Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/136/12. The contractual start date was in February 2017. The final report began editorial review in June 2019 and was accepted for publication in October 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Jon M Dickson reports grants from UCB Pharma Ltd (Slough, UK) outside the submitted work. Steve Goodacre is deputy director of the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme, chairperson of the NIHR HTA Commissioning Committee and a member of the NIHR HTA Funding Board Policy Group. Miranda Phillips reports grants from NIHR during the conduct of the study and grants from The King’s Fund, Nuffield Trust and Public Health England outside the submitted work. Joanne Turnbull reports grants from the NIHR Health Services and Delivery Research (HSDR) programme for project 14/19/16 outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by O’Cathain et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
High demand for emergency and urgent care
Internationally, policy-makers, providers of health services and researchers have expressed concerns about the high demand for emergency ambulance services and emergency departments (EDs). 1 General practice, which deals with a large proportion of patients seeking urgent care,2 also suffers from high demand. 3,4 In England, these three services have been identified as under pressure because of both high demand and workforce challenges;5 that is, there are problems with the supply of these services as well as with the demand for them.
Definition of ‘clinically unnecessary’ use of services
Researchers have often focused on demand for emergency and urgent care services from patients who do not need the clinical resources provided by, or the acuity level of, those services;6 for example, ED attenders who could have been treated at their general practice, or patients seeking urgent appointments with their general practitioner (GP) for problems that could have been dealt with using self-care. A variety of terms have been used in reference to these patients: ‘low acuity conditions’,7,8 ‘medically unnecessary’,6,9 ‘unnecessary use’,10 ‘non-urgent’,11–14 triaged as ‘low acuity’,15 ‘potentially preventable use’,16 use of emergency care for ‘primary care sensitive conditions’17 and ‘inappropriate users’. 18 In this report, the term ‘clinically unnecessary’ defines use that doctors, nurses and paramedics assess as not requiring the level or urgency of clinical care provided by their service. That is, ‘clinically unnecessary’ users may have clinical needs that could be dealt with by a lower-acuity service. ‘Clinically unnecessary’ users can also be frequent users, but these concepts differ. An individual can make ‘clinically unnecessary’ use of a service infrequently. The study focuses on ‘clinically unnecessary’ users, some of whom may also be frequent users.
‘Clinically unnecessary’ use: a contentious area
The concept of ‘clinically unnecessary’ use of health services is contentious. 19,20 Patients face a moral dilemma when help-seeking, as they may be anxious not only about taking responsibility for their health but also about being judged as wasting the time of a service. 21,22 Pope et al. ’s22 recent study highlights the general public’s confusion about the terms ‘emergency’ and ‘urgent’, which problems fall into which category, which services are appropriate to meet them and where the boundary between the categories lies. The authors emphasise the need for clear, consistent messages from service providers around these questions, as well as a more nuanced understanding of how people and communities make decisions about service use, as key prerequisites to changing help-seeking behaviour. Additionally, individual staff judgements about what constitutes a legitimate reason for service use may vary. For example, some staff may view difficulty getting a routine appointment with a GP as a legitimate reason for using urgent care, whereas others may not. 23
Context of supply–demand mismatch
It is also the case that judgements about the clinical necessity of demand may be shaped by the supply of services. 20 Judgements about the necessity of demand become harsher as demand outstrips supply. Indeed, the issue of ‘clinically unnecessary’ demand for emergency and urgent care services may been seen as relevant only if supply does not keep up with demand.
Prevalence of ‘clinically unnecessary’ use
The prevalence of ‘clinically unnecessary’ use of emergency and urgent care varies widely depending on the definition used. 14 In a systematic review,14 the prevalence of ED use for non-urgent conditions was 37%, ranging from 8% to 62% in different studies. Another review identified a range of 5–90%. 13
Interventions to address ‘clinically unnecessary’ use
Owing to widespread concern about the pressure on some emergency and urgent care services, a considerable amount of research has been undertaken to identify and test interventions to address the problem. These interventions have taken a variety of forms to target different aspects of the problem. A recent review by Van den Heede and Van de Voorde24 of 23 systematic reviews that specifically focused on reducing ED use identified six types of intervention:
-
patient education and self-management support
-
strengthening primary care services (including improving GP access and providing alternative primary care options)
-
pre-hospital diversion strategies, including telephone triage
-
co-ordination and case management
-
introducing barriers to access
-
payment from patients.
Despite the large number of primary studies, the authors concluded that evidence is still insufficient for the effectiveness of any particular intervention, partly because of the heterogeneity of the research, including the health-care system context and the target population. They propose that the complexity of the problem will require a multifaceted approach, suggesting that this is likely to include the co-location of GPs and EDs, together with a well-designed and appropriately staffed telephone triage system, although this solution is not fully evidence based.
Policy-makers in England have taken an organisational intervention approach to manage the demand for emergency and urgent care services by introducing new services. Telephone advice and triage have been introduced via NHS Direct and then NHS 111 and 111 Online to address the lack of awareness among the general population about the services available and people’s ability to make judgements about which service is best for their problem. Both NHS Direct and NHS 111 were shown to have had minimal impact on reducing demand for emergency services when they were piloted,25,26 despite NHS 111 receiving 17 million calls per year. New alternatives for access to urgent care, such as walk-in centres (WICs), have been introduced to address the issue that a lack of alternatives to urgent care may increase the use of emergency services. The evidence is mixed about the impact that WICs have on the use of EDs but, even where the effect has been positive, it has been very small, and the new centres have increased the overall use of urgent care services. 27 Organisational changes under evaluation currently include co-locating GP expertise in EDs. Policy-makers have also focused on improving population self-management and understanding about where to seek help for different problems. For example, the ‘Choose Well’ education campaign informs people about the range of available services, including alternatives to EDs.
Research gap
This study focuses on understanding what drives ‘clinically unnecessary’ demand for three emergency and urgent care services currently under pressure in England. It is important to gain an in-depth understanding from patients’ perspectives about why they make decisions that are judged ‘clinically unnecessary’ because this may help to develop interventions that reduce demand on overloaded health services.
A number of reviews have explored the reasons why people choose to use emergency and urgent care services, although some of these have not focused specifically on ‘clinically unnecessary’ use. Coster et al. ’s28 rapid review of a broad range of studies undertaken mainly in the USA and the UK focused largely on EDs and identified six reasons why people used emergency and urgent care:
-
lack of access to and/or confidence in primary care
-
perceptions of urgency or anxiety creating a need for reassurance
-
recommendations from friends, family members or health-care professionals
-
convenience, for example better opening hours or nearer to home
-
patient socioeconomic factors, such as lower costs to using specific services or unavailability of transport
-
perceived need for treatment and investigations available at a hospital only.
A similar set of issues was identified in Kraaijvanger’s29 recent systematic review of reasons why patients self-refer to EDs. Some overlap with Coster et al. ’s28 findings was also identified in Booker et al. ’s17 systematic review of patients’ use of ambulance services for primary care-sensitive conditions. This latter review included the perspectives of health professionals and service managers as well as that of patients, and identified the following factors:
-
poor physical health, including comorbidities and mental health
-
personal anxiety and risk management
-
health knowledge
-
caregivers and bystanders encouraging use of ambulances, particularly for children
-
sociodemographic and economic issues, including deprivation and lack of own transport
-
poor access to primary care.
Although these systematic reviews provide valuable high-quality evidence about the overall use of high-demand emergency and urgent care services, a more detailed exploration is needed of the motivations of patients whom those services have identified as ‘clinically unnecessary’ users. Existing reviews focusing on this issue are limited either because they focus on a single service17,29 or because they include health professional perspectives as well as patient perspectives. 17 Therefore, there is a need for a broader review encompassing the range of services providing emergency and urgent care that specifically explores patients’ perspectives on and reasons for using these services. Realist synthesis, which focuses on the mechanisms that bring about particular outcomes and the contexts in which these processes take place, would complement recent reviews by offering a more in-depth and nuanced understanding of patients’ decision-making in relation to this important issue.
Reviews show that ‘clinically unnecessary’ use of emergency and urgent care differs by population subgroup, although the findings are not consistent. There is a need to explore perceptions, experiences and attitudes by population subgroup. There is also a need to identify potential interventions that might address demand. Drivers and solutions may differ by subgroup, so considering different groups of ‘clinically unnecessary’ users may highlight interventions specific to those groups. Given that population attitudes can affect demand for emergency and urgent care, exploring these attitudes and how they differ by subgroup may improve understanding of the drivers of demand.
Conceptual framework
Three conceptual issues are relevant to this study. First, as recommended in a recent evidence review,30 this study takes an emergency and urgent care system-wide perspective rather than focusing on demand for a single service; the focus is on emergency ambulance, EDs and general practice because these services have been identified as suffering from high demand in England. Second, the focus is on patient and population perceptions of seeking emergency and urgent care rather than on the perspectives of health professionals or policy-makers. This is because it is important to gain an in-depth understanding of people’s attitudes and behaviour in order to understand how best to address these. Third, the focus is on factors operating at micro (person, family), meso (community) and macro (nation, society) levels. Therefore, an ecological model encompassing these levels shapes the study in the context of policy, organisational and societal issues affecting people’s decision-making, as well as individual behaviour.
There is no conceptual model of demand for the emergency and urgent care system as a whole. Three conceptual models focus on parts of the system. One model encapsulates demand for EDs,31 drawing attention to the role of the health-care system and policy factors, as well as the micro-level factor of individual perceptions of severity of illness, quality of care and benefit. A second model of the use of ambulance services for ‘primary care sensitive conditions’ is constructed as an ecological model of infrastructure, population and health professional factors. 17 A third model of the use of ambulance services recognises that the immediate factor of perceived seriousness is influenced by health status, belief in one’s ability to control a situation (self-efficacy), social support and trust in the system, which, in turn, are affected by sociodemographic factors. Rational choice involves weighing up the risks against the benefits and costs of contacting a service, which can be influenced by previous experience. 32 Andersen’s33 model of health service use is also relevant here, explaining the use of all services, not simply the use of emergency and urgent care. This model highlights the three dynamics of predisposing factors (e.g. ethnicity, age and health beliefs), enabling factors (e.g. family support and access to health insurance) and both perceived and actual need for health-care services. Together, these models highlight the types and range of factors likely to affect ‘clinically unnecessary’ demand for emergency and urgent care.
Aim and objectives
The study aim and objectives are articulated slightly differently from in the original proposal to clarify the focus on ‘clinically unnecessary’ demand for three health services offering emergency and urgent care. Appendix 1 provides the original objectives.
Aim
The aim of the study is to identify the drivers of ‘clinically unnecessary’ use of emergency and urgent care using patient and population perceptions.
Objectives
-
To identify the drivers of ‘clinically unnecessary’ use of emergency and urgent care using a realist review and qualitative interview study.
-
To understand how different subgroups of the population make decisions about help-seeking using a qualitative interview study.
-
To identify potential intervention strategies using a focus group study.
-
To measure the prevalence of attitudes to seeking urgent care, and how these vary in different circumstances, and by different subgroups of the population, using a population survey.
-
To identify the characteristics of people with a tendency to make ‘clinically unnecessary’ use of emergency and urgent care, using vignettes within a population survey.
Chapter 2 Overview of the study
Study design
We undertook a sequential mixed-methods study with three work packages (WPs) in the following order: a realist review (WP1), a qualitative interview study of individual interviews and focus groups with three patient subgroups (WP2) and a population survey (WP3) (Figure 1). Integration occurred throughout the study, with findings from WP1 identifying subgroups for studying in WP2, and findings from WP1 and WP2 informing the development of the questionnaire for WP3. Further integration of findings from different components was undertaken, and this is reported in Chapter 7.
FIGURE 1.
Design of the study.

Setting
The setting for the study varied by WP. The realist review was international, with attention paid to articles’ geographical context to assess their relevance to England. The interview study was based in two geographical areas in England with different emergency and urgent care system configurations. The survey was of a representative sample of the British population.
Patient and public involvement
Sheffield Emergency Care Forum (SECF) is an established group of members of the public who have experience of emergency and urgent care services and who offer patient and public involvement (PPI) to research studies. 34 At the planning stage, SECF supported the focus of the study, in particular the proposed focus on the subgroups of parents with young children and young adults. They emphasised the need to avoid a judgemental stance in the research and to ensure that interviewees were not aware that they had been selected because they had been deemed to use urgent or emergency care services unnecessarily. They also recommended offering financial incentives, suggesting that participants may be hard to recruit. They were particularly interested in potential solutions, and raised the importance of education at school about how to make best use of health services.
During the study, three SECF members and co-authors of the report (LA, SB and EH) attended Project Management Group meetings and commented on the evolving findings. Sometimes additional SECF members attended these meetings when we were presenting detailed findings. Two SECF representatives (Alice Riddell and Beryl Darlison) were members of the Project Advisory Group. Members of the Project Management Group and the Project Advisory Group were invited to comment on the draft report and Scientific summary, respectively, and two members (SB and LA) were involved in drafting the Plain English summary.
Patient and public involvement members (LA and SB) contributed to the development of the topic guide and to the interpretation of qualitative data in WP2, via management group meetings and ad hoc meetings specifically to discuss emerging findings. We held a large PPI event with members of the wider public to consider the draft survey in WP3. We report details of this event in Chapter 6.
Patient and public involvement members were reimbursed in payment or vouchers in recognition of their contribution.
Overall, PPI members provided invaluable input into the study. All of those who were part of the SECF had experience of being involved in research and were confident in contributing to discussions and providing feedback on written materials. The wider PPI event we held as part of the questionnaire development for WP3 drew on a more diverse group, including members of the public with no previous experience of research. The success of this event means that we are likely to hold more PPI events of this type in the future.
Project Advisory Group
A Project Advisory Group was convened whose members had operational roles in general practice, the ED or the ambulance service (Philip Foster, Matthew Booker, Kirsten Clinton and Andrew Hodge), a commissioning role (Daniel Mason) or expert knowledge of the emergency and urgent care system (Matthew Cooke), or were service users themselves (Alice Riddell and Beryl Darlison). The group was chaired by Matthew Cooke and met four times during the study.
Ethics approval: interviews and national survey
The realist review (WP1) did not require ethics approval. Ethics approval was sought for the qualitative interview study (WP2) and this was obtained from London – Brent REC (reference 14/LO/1228). The population survey (WP3) was conducted by the National Centre for Social Research (NatCen) (London, UK), which obtained ethics approval through its standard procedures.
Chapter 3 Realist review
Aim and objectives
The aim of this review was to use realist synthesis to identify patients’ perspectives on why they make what is judged to be ‘clinically unnecessary’ use of emergency and urgent care services. The objectives were to identify:
-
programme theories to explain ‘clinically unnecessary’ use of three emergency and urgent care services
-
subgroups of the population about whom more research is needed
-
interventions recommended by researchers.
Methods
Realist synthesis
Realist synthesis was chosen because it enables an understanding of complex social programmes that involve human decisions and actions. 35 Although generally used to explore interventions and how their outcomes are achieved, realist reviews have been used to study other issues, such as access to care. 36,37 Therefore, ‘clinically unnecessary’ use of emergency and urgent care services was considered an appropriate topic for a realist review.
The review had two phases. In the first phase, we developed and refined a set of programme theories (or proposed explanations of patients’ behaviour) that were based on published qualitative research of patients’ perspectives on why they use emergency and urgent care services for reasons judged to be ‘clinically unnecessary’. We had initially intended to draw on multiple types of information, as is common in realist reviews,35 but as the intention of the review was to develop programme theories that were grounded in in-depth patients’ perspectives, we decided to change this approach and to focus only on qualitative journal articles reporting patients’ perspectives. The development of the programme theories was also informed by discussions with our Project Management Group. In the second phase of the review, we tested the programme theories in two ways:
-
Using existing theories of health behaviour, in particular health decision-making, to gain a more in-depth understanding of how these related to this extensive wider literature.
-
Identifying any existing quantitative research that could support or refute these theories.
We registered the proposal with PROSPERO 2017: CRD42017056273. We used the RAMESES (Realist and Meta-narrative Evidence Syntheses: Evolving Standards) reporting guidelines. 35
Phase 1: developing and refining the programme theories
The review question and initial theoretical framework
We focused on three services: emergency ambulance, EDs and general practice. The research question was ‘What are patients’ perspectives of why they make use of services providing emergency and urgent care that is judged subsequently by health professionals to be “clinically unnecessary”?’.
Realist synthesis allows the initial theoretical framework or rough programme theories to be identified in different ways. 38 Coster et al. ’s28 recent review of the demand for emergency and urgent care offered a set of potential rough programme theories, but it was based on qualitative and quantitative research of all users of a range of emergency and urgent care services. Because this did not focus solely on those patients who were judged to have made ‘clinically unnecessary’ use of services, we decided not to use these theories as the basis for developing our programme theories, but rather as a theoretical framework to guide our exploration.
Identifying and selecting primary studies for inclusion
Although we could have identified our literature through database searches, we decided not to do this as we were aware of a number of high-quality reviews of demand for emergency and urgent care that were likely to include the literature we were seeking. We therefore selected three recently published, complementary reviews that were likely to contain relevant articles about emergency ambulance service demand,17 ED demand29 and emergency and urgent care,28,30 together with one ongoing review by a member of our team (Joanne Turnbull). 39 These reviews focused on demand for emergency and urgent care generally, self-referred ED users or the use of ambulance services for ‘primary care sensitive conditions’. We identified the studies in these four reviews and requested copies of the articles from their lead authors. In addition, in February 2017 we updated these searches by using MEDLINE and Google ScholarTM (Google, Inc., Mountain View, CA, USA) to identify material published during 2015 and 2016. Finally, because of a lack of articles identified that focused on ‘clinically unnecessary’ use of same-day GP appointments, in April 2017 we undertook specific searches in MEDLINE and Google Scholar for relevant general practice-focused studies from the start of each database to March 2017. All articles were in English as this was an inclusion criterion of the four reviews, and we applied this to the updated searches. All countries were included. Figure 2 summarises the search processes and the selection of studies, and Appendix 2 provides the search strategies.
FIGURE 2.
Summary of search processes and selection and extraction of articles.

Quality appraisal
The nature of realist reviews means that the formal quality assessment process that is associated with other review types is not used. 35 The study proposal outlined our intention to assess the relevance, context and methodological rigour of potential literature. As part of this process, the relevance of all literature identified from the reviews and additional searches was appraised and we included only literature related to ‘clinically unnecessary’ use of our three services. We identified studies as relevant if they focused on ‘appropriate use of services’, ‘non-urgent ED users’, ‘ED users who could be managed in alternative urgent care services’, ‘ambulance users or ED users with primary care conditions’ or ‘service use for minor disorders/ailments’, or when it was established in the paper that a group made high levels of contact with a service when they could have used alternative services (e.g. ‘use of out-of-hours services for febrile child’). For the qualitative evidence, we then undertook an assessment of how well the context of each included study was reported (see Appendix 3, Table 15) and assessed the study’s methodological rigour using the Critical Appraisal Skills Programme (see Appendix 4, Table 16). 40 We had initially stated that we would exclude studies based on the detail of their reporting of context but not on rigour, but we later decided not to exclude for either reason to ensure that all relevant literature was included. Poorly described context and low methodological rigour tended to coincide, and we took account of these issues in the analysis so that programme theories were not based solely on poorer-quality articles.
Data extraction
For the qualitative evidence, each article identified in the first search iteration was coded by context (year, country, service and type of user, e.g. not clinically necessary, common user, frequent user) and subgroup (e.g. young adults). We also identified key themes, which are reported in Appendix 5, Table 17. We then identified provisional context (C) and mechanism (M) chains for the outcome (O) of using a higher-acuity service than was considered clinically necessary. We defined the mechanism as the trigger for or driver of the decision, which arose from an ongoing situation that we defined as the context. As has been found in other realist reviews, it was often difficult to distinguish context from mechanism41,42 because of the multiple mechanisms operating that were often contexts for further mechanisms. In the early stages of the process, we undertook duplicate data extraction of some articles and discussed context–mechanism–outcome chains and potential programme theories among our team (JCon, JCos, JL and AOC). We supported the findings with direct quotations from participants in the included studies.
Developing and refining programme theories
During team discussions, we sought to identify chains of inference and connections across the data. Our initial proposal stated that we would identify between three and six rough programme theories to refine and test, but as the review progressed we decided to retain all of the programme theories we identified, as we considered them to be of equal importance and too inter-related for any to be appropriately excluded. We had multiple long team discussions (JCon, JL, JCos and AOC), as well as further discussion with the wider team and PPI members in the Project Management Group, to refine the context–mechanism–outcome chains until we had finalised 10 detailed programme theories. We further developed our understanding by focusing on what created an urgent need to contact a service within each programme theory, and developed six mechanisms across the 10 programme theories to account for this urgency. We presented the programme theories at a conference and to our Project Advisory Group for external validation.
Phase 2: testing the programme theories
In parallel with the development and refinement of the programme theories, in September 2017 Jaqui Long and Alicia O’Cathain began searching for existing theories and conceptual models that were applicable to our work using two approaches. Where our included articles referred directly to relevant theoretical work, these references were followed up by Jaqui Long, who then identified further literature around this theory or model, particularly any research applying it to ‘clinically unnecessary’ use of emergency and urgent care. This approach was used in relation to perceptions of risk, coping under stress and perceptions of service provision. When our literature contained no or few references to theoretical material related to an evolving programme theory (fear or anxiety, uncertainty, influence of family and friends), Alicia O’Cathain and Jaqui Long undertook Google searches to identify relevant literature. As part of these searches, a key article was identified43 that integrated three existing theories of how people respond to symptoms to create a new model to understand health-related help-seeking behaviour.
In addition to testing the programme theories in relation to existing theoretical material, we explored the relationship of these theories to relevant quantitative research. In September 2018, Alicia O’Cathain reviewed the quantitative material from the original searches and purposively sampled recent articles focusing on ‘clinically unnecessary’ use of different health services as follows: ambulance (6/14 articles), EDs (11/49), paediatric use of EDs (6/16), and general practice, predominantly GP out-of-hours services (6/9). These articles were read to identify evidence that supported or refuted the programme theories. The evidence was found to consist mostly of cross-sectional surveys of service users labelled ‘clinically unnecessary’. There was little research comparing ‘clinically unnecessary’ users with clinically necessary users, which might have enabled us to distinguish the mechanisms and contexts associated with ‘clinically unnecessary’ use. Even those articles that did explore these differences tested only a limited number of variables that were generally not related to our programme theories. Therefore, this process highlighted significant gaps in the quantitative evidence.
Findings
Programme theories
Description of the qualitative evidence base
We included 32 qualitative articles in the review and rated their relevance to the research question. Eighteen were rated 1, directly relevant, and 14 were rated 2, partially relevant (see Appendix 3, Table 15, for details of the relevance ratings). Articles predominantly focused on EDs, either adult/mixed (n = 16) or specialist paediatric (n = 7). Only four studies focused on GP out-of-hours services and two focused on emergency ambulance services. No studies considered daytime general practice. Most articles were from the USA (n = 12) or the UK (n = 10), with others from continental Europe (n = 5), Australia, Canada and the Caribbean. Almost all were from high-income countries, although some explored the perspectives of communities with high levels of deprivation in those countries. The health-care context varied widely between countries, particularly in relation to how patients paid for services.
Mechanisms and programme theories
An overview of our six underlying mechanisms and 10 inter-related programme theories for seeking ‘clinically unnecessary’ emergency and urgent care, together with their potential relevance to particular subgroups, is shown in Table 1.
| Underlying mechanism for urgency | PT label | PT detail | Subgroups most relevant to |
|---|---|---|---|
| Risk minimisation | 1, uncertainty about symptoms causing anxiety | When there is uncertainty about symptoms (M) because they do not fit with people’s expectations or experience (e.g. they last longer, are more severe, are unfamiliar or do not respond to self-care in the expected time scale) (C/M), this increases the perception that the problem may be serious (M) and results in an immediate need to establish what is wrong and receive reassurance (M). This concern prompts the use of the ED (O), where it is perceived that the most appropriate resources and expertise required to establish cause can be accessed quickly (C), often in the context of a lack of timely or satisfactory answers from primary care services (C) | |
| 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety | When people have experienced traumatic health incidents (e.g. delayed help-seeking leading to serious consequences) or are aware of such incidents experienced by others or reported in the media (C), they have increased anxiety and awareness of danger (C/M) and reduced confidence in their own judgement (M). They are therefore unwilling to take risks when a health problem arises (M), leading them to seek immediate help and advice from an expert in the form of emergency care, including ambulance services and EDs (O) | ||
| 3, fear of consequences when responsible for others | When people are in a position of responsibility for someone else, they are less willing to take risks with that person’s health than with their own, and they fear the consequences (e.g. distress/guilt, dismissal, litigation) (M) of not doing ‘the right thing’. This leads them to seek or to recommend seeking urgent care, particularly at the ED (O) | Parents, carers of vulnerable elderly people, people with chronic conditions, health service or other service professionals (e.g. teachers) | |
| Need for speed | 4, inability to get on with daily life | When people are prevented from undertaking their normal lives, roles or responsibilities (e.g. paid work, childcare) (C), this creates a need to get back to normal quickly (M) and to get on with their lives and discharge their responsibilities. This prompts their use of urgent care (O) because it can resolve a problem quickly by being both more accessible and more efficient than alternatives (C) | Parents of young children, people working in jobs who cannot afford or find it difficult to take time off |
| 5, need for immediate pain relief | When people are in pain or discomfort that they find intolerable (C/M), and they believe or have experienced that no primary care appointments are available within an acceptable time (C), they seek care from a more urgent service – usually the ED (O) – because of a need to obtain prompt relief from their distress (M) | ||
| 6, waited long enough for things to improve | When people delay seeking primary care treatment (for various reasons including deliberation and indecision, cost of treatment, lack of transport, complex living situations, mistrust of health services and work responsibilities) (C), they wait, often while using self-help measures, and hope the situation will improve or resolve (C). The condition reaches a ‘tipping point’ where either it is no longer tolerable (M) or other circumstances force a decision (M), and people feel that they cannot wait any longer (M). At this point, if a primary care service is unavailable to them (C), they feel they have no choice but to use an emergency service (O) | ||
| Low effort required for help-seeking | 7, stressful lives/cannot cope | When people are already experiencing significant stresses that have an impact on the internal and external resources available to them (e.g. money, time) (C), they have less capacity to cope with the additional challenge of a new or changed health problem. Symptoms are therefore likely to trigger emotional distress, including feelings of loss of control and helplessness (M), leading them to use emergency services because this is less burdensome than making an appointment with a GP. This is more likely to occur when people cannot easily or quickly access a primary care service (C) | People with low socioeconomic status, parents, people who are isolated, people with demanding work, people with mental health problems |
| Compliance | 8, following advice of trusted others | When people are anxious or concerned about a health problem and have sought the advice of trusted others (C) – either those in their social network (e.g. family) or health professionals (particularly primary care staff) – and have been advised to seek urgent care, particularly the ED (M), they are likely to then use those emergency services (O) | |
| Availability and quality of care | 9, perceptions or prior experiences of services | When people have individual experience or knowledge, or cultural beliefs, about the differing quality or availability of primary and emergency services, such as primary care offering inadequate diagnosis and care or discrimination (US context only), or EDs having better resources, expertise or more thorough care (C), they are likely to choose emergency care, particularly the ED (O), in which they have more trust and confidence (M) | People previously referred to emergency services by primary care staff, parents of young children, people with chronic conditions |
| Frustration with access to GP | 10, poor access to a GP | When people are unable to obtain an appointment with a primary care practitioner (C/M), this can further exacerbate feelings of anxiety and cause panic (M). Individuals can experience frustration (M), mistrust (M) and the perception of an uncaring service (M), feeling that they have no choice (M) but to contact an emergency service (O) |
Testing the programme theories
There was considerable support for all of the programme theories from existing theories. Only some of the programme theories were supported by quantitative research, and this was largely from cross-sectional quantitative studies rather than comparative studies (Table 2).
| PT | Evidence from qualitative papers | Links to existing theories/models | Evidence from quantitative papers |
|---|---|---|---|
| 1, uncertainty about symptoms causing anxiety: ‘I am worried because I do not know what is wrong’ | 7,44–57 |
Leventhal et al. :58 common sense model Mishel and Braden:59 role of uncertainty in decision-making |
Cross-sectional surveys of ED and GP OOH service users showed that some, but not all, were worried or anxious or thought that they had a serious problem60–64 |
| 2, heightened awareness of risk as a result of experience/knowledge of traumatic health events leading to anxiety: ‘After what happened before I daren’t risk it’ | 44,47,49,51–53,57,65–69 |
Leventhal et al. :58 common sense model Beck:70 risk society Pescosolido:71 network episode model |
– |
| 3, fear of consequences when responsible for others: ‘In my position, it’s better to be safe than sorry’ | 45,46,49,50,52,53,57,72,73 |
Leventhal et al. :58 common sense model Beck: risk society70 Dixon-Woods et al. :74 candidacy Dingwall and Murray:75 categorisation of patients |
There was little evidence, only a related issue of autistic children having higher rates of non-urgent use of EDs76 |
| 4, inability to get on with daily life: ‘I need to get back to normal’ | 56,77 |
Dingwall:78 illness action model Leventhal et al. :58 common sense model Zola:79 pathways to the doctor Beck:70 risk society |
This issue was not addressed explicitly but may have been described as using services for convenience80 |
| 5, need for immediate pain relief: ‘It’s urgent because it hurts’ | 7,45,50,55,56,65,68,77,81–84 |
Leventhal et al. :58 common sense model Andersen:33 behavioural model of health-care utilisation Beck:70 risk society |
– |
| 6, waited long enough for things to improve: ‘I can’t delay this any longer, I need to deal with it now’ | 7,48,51,54,55,65,67,72,77,81–85 |
Andersen:33 behavioural model of health-care utilisation Leventhal et al. :58 common sense model Mishel and Braden:59 role of uncertainty in decision-making Zola: pathways to the doctor79 |
Cross-sectional studies showed that people delayed attending services and tried to self-manage problems, and that duration of symptoms was an issue for ED users. Users of ED and GP OOH services had used over-the-counter remedies beforehand. In a comparative study, medically unnecessary users of GP OOH had longer-lasting problems than medically necessary users8,60–62,64,80,86–88 |
| 7, stressful lives: ‘I just can’t cope with the illness or making an appointment’ | 47,49,52,55,66,67,69,73,77,81,83,84 |
Andersen:33 behavioural model of health-care utilisation Antonovsky and Sagy:89 sense of coherence/generalised resistance resources Dixon-Woods et al. :74 candidacy Mishel and Braden:59 role of uncertainty in decision-making |
People arriving at EDs by ambulance and classed as non-urgent were more likely to be homeless and to have mental health problems. People who were more likely to use an ambulance in a hypothetical situation that did not require an ambulance had no car or lived alone6,61,90 Against: one review concluded there was little evidence of an association between coping mechanisms and the use of EDs, and another concluded that affluent groups were more likely to use EDs for minor problems14,86 |
| 8, following advice of trusted others: ‘That’s what they said to do, and they know better than me’ | 45–51,54–56,66,68,73,77,82,91,92 |
Pescosolido:71 network episode model Leventhal et al. :58 common sense model Andersen:33 behavioural model of health-care utilisation Dixon-Woods et al. :74 candidacy |
Cross-sectional studies showed that people followed the advice of family friends and health professionals when attending EDs. It was common to follow instructions from primary care staff, with at least one-quarter of ED users referred to an ED by a GP12,14,60–62,64,93 |
| 9, perceptions or prior experiences of services: ‘I’ll get a better and faster service from the hospital/ambulance’ | 7,45,46,49,50,54,55,57,66–68,72,73,81–85,91,92,94 |
Rogers and Nicolaas:95 recursivity Andersen:33 behavioural model of health-care utilisation Zimmerman:96 multilevel theory of population health Nilsen et al. :97 role of habit Dixon-Woods et al. :74 candidacy Pescosolido:71 network episode model |
Cross-sectional studies showed the attraction of the tests available and the quality of care at EDs, as well as the ease of getting tests and treatments and the preference for a specialist within paediatric EDs. Concerns about poor-quality general practice were related largely to a lack of tests, such as X-rays, and accessibility8,10,12,15,60,62,86,93 |
| 10, poor access to a GP: ‘I can’t get an appointment quickly enough’ | 7,45,49,50,56,57,65,66,68,72,73,77,81,91,98 | Andersen:33 behavioural model of health-care utilisation | Cross-sectional studies showed that perceived or actual difficulty accessing a GP in the time frame required by patients affected their use of EDs and GP OOH services. Lack of access was sometimes because of the time of day, when primary care was closed. In some studies, a sizeable minority of patients had attempted to contact the GP before going to an ED8,10,12,14,15,62,80,86–88,99–101 |
Population subgroups
The programme theories based on qualitative research were particularly relevant to parents of young children, carers, people living with chronic conditions and people leading complex or stressful lives in terms of experiencing isolation or mental health problems. However, the qualitative research focused explicitly on parents of young children only. We also read systematic reviews and quantitative articles in the review and found subgroups highlighted as more likely to be ‘clinically unnecessary’ users. However, we were concerned about this evidence base because it sometimes identified the characteristics of a cross-sectional study of ‘clinically unnecessary’ users (which may have simply corresponded to the characteristics of users) and less commonly compared ‘clinically unnecessary’ with clinically necessary users, and the results were not always consistent. There was some evidence that the following subgroups were more likely to be ‘clinically unnecessary’ users: men, people born outside the country of study, people living in areas of deprivation, people with some clinical complaints, people living a short distance from an ED, children, adults aged < 40 years and older people.
Recommended interventions to address ‘clinically unnecessary’ use of services
Jaqui Long reviewed the included qualitative articles to identify and extract specific recommendations or observations about interventions to address ‘clinically unnecessary’ use of services. We focused on the qualitative literature to ensure that the recommended interventions were based on an in-depth understanding of patients’ decision-making processes. Almost all of the papers contained relevant information, with only three making no specific comment about potential interventions. We inductively identified seven broad categories of interventions (Table 3). All of the recommendations came from the articles’ authors rather than from the study participants.
| Categorya | Examples | Articles |
|---|---|---|
| Provide patient education about management of health problems and service use |
Clear, consistent advice from health professionals and through public education about self-care, managing non-urgent problems and preventing exacerbations of existing conditions Prior agreement between GPs and patients on how to respond to particular acute problems Education on use of services: what is an emergency Education about the capacity and scope of different services Education about the benefits of continuity of care Promotion of services available through primary care |
48–50,52,54–56,66,68,72,73,81–84,98 |
| Recognise the influence of personal and social context on decision-making | Acknowledge and understand the impact of the following on people’s perceptions of a situation and their choice of service, and provide support to overcome barriers where possible:
|
7,44,48,50–53,55,67–69,73,77,83,85,98 |
| Improve primary care provision, including OOH support |
Improved quality and efficiency of services Simplified appointments system Extended hours/OOH clinics Open access Fast-track option for urgent problems OOH telephone service Internet/e-mail access Wider range of services and tests More co-ordination of care: access to specialist staff |
47,49,50,55,56,66,67,72,83,84,91,92,94,98 |
| Make changes to the structure of care provision in ED |
Locate ED and primary care on the same site Introduce fast track within ED Provide specialist open-access clinics for managing exacerbations of long-term conditions (e.g. asthma) Triage non-urgent patients to community resources/appointments Treatment of minor injuries/illnesses by nurse advisers Provide advocates/social workers for vulnerable patients Provide specialist co-ordinated care for frequent attenders with multiple problems |
7,49,50,54,69,77,91,92 |
| Improve the relationship between primary care and patients |
Address negative attitudes and behaviour of staff to improve patient experience Improve communication regarding appointment systems Involve/collaborate with patients in service design Support self-management and build confidence Provide support for vulnerable patients to navigate and access services (e.g. those with low literacy, deprivation, poor health) |
50,66,67,83,84,98 |
| New/alternative patterns of care provision in the community |
Integrate services to assess and manage urgent problems in the community/at home Provide more urgent care away from ED, including for pain, minor trauma and children’s minor illnesses Provide a nurse-staffed telephone line for non-urgent callers to emergency ambulance service |
49,72,84,91 |
| Reduce primary care referral to ED | Educate primary care staff on when to refer patients to the ED (only in papers published in USA) | 47,66,91 |
Discussion
Summary of findings
Using qualitative research that was focused largely on EDs, we identified 10 inter-related programme theories to explain why patients make ‘clinically unnecessary’ use of emergency and urgent care. These included programme theories related to symptoms (e.g. anxiety due to uncertainty about the seriousness of symptoms), patients (e.g. need for low treatment-seeking burden, caused by an inability to cope as a result of complex or stressful lives) and services (e.g. EDs were perceived to offer the desired tests and expertise when contrasted with primary care, services directed patients to EDs). Multiple mechanisms could operate for an individual. There was considerable support for these programme theories from existing theories of health behaviour but little quantitative evidence of the programme theories operating more in ‘clinically unnecessary’ users than in clinically necessary users.
Links to existing literature
Some of our programme theories aligned with the findings in the original reviews from which we identified our studies. There were clear links to the following ideas: uncertainty causing anxiety and a need to obtain reassurance to manage risk;17,28,29 a fear of consequences, particularly in relation to children and ambulance use;17 the role of stress and social deprivation in driving a need for ease of access to care;17 the influence of others, including professionals, on people’s service use;17,28,29 and consumer satisfaction, expressed positively in relation to EDs offering a range of tests and interventions in one place17,28,29 and negatively in relation to a lack of confidence in GPs28,29 or frustration with a lack of access to primary care. 17,28,29 Wider research on the demand for emergency and urgent care also supported some of the programme theories, in particular highlighting how poor access to GPs is associated with higher use of EDs for all emergency and urgent care, not just that considered ‘clinically unnecessary’. This link has been identified in numerous studies, including a large-scale survey of GP patients in 34 countries. 102
The realist review also identified some programme theories that were not evident in the original reviews. In particular, we highlighted the influence of the following on people’s decision-making: the role of previous traumatic health events in increasing anxiety, the need for immediate relief of intolerable pain, the concern about returning to normal to fulfil responsibilities such as work or child care, and the sense of a ‘tipping point’ triggering a need for urgent care following a period of self-imposed delay.
Our programme theories did not include a number of issues that were highlighted in other reviews (including our original four) or quantitative research into ‘clinically unnecessary’ use. These issues included convenience in terms of a shorter journey to a particular service;12,15,29,63,103 awareness of services;12,87 health knowledge;17 misunderstanding of the role of a service;19,88 differences between urban and rural settings;80 lack of a GP;88 a desire to take control;19 and financial considerations discussed within the US literature. 29 As these issues did not feature strongly within our included qualitative literature, they did not form part of our programme theories. We also did not develop a programme theory around the role of convenience in patients’ decisions to use emergency and urgent care, a key issue identified in other research. 14,28,29,62,93
Strengths and limitations
The lengthy and careful process used by the team to develop and refine the programme theories is a key strength of our study. The specific focus on qualitative research ensured that these theories were grounded in patients’ views and experiences. Linking our programme theories, developed in relation to a particular context of service use, to existing wider theories of health behaviour, also strengthens the review and its findings. The use of a realist approach enabled us to identify similar findings to previous research, but to significantly extend and deepen them by exploring the reasons behind the findings; for example, it confirmed the importance of anxiety, but also identified why people felt anxious. In addition to supporting existing findings, the review identified new issues driving people’s help-seeking, such as a need for immediate pain relief and the impact of previous traumatic experiences.
The review had some limitations. First, the included articles focused largely on the use of EDs. Second, the programme theories are based on qualitative interviews with patients who may have been concerned about portraying themselves as responsible and appropriate users of services. 20 However, even if this was the case, it is important to understand these representations, and we provide valuable insights into how patients describe their decision-making. Third, the included studies used a wide variety of definitions of ‘clinically unnecessary’ or ‘non-urgent’ in their recruitment of participants, and, therefore, our programme theories have not been developed in relation to a consistently defined group, as is the case in other reviews. Fourth, the included studies did not always provide enough detail to give an insight into the interaction of different issues within individuals, or where this particular service use was located in an individual’s overall help-seeking journey (e.g. whether or not they had tried other options). Fifth, the age of many of the included studies meant that very few references were made to online health-care advice, which is being used increasingly as a help-seeking strategy. Finally, our ability to test the programme theories against the quantitative literature was constrained by the limitations of this material, as it frequently did not necessarily measure issues or variables relevant to our findings.
Implications
Our findings highlight how the use of emergency and urgent services that is deemed ‘clinically unnecessary’ may be considered reasonable once details of a patient’s situation are fully taken into account. This conclusion of behaviour being rational was also reached in some of the research included in our review. 7,55,62,104 If patients are in fact generally acting rationally, this implies that interventions need to focus on educating policy-makers and service providers to better understand patients’ decision-making processes. For example, although a clinician may consider that a patient who has had symptoms for some weeks does not require urgent care, it is important to understand that it is precisely this duration that leads the patient to perceive that the situation is urgent. However, although a better understanding may change clinicians’ judgements, it is important to recognise the wider context of demand outstripping supply in many services. In addition to the ‘individual patient perspective’, there is a need to consider interventions with a view to ensuring that services are sustainable in the future.
The review highlights the importance of the impact of social circumstances on people’s ability to cope with even minor health problems. Interventions to bring about changes in service use by people in such circumstances may require wide public health approaches, including reductions in poverty, improvements to child-care support and changes in workplaces to reduce the stress caused by being unable, or feeling unable, to take time off work to seek health care.
An implication for further research is the need to compare the drivers identified here for ‘clinically unnecessary’ users and clinically necessary users to identify the size of effect of these drivers and their variation in different population subgroups.
Implications for work packages 2 and 3
Our review contributed to the selection of subgroups for WP2 (see Chapter 4).
Although data collection and early analysis of the interviews in WP2 was not directly informed by the findings from WP1, later analysis explored the relationship of the 10 programme theories to the experiences described by interviewees, including the number and patterns of programme theories present and any refinements of or challenges to them (see Chapter 4, Methods).
We tested the programme theories in the WP3 survey, including at least one item in the questionnaire relating to each programme theory.
Chapter 4 Qualitative interview study of decision-making with three subgroups of the population
Introduction
In the WP1 review, we identified that there have been many qualitative studies of ‘clinically unnecessary’ users of EDs, but not many studies that focused on users of emergency ambulances or same-day GP appointments. Some of the studies identified were not based on in-depth qualitative analyses. In addition, given that drivers may differ by subgroup, not much of the qualitative research focused on specific subgroups. We concluded that further qualitative research was needed that explored patients’ decision-making processes in depth, including their use of these three services, and that focused on specific subgroups.
Aim
The aim was to identify the drivers of ‘clinically unnecessary’ use of emergency ambulances, EDs and general practice by different subgroups of the population.
Methods
Selecting subgroups
We planned to select the subgroups using the following criteria:
-
those more likely to be ‘clinically unnecessary’ users based on the literature
-
those more likely to be ‘clinically unnecessary’ users based on the views of our Project Advisory Group
-
those on whom a lack of qualitative research has been undertaken.
To identify potential subgroups, Emma Knowles and Alicia O’Cathain read reviews and quantitative papers from the WP1 literature. Articles reported sociodemographic status (age, sex, ethnicity, relationship status), socioeconomic status (income, education level, employment status, housing tenure), presenting clinical complaint, health-care utilisation (registered with a GP, prior use of care, attendance by day/time, arrival mode) and distance to care. The findings from the literature were sometimes inconsistent, so we used them to identify a list of candidate subgroups to be discussed with our Project Advisory Group. Following consideration of the candidate subgroups, the group identified the following as of interest to them: people of Eastern European origin, individuals living in socially deprived areas, ambulatory ED patients, parents with young families, young adults and care home residents. We decided not to focus on Eastern European people, as an ongoing study was focusing on their help-seeking behaviour relating to urgent care services such as WICs,22 ambulatory ED patients, because we were interested in three services rather than EDs only, or care home residents, because the decision to seek care was likely to be taken by a third party rather than the patient. The Project Advisory Group members strongly supported focusing on people from socially deprived areas and parents of young children. They identified young adults as an interesting group to study because they viewed this group as accessing care for convenience. Some relevant qualitative research had been undertaken on these subgroups, particularly on parents of young children, but this had been undertaken largely outside the UK.
We decided that our qualitative research should focus on the following three subgroups.
-
Young adults: people aged 18–25 years (later expanded to 18–30 years). Reviews in WP1 identified that younger adults were more likely to be ‘clinically unnecessary’ users of EDs,13,14,86 and a study of medically unnecessary GP out-of-hours users showed that they were more likely to be aged 25–44 years. 88 This choice of subgroup was supported later in our study, when a UK-based research study was published showing that those aged 16–44 were more likely to use EDs for non-urgent reasons105 and a media study identified young people aged 18–29 as more likely than older working-age groups to use EDs and less likely to visit their GP. 106 None of the qualitative research identified in our WP1 review had focused on this subgroup.
-
Socially deprived: people residing in postcodes with an Index of Multiple Deprivation (IMD) score of ≤ 3. Reviews in WP1 identified that use of ambulance services for non-urgent conditions was higher in deprived areas17 and that people from deprived communities may prefer to access EDs rather than GPs. 28 A review of ‘clinically unnecessary’ use of EDs agreed with this,14 but two other reviews identified that affluent groups were more likely to be ‘clinically unnecessary’ users of EDs. 13,86 Although the evidence was conflicting, our Project Advisory Group members also identified those who are socially deprived as ‘clinically unnecessary’ users. A few of our qualitative articles in WP1 focused on this subgroup, but these were mainly US based.
-
Parents of young children: parents (aged ≥ 18 years) attending on behalf of a child aged 0–5 years (later expanded to 0–10 years). The odds of being a ‘clinically unnecessary’ ED user were found to be 1.5 among children aged 0–2 years. 107 One-third of children attending EDs in London received reassurance only rather than investigations, and researchers concluded that many could have been managed without attending an ED. 108 Our Project Advisory Group identified this as an important group to study. However, a number of the qualitative studies identified in our WP1 review focused on parents of young children attending paediatric EDs, EDs or GP out-of-hours services. We decided to focus on this subgroup because most of these qualitative studies were US based and so did not apply to the UK.
Service and setting selection
We focused on the three service settings of emergency ambulance, ED and daytime general practice. In the original proposal we also said that we would work with one WIC to identify people who were not registered with a GP, if that service was part of the service configuration in that area. However, we did not do this because we focused the study on the three key services currently facing pressures in the UK.
We recruited interviewees in two geographical areas: Sheffield and Wolverhampton. We chose these areas because they offered different service configurations and we wanted to consider whether or not these had an impact on people’s decision-making. Sheffield has a children’s ED but Wolverhampton does not, instead using a self-contained section of its main ED. Additionally, Wolverhampton had recently introduced a pilot to integrate some general practices with the NHS acute trust (vertical integration), and we planned to work with a general practice taking part in this pilot.
Identification and recruitment of potentially eligible patients
Our aim was to recruit recent users of emergency ambulances, EDs or same-day GP appointments whom clinicians had identified as having made ‘clinically unnecessary’ use of that service, that is, they could have accessed a lower-acuity service or used self-care to deal with their health problem. We did not predefine ‘clinically unnecessary’ more specifically but left clinicians to make that decision. We excluded patients who had a known history of violence at the service where they had been identified, lacked the capacity to participate in the study, were < 18 years old or were unable to speak English. When we approached patients, we did not inform them that they were considered ‘clinically unnecessary’ users of the service, and explained the study in terms of wanting to understand how people made decisions about getting help when they had a health problem. We based our selection on clinicians’ views of clinical necessity. The interviewers were not clinicians and did not make checks at interview. However, when the interviewers made follow-up contact with emergency ambulance and ED participants, a very small number had been admitted to hospital and these people were excluded from the research.
Our intention was to complete 16 interviews for each subgroup, making a total of 48 interviews. The processes of identifying and recruiting patients to the study varied between services, and to a lesser extent, between subgroups and geographical areas. Although we had originally anticipated that recruitment in each service would take a short time only, a number of challenges meant that the process was considerably more complex and time-consuming and required significantly greater research team input than planned. We struggled to recruit enough parents of young children and enough young adults. To improve recruitment, we extended the age range from 0–5 to 0–10 years for children, and from 18–25 to 18–30 years for young adults. Whereas extending the age range for young children resulted in only two additional recruits in the older age bracket (i.e. those > 5 years old), another eight young adults were recruited by including those aged between 26 and 30 years. These decisions were supported by the literature, as children included in studies from our realist review were sometimes aged up to 16 years,50,53 and young adults included those aged up to 44 years in studies identifying ‘clinically unnecessary’ use of EDs. 105
Emergency ambulance service
In the two ambulance service areas (Sheffield and Wolverhampton), ‘clinically unnecessary’ users were defined as patients who received only telephone advice or were referred to another service by clinical staff, that is cases where an ambulance was not sent. We briefed relevant staff about the study, and they asked patients before the end of a call if they would be interested in participating in the study and willing to have their contact details passed to the research team. It was not possible for staff to ascertain whether or not someone was living in an area of deprivation based on our criteria (i.e. IMD score of 1–3). As a result, staff were asked to invite all patients who were not excluded and to establish the age of young adults and of young children whose parents were calling on their behalf, and the postcodes of all callers who agreed to be contacted. This information, together with patients’ contact details (usually a telephone number), was telephoned to the research team so that we could check eligibility with regard to deprivation. Once ineligible patients were excluded, a member of the research team attempted to contact those remaining to explain more about the study and arrange to post or e-mail further information (for copies of the letter of invitation, participant information sheet and consent form, see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). A follow-up call was made a few days later to find out if the person was still interested and, if so, to arrange a convenient time for the interview. We confirmed this by letter or e-mail.
We faced considerable challenges in recruiting from the two ambulance service areas. Whereas managers were supportive of the study, front-line staff assessing patients were initially unaware of the study or their role in it. Owing to the pressured environment of the control centre, which operates tightly structured procedures, it was also challenging to introduce a new element into staff contact with patients. As a result, the researchers spent considerably more time liaising with front-line staff to establish effective procedures for patient contact and passing on information, and to keep the study in their awareness. Despite these measures, recruitment remained difficult, particularly in Sheffield, where it did not prove possible to establish a successful system for ongoing recruitment. We encountered specific difficulties with two subgroups. As ambulances are usually dispatched when a call relates to a young child, very few parents of young children were identified to be contacted. Recruitment of young adults also proved extremely difficult. These difficulties led to the expansion of recruitment from the original Sheffield and Wolverhampton areas to include the whole of South Yorkshire and the entire West Midlands region.
Emergency departments
Recruitment strategies varied between the hospitals involved in the study depending on the way in which staff identified relevant patients. A researcher (JL or LBE) was based at each ED for a number of sessions and liaised with relevant staff to identify potential recruits. Recruitment was generally undertaken during the ‘in hours’ period, but some attempts were made to recruit over the weekend or during the early evening.
The definition of ‘clinically unnecessary’ was more complex than that used in the ambulance service, as staff with a triage role were asked to identify patients whom they considered could have used an alternative service or self-care to manage their presenting problem, or, if they had used an emergency ambulance to access the ED, could have arrived by another means.
Sheffield emergency department
During each recruitment session, the researcher (JL) was introduced to the nurse in charge and relevant triage and reception staff by a research nurse, who had briefed the staff about the study. The researcher explained the study and discussed how to establish systems for identifying ‘clinically unnecessary’ users of the department. All patients referred to the GP collaborative were considered ‘clinically unnecessary’ users of an ED, as were other patients whom triage nurses considered could have used a different service or a different mode of transport (i.e. not an emergency ambulance). During the recruitment period, procedures within the department changed to enable reception staff to refer patients with minor injuries directly to a nurse practitioner, and we also approached these patients about the study. When a relevant patient was identified, the researcher met them briefly to explain the study and, if the patient was interested, provide them with written information. If the patient was eligible, the researcher contacted them a few days later to find out if they were still interested and, if so, to arrange a convenient time for an interview.
As with the ambulance service, recruitment took considerably longer than had been anticipated. Although staff were confident that many ‘clinically unnecessary’ patients were visiting the ED, it was difficult for them to keep the study in mind and recruitment tended to be through the GP collaborative referral only, which did not require them to change their existing procedures or to make a difficult decision about whether or not a patient’s use of the department was appropriate. Some staff were initially concerned about including patients who were referred directly to the nurse practitioner, but, as this treatment could also be obtained by going to a WIC or minor injuries unit (MIU), it was agreed that attendance at a type 1 ED could be considered clinically unnecessary. Including this group of patients significantly improved the rate of recruitment, in particular enabling us to recruit the remaining young adults.
Sheffield children’s emergency department
The researcher (LBE) worked closely with the research nurses in the hospital during the recruitment period. During each recruitment session in which the researcher was present, the research nurses screened the details of patients who were being triaged and identified parents whom they considered had made a ‘clinically unnecessary’ decision to attend the ED with their child. Parents were then approached by the researcher and followed up, as described in the previous section.
Wolverhampton emergency department
For each recruitment session, the researcher (JL) was introduced to relevant triage and reception staff by a consultant in the ED. Research nurses at the hospital had no involvement in recruitment at this site. The researcher explained the study and asked staff to give laminated cards to potentially eligible patients and direct them to the reception desk, where the researcher was based. When a patient was identified, the researcher approached them and followed them up, as described above.
As in the Sheffield ED, although the study was positively received by staff, recruitment was slower than expected, with similar problems of triage staff forgetting to mention the study or finding it more difficult than expected to categorise patients as ‘clinically unnecessary’. Variable shift patterns also meant that new staff had to be identified and briefed regularly. Eligibility was frequently confined to patients who were redirected to the independently managed urgent care centre (which treated only a limited range of conditions) and did not include those who were treated in the department. Parents of young children were also initially difficult to identify, as the children’s section of the ED operated very separately from the rest of the department. This was addressed by the researcher working directly with paediatric staff for one recruitment session.
General practitioners
The researchers established links with a particular general practice in each area (LBE in Sheffield and JL in Wolverhampton) that agreed to be recruited to the study. Both general practices were in areas of social deprivation to increase the likelihood of finding participants from this group. We asked GPs and practice nurses to identify patients whom they considered had made ‘clinically unnecessary’ use of same-day/urgent contact, either in a face-to-face consultation or by a telephone call, and whom they believed could have managed their problem through either self-care or a routine appointment. To reduce the impact on GPs’ time, they were not asked to speak to patients about the study but were asked to pass the patient’s details to a research nurse or the practice manager at the end of their session. The research nurse or practice manager then telephoned the patient to ask if they were interested in the study and willing to have their contact details passed to the research team. Details of potentially eligible patients were then telephoned through to the team, who screened the patient for eligibility and made contact, as described previously. Different general practices employed slightly different approaches to identifying ‘clinically unnecessary’ users, so the inclusion criteria varied to some extent between practices as well as between GPs.
As with the other services, recruitment was much slower than anticipated, with a number of difficulties encountered, especially in Wolverhampton. GPs, particularly those with less experience, found it challenging to categorise patients as ‘clinically unnecessary’, and engagement with the recruitment process varied among GPs in each practice. Practices also struggled to find time to make the follow-up calls to patients at certain points. The recruitment of young adults proved particularly challenging, which led to it being extended to a second practice in Sheffield that had a younger and more affluent demographic.
Topic guide
The qualitative researchers developed a draft of the topic guide. The topic guide was not based on the programme theories from the WP1 review; it asked about the events leading up to the patient’s contact with the health service from which they were recruited (e.g. advice sought, steps taken). We also explored patients’ experiences and perceptions of other services in the emergency and urgent care system more generally. Interviewees were also asked if any changes could be made to the current health system that would improve their access to health care. To ensure that the interview questions did not convey any sense of judgement about participants’ decisions, we piloted the topic guide with two PPI co-authors (LA and SB), who were asked to respond based on either a real or an imagined experience of using an emergency or urgent service. Feedback from this process led to some revisions to the sequence and structure of the questions. The resulting topic guide was in a semistructured format, based around nine main questions, each with a number of prompts to minimise the risk of missing key information. A brief introduction explained that the purpose of the interview was to understand the participants’ process of deciding how and where to seek help for a health problem. The topic guide was used flexibly during the interview to enable particular areas of interest to be explored in more depth (for a copy of the topic guide see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). At the end of the interview, we asked participants to complete demographic information, as well as questions from two domains of the Health Literacy Questionnaire (HLQ) in preparation for its intended use in the survey aspect of our work (see Chapter 6).
Data collection
The researchers who had been involved in recruitment (JL and LBE) conducted the interviews; where possible, they interviewed the people who they had recruited. Both were experienced female qualitative researchers. We tried to conduct interviews within 2 weeks of the health episode to facilitate greater recall, but on some occasions difficulties in making contact or arranging a convenient date meant that this was not possible. All but one interview took place face to face, usually in the patient’s home. Interviews lasted between 21 and 72 minutes (mean 40.5 minutes). We gave Sheffield-based participants the option to be interviewed in a meeting room at the University of Sheffield, and offered to pay return taxi fares to avoid any attendance barriers for those on low incomes. For logistical reasons, all Wolverhampton interviews took place in the patient’s home. Details of interview locations are available on the project web page (www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020).
Data analysis
We audio-recorded each interview and transcribed it verbatim. Transcripts were checked for accuracy. Interviewers added a short summary to each transcript, providing any background information that would not be apparent in the transcript and any comments or conversations before or after recording. We uploaded finalised transcripts and summaries into NVivo 12 (QSR International, Warrington, UK), which was used throughout to facilitate data management and retrieval.
Data collection and analysis was an iterative process, with review of early transcripts informing later interviews. Members of the research team (EK, JL, LBE and AOC) met regularly to discuss the process and the findings of the analysis. We applied the key principles of interpretative phenomenological analysis (IPA)109,110 to our analysis.
Interpretive phenomenological analysis aims to explore individuals’ lived experience in a particular context, focusing on their perceptions of events and how they make sense of their experience. 110 Each individual’s case is analysed as a whole using a predominantly inductive approach, which allows the essence of their experience to be identified without imposing a pre-existing framework of understanding. 109,110 These principles clearly reflected the approach that we wanted to take to understanding how interviewees had come to a decision regarding help-seeking for their health problem. Although IPA is generally used with small sample sizes, it is recognised to offer ‘a set of flexible guidelines’111 and can be adapted for use with larger samples. 109,110 There are a number of instances of the method being used to inform the analysis of patients’, carers’ and health-care professionals’ experiences in a range of health-care contexts with samples of between 17 and 55 people. 112–115
In our analysis, we drew on the key principles of IPA while adapting the method to our sample size of 48. For each interviewee, we created a memo and a diagram to identify and represent the drivers of their decision-making in relation to the incident discussed in the interview. To establish some common understanding and terminology within this process, all members of the team independently read the first few transcripts and then met to discuss and reflect on the themes that they had identified. Four members of the research team (EK, JL, LBE and AOC) were involved in this process. Two researchers created each memo, acting as either primary or secondary coder. One of the coders was the researcher who interviewed the participant, which ensured that any contextual factors not in the transcript could be taken into account. Primary coders read the transcript, identifying the drivers of (1) seeking health care (i.e. why the person made contact with a health service), (2) seeking health care at the service where the person presented (i.e. why they had made contact with a specific health service) and (3) seeking care urgently. In many cases, the same driver influenced more than one aspect of the decision (e.g. reason for seeking health care and reason for seeking care urgently).
We also sought to establish the strength of influence of each driver on the decision-making process by differentiating between what we termed ‘primary’ and ‘secondary’ drivers. We defined primary drivers as those factors that appeared to be key to the interviewee’s decision, that is the things that tipped them into taking a particular course of action, either whether or not to seek help or to seek help from a particular service. We defined secondary drivers as factors that had an influence on the process but appeared to be of less direct importance. Secondary drivers sometimes contributed significantly to the primary drivers and sometimes acted independently, but were integral to a complete understanding of the complexity of an individual’s actions. Differentiating primary from secondary drivers was not always easy, and the same driver could feature as either a primary or a secondary factor for different individuals.
The complexity of many participants’ drivers, and particularly the inter-relationships between the drivers, could not be represented adequately by the memos, and we found it helpful to draw diagrams to illustrate relationships between drivers for each interviewee (Figure 3 gives examples of diagrams for two interviews), an approach that is suggested for use in IPA to enable relationships between themes to be identified. 109 This process allowed us to reflect on the interviewees’ decision-making processes, and, in particular, to question the strength of the drivers and the relationships between them. We uploaded the final versions of the memos into NVivo.
FIGURE 3.
Examples of diagrams used for qualitative analysis. (a) Interviewee P7 (deprived, 999); and (b) interviewee P31 (parent, GP, deprived). P, participant. Dark blue, why sought help; orange, why sought help at that particular time; light blue, why sought help at the service they were recruited from; solid line, primary driver; dashed line, secondary driver.


As WP1 had been partially completed by the time WP2 data collection and analysis began, we had to consider the most appropriate approach to using the emerging programme theories in the IPA. We considered two alternatives:
-
to use the programme theories to guide the IPA (i.e. read them and use them to inform and structure the IPA coding)
-
to take an inductive approach to the coding, without reference to the programme theories, and reflect on the programme theories following completion of the definitive memo.
To be consistent with the principles of IPA, it was important to ensure that we focused on the interviewees’ experiences; therefore, given that we considered it would not be appropriate to approach the analysis with a predefined structure, we chose the second approach. One of the researchers (JL) was involved in both developing the programme theories and undertaking interviews and analysis, and a second researcher (AOC) was involved in all aspects of the research, so it is likely that knowledge of the programme theories influenced the analysis. However, Emma Knowles and Lindsey Bishop-Edwards were not involved in WP1 and could base their analysis on the interview data only. Towards the end of the analysis, we considered the findings in relation to the WP1 programme theories and considered how the interviews could be used to refine the programme theories (see Chapter 7).
Reporting guidelines
We completed the COREQ (Consolidated criteria for reporting qualitative research) reporting guidelines. 116
Findings
Sample size
We planned to undertake 48 interviews. We identified 130 individuals to take part in the study. Twenty-nine individuals declined to participate and another 53 did not respond to follow-up messages or were not contactable. We conducted 48 interviews: 37 in Sheffield and 11 in Wolverhampton.
The relatively small number of participants recruited in Wolverhampton did not enable us to carry out the planned comparison of interviewees’ decision-making between the two emergency and urgent care systems. Interviewees were mainly from EDs and GPs, with few recruited from ambulance services (Table 4).
| Service | Setting | Subgroup (n) | Total (n) | ||
|---|---|---|---|---|---|
| Parents | Young adults | Social deprivation | |||
| Ambulance service (n = 6) | Sheffield | 0 | 0 | 1 | 1 |
| West Midlands | 1 | 1 | 3 | 5 | |
| ED (n = 23) | Sheffield (adults only) | – | 9a | 4a | 13 |
| Sheffield (children only) | 6 | – | – | 6 | |
| Wolverhampton | 3 | 0 | 1 | 4 | |
| General practice (n = 19) | Sheffield (area of deprivation) | 4 | 1 | 5 | 10 |
| Sheffield (affluent area) | 2 | 5 | – | 7 | |
| Wolverhampton | 0 | 0 | 2 | 2 | |
| Total | 16 | 16 | 16 | 48 | |
Description of interviewees
The majority of interviewees were female (n = 33) and white British (n = 33) and half were in paid work. Interviewees reported contacting services about a range of concerns, including chest pain, back pain, sore throats, injuries, rash and coughs. For some interviewees, these concerns were part of an ongoing problem but others were experiencing an unfamiliar symptom or problem (Table 5). Health literacy scores ranged across the spectrum (for further interviewee descriptors, see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). The characteristics of interviewees in each subgroup are discussed in more detail below.
| Subgroup | Service | Reason for contact |
|---|---|---|
| D | 999 | Chest/abdominal pain for 24 hours |
| D | 999 | Possible anxiety attack, part of ongoing problem |
| D | 999 | Wife’s confusion, part of ongoing problem |
| D | 999 | Care home resident’s unexplained injury and changed behaviour |
| D | ED via ambulance | Chest pain for 2 weeks |
| D | ED | Back pain, recurrence of previous problem |
| D | ED | Back pain after fall some days before |
| D | ED | Back/shoulder pain, breathing problems, ongoing problem |
| D | ED | Enlarged glands and sore throat |
| D | GP | Headache after known injury |
| D | GP | Sore throat, with general ill health from ongoing problem |
| D | GP | Ear infection and general unwellness after some weeks of illness |
| D | GP | Sore throat, with underlying health anxiety |
| D | GP | Flickering eye and feeling run down |
| D | GP | Older child’s tonsillitis |
| D | GP | Requesting report for benefits assessment |
| YA | 999 | Breathing problems after chest infection |
| YA | ED via 999 | Confusion, head pain and possible concussion |
| YA | ED | Vomiting blood after hangover |
| YA | ED | Neck/back pain and stiffness after car accident |
| YA | ED | Painful, swollen foot after fall |
| YA | ED | Painful wrist from known injury/sprain |
| YA | ED | Ankle/foot injury after fall |
| YA | ED | Joint pain/lack of mobility, part of ongoing problem |
| YA | ED | Rectal bleeding and pain, part of ongoing problem |
| YA | ED | Suspected miscarriage, concern regarding complications |
| YA | GP | Prolonged severe headache, part of ongoing problem |
| YA | GP | Stomach/digestive problems, part of ongoing problem |
| YA | GP | Fatigue and other symptoms for some weeks |
| YA | GP | Exacerbation of anxiety, impacting on function |
| YA | GP | Needing repeat asthma medication |
| YA | GP | Needing contraceptive pill to manage symptoms |
| P | 999 | Child’s head injury, not witnessed |
| P | ED | Child’s unexplained rash |
| P | ED | Child’s raised temperature after previous episode of convulsions |
| P | ED | Child’s cough, vomiting mucus and struggling for breath |
| P | ED | Child’s cough and vomiting mucus |
| P | ED | Child’s vomiting and inflamed tonsils, part of ongoing problem |
| P | ED | Child’s prolonged nosebleed, behaviour change |
| P | ED | Child’s ear infection |
| P | ED | Child’s sore eye, after being generally unwell |
| P | ED | Child’s constipation, part of ongoing problem |
| P | GP | Child’s rash |
| P | GP | Child’s raised temperature, rash and changed behaviour |
| P | GP | Child’s cough after being generally unwell including rash |
| P | GP | Child’s raised temperature and distress after generally being unwell |
| P | GP | Child’s cold, temperature and green phlegm |
| P | GP | Child’s prolonged diarrhoea and behaviour change |
Order of presentation of themes
Where possible, for clarity, the drivers of help-seeking are listed in the same order for each subgroup. Some drivers were more important in certain subgroups, in which case these are presented first.
Parents of young children subgroup
Sample characteristics
Sixteen parents were recruited, ranging in age from 22 to 42 years (mean 33 years). The sample predominantly consisted of interviewees with either high or low deprivation IMD scores, rather than medium scores. Seven had a score of between 1 and 3 (i.e. indicating that they lived in an area of social deprivation, according to our study criteria), whereas another seven had a score of 8–10 (indicating affluence). All but two of the interviewees were female and were accessing care for the child in their role as the child’s mother. Just over half of the interviewees described themselves as white British, with four identifying as black African or Caribbean, two as other white and one as Asian. Twelve interviewees indicated that they were married or living as married, and the other four indicated that they were single or not married. Parents in the sample had between one and five children, with six having one child. The children in the sample were predominantly at the young end of our age range, with nine aged ≤ 2 years and another four aged 3–5 years, and only two aged > 5 years. Of the 16 parents interviewed, one had been recruited following contact with the emergency ambulance service, nine had been recruited following contact with an ED and six had been recruited following contact with a general practice. All but one of the interviewees who were living in areas of deprivation had used emergency ambulance or EDs, whereas those with higher IMD scores had been recruited from their GP.
Overview of findings for parents of young children
Two key drivers were most evident in parents’ decision-making regarding seeking health care: (1) concerns about the seriousness of symptoms that the child was experiencing and (2) a complex interlinking of a sense of responsibility as a parent of a young child and a lower threshold of concern regarding children’s health. In many cases, these concerns prompted a need for some form of reassurance from a health-care provider. There was a strong sense of interaction between these drivers, with each potentially triggering the other. Although these drivers were most prevalent, a number of other factors were also present and contributed to the decision to seek care: in particular, the perceptions or experiences of services, the influence of others and the timing of the incident.
Concern regarding seriousness of symptoms
For all parents in the sample, concern about their child’s symptoms was a key driver of their decision to seek care. A variety of symptoms were reported, including raised temperature, diarrhoea or constipation, head injury, cough, cold, ear infection, rashes, vomiting, sore eye and prolonged nosebleed. Reflecting programme theory 1, uncertainty about symptoms causing anxiety, parents described their concerns in terms of unfamiliar symptoms, prolonged or worsening symptoms, or a change in their child’s behaviour that triggered a belief that the problem might be serious:
I don’t know whether it was affecting his breathing or not but sometimes I felt like he was struggling, while he was coughing, in the breathing. With the cold and a virus, I’m quite confident to say that’s what it is. So if he is ill with a cold then I wouldn’t ring the GP, to say ‘oh he’s got a cold’. It was the cough that worried me most with it being either whooping cough, or croup or anything like that. With him being so young, it was the cough that worried me, more than anything really.
Participant (P) 25, parent, GP
The type of illness or injury could also exacerbate concerns, with head injury or rashes described as particularly worrying. Aligned with programme theory 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety, this concern was linked to a belief that these symptoms could escalate quickly and have serious consequences for the child’s health:
[Child] came out in a rash on his thigh and his back and, just under his arm, and because we had been to [place] I thought that it might have been meningitis or something although he has had his jabs, before we went. It looked sort of like meningitis, same sort of symptoms, bruising, purple and red that’s why we were really concerned about him.
P20, parent, ED
All three services in the study were used by parents who were concerned about symptoms. The need for reassurance was a key driver and different services appeared to offer this in different ways. Linked with both programme theory 1, uncertainty about symptoms causing anxiety, and, to a lesser degree, programme theory 6, waited long enough for things to improve, some parents’ concerns led them to feel that they could not delay seeking care any longer and needed some form of reassurance from a health-care provider. In a few instances, the inability to delay could be driven by a sense of panic and need for immediate reassurance, which was evident in the account of the one interviewee who made contact with the emergency ambulance service. Highlighting the influence of programme theory 7, stressful lives and difficulty coping, the interviewee described how she had discovered her child’s earlier injury late in the evening; the fact that she was a single parent of a number of young children with no access to a car exacerbated her existing anxiety about her children and prompted her to seek help from the only service she perceived that she could access at that particular time of day:
I was thinking ‘oh god, what am I going to do’, so I was thinking the only people that I could think of was the ambulance people and thinking I need to tell them, because I can’t go to sleep, and sort it out the next day, it needs to be sorted today. I need to speak to them just in case with a head injury . . . ‘cause we don’t know how sharp the thing was [that caused the injury], if it went in, if it was a pin, we don’t know. So, and it could have been something that is dirty you know, loads of things were going through my head.
P11, parent, emergency ambulance
However, the majority of parents experienced a situation less intense than this one, and they expressed their need for reassurance in terms of wanting a health-care professional to confirm their feeling that their symptoms did not indicate a serious problem rather than because they were concerned that the problem was serious. In these instances, the GP was frequently interviewees’ preferred service choice. Additionally, some wanted their child to be physically examined, meaning that a telephone-based service (such as NHS 111) would not meet their needs:
[Going to the GP] was going to rule out anything serious, and it was going to give me peace of mind, so that I didn’t have to worry about it ‘cause as soon as I left that surgery, she’s been checked so it’s like, she’s fine . . . it felt like a big weight had been lifted, almost, which is stupid really isn’t it but yes . . . you just know somebody who’s qualified has looked at her and has ruled out anything serious.
P32, parent, GP
Many parents in the sample described themselves as well informed about health care or appeared to the interviewer to be well informed. This was reflected in the higher HLQ scores in this subgroup than in the other two subgroups. Parents often described administering oral medications, including for pain, in the lead-up to help-seeking, and they generally seemed confident in doing so. They often described a period of monitoring and self-care prior to seeking help, rather than seeking care on the day that the symptoms were first noticed. Aligned with programme theory 6, waited long enough for things to improve, they became concerned when these strategies did not appear to alleviate the symptoms. By contrast, one parent appeared reluctant to medicate her child during the incident, despite using that medication previously, and this was consistent with an overall sense during the interview that she had difficulty absorbing medical information, which may have increased her uncertainty about managing the situation.
Sense of responsibility as a parent of a young child
In many instances, concern about symptoms and a decision to seek help were affected significantly by the parent–child relationship in a number of ways. Corresponding to programme theory 3, fear of consequences when responsible for others, some interviewees explicitly identified their specific sense of responsibility as being a parent; this was expressed particularly strongly by one single parent in the sample:
I’m her mother and I’m the only person who can help her so, going back to that panic you know what’s right, but she’s my daughter, so I need to make the right decision.
P29, parent, ED
Parents often described seeking care quickly because they did not want to take risks with their children’s health. This was often at odds with how they approached decision-making about their own health, for which they described ‘putting up with things’ for longer. In addition to the sense of responsibility, there was an underlying perception that less risk was involved in delaying care for adults than in doing so for children. Aligned with programme theory 3, fear of consequences when responsible for others, parents also described how their distress at seeing their child suffering exacerbated their concerns about symptoms:
I just don’t worry that much about myself when I get ill, like I mean I got a bit ill OK, just take some paracetamols, you know. But when it is [name of child #1] I’m like thinking how she feels or she probably feels pain or is she struggling, oh poor girl you know, you want to comfort her, and kiss her and everything, and you just worry, you want her to get better quickly.
P30, parent, ED
Lower threshold of concern regarding children’s health
Closely connected to the sense of parental responsibility, many participants also described a more general concern about managing their children’s health. In general, parents in the sample did not appear to be excessively anxious to the researchers, but expressed concern or anxiety driven by a belief that there was a need for a lower threshold for seeking help for a child. There was a perception that children’s health could be unpredictable and deteriorate quickly, which could be seen as an aspect of programme theory 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety. In one specific instance of this programme theory, a parent who identified herself as a ‘worrier’ felt that her anxiety had been exacerbated because she knew about a situation in which a delay in seeking care had resulted in a long-term health problem. More generally, a number of parents described a particular anxiety in relation to babies and young children, as a child’s inability to explain what or how they were feeling increased the sense of uncertainty described above and reflects programme theory 1, uncertainty about symptoms causing anxiety. In this context, some parents noted that they would have taken a different course of action had the problem related to an older child. Although the age of the child was a significant factor in increasing the sense of urgency to take action, there was no apparent relationship in our sample between the child’s age and the parents’ choice of service, with children aged ≤ 2 years going to both the GP and the ED. Being a first-time parent was also not identified as having a significant impact on help-seeking in most cases. Although six of the parents in the sample had only one child, this was described as significant by only one parent in terms of increasing her concern because of her lack of experience. However, most of the parents in this group had children aged 3 or 4 years, and so they were not new to the experience of being a parent. By contrast, one parent whose two children had a wide age gap described feeling the anxiety of being a new parent again and taking her 2-year-old to the ED:
They have 9 years’ difference so [name of child] when she was born was like first, ‘cause I really forgot everything.
P30, parent, ED
Aligned with programme theory 7, stressful lives and difficulty coping, a few parents described how ongoing health worries about their child had increased their concern and led to their decision to take action in relation to this particular incident. These parents described their children being frequently ill with minor problems, or experiencing longer-term health problems; in both circumstances, there was a sense that this affected the parents’ willingness to wait for the situation to resolve. Highlighting another aspect of programme theory 7, stressful lives and difficulty coping, one parent described being ill at the same time as her child and how this had affected her sleep. She recognised how this, in turn, had reduced her coping capacity, making the situation feel more urgent.
Perceptions and experiences of health services
Aligned with programme theory 9, perceptions or experiences of services, interviewees’ opinions of different health services had a significant impact on where they decided to seek help, with positive and negative views of their general practice being particularly influential. Most parents in the sample who sought care from the GP described their confidence in being able to access a same-day appointment or telephone advice for their child as a key factor in their decision-making. This was often based on previous positive experiences of such access:
In the past if I’ve rung up [the GP] for [name of child], I could ring at 2 o’clock say it’s for my son who’s a toddler and they will ring back within probably 15–20 minutes to get us an appointment, so they’re really, I’ve never had to do it for myself but with kids especially they’re really good, they will get you in that day.
P23, parent, GP
Notably, a number of these parents did not believe that they could access an appointment for themselves in this way, and felt that GPs tended to provide appointments for children because the risks to children’s health were perceived to be greater, suggesting the possible influence of programme theory 3, fear of consequences when responsible for others, and programme theory 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety. Even when appointment access was enhanced for children, these parents highlighted the challenges of booking a GP appointment, particularly because the timing of doing this often coincided with taking children to school. However, for other parents, their negative experiences or views about access to general practice were significant drivers in their decision to go to an ED. Corresponding with programme theory 10, frustration with access to a GP, parents described unsuccessfully trying to get a GP appointment on the occasion in question, as well as previous failed attempts that had created their perception that no appointments would be available within the time frame required:
They [GP] didn’t have any appointments. Usually if I ring from 8.30 they give me appointment, probably because it is a child they give me the same day but it was a bit too late, I called at 10 o’clock as I said she felt a little bit better and I thought OK let’s leave it, then I called like at 10 o’clock and they didn’t have any appointments.
P30, parent, ED
In addition to access problems, one interviewee described how a poor relationship with her GP influenced her decision to seek care at an ED. She reported not being satisfied with the care, examinations and treatment that her daughter had received from the GP on previous occasions, offering no resolution to her ongoing health problems. In another instance, two previous poor experiences of GP out-of-hours care left an interviewee unwilling to consider using this service again:
. . . if you even go to the GP, they just spend 5 minutes with you, it’s like you don’t feel like you’ve been heard properly. So I thought if I go to A&E [accident and emergency] they might take it further, and help her.
P21, parent, ED
Programme theory 9, perceptions or prior experiences of services, also operated in terms of positive views of the ED, whereby parents believed that only a particular service could provide the skills, resources and speed to offer reassurance or resolve their child’s health problem. Parents described the ED as having more doctors with greater levels of expertise and specialism, who had access to equipment and were able to carry out investigations:
. . . what was the thing [the ED] could offer over everything else?
To keep [name of child] safe, and offer equipment and medical things, and decisions that I couldn’t make for her.
Most of the parents in the sample who had accessed an ED said that they had used it on at least one previous occasion, and this positive experience of and familiarity with the ED may have influenced their decision to access the ED on the day in question; that is, there was some evidence of recursivity at play.
Influence of others
Although family, social networks and health-care professionals did not appear to significantly affect the decision to seek care among this sample, they did have some influence on where care was sought. Aligned with programme theory 8, following the advice of trusted others, around one-third of the sample appeared to have been directly influenced by someone else when deciding to seek care from a particular service. Most often this was advice to attend an ED, but in one instance an interviewee described following her mother’s advice to seek care at the GP, noting that she trusted her mother’s judgement because of her mother’s experience of bringing up her and her siblings. Parents in the sample identified a range of people who had advised them to attend an ED, including GPs, nursery staff and, in the case of one man, his wife, who was also a health professional; in some instances more than one source of advice was present. The two interviewees who had been advised by a GP to attend an ED had different experiences. In one instance, the GP had physically assessed the child and, in advising the interviewee to attend an ED, had been following advice that they had received from a specialist department at the hospital. That is, the GP was indirectly following advice of a trusted other. The other interviewee, whose child had an unexplained rash, received advice from a GP over the telephone; highlighting the influence of programme theory 3, fear of consequences when responsible for others on health-care professionals, the GP advised attendance at an ED because they were unable to confidently rule out the risk of something serious without undertaking a physical examination.
The indirect influence of others was also apparent in nearly half of the sample, highlighting a refinement of programme theory 8, following the advice of trusted others, in terms of the broader influence of social networks. This influence took the form of support or encouragement for interviewees’ decisions, and came from partners, other family members, a colleague and, in one instance, NHS 111. All interviewees described or indicated having some form of social support, with most being married or living as married, and others mentioning partners, family members, friends or neighbours in their support network.
In an extension of programme theory 8, following the advice of trusted others, parents discussed how they generally used the internet to obtain health advice and rule out possible diagnoses. This strategy did not appear to exacerbate their concerns or heighten their anxiety. In relation to the specific incident being discussed during the interview, just one interviewee described that the internet had directly influenced her decision to seek care, having read advice from an NHS online source that recommended that a child of her child’s age, with the particular symptoms her child had, should receive medical care. Although this source did not appear to suggest using a particular service, she also considered advice from her child’s nursery to attend an ED.
Timing of incident
For a small number of parents in the sample, the timing of the incident intersected with other concerns to affect their decision about the choice of service. As already noted, the lack of support and resources available to one parent affected their decision to call an emergency ambulance in the evening. In another instance, a problem late on a Friday afternoon prompted one parent to attend an ED, as they believed that a GP appointment would be unavailable and were unwilling to use the GP out-of-hours service. In relation to seeking GP care, two parents made contact on a Friday, with both expressing the sense that this was their last opportunity to contact their own doctor before the weekend. That is, the timing of the episode added to parents’ anxiety levels, leading them to seek care immediately. Neither parent was averse to contacting other services but felt that seeking care over the weekend could be more complicated:
. . . you think if I don’t get in at the doctors before the weekend, we could end up with a pickle over the weekend, so we best get this checked out.
P32, parent, GP
Young adults subgroup
Sample characteristics
Sixteen young adults were recruited, ranging in age from 18 to 30 years (mean 25 years). Most interviewees described themselves as white British, with two being Asian (one Chinese and one Pakistani). Approximately two-thirds of the young adults were female, and all but one had lived in the city from which they were recruited for > 1 year, with most living there for > 5 years. The majority were occupied full-time as students and/or employed full- or part-time. Three described themselves as unemployed because of health problems. Five interviewees were recruited from a general practice in an affluent area and were working full- or part-time, whereas the interviewee recruited from an area of deprivation was unemployed. Half of the sample (n = 8) were living in areas of deprivation (IMD quintile 1 or 2), and, although their child was not the focus of their service contact, four were also parents. All four parents were from areas of deprivation.
Interviewees sought help for a wide range of reasons, and sometimes included more than one reason. Reasons included pain after injuries (n = 4); exacerbations of chronic or ongoing symptoms, including pain, bleeding, digestive problems, fatigue and anxiety (n = 8); breathing difficulties; suspected concussion; vomiting blood after drinking alcohol; suspected miscarriage; and seeking medication to manage anticipated rather than actual symptoms (n = 2). The interviews focused mostly on contact with an ED (n = 8) or a GP (n = 6), with only two relating to emergency ambulance use. The service contact in this sample seemed to be differentiated by sex and deprivation. All of the men had used the ED or emergency ambulance service, whereas just over half of the women had been recruited after contact with the GP. Almost all of the young adults living in areas of deprivation (7 out of 8) had contacted the ED or emergency ambulance service and only one had contacted the GP; both of the young adults who received care from the emergency ambulance service were living in areas of deprivation and were unemployed because of long-term health problems, particularly mental health. By contrast, five of the young adults living in more affluent areas had used a GP and only three had used the ED.
Overview of findings for young adults
Three drivers were most evident in young adults’ decisions to seek health care: concerns about the meaning/seriousness of the symptoms that they were experiencing; an unwillingness to further delay care-seeking; and perceptions or experiences of services. Although these drivers were the most significant among this sample, a number of other factors were also frequently present, notably the influence of others, particularly those in their social network, and the impact of poor mental health. Most interviewees identified between two and four drivers of their decision to seek care, which were usually interconnected.
Concern about seriousness of symptoms
Around half of the sample had sought health care because they had been concerned that their symptoms could indicate a serious health problem. This concern aligned clearly with programme theory 1, uncertainty about symptoms causing anxiety, and could be prompted by a number of aspects of their situation and experiences. Unfamiliarity with a symptom was a particularly significant trigger, which in some instances was exacerbated by seeking information online:
I was concerned and thinking maybe I had something severely wrong with me or a bit paranoid maybe because, I mean like the daft decision is searching the symptoms online, and it just freaked me out [. . .] just, all sorts of like, I don’t know, just big stomach issues, something like ulcers or obviously cancer is always on it.
P3, young adult, ED
Although unfamiliarity with a symptom was a frequent driver among this sample, experiencing recognisable symptoms could also prompt concern. Although this driver featured less strongly here than it did in the parent group, it could increase the urgency to seek help, either because it suggested the return of a previous problem or illness or because the young adult was aware of the serious consequences that similar symptoms had had for someone else. That is, programme theory 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety, could contribute to their concerns:
. . . that’s why I rang up, that’s why when [P36]’s head so hurting, and he said it had been for 3 days, and I remembered a story he told me about a girl who had had a headache and went into hospital and they said it was a migraine, [P36: and they sent her home] and the next few days it wouldn’t go away [P36: and she died, with a bleed on the brain] and then she died of a blood clot.
P36 and girlfriend – both present for interview, young adults, emergency ambulance
The severity of symptoms could be another key trigger of concern, most commonly in relation to injury rather than illness. Sometimes this was a progressive worsening of pain or other aspects of the problem despite self-care measures, and it was this worsening that prompted the search for help because it introduced an element of unfamiliarity. On other occasions the severity was immediately apparent and was itself sufficient to trigger action:
As I fell off I landed awkwardly on my right ankle and just completely rolled it. And then at that point it felt – it kind of just went straight away it went really hard – and as dramatic as it sounds I thought there was a bone sticking out. I couldn’t dare look because it just hurt.
P47, young adult, ED
In instances such as this, anxiety about the nature of the symptoms and their potential seriousness also had a clear impact on service choice, in this case (see above) prompting the decision to use the ED. A similar process was evident for both of the young adults who contacted the emergency ambulance service, when their concern triggered a need for a speedy response that only this service was perceived to offer. In all of these decisions, programme theory 1, uncertainty about symptoms causing anxiety, can be seen to operate in combination with programme theory 9, perceptions or prior experiences of services, to drive both the decision to seek help and the choice of service.
Concern about the severity of symptoms was sometimes accompanied by a desire for reassurance. In a number of these instances, young adults echoed our sample of parents in describing how they thought that their problem was unlikely to be serious, but wanted to allay their nagging concern:
. . . I was like, I want to make, I want to double check that it is not like a break or a twist or like a torn thing or they are going to put me on stronger medication ‘cause I was in a lot of pain.
P6, young adult, ED
Unwillingness to further delay care-seeking
Around half of the young adults in this sample had sought care because they either were unwilling to delay seeking care further or could not tolerate their health problem any longer. This driver, which aligned with programme theory 6, waited long enough for things to improve, always operated in conjunction with other drivers. In some instances, the other driver was interviewees’ concern about the seriousness of the symptoms, as discussed above, but a number of other factors were also found to contribute to this sense of urgency. The most common of these in this sample was a concern about the impact, or the potential impact, of their symptoms on their ability to function, including work, study, child-care responsibilities and leisure activities:
I’ve been feeling under the weather generally for a little while but that particular week I’d just had a really difficult week, I couldn’t, I was so tired and fatigued and I couldn’t really eat, do my job properly, so I was struggling with driving and just being at work so I wanted to try and get it looked at.
P38, young adult, GP
This concern about the impact that symptoms could have on functioning corresponds with programme theory 4, inability to get on with daily life, and was particularly prevalent among the young adult sample. Our findings also offer a refinement of this programme theory by highlighting the influence of anticipated, rather than actual, impact on interviewees’ decision-making.
In a number of instances, as is apparent in the above interviewee’s account, the concern about the impact on function did not arise out of an isolated incident of illness or injury, but was part of a longer-term health problem for which they were seeking resolution. In these cases, the decision to seek care generally had followed attempts to deal with the problem through self-care, including taking over-the-counter medication, and was also sometimes part of a continuing process of medical consultation. This would seem to be an additional dimension of programme theory 6, waited long enough for things to improve, and perhaps an extension of programme theory 10, frustration with access to GP, in that it arose from frustration with the ongoing care from a GP rather than a lack of access to a GP. The issue was more that the failure of previous help-seeking to resolve the situation had prompted further action to try to deal with the problem:
[I was] really sick of it, really, and just having all these symptoms, and for all these tests that I’ve had to come back clear. It’s like well there is something wrong with me so it’s not, if it’s not about these foreign bugs or if it’s not about gluten or whatever, there is something wrong. I need to pursue it, and try and find out [what was wrong].
P44, young adult, GP
A need for pain relief was also an important reason why some did not want to delay care, specifically prompting action at that time. This aligned with programme theory 5, need for immediate pain relief, and, although this was important, it always featured in combination with a range of other factors, as is evidenced in the following account:
. . . the night before I’d had a headache and I woke up and it was even worse, so I just rang them [GP] up and just said you know I can’t, can’t deal with this now. I’ve got a toddler to look after, is there anything that I can do now.
P35, young adult, GP
There was also evidence in this sample of issues that could expand programme theory 6, waited long enough for things to improve, into areas that might be judged externally as unacceptable reasons for contacting services urgently: impatience and lack of organisation. In one instance, a general impatience and intolerance of waiting was evident in the account of the decision-making process, and in the person’s behaviour both during recruitment and in the interview. It is likely that this impatience contributed to their decision to call an emergency ambulance in this instance.
In two cases, no symptoms were present at the time the interviewee made contact, but familiarity with their existing health conditions had prompted them to seek help in the form of obtaining prescribed medication. One interviewee had run out of essential medication and, unexpectedly, had been unable to access it through the usual route. The other interviewee needed a new prescription so that they could manage potentially troublesome and distressing symptoms during an upcoming holiday. These two issues could be viewed as a lack of organisation. However, it might also be the case that, in the first situation, programme theory 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety, was operating in terms of the interviewee’s concern to avoid a recurrence of symptoms managed by the medication. Programme theory 4, inability to get on with daily life, was operating in the second situation, although essential aspects of daily life, such as working or looking after children, were perhaps not affected.
Perceptions and experiences of health services
Interviewees’ perceptions of different services were a significant driver of their decision-making in relation to choice of service. Aligning closely with programme theory 9, perceptions or prior experiences of services, these were both positive and negative and related to a variety of emergency and urgent care services.
Contact with the emergency ambulance service in this sample was related to its positive characteristics. One interviewee described her confidence in the speed and skills of the ambulance service to assess and deal with her problem, which was driven partly by previous positive experiences, including the service’s reassurance that she had ‘done the right thing’ (programme theory 9) to call. That is, recursivity was at play in her decision-making based on the positive reinforcement of her previous decision. She also noted learning subsequently that NHS 111 was able to contact an ambulance if this was deemed necessary, and that this would change her future help-seeking behaviour. Another positive characteristic of the emergency ambulance service was that it was a source of transport, offering a safe, easy and rapid way of getting to hospital.
The majority of interviewees in the sample who sought care in an ED did so because of either a positive belief that it offered the best and/or most appropriate service or a negative perception that other services could not meet their particular needs. Positive characteristics of the ED were that it offered quick access to help and had a wide range of resources and facilities, and that its doctors and nurses were able to deal with serious problems. Proximity of the ED to their home or workplace was also a secondary consideration for a few interviewees who lived within 2 miles of the hospital. One of these interviewees, who lived in an area of deprivation, cited the cost of transport as a factor in their decision to choose the ED instead of the WIC; that is, for this interviewee, choosing the ED was a matter not of convenience but of cost. This could be aligned with programme theory 7, stressful lives and difficulty coping, in that limited financial resources affected decision-making. The influence of proximity of service is not included in any of the existing programme theories.
In some instances, interviewees’ decisions to contact an ED were framed as resulting from negative features of other services, particularly general practice, where delays or difficulties in access were a particular concern, aligned with programme theory 10, frustration with access to a GP. Negative perceptions of general practice were related not only to access. Two interviewees had specific difficulties with their relationship with their GP. One felt that the departure of her previous GP meant that nobody at the practice understood her complex situation well enough to meet her needs, whereas the other’s previous negative experience with her GP contributed to her reluctance to contact this service for her particular symptom. By contrast, all interviewees who had been recruited because they had successfully obtained care from the GP perceived that general practice was the most appropriate service to address their needs. A range of reasons for this perception was given, including that the GP provided an opportunity to discuss concerns about ongoing or recurrent health problems or to obtain a diagnostic label, as well as the practice being the only or most appropriate place to obtain repeat prescriptions or to review existing prescribed medication. Some interviewees saw the GP as a trusted source of knowledge, and in one case this was because the interviewee had an established positive relationship with a specific doctor. For this individual, the GP also represented the quickest and most accessible route to help, important considerations that linked with many of the factors explored previously in relation to an unwillingness to further delay care-seeking (programme theory 6) and the influence of proximity of service on help-seeking behaviour.
Experiences of trying to access a GP were sometimes also a significant factor in deciding where to seek care. A few interviewees described how they had attempted to make contact with their GP, but their inability to get an appointment or to speak to someone quickly enough had prompted them to seek help elsewhere. This frustration aligned with programme theory 10, frustration with access to a GP, but was also related to programme theory 6, waited long enough for things to improve, because people wanted a same-day GP appointment. Individuals sought a same-day appointment either because they wanted to be seen urgently or because they had not been able to book an appointment in advance that allowed them to attend to their work responsibilities, which then led to a sense of having waited long enough. By contrast, two interviewees described their confidence that they could obtain same-day GP appointments when needed and so they chose this approach to seeking help:
If I’m feeling a bit run down at all, or cold, or my chest is bad then they will get me in, on that same day regardless ‘cause obviously it’s a bit more of a medical emergency I guess, more urgent . . .
P40, young adult, GP
A lack of awareness of other potentially appropriate services also contributed to the decision-making process. This particularly related to the MIU, which could probably have met the needs of three of the interviewees who accessed help from the ED but was not considered as an option either by them or by those who gave them advice.
Influence of others
For all but three young adults in the sample, other people had some degree of influence on their decision to seek care or on the service that they accessed. In a few instances, a direct influence was evident, corresponding with programme theory 8, following advice of trusted others. Two interviewees had been advised by health-care professionals specifically to attend the ED, one during a consultation with their GP and the other through a contact with NHS 111 as a result of being unable to speak to their GP:
(. . .) the 111 lady spoke to a nurse that – to get a bit of advice about whether I could go to the walk-in centre, she said you wouldn’t be able to go to the walk-in centre but actually we would say go straight to the hospital for stuff like that.
P46, young adult, ED
Direction to go a specific service could come from family and friends as well as from health professionals, and this was sometimes based on those others’ experiences. This was particularly the case for direction to go to an ED, perhaps indicative of social norms about where to seek care for particular types of health problems. For example, a colleague’s opinion about the diagnostic tools available at an ED (i.e. programme theory 9, perceptions or prior experiences of services) had determined where the following interviewee went for care:
I’d knew that one of my colleagues a couple of months ago had done similar thing and sprained it, I asked him where he went because I didn’t right know, I were gonna go to walk-in centre but then he said ‘there’s no point because they don’t do X-rays I don’t think, which you’d need’ so that’s when I went to [ED].
P45, young adult, ED
(. . .) with it being a year, and I have had other symptoms, I’ve been in hospital because of it, they’re taking that long to get this operation so I think they [partner and mum] were just fed up and they were like just ‘let’s go to place’ because we could’ve gone into [local town] but they thought, we just thought ‘let’s go to [place] where the main thing is because we’re gonna be waiting wherever we go so we might as well go there’.
P43, young adult, ED
Sometimes the family member or friend made the decision on behalf of the patient if they felt that the patient was not fit to make it, or they encouraged the patient to take a particular action (as detailed above). Their influence could also take a more advisory, less directive form; for example, a shared decision between a young adult with a learning disability and their mother, or support from family, partner, friends or colleagues for an interviewee’s decision to seek help. A negative example of this theme was one interviewee’s lack of social support. Their problem occurred late at night, making it difficult for them to draw on their usual social network, exacerbating their uncertainty and driving an urgent need for reassurance, which led them to call the emergency ambulance service:
I honestly thought I was going to die. I really, really thought I was going to die because I’d never felt like that in my life. Like I said, being on my own as well, nobody to speak to, nobody to reassure me. It was just so scary.
P9, young adult, emergency ambulance
This impact of lack of support due to timing of the incident is not represented explicitly in the programme theories but could be related to programme theory 7, inability to cope due to stressful lives.
Poor mental health and stressful lives
Although the majority of young adults presented to a service because of physical concerns, around one-third of those in the sample made some reference to also having mental health problems, particularly generalised anxiety and depression. These influenced their decision-making in a variety of ways. One interviewee’s acute exacerbation of mental health problems was the direct trigger for help-seeking, with programme theory 1, uncertainty about symptoms causing anxiety, evident in her account:
I just didn’t know what was wrong with me at the time it was just really scary . . . I was just frightened it had just not sort of happened before . . . Just a really heightened sense of fear and the whole sense of doom thing was happening and – at the time – it felt very urgent. Yeah I’d, I’d never had it like that before so it’s just totally new.
P39, young adult, GP
Others described a complex interplay between their mental and their physical health. Illustrating the difficulties described in programme theory 7, stressful lives and inability to cope, interviewees’ ongoing struggle with mental health negatively affected their ability to function and to cope with the challenges of additional physical symptoms. In a number of instances, this driver could be seen to operate in conjunction with programme theory 1, uncertainty about symptoms causing anxiety, with interviewees’ overall increased levels of anxiety prompting a need for urgent help and reassurance about their symptoms. In one case, a more complex need for validation was related to mental health problems:
I’m not always as confident in, what I know I’m feeling and, I know I’m feeling it, but when I go to the doctors, the hospital and I explain to them and that like no, you are not just like, making it seem worse. It is bad. But we know what you are dealing with and we are going to try and help, so generally that is why I go to the hospital, if I ever go. So I need the reassurance that I’m not just like making it seem worse than it is and that there is something and that they can help.
P6, young adult, ED
Mental health problems could also have an impact on the particular service that interviewees decided to contact, with programme theory 9, perceptions or prior experiences of services, sometimes evident in the choice to use the ED or emergency ambulance because of the perception that these services would respond more quickly. A more complex influence was potentially present for one interviewee, whose anxieties made it difficult for her to leave home unaccompanied and may have influenced her decision to call an emergency ambulance. This is aligned with programme theory 7, stressful lives and inability to cope. In addition to mental health problems acting as drivers of urgent care seeking, and influencing which service was contacted, high levels of stress from daily living could also have an impact on the urgency of help-seeking in different ways. First, these could trigger an exacerbation of existing physical symptoms to an intolerable level. Second, they could influence which service was contacted by prompting people to seek a service that they felt did not add to their already high levels of stress. For example, the interviewee providing the following quotation had unpredictable work commitments that made it impossible for them to book appointments very far ahead; therefore, they took advantage of unscheduled time off to access help via a same-day GP appointment:
. . . just like work relationship, stress you know, all that stuff, so I know that that is what has been making it a trillion times worse.
P44, young adult, GP
By contrast, depression seemed to decrease one interviewee’s motivation to take action, which may have contributed to the fact that the decision to seek help was taken by someone else on their behalf.
Social deprivation subgroup
Sample characteristics
Sixteen individuals residing in areas of social deprivation were recruited, ranging in age from 32 to 80 years (mean 57 years). The majority of interviewees (n = 9) resided in an area with an IMD score of 1 (the highest level of deprivation). All but one interviewee had lived in the city in which we recruited them for > 5 years; the other interviewee had lived in the city for > 1 year. The sample was evenly split between men and women. Interviewees predominantly identified their ethnicity as white (n = 11); four other interviewees were Asian/Asian British (Kashmiri, Indian, Pakistani and Afghan) and one was black African. Nine interviewees described themselves as married, three separated or divorced, three single and one widowed. Half of this sample were retired (n = 8), with one other describing being both retired and working part-time. Four other interviewees were working full-time or part-time, two were full-time homemakers and one was permanently unemployed.
Of the 16 interviewees, five were recruited following contact with the emergency ambulance service, four were recruited following contact with an ED and seven were recruited following contact with a general practice. More people in this subgroup (n = 4) had used an emergency ambulance than in the other subgroups (young adults, n = 2; parents, n = 1), and one had been taken to the ED by ambulance following a call to NHS 111. Concerns prompting contact varied widely across this sample, and included chest, abdominal or back pain (n = 4), sometimes as part of an ongoing problem; illness, injury or confusion of someone they had caring responsibility for (n = 3); ear, throat and eye problems (n = 5), sometimes as part of a longer-term period of ill-health and other times prompted by health anxiety; anxiety attack; and headache after an injury.
Overview of findings for people living in areas of social deprivation
There was no single dominant driver of interviewees’ decision-making about seeking health care. Instead, a number of key drivers were evident, including concerns about the severity of their symptoms, an unwillingness to further delay care-seeking, and their perceptions and experiences of services. The influences of others and of social isolation were also significant drivers for different participants in this subgroup, together with poor mental health and geographical proximity. Most interviewees in this sample had between two and five drivers, with only one interviewee having a single driver evident in their decision to seek care. With regard to making contact with a particular service, a lack of access (either perceived or real) or dissatisfaction with general practice were factors for all interviewees in their decision to contact either the emergency ambulance service or an ED. Conversely, positive experiences of general practice, or negative perceptions about urgent care services such as WICs, were the predominant factors in the decision to access general practice. The influence of others, either within a social network or health-care professionals, could also determine whether or not an interviewee sought help, or where help was sought from.
Concern regarding seriousness of symptoms
Some of the interviewees sought care because they were concerned about physical symptoms. They described unfamiliar, or worsening, symptoms that they believed might indicate a serious problem; these concerns correspond to programme theory 1, uncertainty about symptoms causing anxiety. Two interviewees who reported concerns about symptoms had sought care on behalf of another person, and, in both instances, programme theory 3, fear of consequences when responsible for others, was clearly evident. One interviewee was a care home manager and her decision-making had been clearly influenced by this role. Although concerned that the symptoms and unusual behaviour of a resident could indicate a more serious problem, she had also been driven to act because she felt a duty of care for the resident and was unwilling to take risks with the health of someone for whom she had responsibility. This was exacerbated by her belief, based on her experience of caring for elderly people, that their health is prone to deteriorating quickly. Another interviewee had sought care on behalf of her teenage daughter, and risk aversion was again apparent. The parent had been unwilling to leave her child’s symptoms untreated, and had been reluctant to medicate her child unless advised by a doctor, highlighting the role of confidence in medication use, which is not currently encompassed in the programme theories.
Unwilling to further delay care-seeking
For around half of the interviewees who were living in areas of deprivation, a key driver of seeking care was their unwillingness to tolerate further delays in doing so. As with the young adults group, this driver, which corresponds to programme theory 6, waited long enough for things to improve, was sometimes also linked to programme theory 5, need for immediate pain relief. Interviewees described being in increasing amounts of pain that could no longer be tolerated, and believing that seeking care could provide the urgent pain relief that they needed. Interviewees described using self-care strategies to alleviate their pain, but these were perceived as ineffective. In some instances, it appeared that there had been a reluctance to self-administer pain medication, or that there was a lack of medication knowledge, which had limited their use of medication in the period before seeking care. This limited engagement with medication is not represented in the existing programme theories:
You are in so much pain you just think, you are thinking about the pain all the time . . . [the pain] had lasted for 24 hours, and I did say to [call handler at 999], you know, I can’t put up with this much longer . . . I thought I’ve put up with it long enough . . . I thought when is it going to end [. . .] I’m not a tablet person, I’ve got, if I was to try and put a number of tablets that I have taken in my life [aged 70+ years] and if you want to include Rennies, I think it must be, around the hundred mark.
P1, social deprivation, emergency ambulance
There was some evidence that pain also led to increased anxiety about symptoms, which was aligned with programme theory 1, uncertainty about symptoms causing anxiety, or had a negative impact on the ability to care for family, which was aligned with programme theory 4, inability to get on with daily life, both of which acted as further key drivers of care-seeking. An unwillingness to delay care further was an important driver for some of the interviewees who sought care from the emergency ambulance service or in the ED. This decision was generally related to unmanageable pain and a need to obtain urgent pain relief, but for one interviewee who was experiencing acute mental health symptoms the 999 call was in reaction to needing an immediate response to these symptoms, suggesting a need to extend programme theory 5, need for immediate pain relief, to include a wider range of acute symptoms. This driver did not appear important to those seeking GP care in this sample.
Others’ unwillingness to delay seeking care was related not to pain but to an inability to manage the symptoms, or the situation, any longer. One interviewee felt that she had delayed seeking care for persistent symptoms for long enough and had reached a point of wanting to get things sorted that day:
. . . so I tell him I got this infection since 3 or 4 weeks. I was suffering, and I got no appointment, so that’s why I say it should be (. . .) that’s why I want to go appointment because I’m not well.
P24, social deprivation, GP
Perceptions and experiences of health services
The influence of both positive and negative experiences of services was evident in interviewees’ decision-making, aligning clearly with programme theory 9, perceptions or prior experiences of services. All interviewees who had made their own decision to access the emergency ambulance service or the ED, rather than doing so on advice from a health-care professional, offered a negative view of some aspect of general practice. Interviewees described trying to make contact with the GP but the telephone was repeatedly engaged, or that they had made contact with their GP but had not been offered care that met their needs or within a timescale that would meet their needs, or that they had not attempted to contact their GP because they believed that an appointment would not be available. This combination of experiences and perceptions corresponded to programme theory 10, frustration with access to a GP, as well as to programme theory 9:
I phoned the doctors to ask for some medication, I thought probably they may, might have come to see me ‘cause I couldn’t get to see them, but they are very reluctant now to come out as well, aren’t they? Yes, and probably that would have saved me a visit up to the hospital.
P4, social deprivation, ED
Some interviewees felt that it might take weeks to obtain a GP appointment for a routine problem, and indicated that they would try to obtain a same-day appointment regardless of how urgent they thought the problem was, thereby effectively using ‘urgent’ appointments for more routine health problems. For one interviewee, this course of action appeared to be endorsed by the GP receptionist as a way to access their preferred GP, illustrating the role of programme theory 8, following advice of trusted others in the decision-making process. The process of trying to obtain a same-day GP appointment was discussed, with many interviewees describing how they needed to call the GP surgery first thing in the morning to do this. For some interviewees this was problematic; for example, if they had taken the decision to seek care later in the day, by which time they believed, or knew, that no same-day appointments would be available. Others found it difficult to call first thing in the morning while feeling unwell:
I find it very frustrating, that you have to call the GP surgery at half past eight when it opens, because it’s just a free-for-all. Obviously everybody, everybody rings at the same time and it’s a little bit like a radio phone-in, you know, the fifth caller wins. The phone is just engaged and engaged and engaged so you have to just constantly keep trying and you can get through at, sometimes at quarter to 9, 15 minutes later and all the appointments have gone and it’s the first, it’s like you know, trying to buy concert tickets.
P26, social deprivation, GP
Others described an unfamiliar triage system at their GP surgery. Although interviewees were not explicit about whether or not this was a factor in their opting to contact a different service, it may have influenced their decision if they felt that they needed help urgently.
A small number of interviewees expressed dissatisfaction with the care that they received from their general practice, which may have influenced their decision not to contact a GP; this again corresponded to programme theory 9, perceptions or prior experiences of services. There appeared to be a lack of confidence in the care provided, with one interviewee recounting a previous occasion when their GP’s inability to make a clinical diagnosis had given them the perception that the GP had not assessed them properly, and another describing inconsistency of care because of the use of locum GPs:
. . . at the minute my doctor’s pretty terrible. It’s kind of, he is an old guy, so I don’t know if he is going through health issues, you know he is in his eighties. His wife is absolutely terrible but the less said about that the better . . . they’ve got a lot of locums in, so I’m again, you can’t judge, for me I like to have consistency. You know if I’ve had a doctor that has known me for a while, it’s good for me to see him on a relatively regular basis, if they’ve got a locum it’s a bit like I don’t know who I’m going to be seeing today. They can look at your paperwork and they can look at your medical records but it doesn’t feel the same, do you know what I mean? So it’s been difficult really.
P19, social deprivation, ED
By contrast, all of the interviewees who had used their GP on the occasion in question identified positive perceptions of their general practice as a key driver of their decision. Interviewees spoke about a range of factors that gave them confidence in, and satisfaction with, their general practice: access to the service, the knowledge and professionalism of their GP, the thoroughness of assessment, the ability to receive reassurance and communicate effectively, and their often well-established relationship with their GP:
I think we’ve got an amazing surgery, I noticed it’s been voted one of the top surgeries in last year’s poll . . . You can ring every morning at half past 8 and they answer or somebody will always ring you back. If you explain that you can’t get in until a certain time they try and fit you in at that time. They’re amazing.
P15, social deprivation, GP
I am a worrier about my health . . . the guy [GP] was very understanding, you know in this particular appointment, good bedside manner if you will, he was very reassuring. He examined me and said that there was nothing to worry about, but very reassuring, wasn’t vague or ambiguous in what he was saying, he was very to the point. There is nothing wrong you know and that sometimes well, all the time, that’s what I need to hear if you see what I mean.
P26, social deprivation, GP
Similarly, some interviewees who accessed an ED had a positive view of the service. They felt that an ED was more likely than a general practice to offer what they needed on that particular occasion, such as making a diagnosis when a GP had failed to make one, providing pain relief quicker than a GP could (which links with programme theory 5, need for immediate pain relief), and giving better information than a GP that they were dissatisfied with.
There were also negative perceptions about urgent care services such as WICs, NHS 111 and pharmacies, which appeared to particularly influence the interviewees who were recruited into the study via general practice, suggesting that these people were less likely to use those services when seeking health care. Some interviewees were unaware of these services or the facilities that they provided, but others felt that they were not appropriate for their clinical needs, had been dissatisfied after using them on a previous occasion or had difficulties accessing them.
Influence of others
In contrast to those experiencing social isolation, other interviewees appeared supported and indicated that family members had influenced or supported their decision to seek care or to seek care from a specific service. This influence corresponds to programme theory 8, following advice of trusted others, although this would need to be modified to recognise the varying degrees of influence of people’s social networks. The motivation of family influence could be worry about the symptoms, corresponding with programme theory 1, uncertainty about symptoms causing anxiety, as well as with programme theory 3, fear of consequences when responsible for others:
. . . why did your family encourage you to make contact with a health service?
probably the fact that I live on my own, and that I was in pain. I think that would probably be the reason. And my granddaughter she works with a lot of elderly people anyway do you know what I mean and yes ‘oh you should be going . . .’
So if you’d just been left to your own devices and your daughter hadn’t intervened, what do you think you would have done, in the next day or whatever?
Just carried on probably with the stronger painkillers.
In other instances, health-care professionals influenced interviewees’ course of action. Some of our interviewees had accessed a lower-acuity service prior to contacting the service from which they had been recruited, and around one-third had followed the advice of a health-care professional in then contacting a higher-acuity service. Aligned with programme theory 8, following advice of trusted others, one interviewee described how NHS 111 had arranged an emergency ambulance for them, and another explained that NHS 111 had obtained a GP appointment for them after they had tried unsuccessfully to do so themselves. Other interviewees described being given advice from a health-care professional rather than having a contact arranged. One interviewee’s GP suggested that they could call the emergency ambulance service about their problem and another had been advised by an optician to contact their GP. In a third instance, general practice surgery staff advised the interviewee to access their chosen GP by requesting a same-day appointment. Some interviewees found that this advice matched their perception of who they should contact, but both interviewees who were assessed by the emergency ambulance service questioned whether this might be a higher-acuity service than necessary. None of our interviewees received advice from a health-care professional to attend an ED.
Social isolation
Although for some interviewees in this sample other people had an impact on their decision-making, around one-third appeared to experience varying degrees of social isolation or a lack of support, aligning with programme theory 7, stressful lives, difficulty coping. For some, this was a key driver of why they sought care, but more often it was a secondary driver of their decision-making when seeking care on that particular occasion. Lack of support related to a general lack of support in their lives from informal/formal networks, rather than a lack of support specifically at the time of the incident (e.g. being alone at the time or unable to contact a usual provider of support). Those describing a general lack of support tended to be older, ranging in age from 64 to 80 years. Two of these interviewees said that they were the main carer for their spouse, with little or no extended family input, whereas the others lived alone or in sheltered housing. In common, they described having no extended family, or none living nearby, or a lack of positive interaction with family. Some identified a network of people around them, such as neighbours, but did not describe these people in terms of friendship or support. In some of these individuals the interviewer perceived a sense of loneliness and a desire to connect during the interview, which had possibly been a reason that they had agreed to take part:
[I have] two [sons] . . . they don’t keep in touch, I’ve not seen them since the divorce [10+ years ago] . . . I phoned them, they never reply, they don’t reply, they don’t reply to texts or anything, I don’t even know if they have got the same number . . . I said I may as well text to the brick wall next door to me, because I’m getting the same response, if you need me at any time, I’m there and I’ve never heard, very sad really.
P1, social deprivation, emergency ambulance
The lack of support or the social isolation appeared to contribute to some interviewees’ inability to manage their symptoms any longer, corresponding to programme theory 7, stressful lives and difficulty coping. This programme theory was also evident in the practical impact of isolation for one interviewee, who did not have anyone to offer them transport to the ED and, without having the financial means of paying for a taxi, going to the ED by ambulance was seen as the only option.
Some interviewees seemed to perceive that, although a degree of informal or formal support was available, this could not provide the advice or kind of support needed. One interviewee felt that they were more knowledgeable about health than those in their support network, and another believed that formal carers would be unable to help within the time frame required, the latter belief potentially aligning with programme theory 9, perceptions or prior experiences of services.
Poor mental health
Although the primary reason for seeking care related predominantly to physical problems, existing mental health problems were mentioned by half of the sample. Interviewees spoke openly about their mental health. They described generalised anxiety, specific health anxiety, separation anxiety, panic attacks and agoraphobia, many of which were longstanding problems for which professional care was being accessed. Mental health problems, which could be understood as an aspect of programme theory 7, stressful lives and difficulty coping, appeared to influence decision-making in a number of ways. Generalised anxiety could contribute to the urgency required when seeking help, where, for example, the onset of a physical symptom could prompt an underlying anxiety that escalated the need to be assessed by a health-care professional urgently. The duration and the nature of symptoms could also trigger or exacerbate health anxiety, prompting a need to seek care to receive reassurance from a health-care professional that the problem was not serious. One interviewee, against the advice of her GP, undertook a symptom-related internet search before she sought care, which further added to her health anxiety; the information gathered during the internet search led her to believe that the physical health problem could be more serious than she had initially perceived. For some, although they made light of the situation, it was clear that the physical symptoms instilled a genuine fear about the severity of the problem, aligned with programme theory 1, uncertainty about symptoms causing anxiety:
I just thought I don’t want to die [laughs]. I don’t know, maybe I was taking it a bit too far, but I was, I’ve never had anything like this before. So when I have spoken to people afterwards they said ‘oh they’ve had swollen lymph when they have been ill this that and the other’, but me I was like ‘damn, I don’t like this’ you know . . . it was scary for me.
P19, social deprivation, ED
In the case of one interviewee who exhibited significant anxiety in the interview, the relationship between key drivers was particularly complex, with social isolation appearing to feed a general anxiety, and a history of serious health problems being associated with health-related anxiety and a fear of death. The onset of an apparent minor health problem exacerbated these beliefs and the need for urgent help.
When mental health problems were described, care was accessed from all three services in our study. Interviewees who opted to seek care from a GP described having a positive and established relationship with their GP (one interviewee described the relationship in terms of a friendship) or perceived that only a doctor had the clinical skills that would allay their concerns. Their trust in their general practice was apparent, and the influence of these perceptions corresponds closely to programme theory 9, perceptions or prior experiences of services:
I’d had a problem with my throat I’d sort of convinced myself that I had a little lump, my throat looked abnormal when I looked in the mirror. I’d had a sore throat and I was checking around and I thought ‘oh that doesn’t look right’, so then the way my brain works is, I automatically need some sort of reassurance, obviously the doctors are the best people to do that, professionally. Knowing how I, what I’m like with my worrying about my health, I feel like I instantly need some, some form of reassurance that could only really come from [the GP].
P26, social deprivation, GP
Geographical proximity to a service
Although not a driver for most, two interviewees described the proximity to a particular service as an important factor in their decision to access it. This factor, which is not represented in existing programme theories, often worked in combination with other drivers. For example, one interviewee described needing to obtain pain relief quickly and, as they lived close to the ED and believed that the ED was an appropriate service for their care, considered themselves to be in too much pain to travel to a service further away. The link between proximity and programme theory 5, need for immediate pain relief, is clearly evident here. Most interviewees lived near a general practice. One interviewee described the general practice as being located within 1 minute’s walk from home and described how they booked appointments in person, rather than over the telephone, such was the convenience of the location. The proximity of the service, combined with these other factors, were significant drivers of why GP care was sought.
Summary of drivers of seeking care from specific services across the three subgroups
We focused on why people sought care from different services across the three subgroups.
Among the eight interviewees who were recruited following contact with the emergency ambulance service, the key drivers were concern about symptoms or an inability to tolerate symptoms any longer; problems with gaining timely access to a GP; and the influence of others (NHS 111 advised calling 999, a GP advised calling 999, or family made the decision to call 999). Other influences included positive perceptions about the ambulance service; a lack of financial means to be able to travel to the ED; a lack of knowledge of or confidence in lower-acuity services; anxiety prompted by the episode occurring overnight while the participant was alone; or an indication that the decision-maker had a general impatience and intolerance of waiting.
Among the 21 interviewees who were recruited following contact with an ED, most drivers related to negative aspects of general practice: a perceived inability to access timely GP care or dissatisfaction with GP care. In addition, EDs had characteristics that many interviewees sought, including speed and range of clinical facilities, or were perceived to be able to resolve their problem. Although the familiarity with, or proximity to, the ED was not a key driver, it was an influential reason for seeking care there. Another key driver was the influence of others, including being advised by service providers in general practice, NHS 111 or people in their social network.
All of the 19 participants recruited following contact at a general practice had positive perceptions of general practice, including having a good relationship with their GP, having good access to GP care in terms of the ease with which they could obtain a same-day appointment, the proximity of the practice, having a desire to obtain reassurance from a professional, and having the sense that it was appropriate to contact a GP with their particular health problem. Following the advice of someone else, such as staff at general practice, NHS 111, an optician, and family and friends, was a key driver of seeking care from a GP.
Discussion
Summary of findings
There was some commonality across the subgroups with respect to decision-making about seeking emergency and urgent care, as well as distinct areas of difference. As might be expected, concerns about symptoms were prevalent in all subgroups. However, the groups differed in the factors that prompted or exacerbated these concerns. Parents specifically placed the child at the centre of this decision-making, in relation to either their sense of responsibility for the child or their lower threshold for tolerating risk concerning the child’s health. Seeking professional care eased parents’ burden of responsibility and met a need for reassurance that was a clear and dominant driver in this subgroup, with other factors not having the same amount of influence.
Among young adults and those living in areas of deprivation, concerns about symptoms were also present, but these were driven by, and one of a more diverse range of, factors that influenced their decision. An unwillingness to delay seeking care was also expressed more frequently in these groups than in the parent sample. This could be driven by a range of factors, including an inability to manage the symptoms, a need for urgent pain relief or, particularly among young adults, a concern about the impact of the symptoms on their functioning, probably reflecting the higher proportion in this group who were working or studying. Poor mental health also influenced decision-making for young adults and those in the social deprivation sample, and social isolation was another factor for some in the latter group. Both of these factors may have had an impact on interviewees’ coping capacity and subsequent decision-making.
All subgroups were heavily influenced in their decisions to make contact with specific services by perceptions or previous experiences of health services. Influences could be positive (i.e. prompting a choice to contact a particular service) or negative (i.e. choosing not to access a specific service). The influence of other people was also apparent in all subgroups, more so on the choice of service rather than on the decision to seek care. This influence could come from health-care professionals, but was most frequently from interviewees’ social networks, where family members’, friends’ and colleagues’ perceptions of services or concerns regarding the seriousness of the symptoms could direct or support help-seeking decisions.
Links to programme theories
Evidence of all 10 programme theories was found in the interviewees’ accounts and, mirroring the findings discussed above, some were present more frequently and to varying degrees across the subgroups (see Appendix 6, Table 18). Reflecting the areas of commonality identified above, three programme theories featured strongly in all three groups: programme theory 1, uncertainty about symptoms causing anxiety, programme theory 8, following advice of trusted others, and programme theory 9, perceptions or experiences of services. Parents’ particular concerns regarding their responsibility for their child and lower threshold of concern for their child’s health are apparent in the much more frequent evidence in this subgroup of programme theory 3, fear of consequences when responsible for others, and programme theory 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety. By contrast, programme theory 6, waited long enough for things to improve, and programme theory 7, stressful lives and difficulty coping, are more apparent in the young adult and social deprivation subgroups, the latter perhaps reflecting the impact of mental health problems and social isolation. Young adults’ concerns about the impact of symptoms on their ability to function are evident in the more frequent occurrence in this subgroup of programme theory 4, inability to get on with daily life. The number and range of programme theories in many of interviewees’ accounts also highlights the complexity of individuals’ experiences. Only seven interviewees showed indications for fewer than four programme theories and 10 interviewees had evidence of six or seven of the theories.
Our findings add new insights to the existing programme theories, indicating areas where these need to be refined or extended to more accurately reflect the diversity of experiences in the data (Table 6). Interviewees’ accounts also identify further drivers of their decision-making that are not reflected in the existing programme theories, particularly in relation to the influence of the timing of the event and the proximity of services, which suggests that there is a need for additional programme theories.
| PT developed in WP1 | Suggested refinements or proposed new theories from WP2 | Suggested revisions |
|---|---|---|
| 1, uncertainty about symptoms causing anxiety |
Degree of vulnerability of person – age – or is this PT2? Or someone else’s uncertainty who made the decision? Need for validation – is this PT1? |
Uncertainty about meaning and seriousness of symptoms causing anxiety |
| 2, heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety |
General beliefs about children’s health quickly deteriorating – or is this PT8 refined? Similarly, elderly people can decline quickly Previous symptoms – chronic conditions or recurrent illness – not exactly trauma but increases concern. Also anticipate return of symptoms if run out of medication |
Heightened awareness of risk to health as a result of personal experience or knowledge causing anxiety |
| 3, fear of consequences when responsible for others |
Distress at seeing the person they are responsible for suffering Duty of care in professional role |
Responsibility and/or care for others causing distress and fear of consequences of not acting |
| 4, inability to get on with daily life |
Anticipated impact on function – trying to avoid a problem Impatience – less well-defined tasks – or does this go in PT6? |
Concern about actual or anticipated impact on daily activities/functioning |
| 5, need for immediate pain relief | Widen to include other acute symptoms (e.g. panic attack/mental health symptoms) | Need for immediate relief of intolerable/unbearable symptoms (including pain) |
| 6, waited long enough for things to improve |
Help-seeking so far has not produced desired outcome so try going somewhere else (e.g. GP has not resolved it) Impatience, intolerance of waiting Tipping point |
Unwillingness to continue current approach to managing symptoms (waiting/self-care/help-seeking) due to lack of resolution of the problem |
| 7, stressful lives |
Needs to include lack of access to resources (e.g. car, support). This could link to time of day in some cases Wider lack of social support, not necessarily incident-specific – impact on decision-making Ongoing health worries increasing concern Own illness affecting coping capacity and managing that of someone else Mental health – additional stress. Can also change perception of seriousness PT1 if have health anxiety Stressful work triggering symptoms and also need for easy access to help Lack of money – affects choice of service |
Reduced coping capacity due to physical and mental illness, stress and/or lack of access to resources |
| 8, following the advice of trusted others |
Influence of social networks and norms Support, encouragement and suggestions from peers, rather than direct advice Use of internet to obtain health advice and information |
Directly or indirectly influenced by the advice or support of others, including social networks, health-care professionals and internet sources |
| 9, perceptions or prior experiences of services |
Can include use of GP for urgent care due to positive experience reinforced by reassurance from health professional that previous use was right Or others’ perceptions – link to PT8 Awareness of other services – could expand PT9? |
Perceptions, prior experiences and/or awareness/knowledge of services |
| 10, frustration with access to a GP |
Need to take account of the fact that some of them did go to GP May have repeatedly tried to get appointment, or cannot wait long enough for routine appt |
Frustration with inability to access an appropriate GP appointment |
| Location – potentially links to cost or other resource issues – PT7 at least sometimes | Proximity or ease of access to particular services | |
|
Timing, e.g. Friday, late at night – this links to PT7 and lack of support Later in the day – no GP appointments left, or perception of PT9 |
Timing of event creating perceived, actual or anticipated unavailability of alternative services | |
| Limited engagement with/confidence in medication use | Lack of knowledge of and/or confidence to use medication to self-manage symptoms |
Links to existing theories
A number of the existing theories and models explored in the WP1 review are evident in the interview findings. For all three subgroups, concern about the seriousness of the symptoms links clearly with Leventhal’s58 self-regulation model, which recognises the importance of both cognitive and emotional dimensions of the experience of illness. In relation to the cognitive dimension, all of Leventhal’s five domains of illness, namely identity (label/name), consequences (including impact on function), timeline (including duration), cause and controllability, can be seen to varying degrees in many aspects of interviewees’ accounts of their symptoms. Uncertainty about the meaning of symptoms, which was a frequent concern for interviewees, has been identified by Mishel and Braden59 as having a significant impact on help-seeking; they also identify the role of social support in coping with uncertainty. All three subgroups frequently identified the influence of others on their decision-making, and Pescosolido’s71 network episode model, recognising both the direct and the indirect impact of social networks, is evident in our findings. The role of recursivity95 and candidacy74 is also evident in this context.
For parents and others in a caring role, the sense of responsibility can be understood partly in relation to Beck’s70 work on the Risk Society, where blame is avoided by acting responsibly, including in relation to health. Dingwall and Murray75 also highlight how children are considered as a different category of patient, with an accepted lower threshold for help-seeking. For those experiencing a range of stresses, which is seen in both the young adults and the social deprivation groups, including poor mental health and social isolation, Antontovsky and Sagy’s89 work recognises how a lack of ‘generalised resistance resources’ can have an impact on people’s ability to cope with additional challenges, including illness. The overall complexity of drivers, including both individual and contextual factors, is recognised in Andersen’s33 model of health-care utilisation, with later iterations increasingly acknowledging many of the social and structural influences on decision-making evident in interviewees’ accounts.
Link to wider literature
The clear correspondences between our findings and the programme theories developed from the realist review inevitably mean that there is a significant overlap with the literature on which the programme theories are based. In particular, our findings support existing qualitative evidence that highlights the influence of uncertainty about symptoms, fear of consequences when responsible for others, need for immediate pain relief, the impact of stressful lives, the advice of others, and perceptions and experiences of services. More recently published work suggests further overlap. Although focusing on different population subgroups, Pope et al. ’s22 research found that perceived risk, anxiety and a need for reassurance were common motivations for accessing urgent care services. Similarly, Pope et al. 22 also found a heightened sense of risk associated with children and babies, corresponding to Kai’s117 work, published over 20 years ago, which describes parents’ experiences of managing young children’s acute illness. His findings identified parental worry about the nature of symptoms, the threat that these symptoms might pose to their child’s health and the responsibility that parents felt to keep their child safe, which mirror the accounts of parents in our study. Given that we found a number of qualitative articles focusing on children using GP out-of-hours services and paediatric EDs in our review, we reflected on our additional contribution to knowledge for this subgroup. We feel that we more clearly identified the difference between people’s behaviour with regard to their own health and their behaviour with regard to the health of their child, how problems with children’s ongoing health creates an anxiety and unwillingness to wait, how a parent’s own illness can have an impact on their coping capacity, and the influence of family on decision-making. In addition, in the literature there is a general perception or experience of not being able to access GP appointments or of a dissatisfaction with GPs, but our inclusion of people accessing same-day GP appointments shows the ease of access for some parents of young children.
The evidence from the realist review showed how a range of social and psychological stressors could have an impact on individuals’ help-seeking, reducing their coping capacity and increasing their use of emergency and urgent care. Although poor mental health was identified as one of these stressors, the findings from our interviews suggest that this specific issue was often more dominant and was frequently a significant driver of seeking care. Although interviewees’ overall physical and mental health was not explored routinely during the interviews, a number described mental health symptoms for which they were being treated or seeking treatment through their GP, and a very small number reported more severe mental health problems. It was clear that, even for those whose problems were less severe, their symptoms or associated reduced coping capacity were frequently a factor in their help-seeking, although the problem for which they were seeking help was frequently a physical one.
Recent research supports our findings, identifying that those with a mental health diagnosis (classified as mild, moderate or severe) are more likely to use EDs than those without a diagnosis, with more severe problems associated with more frequent visits. 118 Other studies from the USA and Australia identify increases in both the absolute numbers and the proportion of ED use that were linked to mental health problems,119–121 particularly in adolescents/young adults121–123 and those with lower incomes. 119 Although most of this use is for problems requiring urgent attention, Hsia and Niedzwiecki124 also identified that 6.8% of all ‘avoidable visits’ to US EDs were for mental health conditions, and that mood disorders resulted in the highest proportion of avoidable visits by diagnostic grouping. In relation to the emergency ambulance service, two recent studies in the UK125 and Australia126 identified that approximately 10% of calls are related to mental health problems. Both studies emphasise the need for alternative solutions, particularly more community-based provision, transportation level of < 50% for those with less severe problems126 and high levels of re-attendance. 125
Mental health problems have also been found to have an impact on levels of primary care use. Lockett et al. 127 found that people with anxiety, depression or bipolar disorder were more likely to use primary care in New Zealand but were also more likely to report having unmet needs and a less positive experience with their GP. Even among those without a diagnosed mental health problem, self-perceived stress has been found to increase use of primary care, with higher stress levels associated with greater numbers of people having visited their GP in the past year in a Danish population study. 128 Notably, stress was also associated with greater use of out-of-hours services and, among those with multimorbidity, with decreased use of chronic care services. This reflects the findings from our interviews, suggesting that poor mental health can have am impact on help-seeking behaviour, even when not at a clinically recognised level.
Convenience has been identified as a driver of navigating emergency and urgent care services. 22,28 For example, an ED may be perceived as offering more availability or accessibility. Although there was some evidence of this in our study, convenience did not appear to play a significant part in decision-making among our participants. It is possible that interviewees did not want to appear to be inappropriate users of health care, but the researchers also perceived that convenience did not generally seem to be an important consideration. A far stronger driver of accessing ED services in our sample was the perceived lack of access to primary care services. This is widely supported in the existing research literature, has been shared in a patient perspective editorial34 and was evident in the recent NHS GP Patient Survey,129 in which around one in five patients (21.6%) reported that they had tried to contact an NHS service in the previous 12 months when they had wanted to see a GP but could not because their general practice was closed.
Strengths and limitations
A key strength of this part of the study is the collection of in-depth qualitative data eliciting drivers of decision-making among three population subgroups that were identified as having a tendency for ‘clinically unnecessary’ use of services. The inclusion in the study of three service settings, in particular same-day GP appointments, also extends the existing literature in this area, which has until now focused largely on ED use, with limited material relating to use of emergency ambulance and GP services. The process of data analysis, particularly the use of the principles of IPA, helped us to identify the complexity of the decision-making process. The findings highlight how, rather than being prompted by one single driver, an individual’s decision both to seek care and to use a particular service to obtain it is influenced by the interaction of multiple drivers. Providing insights into this complexity is vital in understanding and addressing ‘clinically unnecessary’ use.
We encountered a number of difficulties with recruitment that had an impact on the composition of the final sample. Most significantly, despite extending recruitment by a number of months, we recruited considerably fewer participants from the ambulance service than originally planned. Study set-up meetings led us to feel confident that we could recruit our relatively small sample from the large pool of patients calling the ambulance service and receiving telephone advice only. Initial engagement by staff at the ambulance services was also encouraging, but lessened in one service over time. Staff reported that pressures of demand on the service (we attempted to recruit between the months of November 2017 and June 2018) were a barrier to recruitment, and the lack of a researcher present regularly on site is also likely to have affected engagement with the study. To address the lower levels of recruitment via this route, we also recruited a few patients at the ED who had been conveyed by ambulance but whose transportation had been considered unnecessary by ED staff. We also encountered difficulties in recruiting in both the ED and the GP setting in Wolverhampton and, because of time pressure, had to recruit more than half of the overall sample in Sheffield. As a result, it has not been possible to make comparisons between two operationally different emergency and urgent care systems.
The study recruitment processes meant that the majority of participants were recruited between 09:00 and 18:00, with recruitment from only the emergency ambulance service occurring 24/7 (i.e. 24 hours per day, 7 days per week). An attempt to recruit at the ED during the weekend was not successful, and we did not attempt to recruit from this setting overnight. Therefore, there may be some differences between our interviewees and those using the services at other times of the day. For example, the lack of availability of other services or a reduction in social support at night may have an impact on the levels of anxiety that drive help-seeking.
Participants in the qualitative research were not aware that they had been included in the study because they had been identified as ‘clinically unnecessary’ users of a health service; our interest was in the decision-making that led to this contact. This approach was recommended by PPI members and approved by the ethics committee. To have been explicit about this with participants at the recruitment phase may have had an impact on the study in two ways. First, it may have had a negative impact on recruitment if potential participants felt that they had been perceived as using health services inappropriately. Second, if recruited participants felt that they were being labelled as ‘clinically unnecessary’ users, this may have affected their openness during the interviews, and, subsequently, the integrity of the data. The presence of the interviewer and the topic being discussed may have affected interviewees’ responses, prompting them to offer more socially acceptable reasons for their decision-making to avoid being judged. This may have been particularly evident for parents wanting to present themselves as ‘good parents’ who were doing the ‘right thing’ for their child. Although this cannot be ruled out, the researchers did not feel that it was an issue during the interviews.
Interviewees were recruited for their membership of a particular subgroup, but a significant number also belonged to one or even both of the other subgroups. For instance, eight young adults were also living in areas of deprivation, four of whom were parents. This means that there is some overlap between the subgroups. However, analysis was conducted both on those recruited to a particular subgroup and on those who had the characteristic of that subgroup, and this was not found to significantly influence the findings.
Implications
The programme theories identified in WP1 were clearly apparent in the three subgroups, and we refined some programme theories based on the interviews reported in this chapter. The drivers were largely similar across the subgroups but there were differences between subgroups in the strength of the drivers. This implies that potential interventions may need to be different for population subgroups.
Chapter 5 Interventions to address drivers of ‘clinically unnecessary’ use
Aim
Our aim was to identify patients’ views about potential interventions to reduce ‘clinically unnecessary’ use of emergency and urgent services. The term ‘intervention’ in this context means any initiative that could change decision-making about health service use, including reconfiguration of or changes to the delivery of services as well as campaigns to increase knowledge and awareness of services and service use.
Methods
The design was a focus group study with patients identified as ‘clinically unnecessary’ users to identify, discuss and prioritise potential interventions. We held three focus groups, one with each subgroup. We supplemented findings from the focus groups with analysis of recommendations for service improvements made by interviewees during individual interviews (see Chapter 4). We reviewed these findings in the light of recommendations for interventions made in the qualitative literature included in the realist review (see Chapter 3).
Sample
Owing to logistical challenges with recruitment and organisation, we recruited focus group participants in Sheffield only. We considered potential participants eligible if they had been identified as ‘clinically unnecessary’ users of an urgent or emergency care service and were a member of one of the three subgroups identified for the interviews: parents of young children, young adults and people living in areas of deprivation. We used two approaches to recruit participants. First, as the discussion about interventions during the interviews had been very brief, we invited the interviewees to take part in the focus groups. We approached all of the interviewees to determine their interest in taking part in a focus group. We sent participant information sheets and consent forms to those who expressed an interest (see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). Once a date and time had been set, we contacted the participant to confirm their availability and attendance. Second, to broaden the range of perspectives, we also sought to recruit additional patients considered to have made ‘clinically unnecessary’ use of an ED. This was done differently depending on the subgroup, as outlined below. We aimed to recruit a total of 24 participants (eight in each group), but owing to recruitment difficulties we were able to recruit only 15 participants.
Additional parents were recruited at Sheffield Children’s Hospital. This was done by a researcher (LBE) attending the hospital on 4 days, totalling approximately 19 hours. Additional people in the young adult and social deprivation subgroups were recruited at the Northern General Hospital ED, with recruitment for both groups taking place at the same time. This was done by a researcher (JL) attending the hospital on 4 occasions for a total of approximately 25 hours.
Data collection
To develop the topic guide for the focus groups, two researchers (EK and LBE) reviewed the interview transcripts, particularly the responses to a concluding question about the changes in service provision that participants would like to see to make it easier to access health care (see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). The topic guide was structured in two sections. In the first section, questions encouraged a general discussion about positive and negative perceptions and experiences of the emergency ambulance service, the ED and the GP. In the second section, participants were invited to offer and discuss potential reasons for using particular services and to suggest interventions or alternatives that might help individuals to decide to use a different, lower-acuity service or to try self-care. In this section, the focus was on participants’ views of how others in their subgroup (i.e. parents of young children or young adults) might respond rather than on their own individual behaviour. The exception to this was the social deprivation group, as noted below. Focus groups lasted approximately 2.5 hours, including a break for refreshments.
The parents focus group was held at a university building on a weekday morning; this time was based on a consensus from potential participants and to allow parents to take older children to school if necessary. The young adults focus group was held at a university building in the late afternoon/early evening of a weekday; this time was selected to suit the participants’ commitments, primarily work or study. The focus group of people from socially deprived communities was held in a university building on a weekday morning to suit the participants’ availability. As participants were not aware that their inclusion was on the basis of their IMD score, the discussion explored participants’ own views and their perceptions of the wider population, rather than asking specifically about people living in socially deprived communities.
Two experienced female researchers facilitated each focus group (EK and JL/LBE). Refreshments were offered on arrival, and participants completed and signed consent forms (see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). One researcher (EK) facilitated each focus group, keeping the discussion on track and probing further when appropriate. The other researcher (JL/LBE) supported this process by taking notes and joining the discussion if she felt that a particular aspect of the discussion could be expanded on. The discussion was digitally recorded. Detailed notes were made during each focus group about the interventions that participants highlighted during discussion. Towards the end of discussion, these interventions were shared with the group, who were asked if they could prioritise the interventions that they considered were most likely to change decision-making among those in their specific subgroup.
Data analysis
Following each focus group, the assistant moderator created a document based on the notes made during the discussion, in particular the specific positive and negative points relating to each service: ED, GP and out-of-hours provision, WIC, emergency ambulance service, NHS 111 and pharmacies. In addition, the interventions identified and prioritised by the focus group participants in the second part of the discussion were written up and, as the purpose of the focus groups was to identify specific interventions that could change decision-making, this list of recommendations and priorities formed the primary data for the analysis. These topics formed the themes for the analysis, and, owing to the nature of the data, formal coding within NVivo was not undertaken. Each focus group recording was also transcribed verbatim and checked by a member of the team prior to analysis. The transcripts were read by the researchers and used to support or challenge the analysis of the primary data, and to identify illustrative quotations. Analysis was undertaken by two researchers (EK and JL), initially for each focus group and then across the three groups, exploring the similarities and differences in their recommendations and priorities in relation to each service and other wider interventions. This information was then used to identify issues and recommendations specific to each service, and in relation to education, awareness and support.
Inclusion of data from interviews
During the interviews (see Chapter 4), interviewees referred to difficulties that they experienced or perceived in using different health services. They also identified specific changes in service provision that might make it easier for them to access health care differently. Although this did not specifically focus on interventions to encourage interviewees to change their choice of service, it did identify barriers to using particular services that could influence their decision-making process. All data relating to this topic were coded in NVivo to an overarching code of ‘Interventions which may have changed the decision-making’, with a number of specific subcodes also identified. Researchers reviewed this code to identify areas of concern, with the data divided by subgroup and by service. Twenty-four participants made one or more recommendation: 10 parents, nine young adults and five interviewees from socially deprived communities. These recommendations were used to supplement the data from the focus groups rather than be considered as a separate source; there was considerable overlap in the findings at least partly because the majority of focus groups participants had also participated in the interviews.
Reporting guidelines
We completed the COREQ reporting guidelines. 116
Findings
Five parents took part in the first focus group; three had taken part in an interview and two had been recruited specifically for the focus group. Six young adults took part in the second focus group; four had taken part in an interview and two had been recruited specifically for the focus group. Five people living in socially deprived communities were booked to attend the third focus group, but one did not arrive and could not be contacted, so four people took part in the discussion. Three had taken part in an interview and one had been recruited specifically for the focus group. Sociodemographic details are reported in Appendix 7, Table 19.
Parents of young children subgroup
Recommendations made by this group were tailored more to their particular situation (i.e. as parents) than those that were made by the other two groups, and often focused on child-specific service changes.
Changes in service provision
The group viewed improvements to GP provision as key, which was also echoed in the interview data. Better availability of GP appointments was a key priority, with interview participants identifying a number of specific suggestions, including more weekend, early morning and evening appointments, quicker access to appointments for non-urgent problems (i.e. within a few days rather than a number of weeks) and the ability to book appointments further ahead (e.g. 2–3 months). Focus group parents also considered that there should be prioritisation of urgent appointments for children, a point echoed by interview participants, who variously suggested specific appointments, telephone calls or drop-in sessions for children. Six-monthly GP appointments for children were also suggested, providing regular opportunities to discuss health concerns, gain knowledge and reassurance, and build a helpful relationship with an expert in child health.
In relation to accessing appointments, the group described diverse experiences, with some reporting that their GP ‘always sees my children on that day’ [focus group (FG) P3] and others describing the frustration of repeatedly trying to book an appointment:
They tell you to call at 8:30 for my GP. You call, by the time it’s 9 o’clock they’ll be like ‘Oh sorry, we’re out of . . . appointments’ and then, they’re all ‘Call in tomorrow’ you do the same thing for the whole week and then I’m like ‘Oh yeah . . . can I book it for next week?’ and they’ll be like ‘Oh no, there’s no appointments, call in on the day’. It’s just always ‘Call in on the day’ [agreement from group] and you never find one.
P4, parent, FG
Interview participants echoed these frustrations, which were heightened by the fact that the phone-in time was often when they were taking children to school. Suggestions for improvement included an online or app-based booking system for same-day GP appointments and/or call-back requests, and the ability to book an urgent appointment for the next day rather than have to telephone repeatedly each morning.
Recognising that parents’ sense of urgency, combined with the lack of access to GP appointments, may prompt them to use the ED, locating a GP service at the ED was recommended, allowing non-urgent problems to be dealt with via another route, which would also reduce demand on local GPs. The specialist skills available in the ED were also seen to be a significant driver of parents’ decision-making, particularly in the context of there being a children’s hospital in the city, with one parent observing that ‘if your kids are seen by a paediatrician, a specialist (. . .) I feel more you know, more safe’ (P1 FG). Therefore, the group recommended introducing specialist GPs for children, based either in a general practice or in a WIC, suggesting that parents’ greater confidence in the skills of these professionals could reduce their perceived need to use the ED. This suggestion was also made by an interview participant who did not take part in the focus group, and this seems to have been based on their experience in their country of origin. Interview participants also highlighted the need for better information about how to access urgent GP appointments out of hours or when no same-day GP appointments are available, together with increasing out-of-hours capacity to avoid attending an ED because of lack of GP appointments.
Focus group parents identified a number of other service changes that could potentially reduce the pressure that GPs were under. An increased role for pharmacists was suggested, including offering follow-up appointments. Some parent-specific changes to the WIC were also identified, many of which focused on minimising the length of the visit when bringing young children for treatment. These included having a priority system for children, having a separate WIC for children, reducing waiting times and introducing an appointment system to avoid the need to sit in a waiting room with an ill child for long periods. The location of the current WIC was seen as problematic, with the group suggesting that a more child-friendly location, and the introduction of local centres rather than one central service, could encourage greater use. Interview participants also recommended an increase in the number of WICs, enabling people to drop in and guarantee being seen at a convenient location.
More broadly, the group saw increased support, particularly for first-time parents, as essential, including more proactive engagement by health visitors and other community services, and offering parenting lessons in schools. The group also felt that there was a need to improve patient experience across the services and highlighted that a specific priority should be to offer language assistance at other services apart from the ED, as this could be a significant determinant of where to seek help:
. . . I don’t think they had anybody that would translate at certain GPs but in the A&E there’s always somebody (. . .) ‘cause there’s Somali doctors and there’s so many different doctors and nurses, so I think that’s why A&E’s more helpful.
P4, parent, FG
Education/awareness
Improving publicity about the alternatives to emergency and urgent care was seen as important, including promoting the GP out-of-hours service; encouraging the use of NHS 111 and emphasising its value in increasing parents’ health knowledge; and highlighting the knowledge, training and skills of pharmacists and their role in offering advice:
Explain what advice and what they [pharmacists] can actually offer advice on. Do they know about rashes? Do they know about different temperatures? Do they know about the actual symptoms of what my child is getting? Or do they – I don’t really know what they can fully offer, apart from just general advice on ‘Do I use this medicine or do I use this medicine?’
P3, parent, FG
Promoting the services offered by family centres was also seen as important in facilitating access to additional resources to help parents gain the skills and confidence to manage their children’s health.
Young adults subgroup
Changes in service provision
The key service priority identified by this group was the need to significantly improve mental health provision, a concern that may have been driven by at least half of the group having experienced significant mental health problems, as well as the prevalence of such issues in their friendship groups. Improvements in the range, quality and speed of access to mental health services were seen as important aspects of this, with the current gaps in provision leaving people with no option but to use other services, particularly at times of crisis. Lack of appropriate mental health support was also seen to have an impact on decision-making about physical illness, making them likely either to inappropriately delay seeking help or to ‘panic and try to grab out for every service’ (FG P12). In this context, the group suggested that a specific mental health ED should be introduced to provide urgent specialist support and advice, significantly improving patients’ experience and reducing pressure on the main ED (which patients are currently advised to use in crisis):
. . . it doesn’t seem like maybe the best use of the time for the people in A&E because they can’t really do anything really that practical to help, but also the person who’s feeling that way to be sat in there for how many hours to just go home again at the end of it.
P10, young adult, FG
Better support for mental health distress was also highlighted by interview participants, who emphasised the need to improve the quality and speed of access to mental health services, and how the current lack of provision contributed to increased use of the ED. The need for a more sympathetic response from clinical and reception general practice staff over the telephone was also suggested, together with clearer information on how to access immediate support.
Reflecting the concerns raised by parents, easier access to GP appointments was highlighted as important in encouraging people to reduce their use of the ED, with more availability of appointments outside working hours (i.e. early mornings, evenings and weekends) being a particular issue:
I think my GP does one day, where it’s like a late opening I think. But that’s no good if they’re all booked up, so then it’s like you’re going back into the week cycle aren’t you, waiting for the next appointment.
P13, young adult, FG
Interview participants also focused on the need for improvements to GP provision, including having extended opening hours, more same-day appointments and shorter waiting times for non-urgent appointments, introducing drop-in sessions and using a triage system to prioritise urgent cases. A text-reminder system for medication reviews was seen as valuable in preventing urgent appointments.
A number of uses of online technology were proposed by this focus group. One GP-related initiative was the establishment of an online database of GP appointments available across the city, which would allow people to travel to another practice to access a convenient appointment:
(. . .) particularly if younger people are more able to travel around that if they could somehow make, sharing of notes a little bit easier, and maybe people could, opt to travel to get an appointment, rather than going to their same GP and also it prevents, empty appointments going wasted [agreement].
P12, young adult, FG
Other proposed online interventions included improving the accessibility of GP services by using SkypeTM (Microsoft Corporation, Redmond, WA, USA) or online GP consultations, although not all of the interviewees favoured this option. Views were also mixed on other internet-based consultation services, particularly in terms of potential health and privacy/confidentiality risks. However, extending NHS 111, a service known to be credible, to include an online chat facility was seen as having the potential to increase use of this service, particularly among younger people, although the detailed questioning process was identified as a barrier by some.
Young adults taking part in interviews also made suggestions relating to other services, although these were a small proportion of the total. As in the parents group, increasing the number of local WICs was seen as important in improving access to this service. Additionally, co-locating GP and ED provision was recommended, which would enable people to be readily transferred to the service most appropriate to meet their needs.
Education/awareness
The importance of education and awareness raising was a key focus in this group, with significantly more recommendations relating to this rather than to changes in service provision. There was a strong feeling that many people, including young adults, were unaware of the services available and what these can offer, thus making appropriate decision-making difficult. In particular, the group considered that raising awareness of the range and scope of alternative services, including NHS 111, MIUs, WICs and pharmacies, was a key priority:
I think a lot of the problem is people don’t know these things exist, or don’t know what they’re for, and so they know A&E exists, they know something’s wrong, they just go to A&E because it’s probably fine. Some people I think are under the impression that you can’t walk in to A&E, that you have to be ambulanced in so the only way to get to A&E is by ambulance. And I just feel like there needs to be more education and publicity and, ‘These things exist, here’s how you can access them [pauses] there you go’.
P10, young adult, FG
Promoting NHS 111 on social media, in television adverts and by other routes was recommended, including gaining celebrity endorsement. Interview participants also echoed the need for greater publicity of NHS 111. Those in the focus group emphasised the importance of placing publicity in non-clinical locations, noting that ‘most posters about medical services are in the hospital when you are already waiting for one service’ (P15 FG), at which point it is too late to inform people. Specifically, they recommended promoting MIUs as an alternative to the ED, focusing on locations where people are more likely to need this service such as gyms or sports facilities. Increasing awareness of the skills and knowledge of pharmacists, and promoting their role in providing advice, was also highlighted as important in potentially reducing GP use in particular. Specifically, the group recommended that GPs and other practice staff advise patients whose needs could have been addressed by pharmacists about this option for future consultations.
Considering the issue on a wider level, the group felt that there was a need for education around what constitutes an emergency or urgent health problem, as this lack of understanding obviously has an impact on people’s decision-making. The importance of beginning the process of education in schools was emphasised, in terms of informing children about what should be considered an emergency and about the appropriate use of different health services:
I think like the more we’ve talked about it the more like educating in school seem the most plausible [agreement] because we keep going, ‘Oh, more publicity, more publicity’ there’s only so much money in the NHS anyway and it’s, you can’t just throw it out for every single service all the time can you?
It’s just starting people young isn’t it? [agreement] getting them educated.
An app or another online resource to help decision-making was also seen as a key tool to support change in service use, helping people decide on when and how to use different services:
(. . .) mainly directing to the right kind of place. Like if there could be some sort of red flag system of like, ‘Oh you’ve got that symptoms, that’s serious’. You know for people who’ve got a cold and like automatically worry that they’ve maybe got meningitis or something, like some sort of, ‘Have you got any of these three symptoms that would indicate meningitis?’ [agreement] OK, you do? Then yes, you do need a GP appointment. Yes, you do need to go to A&E.
P10, young adult, FG
Addressing the problem of inappropriate use, the group suggested raising awareness of the cost of service use and missed appointments, and explored the issue of penalties for misuse, although they acknowledged the difficulties that prevented this being a viable option. Finally, encouraging people to take more responsibility for their own health was emphasised, as this would ultimately lead to less service use overall. Returning to the concern around mental health, the group felt that improving mental health literacy was a priority, enabling people to identify and address their symptoms before they need urgent or emergency help.
Social deprivation subgroup
Service provision
In common with the other subgroups, accessibility and availability of GP appointments was highlighted as a key priority in changing decision-making. In relation to access, a number of participants reported difficulties in either getting through to their practice to make an appointment or being able to access a timely appointment once they did get through to their practice, leaving them feeling that they had no option but to use another service:
You either go there or you wait to phone your GP then you don’t get through so in the end you go to A&E. Then you’re getting worse so you might as well just go.
P9, social deprivation, FG
Reflecting the concerns raised by young adults, both the focus group and the interview participants emphasised the need for more appointments outside normal office hours and greater availability of appointments within a few days of making contact, rather than the current dichotomy of same-day appointments or waiting several weeks. Summing up a problem experienced by many, one interview participant highlighted how this dichotomy prompted her to leave things until they became urgent rather than book an appointment for some weeks ahead, by which time the problem may have resolved. Interview participants focused almost exclusively on issues relating to general practice and made a wide range of suggestions for improvement, including having drop-in appointments for children; reviewing the current same-day appointment booking system, including offering the option to book a next-day urgent appointment rather than having to telephone each day; being able to book appointments in person rather than over the telephone, which was important for those not confident about speaking English; having greater continuity of care from an individual GP; being able to speak directly to a doctor about a problem rather than communication being mediated by reception staff; having priority appointments for elderly people; and removing the triage system so that appointments could be allocated on request rather than being based on potentially inaccurate information.
One recommendation made in the focus group to reduce the use of GPs was increasing the prescribing role of pharmacists, which could particularly have an impact on those who obtain their prescriptions free of charge:
. . . it sounds really mercenary but some of time, because I get my prescriptions free, I’m over 60, I think I’m going to pharmacist but then, whatever they prescribe you, you’ve got to pay for. And you can go to your doctor and you can get on prescription and I know that sounds really awful (. . .) but that is one of things that goes through me mind (. . .) I’m sure it would be for a lot of these people who are, if they’re on benefits they get free prescriptions anyway don’t they but I certainly think that is a stumbling block for some people, ‘Why should I pay when I can get it free?’
P8, social deprivation, FG
Improvements to the consultation space in pharmacies were also seen as essential in this context, with privacy being a particular concern.
Although NHS 111 was valued, and promoting it more widely was seen as a priority, changes to improve the NHS 111 service were considered a prerequisite. In particular, echoing concerns raised by young adults, the group felt that there was a need to streamline the assessment process, with staff able to access patients’ clinical records so that they could avoid the lengthy questioning that currently discouraged people from using the service:
I think where it’s fallen down is, there’s a boring, protracted rigmarole whereby you’ve got to speak to somebody for 10 minutes and give your details and your favourite colour and everything before you can actually get to the point of the call. If they, you know, streamlined that service and made it more efficient then I think that would be a viable option.
P7, social deprivation, FG
Similarly, although increasing the number of WICs was recommended, there was a perception that the skill and specialism of practitioners based in them needed to be improved if people were to have sufficient confidence in this service for it to become an alternative to the ED. Combining the accessibility of WICs with the quality of GP services was also identified by interview participants.
Perhaps reflecting poorer availability of their own transport, access was a key concern in this group, potentially driving the recommendation to co-locate a wide range of services within a number of local centres, such as the ED, WICs, MIUs, general practices and baby clinics.
. . . instead of just having one central minor injuries, whatever, A&E, you know, Sheffield’s a big city, people have to travel from really far places, you know, so we could have something as (name) said east, west, north and south (. . .) So it would be really good to have something like that around the city where you have so many services at one building.
P9, social deprivation, FG
However, the group also highlighted the widespread confusion about the range and scope of different services available, and the consequent difficulty of making an informed decision. Rather than promoting this diversity, one suggestion was to significantly simplify provision to offer only the familiar, more clearly delineated services of the GP and ED and thereby reduce the complexity of decision-making.
Education and awareness
As noted in the previous section, the group considered it a priority to address the widespread confusion about when and how different services should be used, in particular by raising awareness of what each health service can offer, including the type and severity of conditions it can deal with, and when and how it can be accessed. In particular, the need to raise awareness of the NHS 111 service was emphasised to enable it to be promoted as an alternative source of advice when a GP appointment could not be accessed, with one participant observing:
. . . there’s only four of us and we’ve all got individual ideas. Like to me it’s just an out-of-hours service. I wouldn’t dream of calling it [NHS 111] in the day, if your GP’s open (. . .) We’ve all got such different, it’s just amazing for such a small group (. . .) So if four of us have got our own opinions, you can imagine what 40 would have. So it certainly needs something to get people a lot more aware of.
P8, social deprivation, FG
Promoting the role of pharmacies was also mentioned. Echoing comments made by the young adults’ group, the need to raise awareness about service use in non-clinical locations was highlighted, rather than this being done at a point when individuals had already made a decision about where to seek care:
. . . it seems like closing the stable door after the horse has bolted because you’re already there (. . .) but also a lot of people are worried when they’re in waiting rooms and I don’t think it’s necessarily the best time to be reading things. I mean you’re not at your most perceptive, when you’re about to go into an appointment that you’re concerned about, so I think that more needs to be done to get people before they’re in that situation.
P7, social deprivation, FG
Concern and frustration were also expressed about the misuse of services, prompting the group to recommend greater education to encourage people to take responsibility for managing their health, and to also consider applying penalties to ‘repeat offenders’, although the highly problematic nature of this was also acknowledged.
Overview of findings by service
Although the analysis focused on exploring the perspectives of the different subgroups, it became clear that there was significant overlap in their recommendations relating to particular services and approaches. We drew diagrams to clearly identify these areas of overlap and the distinctive perspectives of each subgroup (see Figures 4–7). The largest number of recommendations related to changes in general practice. Figure 4 highlights how all three subgroups emphasised that improving access to GP appointments was key to reducing the use of higher-acuity services, and each group also made at least one other recommendation. Figure 5 highlights how WICs were discussed in some detail, with both parents and participants from socially deprived areas making recommendations.
FIGURE 4.
Interventions recommended related to general practice. Bold outlines denote the priority recommendation.

FIGURE 5.
Interventions recommended related to WICs. Bold outlines denote the priority recommendation.
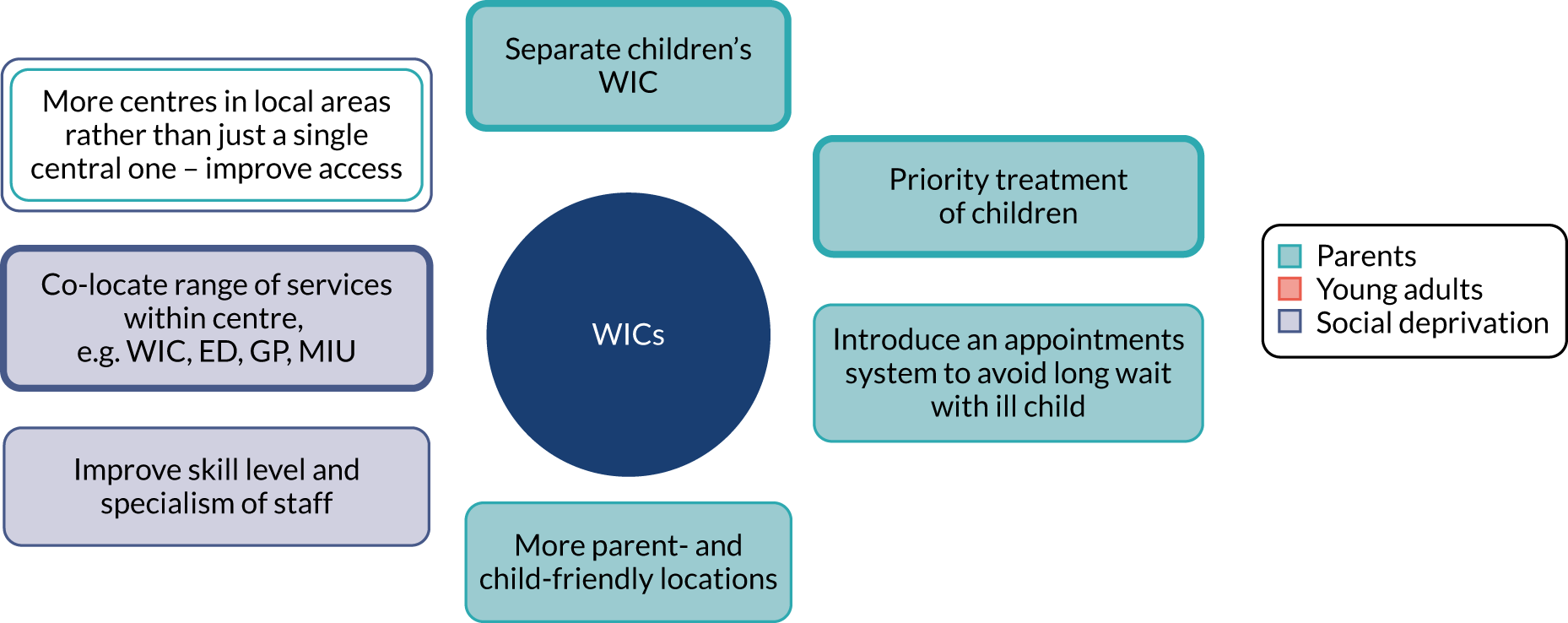
Other services were discussed in less detail, but there was a consensus across the groups that there was a need to better promote services that could provide alternatives to the emergency ambulance service, ED or urgent GP appointments. In particular, all groups highlighted raising awareness of the role of pharmacists and encouraging the use of NHS 111 as part of a broader recommendation to publicise and clarify the scope of each service and how and when it can be accessed. As can be seen in Figure 6, education and raising awareness was a shared area of concern, but a particular focus among the young adults subgroup.
FIGURE 6.
Interventions recommended related to education and awareness. Bold outlines denote the priority recommendation. OOH, out of hours.

The final area of intervention around which there was considerable shared interest was the need to encourage and support people to take responsibility for managing their own and their family’s health. As shown in Figure 7, both young adults and parents of young children had a number of specific recommendations relating to this topic.
FIGURE 7.
Interventions recommended in relation to supporting individuals. Bold outlines denote the priority recommendation.
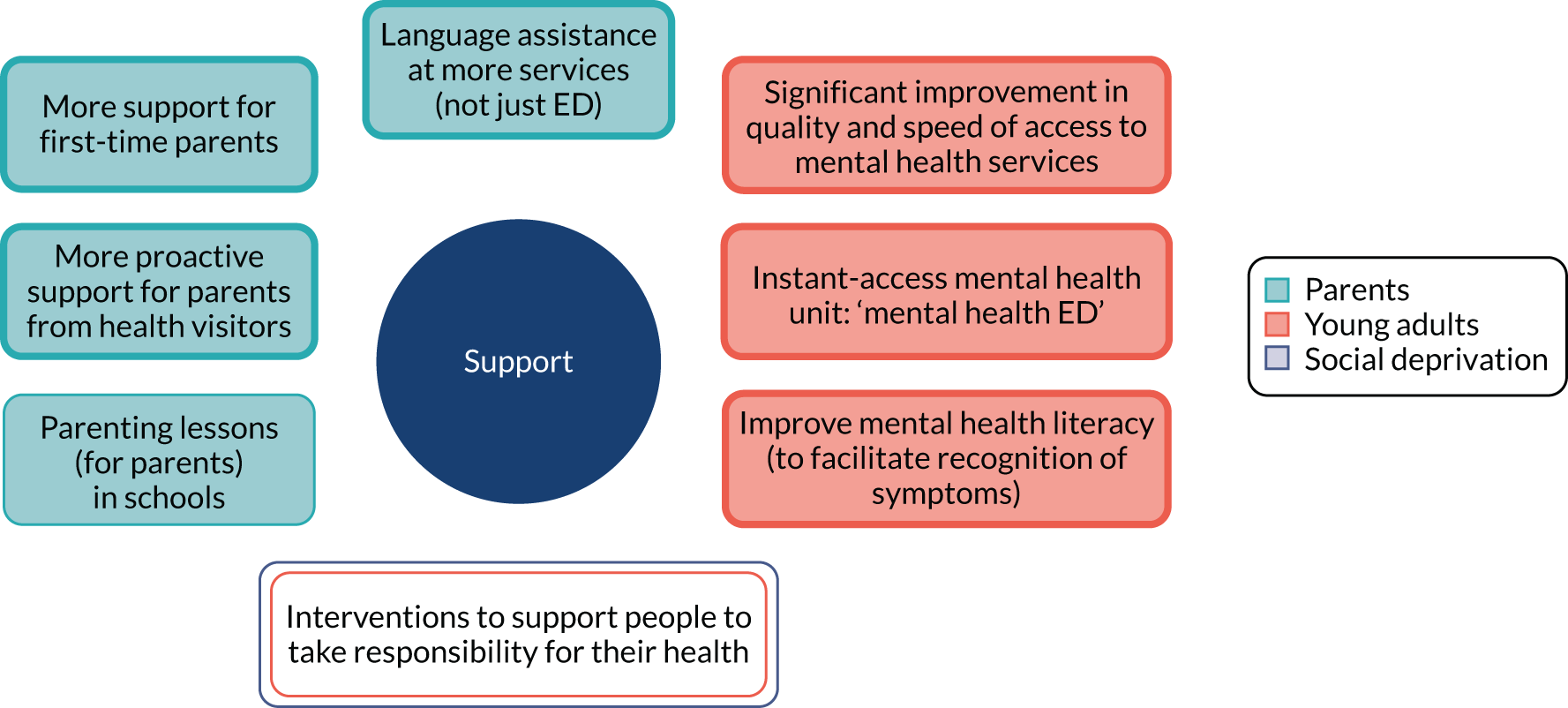
Discussion
Summary of findings
Participants in the focus groups and interviews presented a clear picture of their experiences and views about emergency and urgent care services, and what action could be taken to increase the use of alternative services. Although each subgroup focused their concerns on specific issues and needs, there were also many areas of agreement about where interventions should be focused. In particular, for parents of young children, services needed to offer quick access and have appropriate knowledge and skills in relation to children’s health to address the anxieties and the sense of responsibility that parents experienced. An awareness that young children are more vulnerable drove a number of recommendations for services to prioritise or focus on treatment of this group. Young adults highlighted how inadequate mental health provision could increase the use of emergency and urgent care services for physical problems as a result of raised anxiety, and recommended improvements to these services. The need for education and greater use of online resources and social media was also emphasised by this group. Concerns among the social deprivation group were more universal, but there was a greater focus on improved access to services, including co-locating services at a number of local centres. Although these differences were apparent, there were also clear areas of agreement, with a number of priorities being shared by all three groups. In particular, improved access to and availability of GP appointments was a key priority, together with raising awareness and knowledge of the range and scope of services that could be an alternative to emergency and urgent care. Interventions to enable people to manage their own health and use services more effectively were also highlighted by all three subgroups.
Link to interventions recommended by authors of articles in work package 1
The recommendations made by the focus group and the interview participants clearly related to the different categories of interventions identified by authors of the literature that was included in the review in WP1, as shown in Table 7. The only category of intervention raised in WP1 and not present during the focus group discussions related to reductions in primary care referrals to the ED, although the role of both NHS 111 and the GP in some participants’ service use was mentioned during both the focus groups and the interviews.
| Category of recommended intervention | Parents | Young adults | Social deprivation |
|---|---|---|---|
| Patient education regarding management of health problems and service use | Priority | Priority | Priority |
| Recognition of the influence of personal and social context on decision-making | Priority | Priority | Priority |
| Improve primary care provision, including out-of-hours support | Priority | Priority | Priority |
| Changes to the structure of care provision in the ED | Priority | Priority | Priority |
| Improve the relationship between primary care and patients | Yes | Yes | Yes |
| New/alternative patterns of care provision in the community | Priority | Yes | Priority |
| Reduce primary care referral to the ED | – | – | – |
Strengths and limitations
The findings from this part of the study are based directly on the experiences and views of patients who were deemed by the service that they used to have made a ‘clinically unnecessary’ decision. This is a particular strength, as it allows those patients who were considered to be contributing to ‘clinically unnecessary’ use of three pressurised emergency and urgent care services to identify interventions that could change this behaviour. The findings are limited by the size of the sample, including a substantial overlap between interviewees and focus group participants. This was because recruitment to a focus group proved to be very challenging in terms of both asking people to participate and getting them in a room together at the same time. The recruitment methods also mean that participants were drawn only from the three subgroups considered in this study, and were also self-selecting. Therefore, it cannot be assumed that their views represent those of all patients who make ‘clinically unnecessary’ decisions. Future research needs to extend the findings here by drawing on a larger, more diverse sample of patients, and to explore these ideas using a greater number of focus groups or other methods.
Link to wider literature
Policy-makers have instigated some of the interventions identified here, for example the Choose Well campaign to inform people about alternative options to EDs and GPs, NHS Direct (in the past) to offer reassurance to anxious patients, NHS 111 to direct people to the most appropriate service or self-care and WICs to offer appointment-free, easy-access primary care. As noted in Aim, the research evidence about the variety of interventions tested is largely inconclusive. 24 This leaves the way forward challenging. What is clear is that one intervention alone is unlikely to work because of the diversity and complexity of problems that need to be addressed. The area around which there was the greatest consensus and clearest priority for intervention in the focus group findings was improving access to GP appointments. Participants’ frustrations and challenges with GP appointments in the UK are also highlighted by MacKichan et al. ,98 who identify how factors such as complex systems, limited appointment availability and the requirement to communicate by telephone prompt patients to seek care at the ED. Reflecting on our focus group with parents, speed of access to care has also been seen as particularly important in relation to children’s health. 98 There is some evidence that extended general practice opening hours can reduce ED attendance for minor conditions, and, although cost-effectiveness and long-term feasibility were not established conclusively, our findings suggest that this could be explored further. 130 In addition, the variation in recommendations between the three subgroups highlights the importance of tailoring interventions to different subgroups’ needs. For example, a comprehensive strategy may need to include the introduction of child-specific services, improved mental health service provision and more localised co-located health-care services to address the perceived needs of the three subgroups studied here.
Implications
A range of interventions, rather than one intervention, is likely to be necessary to address ‘clinically unnecessary’ use of emergency and urgent care, with tailoring to specific population subgroups. Evaluation of interventions will be essential owing to the lack of a strong evidence base for such interventions. Strengthening general practice, with an emphasis on access and appointment systems, is worth pursuing as an intervention to reduce the use of EDs.
Chapter 6 Survey of general population
Introduction
Population attitudes and beliefs can shape the use of emergency and urgent care services. For example, leading researchers have concluded that policies to reduce demand for emergency ambulances need to address population opinions and attitudes,1 and researchers have attempted to reduce demand for ambulances by using mass media campaigns to change population attitudes and behaviour. 131
Researchers have undertaken population surveys to explore population attitudes towards emergency and urgent health services. 132 They sometimes use vignettes within these population surveys to identify the characteristics of those who have a tendency to make ‘clinically unnecessary’ use of emergency and urgent health services. 6,133,134
Aim and objectives
Our aim was to explore population attitudes and beliefs about seeking urgent care. The objectives were:
-
to measure the prevalence of population perceptions of seeking urgent care, and how these vary in different circumstances, and by different population subgroups
-
to identify the characteristics of people with a tendency to make ‘clinically unnecessary’ use of emergency and urgent care using vignettes.
Methods
British Social Attitudes Survey
The design was a cross-sectional general population survey undertaken by NatCen. NatCen conducts an annual survey in Britain, the British Social Attitudes Survey, to measure social attitudes. It designs the survey to yield a representative sample of adults aged ≥ 18 years.
In 2018, NatCen undertook a multistage design in three stages. First, it selected 395 postcode sectors, with probability proportional to the number of addresses in each sector. Prior to selection, all sectors were stratified by region, population density and percentage owner-occupied. These sectors covered Great Britain but not Northern Ireland, which is part of the UK. Second, it selected 26 addresses in each sector to produce 10,270 addresses. Third, interviewers called at each address and listed all those aged ≥ 18 years before randomly selecting one adult to interview. For practical reasons, the sample was confined to those living in private households, thus excluding people living in institutions. In 2018, the sample was divided into four parts, with each part (of around 1000 respondents) being nationally representative in its own right. The University of Sheffield used funding from the National Institute for Health Research (NIHR) to purchase a set of questions in three parts of the survey, that is, a sample size of around 3000. We chose this sample size because it offered sufficient statistical power for subgroup analyses.
The main mode of administration was face-to-face computer-assisted interview. Before an interviewer called at an address, a letter was sent to each selected household informing residents that an interviewer would visit and giving an unconditional financial incentive of a voucher. Interviewers then visited and completed most of the questionnaire face to face. A minority of questions were asked through a self-completed questionnaire, which was then collected by the interviewer or posted by the respondent. Data collection was undertaken from July to November 2018.
Developing the questionnaire
In 2018, the full British Attitudes Survey questionnaire covered a range of topics, such as attitudes to welfare, health, housing and education. Sociodemographic questions that were asked as part of the wider questionnaire were available for analysis in our study. We purchased a 60-item module exploring population views of seeking urgent care. The module used language that members of the public could understand, asking about seeking help for ‘unexpected health problems that were not life-threatening’. Items included three pairs of vignettes, questions related to the 10 programme theories from WP1 and attitudes towards the use of emergency and urgent care services. The module was based on findings from the WP1 realist review, literature about the use of emergency and urgent care in general, early findings from the WP2 qualitative study and a workshop with 13 members of the public at which potential questions were presented and discussed in small groups (see the next section). NatCen undertook two consecutive pilots of draft questionnaires on around 50 members of the public prior to finalising the questionnaire.
Patient and public involvement workshop
In the original proposal we planned to develop the content of the questionnaire at a PPI event with 20 members of the public; we held an event in January 2018. The event was designed to provide feedback on some of the questions that we were intending to use as part of the survey, and on the health literacy instruments that we were considering incorporating into the questionnaire. We publicised the event via existing PPI networks and on flyers placed in a variety of locations, including the local WIC and ED waiting rooms. The flyers identified the purpose of the event (to contribute to development of content of a national survey), the date and venue of the event, and that attendees would receive refreshments on the day along with a £30 shopping voucher. We invited interested members of the public to contact a researcher (EK) to obtain further details about the event. We asked those who confirmed that they would attend a small number of demographic questions to allow us to include a diverse range of people. Twenty members of the general public confirmed their attendance. On the night before the event, heavy snowfall occurred, and this resulted in fewer people at the event than anticipated. Thirteen members of the general public spent a day looking at different sections of the proposed questionnaire. A member of the research team (EK, AOC, LBE) facilitated discussion in three smaller groups. In each group, people tried to complete sections of the draft questionnaire and then discussed the content. We tested two ways of measuring health literacy. The conclusions included:
-
Our planned way of measuring health literacy was off-putting because it felt like a test. An alternative, measuring subjective views of health literacy, was preferred.
-
People did not like the use of names in vignettes and were frustrated by the lack of information in the vignettes, but also liked the shorter vignettes.
-
People were concerned that asking why they ticked ‘go to an ED’ for the vignettes would make this stand out as an option and alter later vignette answers.
-
People did not like having a long list of questions to complete using the same response set and asked us to use shorter sets of questions.
We redrafted the questionnaire after this event and sent it to NatCen for piloting.
Questionnaire content
A copy of the final questionnaire is available on the project web page (www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). There were four sets of questions:
-
sociodemographic characteristics
-
vignettes to measure tendency to use higher-acuity services than clinically necessary
-
ten programme theories from the WP1 realist review
-
other issues from the literature influencing ‘clinically unnecessary’ demand.
Sociodemographic characteristics
NatCen collect a range of characteristics of respondents within the British Social Attitudes Survey. We considered the effects of:
-
sociodemographics – age, sex, ethnicity, region, household with children aged < 5 years, deprivation as measured using the IMD, social class and rurality
-
resources – car ownership and access to internet
-
health – long-term limiting illness and general health
Deprivation and rurality were not asked about in the questionnaire but were added to our data set by NatCen from background information held for sampling purposes.
Vignettes
Vignettes used in emergency and urgent care population surveys have varied in terms of whether they focus on a third party or ask an individual to say what they would do, the amount of detail in the vignettes, and the potential seriousness of the problems addressed within them. 6,134,135 For example, some focus on chest pain and finding a lump,135 whereas others focus on less serious issues of an ankle sprain/bruise on leg after a fall and a child with a cold. 6
In the proposal we said that we would construct three vignettes: one in which care is needed immediately from an urgent care service (e.g. NHS 111, GP in hours same day, GP out of hours, WIC), one in which care is needed from a GP within a few days for a non-urgent problem and one in which self-care could be undertaken. In practice we constructed three pairs of vignettes, with a half of the sample receiving the same three vignettes. This allowed us to assess the effect of different symptoms and different times at which events occurred. We constructed these vignettes with clinical input from Steve Goodacre, who is an academic ED consultant, and Jon Dickson, who is an academic GP. Our PPI members and attendees at our large PPI event commented on the evolving versions of these vignettes.
We focused the vignettes on minor health problems. We identified a pair of illness vignettes with an expected action of self-care or pharmacy. We identified use of an emergency ambulance, ED or GP as ‘clinically unnecessary’:
-
Illness 1: imagine you have had a cough and sore throat for 3 days.
-
Illness 2: imagine you have had diarrhoea and vomiting for 2 days.
We identified a pair of injury vignettes where we expected respondents to contact a GP, contact an urgent care service such as an urgent care centre or a MIU, self-care or use a pharmacy. We identified use of an emergency ambulance or ED as ‘clinically unnecessary’:
-
Injury 1: imagine you have fallen and have a very painful rib. It is 8.30 in the evening.
-
Injury 2: imagine you have had back pain for 2 weeks and have not been able to sleep.
We identified a pair of child vignettes where we expected respondents to contact a GP in or out of hours, contact an urgent care service such as a WIC, self-care or use a pharmacy. We identified use of an emergency ambulance or ED as ‘clinically unnecessary’:
-
Child 1: imagine your young child or a young child in your care has a high temperature and cried throughout yesterday and last night. Today, which is a Saturday, you do not think the child has improved.
-
Child 2: imagine your young child or a young child in your care has a high temperature and cried throughout yesterday and last night. Today, which is a Wednesday, you do not think the child has improved.
We explored these symptoms on the NHS Choices website and this validated our conclusions about the clinically recommended actions to take. In the case of all of these symptoms, NHS Choices confirmed they are unlikely to be serious and that self-care is usually adequate. We show summaries of the advice offered by NHS Choices in Appendix 8. The response options offered for each vignette are shown in the questionnaire available on the project web page (www.journalslibrary.nihr.ac.uk/programmes/hsdr/1513612/#/; accessed 5 February 2020). In the proposal we said that if a respondent selected an emergency service we would ask why. However, attendees at our wider PPI event and NatCen expressed concern about this because it might have alerted respondents to what was considered to be a right or wrong answer.
Ten programme theories from work package 1 realist review
We included questions to measure aspects of the 10 programme theories identified in WP1. We struggled to construct questions that measured some of the programme theories (see Results, Description of programme theories).
Other influences
Some issues in the literature did not become programme theories but we felt that they were important enough to be included in the questionnaire:
-
Awareness of services because it appeared in articles in the review.
-
Recursivity, in that patients learn to attend services because services have sanctioned previous decisions,68 because it is a relatively new issue identified in emergency care literature.
-
Health literacy because it is a relatively new issue identified in the emergency care literature. In the proposal we highlighted that researchers in the USA were studying the effect of low health literacy on ED use and developing interventions to address this. 136 Although health literacy is associated with social class and educational attainment, 29% of people attending EDs for non-urgent issues have a college education and low health literacy. 137 We explored the use of two validated instruments to assess health literacy: Newest Vital Sign (NVS) and HLQ. We had originally intended to use the NVS in the first pilot because Duell et al. 138 undertook a systematic review of measuring health literacy in a clinical environment and found that using the NVS was the most acceptable approach. We identified an alternative because of concerns expressed by NatCen about NVS. The HLQ was developed and validated in Australia139 and consists of nine domains of health literacy. We selected two five-item domains most relevant to our study: domain 6, ‘ability to actively engage with health-care providers’ (we labelled this ABILITY), and domain 9, ‘understand health information well enough to know what to do’ (we labelled this UNDERSTAND). Its strengths were that it addressed two aspects of health literacy and was preferred over the NVS at the PPI event, and the attendees at the wider PPI event found it very easy to complete.
We also wanted to take account of the following:
-
Recent use of health care because people recently using a service may be more likely to base their answers on experience. We used the question from the General Practitioner Patient Survey 2017140 and adapted it to ask about emergency ambulance and ED use as well as general practice.
-
Beliefs about overuse of services because we were interested in whether or not the population shared views about ‘clinically unnecessary’ use of services.
Analysis
Weighting
NatCen uses a robust sampling and weighting method, with weights applied for unequal selection probabilities and non-response and then calibration weights. Therefore, it enables analysts to make generalisations to the population at large. NatCen produced separate weights for interviewer-administered questions and self-completed questions because of differential response rates:
-
We used both unweighted and weighted data when presenting descriptions of variables and simple bivariate analyses.
-
We used unweighted data in the logistic regressions because we could not undertake this type of regression in SPSS (IBM Corporation, Armonk, NY, USA) or Stata (Stata Press, College Station, TX, USA) using weights.
Description of attitudes and tendency
We summarised the responses to questions to display the prevalence of population attitudes. This included a summary of responses to each pair of vignettes, comparing responses to show how different characteristics, such as symptoms, age and day of the week, affected tendency.
Differences by subgroups
We compared items related to the 10 programme theories by different sociodemographic characteristics using chi-squared tests. We limited this testing to variables related to the three subgroups from WP2 (young adults, parents of young children, deprivation levels) and a subgroup identified commonly in our programme theories in WP1 (presence of chronic conditions).
Explaining the tendency to make ‘clinically unnecessary’ use of services
We considered fitting a multinomial model comparing ambulance, ED and GP use with pharmacy/self-care, but were concerned about the difficulty of interpreting the results of multinomial analyses. Instead, we undertook a logistic regression on a series of binary comparisons. We considered the tendency to make ‘clinically unnecessary’ use of six health services: emergency ambulance, ED adults, ED children, ED all, GP and any service. We divided ED into adult and child because of the radically different answers to the child and adult vignettes. We wanted to do this for the ambulance analysis also, but the numbers were too small. We created binary variables based on whether or not the respondents chose ‘clinically unnecessary’ options in the vignettes. In the proposal, we planned to measure the proportion of people selecting a higher or lower level of care recommended for each scenario. In practice we selected only a higher level of care because of our focus on ‘clinically unnecessary’ demand.
We undertook a logistic regression comparing those ticking ‘clinically unnecessary’ options for a vignette with those who did not. We used SPSS version 25. First, we conducted a univariate analysis on each of the binary tendency outcomes, testing 54 independent variables. We then tested only the significant independent variables in a complete-case multivariable logistic regression using backwards elimination with a cut-off point of 0.05 for selection. We calculated the number of events per variable: the number of events divided by the number of degrees of freedom required to represent all of the variables in the model. The events per variable need to be at least 10 and preferably 20 for reliable parameter estimation. If fewer than this, there is an increased risk of overfitting of the models. Backwards elimination has advantages over forward selection when variables are correlated. 141 We collapsed some categories of some variables for the regression where numbers were small. We present odds ratios and 95% confidence intervals (CIs).
Once we had our final multivariable regressions we tested for multicolinearity by calculating generalised variance inflation factors using the statistical package R (The R Foundation for Statistical Computing, Vienna, Austria). We could not use SPSS because this software calculates variance inflation factors for linear regressions only. The variance inflation factors for each of the six regressions ranged from 1 to 1.7, well within the limit of < 5, indicating that multicolinearity was not at play.
We took the final multivariate regressions and tested whether or not the results depended on which vignettes were completed. We tested interactions between factors in each final regression and the two samples that completed different vignettes (cough/rib/Saturday and vomiting/back/Wednesday).
Missing data
As the number of missing data was small (apart from the missing values for self completion questions), missing data were treated as missing and no methods of imputation were used. However, in some cases, missing data were recoded as a category ‘missing’ to increase the sample size in the analysis.
Reporting guidelines
We completed the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) reporting guidelines. 142
Results
Response rate and non-response bias
The overall survey response was 42%, with 2906 respondents completing our module during face-to-face administration. In total, 79% of those interviewed returned the self-completed part of the questionnaire, that is, 2309 individuals. There was non-response bias for the self-completion questionnaire compared with the face-to-face interview. People from black, Asian and minority ethnic (BAME) groups, people with fewer educational qualifications and people with lower levels of political interest were less likely to return it.
Description of respondents
We describe respondents in Table 8. We show the distribution of respondents based on both weighted and unweighted data. Among the subgroups relevant to our study (see WP2), 169 respondents were aged 18–24 years, 300 respondents were living in households with children aged < 5 years (a proxy for parents of young children) and 576 were living in the most deprived quintile.
| Variable | Numbers (%) unweighted | Weighted (%) | Source | Numbers missing |
|---|---|---|---|---|
| Age group (years) | ||||
| 18–24 | 169 (5.8) | 11 | IA | 5 |
| 25–34 | 384 (13.2) | 17 | ||
| 35–44 | 467 (16.1) | 16 | ||
| 45–54 | 469 (16.1) | 18 | ||
| 55–64 | 508 (17.5) | 16 | ||
| 65–74 | 499 (17.2) | 13 | ||
| ≥ 75 | 405 (13.9) | 10 | ||
| Sex | ||||
| Male | 1257 (43.3) | 48 | IA | – |
| Female | 1649 (56.7) | 52 | ||
| Ethnicity | ||||
| White origin | 2572 (88.5) | 85 | IA | – |
| BAME | 334 (11.5) | 15 | ||
| Region | ||||
| North | 474 (16.3) | 16 | IA | – |
| Midlands | 796 (27.3) | 25 | ||
| South | 957 (32.9) | 32 | ||
| London | 395 (13.6) | 14 | ||
| Wales | 132 (4.5) | 5 | ||
| Scotland | 264 (9.1) | 9 | ||
| Households with children aged < 5 years | ||||
| 0 | 2591 (89.6) | 88 | IA | 15 |
| ≥ 1 | 300 (10.4) | 12 | ||
| Social class | ||||
| I | 214 (7.6) | 7.5 | IA | 92 |
| II | 1039 (36.9) | 36 | ||
| III (non-manual) | 569 (20.2) | 21 | ||
| III (manual) | 416 (14.8) | 15 | ||
| IV/V | 524 (18.6) | 19 | ||
| Armed forces | 52 (1.8) | 2 | ||
| Social deprivation (IMD quintiles) | ||||
| 1 (most deprived) | 576 (19.8) | 22 | IA | – |
| 2 | 545 (18.8) | 20 | ||
| 3 | 536 (18.4) | 18 | ||
| 4 | 638 (22.0) | 20 | ||
| 5 (affluent) | 611 (21.0) | 20 | ||
| Urban–rural categorisation | ||||
| Urban | 2241 (77.1) | 80 | IA | – |
| Rural | 665 (22.9) | 20 | ||
| Access to internet | ||||
| Yes | 2542 (87.5) | 91 | IA | – |
| No | 364 (12.5) | 9 | ||
| Car ownership | ||||
| 0 | 428 (14.7) | 13 | IA | 995 not asked but included in variable as not known |
| ≥ 1 | 1478 (50.9) | 52 | ||
| Not known | 1000 (34.4) | 35 | ||
| Long-term limiting illness | ||||
| None | 1766 (60.8) | 64 | IA | – |
| Non-limiting | 586 (20.2) | 19 | ||
| Limiting | 541 (18.6) | 16 | ||
| Don’t know, refusal | 13 (0.4) | 0.4 | ||
| General health | ||||
| Excellent | 223 (9.7) | 11 | SC | 597 |
| Very good | 725 (31.4) | 31 | ||
| Good | 799 (34.6) | 35 | ||
| Fair | 360 (15.6) | 15 | ||
| Poor | 163 (7.1) | 6 | ||
| Can’t choose/not answered | 39 (1.7) | 2 | ||
Description of vignette responses
Each respondent completed three vignettes. Respondents could tick more than one option when answering each vignette. All options are shown in Table 9. Those ticking more than one option were asked which would be their first action. A minority of respondents selected more than one option (between 12% and 27%, depending on the vignette). Self-care was a commonly selected first option when ticking more than one option for some of the vignettes: 60% for the cough vignette, 44% for the diarrhoea and vomiting vignette and 25% for the injuries vignettes. Calling NHS 111 was a common first option when ticking more than one option for the child vignettes: 38% for the Saturday vignette and 23% for the Wednesday vignette. When identifying respondents with a tendency to seek ‘clinically unnecessary’ care, we selected those ticking a service used at any point in their help-seeking rather than their first option.
| Option selected | Adult illness, n (%) | Adult injury, n (%) | Child illness, n (%) | Any, (N = 2906)b n (%) | |||
|---|---|---|---|---|---|---|---|
| Cough (N = 1471) | Diarrhoea and vomiting (N = 1435) | Sore rib (N = 1471) | Back pain (N = 1435) | Saturday (N = 1471) | Wednesday (N = 1435) | ||
| Call 999 for an ambulance | 4 (0.3) | 22 (1.5) | 79 (5) | 13 (1) | 129 (9) | 120 (8) | 328 (11) |
| Go to A&E | 17 (1.2) | 73 (5) | 366 (25) | 89 (6) | 504 (34) | 445 (31) | 1216 (42) |
| Contact a GP including GP OOH | 320 (22) | 641 (45) | 174 (12) | 1001 (70) | 417 (28) | 718 (50) | 1972 (68)c |
| Another NHS service (e.g. pharmacist) | 262 (18) | 260 (18) | 278 (19) | 247 (17) | 354 (24) | 270 (19) | 1223 (42) |
| Call urgent telephone helpline, NHS 111 | 42 (3) | 229 (16) | 326 (22) | 93 (6) | 439 (30) | 302 (21) | 1088 (37) |
| Self-care | 1026 (70) | 693 (48) | 379 (26) | 279 (19) | 45 (3) | 43 (3) | 1882 (65) |
| None of these options | 45 | 14 | 71 | 30 | 8 | 16 | 160 |
| Refusal/don’t know/missing | 10 | 7 | 11 | 8 | 18 | 13 | 34 |
| Percentage of respondents ticking ‘clinically unnecessary’ options | 23% | 49% | 30% | 7% | 42% | 37% | 64% |
Propensities for taking different actions differed by vignette (see Table 9). Tendency varied by symptom, and to some extent by time: cough (23%), diarrhoea and vomiting (49%), rib (30%), back pain (7%), child illness on a Saturday (42%) and child illness on a Wednesday (37%). The key findings were:
-
The two adult illness vignettes had different responses. The ‘clinically unnecessary’ options were ambulance service, ED and GP. Diarrhoea and vomiting resulted in a much higher tendency for ‘clinically unnecessary’ use than a cough (49% vs. 23%). This was the case for all services: ambulance, ED and GP.
-
The two adult injury vignettes also had different responses. The ‘clinically unnecessary’ options were ambulance service and ED. Sore rib resulted in a much higher tendency for ‘clinically unnecessary’ use than back pain (30% vs. 7%). The need for an X-ray may have been in people’s minds when responding to the rib vignette, even though NHS Choices says that an X-ray may not be needed (see Appendix 8).
-
The two child vignettes resulted in surprisingly similar answers. The ‘clinically unnecessary’ options were ambulance service and ED. The difference between the percentage of respondents ticking ‘clinically unnecessary’ options for the Saturday and Wednesday vignettes was 42% versus 37%, with respondents more likely to try another service or call NHS 111 on a Saturday.
-
The proportion of ‘clinically unnecessary’ use was considerably higher among responses to the child vignettes than among responses to the adult ones, with considerable use of emergency ambulance for the child vignettes (8% to 9%). This fits with our programme theory ‘fear of consequences when responsible for others’ (see WP1) and our qualitative research showing that parents feel high anxiety about symptoms in children (see WP2).
-
Calling NHS 111 was a commonly chosen option: between 3% and 30% of respondents ticked this option depending on the vignette.
-
Only a small proportion of respondents (5%) ticked a ‘clinically unnecessary’ option for all three vignettes that were presented to them. We had considered undertaking a logistic regression on this group, but the numbers were too small.
Description of programme theories
Operationalising some of the programme theories was difficult, but the variables used to explore each programme theory are shown Table 10. The key findings for each programme theory were:
-
Programme theory 1, uncertainty and anxiety about seriousness. We asked two questions to address this programme theory. Fourteen per cent of respondents were very likely to worry that pain was a sign of something serious and 4% were not confident about deciding when to see a doctor and when to self-care. The latter question had a large number of missing values because it was self-completed.
-
Programme theory 2, previous traumatic event. We asked one question to address this programme theory. Twenty-four per cent of respondents had not gone to the doctors at first for a previous problem and it had turned out to be serious.
-
Programme theory 3, responsibility for others. We measured this by asking about adult and child vignettes and showed that respondents had a higher tendency select ‘clinically unnecessary’ options in response to the child vignettes. We could not include this in the logistic regressions later in the analysis so this programme theory was not tested further.
-
Programme theory 4, need to get back to normal functioning/daily living. We asked three questions related to this programme theory. There was strong support for this programme theory in that an increasing percentage of people would contact a doctor or nurse immediately depending on whether or not and how a health problem affected daily activities, from 9% if the problem was not affecting daily activities to 67% if it was affecting an ability to attend to responsibilities of looking after family or going to work. There was an issue about how to represent this in the logistic regressions. We decided not to use these three variables in the logistic regression but to compute two new variables from these three questions to identify people who would contact a doctor or nurse only if they lost sleep or if they could not fulfil their responsibilities around family or work.
-
Programme theory 5, need for pain relief. We asked three questions about whether or not respondents would worry if a problem was serious if they had pain, whether or not they would seek a doctor urgently if they were in pain, and whether or not they would take medication if in pain. None of these questions directly addressed the issue of seeking care for pain relief. We felt that the first question measured programme theory 1, uncertainty and anxiety about seriousness of the problem, so we included it in programme theory 1. On reflection, we felt that the second question was too generic and might simply be another way of measuring tendency to make ‘clinically unnecessary’ use of services. Eighteen per cent of respondents reported that they would be unlikely to take medication for that pain. We used this variable with the rationale that people who did not take medication might seek pain relief from services.
-
Programme theory 6, delayed long enough. We asked one question to address this, concerning whether or not people wanted to see a doctor straight away once they had made the decision to get help; 22% of respondents strongly agreed with this. On reflection, we had concerns about the extent to which this question addressed the programme theory because it did not include delaying seeking health care. We decided not to use it in the logistic regression because we felt that it was measuring a more generic issue than the one we had tried to measure.
-
Programme theory 7, stressful lives leading to difficulty coping and need for low-burden services. We asked two sets of questions to address this programme theory. The first focused on stress and ability to cope, and the second focused on the burden attached to seeking care. We asked three questions about stressful lives and coping: 14% of respondents felt overwhelmed when faced with an unexpected health problem, 10% generally found their lives very stressful, and 12% probably had no one to look after them if they were ill. Two of these questions had a large number of missing values owing self-completion. We asked six questions related to burden of seeking care and found that, for example, 36% preferred services without appointments.
-
Programme theory 8, compliance with family or friends. We asked one question about how likely people would be to check with family or friends about the action that they should take; 19% of respondents were very likely to do this.
-
Programme theory 9, perceptions and experiences of services. We asked three questions to address this programme theory, all of which were self-completed and so had missing values. For example, 15% strongly agreed/agreed that they preferred EDs because they could have tests done quickly.
-
Programme theory 10, frustration with access to GP. We asked four questions related to this programme theory and found that, for example, 49% reported having difficulty getting a GP appointment at their surgery.
| PT and question | Numbers (%) unweighted | Weighted (%) | Source | Numbers missing |
|---|---|---|---|---|
| 1, Risk: uncertainty causes anxiety | ||||
| Worry that pain is a sign of something serious | IA | |||
| Very likely | 415 (14) | 14 | ||
| Fairly likely | 876 (30) | 31 | ||
| Not very likely | 1138 (39) | 40 | ||
| Not likely at all | 358 (12) | 12 | ||
| Depends | 119 (4) | 4 | ||
| Confident in deciding to see a doctor or self-care | SC | 597 | ||
| Very confident | 993 (34) | 40 | ||
| Fairly confident | 1130 (49) | 50 | ||
| Not very confident | 89 (4) | 5 | ||
| Never had problem | 97 (4) | 5 | ||
| 2, Risk: previous traumatic event | ||||
| Had problem, did not see doctor and was serious | IA | 1 | ||
| Yes | 687 (24) | 23 | ||
| No | 2219 (76) | 77 | ||
| 3, Risk: responsibility for others (see vignettes in Table 8) | ||||
| 4, Speed: need to get back to normal | ||||
| Action if not affecting daily activities | IA | |||
| Contact doctor or nurse | 262 (9) | 10 | ||
| Wait and see | 1617 (56) | 57 | ||
| Deal with it myself | 963 (33) | 32 | ||
| Depends | 64 (2) | 2 | ||
| Action if stopping sleep | IA | |||
| Contact doctor or nurse | 831 (29) | 30 | ||
| Wait and see | 1430 (49) | 49 | ||
| Deal with it myself | 604 (21) | 19 | ||
| Depends | 41 (1) | 1 | ||
| Action if affecting family or work | IA | |||
| Contact doctor or nurse | 1938 (67) | 69 | ||
| Wait and see | 736 (25) | 25 | ||
| Deal with it myself | 143 (5) | 5 | ||
| Depends | 89 (3) | 2 | ||
| Sleep | Computed for DEUCE | |||
| Do not see doctor | 2010 (69) | |||
| See doctor if sleep loss | 634 (22) | |||
| See doctor if other loss | 262 (9) | |||
| Work | Computed for DEUCE | |||
| Do not see doctor | 935 (32) | |||
| See doctor if work loss | 1709 (59) | |||
| See doctor if other loss | 262 (9) | |||
| 5, Speed: need to seek pain relief | ||||
| See a doctor urgently for pain | IA | |||
| Very likely | 294 (10) | 10 | ||
| Fairly likely | 691 (24) | 25 | ||
| Not very likely | 1269 (44) | 43 | ||
| Not at all likely | 554 (19) | 18 | ||
| Depends | 98 (3) | 3 | ||
| Likely to take medication to stop the pain | IA | |||
| Very likely | 1081 (37) | 37 | ||
| Fairly likely | 1257 (43) | 44 | ||
| Not very likely | 376 (13) | 13 | ||
| Not at all likely | 135 (5) | 5 | ||
| Depends | 57 (2) | 2 | ||
| 6, Speed: waited long enough | ||||
| Once I’ve made a decision I want to see the doctor straightaway | IA | |||
| Strongly agree | 629 (22) | 21 | ||
| Agree | 1525 (53) | 53 | ||
| Neither | 400 (14) | 14 | ||
| Disagree/strongly disagree | 352 (12) | 11 | ||
| 7a, Stressful lives | ||||
| Overwhelmed when have health problem | SC | 597 | ||
| Strongly agree/agree | 314 (14) | 17 | ||
| Neither | 537 (23) | 24 | ||
| Disagree | 872 (38) | 35 | ||
| Strongly disagree/disagree | 487 (17) | 20 | ||
| Never had problem | 99 (4) | 4 | ||
| Find life stressful | IA | |||
| Very | 297 (10) | 10 | ||
| Quite | 637 (22) | 24 | ||
| A bit | 1316 (45) | 46 | ||
| Not at all | 637 (22) | 20 | ||
| Don’t know | 19 (1) | 1 | ||
| Someone to care for them if they are ill | SC | 597 | ||
| Definitely | 1240 (54) | 54 | ||
| Probably | 697 (30) | 31 | ||
| Probably not | 280 (12) | 10 | ||
| Don’t know | 92 (4) | 5 | ||
| 7b, Low burden | ||||
| Can take time off work to see GP | IA | |||
| Yes | 1078 (37) | 41 | ||
| Yes but not easy | 275 (10) | 10 | ||
| No | 127 (4) | 5 | ||
| N/A or missing | 1426 (49) | 44 | ||
| Travel to ED | IA | |||
| Very difficult | 610 (21) | 19 | ||
| Neither | 269 (9) | 10 | ||
| Fairly easy | 1172 (40) | 42 | ||
| Very easy | 855 (29) | 30 | ||
| Opening hours a problem | SC | 597 | ||
| Strongly agree/agree | 603 (26) | 27 | ||
| Neither | 608 (26) | 26 | ||
| Disagree/strongly disagree | 1098 (48) | 46 | ||
| Prefer no appointments | SC | 597 | ||
| Strongly agree/agree | 825 (36) | 36 | ||
| Neither | 799 (35) | 34 | ||
| Disagree/strongly disagree | 685 (30) | 30 | ||
| Want convenient times | SC | 597 | ||
| Strongly agree/agree | 1348 (58) | 59 | ||
| Neither | 708 (31) | 30 | ||
| Disagree/strongly disagree | 253 (11) | 11 | ||
| Willing to wait in waiting room | IA | |||
| Strongly agree/agree | 2351 (81) | 80 | ||
| Neither | 194 (7) | 7 | ||
| Disagree/strongly disagree | 361 (12) | 13 | ||
| 8, Compliance with family/friends | ||||
| Check with family and friends for what to do | IA | |||
| Very likely | 554 (19) | 21 | ||
| Fairly likely | 1061 (37) | 39 | ||
| Not very likely | 746 (26) | 24 | ||
| Not at all likely | 545 (19) | 17 | ||
| 9, Perceptions and experiences of services | ||||
| Prefer ED: I can get tests done quickly | SC | 597 | ||
| Strongly agree/agree | 353 (15) | 17 | ||
| Neither | 797 (35) | 35 | ||
| Strongly disagree/disagree | 1159 (50) | 48 | ||
| ED doctors know more than GPs | SC | 597 | ||
| Strongly agree/agree | 418 (18) | 19 | ||
| Neither | 1041 (45) | 45 | ||
| Strongly disagree/disagree | 850 (37) | 36 | ||
| No confidence in GP | SC | 597 | ||
| Strongly agree | 76 (3) | 4 | ||
| Agree | 165 (7) | 7 | ||
| Neither | 446 (19) | 20 | ||
| Disagree | 1008 (44) | 43 | ||
| Strongly disagree | 538 (23) | 22 | ||
| Other | 76 (3) | 3 | ||
| 10, Frustration with access to GP | ||||
| Hard to get GP appointment at my surgery | SC | 597 | ||
| Strongly agree/agree | 1137 (49) | 51 | ||
| Neither | 353 (15) | 16 | ||
| Disagree/strongly disagree | 819 (36) | 33 | ||
| Registered with GP | IA | 1 | ||
| Yes | 2840 (98) | 97 | ||
| No | 65 (2) | 3 | ||
| Work or looking after family makes it difficult to see GP | SC | 597 | ||
| Strongly agree/agree | 410 (18) | 21 | ||
| Neither | 455 (20) | 21 | ||
| Strongly disagree/disagree | 1197 (52) | 50 | ||
| N/A | 247 (11) | 8 | ||
| Believe people use ED because they cannot get GP appointment | IA | |||
| Strongly agree/agree | 2441 (84) | 83 | ||
| Neither | 339 (12) | 12 | ||
| Disagree/strongly disagree | 126 (4) | 5 | ||
The programme theories varied in prevalence among the population, from 4% not feeling confident about when to contact a doctor or to look after the problem themselves (programme theory 1) to 74% feeling that they wanted to see a doctor immediately once they had made up their minds to do so (programme theory 6).
Variation in programme theories by subgroup of the population
We tested for differences in the prevalence of each programme theory by four subgroups of age group, households with children aged < 5 years (to represent parents of young children), deprivation quintile and chronic illness status. We selected one variable only to represent each programme theory (Table 11). The main findings were:
-
We expected to see young adults, households with children aged < 5 years, people living in deprived communities and people with long-term limiting illness reporting a higher prevalence of programme theories based on our WP1 review. This expectation was met for many of the programme theories (see Table 11). Strikingly, those in the most deprived quintile were three times more likely to feel overwhelmed when faced with a health problem than those in the most affluent quintile, and twice as likely to contact a doctor or nurse if a health problem was affecting their work or sleep.
-
Individuals reported a mean of 2.3 programme theories. Some subgroups had higher means in the unweighted and weighted analysis (weighted reported): people in the most deprived quintile (mean 2.8; p < 0.001), people with limiting long-term illness (mean 2.9; p < 0.001) and people aged < 45 years (mean 2.4; p = 0.03). There were no differences in the mean number of programme theories by parental status.
| PT | Focus of PT | Variable used to represent PT | Prevalence, n/N (%) | Age group (years) (%) | Household with children aged < 5 years (%) | Deprivation groups (%) | Long-term limiting illness (%) |
|---|---|---|---|---|---|---|---|
| 1 | Uncertainty | Not confident in deciding when to go to a doctor | 89/2309 (4) | 18–24 (10) | No (5) | 1 (most) (9) | No (4) |
| 25–34 (5) | Children (4) | 2 (3) | Non-limiting (5) | ||||
| 35–44 (4) | (p = 0.77) | 3 (3) | Limiting (7) | ||||
| 45–54 (4) | 4 (3) | Don’t know (0) | |||||
| 55–64 (5) | 5 (affluent) (5) | (p = 0.43) | |||||
| 65–74 (4) | (p = 0.001) | ||||||
| ≥ 75 (3) | |||||||
| (p = 0.05) | |||||||
| 2 | Previous traumatic event | Did not see a doctor previously when it was serious | 689/2906 (24) | 18–24 (21) | No (23) | 1 (most) (22) | No (16) |
| 25–34 (22) | Children (23) | 2 (26) | Non-limiting (30) | ||||
| 35–44 (23) | (p = 0.93) | 3 (22) | Limiting (44) | ||||
| 45–54 (24) | 4 (24) | Don’t know (12) | |||||
| 55–64 (25) | 5 (affluent) (22) | (p < 0.001) | |||||
| 65–74 (26) | (p = 0.64) | ||||||
| ≥ 75 (19) | |||||||
| (p = 0.48) | |||||||
| 3 | Fear of consequences | 999 or ED for a child but not for adult illness vignette | 1148/2906 (40) | 18–24 (31) | No (40) | 1 (most) (45) | No (37) |
| 25–34 (36) | Children (33) | 2 (42) | Non-limiting (40) | ||||
| 35–44 (34) | (p = 0.02) | 3 (35) | Limiting (49) | ||||
| 45–54 (42) | 4 (40) | Don’t know (18) | |||||
| 55–64 (46) | 5 (affluent) (35) | (p < 0.001) | |||||
| 65–74 (46) | (p = 0.006) | ||||||
| ≥ 75 (43) | |||||||
| (p < 0.001) | |||||||
| 4 | Back to normal | Would go to doctor if losing sleep or work only | 262/2906 (9) | 18–24 (11) | No (9) | 1 (most) (18) | No (10) |
| 25–34 (10) | Children (13) | 2 (8) | Non-limiting (6) | ||||
| 35–44 (10) | (p = 0.03) | 3 (8) | Limiting (11) | ||||
| 45–54 (8) | 4 (8) | Don’t know (15) | |||||
| 55–64 (8) | 5 (affluent) (7) | (p = 0.04) | |||||
| 65–74 (6) | (p < 0.001) | ||||||
| ≥ 75 (14) | |||||||
| (p = 0.10) | |||||||
| 5 | Pain relief | Try to see a doctor urgently with pain without taking medication | 104/2906 (4) | 18–24 (2) | No (4) | 1 (most) (2) | No (4) |
| 25–34 (4) | Children (4) | 2 (4) | Non-limiting (3) | ||||
| 35–44 (5) | (p = 0.81) | 3 (4) | Limiting (3) | ||||
| 45–54 (3) | 4 (4) | Don’t know (0) | |||||
| 55–64 (4) | 5 (affluent) (4) | (p = 0.76) | |||||
| 65–74 (3) | (p = 0.48) | ||||||
| ≥ 75 (5) | |||||||
| (p = 0.30) | |||||||
| 6 | Delayed long enough | Once I’ve made up my mind I want to see the doctor immediately | 2154/2906 (74) | 18–24 (70) | No (74) | 1 (most) (78) | No (76) |
| 25–34 (73) | Children (75) | 2 (70) | Non-limiting (71) | ||||
| 35–44 (76) | (p = 0.89) | 3 (70) | Limiting (75) | ||||
| 45–54 (73) | 4 (77) | Don’t know (31) | |||||
| 55–64 (77) | 5 (affluent) (77) | (p = 0.002) | |||||
| 65–74 (75) | (p = 0.009) | ||||||
| ≥ 75 (77) | |||||||
| (p = 0.41) | |||||||
| 7 | Stressful lives | Overwhelmed when have an unexpected health problem | 314/2309 (15) | 18–24 (17) | No (15) | 1 (most) (25) | No (14) |
| 25–34 (22) | Children (21) | 2 (19) | Non-limiting (12) | ||||
| 35–44 (19) | (p = 0.04) | 3 (13) | Limiting (24) | ||||
| 45–54 (12) | 4 (12) | Don’t know (45) | |||||
| 55–64 (15) | 5 (affluent) (8) | (p < 0.001) | |||||
| 65–74 (12) | (p < 0.001) | ||||||
| ≥ 75 (10) | |||||||
| (p = 0.003) | |||||||
| 8 | Compliance with advice | Check with family and friends | 554/2906 (19) | 18–24 (28) | No (20) | 1 (most) (26) | No (20) |
| 25–34 (26) | Children (26) | 2 (23) | Non-limiting (21) | ||||
| 35–44 (23) | (p = 0.02) | 3 (17) | Limiting (22) | ||||
| 45–54 (15) | 4 (18) | Don’t know (9) | |||||
| 55–64 (17) | 5 (affluent) (18) | (p = 0.62) | |||||
| 65–74 (17) | (p = 0.02) | ||||||
| ≥ 75 (17) | |||||||
| (p < 0.001) | |||||||
| 9 | Perceptions and prior experiences of care | Preference for ED due to tests | 353/2309 (15) | 18–24 (21) | No (16) | 1 (most) (26) | No (17) |
| 25–34 (18) | Children (19) | 2 (19) | Non-limiting (13) | ||||
| 35–44 (20) | (p = 0.28) | 3 (13) | Limiting (19) | ||||
| 45–54 (12) | 4 (11) | Don’t know (0) | |||||
| 55–64 (16) | 5 (affluent) (12) | (p = 0.20) | |||||
| 65–74 (12) | (p < 0.001) | ||||||
| ≥ 75 (17) | |||||||
| (p = 0.07) | |||||||
| 10 | Frustration with GP access | Hard to get GP appointment | 1137/2309 (49) | 18–24 (54) | No (49) | 1 (most) (57) | No (17) |
| 25–34 (53) | Children (63) | 2 (52) | Non-limiting (13) | ||||
| 35–44 (55) | (p < 0.001) | 3 (50) | Limiting (19) | ||||
| 45–54 (54) | 4 (48) | Don’t know (0) | |||||
| 55–64 (50) | 5 (affluent) (47) | (p = 0.07) | |||||
| 65–74 (43) | (p = 0.07) | ||||||
| ≥ 75 (42) | |||||||
| (p = 0.02) |
Description of other influences
The distribution of other influences is shown in Table 12. The key findings were:
-
Awareness of services. We asked six questions related to awareness of services. Four questions showed that a small percentage of respondents lacked confidence in knowing the range of NHS services that they could use (10%), knowing when services are open or how they can easily find this out (9%), and especially knowing what tests could be undertaken in different NHS services (22%) and how to contact a GP out of hours (18%). We also asked two questions about using the internet to diagnose problems or to find out what action to take; 49% were not likely to look things up on the internet to see what the problem was and 58% were not likely to use it to see what to do. This large proportion of non-internet users for health has implications for new digital NHS services, such as 111 Digital.
-
Recursivity. We asked one question to address learnt behaviour; 54% of people felt that they were right to contact a service if that service carried out tests on them.
-
Health literacy. The full range of health literacy scores were seen for both domains.
-
Recent use of services. We asked people if they had used the three services recently for themselves or for someone else (e.g. calling 999 to request an ambulance for their elderly parent). Recent use varied by service: 15% had used the ambulance service within the past 12 months, 14% had used an ED and 83% had used a GP in their practice.
-
Overuse of services. We asked three questions about this: one about each service. The majority of respondents agreed or strongly agreed that the three services were used by people who did not need them. Only a small percentage disagreed or strongly disagreed about this (3%, 3% and 9% for ambulance, ED and GP, respectively). NatCen recommended that we ask a question to counterbalance these three questions. We asked if respondents felt that people were reluctant to use an ED for an urgent problem; 46% of respondents agreed, highlighting that people perceive that both overuse and underuse of services may be seen as a problem.
| Influence and question | Numbers (%) unweighted | Numbers (%) weighted | Source | Numbers missing |
|---|---|---|---|---|
| Awareness of services | ||||
| Know the range of NHS services to use | IA | 1 | ||
| Very confident | 1436 (49) | 48 | ||
| Fairly confident | 1189 (41) | 42 | ||
| Can find out when NHS services are open | IA | 1 | ||
| Very confident | 1487 (51) | 51 | ||
| Fairly confident | 1163 (40) | 40 | ||
| Not/not at all | 255 (9) | 9 | ||
| Can find out what tests are available at different NHS services | IA | 1 | ||
| Very confident | 963 (33) | 32 | ||
| Fairly confident | 1307 (45) | 45 | ||
| Not at all | 635 (22) | 22 | ||
| How to contact GP OOH | IA | 1 | ||
| Very confident | 1338 (46) | 44 | ||
| Fairly confident | 1056 (36) | 37 | ||
| Not very confident | 389 (13) | 15 | ||
| Not at all confident | 122 (4) | 4 | ||
| Look on internet to see what the problem is | IA | |||
| Very likely | 667 (23) | 24 | ||
| Fairly likely | 797 (27) | 30 | ||
| Not very likely | 472 (16) | 17 | ||
| Not at all likely | 940 (32) | 29 | ||
| (Never had problem) | 30 (1) | 1 | ||
| Look on internet to decide what to do | IA | |||
| Very likely | 428 (15) | 15 | ||
| Fairly likely | 752 (26) | 28 | ||
| Not very likely | 680 (23) | 26 | ||
| Not at all likely | 1016 (35) | 30 | ||
| (Never had problem) | 30 (1) | 1 | ||
| Recursivity | ||||
| If tests are done I was right to contact the service | SC | 597 | ||
| Strongly agree/agree | 1236 (54) | 52 | ||
| Neither | 793 (34) | 36 | ||
| Disagree/strongly disagree | 280 (12) | 12 | ||
| Health literacy | ||||
| Ability to communicate (mean, SD and range) | 3.9, SD 0.66 (range 1–5) | SC | 637 | |
| Understand information (mean and range) | 4.0, SD 0.64 (range 1–5) | SC | 637 | |
| Recent use of services for self or someone else | ||||
| Ambulance use | IA | 1 | ||
| Never | 1349 (46) | 46 | ||
| ≥ 12 months | 1108 (38) | 38 | ||
| < 12 months | 448 (15) | 16 | ||
| Ambulance frequent user | IA | 1 | ||
| 0–3 times in 12 months | 2842 (98) | 98 | ||
| ≥ 3 times in 12 months | 64 (2) | 2 | ||
| ED use | IA | 1 | ||
| Never | 411 (14) | 15 | ||
| ≥ 12 months | 1478 (51) | 49 | ||
| 6–12 months | 366 (13) | 13 | ||
| 3–6 months | 234 (8) | 9 | ||
| < 3 months | 416 (14) | 15 | ||
| ED frequent user | IA | 1 | ||
| 0–3 times in 12 months | 2738 (94) | 94 | ||
| ≥ 3 times in 12 months | 167 (6) | 6 | ||
| Contacted GP | IA | 1 | ||
| Never | 65 (2) | 3 | ||
| ≥ 12 months | 454 (16) | 16 | ||
| 6–12 months | 484 (17) | 17 | ||
| 3–6 months | 518 (18) | 18 | ||
| < 3 months | 1384 (48) | 46 | ||
| Perceptions of service overuse | ||||
| Too many use ambulance when not needed | IA | |||
| Strongly agree/agree | 2516 (87) | 86 | ||
| Neither | 313 (11) | 11 | ||
| Disagree/strongly disagree | 77 (3) | 3 | ||
| Too many use ED when not needed | IA | |||
| Strongly agree/agree | 2515 (87) | 86 | ||
| Neither | 291 (10) | 10 | ||
| Disagree/strongly disagree | 100 (3) | 4 | ||
| Too many use GP when not needed | IA | |||
| Strongly agree/agree | 2082 (72) | 70 | ||
| Neither | 577 (20) | 20 | ||
| Disagree/strongly disagree | 247 (8) | 9 | ||
| Reluctance to use ED with urgent problem | IA | |||
| Strongly agree/agree | 1348 (46) | 48 | ||
| Neither | 734 (25) | 25 | ||
| Disagree/strongly disagree | 824 (28) | 28 | ||
Explaining tendency to seek ‘clinically unnecessary’ care
We present the regressions explaining the tendency to contact six services: emergency ambulance, ED adult, ED child, ED all, GP and any of these services. We present a univariate analysis first, followed by a multivariable analysis. Below, we display variables by groups representing similar concepts because one variable within a group might be selected instead of another correlated variable.
Tendency to call the emergency ambulance service (adult or child)
A total of 11% (328/2906) of respondents ticked ‘call an ambulance’ for any of the six vignettes. In a univariate analysis respondents had a higher tendency to call an ambulance if any of the following applied (see Appendix 9, Table 20):
-
sociodemographic characteristics – male, BAME
-
resources – social classes III manual/IV/V, most deprived communities, no personal access to the internet, no car
-
health – in fair/poor health, with limiting long-term illness
-
programme theories – worry if in pain (programme theory 1), if losing sleep or loss of daily activities (programme theory 4), if overwhelmed when faced with health problem (programme theory 7), do not have someone to care for them when they are ill (programme theory 7), find it difficult to travel to the ED (programme theory 7), prefer service with no appointments (programme theory 7), prefer the ED for getting tests done quickly (programme theory 9), think ED doctors know more than GPs (programme theory 9) and have no confidence in their GP (programme theory 9)
-
awareness of services – not confident about finding out when NHS services are open, unlikely to look up on the internet what a problem is or what to do about it
-
recursivity – feeling that if tests are undertaken they were right to contact a service
-
health literacy – low levels of understanding information and ability to engage with health professionals
-
recent service use – recent use of ambulance, frequent use of ambulance, frequent use of ED
-
attitudes to overuse of services – disagree that too many people use EDs and GPs when not needed.
There were some unusual findings:
-
People who did not have work or family responsibilities that made seeing their GP difficult had a higher tendency to call an ambulance.
-
People who disagreed that people use an ED because they cannot get a GP appointment were more likely to call an ambulance.
Based on a complete-case analysis of 2203 out of 2906 (76%) of the data set, the full model containing all of the statistically significant variables identified above is given in Appendix 9, Table 21. The events per variable was 8.7 (235/27), showing that there was some risk of overfitting within this model. The following variables made an independent contribution in a multivariable analysis, with the following groups having a higher tendency to contact an emergency ambulance (see Appendix 9, Table 21):
-
sociodemographic characteristics – male, BAME, social class III manual
-
resources – households with no car, no personal access to the internet
-
programme theories – programme theory 1, people who worry that a pain is sign of something serious, and programme theory 7, people who feel overwhelmed when they have an unexpected health problem. Findings for programme theory 8 and programme theory 10 were not straightforward. People who were fairly likely to check with family and friends had a lower tendency than those who were not likely to do this; this finding was not similar for those ticking very likely, as might be expected. Programme theory 10, work or looking after family make it difficult to see a GP, was the opposite of what might be expected, in that people who did not face this problem had a higher tendency to contact the ambulance service
-
health literacy – people with low understanding of information
-
recent service use – people who have used an emergency ambulance, particularly in the past year.
All six vignettes were included here, but the tendency to call an ambulance was dominated by the child vignettes in that around three-quarters of those with this tendency had ticked a child vignette. There were no statistically significant interactions between the samples completing the cough/rib/Saturday and the samples completing the vomiting/back pain/Wednesday vignettes.
In summary, the key findings were:
-
The two child vignettes dominated the tendency to call an ambulance.
-
A large number of variables related to people having low resources, including social class, low health literacy and feeling overwhelmed when faced with a health problem.
-
Lack of a car featured here, indicating that an ambulance may act as transportation to an ED for people with low resources.
-
People who had used the ambulance recently had a higher tendency to select it in the vignettes. This could be explained by someone having an ongoing health problem or by learnt behaviour in that having used it once, they feel happier to use it again.
Tendency to attend an emergency department for an adult
In total, 18% (512/2906) of respondents ticked ‘go to an ED’ for any of the four adult vignettes. In a univariate analysis respondents had a higher tendency to go to an ED for adults if any of the following applied (see Appendix 9, Table 22):
-
sociodemographic characteristics – male, BAME, social classes III manual/IV/V, most deprived quintile, urban areas
-
resources – none
-
health – none
-
programme theories – very likely to worry that pain was a sign of something serious (programme theory 1), lost functioning of daily living such as work or sleep (programme theory 4), overwhelmed when they have health problem (programme theory 7), very likely to check with family or friends if they are ill (programme theory 8), prefer EDs because can get tests done quickly (programme theory 9) and think ED doctors know more than GPs (programme theory 9)
-
awareness of services – none
-
recursivity – if tests are done they were right to go to a service
-
health literacy – none
-
recent service use – recent and frequent use of ED
-
overuse of services – think that too many people use ambulance and ED.
Based on a complete-case analysis of 2309 out of 2906 (80%) of the data set, the full model containing all of the statistically significant variables identified above is given in Appendix 9, Table 23. The events per variable was 32.4 (389/12), showing that there was little risk of overfitting for this model. The following variables made an independent contribution in a multivariable analysis, with the following groups more likely to have a tendency to contact an ED for an adult (see Appendix 9, Table 23):
-
sociodemographic characteristics – male, BAME
-
programme theories – loss of functioning, specifically work (programme theory 4), prefer EDs because can get tests done quickly (programme theory 9)
-
recursivity – think that if tests are done they were right to go to a service
-
beliefs about overuse – if people do not think there is a problem with too much use of EDs and do not think people are reluctant to use an ED.
Four vignettes were included here, but the tendency to attend an ED was dominated by the painful rib vignettes in that around two-thirds of those with a tendency had ticked the rib vignette. There was only one statistically significant interaction between the samples completing the cough/rib/Saturday and those completing the vomiting/back pain/Wednesday vignettes in the final model. This occurred with ethnic group (p = 0.012). People from BAME communities were more likely to tick ‘clinically unnecessary’ options for the cough/rib/Saturday vignettes than white people. White people were more likely to tick ‘clinically unnecessary’ options for the cough/rib/Saturday vignettes than for the diarrhoea/back/Wednesday vignettes. People from BAME communities were slightly less likely to tick ‘clinically unnecessary’ options for the diarrhoea/back/Wednesday vignettes than white people were to tick ‘clinically unnecessary’ options for the cough/rib/Saturday vignettes. Interactions should be interpreted with caution.
When the binary comparison was limited to those ticking attending an ED compared with those selecting lower levels of care only, the results were very similar. All of the variables in the original model featured in this model except programme theory 4, loss of functioning. There were some additional variations by geographical region (no specific region was statistically significantly different): programme theory 1, pain is a sign of something serious, and that too many people call 999 when they do not need to.
In summary, the key findings were:
-
There was evidence of the influence of preference for EDs, getting positive feedback about the validity of contacting a service if tests are undertaken by that service and beliefs that EDs are not overused.
Tendency to attend an emergency department for a child
In total, 33% (949/2906) of respondents ticked ‘go to an ED’ for any of the two child vignettes. In a univariate analysis respondents had a higher tendency to an ED for a child if any of the following applied (see Appendix 9, Table 24):
-
sociodemographic characteristics – aged 55–74 years, male, BAME, Wales and Scotland
-
resources – none
-
health – none
-
programme theories – previous traumatic event (programme theory 2), sleep loss (programme theory 4), loss of work (programme theory 4), not very likely to take medication (programme theory 5), prefer no appointments (programme theory 7), willing to wait in the waiting room if it means being seen that day (programme theory 7) and prefer an ED because get tests more quickly (programme theory 9)
-
awareness of services – none
-
recursivity – tests are carried out then think it was right to contact the service
-
recent service use – used ED recently
-
beliefs about overuse of services – believe too many people use ED when not needed.
There were some unusual findings:
-
Households with children aged < 5 years had a lower tendency to go to an ED for children.
-
In the responses to look up on the internet to find out what to do, the ‘missing’ category is statistically significant.
Based on a complete-case analysis of 2304 out of 2906 (79%) of the data set, the full model containing all of the statistically significant variables identified above is given in Appendix 9, Table 25. The events per variable was 44.4 (754/17), showing that there was little risk of overfitting for this model. The following variables made an independent contribution in a multivariable analysis, with the following groups more likely to have a tendency to contact an ED for a child (see Appendix 9, Table 25):
-
sociodemographic characteristics – aged 45–74 years, male, BAME, Wales and Scotland
-
programme theories – willing to wait in the waiting room if it means being seen that day (programme theory 7), prefer ED because get tests more quickly (programme theory 9).
Two vignettes were included here: the tendency to attend an ED was evenly distributed across the Wednesday and Saturday child vignettes. There were no statistically significant interactions between the samples completing the two child vignettes in the final model.
When the binary comparison was limited to those ticking attending an ED compared with those selecting lower levels of care only, the results were very similar. All the variables in the original model featured in this model. There were some additional variables of looking on the internet to decide what to do and thinking that too many people go the ED.
In summary, the key findings were:
-
The attraction of the ED is prominent here for allowing same-day contact and access to tests.
-
The high tendency in Wales and Scotland to attend an ED is difficult to explain.
Tendency to attend an emergency department (all)
In total, 42% (1216/2906) of respondents ticked ‘go to an ED’ for any of the six vignettes. In a univariate analysis respondents had a higher tendency to an ED if any of the following applied (see Appendix 9, Table 26):
-
sociodemographic characteristics – male, BAME, social classes III manual/IV/V, from Wales or Scotland, were not in a household with children aged < 5 years
-
resources – none
-
health – none
-
programme theories – loss of functioning (programme theory 4), preference for no appointments (programme theory 7), willing to wait in a waiting room to be seen that day (programme theory 7), preference for ED because can get tests quickly (programme theory 9), think ED doctors know more than GPs (programme theory 9)
-
awareness of services – none
-
recursivity – if test were done they were right to contact that service
-
health literacy – none
-
recent service use – recent and frequent use of ED
-
beliefs about overuse of services – do not think that too many people use ambulance and ED when not needed.
There were some unusual findings:
-
If they were not likely to take medication, then they had a lower tendency.
-
If they were ‘missing’ for looking things up on the internet, then they had a lower tendency.
Based on a complete-case analysis of 2304 out of 2906 (79%) of the data set, the full model containing all the statistically significant variables identified above is given in Appendix 9, Table 27. The events per variable was 45.6 (959/21) showing that there was little risk of overfitting for this model. The following variables made an independent contribution in a multivariable analysis, with the following groups more likely to have a tendency to contact an ED:
-
sociodemographic characteristics – male, BAME, Wales and Scotland
-
programme theories – loss of daily activities (programme theory 4), willing to wait in a waiting room to be seen that day (programme theory 7), prefer ED because can get tests quickly (programme theory 9)
-
beliefs about overuse of services – do not think that too many people use EDs when not needed.
All six vignettes were included here but the tendency to attend an ED was dominated by both of the child vignettes and the painful rib vignette. There were no statistically significant interactions between the samples completing the cough/rib/Saturday and those completing the vomiting/back pain/Wednesday vignettes in the final model.
The analysis above compared ED with ‘not ED’. The ‘not ED’ group included people who called an emergency ambulance as well as those calling less urgent options than the ED. Another analysis comparing only those ticking ED with those ticking the less urgent options gave very similar results. Age was included, with older people having a higher tendency, and programme theory 7, willingness to wait in a waiting room to be seen that day, was not included.
In summary, the key findings were:
-
People who are attracted by characteristics of EDs and want to address loss of daily activities such as work and sleep have a higher tendency to contact an ED.
-
Interestingly, negative views of GPs did not feature here.
-
The high tendency to attend an ED in Wales and Scotland is difficult to explain.
Tendency to call a general practitioner
In total, 33% (961/2906) of respondents ticked ‘go to GP’ for the two adult illness vignettes. In a univariate analysis respondents had a higher tendency to contact a GP if any of the following applied (see Appendix 9, Table 28):
-
sociodemographic characteristics – aged over 65 years, BAME, different regions/countries of Britain including Wales, Scotland and London
-
resources – no car, no access to internet
-
health – fair/poor health and with limiting long-term illness
-
programme theories – likely to worry that pain was sign of something serious (programme theory 1), not confident in deciding to see a doctor or self-care (programme theory 1), loss of functioning for daily activities (programme theory 4), feeling overwhelmed when faced with health problems (programme theory 7), travel to ED difficult (programme theory 7), prefer no appointments (programme theory 7), willing to wait in waiting room if can be seen that day (programme theory 7), very likely to check with family or friends about what to do (programme theory 8), prefer ED for quick tests (programme theory 9), registered with a GP (opposite of programme theory 10)
-
awareness of services – not confident in finding out when services are open, not confident in how to contact GP out of hours, would not look up on the internet about what to do about a health problem
-
recursivity – if tests are done they feel right to contact that service
-
health literacy – people with low health literacy
-
recent service use – frequent ambulance use, recent use of GP
-
beliefs about overuse of services – do not think too many people use GP when do not need to, think people are reluctant to use EDs.
Based on a complete-case analysis of 2264 out of 2906 (78%) of the data set, the full model containing all of the statistically significant variables identified above is displayed in Appendix 9, Table 29. The events per variable was 24.9 (746/30), showing that there was little risk of overfitting for this model. The following variables made an independent contribution in a multivariable analysis, with the following groups more likely to have a tendency to contact a GP (see Appendix 9, Table 29):
-
sociodemographic characteristics – > 75 years old, BAME, Wales and Scotland and south of England
-
programme theories – worry that pain is a sign of something serious (programme theory 1), feeling overwhelmed when faced with a health problem (programme theory 7), ease of access to GP (opposite of programme theory 10)
-
recursivity – if tests are done then right to contact that service
-
health literacy – people with low health literacy in terms of understanding information
-
recent service use – recent use of GP but the variable does show consistent pattern.
Only two vignettes were included here, with a tendency to contact a GP dominated by the diarrhoea/vomiting vignette in that two-thirds of people with a tendency for ‘clinically unnecessary’ use of a GP ticked this vignette rather than the cough vignette. There were only two statistically significant interactions by vignette in the final model. The first was with age (p = 0.013) but none of the interaction levels was statistically significant. The second was with people who thought that having tests was a sign that they were right to attend a service (recursivity). People who experienced recursivity were much more likely to tick the cough/rib/Saturday vignettes than people not experiencing recursivity. People who did not experience recursivity were more likely to not experience it for the diarrhoea/back/Wednesday vignettes than for the cough/rib/Saturday vignettes. People who experienced recursivity were more likely to do so for diarrhoea/back/Wednesday vignettes than were those not experiencing it for cough/rib/Saturday vignettes. Caution is needed when interpreting interactions.
The analysis above compared GP with ‘not GP’. The ‘not GP’ group included people who ticked an emergency ambulance or attendance at an ED, as well as those calling less urgent options than ED. Another analysis comparing only those ticking GP with those ticking the less urgent options of another NHS service, NHS 111 or self-care gave a similar regression. Region was replaced by BAME and the belief that too many people use GPs.
In summary, the key findings were:
-
Older people, people with low health literacy and who feel overwhelmed when faced with a health problem, and people who do not have access difficulties to general practice, have a higher tendency to use a GP.
Tendency to make any ‘clinically unnecessary’ demand for any service
In total, 66% (1841/2906) of respondents ticked a ‘clinically unnecessary’ option for any of the six vignettes. In a univariate analysis respondents had a higher tendency to do this if any of the following applied (see Appendix 9, Table 30):
-
sociodemographic characteristics –aged > 65 years, male, BAME, social classes III non-manual–V, London or Scotland, not living in households with children aged < 5 years
-
resources – no car, no personal access to the internet
-
health – poor health, limiting long-term illness
-
programme theories – worry that pain is a sign of something serious (programme theory 1), never had to decide about seeing a doctor (programme theory 1), loss of functioning in daily activities (programme theory 4), likely to take medication if in pain (opposite of programme theory 5), overwhelmed when have a health problem (programme theory 7), do not know if someone would care for them if ill (programme theory 7), find it difficult to travel to an ED (opposite of programme theory 7), prefer services with no appointments (programme theory 7), willing to wait in waiting room if seen that day (programme theory 7), check with family or friends for what to do (programme theory 8), prefer EDs for access to quick tests (programme theory 9), believe that ED doctors know more than GPs (programme theory 9), registered at GP (programme theory 10), family and work do not make it difficult to see GP (opposite of programme theory 10)
-
awareness of services – not confident in finding out when NHS services are open, not confident in knowing how to contact GP out of hours, unlikely to look up on the internet what a problem is or what to do about it
-
recursivity – if tests are carried out then this validates service use
-
health literacy – lower health literacy levels for understanding information and ability to communicate with health professionals
-
recent service use – frequent ED user, recent user of GP
-
beliefs about overuse of services – too many people use ED and GP, think that people are reluctant to use EDs.
Based on a complete-case analysis of 2297 out of 2906 (79%) of the data set, the full model containing all of the statistically significant variables identified above is given in Appendix 9, Table 31. The events per variable was 22.6 (859/38), showing that there was little risk of overfitting for this model. The following variables made an independent contribution in a multivariable analysis, with the following groups more likely to have a tendency to make ‘clinically unnecessary’ use of services (see Appendix 9, Table 31):
-
sociodemographic characteristics – aged 65–74 years, male, BAME
-
health – limiting long-term illness
-
programme theories – worry pain is a sign of something serious (programme theory 1), loss of functioning of daily activities (programme theory 4), overwhelmed when faced with a health problem (programme theory 7), prefer ED because get test quickly (programme theory 9), work and looking after family does not make it difficult to see a GP (opposite of programme theory 10)
-
awareness of services – not confident in contacting GP out of hours, unlikely to look up on the internet what to do about a health problem
-
recursivity – if tests are done then this validates service use
-
recent service use – recent use of GP.
All six vignettes were included here but the back pain vignette did not feature strongly in this analysis compared with other vignettes. There was only one statistically significant interaction between the samples completing the cough/rib/Saturday and those completing the vomiting/back pain/Wednesday vignettes in the final model. People were likely to experience recursivity than not for the cough/rib/Saturday vignettes. People were more likely not to experience recursivity for the diarrhoea/back/Wednesday than for the cough/rib/Saturday vignettes. People were more likely to experience recursivity for the diarrhoea/back/Wednesday vignettes than not experience it for the cough/rib/Saturday vignettes. Caution is needed when interpreting interactions.
In summary, the key findings were:
-
Many of the variables from the individual service analyses appeared within the univariate and multivariable analyses for tendency to contact any service.
Discussion
Summary of findings
The vignettes elicited different responses, with the tendency for ‘clinically unnecessary’ use of services varying between 7% and 49%. In particular, respondents had a higher tendency for ‘clinically unnecessary’ use of services for the child vignettes than the adult vignettes, supporting programme theory 3, responsibility for others. The prevalence of the 10 programme theories from WP1 varied within the population. Most programme theories varied by the population subgroups tested, with young adults, parents of young children, people living in deprived communities and people with chronic conditions more likely to display a number of the programme theories. Individuals from deprived communities and those with chronic conditions reported greater numbers of programme theories. Surprisingly, these subgroups did not feature in the tendency models. Subgroups of the population that did appear consistently as having a higher tendency for ‘clinically unnecessary’ use of services in the tendency models were older people, male people and people from BAME communities. Programme theories commonly explaining ‘clinically unnecessary’ use included programme theory 1, uncertainty, programme theory 4, inability to get on with daily life, programme theory 7, stressful lives and inability to cope, and programme theory 9, perceptions of quality of services where the attraction of EDs featured. There was evidence of recursivity at play, where people learnt that attending a service was the right thing to do. Low health literacy was associated with a tendency for ‘clinically unnecessary’ use of ambulances and general practice.
Links to programme theories
The survey results strongly supported four of the programme theories (Table 13): uncertainty of symptoms causing anxiety (programme theory 1), inability to get on with daily life (programme theory 4), stressful lives causing difficulty coping (programme theory 7) and the attraction of EDs (programme theory 9). Surprisingly, frustration with access to a GP appointment (programme theory 10) was not a prominent issue.
| PT developed in WP1 | Revised PT after WP2 | Support for programme theory after WP3 | Conclusion |
|---|---|---|---|
| 1, Uncertainty about symptoms causing anxiety | Uncertainty about meaning and seriousness of symptoms causing anxiety |
Different symptoms addressed in vignettes but the level of certainty respondents had about these symptoms was not measured Each symptom elicited different propensities so shows effect of symptoms on decision-making In total, 14% likely to worry that pain is serious. Young adults aged 18–24 years three times more likely than older adults and deprived twice as likely as affluent to think this. More likely to call ambulance (univariate and multivariable), attend ED for adult (univariate) and attend GP (univariate and multivariable) |
Important PT affecting use of ambulance, ED and GP |
| 2, Heightened awareness of risk as a result of experience or knowledge of traumatic health events leading to anxiety | Heightened awareness of risk to health as a result of personal experience or knowledge causing anxiety |
In total, 24% of population have missed a serious event. People with a chronic condition are three times more likely than those without to report this More likely to attend ED for child (univariate) |
Limited support |
| 3, Fear of consequences when responsible for others | Responsibility and/or care for others causing distress and fear of consequences of not acting |
Difference between options chosen for adult and child vignettes. Aged 55–74 years, people without small children, most deprived and people with chronic condition more likely to take ‘clinically unnecessary’ option Could not be measured in logistic regression |
Not adequately tested |
| 4, Inability to get on with daily life | Concern about actual or anticipated impact on daily activities/functioning |
Any symptom affecting daily activity such as work or family responsibilities makes people go to doctor or nurse People with small children more likely and most deprived people at least twice as likely to have this programme theory More likely to call ambulance (univariate), ED adult (univariate and multivariable), ED child (univariate) and GP (univariate) |
Important PT affecting use of ambulance, ED and GP |
| 5, Need for immediate pain relief | Need for immediate relief of intolerable/unbearable symptoms (including pain) |
Not measured well. 18% of population would not take medication if in pain. No subgroup differences More likely to attend ED for a child (univariate) |
Not adequately tested |
| 6, Waited long enough for things to improve | Unwillingness to continue current approach to managing symptoms (waiting/self-care/help-seeking) due to lack of resolution of the problem |
Challenging to capture this in a question or set of questions and we did not measure it well. No clear subgroup differences Not tested in logistic regression |
Not tested |
| 7, Stressful lives, difficulty coping, so want ease of access to services | Reduced coping capacity due to physical and mental illness, stress and/or lack of access to resources |
In total, 10% found life stressful and 14% were overwhelmed when faced with health problem. Young adults aged 18–44 years, people with young children and people with chronic conditions more likely to report this. Most deprived three times more likely than affluent In total, 36% prefer services with no appointments More likely to call ambulance (univariate and multivariable), ED for adult (univariate) and GP (univariate and multivariable) |
Important PT affecting use of ambulance, ED and GP |
| 8, Following the advice of trusted others | Directly or indirectly influenced by the advice or support of others, including social networks, health-care professionals and internet sources |
In total, 19% were likely to ask family and friends if ill. Young adults aged 18–44 years, people with children and most deprived were more likely to do this More likely to attend ED adult (univariate) and GP (univariate) |
Limited support |
| 9, Perceptions or prior experiences of services | Perceptions, prior experiences and/or awareness/knowledge of services |
In total, 15% prefer ED to get tests done quickly. Young adults aged 18–44 years were more likely than and most deprived were twice as likely as affluent people to report this More likely to call ambulance if attracted to ED and had no confidence in GP (univariate), more likely to attend ED for adult if attracted to ED (univariate and multivariable), ED for child if attracted to ED (univariate and multivariable regression) and GP if attracted to ED (univariate) |
Important PT with support for attraction of ED affecting use of ED |
| 10, Frustration with access to a GP | Frustration with inability to access an appropriate GP appointment |
In total, 49% reported difficulty getting GP appointment. Adults aged 18–54 years and people with young children were more likely to report this More likely to use GP if there is ease of access to GP |
Not everyone is frustrated by access to GP |
Links to wider literature
To our knowledge, few population surveys have been undertaken related to this topic. Our results are supported by the three population survey-based studies that we found. A population survey of 1256 people in Australia showed that 21% had used EDs in the previous year (compared with 35% of our population who were asked if they had attended for themselves or someone else); that decisions were made by health-care professionals in one-third of cases and by others in one-fifth (aligning with our programme theory 8, compliance with the advice of trusted others); and that they attended because of the severity of their condition, because they could not find alternatives and because they felt that they would receive better care there (aligning with programme theory 9, perceptions of quality of care). 132
The majority of our respondents felt that too many people use emergency services and general practice when they do not need to (87% and 72%, respectively). In 2003, a survey in a single UK general practice identified a similarly high percentage of the population (66%) who felt that people use EDs or GPs inappropriately. 135
Our vignette results were similar to those of a vignette study of unnecessary ambulance use in Japan, where respondents were more likely to select the option of calling an emergency ambulance if they were male, elderly, did not have a car and were not hesitant about using ambulances. 6 The authors estimated that socioeconomic factors increased unnecessary ambulance use by an estimated 10–20%. 6 Although this was not a population survey, the results were also similar to those of a cross-sectional survey of over 900 ambulance users compared with those arriving at an ED themselves in Australia, which showed that ambulance users had higher self-rated sense of urgency, felt that the problem was serious, were in pain, felt that the ambulance service was for everyone regardless of the severity of the problem, and had used an ambulance in the past 6 months. 1 Reasons for using an ambulance included the urgency and severity of their condition, requiring special care, not having a car and financial concerns. 1 This reflects our findings that a lack of a car and socioeconomic issues affect ‘clinically unnecessary’ use of ambulances.
The role of anxiety in help-seeking has also been found in a vignette study, although the vignette addressed a much more serious issue of finding a lump and so did not explore the types of symptoms that we were interested in. 135
Strengths and limitations
The survey was of a representative sample of the British population and, to our knowledge, is the first survey of population attitudes to emergency and urgent care in Britain. The response rate of 42% is lower than historical survey response rates, but is not unusual for similar health surveys undertaken in the UK. There are always issues with non-response bias in surveys; weighting was undertaken to address this for some of the analyses reported here. Weighting made little difference to the findings. The vignette approach used in the survey has not been used extensively when exploring population or patient perceptions in the field of emergency and urgent care research and is a useful way of testing a wide range of factors. However, it had some limitations. It identified tendency rather than actual ‘clinically unnecessary’ use of services and people may act differently in practice. For example, people may believe that their access to a GP appointment is poor but may be able to obtain a GP appointment when needed in practice, or they may believe that they would have no problem accessing a timely GP appointment but be surprised and frustrated when trying to do so for a specific health problem. We were unable to test two of the programme theories in the logistic regressions of the vignettes: programme theory 3, responsibility for others, and programme theory 6, waited long enough for things to improve. Finally, the ambulance model suffered from overfitting.
Implications
There was considerable support for four of the programme theories related to symptoms, personal circumstances and service characteristics, and other factors such as sociodemographic and personal characteristics (male, BAME, low health literacy) and service-related characteristics (recursivity). This highlights that multiple interventions are likely to be necessary because factors operate at a symptom, patient and service level.
Chapter 7 Integration from three work packages
Introduction
Integration has been carried out throughout this sequential mixed-methods study. The realist review (WP1) informed the subgroups selected for the qualitative interview study (WP2) and the interpretation of the findings in WP2. Findings from WP1 and WP2 informed the content of the WP3 population survey. It is also important to bring together findings from all of the WPs to identify overall learning about drivers of demand for ‘clinically unnecessary’ use of emergency and urgent care.
Methods
We used an adapted triangulation protocol143 to bring together the key findings from each component of the study and to identify the overarching conclusions and recommendations from the whole study. First, we identified drivers and other key findings from each study component. Then we presented findings that were related to the same driver/factor from each component on the same page and considered how the findings converged, complemented each other or disagreed, or where there was no finding from a component when we might have expected one.
We also took the opportunity to refine the programme theories developed in WP1 after considering the findings from WP2 and WP3.
Results
The integration grid is shown in Appendix 10, Table 32. After constructing the grid, we considered the types of drivers and decided to summarise the findings as symptom related, patient related and health service related.
The final programme theories with support from all three WPs are displayed in Table 14. Programme theory 10, frustration with poor access to a GP, has been included despite it not being supported strongly in the WP3 vignette analysis because it played such as powerful role in the WP2 interviews.
| PT label | PT detail |
|---|---|
| 1, Uncertainty about symptoms causing anxiety | When there is uncertainty about the meaning and seriousness of symptoms (M) because they do not fit with people’s expectations or prior experience (e.g. they last longer, are more severe, are unfamiliar or do not respond to self-care in the expected timescale) (C/M), this increases anxiety about the perceived risk (M) and an immediate need to establish what is wrong and obtain reassurance (M). This concern prompts the use of the ambulance, ED and GP (O), where it is perceived that the most appropriate resources and expertise required to establish cause can be accessed quickly (C). The ED is used in the context of timely or satisfactory answers not having been received from primary care services (C) |
| 4, Inability to get on with daily life | When people are prevented from undertaking their normal lives, roles or responsibilities (e.g. paid work, child care) (C), or anticipate that this may occur, this creates a need to get back to normal quickly (M), to get on with their lives and discharge their responsibilities. This prompts use of ambulance, ED or GP (O) because the service can resolve a problem quickly by being accessible and efficient (C) |
| 7, Stressful lives/cannot cope | When people are already experiencing significant stresses due to physical or mental illness, stress or lack of access to resources (e.g. money, time) (C) they have less capacity to cope with the additional challenge of a new or changed health problem. Symptoms are, therefore, likely to trigger emotional distress, including feelings of loss of control and helplessness (M), leading them to use services with lower burden of access |
| 9, Perceptions or prior experiences of services | When people have individual experience or knowledge, or cultural beliefs, about the differing quality or availability of primary and emergency services, or lack of awareness of the range of services available, they are likely to choose emergency care, particularly the ED (O), which they see as having the tests and expertise necessary (C) |
| 10, Poor access to a GP | When people are unable to obtain an appointment with a primary care practitioner (C/M), this can further exacerbate feelings of anxiety and cause panic (M). Individuals can experience feelings of frustration (M), mistrust (M), and the perception of an uncaring service (M), feeling that they have no other choice (M) but to contact an emergency service (O) |
Chapter 8 Discussion
We have discussed findings at the end of each chapter. Here we provide discussion of key points across the whole study.
Summary
In the review we identified 10 drivers of ‘clinically unnecessary’ use of ambulances, EDs and general practice that were further expanded in the interview study and tested in the survey. Multiple, interacting drivers operated in individuals’ decision-making, which could be grouped into symptom-related drivers, patient-related drivers and health service-related drivers. Symptom-related drivers included anxiety or the need for reassurance caused by uncertainty about the seriousness of symptoms, concern about the impact of symptoms on daily activities and a need for immediate relief of intolerable symptoms, particularly pain. Patient-related drivers included reduced coping capacity due to illness, stress or limited resources; fear of consequences when responsible for another person’s health, particularly children; and the influence of social networks. Health service-related drivers included perceptions, prior experiences and awareness of different services, lack of timely access to a GP appointment, and compliance with health service staff’s advice to attend an ED. We do not know if these drivers differed between ‘clinically unnecessary’ users and those who attended services and were classed as ‘clinically unnecessary’.
Strengths and limitations
The study had five strengths. First, we undertook a more in-depth piece of research than much of the previous work in the area, including an in-depth synthesis of previous research, an in-depth analysis of qualitative research and quantitative testing of a wide range of potential drivers. Second, we focused on a range of services facing considerable demand in England currently: emergency ambulances, EDs and urgent daytime general practice. The inclusion of emergency ambulances and general practice enabled us to explore drivers that had previously been generated largely from the experience of ED users. Third, we focused fully on patient and population perceptions to understand the issues from their perspectives. Fourth, the sequential approach allowed each WP to inform the next. In our review we found that many studies did not always provide enough detail to give an insight into the interaction of different issues in individuals’ lives, or where particular service use was located in their overall help-seeking journey. Using the principles of IPA for the analysis of the interview data provided depth in describing user behaviour, demonstrating the complexity of decision-making. Fifth, the focus on ‘clinically unnecessary’ users’ views of interventions to address their behaviour is a new addition to the evidence base.
There were three limitations. First, the study did not add as much to the evidence base about use of ambulance services as planned. There were few relevant articles included in the review and we struggled to recruit these users to our qualitative component. Booker’s19 review, encompassing patient and health professional perspectives, still offers the most in-depth understanding of ‘clinically unnecessary’ use of ambulance services. However, our testing of factors affecting the tendency to use emergency ambulances is an excellent contribution to the ambulance service evidence base. Second, we recruited fewer patients to our qualitative component from one of the two geographical areas in our study and so were unable to undertake our planned comparison between two, operationally different, emergency and urgent care systems. Third, it was challenging to measure some of our programme theories in our survey.
What DEUCE adds to the evidence base
In summary:
-
We synthesised the existing evidence and produced a comprehensive set of programme theories that identify the factors at play when patients make use of services providing emergency and urgent care that is judged to be ‘clinically unnecessary’. We have tested these programme theories using qualitative and quantitative methodologies and established a refined set of programme theories built on this evidence. Some of these programme theories were new, such as the way in which delaying seeking care using self-care adds to the urgency of help-seeking.
-
The evidence used in the realist review was largely non-UK based and largely focused on EDs. We have added UK specific evidence and considered a wider part of the emergency care system by focusing on ambulance and GP use as well as ED use.
-
Our qualitative interview study has added to the existing evidence base by focusing on two subgroups of users in whom there is little qualitative research (young adults and people from socially deprived communities) or little qualitative research undertaken in the UK (parents of young children). We found that a number of factors often occur during an individual help-seeking episode and together interact to determine whether or not a service will be used and, if so, which service.
-
We highlighted the extent to which social circumstances related to complex lives, stress, lack of resources and mental health affect help-seeking behaviour. This was a programme theory from the realist review, was shown to be a driver during our interviews with young adults and people living in socially deprived communities, and was identified as a consistent factor explaining a tendency to make ‘clinically unnecessary’ use of ambulances, EDs and general practice in our survey vignettes.
-
The existing evidence base on interventions to address demand for EDs is largely inconclusive. In our qualitative research we identified a range of potential interventions. An important intervention for patients was improving access to GPs and the GP appointment systems that determine access. However, patients’ views on improving the quality and location of alternative services such as WICs and prescriptions/pharmacy highlight the variation in recommendations among the three subgroups and the importance of tailoring interventions to specific subgroups.
Implications
Changing patient behaviour
A 2013 policy document144 set out a vision for supporting the population to facilitate self-care. Six years on, our study shows that, although people are active in undertaking self-care when faced with an urgent problem, many reach a point at which they perceive that care is needed from a higher-acuity health service than necessary. Understanding how people arrive at a decision to seek care, and why they choose a particular service from which to seek it, is an important consideration for the NHS as it plans the configuration of services to meet the needs of the population.
Our study found that patients’ social circumstances play a key role in shaping decision-making. Some of the population may be affected by a complex set of social circumstances that combine, or work in isolation, to have an impact on their coping abilities and decision-making. This may be particularly challenging when a person is experiencing an acute episode of illness. Reducing this complexity is challenging, but it is clear that this complexity is a strong driver of ‘clinically unnecessary’ use of GPs, EDs and the ambulance service.
There are likely to be groups of people who are habitually labelled as seeking ‘clinically unnecessary’ use of emergency and urgent care, for example people who have difficulty coping (see programme theory 7). It is also highly likely that any individual may be labelled as making ‘clinically unnecessary’ use of emergency and urgent care at some point in their life because, for example, a specific symptom or circumstance causes high levels of anxiety. Interventions will need to consider both of these scenarios.
Interventions need to focus on services, not just patient behaviour
Some patients try to take a route through the system of care that is commensurate with their clinical need by contacting their GP before attending an ED. However, it appears that GPs and other services (such as NHS 111) advise some patients to go a higher-acuity service. Our study focused on patient decision-making, rather than attempting to understand the decision-making process from a health-care professional perspective. Interventions will be needed to focus on this contribution to demand.
Emergency and urgent care services are under sustained pressure in terms of supply of workforce as well as demand from patients. Increasing workforces may reduce concerns about demand for services. A key consideration here is general practice. Some patients in our study used same-day GP appointments because of ease of access, the location and a perception that the general practice was the best place to seek care. However, others used EDs after they had attempted to use their general practice but found themselves frustrated by the system of either obtaining a same-day appointment or having to wait > 7 days for a routine appointment. Strengthening general practice by improving access to appointments with a GP might, therefore, alleviate some of the ‘clinically unnecessary’ demand on EDs. Recent evidence of the falling number of GPs relative to the size of the population, and a disproportionate workload faced by GPs in deprived areas,145 may have ongoing implications for patient access to general practice appointments and the use of higher-acuity services than necessary.
Some people felt that urgent care alternatives introduced to improve patient choice and access to care, such as WICs, MIUs and NHS 111, were not acceptable. Uncertainty about service provision, dissatisfaction based on previous experiences and a perception that the service was inferior (when compared with higher-acuity services) contributed to a reluctance to use these services. Improvements in these services could change patient behaviour.
Strengthening primary care and improving urgent care alternatives could have some impact on the demand for EDs, but it is unlikely to alleviate all ‘clinically unnecessary’ demand because some patients feel strongly that they need the facilities offered by ED, particularly X-rays. Service reconfiguration may, therefore, be required to offer X-rays in other services or it may be necessary to educate the population about when these facilities are unlikely to be necessary (e.g. for a rib injury).
Our interview participants were identified by service providers as making ‘clinically unnecessary’ contact with a particular service. However, interviewees did not describe this view being shared during the clinician–patient encounter. Health services themselves may reinforce ‘clinically unnecessary’ use by offering tests or reassuring patients that ‘they have done the right thing’ by making contact with them. If the clinician thinks that a patient could have used a lower-acuity service, then communicating this to the patient may help them to make better decisions in the future and avoid validating service use that may perpetuate further ‘clinically unnecessary’ use by both the individual and those in their social network. We understand the challenges of doing this in terms of the time it might take for busy clinicians, but it could be explored as a potential intervention to reduce ‘clinically unnecessary’ use.
Priorities for research
We identified a number of opportunities for further research:
-
Patients who had been labelled as making ‘clinically unnecessary’ use of services identified a number of interventions that had the potential to change the behaviour of patients seeking care for an urgent health problem. New interventions addressing ‘clinically unnecessary’ use of emergency ambulances and EDs should be evaluated. These include interventions that strengthen capacity in primary care, change GP appointment systems, reduce practices in EDs that encourage further ‘clinically unnecessary’ use, improve health literacy, improve population mental health and increase low resources in the population.
-
Evaluate new interventions to address ‘clinically unnecessary’ use of general practice, including educating the population about pharmacies, improving access to free prescriptions in pharmacies and improving patients’ confidence in self-managing minor illnesses.
-
Evaluate new interventions tailored to different population subgroups, such as education and support aimed at parents of young children.
-
Understand drivers of ‘clinically unnecessary’ use for other subgroups identified in the survey, in particular men and BAME groups.
-
Some service users described that they had been signposted to higher-acuity services by general practice or by urgent care services such as NHS 111. Service users were not in a position to offer a view on why this occurred. Seeking health-care professionals’ perspectives on this would be helpful in understanding how this driver could be best addressed.
Conclusions
‘Clinically unnecessary’ use of emergency and urgent care is of interest when supply fails to match demand. Patients use emergency ambulances, EDs and same-day GP appointments when they do not need the level of clinical care provided by those services for a multitude of inter-related reasons that sometimes differ by population subgroup. Some of these reasons relate to health services in terms of difficulty accessing general practice leading to use of EDs, and population-learnt behaviour concerning the positive attributes of EDs, rather than to patient characteristics. Social circumstances, such as complex and stressful lives, limited resources, the need to attend to responsibilities such as family and work, and parental anxiety, influence help-seeking behaviour in relation to all three services. Demand may be ‘clinically unnecessary’ but completely understandable when general practice accessibility and patients’ social circumstances are considered.
Acknowledgements
We would like to thank everyone who took part in our PPI activities for the insights they gave, and the members of our Project Advisory Group, chaired by Professor Matthew Cooke, for their help and advice.
We are enormously grateful to the NHS organisations that agreed to be study sites, the staff who facilitated our access to potential study participants and the patients who participated in our qualitative research.
We acknowledge the role of NatCen in designing and delivering the survey. We thank the survey participants who completed the questionnaire.
We acknowledge the support of the NIHR Clinical Research Network.
We thank Sue Ridgway and Veronica Fibisan for the administrative support provided during the study.
Contributions of authors
Alicia O’Cathain (https://orcid.org/0000-0003-4033-506X) (Professor of Health Services Research) was the principal investigator with oversight of all aspects of the study. She designed the study, contributed to all WPs and led WP1 and WP3. She wrote the first draft of Chapters 1–3 and Chapters 6 and 7.
Emma Knowles (https://orcid.org/0000-0003-3372-1245) (Senior Research Fellow) was the study manager. A co-applicant, she contributed to the initial design of the study, led WP2, supported the development of the survey instrument in WP3, led the PPI workshop, and wrote the first draft of Chapters 4 and 8.
Jaqui Long (https://orcid.org/0000-0002-6889-6195) (Research Associate) tested and refined the programme theories in WP1, contributed to data collection and analysis in WP2, wrote the first draft of Chapter 5 and contributed significantly to the writing of other chapters.
Janice Connell (https://orcid.org/0000-0003-4609-3911) (Research Associate) led the data extraction and development of the programme theories in WP1, and contributed to writing Chapter 3.
Lindsey Bishop-Edwards (https://orcid.org/0000-0002-2136-5557) (Research Associate) contributed to the data collection in WP2 and early stages of analysis before commencing maternity leave in November 2018.
Rebecca Simpson (https://orcid.org/0000-0003-1677-5938) (Research Associate) undertook the analysis of WP3 data.
Joanne Coster (https://orcid.org/0000-0002-0599-4222) (Research Fellow) was a co-applicant, contributing to searches, selection and early analysis of articles included in WP1.
Linda Abouzeid (https://orcid.org/0000-0003-4215-7367) (PPI member) was a co-applicant, appraising findings throughout the study, especially the analysis of WP2. She contributed to the Plain English summary.
Shan Bennett (https://orcid.org/0000-0001-5597-3254) (PPI member) was a co-applicant, appraising findings throughout the study, especially the analysis of WP2. She contributed to the Plain English summary.
Elizabeth Croot (https://orcid.org/0000-0002-3666-6264) (Senior Research Fellow) was a co-applicant, advising on the WP1 realist synthesis.
Jon M Dickson (https://orcid.org/0000-0002-1361-2714) (Senior Clinical Lecturer) was a co-applicant, contributing to the design of the vignettes in WP3.
Steve Goodacre (https://orcid.org/0000-0003-0803-8444) (Professor of Emergency Medicine) was a co-applicant, contributing to the design of the vignettes in WP3.
Enid Hirst (https://orcid.org/0000-0003-2230-5123) (PPI member) designed the PPI workshop and contributed to interpretation of the findings.
Richard Jacques (https://orcid.org/0000-0001-6710-5403) (Lecturer) was a co-applicant, advising on the analysis of WP3.
Miranda Phillips (https://orcid.org/0000-0001-6318-2233) (Research Director) was a co-applicant, contributing to the design of the questionnaire in WP3 and leading the British Social Attitudes survey.
Joanne Turnbull (https://orcid.org/0000-0002-5006-4438) (Senior Research Fellow) was a co-applicant, advising on how our project complemented and learnt from an ongoing NIHR project in a related field.
Janette Turner (https://orcid.org/0000-0003-3884-7875) (Reader in Emergency and Urgent Care Research) was a co-applicant, advising on how our project findings related to the evidence base and current policy initiatives.
All authors attended project management meetings to discuss the findings of each WP, and commented on the draft report.
Approvals
Ethics approval was sought for the qualitative interview study (WP2) and approval obtained from London – Brent REC (reference 14/LO/1228). The population survey (WP3) was conducted by NatCen and it obtained ethics approval through its standard procedures.
Publications
NatCen published a report of its 2019 British Social Attitudes survey in July 2019. The findings from our module of the survey were published separately in August 2019 focusing on aspects of seeking emergency and urgent care that complement rather than repeat the findings reported here.
Curtice J, Clery E, Perry J, Phillips M, Rahim N. Emergency Care: What do Attitudes Tell us About Demand for Services and how it Might be Reduced? London: The National Centre for Social Research; 2019.
Articles
O’Cathain A, Connell J, Long J, Coster J. ‘Clinically unnecessary’ use of emergency and urgent care: a realist review of patients’ decision making. Health Expect 2020;23:19–40.
O’Cathain A, Simpson R, Phillips M, Dickson J. Tendency to contact general practice instead of self care: population vignette study in Britain. BJGP Open 2020; in press.
Oral conference presentations
O’Cathain A, Connell J, Long J, Coster J. Understanding why Patients Make Clinically Unnecessary Use of Emergency and Urgent Care Services. HSRUK Conference 2018, 4–5 July 2018, Nottingham, UK.
Long J, Knowles EL, Bishop-Edwards, L, O’Cathain A. Interventions to Improve Service Use and Self-care Decision-Making in Patients Making Clinically Unnecessary Use of Urgent and Emergency Care. HSRUK Conference 2019, 2–3 July 2019, Manchester, UK.
O’Cathain A, Simpson R, Knowles EL, Phillips M. The Propensity to Make Clinically Unnecessary Use of Emergency Departments: A Vignette Study. HSRUK Conference 2019, 2–3 July 2019, Manchester, UK.
Data-sharing statement
Any queries or data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review. NatCen makes the data from the British Social Attitudes survey available using its own data-sharing processes.
Disclaimers
This report presents independent research funded by NIHR. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Toloo GS, FitzGerald GJ, Aitken PJ, Ting JY, McKenzie K, Rego J, et al. Ambulance use is associated with higher self-rated illness seriousness: user attitudes and perceptions. Acad Emerg Med 2013;20:576-83. https://doi.org/10.1111/acem.12149.
- O’Cathain A, Knowles E, Munro J, Nicholl J. Exploring the effect of changes to service provision on the use of unscheduled care in England: population surveys. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-61.
- Hobbs FDR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Iacobucci G. GPs forced to turn away patients because of winter pressures. BMJ 2018;360. https://doi.org/10.1136/bmj.k81.
- Kay I. Ambulance Quality Indicators. London: NHS England; 2017.
- Kawakami C, Ohshige K, Kubota K, Tochikubo O. Influence of socioeconomic factors on medically unnecessary ambulance calls. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-120.
- Durand AC, Palazzolo S, Tanti-Hardouin N, Gerbeaux P, Sambuc R, Gentile S. Nonurgent patients in emergency departments: rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res Notes 2012;5. https://doi.org/10.1186/1756-0500-5-525.
- Farion KJ, Wright M, Zemek R, Neto G, Karwowska A, Tse S, et al. Understanding low-acuity visits to the pediatric emergency department. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0128927.
- Patterson PD, Baxley EG, Probst JC, Hussey JR, Moore CG. Medically unnecessary emergency medical services (EMS) transports among children ages 0 to 17 years. Matern Child Health J 2006;10:527-36. https://doi.org/10.1007/s10995-006-0127-6.
- Faulkner D, Law J. The ‘unnecessary’ use of emergency departments by older people: findings from hospital data, hospital staff and older people. Aust Health Rev 2015;39:544-51. https://doi.org/10.1071/AH14185.
- Allen L, Cummings J. Emergency department use among Hispanic Adults: the role of acculturation. Med Care 2016;54:449-56. https://doi.org/10.1097/MLR.0000000000000511.
- Atenstaedt R, Gregory J, Price-Jones C, Newman J, Roberts L, Turner J. Why do patients with nonurgent conditions present to the emergency department despite the availability of alternative services?. Eur J Emerg Med 2015;22:370-3. https://doi.org/10.1097/MEJ.0000000000000224.
- Durand AC, Gentile S, Devictor B, Palazzolo S, Vignally P, Gerbeaux P, et al. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med 2011;29:333-45. https://doi.org/10.1016/j.ajem.2010.01.003.
- Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Deciding to visit the emergency department for non-urgent conditions: a systematic review of the literature. Am J Manag Care 2013;19:47-59.
- Cheek C, Allen P, Shires L, Parry D, Ruigrok M. Low-acuity presentations to regional emergency departments: what is the issue?. Emerg Med Australas 2016;28:145-52. https://doi.org/10.1111/1742-6723.12526.
- Schumacher JR, Hall AG, Davis TC, Arnold CL, Bennett RD, Wolf MS, et al. Potentially preventable use of emergency services: the role of low health literacy. Med Care 2013;51:654-8. https://doi.org/10.1097/MLR.0b013e3182992c5a.
- Booker MJ, Shaw AR, Purdy S. Why do patients with ‘primary care sensitive’ problems access ambulance services? A systematic mapping review of the literature. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-007726.
- Bell C. Does Peppa Pig encourage inappropriate use of primary care resources?. BMJ 2017;359. https://doi.org/10.1136/bmj.j5397.
- Booker MJ, Purdy S, Shaw ARG. Seeking ambulance treatment for ‘primary care’ problems: a qualitative systematic review of patient, carer and professional perspectives. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016832.
- Llanwarne N, Newbould J, Burt J, Campbell JL, Roland M. Wasting the doctor’s time? A video-elicitation interview study with patients in primary care. Soc Sci Med 2017;176:113-22. https://doi.org/10.1016/j.socscimed.2017.01.025.
- Goode J, Greatbatch D, O’Cathain A, Luff D, Hanlon G, Strangleman T. Risk and the responsible health consumer: the problematics of entitlement among callers to NHS Direct. Crit Soc Policy 2004;24:210-32. https://doi.org/10.1177/0261018304041951.
- Pope C, McKenna G, Turnbull J, Prichard J, Rogers A. Navigating and making sense of urgent and emergency care processes and provision. Health Expect 2019;22:435-43. https://doi.org/10.1111/hex.12866.
- Greenfield G, Ignatowicz A, Gnani S, Bucktowonsing M, Ladbrooke T, Millington H, et al. Staff perceptions on patient motives for attending GP-led urgent care centres in London: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-007683.
- Van den Heede K, Van de Voorde C. Interventions to reduce emergency department utilisation: a review of reviews. Health Policy 2016;120:1337-49. https://doi.org/10.1016/j.healthpol.2016.10.002.
- Munro J, Nicholl J, O’Cathain A, Knowles E. Impact of NHS direct on demand for immediate care: observational study. BMJ 2000;321:150-3. https://doi.org/10.1136/bmj.321.7254.150.
- Turner J, O’Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003451.
- Arain M, Campbell MJ, Nicholl JP. Impact of a GP-led walk-in centre on NHS emergency departments. Emerg Med J 2015;32:295-300. https://doi.org/10.1136/emermed-2013-202410.
- Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med 2017;24:1137-49. https://doi.org/10.1111/acem.13220.
- Kraaijvanger N, van Leeuwen H, Rijpsma D, Edwards M. Motives for self-referral to the emergency department: a systematic review of the literature. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1935-z.
- Turner J, Coster J, Chambers D, Cantrell A, Phung V, Knowles E, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03430.
- He J, Hou XY, Toloo S, Patrick JR, Fitz Gerald G. Demand for hospital emergency departments: a conceptual understanding. World J Emerg Med 2011;2:253-61. https://doi.org/10.5847/wjem.j.1920-8642.2011.04.002.
- Toloo S, FitzGerald G, Aitken P, Ting J, Tippett V, Chu K. Emergency Health Services: Demand and Service Delivery Models. Monograph 1: Literature Review and Activity Trends. Brisbane, QLD: Queensland University of Technology; 2011.
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter?. J Health Soc Behav 1995;36:1-10. https://doi.org/10.2307/2137284.
- Weber EJ, Hirst E, Marsh M. The patient’s dilemma: attending the emergency department with a minor illness. BMJ 2017;357. https://doi.org/10.1136/bmj.j1941.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Bunn F, Goodman C, Reece Jones P, Russell B, Trivedi D, Sinclair A, et al. What works for whom in the management of diabetes in people living with dementia: a realist review. BMC Med 2017;15. https://doi.org/10.1186/s12916-017-0909-2.
- Ford JA, Wong G, Jones AP, Steel N. Access to primary care for socioeconomically disadvantaged older people in rural areas: a realist review. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010652.
- Shearn K, Allmark P, Piercy H, Hirst J. Building realist program theory for large complex and messy interventions. Int J Qual Methods 2017;16:1-11. https://doi.org/10.1177/1609406917741796.
- Turnbull J, McKenna G, Prichard J, Rogers A, Crouch R, Lennon A, et al. Sense-making strategies and help-seeking behaviours associated with urgent care services: a mixed-methods study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07260.
- Critical Appraisal Skills Programme . CASP Qualitative Checklist 2019. https://casp-uk.net/casp-tools-checklists/ (accessed 17 May 2019).
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Shaw J, Gray CS, Baker GR, Denis JL, Breton M, Gutberg J, et al. Mechanisms, contexts and points of contention: operationalizing realist-informed research for complex health interventions. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0641-4.
- Wyke S, Adamson J, Dixon D, Hunt K. Consultation and illness behaviour in response to symptoms: a comparison of models from different disciplinary frameworks and suggestions for future research directions. Soc Sci Med 2013;86:79-87. https://doi.org/10.1016/j.socscimed.2013.03.007.
- Becker G, Janson-Bjerklie S, Benner P, Slobin K, Ferketich S. The dilemma of seeking urgent care: asthma episodes and emergency service use. Soc Sci Med 1993;37:305-13. https://doi.org/10.1016/0277-9536(93)90262-3.
- Brousseau DC, Nimmer MR, Yunk NL, Nattinger AB, Greer A. Nonurgent emergency-department care: analysis of parent and primary physician perspectives. Pediatrics 2011;127:e375-81. https://doi.org/10.1542/peds.2010-1723.
- Calnan M. Managing ‘minor’ disorders: pathways to a hospital accident and emergency department. Sociol Health Illn 1983;5:149-67. https://doi.org/10.1111/1467-9566.ep10491503.
- Chin NP, Goepp JG, Malia T, Harris L, Poordabbagh A. Nonurgent use of a pediatric emergency department: a preliminary qualitative study. Pediatr Emerg Care 2006;22:22-7. https://doi.org/10.1097/01.pec.0000195756.74328.21.
- de Bont EG, Loonen N, Hendrix DA, Lepot JM, Dinant GJ, Cals JW. Childhood fever: a qualitative study on parents’ expectations and experiences during general practice out-of-hours care consultations. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0348-0.
- Fieldston ES, Alpern ER, Nadel FM, Shea JA, Alessandrini EA. A qualitative assessment of reasons for nonurgent visits to the emergency department: parent and health professional opinions. Pediatr Emerg Care 2012;28:220-5. https://doi.org/10.1097/PEC.0b013e318248b431.
- Guttman N, Zimmerman DR, Nelson MS. The many faces of access: reasons for medically nonurgent emergency department visits. J Health Polit Policy Law 2003;28:1089-120. https://doi.org/10.1215/03616878-28-6-1089.
- Hopton J, Hogg R, McKee I. Patients’ accounts of calling the doctor out of hours: qualitative study in one general practice. BMJ 1996;313:991-4. https://doi.org/10.1136/bmj.313.7063.991.
- Houston AM, Pickering AJ. ‘Do I don’t I call the doctor’: a qualitative study of parental perceptions of calling the GP out-of-hours. Health Expect 2000;3:234-42. https://doi.org/10.1046/j.1369-6513.2000.00109.x.
- Hugenholtz M, Bröer C, van Daalen R. Apprehensive parents: a qualitative study of parents seeking immediate primary care for their children. Br J Gen Pract 2009;59:173-9. https://doi.org/10.3399/bjgp09X394996.
- McGuigan T, Watson P. Non-urgent attendance at emergency departments. Emerg Nurse 2010;18:34-8. https://doi.org/10.7748/en.18.6.34.s18.
- Shaw EK, Howard J, Clark EC, Etz RS, Arya R, Tallia AF. Decision-making processes of patients who use the emergency department for primary care needs. J Health Care Poor Underserved 2013;24:1288-305. https://doi.org/10.1353/hpu.2013.0140.
- Stafford V, Greenhalgh S, Davidson I. Why do patients with simple mechanical back pain seek urgent care?. Physiotherapy 2014;100:66-72. https://doi.org/10.1016/j.physio.2013.08.001.
- Woolfenden S, Ritchie J, Hanson R, Nossar V. Parental use of a paediatric emergency department as an ambulatory care service. Aust N Z J Public Health 2000;24:204-6. https://doi.org/10.1111/j.1467-842x.2000.tb00144.x.
- Leventhal H, Brissette I, Leventhal E, Cameron L, Leventhal H. The Self-regulation of Health and Illness Behaviour. London: Routledge; 2003.
- Mishel MH, Braden CJ. Uncertainty. A mediator between support and adjustment. West J Nurs Res 1987;9:43-57. https://doi.org/10.1177/019394598700900106.
- Freed GL, Allen AR, Turbitt E, Nicolas C, Oakley E. Parent perspectives and reasons for lower urgency paediatric presentations to emergency departments. Emerg Med Australas 2016;28:211-15. https://doi.org/10.1111/1742-6723.12544.
- Kallestrup P, Bro F. Parents’ beliefs and expectations when presenting with a febrile child at an out-of-hours general practice clinic. Br J Gen Pract 2003;53:43-4.
- Walsh M. The health belief model and use of accident and emergency services by the general public. J Adv Nurs 1995;22:694-9. https://doi.org/10.1046/j.1365-2648.1995.22040694.x.
- Watson MC, Ferguson J, Barton GR, Maskrey V, Blyth A, Paudyal V, et al. A cohort study of influences, health outcomes and costs of patients’ health-seeking behaviour for minor ailments from primary and emergency care settings. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006261.
- Williams A, O’Rourke P, Keogh S. Making choices: why parents present to the emergency department for non-urgent care. Arch Dis Child 2009;94:817-20. https://doi.org/10.1136/adc.2008.149823.
- Ahl C, Nyström M, Jansson L. Making up one’s mind: – patients’ experiences of calling an ambulance. Accid Emerg Nurs 2006;14:11-9. https://doi.org/10.1016/j.aaen.2005.10.002.
- Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study. Ambul Pediatr 2008;8:360-7. https://doi.org/10.1016/j.ambp.2008.07.001.
- Capp R, Kelley L, Ellis P, Carmona J, Lofton A, Cobbs-Lomax D, et al. Reasons for frequent emergency department use by Medicaid enrollees: a qualitative study. Acad Emerg Med 2016;23:476-81. https://doi.org/10.1111/acem.12952.
- Hunter C, Chew-Graham C, Langer S, Stenhoff A, Drinkwater J, Guthrie E, et al. A qualitative study of patient choices in using emergency health care for long-term conditions: the importance of candidacy and recursivity. Patient Educ Couns 2013;93:335-41. https://doi.org/10.1016/j.pec.2013.06.001.
- Olsson M, Hansagi H. Repeated use of the emergency department: qualitative study of the patient’s perspective. Emerg Med J 2001;18:430-4. https://doi.org/10.1136/emj.18.6.430.
- Beck U. Risk Society: Towards a New Modernity. London: SAGE Publications Ltd; 1992.
- Pescosolido B. Beyond rational choice: the social dynamics of how people seek help. Am J Sociol 1992;97:1096-138. https://doi.org/10.1086/229863.
- Agarwal S, Banerjee J, Baker R, Conroy S, Hsu R, Rashid A, et al. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emerg Med J 2012;29. https://doi.org/10.1136/emermed-2011-200585.
- Booker MJ, Simmonds RL, Purdy S. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emerg Med J 2014;31:448-52. https://doi.org/10.1136/emermed-2012-202124.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. https://doi.org/10.1186/1471-2288-6-35.
- Dingwall R, Murray T. Categorization in accident departments: ‘good’ patients, ‘bad’ patients and ‘children’. Sociol Health Illn 1983;5:127-48. https://doi.org/10.1111/1467-9566.ep10491496.
- Deavenport-Saman A, Lu Y, Smith K, Yin L. Do children with autism overutilize the emergency department? Examining visit urgency and subsequent hospital admissions. Matern Child Health J 2016;20:306-14. https://doi.org/10.1007/s10995-015-1830-y.
- Koziol-McLain J, Price DW, Weiss B, Quinn AA, Honigman B. Seeking care for nonurgent medical conditions in the emergency department: through the eyes of the patient. J Emerg Nurs 2000;26:554-63. https://doi.org/10.1067/men.2000.110904.
- Dingwall R. Aspects of Illness (Medicine in Society). Farnham: Ashgate Publishing; 2001.
- Zola IK. Pathways to the doctor-from person to patient. Soc Sci Med 1973;7:677-89. https://doi.org/10.1016/0037-7856(73)90002-4.
- Hodgins MJ, Wuest J. Uncovering factors affecting use of the emergency department for less urgent health problems in urban and rural areas. Can J Nurs Res 2007;39:78-102.
- Mostajer Haqiqi A, Bedos C, Macdonald ME. The emergency department as a ‘last resort’: why parents seek care for their child’s nontraumatic dental problems in the emergency room. Community Dent Oral Epidemiol 2016;44:493-50. https://doi.org/10.1111/cdoe.12239.
- Keizer Beache S, Guell C. Non-urgent accident and emergency department use as a socially shared custom: a qualitative study. Emerg Med J 2016;33:47-51. https://doi.org/10.1136/emermed-2014-204039.
- Neill SJ, Jones CH, Lakhanpaul M, Roland DT, Thompson MJ. Parents’ help-seeking behaviours during acute childhood illness at home: a contribution to explanatory theory. J Child Health Care 2016;20:77-86. https://doi.org/10.1177/1367493514551309.
- Wilkin H, Cohen E, Tannebaum M. How low-income residents decide between emergency and primary health care for non-urgent treatment. Howard J Commun 2012;23:157-74. https://doi.org/10.1080/10646175.2012.667725.
- Goepp JG, Chin NP, Massad J, Edwards LA. Pediatric emergency department outreach: solving medical problems or revealing community solutions?. J Health Care Poor Underserved 2004;15:522-9. https://doi.org/10.1353/hpu.2004.0060.
- Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad Saude Publica 2009;25:7-28. https://doi.org/10.1590/S0102-311X2009000100002.
- Diserens L, Egli L, Fustinoni S, Santos-Eggimann B, Staeger P, Hugli O. Emergency department visits for non-life-threatening conditions: evolution over 13 years in a Swiss urban teaching hospital. Swiss Med Wkly 2015;145. https://doi.org/10.4414/smw.2015.14123.
- Keizer E, Smits M, Peters Y, Huibers L, Giesen P, Wensing M. Contacts with out-of-hours primary care for nonurgent problems: patients’ beliefs or deficiencies in healthcare?. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0376-9.
- Antonovsky H, Sagy S. The development of a sense of coherence and its impact on responses to stress situations. J Soc Psychol 1986;126:213-25.
- Durant E, Fahimi J. Factors associated with ambulance use among patients with low-acuity conditions. Prehosp Emerg Care 2012;16:329-37. https://doi.org/10.3109/10903127.2012.670688.
- Howard MS, Davis BA, Anderson C, Cherry D, Koller P, Shelton D. Patients’ perspective on choosing the emergency department for nonurgent medical care: a qualitative study exploring one reason for overcrowding. J Emerg Nurs 2005;31:429-35. https://doi.org/10.1016/j.jen.2005.06.023.
- Lawson CC, Carroll K, Gonzalez R, Priolo C, Apter AJ, Rhodes KV. ‘No other choice’: reasons for emergency department utilization among urban adults with acute asthma. Acad Emerg Med 2014;21:1-8. https://doi.org/10.1111/acem.12285.
- Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department?. Emerg Med J 2012;29:487-91. https://doi.org/10.1136/emj.2010.107276.
- Goeman DP, Aroni RA, Sawyer SM, Stewart K, Thien FC, Abramson MJ, et al. Back for more: a qualitative study of emergency department reattendance for asthma. Med J Aust 2004;180:113-17. https://doi.org/10.5694/j.1326-5377.2004.tb05831.x.
- Rogers A, Nicolaas G. Understanding the patterns and processes of primary care use: a combined quantitative and qualitative approach. Sociol Res Online 1998;3:1-13. https://doi.org/10.5153/sro.192.
- Zimmerman FJ. Habit, custom, and power: a multi-level theory of population health. Soc Sci Med 2013;80:47-56. https://doi.org/10.1016/j.socscimed.2012.12.029.
- Nilsen P, Roback K, Broström A, Ellström PE. Creatures of habit: accounting for the role of habit in implementation research on clinical behaviour change. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-53.
- MacKichan F, Brangan E, Wye L, Checkland K, Lasserson D, Huntley A, et al. Why do patients seek primary medical care in emergency departments? An ethnographic exploration of access to general practice. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013816.
- Drummond N, McConnachie A, O’Donnell C, Moffat K, Wilson P, Ross S. Social variation in reasons for contacting general practice out-of-hours: implications for daytime service provision?. Br J Gen Pract 2000;50:460-4.
- Thornton V, Fogarty A, Jones P, Ragaban N, Simpson C. Why do patients self-present to Middlemore Hospital Emergency Department?. N Z Med J 2014;127:19-30.
- Zhou Y, Abel G, Warren F, Roland M, Campbell J, Lyratzopoulos G. Do difficulties in accessing in-hours primary care predict higher use of out-of-hours GP services? Evidence from an English National Patient Survey. Emerg Med J 2015;32:373-8. https://doi.org/10.1136/emermed-2013-203451.
- van den Berg MJ, van Loenen T, Westert GP. Accessible and continuous primary care may help reduce rates of emergency department use. An international survey in 34 countries. Fam Pract 2016;33:42-50. https://doi.org/10.1093/fampra/cmv082.
- Benahmed N, Laokri S, Zhang WH, Verhaeghe N, Trybou J, Cohen L, et al. Determinants of nonurgent use of the emergency department for pediatric patients in 12 hospitals in Belgium. Eur J Pediatr 2012;171:1829-37. https://doi.org/10.1007/s00431-012-1853-y.
- Moll van Charante EP, ter Riet G, Bindels P. Self-referrals to the A.E department during out-of-hours: patients’ motives and characteristics. Patient Educ Couns 2008;70:256-65. https://doi.org/10.1016/j.pec.2007.10.012.
- O’Keeffe C, Mason S, Jacques R, Nicholl J. Characterising non-urgent users of the emergency department (ED): a retrospective analysis of routine ED data. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0192855.
- Butcher B. Sex, drugs and A&E: 10 charts on how the under-30s use the NHS. BBC News 2018. www.bbc.co.uk/news/uk-44456571 (accessed 25 February 2020).
- McHale P, Wood S, Hughes K, Bellis MA, Demnitz U, Wyke S. Who uses emergency departments inappropriately and when – a national cross-sectional study using a monitoring data system. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-258.
- Viner RM, Blackburn F, White F, Mannie R, Parr T, Nelson S, et al. The impact of out-of-hospital models of care on paediatric emergency department presentations. Arch Dis Child 2018;103:128-36. https://doi.org/10.1136/archdischild-2017-313307.
- Smith J, Jarman M, Osborn M, Murray M, Chamberlain K. Qualitative Health Psychology: Theories and Methods. London: SAGE Publications Ltd; 1999.
- Smith J. Reflecting on the development of interpretative phenomenological analysis and its contribution to qualitative research in psychology. Qual Res Psychol 2004;1:39-54.
- Pietkiewicz I, Smith J. A practical guide to using interpretative phenomenological analysis in qualitative research psychology. Psychol J 2014;20:7-14. https://doi.org/10.14691/CPPJ.20.1.7.
- Collins A, McLachlan SA, Philip J. Initial perceptions of palliative care: an exploratory qualitative study of patients with advanced cancer and their family caregivers. Palliat Med 2017;31:825-32. https://doi.org/10.1177/0269216317696420.
- Kelly CA, O’Brien MR. Difficult decisions: an interpretative phenomenological analysis study of healthcare professionals’ perceptions of oxygen therapy in palliative care. Palliat Med 2015;29:950-8. https://doi.org/10.1177/0269216315584864.
- McCann TV, Lubman DI, Boardman G, Flood M. Affected family members’ experience of, and coping with, aggression and violence within the context of problematic substance use: a qualitative study. BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1374-3.
- Rifshana F, Breheny M, Taylor J, Ross K. The parental experience of caring for a child with type 1 diabetes. J Child Fam Stud 2017;26:3226-36. https://doi.org/10.1007/s10826-017-0806-5.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health C 2007;19:349-57. https://doi.org/10.1093/intqhc/mzm042.
- Kai J. What worries parents when their preschool children are acutely ill, and why: a qualitative study. BMJ 1996;313:983-6. https://doi.org/10.1136/bmj.313.7063.983.
- Niedzwiecki MJ, Sharma PJ, Kanzaria HK, McConville S, Hsia RY. Factors associated with emergency department use by patients with and without mental health diagnoses. JAMA Netw Open 2018;1. https://doi.org/10.1001/jamanetworkopen.2018.3528.
- Ballou S, Mitsuhashi S, Sankin LS, Petersen TS, Zubiago J, Lembo C, et al. Emergency department visits for depression in the United States from 2006 to 2014. Gen Hosp Psychiatry 2019;59:14-9. https://doi.org/10.1016/j.genhosppsych.2019.04.015.
- Hooker EA, Mallow PJ, Oglesby MM. Characteristics and trends of emergency department visits in the United States (2010-2014). J Emerg Med 2019;56:344-51. https://doi.org/10.1016/j.jemermed.2018.12.025.
- Perera J, Wand T, Bein KJ, Chalkley D, Ivers R, Steinbeck KS, et al. Presentations to NSW emergency departments with self-harm, suicidal ideation, or intentional poisoning, 2010–2014. Med J Aust 2018;208:348-53. https://doi.org/10.5694/mja17.00589.
- Hiscock H, Neely RJ, Lei S, Freed G. Paediatric mental and physical health presentations to emergency departments, Victoria, 2008-15. Med J Aust 2018;208:343-8. https://doi.org/10.5694/mja17.00434.
- Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics 2019;143. https://doi.org/10.1542/peds.2018-2192.
- Hsia RY, Niedzwiecki M. Avoidable emergency department visits: a starting point. Int J Qual Health Care 2017;29:642-5. https://doi.org/10.1093/intqhc/mzx081.
- Duncan EAS, Best C, Dougall N, Skar S, Evans J, Corfield AR, et al. Epidemiology of emergency ambulance service calls related to mental health problems and self harm: a national record linkage study. Scand J Trauma Resusc Emerg Med 2019;27. https://doi.org/10.1186/s13049-019-0611-9.
- Roggenkamp R, Andrew E, Nehme Z, Cox S, Smith K. Descriptive analysis of mental health-related presentations to emergency medical services. Prehosp Emerg Care 2018;22:399-405. https://doi.org/10.1080/10903127.2017.1399181.
- Lockett H, Lai J, Tuason C, Jury A, Fergusson D. Primary healthcare utilisation among adults with mood and anxiety disorders: an analysis of the New Zealand Health Survey. J Prim Health Care 2018;10:68-75. https://doi.org/10.1071/HC17077.
- Prior A, Vestergaard M, Larsen KK, Fenger-Grøn M. Association between perceived stress, multimorbidity and primary care health services: a Danish population-based cohort study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-018323.
- NHS England . GP Patient Survey 2018 2018. www.england.nhs.uk/statistics/2018/08/09/gp-patient-survey-2018/ (accessed 7 October 2019).
- Whittaker W, Anselmi L, Kristensen SR, Lau YS, Bailey S, Bower P, et al. Associations between extending access to primary care and emergency department visits: a difference-in-differences analysis. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1002113.
- Borg K, Wright B, Sannen L, Dumas D, Walker T, Bragge P. Ambulances are for emergencies: shifting attitudes through a research-informed behaviour change campaign. Health Res Policy Syst 2019;17. https://doi.org/10.1186/s12961-019-0430-5.
- FitzGerald G, Toloo GS, Aitken P, Keijzers G, Scuffham P. Public use and perceptions of emergency departments: a population survey. Emerg Med Australas 2015;27:336-42. https://doi.org/10.1111/1742-6723.12420.
- Adamson J, Ben-Shlomo Y, Chaturvedi N, Donovan J. Ethnicity, socio-economic position and gender--do they affect reported health-care seeking behaviour?. Soc Sci Med 2003;57:895-904. https://doi.org/10.1016/S0277-9536(02)00458-6.
- Kirkby HM, Roberts LM. Inappropriate 999 calls: an online pilot survey. Emerg Med J 2012;29:141-6. https://doi.org/10.1136/emj.2010.092346.
- Adamson J, Ben-Shlomo Y, Chaturvedi N, Donovan J. Exploring the impact of patient views on ‘appropriate’ use of services and help seeking: a mixed method study. Br J Gen Pract 2009;59:e226-33. https://doi.org/10.3399/bjgp09X453530.
- Schumacher J, Hendry P, Hall A, Lutz B, Carden D. EMF-250 An emergency department-to-home intervention to improve patient activation. Ann Emerg Med 2014;64:S89-90. https://doi.org/10.1016/j.annemergmed.2014.07.277.
- Morrison AK, Schapira MM, Gorelick MH, Hoffmann RG, Brousseau DC. Low caregiver health literacy is associated with higher pediatric emergency department use and nonurgent visits. Acad Pediatr 2014;14:309-14. https://doi.org/10.1016/j.acap.2014.01.004.
- Duell P, Wright D, Renzaho AM, Bhattacharya D. Optimal health literacy measurement for the clinical setting: a systematic review. Patient Educ Couns 2015;98:1295-307. https://doi.org/10.1016/j.pec.2015.04.003.
- Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-658.
- NHS England . GP Patient Survey – Technical Annex 2017.
- Chatterjee S, Price B. Regression Analysis by Example. New York, NY: John Wiley and Sons; 1977.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335. https://doi.org/10.1136/bmj.39335.541782.A.
- Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res 2006;16:377-94. https://doi.org/10.1177/1049732305285708.
- NHS England . Transforming Urgent and Emergency Care Services in England. Urgent and Emergency Care Review. End of Phase 1 Report 2013.
- Gershlick B, Fisher R. A Worrying Cycle of Pressure for GPs in Deprived Areas. London: The Health Foundation; 2019.
- Ahl C, Nyström M. To handle the unexpected – the meaning of caring in pre-hospital emergency care. Int Emerg Nurs 2012;20:33-41. https://doi.org/10.1016/j.ienj.2011.03.001.
- Goeman DP, Aroni RA, Stewart K, Sawyer SM, Thien FC, Abramson MJ, et al. Patients’ views of the burden of asthma: a qualitative study. Med J Aust 2002;177:295-9.
Appendix 1 Objectives specified in the proposal
The objectives specified in the proposal were to:
-
identify drivers of demand for urgent care from the range of emergency, urgent and routine health services available, in particular the drivers of the propensity to seek care from a higher-acuity service than is clinically necessary (evidence synthesis and qualitative interview study)
-
understand how different subgroups of the population make decisions about help-seeking to inform potential intervention strategies (evidence synthesis, qualitative interview study and general population survey)
-
measure the prevalence of public attitudes towards seeking urgent care, and how these vary in different circumstances and by different subgroups of the population (general population survey).
Appendix 2 Search strategies and terms used in reviews for realist review
Coster et al. 28 searched MEDLINE, EMBASE, The Cochrane Library, Web of Science™ (Clarivate Analytics, Philadelphia, PA, USA) and CINAHL (Cumulative Index to Nursing and Allied Health Literature) from 1995 to 2016. Keywords related to emergency and urgent care services, health service demand and factors relating to rising demand. The search terms included ambulance, ED, appropriate care, utilization and urgent care.
Kraaijvanger et al. 29 searched MEDLINE, EMBASE, The Cochrane Library, CINAHL and PubMed up to February 2015. Searches used a combination of the following terms: ED, self-referred, referral, walk-in, motives and reasons. Studies were included if participants were self-referred to the ED.
Booker et al. 17 searched MEDLINE, EMBASE, PsycINFO, Web of Science and CINAHL from 1980 to June 2014. Search terms related to ‘primary care sensitive clinical conditions’ and ‘health care from ambulance services’ were used. Readers are referred to the PROSPERO register for details, although specific search terms are not included in the register. The ‘primary care-related’ aspects of included papers required explicit reference to terms related to primary care or family medicine, or focused on some of a list of indicator presentations.
Turnbull et al. 39 searched policy and published research MEDLINE, EMBASE, Web of Science, CINAHL and PsycINFO from 1990 to 2017; their search only included articles up to 2016 at the time they shared their database with us in February 2017. The strategy combined terms relating to urgent care and non-urgent use of emergency care services and terms relating to patient experiences, for example patient help-seeking and decision-making.
Appendix 3 Relevance and context appraisal of included qualitative articles
| Authors and year of publication | Relevance code | Definition of sample/participants as described in the paper, and where description(s) can be found (title/abstract/methods) | Service | Comments | Adequacy of description of key aspects of context | ||
|---|---|---|---|---|---|---|---|
| Service | Geographical setting | Demographic details | |||||
| Agarwal et al., 201272 | 1 |
Title: ‘Potentially avoidable ED attendance’ Abstract: ‘could have been managed in an alternative service’ Methods: ‘Suitable to be cared for in an alternative urgent care provider service including primary care’/’attending the ED with urgent care needs that could be managed in other urgent care environments locally’ |
ED, two-thirds arriving by ambulance | ‘Non-urgent’ defined to include referral of relatively serious problems (e.g. chest pain, collapse) to a centre staffed by doctors, nurses and emergency practitioners | Yes | No | Yes |
| Ahl et al. 200665 | 1 |
Methods: ‘had used ambulance care within the past 3 months . . . selected in order to achieve a large variation in . . . emergency priorities and medical diagnosis’ Background of 2012 paper: ‘pre-hospital care situations that are not defined as traumatic or life threatening’ |
Ambulance | – | Yes | Poor | Poor |
| Becker et al. 199344 | 2 | Methods: ‘adults with physician-diagnosed and documented asthma’, studying ‘individuals’ response to asthma’ | Mixed emergency/urgent care: service unclear, mostly ED | – | Poor | No | Yes |
| Berry et al. 200866 | 1 |
Title: ‘bring children to the ED for nonurgent conditions’ Abstract: ‘choosing the ED over their PCP for nonurgent paediatric care’ Methods: child ‘assigned a nurse triage level of 5 on a 1 to 5 scale (with 5 indicating “no resources likely to be utilized” or a non-urgent problem)’/brought child to ED ‘during hours when physicians’ offices are routinely open’ |
PED | – | Yes | Yes | Yes |
| Booker et al. 201473 | 1 |
Title: ‘call emergency ambulances for primary care problems’ Abstract: ‘called an ambulance for a primary care-appropriate health problem’ Methods: ‘likely to have been managed successfully in primary care’ |
Ambulance | – | Yes | No | Yes |
| Brousseau et al. 201145 | 1 |
Abstract: ‘presenting for non-urgent care at a children's hospital ED’ Methods: ‘triaged as nonurgent by the ED triage nurse’ |
PED | Some data relate to HCPs’ perceptions | Yes | No | Yes |
| Calnan 198346 | 1 | Methods: ‘minor condition . . . according to both the level of medical skill needed to treat the complaint and the facilities available to treat the condition’ – minor cuts ‘requiring cleaning and dressing only which could be carried out by a [nurse] alone’ – and minor illnesses ‘complaints of a non-traumatic nature which could have been treated by a GP’ | ED | – | Yes | No | No |
| Capp et al. 201667 | 2 | Abstract: ‘Frequent ED users’ (4–18 visits in past year, if most visits not for mental health or substance abuse reasons) | ED | Sample participating in RCT ‘to improve[e] primary care utilization’ | Yes | Yes | Yes |
| Chin et al. 200647 | 1 |
Title: ‘Nonurgent use of a PED’ Abstract: ‘presenting to a PED for nonacute care’ Methods: ‘in the PED whose visits were of low acuity as defined as score of 5 on 5 point Emergency Severity Index’ |
PED | Some data relate to HCPs’ perceptions | Poor | Poor | Yes |
| de Bont et al. 201548 | 2 | Methods: ‘presenting to the GP OOH centre with a febrile child under the age of 12’ | OOH – delivered by co-op | – | Yes | Yes | Yes |
| Durand et al. 20127 | 1 |
Title: ‘Nonurgent patients in ED’ Methods: ‘triaged as nonurgent upon their arrival to the ED by the triage nurse’, nonurgent defined as ‘problem could be taken care of by primary care physician’ |
ED | Some data relate to HCPs’ perceptions | Yes | No | Yes |
| Fieldston et al. 201249 | 2 |
Title: ‘Nonurgent visits to the ED’ Methods: exploring and describing ‘reasons for nonurgent pediatric ED visits independent of a particular ED visit’ |
PED | Some data relate to HCPs’ perceptions | Poor | Yes | Yes |
| Goeman et al. 200494 | 2 |
Title: ‘ED reattendance for asthma’ Methods: people with asthma not controlled by their current therapy who ‘reattended emergency departments within 12 months’ |
ED | Part of a larger sample where others did not reattend | Yes | Poor | Yes |
| Goepp et al. 200485 | 2 |
Results: families from ‘among residents of the East Baltimore neighbour-hoods’ (area with high poverty levels) Conclusions: ‘low-income patients, especially those belonging to minority groups’ |
Health service use, particularly PED | Some data ethnographic observations and community support workers’ perceptions and experiences | Yes | Poor | Poor |
| Guttman et al. 200350 | 1 |
Title: ‘Medically nonurgent ED visits’ Methods: visit ‘considered medically nonurgent’ by ED triage staff’ |
Adult and PED | – | Yes | Poor | Yes |
| Mostajer Haqiqi et al. 201681 | 1 | Abstract: parents of child under 10 ‘seeking care for nontraumatic dental problems in the ED’ of a paediatric hospital | PED | – | Yes | Yes | Yes |
| Hopton et al. 199651 | 2 | Abstract: adults (or calling on behalf of another adult) or parents ‘who called their doctors out of hours’ | OOH – delivered by general practice | – | Yes | Yes | Poor |
| Houston and Pickering 200052 | 2 |
Methods: parents of child under 10; three categories sampled: ‘Frequent users . . . used the service twice or more in the previous 6 months or four times or more in the previous year . . . One-off callers . . . one or more call in the past 6 months and none in the prior 3 years’ ‘Non-callers . . . not used the service in the previous 3 years’ |
OOH – delivered by general practice | – | Yes | Yes | Yes |
| Howard et al. 200591 | 1 |
Title: ‘choosing the ED for non-urgent medical care’ Methods: ‘seeking treatment in the emergency department for care of a nonurgent complaint and who could articulate the reasons for choosing this source of care as opposed to their PCP’ |
ED | – | Yes | Yes | Yes |
| Hugenholtz et al. 200953 | 2 |
Title: ‘seeking immediate primary care for their children’ Abstract: ‘ask for immediate medical attention for their children’ Methods: ‘had visited the cooperative with a sick child’. Most coded as U3 by triaging assistant ‘urgent, assess within several hours for medical or emotional reasons’ but, after examination, half needed no treatment or only advice about self-treatment |
OOH – delivered by co-op | Second group purposively sampled – ‘children had required immediate referral to hospital care’ – to compare decision-making in two groups | Yes | Poor | Poor |
| Hunter et al. 201368 | 2 | Methods: ‘patients with one or more of four LTCs’ – chronic obstructive pulmonary disease, coronary heart disease, asthma and diabetes | Mixed emergency care: ED, WIC and OOH | – | Poor | Poor | Yes |
| Keizer Beache and Guell 201682 | 1 |
Title: ‘Nonurgent accident and emergency department use’ Methods: ‘patients who had been triaged as non-urgent by the AED nurse’ |
ED | – | Yes | Yes | Yes |
| Koziol-McLain et al. 200077 | 1 |
Title: ‘Seeking care for nonurgent medical conditions in the ED’ Methods: ‘discharged from the ED; and . . . triaged as nonurgent upon their arrival in the ED . . . based on a triage category of greater than 2 (triage categories range from 1 (life threatening) to 4)’ |
ED | – | Yes | Poor | Poor |
| Lawson et al. 201492 | 2 | Methods: ‘patients with documented histories of asthma who were presenting with . . . asthma, shortness of breath, cough, or chest pain’ | ED | – | Yes | Poor | Yes |
| MacKichan et al. 201798 | 1 | Methods: ‘Patients who had self-referred to the ED, who attended the ED during GP practice opening hours, who had no investigations while at the ED and/or were discharged with “advice/guidance only”’ | ED | Some data ethnographic observations and staff experiences | Yes | Yes | Yes |
| McGuigan and Watson 201054 | 1 |
Title: ‘Nonurgent attendance at EDs’ Methods: ‘non-urgent attenders who had been recorded as “self-referral” by receptionists at . . . ED . . . for whom the ED was the first choice for care’ |
ED | – | Poor | No | No |
| Neill et al. 201683 | 2 |
Abstract: ‘parents of children under five years, from a range of socioeconomic groups’ Methods: ‘parents in communities with differing social, economic and ethnic profiles’ |
Health service use | – | Yes | Yes | Yes |
| Olsson and Hansagi 200169 | 2 |
Title: ‘Repeated use of the ED’ Methods: ‘frequent visitor’ defined as ‘a patient who has made four or more visits during the previous 12 months’, focusing on ‘patients who did not require particularly specialised medical care, which is why we used the patient database . . . for general surgery and internal medicine’ (i.e. not gynaecology, ENT, paediatric, psychiatry, etc.) |
ED | – | Yes | Poor | Yes |
| Shaw et al. 201355 | 1 |
Title: ‘patients who use the ED for primary care needs’ Abstract: ‘patients who were discharged from the low acuity area of a university hospital ED’ Methods: ‘patients who sought treatment in the ED and were triaged to the non-urgent area’ based on the Emergency Severity Index – levels 4 and 5 |
ED | – | Yes | Poor | Yes |
| Stafford et al. 201456 | 1 |
Abstract: ‘inappropriate attendances at urgent care facilities’ Methods: ‘patients presenting to urgent care . . . diagnosed with simple mechanical back pain by their urgent care clinician’ and meeting the inclusion criterion of ‘requiring only advice and analgesia’ |
Mixed emergency/urgent care: ED, WIC and OOH service | – | Poor | No | No |
| Wilkin et al. 201284 | 2 | Methods: members of a local community with ‘the second highest rates of calls to 911’ according to hospital data. Some of the participants ‘were identified as 911 users in a previous research project’ | ED | – | No | Yes | Yes |
| Woolfenden et al. 200057 | 1 |
Title: ‘use of a paediatric ED as an ambulatory care service’ Methods: ‘parents of children who presented with non-urgent illnesses to a tertiary PED’ |
PED | – | Yes | No | Poor |
Appendix 4 Methodological rigour of included qualitative articles: Critical Appraisal Skills Programme items
| Authors and year of publication | Quality appraisal | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1: Clear aim? | 2: Qualitative method appropriate? | 3: Design appropriate to aims? | 4: Recruitment strategy appropriate to aims? | 5: Data collection addressed research issue? | 6: Researcher/participant relationship considered? | 7: Ethics issues considered? | 8: Analysis sufficiently rigorous? | 9: Clear findings? | 10: Research valuable? (New insights? Links to existing literature? Links to policy/practice? Further research? Transferability of findings?) | |
| Agarwal et al. 201272 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| aAhl et al. 200665 | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes | Yes | Yes |
| Becker et al. 199344 | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Can’t tell | Can’t tell | Yes | Yes |
| Berry et al. 200866 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Booker et al. 201473 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Brousseau et al. 201145 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Yes |
| Calnan 198346 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Can’t tell | Yes | Limited |
| Capp et al. 201667 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Limited | Limited |
| Chin et al. 200647 | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Can’t tell | Limited | Yes |
| de Bont et al. 201548 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Durand et al. 20127 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Fieldston et al. 201249 | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Can’t tell | Can’t tell | Limited | Yes |
| bGoeman et al. 200494 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Limited | Yes |
| Goepp et al. 200485 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes |
| Guttman et al. 200350 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes | Yes |
| Mostajer Haqiqi et al. 201681 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Hopton et al. 199651 | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes |
| Houston and Pickering 200052 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Can’t tell | Yes | Yes |
| Howard et al. 200591 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Hugenholtz et al. 200953 | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes |
| Hunter et al. 201368 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Keizer Beache and Guell 201682 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Koziol-McLain et al. 200077 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Yes |
| Lawson et al. 201492 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Limited | Yes |
| MacKichan et al. 201798 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| McGuigan and Watson 201054 | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Can’t tell | Limited | Limited |
| Neill et al. 201683 | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Olsson and Hansagi 200169 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Shaw et al. 201355 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Stafford et al. 201456 | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Wilkin et al. 201284 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes | Yes |
| Woolfenden et al. 200057 | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Can’t tell | Can’t tell | Limited | Limited |
Appendix 5 Data extraction for included qualitative articles
| Authors, year of publication and country | Service | Stated aim/objective, plus additional text where this provides justification for inclusion of the paper | Data collection method; number of participants | Identified subgroup and degree of focus in paper | Key themes/issues identified | Formal theories explicitly named in text and informing methods and/or discussion |
|---|---|---|---|---|---|---|
| Agarwal et al. 2012, UK72 | ED and urgent care centre; two-thirds arriving via ambulance | To explore the reasons for attendance at the ED by patients who could have been managed in an alternative service | Semistructured interviews; 23 adult patients and/or their carers | LTCs – mentioned briefly in findings |
|
– |
| aAhl et al. 2006, Sweden65 | Ambulance, including pre-hospital care | To analyse and describe patients’ experiences related to the decision to call an ambulance and when waiting for it to arrive:The issue of inappropriate use of ambulance transport [. . .] To further understand whether or not patients use ambulance care in an inappropriate manner | Exploratory interviews; 20 adult patients | No |
1. Making up one’s mind: major decision, others often involved – situation experienced as intolerable, must get immediate help; someone else points out urgency of need; realising that other options have been exhausted after trying to manage on their own; overcoming hesitancy; ambulance fastest, most safe and secure form of transport, enabling immediate access to care; emphasising the need for care, including to others 2. Waiting for help: experiencing the wait as long; desire immediate help; alone with one’s feelings – anxious, afraid, neglected, lonely; avoiding/handing over responsibility – feeling of relief; sense of safety and trust |
Morse and O’Brien: impact of sudden illness on ability to communicate – mentioned in discussion |
| Becker et al. 1993, USA44 | Mixed emergency/urgent care: range of services unclear, mostly ED | To study the significant variables related to individuals’ response to asthma:. . . an ethos (. . .) surrounds ED use by asthma patients . . . Eighty-five percent of all visits to EDs have been found to be for non-life-threatening reasons . . . staff may regard persons whose lives do not appear to be in danger as wasting their time | Monthly semistructured interviews (×3) and symptom diary; 95 adult patients | LTC (asthma) – focus of the paper |
|
– |
| Berry et al., 2008, USA66 | PED | To identify parents’ reasons for choosing the ED over their PCP for non-urgent paediatric care | Semistructured ethnographic interviews; 31 families (37 parents) of children (age limit not specified) | Parents: focus of the paper |
|
Andersen and Aday behavioural model of health-care utilisation: interview schedule based on this, but not explored in the discussion |
| Booker et al. 2014, UK73 | Ambulance | To explore and understand patient and carer decision-making around calling an ambulance for primary care-appropriate health problems | Semistructured interviews; 16 adult patients or carers of adults | No |
Main theme: patient and carer anxiety in urgent care decision-making Subthemes: |
– |
| Brousseau et al. 2011, USA45 | PED | To better understand parental decisions to seek care for their children and physician perceptions of parents’ decisions to seek non-urgent ED care | In-depth interviews of 26 parents within 20 PCPs; children’s age limit not specified | Parents: focus of the paper |
|
– |
| Calnan 1983, UK46 | ED | A comparison of the processes involved in the decision to seek medical care for sufferers with different types of complaint:Explanations of patient use of the hospital accident and emergency department have, until recently, been coloured by provider’s conceptions of how the service ought to be used. Emphasis has been placed on examining why patients did not go to their GP | Semistructured interviews; 575 adult patients | No |
|
Bloor, drawing on Schutz’s work (not referenced in Calnan’s paper) re ‘systems of relevance and the attribution of meaning’ – differences in cognitive process between novel and routine decision-making: explored in discussion |
| Capp et al. 2016, USA67 | ED | To clarify from the patient’s perspective why adult Medicaid enrollees who want to receive care co-ordination services to improve primary care utilisation frequently use the ED | Secondary analysis of one- to two-page interview summaries from RCT; 100 adult patients | Deprivation: adults with active Medicaid insurance – focus of the paper |
|
– |
| Chin et al. 2006, USA47 | PED | To understand patterns of decision making among families presenting to a PED for non-acute care and to understand PED staff responses | In-depth semistructured interviews; 12 family caregivers of child (age limit not specified) (and 19 ED and paediatric ED staff members) | Parents/caregivers: focus of the paper. Also deprivation – from PCPs in medically underserved areas (inner city and rural): unintentional but noted as finding |
|
– |
| de Bont et al. 2015, the Netherlands48 | OOH – delivered by co-op | To explore experiences of parents when having visited GP OOH services with their febrile child | Semistructured interviews; 20 parents of child under 12 years old | Parents: focus of the paper |
|
– |
| Durand et al. 2012, France7 | ED | To explore the reasons why people with non-urgent complaints choose to come to EDs, and how ED health-care professionals perceive the phenomenon of ‘non-urgency’ | Semistructured interviews; 87 adult patients (and 34 ED staff) across 10 EDs | No |
|
– |
| Fieldston et al. 2012, USA49 | PED | To elicit and to describe guardians’ and health-care professionals’ opinions of reasons for non-urgent PED visits | Focus groups: three groups of guardians of child under 5 years old (n = 25) – most had taken a child to ED, but no indication of appropriateness of visit [and three groups of paediatric health professionals (n = 42)] | Parents and deprivation: target group – sample recruited from services for families at risk/on low incomes |
|
– |
| bGoeman et al. 2004, Australia94 | ED | To explore the reasons why individuals recurrently present with asthma to hospital EDs:Episodes of severe asthma should be mostly preventable with current best treatment, yet asthma remains one of the most common reasons why patients seek emergency care . . . A number of ideas have been proposed as to why some individuals recurrently seek emergency care for asthma | In-depth semistructured interviews; 32 adult patients | LTC: asthma not controlled by current therapy – focus of the paper |
|
– |
| Goepp et al. 2004, USA85 | Service use decisions, particularly PED | Low acuity use of EDs is often viewed as misuse or abuse. We designed a program to help users access services more efficiently | Participatory action model and ethnographic study: observation, interviews, groups; 90 families (interviews and focus groups with workers) | Deprivation and parents: families on low income, minority groups |
Initially designed a programme using lay community workers to educate families about the health-care system and measure change in use of PCP and PED Negative reaction from participants and recognition of their needs led to change to qualitative methods to understand factors driving people’s health-seeking behaviour in order to educate health-care professionals. Findings of ethnographic evaluation: |
– |
| Guttman et al. 2003, USA50 | ED and PED | To identify reasons for medically non-urgent ED visits from the users’ perspective and to identify through their reasons what may have prompted them to use the ED for medical care they could have ostensibly received in primary care sites | Structured interview protocol with open-ended questions and scaled items regarding decision; 331 parents/guardians of child up to 18 years old and 77 adult patients | Parents: majority of the data relate to this group, although 11 out of 12 themes were found in both groups | 1. Conceptions of needs:
|
– |
| Mostajer Haqiqi et al. 2016, Canada81 | PED | To explore the reasons that lead parents to select the ED over a dental clinic for their child’s non-traumatic dental problem | Semistructured interviews; 15 parents of a child under 10 years old | Parents: focus of the paper | 1. Family-related barriers:
|
Grembowski: dental care process model: used as conceptual framework for study |
| Hopton et al. 1996, UK51 | OOH: delivered by general practice | To investigate patients’ accounts of calling the doctor OOH:Alongside the debate about factors influencing demand for out of hours care is debate about the appropriateness of the demand. [. . .] Despite this evidence and calls for patient education as a means of tackling increasing demand and inappropriate use, patients’ perspectives on out of hours calls have been neglected | Semistructured interviews; 23 adult patients or calling on behalf of an adult and 23 parents of child under 16 years old | Deprivation: product of geographical area where research was carried out – area of high deprivation |
|
– |
| Houston and Pickering 2000, UK52 | OOH: delivered by general practice | To investigate how parents use the GP OOH service:The apparent increase in out-of-hours GP consultations is a source of considerable concern and debate. The underlying premise of much of this concern is that many of these calls are unnecessary | In-depth semistructured interviews; 29 families of child under 10 years old | Parents: focus of the paper |
|
Antonovsky: work regarding coping mechanisms and Sense of Coherence: explored in results and discussion |
| Howard et al. 2005, USA91 | ED | Why do people choose to come to the ED instead of their PCP with nonurgent medical complaints? | Interviews using open-ended interview tool modified from survey questionnaire; 31 adult patients (aged 18–50 years) | No |
|
– |
| Hugenholtz et al. 2009, the Netherlands53 | OOH: delivered by co-op | To gain insight into the health-seeking behaviour of parents who ask for immediate medical attention for their children:Data from GP co-operatives . . . show that children make more use of OOH care than members of other age groups, although the health problems . . . are less urgent from a medical point of view | Semistructured interviews; 27 parents of child up to 16 years old – 19 with minor illness; eight requiring immediate referral to hospital | Parents: focus of the paper |
|
Beck; Giddens – Risk Society: explored in discussion |
| Hunter et al. 2013, UK68 | Mixed emergency care: ED, OOH and WIC | To elaborate on the processes by which patients with long-term conditions choose between available options for care in response to a health crisis, to inform the development of future policy and guidance on modifying emergency care use:. . . health policy in many countries seeks to constrain and shape patients’ care decisions in order to ensure that the service accessed reflects the level of medical need | Semistructured interviews; 50 adult patients | LTC (asthma/chronic obstructive pulmonary disease/coronary heart disease/diabetes): focus of the paper |
1. Patients framed instances of emergency care as unavoidable: reluctant to use, do not want to be a burden, no other option because of seriousness of problem 2. Previous experiences shape future emergency care use: |
Dixon-Woods: candidacy Rogers, Hassell and Nicolaas: recursivity– discussion framed around these concepts (Rogers et al. consider how people’s experience of service use influences future help-seeking, but do not actually conceptualise it as ‘recursivity’, and this word is not in the book’s index) |
| Keizer Beache and Guell 2016, St Vincent and the Grenadines82 | ED | To explore attitudes of non-urgent accident and emergency department patients in a middle income health-care setting and to understand how and why they decide to seek emergency care and resist using primary care facilities | Semistructured interviews; 12 adult patients | No |
|
Andersen model of health service use: informed interview guide and mentioned in discussion Nilsen et al: role of habit in decision-making; Zimmerman multilevel theory of population health: role of habit, custom and power in decision-making – explored in discussion |
| Koziol-McLain et al. 2000, USA77 | ED | To gain an understanding of the context in which patients choose to seek health care in an ED:The policy goal of shifting nonurgent visits from the ED to nonemergency health care settings is commonly devised, planned and implemented without considering patients’ perspectives | Unstructured interviews; 30 adults | Uninsured patients: can we assume deprivation? |
Toughing it out: putting up with things before going to ED Symptoms overwhelming self-care measures: mostly use of over-the-counter medicines; decision made when problem began to have an impact on function Calling a friend: seeking support and advice from friends and relatives, especially mothers Nowhere else to go: could not access non-emergency care; being referred to ED by other health-care providers Convenience: work schedules, child care and transportation barriers affecting choice of ED |
Malone: ED’s hidden role as almshouse (giving social care) impacted by changing service context (higher volume and acuity in ED, medicalisation of problems, less community support services) → frequent users seen as problem rather than system – paper framed around this Cassel; Sacks: impact of illness on whole self, contrasted with medical approach of treating a symptom |
| Lawson et al. 2014, USA92 | ED | To explore the reasons for asthma-related ED use among adults:ED visits for asthma have long been considered ‘avoidable’ yet exacerbations remain common . . . it has never been more important for health systems to find new ways to reduce the number of ED visits and hospitalisations for asthma | Semistructured interviews; 26 adults | LTC (asthma) | 1. Reasons for ED utilisation:
|
– |
| MacKichan et al., 2017, UK98 | ED | To describe how processes of primary care access influence decisions to seek help at the ED:Given that a significant proportion of ED attendances . . . are discharged with ‘advice only’ . . . and that ED attendances peak during the working day on Monday, it is presumed that better access to primary care will relieve pressure on EDs | Ethnographic study of six GP practices: observation of reception areas, document analysis, interviews; 20 patients and nine parent/carers (19 clinical and non-clinical staff) | Parents: brief reference in results to particular experiences |
|
Dixon-Woods: candidacy; Rogers et al.: recursivity – explored in discussion (see note in Hunter re ‘recursivity’) |
| McGuigan and Watson 2010, UK54 | ED | To discover the factors influencing patient decisions to attend EDs for non-urgent treatment | Short, semistructured telephone interviews (mean length 3 minutes); 196 adults | No | Reasons for attendance:
|
Zola: five triggers for seeking help when ill or injured |
| Neill et al. 2016, UK83 | Service use decisions | To examine how parents of children aged under 5 years from a range of socioeconomic groups use information to make decisions during acute childhood illness at home:Consultation rates for children are rising, yet little is known about factors that influence parents’ help-seeking behaviours . . .Professional and political solutions have not reduced demand; therefore collaborative approaches . . . are now needed to improve parents’ access to informationOngoing epidemiological research aims to identify those most likely to consult, so interventions can be targeted at these groups. This must be balanced with concerns about discouraging service use by children who need urgent care | Focus groups and interviews; 27 parents from South Asia, travelling and white British communities | Parents: focus of the paper |
|
– |
| Olsson and Hansagi 2001, Sweden69 | ED |
To explore what lies behind repeated ED use from the patients’ own perspectives: A subgroup of patients make frequent use of hospital EDs, thereby accounting for a substantial portion of the total number of visits to these facilities . . . Repeated visits may frustrate the staff . . . as these patients’ complaints are often judged as non-urgent and inappropriate for ED care |
In-depth interviews; 10 adult patients | Deprivation not deliberately targeted but sample ‘all . . . outside or on the periphery of the labour market . . . working lives . . . severely disrupted by their health problems’ | Key points:
|
Brief exploration of how patients’ presentation of their problems and match with the services provided affects staff attitudes and how well needs are met. References include Dingwall: categorisation of ‘good patients, bad patients and children’ |
| Shaw et al. 2013, USA55 | ED | Exploring the decision-making processes to use the ED for non-urgent needs of medically underserved patients | Semistructured interviews; 30 adult patients | No: half unemployed but no discussion of deprivation |
Two subgroups: with and without knowledge of alternatives 1. No knowledge of alternative primary care options: no PCP; belief that ED available only if had no insurance 2. Knowledge of alternatives: |
Andersen: behavioural model of health services use – explored and elaborated in discussion |
| Stafford et al. 2014, UK56 | Mixed emergency/urgent care: ED, WIC OOH service | To explore why patients with simple mechanical back pain seek urgent care | Semistructured interviews; 11 adult patients | Simple mechanical back pain: focus of the paper |
|
– |
| Wilkin et al. 2012, USA84 | ED | What factors influence residents’ [in a low-income urban community] decisions to use emergency versus primary care? | Community forum discussions; three groups of 12–21 adults from area with high 911 use (only some participants identified as 911 users) | Deprivation: community with low socioeconomic status, poor health – focus of the paper |
|
– |
| Woolfenden et al. 2000, Australia57 | PED | Explored the parental attitudes, perceptions and beliefs that play a role in the use of a tertiary PED when a child has a non-urgent illness | In-depth semistructured interviews; 25 parents of children (age range not specified, sample includes up to 14) | Parents – focus of the paper |
|
– |
Appendix 6 Programme theories in interviews
| Participants | Programme theory | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Parents | ||||||||||
| 11 – 999 | ||||||||||
| 13 – ED | ||||||||||
| 14 – ED | ||||||||||
| 17 – GP | ||||||||||
| 18 – ED | ||||||||||
| 20 – ED | ||||||||||
| 21 – ED | ||||||||||
| 23 – GP | ||||||||||
| 25 – GP | ||||||||||
| 29 – ED | ||||||||||
| 30 – ED | ||||||||||
| 31 – GP | ||||||||||
| 32 – GP | ||||||||||
| 33 – ED | ||||||||||
| 42 – GP | ||||||||||
| 48 – ED | ||||||||||
| Young adults | ||||||||||
| 3 – ED | ||||||||||
| 5 – ED | ||||||||||
| 6 – ED | ||||||||||
| 9 – 999 | ||||||||||
| 34 – GP | ||||||||||
| 35 – GP | ||||||||||
| 36 – ED | ||||||||||
| 37 – ED | ||||||||||
| 38 – GP | ||||||||||
| 39 – GP | ||||||||||
| 40 – GP | ||||||||||
| 43 – ED | ||||||||||
| 44 – GP | ||||||||||
| 45 – ED | ||||||||||
| 46 – ED | ||||||||||
| 47 – ED | ||||||||||
| Deprived communities | ||||||||||
| 1 – 999 | ||||||||||
| 2 – ED | ||||||||||
| 4 – ED | ||||||||||
| 7 – 999 | ||||||||||
| 8 – 999 | ||||||||||
| 10 – 999 | ||||||||||
| 12 – GP | ||||||||||
| 15 – GP | ||||||||||
| 16 – GP | ||||||||||
| 19 – ED | ||||||||||
| 22 – GP | ||||||||||
| 24 – GP | ||||||||||
| 26 – GP | ||||||||||
| 27 – ED | ||||||||||
| 28 – GP | ||||||||||
| 41 – ED | ||||||||||
Appendix 7 Sociodemographic details of focus group attendees
| Characteristic | Focus group attendees (n) | Total (n) | ||
|---|---|---|---|---|
| Parents | Young adults | Socially deprived | ||
| Sex | ||||
| Male | 0 | 2 | 2 | 4 |
| Female | 5 | 4 | 2 | 11 |
| Age (years) | ||||
| 18–20 | 0 | 1 | 0 | 1 |
| 21–30 | 2 | 5 | 0 | 7 |
| 31–40 | 2 | 0 | 1 | 3 |
| 41–50 | 0 | 0 | 0 | 0 |
| 51–60 | 0 | 0 | 1 | 1 |
| ≥ 60 | 0 | 0 | 2 | 2 |
| Missing data | 1 | 0 | 0 | 1 |
| Length of residence in city (years) | ||||
| < 1 | 0 | 0 | 0 | 0 |
| 1–5 | 1 | 4 | 0 | 5 |
| > 5 | 3 | 2 | 4 | 9 |
| Missing data | 1 | 0 | 0 | 1 |
| Ethnicity | ||||
| White British | 1 | 5 | 3 | 9 |
| White other | 1 | 0 | 0 | 1 |
| Black British | 0 | 0 | 1 | 1 |
| Black African | 1 | 0 | 0 | 1 |
| Chinese | 0 | 1 | 0 | 1 |
| Pakistani | 1 | 0 | 0 | 1 |
| Missing data | 1 | 0 | 0 | 1 |
| Marital status | ||||
| Married/living as married | 3 | 1 | 2 | 6 |
| Separated/divorced | 0 | 0 | 1 | 1 |
| Single/not married | 1 | 5 | 1 | 7 |
| Missing data | 1 | 0 | 0 | 1 |
| Children? | ||||
| Yes | 5 | 0 | 3 | 8 |
| No | 0 | 6 | 1 | 7 |
| Employment status | ||||
| Working full time | 0 | 2 | 1 | 3 |
| Working part time | 3 | 2a | 2a | 7a |
| Homemaker full time | 1 | 0 | 0 | 1 |
| Retired | 0 | 0 | 1a | 1a |
| Student (full time) | 0 | 3a | 0 | 3a |
| Missing data | 1 | 0 | 0 | 1 |
Appendix 8 NHS Choices advice for symptoms in vignettes
Below we summarise what NHS Choices says about the six symptoms that we used in our vignettes.
Cough
URL: www.nhs.uk/conditions/cough (accessed 25 February 2020)
They go away in 3 weeks and there is no need to see a GP.
A pharmacist can help.
See a GP only if you have chest pain, it’s hard to breathe or you have had it for > 3 weeks.
Diarrhoea and vomiting
URL: www.nhs.uk/conditions/diarrhoea-and-vomiting/ (accessed 25 February 2020)
Common in adults, children and babies.
Usually treat it at home.
Take paracetamol but check the leaflet before giving to a child.
Diarrhoea usually stops within 5–7 days and vomiting usually stops in 1 or 2 days.
A pharmacist can help.
Call NHS 111 for children under some circumstances.
Go to A&E if have sudden severe headache or vomit blood.
Bruised ribs
URL: www.nhs.uk/conditions/broken-or-bruised-ribs/ (accessed 25 February 2020)
Ribs cannot be easily splinted or supported like other bones, so they are usually left to heal naturally.
There’s often no need for an X-ray.
Take painkillers.
Call NHS 111 if not improved in a few weeks or if you have a high temperature.
Call 999 or go to A&E if caused by a serious accident or coughing up blood.
Back pain
URL: www.nhs.uk/conditions/back-pain/ (accessed 25 February 2020)
It is very common and normally improves within a few weeks or months.
Usually not serious and will get better over time.
Take painkillers.
Get help if pain does not start to improve in a few weeks, pain stops day-to-day activities, pain is severe and getting worse or struggling to cope.
Contact GP or NHS 111 if have numbness in buttocks, a high temperature or if it started after a serious accident.
Fever in children
URL: www.nhs.uk/conditions/fever-in-children/ (accessed 25 February 2020)
High temperature is very common in young children.
You can usually look after your child or baby at home. The temperature should go down over 3 or 4 days.
Give them paracetamol or ibuprofen depending on their age.
See GP if child is under 3 months old and has a temperature of ≥ 38 °C, 3–6 months with temperature of ≥ 39 °C, has rash, high temperature has lasted > 5 days, is not their usual self or has high temperature that does not come down with drugs.
It’s quite rare for fever to be a sign of anything serious but call 999 or go to A&E if the child has a rash that does not fade, has a stiff neck or has a weak high-pitched cry that is not their normal cry.
Call NHS 111 if cannot speak to GP and do not know what to do.
Appendix 9 Results of logistic regressions for tendency to make ‘clinically unnecessary’ use of a service
| Variable | Univariate | Final multivariable model | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | n | p-value | Odds ratio (95% CI) | p-value | |
| Sociodemographic characteristics | |||||
| Age (years) | 0.000 | ||||
| 18–24 | 1 | 169 | |||
| 25–34 | 0.9 (0.5 to 1.6) | 384 | |||
| 35–44 | 0.8 (0.4 to 1.4) | 467 | |||
| 45–54 | 0.6 (0.3 to 1.1) | 469 | |||
| 55–64 | 0.9 (0.5 to 1.6) | 508 | |||
| 65–74 | 1.3 (0.8 to 2.3) | 499 | |||
| ≥ 75 | 1.6 (0.9 to 2.8) | 405 | |||
| Sex | 0.018 | 0.015 | |||
| Female | 1 | 1649 | 1 | ||
| Male | 1.3 (1.1 to 1.7) | 1257 | 1.5 (1.1 to 2.0) | ||
| Ethnicity | 0.000 | 0.005 | |||
| White | 1 | 2572 | 1 | ||
| BAME | 2.0 (1.5 to 2.7) | 334 | 1.9 (1.2 to 3.0) | ||
| Social class | 0.000 | 0.004 | |||
| I | 1 | 214 | 1 | ||
| II | 1.7 (0.9 to 3.3) | 1039 | 1.6 (0.7 to 3.6) | ||
| III non-manual | 2.0 (0.98 to 3.95) | 569 | 1.3 (0.5 to 3.0) | ||
| III manual | 4.3 (2.2 to 8.6) | 416 | 3.0 (1.3 to 7.1) | ||
| IV and V | 4.5 (2.3 to 8.9) | 524 | 2.0 (0.8 to 4.6) | ||
| Armed forces | 2.2 (0.7 to 6.6) | 52 | 1.1 (0.2 to 3.0) | ||
| Deprivation | 0.000 | ||||
| 5 (affluent) | 1 | 611 | |||
| 4 | 1.0 (0.6 to 1.4) | 638 | |||
| 3 | 1.0 (0.7 to 1.5) | 536 | |||
| 2 | 1.5 (1.0 to 2.2) | 545 | |||
| 1 (most deprived) | 1.8 (1.3 to 2.6) | 576 | |||
| Rurality | 0.087 | ||||
| Rural | 1 | 665 | |||
| Urban | 1.3 (0.96 to 1.7) | 2241 | |||
| Region | 0.473 | ||||
| North England | 1 | 474 | |||
| Midlands | 0.9 (0.6 to 1.3) | 794 | |||
| South England | 0.9 (0.6 to 1.2) | 957 | |||
| London | 1.3 (0.8 to 2.0) | 285 | |||
| Wales | 1.0 (0.6 to 1.9) | 132 | |||
| Scotland | 0.9 (0.5 to 1.4) | 264 | |||
| In household with children aged < 5 years old | 0.119 | ||||
| No | 1 | 2591 | |||
| Yes | 0.7 (0.5 to 1.1) | 300 | |||
| Resources available | |||||
| Car ownership | 0.000 | 0.000 | |||
| ≥ 1 car | 1 | 1478 | 1 | ||
| No car | 3.3 (2.4 to 4.4) | 428 | 2.1 (1.4 to 3.2) | ||
| Missing | 1.4 (1.0 to 1.8) | 1000 | 1.7 (1.2 to 2.4) | ||
| Personal access to the internet | 0.000 | 0.004 | |||
| Yes | 1 | 2542 | 1 | ||
| No | 2.9 (2.2 to 3.8) | 364 | 1.8 (1.2 to 2.6) | ||
| Health | |||||
| General health | 0.000 | ||||
| Excellent | 1 | 223 | |||
| Very good | 0.7 (0.4 to 1.3) | 725 | |||
| Good | 1.1 (0.7 to 1.9) | 799 | |||
| Fair | 2.2 (1.3 to 3.8) | 360 | |||
| Poor | 2.3 (1.2 to 4.2) | 163 | |||
| Can’t choose | 2.2 (0.9 to 5.7) | 39 | |||
| Missing/not included | 597 | ||||
| Long-term limiting illness | 0.000 | ||||
| None | 1 | 1766 | |||
| Non-limiting | 1.3 (0.96 to 1.7) | 586 | |||
| Limiting | 2.0 (1.6 to 2.7) | 541 | |||
| Programme theories | |||||
| 1, Risk: uncertainty causes anxiety | |||||
| Worry pain is a sign of something serious | 0.000 | 0.001 | |||
| Not likely at all | 1 | 358 | 1 | ||
| Not likely | 0.7 (0.5 to 1.03) | 1138 | 0.7 (0.4 to 2.3) | ||
| Fairly likely | 1.4 (0.9 to 2.0) | 876 | 1.6 (0.9 to 2.7) | ||
| Very likely | 2.1 (1.4 to 3.3) | 415 | 1.6 (0.9 to 2.9) | ||
| It depends | 1.4 (0.7 to 2.6) | 119 | 1.5 (0.7 to 3.5) | ||
| Confident in deciding to see a doctor or self-care | 0.038 | ||||
| Very confident | 1 | 993 | |||
| Fairly | 1.2 (0.9 to 1.7) | 1130 | |||
| Not very | 1.7 (0.9 to 3.1) | 89 | |||
| Never had problem | 2.1 (1.2 to 3.7) | 97 | |||
| 2, Risk: previous traumatic event | |||||
| Had problem, did not see doctor and was serious | 0.114 | ||||
| No | 1 | 2219 | |||
| Yes | 1.2 (0.95 to 1.6) | 687 | |||
| 3, Risk: responsibility for others | |||||
| Variable not tested this in regression | |||||
| 4, Speed: need to get back to normal | |||||
| Sleep | 0.000 | ||||
| Do not see doctor | 1 | 2010 | |||
| See doctor if sleep loss | 1.9 (1.4 to 2.5) | 634 | |||
| See doctor if any loss | 3.4 (2.5 to 4.7) | 262 | |||
| Work | 0.000 | ||||
| Do not see doctor | 1 | 935 | |||
| See doctor if work loss | 1.3 (0.97 to 1.7) | 1709 | |||
| See doctor if any loss | 3.3 (2.3 to 4.8) | 262 | |||
| 5, Speed: need to seek pain relief | |||||
| Likely to take medication | 0.106 | ||||
| Very likely | 1 | 1081 | |||
| Fairly | 0.7 (0.6 to 0.97) | 1257 | |||
| Not very | 0.8 (0.5 to 1.2) | 376 | |||
| Not at all | 1.3 (0.8 to 2.1) | 135 | |||
| Depends | 0.8 (0.3 to 1.9) | 57 | |||
| 6, Speed: waited long enough | |||||
| Variable not included | |||||
| 7a, Stressful lives | |||||
| Overwhelmed when have health problem | 0.000 | ||||
| Strongly disagree | 1 | 487 | 0.000 | 1 | |
| Disagree | 1.3 (0.8 to 2.0) | 872 | 1.1 (0.6 to 1.7) | ||
| Neither | 3.1 (2.0 to 4.9) | 537 | 2.3 (1.4 to 3.8) | ||
| Strongly agree/agree | 4.4 (2.7 to 7.0) | 314 | 2.2 (1.3 to 3.8) | ||
| Never had problem | 1.4 (0.6 to 3.3) | 99 | 1.5 (0.6 to 3.6) | ||
| Find life stressful | 0.095 | ||||
| No | 1 | 637 | |||
| A bit | 0.8 (0.6 to 1.1) | 1316 | |||
| Quite | 0.9 (0.6 to 1.2) | 637 | |||
| Very | 1.4 (0.9 to 2.1) | 297 | |||
| Don’t know | 0.9 (0.2 to 3.8) | 19 | |||
| Someone to care for them if they are ill | 0.000 | ||||
| Definitely | 1 | 1240 | |||
| Probably | 1.0 (0.7 to 1.3) | 697 | |||
| Probably not | 1.6 (1.1 to 2.3) | 280 | |||
| Don’t know | 2.9 (1.7 to 4.9) | 92 | |||
| Can take time off work for GP | 0.000 | ||||
| Yes | 1 | 1078 | |||
| Yes but not easy | 0.7 (0.4 to 1.2) | 275 | |||
| No | 1.0 (0.5 to 2.0) | 127 | |||
| Not applicable/missing | 2.2 (1.7 to 2.9) | 1426 | |||
| 7b, Low burden | |||||
| Travel to ED | 1 | 0.000 | |||
| Very difficult | 0.7 (0.5 to 1.1) | 610 | |||
| Neither | 0.6 (0.4 to 0.7) | 269 | |||
| Fairly easy | 0.4 (0.3 to 0.6) | 1172 | |||
| Very easy | 1 | 855 | |||
| Opening hours a problem | 0.009 | ||||
| Disagree/strongly disagree | 1 | 1098 | |||
| Neither | 1.6 (1.2 to 2.2) | 608 | |||
| Strongly agree/agree | 1.1 (0.8 to 1.5) | 603 | |||
| Prefer no appointments | 0.000 | ||||
| Disagree/strongly disagree | 1 | 685 | |||
| Neither | 1.3 (0.9 to 1.8) | 799 | |||
| Strongly agree/agree | 1.9 (1.3 to 2.7) | 825 | |||
| Want convenient times | 0.905 | ||||
| Disagree/strongly disagree | 1 | 253 | |||
| Neither | 1.0 (0.6 to 1.5) | 708 | |||
| Strongly agree/agree | 0.9 (0.6 to 1.4) | 1348 | |||
| Willing to wait in waiting room | 0.170 | ||||
| Disagree/strongly disagree | 1 | 361 | |||
| Neither | 1.0 (0.5 to 1.8) | 194 | |||
| Strongly agree/agree | 1.3 (0.9 to 1.9) | 2351 | |||
| 8, Compliance with family/friends | |||||
| Check with family and friends for what to do | 0.010 | 0.022 | |||
| Not very likely | 1 | 545 | 1 | ||
| Not likely | 0.8 (0.5 to 1.1) | 746 | 0.9 (0.5 to 1.3) | ||
| Fairly likely | 0.7 (0.5 to 0.98) | 1061 | 0.6 (0.4 to 0.9) | ||
| Very likely | 1.2 (0.8 to 1.6) | 554 | 1.1 (0.7 to 1.8) | ||
| 9, Views of services | |||||
| Prefer ED for quick tests | 0.000 | ||||
| Disagree/strongly disagree | 1 | 1159 | |||
| Neither | 1.9 (1.4 to 2.6) | 797 | |||
| Strongly agree/agree | 2.8 (2.0 to 4.0) | 353 | |||
| Missing, self-complete | 0 | ||||
| Doctors know more at ED | 0.001 | ||||
| Disagree/strongly disagree | 1 | 850 | |||
| Neither | 1.5 (1.1 to 2.1) | 1041 | |||
| Strongly agree/agree | 2.0 (1.4 to 2.9) | 418 | |||
| Missing, self-complete | 0 | ||||
| No confidence in GP | 0.203 | ||||
| Strongly disagree | 1 | 538 | |||
| Disagree | 1.3 (0.9 to 1.9) | 1008 | |||
| Neither | 1.6 (1.0 to 2.4) | 446 | |||
| Agree | 1.8 (1.1 to 3.1) | 165 | |||
| Strongly agree | 1.3 (0.6 to 2.9) | 76 | |||
| Don’t know | 2.2 (0.9 to 5.4) | 42 | |||
| Missing | 1.9 (0.7 to 5.3) | 34 | |||
| Missing, self-complete | 0 | ||||
| 10, Frustration with access to GP | |||||
| Hard to get GP appointment | 0.543 | ||||
| Disagree/strongly disagree | 1 | 819 | |||
| Neither | 1.2 (0.8 to 1.7) | 353 | |||
| Strongly agree/agree | 1.0 (0.8 to 1.3) | 1137 | |||
| Missing, self-complete | 0 | ||||
| Registered with GP | 0.329 | ||||
| Yes | 1 | 2840 | |||
| No | 0.6 (0.3 to 1.6) | 65 | |||
| Work or looking after family makes it difficult to see GP | 0.000 | 0.000 | |||
| Disagree/strongly disagree | 1 | 1197 | 1 | ||
| Neither | 1.3 (0.9 to 1.8) | 455 | 1.0 (0.7 to 1.4) | ||
| Strongly agree/agree | 0.5 (0.3 to 0.8) | 410 | 0.4 (0.2 to 0.6) | ||
| Not applicable | 1.6 (1.1 to 2.4) | 247 | 1.4 (0.9 to 2.2) | ||
| Believe people use ED because can’t get GP appointment | 0.021 | ||||
| Strongly agree/agree | 1 | 2441 | |||
| Neither | 1.2 (0.9 to 1.8) | 339 | |||
| Disagree/strongly disagree | 1.9 (1.2 to 3.0) | 126 | |||
| Awareness of services | |||||
| Know range of NHS services to use | 0.573 | ||||
| Very confident | 1 | 1436 | |||
| Fairly confident | 1.1 (0.9 to 1.4) | 1189 | |||
| Not confident/not at all | 1.0 (0.7 to 1.6) | 280 | |||
| Can find out when NHS services are open | 0.048 | ||||
| Very confident | 1 | 1487 | |||
| Fairly confident | 1.2 (0.96 to 1.6) | 1163 | |||
| Not confident/not at all | 1.6 (1.1 to 2.3) | 255 | |||
| Can find out what test available at services | 0.440 | ||||
| Very confident | 1 | 963 | |||
| Fairly confident | 0.8 (0.7 to 1.1) | 1307 | |||
| Not confident/not at all | 0.96 (0.7 to 1.3) | 635 | |||
| How to contact GP OOH | 0.716 | ||||
| Very | 1 | 1338 | |||
| Fairly | 1.1 (0.8 to 1.4) | 1056 | |||
| Not very confident | 1.1 (0.7 to 1.5) | 389 | |||
| Not at all | 1.3 (0.8 to 2.3) | 122 | |||
| Will look up on the internet to see what to do | 0.000 | ||||
| Very likely | 1 | 428 | |||
| Fairly likely | 0.7 (0.5 to 1.1) | 752 | |||
| Not very likely | 1.0 (0.7 to 1.5) | 680 | |||
| Not at all | 1.6 (1.1 to 2.3) | 1016 | |||
| Missing | 1.0 (0.3 to 3.4) | 30 | |||
| Will look up on the internet to decide what problem is | 0.000 | ||||
| Very likely | 1 | 667 | |||
| Fairly likely | 0.7 (0.5 to 0.9) | 797 | |||
| Not very likely | 0.9 (0.6 to 1.3) | 472 | |||
| Not at all | 1.5 (1.1 to 2.1) | 940 | |||
| Missing | 0.9 (0.3 to 3.1) | 30 | |||
| Recursivity | |||||
| If tests are done I was right to make contact | 0.000 | ||||
| Disagree/strongly disagree | 1 | 280 | |||
| Neither | 1.1 (0.7 to 1.8) | 793 | |||
| Strongly agree/agree | 1.9 (1.2 to 3.0) | 1236 | |||
| Missing, self-complete | 0 | ||||
| Health literacy | |||||
| Lower health literacy compared with higher health literacy – understand information | 2.1 (1.8 to 2.6) | 2269 | 0.000 | 1.7 (1.3 to 2.0) | 0.000 |
| Lower health literacy compared with higher health literacy – ability to communicate | 1.7 (1.4 to 2.0) | 2269 | 0.000 | ||
| Recent use of health care | |||||
| Ambulance use | 0.000 | 0.000 | |||
| Never | 1 | 1349 | 1 | ||
| ≥ 12 months | 1.2 (0.9 to 1.6) | 1108 | 1.4 (1.0 to 1.9) | ||
| < 12 months | 2.2 (1.6 to 3.0) | 448 | 2.5 (1.7 to 3.8) | ||
| Ambulance frequent user | 0.002 | ||||
| < 3 times | 1 | 2842 | |||
| ≥ 3 times in 12 months | 2.7 (1.5 to 4.8) | 64 | |||
| ED use | 0.096 | ||||
| Never | 1 | 411 | |||
| ≥ 12 months | 0.8 (0.5 to 1.1) | 1478 | |||
| 6–12 months | 0.9 (0.6 to 1.4) | 366 | |||
| 3–6 months | 1.2 (0.8 to 1.9) | 234 | |||
| < 3 months | 1.0 (0.7 to 1.5) | 416 | |||
| ED frequent user | 0.000 | ||||
| < 3 times | 1 | 2577 | |||
| ≥ 3 times in 12 months | 2.4 (1.6 to 3.5) | 328 | |||
| Contacted GP | 0.115 | ||||
| Never | 1 | 65 | |||
| ≥ 12 months | 0.4 (0.2 to 0.9) | 454 | |||
| 6–12 months | 0.5 (0.3 to 1.1) | 484 | |||
| 3–6 months | 0.4 (0.2 to 0.9) | 518 | |||
| < 3 months | 0.5 (0.3 to 0.99) | 1384 | |||
| Attitudes towards overuse of health services | |||||
| Too many use 999 | 0.657 | ||||
| Strongly agree/agree | 1 | 2516 | |||
| Neither | 1.1 (0.7 to 1.5) | 313 | |||
| Disagree/strongly disagree | 1.3 (0.7 to 2.6) | 77 | |||
| Too many use ED | 0.032 | ||||
| Strongly agree/agree | 1 | 2515 | |||
| Neither | 1.3 (0.9 to 1.9) | 291 | |||
| Disagree/strongly disagree | 1.8 (1.1 to 3.1) | 100 | |||
| Too many use GP | 0.071 | ||||
| Strongly agree/agree | 1 | 2082 | |||
| Neither | 1.1 (0.9 to 1.5) | 577 | |||
| Disagree/strongly disagree | 1.5 (1.1 to 2.2) | 247 | |||
| Reluctance to use ED | 0.000 | ||||
| Strongly agree/agree | 1 | 1348 | |||
| Neither | 0.7 (0.5 to 0.9) | 734 | |||
| Disagree/strongly disagree | 0.5 (0.3 to 0.6) | 824 | |||
| Variables | Significance | Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age of respondent(grouped) < 7 category > dv | 0.542 | |||
| Age of respondent(grouped) < 7 category > dv(1) | 0.286 | 1.650 | 0.657 | 4.143 |
| Age of respondent(grouped) < 7 category > dv(2) | 0.880 | 1.075 | 0.418 | 2.765 |
| Age of respondent(grouped) < 7 category > dv(3) | 0.730 | 1.180 | 0.462 | 3.015 |
| Age of respondent(grouped) < 7 category > dv(4) | 0.342 | 1.551 | 0.628 | 3.833 |
| Age of respondent(grouped) < 7 category > dv(5) | 0.171 | 1.910 | 0.756 | 4.823 |
| Age of respondent(grouped) < 7 category > dv(6) | 0.321 | 1.640 | 0.618 | 4.353 |
| Sex of respondent(1) | 0.017 | 0.664 | 0.475 | 0.930 |
| Limiting long term condition or disability dv | 0.602 | |||
| Limiting long term condition or disability dv(1) | 0.484 | 1.157 | 0.769 | 1.743 |
| Limiting long term condition or disability dv(2) | 0.701 | 0.911 | 0.567 | 1.465 |
| Respondent: social class [pre-SOC2000] best estimate dv | 0.016 | |||
| Respondent: social class [pre-SOC2000] best estimate dv(1) | 0.300 | 1.588 | 0.662 | 3.811 |
| Respondent: social class [pre-SOC2000] best estimate dv(2) | 0.616 | 1.267 | 0.503 | 3.194 |
| Respondent: social class [pre-SOC2000] best estimate dv(3) | 0.020 | 2.938 | 1.184 | 7.290 |
| Respondent: social class [pre-SOC2000] best estimate dv(4) | 0.106 | 2.110 | 0.854 | 5.213 |
| Respondent: social class [pre-SOC2000] best estimate dv(5) | 0.724 | 1.328 | 0.275 | 6.423 |
| IMD_ALL | 0.253 | |||
| IMD_ALL(1) | 0.128 | 1.451 | 0.899 | 2.344 |
| IMD_ALL(2) | 0.477 | 1.209 | 0.716 | 2.040 |
| IMD_ALL(3) | 0.887 | 1.038 | 0.618 | 1.745 |
| IMD_ALL(4) | 0.074 | 1.621 | 0.955 | 2.751 |
| DV To which of these racial groups do you consider you belong? (compressed)(1) | 0.009 | 1.938 | 1.176 | 3.194 |
| When did you last see or speak to the 999 ambulance service (for yourself or someone else)? | 0.000 | |||
| When did you last see or speak to the 999 ambulance service (for yourself or someone else)?(1) | 0.005 | 0.551 | 0.362 | 0.839 |
| When did you last see or speak to the 999 ambulance service (for yourself or someone else)?(2) | 0.000 | 0.399 | 0.259 | 0.614 |
| Do you personally have internet access at home/work/elsewhere or on a smartphone/tablet/mobile device?(1) | 0.177 | 1.389 | 0.862 | 2.239 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be | 0.191 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(1) | 0.027 | 0.519 | 0.290 | 0.929 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(2) | 0.115 | 0.568 | 0.281 | 1.147 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(3) | 0.629 | 0.809 | 0.343 | 1.909 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(4) | 0.698 | 1.743 | 0.106 | 28.792 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do | 0.695 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(1) | 0.330 | 1.385 | 0.719 | 2.669 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(2) | 0.332 | 1.436 | 0.692 | 2.979 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(3) | 0.670 | 1.225 | 0.482 | 3.112 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(4) | 0.431 | 0.323 | 0.019 | 5.386 |
| How many, if any, cars or vans does your household own or have the regular use of? <summary> | 0.001 | |||
| How many, if any, cars or vans does your household own or have the regular use of? <summary>(1) | 0.001 | 0.469 | 0.297 | 0.739 |
| How many, if any, cars or vans does your household own or have the regular use of? <summary>(2) | 0.422 | 0.834 | 0.536 | 1.299 |
| In general, would you say your health is . . . (excellent to poor) | 0.118 | |||
| In general, would you say your health is . . . (excellent to poor)(1) | 0.593 | 0.841 | 0.445 | 1.587 |
| In general, would you say your health is . . . (excellent to poor)(2) | 0.567 | 0.834 | 0.447 | 1.555 |
| In general, would you say your health is . . . (excellent to poor)(3) | 0.294 | 1.434 | 0.732 | 2.812 |
| In general, would you say your health is . . . (excellent to poor)(4) | 0.850 | 0.924 | 0.406 | 2.103 |
| In general, would you say your health is . . . (excellent to poor)(5) | 0.250 | 2.197 | 0.575 | 8.392 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D | 0.514 | |||
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(1) | 0.402 | 0.857 | 0.597 | 1.230 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(2) | 0.162 | 0.572 | 0.261 | 1.252 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(3) | 0.495 | 0.743 | 0.317 | 1.742 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do | 0.030 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(1) | 0.008 | 0.545 | 0.348 | 0.855 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(2) | 0.519 | 0.856 | 0.534 | 1.372 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(3) | 0.872 | 0.959 | 0.574 | 1.601 |
| HPrbDr13 | 0.239 | |||
| HPrbDr13(1) | 0.221 | 1.259 | 0.870 | 1.822 |
| HPrbDr13(2) | 0.109 | 1.573 | 0.904 | 2.735 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D | 0.006 | |||
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(1) | 0.004 | 2.516 | 1.341 | 4.720 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(2) | 0.001 | 2.732 | 1.498 | 4.983 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(3) | 0.001 | 3.336 | 1.632 | 6.820 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious | 0.001 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(1) | 0.621 | 1.120 | 0.714 | 1.757 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(2) | 0.003 | 0.488 | 0.302 | 0.790 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(3) | 0.345 | 0.739 | 0.394 | 1.385 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(4) | 0.541 | 1.291 | 0.569 | 2.929 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)? | 0.266 | |||
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(1) | 0.593 | 0.849 | 0.465 | 1.548 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(2) | 0.459 | 1.164 | 0.779 | 1.740 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(3) | 0.301 | 0.778 | 0.483 | 1.253 |
| The opening hours for some NHS services are a problem for me SC: B, C, D | 0.196 | |||
| The opening hours for some NHS services are a problem for me SC: B, C, D(1) | 0.508 | 1.163 | 0.744 | 1.818 |
| The opening hours for some NHS services are a problem for me SC: B, C, D(2) | 0.348 | 0.814 | 0.529 | 1.252 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D | 0.500 | |||
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(1) | 0.258 | 0.801 | 0.545 | 1.177 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(2) | 0.889 | 0.970 | 0.636 | 1.481 |
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D | 0.353 | |||
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D(1) | 0.422 | 0.856 | 0.585 | 1.252 |
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D(2) | 0.338 | 1.255 | 0.788 | 2.000 |
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D(3) | 0.347 | 1.470 | 0.659 | 3.283 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D | 0.004 | |||
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(1) | 0.888 | 1.033 | 0.656 | 1.628 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(2) | 0.005 | 0.500 | 0.309 | 0.807 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(3) | 0.016 | 0.480 | 0.264 | 0.872 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(4) | 0.353 | 0.658 | 0.272 | 1.590 |
| Can you take time away from your work, during working hours, to see a GP? | 0.694 | |||
| Can you take time away from your work, during working hours, to see a GP?(1) | 0.325 | 0.671 | 0.303 | 1.485 |
| Can you take time away from your work, during working hours, to see a GP?(2) | 0.786 | 1.134 | 0.459 | 2.802 |
| Can you take time away from your work, during working hours, to see a GP?(3) | 0.699 | 1.091 | 0.702 | 1.694 |
| I think doctors at A&E know more than GPs SC: B, C, D | 0.927 | |||
| I think doctors at A&E know more than GPs SC: B, C, D(1) | 0.760 | 1.069 | 0.696 | 1.641 |
| I think doctors at A&E know more than GPs SC: B, C, D(2) | 0.994 | 0.998 | 0.622 | 1.602 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D | 0.215 | |||
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(1) | 0.913 | 0.975 | 0.617 | 1.540 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(2) | 0.159 | 0.705 | 0.433 | 1.147 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D | 0.159 | |||
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(1) | 0.087 | 0.712 | 0.483 | 1.050 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(2) | 0.658 | 1.135 | 0.647 | 1.990 |
| Ability | 0.790 | 0.952 | 0.661 | 1.371 |
| Understand | 0.047 | 0.690 | 0.478 | 0.996 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open | 0.216 | |||
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open(1) | 0.401 | 1.160 | 0.821 | 1.638 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open(2) | 0.227 | 0.689 | 0.376 | 1.261 |
| I think too many people use A&E when they do not need to | 0.639 | |||
| I think too many people use A&E when they do not need to(1) | 0.648 | 0.879 | 0.505 | 1.529 |
| I think too many people use A&E when they do not need to(2) | 0.428 | 1.390 | 0.616 | 3.140 |
| Many people use A&E because they cannot get a GP appointment easily | 0.207 | |||
| Many people use A&E because they cannot get a GP appointment easily(1) | 0.157 | 1.443 | 0.868 | 2.397 |
| Many people use A&E because they cannot get a GP appointment easily(2) | 0.220 | 1.579 | 0.761 | 3.275 |
| Many people are reluctant to use A&E when they have an urgent health problem | 0.121 | |||
| Many people are reluctant to use A&E when they have an urgent health problem(1) | 0.466 | 0.864 | 0.583 | 1.280 |
| Many people are reluctant to use A&E when they have an urgent health problem(2) | 0.040 | 0.660 | 0.444 | 0.981 |
| Constant | 0.823 | 0.808 | ||
| Variables | Univariate | Final multivariable model | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | n | p-value | Odds ratio (95% CI) | p-value | |
| Sociodemographic characteristics | |||||
| Age (years) | 0.977 | ||||
| 18–24 | 1 | 169 | |||
| 25–34 | 1.0 (0.6 to 1.5) | 384 | |||
| 35–44 | 1.0 (0.6 to 1.5) | 467 | |||
| 45–54 | 0.9 (0.6 to 1.4) | 469 | |||
| 55–64 | 0.9 (0.6 to 1.4) | 508 | |||
| 65–74 | 0.9 (0.7 to 1.5) | 499 | |||
| ≥ 75 | 0.8 (0.6 to 1.5) | 405 | |||
| Sex | 0.001 | 1 | 0.015 | ||
| Female | 1 | 1649 | |||
| Male | 1.4 (1.1 to 1.7) | 1257 | 1.3 (1.0 to 1.6) | ||
| Ethnicity | < 0.001 | 0.003 | |||
| White | 1 | 2572 | 1 | ||
| BAME | 2.1 (1.6 to 2.7) | 334 | 1.7 (1.2 to 2.4) | ||
| Social class | 0.034 | ||||
| I | 1 | 214 | |||
| II | 1.6 (1.0 to 2.5) | 1039 | |||
| III non-manual | 1.6 (0.97 to 2.5) | 569 | |||
| III manual | 2.0 (1.2 to 3.3) | 416 | |||
| IV and V | 1.8 (1.1 to 2.9) | 524 | |||
| Armed forces | 2.9 (1.4 to 6.1) | 52 | |||
| Deprivation | 0.051 | ||||
| 5 (affluent) | 1 | 611 | |||
| 4 | 1.0 (0.7 to 1.3) | 638 | |||
| 3 | 0.9 (0.7 to 1.3) | 536 | |||
| 2 | 1.0 (0.7 to 1.3) | 545 | |||
| 1 (most deprived) | 1.4 (1.0 to 1.8) | 576 | |||
| Rurality | 0.004 | ||||
| Rural | 1 | 665 | |||
| Urban | 1.4 (1.1 to 1.8) | 2241 | |||
| Region | 0.09 | ||||
| North England | 1 | 474 | |||
| Midlands | 1.0 (0.7 to 1.3) | 794 | |||
| South England | 0.9 (0.7 to 1.2) | 957 | |||
| London | 1.4 (0.95 to 2.0) | 285 | |||
| Wales | 1.4 (0.9 to 2.3) | 132 | |||
| Scotland | 1.2 (0.8 to 1.8) | 264 | |||
| In household with children aged < 5 years old | 0.503 | ||||
| No | 1 | 2591 | |||
| Yes | 1.1 (0.8 to 1.5) | 300 | |||
| Resources available | |||||
| Car ownership | 1 | 0.561 | |||
| ≥ 1 cars | 1.2 (0.9 to 1.5) | 1478 | |||
| No car | 1.1 (0.9 to 1.3) | 428 | |||
| Missing | 1 | 1000 | |||
| Personal access to internet | 0.393 | ||||
| Yes | 1 | 2542 | |||
| No | 1.1 (0.9 to 1.5) | 364 | |||
| Health | |||||
| General health | 0.775 | ||||
| Excellent | 1 | 223 | |||
| Very good | 0.8 (0.5 to 1.2) | 725 | |||
| Good | 1.0 (0.6 to 1.4) | 799 | |||
| Fair | 1.0 (0.6 to 1.5) | 360 | |||
| Poor | 0.9 (0.5 to 1.5) | 163 | |||
| Can’t choose | 0.8 (0.3 to 2.1) | 39 | |||
| Missing/not included | 0 | ||||
| Long-term limiting illness | 0.549 | ||||
| None | 1 | 1766 | |||
| Non-limiting | 0.9 (0.7 to 1.1) | 586 | |||
| Limiting | 1.0 (0.8 to 1.3) | 541 | |||
| Don’t know | 0.8 (0.2 to 3.8) | 13 | |||
| Programme theories | |||||
| 1, Risk: uncertainty causes anxiety | |||||
| Worry pain is a sign of something serious | < 0.001 | ||||
| Not likely at all | 1 | 358 | |||
| Not likely | 1.1 (0.8 to 1.6) | 1138 | |||
| Fairly likely | 1.4 (0.97 to 1.9) | 876 | |||
| Very likely | 2.0 (1.4 to 2.9) | 415 | |||
| It depends | 0.9 (0.5 to 1.6) | 119 | |||
| Confident in deciding to see a doctor or self-care | 0.283 | ||||
| Very confident | 1 | 993 | |||
| Fairly confident | 1.2 (0.98 to 1.5) | 1130 | |||
| Not very confident | 1.4 (0.8 to 2.4) | 89 | |||
| Never had problem | 1.1 (0.6 to 1.9) | 97 | |||
| 2, Risk: previous traumatic event | |||||
| Had problem, did not see doctor and was serious | 0.562 | ||||
| No | 1 | 2219 | |||
| Yes | 0.9 (0.7 to 1.2) | 687 | |||
| 3, Risk: responsibility for others | |||||
| 4, Speed: need to get back to normal | |||||
| Sleep | < 0.001 | ||||
| Do not see doctor | 1 | 2010 | |||
| See doctor if sleep loss | 1.9 (1.5 to 2.4) | 634 | |||
| See doctor if any loss | 1.8 (1.3 to 2.5) | 262 | |||
| Work | |||||
| Do not see doctor | 1 | 935 | < 0.001 | 1 | 0.037 |
| See doctor if work loss | 1.6 (1.3 to 2.0) | 1709 | 1.4 (1.1 to 1.8) | ||
| See doctor if any loss | 2.1 (1.5 to 2.9) | 262 | 1.3 (0.9 to 2.1) | ||
| 5, Speed: need to seek pain relief | |||||
| Likely to take medication | 0.162 | ||||
| Very likely | 1 | 1081 | |||
| Fairly likely | 0.8 (0.6 to 0.99) | 1257 | |||
| Not very likely | 0.9 (0.7 to 1.3) | 376 | |||
| Not at all likely | 0.6 (0.4 to 1.1) | 135 | |||
| Depends | 0.8 (0.4 to 1.6) | 57 | |||
| 6, Speed: waited long enough | |||||
| 7a, Stressful lives | |||||
| Overwhelmed when have health problem | 0.005 | ||||
| Strongly disagree | 1 | 487 | |||
| Disagree | 1.4 (1.0 to 2.0) | 872 | |||
| Neither | 1.8 (1.3 to 2.5) | 537 | |||
| Strongly agree/agree | 1.9 (1.3 to 2.8) | 314 | |||
| Never had problem | 1.3 (0.7 to 2.4) | 99 | |||
| Find life stressful | 0.192 | ||||
| No | 1 | 637 | |||
| A bit | 1.2 (0.97 to 1.6) | 1316 | |||
| Quite | 1.0 (0.7 to 1.3) | 637 | |||
| Very | 1.1 (0.8 to 1.6) | 297 | |||
| Don’t know | 0.6 (0.1 to 2.7) | 19 | |||
| Someone to care for them if they are ill | 0.165 | ||||
| Definitely | 1 | 1240 | |||
| Probably | 0.8 (0.6 to 0.97) | 697 | |||
| Probably not | 0.9 (0.6 to 1.2) | 280 | |||
| Don’t know | 1.0 (0.6 to 1.8) | 92 | |||
| Can take time off work for GP | 0.270 | ||||
| Yes | 1 | 1078 | |||
| Yes but not easy | 1.0 (0.7 to 1.5) | 275 | |||
| No | 0.6 (0.4 to 1.1) | 127 | |||
| Not applicable/missing | 1.1 (0.9 to 1.3) | 1426 | |||
| 7b, Low burden | |||||
| Travel to ED | 0.251 | ||||
| Very difficult | 1 | 610 | |||
| Neither | 0.9 (0.6 to 1.3) | 269 | |||
| Fairly easy | 1.1 (0.8 to 1.4) | 1172 | |||
| Very easy | 0.9 (0.7 to 1.2) | 855 | |||
| Opening hours a problem | 0.974 | ||||
| Disagree/strongly disagree | 1 | 1098 | |||
| Neither | 1.0 (0.8 to 1.3) | 608 | |||
| Strongly agree/agree | 1.0 (0.8 to 1.3) | 603 | |||
| Prefer no appointments | 0.553 | ||||
| Disagree/strongly disagree | 1 | 685 | |||
| Neither | 1.0 (0.8 to 1.5) | 799 | |||
| Strongly agree/agree | 1.2 (0.9 to 1.5) | 825 | |||
| Want convenient times | 0.899 | ||||
| Disagree/strongly disagree | 1 | 253 | |||
| Neither | 0.9 (0.6 to 1.4) | 708 | |||
| Strongly agree/agree | 0.9 (0.6 to 1.3) | 1348 | |||
| Willing to wait in waiting room | 0.222 | ||||
| Disagree/strongly disagree | 1 | 361 | |||
| Neither | 1.0 (0.6 to 1.6) | 194 | |||
| Strongly agree/agree | 1.2 (0.9 to 1.7) | 2351 | |||
| 8, Compliance with family/friends | |||||
| Check with family and friends for what to do | 0.019 | ||||
| Not very likely | 1 | 545 | |||
| Not likely | 1.2 (0.9 to 1.7) | 746 | |||
| Fairly likely | 1.2 (0.9 to 1.5) | 1061 | |||
| Very likely | 1.6 (1.2 to 2.2) | 554 | |||
| 9, Views of services | |||||
| Prefer ED for quick tests | < 0.001 | 0.003 | |||
| Disagree/strongly disagree | 1 | 1159 | 1 | ||
| Neither | 1.3 (0.99 to 1.6) | 797 | 1.2 (0.9 to 1.5) | ||
| Strongly agree/agree | 2.2 (1.5 to 2.7) | 353 | 1.7 (1.3 to 2.3) | ||
| Missing, self-complete | 0 | ||||
| Doctors know more at ED | 0.007 | ||||
| Disagree/strongly disagree | 1 | 850 | |||
| Neither | 1.4 (1.1 to 1.8) | 1041 | |||
| Strongly agree/agree | 1.6 (1.1 to 2.1) | 418 | |||
| Missing, self-complete | 0 | ||||
| No confidence in GP | 0.186 | ||||
| Strongly disagree | 1 | 538 | |||
| Disagree | 1.2 (0.9 to 1.6) | 1088 | |||
| Neither | 1.6 (1.1 to 2.2) | 446 | |||
| Agree | 1.4 (0.9 to 2.2) | 165 | |||
| Strongly agree | 0.9 (0.4 to 1.9) | 76 | |||
| Don’t know | 1.7 (0.8 to 3.6) | 42 | |||
| Missing | 1.0 (0.4 to 2.8) | 34 | |||
| Missing, self-complete | 0 | ||||
| 10, Frustration with access to GP | |||||
| Hard to get GP appointment | 0.636 | ||||
| Disagree/strongly disagree | 1 | 819 | |||
| Neither | 1.0 (0.7 to 1.4) | 353 | |||
| Strongly agree/agree | 0.9 (0.7 to 1.1) | 1137 | |||
| Missing, self-complete | 0 | ||||
| Registered with GP | 0.611 | ||||
| Yes | 1 | 2840 | |||
| No | 1.2 (0.6 to 2.2) | 65 | |||
| Work or looking after family makes it difficult to see GP | 0.138 | ||||
| Disagree/strongly disagree | 1 | 1197 | |||
| Neither | 1.1 (0.8 to 1.5) | 455 | |||
| Strongly agree/agree | 0.7 (0.5 to 1.0) | 410 | |||
| Not applicable | 0.9 (0.6 to 1.3) | 247 | |||
| Believe people use ED because they can’t get GP appointment | 0.541 | ||||
| Strongly agree/agree | 1 | 2441 | |||
| Neither | 1.2 (0.9 to 1.6) | 339 | |||
| Disagree/strongly disagree | 1.0 (0.6 to 1.5) | 126 | |||
| Awareness of services | |||||
| Know range of NHS services to use | 0.349 | ||||
| Very confident | 1 | 1436 | |||
| Fairly confident | 1.0 (0.8 to 1.2) | 1189 | |||
| Not confident/not at all | 1.2 (0.9 to 1.7) | 280 | |||
| Can find out when NHS services are open | 0.875 | ||||
| Very confident | 1 | 1487 | |||
| Fairly confident | 1.0 (0.8 to 1.2) | 1163 | |||
| Not confident/not at all | 0.9 (0.6 to 1.3) | 255 | |||
| Can find out what test available at services | 0.520 | ||||
| Very confident | 1 | 963 | |||
| Fairly confident | 0.9 (0.8 to 1.2) | 1307 | |||
| Not confident/not at all | 0.9 (0.7 to 1.1) | 635 | |||
| How to contact GP OOH | 0.105 | ||||
| Very confident | 1 | 1338 | |||
| Fairly confident | 0.9 (0.7 to 1.1) | 1056 | |||
| Not very confident | 1.2 (0.9 to 1.6) | 389 | |||
| Not at all confident | 0.7 (0.4 to 1.3) | 122 | |||
| Will look up on the internet to see what to do | 0.069 | ||||
| Very likely | 1 | 428 | |||
| Fairly likely | 1.0 (0.8 to 1.4) | 752 | |||
| Not very likely | 1.4 (1.0 to 1.9) | 680 | |||
| Not at all | 1.0 (0.7 to 1.4) | 1016 | |||
| Missing | 30 | ||||
| Will look up on the internet to decide what problem is | 0.063 | ||||
| Very likely | 1 | 667 | |||
| Fairly likely | 0.7 (0.6 to 0.97) | 797 | |||
| Not very likely | 1.0 (0.8 to 1.4) | 472 | |||
| Not at all | 0.8 (0.6 to 1.1) | 940 | |||
| Missing | 0.5 (0.1 to 1.5) | 30 | |||
| Recursivity | |||||
| If tests are done I was right to make contact | 0.005 | 0.05 | |||
| Disagree/strongly disagree | 1 | 280 | 1 | ||
| Neither | 1.4 (0.9 to 2.1) | 793 | 1.2 (0.8 to 1.8) | ||
| Strongly agree/agree | 1.7 (1.2 to 2.6) | 1236 | 1.5 (1.0 to 2.3) | ||
| Missing, self-complete | 0 | ||||
| Health literacy | |||||
| Lower health literacy compared with higher health literacy – understand information | 1.1 (0.97 to 1.4) | 2269 | 0.108 | ||
| Lower health literacy compared with higher health literacy – ability to communicate | 1.0 (0.9 to 1.2) | 2269 | 0.884 | ||
| Recent use of health care | 0.436 | ||||
| Ambulance use | |||||
| Never | 1 | 1349 | |||
| ≥ 12 months | 0.9 (0.8 to 1.1) | 1108 | |||
| < 12 months | 1.1 (0.8 to 1.5) | 448 | |||
| Ambulance frequent user | 0.366 | ||||
| < 3 times | 1 | 2842 | |||
| ≥ 3 times in 12 months | 1.3 (0.7 to 2.4) | 64 | |||
| ED use | < 0.001 | ||||
| Never | 1 | 411 | |||
| ≥ 12 months | 1.0 (0.7 to 1.3) | 1478 | |||
| 6–12 months | 1.2 (0.8 to 1.8) | 366 | |||
| 3–6 months | 2.0 (1.4 to 3.0) | 234 | |||
| < 3 months | 1.3 (0.9 to 1.9) | 416 | |||
| ED frequent user | < 0.001 | ||||
| < 3 times | 1 | 2738 | |||
| ≥ 3 times in 12 months | 2.2 (1.6 to 3.2) | 167 | |||
| Contacted GP | 0.544 | ||||
| Never | 1 | 65 | |||
| ≥ 12 months | 1.2 (0.6 to 2.6) | 454 | |||
| 6–12 months | 1.2 (0.6 to 2.5) | 484 | |||
| 3–6 months | 1.4 (0.7 to 2.9) | 518 | |||
| < 3 months | 1.4 (0.7 to 2.9) | 1384 | |||
| Attitudes towards overuse of health services | |||||
| Too many use 999 | 0.001 | ||||
| Strongly agree/agree | 1 | 2516 | |||
| Neither | 1.7 (1.3 to 2.2) | 313 | |||
| Disagree/strongly disagree | 1.4 (0.8 to 2.5) | 77 | |||
| Too many use ED | < 0.001 | < 0.001 | |||
| Strongly agree/agree | 1 | 2515 | 1 | ||
| Neither | 1.5 (1.1 to 2.1) | 291 | 1.4 (1.0 to 2.0) | ||
| Disagree/strongly disagree | 2.6 (1.7 to 4.0) | 100 | 3.1 (1.9 to 5.3) | ||
| Too many use GP | 0.541 | ||||
| Strongly agree/agree | 1 | 2441 | |||
| Neither | 1.2 (0.9 to 1.6) | 339 | |||
| Disagree/strongly disagree | 1.0 (0.6 to 1.5) | 126 | |||
| Reluctance to use ED | 0.028 | 0.012 | |||
| Strongly agree/agree | 1 | 1348 | 1 | ||
| Neither | 1.4 (1.1 to 1.7) | 734 | 1.5 (1.1 to 2.0) | ||
| Disagree/strongly disagree | 1.1 (0.8 to 1.4) | 824 | 1.3 (1.0 to 1.7) | ||
| Variables | Significance | Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Sex of respondent(1) | 0.031 | 0.765 | 0.600 | 0.976 |
| Respondent: social class [pre-SOC2000] best estimate dv | 0.421 | |||
| Respondent: social class [pre-SOC2000] best estimate dv(1) | 0.122 | 1.542 | 0.890 | 2.670 |
| Respondent: social class [pre-SOC2000] best estimate dv(2) | 0.105 | 1.617 | 0.904 | 2.894 |
| Respondent: social class [pre-SOC2000] best estimate dv(3) | 0.048 | 1.836 | 1.006 | 3.351 |
| Respondent: social class [pre-SOC2000] best estimate dv(4) | 0.176 | 1.512 | 0.831 | 2.750 |
| Respondent: social class [pre-SOC2000] best estimate dv(5) | 0.097 | 2.320 | 0.860 | 6.263 |
| IMD_ALL | 0.421 | |||
| IMD_ALL(1) | 0.069 | 0.701 | 0.477 | 1.029 |
| IMD_ALL(2) | 0.392 | 0.846 | 0.577 | 1.241 |
| IMD_ALL(3) | 0.263 | 0.806 | 0.552 | 1.177 |
| IMD_ALL(4) | 0.658 | 0.919 | 0.633 | 1.336 |
| DV To which of these racial groups do you consider you belong? (compressed)(1) | 0.020 | 0.635 | 0.432 | 0.932 |
| UrbRur_ALL(1) | 0.211 | 0.828 | 0.617 | 1.113 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)? | 0.558 | |||
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(1) | 0.300 | 1.285 | 0.799 | 2.066 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(2) | 0.830 | 0.953 | 0.617 | 1.473 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(3) | 0.577 | 0.907 | 0.643 | 1.279 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(4) | 0.627 | 0.895 | 0.572 | 1.400 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do | 0.314 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(1) | 0.066 | 0.734 | 0.528 | 1.020 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(2) | 0.355 | 0.848 | 0.598 | 1.202 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(3) | 0.522 | 0.882 | 0.600 | 1.296 |
| HPrbDr13 | 0.047 | |||
| HPrbDr13(1) | 0.014 | 1.404 | 1.071 | 1.840 |
| HPrbDr13(2) | 0.429 | 1.207 | 0.757 | 1.926 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious | 0.735 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(1) | 0.233 | 0.802 | 0.557 | 1.153 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(2) | 0.215 | 0.794 | 0.551 | 1.144 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(3) | 0.589 | 0.877 | 0.546 | 1.411 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(4) | 0.400 | 0.743 | 0.372 | 1.483 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D | 0.376 | |||
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(1) | 0.907 | 0.978 | 0.668 | 1.432 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(2) | 0.921 | 0.981 | 0.676 | 1.424 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(3) | 0.120 | 0.703 | 0.452 | 1.096 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(4) | 0.590 | 0.836 | 0.435 | 1.605 |
| I think doctors at A&E know more than GPs SC: B, C, D | 0.415 | |||
| I think doctors at A&E know more than GPs SC: B, C, D(1) | 0.643 | 1.082 | 0.776 | 1.507 |
| I think doctors at A&E know more than GPs SC: B, C, D(2) | 0.537 | 0.892 | 0.620 | 1.283 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D | 0.067 | |||
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(1) | 0.057 | 0.709 | 0.497 | 1.011 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(2) | 0.023 | 0.662 | 0.464 | 0.945 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D | 0.155 | |||
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(1) | 0.144 | 0.823 | 0.634 | 1.069 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(2) | 0.117 | 0.711 | 0.464 | 1.089 |
| I think too many people call 999 for an ambulance when they do not need to | 0.038 | |||
| I think too many people call 999 for an ambulance when they do not need to(1) | 0.018 | 1.621 | 1.085 | 2.423 |
| I think too many people call 999 for an ambulance when they do not need to(2) | 0.521 | 0.779 | 0.363 | 1.671 |
| I think too many people use A&E when they do not need to | 0.005 | |||
| I think too many people use A&E when they do not need to(1) | 0.542 | 1.144 | 0.743 | 1.762 |
| I think too many people use A&E when they do not need to(2) | 0.001 | 2.927 | 1.525 | 5.616 |
| I think too many people go to their GP when they do not need to | 0.727 | |||
| I think too many people go to their GP when they do not need to(1) | 0.510 | 1.110 | 0.814 | 1.514 |
| I think too many people go to their GP when they do not need to(2) | 0.759 | 0.931 | 0.592 | 1.466 |
| Many people are reluctant to use A&E when they have an urgent health problem | 0.028 | |||
| Many people are reluctant to use A&E when they have an urgent health problem(1) | 0.019 | 1.420 | 1.059 | 1.905 |
| Many people are reluctant to use A&E when they have an urgent health problem(2) | 0.033 | 1.356 | 1.024 | 1.795 |
| Constant | 0.038 | 0.398 | ||
| Variable | Univariate | Final multivariable model | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | n | p-value | Odds ratio (95% CI) | p-value | |
| Sociodemographic characteristics | |||||
| Age (years) | < 0.001 | < 0.001 | |||
| 18–24 | 1 | 169 | 1 | ||
| 25–34 | 1.0 (0.6 to 1.4) | 384 | 0.9 (0.6 to 1.5) | ||
| 35–44 | 1.0 (0.6 to 1.4) | 467 | 1.1 (0.7 to 1.7) | ||
| 45–54 | 1.4 (0.9 to 2.1) | 469 | 1.6 (1.0 to 2.5) | ||
| 55–64 | 1.7 (1.1 to 2.4) | 508 | 1.9 (1.2 to 3.0) | ||
| 65–74 | 1.6 (1.1 to 2.3) | 499 | 1.7 (1.1 to 2.7) | ||
| ≥ 75 | 1.1 (0.7 to 1.6) | 405 | 1.1 (0.7 to 1.8) | ||
| Sex | 0.002 | 0.007 | |||
| Female | 1 | 1649 | 1 | ||
| Male | 1.3 (1.1 to 1.5) | 1257 | 1.3 (1.1 to 1.5) | ||
| Ethnicity | 0.038 | 0.003 | |||
| White | 1 | 2572 | 1 | ||
| BAME | 1.3 (1.0 to 1.6) | 334 | 1.6 (1.2 to 2.3) | ||
| Social class | 0.072 | ||||
| I | 1 | 214 | |||
| II | 1.0 (0.7 to 1.4) | 1039 | |||
| III non-manual | 0.9 (0.6 to 1.3) | 569 | |||
| III manual | 1.3 (0.9 to 1.8) | 416 | |||
| IV and V | 1.2 (0.9 to 1.7) | 524 | |||
| Armed forces | 1.0 (0.5 to 1.8) | 52 | |||
| Deprivation | 0.357 | ||||
| 5 (affluent) | 1 | 611 | |||
| 4 | 1.2 (0.9 to 1.5) | 638 | |||
| 3 | 1.0 (0.8 to 1.3) | 536 | |||
| 2 | 1.0 (0.8 to 1.3) | 545 | |||
| 1 (most deprived) | 1.2 (0.9 to 1.5) | 576 | |||
| Rurality | 0.988 | ||||
| Rural | 1 | 665 | |||
| Urban | 1.0 (0.8 to 1.2) | 2241 | |||
| Region | < 0.001 | < 0.001 | |||
| North England | 1 | 474 | 1 | ||
| Midlands | 1.1 (0.9 to 1.4) | 794 | 1.1 (0.9 to 1.5) | ||
| South England | 1.0 (0.8 to 1.2) | 957 | 1.0 (0.7 to 1.2) | ||
| London | 1.0 (0.7 to 1.4) | 285 | 0.8 (0.5 to 1.1) | ||
| Wales | 2.0 (1.3 to 2.9) | 132 | 1.9 (1.2 to 3.0) | ||
| Scotland | 1.7 (1.2 to 2.3) | 264 | 1.7 (1.2 to 2.4) | ||
| In household with children aged < 5 years old | 0.01 | ||||
| No | 1 | 2591 | |||
| Yes | 0.7 (0.5 to 0.9) | 300 | |||
| Resources available | |||||
| Car ownership | 1 | 0.652 | |||
| ≥ 1 cars | 0.9 (0.7 to 1.1) | 1478 | |||
| No car | 1.0 (0.8 to 1.2) | 428 | |||
| Missing | 1 | 1000 | |||
| Personal access to the internet | 0.643 | ||||
| Yes | 1 | 2542 | |||
| No | 0.9 (0.7 to 1.2) | 364 | |||
| Health | 0.378 | ||||
| General health | |||||
| Excellent | 1 | 223 | |||
| Very good | 1.1 (0.8 to 1.5) | 725 | |||
| Good | 1.0 (0.7 to 1.3) | 799 | |||
| Fair | 1.2 (0.8 to 1.7) | 360 | |||
| Poor | 1.3 (0.8 to 2.0) | 163 | |||
| Can’t choose | 0.7 (0.3 to 1.6) | 39 | |||
| Missing/not included | 1 | 597 | |||
| Long-term limiting illness | 0.129 | ||||
| None | 1 | 1766 | |||
| Non-limiting | 1.1 (0.9 to 1.4) | 586 | |||
| Limiting | 1.2 (0.99 to 1.5) | 541 | |||
| Don’t know | 0.4 (0.1 to 1.8) | 13 | |||
| Programme theories | |||||
| 1, Risk: uncertainty causes anxiety | |||||
| Worry pain is a sign of something serious | 0.998 | ||||
| Not likely at all | 1 | 358 | |||
| Not likely | 1.0 (0.8 to 1.3) | 1138 | |||
| Fairly likely | 1.0 (0.8 to 1.3) | 876 | |||
| Very likely | 1.0 (0.8 to 1.4) | 415 | |||
| It depends | 1.0 (0.6 to 1.5) | 119 | |||
| Confident in deciding to see a doctor or self-care | 0.381 | ||||
| Very confident | 1 | 993 | |||
| Fairly | 1.0 (0.9 to 1.2) | 1130 | |||
| Not very | 1.4 (0.9 to 2.2) | 89 | |||
| Never had problem | 1.2 (0.8 to 1.9) | 97 | |||
| 2, Risk: previous traumatic event | |||||
| Had problem, did not see doctor and was serious | 0.029 | ||||
| No | 1 | 2219 | |||
| Yes | 1.2 (1.0 to 1.5) | 687 | |||
| 3, Risk: responsibility for others | |||||
| 4, Speed: need to get back to normal | |||||
| Sleep | 0.007 | ||||
| Do not see doctor | 1 | 2010 | |||
| See doctor if sleep loss | 1.3 (1.1 to 1.6) | 634 | |||
| See doctor if any loss | 0.9 (0.7 to 1.3) | 262 | |||
| Work | 0.045 | ||||
| Do not see doctor | 1 | 935 | |||
| See doctor if work loss | 1.2 (1.0 to 1.5) | 1709 | |||
| See doctor if any loss | 1.0 (0.7 to 1.4) | 262 | |||
| 5, Speed: need to seek pain relief | |||||
| Likely to take medication | 0.043 | ||||
| Very likely | 1 | 1081 | |||
| Fairly | 0.8 (0.7 to 0.95) | 1257 | |||
| Not very | 0.7 (0.5 to 0.9) | 376 | |||
| Not at all | 0.9 (0.6 to 1.3) | 135 | |||
| Depends | 0.8 (0.5 to 1.5) | 57 | |||
| 6, Speed: waited long enough | |||||
| 7a, Stressful lives | |||||
| Overwhelmed when have health problem | 0.367 | ||||
| Strongly disagree | 1 | 487 | |||
| Disagree | 0.9 (0.7 to 1.1) | 872 | |||
| Neither | 1.1 (0.8 to 1.4) | 537 | |||
| Strongly agree/agree | 0.9 (0.7 to 1.2) | 314 | |||
| Never had problem | 1.3 (0.8 to 2.0) | 99 | |||
| Find life stressful | 0.770 | ||||
| No | 1 | 637 | |||
| A bit | 1.0 (0.8 to 1.2) | 1316 | |||
| Quite | 0.9 (0.7 to 1.2) | 637 | |||
| Very | 0.9 (0.7 to 1.2) | 297 | |||
| Don’t know | 0.5 (0.2 to 1.6) | 19 | |||
| Someone to care for them if they are ill | 0.979 | ||||
| Definitely | 1 | 1240 | |||
| Probably | 1.0 (0.8 to 1.2) | 697 | |||
| Probably not | 1.0 (0.8 to 1.4) | 280 | |||
| Don’t know | 0.9 (0.6 to 1.5) | 92 | |||
| Can take time off work for GP | 0.627 | ||||
| Yes | 1 | 1078 | |||
| Yes but not easy | 1.0 (0.8 to 1.3) | 275 | |||
| No | 0.8 (0.6 to 1.3) | 127 | |||
| Not applicable/missing | 1.1 (0.9 to 1.3) | 1426 | |||
| 7b, Low burden | |||||
| Travel to ED | 0.554 | ||||
| Very difficult | 1 | 610 | |||
| Neither | 0.9 (0.7 to 1.2) | 269 | |||
| Fairly easy | 0.9 (0.7 to 1.1) | 1172 | |||
| Very easy | 0.9 (0.7 to 1.1) | 855 | |||
| Opening hours a problem | 0.084 | ||||
| Disagree/strongly disagree | 1 | 1098 | |||
| Neither | 1.3 (1.0 to 1.6) | 608 | |||
| Strongly agree/agree | 1.0 (0.8 to 1.3) | 603 | |||
| Prefer no appointments | 0.005 | ||||
| Disagree/strongly disagree | 1 | 685 | |||
| Neither | 1.2 (0.9 to 1.4) | 799 | |||
| Strongly agree/agree | 1.4 (1.1 to 1.8) | 825 | |||
| Want convenient times | 0.847 | ||||
| Disagree/strongly disagree | 1 | 253 | |||
| Neither | 1.1 (0.7 to 1.4) | 708 | |||
| Strongly agree/agree | 1.0 (0.7 to 1.3) | 1348 | |||
| Willing to wait in waiting room | < 0.001 | 0.029 | |||
| Disagree/strongly disagree | 1 | 361 | 1 | ||
| Neither | 0.7 (0.5 to 1.1) | 194 | 0.8 (0.5 to 1.2) | ||
| Strongly agree/agree | 1.4 (1.1 to 1.8) | 2351 | 1.3 (0.96 to 1.7) | ||
| 8, Compliance with family/friends | |||||
| Check with family and friends for what to do | 0.171 | ||||
| Not very likely | 1 | 545 | |||
| Not likely | 0.9 (0.7 to 1.2) | 746 | |||
| Fairly likely | 0.8 (0.6 to 1.0) | 1061 | |||
| Very likely | 0.9 (0.7 to 1.1) | 554 | |||
| 9, Views of services | |||||
| Prefer ED for quick tests | 0.001 | 0.003 | |||
| Disagree/strongly disagree | 1 | 1159 | 1 | ||
| Neither | 1.2 (1.0 to 1.5) | 797 | 1.2 (0.99 to 1.5) | ||
| Strongly agree/agree | 1.6 (1.2 to 2.0) | 353 | 1.5 (1.2 to 2.0) | ||
| Missing, self-complete | 0 | ||||
| Doctors know more at ED | 0.118 | ||||
| Disagree/strongly disagree | 1 | 850 | |||
| Neither | 1.2 (0.99 to 1.5) | 1041 | |||
| Strongly agree/agree | 1.2 (0.96 to 1.6) | 418 | |||
| Missing, self-complete | 0 | ||||
| No confidence in GP | 0.847 | ||||
| Strongly disagree | 1 | 538 | |||
| Disagree | 0.9 (0.7 to 1.1) | 1008 | |||
| Neither | 0.9 (0.7 to 1.1) | 446 | |||
| Agree | 0.9 (0.6 to 1.3) | 165 | |||
| Strongly agree | 1.0 (0.6 to 1.6) | 76 | |||
| Don’t know | 0.7 (0.4 to 1.5) | 42 | |||
| Missing | 0.8 (0.4 to 1.6) | 34 | |||
| Missing, self-complete | 0 | ||||
| 10, Frustration with access to GP | |||||
| Hard to get GP appointment | 0.905 | ||||
| Disagree/strongly disagree | 1 | 819 | |||
| Neither | 1.0 (0.7 to 1.3) | 353 | |||
| Strongly agree/agree | 1.0 (0.9 to 1.2) | 1137 | |||
| Missing, self-complete | 0 | ||||
| Registered with GP | 0.320 | ||||
| Yes | 1 | 2840 | |||
| No | 1.3 (0.8 to 2.1) | 65 | |||
| Work or looking after family makes it difficult to see GP | 0.795 | ||||
| Disagree/strongly disagree | 1 | 1197 | |||
| Neither | 1.1 (0.9 to 1.4) | 455 | |||
| Strongly agree/agree | 1.0 (0.8 to 1.3) | 410 | |||
| Not applicable | 1.0 (0.7 to 1.3) | 247 | |||
| Believe people use ED because can’t get GP appointment | 0.328 | ||||
| Strongly agree/agree | 1 | 2441 | |||
| Neither | 0.8 (0.6 to 1.1) | 339 | |||
| Disagree/strongly disagree | 0.9 (0.6 to 1.4) | 126 | |||
| Awareness of services | |||||
| Know range of NHS services to use | 0.978 | ||||
| Very confident | 1 | 1436 | |||
| Fairly confident | 1.0 (0.9 to 1.2) | 1189 | |||
| Not confident/not at all | 1.0 (0.7 to 1.3) | 280 | |||
| Can find out when NHS services are open | 0.761 | ||||
| Very confident | 1 | 1487 | |||
| Fairly confident | 1.0 (0.9 to 1.2) | 1163 | |||
| Not confident/not at all | 1.1 (0.8 to 1.5) | 255 | |||
| Can find out what tests available at services | 0.402 | ||||
| Very confident | 1 | 963 | |||
| Fairly confident | 0.9 (0.8 to 1.1) | 1307 | |||
| Not confident/not at all | 1.0 (0.8 to 1.2) | 635 | |||
| How to contact GP OOH | 0.837 | ||||
| Very confident | 1 | 1338 | |||
| Fairly confident | 1.0 (0.8 to 1.2) | 1056 | |||
| Not very confident | 1.1 (0.9 to 1.4) | 389 | |||
| Not at all confident | 1.0 (0.7 to 1.5) | 122 | |||
| Will look up on the internet to see what to do | 0.003 | ||||
| Very likely | 1 | 428 | |||
| Fairly likely | 0.8 (0.7 to 1.1) | 752 | |||
| Not very likely | 1.2 (0.9 to 1.5) | 680 | |||
| Not at all | 1.1 (0.9 to 1.4) | 1016 | |||
| Missing | 0.3 (0.1 to 0.9) | 30 | |||
| Will look up on the internet to decide what problem is | 0.143 | ||||
| Very likely | 1 | 667 | |||
| Fairly likely | 0.9 (0.7 to 1.1) | 797 | |||
| Not very likely | 1.1 (0.8 to 1.4) | 472 | |||
| Not at all | 1.1 (0.9 to 1.3) | 940 | |||
| Missing | 0.4 (0.2 to 1.1) | 30 | |||
| Recursivity | |||||
| If tests are done I was right to make contact | 0.037 | ||||
| Disagree/strongly disagree | 1 | 280 | |||
| Neither | 1.1 (0.8 to 1.5) | 793 | |||
| Strongly agree/agree | 1.3 (0.99 to 1.8) | 1236 | |||
| Missing, self-complete | 0 | ||||
| Health literacy | |||||
| Lower health literacy compared with higher health literacy – understand information | 0.9 (0.8 to 1.1) | 2269 | 0.469 | ||
| Lower health literacy compared with higher health literacy – ability to communicate | 0.9 (0.8 to 1.1) | 2269 | 0.332 | ||
| Recent use of health care | |||||
| Ambulance use | 0.781 | ||||
| Never | 1 | 1349 | |||
| ≥ 12 months | 1.1 (0.9 to 1.2) | 1108 | |||
| < 12 months | 1.1 (0.9 to 1.3) | 448 | |||
| Ambulance frequent user | 0.429 | ||||
| < 3 times | 1 | 2842 | |||
| ≥ 3 times in 12 months | 0.8 (0.5 to 1.4) | 64 | |||
| ED use | 0.027 | ||||
| Never | 1 | 411 | |||
| ≥ 12 months | 1.3 (1.0 to 1.6) | 1478 | |||
| 6–12 months | 1.3 (0.96 to 1.8) | 366 | |||
| 3–6 months | 1.3 (0.9 to 1.9) | 234 | |||
| < 3 months | 1.6 (1.2 to 2.2) | 416 | |||
| ED frequent user | 0.278 | ||||
| < 3 times | 1 | 1959 | |||
| ≥ 3 times in 12 months | 1.2 (0.9 to 1.7) | 949 | |||
| Contacted GP | 0.322 | ||||
| Never | 1 | 65 | |||
| ≥ 12 months | 1.7 (0.9 to 3.1) | 454 | |||
| 6–12 months | 1.5 (0.8 to 2.7) | 484 | |||
| 3–6 months | 1.7 (0.95 to 3.2) | 518 | |||
| < 3 months | 1.6 (0.9 to 2.9) | 1384 | |||
| Attitudes towards overuse of health services | |||||
| Too many use 999 | 0.126 | ||||
| Strongly agree/agree | 1 | 2516 | |||
| Neither | 1.3 (1.0 to 1.6) | 313 | |||
| Disagree/strongly disagree | 1.2 (0.8 to 2.0) | 77 | |||
| Too many use ED | 0.038 | ||||
| Strongly agree/agree | 1 | 2515 | |||
| Neither | 1.3 (1.0 to 1.7) | 291 | |||
| Disagree/strongly disagree | 1.3 (0.9 to 2.0) | 100 | |||
| Too many use GP | 0.890 | ||||
| Strongly agree/agree | 1 | 2082 | |||
| Neither | 1.0 (0.9 to 1.3) | 577 | |||
| Disagree/strongly disagree | 1.0 (0.7 to 1.3) | 247 | |||
| Reluctance to use ED | 0.495 | ||||
| Strongly agree/agree | 1 | 1348 | |||
| Neither | 1.1 (0.9 to 1.3) | 734 | |||
| Disagree/strongly disagree | 1.1 (0.9 to 1.4) | 824 | |||
| Variables | Significance | Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age of respondent(grouped) < 7 category > dv | 0.000 | |||
| Age of respondent(grouped) < 7 category > dv(1) | 0.905 | 0.970 | 0.590 | 1.595 |
| Age of respondent(grouped) < 7 category > dv(2) | 0.641 | 1.119 | 0.697 | 1.796 |
| Age of respondent(grouped) < 7 category > dv(3) | 0.028 | 1.671 | 1.056 | 2.645 |
| Age of respondent(grouped) < 7 category > dv(4) | 0.002 | 2.038 | 1.291 | 3.218 |
| Age of respondent(grouped) < 7 category > dv(5) | 0.008 | 1.873 | 1.179 | 2.975 |
| Age of respondent(grouped) < 7 category > dv(6) | 0.378 | 1.251 | 0.760 | 2.060 |
| Sex of respondent(1) | 0.019 | 0.801 | 0.666 | 0.964 |
| DV To which of these racial groups do you consider you belong? (compressed)(1) | 0.003 | 1.656 | 1.181 | 2.321 |
| 2007 version: Government office region | 0.001 | |||
| 2007 version: Government office region(1) | 0.299 | 1.164 | 0.874 | 1.549 |
| 2007 version: Government office region(2) | 0.782 | 0.962 | 0.729 | 1.268 |
| 2007 version: Government office region(3) | 0.293 | 0.804 | 0.536 | 1.207 |
| 2007 version: Government office region(4) | 0.006 | 1.883 | 1.195 | 2.968 |
| 2007 version: Government office region(5) | 0.006 | 1.684 | 1.163 | 2.438 |
| Number of Respondents children in HH aged 0–4yrs – dv(1) | 0.816 | 0.957 | 0.661 | 1.386 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)? | 0.232 | |||
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(1) | 0.533 | 0.881 | 0.592 | 1.312 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(2) | 0.466 | 0.879 | 0.622 | 1.242 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(3) | 0.180 | 0.831 | 0.634 | 1.089 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(4) | 0.020 | 0.654 | 0.457 | 0.937 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do | 0.047 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(1) | 0.118 | 0.781 | 0.574 | 1.064 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(2) | 0.599 | 1.086 | 0.799 | 1.474 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(3) | 0.810 | 0.964 | 0.713 | 1.303 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(4) | 0.068 | 0.234 | 0.049 | 1.115 |
| Have you ever had a health problem where you did not go to see a doctor at first and it turned out to be serious?(1) | 0.273 | 0.888 | 0.719 | 1.098 |
| HPrbDr13 | 0.154 | |||
| HPrbDr13(1) | 0.091 | 1.194 | 0.972 | 1.467 |
| HPrbDr13(2) | 0.830 | 0.960 | 0.658 | 1.399 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain | 0.182 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(1) | 0.281 | 0.893 | 0.728 | 1.097 |
| For unexpected non-life-threatening g pain, how likely is it you would . . . take medication to stop the pain(2) | 0.016 | 0.689 | 0.509 | 0.934 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(3) | 0.447 | 0.836 | 0.528 | 1.325 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(4) | 0.785 | 1.104 | 0.542 | 2.246 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious | 0.563 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(1) | 0.178 | 1.231 | 0.910 | 1.665 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(2) | 0.248 | 1.190 | 0.886 | 1.599 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(3) | 0.321 | 1.209 | 0.831 | 1.761 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(4) | 0.132 | 1.522 | 0.881 | 2.629 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D | 0.348 | |||
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(1) | 0.312 | 0.891 | 0.713 | 1.114 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(2) | 0.164 | 0.845 | 0.666 | 1.071 |
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day | 0.096 | |||
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day(1) | 0.055 | 0.660 | 0.432 | 1.010 |
| For unexpected non-life-threatening health problem... I’m willing to wait a few hours in a waiting room if it means I can be seen that day(2) | 0.233 | 0.837 | 0.625 | 1.121 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D | 0.019 | |||
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(1) | 0.210 | 0.835 | 0.631 | 1.106 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(2) | 0.008 | 0.690 | 0.525 | 0.907 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D | 0.438 | |||
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(1) | 0.199 | 0.872 | 0.708 | 1.075 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(2) | 0.730 | 0.947 | 0.695 | 1.290 |
| I think too many people use A&E when they do not need to | 0.047 | |||
| I think too many people use A&E when they do not need to(1) | 0.023 | 1.433 | 1.052 | 1.952 |
| I think too many people use A&E when they do not need to(2) | 0.257 | 1.358 | 0.800 | 2.306 |
| Constant | 0.090 | 0.561 | ||
| Variable | Univariate | Final multivariable model | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | n | p-value | Odds ratio (95% CI) | p-value | |
| Sociodemographic characteristics | |||||
| Age (years) | 0.001 | < 0.001 | |||
| 18–24 | 1 | 169 | 1 | ||
| 25–34 | 0.8 (0.6 to 1.2) | 384 | 0.8 (0.5 to 1.2) | ||
| 35–44 | 0.8 (0.6 to 1.2) | 467 | 0.9 (0.6 to 1.4) | ||
| 45–54 | 1.2 (0.8 to 1.7) | 469 | 1.3 (0.9 to 2.0) | ||
| 55–64 | 1.3 (0.9 to 1.8) | 508 | 1.4 (0.9 to 2.1) | ||
| 65–74 | 1.3 (0.9 to 1.8) | 499 | 1.4 (0.9 to 2.1) | ||
| ≥ 75 | 0.9 (0.6 to 1.3) | 405 | 1.0 (0.6 to 1.5) | ||
| Sex | < 0.001 | 0.001 | |||
| Female | 1 | 1649 | 1 | ||
| Male | 1.4 (1.2 to 1.6) | 1257 | 1.4 (1.1 to 1.6) | ||
| Ethnicity | 0.001 | 0.005 | |||
| White | 1 | 2572 | 1 | ||
| BAME | 1.5 (1.2 to 1.8) | 334 | 1.5 (1.1 to 2.0) | ||
| Social class | 0.027 | ||||
| I | 1 | 214 | |||
| II | 1.2 (0.8 to 1.6) | 1039 | |||
| III non-manual | 1.2 (0.9 to 1.6) | 569 | |||
| III manual | 1.6 (1.1 to 2.2) | 416 | |||
| IV and V | 1.5 (1.1 to 2.1) | 524 | |||
| Armed forces | 1.3 (0.7 to 2.4) | 52 | |||
| Deprivation | 0.183 | ||||
| 5 (affluent) | |||||
| 4 | |||||
| 3 | |||||
| 2 | |||||
| 1 (most deprived) | |||||
| Rurality | 0.201 | ||||
| Rural | |||||
| Urban | |||||
| Region | 0.001 | < 0.001 | |||
| North England | 1 | 474 | 1 | ||
| Midlands | 0.9 (0.7 to 1.2) | 794 | 0.9 (0.7 to 1.2) | ||
| South England | 0.8 (0.7 to 1.0) | 957 | 0.8 (0.6 to 1.0) | ||
| London | 1.0 (0.7 to 1.3) | 285 | 0.8 (0.5 to 1.1) | ||
| Wales | 1.6 (1.1 to 2.3) | 132 | 1.6 (1.0 to 2.5) | ||
| Scotland | 1.4 (1.0 to 1.9) | 264 | 1.4 (0.95 to 1.9) | ||
| In household with children aged < 5 years old | 0.041 | ||||
| No | 1 | 2591 | |||
| Yes | 0.8 (0.6 to 0.99) | 300 | |||
| Resources available | |||||
| Car ownership | 0.424 | ||||
| ≥ 1 cars | |||||
| No car | |||||
| Missing | |||||
| Personal access to the internet | 0.706 | ||||
| Yes | |||||
| No | |||||
| Health | |||||
| General health | 0.489 | ||||
| Excellent | |||||
| Very good | |||||
| Good | |||||
| Fair | |||||
| Poor | |||||
| Can’t choose | |||||
| Missing/not included | |||||
| Long-term limiting illness | 0.075 | ||||
| None | |||||
| Non-limiting | |||||
| Limiting | |||||
| Don’t know | |||||
| Programme theories | |||||
| 1, Risk: uncertainty causes anxiety | |||||
| Worry pain is a sign of something serious | 0.071 | ||||
| Not likely at all | |||||
| Not likely | |||||
| Fairly likely | |||||
| Very likely | |||||
| It depends | |||||
| Confident in deciding to see a doctor or self-care | 0.316 | ||||
| Very confident | |||||
| Fairly | |||||
| Not very | |||||
| Never had problem | |||||
| 2, Risk: previous traumatic event | |||||
| Had problem, did not see doctor and was serious | 0.170 | ||||
| No | |||||
| Yes | |||||
| 3, Risk: responsibility for others | |||||
| 4, Speed: need to get back to normal | |||||
| Sleep | < 0.001 | ||||
| Do not see doctor | 1 | 2010 | |||
| See doctor if sleep loss | 1.5 (1.3 to 1.8) | 634 | |||
| See doctor if any loss | 1.2 (0.9 to 1.5) | 262 | |||
| Work | 0.002 | 0.04 | |||
| Do not see doctor | 1 | 935 | 1 | ||
| See doctor if work loss | 1.3 (1.1 to 1.6) | 1709 | 1.3 (1.0 to 1.5) | ||
| See doctor if any loss | 1.3 (1.0 to 1.7) | 262 | 1.1 (0.8 to 1.6) | ||
| 5, Speed: need to seek pain relief | |||||
| Likely to take medication | 0.050 | ||||
| Very likely | 1 | 1081 | |||
| Fairly | 0.8 (0.7 to 0.95) | 1257 | |||
| Not very | 0.8 (0.6 to 0.97) | 376 | |||
| Not at all | 0.8 (0.6 to 1.1) | 135 | |||
| Depends | 0.7 (0.4 to 1.2) | 57 | |||
| 6, Speed: waited long enough | |||||
| 7a, Stressful lives | |||||
| Overwhelmed when have health problem | 0.263 | ||||
| Strongly disagree | |||||
| Disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Never had problem | |||||
| Find life stressful | 0.286 | ||||
| No | |||||
| A bit | |||||
| Quite | |||||
| Very | |||||
| Don’t know | |||||
| Someone to care for them if they are ill | 0.374 | ||||
| Definitely | |||||
| Probably | |||||
| Probably not | |||||
| Don’t know | |||||
| Can take time off work for GP | 0.281 | ||||
| Yes | |||||
| Yes but not easy | |||||
| No | |||||
| Not applicable/missing | |||||
| 7b, Low burden | |||||
| Travel to ED | 0.521 | ||||
| Very difficult | |||||
| Neither | |||||
| Fairly easy | |||||
| Very easy | |||||
| Opening hours a problem | 0.143 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Prefer no appointments | 0.005 | ||||
| Disagree/strongly disagree | 1 | 685 | |||
| Neither | 1.2 (0.9 to 1.4) | 799 | |||
| Strongly agree/agree | 1.4 (1.1 to 1.7) | 825 | |||
| Want convenient times | 0.875 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Willing to wait in waiting room | < 0.001 | 0.012 | |||
| Disagree/strongly disagree | 1 | 361 | 1 | ||
| Neither | 0.7 (0.5 to 1.0) | 194 | 0.7 (0.4 to 1.1) | ||
| Strongly agree/agree | 1.3 (1.1 to 1.7) | 2351 | 1.2 (0.9 to 1.5) | ||
| 8, Compliance with family/friends | |||||
| Check with family and friends for what to do | 0.112 | ||||
| Not very likely | |||||
| Not likely | |||||
| Fairly likely | |||||
| Very likely | |||||
| 9, Views of services | |||||
| Prefer ED for quick tests | < 0.001 | < 0.001 | |||
| Disagree/strongly disagree | 1 | 1159 | 1 | ||
| Neither | 1.3 (1.1 to 1.6) | 797 | 1.3 (1.0 to 1.5) | ||
| Strongly agree/agree | 1.8 (1.4 to 2.3) | 353 | 1.7 (1.4 to 2.2) | ||
| Missing, self-complete | 0 | ||||
| Doctors know more at ED | 0.029 | ||||
| Disagree/strongly disagree | 1 | 850 | |||
| Neither | 1.2 (1.0 to 1.5) | 1041 | |||
| Strongly agree/agree | 1.3 (1.0 to 1.7) | 418 | |||
| Missing, self-complete | 0 | ||||
| No confidence in GP | 0.925 | ||||
| Strongly disagree | |||||
| Disagree | |||||
| Neither | |||||
| Agree | |||||
| Strongly agree | |||||
| Don’t know | |||||
| Missing | |||||
| Missing, self-complete | |||||
| 10, Frustration with access to GP | |||||
| Hard to get GP appointment | 0.994 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Missing, self-complete | 0 | ||||
| Registered with GP | 0.958 | ||||
| Yes | |||||
| No | |||||
| Work or looking after family makes it difficult to see GP | 0.246 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Not applicable | |||||
| Believe people use ED because can’t get GP appointment | 0.710 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Awareness of services | 0.887 | ||||
| Know range of NHS services to use | |||||
| Very confident | |||||
| Fairly confident | |||||
| Not confident/not at all | |||||
| Can find out when NHS services are open | 0.825 | ||||
| Very confident | |||||
| Fairly confident | |||||
| Not confident/not at all | |||||
| Can find out what tests available at services | 0.483 | ||||
| Very confident | |||||
| Fairly confident | |||||
| Not confident/not at all | |||||
| How to contact GP OOH | 0.546 | ||||
| Very | |||||
| Fairly | |||||
| Not very confident | |||||
| Not at all | |||||
| Will look up on the internet to see what to do | 0.001 | ||||
| Very likely | 1 | 428 | |||
| Fairly likely | 0.8 (0.7 to 1.1) | 752 | |||
| Not very likely | 1.1 (0.9 to 1.5) | 680 | |||
| Not at all | 1.0 (0.8 to 1.3) | 1016 | |||
| Missing | 0.3 (0.1 to 0.9) | 30 | |||
| Will look up on the internet to decide what problem is | 0.035 | ||||
| Very likely | 1 | 667 | |||
| Fairly likely | 0.8 (0.7 to 1.0) | 797 | |||
| Not very likely | 1.1 (0.8 to 1.3) | 472 | |||
| Not at all | 1.0 (0.8 to 1.2) | 940 | |||
| Missing | 0.4 (0.2 to 0.9) | 30 | |||
| Recursivity | |||||
| If tests are done I was right to make contact | 0.002 | ||||
| Disagree/strongly disagree | 1 | 280 | |||
| Neither | 1.1 (0.9 to 1.5) | 793 | |||
| Strongly agree/agree | 1.5 (1.1 to 1.9) | 1236 | |||
| Missing, self-complete | 0 | ||||
| Health literacy | |||||
| Lower health literacy compared with higher health literacy – understand information | 0.995 | ||||
| Lower health literacy compared with higher health literacy – ability to communicate | 0.291 | ||||
| Recent use of health care | |||||
| Ambulance use | 0.473 | ||||
| Never | |||||
| ≥ 12 months | |||||
| < 12 months | |||||
| Ambulance frequent user | 0.755 | ||||
| < 3 times | |||||
| ≥ 3 times in 12 months | |||||
| ED use | 0.009 | ||||
| Never | 1 | 411 | |||
| ≥ 12 months | 1.2 (0.97 to 1.5) | 416 | |||
| 6–12 months | 1.3 (0.99 to 1.8) | 234 | |||
| 3–6 months | 1.6 (1.2 to 2.3) | 366 | |||
| < 3 months | 1.5 (1.2 to 2.0) | 1478 | |||
| ED frequent user | 0.001 | ||||
| < 3 times | 1 | 2738 | |||
| ≥ 3 times in 12 months | 1.7 (1.3 to 2.4) | 167 | |||
| Contacted GP | 0.345 | ||||
| Never | |||||
| ≥ 12 months | |||||
| 6–12 months | |||||
| 3–6 months | |||||
| < 3 months | |||||
| Attitudes towards overuse of health services | |||||
| Too many use 999 | 0.039 | ||||
| Strongly agree/agree | 1 | 2516 | |||
| Neither | 1.3 (1.1 to 1.7) | 313 | |||
| Disagree/strongly disagree | 1.2 (0.8 to 1.9) | 77 | |||
| Too many use ED | 0.003 | 0.003 | |||
| Strongly agree/agree | 1 | 2515 | 1 | ||
| Neither | 1.4 (1.1 to 1.8) | 291 | 1.4 (1.0 to 1.9) | ||
| Disagree/strongly disagree | 1.6 (1.1 to 2.5) | 100 | 2.0 (1.2 to 3.4) | ||
| Too many use GP | 0.357 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Reluctance to use ED | 0.236 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Variables | Significance | Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age of respondent(grouped) < 7 category > dv | 0.002 | |||
| Age of respondent(grouped) < 7 category > dv(1) | 0.387 | 0.802 | 0.486 | 1.322 |
| Age of respondent(grouped) < 7 category > dv(2) | 0.658 | 0.897 | 0.554 | 1.452 |
| Age of respondent(grouped) < 7 category > dv(3) | 0.172 | 1.389 | 0.867 | 2.224 |
| Age of respondent(grouped) < 7 category > dv(4) | 0.155 | 1.407 | 0.879 | 2.252 |
| Age of respondent(grouped) < 7 category > dv(5) | 0.169 | 1.395 | 0.868 | 2.242 |
| Age of respondent(grouped) < 7 category > dv(6) | 0.877 | 0.961 | 0.580 | 1.593 |
| Sex of respondent(1) | 0.003 | 0.754 | 0.625 | 0.910 |
| Respondent: social class [pre-SOC2000] best estimate dv | 0.430 | |||
| Respondent: social class [pre-SOC2000] best estimate dv(1) | 0.676 | 1.081 | 0.752 | 1.554 |
| Respondent: social class [pre-SOC2000] best estimate dv(2) | 0.369 | 1.196 | 0.809 | 1.769 |
| Respondent: social class [pre-SOC2000] best estimate dv(3) | 0.169 | 1.337 | 0.884 | 2.021 |
| Respondent: social class [pre-SOC2000] best estimate dv(4) | 0.136 | 1.357 | 0.909 | 2.027 |
| Respondent: social class [pre-SOC2000] best estimate dv(5) | 0.884 | 1.062 | 0.471 | 2.395 |
| DV To which of these racial groups do you consider you belong? (compressed)(1) | 0.014 | 1.536 | 1.091 | 2.161 |
| 2007 version: Government office region | 0.004 | |||
| 2007 version: Government office region(1) | 0.515 | 0.913 | 0.694 | 1.201 |
| 2007 version: Government office region(2) | 0.127 | 0.814 | 0.625 | 1.060 |
| 2007 version: Government office region(3) | 0.809 | 0.954 | 0.652 | 1.397 |
| 2007 version: Government office region(4) | 0.046 | 1.586 | 1.009 | 2.493 |
| 2007 version: Government office region(5) | 0.068 | 1.411 | 0.975 | 2.041 |
| Number of Respondents children in HH aged 0–4yrs – dv(1) | 0.756 | 0.946 | 0.666 | 1.343 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)? | 0.323 | |||
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(1) | 0.720 | 1.073 | 0.729 | 1.581 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(2) | 0.591 | 0.912 | 0.651 | 1.277 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(3) | 0.381 | 0.888 | 0.682 | 1.158 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(4) | 0.071 | 0.726 | 0.513 | 1.028 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be | 0.844 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(1) | 0.400 | 0.871 | 0.630 | 1.202 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(2) | 0.375 | 0.840 | 0.570 | 1.236 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(3) | 0.561 | 0.867 | 0.536 | 1.403 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(4) | 0.600 | 1.703 | 0.233 | 12.435 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do | 0.138 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(1) | 0.726 | 0.937 | 0.649 | 1.351 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(2) | 0.198 | 1.298 | 0.873 | 1.929 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(3) | 0.622 | 1.137 | 0.683 | 1.892 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(4) | 0.199 | 0.251 | 0.030 | 2.072 |
| HPrbDr13 | 0.080 | |||
| HPrbDr13(1) | 0.028 | 1.250 | 1.024 | 1.526 |
| HPrbDr13(2) | 0.702 | 1.074 | 0.745 | 1.549 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain | 0.538 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(1) | 0.154 | 0.865 | 0.708 | 1.056 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(2) | 0.180 | 0.823 | 0.618 | 1.094 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(3) | 0.425 | 0.837 | 0.542 | 1.295 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(4) | 0.884 | 1.052 | 0.535 | 2.065 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D | 0.560 | |||
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(1) | 0.420 | 0.914 | 0.734 | 1.138 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(2) | 0.314 | 0.888 | 0.705 | 1.119 |
| For unexpected non-life threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day | 0.061 | |||
| For unexpected non-life threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day(1) | 0.021 | 0.615 | 0.406 | 0.930 |
| For unexpected non-life threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day(2) | 0.447 | 0.899 | 0.683 | 1.183 |
| I think doctors at A&E know more than GPs SC: B, C, D | 0.791 | |||
| I think doctors at A&E know more than GPs SC: B, C, D(1) | 0.590 | 1.075 | 0.827 | 1.397 |
| I think doctors at A&E know more than GPs SC: B, C, D(2) | 0.499 | 1.102 | 0.832 | 1.458 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D | 0.002 | |||
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(1) | 0.048 | 0.744 | 0.556 | 0.997 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(2) | 0.000 | 0.594 | 0.444 | 0.795 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D | 0.210 | |||
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(1) | 0.103 | 0.844 | 0.689 | 1.035 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(2) | 0.254 | 0.839 | 0.621 | 1.134 |
| I think too many people call 999 for an ambulance when they do not need to | 0.121 | |||
| I think too many people call 999 for an ambulance when they do not need to(1) | 0.048 | 1.407 | 1.003 | 1.974 |
| I think too many people call 999 for an ambulance when they do not need to(2) | 0.774 | 0.915 | 0.498 | 1.680 |
| I think too many people use A&E when they do not need to | 0.057 | |||
| I think too many people use A&E when they do not need to(1) | 0.164 | 1.277 | 0.905 | 1.802 |
| I think too many people use A&E when they do not need to(2) | 0.033 | 1.865 | 1.050 | 3.312 |
| Constant | 0.929 | 1.033 | ||
| Variables | Univariate | Final multivariable model | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | n | p-value | Odds ratio (95% CI) | p-value | |
| Sociodemographic characteristics | |||||
| Age (years) | < 0.001 | < 0.001 | |||
| 18–24 | 1 | 169 | 1 | ||
| 25–34 | 1.0 (0.7 to 1.5) | 384 | 1.0 (0.6 to 1.5) | ||
| 35–44 | 1.0 (0.7 to 1.5) | 467 | 0.9 (0.6 to 1.4) | ||
| 45–54 | 0.9 (0.6 to 1.3) | 469 | 0.8 (0.5 to 1.3) | ||
| 55–64 | 1.1 (0.8 to 1.7) | 508 | 1.3 (0.8 to 2.0) | ||
| 65–74 | 1.5 (1.0 to 2.1) | 499 | 1.3 (0.8 to 2.0) | ||
| ≥ 75 | 1.9 (1.3 to 2.8) | 405 | 1.8 (1.1 to 2.9) | ||
| Sex | 0.09 | ||||
| Female | |||||
| Male | |||||
| Ethnicity | < 0.001 | < 0.001 | |||
| White | 1 | 2572 | 1 | ||
| BAME | 1.6 (1.3 to 2.1) | 334 | 2.1 (1.5 to 2.9) | ||
| Social class | 0.302 | ||||
| I | |||||
| II | |||||
| III non-manual | |||||
| III manual | |||||
| IV and V | |||||
| Armed forces | |||||
| Deprivation | 0.571 | ||||
| 5 (affluent) | |||||
| 4 | |||||
| 3 | |||||
| 2 | |||||
| 1 (most deprived) | |||||
| Rurality | 0.784 | ||||
| Rural | |||||
| Urban | |||||
| Region | 0.010 | 0.026 | |||
| North England | 1 | 474 | 1 | ||
| Midlands | 1.1 (0.8 to 1.4) | 794 | 1.1 (0.8 to 1.4) | ||
| South England | 1.3 (1.0 to 1.6) | 957 | 1.4 (1.0 to 1.8) | ||
| London | 1.5 (1.1 to 1.0) | 285 | 1.3 (0.9 to 1.9) | ||
| Wales | 1.5 (1.0 to 2.3) | 132 | 1.7 (1.0 to 2.7) | ||
| Scotland | 1.5 (1.1 to 2.1) | 264 | 1.7 (1.1 to 2.4) | ||
| In household with children aged < 5 years old | 0.341 | ||||
| No | |||||
| Yes | |||||
| Resources available | |||||
| Car ownership | 0.010 | ||||
| ≥ 1 cars | 1 | 1478 | |||
| No car | 1.4 (1.1 to 1.8) | 428 | |||
| Missing | 1.1 (0.9 to 1.3) | 1000 | |||
| Personal access to the internet | < 0.001 | ||||
| Yes | 1 | 2542 | |||
| No | 1.7 (1.3 to 2.1) | 364 | |||
| Health | |||||
| General health | 0.003 | ||||
| Excellent | 1 | 223 | |||
| Very good | 1.0 (0.7 to 1.4) | 725 | |||
| Good | 1.3 (0.9 to 1.8) | 799 | |||
| Fair | 1.4 (1.0 to 2.0) | 360 | |||
| Poor | 1.8 (1.2 to 2.8) | 163 | |||
| Can’t choose | 2.4 (1.2 to 4.7) | 39 | |||
| Missing/not included | 1 | 597 | |||
| Long-term limiting illness | 0.032 | ||||
| None | 1 | 1766 | |||
| Non-limiting | 1.0 (0.8 to 1.2) | 586 | |||
| Limiting | 1.3 (1.1 to 1.6) | 541 | |||
| Don’t know | 1.3 (0.4 to 4.1) | 13 | |||
| Programme theories | |||||
| 1, Risk: uncertainty causes anxiety | |||||
| Worry pain is a sign of something serious | < 0.001 | < 0.001 | |||
| Not likely at all | 1 | 358 | 1 | ||
| Not likely | 1.4 (1.0 to 1.8) | 1138 | 1.3 (0.9 to 1.8) | ||
| Fairly likely | 1.9 (1.5 to 2.6) | 876 | 1.8 (1.3 to 2.5) | ||
| Very likely | 2.8 (2.1 to 3.9) | 415 | 2.0 (1.4 to 3.0) | ||
| It depends | 1.2 (0.8 to 2.0) | 119 | 1.2 (0.6 to 2.1) | ||
| Confident in deciding to see a doctor or self-care | 0.029 | ||||
| Very confident | 1 | 993 | |||
| Fairly | 1.2 (1.0 to 1.4) | 1130 | |||
| Not very | 1.2 (0.8 to 1.9) | 89 | |||
| Never had problem | 1.8 (1.2 to 2.8) | 97 | |||
| 2, Risk: previous traumatic event | |||||
| Had problem, did not see doctor and was serious | 0.767 | ||||
| No | |||||
| Yes | |||||
| 3, Risk: responsibility for others | |||||
| 4, Speed: need to get back to normal | |||||
| Sleep | < 0.001 | ||||
| Do not see doctor | 1 | 2010 | |||
| See doctor if sleep loss | 1.7 (1.4 to 2.0) | 634 | |||
| See doctor if any loss | 2.2 (1.7 to 2.8) | 262 | |||
| Work | < 0.001 | ||||
| Do not see doctor | 1 | 935 | |||
| See doctor if work loss | 1.2 (1.0 to 1.4) | 1709 | |||
| See doctor if any loss | 2.2 (1.6 to 2.9) | 262 | |||
| 5, Speed: need to seek pain relief | |||||
| Likely to take medication | 0.006 | ||||
| Very likely | 1 | 1081 | |||
| Fairly | 0.9 (0.8 to 1.1) | 1257 | |||
| Not very | 0.7 (0.5 to 0.9) | 376 | |||
| Not at all | 0.6 (0.4 to 0.9) | 135 | |||
| Depends | 0.9 (0.5 to 1.6) | 57 | |||
| 6, Speed: waited long enough | |||||
| 7a, Stressful lives | |||||
| Overwhelmed when have health problem | < 0.001 | 0.012 | |||
| Strongly disagree | 1 | 487 | 1 | ||
| Disagree | 1.5 (1.2 to 2.0) | 872 | 1.3 (0.97 to 1.6) | ||
| Neither | 2.2 (1.7 to 2.9) | 537 | 1.7 (1.2 to 2.2) | ||
| Strongly agree/agree | 2.0 (1.5 to 2.8) | 314 | 1.4 (0.96 to 1.9) | ||
| Never had problem | 2.1 (1.3 to 3.3) | 99 | 1.7 (1.0 to 2.8) | ||
| Find life stressful | 0.055 | ||||
| No | |||||
| A bit | |||||
| Quite | |||||
| Very | |||||
| Don’t know | |||||
| Someone to care for them if they are ill | 0.257 | ||||
| Definitely | |||||
| Probably | |||||
| Probably not | |||||
| Don’t know | |||||
| Can take time off work for GP | < 0.001 | ||||
| Yes | 1 | 1078 | |||
| Yes but not easy | 0.8 (0.6 to 1.1) | 275 | |||
| No | 0.7 (0.4 to 1.1) | 127 | |||
| Not applicable/missing | 1.6 (1.3 to 1.8) | 1426 | |||
| 7b, Low burden | |||||
| Travel to ED | < 0.001 | ||||
| Very difficult | 1 | 620 | |||
| Neither | 1.0 (0.7 to 1.3) | 269 | |||
| Fairly easy | 0.8 (0.6 to 0.97) | 1172 | |||
| Very easy | 0.6 (0.4 to 0.7) | 855 | |||
| Opening hours a problem | 0.423 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Prefer no appointments | 0.017 | ||||
| Disagree/strongly disagree | 1 | 685 | |||
| Neither | 1.1 (0.9 to 1.4) | 799 | |||
| Strongly agree/agree | 1.4 (1.1 to 1.7) | 825 | |||
| Want convenient times | 0.549 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Willing to wait in waiting room | < 0.001 | ||||
| Disagree/strongly disagree | 1 | 361 | |||
| Neither | 1.4 (0.97 to 2.1) | 194 | |||
| Strongly agree/agree | 1.7 (1.3 to 2.2) | 2351 | |||
| 8, Compliance with family/friends | |||||
| Check with family and friends for what to do | < 0.001 | ||||
| Not very likely | 1 | 545 | |||
| Not likely | 1.3 (0.99 to 1.6) | 746 | |||
| Fairly likely | 1.4 (1.1 to 1.8) | 1061 | |||
| Very likely | 1.8 (1.4 to 2.3) | 554 | |||
| 9, Views of services | |||||
| Prefer ED for quick tests | 0.013 | ||||
| Disagree/strongly disagree | 1 | 1159 | |||
| Neither | 1.2 (1.0 to 1.5) | 797 | |||
| Strongly agree/agree | 1.4 (1.1 to 1.8) | 353 | |||
| Missing, self-complete | |||||
| Doctors know more at ED | 0.392 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Missing, self-complete | |||||
| No confidence in GP | 0.652 | ||||
| Strongly disagree | |||||
| Disagree | |||||
| Neither | |||||
| Agree | |||||
| Strongly agree | |||||
| Don’t know | |||||
| Missing | |||||
| Missing, self-complete | |||||
| 10, Frustration with access to GP | |||||
| Hard to get GP appointment | 0.689 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Missing, self-complete | |||||
| Registered with GP | 0.038 | ||||
| Yes | 1 | 2840 | |||
| No | 0.5 (0.3 to 0.99) | 65 | |||
| Work or looking after family makes it difficult to see GP | 0.003 | 0.027 | |||
| Disagree/strongly disagree | 1 | 1197 | 1 | ||
| Neither | 1.0 (0.8 to 1.2) | 455 | 0.8 (0.6 to 1.0) | ||
| Strongly agree/agree | 0.6 (0.5 to 0.8) | 410 | 0.7 (0.5 to 0.9) | ||
| Not applicable | 1.1 (0.8 to 1.4) | 247 | 0.8 (0.6 to 1.1) | ||
| Believe people use ED because can’t get GP appointment | 0.901 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Awareness of services | |||||
| Know range of NHS services to use | 0.061 | ||||
| Very confident | |||||
| Fairly confident | |||||
| Not confident/not at all | |||||
| Can find out when NHS services are open | 0.008 | ||||
| Very confident | 1 | 1487 | |||
| Fairly confident | 1.3 (1.1 to 1.5) | 1163 | |||
| Not confident/not at all | 1.3 (1.0 to 1.8) | 255 | |||
| Can find out what tests available at services | 0.105 | ||||
| Very confident | |||||
| Fairly confident | |||||
| Not confident/not at all | |||||
| How to contact GP OOH | 0.007 | ||||
| Very confident | 1 | 1338 | |||
| Fairly confident | 1.3 (1.1 to 1.5) | 1056 | |||
| Not very confident | 1.3 (1.1 to 1.7) | 389 | |||
| Not at all confident | 1.0 (0.6 to 1.5) | 122 | |||
| Will look up on the internet to see what to do | 0.02 | ||||
| Very likely | 1 | 428 | |||
| Fairly likely | 0.9 (0.7 to 1.2) | 752 | |||
| Not very likely | 1.2 (0.9 to 1.5) | 680 | |||
| Not at all | 1.3 (1.0 to 1.6) | 1016 | |||
| Missing | 1.1 (0.5 to 2.4) | 30 | |||
| Will look up on the internet to decide what problem is | 0.073 | ||||
| Very likely | |||||
| Fairly likely | |||||
| Not very likely | |||||
| Not at all | |||||
| Missing | |||||
| Recursivity | |||||
| If tests are done I was right to make contact | < 0.001 | 0.004 | |||
| Disagree/strongly disagree | 1 | 280 | 1 | ||
| Neither | 1.8 (1.3 to 2.4) | 793 | 1.5 (1.1 to 2.1) | ||
| Strongly agree/agree | 2.3 (1.7 to 3.2) | 1236 | 1.7 (1.2 to 2.4) | ||
| Missing, self-complete | 0 | ||||
| Health literacy | |||||
| Lower health literacy compared with higher health literacy – understand information | 1.4 (1.2 to 1.6) | 2269 | < 0.001 | 1.24 (1.1 to 1.4) | 0.005 |
| Lower health literacy compared with higher health literacy – ability to communicate | 1.2 (1.0 to 1.3) | 2269 | 0.013 | ||
| Recent use of health care | |||||
| Ambulance use | 0.618 | ||||
| Never | |||||
| ≥ 12 months | |||||
| < 12 months | |||||
| Ambulance frequent user | 0.040 | ||||
| < 3 times | 1 | 2842 | |||
| ≥ 3 times in 12 months | 1.7 (1.0 to 2.8) | 64 | |||
| ED use | 0.006 | ||||
| Never | 1 | 411 | |||
| ≥ 12 months | 0.7 (0.5 to 0.8) | 1478 | |||
| 6–12 months | 0.6 (0.5 to 0.9) | 366 | |||
| 3–6 months | 0.7 (0.5 to 0.98) | 234 | |||
| < 3 months | 0.8 (0.6 to 1.0) | 416 | |||
| ED frequent user | 0.072 | ||||
| < 3 times | |||||
| ≥ 3 times in 12 months | |||||
| Contacted GP | < 0.001 | 0.016 | |||
| ≥ 12 months | 1 | 1 | |||
| Never | 1.0 (0.6 to 1.8) | 1.0 (0.5 to 2.1) | |||
| 6–12 months | 1.5 (1.1 to 2.0) | 1.5 (1.1 to 2.1) | |||
| 3–6 months | 1.2 (0.9 to 1.6) | 0.9 (0.7 to 1.3) | |||
| < 3 months | 1.6 (1.3 to 2.1) | 1.3 (0.98 to 1.7) | |||
| Attitudes towards overuse of health services | |||||
| Too many use 999 | 0.571 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Too many use ED | 0.097 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Too many use GP | < 0.001 | ||||
| Strongly agree/agree | 1 | 2082 | |||
| Neither | 1.3 (1.1 to 1.7) | 577 | |||
| Disagree/strongly disagree | 1.5 (1.1 to 1.9) | 247 | |||
| Reluctance to use ED | 0.022 | ||||
| Strongly agree/agree | 1 | 1348 | |||
| Neither | 0.9 (0.7 to 1.0) | 734 | |||
| Disagree/strongly disagree | 0.8 (0.6 to 0.9) | 824 | |||
| Variables | Sig. | Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age of respondent(grouped) < 7 category > dv | 0.053 | |||
| Age of respondent(grouped) < 7 category > dv(1) | 0.654 | 1.116 | 0.689 | 1.808 |
| Age of respondent(grouped) < 7 category > dv(2) | 0.952 | 0.985 | 0.612 | 1.588 |
| Age of respondent(grouped) < 7 category > dv(3) | 0.900 | 0.969 | 0.599 | 1.569 |
| Age of respondent(grouped) < 7 category > dv(4) | 0.091 | 1.501 | 0.938 | 2.402 |
| Age of respondent(grouped) < 7 category > dv(5) | 0.274 | 1.309 | 0.808 | 2.120 |
| Age of respondent(grouped) < 7 category > dv(6) | 0.049 | 1.695 | 1.003 | 2.866 |
| Limiting long-term condition or disability dv | 0.902 | |||
| Limiting long-term condition or disability dv(1) | 0.578 | 0.930 | 0.721 | 1.200 |
| Limiting long-term condition or disability dv(2) | 0.884 | 1.024 | 0.748 | 1.402 |
| Limiting long-term condition or disability dv(3) | 0.734 | 1.377 | 0.218 | 8.708 |
| DV To which of these racial groups do you consider you belong? (compressed)(1) | 0.001 | 1.845 | 1.306 | 2.607 |
| 2007 version: Government office region | 0.045 | |||
| 2007 version: Government office region(1) | 0.753 | 1.050 | 0.775 | 1.422 |
| 2007 version: Government office region(2) | 0.034 | 1.370 | 1.024 | 1.832 |
| 2007 version: Government office region(3) | 0.263 | 1.264 | 0.839 | 1.904 |
| 2007 version: Government office region(4) | 0.039 | 1.669 | 1.026 | 2.715 |
| 2007 version: Government office region(5) | 0.030 | 1.545 | 1.043 | 2.291 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)? | 0.678 | |||
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(1) | 0.539 | 0.876 | 0.573 | 1.338 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(2) | 0.335 | 0.834 | 0.578 | 1.206 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(3) | 0.588 | 0.923 | 0.691 | 1.233 |
| When did you last see or speak to an accident and emergency department (A&E) (for yourself or someone else)?(4) | 0.685 | 1.079 | 0.747 | 1.559 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)? | 0.033 | |||
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(1) | 0.029 | 0.740 | 0.564 | 0.970 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(2) | 0.211 | 1.185 | 0.908 | 1.548 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(3) | 0.166 | 0.802 | 0.587 | 1.096 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(4) | 0.568 | 0.796 | 0.364 | 1.741 |
| Do you personally have internet access at home/work/elsewhere or on a smartphone/tablet/mobile device?(1) | 0.681 | 1.074 | 0.765 | 1.508 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do | 0.201 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(1) | 0.572 | 1.100 | 0.791 | 1.529 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(2) | 0.072 | 1.352 | 0.974 | 1.877 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(3) | 0.106 | 1.314 | 0.943 | 1.831 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(4) | 0.498 | 0.640 | 0.176 | 2.325 |
| How many, if any, cars or vans does your household own or have the regular use of? <summary> | 0.561 | |||
| How many, if any, cars or vans does your household own or have the regular use of? <summary>(1) | 0.672 | 1.068 | 0.787 | 1.449 |
| How many, if any, cars or vans does your household own or have the regular use of? <summary>(2) | 0.339 | 1.163 | 0.854 | 1.583 |
| In general, would you say your health is . . . (excellent to poor) | 0.914 | |||
| In general, would you say your health is . . . (excellent to poor)(1) | 0.684 | 0.928 | 0.648 | 1.330 |
| In general, would you say your health is . . . (excellent to poor)(2) | 0.984 | 1.004 | 0.696 | 1.448 |
| In general, would you say your health is . . . (excellent to poor)(3) | 0.720 | 0.925 | 0.602 | 1.420 |
| In general, would you say your health is . . . (excellent to poor)(4) | 0.855 | 1.052 | 0.612 | 1.807 |
| In general, would you say your health is . . . (excellent to poor)(5) | 0.461 | 1.485 | 0.519 | 4.250 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D | 0.563 | |||
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(1) | 0.213 | 0.871 | 0.701 | 1.082 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(2) | 0.497 | 0.835 | 0.497 | 1.405 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(3) | 0.789 | 1.076 | 0.629 | 1.839 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do | 0.376 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(1) | 0.592 | 0.927 | 0.703 | 1.222 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(2) | 0.210 | 0.824 | 0.608 | 1.116 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(3) | 0.118 | 0.763 | 0.543 | 1.071 |
| HPrbDr13 | 0.471 | |||
| HPrbDr13(1) | 0.330 | 1.112 | 0.898 | 1.379 |
| HPrbDr13(2) | 0.279 | 1.232 | 0.844 | 1.798 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D | 0.056 | |||
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(1) | 0.563 | 1.106 | 0.786 | 1.556 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(2) | 0.027 | 1.408 | 1.041 | 1.906 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(3) | 0.707 | 1.083 | 0.715 | 1.640 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain | 0.568 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(1) | 0.979 | 0.997 | 0.802 | 1.239 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(2) | 0.309 | 0.850 | 0.621 | 1.163 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(3) | 0.184 | 0.698 | 0.412 | 1.185 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(4) | 0.791 | 1.105 | 0.530 | 2.304 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious | 0.014 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(1) | 0.318 | 0.857 | 0.632 | 1.161 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(2) | 0.007 | 0.657 | 0.485 | 0.890 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(3) | 0.009 | 0.578 | 0.383 | 0.872 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(4) | 0.068 | 0.577 | 0.320 | 1.040 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)? | 0.326 | |||
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(1) | 0.960 | 0.990 | 0.681 | 1.440 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(2) | 0.447 | 0.905 | 0.700 | 1.170 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(3) | 0.084 | 0.778 | 0.585 | 1.035 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D | 0.663 | |||
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(1) | 0.390 | 0.903 | 0.715 | 1.140 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(2) | 0.511 | 0.920 | 0.718 | 1.180 |
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day | 0.297 | |||
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day(1) | 0.995 | 1.001 | 0.666 | 1.506 |
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day(2) | 0.122 | 0.781 | 0.572 | 1.068 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D | 0.089 | |||
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(1) | 0.220 | 1.224 | 0.887 | 1.689 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(2) | 0.768 | 0.953 | 0.695 | 1.309 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(3) | 0.204 | 0.784 | 0.539 | 1.141 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(4) | 0.592 | 1.159 | 0.675 | 1.993 |
| Can you take time away from your work, during working hours, to see a GP? | 0.118 | |||
| Can you take time away from your work, during working hours, to see a GP?(1) | 0.418 | 0.854 | 0.583 | 1.251 |
| Can you take time away from your work, during working hours, to see a GP?(2) | 0.072 | 0.595 | 0.338 | 1.047 |
| Can you take time away from your work, during working hours, to see a GP?(3) | 0.291 | 1.153 | 0.885 | 1.501 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D | 0.995 | |||
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(1) | 0.917 | 1.016 | 0.756 | 1.366 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(2) | 0.934 | 1.013 | 0.754 | 1.360 |
| Are you registered with a GP?(1) | 0.810 | 0.911 | 0.429 | 1.938 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D | 0.040 | |||
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(1) | 0.349 | 0.901 | 0.725 | 1.120 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(2) | 0.012 | 0.640 | 0.452 | 0.905 |
| Ability | 0.999 | 1.000 | 0.797 | 1.255 |
| Understand | 0.242 | 0.868 | 0.686 | 1.100 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open | 0.928 | |||
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open(1) | 0.756 | 0.964 | 0.763 | 1.218 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open(2) | 0.919 | 1.021 | 0.687 | 1.517 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours | 0.256 | |||
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours(1) | 0.053 | 1.269 | 0.996 | 1.616 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours(2) | 0.188 | 1.246 | 0.898 | 1.730 |
| For unexpected non non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours(3) | 0.778 | 1.081 | 0.629 | 1.859 |
| I think too many people go to their GP when they do not need to | 0.137 | |||
| I think too many people go to their GP when they do not need to(1) | 0.058 | 1.261 | 0.992 | 1.604 |
| I think too many people go to their GP when they do not need to(2) | 0.364 | 1.177 | 0.828 | 1.673 |
| Many people are reluctant to use A&E when they have an urgent health problem | 0.780 | |||
| Many people are reluctant to use A&E when they have an urgent health problem(1) | 0.814 | 0.972 | 0.765 | 1.234 |
| Many people are reluctant to use A&E when they have an urgent health problem(2) | 0.481 | 0.921 | 0.733 | 1.158 |
| Constant | 0.449 | 0.659 | ||
| Variables | Univariate | Final multivariable model | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | n | p-value | Odds ratio (95% CI) | p-value | |
| Sociodemographic characteristics | |||||
| Age (years) | < 0.001 | < 0.001 | |||
| 18–24 | 1 | 169 | 1 | ||
| 25–34 | 0.8 (0.5 to 1.1) | 384 | 0.8 (0.5 to 1.2) | ||
| 35–44 | 0.7 (0.5 to 0.97) | 467 | 0.6 (0.4 to 1.0) | ||
| 45–54 | 0.9 (0.7 to 1.4) | 469 | 1.1 (0.7 to 1.6) | ||
| 55–64 | 1.2 (0.8 to 1.7) | 508 | 1.3 (0.8 to 2.0) | ||
| 65–74 | 1.5 (1.1 to 2.2) | 499 | 1.6 (1.0 to 2.5) | ||
| ≥ 75 | 1.3 (0.9 to 1.9) | 405 | 1.2 (0.7 to 1.9) | ||
| Sex | < 0.001 | < 0.001 | |||
| Female | 1 | 1649 | 1 | ||
| Male | 1.4 (1.2 to 1.6) | 1257 | 1.5 (1.2 to 1.8) | ||
| Ethnicity | < 0.001 | < 0.001 | |||
| White | 1 | 2572 | 1 | ||
| BAME | 2.2 (1.7 to 2.9) | 334 | 2.6 (1.8 to 3.8) | ||
| Social class | < 0.001 | ||||
| I | 1 | 214 | |||
| II | 1.2 (0.9 to 1.6) | 1039 | |||
| III non-manual | 1.5 (1.1 to 2.0) | 569 | |||
| III manual | 2.0 (1.4 to 2.8) | 416 | |||
| IV and V | 1.8 (1.3 to 2.5) | 524 | |||
| Armed forces | 1.2 (0.7 to 2.3) | 52 | |||
| Deprivation | 0.585 | ||||
| 5 (affluent) | |||||
| 4 | |||||
| 3 | |||||
| 2 | |||||
| 1 (most deprived) | |||||
| Rurality | 0.505 | ||||
| Rural | |||||
| Urban | |||||
| Region | 0.003 | ||||
| North England | 1 | 474 | |||
| Midlands | 1.0 (0.8 to 1.3) | 794 | |||
| South England | 1.1 (0.8 to 1.3) | 957 | |||
| London | 1.5 (1.1 to 2.1) | 285 | |||
| Wales | 1.4 (0.9 to 2.1) | 132 | |||
| Scotland | 1.6 (1.2 to 2.2) | 264 | |||
| In household with children aged < 5 years old | 0.006 | ||||
| No | 1 | 2591 | |||
| Yes | 0.7 (0.6 to 0.9) | 300 | |||
| Resources available | |||||
| Car ownership | 0.002 | ||||
| ≥ 1 cars | 1 | 1478 | |||
| No car | 1.5 (1.2 to 1.9) | 428 | |||
| Missing | 1.1 (0.9 to 1.3) | 1000 | |||
| Personal access to the internet | < 0.001 | ||||
| Yes | 1 | 2542 | |||
| No | 1.7 (1.4 to 2.2) | 364 | |||
| Health | |||||
| General health | < 0.001 | ||||
| Excellent | 1 | 223 | |||
| Very good | 0.9 (0.6 to 1.1) | 725 | |||
| Good | 1.0 (0.8 to 1.4) | 799 | |||
| Fair | 1.4 (0.97 to 2.0) | 360 | |||
| Poor | 1.6 (1.0 to 2.4) | 163 | |||
| Can’t choose | 1.6 (0.7 to 3.3) | 39 | |||
| Missing/not included | 1 | ||||
| Long-term limiting illness | < 0.001 | 0.001 | |||
| None | 1 | 1766 | 1 | ||
| Non-limiting | 0.9 (0.8 to 1.1) | 586 | 0.8 (0.7 to 1.1) | ||
| Limiting | 1.6 (1.3 to 2.0) | 541 | 1.5 (1.1 to 2.0) | ||
| Don’t know | 0.5 (0.2 to 1.6) | 13 | 0.5 (0.1 to 2.6) | ||
| Programme theories | |||||
| 1, Risk: uncertainty causes anxiety | |||||
| Worry pain is a sign of something serious | < 0.001 | 0.026 | |||
| Not likely at all | 1 | 358 | 1 | ||
| Not likely | 1.1 (0.9 to 1.4) | 1138 | 1.0 (0.8 to 1.4) | ||
| Fairly likely | 1.5 (1.2 to 1.9) | 876 | 1.3 (0.95 to 1.8) | ||
| Very likely | 2.5 (1.8 to 3.4) | 415 | 1.6 (1.1 to 2.4) | ||
| It depends | 119 | 1.3 (0.8 to 2.3) | |||
| Confident in deciding to see a doctor or self-care | 0.003 | ||||
| Very confident | 1 | 993 | |||
| Fairly confident | 1.1 (0.9 to 1.3) | 1130 | |||
| Not very confident | 1.6 (0.98 to 2.5) | 89 | |||
| Never had problem | 2.2 (1.3 to 3.6) | 97 | |||
| 2, Risk: previous traumatic event | |||||
| Had problem, did not see doctor and was serious | 0.375 | ||||
| No | |||||
| Yes | |||||
| 3, Risk: responsibility for others | |||||
| 4, Speed: need to get back to normal | |||||
| Sleep | < 0.001 | ||||
| Do not see doctor | 1 | 2010 | |||
| See doctor if sleep loss | 1.8 (1.5 to 2.2) | 634 | |||
| See doctor if any loss | 2.5 (1.9 to 3.5) | 262 | |||
| Work | < 0.001 | 0.023 | |||
| Do not see doctor | 1 | 935 | 1 | ||
| See doctor if work loss | 1.3 (1.1 to 1.6) | 1709 | 1.2 (1.0 to 1.5) | ||
| See doctor if any loss | 2.7 (1.9 to 3.7) | 262 | 1.7 (1.1 to 2.5) | ||
| 5, Speed: need to seek pain relief | |||||
| Likely to take medication | 0.028 | ||||
| Very likely | 1 | 1081 | |||
| Fairly | 0.9 (0.7 to 1.1) | 1257 | |||
| Not very | 0.7 (0.5 to 0.9) | 376 | |||
| Not at all | 0.7 (0.5 to 1.1) | 135 | |||
| Depends | 0.7 (0.4 to 1.2) | 57 | |||
| 6, Speed: waited long enough | |||||
| 7a, Stressful lives | |||||
| Overwhelmed when have health problem | < 0.001 | 0.031 | |||
| Strongly disagree | 1 | 487 | 1 | ||
| Disagree | 1.2 (0.98 to 1.5) | 872 | 1.0 (0.8 to 1.3) | ||
| Neither | 2.0 (1.5 to 2.6) | 537 | 1.4 (1.1 to 1.9) | ||
| Strongly agree/agree | 2.1 (1.6 to 2.9) | 314 | 1.3 (0.9 to 1.8) | ||
| Never had problem | 2.0 (1.2 to 3.1) | 99 | 1.7 (1.0 to 2.8) | ||
| Find life stressful | 0.012 | ||||
| No | 1 | 637 | |||
| A bit | 1.0 (0.8 to 1.2) | 1316 | |||
| Quite | 0.8 (0.6 to 1.0) | 637 | |||
| Very | 0.9 (0.7 to 1.2) | 297 | |||
| Don’t know | 0.2 (0.1 to 0.7) | 19 | |||
| Someone to care for them if they are ill | 0.004 | ||||
| Definitely | 1 | 1240 | |||
| Probably | 0.9 (0.8 to 1.1) | 697 | |||
| Probably not | 1.1 (0.8 to 1.4) | 280 | |||
| Don’t know | 2.3 (1.4 to 3.9) | 92 | |||
| Can take time off work for GP | < 0.001 | ||||
| Yes | 1 | 1078 | |||
| Yes but not easy | 0.8 (0.6 to 1.0) | 275 | |||
| No | 0.7 (0.5 to 1.0) | 127 | |||
| Not applicable/missing | 1.5 (1.3 to 1.8) | 1426 | |||
| 7b, Low burden | |||||
| Travel to ED | < 0.001 | ||||
| Very difficult | 1 | 610 | |||
| Neither | 0.7 (0.5 to 0.96) | 269 | |||
| Fairly easy | 0.7 (0.6 to 0.9) | 1172 | |||
| Very easy | 0.6 (0.5 to 0.7) | 855 | |||
| Opening hours a problem | 0.239 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Prefer no appointments | < 0.001 | ||||
| Disagree/strongly disagree | 1 | 685 | |||
| Neither | 1.2 (1.0 to 1.5) | 799 | |||
| Strongly agree/agree | 1.6 (1.3 to 2.0) | 825 | |||
| Want convenient times | 0.737 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Willing to wait in waiting room | < 0.001 | ||||
| Disagree/strongly disagree | 1 | 361 | |||
| Neither | 0.9 (0.7 to 1.3) | 194 | |||
| Strongly agree/agree | 1.6 (1.3 to 2.0) | 2351 | |||
| 8, Compliance with family/friends | |||||
| Check with family and friends for what to do | 0.027 | ||||
| Not very likely | 1 | 545 | |||
| Not likely | 1.0 (0.8 to 1.3) | 746 | |||
| Fairly likely | 1.1 (0.9 to 1.3) | 1061 | |||
| Very likely | 1.4 (1.1 to 1.8) | 554 | |||
| 9, Views of services | |||||
| Prefer ED for quick tests | < 0.001 | < 0.001 | |||
| Disagree/strongly disagree | 1 | 1159 | 1 | ||
| Neither | 1.6 (1.3 to 1.9) | 797 | 1.3 (1.1 to 1.7) | ||
| Strongly agree/agree | 2.6 (1.9 to 3.3) | 353 | 1.9 (1.4 to 2.6) | ||
| Missing, self-complete | 0 | ||||
| Doctors know more at ED | < 0.001 | ||||
| Disagree/strongly disagree | 1 | 850 | |||
| Neither | 1.5 (1.2 to 1.8) | 1041 | |||
| Strongly agree/agree | 1.4 (1.1 to 1.8) | 418 | |||
| Missing, self-complete | 0 | ||||
| No confidence in GP | 0.895 | ||||
| Strongly disagree | |||||
| Disagree | |||||
| Neither | |||||
| Agree | |||||
| Strongly agree | |||||
| Don’t know | |||||
| Missing | |||||
| Missing, self-complete | |||||
| 10, Frustration with access to GP | |||||
| Hard to get GP appointment | 0.940 | ||||
| Disagree/strongly disagree | |||||
| Neither | |||||
| Strongly agree/agree | |||||
| Missing, self-complete | |||||
| Registered with GP | 0.019 | ||||
| Yes | 1 | 2840 | |||
| No | 0.6 (0.3 to 0.9) | 65 | |||
| Work or looking after family makes it difficult to see GP | < 0.001 | 0.040 | |||
| Disagree/strongly disagree | 1 | 1197 | 1 | ||
| Neither | 1.2 (0.98 to 1.5) | 455 | 1.0 (0.8 to 1.3) | ||
| Strongly agree/agree | 0.7 (0.5 to 0.8) | 410 | 0.7 (0.5 to 0.9) | ||
| Not applicable | 1.2 (0.9 to 1.6) | 247 | 0.9 (0.7 to 1.3) | ||
| Believe people use ED because can’t get GP appointment | 0.499 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Awareness of services | |||||
| Know range of NHS services to use | 0.118 | ||||
| Very confident | |||||
| Fairly confident | |||||
| Not confident/not at all | |||||
| Can find out when NHS services are open | 0.007 | ||||
| Very confident | 1 | 1487 | |||
| Fairly confident | 1.2 (1.1 to 1.5) | 1163 | |||
| Not confident/not at all | 1.4 (1.0 to 1.8) | 255 | |||
| Can find out what tests available at services | 0.753 | ||||
| Very confident | |||||
| Fairly confident | |||||
| Not confident/not at all | |||||
| How to contact GP OOH | 0.008 | 0.043 | |||
| Very confident | 1 | 1338 | 1 | ||
| Fairly confident | 1.1 (0.96 to 1.3) | 1056 | 1.1 (0.9 to 1.4) | ||
| Not very confident | 1.5 (1.2 to 1.9) | 389 | 1.5 (1.1 to 2.0) | ||
| Not at all confident | 0.9 (0.6 to 1.4) | 122 | 0.8 (0.5 to 1.3) | ||
| Will look up on the internet to see what to do | < 0.001 | 0.015 | |||
| Very likely | 1 | 428 | 1 | ||
| Fairly likely | 0.8 (0.7 to 1.1) | 752 | 1.0 (0.7 to 1.3) | ||
| Not very likely | 1.3 (1.0 to 1.7) | 680 | 1.3 (1.0 to 1.8) | ||
| Not at all | 1.4 (1.1 to 1.7) | 1016 | 1.3 (1.0 to 1.8) | ||
| Missing | 0.7 (0.3 to 1.4) | 30 | 0.5 (0.2 to 1.5) | ||
| Will look up on the internet to decide what problem is | < 0.001 | ||||
| Very likely | 1 | 667 | |||
| Fairly likely | 0.9 (0.7 to 1.1) | 797 | |||
| Not very likely | 1.2 (0.95 to 1.6) | 472 | |||
| Not at all | 1.4 (1.1 to 1.7) | 940 | |||
| Missing | 0.6 (0.3 to 1.2) | 30 | |||
| Recursivity | |||||
| If tests are done I was right to make contact | < 0.001 | 0.002 | |||
| Disagree/strongly disagree | 1 | 280 | 1 | ||
| Neither | 1.8 (1.3 to 2.3) | 793 | 1.4 (1.0 to 1.9) | ||
| Strongly agree/agree | 2.5 (1.9 to 3.2) | 1236 | 1.7 (1.2 to 2.2) | ||
| Missing, self-complete | 0 | ||||
| Health literacy | |||||
| Lower health literacy compared with higher health literacy – understand information | 1.5 (1.3 to 1.7) | < 0.001 | |||
| Lower health literacy compared with higher health literacy – ability to communicate | 1.2 (1.1 to 1.4) | 0.005 | |||
| Recent use of health care | |||||
| Ambulance use | 0.238 | ||||
| Never | |||||
| ≥ 12 months | |||||
| < 12 months | |||||
| Ambulance frequent user | 0.235 | ||||
| < 3 times | |||||
| ≥ 3 times in 12 months | |||||
| ED use | 0.450 | ||||
| Never | |||||
| ≥ 12 months | |||||
| 6–12 months | |||||
| 3–6 months | |||||
| < 3 months | |||||
| ED frequent user | 0.017 | ||||
| < 3 times | 1 | 2738 | |||
| ≥ 3 times in 12 months | 1.5 (1.1 to 2.1) | 167 | |||
| Contacted GP | 0.015 | 0.043 | |||
| ≥ 12 months | 454 | 1 | |||
| Never | 0.8 (0.5 to 1.4) | 65 | 0.7 (0.4 to 1.5) | ||
| 6–12 months | 1.3 (0.98 to 1.7) | 484 | 1.5 (1.1 to 2.1) | ||
| 3–6 months | 1.2 (0.9 to 1.5) | 518 | 1.1 (0.8 to 1.6) | ||
| < 3 months | 1.4 (1.1 to 1.7) | 1384 | 1.4 (0.98 to 1.7) | ||
| Attitudes towards overuse of health services | |||||
| Too many use 999 | 0.112 | ||||
| Strongly agree/agree | |||||
| Neither | |||||
| Disagree/strongly disagree | |||||
| Too many use ED | 0.015 | ||||
| Strongly agree/agree | 1 | 2515 | |||
| Neither | 1.4 (1.1 to 1.8) | 291 | |||
| Disagree/strongly disagree | 1.5 (0.95 to 2.3) | 100 | |||
| Too many use GP | 0.017 | ||||
| Strongly agree/agree | 1 | 2082 | |||
| Neither | 1.3 (1.0 to 1.5) | 577 | |||
| Disagree/strongly disagree | 1.3 (1.0 to 1.8) | 247 | |||
| Reluctance to use ED | 0.043 | ||||
| Strongly agree/agree | 1 | 1348 | |||
| Neither | 0.9 (0.8 to 1.1) | 734 | |||
| Disagree/strongly disagree | 0.8 (0.7 to 0.95) | 824 | |||
| Variables | Sig. | Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age of respondent(grouped) < 7 category > dv | 0.000 | |||
| Age of respondent(grouped) < 7 category > dv(1) | 0.828 | 0.943 | 0.555 | 1.602 |
| Age of respondent(grouped) < 7 category > dv(2) | 0.320 | 0.770 | 0.461 | 1.288 |
| Age of respondent(grouped) < 7 category > dv(3) | 0.222 | 1.379 | 0.824 | 2.308 |
| Age of respondent(grouped) < 7 category > dv(4) | 0.051 | 1.678 | 0.998 | 2.820 |
| Age of respondent(grouped) < 7 category > dv(5) | 0.014 | 2.007 | 1.154 | 3.491 |
| Age of respondent(grouped) < 7 category > dv(6) | 0.301 | 1.375 | 0.752 | 2.514 |
| Sex of respondent(1) | 0.000 | 0.667 | 0.538 | 0.827 |
| Limiting long-term condition or disability dv | 0.003 | |||
| Limiting long-term condition or disability dv(1) | 0.132 | 0.822 | 0.636 | 1.061 |
| Limiting long-term condition or disability dv(2) | 0.013 | 1.544 | 1.095 | 2.178 |
| Limiting long-term condition or disability dv(3) | 0.190 | 0.233 | 0.026 | 2.063 |
| Respondent: social class [pre-SOC2000] best estimate dv | 0.395 | |||
| Respondent: social class [pre-SOC2000] best estimate dv(1) | 0.333 | 1.203 | 0.827 | 1.750 |
| Respondent: social class [pre-SOC2000] best estimate dv(2) | 0.157 | 1.346 | 0.892 | 2.029 |
| Respondent: social class [pre-SOC2000] best estimate dv(3) | 0.055 | 1.555 | 0.991 | 2.440 |
| Respondent: social class [pre-SOC2000] best estimate dv(4) | 0.094 | 1.453 | 0.938 | 2.251 |
| Respondent: social class [pre-SOC2000] best estimate dv(5) | 0.861 | 1.083 | 0.445 | 2.638 |
| IMD_ALL | 0.514 | |||
| IMD_ALL(1) | 0.725 | 1.063 | 0.757 | 1.493 |
| IMD_ALL(2) | 0.398 | 1.157 | 0.825 | 1.624 |
| IMD_ALL(3) | 0.415 | 1.147 | 0.825 | 1.595 |
| IMD_ALL(4) | 0.098 | 1.333 | 0.949 | 1.874 |
| DV To which of these racial groups do you consider you belong? (compressed)(1) | 0.000 | 2.431 | 1.574 | 3.753 |
| 2007 version: Government office region | 0.095 | |||
| 2007 version: Government office region(1) | 0.934 | 0.987 | 0.731 | 1.333 |
| 2007 version: Government office region(2) | 0.755 | 0.954 | 0.711 | 1.280 |
| 2007 version: Government office region(3) | 0.111 | 1.428 | 0.921 | 2.212 |
| 2007 version: Government office region(4) | 0.235 | 1.375 | 0.813 | 2.325 |
| 2007 version: Government office region(5) | 0.079 | 1.457 | 0.957 | 2.219 |
| Number of Respondents children in HH aged 0–4yrs – dv(1) | 0.540 | 1.120 | 0.779 | 1.609 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)? | 0.061 | |||
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(1) | 0.344 | 0.880 | 0.674 | 1.147 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(2) | 0.396 | 1.127 | 0.855 | 1.486 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(3) | 0.029 | 0.713 | 0.526 | 0.966 |
| When did you last see or speak to a GP from your GP surgery (for yourself or someone else)?(4) | 0.191 | 0.593 | 0.272 | 1.296 |
| Do you personally have internet access at home/work/elsewhere or on a smartphone/tablet/mobile device?(1) | 0.420 | 1.177 | 0.792 | 1.751 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be | 0.989 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(1) | 0.877 | 0.973 | 0.687 | 1.378 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(2) | 0.762 | 0.937 | 0.613 | 1.431 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(3) | 0.604 | 0.869 | 0.512 | 1.476 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what the problem might be(4) | 0.792 | 0.771 | 0.111 | 5.338 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do | 0.239 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(1) | 0.935 | 1.017 | 0.686 | 1.507 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(2) | 0.170 | 1.356 | 0.878 | 2.094 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(3) | 0.194 | 1.445 | 0.829 | 2.521 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . look on the internet to decide what to do(4) | 0.465 | 0.481 | 0.068 | 3.423 |
| How many, if any, cars or vans does your household own or have the regular use of? <summary> | 0.820 | |||
| How many, if any, cars or vans does your household own or have the regular use of? <summary>(1) | 0.998 | 1.000 | 0.712 | 1.405 |
| How many, if any, cars or vans does your household own or have the regular use of? <summary>(2) | 0.710 | 1.069 | 0.753 | 1.516 |
| In general, would you say your health is . . . (excellent to poor) | 0.424 | |||
| In general, would you say your health is . . . (excellent to poor)(1) | 0.101 | 0.743 | 0.521 | 1.059 |
| In general, would you say your health is . . . (excellent to poor)(2) | 0.261 | 0.809 | 0.560 | 1.170 |
| In general, would you say your health is . . . (excellent to poor)(3) | 0.364 | 0.814 | 0.521 | 1.270 |
| In general, would you say your health is . . . (excellent to poor)(4) | 0.059 | 0.568 | 0.316 | 1.022 |
| In general, would you say your health is . . . (excellent to poor)(5) | 0.750 | 0.813 | 0.228 | 2.903 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D | 0.558 | |||
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(1) | 0.170 | 0.855 | 0.684 | 1.070 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(2) | 0.861 | 0.949 | 0.530 | 1.699 |
| How confident are you in deciding when to see a doctor, or deal with the problem yourself, for an unexpected non-life-threatening health problem? SC: B, C, D(3) | 0.886 | 1.053 | 0.519 | 2.135 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do | 0.534 | |||
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(1) | 0.141 | 0.801 | 0.597 | 1.076 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(2) | 0.377 | 0.866 | 0.629 | 1.192 |
| For unexpected non-life-threatening health problem, how likely is it you would . . . check what family or friends think you should do(3) | 0.405 | 0.861 | 0.605 | 1.225 |
| HPrbDr13 | 0.085 | |||
| HPrbDr13(1) | 0.086 | 1.205 | 0.974 | 1.491 |
| HPrbDr13(2) | 0.058 | 1.557 | 0.984 | 2.464 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D | 0.058 | |||
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(1) | 0.033 | 1.453 | 1.032 | 2.047 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(2) | 0.008 | 1.489 | 1.109 | 1.997 |
| My work or looking after my family makes it difficult to see a GP SC: B, C, D(3) | 0.077 | 1.475 | 0.959 | 2.267 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain | 0.697 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(1) | 0.752 | 0.965 | 0.772 | 1.206 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(2) | 0.182 | 0.810 | 0.594 | 1.104 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(3) | 0.454 | 0.835 | 0.520 | 1.340 |
| For unexpected non-life-threatening pain, how likely is it you would . . . take medication to stop the pain(4) | 0.700 | 0.860 | 0.400 | 1.850 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious | 0.140 | |||
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(1) | 0.203 | 0.799 | 0.566 | 1.129 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(2) | 0.014 | 0.654 | 0.466 | 0.919 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(3) | 0.070 | 0.677 | 0.444 | 1.033 |
| For unexpected non-life-threatening pain, how likely is it you would . . . worry that it is a sign of something serious(4) | 0.420 | 0.780 | 0.426 | 1.427 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)? | 0.228 | |||
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(1) | 0.112 | 0.723 | 0.484 | 1.079 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(2) | 0.414 | 0.892 | 0.678 | 1.174 |
| How easy or difficult would you find it to travel to an accident and emergency department (A&E)?(3) | 0.086 | 0.773 | 0.576 | 1.037 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D | 0.598 | |||
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(1) | 0.427 | 0.906 | 0.710 | 1.156 |
| I prefer NHS services where I don’t need to make an appointment SC: B, C, D(2) | 0.345 | 0.885 | 0.688 | 1.140 |
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day | 0.304 | |||
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day(1) | 0.150 | 0.735 | 0.484 | 1.118 |
| For unexpected non-life-threatening health problem . . . I’m willing to wait a few hours in a waiting room if it means I can be seen that day(2) | 0.482 | 0.900 | 0.671 | 1.207 |
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D | 0.110 | |||
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D(1) | 0.053 | 0.799 | 0.637 | 1.003 |
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D(2) | 0.556 | 0.909 | 0.662 | 1.249 |
| Do you have family, friends or a partner who could look after them if have an unexpected non-life-threatening health problem? SC: B, C, D(3) | 0.212 | 1.602 | 0.765 | 3.356 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D | 0.070 | |||
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(1) | 0.491 | 1.137 | 0.790 | 1.636 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(2) | 0.242 | 0.814 | 0.576 | 1.150 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(3) | 0.196 | 0.773 | 0.524 | 1.142 |
| When I have an unexpected health problem that is not life-threatening, I tend to feel overwhelmed SC: B, C, D(4) | 0.497 | 1.229 | 0.677 | 2.232 |
| Generally, do you find your life stressful? | 0.989 | |||
| Generally, do you find your life stressful?(1) | 0.664 | 1.059 | 0.816 | 1.375 |
| Generally, do you find your life stressful?(2) | 0.708 | 1.062 | 0.775 | 1.456 |
| Generally, do you find your life stressful?(3) | 0.878 | 1.032 | 0.687 | 1.552 |
| Generally, do you find your life stressful?(4) | 0.791 | 0.803 | 0.159 | 4.062 |
| Can you take time away from your work, during working hours, to see a GP? | 0.414 | |||
| Can you take time away from your work, during working hours, to see a GP?(1) | 0.827 | 1.040 | 0.732 | 1.477 |
| Can you take time away from your work, during working hours, to see a GP?(2) | 0.109 | 0.662 | 0.399 | 1.097 |
| Can you take time away from your work, during working hours, to see a GP?(3) | 0.997 | 1.000 | 0.761 | 1.314 |
| I think doctors at A&E know more than GPs SC: B, C, D | 0.059 | |||
| I think doctors at A&E know more than GPs SC: B, C, D(1) | 0.022 | 1.402 | 1.049 | 1.873 |
| I think doctors at A&E know more than GPs SC: B, C, D(2) | 0.039 | 1.380 | 1.016 | 1.874 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D | 0.000 | |||
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(1) | 0.012 | 0.639 | 0.452 | 0.904 |
| I prefer A&E to a GP because I can get tests done quickly SC: B, C, D(2) | 0.000 | 0.476 | 0.336 | 0.674 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D | 0.026 | |||
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(1) | 0.205 | 0.866 | 0.693 | 1.082 |
| If a service does tests on me, it shows I was right to go to that service SC: B, C, D(2) | 0.008 | 0.653 | 0.477 | 0.893 |
| Ability | 0.916 | 1.013 | 0.803 | 1.278 |
| Understand | 0.474 | 0.912 | 0.710 | 1.172 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open | 0.644 | |||
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open(1) | 0.582 | 0.935 | 0.737 | 1.187 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, when NHS services are open(2) | 0.592 | 1.127 | 0.728 | 1.747 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours | 0.018 | |||
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours(1) | 0.134 | 1.206 | 0.944 | 1.541 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours(2) | 0.005 | 1.663 | 1.168 | 2.367 |
| For unexpected non-life-threatening health problem, how confident are you that . . . you know, or can easily find out, how to contact GP out of hours(3) | 0.488 | 0.822 | 0.473 | 1.429 |
| I think too many people use A&E when they do not need to | 0.366 | |||
| I think too many people use A&E when they do not need to(1) | 0.193 | 1.285 | 0.881 | 1.875 |
| I think too many people use A&E when they do not need to(2) | 0.498 | 1.248 | 0.657 | 2.373 |
| I think too many people go to their GP when they do not need to | 0.173 | |||
| I think too many people go to their GP when they do not need to(1) | 0.066 | 1.284 | 0.983 | 1.675 |
| I think too many people go to their GP when they do not need to(2) | 0.490 | 1.148 | 0.776 | 1.698 |
| Many people are reluctant to use A&E when they have an urgent health problem | 0.929 | |||
| Many people are reluctant to use A&E when they have an urgent health problem(1) | 0.820 | 0.972 | 0.759 | 1.245 |
| Many people are reluctant to use A&E when they have an urgent health problem(2) | 0.710 | 0.958 | 0.762 | 1.204 |
| Constant | 0.093 | 3.014 | ||
Appendix 10 Integration grid
| Themes | WP1 realist review | WP2 qualitative interviews | WP2 focus groups | WP3 survey | Convergence, complementarity, disagreement, and silence |
|---|---|---|---|---|---|
| PT1 Uncertainty causing anxiety | When there is uncertainty surrounding symptoms (M) because they do not fit with people’s expectations or prior experience (e.g. last longer, are more severe, are unfamiliar or do not respond to self-care in the expected timescale) (C/M), this increases the perceived risk that the problem may be serious (M) and an immediate need to establish what is wrong and obtain reassurance (M). This concern prompts the use of the ED (O), where it is perceived that the most appropriate resources and expertise required to establish cause can be accessed quickly (C), often in the context of timely or satisfactory answers not having been received from primary care services (C) |
|
Yes | Tendency to use ambulance, GP and any service | Convergence |
| PT2 Previous traumatic event | When people have experience of previous traumatic health incidents (e.g. delayed help-seeking leading to serious consequences), or have awareness of such incidents experienced by others or in the media (C), they have increased anxiety and awareness of danger (C/M) and reduced confidence in their own judgement (M). They are therefore unwilling to take risks when a health problem arises (M), leading them to seek immediate help and advice from an expert in the form of emergency care, including ambulance services and EDs (O) |
|
– | No | Disagreement: may simply be part of PT1, no support for this in survey but review highlights that people may not be aware of it. Also did we measure it well enough in the survey? |
| PT3 Responsibility for others | When people are in a position of responsibility for others they are less willing to take risks with someone else’s health than with their own, and fear the consequences (e.g. distress/guilt, dismissal, litigation) (M) of not doing ‘the right thing’. This leads them to seek or to recommend seeking urgent care, particularly the ED (O) |
|
Yes |
|
Some convergence: strongly present for parents of young children |
| PT4 Inability to function normally | When people are prevented them from undertaking their normal lives, roles or responsibilities (e.g. paid work, child care) (C), this creates a need to get back to normal quickly (M), to get on with their lives and discharge their responsibilities. This prompts use of urgent care (O) because it can resolve a problem quickly by being both more accessible and more efficient than alternatives (C) |
|
Yes |
|
Convergence |
| PT5 Need for immediate pain relief | When people are in pain or discomfort which they find intolerable (C/M), and they believe or experience that no primary care appointments are available within an acceptable time period (C), they seek care from a more urgent service – usually the ED (O) – because of a need to obtain prompt relief from their distress (M) |
|
Pharmacists offer free prescriptions not just GPs (DEP) | No | Some convergence but not supported by survey. However, we did not measure this well |
| PT6 Delayed already so cannot wait longer | When people delay seeking primary care treatment (for various reasons, including deliberation and indecision, cost of treatment, lack of transport, complex living situations, mistrust of health services and work responsibilities) (C), they wait, often using self-help measures, and hope that the situation will improve or go away (C). The condition reaches a ‘tipping point’ where either it is no longer tolerable (M) or other circumstances force a decision (M), and people feel they cannot wait any longer (M). At this point, if a primary care service is unavailable to them (C), they feel they have no choice but to use an emergency service (O) |
|
Yes | Not tested in regression | Some convergence but not tested in regression |
| PT7 Complex/stressful lives and inability to cope | When people are already experiencing significant stresses which impact on the internal and external resources available to them (money, time) (C) they have less capacity to cope with the additional challenge of a new or changed health problem. Symptoms are therefore likely to trigger emotional distress, including feelings of loss of control and helplessness (M), leading them to use emergency services because this is less burdensome than making an appointment with a GP. This is more likely to occur when people cannot easily or quickly access a primary care service (C) |
|
|
Tendency for ambulance, ED, GP and any service |
|
| PT8 Compliance: following advice of trusted others | When people are anxious or concerned about a health problem and have sought the advice of trusted others (C), either in their social network (e.g. family) or health professionals (particularly primary care staff), and have been advised to seek urgent care, particularly the ED (M), they are likely to then use those emergency services (O) |
Featured for YP, with lots of shared decision-making (YP) Social network norms about attending ED (YP, PAR) |
Yes | Features in a number of the univariate analyses but not the multivariable | Convergence but not as one of the strongest drivers |
| PT9 Availability and quality of service | When people have individual experience or knowledge, or cultural beliefs about the differing quality or availability of primary and emergency services [e.g. primary care offering inadequate diagnosis and care or discrimination (US context only)], or EDs having better resources, expertise or more thorough care (C), they are likely to choose emergency care, particularly the ED (O) in which they have more trust and confidence (M) |
|
Yes | Tendency for ED based on attraction of ED rather than problems with GP | Some disagreement: review, interviews and focus groups show unhappiness with GP but it is attraction of ED that explains tendency |
| PT10 Frustration with access to GP | When people are unable to obtain an appointment with a primary care practitioner (C/M) this can further exacerbate the feelings of anxiety and cause panic (M). Individuals can experience feelings of frustration (M), mistrust (M), and the perception of an uncaring service (M), feeling they have no other choice (M) but to contact an emergency service (O) |
|
|
Did not explain tendency |
|
| Other drivers | |||||
| Awareness of services | Lack of awareness of alternatives appeared in some reviews and articles but not strongly enough to be a PT |
|
|
Awareness of how to contact GP OOH explains tendency to use any service | Some disagreement. Big topic of conversation in the focus groups but did not feature strongly in other components. Is this because it is not a strong driver? |
| Problems with other services such as NHS 111, WIC and MIU | – | Did not necessarily like alternatives (DEP) |
|
– | The focus groups identified details about this issue even though in the interviews we asked why they did not use alternatives |
| Recursivity: learnt behaviour | In qualitative study about chronic conditions |
|
Tendency to use ED, GP and any service |
|
|
| Health literacy | Some evidence in recent quantitative publications about EDs |
|
|
Tendency to use ambulance and GP | Some convergence but difficult to see it in the interviews |
| Recent use of services | – | – | – |
|
This factor was tested because we felt that people who had used services recently would base their vignette answers on experience. It could explain tendency because people are ill, or this could be related to recursivity in that it is easier to use it a second time if use recently? |
| Attitudes towards health service misuse | A couple of quantitative articles identified population views of this, showing high levels of agreement about misuse | – | Educate or punish offenders and misusers (YP, DEP) | People who do not think services are misused tend to be ‘clinically unnecessary’ users in univariate analyses for all the services but may be correlated with other variables because does not appear in most of the multivariable regressions | Not enough information about this but certainly worth exploring further |
| Convenience | Appears frequently in different reviews |
|
Co-locate services in local areas (DEP) | Not explicitly addressed | PT4 and PT7 could appear to be convenience, and interviewees may give accounts of being appropriate users, but little evidence of misuse for convenience. Cost of travel is an issue for people with little money |
| Digital use | – |
|
Develop app to direct people to best care (YP) | Lack of access to the internet increased tendency to use ambulance | Not many findings about this but could be explored further as an intervention (e.g. NHS 111 Online) |
| Time of day/day of week | Evident in some reviews |
|
GP wanted outside office hours (YP, DEP) | No real difference between Wednesday and Saturday in child vignettes |
|
| Population subgroups | |||||
| Young people | Nothing in qualitative studies but identified as non-urgent users of EDs in quantitative studies | See above | See above |
|
Disagreement |
| Parents |
|
See above | See above |
|
Disagreement |
| Deprivation/social class/car ownership |
|
See above | See above |
|
Disagreement for ED and GP |
| Ethnicity | Mixed findings in reviews and quantitative studies | – | – | BAME consistently explains ‘clinically unnecessary’ use of all services | Relies on survey to show BAME consistently explains ‘clinically unnecessary’ use of all services |
| Age | – | – | – | Those aged > 65 years more likely to contact GP; those aged 55–74 years more likely to contact ED for a child | Relies on survey to show that older people have higher tendency for some services in some situations |
| Sex | Mixed findings in reviews and quantitative studies | – | – | Males consistently have higher tendency for emergency services, not for GPs | Relies on survey to show that males consistently have higher ‘clinically unnecessary’ use of emergency services |
| Chronic conditions | Appear strongly in PT3, PT9 | PT7 | – | No | Little to say here |
| Region | – | Not addressed | Not addressed | Scotland, Wales, London appear to have higher tendency for ED and GP | WP1 was international, mainly the USA and Australia. WP2 was in two regions in the north/midlands of England so cannot explain why these regional differences appeared consistently for ED and GP use |
| Service-specific drivers | |||||
| Emergency ambulance | Not a lot of qualitative studies but a review based on health professional as well as patient view | Not a lot of interviews | – | Lack of resources is a major issue – no car, no internet access, low health literacy, manual social class | Relies heavily on the survey to show lack of resources an issue |
| ED | Lots of studies identifying the attraction of the ED and poor access to GP |
|
– | Need to get back to normal, stress, attraction of ED with tests and expertise | Convergence of WPs around attraction of ED |
| General practice | Not a lot of qualitative studies | Good access and relationship, best place, proximity | – | Attend if uncertain, have stressful lives, low health literacy | Highlights that people do access GPs in a timely way, use GP and appreciate GP |
Glossary
- ‘Clinically unnecessary’ use
- When patients do not need the level of clinical care or urgency of care provided by the service that they contact.
- Programme theory
- In this study, a proposed explanation of patients’ behaviour.
List of abbreviations
- A&E
- accident and emergency
- BAME
- Black, Asian and minority ethnic
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- ED
- emergency department
- GP
- general practitioner
- HLQ
- Health Literacy Questionnaire
- IMD
- Index of Multiple Deprivation
- IPA
- interpretative phenomenological analysis
- MIU
- minor injuries unit
- NatCen
- National Centre for Social Research
- NIHR
- National Institute for Health Research
- NVS
- Newest Vital Sign
- PPI
- patient and public involvement
- SECF
- Sheffield Emergency Care Forum
- WIC
- walk-in centre
- WP
- work package
