terminology creates a mix of approaches to reducing immigrant women and their complex cultures, ethnicities and lives to particular contexts or situations. Although a range of identifiers are used, we noted a pattern of identifying immigrant women by their situation or context (such as the use of ‘asylum seeking’), as well as the use of ‘immigrant’ woman as a generic demarcation of a non-British or non-white woman. In sociological terms, this creates a process of ‘othering’ of some of the most vulnerable women in UK society.
Specific challenges existed in extrapolating the findings specifically for immigrant women, when studies used mixed samples of immigrants and non-immigrants. We rejected papers in which no clear findings were presented about the immigrant women in mixed population samples. We also employed as a ‘proxy’ for immigrant status, the use of an interpreter in the data collection processes, or the clear identification of a place of origin for the participants that was outside the UK.
Most of the included studies focused on women’s perspectives on maternity care service, as women’s views were critical in understanding the access and acceptability of maternity care services delivered in the UK. We also included a small number of studies that captured the perspectives of both HCPs and immigrant women, but we largely excluded studies that provided only the views of HCPs on the topic.
Some challenges existed in determining the temporal dimensions of all the included studies. It was not always clear in which phase of maternity the data were collected (e.g. antenatal, intranatal or postnatal). The included studies focusing on the postnatal period also presented a challenge; our operational definition of the postnatal period concluded at 6 weeks, whereas one study included the postnatal phase as the period immediately following birth until 13 months post partum.
The number of interventions evaluated by rigorous research methodologies was quite limited. Although we became aware of a wide range of interventions through our key stakeholder events, most of these have not been subjected to scientific appraisal.
A review of this nature does not include a meta-synthesis data analysis as might occur in a classical systematic review. However, Popay et al. ’s 86 original work included conducting a review using a classical genre and a NS review on one topic; and the findings of both reviews were highly congruent in their conclusions.
We experienced technical challenges with the shared use of EndNote, which created a time lag requiring remedial actions. These problems have been relayed to the producers of EndNote.
Priority and key areas for future research
Studies are needed regarding interventions and their effectiveness in enhancing the accessibility to, and the utilisation of, maternity care for immigrant women. We also need studies that address the factors associated with negative and positive relationships between HCPs and immigrant women by using social and psychological theories of ‘otherness’ and ‘difference’. Additionally, there is a lack of research emphasis on the structural dynamics within health systems that may encourage or even foster negative relationships between service users and HCPs. The high-risk intrapartum phase is a critical phase of maternity, but studies focusing on communication challenges and interventions in this phase are almost absent. Many of the existing studies regarding communication were conducted several decades ago. In the current period of superdiversity with new and more diverse ethnocultural groups in the UK, more contemporary evidence is required. We also see a lack of complete strategies, at scale, that consider interventions as part of an integrated system of approaches and care. Most immigrant women come from countries where breastfeeding is a cultural norm, but more research is needed on how we can maintain their existing breastfeeding practices in the UK; the health benefits are substantial and contribute to the health of the nation. The impact of limited legal rights on the health of the mother and infant also needs more study. To our knowledge, no intervention has been reported that focuses on addressing discrimination and stereotyping, eradicating racism, and reducing cultural insensitively to improve maternity care for immigrant women.
Development and evaluation of online antenatal education resources in multiple languages could be explored and obviate the need for written materials and expensive interpreter time. Software exists that will translate online materials into different languages. Development and appraisal of education packages for HCPs, focused on the provision of culturally safe maternity care for the UK’s diverse population, should also be considered.
Significantly, the NHS in the UK has a hugely diverse workforce, with a vast untapped linguistic resource. Strategies might be developed to harness this resource in a non-exploitative fashion, ensuring that NHS staff are correctly remunerated for this activity.
More research is required into the term ‘immigrant’, how it is used and the changes in its use over time that may affect immigrant women’s care. At present, the term is used very broadly and simplistically, which masks its inherent heterogeneity. Furthermore, more research is needed to understand how the intersections of particular characteristics – such as gender, education status, time in the UK, immigration status, wealth and country of origin – may influence or alter the experiences of these women in their maternity care.
Review conclusions
The experiences of immigrant women in accessing and using maternity care services in the UK are mixed; however, these women often have poor experiences. Factors contributing to poor experiences include lack of language support, cultural insensitivity, discrimination, poor relationships between immigrant women and HCPs, legal entitlements and guidelines on the provision of welfare support to immigrants.
The evidence indicates that very few evaluated interventions have been implemented to address inequalities in access to, and quality in, maternity care for immigrant women. However, participants in our national research symposium shared details of many local initiatives not evaluated by rigorous research methodologies. To our knowledge no single study exists on economic evaluations of interventions, which is an important requirement for implementation. Likewise, to our knowledge, postnatal checks by a GP have also not been studied. Researchers may be missing opportunities to connect maternal care with a future holistic approach to improve the mental and physical health of immigrant women and ultimately the health and well-being of future UK citizens.
We suggest that a focus on cultural safety and competence could provide vehicles and mechanisms for improving maternity care services for immigrant women in the UK.
Gaps in the evidence in this review
In the current period of superdiversity in the UK, more contemporary evidence is required. We need complete strategies, at scale, that see interventions as part of an integrated system of approaches and care. In concluding, and as noted earlier, studies are lacking on interventions and their effectiveness in enhancing accessibility and utilisation of maternity care for immigrant women. Studies addressing factors associated with negative and positive relationships between HCPs and immigrant women using social and psychological theories of ‘otherness’ and ‘difference’ are also needed.
Intrapartum/delivery is high risk and is a critical phase of maternity, but studies focusing on communication challenges and interventions are almost absent. Many of the existing studies on such communication were conducted several decades ago. Most immigrant women come from countries in which breastfeeding is a cultural norm, but it is not in the UK. Therefore, more research is needed on how to maintain their existing breastfeeding practices, as the health benefits are substantial and contribute to the health of the nation. For asylum-seeking mothers, the impact of limited legal rights on the health of the mother and infant also needs more study. No intervention has been reported that focuses on addressing discrimination and stereotyping, eradicating racism and reducing cultural insensitivity to improve maternity care for immigrant women.
Additionally, the structural dynamics within health systems have not been emphasised as yet, even though they may encourage or even foster negative relationships between service users and HCPs.
Knowledge transfer
Who should know the implications?
The target list includes policy-makers, commissioners, women in communities, academics, midwives, clinical trainers, HCPs, maternity action groups, migrant women’s rights services, GPs, students in health-care programmes, volunteer and community services organisations, organisations working with migrant women, maternity voice partnerships, the Department of Health and Social Care, UK Visas and Immigration, the Royal College of Midwives, the Royal College of Nursing, Public Health England, the World Health Organization, support agencies in other countries, migrant refugee organisations, religious leaders, local councils, pressure groups, Unite Community Practitioners and Health Visitors Association and, indeed, everyone.
Activities undertaken
-
Publication of the review protocol.
-
National research symposium with key stakeholders.
-
Oral presentation at the Healthy Mothers and Babies Conference, Vancouver, Canada, 1 March 2018.
-
Oral presentation to GPs and primary care nurses at the Academic Unit of Primary Care, University of Sheffield, Sheffield, UK, 19 September 2018.
Further activities
Publication of the findings paper in an academic journal. Contributions to theory and practice will occur via publication of findings in high-impact international journals, such as the Journal of Immigrant and Minority Health, Sociology of Health and Illness, Journal of Health Services Research and Policy and Social Science and Medicine, as well as open-access journals such as BMC Pregnancy and Childbirth and BMJ Open Access. The PAG will be invited as co-authors.
Knowledge translation and impact
GH is invited to participate in a multidisciplinary, international Delphi Expert Panel that will select a core set of validated items that can measure mistreatment in medium and high resource countries and align with the World Health Organization Quality of Maternal and Newborn Care framework.
Supported by the Canadian Institutes of Health Research 5-year grant we will study respectful maternity care and mistreatment of pregnant families across Canada, using a participatory research methodology.
GH is invited to participate as an external (independent) International Advisory Group member for the recently funded NIHR Research Global Health Research Group on Preterm Birth, University of Sheffield, along with PAG member Dr Caroline Mitchell. Principal investigator Professor Dilly Anumba. Funding: £2M. Capacity building has resulted from this review as CM (PAG member) is leading the knowledge synthesis strand of this significant study.
GH is invited to provide a methodological workshop on NS at the University of Middlesex on the 16 October 2018.
Acknowledgements
This project was funded by the UK NIHR Health Services and Delivery Research programme. Along with this funding, the NIHR contributed by peer-reviewing the funding proposal. We gratefully acknowledge valuable input from the members of our PAG. Their input has been very helpful in making possible the successful completion and the high quality of this review. The following people kindly consented to be members:
-
Jim Thornton, Professor of Obstetrics and Gynaecology, Faculty of Medicine and Health Sciences, University of Nottingham (member of the NIHR Health Technology Assessment and Efficacy and Mechanism Evaluation Editorial Board)
-
Caroline Mitchell, GP/Senior Clinical Lecturer, Clinical Academic Training Programme Lead, Academic Unit of Primary Medical Care, University of Sheffield
-
Jane Mischenko, Commissioning Lead, Children and Maternity Services, NHS Leeds
-
Carol McCormack, Specialist Midwife, Nottingham University Hospitals NHS Trust.
We also thank following immigrant women for their input in the conceptualisation of this review:
-
Valentine Nkoyo, Director of Mojatu, Nottingham
-
Kinsi Clarke, Nottingham Refugee Forum, Nottingham.
Contributions of authors
Gina MA Higginbottom (Emeritus Professor, School of Health Sciences) was principal investigator. Initiated the project and oversaw all stages. She led the interpretation/synthesis phases and drafted all chapters of the report.
Catrin Evans (Associate Professor, Nursing, Director of the Centre for Evidence Based Health Care) contributed to all stages of the review, provided expert methodological advice, acted as second reviewer for quality appraisal and development of the synthesis. She contributed to the review of the final report.
Myfanwy Morgan (Professor Emerita King’s College, London) contributed to all stages of the review, provided expert methodological advice, acted as second reviewer for quality appraisal and development of the synthesis. She contributed to the review of the final report.
Kuldip K Bharj (Retired Director of Midwifery, University of Leeds) contributed to all stages of the review, provided clinical and policy perspectives, contributed to formulation of the implications and recommendation.
Jeanette Eldridge (Information Specialist) designed the literature search strategy, advised the team on all aspects of information retrieval and undertook the main database searches.
Basharat Hussain (Senior Research Fellow) contributed to all stages of the review and led the data extraction, coding, quality appraisal and drafting of preliminary chapters of the research report.
Karen Salt (Director of the Centre for Research into Race and Right, University of Nottingham) contributed to the review of the final report.
Publications
Higginbottom G, Evans C, Morgan M, Bharj K, Eldridge J, Hussain B. Interventions that improve maternity care for immigrant women in the UK: protocol for a narrative synthesis systematic review. BMJ Open 2017;7:e01698.
Higginbottom GMA, Evans C, Morgan M, Bharj KK, Eldridge J, Hussain B. Experience of and access to maternity care in the UK by immigrant women: a narrative synthesis systematic review. BMJ Open 2019;9:e029478.
Data-sharing statement
Most of the data used in this report came from published papers that are therefore already available to all, subject to the usual copyright and in some cases paywall restrictions. Any other queries should be addressed to the corresponding author for consideration.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/five-year-forward-view/ (accessed 10 October 2018).
- Office for National Statistics . Birth in England and Wales by Parents’ Country of Birth (2013) 2014. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/parentscountryofbirthenglandandwales/2014-08-28 (accessed 20 November 2018).
- Phillimore J. Migrant maternity in an era of superdiversity: New migrants’ access to, and experience of, antenatal care in the West Midlands, UK. Soc Sci Med 2016;148:152-9. https://doi.org/10.1016/j.socscimed.2015.11.030.
- Binder P, Johnsdotter S, Essén B. Conceptualising the prevention of adverse obstetric outcomes among immigrants using the ‘three delays’ framework in a high-income context. Soc Sci Med 2012;75:2028-36. https://doi.org/10.1016/j.socscimed.2012.08.010.
- Knight MBK, Tuffnell D, Jayakody H, Shakespeare J, Kotnis R, Kenyon S, et al. Saving Lives, Improving Mothers’ Care – Lessons Learned to Inform Maternity Care From the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2014–16 2018.
- NHS England . National Maternity Review. Better Births; Improving Outcomes of Maternity Services in England 2016. www.england.nhs.uk/wp-content/uploads/2016/02/national-maternity-review-report.pdf (accessed 8 August 2018).
- Vertovec S. Super-diversity and its implications. Ethn Racial Stud 2007;30:1024-54. https://doi.org/10.1080/01419870701599465.
- Small R, Roth C, Raval M, Shafiei T, Korfker D, Heaman M, et al. Immigrant and non-immigrant women’s experiences of maternity care: a systematic and comparative review of studies in five countries. BMC Pregnancy Childbirth 2014;14. https://doi.org/10.1186/1471-2393-14-152.
- Bharj K, Salway S. Addressing Ethnic Inequalities in Maternity Service Experiences and Outcomes: Responding to Women’s Needs and Preferences 2008. http://raceequalityfoundation.org.uk/health-care/addressing-ethnic-inequalities-in-maternity-service-experiences-and-outcomes-responding-to-womens-needs-and-preferences/ (accessed July 2019).
- Higginbottom G, Reime B, Bharj K, Chowbey P, Ertan K, Foster-Boucher C, et al. Migration and maternity: insights of context, health policy, and research evidence on experiences and outcomes from a three country preliminary study across Germany, Canada, and the United Kingdom. Health Care Women Int 2013;34:936-65. https://doi.org/10.1080/07399332.2013.769999.
- Knight M, Kurinczuk JJ, Spark P, Brocklehurst P. UKOSS . Inequalities in maternal health: national cohort study of ethnic variation in severe maternal morbidities. BMJ 2009;338. https://doi.org/10.1136/bmj.b542.
- Salway SM, Higginbottom G, Reime B, Bharj KK, Chowbey P, Foster C, et al. Contributions and challenges of cross-national comparative research in migration, ethnicity and health: insights from a preliminary study of maternal health in Germany, Canada and the UK. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-514.
- Urquia ML, Frank JW, Glazier RH, Moineddin R. Birth outcomes by neighbourhood income and recent immigration in Toronto. Health Rep 2007;18:21-30.
- Cresswell JA, Yu G, Hatherall B, Morris J, Jamal F, Harden A, et al. Predictors of the timing of initiation of antenatal care in an ethnically diverse urban cohort in the UK. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-103.
- Renzaho AM, Skouteris H, Oldroyd J. Preventing gestational diabetes mellitus among migrant women and reducing obesity and type 2 diabetes in their offspring: a call for culturally competent lifestyle interventions in pregnancy. J Am Diet Assoc 2010;110:1814-17. https://doi.org/10.1016/j.jada.2010.09.017.
- Latif Z. The Maternal Mental Health of Migrant Women 2014. https://raceequalityfoundation.org.uk/health-care/the-maternal-mental-health-of-migrant-women/ (accessed July 2019).
- Guendelman S, Buekens P, Blondel B, Kaminski M, Notzon FC, Masuy-Stroobant G. Birth outcomes of immigrant women in the United States, France, and Belgium. Matern Child Health J 1999;3:177-87. https://doi.org/10.1023/A:1022328020935.
- Bollini P, Pampallona S, Wanner P, Kupelnick B. Pregnancy outcome of migrant women and integration policy: a systematic review of the international literature. Soc Sci Med 2009;68:452-61. https://doi.org/10.1016/j.socscimed.2008.10.018.
- Urquia M, Glazier RH, Berger H, Ying I, De Souza L, Ray JG. Gestational diabetes among immigrant women. Epidemiology 2011;22:879-80. https://doi.org/10.1097/EDE.0b013e31823199ee.
- Phillimore J. Delivering maternity services in an era of superdiversity: the challenges of novelty and newness. Ethn Racial Stud 2015;38:568-82. https://doi.org/10.1080/01419870.2015.980288.
- Department of Health and Social Care . Equity and Excellence: Liberating the NHS 2010. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213823/dh_117794.pdf (accessed 8 October 2018).
- Department of Health and Social Care . Midwifery 2020: Delivering Expectations 2010. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216029/dh_119470.pdf (accessed 8 October 2018).
- Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, et al. What does ‘access to health care’ mean?. J Health Serv Res Policy 2002;7:186-8. https://doi.org/10.1258/135581902760082517.
- Higginbottom GMA, Evans C, Morgan M, Bharj KK, Eldridge J, Hussain B. Experience of and access to maternity care in the UK by immigrant women: a narrative synthesis systematic review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-029478.
- National Institute for Health and Care Excellence . Pregnancy and Complex Social Factors: A Model for Service Provision for Pregnant Women With Complex Social Factors 2010. www.nice.org.uk/guidance/cg110 (accessed 17 March 2018).
- Coast E, Jones E, Portela A, Lattof SR. Maternity care services and culture: a systematic global mapping of interventions. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0108130.
- Oakley L, Gray R, Kurinczuk J, Brocklehurst P, Hollowell J. P14 interventions to increase the early initiation of antenatal care in socially disadvantaged and vulnerable women: a systematic review. J Epidemiol Community Health 2010;64. https://doi.org/10.1136/jech.2010.120477.14.
- Davies MM, Bath PA. The maternity information concerns of Somali women in the United Kingdom. J Adv Nurs 2001;36:237-45. https://doi.org/10.1046/j.1365-2648.2001.01964.x.
- Nápoles-Springer AM, Santoyo J, Houston K, Pérez-Stable EJ, Stewart AL. Patients’ perceptions of cultural factors affecting the quality of their medical encounters. Health Expect 2005;8:4-17. https://doi.org/10.1111/j.1369-7625.2004.00298.x.
- Karlsen S, Nazroo JY. Agency and structure: the impact of ethnic identity and racism on the health of ethnic minority people. Sociol Health Illn 2002;24:1-20. https://doi.org/10.1111/1467-9566.00001.
- Henderson J, Gao H, Redshaw M. Experiencing maternity care: the care received and perceptions of women from different ethnic groups. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-196.
- Mumtaz Z, O’Brien B, Higginbottom G. Navigating maternity health care: a survey of the Canadian prairie newcomer experience. BMC Pregnancy Childbirth 2014;14. https://doi.org/10.1186/1471-2393-14-4.
- Rowe RE, Garcia J. Social class, ethnicity and attendance for antenatal care in the United Kingdom: a systematic review. J Public Health Med 2003;25:113-19. https://doi.org/10.1093/pubmed/fdg025.
- Fisher J, Hinchliff S. Immigrant women’s perceptions of their maternity care: a review of the literature. Part 2. Pract Midwife 2013;16:32-4.
- Higginbottom GM, Safipour J, Yohani S, O’Brien B, Mumtaz Z, Paton P. An ethnographic study of communication challenges in maternity care for immigrant women in rural Alberta. Midwifery 2015;31:297-304. https://doi.org/10.1016/j.midw.2014.09.009.
- Manktelow B, Smith L, Seaton S, Hyman-Taylor P, Kurinczuk J, Field D, et al. MBRRACE-UK Perinatal Mortality Surveillance Report, UK Perinatal Deaths for Births from January to December 2014 2016. www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/MBRRACE-UK-PMS-Report-2014.pdf (accessed 6 July 2018).
- Urquia ML, Frank JW, Moineddin R, Glazier RH. Immigrants’ duration of residence and adverse birth outcomes: a population-based study. BJOG 2010;117:591-60. https://doi.org/10.1111/j.1471-0528.2010.02523.x.
- Hollowell J, Oakley L, Vigurs C, Barnett-Page E, Kavanagh J, Oliver S. Increasing the Early Initiation of Antenatal Care by Black and Minority Ethnic Women in the United Kingdom: A Systematic Review and Mixed Methods Synthesis of Women’s Views and the Literature on Intervention Effectiveness 2012. www.npeu.ox.ac.uk/downloads/files/infant-mortality/Infant-Mortality---DIVA-final-report-Oct-2012.pdf (accessed 8 October 2018).
- Hammoud MM, White CB, Fetters MD. Opening cultural doors: providing culturally sensitive healthcare to Arab American and American Muslim patients. Am J Obstet Gynecol 2005;193:1307-11. https://doi.org/10.1016/j.ajog.2005.06.065.
- Hyman I, Dussault G. Negative consequences of acculturation on health behaviour, social support and stress among pregnant Southeast Asian immigrant women in Montreal: an exploratory study. Can J Public Health 2000;91:357-60.
- Gagnon AJ, Zimbeck M, Zeitlin J, Alexander S, Blondel B, Buitendijk S, et al. Migration to western industrialised countries and perinatal health: a systematic review. Soc Sci Med 2009;69:934-46. https://doi.org/10.1016/j.socscimed.2009.06.027.
- Chalmers B, Omer-Hashi K. What Somali women say about giving birth in Canada. J Reprod Infant Psychol 2002;20:267-82. https://doi.org/10.1080/0264683021000033183.
- Sword W, Watt S, Krueger P. Postpartum health, service needs, and access to care experiences of immigrant and Canadian-born women. J Obstet Gynecol Neonatal Nurs 2006;35:717-27. https://doi.org/10.1111/j.1552-6909.2006.00092.x.
- Small R, Yelland J, Lumley J, Brown S, Liamputtong P. Immigrant women’s views about care during labor and birth: an Australian study of Vietnamese, Turkish, and Filipino women. Birth 2002;29:266-77. https://doi.org/10.1046/j.1523-536X.2002.00201.x.
- Carolan M, Cassar L. Antenatal care perceptions of pregnant African women attending maternity services in Melbourne, Australia. Midwifery 2010;26:189-201. https://doi.org/10.1016/j.midw.2008.03.005.
- Essén B, Johnsdotter S, Hovelius B, Gudmundsson S, Sjöberg NO, Friedman J, et al. Qualitative study of pregnancy and childbirth experiences in Somalian women resident in Sweden. BJOG 2000;107:1507-12. https://doi.org/10.1111/j.1471-0528.2000.tb11676.x.
- Shortall C, McMorran J, Taylor K, Traianou A, Garcia de Frutos M, Jones L, et al. Experiences of Pregnant Migrant Women Receiving Ante Peri and Postnatal Care in the UK: A Doctors of the World Report on the Experiences of Attendees at Their London Drop-In Clinic 2015. https://b.3cdn.net/droftheworld/08303864eb97b2d304_lam6brw4c.pdf (accessed March 2018).
- Higginbottom GM, Safipour J, Mumtaz Z, Chiu Y, Paton P, Pillay J. ‘I have to do what I believe’: Sudanese women’s beliefs and resistance to hegemonic practices at home and during experiences of maternity care in Canada. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-51.
- Rowe RE, Magee H, Quigley MA, Heron P, Askham J, Brocklehurst P. Social and ethnic differences in attendance for antenatal care in England. Public Health 2008;122:1363-72. https://doi.org/10.1016/j.puhe.2008.05.011.
- Ramsden I. Cultural Safety and Nursing Education in Aotearoa and Te Waipounamu 2002.
- Ramsden I. Binan Goonj: Bridging Cultures in Aboriginal Health. Sydney, NSW: Elsevier; 2009.
- Leininger M. Culture care theory, research, and practice. Nurs Sci Q 1996;9:71-8. https://doi.org/10.1177/089431849600900208.
- Robinson K, Kearns R, Dyck I. Cultural safety, biculturalism and nursing education in Aotearoa/New Zealand. Health Soc Care Community 1996;4:371-80. https://doi.org/10.1111/j.1365-2524.1996.tb00084.x.
- Mixer SJ. Use of the Culture Care Theory and ethnonursing method to discover how nursing faculty teach culture care. Contemp Nurse 2008;28:23-36. https://doi.org/10.5172/conu.673.28.1-2.23.
- Higginbottom GM, Richter MS, Mogale RS, Ortiz L, Young S, Mollel O. Identification of nursing assessment models/tools validated in clinical practice for use with diverse ethno-cultural groups: an integrative review of the literature. BMC Nurs 2011;10. https://doi.org/10.1186/1472-6955-10-16.
- Culley L. A critique of multiculturalism in heath care: the challenge for nurse education. J Adv Nurs 1996;23:564-70. https://doi.org/10.1111/j.1365-2648.1996.tb00020.x.
- Mulholland J. Nursing, humanism and transcultural theory: the ‘bracketing-out’ of reality. J Adv Nurs 1995;22:442-9. https://doi.org/10.1046/j.1365-2648.1995.22030442.x.
- Serrant-Green L. Transcultural nursing education: a view from within. Nurse Educ Today 2001;21:670-8. https://doi.org/10.1054/nedt.2001.0663.
- Salway SHG. Development of a Digital Learning Resource for Cultural Competence Training 2009.
- Springer KW, Hankivsky O, Bates LM. Gender and health: Relational, intersectional, and biosocial approaches. Soc Sci Med 2012;74:1661-6. https://doi.org/10.1016/j.socscimed.2012.03.001.
- Brascoupé S, Waters C. Cultural safety: exploring the applicability of the concept of cultural safety to Aboriginal health and community wellness. Int J Indig Health 2009;5.
- Aboriginal Nurses Association of Canada . Cultural Competence and Cultural Safety in Nursing Education: A Framework for First Nations, Inuit and Métis Nursing n.d. www.cna-aiic.ca/∼/media/cna/page-content/pdf-en/first_nations_framework_e.pdf (accessed 26 February 2018).
- Papps E, Ramsden I. Cultural safety in nursing: the New Zealand experience. Int J Qual Health Care 1996;8:491-7. https://doi.org/10.1093/intqhc/8.5.491.
- Nursing Council of New Zealand . Guidelines for Cultural Safety, the Treaty of Waitangi, and Maori Health in Nursing and Midwifery Education and Practice n.d. www.nursingcouncil.org.nz/Publications/Standards-and-guidelines-for-nurses (accessed 26 February 2018).
- Giger J, Davidhizar RE, Purnell L, Harden JT, Phillips J, Strickland O. American Academy of Nursing . American Academy of Nursing Expert Panel report: developing cultural competence to eliminate health disparities in ethnic minorities and other vulnerable populations. J Transcult Nurs 2007;18:95-102. https://doi.org/10.1177/1043659606298618.
- Canadian Council for Refugees . Refugees and Immigrants: A Glossary 2017.
- United Nations Statistics Division . Recommendations on Statistics of International Migration. Revision 1 1998. https://unstats.un.org/unsd/iiss/Recommendations-on-Statistics-of-International-Migration-Revision-1.ashx (accessed 8 November 2018).
- Australian Bureau of Statistics . Australian Historical Population Statistics n.d. www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/3105.0.65.001Main+Features12014?OpenDocument (accessed 8 August 2018).
- United States Census Bureau . Glossary n.d. www.census.gov/glossary/ (accessed 8 August 2018).
- Anderson B, Blinder S. Who Counts As a Migrant? Definitions and Their Consequences n.d. www.migrationobservatory.ox.ac.uk/resources/briefings/who-counts-as-a-migrant-definitions-and-their-consequences/ (accessed 26 February 2018).
- Office for National Statistics . Annual Population Survey (APS) QMI 2012. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/methodologies/annualpopulationsurveyapsqmi (accessed August 2018).
- Mullins T, Hussain B. Definition of ‘Immigrant’ 2017. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/internationalmigration/bulletins/migrationstatisticsquarterlyreport/november2017 (accessed August 2018).
- The King’s Fund . What Do We Know About the Impact of Immigration on the NHS? n.d. www.kingsfund.org.uk/projects/verdict/what-do-we-know-about-impact-immigration-nhs (accessed 8 August 2018).
- Jayaweera H. Health of Migrants in the UK: What Do We Know? 2011. https://migrationobservatory.ox.ac.uk/resources/briefings/health-of-migrants-in-the-uk-what-do-we-know/ (accessed 8 August 2018).
- Giuntella O, Nicodemo C, Vargas-Silva C. The effects of immigration on NHS waiting times. J Health Econ 2018;58:123-43. https://doi.org/10.1016/j.jhealeco.2018.02.001.
- Urquia ML, Gagnon AJ. Glossary: migration and health. J Epidemiol Community Health 2011;65:467-72. https://doi.org/10.1136/jech.2010.109405.
- Degni F, Suominen SB, El Ansari W, Vehviläinen-Julkunen K, Essen B. Reproductive and maternity health care services in Finland: perceptions and experiences of Somali-born immigrant women. Ethn Health 2014;19:348-66. https://doi.org/10.1080/13557858.2013.797567.
- Salt J. International Migration and the United Kingdom 2015. www.geog.ucl.ac.uk//research/research-centres/migration-research-unit/pdfs/Sopemi_UK_2015.pdf (accessed 8 August 2018).
- Derose KP, Bahney BW, Lurie N, Escarce JJ. Review: immigrants and health care access, quality, and cost. Med Care Res Rev 2009;66:355-408. https://doi.org/10.1177/1077558708330425.
- Drewniak D, Krones T, Wild V. Do attitudes and behavior of health care professionals exacerbate health care disparities among immigrant and ethnic minority groups? An integrative literature review. Int J Nurs Stud 2017;70:89-98. https://doi.org/10.1016/j.ijnurstu.2017.02.015.
- Tobin CL, Di Napoli P, Beck CT. Refugee and immigrant women’s experience of postpartum depression: a meta-synthesis. J Transcult Nurs 2017;29:84-100. https://doi.org/10.1177/1043659616686167.
- Jentsch B, Durham R, Hundley V, Hussein J. Creating consumer satisfaction in maternity care: the neglected needs of migrants, asylum seekers and refugees. Int J Consum Stud 2007;31:128-34. https://doi.org/10.1111/j.1470-6431.2006.00582.x.
- Collins CH, Zimmerman C, Howard LM. Refugee, asylum seeker, immigrant women and postnatal depression: rates and risk factors. Arch Womens Ment Health 2011;14:3-11. https://doi.org/10.1007/s00737-010-0198-7.
- Higginbottom GMA, Evans C, Morgan M, Kaur Bharj K, Eldridge J, Hussain B. Interventions that improve maternity care for immigrant women in the UK: protocol for a narrative synthesis systematic review. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016988.
- Booth A. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions 2016.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews 2006. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.178.3100&rep=rep1&type=pdf (accessed June 2018).
- Higginbottom GM, Morgan M, O’Mahony J, Chiu Y, Kocay D, Alexandre M, et al. Immigrant women’s experiences of postpartum depression in Canada: a protocol for systematic review using a narrative synthesis. Syst Rev 2013;2. https://doi.org/10.1186/2046-4053-2-65.
- Paterson BL, Hannes K, Lockwood C. Synthesizing Qualitative Research: Choosing the Right Approach. Hoboken, NJ: John Wiley & Sons; 2012.
- National Information Center on Health Services Research and Health Care Technology . Health Services Research and Health Policy Grey Literature Project: Summary Report 2006. www.nlm.nih.gov/nichsr/greylitreport_06.html (accessed March 2017).
- Intervention MICA . Building Healthy Communities. What Is an Intervention n.d. http://health.mo.gov/data/interventionmica/ (accessed 15 February 2018).
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Carr S, Coren E. SCIE Research Resource 02: Collection of Examples of Service User and Carer Participation in Systematic Reviews n.d. www.scie.org.uk/publications/researchresources/rr02.asp (accessed 26 February 2018).
- McGrath Y, Sumnall H, Edmonds K, McVeigh J, Bellis M. Review of Grey Literature on Drug Prevention Among Young People 2006. www.cph.org.uk/wp-content/uploads/2012/08/review-of-grey-literature-on-drug-prevention-among-young-people-review-summary.pdf (accessed 6 March 2018).
- Higginbottom GM, Morgan M, Alexandre M, Chiu Y, Forgeron J, Kocay D, et al. Immigrant women’s experiences of maternity-care services in Canada: a systematic review using a narrative synthesis. Syst Rev 2015;4. https://doi.org/10.1186/2046-4053-4-13.
- Miles M, Huberman AM, Saldana J. Qualitative Data Analysis. Thousand Oaks, CA: Sage Publications; 1994.
- Roper JM, Shapira J. Ethnography in Nursing Research. Thousand Oaks, CA: Sage Publications; 2000.
- Tashakorri C, Teddlie A. Foundations in Mixed Methods Research; Integrating Quantitative and Qualitative Approaches in the Social and Behavioral Sciences. Thousand Oaks, CA: Sage Publications; 2008.
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009;9. https://doi.org/10.1186/1471-2288-9-59.
- Hannes K, Booth A, Harris J, Noyes J. Celebrating methodological challenges and changes: reflecting on the emergence and importance of the role of qualitative evidence in Cochrane reviews. Syst Rev 2013;2. https://doi.org/10.1186/2046-4053-2-84.
- Lincoln YS, Guba EG, Pilotta JJ. Naturalistic Inquiry. Thousand Oaks, CA: Sage Publications; 1985.
- Carroll C, Booth A, Lloyd-Jones M. Should we exclude inadequately reported studies from qualitative systematic reviews? An evaluation of sensitivity analyses in two case study reviews. Qual Health Res 2012;22:1425-34. https://doi.org/10.1177/1049732312452937.
- Center for Evidence-Based Management . Critical Appraisal Tools &Amp; Questionnaires n.d. www.cebma.org/ (accessed 15 February 2018).
- O’Cathain A, Andrew S, Halcomb EJ. Mixed Methods Research for Nursing and the Health Sciences. London: Blackwell; 2009.
- Booth A, Lewin S, Glenton C, Munthe-Kaas H, Toews I, Noyes J, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 7: understanding the potential impacts of dissemination bias. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0694-5.
- Murphy EDR, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technol Assess 1998;2. https://doi.org/10.3310/hta2160.
- Cheung NF. The cultural and social meanings of childbearing for Chinese and Scottish women in Scotland. Midwifery 2002;18:279-95. https://doi.org/10.1054/midw.2002.0328.
- Jomeen J, Redshaw M. Ethnic minority women’s experience of maternity services in England. Ethn Health 2013;18:280-96. https://doi.org/10.1080/13557858.2012.730608.
- Bulman KH, McCourt C. Somali refugee women’s experiences of maternity care in west London: a case study. Crit Public Health 2002;12:365-80. https://doi.org/10.1080/0958159021000029568.
- McLeish J. Maternity experiences of asylum seekers in England. Br J Midwifery 2005;13:782-5. https://doi.org/10.12968/bjom.2005.13.12.20125.
- Briscoe L, Lavender T. Exploring maternity care for asylum seekers and refugees. Br J Midwifery 2009;17:17-24. https://doi.org/10.12968/bjom.2009.17.1.37649.
- Raine R, Cartwright M, Richens Y, Mahamed Z, Smith D. A qualitative study of women’s experiences of communication in antenatal care: identifying areas for action. Matern Child Health J 2010;14:590-9. https://doi.org/10.1007/s10995-009-0489-7.
- Essén B, Binder P, Johnsdotter S. An anthropological analysis of the perspectives of Somali women in the West and their obstetric care providers on caesarean birth. J Psychosom Obstet Gynaecol 2011;32:10-8. https://doi.org/10.3109/0167482X.2010.547966.
- Binder P, Borné Y, Johnsdotter S, Essén B. Shared language is essential: communication in a multiethnic obstetric care setting. J Health Commun 2012;17:1171-86. https://doi.org/10.1080/10810730.2012.665421.
- Feldman R. When maternity doesn’t matter: dispersing pregnant women seeking asylum. Br J Midwifery 2014;22:23-8. https://doi.org/10.12968/bjom.2014.22.1.23.
- Greenhalgh T, Clinch M, Afsar N, Choudhury Y, Sudra R, Campbell-Richards D, et al. Socio-cultural influences on the behaviour of South Asian women with diabetes in pregnancy: qualitative study using a multi-level theoretical approach. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0360-1.
- Hufton E, Raven J. Exploring the infant feeding practices of immigrant women in the North West of England: a case study of asylum seekers and refugees in Liverpool and Manchester. Matern Child Nutr 2016;12:299-313. https://doi.org/10.1111/mcn.12145.
- Moxey JM, Jones LL. A qualitative study exploring how Somali women exposed to female genital mutilation experience and perceive antenatal and intrapartum care in England. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009846.
- Lephard E, Haith-Cooper M. Pregnant and seeking asylum: exploring women’s experiences’ from booking to baby. Br J Midwifery 2016;4:130-6. https://doi.org/10.12968/bjom.2016.24.2.130.
- de Chavez AC, Ball HL, Ward-Platt M. Bi-ethnic infant thermal care beliefs in Bradford, UK. Int J Hum Rights Healthc 2016;9:120-34. https://doi.org/10.1108/IJHRH-06-2015-0019.
- Warrier S. Consumer Empowerment: A Qualitative Study of Linkworker and Advocacy Services for Non-English Speaking Users of Maternity Services. London: The Maternity Alliance; 1996.
- Ali N. Experiences of Maternity Services: Muslim Women’s Perspectives 2004. www.maternityaction.org.uk/wp-content/uploads/2013/09/muslimwomensexperiencesofmaternityservices.pdf (accessed 10 April 2018).
- Nabb J. Pregnant asylum-seekers: perceptions of maternity service provision. Evid Based Midwifery 2006;4:89-96.
- Bawadi HA. Migrant Arab Muslim Women’s Experiences of Childbirth in the UK 2009.
- Lee JY. ‘My Body Is Korean, But Not My Child’s . . .’ : A Foucauldian Approach to Korean Migrant Women’s Health-Seeking Behaviours in the UK 2010.
- Baldeh F. Obstetric Care in Scotland: The Experience of Women Who Have Undergone Female Genital Mutilation (FGM) 2013.
- Lamba R. A Qualitative Study Exploring Migrant Pakistani-Muslim Women’s Lived Experiences and Understanding of Postnatal Depression 2015.
- Goodwin L. The Midwife–Woman Relationship in a South Wales Community: A Focused Ethnography of the Experiences of Midwives and Migrant Pakistani Women in Early Pregnancy 2016. https://doi.org/10.1111/hex.12629.
- Hicks C, Hayes L. Linkworkers in antenatal care: facilitators of equal opportunities in health provision or salves for the management conscience?. Health Serv Manage Res 1991;4:89-93. https://doi.org/10.1177/095148489100400202.
- Hawkins SS, Lamb K, Cole TJ, Law C. Millennium Cohort Study Child Health Group . Influence of moving to the UK on maternal health behaviours: prospective cohort study. BMJ 2008;336:1052-5. https://doi.org/10.1136/bmj.39532.688877.25.
- Tucker A, Ogutu D, Yoong W, Nauta M, Fakokunde A. The unbooked mother: a cohort study of maternal and foetal outcomes in a North London Hospital. Arch Gynecol Obstet 2010;281:613-16. https://doi.org/10.1007/s00404-009-1152-7.
- Gorman DR, Katikireddi SV, Morris C, Chalmers JW, Sim J, Szamotulska K, et al. Ethnic variation in maternity care: a comparison of Polish and Scottish women delivering in Scotland 2004–2009. Public Health 2014;128:262-7. https://doi.org/10.1016/j.puhe.2013.11.008.
- Pershad P, Tyrrell H. Access to Antenatal and Postnatal Services for Asian Women Living in East Pollokshields, Glasgow. Save the Children; 1995.
- Redshaw M, Rowe R, Hockley C, Brocklehurst P. Recorded Delivery: A National Survey of Women’s Experience of Maternity Care 2006 2007. www.npeu.ox.ac.uk/recorded-delivery (accessed 16 May 2018).
- Duff LA, Lamping DL, Ahmed LB. Evaluating satisfaction with maternity care in women from minority ethnic communities: development and validation of a Sylheti questionnaire. Int J Qual Health Care 2001;13:215-30. https://doi.org/10.1093/intqhc/13.3.215.
- Ahmed S, Macfarlane A, Naylor J, Hastings J. Evaluating bilingual peer support for breastfeeding in a local sure start. Br J Midwifery 2006;14:467-70. https://doi.org/10.12968/bjom.2006.14.8.21640.
- Cross-Sudworth F, Williams A, Herron-Marx S. Maternity services in multi-cultural Britain: using Q methodology to explore the views of first- and second-generation women of Pakistani origin. Midwifery 2011;27:458-68. https://doi.org/10.1016/j.midw.2010.03.001.
- O’Shaughnessy R, Nelki J, Chiumento A, Hassan A, Rahman A. Sweet mother: evaluation of a pilot mental health service for asylum-seeking mothers and babies. J Public Ment Health 2012;11:214-28. https://doi.org/10.1108/17465721211289392.
- Leeds Family Health . Research Into the Uptake of Maternity Services As Provided by Primary Health Care Teams to Women from Black and Minorities 1992.
- Almalik M. A Comparative Evaluation of Postnatal Care for Migrant and UK-Born Women 2011.
- BEMIS Scotland and Community Food and Health (Scotland) . Strengthening Food Work Across Ethnic Minority Communities: A Focus on Maternal and Infant Nutrition 2013. www.communityfoodandhealth.org.uk/publications/strengthening-food-work-ethnic-minority-communities-focus-maternal-infant-nutrition/ (accessed 12 August 2018).
- Edge D. Falling through the net – black and minority ethnic women and perinatal mental healthcare: health professionals’ views. Gen Hosp Psychiatry 2010;32:17-25. https://doi.org/10.1016/j.genhosppsych.2009.07.007.
- Thomas VN, Saleem T, Abraham R. Barriers to effective uptake of cancer screening among Black and minority ethnic groups. Int J Palliat Nurs 2005;11. https://doi.org/10.12968/ijpn.2005.11.11.20096.
- Ahmad W, Bradby H. Ethnicity and health: key themes in a developing field. Curr Sociol 2008;56:47-56. https://doi.org/10.1177/0011392107084378.
- Green G, Bradby H, Chan A, Lee M. ‘We are not completely Westernised’: dual medical systems and pathways to health care among Chinese migrant women in England. Soc Sci Med 2006;62:1498-509. https://doi.org/10.1016/j.socscimed.2005.08.014.
- Taylor SP, Nicolle C, Maguire M. Cross-cultural communication barriers in health care. Nurs Stand 2013;27:35-43. https://doi.org/10.7748/ns2013.04.27.31.35.e7040.
- Department of Health and Social Care . Safer Maternity Care: Next Steps Towards the National Maternity Ambition 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/560491/Safer_Maternity_Care_action_plan.pdf (accessed 24 October 2019).
- Redshaw M, Heikkilä K. Ethnic differences in women’s worries about labour and birth. Ethn Health 2011;16:213-23. https://doi.org/10.1080/13557858.2011.561302.
- Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved 1998;9:117-25. https://doi.org/10.1353/hpu.2010.0233.
- Foronda CL. A concept analysis of cultural sensitivity. J Transcult Nurs 2008;19:207-12. https://doi.org/10.1177/1043659608317093.
- Cohen AL, Rivara F, Marcuse EK, McPhillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients?. Pediatrics 2005;116:575-79. https://doi.org/10.1542/peds.2005-0521.
- Mehrabian A. Nonverbal Communication. New Brunswick, NJ: Transaction Publishers; 1972.
- Agency for Healthcare Research and Quality . National Healthcare Disparities Report 2005. https://archive.ahrq.gov/qual/nhdr05/nhdr05.pdf (accessed 12 February 2018).
- The Home Office . The Stephen Lawrence Inquiry 1999. www.gov.uk/government/publications/the-stephen-lawrence-inquiry (accessed July 2017).
- Steele CM, Aronson J. Stereotype threat and the intellectual test performance of African Americans. J Pers Soc Psychol 1995;69:797-811. https://doi.org/10.1037/0022-3514.69.5.797.
- Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health 2000;90:1212-15. https://doi.org/10.2105/AJPH.90.8.1212.
- Mohammadi N, Evans D, Jones T. Muslims in Australian hospitals: the clash of cultures. Int J Nurs Pract 2007;13:310-15. https://doi.org/10.1111/j.1440-172X.2007.00643.x.
- Betancourt JR, Green AR, Carrillo JE. Cultural Competence in Health Care: Emerging Frameworks and Practical Approaches. Washington, DC: Commonwealth Fund; 2002.
- Department of Health, Social Services and Public Safety . A Strategy for Maternity Care in Northern Ireland 2012–2018 n.d. www.health-ni.gov.uk/publications/strategy-maternity-care-northern-ireland-2012-2018 (accessed 22 October 2019).
- The Maternity Services Action Group . A Refreshed Framework for Maternity Care in Scotland 2011. www2.gov.scot/resource/doc/337644/0110854.pdf (accessed 22 October 2019).
- Welsh Government . Strategic Vision for Maternity Services in Wales 2011. www.wales.nhs.uk/documents/A%20Strategic%20Vision%20for%20Maternity%20Services%20in%20Wales%20-%20September%202011.pdf (accessed 10 October 2018).
- NHS England . Spotlight on Maternity: Contributing to the Government’s National Ambition to Halve the Rates of Stillbirths, Neonatal and Maternal Deaths and Intrapartum Brain Injuries by 2030 2016. www.england.nhs.uk/signuptosafety/wp-content/uploads/sites/16/2015/11/spotlight-on-maternity-guide.pdf (accessed 25 September 2019).
- Spector RE. Cultural diversity in health and illness. J Transcult Nurs 2002;13:197-9. https://doi.org/10.1177/10459602013003007.
- Cross TL. Towards a Culturally Competent System of Care: A Monograph on Effective Services for Minority Children Who Are Severely Emotionally Disturbed. Washington, DC: CASSP Technical Assistance Center, Georgetown University Child Development Center; 1989.
- Betancourt JR. Cultural competence and medical education: many names, many perspectives, one goal. Acad Med 2006;81:499-501. https://doi.org/10.1097/01.ACM.0000225211.77088.cb.
- Crombie IK. The Pocket Guide to Critical Appraisal. London: British Medical Journal Publishing Group; 1996.
Appendix 1 Review search strategy: MEDLINE
| Search | MeSH terms | Number recieved | Notes |
|---|---|---|---|
| 1 | Maternal Health Services/or Postnatal Care/or Preconception Care/or Prenatal Care/or Perinatal Care/or Infant Care/or Midwifery/or Obstetrics/or General Practitioners/or Primary Health Care/or Family Health/ | 162,335 | |
| 2 | ((maternal or child* or baby or babies or fetus* or fetal* or embryo* or obstetric*) adj3 (health* or nurs* or care or service*)).ti,ab. | 119,288 | Field modified from.mp. to.ti,ab. |
| 3 | ((birth* or matern* or mother* or pregnan* or childbearing or child-bearing or prenatal or pre-natal or postnatal or post-natal or perinatal or peri-natal or preconception or pre-conception or antenatal or ante-natal or postpartum or puerperium) adj3 (health* or nurs* or care or service*)).ti,ab. | 65,240 | Field modified from.mp. to.ti,ab. |
| 4 | exp Midwifery/or exp Obstetric Nursing/or exp Community Health Nursing/or (midwif* or midwiv*).ti,ab. | 47,851 | Field modified from.mp. to. ti, ab. |
| 5 | exp Health Services Accessibility/or exp Healthcare Disparities/or exp Health Services/ | 1,829,149 | |
| 6 | 5 and (matern* or child* or baby or babies or fetus* or fetal* or embryo* or obstetric* or birth* or mother* or pregnan* or childbearing or child-bearing or prenatal or pre-natal or postnatal or post-natal or perinatal or peri-natal or preconception or pre-conception or antenatal or ante-natal or postpartum or puerperium). ti, ab. | 253,992 | Limit 5 to female did not sufficiently focus previous search strategy so text terms used instead; Field modified from.mp. to. ti, ab. |
| 7 | 1 or 2 or 3 or 4 or 6 | 490,776 | |
| 8 | (‘use’ or access* or utili* or consum* or block* or hurdl* or barrier* or hindr* or hinder* or obstacle* or exclu* or discrimin* or disparit* or disproportion* or inequal* or unequal* or inadequat* or insuffic* or stratif* or limit* or lack* or unreliab* or poor* or poverty* or depriv* or disadvantag* or insecur* or insensit* or status* or entitl* or uninform* or ill-inform* or benefit* or interven* or deliver* or effective* or cost effective*).ti,ab. | 8,190,143 | |
| 9 | 5 and 8 | 761,677 | Use of/access to health services |
| 10 | ‘Emigrants and Immigrants’/or Refugees/or ‘Transients and Migrants’/or ‘Emigration and Immigration’/ | 42,486 | |
| 11 | (((established or ‘first generation*’ or new* or recent* or current*) adj3 (migrant* or migrat* or immigrant* or immigrat* or emigrant* or emigrat* or emigre* or expat* or (ex adj pat*) or transient* or alien*)) or newcomer* or (new adj comer*) or incomer* or (in adj omer*)).ti,ab. | 14,965 | Revised to focus on established or new immigrant groups; Field modified from.mp. to. ti, ab. |
| 12 | (refugee* or (asylum adj seek*) or asylee* or (refused adj3 (asylum* or refugee*)) or (displaced adj person*) or exile* or (new adj arrival) or (country adj2 (birth or origin)) or transnational*). ti, ab. | 13,603 | Field modified from.mp. to. ti, ab. |
| 13 | (foreigner* or (foreign adj (born or citizen* or national* or origin*)) or (non adj (citizen* or native*)) or ((adoptive or naturali#ed) adj (citizen* or resident*)) or overstay* or trafficked or ‘spousal migrant*’). ti, ab. | 10,542 | Additional migrants terminology; Field modified from.mp. to.ti,ab. |
| 14 | (‘non-UK-born’ or ‘born outside the UK’ or ‘length of residence in the UK’ or ((‘not lawful*’ or ‘not legal*’ or unlawful* or illegal* or unauthori#ed* or ‘not authori#ed’ or uncertain or insecure or illegal or legal or irregular* or refused or undocumented) adj3 (residen* or immigrant* or imigrat* or migrant* or migrat*))).ti,ab. | 1375 | Additional migrants terminology; Field modified from.mp. to.ti,ab. |
| 15 | exp Ethnic Groups/or (ethnic* or ethno* or race or racial*). ti, ab. | 282,908 | Expanded ethnic terminology; Field modified from.mp. to. ti, ab. |
| 16 | exp african continental ancestry group/or exp asian continental ancestry group/or exp Caribbean Region/ | 152,457 | Additional ethnic terminology to specify South Asian and African Caribbean groups; Field modified from.mp. to. ti, ab. |
| 17 | exp Vulnerable Populations/or ((vulnerab* or disadvantag* or minorit*) adj3 (individ* or person* or people* or population* or communit* or group*)). ti, ab. | 35,822 | Expanded vulnerable populations terminology; Field modified from.mp. to. ti, ab. |
| 18 | (‘Black and Minority Ethnic’ or ‘Black & Minority ethnic’ or BME or african caribbean* or afro caribbean* or black african* or (west adj (indies or indian*))). ti, ab. | 7587 | Expanded ethnic terminology; Field modified from.mp. to. ti, ab. |
| 19 | (south asia* or afghan* or bangladesh* or bengal* or bhutan* or india* or maldiv* or nepal* or pakistan* or sri lanka*). ti, ab. | 163,384 | Additional ethnic terminology; Field modified from.mp. to. ti, ab.; specific South Asian countries and ethnicities identified from Migration Observatory the UK: An Overview and Migration Observatory: Health of Migrants in the UK |
| 20 | 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 | 589,408 | All ethnic/migrant groups |
| 21 | 7 and 9 and 20 | 20,754 | Maternity health services AND use of/access to health services AND All ethnic/migrant groups |
| 22 | limit 21 to yr = ’1990 -Current’ | 18,783 | Time range expanded |
| 23 | higginbottom*.au. | 214 | |
| 24 | 22 and 23 | 9 | Check of strategy retrieval of known relevant records |
Appendix 2 Master table of included studies
| Study | Study aim | Region | Methodology | Theory or framework | Setting | Data analysis | Sample and mode of recruitment |
|---|---|---|---|---|---|---|---|
| Hick and Hayes128 | To establish efficacy of linkworker services (an intervention) introduced for non-English-speaking Asian women in multiracial health districts | Not specified | Quantitative survey: 21-item questionnaire | Not specified | Qualitative: content analysis | Questionnaire to the heads of midwifery services in 30 multiracial district health authorities. Twenty responded. Sample is not immigrant women; however, this is an evaluation of an intervention | |
| Duff et al.134 | To develop a reliable and valid questionnaire to evaluate satisfaction with maternity care in Sylheti-speaking Bangladeshi women | London | Mixed methods: two-stage psychometric study. First, a Sylheti-language questionnaire regarding Bangladeshi women’s experiences of maternity services was translated and culturally adapted from an English-language questionnaire, using focus groups, in-depth interviews and iterative methods. Second, quantitative psychometric methods were used to field test and evaluate the acceptability, reliability and validity of this questionnaire | Not specified | Not specified | Qualitative: thematical analysis. Quantitative: validity of an instrument | Located at four hospitals providing maternity services in London, UK. Study participants included 242 women from the London Bangladeshi communities who were in the antenatal (at least 4 months’ pregnant) or postnatal phase (up to 6 months after delivery). The women spoke Sylheti, a language with no accepted written form. In stage 1, purposive samples of 40 women in the antenatal or postnatal phase participated, along with one convenience sample of six women in the antenatal phase and three consecutive samples of 60 women in the postnatal phase. In stage 2, 135 women (main sample) completed the questionnaire 2 months after delivery (82% response rate), and 50 women (retest sample) from the main sample completed a second questionnaire 2 weeks later (96% response rate) |
| Bulman and McCourt108 | To study the maternity care experiences of Somali refugee women in an area of West London. This article focused particularly on findings relating to the language barrier, which to a large degree underpinned or at least aggravated other problems the women experienced | West London | Qualitative: case study. Six semistructured interviews and two focus groups (with six participants each) | Not specified | Not specified | Qualitative: thematical analysis | Snowball sampling: 12 Somali women were selected from a larger survey involving 1400 women |
| McLeish109 | To undertake a qualitative study of the maternity experiences of 33 asylum seekers | London, Plymouth, Hastings, Brighton, Oxford, Manchester, and King’s Lynn | Qualitative | Not specified | Home or a neutral location | Qualitative: content analysis | Convenience and snowball sampling of recent asylum seekers. Based on semistructured interviews carried out in seven English cities |
| Ahmed et al.135 | A Sure Start local programme had funded a Bangladeshi support worker to provide bilingual breastfeeding support to childbearing Bangladeshi women, many of whom were not fluent in English. This study aimed to conduct a short evaluation of the impact of this work on the uptake and duration of breastfeeding among these women | Tower Hamlets | Mixed methods: the survey questionnaire included some open and closed questions about the women’s intention to feed; their current feeding methods; the breastfeeding support and information they received antenatally, during the hospital stay and postnatally; overall views on the information and support received; and some demographic details. Eleven interviews were conducted by telephone in Sylheti (a dialect that has no written format), three in English and one in Urdu (using a female family member to translate). Interviews took between 15 and 30 minutes to complete | Not specified | Not specified (survey conducted by telephone) | Qualitative: content analysis of a questionnaire (open and closed questions) | The two midwives and the support worker had provided breastfeeding support to 194 women during a 1-year period (September 2001 to August 2002). Of these, 80 women received help from the support worker alone. The majority of these 80 women were Bangladeshi. For the evaluation, 15 women were randomly selected from these 80 women |
| Rowe et al.49 | To identify any social or ethnic differences in access to antenatal care and to quantify the effects of any such differences using data collected in a survey of women’s experiences of antenatal screening | England | Quantitative: a cross-sectional survey using a postal questionnaire | Not specified | Not specified | Quantitative: cross-sectional analysis | A stratified clustered random sampling strategy was used. Hospitals in England were stratified according to ethnic mix. To ensure inclusion of an adequate number of women from BME backgrounds, hospitals with ≥ 15% of women of BME origin were oversampled. Pregnant women aged ≥ 16 years and receiving care in 15 participating hospitals were sent a postal questionnaire at 27–31 weeks of gestation |
| Hawkins et al.129 | To compare the health behaviours both antenatally (smoking and alcohol consumption) and postnatally (initiation and duration of breastfeeding) of mothers who have white British or Irish heritage with those of mothers from ethnic minority groups, and to examine in mothers from ethnic minority groups whether or not indicators of acculturation (generational status, language spoken at home and length of residency in the UK) were associated with these health behaviours | England | Quantitative: a prospective nationally representative cohort study | Not specified | Not specified | Quantitative: cohort study | Stratified clustered sampling framework to over-represent mothers from ethnic minority groups and disadvantaged areas produced 6478 white British or Irish mothers and 2110 mothers from ethnic minority groups. Of those from ethnic minority groups, 681 (33%) were first generation and 55 (4%) were second generation |
| Briscoe and Lavender110 | To explore and synthesise the maternity care experiences of female asylum seekers and refugees | UK | Qualitative: multiple exploratory longitudinal case studies that used a series of interviews, photographs taken by the women, field notes and observational methods to contextualise data obtained during 2002 and 2003 | Theory of interactions and transformational educational theory | Hospital settings or women’s homes | Qualitative: thematical analysis | Women were approached if the status of ‘asylum seeker’ or ‘refugee’ was written in the hospital notes taken at their booking appointment. Fourteen women were approached, but nine women declined to participate. Five women consented, but one woman was dispersed before 20 weeks’ gestation and therefore was not included in the study. Of the remaining four participating women, three were asylum seekers and one was a refugee. The sampling technique was not clearly reported |
| Raine et al.111 | To identify key features of communication across antenatal care and whether they are evaluated positively or negatively by service users | Central London | Qualitative: used six focus groups of 15 participants each and conducted 15 semistructured interviews. Non-English-speaking focus groups and interviews were conducted in standard Bengali, Sylheti or Somali | Not specified | Focus groups: hospitals and university meeting rooms. Semistructured interviews: various locations to suit the needs of the women | Qualitative: thematical analysis | The sampling technique was not clearly reported, but they recruited 30 pregnant women from diverse social and ethnic backgrounds affiliated with one NHS trust (i.e. hospital) in central London. Participants were recruited within this hospital, in eight community antenatal clinics situated in socially and ethnically diverse areas, via a community parenting group for Somali women and via a Bengali Women’s Health Project. Within the hospital, participants were recruited from the antenatal waiting room (which services low- and high-risk pregnancies), the ultrasound clinic and the glucose tolerance testing clinic |
| Bharj and Salway9 | To determine the pregnancy outcomes of women of similar parity and ethnic background who received antenatal care (‘booked’), compared those who did not (‘unbooked’) over a period of 18 months | North Middlesex University Hospital, London | Quantitative: a retrospective cohort study from September 2006 to March 2008 comparing the sociodemographics and the fetal and maternal outcomes of pregnancies of unbooked vs. booked women | Not specified | Not specified | Quantitative: a retrospective cohort study | Women who received no antenatal care or who delivered within 3 days of their initial booking visit were categorised as ‘unbooked’. In each case, the woman who had delivered next on the labour ward register (matched for ethnicity and parity) and who had received antenatal care prior to the second trimester served as a comparison |
| Cross-Sudworth et al.136 | To explore the perspectives of first- and second-generation women of Pakistani origin on maternity care and to make recommendations for culturally appropriate support and care from maternity services | West Midlands | Mixed methods: a retrospective Q-methodology study of Pakistani women following childbirth | Retrospective Q- methodology study | Not specified | Qualitative: Q-methodology | A purposive sampling strategy was used. Postnatal first- and second-generation Pakistani women were self-identified by their responses to information leaflets disseminated at local children’s centres across an inner city in the West Midlands |
| Essén et al.112 | To study the relationships between Somali women and their Western obstetric care providers. The attitudes, perceptions, beliefs and experiences of both groups were explored in relation to caesarean sections, particularly to identify factors that might lead to adverse obstetric outcomes | Greater London | Qualitative: in-depth individual and focus group interviews | Framework of naturalistic enquiry, emic/etic model | Not specified | Qualitative: emic/etic analysis | Selected 39 Somali women by snowball sampling, 36 from the community and three purposively from a hospital |
| Binder et al.113 | To address the postulates that immigrant women experience sensitive care through the use of an ethnically congruent interpreter and that such women prefer to meet health providers of the same ethnic and gender profile when in a multiethnic obstetrics care setting | Greater London | Qualitative: in-depth individual and focus group interviews. Open-ended questions were presented by an obstetrician and an anthropologist | Framework of naturalistic enquiry | Not specified | Qualitative: naturalistic inquiry | Participants were recruited throughout Greater London between 2005 and 2006. Snowball sampling was used to recruit 36 immigrant Somali women, and another three were selected by a by-purposive technique for a total of 39 women. A purposive technique was used to select a further 11 Ghanaian women who had delivered at least one child within the British health-care system and who were living within the study area at the time of data collection |
| O’Shaughnessy et al.137 | To evaluate a pilot mental health service for asylum-seeking mothers and babies | UK (not clear) | Mixed methods: evaluation within a participatory action research framework | Participatory action research framework | Not specified | Qualitative: thematical analysis. Quantitative: the CARE-Index | An active outreach recruitment strategy was adopted by psychologists, who embedded themselves in a drop-in community group, the Merseyside Refugee & Asylum Seekers & Asylum Seekers Pre & Postnatal Support Group. Participants were West African women who were asylum seekers or refugees and who were either pregnant or had a young baby. They originated from The Gambia, Sierra Leone, Ivory Coast and Nigeria. All spoke English. Their ages ranged from 17 years to 32 years, and all babies were aged < 6 months at the point of initial contact, with three babies not yet born. Attendance at the 21 therapeutic group sessions ranged between 4 and 12 mothers (with their babies). Seven mothers attended a significant proportion or all group sessions. An additional six mothers attended one to four group sessions |
| Binder et al.4 | To apply the ‘three delays’ framework (developed for low-income African contexts) to a high-income Western scenario, to identify delay-causing influences in the pathway to optimal facility treatment | Greater London | Qualitative: individual and focus group interviews | ‘Three delays’ framework | Not specified | Constructivist hermeneutic naturalistic study | Purposive and snowball sampling was used to recruit 54 immigrant women originally from sub-Saharan regions in Africa (Somalia, Ghana, Nigeria, Senegal and Eritrea) living in London and to recruit 32 maternal providers |
| Cresswell et al.14 | To identify predictors of late initiation of antenatal care within an ethnically diverse cohort | Newham, East London | Quantitative: a cross-sectional analysis of routinely collected electronic patient records from Newham University Hospital NHS Trust | Not specified | Not specified | Quantitative: cross-sectional analysis | All women who attended their antenatal booking appointment within Newham University Hospital NHS Trust between 1 January 2008 and 24 January 2011 were included in this study. The main outcome measure was late antenatal booking, defined as attendance at the antenatal booking appointment after 12 weeks’ (+ 6 days’) gestation. The sample included women from Somalia, Eastern Europe, Africa, the Caribbean and South Asia |
| Jomeen et al.107 | To explore BME women’s experiences of contemporary maternity care in England | England | Qualitative data collected from a large cross-sectional survey using three open-ended questions that encouraged participants to articulate their experience of maternity care in their own words | Not specified | Not specified | Qualitative: thematic analysis | A random sample of 4800 women was selected using ONS birth registration records. The overall response rate was 63%, but was only 3% from BME groups. A total of 368 women self-identified as coming from BME groups. Of those, 219 (60%) responded with open text and 132 (60%) were born outside the UK |
| Feldman114 | To investigate women’s experiences of dispersal in pregnancy and to explore the effects of dispersal on the health and maternity care of women asylum seekers who were dispersed during pregnancy in the light of NICE guidelines on antenatal, intrapartum and postnatal care | London, south of England, Midlands and east of England, North West, North East and Wales | Qualitative: interviews were conducted with 19 women who had been dispersed during their pregnancies and with one woman kept in an initial accommodation centre | Not specified | Not specified | Qualitative (not clear) | The sampling technique was not mentioned clearly. The women interviewed came from 14 different countries and had been dispersed or relocated to or within six regions of the UK. At the time of dispersal, 14 women had been awaiting a decision on their asylum claim and six women had been refused asylum |
| Gorman et al.131 | To compare the maternal and birth outcomes of Polish and Scottish women having babies in Scotland and to describe any differences in clinical profiles and service use associated with migration from Poland | All over Scotland | Quantitative: a population-based epidemiological study of linked maternal country of birth, maternity and birth outcomes. Scottish maternity and neonatal records linked to birth registrations were analysed for differences in modes of delivery and pregnancy outcomes between Polish migrants and Scots. These outcomes were also compared with Polish Health Fund and survey data | Not specified | Not specified | Quantitative: statistical analysis | The study analysed 119,698 Scottish and 3105 Polish births to primiparous women in Scotland in 2004–9, using routinely collected administrative data on maternal country of birth and birth outcome |
| Greenhalgh et al.115 | To understand the multiple influences on behaviour and hence the risks to metabolic health of South Asian mothers and their unborn children, to theorise how these influences interact and build over time and to inform the design of culturally congruent, multilevel interventions | London boroughs, Tower Hamlets and Newham | Qualitative: group story-sharing sessions and individual biographical life-narrative interviews | Multilevel ecological models | All but four interviews were in the participants’ homes | Qualitative: phenomenology | The study recruited from diabetes and antenatal services in two deprived London boroughs. Forty-five women of Bangladeshi, Indian, Sri Lankan or Pakistani origin, aged 21–45 years with histories of diabetes in pregnancy. Overall, 17 women shared their experiences of diabetes, pregnancy, and health services in group discussions and 28 women gave individual narrative interviews (facilitated by multilingual researchers). All were audio-recorded, translated and transcribed |
| Phillimore20 | To understand the nature of need in super-diverse areas and to examine the emergent challenges for effective maternity service delivery in an era of superdiversity | West Midlands | Mixed methods: the study used a semistructured questionnaire and held narrative interviews of newcomer women. The findings were then triangulated with interviews of professionals who regularly worked with such women | Not specified | Not specified | Qualitative: systematic thematic analysis. Quantitative: triangulation of findings. | Sampling was not described clearly. However, the study used a semistructured questionnaire that was designed in collaboration with maternity professionals and community researchers to explore the views and maternity experiences of newcomer women. Experienced multilingual female community researchers completed 82 questionnaires with interviewees in a range of different languages. Narrative interviews were also held with 13 women to further explore issues. The findings were triangulated with 18 interviews of professionals who regularly worked with migrant women |
| Moxey and Jones117 | To explore how Somali women with FGM, with experienced and perceived antenatal and intrapartum care in England | Birmingham | Qualitative: a descriptive, exploratory study, using face-to-face semistructured interviews that were audio-recorded | Not specified | Private room | Qualitative: thematical analysis | The study used convenience and snowball sampling of 10 Somali women in Birmingham who had received antenatal care in England in the past 5 years |
| de Chavez et al.119 | To explore differences in infant thermal care beliefs between mothers of South Asian and white British origin in Bradford | Bradford District, West Yorkshire | Mixed methods: mothers were interviewed using a questionnaire with structured and unstructured questions | Not specified | The women chose the location of the interview | Qualitative: thematical analysis | A total of 102 mothers (51 South Asian and 51 white British) were recruited in Bradford District, West Yorkshire, UK. The inclusion criteria specified infants aged ≤ 13 months a parent of South Asian or white British cultural origin who lived in the Bradford District. South Asia was defined as including the countries of Pakistan, India, Afghanistan, Sri Lanka and Nepal. Recruitment was aided by local community organisations, children’s centres and community contacts. Urdu- and Punjabi-speaking interpreters were requested and provided for 69% of the first-generation South Asian mothers (n = 26) in the sample |
| Hufton and Raven116 | To gain an understanding of infant feeding practices among a group of UK-based refugee mothers | Liverpool and Manchester | Qualitative: two focus group discussions and 15 semistructured interviews | Not specified | HCPs: private offices or clinics. Refugee women: private rooms or discrete areas at the support venue (community centre or church hall) | Qualitative: thematical analysis | The study purposively selected 30 refugee mothers from 19 countries who now resided in Liverpool or Manchester and were at least 6 months pregnant or had a child who had been born in the UK in the last 4 years. Of these 30 women, 19 were HIV negative and 11 were HIV positive |
| Phillimore3 | To provide insights into possible causes of poor maternity outcomes for new migrants in the West Midlands region of the UK and to develop recommendations that could help improve maternity services for these migrants | West Midlands | Mixed methods: a semistructured questionnaire and in-depth interviews | Not specified | Not specified | Qualitative: systematic thematical approach. Quantitative: triangulation of the findings | A non-probability purposive sample was generated by selecting 82 women who had moved to the UK within the past 5 years and had subsequently utilised maternity services. Of these women, 13 underwent in-depth interviews as well |
| Lephard and Haith-Cooper118 | To explore the maternity care experiences of pregnant asylum-seeking women in West Yorkshire to inform service development | West Yorkshire | Qualitative: interpretative approach within the tradition of hermeneutic phenomenology | Not specified | Not specified | Qualitative: interpretive approach with hermeneutic phenomenology analysis | Purposive sampling was performed through the voluntary sector and a children’s centre. In addition, word of mouth led to an element of snowball sampling. Six women were recruited |
| Leeds Family Health138 | To provide locally applicable data on the needs of BME women in relation to their uptake of maternity and neonatal care provision by primary health-care teams in Leeds | Leeds | Mixed methods: questionnaires and focus groups. Interpreters were used when necessary for data collection. A questionnaire was translated into Urdu for some women | Not specified | Local community centres and in the participants’ homes | Qualitative: content analysis. Quantitative: survey (not clear) | A total of 97 questionnaires were completed. Of which, 50 were completed through informal links at community centres, schools and in women’s homes. The remaining 47 questionnaires were completed when the researcher attended various antenatal clinics in the community |
| Warrier120 | To study the effectiveness of three linkworker and advocacy schemes that were designed to empower minority ethnic community users of maternity services | Birmingham | Qualitative: focus group discussions, semistructured interviews and non-directive interviews | Not specified | Antenatal clinics in hospitals and health centres, community group settings and participants’ homes | Qualitative: not clear, thematical analysis? | Individual interviews were conducted with 66 Asian women who had received support from linkworker and advocacy services during their pregnancy and postnatally. Of these women, 28 were from Birmingham, 13 from Leeds and 25 from Wandsworth, London. A semistructured interview guide was translated into five Asian languages: Hindi, Punjabi, Gujarati, Urdu and Tamil. The study also included 10 focus groups made up of 60 women who had not used linkworker or advocacy services. All participants were recruited with the help of various minority ethnic women’s groups and community organisations. Interpreters assisted 11 personal interviews with non-users from Vietnamese and Chinese backgrounds |
| Pershad and Tyrrell132 | To determine the nature of the barriers confronting women when they used antenatal and postnatal services | Pollokshields, Glasgow | Qualitative: semistructured questionnaire | Not specified | Not specified | Qualitative: thematic analysis | Twenty women were interviewed in depth by the centre’s health development worker. Of these women, 17 were born outside the UK |
| Ali121 | To study the maternity services experiences of Muslim parents in England | UK: not specified | Qualitative: focus groups with Muslim mothers to explore their experiences of, and views about, maternity services; questionnaires with Muslim fathers; and interviews with HCPs | Not specified | Not specified | Qualitative: content analysis | A mixed sample of 43 immigrants and non-immigrants were recruited via their project advisory groups. The focus groups were conducted in various locations around the UK, with two focus group discussions in a language other than English. A total of eight HPCs were interviewed: six midwives (two of whom worked for Sure Start programmes), a health visitor and a consultant obstetrician |
| Redshaw133 | To determine the current clinical practice of maternity care in England, including the service provision and organisations that underpin care, from the perspective of women needing the care; to identify the key areas of concern for women receiving maternity care in England; and to determine if, and in what ways, women’s experiences and perceptions of care have changed over the last 10 years | England: not specified | Quantitative: survey | Not specified | Survey: not specified | Quantitative: cross-sectional design | Random samples of women selected for the pilot and main studies were identified by staff at the ONS, using live birth registrations for births within 2 specific weeks: 2–8 January 2006 (pilot) and 4–10 March 2006 (main study). The same method of sampling was used as had been employed in 1995 to enable direct comparisons. Random samples of 400 women for the pilot survey and 4800 women for the main survey who were aged ≥ 16 years and who had delivered their baby in a 1-week period in England were selected. The sampling was stratified on the basis of births in different geographical areas (Government Office Regions). No subgroups were oversampled. The usable response rate was 60% for the pilot survey and 63% for the main survey. The samples included 229 women of BME born outside the UK |
| Nabb122 | To explore the perceptions of pregnant asylum seekers in relation to the provision of their maternity care while in emergency accommodation in the UK | South-east of England | Qualitative: an exploratory approach using unstructured interviews with five HCPs and semistructured interviews with 10 pregnant asylum-seeking women | Not specified | Participants’ emergency accommodations | Qualitative: thematical analysis | Purposive sampling of those providing maternity care for asylum-seeking women produced a sample comprising two midwives, one GP, one hospital consultant and one nurse, all based in south coast health centres and hospitals. A total of 15 pregnant asylum-seeking women were approached to participate in the study. These women entered the UK through a south coast port over a 3-month period. Their countries of origin were Algeria, Congo, Angola, Nigeria, Somalia and Iraq, and they spoke French, Portuguese, Yoruba, Arabic and Kurdish. Translated information letters and consent forms were distributed to pregnant asylum-seeking women via the refugee helpline, which also returned signed consent forms. This constitutes non-probability, purposive sampling |
| Bawadi123 | To explore the meanings attributed by migrant Arab Muslim women to their experiences of childbirth in the UK. In particular, to explore migrant Arab Muslim women’s experiences of maternity services in the UK; to examine the traditional childbearing beliefs and practices of Arab Muslim society; and to suggest ways to provide culturally sensitive care for this group of women | UK: not specified | Qualitative: an interpretive ontological–phenomenological perspective, informed by the philosophical tenets of Heidegger (1927/1962) | Heideggerian hermeneutic phenomenology | All interviews were in the participants’ homes, except for one which took place in a restaurant after 10 p.m. | Qualitative: thematical analysis | Purposive sampling found eight Arab Muslim women who had migrated to one multicultural city in the Midlands |
| Lee124 | To examine the health-seeking behaviours of Korean migrant women living in the UK | London | Qualitative: 21 semistructured interviews | Foucauldian approach | Not clear | Qualitative: not clear | Women were recruited from New Malden via Korean community contacts |
| Almalik139 | To explore perinatal clinical indicators and experiences of postnatal care among European and Middle Eastern migrant women and to compare them with those of British women at a tertiary hospital in the north-east of Scotland | North-east of Scotland |
Mixed methods Phase 1 of the research was a secondary analysis of routine data for 15,030 consecutive deliveries at Aberdeen Maternity Hospital Phase 2 was a retrospective study of 26 European, Middle Eastern and British mothers in this hospital. After the women had given birth, verbal data were collected using face-to-face semistructured interviews |
Not clear | Phase 2: 24 interviews were conducted in the homes of participants and two interviews at the university department | Qualitative: thematical analysis. Quantitative: phase 1 was a secondary analysis of routine data for 15,030 consecutive deliveries at Aberdeen Maternity Hospital; and phase 2 was a retrospective study of women |
Phase 1: the 15,030 deliveries included all births at Aberdeen Maternity Hospital over the financial years 2004–8, in which maternal nationalities were identified and gestation was ≥ 24 weeks. Both singleton and multiple births were included. The clinical data were harvested from the Patient Administration System and the PROTOS maternity information system. In the case of women with multiple order births during the study, all births were included Phase 2 of the research was a retrospective study of a few of the mothers who had given birth at this hospital. Eight European and five Middle Eastern women were semi-matched with 13 British women |
| BEMIS Scotland and Community Food and Health (Scotland)140 | To assess the mechanisms of support available to ethnic minority communities from community and voluntary sector organisations in relation to maternal and infant nutrition (a mapping exercise); to explore the experiences of the targeted client groups in seeking and receiving such support; and to identify gaps and opportunities to enhance support mechanisms and engagement with diverse ethnic minority communities | Glasgow, Edinburgh, Aberdeen, Stirling, Fife, Dundee and Inverness | Mixed methods: an online questionnaire survey of organisations working with ethnic minority communities, focus groups and telephone interviews with ethnic minority women | Not specified | Not specified | Qualitative: thematical analysis | The study identified 65 community organisations that potentially provided food and health services across ethnic minority communities in Scotland. In total, 37 organisations replied to the survey. Of those organisations, 15 indicated that they are providing services in the area of maternal and infant nutrition. A further 12 indicated that despite working with ethnic minority communities, they do not provide services in maternal and infant nutrition or healthy eating, in general. An additional 10 organisations confirmed by telephone that they were or had been working with ethnic minority women, but were unable to undertake the survey. The majority of interviewees for the focus groups and interviews were selected in response to a request sent by Black and Ethnic Minorities Infrastructure in Scotland to community organisations. Snowball sampling was used to provide further contacts. In total, four focus groups were conducted with Polish, Roma, Czech and African mothers. In addition, six telephone interviews were conducted with Polish mothers. We focused on Polish mothers because they were the largest new ethnic group in Scotland since 2004 |
| Baldeh125 | To explore the experiences of obstetric care in Scotland among women who have undergone FGM | Glasgow and Edinburgh | Qualitative: personal experiences of FGM and interviews | Interpretivism paradigm and feminist perspective | The Dignity Alert & Research Forum office or in the participant’s home | Qualitative: thematical analysis | Convenience and purposive sampling resulted in a total number of seven women taking part in this study. All women were of African origin, living in Scotland (three in Glasgow and four in Edinburgh). The inclusion criteria for the study were women who have undergone FGM and had experienced childbirth in Scotland. Three women were originally from Somalia, two from The Gambia, one from Ghana and one from Sudan. Six of them were Muslims and one was Christian. All women had undergone FGM in their countries of origin. Four women had been infibulated and the remaining three could not tell if they have had FGM type 2 or 3 |
| Lamba126 | To gain a rich understanding of migrant Pakistani Muslim women’s experiences of postnatal depression within motherhood; to inform clinical practice; and to suggest ways of improving supportive services for this group | East London | Qualitative: interpretative phenomenology | Interpretative phenomenological analysis theory | Not specified | Qualitative: interpretative phenomenology | Purposive sampling resulted in the recruitment of four migrant Pakistani Muslim women from London, aged 27–39 years |
| Shortall et al.47 | To explore the health-care experience of vulnerable pregnant migrant women | London | Mixed methods: participants were contacted by telephone (using a three-way interpreter call if appropriate) and interviewed using a pro forma questionnaire designed to determine their access to antenatal care; barriers to that access; and their experiences during pregnancy, labour and the immediate postnatal period. Further data were extracted from their records at the Doctors of the World clinic to see how they had accessed the clinic | Not specified | Telephone survey | Qualitative: thematical analysis. Quantitative: not clear | Pregnant women who presented to the drop-in clinic of the Doctors of the World in London were approached between January 2013 and June 2014 |
| Goodwin127 | To explore relationships between first-generation migrant Pakistani women and midwives in the South Wales region, focusing on the factors that contribute to these relationships and the ways that these factors might affect the women’s experiences of care | South Wales | Qualitative: a focused ethnography | Symbolic interactionism | Midwives: at lunch break or between clinics. Pakistani women: not clear | Qualitative: thematical analysis | Purposive sampling, through midwife gatekeepers, was selected for the initial recruitment of pregnant migrant Pakistani women: e-mails were sent to all midwives working with migrant women in South Wales. Snowballing was then used to recruit other midwives eligible for participation. Focused, non-participant observations of antenatal booking appointments took place in antenatal clinics across the local health board region over a period of 3–6 months. A total of seven midwives and 15 women were observed during these appointments, which lasted 20–60 minutes each |
Appendix 3 Excluded studies with reasons for exclusion
| Exclusion number | Reference | Reasons for exclusion |
|---|---|---|
| 1 | Bowler I. ‘They’re not the same as us’: midwives’ stereotypes of South Asian descent maternity patients. Sociol Health Illn 1993;15:157–78 | Presented professionals’ perspectives: focused on midwife interviews and observational data on midwives |
| 2 | Straus L, McEwen A, Hussein FM. Somali women’s experience of childbirth in the UK: perspectives from Somali health workers. Midwifery 2009;25:181–6 | Presented professionals’ perspectives: interviewed Somali health workers and not the immigrant women |
| 3 | Bowler IM. Stereotypes of women of Asian descent in midwifery: some evidence. Midwifery 1993;9:7–16 | Presented professionals’ perspectives: interviewed midwives |
| 4 | Haith-Cooper M, Bradshaw G. Meeting the health and social needs of pregnant asylum seekers: midwifery students’ perspectives. Part 2: dominant discourses and approaches to care. Nurse Educ Today 2013;33:772–7 | Presented professionals’ perspectives: focused on midwifery students’ perceptions |
| 5 | Haith-Cooper M, Bradshaw G. Meeting the health and social care needs of pregnant asylum seekers; midwifery students’ perspectives: part 3; the pregnant woman within the global context; an inclusive model for midwifery education to address the needs of asylum-seeking women in the UK. Nurse Educ Today 2013;33:1045–50 | Presented professionals’ perspectives: interviewed midwives |
| 6 | Balaam MC, Kingdon C, Thomson G, Finlayson K, Downe S. ‘We make them feel special’: the experiences of voluntary sector workers supporting asylum-seeking and refugee women during pregnancy and early motherhood. Midwifery 2016;34:133–40 | Presented professionals’ perspectives |
| 7 | Richards J, Kliner M, Brierley S, Stroud L. Maternal and infant health of Eastern Europeans in Bradford, UK: a qualitative study. Community Practitioner 2014;87:33 | Presented professionals’ perspectives |
| 8 | Redshaw M, Heikkilä K. Ethnic differences in women’s worries about labour and birth. Ethn Health 2011;16:213–23 | Mixed sample of UK-born BME and immigrant women, with no separate findings reported for immigrant women |
| 9 | Darwin Z, Green J, McLeish J, Willmot H, Spiby H. Evaluation of trained volunteer doula services for disadvantaged women in five areas in England: women’s experiences. Health Social Care Community 2017;25:466–77 | Mixed sample of UK-born BME and immigrant women with no separate findings reported for immigrant women |
| 10 | Dunne FP, Brydon PA, Proffitt M, Smith T, Gee H, Holder RL. Fetal and maternal outcomes in Indo-Asian compared to Caucasian women with diabetes in pregnancy. QJM 2000;93:813–18 | Mixed sample of Indo-Asian women born inside and outside the UK, with no separate findings for immigrant women |
| 11 | Ball HL, Moya E, Fairley L, Westman J, Oddie S, Wright J. Infant care practices related to sudden infant death syndrome in South Asian and White British families in the UK. Paediatr Perinat Epidemiol 2012;26:3–12 | Focused on care of infants aged 2–4 months, but our chosen limit of maternity care was only up to 6 weeks after birth. Mixed sample of UK-born and non-UK-born women, with no separate findings for immigrant women |
| 12 | McCarthy R, Haith-Cooper M. Evaluating the impact of befriending for pregnant asylum-seeking and refugee women. Br J Midwifery 2013;21:404–9 | Not an empirical study: the study does not report its methodology, sampling, or data analysis |
| 13 | Streetly A, Grant C, Bickler G, Eldridge P, Bird S, Griffiths W. Variation in coverage by ethnic group of neonatal (Guthrie) screening programme in south London. BMJ 1994;309:372–4 | Mixed sample of ethnic groups, with no separate findings for immigrant women |
| 14 | Burchill J, Pevalin DJ. Demonstrating cultural competence within health-visiting practice: working with refugee and asylum-seeking families. Divers Equal Health Care 2014;11 | Weak focus on maternity care: just two quotes on the influence of cultural sensitivity training and on addressing FGM in maternity |
| 15 | Dormandy E, Michie S, Hooper R, Marteau TM. Low uptake of prenatal screening for Down syndrome in minority ethnic groups and socially deprived groups: a reflection of women’s attitudes or a failure to facilitate informed choices? Int J Epidemiol 2005;34:346–52 | Not clear if sample was composed of immigrant women: no separate findings for immigrant women |
| 16 | Henderson J, Gao H, Redshaw M. Experiencing maternity care: the care received and perceptions of women from different ethnic groups. BMC Pregnancy Childbirth 2013;13:196 | Not clear if sample was composed of immigrant women: no separate findings for immigrant women |
| 17 | Ingram J, Cann K, Peacock J, Potter B. Exploring the barriers to exclusive breastfeeding in Black and minority ethnic groups and young mothers in the UK. Matern Child Nutr 2008;4:171–80 | Mixed sample of UK-born and immigrant women, with no separate findings for immigrant women |
| 18 | Parsons L, Day S. Improving obstetric outcomes in ethnic minorities: an evaluation of health advocacy in Hackney. J Public Health 1992;14:183–91 | Not clear if sample was composed of immigrant women |
| 19 | Knight M, Kurinczuk JJ, Spark P, Brocklehurst P. Inequalities in maternal health: national cohort study of ethnic variation in severe maternal morbidities. BMJ 2009;338:b542 | Mixed sample of both UK- and foreign-born BME women, with no separate findings for immigrant women |
| 20 | Almond P, Lathlean J. Inequity in provision of and access to health-visiting postnatal depression services. J Adv Nurs 2011;67:2350–62 | Focused on professionals’ perspective. Eight of the nine participants were immigrant women, but just three brief quotes were reported from immigrant Bangladeshi women. Authors did not reply to our request for clarification of the immigrant status of the sample |
| 21 | Row MA, Nevill AM, Young DB, Adamson-Macedo EN. Promoting positive postpartum mental health through exercise in ethnically diverse priority groups. Divers Equal Health Care 2013;10:185–95 | Mixed sample of minority ethnicity women born in and outside the UK, with no separate findings for immigrant women |
| 22 | Hemingway H, Saunders D, Parsons L. Social class, spoken language and pattern of care as determinants of continuity of carer in maternity services in east London. J Public Health 1997;19:156–61 | Mixed sample of women with and without English as a first language. We used lack of English as a proxy for immigrant, but only one finding was reported for a non-English sample (i.e. the presence of an advocate who could translate for women visiting midwives or doctors). Did not receive a reply from the authors regarding the immigrant status of the sample |
| 23 | Ingram J, Johnson D, Hamid N. South Asian grandmothers’ influence on breast feeding in Bristol. Midwifery 2003;19:318–27 | No clarity on the immigrant status of the sample and no separate findings for immigrant women. Did not receive a reply from the authors on the immigrant status of the sample |
| 24 | Gardner PL, Bunton P, Edge D, Wittkowski A. The experience of postnatal depression in West African mothers living in the United Kingdom: a qualitative study. Midwifery 2014;30:756–63 | No clarity on the immigrant status of the sample and no separate findings for immigrant women |
| 25 | Kelly Y, Panico L, Bartley M, Marmot M, Nazroo J, Sacker A. Why does birthweight vary among ethnic groups in the UK? Findings from the Millennium Cohort Study. J Public Health 2008;31:131–7 | Not clear if participants included immigrant women. Did not receive a reply from the authors on the immigrant status of the sample |
| 26 | Beake S, McCourt C, Bick D. Women’s views of hospital and community-based postnatal care: the good, the bad and the indifferent. Evid Based Midwifery 2005;3:80–7 | Not clear if participants included immigrant women. Did not receive a reply from the authors on the immigrant status of the sample |
| 27 | Ahmed S, Green J, Hewison J. Antenatal thalassaemia carrier testing: women’s perceptions of information and consent. J Med Screen 2005;12:69–77 | Weak focus on maternity care: main focus was on an ancestry issue |
| 28 | Dyson SM, Cochran F, Culley L, Dyson SE, Kennefick A, Kirkham M, et al. Ethnicity questions and antenatal screening for sickle cell/thalassaemia (EQUANS) in England: observation and interview study. Crit Public Health 2007;17:31–43 | Not clear if participants included immigrant women |
| 29 | Baker D, Garrow A, Shiels C. Inequalities in immunisation and breast feeding in an ethnically diverse urban area: cross-sectional study in Manchester, UK. J Epidemiol Community Health 2011;65:346–52 | Not clear if participants included immigrant women and not focused on maternity care. Did not receive a reply from the authors on the immigrant status of the sample |
| 30 | Dyson SM, Chambers K, Gawler S, Hubbard S, Jivanji V, Sutton F, Squire P. Lessons for intermediate- and low-prevalence areas in England from the Ethnicity Questions and Antenatal Screening for sickle cell/thalassaemia (EQUANS) study. Divers Health Social Care 2007;4 | Not clear if participants included immigrant women and not focused on maternity care |
| 31 | Sim JA, Ulanika AA, Katikireddi SV, Gorman D. ‘Out of two bad choices, I took the slightly better one’: Vaccination dilemmas for Scottish and Polish migrant women during the H1N1 influenza pandemic. Public Health 2011;125:505–11 | Not focused on maternity care |
| 32 | Wittkowski A, Zumla A, Glendenning S, Fox JR. The experience of postnatal depression in South Asian mothers living in Great Britain: a qualitative study. J Reprod Infant Psychol 2011;29:480–92 | Mixed sample with only two quotes related to immigrant women |
| 33 | McFadden A, Atkin K, Renfrew MJ. The impact of transnational migration on intergenerational transmission of knowledge and practice related to breast feeding. Midwifery 2014;30:439–46 | Not focused on maternity care |
| 34 | Datta S, Alfaham M, Davies DP, Dunstan F, Woodhead S, Evans J, Richards B. Vitamin D deficiency in pregnant women from a non-European ethnic minority population – an interventional study. BJOG 2002;109:905–8 | Not clear if participants included immigrant women. Did not receive a reply from the authors on the immigrant status of the sample |
| 35 | McLeish J, Redshaw M. ‘I didn’t think we’d be dealing with stuff like this’: a qualitative study of volunteer support for very disadvantaged pregnant women and new mothers. Midwifery 2017;45:36–43 | Mixed sample with no separate findings for immigrant women |
Appendix 4 Sample of a textual summary of an included study
Reference: Phillimore J. Migrant maternity in an era of superdiversity: new migrants’ access to, and experience of, antenatal care in the West Midlands, UK. Soc Sci Med 2016;148:152–9.
Qualitative/quantitative/mixed method
Mixed methods.
What is the research question or aim?
The project aimed to provide insights into possible causes of poor migrant maternity outcomes in the West Midlands region of the UK and to develop recommendations that could help improve maternity services for migrants. The project focused on new migrants.
What is the design methodology?
A semistructured questionnaire (n = 82) and in-depth interviews (n = 13).
Sampling
A non-probability, purposive sample was generated as we selected individuals based on particular characteristics, namely women who had moved to the UK within the past 5 years and subsequently utilised maternity services.
Data analysis
The data were analysed in two parts. Qualitative responses (questions such as what provision was made to meet your cultural or religious needs?) were themed using a systematic thematic analysis approach. This involved interpretive code-and-retrieve methods, wherein the qualitative data were transcribed and read by the research team who together identified codes and then undertook an interpretative thematic analysis. Quantitative responses (questions such as how many weeks pregnant were you when you first informed a health professional that you were pregnant?) were analysed in Statistical Product and Service Solutions (SPSS) (IBM Corporation, Armonk, NY, USA). We used the frequency function to identify the most common barriers and challenges faced by migrant women, followed by cross-tabulation to identify the characteristics of the women experiencing problems.
Findings
Migrant maternity and infant mortality in the West Midlands
Perinatal mortality rates in wards with large concentrations of migrants exceed the regional average, with the most deprived super-diverse wards housing large proportions of migrant women being among the highest in the UK (17 per 1000 vs. 7.6 per 1000 for England and Wales).
Initial booking
Some 82% of respondents (n = 67) accessed some kind of service when < 12 weeks pregnant. Nine (11%) respondents attended between 12 and 16 weeks, two (2%) respondents between 17 and 20 weeks, one respondent between 21 and 30 weeks and three (4%) respondents after 31 weeks. Late bookers tended to be asylum seekers, refugees and spousal migrants. The first services accessed were the GP (n = 56), referral to a midwife for nutrition advice (n = 53) or being offered advice about antenatal tests (n = 47). Some 53 women had antenatal tests before 12 weeks, whereas 15 women did not. Women booked late for a range of reasons, including not having sufficient information about services (n = 8), not understanding the services available (n = 5), lack of translated materials (n = 4) lack of an interpreter (n = 4) or not being registered with a GP (n = 2). For example, a Chinese refugee in Birmingham wanted to register her pregnancy but did not know who to contact, ‘. . . my friend told me who to first contact. It is different to China where all health-related services take place in a hospital’. Respondents who had received advice about how to access maternity services gained information from a community midwife (n = 46), GP (n = 31), family and friends (n = 8) or community organisation (n = 7). Basic information about procedures and routines was not readily available to migrant women and rarely translated into new migrant languages. One refugee did not understand why she was told to have a blood test and sought advice via transnational networks. Several women respondents could not find information about maintaining a healthy pregnancy and sought such help from friends and family. Lack of knowledge about pregnancy monitoring processes left women fearful of scans and tests, and unsure whether or not they should consent to procedures. Women with immigration problems told how they worried that they would be tracked by immigration authorities and their babies removed if they registered with maternity services believing their presence in the UK would be evident if their name was entered into an electronic database. Indeed, a small number of women respondents felt unable to share their anxieties with their midwife, as the professionals seemed rushed. Family members were frequently used for interpretation, but such practice often excluded women from conversations about their care, a situation repeatedly raised as a concern by women.
Follow on
Having made initial contact with maternity services some 65 women (80%) were able to attend all the appointments they were offered, whereas 16 (20%) were not. Reasons women gave for non-attendance included no transport (n = 11) or inability to afford transport (n = 8), not being well (n = 6), inability to communicate (n = 3), dispersal (n = 2) or domestic responsibilities (n = 2). All but two respondents in the rural areas attended their appointments, whereas attendance in urban areas was patchier, with between one-third and all respondents in the different cities not attending follow-ups. A8 migrants were most likely to attend (94%), whereas 50% of South Asian respondents and two-thirds of African respondents attended. Failed asylum seekers, NRPF and spousal migrants were the least likely to attend all follow-up appointments. Some failed asylum seekers in the UK receive Section 4 support, set at 60% of income support levels, which themselves are already acknowledged to be too low to keep recipients above poverty lines. Section 4 payments are made via the Azure card and previously by vouchers which could only be used in certain shops. Respondents had no flexibility and choice, were unable to use cheaper shops and markets and could not travel. Some failed asylum seekers and irregular migrants with NRPF are not permitted to work; therefore, they had no income whatsoever and depended on friends for food and/or cash for travel. Women on low incomes could reclaim the costs of travelling to appointments, but claims could only be made retrospectively. Respondents were unaware of the possibility of reclaiming costs. Women said they sometimes stopped attending appointments because they felt attendance was pointless; for example, if their husbands did not explain procedures or communicate their concerns. Others were unable to access a telephone to make an appointment or could not find the hospital or identify which bus to catch. Economic migrants sometimes skipped one or more follow-ups because their employers were reluctant to release them and they feared losing their job. Asylum seekers and failed asylum seekers wanted to attend appointments but were detained or dispersed by immigration services to areas away from their midwife. One asylum seeker with HIV stated that when she was detained for 2 months, she was denied access to maternity care and retroviral medication. Asylum-seeking women were sometimes preoccupied with resolving immediate crises, or attending solicitors’ appointments to discuss their asylum case, and tended to prioritise these matters over attending antenatal follow-ups. New migrant women often moved home frequently, sometimes at short notice. Sometimes they forgot, or lacked time, to notify maternity services about their change of address and could not be contacted to arrange follow-ups. Lack of continuity of care influenced the quality of patient–midwife relationships and sometimes affected women’s confidence to attend follow-ups. Some 50% of women respondents reported not having the name of a midwife they could contact when needed. Lack of continuity made appointments less effective than those in which a prior relationship with women existed. Only 21 women (26%) attended antenatal classes. African respondents were least likely to attend (13%) and A8 migrants most likely to attend (50%). Lack of information about classes (44%), being unable to communicate with health-care staff (25%), and lack of transport (21%) or affordable transport (12%) presented the main barriers to attendance. Particular problems attending classes were experienced by asylum seekers and those who were undocumented and hiding to avoid deportation.
Limitation
Accessed respondents via community groups, may well have omitted those who were most isolated, least likely to book and perhaps having even greater needs than in this study.
Quality
Medium.
Relevance
High.
Appendix 5 Critical appraisal tool: an exemplar
We based our appraisal on the following approaches: Crombie,165 the critical appraisal approach used by the Oxford Centre for Evidence-Based Medicine, checklists of the Dutch Cochrane Centre, British Medical Journal editor’s checklists and the checklists of the EPPI-Centre.
| Critical appraisal of a cross-sectional study (survey) | |||
|---|---|---|---|
| Appraisal questions | Yes | Can’t tell | No |
| 1. Did the study address a clearly focused question/issue? | |||
| 2. Is the research method (study design) appropriate for answering the research question? | |||
| 3. Is the method of selection of the subjects (employees, teams, divisions, organisations) clearly described? | |||
| 4. Could the way the sample was obtained introduce (selection) bias? | |||
| 5. Was the sample of subjects representative with regard to the population to which the findings will be referred? | |||
| 6. Was the sample size based on pre-study considerations of statistical power? | |||
| 7. Was a satisfactory response rate achieved? | |||
| 8. Are the measurements (questionnaires) likely to be valid and reliable? | |||
| 9. Was the statistical significance assessed? | |||
| 10. Are confidence intervals given for the main results? | |||
| 11. Could there be confounding factors that haven’t been accounted for? | |||
| 12. Can the results be applied to your organisation? | |||
Appendix 6 Distribution of studies across the themes
| Study | Theme | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| n = 23 | n = 23 | n = 23 | n = 11 | n = 12 | |
| Badawi H. Migrant Arab Muslim Women’s Experiences of Childbirth in the UK. PhD thesis. Leicester: De Montfort University; 2009 | ✗ | ✗ | ✗ | ✗ | |
| Goodwin L. The Midwife–Woman Relationship in a South Wales Community: A Focused Ethnography of the Experiences of Midwives and Migrant Pakistani Women in Early Pregnancy. PhD thesis. Cardiff: Cardiff University; 2016 | ✗ | ✗ | ✗ | ||
| Hicks C, Hayes L. Linkworkers in antenatal care: facilitators of equal opportunities in health provision or salves for the management conscience? Health Serv Manage Res 1991;4:89–93 | ✗ | ✗ | ✗ | ||
| Leeds Family Health. Research Into the Uptake of Maternity Services as Provided by Primary Health Care Teams to Women from Black and Minorities. 1992. London: Leeds FHSA; 1992 | ✗ | ✗ | ✗ | ||
| Pershad P, Tyrrell H. Access to Antenatal and Postnatal Services for Asian Women Living in East Pollokshields, Glasgow. Save the Children; 1995 | ✗ | ✗ | ✗ | ✗ | |
| Warrier S. Consumer Empowerment: A Qualitative Study of Linkworker and Advocacy Services for Non-English Speaking Users of Maternity Services. London: The Maternity Alliance; 1996 | ✗ | ✗ | ✗ | ✗ | |
| Duff LA, Lamping DL, Ahmed LB. Evaluating satisfaction with maternity care in women from minority ethnic communities: development and validation of a Sylheti questionnaire. Int J Qual Health Care 2001;13:215–30 | ✗ | ✗ | |||
| Bulman KH, McCourt C. Somali refugee women’s experiences of maternity care in west London: a case study. Crit Public Health 2002;12:365–80 | ✗ | ✗ | ✗ | ✗ | ✗ |
| Ali N. Experiences of Maternity Services: Muslim Women’s Perspectives. 2004. URL: www.maternityaction.org.uk/wp-content/uploads/2013/09/muslimwomensexperiencesofmaternityservices.pdf (accessed 10 April 2018) | ✗ | ✗ | ✗ | ✗ | ✗ |
| McLeish J. Maternity experiences of asylum seekers in England. Br J Midwifery 2005;13:782–5 | ✗ | ✗ | ✗ | ✗ | ✗ |
| Ahmed S, Macfarlane A, Naylor J, Hastings J. Evaluating bilingual peer support for breastfeeding in a local sure start. Br J Midwifery 2006;14:467–70 | ✗ | ✗ | ✗ | ✗ | |
| Redshaw M, Rowe R, Hockley C, Brocklehurst P. Recorded Delivery: a National Survey of Women’s Experience of Maternity Care 2006. 2007. URL: www.npeu.ox.ac.uk/recorded-delivery (accessed 16 May 2018) | ✗ | ✗ | ✗ | ||
| Nabb J. Pregnant asylum-seekers: perceptions of maternity service provision. Evid Based Midwifery 2006;4:89–96 | ✗ | ✗ | ✗ | ||
| Rowe RE, Magee H, Quigley MA, Heron P, Askham J, Brocklehurst P. Social and ethnic differences in attendance for antenatal care in England. Public Health 2008;122:1363–72 | ✗ | ||||
| Hawkins SS, Lamb K, Cole TJ, Law C, Millennium Cohort Study Child Health Group. Influence of moving to the UK on maternal health behaviours: prospective cohort study. BMJ 2008;336:1052–5 | ✗ | ✗ | |||
| Briscoe L, Lavender T. Exploring maternity care for asylum seekers and refugees. Br J Midwifery 2009;17:17–24 | ✗ | ✗ | |||
| Raine R, Cartwright M, Richens Y, Mahamed Z, Smith D. A qualitative study of women’s experiences of communication in antenatal care: identifying areas for action. Matern Child Health J 2010;14:590–9 | ✗ | ✗ | ✗ | ||
| Tucker A, Ogutu D, Yoong W, Nauta M, Fakokunde A. The unbooked mother: a cohort study of maternal and foetal outcomes in a North London Hospital. Arch Gynecol Obstet 2010;281:613–16 | ✗ | ✗ | |||
| Lee JY. ‘My Body is Korean, But Not My Child’s . . .’ : a Foucauldian Approach to Korean Migrant Women’s Health-Seeking Behaviours in the UK. PhD thesis. Nottingham: University of Nottingham; 2010 | ✗ | ✗ | |||
| Cross-Sudworth F, Williams A, Herron-Marx S. Maternity services in multi-cultural Britain: using Q methodology to explore the views of first- and second-generation women of Pakistani origin. Midwifery 2011;27:458–68 | ✗ | ✗ | ✗ | ||
| Essén B, Binder P, Johnsdotter S. An anthropological analysis of the perspectives of Somali women in the West and their obstetric care providers on caesarean birth. J Psychosom Obstet Gynaecol 2011;32:10–18 | ✗ | ||||
| Almalik M. A Comparative Evaluation of Postnatal Care for Migrant and UK-Born Women. PhD thesis. Aberdeen: University of Aberdeen; 2011 | ✗ | ✗ | ✗ | ✗ | |
| Binder P, Johnsdotter S, Essén B. Conceptualising the prevention of adverse obstetric outcomes among immigrants using the ‘three delays’ framework in a high-income context. Soc Sci Med 2012;75:2028–36 | ✗ | ✗ | ✗ | ✗ | |
| O’Shaughnessy R, Nelki J, Chiumento A, Hassan A, Rahman A. Sweet mother: evaluation of a pilot mental health service for asylum-seeking mothers and babies. J Public Ment Health 2012;11:214–28 | ✗ | ||||
| Binder P, Borné Y, Johnsdotter S, Essén B. Shared language is essential: communication in a multiethnic obstetric care setting. J Health Commun 2012;17:1171–86 | ✗ | ✗ | |||
| Cresswell JA, Yu G, Hatherall B, Morris J, Jamal F, Harden A, Renton A. Predictors of the timing of initiation of antenatal care in an ethnically diverse urban cohort in the UK. BMC Pregnancy Childbirth 2013;13:103 | ✗ | ✗ | |||
| Jomeen J, Redshaw M. Ethnic minority women’s experience of maternity services in England. Ethn Health 2013;18:280–96 | ✗ | ✗ | ✗ | ||
| BEMIS Scotland and Community Food and Health (Scotland). Strengthening Food Work Across Ethnic Minority Communities: A Focus on Maternal and Infant Nutrition. 2013. URL: www.communityfoodandhealth.org.uk/publications/strengthening-food-work-ethnic-minority-communities-focus-maternal-infant-nutrition/ (accessed 12 August 2018) | ✗ | ✗ | ✗ | ||
| Baldeh F. Obstetric Care in Scotland: The Experience of Women Who Have Undergone Female Genital Mutilation (FGM). MSc thesis. Edinburgh: Queen Margaret University; 2013 | ✗ | ✗ | ✗ | ||
| Feldman R. When maternity doesn’t matter: dispersing pregnant women seeking asylum. Br J Midwifery 2014;22:23–8 | ✗ | ✗ | |||
| Gorman DR, Katikireddi SV, Morris C, Chalmers JW, Sim J, Szamotulska K, et al. Ethnic variation in maternity care: a comparison of Polish and Scottish women delivering in Scotland 2004–2009. Public Health 2014;128:262–7 | ✗ | ||||
| Greenhalgh T, Clinch M, Afsar N, Choudhury Y, Sudra R, Campbell-Richards D, et al. Socio-cultural influences on the behaviour of South Asian women with diabetes in pregnancy: qualitative study using a multi-level theoretical approach. BMC Med 2015;13:120 | ✗ | ||||
| Phillimore J. Delivering maternity services in an era of superdiversity: the challenges of novelty and newness. Ethn Racial Stud 2015;38:568–82 | ✗ | ✗ | ✗ | ✗ | ✗ |
| Lamba R. A Qualitative Study Exploring Migrant Pakistani-Muslim Women’s Lived Experiences and Understanding of Postnatal Depression. PhD thesis. London: University of East London; 2015 | ✗ | ✗ | |||
| Shortall C, McMorran J, Taylor K, Traianou A, Garcia de Frutos M, Jones L, et al. Experiences of Pregnant Migrant Women Receiving Ante/Peri and Postnatal Care in the UK: A Doctors of the World Report on the Experiences of Attendees at their London Drop-In Clinic. 2015. URL: https://b.3cdn.net/droftheworld/08303864eb97b2d304_lam6brw4c.pdf | ✗ | ✗ | ✗ | ||
| Moxey JM, Jones LL. A qualitative study exploring how Somali women exposed to female genital mutilation experience and perceive antenatal and intrapartum care in England. BMJ Open 2016;6:e009846 | ✗ | ✗ | ✗ | ✗ | |
| Chavez AC, Ball HL, Ward-Platt M. Bi-ethnic infant thermal care beliefs in Bradford, UK. Int J Hum Rights Healthc 2016;9:120–34 | ✗ | ||||
| Hufton E, Raven J. Exploring the infant feeding practices of immigrant women in the North West of England: a case study of asylum seekers and refugees in Liverpool and Manchester. Matern Child Nutr 2016;12:299–313 | ✗ | ✗ | |||
| Phillimore J. Migrant maternity in an era of superdiversity: New migrants’ access to, and experience of, antenatal care in the West Midlands, UK. Soc Sci Med 2016;148:152–9 | ✗ | ✗ | |||
| Lephard E, Haith-Cooper M. Pregnant and seeking asylum: exploring women’s experiences’ from booking to baby. Br J Midwifery 2016;4:130–6 | ✗ | ✗ | ✗ | ✗ | ✗ |
List of abbreviations
- BME
- black and minority ethnic
- CEBMa
- Center for Evidence-Based Management
- CERQual
- Confidence in the Evidence from Reviews of Qualitative Research
- FGM
- female genital mutilation
- GP
- general practitioner
- GRAMMS
- Good Reporting of A Mixed Methods Study
- HCP
- health-care professional
- HIV
- human immunodeficiency virus
- MeSH
- medical subject heading
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NRPF
- no recourse to public funds
- NS
- narrative synthesis
- ONS
- Office for National Statistics
- OR
- odds ratio
- PAG
- Project Advisory Group
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- UN
- United Nations
Notes
-
Grey literature search, tabulation and clustering of included studies
-
Research symposium programme, research symposium attendees and research symposium participants views
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08140).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
